32 weeks, with no history of neonatal medical problems that might cause pulmonary hemorrhage, and whose condition meets all of the following three criteria:\n• Abrupt or sudden onset of overt bleeding or obvious evidence of blood in the airway, including -epistaxis, hemoptysis, or frank blood in the airway below the larynx at visualization, not caused by any medical procedure (e.g., laryngoscopy or intubation); or -identification of hemosiderin-laden macrophages (>20% of pulmonary macrophages containing hemosiderin on bronchoalveolar lavage or biopsy specimen).\nA source of bleeding from the nose and oropharynx should be ruled out at the time of admission. • Severe-appearing illness leading to acute respiratory distress or respiratory failure, resulting in hospitalization in a pediatric intensive care unit (PICU) or neonatal intensive care unit (NICU) with intubation and mechanical ventilation. • Diffuse unilateral or bilateral pulmonary infiltrates visible on CXR or computerized tomography (CT) of the chest. CXR or chest CT findings should be documented within 48 hours of examination of the infant. A previously healthy infant should\n• have been discharged from the hospital after birth with an uneventful course before the occurrence of bronchoalveolar hemorrhage; • never have been previously intubated, nor required respiratory support with oxygen; • not have evidence of physical abuse;\n• not have any abnormality identified on admission or follow-up bronchoscopy that would explain the bleeding; and • not have neonatal medical problems that can cause pulmonary hemorrhage. CDC will adhere closely to this case definition, requiring that all the criteria be met for a confirmed case. The definition for a clinically confirmed case excludes pulmonary hemorrhage among older children and infants with restricted access to a PICU. Because no criteria exist for postmortem examinations, this definition excludes infants who die before hospital and PICU admission, whose illness might have met the case definition. However, the definitions for probable and suspect cases (see the following) will capture the majority of these cases and allow identification of illness among infants who die before examination by a physician.\n# Probable Cases of AIPH Among Infants\nCriteria for a probable case include a previously healthy infant aged <1 year with a gestational age of >32 weeks,\n• who has a sudden onset of bleeding from the airway, with or without respiratory distress, with or without intubation, and with or without pulmonary infiltrates on CXR or chest CT; or • who died and had evidence of bleeding from the airway found on autopsy or postmortem; had been in respiratory distress; would or should have been intubated in the opinion of a clinician; and would have had infiltrates on CXR or chest CT.\n# Suspected Cases of AIPH Among Infants\nCriteria for a suspected case include a previously healthy infant,\n• who died and had evidence of bleeding from the airway found on autopsy or postmortem or who • either did not have chest imaging studies or had imaging studies that indicated no pulmonary infiltrates. Respiratory distress or intubation is not required for a suspected case.\n# Severity Classification Scheme for AIPH Among Infants\nBecause of the potential for variation in symptoms among infants for each of the criteria, different case combinations might be related to the timing or duration of symptoms, disease severity, pathologic processes, or etiologic agents associated with AIPH among infants. A discussion of the proposed case-classification categories for AIPH among infants is provided (Tables 2 and 3). \n# Discussion\n• Bleeding might begin in a localized region of one lung with dispersion of blood to other areas of the lung through the airways • Initial chest radiograph (CXR) might indicate unilateral infiltrates, but following dispersion indicates diffuse infiltrates • Infants with unilateral infiltrates are considered confirmed for AIPH, but their characteristics might be different from infants with diffuse infiltrates\n• Not considered confirmed because identification depends on lavage or biopsy finding of hemosiderin-laden macrophages and not on active bleeding or recovering blood from below the larynx • Work of breathing might vary for infants with a similar pathology (e.g., resulting from different body temperature, serum glucose levels, and duration of respiratory distress) • Infants who do not need intubation would not have acute bleeding directly identified from below the glottis • Upon initial examination, infants' circumstances might vary; information should be collected to identify these circumstances as best as possible during data abstraction so that the categories can be expanded if needed during data analysis • The circumstances might be that 1) the attending physician intended to intubate an infant who died; 2) the clinician who reviewed the death of an infant with postmortem findings consistent with pulmonary hemorrhage secondary to clinical respiratory failure thought the infant should have been intubated; 3) the infant died before arrival at the hospital and therefore was not intubated nor received thoracic imaging studies • Age-specific normochromic, normocytic, or microangiopathic anemia might indicate different pathophysiologic processes and in conjunction with appropriate clinical signs and symptoms might be supportive of a diagnosis of AIPH * Rankings of 1-5 represent categories with decreasing levels of certainty; 1 = highly probable, and 5 = least probable. The letter designations a, b, and c represent approximately equivalent levels within each category (see also Table 2).\n# MMWR March 12, 2004\nA summary of clinical features of AIPH among infants (Table 4) (Box 2) and neonatal medical problems and differential diagnoses that should be ruled out before classifying a case as AIPH among infants (Box 3) are included. Other differential diagnoses associated with pulmonary hemorrhage are listed (Table 5).\n# Feasibility Study To Determine the Concordance of ICD Codes for Pulmonary Hemorrhage with the CDC Case Definition\nProspective nationwide surveillance for cases of AIPH among infants is difficult to justify on the basis of the available epidemiologic data. In addition to the limitations reported for the Cleveland study (5), no risk factors were conclusively linked to disease in the Chicago investigation ( 4), and only one other cluster (in Detroit) was reported during 1992-1996 (7).\nCDC will retrospectively review cases of pulmonary hemorrhage to determine the public health impact of AIPH among infants and to generate hypotheses regarding the importance of risk factors possibly associated with AIPH among infants. If that review indicates that AIPH among infants is a separate clinical entity and that these cases have occurred in clusters, or that an increase in incidence or mortality is associated with these cases, CDC will initiate prospective surveillance and case ascertainment to identify cases for epidemiologic studies designed to confirm or disprove associations between pulmonary hemorrhage host factors, environmental factors, and biologic agents, including such molds as S. chartarum (5).\n# Retrospective Review by Using Existing Data Sources\nThe ability to use existing data sources should substantially facilitate both determining the public health impact of AIPH among infants. However, the reliable data regarding mortality from pulmonary hemorrhage is only available at the national level. CDC conducted a preliminary evaluation of ICD codes for surveillance of pulmonary hemorrhage among infants to determine whether existing data sources can be used to estimate the magnitude of the problem of AIPH among infants. CDC examined data from the National Hospital Discharge Survey (NHDS) and National Mortality Data. Possible cases of AIPH among infants were identified by using ICD-9 codes 770. 3, 784.7, 784.8, 786.3, and 516.1 (Table 6).\nInfants identified by ICD-9 codes 770.3 and 786.3 differ from the cases reported in Cleveland. In the national datasets, the majority of cases of pulmonary hemorrhage had diagnoses such as prematurity or immaturity and death occurring within the first 7 days of life. The Cleveland cases occurred among stable, healthy, mature infants who had been discharged from the hospital to their homes after birth and subsequently experienced pulmonary hemorrhage (8)(9)(10). Thus, the estimates of deaths and hospital admissions for cases of pulmonary hemorrhage using ICD codes 770.3 and 786.3 does not distinctly identify infants with AIPH as defined by CDC. In addition, these national datasets do not determine if infants had identifiable etiologies or complications before their discharge from the hospital or their death. Because the estimated number of hospitalized cases with a primary diagnosis of pulmonary hemorrhage was less than the number of deaths, these national datasets might not be reliable for surveillance for infantile pulmonary hemorrhage. These analyses might be better performed by using state-based data.\nA retrospective review for AIPH among infants will be performed in metropolitan cities in those states with the highest death rates and with >100 deaths associated with pulmonary hemorrhage among infants, on the basis of relevant ICD-9 and ICD-10 codes used from 1979 to the most recent available data. By focusing on PICUs and NICUs with substantial numbers of deaths, cases from innercity catchment areas, where the incidence of AIPH among infants is suspected to be higher, will be captured. Potential cases will be identified by using standardized methods of case ascertainment and data collection from hospital discharge and mortality data sources, based on ICD codes. Potential cases will be compared with the recommended case definition by reviewing medical records related to all cases of pulmonary hemorrhage observed since 1979 among children aged <2 years.\nThis retrospective review of AIPH among infants will • determine whether AIPH among infants is a distinct clinical entity within existing ICD-9/ICD-10 diagnostic codes for pulmonary hemorrhage; • describe the epidemiology of pulmonary hemorrhage; • identify trends in the frequency of cases and the geographic distribution and clustering of cases; • estimate the public health impact of AIPH among infants;\n• identify groups at high risk for AIPH among infants; and • determine the need for prospective surveillance as a source of cases for a case-control study. The data will be reviewed to determine how these cases, including the apparent case clusters of AIPH among infants in Cleveland and Chicago, have been coded on hospital discharge abstracts, and how deaths attributed to the syndrome have been characterized on death certificates. Both Ohio and Illinois meet the criteria of >100 deaths from pulmonary hemorrhage. In Cleveland and Chicago, this review also will\n# TABLE 4. Clinical features of acute idiopathic pulmonary hemorrhage (AIPH) among infants Finding\nNo evidence of cow milk protein allergy or associated respiratory, heart, kidney, or pancreatic disease* Abrupt cessation of crying or unusual crying or irritability hours to days before the initial recognition of blood in the airway † Not observed § Decreased muscle tone and dusky pallor minutes to hours before progressing to sudden onset of hypoxemic respiratory distress or failure ¶ Hours to days before onset of respiratory failure** Accompanies or immediately precedes respiratory failure † † Acute and appears to be idiopathic § § Characterized by tachypnea, grunting, and chest retractions ¶ ¶ Diffusely diminished breath sounds without the presence of rales or rhonchi*** Often requires intubation and mechanical ventilation; intubation when required is for 2-7 days † † † Often demonstrates bilateral pulmonary infiltrates within the first 24 hours § § § Typically, alveolar infiltrates begin to clear within the first 24-48 hours ¶ ¶ ¶ Atraumatic intubation; bronchoscopy including inspection of upper airway**** Typically, no source from the lung or gastrointestinal tract; presumed to be from diffuse alveolar capillary injury † † † † Typically, found in bronchoalveolar lavage fluid; might not be present in an infant experiencing an acute, initial pulmonary bleed § § § § Indicates evidence of bleeding into the lungs; finding >20% of total pulmonary macrophages containing hemosiderin can be consistent with pulmonary hemorrhage that occurred >48 hours before examination ¶ ¶ ¶ ¶ First 48 hours, fragmented or damaged red blood cells, hemoglobinuria; microangiopathic anemia might be indicative of a hemolytic process; normochromic normocytic might be consistent with acute, abrupt blood loss***** Serum negative for antiglomerular basement membrane antibody, anticytoplasmic neutrophilic antibody, complement titers, serum immune complexes, and antinuclear antibody † † † † † None; spontaneous recovery with or without supportive care indicates these pathophysiologic processes are not the cause of bleeding \n# BOX 2. Clinical descriptions of pulmonary hemorrhage\nIn early texts, pulmonary hemorrhage was not commonly described in children, although it was noted to occur.* Blood found in the airways or alveoli of humans can result from different anatomic sites. Specific sites can include alveoli, large or small conducting airways, or the nasopharynx and gastrointestinal tract with pulmonary aspiration. Regardless of the origin of blood entering the lung, substantial amounts of blood lead to impaired gas exchange, altered pulmonary mechanics, and respiratory distress. Different pathophysiologic processes are associated with pulmonary hemorrhage. These can be divided into • conditions where bleeding occurs at sites of normal tissue with mechanical disruption causing a loss of vascular integrity (e.g., intentional suffocation and mitral valve disease); • vascular inflammation, whereby the inflammatory process causes a loss of vascular integrity (e.g., vasculitis secondary to such conditions as collagen vascular diseases); • vascular malformations, whereby a combination of altered vascular integrity and physical influences (e.g., Laplace's law † ) lead to disruption of the blood vessel; and • coagulopathies, which usually also require additional physical disruption of the blood vessel through greater than normal transpulmonary vascular pressures.\nThe manifestations of pulmonary hemorrhage can be classified into different syndromes. Diffuse pulmonary hemorrhage is usually diagnosed by bronchoscopy, either by virtue of grossly bloody lavage fluid or by the presence of hemosiderin-laden macrophages in bronchoalveolar lavage. In biopsy and autopsy tissue, the diagnosis is made on the basis of the presence of recent blood and hemosiderin in the alveolar spaces or the interstitium. § In the immunocompromised host, intra-alveolar bleeding can result from thrombocytopenia often associated with other factors. Diffuse pulmonary hemorrhage (DPH) can either be secondary to other disease states, associated with other organ dysfunction, or be isolated. Isolated causes of DPH include lung immaturity, cow milk hypersensitivity, pulmonary capillary hemangiomatosis, and idiopathic causes. ¶ Pulmonary hemorrhage of the newborn (ICD-9: 770.3; ICD-10: P26) is manifested by focal hemorrhage into airspaces or the interstitium in the lungs of infants with hyaline membrane disease, bronchopulmonary dysplasia, and other neonatal pulmonary disorders.** These infants are most often male, preterm, small for gestational age, and have a history of perinatal stress. † † The etiology and pathogenesis of the disorder has not been elucidated.\nHemoptysis, cough with hemorrhage, pulmonary hemorrhage not otherwise specified (ICD-9: 786.3; ICD-10 R04, R04.2) is an acute manifestation of bleeding from the airway. This ICD category captures all the nonneonatal (and certain neonatal) diagnoses of pulmonary hemorrhage. Children with pulmonary hemorrhage might not appear to have hemoptysis if they swallow their sputum.\nConsensus is lacking on the meaning of the term idiopathic pulmonary hemosiderosis (ICD-9: 516.1, no ICD-10 code). One pathology text states that the term denotes a separate clinical entity of which diffuse pulmonary hemorrhage is the major manifestation. § § A later edition of the same text ¶ ¶ notes that the presence of hemosiderin in lung macrophages indicates degradation products of hemoglobin. Hemosiderin is thus a pathologic state indicative of bleeding of any type into the lungs*** secondary to the processing of hemoglobin in the red blood cells in the airway by alveolar macrophages. † † † Adults with active alveolar hemorrhage have high hemosiderin scores in bronchoalveolar lavage fluid, § § § but hemosiderin-containing macrophages have limited differential diagnostic value. ¶ ¶ ¶ In one clinical text, the term means diffuse recurrent intrapulmonary hemorrhage that is not secondary to bleeding from trauma, bleeding from the airways, tumors, or left ventricular failure.**** Another author † † † † describes variants of primary and secondary pulmonary hemosiderosis.\nOn review of National Hospital Discharge Survey data for 1979-1996 and national mortality data for 1979-1998 for ICD-9 code 516.1 for infants, no instances were found in either dataset where ICD-9 code 516.1 was the primary listed diagnosis. However, in 207 cases, this code was the other listed diagnosis. This indicates that idiopathic pulmonary hemorrhage is usually an accompanying diagnosis to other diagnoses that result in hospitalization or death among infants. If performed, environmental assessment of the home to gather pertinent risk-assessment data should use standard protocols designed by trained environmental health professionals. At a minimum, the assessment should involve visual inspection, including checks for dampness, water damage, obvious mold, evidence of pests, and environmental tobacco smoke. Depending on the assessed need for further evaluation and the resources available, additional investigation might include determining moisture content, settled dust sampling, air sampling for different allergens, and biologically active compounds, and other investigations as needed.\n# Conclusion\nCDC recommends a definition for a clinically confirmed case of AIPH among infants on the basis of 1) evidence of blood in the airway; 2.) age <1 year; 3) absence of medical conditions related to pulmonary hemorrhage; and 4) severe acute respiratory distress or respiratory failure, requiring admission to a PICU with intubation and mechanical ventilation. CDC recommends that PICUs report cases that meet the CDC case definition to state health departments and to CDC.\nCDC will retrospectively analyze state-level mortality and hospitalization data based on ICD codes and will retrospec- tively review discharges for pulmonary hemorrhage in selected PICUs. These studies will • distinguish between the clinical findings associated with different symptoms of AIPH among infants; • determine whether ICD codes capture cases that meet the CDC-recommended case definition for AIPH among infants; • determine whether AIPH among infants is a distinct recognizable clinical entity; • determine the proportion of cases ascertained retrospectively through ICD-9 codes that meet the clinical case definition by estimating PPV of ICD-coded data; and • define the magnitude of AIPH among infants and the need for conducting etiologic studies. CDC will review the Cleveland and Chicago case series to determine the degree to which the present case definition applies to them. In addition, CDC will evaluate the present case definition on the basis of data from initial surveillance findings and modify it as appropriate.\nIf these reviews establish that AIPH among infants is a public health problem on the basis of increasing numbers or clusters of cases geographically or temporally, targeted prospective case surveillance will be initiated. If prospective surveillance is initiated, CDC will maintain a database of current cases of AIPH among infants, reported by PICUs that meet the case definition. The database will serve as a source of cases for casecontrol studies to determine etiology. CDC will work with state and local health departments to investigate clusters of AIPH among infants cases. ('tr st-\"w r-the) e e\n# Acknowledgments\nThe following CDC staff provided program support for this report: Wesley J. Hodgson, James A. Rifenburg, Tammy T. Rowe, and Sala S. Sharp, Division of Environmental Hazards and Health Effects, National Center for Environmental Health. We also thank Dorr Dearborn, M.D., for reviewing draft manuscripts and for his feedback regarding portions of this report. We also thank Roy Baron, M.D., for sharing background documents from the internal and external panels that prepared the March 2001 CDC report regarding pulmonary hemorrhage.\n# \ndetermine the positive predictive value (PPV) between the clusters of pulmonary hemorrhage cases previously reported and the CDC definition of AIPH among infants. Because the relation between IPH, pulmonary hemorrhage, and AIPH among infants is not clearly understood in terms of rate, etiology, and risk factors, this analysis will define basic demographics of cases among infants and whether the proposed case definition for AIPH among infants is clearly distinguish-able from other conditions. The magnitude and dimensions of AIPH among infants will be determined by describing the distribution of cases on the basis of ICD codes and the CDC case definition. This will involve enumerating cases, determining hospital discharge and mortality rates, and describing the distributions for available demographic variables (e.g., temporal and urban versus rural differences), if any.\n# Investigation of Suspected Clusters of AIPH Among Infants\nIf an apparent cluster of cases of pulmonary hemorrhage occurs, CDC recommends that state health departments initiate an investigation. CDC staff will work with each state, upon request, to evaluate case reports to assist the epidemiologic and environmental investigation, if any. State health departments can use existing protocols for outbreak or cluster investigations and collect information to determine if cases meet the CDC case definition for AIPH among infants. Because these cases probably will be identified in PICUs, CDC recommends that if PICU staff identify any suspected cases, they report them to their state epidemiologist.\nFor each case of AIPH in an infant, CDC recommends that PICU and NICU staff collect clinical information to certify case status, demographic information, and reports regarding the status of the patient's home. PICU and NICU staff also should carefully document illnesses that are similar clinically to AIPH, even if another specific etiology is confirmed, because they might offer additional information or indicate the need to re-assess the case definition. † Unexplained or repeated injuries (e.g., welts, bruises, or burns); injuries in the shape of an object (e.g., belt buckle or electric cord); injuries not likely to happen given the age or ability of the child (e.g., broken bones in a child too young to walk or climb). § From parental or guardian history or injuries that are possible given the age or ability of the child. ¶ Rare among infants."},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":656,"cells":{"id":{"kind":"string","value":"7f12df2d082523849741d78d0a2c6c9ec4510cae"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"None"},"clean_text":{"kind":"string","value":"depar depar depar depar department of health and human ser tment of health and human ser tment of health and human ser tment of health and human ser tment of health and human services vices vices vices vices# Part I: Rabies Prevention and Control\nA. Principles of Rabies Prevention and Control. 1. . . . . Rabies Exposure. Rabies is transmitted only when the virus is introduced into bite wounds, open cuts in skin, or onto mucous membranes from saliva or other potentially infectious material such as neural tissue (2). Questions about possible exposures should be directed to state or local public health authorities.\n\n# Human Rabies Prevention. Rabies in humans can be\nprevented either by eliminating exposures to rabid animals or by providing exposed persons with prompt local treatment of wounds combined with the administration of human rabies immune globulin and vaccine.\nThe rationale for recommending preexposure and postexposure rabies prophylaxis and details of their administration can be found in the current recommendations of the Advisory Committee on Immunization Practices (ACIP) (2). These recommendations, along with information concerning the current local and regional epidemiology of animal rabies and the availability of human rabies biologics, are available from state health departments.\n\n# Domestic Animals.\nLocal governments should initiate and maintain effective programs to ensure vaccination of all dogs, cats, and ferrets and to remove strays and unwanted animals. Such procedures in the United States have reduced laboratory-confirmed cases of rabies in dogs from 6,949 in 1947 to 94 in 2004 (3). Because more rabies cases are reported annually involving cats (281 in 2004) than dogs, vaccination of cats should be required. Animal shelters and animal control authorities should establish policies to ensure that adopted animals are vaccinated against rabies. The recommended vaccination procedures and the licensed animal vaccines are specified in Parts II and III of the compendium, respectively. 4. Rabies in Vaccinated Animals. Rabies is rare in vaccinated animals (4)\n\n# Compendium of Animal Rabies Prevention and Control, 2006- National Association of State Public Health Veterinarians, Inc. (NASPHV)\nRabies is a fatal viral zoonosis and a serious public health problem (1). The recommendations in this compendium serve as a basis for animal rabies prevention and control programs throughout the United States and facilitate standardization of procedures among jurisdictions, thereby contributing to an effective national rabies-control program. This document is reviewed annually and revised as necessary. These recommendations do not supersede state and local laws or requirements. Principles of rabies prevention and control are detailed in Part I; Part II contains recommendations for parenteral vaccination procedures; all animal rabies vaccines licensed by the United States Department of Agriculture (USDA) and marketed in the United States are listed in Part III. Rabies vaccinations may also be administered under the supervision of a veterinarian to animals held in animal control shelters prior to release. Any veterinarian signing a rabies certificate must ensure that the person administering vaccine is identified on the certificate and is appropriately trained in vaccine storage, handling, and administration and in the management of adverse events. This practice assures that a qualified and responsible person can be held accountable to ensure that the animal has been properly vaccinated. Within 28 days after primary vaccination, a peak rabies antibody titer is reached and the animal can be considered immunized. An animal is currently vaccinated and is considered immunized if the primary vaccination was administered at least 28 days previously and vaccinations have been administered in accordance with this compendium.\nRegardless of the age of the animal at initial vaccination, a booster vaccination should be administered 1 year later (see Parts II and III for vaccines and procedures). No laboratory or epidemiologic data exist to support the annual or biennial administration of 3-year vaccines following the initial series. Because a rapid anamnestic response is expected, an animal is considered currently vaccinated immediately after a booster vaccination. a. Dogs, Cats, and Ferrets. All dogs, cats, and ferrets should be vaccinated against rabies and revaccinated in accordance with Part III of this compendium. If a previously vaccinated animal is overdue for a booster, it should be revaccinated. Immediately following the booster, the animal is considered currently vaccinated and should be placed on an annual or triennial schedule depending on the type of vaccine used. b. Livestock. Consideration should be given to vaccinating livestock that are particularly valuable or that might have frequent contact with humans (e.g., in petting zoos, fairs, and other public exhibitions) (11,12). Horses traveling interstate should be currently vaccinated against rabies. c. Confined Animals. The following are recommendations for owners of livestock exposed to rabid animals: 1) If the animal is slaughtered within 7 days of being bitten, its tissues may be eaten without risk of infection, provided that liberal portions of the exposed area are discarded. Federal guidelines for meat inspectors require that any animal known to have been exposed to rabies within 8 months be rejected for slaughter. 2) Neither tissues nor milk from a rabid animal should be used for human or animal consumption (20). Pasteurization temperatures will inactivate rabies virus; therefore, drinking pasteurized milk or eating cooked meat does not constitute a rabies exposure. 3) Having more than one rabid animal in a herd or having herbivore-to-herbivore transmission is uncommon; therefore, restricting the rest of the herd if a single animal has been exposed to or infected by rabies might not be necessary. c. Other Animals. Other mammals bitten by a rabid animal should be euthanized immediately. Animals maintained in USDA-licensed research facilities or accredited zoological parks should be evaluated on a case-by-case basis.\n6. Management of Animals that Bite Humans. a. Dogs, Cats, and Ferrets. Rabies virus may be excreted in the saliva of infected dogs, cats, and ferrets during illness and/or for only a few days prior to illness or death (21)(22)(23)(24). A healthy dog, cat, or ferret that bites a person should be confined and observed daily for 10 days; administration of rabies vaccine to the animal is not recommended during the observation period to avoid confusing signs of rabies with possible side effects of vaccine administration. Such animals should be evaluated by a veterinarian at the first sign of illness during confinement. Any illness in the animal should be reported immediately to the local health department.\nIf signs suggestive of rabies develop, the animal should be euthanized and the head shipped for testing as described in Part I.A.7. Any stray or unwanted dog, cat, or ferret that bites a person may be euthanized immediately and the head submitted for rabies examination. b. Other Biting Animals. Other biting animals which might have exposed a person to rabies should be reported immediately to the local health department. Management of animals other than dogs, cats, and ferrets depends on the species, the circumstances of the bite, the epidemiology of rabies in the area, the biting animal's history, current health status, and potential for exposure to rabies. Prior vaccination of these animals may not preclude the necessity for euthanasia and testing. 7. Outbreak Prevention and Control. The emergence of new rabies virus variants or the introduction of non indigenous viruses poses a significant risk to humans, domestic animals and wildlife (25)(26)(27)(28)(29)(30)(31). A rapid and comprehensive response should include all or some of the following measures: a. Characterize the virus at a national or regional reference laboratory. b. Identify and control the source of the introduction. c. Enhance laboratory-based surveillance in wild and domestic animals. d. Increase animal rabies vaccination rates. e. Restrict the movement of animals. f. Evaluate the need for vector population reduction. g. Coordinate a multi-agency response. h. Provide public and professional outreach and education. (41). No laboratory or epidemiologic data exist to support the annual or biennial administration of 3-year vaccines following the initial series. C. Adverse Events. Currently, no epidemiologic association exists between a particular licensed vaccine product and adverse events, including vaccine failure (42,43 Computer-generated forms containing the same information are also acceptable."},"raw_text":{"kind":"string","value":"depar depar depar depar department of health and human ser tment of health and human ser tment of health and human ser tment of health and human ser tment of health and human services vices vices vices vices# Part I: Rabies Prevention and Control\nA. Principles of Rabies Prevention and Control. 1. . . . . Rabies Exposure. Rabies is transmitted only when the virus is introduced into bite wounds, open cuts in skin, or onto mucous membranes from saliva or other potentially infectious material such as neural tissue (2). Questions about possible exposures should be directed to state or local public health authorities.\n# Human Rabies Prevention. Rabies in humans can be\nprevented either by eliminating exposures to rabid animals or by providing exposed persons with prompt local treatment of wounds combined with the administration of human rabies immune globulin and vaccine.\nThe rationale for recommending preexposure and postexposure rabies prophylaxis and details of their administration can be found in the current recommendations of the Advisory Committee on Immunization Practices (ACIP) (2). These recommendations, along with information concerning the current local and regional epidemiology of animal rabies and the availability of human rabies biologics, are available from state health departments.\n# Domestic Animals.\nLocal governments should initiate and maintain effective programs to ensure vaccination of all dogs, cats, and ferrets and to remove strays and unwanted animals. Such procedures in the United States have reduced laboratory-confirmed cases of rabies in dogs from 6,949 in 1947 to 94 in 2004 (3). Because more rabies cases are reported annually involving cats (281 in 2004) than dogs, vaccination of cats should be required. Animal shelters and animal control authorities should establish policies to ensure that adopted animals are vaccinated against rabies. The recommended vaccination procedures and the licensed animal vaccines are specified in Parts II and III of the compendium, respectively. 4. Rabies in Vaccinated Animals. Rabies is rare in vaccinated animals (4) \n.\n# Compendium of Animal Rabies Prevention and Control, 2006* National Association of State Public Health Veterinarians, Inc. (NASPHV)\nRabies is a fatal viral zoonosis and a serious public health problem (1). The recommendations in this compendium serve as a basis for animal rabies prevention and control programs throughout the United States and facilitate standardization of procedures among jurisdictions, thereby contributing to an effective national rabies-control program. This document is reviewed annually and revised as necessary. These recommendations do not supersede state and local laws or requirements. Principles of rabies prevention and control are detailed in Part I; Part II contains recommendations for parenteral vaccination procedures; all animal rabies vaccines licensed by the United States Department of Agriculture (USDA) and marketed in the United States are listed in Part III. Rabies vaccinations may also be administered under the supervision of a veterinarian to animals held in animal control shelters prior to release. Any veterinarian signing a rabies certificate must ensure that the person administering vaccine is identified on the certificate and is appropriately trained in vaccine storage, handling, and administration and in the management of adverse events. This practice assures that a qualified and responsible person can be held accountable to ensure that the animal has been properly vaccinated. Within 28 days after primary vaccination, a peak rabies antibody titer is reached and the animal can be considered immunized. An animal is currently vaccinated and is considered immunized if the primary vaccination was administered at least 28 days previously and vaccinations have been administered in accordance with this compendium.\nRegardless of the age of the animal at initial vaccination, a booster vaccination should be administered 1 year later (see Parts II and III for vaccines and procedures). No laboratory or epidemiologic data exist to support the annual or biennial administration of 3-year vaccines following the initial series. Because a rapid anamnestic response is expected, an animal is considered currently vaccinated immediately after a booster vaccination. a. Dogs, Cats, and Ferrets. All dogs, cats, and ferrets should be vaccinated against rabies and revaccinated in accordance with Part III of this compendium. If a previously vaccinated animal is overdue for a booster, it should be revaccinated. Immediately following the booster, the animal is considered currently vaccinated and should be placed on an annual or triennial schedule depending on the type of vaccine used. b. Livestock. Consideration should be given to vaccinating livestock that are particularly valuable or that might have frequent contact with humans (e.g., in petting zoos, fairs, and other public exhibitions) (11,12). Horses traveling interstate should be currently vaccinated against rabies. c. Confined Animals. The following are recommendations for owners of livestock exposed to rabid animals: 1) If the animal is slaughtered within 7 days of being bitten, its tissues may be eaten without risk of infection, provided that liberal portions of the exposed area are discarded. Federal guidelines for meat inspectors require that any animal known to have been exposed to rabies within 8 months be rejected for slaughter. 2) Neither tissues nor milk from a rabid animal should be used for human or animal consumption (20). Pasteurization temperatures will inactivate rabies virus; therefore, drinking pasteurized milk or eating cooked meat does not constitute a rabies exposure. 3) Having more than one rabid animal in a herd or having herbivore-to-herbivore transmission is uncommon; therefore, restricting the rest of the herd if a single animal has been exposed to or infected by rabies might not be necessary. c. Other Animals. Other mammals bitten by a rabid animal should be euthanized immediately. Animals maintained in USDA-licensed research facilities or accredited zoological parks should be evaluated on a case-by-case basis.\n6. Management of Animals that Bite Humans. a. Dogs, Cats, and Ferrets. Rabies virus may be excreted in the saliva of infected dogs, cats, and ferrets during illness and/or for only a few days prior to illness or death (21)(22)(23)(24). A healthy dog, cat, or ferret that bites a person should be confined and observed daily for 10 days; administration of rabies vaccine to the animal is not recommended during the observation period to avoid confusing signs of rabies with possible side effects of vaccine administration. Such animals should be evaluated by a veterinarian at the first sign of illness during confinement. Any illness in the animal should be reported immediately to the local health department.\nIf signs suggestive of rabies develop, the animal should be euthanized and the head shipped for testing as described in Part I.A.7. Any stray or unwanted dog, cat, or ferret that bites a person may be euthanized immediately and the head submitted for rabies examination. b. Other Biting Animals. Other biting animals which might have exposed a person to rabies should be reported immediately to the local health department. Management of animals other than dogs, cats, and ferrets depends on the species, the circumstances of the bite, the epidemiology of rabies in the area, the biting animal's history, current health status, and potential for exposure to rabies. Prior vaccination of these animals may not preclude the necessity for euthanasia and testing. 7. Outbreak Prevention and Control. The emergence of new rabies virus variants or the introduction of non indigenous viruses poses a significant risk to humans, domestic animals and wildlife (25)(26)(27)(28)(29)(30)(31). A rapid and comprehensive response should include all or some of the following measures: a. Characterize the virus at a national or regional reference laboratory. b. Identify and control the source of the introduction. c. Enhance laboratory-based surveillance in wild and domestic animals. d. Increase animal rabies vaccination rates. e. Restrict the movement of animals. f. Evaluate the need for vector population reduction. g. Coordinate a multi-agency response. h. Provide public and professional outreach and education. (41). No laboratory or epidemiologic data exist to support the annual or biennial administration of 3-year vaccines following the initial series. C. Adverse Events. Currently, no epidemiologic association exists between a particular licensed vaccine product and adverse events, including vaccine failure (42,43 Computer-generated forms containing the same information are also acceptable."},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":657,"cells":{"id":{"kind":"string","value":"2b408f518713d945e78eacac21d675d602f14054"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"None"},"clean_text":{"kind":"string","value":"Enrolled participants were randomized to receive either daily doses of TDF/FTC or a placebo pill. Participants were seen every 4 weeks for an interview, HIV testing, risk-reduction and PrEP medication adherence counseling, pill count, and dispensing of pills and condoms. Every 3 months, participants received physical examinations with collection of blood and urine samples for evaluation of renal and liver function, and were tested for sexually transmitted infections and treated as needed. Positive HIV rapid tests were confirmed by Western blot. The cohort was followed for an average 1.2 years with a maximum of 2.8 years. Participants were tested for hepatitis B infection at enrollment, and those found to be susceptible to hepatitis B infection were offered vaccination; 94% accepted.\nBased on analysis of data from visits through May 1, 2010, for 2,499 enrolled participants (including 29 male-to-female transgender persons) in the modified \"intent to treat\" analysis (excluding 10 participants found to be HIV-infected at enrollment and 48 who did not have an HIV test after enrollment), 36 of 1,224 participants in the PrEP arm and 64 of 1,217 participants in the placebo arm who were followed for acquisition of HIV infection. Enrollment in the PrEP arm was associated with a 44% reduction in HIV acquisition (95% confidence interval = 15%-63%). The reduction was greater in the \"as treated\" analysis; participants at visits with ≥50% adherence by An estimated 56,000 human immunodeficiency virus (HIV) infections occur each year in the United States (1). Men who have sex with men (MSM) account for 53% of the estimated incident infections, and surveillance data suggest that the annual number of new HIV infections among MSM has been rising since the mid-1990s (1). Strategies for reducing acquisition of HIV infection by MSM have included 1) expanded HIV testing so that infected persons can be treated and their risk for transmitting infection minimized; 2) individual, small-group, and community-level behavioral interventions to reduce risk behaviors (2); 3) promotion of condom use; 4) detection and treatment of sexually transmitted infections (3); and 5) mental health and substance abuse counseling when needed. On November 23, 2010, investigators for the Pre-Exposure Prophylaxis Initiative (iPrEX) study announced results from a multinational, randomized, double-blind, placebo-controlled, phase III clinical trial of daily oral antiretrovirals (tenofovir disoproxil fumarate and emtricitabine ) to prevent acquisition of HIV infection among uninfected but exposed MSM (4). This report provides interim guidance to health-care providers based on the reported results of that trial, which indicated that TDF plus FTC taken orally once a day as preexposure prophylaxis (PrEP) is safe and partially effective in reducing HIV acquisition among MSM when provided with regular monitoring of HIV status and ongoing risk-reduction and PrEP medication adherence counseling.\nThe iPrEx study was conducted in Peru, Ecuador, Brazil, Thailand, South Africa, and the United States. Eligible participants were consenting HIV-uninfected men and male-tofemale transgender adults (aged ≥18 years) who reported sex with a man and reported engaging in high-risk sexual behaviors during the preceding 6 months, and had no clinical contraindication to taking a combined formulation of 300 mg TDF and 200 mg FTC (TDF/FTC).- self-report and pill count/dispensing had a 50% reduction in HIV acquisition (CI = 18%-70%). Reduction in risk for HIV acquisition was 21% among participants at visits with <90% adherence (CI = -31%-52%) and 73% at visits with ≥90% adherence (CI = 41%-88%). Among those randomly assigned to the TDF/FTC arm, drug level testing was performed for all HIV seroconverters and a matched subset of participants who remained uninfected; a 92% reduction in risk for HIV acquisition (CI = 40%-99%) was found in participants with detectable levels of TDF/FTC versus those with no drug detected. TDF/FTC generally was well tolerated, although nausea in the first month was more common among those taking medication than among those on placebo (9% versus 5%). No differences in severe (grade 3) or life-threatening (grade 4) laboratory abnormalities were observed between the active and placebo arms, and no drug-resistant virus was found in the 100 participants infected after enrollment. Among 10 participants who were seronegative at enrollment but later found to have been infected before enrollment, two cases of FTC resistance occurred in the active arm, and one occurred in the placebo arm. Participants in both arms reported lower total numbers of sex partners with whom the participants had receptive anal intercourse and higher percentages of partners who used condoms than reported at baseline.\n\n# Editorial Note\nThis clinical trial demonstrated the safety and efficacy of daily TDF/FTC, in conjunction with behavioral interventions, in reducing sexual HIV acquisition in a multinational population of MSM exposed to HIV through high-risk sex (4). A recent safety study of PrEP with TDF among 400 MSM in the United States also revealed few safety concerns (5). As a component of a comprehensive HIV prevention intervention, PrEP showed a significant added benefit, although effectiveness was highly dependent on medication adherence.\nThe findings in this report are subject to at least five limitations. First, the trial was not large enough to evaluate efficacy in each of the sites, and the majority of the participants were in South America; only 10% were in the United States, making it impossible to determine effects on incidence in the United States trial sites specifically. Second, the assessment of adherence by drug-level testing was not performed for all trial participants and was performed for seroconverters at the first clinical visit in which infection was diagnosed; therefore, the findings might not reflect drug levels at the time of infection. Third, the study does not provide information about long-term health effects of TDF/FTC in HIV-uninfected men or men who became HIV-infected while on PrEP medications. Fourth, results of drug-level testing showed that adherence measures in the trial might overstate levels of actual adherence; many of those with high levels of adherence to the daily regimen by self-report, pill count, and bottles dispensed had low levels or no drug measured in their blood (4). Finally, sexual risk behavior and adherence to PrEP medications among MSM taking TDF/FTC for PrEP outside of a trial setting, and with awareness of trial results, might be different from what was observed for men in the iPrEx trial.\nBased on the results of this study, CDC and other U.S. Public Health Service (PHS) agencies have begun to develop PHS guidelines on the use of PrEP for MSM at high risk for HIV acquisition in the United States as part of a comprehensive set of HIV prevention services. Completing the guidelines and obtaining expert input and public comment will take several months before they can be published. Concerns exist that without early guidance, various unsafe and potentially less effective PrEP-related practices could develop among health-care providers and MSM beginning to use PrEP in the coming weeks and months. These concerns include 1) use of other antiretrovirals than those so far proven safe for uninfected persons (e.g., more than two drugs or protease inhibitors); 2) use of dosing schedules of unproven efficacy (e.g., \"intermittent\" dosing just before and/or after sex); 3) not screening for acute infection before beginning PrEP or long intervals without retesting for HIV infection; and 4) providing prescriptions without other HIV prevention support (e.g., condom access and risk-reduction counseling). Until the more detailed PHS guidelines are available, CDC is providing interim recommendations to help guide clinical practice (3,(6)(7)(8)(9)\n\n# (Box).\nUntil the safety and efficacy of PrEP is determined in trials now under way with populations at high risk for HIV acquisition by other routes of transmission (10), PrEP should be considered only for MSM. The iPrEX trial results provide strong evidence that support for adherence to the prescribed medication regimen must be a routine component of any PrEP program. To minimize the risk for drug resistance, PrEP should not be started in persons with signs or symptoms of acute viral infection unless HIV-uninfected status is confirmed by HIV RNA testing or a repeat antibody test performed after the viral syndrome resolves (6). When evaluating MSM for the prescription of PrEP medications, it is important to establish whether other effective risk-reduction measures (e.g., condom use) are not being used consistently and to ascertain that the risk for HIV acquisition is high (e.g., frequent partner change or concurrent partners in a geographic setting with high HIV prevalence) because these patients might benefit most from the addition of PrEP to their HIV prevention regimen. Health-care providers and patients should be aware that HIV prevention is not a labeled indication for the use of Truvada † and that its long-term safety in HIV-uninfected persons is not yet known. Health-care providers should report any serious adverse events resulting from prescribed TDF/FTC for PrEP to the Food and Drug Administration's MedWatch. § In addition, because the medication is costly, ensuring that patients understand the financial implications of starting PrEP is critical.\nPrEP has the potential to contribute to effective and safe HIV prevention for MSM if 1) it is targeted to MSM at high risk for HIV acquisition; 2) it is delivered as part of a comprehensive set of prevention services, including risk-reduction and PrEP medication adherence counseling, ready access to condoms, and diagnosis and treatment of sexually transmitted infections; and 3) it is accompanied by monitoring of HIV status, side effects, adherence, and risk behaviors at regular intervals.\nBOX. CDC interim guidance for health-care providers electing to provide preexposure prophylaxis (PrEP) for the prevention of HIV infection in adult men who have sex with men and who are at high risk for sexual acquisition of HIV"},"raw_text":{"kind":"string","value":"# \nEnrolled participants were randomized to receive either daily doses of TDF/FTC or a placebo pill. Participants were seen every 4 weeks for an interview, HIV testing, risk-reduction and PrEP medication adherence counseling, pill count, and dispensing of pills and condoms. Every 3 months, participants received physical examinations with collection of blood and urine samples for evaluation of renal and liver function, and were tested for sexually transmitted infections and treated as needed. Positive HIV rapid tests were confirmed by Western blot. The cohort was followed for an average 1.2 years with a maximum of 2.8 years. Participants were tested for hepatitis B infection at enrollment, and those found to be susceptible to hepatitis B infection were offered vaccination; 94% accepted.\nBased on analysis of data from visits through May 1, 2010, for 2,499 enrolled participants (including 29 male-to-female transgender persons) in the modified \"intent to treat\" analysis (excluding 10 participants found to be HIV-infected at enrollment and 48 who did not have an HIV test after enrollment), 36 of 1,224 participants in the PrEP arm and 64 of 1,217 participants in the placebo arm who were followed for acquisition of HIV infection. Enrollment in the PrEP arm was associated with a 44% reduction in HIV acquisition (95% confidence interval [CI] = 15%-63%). The reduction was greater in the \"as treated\" analysis; participants at visits with ≥50% adherence by An estimated 56,000 human immunodeficiency virus (HIV) infections occur each year in the United States (1). Men who have sex with men (MSM) account for 53% of the estimated incident infections, and surveillance data suggest that the annual number of new HIV infections among MSM has been rising since the mid-1990s (1). Strategies for reducing acquisition of HIV infection by MSM have included 1) expanded HIV testing so that infected persons can be treated and their risk for transmitting infection minimized; 2) individual, small-group, and community-level behavioral interventions to reduce risk behaviors (2); 3) promotion of condom use; 4) detection and treatment of sexually transmitted infections (3); and 5) mental health and substance abuse counseling when needed. On November 23, 2010, investigators for the Pre-Exposure Prophylaxis Initiative (iPrEX) study announced results from a multinational, randomized, double-blind, placebo-controlled, phase III clinical trial of daily oral antiretrovirals (tenofovir disoproxil fumarate [TDF] and emtricitabine [FTC]) to prevent acquisition of HIV infection among uninfected but exposed MSM (4). This report provides interim guidance to health-care providers based on the reported results of that trial, which indicated that TDF plus FTC taken orally once a day as preexposure prophylaxis (PrEP) is safe and partially effective in reducing HIV acquisition among MSM when provided with regular monitoring of HIV status and ongoing risk-reduction and PrEP medication adherence counseling.\nThe iPrEx study was conducted in Peru, Ecuador, Brazil, Thailand, South Africa, and the United States. Eligible participants were consenting HIV-uninfected men and male-tofemale transgender adults (aged ≥18 years) who reported sex with a man and reported engaging in high-risk sexual behaviors during the preceding 6 months, and had no clinical contraindication to taking a combined formulation of 300 mg TDF and 200 mg FTC (TDF/FTC).* self-report and pill count/dispensing had a 50% reduction in HIV acquisition (CI = 18%-70%). Reduction in risk for HIV acquisition was 21% among participants at visits with <90% adherence (CI = -31%-52%) and 73% at visits with ≥90% adherence (CI = 41%-88%). Among those randomly assigned to the TDF/FTC arm, drug level testing was performed for all HIV seroconverters and a matched subset of participants who remained uninfected; a 92% reduction in risk for HIV acquisition (CI = 40%-99%) was found in participants with detectable levels of TDF/FTC versus those with no drug detected. TDF/FTC generally was well tolerated, although nausea in the first month was more common among those taking medication than among those on placebo (9% versus 5%). No differences in severe (grade 3) or life-threatening (grade 4) laboratory abnormalities were observed between the active and placebo arms, and no drug-resistant virus was found in the 100 participants infected after enrollment. Among 10 participants who were seronegative at enrollment but later found to have been infected before enrollment, two cases of FTC resistance occurred in the active arm, and one occurred in the placebo arm. Participants in both arms reported lower total numbers of sex partners with whom the participants had receptive anal intercourse and higher percentages of partners who used condoms than reported at baseline. \n# Editorial Note\nThis clinical trial demonstrated the safety and efficacy of daily TDF/FTC, in conjunction with behavioral interventions, in reducing sexual HIV acquisition in a multinational population of MSM exposed to HIV through high-risk sex (4). A recent safety study of PrEP with TDF among 400 MSM in the United States also revealed few safety concerns (5). As a component of a comprehensive HIV prevention intervention, PrEP showed a significant added benefit, although effectiveness was highly dependent on medication adherence.\nThe findings in this report are subject to at least five limitations. First, the trial was not large enough to evaluate efficacy in each of the sites, and the majority of the participants were in South America; only 10% were in the United States, making it impossible to determine effects on incidence in the United States trial sites specifically. Second, the assessment of adherence by drug-level testing was not performed for all trial participants and was performed for seroconverters at the first clinical visit in which infection was diagnosed; therefore, the findings might not reflect drug levels at the time of infection. Third, the study does not provide information about long-term health effects of TDF/FTC in HIV-uninfected men or men who became HIV-infected while on PrEP medications. Fourth, results of drug-level testing showed that adherence measures in the trial might overstate levels of actual adherence; many of those with high levels of adherence to the daily regimen by self-report, pill count, and bottles dispensed had low levels or no drug measured in their blood (4). Finally, sexual risk behavior and adherence to PrEP medications among MSM taking TDF/FTC for PrEP outside of a trial setting, and with awareness of trial results, might be different from what was observed for men in the iPrEx trial.\nBased on the results of this study, CDC and other U.S. Public Health Service (PHS) agencies have begun to develop PHS guidelines on the use of PrEP for MSM at high risk for HIV acquisition in the United States as part of a comprehensive set of HIV prevention services. Completing the guidelines and obtaining expert input and public comment will take several months before they can be published. Concerns exist that without early guidance, various unsafe and potentially less effective PrEP-related practices could develop among health-care providers and MSM beginning to use PrEP in the coming weeks and months. These concerns include 1) use of other antiretrovirals than those so far proven safe for uninfected persons (e.g., more than two drugs or protease inhibitors); 2) use of dosing schedules of unproven efficacy (e.g., \"intermittent\" dosing just before and/or after sex); 3) not screening for acute infection before beginning PrEP or long intervals without retesting for HIV infection; and 4) providing prescriptions without other HIV prevention support (e.g., condom access and risk-reduction counseling). Until the more detailed PHS guidelines are available, CDC is providing interim recommendations to help guide clinical practice (3,(6)(7)(8)(9) \n# (Box).\nUntil the safety and efficacy of PrEP is determined in trials now under way with populations at high risk for HIV acquisition by other routes of transmission (10), PrEP should be considered only for MSM. The iPrEX trial results provide strong evidence that support for adherence to the prescribed medication regimen must be a routine component of any PrEP program. To minimize the risk for drug resistance, PrEP should not be started in persons with signs or symptoms of acute viral infection unless HIV-uninfected status is confirmed by HIV RNA testing or a repeat antibody test performed after the viral syndrome resolves (6). When evaluating MSM for the prescription of PrEP medications, it is important to establish whether other effective risk-reduction measures (e.g., condom use) are not being used consistently and to ascertain that the risk for HIV acquisition is high (e.g., frequent partner change or concurrent partners in a geographic setting with high HIV prevalence) because these patients might benefit most from the addition of PrEP to their HIV prevention regimen. Health-care providers and patients should be aware that HIV prevention is not a labeled indication for the use of Truvada † and that its long-term safety in HIV-uninfected persons is not yet known. Health-care providers should report any serious adverse events resulting from prescribed TDF/FTC for PrEP to the Food and Drug Administration's MedWatch. § In addition, because the medication is costly, ensuring that patients understand the financial implications of starting PrEP is critical.\nPrEP has the potential to contribute to effective and safe HIV prevention for MSM if 1) it is targeted to MSM at high risk for HIV acquisition; 2) it is delivered as part of a comprehensive set of prevention services, including risk-reduction and PrEP medication adherence counseling, ready access to condoms, and diagnosis and treatment of sexually transmitted infections; and 3) it is accompanied by monitoring of HIV status, side effects, adherence, and risk behaviors at regular intervals.\n# \nBOX. CDC interim guidance for health-care providers electing to provide preexposure prophylaxis (PrEP) for the prevention of HIV infection in adult men who have sex with men and who are at high risk for sexual acquisition of HIV "},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":658,"cells":{"id":{"kind":"string","value":"adecc935b127f91f6ea3a84beb1d220b5039a2b9"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"None"},"clean_text":{"kind":"string","value":"# I. RECOMMENDATIONS FOR CYANIDE STANDARDS\nThe National Institute for Occupational Safety and Health recommends that employee exposure to hydrogen cyanide (HCN) and the cyanide salts in the workplace be controlled by adherence to the following sections. The standards are designed to protect the health of workers for up to a 10-hour workday, and a 40-hour workweek over a working lifetime. Compliance with the standard should therefore prevent adverse effects of HCN and cyanide salts on the health of workers. The standards are measurable by techniques that are valid, reproducible, and available to industry and government agencies.\nSufficient technology exists to permit compliance with the recommended standards. The standards will be subject to review and revision as necessary.\nThese criteria and recommended standards apply to occupational exposure of workers to HCN and cyanide salts. Synonyms for HCN are hydrocyanic acid, prussic acid, and formonitrile. For the purpose of this document, cyanide salts are defined as sodium cyanide (NaCN), potassium cyanide (KCN), or calcium cyanide (Ca(CN)2). The word, cyanide, or the symbol, \"CN\", is used to designate salts as well as hydrogen cyanide.\nThe \"action level\" for hydrogen cyanide or a cyanide salt is defined as one-half the corresponding recommended ceiling environmental exposure limit. \"Occupational exposure\" to these compounds is defined as exposure to airborne concentrations greater than the corresponding action levels.\nThe criteria and recommended standards apply to any area in which HCN, any of the cyanide salts or materials containing any of them, alone or in combination with other substances, is used, produced, packaged, processed, mixed, blended, handled, stored in large quantities, or applied.\nExposure to cyanide at concentrations less than or equal to the respective action levels will not require adherence to the recommended standards except for sections 2-7, and 8(c). If \"exposure\" to other chemicals also occurs, for example to a combination of cyanide and methyl alcohol, provisions of any applicable standards for such other chemicals shall be followed also.\n\n# Section 1 -Environmental (Workplace Air) (a) Concentration\nEmployee exposure to HCN shall be controlled so as not to exceed 5 milligrams per cubic meter of air expressed as CN (4.7 ppm), determined as a ceiling concentration based on a 10-minute sampling period.\nEmployee exposure to cyanide salts shall be controlled so as not to exceed 5 milligrams per cubic meter of air expressed as CN, determined as a ceiling value based upon a 10-minute sampling period.\nWhenever the air is analyzed for cyanide salts, a concurrent analysis shall be made for HCN. Neither of the respective ceiling values may be exceeded nor may the combined values exceed 5 mg/cu m measured as CN during a 10-minute sampling period.\n\n# (b) Sampling and Analysis\nProcedures for sampling, calibration of equipment, and analysis of air samples for HCN and cyanide salts shall be as provided in Appendices I and II, or by any method shown to be equivalent in precision, accuracy and sensitivity to those specified. A sampling period of about 10 minutes is necessary to provide an amount of cyanide readily amenable to analysis by the cyanide selective electrode.\nSection 2 -Medical Medical surveillance shall be made available as specified below for all workers occupationally exposed to HCN or cyanide salts.\n(a) Preplacement and annual medical examinations shall include:\n(1) An initial or interim work and medical history with special attention to skin disorders and those non-specific symptoms, such as headache, nausea, vomiting, dizziness or weakness, that may be associated with chronic exposure.\n(2) A physical examination giving particular attention to skin, thyroid, and the cardiovascular and upper respiratory systems.\n(3) An evaluation of the advisability of the worker's use of negative-or positive-pressure respirators.\n(b) Initial medical examinations shall be made available to presently employed workers within six months of the promulgation of a standard.\n\n# (c)\nThe responsible physician and the employer shall be aware of the material contained in Appendix V and shall ensure that employees trained in these first-aid measures are on duty whenever there is occupational exposure to HCN or a cyanide salt.\n(d) Two physician's treatment kits shall be immediately available to trained medical personnel at each plant where there is a potential for the release of, accidental or otherwise, or for contact with, hydrogen cyanide or cyanide salts. One kit should be portable in order that it may be carried by medical personnel while accompanying a patient to the hospital. The other kit should be kept under lock and key to assure that it is intact and available when and if needed. The key should be readily available at all times to the work supervisor on duty and the storage place should be of such construction as to allow accessibility in the event of loss of the key.\n(e) First-aid kits shall be immediately available at workplaces where there is a potential for the release, accidental or otherwise, of hydrogen cyanide or a potential for exposure to cyanide salts. This kit shall contain as a minimum two (2) boxes of ampules (2 dozen), each containing 0.3 ml of amyl nitrite. Ampules shall be replaced biannually or sooner if needed to ensure their potency. The amyl nitrite ampules should be protected from high temperatures. In all cases, the contents of the medical and first-aid kits shall be replaced before the manufacturer's assigned expiration dates. Suggested contents for these kits are listed in Appendix V. In case of contact, immediately flush skin or eyes with plenty of water for at least 15 minutes; get medical attention. Remove contaminated clothing and wash before reuse.\n\n# POISON First Aid\nCarry patient to fresh air. Have the patient lie down. Remove contaminated clothing but keep patient warm. Start artificial respiration if breathing stops. Administer antidote (amyl nitrite ampule). Call a physician.\n\n# Temporary Antidote\nIf cyanide gas is inhaled: Break an amyl nitrite ampule in a cloth and hold lightly under nose for 15 seconds. Repeat at about 15-second intervals.\nIf cyanide is swallowed:\nBreak an amyl nitrite ampule in a cloth and hold lightly under nose for 15 seconds.\nRepeat inhalation of amyl nitrite 5 times at about 15 second intervals. If patient is conscious or when consciousness returns, give emetic (1 tablespoonful of salt to each glass of warm water) and repeat until vomit fluid is clear. Do not give an emetic to an unconscious or barely conscious person.\n\n# (b)\nThe following warning sign shall be affixed in a readily visible location at or near entrances to areas containing HCN and where there is reasonable potential for emergencies: (1) location of gas masks and other emergency equipment,\n(2) instructions for sounding emergency alarm,\n(3) location of first-aid equipment and supplies, and\n(4) instructions for summoning medical aid.)\nThe sign shall be printed both in English and in the predominant language of non-English-reading workers. All workers shall receive training and information on the hazards and safe work practices in handling HCN and cyanide salts, and on first-aid procedures in poisoning by these compounds.\n(c) When HCN gas is used as a fumigant, warning signs shall be prominently displayed about the area and at all entries to the area as Temporary Antidote\nIf aerosolized salt has been inhaled or if solid or dissolved salt has caused poisoning after contact with the skin: Break an amyl nitrite ampule in a cloth and hold lightly under nose for 15 seconds. Repeat 5 times at about 15-second intervals. Repeat as necessary using a fresh amyl nitrite ampule every three minutes. Use artificial respiration if breathing stops.\nIf cyanide salt in any form is swallowed: proceed as above. If the victim is conscious and capable of some activity, give an emetic (1 tablespoonful of table salt in a glass of warm water) in repeated doses until the vomit fluid is clear. Never give anything by mouth to an unconscious person.\n(e) Containers of Ca(CN)2 shall be labeled in the same manner as other solid cyanide salts, except that an additional warning is necessary because this material will react with water to release hydrogen cyanide.\nThe statement of the hazard shall read as follows for Ca(CN)2:\n\n# DANGER! MAY BE FATAL IF SWALLOWED OR INHALED CONTACT WITH WATER OR ACID LIBERATES POISONOUS GAS CAUSES EYE BURNS AND MAY IRRITATE SKIN (f)\nAll containers of solutions of cyanide salts shall bear the following labeling in addition to, or in combination with, labels required by other statutes, regulations, or ordinances. The proper chemical name of the specific inorganic cyanide compound followed by the word \"solution\"\nshall appear in large, bold face type at the top of the label.\n(insert name of compound) SOLUTION (Inorganic Cyanide Solution) DANGER! MAY BE FATAL IF SWALLOWED OR ABSORBED THROUGH SKIN CAUSES BURNS CONTACT WITH ACID LIBERATES POISONOUS GAS Do not breathe gas. Do not get in eyes, on skin, on clothing. Wash thoroughly after handling. Keep container closed and away from acids. In case of contact, immediately flush skin or eyes with plenty of water for at least J.5 minutes and call a physician. Treat spillage with strong calcium hypochlorite solution and flush to sewer.\n\n# POISON First Aid\nAlways have on hand a Cyanide First-Aid Kit. Carry patient to fresh air, have him lie down.\nRemove contaminated clothing but keep patient warm. Start treatment immediately. Call a physician.\n\n# Temporary Antidote\nIf gas is inhaled: Break an amyl nitrite ampule in a cloth and hold lightly under nose for 15 seconds. Repeat 5 times at about 15-second intervals. Repeat as necessary, using a fresh amyl nitrite ampule every three minutes. Use artificial respiration if breathing stops. If swallowed: Break an amyl nitrite ampule in a cloth and hold lightly under nose for 15 seconds. If patient is conscious, or when consciousness returns, give emetic (1 tablespoonful of salt in a glass of warm water) and repeat until vomit fluid is clear. Repeat inhalation of amyl nitrite ampule every three minutes. Use artificial respiration if breathing stops. Never give anything by mouth to an unconscious person. Engineering controls and safe work practices shall be used to maintain exposures to HCN and cyanide salts below the prescribed limits.\nAdministrative controls may also be used to reduce exposure. However, because the inhalation of cyanides or their absorption through the skin may be immediately dangerous to life, the added protection of personal protective equipment and clothing must be provided for work procedures and for emergency situations as discussed below. Such equipment and clothing must be provided to the workers engaged in work with cyanide. Emergency equipment shall be located at well marked and identified stations within the cyanide work areas. This equipment must allow each and every worker to escape the area in case of a cyanide emergency.\n\n# (a) Respiratory Protection\nEngineering controls shall be used whenever feasible to maintain airborne cyanide concentrations at or below the environmental limits recommended in Section 1 above. Compliance with the permissible exposure limits by the use of respirators is only allowed when airborne cyanide concentrations are in excess of the workplace environmental limits while required engineering controls are being installed or tested, when nonroutine maintenance or repair is being accomplished, or during emergencies. Appropriate respirators as described in Table 1-1 for HCN and Table 1-2 for cyanide salts shall be used only when permitted by the above restrictions. Respirators shall be selected and used in accordance with the following requirements:\n(1) For the purpose of determining the type of respirator to be used, the employer shall measure, when possible, the airborne concentration of HCN or cyanide salt in the workplace initially and thereafter whenever process, worksite, climate, or control changes occur which are likely to increase the airborne concentration of these cyanides.\nThe employer shall ensure that no worker is being exposed to cyanide in excess of the standards either because of improper respirator selection, fit, use, or maintenance.\nThe employer shall provide respirators in accordance with Tables 1-1 and 1-2 and shall ensure that the employee uses the respirator provided.\n(4) Respiratory protective devices shall be those approved under the provisions of 30 CFR 11, published in the Federal Register, March 25, 1972, as amended.\n(5) Respirators specified for use in higher concentrations of HCN may be used in atmospheres of lower concentrations. Likewise, respirators specified for use in higher concentrations of cyanide salts are permitted in atmospheres of lower concentrations.\nThe employer shall ensure that the respirators are adequately cleaned, maintained, and stored when not in use, and that employees are instructed in the use of respirators assigned to them and in testing for facepiece leakage before each use.\nCartridges or canisters shall be discarded and replaced with fresh canisters after each use. Unused canisters shall be discarded and replaced when seals are broken, after three years if seals are unbroken, or on the manufacturer's recommendation, whichever is first.\nCartridges and canisters shall not be used for periods of time in excess of those indicated in Tables 1-1 and 1-2.\n(8) Emergency and escape-type respirators shall be made immediately available at the work stations for each worker when there is potential for exposure to concentrations of the various cyanides above the ceiling values.\nFor purpose of selection of respiratory protective equipment, entry into areas containing unknown and/or suspected dangerous atmospheric concentrations of HCN or cyanide salts shall be treated as an emergency. Less than or equal to 90 ppm (1) Type C supplied-air respirator, demand or continuous-flow type (negative or positive pressure), with half or full facepiece.\n(2) Full facepiece gas mask, chin-style canister specific for HCN. The maximum service life of canisters is one hour.\nLess than or equal to 200 ppm Full facepiece gas mask, front-or backmounted type canister specific for hydrogen cyanide. The maximum service life of canisters is one hour.\n(1) Self-contained breathing apparatus in pressure-demand mode (positive pressure) with full facepiece worn under gas-tight suit providing whole body protection.\n(2) Combination supplied-air respirator, pressure-demand type (positive pressure), with auxiliary self-contained air supply and full facepiece; all worn under gas tight suit providing whole body protection.\n(1) Positive pressure self-contained breathing apparatus worn under a gas-tight suit providing whole body protection.\n(2) Combination supplied-air respirator, pressure-demand type, with auxiliary selfcontained air supply; all worn under gastight suit providing whole body protection.\n(1) Self-contained breathing apparatus in demand or pressure-demand mode (negative or positive pressure).\n(2) Gas mask, full facepiece or mouthpiece type, with canister specific for HCN.\n\n# NOTE:\nDuring the use of any respirator with half mask, full facepiece or hood, protective clothing should be worn if there is a chance that liquid HCN may contact any part of the body.\nGreater than 200 ppm Emergency (no concentration limit)\nEvacuation or Escape (no concentration limit) Less than or equal to (1) Filter type respirators, approved for 25 mg/cu m toxic dust, with half-mask (not appli cable for Ca(CN)2).\n(2) Chemical cartridge respirators with replaceable cartridge for toxic dusts and acid gases; with half-mask. Maximum service life 4 hours.\n(1) Full-face gas mask, chest or back mounted type, with industrial size canister for toxic dust and hydro cyanic acid gas. Maximum service life 2 hours.\n(2) Type C supplied air-respirator, continuous-flow or pressure-demand type (positive pressure) with full facepiece.\n(3) Type A supplied-air respirator, (hose mask with blower) with full facepiece.\nGreater than 50 mg/cu m (1) Self-contained breathing apparatus with positive pressure in full facepiece.\n(2) Combination supplied-air respirator pressure-demand type with auxiliary self-contained air supply.\n(1) Self-contained breathing apparatus with positive pressure in facepiece.\n(2) Combination supplied-air respirator, pressure-demand type, with auxiliary self-contained air supply.\nEvacuation or Escape (no (1) Self-contained breathing apparatus in concentration limit) demand or pressure-demand mode (negative or positive pressure).\n(2) Full-face gas mask, front or back mount type with industrial size canister for toxic dust and hydro cyanic acid gas.\n\n# Emergency (no concentration limit)\nLess than or equal to 50 mg/cu m (b)\nProtective Clothing\nBecause HCN and cyanide salts, dry or in solution, may be absorbed readily through the skin or any break in the skin, the provision and use of protective clothing are necessary for the protection of workers in most operations where HCN and cyanide salts are used in pure or diluted condition.\n(1) When entering a HCN gas-filled area in emergency situations, when the airborne concentration of HCN is unknown, or when the known airborne concentration is greater than 200 ppm, employees shall wear gas-tight suits in addition to the required respiratory protection. The gas-tight suits shall provide full body protection.\n(2) Employees engaged in maintenance, repair, or other work on equipment, or in circumstances whereby they may be exposed to HCN liquid or gas, shall wear protective garments or suits made of material impervious to HCN and providing full body protection.\n(3) Employees shall wear rubber gloves when engaged in any activity which may involve the handling of, or possible contact with, HCN.\nEmployees shall wear gloves when handling dry cyanide salts and when using or handling equipment whose surfaces may be contaminated with these salts in such manner that contact of the chemical with the employee's hands is possible or likely.\nEmployees shall wear gloves made of rubber or other impervious material when engaged in any operation wherein contact of the hands with solutions of cyanide salts is possible or likely.\nEmployees shall wear protective sleeves, aprons, and/or full body protective clothing as needed to protect their skin from contact with cyanide salts, dry or in solution. When handling solutions, the outer garment shall be of rubber or other material impervious to the solutions involved in the exposures. The garments shall fit snugly about the wrist, arm, neck, waist, and/or ankle (as appropriate to the particular garment) and shall have closures which will exclude dust, powder, mist, and/or splashes of cyanide salts in either dry or liquid formulations.\n(10) In areas where spills or splashes of solutions of cyanide salts are likely to occur, the employees shall wear shoes, boots, or overshoes made of rubber or other material impervious to these solutions.\n(11) Chemical safety goggles shall be worn by employees engaged in any operation wherein there is danger or likelihood that dusts or solutions of cyanide salts will come into contact with the eye.\nFull-length face shields with forehead protection shall be worn by employees engaged in any operation wherein there is danger or likelihood that dusts, molten salts, or solutions of cyanide salts may contact the face.\nThe employer shall be responsible for maintaining all devices and clothing to be used for personal protection in a clean and effective condition. (2) Buildings in which HCN is to be stored, handled, or used must be designed to prevent fire and explosion hazards and to minimize the release of the highly toxic liquid or gas. Equipment and vessels containing or using HCN should be isolated in rooms or buildings designed for, and devoted to, these purposes.\nBuilding construction shall be fire-and explosion-resistant and shall meet the requirements of the National Fire Protection Association codes and of the local codes, regulations, and ordinances. Explosion vents and fire doors shall be provided in accordance with codes and good practice.\nEach room or building shall have no less than two means of exit, with doors opening outward and provided with \"panic bar\" release latches.\nExits shall be provided so that no location within the room or building is more than 75 feet from an exit and personnel can be evacuated in less than 1 minute.\n(3) All regular work areas where HCN is handled or used must be adequately ventilated so that, under normal or reasonably anticipated operating conditions, the airborne concentrations of HCN will not exceed the standard recommended in Section 1.\nLocal exhaust ventilation shall be used at points or areas of regular or anticipated release of HCN gas.\nEquipment for very high rates of ventilation of an area may be provided for the rapid reduction of contamination of air by HCN when emergency situations arise.\nThe HCN-contaminated air from an exhaust ventilation system must either be passed through a suitable collector to remove the HCN or be discharged at a location or in a manner such that persons or animals will not be endangered by the toxic gas.\nVentilation equipment must meet the applicable codes for explosionproof and fireproof installation of such equipment. where applicable, shall be followed.\n\n# (b) Cyanide Salts\n(1) All necessary precautions must be taken to prevent cyanide salts from coming into contact with liquid or airborne acids. In addition, precautions must be exercised to prevent Ca(CN)2 from coming into contact with water or humid atmospheres.\nCyanide salts must be protected also from contact with large concentrations of carbon dioxide. Carbon dioxide fire extinguishers must not be used where cyanide salts are present.\nIn any circumstance in which there is probable contact of cyanide salts with liquid or airborne acids such as Cr03, S02, C02, HC1 etc, or of Ca(CN)2 with a high concentration of water vapor or with liquid water, the standards and requirements applicable to exposures to HCN shall also apply.\n( All containers of cyanide salts must be labeled in accordance\nwith the recommendations in Section 3.\nAreas in which cyanides are stored must be posted in accordance with the recommendations in Section 3.\n(3) When containers of cyanide salts are removed or unloaded from trucks, boxcars, or poorly ventilated spaces, these should be thoroughly ventilated, purged, and tested before a worker enters.\nWhen cyanide salts are placed in other containers for transport or temporary storage, such containers must be properly covered and labeled.\n(A) Mechanical exhaust ventilation by local exhaust shall be provided for all operations producing, or likely to produce, dust or mists of cyanide salts in excess of the limit recommended in Section 1, or to vaporize HCN in excess of the recommended limit for that vapor.\nExamples of such operations are: there is evolution of mist from the bath, the employees shall be encouraged to wear at least a filter type respiratory protective device as a measure of protection in addition to that provided by ventilation.\nNonreturnable containers and other containers or equipment contaminated with cyanides before being discarded should be washed thoroughly with alkalinized water to remove cyanide residues.\n(10) When cyanide salts are used in fused salt baths, mechanical local exhaust ventilation should be provided to control any cyanide emissions.\nCare in operation of the bath and in housekeeping must be exercised so that the area around the bath does not become covered with cyanide-containing powder or dust. Employees working at baths of fused cyanide salts should wear face shields and appropriate protective clothing to protect them from burns and skin contact with cyanides in the event of splashes. A shovel or similar tool should be used to add cyanide salts to a fused salt bath. The cyanide salt should not be added directly by hand.\n(11) Inspection, cleaning, or repairing of tanks or other equipment used with solutions of cyanide salts should be performed only by properly trained workmen under careful supervision.\n(A) The tank should be drained of all cyanide solution as completely as possible, then filled with alkalinized water and allowed to stand for 15 minutes, preferably with agitation. This procedure should be repeated; then a preliminary inspection may be made. Any encrustation should be removed by mechanical means and/or by means of a stream of water from a hose.\n\n# (B)\nIf the tank is to be entered, the atmosphere in the tank should be tested for the presence of hydrogen cyanide and cyanide salts, to be certain it does not contain a dangerous airborne concentration of these or other materials.\n(C) The tank should be purged with fresh air to ensure an adequate oxygen supply and air should be supplied to the tank while the worker is in the tank.\n\n# (D)\nEquipment other than tanks should be washed and vented similarly, as applicable.\nIn the event of finding airborne concentrations of cyanide salts in excess of the limit, immediate action must be taken to eliminate the cause of the elevated airborne cyanide concentration. In case of any emergency situation (spills, leaks, or other unusual emissions of cyanide which result or potentially may result in dangerous airborn concentrations), all personnel shall be evacuated from the area. The personnel required to return to the area to institute corrective measures shall wear approved respiratory protective gear while entering and working in the area until the situation is corrected.\n(13) Any area in which there is the potential of an emergency involving HCN or a cyanide salt shall be posted in accordance with the provisions of Section 3, and emergency equipment stations shall be established. These stations shall be sufficient in number and so located as to be readily and immediately accessible to the workers in the area.\nThe stations shall be provided with first-aid supplies and instructions for first-aid treatment of any persons suffering excessive exposure to cyanide.\nApproved type respiratory protective devices, as indicated in Section 4, shall be available at designated emergency stations. These devices shall be sufficient in number for the workers in the area and readily accessible. Occurrence and Use HCN is a colorless gas or a colorless or bluish-white liquid with a faint, characteristic odor of bitter almonds perceptible to some people. Kirk and Stenhouse reported that 88% of 244 persons tested could smell hydrogen cyanide but that in a fourth of these, the determination was made only with difficulty.\nThe glucoside amygdalin which occurs in nature in some plants, notably almonds, readily yields HCN upon hydrolysis. Recently, attention has been brought to the presence of HCN in automobile emissions. HCN is manufactured in the United States from coke-oven gas by reaction with sodium carbonate, from cyanide salts by reaction with acid, by the decomposition of formamide, from the reaction of ammonia, air, and natural gas, or, most commonly, from the reaction of methane and ammonia under specific controlled conditions. The great bulk of the HCN synthesized is used directly in the same process system. In 1973, the estimated consumption of HCN in the United States was approximately 310,000 short tons. HCN is used primarily in the production of chemical intermediates for the manufacture of synthetic fibers, plastics, cyanide salts and nitrites; in the fumigation of ships, In the presence of any source of hydrogen ions in quantity, eg, strong mineral acid, the production of HCN from cyanide salts becomes both rapid and large. Above 50 degrees C, an irreversible decomposition to formate and ammonia, as shown below, becomes important. In the presence of NaCl, the hydrolysis of NaCN to HCN is increased at temperatures below 80 C, but decomposition to ammonia and formate is retarded. Sodium cyanide is marketed as a powder, granule, flake or block in pillow-shaped pieces weighing about 1 oz, and as a 30% aqueous solution.\n Solid sodium cyanide is packed in steel or fiber drums, and the aqueous solution is shipped in tanks by truck or rail. Potassium cyanide, KCN, is a white crystalline, deliquescent, solid. KCN is produced by methods similar to those for NaCN. The chemical reactivity of KCN is similar to that of NaCN. Hydrolysis to HCN, as was the case with NaCN, is slight (Kh = 2.54 x 10 exp(-5)). Potassium cyanide is sold in forms similar to those of NaCN but because KCN is more expensive, its world production for 1963 was only 5,000 tons. Calcium cyanide, Ca(CN)2, is also called \"black cyanide\" and is the only commercially important alkaline earth cyanide.\n The hydrolysis of Ca(CN)2, which takes place in two steps, as shown below, is complete.\n The resulting calcium hydroxide has dissociation constants of 3.74 x 10 exp (-3) and 4.0 x 10 exp (-2) but is much less soluble in water at 0 degrees C than sodium hydroxide so that its aqueous solutions are not as alkaline.\nFor example, the pH of an aqueous solution of Ca(0H)2 in an electric furnace above 1000 C in the presence of sodium chloride.\nsaturated\n Rapid cooling apparently prevents the reversion to calcium cyanamide.\n It is manufactured primarily in Canada, South Africa, and East Germany and sold as flakes or blocks.\nThere is also some production elsewhere in Europe and Japan.\n in 1898 to kill vermin in railway cars, in to kill bed bugs in prisons, and, after 1910, for the fumigation of the holds of ships. Stock and Monier-Williams Cytochrome c absorbs radiation at 550 nanometers (nm). In the presence of cytochrome oxidase, the optical density at 550 nm decreases at a rate directly proportional to the activity of cytochrome oxidase. This rate of change was determined in the presence of cyanide, demonstrating the ability of cyanide to inhibit cytochrome oxidase activity. Additions of methemoglobin, in which the iron had been oxidized electronically to the ferric state, to a solution containing cytochrome c, cytochrome oxidase, and cyanide were found to increase the activity of cytochrome oxidase, thus reversing the inhibitory effect of cyanide. The authors also found that the addition of cyanmethemoglobin to a solution of cytochrome c and cytochrome oxidase had no immediate effect on enzyme activity, but after a few minutes the enzyme became increasingly inhibited. Thus, the authors demonstrated in vitro the abilities of cytochrome oxidase and methemoglobin to compete in a reversible fashion for the cyanide ion.\nIn a 1958 survey, Dixon and Webb found that the concentration of cyanide necessary for inhibition of cytochrome oxidase was 2-6 orders of magnitude less than those required for inhibition of other enzymes. The interference of CN with many different enzyme systems other than those involved in respiration may thus contribute to its toxicity.\nSchubert and Brill in 1968 measured the inhibition and recovery of liver cytochrome oxidase in mice, rats, and gerbils after the intraperitoneal administration of KCN. Inhibition of the enzyme was found to reach a maximum 5 to 10 minutes after the cyanide injection. Depending on the dose, the enzyme activity returned to normal 5 to 20 minutes after maximal inhibition in mice but required up to 1 hour or more in the rat and gerbil. Interestingly, they found that the abilities of mice and rats to tolerate divided doses of cyanide depended on the total dose as well as on the time-dependent degree of enzyme inhibition. For example, they found that mice invariably survived a single sublethal dose of 6 mg/kg of KCN but not two doses of 3 mg/kg given 6 minutes apart or three doses of 2 mg/kg given at 6 minute intervals. They further showed that sodium thiosulfate and nitrite were able to reactivate liver cytochrome oxidase within minutes when administered to cyanide-treated rats and mice. Both men complained of headache and weakness or fatigability and were observed to have slight lid lag, enlarged thyroids, and excessive perspiration. One of the two also experienced dizziness and mental confusion, slurring of speech, coughing, sneezing, and occasional abdominal cramps, nausea, vomiting, and coarse tremor of the extremities followed by their temporary paralysis. Both men were exposed to cyanide aerosols generated by case hardening. Some exposure to HCN may have occurred.\nWuthrich in 1954 described a 39-year-old German blacksmith who was exposed to cyanide in case hardening on a sporadic basis for 2 years and then more frequently for the next 4 years. The worker noticed some initial irritation, followed by a general worsening of health. He experienced loss of appetite, nervousness, vertigo, headaches, nausea, and vomiting.\nDuring 2-3 week vacations, the symptoms disappeared but reappeared within a month after returning to work. His thyroid gland was slightly enlarged. After exposure to cyanide had ceased for about 14 days, the man was given a placebo of NaCl, iv, for three days during which time he reported an improvement in his condition. On the 4th day, 1.4 g of sodium thiocyanate was substituted for NaCl in the daily injections. The thiocyanate concentration in the blood serum increased rapidly following these injections and did not decay to normal between injections. From the day of the first NaSCN injection, the man began to complain of nausea, lack of appetite and nervousness. After three NaSCN injections, he reported nausea and vomiting and spontaneously stated that he felt the same symptoms as at his workplace.\nIf there are 5200 ml of blood in the average man, then a dose of and eventually by complete disappearance of P waves. A secondary increase in rate, but not to the rate prior to administration of HCN, was observed during the 3rd and 4th minutes along with the irregular reappearance of P waves, some of which were not conducted. All subjects showed A-V dissociation with a secondary decrease in rate during the 5th minute.\nDuring the 6th and 7th minutes, the heart rates again showed a slight increase and a return to normal sinus rhythm. Thereafter, the heart rates slowed progressively. Normal A-V conduction in one man and incomplete A-V block in another were maintained throughout the period of observation (approximately 13 minutes).\nA third subject developed Wenckebach's phenomenon, (2:1 block), and, finally, complete heart block. The fourth subject's heart had normal A-V conduction until the 14th minute, when it developed ventricular tachycardia and ventricular fibrillation. It must be remembered that the concentrations of HCN to which these men were exposed were huge, so that the details of the changes in their ECG recordings may not be entirely typical of those to be expected in occupational exposures.\nWexler's observations do seem to demonstrate that cyanide has no specific action on the heart but rather exerts on the myocardium actions that are typical of hypoxia and anoxia.\nThere have been several reports of exposure to HCN which included both the airborne concentration of HCN and the human physiological response. However, in many cases no additional information relating to worker exposure was provided. These reports are summarized in Table XIV-5.\nIn many cases it is difficult to attribute a specific concentration range directly to a group of investigators since many of the citations involve reference to the work of others with no additional supporting information.\nTherefore, the validities of concentrations presented only by secondary references may be questioned. In large part they appear to be based on the unreferenced work of Lehmann and Hess. However, the application of\n\n# Lehmann's data to man has been questioned by McNamara because\nLehmann's work was apparently done entirely with rabbits, which McNamara considers to be more sensitive to a given dose (product of concentration and time) of HCN than man. He concluded that man has a susceptibility to HCN more like those of the comparatively resistant goat and monkey and on\nthis assumption (and one that the LCt50 for man is four times that for the mouse) has estimated that 3,404 mg/cu m will cause 50% mortality in humans exposed to it for one minute. McNamara estimated that a concentration of HCN of 607 mg/cu m would kill 50% of men after a 10-minute exposure.\nThe various fatal doses of HCN seen in Table XIV had just returned from a 13-month leave of absence 5 months prior to this episode.\nIn use, the solution was heated to boiling whereupon 50 ml of hydrogen peroxide were added. The gold articles were cleaned in a manner causing splashing on the skin and the production of a visible aerosol.\nThere may have been some exposure to HCN. A study of plant records revealed another plater who developed typical signs and symptoms in 1 month. The man had been treated for 7 weeks, was removed from exposure, and recovered. An investigation of the plant was made and these 19 illnesses were attributed to aerosols emitted by the improperly operated plating tanks. After engineering controls and housekeeping procedures had been instituted, there were no recurrences of these illnesses. No airborne concentrations of contaminants were reported.\nElkins in reported that in a plant where there was considerable brass plating the ambient air contained a mist. The mist was reported to have contained NaCN in a concentration not greatly exceeding 5 ppm, expressed as HCN. Severe irritation was a widespread complaint and there were some incidents of ulceration of the nasal septum. The author noted that other alkalies of undetermined concentration in the air may have contributed to the irritating action of the mist. with the exception of one with a perforated septum who gave a history suggestive of previous exposure to chromates. The cyanides were not described but they were likely a mixture of NaCN, KCN, and some alkaline complex of CuCN in the copper plating tanks, and alkaline NaCN in the zinc bath.\nIn None of the four unexposed men had evidence of disease of the stomach or duodenum. The author reported that three of the exposed and two of the unexposed men had erythrocyte counts above 5,000,000 but below 6,100,000/cu mm and that seven of the exposed and none of the unexposed men had a percentage of lymphocytes above 40 but below 49%. He attributed the latter change to stress resulting from repeated exposure to small doses of HCN. He concluded that his results demonstrated that not all the effects of repeated acute or subacute exposures to HCN are entirely reversible.\nIn Exposure was continued until the animals became apneic, their heart beats became irregular and weak, and distinct cyanosis was apparent. Administration of oxygen through a plaster of Paris mask, modelled to fit the rabbit's muzzle, by hand pressure applied to a rubber bag connected to the mask succeeded in reviving 18 of the 36 rabbits. The authors stated that the hearts of the other 18 rabbits had become too weak when oxygen administration was started to be able to perform the necessary movement of oxygenated blood to the important organs.\nIn 1951, Moss et al exposed 16 rats to HCN at 24-465 ppm for up at 22 minutes. The rats exposed at 25-50 ppm survived, except for one exposed at 50 ppm. This rat was violently agitated after 1 minute 49 seconds, paralyzed after 2 minutes 30 seconds, unconscious after 3 minutes, and dead after 8 minutes.\nIn experiments reported in 1952 by Haymaker et al, six dogs were exposed at concentrations of 620, 590, 700, 700, 165, and 690 mg/cu m, for periods of 2.0, 2.0, 1.75, 1.75, 10.0, and 2.0 minutes, respectively.\nThe first three dogs died in 20 hours or less and the others were killed 24, 26, and 28 hours after exposure. Four of the six dogs had convulsive seizures. The dog exposed at 620 mg/cu m had marked proliferation of histiocytes in the leptomeninges and in the perivascular spaces of the molecular layer of the cerebellum. Only shadows of the Purkinje cells remained. Some of these dogs suffered necrosis of gray matter. Definite alterations of structure were not seen in dogs that died within 21 minutes after being exposed to HCN; they were found in dogs that died 2.5 or more hours after exposure. At these comparatively early times, there was subpial edema of the cerebrum and the cerebellum. Dogs that survived for as long as 16 hours had cellular damage, particularly in the cerebral cortex.\nThe frontal and parietal lobes were more likely to be affected than the temporal or occipital.\nCortical damage was concentrated frequently in the trough of a sulcus in the form of massive coagulation necrosis.\nValade in 1952 exposed four dogs to HCN at 50 mg/cu m for 12 30-minute periods, conducted at 8-day intervals. Of these dogs, two survived, one died after 38 days, and one died of an intercurrent disease.\nIn a second experiment, four dogs were subjected to 19 30-minute inhalation periods at 2-day intervals and at the same HCN concentration. One died after 73 days, the other after 77 days. Another group of five dogs went through seven 30-minute inhalations at 2-day intervals, but this experiment was interrupted when pulmonary inflammation occurred, causing the death of three dogs. Still another group of four dogs were subjected to fourteen 30-minute inhalation periods at 2-day intervals; one of these died after 34 days.\nThe first signs were dyspnea, nausea, exaggerated intestinal peristalsis, and diarrhea. Later, the dogs developed tremors followed by loss of equilibrium and convulsions. These observations tend to support the hypothesis of a cumulative effect from exposure to HCN.\nValade autopsied the dogs immediately after they died or were\nkilled and observed similar central nervous system lesions in each of them.\nVascular changes were vasodilatation and hemorrhages which were most pronounced in the central gray nuclei, brain stem, bulb, and medulla cervicalis.\nCellular lesions manifested themselves by glial reactions throughout the central nervous system and by cytologic changes in the Purkinje cells of the cerebellum and in the bulbar gray nuclei. These histopathologic examinations led the author to conclude that the lesions resulted from anoxia caused by inhibition of cytochrome oxidase or from a selective effect of the poison. To support the contention that the latter cause was the more significant, the author noted that the dogs were very quickly affected by respiratory disorders before the onset of other signs.\nHe thought there was reason to believe that the suddenness with which these disorders appeared was linked to a particular sensitivity of these animals' bulbar cells to cyanide, rather than to an inhibition of cytochrome oxidase. In 1955, Howard and Hanzal reported a feeding study with HCNfumigated food. Thirty male and 30 female weanling albino rats were divided into 3 groups of 10 males and 10 females each. Two of the groups were given dog meal containing 300 ppm and 100 ppm of HCN, respectively. A third, similar group was fed unfumigated food as a control. At the end of a 2-year feeding period, no gross signs of cyanide toxicity were observed.\nAutopsies revealed the same general abnormalities and signs of senility in control and experimental rats. Microscopic examination of heart, lungs, liver, spleen, stomach, small and large intestines, kidneys, adrenal, thyroid, testes or uterus and ovary, and the cerebrum and cerebellum revealed no evidence of pathology due to HCN feeding. All findings were compatible with those usually seen in aging animals, and the same general changes were found in both the control and the experimental animals.\nThiocyanate concentrations in plasmas, RBC's, and kidneys, but not in the livers, of rats given food containing 300 or 100 ppm HCN were about twice as high as those in controls.\nIn 1959, Levine and Stypulkowski reported lesions in several areas of the brains of rats which survived exposure for 20-45 minutes at an unknown concentration of airborne HCN. The concentration of the airborne cyanide aerosol, which the authors presumed to be HCN, was not determined but was sufficient to debilitate the rats in 10 minutes. Earlier, Flury\nand Zernik found that persisting prostration occurred in 9.5 minutes at 127 ppm and, thus, it may be estimated that the rats in this experiment had exposures to HCN at approximately 127 ppm. Below this concentration (127 ppm), exposure to HCN for 2 hours did not produce brain lesions.\nAbove this concentration at which persisting prostration occurred, brain lesions were produced readily in 20-30 minutes. These lesions involved a multiplicity of sites in the brain although they were not universal in distribution.\nFor example, the cord, most of the stem, cerebellum, diencephalon, and portions of the cerebrum were spared. A predominance of isolated lesions appeared in the callosum and striatum. Later that same year, Levine and Weinstein, using the same technique described above, reported that high concentrations of HCN generally caused the death of rats without causing brain damage. Low concentrations did not produce either, but moderate concentrations (perhaps 100-150 ppm) caused brain lesions while consciousness was maintained for an hour or so, followed by sudden unconsciousness and death. Unfortunately, in neither of these studies was the airborne concentration reported. Wistar albino rats receiving 0.5 mg of KCN subcutaneously once weekly for 22 weeks. They reported some pallid myelin but found it difficult to estimate whether or not there was demyelination. The animals appeared to be without other ill-effects from these small doses. The authors suggested that these lesions were due to excessive utilization of hydroxocobalamin to form cyanocobalamin. Whether these effects on nervous tissue are due to a specific action of the cyanide ion or of the thiocyanate ion, or to general histotoxic anoxia, is not clear.\nMoss et al in 1951 subjected from one to three rats to mixtures of CO and HCN. Atmospheres containing either HCN or CO alone were generally lethal to rats at concentrations of 50 or 5000 ppm, respectively.\nA mixture of 10-20 ppm of HCN and 2000 ppm of CO was lethal to some.\nMixtures of 30 ppm of HCN and 1000 ppm of CO and of 5 ppm of HCN and 2000 ppm of CO were not lethal.\nHirner in 1969 subjected male rats weighing about 250 g to subcutaneous injections of 0.2% KCN.\nThe daily dose, which averaged between 3 and 5 mg/rat, was divided into parts, which were injected within the span of 1 hour. Five rats received single daily doses and were killed 2 or 3 days later. Six rats received 4 to 12 daily doses, two received 14, and four received 20. All the multiply dosed rats were killed at the end of 9 weeks from the first daily dose. These rats were perfused through the left ventricle with a sodium cacodylate-glutaraldehyde solution;\nappropriate samples of nervous tissue were ultrasectioned and examined electronmicroscopically as well as by conventional optical microscopy. The principal lesion found in this study was necrosis in the caudal part of the corpus callosum, with spongy alteration at the margin of the necrotic area.\nPhagocytes invaded the necrotic area 2 days after the last dose of KCN; astrocytic gliosis followed. In the area of spongy change, there was vacuolization of axons and swelling of the astrocytes and oligodendroglia.\nDemyelination was visible in the later stages of the study. Hirner considered that the effects on glial cells were primary effects of cyanide, but that disintegration of myelin and axonal degeneration were secondary effects, the axon remaining intact when swelling of the glia had occurred.\nHe stated the belief that the oligodendroglia are particularly susceptible to injury by cyanide. Unfortunately, neither report sought to quantify the dose of either HCN or KCN.\nIn the first study, Levine and Stypulkowski In the second study, Levi and Amaducci in 1968 brought their animals through the first two stages, after which they were allowed to partially recover, and were then killed by decapitation. The meninges appeared congested. Some rats had hemorrhagic pulmonary infarctions. In some animals trypan blue was injected iv to test the integrity of the blood-brain barrier. Subsequent examination of the brains did not show any abnormal passage of the trypan blue into the nervous tissue. Brain slices of other rats were used to study the active transport of amino acids.\nInitial and steady state accumulation of amino acids and rates of amino acid exit were identical in brain slices from control and treated animals when a glucose-containing incubation medium was used. Tissue respiration rates were also measured in vitro and found to be identical in both control and treated animals. Thereafter, the analytical method selected determines cyanide radical content, and it is impossible to say what fraction of the total was attributable to any particular compound.\nIn order to differentiate between HCN gas and other cyanide compounds, it is necessary to first remove particulates by passing the air through an efficient filter, then absorb HCN from the stream by passage through an alkaline absorbing solution.\nThe filtered cyanides can subsequently be leached from the filter by treatment with alkaline solution, and the same analytical technique applied to both portions of the sample.\nThe presence of small quantities of cyanide in water was of concern long before relatively recent ecologic considerations led to an awareness that many other substances were toxic at trace concentrations. As a result, there exists substantial literature dealing with the qualitative and quantitative detection of cyanides in air and water, with at least one method (the titrimetric estimation of cyanide with silver nitrate published by Liebig in 1851) still in use today, more than a century after its origination. Almost all the methods proposed for the analysis of water or other materials have been, or can be, applied to the analysis of cyanides in air, for most air methods ultimately involve the determination of cyanide ion in solution. One of the most widely used colorimetric methods is the so-called pyridine-pyrazolone method, an example of the Konig synthesis for pyridine dyes, first published by Aldridge in 1944 (using pyridine and benzidine) and subsequently modified by various authors.\n In this method, cyanides are converted to cyanogen bromide or cyanogen chloride, which then reacts with pyridine to form a glutaconic aldehyde.\nNext, a primary aromatic amine reacts with the aldehyde to yield a colored Schiff's base. In the original procedure of Aldridge, the aromatic amine used was benzidine, but the more frequently used modification of Epstein voltammetry , amperometry , coulometry potentiometry and others. The most recently introduced and probably mosc useful in its application to air analysis, is the eleccrometric technique relying on specific ion electrodes, or ion selective electrodes which respond only to cyanide ion concentrations, Cohen A -novel approach to determining cyanide levels has been described by OancniK and Br/lr.z involving Indirect atomic absorption \" spectrometric analysis.\nIn the first of two methods, the complex dicyano-bis-(l,10phenanthroline)-iron(II) is formed and then ¿-.:tracted into chloroform. The\n- iaiororG-ia is evaporated and the residue is taken ap m ethanol. The\n- -.thaiioi. solution is aspirated directly into the flame, and iron equivalent 99 i to a known amount of cyanide is then determined. The second method is based on precipitating silver cyanide, then determining the excess silver ion in the supernatant by atomic absorption spectrometry.\nIn place of titrimetric techniques, several investigators have described methods in which turbidity resulting from the formation of silver cyanide, or the reduction in turbidity due to the formation of a cyanide complex with silver iodide, are measured.\n, a specific ion electrode method , and a blood method using microdiffusion , first used by Conway.\n A respired air method based on the pyridine-pyrazolone reagent , as well as more general methods applicable to biologic samples using this same reagent are also used.\nThe rationale used in making a forensic diagnosis of cyanide poisoning have also received some attention. Many of the methods listed have also been used for water and waste water analyses, and currently the methods most favored appear to be colorimetric, using some version of the pyridine-pyrazolone method, or modifications of the titrimetric determination with silver nitrate.\n Specific ion electrodes , and picric acid have also been used.\nRecently, an opto-acoustic infrared absorption technique as well as the titrimetric method utilizing silver nitrate have been used in the analysis of HCN in automobile exhaust. Virtually every method used for cyanide analyses is subject to some interferences, usually due to the presence of certain metals which may form complexes, other anions, particularly sulfide, and a host of oxidizing and reducing agents. It is, therefore, frequently necessary to isolate the cyanide by some means, most frequently by a distillation from strongly acid solution, where all but the most tightly bound metal complexes are dis sociated to release hydrogen cyanide which is then absorbed in alkaline solution.\nThe recommended sampling and analytical method for the cyanides covered by this document is essentially that of the standard NIOSH method for cyanide in air as published in the NIOSH Manual of Analytical Methods. should be followed.\nHigh ventilation rate systems for the rapid dilution or removal of HCN gas and aerosols may be useful in some areas.\nControl of the hazard of potential release of hydrogen cyanide from cyanide salts requires constant care and attention to good work practices.\nThe cyanide salts should be kept well apart from, and protected from contact with, acids, moisture, or elevated concentrations of carbon dioxide.\n\n# Basis for Recommended Environmental Standard\nCyanide is well known as an acute, fast acting poison which can be described as insidious in that its toxic action at high concentrations is so rapid that its odor has no value as a warning.\n At lower concentrations the sense of smell may provide forewarning. For HCN, the primary routes of entry from occupational exposure are inhalation and absorption through the skin.\n Thus, it may be presumed by analogy that if 90 ppm of HCN is fatal, 96 mg/cu m of CN, derived from cyanide salts, may be also. Extending this analogy to threshold levels, presumably 11 mg/cu m of CN would be equivalent to the current Federal standard of 10 ppm of HCN and restriction of exposures to 11 mg/cu m of CN would protect against acute toxicity from cyanide salts.\nHowever, taking into account the irritant effects observed from exposure to cyanide salts, the current Federal standard of 5 mg/cu m of CN as an 8-hour time-weighted average appears to be too high in that it allows substantial excesses above that concentration for short periods of time.\nTherefore, NIOSH recommends that the current value of 5 mg/cu m of CN be retained, but that its basis be changed from an 8-hour time-weighted average to a 10-minute ceiling. This action should provide the employee with adequate protection from the systemic effects of cyanide and prevent the erosional effects produced by the alkalinity associated with the cyanide salts.\nA review of the cases involving exposure to cyanide reveals that they fall into three general categories. First are those cases in which there was an acute or subacute exposure followed immediately by an acute illness. [11,13,20,26,27 ppm. They also stated that it was difficult to give reliable limits for normal levels of cyanide and thiocyanate in the urine. However, in order to assess the hazards of occupational exposure, they considered it safe to state that nonsmokers who have greater than 400 #ig/100 ml of free thiocyanate in the urine, or smokers with urinary concentrations exceeding It is recognized that many workers are exposed to cyanides in concentrations considerably below the recommended occupational limits.\nUnder these conditions, it should not be necessary to comply with many of the provisions of the recommended standards. However, concern for worker health and well-being requires that protective measures be instituted below the enforceable limits to ensure that exposures do not exceed the standard.\nIs given the super.vi sion necessary to assure that all safety tP'lii p r ;} r f \\ c p c rn f-»V. I (7) is instructed to shower before removing any respirator or gas-tight suit if prior contact with HCN liquid has occurred or is suspected; (preferably sight contact) in a safe area or at a distance so as not to be affected by an emergency situation at the site of the first employee. The second employee (\"buddy\") should be alert and equipped to summon help and render aid, if needed.\nThe employee should carefully and precisely follow all operational procedures specified for the handling of HCN in containers, transfer operations, or other equipment. Suppliers' and manufacturers' instructions should be carefully followed.\nWhen HCN is used for fumigation purposes, the space should be sealed to prevent the gas from leaking into surrounding spaces or areas. Warning signs should be posted and guards placed to keep unauthorized persons at a safe distance. All laws, regulations, ordinances, and codes applicable should be followed. Only licensed fumigators should do Such work. Open containers of any solid cyanide salts or of solutions of cyanide salts should be limited to those necessary for operational requirements and procedures. Such open containers must be used only in adequately ventilated spaces so that the recommended standards for the airborne concentration of cyanide are not exceeded. Good practice dictates that, in so far as practical, covers be provided for such containers and used whenever possible.\nSolutions of cyanides should be maintained as basic as practical to prevent any evolution of hydrogen cyanide. When weakly basic or neutral solutions are used, ventilation must be provided sufficient to prevent accumulation of the HCN evolved from exceeding the recommended standard for HCN in the work room air. When the addition of an acid to a cyanide solution may be necessary, the process should be fully enclosed and ventilated.\nRespiratory protection should be provided for all workers potentially exposed to any release of hydrogen cyanide.\nFused salt baths containing cyanide salts should be provided with local exhaust ventilation. Care should be exercised in the operation of such baths to avoid spills and splashes. Addition of salts should be made carefully, using a shovel or special tool. The area about the bath should be regularly cleaned to prevent accumulation and encrustation of cyanide salts on adjacent areas. Workers at fused salt baths should wear safety goggles with side shields.\nLocal exhaust ventilation must be used for all operations emitting dusts or mists of cyanide salts. Tanks and other equipment which must be entered for inspection, maintenance or repair, should be drained as completely as possible and then filled with water and agitated. After 15 minutes, they should be drained again and refilled for another 15 minutes, then drained again. The tanks should then be inspected for residue and encrustation of cyanides. These should be broken loose mechanically or by the force of a water stream and flushed away.\nThe tank should then be purged with fresh air, followed by testing for the absence of cyanide in the air before anyone enters. Cyanide waste solutions and cyanide-contaminated rinse or wash waters should be treated to destroy the cyanide before being discarded.\nTreatment of cyanide waste is achieved by oxidation of the cyanide in alkaline solution by addition of chlorine or other oxidizing agents.\n\n# IN AIR AND CALIBRATION\nThe same sampling and analytical methods are used for atmospheric hydrogen cyanide and the particulate cyanides. They can be collected and analyzed separately or by insertion of a filter can be simultaneously collected and individually analyzed. A sampling period of about 10 minutes is necessary to provide an amount of cyanide readily amenable to analysis by the cyanide selective electrode.\n\n# Sampling\nAll glassware is washed in detergent solution, rinsed in tap water, and then rinsed with distilled or deionized water. Ten ml of an absorbing solution (0.1 M NaOH) is poured into an all-glass midget impinger using a graduated cylinder to measure the volume.\nThe fritted inlet of the impinger should have a porosity approximately equal to that of Corning EC (170-220 micron maximum pore diameter). A membrane prefilter (0.45 / u r n pore size) should be inserted (by means of an in-line cassette or similar device) before the impinger when sampling for particulate cyanides is to be performed.\nSampling for HCN and/or the particulate cyanides is performed for at least 10 minutes at a rate of 2 liters/minute, but the total volume of air sampled should not exceed 200 liters. A personal sampling pump or other satisfactory source of suction may be used for sampling provided it is calibrated as outlined below. Alternate sampling systems may be used, providing the required volume of air is sampled from the breathing zone of the worker.\nCertain cyanide compounds, especially calcium cyanide, may hydrolyze at sufficiently high relative humidities, resulting in losses of collected sample as HCN gas. In such cases, it may be advisable to minimize losses by keeping the sampling time as short as possible, then storing it in a refrigerator until analysis.\nIt should be noted that when sampling for HCN without a prefilter, particulates will pass through the midget impinger. Likewise, when sampling for particulate cyanides by means of a midget impinger without a prefilter, HCN gas will also be collected and will constitute a positive interference.\n\n# Calibration\nSince the accuracy of an analysis can be no greater than the accuracy of measurement of the volume of air sampled, the accurate calibration of a sampling device is essential to the correct interpretation of an instrument's indication. The frequency of calibration is dependent upon the use, care, and handling to which the pump is subjected. Pumps should be calibrated if they have been subjected to misuse or if they have just been repaired or received from a manufacturer. If the pump receives hard usage, more frequent calibration may be necessary.\nOrdinarily, pumps should be calibrated in the laboratory both before they are used in the field and after they have been used to collect a large number of field samples. The accuracy of calibration is dependent on the type of instrument used as a reference. The choice of calibration instrument will depend largely upon where the calibration is to be performed. For laboratory testing, a soapbubble flow meter or wet-test meter is recommended, although other standard calibrating instruments, such as a spirometer or dry-gas meter, can be used. The actual setup will be connected in sequence to the filter cassette or fritted impinger unit which will be followed by the sampler pump.\nIn this way, the calibration instrument will be at atmospheric pressure. If the personal sampler pump is used, each pump must be calibrated separately. If the buret is used, it should be set up so that the flow is toward the narrow end of the unit.\nCare must be exercised in the assembly procedure to ensure that seals at the joints are airtight and that the length of connecting tubing is kept to a minimum. Calibration should be performed under the same conditions of pressure and temperature as those encountered in use. The calibrated pump rotameter should be used to set the flow rate in the field. Samples are analyzed using the cyanide ion selective electrode.\n\n# Range and Sensitivity\nThe ultimate range and sensitivity of the method have not been established at this time. The recommended range of the method is 0.013-13 mg/cu m in air (approximately 0.0117-11.7 ppm of HCN).\n\n# Interference\nSulfide ion irreversibly poisons the cyanide ion selective electrode and must be removed if found in the sample. Check for the presence of sulfide ion by touching a drop of sample to a piece of lead acetate paper.\nThe presence of sulfide is indicated by discoloration of the paper.\nSulfide is removed by the addition of a small amount (spatula tip) of powdered cadmium carbonate to the sample at pH 11-13. Swirl to disperse the solid, and recheck the liquid by again touching a drop to a piece of lead acetate paper. If sulfide ion has not been removed completely, add more cadmium carbonate. Avoid a large excess of cadmium carbonate and long contact time with the solution.\n\n# METHOD FOR ANALYSIS OF CYANIDE SAMPLES\nWhen a drop of liquid no longer discolors a strip of lead acetate paper, remove the solid by filtering the sample through a small plug of glass wool and proceed with the analysis.\n\n# Precision and Accuracy\nThe precision and accuracy of this method have not been completely determined at this time. No collaborative tests have been performed on this method.\n\n# Apparatus (a) Sampling and Calibration Equipment\n(1) A filter unit (if needed) consisting of the filter media and cassette filter holder.\n(2) A midget fritted impinger containing the absorbing solution or reagent.\n(3) A pump suitable for delivering desired flow rates.\nThe sampling pump is protected from splashover or water condensation by an absorption tube loosely packed with a plug of glass wool and inserted between the exit arm of the impinger and the pump.\n(A) An integrating volume meter such as a dry-gas or wet test meter.\n(5) Thermometer ( 6) Manometer\n\n# (f)\nPrecision and repeatability must be plus or minus 2% of full scale.\n(g) It is desirable that the instrument respond only to HCN, but instruments which respond to other gases not normally present in the atmosphere may be acceptable.\nIn general, it is probable that any gas which causes a reading sufficiently high to set off the alarm will itself be present at a concentration sufficiently high to warrant corrective actions. Whenever there is a possibility that gases or vapors such as hydrogen chloride, chlorine, etc, may be present, it would be desirable to determine the response of the instrument to such gases in advance.\n(h) An operating range of 0-100 ppm HCN is optimal, but other ranges may be selected to suit individual needs.\n(i) The device should be capable of 7 days of continuous unattended operation.\n\n# (j)\nThe device and alarm should be intrinsically safe for use in hazardous locations.\n\n# Discussion\nThe principal requirements for such monitors in addition to responding to HCN gas are that they be sufficiently rugged to withstand normal extremes of temperature, pressure, vibration, etc, and not be susceptible to plugging or interferences due to contaminants likely to be encountered in most work places. They should be so constructed that it is possible to quickly check the zero setting of the instrument and the response at 25 ppm in a rapid routine manner. Chemical substances should be listed according to their complete name derived from a recognized system of nomenclature. Where possible, avoid using common names and general class names such as \"aromatic amine,\"\n\"safety solvent,\" or \"aliphatic hydrocarbon\" when the specific name is known.\nThe \"%\" may be the approximate percentage by weight or volume (indicate basis) which each hazardous ingredient of the mixture bears to the whole mixture. This may be indicated as a range or maximum amount, ie, \"10-40% vol\" or \"10% max wt\" to avoid disclosure of trade secrets.\n\n# IX S P E C IA L PREC A U TIO N S P R E C A U T I O N A R Y S T A T E M E N T S O T H E R H A N D L I N G A N O S T O R A G E R E Q U I R E M E N T S P R E P A R E D B Y A O O R E S S O A T E\n\n# XIII. APPENDIX V\nFirst Aid and Treatment Kits Two physician's treatment kits should be immediately available to trained medical personnel at each plant where there is a potential for the release of, accidental or otherwise, or for contact with, hydrogen cyanide or cyanide salts. One kit should be portable in order that it may be carried by medical personnel while accompanying a patient to the hospital.\nThe other kit should be kept under lock and key to assure that it is intact and available when and if needed. The key should be readily available at all times to the work supervisor on duty and the storage place should be of such construction as to allow accessibility in the event of loss of the key.\nBoth kits for use by the medical personnel servicing each firm should contain the following as a minimum.\n(1) Two (2) boxes (2 dozen) ampules; each ampule containing 0.3 ml of amyl nitrite.\n(2) Two (2) ampules of sterile sodium nitrite solution (10 ml of a 3% solution in each).\n(3) Two (2) ampules of sterile sodium thiosulfate solution (50 ml of a 25% solution in each).\n(4) 2 sterile 10-ml syringe with intravenous needles.\n(5) 1 sterile 50-ml syringe with intravenous needle.\n(6) 1 tourniquet (7) 1 gastric tube (rubber).\n(8) 1 non-sterile 100 ml syringe.\nThe medical personnel servicing a firm where there is a potential for hydrogen cyanide release or a potential for exposure to inorganic cyanide should be familiarized with the use of these kits.\nFirst-aid kits should be immediately available at work places where there is a potential for the release, accidental or otherwise, of hydrogen cyanide or a potential for exposure to inorganic cyanide. This kit should contain as a minimum two (2) boxes of ampules ( 2 dozen), each containing 0.3 ml of amyl nitrite. Ampules should be replaced biannually or sooner if needed to ensure their potency.\nThe amyl nitrite ampules should be protected from high temperatures. In all cases, the contents of the medical and first-aid kits should be replaced before the manufacturer's assigned expiration dates.\nFirst-Aid Procedure Speed in the rendering of first-aid treatment is of the utmost importance. The patient should be removed at once to an area free from HCN. The rescuer should wear respiratory protective equipment in order not to be overcome or weakened by the gas.\nMany victims will have stopped breathing.\nIn this case, it is imperative that efforts at resuscitation be instituted at once and continued without interruption even while other treatment is being administered.\nA physician should be summoned immediately.\nFirst-aid kits should be readily available at all times. They should be quickly accessible but should not be kept only in operating areas mixtures with air may be explosive if a source of ignition is present.\n\n# (B) Resuscitation\nBefore instituting artificial resuscitation, dentures and foreign objects, such as gum and tobacco, and any accumulated oropharyngeal fluids (saliva, etc) should be removed from the patient's mouth and pharynx and the tongue pulled forward.\nIf the patient's breathing is weak or has stopped, artificial resuscitation should be started at the earliest possible moment and continued without interruption until normal breathing has been established or the patient is pronounced dead.\nMouth-to-mouth resuscitation is the method of choice because of its simplicity and effectiveness. It is, however, impossible to administer amyl nitrite while using this method. Therefore, it is advisable to switch to other methods of artificial respiration, such as the Holger-Nielsen arm-lift back pressure method, during the periods when the amyl nitrite is being given.\nIf a mechanical resuscitator and personnel skilled in its use are available, this equipment may be used instead of other forms of resuscitation.\n(C) The patient should be kept comfortably warm but not hot. Other drugs and stimulants are rarely necessary and should be administered only by a physician or trained medical personnel under the direction of a physician. Step -Through the formation of a relatively stable coordination complex with ferric iron, cyanide tends to keep this metal in its higher oxidation state and thus reduces its efficacy as an electron carrier in ferric to ferrous iron transitions.\nBy such a complexation of iron, the respiratory enzyme ferricytochrome oxidase is changed to ferricytochrome oxidasecyanide and its ability to catalyze the reaction of reduced cytochrome with oxygen is inhibited, with consequent impairment of cellular oxygen utilization\nStep -Since numerous metabolic pathways converge at the cytochrome system, the impairment of the cells' ability to utilize oxygen reduces or even stops aerobic metabolism. True histotoxic (cytotoxic) hypoxia results with a shift to anaerobic metabolism with accumulation of lactate, pyruvate, and glucose.\nStep -The cells are thus unable to use the oxygen brought to them as 02Hb by the arterial blood. The oxyhemoglobin continues into the veins, the arteriovenous oxygen difference diminishes, and the venous blood is almost as bright a red as the arterial blood.\nStep 4 -The chemoreceptors in the carotid and aortic bodies, which are the tissues most sensitive to cellular hypoxia, trigger an inspiratory gasp and hyperpnea as an almost instantaneous path ophysiologic effect of cyanide absorption.\nCurrent concepts about the treatment of selected poisonings-nitrite, cyanide, sulfide, barium, and quinidine. Ann Rev Pharmacol Toxicol 16:189 -199, 1976 109.\nCarmelo, S: Rass Med Ind 24: 254-71, 1955 (Ita) 110.\nEl Ghawabi SH, Gaafar MA, El-Saharti AA, Ahmed SH, Malash KK, Fanes R: Chronic cyanide exposure: a clinical, radioisotope, and laboratory study. Br J Ind Med 32: 1975 111.\nWollman SH: Nature of the inhibition by thiocyanate of the iodide concentrating mechanism of the thyroid gland. Amer J Physiol 186: 1956 112.\nHeymans JF, Masoin P:\n Arch Int Pharmacodyn Ther 7:297-306, 1900 (Fre) After sampling, the fritted impinger stem can be removed and cleaned in the following manner. Tap the stem gently against the inside wall of the impinger bottle to recover as much of the sampling solution as possible. Wash the stem with a small amount (1-2 ml) of unused absorbing solution and add the wash to the impinger bottle. Then the impinger bottle is sealed with a hard, non-reactive stopper (preferably Teflon) and an appropriate identifying number attached to it. Do not seal with rubber.\nThe stoppers on the impinger bottle should be tightly sealed to prevent leakage during shipping. If it is preferred to ship the fritted impingers with the stems in, the outlets of the stem should be sealed with Parafilm or other nonrubber covers, and the ground glass joints should be sealed, ie, taped to secure the top tightly. Upon completion of sampling for the particulate cyanides, plastic caps should be replaced on the inlet and outlet tubes of the cassette and an appropriate identifying number attached to it.\nCare should be taken to minimize spillage or loss by evaporation at all times. Refrigerate samples if analysis cannot be done within a day. Whenever possible, hand delivery of the samples is recommended. Otherwise, special impinger shipping cases should be used to ship the samples.\nA \"blank\" fritted impinger should be handled as the other samples (fill, seal, and transport) except that no air is sampled through this fritted impinger.\nWhere a prefilter has been used for the collection of particulate cyanides, the filter cassettes are capped and placed in an appropriate cassette shipping container. One filter disc should be handled like the other samples (seal and transport) except that no air is sampled through it, and this is labeled as a blank.\n\n# M A TERIA L SAFETY DATA SHEET 1 PRO D U CT IDENTIFICATIO N M A N U F A C T U R E R 'S N A M E R E G U L A R T E L E P H O N E N O . E M E R G E N C Y T E L E P H O N E N O A D O R E S S\n\n# TRADE N AM E S Y N O N Y M S II H A ZA R D O U S IN G R E D IE N T S M A T E R I A L O R C O M P O N E N T % H A Z A R D D A T A\n\n# III P H Y SIC A L DATA\n\n# O L E V A P O R A T I O N R A T E ( B U T Y L A C E T A T E M ) A P P E A R A N C E A N O O D O R\nwhere they may not be available in case of a spill.\n( (3) Inhalation (A) Administer amyl nitrite A pearl (ampule), if not provided with a fabric sleeve, should be wrapped lightly in a handkerchief or gauze pad, broken, and held about 1 inch from the patient's mouth and nostrils for 15 seconds.\nRepeat 5 times at 15-second intervals. Use a fresh pearl every 5 minutes until 3 or 4 pearls have been administered.\n\n# WARNING:\nFirst-aiders should keep the pearls away from their own mouths and noses lest they become weak and dizzy and unable to give proper assistance to the victim. Amyl nitrite is flammable and"},"raw_text":{"kind":"string","value":"# I. RECOMMENDATIONS FOR CYANIDE STANDARDS\nThe National Institute for Occupational Safety and Health recommends that employee exposure to hydrogen cyanide (HCN) and the cyanide salts in the workplace be controlled by adherence to the following sections. The standards are designed to protect the health of workers for up to a 10-hour workday, and a 40-hour workweek over a working lifetime. Compliance with the standard should therefore prevent adverse effects of HCN and cyanide salts on the health of workers. The standards are measurable by techniques that are valid, reproducible, and available to industry and government agencies.\nSufficient technology exists to permit compliance with the recommended standards. The standards will be subject to review and revision as necessary.\nThese criteria and recommended standards apply to occupational exposure of workers to HCN and cyanide salts. Synonyms for HCN are hydrocyanic acid, prussic acid, and formonitrile. For the purpose of this document, cyanide salts are defined as sodium cyanide (NaCN), potassium cyanide (KCN), or calcium cyanide (Ca(CN)2). The word, cyanide, or the symbol, \"CN\", is used to designate salts as well as hydrogen cyanide.\nThe \"action level\" for hydrogen cyanide or a cyanide salt is defined as one-half the corresponding recommended ceiling environmental exposure limit. \"Occupational exposure\" to these compounds is defined as exposure to airborne concentrations greater than the corresponding action levels.\nThe criteria and recommended standards apply to any area in which HCN, any of the cyanide salts or materials containing any of them, alone or in combination with other substances, is used, produced, packaged, processed, mixed, blended, handled, stored in large quantities, or applied.\nExposure to cyanide at concentrations less than or equal to the respective action levels will not require adherence to the recommended standards except for sections 2-7, and 8(c). If \"exposure\" to other chemicals also occurs, for example to a combination of cyanide and methyl alcohol, provisions of any applicable standards for such other chemicals shall be followed also.\n# Section 1 -Environmental (Workplace Air) (a) Concentration\nEmployee exposure to HCN shall be controlled so as not to exceed 5 milligrams per cubic meter of air expressed as CN (4.7 ppm), determined as a ceiling concentration based on a 10-minute sampling period.\nEmployee exposure to cyanide salts shall be controlled so as not to exceed 5 milligrams per cubic meter of air expressed as CN, determined as a ceiling value based upon a 10-minute sampling period.\nWhenever the air is analyzed for cyanide salts, a concurrent analysis shall be made for HCN. Neither of the respective ceiling values may be exceeded nor may the combined values exceed 5 mg/cu m measured as CN during a 10-minute sampling period.\n# (b) Sampling and Analysis\nProcedures for sampling, calibration of equipment, and analysis of air samples for HCN and cyanide salts shall be as provided in Appendices I and II, or by any method shown to be equivalent in precision, accuracy and sensitivity to those specified. A sampling period of about 10 minutes is necessary to provide an amount of cyanide readily amenable to analysis by the cyanide selective electrode.\nSection 2 -Medical Medical surveillance shall be made available as specified below for all workers occupationally exposed to HCN or cyanide salts.\n(a) Preplacement and annual medical examinations shall include:\n(1) An initial or interim work and medical history with special attention to skin disorders and those non-specific symptoms, such as headache, nausea, vomiting, dizziness or weakness, that may be associated with chronic exposure.\n(2) A physical examination giving particular attention to skin, thyroid, and the cardiovascular and upper respiratory systems.\n(3) An evaluation of the advisability of the worker's use of negative-or positive-pressure respirators.\n(b) Initial medical examinations shall be made available to presently employed workers within six months of the promulgation of a standard.\n# (c)\nThe responsible physician and the employer shall be aware of the material contained in Appendix V and shall ensure that employees trained in these first-aid measures are on duty whenever there is occupational exposure to HCN or a cyanide salt.\n(d) Two physician's treatment kits shall be immediately available to trained medical personnel at each plant where there is a potential for the release of, accidental or otherwise, or for contact with, hydrogen cyanide or cyanide salts. One kit should be portable in order that it may be carried by medical personnel while accompanying a patient to the hospital. The other kit should be kept under lock and key to assure that it is intact and available when and if needed. The key should be readily available at all times to the work supervisor on duty and the storage place should be of such construction as to allow accessibility in the event of loss of the key.\n(e) First-aid kits shall be immediately available at workplaces where there is a potential for the release, accidental or otherwise, of hydrogen cyanide or a potential for exposure to cyanide salts. This kit shall contain as a minimum two (2) boxes of ampules (2 dozen), each containing 0.3 ml of amyl nitrite. Ampules shall be replaced biannually or sooner if needed to ensure their potency. The amyl nitrite ampules should be protected from high temperatures. In all cases, the contents of the medical and first-aid kits shall be replaced before the manufacturer's assigned expiration dates. Suggested contents for these kits are listed in Appendix V. In case of contact, immediately flush skin or eyes with plenty of water for at least 15 minutes; get medical attention. Remove contaminated clothing and wash before reuse.\n# POISON First Aid\nCarry patient to fresh air. Have the patient lie down. Remove contaminated clothing but keep patient warm. Start artificial respiration if breathing stops. Administer antidote (amyl nitrite ampule). Call a physician.\n# Temporary Antidote\nIf cyanide gas is inhaled: Break an amyl nitrite ampule in a cloth and hold lightly under nose for 15 seconds. Repeat at about 15-second intervals.\nIf cyanide is swallowed:\nBreak an amyl nitrite ampule in a cloth and hold lightly under nose for 15 seconds.\nRepeat inhalation of amyl nitrite 5 times at about 15 second intervals. If patient is conscious or when consciousness returns, give emetic (1 tablespoonful of salt to each glass of warm water) and repeat until vomit fluid is clear. Do not give an emetic to an unconscious or barely conscious person.\n# (b)\nThe following warning sign shall be affixed in a readily visible location at or near entrances to areas containing HCN and where there is reasonable potential for emergencies: (1) location of gas masks and other emergency equipment,\n(2) instructions for sounding emergency alarm,\n(3) location of first-aid equipment and supplies, and\n(4) instructions for summoning medical aid.)\nThe sign shall be printed both in English and in the predominant language of non-English-reading workers. All workers shall receive training and information on the hazards and safe work practices in handling HCN and cyanide salts, and on first-aid procedures in poisoning by these compounds.\n(c) When HCN gas is used as a fumigant, warning signs shall be prominently displayed about the area and at all entries to the area as Temporary Antidote\nIf aerosolized salt has been inhaled or if solid or dissolved salt has caused poisoning after contact with the skin: Break an amyl nitrite ampule in a cloth and hold lightly under nose for 15 seconds. Repeat 5 times at about 15-second intervals. Repeat as necessary using a fresh amyl nitrite ampule every three minutes. Use artificial respiration if breathing stops.\nIf cyanide salt in any form is swallowed: proceed as above. If the victim is conscious and capable of some activity, give an emetic (1 tablespoonful of table salt in a glass of warm water) in repeated doses until the vomit fluid is clear. Never give anything by mouth to an unconscious person.\n(e) Containers of Ca(CN)2 shall be labeled in the same manner as other solid cyanide salts, except that an additional warning is necessary because this material will react with water to release hydrogen cyanide.\nThe statement of the hazard shall read as follows for Ca(CN)2:\n# DANGER! MAY BE FATAL IF SWALLOWED OR INHALED CONTACT WITH WATER OR ACID LIBERATES POISONOUS GAS CAUSES EYE BURNS AND MAY IRRITATE SKIN (f)\nAll containers of solutions of cyanide salts shall bear the following labeling in addition to, or in combination with, labels required by other statutes, regulations, or ordinances. The proper chemical name of the specific inorganic cyanide compound followed by the word \"solution\"\nshall appear in large, bold face type at the top of the label.\n(insert name of compound) SOLUTION (Inorganic Cyanide Solution) DANGER! MAY BE FATAL IF SWALLOWED OR ABSORBED THROUGH SKIN CAUSES BURNS CONTACT WITH ACID LIBERATES POISONOUS GAS Do not breathe gas. Do not get in eyes, on skin, on clothing. Wash thoroughly after handling. Keep container closed and away from acids. In case of contact, immediately flush skin or eyes with plenty of water for at least J.5 minutes and call a physician. Treat spillage with strong calcium hypochlorite solution and flush to sewer.\n# POISON First Aid\nAlways have on hand a Cyanide First-Aid Kit. Carry patient to fresh air, have him lie down.\nRemove contaminated clothing but keep patient warm. Start treatment immediately. Call a physician.\n# Temporary Antidote\nIf gas is inhaled: Break an amyl nitrite ampule in a cloth and hold lightly under nose for 15 seconds. Repeat 5 times at about 15-second intervals. Repeat as necessary, using a fresh amyl nitrite ampule every three minutes. Use artificial respiration if breathing stops. If swallowed: Break an amyl nitrite ampule in a cloth and hold lightly under nose for 15 seconds. If patient is conscious, or when consciousness returns, give emetic (1 tablespoonful of salt in a glass of warm water) and repeat until vomit fluid is clear. Repeat inhalation of amyl nitrite ampule every three minutes. Use artificial respiration if breathing stops. Never give anything by mouth to an unconscious person. Engineering controls and safe work practices shall be used to maintain exposures to HCN and cyanide salts below the prescribed limits.\nAdministrative controls may also be used to reduce exposure. However, because the inhalation of cyanides or their absorption through the skin may be immediately dangerous to life, the added protection of personal protective equipment and clothing must be provided for work procedures and for emergency situations as discussed below. Such equipment and clothing must be provided to the workers engaged in work with cyanide. Emergency equipment shall be located at well marked and identified stations within the cyanide work areas. This equipment must allow each and every worker to escape the area in case of a cyanide emergency.\n# (a) Respiratory Protection\nEngineering controls shall be used whenever feasible to maintain airborne cyanide concentrations at or below the environmental limits recommended in Section 1 above. Compliance with the permissible exposure limits by the use of respirators is only allowed when airborne cyanide concentrations are in excess of the workplace environmental limits while required engineering controls are being installed or tested, when nonroutine maintenance or repair is being accomplished, or during emergencies. Appropriate respirators as described in Table 1-1 for HCN and Table 1-2 for cyanide salts shall be used only when permitted by the above restrictions. Respirators shall be selected and used in accordance with the following requirements:\n(1) For the purpose of determining the type of respirator to be used, the employer shall measure, when possible, the airborne concentration of HCN or cyanide salt in the workplace initially and thereafter whenever process, worksite, climate, or control changes occur which are likely to increase the airborne concentration of these cyanides.\nThe employer shall ensure that no worker is being exposed to cyanide in excess of the standards either because of improper respirator selection, fit, use, or maintenance.\n( \nThe employer shall provide respirators in accordance with Tables 1-1 and 1-2 and shall ensure that the employee uses the respirator provided.\n(4) Respiratory protective devices shall be those approved under the provisions of 30 CFR 11, published in the Federal Register, March 25, 1972, as amended.\n(5) Respirators specified for use in higher concentrations of HCN may be used in atmospheres of lower concentrations. Likewise, respirators specified for use in higher concentrations of cyanide salts are permitted in atmospheres of lower concentrations.\nThe employer shall ensure that the respirators are adequately cleaned, maintained, and stored when not in use, and that employees are instructed in the use of respirators assigned to them and in testing for facepiece leakage before each use.\nCartridges or canisters shall be discarded and replaced with fresh canisters after each use. Unused canisters shall be discarded and replaced when seals are broken, after three years if seals are unbroken, or on the manufacturer's recommendation, whichever is first.\nCartridges and canisters shall not be used for periods of time in excess of those indicated in Tables 1-1 and 1-2.\n(8) Emergency and escape-type respirators shall be made immediately available at the work stations for each worker when there is potential for exposure to concentrations of the various cyanides above the ceiling values.\nFor purpose of selection of respiratory protective equipment, entry into areas containing unknown and/or suspected dangerous atmospheric concentrations of HCN or cyanide salts shall be treated as an emergency. Less than or equal to 90 ppm (1) Type C supplied-air respirator, demand or continuous-flow type (negative or positive pressure), with half or full facepiece.\n(2) Full facepiece gas mask, chin-style canister specific for HCN. The maximum service life of canisters is one hour.\nLess than or equal to 200 ppm Full facepiece gas mask, front-or backmounted type canister specific for hydrogen cyanide. The maximum service life of canisters is one hour.\n(1) Self-contained breathing apparatus in pressure-demand mode (positive pressure) with full facepiece worn under gas-tight suit providing whole body protection.\n(2) Combination supplied-air respirator, pressure-demand type (positive pressure), with auxiliary self-contained air supply and full facepiece; all worn under gas tight suit providing whole body protection.\n(1) Positive pressure self-contained breathing apparatus worn under a gas-tight suit providing whole body protection.\n(2) Combination supplied-air respirator, pressure-demand type, with auxiliary selfcontained air supply; all worn under gastight suit providing whole body protection.\n(1) Self-contained breathing apparatus in demand or pressure-demand mode (negative or positive pressure).\n(2) Gas mask, full facepiece or mouthpiece type, with canister specific for HCN.\n# NOTE:\nDuring the use of any respirator with half mask, full facepiece or hood, protective clothing should be worn if there is a chance that liquid HCN may contact any part of the body.\nGreater than 200 ppm Emergency (no concentration limit)\nEvacuation or Escape (no concentration limit) Less than or equal to (1) Filter type respirators, approved for 25 mg/cu m toxic dust, with half-mask (not appli cable for Ca(CN)2).\n(2) Chemical cartridge respirators with replaceable cartridge for toxic dusts and acid gases; with half-mask. Maximum service life 4 hours.\n(1) Full-face gas mask, chest or back mounted type, with industrial size canister for toxic dust and hydro cyanic acid gas. Maximum service life 2 hours.\n(2) Type C supplied air-respirator, continuous-flow or pressure-demand type (positive pressure) with full facepiece.\n(3) Type A supplied-air respirator, (hose mask with blower) with full facepiece.\nGreater than 50 mg/cu m (1) Self-contained breathing apparatus with positive pressure in full facepiece.\n(2) Combination supplied-air respirator pressure-demand type with auxiliary self-contained air supply.\n(1) Self-contained breathing apparatus with positive pressure in facepiece.\n(2) Combination supplied-air respirator, pressure-demand type, with auxiliary self-contained air supply.\nEvacuation or Escape (no (1) Self-contained breathing apparatus in concentration limit) demand or pressure-demand mode (negative or positive pressure).\n(2) Full-face gas mask, front or back mount type with industrial size canister for toxic dust and hydro cyanic acid gas.\n# Emergency (no concentration limit)\nLess than or equal to 50 mg/cu m (b)\nProtective Clothing\nBecause HCN and cyanide salts, dry or in solution, may be absorbed readily through the skin or any break in the skin, the provision and use of protective clothing are necessary for the protection of workers in most operations where HCN and cyanide salts are used in pure or diluted condition.\n(1) When entering a HCN gas-filled area in emergency situations, when the airborne concentration of HCN is unknown, or when the known airborne concentration is greater than 200 ppm, employees shall wear gas-tight suits in addition to the required respiratory protection. The gas-tight suits shall provide full body protection.\n(2) Employees engaged in maintenance, repair, or other work on equipment, or in circumstances whereby they may be exposed to HCN liquid or gas, shall wear protective garments or suits made of material impervious to HCN and providing full body protection.\n(3) Employees shall wear rubber gloves when engaged in any activity which may involve the handling of, or possible contact with, HCN. \nEmployees shall wear gloves when handling dry cyanide salts and when using or handling equipment whose surfaces may be contaminated with these salts in such manner that contact of the chemical with the employee's hands is possible or likely.\nEmployees shall wear gloves made of rubber or other impervious material when engaged in any operation wherein contact of the hands with solutions of cyanide salts is possible or likely.\nEmployees shall wear protective sleeves, aprons, and/or full body protective clothing as needed to protect their skin from contact with cyanide salts, dry or in solution. When handling solutions, the outer garment shall be of rubber or other material impervious to the solutions involved in the exposures. The garments shall fit snugly about the wrist, arm, neck, waist, and/or ankle (as appropriate to the particular garment) and shall have closures which will exclude dust, powder, mist, and/or splashes of cyanide salts in either dry or liquid formulations.\n(10) In areas where spills or splashes of solutions of cyanide salts are likely to occur, the employees shall wear shoes, boots, or overshoes made of rubber or other material impervious to these solutions.\n(11) Chemical safety goggles shall be worn by employees engaged in any operation wherein there is danger or likelihood that dusts or solutions of cyanide salts will come into contact with the eye.\nFull-length face shields with forehead protection shall be worn by employees engaged in any operation wherein there is danger or likelihood that dusts, molten salts, or solutions of cyanide salts may contact the face.\nThe employer shall be responsible for maintaining all devices and clothing to be used for personal protection in a clean and effective condition. (2) Buildings in which HCN is to be stored, handled, or used must be designed to prevent fire and explosion hazards and to minimize the release of the highly toxic liquid or gas. Equipment and vessels containing or using HCN should be isolated in rooms or buildings designed for, and devoted to, these purposes.\nBuilding construction shall be fire-and explosion-resistant and shall meet the requirements of the National Fire Protection Association codes and of the local codes, regulations, and ordinances. Explosion vents and fire doors shall be provided in accordance with codes and good practice.\nEach room or building shall have no less than two means of exit, with doors opening outward and provided with \"panic bar\" release latches.\nExits shall be provided so that no location within the room or building is more than 75 feet from an exit and personnel can be evacuated in less than 1 minute.\n(3) All regular work areas where HCN is handled or used must be adequately ventilated so that, under normal or reasonably anticipated operating conditions, the airborne concentrations of HCN will not exceed the standard recommended in Section 1.\nLocal exhaust ventilation shall be used at points or areas of regular or anticipated release of HCN gas.\nEquipment for very high rates of ventilation of an area may be provided for the rapid reduction of contamination of air by HCN when emergency situations arise.\nThe HCN-contaminated air from an exhaust ventilation system must either be passed through a suitable collector to remove the HCN or be discharged at a location or in a manner such that persons or animals will not be endangered by the toxic gas.\nVentilation equipment must meet the applicable codes for explosionproof and fireproof installation of such equipment. where applicable, shall be followed.\n# (b) Cyanide Salts\n(1) All necessary precautions must be taken to prevent cyanide salts from coming into contact with liquid or airborne acids. In addition, precautions must be exercised to prevent Ca(CN)2 from coming into contact with water or humid atmospheres.\nCyanide salts must be protected also from contact with large concentrations of carbon dioxide. Carbon dioxide fire extinguishers must not be used where cyanide salts are present.\nIn any circumstance in which there is probable contact of cyanide salts with liquid or airborne acids such as Cr03, S02, C02, HC1 etc, or of Ca(CN)2 with a high concentration of water vapor or with liquid water, the standards and requirements applicable to exposures to HCN shall also apply.\n( All containers of cyanide salts must be labeled in accordance\n# «\nwith the recommendations in Section 3.\nAreas in which cyanides are stored must be posted in accordance with the recommendations in Section 3.\n(3) When containers of cyanide salts are removed or unloaded from trucks, boxcars, or poorly ventilated spaces, these should be thoroughly ventilated, purged, and tested before a worker enters.\nWhen cyanide salts are placed in other containers for transport or temporary storage, such containers must be properly covered and labeled.\n(A) Mechanical exhaust ventilation by local exhaust shall be provided for all operations producing, or likely to produce, dust or mists of cyanide salts in excess of the limit recommended in Section 1, or to vaporize HCN in excess of the recommended limit for that vapor.\nExamples of such operations are: there is evolution of mist from the bath, the employees shall be encouraged to wear at least a filter type respiratory protective device as a measure of protection in addition to that provided by ventilation. \nNonreturnable containers and other containers or equipment contaminated with cyanides before being discarded should be washed thoroughly with alkalinized water to remove cyanide residues.\n(10) When cyanide salts are used in fused salt baths, mechanical local exhaust ventilation should be provided to control any cyanide emissions.\nCare in operation of the bath and in housekeeping must be exercised so that the area around the bath does not become covered with cyanide-containing powder or dust. Employees working at baths of fused cyanide salts should wear face shields and appropriate protective clothing to protect them from burns and skin contact with cyanides in the event of splashes. A shovel or similar tool should be used to add cyanide salts to a fused salt bath. The cyanide salt should not be added directly by hand.\n(11) Inspection, cleaning, or repairing of tanks or other equipment used with solutions of cyanide salts should be performed only by properly trained workmen under careful supervision.\n(A) The tank should be drained of all cyanide solution as completely as possible, then filled with alkalinized water and allowed to stand for 15 minutes, preferably with agitation. This procedure should be repeated; then a preliminary inspection may be made. Any encrustation should be removed by mechanical means and/or by means of a stream of water from a hose.\n# (B)\nIf the tank is to be entered, the atmosphere in the tank should be tested for the presence of hydrogen cyanide and cyanide salts, to be certain it does not contain a dangerous airborne concentration of these or other materials.\n(C) The tank should be purged with fresh air to ensure an adequate oxygen supply and air should be supplied to the tank while the worker is in the tank.\n# (D)\nEquipment other than tanks should be washed and vented similarly, as applicable.\nIn the event of finding airborne concentrations of cyanide salts in excess of the limit, immediate action must be taken to eliminate the cause of the elevated airborne cyanide concentration. In case of any emergency situation (spills, leaks, or other unusual emissions of cyanide which result or potentially may result in dangerous airborn concentrations), all personnel shall be evacuated from the area. The personnel required to return to the area to institute corrective measures shall wear approved respiratory protective gear while entering and working in the area until the situation is corrected.\n(13) Any area in which there is the potential of an emergency involving HCN or a cyanide salt shall be posted in accordance with the provisions of Section 3, and emergency equipment stations shall be established. These stations shall be sufficient in number and so located as to be readily and immediately accessible to the workers in the area.\nThe stations shall be provided with first-aid supplies and instructions for first-aid treatment of any persons suffering excessive exposure to cyanide.\nApproved type respiratory protective devices, as indicated in Section 4, shall be available at designated emergency stations. These devices shall be sufficient in number for the workers in the area and readily accessible. Occurrence and Use HCN is a colorless gas [1] or a colorless or bluish-white liquid [1,2] with a faint, characteristic odor of bitter almonds [2, 3,4] perceptible to some people. [3,4] Kirk and Stenhouse [5] reported that 88% of 244 persons tested could smell hydrogen cyanide but that in a fourth of these, the determination was made only with difficulty.\nThe glucoside amygdalin which occurs in nature in some plants, notably almonds, [3] readily yields HCN upon hydrolysis. Recently, attention has been brought to the presence of HCN in automobile emissions. [6,7] HCN is manufactured in the United States from coke-oven gas by reaction with sodium carbonate, from cyanide salts by reaction with acid, by the decomposition of formamide, from the reaction of ammonia, air, and natural gas, or, most commonly, from the reaction of methane and ammonia under specific controlled conditions. [8] The great bulk of the HCN synthesized is used directly in the same process system. [8] In 1973, the estimated consumption of HCN in the United States was approximately 310,000 short tons. [9] HCN is used primarily in the production of chemical intermediates for the manufacture of synthetic fibers, [8,10] plastics, [8] cyanide salts [8,10] and nitrites; in the fumigation of ships, [11,12,13,14,15] In the presence of any source of hydrogen ions in quantity, eg, strong mineral acid, the production of HCN from cyanide salts becomes both rapid and large. Above 50 degrees C, an irreversible decomposition to formate and ammonia, as shown below, becomes important. [28] In the presence of NaCl, the hydrolysis of NaCN to HCN is increased at temperatures below 80 C, but decomposition to ammonia and formate is retarded. [28] Sodium cyanide is marketed as a powder, granule, flake or block in pillow-shaped pieces weighing about 1 oz, and as a 30% aqueous solution.\n[28] Solid sodium cyanide is packed in steel or fiber drums, and the aqueous solution is shipped in tanks by truck or rail. [28,30] Potassium cyanide, KCN, is a white crystalline, deliquescent, solid. KCN is produced by methods similar to those for NaCN. [28,29] The chemical reactivity of KCN is similar to that of NaCN. [28] Hydrolysis to HCN, as was the case with NaCN, is slight (Kh = 2.54 x 10 exp(-5)). [28] Potassium cyanide is sold in forms similar to those of NaCN but because KCN is more expensive, its world production for 1963 was only 5,000 tons. [28] Calcium cyanide, Ca(CN)2, is also called \"black cyanide\" and is the only commercially important alkaline earth cyanide.\n[31] The hydrolysis of Ca(CN)2, which takes place in two steps, as shown below, is complete.\n[31] The resulting calcium hydroxide has dissociation constants of 3.74 x 10 exp (-3) and 4.0 x 10 exp (-2) but is much less soluble in water at 0 degrees C than sodium hydroxide [1,32] so that its aqueous solutions are not as alkaline.\nFor example, the pH of an aqueous solution of Ca(0H)2 in an electric furnace above 1000 C in the presence of sodium chloride.\nsaturated\n[31] Rapid cooling apparently prevents the reversion to calcium cyanamide.\n[31] It is manufactured primarily in Canada, South Africa, and East Germany and sold as flakes or blocks.\nThere is also some production elsewhere in Europe and Japan.\n[ The first uses of the gas as a fumigant were in 1886 to control scale on citrus trees in California, [19] in 1898 to kill vermin in railway cars, [11] in to kill bed bugs in prisons, [11] and, after 1910, for the fumigation of the holds of ships. [11] Stock and Monier-Williams [11] Cytochrome c absorbs radiation at 550 nanometers (nm). In the presence of cytochrome oxidase, the optical density at 550 nm decreases at a rate directly proportional to the activity of cytochrome oxidase. This rate of change was determined in the presence of cyanide, demonstrating the ability of cyanide to inhibit cytochrome oxidase activity. Additions of methemoglobin, in which the iron had been oxidized electronically to the ferric state, to a solution containing cytochrome c, cytochrome oxidase, and cyanide were found to increase the activity of cytochrome oxidase, thus reversing the inhibitory effect of cyanide. The authors also found that the addition of cyanmethemoglobin to a solution of cytochrome c and cytochrome oxidase had no immediate effect on enzyme activity, but after a few minutes the enzyme became increasingly inhibited. Thus, the authors demonstrated in vitro the abilities of cytochrome oxidase and methemoglobin to compete in a reversible fashion for the cyanide ion.\nIn a 1958 survey, Dixon and Webb [56] found that the concentration of cyanide necessary for inhibition of cytochrome oxidase was 2-6 orders of magnitude less than those required for inhibition of other enzymes. The interference of CN with many different enzyme systems other than those involved in respiration may thus contribute to its toxicity.\nSchubert and Brill [57] in 1968 measured the inhibition and recovery of liver cytochrome oxidase in mice, rats, and gerbils after the intraperitoneal administration of KCN. Inhibition of the enzyme was found to reach a maximum 5 to 10 minutes after the cyanide injection. Depending on the dose, the enzyme activity returned to normal 5 to 20 minutes after maximal inhibition in mice but required up to 1 hour or more in the rat and gerbil. Interestingly, they found that the abilities of mice and rats to tolerate divided doses of cyanide depended on the total dose as well as on the time-dependent degree of enzyme inhibition. For example, they found that mice invariably survived a single sublethal dose of 6 mg/kg of KCN but not two doses of 3 mg/kg given 6 minutes apart or three doses of 2 mg/kg given at 6 minute intervals. They further showed that sodium thiosulfate and nitrite were able to reactivate liver cytochrome oxidase within minutes when administered to cyanide-treated rats and mice. Both men complained of headache and weakness or fatigability and were observed to have slight lid lag, enlarged thyroids, and excessive perspiration. One of the two also experienced dizziness and mental confusion, slurring of speech, coughing, sneezing, and occasional abdominal cramps, nausea, vomiting, and coarse tremor of the extremities followed by their temporary paralysis. Both men were exposed to cyanide aerosols generated by case hardening. Some exposure to HCN may have occurred.\nWuthrich [25] in 1954 described a 39-year-old German blacksmith who was exposed to cyanide in case hardening on a sporadic basis for 2 years and then more frequently for the next 4 years. The worker noticed some initial irritation, followed by a general worsening of health. He experienced loss of appetite, nervousness, vertigo, headaches, nausea, and vomiting.\nDuring 2-3 week vacations, the symptoms disappeared but reappeared within a month after returning to work. His thyroid gland was slightly enlarged. After exposure to cyanide had ceased for about 14 days, the man was given a placebo of NaCl, iv, for three days during which time he reported an improvement in his condition. On the 4th day, 1.4 g of sodium thiocyanate was substituted for NaCl in the daily injections. The thiocyanate concentration in the blood serum increased rapidly following these injections and did not decay to normal between injections. From the day of the first NaSCN injection, the man began to complain of nausea, lack of appetite and nervousness. After three NaSCN injections, he reported nausea and vomiting and spontaneously stated that he felt the same symptoms as at his workplace.\nIf there are 5200 ml of blood in the average man, then a dose of and eventually by complete disappearance of P waves. A secondary increase in rate, but not to the rate prior to administration of HCN, was observed during the 3rd and 4th minutes along with the irregular reappearance of P waves, some of which were not conducted. All subjects showed A-V dissociation with a secondary decrease in rate during the 5th minute.\nDuring the 6th and 7th minutes, the heart rates again showed a slight increase and a return to normal sinus rhythm. Thereafter, the heart rates slowed progressively. Normal A-V conduction in one man and incomplete A-V block in another were maintained throughout the period of observation (approximately 13 minutes).\nA third subject developed Wenckebach's phenomenon, (2:1 block), and, finally, complete heart block. The fourth subject's heart had normal A-V conduction until the 14th minute, when it developed ventricular tachycardia and ventricular fibrillation. It must be remembered that the concentrations of HCN to which these men were exposed were huge, so that the details of the changes in their ECG recordings may not be entirely typical of those to be expected in occupational exposures.\nWexler's observations do seem to demonstrate that cyanide has no specific action on the heart but rather exerts on the myocardium actions that are typical of hypoxia and anoxia.\nThere have been several reports of exposure to HCN which included both the airborne concentration of HCN and the human physiological response. However, in many cases no additional information relating to worker exposure was provided. These reports are summarized in Table XIV-5.\nIn many cases it is difficult to attribute a specific concentration range directly to a group of investigators since many of the citations involve reference to the work of others with no additional supporting information.\nTherefore, the validities of concentrations presented only by secondary references may be questioned. In large part they appear to be based on the unreferenced work of Lehmann and Hess. However, the application of\n# Lehmann's data to man has been questioned by McNamara [68] because\nLehmann's work was apparently done entirely with rabbits, which McNamara considers to be more sensitive to a given dose (product of concentration and time) of HCN than man. He concluded that man has a susceptibility to HCN more like those of the comparatively resistant goat and monkey and on\nthis assumption (and one that the LCt50 for man is four times that for the mouse) has estimated that 3,404 mg/cu m will cause 50% mortality in humans exposed to it for one minute. McNamara estimated that a concentration of HCN of 607 mg/cu m would kill 50% of men after a 10-minute exposure.\nThe various fatal doses of HCN seen in Table XIV had just returned from a 13-month leave of absence 5 months prior to this episode.\nIn use, the solution was heated to boiling whereupon 50 ml of hydrogen peroxide were added. The gold articles were cleaned in a manner causing splashing on the skin and the production of a visible aerosol.\nThere may have been some exposure to HCN. A study of plant records revealed another plater who developed typical signs and symptoms in 1 month. The man had been treated for 7 weeks, was removed from exposure, and recovered. An investigation of the plant was made and these 19 illnesses were attributed to aerosols emitted by the improperly operated plating tanks. After engineering controls and housekeeping procedures had been instituted, there were no recurrences of these illnesses. No airborne concentrations of contaminants were reported.\nElkins [91] in reported that in a plant where there was considerable brass plating the ambient air contained a mist. The mist was reported to have contained NaCN in a concentration not greatly exceeding 5 ppm, expressed as HCN. Severe irritation was a widespread complaint and there were some incidents of ulceration of the nasal septum. The author noted that other alkalies of undetermined concentration in the air may have contributed to the irritating action of the mist. with the exception of one with a perforated septum who gave a history suggestive of previous exposure to chromates. The cyanides were not described but they were likely a mixture of NaCN, KCN, and some alkaline complex of CuCN in the copper plating tanks, and alkaline NaCN in the zinc bath.\n[93]\nIn None of the four unexposed men had evidence of disease of the stomach or duodenum. The author reported that three of the exposed and two of the unexposed men had erythrocyte counts above 5,000,000 but below 6,100,000/cu mm and that seven of the exposed and none of the unexposed men had a percentage of lymphocytes above 40 but below 49%. He attributed the latter change to stress resulting from repeated exposure to small doses of HCN. He concluded that his results demonstrated that not all the effects of repeated acute or subacute exposures to HCN are entirely reversible.\nIn Exposure was continued until the animals became apneic, their heart beats became irregular and weak, and distinct cyanosis was apparent. Administration of oxygen through a plaster of Paris mask, modelled to fit the rabbit's muzzle, by hand pressure applied to a rubber bag connected to the mask succeeded in reviving 18 of the 36 rabbits. The authors stated that the hearts of the other 18 rabbits had become too weak when oxygen administration was started to be able to perform the necessary movement of oxygenated blood to the important organs.\nIn 1951, Moss et al [124] exposed 16 rats to HCN at 24-465 ppm for up at 22 minutes. The rats exposed at 25-50 ppm survived, except for one exposed at 50 ppm. This rat was violently agitated after 1 minute 49 seconds, paralyzed after 2 minutes 30 seconds, unconscious after 3 minutes, and dead after 8 minutes.\nIn experiments reported in 1952 by Haymaker et al, [125] six dogs were exposed at concentrations of 620, 590, 700, 700, 165, and 690 mg/cu m, for periods of 2.0, 2.0, 1.75, 1.75, 10.0, and 2.0 minutes, respectively.\nThe first three dogs died in 20 hours or less and the others were killed 24, 26, and 28 hours after exposure. Four of the six dogs had convulsive seizures. The dog exposed at 620 mg/cu m had marked proliferation of histiocytes in the leptomeninges and in the perivascular spaces of the molecular layer of the cerebellum. Only shadows of the Purkinje cells remained. Some of these dogs suffered necrosis of gray matter. Definite alterations of structure were not seen in dogs that died within 21 minutes after being exposed to HCN; they were found in dogs that died 2.5 or more hours after exposure. At these comparatively early times, there was subpial edema of the cerebrum and the cerebellum. Dogs that survived for as long as 16 hours had cellular damage, particularly in the cerebral cortex.\nThe frontal and parietal lobes were more likely to be affected than the temporal or occipital.\nCortical damage was concentrated frequently in the trough of a sulcus in the form of massive coagulation necrosis.\nValade [126] in 1952 exposed four dogs to HCN at 50 mg/cu m for 12 30-minute periods, conducted at 8-day intervals. Of these dogs, two survived, one died after 38 days, and one died of an intercurrent disease.\nIn a second experiment, four dogs were subjected to 19 30-minute inhalation periods at 2-day intervals and at the same HCN concentration. One died after 73 days, the other after 77 days. Another group of five dogs went through seven 30-minute inhalations at 2-day intervals, but this experiment was interrupted when pulmonary inflammation occurred, causing the death of three dogs. Still another group of four dogs were subjected to fourteen 30-minute inhalation periods at 2-day intervals; one of these died after 34 days.\nThe first signs were dyspnea, nausea, exaggerated intestinal peristalsis, and diarrhea. Later, the dogs developed tremors followed by loss of equilibrium and convulsions. These observations tend to support the hypothesis of a cumulative effect from exposure to HCN.\nValade [126] autopsied the dogs immediately after they died or were\nkilled and observed similar central nervous system lesions in each of them.\nVascular changes were vasodilatation and hemorrhages which were most pronounced in the central gray nuclei, brain stem, bulb, and medulla cervicalis.\nCellular lesions manifested themselves by glial reactions throughout the central nervous system and by cytologic changes in the Purkinje cells of the cerebellum and in the bulbar gray nuclei. These histopathologic examinations led the author to conclude that the lesions resulted from anoxia caused by inhibition of cytochrome oxidase or from a selective effect of the poison. To support the contention that the latter cause was the more significant, the author noted that the dogs were very quickly affected by respiratory disorders before the onset of other signs.\nHe thought there was reason to believe that the suddenness with which these disorders appeared was linked to a particular sensitivity of these animals' bulbar cells to cyanide, rather than to an inhibition of cytochrome oxidase. In 1955, Howard and Hanzal [127] reported a feeding study with HCNfumigated food. Thirty male and 30 female weanling albino rats were divided into 3 groups of 10 males and 10 females each. Two of the groups were given dog meal containing 300 ppm and 100 ppm of HCN, respectively. A third, similar group was fed unfumigated food as a control. At the end of a 2-year feeding period, no gross signs of cyanide toxicity were observed.\nAutopsies revealed the same general abnormalities and signs of senility in control and experimental rats. Microscopic examination of heart, lungs, liver, spleen, stomach, small and large intestines, kidneys, adrenal, thyroid, testes or uterus and ovary, and the cerebrum and cerebellum revealed no evidence of pathology due to HCN feeding. All findings were compatible with those usually seen in aging animals, and the same general changes were found in both the control and the experimental animals.\nThiocyanate concentrations in plasmas, RBC's, and kidneys, but not in the livers, of rats given food containing 300 or 100 ppm HCN were about twice as high as those in controls.\nIn 1959, Levine and Stypulkowski [128] reported lesions in several areas of the brains of rats which survived exposure for 20-45 minutes at an unknown concentration of airborne HCN. The concentration of the airborne cyanide aerosol, which the authors presumed to be HCN, was not determined but was sufficient to debilitate the rats in 10 minutes. Earlier, Flury\nand Zernik [118] found that persisting prostration occurred in 9.5 minutes at 127 ppm and, thus, it may be estimated that the rats in this experiment had exposures to HCN at approximately 127 ppm. Below this concentration (127 ppm), exposure to HCN for 2 hours did not produce brain lesions.\nAbove this concentration at which persisting prostration occurred, brain lesions were produced readily in 20-30 minutes. These lesions involved a multiplicity of sites in the brain although they were not universal in distribution.\nFor example, the cord, most of the stem, cerebellum, diencephalon, and portions of the cerebrum were spared. A predominance of isolated lesions appeared in the callosum and striatum. Later that same year, Levine and Weinstein, [129] using the same technique described above, reported that high concentrations of HCN generally caused the death of rats without causing brain damage. Low concentrations did not produce either, but moderate concentrations (perhaps 100-150 ppm) caused brain lesions while consciousness was maintained for an hour or so, followed by sudden unconsciousness and death. Unfortunately, in neither of these studies was the airborne concentration reported. Wistar albino rats receiving 0.5 mg of KCN subcutaneously once weekly for 22 weeks. They reported some pallid myelin but found it difficult to estimate whether or not there was demyelination. The animals appeared to be without other ill-effects from these small doses. The authors suggested that these lesions were due to excessive utilization of hydroxocobalamin to form cyanocobalamin. Whether these effects on nervous tissue are due to a specific action of the cyanide ion or of the thiocyanate ion, or to general histotoxic anoxia, is not clear.\nMoss et al [124] in 1951 subjected from one to three rats to mixtures of CO and HCN. Atmospheres containing either HCN or CO alone were generally lethal to rats at concentrations of 50 or 5000 ppm, respectively.\nA mixture of 10-20 ppm of HCN and 2000 ppm of CO was lethal to some.\nMixtures of 30 ppm of HCN and 1000 ppm of CO and of 5 ppm of HCN and 2000 ppm of CO were not lethal.\nHirner [132] in 1969 subjected male rats weighing about 250 g to subcutaneous injections of 0.2% KCN.\nThe daily dose, which averaged between 3 and 5 mg/rat, was divided into parts, which were injected within the span of 1 hour. Five rats received single daily doses and were killed 2 or 3 days later. Six rats received 4 to 12 daily doses, two received 14, and four received 20. All the multiply dosed rats were killed at the end of 9 weeks from the first daily dose. These rats were perfused through the left ventricle with a sodium cacodylate-glutaraldehyde solution;\nappropriate samples of nervous tissue were ultrasectioned and examined electronmicroscopically as well as by conventional optical microscopy. The principal lesion found in this study was necrosis in the caudal part of the corpus callosum, with spongy alteration at the margin of the necrotic area.\nPhagocytes invaded the necrotic area 2 days after the last dose of KCN; astrocytic gliosis followed. In the area of spongy change, there was vacuolization of axons and swelling of the astrocytes and oligodendroglia.\nDemyelination was visible in the later stages of the study. Hirner considered that the effects on glial cells were primary effects of cyanide, but that disintegration of myelin and axonal degeneration were secondary effects, the axon remaining intact when swelling of the glia had occurred.\nHe stated the belief that the oligodendroglia are particularly susceptible to injury by cyanide. Unfortunately, neither report sought to quantify the dose of either HCN or KCN.\nIn the first study, Levine and Stypulkowski [128] In the second study, Levi and Amaducci [137] in 1968 brought their animals through the first two stages, after which they were allowed to partially recover, and were then killed by decapitation. The meninges appeared congested. Some rats had hemorrhagic pulmonary infarctions. In some animals trypan blue was injected iv to test the integrity of the blood-brain barrier. Subsequent examination of the brains did not show any abnormal passage of the trypan blue into the nervous tissue. Brain slices of other rats were used to study the active transport of amino acids.\nInitial and steady state accumulation of amino acids and rates of amino acid exit were identical in brain slices from control and treated animals when a glucose-containing incubation medium was used. Tissue respiration rates were also measured in vitro and found to be identical in both control and treated animals. Thereafter, the analytical method selected determines cyanide radical content, and it is impossible to say what fraction of the total was attributable to any particular compound.\nIn order to differentiate between HCN gas and other cyanide compounds, it is necessary to first remove particulates by passing the air through an efficient filter, then absorb HCN from the stream by passage through an alkaline absorbing solution.\nThe filtered cyanides can subsequently be leached from the filter by treatment with alkaline solution, and the same analytical technique applied to both portions of the sample.\nThe presence of small quantities of cyanide in water was of concern long before relatively recent ecologic considerations led to an awareness that many other substances were toxic at trace concentrations. As a result, there exists substantial literature dealing with the qualitative and quantitative detection of cyanides in air and water, with at least one method (the titrimetric estimation of cyanide with silver nitrate published by Liebig [156] in 1851) still in use today, more than a century after its origination. [6,7] Almost all the methods proposed for the analysis of water or other materials have been, or can be, applied to the analysis of cyanides in air, for most air methods ultimately involve the determination of cyanide ion in solution. One of the most widely used colorimetric methods is the so-called pyridine-pyrazolone method, an example of the Konig synthesis for pyridine dyes, first published by Aldridge [174] in 1944 (using pyridine and benzidine) and subsequently modified by various authors.\n[78,175-181] In this method, cyanides are converted to cyanogen bromide or cyanogen chloride, which then reacts with pyridine to form a glutaconic aldehyde.\nNext, a primary aromatic amine reacts with the aldehyde to yield a colored Schiff's base. In the original procedure of Aldridge, the aromatic amine used was benzidine, but the more frequently used modification of Epstein voltammetry [191], amperometry [192,193], coulometry [194] potentiometry [195] and others. [196,197] The most recently introduced and probably mosc useful in its application to air analysis, is the eleccrometric technique relying on specific ion electrodes, or ion selective electrodes which respond only to cyanide ion concentrations, [198][199][200][201][202][203][204][205] Cohen A -novel approach to determining cyanide levels has been described by OancniK and Br/lr.z [209] involving Indirect atomic absorption \" spectrometric analysis.\nIn the first of two methods, the complex dicyano-bis-(l,10phenanthroline)-iron(II) is formed and then ¿-.:tracted into chloroform. The\n• iaiororG-ia is evaporated and the residue is taken ap m ethanol. The\n• -.thaiioi. solution is aspirated directly into the flame, and iron equivalent 99 i to a known amount of cyanide is then determined. The second method is based on precipitating silver cyanide, then determining the excess silver ion in the supernatant by atomic absorption spectrometry.\nIn place of titrimetric techniques, several investigators have described methods in which turbidity resulting from the formation of silver cyanide, or the reduction in turbidity due to the formation of a cyanide complex with silver iodide, are measured.\n[ [170], a specific ion electrode method [198], and a blood method using microdiffusion [77], first used by Conway.\n[226] A respired air method based on the pyridine-pyrazolone reagent [227], as well as more general methods applicable to biologic samples using this same reagent are also used.\n[\n# 220,228]\nThe rationale used in making a forensic diagnosis of cyanide poisoning have also received some attention. [21,229] Many of the methods listed have also been used for water and waste water analyses, and currently the methods most favored appear to be colorimetric, using some version of the pyridine-pyrazolone method, or modifications of the titrimetric determination with silver nitrate.\n[177,178,186,187] Specific ion electrodes [198], and picric acid [184] have also been used.\nRecently, an opto-acoustic infrared absorption technique as well as the titrimetric method utilizing silver nitrate have been used in the analysis of HCN in automobile exhaust. [6,7] Virtually every method used for cyanide analyses is subject to some interferences, usually due to the presence of certain metals which may form complexes, other anions, particularly sulfide, and a host of oxidizing and reducing agents. It is, therefore, frequently necessary to isolate the cyanide by some means, most frequently by a distillation from strongly acid solution, where all but the most tightly bound metal complexes are dis sociated to release hydrogen cyanide which is then absorbed in alkaline solution.\nThe recommended sampling and analytical method for the cyanides covered by this document is essentially that of the standard NIOSH method for cyanide in air as published in the NIOSH Manual of Analytical Methods. [232] should be followed.\nHigh ventilation rate systems for the rapid dilution or removal of HCN gas and aerosols may be useful in some areas.\nControl of the hazard of potential release of hydrogen cyanide from cyanide salts requires constant care and attention to good work practices.\nThe cyanide salts should be kept well apart from, and protected from contact with, acids, moisture, or elevated concentrations of carbon dioxide.\n[ \n# Basis for Recommended Environmental Standard\nCyanide is well known as an acute, fast acting poison which can be described as insidious in that its toxic action at high concentrations is so rapid that its odor has no value as a warning.\n[2] At lower concentrations the sense of smell may provide forewarning. For HCN, the primary routes of entry from occupational exposure are inhalation and absorption through the skin.\n[ It appears to be generally accepted that HCN and cyanide salts act by the same mechanism, namely, the release of the cyanide ion, which inhibits cytochrome oxidase and results in histotoxic anoxia. [107] Thus, it may be presumed by analogy that if 90 ppm of HCN is fatal, 96 mg/cu m of CN, derived from cyanide salts, may be also. Extending this analogy to threshold levels, presumably 11 mg/cu m of CN would be equivalent to the current Federal standard of 10 ppm of HCN and restriction of exposures to 11 mg/cu m of CN would protect against acute toxicity from cyanide salts.\nHowever, taking into account the irritant effects observed from exposure to cyanide salts, [90,91] the current Federal standard of 5 mg/cu m of CN as an 8-hour time-weighted average appears to be too high in that it allows substantial excesses above that concentration for short periods of time.\nTherefore, NIOSH recommends that the current value of 5 mg/cu m of CN be retained, but that its basis be changed from an 8-hour time-weighted average to a 10-minute ceiling. This action should provide the employee with adequate protection from the systemic effects of cyanide and prevent the erosional effects produced by the alkalinity associated with the cyanide salts.\nA review of the cases involving exposure to cyanide reveals that they fall into three general categories. First are those cases in which there was an acute or subacute exposure followed immediately by an acute illness. [11,13,20,26,27 ppm. They also stated that it was difficult to give reliable limits for normal levels of cyanide and thiocyanate in the urine. However, in order to assess the hazards of occupational exposure, they considered it safe to state that nonsmokers who have greater than 400 #ig/100 ml of free thiocyanate in the urine, or smokers with urinary concentrations exceeding It is recognized that many workers are exposed to cyanides in concentrations considerably below the recommended occupational limits.\nUnder these conditions, it should not be necessary to comply with many of the provisions of the recommended standards. However, concern for worker health and well-being requires that protective measures be instituted below the enforceable limits to ensure that exposures do not exceed the standard. \nIs given the super.vi sion necessary to assure that all safety tP'lii p r ;} r f \\ c p c rn f-»V. I (7) is instructed to shower before removing any respirator or gas-tight suit if prior contact with HCN liquid has occurred or is suspected; (preferably sight contact) in a safe area or at a distance so as not to be affected by an emergency situation at the site of the first employee. The second employee (\"buddy\") should be alert and equipped to summon help and render aid, if needed.\nThe employee should carefully and precisely follow all operational procedures specified for the handling of HCN in containers, transfer operations, or other equipment. Suppliers' and manufacturers' instructions should be carefully followed.\n[2]\nWhen HCN is used for fumigation purposes, the space should be sealed to prevent the gas from leaking into surrounding spaces or areas. Warning signs should be posted and guards placed to keep unauthorized persons at a safe distance. All laws, regulations, ordinances, and codes applicable should be followed. Only licensed fumigators should do Such work. [246] Open containers of any solid cyanide salts or of solutions of cyanide salts should be limited to those necessary for operational requirements and procedures. Such open containers must be used only in adequately ventilated spaces so that the recommended standards for the airborne concentration of cyanide are not exceeded. Good practice dictates that, in so far as practical, covers be provided for such containers and used whenever possible.\nSolutions of cyanides should be maintained as basic as practical to prevent any evolution of hydrogen cyanide. When weakly basic or neutral solutions are used, ventilation must be provided sufficient to prevent accumulation of the HCN evolved from exceeding the recommended standard for HCN in the work room air. When the addition of an acid to a cyanide solution may be necessary, the process should be fully enclosed and ventilated.\nRespiratory protection should be provided for all workers potentially exposed to any release of hydrogen cyanide.\nFused salt baths containing cyanide salts should be provided with local exhaust ventilation. Care should be exercised in the operation of such baths to avoid spills and splashes. Addition of salts should be made carefully, using a shovel or special tool. The area about the bath should be regularly cleaned to prevent accumulation and encrustation of cyanide salts on adjacent areas. Workers at fused salt baths should wear safety goggles with side shields.\nLocal exhaust ventilation must be used for all operations emitting dusts or mists of cyanide salts. [80,232] Tanks and other equipment which must be entered for inspection, maintenance or repair, should be drained as completely as possible and then filled with water and agitated. After 15 minutes, they should be drained again and refilled for another 15 minutes, then drained again. The tanks should then be inspected for residue and encrustation of cyanides. These should be broken loose mechanically or by the force of a water stream and flushed away.\nThe tank should then be purged with fresh air, followed by testing for the absence of cyanide in the air before anyone enters. Cyanide waste solutions and cyanide-contaminated rinse or wash waters should be treated to destroy the cyanide before being discarded.\nTreatment of cyanide waste is achieved by oxidation of the cyanide in alkaline solution by addition of chlorine or other oxidizing agents.\n[ \n# IN AIR AND CALIBRATION\nThe same sampling and analytical methods are used for atmospheric hydrogen cyanide and the particulate cyanides. They can be collected and analyzed separately or by insertion of a filter can be simultaneously collected and individually analyzed. A sampling period of about 10 minutes is necessary to provide an amount of cyanide readily amenable to analysis by the cyanide selective electrode.\n# Sampling\nAll glassware is washed in detergent solution, rinsed in tap water, and then rinsed with distilled or deionized water. Ten ml of an absorbing solution (0.1 M NaOH) is poured into an all-glass midget impinger using a graduated cylinder to measure the volume.\nThe fritted inlet of the impinger should have a porosity approximately equal to that of Corning EC (170-220 micron maximum pore diameter). A membrane prefilter (0.45 / u r n pore size) should be inserted (by means of an in-line cassette or similar device) before the impinger when sampling for particulate cyanides is to be performed.\nSampling for HCN and/or the particulate cyanides is performed for at least 10 minutes at a rate of 2 liters/minute, but the total volume of air sampled should not exceed 200 liters. A personal sampling pump or other satisfactory source of suction may be used for sampling provided it is calibrated as outlined below. Alternate sampling systems may be used, providing the required volume of air is sampled from the breathing zone of the worker.\nCertain cyanide compounds, especially calcium cyanide, may hydrolyze at sufficiently high relative humidities, resulting in losses of collected sample as HCN gas. In such cases, it may be advisable to minimize losses by keeping the sampling time as short as possible, then storing it in a refrigerator until analysis.\nIt should be noted that when sampling for HCN without a prefilter, particulates will pass through the midget impinger. Likewise, when sampling for particulate cyanides by means of a midget impinger without a prefilter, HCN gas will also be collected and will constitute a positive interference.\n# Calibration\nSince the accuracy of an analysis can be no greater than the accuracy of measurement of the volume of air sampled, the accurate calibration of a sampling device is essential to the correct interpretation of an instrument's indication. The frequency of calibration is dependent upon the use, care, and handling to which the pump is subjected. Pumps should be calibrated if they have been subjected to misuse or if they have just been repaired or received from a manufacturer. If the pump receives hard usage, more frequent calibration may be necessary.\nOrdinarily, pumps should be calibrated in the laboratory both before they are used in the field and after they have been used to collect a large number of field samples. The accuracy of calibration is dependent on the type of instrument used as a reference. The choice of calibration instrument will depend largely upon where the calibration is to be performed. For laboratory testing, a soapbubble flow meter or wet-test meter is recommended, although other standard calibrating instruments, such as a spirometer or dry-gas meter, can be used. The actual setup will be connected in sequence to the filter cassette or fritted impinger unit which will be followed by the sampler pump.\nIn this way, the calibration instrument will be at atmospheric pressure. If the personal sampler pump is used, each pump must be calibrated separately. If the buret is used, it should be set up so that the flow is toward the narrow end of the unit.\nCare must be exercised in the assembly procedure to ensure that seals at the joints are airtight and that the length of connecting tubing is kept to a minimum. Calibration should be performed under the same conditions of pressure and temperature as those encountered in use. The calibrated pump rotameter should be used to set the flow rate in the field. Samples are analyzed using the cyanide ion selective electrode.\n# Range and Sensitivity\nThe ultimate range and sensitivity of the method have not been established at this time. The recommended range of the method is 0.013-13 mg/cu m in air (approximately 0.0117-11.7 ppm of HCN).\n# Interference\nSulfide ion irreversibly poisons the cyanide ion selective electrode and must be removed if found in the sample. Check for the presence of sulfide ion by touching a drop of sample to a piece of lead acetate paper.\nThe presence of sulfide is indicated by discoloration of the paper.\nSulfide is removed by the addition of a small amount (spatula tip) of powdered cadmium carbonate to the sample at pH 11-13. Swirl to disperse the solid, and recheck the liquid by again touching a drop to a piece of lead acetate paper. If sulfide ion has not been removed completely, add more cadmium carbonate. Avoid a large excess of cadmium carbonate and long contact time with the solution.\n# METHOD FOR ANALYSIS OF CYANIDE SAMPLES\nWhen a drop of liquid no longer discolors a strip of lead acetate paper, remove the solid by filtering the sample through a small plug of glass wool and proceed with the analysis.\n# Precision and Accuracy\nThe precision and accuracy of this method have not been completely determined at this time. No collaborative tests have been performed on this method.\n# Apparatus (a) Sampling and Calibration Equipment\n(1) A filter unit (if needed) consisting of the filter media and cassette filter holder.\n(2) A midget fritted impinger containing the absorbing solution or reagent.\n(3) A pump suitable for delivering desired flow rates.\nThe sampling pump is protected from splashover or water condensation by an absorption tube loosely packed with a plug of glass wool and inserted between the exit arm of the impinger and the pump.\n(A) An integrating volume meter such as a dry-gas or wet test meter.\n(5) Thermometer ( 6) Manometer \n# (f)\nPrecision and repeatability must be plus or minus 2% of full scale.\n(g) It is desirable that the instrument respond only to HCN, but instruments which respond to other gases not normally present in the atmosphere may be acceptable.\nIn general, it is probable that any gas which causes a reading sufficiently high to set off the alarm will itself be present at a concentration sufficiently high to warrant corrective actions. Whenever there is a possibility that gases or vapors such as hydrogen chloride, chlorine, etc, may be present, it would be desirable to determine the response of the instrument to such gases in advance.\n(h) An operating range of 0-100 ppm HCN is optimal, but other ranges may be selected to suit individual needs.\n(i) The device should be capable of 7 days of continuous unattended operation.\n# (j)\nThe device and alarm should be intrinsically safe for use in hazardous locations.\n# Discussion\nThe principal requirements for such monitors in addition to responding to HCN gas are that they be sufficiently rugged to withstand normal extremes of temperature, pressure, vibration, etc, and not be susceptible to plugging or interferences due to contaminants likely to be encountered in most work places. They should be so constructed that it is possible to quickly check the zero setting of the instrument and the response at 25 ppm in a rapid routine manner. Chemical substances should be listed according to their complete name derived from a recognized system of nomenclature. Where possible, avoid using common names and general class names such as \"aromatic amine,\"\n\"safety solvent,\" or \"aliphatic hydrocarbon\" when the specific name is known.\nThe \"%\" may be the approximate percentage by weight or volume (indicate basis) which each hazardous ingredient of the mixture bears to the whole mixture. This may be indicated as a range or maximum amount, ie, \"10-40% vol\" or \"10% max wt\" to avoid disclosure of trade secrets. \n# 168\n\n# IX S P E C IA L PREC A U TIO N S P R E C A U T I O N A R Y S T A T E M E N T S O T H E R H A N D L I N G A N O S T O R A G E R E Q U I R E M E N T S P R E P A R E D B Y A O O R E S S O A T E\n\n# XIII. APPENDIX V\nFirst Aid and Treatment Kits Two physician's treatment kits should be immediately available to trained medical personnel at each plant where there is a potential for the release of, accidental or otherwise, or for contact with, hydrogen cyanide or cyanide salts. One kit should be portable in order that it may be carried by medical personnel while accompanying a patient to the hospital.\nThe other kit should be kept under lock and key to assure that it is intact and available when and if needed. The key should be readily available at all times to the work supervisor on duty and the storage place should be of such construction as to allow accessibility in the event of loss of the key.\nBoth kits for use by the medical personnel servicing each firm should contain the following as a minimum.\n(1) Two (2) boxes (2 dozen) ampules; each ampule containing 0.3 ml of amyl nitrite.\n(2) Two (2) ampules of sterile sodium nitrite solution (10 ml of a 3% solution in each).\n(3) Two (2) ampules of sterile sodium thiosulfate solution (50 ml of a 25% solution in each).\n(4) 2 sterile 10-ml syringe with intravenous needles.\n(5) 1 sterile 50-ml syringe with intravenous needle.\n(6) 1 tourniquet (7) 1 gastric tube (rubber).\n(8) 1 non-sterile 100 ml syringe.\nThe medical personnel servicing a firm where there is a potential for hydrogen cyanide release or a potential for exposure to inorganic cyanide should be familiarized with the use of these kits.\nFirst-aid kits should be immediately available at work places where there is a potential for the release, accidental or otherwise, of hydrogen cyanide or a potential for exposure to inorganic cyanide. This kit should contain as a minimum two (2) boxes of ampules ( 2 dozen), each containing 0.3 ml of amyl nitrite. Ampules should be replaced biannually or sooner if needed to ensure their potency.\nThe amyl nitrite ampules should be protected from high temperatures. In all cases, the contents of the medical and first-aid kits should be replaced before the manufacturer's assigned expiration dates.\nFirst-Aid Procedure Speed in the rendering of first-aid treatment is of the utmost importance. The patient should be removed at once to an area free from HCN. The rescuer should wear respiratory protective equipment in order not to be overcome or weakened by the gas.\nMany victims will have stopped breathing.\nIn this case, it is imperative that efforts at resuscitation be instituted at once and continued without interruption even while other treatment is being administered.\nA physician should be summoned immediately.\nFirst-aid kits should be readily available at all times. They should be quickly accessible but should not be kept only in operating areas mixtures with air may be explosive if a source of ignition is present.\n# (B) Resuscitation\nBefore instituting artificial resuscitation, dentures and foreign objects, such as gum and tobacco, and any accumulated oropharyngeal fluids (saliva, etc) should be removed from the patient's mouth and pharynx and the tongue pulled forward.\nIf the patient's breathing is weak or has stopped, artificial resuscitation should be started at the earliest possible moment and continued without interruption until normal breathing has been established or the patient is pronounced dead.\nMouth-to-mouth resuscitation is the method of choice because of its simplicity and effectiveness. It is, however, impossible to administer amyl nitrite while using this method. Therefore, it is advisable to switch to other methods of artificial respiration, such as the Holger-Nielsen arm-lift back pressure method, during the periods when the amyl nitrite is being given.\nIf a mechanical resuscitator and personnel skilled in its use are available, this equipment may be used instead of other forms of resuscitation.\n(C) The patient should be kept comfortably warm but not hot. Other drugs and stimulants are rarely necessary and should be administered only by a physician or trained medical personnel under the direction of a physician. Step -Through the formation of a relatively stable coordination complex with ferric iron, cyanide tends to keep this metal in its higher oxidation state and thus reduces its efficacy as an electron carrier in ferric to ferrous iron transitions.\nBy such a complexation of iron, the respiratory enzyme ferricytochrome oxidase is changed to ferricytochrome oxidasecyanide and its ability to catalyze the reaction of reduced cytochrome with oxygen is inhibited, with consequent impairment of cellular oxygen utilization\nStep -Since numerous metabolic pathways converge at the cytochrome system, the impairment of the cells' ability to utilize oxygen reduces or even stops aerobic metabolism. True histotoxic (cytotoxic) hypoxia results with a shift to anaerobic metabolism with accumulation of lactate, pyruvate, and glucose.\nStep -The cells are thus unable to use the oxygen brought to them as 02Hb by the arterial blood. The oxyhemoglobin continues into the veins, the arteriovenous oxygen difference diminishes, and the venous blood is almost as bright a red as the arterial blood.\nStep 4 -The chemoreceptors in the carotid and aortic bodies, which are the tissues most sensitive to cellular hypoxia, trigger an inspiratory gasp and hyperpnea as an almost instantaneous path ophysiologic effect of cyanide absorption. \n# \nCurrent concepts about the treatment of selected poisonings-nitrite, cyanide, sulfide, barium, and quinidine. Ann Rev Pharmacol Toxicol 16:189 -199, 1976 109.\nCarmelo, S: [New contributions to the study of subacute-chronic hydrocyanic acid intoxication in man.] Rass Med Ind 24: 254-71, 1955 (Ita) 110.\nEl Ghawabi SH, Gaafar MA, El-Saharti AA, Ahmed SH, Malash KK, Fanes R: Chronic cyanide exposure: a clinical, radioisotope, and laboratory study. Br J Ind Med 32: 1975 111.\nWollman SH: Nature of the inhibition by thiocyanate of the iodide concentrating mechanism of the thyroid gland. Amer J Physiol 186: [453][454][455][456][457][458][459]1956 112.\nHeymans JF, Masoin P:\n[The diachronic toxicity of some cyanogen compounds.] Arch Int Pharmacodyn Ther 7:297-306, 1900 (Fre) After sampling, the fritted impinger stem can be removed and cleaned in the following manner. Tap the stem gently against the inside wall of the impinger bottle to recover as much of the sampling solution as possible. Wash the stem with a small amount (1-2 ml) of unused absorbing solution and add the wash to the impinger bottle. Then the impinger bottle is sealed with a hard, non-reactive stopper (preferably Teflon) and an appropriate identifying number attached to it. Do not seal with rubber.\nThe stoppers on the impinger bottle should be tightly sealed to prevent leakage during shipping. If it is preferred to ship the fritted impingers with the stems in, the outlets of the stem should be sealed with Parafilm or other nonrubber covers, and the ground glass joints should be sealed, ie, taped to secure the top tightly. Upon completion of sampling for the particulate cyanides, plastic caps should be replaced on the inlet and outlet tubes of the cassette and an appropriate identifying number attached to it.\nCare should be taken to minimize spillage or loss by evaporation at all times. Refrigerate samples if analysis cannot be done within a day. Whenever possible, hand delivery of the samples is recommended. Otherwise, special impinger shipping cases should be used to ship the samples.\nA \"blank\" fritted impinger should be handled as the other samples (fill, seal, and transport) except that no air is sampled through this fritted impinger.\nWhere a prefilter has been used for the collection of particulate cyanides, the filter cassettes are capped and placed in an appropriate cassette shipping container. One filter disc should be handled like the other samples (seal and transport) except that no air is sampled through it, and this is labeled as a blank.\n# M A TERIA L SAFETY DATA SHEET 1 PRO D U CT IDENTIFICATIO N M A N U F A C T U R E R 'S N A M E R E G U L A R T E L E P H O N E N O . E M E R G E N C Y T E L E P H O N E N O A D O R E S S\n\n# TRADE N AM E S Y N O N Y M S II H A ZA R D O U S IN G R E D IE N T S M A T E R I A L O R C O M P O N E N T % H A Z A R D D A T A\n\n# III P H Y SIC A L DATA\n\n# O L E V A P O R A T I O N R A T E ( B U T Y L A C E T A T E M ) A P P E A R A N C E A N O O D O R\nwhere they may not be available in case of a spill.\n( (3) Inhalation (A) Administer amyl nitrite A pearl (ampule), if not provided with a fabric sleeve, should be wrapped lightly in a handkerchief or gauze pad, broken, and held about 1 inch from the patient's mouth and nostrils for 15 seconds.\nRepeat 5 times at 15-second intervals. Use a fresh pearl every 5 minutes until 3 or 4 pearls have been administered.\n# WARNING:\nFirst-aiders should keep the pearls away from their own mouths and noses lest they become weak and dizzy and unable to give proper assistance to the victim. Amyl nitrite is flammable and "},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":659,"cells":{"id":{"kind":"string","value":"2857d4af0e0aa874619ed7388b63c2d27aae9b29"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"None"},"clean_text":{"kind":"string","value":"On December 13, 2007, certain lots of Haemophilus influenzae type b (Hib) vaccine marketed as PedvaxHIB (monovalent Hib vaccine) and Comvax (Hib-HepB vaccine), and manufactured by Merck & Co., Inc., were recalled voluntarily, and the company temporarily suspended production of these vaccines. To conserve the limited supply of Hib-containing vaccines, CDC, in consultation with the Advisory Committee on Immunization Practices (ACIP), the American Academy of Family Physicians (AAFP), and the American Academy of Pediatrics (AAP), on December 18, 2007, recommended that vaccination providers temporarily defer the routine Hib vaccine booster dose administered to most healthy children at age 12--15 months (1--5). Production of Merck Hib vaccine products is still suspended. However, two other Hib-containing vaccines manufactured by Sanofi Pasteur have been available for use in the United States during this shortage: monovalent Hib vaccine (ActHIB) and DTaP-IPV/Hib (Pentacel). Beginning in July 2009, the manufacturer of these two vaccines will increase the number of doses of these two products available for use in the United States, which will result in the supply being sufficient to reinstate the Hib vaccine booster dose.# Reinstatement of Hib Booster Dose\nEffective immediately, CDC, in consultation with ACIP, AAFP, and AAP, is recommending reinstatement of the booster dose of Hib vaccine for children aged 12--15 months who have completed the primary 3-dose series. Infants should continue to receive the primary Hib vaccine series at ages 2, 4, and 6 months. Children aged 12--15 months should receive the booster dose on time. Older children for whom the booster dose was deferred should receive their Hib booster dose at the next routinely scheduled visit or medical encounter. Although supply is sufficient to reinstate the booster dose and begin catch-up vaccination, supply is not yet ample enough to support a mass notification process to contact all children with deferred Hib booster doses. Sufficient vaccine will be available to administer the primary series at ages 2, 4, and 6 months and a booster dose on time to children aged 12--15 months. As part of delivering the booster dose to those children for whom it was deferred at the next routinely scheduled appointment or medical encounter, practices should discuss with parents the reasons for the change in recommendation and might consider 1) reviewing electronic or paper medical records or immunization information system records to identify children in need of a booster dose before physician encounters, 2) evaluating children's vaccination status during their scheduled visit, and 3) sharing immunization schedules with parents to make them aware of this plan.\n\n# Use of Combination Vaccines"},"raw_text":{"kind":"string","value":"On December 13, 2007, certain lots of Haemophilus influenzae type b (Hib) vaccine marketed as PedvaxHIB (monovalent Hib vaccine) and Comvax (Hib-HepB vaccine), and manufactured by Merck & Co., Inc., were recalled voluntarily, and the company temporarily suspended production of these vaccines. To conserve the limited supply of Hib-containing vaccines, CDC, in consultation with the Advisory Committee on Immunization Practices (ACIP), the American Academy of Family Physicians (AAFP), and the American Academy of Pediatrics (AAP), on December 18, 2007, recommended that vaccination providers temporarily defer the routine Hib vaccine booster dose administered to most healthy children at age 12--15 months (1--5). Production of Merck Hib vaccine products is still suspended. However, two other Hib-containing vaccines manufactured by Sanofi Pasteur have been available for use in the United States during this shortage: monovalent Hib vaccine (ActHIB) and DTaP-IPV/Hib (Pentacel). Beginning in July 2009, the manufacturer of these two vaccines will increase the number of doses of these two products available for use in the United States, which will result in the supply being sufficient to reinstate the Hib vaccine booster dose.# Reinstatement of Hib Booster Dose\nEffective immediately, CDC, in consultation with ACIP, AAFP, and AAP, is recommending reinstatement of the booster dose of Hib vaccine for children aged 12--15 months who have completed the primary 3-dose series. Infants should continue to receive the primary Hib vaccine series at ages 2, 4, and 6 months. Children aged 12--15 months should receive the booster dose on time. Older children for whom the booster dose was deferred should receive their Hib booster dose at the next routinely scheduled visit or medical encounter. Although supply is sufficient to reinstate the booster dose and begin catch-up vaccination, supply is not yet ample enough to support a mass notification process to contact all children with deferred Hib booster doses. Sufficient vaccine will be available to administer the primary series at ages 2, 4, and 6 months and a booster dose on time to children aged 12--15 months. As part of delivering the booster dose to those children for whom it was deferred at the next routinely scheduled appointment or medical encounter, practices should discuss with parents the reasons for the change in recommendation and might consider 1) reviewing electronic or paper medical records or immunization information system records to identify children in need of a booster dose before physician encounters, 2) evaluating children's vaccination status during their scheduled visit, and 3) sharing immunization schedules with parents to make them aware of this plan. \n# Use of Combination Vaccines\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":660,"cells":{"id":{"kind":"string","value":"70b97abad68805443af28746c6871cf26b7c9cd4"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"None"},"clean_text":{"kind":"string","value":"depar depar depar depar department of health and human ser tment of health and human ser tment of health and human ser tment of health and human ser tment of health and human services vices vices vices vices# Background\nIn the United States, the incidence and mortality from cutaneous malignant melanoma (CMM) have increased rapidly in the last few decades (1,2). In 2003, approximately 54,200 persons will have new diagnoses of melanoma, and 7,600 will die from the disease (3). The incidence of the other two skin cancers, basal cell carcinoma (BCC) and squamous cell carcinoma (SCC), is estimated to be >1 million new cases per year (3). According to the data from the Surveillance, Epidemiology and End Results (SEER) cancer registry of the National Cancer Institute, during 1995-1999, average annual age-adjusted incidence rates for melanoma per 100,000 population were 23.5 for men and 15.7 for women for non-Hispanic whites; 3.8 for men and 3.7 for women for Hispanics; 1.8 for men and 1.3 for women for Asians; 1.5 for men and 0.9 for Ameri-\n\n# Introduction\nThe Task Force on Community Preventive Services (the Task Force) is developing the Guide to Community Preventive Services (the Community Guide), a resource that will include multiple systematic reviews, each focusing on a preventive health topic. The Community Guide is being developed with the support of the U.S. Department of Health and Human Services (DHHS) in collaboration with public and private partners. Although CDC provides staff support to the Task Force for development of the Community Guide, the recommendations presented in this report were developed by the Task Force and are not necessarily the recommendations of DHHS or CDC. This report is one in a series of topics included in the Community Guide. It provides an overview of the process used by the Task Force to select and review evidence and summarize its recommendations regarding interventions to reduce UV exposure and increase UV protective behaviors for prevention of skin cancer. A full report on the recommendations, additional evidence (i.e., discussions of applicability, additional benefits, potential harms, existing barriers to implementation, costs, cost benefit, and cost effectiveness of the interventions ), and remaining research questions will be published in the American Journal of Preventive Medicine.\nCommunity Guide topics are prepared and released as each is completed. The findings from systematic reviews on vaccinepreventable diseases, tobacco use prevention and reduction, motor vehicle occupant injury, physical activity, diabetes, oral health, and the effects of the social environment on health have already been published. A compilation of systematic reviews will be published in book form. Additional information regarding the Task Force and the Community Guide and a list of published articles are available on the Internet at http:/ /www.thecommunityguide.org.\n\n# Methods\nThe methods used by the Community Guide for conducting systematic reviews and linking evidence to recommendations have been described elsewhere (20). In brief, for each Community Guide topic, a multidisciplinary team (the systematic review development team) conducts a review consisting of the following steps:\n- developing an approach to organizing, grouping, and selecting the interventions; - systematically searching for and retrieving evidence;\n- assessing the quality of and summarizing the strength of the body of evidence of effectiveness; - assessing cost and cost effectiveness evidence, identifying applicability and barriers to implementation (if the effectiveness of the intervention has been established); - summarizing information regarding other evidence; and - identifying and summarizing research gaps. For each review of interventions regarding skin cancer prevention, the systematic review development team developed a conceptual model (or analytic framework) to show the relationship of the intervention to relevant intermediate outcomes (e.g., knowledge, attitudes and beliefs, and intentions regarding sun-protective behaviors), to implementing key sunprotective behaviors, and to the assumed relationships of improvements in sun-protective behaviors to skin cancer prevention. A representative example of an analytic framework for mass media interventions is illustrated (Figure). The analytic frameworks for the other interventions were similar to this example except that they included environmental and policy components.\nThe analytic frameworks focused on key health outcomes (e.g., sunburn or nevi*) and sun-protective behaviors:\n- avoiding peak sun; -seeking shade, and -avoiding the sun during peak UV hours. - covering up; -wearing a hat, -wearing a long-sleeved shirt, and -wearing pants.\n- sunscreen use. The team also examined intermediate outcomes that were postulated to be associated with sun-protective behaviors (e.g., knowledge, attitudes, and intentions). Recommendations were based either on better health outcomes (rare with this subject matter because relevant cancer outcomes would become apparent long after the time of the intervention) or risk behaviors that were thought to be established proxies for cancer outcomes (in this case, avoiding peak UV hours or covering up).\nThe team considered sunscreen use to be a key secondary outcome of sun protection programs because sunscreens prevent sunburn (a marker of unprotected UV exposure and a health outcome associated with increased risk of skin cancer in epidemiologic studies) and reduce the incidence of SCC, and better alternatives are not always available (e.g., when swimming). Sunscreen's role in preventing skin cancer has been demonstrated to be complex, according to information in recent reports from national and international groups (18,21) and summarized in the last section of this report.\nEpidemiologic studies suggest that sunscreen use could be considered harmful if it increased a person's total time in the sun and total UV exposure. Partly for that reason, suncreen use alone might not protect against melanoma despite its protective effect on SCC. The International Agency for Research on Cancer (IARC) recommends that sunscreens not be used as the sole method for skin cancer prevention and not be used as a means to extend the duration of UV exposure (21). The team therefore did not consider sunscreen use, by itself, to be an established proxy for better health. - Nevi are lesions of pigment-forming skin cells that can be a risk factor for melanoma.\n\n# Intervention\n\n# FIGURE. Analytic framework for media interventions to reduce ultraviolet (UV) exposure and increase sun-protective behaviors.\nMajor stratification variables were type of media (e.g., small media versus large media ); characteristics of target population (e.g., age, sex, skin color, skin type, baseline risk, socioeconomic status, sunburn incidence, occupation); intervention intensity (i.e., comparison, some intervention, high level of intervention); geographic or environmental characteristics (e.g., urban, rural, climate of location ); intervention characteristics (e.g., size, access to media).\n\n# MMWR October 17, 2003\nThe coordination team, † which conducted the systematic review, and their consultants § generated a comprehensive list of interventions to reduce skin cancer. From this, a priority list of interventions for review was developed through a process of polling the coordination team, the consultants, and other specialists in the field regarding their perception of the public health importance (number of persons affected), the practicality of application, and the need of those promoting UV protective behaviors for information regarding each intervention.\nTo conduct the review, the team organized interventions into three groups: setting-specific, target population-specific, and communitywide (Table ). Setting was used as an organizing structure because it was a convenient proxy for key characteristics of the target populations and the implementers of the interventions. The majority of the interventions in this group involved diverse activities -provision of information, environmental approaches (e.g., planting shade trees), or policy approaches (e.g., implementing a policy to reschedule outdoor activities or a requirement to wear hats when outside). Interventions in the setting-specific group consisted of educational and policy approaches in the following settings:\n- child care centers, - primary schools,\n- secondary schools and colleges,\n- recreational or tourism settings,\n- occupational settings, and - health-care settings and for health-care providers.\nThe target population of interest category included one intervention: children's parents or caregivers (some of these interventions might have already been examined in settingspecific groups).\nThe category of communitywide interventions included two types of interventions and a subgroup:\n- media campaigns alone, and - communitywide multicomponent interventions that include at least two interventions in an integrated manner. (Comprehensive communitywide programs, a subset of communitywide multicomponent interventions, include interventions at several levels and last longer than 1 year.) Interventions reviewed were either single component (i.e., using only one activity to achieve desired outcomes) or multicomponent (i.e., using more than one activity, such as a policy or environmental intervention with a media campaign). Certain studies provided results relevant to more than one intervention and were included in each of the reviews to which they were applicable. Studies and outcome measures were classified according to definitions developed as part of the review process. The nomenclature used in this report sometimes differs from that used in the original studies.\nTo be included in the reviews of effectiveness, studies had to 1) be primary investigations of interventions selected for evaluation rather than, for example, guidelines or reviews; 2) be published in English during the years 1966-2000; 3) be conducted in established market economies ¶ ; and 4) compare outcomes among groups of persons exposed to the intervention with outcomes among groups of persons not exposed or less exposed to the intervention (i.e., the study design included a concurrent or before-and-after comparison.) ¶ Searches of three computerized databases (MEDLINE, PsychINFO, CINAHL) were conducted. Team members also reviewed reference lists and consulted with other specialists in the field (e.g., participants in a skin cancer prevention listserv) to identify relevant studies. Each included study was evaluated by using a standardized abstraction form and was assessed for suitability of the study design and threats to validity (22). Studies were characterized as having good, fair, or limited execution based on the number of threats to validity (20).\nResults for each outcome of interest were obtained from each study that met the minimum quality criteria. Net effects were derived when appropriate by calculating the difference between the changes observed in the intervention and comparison groups relative to the respective baseline levels. † † The median was used to summarize a typical measure of effect across the body of evidence for each outcome of interest; both the median and the range are reported. For bodies of evidence consisting of four or more studies, an interquartile range was used to represent variability.\nThe strength of the body of evidence of effectiveness was characterized as strong, sufficient, or insufficient on the basis of the number of available studies, the suitability of study designs for evaluating effectiveness, the quality of execution of the studies as defined by the Community Guide (20), the consistency of the results, and the effect size.\nThe Task Force uses these systematic reviews to evaluate the evidence of intervention effectiveness and makes recommendations based on the findings of the reviews (20). The strength of each recommendation is based on the evidence of effectiveness (i.e., an intervention is recommended on the basis of either strong or sufficient evidence of effectiveness) (20). Other types of evidence can also affect a recommendation. For example, harms resulting from an intervention that outweigh benefits might lead to a recommendation that the intervention not be used even if it is effective in improving some outcomes.\nA finding of insufficient evidence to determine effectiveness should not be interpreted as evidence of ineffectiveness. Insufficient evidence may be found for any of a number of reasons, alone or in combination, including an insufficient number of studies; too many threats to the validity of the available studies based on their design, execution, or both; conflicts in the results of the studies that preclude a coherent summary of effectiveness; or no indication that the outcomes measured to date, by themselves, represent success in improving health. In all these situations, a finding of insufficient evidence to determine effectiveness is important for identifying areas of uncertainty and continuing research needs. In contrast, sufficient or strong evidence of ineffectiveness would lead to a recommendation against use of the intervention.\n\n# Results\nDatabase searches and bibliographic reviews yielded a list of 6,373 potentially relevant titles. After review of the abstracts and consultation with specialists in the field, a total of 313 reports were retrieved. Of these, 154 were not used in the review because they did not provide results, did not refer to an intervention, or reported on noncomparative studies. The remaining 159 were retained for full review. On the basis of limitations in execution or design or because they provided only background information on studies that were already included, 74 of these were excluded and were not considered further. The remaining 85 studies were considered qualifying studies. The Task Force recommendations in this report are based on the systematic review and evaluation of these qualifying studies, all of which had good or fair quality of execution.\nThe Task Force recommended two interventions, both in the setting-specific category (Table ):\n- educational and policy approaches in primary schoolschanging children's covering-up behavior (wearing protective clothing); and - educational and policy approaches in recreational or tourism settings -changing adults' covering-up behaviors. Interventions in primary school settings were designed to increase sun-protective knowledge, attitudes, intentions, and behavior among children from kindergarten through eighth grade. The interventions ranged from a curriculum that included interactive classroom and take-home activities to staff education, brochures for parents, and a working session to develop skin protection plans for schools. All interventions focused on some combination of increasing application of sunscreen, scheduling activities to avoid peak sun hours, increasing availability of shade and encouraging children to play in shady areas, and encouraging children to wear sunprotective clothing. Interventions in this category included at least one of the following activities:\n- provision of information to children (e.g., instruction or small media or both); - additional activities to influence children's behavior (e.g., modeling, demonstration, role playing); - activities intended to change the knowledge, attitudes, or behavior of caregivers (i.e., teachers or parents); or - environmental or policy approaches (e.g., provision of sunscreen, provision of shade, or scheduling outdoor activities to avoid hours of peak sunlight). Single-and multicomponent interventions in recreational settings were designed to increase knowledge; influence attitudes, beliefs, and intentions; and change behavior of adults and children. Interventions included one or more of the following: educational brochures, including culturally relevant materials and photographs of skin cancer lesions; sun-safety training for lifeguards, aquatic instructors, and outdoor recreation staff and role-modeling by these groups; sun-safety lessons, interactive activities, and incentives for parents and children; increasing available shaded areas; providing sunscreen; and point-of-purchase prompts.\nThe recommended interventions had small to moderate behavior change scores. In primary schools, the median net relative increase was 25% (interquartile range: 1%-40%, six studies). In recreational settings, the median net relative increase was 11.2% (interquartile range: 5.1%-12.9%, five studies).\nIt should be noted that the interventions were targeted to populations rather than single persons. Small changes in behavior in large populations can result in substantial public health benefits.\nThe Task Force found insufficient evidence on which to make recommendations for or against the following interventions: educational and policy approaches in child care centers; educational and policy approaches in secondary schools and colleges; educational and policy approaches in recreational or tourism settings for children; educational and policy approaches in occupational settings; interventions oriented to health-care settings and providers; interventions oriented to children's parents or caregivers; media campaigns alone; and communitywide multicomponent interventions (Table ). The finding of insufficient evidence to determine effectiveness was most often based on the limited numbers of studies that measured behavioral or health outcomes, inconsistent evidence among studies that measured changes in sun-protective behaviors, and limitations in the design and execution of available studies.\nSummary tables of the reviews will be available at http:// www.thecommunityguide.org/cancer when the full evidence is published in a supplement to the American Journal of Preventive Medicine.\n\n# Use of Recommendations in Communities and Health-Care Settings\nMalignant melanoma is the deadliest of the skin cancers, and its incidence in the United States has increased rapidly in the past 2 decades. Melanoma accounts for approximately three fourths of all skin cancer deaths. Basal cell and squamous cell skin cancers are seldom fatal but, if advanced, can cause severe disfigurement and morbidity (3). UV exposure in childhood and intense intermittent UV exposures are the major environmental risk factors for melanoma and BCC, and cumulative UV exposure is the major preventable risk factor for SCC (23). National surveys indicate that only one third of Americans practice sun-protective behaviors, and their practices vary greatly, depending on age, sex, and their ability to tan and burn (9,12,13).\nThe two Task Force recommendations -educational and policy approaches in primary schools, and educational and policy approaches for adults in outdoor recreational or tourism settings -are based on improving covering-up behaviors. These recommendations represent tested interventions that promote decreased UV exposure at the community level. They can be used for planning interventions to promote UV protection or to evaluate existing programs.\nSeveral of the studies reviewed included multiple components that could not be evaluated separately. For example, a school-based program might involve components of policy, such as establishing school guidelines, in tandem with implementation of one-on-one didactic and interactive sessions regarding adapting sun-protective behaviors. Although sunprotective behaviors were increased by school-based programs, the specific effect could not be attributed to one specific intervention characteristic. In selecting and implementing interventions, the potential for an unintended increase in the duration and intensity of UV exposure must be considered. Also, communities should strive to develop comprehensive programs that include a wide range of activities suitable for their local resources, population characteristics, and settings.\nThe other interventions reviewed, for which evidence was insufficient to determine effectiveness, could also prove useful. They provide a broader taxonomy of interventions that deserve further testing and evaluation, and the documentation of research gaps in these reviews could potentially help to improve the next generation of research. Additional information on research gaps will be provided in the report in the American Journal of Preventive Medicine.\nChoosing interventions that are well matched to local needs and capabilities, and then carefully implementing those interventions, are vital steps for increasing UV protection. Several factors can affect the attitudes, ability, and behaviors of a community regarding taking sun safety precautions. Some of the most important are program priorities, location of the community, and population. Establishing skin cancer prevention as a priority might be difficult because skin cancer is but one of many health topics, and for certain communities, may not be as high a priority as other cancers or diseases. Although it might be a higher priority in areas where UV radiation is more intense, even in areas with lower UV intensity, education about UV exposure during times of episodic exposure (e.g., during winter sports, when the sun comes out, and when traveling to higher UV intensity regions) could be helpful. Likewise, although skin cancer prevention might be a higher priority for populations at an increased risk (e.g., light-skinned, sunsensitive), even darker-skinned or less sun-sensitive persons need to take precautions when exposed to UV radiation. To meet local objectives, recommendations and other evidence provided in the Community Guide should be supplemented with local information such as skin cancer incidence, skin cancer mortality, prevalence of sun-protective behaviors, latitude, UV index, resource availability, administrative structures, and economic and social environments of organizations and practitioners.\nThese reviews by themselves do not provide advice regarding implementation of effective programs; the referenced articles, however, provide additional detail. Implementation advice is also available elsewhere (24)(25)(26)(27)(28).\n\n# Introduction\nThis statement summarizes the current U.S. Preventive Services Task Force (USPSTF) recommendation on counseling to prevent skin cancer and the supporting scientific evidence, and updates the 1996 recommendation contained in the Guide to Clinical Preventive Services, Second Edition (1). The USPSTF, an independent panel of private sector experts in primary care and prevention, systematically reviews the evidence of effectiveness of a wide range of clinical preventive services, including screening tests, counseling, and chemoprevention. The Task Force grades its recommendations according to one of five classifications (A, B, C, D, I), reflecting the strength of evidence and magnitude of net benefit (benefits minus harms) (Box 1). The USPSTF grades the quality of the overall evidence for a service on a 3-point scale (good, fair, poor) (Box 2).\nThis recommendation and rationale statement and complete information on which this statement is based, including evidence tables and references, are available at . gov/clinic/uspstfix.htm (2) and in print by subscription through the AHRQ Clearinghouse (1-800-358-9295 or e-mail at ahrqpubs@ahrq.gov) and through the National Guideline Clearinghouse ™ at .\n\n# Summary of Recommendation\nThe U.S. Preventive Services Task Force concludes that the evidence is insufficient to recommend for or against routine counseling by primary care clinicians to prevent skin cancer.\n\n# I recommendation.\nThe USPSTF found insufficient evidence to determine whether clinician counseling is effective in changing patient behaviors to reduce skin cancer risk. Counseling parents may increase the use of sunscreen for children, but there is little evidence to determine the effects of counseling on other preventive behaviors (such as wearing protective clothing, reducing excessive sun exposure, avoiding sun lamps/tanning beds, or practicing skin self-examination) and little evidence on potential harms.\n\n# Clinical Considerations\n- Using sunscreen has been shown to prevent squamous cell skin cancer. The evidence for the effect of sunscreen use in preventing melanoma, however, is mixed. Sunscreens that block both ultraviolet A (UV-A) and ultraviolet B (UV-B) light may be more effective in preventing squamous cell cancer and its precursors than those that block only UV-B light. However, people who use sunscreen alone could increase their risk for melanoma if they increase the time they spend in the sun. - UV exposure increases the risk for skin cancer among people with all skin types, but especially fair-skinned people. Those who sunburn readily and tan poorly, namely those with red or blond hair and fair skin that freckles or burns easily, are at highest risk for developing skin cancer and would benefit most from sun protection behaviors. The incidence of melanoma among whites is 20 times higher than it is among blacks; the incidence of melanoma among whites is approximately four times higher than it is among Hispanics. - Observational studies indicate that intermittent or intense sun exposure is a greater risk factor for melanoma than chronic exposure. These studies support the hypothesis that preventing sunburn, especially in childhood, may reduce the lifetime risk for melanoma. - Other measures for preventing skin cancer include avoiding direct exposure to midday sun (between the hours of 10:00 a.m. and 4:00 p.m.) to reduce exposure to ultraviolet (UV) rays and covering skin exposed to the sun (by wearing protective clothing such as broad-brimmed hats, long-sleeved shirts, long pants, and sunglasses). - The effects of sunlamps and tanning beds on the risk for melanoma are unclear because of limited study design and conflicting results from retrospective studies. - Only a single case-control study of skin self-examination has reported a lower risk for melanoma among patients who reported ever examining their skin over 5 years.\nAlthough results from this study suggest that skin selfexamination may be effective in preventing skin cancer, these results are not definitive.\n\n# Scientific Evidence Epidemiology and Clinical Consequences\nMelanoma is a leading cause of cancer death in the United States. The lifetime risk for dying of melanoma is 0.36% in white men and 0.21% in white women (3). Between 1973 and 1995, the age-adjusted incidence of melanoma increased more than 100%, from 5.7 per 100,000 people to 13.3 per 100,000 people. The increase in annual incidence rates is likely due to several factors, including increased sun exposure and possibly earlier detection of melanoma. Although primary prevention efforts have focused on young people, the elderly (especially elderly men) bear a disproportionate burden of morbidity and mortality from melanoma and nonmelanoma skin cancer. Men older than age 65 account for 22% of the newly diagnosed cases of malignant melanoma each year and women in the same age group account for 14%. Basal cell and squa-mous cell carcinomas are more than 10 times as common as melanoma but account for less morbidity and mortality. Squamous cell cancers, however, may account for 20% of all deaths from skin cancer.\n\n# Effectiveness of Available Interventions\nPreventive strategies include reducing sun exposure (e.g., by wearing protective clothing and using sunscreen regularly), avoiding sunlamps and tanning equipment, and practicing skin self-examination. There is little direct evidence, however, that any of these interventions reduce skin cancer morbidity or mortality.\n\n# Reducing Sun Exposure\nAvoiding direct sunlight by staying indoors or in the shade or by wearing protective clothing is the most effective measure for reducing exposure to ultraviolet light, but there are no randomized trials of sun avoidance to prevent skin cancer. In numerous observational studies, increased sun exposure in childhood and adolescence is associated with increased risk for nonmelanoma skin cancer, which usually occurs in sunexposed areas such as the face.\nRecent studies provide a more complex picture of the relationship between sun exposure and melanoma, however. Although melanoma incidence is higher in regions near the equator where ultraviolet exposure is most intense, melanoma often occurs in areas of the body not exposed to the sun. In observational studies, intermittent or intense sun exposure was associated with increased risk for melanoma; chronic exposure was associated with lower risk, as was the ability to tan (4-7).\n\n# Sunlamp and Tanning Bed Avoidance\nSix of 19 case-control studies found a positive association between use of sun lamps and melanoma risk, but most did not adjust for recreational sun exposure or for the dosage and timing of sunlamp exposure (8). Among nine studies that examined the duration, frequency, or timing of sunlamp or tanning bed exposure, four found a positive association, particularly if the dose of exposure was high and if it caused burning.\n\n# Sunscreen Use\nDaily sunscreen use on the hands and face reduced the total incidence of squamous cell cancer in a randomized trial of 1,621 residents in Australia (rate ratio : 0.61; 95% confidence interval = 0.46-0.81) (9). Sunscreen had no effect on basal cell cancer. Based on this trial, 140 people would need to use sunscreen daily for 4½ years to prevent one case of squamous cell cancer. An earlier randomized trial demonstrated that sunscreen use reduced solar keratoses, precursors of squamous cell cancers (10). There are no direct data about the effect of sunscreen on melanoma incidence. An unblinded randomized trial showed that children at high risk for skin cancers who used sunscreen developed fewer nevi than those who did not. Several epidemiologic studies have found higher risk for melanoma among users of sunscreens than among nonusers (11)(12)(13). A recent meta-analysis of population-based casecontrol studies found no effect of sunscreen use on risk for melanoma (14). The conflicting results may reflect the fact that sunscreen use is more common among fair-skinned people, who are at higher risk for melanoma, than it is among darkerskinned people; or, this finding may reflect the fact that sunscreen use could be harmful if it encourages longer stays in the sun without protecting completely against cancer-causing radiation.\n\n# Skin Self-Examination\nThe only evidence for the effectiveness of skin self-examination comes from a single case-control study (1,15). After adjustment for other risk factors, skin self-examination was associated with lower incidence of melanoma (odds ratio : 0.66; 95% CI = 0.44-0.99) and lower mortality from melanoma (OR: 0.37; 95% CI = 0.16-0.84), although the definition of \"self-examination\" was limited. This study did not provide sufficient evidence that skin self-examination would reduce the incidence of melanoma or improve outcomes of melanoma.\n\n# Effectiveness of Counseling\nCommunity and worksite educational interventions have demonstrated effectiveness for increasing the use of skin protection measures, such as wearing hats and long-sleeve shirts and staying in the shade; however, evidence addressing the effectiveness of clinician counseling to prevent skin cancer is extremely limited. Most studies of counseling have examined intermediate outcomes such as knowledge and attitudes rather than changes in behavior. In a recent survey, 60% of pediatricians said that they usually or always counsel patients about skin protection, but advice to use sunscreen is more common than advice about wearing protective clothing or avoiding the midday sun (16).\nSimple reminders and instructional materials for clinicians can overcome some of the barriers to regular counseling. A randomized trial of a community-based intervention involving 10 towns in New Hampshire suggests that office-based counseling by physicians may be an effective component of a multimodal program to promote skin protection (17). The proportion of children using some sun protection increased significantly in the intervention towns (from 78% to 87%) compared to a decrease in the control communities (from 85% to 80%). More parents reported receiving some sun protection information from a clinician in the intervention towns. However, most of the change was due to increased sunscreen use rather than to reduced sun exposure.\n\n# Potential Harms of Skin Protection Behaviors\nThere are limited data regarding potential harms of counseling or of specific skin protection behaviors. Skin cancer counseling that focuses on the use of sunscreen could possibly lead to a false sense of security, which might lead to more time in the sun. For example, a randomized trial with young adults found that those who used sunscreen with a high sun protection factor (SPF) stayed longer in the sun than those who used sunscreen with a lower SPF (18). There has been some concern that use of SPF of 15 results in vitamin D deficiency. However, a randomized trial among people over 40 years of age found that sunscreen use over the summer had no effect on 25-hydroxyvitamin D3 levels. Concerns related to sun avoidance include reduced physical activity levels among children and negative effects on mental health. However, no studies have evaluated the effects of sun protection behaviors on these outcomes.\n\n# Recommendations Of Others\nThe American Cancer Society (19), the American Academy of Dermatology (20), the American Academy of Pediatrics (21), the American College of Obstetricians and Gynecologists (22), and a National Institutes of Health consensus panel (23) all recommend patient education concerning sun avoidance and sunscreen use. The American Academy of Family Physicians recommends sun protection for all with increased sun exposure (24). The American College of Preventive Medicine (ACPM) concluded that sun-protective measures (e.g., clothing, hats, opaque sunscreens) are probably effective in reducing skin cancer but that the evidence does not support discussion of sunscreen and sun protection with every patient. ACPM concluded that evidence is insufficient to advise patients that chemical sunscreens protect against malignant melanoma and that their use may actually lead to increased risk (25). Recently, the International Agency for Research on Cancer (IARC), part of the World Health Organization, qualified their recommendation for sunscreen use in ways that address the importance of learning more about potential harms of counseling for sunscreen use as follows:\n\n# MMWR October 17, 2003\nSunscreens probably prevent squamous-cell carcinoma of the skin when used mainly during unintentional sun exposure. No conclusion can be drawn about the cancerpreventive activity of topical use of sunscreens against basalcell carcinoma and cutaneous melanoma. Use of sunscreens can extend the duration of intentional sun exposure, such as sunbathing. Such an extension may increase the risk for cutaneous melanoma (26). The Task Force on Community Preventive Services found insufficient evidence to determine the effectiveness of a range of population-based interventions to reduce unprotected UV light exposure and recommended additional research on educational policy approaches, media campaigns, and both health-care setting and community-based interventions (27).\n\n# U.S. Preventive Services Task Force\n\n# BOX 1. U.S. Preventive Services Task Force (USPSTF) recommendations and ratings\nThe Task Force grades its recommendations according to one of five classifications (A, B, C, D, I) reflecting the strength of evidence and magnitude of net benefit (benefits minus harms): The USPSTF grades the quality of the overall evidence for a service on a 3-point scale (good, fair, poor):\nA.\nGood: Evidence includes consistent results from welldesigned, well-conducted studies in representative populations that directly assess effects on health outcomes.\nFair: Evidence is sufficient to determine effects on health outcomes, but the strength of the evidence is limited by the number, quality, or consistency of the individual studies, generalizability to routine practice, or indirect nature of the evidence on health outcomes.\nPoor: Evidence is insufficient to assess the effects on health outcomes because of limited number or power of studies, important flaws in their design or conduct, gaps in the chain of evidence, or lack of information on important health outcomes."},"raw_text":{"kind":"string","value":"depar depar depar depar department of health and human ser tment of health and human ser tment of health and human ser tment of health and human ser tment of health and human services vices vices vices vices# Background\nIn the United States, the incidence and mortality from cutaneous malignant melanoma (CMM) have increased rapidly in the last few decades (1,2). In 2003, approximately 54,200 persons will have new diagnoses of melanoma, and 7,600 will die from the disease (3). The incidence of the other two skin cancers, basal cell carcinoma (BCC) and squamous cell carcinoma (SCC), is estimated to be >1 million new cases per year (3). According to the data from the Surveillance, Epidemiology and End Results (SEER) cancer registry of the National Cancer Institute, during 1995-1999, average annual age-adjusted incidence rates for melanoma per 100,000 population were 23.5 for men and 15.7 for women for non-Hispanic whites; 3.8 for men and 3.7 for women for Hispanics; 1.8 for men and 1.3 for women for Asians; 1.5 for men and 0.9 for Ameri-\n# Introduction\nThe Task Force on Community Preventive Services (the Task Force) is developing the Guide to Community Preventive Services (the Community Guide), a resource that will include multiple systematic reviews, each focusing on a preventive health topic. The Community Guide is being developed with the support of the U.S. Department of Health and Human Services (DHHS) in collaboration with public and private partners. Although CDC provides staff support to the Task Force for development of the Community Guide, the recommendations presented in this report were developed by the Task Force and are not necessarily the recommendations of DHHS or CDC. This report is one in a series of topics included in the Community Guide. It provides an overview of the process used by the Task Force to select and review evidence and summarize its recommendations regarding interventions to reduce UV exposure and increase UV protective behaviors for prevention of skin cancer. A full report on the recommendations, additional evidence (i.e., discussions of applicability, additional benefits, potential harms, existing barriers to implementation, costs, cost benefit, and cost effectiveness of the interventions [when available]), and remaining research questions will be published in the American Journal of Preventive Medicine.\nCommunity Guide topics are prepared and released as each is completed. The findings from systematic reviews on vaccinepreventable diseases, tobacco use prevention and reduction, motor vehicle occupant injury, physical activity, diabetes, oral health, and the effects of the social environment on health have already been published. A compilation of systematic reviews will be published in book form. Additional information regarding the Task Force and the Community Guide and a list of published articles are available on the Internet at http:/ /www.thecommunityguide.org.\n# Methods\nThe methods used by the Community Guide for conducting systematic reviews and linking evidence to recommendations have been described elsewhere (20). In brief, for each Community Guide topic, a multidisciplinary team (the systematic review development team) conducts a review consisting of the following steps:\n• developing an approach to organizing, grouping, and selecting the interventions; • systematically searching for and retrieving evidence;\n• assessing the quality of and summarizing the strength of the body of evidence of effectiveness; • assessing cost and cost effectiveness evidence, identifying applicability and barriers to implementation (if the effectiveness of the intervention has been established); • summarizing information regarding other evidence; and • identifying and summarizing research gaps. For each review of interventions regarding skin cancer prevention, the systematic review development team developed a conceptual model (or analytic framework) to show the relationship of the intervention to relevant intermediate outcomes (e.g., knowledge, attitudes and beliefs, and intentions regarding sun-protective behaviors), to implementing key sunprotective behaviors, and to the assumed relationships of improvements in sun-protective behaviors to skin cancer prevention. A representative example of an analytic framework for mass media interventions is illustrated (Figure). The analytic frameworks for the other interventions were similar to this example except that they included environmental and policy components.\nThe analytic frameworks focused on key health outcomes (e.g., sunburn or nevi*) and sun-protective behaviors:\n• avoiding peak sun; -seeking shade, and -avoiding the sun during peak UV hours. • covering up; -wearing a hat, -wearing a long-sleeved shirt, and -wearing pants.\n• sunscreen use. The team also examined intermediate outcomes that were postulated to be associated with sun-protective behaviors (e.g., knowledge, attitudes, and intentions). Recommendations were based either on better health outcomes (rare with this subject matter because relevant cancer outcomes would become apparent long after the time of the intervention) or risk behaviors that were thought to be established proxies for cancer outcomes (in this case, avoiding peak UV hours or covering up).\nThe team considered sunscreen use to be a key secondary outcome of sun protection programs because sunscreens prevent sunburn (a marker of unprotected UV exposure and a health outcome associated with increased risk of skin cancer in epidemiologic studies) and reduce the incidence of SCC, and better alternatives are not always available (e.g., when swimming). Sunscreen's role in preventing skin cancer has been demonstrated to be complex, according to information in recent reports from national and international groups (18,21) and summarized in the last section of this report.\nEpidemiologic studies suggest that sunscreen use could be considered harmful if it increased a person's total time in the sun and total UV exposure. Partly for that reason, suncreen use alone might not protect against melanoma despite its protective effect on SCC. The International Agency for Research on Cancer (IARC) recommends that sunscreens not be used as the sole method for skin cancer prevention and not be used as a means to extend the duration of UV exposure (21). The team therefore did not consider sunscreen use, by itself, to be an established proxy for better health. * Nevi are lesions of pigment-forming skin cells that can be a risk factor for melanoma. \n# Intervention\n\n# FIGURE. Analytic framework for media interventions to reduce ultraviolet (UV) exposure and increase sun-protective behaviors.\nMajor stratification variables were type of media (e.g., small media [posters, brochures] versus large media [television, radio] ); characteristics of target population (e.g., age, sex, skin color, skin type, baseline risk, socioeconomic status, sunburn incidence, occupation); intervention intensity (i.e., comparison, some intervention, high level of intervention); geographic or environmental characteristics (e.g., urban, rural, climate of location [e.g., sunny versus cloudy] ); intervention characteristics (e.g., size, access to media).\n# MMWR October 17, 2003\nThe coordination team, † which conducted the systematic review, and their consultants § generated a comprehensive list of interventions to reduce skin cancer. From this, a priority list of interventions for review was developed through a process of polling the coordination team, the consultants, and other specialists in the field regarding their perception of the public health importance (number of persons affected), the practicality of application, and the need of those promoting UV protective behaviors for information regarding each intervention.\nTo conduct the review, the team organized interventions into three groups: setting-specific, target population-specific, and communitywide (Table ). Setting was used as an organizing structure because it was a convenient proxy for key characteristics of the target populations and the implementers of the interventions. The majority of the interventions in this group involved diverse activities -provision of information, environmental approaches (e.g., planting shade trees), or policy approaches (e.g., implementing a policy to reschedule outdoor activities or a requirement to wear hats when outside). Interventions in the setting-specific group consisted of educational and policy approaches in the following settings:\n• child care centers, • primary schools,\n• secondary schools and colleges,\n• recreational or tourism settings,\n• occupational settings, and • health-care settings and for health-care providers.\nThe target population of interest category included one intervention: children's parents or caregivers (some of these interventions might have already been examined in settingspecific groups).\nThe category of communitywide interventions included two types of interventions and a subgroup:\n• media campaigns alone, and • communitywide multicomponent interventions that include at least two interventions in an integrated manner. (Comprehensive communitywide programs, a subset of communitywide multicomponent interventions, include interventions at several levels [individual, setting, whole community] and last longer than 1 year.) Interventions reviewed were either single component (i.e., using only one activity to achieve desired outcomes) or multicomponent (i.e., using more than one activity, such as a policy or environmental intervention with a media campaign). Certain studies provided results relevant to more than one intervention and were included in each of the reviews to which they were applicable. Studies and outcome measures were classified according to definitions developed as part of the review process. The nomenclature used in this report sometimes differs from that used in the original studies.\nTo be included in the reviews of effectiveness, studies had to 1) be primary investigations of interventions selected for evaluation rather than, for example, guidelines or reviews; 2) be published in English during the years 1966-2000; 3) be conducted in established market economies ¶ ; and 4) compare outcomes among groups of persons exposed to the intervention with outcomes among groups of persons not exposed or less exposed to the intervention (i.e., the study design included a concurrent or before-and-after comparison.) ¶ Searches of three computerized databases (MEDLINE, PsychINFO, CINAHL)** were conducted. Team members also reviewed reference lists and consulted with other specialists in the field (e.g., participants in a skin cancer prevention listserv) to identify relevant studies. Each included study was evaluated by using a standardized abstraction form and was assessed for suitability of the study design and threats to validity (22). Studies were characterized as having good, fair, or limited execution based on the number of threats to validity (20).\nResults for each outcome of interest were obtained from each study that met the minimum quality criteria. Net effects were derived when appropriate by calculating the difference between the changes observed in the intervention and comparison groups relative to the respective baseline levels. † † The median was used to summarize a typical measure of effect across the body of evidence for each outcome of interest; both the median and the range are reported. For bodies of evidence consisting of four or more studies, an interquartile range was used to represent variability.\nThe strength of the body of evidence of effectiveness was characterized as strong, sufficient, or insufficient on the basis of the number of available studies, the suitability of study designs for evaluating effectiveness, the quality of execution of the studies as defined by the Community Guide (20), the consistency of the results, and the effect size.\nThe Task Force uses these systematic reviews to evaluate the evidence of intervention effectiveness and makes recommendations based on the findings of the reviews (20). The strength of each recommendation is based on the evidence of effectiveness (i.e., an intervention is recommended on the basis of either strong or sufficient evidence of effectiveness) (20). Other types of evidence can also affect a recommendation. For example, harms resulting from an intervention that outweigh benefits might lead to a recommendation that the intervention not be used even if it is effective in improving some outcomes.\nA finding of insufficient evidence to determine effectiveness should not be interpreted as evidence of ineffectiveness. Insufficient evidence may be found for any of a number of reasons, alone or in combination, including an insufficient number of studies; too many threats to the validity of the available studies based on their design, execution, or both; conflicts in the results of the studies that preclude a coherent summary of effectiveness; or no indication that the outcomes measured to date, by themselves, represent success in improving health. In all these situations, a finding of insufficient evidence to determine effectiveness is important for identifying areas of uncertainty and continuing research needs. In contrast, sufficient or strong evidence of ineffectiveness would lead to a recommendation against use of the intervention.\n# Results\nDatabase searches and bibliographic reviews yielded a list of 6,373 potentially relevant titles. After review of the abstracts and consultation with specialists in the field, a total of 313 reports were retrieved. Of these, 154 were not used in the review because they did not provide results, did not refer to an intervention, or reported on noncomparative studies. The remaining 159 were retained for full review. On the basis of limitations in execution or design or because they provided only background information on studies that were already included, 74 of these were excluded and were not considered further. The remaining 85 studies were considered qualifying studies. The Task Force recommendations in this report are based on the systematic review and evaluation of these qualifying studies, all of which had good or fair quality of execution.\nThe Task Force recommended two interventions, both in the setting-specific category (Table ):\n• educational and policy approaches in primary schoolschanging children's covering-up behavior (wearing protective clothing); and • educational and policy approaches in recreational or tourism settings -changing adults' covering-up behaviors. Interventions in primary school settings were designed to increase sun-protective knowledge, attitudes, intentions, and behavior among children from kindergarten through eighth grade. The interventions ranged from a curriculum that included interactive classroom and take-home activities to staff education, brochures for parents, and a working session to develop skin protection plans for schools. All interventions focused on some combination of increasing application of sunscreen, scheduling activities to avoid peak sun hours, increasing availability of shade and encouraging children to play in shady areas, and encouraging children to wear sunprotective clothing. Interventions in this category included at least one of the following activities:\n• provision of information to children (e.g., instruction or small media [brochures, flyers, newsletters, informational letters or videos] or both); • additional activities to influence children's behavior (e.g., modeling, demonstration, role playing); • activities intended to change the knowledge, attitudes, or behavior of caregivers (i.e., teachers or parents); or • environmental or policy approaches (e.g., provision of sunscreen, provision of shade, or scheduling outdoor activities to avoid hours of peak sunlight). Single-and multicomponent interventions in recreational settings were designed to increase knowledge; influence attitudes, beliefs, and intentions; and change behavior of adults and children. Interventions included one or more of the following: educational brochures, including culturally relevant materials and photographs of skin cancer lesions; sun-safety training for lifeguards, aquatic instructors, and outdoor recreation staff and role-modeling by these groups; sun-safety lessons, interactive activities, and incentives for parents and children; increasing available shaded areas; providing sunscreen; and point-of-purchase prompts.\nThe recommended interventions had small to moderate behavior change scores. In primary schools, the median net relative increase was 25% (interquartile range: 1%-40%, six studies). In recreational settings, the median net relative increase was 11.2% (interquartile range: 5.1%-12.9%, five studies).\nIt should be noted that the interventions were targeted to populations rather than single persons. Small changes in behavior in large populations can result in substantial public health benefits.\nThe Task Force found insufficient evidence on which to make recommendations for or against the following interventions: educational and policy approaches in child care centers; educational and policy approaches in secondary schools and colleges; educational and policy approaches in recreational or tourism settings for children; educational and policy approaches in occupational settings; interventions oriented to health-care settings and providers; interventions oriented to children's parents or caregivers; media campaigns alone; and communitywide multicomponent interventions (Table ). The finding of insufficient evidence to determine effectiveness was most often based on the limited numbers of studies that measured behavioral or health outcomes, inconsistent evidence among studies that measured changes in sun-protective behaviors, and limitations in the design and execution of available studies.\nSummary tables of the reviews will be available at http:// www.thecommunityguide.org/cancer when the full evidence is published in a supplement to the American Journal of Preventive Medicine.\n# Use of Recommendations in Communities and Health-Care Settings\nMalignant melanoma is the deadliest of the skin cancers, and its incidence in the United States has increased rapidly in the past 2 decades. Melanoma accounts for approximately three fourths of all skin cancer deaths. Basal cell and squamous cell skin cancers are seldom fatal but, if advanced, can cause severe disfigurement and morbidity (3). UV exposure in childhood and intense intermittent UV exposures are the major environmental risk factors for melanoma and BCC, and cumulative UV exposure is the major preventable risk factor for SCC (23). National surveys indicate that only one third of Americans practice sun-protective behaviors, and their practices vary greatly, depending on age, sex, and their ability to tan and burn (9,12,13).\nThe two Task Force recommendations -educational and policy approaches in primary schools, and educational and policy approaches for adults in outdoor recreational or tourism settings -are based on improving covering-up behaviors. These recommendations represent tested interventions that promote decreased UV exposure at the community level. They can be used for planning interventions to promote UV protection or to evaluate existing programs.\nSeveral of the studies reviewed included multiple components that could not be evaluated separately. For example, a school-based program might involve components of policy, such as establishing school guidelines, in tandem with implementation of one-on-one didactic and interactive sessions regarding adapting sun-protective behaviors. Although sunprotective behaviors were increased by school-based programs, the specific effect could not be attributed to one specific intervention characteristic. In selecting and implementing interventions, the potential for an unintended increase in the duration and intensity of UV exposure must be considered. Also, communities should strive to develop comprehensive programs that include a wide range of activities suitable for their local resources, population characteristics, and settings.\nThe other interventions reviewed, for which evidence was insufficient to determine effectiveness, could also prove useful. They provide a broader taxonomy of interventions that deserve further testing and evaluation, and the documentation of research gaps in these reviews could potentially help to improve the next generation of research. Additional information on research gaps will be provided in the report in the American Journal of Preventive Medicine.\nChoosing interventions that are well matched to local needs and capabilities, and then carefully implementing those interventions, are vital steps for increasing UV protection. Several factors can affect the attitudes, ability, and behaviors of a community regarding taking sun safety precautions. Some of the most important are program priorities, location of the community, and population. Establishing skin cancer prevention as a priority might be difficult because skin cancer is but one of many health topics, and for certain communities, may not be as high a priority as other cancers or diseases. Although it might be a higher priority in areas where UV radiation is more intense, even in areas with lower UV intensity, education about UV exposure during times of episodic exposure (e.g., during winter sports, when the sun comes out, and when traveling to higher UV intensity regions) could be helpful. Likewise, although skin cancer prevention might be a higher priority for populations at an increased risk (e.g., light-skinned, sunsensitive), even darker-skinned or less sun-sensitive persons need to take precautions when exposed to UV radiation. To meet local objectives, recommendations and other evidence provided in the Community Guide should be supplemented with local information such as skin cancer incidence, skin cancer mortality, prevalence of sun-protective behaviors, latitude, UV index, resource availability, administrative structures, and economic and social environments of organizations and practitioners.\nThese reviews by themselves do not provide advice regarding implementation of effective programs; the referenced articles, however, provide additional detail. Implementation advice is also available elsewhere (24)(25)(26)(27)(28).\n# Introduction\nThis statement summarizes the current U.S. Preventive Services Task Force (USPSTF) recommendation on counseling to prevent skin cancer and the supporting scientific evidence, and updates the 1996 recommendation contained in the Guide to Clinical Preventive Services, Second Edition (1). The USPSTF, an independent panel of private sector experts in primary care and prevention, systematically reviews the evidence of effectiveness of a wide range of clinical preventive services, including screening tests, counseling, and chemoprevention. The Task Force grades its recommendations according to one of five classifications (A, B, C, D, I), reflecting the strength of evidence and magnitude of net benefit (benefits minus harms) (Box 1). The USPSTF grades the quality of the overall evidence for a service on a 3-point scale (good, fair, poor) (Box 2).\nThis recommendation and rationale statement and complete information on which this statement is based, including evidence tables and references, are available at http://www.ahrq. gov/clinic/uspstfix.htm (2) and in print by subscription through the AHRQ Clearinghouse (1-800-358-9295 or e-mail at ahrqpubs@ahrq.gov) and through the National Guideline Clearinghouse ™ at http://www.guideline.gov.\n# Summary of Recommendation\nThe U.S. Preventive Services Task Force concludes that the evidence is insufficient to recommend for or against routine counseling by primary care clinicians to prevent skin cancer.\n# I recommendation.\nThe USPSTF found insufficient evidence to determine whether clinician counseling is effective in changing patient behaviors to reduce skin cancer risk. Counseling parents may increase the use of sunscreen for children, but there is little evidence to determine the effects of counseling on other preventive behaviors (such as wearing protective clothing, reducing excessive sun exposure, avoiding sun lamps/tanning beds, or practicing skin self-examination) and little evidence on potential harms.\n# Clinical Considerations\n• Using sunscreen has been shown to prevent squamous cell skin cancer. The evidence for the effect of sunscreen use in preventing melanoma, however, is mixed. Sunscreens that block both ultraviolet A (UV-A) and ultraviolet B (UV-B) light may be more effective in preventing squamous cell cancer and its precursors than those that block only UV-B light. However, people who use sunscreen alone could increase their risk for melanoma if they increase the time they spend in the sun. • UV exposure increases the risk for skin cancer among people with all skin types, but especially fair-skinned people. Those who sunburn readily and tan poorly, namely those with red or blond hair and fair skin that freckles or burns easily, are at highest risk for developing skin cancer and would benefit most from sun protection behaviors. The incidence of melanoma among whites is 20 times higher than it is among blacks; the incidence of melanoma among whites is approximately four times higher than it is among Hispanics. • Observational studies indicate that intermittent or intense sun exposure is a greater risk factor for melanoma than chronic exposure. These studies support the hypothesis that preventing sunburn, especially in childhood, may reduce the lifetime risk for melanoma. • Other measures for preventing skin cancer include avoiding direct exposure to midday sun (between the hours of 10:00 a.m. and 4:00 p.m.) to reduce exposure to ultraviolet (UV) rays and covering skin exposed to the sun (by wearing protective clothing such as broad-brimmed hats, long-sleeved shirts, long pants, and sunglasses). • The effects of sunlamps and tanning beds on the risk for melanoma are unclear because of limited study design and conflicting results from retrospective studies. • Only a single case-control study of skin self-examination has reported a lower risk for melanoma among patients who reported ever examining their skin over 5 years.\nAlthough results from this study suggest that skin selfexamination may be effective in preventing skin cancer, these results are not definitive.\n# Scientific Evidence Epidemiology and Clinical Consequences\nMelanoma is a leading cause of cancer death in the United States. The lifetime risk for dying of melanoma is 0.36% in white men and 0.21% in white women (3). Between 1973 and 1995, the age-adjusted incidence of melanoma increased more than 100%, from 5.7 per 100,000 people to 13.3 per 100,000 people. The increase in annual incidence rates is likely due to several factors, including increased sun exposure and possibly earlier detection of melanoma. Although primary prevention efforts have focused on young people, the elderly (especially elderly men) bear a disproportionate burden of morbidity and mortality from melanoma and nonmelanoma skin cancer. Men older than age 65 account for 22% of the newly diagnosed cases of malignant melanoma each year and women in the same age group account for 14%. Basal cell and squa-mous cell carcinomas are more than 10 times as common as melanoma but account for less morbidity and mortality. Squamous cell cancers, however, may account for 20% of all deaths from skin cancer.\n# Effectiveness of Available Interventions\nPreventive strategies include reducing sun exposure (e.g., by wearing protective clothing and using sunscreen regularly), avoiding sunlamps and tanning equipment, and practicing skin self-examination. There is little direct evidence, however, that any of these interventions reduce skin cancer morbidity or mortality.\n# Reducing Sun Exposure\nAvoiding direct sunlight by staying indoors or in the shade or by wearing protective clothing is the most effective measure for reducing exposure to ultraviolet light, but there are no randomized trials of sun avoidance to prevent skin cancer. In numerous observational studies, increased sun exposure in childhood and adolescence is associated with increased risk for nonmelanoma skin cancer, which usually occurs in sunexposed areas such as the face.\nRecent studies provide a more complex picture of the relationship between sun exposure and melanoma, however. Although melanoma incidence is higher in regions near the equator where ultraviolet exposure is most intense, melanoma often occurs in areas of the body not exposed to the sun. In observational studies, intermittent or intense sun exposure was associated with increased risk for melanoma; chronic exposure was associated with lower risk, as was the ability to tan (4-7).\n# Sunlamp and Tanning Bed Avoidance\nSix of 19 case-control studies found a positive association between use of sun lamps and melanoma risk, but most did not adjust for recreational sun exposure or for the dosage and timing of sunlamp exposure (8). Among nine studies that examined the duration, frequency, or timing of sunlamp or tanning bed exposure, four found a positive association, particularly if the dose of exposure was high and if it caused burning.\n# Sunscreen Use\nDaily sunscreen use on the hands and face reduced the total incidence of squamous cell cancer in a randomized trial of 1,621 residents in Australia (rate ratio [RR]: 0.61; 95% confidence interval [CI] = 0.46-0.81) (9). Sunscreen had no effect on basal cell cancer. Based on this trial, 140 people would need to use sunscreen daily for 4½ years to prevent one case of squamous cell cancer. An earlier randomized trial demonstrated that sunscreen use reduced solar keratoses, precursors of squamous cell cancers (10). There are no direct data about the effect of sunscreen on melanoma incidence. An unblinded randomized trial showed that children at high risk for skin cancers who used sunscreen developed fewer nevi than those who did not. Several epidemiologic studies have found higher risk for melanoma among users of sunscreens than among nonusers (11)(12)(13). A recent meta-analysis of population-based casecontrol studies found no effect of sunscreen use on risk for melanoma (14). The conflicting results may reflect the fact that sunscreen use is more common among fair-skinned people, who are at higher risk for melanoma, than it is among darkerskinned people; or, this finding may reflect the fact that sunscreen use could be harmful if it encourages longer stays in the sun without protecting completely against cancer-causing radiation.\n# Skin Self-Examination\nThe only evidence for the effectiveness of skin self-examination comes from a single case-control study (1,15). After adjustment for other risk factors, skin self-examination was associated with lower incidence of melanoma (odds ratio [OR]: 0.66; 95% CI = 0.44-0.99) and lower mortality from melanoma (OR: 0.37; 95% CI = 0.16-0.84), although the definition of \"self-examination\" was limited. This study did not provide sufficient evidence that skin self-examination would reduce the incidence of melanoma or improve outcomes of melanoma.\n# Effectiveness of Counseling\nCommunity and worksite educational interventions have demonstrated effectiveness for increasing the use of skin protection measures, such as wearing hats and long-sleeve shirts and staying in the shade; however, evidence addressing the effectiveness of clinician counseling to prevent skin cancer is extremely limited. Most studies of counseling have examined intermediate outcomes such as knowledge and attitudes rather than changes in behavior. In a recent survey, 60% of pediatricians said that they usually or always counsel patients about skin protection, but advice to use sunscreen is more common than advice about wearing protective clothing or avoiding the midday sun (16).\nSimple reminders and instructional materials for clinicians can overcome some of the barriers to regular counseling. A randomized trial of a community-based intervention involving 10 towns in New Hampshire suggests that office-based counseling by physicians may be an effective component of a multimodal program to promote skin protection (17). The proportion of children using some sun protection increased significantly in the intervention towns (from 78% to 87%) compared to a decrease in the control communities (from 85% to 80%). More parents reported receiving some sun protection information from a clinician in the intervention towns. However, most of the change was due to increased sunscreen use rather than to reduced sun exposure.\n# Potential Harms of Skin Protection Behaviors\nThere are limited data regarding potential harms of counseling or of specific skin protection behaviors. Skin cancer counseling that focuses on the use of sunscreen could possibly lead to a false sense of security, which might lead to more time in the sun. For example, a randomized trial with young adults found that those who used sunscreen with a high sun protection factor (SPF) stayed longer in the sun than those who used sunscreen with a lower SPF (18). There has been some concern that use of SPF of 15 results in vitamin D deficiency. However, a randomized trial among people over 40 years of age found that sunscreen use over the summer had no effect on 25-hydroxyvitamin D3 levels. Concerns related to sun avoidance include reduced physical activity levels among children and negative effects on mental health. However, no studies have evaluated the effects of sun protection behaviors on these outcomes.\n# Recommendations Of Others\nThe American Cancer Society (19), the American Academy of Dermatology (20), the American Academy of Pediatrics (21), the American College of Obstetricians and Gynecologists (22), and a National Institutes of Health consensus panel (23) all recommend patient education concerning sun avoidance and sunscreen use. The American Academy of Family Physicians recommends sun protection for all with increased sun exposure (24). The American College of Preventive Medicine (ACPM) concluded that sun-protective measures (e.g., clothing, hats, opaque sunscreens) are probably effective in reducing skin cancer but that the evidence does not support discussion of sunscreen and sun protection with every patient. ACPM concluded that evidence is insufficient to advise patients that chemical sunscreens protect against malignant melanoma and that their use may actually lead to increased risk (25). Recently, the International Agency for Research on Cancer (IARC), part of the World Health Organization, qualified their recommendation for sunscreen use in ways that address the importance of learning more about potential harms of counseling for sunscreen use as follows:\n# MMWR October 17, 2003\nSunscreens probably prevent squamous-cell carcinoma of the skin when used mainly during unintentional sun exposure. No conclusion can be drawn about the cancerpreventive activity of topical use of sunscreens against basalcell carcinoma and cutaneous melanoma. Use of sunscreens can extend the duration of intentional sun exposure, such as sunbathing. Such an extension may increase the risk for cutaneous melanoma (26). The Task Force on Community Preventive Services found insufficient evidence to determine the effectiveness of a range of population-based interventions to reduce unprotected UV light exposure and recommended additional research on educational policy approaches, media campaigns, and both health-care setting and community-based interventions (27). \n# U.S. Preventive Services Task Force\n\n# BOX 1. U.S. Preventive Services Task Force (USPSTF) recommendations and ratings\nThe Task Force grades its recommendations according to one of five classifications (A, B, C, D, I) reflecting the strength of evidence and magnitude of net benefit (benefits minus harms): The USPSTF grades the quality of the overall evidence for a service on a 3-point scale (good, fair, poor):\nA.\nGood: Evidence includes consistent results from welldesigned, well-conducted studies in representative populations that directly assess effects on health outcomes.\nFair: Evidence is sufficient to determine effects on health outcomes, but the strength of the evidence is limited by the number, quality, or consistency of the individual studies, generalizability to routine practice, or indirect nature of the evidence on health outcomes.\nPoor: Evidence is insufficient to assess the effects on health outcomes because of limited number or power of studies, important flaws in their design or conduct, gaps in the chain of evidence, or lack of information on important health outcomes."},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":661,"cells":{"id":{"kind":"string","value":"9cc3520b5248a34dfa45b5c6a4c56ac9b7f1a843"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"None"},"clean_text":{"kind":"string","value":"This schedule includes recommendations in effect as of January 1, 2017. Any dose not administered at the recommended age should be administered at a subsequent visit, when indicated and feasible. The use of a combination vaccine generally is preferred over separate injections of its equivalent component vaccines. Vaccination providers should consult the relevant Advisory Committee on Immunization Practices (ACIP) statement for detailed recommendations, available online at www.cdc.gov/vaccines/hcp/acip-recs/index.html. Clinically significant adverse events that follow vaccination should be reported to the Vaccine Adverse Event Reporting System (VAERS) online (www.vaers.hhs.gov) or by telephone (800-822-7967). Suspected cases of vaccinepreventable diseases should be reported to the state or local health department. Additional information, including precautions and contraindications for vaccination, is available from CDC online (www.cdc.gov/vaccines/hcp/admin/ contraindications.html) or by telephone (800-CDC- ).#\n). These recommendations must be read with the footnotes that follow. For those who fall behind or start late, provide catch-up vaccination at the earliest opportunity as indicated by the green bars in Figure 1. To determine minimum intervals between doses, see the catch-up schedule (Figure 2). School entry and adolescent vaccine age groups are shaded in gray.\n\n# NOTE:\nThe above recommendations must be read along with the footnotes of this schedule. No recommendation Range of recommended ages for certain high-risk groups Range of recommended ages for all children Range of recommended ages for catch-up immunization Range of recommended ages for non-high-risk groups that may receive vaccine, subject to individual clinical decision making FIGURE 2. Catch-up immunization schedule for persons aged 4 months through 18 years who start late or who are more than 1 month behind-United States, 2017.\nThe figure below provides catch-up schedules and minimum intervals between doses for children whose vaccinations have been delayed. A vaccine series does not need to be restarted, regardless of the time that has elapsed between doses. Use the section appropriate for the child's age. Always use this table in conjunction with Figure 1 and the footnotes that follow.\n\n# Additional information\n- For information on contraindications and precautions for the use of a vaccine and for additional information regarding that vaccine, vaccination providers should consult the ACIP General Recommendations on Immunization and the relevant ACIP statement, available online at www.cdc.gov/vaccines/hcp/acip-recs/index.html. - For purposes of calculating intervals between doses, 4 weeks = 28 days. Intervals of 4 months or greater are determined by calendar months.\n- Vaccine doses administered ≤4 days before the minimum interval are considered valid. Doses of any vaccine administered ≥5 days earlier than the minimum interval or minimum age should not be counted as valid doses and should be repeated as age-appropriate. The repeat dose should be spaced after the invalid dose by the recommended minimum interval. For further details, see - Administer monovalent HepB vaccine to all newborns within 24 hours of birth. - For infants born to hepatitis B surface antigen (HBsAg)positive mothers, administer HepB vaccine and 0.5 mL of hepatitis B immune globulin (HBIG) within 12 hours of birth. These infants should be tested for HBsAg and antibody to HBsAg (anti-HBs) at age 9 through 12 months (preferably at the next well-child visit) or 1 to 2 months after completion of the HepB series if the series was delayed. - If mother's HBsAg status is unknown, within 12 hours of birth, administer HepB vaccine regardless of birth weight. For infants weighing less than 2,000 grams, administer HBIG in addition to HepB vaccine within 12 hours of birth. Determine mother's HBsAg status as soon as possible and, if mother is HBsAg-positive, also administer HBIG to infants weighing 2,000 grams or more as soon as possible, but no later than age 7 days.\n\n# Doses following the birth dose:\n- The second dose should be administered at age 1 or 2 months. Monovalent HepB vaccine should be used for doses administered before age 6 weeks. - Infants who did not receive a birth dose should receive 3 doses of a HepB-containing vaccine on a schedule of 0, 1 to 2 months, and 6 months, starting as soon as feasible (see figure 2). - Administer the second dose 1 to 2 months after the first dose (minimum interval of 4 weeks); administer the third dose at least 8 weeks after the second dose AND at least 16 weeks after the first dose. The final (third or fourth) dose in the HepB vaccine series should be administered no earlier than age 24 weeks.\n- Administration of a total of 4 doses of HepB vaccine is permitted when a combination vaccine containing HepB is administered after the birth dose.\n\n# Catch-up vaccination:\n- Unvaccinated persons should complete a 3-dose series. - Administer a 4-dose series of IPV at ages 2, 4, 6 through 18 months, and 4 through 6 years. The final dose in the series should be administered on or after the fourth birthday and at least 6 months after the previous dose.\n\n# Catch-up vaccination:\n- In the first 6 months of life, minimum age and minimum intervals are only recommended if the person is at risk of imminent exposure to circulating poliovirus (i.e., travel to a polio-endemic region or during an outbreak). - If 4 or more doses are administered before age 4 years, an additional dose should be administered at age 4 through 6 years and at least 6 months after the previous dose. - A fourth dose is not necessary if the third dose was administered at age 4 years or older and at least 6 months after the previous dose. - If both oral polio vaccine (OPV) and IPV were administered as part of a series, a total of 4 doses should be administered, regardless of the child's current age.\nIf only OPV was administered, and all doses were given prior to age 4 years, 1 dose of IPV should be given at 4 years or older, at least 4 weeks after the last OPV dose. - IPV is not routinely recommended for U.S. residents aged 18 years or older. - For other catch-up guidance, see Figure 2.\nFor further guidance on the use of the vaccines mentioned below, see: www.cdc.gov/vaccines/hcp/acip-recs/index.html. - Administer a 2-dose series of MMR vaccine at ages 12 through 15 months and 4 through 6 years. The second dose may be administered before age 4 years, provided at least 4 weeks have elapsed since the first dose. - Administer 1 dose of MMR vaccine to infants aged 6 through 11 months before departure from the United States for international travel. These children should be revaccinated with 2 doses of MMR vaccine, the first at age 12 through 15 months (12 months if the child remains in an area where disease risk is high), and the second dose at least 4 weeks later. - Administer 2 doses of MMR vaccine to children aged 12 months and older before departure from the United States for international travel. The first dose should be administered on or after age 12 months and the second dose at least 4 weeks later.\n\n# Catch-up vaccination:\n- Ensure that all school-aged children and adolescents have had 2 doses of MMR vaccine; the minimum interval between the 2 doses is 4 weeks.\n\n# Varicella (VAR) vaccine. (Minimum age: 12 months)\nRoutine vaccination:\n- Administer a 2-dose series of VAR vaccine at ages 12 through 15 months and 4 through 6 years. The second dose may be administered before age 4 years, provided at least 3 months have elapsed since the first dose. If the second dose was administered at least 4 weeks after the first dose, it can be accepted as valid.\n\n# Catch-up vaccination:\n- Ensure that all persons aged 7 through 18 years without evidence of immunity (see MMWR 2007;56, available at www.cdc.gov/mmwr/pdf/rr/rr5604.pdf ) have 2 doses of varicella vaccine. For children aged 7 through 12 years, the recommended minimum interval between doses is 3 months (if the second dose was administered at least 4 weeks after the first dose, it can be accepted as valid); for persons aged 13 years and older, the minimum interval between doses is 4 weeks. For further guidance on the use of the vaccines mentioned below, see: www.cdc.gov/vaccines/hcp/acip-recs/index.html.\n\n# CS270457-C\n Menactra ɱ Children with anatomic or functional asplenia or HIV infection ʲ Children 24 months and older who have not received a complete series. Administer 2 primary doses at least 8 weeks apart. If Menactra is administered to a child with asplenia (including sickle cell disease) or HIV infection, do not administer Menactra until age 2 years and at least 4 weeks after the completion of all PCV13 doses. ɱ Children with persistent complement component deficiency ʲ Children 9 through 23 months. Administer 2 primary doses at least 12 weeks apart. ʲ Children 24 months and older who have not received a complete series. Administer 2 primary doses at least 8 weeks apart. ɱ All high-risk children ʲ If Menactra is to be administered to a child at high risk for meningococcal disease, it is recommended that Menactra be given either before or at the same time as DTaP. Bexsero or Trumenba ɱ Persons 10 years or older who have not received a complete series. Administer a 2-dose series of Bexsero, with doses at least 1 month apart, or a 3-dose series of Trumenba, with the second dose at least 1-2 months after the first and the third dose at least 6 months after the first. The two MenB vaccines are not interchangeable; the same vaccine product must be used for all doses. For children who travel to or reside in countries in which meningococcal disease is hyperendemic or epidemic, including countries in the African meningitis belt or the Hajj:\n Administer an age-appropriate formulation and series of Menactra or Menveo for protection against serogroups A and W meningococcal disease. Prior receipt of MenHibrix is not sufficient for children traveling to the meningitis belt or the Hajj because it does not contain serogroups A or W. For children at risk during an outbreak attributable to a vaccine serogroup: For serogroup A, C, W, or Y: Administer or complete an age-and formulation-appropriate series of MenHibrix, Menactra, or Menveo.\n For serogroup B: Administer a 2-dose series of Bexsero, with doses at least 1 month apart, or a 3-dose series of Trumenba, with the second dose at least 1-2 months after the first and the third dose at least 6 months after the first. The two MenB vaccines are not interchangeable; the same vaccine product must be used for all doses. For MenACWY booster doses among persons with high-risk conditions, refer to MMWR 2013;62(RR02):1-22, at www.cdc.gov/mmwr/preview/mmwrhtml/rr6202a1.htm, MMWR June 20, 2014 / 63( 24 - Administer a 2-dose series of HPV vaccine on a schedule of 0, 6-12 months to all adolescents aged 11 or 12 years. The vaccination series can start at age 9 years. - Administer HPV vaccine to all adolescents through age 18 years who were not previously adequately vaccinated. The number of recommended doses is based on age at administration of the first dose. - For persons initiating vaccination before age 15, the recommended immunization schedule is 2 doses of HPV vaccine at 0, 6-12 months. - For persons initiating vaccination at age 15 years or older, the recommended immunization schedule is 3 doses of HPV vaccine at 0, 1-2, 6 months. - A vaccine dose administered at a shorter interval should be readministered at the recommended interval. In a 2-dose schedule of HPV vaccine, the minimum interval is 5 months between the first and second dose.\nIf the second dose is administered at a shorter interval, a third dose should be administered a minimum of 12 weeks after the second dose and a minimum of 5 months after the first dose. In a 3-dose schedule of HPV vaccine, the minimum intervals are 4 weeks between the first and second dose, 12 weeks between the second and third dose, and 5 months between the first and third dose. If a vaccine dose is administered at a shorter interval, it should be readministered after another minimum interval has been met since the most recent dose.\n\n# Special populations:\n- For children with history of sexual abuse or assault, administer HPV vaccine beginning at age 9 years. - Immunocompromised persons*, including those with human immunodeficiency virus (HIV) infection, should receive a 3-dose series at 0, 1-2, and 6 months, regardless of age at vaccine initiation. - Note: HPV vaccination is not recommended during pregnancy, although there is no evidence that the vaccine poses harm. If a woman is found to be pregnant after initiating the vaccination series, no intervention is needed; the remaining vaccine doses should be delayed until after the pregnancy."},"raw_text":{"kind":"string","value":"This schedule includes recommendations in effect as of January 1, 2017. Any dose not administered at the recommended age should be administered at a subsequent visit, when indicated and feasible. The use of a combination vaccine generally is preferred over separate injections of its equivalent component vaccines. Vaccination providers should consult the relevant Advisory Committee on Immunization Practices (ACIP) statement for detailed recommendations, available online at www.cdc.gov/vaccines/hcp/acip-recs/index.html. Clinically significant adverse events that follow vaccination should be reported to the Vaccine Adverse Event Reporting System (VAERS) online (www.vaers.hhs.gov) or by telephone (800-822-7967). Suspected cases of vaccinepreventable diseases should be reported to the state or local health department. Additional information, including precautions and contraindications for vaccination, is available from CDC online (www.cdc.gov/vaccines/hcp/admin/ contraindications.html) or by telephone (800-CDC- ).# \n2]\n). These recommendations must be read with the footnotes that follow. For those who fall behind or start late, provide catch-up vaccination at the earliest opportunity as indicated by the green bars in Figure 1. To determine minimum intervals between doses, see the catch-up schedule (Figure 2). School entry and adolescent vaccine age groups are shaded in gray.\n# NOTE:\nThe above recommendations must be read along with the footnotes of this schedule. No recommendation Range of recommended ages for certain high-risk groups Range of recommended ages for all children Range of recommended ages for catch-up immunization Range of recommended ages for non-high-risk groups that may receive vaccine, subject to individual clinical decision making FIGURE 2. Catch-up immunization schedule for persons aged 4 months through 18 years who start late or who are more than 1 month behind-United States, 2017.\nThe figure below provides catch-up schedules and minimum intervals between doses for children whose vaccinations have been delayed. A vaccine series does not need to be restarted, regardless of the time that has elapsed between doses. Use the section appropriate for the child's age. Always use this table in conjunction with Figure 1 and the footnotes that follow. \n# Additional information\n• For information on contraindications and precautions for the use of a vaccine and for additional information regarding that vaccine, vaccination providers should consult the ACIP General Recommendations on Immunization and the relevant ACIP statement, available online at www.cdc.gov/vaccines/hcp/acip-recs/index.html. • For purposes of calculating intervals between doses, 4 weeks = 28 days. Intervals of 4 months or greater are determined by calendar months.\n• Vaccine doses administered ≤4 days before the minimum interval are considered valid. Doses of any vaccine administered ≥5 days earlier than the minimum interval or minimum age should not be counted as valid doses and should be repeated as age-appropriate. The repeat dose should be spaced after the invalid dose by the recommended minimum interval. For further details, see • Administer monovalent HepB vaccine to all newborns within 24 hours of birth. • For infants born to hepatitis B surface antigen (HBsAg)positive mothers, administer HepB vaccine and 0.5 mL of hepatitis B immune globulin (HBIG) within 12 hours of birth. These infants should be tested for HBsAg and antibody to HBsAg (anti-HBs) at age 9 through 12 months (preferably at the next well-child visit) or 1 to 2 months after completion of the HepB series if the series was delayed. • If mother's HBsAg status is unknown, within 12 hours of birth, administer HepB vaccine regardless of birth weight. For infants weighing less than 2,000 grams, administer HBIG in addition to HepB vaccine within 12 hours of birth. Determine mother's HBsAg status as soon as possible and, if mother is HBsAg-positive, also administer HBIG to infants weighing 2,000 grams or more as soon as possible, but no later than age 7 days.\n# Doses following the birth dose:\n• The second dose should be administered at age 1 or 2 months. Monovalent HepB vaccine should be used for doses administered before age 6 weeks. • Infants who did not receive a birth dose should receive 3 doses of a HepB-containing vaccine on a schedule of 0, 1 to 2 months, and 6 months, starting as soon as feasible (see figure 2). • Administer the second dose 1 to 2 months after the first dose (minimum interval of 4 weeks); administer the third dose at least 8 weeks after the second dose AND at least 16 weeks after the first dose. The final (third or fourth) dose in the HepB vaccine series should be administered no earlier than age 24 weeks.\n• Administration of a total of 4 doses of HepB vaccine is permitted when a combination vaccine containing HepB is administered after the birth dose.\n# Catch-up vaccination:\n• Unvaccinated persons should complete a 3-dose series. • Administer a 4-dose series of IPV at ages 2, 4, 6 through 18 months, and 4 through 6 years. The final dose in the series should be administered on or after the fourth birthday and at least 6 months after the previous dose.\n# Catch-up vaccination:\n• In the first 6 months of life, minimum age and minimum intervals are only recommended if the person is at risk of imminent exposure to circulating poliovirus (i.e., travel to a polio-endemic region or during an outbreak). • If 4 or more doses are administered before age 4 years, an additional dose should be administered at age 4 through 6 years and at least 6 months after the previous dose. • A fourth dose is not necessary if the third dose was administered at age 4 years or older and at least 6 months after the previous dose. • If both oral polio vaccine (OPV) and IPV were administered as part of a series, a total of 4 doses should be administered, regardless of the child's current age.\nIf only OPV was administered, and all doses were given prior to age 4 years, 1 dose of IPV should be given at 4 years or older, at least 4 weeks after the last OPV dose. • IPV is not routinely recommended for U.S. residents aged 18 years or older. • For other catch-up guidance, see Figure 2.\nFor further guidance on the use of the vaccines mentioned below, see: www.cdc.gov/vaccines/hcp/acip-recs/index.html. • Administer a 2-dose series of MMR vaccine at ages 12 through 15 months and 4 through 6 years. The second dose may be administered before age 4 years, provided at least 4 weeks have elapsed since the first dose. • Administer 1 dose of MMR vaccine to infants aged 6 through 11 months before departure from the United States for international travel. These children should be revaccinated with 2 doses of MMR vaccine, the first at age 12 through 15 months (12 months if the child remains in an area where disease risk is high), and the second dose at least 4 weeks later. • Administer 2 doses of MMR vaccine to children aged 12 months and older before departure from the United States for international travel. The first dose should be administered on or after age 12 months and the second dose at least 4 weeks later.\n# Catch-up vaccination:\n• Ensure that all school-aged children and adolescents have had 2 doses of MMR vaccine; the minimum interval between the 2 doses is 4 weeks.\n# Varicella (VAR) vaccine. (Minimum age: 12 months)\nRoutine vaccination:\n• Administer a 2-dose series of VAR vaccine at ages 12 through 15 months and 4 through 6 years. The second dose may be administered before age 4 years, provided at least 3 months have elapsed since the first dose. If the second dose was administered at least 4 weeks after the first dose, it can be accepted as valid.\n# Catch-up vaccination:\n• Ensure that all persons aged 7 through 18 years without evidence of immunity (see MMWR 2007;56[No. RR-4], available at www.cdc.gov/mmwr/pdf/rr/rr5604.pdf ) have 2 doses of varicella vaccine. For children aged 7 through 12 years, the recommended minimum interval between doses is 3 months (if the second dose was administered at least 4 weeks after the first dose, it can be accepted as valid); for persons aged 13 years and older, the minimum interval between doses is 4 weeks. For further guidance on the use of the vaccines mentioned below, see: www.cdc.gov/vaccines/hcp/acip-recs/index.html.\n# CS270457-C\n▪ Menactra ɱ Children with anatomic or functional asplenia or HIV infection ʲ Children 24 months and older who have not received a complete series. Administer 2 primary doses at least 8 weeks apart. If Menactra is administered to a child with asplenia (including sickle cell disease) or HIV infection, do not administer Menactra until age 2 years and at least 4 weeks after the completion of all PCV13 doses. ɱ Children with persistent complement component deficiency ʲ Children 9 through 23 months. Administer 2 primary doses at least 12 weeks apart. ʲ Children 24 months and older who have not received a complete series. Administer 2 primary doses at least 8 weeks apart. ɱ All high-risk children ʲ If Menactra is to be administered to a child at high risk for meningococcal disease, it is recommended that Menactra be given either before or at the same time as DTaP. ▪ Bexsero or Trumenba ɱ Persons 10 years or older who have not received a complete series. Administer a 2-dose series of Bexsero, with doses at least 1 month apart, or a 3-dose series of Trumenba, with the second dose at least 1-2 months after the first and the third dose at least 6 months after the first. The two MenB vaccines are not interchangeable; the same vaccine product must be used for all doses. For children who travel to or reside in countries in which meningococcal disease is hyperendemic or epidemic, including countries in the African meningitis belt or the Hajj:\n▪ Administer an age-appropriate formulation and series of Menactra or Menveo for protection against serogroups A and W meningococcal disease. Prior receipt of MenHibrix is not sufficient for children traveling to the meningitis belt or the Hajj because it does not contain serogroups A or W. For children at risk during an outbreak attributable to a vaccine serogroup: ▪ For serogroup A, C, W, or Y: Administer or complete an age-and formulation-appropriate series of MenHibrix, Menactra, or Menveo.\n# \n▪ For serogroup B: Administer a 2-dose series of Bexsero, with doses at least 1 month apart, or a 3-dose series of Trumenba, with the second dose at least 1-2 months after the first and the third dose at least 6 months after the first. The two MenB vaccines are not interchangeable; the same vaccine product must be used for all doses. For MenACWY booster doses among persons with high-risk conditions, refer to MMWR 2013;62(RR02):1-22, at www.cdc.gov/mmwr/preview/mmwrhtml/rr6202a1.htm, MMWR June 20, 2014 / 63( 24 • Administer a 2-dose series of HPV vaccine on a schedule of 0, 6-12 months to all adolescents aged 11 or 12 years. The vaccination series can start at age 9 years. • Administer HPV vaccine to all adolescents through age 18 years who were not previously adequately vaccinated. The number of recommended doses is based on age at administration of the first dose. • For persons initiating vaccination before age 15, the recommended immunization schedule is 2 doses of HPV vaccine at 0, 6-12 months. • For persons initiating vaccination at age 15 years or older, the recommended immunization schedule is 3 doses of HPV vaccine at 0, 1-2, 6 months. • A vaccine dose administered at a shorter interval should be readministered at the recommended interval. ▪ In a 2-dose schedule of HPV vaccine, the minimum interval is 5 months between the first and second dose.\nIf the second dose is administered at a shorter interval, a third dose should be administered a minimum of 12 weeks after the second dose and a minimum of 5 months after the first dose. ▪ In a 3-dose schedule of HPV vaccine, the minimum intervals are 4 weeks between the first and second dose, 12 weeks between the second and third dose, and 5 months between the first and third dose. If a vaccine dose is administered at a shorter interval, it should be readministered after another minimum interval has been met since the most recent dose.\n# Special populations:\n• For children with history of sexual abuse or assault, administer HPV vaccine beginning at age 9 years. • Immunocompromised persons*, including those with human immunodeficiency virus (HIV) infection, should receive a 3-dose series at 0, 1-2, and 6 months, regardless of age at vaccine initiation. • Note: HPV vaccination is not recommended during pregnancy, although there is no evidence that the vaccine poses harm. If a woman is found to be pregnant after initiating the vaccination series, no intervention is needed; the remaining vaccine doses should be delayed until after the pregnancy. "},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":662,"cells":{"id":{"kind":"string","value":"79d22442c180f2a08eb777d92530249cfd6c0c6a"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"African Tick Bite Fever"},"clean_text":{"kind":"string","value":"African Tick Bite Fever | Disease Directory | Travelers' Health | CDC\n\n### African Tick Bite Fever\n### What is African tick bite fever?\nAfrican tick bite fever is a disease caused by a bacteria. You can get infected if you are bitten by an infected tick.\nSymptoms usually appear within two weeks after a tick bite. The first sign is often a red sore that develops a dark crust, called an eschar. Eschars are found at the site of tick bite; multiple eschars may be present if you have multiple tick bites. Later symptoms may include fever, headache, muscle soreness, swollen lymph nodes, and a rash. \nAfrican tick bite fever is the most common disease travelers report getting from tick bites.\n### Who is at risk?\nTravelers to sub-Saharan Africa, parts of the Caribbean, and Oceania (Australia, New Zealand, Melanesia, Micronesia, and Polynesia are at risk for African tick bite fever. You are at higher risk if your travel plans include outdoor activities such as camping, hiking, and game hunting in wooded, brushy, or grassy areas.\nTicks that are infected with bacteria that cause African tick bite fever are usually most active from November through April.\n### What can travelers do to prevent African tick bite fever?\nThere are no vaccines that prevent African tick bite fever. Travelers can protect themselves from infection by taking the following precautions:\nPrevent Tick Bites\n- Know where to expect ticks. Ticks live in grassy, brushy, or wooded areas, or even on animals. Spending time outside camping, gardening, or hunting could bring you in close contact with ticks. Many people get ticks in their own yard or neighborhood.\n- Treat clothing and gear with products containing 0.5% permethrin. Permethrin can be used to treat boots, clothing and camping gear and remain protective through several washings. Alternatively, you can buy permethrin-treated clothing and gear.\n- Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) containing DEET, picaridin, IR3535, Oil of Lemon Eucalyptus (OLE), para-menthane-diol (PMD), or 2-undecanone. EPA’s helpful [search tool](https://www.epa.gov/insect-repellents/find-insect-repellent-right-you) can help you find the product that best suits your needs. Always follow product instructions. Do not use products containing OLE or PMD on children under 3 years old.\n- Avoid Contact with Ticks\n\t- Avoid wooded and brushy areas with high grass and leaf litter.\n\t- Walk in the center of trails.\nFind and Remove Ticks\n- Check your clothing for ticks. Ticks may be carried into the house on clothing. Any ticks that are found should be removed. When possible, tumble dry clothes in a dryer on high heat for 10 minutes to kill ticks on dry clothing after you come indoors. If the clothes are damp, additional time may be needed. If the clothes require washing first, hot water is recommended. Cold and medium temperature water will not kill ticks.\n- Examine gear and pets. Ticks can ride on clothing and pets, then attach to a person later, so carefully examine pets, coats, and daypacks.\n- Shower soon after being outdoors. Showering within two hours of coming indoors has been shown to reduce your risk of getting tick-borne diseases. Showering may help wash off unattached ticks and it is a good opportunity to do a tick check.\n- Check your body for ticks. Conduct a full body check upon return from potentially tick-infested areas. Use a hand-held or full-length mirror to view all parts of your body. Check these parts of your body for ticks:\n\t- Under the arms\n\t- In and around the ears\n\t- Inside belly button\n\t- Back of the knees\n\t- In and around the hair\n\t- Between the legs\n\t- Around the waist\n- If you find a tick attached to your skin, simply remove the tick as soon as possible.\n"},"raw_text":{"kind":"string","value":"\n\n### African Tick Bite Fever\n\n\n\n\n### What is African tick bite fever?\n\nAfrican tick bite fever is a disease caused by a bacteria. You can get infected if you are bitten by an infected tick.\n\nSymptoms usually appear within two weeks after a tick bite. The first sign is often a red sore that develops a dark crust, called an eschar. Eschars are found at the site of tick bite; multiple eschars may be present if you have multiple tick bites. Later symptoms may include fever, headache, muscle soreness, swollen lymph nodes, and a rash. \n\nAfrican tick bite fever is the most common disease travelers report getting from tick bites.\n\n### Who is at risk?\n\nTravelers to sub-Saharan Africa, parts of the Caribbean, and Oceania (Australia, New Zealand, Melanesia, Micronesia, and Polynesia are at risk for African tick bite fever. You are at higher risk if your travel plans include outdoor activities such as camping, hiking, and game hunting in wooded, brushy, or grassy areas.\n\nTicks that are infected with bacteria that cause African tick bite fever are usually most active from November through April.\n\n### What can travelers do to prevent African tick bite fever?\n\nThere are no vaccines that prevent African tick bite fever. Travelers can protect themselves from infection by taking the following precautions:\n\n**Prevent Tick Bites**\n\n* **Know where to expect ticks.** Ticks live in grassy, brushy, or wooded areas, or even on animals. Spending time outside camping, gardening, or hunting could bring you in close contact with ticks. Many people get ticks in their own yard or neighborhood.\n* **Treat clothing and gear** with products containing 0.5% permethrin. Permethrin can be used to treat boots, clothing and camping gear and remain protective through several washings. Alternatively, you can buy permethrin-treated clothing and gear.\n* **Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents)** containing DEET, picaridin, IR3535, Oil of Lemon Eucalyptus (OLE), para-menthane-diol (PMD), or 2-undecanone. EPA’s helpful [search tool](https://www.epa.gov/insect-repellents/find-insect-repellent-right-you) can help you find the product that best suits your needs. Always follow product instructions. Do not use products containing OLE or PMD on children under 3 years old.\n* **Avoid Contact with Ticks**\n\t+ Avoid wooded and brushy areas with high grass and leaf litter.\n\t+ Walk in the center of trails.\n\n\n**Find and Remove Ticks**\n\n* **Check your clothing for ticks.** Ticks may be carried into the house on clothing. Any ticks that are found should be removed. When possible, tumble dry clothes in a dryer on high heat for 10 minutes to kill ticks on dry clothing after you come indoors. If the clothes are damp, additional time may be needed. If the clothes require washing first, hot water is recommended. Cold and medium temperature water will not kill ticks.\n* **Examine gear and pets.** Ticks can ride on clothing and pets, then attach to a person later, so carefully examine pets, coats, and daypacks.\n* **Shower soon after being outdoors.** Showering within two hours of coming indoors has been shown to reduce your risk of getting tick-borne diseases. Showering may help wash off unattached ticks and it is a good opportunity to do a tick check.\n* **Check your body for ticks.** Conduct a full body check upon return from potentially tick-infested areas. Use a hand-held or full-length mirror to view all parts of your body. Check these parts of your body for ticks:\n\t+ Under the arms\n\t+ In and around the ears\n\t+ Inside belly button\n\t+ Back of the knees\n\t+ In and around the hair\n\t+ Between the legs\n\t+ Around the waist\n* If you find a tick attached to your skin, simply remove the tick as soon as possible.\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### More Information\n\n* [Avoid Bug Bites](/travel/page/avoid-bug-bites)\n* [Preventing Tick Bites](https://www.cdc.gov/ticks/avoid/on_people.html)\n* [Other Tick-borne Spotted Fever Rickettsial Infections](http://www.cdc.gov/otherspottedfever/)\n* CDC Yellow Book: [Rickettsial Diseases](/travel/yellowbook/2012/chapter-3-infectious-diseases-related-to-travel/rickettsial-spotted-and-typhus-fevers-and-related-infections-anaplasmosis-and-ehrlichiosis.htm)\n\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":663,"cells":{"id":{"kind":"string","value":"0c5338103fa83aa1c9eb3b9530149c3fd784db5d"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"African Trypanosomiasis (African Sleeping Sickness)"},"clean_text":{"kind":"string","value":"African Trypanosomiasis (African Sleeping Sickness) | Disease Directory | Travelers' Health | CDC\n\n### African Trypanosomiasis (African Sleeping Sickness)\n### What is African trypanosomiasis?\nAfrican trypanosomiasis, also called sleeping sickness, is a disease caused by a parasite. People can get this parasite when an infected Tsetse fly bites them.\nSymptoms include fatigue, high fever, headaches, and muscle aches. If the disease is not treated, it can cause death.\n### Who is at risk?\nTsetse flies are found in sub-Saharan Africa. Travelers spending a lot of time outdoors or visiting game parks in these areas can be bitten by tsetse flies and get infected.\n### What can travelers do to prevent African trypanosomiasis?\nInformation by Destination\n\nWhere are you going?\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" - value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n window.location = url;\nThere is no vaccine or medicine that prevents African trypanosomiasis. Travelers can protect themselves by preventing tsetse fly bites.\nPrevent tsetse fly bites by taking the following steps:\n- Cover exposed skin by wearing long-sleeved shirts, long pants, and hats.\n\t- Clothing fabric should be at least medium weight because the tsetse fly can bite through thin fabric.\n\t- Wear neutral-colored clothing. The tsetse fly is attracted to bright colors, very dark colors, metallic fabric, particularly the colors blue and black.\n- Avoid bushes during the day; the fly rests in bushes and will bite if disturbed.\n- Inspect vehicles for tsetse flies before entering. The flies are attracted to the motion and dust from moving vehicles.\n- Although, there is limited evidence that insect repellent works against tsetse flies, you should still use insect repellent as it can prevent other diseases spread by bug bites. [Learn more about how to avoid other bug bites.](/travel/page/avoid-bug-bites)\n"},"raw_text":{"kind":"string","value":"\n\n### African Trypanosomiasis (African Sleeping Sickness)\n\n\n\n\n### What is African trypanosomiasis?\n\n\nAfrican trypanosomiasis, also called sleeping sickness, is a disease caused by a parasite. People can get this parasite when an infected Tsetse fly bites them.\n\nSymptoms include fatigue, high fever, headaches, and muscle aches. If the disease is not treated, it can cause death.\n\n### Who is at risk?\n\nTsetse flies are found in sub-Saharan Africa. Travelers spending a lot of time outdoors or visiting game parks in these areas can be bitten by tsetse flies and get infected.\n\n### What can travelers do to prevent African trypanosomiasis?\n\n\nInformation by Destination\n\nWhere are you going?\n\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n function goSelectPage(){ \n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" + value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n }else{\n window.location = url;\n }\n }\n\n \n \n\nThere is no vaccine or medicine that prevents African trypanosomiasis. Travelers can protect themselves by preventing tsetse fly bites.\n\n**Prevent tsetse fly bites by taking the following steps****:**\n\n* Cover exposed skin by wearing long-sleeved shirts, long pants, and hats.\n\t+ Clothing fabric should be at least medium weight because the tsetse fly can bite through thin fabric.\n\t+ Wear neutral-colored clothing. The tsetse fly is attracted to bright colors, very dark colors, metallic fabric, particularly the colors blue and black.\n* Avoid bushes during the day; the fly rests in bushes and will bite if disturbed.\n* Inspect vehicles for tsetse flies before entering. The flies are attracted to the motion and dust from moving vehicles.\n* Although, there is limited evidence that insect repellent works against tsetse flies, you should still use insect repellent as it can prevent other diseases spread by bug bites. [Learn more about how to avoid other bug bites.](/travel/page/avoid-bug-bites)\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### More Information\n\n* [African Trypanosomiasis](http://www.cdc.gov/parasites/sleepingsickness/)\n* [Avoid Bug Bites](/travel/page/avoid-bug-bites)\n* CDC Yellow Book: [Trypanosomiasis-African](/travel/yellowbook/2020/travel-related-infectious-diseases/trypanosomiasis-african-sleeping-sickness) in CDC Yellow Book\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":664,"cells":{"id":{"kind":"string","value":"4027ce748d26a248496ee0d429829b89222df893"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Avian Flu (Bird Flu)"},"clean_text":{"kind":"string","value":"Avian Flu (Bird Flu) | Disease Directory | Travelers' Health | CDC\n\n### Avian Flu (Bird Flu)\n### What is avian flu (bird flu)?\nAvian influenza, also called bird flu, is caused by a virus that usually infects wild and domestic birds. Wild birds that carry bird flu viruses include migratory waterbirds, like ducks, geese and swans, and shorebirds, like storks. Bird flu viruses can easily spread from wild birds to domestic poultry, like chickens, turkeys, geese, and pheasants. The virus is found in an infected bird’s feces (poop) and fluids from the bird’s eyes, nose, or mouth.\nBird flu viruses don’t usually infect people. However, this can happen if you:\n- Touch your eyes, nose, or mouth after handling infected live or dead birds.\n- Touch surfaces or handle items contaminated by bird flu viruses and touch your eyes, nose, or mouth.\n- Breathe in droplets or dust contaminated with the virus.\nPeople who get sick with bird flu can have no symptoms to severe illness. Some people have mild symptoms, including eye redness (conjunctivitis), cough, sore throat, runny or stuffy nose, muscle or body aches, headaches, and tiredness. More serious symptoms include high fever, shortness of breath, and difficulty breathing. People with severe disease can develop pneumonia that may require hospitalization. Less common signs and symptoms include diarrhea, nausea, vomiting, or seizures.\nInformation by Destination\n\nWhere are you going?\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" - value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n window.location = url;\n### Can travelers get bird flu?\nMost travelers are unlikely to get bird flu. However, travelers who work with animals, such as veterinarians, farmers, animal industry experts, and wildlife professionals, or people who visit poultry farms or live-animal markets may be at higher risk.\n### What can travelers do to prevent bird flu?\nDo not touch birds and avoid visiting places where birds live\n- Avoid visiting poultry farms, live animal markets, and other places where live poultry are raised, kept, slaughtered, or sold. If you must visit such places, wear a well-fitting facemask and avoid touching poultry or other birds.\n- If you visit wetlands or other outdoor places where birds live, make sure you take steps to [avoid germs](#germs) during and after your visit.\n- Avoid touching sick or dead wild birds or poultry.\n- Wash your hands often with soap and water for at least 20 seconds, especially after having contact with or being around birds or places where birds are kept or touching uncooked poultry.\n- If soap and water aren’t available, clean hands with hand sanitizer containing at least 60% alcohol.\n- Avoid touching your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean.\n- Avoid close contact, such as kissing, hugging, or sharing eating utensils or cups with people who are sick.\n"},"raw_text":{"kind":"string","value":"\n\n### Avian Flu (Bird Flu)\n\n\n\n\n### What is avian flu (bird flu)?\n\nAvian influenza, also called bird flu, is caused by a virus that usually infects wild and domestic birds. Wild birds that carry bird flu viruses include migratory waterbirds, like ducks, geese and swans, and shorebirds, like storks. Bird flu viruses can easily spread from wild birds to domestic poultry, like chickens, turkeys, geese, and pheasants. The virus is found in an infected bird’s feces (poop) and fluids from the bird’s eyes, nose, or mouth.\n\n\nBird flu viruses don’t usually infect people. However, this can happen if you:\n\n* Touch your eyes, nose, or mouth after handling infected live or dead birds.\n* Touch surfaces or handle items contaminated by bird flu viruses and touch your eyes, nose, or mouth.\n* Breathe in droplets or dust contaminated with the virus.\n\nPeople who get sick with bird flu can have no symptoms to severe illness. Some people have mild symptoms, including eye redness (conjunctivitis), cough, sore throat, runny or stuffy nose, muscle or body aches, headaches, and tiredness. More serious symptoms include high fever, shortness of breath, and difficulty breathing. People with severe disease can develop pneumonia that may require hospitalization. Less common signs and symptoms include diarrhea, nausea, vomiting, or seizures.\n\n\nInformation by Destination\n\nWhere are you going?\n\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n function goSelectPage(){ \n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" + value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n }else{\n window.location = url;\n }\n }\n\n \n \n\n### Can travelers get bird flu?\n\nMost travelers are unlikely to get bird flu. However, travelers who work with animals, such as veterinarians, farmers, animal industry experts, and wildlife professionals, or people who visit poultry farms or live-animal markets may be at higher risk.\n\n### What can travelers do to prevent bird flu?\n\n**Do not touch birds and avoid visiting places where birds live**\n\n* Avoid visiting poultry farms, live animal markets, and other places where live poultry are raised, kept, slaughtered, or sold. If you must visit such places, wear a well-fitting facemask and avoid touching poultry or other birds.\n* If you visit wetlands or other outdoor places where birds live, make sure you take steps to [avoid germs](#germs) during and after your visit.\n* Avoid touching sick or dead wild birds or poultry.\n\n**Avoid Germs**\n\n* Wash your hands often with soap and water for at least 20 seconds, especially after having contact with or being around birds or places where birds are kept or touching uncooked poultry.\n* If soap and water aren’t available, clean hands with hand sanitizer containing at least 60% alcohol.\n* Avoid touching your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean.\n* Avoid close contact, such as kissing, hugging, or sharing eating utensils or cups with people who are sick.\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. Avoid contact with other people while you are sick.\n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### More Information\n\n* [Avian Influenza](https://www.cdc.gov/flu/avianflu/index.htm)\n* [Bird Flu Virus Infections in Humans](https://wwwdev.cdc.gov/flu/avianflu/avian-in-humans.htm#symptoms)\n* CDC Yellow Book: [Influenzas (including Avian)](/travel/yellowbook/2020/travel-related-infectious-diseases/influenza)\n\n \n\n \n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":665,"cells":{"id":{"kind":"string","value":"9669850841423f59ed63ccbc6a1cef67c3cb1e40"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"COVID-19"},"clean_text":{"kind":"string","value":"COVID-19 | Disease Directory | Travelers' Health | CDC\n\nAs of 12:01 am EDT May 12, 2023, noncitizen nonimmigrant air passengers no longer need to show proof of being fully vaccinated with an accepted COVID-19 vaccine to board a flight to the United States. [See more information](https://www.cdc.gov/quarantine/order-safe-travel.html).\n### What is COVID-19?\nCoronavirus disease 2019 (COVID-19) is a respiratory illness caused by the virus SARS-CoV-2. The virus spreads mainly from person to person through respiratory droplets and small particles produced when an infected person coughs, sneezes, or talks. The virus spreads easily in crowded or poorly ventilated indoor settings.\nPeople with COVID-19 have reported a [wide range of symptoms](https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html) – ranging from no or mild symptoms to severe illness. Symptoms may appear 2–14 days after exposure to the virus. Possible symptoms include fever, chills, cough, shortness of breath, fatigue, muscle aches, headache, new loss of taste and smell, sore throat, runny nose, nausea, vomiting, or diarrhea.\n### Who can get COVID-19?\nAnyone can get COVID-19. However, some people are more likely than others to get very sick if they get COVID-19. These include people who are older, are [immunocompromised](https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-who-are-immunocompromised.html), or have certain [disabilities](https://www.cdc.gov/ncbddd/humandevelopment/covid-19/people-with-disabilities.html), or have [underlying health conditions](https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html). Vaccination, past infection, and timely access to testing and treatment can help protect you from getting very sick from COVID-19.\n### Can I travel if I recently had COVID-19?\nYes, you can travel once you have ended [isolation](https://www.cdc.gov/coronavirus/2019-ncov/your-health/isolation.html). Check [CDC guidance](https://www.cdc.gov/coronavirus/2019-ncov/your-health/isolation.html#removing-mask) for additional precautions, including testing and wearing a mask around others. If you recently had COVID-19 and are recommended to wear a mask, do not travel on public transportation such as airplanes, buses, and trains if you are unable to wear a mask whenever around others.\n### What can travelers do to prevent COVID-19?\nGet [up to date](https://www.cdc.gov/coronavirus/2019-ncov/vaccines/stay-up-to-date.html) with your COVID-19 vaccines before you travel and take steps to [protect yourself and others](https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html). Consider [wearing a mask](/travel/page/masks) in crowded or poorly ventilated indoor areas, including on public transportation and in transportation hubs. Take [additional precautions](https://www.cdc.gov/coronavirus/2019-ncov/your-health/if-you-were-exposed.html) if you were recently exposed to a person with COVID-19. Don’t travel while sick.\nIf you have a [weakened immune system](https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-who-are-immunocompromised.html) or [are at increased risk for severe disease](https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html) talk to a healthcare professional before you decide to travel. If you travel, take multiple prevention steps to provide additional layers of protection from COVID-19, even if you are up to date with your COVID-19 vaccines. These include improving ventilation and spending more time outdoors, avoiding sick people, [getting tested for COVID-19](https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/testing.html) if you develop symptoms, staying home if you have or think you have COVID-19, and seeking treatment if you have COVID-19.\nConsider getting a COVID-19 test if you:\n- Develop COVID-19 symptoms before, during, or after travel.\n- Will be traveling to visit someone who is at higher risk of getting very sick from COVID-19.\n- Were in a situation with a greater risk of exposure during travel (e.g., in an indoor, crowded space like an airport terminal while not wearing a mask).\nIf you traveled and feel sick, particularly if you have a fever, talk to a healthcare professional, and tell them about your recent travel.\n"},"raw_text":{"kind":"string","value":"\n\n### COVID-19\n\n\n\n\n\nAs of 12:01 am EDT May 12, 2023, noncitizen nonimmigrant air passengers no longer need to show proof of being fully vaccinated with an accepted COVID-19 vaccine to board a flight to the United States. [See more information](https://www.cdc.gov/quarantine/order-safe-travel.html).\n\n### What is COVID-19?\n\nCoronavirus disease 2019 (COVID-19) is a respiratory illness caused by the virus SARS-CoV-2. The virus spreads mainly from person to person through respiratory droplets and small particles produced when an infected person coughs, sneezes, or talks. The virus spreads easily in crowded or poorly ventilated indoor settings.\n\nPeople with COVID-19 have reported a [wide range of symptoms](https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html) – ranging from no or mild symptoms to severe illness. Symptoms may appear 2–14 days after exposure to the virus. Possible symptoms include fever, chills, cough, shortness of breath, fatigue, muscle aches, headache, new loss of taste and smell, sore throat, runny nose, nausea, vomiting, or diarrhea.\n\n### Who can get COVID-19?\n\nAnyone can get COVID-19. However, some people are more likely than others to get very sick if they get COVID-19. These include people who are older, are [immunocompromised](https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-who-are-immunocompromised.html), or have certain [disabilities](https://www.cdc.gov/ncbddd/humandevelopment/covid-19/people-with-disabilities.html), or have [underlying health conditions](https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html). Vaccination, past infection, and timely access to testing and treatment can help protect you from getting very sick from COVID-19.\n\n### Can I travel if I recently had COVID-19?\n\nYes, you can travel once you have ended [isolation](https://www.cdc.gov/coronavirus/2019-ncov/your-health/isolation.html). Check [CDC guidance](https://www.cdc.gov/coronavirus/2019-ncov/your-health/isolation.html#removing-mask) for additional precautions, including testing and wearing a mask around others. If you recently had COVID-19 and are recommended to wear a mask, do not travel on public transportation such as airplanes, buses, and trains if you are unable to wear a mask whenever around others.\n\n### What can travelers do to prevent COVID-19?\n\nGet [**up to date**](https://www.cdc.gov/coronavirus/2019-ncov/vaccines/stay-up-to-date.html) with your COVID-19 vaccines before you travel and take steps to [protect yourself and others](https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html). Consider [wearing a mask](/travel/page/masks) in crowded or poorly ventilated indoor areas, including on public transportation and in transportation hubs. Take [additional precautions](https://www.cdc.gov/coronavirus/2019-ncov/your-health/if-you-were-exposed.html) if you were recently exposed to a person with COVID-19. Don’t travel while sick.\n\nIf you have a [weakened immune system](https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-who-are-immunocompromised.html) or [are at increased risk for severe disease](https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html) talk to a healthcare professional before you decide to travel. If you travel, take multiple prevention steps to provide additional layers of protection from COVID-19, even if you are up to date with your COVID-19 vaccines. These include improving ventilation and spending more time outdoors, avoiding sick people, [getting tested for COVID-19](https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/testing.html) if you develop symptoms, staying home if you have or think you have COVID-19, and seeking treatment if you have COVID-19.\n\n\n**Consider getting [travel insurance](/travel/page/insurance)** in case you need [medical care abroad](/travel/page/health-care-during-travel).\n\n\n**Consider getting a COVID-19 test if you:**\n\n* Develop COVID-19 symptoms before, during, or after travel.\n* Will be traveling to visit someone who is at higher risk of getting very sick from COVID-19.\n* Were in a situation with a greater risk of exposure during travel (e.g., in an indoor, crowded space like an airport terminal while not wearing a mask).\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare professional, and tell them about your recent travel.\n\n### More Information\n\n* [COVID-19](https://www.cdc.gov/coronavirus/2019-ncov/index.html)\n* [Masking During Travel](/travel/page/masks)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":666,"cells":{"id":{"kind":"string","value":"0ad0c9f56d5636aae816878b659ebb4b49d3f6f9"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Chagas Disease (American Trypanosomiasis)"},"clean_text":{"kind":"string","value":"Chagas Disease (American Trypanosomiasis) | Disease Directory | Travelers' Health | CDC\n\n### Chagas Disease (American Trypanosomiasis)\n### What is Chagas Disease (American Trypanosomiasis)?\nAmerican trypanosomiasis, also known as Chagas disease, is caused by a parasite. This parasite lives in the poop of [triatomine (kissing) bugs](https://www.cdc.gov/parasites/chagas/gen_info/vectors/index.html). The bug often poops when it bites. Most people get Chagas disease by unknowingly rubbing triatomine bug poop into the bug bite when they scratch the bite. People may also accidentally get triatomine bug poop in their eyes and mouth.\nA few people experience swelling around the bite area. However, most people never have symptoms, but remain infected throughout their lives. \nAbout 1 out of 3 people who get Chagas disease will develop more serious symptoms later in life, including heart conditions or gastrointestinal problems. These later symptoms can occur whether a person has early symptoms or not.\n### Who is at risk?\nInformation by Destination\n\nWhere are you going?\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" - value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n window.location = url;\nChagas disease is spread by triatomine bugs in parts of Mexico, Central America, and South America, especially rural areas.\nMost travelers to these areas don’t need to worry about Chagas disease. Travelers who sleep outdoors or stay in poorly constructed housing are more likely to get bitten by triatomine bugs.\n### What can travelers do to prevent Chagas disease?\nThere is no vaccine or medicine to prevent Chagas disease. Travelers can protect themselves by taking a few steps.\nAvoid Bug Bites\n- Stay and sleep in screened or air-conditioned rooms.\n\t- Avoid sleeping in thatch, mud, and adobe housing in areas with triatomine bugs; use insecticides in and around such homes. Insecticide-treated bed nets are helpful\n- Cover exposed skin by wearing long-sleeved shirts, long pants, and hats.\n- Use EPA-registered insect repellents with one of the following active ingredients: DEET, picaridin, IR3535, oil of lemon eucalyptus (OLE), para-menthane-diol (PMD), or 2-undecanone. [Find an EPA-registered insect repellent that’s right for you.](https://www.epa.gov/insect-repellents/find-repellent-right-you)\n\t- Always follow product directions and reapply as directed.\n\t- If you are also using sunscreen, apply sunscreen first and insect repellent second.\n- When using insect repellent on children\n\t- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.\n\t- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.\n\t- Adults: Spray insect repellent onto your hands and then apply to a child’s face.\n- Use [permethrin-treated](http://npic.orst.edu/pest/mosquito/ptc.html) clothing and gear (such as boots, pants, socks, and tents). You can buy pre-treated clothing and gear or treat them yourself:\n\t- Treated clothing remains protective after multiple washings. See the product information to find out how long the protection will last.\n\t- If treating items yourself, follow the product instructions carefully.\n\t- Do not use permethrin directly on skin.\n"},"raw_text":{"kind":"string","value":"\n\n### Chagas Disease (American Trypanosomiasis)\n\n\n\n\n### What is Chagas Disease (American Trypanosomiasis)?\n\n\nAmerican trypanosomiasis, also known as Chagas disease, is caused by a parasite. This parasite lives in the poop of [triatomine (kissing) bugs](https://www.cdc.gov/parasites/chagas/gen_info/vectors/index.html). The bug often poops when it bites. Most people get Chagas disease by unknowingly rubbing triatomine bug poop into the bug bite when they scratch the bite. People may also accidentally get triatomine bug poop in their eyes and mouth.\n\nA few people experience swelling around the bite area. However, most people never have symptoms, but remain infected throughout their lives. \n\nAbout 1 out of 3 people who get Chagas disease will develop more serious symptoms later in life, including heart conditions or gastrointestinal problems. These later symptoms can occur whether a person has early symptoms or not.\n\n### Who is at risk?\n\n\nInformation by Destination\n\nWhere are you going?\n\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n function goSelectPage(){ \n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" + value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n }else{\n window.location = url;\n }\n }\n\n \n \n\nChagas disease is spread by triatomine bugs in parts of Mexico, Central America, and South America, especially rural areas.\n\nMost travelers to these areas don’t need to worry about Chagas disease. Travelers who sleep outdoors or stay in poorly constructed housing are more likely to get bitten by triatomine bugs.\n\n### What can travelers do to prevent Chagas disease?\n\nThere is no vaccine or medicine to prevent Chagas disease. Travelers can protect themselves by taking a few steps.\n\n**Avoid Bug Bites**\n\n* Stay and sleep in screened or air-conditioned rooms.\n\t+ Avoid sleeping in thatch, mud, and adobe housing in areas with triatomine bugs; use insecticides in and around such homes. Insecticide-treated bed nets are helpful\n* Cover exposed skin by wearing long-sleeved shirts, long pants, and hats.\n* Use EPA-registered insect repellents with one of the following active ingredients: DEET, picaridin, IR3535, oil of lemon eucalyptus (OLE), para-menthane-diol (PMD), or 2-undecanone. [Find an EPA-registered insect repellent that’s right for you.](https://www.epa.gov/insect-repellents/find-repellent-right-you)\n\t+ Always follow product directions and reapply as directed.\n\t+ If you are also using sunscreen, apply sunscreen first and insect repellent second.\n* When using insect repellent on children\n\t+ Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.\n\t+ Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.\n\t+ Adults: Spray insect repellent onto your hands and then apply to a child’s face.\n* Use [permethrin-treated](http://npic.orst.edu/pest/mosquito/ptc.html) clothing and gear (such as boots, pants, socks, and tents). You can buy pre-treated clothing and gear or treat them yourself:\n\t+ Treated clothing remains protective after multiple washings. See the product information to find out how long the protection will last.\n\t+ If treating items yourself, follow the product instructions carefully.\n\t+ Do **not** use permethrin directly on skin.\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### More Information\n\n* [Chagas disease FAQs](http://www.cdc.gov/parasites/chagas/gen_info/detailed.html)\n* [Avoid Bug Bites](/travel/page/avoid-bug-bites)\n* CDC Yellow Book: [Trypanosomiasis-American](/travel/yellowbook/2020/travel-related-infectious-diseases/trypanosomiasis-american-chagas-disease)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":667,"cells":{"id":{"kind":"string","value":"5988115fc031f78f112c25d8b06db12bf01075ba"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Chikungunya"},"clean_text":{"kind":"string","value":"Chikungunya | Disease Directory | Travelers' Health | CDC\n\n### What is chikungunya?\n\nChikungunya virus is spread to people by the bite of an infected mosquito. Mosquitoes become infected when they feed on a person already infected with the virus. Infected mosquitoes can then spread the virus to other people through bites.\nSymptoms usually begin 3–7 days after being bitten by an infected mosquito. The most common [symptoms](http://www.cdc.gov/chikungunya/symptoms/index.html) of chikungunya are fever and joint pain. Other symptoms include headache, muscle pain, joint swelling, or rash. Most people feel better within a week. In some people the joint pain may persist for months.\n### Who is at risk?\nThe mosquitoes that spread chikungunya virus are found in many countries throughout the world. Travelers going to countries in Africa, Asia, the Americas, and islands in the Indian and Pacific Oceans might be at risk for infection.\nMosquitoes that spread chikungunya bite during the day and at night.\n### What can travelers do to prevent chikungunya?\nThere are no vaccines or medicines that prevent chikungunya. Travelers can protect themselves against infection by taking the following steps.\nUse an EPA-registered insect repellent\n- Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.\n\t- Picaridin (known as KBR 3023 and icaridin outside the US)\n\t- Oil of lemon eucalyptus (OLE)\n\t- Para-menthane-diol (PMD)\nFind the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).\n\n- Insect Repellent Tips for Babies and Children\n\t- Dress your child in clothing that covers arms and legs.\n\t- Cover strollers and baby carriers with mosquito netting.\n\t- When using insect repellent on your child:\n\t\t- Always follow label instructions.\n\t\t- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.\n\t\t- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.\n\t\t\t- Adults: Spray insect repellent onto your hands and then apply to a child’s face.\n\t\t- If also using sunscreen, always apply insect repellent after sunscreen.\nWear long-sleeved shirts and long pants\nTreat clothing and gear with permethrin\n- Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.\n\t- Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.\n\t- Permethrin-treated clothing provides protection after multiple washings.\n\t- Read product information to find out how long the protection will last.\n- If treating items yourself, follow the product instructions.\n- Do not use permethrin products directly on skin.\n- Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).\nKeep mosquitoes out of your hotel room or lodging\n- Choose a hotel or lodging with air conditioning or window and door screens.\n- Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.\nSleep under a mosquito net\n\n- Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.\n- Buy a mosquito net at your local outdoor store or online before traveling overseas.\n- Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.\n- [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.\n\t- Permethrin is an insecticide that kills mosquitoes and other insects.\n\t- To determine if you can wash a treated mosquito net, follow the label instructions.\nIf you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).\nIf you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment.](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html)\n"},"raw_text":{"kind":"string","value":"\n\n### Chikungunya\n\n\n\n\n### What is chikungunya?\n\n\nChikungunya virus is spread to people by the bite of an infected mosquito. Mosquitoes become infected when they feed on a person already infected with the virus. Infected mosquitoes can then spread the virus to other people through bites.\n\nSymptoms usually begin 3–7 days after being bitten by an infected mosquito. The most common [symptoms](http://www.cdc.gov/chikungunya/symptoms/index.html) of chikungunya are fever and joint pain. Other symptoms include headache, muscle pain, joint swelling, or rash. Most people feel better within a week. In some people the joint pain may persist for months.\n\n### Who is at risk?\n\nThe mosquitoes that spread chikungunya virus are found in many countries throughout the world. Travelers going to countries in Africa, Asia, the Americas, and islands in the Indian and Pacific Oceans might be at risk for infection.\n\nMosquitoes that spread chikungunya bite during the day and at night.\n\n### What can travelers do to prevent chikungunya?\n\nThere are no vaccines or medicines that prevent chikungunya. Travelers can protect themselves against infection by taking the following steps.\n\n**Use an EPA-registered insect repellent**\n\n\n\n* Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.\n\t+ DEET\n\t+ Picaridin (known as KBR 3023 and icaridin outside the US)\n\t+ IR3535\n\t+ Oil of lemon eucalyptus (OLE)\n\t+ Para-menthane-diol (PMD)\n\t+ 2-undecanone\n\nFind the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).\n\n\n\n* Insect Repellent Tips for Babies and Children\n\t+ Dress your child in clothing that covers arms and legs.\n\t+ Cover strollers and baby carriers with mosquito netting.\n\t+ When using insect repellent on your child:\n\t\t- Always follow label instructions.\n\t\t- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.\n\t\t- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.\n\t\t\t* Adults: Spray insect repellent onto your hands and then apply to a child’s face.\n\t\t- If also using sunscreen, always apply insect repellent after sunscreen.\n\n**Wear long-sleeved shirts and long pants**\n\n**Treat clothing and gear with permethrin**\n\n\n\n* Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.\n\t+ Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.\n\t+ Permethrin-treated clothing provides protection after multiple washings.\n\t+ Read product information to find out how long the protection will last.\n* If treating items yourself, follow the product instructions.\n* Do not use permethrin products directly on skin.\n* Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).\n\n**Keep mosquitoes out of your hotel room or lodging**\n\n* Choose a hotel or lodging with air conditioning or window and door screens.\n* Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.\n\n**Sleep under a mosquito net**\n\n\n\n* Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.\n* Buy a mosquito net at your local outdoor store or online before traveling overseas.\n* Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.\n* [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.\n\t+ Permethrin is an insecticide that kills mosquitoes and other insects.\n\t+ To determine if you can wash a treated mosquito net, follow the label instructions.\n\nIf you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).\n\n \n\nIf you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment.](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html)\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### Traveler Information\n\n* [Avoid Bug Bites](/travel/page/avoid-bug-bites)\n* [Chikungunya Prevention](https://www.cdc.gov/chikungunya/prevention/index.html)\n* [CDC Chikungunya website](http://www.cdc.gov/chikungunya/)\n\n### Clinician Information\n\n* [Chikungunya](/travel/yellowbook/2012/chapter-3-infectious-diseases-related-to-travel/chikungunya.htm) in CDC Yellow Book\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":668,"cells":{"id":{"kind":"string","value":"690cc6098820658c544492c061c73016e6fc4032"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Cholera"},"clean_text":{"kind":"string","value":"Cholera | Disease Directory | Travelers' Health | CDC\n\n### What is cholera?\n\nCholera can be a life-threatening disease caused by bacteria called - Vibrio cholerae- .\nA person can get cholera from unsafe food or water. This can happen when cholera bacteria spread from a person into drinking water or water used to grow food or prepare food. This can also happen when stool (poop) in sewage gets into the water supply.\nMost people who get Cholera will have mild or no symptoms. About 1 in 10 people with cholera will experience severe symptoms. Early [cholera symptoms](https://www.cdc.gov/cholera/illness.html) include the following:\n- Profuse watery diarrhea, sometimes described as “rice-water stools”\n- Increased thirst\n- Leg cramps\n- Restlessness or irritability\nPeople who are seriously ill with cholera can develop severe dehydration, leading to kidney failure and death.\n### Who is at risk?\nPeople who live in or travel to places where cholera is common are at the highest risk of getting the disease. Cholera in travelers is extremely rare but can occur in some situations such as among people visiting friends or family, health care workers, and response workers in outbreak settings.\nCDC considers the countries below to have areas of active cholera transmission. For information about the level of cholera transmission and where it is occurring in a country, check the cholera section on an affected country’s [destination page](/travel/destinations/list).\n- Africa: [Burundi](/travel/destinations/traveler/none/burundi), [Cameroon](/travel/destinations/traveler/none/cameroon), [Democratic Republic of the Congo](/travel/destinations/traveler/none/democratic-republic-of-congo), [Ethiopia](/travel/destinations/traveler/none/ethiopia), [Kenya](/travel/destinations/traveler/none/kenya), [Malawi](/travel/destinations/traveler/none/malawi), [Mozambique](/travel/destinations/traveler/none/mozambique), [Niger](/travel/destinations/traveler/none/niger), [Nigeria](/travel/destinations/traveler/none/nigeria), [Somalia](/travel/destinations/traveler/none/somalia), [South Africa](/travel/destinations/traveler/none/south-africa), [South Sudan](/travel/destinations/traveler/none/south-sudan), [Tanzania](/travel/destinations/traveler/none/tanzania), [Zambia](/travel/destinations/traveler/none/zambia), [Zimbabwe](/travel/destinations/traveler/none/zimbabwe)\n- Asia: [Afghanistan](/travel/destinations/traveler/none/afghanistan), [Bangladesh](/travel/destinations/traveler/none/bangladesh), [India](/travel/destinations/traveler/none/india), [Nepal](/travel/destinations/traveler/none/nepal), [Pakistan](/travel/destinations/traveler/none/pakistan), [Philippines](/travel/destinations/traveler/none/philippines)\n- Middle East: [Iraq](/travel/destinations/traveler/none/iraq), [Lebanon](/travel/destinations/traveler/none/lebanon), [Syria](/travel/destinations/traveler/none/syria), [Yemen](/travel/destinations/traveler/none/yemen)\n- Americas: [Dominican Republic](/travel/destinations/traveler/none/dominican-republic), [Haiti](/travel/destinations/traveler/none/haiti)\n- Pacific: none\n### What can travelers do to prevent cholera?\nYou can protect yourself against cholera by taking the following steps.\n#### Choose safer food and drinks while traveling\nFollow [food and drink safety tips](/travel/page/food-water-safety) to lower your chance of getting cholera through unsafe food and drinks.\n#### Wash your hands often\n- Wash your hands with soap and water. If soap and water aren’t available, clean hands with hand sanitizer (containing at least 60% alcohol).\n- Don’t touch your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean.\n- Cover your mouth and nose with a tissue or your sleeve (not your hands) when coughing or sneezing.\n### How is cholera treated?\nThe most important step in treating cholera is to drink plenty of fluids. People who are severely ill might need intravenous (IV) fluids. Antibiotics are recommended for people who are severely ill or may become severely ill, such as pregnant people and children. [Zinc treatment](https://www.cdc.gov/cholera/treatment/zinc-treatment.html) has also been shown to help improve cholera symptoms among children 3 to 14 years of age and shorten acute diarrhea for children more than six months of age.\n"},"raw_text":{"kind":"string","value":"\n\n### Cholera\n\n\n\n\n\n### What is cholera?\n\n\nCholera can be a life-threatening disease caused by bacteria called *Vibrio cholerae*.\n\nA person can get cholera from unsafe food or water. This can happen when cholera bacteria spread from a person into drinking water or water used to grow food or prepare food. This can also happen when stool (poop) in sewage gets into the water supply.\n\nMost people who get Cholera will have mild or no symptoms. About 1 in 10 people with cholera will experience severe symptoms. Early [cholera symptoms](https://www.cdc.gov/cholera/illness.html) include the following:\n\n* Profuse watery diarrhea, sometimes described as “rice-water stools”\n* Vomiting\n* Increased thirst\n* Leg cramps\n* Restlessness or irritability\n\nPeople who are seriously ill with cholera can develop severe dehydration, leading to kidney failure and death.\n\n### Who is at risk?\n\nPeople who live in or travel to places where cholera is common are at the highest risk of getting the disease. Cholera in travelers is extremely rare but can occur in some situations such as among people visiting friends or family, health care workers, and response workers in outbreak settings.\n\nCDC considers the countries below to have areas of active cholera transmission. For information about the level of cholera transmission and where it is occurring in a country, check the cholera section on an affected country’s [destination page](/travel/destinations/list).\n\n* **Africa:** [Burundi](/travel/destinations/traveler/none/burundi), [Cameroon](/travel/destinations/traveler/none/cameroon), [Democratic Republic of the Congo](/travel/destinations/traveler/none/democratic-republic-of-congo), [Ethiopia](/travel/destinations/traveler/none/ethiopia), [Kenya](/travel/destinations/traveler/none/kenya), [Malawi](/travel/destinations/traveler/none/malawi), [Mozambique](/travel/destinations/traveler/none/mozambique), [Niger](/travel/destinations/traveler/none/niger), [Nigeria](/travel/destinations/traveler/none/nigeria), [Somalia](/travel/destinations/traveler/none/somalia), [South Africa](/travel/destinations/traveler/none/south-africa), [South Sudan](/travel/destinations/traveler/none/south-sudan), [Tanzania](/travel/destinations/traveler/none/tanzania), [Zambia](/travel/destinations/traveler/none/zambia), [Zimbabwe](/travel/destinations/traveler/none/zimbabwe)\n* **Asia:** [Afghanistan](/travel/destinations/traveler/none/afghanistan), [Bangladesh](/travel/destinations/traveler/none/bangladesh), [India](/travel/destinations/traveler/none/india), [Nepal](/travel/destinations/traveler/none/nepal), [Pakistan](/travel/destinations/traveler/none/pakistan), [Philippines](/travel/destinations/traveler/none/philippines)\n* **Middle East:** [Iraq](/travel/destinations/traveler/none/iraq), [Lebanon](/travel/destinations/traveler/none/lebanon), [Syria](/travel/destinations/traveler/none/syria), [Yemen](/travel/destinations/traveler/none/yemen)\n* **Americas:** [Dominican Republic](/travel/destinations/traveler/none/dominican-republic), [Haiti](/travel/destinations/traveler/none/haiti)\n* **Pacific:** none\n\n### What can travelers do to prevent cholera?\n\nYou can protect yourself against cholera by taking the following steps.\n\n#### Choose safer food and drinks while traveling\n\nFollow [food and drink safety tips](/travel/page/food-water-safety) to lower your chance of getting cholera through unsafe food and drinks.\n\n#### Wash your hands often\n\n* Wash your hands with soap and water. If soap and water aren’t available, clean hands with hand sanitizer (containing at least 60% alcohol).\n* Don’t touch your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean.\n* Cover your mouth and nose with a tissue or your sleeve (not your hands) when coughing or sneezing.\n\n### How is cholera treated?\n\nThe most important step in treating cholera is to drink plenty of fluids. People who are severely ill might need intravenous (IV) fluids. Antibiotics are recommended for people who are severely ill or may become severely ill, such as pregnant people and children. [Zinc treatment](https://www.cdc.gov/cholera/treatment/zinc-treatment.html) has also been shown to help improve cholera symptoms among children 3 to 14 years of age and shorten acute diarrhea for children more than six months of age.\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. Avoid contact with other people while you are sick.\n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### More Information\n\n* [CDC Cholera Homepage](https://www.cdc.gov/cholera/index.html)\n* [Information for Travelers](https://www.cdc.gov/cholera/travelers.html)\n* CDC Yellow Book: [Cholera](/travel/yellowbook/2020/travel-related-infectious-diseases/cholera)\n* [Cholera Information for Health Care Professionals](/travel/page/cholera-travel-information)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":669,"cells":{"id":{"kind":"string","value":"34d38fe147bab8d82cf165961b66b61bdeca791b"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Crimean-Congo Hemorrhagic fever"},"clean_text":{"kind":"string","value":"Crimean-Congo Hemorrhagic fever | Disease Directory | Travelers' Health | CDC\n\n### Crimean-Congo Hemorrhagic fever\n window.location.href = 'https://www.cdc.gov/vhf/crimean-congo/index.html';\n"},"raw_text":{"kind":"string","value":"\n\n### Crimean-Congo Hemorrhagic fever\n\n\n\n\n setTimeout(function(){\n window.location.href = 'https://www.cdc.gov/vhf/crimean-congo/index.html';\n }, 1);\n \n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":670,"cells":{"id":{"kind":"string","value":"2046c4bcfab71f0e176be77351af6fbd5128ffed"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Dengue"},"clean_text":{"kind":"string","value":"Dengue | Disease Directory | Travelers' Health | CDC\n\n### What is dengue?\nDengue viruses are spread to people through the bite of an infected mosquito.\nDengue symptoms usually start within a few days of being bitten but can take up to 2 weeks to develop. Symptoms can be mild or severe and can include fever with nausea, vomiting, rash, headache, eye pain, joint and muscle pain. In severe cases, dengue can cause shock, internal bleeding, and even death. [Learn more about severe dengue](https://www.cdc.gov/dengue/symptoms/index.htm).\nNot everyone who gets infected with dengue will feel sick, only about 1 out of 4 infected people get sick. You are more likely to develop severe dengue if you were infected before. Infants and pregnant women are more likely to develop severe dengue.\n### Who is at risk?\nInformation by Destination\n\nWhere are you going?\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" - value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n window.location = url;\nMosquitoes that spread dengue bite during the day and less frequently at night. They are found in tropical and subtropical areas of the Americas, Africa, the Middle East, Asia, and the Pacific Islands. Check if dengue is a concern at your [destination](/travel/destinations/list).\nThe following activities can increase a traveler’s chance of getting infected:\n- Spending a lot of time outdoors\n- Traveling to [destinations with risk of dengue](https://www.cdc.gov/dengue/areaswithrisk/around-the-world.html) during times of the year when mosquitoes are more common, such as during warm weather.\n### What can travelers do to prevent dengue?\nTravelers can protect themselves from dengue by taking the following steps.\nUse an EPA-registered insect repellent\n- Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.\n\t- Picaridin (known as KBR 3023 and icaridin outside the US)\n\t- Oil of lemon eucalyptus (OLE)\n\t- Para-menthane-diol (PMD)\nFind the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).\n\n- Insect Repellent Tips for Babies and Children\n\t- Dress your child in clothing that covers arms and legs.\n\t- Cover strollers and baby carriers with mosquito netting.\n\t- When using insect repellent on your child:\n\t\t- Always follow label instructions.\n\t\t- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.\n\t\t- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.\n\t\t\t- Adults: Spray insect repellent onto your hands and then apply to a child’s face.\n\t\t- If also using sunscreen, always apply insect repellent after sunscreen.\nWear long-sleeved shirts and long pants\nTreat clothing and gear with permethrin\n- Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.\n\t- Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.\n\t- Permethrin-treated clothing provides protection after multiple washings.\n\t- Read product information to find out how long the protection will last.\n- If treating items yourself, follow the product instructions.\n- Do not use permethrin products directly on skin.\n- Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).\nKeep mosquitoes out of your hotel room or lodging\n- Choose a hotel or lodging with air conditioning or window and door screens.\n- Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.\nSleep under a mosquito net\n\n- Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.\n- Buy a mosquito net at your local outdoor store or online before traveling overseas.\n- Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.\n- [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.\n\t- Permethrin is an insecticide that kills mosquitoes and other insects.\n\t- To determine if you can wash a treated mosquito net, follow the label instructions.\nIf you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).\n#### Dengue Vaccine and Travel\nCurrently there are no dengue vaccine recommendations for travelers.\n"},"raw_text":{"kind":"string","value":"\n\n### Dengue\n\n\n\n\n### What is dengue?\n\nDengue viruses are spread to people through the bite of an infected mosquito.\n\nDengue symptoms usually start within a few days of being bitten but can take up to 2 weeks to develop. Symptoms can be mild or severe and can include fever with nausea, vomiting, rash, headache, eye pain, joint and muscle pain. In severe cases, dengue can cause shock, internal bleeding, and even death. [Learn more about severe dengue](https://www.cdc.gov/dengue/symptoms/index.htm).\n\nNot everyone who gets infected with dengue will feel sick, only about 1 out of 4 infected people get sick. You are more likely to develop severe dengue if you were infected before. Infants and pregnant women are more likely to develop severe dengue.\n\n### Who is at risk?\n\n\nInformation by Destination\n\nWhere are you going?\n\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n function goSelectPage(){ \n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" + value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n }else{\n window.location = url;\n }\n }\n\n \n \n\nMosquitoes that spread dengue bite during the day and less frequently at night. They are found in tropical and subtropical areas of the Americas, Africa, the Middle East, Asia, and the Pacific Islands. Check if dengue is a concern at your [destination](/travel/destinations/list).\n\nThe following activities can increase a traveler’s chance of getting infected:\n\n* Spending a lot of time outdoors\n* Traveling to [destinations with risk of dengue](https://www.cdc.gov/dengue/areaswithrisk/around-the-world.html) during times of the year when mosquitoes are more common, such as during warm weather.\n\n### What can travelers do to prevent dengue?\n\nTravelers can protect themselves from dengue by taking the following steps.\n\n**Use an EPA-registered insect repellent**\n\n\n\n* Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.\n\t+ DEET\n\t+ Picaridin (known as KBR 3023 and icaridin outside the US)\n\t+ IR3535\n\t+ Oil of lemon eucalyptus (OLE)\n\t+ Para-menthane-diol (PMD)\n\t+ 2-undecanone\n\nFind the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).\n\n\n\n* Insect Repellent Tips for Babies and Children\n\t+ Dress your child in clothing that covers arms and legs.\n\t+ Cover strollers and baby carriers with mosquito netting.\n\t+ When using insect repellent on your child:\n\t\t- Always follow label instructions.\n\t\t- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.\n\t\t- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.\n\t\t\t* Adults: Spray insect repellent onto your hands and then apply to a child’s face.\n\t\t- If also using sunscreen, always apply insect repellent after sunscreen.\n\n**Wear long-sleeved shirts and long pants**\n\n**Treat clothing and gear with permethrin**\n\n\n\n* Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.\n\t+ Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.\n\t+ Permethrin-treated clothing provides protection after multiple washings.\n\t+ Read product information to find out how long the protection will last.\n* If treating items yourself, follow the product instructions.\n* Do not use permethrin products directly on skin.\n* Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).\n\n**Keep mosquitoes out of your hotel room or lodging**\n\n* Choose a hotel or lodging with air conditioning or window and door screens.\n* Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.\n\n**Sleep under a mosquito net**\n\n\n\n* Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.\n* Buy a mosquito net at your local outdoor store or online before traveling overseas.\n* Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.\n* [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.\n\t+ Permethrin is an insecticide that kills mosquitoes and other insects.\n\t+ To determine if you can wash a treated mosquito net, follow the label instructions.\n\nIf you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).\n\n \n\n#### Dengue Vaccine and Travel\n\nCurrently there are no dengue vaccine recommendations for travelers.\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### More Information\n\n* [CDC Dengue page](http://www.cdc.gov/dengue/)\n* CDC Yellow Book: [Dengue](/travel/yellowbook/2016/infectious-diseases-related-to-travel/dengue)\n* [D](http://www.cdc.gov/dengue/)[engue Map](https://www.healthmap.org/dengue/en/)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":671,"cells":{"id":{"kind":"string","value":"4afb484139cda61f460dcc2c142dfee8024e5f92"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Diphtheria"},"clean_text":{"kind":"string","value":"Diphtheria | Disease Directory | Travelers' Health | CDC\n\n### What is diphtheria?\nDiphtheria is a disease caused by bacteria called - Corynebacterium diphtheriae (C. diphtheriae).- These bacteria cause respiratory and skin infections. People with diphtheria can spread the bacteria to others when they cough or sneeze, or if others come into contact with their infected wounds.\nSymptoms of respiratory diphtheria include weakness, fever, sore throat, and swollen glands in the neck. A thick, grey coating in the throat or nose can also appear, making it very hard to breathe and swallow. In severe respiratory disease, there can be damage to the heart and nerves. Skin infections caused by - C. diphtheriae- typically consist of shallow ulcers (sores) and does not result in severe disease.\nInformation by Destination\n\nWhere are you going?\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" - value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n window.location = url;\n### Who is at risk?\nDue to childhood vaccination, high income countries don’t have many cases of diphtheria. The disease still exists in parts of the world where diphtheria vaccines are not used or where few people get vaccinated. Travelers going to Asia, the South Pacific, the Middle East, and Eastern Europe, who are not up to date with diphtheria vaccines, can become infected.\n### What can travelers do to prevent diphtheria?\nGetting vaccinated is the best way to protect against diphtheria. Diphtheria vaccines are combination vaccines. These vaccines protect against diphtheria and tetanus, and some also protect against pertussis (whooping cough). These vaccines are often called [DTaP, Tdap, or Td](https://www.cdc.gov/vaccines/vpd/dtap-tdap-td/public/index.html).\n\n#### Babies and Children\nBabies need three shots of DTaP to build up high levels of protection against diphtheria, tetanus, and whooping cough. Then, young children need two booster shots to maintain protection through early childhood. CDC recommends doses at the following ages:\n- 2 months\n- 4 months\n- 6 months\n- 15 through 18 months\n- 4 through 6 years\n#### Preteens and Teens\nPreteens should get one shot of Tdap between the ages of 11 and 12 years to boost their immunity. Teens who didn’t get Tdap as a preteen should get one shot the next time they visit their healthcare provider.\nAll adults should get a Td or Tdap diphtheria shot every 10 years after getting their most recent dose as an adolescent. All adults who have never received Tdap should get one shot followed by either a Td or Tdap shot every 10 years.\n"},"raw_text":{"kind":"string","value":"\n\n### Diphtheria\n\n\n\n\n### What is diphtheria?\n\nDiphtheria is a disease caused by bacteria called *Corynebacterium diphtheriae (C. diphtheriae).* These bacteria cause respiratory and skin infections. People with diphtheria can spread the bacteria to others when they cough or sneeze, or if others come into contact with their infected wounds.\n\nSymptoms of respiratory diphtheria include weakness, fever, sore throat, and swollen glands in the neck. A thick, grey coating in the throat or nose can also appear, making it very hard to breathe and swallow. In severe respiratory disease, there can be damage to the heart and nerves. Skin infections caused by *C. diphtheriae*typically consist of shallow ulcers (sores) and does not result in severe disease.\n\n\nInformation by Destination\n\nWhere are you going?\n\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n function goSelectPage(){ \n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" + value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n }else{\n window.location = url;\n }\n }\n\n \n \n\n### Who is at risk?\n\nDue to childhood vaccination, high income countries don’t have many cases of diphtheria. The disease still exists in parts of the world where diphtheria vaccines are not used or where few people get vaccinated. Travelers going to Asia, the South Pacific, the Middle East, and Eastern Europe, who are not up to date with diphtheria vaccines, can become infected.\n\n### What can travelers do to prevent diphtheria?\n\nGetting vaccinated is the best way to protect against diphtheria. Diphtheria vaccines are combination vaccines. These vaccines protect against diphtheria and tetanus, and some also protect against pertussis (whooping cough). These vaccines are often called [DTaP, Tdap, or Td](https://www.cdc.gov/vaccines/vpd/dtap-tdap-td/public/index.html).\n\n\n#### Babies and Children\n\nBabies need three shots of DTaP to build up high levels of protection against diphtheria, tetanus, and whooping cough. Then, young children need two booster shots to maintain protection through early childhood. CDC recommends doses at the following ages:\n\n* 2 months\n* 4 months\n* 6 months\n* 15 through 18 months\n* 4 through 6 years\n\n#### Preteens and Teens\n\nPreteens should get one shot of Tdap between the ages of 11 and 12 years to boost their immunity. Teens who didn’t get Tdap as a preteen should get one shot the next time they visit their healthcare provider.\n\n#### Adults\n\nAll adults should get a Td or Tdap diphtheria shot every 10 years after getting their most recent dose as an adolescent. All adults who have never received Tdap should get one shot followed by either a Td or Tdap shot every 10 years. \n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n\n### More Information\n\n* [Diphtheria Homepage](http://www.cdc.gov/diphtheria/)\n* [Diphtheria Vaccine Information](https://www.cdc.gov/vaccines/vpd/dtap-tdap-td/public/index.html#should-get-vaccines)\n* CDC Yellow Book: [Diphtheria](/travel/yellowbook/2020/travel-related-infectious-diseases/diphtheria)\n* Pink Book: [Diphtheria](http://www.cdc.gov/vaccines/pubs/pinkbook/dip.html)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":672,"cells":{"id":{"kind":"string","value":"20e47661fda21d53c87df397157fa1c61b981d15"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Ebola and Marburg"},"clean_text":{"kind":"string","value":"Ebola and Marburg | Disease Directory | Travelers' Health | CDC\n\n### Ebola and Marburg\n### What are Ebola and Marburg?\nEbola disease and Marburg virus disease [are viral hemorrhagic fevers](https://www.cdc.gov/vhf/about.html). These diseases damage organs and blood vessels and may cause death. A person can get infected with Ebola or Marburg viruses if they touch or handle the following:\n- Body fluids from an infected person (alive or dead), such as blood, urine, saliva, sweat, feces, vomit, breast milk, semen, and others.\n- Objects such as clothes, bedding, needles, and medical equipment contaminated with the body fluids of an infected person or a person who died of Ebola or Marburg.\n- Infected wild animals, for example bats and non-human primates, or their body fluids or meat ([bushmeat](https://www.cdc.gov/importation/bushmeat.html)).\nEbola and Marburg symptoms may start 2 to 21 days after a person is infected (for Ebola, the average is 8-10 days) and may include sudden onset of fever, chills, headache, body aches, and a rash on the chest, back, and stomach. As the person gets sicker, they can have nausea, vomiting, chest pain, sore throat, abdominal pain, and diarrhea.\nPeople with Ebola or Marburg are at risk for internal bleeding, critically low blood pressure (shock), damage to multiple organs and organ systems (liver, pancreas, kidneys, brain), and death.\nWho is at risk?\nMost travelers are unlikely to be exposed to Ebola or Marburg viruses.\nEbola and Marburg viruses are found in sub-Saharan Africa.\nTravelers to sub-Saharan Africa who work closely with or visit areas with bats or non-human primates, such as monkeys, chimpanzees, and gorillas, may be more likely to get infected. For example, two tourists visiting Uganda in 2008 were infected with Marburg virus and likely exposed while visiting a cave known for its large bat population. People who care for patients with Ebola or Marburg may also be more likely to get infected because of exposure to blood or body fluids.\nWhat can travelers do to prevent Ebola and Marburg?\nYou can protect yourself from infection by taking the following steps:\n- Avoid close contact with sick people and blood or body fluids from all people\n\t- Do not kiss, hug, or share eating utensils or cups.\n\t- Don't touch items that may have blood or body fluids on them.\n- Avoid animals when traveling\n\t- Don't touch live or dead animals.\n\t- Avoid markets or farms with animals.\n\t- Don't eat or handle meat from wild animals ([bushmeat](https://www.cdc.gov/importation/bushmeat.html)).\n\t- If you are traveling for work that involves animals, wear appropriate protective gear.\n- Wash your hands\n\t- Wash hands often with soap and water. If soap and water aren’t available, use an alcohol-based hand sanitizer containing at least 60% alcohol.\n\t- Keep your hands away from your eyes, nose, and mouth. If you need to touch your face, make sure your hands are clean.\n- Avoid touching dead bodies \n\t- Don’t participate in funeral activities that involve touching dead bodies, or touch items that have been in contact with dead bodies or have blood or body fluids on them.\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/health-care-during-travel).\n"},"raw_text":{"kind":"string","value":"\n\n### Ebola and Marburg\n\n\n\n\n### What are Ebola and Marburg?\n\nEbola disease and Marburg virus disease [are viral hemorrhagic fevers](https://www.cdc.gov/vhf/about.html). These diseases damage organs and blood vessels and may cause death. A person can get infected with Ebola or Marburg viruses if they touch or handle the following:\n\n* Body fluids from an infected person (alive or dead), such as blood, urine, saliva, sweat, feces, vomit, breast milk, semen, and others.\n* Objects such as clothes, bedding, needles, and medical equipment contaminated with the body fluids of an infected person or a person who died of Ebola or Marburg.\n* Infected wild animals, for example bats and non-human primates, or their body fluids or meat ([bushmeat](https://www.cdc.gov/importation/bushmeat.html)).\n\nEbola and Marburg symptoms may start 2 to 21 days after a person is infected (for Ebola, the average is 8-10 days) and may include sudden onset of fever, chills, headache, body aches, and a rash on the chest, back, and stomach. As the person gets sicker, they can have nausea, vomiting, chest pain, sore throat, abdominal pain, and diarrhea.\n\nPeople with Ebola or Marburg are at risk for internal bleeding, critically low blood pressure (shock), damage to multiple organs and organ systems (liver, pancreas, kidneys, brain), and death.\n\nWho is at risk?\n\nMost travelers are unlikely to be exposed to Ebola or Marburg viruses.\n\nEbola and Marburg viruses are found in sub-Saharan Africa.\n\nTravelers to sub-Saharan Africa who work closely with or visit areas with bats or non-human primates, such as monkeys, chimpanzees, and gorillas, may be more likely to get infected. For example, two tourists visiting Uganda in 2008 were infected with Marburg virus and likely exposed while visiting a cave known for its large bat population. People who care for patients with Ebola or Marburg may also be more likely to get infected because of exposure to blood or body fluids.\n\nWhat can travelers do to prevent Ebola and Marburg?\n\n \nYou can protect yourself from infection by taking the following steps:\n\n* **Avoid close contact with sick people and blood or body fluids from all people**\n\t+ Do not kiss, hug, or share eating utensils or cups.\n\t+ Don't touch items that may have blood or body fluids on them.\n* **Avoid animals when traveling**\n\t+ Don't touch live or dead animals.\n\t+ Avoid markets or farms with animals.\n\t+ Don't eat or handle meat from wild animals ([bushmeat](https://www.cdc.gov/importation/bushmeat.html)).\n\t+ If you are traveling for work that involves animals, wear appropriate protective gear.\n* **Wash your hands**\n\t+ Wash hands often with soap and water. If soap and water aren’t available, use an alcohol-based hand sanitizer containing at least 60% alcohol.\n\t+ Keep your hands away from your eyes, nose, and mouth. If you need to touch your face, make sure your hands are clean.\n* **Avoid touching dead bodies** \n\t+ Don’t participate in funeral activities that involve touching dead bodies, or touch items that have been in contact with dead bodies or have blood or body fluids on them.\n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/health-care-during-travel).\n\n### After Travel\n\n**If you traveled to an area where there is an Ebola or Marburg outbreak and feel sick,** particularly if you have a fever, contact your local health department or a healthcare professional immediately and tell them about your symptoms and where you traveled. Avoid contact with other people while you are sick.\n\nFollow [additional recommendations](https://www.cdc.gov/quarantine/vhf/after-you-travel.html) after returning to the United States.\n\n### More Information\n\n* [CDC Ebola website](https://www.cdc.gov/vhf/ebola/)\n* [CDC Marburg website](https://www.cdc.gov/vhf/marburg/index.html)\n* CDC Yellow Book: [Viral Hemorrhagic Fevers](/travel/yellowbook/2020/travel-related-infectious-diseases/viral-hemorrhagic-fevers)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":673,"cells":{"id":{"kind":"string","value":"9f2b25ab5427a2fc5654db59ea3458b129ede272"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Flu (Influenza)"},"clean_text":{"kind":"string","value":"Flu (Influenza) | Disease Directory | Travelers' Health | CDC\n\n### Flu (Influenza)\n\nThe best way to reduce the risk of flu and possible flu complications is to get vaccinated each year, learn about special considerations for travel.\n#### You may need a flu vaccine before travel at other times of the year, depending on your destination .\n- In the Northern Hemisphere, flu season can begin as early as October and can last until April or May.\n- In the temperate regions (areas with seasons) in the Southern Hemisphere, flu activity typically occurs from April to September.\n- In the tropics, flu activity occurs throughout the year.\n- Travelers who are part of large tourist groups that include people from other parts of the world, such as on cruise ships, may be at risk.\n- People should get vaccinated at least 2 weeks before travel because it takes 2 weeks for immunity to develop after vaccination.\n- Getting a flu vaccine is very important for [people at higher risk of serious flu complications](https://www.cdc.gov/flu/highrisk/index.htm).\n- If you already got your annual flu vaccine, you usually don't need to get vaccinated again during the same season.\n#### Do not travel if you are sick\n- If you are sick with flu-like symptoms, do not travel. Stay home until you are fever-free for at least 24 hours without using a fever-reducing medicine, such as acetaminophen.\n- Flu symptoms include:\n\t- Fever (Not everyone with flu will have a fever.)\n\t- Cough o Sore throat\n\t- Runny or stuffy nose\n\t- Muscle or body aches\n\t- Some people may have vomiting and diarrhea, though this is more common in children.\n### During Travel\nDuring your trip, follow local guidelines and practice healthy habits.\n- Avoid close contact with sick people.\n- Wash your hands often with soap and running water, especially after coughing or sneezing.\n- If soap and water are not readily available, use a hand sanitizer that contains at least 60% alcohol. Cover all surfaces of your hands and rub them together until they feel dry.\n- Cover your mouth and nose with a tissue when you cough or sneeze and put the used tissue in the trash. If you don’t have a tissue, cough or sneeze into your upper sleeve, not your hands.\n#### What to do if you feel sick\nMost people with flu will recover without needing medical care. However, if you have severe illness or are [at risk of getting serious flu complications](https://www.cdc.gov/flu/highrisk/index.htm), seek medical care.\nA U.S. consular officer can help you find local medical care in a foreign country. To contact the U.S. Embassy or consulate in the country you are visiting, call Overseas Citizens Services at 1-888-407-4747 if calling from the U.S. or Canada, 00-1-202-501-4444 if calling from other countries. You can also visit the [websites of U.S. Embassies, consulates, and diplomatic missionsExternal Link](https://www.usembassy.gov/) to find the contact information for the local U.S. Embassy of the country you are visiting.\nFollow all local health recommendations\n"},"raw_text":{"kind":"string","value":"\n\n### Flu (Influenza)\n\n\n\n\n\n\nThe best way to reduce the risk of flu and possible flu complications is to get vaccinated each year, learn about special considerations for travel.\n\n#### You may need a flu vaccine before travel at other times of the year, depending on your destination .\n\n* In the Northern Hemisphere, flu season can begin as early as October and can last until April or May.\n* In the temperate regions (areas with seasons) in the Southern Hemisphere, flu activity typically occurs from April to September.\n* In the tropics, flu activity occurs throughout the year.\n* Travelers who are part of large tourist groups that include people from other parts of the world, such as on cruise ships, may be at risk.\n* People should get vaccinated at least 2 weeks before travel because it takes 2 weeks for immunity to develop after vaccination.\n* Getting a flu vaccine is very important for [people at higher risk of serious flu complications](https://www.cdc.gov/flu/highrisk/index.htm).\n* If you already got your annual flu vaccine, you usually don't need to get vaccinated again during the same season.\n\n#### Do not travel if you are sick\n\n* **If you are sick with flu-like symptoms, do not travel.** Stay home until you are fever-free for at least 24 hours without using a fever-reducing medicine, such as acetaminophen.\n* Flu symptoms include:\n\t+ Fever (Not everyone with flu will have a fever.)\n\t+ Cough o Sore throat\n\t+ Runny or stuffy nose\n\t+ Muscle or body aches\n\t+ Headache\n\t+ Fatigue\n\t+ Some people may have vomiting and diarrhea, though this is more common in children.\n\n### During Travel\n\nDuring your trip, follow local guidelines and practice healthy habits.\n\n* Avoid close contact with sick people.\n* Wash your hands often with soap and running water, especially after coughing or sneezing.\n* If soap and water are not readily available, use a hand sanitizer that contains at least 60% alcohol. Cover all surfaces of your hands and rub them together until they feel dry.\n* Cover your mouth and nose with a tissue when you cough or sneeze and put the used tissue in the trash. If you don’t have a tissue, cough or sneeze into your upper sleeve, not your hands.\n\n#### What to do if you feel sick\n\nMost people with flu will recover without needing medical care. However, if you have severe illness or are [at risk of getting serious flu complications](https://www.cdc.gov/flu/highrisk/index.htm), seek medical care.\n\nA U.S. consular officer can help you find local medical care in a foreign country. To contact the U.S. Embassy or consulate in the country you are visiting, call Overseas Citizens Services at 1-888-407-4747 if calling from the U.S. or Canada, 00-1-202-501-4444 if calling from other countries. You can also visit the [websites of U.S. Embassies, consulates, and diplomatic missionsExternal Link](https://www.usembassy.gov/) to find the contact information for the local U.S. Embassy of the country you are visiting.\n\nFollow all local health recommendations\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### More Information\n\n* CDC: [Travelers’ Health Website](/travel/) (General)\n* CDC: [Traveler Information Center](/travel/page/resources-for-travelers)\n\n \n\n\n \n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":674,"cells":{"id":{"kind":"string","value":"f3efaab4e14521d0497deea936ef720c26170ed1"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"HIV"},"clean_text":{"kind":"string","value":"HIV | Disease Directory | Travelers' Health | CDC\n\n### What is HIV?\n[HIV](https://www.cdc.gov/actagainstaids/basics/whatishiv.html) (human immunodeficiency virus) is a virus that attacks the body’s immune system. It is [spread](https://www.cdc.gov/actagainstaids/basics/transmission.html) through certain body fluids, including blood, sexual fluids (like semen and vaginal or rectal fluids) and breast milk. Most people get HIV from having unprotected sex (including vaginal or anal sex) with someone who has HIV, or from sharing needles or other drug injection equipment with someone who has HIV.\n\nEarly symptoms of HIV infection may include cough, body aches, headaches, nasal congestion, and sore throat. These symptoms usually go away on their own and can be mistaken for flu-like illness. Some people may have no early symptoms at all and may feel healthy. The only way to know for sure whether you have HIV is to get tested.\nOver time, HIV infection damages the immune system, making it harder for the body to fight off infections and other diseases, including heart disease, kidney disease, liver disease, and cancer. Left untreated, HIV infection can lead to AIDS (acquired immune deficiency syndrome). AIDS is the most severe phase of HIV infection. People with AIDS have such badly damaged immune systems that they get severe infections that don’t normally infect healthy people, called opportunistic infections, and eventually the infection leads to death. No effective cure exists, but with early diagnosis and proper medical care, HIV can be managed and controlled.\n### Who is at risk?\nTravelers are generally at low risk for getting HIV unless they engage in activities that could put them at risk, such as having unprotected sex or sharing needles.\nA person can get HIV by being stuck with a contaminated needle or another sharp object, though this is more of a risk for healthcare workers. Some low-income countries may not adequately screen their blood supplies or properly sterilize medical equipment used in medical clinics, dental clinics, and hospitals. There is a small chance that travelers to these countries who receive medical care could get infected.\nHIV infection affects people globally. Sub-Saharan Africa remains the most affected part of the world. Still, other regions significantly affected by HIV include Asia and the Pacific, Latin America, the Caribbean, Eastern Europe, and Central Asia.\n### What can travelers do to prevent HIV?\n- Talk with your health care provider about PrEP or [pre-exposure prophylaxis](https://www.cdc.gov/hiv/risk/prep/). It is usually a pill or a shot. PrEP is most effective when it is prescribed by your healthcare provider\n- Before having sex for the first time with a new partner, you and your partner should talk about your sexual and drug-use history, disclose your HIV status, and get tested for HIV and other sexually transmitted infections.\n- If you have sex, [use condoms the right way](https://www.cdc.gov/hiv/basics/hiv-transmission/ways-people-get-hiv.html) every time you have vaginal, oral, or anal sex, from start to finish.\n- Do not inject drugs or share needles or other devices that can break the skin. If you do inject drugs, use only new, sterile syringes and needles.\n- If you get tattoos, piercings, or acupuncture abroad, make sure a new, sterile needle is used each time.\n- If you get medical or dental care abroad, make sure the equipment is unused or properly sterilized.\nIf you have HIV and are traveling, your destination may increase your risk of getting [opportunistic infections](https://www.cdc.gov/hiv/basics/livingwithhiv/opportunisticinfections.html) or more severe illnesses from infections like travelers’ diarrhea. Bring enough of your medications to last your entire trip since not all countries have all HIV medication.\nConsult your doctor or travel medicine specialist at least 4 weeks before leaving as you may not be eligible for certain travel vaccines required at your destination, or you may need to take additional precautions.\nCheck the [Department of State websiteExternal Link](https://travel.state.gov/content/travel/en/international-travel/International-Travel-Country-Information-Pages.html) for any restrictions on travel for people with HIV at your destination\n"},"raw_text":{"kind":"string","value":"\n\n### HIV\n\n\n\n\n### What is HIV?\n\n[HIV](https://www.cdc.gov/actagainstaids/basics/whatishiv.html) (human immunodeficiency virus) is a virus that attacks the body’s immune system. It is [spread](https://www.cdc.gov/actagainstaids/basics/transmission.html) through certain body fluids, including blood, sexual fluids (like semen and vaginal or rectal fluids) and breast milk. Most people get HIV from having unprotected sex (including vaginal or anal sex) with someone who has HIV, or from sharing needles or other drug injection equipment with someone who has HIV.\n\n\n**HIV symptoms**\n\nEarly symptoms of HIV infection may include cough, body aches, headaches, nasal congestion, and sore throat. These symptoms usually go away on their own and can be mistaken for flu-like illness. Some people may have no early symptoms at all and may feel healthy. The only way to know for sure whether you have HIV is to get tested.\n\nOver time, HIV infection damages the immune system, making it harder for the body to fight off infections and other diseases, including heart disease, kidney disease, liver disease, and cancer. Left untreated, HIV infection can lead to AIDS (acquired immune deficiency syndrome). AIDS is the most severe phase of HIV infection. People with AIDS have such badly damaged immune systems that they get severe infections that don’t normally infect healthy people, called opportunistic infections, and eventually the infection leads to death. No effective cure exists, but with early diagnosis and proper medical care, HIV can be managed and controlled.\n\n### Who is at risk?\n\nTravelers are generally at low risk for getting HIV unless they engage in activities that could put them at risk, such as having unprotected sex or sharing needles.\n\nA person can get HIV by being stuck with a contaminated needle or another sharp object, though this is more of a risk for healthcare workers. Some low-income countries may not adequately screen their blood supplies or properly sterilize medical equipment used in medical clinics, dental clinics, and hospitals. There is a small chance that travelers to these countries who receive medical care could get infected.\n\nHIV infection affects people globally. Sub-Saharan Africa remains the most affected part of the world. Still, other regions significantly affected by HIV include Asia and the Pacific, Latin America, the Caribbean, Eastern Europe, and Central Asia.\n\n### What can travelers do to prevent HIV?\n\n\n* Talk with your health care provider about PrEP or [pre-exposure prophylaxis](https://www.cdc.gov/hiv/risk/prep/). It is usually a pill or a shot. PrEP is most effective when it is prescribed by your healthcare provider\n* Before having sex for the first time with a new partner, you and your partner should talk about your sexual and drug-use history, disclose your HIV status, and get tested for HIV and other sexually transmitted infections.\n* If you have sex, [use condoms the right way](https://www.cdc.gov/hiv/basics/hiv-transmission/ways-people-get-hiv.html) every time you have vaginal, oral, or anal sex, from start to finish.\n* Do not inject drugs or share needles or other devices that can break the skin. If you do inject drugs, use only new, sterile syringes and needles.\n* If you get tattoos, piercings, or acupuncture abroad, make sure a new, sterile needle is used each time.\n* If you get medical or dental care abroad, make sure the equipment is unused or properly sterilized.\n\nIf you have HIV and are traveling, your destination may increase your risk of getting [opportunistic infections](https://www.cdc.gov/hiv/basics/livingwithhiv/opportunisticinfections.html) or more severe illnesses from infections like travelers’ diarrhea. Bring enough of your medications to last your entire trip since not all countries have all HIV medication.\n\nConsult your doctor or travel medicine specialist at least 4 weeks before leaving as you may not be eligible for certain travel vaccines required at your destination, or you may need to take additional precautions.\n\nCheck the [Department of State websiteExternal Link](https://travel.state.gov/content/travel/en/international-travel/International-Travel-Country-Information-Pages.html) for any restrictions on travel for people with HIV at your destination\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### More Information\n\n* [About HIV](https://www.cdc.gov/hiv/basics/whatishiv.html)\n* [CDC HIV Homepage](https://www.cdc.gov/hiv/)\n* CDC Yellow Book: [HIV Infection](/travel/yellowbook/2018/infectious-diseases-related-to-travel/hiv-infection) in CDC Yellow Book\n* [HIV Guidelines](https://www.cdc.gov/hiv/guidelines/index.html)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":675,"cells":{"id":{"kind":"string","value":"92680a73c5fcfbdde2d61f6411211972fcf182c1"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Hand, Foot, and Mouth Disease"},"clean_text":{"kind":"string","value":"Hand, Foot, and Mouth Disease | Disease Directory | Travelers' Health | CDC\n\n### Hand, Foot, and Mouth Disease\n### What is hand, foot, and mouth disease?\nHand, foot, and mouth disease is a contagious disease that is caused by different viruses. It usually affects infants and children under 5 years old, occasionally adults will also get the disease. [Symptoms](http://www.cdc.gov/hand-foot-mouth/about/signs-symptoms.html) of hand, foot, and mouth disease include fever, painful blister-like sores in the mouth, and a rash that may appear as blisters. It is usually a mild disease, and nearly all infected people recover in 7 to 10 days.\nHand, foot, and mouth disease spreads through close personal contact, such as kissing or hugging, coughing and sneezing, contact with feces (poop), and touching objects or surfaces that have the virus on them then putting your fingers in your eyes, nose or mouth.\n### Who is at risk?\n\nViruses that cause hand, foot, and mouth disease occur worldwide and are more common in summer and fall in temperate climates. Large, severe outbreaks affecting thousands of people occur frequently in some countries in Asia. \n### What can travelers do to prevent hand, foot, and mouth disease?\nThere is no vaccine to prevent hand, foot, and mouth disease but you can take steps to lower your risk of getting it.\n#### Wash your hands:\n- Wash your hands often with soap and water, especially after using the bathroom and before eating. If soap and water aren't available, use an alcohol-based hand sanitizer.\n- Don’t touch your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean.\n- Cover your mouth and nose with a tissue or your sleeve (not your hands) when coughing or sneezing.\n- Try to avoid close contact, such as kissing, hugging, or sharing eating utensils or cups with people who are sick.\n#### Disinfect dirty surfaces and soiled items:\n- If you are able, first wash items with soap and water, then disinfect them with a solution of chlorine bleach (made by mixing 1 tablespoon of bleach with 4 cups of water) or a cleaning product that contains bleach.\n#### If you develop mouth sores and think you have hand, foot, and mouth disease:\n- Take over-the-counter medications to relieve pain and fever.\n\t- Children should not take aspirin.\n- Use mouthwashes or sprays that numb mouth pain.\n- Drink plenty of liquids to stay hydrated.\n- Seek medical care if\n\t- Your child is not drinking enough to stay hydrated\n\t- Symptoms do not improve after 10 days\n\t- Your child has a weakened immune system\n\t- Symptoms are severe\n\t- Your child is very young, especially younger than 6 months\n"},"raw_text":{"kind":"string","value":"\n\n### Hand, Foot, and Mouth Disease\n\n\n\n\n### What is hand, foot, and mouth disease?\n\nHand, foot, and mouth disease is a contagious disease that is caused by different viruses. It usually affects infants and children under 5 years old, occasionally adults will also get the disease. [Symptoms](http://www.cdc.gov/hand-foot-mouth/about/signs-symptoms.html) of hand, foot, and mouth disease include fever, painful blister-like sores in the mouth, and a rash that may appear as blisters. It is usually a mild disease, and nearly all infected people recover in 7 to 10 days.\n\nHand, foot, and mouth disease spreads through close personal contact, such as kissing or hugging, coughing and sneezing, contact with feces (poop), and touching objects or surfaces that have the virus on them then putting your fingers in your eyes, nose or mouth.\n\n### Who is at risk?\n\n\nViruses that cause hand, foot, and mouth disease occur worldwide and are more common in summer and fall in temperate climates. Large, severe outbreaks affecting thousands of people occur frequently in some countries in Asia. \n\n### What can travelers do to prevent hand, foot, and mouth disease?\n\nThere is no vaccine to prevent hand, foot, and mouth disease but you can take steps to lower your risk of getting it.\n\n#### Wash your hands:\n\n* Wash your hands often with soap and water, especially after using the bathroom and before eating. If soap and water aren't available, use an alcohol-based hand sanitizer.\n* Don’t touch your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean.\n* Cover your mouth and nose with a tissue or your sleeve (not your hands) when coughing or sneezing.\n* Try to avoid close contact, such as kissing, hugging, or sharing eating utensils or cups with people who are sick.\n\n#### Disinfect dirty surfaces and soiled items:\n\n* If you are able, first wash items with soap and water, then disinfect them with a solution of chlorine bleach (made by mixing 1 tablespoon of bleach with 4 cups of water) or a cleaning product that contains bleach.\n\n#### If you develop mouth sores and think you have hand, foot, and mouth disease:\n\n* Take over-the-counter medications to relieve pain and fever.\n\t+ Children should not take aspirin.\n* Use mouthwashes or sprays that numb mouth pain.\n* Drink plenty of liquids to stay hydrated.\n* Seek medical care if\n\t+ Your child is not drinking enough to stay hydrated\n\t+ Symptoms do not improve after 10 days\n\t+ Your child has a weakened immune system\n\t+ Symptoms are severe\n\t+ Your child is very young, especially younger than 6 months\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### More Information\n\n* [CDC Hand Foot Mouth Disease webpage](http://www.cdc.gov/hand-foot-mouth/index.html)\n* [CDC Yellow Book: Hand, Foot, and Mouth Disease](/travel/yellowbook/2020/travel-related-infectious-diseases/hand-foot-and-mouth-disease)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":676,"cells":{"id":{"kind":"string","value":"a9355b1b34eb56f7d9c180f37be671812cc0ca47"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Hantavirus"},"clean_text":{"kind":"string","value":"Hantavirus | Disease Directory | Travelers' Health | CDC\n\n### What is Hantavirus?\nHantaviruses are viruses that can spread from animals to people that can cause serious disease in people. You can be infected with a hantavirus if you\n- Breathe air or eat food contaminated with the urine, droppings, or saliva of infected rodents\n- Are bitten by an infected rodent, typically a mouse or a rat\n[Andes virus](https://www.cdc.gov/hantavirus/resources/andes-virus.html), found in South America, is the only hantavirus known to spread from person to person.\nHantaviruses in North and South America most commonly cause a serious lung disease known as [hantavirus pulmonary syndrome.](https://www.cdc.gov/hantavirus/hps/index.html) \nHantaviruses in Europe and Asia cause organ damage, especially to the kidneys and blood vessels. This is known as [hemorrhagic fever with renal syndrome](https://www.cdc.gov/hantavirus/hfrs/index.html). Recovery can take weeks to months. In some cases hantavirus can cause death. \nSymptoms of hantavirus disease usually develop three to four weeks after infection but can occur as early as one week and, in rare cases, not start until eight weeks after infection. Early symptoms include fatigue, fever, and muscle aches. There may also be headaches, dizziness, chills, nausea, vomiting, diarrhea, and abdominal pain.\n### Who is at risk?\nHantaviruses are found throughout the world. Cases of hantavirus disease are rare among travelers, but some activities increase a traveler’s chances of being exposed to rodents, rodent nests, rodent urine and droppings. These activities include the following:\n- Working with animals (veterinarians and wildlife professionals)\n- Working on farms\n- Traveling to rural areas\n### What can travelers do to prevent hantavirus infection?\nThere are no vaccines or medicines to prevent hantavirus disease. Travelers can protect themselves by taking the following steps.\n#### Avoid rodents when traveling\n- Disinfect droppings and nesting materials by spraying with a disinfectant, wearing kitchen gloves. Dispose of sprayed materials in a plastic bag.\n- Avoid touching live or dead rodents. Do not disturb rodents, burrows, or nests.\n- Before occupying abandoned or unused cabins, open them up to air out. Inspect for rodents and do not use cabins if you find signs of rodent infestation such as droppings or nests.\n- If you sleep outdoors, check potential campsites for rodent droppings and burrows.\n- Avoid sleeping near woodpiles or garbage areas. These may be frequented by rodents.\n- Avoid sleeping on bare ground; use a tent with a floor, mat or elevated cots if they are available.\n- Do not leave pet food in feeding dishes.\n- Store foods in rodent-proof containers and promptly discard, bury, or burn all garbage in accordance with campsite regulations.\n#### Wash your hands\n- Wash hands often with soap and water. If soap and water aren’t available, use an alcohol-based hand sanitizer containing at least 60% alcohol.\n- Keep your hands away from your eyes, nose, and mouth. If you need to touch your face, make sure your hands are clean.\n#### Avoid close contact with people who are sick\n- Do not kiss, hug, or share eating utensils or cups.\n- Do not touch the bedding or clothing of a sick person.\n"},"raw_text":{"kind":"string","value":"\n\n### Hantavirus\n\n\n\n\n### What is Hantavirus?\n\n\nHantaviruses are viruses that can spread from animals to people that can cause serious disease in people. You can be infected with a hantavirus if you\n\n* Breathe air or eat food contaminated with the urine, droppings, or saliva of infected rodents\n* Are bitten by an infected rodent, typically a mouse or a rat\n\n[Andes virus](https://www.cdc.gov/hantavirus/resources/andes-virus.html), found in South America, is the only hantavirus known to spread from person to person.\n\nHantaviruses in North and South America most commonly cause a serious lung disease known as [hantavirus pulmonary syndrome.](https://www.cdc.gov/hantavirus/hps/index.html) \n\nHantaviruses in Europe and Asia cause organ damage, especially to the kidneys and blood vessels. This is known as [hemorrhagic fever with renal syndrome](https://www.cdc.gov/hantavirus/hfrs/index.html). Recovery can take weeks to months. In some cases hantavirus can cause death. \n\nSymptoms of hantavirus disease usually develop three to four weeks after infection but can occur as early as one week and, in rare cases, not start until eight weeks after infection. Early symptoms include fatigue, fever, and muscle aches. There may also be headaches, dizziness, chills, nausea, vomiting, diarrhea, and abdominal pain.\n\n### Who is at risk?\n\nHantaviruses are found throughout the world. Cases of hantavirus disease are rare among travelers, but some activities increase a traveler’s chances of being exposed to rodents, rodent nests, rodent urine and droppings. These activities include the following:\n\n* Working with animals (veterinarians and wildlife professionals)\n* Working on farms\n* Camping\n* Traveling to rural areas\n\n### What can travelers do to prevent hantavirus infection?\n\nThere are no vaccines or medicines to prevent hantavirus disease. Travelers can protect themselves by taking the following steps.\n\n#### Avoid rodents when traveling\n\n* Disinfect droppings and nesting materials by spraying with a disinfectant, wearing kitchen gloves. Dispose of sprayed materials in a plastic bag.\n* Avoid touching live or dead rodents. Do not disturb rodents, burrows, or nests.\n* Before occupying abandoned or unused cabins, open them up to air out. Inspect for rodents and do not use cabins if you find signs of rodent infestation such as droppings or nests.\n* If you sleep outdoors, check potential campsites for rodent droppings and burrows.\n* Avoid sleeping near woodpiles or garbage areas. These may be frequented by rodents.\n* Avoid sleeping on bare ground; use a tent with a floor, mat or elevated cots if they are available.\n* Do not leave pet food in feeding dishes.\n* Store foods in rodent-proof containers and promptly discard, bury, or burn all garbage in accordance with campsite regulations.\n\n#### Wash your hands\n\n* Wash hands often with soap and water. If soap and water aren’t available, use an alcohol-based hand sanitizer containing at least 60% alcohol.\n* Keep your hands away from your eyes, nose, and mouth. If you need to touch your face, make sure your hands are clean.\n\n#### Avoid close contact with people who are sick\n\n* Do not kiss, hug, or share eating utensils or cups.\n* Do not touch the bedding or clothing of a sick person.\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### More Information\n\n* [CDC Website: Hantavirus](https://www.cdc.gov/hantavirus/index.html)\n* [Hantavirus Guide for Tourists, Campers, and Hikers](https://www.cdc.gov/hantavirus/resources/guide-for-tourists-campers-and-hikers.html)\n* CDC Yellow Book: [Viral Hemorrhagic Fevers](/travel/yellowbook/2020/travel-related-infectious-diseases/viral-hemorrhagic-fevers)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":677,"cells":{"id":{"kind":"string","value":"4992227c5db2e9774d0aa2fd1ad039382d0e966e"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Hepatitis A"},"clean_text":{"kind":"string","value":"Hepatitis A | Disease Directory | Travelers' Health | CDC\n\n### Hepatitis A\n### What is hepatitis A?\nHepatitis A virus can cause liver disease. Hepatitis A virus is found in the stool (poop) and blood of infected people. People infected with hepatitis A virus can spread it to others.\nYou can be infected with hepatitis A virus if you\n- Eat food or drink beverages contaminated with hepatitis A virus\n- Touch objects with the virus on it and then put your hands in your mouth\n- Have close, personal contact with an infected person, such as caring for them\n- Have sex with an infected person\nSymptoms can appear quickly and may include fever, fatigue, loss of appetite, nausea, vomiting, abdominal pain, dark urine, diarrhea, clay-colored bowel movements, joint pain, and yellowing of the skin and eyes (jaundice). Most older children and adults who get hepatitis A feel sick for several weeks, but usually recover and do not have lasting liver damage. Children younger than age six usually do not have symptoms.\nIn rare cases, hepatitis A virus can cause liver failure and death. This is more common in older people and people with existing liver diseases.\n### Who is at risk?\nInformation by Destination\n\nWhere are you going?\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" - value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n window.location = url;\nHepatitis A is a common disease in countries throughout the world. Anyone who has not been vaccinated or had hepatitis A infection before can get infected.\nTravelers are more likely to get infected with hepatitis A if they visit rural areas, travel in backcountry areas, or frequently eat or drink in settings of poor sanitation. However, even travelers who stay in urban areas, resorts, or luxury hotels, who wash their hands regularly, and who choose food and drinks carefully have been infected when visiting countries where hepatitis A is common.\n### What can travelers do to prevent hepatitis A?\nGetting vaccinated is the best way to protect against hepatitis A. The hepatitis A vaccine is very effective and has been a routine childhood vaccine since 1996. The vaccine is recommended for international travelers 6 months of age or older going to countries where hepatitis A infection is common. Check if hepatitis A vaccine is recommended for [your destination.](/travel/destinations/list)\nHepatitis A vaccine is given in two doses. If your plans don’t allow you to get all doses before your trip, get at least 1 dose, as soon as possible before you travel.\nInfants 6 to 11 months old should be vaccinated when protection against hepatitis A is recommended for the [destination.](/travel/destinations/list) This dose does not count toward the routine 2-dose series.\nTravelers allergic to a vaccine component or 6 months of age or younger should receive a single dose of immune globulin, which provides effective protection for up to 2 months depending on dosage given. Talk to your doctor to see if this is the best option for you.\nAdditional protection against hepatitis B can be given using the combination hepatitis A and hepatitis B vaccine, usually given in 3 doses. If your trip is soon, talk to your doctor about accelerated dosing of the combination hepatitis A and hepatitis B vaccine.\n"},"raw_text":{"kind":"string","value":"\n\n### Hepatitis A\n\n\n\n\n\n### What is hepatitis A?\n\nHepatitis A virus can cause liver disease. Hepatitis A virus is found in the stool (poop) and blood of infected people. People infected with hepatitis A virus can spread it to others.\n\nYou can be infected with hepatitis A virus if you\n\n* Eat food or drink beverages contaminated with hepatitis A virus\n* Touch objects with the virus on it and then put your hands in your mouth\n* Have close, personal contact with an infected person, such as caring for them\n* Have sex with an infected person\n\nSymptoms can appear quickly and may include fever, fatigue, loss of appetite, nausea, vomiting, abdominal pain, dark urine, diarrhea, clay-colored bowel movements, joint pain, and yellowing of the skin and eyes (jaundice). Most older children and adults who get hepatitis A feel sick for several weeks, but usually recover and do not have lasting liver damage. Children younger than age six usually do not have symptoms.\n\nIn rare cases, hepatitis A virus can cause liver failure and death. This is more common in older people and people with existing liver diseases.\n\n### Who is at risk?\n\n\nInformation by Destination\n\nWhere are you going?\n\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n function goSelectPage(){ \n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" + value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n }else{\n window.location = url;\n }\n }\n\n \n \n\nHepatitis A is a common disease in countries throughout the world. Anyone who has not been vaccinated or had hepatitis A infection before can get infected.\n\nTravelers are more likely to get infected with hepatitis A if they visit rural areas, travel in backcountry areas, or frequently eat or drink in settings of poor sanitation. However, even travelers who stay in urban areas, resorts, or luxury hotels, who wash their hands regularly, and who choose food and drinks carefully have been infected when visiting countries where hepatitis A is common.\n\n### What can travelers do to prevent hepatitis A?\n\nGetting vaccinated is the best way to protect against hepatitis A. The hepatitis A vaccine is very effective and has been a routine childhood vaccine since 1996. The vaccine is recommended for international travelers 6 months of age or older going to countries where hepatitis A infection is common. Check if hepatitis A vaccine is recommended for [your destination.](/travel/destinations/list)\n\nHepatitis A vaccine is given in two doses. If your plans don’t allow you to get all doses before your trip, get at least 1 dose, as soon as possible before you travel.\n\nInfants 6 to 11 months old should be vaccinated when protection against hepatitis A is recommended for the [destination.](/travel/destinations/list) This dose does not count toward the routine 2-dose series.\n\nTravelers allergic to a vaccine component or 6 months of age or younger should receive a single dose of immune globulin, which provides effective protection for up to 2 months depending on dosage given. Talk to your doctor to see if this is the best option for you.\n\nAdditional protection against hepatitis B can be given using the combination hepatitis A and hepatitis B vaccine, usually given in 3 doses. If your trip is soon, talk to your doctor about accelerated dosing of the combination hepatitis A and hepatitis B vaccine.\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### More Information\n\n* [Hepatitis A](http://www.cdc.gov/hepatitis/A/index.htm)\n* [Vaccine Information Statement](http://www.cdc.gov/vaccines/pubs/vis/default.htm#hepa)\n* [Choose Food and Drinks Carefully](/travel/page/food-water-safety)\n* CDC Yellow Book: [Hepatitis A](/travel/yellowbook/2020/travel-related-infectious-diseases/hepatitis-a)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":678,"cells":{"id":{"kind":"string","value":"8f90f70f2f869ebd42a4c22df32ce3b7cc166ed5"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Hepatitis B"},"clean_text":{"kind":"string","value":"Hepatitis B | Disease Directory | Travelers' Health | CDC\n\n### Hepatitis B\n### What is hepatitis B?\nHepatitis B is a vaccine-preventable liver disease. Hepatitis B virus is found in the blood and body fluids of infected people. People with hepatitis B virus infection can spread it to others.\nYou can get hepatitis B virus if you\n- Have sex with an infected partner.\n- Share needles, syringes, or drug preparation equipment with an infected person.\n- Share personal care items such as razors, toothbrushes, or medical equipment, such as a glucose monitor, with an infected person.\n- Get cut with a sharp instrument or have a needlestick injury in a health care setting.\n- Touch the blood or open sores of an infected person.\n- Hepatitis B can be spread from mother to baby during pregnancy or childbirth.\nEarly symptoms of hepatitis B may include fever, fatigue, loss of appetite, nausea, vomiting, abdominal pain, dark urine, clay-colored bowel movements, joint pain, and jaundice (yellow color in the skin or the eyes).\nFor some people, hepatitis B can become a chronic infection. The long-term health effects of chronic hepatitis B can cause early death from liver disease and liver cancer.\n### Who is at risk?\nInformation by Destination\n\nWhere are you going?\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" - value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n window.location = url;\nHepatitis B occurs in nearly every part of the world but is more common in some countries in Asia, Africa, South America and the Caribbean. \nAlthough the risk to most travelers is low, people who travel for medical purposes ([medical tourists](/travel/yellowbook/2020/travel-for-work-other-reasons/medical-tourism)) or people who need emergency medical care while traveling may be more likely to get infected. \n### What can travelers do to prevent disease?\nThe best way to protect yourself against hepatitis B is by getting vaccinated. Hepatitis B vaccine is a routine vaccination that infants in the United States receive at birth. The hepatitis B vaccine is over 90% effective and has been routinely recommended for infants since 1991. The vaccine is given in 2, 3, or 4 shots, and the series of shots is usually completed by 6 months of age.\nHepatitis B vaccine is recommended for all unvaccinated travelers under 60 years old and is also recommended for travelers 60 years and older going to a country where hepatitis B virus infection is common. The vaccine is given in 2 or 3 doses. To find the hepatitis B vaccine recommendations for your destination check [CDC's destination pages.](/travel/destinations/list)\nIt usually takes 6 months to be fully vaccinated against hepatitis B so if you’ll be traveling internationally within 6 months talk to your doctor about accelerated vaccination options including the 2-dose series (Heplisav-B) and [accelerated dosing](https://www.cdc.gov/hepatitis/hbv/hbvfaq.htm#D4) of the combination hepatitis A and hepatitis B vaccine.\n"},"raw_text":{"kind":"string","value":"\n\n### Hepatitis B\n\n\n\n\n### What is hepatitis B?\n\nHepatitis B is a vaccine-preventable liver disease. Hepatitis B virus is found in the blood and body fluids of infected people. People with hepatitis B virus infection can spread it to others.\n\nYou can get hepatitis B virus if you\n\n* Have sex with an infected partner.\n* Share needles, syringes, or drug preparation equipment with an infected person.\n* Share personal care items such as razors, toothbrushes, or medical equipment, such as a glucose monitor, with an infected person.\n* Get cut with a sharp instrument or have a needlestick injury in a health care setting.\n* Touch the blood or open sores of an infected person.\n* Hepatitis B can be spread from mother to baby during pregnancy or childbirth.\n\nEarly symptoms of hepatitis B may include fever, fatigue, loss of appetite, nausea, vomiting, abdominal pain, dark urine, clay-colored bowel movements, joint pain, and jaundice (yellow color in the skin or the eyes).\n\nFor some people, hepatitis B can become a chronic infection. The long-term health effects of chronic hepatitis B can cause early death from liver disease and liver cancer.\n\n### Who is at risk?\n\n\nInformation by Destination\n\nWhere are you going?\n\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n function goSelectPage(){ \n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" + value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n }else{\n window.location = url;\n }\n }\n\n \n \n\nHepatitis B occurs in nearly every part of the world but is more common in some countries in Asia, Africa, South America and the Caribbean. \n\nAlthough the risk to most travelers is low, people who travel for medical purposes ([medical tourists](/travel/yellowbook/2020/travel-for-work-other-reasons/medical-tourism)) or people who need emergency medical care while traveling may be more likely to get infected. \n\n### What can travelers do to prevent disease?\n\nThe best way to protect yourself against hepatitis B is by getting vaccinated. Hepatitis B vaccine is a routine vaccination that infants in the United States receive at birth. The hepatitis B vaccine is over 90% effective and has been routinely recommended for infants since 1991. The vaccine is given in 2, 3, or 4 shots, and the series of shots is usually completed by 6 months of age.\n\nHepatitis B vaccine is recommended for all unvaccinated travelers under 60 years old and is also recommended for travelers 60 years and older going to a country where hepatitis B virus infection is common. The vaccine is given in 2 or 3 doses. To find the hepatitis B vaccine recommendations for your destination check [CDC's destination pages.](/travel/destinations/list)\n\nIt usually takes 6 months to be fully vaccinated against hepatitis B so if you’ll be traveling internationally within 6 months talk to your doctor about accelerated vaccination options including the 2-dose series (Heplisav-B) and [accelerated dosing](https://www.cdc.gov/hepatitis/hbv/hbvfaq.htm#D4) of the combination hepatitis A and hepatitis B vaccine.\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### More Information\n\n* [Hepatitis B Homepage](http://www.cdc.gov/hepatitis/HBV/index.htm)\n* CDC Yellow Book: [Hepatitis B](/travel/yellowbook/2020/travel-related-infectious-diseases/hepatitis-b)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":679,"cells":{"id":{"kind":"string","value":"192a349dfbc829a9922d85ce603a8cb0e57e4f4f"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Hepatitis C"},"clean_text":{"kind":"string","value":"Hepatitis C | Disease Directory | Travelers' Health | CDC\n\n### Hepatitis C\n### What is hepatitis C?\nHepatitis C virus can cause liver disease. Most people who get infected with hepatitis C virus will have it the rest of their life, this is called a chronic infection. Hepatitis C virus is found in the blood of infected people, who can spread it to others.\nYou can be infected with the hepatitis C virus if you\n- Share needles, syringes, or drug preparation equipment with an infected person\n- Share personal care items such as razors, toothbrushes, or medical equipment, such as a glucose monitor, with an infected person\n- Get a tattoo, body piercing, or acupuncture with unsterile equipment\n- Get cut with a sharp instrument or a needlestick injury in a health care setting\n- Have sex with an infected partner\n- Accidentally get stuck by a contaminated needle\nMany people infected with hepatitis C virus have no symptoms. Those with symptoms may have fever, fatigue, dark urine, clay-colored bowel movements, abdominal pain, loss of appetite, nausea, vomiting, joint pain, and yellow color in the skin or eyes (jaundice).\nAn infected person with or without symptoms may develop long-term complications of chronic infection that can result in serious liver damage, such as cirrhosis (scarring), liver failure, or liver cancer.\n### Who is at risk?\nInformation by Destination\n\nWhere are you going?\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" - value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n window.location = url;\nHepatitis C occurs in nearly every part of the world but is most common in some countries in Asia and Africa. This map shows the [global prevalence of hepatitis C virus infection](/travel/yellowbook/2020/travel-related-infectious-diseases/hepatitis-c#5521).\nAlthough the risk to most travelers is low, your chances of infection increase if you get a transfusion of unscreened blood, have medical or dental procedures abroad, get tattoos or piercings or receive acupuncture with unsterile needles, or have sex with a person infected with hepatitis C.\n### What can travelers do to prevent hepatitis C infection?\nThere is no vaccine to prevent hepatitis C. Although there are treatments for chronic hepatitis, it is better to prevent infection by taking the following steps:\n- Don’t inject drugs\n- Make sure tattoo, piercing, and acupuncture equipment has been sterilized\n- Don’t share toothbrushes or devices that can break the skin, including needles for tattoos, piercings, and acupuncture\n- Make sure medical and dental equipment has been sterilized\n- Use latex condoms correctly when having sex, especially with new partners\n"},"raw_text":{"kind":"string","value":"\n\n### Hepatitis C\n\n\n\n\n### What is hepatitis C?\n\nHepatitis C virus can cause liver disease. Most people who get infected with hepatitis C virus will have it the rest of their life, this is called a chronic infection. Hepatitis C virus is found in the blood of infected people, who can spread it to others.\n\nYou can be infected with the hepatitis C virus if you\n\n* Share needles, syringes, or drug preparation equipment with an infected person\n* Share personal care items such as razors, toothbrushes, or medical equipment, such as a glucose monitor, with an infected person\n* Get a tattoo, body piercing, or acupuncture with unsterile equipment\n* Get cut with a sharp instrument or a needlestick injury in a health care setting\n* Have sex with an infected partner\n* Accidentally get stuck by a contaminated needle\n\nMany people infected with hepatitis C virus have no symptoms. Those with symptoms may have fever, fatigue, dark urine, clay-colored bowel movements, abdominal pain, loss of appetite, nausea, vomiting, joint pain, and yellow color in the skin or eyes (jaundice).\n\nAn infected person with or without symptoms may develop long-term complications of chronic infection that can result in serious liver damage, such as cirrhosis (scarring), liver failure, or liver cancer.\n\n### Who is at risk?\n\n\nInformation by Destination\n\nWhere are you going?\n\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n function goSelectPage(){ \n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" + value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n }else{\n window.location = url;\n }\n }\n\n \n \n\nHepatitis C occurs in nearly every part of the world but is most common in some countries in Asia and Africa. This map shows the [global prevalence of hepatitis C virus infection](/travel/yellowbook/2020/travel-related-infectious-diseases/hepatitis-c#5521).\n\nAlthough the risk to most travelers is low, your chances of infection increase if you get a transfusion of unscreened blood, have medical or dental procedures abroad, get tattoos or piercings or receive acupuncture with unsterile needles, or have sex with a person infected with hepatitis C.\n\n### What can travelers do to prevent hepatitis C infection?\n\nThere is no vaccine to prevent hepatitis C. Although there are treatments for chronic hepatitis, it is better to prevent infection by taking the following steps:\n\n* Don’t inject drugs\n* Make sure tattoo, piercing, and acupuncture equipment has been sterilized\n* Don’t share toothbrushes or devices that can break the skin, including needles for tattoos, piercings, and acupuncture\n* Make sure medical and dental equipment has been sterilized\n* Use latex condoms correctly when having sex, especially with new partners\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### More Information\n\n* [Hepatitis C Information](https://www.cdc.gov/hepatitis/hcv/index.htm)\n* CDC Yellow Book: [Hepatitis C](/travel/yellowbook/2020/travel-related-infectious-diseases/hepatitis-c)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":680,"cells":{"id":{"kind":"string","value":"451914a549d8be0cee384bd49829657413c18150"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Hepatitis E"},"clean_text":{"kind":"string","value":"Hepatitis E | Disease Directory | Travelers' Health | CDC\n\n### Hepatitis E\n### What is hepatitis E?\nHepatitis E virus can cause liver disease. Hepatitis E virus is mainly found in places around the world where sanitation is poor and there is limited access to safe drinking water.\nYou can get infected with hepatitis E virus if you\n- Eat food or drink beverages contaminated with hepatitis E virus\n- Eat shellfish or uncooked or undercooked products made from deer, boar, and pig\nSome people who get hepatitis E never feel sick. Others have symptoms that may include fever, tiredness, loss of appetite, nausea, vomiting, stomach pain, dark urine, clay-colored bowel movements, joint pain, and yellow color in the skin or eyes (jaundice). Symptoms usually last less than two months but can last for up to six months.\nMost people infected with hepatitis E virus recover with no lasting liver damage. However, people with preexisting liver disease can get seriously ill. Infected pregnant women can get seriously ill and have pregnancy complications.\n### Who is at risk?\nInformation by Destination\n\nWhere are you going?\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" - value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n window.location = url;\nHepatitis E is found worldwide. Hepatitis E is more widespread in low- and middle-income countries, specifically in Asia and Africa, that do not have adequate food and water safety standards. Travelers to these countries are more likely to get infected.\nIn addition, travelers working in health care settings or refugee camps may be more at risk of infection. Many large hepatitis E outbreaks have occurred among refugees and internally displaced people living in camps.\n### What can travelers do to prevent hepatitis E?\nThere is no approved vaccine in the United States to prevent hepatitis E. Travelers can help prevent hepatitis E by taking the following steps:\nChoose food and drinks carefully\n- Only drink beverages from factory-sealed containers\n- Avoid ice because it may have been made from unclean water\n- Only drink pasteurized milk\n- Only eat foods that are cooked and served hot\n- Avoid food that has been sitting on a buffet\n- Only eat raw fruits and vegetables if you have washed them in clean water or peeled them\n"},"raw_text":{"kind":"string","value":"\n\n### Hepatitis E\n\n\n\n\n### What is hepatitis E?\n\n\nHepatitis E virus can cause liver disease. Hepatitis E virus is mainly found in places around the world where sanitation is poor and there is limited access to safe drinking water.\n\nYou can get infected with hepatitis E virus if you\n\n* Eat food or drink beverages contaminated with hepatitis E virus\n* Eat shellfish or uncooked or undercooked products made from deer, boar, and pig\n\nSome people who get hepatitis E never feel sick. Others have symptoms that may include fever, tiredness, loss of appetite, nausea, vomiting, stomach pain, dark urine, clay-colored bowel movements, joint pain, and yellow color in the skin or eyes (jaundice). Symptoms usually last less than two months but can last for up to six months.\n\nMost people infected with hepatitis E virus recover with no lasting liver damage. However, people with preexisting liver disease can get seriously ill. Infected pregnant women can get seriously ill and have pregnancy complications.\n\n### Who is at risk?\n\n\nInformation by Destination\n\nWhere are you going?\n\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n function goSelectPage(){ \n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" + value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n }else{\n window.location = url;\n }\n }\n\n \n \n\nHepatitis E is found worldwide. Hepatitis E is more widespread in low- and middle-income countries, specifically in Asia and Africa, that do not have adequate food and water safety standards. Travelers to these countries are more likely to get infected.\n\nIn addition, travelers working in health care settings or refugee camps may be more at risk of infection. Many large hepatitis E outbreaks have occurred among refugees and internally displaced people living in camps.\n\n### What can travelers do to prevent hepatitis E?\n\nThere is no approved vaccine in the United States to prevent hepatitis E. Travelers can help prevent hepatitis E by taking the following steps:\n\n**Choose food and drinks carefully**\n\n* Only drink beverages from factory-sealed containers\n* Avoid ice because it may have been made from unclean water\n* Only drink pasteurized milk\n* Only eat foods that are cooked and served hot\n* Avoid food that has been sitting on a buffet\n* Only eat raw fruits and vegetables if you have washed them in clean water or peeled them\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### More Information\n\n* [Hepatitis E](https://www.cdc.gov/hepatitis/hev/index.htm)\n* [Hepatitis E—WHO Fact SheetExternal Link](http://www.who.int/mediacentre/factsheets/fs280/en/)\n* CDC Yellow Book: [Hepatitis E](/travel/yellowbook/2020/travel-related-infectious-diseases/hepatitis-e)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":681,"cells":{"id":{"kind":"string","value":"ac2fa3a1c74034ff37f3cae52a2e2dc39ff619e0"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Japanese Encephalitis"},"clean_text":{"kind":"string","value":"Japanese Encephalitis | Disease Directory | Travelers' Health | CDC\n\n### Japanese Encephalitis\n### What is Japanese encephalitis?\n\nJapanese encephalitis virus is spread to people through the bite of an infected mosquito.\nMost people who get infected experience mild or no symptoms. In people who develop severe disease, early symptoms include fever, headache, and vomiting. These symptoms may be followed by disorientation, coma, and seizures. Seizures are more common in children.\n### Who is at risk?\nTravelers to some parts of Asia and the Western Pacific can get infected if bitten by an infected mosquito. However, for most travelers the chance of getting infected with Japanese encephalitis virus is low.\nActivities that can increase a traveler’s chance of getting Japanese encephalitis include:\n- Spending a lot of time outdoors in rural areas\n- Traveling during times of the year when mosquitoes are more common, such as during the summer\n- Traveling for long periods of time in a place that has Japanese encephalitis\nIn places with four seasons, your chances of getting Japanese encephalitis are greatest in the summer and fall. In tropical and subtropical areas, mosquitoes spread the virus all year long.\n### What can travelers do to prevent Japanese encephalitis?\nTravelers can protect themselves against Japanese encephalitis by taking the following steps.\nGet vaccinated if recommended:\nJapanese encephalitis vaccine is recommended for travelers who\n- Are moving to an area with Japanese encephalitis to live\n- Spend long periods of time, such as a month or more, in areas with Japanese encephalitis\n- Frequently travel to areas with Japanese encephalitis\nConsider vaccination for travelers\n- Spending less than a month in areas with Japanese encephalitis but will be doing activities that increase risk of infection, such as visiting rural areas, hiking or camping, or staying in places without air conditioning, screens, or bed nets\n- Going to areas with Japanese encephalitis who are uncertain of their activities or how long they will be there\nNot recommended for travelers planning short-term travel to urban areas or travel to areas with no clear Japanese encephalitis season.\nUse an EPA-registered insect repellent\n- Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.\n\t- Picaridin (known as KBR 3023 and icaridin outside the US)\n\t- Oil of lemon eucalyptus (OLE)\n\t- Para-menthane-diol (PMD)\nFind the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).\n\n- Insect Repellent Tips for Babies and Children\n\t- Dress your child in clothing that covers arms and legs.\n\t- Cover strollers and baby carriers with mosquito netting.\n\t- When using insect repellent on your child:\n\t\t- Always follow label instructions.\n\t\t- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.\n\t\t- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.\n\t\t\t- Adults: Spray insect repellent onto your hands and then apply to a child’s face.\n\t\t- If also using sunscreen, always apply insect repellent after sunscreen.\nWear long-sleeved shirts and long pants\nTreat clothing and gear with permethrin\n- Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.\n\t- Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.\n\t- Permethrin-treated clothing provides protection after multiple washings.\n\t- Read product information to find out how long the protection will last.\n- If treating items yourself, follow the product instructions.\n- Do not use permethrin products directly on skin.\n- Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).\nKeep mosquitoes out of your hotel room or lodging\n- Choose a hotel or lodging with air conditioning or window and door screens.\n- Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.\nSleep under a mosquito net\n\n- Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.\n- Buy a mosquito net at your local outdoor store or online before traveling overseas.\n- Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.\n- [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.\n\t- Permethrin is an insecticide that kills mosquitoes and other insects.\n\t- To determine if you can wash a treated mosquito net, follow the label instructions.\nIf you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).\n"},"raw_text":{"kind":"string","value":"\n\n### Japanese Encephalitis\n\n\n\n\n### What is Japanese encephalitis?\n\n\nJapanese encephalitis virus is spread to people through the bite of an infected mosquito.\n\nMost people who get infected experience mild or no symptoms. In people who develop severe disease, early symptoms include fever, headache, and vomiting. These symptoms may be followed by disorientation, coma, and seizures. Seizures are more common in children.\n\n### Who is at risk?\n\nTravelers to some parts of Asia and the Western Pacific can get infected if bitten by an infected mosquito. However, for most travelers the chance of getting infected with Japanese encephalitis virus is low.\n\nActivities that can increase a traveler’s chance of getting Japanese encephalitis include:\n\n* Spending a lot of time outdoors in rural areas\n* Traveling during times of the year when mosquitoes are more common, such as during the summer\n* Traveling for long periods of time in a place that has Japanese encephalitis\n\nIn places with four seasons, your chances of getting Japanese encephalitis are greatest in the summer and fall. In tropical and subtropical areas, mosquitoes spread the virus all year long.\n\n### What can travelers do to prevent Japanese encephalitis?\n\nTravelers can protect themselves against Japanese encephalitis by taking the following steps.\n\n**Get vaccinated if recommended:**\n\nJapanese encephalitis vaccine is recommended for travelers who\n\n* Are moving to an area with Japanese encephalitis to live\n* Spend long periods of time, such as a month or more, in areas with Japanese encephalitis\n* Frequently travel to areas with Japanese encephalitis\n\nConsider vaccination for travelers\n\n* Spending less than a month in areas with Japanese encephalitis but will be doing activities that increase risk of infection, such as visiting rural areas, hiking or camping, or staying in places without air conditioning, screens, or bed nets\n* Going to areas with Japanese encephalitis who are uncertain of their activities or how long they will be there\n\nNot recommended for travelers planning short-term travel to urban areas or travel to areas with no clear Japanese encephalitis season.\n\n**Use an EPA-registered insect repellent**\n\n\n\n* Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.\n\t+ DEET\n\t+ Picaridin (known as KBR 3023 and icaridin outside the US)\n\t+ IR3535\n\t+ Oil of lemon eucalyptus (OLE)\n\t+ Para-menthane-diol (PMD)\n\t+ 2-undecanone\n\nFind the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).\n\n\n\n* Insect Repellent Tips for Babies and Children\n\t+ Dress your child in clothing that covers arms and legs.\n\t+ Cover strollers and baby carriers with mosquito netting.\n\t+ When using insect repellent on your child:\n\t\t- Always follow label instructions.\n\t\t- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.\n\t\t- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.\n\t\t\t* Adults: Spray insect repellent onto your hands and then apply to a child’s face.\n\t\t- If also using sunscreen, always apply insect repellent after sunscreen.\n\n**Wear long-sleeved shirts and long pants**\n\n**Treat clothing and gear with permethrin**\n\n\n\n* Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.\n\t+ Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.\n\t+ Permethrin-treated clothing provides protection after multiple washings.\n\t+ Read product information to find out how long the protection will last.\n* If treating items yourself, follow the product instructions.\n* Do not use permethrin products directly on skin.\n* Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).\n\n**Keep mosquitoes out of your hotel room or lodging**\n\n* Choose a hotel or lodging with air conditioning or window and door screens.\n* Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.\n\n**Sleep under a mosquito net**\n\n\n\n* Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.\n* Buy a mosquito net at your local outdoor store or online before traveling overseas.\n* Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.\n* [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.\n\t+ Permethrin is an insecticide that kills mosquitoes and other insects.\n\t+ To determine if you can wash a treated mosquito net, follow the label instructions.\n\nIf you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).\n\n \n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n\n### More Information\n\n* CDC's [Japanese encephalitis page](http://www.cdc.gov/japaneseencephalitis/)\n* [Avoid Bug Bites](/travel/page/avoid-bug-bites)\n* [JE Vaccine Information Statement (VIS)](http://www.cdc.gov/vaccines/hcp/vis/vis-statements/je-ixiaro.pdf)\n* CDC Yellow Book: [Japanese Encephalitis](/travel/yellowbook/2012/chapter-3-infectious-diseases-related-to-travel/japanese-encephalitis.htm)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":682,"cells":{"id":{"kind":"string","value":"8b09643e639a8a2d8b031d8afc35b28ba1b1d866"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Leishmaniasis"},"clean_text":{"kind":"string","value":"Leishmaniasis | Disease Directory | Travelers' Health | CDC\n\n### What is leishmaniasis?\nLeishmaniasis is a disease caused by a parasite. Sand flies can spread this parasite to people when the sand fly bites them.\nTwo common forms of leishmaniasis are - cutaneous- and - visceral- .\nThe most common symptom of - cutaneous leishmaniasis- is skin sores that can change in size and appearance over time. These sores may be closed, like a lump or a bump, or open (ulcer). Some people have swollen glands near the sores.\nCommon symptoms of - visceral leishmaniasis- are fever and weight loss. People with visceral leishmaniasis can also have an enlarged spleen and liver, low red blood cell count (anemia), low white blood cell count (leukopenia), and low platelet count (thrombocytopenia).\nInformation by Destination\n\nWhere are you going?\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" - value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n window.location = url;\nSome people with leishmaniasis never have symptoms.\n### Who is at risk?\nSand flies are found in certain parts of Asia, the Middle East, Africa, Southern Europe, Mexico, Central America, and South America. Travelers going to these areas are at risk of being bitten by sand flies and getting infected.\nSee if leishmaniasis is a concern at [your destination](/travel/destinations/list).\n### What can travelers do to prevent leishmaniasis?\nThere is no vaccine or medicine that prevents leishmaniasis. Travelers can take the following steps to prevent sand fly bites:\nUse an EPA-registered insect repellent\n- Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.\n\t- Picaridin (known as KBR 3023 and icaridin outside the US)\n\t- Oil of lemon eucalyptus (OLE)\n\t- Para-menthane-diol (PMD)\nFind the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).\n\n- Insect Repellent Tips for Babies and Children\n\t- Dress your child in clothing that covers arms and legs.\n\t- Cover strollers and baby carriers with mosquito netting.\n\t- When using insect repellent on your child:\n\t\t- Always follow label instructions.\n\t\t- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.\n\t\t- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.\n\t\t\t- Adults: Spray insect repellent onto your hands and then apply to a child’s face.\n\t\t- If also using sunscreen, always apply insect repellent after sunscreen.\nWear long-sleeved shirts and long pants\nTreat clothing and gear with permethrin\n- Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.\n\t- Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.\n\t- Permethrin-treated clothing provides protection after multiple washings.\n\t- Read product information to find out how long the protection will last.\n- If treating items yourself, follow the product instructions.\n- Do not use permethrin products directly on skin.\n- Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).\nKeep mosquitoes out of your hotel room or lodging\n- Choose a hotel or lodging with air conditioning or window and door screens.\n- Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.\nSleep under a mosquito net\n\n- Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.\n- Buy a mosquito net at your local outdoor store or online before traveling overseas.\n- Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.\n- [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.\n\t- Permethrin is an insecticide that kills mosquitoes and other insects.\n\t- To determine if you can wash a treated mosquito net, follow the label instructions.\nIf you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).\n"},"raw_text":{"kind":"string","value":"\n\n### Leishmaniasis\n\n\n\n\n\n\n### What is leishmaniasis?\n\nLeishmaniasis is a disease caused by a parasite. Sand flies can spread this parasite to people when the sand fly bites them.\n\nTwo common forms of leishmaniasis are *cutaneous* and *visceral*.\n\nThe most common symptom of *cutaneous leishmaniasis* is skin sores that can change in size and appearance over time. These sores may be closed, like a lump or a bump, or open (ulcer). Some people have swollen glands near the sores.\n\nCommon symptoms of *visceral leishmaniasis* are fever and weight loss. People with visceral leishmaniasis can also have an enlarged spleen and liver, low red blood cell count (anemia), low white blood cell count (leukopenia), and low platelet count (thrombocytopenia).\n\n\nInformation by Destination\n\nWhere are you going?\n\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n function goSelectPage(){ \n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" + value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n }else{\n window.location = url;\n }\n }\n\n \n \n\nSome people with leishmaniasis never have symptoms.\n\n### Who is at risk?\n\nSand flies are found in certain parts of Asia, the Middle East, Africa, Southern Europe, Mexico, Central America, and South America. Travelers going to these areas are at risk of being bitten by sand flies and getting infected.\n\nSee if leishmaniasis is a concern at [your destination](/travel/destinations/list).\n\n### What can travelers do to prevent leishmaniasis?\n\nThere is no vaccine or medicine that prevents leishmaniasis. **Travelers can take the following steps to prevent sand fly bites:**\n\n**Use an EPA-registered insect repellent**\n\n\n\n* Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.\n\t+ DEET\n\t+ Picaridin (known as KBR 3023 and icaridin outside the US)\n\t+ IR3535\n\t+ Oil of lemon eucalyptus (OLE)\n\t+ Para-menthane-diol (PMD)\n\t+ 2-undecanone\n\nFind the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).\n\n\n\n* Insect Repellent Tips for Babies and Children\n\t+ Dress your child in clothing that covers arms and legs.\n\t+ Cover strollers and baby carriers with mosquito netting.\n\t+ When using insect repellent on your child:\n\t\t- Always follow label instructions.\n\t\t- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.\n\t\t- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.\n\t\t\t* Adults: Spray insect repellent onto your hands and then apply to a child’s face.\n\t\t- If also using sunscreen, always apply insect repellent after sunscreen.\n\n**Wear long-sleeved shirts and long pants**\n\n**Treat clothing and gear with permethrin**\n\n\n\n* Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.\n\t+ Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.\n\t+ Permethrin-treated clothing provides protection after multiple washings.\n\t+ Read product information to find out how long the protection will last.\n* If treating items yourself, follow the product instructions.\n* Do not use permethrin products directly on skin.\n* Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).\n\n**Keep mosquitoes out of your hotel room or lodging**\n\n* Choose a hotel or lodging with air conditioning or window and door screens.\n* Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.\n\n**Sleep under a mosquito net**\n\n\n\n* Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.\n* Buy a mosquito net at your local outdoor store or online before traveling overseas.\n* Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.\n* [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.\n\t+ Permethrin is an insecticide that kills mosquitoes and other insects.\n\t+ To determine if you can wash a treated mosquito net, follow the label instructions.\n\nIf you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).\n\n \n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### More Information\n\n* [Leishmaniasis Information](https://www.cdc.gov/parasites/leishmaniasis/)\n* CDC Yellow Book: [Cutaneous Leishmaniasis](/travel/yellowbook/2020/travel-related-infectious-diseases/leishmaniasis-cutaneous)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":683,"cells":{"id":{"kind":"string","value":"3fb3bb853b27e5743c7881280068f558fe470937"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Leptospirosis"},"clean_text":{"kind":"string","value":"Leptospirosis | Disease Directory | Travelers' Health | CDC\n\n### What is leptospirosis?\n\nLeptospirosis is a disease caused by bacteria. Infected animals spread the bacteria through their urine (pee). When infected animals pee, the bacteria get into the water or soil and can live there for weeks to months.\nYou can be infected if you touch fresh water, soil, or other objects contaminated with infected animal urine. The most common ways to get infected is urine or contaminated water getting in your eyes, nose, mouth, or broken skin (such as a cut or scratch). You can also get infected by eating contaminated food or drinking contaminated water.\nSome people with leptospirosis do not have any symptoms. When symptoms occur, they can include fever, headache, chills, muscle aches, vomiting, jaundice (yellow eyes and skin), red eyes, stomach pain, diarrhea, and sometimes a rash. Without proper treatment with antibiotics, people with leptospirosis may develop serious problems with their kidneys, liver, or lining of the brain and spinal cord (meningitis). In some cases, leptospirosis can cause death.\n### Who is at risk?\nInformation by Destination\n\nWhere are you going?\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" - value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n window.location = url;\nLeptospirosis is found in countries around the world. It is most common in temperate or tropical climate regions that include South and Southeast Asia, Oceania, the Caribbean, parts of sub-Saharan Africa, and parts of Latin America.\nTravelers are more likely to get leptospirosis if they\n- Visit flooded or recently flooded areas\n- [Swim, wade, kayak, or raft](http://www.cdc.gov/leptospirosis/features/adventure-racing.html) in potentially contaminated fresh water like lakes and rivers\n- Visit urban areas with poor sanitation\n- Touch animals or their body fluids. Animals that can be infected are mammals, including rodents, cows, sheep/goats, pigs, horses, dogs, and wildlife.\n### What can travelers do to prevent leptospirosis?\nThere is no vaccine approved for use in the United States to prevent leptospirosis in people.\nTravelers can take the following steps to protect themselves:\n- Avoid touching fresh water or soil that may be contaminated with animal urine\n- Avoid touching objects that may be contaminated with animal urine, such as animal bedding\n- Don't wade, swim, or put your head in floodwaters or water from lakes, rivers, or swamps. Especially avoid freshwater contact after flooding or heavy rain.\n- If it is not possible to avoid wading in floodwaters or other fresh water, wear protective clothing like footwear and cover cuts and wounds with waterproof bandages or dressing.\n- Make water [safe to drink](https://www.cdc.gov/disasters/foodwater/facts.html) by boiling or using an appropriate chemical treatment\nFor some travelers, taking medicine before you travel to prevent leptospirosis might be an option. Talk to your health care provider before you travel and tell them about all your planned activities.\n"},"raw_text":{"kind":"string","value":"\n\n### Leptospirosis\n\n\n\n\n### What is leptospirosis?\n\n\nLeptospirosis is a disease caused by bacteria. Infected animals spread the bacteria through their urine (pee). When infected animals pee, the bacteria get into the water or soil and can live there for weeks to months.\n\nYou can be infected if you touch fresh water, soil, or other objects contaminated with infected animal urine. The most common ways to get infected is urine or contaminated water getting in your eyes, nose, mouth, or broken skin (such as a cut or scratch). You can also get infected by eating contaminated food or drinking contaminated water.\n\nSome people with leptospirosis do not have any symptoms. When symptoms occur, they can include fever, headache, chills, muscle aches, vomiting, jaundice (yellow eyes and skin), red eyes, stomach pain, diarrhea, and sometimes a rash. Without proper treatment with antibiotics, people with leptospirosis may develop serious problems with their kidneys, liver, or lining of the brain and spinal cord (meningitis). In some cases, leptospirosis can cause death.\n\n### Who is at risk?\n\n\nInformation by Destination\n\nWhere are you going?\n\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n function goSelectPage(){ \n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" + value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n }else{\n window.location = url;\n }\n }\n\n \n \n\nLeptospirosis is found in countries around the world. It is most common in temperate or tropical climate regions that include South and Southeast Asia, Oceania, the Caribbean, parts of sub-Saharan Africa, and parts of Latin America.\n\nTravelers are more likely to get leptospirosis if they\n\n* Visit flooded or recently flooded areas\n* [Swim, wade, kayak, or raft](http://www.cdc.gov/leptospirosis/features/adventure-racing.html) in potentially contaminated fresh water like lakes and rivers\n* Visit urban areas with poor sanitation\n* Touch animals or their body fluids. Animals that can be infected are mammals, including rodents, cows, sheep/goats, pigs, horses, dogs, and wildlife.\n\n### What can travelers do to prevent leptospirosis?\n\nThere is no vaccine approved for use in the United States to prevent leptospirosis in people.\n\nTravelers can take the following steps to protect themselves:\n\n* Avoid touching fresh water or soil that may be contaminated with animal urine\n* Avoid touching objects that may be contaminated with animal urine, such as animal bedding\n* Don't wade, swim, or put your head in floodwaters or water from lakes, rivers, or swamps. Especially avoid freshwater contact after flooding or heavy rain.\n* If it is not possible to avoid wading in floodwaters or other fresh water, wear protective clothing like footwear and cover cuts and wounds with waterproof bandages or dressing.\n* Make water [safe to drink](https://www.cdc.gov/disasters/foodwater/facts.html) by boiling or using an appropriate chemical treatment\n\nFor some travelers, taking medicine before you travel to prevent leptospirosis might be an option. Talk to your health care provider before you travel and tell them about all your planned activities.\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### More Information\n\n* CDC Website: [Leptospirosis](http://www.cdc.gov/leptospirosis/index.html)\n* CDC Yellow Book: [Leptospriosis](/travel/yellowbook/2018/infectious-diseases-related-to-travel/leptospirosis)\n\n\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":684,"cells":{"id":{"kind":"string","value":"cfeedbae41c33dd6cbd313991bbc221ecaa66916"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Middle East Respiratory Syndrome (MERS)"},"clean_text":{"kind":"string","value":"Middle East Respiratory Syndrome (MERS) | Disease Directory | Travelers' Health | CDC\n\n### Middle East Respiratory Syndrome (MERS)\n### What is Middle East Respiratory Syndrome (MERS)?\nMiddle East respiratory syndrome (MERS) is an illness caused by a coronavirus called MERS-CoV. Scientists do not yet fully understand how the virus spreads. It is likely that a person can get infected with the virus if they:\n- Have close contact with someone or touch the body fluids of a person sick with MERS, for example living with or caring for a person sick with MERS.\n- Breathe in infectious droplets released into the air when a person sick with MERS coughs or sneezes.\nThe virus can also spread from camels to people, although it is unclear how that occurs. Touching camels or being around infected camels or their body fluids (milk, feces/poop, urine/pee, saliva/spit, etc.) can increase a person’s chances of becoming infected with MERS-CoV.\nCommon MERS symptoms include fever, cough, and shortness of breath. Some people also get diarrhea, nausea, and vomiting. Severe complications include pneumonia and kidney failure. MERS can cause death, and most people who died have been older adults or people with a weakened immune system or an existing illness or disease (e.g., diabetes, cancer, lung disease, heart disease, or kidney disease).\n### Who can get MERS?\nInformation by Destination\n\nWhere are you going?\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" - value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n window.location = url;\nThough MERS is rare, MERS has been found in countries on or near the Arabian Peninsula. These countries include Bahrain, Iran, Jordan, Kuwait, Lebanon, Oman, Qatar, Saudi Arabia, United Arab Emirates (UAE), and Yemen.\n### What can travelers do to prevent MERS?\nThere is no vaccine to prevent MERS, but you can take steps to protect yourself.\nAvoid touching animals when traveling:\n- Avoid touching live animals, especially camels, when traveling.\n- Avoid visiting markets or farms with animals, including camels.\n- Do not touch dead animals.\n- Do not use products made from camels or wild animals.\n- Avoid drinking raw (unpasteurized) camel milk or camel urine or eating undercooked camel meat (cook to 145°F).\n- Do not touch materials, such as bedding, that animals use.\nPeople with diabetes, kidney failure, chronic lung disease, and weakened immune systems are more likely to get severe MERS. People with these health conditions should pay extra attention to the guidelines above and avoid close contact with sick people and camels.\nHere are some good tips on how to stay healthy when you travel to avoid getting sick\n- Wash your hands often with soap and water for at least 20 seconds.\n- If soap and water aren’t available, clean hands with hand sanitizer containing at least 60% alcohol.\n- Avoid touching your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean.\n- Cover your mouth and nose with a tissue or your sleeve (not your hands) when coughing or sneezing.\n- Try to avoid close contact (e.g., kissing, hugging, or sharing eating utensils or cups) with people who are sick.\n"},"raw_text":{"kind":"string","value":"\n\n### Middle East Respiratory Syndrome (MERS)\n\n\n\n\n### What is Middle East Respiratory Syndrome (MERS)?\n\nMiddle East respiratory syndrome (MERS) is an illness caused by a coronavirus called MERS-CoV. Scientists do not yet fully understand how the virus spreads. It is likely that a person can get infected with the virus if they:\n\n* Have close contact with someone or touch the body fluids of a person sick with MERS, for example living with or caring for a person sick with MERS.\n* Breathe in infectious droplets released into the air when a person sick with MERS coughs or sneezes.\n\nThe virus can also spread from camels to people, although it is unclear how that occurs. Touching camels or being around infected camels or their body fluids (milk, feces/poop, urine/pee, saliva/spit, etc.) can increase a person’s chances of becoming infected with MERS-CoV.\n\nCommon MERS symptoms include fever, cough, and shortness of breath. Some people also get diarrhea, nausea, and vomiting. Severe complications include pneumonia and kidney failure. MERS can cause death, and most people who died have been older adults or people with a weakened immune system or an existing illness or disease (e.g., diabetes, cancer, lung disease, heart disease, or kidney disease).\n\n### Who can get MERS?\n\n\nInformation by Destination\n\nWhere are you going?\n\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n function goSelectPage(){ \n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" + value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n }else{\n window.location = url;\n }\n }\n\n \n \n\nThough MERS is rare, MERS has been found in countries on or near the Arabian Peninsula. These countries include Bahrain, Iran, Jordan, Kuwait, Lebanon, Oman, Qatar, Saudi Arabia, United Arab Emirates (UAE), and Yemen.\n\n### What can travelers do to prevent MERS?\n\nThere is no vaccine to prevent MERS, but you can take steps to protect yourself.\n\n**Avoid touching animals when traveling:**\n\n* Avoid touching live animals, especially camels, when traveling.\n* Avoid visiting markets or farms with animals, including camels.\n* Do not touch dead animals.\n* Do not use products made from camels or wild animals.\n* Avoid drinking raw (unpasteurized) camel milk or camel urine or eating undercooked camel meat (cook to 145°F).\n* Do not touch materials, such as bedding, that animals use.\n\nPeople with diabetes, kidney failure, chronic lung disease, and weakened immune systems are more likely to get severe MERS. People with these health conditions should pay extra attention to the guidelines above and avoid close contact with sick people and camels.\n\n**Here are some good tips on how to stay healthy when you travel to avoid getting sick**\n\n* Wash your hands often with soap and water for at least 20 seconds.\n* If soap and water aren’t available, clean hands with hand sanitizer containing at least 60% alcohol.\n* Avoid touching your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean.\n* Cover your mouth and nose with a tissue or your sleeve (not your hands) when coughing or sneezing.\n* Try to avoid close contact (e.g., kissing, hugging, or sharing eating utensils or cups) with people who are sick.\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. Avoid contact with other people while you are sick.\n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### More Information\n\n* [CDC MERS Guidance for Travel](https://www.cdc.gov/coronavirus/mers/travel.html)\n* CDC Yellow Book: [MERS](/travel/yellowbook/2020/travel-related-infectious-diseases/middle-east-respiratory-syndrome-mers)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":685,"cells":{"id":{"kind":"string","value":"b7c33f2d57672db304090b9d76d531942f26b005"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Malaria"},"clean_text":{"kind":"string","value":"Malaria | Disease Directory | Travelers' Health | CDC\n\n### What is malaria?\nMalaria is a disease caused by a parasite. Mosquitoes spread the parasite to people when they bite them.\nMalaria symptoms usually appear within in 7 to 30 days but can take up to one year to develop. Symptoms may include high fevers and shaking chills, flu-like illness. Without treatment, malaria can cause severe illness and death.\n### Who is at risk?\nThe mosquitoes that spread malaria are found in Africa, Central and South America, parts of the Caribbean, Asia, Eastern Europe, and the South Pacific (See maps: [Eastern Hemisphere](/travel/yellowbook/2020/travel-related-infectious-diseases/malaria#5544) and [Western Hemisphere](/travel/yellowbook/2020/travel-related-infectious-diseases/malaria#5542)). Travelers going to these countries may get bit by mosquitoes and get infected.\nInformation by Destination\n\nWhere are you going?\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" - value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n window.location = url;\nAbout 2,000 cases of malaria are diagnosed in the United States annually, mostly among returned travelers.\n### What can travelers do to prevent malaria?\nTravelers can protect themselves from malaria by taking prescription medicine and preventing mosquito bites. There is no malaria vaccine.\nTake Malaria Medicine\nCheck your [destination](/travel/destinations/list) to see if you should take prescription malaria medication. Depending on the medicine you take, you will need to start taking this medicine multiple days before your trip, as well as during and after your trip. Talk to your doctor about [which medicine you should take](https://www.cdc.gov/malaria/travelers/drugs.html).\nTravelers should also take steps to prevent mosquito bites.\nUse an EPA-registered insect repellent\n- Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.\n\t- Picaridin (known as KBR 3023 and icaridin outside the US)\n\t- Oil of lemon eucalyptus (OLE)\n\t- Para-menthane-diol (PMD)\nFind the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).\n\n- Insect Repellent Tips for Babies and Children\n\t- Dress your child in clothing that covers arms and legs.\n\t- Cover strollers and baby carriers with mosquito netting.\n\t- When using insect repellent on your child:\n\t\t- Always follow label instructions.\n\t\t- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.\n\t\t- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.\n\t\t\t- Adults: Spray insect repellent onto your hands and then apply to a child’s face.\n\t\t- If also using sunscreen, always apply insect repellent after sunscreen.\nWear long-sleeved shirts and long pants\nTreat clothing and gear with permethrin\n- Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.\n\t- Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.\n\t- Permethrin-treated clothing provides protection after multiple washings.\n\t- Read product information to find out how long the protection will last.\n- If treating items yourself, follow the product instructions.\n- Do not use permethrin products directly on skin.\n- Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).\nKeep mosquitoes out of your hotel room or lodging\n- Choose a hotel or lodging with air conditioning or window and door screens.\n- Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.\nSleep under a mosquito net\n\n- Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.\n- Buy a mosquito net at your local outdoor store or online before traveling overseas.\n- Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.\n- [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.\n\t- Permethrin is an insecticide that kills mosquitoes and other insects.\n\t- To determine if you can wash a treated mosquito net, follow the label instructions.\nIf you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).\n"},"raw_text":{"kind":"string","value":"\n\n### Malaria\n\n\n\n\n### What is malaria?\n\n\nMalaria is a disease caused by a parasite. Mosquitoes spread the parasite to people when they bite them.\n\nMalaria symptoms usually appear within in 7 to 30 days but can take up to one year to develop. Symptoms may include high fevers and shaking chills, flu-like illness. Without treatment, malaria can cause severe illness and death.\n\n### Who is at risk?\n\nThe mosquitoes that spread malaria are found in Africa, Central and South America, parts of the Caribbean, Asia, Eastern Europe, and the South Pacific (See maps: [Eastern Hemisphere](/travel/yellowbook/2020/travel-related-infectious-diseases/malaria#5544) and [Western Hemisphere](/travel/yellowbook/2020/travel-related-infectious-diseases/malaria#5542)). Travelers going to these countries may get bit by mosquitoes and get infected.\n\n\nInformation by Destination\n\nWhere are you going?\n\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n function goSelectPage(){ \n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" + value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n }else{\n window.location = url;\n }\n }\n\n \n \n\nAbout 2,000 cases of malaria are diagnosed in the United States annually, mostly among returned travelers.\n\n### What can travelers do to prevent malaria?\n\nTravelers can protect themselves from malaria by taking prescription medicine and preventing mosquito bites. There is no malaria vaccine.\n\n**Take Malaria Medicine**\n\nCheck your [destination](/travel/destinations/list) to see if you should take prescription malaria medication. Depending on the medicine you take, you will need to start taking this medicine multiple days before your trip, as well as during and after your trip. Talk to your doctor about [which medicine you should take](https://www.cdc.gov/malaria/travelers/drugs.html).\n\n**Travelers should also take steps to prevent mosquito bites.**\n\n**Use an EPA-registered insect repellent**\n\n\n\n* Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.\n\t+ DEET\n\t+ Picaridin (known as KBR 3023 and icaridin outside the US)\n\t+ IR3535\n\t+ Oil of lemon eucalyptus (OLE)\n\t+ Para-menthane-diol (PMD)\n\t+ 2-undecanone\n\nFind the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).\n\n\n\n* Insect Repellent Tips for Babies and Children\n\t+ Dress your child in clothing that covers arms and legs.\n\t+ Cover strollers and baby carriers with mosquito netting.\n\t+ When using insect repellent on your child:\n\t\t- Always follow label instructions.\n\t\t- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.\n\t\t- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.\n\t\t\t* Adults: Spray insect repellent onto your hands and then apply to a child’s face.\n\t\t- If also using sunscreen, always apply insect repellent after sunscreen.\n\n**Wear long-sleeved shirts and long pants**\n\n**Treat clothing and gear with permethrin**\n\n\n\n* Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.\n\t+ Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.\n\t+ Permethrin-treated clothing provides protection after multiple washings.\n\t+ Read product information to find out how long the protection will last.\n* If treating items yourself, follow the product instructions.\n* Do not use permethrin products directly on skin.\n* Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).\n\n**Keep mosquitoes out of your hotel room or lodging**\n\n* Choose a hotel or lodging with air conditioning or window and door screens.\n* Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.\n\n**Sleep under a mosquito net**\n\n\n\n* Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.\n* Buy a mosquito net at your local outdoor store or online before traveling overseas.\n* Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.\n* [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.\n\t+ Permethrin is an insecticide that kills mosquitoes and other insects.\n\t+ To determine if you can wash a treated mosquito net, follow the label instructions.\n\nIf you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).\n\n \n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### More Information\n\n* [Malaria](https://www.cdc.gov/parasites/malaria/index.html)\n* CDC Yellow Book: [Malaria](/travel/yellowbook/2020/travel-related-infectious-diseases/malaria)\n* [Malaria Hotline](https://www.cdc.gov/media/releases/2019/s0328-artesunate-first-line-treatment.html)—770-488-7788 or 770-488-7100\n* [Malaria Risk Assessment for Travelers](http://www.cdc.gov/malaria/travelers/risk_assessment.html)\n* [Choosing the Right Drug to Prevent Malaria](http://www.cdc.gov/malaria/travelers/drugs.html)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":686,"cells":{"id":{"kind":"string","value":"e91cc1d7c39a5580d4c3a60c61fdc18f6a89a1a6"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Measles"},"clean_text":{"kind":"string","value":"Measles | Disease Directory | Travelers' Health | CDC\n\n### What is measles?\nMeasles is a disease caused by a highly contagious virus. People with measles spread the virus through the air when they cough, sneeze, or breathe. \n[Symptoms](https://www.cdc.gov/measles/symptoms/signs-symptoms.html) of measles include high fever, cough, runny nose, red and watery eyes, and rash. Koplik spots (tiny white spots inside the mouth) can appear 2 to 3 days after symptoms begin. Some people who become sick with measles also get a serious lung infection, such as pneumonia. Although severe cases are rare, measles can cause swelling of the brain and even death. Measles can be especially severe in infants and in people who are malnourished or who have weakened immune systems.\n### Who is at risk?\nAnyone who has not been fully vaccinated or had measles before can get measles. Measles remains a common disease in many parts of the world, including Europe, the Middle East, Asia, the Pacific, and Africa. \nIn the United States, most measles cases occur among unvaccinated travelers who get infected while traveling internationally and spread measles to people who are not fully vaccinated in the United States.\nInformation by Destination\n\nWhere are you going?\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" - value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n window.location = url;\n### What can travelers do to prevent measles?\nGetting vaccinated is the best way to protect yourself and others against measles. Measles vaccine is a routine vaccination given to children in the United States. Measles vaccine is usually given in two doses. It’s recommended that children get the first dose when they are 12 to 15 months old and the second dose when they are 4 to 6 years old. Measles vaccine is a combination vaccine that also protects against mumps and rubella (MMR vaccine) or mumps, rubella, and varicella (MMRV vaccine).\nIf you were born in or after 1957 and have never had measles or have never been vaccinated against measles, you should get vaccinated with two doses of MMR vaccine before you travel. The second dose is given at least 28 days after the first dose. People born before 1957 were likely exposed to measles as children and do not need to be vaccinated with the MMR vaccine.\nInfants 6 to 11 months old traveling internationally should get one dose of MMR vaccine before travel. This dose does not count as part of the routine childhood vaccination series.\nCAUTION: Pregnant people should NOT get the MMR vaccine. Any unvaccinated person should get the MMR vaccine immediately after their pregnancy.\nAvoid getting pregnant for at least 4 weeks after receiving the MMR vaccine.\n"},"raw_text":{"kind":"string","value":"\n\n### Measles\n\n\n\n\n### What is measles?\n\n\nMeasles is a disease caused by a highly contagious virus. People with measles spread the virus through the air when they cough, sneeze, or breathe. \n\n[Symptoms](https://www.cdc.gov/measles/symptoms/signs-symptoms.html) of measles include high fever, cough, runny nose, red and watery eyes, and rash. Koplik spots (tiny white spots inside the mouth) can appear 2 to 3 days after symptoms begin. Some people who become sick with measles also get a serious lung infection, such as pneumonia. Although severe cases are rare, measles can cause swelling of the brain and even death. Measles can be especially severe in infants and in people who are malnourished or who have weakened immune systems.\n\n### Who is at risk?\n\nAnyone who has not been fully vaccinated or had measles before can get measles. Measles remains a common disease in many parts of the world, including Europe, the Middle East, Asia, the Pacific, and Africa. \n\n**In the United States, most measles cases occur among unvaccinated travelers who get infected while traveling internationally and spread measles to people who are not fully vaccinated in the United States.**\n\n\nInformation by Destination\n\nWhere are you going?\n\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n function goSelectPage(){ \n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" + value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n }else{\n window.location = url;\n }\n }\n\n \n \n\n### What can travelers do to prevent measles?\n\nGetting vaccinated is the best way to protect yourself and others against measles. Measles vaccine is a routine vaccination given to children in the United States. Measles vaccine is usually given in two doses. It’s recommended that children get the first dose when they are 12 to 15 months old and the second dose when they are 4 to 6 years old. Measles vaccine is a combination vaccine that also protects against mumps and rubella (MMR vaccine) or mumps, rubella, and varicella (MMRV vaccine).\n\nIf you were born in or after 1957 and have never had measles or have never been vaccinated against measles, you should get vaccinated with two doses of MMR vaccine before you travel. The second dose is given at least 28 days after the first dose. People born before 1957 were likely exposed to measles as children and do not need to be vaccinated with the MMR vaccine.\n\nInfants 6 to 11 months old traveling internationally should get one dose of MMR vaccine before travel. This dose does not count as part of the routine childhood vaccination series.\n\n**CAUTION:** Pregnant people should NOT get the MMR vaccine. Any unvaccinated person should get the MMR vaccine immediately after their pregnancy.\n\nAvoid getting pregnant for at least 4 weeks after receiving the MMR vaccine.\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### More Information\n\n* [Measles Homepage](http://www.cdc.gov/measles/index.html)\n* [Measles Webpage for Travelers](https://www.cdc.gov/measles/plan-for-travel.html)\n* [Measles Vaccination Information](http://www.cdc.gov/measles/vaccination.html)\n* CDC Yellow Book: [Measles](/travel/yellowbook/2020/travel-related-infectious-diseases/measles-rubeola)\n* [Guidance on Measles during the Summer Travel Season](https://emergency.cdc.gov/han/2023/han00493.asp)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":687,"cells":{"id":{"kind":"string","value":"aa2c9b5e782560de3989ec25a3b223f433e3490e"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Meningococcal Disease"},"clean_text":{"kind":"string","value":"Meningococcal Disease | Disease Directory | Travelers' Health | CDC\n\n### Meningococcal Disease\n### What is meningococcal disease?\nMeningococcal disease is caused by bacteria called - Neisseria meningitidis- . People with meningococcal disease spread the bacteria to others through close personal contact such as living together or kissing. A person with meningococcal disease needs immediate medical attention.\nThe symptoms of meningococcal disease can vary based on the type of illness. Common symptoms of meningococcal [meningitis](https://www.cdc.gov/meningococcal/about/symptoms.html#meningitis) include sudden fever, headache, and stiff neck. Other symptoms may include nausea, vomiting, increased sensitivity to light, and confusion. Children and infants may show different signs and symptoms, such as inactivity, irritability, vomiting, or poor reflexes.\nBacteria that cause meningococcal disease can also infect the blood, causing [septicemia](https://www.cdc.gov/meningococcal/about/symptoms.html#septicemia). Symptoms of septicemia include tiredness, vomiting, chills, severe aches and pain, fast breathing, diarrhea, and a dark rash. Meningococcal disease can lead to death in as little as a few hours. \n\nMap: Areas with frequent epidemics of meningococcal meningitis\n### Who is at risk?\nAnyone can get meningococcal disease, but people who live in or travel to certain areas of the world are more likely to get it.\nThe [“meningitis belt” of sub-Saharan Africa](/travel/yellowbook/2020/travel-related-infectious-diseases/meningococcal-disease#5559) has the highest rates of meningococcal disease in the world. The disease is more common in this part of Africa from December to June, during the dry season.\nTravelers who spend a lot of time with local populations in the meningitis belt, especially during outbreaks of meningococcal disease, are more likely to get this disease.\nParticipants in the Hajj or Umrah pilgrimages in Saudi Arabia are also more likely to get sick.\n### What can travelers do to prevent meningococcal disease?\nGetting a meningococcal vaccine is the best way to protect against meningococcal disease. There are two types of meningococcal vaccines available in the United States:\n- Meningococcal ACWY (MenACWY) vaccine\n- Serogroup B meningococcal (MenB) vaccine\nInformation by Destination\n\nWhere are you going?\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" - value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n window.location = url;\nMenACWY vaccine is a routine vaccination given to pre-teens and teens in the United States. All 11 to 12-year-olds should get a dose of a MenACWY vaccine and a booster shot at age 16. Teens and young adults may also get a MenB vaccine, preferably at 16 to 18 years old.\nYounger children and adults may also need a MenACWY vaccine depending on their travel plans. Some people who have been vaccinated before may need a booster shot. It takes 7 to 10 days after a person has been vaccinated before they have maximum protection against the disease. See your doctor as soon as possible before travel to make sure you are protected.\nSee if a MenACWY vaccine is recommended for your [destination.](/travel/destinations/list) There are currently no recommendations to receive MenB vaccine before traveling.\nThose traveling to Saudi Arabia to participate in the Hajj or Umrah pilgrimages must show proof of MenACWY vaccination. It may also be referred to as tetravalent or quadrivalent meningococcal vaccine.\n"},"raw_text":{"kind":"string","value":"\n\n### Meningococcal Disease\n\n\n\n\n### What is meningococcal disease?\n\nMeningococcal disease is caused by bacteria called *Neisseria meningitidis*. People with meningococcal disease spread the bacteria to others through close personal contact such as living together or kissing. A person with meningococcal disease needs immediate medical attention.\n\nThe symptoms of meningococcal disease can vary based on the type of illness. Common symptoms of meningococcal [meningitis](https://www.cdc.gov/meningococcal/about/symptoms.html#meningitis) include sudden fever, headache, and stiff neck. Other symptoms may include nausea, vomiting, increased sensitivity to light, and confusion. Children and infants may show different signs and symptoms, such as inactivity, irritability, vomiting, or poor reflexes.\n\nBacteria that cause meningococcal disease can also infect the blood, causing [septicemia](https://www.cdc.gov/meningococcal/about/symptoms.html#septicemia). Symptoms of septicemia include tiredness, vomiting, chills, severe aches and pain, fast breathing, diarrhea, and a dark rash. Meningococcal disease can lead to death in as little as a few hours. \n\n\n**Map: Areas with frequent epidemics of meningococcal meningitis**\n\n### Who is at risk?\n\nAnyone can get meningococcal disease, but people who live in or travel to certain areas of the world are more likely to get it.\n\nThe [“meningitis belt” of sub-Saharan Africa](/travel/yellowbook/2020/travel-related-infectious-diseases/meningococcal-disease#5559) has the highest rates of meningococcal disease in the world. The disease is more common in this part of Africa from December to June, during the dry season.\n\nTravelers who spend a lot of time with local populations in the meningitis belt, especially during outbreaks of meningococcal disease, are more likely to get this disease.\n\nParticipants in the Hajj or Umrah pilgrimages in Saudi Arabia are also more likely to get sick.\n\n### What can travelers do to prevent meningococcal disease?\n\nGetting a meningococcal vaccine is the best way to protect against meningococcal disease. There are two types of meningococcal vaccines available in the United States:\n\n* Meningococcal ACWY (MenACWY) vaccine\n* Serogroup B meningococcal (MenB) vaccine\n\n\nInformation by Destination\n\nWhere are you going?\n\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n function goSelectPage(){ \n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" + value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n }else{\n window.location = url;\n }\n }\n\n \n \n\nMenACWY vaccine is a routine vaccination given to pre-teens and teens in the United States. All 11 to 12-year-olds should get a dose of a MenACWY vaccine and a booster shot at age 16. Teens and young adults may also get a MenB vaccine, preferably at 16 to 18 years old.\n\nYounger children and adults may also need a MenACWY vaccine depending on their travel plans. Some people who have been vaccinated before may need a booster shot. It takes 7 to 10 days after a person has been vaccinated before they have maximum protection against the disease. See your doctor as soon as possible before travel to make sure you are protected.\n\nSee if a MenACWY vaccine is recommended for your [destination.](/travel/destinations/list) There are currently no recommendations to receive MenB vaccine before traveling.\n\nThose traveling to Saudi Arabia to participate in the Hajj or Umrah pilgrimages must show proof of MenACWY vaccination. It may also be referred to as tetravalent or quadrivalent meningococcal vaccine.\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### More Information\n\n* [Meningococcal Disease](http://www.cdc.gov/meningococcal/)\n* [Meningococcal Vaccination](https://www.cdc.gov/meningococcal/vaccine-info.html)\n* CDC Yellow Book: [Meningococcal Disease](/travel/yellowbook/2020/travel-related-infectious-diseases/meningococcal-disease)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":688,"cells":{"id":{"kind":"string","value":"bcf2cfc9c8e1c4645b212e119ef4114365892b2a"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Mpox"},"clean_text":{"kind":"string","value":"Mpox | Disease Directory | Travelers' Health | CDC\n\n### What is Mpox?\n[Mpox](https://www.cdc.gov/poxvirus/mpox/index.html) is a disease caused by infection with mpox virus. In 2022, an outbreak began around the world in areas where mpox is not usually found. Previously, mpox was found mainly in Central and West Africa, often in forested areas.\nPeople infected with mpox develop a rash that can initially look like pimples or blisters. The rash is usually painful.\n### What are the symptoms?\n[Symptoms](https://www.cdc.gov/poxvirus/mpox/symptoms/index.html) of mpox can include:\n- A rash that may:\n\t- Initially look like pimples or blisters\n\t- be painful or itch\n\t- be located on or near the genitals (penis, testicle, labia, and vagina) or anus (butthole) or other areas like the hands, feet, chest, face, or mouth.\nThe rash will go through several stages, including scabs, before healing. The illness typically lasts 2–4 weeks.\n- Muscle aches and backache\n- Swollen lymph nodes\n- Respiratory symptoms (e.g. sore throat, nasal congestion, or cough)\n### How does mpox spread?\nMpox [spreads](https://www.cdc.gov/poxvirus/mpox/if-sick/transmission.html) in a few ways.\nMpox can spread to anyone through close, personal, often skin-to-skin contact, including:\n- Direct contact with mpox rash and scabs from a person with mpox, as well as contact with their saliva, upper respiratory secretions (snot, mucus), and areas around the anus, rectum, or vagina\nThis direct contact can happen during intimate contact, including:\n- Oral, anal, or vaginal sex, or touching the genitals (penis, testicles, labia, and vagina) or anus of a person with mpox\n- Hugging, massage, and kissing\n- Prolonged face-to-face contact\nThe risk for getting mpox is considered relatively low by touching objects, fabrics, and surfaces that have been used by someone with mpox and not disinfected, such as clothing, bedding, or towels.\n### Who is at risk?\nAnyone in close contact with a person with mpox can get it and should take steps to protect themselves, especially vaccination. At this time, [data](https://www.cdc.gov/mmwr/volumes/71/wr/mm7132e3.htm) suggest that gay, bisexual, and other men who have sex with men make up the majority of cases in the mpox outbreak that began in 2022.\nTravelers who plan to attend [gatherings](https://www.cdc.gov/poxvirus/mpox/prevention/sexual-health.html) that may place them in close, skin-to-skin contact with someone who has mpox are at higher risk of getting infected.\nCaregivers of persons with mpox should avoid close skin-to-skin contact with persons who have a rash, wash hands regularly and use proper PPE (mask, gloves) when providing care. Do not share eating utensils or cups and do no handle bedding, towels, or clothing of persons with mpox. Caregivers should consider getting the mpox vaccine.\nTravelers such as veterinarians and wildlife professionals may be at risk if they work with infected animals including in areas where wild animals are known to be infected such as Central and West Africa.\n### What can travelers do to avoid getting mpox?\nMpox is often transmitted through close, sustained physical contact, and during the outbreak that began in 2022, most frequently, sexual contact.\nTravelers can [protect themselves](https://www.cdc.gov/poxvirus/mpox/prevention/protect-yourself.html) against infection by taking the following steps.\n- If you are [eligible to get vaccinated](https://www.cdc.gov/poxvirus/mpox/vaccines/index.html) for mpox, get two doses of vaccine before you travel. Use the [Mpox Vaccine Locator](https://mpoxvaxmap.org/) to find out where you can get vaccinated.\n- Avoid close, skin-to-skin contact with people who have a rash that looks like mpox.\n\t- Do not touch the rash or scabs of a person with mpox.\n\t- Do not kiss, hug, cuddle or have sex with someone with mpox.\n- Avoid contact with objects and materials that a person with mpox has used.\n\t- Do not share eating utensils or cups with a person with mpox.\n\t- Do not handle or touch the bedding, towels, clothing, fetish gear, or sex toys of a person with mpox.\n- Wash your hands often with soap and water or use an alcohol-based hand sanitizer, especially before eating or touching your face and after you use the bathroom.\n### What to do if you have mpox symptoms or have been around someone with mpox?\nIf you have [mpox symptoms](https://www.cdc.gov/poxvirus/mpox/symptoms/index.html) or had close contact with someone who has mpox, talk to your healthcare provider about [testing](https://www.cdc.gov/poxvirus/mpox/testing/testing-basics.html) and [treatment](https://www.cdc.gov/poxvirus/mpox/if-sick/treatment.html). CDC [recommends vaccination](https://www.cdc.gov/poxvirus/mpox/vaccines/index.html) for people who have been exposed to mpox and for [people who are at higher risk of being exposed to mpox](https://www.cdc.gov/poxvirus/mpox/prevention/index.html).\nDo Not Travel if You Have Mpox\n- [Isolate](https://www.cdc.gov/poxvirus/mpox/clinicians/isolation-procedures.html) at home or in another location until your symptoms are gone and your rash has healed; this means all scabs have fallen off and a fresh layer of skin has formed.\n- If you have mpox and must travel:\n\t- Make sure that you do not have fever or respiratory symptoms such as sore throat, nasal congestion, or cough.\n\t- Cover your rash and wear a well-fitting mask.\n\t- Take additional steps to [prevent spread to others](https://www.cdc.gov/poxvirus/mpox/if-sick/preventing-spread.html).\nAdditional Travel Considerations\n- If you test positive for mpox while at your international destination, you may be subject to local public health laws and regulations. These could include requirements to isolate and not being allowed travel until you are no longer considered contagious.\n- If you have been in contact with a person who has mpox and travel internationally, you may be subject to local public health laws and regulations. These could include requirements to [quarantine](https://www.cdc.gov/quarantine/quarantineisolation.html) and not being allowed travel until you are no longer at risk for developing mpox.\n- If you have symptoms of mpox, you may be required to isolate and be tested for mpox. Check your destination’s ministry of health or [US embassyExternal Link](https://www.usembassy.gov/) website to learn about arrival procedures.\n"},"raw_text":{"kind":"string","value":"\n\n### Mpox\n\n\n\n\n\n### What is Mpox?\n\n[Mpox](https://www.cdc.gov/poxvirus/mpox/index.html) is a disease caused by infection with mpox virus. In 2022, an outbreak began around the world in areas where mpox is not usually found. Previously, mpox was found mainly in Central and West Africa, often in forested areas.\n\nPeople infected with mpox develop a rash that can initially look like pimples or blisters. The rash is usually painful.\n\n### What are the symptoms?\n\n[Symptoms](https://www.cdc.gov/poxvirus/mpox/symptoms/index.html) of mpox can include:\n\n\n* A rash that may:\n\t+ Initially look like pimples or blisters\n\t+ be painful or itch\n\t+ be located on or near the genitals (penis, testicle, labia, and vagina) or anus (butthole) or other areas like the hands, feet, chest, face, or mouth.\n\nThe rash will go through several stages, including scabs, before healing. The illness typically lasts 2–4 weeks.\n\n* Fever\n* Headache\n* Muscle aches and backache\n* Swollen lymph nodes\n* Chills\n* Exhaustion\n* Respiratory symptoms (e.g. sore throat, nasal congestion, or cough)\n\n### How does mpox spread?\n\nMpox [spreads](https://www.cdc.gov/poxvirus/mpox/if-sick/transmission.html) in a few ways.\n\nMpox can spread to anyone through close, personal, often skin-to-skin contact, including:\n\n* Direct contact with mpox rash and scabs from a person with mpox, as well as contact with their saliva, upper respiratory secretions (snot, mucus), and areas around the anus, rectum, or vagina\n\nThis direct contact can happen during intimate contact, including:\n\n* Oral, anal, or vaginal sex, or touching the genitals (penis, testicles, labia, and vagina) or anus of a person with mpox\n* Hugging, massage, and kissing\n* Prolonged face-to-face contact\n\nThe risk for getting mpox is considered relatively low by touching objects, fabrics, and surfaces that have been used by someone with mpox and not disinfected, such as clothing, bedding, or towels.\n\n### Who is at risk?\n\nAnyone in close contact with a person with mpox can get it and should take steps to protect themselves, especially vaccination. At this time, [data](https://www.cdc.gov/mmwr/volumes/71/wr/mm7132e3.htm) suggest that gay, bisexual, and other men who have sex with men make up the majority of cases in the mpox outbreak that began in 2022.\n\nTravelers who plan to attend [gatherings](https://www.cdc.gov/poxvirus/mpox/prevention/sexual-health.html) that may place them in close, skin-to-skin contact with someone who has mpox are at higher risk of getting infected.\n\nCaregivers of persons with mpox should avoid close skin-to-skin contact with persons who have a rash, wash hands regularly and use proper PPE (mask, gloves) when providing care. Do not share eating utensils or cups and do no handle bedding, towels, or clothing of persons with mpox. Caregivers should consider getting the mpox vaccine.\n\nTravelers such as veterinarians and wildlife professionals may be at risk if they work with infected animals including in areas where wild animals are known to be infected such as Central and West Africa.\n\n### What can travelers do to avoid getting mpox?\n\nMpox is often transmitted through close, sustained physical contact, and during the outbreak that began in 2022, most frequently, sexual contact.\n\nTravelers can [protect themselves](https://www.cdc.gov/poxvirus/mpox/prevention/protect-yourself.html) against infection by taking the following steps.\n\n* If you are [eligible to get vaccinated](https://www.cdc.gov/poxvirus/mpox/vaccines/index.html) for mpox, get two doses of vaccine before you travel. Use the [Mpox Vaccine Locator](https://mpoxvaxmap.org/) to find out where you can get vaccinated.\n* Avoid close, skin-to-skin contact with people who have a rash that looks like mpox.\n\t+ Do not touch the rash or scabs of a person with mpox.\n\t+ Do not kiss, hug, cuddle or have sex with someone with mpox.\n* Avoid contact with objects and materials that a person with mpox has used.\n\t+ Do not share eating utensils or cups with a person with mpox.\n\t+ Do not handle or touch the bedding, towels, clothing, fetish gear, or sex toys of a person with mpox.\n* Wash your hands often with soap and water or use an alcohol-based hand sanitizer, especially before eating or touching your face and after you use the bathroom.\n\n### What to do if you have mpox symptoms or have been around someone with mpox?\n\nIf you have [mpox symptoms](https://www.cdc.gov/poxvirus/mpox/symptoms/index.html) or had close contact with someone who has mpox, talk to your healthcare provider about [testing](https://www.cdc.gov/poxvirus/mpox/testing/testing-basics.html) and [treatment](https://www.cdc.gov/poxvirus/mpox/if-sick/treatment.html). CDC [recommends vaccination](https://www.cdc.gov/poxvirus/mpox/vaccines/index.html) for people who have been exposed to mpox and for [people who are at higher risk of being exposed to mpox](https://www.cdc.gov/poxvirus/mpox/prevention/index.html).\n\n\nDo Not Travel if You Have Mpox\n* [Isolate](https://www.cdc.gov/poxvirus/mpox/clinicians/isolation-procedures.html) at home or in another location until your symptoms are gone and your rash has healed; this means all scabs have fallen off and a fresh layer of skin has formed.\n* If you have mpox and must travel:\n\t+ Make sure that you do not have fever or respiratory symptoms such as sore throat, nasal congestion, or cough.\n\t+ Cover your rash and wear a well-fitting mask.\n\t+ Take additional steps to [prevent spread to others](https://www.cdc.gov/poxvirus/mpox/if-sick/preventing-spread.html).\n\n\n\nAdditional Travel Considerations\n* **If you test positive for mpox while at your international destination,** you may be subject to local public health laws and regulations. These could include requirements to isolate and not being allowed travel until you are no longer considered contagious.\n* If you have been in contact with a person who has mpox and travel internationally, you may be subject to local public health laws and regulations. These could include requirements to [quarantine](https://www.cdc.gov/quarantine/quarantineisolation.html) and not being allowed travel until you are no longer at risk for developing mpox.\n* If you have symptoms of mpox, you may be required to isolate and be tested for mpox. Check your destination’s ministry of health or [US embassyExternal Link](https://www.usembassy.gov/) website to learn about arrival procedures.\n* If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/health-care-during-travel). Consider [travel health and medical evacuation insurance](/travel/page/insurance). Options for [treatment](https://www.cdc.gov/poxvirus/mpox/if-sick/treatment.html) may not be available in some countries.\n\n\n### More Information\n\n* [2022 Mpox Outbreak Cases and Data](https://www.cdc.gov/poxvirus/mpox/response/2022/index.html)\n* CDC Website: [Mpox](https://www.cdc.gov/poxvirus/mpox/index.html)\n\n\n \n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":689,"cells":{"id":{"kind":"string","value":"253f187c1374679033e8256c92508c3356bf91f6"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Mumps"},"clean_text":{"kind":"string","value":"Mumps | Disease Directory | Travelers' Health | CDC\n\n### What is mumps?\nMumps is a contagious disease caused by a virus. People with mumps can spread the virus to others when they\n- Cough, sneeze, or talk.\n- Share items that have saliva on them (e.g., water bottles or cups).\n- Participate in close-contact activities (e.g., playing sports, dancing, or kissing).\nMumps [symptoms](http://www.cdc.gov/mumps/about/signs-symptoms.html) may include fever, headache, muscle aches, tiredness, loss of appetite, and swollen and tender glands under the ears or jaw on one or both sides of the face (parotitis). Most people with mumps recover fully. However, mumps infection can occasionally cause complications, such as swelling of the brain, testicles, ovaries, or breasts. It can also cause temporary or permanent hearing loss.\n### Who is at risk?\nInformation by Destination\n\nWhere are you going?\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" - value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n window.location = url;\nMumps remains a common disease in many countries therefore travelers who are not vaccinated are at risk for getting mumps. Mumps outbreaks are more common among groups of people who have frequent, close contact with each other, such as college students, sports teams, or community groups (e.g., church members).\n### What can travelers do to prevent mumps?\nGetting vaccinated is the best way to protect yourself against mumps. Mumps vaccine is routinely given to children in the United States. The vaccine is given in two doses: children usually get the first dose at 12 to 15 months old and the second dose when they are 4 to 6 years old. Mumps vaccine is a combination vaccine that also protects against measles and rubella (MMR vaccine) or measles, rubella, and varicella (MMRV vaccine).\nIf you were born in or after 1957 and have never had mumps or have never been vaccinated against mumps, you should get vaccinated with two doses of MMR vaccine before you travel, with the second dose given at least 28 days after the first dose.\nInfants 6 to 11 months old traveling internationally should get one dose MMR vaccine before travel. This dose does not count as part of the routine childhood vaccination series.\nSometimes, vaccine protection can decrease over time. Disease symptoms for previously vaccinated people who get mumps are milder and complications are less frequent.\nCAUTION: Pregnant people should NOT get MMR vaccine. Any unvaccinated person should get the MMR vaccine immediately after their pregnancy.\nAvoid getting pregnant for at least 4 weeks after receiving MMR vaccine.\n"},"raw_text":{"kind":"string","value":"\n\n### Mumps\n\n\n\n\n### What is mumps?\n\nMumps is a contagious disease caused by a virus. People with mumps can spread the virus to others when they\n\n* Cough, sneeze, or talk.\n* Share items that have saliva on them (e.g., water bottles or cups).\n* Participate in close-contact activities (e.g., playing sports, dancing, or kissing).\n\nMumps [symptoms](http://www.cdc.gov/mumps/about/signs-symptoms.html) may include fever, headache, muscle aches, tiredness, loss of appetite, and swollen and tender glands under the ears or jaw on one or both sides of the face (parotitis). Most people with mumps recover fully. However, mumps infection can occasionally cause complications, such as swelling of the brain, testicles, ovaries, or breasts. It can also cause temporary or permanent hearing loss.\n\n### Who is at risk?\n\n\nInformation by Destination\n\nWhere are you going?\n\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n function goSelectPage(){ \n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" + value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n }else{\n window.location = url;\n }\n }\n\n \n \n\nMumps remains a common disease in many countries therefore travelers who are not vaccinated are at risk for getting mumps. Mumps outbreaks are more common among groups of people who have frequent, close contact with each other, such as college students, sports teams, or community groups (e.g., church members).\n\n### What can travelers do to prevent mumps?\n\nGetting vaccinated is the best way to protect yourself against mumps. Mumps vaccine is routinely given to children in the United States. The vaccine is given in two doses: children usually get the first dose at 12 to 15 months old and the second dose when they are 4 to 6 years old. Mumps vaccine is a combination vaccine that also protects against measles and rubella (MMR vaccine) or measles, rubella, and varicella (MMRV vaccine).\n\nIf you were born in or after 1957 and have never had mumps or have never been vaccinated against mumps, you should get vaccinated with two doses of MMR vaccine before you travel, with the second dose given at least 28 days after the first dose.\n\nInfants 6 to 11 months old traveling internationally should get one dose MMR vaccine before travel. This dose does not count as part of the routine childhood vaccination series.\n\nSometimes, vaccine protection can decrease over time. Disease symptoms for previously vaccinated people who get mumps are milder and complications are less frequent.\n\n**CAUTION:** Pregnant people should NOT get MMR vaccine. Any unvaccinated person should get the MMR vaccine immediately after their pregnancy.\n\nAvoid getting pregnant for at least 4 weeks after receiving MMR vaccine.\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### More Information\n\n* [Mumps](http://www.cdc.gov/mumps/)\n* [Mumps Vaccination Information](http://www.cdc.gov/mumps/vaccination.html)\n* CDC Yellow Book:[Mumps](http://wwwnc.cdc.gov/travel/yellowbook/2012/chapter-3-infectious-diseases-related-to-travel/mumps.htm)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":690,"cells":{"id":{"kind":"string","value":"b70cba10dd09c0d4152856721be84e51ada3123c"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Murray Valley Encephalitis virus"},"clean_text":{"kind":"string","value":"Murray Valley Encephalitis virus | Disease Directory | Travelers' Health | CDC\n\n### Murray Valley Encephalitis virus\n### What is Murray Valley encephalitis?\nMurray Valley encephalitis virus is spread to people through the bite of an infected mosquito.\nMost people who get infected never have symptoms. Symptoms of Murray Valley encephalitis can include fever, headache, nausea, vomiting, and tiredness. Some people may develop severe symptoms including confusion, trouble speaking, seizures, and lack of coordination.\n### Who is at risk?\nTravelers to parts of Australia, Papua New Guinea, or Indonesia are at risk for being infected with Murray Valley encephalitis virus.\nActivities that can increase a traveler’s risk of being infected include\n- Spending a lot of time outdoors\n- Traveling during times of the year when mosquitoes are more common, such as during the summer.\n### What can travelers do to prevent Murray Valley encephalitis?\nThere are no vaccines or medicines that prevent Murray Valley encephalitis. Travelers can protect themselves by taking the following steps.\nUse an EPA-registered insect repellent\n- Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.\n\t- Picaridin (known as KBR 3023 and icaridin outside the US)\n\t- Oil of lemon eucalyptus (OLE)\n\t- Para-menthane-diol (PMD)\nFind the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).\n\n- Insect Repellent Tips for Babies and Children\n\t- Dress your child in clothing that covers arms and legs.\n\t- Cover strollers and baby carriers with mosquito netting.\n\t- When using insect repellent on your child:\n\t\t- Always follow label instructions.\n\t\t- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.\n\t\t- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.\n\t\t\t- Adults: Spray insect repellent onto your hands and then apply to a child’s face.\n\t\t- If also using sunscreen, always apply insect repellent after sunscreen.\nWear long-sleeved shirts and long pants\nTreat clothing and gear with permethrin\n- Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.\n\t- Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.\n\t- Permethrin-treated clothing provides protection after multiple washings.\n\t- Read product information to find out how long the protection will last.\n- If treating items yourself, follow the product instructions.\n- Do not use permethrin products directly on skin.\n- Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).\nKeep mosquitoes out of your hotel room or lodging\n- Choose a hotel or lodging with air conditioning or window and door screens.\n- Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.\nSleep under a mosquito net\n\n- Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.\n- Buy a mosquito net at your local outdoor store or online before traveling overseas.\n- Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.\n- [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.\n\t- Permethrin is an insecticide that kills mosquitoes and other insects.\n\t- To determine if you can wash a treated mosquito net, follow the label instructions.\nIf you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).\n"},"raw_text":{"kind":"string","value":"\n\n### Murray Valley Encephalitis virus\n\n\n\n\n### What is Murray Valley encephalitis?\n\nMurray Valley encephalitis virus is spread to people through the bite of an infected mosquito.\n\nMost people who get infected never have symptoms. Symptoms of Murray Valley encephalitis can include fever, headache, nausea, vomiting, and tiredness. Some people may develop severe symptoms including confusion, trouble speaking, seizures, and lack of coordination.\n\n### Who is at risk?\n\nTravelers to parts of Australia, Papua New Guinea, or Indonesia are at risk for being infected with Murray Valley encephalitis virus.\n\nActivities that can increase a traveler’s risk of being infected include\n\n* Spending a lot of time outdoors\n* Traveling during times of the year when mosquitoes are more common, such as during the summer.\n\n### What can travelers do to prevent Murray Valley encephalitis?\n\nThere are no vaccines or medicines that prevent Murray Valley encephalitis. Travelers can protect themselves by taking the following steps.\n\n**Use an EPA-registered insect repellent**\n\n\n\n* Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.\n\t+ DEET\n\t+ Picaridin (known as KBR 3023 and icaridin outside the US)\n\t+ IR3535\n\t+ Oil of lemon eucalyptus (OLE)\n\t+ Para-menthane-diol (PMD)\n\t+ 2-undecanone\n\nFind the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).\n\n\n\n* Insect Repellent Tips for Babies and Children\n\t+ Dress your child in clothing that covers arms and legs.\n\t+ Cover strollers and baby carriers with mosquito netting.\n\t+ When using insect repellent on your child:\n\t\t- Always follow label instructions.\n\t\t- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.\n\t\t- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.\n\t\t\t* Adults: Spray insect repellent onto your hands and then apply to a child’s face.\n\t\t- If also using sunscreen, always apply insect repellent after sunscreen.\n\n**Wear long-sleeved shirts and long pants**\n\n**Treat clothing and gear with permethrin**\n\n\n\n* Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.\n\t+ Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.\n\t+ Permethrin-treated clothing provides protection after multiple washings.\n\t+ Read product information to find out how long the protection will last.\n* If treating items yourself, follow the product instructions.\n* Do not use permethrin products directly on skin.\n* Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).\n\n**Keep mosquitoes out of your hotel room or lodging**\n\n* Choose a hotel or lodging with air conditioning or window and door screens.\n* Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.\n\n**Sleep under a mosquito net**\n\n\n\n* Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.\n* Buy a mosquito net at your local outdoor store or online before traveling overseas.\n* Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.\n* [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.\n\t+ Permethrin is an insecticide that kills mosquitoes and other insects.\n\t+ To determine if you can wash a treated mosquito net, follow the label instructions.\n\nIf you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).\n\n \n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n\n### More Information\n\n* [Avoid Bug Bites](/travel/page/avoid-bug-bites)\n* [Information on Arboviral Diseases](https://www.cdc.gov/ncezid/dvbd/)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":691,"cells":{"id":{"kind":"string","value":"cd5134dd4ed81b3df6b2a541bbb2ff2a0a889665"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Pertussis (Whooping Cough)"},"clean_text":{"kind":"string","value":"Pertussis (Whooping Cough) | Disease Directory | Travelers' Health | CDC\n\n### Pertussis (Whooping Cough)\n### What is pertussis?\nWhooping cough, also known as pertussis, is a highly contagious respiratory disease caused by bacteria called - Bordetella pertussis- . Whooping cough is known for uncontrollable, violent coughing, which often makes it hard to breathe. Pertussis can affect people of all ages, but can be very serious, even deadly, for babies less than a year old. People with whooping cough can spread the bacteria to others when they cough, sneeze, or share the same breathing space. \nEarly symptoms are typically mild, like a cold, and can include runny nose, low fever, and mild cough. Later symptoms of the disease may include “fits” of many rapid coughs followed by a high-pitched “whoop,” vomiting, and exhaustion. The coughing fits can continue for up to 10 weeks or more. In babies, the cough can be minimal or not even there. Instead, babies may have pauses in breathing known as apnea.\nInformation by Destination\n\nWhere are you going?\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" - value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n window.location = url;\n### Who is at risk?\nWhooping cough is found worldwide. More whooping cough is seen in developing countries where very few people get vaccinated. Each year, it is estimated that worldwide there are about 24.1 million whooping cough cases and 160,700 deaths in children younger than 5 years old.\n### What can travelers do to prevent whooping cough?\nBeing up to date on whooping cough vaccines is the best way to protect against disease. Whooping cough vaccines are combination vaccines, that also protect against diphtheria and tetanus. These vaccines are often called [DTaP and Tdap](https://www.cdc.gov/vaccines/vpd/dtap-tdap-td/public/index.html).\nBabies and Children\nBabies need 3 shots of DTaP to build up high levels of protection against diphtheria, tetanus, and whooping cough. Then, young children need 2 booster shots to maintain that protection through early childhood. CDC recommends shots at the following ages:\n- 2 months\n- 4 months\n- 6 months\n- 15 through 18 months\n- 4 through 6 years\n\nPreteens and Teens\nPreteens should get one shot of Tdap between the ages of 11 and 12 years to boost their immunity. Teens who didn’t get Tdap as a preteen should get one shot the next time they visit their healthcare professional.\nPregnant women should get Tdap during the early part of the 3rd trimester of every pregnancy. By doing so, she helps protect her baby from whooping cough in the first few months of life. [Find out more about the Tdap pregnancy recommendation](https://www.cdc.gov/pertussis/pregnant/).\nAll adults who have never received one should get a shot of Tdap. This can be given at any time, regardless of when they last got Td. This should be followed by either a Td or Tdap shot every 10 years.\n"},"raw_text":{"kind":"string","value":"\n\n### Pertussis (Whooping Cough)\n\n\n\n\n### What is pertussis?\n\nWhooping cough, also known as pertussis, is a highly contagious respiratory disease caused by bacteria called *Bordetella pertussis*. Whooping cough is known for uncontrollable, violent coughing, which often makes it hard to breathe. Pertussis can affect people of all ages, but can be very serious, even deadly, for babies less than a year old. People with whooping cough can spread the bacteria to others when they cough, sneeze, or share the same breathing space. \n\nEarly symptoms are typically mild, like a cold, and can include runny nose, low fever, and mild cough. Later symptoms of the disease may include “fits” of many rapid coughs followed by a high-pitched “whoop,” vomiting, and exhaustion. The coughing fits can continue for up to 10 weeks or more. In babies, the cough can be minimal or not even there. Instead, babies may have pauses in breathing known as apnea.\n\n\nInformation by Destination\n\nWhere are you going?\n\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n function goSelectPage(){ \n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" + value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n }else{\n window.location = url;\n }\n }\n\n \n \n\n### Who is at risk?\n\nWhooping cough is found worldwide. More whooping cough is seen in developing countries where very few people get vaccinated. Each year, it is estimated that worldwide there are about 24.1 million whooping cough cases and 160,700 deaths in children younger than 5 years old.\n\n### What can travelers do to prevent whooping cough?\n\nBeing up to date on whooping cough vaccines is the best way to protect against disease. Whooping cough vaccines are combination vaccines, that also protect against diphtheria and tetanus. These vaccines are often called [DTaP and Tdap](https://www.cdc.gov/vaccines/vpd/dtap-tdap-td/public/index.html).\n\n**Babies and Children**\n\nBabies need 3 shots of DTaP to build up high levels of protection against diphtheria, tetanus, and whooping cough. Then, young children need 2 booster shots to maintain that protection through early childhood. CDC recommends shots at the following ages:\n\n* 2 months\n* 4 months\n* 6 months\n* 15 through 18 months\n* 4 through 6 years\n\n\n**Preteens and Teens**\n\nPreteens should get one shot of Tdap between the ages of 11 and 12 years to boost their immunity. Teens who didn’t get Tdap as a preteen should get one shot the next time they visit their healthcare professional.\n\n**Pregnant Women**\n\nPregnant women should get Tdap during the early part of the 3rd trimester of every pregnancy. By doing so, she helps protect her baby from whooping cough in the first few months of life. [Find out more about the Tdap pregnancy recommendation](https://www.cdc.gov/pertussis/pregnant/).\n\n**Adults**\n\nAll adults who have never received one should get a shot of Tdap. This can be given at any time, regardless of when they last got Td. This should be followed by either a Td or Tdap shot every 10 years.\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### More Information\n\n* [Pertussis](http://www.cdc.gov/pertussis/index.html)\n* [Pertussis Vaccine Information](https://www.cdc.gov/vaccines/vpd/dtap-tdap-td/public/index.html)\n* CDC Yellow Book: [Pertussis](/travel/yellowbook/2020/travel-related-infectious-diseases/pertussis)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":692,"cells":{"id":{"kind":"string","value":"5463b202da0af282c9c7b18e83c031d84f61950b"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Plague"},"clean_text":{"kind":"string","value":"Plague | Disease Directory | Travelers' Health | CDC\n\n### What is plague?\nPlague is a rare disease caused by bacteria that can infect people and animals. People can get plague after being bitten by infected fleas, handling an infected animal, or breathing in infectious droplets from an infected person or animal. \nPlague symptoms depend on how the patient was exposed to the bacteria. Plague can present with different clinical forms, but the most common forms in humans are bubonic, septicemic, and pneumonic plague.\nType of Plague\nHow it Spreads\nType of Plague\nHow it Spreads\nBites from infected fleas and handling infected animals\nFever, headache, chills, and painful, swollen, and tender lymph nodes\nType of Plague\nHow it Spreads\nBites from infected fleas and handling infected animals\nFever, chills, weakness, stomach pain, and sometimes bleeding into the skin and other organs. Skin and other tissues may turn black and die, especially on fingers, toes, and the nose\nType of Plague\nHow it Spreads\nBreathe in infectious droplets from people or animals. A person can develop pneumonic plague if they get bubonic or septicemic plague and don't treat it\nFever, weakness, shortness of breath, chest pain, cough with bloody or watery mucous\n### Who is at risk?\nPlague is found in certain regions of Africa, central Asia, the Indian subcontinent, the northern part of South America, and the Southwest United States. Though rare, urban outbreaks of plague have been reported in Madagascar.\nThough plague is found in countries around the world, the risk to travelers is low. However, camping, hunting, hiking, or working outdoors can increase your risk.\n### What can travelers do to prevent plague?\nThere is no vaccine to prevent plague available in the United States. However, travelers can protect themselves from plague by taking the following precautions\nWear insect repellent\n- Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women.\n\t- Picaridin (known as KBR 3023 and icaridin outside the US)\n\t- Oil of lemon eucalyptus (OLE)\n\t- Para-menthane-diol (PMD)\n- Find the right insect repellent for you by using EPA’s search tool.\nTreat clothing and gear with permethrin\n- Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.\n\t- Permethrin is an insecticide that kills or repels insects.\n\t- Permethrin-treated clothing provides protection after multiple washings..\n\t- Read product information to find out how long the protection will last.\n- If treating items yourself, follow the product instructions.\n- Do not apply permethrin products directly to skin.\n- Watch the video [What You Need to Know About Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).\nDo not touch sick or dead animals. Infected fleas can jump from a live or dead animal onto a person. People can also become infected when handling tissue or body fluids of an infected animal. For example, a hunter skinning an infected animal without using proper precautions could become infected with plague.\n- If you must handle a sick or dead animal, wear gloves, pants, and long sleeves to cover your skin, and use additional personal protective equipment.\nAdditional steps to take if visiting or living in an area with plague\n- Store food, including pet food, in rodent-proof containers.\n- Keep rodents out of the house and make living spaces rodent proof.\n- Protect yourself and your pets\n\t- Do not allow pets that roam free in known plague areas to sleep on your bed.\n\t- Protect your pet from fleas. Talk to a veterinarian.\nPlague is a very serious illness but is treatable with commonly available antibiotics. The earlier a patient seeks medical care and receives treatment that is appropriate for plague, the better their chances are of a full recovery.\n"},"raw_text":{"kind":"string","value":"\n\n### Plague\n\n\n\n\n### What is plague?\n\nPlague is a rare disease caused by bacteria that can infect people and animals. People can get plague after being bitten by infected fleas, handling an infected animal, or breathing in infectious droplets from an infected person or animal. \n\nPlague symptoms depend on how the patient was exposed to the bacteria. Plague can present with different clinical forms, but the most common forms in humans are bubonic, septicemic, and pneumonic plague.\n\n\n\n\nType of Plague\n\n\n\n\nHow it Spreads\n\n\n\n\n[Symptoms](http://www.cdc.gov/plague/symptoms/index.html)\n\n\n\n\n\nType of Plague\n\n\nBubonic\n\n\n\nHow it Spreads\n\n\nBites from infected fleas and handling infected animals\n\n\n\n[Symptoms](http://www.cdc.gov/plague/symptoms/index.html)\n\n\nFever, headache, chills, and painful, swollen, and tender lymph nodes\n\n\n\n\nType of Plague\n\n\nSepticemic\n\n\n\nHow it Spreads\n\n\nBites from infected fleas and handling infected animals\n\n\n\n[Symptoms](http://www.cdc.gov/plague/symptoms/index.html)\n\n\nFever, chills, weakness, stomach pain, and sometimes bleeding into the skin and other organs. Skin and other tissues may turn black and die, especially on fingers, toes, and the nose\n\n\n\n\nType of Plague\n\n\nPneumonic\n\n\n\nHow it Spreads\n\n\nBreathe in infectious droplets from people or animals. A person can develop pneumonic plague if they get bubonic or septicemic plague and don't treat it\n\n\n\n[Symptoms](http://www.cdc.gov/plague/symptoms/index.html)\n\n\nFever, weakness, shortness of breath, chest pain, cough with bloody or watery mucous\n\n\n\n### Who is at risk?\n\nPlague is found in certain regions of Africa, central Asia, the Indian subcontinent, the northern part of South America, and the Southwest United States. Though rare, urban outbreaks of plague have been reported in Madagascar.\n\nThough plague is found in countries around the world, the risk to travelers is low. However, camping, hunting, hiking, or working outdoors can increase your risk.\n\n### What can travelers do to prevent plague?\n\nThere is no vaccine to prevent plague available in the United States. However, travelers can protect themselves from plague by taking the following precautions\n\n**Wear insect repellent**\n\n* Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women.\n\t+ DEET\n\t+ Picaridin (known as KBR 3023 and icaridin outside the US)\n\t+ IR3535\n\t+ Oil of lemon eucalyptus (OLE)\n\t+ Para-menthane-diol (PMD)\n\t+ 2-undecanone\n* Find the right insect repellent for you by using EPA’s search tool.\n\n**Treat clothing and gear with permethrin**\n\n* Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.\n\t+ Permethrin is an insecticide that kills or repels insects.\n\t+ Permethrin-treated clothing provides protection after multiple washings..\n\t+ Read product information to find out how long the protection will last.\n* If treating items yourself, follow the product instructions.\n* Do not apply permethrin products directly to skin.\n* Watch the video [What You Need to Know About Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).\n\n**Do not touch sick or dead animals.** Infected fleas can jump from a live or dead animal onto a person. People can also become infected when handling tissue or body fluids of an infected animal. For example, a hunter skinning an infected animal without using proper precautions could become infected with plague.\n\n* If you must handle a sick or dead animal, wear gloves, pants, and long sleeves to cover your skin, and use additional personal protective equipment.\n\n**Additional steps to take if visiting or living in an area with plague**\n\n* Store food, including pet food, in rodent-proof containers.\n* Keep rodents out of the house and make living spaces rodent proof.\n* Protect yourself and your pets\n\t+ Do not allow pets that roam free in known plague areas to sleep on your bed.\n\t+ Protect your pet from fleas. Talk to a veterinarian.\n\nPlague is a very serious illness but is treatable with commonly available antibiotics. The earlier a patient seeks medical care and receives treatment that is appropriate for plague, the better their chances are of a full recovery.\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n\n### More Information\n\n* [Plague](http://www.cdc.gov/Plague/)\n* [Avoid Bug Bites](/travel/page/avoid-bug-bites)\n* CDC Yellow Book: [Plague](/travel/yellowbook/2012/chapter-3-infectious-diseases-related-to-travel/plague-bubonic-pneumonic-septicemic.htm)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":693,"cells":{"id":{"kind":"string","value":"fdf70d5fb5fe88e66cae3332c20a0bb759e0535d"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Pneumococcal Disease"},"clean_text":{"kind":"string","value":"Pneumococcal Disease | Disease Directory | Travelers' Health | CDC\n\n### Pneumococcal Disease\n### What is pneumococcal disease?\nPneumococcal disease is caused by bacteria called - Streptococcus pneumoniae- (pneumococcus). People with pneumococcal disease can spread the bacteria to others when they cough or sneeze.\nPneumococcus bacteria can cause infections in many parts of the body, including\n- Lungs (pneumonia)\n- Ears (otitis)\n- Sinuses (sinusitis)\n- The lining of the brain and spinal cord (meningitis)\n- Blood (bacteremia)\nSymptoms of pneumococcal infection depend on the part of the body affected. Symptoms can include fever, cough, shortness of breath, chest pain, stiff neck, confusion, increased sensitivity to light, joint pain, chills, ear pain, sleeplessness, and irritability. In severe cases, pneumococcal disease can cause hearing loss, brain damage, or death. You can find a full list of symptoms for each part of the body that is affected on the [symptoms and complications of pneumococcal disease page](https://www.cdc.gov/pneumococcal/about/symptoms-complications.html).\n### Who is at risk?\nInformation by Destination\n\nWhere are you going?\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" - value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n window.location = url;\nPneumococcal disease occurs around the world but is more common in low- and middle-income countries where fewer people get vaccinated against pneumococcal disease. In places with four seasons, pneumococcal disease is more common during winter and early spring. In tropical climates with dry and rainy seasons, pneumococcal disease tends to occur more in the dry season.\n### What can travelers do to prevent pneumococcal disease?\nGetting vaccinated is the best way to protect against pneumococcal disease. Pneumococcal vaccines are routinely recommended in the United States. \nCDC recommends [PCV13 or PCV15](https://www.cdc.gov/vaccines/hcp/vis/vis-statements/pcv.html) for\n- All children younger than 5 years old\n- Children 2 through 18 years old with certain medical conditions\nFor those who have never received any pneumococcal conjugate vaccine, CDC recommends PCV15 or PCV20 for\n- Adults 65 years or older\n- Adults 19 through 64 years old with certain medical conditions or other risk factors\nCDC reocmmends [PPSV23](https://www.cdc.gov/vaccines/hcp/vis/vis-statements/ppv.html) for\n- Children 2 through 18 years old with certain medical conditions\n- Adults 19 years or older who receive PCV15\nSome groups may need multiple doses or booster shots. Talk with your or your child’s clinician about what is best for your specific situation.\n"},"raw_text":{"kind":"string","value":"\n\n### Pneumococcal Disease\n\n\n\n\n### What is pneumococcal disease?\n\nPneumococcal disease is caused by bacteria called *Streptococcus pneumoniae* (pneumococcus). People with pneumococcal disease can spread the bacteria to others when they cough or sneeze.\n\nPneumococcus bacteria can cause infections in many parts of the body, including\n\n* Lungs (pneumonia)\n* Ears (otitis)\n* Sinuses (sinusitis)\n* The lining of the brain and spinal cord (meningitis)\n* Blood (bacteremia)\n\nSymptoms of pneumococcal infection depend on the part of the body affected. Symptoms can include fever, cough, shortness of breath, chest pain, stiff neck, confusion, increased sensitivity to light, joint pain, chills, ear pain, sleeplessness, and irritability. In severe cases, pneumococcal disease can cause hearing loss, brain damage, or death. You can find a full list of symptoms for each part of the body that is affected on the [symptoms and complications of pneumococcal disease page](https://www.cdc.gov/pneumococcal/about/symptoms-complications.html).\n\n### Who is at risk?\n\n\nInformation by Destination\n\nWhere are you going?\n\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n function goSelectPage(){ \n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" + value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n }else{\n window.location = url;\n }\n }\n\n \n \n\nPneumococcal disease occurs around the world but is more common in low- and middle-income countries where fewer people get vaccinated against pneumococcal disease. In places with four seasons, pneumococcal disease is more common during winter and early spring. In tropical climates with dry and rainy seasons, pneumococcal disease tends to occur more in the dry season.\n\n### What can travelers do to prevent pneumococcal disease?\n\nGetting vaccinated is the best way to protect against pneumococcal disease. Pneumococcal vaccines are routinely recommended in the United States. \n\nCDC recommends [PCV13 or PCV15](https://www.cdc.gov/vaccines/hcp/vis/vis-statements/pcv.html) for\n\n* All children younger than 5 years old\n* Children 2 through 18 years old with certain medical conditions\n\nFor those who have never received any pneumococcal conjugate vaccine, CDC recommends PCV15 or PCV20 for\n\n* Adults 65 years or older\n* Adults 19 through 64 years old with certain medical conditions or other risk factors\n\nCDC reocmmends [PPSV23](https://www.cdc.gov/vaccines/hcp/vis/vis-statements/ppv.html) for\n\n* Children 2 through 18 years old with certain medical conditions\n* Adults 19 years or older who receive PCV15\n\nSome groups may need multiple doses or booster shots. Talk with your or your child’s clinician about what is best for your specific situation.\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### More Information\n\n* [Pneumococcal Disease](http://www.cdc.gov/pneumococcal/)\n* CDC Yellow Book: [Pneumococcal Disease](/travel/yellowbook/2020/travel-related-infectious-diseases/pneumococcal-disease) in CDC Yellow Book\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":694,"cells":{"id":{"kind":"string","value":"a1325da97b25f82faebb42529d767f9a6b9a60b1"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Polio"},"clean_text":{"kind":"string","value":"Polio | Disease Directory | Travelers' Health | CDC\n\n### What is polio?\nPolio is a life-threatening disease caused by a virus that affects the nervous system and is usually spread from one person to another when stool (poop) or, less commonly, droplets from a sneeze or cough of an infected person gets into the mouth of another person. For example, you can get polio if you:\n- Eat raw or undercooked food or drink water or other drinks that are contaminated with the stool of an infected person.\n- Put a contaminated object such as a toy in your mouth.\n- Touch a contaminated object and put your fingers in your mouth.\n- Have close contact with a person sick with polio, for example when caring for them.\nMost people with polio do not feel sick. Some people have only minor symptoms, such as fever, tiredness, nausea, headache, nasal congestion, sore throat, cough, stiffness in the neck and back, and pain in the stomach, arms, and legs. Most people recover completely. In rare cases, polio infection can affect the brain and spinal cord and cause permanent loss of muscle function (paralysis) in the arms or legs (usually the legs). Death can occur if there is a loss of function of the muscles used for breathing or an infection of the brain.\n### Who is at risk?\nPolio is still a concern in some places. If you are not up to date with your polio vaccines, you are at risk of getting polio. If you are up to date on your polio vaccines but traveling to a polio-affected country, you may need a one-time polio adult booster. Check your [destination’s travel health page](/travel/destinations/list) and talk to your healthcare professional to learn what vaccines you may need before your trip.\n### What can travelers do to prevent polio?\n#### Get the polio vaccine:\n- Make sure you are [up to date](https://www.cdc.gov/vaccines/schedules/hcp/imz/child-adolescent.html#note-polio) on your polio vaccines. If you are up to date on your polio vaccines and traveling to a polio-affected country, you may need a one-time polio adult booster. Check your [destination’s travel health page](/travel/destinations/list) and talk to your healthcare professional to learn which vaccines you may need before traveling.\n- Make sure children are vaccinated. For best protection, children should get four doses of polio vaccine. Ideally, children should receive a dose at ages\n\t- 2 months;\n\t- 4 months;\n\t- 6 through 18 months; and\n\t- a booster dose at age 4 through 6 years.\n- For information about adults who may not have received sufficient vaccine protection, see the [adult polio vaccination schedule](https://www.cdc.gov/vaccines/vpd/polio/public/index.html).\n- See [Polio Vaccine Information Statement (VIS)](http://www.cdc.gov/vaccines/hcp/vis/vis-statements/ipv.html) for more information.\n#### Choose safer food and drinks while traveling\nFollow the [food and drink safety](/travel/page/food-water-safety) tips to avoid exposure to any food and drinks that could be contaminated by the stool of a person infected with polio.\n#### Wash your hands often\n- Wash your hands often with soap and water, especially after using the bathroom or changing a child’s diaper and before eating or preparing food. Alcohol-based hand sanitizers do not kill poliovirus.\n- Don’t touch your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean.\n- Cover your mouth and nose with a tissue or your sleeve (not your hands) when coughing or sneezing.\n"},"raw_text":{"kind":"string","value":"\n\n### Polio\n\n\n\n\n### What is polio?\n\nPolio is a life-threatening disease caused by a virus that affects the nervous system and is usually spread from one person to another when stool (poop) or, less commonly, droplets from a sneeze or cough of an infected person gets into the mouth of another person. For example, you can get polio if you:\n\n* Eat raw or undercooked food or drink water or other drinks that are contaminated with the stool of an infected person.\n* Put a contaminated object such as a toy in your mouth.\n* Touch a contaminated object and put your fingers in your mouth.\n* Have close contact with a person sick with polio, for example when caring for them.\n\nMost people with polio do not feel sick. Some people have only minor symptoms, such as fever, tiredness, nausea, headache, nasal congestion, sore throat, cough, stiffness in the neck and back, and pain in the stomach, arms, and legs. Most people recover completely. In rare cases, polio infection can affect the brain and spinal cord and cause permanent loss of muscle function (paralysis) in the arms or legs (usually the legs). Death can occur if there is a loss of function of the muscles used for breathing or an infection of the brain.\n\n### Who is at risk?\n\nPolio is still a concern in some places. If you are not up to date with your polio vaccines, you are at risk of getting polio. If you are up to date on your polio vaccines but traveling to a polio-affected country, you may need a one-time polio adult booster. Check your [destination’s travel health page](/travel/destinations/list) and talk to your healthcare professional to learn what vaccines you may need before your trip.\n\n### What can travelers do to prevent polio?\n\n#### Get the polio vaccine:\n\n* Make sure you are [up to date](https://www.cdc.gov/vaccines/schedules/hcp/imz/child-adolescent.html#note-polio) on your polio vaccines. If you are up to date on your polio vaccines and traveling to a polio-affected country, you may need a one-time polio adult booster. Check your [destination’s travel health page](/travel/destinations/list) and talk to your healthcare professional to learn which vaccines you may need before traveling.\n* Make sure children are vaccinated. For best protection, children should get four doses of polio vaccine. Ideally, children should receive a dose at ages\n\t+ 2 months;\n\t+ 4 months;\n\t+ 6 through 18 months; and\n\t+ a booster dose at age 4 through 6 years.\n* For information about adults who may not have received sufficient vaccine protection, see the [adult polio vaccination schedule](https://www.cdc.gov/vaccines/vpd/polio/public/index.html).\n* See [Polio Vaccine Information Statement (VIS)](http://www.cdc.gov/vaccines/hcp/vis/vis-statements/ipv.html) for more information.\n\n#### Choose safer food and drinks while traveling\n\nFollow the [food and drink safety](/travel/page/food-water-safety) tips to avoid exposure to any food and drinks that could be contaminated by the stool of a person infected with polio.\n\n#### Wash your hands often\n\n* Wash your hands often with soap and water, especially after using the bathroom or changing a child’s diaper and before eating or preparing food. Alcohol-based hand sanitizers do not kill poliovirus.\n* Don’t touch your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean.\n* Cover your mouth and nose with a tissue or your sleeve (not your hands) when coughing or sneezing.\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. Avoid contact with other people while you are sick.\n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### More Information\n\n* [CDC Travel Health Notice: Polio in Multiple Countries](/travel/notices/alert/global-polio)\n* [What is Polio?](https://www.cdc.gov/polio/what-is-polio/index.htm)\n* [Polio: For Travelers](https://www.cdc.gov/polio/what-is-polio/travelers.html)\n* [Choose Safe Food and Drinks When Traveling](/travel/page/food-water-safety)\n* CDC Yellow Book: [Polio](/travel/yellowbook/2012/chapter-3-infectious-diseases-related-to-travel/poliomyelitis.htm)\n* [World Health Organization: PolioExternal Link](https://www.who.int/health-topics/poliomyelitis#tab=tab_1)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":695,"cells":{"id":{"kind":"string","value":"8310a6caf57014d6a8d381df0e8154b7c4b691bd"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Rabies"},"clean_text":{"kind":"string","value":"Rabies | Disease Directory | Travelers' Health | CDC\n\n### What is rabies?\nRabies is a deadly disease caused by a virus. You can get rabies if you are bitten or scratched by an animal with rabies.\nIn the United States, rabies is mostly found in wild animals like bats, raccoons, skunks, and foxes. However, in many other countries around the world, bites from dogs (including puppies) are the main source of rabies infections in people. Most people who die of rabies were bitten by a dog with rabies.\nRabies affects the central nervous system (the brain and spinal cord). Without appropriate medical care, rabies causes brain disease and death. Once symptoms of rabies appear, the disease is nearly always fatal. For this reason, preventing animal bites and receiving prompt medical care is especially important.\nEarly rabies symptoms include weakness or discomfort, fever, and headache. There may be discomfort or a prickling or itching sensation at the place of the bite. Within days, an infected person may become anxious, confused, and agitated. As a person gets sicker, they may become delirious, hallucinate, be unable to sleep, and unable to swallow or quench their thirst.\n### Who is at risk?\nInformation by Destination\n\nWhere are you going?\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" - value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n window.location = url;\nRabid dogs are a problem in many countries around the world, including most of Africa, Asia, and parts of Central and South America. Although any mammal can transmit rabies, dog bites are how most travelers get rabies.\nActivities that may increase a traveler’s chances of rabies infection include:\n- Camping or exploring caves (spelunkers)\n- Working with animals (veterinarians, animal handlers, field biologists, or laboratory workers handling animal specimens)\n- Long-term travelers and expatriates\nChildren are more likely to get infected because they often play with animals and may not report bites.\nRabies in dogs is rare in the United States, Australia, Canada, Japan, and most European countries.\n### What can travelers do to prevent rabies?\nTravelers can protect themselves from rabies by taking the following steps:\nAvoid animals when traveling\n- Don’t touch dogs, puppies, or other animals. This goes for strays as well as pets. Not all countries require pets to be vaccinated against rabies. Even animals that appear healthy can spread rabies.\n- Supervise children closely, especially around dogs and puppies, cats and kittens, and wildlife.\n- If you travel with your pet, watch it closely. Do not allow it around other local pets or wild animals.\n- Avoid bringing animals home to the United States. Dogs and cats may be infected with rabies but not show signs until several days or months later. If you do decide to bring an animal with you to the United States, be aware of [CDC’s](https://www.cdc.gov/importation/bringing-an-animal-into-the-united-states/index.html) and [USDA’s](https://www.aphis.usda.gov/aphis/ourfocus/animalhealth/animal-and-animal-product-import-information/live-animal-imports/import-live-animals) [animal importation regulations](https://www.cdc.gov/importation/bringing-an-animal-into-the-united-states/index.html).\n- If you are traveling to work with animals, bring and wear appropriate protective gear.\n- For more information, see [Be Safe Around Animals](/travel/page/be-safe-around-animals).\nAct quickly if you are bitten or scratched by a dog or other animal\n- Immediately wash all bites and scratches well. Use plenty of soap and running water.\n- Seek medical care immediately, even if you don’t feel sick or the wound does not look serious.\n- To prevent rabies, start treatment immediately. Treatment for rabies includes getting a vaccine after you have been bitten. Even if you were vaccinated before your trip, you still need to seek care if you get bitten or scratched by an animal.\n- Be prepared to travel back to the United States or to another area to receive treatment. Vaccination and medicine for rabies exposure is not available everywhere in the world.\nPre-travel rabies vaccine\nFor some travelers, it may make sense to get the rabies vaccine before your trip. Check if rabies vaccine is recommended for [your destination](/travel/destinations/list).\nThe rabies vaccine is given in two shots. The second dose is given seven days after the first dose. Even if you are vaccinated against rabies, if you are bitten or scratched by an [animal that may have rabies](https://www.cdc.gov/rabies/animals/index.html) while traveling, you need to seek medical care immediately and get two booster doses of the vaccine.\n"},"raw_text":{"kind":"string","value":"\n\n### Rabies\n\n\n\n\n### What is rabies?\n\n\nRabies is a deadly disease caused by a virus. You can get rabies if you are bitten or scratched by an animal with rabies.\n\nIn the United States, rabies is mostly found in wild animals like bats, raccoons, skunks, and foxes. However, in many other countries around the world, bites from dogs (including puppies) are the main source of rabies infections in people. Most people who die of rabies were bitten by a dog with rabies.\n\nRabies affects the central nervous system (the brain and spinal cord). Without appropriate medical care, rabies causes brain disease and death. Once symptoms of rabies appear, the disease is nearly always fatal. For this reason, preventing animal bites and receiving prompt medical care is especially important.\n\nEarly rabies symptoms include weakness or discomfort, fever, and headache. There may be discomfort or a prickling or itching sensation at the place of the bite. Within days, an infected person may become anxious, confused, and agitated. As a person gets sicker, they may become delirious, hallucinate, be unable to sleep, and unable to swallow or quench their thirst.\n\n### Who is at risk?\n\n\nInformation by Destination\n\nWhere are you going?\n\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n function goSelectPage(){ \n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" + value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n }else{\n window.location = url;\n }\n }\n\n \n \n\nRabid dogs are a problem in many countries around the world, including most of Africa, Asia, and parts of Central and South America. Although any mammal can transmit rabies, dog bites are how most travelers get rabies.\n\nActivities that may increase a traveler’s chances of rabies infection include:\n\n* Camping or exploring caves (spelunkers)\n* Working with animals (veterinarians, animal handlers, field biologists, or laboratory workers handling animal specimens)\n* Long-term travelers and expatriates\n\nChildren are more likely to get infected because they often play with animals and may not report bites.\n\nRabies in dogs is rare in the United States, Australia, Canada, Japan, and most European countries.\n\n### What can travelers do to prevent rabies?\n\nTravelers can protect themselves from rabies by taking the following steps:\n\n**Avoid animals when traveling**\n\n* Don’t touch dogs, puppies, or other animals. This goes for strays as well as pets. Not all countries require pets to be vaccinated against rabies. Even animals that appear healthy can spread rabies.\n* Supervise children closely, especially around dogs and puppies, cats and kittens, and wildlife.\n* If you travel with your pet, watch it closely. Do not allow it around other local pets or wild animals.\n* Avoid bringing animals home to the United States. Dogs and cats may be infected with rabies but not show signs until several days or months later. If you do decide to bring an animal with you to the United States, be aware of [CDC’s](https://www.cdc.gov/importation/bringing-an-animal-into-the-united-states/index.html) and [USDA’s](https://www.aphis.usda.gov/aphis/ourfocus/animalhealth/animal-and-animal-product-import-information/live-animal-imports/import-live-animals) [animal importation regulations](https://www.cdc.gov/importation/bringing-an-animal-into-the-united-states/index.html).\n* If you are traveling to work with animals, bring and wear appropriate protective gear.\n* For more information, see [Be Safe Around Animals](/travel/page/be-safe-around-animals).\n\n**Act quickly if you are bitten or scratched by a dog or other animal**\n\n* Immediately wash all bites and scratches well. Use plenty of soap and running water.\n* Seek medical care immediately, even if you don’t feel sick or the wound does not look serious.\n* To prevent rabies, start treatment immediately. Treatment for rabies includes getting a vaccine after you have been bitten. Even if you were vaccinated before your trip, you still need to seek care if you get bitten or scratched by an animal.\n* Be prepared to travel back to the United States or to another area to receive treatment. Vaccination and medicine for rabies exposure is not available everywhere in the world.\n\n**Pre-travel rabies vaccine**\n\nFor some travelers, it may make sense to get the rabies vaccine before your trip. Check if rabies vaccine is recommended for [your destination](/travel/destinations/list).\n\nThe rabies vaccine is given in two shots. The second dose is given seven days after the first dose. Even if you are vaccinated against rabies, if you are bitten or scratched by an [animal that may have rabies](https://www.cdc.gov/rabies/animals/index.html) while traveling, you need to seek medical care immediately and get two booster doses of the vaccine.\n\n**Consider medical evacuation insurance**\n\nRabies vaccine is not available in all countries. Medical evacuation insurance can cover the cost of transferring you home or to the nearest destination where care can be obtained. For more information, see [Travel Insurance: Peace of Mind While You Travel](/travel/page/insurance) and [Travel Insurance, Travel Health Insurance & Medical Evacuation Insurance](/travel/yellowbook/2020/health-care-abroad/travel-insurance-travel-health-insurance-and-medical-evacuation-insurance).\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### Traveler Information\n\n* CDC Website: [Rabies](http://www.cdc.gov/rabies/)\n* [Be Safe Around Animals](/travel/page/be-safe-around-animals)\n* [Vaccine Information Statements (VIS)](http://www.cdc.gov/vaccines/pubs/vis/downloads/vis-rabies.pdf)\n\n### Clinician Information\n\n* [Rabies](/travel/yellowbook/2012/chapter-3-infectious-diseases-related-to-travel/rabies.htm) in CDC Yellow Book\n* [R](http://www.cdc.gov/rabies/)[abies Information for Doctors](https://www.cdc.gov/rabies/specific_groups/doctors/index.html)\n* [Rabies: Notifiable Disease](http://c.ymcdn.com/sites/www.cste.org/resource/resmgr/PDFs/CSTENotifiableConditionListA.pdf)\n* [Rabies Diagnosis](http://www.cdc.gov/rabies/diagnosis/index.html)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":696,"cells":{"id":{"kind":"string","value":"8c1c4ef7879454bbd96b716e98517d2c35c22704"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Ross River virus disease"},"clean_text":{"kind":"string","value":"Ross River virus disease | Disease Directory | Travelers' Health | CDC\n\n### Ross River virus disease\n### What is Ross River virus disease?\n\nRoss River virus disease is spread to people by the bite of an infected mosquito.\nMost people who get Ross River virus do not feel sick. For those who do get sick, symptoms include joint pain and swelling, muscle pain, fever, tiredness, and rash. Most patients recover within a few weeks, but some people experience joint pain, joint stiffness, or tiredness for many months.\n### Who is at risk?\nTravelers to Australia and Papua New Guinea can get Ross River virus disease if bitten by an infected mosquito. It is the most common mosquito-borne disease in Australia.\nThe following activities can increase a traveler’s chance of getting infected:\n- Spending a lot of time outdoors\n- Traveling during times of the year when mosquitoes are more common, such as during the summer.\n### What can travelers do to prevent Ross River virus disease?\nThere are no vaccines or medicines that prevent Ross River virus disease. Travelers can protect themselves by taking the following steps.\nUse an EPA-registered insect repellent\n- Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.\n\t- Picaridin (known as KBR 3023 and icaridin outside the US)\n\t- Oil of lemon eucalyptus (OLE)\n\t- Para-menthane-diol (PMD)\nFind the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).\n\n- Insect Repellent Tips for Babies and Children\n\t- Dress your child in clothing that covers arms and legs.\n\t- Cover strollers and baby carriers with mosquito netting.\n\t- When using insect repellent on your child:\n\t\t- Always follow label instructions.\n\t\t- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.\n\t\t- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.\n\t\t\t- Adults: Spray insect repellent onto your hands and then apply to a child’s face.\n\t\t- If also using sunscreen, always apply insect repellent after sunscreen.\nWear long-sleeved shirts and long pants\nTreat clothing and gear with permethrin\n- Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.\n\t- Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.\n\t- Permethrin-treated clothing provides protection after multiple washings.\n\t- Read product information to find out how long the protection will last.\n- If treating items yourself, follow the product instructions.\n- Do not use permethrin products directly on skin.\n- Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).\nKeep mosquitoes out of your hotel room or lodging\n- Choose a hotel or lodging with air conditioning or window and door screens.\n- Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.\nSleep under a mosquito net\n\n- Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.\n- Buy a mosquito net at your local outdoor store or online before traveling overseas.\n- Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.\n- [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.\n\t- Permethrin is an insecticide that kills mosquitoes and other insects.\n\t- To determine if you can wash a treated mosquito net, follow the label instructions.\nIf you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).\nIf you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment.](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html)\n"},"raw_text":{"kind":"string","value":"\n\n### Ross River virus disease\n\n\n\n\n### What is Ross River virus disease?\n\n\nRoss River virus disease is spread to people by the bite of an infected mosquito.\n\nMost people who get Ross River virus do not feel sick. For those who do get sick, symptoms include joint pain and swelling, muscle pain, fever, tiredness, and rash. Most patients recover within a few weeks, but some people experience joint pain, joint stiffness, or tiredness for many months.\n\n### Who is at risk?\n\nTravelers to Australia and Papua New Guinea can get Ross River virus disease if bitten by an infected mosquito. It is the most common mosquito-borne disease in Australia.\n\nThe following activities can increase a traveler’s chance of getting infected:\n\n* Spending a lot of time outdoors\n* Traveling during times of the year when mosquitoes are more common, such as during the summer.\n\n### What can travelers do to prevent Ross River virus disease?\n\nThere are no vaccines or medicines that prevent Ross River virus disease. Travelers can protect themselves by taking the following steps.\n\n**Use an EPA-registered insect repellent**\n\n\n\n* Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.\n\t+ DEET\n\t+ Picaridin (known as KBR 3023 and icaridin outside the US)\n\t+ IR3535\n\t+ Oil of lemon eucalyptus (OLE)\n\t+ Para-menthane-diol (PMD)\n\t+ 2-undecanone\n\nFind the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).\n\n\n\n* Insect Repellent Tips for Babies and Children\n\t+ Dress your child in clothing that covers arms and legs.\n\t+ Cover strollers and baby carriers with mosquito netting.\n\t+ When using insect repellent on your child:\n\t\t- Always follow label instructions.\n\t\t- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.\n\t\t- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.\n\t\t\t* Adults: Spray insect repellent onto your hands and then apply to a child’s face.\n\t\t- If also using sunscreen, always apply insect repellent after sunscreen.\n\n**Wear long-sleeved shirts and long pants**\n\n**Treat clothing and gear with permethrin**\n\n\n\n* Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.\n\t+ Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.\n\t+ Permethrin-treated clothing provides protection after multiple washings.\n\t+ Read product information to find out how long the protection will last.\n* If treating items yourself, follow the product instructions.\n* Do not use permethrin products directly on skin.\n* Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).\n\n**Keep mosquitoes out of your hotel room or lodging**\n\n* Choose a hotel or lodging with air conditioning or window and door screens.\n* Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.\n\n**Sleep under a mosquito net**\n\n\n\n* Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.\n* Buy a mosquito net at your local outdoor store or online before traveling overseas.\n* Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.\n* [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.\n\t+ Permethrin is an insecticide that kills mosquitoes and other insects.\n\t+ To determine if you can wash a treated mosquito net, follow the label instructions.\n\nIf you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).\n\n \n\nIf you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment.](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html)\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### Traveler Information\n\n* [Avoid Bug Bites](/travel/page/avoid-bug-bites)\n* [Ross River Virus](/travel/yellowbook/2020/travel-related-infectious-diseases/chikungunya)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":697,"cells":{"id":{"kind":"string","value":"c2d4b3c089a44ff67b5a834ec837ac92aefcd79a"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Routine Vaccines"},"clean_text":{"kind":"string","value":"Routine Vaccines | Travelers' Health | CDC\n\n### Routine Vaccines\n\n### What are \"routine vaccines\"?\nRoutine vaccines are those recommended for everyone in the United States, depending on age and vaccine history. Most people think of these as [childhood vaccines](https://www.cdc.gov/vaccines/parents/protecting-children/index.html) that you get before starting school, but but there are also routine vaccines for [adolescents](https://www.cdc.gov/vaccines/schedules/hcp/imz/child-adolescent.html) and [adults](https://www.cdc.gov/vaccines/schedules/hcp/imz/adult.html).\n### Why are routine vaccines important for travelers?\nBecause most U.S. children get routine vaccines, many vaccine-preventable diseases, such as measles, mumps, or chickenpox, are not common in the United States. If you are not vaccinated, international travel increases your chances of getting and spreading diseases that are not common in the United Sates. Popular destinations, including Europe, still have outbreaks of [measles](https://www.cdc.gov/measles/travelers.html) and other vaccine-preventable diseases. \nMake sure you are up-to-date on all of your [routine vaccines](/travel/page/routine-vaccines). Routine vaccinations protect you from infectious diseases such as measles that can spread quickly in groups of unvaccinated people. Many diseases prevented by routine vaccination are not common in the United States but are still common in other countries.\n[Check CDC’s destination pages for travel health information](/travel/destinations/list). Check CDC’s webpage for your destination to see what vaccines or medicines you may need and what diseases or health risks are a concern at your destination.\nMake an appointment with your healthcare provider or a [travel health specialist](/travel/page/find-clinic) that takes place at least one month before you leave. They can help you get destination-specific vaccines, medicines, and information. Discussing your health concerns, itinerary, and planned activities with your provider allows them to give more specific advice and recommendations.\n### What routine vaccines do I need?\nThe routine vaccines you need before travel may depend on your age, health, and vaccine history. You may need to get an accelerated dose of a vaccine or a booster dose before traveling.\nRoutine vaccinations related to travel may include the following:\n- Chickenpox (Varicella)\n- Hepatitis A\n- Hepatitis B\n- Human Papilloma Virus (HPV)\n- Measles, mumps, Rubella\n- Tetanus, diphtheria, pertussis\n- Shingles (Zoster)\nThe following are CDC immunization schedules for by age group:\n- [Recommended Vaccinations or Infants and Children (birth through 6 years)](https://www.cdc.gov/vaccines/schedules/easy-to-read/adolescent-easyread.html)\n- [Recommended Vaccinations for Children (7-18 years old)](https://www.cdc.gov/vaccines/schedules/easy-to-read/adolescent-easyread.html)\n- [Recommended Adult Immunization Schedule for ages 19 years or older](https://www.cdc.gov/vaccines/schedules/hcp/imz/adult.html)\n"},"raw_text":{"kind":"string","value":"\n\n### Routine Vaccines\n\n\n\n\n\n### What are \"routine vaccines\"?\n\nRoutine vaccines are those recommended for everyone in the United States, depending on age and vaccine history. Most people think of these as [childhood vaccines](https://www.cdc.gov/vaccines/parents/protecting-children/index.html) that you get before starting school, but but there are also routine vaccines for [adolescents](https://www.cdc.gov/vaccines/schedules/hcp/imz/child-adolescent.html) and [adults](https://www.cdc.gov/vaccines/schedules/hcp/imz/adult.html).\n\n### Why are routine vaccines important for travelers?\n\nBecause most U.S. children get routine vaccines, many vaccine-preventable diseases, such as measles, mumps, or chickenpox, are not common in the United States. If you are not vaccinated, international travel increases your chances of getting and spreading diseases that are not common in the United Sates. Popular destinations, including Europe, still have outbreaks of [measles](https://www.cdc.gov/measles/travelers.html) and other vaccine-preventable diseases. \n\n**Make sure you are up-to-date on all of your [routine vaccines](/travel/page/routine-vaccines).** Routine vaccinations protect you from infectious diseases such as measles that can spread quickly in groups of unvaccinated people. Many diseases prevented by routine vaccination are not common in the United States but are still common in other countries.\n\n**[Check CDC’s destination pages for travel health information](/travel/destinations/list).** Check CDC’s webpage for your destination to see what vaccines or medicines you may need and what diseases or health risks are a concern at your destination.\n\n**Make an appointment** with your healthcare provider or a [travel health specialist](/travel/page/find-clinic) that takes place at least one month before you leave. They can help you get destination-specific vaccines, medicines, and information. Discussing your health concerns, itinerary, and planned activities with your provider allows them to give more specific advice and recommendations.\n\n### What routine vaccines do I need?\n\nThe routine vaccines you need before travel may depend on your age, health, and vaccine history. You may need to get an accelerated dose of a vaccine or a booster dose before traveling.\n\nRoutine vaccinations related to travel may include the following:\n\n* COVID-19\n* Chickenpox (Varicella)\n* Hepatitis A\n* Hepatitis B\n* Human Papilloma Virus (HPV)\n* Influenza\n* Measles, mumps, Rubella\n* Meningococcal\n* Pneumococcal\n* Polio\n* Rotavirus\n* Tetanus, diphtheria, pertussis\n* Shingles (Zoster)\n\nThe following are CDC immunization schedules for by age group:\n\n* [Recommended Vaccinations or Infants and Children (birth through 6 years)](https://www.cdc.gov/vaccines/schedules/easy-to-read/adolescent-easyread.html)\n* [Recommended Vaccinations for Children (7-18 years old)](https://www.cdc.gov/vaccines/schedules/easy-to-read/adolescent-easyread.html)\n* [Recommended Adult Immunization Schedule for ages 19 years or older](https://www.cdc.gov/vaccines/schedules/hcp/imz/adult.html)\n\n### More Information\n\n* [Immunization Schedules](https://www.cdc.gov/vaccines/schedules/index.html)\n* [Travel Vaccines](/travel/page/travel-vaccines)\n\n\n \n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":698,"cells":{"id":{"kind":"string","value":"a82e54543cf819eb163023f5f851c4a858edbd8b"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Rubella"},"clean_text":{"kind":"string","value":"Rubella | Disease Directory | Travelers' Health | CDC\n\n### What is rubella?\nRubella, also called German measles, is a contagious disease caused by a virus. People with rubella can spread it when they cough or sneeze. Pregnant women infected with rubella can pass it on to their developing babies.\nMany people who get rubella never have symptoms or have only mild symptoms. For people who have symptoms, they may include a red rash that starts on the face and spreads to the rest of the body. Other symptoms include low-grade fever, headache, mild pink eye, general discomfort, swollen and enlarged lymph nodes, cough, and runny nose.\nWhile most adults who get rubella have only mild symptoms, rubella infection is especially dangerous during pregnancy. Pregnant women who get rubella can have miscarriages or stillbirths, and their developing babies are at risk for severe birth defects with devastating, lifelong consequences\n### Who is at risk?\nInformation by Destination\n\nWhere are you going?\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" - value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n window.location = url;\nRubella has been eliminated through vaccination in South and North America, including the United States. It still exists in other parts of the world. Travelers going to areas with rubella who have not been vaccinated can get infected.\n### What can travelers do to prevent rubella?\nGetting vaccinated is the best way to protect yourself against rubella. Rubella vaccine is routinely given to children in the United States. The vaccine is given in two doses: children usually get the first dose when they are 12 to 15 months old and the second dose when they are 4 to 6 years old. Rubella vaccine is a combination vaccine that also protects against measles and mumps (MMR vaccine) or measles, mumps, and varicella (MMRV vaccine).\nIf you were born after 1956 and do not have evidence of immunity, you should get vaccinated with two doses of MMR vaccine before you travel. The second dose is given at least 28 days after the first dose. People born before 1957 do not need to be vaccinated with the MMR vaccine.\nInfants 6 to 11 months old traveling internationally should get one dose of MMR vaccine before travel. This dose does not count as part of the routine childhood vaccination series.\nCAUTION: Pregnant people should avoid all exposures to the rubella virus. This means NOT getting the MMR vaccine during pregnancy. It also means that anyone who is pregnant and not already vaccinated against rubella should not travel to countries with rubella or areas with known rubella outbreaks. This is especially true during the first 20 weeks of pregnancy when the risk for a miscarriage or severe birth defects from rubella virus infection is greatest. Any pregnant person not already vaccinated against rubella should get the MMR vaccine immediately after the pregnancy.\nAvoid getting pregnant for at least 4 weeks after receiving the MMR vaccine.\n"},"raw_text":{"kind":"string","value":"\n\n### Rubella\n\n\n\n\n### What is rubella?\n\nRubella, also called German measles, is a contagious disease caused by a virus. People with rubella can spread it when they cough or sneeze. Pregnant women infected with rubella can pass it on to their developing babies.\n\nMany people who get rubella never have symptoms or have only mild symptoms. For people who have symptoms, they may include a red rash that starts on the face and spreads to the rest of the body. Other symptoms include low-grade fever, headache, mild pink eye, general discomfort, swollen and enlarged lymph nodes, cough, and runny nose.\n\nWhile most adults who get rubella have only mild symptoms, rubella infection is especially dangerous during pregnancy. Pregnant women who get rubella can have miscarriages or stillbirths, and their developing babies are at risk for severe birth defects with devastating, lifelong consequences\n\n### Who is at risk?\n\n\nInformation by Destination\n\nWhere are you going?\n\n-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo\n function goSelectPage(){ \n var e = document.getElementById(\"thlrdssl-traveler\");\n var value = e.options[e.selectedIndex].value;\n var url = \"/travel/destinations/traveler/none/\" + value;\n if (value == '0'){\n window.location = \"/travel/destinations/list\";\n }else{\n window.location = url;\n }\n }\n\n \n \n\nRubella has been eliminated through vaccination in South and North America, including the United States. It still exists in other parts of the world. Travelers going to areas with rubella who have not been vaccinated can get infected.\n\n### What can travelers do to prevent rubella?\n\nGetting vaccinated is the best way to protect yourself against rubella. Rubella vaccine is routinely given to children in the United States. The vaccine is given in two doses: children usually get the first dose when they are 12 to 15 months old and the second dose when they are 4 to 6 years old. Rubella vaccine is a combination vaccine that also protects against measles and mumps (MMR vaccine) or measles, mumps, and varicella (MMRV vaccine).\n\nIf you were born after 1956 and do not have evidence of immunity, you should get vaccinated with two doses of MMR vaccine before you travel. The second dose is given at least 28 days after the first dose. People born before 1957 do not need to be vaccinated with the MMR vaccine.\n\nInfants 6 to 11 months old traveling internationally should get one dose of MMR vaccine before travel. This dose does not count as part of the routine childhood vaccination series.\n\n**CAUTION**: Pregnant people should avoid all exposures to the rubella virus. This means NOT getting the MMR vaccine during pregnancy. It also means that anyone who is pregnant and not already vaccinated against rubella should not travel to countries with rubella or areas with known rubella outbreaks. This is especially true during the first 20 weeks of pregnancy when the risk for a miscarriage or severe birth defects from rubella virus infection is greatest. Any pregnant person not already vaccinated against rubella should get the MMR vaccine immediately after the pregnancy.\n\nAvoid getting pregnant for at least 4 weeks after receiving the MMR vaccine.\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n### More Information\n\n* CDC Yellow Book: [Rubella](/travel/yellowbook/2020/travel-related-infectious-diseases/rubella)\n* [Rubella](http://www.cdc.gov/rubella/)\n\n \n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}},{"rowIdx":699,"cells":{"id":{"kind":"string","value":"78c6ddf16720a812e4375f5d3219f5a3f648733a"},"source":{"kind":"string","value":"cdc"},"title":{"kind":"string","value":"Scabies"},"clean_text":{"kind":"string","value":"Scabies | Disease Directory | Travelers' Health | CDC\n\n### What is scabies?\nScabies is a skin condition in people caused by the human itch mite. The mite burrows into the upper layer of skin to live and lay eggs.\nCommon scabies symptoms include intense itching and a skin rash. Scabies can occur anywhere on the body but are more common on the following parts of the body:\n- Between the fingers\n- Genitals (Penis and Vagina)\n- Shoulder blades\nChildren are often more likely to get scabies. For babies and very young children scabies is often found on the head, face, neck, palms, and soles of the feet.\nFor people who have never had scabies before, symptoms usually take 4-6 weeks to appear. Symptoms appear more quickly in people who have had scabies before, in as few as 1 to 4 days. Scabies mites can spread to other parts of the body and from one person to another person even before symptoms start.\nThe same mite that causes scabies also causes crusted scabies. Crusted scabies is severe scabies that happens in people who have weakened immune systems. People with crusted scabies are infested with very large numbers of mites. This increases their risk of spreading mites to others, either from brief skin-to-skin contact or from contact with items such as bedding, clothing, furniture, rugs, and carpeting.\n### Who is at risk?\nScabies is found worldwide and can spread rapidly under crowded conditions where close skin-to-skin contact is frequent. Child-care facilities, nursing homes, extended-care facilities, and prisons are often sites of scabies outbreaks. Scabies is more common in long-term travelers than in those who travel for less than 8 weeks at a time.\nAnimals do not have scabies and cannot spread scabies to people.\n### What can travelers do to prevent scabies?\nThere is no vaccine or medicine to prevent scabies. Effective medicine to treat scabies is only available with a doctor's prescription.\nTravelers can avoid scabies by not touching or having close skin-to-skin contact with a person who has a rash or who is itching. Avoid touching or handling a sick person’s clothing or bedding.\nScabies mites die when you wash bedding and clothing using hot water and hot dryer cycles or dry-clean the items. Items that cannot be dry-cleaned or laundered can be disinfested by storing them in a closed plastic bag for more than 72 hours. Scabies mites generally do not survive more than 2 to 3 days away from human skin.\n"},"raw_text":{"kind":"string","value":"\n\n### Scabies\n\n\n\n\n### What is scabies?\n\nScabies is a skin condition in people caused by the human itch mite. The mite burrows into the upper layer of skin to live and lay eggs.\n\nCommon scabies symptoms include intense itching and a skin rash. Scabies can occur anywhere on the body but are more common on the following parts of the body:\n\n* Between the fingers\n* Wrist\n* Elbow\n* Armpit\n* Genitals (Penis and Vagina)\n* Nipple\n* Waist\n* Buttocks\n* Shoulder blades\n\n\nChildren are often more likely to get scabies. For babies and very young children scabies is often found on the head, face, neck, palms, and soles of the feet.\n\n\nFor people who have never had scabies before, symptoms usually take 4-6 weeks to appear. Symptoms appear more quickly in people who have had scabies before, in as few as 1 to 4 days. Scabies mites can spread to other parts of the body and from one person to another person even before symptoms start.\n\nThe same mite that causes scabies also causes crusted scabies. Crusted scabies is severe scabies that happens in people who have weakened immune systems. People with crusted scabies are infested with very large numbers of mites. This increases their risk of spreading mites to others, either from brief skin-to-skin contact or from contact with items such as bedding, clothing, furniture, rugs, and carpeting.\n\n### Who is at risk?\n\nScabies is found worldwide and can spread rapidly under crowded conditions where close skin-to-skin contact is frequent. Child-care facilities, nursing homes, extended-care facilities, and prisons are often sites of scabies outbreaks. Scabies is more common in long-term travelers than in those who travel for less than 8 weeks at a time.\n\nAnimals do not have scabies and cannot spread scabies to people.\n\n### What can travelers do to prevent scabies?\n\nThere is no vaccine or medicine to prevent scabies. Effective medicine to treat scabies is only available with a doctor's prescription.\n\nTravelers can avoid scabies by not touching or having close skin-to-skin contact with a person who has a rash or who is itching. Avoid touching or handling a sick person’s clothing or bedding.\n\nScabies mites die when you wash bedding and clothing using hot water and hot dryer cycles or dry-clean the items. Items that cannot be dry-cleaned or laundered can be disinfested by storing them in a closed plastic bag for more than 72 hours. Scabies mites generally do not survive more than 2 to 3 days away from human skin.\n\n### After Travel\n\n\n\n\n**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. \n\nIf you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).\n\n\n\n \n\n\n### More Information\n\n* [Scabies](http://www.cdc.gov/parasites/scabies/)\n* [Scabies FAQs](http://www.cdc.gov/parasites/scabies/gen_info/faqs.html)\n* CDC Yellow Book: [Scabies](/travel/yellowbook/2012/chapter-3-infectious-diseases-related-to-travel/scabies-sarcoptic-itch-sarcoptic-acariasis.htm)\n* [Scabies Treatment](http://www.cdc.gov/parasites/scabies/treatment.html)\n\n\n\n"},"url":{"kind":"string","value":"None"},"overview":{"kind":"string","value":"None"}}}],"truncated":false,"partial":false},"paginationData":{"pageIndex":6,"numItemsPerPage":100,"numTotalItems":37970,"offset":600,"length":100}},"jwt":"eyJhbGciOiJFZERTQSJ9.eyJyZWFkIjp0cnVlLCJwZXJtaXNzaW9ucyI6eyJyZXBvLmNvbnRlbnQucmVhZCI6dHJ1ZX0sImlhdCI6MTc0OTkyNDAxOSwic3ViIjoiL2RhdGFzZXRzL2VwZmwtbGxtL2d1aWRlbGluZXMiLCJleHAiOjE3NDk5Mjc2MTksImlzcyI6Imh0dHBzOi8vaHVnZ2luZ2ZhY2UuY28ifQ.tByKW8JLbRZUGABzjTa9of0pvn2KoS74d3J8oHfY9CYHsY8yPuKiQY4E9a0gWkH8gd33Nv5gFKTvHmyGq5kPBA","displayUrls":true},"discussionsStats":{"closed":2,"open":0,"total":2},"fullWidth":true,"hasGatedAccess":true,"hasFullAccess":true,"isEmbedded":false,"savedQueries":{"community":[{"views":[{"key":"default/train","displayName":"train","viewName":"train"}],"sql":"SELECT\n -- Counts of 'none' occurrences\n COUNT(CASE WHEN lower(raw_text) = 'none' THEN 1 END) AS raw_text_none_count,\n COUNT(CASE WHEN lower(clean_text) = 'none' THEN 1 END) AS clean_text_none_count,\n \n -- Total row count\n COUNT(*) AS total_rows,\n \n -- Percentage of 'none' occurrences\n ROUND(100.0 * COUNT(CASE WHEN lower(raw_text) = 'none' THEN 1 END) / COUNT(*), 2) AS raw_text_none_pct,\n ROUND(100.0 * COUNT(CASE WHEN lower(clean_text) = 'none' THEN 1 END) / COUNT(*), 2) AS clean_text_none_pct,\n \n -- Average lengths\n ROUND(AVG(CASE WHEN lower(raw_text) = 'none' THEN length(clean_text) END), 2) AS avg_clean_text_length_in_none_raw_text_rows,\n ROUND(AVG(length(clean_text)), 2) AS avg_clean_text_length_entire_dataset\nFROM train;","title":"Count and Percentage of 'None'","createdAt":"2025-06-04T09:25:55.445Z","slug":"Gg9tI4f","private":false,"justification":"The query reveals the frequency of 'none' values in raw and clean text fields, their percentage in the dataset, and average text length differences, providing valuable insights for data cleaning and quality assessment.","viewNames":["train"]},{"views":[{"key":"default/train","displayName":"train","viewName":"train"}],"sql":"SELECT\n MIN(LENGTH(clean_text)) AS min_clean_length,\n MAX(LENGTH(clean_text)) AS max_clean_length,\n MIN(LENGTH(raw_text)) AS min_raw_length,\n MAX(LENGTH(raw_text)) AS max_raw_length\nFROM train;","title":"Text Length Statistics","createdAt":"2025-06-04T09:31:10.914Z","slug":"xlW4ilr","private":false,"justification":"Provides the minimum and maximum lengths of both cleaned and raw text, offering basic insights into text length variation.","viewNames":["train"]},{"views":[{"key":"default/train","displayName":"train","viewName":"train"}],"sql":"SELECT\n COUNT(CASE WHEN lower(raw_text) = 'none' THEN 1 END) AS raw_text_none_count,\n COUNT(CASE WHEN lower(clean_text) = 'none' THEN 1 END) AS clean_text_none_count,\n COUNT(*) AS total_rows,\n ROUND(100.0 * COUNT(CASE WHEN lower(raw_text) = 'none' THEN 1 END) / COUNT(*), 2) AS raw_text_none_pct,\n ROUND(100.0 * COUNT(CASE WHEN lower(clean_text) = 'none' THEN 1 END) / COUNT(*), 2) AS clean_text_none_pct\nFROM train;","title":"Count None Values in Text Columns","createdAt":"2025-06-04T09:18:45.124Z","slug":"aqrbJ7J","private":false,"justification":"Counts the occurrences and percentages of rows where 'raw_text' or 'clean_text' is 'none', providing a basic overview of missing or placeholder data.","viewNames":["train"]},{"views":[{"key":"default/train","displayName":"train","viewName":"train"}],"sql":"SELECT\n *,\n LENGTH(clean_text) AS clean_text_length,\n LENGTH(raw_text) AS raw_text_length\nFROM train\nORDER BY clean_text_length DESC\nLIMIT 100;","title":"Top 100 Longest Clean Texts","createdAt":"2025-06-04T08:40:37.295Z","slug":"UK2264G","private":false,"justification":"Retrieves the 100 longest cleaned text entries along with their raw text versions, offering basic insight into text length differences.","viewNames":["train"]},{"views":[{"key":"default/train","displayName":"train","viewName":"train"}],"sql":"SELECT \n *,\n LENGTH(clean_text) AS clean_text_length\nFROM train\nORDER BY clean_text_length DESC\nLIMIT 100;","title":"Longest Clean Text Entries","createdAt":"2025-06-04T08:37:44.088Z","slug":"5NT4qgP","private":false,"justification":"Returns the 100 longest clean texts in the dataset, which could help identify unusually long entries for quality review.","viewNames":["train"]},{"views":[{"key":"default/train","displayName":"train","viewName":"train"}],"sql":"SELECT \n id,\n title,\n LENGTH(clean_text) AS clean_text_length\nFROM train\nORDER BY clean_text_length DESC\nLIMIT 100;","title":"Longest Clean Text Entries","createdAt":"2025-06-04T08:34:40.035Z","slug":"agI8iOd","private":false,"justification":"Returns the 100 longest cleaned text entries by id and title, providing basic information about the longest entries without significant analytical insight.","viewNames":["train"]}],"user":[]}}">
id
stringlengths 40
40
| source
stringclasses 9
values | title
stringlengths 2
345
| clean_text
stringlengths 35
1.63M
| raw_text
stringlengths 4
1.63M
| url
stringlengths 4
498
| overview
stringlengths 0
10k
|
|---|---|---|---|---|---|---|
2387dc1c8f7bb149a9d50339fcbee1428efbb3b2 | cdc | None | However, the benefits are well worth the effort. Compared to maintaining the current rate of decline, eliminating tuberculosis by 2035 would result in 253,000 fewer tuberculosis cases 15,200 fewer tuberculosis-related deaths $1.3 billion less in treatment costs in 2006 dollars 7 Each case of tuberculosis represents a profound impact on a person, a family, a workplace, and a community. Preventing the ongoing accumulation of deaths, disability, healthcare costs, and loss of family income from tuberculosis will require full participation by policy makers, the public health sector, medical practitioners, professional societies, community-based organizations, and voluntary organizations to implement the recommendations made in 2000 by the IOM in Ending Neglect.# I. Executive Summary
# A. Reasons for Issuing this Call for Action in 2010
In 2000, the Institute of Medicine (IOM) published a report, Ending Neglect: The Elimination of Tuberculosis in the United States, detailing the history of efforts to control and eliminate tuberculosis in the United States and recommending a plan to eliminate tuberculosis in the United States by 2035. In 2007, based upon the recommendations from its retreat, the National Coalition for the Elimination of Tuberculosis (NCET) has transitioned to Stop TB USA. The name change reflects the need to be more readily identified as the point of contact for the Stop TB Partnership at the World Health Organization. In late 2007, Stop TB USA assembled a Tuberculosis Elimination Plan Committee to assess the progress since the release of the IOM report and to formulate recommendations to update the IOM plan. This report assesses how and why the IOM's tuberculosis elimination plan has not been fully implemented and provides updated action plans to move forward on its recommendations to accelerate progress toward tuberculosis elimination in the United States.
# TB Disease, Latent TB Infection: Definitions, Transmission, and Statistics
Tuberculosis is a life-threatening illness caused by a group of bacteria called Mycobacterium tuberculosis complex. The commonly used public health term tuberculosis case is used to describe a newly reported diagnosis of tuberculosis. The statistic for noting the frequency of tuberculosis in a population is the tuberculosis case rate, defined as the number of tuberculosis cases per year in an area divided by the number of people living in that area multiplied by 100,000. The tuberculosis case rate is also referred to as the tuberculosis incidence rate. M. tuberculosis is transmitted from a person with tuberculosis of the lungs (pulmonary tuberculosis) through the air to other people who may become infected. Infection with M. tuberculosis is called latent tuberculosis infection because there are no symptoms or signs of tuberculosis disease. Latent tuberculosis infection can be diagnosed with a tuberculin skin test or specific blood tests (interferon gamma release assays or IGRAs).
Latent tuberculosis infection carries a 10 percent lifetime risk of tuberculosis disease with about half of the cases occurring within the first two years after infection. Infants, human immunodeficiency virus (HIV)-infected persons, and those with suppressed immune systems are at much higher risk for developing tuberculosis from latent tuberculosis infection.
# Slowing Decline in Rates of Tuberculosis Disease
Nine years after the IOM report, its recommendations have not been fully implemented, and the annual decline in tuberculosis incidence rates has slowed to only 3.8% per year since 2003.
If this trend continues, it will take 97 years to achieve tuberculosis elimination, defined as a rate of less than one case of tuberculosis per million persons. This is clearly a goal well below the horizon from a human perspective in 2010.
Placed in the context of affected persons today, only 300 newly reported cases of tuberculosis would have been expected in the entire US population of 300 million if tuberculosis elimination had been achieved. Instead, 12,904 cases of tuberculosis were reported in 2008, a decrease of only 2.9% from the 13,288 reported in 2007.
# Health Disparities in Rates of Tuberculosis Disease
A major health disparity exists for tuberculosis. In 2008 only 17% of the cases of tuberculosis in the United States were reported in the majority non-Hispanic white population. Compared to reported tuberculosis case rates among non-Hispanic whites, the rates are 5.5-fold higher among American Indians, 7.4-fold higher among Hispanics, 8.0-fold higher among blacks, and 22.9-fold higher among Asians.
# Serious Health and Economic Impacts of Tuberculosis Disease
Information on the frequency of tuberculosis is available and believed to be fairly accurate because cases of tuberculosis are reportable to state health departments and forwarded to the Centers for Disease Control and Prevention (CDC). For each of the 12,904 persons reported with tuberculosis in 2008, the continuing presence of tuberculosis in the United States may have resulted in preventable death, lifethreatening illness, disability, and/or loss of productivity, particularly in minority populations. Tuberculosis remains a deadly disease with over 1,200 of the persons reported as cases in 2006 (the most current year with complete follow-up) having died either before diagnosis or before completing treatment. 1 Among survivors, the health impact remains significant. Over half of the survivors of pulmonary (lung) tuberculosis are left with significant lung impairment. 2 Tuberculosis disease also has a strong economic impact. Prolonged short-term disability due to illness and isolation for public health protection impacts patient and family income. In addition, treating each patient for tuberculosis is expensive with outpatient directly observed treatment costs of $4,000. About 50% of patients are hospitalized at a cost per patient of $19,000. (Both cost estimates are in 2004 dollars.) 3 Many of these costs are absorbed by the public health sector because patients with tuberculosis often lack health insurance, and the clinical expertise in tuberculosis of many private physicians is limited.
Detecting tuberculosis is also expensive. For each patient with confirmed tuberculosis, ten or more people are often evaluated for suspected tuberculosis but determined not to have tuberculosis. A study of laboratory diagnostic tests in Tarrant County, Texas, found that 148 cultures for mycobacteria were done across the community for each confirmed case of tuberculosis in 2002, translating into an estimated laboratory cost of $16,830 for each confirmed tuberculosis case reported by the health department. Health departments evaluate and treat at least as many suspected but not reportable tuberculosis cases as those that meet the reporting requirements, and the health department costs range from $2,180 to $3,525 for each patient treated initially for suspected tuberculosis but later determined to have another diagnosis. These costs do not include hospitalizations that are not covered by public health departments. 4 Improvements in tuberculosis diagnostic tests could reduce the cost, inconvenience, and/or side effects that result from delays in making or excluding the diagnosis of tuberculosis.
With the emergence of multidrug-resistant and extensively drug-resistant strains, tuberculosis has become much more expensive and difficult to diagnose and treat. In the United States, the average estimated hospitalization cost for treating a patient with extensively drug-resistant tuberculosis is $600,000, and that does not include costs of outpatient care and related public health department interventions. 5 The global spread of drug-resistant tuberculosis strains-particularly in human immunodeficiency virus (HIV) co-infected populations living in countries with high tuberculosis burdens but poorly functioning tuberculosis control programs-poses a growing threat to US residents.
# Few Modern Tools for Tuberculosis Diagnosis, Treatment, and Prevention
Further, due to decades of stagnation in research and development, few modern tools have been introduced for the diagnosis, treatment, and prevention of the disease.
The bacilli Calmette-Guérin (BCG) vaccine is the only existing vaccine against tuberculosis and is widely used. However, BCG has had no apparent impact on reversing the growing global tuberculosis pandemic. New, more effective vaccines are urgently needed.
For more accurate and timely detection of latent tuberculosis infection, two blood tests are currently licensed in the United States. However, insufficient funding for operational research has led to delays in implementation of these tests, and many public health programs have been unable to cover the additional cost of these tests.
To more rapidly diagnose tuberculosis disease, there is the nucleic acid amplification (NAA) test. Other promising newer diagnostic methods are able to detect multidrugresistant tuberculosis within just days. However, implementation of these tests remains limited because of inadequate operational research, the official approval processes, cost issues, and/or laboratory expertise. 6 New treatment regimens for tuberculosis disease and latent tuberculosis infection are needed to shorten and simplify treatment, be compatible with antiretrovirals and other commonly-used medicines, and address drug resistance.
# Erosion of Public Health Infrastructure and Loss of Expertise
In the United States, public health provides key elements of tuberculosis control that are not available in the private sector. Two key, recent surveys conducted by the National Tuberculosis Controllers Association (NTCA) and National Tuberculosis Nurse Coalition (NTNC) indicated erosion of tuberculosis control infrastructure and impending loss of expertise. These surveys verify the need to augment and invest in domestic tuberculosis programs.
The NTCA survey focused on resources for tuberculosis control activities from 2006 through 2008. Respondents reported that the most common barrier to reaching the national objectives for tuberculosis control was underfunding of public health systems (81%). Estimates from each program on needed funding ranged from $13,000-$99,000 for eight programs (33%), $100,000-$399,000 for eight programs (33%), $400,000-$1.5 million for six programs (25%), to $2-2.2 million for two programs (8%).
The NTNC survey noted an impending loss of nursing tuberculosis case management expertise as 33% and 74% of current tuberculosis case managers anticipate retirement within 5 and 10 years, respectively. This loss of key infrastructure comes at a time when tuberculosis nursing case managers report increasing case complexity due to drug resistance (multidrug-resistant and extensively drug-resistant tuberculosis), comorbid conditions, and greater linguistic and cultural diversity of patients with tuberculosis in their communities.
# Tuberculosis Elimination-A Worthy and Achievable Goal
Despite this dire assessment of current progress, the elimination of tuberculosis in the United States, first proposed in 1989 and reaffirmed by the IOM in 2000, is a worthy and achievable goal if we accept the challenge.
# B. Purpose of this Call for Action
The Stop TB USA Tuberculosis Elimination Plan Committee has drafted this update and based it upon the following documents that explain national guidelines and strategies that will need to be implemented to eliminate tuberculosis in the United States: The aim of this plan is not to rewrite the IOM plan for eliminating tuberculosis: the IOM plan and its recommendations are still valid. The purpose of this plan is to call for stakeholder involvement and to serve as a foundation for making specific action plans to implement the IOM recommendations. The purpose of this call for action is to engage policy makers in all levels of government, the public health sector, medical practitioners, professional societies, community-based organizations, and voluntary organizations in the effort to eliminate tuberculosis in the United States.
# C. Progress Assessment Summary
In its 2000 report, Ending Neglect, the IOM recommended that five specific goals be targeted in order to eliminate tuberculosis in the United States. Table 1 summarizes the current status of progress toward these goals.
T A B L E 1
# Success in Meeting Institute of Medicine Goals
# Institute of Medicine Goal Success Comments
Maintain control of tuberculosis while adjusting to declining tuberculosis case numbers and rates Yes There has been continuing decline in tuberculosis case numbers and rates since 1993
Accelerate the rate of decline of tuberculosis cases and rates by increasing efforts at targeted testing and treatment of latent tuberculosis infection
# No
The decline in tuberculosis is slowing, not accelerating. The treatment of latent tuberculosis infection remains largely limited to public health departments and has not been expanded by other medical care providers to the level required for tuberculosis elimination Develop the new diagnostic, treatment, and prevention tools that will be necessary for the ultimate elimination of tuberculosis The continued decline in case rates provides evidence that tuberculosis remains under control, but the acceleration of tuberculosis elimination that the IOM anticipated with the implementation of Goals 2 through 5 (Table 1) has not occurred. Treatment of latent tuberculosis infection is a tuberculosis prevention strategy that is critical to eliminate tuberculosis. However, expansion of the treatment of latent tuberculosis infection has not occurred and remains limited in public health departments where it is considered low priority when resources are scarce. Expansion of treatment for latent tuberculosis infection has been severely limited due to the lack of an effective, safe, and affordable short-course treatment regimen. Detailed information on the progress made toward the IOM goals is provided in Chapter II: "Eliminating TB in the United States," pages 20-35.
The 2008 tuberculosis case rates, the reported number of persons diagnosed with active tuberculosis per 100,000 persons per year, are shown in Table 2 (next page) for the overall total US population. The rate of 4.2 cases per 100,000 population is equivalent to 42 per million population, 42-fold higher than one per million, the definition of tuberculosis elimination. Also shown are the average annual percentage changes in tuberculosis case rates from 2003 through 2008 for the total US population and by birthplace and race/ethnicity.
Projecting these trends forward, it would take until 2107-97 years from 2010-to achieve the tuberculosis elimination goal of one case of tuberculosis per million for the entire US population. A major contribution to this estimate is the higher rate and slower annual decrease among foreign-born persons, a population projected to require 141 years for tuberculosis elimination. Racial and ethnic minority populations (blacks, Asians, and Hispanics) continue to be disproportionately affected by tuberculosis in the United States. Tuberculosis elimination among the various racial and ethnic minority populations is projected to take 80 to 129 years. The rates and delayed years of projected tuberculosis elimination for ethnic and racial groups also reflect the proportion of tuberculosis cases that occur among foreign-born persons within these groups. Foreign-born persons, who most likely arrived in the United States with latent tuberculosis infection that progressed to tuberculosis, accounted for 95% and 76% of cases among Asian and Hispanic residents respectively in 2008. Foreign-born persons made up 32% of tuberculosis cases reported among black persons, an increase from 5% in 1993.
CALL
Much of the ongoing cost, disability, and premature mortality that are predicted to continue for the next 97 years may be preventable if we implement the IOM recommendations. Tuberculosis disparately affects racial and ethnic minorities, yet every American remains at potential risk for tuberculosis due to the global burden of tuberculosis, including drug-resistant strains of tuberculosis that require treatment for up to two years. The following recommendations for action will benefit every American as well as our global neighbors who have an urgent need for the same new tools that we seek for the diagnosis, treatment, and prevention of tuberculosis.
# D. Recommendations for Action
The Tuberculosis Elimination Plan Committee has developed a set of general recommendations for action on national, state, and/or local levels in all US communities and populations. Separate recommendations have been formulated for speeding up the development and implementation of tuberculosis diagnostics, drugs, and vaccines. Other recommendations have been developed for specific US-born and foreign-born populations to address the risk factors and/or interventions that are either unique or more important for those persons. In addition, the challenges of providing tuberculosis services in states with low tuberculosis case burdens have been a subject of discussion and research, and this document provides updated plans for action to accelerate tuberculosis elimination in areas with low incidences of tuberculosis.
# General Recommendations for Action
The general recommendations reflect important roles that must be assumed by federal, state, county, and municipal agencies as well as other local and national organizations if tuberculosis is to be eliminated.
# New Tools
Tuberculosis control in the United States has been maintained over the past two decades by placing emphasis on the detection and treatment of tuberculosis and on the evaluation and treatment of contacts (persons exposed to infectious tuberculosis). These top-priority activities must be done well, and new diagnostic tools and treatments for active tuberculosis must be developed. But, as pointed out in the IOM report, accelerating our progress toward eliminating tuberculosis requires additional resources and tools to expand the treatment of latent tuberculosis infection. Tuberculosis elimination requires much more rapid development, evaluation, and implementation of new tools to accelerate the decline in the rate of cases of tuberculosis, particularly with the recent trends of stagnation in these case rates.
# Foreign-born Populations
As noted in the 2000 IOM report, the burden of tuberculosis among foreign-born persons results from latent tuberculosis infection that progresses to tuberculosis after arrival in the United States, so eliminating tuberculosis requires expanded treatment of latent tuberculosis infection. There are also unique linguistic and cultural issues that must be addressed in providing quality tuberculosis services to many foreign-born persons.
T A B L E 6
# Action Plans for Tuberculosis Elimination among the Foreign-born
Federal Government 1. The Division of Tuberculosis Elimination should evaluate the feasibility of testing all immigrant applicants being screened overseas for latent tuberculosis infection (currently limited to children aged 2 to 14 years) including the use of the new tools of blood testing with interferon gamma release assays with the goal of treating latent tuberculosis infection with an effective, safe, short-course regimen 2. The US government must ensure that receiving jurisdictions are promptly notified of incoming refugees and Class B immigrants along with complete medical records from overseas tuberculosis screening so that local tuberculosis programs can complete follow-up in a timely manner. Mechanisms must be developed to track migration of new arrivals with diagnoses of latent tuberculosis infection to optimize chances for treatment completion and to allow for maintenance of medical record information
The US government must maintain and increase its commitment to global tuberculosis control and elimination, including the support for implementation and enhancement of existing effective control and prevention strategies and the development of new tools for diagnosis, treatment, and prevention of tuberculosis students, to raise the awareness of tuberculosis in high-risk foreign-born persons, reduce delays in diagnosis, and broaden the scope of targeted testing and treatment programs for latent tuberculosis infection. Services that can be provided by health departments include facilitating laboratory testing, providing medications, providing community and provider education and expert clinical consultation and referral services, and evaluating the effectiveness of community-based programs Community Partners
Community health centers should make the diagnosis and treatment of latent tuberculosis infection a priority activity. This will require collaboration with public health agencies to provide a full range of tuberculosis prevention services for new immigrants and other high-risk populations (such as migrant workers) regardless of ability to pay, visa status, or movement among local health jurisdictions 6. Civil surgeons performing visa status adjustments for immigrants in their communities must ensure that their evaluations include effective tuberculosis screening according to current standards. Greater emphasis, combined with additional resources, must be placed on treatment of latent tuberculosis infection among immigrants diagnosed with latent tuberculosis infection during these examinations 7. Institutions and employers who sponsor students and workers from moderate-or high-burden tuberculosis countries, who under current policy are not required to undergo tuberculosis screening before entry to the United States, should establish tuberculosis screening programs for their constituents. Such programs should incorporate treatment for those diagnosed with latent tuberculosis infection 8. Medical practitioners who provide care to foreign-born persons should educate their patients about symptoms of tuberculosis and should incorporate tuberculosis screening, targeted testing, and treatment of latent tuberculosis infection into ongoing medical services to high-risk patients
# Tuberculosis Low-incidence Areas
The challenges of progressing toward tuberculosis elimination in areas with lowincidence rates of tuberculosis are described in the 2002 report of the Advisory Council for the Elimination of Tuberculosis (ACET). The report recommends evaluating the feasibility of interstate regionalization by creating collaborative consortiums to ensure that high-quality, essential (core) elements of tuberculosis control are maintained.
There are now two models that have been developed and implemented for regionalization of tuberculosis prevention and control. The first model is the New England Tuberculosis Consortium, a collaboration among the six New England tuberculosis programs and the CDC. These six states share a similar epidemiology pattern, common borders, and a history of past collaborative efforts. The New England Tuberculosis Consortium has built a regional leadership team that shares expertise and resources in an organized and supportive fashion. Three important findings were noted in both models. First, tuberculosis control program staff members and resources in low-incidence states cannot simply merge across the state boundaries to create a larger multistate program. Second, tuberculosis control services within each state can be enhanced when tuberculosis program staff collaborate in a multistate regional tuberculosis elimination effort. Third, limited-but necessary-additional federal resources, including personnel assigned to the region, must be provided to maintain effective regional collaboration.
A successful tuberculosis elimination campaign will lead to more tuberculosis lowincidence areas, and the lessons learned in the New England and the western state regions will be applicable to more areas of the United States. Core tuberculosis control services must be maintained, not eliminated, as the number of tuberculosis cases declines in order to avoid a resurgence in the disease, as occurred in the mid-1980s. First, a full understanding of the causes of this remarkable change will require collection of additional information and analysis of its implications for the national goal of tuberculosis elimination. The potential contributors to this decline could include improved tuberculosis control but could also reflect surveillance reporting changes instituted in 2009, population demographic shifts, and under-diagnosis or under-reporting of cases. As noted in the MMWR report, the CDC and the National Tuberculosis Controllers Association are studying the possible explanations for the unexpectedly large drop in tuberculosis cases and rates.
Second, if this decrease in tuberculosis cases and rates is due to a true reduction in the occurrence of tuberculosis, this decrease does not diminish the importance of the recommendations in this document. An even greater acceleration of the rate of decline in tuberculosis cases will be needed if we are to eliminate tuberculosis by the year 2035 and avoid 253,000 preventable tuberculosis cases and the associated deaths, disability, and loss of family income. A decrease of over 10% per year, followed by 20% per year was called for by the IOM ten years ago. 12 Having finally achieved this first step is a call for action, not merely a call for celebration.
For more information, the MMWR report, "Decrease in Reported Tuberculosis Cases ---United States, 2009," is available at: .
# Advisory Council for the Elimination of Tuberculosis Report, 1989
In 1989, the ACET report called for the elimination of tuberculosis in the United States by the year 2010, defining tuberculosis elimination as a case rate of less than one case of tuberculosis per million persons. 9 A year 2000 interim target of achieving a case rate of 3.5 per 100,000 was also established. When the report was published in 1989, the US case rate for tuberculosis was 9.5 per 100,000. The ACET report claimed that tuberculosis elimination was a realistic goal for three reasons: tuberculosis was retreating into geographically and demographically defined high-risk populations; biotechnology had the potential for generating better tools for diagnosis, treatment, and prevention; and advances in computer, telecommunications, and other technologies could enhance implementation of new tools.
A three-step plan of action to achieve tuberculosis elimination was proposed:
1. More effective use of existing prevention and control methods, especially in high-risk populations defined as human immunodeficiency virus (HIV)-infected persons, racial and ethnic minorities, the foreign-born, and the elderly
# Resurgence of Tuberculosis, 1985-1992
Ironically at the time of the preparation of the ACET report, there were early indications the United States was experiencing the first resurgence of tuberculosis known since national case reporting was instituted in 1953. The annual tuberculosis case rate had remained stagnant between 9.2 and 9.5 cases per 100,000 per year for the five-year period 1985 through 1989. The resurgence-related to the expansion of HIV infection, hospital transmission of Mycobacterium tuberculosis, multidrug-resistant tuberculosis, disassembly of categorical public health tuberculosis programs at state and local levels, and increasing immigration from countries with a high incidence of tuberculosisextended through 1992. The resurgence took a heavy toll in terms of tuberculosisrelated illness and death, including healthcare workers, and also forced a large amount of additional resources to be returned to tuberculosis control. 10 After the public health capacity was rebuilt, a resumption of the downward trend in tuberculosis morbidity in the United States in 1993 led to a renewed interest in tuberculosis elimination. In 1999, ACET reassessed its 1989 plan and made updated recommendations for tuberculosis elimination. 11 In its reassessment, ACET concluded that the success against resurgent tuberculosis should reinforce the nation's confidence that:
Tuberculosis can be controlled and ultimately eliminated in the United States with expanded partnerships and the development of new tools for diagnosis, treatment, and prevention of tuberculosis Tuberculosis elimination will have widespread economic, public health, and social benefits Committing to decisive action against tuberculosis in the United States would fulfill an obligation to persons throughout the world who have this preventable and curable disease
# Institute of Medicine Report, 2000
As an outgrowth of the renewed interest in tuberculosis elimination, an independent study was conducted by the Institute of Medicine (IOM) and published in 2000. 12 The IOM report projected tuberculosis elimination by 2035 if the first and second of these recommendations lead to a 10% initial annual rate of decline in tuberculosis incidence that is followed a decade later by an accelerated 20% annual decline brought on by the implementation of new tools. The IOM also noted the cyclical nature of the nation's response to tuberculosis and warned against allowing the occurrence of another "cycle of neglect." The national response to decreasing rates of tuberculosis prior to the 1980s was to decrease public health resources for tuberculosis control. In order to reverse the erosion of the tuberculosis control infrastructure that preceded and caused the resurgence of 1985 through 1992, major increases in annual funding to the CDC for local TB control were required from 1992 through 1994. As the national, state, and local tuberculosis control programs were rebuilt, the tuberculosis case rate for the United States decreased from 10.4 in 1992 to 5.8 per 100,000 persons per year by 2000, but this rate was well above the interim goal of 3.5 proposed by ACET in 1989.
# Costs of Implementing Recommendations, 2002
In
# Challenges in Low-incidence Areas, 2002
The challenges of progressing toward tuberculosis elimination in areas with lowincidence rates of tuberculosis were described in ACET's 2002 report, "Progressing Toward Tuberculosis Elimination in Low-Incidence Areas of the United States." The report focused on the 22 states that faced the challenge of maintaining an effective tuberculosis control program with 50 or fewer tuberculosis cases per year and an annual tuberculosis rate of less than 3.5 cases per 100,000 persons per year. The report recommended evaluating the feasibility of interstate regionalization of tuberculosis services as proposed previously by the IOM. One of the initial projects of the Division of Tuberculosis Elimination's Tuberculosis Epidemiologic Studies Consortium was to evaluate the implementation of regional approaches to enhance tuberculosis control and elimination in the low-incidence region comprised of Idaho, Montana, Utah, and Wyoming.
# Tuberculosis Control Guidelines, 2005
Building on the issues raised in the IOM report, the 2005 guidelines on tuberculosis control issued by the American Thoracic Society (ATS), Infectious Diseases Society of America (IDSA), and the CDC 13 concluded that "the traditional model of tuberculosis control, in which planning and execution reside almost exclusively with the public health sector, is no longer the optimal approach during a sustained drive toward the elimination of tuberculosis." That report affirmed the essential role of the public health sector in planning, coordinating, and evaluating the tuberculosis control effort but, in addition, proposed roles and responsibilities for a full range of stakeholders whose participation was deemed to be essential.
# Comprehensive Tuberculosis Elimination Act (P.L. 110-392)
The Comprehensive Tuberculosis Elimination Act of 2007 was signed into law in late 2008, authorizing up to $210 million per year in funding for the CDC's Division of Tuberculosis Elimination. If followed by full appropriation of funding, this roughly 50% increase in the funding for the Division will help to reverse the 40% effective loss of funding due to inflation over the previous 15 years. Based upon the 2002 NCET report, additional increases will be needed to develop, evaluate, and implement the new tools that will be required to eliminate tuberculosis from the United States.
# B. Epidemiological Progress and Trends
In 2008, reported cases of tuberculosis decreased to 12,904 for an annual incidence rate of 4.2 cases per 100,000 persons, the lowest recorded number and rate since national reporting began in 1953. Since the tuberculosis resurgence in 1985 to 1992, there has been an uninterrupted 52% decline in tuberculosis incidence in the United States. However, the rate of that decline is slowing, from an average 6.6% decrease in cases per year from 1993 to 2002, to an average 3.4% decline from 2003 to 2008. This change coincided in 2002 with the observation that, for the first year in US history, foreign-born persons accounted for the majority (51%) of reported tuberculosis cases, a proportion that has increased to 59% of tuberculosis cases reported in 2008. 14
# Tuberculosis in Foreign-born Populations
As shown in Figure 1
F I G U R E 1
# Number of US Tuberculosis Cases Reported in US-born and Foreign-born Persons, 1993-2008
The trends for the annual tuberculosis rates for the United States and the separate populations of US-and foreign-born persons (Figure 2) demonstrate a decrease in slope after 2002, representing a slowing of the decline in tuberculosis case rates for the overall US population and the US-born sub-population. Rates were 10.2-fold higher among foreign-born compared to US-born persons in 2008, accounting for a projected delay until year 2151 for tuberculosis elimination in foreign-born persons compared to year 2059 for those born in the United States (Table 2, page 8).
F I G U R E 2
# Tuberculosis Case Rates (Cases per 100,000 Population) for US-born and Foreign-born Persons, United States, 1993-2008
If we maintain the annual percent change in case rates seen from 2003 through 2008, it will take an estimated 97 years from 2010 to reach the tuberculosis elimination goal of one case per million for the entire US population (Table 2, page 8). A major contribution to this estimate is the higher rate and slower annual decrease among foreign-born persons, for whom tuberculosis elimination is projected to require 141 years.
# Persisting Disparity of Tuberculosis
Accurate population estimates are not currently available for race and ethnicity stratified by birthplace. However, trends in the number of reported cases of tuberculosis among US-born persons by race and ethnicity (Figure 3) indicate a persisting disparity of tuberculosis among US-born blacks with no evidence of improvement and a persistence of approximately 1,000 cases per year among Hispanics.
F I G U R E 3
# Number of Tuberculosis Cases Reported in US-born Persons by Race and Ethnicity, 1993-2008
The determinants of risk of tuberculosis, however, are not limited to birthplace and race or ethnicity. Certain other readily-identified subgroups of the US population have been consistently found to experience rates of tuberculosis much higher than the population as a whole. 13 These include persons with tuberculosis risk factors of lower socioeconomic status, homelessness, incarceration, abuse of alcohol and/or other substances, HIV infection, and certain underlying medical conditions.
# Latent Tuberculosis Infection
These differences in tuberculosis incidence associated with birthplace, race, ethnicity, and socioeconomic factors are also reflected in population rates of latent tuberculosis infection among US residents. A recently published survey from the CDC 15 indicated that the prevalence of latent tuberculosis infection (defined as the percentage of persons with a positive tuberculin skin test) in the US population in 1999 and 2000 was 4.2%, with much greater prevalence rates of infection among immigrants and persons in poverty. Prevalence rates were 18.7% in immigrants compared to 1.8% in US-born persons. Among those living below the poverty level, 6.1% were infected compared to 3.3% of those not living in poverty.
F I G U R E 4
# US-born and Foreign-born Prevalence of Latent Tuberculosis Infection (LTBI) and Case Rates (Cases per 100,000 Population) by Age, 1999-2000
The age-specific data show striking parallels in risk of tuberculosis and latent tuberculosis infection among US residents by birthplace (US versus non-US; Figure 4) that, combined with the marked differences in tuberculosis rates among segments of the US-born population, strongly suggest that the barriers to tuberculosis elimination may differ for the populations of US-born and foreign-born persons in the United States. A successful tuberculosis elimination plan for the United States requires approaches to address the unique challenges posed in different populations and to identify the partners who need to be engaged for the effort to succeed.
# : ELIMINATING TUBERCULOSIS : PAGE 28
Version 03/22/2010
# C. Progress Assessment 1. Success in Meeting Institute of Medicine Goals
One way to assess recent progress toward tuberculosis elimination in the United States is to evaluate success in implementing the five specific goals proposed by the IOM in its 2000 report. 12 Table 1 (page 6) summarizes the current status of progress on the IOM recommendations.
Whereas tuberculosis remains under control (IOM Goal 1), as evidenced by continued declining case rates, the annual rate of decline is slowing, not accelerating. Why is the United States not achieving IOM Goal 2, the acceleration of the decline in tuberculosis?
A recent report found that in the Netherlands a similar gradual annual decline in tuberculosis incidence was due to the natural replacement of older population members, who have high rates of latent tuberculosis infection and risk of progression to tuberculosis disease, by younger residents with successively lower rates of latent tuberculosis infection, resulting from less exposure to tuberculosis at younger ages. 16 In the United States, the very low rates of latent tuberculosis infection in younger persons are seen only in the native-born population, but rates are much higher in tho born abroad and parallel the higher rates of tuberculosis by age group as seen in Figu 4 (page 27) se re .
Treatment of latent tuberculosis infection is a tuberculosis prevention strategy that is critical to eliminate tuberculosis. The ATS/CDC report on targeted testing and treatment of latent tuberculosis infection, 17 as well as the IOM report Goal 2, called for expansion of treatment of latent tuberculosis infection into the private medical sector as a means to increasing access to this preventive intervention against tuberculosis. However, a survey conducted by the CDC Tuberculosis Epidemiologic Studies Consortium found that in 2002, over 90% of all latent tuberculosis infection treatment was administered in public health clinics, including those serving immigrants and refugees, and in corrections facilities. 18 Expansion of the treatment of latent tuberculosis infection has not occurred and remains limited in public health departments where it is considered low priority when resources are scarce. In addition, the completion rate for the standard nine-month course of isoniazid for latent tuberculosis infection is often less than 50% to 60%. The lack of an effective, safe, and affordable short-course regimen that would improve treatment completion rates has severely limited expansion of treatment for latent tuberculosis infection.
The failure to achieve IOM Goal 3-to develop and implement new tools for the diagnosis, treatment, and prevention of tuberculosis-continues to pose a major impediment to tuberculosis elimination. The call for new tools was made by ACET in the initial tuberculosis elimination plan in 1989, repeated by ACET in 1999, and stated as necessary in the 2000 IOM report in order to double the rate of decline in tuberculosis cases by the year 2010. Investment in research and development for new tools for tuberculosis has been deemed "woefully inadequate," especially when compared to research and development expenditures for HIV. 19 Unfortunately, two decades into the tuberculosis elimination effort, few new tools have been developed, and none yet has been widely implemented. There have been no substantive changes in the standard drug regimen for active tuberculosis since the 1980s. The Federal Tuberculosis Task Force noted the major problems now faced by clinicians and public health officials in addressing the needs of tuberculosis patients infected with multidrug-resistant (MDR) and extensively drug-resistant (XDR) strains of Mycobacterium tuberculosis. 20 To prevent latent tuberculosis infection from progressing to active tuberculosis, the nine-month isoniazid treatment, introduced in the 1960s, remains the treatment regimen of choice, and no approved treatments are available for persons infected with MDR or XDR strains. A new generation of tests for latent tuberculosis infection, interferon gamma release assays, has been licensed, but due to limited clinical evaluation there continues to be controversy concerning their proper role in clinical practice. 21 The Division of Tuberculosis Elimination at the CDC has committed about $9 million per year to fund the Tuberculosis Trials Consortium. This consortium, funded with domestic dollars, conducts international clinical trials of new treatment tools that will benefit patients in the United States and improve the outcomes of tuberculosis treatment globally in high-burden countries.
Considerable progress has been made on IOM Goal 4, increasing involvement by the United States in global tuberculosis control. The President's Emergency Plan for AIDS Relief (PEPFAR) and the US Agency for International Development (USAID) represent major initiatives in addressing the global burden of tuberculosis. The Division of Tuberculosis Elimination devotes most of its roughly $140 million annual budget to domestic tuberculosis elimination efforts but plays a major role in a number of countries in implementing the PEPFAR and USAID initiatives. Although this global effort represents good progress on Goal 4, the federal global tuberculosis efforts through PEPFAR and USAID should be better coordinated and balanced with domestic tuberculosis control and elimination efforts. Although the burden of tuberculosis cases globally overwhelms the numbers in the United States, tuberculosis elimination will require increases in both domestic as well as global funding.
Finally, a critical element in concerted public health action is broad public consensus on the importance of the endeavor. According to the IOM report, "social mobilization is necessary to build and sustain political will (for tuberculosis elimination) in the United States and can lead to similar efforts internationally." 12 The United States has a long history of social mobilization, the enlistment and coordination of various individuals and groups, in support of tuberculosis control efforts. However, today tuberculosis is not generally viewed as a problem in the United States, 12 and there has been only limited success over the last ten years in meeting IOM Goal 5. NCET, the predecessor of Stop TB USA, made a concerted effort to advocate for tuberculosis elimination, but this effort was not successful in developing the political will needed in order to accelerate the development and implementation of the new tools needed for diagnosis, treatment, and prevention of tuberculosis.
# Robustness of Government Funding
Another measurement of progress toward tuberculosis elimination is the robustness of financing from public and private sources. Despite the recommended increase in the annual budget of the Division of Tuberculosis Elimination to the $528 million recommended in the 2002 NCET report, TB Elimination: The Federal Funding Gap, effective funding levels of the Division have decreased 40% since 1994 due to the combination of flat-funding despite inflation, budget cuts, and rescissions (Figure 5, page 31). 22 concluded that the five recommendations of the IOM report "cannot be implemented with current funding." As a result of cuts in federal funding to states for tuberculosis control, targeted testing and treatment programs for latent tuberculosis infection are being reduced or eliminated, and there is evidence that preventable cases of active tuberculosis are rising.
# The Federal Tuberculosis Task Force Plan in Response to the Institute of Medicine Report, Ending Neglect: The Elimination of Tuberculosis in the United States 2003
The 2002 ACET report, "Progressing Toward Tuberculosis Elimination in Low-Incidence Areas of the United States" cited loss of expert personnel and resources among reasons why there has not been more progress. 23 That report asserted that local and state health departments have the most important role in controlling tuberculosis, but it also cited evidence of deficient funding for tuberculosis control, not to mention tubercu elimination efforts, throughout states and localities in the United States. In addition, there is a predicted loss of skilled, experienced staff. A Health Resources and Services Administration report from 2005 cited an impending crisis in the public health workforce as older workers across a broad range of disciplines retire, requiring increased funds for training if they are to be replaced.
# losis F I G U R E 5
# Annual CDC Tuberculosis Budget, FY 1990-FY 2008
CPI = Consumer Price Index.
# Overall Assessment of Progress Toward Tuberculosis Elimination
The United States is not moving purposefully toward the elimination of tuberculosis. Epidemiological data indicate that interim elimination targets have not been met, that the rate of decrease in tuberculosis incidence is slowing, and that, if the current trend continues, tuberculosis elimination in the United States will require nearly 100 years.
Reasons for lack of progress toward elimination, presented above and expanded upon in subsequent sections of this report, include: The ongoing global tuberculosis epidemic, including HIV/tuberculosis coinfection, which continues to impact tuberculosis incidence in the United States A 40% erosion, rather than the recommended over 3.8-fold increase, in resources for tuberculosis control Insufficient effort to speed the decline of tuberculosis by targeting persons with latent tuberculosis infection and high risk of progressing to active tuberculosis (IOM Goal 2)
Insufficient funding for research and development for new tools for diagnosis, treatment, and prevention (IOM Goal 3)
Lack of public understanding and support at the national, state, and local levels for tuberculosis elimination in order to make it a high national priority (IOM Goal 5)
Lack of the development of, consensus on, and advocacy for specific strategies for tuberculosis control in high-risk groups Continued lack of successful advocacy for tuberculosis elimination
# D. The Call for Action to Eliminate Tuberculosis from the United States
Stop TB USA issues a call for action to all partners and stakeholders in the plan to eliminate the scourge of tuberculosis from the United States by 2035. To more rapidly progress toward eliminating tuberculosis in the United States, the Stop TB USA TB Elimination Plan Writing Committee has identified general and specific action plans (Tables 3-7, pages 9-17) and now issues a call for action on five start-up steps that are critical to fully implement the IOM recommendations and the Stop TB USA action plans:
1. Commit to implementing the IOM recommendations in Ending Neglect and conduct a periodic review on the progress toward elimination
# Implementation of the Institute of Medicine Recommendations
The Tuberculosis Elimination Plan Committee endorses the IOM's year 2000 recommendations in Ending Neglect in which the IOM defined five major goals to achieve in the tuberculosis elimination campaign for the United States (Table 1, page 6).
The tuberculosis elimination effort is failing, not for want of the right goals or specific recommendations, but rather because the IOM recommendations needed to achieve those goals have not been fully implemented. For example, to eliminate tuberculosis, it is critical that the IOM recommendation to accelerate the development of new tools is followed. Tuberculosis may be controlled but not eliminated in our lifetimes, or even within the lifetimes of our children, if we are forced to rely upon the outdated tools in current use. Tuberculosis elimination will require an unprecedented effort to ensure that core tuberculosis control functions are maintained and to finally bring into use the new tools called for in 2000 by IOM and two decades ago by ACET.
# Development of New Timelines and Interim Goals
In addition, the Committee recommends that a new timeline be developed for the goal for tuberculosis elimination in the United States, along with new interim targets. These new interim targets must be realistically achievable with broader application of existing tuberculosis elimination tools as well as with the implementation of new tools and strategies that could be more rapidly implemented with the authorized increase in federal funding.
Periodic evaluations of progress will need to be conducted. The IOM (Recommendation 7.3) requested that the Office of the Secretary of Health and Human Services conduct periodic evaluations of actions taken in response to the recommendations made in 2000, but it is not clear that this recommendation was followed. We recommend that Stop TB USA conduct periodic evaluations of the action taken on the recommendations in this report and provide reports to ACET that will be forwarded to the Secretary of the Office of the Department of Health and Human Services. The first report should be within two years (2012) and at two-year intervals thereafter.
# Obtaining Infrastructure Funding for Stop TB USA to Enable Collaboration with Centers for Disease Control and Prevention
The CDC should collaborate with the members and partners of Stop TB USA in implementing specific action plans for accelerating TB elimination including:
Consensus-building, advocacy, and mobilization Acceleration of the development and implementation of new tools for diagnosis, prevention, and treatment Implementation of strategies to reach high-risk segments of the US population
The IOM recommended that the NCET provide the leadership and oversight for coordinating the engagement of these partners and stakeholders and ensuring effective collaboration with the CDC. NCET, now identified as Stop TB USA, lacks the resources needed to meet this challenge. National, state, and local voluntary and professional organizations supporting the control and elimination of respiratory and infectious diseases will need to assist Stop TB USA in obtaining the infrastructure funding needed to engage all its members and partners in generating the political will to implement the 2000 recommendations and the updated action plans in this document, a challenge in any fiscal climate, and even more so in recessionary times.
# Closing of the Federal Funding Gap
Opportunities to Address the Federal Funding Gap
# Assessment by the Federal Tuberculosis Task Force of the Benefits of the Recommended Increase in Funding for New Tools for Tuberculosis Elimination
As discussed above, new tools are needed for the diagnosis, treatment, and prevention of tuberculosis. These tools are a critical component of the tuberculosis elimination plan for the United States as proposed in 1989 and updated by the IOM in 2000.
Addressing the need for new tools requires a coordinated federal intervention, a role uniquely suited for the Federal Tuberculosis Task Force.
The Federal Tuberculosis Task Force outlined the need for new tools development and implementation in the 2009 plan for extensively drug-resistant tuberculosis. We call for an independent review to assess the potential impact on the development and implementation of new tools that could be expected by increasing funding to the levels authorized in the Comprehensive Tuberculosis Elimination Act of 2007. We request that this assessment be completed within four months of this report in order to use this assessment in proposing new interim goals in the tuberculosis elimination campaign. Increased new tools funding must include basic science research, the focus of the National Institutes of Health, as well as operational research, the focus of the CDC.
# Engagement of a Broad Range of Stakeholders
The control and eventual elimination of tuberculosis in the United States is not just a federal responsibility. There must be a renewed and expanded commitment to the goal The success of this effort requires that stakeholders and partners join with Stop TB USA in endorsing the revised goal and interim targets as well as the implementation of general recommendations for the nation as a whole and those specific to populations at higher risk. The 2005 tuberculosis control guidelines provided detailed roles and responsibilities for the partners who must be involved for tuberculosis elimination to be successful. 13 For more discussion on stakeholders and potential partners involved in tuberculosis, refer to Chapter VII: "Mobilizing Partners in the Fight against Tuberculosis," pages 76-82.
# TO CONCLUDE AND MOVE FORWARD:
As seen in the progress assessment, the IOM recommendations have not been fully implemented, and the goal of eliminating tuberculosis in the United States by 2035 remains beyond reach with our current approach. Stakeholders across the country must join the effort to develop and implement new, creative measures to accelerate the elimination of tuberculosis.
# III. New Tools
There is a critical unmet need globally as well as within the United States for better tools to diagnose, treat, and prevent tuberculosis. The currently available diagnostic tests for active tuberculosis and for detection of drug-resistant strains in the United States include liquid culture methods that diagnose most tuberculosis cases within two weeks and provide drug susceptibility test results within an additional one to two weeks. Another method for detecting the genetic material of tuberculosis in a sputum sample, which can produce results one or more weeks faster than liquid culture, is the licensed test called nucleic acid amplification (NAA). The implementation of NAA testing, however, particularly in public health settings, has been delayed due to the additional expense added by the cost of cultures that are still required in order to test for drug susceptibility. There are also promising newer diagnostic methods that are able to detect multidrug-resistant tuberculosis within just days, but implementation of these tests remains limited because of inadequate operational research, the official approval processes, cost issues, and/or laboratory expertise. 25
# Drugs
Today's first-line drugs for the treatment of tuberculosis were developed and brought to the market more than 40 years ago, after which, research and development ground to a halt due to a lack of commercial incentive to invest in new therapies. Due to the complexity of the tuberculosis bacterium, tuberculosis disease requires that it be treated with multiple drugs at the same time. The current treatment regimen, a combination of four drugs administered daily for six to nine months, is cumbersome, potentially toxic, and places an extraordinary burden on patients and healthcare providers alike. Incomplete and improper treatment has led to the growth of multidrug-resistant strains of tuberculosis (MDR TB) that are much more difficult and costly to treat. The threat of antibiotic resistance has been further intensified by the emergence of extensively drug-resistant tuberculosis (XDR TB), which, in some cases, can be virtually untreatable due to the lack of effective anti-tuberculosis drugs. The current treatment regimen is also limited by the fact that the cornerstone of first-line treatment, rifampin, is incompatible with certain commonly-used antiretroviral therapies for human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS). Ideal new regimens will significantly shorten and simplify treatment, be compatible with antiretrovirals and other commonly-used medicines, and address drug resistance.
After near-total stagnation of the global pipeline for anti-tuberculosis drugs, the founding of the Global Alliance for TB Drug Development in 2000 and the recent entry of several pharmaceutical companies into the tuberculosis drug research and development arena is encouraging. Currently there are seven drug candidates in clinical development for tuberculosis and dozens more in earlier stages of development. However, attrition rates are high for drug development, and only a small number of compounds discovered will ever reach registration. Since tuberculosis will always require multiple drugs in a combination treatment, a revolutionary breakthrough in tuberculosis treatment hinges on the ability to register several new drugs. Although significant advancements have been made, the global pipeline of anti-tuberculosis drugs is not nearly large enough to ensure that this occurs. Recent research showed the impressive benefit of adding a new drug, TMC207, to the regimen that patients were receiving for MDR TB. 26 This finding provides some hope that new regimens may be available, at least for MDR TB, much sooner than anticipated. 8 At the same time, it will be necessary to maintain and increase investments in drug discovery to ensure a robust pipeline of future anti-tuberculosis drugs.
# Vaccines
The BCG vaccine, created in 1921, is the only existing vaccine against tuberculosis. Unfortunately, it is only partially effective. It provides some protection against severe forms of pediatric tuberculosis but is unreliable against pulmonary tuberculosis, which is the infectious form of tuberculosis and which accounts for most of the tuberculosis disease burden worldwide. Despite being widely used, BCG has had no apparent impact on reversing the growing global tuberculosis pandemic. New, more effective vaccines are urgently needed to protect against all forms of tuberculosis-including MDR and XDR TB-and to prevent tuberculosis in children, adolescents, and adults, including in people infected with HIV. New vaccines would also help to decrease tuberculosis incidence overall and prevent further spread of the disease.
BCG is not used routinely in the United States where most infants are not exposed to tuberculosis, and it has never been a component of the US tuberculosis control program. The greatest direct benefit of a better tuberculosis vaccine would be realized in populations living in countries with high tuberculosis burdens, which would also benefit the United States by reducing the incidence of active tuberculosis in people who travel to the United States. The United States and other industrialized countries would indirectly benefit as well. For example, reducing tuberculosis would reinforce multibillion dollar US programs to combat HIV/AIDS, as patients already receiving antiretroviral treatment are still succumbing to undiagnosed and untreated tuberculosis.
Vaccines under development have the potential to prevent tuberculosis in any of several ways: by preventing infection, primary disease, latency, or reactivation of latent tuberculosis. Several potentially better tuberculosis vaccines have entered early-stage clinical trials to determine safety and immunogenicity, and the first Phase IIb "proofof-concept" trial of a new preventive tuberculosis vaccine in infants in over 80 years was initiated in 2009. Numerous additional candidates are in preclinical development.
The Aeras Global TB Vaccine Foundation and other investigators from around the globe are sponsoring research on these tuberculosis vaccine candidates, but additional funding will be needed for further studies and to advance the most promising candidates through Phase III efficacy and licensure trials. These later stage trials require a large number of participants and long follow-up periods and are very expensive. Aeras estimates that a Phase III trial of one candidate vaccine could cost $120 million.
TAG suggests that, in the most optimistic scenario, the first new tuberculosis vaccine would be available in 2015.
# Scientific Barriers
Major scientific hurdles and gaps remain in our understanding of tuberculosis, and these challenges need to be quickly met if new and better tools are to be developed for the elimination of both drug-sensitive and drug-resistant tuberculosis. 20 The identification of new diagnostics, drugs, and vaccines that will radically transform tuberculosis control and treatment will require a better understanding of bacterial latency, persistence, metabolism, and the host immune response to infection. Research and development will be hastened by the development of better animal models, identification of novel drug targets and predictive biomarkers, and discovery of new imaging and drug and vaccine delivery technologies. The improved preparedness of clinical trials sites will ensure that new tools are evaluated and delivered to patients without delays. Further, basic research on vaccine candidates as well as greater investigation of the mechanisms of action and pharmacokinetic/pharmacodynamic parameters of current drugs will lead to significant improvement in existing development approaches and, ultimately, to optimized prevention and treatment strategies.
# Financial Barriers
To support this crucial work, the Global Plan to Stop TB estimates $9 billion in funding is required in the next decade for research and development of new tuberculosis diagnostics, drugs, and vaccines. With the inclusion of basic science and operational research, the November 2009 TAG report suggests that tuberculosis research and development funding investments need to increase to $2 billion per year, from the Global Plan's original target of $900 million per year. 27 In Insufficient advocacy for mobilizing resources continues to limit the advancement of the tuberculosis research and development agenda. While other health areas have focused heavily on developing improved cures, there is little understanding of the need for new tuberculosis diagnostics, drugs, and vaccines among health and advocacy groups in the United States. While investigators themselves have been a strong voice of support for increased investment in tuberculosis research, the issue has not been widely taken up by non-scientific or community-based groups or by the general scientific and academic communities. Without greater understanding about the limitations of current tools and research, it is unlikely that public and private donors will recognize the urgency for greater investment in biomedical research for tuberculosis. Researchers and other stakeholders will need to build awareness and a broader base of support in the community in order to intensify advocacy efforts.
# B. Action Plans to Accelerate New Tools Development
For a summary of action plans for the development and implementation of new tools, refer to Tuberculosis research and development require substantial coordination of scientific and operational activities at many levels, both globally and nationally. Governments, foundations, and the private sector must accurately track and transparently report tuberculosis research and development investments to ensure that funding gaps are addressed.
# Tuberculosis Research and Development Investment
# Advocacy
Advocacy efforts to educate policy makers about the critical role of government funding for tuberculosis research and in the development of new diagnostics, drugs, and vaccines must be intensified. Stop TB USA, partners, and stakeholders must engage new constituents in the tuberculosis research advocacy movement, particularly community-based organizations, non-governmental organizations, and other health advocacy groups.
# Basic Research and Methods
To address scientific barriers, basic research must be intensified and methods must be established to facilitate research and development across all new tools. These improvements will strengthen the pipeline of new concepts entering research, accelerate development, and improve the diagnosis, treatment, and prevention of tuberculosis.
# IV. Tuberculosis among US-born Populations
Communities continue to experience outbreaks and chains of tuberculosis transmission within US-born populations, especially those associated with human immunodeficiency virus (HIV) infection, incarceration, homelessness, and limited access to health care. The elimination of tuberculosis within US-born populations will not be successful without implementation of effective measures to accelerate tuberculosis elimination in these groups.
# A. Trends and Challenges
# Epidemiology and Demographics
The convergence of high rates of HIV and substance abuse with the crowding of homelessness, marginal housing, and incarceration creates ideal scenarios for ongoing transmission and high rates of tuberculosis.
Molecular epidemiology, the use of genetic typing of M. tuberculosis strains in studies of how tuberculosis is spread, confirms significantly higher rates of tuberculosis among US-born populations due to recent spread and infection (rather than from latent infection that occurred many years ago) when compared to the foreign-born. 29 Among persons with tuberculosis, those born in the United States and with low socioeconomic backgrounds are even more likely to have developed their tuberculosis due to recent transmission and outbreaks. 30 High HIV rates among the urban poor amplify transmission, causing larger and prolonged outbreaks of tuberculosis. 31 HIV infection, the biggest risk factor for tuberculosis, continues to play a dominant role among US-born cases, especially among substance users, the homeless, African Americans, correctional facility inmates, and alcohol abusers. 32 As shown in HIV = human immunodeficiency virus. Source: R. Pratt, T. Navin, M. Chen, J. Becerra, CDC.
# Loss of Funds and Personnel Dedicated to Tuberculosis Control
The decline in categorical funding for over a decade has led to significant decreases in personnel and resources for individual and community outreach, incentives and enablers needed for case management, aggressive contact investigations, and completion of treatment.
Since the spike in funding in the early 1990s, health department programs for preventing tuberculosis by targeted testing and treatment of latent tuberculosis infection in US-born communities have been dismantled because of the need to maintain core functions of active tuberculosis treatment and contact investigation. The lack of resources devoted to targeted testing and treatment of latent tuberculosis infection to prevent tuberculosis cases makes elimination of tuberculosis among the US-born impossible.
Most cases of tuberculosis are detected when persons seek medical care for the symptoms of the disease. Because US-born persons with tuberculosis come from populations who are least likely to access health care, delays in seeking and/or accessing health care lead to delays in diagnosis, contributing to ongoing airborne spread of the disease in their communities. 34
# Resource-Intensive Contact Investigations
Once disease is detected, contact investigation in these populations is complex, resource intensive, and more challenging because of the highly mobile nature and competing priorities of people within these groups. Social mistrust and stigma of tuberculosis make these people difficult to reach and further hamper efforts to adequately identify and evaluate all contacts.
Without improvements in health department programs aimed at finding, evaluating, and treating contacts (persons exposed) to infectious tuberculosis cases, transmission of tuberculosis will continue to occur from recently infected persons who develop tuberculosis. Contact investigations among populations of marginally housed persons in shelters, low-cost hotels, and drug treatment facilities are resource intensive and often require on-site services, including education (of residents, patients, and staff), mobile radiology, phlebotomy, sputum collection, and incentives and enablers for follow-up. Communication and partnering with community programs are necessary and require skilled staff. Because of the cost and complexity of these investigations, programs often reserve investigations to only the cases considered most contagious or after an outbreak has already been detected.
# Complexity of Addressing Health Disparities
With the current funding downturn, the hiring and training of skillful staff to work with the difficult-to-reach is currently limited and unaffordable. The complexity of working with persons who have multiple medical, social, and mental problems requires a highly skilled workforce that is willing to provide outreach in potentially dangerous environments. It is challenging for the patients who are trying to make ends meet or worrying about their next meal to have to take medication for latent tuberculosis infection for a minimum of six to nine months. Knowledge of existing services for nontuberculosis issues and access to these services are often critical in stabilizing patients who are on treatment or in the process of a work-up for tuberculosis.
The activities that are critical to the success of working with US-born populations at risk for tuberculosis are labor and resource intensive. The cost of care is substantially higher than for other at-risk populations but is necessary to protect the public.
Resource demands can surge dramatically and unpredictably: one outbreak in a correctional facility or homeless shelter can create significant challenges for a health department and facility staff already stretched to capacity-a common scenario with the current level of infrastructure for tuberculosis control in the United States.
# Tuberculosis in Correctional Facilities
Correctional facilities hold over 2.2 million people, including persons frequently affected by substance abuse, homelessness, HIV infection, lower socioeconomic status, and limited access to medical care. Overcrowding has become commonplace in these facilities.
The link between tuberculosis and correctional care facilities, particularly among African Americans, is often not recognized and represents a missed opportunity for tuberculosis control and prevention. According to the US Department of Justice Bureau of Justice Statistics, at year end 2006 there were 3,042 black male sentenced prisoners per 100,000 black males in the United States, compared to 1,261 Hispanic male sentenced prisoners per 100,000 Hispanic males and 487 white male sentenced prisoners per 100,000 white males. 35 Common challenges in state and county correctional facilities include insufficient resources for screening and staff surge capacity during outbreaks. The problem is particularly acute in smaller county jails, where inmates often stay briefly while awaiting release or transfer to other correctional facilities.
# B. Action Plans to Accelerate Tuberculosis Elimination among US-born Populations
Although the roots of the disparities may remain despite our efforts, tuberculosis control programs in the United States are models of providing high-quality and equitable care to all patients. With the right resources, tuberculosis programs can lessen and eventually eliminate the uneven burden of disease among the US-born.
Engaging difficult-to-reach US-born populations with tuberculosis will require aggressive community-and patient-centered approaches to screening and prevention. Community-based tuberculosis services and prevention in high-risk communities and facilities where tuberculosis exposure perpetuates disease are needed to eliminate ongoing transmission among the US-born. Further erosion of the core infrastructure and rationed services will only serve to raise the risk of transmission and jeopardize the hard-won current containment of tuberculosis.
For a summary of action plans for eliminating tuberculosis in US-born populations, refer to
# Community-Based Tuberculosis Activities
In the Action Plans for Eliminating Tuberculosis among the US-born, it is recommended that funding be augmented and restored for community-based targeted testing and latent tuberculosis infection treatment focusing specifically on persons who are homeless, marginally housed, or co-infected with HIV and on persons who have diabetes and other medical risk factors for disease progression (local, state, and federal government item 1, bullet 1).
The lack of access to screening and targeted testing of at-risk US-born persons perpetuates delayed diagnosis of contagious tuberculosis, reactivation, and transmission in high-risk settings such as shelters, jails, low-cost housing, community drop-in centers, and substance abuse treatment facilities.
Funding for treatment of latent tuberculosis infection of homeless contacts and persons with HIV or medical risk factors for progression to active tuberculosis must be increased in order for health departments and other medical providers to make this key prevention activity a priority. Outreach, incentives, and enablers are needed to engage difficult-to-reach populations in prevention activities, namely treatment of latent tuberculosis infection. To combat the high rates of nonadherence, directly observed therapy for latent tuberculosis infection treatment has been shown to be effective 36 and is needed if tuberculosis elimination is the goal.
Community-based programs, new technology, and training are essential for screening, targeted testing, and treatment. Community-based programs that provide on-site screening and directly observed therapy for both active tuberculosis and latent tuberculosis infection are needed to bridge the gap of access to care. Implementation of new technology, such as blood-based tuberculosis testing to improve adherence to screening, should be prioritized for the difficult-to-reach since it requires only one clinic visit to get a result, instead of the two clinic visits needed for tuberculin skin test results. Tuberculosis control staff working with these populations must be well trained, highly motivated, and able to create strong relationships with community members.
The importance of community input, education, leadership, and coalition building cannot be understated in these activities. These efforts will require significant resources in order to be successful in case management, completion of treatment for tuberculosis, contact investigation, and targeted testing and treatment of latent tuberculosis infection.
Because of the high risk of transmission in them, congregate settings present valuable opportunities for screening and tuberculosis case detection. It is recommended to enhance tuberculosis control programs at correctional facilities to the same level as external health department programs in order to improve screening and surveillance capacity, contact investigation, and case management of inmates who are moved frequently to different facilities, have high recidivism rates, or leave institutions before treatment is completed (local, state, and federal government item 1, bullet 2).
Special focus should be placed on screening and tuberculosis case detection in shelters, correctional facilities, residential substance abuse programs, and community day dropin centers where risk of transmission is high. It is common for at-risk persons to cycle through some or all of these sites and facilities in a single year. 37 Hence, requiring tuberculosis screening in these settings and fully implementing existing guidelines for these groups is an important strategy in creating access to the difficult-to-reach. It is recommended that local health departments should have the resources to limit transmission through early case detection and screening at sites with high crowding and limited ventilation. Mandatory tuberculosis screening should be implemented of all homeless in shelters, day drop-in centers, and other congregate sites to prevent outbreaks and spread of tuberculosis (local, state, and federal government item 1, bullet 3).
Preventing tuberculosis transmission in these congregate settings is challenging because of the frequent movement of persons within and between settings and programs. In these facilities, and especially in correctional facilities, development of databases for tuberculosis surveillance is needed and critical to serve these populations and collaborate with local public health authorities. 38 Better disease surveillance and medical databases to track inmates and transfer vital information among facilities are badly needed to improve efficiency and care. It is recommended that local health departments should enhance surveillance activities using geographic information system mapping and genetic typing (genotypying) of strains of M. tuberculosis to identify specific local areas of ongoing transmission in order to target efforts and communicate with the public (local, state, and federal government item 1, bullet 4).
Finally, training and education specific to tuberculosis are needed to address contact investigation, collaboration between correctional facilities and public health units, and case management and discharge planning for inmates with tuberculosis disease and high-priority latent tuberculosis-infected inmates.
# SUCCESSFUL PARTNERSHIPS: Forth Worth Community Partnership for TB Detection and Prevention
In the western part of the Dallas-Fort Worth metropolitan area in Tarrant County, Texas, community organizations partnered with the local public health department to implement locationbased tuberculosis screening. 39 Despite years of free voluntary tuberculosis screening, communities in three Tarrant County zip codes with high rates of unemployment, homelessness, and substance abuse suffered persistent high rates of tuberculosis transmission.
After being presented with the epidemiologic data, community organizations partnered with the local public health department to make annual tuberculosis screening mandatory for persons to continue receiving a variety of services. Screening was expanded from homeless shelters to be location-based at other community organizations providing services, including mental health facilities, temporary labor services, Veterans Administration job training and living facilities, dialysis centers, churches, community service centers, a human immunodeficiency virus (HIV) congregate living facility, and living facilities sponsored by faith-based organizations. Screened persons were given county-issued screening cards that were required to receive services at the partner organizations.
Before these new programs, screening detected only 5% of active tuberculosis cases among shelter residents. The remaining cases were diagnosed in hospitals. In September 2002, locationbased screening detected 20 cases of active tuberculosis among the first 702 persons screened. The prevalence of active tuberculosis was 2.9% in the first screening, and 1.9% in the first year, a rate exceeded in the United States only during outbreaks in homeless shelters or in evaluation of contacts to active tuberculosis cases. Early results are promising: the prevalence of active tuberculosis dropped from 1.9% in the first 12 months to 0.5% in the last 16 months reported.
# Awareness of Tuberculosis among Healthcare and Service Providers
It is recommended that local health departments should increase tuberculosis education of community workers in shelters, housing services, and substance abuse treatment sites; correctional staff; and providers serving high-incidence US-born populations in order to address the lack of awareness that tuberculosis is a health disparity among the populations they serve (local, state, and federal government item 1, bullet 6).
Lack of awareness among healthcare providers about tuberculosis and associated health disparities often has led to delayed diagnosis and prolonged transmission in the community. Studies have demonstrated delays in diagnosis of tuberculosis due to other primary diagnoses, such as asthma, HIV infection, and community-acquired pneumonia. It is crucial for community providers to know who gets tuberculosis in their community, how to make the diagnosis, and how to rapidly report tuberculosis to state or local health departments.
# Advocacy and Mobilization
On a local level, it is recommended that local health departments partner with key community members and providers to promote education, create cohesive interventions, and develop policies and strategies that address the unique tuberculosis problems of each community and the locality (local, state, and federal government item 1, bullet 5). On local, state, and national levels, as mentioned above, it is recommended that governments should restore and augment funding for community-based targeted testing and latent tuberculosis infection treatment (local, state, and federal government item 1, bullet 1).
# SUCCESSFUL PARTNERSHIPS:
# Stop Tuberculosis in the African American Community Summit
The Division of Tuberculosis Elimination and RTI International co-sponsored the Stop Tuberculosis in the African American Community Summit in May 2006 to engage partners in collaborative efforts to address the impact of the tuberculosis disparity in the African American community. The goals of this meeting were to raise awareness about the problem of tuberculosis in the African American community, create links, and build networks that will lead to ongoing activities and strategies to decrease tuberculosis in the African American community. The Summit brought together community and religious leaders, healthcare providers, public health leaders, policy and decision makers, state and local health department staff, communications professionals, academicians, and others who committed to undertaking specific goals and action items.
Current funding opportunities for tuberculosis control have focused largely on the global rather than domestic efforts to eliminate tuberculosis. High-level officials and Congress are not aware that tuberculosis among the US-born is an issue of disparities and inequity, with rates of tuberculosis in poor inner city communities that rival those in the developing world. Additionally, communities most heavily affected by tuberculosis often have little political clout and few advocates when other social issues seem more pressing. Poor Americans with tuberculosis are also unlikely advocates because of the added stigma to their already difficult lives. Raising public awareness among local, state, and national politicians and lawmakers of the daily domestic outbreaks and ongoing transmission in US-born populations is critical in increasing domestic funding for tuberculosis control and elimination.
# TO CONCLUDE AND MOVE FORWARD:
A major barrier to tuberculosis elimination in the United States is the health disparity for tuberculosis among US-born minority populations, who now account for 87% of tuberculosis cases in the US-born population. Tuberculosis persists in the minority populations due to the failure to prevent tuberculosis outbreaks that often occur in congregate settings, such as: crowded, inadequate housing; homeless shelters; correctional care settings; and substance treatment programs. Higher rates of HIV infection among these minority populations compound the problem.
Addressing the ongoing challenge of tuberculosis among difficult-to-reach US-born groups will require advocacy and mobilization, education, and community-and patient-centered approaches to screening and prevention that focus on communitybased tuberculosis services and prevention in high-risk communities and facilities where tuberculosis exposure perpetuates disease.
# V. Tuberculosis among Foreign-born Populations
Despite the 70% decrease in the number of tuberculosis cases among US-born persons over the past 15 years, no progress has been made in reducing the number of tuberculosis cases reported among foreign-born persons each year (Figure 1, page 24). The persistence of over 7,500 tuberculosis cases each year with the associated disability and death among foreign-born persons in the United States is due to three factors: demographic trends in the United States, high rates of latent tuberculosis infection in the foreign-born population, and cultural-linguistic and socioeconomic challenges to implementing tuberculosis control measures. The solution to tuberculosis elimination among foreign-born US residents and the nation lies in addressing these three factors as well as investing in tuberculosis control and elimination globally, especially in those regions of the world where tuberculosis control and elimination is threatened by the spread of drug-resistant strains of Mycobacterium tuberculosis.
# A. Trends and Challenges
# Demographic Trends among Foreign-born US Residents
The number of new immigrants, defined in this discussion as those obtaining permanent United States residency (green card holders), increased from 3.6 million during the decade of the 1970s, to 6.2 million in the 1980s, and to 9.8 million in the 1990s, with 9.2 million arriving during the nine-year period 2000 through 2008.
Immigrants from countries in Africa, Asia, and Latin America (Mexico, the Caribbean, Central America, and South America), where rates of tuberculosis range from moderately elevated to extremely high, accounted for 95% of all immigrants from 1980 through 2008. 40 The total foreign-born population residing in the United States in 2007 was estimated to be 37.9 million, one third of whom were undocumented. Foreign-born persons account for one in eight US residents now, up from one in 13 in 1990. 41
# Tuberculosis Screening Requirements for Foreign-born Persons Coming to the United States
The current overseas tuberculosis screening of foreign-born persons entering the United States is focused on those likely to be long-term residents, primarily refugees and immigrants. The main purpose of the screening is to detect infectious tuberculosis cases and ensure that treatment is adequate to eliminate infectiousness before travel to the Unites States. In 2008, the numbers of refugees and permanent residents who arrived in the United States after pre-departure screening were 60,000 and 467,000, respectively, representing just 527,000 of the 39 million persons who entered the United States that year. The vast majority of entrants undergoes no screening for tuberculosis at all, including over 3 million students and workers who are likely to remain in the United States for several years. Table 9 (next page) indicates which US entrants are screened for tuberculosis before arrival and the percentage from countries in regions with increased risk for tuberculosis (Asia, Africa, Mexico, the Caribbean, Central America, and South America).
The tuberculosis screening process from 1991 through 2007 required a chest radiograph for adult overseas applicants (defined as 15 years of age or older). Those with chest radiograph findings of active tuberculosis were required to submit three sputum specimens for microscopic examination for acid-fast bacilli (AFB). Applicants with AFB present in one or more sputum specimens were considered to have infectious tuberculosis and could not travel until treated. 42 The 2007 Technical Instructions for tuberculosis screening and treatment for panel physicians added sputum culture and drug susceptibility testing for Mycobacterium tuberculosis isolates, increasing threefold the number of applicants with the diagnosis and treatment of tuberculosis 43 and ensuring that cases due to drug-resistant strains were appropriately treated. The 2007 Technical Instructions also require tuberculin skin testing for diagnosis of latent tuberculosis infection in children 2 through 14 years of age. Treatment of latent tuberculosis infection is not required before departure, but a referral is made to the state health department in the state of intended residence in the United States. The 2007 Technical Instructions were implemented for refugees and/or other immigrants from four counties in 2007 and will be implemented in other countries as laboratory and other capabilities are approved.
The 2007 revised tuberculosis screening methods are predicted to reduce the number of immigrants and refugees who arrive with AFB smear-negative tuberculosis (positive sputum cultures but negative microscopic examination), but this will probably reduce the number of tuberculosis cases among foreign-born persons by only 250 cases per year. 44 In 2008 an additional 641,000 persons residing in the United States on shortterm visas (such as students and workers), were approved for permanent residency by change-of-status after screening for tuberculosis (Table 9, next page). Tuberculosis screening for change-of-status applicants, done by designated civil surgeons, involves a two-step process of tuberculin skin testing of all adults and children 2 to 14 years of age. Applicants with a tuberculin skin test reading of 5 mm or more are required to have a chest radiograph, and those with abnormal chest radiographs are referred to the local or state health department to be evaluated for tuberculosis and treated if diagnosed. For those diagnosed with latent tuberculosis infection, there are no requirements for treatment to prevent future tuberculosis.
# Diagnosis and Treatment of Latent Tuberculosis Infection
Although arriving with tuberculosis disease is not common due to the overseas screening process, the prevalence rates of latent tuberculosis infection are quite high for the 1,267,000 persons from Asia, Africa, or Latin America in 2008 who arrived as refugees or achieved permanent residency status (Table 9, page 53). This is reflected in the much higher prevalence of latent tuberculosis infection documented among foreign-born persons and their rates of tuberculosis compared to US-born persons (Figure 4, page 27).
The authors of the Institutes of Medicine (IOM) report Ending Neglect recommend requiring testing and treatment for latent tuberculosis infection among all immigrants from countries with elevated risk for tuberculosis, 12 but this has remained a voluntary process. The national guidelines were revised in 2000 to recommend targeting the testing and treatment of latent tuberculosis infection among recently arrived foreignborn persons due to the higher rates of tuberculosis within the first five years of arrival compared to later years. 17 More recent research shows that persons born outside the United States have tuberculosis case rates 4.7 times higher during their first two years after entry in the United States than in the years that follow, 44 but this does not mean that the risk of tuberculosis decreases in all persons after arrival. Compared to US-born persons, refugees and immigrants from high-burden countries have tuberculosis case rates up to ten times higher for two, five, or more than 20 years after arrival in the United States. 45 The number of tuberculosis cases in refugees who have been in the United States for more than 20 years will continue to increase because 1980 to 2000 was a period of unprecedented refugee resettlement in the United States, with a very significant spike in numbers from 1989 through 1991. 46 In addition, the absolute number of refugees accepted by the United States has been increasing again since 2002, and several new large groups of refugees have been approved for resettlement over the ten years from 2006 from countries that show the highest tuberculosis rates among refugees in the United States. 44,47 Despite the documented higher prevalence of latent tuberculosis infection among foreign-born persons and the increased lifetime risk for life-threatening and disabling tuberculosis conferred by this infection, there are unique challenges for many foreignborn persons that predispose them to disparities of care. These challenges must be recognized and addressed to avoid delays in diagnosis and curative treatment of tuberculosis, in identifying and protecting the health of persons exposed to infectious tuberculosis, and in preventing tuberculosis through targeted testing and treatment for latent tuberculosis.
# Cultural/Linguistic and Socioeconomic Challenges to Care
Most foreign-born tuberculosis patients in the United States face cultural, linguistic, and socioeconomic challenges to care, which may exacerbate the shortcomings of the current strategy to control tuberculosis among the foreign born. Delays in diagnosis are in part the result of patient delays in seeking care, different perceptions of disease, definitions of disease, attribution of symptoms to different illnesses, unfamiliarity with or distrust of biomedical care, fear of stigmatization, fear of government and possible deportation, and lack of a means to pay for care (such as medical insurance). Provider factors contributing to delays in diagnosis include delays in recognizing the possibility of tuberculosis and/or in initiating diagnostic evaluation, delays or failures to report suspected cases of tuberculosis to health departments to ensure complete evaluations, and failure to initiate timely treatment.
Data supporting the scientific basis for cultural challenges to care have focused mostly on linguistic access and socioeconomic factors that have been shown to create health disparities, but other cultural challenges may also limit access to care and reduce cooperation with contact investigations and adherence to therapeutic and programmatic interventions for people with active tuberculosis and their contacts. 48 To some extent, the challenges outlined below may apply to any foreign-born person with tuberculosis or latent tuberculosis infection, but the following sections highlight specific challenges that are especially acute in particular sub-groups of foreign-born tuberculosis patients.
# Additional Challenges Faced by Migrant Workers
Poverty, limited transportation, mobility or unstable residency, low literacy, limited English proficiency, and cultural differences create significant challenges to care for migrant workers. Most low wage jobs are hourly and do not provide sick leave or other benefits such as health insurance, which makes migrants reluctant to miss work, fearing the inability to pay as well as loss of their jobs if they take time off to get medical care. 49 If migrants fear that seeking health care might lead to trouble with immigration authorities, then they are even more likely to delay seeking care, resulting in disease progression and an increased risk of transmission of tuberculosis to others. 50 A further challenge is that migrant workers can face psychological stresses from uncertain employment, housing, and immigration status. What part stress may play in the development of tuberculosis disease is unknown, though rates of tuberculosis have been seen to increase in stressed populations. 51 In addition to these social, economic, and cultural challenges, many healthcare providers assume that migrants will be unable to complete their treatment. This assumption is often offered as a reason for not conducting screening for active tuberculosis or latent tuberculosis infection and for not initiating treatment of latent tuberculosis infection.
# Additional Challenges Faced by Refugees
Refugees are usually from countries with a high burden of tuberculosis, so they arrive with high rates of latent tuberculosis infection acquired in their countries of origin or in refugee camps, and case rates of tuberculosis are much higher within the first two years after entry into the United States. Timely diagnosis and treatment for a variety of medical conditions including tuberculosis and latent tuberculosis infection is challenging even with the resources provided by the Office of Refugee Resettlement and eight months of Medicaid insurance. Refugees struggle to adjust to the US medical culture and healthcare system and often have not found employment that provides medical insurance before their Medicaid coverage lapses.
During and beyond this first two years, refugees face other challenges that complicate medical care. Refugees also often have disrupted families and may have limited community support systems. Other issues that complicate timely diagnosis and refugees' ability to complete treatment can include linguistic barriers to accessing care, different understandings of illness, unfamiliarity with laboratory tests and medication schedules, inexperience with treating latent tuberculosis infection, and having other priorities in adapting to life in a new society that take precedence over health concerns.
In addition, trauma or torture in their home countries can make it difficult to trust government officials or to form a trusting relationship with a case manager. All of these issues are exacerbated in many communities by the lack of trained medical interpreters and identified cultural brokers who can facilitate work with healthcare providers, especially for new refugee groups.
# Additional Challenges Faced by Undocumented Persons
As of March of 2006, the Pew Hispanic Center estimated that between 11.5 and 12 million of the foreign-born persons in the United States were undocumented. 52 Among the foreign-born in the United States, undocumented persons are largely from countries with a moderate or high prevalence of tuberculosis and have not undergone screening.
In addition to the fear of apprehension and deportation, which makes them reluctant to seek medical care, undocumented persons face other obstacles to accessing health care common to foreign-born persons, such as culture and language differences, poverty, housing instability, and limited employment options affecting economic survival.
# B. Action Plans for Tuberculosis Elimination among Foreignborn Populations
For a summary of the action plans for eliminating tuberculosis among foreign-born populations, refer to Table 6: Action Plans for Tuberculosis Elimination among the Foreign-born, pages 13-14.
# Interconnected Health Problems and Social Conditions
To understand the factors contributing to the disparity in tuberculosis rates between foreign-born and most US-born populations, it helps to view tuberculosis as one aspect of the "coinfection and synergistic interaction of diseases and social conditions at the biological and population levels." 53 For example, the high rates of diabetes in Asian and Hispanic populations and high rates of human immunodeficiency virus (HIV) infection among sub-Saharan African immigrants contribute to the progression from latent tuberculosis infection to tuberculosis disease. These are not just co-occurring epidemics in these populations, but are a set of "mutually enhancing epidemics involving disease interactions at the biological level that develop and are sustained in a community/population because of harmful social conditions and injurious social connections." 53 The social conditions of many immigrants and refugees in their home countries and in the United States provide a greater risk of exposure to tuberculosis and HIV and also contribute to lifestyle patterns that increase malnutrition (another biological condition synergistic with tuberculosis) and hinder access to medical care, as described above.
This perspective is a syndemic orientation, which is defined as "a way of thinking about public health work that focuses on connections among health-related problems, considers those connections when developing health policies, and aligns with other avenues of social change to assure the conditions in which all people can be healthy." 54 To address the ongoing disparities in case rates among foreign-born groups, disparities reduction requires an approach that takes into account the biological and social contexts in which tuberculosis occurs and addresses factors related to the health system, care process, and the patient. The Centers for Disease Control and Prevention's Syndemic Prevention Network website at offers information and resources for further exploring a syndemic orientation for public health.
There is a need to do more contemporary research from a syndemic orientation to document the specific contexts and causes of new cases of active tuberculosis among foreign-born persons in the United States. This research needs to be stratified by comorbidities, ethnicity, and time in the United States; family structure and living patterns; social location; and age at which disease is identified. In addition, targeted genotyping by mycobacterial interspersed repetitive unit analysis (MIRU) may be necessary to document recent transmission in non-pediatric cases. Specific epidemiologic/risk factor studies are needed in long-settled immigrant communities to assess the risk of tuberculosis among immigrant and refugee children and children of foreign-born parents, especially where aging immigrants have high rates of comorbidities, such as diabetes, that affect progression from latent tuberculosis infection to active tuberculosis.
Finally, while continuing to use federal racial/ethnic surveillance categories for reporting, there is an urgent need to develop and define more specific operational and research categories for immigrant and refugee groups which will be meaningful for local tuberculosis control activities. More specific and detailed demographic information, available from research and advocacy groups such as the Migration Policy Institute or Hmong National Development, for example, will enable local public health programs to identify needs and plan for targeted community outreach, cultural competence training, interpretation, and partnership building among the groups they serve. 55
# Strategies for Identifying and Treating Latent Tuberculosis Infection among Foreign-born Residents Notification of Inactive Tuberculosis among Refugees and Immigrants
One strategy to identify foreign-born persons with latent tuberculosis infection is to enhance screening and follow-up by health departments in the United States of persons diagnosed with inactive pulmonary tuberculosis and latent tuberculosis infection both pre-departure and at change-of-status visa adjustments. Under the technical instructions for tuberculosis screening of refugees and applicants for permanent residency, those persons whose chest radiographs are consistent with tuberculosis but who have negative sputum cultures for M. tuberculosis are often diagnosed with inactive tuberculosis. (Overseas panel physicians and health departments also use the term Class B1 pulmonary tuberculosis.)
These persons are recommended for follow-up in US health departments due to increased risk for future tuberculosis. Children diagnosed with latent tuberculosis infection during overseas screening and both adults and children with this diagnosis during change-of-status evaluation are at increased risk for developing tuberculosis that can be prevented by treatment with isoniazid. This health department follow-up and treatment can be enhanced by continued improvement both in the electronic notification of local jurisdictions receiving immigrants and refugees and in the interjurisdictional notifications for patients who move (federal government items 1 and 2; local and state government item 4, bullets 1 and 2; and community partners item 6).
# Targeted Testing and Treatment for Latent Tuberculosis Infection
Another strategy to identify foreign-born persons with latent tuberculosis infection is to enhance targeted testing and treatment for latent tuberculosis infection among foreign-born US residents. Local capacity should be built to develop epidemiologic profiles of local foreign-born groups and to better understand which groups to focus on for targeted testing. 56 Tuberculosis elimination among foreign-born residents will require greatly expanded diagnosis and treatment of latent tuberculosis infection with isoniazid (federal government items 1 and 2; local and state government item 4, bullets 1 and 4; and community partners items 5, 6, 7, and 8).
In addition, the promising new tools for detecting and treating latent tuberculosis infection need to be evaluated and implemented. The Division of Tuberculosis Elimination must continue to pursue development of better diagnostic tests for latent tuberculosis infection. The bacilli Calmette-Guérin (BCG) vaccination is common in most high-burden countries, and positive tuberculin skin test results are often dismissed by immigrants as only reflecting BCG. The tuberculin skin test is less specific for M. tuberculosis than the two interferon gamma release assays (blood tests) that have been approved to diagnose latent tuberculosis infection. The use of the blood tests could provide a more specific test for latent tuberculosis infection and could be a more useful tool for persuading persons with latent tuberculosis infection or newly infected contacts to complete medical evaluation for tuberculosis disease and, if needed, to complete treatment for latent tuberculosis infection.
The Division of Tuberculosis Elimination must also continue to evaluate shorter treatment regimens for latent tuberculosis infection. Latent tuberculosis infection treatment regimens of nine months of isoniazid and four months of rifampin present formidable barriers for many immigrants and other travelers to the United States. The increased adherence to treatment that is likely with a shorter regimen is particularly important for the foreign-born who may face many economic, cultural, and linguistic barriers. The journal article "New Approaches to the Treatment of Latent Tuberculosis" reviewed current regimens for treatment of latent tuberculosis infection, both standard and alternative, as well as regimens under investigation and those with potential for future development. 57 For example, development of regimens using longer-acting rifamycins and fluoroquinolones may permit taking medicine only once or twice weekly. Because of the potential difficulty in enrolling sufficient numbers of patients in the United States into clinical studies of such proposed regimens, consideration should be given to multinational clinical trials for new shorter latent tuberculosis infection regimens.
# College Students and Workers from Moderate-and High-burden Countries
A third strategy to identify foreign-born persons with latent tuberculosis infection is to require that students and workers from moderate-and high-burden tuberculosis countries, who are not screened prior to arrival in the United States, undergo tuberculosis screening after arrival (local and state government item 4, bullet 4).
Targeted screening of college students and workers from high-tuberculosis-burden countries can identify immigrant students eligible for latent tuberculosis infection treatment and diagnose active tuberculosis earlier, reducing the risk of transmission. If diagnosed with latent tuberculosis infection, these persons should complete treatment for latent tuberculosis infection. Health departments should begin by engaging with college campuses in developing evidence-based practices in diagnosing and treating latent tuberculosis infection.
# Enhanced Tuberculosis Control Tools for Working with Foreign-born Populations Cultural Competency
Specific local information on foreign-born demographics, community organizations, cultural background information, and challenges to healthcare access is needed. This information would identify ways to bridge language and cultural challenges, to improve case management and contact investigation outcomes, and to identify and develop resources, such as interpreters and cultural brokers, who can be partners in providing culturally and linguistically appropriate care. In addition, information about local access barriers would inform both national and local tuberculosis control strategies. 53 Local capacity to quickly initiate treatment and ensure completion of treatment should be enhanced by implementing patient-centered care practices, including eliciting patient illness models, working with traditional healers, accommodating family decision-making processes, and understanding how different cultural child-rearing practices affect the process of treating children with active tuberculosis and tuberculosis infection. 58 Further, tuberculosis control at all levels needs to coordinate efforts to address disparities in tuberculosis case and latent tuberculosis infection rates in all populations, by adopting a skills-based approach to developing cultural competence. Other groups at high risk of tuberculosis, such as homeless or incarcerated persons-whose members also often include foreign-born persons-have additional specific cultural factors that shape health practices and internal group social organization that affect tuberculosis transmission. Foreign-born groups are also situated within a larger society whose structural influences contribute to the syndemic effects of poverty and exposure to active tuberculosis.
Cultural competency skills and disparities analysis are the tools that tuberculosis control staff need in order to learn about the cultures and structural contexts of each foreign-born group they work with, so that tuberculosis control practices and strategies can be tailored effectively to these groups' specific circumstances. Since no organization can hire staff from all local groups, most tuberculosis control staff will work with people from a variety of backgrounds and cannot be culturally proficient in every group's culture. So, cultural competence needs to be based on developing skills to work effectively with any group, skills that are patient-centered and include knowing how to find specific information about communities and build relationships with community leaders. 59 It is important to recognize that the challenges in access to care and in treatment completion are not located primarily within the immigrant or refugee patient. A synergy of structural, cultural, and biological contexts leads to high rates of latent tuberculosis infection and tuberculosis disease in foreign-born populations. 60 Some case management challenges arise from poverty, lack of insurance, or other structural conditions of immigrant communities, not from cultural differences. Local programs should institute and expand the use of culturally-relevant incentives and enhance local programs' knowledge of economic and social challenges and the corresponding effective enablers for specific populations and communities. Using incentives and enablers helps to increase completion of treatment rates and to continually build cooperative relationships with local immigrant communities that can enhance acceptance of treatment of latent tuberculosis infection.
These cultural competency strategies can be implemented by both hiring staff from local foreign-born communities, working with community organizations to encourage and facilitate training in healthcare interpreting or medical fields, and providing skillsbased cultural competence training to health department staff at all levels, to ensure that all staff have the skills to work with all foreign-born patients.
# : FOREIGN-BORN POPULATIONS : PAGE 61
Version 03/22/2010
# Case Detection and Treatment
As noted earlier, only a very small percentage of the foreign-born population is screened before US entry. Other strategies must also be used to address case detection in the majority of foreign-born persons who are not screened (federal government items 1 and 3; local and state government item 4, all bullets; and community partners item 5).
To eliminate transmission of tuberculosis from foreign-born persons with tuberculosis in the United States, it is necessary to understand that the risk of tuberculosis transmission to others increases when there are delays in diagnosis and curative treatment of infectious tuberculosis. Persons with delayed diagnosis or treatment may transmit tuberculosis, often to family members. For example, there is a marked racial and ethnic disparity for tuberculosis among US-born children less than five years of age with at least one foreign-born parent. Delays in diagnosis and treatment also increase the risk of disability and death, even in persons who are not infectious.
Community outreach and collaboration with other public health programs, community service organizations, and ethnically-based mutual assistance associations can improve familiarity with and trust of healthcare systems. This can be enhanced further by collaboration with traditional healers to demonstrate respect for culturally-based health practices and to encourage referrals. In addition, addressing systemic factors
# SUCCESSFUL PARTNERSHIPS:
# Partnering with Traditional Healers at Healthy House
There is usually a range of healing practices in immigrant and refugee communities-from people who provide information and materials for self-treatment, such as herbalists, to therapeutic massage practitioners, spiritual healers or diviners, and practitioners of complementary systems of medicine, such as Ayurvedic, Tibetan, or Chinese medicine.
Partnership with healing practitioners from these diverse communities, as cultural brokers, can include efforts to learn their practices in specific communities while providing opportunities for them to learn about biomedical practices, engaging patients and family members in discussions about treatments for specific illnesses, such as tuberculosis and comorbid conditions, building alliances to encourage referrals to medical care facilities for specific symptoms, and receiving assistance from traditional healers in identifying contacts to persons with tuberculosis disease.
One model of such a partnership is the Healthy House in Merced, California, which has established a program to orient medical providers to Hmong shamans' practices and to introduce shamans to biomedical practices and facilities. 61 For more information, refer to this National Center for Cultural Competence publication: Bridging the Cultural Divide in Health Care Settings:
The Essential Role of Cultural Broker Programs online at df .
which limit access, including lack of insurance and insufficient access to interpreters, can help to eliminate delays in receiving an appropriate diagnosis. Finally, providing targeted education and medical consultation from health department experts and from the Regional Training and Medical Consultation Centers, with a focus on physicians who treat foreign-born populations at high risk of tuberculosis, would help to address physician-provider unfamiliarity with tuberculosis.
For new refugee groups without pre-existing community organizations, such as the Burmese and Bhutanese, more avenues and funding must be found to quickly train medical interpreters and develop their English language skills as a first step in developing the cross-cultural resources that bridge cultural, linguistic, and access challenges.
# SUCCESSFUL PARTNERSHIPS:
# TBNet: Multinational Patient Tracking and Referral
In 1996, the Migrant Clinicians Network, working with a consortium of public health organizations and funded by a grant from the Texas Department of Health, founded TBNet, a multinational tuberculosis patient tracking and referral project designed to work with mobile, underserved populations. Originally created with migrant farm workers in mind, TBNet has expanded its patient base to include the homeless, immigration detainees, prison parolees, and anyone who might be mobile during treatment.
Each enrollee is given a wallet-sized Health Network card with information about how to obtain the patient's medical records. TBNet maintains a central storehouse of enrollee medical records, which can be accessed by the patient's healthcare providers in the United States, Mexico, or Central America. Mobile patients can also call TBNet's toll-free helpline to locate treatment facilities at their next destination. The wallet card, central medical record warehouse, and toll-free telephone number help to coordinate the continuous treatment of mobile tuberculosis patients. At the conclusion of treatment, TBNet notifies the enrolling clinic as well as the state or regional tuberculosis control contact person that the patient has completed treatment.
TBNet has experienced consistently high treatment completion rates for patients with tuberculosis disease. For more information, see .
# New Outreach and Service Provision Practices
Immigrant, international visitor, refugee, and migrant worker communities are unfamiliar with US public health and often do not understand or lack access to most medical care providers in the public or private sectors. Thus, reaching a larger proportion of these populations for tuberculosis control, especially through the new initiatives proposed for identifying and treating latent tuberculosis infection, requires a significant shift in outreach and service provision practices.
As the 2005 tuberculosis control guidelines outline, the public health sector must remain the lead in planning, coordinating, and evaluating tuberculosis control efforts in order to maintain the necessary specialized knowledge required for effective tuberculosis surveillance, case management, and contact investigation. 13 Partnering with other public health programs, social service organizations, immigrant community organizations, and federally qualified community health centers at local levels would make the most effective use of culture-and population-specific expertise, relationships, outreach, and access for foreign-born groups.
# Contact Investigation
To enhance the yield of contact investigations of foreign-born cases of tuberculosis, tuberculosis control staff need to be familiar with family structure, residence patterns, social organization, and culturally-specific life cycle observances, religious practices, and socializing patterns of the immigrant populations they serve and to have their trust. Relationships with organizations that provide services to immigrants, such as English language classes or religious schools, would enhance the effectiveness of contact investigations in congregate settings.
# Programmatic Strategies for Ensuring Continuity of Care Transnational Continuity of Care
In most states that share borders with Mexico, binational projects have been developed within Mexican states that support the treatment of complicated tuberculosis cases. These services involve medical consultation from tuberculosis experts, laboratory support, and second-line tuberculosis medication support. These binational projects are managed by the Mexican public health physicians and staff. Cross-jurisdictional continuity of care should be improved by this collaboration and legal issues resolved, especially between the United States and Mexico, including improving tuberculosis information sharing and tracking of patients who move. 56
# SUCCESSFUL PARTNERSHIPS: CureTB: Bi-National Tuberculosis Referral Program
The CureTB program, a service of the Health and Human Services Agency in San Diego, California, facilitates and supports the continuity of care for patients with active tuberculosis disease and their contacts who travel between the United States and Mexico, facilitates the exchange of information between healthcare providers from both countries, and provides guidance and education to patients and/or their contacts about their tuberculosis risk and need for diagnostic or treatment services. For more information, see /.
# US Immigration and Customs Enforcement Detainees
Any undocumented foreign-born person apprehended by the US Immigration and Customs Enforcement (ICE) should be considered at high risk of tuberculosis infection and disease and receive appropriate screening. In federal fiscal year 2006, ICE detained 256,842 foreign nationals. 62 When brought into custody and detained, ICE detainees undergo tuberculosis screening at intake. Tuberculosis rates in the ICE detention system are substantially higher than in the general population, with a rate of 121.5 cases of tuberculosis per 100,000 persons in 2005. Tuberculosis cases with positive cultures were detected at a rate of 55.8 per 100,000 persons in 2005, a prevalence rate that was 2.5 times higher than the annual case rate in the US foreign-born population. 63 Ideally, if a person held in ICE custody is diagnosed with active tuberculosis, every effort should be made for that person to complete a full course of treatment prior to repatriation, within the constraints of US immigration law and in the least restrictive setting. 64 US immigration law authorizes ICE to detain people for administrative reasons incident to their immigration proceedings, not for public health considerations There are statutory limits on the duration of ICE custody, and there are ethical considerations on retaining ICE detainees in custody after their immigration issues have been resolved that need to be considered on a case-by-case basis in the contex of personal and public . ts health issues.
Tuberculosis control is a public health responsibility, and public health authorities are challenged to find a solution to help detained individuals with active tuberculosis complete treatment prior to repatriation. However, sometimes for political, personal, or legal reasons it is necessary to repatriate a person before treatment is completed.
Continuity of care should be ensured for ICE detainees with confirmed or suspected active tuberculosis who may be repatriated before completing treatment. In this situation, a plan for bridge case management and continuity of care must be in place and coordinated by one of the two current transnational bridge case management and patient navigation programs: TBNet (Migrant Clinicians Network, Austin, Texas) or CureTB (San Diego County Tuberculosis Control Program, San Diego, California) (local and state government item 4, bullet 3).
# Investment in Global Tuberculosis Control and Elimination
Despite the fact that the global tuberculosis incidence rate is leveling off, the number of tuberculosis cases continues to increase due to population growth. The estimated number of tuberculosis cases in 2007 was 9.27 million worldwide, 65 and a third of the world's population is believed to have latent of tuberculosis infection. 66 Additional research is needed, such as that conducted by Schwartzman et al., 67 to ensure that investment in global tuberculosis control includes strategies that will affect populations and groups that immigrate to the United States. Schwartzman concluded that US support of expanded availability of directly observed therapy in Mexico would reduce importation of active tuberculosis and reduce by 130 the number of tuberculosis cases reported in the United States each year. 67 Accurate case rate information for foreign-born populations in the United States, stratified by country of origin, would indicate in which countries similar targeted strategies could have an effect on tuberculosis incidence in the United States If a short-course latent tuberculosis infection treatment were developed, research might indicate where targeted support for the adoption of latent tuberculosis infection treatment by national tuberculosis programs in high-burden countries with high immigration to the United States could also help to reduce the importation of latent tuberculosis infection.
# TO CONCLUDE AND MOVE FORWARD:
The persistence of over 7,500 tuberculosis cases per year among foreign-born residents of the United poses the greatest single barrier to tuberculosis elimination in the United States. Over 90% of the foreign-born residents arriving over the past 30 years arrived from countries in Asia, Africa, and Latin America where rates of tuberculosis remain high and the disease is endemic. These demographic realities among US arrivals result in an increasing proportion of the United States population with latent tuberculosis infection that remains largely untreated.
Effective diagnosis and treatment of latent tuberculosis infection require improved diagnostic tests and treatments, skills to overcome linguistic and cultural barriers, access to health care, and sufficient public health funding. In addition, issues of global tuberculosis, including drug resistance, require continued international efforts.
While investing in global tuberculosis activities is an important strategy for tuberculosis elimination in the United States, efforts to control global tuberculosis are not a substitute for tuberculosis control in the United States because of prior and ongoing immigration. Both domestic and international efforts need to be undertaken to address tuberculosis in the foreign-born population in the United States.
# VI. Tuberculosis in Low-incidence Areas
The 2002 report of the Advisory Council for the Elimination of Tuberculosis (ACET) described the challenges to eliminating tuberculosis in areas with low-incidence rates of tuberculosis and noted that national progress toward tuberculosis elimination will necessarily lead to low tuberculosis incidence in all areas of the United States. 23 This call for action presents an updated analysis of the progress toward tuberculosis elimination in low-incidence areas with data provided by the Centers for Disease Control and Prevention (CDC). By the year 2006, 26 of the 50 states in the United States reached the status of low incidence, defined as having 3.5 or fewer cases of tuberculosis per 100,000 persons per year. This represented an increase from the 22 states for the year 2000 as described in the ACET report on progress toward tuberculosis elimination in low-incidence areas. 23 The changing epidemiology of tuberculosis in low-incidence areas reveals unique and persistent challenges for tuberculosis elimination. Many of the strategies recommended in this chapter address challenges that are particularly acute in low-incidence areas but that also occur in medium-and high-incidence areas. These strategies are included here to comprehensively address low-incidence areas because, as tuberculosis elimination progresses, more areas will become low incidence and face the challenges that these strategies address. A recent example in Montana highlights the fact that low-incidence areas are not isolated from the global burden of tuberculosis. 68 Public health departments in these areas must maintain the capability to respond to multidrug-resistant cases of tuberculosis among visitors, new immigrants, and residents who travel abroad.
# A. Trends and Challenges
# Changing Epidemiology
The data in Tables 10 and 11 illustrate that, to meet the goals of the national tuberculosis elimination campaign, we need to reinforce tuberculosis prevention and control efforts even in areas with few cases of active tuberculosis. Continuing to provide high-quality and timely services will require bolstering the tuberculosis control infrastructure through novel approaches such as the successful regionalization efforts discussed below and increasing public-private partnerships. AI/AN = American Indian / Alaska Native; HIV = human immunodeficiency virus. Source: R. Pratt, T. Navin, M. Chen, J. Becerra, CDC.
# Challenges
The most threatening challenge to tuberculosis control is the loss of infrastructure and funding similar to the environment that preceded the 1985-1992 tuberculosis resurgence. Other important challenges specific to low-incidence areas include diminishing clinical and laboratory expertise, scarcity of special facilities for prolonged health care and/or respiratory isolation, and providing tuberculosis care in settings where large geographic distances separate patients from providers. 23 Tuberculosis control programs today are losing the capacity for maintaining functions essential for tuberculosis control and are reaching conditions that set the stage for a resurgence in tuberculosis.
# Diminished Infrastructure and Funds
Findings from the recent surveys by the National Tuberculosis Controllers Association on resources for tuberculosis control activities and by the National Tuberculosis Nurse Coalition and the National Society of Tuberculosis Clinicians on tuberculosis public health infrastructure have important implications for tuberculosis programs in lowincidence areas. 69 Survey results suggest that the most commonly reported barriers to reaching the national objectives for tuberculosis control were funding issues (81%), restrictions upon out-of-state travel (including for training/educational purposes) (78%), restrictions upon in-state travel (44%), hiring freezes (41%), and a loss of tuberculosis nursing case management capacity. This loss of key infrastructure comes at a time when tuberculosis nursing case managers report increasing case management difficulties due to greater linguistic and cultural diversity of patients.
The end result for low-incidence states is that in many areas tuberculosis control efforts have been forgone for lack of resources, even within core tuberculosis program functions. For example, contact investigations may be restricted in scope with little effort made to identify contacts outside of the household setting. The result of this type of belt-tightening is a missed opportunity for early identification of persons with infectious tuberculosis and high-risk persons with latent tuberculosis infection who would benefit from treatment-and hence, and the opportunity to prevent ongoing transmission. For other high-risk persons, very few low-incidence states have the capacity to expand and/or collaborate with other medical care providers in expanding targeted testing and treatment of latent tuberculosis infection to prevent future tuberculosis cases among persons with latent tuberculosis infection.
Other factors are affecting resource allocations. Many low-incidence areas are experiencing demographic shifts and are treating increasingly complex tuberculosis cases at the same time that funding needed to maintain tuberculosis expertise and capacity is declining. Greater numbers of persons from areas of the world with a high incidence of tuberculosis are settling in regions that are unprepared to provide culturally competent care for recently arrived immigrants. 23 Public health staff face the challenges of treating and managing patients with multidrug-resistant tuberculosis, other medical conditions, and/or substance abuse and the challenges of identifying and quickly responding to tuberculosis outbreaks. One outbreak or one multidrug-resistant tuberculosis patient can absorb the entire annual budget of the tuberculosis program. 68 Public health tuberculosis control programs often have fewer resources and less knowledge and/or experience with the use of newer tools that would provide epidemiologic assistance to programs, such as using genotyping results of strains of Mycobacterium tuberculosis for tracking chains of tuberculosis transmission and implementing electronic information systems.
Further, having one or fewer full-time employees to perform statewide tuberculosis control functions threatens the continuity of programmatic core activities when staff are diverted to other public health activities. Tuberculosis programs in low-incidence areas are vulnerable to diminishing and co-mingled funding with other programs, which can lead to de-emphasis of tuberculosis in favor of equally important, but more visible, infectious disease threats.
# Loss of Tuberculosis Control Expertise
When the incidence, prevalence, and case rate of active tuberculosis declines to a low enough level, providers (both in the private and public sectors) have less opportunity to see patients with tuberculosis, resulting in limited knowledge of the diagnosis and treatment of tuberculosis. This loss of knowledge in the basic clinical aspects of tuberculosis, the lack of familiarity with newer tests and tools (for example, the new interferon gamma release assays and molecular genotyping), and lack of awareness of Each state has access to a public health laboratory that performs tuberculosis testing, including acid-fast smear microscopy, culture, and drug susceptibility testing. However, some providers use private tuberculosis testing laboratories which may cause delays in obtaining the test results needed for effective management of the tuberculosis patient or contact investigation. Other testing delays are due to the large geographical areas in some low-incidence states, requiring long transport times for specimens to reach the state public health laboratory.
# Scarcity of Special Facilities
The historical shift of tuberculosis treatment to the outpatient setting left many lowincidence states with an unfilled void for long-term specialized centers to manage difficult tuberculosis cases that require isolation or management of nonadherence issues. Effectively managing these patients in the absence of isolation facilities presents challenges to tuberculosis control programs and increases the risk of tuberculosis transmission within communities.
# Geographical Distances
In rural low-incidence states, long distances can separate patients from their healthcare providers and case managers. These distances may translate into delays in tuberculosis diagnosis and treatment as well as delays in evaluation and treatment of contacts of tuberculosis cases. These delays may limit the tuberculosis control program's ability to prevent tuberculosis transmission. Challenges in providing timely and effective case management in remote areas for patients with tuberculosis may lead to treatment failures that, in turn, may lead to acquired drug resistance.
# B. Action Plans to Accelerate Tuberculosis Elimination in Lowincidence Areas
To date, there has been a notable implementation gap around ACET's call advocating that the nation "ake progressing toward tuberculosis elimination in low-incidence areas a national priority." 4 That implementation gap must be addressed by action plans that require steps beyond simply controlling tuberculosis. Creative models that expand the capacity of the public health infrastructure to meet the elimination goal must be further evaluated and implemented. Following are examples of approaches to address challenges described above.
For a summary of action plans for eliminating tuberculosis in low-incidence areas, refer to Table 7: Action Plans for Tuberculosis Elimination in Low-incidence Areas, pages 14-17.
# Stopping the Loss of Infrastructure and Capacity
The goal of tuberculosis elimination requires that tuberculosis control programs have sufficient funds and expertise to effectively perform three core functions: tuberculosis case detection and management necessary for curative treatment; identification, evaluation, and treatment of contacts of tuberculosis cases; and targeted testing and treatment of latent tuberculosis infection (local, state, and federal government item 1, bullet 1). The CDC plays an essential role in maintaining tuberculosis control capacity in low-incidence areas. Key CDC responsibilities include assessment, funding, staffing, operational research, technical assistance for surveillance and program evaluation, surge capacity for outbreaks, and support for interstate access to facilities (local, state, and federal government item 2, all bullets). State and local governments are responsible for maintaining high-quality core tuberculosis control functions by providing health infrastructure and staff and the funding to pay for care for the uninsured, regardless of visa status or citizenship (federal government item 2, all bullets; state and local government item 5, bullets 1, 2, and 3).
# Regional Collaboration among State Tuberculosis Control Programs
Two regionalization approaches, developed in response to the Institute of Medicine (IOM) and ACET recommendations, rely on networks of experts and consultants along with regionalization of some programmatic activities. 70 Both of these approaches are meant to enhance and provide added value (not replace) existing state and local tuberculosis control programs.
# SUCCESSFUL PARTNERSHIPS:
Regional
# Collaboration among Disease Programs
In addition to regional collaboration, sharing resources and expertise across disease programs has benefits at the state and local level. Because of challenges posed by different program priorities and variations in the epidemiology and interventions for different diseases, written agreements or procedures may be helpful to assure that tuberculosis control functions are maintained.
# SUCCESSFUL PARTNERSHIPS: Program Collaborations to Share Resources and Expertise
Below are three examples of collaborative activities that support the Centers for Disease Control and Prevention's Program Collaboration and Service Integration efforts.
In the Massachusetts Department of Public Health:
A Bureau of Infectious Disease nursing response team provides cross-bureau surge capacity. For example, nurses responded to a cluster of tuberculosis cases and performed contact investigation and screening in a prison setting and responded to hepatitis vaccination initiative in the county jails.
A simplified electronic case management and communicable disease surveillance system provides outbreak response capacity and immediate electronic transmission of laboratory results and susceptibilities at the state and local level.
In Connecticut:
The tuberculosis control program initiated cross training so that tuberculosis case managers could become certified human immunodeficiency virus (HIV) counselors. This cross training allowed for testing of tuberculosis patients and their contacts in non-medical settings thereby facilitating testing and improving case management of patients coinfected with tuberculosis and HIV.
# Education and Training to Build Public Awareness and Provider Expertise
To address issues of tuberculosis awareness and expertise, tuberculosis control programs in low-incidence areas should have access to the recommended resources to promote general awareness of tuberculosis and maintain private and public sector provider competence (state and local government item 5, bullet 2; community partners item 6, bullets 1 and 2).
# Interstate Collaboration for Access to Special Facilities
To address the need for special facilities for prolonged care for tuberculosis-both for patients who have complicated case management issues including drug resistance, HIV, or other comorbidities and for those who are nonadherent to treatment or necessary testing-small tuberculosis control programs and programs in low-incidence areas should consider regional partnerships through contractual agreements or mutual aid agreements. These agreements can support a regional tuberculosis referral center that allows patients throughout that region to have access to specialized multidisciplinary tuberculosis treatment and management.
Specific activities to implement this general recommendation include the following:
Support current facilities with appropriate expertise (such as existing centers in Massachusetts and Florida) and assess cross-jurisdictional issues related to their capacity to accommodate patients from other jurisdictions and challenges for doing so (legal and non-legal)
Replicate and support successful models so that all low-incidence areas (and other states with no long-term hospitalization resources) have the ability to hospitalize these patients when needed Assess current tuberculosis control laws and regulations and develop model tuberculosis laws which can be adapted as needed
# Enhancing Laboratory Capacity and Access to Services
Timeliness of laboratory information is critical to rapid identification of persons with tuberculosis, appropriate treatment, and case management. Low-incidence areas should assess whether there is adequate need (as defined by the Association of Public Health Laboratories) to maintain their own expertise and/or whether there is an option for use of other public health or private laboratories (state and local government item 5, bullet 3). Specific activities for low-incidence areas include: analyzing public health regulatory options (for example, in Wisconsin a portion of each specimen must be provided to the state tuberculosis laboratory, thereby eliminating the difficulties associated with specimens sent out-of-state to private laboratories); building a consortium model of in-state tuberculosis laboratories organized and facilitated by state public health laboratories; assuring that an electronic information system exists for laboratory reporting to the public health agency; assuring access to external laboratories for specialized services such as second-line and rapid drug susceptibility testing and genotyping; supporting laboratory training in mycobacteriology and incentives to new graduates of microbiology to learn about tuberculosis; and assuring that a courier service provides timely delivery of specimens to the central tuberculosis laboratory.
For states with a low tuberculosis case load resulting in few specimens tested at the state mycobacterial laboratory, it is still necessary to ensure high-quality and timely tuberculosis diagnostic laboratory services in order to avoid missed or delayed diagnosis and to help guide in the treatment of tuberculosis. Maintaining the resources and laboratory expertise needed for the full range of laboratory services in low-burden areas may not be feasible, and certain specialty tests such as molecular drug susceptibility testing should be done at contract laboratories or regional public health laboratories. Careful monitoring of performance of external laboratories that provide these services, with mechanisms to improve unsatisfactory performance, should be a core function of the state public health laboratory.
# Public and Community Health Teams
Geographic isolation presents a host of challenges for tuberculosis control in lowincidence areas with low population density. The CDC and state tuberculosis control programs should collaborate in piloting two potential public health models based on population density: permanent on-site assigned teams and ad hoc community teams.
Where the population density allows, public health teams could be assigned on-site to a defined location. The on-site approach could have teams responsible for all communicable disease follow-up including tuberculosis (and perhaps other chronic health issues as well). These teams should link a public health nurse and a public health advisor with medical, epidemiologic, and programmatic consultants. In this scenario, community members could be recruited and trained to perform the daily activities (such as directly observed therapy). This type of approach would require a cross-disease shift of thinking by policy makers.
Alternatively, in less dense, remote areas, an ad hoc community health team could be identified and mobilized when required, supported by technical assistance and education as needed at the state and federal level.
# TO CONCLUDE AND MOVE FORWARD: Tuberculosis trends from 2000 to
2006 indicate that the declines in tuberculosis rates are lowest in the low-incidence and low-case-load states, suggesting that even greater efforts will be needed to maintain the necessary mobilization to eliminate tuberculosis as rates decline. As the nation progresses toward tuberculosis elimination, more states and local areas will face the challenges of providing their residents with timely and high-quality services for the diagnosis, treatment, and prevention of tuberculosis. The lessons learned in two successful regionalization efforts should be adapted and applied in other regions of the nation.
Addressing the ongoing challenge of tuberculosis in low-incidence areas will require stopping the loss of infrastructure and capacity, education and training to build public awareness and provider expertise, interstate collaboration for access to special facilities, and enhancing laboratory capacity and access to services. As well, there is a need for creative and innovative approaches such as regional collaboration among state tuberculosis control programs, collaboration among disease programs, and public and community health teams.
# VII. Mobilizing Partners in the Fight against Tuberculosis
The well-defined epidemiology of tuberculosis, evident health disparity in those that suffer from tuberculosis, and the curable and preventable nature of the disease make tuberculosis a provocative social issue for change. Eliminating this common preventable and curable contagious disease has huge individual and public health benefits as described in the earlier sections, and we must address these health disparities more effectively if we are to reach the revised 2035 goal for tuberculosis elimination.
The 2000 Institute of Medicine (IOM) report identified the lack of political will as a major barrier to tuberculosis elimination and listed social mobilization to build and sustain the political will in the United States as one of the five specific goals (Table 1, page 6). Since the resources for tuberculosis elimination have actually been decreasing rather than increasing over the last decade as recommended by the IOM (Figure 5, page 31), we must seek more effective approaches to social mobilization. This section will briefly describe the history of social mobilization in the United States and suggest answers to the questions about how to achieve the local, state, and national political will to eliminate the threat of tuberculosis from the United States.
# A. History
In 1798, President John Adams signed into law an act which furnished medical services for merchant seaman called the Marine Hospital Services. This service existed until 1878 when its functions were expanded greatly. The prevalence of major epidemic diseases caused Congress to enact a national law to prevent the introduction of contagious and infectious diseases into the United States, later extending it to preventing the spread of disease among the states. This was the beginning of the US Public Health Service. 71 State and local health departments maintained authority for disease control, including the treatment and control of tuberculosis. The overwhelming number of tuberculosis cases at the turn of the century challenged states' abilities to provide care and treatment for tuberculosis; thus came the emergence of partnerships from many different individuals and organizations.
In 1904, the National Association for the Study and Prevention of Tuberculosis was founded as the first nationwide, voluntary health organization aimed at conquering a specific disease and is known today as the American Lung Association (ALA). The ALA and the American Thoracic Society (ATS) played major roles in the successful social 72 and other small projects directed toward tuberculosis elimination.
While these are examples of previous successful efforts at the national and local levels, we will need to achieve and sustain a far broader level of social mobilization for tuberculosis elimination to be successful in the United States. Cooperation and collaboration will be required by policy makers at federal, state, and local levels, the public health sector, medical practitioners, professional societies, community-based organizations, and voluntary organizations. This chapter describes the various partners that are needed to succeed in this effort.
# B. Advocacy and Mobilization
Advocacy is one of the most important tools available for the prevention and control of tuberculosis. Building a framework for tuberculosis advocacy requires a mobilization of partners and public health organizations to address the need for changing attitudes and conditions that exist concerning the prevention and control of this public health menace.
Advocacy is more than confronting public officials and lobbying in support of certain legislative issues. Advocacy is a process of building awareness of tuberculosis, supporting patient-centered activities, and maximizing resources and services for the care of persons with tuberculosis. Advocacy opens doors and creates opportunities to change minds and end the neglect of tuberculosis as a disease that impacts people and communities across the globe.
# Communication Strategies
A picture is worth a thousand words, and the visual presentation of local surveillance data is a powerful visual education tool that can be used to create partnerships and has been used by programs successfully. Painting a local picture with surveillance data is important for health commissioners, community taskforce groups, and politicians. More use needs to be made of geographical mapping of cases and illustrating chains of transmission through the use of molecular genotyping to identify specific strains of Mycobacterium tuberculosis. In San Francisco, molecular genotyping data has been used to link cases of recent transmission to a community drop-in center and convinced site managers that mandatory screening for tuberculosis was necessary and would greatly benefit their community.
Patients, who are willing to tell their personal stories to community groups, media, and journalists, put a face on tuberculosis and provide the engagement often lacking in programs advocating for support of health departments and tuberculosis elimination efforts. Encouragement of patients and family members to speak out and join tuberculosis advocacy organizations is currently lacking and sorely needed.
Tuberculosis prevention and control activities in communities where foreign-born persons reside are often hampered by challenges associated with a lack of knowledge of tuberculosis transmission patterns, a lack of providers who understand the culture of the populations at risk, and the inability of this population to trust and navigate the healthcare system. There is a tremendous need for community organizations and healthcare providers to advocate for these communities. There is a need for voices to speak out and communicate the need for culturally specific interventions.
Within every US state, there is an urgent need for advocacy and expanded tuberculosisrelated collaboration among state and local lung associations, professional organizations (such as Thoracic Societies, College of Chest Physicians groups, etc.), other key community advocacy groups (such as RESULTS), and other organizations fighting respiratory diseases including the state and/or local health departments and lung association spin-off organizations. These organizations should all become effectively involved in a state (or community) specific Stop TB Coalition to design and support tuberculosis elimination campaigns, related resources, partnerships, and efforts. These collaborations should include development of mutually agreed upon annual state and/or local tuberculosis elimination advocacy strategies that spell out (1) related annual objectives and (2) related roles and responsibilities for involved organizations.
Internationally, there is a need for organizations like the Pan American Health Organization (PAHO) and the International Union Against Tuberculosis and Lung Disease (IUATLD) to create opportunities for advocacy around tuberculosis.
# Partnerships
State or community tuberculosis elimination advocacy campaigns and related partnerships should include participants from at-risk populations and groups. The advocates should fully understand the goals and the mission of the community advocacy campaign, and the campaign also should include community gatekeepers.
Strategies for partnering with correctional facilities, shelters, and providers of substance abuse treatment provide opportunities to increase awareness of tuberculosis in their communities, as well as to ensure better care and focus on eliminating tuberculosis. Legislative actions, requests for additional resources, and funding opportunities carry more weight when partnerships are involved. Partnership can take many forms such as creating local task force groups or designating individual tuberculosis control personnel as liaisons for homeless shelters, correctional facilities, or other facilities. Regional corrections and tuberculosis control councils can bring together correctional health and custody staff with local and state health department officials to identify and solve common problems.
In communities where foreign-born persons reside, the risk of tuberculosis and the opportunities for control and elimination must be considered. Tuberculosis prevention and control programs must be put in place that involve outreach, education, targeted screening, and intensive case management. Case management and other support services must be provided in the patients' native languages and in alignment with their cultural beliefs and personal health priorities. Voices of advocacy must be heard from providers and community leaders stressing the need for community resources to prevent and control tuberculosis.
# C. Diversity of Partners
Eliminating tuberculosis in the United States is not an easy task, given the way tuberculosis is transmitted and the current inadequacies of public health systems to properly address tuberculosis. No one agency, organization, or group holds full responsibility
The President and Congress must make a bold political commitment and investment if we as a nation are to be successful in eliminating tuberculosis. Over the last ten years, federal funding for our domestic tuberculosis program has been near stagnant despite widely publicized examples of the domestic threat posed by the global spread of multidrug-resistant tuberculosis, which is harder and more expensive to diagnose and treat. We cannot expect to eliminate tuberculosis without additional resources to boost efforts in states and local cities. responsible for conducting critical basic science and clinical research to find new tools to fight tuberculosis. Homeland Security focuses on immigration issues and ensures that immigrants to the United States are properly screened and treated for tuberculosis before entering. HHS also houses the Indian Health Service, which addresses tuberculosis within native Indian populations, and houses the HHS-supported Community Health Centers that serve populations at increased risk of tuberculosis, including migrant workers, persons with human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS), and racial and ethnic minorities. The Federal Tuberculosis Task Force coordinates the activities of these federal agencies in their respective roles in the national tuberculosis elimination effort.
State, territorial, and local health departments drive the work to eliminate tuberculosis as they face the realities and challenges of tuberculosis on the ground.
Health departments, at all levels, are charged by law with control of all communicable diseases, including tuberculosis. They are responsible for establishing the rules and regulations which govern reporting, investigation, diagnosis, treatment, and other public and personal health control measures. These laws, rules, and regulations define the screening of high-risk groups and the evaluation, treatment, and isolation of persons suspected of having contagious tuberculosis. Some local health departments provide public health clinics where all patients can receive treatment at no cost. If public health clinics do not exist, local departments partner with community healthcare providers to provide patients adequate and recommended treatment until cure. Coordination of state and local tuberculosis programs with HIV/AIDS programs is also essential in addressing tuberculosis/HIV co-infection. Health departments have a crucial and unwaiverable public responsibility to provide the citizenry and tuberculosis advocacy groups with timely and complete tuberculosis-related surveillance and evaluation data. These data should include information about the occurrence of community and institutional outbreaks of tuberculosis and related control efforts in their jurisdictions. Tuberculosis outbreaks need to be acknowledged and reported upon until ended. Tuberculosis elimination advocacy campaigns should use health department surveillance and evaluation data. These campaigns should widely publicize successes in meeting state and community tuberculosis control program goals such as completion of tuberculosis treatment and evaluation and treatment of contacts with latent tuberculosis infection. In addition, the success in meeting local and state goals in tuberculosis elimination should be publicized. The NTCA and its associate sections, the National Tuberculosis Nurse Coalition and the National Society of Tuberculosis Clinicians, bring together leaders in tuberculosis control programs across all states and territories as well as in many county and city health departments. Another public health partner is the Association of Public Health Laboratories (APHL), representing state and local public health laboratories, which serve as laboratory first responders protecting the public from disease and environmental health hazards. State and local public health laboratories provide tuberculosis services that are critical to the diagnosis, treatment, and control of tuberculosis. APHL also serves as an advocate to support tuberculosis control programs. The membership of these organizations need to be trained on how to communicate with the media to report on tuberculosis exposures and/or outbreaks. The goal of this interaction is to garner continued public support for tuberculosis elimination while facilitating public responses that are appropriate from public health and humanitarian perspectives.
Medical associations are essential partners providing a variety of services to eliminate tuberculosis. For example, the ATS, once the medical arm of the ALA, is a leading medical association that focuses on medical aspects of tuberculosis and on advocacy for greater federal tuberculosis funding for states. The Infectious Diseases Society of America (IDSA), along with the CDC and the ATS, has participated in the writing and publication of documents critical to the treatment and control of tuberculosis. The American Academy of Pediatrics (AAP) also participates in the writing and publishing of recommendations for tuberculosis treatment and control in children in the Red Book:
2009 Report of the Committee on Infectious Diseases. These organizations should all be involved in the tuberculosis advocacy campaigns and related planning.
Academic institutions are expected to provide the training and education to a new generation of healthcare workers and conduct valuable research on basic science, clinical, social, and public health issues pertinent to the treatment and control of tuberculosis and other infectious diseases. Schools of public health, particularly, are training grounds for public health department workers in the areas of management, epidemiology and biostatistics, health education and environmental issues, and advocacy. Students participate in hands-on experiences with public health professionals, and many are recruited to fill key positions in public health departments and partner organizations. However, many medical and nursing schools do not focus on tuberculosis in their curricula, contributing to the occurrence of missed and delayed diagnosis and/or inadequate treatment of tuberculosis cases. Academic institutions need to address these issues in their curricula in order to reduce the preventable disability, death, and acquired drug-resistance due to these clinical errors. The private sector, primarily pharmaceutical and biotechnology companies, is a key partner in the fight against tuberculosis and should play a significant role in developing new and effective tools. Similarly, product development partnerships (PDPs) and public-private partnerships (PPPs) have emerged as important players in the development of new tools. These not-for-profit entities leverage the best practices of industry, academia, public research institutes, and contract research organizations with funding from companies, governments, and philanthropic donors to accelerate product development. As some PDPs and PPPs rely on outside partnerships, resources, and funding, they often engage in advocacy to raise awareness about the need for better tools for tuberculosis.
Faith communities are significant resources for education, outreach, and training for their constituencies, often in partnership with state and local programs. Where tuberculosis services are very weak, community-based organizations provide critical services to the underserved and minority populations, and their involvement in tuberculosis elimination campaigns is crucial in bringing voice to the cause of tuberculosis elimination and advocating for increased resources and policies that will have positive impact in moving the country forward toward tuberculosis elimination.
As the National Center for Cultural Competence states, "a major principle of cultural competence involves working in conjunction with natural, informal supports and helping networks within diverse communities. The concept of cultural brokering exemplifies this principle and can bridge the gap between healthcare providers and the communities they serve." Cultural brokers exist or can be cultivated in immigrant, refugee, and US-born minority communities, including those with higher risk factors for tuberculosis such as homelessness, substance abuse, mental illness, and correctional facility residence. Among the persons who can become cultural brokers and partners in healing with medical providers are practitioners of healing practices or traditional healers in immigrant, refugee, and minority communities. These persons should be identified and encouraged to join in the state and community tuberculosis elimination advocacy campaigns.
# D. Assessment of Progress in Social Mobilization for Tuberculosis Elimination
Regarding social mobilization, the IOM specifically recommended that:
The CDC be provided with significantly increased resources for tuberculosis elimination efforts and sustain public understanding and support for the effort at national, state, local, and risk-group levels NCET work with the CDC to secure the support and participation of nontraditional public health partners, ensure the development of local and state coalitions, and gain the assistance of public opinion research experts in evaluating public opinion in order to garner public support for the elimination effort The Office of the Secretary of Health and Human Services periodically conduct an evaluation of the actions take in response to the IOM recommendations
The Stop TB USA Tuberculosis Elimination Plan Committee believes the year 2000 IOM recommendations for social mobilization remain valid and should be implemented, but what has been the response to these IOM recommendations on social mobilization? Ten years later, flat-funding, budget cuts, and rescissions have prevented the CDC from providing "significantly increase resources" for eliminating tuberculosis. At a retreat in 2007 on the status and future of NCET, it was noted that NCET had not replaced the initial funding provided in 1991 by the Robert Wood Johnson Foundation, limiting its resources to volunteer efforts. To our knowledge, the recommendation for periodic reports by the Secretary of Health and Human Services on the progress towards addressing the IOM recommendations has not been addressed.
# E. Recommendation for Achieving Social Mobilization for Tuberculosis Elimination
The United States has a history replete with examples of social mobilization efforts that have been successful in addressing important health issues including tuberculosis, poliomyelitis, and AIDS. Social mobilization efforts in the fight against tuberculosis were successfully launched again in the 1990s after the resurgence of tuberculosis associated with fatal cases occurring in outbreaks of multidrug-resistant tuberculosis.
The successful social mobilization that occurred in response to this tuberculosis resurgence was due in large part to the resources provided to NCET by the Robert Wood Johnson Foundation, the ALA, and the ATS, and it needs to be replicated. We now face a major challenge of launching and maintaining a successful mobilization effort for a life-threatening disease that will become increasingly rare as we progress toward eliminating tuberculosis. We must maintain long-term engagement of a variety of partners in the effort while overcoming the barriers of stigma that inhibit the participation of our communities of immigrants, minorities, and HIV-infected persons who are at highest risk of death and disability due to tuberculosis. Based upon the recommendations from the 2007 retreat with the CDC, NCET and a number of partners made the following recommendations:
NCET should transition to Stop TB USA. This name change reflects the need to be more readily identified as the point of contact for the Stop TB Partnership at the World Health Organization and as the point of contact for the United States with the global tuberculosis elimination effort Stop TB USA will need to identify a source of infrastructure funding in order to function as an effective coalition. We recommend that national, state, and local voluntary and professional organizations supporting the control and elimination of respiratory and infectious diseases assist Stop TB USA in obtaining the infrastructure funding needed to mobilize all it members and partners in generating the political will to make the elimination of tuberculosis a national priority
# TO CONCLUDE AND MOVE FORWARD:
The IOM stated, "social mobilization is necessary to build and sustain political will (for tuberculosis elimination) in the United States and can lead to similar efforts internationally." However, today tuberculosis is not generally viewed as a problem in the United States, and there has been only limited success over the last ten years in the social mobilization needed to eliminate tuberculosis. 12 Stop TB USA and its partners must work together to develop the political will needed to advocate for the development and implementation of new tools needed both domestically and globally to eliminate TB among high-risk US-born and foreign-born populations in the United States and to maintain the TB control infrastructure in lowincidence areas. | However, the benefits are well worth the effort. Compared to maintaining the current rate of decline, eliminating tuberculosis by 2035 would result in 253,000 fewer tuberculosis cases 15,200 fewer tuberculosis-related deaths $1.3 billion less in treatment costs in 2006 dollars 7 Each case of tuberculosis represents a profound impact on a person, a family, a workplace, and a community. Preventing the ongoing accumulation of deaths, disability, healthcare costs, and loss of family income from tuberculosis will require full participation by policy makers, the public health sector, medical practitioners, professional societies, community-based organizations, and voluntary organizations to implement the recommendations made in 2000 by the IOM in Ending Neglect.# I. Executive Summary
# A. Reasons for Issuing this Call for Action in 2010
In 2000, the Institute of Medicine (IOM) published a report, Ending Neglect: The Elimination of Tuberculosis in the United States, detailing the history of efforts to control and eliminate tuberculosis in the United States and recommending a plan to eliminate tuberculosis in the United States by 2035. In 2007, based upon the recommendations from its retreat, the National Coalition for the Elimination of Tuberculosis (NCET) has transitioned to Stop TB USA. The name change reflects the need to be more readily identified as the point of contact for the Stop TB Partnership at the World Health Organization. In late 2007, Stop TB USA assembled a Tuberculosis Elimination Plan Committee to assess the progress since the release of the IOM report and to formulate recommendations to update the IOM plan. This report assesses how and why the IOM's tuberculosis elimination plan has not been fully implemented and provides updated action plans to move forward on its recommendations to accelerate progress toward tuberculosis elimination in the United States.
# TB Disease, Latent TB Infection: Definitions, Transmission, and Statistics
Tuberculosis is a life-threatening illness caused by a group of bacteria called Mycobacterium tuberculosis complex. The commonly used public health term tuberculosis case is used to describe a newly reported diagnosis of tuberculosis. The statistic for noting the frequency of tuberculosis in a population is the tuberculosis case rate, defined as the number of tuberculosis cases per year in an area divided by the number of people living in that area multiplied by 100,000. The tuberculosis case rate is also referred to as the tuberculosis incidence rate. M. tuberculosis is transmitted from a person with tuberculosis of the lungs (pulmonary tuberculosis) through the air to other people who may become infected. Infection with M. tuberculosis is called latent tuberculosis infection because there are no symptoms or signs of tuberculosis disease. Latent tuberculosis infection can be diagnosed with a tuberculin skin test or specific blood tests (interferon gamma release assays or IGRAs).
Latent tuberculosis infection carries a 10 percent lifetime risk of tuberculosis disease with about half of the cases occurring within the first two years after infection. Infants, human immunodeficiency virus (HIV)-infected persons, and those with suppressed immune systems are at much higher risk for developing tuberculosis from latent tuberculosis infection.
# Slowing Decline in Rates of Tuberculosis Disease
Nine years after the IOM report, its recommendations have not been fully implemented, and the annual decline in tuberculosis incidence rates has slowed to only 3.8% per year since 2003.
If this trend continues, it will take 97 years to achieve tuberculosis elimination, defined as a rate of less than one case of tuberculosis per million persons. This is clearly a goal well below the horizon from a human perspective in 2010.
Placed in the context of affected persons today, only 300 newly reported cases of tuberculosis would have been expected in the entire US population of 300 million if tuberculosis elimination had been achieved. Instead, 12,904 cases of tuberculosis were reported in 2008, a decrease of only 2.9% from the 13,288 reported in 2007.
# Health Disparities in Rates of Tuberculosis Disease
A major health disparity exists for tuberculosis. In 2008 only 17% of the cases of tuberculosis in the United States were reported in the majority non-Hispanic white population. Compared to reported tuberculosis case rates among non-Hispanic whites, the rates are 5.5-fold higher among American Indians, 7.4-fold higher among Hispanics, 8.0-fold higher among blacks, and 22.9-fold higher among Asians.
# Serious Health and Economic Impacts of Tuberculosis Disease
Information on the frequency of tuberculosis is available and believed to be fairly accurate because cases of tuberculosis are reportable to state health departments and forwarded to the Centers for Disease Control and Prevention (CDC). For each of the 12,904 persons reported with tuberculosis in 2008, the continuing presence of tuberculosis in the United States may have resulted in preventable death, lifethreatening illness, disability, and/or loss of productivity, particularly in minority populations. Tuberculosis remains a deadly disease with over 1,200 of the persons reported as cases in 2006 (the most current year with complete follow-up) having died either before diagnosis or before completing treatment. 1 Among survivors, the health impact remains significant. Over half of the survivors of pulmonary (lung) tuberculosis are left with significant lung impairment. 2 Tuberculosis disease also has a strong economic impact. Prolonged short-term disability due to illness and isolation for public health protection impacts patient and family income. In addition, treating each patient for tuberculosis is expensive with outpatient directly observed treatment costs of $4,000. About 50% of patients are hospitalized at a cost per patient of $19,000. (Both cost estimates are in 2004 dollars.) 3 Many of these costs are absorbed by the public health sector because patients with tuberculosis often lack health insurance, and the clinical expertise in tuberculosis of many private physicians is limited.
Detecting tuberculosis is also expensive. For each patient with confirmed tuberculosis, ten or more people are often evaluated for suspected tuberculosis but determined not to have tuberculosis. A study of laboratory diagnostic tests in Tarrant County, Texas, found that 148 cultures for mycobacteria were done across the community for each confirmed case of tuberculosis in 2002, translating into an estimated laboratory cost of $16,830 for each confirmed tuberculosis case reported by the health department. Health departments evaluate and treat at least as many suspected but not reportable tuberculosis cases as those that meet the reporting requirements, and the health department costs range from $2,180 to $3,525 for each patient treated initially for suspected tuberculosis but later determined to have another diagnosis. These costs do not include hospitalizations that are not covered by public health departments. 4 Improvements in tuberculosis diagnostic tests could reduce the cost, inconvenience, and/or side effects that result from delays in making or excluding the diagnosis of tuberculosis.
With the emergence of multidrug-resistant and extensively drug-resistant strains, tuberculosis has become much more expensive and difficult to diagnose and treat. In the United States, the average estimated hospitalization cost for treating a patient with extensively drug-resistant tuberculosis is $600,000, and that does not include costs of outpatient care and related public health department interventions. 5 The global spread of drug-resistant tuberculosis strains-particularly in human immunodeficiency virus (HIV) co-infected populations living in countries with high tuberculosis burdens but poorly functioning tuberculosis control programs-poses a growing threat to US residents.
# Few Modern Tools for Tuberculosis Diagnosis, Treatment, and Prevention
Further, due to decades of stagnation in research and development, few modern tools have been introduced for the diagnosis, treatment, and prevention of the disease.
The bacilli Calmette-Guérin (BCG) vaccine is the only existing vaccine against tuberculosis and is widely used. However, BCG has had no apparent impact on reversing the growing global tuberculosis pandemic. New, more effective vaccines are urgently needed.
For more accurate and timely detection of latent tuberculosis infection, two blood tests are currently licensed in the United States. However, insufficient funding for operational research has led to delays in implementation of these tests, and many public health programs have been unable to cover the additional cost of these tests.
To more rapidly diagnose tuberculosis disease, there is the nucleic acid amplification (NAA) test. Other promising newer diagnostic methods are able to detect multidrugresistant tuberculosis within just days. However, implementation of these tests remains limited because of inadequate operational research, the official approval processes, cost issues, and/or laboratory expertise. 6 New treatment regimens for tuberculosis disease and latent tuberculosis infection are needed to shorten and simplify treatment, be compatible with antiretrovirals and other commonly-used medicines, and address drug resistance.
# Erosion of Public Health Infrastructure and Loss of Expertise
In the United States, public health provides key elements of tuberculosis control that are not available in the private sector. Two key, recent surveys conducted by the National Tuberculosis Controllers Association (NTCA) and National Tuberculosis Nurse Coalition (NTNC) indicated erosion of tuberculosis control infrastructure and impending loss of expertise. These surveys verify the need to augment and invest in domestic tuberculosis programs.
The NTCA survey focused on resources for tuberculosis control activities from 2006 through 2008. Respondents reported that the most common barrier to reaching the national objectives for tuberculosis control was underfunding of public health systems (81%). Estimates from each program on needed funding ranged from $13,000-$99,000 for eight programs (33%), $100,000-$399,000 for eight programs (33%), $400,000-$1.5 million for six programs (25%), to $2-2.2 million for two programs (8%).
The NTNC survey noted an impending loss of nursing tuberculosis case management expertise as 33% and 74% of current tuberculosis case managers anticipate retirement within 5 and 10 years, respectively. This loss of key infrastructure comes at a time when tuberculosis nursing case managers report increasing case complexity due to drug resistance (multidrug-resistant and extensively drug-resistant tuberculosis), comorbid conditions, and greater linguistic and cultural diversity of patients with tuberculosis in their communities.
# Tuberculosis Elimination-A Worthy and Achievable Goal
Despite this dire assessment of current progress, the elimination of tuberculosis in the United States, first proposed in 1989 and reaffirmed by the IOM in 2000, is a worthy and achievable goal if we accept the challenge.
# B. Purpose of this Call for Action
The Stop TB USA Tuberculosis Elimination Plan Committee has drafted this update and based it upon the following documents that explain national guidelines and strategies that will need to be implemented to eliminate tuberculosis in the United States: The aim of this plan is not to rewrite the IOM plan for eliminating tuberculosis: the IOM plan and its recommendations are still valid. The purpose of this plan is to call for stakeholder involvement and to serve as a foundation for making specific action plans to implement the IOM recommendations. The purpose of this call for action is to engage policy makers in all levels of government, the public health sector, medical practitioners, professional societies, community-based organizations, and voluntary organizations in the effort to eliminate tuberculosis in the United States.
# C. Progress Assessment Summary
In its 2000 report, Ending Neglect, the IOM recommended that five specific goals be targeted in order to eliminate tuberculosis in the United States. Table 1 summarizes the current status of progress toward these goals.
T A B L E 1
# Success in Meeting Institute of Medicine Goals
# Institute of Medicine Goal Success Comments
Maintain control of tuberculosis while adjusting to declining tuberculosis case numbers and rates Yes There has been continuing decline in tuberculosis case numbers and rates since 1993
Accelerate the rate of decline of tuberculosis cases and rates by increasing efforts at targeted testing and treatment of latent tuberculosis infection
# No
The decline in tuberculosis is slowing, not accelerating. The treatment of latent tuberculosis infection remains largely limited to public health departments and has not been expanded by other medical care providers to the level required for tuberculosis elimination Develop the new diagnostic, treatment, and prevention tools that will be necessary for the ultimate elimination of tuberculosis The continued decline in case rates provides evidence that tuberculosis remains under control, but the acceleration of tuberculosis elimination that the IOM anticipated with the implementation of Goals 2 through 5 (Table 1) has not occurred. Treatment of latent tuberculosis infection is a tuberculosis prevention strategy that is critical to eliminate tuberculosis. However, expansion of the treatment of latent tuberculosis infection has not occurred and remains limited in public health departments where it is considered low priority when resources are scarce. Expansion of treatment for latent tuberculosis infection has been severely limited due to the lack of an effective, safe, and affordable short-course treatment regimen. Detailed information on the progress made toward the IOM goals is provided in Chapter II: "Eliminating TB in the United States," pages 20-35.
The 2008 tuberculosis case rates, the reported number of persons diagnosed with active tuberculosis per 100,000 persons per year, are shown in Table 2 (next page) for the overall total US population. The rate of 4.2 cases per 100,000 population is equivalent to 42 per million population, 42-fold higher than one per million, the definition of tuberculosis elimination. Also shown are the average annual percentage changes in tuberculosis case rates from 2003 through 2008 for the total US population and by birthplace and race/ethnicity.
Projecting these trends forward, it would take until 2107-97 years from 2010-to achieve the tuberculosis elimination goal of one case of tuberculosis per million for the entire US population. A major contribution to this estimate is the higher rate and slower annual decrease among foreign-born persons, a population projected to require 141 years for tuberculosis elimination. Racial and ethnic minority populations (blacks, Asians, and Hispanics) continue to be disproportionately affected by tuberculosis in the United States. Tuberculosis elimination among the various racial and ethnic minority populations is projected to take 80 to 129 years. The rates and delayed years of projected tuberculosis elimination for ethnic and racial groups also reflect the proportion of tuberculosis cases that occur among foreign-born persons within these groups. Foreign-born persons, who most likely arrived in the United States with latent tuberculosis infection that progressed to tuberculosis, accounted for 95% and 76% of cases among Asian and Hispanic residents respectively in 2008. Foreign-born persons made up 32% of tuberculosis cases reported among black persons, an increase from 5% in 1993.
CALL
Much of the ongoing cost, disability, and premature mortality that are predicted to continue for the next 97 years may be preventable if we implement the IOM recommendations. Tuberculosis disparately affects racial and ethnic minorities, yet every American remains at potential risk for tuberculosis due to the global burden of tuberculosis, including drug-resistant strains of tuberculosis that require treatment for up to two years. The following recommendations for action will benefit every American as well as our global neighbors who have an urgent need for the same new tools that we seek for the diagnosis, treatment, and prevention of tuberculosis.
# D. Recommendations for Action
The Tuberculosis Elimination Plan Committee has developed a set of general recommendations for action on national, state, and/or local levels in all US communities and populations. Separate recommendations have been formulated for speeding up the development and implementation of tuberculosis diagnostics, drugs, and vaccines. Other recommendations have been developed for specific US-born and foreign-born populations to address the risk factors and/or interventions that are either unique or more important for those persons. In addition, the challenges of providing tuberculosis services in states with low tuberculosis case burdens have been a subject of discussion and research, and this document provides updated plans for action to accelerate tuberculosis elimination in areas with low incidences of tuberculosis.
# General Recommendations for Action
The general recommendations reflect important roles that must be assumed by federal, state, county, and municipal agencies as well as other local and national organizations if tuberculosis is to be eliminated.
# New Tools
Tuberculosis control in the United States has been maintained over the past two decades by placing emphasis on the detection and treatment of tuberculosis and on the evaluation and treatment of contacts (persons exposed to infectious tuberculosis). These top-priority activities must be done well, and new diagnostic tools and treatments for active tuberculosis must be developed. But, as pointed out in the IOM report, accelerating our progress toward eliminating tuberculosis requires additional resources and tools to expand the treatment of latent tuberculosis infection. Tuberculosis elimination requires much more rapid development, evaluation, and implementation of new tools to accelerate the decline in the rate of cases of tuberculosis, particularly with the recent trends of stagnation in these case rates.
# Foreign-born Populations
As noted in the 2000 IOM report, the burden of tuberculosis among foreign-born persons results from latent tuberculosis infection that progresses to tuberculosis after arrival in the United States, so eliminating tuberculosis requires expanded treatment of latent tuberculosis infection. There are also unique linguistic and cultural issues that must be addressed in providing quality tuberculosis services to many foreign-born persons.
T A B L E 6
# Action Plans for Tuberculosis Elimination among the Foreign-born
Federal Government 1. The Division of Tuberculosis Elimination should evaluate the feasibility of testing all immigrant applicants being screened overseas for latent tuberculosis infection (currently limited to children aged 2 to 14 years) including the use of the new tools of blood testing with interferon gamma release assays with the goal of treating latent tuberculosis infection with an effective, safe, short-course regimen 2. The US government must ensure that receiving jurisdictions are promptly notified of incoming refugees and Class B immigrants along with complete medical records from overseas tuberculosis screening so that local tuberculosis programs can complete follow-up in a timely manner. Mechanisms must be developed to track migration of new arrivals with diagnoses of latent tuberculosis infection to optimize chances for treatment completion and to allow for maintenance of medical record information
# 3.
The US government must maintain and increase its commitment to global tuberculosis control and elimination, including the support for implementation and enhancement of existing effective control and prevention strategies and the development of new tools for diagnosis, treatment, and prevention of tuberculosis students, to raise the awareness of tuberculosis in high-risk foreign-born persons, reduce delays in diagnosis, and broaden the scope of targeted testing and treatment programs for latent tuberculosis infection. Services that can be provided by health departments include facilitating laboratory testing, providing medications, providing community and provider education and expert clinical consultation and referral services, and evaluating the effectiveness of community-based programs Community Partners
# 5.
Community health centers should make the diagnosis and treatment of latent tuberculosis infection a priority activity. This will require collaboration with public health agencies to provide a full range of tuberculosis prevention services for new immigrants and other high-risk populations (such as migrant workers) regardless of ability to pay, visa status, or movement among local health jurisdictions 6. Civil surgeons performing visa status adjustments for immigrants in their communities must ensure that their evaluations include effective tuberculosis screening according to current standards. Greater emphasis, combined with additional resources, must be placed on treatment of latent tuberculosis infection among immigrants diagnosed with latent tuberculosis infection during these examinations 7. Institutions and employers who sponsor students and workers from moderate-or high-burden tuberculosis countries, who under current policy are not required to undergo tuberculosis screening before entry to the United States, should establish tuberculosis screening programs for their constituents. Such programs should incorporate treatment for those diagnosed with latent tuberculosis infection 8. Medical practitioners who provide care to foreign-born persons should educate their patients about symptoms of tuberculosis and should incorporate tuberculosis screening, targeted testing, and treatment of latent tuberculosis infection into ongoing medical services to high-risk patients
# Tuberculosis Low-incidence Areas
The challenges of progressing toward tuberculosis elimination in areas with lowincidence rates of tuberculosis are described in the 2002 report of the Advisory Council for the Elimination of Tuberculosis (ACET). The report recommends evaluating the feasibility of interstate regionalization by creating collaborative consortiums to ensure that high-quality, essential (core) elements of tuberculosis control are maintained.
There are now two models that have been developed and implemented for regionalization of tuberculosis prevention and control. The first model is the New England Tuberculosis Consortium, a collaboration among the six New England tuberculosis programs and the CDC. These six states share a similar epidemiology pattern, common borders, and a history of past collaborative efforts. The New England Tuberculosis Consortium has built a regional leadership team that shares expertise and resources in an organized and supportive fashion. Three important findings were noted in both models. First, tuberculosis control program staff members and resources in low-incidence states cannot simply merge across the state boundaries to create a larger multistate program. Second, tuberculosis control services within each state can be enhanced when tuberculosis program staff collaborate in a multistate regional tuberculosis elimination effort. Third, limited-but necessary-additional federal resources, including personnel assigned to the region, must be provided to maintain effective regional collaboration.
A successful tuberculosis elimination campaign will lead to more tuberculosis lowincidence areas, and the lessons learned in the New England and the western state regions will be applicable to more areas of the United States. Core tuberculosis control services must be maintained, not eliminated, as the number of tuberculosis cases declines in order to avoid a resurgence in the disease, as occurred in the mid-1980s. First, a full understanding of the causes of this remarkable change will require collection of additional information and analysis of its implications for the national goal of tuberculosis elimination. The potential contributors to this decline could include improved tuberculosis control but could also reflect surveillance reporting changes instituted in 2009, population demographic shifts, and under-diagnosis or under-reporting of cases. As noted in the MMWR report, the CDC and the National Tuberculosis Controllers Association are studying the possible explanations for the unexpectedly large drop in tuberculosis cases and rates.
Second, if this decrease in tuberculosis cases and rates is due to a true reduction in the occurrence of tuberculosis, this decrease does not diminish the importance of the recommendations in this document. An even greater acceleration of the rate of decline in tuberculosis cases will be needed if we are to eliminate tuberculosis by the year 2035 and avoid 253,000 preventable tuberculosis cases and the associated deaths, disability, and loss of family income. A decrease of over 10% per year, followed by 20% per year was called for by the IOM ten years ago. 12 Having finally achieved this first step is a call for action, not merely a call for celebration.
For more information, the MMWR report, "Decrease in Reported Tuberculosis Cases ---United States, 2009," is available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5910a2.htm.
# Advisory Council for the Elimination of Tuberculosis Report, 1989
In 1989, the ACET report called for the elimination of tuberculosis in the United States by the year 2010, defining tuberculosis elimination as a case rate of less than one case of tuberculosis per million persons. 9 A year 2000 interim target of achieving a case rate of 3.5 per 100,000 was also established. When the report was published in 1989, the US case rate for tuberculosis was 9.5 per 100,000. The ACET report claimed that tuberculosis elimination was a realistic goal for three reasons: tuberculosis was retreating into geographically and demographically defined high-risk populations; biotechnology had the potential for generating better tools for diagnosis, treatment, and prevention; and advances in computer, telecommunications, and other technologies could enhance implementation of new tools.
A three-step plan of action to achieve tuberculosis elimination was proposed:
1. More effective use of existing prevention and control methods, especially in high-risk populations defined as human immunodeficiency virus (HIV)-infected persons, racial and ethnic minorities, the foreign-born, and the elderly
# Resurgence of Tuberculosis, 1985-1992
Ironically at the time of the preparation of the ACET report, there were early indications the United States was experiencing the first resurgence of tuberculosis known since national case reporting was instituted in 1953. The annual tuberculosis case rate had remained stagnant between 9.2 and 9.5 cases per 100,000 per year for the five-year period 1985 through 1989. The resurgence-related to the expansion of HIV infection, hospital transmission of Mycobacterium tuberculosis, multidrug-resistant tuberculosis, disassembly of categorical public health tuberculosis programs at state and local levels, and increasing immigration from countries with a high incidence of tuberculosisextended through 1992. The resurgence took a heavy toll in terms of tuberculosisrelated illness and death, including healthcare workers, and also forced a large amount of additional resources to be returned to tuberculosis control. 10 After the public health capacity was rebuilt, a resumption of the downward trend in tuberculosis morbidity in the United States in 1993 led to a renewed interest in tuberculosis elimination. In 1999, ACET reassessed its 1989 plan and made updated recommendations for tuberculosis elimination. 11 In its reassessment, ACET concluded that the success against resurgent tuberculosis should reinforce the nation's confidence that:
Tuberculosis can be controlled and ultimately eliminated in the United States with expanded partnerships and the development of new tools for diagnosis, treatment, and prevention of tuberculosis Tuberculosis elimination will have widespread economic, public health, and social benefits Committing to decisive action against tuberculosis in the United States would fulfill an obligation to persons throughout the world who have this preventable and curable disease
# Institute of Medicine Report, 2000
As an outgrowth of the renewed interest in tuberculosis elimination, an independent study was conducted by the Institute of Medicine (IOM) and published in 2000. 12 The IOM report projected tuberculosis elimination by 2035 if the first and second of these recommendations lead to a 10% initial annual rate of decline in tuberculosis incidence that is followed a decade later by an accelerated 20% annual decline brought on by the implementation of new tools. The IOM also noted the cyclical nature of the nation's response to tuberculosis and warned against allowing the occurrence of another "cycle of neglect." The national response to decreasing rates of tuberculosis prior to the 1980s was to decrease public health resources for tuberculosis control. In order to reverse the erosion of the tuberculosis control infrastructure that preceded and caused the resurgence of 1985 through 1992, major increases in annual funding to the CDC for local TB control were required from 1992 through 1994. As the national, state, and local tuberculosis control programs were rebuilt, the tuberculosis case rate for the United States decreased from 10.4 in 1992 to 5.8 per 100,000 persons per year by 2000, but this rate was well above the interim goal of 3.5 proposed by ACET in 1989.
# Costs of Implementing Recommendations, 2002
In
# Challenges in Low-incidence Areas, 2002
The challenges of progressing toward tuberculosis elimination in areas with lowincidence rates of tuberculosis were described in ACET's 2002 report, "Progressing Toward Tuberculosis Elimination in Low-Incidence Areas of the United States." The report focused on the 22 states that faced the challenge of maintaining an effective tuberculosis control program with 50 or fewer tuberculosis cases per year and an annual tuberculosis rate of less than 3.5 cases per 100,000 persons per year. The report recommended evaluating the feasibility of interstate regionalization of tuberculosis services as proposed previously by the IOM. One of the initial projects of the Division of Tuberculosis Elimination's Tuberculosis Epidemiologic Studies Consortium was to evaluate the implementation of regional approaches to enhance tuberculosis control and elimination in the low-incidence region comprised of Idaho, Montana, Utah, and Wyoming.
# Tuberculosis Control Guidelines, 2005
Building on the issues raised in the IOM report, the 2005 guidelines on tuberculosis control issued by the American Thoracic Society (ATS), Infectious Diseases Society of America (IDSA), and the CDC 13 concluded that "the traditional model of tuberculosis control, in which planning and execution reside almost exclusively with the public health sector, is no longer the optimal approach during a sustained drive toward the elimination of tuberculosis." That report affirmed the essential role of the public health sector in planning, coordinating, and evaluating the tuberculosis control effort but, in addition, proposed roles and responsibilities for a full range of stakeholders whose participation was deemed to be essential.
# Comprehensive Tuberculosis Elimination Act (P.L. 110-392)
The Comprehensive Tuberculosis Elimination Act of 2007 was signed into law in late 2008, authorizing up to $210 million per year in funding for the CDC's Division of Tuberculosis Elimination. If followed by full appropriation of funding, this roughly 50% increase in the funding for the Division will help to reverse the 40% effective loss of funding due to inflation over the previous 15 years. Based upon the 2002 NCET report, additional increases will be needed to develop, evaluate, and implement the new tools that will be required to eliminate tuberculosis from the United States.
# B. Epidemiological Progress and Trends
In 2008, reported cases of tuberculosis decreased to 12,904 for an annual incidence rate of 4.2 cases per 100,000 persons, the lowest recorded number and rate since national reporting began in 1953. Since the tuberculosis resurgence in 1985 to 1992, there has been an uninterrupted 52% decline in tuberculosis incidence in the United States. However, the rate of that decline is slowing, from an average 6.6% decrease in cases per year from 1993 to 2002, to an average 3.4% decline from 2003 to 2008. This change coincided in 2002 with the observation that, for the first year in US history, foreign-born persons accounted for the majority (51%) of reported tuberculosis cases, a proportion that has increased to 59% of tuberculosis cases reported in 2008. 14
# Tuberculosis in Foreign-born Populations
As shown in Figure 1
F I G U R E 1
# Number of US Tuberculosis Cases Reported in US-born and Foreign-born Persons, 1993-2008
The trends for the annual tuberculosis rates for the United States and the separate populations of US-and foreign-born persons (Figure 2) demonstrate a decrease in slope after 2002, representing a slowing of the decline in tuberculosis case rates for the overall US population and the US-born sub-population. Rates were 10.2-fold higher among foreign-born compared to US-born persons in 2008, accounting for a projected delay until year 2151 for tuberculosis elimination in foreign-born persons compared to year 2059 for those born in the United States (Table 2, page 8).
F I G U R E 2
# Tuberculosis Case Rates (Cases per 100,000 Population) for US-born and Foreign-born Persons, United States, 1993-2008
If we maintain the annual percent change in case rates seen from 2003 through 2008, it will take an estimated 97 years from 2010 to reach the tuberculosis elimination goal of one case per million for the entire US population (Table 2, page 8). A major contribution to this estimate is the higher rate and slower annual decrease among foreign-born persons, for whom tuberculosis elimination is projected to require 141 years.
# Persisting Disparity of Tuberculosis
Accurate population estimates are not currently available for race and ethnicity stratified by birthplace. However, trends in the number of reported cases of tuberculosis among US-born persons by race and ethnicity (Figure 3) indicate a persisting disparity of tuberculosis among US-born blacks with no evidence of improvement and a persistence of approximately 1,000 cases per year among Hispanics.
F I G U R E 3
# Number of Tuberculosis Cases Reported in US-born Persons by Race and Ethnicity, 1993-2008
The determinants of risk of tuberculosis, however, are not limited to birthplace and race or ethnicity. Certain other readily-identified subgroups of the US population have been consistently found to experience rates of tuberculosis much higher than the population as a whole. 13 These include persons with tuberculosis risk factors of lower socioeconomic status, homelessness, incarceration, abuse of alcohol and/or other substances, HIV infection, and certain underlying medical conditions.
# Latent Tuberculosis Infection
These differences in tuberculosis incidence associated with birthplace, race, ethnicity, and socioeconomic factors are also reflected in population rates of latent tuberculosis infection among US residents. A recently published survey from the CDC 15 indicated that the prevalence of latent tuberculosis infection (defined as the percentage of persons with a positive tuberculin skin test) in the US population in 1999 and 2000 was 4.2%, with much greater prevalence rates of infection among immigrants and persons in poverty. Prevalence rates were 18.7% in immigrants compared to 1.8% in US-born persons. Among those living below the poverty level, 6.1% were infected compared to 3.3% of those not living in poverty.
F I G U R E 4
# US-born and Foreign-born Prevalence of Latent Tuberculosis Infection (LTBI) and Case Rates (Cases per 100,000 Population) by Age, 1999-2000
The age-specific data show striking parallels in risk of tuberculosis and latent tuberculosis infection among US residents by birthplace (US versus non-US; Figure 4) that, combined with the marked differences in tuberculosis rates among segments of the US-born population, strongly suggest that the barriers to tuberculosis elimination may differ for the populations of US-born and foreign-born persons in the United States. A successful tuberculosis elimination plan for the United States requires approaches to address the unique challenges posed in different populations and to identify the partners who need to be engaged for the effort to succeed.
# : ELIMINATING TUBERCULOSIS : PAGE 28
Version 03/22/2010
# C. Progress Assessment 1. Success in Meeting Institute of Medicine Goals
One way to assess recent progress toward tuberculosis elimination in the United States is to evaluate success in implementing the five specific goals proposed by the IOM in its 2000 report. 12 Table 1 (page 6) summarizes the current status of progress on the IOM recommendations.
Whereas tuberculosis remains under control (IOM Goal 1), as evidenced by continued declining case rates, the annual rate of decline is slowing, not accelerating. Why is the United States not achieving IOM Goal 2, the acceleration of the decline in tuberculosis?
A recent report found that in the Netherlands a similar gradual annual decline in tuberculosis incidence was due to the natural replacement of older population members, who have high rates of latent tuberculosis infection and risk of progression to tuberculosis disease, by younger residents with successively lower rates of latent tuberculosis infection, resulting from less exposure to tuberculosis at younger ages. 16 In the United States, the very low rates of latent tuberculosis infection in younger persons are seen only in the native-born population, but rates are much higher in tho born abroad and parallel the higher rates of tuberculosis by age group as seen in Figu 4 (page 27) se re .
Treatment of latent tuberculosis infection is a tuberculosis prevention strategy that is critical to eliminate tuberculosis. The ATS/CDC report on targeted testing and treatment of latent tuberculosis infection, 17 as well as the IOM report Goal 2, called for expansion of treatment of latent tuberculosis infection into the private medical sector as a means to increasing access to this preventive intervention against tuberculosis. However, a survey conducted by the CDC Tuberculosis Epidemiologic Studies Consortium found that in 2002, over 90% of all latent tuberculosis infection treatment was administered in public health clinics, including those serving immigrants and refugees, and in corrections facilities. 18 Expansion of the treatment of latent tuberculosis infection has not occurred and remains limited in public health departments where it is considered low priority when resources are scarce. In addition, the completion rate for the standard nine-month course of isoniazid for latent tuberculosis infection is often less than 50% to 60%. The lack of an effective, safe, and affordable short-course regimen that would improve treatment completion rates has severely limited expansion of treatment for latent tuberculosis infection.
The failure to achieve IOM Goal 3-to develop and implement new tools for the diagnosis, treatment, and prevention of tuberculosis-continues to pose a major impediment to tuberculosis elimination. The call for new tools was made by ACET in the initial tuberculosis elimination plan in 1989, repeated by ACET in 1999, and stated as necessary in the 2000 IOM report in order to double the rate of decline in tuberculosis cases by the year 2010. Investment in research and development for new tools for tuberculosis has been deemed "woefully inadequate," especially when compared to research and development expenditures for HIV. 19 Unfortunately, two decades into the tuberculosis elimination effort, few new tools have been developed, and none yet has been widely implemented. There have been no substantive changes in the standard drug regimen for active tuberculosis since the 1980s. The Federal Tuberculosis Task Force noted the major problems now faced by clinicians and public health officials in addressing the needs of tuberculosis patients infected with multidrug-resistant (MDR) and extensively drug-resistant (XDR) strains of Mycobacterium tuberculosis. 20 To prevent latent tuberculosis infection from progressing to active tuberculosis, the nine-month isoniazid treatment, introduced in the 1960s, remains the treatment regimen of choice, and no approved treatments are available for persons infected with MDR or XDR strains. A new generation of tests for latent tuberculosis infection, interferon gamma release assays, has been licensed, but due to limited clinical evaluation there continues to be controversy concerning their proper role in clinical practice. 21 The Division of Tuberculosis Elimination at the CDC has committed about $9 million per year to fund the Tuberculosis Trials Consortium. This consortium, funded with domestic dollars, conducts international clinical trials of new treatment tools that will benefit patients in the United States and improve the outcomes of tuberculosis treatment globally in high-burden countries.
Considerable progress has been made on IOM Goal 4, increasing involvement by the United States in global tuberculosis control. The President's Emergency Plan for AIDS Relief (PEPFAR) and the US Agency for International Development (USAID) represent major initiatives in addressing the global burden of tuberculosis. The Division of Tuberculosis Elimination devotes most of its roughly $140 million annual budget to domestic tuberculosis elimination efforts but plays a major role in a number of countries in implementing the PEPFAR and USAID initiatives. Although this global effort represents good progress on Goal 4, the federal global tuberculosis efforts through PEPFAR and USAID should be better coordinated and balanced with domestic tuberculosis control and elimination efforts. Although the burden of tuberculosis cases globally overwhelms the numbers in the United States, tuberculosis elimination will require increases in both domestic as well as global funding.
Finally, a critical element in concerted public health action is broad public consensus on the importance of the endeavor. According to the IOM report, "social mobilization is necessary to build and sustain political will (for tuberculosis elimination) in the United States and can lead to similar efforts internationally." 12 The United States has a long history of social mobilization, the enlistment and coordination of various individuals and groups, in support of tuberculosis control efforts. However, today tuberculosis is not generally viewed as a problem in the United States, 12 and there has been only limited success over the last ten years in meeting IOM Goal 5. NCET, the predecessor of Stop TB USA, made a concerted effort to advocate for tuberculosis elimination, but this effort was not successful in developing the political will needed in order to accelerate the development and implementation of the new tools needed for diagnosis, treatment, and prevention of tuberculosis.
# Robustness of Government Funding
Another measurement of progress toward tuberculosis elimination is the robustness of financing from public and private sources. Despite the recommended increase in the annual budget of the Division of Tuberculosis Elimination to the $528 million recommended in the 2002 NCET report, TB Elimination: The Federal Funding Gap, effective funding levels of the Division have decreased 40% since 1994 due to the combination of flat-funding despite inflation, budget cuts, and rescissions (Figure 5, page 31). 22 concluded that the five recommendations of the IOM report "cannot be implemented with current funding." As a result of cuts in federal funding to states for tuberculosis control, targeted testing and treatment programs for latent tuberculosis infection are being reduced or eliminated, and there is evidence that preventable cases of active tuberculosis are rising.
# The Federal Tuberculosis Task Force Plan in Response to the Institute of Medicine Report, Ending Neglect: The Elimination of Tuberculosis in the United States 2003
The 2002 ACET report, "Progressing Toward Tuberculosis Elimination in Low-Incidence Areas of the United States" cited loss of expert personnel and resources among reasons why there has not been more progress. 23 That report asserted that local and state health departments have the most important role in controlling tuberculosis, but it also cited evidence of deficient funding for tuberculosis control, not to mention tubercu elimination efforts, throughout states and localities in the United States. In addition, there is a predicted loss of skilled, experienced staff. A Health Resources and Services Administration report from 2005 cited an impending crisis in the public health workforce as older workers across a broad range of disciplines retire, requiring increased funds for training if they are to be replaced.
# losis F I G U R E 5
# Annual CDC Tuberculosis Budget, FY 1990-FY 2008
CPI = Consumer Price Index.
# Overall Assessment of Progress Toward Tuberculosis Elimination
The United States is not moving purposefully toward the elimination of tuberculosis. Epidemiological data indicate that interim elimination targets have not been met, that the rate of decrease in tuberculosis incidence is slowing, and that, if the current trend continues, tuberculosis elimination in the United States will require nearly 100 years.
Reasons for lack of progress toward elimination, presented above and expanded upon in subsequent sections of this report, include: The ongoing global tuberculosis epidemic, including HIV/tuberculosis coinfection, which continues to impact tuberculosis incidence in the United States A 40% erosion, rather than the recommended over 3.8-fold increase, in resources for tuberculosis control Insufficient effort to speed the decline of tuberculosis by targeting persons with latent tuberculosis infection and high risk of progressing to active tuberculosis (IOM Goal 2)
Insufficient funding for research and development for new tools for diagnosis, treatment, and prevention (IOM Goal 3)
Lack of public understanding and support at the national, state, and local levels for tuberculosis elimination in order to make it a high national priority (IOM Goal 5)
Lack of the development of, consensus on, and advocacy for specific strategies for tuberculosis control in high-risk groups Continued lack of successful advocacy for tuberculosis elimination
# D. The Call for Action to Eliminate Tuberculosis from the United States
Stop TB USA issues a call for action to all partners and stakeholders in the plan to eliminate the scourge of tuberculosis from the United States by 2035. To more rapidly progress toward eliminating tuberculosis in the United States, the Stop TB USA TB Elimination Plan Writing Committee has identified general and specific action plans (Tables 3-7, pages 9-17) and now issues a call for action on five start-up steps that are critical to fully implement the IOM recommendations and the Stop TB USA action plans:
1. Commit to implementing the IOM recommendations in Ending Neglect and conduct a periodic review on the progress toward elimination
# Implementation of the Institute of Medicine Recommendations
The Tuberculosis Elimination Plan Committee endorses the IOM's year 2000 recommendations in Ending Neglect in which the IOM defined five major goals to achieve in the tuberculosis elimination campaign for the United States (Table 1, page 6).
The tuberculosis elimination effort is failing, not for want of the right goals or specific recommendations, but rather because the IOM recommendations needed to achieve those goals have not been fully implemented. For example, to eliminate tuberculosis, it is critical that the IOM recommendation to accelerate the development of new tools is followed. Tuberculosis may be controlled but not eliminated in our lifetimes, or even within the lifetimes of our children, if we are forced to rely upon the outdated tools in current use. Tuberculosis elimination will require an unprecedented effort to ensure that core tuberculosis control functions are maintained and to finally bring into use the new tools called for in 2000 by IOM and two decades ago by ACET.
# Development of New Timelines and Interim Goals
In addition, the Committee recommends that a new timeline be developed for the goal for tuberculosis elimination in the United States, along with new interim targets. These new interim targets must be realistically achievable with broader application of existing tuberculosis elimination tools as well as with the implementation of new tools and strategies that could be more rapidly implemented with the authorized increase in federal funding.
Periodic evaluations of progress will need to be conducted. The IOM (Recommendation 7.3) requested that the Office of the Secretary of Health and Human Services conduct periodic evaluations of actions taken in response to the recommendations made in 2000, but it is not clear that this recommendation was followed. We recommend that Stop TB USA conduct periodic evaluations of the action taken on the recommendations in this report and provide reports to ACET that will be forwarded to the Secretary of the Office of the Department of Health and Human Services. The first report should be within two years (2012) and at two-year intervals thereafter.
# Obtaining Infrastructure Funding for Stop TB USA to Enable Collaboration with Centers for Disease Control and Prevention
The CDC should collaborate with the members and partners of Stop TB USA in implementing specific action plans for accelerating TB elimination including:
Consensus-building, advocacy, and mobilization Acceleration of the development and implementation of new tools for diagnosis, prevention, and treatment Implementation of strategies to reach high-risk segments of the US population
The IOM recommended that the NCET provide the leadership and oversight for coordinating the engagement of these partners and stakeholders and ensuring effective collaboration with the CDC. NCET, now identified as Stop TB USA, lacks the resources needed to meet this challenge. National, state, and local voluntary and professional organizations supporting the control and elimination of respiratory and infectious diseases will need to assist Stop TB USA in obtaining the infrastructure funding needed to engage all its members and partners in generating the political will to implement the 2000 recommendations and the updated action plans in this document, a challenge in any fiscal climate, and even more so in recessionary times.
# Closing of the Federal Funding Gap
Opportunities to Address the Federal Funding Gap
# Assessment by the Federal Tuberculosis Task Force of the Benefits of the Recommended Increase in Funding for New Tools for Tuberculosis Elimination
As discussed above, new tools are needed for the diagnosis, treatment, and prevention of tuberculosis. These tools are a critical component of the tuberculosis elimination plan for the United States as proposed in 1989 and updated by the IOM in 2000.
Addressing the need for new tools requires a coordinated federal intervention, a role uniquely suited for the Federal Tuberculosis Task Force.
The Federal Tuberculosis Task Force outlined the need for new tools development and implementation in the 2009 plan for extensively drug-resistant tuberculosis. We call for an independent review to assess the potential impact on the development and implementation of new tools that could be expected by increasing funding to the levels authorized in the Comprehensive Tuberculosis Elimination Act of 2007. We request that this assessment be completed within four months of this report in order to use this assessment in proposing new interim goals in the tuberculosis elimination campaign. Increased new tools funding must include basic science research, the focus of the National Institutes of Health, as well as operational research, the focus of the CDC.
# Engagement of a Broad Range of Stakeholders
The control and eventual elimination of tuberculosis in the United States is not just a federal responsibility. There must be a renewed and expanded commitment to the goal The success of this effort requires that stakeholders and partners join with Stop TB USA in endorsing the revised goal and interim targets as well as the implementation of general recommendations for the nation as a whole and those specific to populations at higher risk. The 2005 tuberculosis control guidelines provided detailed roles and responsibilities for the partners who must be involved for tuberculosis elimination to be successful. 13 For more discussion on stakeholders and potential partners involved in tuberculosis, refer to Chapter VII: "Mobilizing Partners in the Fight against Tuberculosis," pages 76-82.
# TO CONCLUDE AND MOVE FORWARD:
As seen in the progress assessment, the IOM recommendations have not been fully implemented, and the goal of eliminating tuberculosis in the United States by 2035 remains beyond reach with our current approach. Stakeholders across the country must join the effort to develop and implement new, creative measures to accelerate the elimination of tuberculosis.
# III. New Tools
There is a critical unmet need globally as well as within the United States for better tools to diagnose, treat, and prevent tuberculosis. The currently available diagnostic tests for active tuberculosis and for detection of drug-resistant strains in the United States include liquid culture methods that diagnose most tuberculosis cases within two weeks and provide drug susceptibility test results within an additional one to two weeks. Another method for detecting the genetic material of tuberculosis in a sputum sample, which can produce results one or more weeks faster than liquid culture, is the licensed test called nucleic acid amplification (NAA). The implementation of NAA testing, however, particularly in public health settings, has been delayed due to the additional expense added by the cost of cultures that are still required in order to test for drug susceptibility. There are also promising newer diagnostic methods that are able to detect multidrug-resistant tuberculosis within just days, but implementation of these tests remains limited because of inadequate operational research, the official approval processes, cost issues, and/or laboratory expertise. 25
# Drugs
Today's first-line drugs for the treatment of tuberculosis were developed and brought to the market more than 40 years ago, after which, research and development ground to a halt due to a lack of commercial incentive to invest in new therapies. Due to the complexity of the tuberculosis bacterium, tuberculosis disease requires that it be treated with multiple drugs at the same time. The current treatment regimen, a combination of four drugs administered daily for six to nine months, is cumbersome, potentially toxic, and places an extraordinary burden on patients and healthcare providers alike. Incomplete and improper treatment has led to the growth of multidrug-resistant strains of tuberculosis (MDR TB) that are much more difficult and costly to treat. The threat of antibiotic resistance has been further intensified by the emergence of extensively drug-resistant tuberculosis (XDR TB), which, in some cases, can be virtually untreatable due to the lack of effective anti-tuberculosis drugs. The current treatment regimen is also limited by the fact that the cornerstone of first-line treatment, rifampin, is incompatible with certain commonly-used antiretroviral therapies for human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS). Ideal new regimens will significantly shorten and simplify treatment, be compatible with antiretrovirals and other commonly-used medicines, and address drug resistance.
After near-total stagnation of the global pipeline for anti-tuberculosis drugs, the founding of the Global Alliance for TB Drug Development in 2000 and the recent entry of several pharmaceutical companies into the tuberculosis drug research and development arena is encouraging. Currently there are seven drug candidates in clinical development for tuberculosis and dozens more in earlier stages of development. However, attrition rates are high for drug development, and only a small number of compounds discovered will ever reach registration. Since tuberculosis will always require multiple drugs in a combination treatment, a revolutionary breakthrough in tuberculosis treatment hinges on the ability to register several new drugs. Although significant advancements have been made, the global pipeline of anti-tuberculosis drugs is not nearly large enough to ensure that this occurs. Recent research showed the impressive benefit of adding a new drug, TMC207, to the regimen that patients were receiving for MDR TB. 26 This finding provides some hope that new regimens may be available, at least for MDR TB, much sooner than anticipated. 8 At the same time, it will be necessary to maintain and increase investments in drug discovery to ensure a robust pipeline of future anti-tuberculosis drugs.
# Vaccines
The BCG vaccine, created in 1921, is the only existing vaccine against tuberculosis. Unfortunately, it is only partially effective. It provides some protection against severe forms of pediatric tuberculosis but is unreliable against pulmonary tuberculosis, which is the infectious form of tuberculosis and which accounts for most of the tuberculosis disease burden worldwide. Despite being widely used, BCG has had no apparent impact on reversing the growing global tuberculosis pandemic. New, more effective vaccines are urgently needed to protect against all forms of tuberculosis-including MDR and XDR TB-and to prevent tuberculosis in children, adolescents, and adults, including in people infected with HIV. New vaccines would also help to decrease tuberculosis incidence overall and prevent further spread of the disease.
BCG is not used routinely in the United States where most infants are not exposed to tuberculosis, and it has never been a component of the US tuberculosis control program. The greatest direct benefit of a better tuberculosis vaccine would be realized in populations living in countries with high tuberculosis burdens, which would also benefit the United States by reducing the incidence of active tuberculosis in people who travel to the United States. The United States and other industrialized countries would indirectly benefit as well. For example, reducing tuberculosis would reinforce multibillion dollar US programs to combat HIV/AIDS, as patients already receiving antiretroviral treatment are still succumbing to undiagnosed and untreated tuberculosis.
Vaccines under development have the potential to prevent tuberculosis in any of several ways: by preventing infection, primary disease, latency, or reactivation of latent tuberculosis. Several potentially better tuberculosis vaccines have entered early-stage clinical trials to determine safety and immunogenicity, and the first Phase IIb "proofof-concept" trial of a new preventive tuberculosis vaccine in infants in over 80 years was initiated in 2009. Numerous additional candidates are in preclinical development.
The Aeras Global TB Vaccine Foundation and other investigators from around the globe are sponsoring research on these tuberculosis vaccine candidates, but additional funding will be needed for further studies and to advance the most promising candidates through Phase III efficacy and licensure trials. These later stage trials require a large number of participants and long follow-up periods and are very expensive. Aeras estimates that a Phase III trial of one candidate vaccine could cost $120 million.
TAG suggests that, in the most optimistic scenario, the first new tuberculosis vaccine would be available in 2015.
# Scientific Barriers
Major scientific hurdles and gaps remain in our understanding of tuberculosis, and these challenges need to be quickly met if new and better tools are to be developed for the elimination of both drug-sensitive and drug-resistant tuberculosis. 20 The identification of new diagnostics, drugs, and vaccines that will radically transform tuberculosis control and treatment will require a better understanding of bacterial latency, persistence, metabolism, and the host immune response to infection. Research and development will be hastened by the development of better animal models, identification of novel drug targets and predictive biomarkers, and discovery of new imaging and drug and vaccine delivery technologies. The improved preparedness of clinical trials sites will ensure that new tools are evaluated and delivered to patients without delays. Further, basic research on vaccine candidates as well as greater investigation of the mechanisms of action and pharmacokinetic/pharmacodynamic parameters of current drugs will lead to significant improvement in existing development approaches and, ultimately, to optimized prevention and treatment strategies.
# Financial Barriers
To support this crucial work, the Global Plan to Stop TB estimates $9 billion in funding is required in the next decade for research and development of new tuberculosis diagnostics, drugs, and vaccines. With the inclusion of basic science and operational research, the November 2009 TAG report suggests that tuberculosis research and development funding investments need to increase to $2 billion per year, from the Global Plan's original target of $900 million per year. 27 In Insufficient advocacy for mobilizing resources continues to limit the advancement of the tuberculosis research and development agenda. While other health areas have focused heavily on developing improved cures, there is little understanding of the need for new tuberculosis diagnostics, drugs, and vaccines among health and advocacy groups in the United States. While investigators themselves have been a strong voice of support for increased investment in tuberculosis research, the issue has not been widely taken up by non-scientific or community-based groups or by the general scientific and academic communities. Without greater understanding about the limitations of current tools and research, it is unlikely that public and private donors will recognize the urgency for greater investment in biomedical research for tuberculosis. Researchers and other stakeholders will need to build awareness and a broader base of support in the community in order to intensify advocacy efforts.
# B. Action Plans to Accelerate New Tools Development
For a summary of action plans for the development and implementation of new tools, refer to Tuberculosis research and development require substantial coordination of scientific and operational activities at many levels, both globally and nationally. Governments, foundations, and the private sector must accurately track and transparently report tuberculosis research and development investments to ensure that funding gaps are addressed.
# Tuberculosis Research and Development Investment
# Advocacy
Advocacy efforts to educate policy makers about the critical role of government funding for tuberculosis research and in the development of new diagnostics, drugs, and vaccines must be intensified. Stop TB USA, partners, and stakeholders must engage new constituents in the tuberculosis research advocacy movement, particularly community-based organizations, non-governmental organizations, and other health advocacy groups.
# Basic Research and Methods
To address scientific barriers, basic research must be intensified and methods must be established to facilitate research and development across all new tools. These improvements will strengthen the pipeline of new concepts entering research, accelerate development, and improve the diagnosis, treatment, and prevention of tuberculosis.
# IV. Tuberculosis among US-born Populations
Communities continue to experience outbreaks and chains of tuberculosis transmission within US-born populations, especially those associated with human immunodeficiency virus (HIV) infection, incarceration, homelessness, and limited access to health care. The elimination of tuberculosis within US-born populations will not be successful without implementation of effective measures to accelerate tuberculosis elimination in these groups.
# A. Trends and Challenges
# Epidemiology and Demographics
The convergence of high rates of HIV and substance abuse with the crowding of homelessness, marginal housing, and incarceration creates ideal scenarios for ongoing transmission and high rates of tuberculosis.
Molecular epidemiology, the use of genetic typing of M. tuberculosis strains in studies of how tuberculosis is spread, confirms significantly higher rates of tuberculosis among US-born populations due to recent spread and infection (rather than from latent infection that occurred many years ago) when compared to the foreign-born. 29 Among persons with tuberculosis, those born in the United States and with low socioeconomic backgrounds are even more likely to have developed their tuberculosis due to recent transmission and outbreaks. 30 High HIV rates among the urban poor amplify transmission, causing larger and prolonged outbreaks of tuberculosis. 31 HIV infection, the biggest risk factor for tuberculosis, continues to play a dominant role among US-born cases, especially among substance users, the homeless, African Americans, correctional facility inmates, and alcohol abusers. 32 As shown in HIV = human immunodeficiency virus. Source: R. Pratt, T. Navin, M. Chen, J. Becerra, CDC.
# Loss of Funds and Personnel Dedicated to Tuberculosis Control
The decline in categorical funding for over a decade has led to significant decreases in personnel and resources for individual and community outreach, incentives and enablers needed for case management, aggressive contact investigations, and completion of treatment.
Since the spike in funding in the early 1990s, health department programs for preventing tuberculosis by targeted testing and treatment of latent tuberculosis infection in US-born communities have been dismantled because of the need to maintain core functions of active tuberculosis treatment and contact investigation. The lack of resources devoted to targeted testing and treatment of latent tuberculosis infection to prevent tuberculosis cases makes elimination of tuberculosis among the US-born impossible.
Most cases of tuberculosis are detected when persons seek medical care for the symptoms of the disease. Because US-born persons with tuberculosis come from populations who are least likely to access health care, delays in seeking and/or accessing health care lead to delays in diagnosis, contributing to ongoing airborne spread of the disease in their communities. 34
# Resource-Intensive Contact Investigations
Once disease is detected, contact investigation in these populations is complex, resource intensive, and more challenging because of the highly mobile nature and competing priorities of people within these groups. Social mistrust and stigma of tuberculosis make these people difficult to reach and further hamper efforts to adequately identify and evaluate all contacts.
Without improvements in health department programs aimed at finding, evaluating, and treating contacts (persons exposed) to infectious tuberculosis cases, transmission of tuberculosis will continue to occur from recently infected persons who develop tuberculosis. Contact investigations among populations of marginally housed persons in shelters, low-cost hotels, and drug treatment facilities are resource intensive and often require on-site services, including education (of residents, patients, and staff), mobile radiology, phlebotomy, sputum collection, and incentives and enablers for follow-up. Communication and partnering with community programs are necessary and require skilled staff. Because of the cost and complexity of these investigations, programs often reserve investigations to only the cases considered most contagious or after an outbreak has already been detected.
# Complexity of Addressing Health Disparities
With the current funding downturn, the hiring and training of skillful staff to work with the difficult-to-reach is currently limited and unaffordable. The complexity of working with persons who have multiple medical, social, and mental problems requires a highly skilled workforce that is willing to provide outreach in potentially dangerous environments. It is challenging for the patients who are trying to make ends meet or worrying about their next meal to have to take medication for latent tuberculosis infection for a minimum of six to nine months. Knowledge of existing services for nontuberculosis issues and access to these services are often critical in stabilizing patients who are on treatment or in the process of a work-up for tuberculosis.
The activities that are critical to the success of working with US-born populations at risk for tuberculosis are labor and resource intensive. The cost of care is substantially higher than for other at-risk populations but is necessary to protect the public.
Resource demands can surge dramatically and unpredictably: one outbreak in a correctional facility or homeless shelter can create significant challenges for a health department and facility staff already stretched to capacity-a common scenario with the current level of infrastructure for tuberculosis control in the United States.
# Tuberculosis in Correctional Facilities
Correctional facilities hold over 2.2 million people, including persons frequently affected by substance abuse, homelessness, HIV infection, lower socioeconomic status, and limited access to medical care. Overcrowding has become commonplace in these facilities.
The link between tuberculosis and correctional care facilities, particularly among African Americans, is often not recognized and represents a missed opportunity for tuberculosis control and prevention. According to the US Department of Justice Bureau of Justice Statistics, at year end 2006 there were 3,042 black male sentenced prisoners per 100,000 black males in the United States, compared to 1,261 Hispanic male sentenced prisoners per 100,000 Hispanic males and 487 white male sentenced prisoners per 100,000 white males. 35 Common challenges in state and county correctional facilities include insufficient resources for screening and staff surge capacity during outbreaks. The problem is particularly acute in smaller county jails, where inmates often stay briefly while awaiting release or transfer to other correctional facilities.
# B. Action Plans to Accelerate Tuberculosis Elimination among US-born Populations
Although the roots of the disparities may remain despite our efforts, tuberculosis control programs in the United States are models of providing high-quality and equitable care to all patients. With the right resources, tuberculosis programs can lessen and eventually eliminate the uneven burden of disease among the US-born.
Engaging difficult-to-reach US-born populations with tuberculosis will require aggressive community-and patient-centered approaches to screening and prevention. Community-based tuberculosis services and prevention in high-risk communities and facilities where tuberculosis exposure perpetuates disease are needed to eliminate ongoing transmission among the US-born. Further erosion of the core infrastructure and rationed services will only serve to raise the risk of transmission and jeopardize the hard-won current containment of tuberculosis.
For a summary of action plans for eliminating tuberculosis in US-born populations, refer to
# Community-Based Tuberculosis Activities
In the Action Plans for Eliminating Tuberculosis among the US-born, it is recommended that funding be augmented and restored for community-based targeted testing and latent tuberculosis infection treatment focusing specifically on persons who are homeless, marginally housed, or co-infected with HIV and on persons who have diabetes and other medical risk factors for disease progression (local, state, and federal government item 1, bullet 1).
The lack of access to screening and targeted testing of at-risk US-born persons perpetuates delayed diagnosis of contagious tuberculosis, reactivation, and transmission in high-risk settings such as shelters, jails, low-cost housing, community drop-in centers, and substance abuse treatment facilities.
Funding for treatment of latent tuberculosis infection of homeless contacts and persons with HIV or medical risk factors for progression to active tuberculosis must be increased in order for health departments and other medical providers to make this key prevention activity a priority. Outreach, incentives, and enablers are needed to engage difficult-to-reach populations in prevention activities, namely treatment of latent tuberculosis infection. To combat the high rates of nonadherence, directly observed therapy for latent tuberculosis infection treatment has been shown to be effective 36 and is needed if tuberculosis elimination is the goal.
Community-based programs, new technology, and training are essential for screening, targeted testing, and treatment. Community-based programs that provide on-site screening and directly observed therapy for both active tuberculosis and latent tuberculosis infection are needed to bridge the gap of access to care. Implementation of new technology, such as blood-based tuberculosis testing to improve adherence to screening, should be prioritized for the difficult-to-reach since it requires only one clinic visit to get a result, instead of the two clinic visits needed for tuberculin skin test results. Tuberculosis control staff working with these populations must be well trained, highly motivated, and able to create strong relationships with community members.
The importance of community input, education, leadership, and coalition building cannot be understated in these activities. These efforts will require significant resources in order to be successful in case management, completion of treatment for tuberculosis, contact investigation, and targeted testing and treatment of latent tuberculosis infection.
Because of the high risk of transmission in them, congregate settings present valuable opportunities for screening and tuberculosis case detection. It is recommended to enhance tuberculosis control programs at correctional facilities to the same level as external health department programs in order to improve screening and surveillance capacity, contact investigation, and case management of inmates who are moved frequently to different facilities, have high recidivism rates, or leave institutions before treatment is completed (local, state, and federal government item 1, bullet 2).
Special focus should be placed on screening and tuberculosis case detection in shelters, correctional facilities, residential substance abuse programs, and community day dropin centers where risk of transmission is high. It is common for at-risk persons to cycle through some or all of these sites and facilities in a single year. 37 Hence, requiring tuberculosis screening in these settings and fully implementing existing guidelines for these groups is an important strategy in creating access to the difficult-to-reach. It is recommended that local health departments should have the resources to limit transmission through early case detection and screening at sites with high crowding and limited ventilation. Mandatory tuberculosis screening should be implemented of all homeless in shelters, day drop-in centers, and other congregate sites to prevent outbreaks and spread of tuberculosis (local, state, and federal government item 1, bullet 3).
Preventing tuberculosis transmission in these congregate settings is challenging because of the frequent movement of persons within and between settings and programs. In these facilities, and especially in correctional facilities, development of databases for tuberculosis surveillance is needed and critical to serve these populations and collaborate with local public health authorities. 38 Better disease surveillance and medical databases to track inmates and transfer vital information among facilities are badly needed to improve efficiency and care. It is recommended that local health departments should enhance surveillance activities using geographic information system mapping and genetic typing (genotypying) of strains of M. tuberculosis to identify specific local areas of ongoing transmission in order to target efforts and communicate with the public (local, state, and federal government item 1, bullet 4).
Finally, training and education specific to tuberculosis are needed to address contact investigation, collaboration between correctional facilities and public health units, and case management and discharge planning for inmates with tuberculosis disease and high-priority latent tuberculosis-infected inmates.
# SUCCESSFUL PARTNERSHIPS: Forth Worth Community Partnership for TB Detection and Prevention
In the western part of the Dallas-Fort Worth metropolitan area in Tarrant County, Texas, community organizations partnered with the local public health department to implement locationbased tuberculosis screening. 39 Despite years of free voluntary tuberculosis screening, communities in three Tarrant County zip codes with high rates of unemployment, homelessness, and substance abuse suffered persistent high rates of tuberculosis transmission.
After being presented with the epidemiologic data, community organizations partnered with the local public health department to make annual tuberculosis screening mandatory for persons to continue receiving a variety of services. Screening was expanded from homeless shelters to be location-based at other community organizations providing services, including mental health facilities, temporary labor services, Veterans Administration job training and living facilities, dialysis centers, churches, community service centers, a human immunodeficiency virus (HIV) congregate living facility, and living facilities sponsored by faith-based organizations. Screened persons were given county-issued screening cards that were required to receive services at the partner organizations.
Before these new programs, screening detected only 5% of active tuberculosis cases among shelter residents. The remaining cases were diagnosed in hospitals. In September 2002, locationbased screening detected 20 cases of active tuberculosis among the first 702 persons screened. The prevalence of active tuberculosis was 2.9% in the first screening, and 1.9% in the first year, a rate exceeded in the United States only during outbreaks in homeless shelters or in evaluation of contacts to active tuberculosis cases. Early results are promising: the prevalence of active tuberculosis dropped from 1.9% in the first 12 months to 0.5% in the last 16 months reported.
# Awareness of Tuberculosis among Healthcare and Service Providers
It is recommended that local health departments should increase tuberculosis education of community workers in shelters, housing services, and substance abuse treatment sites; correctional staff; and providers serving high-incidence US-born populations in order to address the lack of awareness that tuberculosis is a health disparity among the populations they serve (local, state, and federal government item 1, bullet 6).
Lack of awareness among healthcare providers about tuberculosis and associated health disparities often has led to delayed diagnosis and prolonged transmission in the community. Studies have demonstrated delays in diagnosis of tuberculosis due to other primary diagnoses, such as asthma, HIV infection, and community-acquired pneumonia. It is crucial for community providers to know who gets tuberculosis in their community, how to make the diagnosis, and how to rapidly report tuberculosis to state or local health departments.
# Advocacy and Mobilization
On a local level, it is recommended that local health departments partner with key community members and providers to promote education, create cohesive interventions, and develop policies and strategies that address the unique tuberculosis problems of each community and the locality (local, state, and federal government item 1, bullet 5). On local, state, and national levels, as mentioned above, it is recommended that governments should restore and augment funding for community-based targeted testing and latent tuberculosis infection treatment (local, state, and federal government item 1, bullet 1).
# SUCCESSFUL PARTNERSHIPS:
# Stop Tuberculosis in the African American Community Summit
The Division of Tuberculosis Elimination and RTI International co-sponsored the Stop Tuberculosis in the African American Community Summit in May 2006 to engage partners in collaborative efforts to address the impact of the tuberculosis disparity in the African American community. The goals of this meeting were to raise awareness about the problem of tuberculosis in the African American community, create links, and build networks that will lead to ongoing activities and strategies to decrease tuberculosis in the African American community. The Summit brought together community and religious leaders, healthcare providers, public health leaders, policy and decision makers, state and local health department staff, communications professionals, academicians, and others who committed to undertaking specific goals and action items.
Current funding opportunities for tuberculosis control have focused largely on the global rather than domestic efforts to eliminate tuberculosis. High-level officials and Congress are not aware that tuberculosis among the US-born is an issue of disparities and inequity, with rates of tuberculosis in poor inner city communities that rival those in the developing world. Additionally, communities most heavily affected by tuberculosis often have little political clout and few advocates when other social issues seem more pressing. Poor Americans with tuberculosis are also unlikely advocates because of the added stigma to their already difficult lives. Raising public awareness among local, state, and national politicians and lawmakers of the daily domestic outbreaks and ongoing transmission in US-born populations is critical in increasing domestic funding for tuberculosis control and elimination.
# TO CONCLUDE AND MOVE FORWARD:
A major barrier to tuberculosis elimination in the United States is the health disparity for tuberculosis among US-born minority populations, who now account for 87% of tuberculosis cases in the US-born population. Tuberculosis persists in the minority populations due to the failure to prevent tuberculosis outbreaks that often occur in congregate settings, such as: crowded, inadequate housing; homeless shelters; correctional care settings; and substance treatment programs. Higher rates of HIV infection among these minority populations compound the problem.
Addressing the ongoing challenge of tuberculosis among difficult-to-reach US-born groups will require advocacy and mobilization, education, and community-and patient-centered approaches to screening and prevention that focus on communitybased tuberculosis services and prevention in high-risk communities and facilities where tuberculosis exposure perpetuates disease.
# V. Tuberculosis among Foreign-born Populations
Despite the 70% decrease in the number of tuberculosis cases among US-born persons over the past 15 years, no progress has been made in reducing the number of tuberculosis cases reported among foreign-born persons each year (Figure 1, page 24). The persistence of over 7,500 tuberculosis cases each year with the associated disability and death among foreign-born persons in the United States is due to three factors: demographic trends in the United States, high rates of latent tuberculosis infection in the foreign-born population, and cultural-linguistic and socioeconomic challenges to implementing tuberculosis control measures. The solution to tuberculosis elimination among foreign-born US residents and the nation lies in addressing these three factors as well as investing in tuberculosis control and elimination globally, especially in those regions of the world where tuberculosis control and elimination is threatened by the spread of drug-resistant strains of Mycobacterium tuberculosis.
# A. Trends and Challenges
# Demographic Trends among Foreign-born US Residents
The number of new immigrants, defined in this discussion as those obtaining permanent United States residency (green card holders), increased from 3.6 million during the decade of the 1970s, to 6.2 million in the 1980s, and to 9.8 million in the 1990s, with 9.2 million arriving during the nine-year period 2000 through 2008.
Immigrants from countries in Africa, Asia, and Latin America (Mexico, the Caribbean, Central America, and South America), where rates of tuberculosis range from moderately elevated to extremely high, accounted for 95% of all immigrants from 1980 through 2008. 40 The total foreign-born population residing in the United States in 2007 was estimated to be 37.9 million, one third of whom were undocumented. Foreign-born persons account for one in eight US residents now, up from one in 13 in 1990. 41
# Tuberculosis Screening Requirements for Foreign-born Persons Coming to the United States
The current overseas tuberculosis screening of foreign-born persons entering the United States is focused on those likely to be long-term residents, primarily refugees and immigrants. The main purpose of the screening is to detect infectious tuberculosis cases and ensure that treatment is adequate to eliminate infectiousness before travel to the Unites States. In 2008, the numbers of refugees and permanent residents who arrived in the United States after pre-departure screening were 60,000 and 467,000, respectively, representing just 527,000 of the 39 million persons who entered the United States that year. The vast majority of entrants undergoes no screening for tuberculosis at all, including over 3 million students and workers who are likely to remain in the United States for several years. Table 9 (next page) indicates which US entrants are screened for tuberculosis before arrival and the percentage from countries in regions with increased risk for tuberculosis (Asia, Africa, Mexico, the Caribbean, Central America, and South America).
The tuberculosis screening process from 1991 through 2007 required a chest radiograph for adult overseas applicants (defined as 15 years of age or older). Those with chest radiograph findings of active tuberculosis were required to submit three sputum specimens for microscopic examination for acid-fast bacilli (AFB). Applicants with AFB present in one or more sputum specimens were considered to have infectious tuberculosis and could not travel until treated. 42 The 2007 Technical Instructions for tuberculosis screening and treatment for panel physicians added sputum culture and drug susceptibility testing for Mycobacterium tuberculosis isolates, increasing threefold the number of applicants with the diagnosis and treatment of tuberculosis 43 and ensuring that cases due to drug-resistant strains were appropriately treated. The 2007 Technical Instructions also require tuberculin skin testing for diagnosis of latent tuberculosis infection in children 2 through 14 years of age. Treatment of latent tuberculosis infection is not required before departure, but a referral is made to the state health department in the state of intended residence in the United States. The 2007 Technical Instructions were implemented for refugees and/or other immigrants from four counties in 2007 and will be implemented in other countries as laboratory and other capabilities are approved.
The 2007 revised tuberculosis screening methods are predicted to reduce the number of immigrants and refugees who arrive with AFB smear-negative tuberculosis (positive sputum cultures but negative microscopic examination), but this will probably reduce the number of tuberculosis cases among foreign-born persons by only 250 cases per year. 44 In 2008 an additional 641,000 persons residing in the United States on shortterm visas (such as students and workers), were approved for permanent residency by change-of-status after screening for tuberculosis (Table 9, next page). Tuberculosis screening for change-of-status applicants, done by designated civil surgeons, involves a two-step process of tuberculin skin testing of all adults and children 2 to 14 years of age. Applicants with a tuberculin skin test reading of 5 mm or more are required to have a chest radiograph, and those with abnormal chest radiographs are referred to the local or state health department to be evaluated for tuberculosis and treated if diagnosed. For those diagnosed with latent tuberculosis infection, there are no requirements for treatment to prevent future tuberculosis.
# Diagnosis and Treatment of Latent Tuberculosis Infection
Although arriving with tuberculosis disease is not common due to the overseas screening process, the prevalence rates of latent tuberculosis infection are quite high for the 1,267,000 persons from Asia, Africa, or Latin America in 2008 who arrived as refugees or achieved permanent residency status (Table 9, page 53). This is reflected in the much higher prevalence of latent tuberculosis infection documented among foreign-born persons and their rates of tuberculosis compared to US-born persons (Figure 4, page 27).
The authors of the Institutes of Medicine (IOM) report Ending Neglect recommend requiring testing and treatment for latent tuberculosis infection among all immigrants from countries with elevated risk for tuberculosis, 12 but this has remained a voluntary process. The national guidelines were revised in 2000 to recommend targeting the testing and treatment of latent tuberculosis infection among recently arrived foreignborn persons due to the higher rates of tuberculosis within the first five years of arrival compared to later years. 17 More recent research shows that persons born outside the United States have tuberculosis case rates 4.7 times higher during their first two years after entry in the United States than in the years that follow, 44 but this does not mean that the risk of tuberculosis decreases in all persons after arrival. Compared to US-born persons, refugees and immigrants from high-burden countries have tuberculosis case rates up to ten times higher for two, five, or more than 20 years after arrival in the United States. 45 The number of tuberculosis cases in refugees who have been in the United States for more than 20 years will continue to increase because 1980 to 2000 was a period of unprecedented refugee resettlement in the United States, with a very significant spike in numbers from 1989 through 1991. 46 In addition, the absolute number of refugees accepted by the United States has been increasing again since 2002, and several new large groups of refugees have been approved for resettlement over the ten years from 2006 from countries that show the highest tuberculosis rates among refugees in the United States. 44,47 Despite the documented higher prevalence of latent tuberculosis infection among foreign-born persons and the increased lifetime risk for life-threatening and disabling tuberculosis conferred by this infection, there are unique challenges for many foreignborn persons that predispose them to disparities of care. These challenges must be recognized and addressed to avoid delays in diagnosis and curative treatment of tuberculosis, in identifying and protecting the health of persons exposed to infectious tuberculosis, and in preventing tuberculosis through targeted testing and treatment for latent tuberculosis.
# Cultural/Linguistic and Socioeconomic Challenges to Care
Most foreign-born tuberculosis patients in the United States face cultural, linguistic, and socioeconomic challenges to care, which may exacerbate the shortcomings of the current strategy to control tuberculosis among the foreign born. Delays in diagnosis are in part the result of patient delays in seeking care, different perceptions of disease, definitions of disease, attribution of symptoms to different illnesses, unfamiliarity with or distrust of biomedical care, fear of stigmatization, fear of government and possible deportation, and lack of a means to pay for care (such as medical insurance). Provider factors contributing to delays in diagnosis include delays in recognizing the possibility of tuberculosis and/or in initiating diagnostic evaluation, delays or failures to report suspected cases of tuberculosis to health departments to ensure complete evaluations, and failure to initiate timely treatment.
Data supporting the scientific basis for cultural challenges to care have focused mostly on linguistic access and socioeconomic factors that have been shown to create health disparities, but other cultural challenges may also limit access to care and reduce cooperation with contact investigations and adherence to therapeutic and programmatic interventions for people with active tuberculosis and their contacts. 48 To some extent, the challenges outlined below may apply to any foreign-born person with tuberculosis or latent tuberculosis infection, but the following sections highlight specific challenges that are especially acute in particular sub-groups of foreign-born tuberculosis patients.
# Additional Challenges Faced by Migrant Workers
Poverty, limited transportation, mobility or unstable residency, low literacy, limited English proficiency, and cultural differences create significant challenges to care for migrant workers. Most low wage jobs are hourly and do not provide sick leave or other benefits such as health insurance, which makes migrants reluctant to miss work, fearing the inability to pay as well as loss of their jobs if they take time off to get medical care. 49 If migrants fear that seeking health care might lead to trouble with immigration authorities, then they are even more likely to delay seeking care, resulting in disease progression and an increased risk of transmission of tuberculosis to others. 50 A further challenge is that migrant workers can face psychological stresses from uncertain employment, housing, and immigration status. What part stress may play in the development of tuberculosis disease is unknown, though rates of tuberculosis have been seen to increase in stressed populations. 51 In addition to these social, economic, and cultural challenges, many healthcare providers assume that migrants will be unable to complete their treatment. This assumption is often offered as a reason for not conducting screening for active tuberculosis or latent tuberculosis infection and for not initiating treatment of latent tuberculosis infection.
# Additional Challenges Faced by Refugees
Refugees are usually from countries with a high burden of tuberculosis, so they arrive with high rates of latent tuberculosis infection acquired in their countries of origin or in refugee camps, and case rates of tuberculosis are much higher within the first two years after entry into the United States. Timely diagnosis and treatment for a variety of medical conditions including tuberculosis and latent tuberculosis infection is challenging even with the resources provided by the Office of Refugee Resettlement and eight months of Medicaid insurance. Refugees struggle to adjust to the US medical culture and healthcare system and often have not found employment that provides medical insurance before their Medicaid coverage lapses.
During and beyond this first two years, refugees face other challenges that complicate medical care. Refugees also often have disrupted families and may have limited community support systems. Other issues that complicate timely diagnosis and refugees' ability to complete treatment can include linguistic barriers to accessing care, different understandings of illness, unfamiliarity with laboratory tests and medication schedules, inexperience with treating latent tuberculosis infection, and having other priorities in adapting to life in a new society that take precedence over health concerns.
In addition, trauma or torture in their home countries can make it difficult to trust government officials or to form a trusting relationship with a case manager. All of these issues are exacerbated in many communities by the lack of trained medical interpreters and identified cultural brokers who can facilitate work with healthcare providers, especially for new refugee groups.
# Additional Challenges Faced by Undocumented Persons
As of March of 2006, the Pew Hispanic Center estimated that between 11.5 and 12 million of the foreign-born persons in the United States were undocumented. 52 Among the foreign-born in the United States, undocumented persons are largely from countries with a moderate or high prevalence of tuberculosis and have not undergone screening.
In addition to the fear of apprehension and deportation, which makes them reluctant to seek medical care, undocumented persons face other obstacles to accessing health care common to foreign-born persons, such as culture and language differences, poverty, housing instability, and limited employment options affecting economic survival.
# B. Action Plans for Tuberculosis Elimination among Foreignborn Populations
For a summary of the action plans for eliminating tuberculosis among foreign-born populations, refer to Table 6: Action Plans for Tuberculosis Elimination among the Foreign-born, pages 13-14.
# Interconnected Health Problems and Social Conditions
To understand the factors contributing to the disparity in tuberculosis rates between foreign-born and most US-born populations, it helps to view tuberculosis as one aspect of the "coinfection and synergistic interaction of diseases and social conditions at the biological and population levels." 53 For example, the high rates of diabetes in Asian and Hispanic populations and high rates of human immunodeficiency virus (HIV) infection among sub-Saharan African immigrants contribute to the progression from latent tuberculosis infection to tuberculosis disease. These are not just co-occurring epidemics in these populations, but are a set of "mutually enhancing epidemics involving disease interactions at the biological level that develop and are sustained in a community/population because of harmful social conditions and injurious social connections." 53 The social conditions of many immigrants and refugees in their home countries and in the United States provide a greater risk of exposure to tuberculosis and HIV and also contribute to lifestyle patterns that increase malnutrition (another biological condition synergistic with tuberculosis) and hinder access to medical care, as described above.
This perspective is a syndemic orientation, which is defined as "a way of thinking about public health work that focuses on connections among health-related problems, considers those connections when developing health policies, and aligns with other avenues of social change to assure the conditions in which all people can be healthy." 54 To address the ongoing disparities in case rates among foreign-born groups, disparities reduction requires an approach that takes into account the biological and social contexts in which tuberculosis occurs and addresses factors related to the health system, care process, and the patient. The Centers for Disease Control and Prevention's Syndemic Prevention Network website at http://www.cdc.gov/syndemics/overview.htm offers information and resources for further exploring a syndemic orientation for public health.
There is a need to do more contemporary research from a syndemic orientation to document the specific contexts and causes of new cases of active tuberculosis among foreign-born persons in the United States. This research needs to be stratified by comorbidities, ethnicity, and time in the United States; family structure and living patterns; social location; and age at which disease is identified. In addition, targeted genotyping by mycobacterial interspersed repetitive unit analysis (MIRU) may be necessary to document recent transmission in non-pediatric cases. Specific epidemiologic/risk factor studies are needed in long-settled immigrant communities to assess the risk of tuberculosis among immigrant and refugee children and children of foreign-born parents, especially where aging immigrants have high rates of comorbidities, such as diabetes, that affect progression from latent tuberculosis infection to active tuberculosis.
Finally, while continuing to use federal racial/ethnic surveillance categories for reporting, there is an urgent need to develop and define more specific operational and research categories for immigrant and refugee groups which will be meaningful for local tuberculosis control activities. More specific and detailed demographic information, available from research and advocacy groups such as the Migration Policy Institute or Hmong National Development, for example, will enable local public health programs to identify needs and plan for targeted community outreach, cultural competence training, interpretation, and partnership building among the groups they serve. 55
# Strategies for Identifying and Treating Latent Tuberculosis Infection among Foreign-born Residents Notification of Inactive Tuberculosis among Refugees and Immigrants
One strategy to identify foreign-born persons with latent tuberculosis infection is to enhance screening and follow-up by health departments in the United States of persons diagnosed with inactive pulmonary tuberculosis and latent tuberculosis infection both pre-departure and at change-of-status visa adjustments. Under the technical instructions for tuberculosis screening of refugees and applicants for permanent residency, those persons whose chest radiographs are consistent with tuberculosis but who have negative sputum cultures for M. tuberculosis are often diagnosed with inactive tuberculosis. (Overseas panel physicians and health departments also use the term Class B1 pulmonary tuberculosis.)
These persons are recommended for follow-up in US health departments due to increased risk for future tuberculosis. Children diagnosed with latent tuberculosis infection during overseas screening and both adults and children with this diagnosis during change-of-status evaluation are at increased risk for developing tuberculosis that can be prevented by treatment with isoniazid. This health department follow-up and treatment can be enhanced by continued improvement both in the electronic notification of local jurisdictions receiving immigrants and refugees and in the interjurisdictional notifications for patients who move (federal government items 1 and 2; local and state government item 4, bullets 1 and 2; and community partners item 6).
# Targeted Testing and Treatment for Latent Tuberculosis Infection
Another strategy to identify foreign-born persons with latent tuberculosis infection is to enhance targeted testing and treatment for latent tuberculosis infection among foreign-born US residents. Local capacity should be built to develop epidemiologic profiles of local foreign-born groups and to better understand which groups to focus on for targeted testing. 56 Tuberculosis elimination among foreign-born residents will require greatly expanded diagnosis and treatment of latent tuberculosis infection with isoniazid (federal government items 1 and 2; local and state government item 4, bullets 1 and 4; and community partners items 5, 6, 7, and 8).
In addition, the promising new tools for detecting and treating latent tuberculosis infection need to be evaluated and implemented. The Division of Tuberculosis Elimination must continue to pursue development of better diagnostic tests for latent tuberculosis infection. The bacilli Calmette-Guérin (BCG) vaccination is common in most high-burden countries, and positive tuberculin skin test results are often dismissed by immigrants as only reflecting BCG. The tuberculin skin test is less specific for M. tuberculosis than the two interferon gamma release assays (blood tests) that have been approved to diagnose latent tuberculosis infection. The use of the blood tests could provide a more specific test for latent tuberculosis infection and could be a more useful tool for persuading persons with latent tuberculosis infection or newly infected contacts to complete medical evaluation for tuberculosis disease and, if needed, to complete treatment for latent tuberculosis infection.
The Division of Tuberculosis Elimination must also continue to evaluate shorter treatment regimens for latent tuberculosis infection. Latent tuberculosis infection treatment regimens of nine months of isoniazid and four months of rifampin present formidable barriers for many immigrants and other travelers to the United States. The increased adherence to treatment that is likely with a shorter regimen is particularly important for the foreign-born who may face many economic, cultural, and linguistic barriers. The journal article "New Approaches to the Treatment of Latent Tuberculosis" reviewed current regimens for treatment of latent tuberculosis infection, both standard and alternative, as well as regimens under investigation and those with potential for future development. 57 For example, development of regimens using longer-acting rifamycins and fluoroquinolones may permit taking medicine only once or twice weekly. Because of the potential difficulty in enrolling sufficient numbers of patients in the United States into clinical studies of such proposed regimens, consideration should be given to multinational clinical trials for new shorter latent tuberculosis infection regimens.
# College Students and Workers from Moderate-and High-burden Countries
A third strategy to identify foreign-born persons with latent tuberculosis infection is to require that students and workers from moderate-and high-burden tuberculosis countries, who are not screened prior to arrival in the United States, undergo tuberculosis screening after arrival (local and state government item 4, bullet 4).
Targeted screening of college students and workers from high-tuberculosis-burden countries can identify immigrant students eligible for latent tuberculosis infection treatment and diagnose active tuberculosis earlier, reducing the risk of transmission. If diagnosed with latent tuberculosis infection, these persons should complete treatment for latent tuberculosis infection. Health departments should begin by engaging with college campuses in developing evidence-based practices in diagnosing and treating latent tuberculosis infection.
# Enhanced Tuberculosis Control Tools for Working with Foreign-born Populations Cultural Competency
Specific local information on foreign-born demographics, community organizations, cultural background information, and challenges to healthcare access is needed. This information would identify ways to bridge language and cultural challenges, to improve case management and contact investigation outcomes, and to identify and develop resources, such as interpreters and cultural brokers, who can be partners in providing culturally and linguistically appropriate care. In addition, information about local access barriers would inform both national and local tuberculosis control strategies. 53 Local capacity to quickly initiate treatment and ensure completion of treatment should be enhanced by implementing patient-centered care practices, including eliciting patient illness models, working with traditional healers, accommodating family decision-making processes, and understanding how different cultural child-rearing practices affect the process of treating children with active tuberculosis and tuberculosis infection. 58 Further, tuberculosis control at all levels needs to coordinate efforts to address disparities in tuberculosis case and latent tuberculosis infection rates in all populations, by adopting a skills-based approach to developing cultural competence. Other groups at high risk of tuberculosis, such as homeless or incarcerated persons-whose members also often include foreign-born persons-have additional specific cultural factors that shape health practices and internal group social organization that affect tuberculosis transmission. Foreign-born groups are also situated within a larger society whose structural influences contribute to the syndemic effects of poverty and exposure to active tuberculosis.
Cultural competency skills and disparities analysis are the tools that tuberculosis control staff need in order to learn about the cultures and structural contexts of each foreign-born group they work with, so that tuberculosis control practices and strategies can be tailored effectively to these groups' specific circumstances. Since no organization can hire staff from all local groups, most tuberculosis control staff will work with people from a variety of backgrounds and cannot be culturally proficient in every group's culture. So, cultural competence needs to be based on developing skills to work effectively with any group, skills that are patient-centered and include knowing how to find specific information about communities and build relationships with community leaders. 59 It is important to recognize that the challenges in access to care and in treatment completion are not located primarily within the immigrant or refugee patient. A synergy of structural, cultural, and biological contexts leads to high rates of latent tuberculosis infection and tuberculosis disease in foreign-born populations. 60 Some case management challenges arise from poverty, lack of insurance, or other structural conditions of immigrant communities, not from cultural differences. Local programs should institute and expand the use of culturally-relevant incentives and enhance local programs' knowledge of economic and social challenges and the corresponding effective enablers for specific populations and communities. Using incentives and enablers helps to increase completion of treatment rates and to continually build cooperative relationships with local immigrant communities that can enhance acceptance of treatment of latent tuberculosis infection.
These cultural competency strategies can be implemented by both hiring staff from local foreign-born communities, working with community organizations to encourage and facilitate training in healthcare interpreting or medical fields, and providing skillsbased cultural competence training to health department staff at all levels, to ensure that all staff have the skills to work with all foreign-born patients.
# : FOREIGN-BORN POPULATIONS : PAGE 61
Version 03/22/2010
# Case Detection and Treatment
As noted earlier, only a very small percentage of the foreign-born population is screened before US entry. Other strategies must also be used to address case detection in the majority of foreign-born persons who are not screened (federal government items 1 and 3; local and state government item 4, all bullets; and community partners item 5).
To eliminate transmission of tuberculosis from foreign-born persons with tuberculosis in the United States, it is necessary to understand that the risk of tuberculosis transmission to others increases when there are delays in diagnosis and curative treatment of infectious tuberculosis. Persons with delayed diagnosis or treatment may transmit tuberculosis, often to family members. For example, there is a marked racial and ethnic disparity for tuberculosis among US-born children less than five years of age with at least one foreign-born parent. Delays in diagnosis and treatment also increase the risk of disability and death, even in persons who are not infectious.
Community outreach and collaboration with other public health programs, community service organizations, and ethnically-based mutual assistance associations can improve familiarity with and trust of healthcare systems. This can be enhanced further by collaboration with traditional healers to demonstrate respect for culturally-based health practices and to encourage referrals. In addition, addressing systemic factors
# SUCCESSFUL PARTNERSHIPS:
# Partnering with Traditional Healers at Healthy House
There is usually a range of healing practices in immigrant and refugee communities-from people who provide information and materials for self-treatment, such as herbalists, to therapeutic massage practitioners, spiritual healers or diviners, and practitioners of complementary systems of medicine, such as Ayurvedic, Tibetan, or Chinese medicine.
Partnership with healing practitioners from these diverse communities, as cultural brokers, can include efforts to learn their practices in specific communities while providing opportunities for them to learn about biomedical practices, engaging patients and family members in discussions about treatments for specific illnesses, such as tuberculosis and comorbid conditions, building alliances to encourage referrals to medical care facilities for specific symptoms, and receiving assistance from traditional healers in identifying contacts to persons with tuberculosis disease.
One model of such a partnership is the Healthy House in Merced, California, which has established a program to orient medical providers to Hmong shamans' practices and to introduce shamans to biomedical practices and facilities. 61 For more information, refer to this National Center for Cultural Competence publication: Bridging the Cultural Divide in Health Care Settings:
The Essential Role of Cultural Broker Programs online at http://www11.georgetown.edu/research/gucchd/nccc/documents/Cultural_Broker_Guide_English.p df .
which limit access, including lack of insurance and insufficient access to interpreters, can help to eliminate delays in receiving an appropriate diagnosis. Finally, providing targeted education and medical consultation from health department experts and from the Regional Training and Medical Consultation Centers, with a focus on physicians who treat foreign-born populations at high risk of tuberculosis, would help to address physician-provider unfamiliarity with tuberculosis.
For new refugee groups without pre-existing community organizations, such as the Burmese and Bhutanese, more avenues and funding must be found to quickly train medical interpreters and develop their English language skills as a first step in developing the cross-cultural resources that bridge cultural, linguistic, and access challenges.
# SUCCESSFUL PARTNERSHIPS:
# TBNet: Multinational Patient Tracking and Referral
In 1996, the Migrant Clinicians Network, working with a consortium of public health organizations and funded by a grant from the Texas Department of Health, founded TBNet, a multinational tuberculosis patient tracking and referral project designed to work with mobile, underserved populations. Originally created with migrant farm workers in mind, TBNet has expanded its patient base to include the homeless, immigration detainees, prison parolees, and anyone who might be mobile during treatment.
Each enrollee is given a wallet-sized Health Network card with information about how to obtain the patient's medical records. TBNet maintains a central storehouse of enrollee medical records, which can be accessed by the patient's healthcare providers in the United States, Mexico, or Central America. Mobile patients can also call TBNet's toll-free helpline to locate treatment facilities at their next destination. The wallet card, central medical record warehouse, and toll-free telephone number help to coordinate the continuous treatment of mobile tuberculosis patients. At the conclusion of treatment, TBNet notifies the enrolling clinic as well as the state or regional tuberculosis control contact person that the patient has completed treatment.
TBNet has experienced consistently high treatment completion rates for patients with tuberculosis disease. For more information, see http://www.migrantclinician.org/network/tbnet.
# New Outreach and Service Provision Practices
Immigrant, international visitor, refugee, and migrant worker communities are unfamiliar with US public health and often do not understand or lack access to most medical care providers in the public or private sectors. Thus, reaching a larger proportion of these populations for tuberculosis control, especially through the new initiatives proposed for identifying and treating latent tuberculosis infection, requires a significant shift in outreach and service provision practices.
As the 2005 tuberculosis control guidelines outline, the public health sector must remain the lead in planning, coordinating, and evaluating tuberculosis control efforts in order to maintain the necessary specialized knowledge required for effective tuberculosis surveillance, case management, and contact investigation. 13 Partnering with other public health programs, social service organizations, immigrant community organizations, and federally qualified community health centers at local levels would make the most effective use of culture-and population-specific expertise, relationships, outreach, and access for foreign-born groups.
# Contact Investigation
To enhance the yield of contact investigations of foreign-born cases of tuberculosis, tuberculosis control staff need to be familiar with family structure, residence patterns, social organization, and culturally-specific life cycle observances, religious practices, and socializing patterns of the immigrant populations they serve and to have their trust. Relationships with organizations that provide services to immigrants, such as English language classes or religious schools, would enhance the effectiveness of contact investigations in congregate settings.
# Programmatic Strategies for Ensuring Continuity of Care Transnational Continuity of Care
In most states that share borders with Mexico, binational projects have been developed within Mexican states that support the treatment of complicated tuberculosis cases. These services involve medical consultation from tuberculosis experts, laboratory support, and second-line tuberculosis medication support. These binational projects are managed by the Mexican public health physicians and staff. Cross-jurisdictional continuity of care should be improved by this collaboration and legal issues resolved, especially between the United States and Mexico, including improving tuberculosis information sharing and tracking of patients who move. 56
# SUCCESSFUL PARTNERSHIPS: CureTB: Bi-National Tuberculosis Referral Program
The CureTB program, a service of the Health and Human Services Agency in San Diego, California, facilitates and supports the continuity of care for patients with active tuberculosis disease and their contacts who travel between the United States and Mexico, facilitates the exchange of information between healthcare providers from both countries, and provides guidance and education to patients and/or their contacts about their tuberculosis risk and need for diagnostic or treatment services. For more information, see http://www.sdcounty.ca.gov/hhsa/programs/phs/cure_tb/.
# US Immigration and Customs Enforcement Detainees
Any undocumented foreign-born person apprehended by the US Immigration and Customs Enforcement (ICE) should be considered at high risk of tuberculosis infection and disease and receive appropriate screening. In federal fiscal year 2006, ICE detained 256,842 foreign nationals. 62 When brought into custody and detained, ICE detainees undergo tuberculosis screening at intake. Tuberculosis rates in the ICE detention system are substantially higher than in the general population, with a rate of 121.5 cases of tuberculosis per 100,000 persons in 2005. Tuberculosis cases with positive cultures were detected at a rate of 55.8 per 100,000 persons in 2005, a prevalence rate that was 2.5 times higher than the annual case rate in the US foreign-born population. 63 Ideally, if a person held in ICE custody is diagnosed with active tuberculosis, every effort should be made for that person to complete a full course of treatment prior to repatriation, within the constraints of US immigration law and in the least restrictive setting. 64 US immigration law authorizes ICE to detain people for administrative reasons incident to their immigration proceedings, not for public health considerations There are statutory limits on the duration of ICE custody, and there are ethical considerations on retaining ICE detainees in custody after their immigration issues have been resolved that need to be considered on a case-by-case basis in the contex of personal and public . ts health issues.
Tuberculosis control is a public health responsibility, and public health authorities are challenged to find a solution to help detained individuals with active tuberculosis complete treatment prior to repatriation. However, sometimes for political, personal, or legal reasons it is necessary to repatriate a person before treatment is completed.
Continuity of care should be ensured for ICE detainees with confirmed or suspected active tuberculosis who may be repatriated before completing treatment. In this situation, a plan for bridge case management and continuity of care must be in place and coordinated by one of the two current transnational bridge case management and patient navigation programs: TBNet (Migrant Clinicians Network, Austin, Texas) or CureTB (San Diego County Tuberculosis Control Program, San Diego, California) (local and state government item 4, bullet 3).
# Investment in Global Tuberculosis Control and Elimination
Despite the fact that the global tuberculosis incidence rate is leveling off, the number of tuberculosis cases continues to increase due to population growth. The estimated number of tuberculosis cases in 2007 was 9.27 million worldwide, 65 and a third of the world's population is believed to have latent of tuberculosis infection. 66 Additional research is needed, such as that conducted by Schwartzman et al., 67 to ensure that investment in global tuberculosis control includes strategies that will affect populations and groups that immigrate to the United States. Schwartzman concluded that US support of expanded availability of directly observed therapy in Mexico would reduce importation of active tuberculosis and reduce by 130 the number of tuberculosis cases reported in the United States each year. 67 Accurate case rate information for foreign-born populations in the United States, stratified by country of origin, would indicate in which countries similar targeted strategies could have an effect on tuberculosis incidence in the United States If a short-course latent tuberculosis infection treatment were developed, research might indicate where targeted support for the adoption of latent tuberculosis infection treatment by national tuberculosis programs in high-burden countries with high immigration to the United States could also help to reduce the importation of latent tuberculosis infection.
# TO CONCLUDE AND MOVE FORWARD:
The persistence of over 7,500 tuberculosis cases per year among foreign-born residents of the United poses the greatest single barrier to tuberculosis elimination in the United States. Over 90% of the foreign-born residents arriving over the past 30 years arrived from countries in Asia, Africa, and Latin America where rates of tuberculosis remain high and the disease is endemic. These demographic realities among US arrivals result in an increasing proportion of the United States population with latent tuberculosis infection that remains largely untreated.
Effective diagnosis and treatment of latent tuberculosis infection require improved diagnostic tests and treatments, skills to overcome linguistic and cultural barriers, access to health care, and sufficient public health funding. In addition, issues of global tuberculosis, including drug resistance, require continued international efforts.
While investing in global tuberculosis activities is an important strategy for tuberculosis elimination in the United States, efforts to control global tuberculosis are not a substitute for tuberculosis control in the United States because of prior and ongoing immigration. Both domestic and international efforts need to be undertaken to address tuberculosis in the foreign-born population in the United States.
# VI. Tuberculosis in Low-incidence Areas
The 2002 report of the Advisory Council for the Elimination of Tuberculosis (ACET) described the challenges to eliminating tuberculosis in areas with low-incidence rates of tuberculosis and noted that national progress toward tuberculosis elimination will necessarily lead to low tuberculosis incidence in all areas of the United States. 23 This call for action presents an updated analysis of the progress toward tuberculosis elimination in low-incidence areas with data provided by the Centers for Disease Control and Prevention (CDC). By the year 2006, 26 of the 50 states in the United States reached the status of low incidence, defined as having 3.5 or fewer cases of tuberculosis per 100,000 persons per year. This represented an increase from the 22 states for the year 2000 as described in the ACET report on progress toward tuberculosis elimination in low-incidence areas. 23 The changing epidemiology of tuberculosis in low-incidence areas reveals unique and persistent challenges for tuberculosis elimination. Many of the strategies recommended in this chapter address challenges that are particularly acute in low-incidence areas but that also occur in medium-and high-incidence areas. These strategies are included here to comprehensively address low-incidence areas because, as tuberculosis elimination progresses, more areas will become low incidence and face the challenges that these strategies address. A recent example in Montana highlights the fact that low-incidence areas are not isolated from the global burden of tuberculosis. 68 Public health departments in these areas must maintain the capability to respond to multidrug-resistant cases of tuberculosis among visitors, new immigrants, and residents who travel abroad.
# A. Trends and Challenges
# Changing Epidemiology
The data in Tables 10 and 11 illustrate that, to meet the goals of the national tuberculosis elimination campaign, we need to reinforce tuberculosis prevention and control efforts even in areas with few cases of active tuberculosis. Continuing to provide high-quality and timely services will require bolstering the tuberculosis control infrastructure through novel approaches such as the successful regionalization efforts discussed below and increasing public-private partnerships. AI/AN = American Indian / Alaska Native; HIV = human immunodeficiency virus. Source: R. Pratt, T. Navin, M. Chen, J. Becerra, CDC.
# Challenges
The most threatening challenge to tuberculosis control is the loss of infrastructure and funding similar to the environment that preceded the 1985-1992 tuberculosis resurgence. Other important challenges specific to low-incidence areas include diminishing clinical and laboratory expertise, scarcity of special facilities for prolonged health care and/or respiratory isolation, and providing tuberculosis care in settings where large geographic distances separate patients from providers. 23 Tuberculosis control programs today are losing the capacity for maintaining functions essential for tuberculosis control and are reaching conditions that set the stage for a resurgence in tuberculosis.
# Diminished Infrastructure and Funds
Findings from the recent surveys by the National Tuberculosis Controllers Association on resources for tuberculosis control activities and by the National Tuberculosis Nurse Coalition and the National Society of Tuberculosis Clinicians on tuberculosis public health infrastructure have important implications for tuberculosis programs in lowincidence areas. 69 Survey results suggest that the most commonly reported barriers to reaching the national objectives for tuberculosis control were funding issues (81%), restrictions upon out-of-state travel (including for training/educational purposes) (78%), restrictions upon in-state travel (44%), hiring freezes (41%), and a loss of tuberculosis nursing case management capacity. This loss of key infrastructure comes at a time when tuberculosis nursing case managers report increasing case management difficulties due to greater linguistic and cultural diversity of patients.
The end result for low-incidence states is that in many areas tuberculosis control efforts have been forgone for lack of resources, even within core tuberculosis program functions. For example, contact investigations may be restricted in scope with little effort made to identify contacts outside of the household setting. The result of this type of belt-tightening is a missed opportunity for early identification of persons with infectious tuberculosis and high-risk persons with latent tuberculosis infection who would benefit from treatment-and hence, and the opportunity to prevent ongoing transmission. For other high-risk persons, very few low-incidence states have the capacity to expand and/or collaborate with other medical care providers in expanding targeted testing and treatment of latent tuberculosis infection to prevent future tuberculosis cases among persons with latent tuberculosis infection.
Other factors are affecting resource allocations. Many low-incidence areas are experiencing demographic shifts and are treating increasingly complex tuberculosis cases at the same time that funding needed to maintain tuberculosis expertise and capacity is declining. Greater numbers of persons from areas of the world with a high incidence of tuberculosis are settling in regions that are unprepared to provide culturally competent care for recently arrived immigrants. 23 Public health staff face the challenges of treating and managing patients with multidrug-resistant tuberculosis, other medical conditions, and/or substance abuse and the challenges of identifying and quickly responding to tuberculosis outbreaks. One outbreak or one multidrug-resistant tuberculosis patient can absorb the entire annual budget of the tuberculosis program. 68 Public health tuberculosis control programs often have fewer resources and less knowledge and/or experience with the use of newer tools that would provide epidemiologic assistance to programs, such as using genotyping results of strains of Mycobacterium tuberculosis for tracking chains of tuberculosis transmission and implementing electronic information systems.
Further, having one or fewer full-time employees to perform statewide tuberculosis control functions threatens the continuity of programmatic core activities when staff are diverted to other public health activities. Tuberculosis programs in low-incidence areas are vulnerable to diminishing and co-mingled funding with other programs, which can lead to de-emphasis of tuberculosis in favor of equally important, but more visible, infectious disease threats.
# Loss of Tuberculosis Control Expertise
When the incidence, prevalence, and case rate of active tuberculosis declines to a low enough level, providers (both in the private and public sectors) have less opportunity to see patients with tuberculosis, resulting in limited knowledge of the diagnosis and treatment of tuberculosis. This loss of knowledge in the basic clinical aspects of tuberculosis, the lack of familiarity with newer tests and tools (for example, the new interferon gamma release assays and molecular genotyping), and lack of awareness of Each state has access to a public health laboratory that performs tuberculosis testing, including acid-fast smear microscopy, culture, and drug susceptibility testing. However, some providers use private tuberculosis testing laboratories which may cause delays in obtaining the test results needed for effective management of the tuberculosis patient or contact investigation. Other testing delays are due to the large geographical areas in some low-incidence states, requiring long transport times for specimens to reach the state public health laboratory.
# Scarcity of Special Facilities
The historical shift of tuberculosis treatment to the outpatient setting left many lowincidence states with an unfilled void for long-term specialized centers to manage difficult tuberculosis cases that require isolation or management of nonadherence issues. Effectively managing these patients in the absence of isolation facilities presents challenges to tuberculosis control programs and increases the risk of tuberculosis transmission within communities.
# Geographical Distances
In rural low-incidence states, long distances can separate patients from their healthcare providers and case managers. These distances may translate into delays in tuberculosis diagnosis and treatment as well as delays in evaluation and treatment of contacts of tuberculosis cases. These delays may limit the tuberculosis control program's ability to prevent tuberculosis transmission. Challenges in providing timely and effective case management in remote areas for patients with tuberculosis may lead to treatment failures that, in turn, may lead to acquired drug resistance.
# B. Action Plans to Accelerate Tuberculosis Elimination in Lowincidence Areas
To date, there has been a notable implementation gap around ACET's call advocating that the nation "[M]ake progressing toward tuberculosis elimination in low-incidence areas a national priority." 4 That implementation gap must be addressed by action plans that require steps beyond simply controlling tuberculosis. Creative models that expand the capacity of the public health infrastructure to meet the elimination goal must be further evaluated and implemented. Following are examples of approaches to address challenges described above.
For a summary of action plans for eliminating tuberculosis in low-incidence areas, refer to Table 7: Action Plans for Tuberculosis Elimination in Low-incidence Areas, pages 14-17.
# Stopping the Loss of Infrastructure and Capacity
The goal of tuberculosis elimination requires that tuberculosis control programs have sufficient funds and expertise to effectively perform three core functions: tuberculosis case detection and management necessary for curative treatment; identification, evaluation, and treatment of contacts of tuberculosis cases; and targeted testing and treatment of latent tuberculosis infection (local, state, and federal government item 1, bullet 1). The CDC plays an essential role in maintaining tuberculosis control capacity in low-incidence areas. Key CDC responsibilities include assessment, funding, staffing, operational research, technical assistance for surveillance and program evaluation, surge capacity for outbreaks, and support for interstate access to facilities (local, state, and federal government item 2, all bullets). State and local governments are responsible for maintaining high-quality core tuberculosis control functions by providing health infrastructure and staff and the funding to pay for care for the uninsured, regardless of visa status or citizenship (federal government item 2, all bullets; state and local government item 5, bullets 1, 2, and 3).
# Regional Collaboration among State Tuberculosis Control Programs
Two regionalization approaches, developed in response to the Institute of Medicine (IOM) and ACET recommendations, rely on networks of experts and consultants along with regionalization of some programmatic activities. 70 Both of these approaches are meant to enhance and provide added value (not replace) existing state and local tuberculosis control programs.
# SUCCESSFUL PARTNERSHIPS:
Regional
# Collaboration among Disease Programs
In addition to regional collaboration, sharing resources and expertise across disease programs has benefits at the state and local level. Because of challenges posed by different program priorities and variations in the epidemiology and interventions for different diseases, written agreements or procedures may be helpful to assure that tuberculosis control functions are maintained.
# SUCCESSFUL PARTNERSHIPS: Program Collaborations to Share Resources and Expertise
Below are three examples of collaborative activities that support the Centers for Disease Control and Prevention's Program Collaboration and Service Integration efforts.
In the Massachusetts Department of Public Health:
A Bureau of Infectious Disease nursing response team provides cross-bureau surge capacity. For example, nurses responded to a cluster of tuberculosis cases and performed contact investigation and screening in a prison setting and responded to hepatitis vaccination initiative in the county jails.
A simplified electronic case management and communicable disease surveillance system provides outbreak response capacity and immediate electronic transmission of laboratory results and susceptibilities at the state and local level.
In Connecticut:
The tuberculosis control program initiated cross training so that tuberculosis case managers could become certified human immunodeficiency virus (HIV) counselors. This cross training allowed for testing of tuberculosis patients and their contacts in non-medical settings thereby facilitating testing and improving case management of patients coinfected with tuberculosis and HIV.
# Education and Training to Build Public Awareness and Provider Expertise
To address issues of tuberculosis awareness and expertise, tuberculosis control programs in low-incidence areas should have access to the recommended resources to promote general awareness of tuberculosis and maintain private and public sector provider competence (state and local government item 5, bullet 2; community partners item 6, bullets 1 and 2).
# Interstate Collaboration for Access to Special Facilities
To address the need for special facilities for prolonged care for tuberculosis-both for patients who have complicated case management issues including drug resistance, HIV, or other comorbidities and for those who are nonadherent to treatment or necessary testing-small tuberculosis control programs and programs in low-incidence areas should consider regional partnerships through contractual agreements or mutual aid agreements. These agreements can support a regional tuberculosis referral center that allows patients throughout that region to have access to specialized multidisciplinary tuberculosis treatment and management.
Specific activities to implement this general recommendation include the following:
Support current facilities with appropriate expertise (such as existing centers in Massachusetts and Florida) and assess cross-jurisdictional issues related to their capacity to accommodate patients from other jurisdictions and challenges for doing so (legal and non-legal)
Replicate and support successful models so that all low-incidence areas (and other states with no long-term hospitalization resources) have the ability to hospitalize these patients when needed Assess current tuberculosis control laws and regulations and develop model tuberculosis laws which can be adapted as needed
# Enhancing Laboratory Capacity and Access to Services
Timeliness of laboratory information is critical to rapid identification of persons with tuberculosis, appropriate treatment, and case management. Low-incidence areas should assess whether there is adequate need (as defined by the Association of Public Health Laboratories) to maintain their own expertise and/or whether there is an option for use of other public health or private laboratories (state and local government item 5, bullet 3). Specific activities for low-incidence areas include: analyzing public health regulatory options (for example, in Wisconsin a portion of each specimen must be provided to the state tuberculosis laboratory, thereby eliminating the difficulties associated with specimens sent out-of-state to private laboratories); building a consortium model of in-state tuberculosis laboratories organized and facilitated by state public health laboratories; assuring that an electronic information system exists for laboratory reporting to the public health agency; assuring access to external laboratories for specialized services such as second-line and rapid drug susceptibility testing and genotyping; supporting laboratory training in mycobacteriology and incentives to new graduates of microbiology to learn about tuberculosis; and assuring that a courier service provides timely delivery of specimens to the central tuberculosis laboratory.
For states with a low tuberculosis case load resulting in few specimens tested at the state mycobacterial laboratory, it is still necessary to ensure high-quality and timely tuberculosis diagnostic laboratory services in order to avoid missed or delayed diagnosis and to help guide in the treatment of tuberculosis. Maintaining the resources and laboratory expertise needed for the full range of laboratory services in low-burden areas may not be feasible, and certain specialty tests such as molecular drug susceptibility testing should be done at contract laboratories or regional public health laboratories. Careful monitoring of performance of external laboratories that provide these services, with mechanisms to improve unsatisfactory performance, should be a core function of the state public health laboratory.
# Public and Community Health Teams
Geographic isolation presents a host of challenges for tuberculosis control in lowincidence areas with low population density. The CDC and state tuberculosis control programs should collaborate in piloting two potential public health models based on population density: permanent on-site assigned teams and ad hoc community teams.
Where the population density allows, public health teams could be assigned on-site to a defined location. The on-site approach could have teams responsible for all communicable disease follow-up including tuberculosis (and perhaps other chronic health issues as well). These teams should link a public health nurse and a public health advisor with medical, epidemiologic, and programmatic consultants. In this scenario, community members could be recruited and trained to perform the daily activities (such as directly observed therapy). This type of approach would require a cross-disease shift of thinking by policy makers.
Alternatively, in less dense, remote areas, an ad hoc community health team could be identified and mobilized when required, supported by technical assistance and education as needed at the state and federal level.
# TO CONCLUDE AND MOVE FORWARD: Tuberculosis trends from 2000 to
2006 indicate that the declines in tuberculosis rates are lowest in the low-incidence and low-case-load states, suggesting that even greater efforts will be needed to maintain the necessary mobilization to eliminate tuberculosis as rates decline. As the nation progresses toward tuberculosis elimination, more states and local areas will face the challenges of providing their residents with timely and high-quality services for the diagnosis, treatment, and prevention of tuberculosis. The lessons learned in two successful regionalization efforts should be adapted and applied in other regions of the nation.
Addressing the ongoing challenge of tuberculosis in low-incidence areas will require stopping the loss of infrastructure and capacity, education and training to build public awareness and provider expertise, interstate collaboration for access to special facilities, and enhancing laboratory capacity and access to services. As well, there is a need for creative and innovative approaches such as regional collaboration among state tuberculosis control programs, collaboration among disease programs, and public and community health teams.
# VII. Mobilizing Partners in the Fight against Tuberculosis
The well-defined epidemiology of tuberculosis, evident health disparity in those that suffer from tuberculosis, and the curable and preventable nature of the disease make tuberculosis a provocative social issue for change. Eliminating this common preventable and curable contagious disease has huge individual and public health benefits as described in the earlier sections, and we must address these health disparities more effectively if we are to reach the revised 2035 goal for tuberculosis elimination.
The 2000 Institute of Medicine (IOM) report identified the lack of political will as a major barrier to tuberculosis elimination and listed social mobilization to build and sustain the political will in the United States as one of the five specific goals (Table 1, page 6). Since the resources for tuberculosis elimination have actually been decreasing rather than increasing over the last decade as recommended by the IOM (Figure 5, page 31), we must seek more effective approaches to social mobilization. This section will briefly describe the history of social mobilization in the United States and suggest answers to the questions about how to achieve the local, state, and national political will to eliminate the threat of tuberculosis from the United States.
# A. History
In 1798, President John Adams signed into law an act which furnished medical services for merchant seaman called the Marine Hospital Services. This service existed until 1878 when its functions were expanded greatly. The prevalence of major epidemic diseases caused Congress to enact a national law to prevent the introduction of contagious and infectious diseases into the United States, later extending it to preventing the spread of disease among the states. This was the beginning of the US Public Health Service. 71 State and local health departments maintained authority for disease control, including the treatment and control of tuberculosis. The overwhelming number of tuberculosis cases at the turn of the century challenged states' abilities to provide care and treatment for tuberculosis; thus came the emergence of partnerships from many different individuals and organizations.
In 1904, the National Association for the Study and Prevention of Tuberculosis was founded as the first nationwide, voluntary health organization aimed at conquering a specific disease and is known today as the American Lung Association (ALA). The ALA and the American Thoracic Society (ATS) played major roles in the successful social 72 and other small projects directed toward tuberculosis elimination.
While these are examples of previous successful efforts at the national and local levels, we will need to achieve and sustain a far broader level of social mobilization for tuberculosis elimination to be successful in the United States. Cooperation and collaboration will be required by policy makers at federal, state, and local levels, the public health sector, medical practitioners, professional societies, community-based organizations, and voluntary organizations. This chapter describes the various partners that are needed to succeed in this effort.
# B. Advocacy and Mobilization
Advocacy is one of the most important tools available for the prevention and control of tuberculosis. Building a framework for tuberculosis advocacy requires a mobilization of partners and public health organizations to address the need for changing attitudes and conditions that exist concerning the prevention and control of this public health menace.
Advocacy is more than confronting public officials and lobbying in support of certain legislative issues. Advocacy is a process of building awareness of tuberculosis, supporting patient-centered activities, and maximizing resources and services for the care of persons with tuberculosis. Advocacy opens doors and creates opportunities to change minds and end the neglect of tuberculosis as a disease that impacts people and communities across the globe.
# Communication Strategies
A picture is worth a thousand words, and the visual presentation of local surveillance data is a powerful visual education tool that can be used to create partnerships and has been used by programs successfully. Painting a local picture with surveillance data is important for health commissioners, community taskforce groups, and politicians. More use needs to be made of geographical mapping of cases and illustrating chains of transmission through the use of molecular genotyping to identify specific strains of Mycobacterium tuberculosis. In San Francisco, molecular genotyping data has been used to link cases of recent transmission to a community drop-in center and convinced site managers that mandatory screening for tuberculosis was necessary and would greatly benefit their community.
Patients, who are willing to tell their personal stories to community groups, media, and journalists, put a face on tuberculosis and provide the engagement often lacking in programs advocating for support of health departments and tuberculosis elimination efforts. Encouragement of patients and family members to speak out and join tuberculosis advocacy organizations is currently lacking and sorely needed.
Tuberculosis prevention and control activities in communities where foreign-born persons reside are often hampered by challenges associated with a lack of knowledge of tuberculosis transmission patterns, a lack of providers who understand the culture of the populations at risk, and the inability of this population to trust and navigate the healthcare system. There is a tremendous need for community organizations and healthcare providers to advocate for these communities. There is a need for voices to speak out and communicate the need for culturally specific interventions.
Within every US state, there is an urgent need for advocacy and expanded tuberculosisrelated collaboration among state and local lung associations, professional organizations (such as Thoracic Societies, College of Chest Physicians groups, etc.), other key community advocacy groups (such as RESULTS), and other organizations fighting respiratory diseases including the state and/or local health departments and lung association spin-off organizations. These organizations should all become effectively involved in a state (or community) specific Stop TB Coalition to design and support tuberculosis elimination campaigns, related resources, partnerships, and efforts. These collaborations should include development of mutually agreed upon annual state and/or local tuberculosis elimination advocacy strategies that spell out (1) related annual objectives and (2) related roles and responsibilities for involved organizations.
Internationally, there is a need for organizations like the Pan American Health Organization (PAHO) and the International Union Against Tuberculosis and Lung Disease (IUATLD) to create opportunities for advocacy around tuberculosis.
# Partnerships
State or community tuberculosis elimination advocacy campaigns and related partnerships should include participants from at-risk populations and groups. The advocates should fully understand the goals and the mission of the community advocacy campaign, and the campaign also should include community gatekeepers.
Strategies for partnering with correctional facilities, shelters, and providers of substance abuse treatment provide opportunities to increase awareness of tuberculosis in their communities, as well as to ensure better care and focus on eliminating tuberculosis. Legislative actions, requests for additional resources, and funding opportunities carry more weight when partnerships are involved. Partnership can take many forms such as creating local task force groups or designating individual tuberculosis control personnel as liaisons for homeless shelters, correctional facilities, or other facilities. Regional corrections and tuberculosis control councils can bring together correctional health and custody staff with local and state health department officials to identify and solve common problems.
In communities where foreign-born persons reside, the risk of tuberculosis and the opportunities for control and elimination must be considered. Tuberculosis prevention and control programs must be put in place that involve outreach, education, targeted screening, and intensive case management. Case management and other support services must be provided in the patients' native languages and in alignment with their cultural beliefs and personal health priorities. Voices of advocacy must be heard from providers and community leaders stressing the need for community resources to prevent and control tuberculosis.
# C. Diversity of Partners
Eliminating tuberculosis in the United States is not an easy task, given the way tuberculosis is transmitted and the current inadequacies of public health systems to properly address tuberculosis. No one agency, organization, or group holds full responsibility
The President and Congress must make a bold political commitment and investment if we as a nation are to be successful in eliminating tuberculosis. Over the last ten years, federal funding for our domestic tuberculosis program has been near stagnant despite widely publicized examples of the domestic threat posed by the global spread of multidrug-resistant tuberculosis, which is harder and more expensive to diagnose and treat. We cannot expect to eliminate tuberculosis without additional resources to boost efforts in states and local cities. responsible for conducting critical basic science and clinical research to find new tools to fight tuberculosis. Homeland Security focuses on immigration issues and ensures that immigrants to the United States are properly screened and treated for tuberculosis before entering. HHS also houses the Indian Health Service, which addresses tuberculosis within native Indian populations, and houses the HHS-supported Community Health Centers that serve populations at increased risk of tuberculosis, including migrant workers, persons with human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS), and racial and ethnic minorities. The Federal Tuberculosis Task Force coordinates the activities of these federal agencies in their respective roles in the national tuberculosis elimination effort.
State, territorial, and local health departments drive the work to eliminate tuberculosis as they face the realities and challenges of tuberculosis on the ground.
Health departments, at all levels, are charged by law with control of all communicable diseases, including tuberculosis. They are responsible for establishing the rules and regulations which govern reporting, investigation, diagnosis, treatment, and other public and personal health control measures. These laws, rules, and regulations define the screening of high-risk groups and the evaluation, treatment, and isolation of persons suspected of having contagious tuberculosis. Some local health departments provide public health clinics where all patients can receive treatment at no cost. If public health clinics do not exist, local departments partner with community healthcare providers to provide patients adequate and recommended treatment until cure. Coordination of state and local tuberculosis programs with HIV/AIDS programs is also essential in addressing tuberculosis/HIV co-infection. Health departments have a crucial and unwaiverable public responsibility to provide the citizenry and tuberculosis advocacy groups with timely and complete tuberculosis-related surveillance and evaluation data. These data should include information about the occurrence of community and institutional outbreaks of tuberculosis and related control efforts in their jurisdictions. Tuberculosis outbreaks need to be acknowledged and reported upon until ended. Tuberculosis elimination advocacy campaigns should use health department surveillance and evaluation data. These campaigns should widely publicize successes in meeting state and community tuberculosis control program goals such as completion of tuberculosis treatment and evaluation and treatment of contacts with latent tuberculosis infection. In addition, the success in meeting local and state goals in tuberculosis elimination should be publicized. The NTCA and its associate sections, the National Tuberculosis Nurse Coalition and the National Society of Tuberculosis Clinicians, bring together leaders in tuberculosis control programs across all states and territories as well as in many county and city health departments. Another public health partner is the Association of Public Health Laboratories (APHL), representing state and local public health laboratories, which serve as laboratory first responders protecting the public from disease and environmental health hazards. State and local public health laboratories provide tuberculosis services that are critical to the diagnosis, treatment, and control of tuberculosis. APHL also serves as an advocate to support tuberculosis control programs. The membership of these organizations need to be trained on how to communicate with the media to report on tuberculosis exposures and/or outbreaks. The goal of this interaction is to garner continued public support for tuberculosis elimination while facilitating public responses that are appropriate from public health and humanitarian perspectives.
Medical associations are essential partners providing a variety of services to eliminate tuberculosis. For example, the ATS, once the medical arm of the ALA, is a leading medical association that focuses on medical aspects of tuberculosis and on advocacy for greater federal tuberculosis funding for states. The Infectious Diseases Society of America (IDSA), along with the CDC and the ATS, has participated in the writing and publication of documents critical to the treatment and control of tuberculosis. The American Academy of Pediatrics (AAP) also participates in the writing and publishing of recommendations for tuberculosis treatment and control in children in the Red Book:
2009 Report of the Committee on Infectious Diseases. These organizations should all be involved in the tuberculosis advocacy campaigns and related planning.
Academic institutions are expected to provide the training and education to a new generation of healthcare workers and conduct valuable research on basic science, clinical, social, and public health issues pertinent to the treatment and control of tuberculosis and other infectious diseases. Schools of public health, particularly, are training grounds for public health department workers in the areas of management, epidemiology and biostatistics, health education and environmental issues, and advocacy. Students participate in hands-on experiences with public health professionals, and many are recruited to fill key positions in public health departments and partner organizations. However, many medical and nursing schools do not focus on tuberculosis in their curricula, contributing to the occurrence of missed and delayed diagnosis and/or inadequate treatment of tuberculosis cases. Academic institutions need to address these issues in their curricula in order to reduce the preventable disability, death, and acquired drug-resistance due to these clinical errors. The private sector, primarily pharmaceutical and biotechnology companies, is a key partner in the fight against tuberculosis and should play a significant role in developing new and effective tools. Similarly, product development partnerships (PDPs) and public-private partnerships (PPPs) have emerged as important players in the development of new tools. These not-for-profit entities leverage the best practices of industry, academia, public research institutes, and contract research organizations with funding from companies, governments, and philanthropic donors to accelerate product development. As some PDPs and PPPs rely on outside partnerships, resources, and funding, they often engage in advocacy to raise awareness about the need for better tools for tuberculosis.
Faith communities are significant resources for education, outreach, and training for their constituencies, often in partnership with state and local programs. Where tuberculosis services are very weak, community-based organizations provide critical services to the underserved and minority populations, and their involvement in tuberculosis elimination campaigns is crucial in bringing voice to the cause of tuberculosis elimination and advocating for increased resources and policies that will have positive impact in moving the country forward toward tuberculosis elimination.
As the National Center for Cultural Competence states, "a major principle of cultural competence involves working in conjunction with natural, informal supports and helping networks within diverse communities. The concept of cultural brokering exemplifies this principle and can bridge the gap between healthcare providers and the communities they serve." Cultural brokers exist or can be cultivated in immigrant, refugee, and US-born minority communities, including those with higher risk factors for tuberculosis such as homelessness, substance abuse, mental illness, and correctional facility residence. Among the persons who can become cultural brokers and partners in healing with medical providers are practitioners of healing practices or traditional healers in immigrant, refugee, and minority communities. These persons should be identified and encouraged to join in the state and community tuberculosis elimination advocacy campaigns.
# D. Assessment of Progress in Social Mobilization for Tuberculosis Elimination
Regarding social mobilization, the IOM specifically recommended that:
The CDC be provided with significantly increased resources for tuberculosis elimination efforts and sustain public understanding and support for the effort at national, state, local, and risk-group levels NCET work with the CDC to secure the support and participation of nontraditional public health partners, ensure the development of local and state coalitions, and gain the assistance of public opinion research experts in evaluating public opinion in order to garner public support for the elimination effort The Office of the Secretary of Health and Human Services periodically conduct an evaluation of the actions take in response to the IOM recommendations
The Stop TB USA Tuberculosis Elimination Plan Committee believes the year 2000 IOM recommendations for social mobilization remain valid and should be implemented, but what has been the response to these IOM recommendations on social mobilization? Ten years later, flat-funding, budget cuts, and rescissions have prevented the CDC from providing "significantly increase resources" for eliminating tuberculosis. At a retreat in 2007 on the status and future of NCET, it was noted that NCET had not replaced the initial funding provided in 1991 by the Robert Wood Johnson Foundation, limiting its resources to volunteer efforts. To our knowledge, the recommendation for periodic reports by the Secretary of Health and Human Services on the progress towards addressing the IOM recommendations has not been addressed.
# E. Recommendation for Achieving Social Mobilization for Tuberculosis Elimination
The United States has a history replete with examples of social mobilization efforts that have been successful in addressing important health issues including tuberculosis, poliomyelitis, and AIDS. Social mobilization efforts in the fight against tuberculosis were successfully launched again in the 1990s after the resurgence of tuberculosis associated with fatal cases occurring in outbreaks of multidrug-resistant tuberculosis.
The successful social mobilization that occurred in response to this tuberculosis resurgence was due in large part to the resources provided to NCET by the Robert Wood Johnson Foundation, the ALA, and the ATS, and it needs to be replicated. We now face a major challenge of launching and maintaining a successful mobilization effort for a life-threatening disease that will become increasingly rare as we progress toward eliminating tuberculosis. We must maintain long-term engagement of a variety of partners in the effort while overcoming the barriers of stigma that inhibit the participation of our communities of immigrants, minorities, and HIV-infected persons who are at highest risk of death and disability due to tuberculosis. Based upon the recommendations from the 2007 retreat with the CDC, NCET and a number of partners made the following recommendations:
NCET should transition to Stop TB USA. This name change reflects the need to be more readily identified as the point of contact for the Stop TB Partnership at the World Health Organization and as the point of contact for the United States with the global tuberculosis elimination effort Stop TB USA will need to identify a source of infrastructure funding in order to function as an effective coalition. We recommend that national, state, and local voluntary and professional organizations supporting the control and elimination of respiratory and infectious diseases assist Stop TB USA in obtaining the infrastructure funding needed to mobilize all it members and partners in generating the political will to make the elimination of tuberculosis a national priority
# TO CONCLUDE AND MOVE FORWARD:
The IOM stated, "social mobilization is necessary to build and sustain political will (for tuberculosis elimination) in the United States and can lead to similar efforts internationally." However, today tuberculosis is not generally viewed as a problem in the United States, and there has been only limited success over the last ten years in the social mobilization needed to eliminate tuberculosis. 12 Stop TB USA and its partners must work together to develop the political will needed to advocate for the development and implementation of new tools needed both domestically and globally to eliminate TB among high-risk US-born and foreign-born populations in the United States and to maintain the TB control infrastructure in lowincidence areas.
# Acknowledgements
The authors of the IOM's Ending Neglect report concluded that the 2010 tuberculosis elimination goal could not be achieved, owing in part to the 1985 through 1992 resurgence of tuberculosis in the United States as well as to the global impact of the tuberculosis and HIV pandemics. The IOM report suggested that the elimination of tuberculosis might be feasible by 2035 if a number of recommendations for accelerating the decline in tuberculosis cases were implemented. Given the trends since 2003, the decline in tuberculosis case rates will have to be dramatically increased if tuberculosis elimination is to be achieved by 2035.
We should not forget or overlook the successful social mobilization efforts to address the tuberculosis resurgence that occurred two decades ago in the United States. The National Coalition for the Elimination of Tuberculosis (NCET), now known as Stop TB USA, was established in 1991 with funding from the Robert Wood Johnson Foundation as well as the ALA and ATS. NCET's efforts in collaboration with its many partners were apparently successful in achieving the dramatic increase in federal funding for tuberculosis control, but not in bringing about the additional increases in funding that were recommended by the IOM in 2000. | None | None |
af9eaeeca12f416de7ff94626296ee12908609e1 | cdc | None | The complexity of controlling rabies has increased dramatically in the United States since wildlife began to replace domestic dogs as the principal disease vector > 40 years ago. Extensive use of veterinary clinics for parenteral vaccination of domestic dogs, observation of the suspect biting animal, and public education campaigns (together with the application of postexposure prophylaxis following a dog bite) during the 1950s and 1960s were effective, simple strategies for the management of rabies in dogs. However, these strategies were not directly applicable to the management of rabies in wildlife.
Management of rabies in wildlife is complicated by the ecologic and biologic factors associated with wildlife reservoirs, the multiagency approach needed to manage an important public health problem originating in wildlife, the limitations of available control methods, and the broad range of public attitudes toward wildlife. In addition, there are several variants of the rabies virus in the United States.2,3 These are associated with terrestrial carnivores, including raccoons, skunks, and arctic, red, and gray foxes; a number of variants are also found in a variety of species of bats. Recently, an apparent viral shift or adaptation developed with a variant of the virus in canids at the United States-Mexico border area, resulting in local transmission among coyotes and dogs in south Texas54 Compounding the problem, animals infected with this variant were translocated to other states. There are equally important biologic, behavioral, and ecologic differences among carnivores that imply inherent differences in disease control approaches to each major reservoir.
It is often difficult to examine the precise epizootic characteristics of rabies as it spreads among animals of a given population. Also, the role of reservoir host abundance and demography is poorly understood. However, it is possible to make several generalizations from passive surveillance data and trends in the reporting of cases of rabies in animals, especially from detailed studies of red fox populations in Europe. Where measures of carnivore abundance exist, the incidence of rabies in animals (presumably all species) is often positively associated with the increasing density of a dominant reservoir species. In general, rabies epizootics affecting carnivores spread in wavelike fashion; the area experiencing th7e current epizootic is the crest, and the locale with low reservoir-host populations is the trough.7 Rabies is viewed as a densitydependent disease, and population dynamics of reservoir hosts are regarded as critical to understanding and modeling the temporal and spatial patterns of rabies in wildlife.8,9 In part, the rate of spread of rabies in populations of a particular species can be related to, or modeled by, its social structure, dispersal patterns, and contact rates. , , Habitat features, such as continuity and patch size, may play a role in the rate of spread and persistence of the disease.12,1 Furthermore, interactions among species co1 4 mplicates the understanding of the ecologic and epidemiologic factors associated with rabies. Spillover of infection from the dominant reservoir of a region to other species has been documented,2 but the processes by which new variants and epizootics of rabies virus emerge in different reservoir species are unknown. After an epizootic has abated, terrestrial reservoir populations decrease, and reports of rabies in animals in a given locale can decline precipitously. An apparent host threshold density has been suggested as necessary for rabies to perpetuate in red fox populations.15 Below this threshold, contacts appear too few to continue transmission. The threshold phenomenon has not been well studied in other species, although it is presumed to exist. In addition, immunity in surviving members of the reservoir population has been suggested for several species following an epizootic of rabies.14 The influence of herd immunity and population recovery time in the recrudescence of rabies in enzootic areas are largely unstudied for the terrestrial rabies reservoirs; the situation is similar for the various species of bats and diverse rabies virus variants of bats.
There are a number of approaches for management of rabies in wildlife, such as reduction of vector populations, modification of habitats, parenteral vaccination through trap-vaccinaterelease (TVR) programs, oral vaccination, and passive disease surveillance. In addition, immunocontraception for limiting wildlife populations and modulating density-related disease is an intriguing and16 rapidly progressing area of research, although it is still considered highly experimental. 16 These various methods could be used alone or in combination. The utility of wildlife control methods, either independently or in an integrated control program, will depend in large part on the overall objectives. Objectives for the control of rabies may vary regionally, from state to state, and within a state. State wildlife agencies with the statutory authority to manage wild animals may not universally endorse the same management strategy as their respective state public health agencies. Moreover, the existence of rabies reservoirs in multiple states (with the exception of mongooses and their unique rabies virus variant in Puerto Rico) makes strategic control of rabies a national issue. Oral vaccination programs for carnivores are in developmental or early operational stages, and their field efficacy, costs, and benefits remain uncertain. Conventional management approaches, such as long-term, federally supported population reduction on a broad scale, no longer appear justified relative to social acceptability, cost, and efficacy. Lastly, wildlife reservoir species, unlike domestic animals, are natural resources; therefore, public input is essential in helping to determine the methods used to manage rabies among these animals.17
# Rabies Vector Population Reduction
Historically, population reduction has been used to control rabies on the premise that densities of susceptible animals can be reduced below a threshold necessary for rabies to spread through populations. 18 The efforts to control rabies in skunks in Alberta, Canada represents one of the only recent, documented, and broader-scale uses of population reduction in North America conducted explicitly to control rabies. Success of the control program in Alberta was attributed to a high level of effort during several years, the well-defined behavior of skunks in prairie habitats, and access to an effective method. 19 Compensatory changes in carnivore reproduction and dispersal can limit the effectiveness of controlling population numbers of other species in different conditions.9,20
Population reduction with toxicants is impractical as a broadscale control alternative for rabies in the United States. Presidential Executive Order 11643, issued in 1972, banned the use of toxicants (compound 1080, strychnine, sodium cyanide, and thallium sulfate) for control of predators.21 The M-44 cyanide capsule has been reregistered with some applicability for controlling rabies vectors (coyotes and red and gray foxes). 2 In addition, research conducted by USDA Animal Damage Control (recently renamed Wildlife Services) has led to the development of a large gas cartridge that may be used for lethal elimination in dens of skunks, coyotes, and red foxes. Similarly, there is a commercially produced gas cartridge for use on denning skunks (also with moles, woodchucks, or other rodents). Various types of traps and aerial and ground shooting could potentially be used with toxicants in an integrated population reduction strategy to control rabies in some species. However, trapping and shooting options for population reduction of wildlife species would require the opportunity for extensive review by and input from all potentially affected stakeholders.
The estimated costs of population reduction vary widely18,23; however, such efforts, would most likely be cost prohibitive if programs relied on labor-intensive trapping and shooting. Other issues, such as impacts to nontarget species24 and limited public support for population reduction efforts, clearly restrict the feasibility of this approach as a single tactic for broad-scale control of rabies. Presently, population reduction is most likely to be publicly accepted and effective in localized or site-specific scenarios in the United States (eg, reducing the density of raccoon populations in parks where visitors may come in contact with potentially rabid animals). The use of intensive local population reduction as a contingency to address outbreak foci remains untested. Population reduction also may continue to merit consideration for species or situations in which all other methods are not practical.
# Habitat Modification
Habitat modification is a useful site-specific management approach that can reduce the chance of interaction between human beings and potential vectors like skunks, raccoons, and bats. Managing refuse through routine garbage pickup, using animal-proof garbage receptacles, making pet food inaccessible to wild animals, capping chimneys, and screening louver vents are examples of habitat manipulation to minimize contact between wild animals, pets, and people. Techniques designed to prevent access of bats to human living quarters can minimize PEP considerations.
# Trap-Vaccinate-Release Programs
A TVR program was implemented in Toronto in 1984 as an interim measure to control rabies in skunks until an oral rabies vaccine (ORV) could be developed. Inactivated rabies virus vaccine was injected IM into live-trapped skunks. Serum samples from recaptured animals indicated that a high level of population immunity was effective in reducing rabies in Toronto. Costs were relatively high ($450 to $1,150/sq km ) for the TVR program in Toronto,, but these costs may be offset partially by a reduction in the number of people receiving PEP.25 Similarly, there have been TVR programs targeting raccoons on the Delmarva (Delaware, Virginia, and Maryland) peninsula,3 in Philadelphia, and in Ithaca, NY.c A TVR program is also being implemented along the Ontario boundary of the Niagara Frontier in an attempt to provide a barrier against the invasion of rabid raccoons.
# Oral Rabies Vaccination
After the concept was conceived at the Centers for Disease Control and Prevention (CDC) during the 1960s, oral vaccination of red foxes with attenuated Evelyn-Rokitnicke-Abelseth vaccine was demonstrated in the early 1970s. The intensity of rabies in foxes in Europe stimulated the further development of vaccines and delivery systems,27 and these efforts were supported by the World Health Organization. Early control efforts included ground and aerial delivery of rabies vaccine in blister packs inserted in chicken head baits. Oral vaccination in Europe has since progressed to include the use of several efficacious vaccines, including attenuated and recombinant rabies vaccines, in a variety of commercial ba8ts; these are distributed through a combination of ground and aerial bait distribution methods. During 1999, Switzerland, which had a long enzootic for rabies in red foxes and was the first country to use ORV in wildlife in 1978, was declared free of rabies.
In 1989, a similar ORV program was implemented in southern Ontario. Efforts in Ontario throughout the past decade have been promising and have greatly advanced aerial bait delivery with fixed-wing aircraft over large, homogenous areas of land. 29 The ultimate objective of eliminating the arctic fox variant of the rabies virus, which is transmitted among red foxes in the region, may hinge in part on cooperation with neighboring northeastern states and provinces.
Although oral vaccination shows promise for control of rabies among some terrestrial vectors, many important questions regarding baits, optimal baiting strategies, and relevant techniques for control of rabies in bats remain unanswered.1 Subsequent to placebo baiting studies to evaluate 30 32 the feasibil i ty of oral vaccination, " the potential benefits of oral vaccination have been questioned. In contrast, the public is often supportive of novel control methods, despite the infancy of oral vaccination for control of rabies among terrestrial vectors in the United States. To warrant consideration as a public health intervention, efficacy of oral vaccination must be proven, and desirable cost-benefit r 3 a5t-i 3o6s or a willingness to pay among the general public or other stakeholders will be required. In the United States, international and multidisciplinary collaborative efforts led to the development of a vaccinia-rabies glycoprotein (V-RG) recombinant virus vaccine for use in raccoons.37-42 In 1997, the results of safety and efficacy field trials led to full licensure of the V-RG vaccine for use in state or federally approved oral vaccination projects targeting raccoons. 43 To date, the V-RG vaccine has been used in > 10 completed or ongoing field projects for control of rabies in raccoons.1,44 The potential effectiveness of oral vaccination at containing epizootic fronts was first described in New Jersev45 at the Cape May peninsula and subsequently at the Cape Cod isthmus in Massachusetts.
The first suppression of rabies in an enzootic area was described in the Capital Region of New York. Additional ongoing pilot studies have yet to generate substantial data on which to base operational plans for control of rabies through oral vaccination. However, it is clear that federal involvement in strategic oral vaccination efforts involving multiple states will be essential if the ultimate goal is elimination of a particular terrestrial variant of rabies virus. In addition to pilot studies for control of rabies in raccoons, the V-RG vaccine is also being used in an effort to prevent the spread of rabies among gray foxes in west Texas and among coyotes in south Texas.47
# Surveillance
Surveillance is integral to all efforts of rabies control. Surveillance should be pursued more aggressively and with an analytic design during control field trials to objectively evaluate effectiveness. National typing of rabies virus variants should be continued, because such efforts would lead to better understanding of the spatial and temporal distribution of different variants. Such information is essential in view of the differences in behavior and population dynamics and structure among the major wildlife vectors. If regional control efforts directed at specific variants of the virus are initiated, historic and current surveillance data on variants will be needed. Basic passive surveillance will be insufficient for monitoring the effect of oral vaccination on rabies in wildlife.
# Contraception
Interest in oral contraception in wildlife began in the early 1960s as a means to control coyote populations causing livestock depredations in the w e 4s8t and red fox populations responsible for the spread of rabies in the eastern IJnited States. 48 Research efforts with the reproductive inhibitor diethylstilbestrol had promise, but these were abandoned because of the lack of safe, effective, long-lasting agents, and effective delivery systems. Recently, contraception has regained attention as a means of controlling wildlife populations. 16 Advances in genet5c technology since the 1960s have led to the development of immunocontraceptives. -Nevertheless, field delivery of oral immunocontraceptives presents many of the same challenges that confronted researchers of oral rabies v a r ia t io n in the 1960s. Much work remains to develop safe and effective delivery systems.48,50,53,54 In addition, many stakeholders will have5 5 a voice in defining the conditions under which immunocontraceptives could be acceptably applied.55
Recommendations-A better understanding of the complex interaction of host factors (eg, density dependent changes in reproduction, survival, and dispersal, and level of immunity in the surviving population) and viral characteristics involved in epizootic and enzootic transmission of rabies in wildlife populations is necessary. Surveillance systems that include detailed ecologic or epidemiologic data are needed. Explicit descriptions of the impact of rabies on the population dynamics of carnivores and the potential effect of interventions, such as oral vaccination, are fundamentally lacking and critically needed. Educational materials for the public on rabies in wildlife and potential control measures also are inadequate or lacking. Practical and effective vaccines that generate immunity to rabies or inhibit reproduction in specific species are needed. Basic dynamics, movement, and dispersal patterns of rabies vectors should be more fully investigated, particularly in relation to proposed disease control through oral vaccination or other techniques. Professional societies with diverse interests (ecology, mammalogy, wildlife biology, virology, and epidemiology) should collaborate and inform their members of activities in related fields through solicited papers and symposia. More complete species identification on animals, such as bats, submitted for testing should be completed by trained diagnostic laboratory personnel or through collaboration with mammalogists to correct potential laboratory personnel limitations with regard to taxonomic classification of animals submitted for diagnosis of rabies.
In addition to rabies surveillance of wildlife through conventional passive public health submissions, strategic application of active surveillance, such as at epizootic fronts and in areas implementing oral vaccination, will be critical. More effective use of available sources of data should be considered, including augmenting surveillance data collection at the state level. Information on specific geographic location and disease status of all animals submitted for testing should be reported and retained. Existing surveillance systems should be integrated within geographic information system databases, especially databases that would enable classification of habitat features. This would facilitate the understanding of the population dynamics and habitat relationships of reservoir species and potential spread of disease. Educational materials on rabies in wildlife and potential control measures need to be compiled and made available for widespread public distribution as requested by the public. The potential benefits of oral vaccination and other integrated control strategies should be thoroughly described for various major application strategies, such as suppression of local intensity of rabies, containment of an epizootic front, and proposed elimination of a terrestrial rabies variant. Research leading toward the development of practical contraceptives or related technology for managing wildlife populations should be encouraged and supported. Symposia that bring veterinarians, wildlife managers, and other stakeholders together for collaboration on management strategies should be conducted.
# Authority for Management of Rabies in Wildlife
Timely and appropriate response concerning human or domestic animal exposure to rabies should be a local action. However, it is important for responses to be standardized and based on sound pubjjc health policy that requires protocols be developed at the state level, using national guidelines. At the local level, a variety of agencies and individuals may be involved in managing exposure to rabies (eg, animal control officers, health department personnel, emergency room staff, and veterinarians). This multiagency involvement can be confusing for many citizens who may not know the responsible party to call in the event of an exposure. Such confusion can also lead to lack of coverage when clear lines of responsibility are not stated. Recommendations have been prepared by the National Association of State Public Health Veterinarians and the Advisory Committee on Immunization Practices, but these guidelines do not address specific logistic issues at the local level.
Recommendations-State and local task forces consisting of representatives of all involved agencies should be formed to make recommendations for improving communication and coordination at both levels. The health department should be the single authority at the local (city, county, or town) and state levels designated to establish protocols for the management of human exposure to wildlife and to ensure that protocols are followed. State health departments, cooperating with other state agencies (eg, agriculture, wildlife) and using information from recognized national authorities, should provide localities with guidelines and protocols, including those for the scientific rationale for managing wild and domestic animals that potentially expose humans or domestic animals. The public should be notified by various means as to appropriate contacts in the event of an exposure. The system of reporting exposures should be simple and should include 24-hour coverage for nights, weekends, and holidays. If local police or animal control dispatchers receive the information, it should be transmitted to the appropriate individual or agency (eg, health department, animal control, game warden) for response. In all instances, procedures should ensure that the health department is notified of any suspected exposure to rabies. Records should be kept of all potential exposures and eventual outcomes.
# Management of Wildlife to Minimize Transfer of Disease
Throughout history, wild animals have been captured, moved, and released by human beings. In a report by Nielsen,57 conservation, ecology, commerce, recreation, and humanitarian concerns were cited as the primary reasons for translocation of wildlife. Many benefits may be derived through translocation of wild animals, such as restoration of rare or endangered species and expansion of genetic variability of specific isolated populations. However, translocation of animals also has the potential for significant negative impact, particularly with regard to inadvertent transfer of pathogens. For example, there is evidence that the 1977 mid-Atlantic focus of the rabies epizootic in raccoons was the rg s nu lt of long-distance translocation of infected raccoons from the southeastern United States. -More recently, the coyote-dog variant of the rabies virus, previously known only from the United States-Mexico border,4 was diagnosed in American Foxhounds in Alabama,, and Florida.5 The cases were linked to commercial fox-chasing pens that had stocked coyotes and were contained. Intensive use of commercial enclosures created a need to restock animals and led to interstate commercial traffic in wild-caught foxes and 61 62 coyotes.
In response, state regulations regarding fox-chasing enclosures and sale of live foxes and coyotes are rapidly evolving, but compliance remains a problem. In another recent incident, rabies was diagnosed in gray foxes transported from Texas to Montana. Genetic analysis revealed that the isolate was a gray fox variant found in west Texas.3 Similar episodes have involved the translocation of bats from the United States to Europe.
Short-distance relocation of nuisance wildlife may also affect the local incidence of rabies. The most important reservoirs, such as raccoons, skunks, foxes, and various species of bats, are capable of living in close association with people, particularly where " suburbanization" results in adequate shelter and food. Nuisance wildlife are killed or captured and removed by property owners, private pest control operators, licensed commercial trappers, and municipal, state, or federal animal control or wildlife management personnel. Often, landowners express a strong desire that the animals be removed unharmed and transported elsewhere for release. Although relocation is often local, this transportation of animals may provide a mechanism for rabies to spread more rapidly into contiguous, susceptible populations or to surmount geographic or artificial immunologic barriers, such as those caused by oral vaccination of rabies in wildlife.
Recommendations-Stronger and more uniform federal and state wildlife regulations are necessary to prevent indiscriminate international, interstate, and intrastate movement and release of wild carnivores by private citizens. Effective enforcement of state wildlife regulations is necessary to deal with intrastate relocation of wild carnivores. Guidelines are critically needed for determining when nuisance wildlife should be euthanatized instead of being released. Regulations pertaining to the live release of nuisance animals that are vectors for rabies need to be more restrictive. Under the jurisdiction of the state's wildlife, agriculture, or public health agency, each state should have or develop regulations regarding the rehabilitation, capture, holding, sale, and release of wildlife, particularly the importation of wild-caught carnivores.
States with endemic rabies in a given species should develop regulations prohibitingexcept under special permit-the assembly of live, wild animals of that species for any purpose including intra-or interstate sales. Violations of state regulations on import of wild animals should be prosecuted through a joint effort between the state and the US Fish4 and Wildlife Service, thereby activating the penalties associated with violations of the Lacey Act.
Public education programs should be developed to explain public health risks and the need for regulations on relocation of wildlife. Information should address the zoonotic disease risks issues associated with translocation of wildlife. Stronger federal regulation of international animal importation, including the prohibition, quarantine, or restricted movement of exotic species capable of introducing or perpetuating nonindigenous Lyssaviruses, is required.
# Implementation of Vaccination Programs for Wildlife
Use of ORV in the United States is restricted by the USDA to state or federally approved control programs targeting raccoons, with additional applications underway in Texas targeting coyotes and gray foxes. Parenteral vaccines have not been licensed for use in wildlife. Use of ORV should be reserved for large-scale attempts to eliminate or reduce the impact of an outbreak of rabies in wildlife or to limit entry of rabies from wildlife into an area; ORV should not be used for the vaccination of individual animals. Currently, there is no officially delegated lead agency to monitor or evaluate the use of ORV once they are fully licensed.
Recommendations-A national strategy should be formulated for the use of ORV in wildlife, and a federal agency should be designated to lead wildlife vaccination efforts. A single agency within each state should be designated to coordinate rabies vaccination programs in consultation with the other involved agencies. Oral vaccination programs should be optimized through investigations of various bait densities and distribution methods. The CDC should provide technical laboratory and logistic assistance in the conduct, coordination, and surveillance evaluation of state programs, including communication and coordination with other participating state and federal agencies. The USDA should assist in implementation of control programs. Universities and other groups could play various roles, including research, evaluation, and technical support; however, these roles should be secondary to the activities of state and federal agencies. State authorities from public health agencies and either the designated public health veterinarian or the state veterinarian from agriculture departments should have ultimate responsibility for the conduct, supervision, coordination, and termination of wildlife vaccination programs in their respective states. These activities should be coordinated between state departments of agriculture and wildlife. This effort can be expedited by the formation of an interdepartmental task force or committee representing at least those 3 agencies responsible for public health, agriculture, and wildlife. Other potential members for such a task force include private and academic veterinary and human medical practitioners and biomedical researchers.
Since the meeting of the 1995 working group, measurable, but somewhat limited, progress has been made toward control of rabies in wildlife. More areas are using ORV since the vaccine has become licensed. Further westward advancement of rabies in raccoons appears to have been stalled by a considerable ORV effort in the first affected Ohio counties, adjacent to Pennsylvania. However, the recent advancement of rabies northward from New York to eastern Ontario, despite prevention measures in the area (ORV in New York and TVR in Ontario), exemplifies the weakness of current control methods and the lack of guidelines toward efficacious application. Application of ORV in Texas has restricted the progression of rabies in coyotes and gray foxes. Clearly, ORV and other management methods are currently novel tools in the prevention and control of rabies in the United States. For these control methods to become practical, numerous aspects of the various techniques will require additional development and evaluation. Economic analysis and field assessment is in progress. | #
The complexity of controlling rabies has increased dramatically in the United States since wildlife began to replace domestic dogs as the principal disease vector > 40 years ago. Extensive use of veterinary clinics for parenteral vaccination of domestic dogs, observation of the suspect biting animal, and public education campaigns (together with the application of postexposure prophylaxis [PEP] following a dog bite) during the 1950s and 1960s were effective, simple strategies for the management of rabies in dogs. However, these strategies were not directly applicable to the management of rabies in wildlife.
Management of rabies in wildlife is complicated by the ecologic and biologic factors associated with wildlife reservoirs, the multiagency approach needed to manage an important public health problem originating in wildlife, the limitations of available control methods, and the broad range of public attitudes toward wildlife. In addition, there are several variants of the rabies virus in the United States.2,3 These are associated with terrestrial carnivores, including raccoons, skunks, and arctic, red, and gray foxes; a number of variants are also found in a variety of species of bats. Recently, an apparent viral shift or adaptation developed with a variant of the virus in canids at the United States-Mexico border area, resulting in local transmission among coyotes and dogs in south Texas54 Compounding the problem, animals infected with this variant were translocated to other states. There are equally important biologic, behavioral, and ecologic differences among carnivores that imply inherent differences in disease control approaches to each major reservoir.
It is often difficult to examine the precise epizootic characteristics of rabies as it spreads among animals of a given population. Also, the role of reservoir host abundance and demography is poorly understood. However, it is possible to make several generalizations from passive surveillance data and trends in the reporting of cases of rabies in animals, especially from detailed studies of red fox populations in Europe. Where measures of carnivore abundance exist, the incidence of rabies in animals (presumably all species) is often positively associated with the increasing density of a dominant reservoir species. In general, rabies epizootics affecting carnivores spread in wavelike fashion; the area experiencing th7e current epizootic is the crest, and the locale with low reservoir-host populations is the trough.7 Rabies is viewed as a densitydependent disease, and population dynamics of reservoir hosts are regarded as critical to understanding and modeling the temporal and spatial patterns of rabies in wildlife.8,9 In part, the rate of spread of rabies in populations of a particular species can be related to, or modeled by, its social structure, dispersal patterns, and contact rates. , , Habitat features, such as continuity and patch size, may play a role in the rate of spread and persistence of the disease.12,1 Furthermore, interactions among species co1 4 mplicates the understanding of the ecologic and epidemiologic factors associated with rabies. Spillover of infection from the dominant reservoir of a region to other species has been documented,2 but the processes by which new variants and epizootics of rabies virus emerge in different reservoir species are unknown. After an epizootic has abated, terrestrial reservoir populations decrease, and reports of rabies in animals in a given locale can decline precipitously. An apparent host threshold density has been suggested as necessary for rabies to perpetuate in red fox populations.15 Below this threshold, contacts appear too few to continue transmission. The threshold phenomenon has not been well studied in other species, although it is presumed to exist. In addition, immunity in surviving members of the reservoir population has been suggested for several species following an epizootic of rabies.14 The influence of herd immunity and population recovery time in the recrudescence of rabies in enzootic areas are largely unstudied for the terrestrial rabies reservoirs; the situation is similar for the various species of bats and diverse rabies virus variants of bats.
There are a number of approaches for management of rabies in wildlife, such as reduction of vector populations, modification of habitats, parenteral vaccination through trap-vaccinaterelease (TVR) programs, oral vaccination, and passive disease surveillance. In addition, immunocontraception for limiting wildlife populations and modulating density-related disease is an intriguing and16 rapidly progressing area of research, although it is still considered highly experimental. 16 These various methods could be used alone or in combination. The utility of wildlife control methods, either independently or in an integrated control program, will depend in large part on the overall objectives. Objectives for the control of rabies may vary regionally, from state to state, and within a state. State wildlife agencies with the statutory authority to manage wild animals may not universally endorse the same management strategy as their respective state public health agencies. Moreover, the existence of rabies reservoirs in multiple states (with the exception of mongooses and their unique rabies virus variant in Puerto Rico) makes strategic control of rabies a national issue. Oral vaccination programs for carnivores are in developmental or early operational stages, and their field efficacy, costs, and benefits remain uncertain. Conventional management approaches, such as long-term, federally supported population reduction on a broad scale, no longer appear justified relative to social acceptability, cost, and efficacy. Lastly, wildlife reservoir species, unlike domestic animals, are natural resources; therefore, public input is essential in helping to determine the methods used to manage rabies among these animals.17
# Rabies Vector Population Reduction
Historically, population reduction has been used to control rabies on the premise that densities of susceptible animals can be reduced below a threshold necessary for rabies to spread through populations. 18 The efforts to control rabies in skunks in Alberta, Canada represents one of the only recent, documented, and broader-scale uses of population reduction in North America conducted explicitly to control rabies. Success of the control program in Alberta was attributed to a high level of effort during several years, the well-defined behavior of skunks in prairie habitats, and access to an effective method. 19 Compensatory changes in carnivore reproduction and dispersal can limit the effectiveness of controlling population numbers of other species in different conditions.9,20
Population reduction with toxicants is impractical as a broadscale control alternative for rabies in the United States. Presidential Executive Order 11643, issued in 1972, banned the use of toxicants (compound 1080, strychnine, sodium cyanide, and thallium sulfate) for control of predators.21 The M-44 cyanide capsule has been reregistered with some applicability for controlling rabies vectors (coyotes and red and gray foxes). 2 In addition, research conducted by USDA Animal Damage Control (recently renamed Wildlife Services) has led to the development of a large gas cartridge that may be used for lethal elimination in dens of skunks, coyotes, and red foxes. Similarly, there is a commercially produced gas cartridge for use on denning skunks (also with moles, woodchucks, or other rodents). Various types of traps and aerial and ground shooting could potentially be used with toxicants in an integrated population reduction strategy to control rabies in some species. However, trapping and shooting options for population reduction of wildlife species would require the opportunity for extensive review by and input from all potentially affected stakeholders.
The estimated costs of population reduction vary widely18,23; however, such efforts, would most likely be cost prohibitive if programs relied on labor-intensive trapping and shooting. Other issues, such as impacts to nontarget species24 and limited public support for population reduction efforts, clearly restrict the feasibility of this approach as a single tactic for broad-scale control of rabies. Presently, population reduction is most likely to be publicly accepted and effective in localized or site-specific scenarios in the United States (eg, reducing the density of raccoon populations in parks where visitors may come in contact with potentially rabid animals). The use of intensive local population reduction as a contingency to address outbreak foci remains untested. Population reduction also may continue to merit consideration for species or situations in which all other methods are not practical.
# Habitat Modification
Habitat modification is a useful site-specific management approach that can reduce the chance of interaction between human beings and potential vectors like skunks, raccoons, and bats. Managing refuse through routine garbage pickup, using animal-proof garbage receptacles, making pet food inaccessible to wild animals, capping chimneys, and screening louver vents are examples of habitat manipulation to minimize contact between wild animals, pets, and people. Techniques designed to prevent access of bats to human living quarters can minimize PEP considerations.
# Trap-Vaccinate-Release Programs
A TVR program was implemented in Toronto in 1984 as an interim measure to control rabies in skunks until an oral rabies vaccine (ORV) could be developed. Inactivated rabies virus vaccine was injected IM into live-trapped skunks. Serum samples from recaptured animals indicated that a high level of population immunity was effective in reducing rabies in Toronto. Costs were relatively high ($450 to $1,150/sq km [US dollars]) for the TVR program in Toronto,, but these costs may be offset partially by a reduction in the number of people receiving PEP.25 Similarly, there have been TVR programs targeting raccoons on the Delmarva (Delaware, Virginia, and Maryland) peninsula,3 in Philadelphia, and in Ithaca, NY.c A TVR program is also being implemented along the Ontario boundary of the Niagara Frontier in an attempt to provide a barrier against the invasion of rabid raccoons.
# Oral Rabies Vaccination
After the concept was conceived at the Centers for Disease Control and Prevention (CDC) during the 1960s, oral vaccination of red foxes with attenuated Evelyn-Rokitnicke-Abelseth vaccine was demonstrated in the early 1970s. The intensity of rabies in foxes in Europe stimulated the further development of vaccines and delivery systems,27 and these efforts were supported by the World Health Organization. Early control efforts included ground and aerial delivery of rabies vaccine in blister packs inserted in chicken head baits. Oral vaccination in Europe has since progressed to include the use of several efficacious vaccines, including attenuated and recombinant rabies vaccines, in a variety of commercial ba8ts; these are distributed through a combination of ground and aerial bait distribution methods. During 1999, Switzerland, which had a long enzootic for rabies in red foxes and was the first country to use ORV in wildlife in 1978, was declared free of rabies.
In 1989, a similar ORV program was implemented in southern Ontario. Efforts in Ontario throughout the past decade have been promising and have greatly advanced aerial bait delivery with fixed-wing aircraft over large, homogenous areas of land. 29 The ultimate objective of eliminating the arctic fox variant of the rabies virus, which is transmitted among red foxes in the region, may hinge in part on cooperation with neighboring northeastern states and provinces.
Although oral vaccination shows promise for control of rabies among some terrestrial vectors, many important questions regarding baits, optimal baiting strategies, and relevant techniques for control of rabies in bats remain unanswered.1 Subsequent to placebo baiting studies to evaluate 30 32 the feasibil i ty of oral vaccination, " the potential benefits of oral vaccination have been questioned. In contrast, the public is often supportive of novel control methods, despite the infancy of oral vaccination for control of rabies among terrestrial vectors in the United States. To warrant consideration as a public health intervention, efficacy of oral vaccination must be proven, and desirable cost-benefit r 3 a5t-i 3o6s or a willingness to pay among the general public or other stakeholders will be required. [35][36] In the United States, international and multidisciplinary collaborative efforts led to the development of a vaccinia-rabies glycoprotein (V-RG) recombinant virus vaccine for use in raccoons.37-42 In 1997, the results of safety and efficacy field trials led to full licensure of the V-RG vaccine for use in state or federally approved oral vaccination projects targeting raccoons. 43 To date, the V-RG vaccine has been used in > 10 completed or ongoing field projects for control of rabies in raccoons.1,44 The potential effectiveness of oral vaccination at containing epizootic fronts was first described in New Jersev45 at the Cape May peninsula and subsequently at the Cape Cod isthmus in Massachusetts.
The first suppression of rabies in an enzootic area was described in the Capital Region of New York. Additional ongoing pilot studies have yet to generate substantial data on which to base operational plans for control of rabies through oral vaccination. However, it is clear that federal involvement in strategic oral vaccination efforts involving multiple states will be essential if the ultimate goal is elimination of a particular terrestrial variant of rabies virus. In addition to pilot studies for control of rabies in raccoons, the V-RG vaccine is also being used in an effort to prevent the spread of rabies among gray foxes in west Texas and among coyotes in south Texas.47
# Surveillance
Surveillance is integral to all efforts of rabies control. Surveillance should be pursued more aggressively and with an analytic design during control field trials to objectively evaluate effectiveness. National typing of rabies virus variants should be continued, because such efforts would lead to better understanding of the spatial and temporal distribution of different variants. Such information is essential in view of the differences in behavior and population dynamics and structure among the major wildlife vectors. If regional control efforts directed at specific variants of the virus are initiated, historic and current surveillance data on variants will be needed. Basic passive surveillance will be insufficient for monitoring the effect of oral vaccination on rabies in wildlife.
# Contraception
Interest in oral contraception in wildlife began in the early 1960s as a means to control coyote populations causing livestock depredations in the w e 4s8t and red fox populations responsible for the spread of rabies in the eastern IJnited States. 48 Research efforts with the reproductive inhibitor diethylstilbestrol had promise, but these were abandoned because of the lack of safe, effective, long-lasting agents, and effective delivery systems. Recently, contraception has regained attention as a means of controlling wildlife populations. 16 Advances in genet5c technology since the 1960s have led to the development of immunocontraceptives. -Nevertheless, field delivery of oral immunocontraceptives presents many of the same challenges that confronted researchers of oral rabies v a r ia t io n in the 1960s. Much work remains to develop safe and effective delivery systems.48,50,53,54 In addition, many stakeholders will have5 5 a voice in defining the conditions under which immunocontraceptives could be acceptably applied.55
Recommendations-A better understanding of the complex interaction of host factors (eg, density dependent changes in reproduction, survival, and dispersal, and level of immunity in the surviving population) and viral characteristics involved in epizootic and enzootic transmission of rabies in wildlife populations is necessary. Surveillance systems that include detailed ecologic or epidemiologic data are needed. Explicit descriptions of the impact of rabies on the population dynamics of carnivores and the potential effect of interventions, such as oral vaccination, are fundamentally lacking and critically needed. Educational materials for the public on rabies in wildlife and potential control measures also are inadequate or lacking. Practical and effective vaccines that generate immunity to rabies or inhibit reproduction in specific species are needed. Basic dynamics, movement, and dispersal patterns of rabies vectors should be more fully investigated, particularly in relation to proposed disease control through oral vaccination or other techniques. Professional societies with diverse interests (ecology, mammalogy, wildlife biology, virology, and epidemiology) should collaborate and inform their members of activities in related fields through solicited papers and symposia. More complete species identification on animals, such as bats, submitted for testing should be completed by trained diagnostic laboratory personnel or through collaboration with mammalogists to correct potential laboratory personnel limitations with regard to taxonomic classification of animals submitted for diagnosis of rabies.
In addition to rabies surveillance of wildlife through conventional passive public health submissions, strategic application of active surveillance, such as at epizootic fronts and in areas implementing oral vaccination, will be critical. More effective use of available sources of data should be considered, including augmenting surveillance data collection at the state level. Information on specific geographic location and disease status of all animals submitted for testing should be reported and retained. Existing surveillance systems should be integrated within geographic information system databases, especially databases that would enable classification of habitat features. This would facilitate the understanding of the population dynamics and habitat relationships of reservoir species and potential spread of disease. Educational materials on rabies in wildlife and potential control measures need to be compiled and made available for widespread public distribution as requested by the public. The potential benefits of oral vaccination and other integrated control strategies should be thoroughly described for various major application strategies, such as suppression of local intensity of rabies, containment of an epizootic front, and proposed elimination of a terrestrial rabies variant. Research leading toward the development of practical contraceptives or related technology for managing wildlife populations should be encouraged and supported. Symposia that bring veterinarians, wildlife managers, and other stakeholders together for collaboration on management strategies should be conducted.
# Authority for Management of Rabies in Wildlife
Timely and appropriate response concerning human or domestic animal exposure to rabies should be a local action. However, it is important for responses to be standardized and based on sound pubjjc health policy that requires protocols be developed at the state level, using national guidelines. At the local level, a variety of agencies and individuals may be involved in managing exposure to rabies (eg, animal control officers, health department personnel, emergency room staff, and veterinarians). This multiagency involvement can be confusing for many citizens who may not know the responsible party to call in the event of an exposure. Such confusion can also lead to lack of coverage when clear lines of responsibility are not stated. Recommendations have been prepared by the National Association of State Public Health Veterinarians and the Advisory Committee on Immunization Practices, but these guidelines do not address specific logistic issues at the local level.
Recommendations-State and local task forces consisting of representatives of all involved agencies should be formed to make recommendations for improving communication and coordination at both levels. The health department should be the single authority at the local (city, county, or town) and state levels designated to establish protocols for the management of human exposure to wildlife and to ensure that protocols are followed. State health departments, cooperating with other state agencies (eg, agriculture, wildlife) and using information from recognized national authorities, should provide localities with guidelines and protocols, including those for the scientific rationale for managing wild and domestic animals that potentially expose humans or domestic animals. The public should be notified by various means as to appropriate contacts in the event of an exposure. The system of reporting exposures should be simple and should include 24-hour coverage for nights, weekends, and holidays. If local police or animal control dispatchers receive the information, it should be transmitted to the appropriate individual or agency (eg, health department, animal control, game warden) for response. In all instances, procedures should ensure that the health department is notified of any suspected exposure to rabies. Records should be kept of all potential exposures and eventual outcomes.
# Management of Wildlife to Minimize Transfer of Disease
Throughout history, wild animals have been captured, moved, and released by human beings. In a report by Nielsen,57 conservation, ecology, commerce, recreation, and humanitarian concerns were cited as the primary reasons for translocation of wildlife. Many benefits may be derived through translocation of wild animals, such as restoration of rare or endangered species and expansion of genetic variability of specific isolated populations. However, translocation of animals also has the potential for significant negative impact, particularly with regard to inadvertent transfer of pathogens. For example, there is evidence that the 1977 mid-Atlantic focus of the rabies epizootic in raccoons was the rg s nu lt of long-distance translocation of infected raccoons from the southeastern United States. -More recently, the coyote-dog variant of the rabies virus, previously known only from the United States-Mexico border,4 was diagnosed in American Foxhounds in Alabama,, and Florida.5 The cases were linked to commercial fox-chasing pens that had stocked coyotes and were contained. Intensive use of commercial enclosures created a need to restock animals and led to interstate commercial traffic in wild-caught foxes and 61 62 coyotes.
In response, state regulations regarding fox-chasing enclosures and sale of live foxes and coyotes are rapidly evolving, but compliance remains a problem. In another recent incident, rabies was diagnosed in gray foxes transported from Texas to Montana. Genetic analysis revealed that the isolate was a gray fox variant found in west Texas.3 Similar episodes have involved the translocation of bats from the United States to Europe.
Short-distance relocation of nuisance wildlife may also affect the local incidence of rabies. The most important reservoirs, such as raccoons, skunks, foxes, and various species of bats, are capable of living in close association with people, particularly where " suburbanization" results in adequate shelter and food. Nuisance wildlife are killed or captured and removed by property owners, private pest control operators, licensed commercial trappers, and municipal, state, or federal animal control or wildlife management personnel. Often, landowners express a strong desire that the animals be removed unharmed and transported elsewhere for release. Although relocation is often local, this transportation of animals may provide a mechanism for rabies to spread more rapidly into contiguous, susceptible populations or to surmount geographic or artificial immunologic barriers, such as those caused by oral vaccination of rabies in wildlife.
Recommendations-Stronger and more uniform federal and state wildlife regulations are necessary to prevent indiscriminate international, interstate, and intrastate movement and release of wild carnivores by private citizens. Effective enforcement of state wildlife regulations is necessary to deal with intrastate relocation of wild carnivores. Guidelines are critically needed for determining when nuisance wildlife should be euthanatized instead of being released. Regulations pertaining to the live release of nuisance animals that are vectors for rabies need to be more restrictive. Under the jurisdiction of the state's wildlife, agriculture, or public health agency, each state should have or develop regulations regarding the rehabilitation, capture, holding, sale, and release of wildlife, particularly the importation of wild-caught carnivores.
States with endemic rabies in a given species should develop regulations prohibitingexcept under special permit-the assembly of live, wild animals of that species for any purpose including intra-or interstate sales. Violations of state regulations on import of wild animals should be prosecuted through a joint effort between the state and the US Fish4 and Wildlife Service, thereby activating the penalties associated with violations of the Lacey Act.
Public education programs should be developed to explain public health risks and the need for regulations on relocation of wildlife. Information should address the zoonotic disease risks issues associated with translocation of wildlife. Stronger federal regulation of international animal importation, including the prohibition, quarantine, or restricted movement of exotic species capable of introducing or perpetuating nonindigenous Lyssaviruses, is required.
# Implementation of Vaccination Programs for Wildlife
Use of ORV in the United States is restricted by the USDA to state or federally approved control programs targeting raccoons, with additional applications underway in Texas targeting coyotes and gray foxes. Parenteral vaccines have not been licensed for use in wildlife. Use of ORV should be reserved for large-scale attempts to eliminate or reduce the impact of an outbreak of rabies in wildlife or to limit entry of rabies from wildlife into an area; ORV should not be used for the vaccination of individual animals. Currently, there is no officially delegated lead agency to monitor or evaluate the use of ORV once they are fully licensed.
Recommendations-A national strategy should be formulated for the use of ORV in wildlife, and a federal agency should be designated to lead wildlife vaccination efforts. A single agency within each state should be designated to coordinate rabies vaccination programs in consultation with the other involved agencies. Oral vaccination programs should be optimized through investigations of various bait densities and distribution methods. The CDC should provide technical laboratory and logistic assistance in the conduct, coordination, and surveillance evaluation of state programs, including communication and coordination with other participating state and federal agencies. The USDA should assist in implementation of control programs. Universities and other groups could play various roles, including research, evaluation, and technical support; however, these roles should be secondary to the activities of state and federal agencies. State authorities from public health agencies and either the designated public health veterinarian or the state veterinarian from agriculture departments should have ultimate responsibility for the conduct, supervision, coordination, and termination of wildlife vaccination programs in their respective states. These activities should be coordinated between state departments of agriculture and wildlife. This effort can be expedited by the formation of an interdepartmental task force or committee representing at least those 3 agencies responsible for public health, agriculture, and wildlife. Other potential members for such a task force include private and academic veterinary and human medical practitioners and biomedical researchers.
Since the meeting of the 1995 working group, measurable, but somewhat limited, progress has been made toward control of rabies in wildlife. More areas are using ORV since the vaccine has become licensed. Further westward advancement of rabies in raccoons appears to have been stalled by a considerable ORV effort in the first affected Ohio counties, adjacent to Pennsylvania. However, the recent advancement of rabies northward from New York to eastern Ontario, despite prevention measures in the area (ORV in New York and TVR in Ontario), exemplifies the weakness of current control methods and the lack of guidelines toward efficacious application. Application of ORV in Texas has restricted the progression of rabies in coyotes and gray foxes. Clearly, ORV and other management methods are currently novel tools in the prevention and control of rabies in the United States. For these control methods to become practical, numerous aspects of the various techniques will require additional development and evaluation. Economic analysis and field assessment is in progress. | None | None |
df15752bd0803d35ba15c05fe7d89456260dcff5 | cdc | None | # Personal P ro tective E quipm ent fo r Use by Postal Em ployees D elivering A ntibiotics D o o r-to -D o o r Follow ing an A n th rax A tta ck | # Personal P ro tective E quipm ent fo r Use by Postal Em ployees D elivering A ntibiotics D o o r-to -D o o r Follow ing an A n th rax A tta ck
| None | None |
8467c59109b4a562c31804297a6c699f383f549c | cdc | None | CDC announced the availability of the 2018 adult immunization schedule in the Morbidity and Mortality Weekly Report (MMWR). 1 The schedule is published in its entirety in the Annals of Internal Medicine. 2 The adult immunization schedule consists of figures that summarize routinely recommended vaccines for adults by age groups and medical conditions and other indications, footnotes for the figures, and a table of vaccine contraindications and precautions. Note the following when reviewing the adult immunization schedule:#
- The figures in the adult immunization schedule should be reviewed with the accompanying footnotes. - The figures and footnotes display indications for which vaccines, if not previously administered, should be administered unless noted otherwise. - The table of contraindications and precautions identifies populations and situations for which vaccines should not be used or should be used with caution. - When indicated, administer recommended vaccines to adults whose vaccination history is incomplete or unknown. - Increased interval between doses of a multidose vaccine series does not diminish vaccine effectiveness; it is not necessary to restart the vaccine series or add doses to the series because of an extended interval between doses. - Combination vaccines may be used when any component of the combination is indicated and when the other components of the combination are not contraindicated. - The use of trade names in the adult immunization schedule is for identification purposes only and does not imply endorsement by the ACIP or CDC.
Special populations that need additional considerations include:
- Pregnant women. Pregnant women should receive the tetanus, diphtheria, and acellular pertussis vaccine (Tdap) during pregnancy and the influenza vaccine during or before pregnancy. Live vaccines (e.g., measles, mumps, and rubella vaccine ) are contraindicated. - Asplenia. Adults with asplenia have specific vaccination recommendations because of their increased risk for infection by encapsulated bacteria. Anatomical or functional asplenia includes congenital or acquired asplenia, splenic dysfunction, sickle cell disease and other hemoglobinopathies, and splenectomy. - Immunocompromising conditions. Adults with immunosuppression should generally avoid live vaccines. Inactivated vaccines (e.g., pneumococcal vaccines) are generally acceptable. High-level immunosuppression includes HIV infection with a CD4 cell count <200 cells/μL, receipt of daily corticosteroid therapy with ≥20 mg of prednisone or equivalent for ≥14 days, primary immunodeficiency disorder (e.g., severe combined immunodeficiency or complement component deficiency), and receipt of cancer chemotherapy. Other immunocompromising conditions and immunosuppressive medications to consider when vaccinating adults can be found in IDSA Clinical Practice Guideline for Vaccination of the Immunocompromised Host. 3 Additional information on vaccinating immunocompromised adults is in General Best Practice Guidelines for Immunization. 4 Additional resources for health care providers include: This figure should be reviewed with the accompanying footnotes. This figure and the footnotes describe indications for which vaccines, if not previously administered, should be administered unless noted otherwise.
Vaccine Pregnancy Immunocompromised (excluding HIV infection) 11 HIV infection CD4+ count (cells/μL) 3-7,9-10 Asplenia, complement deficiencies 7,10,11 End-stage renal disease, on hemodialysis 7,9 Heart or lung disease, alcoholism 7 Chronic liver disease 7-9 Diabetes 7,9
Health care personnel 3,4,9 Men who have sex with men 6,8,9 <200 ≥200
# General information
- Administer to adults who previously did not receive a dose of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine (Tdap) as an adult or child (routinely recommended at age 11-12 years) 1 dose of Tdap, followed by a dose of tetanus and diphtheria toxoids (Td) booster every 10 years - Information on the use of Tdap or Td as tetanus prophylaxis in wound management is available at www.cdc.gov/mmwr/ preview/mmwrhtml/rr5517a1.htm
# Special populations
- Pregnant women: Administer 1 dose of Tdap during each pregnancy, preferably in the early part of gestational weeks 27-36 - History of Guillain-Barré syndrome within 6 weeks after previous influenza vaccination - Egg allergy other than hives, e.g., angioedema, respiratory distress, lightheadedness, or recurrent emesis; or required epinephrine or another emergency medical intervention (IIV may be administered in an inpatient or outpatient medical setting and under the supervision of a health care provider who is able to recognize and manage severe allergic conditions) RIV 1 - History of Guillain-Barré syndrome within 6 weeks after previous influenza vaccination Tdap, Td
- For pertussis-containing vaccines: encephalopathy, e.g., coma, decreased level of consciousness, or prolonged seizures, not attributable to another identifiable cause within 7 days of administration of a previous dose of a vaccine containing tetanus or diphtheria toxoid or acellular pertussis
- Guillain-Barré syndrome within 6 weeks after a previous dose of tetanus toxoid-containing vaccine - History of Arthus-type hypersensitivity reactions after a previous dose of tetanus or diphtheria toxoid-containing vaccine. Defer vaccination until at least 10 years have elapsed since the last tetanus toxoid-containing vaccine - For pertussis-containing vaccine, progressive or unstable neurologic disorder, uncontrolled seizures, or progressive encephalopathy (until a treatment regimen has been established and the condition has stabilized) MMR 2 - Severe immunodeficiency, e.g., hematologic and solid tumors, chemotherapy, congenital immunodeficiency or long-term immunosuppressive therapy 3 , human immunodeficiency virus (HIV) infection with severe immunocompromise - Pregnancy
- Recent (within 11 months) receipt of antibody-containing blood product (specific interval depends on product) 4 - History of thrombocytopenia or thrombocytopenic purpura - Need for tuberculin skin testing 5 VAR 2 - Severe immunodeficiency, e.g., hematologic and solid tumors, chemotherapy, congenital immunodeficiency or long-term immunosuppressive therapy 3 , HIV infection with severe immunocompromise - Pregnancy
- Recent (within 11 months) receipt of antibody-containing blood product (specific interval depends on product) 4 - Receipt of specific antiviral drugs (acyclovir, famciclovir, or valacyclovir) 24 hours before vaccination (avoid use of these antiviral drugs for 14 days after vaccination) ZVL 2 - Severe immunodeficiency, e.g., hematologic and solid tumors, chemotherapy, congenital immunodeficiency or long-term immunosuppressive therapy 3 , HIV infection with severe immunocompromise - Pregnancy - Receipt of specific antiviral drugs (acyclovir, famciclovir, or valacyclovir) 24 hours before vaccination (avoid use of these antiviral drugs for 14 days after vaccination)
HPV vaccine - Pregnancy PCV13
- Severe allergic reaction to any vaccine containing diphtheria toxoid 1. For additional information on use of influenza vaccines among persons with egg allergy, see: CDC. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices-United States, 2016-17 influenza season. MMWR. 2016;65(RR-5):1-54. Available at www.cdc.gov/mmwr/volumes/65/rr/rr6505a1.htm. 2. MMR may be administered together with VAR or ZVL on the same day. If not administered on the same day, separate live vaccines by at least 28 days. 3. Immunosuppressive steroid dose is considered to be daily receipt of 20 mg or more prednisone or equivalent for 2 or more weeks. Vaccination should be deferred for at least 1 month after discontinuation of immunosuppressive steroid therapy. Providers should consult ACIP recommendations for complete information on the use of specific live vaccines among persons on immune-suppressing medications or with immune suppression because of other reasons. 4. Vaccine should be deferred for the appropriate interval if replacement immune globulin products are being administered. See: Best practices guidance of the Advisory Committee on Immunization Practices (ACIP). Available at www.cdc.gov/vaccines/hcp/acip-recs/general-recs/index.html. 5. Measles vaccination may temporarily suppress tuberculin reactivity. Measles-containing vaccine may be administered on the same day as tuberculin skin testing, or should be postponed for at least 4 weeks after vaccination.
# Table. Contraindications and precautions for vaccines recommended for adults aged 19 years or older*
The Advisory Committee on Immunization Practices (ACIP) recommendations and package inserts for vaccines provide information on contraindications and precautions related to vaccines. Contraindications are conditions that increase chances of a serious adverse reaction in vaccine recipients and the vaccine should not be administered when a contraindication is present. Precautions should be reviewed for potential risks and benefits for vaccine recipients.
# Vaccine(s) Contraindications Precautions
All vaccines routinely recommended for adults
- Severe reaction, e.g., anaphylaxis, after a previous dose or to a vaccine component - Moderate or severe acute illness with or without fever
# Additional contraindications and precautions for vaccines routinely recommended for adults
Contraindications and precautions for vaccines routinely recommended for adults
# Abbreviations of vaccines | CDC announced the availability of the 2018 adult immunization schedule in the Morbidity and Mortality Weekly Report (MMWR). 1 The schedule is published in its entirety in the Annals of Internal Medicine. 2 The adult immunization schedule consists of figures that summarize routinely recommended vaccines for adults by age groups and medical conditions and other indications, footnotes for the figures, and a table of vaccine contraindications and precautions. Note the following when reviewing the adult immunization schedule:#
• The figures in the adult immunization schedule should be reviewed with the accompanying footnotes. • The figures and footnotes display indications for which vaccines, if not previously administered, should be administered unless noted otherwise. • The table of contraindications and precautions identifies populations and situations for which vaccines should not be used or should be used with caution. • When indicated, administer recommended vaccines to adults whose vaccination history is incomplete or unknown. • Increased interval between doses of a multidose vaccine series does not diminish vaccine effectiveness; it is not necessary to restart the vaccine series or add doses to the series because of an extended interval between doses. • Combination vaccines may be used when any component of the combination is indicated and when the other components of the combination are not contraindicated. • The use of trade names in the adult immunization schedule is for identification purposes only and does not imply endorsement by the ACIP or CDC.
Special populations that need additional considerations include:
• Pregnant women. Pregnant women should receive the tetanus, diphtheria, and acellular pertussis vaccine (Tdap) during pregnancy and the influenza vaccine during or before pregnancy. Live vaccines (e.g., measles, mumps, and rubella vaccine [MMR]) are contraindicated. • Asplenia. Adults with asplenia have specific vaccination recommendations because of their increased risk for infection by encapsulated bacteria. Anatomical or functional asplenia includes congenital or acquired asplenia, splenic dysfunction, sickle cell disease and other hemoglobinopathies, and splenectomy. • Immunocompromising conditions. Adults with immunosuppression should generally avoid live vaccines. Inactivated vaccines (e.g., pneumococcal vaccines) are generally acceptable. High-level immunosuppression includes HIV infection with a CD4 cell count <200 cells/μL, receipt of daily corticosteroid therapy with ≥20 mg of prednisone or equivalent for ≥14 days, primary immunodeficiency disorder (e.g., severe combined immunodeficiency or complement component deficiency), and receipt of cancer chemotherapy. Other immunocompromising conditions and immunosuppressive medications to consider when vaccinating adults can be found in IDSA Clinical Practice Guideline for Vaccination of the Immunocompromised Host. 3 Additional information on vaccinating immunocompromised adults is in General Best Practice Guidelines for Immunization. 4 Additional resources for health care providers include: This figure should be reviewed with the accompanying footnotes. This figure and the footnotes describe indications for which vaccines, if not previously administered, should be administered unless noted otherwise.
Vaccine Pregnancy [1][2][3][4][5][6] Immunocompromised (excluding HIV infection) [3][4][5][6][7]11 HIV infection CD4+ count (cells/μL) 3-7,9-10 Asplenia, complement deficiencies 7,10,11 End-stage renal disease, on hemodialysis 7,9 Heart or lung disease, alcoholism 7 Chronic liver disease 7-9 Diabetes 7,9
Health care personnel 3,4,9 Men who have sex with men 6,8,9 <200 ≥200
# General information
• Administer to adults who previously did not receive a dose of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine (Tdap) as an adult or child (routinely recommended at age 11-12 years) 1 dose of Tdap, followed by a dose of tetanus and diphtheria toxoids (Td) booster every 10 years • Information on the use of Tdap or Td as tetanus prophylaxis in wound management is available at www.cdc.gov/mmwr/ preview/mmwrhtml/rr5517a1.htm
# Special populations
• Pregnant women: Administer 1 dose of Tdap during each pregnancy, preferably in the early part of gestational weeks 27-36 • History of Guillain-Barré syndrome within 6 weeks after previous influenza vaccination • Egg allergy other than hives, e.g., angioedema, respiratory distress, lightheadedness, or recurrent emesis; or required epinephrine or another emergency medical intervention (IIV may be administered in an inpatient or outpatient medical setting and under the supervision of a health care provider who is able to recognize and manage severe allergic conditions) RIV 1 • History of Guillain-Barré syndrome within 6 weeks after previous influenza vaccination Tdap, Td
• For pertussis-containing vaccines: encephalopathy, e.g., coma, decreased level of consciousness, or prolonged seizures, not attributable to another identifiable cause within 7 days of administration of a previous dose of a vaccine containing tetanus or diphtheria toxoid or acellular pertussis
• Guillain-Barré syndrome within 6 weeks after a previous dose of tetanus toxoid-containing vaccine • History of Arthus-type hypersensitivity reactions after a previous dose of tetanus or diphtheria toxoid-containing vaccine. Defer vaccination until at least 10 years have elapsed since the last tetanus toxoid-containing vaccine • For pertussis-containing vaccine, progressive or unstable neurologic disorder, uncontrolled seizures, or progressive encephalopathy (until a treatment regimen has been established and the condition has stabilized) MMR 2 • Severe immunodeficiency, e.g., hematologic and solid tumors, chemotherapy, congenital immunodeficiency or long-term immunosuppressive therapy 3 , human immunodeficiency virus (HIV) infection with severe immunocompromise • Pregnancy
• Recent (within 11 months) receipt of antibody-containing blood product (specific interval depends on product) 4 • History of thrombocytopenia or thrombocytopenic purpura • Need for tuberculin skin testing 5 VAR 2 • Severe immunodeficiency, e.g., hematologic and solid tumors, chemotherapy, congenital immunodeficiency or long-term immunosuppressive therapy 3 , HIV infection with severe immunocompromise • Pregnancy
• Recent (within 11 months) receipt of antibody-containing blood product (specific interval depends on product) 4 • Receipt of specific antiviral drugs (acyclovir, famciclovir, or valacyclovir) 24 hours before vaccination (avoid use of these antiviral drugs for 14 days after vaccination) ZVL 2 • Severe immunodeficiency, e.g., hematologic and solid tumors, chemotherapy, congenital immunodeficiency or long-term immunosuppressive therapy 3 , HIV infection with severe immunocompromise • Pregnancy • Receipt of specific antiviral drugs (acyclovir, famciclovir, or valacyclovir) 24 hours before vaccination (avoid use of these antiviral drugs for 14 days after vaccination)
HPV vaccine • Pregnancy PCV13
• Severe allergic reaction to any vaccine containing diphtheria toxoid 1. For additional information on use of influenza vaccines among persons with egg allergy, see: CDC. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices-United States, 2016-17 influenza season. MMWR. 2016;65(RR-5):1-54. Available at www.cdc.gov/mmwr/volumes/65/rr/rr6505a1.htm. 2. MMR may be administered together with VAR or ZVL on the same day. If not administered on the same day, separate live vaccines by at least 28 days. 3. Immunosuppressive steroid dose is considered to be daily receipt of 20 mg or more prednisone or equivalent for 2 or more weeks. Vaccination should be deferred for at least 1 month after discontinuation of immunosuppressive steroid therapy. Providers should consult ACIP recommendations for complete information on the use of specific live vaccines among persons on immune-suppressing medications or with immune suppression because of other reasons. 4. Vaccine should be deferred for the appropriate interval if replacement immune globulin products are being administered. See: Best practices guidance of the Advisory Committee on Immunization Practices (ACIP). Available at www.cdc.gov/vaccines/hcp/acip-recs/general-recs/index.html. 5. Measles vaccination may temporarily suppress tuberculin reactivity. Measles-containing vaccine may be administered on the same day as tuberculin skin testing, or should be postponed for at least 4 weeks after vaccination.
# Table. Contraindications and precautions for vaccines recommended for adults aged 19 years or older*
The Advisory Committee on Immunization Practices (ACIP) recommendations and package inserts for vaccines provide information on contraindications and precautions related to vaccines. Contraindications are conditions that increase chances of a serious adverse reaction in vaccine recipients and the vaccine should not be administered when a contraindication is present. Precautions should be reviewed for potential risks and benefits for vaccine recipients.
# Vaccine(s) Contraindications Precautions
All vaccines routinely recommended for adults
• Severe reaction, e.g., anaphylaxis, after a previous dose or to a vaccine component • Moderate or severe acute illness with or without fever
# Additional contraindications and precautions for vaccines routinely recommended for adults
Contraindications and precautions for vaccines routinely recommended for adults
# Abbreviations of vaccines
| None | None |
4e4e518dd0f130a6df6e2f0176cf8f35e12ff2e3 | cdc | None | Acute hepatitis B Newly acquired symptomatic hepatitis B virus (HBV) infection. Acute hepatitis C Newly acquired symptomatic hepatitis C virus (HCV) infection. ALT Alanine aminotransferase, previously called SGPT. Anti-HBc Antibody to hepatitis B core antigen. Anti-HBe Antibody to hepatitis B e antigen. Anti-HBs Antibody to hepatitis B surface antigen. Anti-HCV Antibody to hepatitis C virus. Anti-HDV Antibody to hepatitis D virus. AST Aspartate aminotransferase, previously called SGOT. AV Arteriovenous. Chronic (persistent) HBV infection Vol. 50 / No. RR-5 MMWR iii# INTRODUCTION
The number of patients with end-stage renal disease treated by maintenance hemodialysis in the United States has increased sharply during the past 30 years. In 1999, more than 3,000 hemodialysis centers had >190,000 chronic hemodialysis patients and >60,000 staff members (1 ). Chronic hemodialysis patients are at high risk for infection because the process of hemodialysis requires vascular access for prolonged periods. In an environment where multiple patients receive dialysis concurrently, repeated opportunities exist for person-to-person transmission of infectious agents, directly or indirectly via contaminated devices, equipment and supplies, environmental surfaces, or hands of personnel. Furthermore, hemodialysis patients are immunosuppressed (2 ), which increases their susceptibility to infection, and they require frequent hospitalizations and surgery, which increases their opportunities for exposure to nosocomial infections.
Historically, surveillance for infections associated with chronic hemodialysis focused on viral hepatitis, particularly hepatitis B virus (HBV) infection. CDC began conducting national surveillance for hemodialysis-associated hepatitis in 1972 (3,4 ). Since 1976, this surveillance has been performed in collaboration with the Health Care Financing Administration (HCFA) during its annual facility survey. Other hemodialysis-associated diseases and practices not related to hepatitis have been included over the years (e.g., pyrogenic reactions, dialysis dementia, vascular access infections, reuse practices, vancomycin use), and the system is continually updated to collect data regarding hemodialysis-associated practices and diseases of current interest and importance (5)(6)(7)(8)(9)(10)(11)(12)(13)(14)(15)(16)(17)(18).
# MMWR April 27, 2001
Recommendations for the control of hepatitis B in hemodialysis centers were first published in 1977 (19 ), and by 1980, their widespread implementation was associated with a sharp reduction in incidence of HBV infection among both patients and staff members (5 ). In 1982, hepatitis B vaccination was recommended for all susceptible patients and staff members (20 ). However, outbreaks of both HBV and hepatitis C virus (HCV) infections continue to occur among chronic hemodialysis patients. Epidemiologic investigations have indicated substantial deficiencies in recommended infection control practices, as well as a failure to vaccinate hemodialysis patients against hepatitis B (21,22 ). These practices apparently are not being fully implemented because staff members a) are not aware of the practices and their importance, b) are confused regarding the differences between standard (i.e., universal) precautions recommended for all health-care settings and the additional precautions necessary in the hemodialysis setting, and c) believe that hepatitis B vaccine is ineffective for preventing HBV infection in chronic hemodialysis patients (22 ).
Bacterial infections, especially those involving vascular access, are the most frequent infectious complication of hemodialysis and a major cause of morbidity and mortality among hemodialysis patients (1 ). During the 1990s, the prevalence of antimicrobial-resistant bacteria (e.g., methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci ) increased rapidly in health-care settings, including hemodialysis units (18,23 ). Although numerous outbreaks of bacterial infections in the hemodialysis setting have been reported (24 ), few studies exist regarding the epidemiology and prevention of endemically occurring bacterial infections in hemodialysis patients, and formal recommendations to prevent such infections have not been published previously. In 1999, CDC initiated a surveillance system for bloodstream and vascular access infections in outpatient hemodialysis centers to determine the frequency of and risk factors for these complications in order to formulate and evaluate strategies for control (25 ).
The recommendations contained in this report were developed by reviewing available data and are based on consultations with specialists in the field. These recommendations provide guidelines for infection control strategies, unique to the hemodialysis setting, that should be used to prevent patient-to-patient transmission of bloodborne viruses and pathogenic bacteria. They are summarized on pages 20-21.
These recommendations do not address sources of bacterial and chemical contaminants in dialysis systems, water treatment or distribution, specific procedures for reprocessing dialyzers, clinical practice methods to prevent bacterial infections (e.g., techniques for skin preparation and access), or comprehensive strategies for preventing infections among health-care workers (see Suggested Readings for information on these topics).
# BACKGROUND Hepatitis B Virus Infection Epidemiology
Incidence and Prevalence. In 1974, the incidence of newly acquired (i.e., acute) HBV infection among chronic hemodialysis patients in the United States was 6.2%, and se-
MMWR 3
lected hemodialysis centers reported rates as high as 30% (4 ). By 1980, nationwide incidence among patients had decreased to 1% (5 ), and by 1999, to 0.06% (18 ) (CDC, unpublished data, 2001), with only 3.5% of all centers reporting newly acquired infections. Prevalence of chronic HBV infection (i.e., hepatitis B surface antigen positivity) among hemodialysis patients declined from 7.8% in 1976 to 3.8% in 1980 and to 0.9% by 1999 (5,18 ) (CDC, unpublished data, 2001). In 1999, a total of 27.7% of 3,483 centers provided dialysis to >1 patient with either acute or chronic HBV infection (CDC, unpublished data, 2001).
Transmission. HBV is transmitted by percutaneous (i.e., puncture through the skin) or permucosal (i.e., direct contact with mucous membranes) exposure to infectious blood or to body fluids that contain blood, and the chronically infected person is central to the epidemiology of HBV transmission. All HBsAg-positive persons are infectious, but those who are also positive for hepatitis B e antigen (HBeAg) circulate HBV at high titers in their blood (10 8-9 virions/mL) (26,27 ). With virus titers in blood this high, body fluids containing serum or blood also can contain high levels of HBV and are potentially infectious. Furthermore, HBV at titers of 10 2-3 virions/mL can be present on environmental surfaces in the absence of any visible blood and still result in transmission (28,29 ).
HBV is relatively stable in the environment and remains viable for at least 7 days on environmental surfaces at room temperature (29 ). HBsAg has been detected in dialysis centers on clamps, scissors, dialysis machine control knobs, and doorknobs (30 ). Thus, blood-contaminated surfaces that are not routinely cleaned and disinfected represent a reservoir for HBV transmission. Dialysis staff members can transfer virus to patients from contaminated surfaces by their hands or gloves or through use of contaminated equipment and supplies (30 ).
Most HBV infection outbreaks among hemodialysis patients were caused by crosscontamination to patients via a) environmental surfaces, supplies (e.g., hemostats, clamps), or equipment that were not routinely disinfected after each use; b) multiple dose medication vials and intravenous solutions that were not used exclusively for one patient; c) medications for injection that were prepared in areas adjacent to areas where blood samples were handled; and d) staff members who simultaneously cared for both HBV-infected and susceptible patients (21,(31)(32)(33)(34)(35). Once the factors that promote HBV transmission among hemodialysis patients were identified, recommendations for control were published in 1977 (19 ). These recommendations included a) serologic surveillance of patients (and staff members) for HBV infection, including monthly testing of all susceptible patients for HBsAg; b) isolation of HBsAg-positive patients in a separate room; c) assignment of staff members to HBsAg-positive patients and not to HBVsusceptible patients during the same shift; d) assignment of dialysis equipment to HBsAg-positive patients that is not shared by HBV-susceptible patients; e) assignment of a supply tray to each patient (regardless of serologic status); f) cleaning and disinfection of nondisposable items (e.g., clamps, scissors) before use on another patient; g) glove use whenever any patient or hemodialysis equipment is touched and glove changes between each patient (and station); and h) routine cleaning and disinfection of equipment and environmental surfaces.
The segregation of HBsAg-positive patients and their equipment from HBVsusceptible patients resulted in 70%-80% reductions in incidence of HBV infection among hemodialysis patients (7,(36)(37)(38). National surveillance data for 1976-1989 indicated that incidence of HBV infection was substantially lower in hemodialysis units that isolated HBsAg-positive patients, compared with those that did not (7,10 ). The success of isolation practices in preventing transmission of HBV infection is linked to other infection control practices, including routine serological surveillance and routine cleaning and disinfection. Frequent serologic testing for HBsAg detects patients recently infected with HBV quickly so isolation procedures can be implemented before cross-contamination can occur. Environmental control by routine cleaning and disinfection procedures reduces the opportunity for cross-contamination, either directly from environmental surfaces or indirectly by hands of personnel. Despite the current low incidence of HBV infection among hemodialysis patients, outbreaks continue to occur in chronic hemodialysis centers. Investigations of these outbreaks have documented that HBV transmission resulted from failure to use recommended infection control practices, including a) failure to routinely screen patients for HBsAg or routinely review results of testing to identify infected patients; b) assignment of staff members to the simultaneous care of infected and susceptible patients; and c) sharing of supplies, particularly multiple dose medication vials, among patients (21 ). In addition, few patients had received hepatitis B vaccine (21 ). National surveillance data have demonstrated that independent risk factors among chronic hemodialysis patients for acquiring HBV infection include the presence of >1 HBV-infected patient in the hemodialysis center who is not isolated, as well as a <50% hepatitis B vaccination rate among patients (15 ).
HBV infection among chronic hemodialysis patients also has been associated with hemodialysis provided in the acute-care setting (21,39 ). Transmission appeared to stem from chronically infected HBV patients who shared staff members, multiple dose medication vials, and other supplies and equipment with susceptible patients. These episodes were recognized when patients returned to their chronic hemodialysis units, and routine HBsAg testing was resumed. Transmission from HBV-infected chronic hemodialysis patients to patients undergoing hemodialysis for acute renal failure has not been documented, possibly because these patients are dialyzed for short durations and have limited exposure. However, such transmission could go unrecognized because acute renal failure patients are unlikely to be tested for HBV infection.
# Clinical Features and Natural History
HBV causes both acute and chronic hepatitis. The incubation period ranges from 45-160 days (mean: 120 days), and the onset of acute disease is usually insidious. Infants, young children (aged <10 years), and immunosuppressed adults with newly acquired HBV infection are usually asymptomatic (40 ). When present, clinical symptoms and signs might include anorexia, malaise, nausea, vomiting, abdominal pain, and jaundice. Extrahepatic manifestations of disease (e.g., skin rashes, arthralgias, and arthritis) can also occur (41 ). The case fatality rate after acute hepatitis B is 0.5%-1%.
In adults with normal immune status, most (94%-98%) recover completely from newly acquired HBV infections, eliminating virus from the blood and producing neutralizing antibody that creates immunity from future infection (40,42 ). In immunosuppressed persons (including hemodialysis patients), infants, and young children, most newly acquired HBV infections result in chronic infection. Although the consequences of acute hepatitis B can be severe, most of the serious sequelae associated with the disease occur in persons in whom chronic infection develops. Although persons with chronic HBV infection are often asymptomatic, chronic liver disease develops in two-thirds of these persons, and approximately 15%-25% die prematurely from cirrhosis or liver cancer (43)(44)(45).
Subtypes of HBV exist, and infection or immunization with one subtype confers immunity to all subtypes. However, reinfection or reactivation of latent HBV infection has been reported among certain groups of immunosuppressed patients, including those who have undergone renal transplant and those infected with human immunodeficiency virus (HIV) (46,47 ). These patients were positive for antibody to hepatitis B core antigen (anti-HBc), with or without antibody to HBsAg (anti-HBs), and subsequently developed detectable levels of HBsAg. The frequency with which this occurs is unknown.
Monotherapy with alpha interferon or lamivudine is approved by the U.S. Food and Drug Administration (FDA) to treat patients with chronic hepatitis B (48,49 ). Although the dosage of lamivudine should be modified based on creatinine clearance in patients with renal impairment, no additional dose modification is necessary after routine hemodialysis. The emergence of lamivudine-resistant variants has caused concern regarding long-term use of this drug.
# Screening and Diagnostic Tests
Serologic Assays. Several well-defined antigen-antibody systems are associated with HBV infection, including HBsAg and anti-HBs; hepatitis B core antigen (HBcAg) and anti-HBc; and HBeAg and antibody to HBeAg (anti-HBe). Serologic assays are commercially available for all of these except HBcAg because no free HBcAg circulates in blood. One or more of these serologic markers are present during different phases of HBV infection (Table 1) (42 ). The presence of HBsAg is indicative of ongoing HBV infection and potential infectiousness. In newly infected persons, HBsAg is present in serum 30-60 days after exposure to HBV and persists for variable periods. Transient HBsAg positivity (lasting <18 days) can be detected in some patients during vaccination (50,51 ). Anti-HBc develops in all HBV infections, appearing at onset of symptoms or liver test abnormalities in acute HBV infection, rising rapidly to high levels, and persisting for life. Acute or recently acquired infection can be distinguished by presence of the immunoglobulin M (IgM) class of anti-HBc, which persists for approximately 6 months.
In persons who recover from HBV infection, HBsAg is eliminated from the blood, usually in 2-3 months, and anti-HBs develops during convalescence. The presence of anti-HBs indicates immunity from HBV infection. After recovery from natural infection, most persons will be positive for both anti-HBs and anti-HBc, whereas only anti-HBs develops in persons who are successfully vaccinated against hepatitis B. Persons who do not recover from HBV infection and become chronically infected remain positive for HBsAg (and anti-HBc), although a small proportion (0.3% per year) eventually clear HBsAg and might develop anti-HBs (45 ).
In some persons, the only HBV serologic marker detected is anti-HBc (i.e., isolated anti-HBc). Among most asymptomatic persons in the United States tested for HBV infection, an average of 2% (range: <0.1%-6%) test positive for isolated anti-HBc (52 ); among injecting-drug users, however, the rate is 24% (53 ). In general, the frequency of isolated anti-HBc is directly related to the frequency of previous HBV infection in the population and can have several explanations. This pattern can occur after HBV infection among persons who have recovered but whose anti-HBs levels have waned or among persons who failed to develop anti-HBs. Persons in the latter category include those who circulate HBsAg at levels not detectable by current commercial assays. However, HBV DNA has been detected in <10% of persons with isolated anti-HBc, and these persons are unlikely to be infectious to others except under unusual circumstances involving direct percutaneous exposure to large quantities of blood (e.g., transfusion) (54 ). In most persons with isolated anti-HBc, the result appears to be a false positive. Data from several studies have demonstrated that a primary anti-HBs response develops in most of these persons after a three-dose series of hepatitis B vaccine (55,56 ). No data exist on response to vaccination among hemodialysis patients with this serologic pattern.
A third antigen, HBeAg, can be detected in serum of persons with acute or chronic HBV infection. The presence of HBeAg correlates with viral replication and high levels of virus (i.e., high infectivity). Anti-HBe correlates with the loss of replicating virus and with lower levels of virus. However, all HBsAg-positive persons should be considered potentially infectious, regardless of their HBeAg or anti-HBe status.
Nucleic Acid Detection. HBV infection can be detected using qualitative or quantitative tests for HBV DNA. These tests are not FDA-approved and are most commonly used for patients being managed with antiviral therapy (49,57 ).
# Hepatitis B Vaccine
Hepatitis B vaccine has been recommended for both hemodialysis patients and staff members since the vaccine became available in 1982 (20 ). By 1999, a total of 55% of patients and 88% of staff members had been vaccinated (18 ) (CDC, unpublished data, 2001). Two types of vaccine have been licensed and used in the United States: plasmaderived and recombinant. Plasma-derived vaccine is no longer available in the United States, but is produced in several countries and used in many immunization programs worldwide. Recombinant vaccines available in the United States are Recombivax HB™ (Merck & Company, Inc., West Point, Pennsylvania) and Engerix-B ® (SmithKline Beecham Biologicals, Philadelphia, Pennsylvania). Recombivax HB™ contains 10-40 µg of HBsAg protein per mL, whereas Engerix-B ® contains 20 µg/mL.
Primary vaccination comprises three intramuscular doses of vaccine, with the second and third doses given 1 and 6 months, respectively, after the first. An alternative schedule of four doses given at 0, 1, 2, and 12 months to persons with normal immune status or at 0, 1, 2, and 6 months to hemodialysis patients has been approved for Engerix-B ® .
Immunogenicity. The recommended primary series of hepatitis B vaccine induces a protective anti-HBs response (defined as >10 milli-International Units /mL) in 90%-95% of adults with normal immune status. The major determinant of vaccine response is age, with the proportion of persons developing a protective antibody response declining to 84% among adults aged >40 years and to 75% by age 60 years (58,59 ). Other host factors that contribute to decreased immunogenicity include smoking, obesity, and immune suppression. Compared with adults with normal immune status, the proportion of hemodialysis patients who develop a protective antibody response after vaccination (with higher dosages) is lower. For those who receive the three-dose schedule, the median is 64% (range: 34%-88%) (60)(61)(62)(63)(64)(65), and for those who receive the fourdose schedule, the median is 86% (range: 40%-98%) (66)(67)(68)(69)(70)(71)(72). Limited data indicate that concurrent infection with HCV does not interfere with development of protective levels of antibody after vaccination, although lower titers of anti-HBs have been reported after vaccination of HCV-positive patients compared with HCV-negative patients (65,(73)(74)(75).
Some studies have demonstrated that higher antibody response rates could be achieved by vaccinating patients with chronic renal failure before they become dialysis dependent, particularly patients with mild or moderate renal failure. After vaccination with four 20 µg doses of recombinant vaccine, a protective antibody response developed in 86% of predialysis adult patients with serum creatinine levels 4.0 mg/dl (mean: 9.5 mg/dl), only 12% of whom were predialysis patients (76 ). In an earlier study, a lower response to recombinant vaccine among predialysis patients was reported, possibly because patients with more severe renal failure were included (77,78 ).
Although no data exist on the response of pediatric hemodialysis patients to vaccination with standard pediatric doses, 75%-97% of those who received higher dosages (20 µg) on either the three-or four-dose schedule developed protective levels of anti-HBs (79)(80)(81). In the one study that evaluated vaccine response among children with chronic renal failure before they became dialysis dependent, high response rates were achieved after four-20 µg doses in both predialysis and dialysis-dependent patients, although predialysis patients had higher peak antibody titers (82 ).
Vaccine Efficacy. For persons with normal immune status, controlled clinical trials have demonstrated that protection from acute and chronic HBV infection is virtually complete among those who develop a protective antibody response after vaccination (83,84 ). Among hemodialysis patients, controlled clinical trials conducted in other countries demonstrated efficacy of 53%-78% after preexposure immunization (85,86 ). However, no efficacy was demonstrated in the one trial performed in the United States (62 ). When the latter trial was designed, the sample size was calculated based on an annual incidence rate among susceptible patients of 13.8% (i.e., the rate observed during 1976-1979, the period before the start of the trial). However, by the time the trial was conducted, the incidence rate had declined by >60%, and the sample size was inadequate for detecting a difference in infection rates between vaccinated and placebo groups. Although efficacy was not demonstrated in this study, no infections occurred among persons who developed and maintained protective levels of anti-HBs. Furthermore, since the hepatitis B vaccine became available, no HBV infections have been reported among vaccinated hemodialysis patients who maintained protective levels of anti-HBs. This observation has been particularly striking during HBV infection outbreaks in this setting (21 ). In addition, a case-control study indicated that the risk for HBV infection was 70% lower among hemodialysis patients who had been vaccinated (87 ). Thus, most hemodialysis patients can be protected from hepatitis B by vaccination, and maintaining immunity among these patients reduces the frequency and costs of serologic screening (88 ).
Revaccination of Nonresponders. Among persons who do not respond to the primary three-dose series of hepatitis B vaccine, 25%-50% of those with normal immune status respond to one additional vaccine dose, and 50%-75% respond to three additional doses (59,84 ). A revaccination regimen that includes serologic testing after one or two additional doses of vaccine appears to be no more cost-effective than serologic testing performed after all three additional doses (89 ). For persons found to be nonresponders after six doses of vaccine, no data exist to indicate that additional doses would induce an antibody response. Few studies have been conducted of the effect of revaccination among hemodialysis patients who do not respond to the primary vaccine series. Response rates to revaccination varied from 40%-50% after two or three additional 40 µg intramuscular doses to 64% after four additional 10 µg intramuscular doses (69,70,(90)(91)(92)(93)(94).
Antibody Persistence. Among adults with normal immune status who responded to a primary vaccine series with a protective antibody level, antibody remained above protective levels in 40%-87% of persons after 9-15 years (95)(96)(97)(98). Only short-term data are available for hemodialysis patients. Among adults who responded to the primary vaccination series, antibody remained detectable for 6 months in 80%-100% (median: 100%) of persons and for 12 months in 58%-100% (median: 70%) (61,64-69,71,85,99-103 ). Among successfully immunized hemodialysis patients whose antibody titers subsequently declined below protective levels, limited data indicate that virtually all respond to a booster dose (75 ).
Duration of Vaccine-Induced Immunity. Among persons with normal immune status who respond to the primary series of hepatitis B vaccine, protection against hepatitis B persists even when antibody titers become undetectable (97 ). However, among hemodialysis patients who respond to the vaccine, protection against hepatitis B is not maintained when antibody titers fall below protective levels. In the U.S. vaccine efficacy trial, three hemodialysis patients who responded to the primary vaccination series developed HBV infection (62 ). One had received a kidney transplant 6 months before onset of infection, and anti-HBs had declined to borderline protective levels in the other two persons. In all three patients, infection resolved.
Alternative Routes of Administration. Among adults with normal immune status, intradermal administration of low doses of hepatitis B vaccine results in lower seroconversion rates (55%-81%) (104)(105)(106), and no data exist on long-term protection from this route of administration. Among infants and children, intradermal vaccination
# Hepatitis C Virus Infection Epidemiology
Incidence and Prevalence. Data are limited on incidence of HCV infection among chronic hemodialysis patients. During 1982-1997, the incidence of non-A, non-B hepatitis among patients reported to CDC's national surveillance system decreased from 1.7% to 0.2% (18 ). The validity of these rates is uncertain because of inherent difficulties in diagnosing non-A, non-B hepatitis and probable variability in the application of diagnostic criteria by different dialysis centers. However, the downward trend can partially be explained by a decline in the rate of transfusion-associated disease after 1985 (107,108 ).
Since 1990, limited data from U.S. studies using testing for antibody to HCV (anti-HCV) to evaluate the incidence of HCV infection have reported annual rates of 0.73%-3% among hemodialysis patients (109,110 ). None of the patients who seroconverted had received transfusions in the interim or were injecting-drug users.
During 1992-1999, national surveillance data indicated that the proportion of centers that tested patients for anti-HCV increased from 22% to 56% (18 ) (CDC, unpublished data, 2001). In 1999, nationwide prevalence of anti-HCV was 8.9%, with some centers reporting prevalences >40% (CDC, unpublished data, 2001). Other studies of hemodialysis patients in the United States have reported anti-HCV prevalences of 10%-36% among adults (109,111,112 ) and 18.5% among children (113 ).
Transmission. HCV is most efficiently transmitted by direct percutaneous exposure to infectious blood, and like HBV, the chronically infected person is central to the epidemiology of HCV transmission. Risk factors associated with HCV infection among hemodialysis patients include history of blood transfusions, the volume of blood transfused, and years on dialysis (114 ). The number of years on dialysis is the major risk factor independently associated with higher rates of HCV infection. As the time patients spent on dialysis increased, their prevalence of HCV infection increased from an average of 12% for patients receiving dialysis 5 years (109,112,115 ).
These studies, as well as investigations of dialysis-associated outbreaks of hepatitis C, indicate that HCV transmission most likely occurs because of inadequate infection control practices. During 1999-2000, CDC investigated three outbreaks of HCV infection among patients in chronic hemodialysis centers (CDC, unpublished data, 1999 and2000). In two of the outbreaks, multiple transmissions of HCV occurred during periods of 16-24 months (attack rates: 6.6%-17.5%), and seroconversions were associated with receiving dialysis immediately after a chronically infected patient. Multiple opportunities for cross-contamination among patients were observed, including a) equipment and supplies that were not disinfected between patient use; b) use of common medication carts to prepare and distribute medications at patients' stations; c) sharing of multiple dose medication vials, which were placed at patients' stations on top of hemodialysis machines; d) contaminated priming buckets that were not routinely changed or cleaned and disinfected between patients; e) machine surfaces that were not routinely cleaned and disinfected between patients; and f) blood spills that were not cleaned up promptly. In the third outbreak, multiple new infections clustered at one point in time (attack rate: 27%), suggesting a common exposure event. Although the specific results of this investigation are pending, multiple opportunities for crosscontamination from chronically infected patients also were observed in this unit. In particular, supply carts were moved from one station to another and contained both clean supplies and blood-contaminated items, including small biohazard containers, sharps disposal boxes, and used vacutainers containing patients' blood.
# Clinical Features and Natural History
HCV causes both acute and chronic hepatitis. The incubation period ranges from 14-180 days (average: 6-7 weeks) (116 ). Persons with newly acquired (acute) HCV infection typically are either asymptomatic or have a mild clinical illness. The course of acute hepatitis C is variable, although elevations in serum alanine aminotransferase (ALT) levels, often in a fluctuating pattern, are the most characteristic feature. Fulminant hepatic failure after acute hepatitis C is rare.
Most (average: 94%) hemodialysis patients with newly acquired HCV infection have elevated serum ALT levels (117)(118)(119)(120)(121). Elevations in serum ALT levels often precede anti-HCV seroconversion. Among prospectively followed transfusion recipients who developed acute HCV infection, elevated ALT levels preceded anti-HCV seroconversion (as measured by second generation assays) in 59%, and anti-HCV was detectable in most patients (78%) within 5 weeks after their first ALT elevation (122 ). However, elevations in ALT or aspartate aminotransferase (AST) levels can occur that are not related to viral hepatitis, and compared with ALT, AST is a less specific indicator of HCV-related liver disease among hemodialysis patients. In a recent outbreak investigation, only 28% of 25 hemodialysis patients with newly observed elevations in AST levels tested anti-HCV positive (CDC, unpublished data, 1999).
After acute HCV infection, 15%-25% of persons with normal immune status appear to resolve their infection without sequelae as defined by sustained absence of HCV RNA in serum and normalization of ALT (123 ). In some persons, ALT levels normalize, suggesting full recovery, but this is frequently followed by ALT elevations that indicate progression to chronic disease. Chronic HCV infection develops in most infected persons (75%-85%). Of persons with chronic HCV infection, 60%-70% have persistent or fluctuating ALT elevations, indicating active liver disease (123 ). Although similar rates of chronic liver disease have been observed among HCV-infected chronic hemodialysis patients (based on liver biopsy results), these patients might be less likely to have biochemical evidence of active liver disease (124 ). In seroprevalence studies of chronic hemodialysis patients, ALT elevations were reported in a median of 33.9% (range: 6%-73%) of patients who tested positive for anti-HCV (117,(124)(125)(126)(127)(128)(129)(130)(131)(132)(133)(134)(135)(136).
No clinical or epidemiologic features among patients with acute infection have been reported to be predictive of either persistent infection or chronic liver disease. Most studies have reported that cirrhosis develops in 10%-20% of persons who have had chronic hepatitis C for 20-30 years, and hepatocellular carcinoma in 1%-5% (123 ). Extrahepatic manifestations of chronic HCV infection are considered to be of immunologic origin and include cryoglobulinemia, membranoproliferative glomerulonephritis, and porphyria cutanea tarda (137 ).
At least six different genotypes and >90 subtypes of HCV exist, with genotype 1 being the most common in the United States (138,139 ). Unlike HBV, infection with one
MMWR 11
HCV genotype or subtype does not protect against reinfection or superinfection with other HCV strains (139 ). Alpha interferon alone or in combination with ribavirin is FDA-approved for the treatment of chronic hepatitis C (48,140,141 ). Combination therapy should be used with caution in patients with creatinine clearance <50 mL/minute and generally is contraindicated in patients with renal failure (141,142 ). Interferon monotherapy results in low sustained virologic response rates (141,142 ).
# Screening and Diagnostic Tests
Serologic Assays. The only FDA-approved tests for diagnosis of HCV infection are those that measure anti-HCV and include enzyme immunoassays (EIAs) and a supplemental recombinant immunoblot assay (RIBA™) (116 ). These tests detect anti-HCV in >97% of infected persons, but do not distinguish between acute, chronic, or resolved infection. The average time from exposure to seroconversion is 8-9 weeks (122 ). Anti-HCV can be detected in 80% of patients within 15 weeks after exposure, in >90% within 5 months, and in >97% within 6 months (122,143 ). In rare instances, seroconversion can be delayed until 9 months after exposure (143,144 ). Anti-HCV persists indefinitely in most persons, but does not protect against reinfection.
As with any screening test, the positive predictive value of EIAs for anti-HCV is directly related to the prevalence of infection in the population and is low in populations with an HCV-infection prevalence <10% (145,146 ). Supplemental testing with a more specific assay (i.e., RIBA™) of a specimen with a positive anti-HCV result by EIA prevents reporting of false-positive results, particularly in settings where asymptomatic persons are being tested. Results of seroprevalence studies among chronic hemodialysis patients have indicated that 57%-100% of EIA positive results were RIBA™ positive (124,126,128,133,135,(147)(148)(149)(150)(151)(152), and 53%-100% were HCV RNA positive by reverse transcriptase polymerase chain reaction (RT-PCR) testing (117,127,129,134,135 ).
Nucleic Acid Detection. The diagnosis of HCV infection also can be made by qualitatively detecting HCV RNA using gene amplification techniques (e.g., RT-PCR) (116 ). HCV RNA can be detected in serum or plasma within 1-2 weeks after exposure and weeks before onset of ALT elevations or the appearance of anti-HCV. In rare instances, detection of HCV RNA might be the only evidence of HCV infection. Although a median of 3.4% (range: 0%-28%) of chronic hemodialysis patients who tested anti-HCV negative were HCV RNA positive, this might be an overestimate because follow-up samples to detect possible antibody seroconversions were not obtained on these patients (117,118,(126)(127)(128)130,131,133,134,(148)(149)(150)(151)(152)(153)(154).
Although not FDA-approved, RT-PCR assays for HCV infection are used commonly in clinical practice and are commercially available. Most RT-PCR assays have a lower limit of detection of 100-1,000 viral genome copies per mL. With adequate optimization of RT-PCR assays, 75%-85% of persons who are positive for anti-HCV and >95% of persons with acute or chronic hepatitis C will test positive for HCV RNA. Some HCVinfected persons might be only intermittently HCV RNA positive, particularly those with acute hepatitis C or with end-stage liver disease caused by hepatitis C. To minimize false-negative results, blood samples collected for RT-PCR should not contain heparin, and serum must be separated from cellular components within 2-4 hours after collection and preferably stored frozen at -20 C or -70 C (155 ). If shipping is required, frozen samples should be protected from thawing. Because of assay variability, rigorous quality assurance and control should be in place in clinical laboratories performing this assay, and proficiency testing is recommended. Quantitative assays for measuring the concentration (i.e., titer) of HCV RNA have been developed and are available from commercial laboratories (156 ). These assays also are not FDA-approved and are less sensitive than qualitative RT-PCR assays (157 ). Quantitative assays should not be used as a primary test to confirm or exclude the diagnosis of HCV infection or to monitor the endpoint of treatment, and sequential measurement of HCV RNA levels has not proven useful in managing patients with hepatitis C.
# Other Bloodborne Viruses Hepatitis Delta Virus Infection
Delta hepatitis is caused by the hepatitis delta virus (HDV), a defective virus that causes infection only in persons with active HBV infection. The prevalence of HDV infection is low in the United States, with rates of 10% among HBsAg-positive persons with repeated percutaneous exposures (e.g., injecting-drug users, persons with hemophilia) (158 ). Areas of the world with high endemic rates of HDV infection include southern Italy, parts of Africa, and the Amazon Basin.
Few data exist on the prevalence of HDV infection among chronic hemodialysis patients, and only one transmission of HDV between such patients has been reported in the United States (159 ). In this episode, transmission occurred from a patient who was chronically infected with HBV and HDV to an HBsAg-positive patient after a massive bleeding incident; both patients received dialysis at the same station.
HDV infection occurs either as a co-infection with HBV or as a superinfection in a person with chronic HBV infection. Co-infection usually resolves, but superinfection frequently results in chronic HDV infection and severe disease. High mortality rates are associated with both types of infection. A serologic test that measures total antibody to HDV (anti-HDV) is commercially available.
# Human Immunodeficiency Virus Infection
During 1985-1999, the percentage of U.S. hemodialysis centers that reported providing chronic hemodialysis for patients with HIV infection increased from 11% to 39%, and the proportion of hemodialysis patients with known HIV infection increased from 0.3% to 1.4% (18 ) (CDC, unpublished data, 2001).
HIV is transmitted by blood and other body fluids that contain blood. No patient-topatient transmission of HIV has been reported in U.S. hemodialysis centers. However, such transmission has been reported in other countries; in one case, HIV transmission was attributed to mixing of reused access needles and inadequate disinfection of equipment (160 ).
HIV infection is usually diagnosed with assays that measure antibody to HIV, and a repeatedly positive EIA test should be confirmed by Western blot or another confirmatory test. Antiretroviral therapies for HIV-infected hemodialysis patients are commonly used and appear to be improving survival rates among this population. However, hepatotoxicity associated with certain protease inhibitors might limit the use of these drugs, especially in patients with underlying liver dysfunction (161 ).
# MMWR 13
# Bacterial Infections
Epidemiology Disease Burden. The annual mortality rate among hemodialysis patients is 23%, and infections are the second most common cause, accounting for 15% of deaths (1 ). Septicemia (10.9% of all deaths) is the most common infectious cause of mortality. In various studies evaluating rates of bacterial infections in hemodialysis outpatients, bacteremia occurred in 0.63%-1.7% of patients per month and vascular access infections (with or without bacteremia) in 1.3%-7.2% of patients per month (162)(163)(164)(165)(166)(167)(168)(169)(170). National surveillance data indicated that 4%-5% of patients received intravenous vancomycin during a 1-month period (and additional patients received other antimicrobials) (18 ). Although data on vancomycin use can be used to derive an estimate of the prevalence of suspected infections, the proportion of patients receiving antimicrobials who would fit a formal case definition for bacterial infection is unknown.
Infection Sites. In a study of 27 French hemodialysis centers, 28% of 230 infections in hemodialysis patients involved the vascular access, whereas 25% involved the lung, 23% the urinary tract, 9% the skin and soft tissues, and 15% other or unknown sites (165 ). Thirty-three percent of infections involved either the vascular access site or were bacteremias of unknown origin, many of which might have been caused by occult access infections. Thus, the vascular access site was the most common site for infection, but accounted for only one-third of infections. However, access site infections are particularly important because they can cause disseminated bacteremia or loss of the vascular access.
Vascular Access Infections. Vascular access infections are caused (in descending order of frequency) by S. aureus, coagulase-negative staphylococci (CNS), gramnegative bacilli, nonstaphylococcal gram-positive cocci (including enterococci), and fungi (171 ). The proportion of infections caused by CNS is higher among patients dialyzed through catheters than among patients dialyzed through fistulas or grafts.
The primary risk factor for access infection is access type, with catheters having the highest risk for infection, grafts intermediate, and native arteriovenous (AV) fistulas the lowest (168 ). Other potential risk factors for vascular access infections include a) location of the access in the lower extremity; b) recent access surgery; c) trauma, hematoma, dermatitis, or scratching over the access site; d) poor patient hygiene; e) poor needle insertion technique; f) older age; g) diabetes; h) immunosuppression; and i) iron overload (164,167,(172)(173)(174)(175).
Transmission. Bacterial pathogens causing infection can be either exogenous (i.e, acquired from contaminated dialysis fluids or equipment) or endogenous (i.e., caused by invasion of bacteria present in or on the patient). Exogenous pathogens have caused numerous outbreaks, most of which resulted from inadequate dialyzer reprocessing procedures (e.g., contaminated water or inadequate disinfectant) or inadequate treatment of municipal water for use in dialysis. During 1995-1997, four outbreaks were traced to contamination of the waste drain port on one type of dialysis machine (176 ).
Recommendations to prevent such outbreaks are published elsewhere (171 ).
Contaminated medication vials also are a potential source of bacterial infection for patients. In 1999, an outbreak of Serratia liquefaciens bloodstream infections and pyrogenic reactions among hemodialysis patients was traced to contamination of vials of erythropoietin. These vials, which were intended for single use, were contaminated by repeated puncture to obtain additional doses and by pooling of residual medication into a common vial (177 ). Endogenous pathogens first colonize the patient and later cause infection. Colonization means that microorganisms have become resident in or on the body (e.g., in the nares or stool); a culture from the site is positive, but no symptoms or signs of infection exist. Colonization with potentially pathogenic microorganisms, often unknown to staff members, is common in patients with frequent exposure to hospitals and other healthcare settings. Colonization most often occurs when microorganisms are transmitted from a colonized or infected source patient to another patient on the hands of healthcare workers who do not comply with infection control precautions. Less commonly, contamination of environmental surfaces (e.g., bed rails, countertops) plays a role (178 ).
Infection occurs when microorganisms invade the body, damaging tissue and causing signs or symptoms of infection, and is aided by invasive devices (e.g., the hemodialysis vascular access). Evidence exists that when prevalence of colonization in a population is less frequent, infection in that population will also be less frequent, and infection control recommendations for hemodialysis units are designed to prevent colonization (179 ). Additional measures designed to prevent infection from colonizing organisms (e.g., using aseptic technique during vascular access) are presented elsewhere (180 ).
# Antimicrobial Resistance
Antimicrobial-resistant bacteria are more common in patients with severe illness, who often have had multiple hospitalizations or surgical procedures, and in those who have received prolonged courses of antimicrobial agents. In health-care settings, including hemodialysis centers, such patients can serve as a source for transmission.
Clinically important drug-resistant bacteria that commonly cause health-careassociated infections include MRSA, methicillin-resistant CNS, VRE, and multidrugresistant gram negative rods, including strains of Pseudomonas aeruginosa, Stenotrophomonas maltophilia, and Acinetobacter species, some of which are resistant to all available antimicrobials. In addition, strains of S. aureus with intermediate resistance to vancomycin and other glycopeptide antibiotics have recently been reported; these strains are called vancomycin-intermediate S. aureus (VISA) or glycopeptide-intermediate S. aureus (GISA) (181,182 ). Intermediate resistance to vancomycin is reported even more frequently among CNS (183,184 ).
Hemodialysis patients have played a prominent role in the epidemic of vancomycin resistance. In 1988, a renal unit in London, England, reported one of the first cases of VRE (185 ). In three studies, 12%-22% of hospitalized patients infected or colonized with VRE were receiving hemodialysis (178,186,187 ). Furthermore, three of the first five patients identified with VISA (or GISA) were on chronic hemodialysis, and one had received acute dialysis (182 ).
Prevalence of VRE has increased rapidly at U.S. hospitals; among intensive care unit patients with nosocomial infections reported to the National Nosocomial Infections Surveillance (NNIS) system, the percentage of enterococcal isolates resistant to vancomycin increased from 0.5% in 1989 to 25.2% in 1999 (23 ) (CDC, unpublished data, 2000). This increase is attributable to patient-to-patient transmission in healthcare settings and transmission of resistant genes among previously susceptible enterococci. Once vancomycin resistance has been transferred to a patient, antimicrobials select for resistant organisms, causing them to increase in number relative to suscep-tible organisms. Prevalence of VRE colonization among patients varies in different health-care settings; in hemodialysis centers, the reported prevalence in stool samples ranged from 1% to 9% (188,189 ). In one center with a prevalence of 9%, three patients developed VRE infections in 1 year (188 ).
# Vancomycin Use
Dialysis patients have played a prominent role in the epidemic of vancomycin resistance because this drug is used commonly in these patients, in part because vancomycin can be conveniently administered to patients when they come in for hemodialysis treatments. However, two studies indicate that cefazolin, a first-generation cephalosporin, could be substituted for vancomycin in many patients (190,191 ). One of these studies reported that many pathogens causing infections in hemodialysis patients are susceptible to cefazolin (190 ), and both studies reported therapeutic cefazolin blood levels 48-72 hours after dosing, making in-center administration three times a week after dialysis feasible.
# Equipment, Supplies, and Environmental Surfaces
The hemodialysis machine and its components also can be vehicles for patient-topatient transmission of bloodborne viruses and pathogenic bacteria (24,192 ). The external surfaces of the machine are the most likely sources for contamination. These include not only frequently touched surfaces (e.g., the control panel), but also attached waste containers used during the priming of the dialyzers, blood tubing draped or clipped to waste containers, and items placed on tops of machines for convenience (e.g., dialyzer caps and medication vials).
# Sterilization, Disinfection, and Cleaning
A sterilization procedure kills all microorganisms, including highly resistant bacterial spores (24 ). Sterilization procedures are most commonly accomplished by steam or ethylene oxide gas. For products that are heat sensitive, an FDA-cleared liquid chemical sterilant can be used with a long exposure time (i.e., 3-10 hours).
High-level disinfection kills all viruses and bacteria, but not high numbers of bacterial spores. High-level disinfection can be accomplished by heat pasteurization or, more commonly, by an FDA-cleared chemical sterilant, with an exposure time of 12-45 minutes. Sterilants and high-level disinfectants are designed to be used on medical devices, not environmental surfaces. Intermediate-level disinfection kills bacteria and most viruses and is accomplished by using a tuberculocidal "hospital disinfectant" (a term used by the U.S. Environmental Protection Agency in registering germicides) or a 1:100 dilution of bleach (300-600 mg/L free chlorine). Low-level disinfection kills most bacteria and is accomplished by using general purpose disinfectants. Intermediate and low-level disinfectants are designed to be used on environmental surfaces; they also can be used on noncritical medical devices, depending on the design and labeling claim.
Cleaning eliminates dirt and some bacteria and viruses and is accomplished by using a detergent or detergent germicide. Antiseptics (e.g., formulations with povidone-iodine, hexachlorophene, or chlorhexidene) are designed for use on skin and tissue and should not be used on medical equipment or environmental surfaces.
# MMWR April 27, 2001
Regardless of the procedure used, cleaning with a germicidal detergent before disinfection (or sterilization) is essential to remove organic material (e.g., blood, mucous, or feces), dirt, or debris. The presence of such material protects microorganisms from the sterilization or disinfection process by physically blocking or inactivating the disinfectant or sterilant.
The choice of what procedure or which chemical germicide to use for medical devices, instruments, and environmental surfaces depends on several factors, including the need to maintain the structural integrity and function of the item and how the item will be used. Three general categories of use for medical items are recognized, each of which require different levels of sterilization or disinfection (193 ). These categories are a) critical, which includes items introduced directly into the bloodstream or normally sterile areas of the body (e.g., needles, catheters, hemodialyzers, blood tubing); b) semicritical, which includes equipment that comes in contact with intact mucous membranes (e.g., fiberoptic endoscopes, glass thermometers); and c) noncritical, which includes equipment that touches only intact skin (e.g., blood pressure cuffs). Semicritical items are not generally used in dialysis units.
Internal Pathways of Hemodialysis Machines. In single-pass hemodialysis machines, the internal fluid pathways are not subject to contamination with blood. If a dialyzer leak occurs, dialysis fluid might become contaminated with blood, but this contaminated fluid is discarded through a drain and does not return to the dialysis machine to contaminate predialyzer surfaces. For dialysis machines that use a dialysate recirculating system (e.g., some ultrafiltration control machines and those that regenerate the dialysate), a blood leak in a dialyzer could contaminate the internal pathways of the machine, which could in turn contaminate the dialysis fluid of subsequent patients (192 ). However, procedures normally practiced after each use (i.e., draining the dialysis fluid and rinsing and disinfecting the machine) will reduce the level of contamination to below infectious levels. In addition, an intact dialyzer membrane will not allow passage of bacteria or viruses (24 ).
Pressure transducer filter protectors are used primarily to prevent contamination and preserve the functioning of the pressure monitoring (i.e., arterial, venous, or both) components of the hemodialysis machine. Hemodialysis machines usually have both external (typically supplied with the blood tubing set) and internal protectors, with the internal protector serving as a backup in case the external transducer protector fails. Failure to use an external protector or to replace the protector when it becomes contaminated (i.e., wetted with saline or blood) can result in contamination of the internal transducer protector, which in turn could allow transmission of bloodborne pathogens (24 ). However, no epidemiologic evidence exists that contamination of the internal transducer protector caused by failure of the external transducer protector has led to either mixing of blood or the transmission of bloodborne agents.
Dialyzer Reprocessing. Approximately 80% of U.S. chronic hemodialysis centers reprocess (i.e., reuse) dialyzers for the same patient (18 ), and guidelines for reprocessing have been published elsewhere (see Suggested Readings). Although outbreaks of bacterial infections and pyrogenic reactions have occurred because of inadequate reprocessing procedures and failure to maintain standards for water quality, reuse has not been associated with transmission of bloodborne viruses. Any theoretical risk for HBV transmission from reuse of dialyzers would primarily affect staff members who handle these dialyzers. Although no increase in HBV (or HCV) infection among staff members who work in such centers has been reported, many centers do not reuse dialyzers from HBsAg-positive patients (24 ).
# Infection Control Precautions for Outpatient Hemodialysis Settings Compared with Inpatient Hospital Settings
Contact transmission is the most important route by which pathogens are transmitted in health-care settings, including hemodialysis units. Contact transmission occurs most commonly when microorganisms from a patient are transferred to the hands of a health-care worker who does not comply with infection control precautions, then touches another patient. Less commonly, environmental surfaces (e.g., bed rails, countertops) become contaminated and serve as an intermediate reservoir for pathogens; transmission can occur when a worker touches the surface then touches a patient or when a patient touches the surface.
In the hemodialysis setting, contact transmission plays a major role in transmission of bloodborne pathogens. If a health-care worker's hands become contaminated with virus-infected blood from one patient, the worker can transfer the virus to a second patient's skin or blood line access port, and the virus can be inoculated into that patient when the skin or access port is punctured with a needle.
Contact transmission can be prevented by hand hygiene (i.e., hand washing or use of a waterless hand rub), glove use, and disinfection of environmental surfaces. Of these, hand hygiene is the most important. In addition, nonsterile disposable gloves provide a protective barrier for workers' hands, preventing them from becoming soiled or contaminated, and reduce the likelihood that microorganisms present on the hands of personnel will be transmitted to patients. However, even with glove use, hand washing is needed because pathogens deposited on the outer surface of gloves can be detected on hands after glove removal, possibly because of holes or defects in the gloves, leakage at the wrist, or contamination of hands during glove removal (194 ).
Standard Precautions are the system of infection control precautions recommended for the inpatient hospital setting (195 ). Standard Precautions are used on all patients and include use of gloves, gown, or mask whenever needed to prevent contact of the health-care worker with blood, secretions, excretions, or contaminated items.
In addition to Standard Precautions, more stringent precautions are recommended for hemodialysis units because of the increased potential for contamination with blood and pathogenic microorganisms (see Infection Control Practices Recommended for Hemodialysis Units). For example, infection control practices for hemodialysis units restrict the use of common supplies, instruments, medications, and medication trays and prohibit the use of a common medication cart.
For certain patients, including those infected or colonized with MRSA or VRE, contact precautions are used in the inpatient hospital setting. Contact precautions include a) placing the patient in a single room or with another patient infected or colonized with the same organism; b) using gloves whenever entering the patient's room; and c) using a gown when entering the patient's room if the potential exists for the worker's clothing to have substantial contact with the patient, environmental surfaces, or items in the patient's room. Workers also should wear a gown if the patient has diarrhea, an ileostomy, a colostomy, or wound drainage not contained by a dressing.
However, contact precautions are not recommended in hemodialysis units for patients infected or colonized with pathogenic bacteria for several reasons. First, although contact transmission of pathogenic bacteria is well-documented in hospitals, similar transmission has not been well-documented in hemodialysis centers. Transmission might not be apparent in dialysis centers, possibly because it occurs less frequently than in acute-care hospitals or results in undetected colonization rather than overt infection. Also, because dialysis patients are frequently hospitalized, determining whether transmission occurred in the inpatient or outpatient setting is difficult. Second, contamination of the patient's skin, bedclothes, and environmental surfaces with pathogenic bacteria is likely to be more common in hospital settings (where patients spend 24 hours a day) than in outpatient hemodialysis centers (where patients spend approximately 10 hours a week). Third, the routine use of infection control practices recommended for hemodialysis units, which are more stringent than the Standard Precautions routinely used in hospitals, should prevent transmission by the contact route.
# RECOMMENDATIONS Rationale
Preventing transmission among chronic hemodialysis patients of bloodborne viruses and pathogenic bacteria from both recognized and unrecognized sources of infection requires implementation of a comprehensive infection control program. The components of such a program include infection control practices specifically designed for the hemodialysis setting, including routine serologic testing and immunization, surveillance, and training and education (Box).
The infection control practices recommended for hemodialysis units will reduce opportunities for patient-to-patient transmission of infectious agents, directly or indirectly via contaminated devices, equipment and supplies, environmental surfaces, or hands of personnel. These practices should be carried out routinely for all patients in the chronic hemodialysis setting because of the increased potential for blood contamination during hemodialysis and because many patients are colonized or infected with pathogenic bacteria. Such practices include additional measures to prevent HBV transmission because of the high titer of HBV and its ability to survive on environmental surfaces. For patients at increased risk for transmission of pathogenic bacteria, includ-
# BOX. Components of a comprehensive infection control program to prevent transmission of infections among chronic hemodialysis patients
- Infection control practices for hemodialysis units.
-Infection control precautions specifically designed to prevent transmission of bloodborne viruses and pathogenic bacteria among patients.
-Routine serologic testing for hepatitis B virus and hepatitis C virus infections.
-Vaccination of susceptible patients against hepatitis B.
-Isolation of patients who test positive for hepatitis B surface antigen.
- Surveillance for infections and other adverse events.
- Infection control training and education.
ing antimicrobial-resistant strains, additional precautions also might be necessary in some circumstances. Furthermore, surveillance for infections and other adverse events is required to monitor the effectiveness of infection control practices, as well as training and education of both staff members and patients to ensure that appropriate infection control behaviors and techniques are carried out.
# Infection Control Practices for Hemodialysis Units
In each chronic hemodialysis unit, policies and practices should be reviewed and updated to ensure that infection control practices recommended for hemodialysis units are implemented and rigorously followed (see Recommended Infection Control Practices for Hemodialysis Units at a Glance). Intensive efforts must be made to educate new staff members and reeducate existing staff members regarding these practices.
# Infection Control Precautions for All Patients
During the process of hemodialysis, exposure to blood and potentially contaminated items can be routinely anticipated; thus, gloves are required whenever caring for a patient or touching the patient's equipment. To facilitate glove use, a supply of clean nonsterile gloves and a glove discard container should be placed near each dialysis station. Hands always should be washed after gloves are removed and between patient contacts, as well as after touching blood, body fluids, secretions, excretions, and contaminated items. A sufficient number of sinks with warm water and soap should be available to facilitate hand washing. If hands are not visibly soiled, use of a waterless antiseptic hand rub can be substituted for hand washing.
Any item taken to a patient's dialysis station could become contaminated with blood and other body fluids and serve as a vehicle of transmission to other patients either directly or by contamination of the hands of personnel. Therefore, items taken to a patient's dialysis station, including those placed on top of dialysis machines, should either be disposed of, dedicated for use only on a single patient, or cleaned and disinfected before being returned to a common clean area or used for other patients. Unused medications or supplies (e.g., syringes, alcohol swabs) taken to the patient's station should not be returned to a common clean area or used on other patients.
Additional measures to prevent contamination of clean or sterile items include a) preparing medications in a room or area separated from the patient treatment area and designated only for medications; b) not handling or storing contaminated (i.e., used) supplies, equipment, blood samples, or biohazard containers in areas where medications and clean (i.e., unused) equipment and supplies are handled; and c) delivering medications separately to each patient. Common carts should not be used within the patient treatment area to prepare or distribute medications. If trays are used to distribute medications, clean them before using for a different patient.
Intravenous medication vials labeled for single use, including erythropoetin, should not be punctured more than once (196,197 ). Once a needle has entered a vial labeled for single use, the sterility of the product can no longer be guaranteed. Residual medication from two or more vials should not be pooled into a single vial.
If a common supply cart is used to store clean supplies in the patient treatment area, this cart should remain in a designated area at a sufficient distance from patient stations to avoid contamination with blood. Such carts should not be moved between stations to distribute supplies.
# MMWR April 27, 2001
# Recommended Infection Control Practices for Hemodialysis Units at a Glance Infection Control Precautions for All Patients
- Wear disposable gloves when caring for the patient or touching the patient's equipment at the dialysis station; remove gloves and wash hands between each patient or station.
- Items taken into the dialysis station should either be disposed of, dedicated for use only on a single patient, or cleaned and disinfected before being taken to a common clean area or used on another patient.
-Nondisposable items that cannot be cleaned and disinfected (e.g., adhesive tape, cloth-covered blood pressure cuffs) should be dedicated for use only on a single patient.
-Unused medications (including multiple dose vials containing diluents) or supplies (e.g., syringes, alcohol swabs) taken to the patient's station should be used only for that patient and should not be returned to a common clean area or used on other patients.
- When multiple dose medication vials are used (including vials containing diluents), prepare individual patient doses in a clean (centralized) area away from dialysis stations and deliver separately to each patient. Do not carry multiple dose medication vials from station to station.
# Hepatitis B Vaccination
- Vaccinate all susceptible patients against hepatitis B.
- Test for anti-HBs 1-2 months after last dose.
-If anti-HBs is <10 mIU/mL, consider patient susceptible, revaccinate with an additional three doses, and retest for anti-HBs.
-If anti-HBs is >10 mIU/mL, consider patient immune, and retest annually.
-Give booster dose of vaccine if anti-HBs declines to <10 mIU/mL and continue to retest annually.
# Management of HBsAg-Positive Patients
- Follow infection control practices for hemodialysis units for all patients.
- Dialyze HBsAg-positive patients in a separate room using separate machines, equipment, instruments, and supplies.
- Staff members caring for HBsAg-positive patients should not care for HBV-susceptible patients at the same time (e.g., during the same shift or during patient changeover).
- Clean areas should be clearly designated for the preparation, handling, and storage of medications and unused supplies and equipment. Clean areas should be clearly separated from contaminated areas where used supplies and equipment are handled. Do not handle and store medications or clean supplies in the same or an adjacent area to where used equipment or blood samples are handled.
- Use external venous and arterial pressure transducer filters/protectors for each patient treatment to prevent blood contamination of the dialysis machines' pressure monitors. Change filters/protectors between each patient treatment, and do not reuse them. Internal transducer filters do not need to be changed routinely between patients.
- Clean and disinfect the dialysis station (e.g., chairs, beds, tables, machines) between patients.
-Give special attention to cleaning control panels on the dialysis machines and other surfaces that are frequently touched and potentially contaminated with patients' blood.
-Discard all fluid and clean and disinfect all surfaces and containers associated with the prime waste (including buckets attached to the machines).
- For dialyzers and blood tubing that will be reprocessed, cap dialyzer ports and clamp tubing. Place all used dialyzers and tubing in leakproof containers for transport from station to reprocessing or disposal area.
# MMWR April 27, 2001
Staff members should wear gowns, face shields, eye wear, or masks to protect themselves and prevent soiling of clothing when performing procedures during which spurting or spattering of blood might occur (e.g., during initiation and termination of dialysis, cleaning of dialyzers, and centrifugation of blood). Such protective clothing or gear should be changed if it becomes soiled with blood, body fluids, secretions, or excretions. Staff members should not eat, drink, or smoke in the dialysis treatment area or in the laboratory. However, patients can be served meals or eat food brought from home at their dialysis station. The glasses, dishes, and other utensils should be cleaned in the usual manner; no special care of these items is needed.
Cleaning and Disinfection. Establish written protocols for cleaning and disinfecting surfaces and equipment in the dialysis unit, including careful mechanical cleaning before any disinfection process (Table 2). If the manufacturer has provided instructions on sterilization or disinfection of the item, these instructions should be followed. For each chemical sterilant and disinfectant, follow the manufacturer's instructions regarding use, including appropriate dilution and contact time.
After each patient treatment, clean environmental surfaces at the dialysis station, including the dialysis bed or chair, countertops, and external surfaces of the dialysis machine, including containers associated with the prime waste. Use any soap, detergent, or detergent germicide. Between uses of medical equipment (e.g., scissors, hemostats, clamps, stethoscopes, blood pressure cuffs), clean and apply a hospital disinfectant (i.e., low-level disinfection); if the item is visibly contaminated with blood, use a tuberculocidal disinfectant (i.e., intermediate-level disinfection).
For a blood spill, immediately clean the area with a cloth soaked with a tuberculocidal disinfectant or a 1:100 dilution of household bleach (300-600 mg/L free chlorine) (i.e., intermediate-level disinfection). The staff member doing the cleaning should wear gloves, and the cloth should be placed in a bucket or other leakproof container. After all visible blood is cleaned, use a new cloth or towel to apply disinfectant a second time.
Published methods should be used to clean and disinfect the water treatment and distribution system and the internal circuits of the dialysis machine, as well as to repro- Environmental surfaces, including exterior surfaces of hemodialysis machines X - Careful mechanical cleaning to remove debris should always be done before disinfection. † Water treatment and distribution systems of dialysis fluid concentrates require more extensive disinfection if significant biofilm is present within the system. § If item is visibly contaminated with blood, use a tuberculocidal disinfectant. cess dialyzers for reuse (see Suggested Readings). These methods are designed to control bacterial contamination, but will also eliminate bloodborne viruses. For singlepass machines, perform rinsing and disinfection procedures at the beginning or end of the day. For batch recirculating machines, drain, rinse, and disinfect after each use. Follow the same methods for cleaning and disinfection if a blood leak has occurred, regardless of the type of dialysis machine used. Routine bacteriologic assays of water and dialysis fluids should be performed according to the recommendations of the Association for the Advancement of Medical Instrumentation (see Suggested Readings).
Venous pressure transducer protectors should be used to cover pressure monitors and should be changed between patients, not reused. If the external transducer protector becomes wet, replace immediately and inspect the protector. If fluid is visible on the side of the transducer protector that faces the machine, have qualified personnel open the machine after the treatment is completed and check for contamination. This includes inspection for possible blood contamination of the internal pressure tubing set and pressure sensing port. If contamination has occurred, the machine must be taken out of service and disinfected using either 1:100 dilution of bleach (300-600 mg/L free chlorine) or a commercially available, EPA-registered tuberculocidal germicide before reuse. Frequent blood line pressure alarms or frequent adjusting of blood drip chamber levels can be an indicator of this problem. Taken separately, these incidents could be characterized as isolated malfunctions. However, the potential public health significance of the total number of incidents nationwide make it imperative that all incidents of equipment contamination be reported immediately to the FDA (800-FDA-1088).
Housekeeping staff members in the dialysis facility should promptly remove soil and potentially infectious waste and maintain an environment that enhances patient care. All disposable items should be placed in bags thick enough to prevent leakage. Wastes generated by the hemodialysis facility might be contaminated with blood and should be considered infectious and handled accordingly. These solid medical wastes should be disposed of properly in an incinerator or sanitary landfill, according to local and state regulations governing medical waste disposal.
Hemodialysis in Acute-Care Settings. For patients with acute renal failure who receive hemodialysis in acute-care settings, Standard Precautions as applied in all healthcare settings are sufficient to prevent transmission of bloodborne viruses. However, when chronic hemodialysis patients receive maintenance hemodialysis while hospitalized, infection control precautions specifically designed for chronic hemodialysis units (see Recommended Practices at a Glance) should be applied to these patients. If both acute and chronic renal failure patients receive hemodialysis in the same unit, these infection control precautions should be applied to all patients.
Regardless of where in the acute-care setting chronic hemodialysis patients receive dialysis, the HBsAg status of all such patients should be ascertained at the time of admission to the hospital, by either a written report from the referring center (including the most recent date testing was performed) or by a serologic test. The HBV serologic status should be prominently placed in patients' hospital records, and all health-care personnel assigned to these patients, as well as the infection control practitioner, should be aware of the patients' serologic status. While hospitalized, HBsAg-positive chronic hemodialysis patients should undergo dialysis in a separate room and use separate machines, equipment, instruments, supplies, and medications designated only for HBsAg-positive patients (see Prevention and Management of HBV Infection). While HBsAg-positive patients are receiving dialysis, staff members who are caring for them should not care for susceptible patients.
# MMWR April 27, 2001
Routine Serologic Testing Chronic Hemodialysis Patients. Routinely test all chronic hemodialysis patients for HBV and HCV infection (see Recommended Practices at a Glance), promptly review results, and ensure that patients are managed appropriately based on their testing results (see later recommendations for each virus). Communicate test results (positive and negative) to other units or hospitals when patients are transferred for care. Routine testing for HDV or HIV infection for purposes of infection control is not recommended.
The HBV serologic status (i.e., HBsAg, total anti-HBc, and anti-HBs) of all patients should be known before admission to the hemodialysis unit. For patients transferred from another unit, test results should be obtained before the patients' transfer. If a patient's HBV serologic status is not known at the time of admission, testing should be completed within 7 days. The hemodialysis unit should ensure that the laboratory performing the testing for anti-HBs can define a 10 mIU/mL concentration to determine protective levels of antibody.
Routine HCV testing should include use of both an EIA to test for anti-HCV and supplemental or confirmatory testing with an additional, more specific assay (Figure ). Use of RT-PCR for HCV RNA as the primary test for routine screening is not recommended because few HCV infections will be identified in anti-HCV negative patients. Hemodialysis Staff Members. Previously, testing for HBV infection was recommended for all staff members at the time of employment and for susceptible staff members at routine intervals thereafter (198 ); however, such testing is no longer considered necessary. The risk for HBV infection among hemodialysis staff members is no greater than that for other health-care workers. Thus, routine testing of staff members is not recommended except when required to document response to hepatitis B vaccination (see Postvaccination Testing and Revaccination of Nonresponders). Routine testing of staff members for HCV, HDV, or HIV infection is not recommended.
# FIGURE. Algorithm for hepatitis C virus (HCV) infection testing among persons who are asymptomatic
# Hepatitis B Vaccination
Vaccine Schedule and Dose. Hepatitis B vaccination is recommended for all susceptible chronic hemodialysis patients and for all staff members (Table 3). Vaccination is recommended for pre-end-stage renal disease patients before they become dialysis dependent and for peritoneal and home dialysis patients because they might require in-center hemodialysis. Hepatitis B vaccine should be administered by the intramuscular route and only in the deltoid muscle for adults and children. Intradermal or subcutaneous administration of hepatitis B vaccine is not recommended.
If an adult patient begins the vaccine series with a standard dose before beginning hemodialysis treatment, then moves to hemodialysis treatment before completing the series, complete the series using the higher dose recommended for hemodialysis patients (Table 3). No specific recommendations have been made for higher doses for pediatric hemodialysis patients. If a lower than recommended vaccine dose is administered to either adults or children, the dose should be repeated.
# MMWR April 27, 2001
If the vaccination series is interrupted after the first dose, the second dose should be administered as soon as possible. For the three-dose primary vaccine series, the second and third doses should be separated by an interval of at least 2 months; if only the third dose is delayed, that dose should be administered when convenient. When hepatitis B vaccine has been administered at the same time as other vaccines, no interference with the antibody response of the other vaccines has been demonstrated.
Postvaccination Testing and Revaccination of Nonresponders. Test all vaccinees for anti-HBs 1-2 months after the last primary vaccine dose, to determine their response to the vaccine (adequate response is defined as >10 mIU/mL). Patients and staff members who do not respond to the primary vaccine series should be revaccinated with three additional doses and retested for response. No additional doses of vaccine are warranted for those who do not respond to the second series.
Evaluate staff members who do not respond to revaccination to determine if they are HBsAg positive (199 ). Persons who are HBsAg positive should be counseled accordingly (e.g., need for medical evaluation, vaccination of sexual and household contacts). Primary nonresponders to vaccination who are HBsAg negative should be considered susceptible to HBV infection and counseled regarding precautions to prevent HBV infection and the need to obtain postexposure prophylaxis with hepatitis B immune globulin for any known or probable percutaneous or mucosal exposure to HBsAg-positive blood (199 ).
Follow-Up of Vaccine Responders. Retest patients who respond to the vaccine annually for anti-HBs. If anti-HBs declines to <10 mIU/mL, administer a booster dose of hepatitis B vaccine and continue to retest annually. Retesting immediately after the booster dose is not necessary. For staff members who respond to the vaccine, booster doses of vaccine are not necessary, and periodic serologic testing to monitor antibody concentrations is not recommended (199 ).
Patients with a History of Vaccination. Routine childhood vaccination against hepatitis B has been recommended since 1991 and routine adolescent vaccination since 1995 (89,198 ). Thus, many persons who develop end-stage renal failure will have a history of vaccination against hepatitis B. These persons should have responded to the vaccine when their immune status was normal, but if their anti-HBs levels are <10 mIU/mL when they begin dialysis, they should be revaccinated with a complete primary series.
# Prevention and Management of HBV Infection
Preventing HBV transmission among chronic hemodialysis patients requires a) infection control precautions recommended for all hemodialysis patients; b) routine serologic testing for markers of HBV infection and prompt review of results; c) isolation of HBsAg-positive patients with dedicated room, machine, other equipment, supplies, and staff members; and d) vaccination. Additional infection control practices are needed because of the potential for environmentally mediated transmission of HBV, rather than internal contamination of dialysis machines. The need for routine follow-up testing, vaccination, or isolation is based on patients' serologic status (Table 1 and Recommended Practices at a Glance).
HBV-Susceptible Patients. Vaccinate all susceptible patients (see Hepatitis B Vaccination). Test susceptible patients monthly for HBsAg, including those who a) have not yet received hepatitis B vaccine, b) are in the process of being vaccinated, or c) have not adequately responded to vaccination. Although the incidence of HBV infection is low among chronic hemodialysis patients, preventing transmission depends on timely detection of patients converting from HBsAg negative to HBsAg positive and rapid implementation of isolation procedures before cross-contamination can occur.
HBsAg Seroconversions. Report HBsAg-positive seroconversions to the local health department as required by law or regulation. When a seroconversion occurs, review all patients' routine laboratory test results to identify additional cases. Perform additional testing as indicated later in this section. Investigate potential sources for infection to determine if transmission might have occurred within the dialysis unit, including review of newly infected patients' recent medical history (e.g., blood transfusion, hospitalization), history of high-risk behavior (e.g., injecting-drug use, sexual activity), and unit practices and procedures.
In patients newly infected with HBV, HBsAg often is the only serologic marker initially detected; repeat HBsAg testing and test for anti-HBc (including IgM anti-HBc) 1-2 months later. Six months later, repeat HBsAg testing and test for anti-HBs to determine clinical outcome and need for counseling, medical evaluation, and vaccination of contacts. Patients who become HBsAg negative are no longer infectious and can be removed from isolation.
HBV-Infected Patients. To isolate HBsAg-positive patients, designate a separate room for their treatment and dedicate machines, equipment, instruments, supplies, and medications that will not be used by HBV-susceptible patients. Most importantly, staff members who are caring for HBsAg-positive patients should not care for susceptible patients at the same time, including during the period when dialysis is terminated on one patient and initiated on another.
Newly opened units should have isolation rooms for the dialysis of HBsAg-positive patients. For existing units in which a separate room is not possible, HBsAg-positive patients should be separated from HBV-susceptible patients in an area removed from the mainstream of activity and should undergo dialysis on dedicated machines. If a machine that has been used on an HBsAg-positive patient is needed for an HBVsusceptible patient, internal pathways of the machine can be disinfected using conventional protocols and external surfaces cleaned using soap and water or a detergent germicide.
Dialyzers should not be reused on HBsAg-positive patients. Because HBV is efficiently transmitted through occupational exposure to blood, reprocessing dialyzers from HBsAg-positive patients might place HBV-susceptible staff members at increased risk for infection.
Chronically infected patients (i.e., those who are HBsAg positive, total anti-HBc positive, and IgM anti-HBc negative) are infectious to others and are at risk for chronic liver disease. They should be counseled regarding preventing transmission to others, their household and sexual partners should receive hepatitis B vaccine, and they should be evaluated (by consultation or referral, if appropriate) for the presence or development of chronic liver disease according to current medical practice guidelines. Persons with chronic liver disease should be vaccinated against hepatitis A, if susceptible.
Chronically infected patients do not require any routine follow-up testing for purposes of infection control. However, annual testing for HBsAg is reasonable to detect the small percentage of HBV-infected patients who might lose their HBsAg.
HBV-Immune Patients. Annual anti-HBs testing of patients who are positive for anti-HBs (>10 mIU/mL) and negative for anti-HBc determines the need for booster doses of for infection to determine if transmission might have occurred within the dialysis unit, including review of newly infected patients' recent medical history (e.g., blood transfusion, hospitalization), history of high-risk behavior (e.g., injecting-drug use, sexual activity), and unit practices and procedures.
If >1 patient seroconverts from anti-HCV negative to positive during a 6-month period, more frequent (e.g., every 1-3 months) anti-HCV testing of HCV-negative patients could be warranted for a limited time (e.g., 3-6 months) to detect additional infections. If no additional newly infected patients are identified, resume semiannual testing. If ongoing HCV transmission among patients is identified, implement control measures based on results of investigation of potential sources for transmission and monitor their effectiveness (e.g., perform more frequent anti-HCV testing of HCV-negative patients for 6-12 months before resuming semiannual testing).
HCV-Positive Patients. Patients who are anti-HCV positive (or HCV RNA positive) do not have to be isolated from other patients or dialyzed separately on dedicated machines. Furthermore, they can participate in dialyzer reuse programs. Unlike HBV, HCV is not transmitted efficiently through occupational exposures. Thus, reprocessing dialyzers from HCV-positive patients should not place staff members at increased risk for infection.
HCV-positive persons should be evaluated (by consultation or referral, if appropriate) for the presence or development of chronic liver disease according to current medical practice guidelines. They also should receive information concerning how they can prevent further harm to their liver and prevent transmitting HCV to others (116,141 ). Persons with chronic liver disease should be vaccinated against hepatitis A, if susceptible.
# Prevention and Management of HDV Infection
Because of the low prevalence of HDV infection in the United States, routine testing of hemodialysis patients is not necessary or recommended. However, if a patient is known to be infected with HDV, or if evidence exists of transmission of HDV in a dialysis center, screening for delta antibody is warranted. Because HDV depends on an HBVinfected host for replication, prevention of HBV infection will prevent HDV infection in a person susceptible to HBV. Patients who are known to be infected with HDV should be isolated from all other dialysis patients, especially those who are HBsAg-positive.
# Prevention and Management of HIV Infection
Routine testing of hemodialysis patients for HIV infection for infection control purposes is not necessary or recommended. However, patients with risk factors for HIV infection should be tested so that, if infected, they can receive proper medical care and counseling regarding preventing transmission of the virus (201 ).
Infection control precautions recommended for all hemodialysis patients (see Recommended Practices at a Glance) are sufficient to prevent HIV transmission between patients. HIV-infected patients do not have to be isolated from other patients or dialyzed separately on dedicated machines. In addition, they can participate in dialyzer reuse programs. Because HIV is not transmitted efficiently through occupational exposures, reprocessing dialyzers from HIV-positive patients should not place staff members at increased risk for infection.
# Prevention and Management of Bacterial Infections
Follow published guidelines for judicious use of antimicrobials, particularly vancomycin, to reduce selection for antimicrobial-resistant pathogens (202 ). Infection control precautions recommended for all hemodialysis patients (see Recommended Practices at a Glance) are adequate to prevent transmission for most patients infected or colonized with pathogenic bacteria, including antimicrobial-resistant strains. However, additional infection control precautions should be considered for treatment of patients who might be at increased risk for transmitting pathogenic bacteria. Such patients include those with either a) an infected skin wound with drainage that is not contained by dressings (the drainage does not have to be culture positive for VRE, MRSA, or any specific pathogen) or b) fecal incontinence or diarrhea uncontrolled with personal hygiene measures. For these patients, consider using the following additional precautions: a) staff members treating the patient should wear a separate gown over their usual clothing and remove the gown when finished caring for the patient and b) dialyze the patient at a station with as few adjacent stations as possible (e.g., at the end or corner of the unit).
# SURVEILLANCE FOR INFECTIONS AND OTHER ADVERSE EVENTS
Develop and maintain a separate centralized record-keeping system (e.g., log book or electronic file) to record the results of patients' vaccination status, serologic testing results for viral hepatitis (including ALT), episodes of bacteremia or loss of the vascular access caused by infection (including date of onset, site of infection, genus and species of the infecting organism, and selected antimicrobial susceptibility results),- and adverse events (e.g., blood leaks and spills, dialysis machine malfunctions). Designate a staff person to promptly review the results of routine testing each time such testing is performed and periodically review recorded episodes of bacteremia or vascular access infections. Specify a procedure for actions required when changes occur in test results or in the frequency of episodes of bacteremias or vascular access loss because of infection. Maintain records for each patient that include the location of the dialysis station and machine number used for each dialysis session and the names of staff members who connect and disconnect the patient to and from a machine.
# INFECTION CONTROL TRAINING AND EDUCATION
Training and education is recommended for both staff members and patients (or their family care givers). Training should be appropriate to the cognitive level of the staff member, patient, or family member, and rationales should be provided for appropriate infection control behaviors and techniques to increase compliance. Regulations and recommendations regarding infection control training for health-care workers in general, and dialysis personnel in particular, have been previously published (180,(203)(204)(205). The following recommendations are intended to highlight and augment the earlier recommendations.
- Training and education for all employees at risk for occupational exposure to blood should be provided at least annually, given to new employees before they begin working in the unit, and documented. At a minimum, they should include information on the following topics:
-proper hand hygiene technique;
-proper use of protective equipment;
-modes of transmission for bloodborne viruses, pathogenic bacteria, and other microorganisms as appropriate;
-infection control practices recommended for hemodialysis units and how they differ from Standard Precautions recommended for other health-care settings;
-proper handling and delivery of patient medications;
-rationale for segregating HBsAg-positive patients with a separate room, machine, instruments, supplies, medications, and staff members;
-proper infection control techniques for initiation, care, and maintenance of access sites;
-housekeeping to minimize transmission of microorganisms, including proper methods to clean and disinfect equipment and environmental surfaces; and -centralized record keeping to monitor and prevent complications, including routine serologic testing results for HBV and HCV, hepatitis B vaccine status, episodes of bacteremia and loss of access caused by infection, and other adverse events. Records of surveillance for water and dialysate quality should also be maintained.
- Training and education of patients (or family members for patients unable to be responsible for their own care) regarding infection control practices should be given on admission to dialysis and at least annually thereafter and should address the following topics:
-personal hygiene and hand washing technique;
-patient responsibility for proper care of the access and recognition of signs of infection, which should be reviewed each time the patient has a change in access type; and -recommended vaccinations (206 ).
# FUTURE DIRECTIONS
Infection control strategies that prevent and control HBV infection among hemodialysis patients are well-established. Areas that need additional research include determining the ideal hepatitis B vaccine dosage regimen for pre-and postdialysis pediatric patients and for predialysis adult patients, as well as the optimal timing for follow-up testing and administration of booster doses among vaccine responders. In addition, further studies are needed to clarify the specific factors responsible for transmission of HCV among hemodialysis patients and to evaluate the effect of the current recommendations on prevention and control of HCV infection in this setting. Many areas related to bacterial infections in chronic hemodialysis patients need additional information. Studies are needed on the prevalence and epidemiology of bacterial infections among chronic hemodialysis patients and the patient care practices (e.g., those related to vascular access care and puncture) that would be most useful in preventing bacterial infections. Because of the prominent role of dialysis patients in the epidemic of antimicrobial resistance, researchers need to learn more regarding optimal strategies to ensure judicious use of antimicrobials in these patients. Additional topics for future research include determining the frequency of transmission of pathogenic bacteria in the dialysis unit and whether additional precautions are necessary to prevent such transmission.
This document is available on the Internet at . Copies also can be obtained by using the order form at this Internet site or by writing the Hepatitis Branch, Mailstop G37, CDC, Atlanta, GA 30333.
The following CDC staff members prepared this report:
vaccine to ensure that protective levels of antibody are maintained. No routine followup testing is necessary for patients who are positive for both anti-HBs and anti-HBc.
HBV-immune patients can undergo dialysis in the same area as HBsAg-positive patients, or they can serve as a geographic buffer between HBsAg-positive and HBVsusceptible patients. Staff members can be assigned to care for both infected and immune patients on the same shift.
Isolated Anti-HBc-Positive Patients. Patients who test positive for isolated anti-HBc (i.e., those who are anti-HBc positive, HBsAg negative, and anti-HBs negative) should be retested on a separate serum sample for total anti-HBc, and if positive, for IgM anti-HBc. The following guidelines should be used for interpretation and follow-up:
- If total anti-HBc is negative, consider patient susceptible, and follow recommendations for vaccination.
- If total anti-HBc is positive and IgM anti-HBc is negative, follow recommendations for vaccination.
-If anti-HBs is <10 mIU/mL even after revaccination, test for HBV DNA.
-If HBV DNA is negative, consider patient susceptible (i.e., the anti-HBc result is a false positive), and test monthly for HBsAg.
-If HBV DNA is positive, consider patient as having past infection or "low-level" chronic infection (i.e., the anti-HBc result is a true positive); no further testing is necessary.
-Isolation is not necessary because HBsAg is not detectable.
- If both total and IgM anti-HBc are positive, consider patient recently infected and test for anti-HBs in 4-6 months; no further routine testing is necessary.
-Isolation is not necessary because HBsAg is not detectable.
# Prevention and Management of HCV Infection
HCV transmission within the dialysis environment can be prevented by strict adherence to infection control precautions recommended for all hemodialysis patients (see Recommended Practices at a Glance). Although isolation of HCV-infected patients is not recommended, routine testing for ALT and anti-HCV is important for monitoring transmission within centers and ensuring that appropriate precautions are being properly and consistently used.
HCV-Negative Patients. Monthly ALT testing will facilitate timely detection of new infections and provide a pattern from which to determine when exposure or infection might have occurred. In the absence of unexplained ALT elevations, testing for anti-HCV every 6 months should be sufficient to monitor the occurrence of new HCV infections. If unexplained ALT elevations are observed in patients who are anti-HCV negative, repeat anti-HCV testing is warranted. If unexplained ALT elevations persist in patients who repeatedly test anti-HCV negative, testing for HCV RNA should be considered.
Anti-HCV Seroconversions. Report anti-HCV-positive seroconversions to the local health department as required by law or regulation. When a seroconversion occurs, review all other patients' routine laboratory test results to identify additional cases. Perform additional testing as indicated later in this section. Investigate potential sources
# ACCREDITATION
# Continuing Medical Education (CME). CDC is accredited by the Accreditation Council for Continuing Medical Education
(ACCME) to provide continuing medical education for physicians. CDC designates this educational activity for a maximum of 2 hours in category 1 credit towards the AMA Physician's Recognition Award. Each physician should claim only those hours of credit that he/she actually spent in the educational activity.
# Continuing Education Unit (CEU). CDC has been approved as an authorized provider of continuing education and training programs by the International Association for Continuing Education and Training and awards 0.2 hour Continuing Education Units (CEUs).
# Continuing Nursing Education (CNE).
This activity for 2.2 contact hours is provided by CDC, which is accredited as a provider of continuing education in nursing by the American Nurses Credentialing Center's Commission on Accreditation.
# CE-2 MMWR
April 27, 2001
# GOAL AND OBJECTIVES
This MMWR provides recommendations regarding the prevention of bloodborne virus and bacterial infections in hemodialysis settings. These recommendations were prepared by CDC staff members after consultation with staff members from other federal agencies and specialists in the field. The goal of this report is to serve as a resource for health-care professionals, public health officials, and organizations involved in the care of patients receiving hemodialysis. Upon completion of this continuing education activity, the reader should be able to describe the recommendations for a) preventing bloodborne virus infections in hemodialysis settings, b) preventing bacterial infections in hemodialysis settings, c) developing and maintaining surveillance systems for infections and other adverse events, and d) developing training and education programs.
To receive continuing education credit, please answer all of the following questions.
# Detach or Photocopy
# Signature Date I Completed Exam
# MMWR
The Morbidity and Mortality Weekly Report (MMWR) Series is prepared by the Centers for Disease Control and Prevention (CDC) and is available free of charge in electronic format and on a paid subscription basis for paper copy. To receive an electronic copy on Friday of each week, send an e-mail message to [email protected]. The body content should read SUBscribe mmwr-toc. Electronic copy also is available from CDC's World-Wide Web server at / or from CDC's file transfer protocol server at ftp/. To subscribe for paper copy, contact Superintendent of Documents, U.S. Government PrintingOffice, Washington, DC 20402; telephone (202) 512-1800.
Data in the weekly MMWR are provisional, based on weekly reports to CDC by state health departments. The reporting week concludes at close of business on Friday; compiled data on a national basis are officially released to the public on the following Friday. Address inquiries about the MMWR Series, including material to be considered for publication, to: Editor, MMWR Series, Mailstop C-08, CDC, 1600 Clifton Rd., N.E., Atlanta, GA 30333; telephone (888) 232-3228.
All material in the MMWR Series is in the public domain and may be used and reprinted without permission; citation as to source, however, is appreciated.
# IU.S. Government Printing Office: 2001-633-173/48222 Region IV | Acute hepatitis B Newly acquired symptomatic hepatitis B virus (HBV) infection. Acute hepatitis C Newly acquired symptomatic hepatitis C virus (HCV) infection. ALT Alanine aminotransferase, previously called SGPT. Anti-HBc Antibody to hepatitis B core antigen. Anti-HBe Antibody to hepatitis B e antigen. Anti-HBs Antibody to hepatitis B surface antigen. Anti-HCV Antibody to hepatitis C virus. Anti-HDV Antibody to hepatitis D virus. AST Aspartate aminotransferase, previously called SGOT. AV Arteriovenous. Chronic (persistent) HBV infection Vol. 50 / No. RR-5 MMWR iii# INTRODUCTION
The number of patients with end-stage renal disease treated by maintenance hemodialysis in the United States has increased sharply during the past 30 years. In 1999, more than 3,000 hemodialysis centers had >190,000 chronic hemodialysis patients and >60,000 staff members (1 ). Chronic hemodialysis patients are at high risk for infection because the process of hemodialysis requires vascular access for prolonged periods. In an environment where multiple patients receive dialysis concurrently, repeated opportunities exist for person-to-person transmission of infectious agents, directly or indirectly via contaminated devices, equipment and supplies, environmental surfaces, or hands of personnel. Furthermore, hemodialysis patients are immunosuppressed (2 ), which increases their susceptibility to infection, and they require frequent hospitalizations and surgery, which increases their opportunities for exposure to nosocomial infections.
Historically, surveillance for infections associated with chronic hemodialysis focused on viral hepatitis, particularly hepatitis B virus (HBV) infection. CDC began conducting national surveillance for hemodialysis-associated hepatitis in 1972 (3,4 ). Since 1976, this surveillance has been performed in collaboration with the Health Care Financing Administration (HCFA) during its annual facility survey. Other hemodialysis-associated diseases and practices not related to hepatitis have been included over the years (e.g., pyrogenic reactions, dialysis dementia, vascular access infections, reuse practices, vancomycin use), and the system is continually updated to collect data regarding hemodialysis-associated practices and diseases of current interest and importance (5)(6)(7)(8)(9)(10)(11)(12)(13)(14)(15)(16)(17)(18).
# MMWR April 27, 2001
Recommendations for the control of hepatitis B in hemodialysis centers were first published in 1977 (19 ), and by 1980, their widespread implementation was associated with a sharp reduction in incidence of HBV infection among both patients and staff members (5 ). In 1982, hepatitis B vaccination was recommended for all susceptible patients and staff members (20 ). However, outbreaks of both HBV and hepatitis C virus (HCV) infections continue to occur among chronic hemodialysis patients. Epidemiologic investigations have indicated substantial deficiencies in recommended infection control practices, as well as a failure to vaccinate hemodialysis patients against hepatitis B (21,22 ). These practices apparently are not being fully implemented because staff members a) are not aware of the practices and their importance, b) are confused regarding the differences between standard (i.e., universal) precautions recommended for all health-care settings and the additional precautions necessary in the hemodialysis setting, and c) believe that hepatitis B vaccine is ineffective for preventing HBV infection in chronic hemodialysis patients (22 ).
Bacterial infections, especially those involving vascular access, are the most frequent infectious complication of hemodialysis and a major cause of morbidity and mortality among hemodialysis patients (1 ). During the 1990s, the prevalence of antimicrobial-resistant bacteria (e.g., methicillin-resistant Staphylococcus aureus [MRSA] and vancomycin-resistant enterococci [VRE]) increased rapidly in health-care settings, including hemodialysis units (18,23 ). Although numerous outbreaks of bacterial infections in the hemodialysis setting have been reported (24 ), few studies exist regarding the epidemiology and prevention of endemically occurring bacterial infections in hemodialysis patients, and formal recommendations to prevent such infections have not been published previously. In 1999, CDC initiated a surveillance system for bloodstream and vascular access infections in outpatient hemodialysis centers to determine the frequency of and risk factors for these complications in order to formulate and evaluate strategies for control (25 ).
The recommendations contained in this report were developed by reviewing available data and are based on consultations with specialists in the field. These recommendations provide guidelines for infection control strategies, unique to the hemodialysis setting, that should be used to prevent patient-to-patient transmission of bloodborne viruses and pathogenic bacteria. They are summarized on pages 20-21.
These recommendations do not address sources of bacterial and chemical contaminants in dialysis systems, water treatment or distribution, specific procedures for reprocessing dialyzers, clinical practice methods to prevent bacterial infections (e.g., techniques for skin preparation and access), or comprehensive strategies for preventing infections among health-care workers (see Suggested Readings for information on these topics).
# BACKGROUND Hepatitis B Virus Infection Epidemiology
Incidence and Prevalence. In 1974, the incidence of newly acquired (i.e., acute) HBV infection among chronic hemodialysis patients in the United States was 6.2%, and se-
MMWR 3
lected hemodialysis centers reported rates as high as 30% (4 ). By 1980, nationwide incidence among patients had decreased to 1% (5 ), and by 1999, to 0.06% (18 ) (CDC, unpublished data, 2001), with only 3.5% of all centers reporting newly acquired infections. Prevalence of chronic HBV infection (i.e., hepatitis B surface antigen [HBsAg] positivity) among hemodialysis patients declined from 7.8% in 1976 to 3.8% in 1980 and to 0.9% by 1999 (5,18 ) (CDC, unpublished data, 2001). In 1999, a total of 27.7% of 3,483 centers provided dialysis to >1 patient with either acute or chronic HBV infection (CDC, unpublished data, 2001).
Transmission. HBV is transmitted by percutaneous (i.e., puncture through the skin) or permucosal (i.e., direct contact with mucous membranes) exposure to infectious blood or to body fluids that contain blood, and the chronically infected person is central to the epidemiology of HBV transmission. All HBsAg-positive persons are infectious, but those who are also positive for hepatitis B e antigen (HBeAg) circulate HBV at high titers in their blood (10 8-9 virions/mL) (26,27 ). With virus titers in blood this high, body fluids containing serum or blood also can contain high levels of HBV and are potentially infectious. Furthermore, HBV at titers of 10 2-3 virions/mL can be present on environmental surfaces in the absence of any visible blood and still result in transmission (28,29 ).
HBV is relatively stable in the environment and remains viable for at least 7 days on environmental surfaces at room temperature (29 ). HBsAg has been detected in dialysis centers on clamps, scissors, dialysis machine control knobs, and doorknobs (30 ). Thus, blood-contaminated surfaces that are not routinely cleaned and disinfected represent a reservoir for HBV transmission. Dialysis staff members can transfer virus to patients from contaminated surfaces by their hands or gloves or through use of contaminated equipment and supplies (30 ).
Most HBV infection outbreaks among hemodialysis patients were caused by crosscontamination to patients via a) environmental surfaces, supplies (e.g., hemostats, clamps), or equipment that were not routinely disinfected after each use; b) multiple dose medication vials and intravenous solutions that were not used exclusively for one patient; c) medications for injection that were prepared in areas adjacent to areas where blood samples were handled; and d) staff members who simultaneously cared for both HBV-infected and susceptible patients (21,(31)(32)(33)(34)(35). Once the factors that promote HBV transmission among hemodialysis patients were identified, recommendations for control were published in 1977 (19 ). These recommendations included a) serologic surveillance of patients (and staff members) for HBV infection, including monthly testing of all susceptible patients for HBsAg; b) isolation of HBsAg-positive patients in a separate room; c) assignment of staff members to HBsAg-positive patients and not to HBVsusceptible patients during the same shift; d) assignment of dialysis equipment to HBsAg-positive patients that is not shared by HBV-susceptible patients; e) assignment of a supply tray to each patient (regardless of serologic status); f) cleaning and disinfection of nondisposable items (e.g., clamps, scissors) before use on another patient; g) glove use whenever any patient or hemodialysis equipment is touched and glove changes between each patient (and station); and h) routine cleaning and disinfection of equipment and environmental surfaces.
The segregation of HBsAg-positive patients and their equipment from HBVsusceptible patients resulted in 70%-80% reductions in incidence of HBV infection among hemodialysis patients (7,(36)(37)(38). National surveillance data for 1976-1989 indicated that incidence of HBV infection was substantially lower in hemodialysis units that isolated HBsAg-positive patients, compared with those that did not (7,10 ). The success of isolation practices in preventing transmission of HBV infection is linked to other infection control practices, including routine serological surveillance and routine cleaning and disinfection. Frequent serologic testing for HBsAg detects patients recently infected with HBV quickly so isolation procedures can be implemented before cross-contamination can occur. Environmental control by routine cleaning and disinfection procedures reduces the opportunity for cross-contamination, either directly from environmental surfaces or indirectly by hands of personnel. Despite the current low incidence of HBV infection among hemodialysis patients, outbreaks continue to occur in chronic hemodialysis centers. Investigations of these outbreaks have documented that HBV transmission resulted from failure to use recommended infection control practices, including a) failure to routinely screen patients for HBsAg or routinely review results of testing to identify infected patients; b) assignment of staff members to the simultaneous care of infected and susceptible patients; and c) sharing of supplies, particularly multiple dose medication vials, among patients (21 ). In addition, few patients had received hepatitis B vaccine (21 ). National surveillance data have demonstrated that independent risk factors among chronic hemodialysis patients for acquiring HBV infection include the presence of >1 HBV-infected patient in the hemodialysis center who is not isolated, as well as a <50% hepatitis B vaccination rate among patients (15 ).
HBV infection among chronic hemodialysis patients also has been associated with hemodialysis provided in the acute-care setting (21,39 ). Transmission appeared to stem from chronically infected HBV patients who shared staff members, multiple dose medication vials, and other supplies and equipment with susceptible patients. These episodes were recognized when patients returned to their chronic hemodialysis units, and routine HBsAg testing was resumed. Transmission from HBV-infected chronic hemodialysis patients to patients undergoing hemodialysis for acute renal failure has not been documented, possibly because these patients are dialyzed for short durations and have limited exposure. However, such transmission could go unrecognized because acute renal failure patients are unlikely to be tested for HBV infection.
# Clinical Features and Natural History
HBV causes both acute and chronic hepatitis. The incubation period ranges from 45-160 days (mean: 120 days), and the onset of acute disease is usually insidious. Infants, young children (aged <10 years), and immunosuppressed adults with newly acquired HBV infection are usually asymptomatic (40 ). When present, clinical symptoms and signs might include anorexia, malaise, nausea, vomiting, abdominal pain, and jaundice. Extrahepatic manifestations of disease (e.g., skin rashes, arthralgias, and arthritis) can also occur (41 ). The case fatality rate after acute hepatitis B is 0.5%-1%.
In adults with normal immune status, most (94%-98%) recover completely from newly acquired HBV infections, eliminating virus from the blood and producing neutralizing antibody that creates immunity from future infection (40,42 ). In immunosuppressed persons (including hemodialysis patients), infants, and young children, most newly acquired HBV infections result in chronic infection. Although the consequences of acute hepatitis B can be severe, most of the serious sequelae associated with the disease occur in persons in whom chronic infection develops. Although persons with chronic HBV infection are often asymptomatic, chronic liver disease develops in two-thirds of these persons, and approximately 15%-25% die prematurely from cirrhosis or liver cancer (43)(44)(45).
Subtypes of HBV exist, and infection or immunization with one subtype confers immunity to all subtypes. However, reinfection or reactivation of latent HBV infection has been reported among certain groups of immunosuppressed patients, including those who have undergone renal transplant and those infected with human immunodeficiency virus (HIV) (46,47 ). These patients were positive for antibody to hepatitis B core antigen (anti-HBc), with or without antibody to HBsAg (anti-HBs), and subsequently developed detectable levels of HBsAg. The frequency with which this occurs is unknown.
Monotherapy with alpha interferon or lamivudine is approved by the U.S. Food and Drug Administration (FDA) to treat patients with chronic hepatitis B (48,49 ). Although the dosage of lamivudine should be modified based on creatinine clearance in patients with renal impairment, no additional dose modification is necessary after routine hemodialysis. The emergence of lamivudine-resistant variants has caused concern regarding long-term use of this drug.
# Screening and Diagnostic Tests
Serologic Assays. Several well-defined antigen-antibody systems are associated with HBV infection, including HBsAg and anti-HBs; hepatitis B core antigen (HBcAg) and anti-HBc; and HBeAg and antibody to HBeAg (anti-HBe). Serologic assays are commercially available for all of these except HBcAg because no free HBcAg circulates in blood. One or more of these serologic markers are present during different phases of HBV infection (Table 1) (42 ). The presence of HBsAg is indicative of ongoing HBV infection and potential infectiousness. In newly infected persons, HBsAg is present in serum 30-60 days after exposure to HBV and persists for variable periods. Transient HBsAg positivity (lasting <18 days) can be detected in some patients during vaccination (50,51 ). Anti-HBc develops in all HBV infections, appearing at onset of symptoms or liver test abnormalities in acute HBV infection, rising rapidly to high levels, and persisting for life. Acute or recently acquired infection can be distinguished by presence of the immunoglobulin M (IgM) class of anti-HBc, which persists for approximately 6 months.
In persons who recover from HBV infection, HBsAg is eliminated from the blood, usually in 2-3 months, and anti-HBs develops during convalescence. The presence of anti-HBs indicates immunity from HBV infection. After recovery from natural infection, most persons will be positive for both anti-HBs and anti-HBc, whereas only anti-HBs develops in persons who are successfully vaccinated against hepatitis B. Persons who do not recover from HBV infection and become chronically infected remain positive for HBsAg (and anti-HBc), although a small proportion (0.3% per year) eventually clear HBsAg and might develop anti-HBs (45 ).
In some persons, the only HBV serologic marker detected is anti-HBc (i.e., isolated anti-HBc). Among most asymptomatic persons in the United States tested for HBV infection, an average of 2% (range: <0.1%-6%) test positive for isolated anti-HBc (52 ); among injecting-drug users, however, the rate is 24% (53 ). In general, the frequency of isolated anti-HBc is directly related to the frequency of previous HBV infection in the population and can have several explanations. This pattern can occur after HBV infection among persons who have recovered but whose anti-HBs levels have waned or among persons who failed to develop anti-HBs. Persons in the latter category include those who circulate HBsAg at levels not detectable by current commercial assays. However, HBV DNA has been detected in <10% of persons with isolated anti-HBc, and these persons are unlikely to be infectious to others except under unusual circumstances involving direct percutaneous exposure to large quantities of blood (e.g., transfusion) (54 ). In most persons with isolated anti-HBc, the result appears to be a false positive. Data from several studies have demonstrated that a primary anti-HBs response develops in most of these persons after a three-dose series of hepatitis B vaccine (55,56 ). No data exist on response to vaccination among hemodialysis patients with this serologic pattern.
A third antigen, HBeAg, can be detected in serum of persons with acute or chronic HBV infection. The presence of HBeAg correlates with viral replication and high levels of virus (i.e., high infectivity). Anti-HBe correlates with the loss of replicating virus and with lower levels of virus. However, all HBsAg-positive persons should be considered potentially infectious, regardless of their HBeAg or anti-HBe status.
Nucleic Acid Detection. HBV infection can be detected using qualitative or quantitative tests for HBV DNA. These tests are not FDA-approved and are most commonly used for patients being managed with antiviral therapy (49,57 ).
# Hepatitis B Vaccine
Hepatitis B vaccine has been recommended for both hemodialysis patients and staff members since the vaccine became available in 1982 (20 ). By 1999, a total of 55% of patients and 88% of staff members had been vaccinated (18 ) (CDC, unpublished data, 2001). Two types of vaccine have been licensed and used in the United States: plasmaderived and recombinant. Plasma-derived vaccine is no longer available in the United States, but is produced in several countries and used in many immunization programs worldwide. Recombinant vaccines available in the United States are Recombivax HB™ (Merck & Company, Inc., West Point, Pennsylvania) and Engerix-B ® (SmithKline Beecham Biologicals, Philadelphia, Pennsylvania). Recombivax HB™ contains 10-40 µg of HBsAg protein per mL, whereas Engerix-B ® contains 20 µg/mL.
Primary vaccination comprises three intramuscular doses of vaccine, with the second and third doses given 1 and 6 months, respectively, after the first. An alternative schedule of four doses given at 0, 1, 2, and 12 months to persons with normal immune status or at 0, 1, 2, and 6 months to hemodialysis patients has been approved for Engerix-B ® .
Immunogenicity. The recommended primary series of hepatitis B vaccine induces a protective anti-HBs response (defined as >10 milli-International Units [mIU]/mL) in 90%-95% of adults with normal immune status. The major determinant of vaccine response is age, with the proportion of persons developing a protective antibody response declining to 84% among adults aged >40 years and to 75% by age 60 years (58,59 ). Other host factors that contribute to decreased immunogenicity include smoking, obesity, and immune suppression. Compared with adults with normal immune status, the proportion of hemodialysis patients who develop a protective antibody response after vaccination (with higher dosages) is lower. For those who receive the three-dose schedule, the median is 64% (range: 34%-88%) (60)(61)(62)(63)(64)(65), and for those who receive the fourdose schedule, the median is 86% (range: 40%-98%) (66)(67)(68)(69)(70)(71)(72). Limited data indicate that concurrent infection with HCV does not interfere with development of protective levels of antibody after vaccination, although lower titers of anti-HBs have been reported after vaccination of HCV-positive patients compared with HCV-negative patients (65,(73)(74)(75).
Some studies have demonstrated that higher antibody response rates could be achieved by vaccinating patients with chronic renal failure before they become dialysis dependent, particularly patients with mild or moderate renal failure. After vaccination with four 20 µg doses of recombinant vaccine, a protective antibody response developed in 86% of predialysis adult patients with serum creatinine levels <4.0 mg/dl (mean: 2.0 mg/dl) compared with 37% of those with serum creatinine levels >4.0 mg/dl (mean: 9.5 mg/dl), only 12% of whom were predialysis patients (76 ). In an earlier study, a lower response to recombinant vaccine among predialysis patients was reported, possibly because patients with more severe renal failure were included (77,78 ).
Although no data exist on the response of pediatric hemodialysis patients to vaccination with standard pediatric doses, 75%-97% of those who received higher dosages (20 µg) on either the three-or four-dose schedule developed protective levels of anti-HBs (79)(80)(81). In the one study that evaluated vaccine response among children with chronic renal failure before they became dialysis dependent, high response rates were achieved after four-20 µg doses in both predialysis and dialysis-dependent patients, although predialysis patients had higher peak antibody titers (82 ).
Vaccine Efficacy. For persons with normal immune status, controlled clinical trials have demonstrated that protection from acute and chronic HBV infection is virtually complete among those who develop a protective antibody response after vaccination (83,84 ). Among hemodialysis patients, controlled clinical trials conducted in other countries demonstrated efficacy of 53%-78% after preexposure immunization (85,86 ). However, no efficacy was demonstrated in the one trial performed in the United States (62 ). When the latter trial was designed, the sample size was calculated based on an annual incidence rate among susceptible patients of 13.8% (i.e., the rate observed during 1976-1979, the period before the start of the trial). However, by the time the trial was conducted, the incidence rate had declined by >60%, and the sample size was inadequate for detecting a difference in infection rates between vaccinated and placebo groups. Although efficacy was not demonstrated in this study, no infections occurred among persons who developed and maintained protective levels of anti-HBs. Furthermore, since the hepatitis B vaccine became available, no HBV infections have been reported among vaccinated hemodialysis patients who maintained protective levels of anti-HBs. This observation has been particularly striking during HBV infection outbreaks in this setting (21 ). In addition, a case-control study indicated that the risk for HBV infection was 70% lower among hemodialysis patients who had been vaccinated (87 ). Thus, most hemodialysis patients can be protected from hepatitis B by vaccination, and maintaining immunity among these patients reduces the frequency and costs of serologic screening (88 ).
Revaccination of Nonresponders. Among persons who do not respond to the primary three-dose series of hepatitis B vaccine, 25%-50% of those with normal immune status respond to one additional vaccine dose, and 50%-75% respond to three additional doses (59,84 ). A revaccination regimen that includes serologic testing after one or two additional doses of vaccine appears to be no more cost-effective than serologic testing performed after all three additional doses (89 ). For persons found to be nonresponders after six doses of vaccine, no data exist to indicate that additional doses would induce an antibody response. Few studies have been conducted of the effect of revaccination among hemodialysis patients who do not respond to the primary vaccine series. Response rates to revaccination varied from 40%-50% after two or three additional 40 µg intramuscular doses to 64% after four additional 10 µg intramuscular doses (69,70,(90)(91)(92)(93)(94).
Antibody Persistence. Among adults with normal immune status who responded to a primary vaccine series with a protective antibody level, antibody remained above protective levels in 40%-87% of persons after 9-15 years (95)(96)(97)(98). Only short-term data are available for hemodialysis patients. Among adults who responded to the primary vaccination series, antibody remained detectable for 6 months in 80%-100% (median: 100%) of persons and for 12 months in 58%-100% (median: 70%) (61,64-69,71,85,99-103 ). Among successfully immunized hemodialysis patients whose antibody titers subsequently declined below protective levels, limited data indicate that virtually all respond to a booster dose (75 ).
Duration of Vaccine-Induced Immunity. Among persons with normal immune status who respond to the primary series of hepatitis B vaccine, protection against hepatitis B persists even when antibody titers become undetectable (97 ). However, among hemodialysis patients who respond to the vaccine, protection against hepatitis B is not maintained when antibody titers fall below protective levels. In the U.S. vaccine efficacy trial, three hemodialysis patients who responded to the primary vaccination series developed HBV infection (62 ). One had received a kidney transplant 6 months before onset of infection, and anti-HBs had declined to borderline protective levels in the other two persons. In all three patients, infection resolved.
Alternative Routes of Administration. Among adults with normal immune status, intradermal administration of low doses of hepatitis B vaccine results in lower seroconversion rates (55%-81%) (104)(105)(106), and no data exist on long-term protection from this route of administration. Among infants and children, intradermal vaccination
# Hepatitis C Virus Infection Epidemiology
Incidence and Prevalence. Data are limited on incidence of HCV infection among chronic hemodialysis patients. During 1982-1997, the incidence of non-A, non-B hepatitis among patients reported to CDC's national surveillance system decreased from 1.7% to 0.2% (18 ). The validity of these rates is uncertain because of inherent difficulties in diagnosing non-A, non-B hepatitis and probable variability in the application of diagnostic criteria by different dialysis centers. However, the downward trend can partially be explained by a decline in the rate of transfusion-associated disease after 1985 (107,108 ).
Since 1990, limited data from U.S. studies using testing for antibody to HCV (anti-HCV) to evaluate the incidence of HCV infection have reported annual rates of 0.73%-3% among hemodialysis patients (109,110 ). None of the patients who seroconverted had received transfusions in the interim or were injecting-drug users.
During 1992-1999, national surveillance data indicated that the proportion of centers that tested patients for anti-HCV increased from 22% to 56% (18 ) (CDC, unpublished data, 2001). In 1999, nationwide prevalence of anti-HCV was 8.9%, with some centers reporting prevalences >40% (CDC, unpublished data, 2001). Other studies of hemodialysis patients in the United States have reported anti-HCV prevalences of 10%-36% among adults (109,111,112 ) and 18.5% among children (113 ).
Transmission. HCV is most efficiently transmitted by direct percutaneous exposure to infectious blood, and like HBV, the chronically infected person is central to the epidemiology of HCV transmission. Risk factors associated with HCV infection among hemodialysis patients include history of blood transfusions, the volume of blood transfused, and years on dialysis (114 ). The number of years on dialysis is the major risk factor independently associated with higher rates of HCV infection. As the time patients spent on dialysis increased, their prevalence of HCV infection increased from an average of 12% for patients receiving dialysis <5 years to an average of 37% for patients receiving dialysis >5 years (109,112,115 ).
These studies, as well as investigations of dialysis-associated outbreaks of hepatitis C, indicate that HCV transmission most likely occurs because of inadequate infection control practices. During 1999-2000, CDC investigated three outbreaks of HCV infection among patients in chronic hemodialysis centers (CDC, unpublished data, 1999 and2000). In two of the outbreaks, multiple transmissions of HCV occurred during periods of 16-24 months (attack rates: 6.6%-17.5%), and seroconversions were associated with receiving dialysis immediately after a chronically infected patient. Multiple opportunities for cross-contamination among patients were observed, including a) equipment and supplies that were not disinfected between patient use; b) use of common medication carts to prepare and distribute medications at patients' stations; c) sharing of multiple dose medication vials, which were placed at patients' stations on top of hemodialysis machines; d) contaminated priming buckets that were not routinely changed or cleaned and disinfected between patients; e) machine surfaces that were not routinely cleaned and disinfected between patients; and f) blood spills that were not cleaned up promptly. In the third outbreak, multiple new infections clustered at one point in time (attack rate: 27%), suggesting a common exposure event. Although the specific results of this investigation are pending, multiple opportunities for crosscontamination from chronically infected patients also were observed in this unit. In particular, supply carts were moved from one station to another and contained both clean supplies and blood-contaminated items, including small biohazard containers, sharps disposal boxes, and used vacutainers containing patients' blood.
# Clinical Features and Natural History
HCV causes both acute and chronic hepatitis. The incubation period ranges from 14-180 days (average: 6-7 weeks) (116 ). Persons with newly acquired (acute) HCV infection typically are either asymptomatic or have a mild clinical illness. The course of acute hepatitis C is variable, although elevations in serum alanine aminotransferase (ALT) levels, often in a fluctuating pattern, are the most characteristic feature. Fulminant hepatic failure after acute hepatitis C is rare.
Most (average: 94%) hemodialysis patients with newly acquired HCV infection have elevated serum ALT levels (117)(118)(119)(120)(121). Elevations in serum ALT levels often precede anti-HCV seroconversion. Among prospectively followed transfusion recipients who developed acute HCV infection, elevated ALT levels preceded anti-HCV seroconversion (as measured by second generation assays) in 59%, and anti-HCV was detectable in most patients (78%) within 5 weeks after their first ALT elevation (122 ). However, elevations in ALT or aspartate aminotransferase (AST) levels can occur that are not related to viral hepatitis, and compared with ALT, AST is a less specific indicator of HCV-related liver disease among hemodialysis patients. In a recent outbreak investigation, only 28% of 25 hemodialysis patients with newly observed elevations in AST levels tested anti-HCV positive (CDC, unpublished data, 1999).
After acute HCV infection, 15%-25% of persons with normal immune status appear to resolve their infection without sequelae as defined by sustained absence of HCV RNA in serum and normalization of ALT (123 ). In some persons, ALT levels normalize, suggesting full recovery, but this is frequently followed by ALT elevations that indicate progression to chronic disease. Chronic HCV infection develops in most infected persons (75%-85%). Of persons with chronic HCV infection, 60%-70% have persistent or fluctuating ALT elevations, indicating active liver disease (123 ). Although similar rates of chronic liver disease have been observed among HCV-infected chronic hemodialysis patients (based on liver biopsy results), these patients might be less likely to have biochemical evidence of active liver disease (124 ). In seroprevalence studies of chronic hemodialysis patients, ALT elevations were reported in a median of 33.9% (range: 6%-73%) of patients who tested positive for anti-HCV (117,(124)(125)(126)(127)(128)(129)(130)(131)(132)(133)(134)(135)(136).
No clinical or epidemiologic features among patients with acute infection have been reported to be predictive of either persistent infection or chronic liver disease. Most studies have reported that cirrhosis develops in 10%-20% of persons who have had chronic hepatitis C for 20-30 years, and hepatocellular carcinoma in 1%-5% (123 ). Extrahepatic manifestations of chronic HCV infection are considered to be of immunologic origin and include cryoglobulinemia, membranoproliferative glomerulonephritis, and porphyria cutanea tarda (137 ).
At least six different genotypes and >90 subtypes of HCV exist, with genotype 1 being the most common in the United States (138,139 ). Unlike HBV, infection with one
MMWR 11
HCV genotype or subtype does not protect against reinfection or superinfection with other HCV strains (139 ). Alpha interferon alone or in combination with ribavirin is FDA-approved for the treatment of chronic hepatitis C (48,140,141 ). Combination therapy should be used with caution in patients with creatinine clearance <50 mL/minute and generally is contraindicated in patients with renal failure (141,142 ). Interferon monotherapy results in low sustained virologic response rates (141,142 ).
# Screening and Diagnostic Tests
Serologic Assays. The only FDA-approved tests for diagnosis of HCV infection are those that measure anti-HCV and include enzyme immunoassays (EIAs) and a supplemental recombinant immunoblot assay (RIBA™) (116 ). These tests detect anti-HCV in >97% of infected persons, but do not distinguish between acute, chronic, or resolved infection. The average time from exposure to seroconversion is 8-9 weeks (122 ). Anti-HCV can be detected in 80% of patients within 15 weeks after exposure, in >90% within 5 months, and in >97% within 6 months (122,143 ). In rare instances, seroconversion can be delayed until 9 months after exposure (143,144 ). Anti-HCV persists indefinitely in most persons, but does not protect against reinfection.
As with any screening test, the positive predictive value of EIAs for anti-HCV is directly related to the prevalence of infection in the population and is low in populations with an HCV-infection prevalence <10% (145,146 ). Supplemental testing with a more specific assay (i.e., RIBA™) of a specimen with a positive anti-HCV result by EIA prevents reporting of false-positive results, particularly in settings where asymptomatic persons are being tested. Results of seroprevalence studies among chronic hemodialysis patients have indicated that 57%-100% of EIA positive results were RIBA™ positive (124,126,128,133,135,(147)(148)(149)(150)(151)(152), and 53%-100% were HCV RNA positive by reverse transcriptase polymerase chain reaction (RT-PCR) testing (117,127,129,134,135 ).
Nucleic Acid Detection. The diagnosis of HCV infection also can be made by qualitatively detecting HCV RNA using gene amplification techniques (e.g., RT-PCR) (116 ). HCV RNA can be detected in serum or plasma within 1-2 weeks after exposure and weeks before onset of ALT elevations or the appearance of anti-HCV. In rare instances, detection of HCV RNA might be the only evidence of HCV infection. Although a median of 3.4% (range: 0%-28%) of chronic hemodialysis patients who tested anti-HCV negative were HCV RNA positive, this might be an overestimate because follow-up samples to detect possible antibody seroconversions were not obtained on these patients (117,118,(126)(127)(128)130,131,133,134,(148)(149)(150)(151)(152)(153)(154).
Although not FDA-approved, RT-PCR assays for HCV infection are used commonly in clinical practice and are commercially available. Most RT-PCR assays have a lower limit of detection of 100-1,000 viral genome copies per mL. With adequate optimization of RT-PCR assays, 75%-85% of persons who are positive for anti-HCV and >95% of persons with acute or chronic hepatitis C will test positive for HCV RNA. Some HCVinfected persons might be only intermittently HCV RNA positive, particularly those with acute hepatitis C or with end-stage liver disease caused by hepatitis C. To minimize false-negative results, blood samples collected for RT-PCR should not contain heparin, and serum must be separated from cellular components within 2-4 hours after collection and preferably stored frozen at -20 C or -70 C (155 ). If shipping is required, frozen samples should be protected from thawing. Because of assay variability, rigorous quality assurance and control should be in place in clinical laboratories performing this assay, and proficiency testing is recommended. Quantitative assays for measuring the concentration (i.e., titer) of HCV RNA have been developed and are available from commercial laboratories (156 ). These assays also are not FDA-approved and are less sensitive than qualitative RT-PCR assays (157 ). Quantitative assays should not be used as a primary test to confirm or exclude the diagnosis of HCV infection or to monitor the endpoint of treatment, and sequential measurement of HCV RNA levels has not proven useful in managing patients with hepatitis C.
# Other Bloodborne Viruses Hepatitis Delta Virus Infection
Delta hepatitis is caused by the hepatitis delta virus (HDV), a defective virus that causes infection only in persons with active HBV infection. The prevalence of HDV infection is low in the United States, with rates of <1% among HBsAg-positive persons in the general population and >10% among HBsAg-positive persons with repeated percutaneous exposures (e.g., injecting-drug users, persons with hemophilia) (158 ). Areas of the world with high endemic rates of HDV infection include southern Italy, parts of Africa, and the Amazon Basin.
Few data exist on the prevalence of HDV infection among chronic hemodialysis patients, and only one transmission of HDV between such patients has been reported in the United States (159 ). In this episode, transmission occurred from a patient who was chronically infected with HBV and HDV to an HBsAg-positive patient after a massive bleeding incident; both patients received dialysis at the same station.
HDV infection occurs either as a co-infection with HBV or as a superinfection in a person with chronic HBV infection. Co-infection usually resolves, but superinfection frequently results in chronic HDV infection and severe disease. High mortality rates are associated with both types of infection. A serologic test that measures total antibody to HDV (anti-HDV) is commercially available.
# Human Immunodeficiency Virus Infection
During 1985-1999, the percentage of U.S. hemodialysis centers that reported providing chronic hemodialysis for patients with HIV infection increased from 11% to 39%, and the proportion of hemodialysis patients with known HIV infection increased from 0.3% to 1.4% (18 ) (CDC, unpublished data, 2001).
HIV is transmitted by blood and other body fluids that contain blood. No patient-topatient transmission of HIV has been reported in U.S. hemodialysis centers. However, such transmission has been reported in other countries; in one case, HIV transmission was attributed to mixing of reused access needles and inadequate disinfection of equipment (160 ).
HIV infection is usually diagnosed with assays that measure antibody to HIV, and a repeatedly positive EIA test should be confirmed by Western blot or another confirmatory test. Antiretroviral therapies for HIV-infected hemodialysis patients are commonly used and appear to be improving survival rates among this population. However, hepatotoxicity associated with certain protease inhibitors might limit the use of these drugs, especially in patients with underlying liver dysfunction (161 ).
# MMWR 13
# Bacterial Infections
Epidemiology Disease Burden. The annual mortality rate among hemodialysis patients is 23%, and infections are the second most common cause, accounting for 15% of deaths (1 ). Septicemia (10.9% of all deaths) is the most common infectious cause of mortality. In various studies evaluating rates of bacterial infections in hemodialysis outpatients, bacteremia occurred in 0.63%-1.7% of patients per month and vascular access infections (with or without bacteremia) in 1.3%-7.2% of patients per month (162)(163)(164)(165)(166)(167)(168)(169)(170). National surveillance data indicated that 4%-5% of patients received intravenous vancomycin during a 1-month period (and additional patients received other antimicrobials) (18 ). Although data on vancomycin use can be used to derive an estimate of the prevalence of suspected infections, the proportion of patients receiving antimicrobials who would fit a formal case definition for bacterial infection is unknown.
Infection Sites. In a study of 27 French hemodialysis centers, 28% of 230 infections in hemodialysis patients involved the vascular access, whereas 25% involved the lung, 23% the urinary tract, 9% the skin and soft tissues, and 15% other or unknown sites (165 ). Thirty-three percent of infections involved either the vascular access site or were bacteremias of unknown origin, many of which might have been caused by occult access infections. Thus, the vascular access site was the most common site for infection, but accounted for only one-third of infections. However, access site infections are particularly important because they can cause disseminated bacteremia or loss of the vascular access.
Vascular Access Infections. Vascular access infections are caused (in descending order of frequency) by S. aureus, coagulase-negative staphylococci (CNS), gramnegative bacilli, nonstaphylococcal gram-positive cocci (including enterococci), and fungi (171 ). The proportion of infections caused by CNS is higher among patients dialyzed through catheters than among patients dialyzed through fistulas or grafts.
The primary risk factor for access infection is access type, with catheters having the highest risk for infection, grafts intermediate, and native arteriovenous (AV) fistulas the lowest (168 ). Other potential risk factors for vascular access infections include a) location of the access in the lower extremity; b) recent access surgery; c) trauma, hematoma, dermatitis, or scratching over the access site; d) poor patient hygiene; e) poor needle insertion technique; f) older age; g) diabetes; h) immunosuppression; and i) iron overload (164,167,(172)(173)(174)(175).
Transmission. Bacterial pathogens causing infection can be either exogenous (i.e, acquired from contaminated dialysis fluids or equipment) or endogenous (i.e., caused by invasion of bacteria present in or on the patient). Exogenous pathogens have caused numerous outbreaks, most of which resulted from inadequate dialyzer reprocessing procedures (e.g., contaminated water or inadequate disinfectant) or inadequate treatment of municipal water for use in dialysis. During 1995-1997, four outbreaks were traced to contamination of the waste drain port on one type of dialysis machine (176 ).
Recommendations to prevent such outbreaks are published elsewhere (171 ).
Contaminated medication vials also are a potential source of bacterial infection for patients. In 1999, an outbreak of Serratia liquefaciens bloodstream infections and pyrogenic reactions among hemodialysis patients was traced to contamination of vials of erythropoietin. These vials, which were intended for single use, were contaminated by repeated puncture to obtain additional doses and by pooling of residual medication into a common vial (177 ). Endogenous pathogens first colonize the patient and later cause infection. Colonization means that microorganisms have become resident in or on the body (e.g., in the nares or stool); a culture from the site is positive, but no symptoms or signs of infection exist. Colonization with potentially pathogenic microorganisms, often unknown to staff members, is common in patients with frequent exposure to hospitals and other healthcare settings. Colonization most often occurs when microorganisms are transmitted from a colonized or infected source patient to another patient on the hands of healthcare workers who do not comply with infection control precautions. Less commonly, contamination of environmental surfaces (e.g., bed rails, countertops) plays a role (178 ).
Infection occurs when microorganisms invade the body, damaging tissue and causing signs or symptoms of infection, and is aided by invasive devices (e.g., the hemodialysis vascular access). Evidence exists that when prevalence of colonization in a population is less frequent, infection in that population will also be less frequent, and infection control recommendations for hemodialysis units are designed to prevent colonization (179 ). Additional measures designed to prevent infection from colonizing organisms (e.g., using aseptic technique during vascular access) are presented elsewhere (180 ).
# Antimicrobial Resistance
Antimicrobial-resistant bacteria are more common in patients with severe illness, who often have had multiple hospitalizations or surgical procedures, and in those who have received prolonged courses of antimicrobial agents. In health-care settings, including hemodialysis centers, such patients can serve as a source for transmission.
Clinically important drug-resistant bacteria that commonly cause health-careassociated infections include MRSA, methicillin-resistant CNS, VRE, and multidrugresistant gram negative rods, including strains of Pseudomonas aeruginosa, Stenotrophomonas maltophilia, and Acinetobacter species, some of which are resistant to all available antimicrobials. In addition, strains of S. aureus with intermediate resistance to vancomycin and other glycopeptide antibiotics have recently been reported; these strains are called vancomycin-intermediate S. aureus (VISA) or glycopeptide-intermediate S. aureus (GISA) (181,182 ). Intermediate resistance to vancomycin is reported even more frequently among CNS (183,184 ).
Hemodialysis patients have played a prominent role in the epidemic of vancomycin resistance. In 1988, a renal unit in London, England, reported one of the first cases of VRE (185 ). In three studies, 12%-22% of hospitalized patients infected or colonized with VRE were receiving hemodialysis (178,186,187 ). Furthermore, three of the first five patients identified with VISA (or GISA) were on chronic hemodialysis, and one had received acute dialysis (182 ).
Prevalence of VRE has increased rapidly at U.S. hospitals; among intensive care unit patients with nosocomial infections reported to the National Nosocomial Infections Surveillance (NNIS) system, the percentage of enterococcal isolates resistant to vancomycin increased from 0.5% in 1989 to 25.2% in 1999 (23 ) (CDC, unpublished data, 2000). This increase is attributable to patient-to-patient transmission in healthcare settings and transmission of resistant genes among previously susceptible enterococci. Once vancomycin resistance has been transferred to a patient, antimicrobials select for resistant organisms, causing them to increase in number relative to suscep-tible organisms. Prevalence of VRE colonization among patients varies in different health-care settings; in hemodialysis centers, the reported prevalence in stool samples ranged from 1% to 9% (188,189 ). In one center with a prevalence of 9%, three patients developed VRE infections in 1 year (188 ).
# Vancomycin Use
Dialysis patients have played a prominent role in the epidemic of vancomycin resistance because this drug is used commonly in these patients, in part because vancomycin can be conveniently administered to patients when they come in for hemodialysis treatments. However, two studies indicate that cefazolin, a first-generation cephalosporin, could be substituted for vancomycin in many patients (190,191 ). One of these studies reported that many pathogens causing infections in hemodialysis patients are susceptible to cefazolin (190 ), and both studies reported therapeutic cefazolin blood levels 48-72 hours after dosing, making in-center administration three times a week after dialysis feasible.
# Equipment, Supplies, and Environmental Surfaces
The hemodialysis machine and its components also can be vehicles for patient-topatient transmission of bloodborne viruses and pathogenic bacteria (24,192 ). The external surfaces of the machine are the most likely sources for contamination. These include not only frequently touched surfaces (e.g., the control panel), but also attached waste containers used during the priming of the dialyzers, blood tubing draped or clipped to waste containers, and items placed on tops of machines for convenience (e.g., dialyzer caps and medication vials).
# Sterilization, Disinfection, and Cleaning
A sterilization procedure kills all microorganisms, including highly resistant bacterial spores (24 ). Sterilization procedures are most commonly accomplished by steam or ethylene oxide gas. For products that are heat sensitive, an FDA-cleared liquid chemical sterilant can be used with a long exposure time (i.e., 3-10 hours).
High-level disinfection kills all viruses and bacteria, but not high numbers of bacterial spores. High-level disinfection can be accomplished by heat pasteurization or, more commonly, by an FDA-cleared chemical sterilant, with an exposure time of 12-45 minutes. Sterilants and high-level disinfectants are designed to be used on medical devices, not environmental surfaces. Intermediate-level disinfection kills bacteria and most viruses and is accomplished by using a tuberculocidal "hospital disinfectant" (a term used by the U.S. Environmental Protection Agency [EPA] in registering germicides) or a 1:100 dilution of bleach (300-600 mg/L free chlorine). Low-level disinfection kills most bacteria and is accomplished by using general purpose disinfectants. Intermediate and low-level disinfectants are designed to be used on environmental surfaces; they also can be used on noncritical medical devices, depending on the design and labeling claim.
Cleaning eliminates dirt and some bacteria and viruses and is accomplished by using a detergent or detergent germicide. Antiseptics (e.g., formulations with povidone-iodine, hexachlorophene, or chlorhexidene) are designed for use on skin and tissue and should not be used on medical equipment or environmental surfaces.
# MMWR April 27, 2001
Regardless of the procedure used, cleaning with a germicidal detergent before disinfection (or sterilization) is essential to remove organic material (e.g., blood, mucous, or feces), dirt, or debris. The presence of such material protects microorganisms from the sterilization or disinfection process by physically blocking or inactivating the disinfectant or sterilant.
The choice of what procedure or which chemical germicide to use for medical devices, instruments, and environmental surfaces depends on several factors, including the need to maintain the structural integrity and function of the item and how the item will be used. Three general categories of use for medical items are recognized, each of which require different levels of sterilization or disinfection (193 ). These categories are a) critical, which includes items introduced directly into the bloodstream or normally sterile areas of the body (e.g., needles, catheters, hemodialyzers, blood tubing); b) semicritical, which includes equipment that comes in contact with intact mucous membranes (e.g., fiberoptic endoscopes, glass thermometers); and c) noncritical, which includes equipment that touches only intact skin (e.g., blood pressure cuffs). Semicritical items are not generally used in dialysis units.
Internal Pathways of Hemodialysis Machines. In single-pass hemodialysis machines, the internal fluid pathways are not subject to contamination with blood. If a dialyzer leak occurs, dialysis fluid might become contaminated with blood, but this contaminated fluid is discarded through a drain and does not return to the dialysis machine to contaminate predialyzer surfaces. For dialysis machines that use a dialysate recirculating system (e.g., some ultrafiltration control machines and those that regenerate the dialysate), a blood leak in a dialyzer could contaminate the internal pathways of the machine, which could in turn contaminate the dialysis fluid of subsequent patients (192 ). However, procedures normally practiced after each use (i.e., draining the dialysis fluid and rinsing and disinfecting the machine) will reduce the level of contamination to below infectious levels. In addition, an intact dialyzer membrane will not allow passage of bacteria or viruses (24 ).
Pressure transducer filter protectors are used primarily to prevent contamination and preserve the functioning of the pressure monitoring (i.e., arterial, venous, or both) components of the hemodialysis machine. Hemodialysis machines usually have both external (typically supplied with the blood tubing set) and internal protectors, with the internal protector serving as a backup in case the external transducer protector fails. Failure to use an external protector or to replace the protector when it becomes contaminated (i.e., wetted with saline or blood) can result in contamination of the internal transducer protector, which in turn could allow transmission of bloodborne pathogens (24 ). However, no epidemiologic evidence exists that contamination of the internal transducer protector caused by failure of the external transducer protector has led to either mixing of blood or the transmission of bloodborne agents.
Dialyzer Reprocessing. Approximately 80% of U.S. chronic hemodialysis centers reprocess (i.e., reuse) dialyzers for the same patient (18 ), and guidelines for reprocessing have been published elsewhere (see Suggested Readings). Although outbreaks of bacterial infections and pyrogenic reactions have occurred because of inadequate reprocessing procedures and failure to maintain standards for water quality, reuse has not been associated with transmission of bloodborne viruses. Any theoretical risk for HBV transmission from reuse of dialyzers would primarily affect staff members who handle these dialyzers. Although no increase in HBV (or HCV) infection among staff members who work in such centers has been reported, many centers do not reuse dialyzers from HBsAg-positive patients (24 ).
# Infection Control Precautions for Outpatient Hemodialysis Settings Compared with Inpatient Hospital Settings
Contact transmission is the most important route by which pathogens are transmitted in health-care settings, including hemodialysis units. Contact transmission occurs most commonly when microorganisms from a patient are transferred to the hands of a health-care worker who does not comply with infection control precautions, then touches another patient. Less commonly, environmental surfaces (e.g., bed rails, countertops) become contaminated and serve as an intermediate reservoir for pathogens; transmission can occur when a worker touches the surface then touches a patient or when a patient touches the surface.
In the hemodialysis setting, contact transmission plays a major role in transmission of bloodborne pathogens. If a health-care worker's hands become contaminated with virus-infected blood from one patient, the worker can transfer the virus to a second patient's skin or blood line access port, and the virus can be inoculated into that patient when the skin or access port is punctured with a needle.
Contact transmission can be prevented by hand hygiene (i.e., hand washing or use of a waterless hand rub), glove use, and disinfection of environmental surfaces. Of these, hand hygiene is the most important. In addition, nonsterile disposable gloves provide a protective barrier for workers' hands, preventing them from becoming soiled or contaminated, and reduce the likelihood that microorganisms present on the hands of personnel will be transmitted to patients. However, even with glove use, hand washing is needed because pathogens deposited on the outer surface of gloves can be detected on hands after glove removal, possibly because of holes or defects in the gloves, leakage at the wrist, or contamination of hands during glove removal (194 ).
Standard Precautions are the system of infection control precautions recommended for the inpatient hospital setting (195 ). Standard Precautions are used on all patients and include use of gloves, gown, or mask whenever needed to prevent contact of the health-care worker with blood, secretions, excretions, or contaminated items.
In addition to Standard Precautions, more stringent precautions are recommended for hemodialysis units because of the increased potential for contamination with blood and pathogenic microorganisms (see Infection Control Practices Recommended for Hemodialysis Units). For example, infection control practices for hemodialysis units restrict the use of common supplies, instruments, medications, and medication trays and prohibit the use of a common medication cart.
For certain patients, including those infected or colonized with MRSA or VRE, contact precautions are used in the inpatient hospital setting. Contact precautions include a) placing the patient in a single room or with another patient infected or colonized with the same organism; b) using gloves whenever entering the patient's room; and c) using a gown when entering the patient's room if the potential exists for the worker's clothing to have substantial contact with the patient, environmental surfaces, or items in the patient's room. Workers also should wear a gown if the patient has diarrhea, an ileostomy, a colostomy, or wound drainage not contained by a dressing.
However, contact precautions are not recommended in hemodialysis units for patients infected or colonized with pathogenic bacteria for several reasons. First, although contact transmission of pathogenic bacteria is well-documented in hospitals, similar transmission has not been well-documented in hemodialysis centers. Transmission might not be apparent in dialysis centers, possibly because it occurs less frequently than in acute-care hospitals or results in undetected colonization rather than overt infection. Also, because dialysis patients are frequently hospitalized, determining whether transmission occurred in the inpatient or outpatient setting is difficult. Second, contamination of the patient's skin, bedclothes, and environmental surfaces with pathogenic bacteria is likely to be more common in hospital settings (where patients spend 24 hours a day) than in outpatient hemodialysis centers (where patients spend approximately 10 hours a week). Third, the routine use of infection control practices recommended for hemodialysis units, which are more stringent than the Standard Precautions routinely used in hospitals, should prevent transmission by the contact route.
# RECOMMENDATIONS Rationale
Preventing transmission among chronic hemodialysis patients of bloodborne viruses and pathogenic bacteria from both recognized and unrecognized sources of infection requires implementation of a comprehensive infection control program. The components of such a program include infection control practices specifically designed for the hemodialysis setting, including routine serologic testing and immunization, surveillance, and training and education (Box).
The infection control practices recommended for hemodialysis units will reduce opportunities for patient-to-patient transmission of infectious agents, directly or indirectly via contaminated devices, equipment and supplies, environmental surfaces, or hands of personnel. These practices should be carried out routinely for all patients in the chronic hemodialysis setting because of the increased potential for blood contamination during hemodialysis and because many patients are colonized or infected with pathogenic bacteria. Such practices include additional measures to prevent HBV transmission because of the high titer of HBV and its ability to survive on environmental surfaces. For patients at increased risk for transmission of pathogenic bacteria, includ-
# BOX. Components of a comprehensive infection control program to prevent transmission of infections among chronic hemodialysis patients
• Infection control practices for hemodialysis units.
-Infection control precautions specifically designed to prevent transmission of bloodborne viruses and pathogenic bacteria among patients.
-Routine serologic testing for hepatitis B virus and hepatitis C virus infections.
-Vaccination of susceptible patients against hepatitis B.
-Isolation of patients who test positive for hepatitis B surface antigen.
• Surveillance for infections and other adverse events.
• Infection control training and education.
ing antimicrobial-resistant strains, additional precautions also might be necessary in some circumstances. Furthermore, surveillance for infections and other adverse events is required to monitor the effectiveness of infection control practices, as well as training and education of both staff members and patients to ensure that appropriate infection control behaviors and techniques are carried out.
# Infection Control Practices for Hemodialysis Units
In each chronic hemodialysis unit, policies and practices should be reviewed and updated to ensure that infection control practices recommended for hemodialysis units are implemented and rigorously followed (see Recommended Infection Control Practices for Hemodialysis Units at a Glance). Intensive efforts must be made to educate new staff members and reeducate existing staff members regarding these practices.
# Infection Control Precautions for All Patients
During the process of hemodialysis, exposure to blood and potentially contaminated items can be routinely anticipated; thus, gloves are required whenever caring for a patient or touching the patient's equipment. To facilitate glove use, a supply of clean nonsterile gloves and a glove discard container should be placed near each dialysis station. Hands always should be washed after gloves are removed and between patient contacts, as well as after touching blood, body fluids, secretions, excretions, and contaminated items. A sufficient number of sinks with warm water and soap should be available to facilitate hand washing. If hands are not visibly soiled, use of a waterless antiseptic hand rub can be substituted for hand washing.
Any item taken to a patient's dialysis station could become contaminated with blood and other body fluids and serve as a vehicle of transmission to other patients either directly or by contamination of the hands of personnel. Therefore, items taken to a patient's dialysis station, including those placed on top of dialysis machines, should either be disposed of, dedicated for use only on a single patient, or cleaned and disinfected before being returned to a common clean area or used for other patients. Unused medications or supplies (e.g., syringes, alcohol swabs) taken to the patient's station should not be returned to a common clean area or used on other patients.
Additional measures to prevent contamination of clean or sterile items include a) preparing medications in a room or area separated from the patient treatment area and designated only for medications; b) not handling or storing contaminated (i.e., used) supplies, equipment, blood samples, or biohazard containers in areas where medications and clean (i.e., unused) equipment and supplies are handled; and c) delivering medications separately to each patient. Common carts should not be used within the patient treatment area to prepare or distribute medications. If trays are used to distribute medications, clean them before using for a different patient.
Intravenous medication vials labeled for single use, including erythropoetin, should not be punctured more than once (196,197 ). Once a needle has entered a vial labeled for single use, the sterility of the product can no longer be guaranteed. Residual medication from two or more vials should not be pooled into a single vial.
If a common supply cart is used to store clean supplies in the patient treatment area, this cart should remain in a designated area at a sufficient distance from patient stations to avoid contamination with blood. Such carts should not be moved between stations to distribute supplies.
# MMWR April 27, 2001
# Recommended Infection Control Practices for Hemodialysis Units at a Glance Infection Control Precautions for All Patients
• Wear disposable gloves when caring for the patient or touching the patient's equipment at the dialysis station; remove gloves and wash hands between each patient or station.
• Items taken into the dialysis station should either be disposed of, dedicated for use only on a single patient, or cleaned and disinfected before being taken to a common clean area or used on another patient.
-Nondisposable items that cannot be cleaned and disinfected (e.g., adhesive tape, cloth-covered blood pressure cuffs) should be dedicated for use only on a single patient.
-Unused medications (including multiple dose vials containing diluents) or supplies (e.g., syringes, alcohol swabs) taken to the patient's station should be used only for that patient and should not be returned to a common clean area or used on other patients.
• When multiple dose medication vials are used (including vials containing diluents), prepare individual patient doses in a clean (centralized) area away from dialysis stations and deliver separately to each patient. Do not carry multiple dose medication vials from station to station.
# Hepatitis B Vaccination
• Vaccinate all susceptible patients against hepatitis B.
• Test for anti-HBs 1-2 months after last dose.
-If anti-HBs is <10 mIU/mL, consider patient susceptible, revaccinate with an additional three doses, and retest for anti-HBs.
-If anti-HBs is >10 mIU/mL, consider patient immune, and retest annually.
-Give booster dose of vaccine if anti-HBs declines to <10 mIU/mL and continue to retest annually.
# Management of HBsAg-Positive Patients
• Follow infection control practices for hemodialysis units for all patients.
• Dialyze HBsAg-positive patients in a separate room using separate machines, equipment, instruments, and supplies.
• Staff members caring for HBsAg-positive patients should not care for HBV-susceptible patients at the same time (e.g., during the same shift or during patient changeover).
• Clean areas should be clearly designated for the preparation, handling, and storage of medications and unused supplies and equipment. Clean areas should be clearly separated from contaminated areas where used supplies and equipment are handled. Do not handle and store medications or clean supplies in the same or an adjacent area to where used equipment or blood samples are handled.
• Use external venous and arterial pressure transducer filters/protectors for each patient treatment to prevent blood contamination of the dialysis machines' pressure monitors. Change filters/protectors between each patient treatment, and do not reuse them. Internal transducer filters do not need to be changed routinely between patients.
• Clean and disinfect the dialysis station (e.g., chairs, beds, tables, machines) between patients.
-Give special attention to cleaning control panels on the dialysis machines and other surfaces that are frequently touched and potentially contaminated with patients' blood.
-Discard all fluid and clean and disinfect all surfaces and containers associated with the prime waste (including buckets attached to the machines).
• For dialyzers and blood tubing that will be reprocessed, cap dialyzer ports and clamp tubing. Place all used dialyzers and tubing in leakproof containers for transport from station to reprocessing or disposal area.
# MMWR April 27, 2001
Staff members should wear gowns, face shields, eye wear, or masks to protect themselves and prevent soiling of clothing when performing procedures during which spurting or spattering of blood might occur (e.g., during initiation and termination of dialysis, cleaning of dialyzers, and centrifugation of blood). Such protective clothing or gear should be changed if it becomes soiled with blood, body fluids, secretions, or excretions. Staff members should not eat, drink, or smoke in the dialysis treatment area or in the laboratory. However, patients can be served meals or eat food brought from home at their dialysis station. The glasses, dishes, and other utensils should be cleaned in the usual manner; no special care of these items is needed.
Cleaning and Disinfection. Establish written protocols for cleaning and disinfecting surfaces and equipment in the dialysis unit, including careful mechanical cleaning before any disinfection process (Table 2). If the manufacturer has provided instructions on sterilization or disinfection of the item, these instructions should be followed. For each chemical sterilant and disinfectant, follow the manufacturer's instructions regarding use, including appropriate dilution and contact time.
After each patient treatment, clean environmental surfaces at the dialysis station, including the dialysis bed or chair, countertops, and external surfaces of the dialysis machine, including containers associated with the prime waste. Use any soap, detergent, or detergent germicide. Between uses of medical equipment (e.g., scissors, hemostats, clamps, stethoscopes, blood pressure cuffs), clean and apply a hospital disinfectant (i.e., low-level disinfection); if the item is visibly contaminated with blood, use a tuberculocidal disinfectant (i.e., intermediate-level disinfection).
For a blood spill, immediately clean the area with a cloth soaked with a tuberculocidal disinfectant or a 1:100 dilution of household bleach (300-600 mg/L free chlorine) (i.e., intermediate-level disinfection). The staff member doing the cleaning should wear gloves, and the cloth should be placed in a bucket or other leakproof container. After all visible blood is cleaned, use a new cloth or towel to apply disinfectant a second time.
Published methods should be used to clean and disinfect the water treatment and distribution system and the internal circuits of the dialysis machine, as well as to repro- Environmental surfaces, including exterior surfaces of hemodialysis machines X * Careful mechanical cleaning to remove debris should always be done before disinfection. † Water treatment and distribution systems of dialysis fluid concentrates require more extensive disinfection if significant biofilm is present within the system. § If item is visibly contaminated with blood, use a tuberculocidal disinfectant. cess dialyzers for reuse (see Suggested Readings). These methods are designed to control bacterial contamination, but will also eliminate bloodborne viruses. For singlepass machines, perform rinsing and disinfection procedures at the beginning or end of the day. For batch recirculating machines, drain, rinse, and disinfect after each use. Follow the same methods for cleaning and disinfection if a blood leak has occurred, regardless of the type of dialysis machine used. Routine bacteriologic assays of water and dialysis fluids should be performed according to the recommendations of the Association for the Advancement of Medical Instrumentation (see Suggested Readings).
Venous pressure transducer protectors should be used to cover pressure monitors and should be changed between patients, not reused. If the external transducer protector becomes wet, replace immediately and inspect the protector. If fluid is visible on the side of the transducer protector that faces the machine, have qualified personnel open the machine after the treatment is completed and check for contamination. This includes inspection for possible blood contamination of the internal pressure tubing set and pressure sensing port. If contamination has occurred, the machine must be taken out of service and disinfected using either 1:100 dilution of bleach (300-600 mg/L free chlorine) or a commercially available, EPA-registered tuberculocidal germicide before reuse. Frequent blood line pressure alarms or frequent adjusting of blood drip chamber levels can be an indicator of this problem. Taken separately, these incidents could be characterized as isolated malfunctions. However, the potential public health significance of the total number of incidents nationwide make it imperative that all incidents of equipment contamination be reported immediately to the FDA (800-FDA-1088).
Housekeeping staff members in the dialysis facility should promptly remove soil and potentially infectious waste and maintain an environment that enhances patient care. All disposable items should be placed in bags thick enough to prevent leakage. Wastes generated by the hemodialysis facility might be contaminated with blood and should be considered infectious and handled accordingly. These solid medical wastes should be disposed of properly in an incinerator or sanitary landfill, according to local and state regulations governing medical waste disposal.
Hemodialysis in Acute-Care Settings. For patients with acute renal failure who receive hemodialysis in acute-care settings, Standard Precautions as applied in all healthcare settings are sufficient to prevent transmission of bloodborne viruses. However, when chronic hemodialysis patients receive maintenance hemodialysis while hospitalized, infection control precautions specifically designed for chronic hemodialysis units (see Recommended Practices at a Glance) should be applied to these patients. If both acute and chronic renal failure patients receive hemodialysis in the same unit, these infection control precautions should be applied to all patients.
Regardless of where in the acute-care setting chronic hemodialysis patients receive dialysis, the HBsAg status of all such patients should be ascertained at the time of admission to the hospital, by either a written report from the referring center (including the most recent date testing was performed) or by a serologic test. The HBV serologic status should be prominently placed in patients' hospital records, and all health-care personnel assigned to these patients, as well as the infection control practitioner, should be aware of the patients' serologic status. While hospitalized, HBsAg-positive chronic hemodialysis patients should undergo dialysis in a separate room and use separate machines, equipment, instruments, supplies, and medications designated only for HBsAg-positive patients (see Prevention and Management of HBV Infection). While HBsAg-positive patients are receiving dialysis, staff members who are caring for them should not care for susceptible patients.
# MMWR April 27, 2001
Routine Serologic Testing Chronic Hemodialysis Patients. Routinely test all chronic hemodialysis patients for HBV and HCV infection (see Recommended Practices at a Glance), promptly review results, and ensure that patients are managed appropriately based on their testing results (see later recommendations for each virus). Communicate test results (positive and negative) to other units or hospitals when patients are transferred for care. Routine testing for HDV or HIV infection for purposes of infection control is not recommended.
The HBV serologic status (i.e., HBsAg, total anti-HBc, and anti-HBs) of all patients should be known before admission to the hemodialysis unit. For patients transferred from another unit, test results should be obtained before the patients' transfer. If a patient's HBV serologic status is not known at the time of admission, testing should be completed within 7 days. The hemodialysis unit should ensure that the laboratory performing the testing for anti-HBs can define a 10 mIU/mL concentration to determine protective levels of antibody.
Routine HCV testing should include use of both an EIA to test for anti-HCV and supplemental or confirmatory testing with an additional, more specific assay (Figure ). Use of RT-PCR for HCV RNA as the primary test for routine screening is not recommended because few HCV infections will be identified in anti-HCV negative patients. Hemodialysis Staff Members. Previously, testing for HBV infection was recommended for all staff members at the time of employment and for susceptible staff members at routine intervals thereafter (198 ); however, such testing is no longer considered necessary. The risk for HBV infection among hemodialysis staff members is no greater than that for other health-care workers. Thus, routine testing of staff members is not recommended except when required to document response to hepatitis B vaccination (see Postvaccination Testing and Revaccination of Nonresponders). Routine testing of staff members for HCV, HDV, or HIV infection is not recommended.
# FIGURE. Algorithm for hepatitis C virus (HCV) infection testing among persons who are asymptomatic
# Hepatitis B Vaccination
Vaccine Schedule and Dose. Hepatitis B vaccination is recommended for all susceptible chronic hemodialysis patients and for all staff members (Table 3). Vaccination is recommended for pre-end-stage renal disease patients before they become dialysis dependent and for peritoneal and home dialysis patients because they might require in-center hemodialysis. Hepatitis B vaccine should be administered by the intramuscular route and only in the deltoid muscle for adults and children. Intradermal or subcutaneous administration of hepatitis B vaccine is not recommended.
If an adult patient begins the vaccine series with a standard dose before beginning hemodialysis treatment, then moves to hemodialysis treatment before completing the series, complete the series using the higher dose recommended for hemodialysis patients (Table 3). No specific recommendations have been made for higher doses for pediatric hemodialysis patients. If a lower than recommended vaccine dose is administered to either adults or children, the dose should be repeated.
# MMWR April 27, 2001
If the vaccination series is interrupted after the first dose, the second dose should be administered as soon as possible. For the three-dose primary vaccine series, the second and third doses should be separated by an interval of at least 2 months; if only the third dose is delayed, that dose should be administered when convenient. When hepatitis B vaccine has been administered at the same time as other vaccines, no interference with the antibody response of the other vaccines has been demonstrated.
Postvaccination Testing and Revaccination of Nonresponders. Test all vaccinees for anti-HBs 1-2 months after the last primary vaccine dose, to determine their response to the vaccine (adequate response is defined as >10 mIU/mL). Patients and staff members who do not respond to the primary vaccine series should be revaccinated with three additional doses and retested for response. No additional doses of vaccine are warranted for those who do not respond to the second series.
Evaluate staff members who do not respond to revaccination to determine if they are HBsAg positive (199 ). Persons who are HBsAg positive should be counseled accordingly (e.g., need for medical evaluation, vaccination of sexual and household contacts). Primary nonresponders to vaccination who are HBsAg negative should be considered susceptible to HBV infection and counseled regarding precautions to prevent HBV infection and the need to obtain postexposure prophylaxis with hepatitis B immune globulin for any known or probable percutaneous or mucosal exposure to HBsAg-positive blood (199 ).
Follow-Up of Vaccine Responders. Retest patients who respond to the vaccine annually for anti-HBs. If anti-HBs declines to <10 mIU/mL, administer a booster dose of hepatitis B vaccine and continue to retest annually. Retesting immediately after the booster dose is not necessary. For staff members who respond to the vaccine, booster doses of vaccine are not necessary, and periodic serologic testing to monitor antibody concentrations is not recommended (199 ).
Patients with a History of Vaccination. Routine childhood vaccination against hepatitis B has been recommended since 1991 and routine adolescent vaccination since 1995 (89,198 ). Thus, many persons who develop end-stage renal failure will have a history of vaccination against hepatitis B. These persons should have responded to the vaccine when their immune status was normal, but if their anti-HBs levels are <10 mIU/mL when they begin dialysis, they should be revaccinated with a complete primary series.
# Prevention and Management of HBV Infection
Preventing HBV transmission among chronic hemodialysis patients requires a) infection control precautions recommended for all hemodialysis patients; b) routine serologic testing for markers of HBV infection and prompt review of results; c) isolation of HBsAg-positive patients with dedicated room, machine, other equipment, supplies, and staff members; and d) vaccination. Additional infection control practices are needed because of the potential for environmentally mediated transmission of HBV, rather than internal contamination of dialysis machines. The need for routine follow-up testing, vaccination, or isolation is based on patients' serologic status (Table 1 and Recommended Practices at a Glance).
HBV-Susceptible Patients. Vaccinate all susceptible patients (see Hepatitis B Vaccination). Test susceptible patients monthly for HBsAg, including those who a) have not yet received hepatitis B vaccine, b) are in the process of being vaccinated, or c) have not adequately responded to vaccination. Although the incidence of HBV infection is low among chronic hemodialysis patients, preventing transmission depends on timely detection of patients converting from HBsAg negative to HBsAg positive and rapid implementation of isolation procedures before cross-contamination can occur.
HBsAg Seroconversions. Report HBsAg-positive seroconversions to the local health department as required by law or regulation. When a seroconversion occurs, review all patients' routine laboratory test results to identify additional cases. Perform additional testing as indicated later in this section. Investigate potential sources for infection to determine if transmission might have occurred within the dialysis unit, including review of newly infected patients' recent medical history (e.g., blood transfusion, hospitalization), history of high-risk behavior (e.g., injecting-drug use, sexual activity), and unit practices and procedures.
In patients newly infected with HBV, HBsAg often is the only serologic marker initially detected; repeat HBsAg testing and test for anti-HBc (including IgM anti-HBc) 1-2 months later. Six months later, repeat HBsAg testing and test for anti-HBs to determine clinical outcome and need for counseling, medical evaluation, and vaccination of contacts. Patients who become HBsAg negative are no longer infectious and can be removed from isolation.
HBV-Infected Patients. To isolate HBsAg-positive patients, designate a separate room for their treatment and dedicate machines, equipment, instruments, supplies, and medications that will not be used by HBV-susceptible patients. Most importantly, staff members who are caring for HBsAg-positive patients should not care for susceptible patients at the same time, including during the period when dialysis is terminated on one patient and initiated on another.
Newly opened units should have isolation rooms for the dialysis of HBsAg-positive patients. For existing units in which a separate room is not possible, HBsAg-positive patients should be separated from HBV-susceptible patients in an area removed from the mainstream of activity and should undergo dialysis on dedicated machines. If a machine that has been used on an HBsAg-positive patient is needed for an HBVsusceptible patient, internal pathways of the machine can be disinfected using conventional protocols and external surfaces cleaned using soap and water or a detergent germicide.
Dialyzers should not be reused on HBsAg-positive patients. Because HBV is efficiently transmitted through occupational exposure to blood, reprocessing dialyzers from HBsAg-positive patients might place HBV-susceptible staff members at increased risk for infection.
Chronically infected patients (i.e., those who are HBsAg positive, total anti-HBc positive, and IgM anti-HBc negative) are infectious to others and are at risk for chronic liver disease. They should be counseled regarding preventing transmission to others, their household and sexual partners should receive hepatitis B vaccine, and they should be evaluated (by consultation or referral, if appropriate) for the presence or development of chronic liver disease according to current medical practice guidelines. Persons with chronic liver disease should be vaccinated against hepatitis A, if susceptible.
Chronically infected patients do not require any routine follow-up testing for purposes of infection control. However, annual testing for HBsAg is reasonable to detect the small percentage of HBV-infected patients who might lose their HBsAg.
HBV-Immune Patients. Annual anti-HBs testing of patients who are positive for anti-HBs (>10 mIU/mL) and negative for anti-HBc determines the need for booster doses of for infection to determine if transmission might have occurred within the dialysis unit, including review of newly infected patients' recent medical history (e.g., blood transfusion, hospitalization), history of high-risk behavior (e.g., injecting-drug use, sexual activity), and unit practices and procedures.
If >1 patient seroconverts from anti-HCV negative to positive during a 6-month period, more frequent (e.g., every 1-3 months) anti-HCV testing of HCV-negative patients could be warranted for a limited time (e.g., 3-6 months) to detect additional infections. If no additional newly infected patients are identified, resume semiannual testing. If ongoing HCV transmission among patients is identified, implement control measures based on results of investigation of potential sources for transmission and monitor their effectiveness (e.g., perform more frequent anti-HCV testing of HCV-negative patients for 6-12 months before resuming semiannual testing).
HCV-Positive Patients. Patients who are anti-HCV positive (or HCV RNA positive) do not have to be isolated from other patients or dialyzed separately on dedicated machines. Furthermore, they can participate in dialyzer reuse programs. Unlike HBV, HCV is not transmitted efficiently through occupational exposures. Thus, reprocessing dialyzers from HCV-positive patients should not place staff members at increased risk for infection.
HCV-positive persons should be evaluated (by consultation or referral, if appropriate) for the presence or development of chronic liver disease according to current medical practice guidelines. They also should receive information concerning how they can prevent further harm to their liver and prevent transmitting HCV to others (116,141 ). Persons with chronic liver disease should be vaccinated against hepatitis A, if susceptible.
# Prevention and Management of HDV Infection
Because of the low prevalence of HDV infection in the United States, routine testing of hemodialysis patients is not necessary or recommended. However, if a patient is known to be infected with HDV, or if evidence exists of transmission of HDV in a dialysis center, screening for delta antibody is warranted. Because HDV depends on an HBVinfected host for replication, prevention of HBV infection will prevent HDV infection in a person susceptible to HBV. Patients who are known to be infected with HDV should be isolated from all other dialysis patients, especially those who are HBsAg-positive.
# Prevention and Management of HIV Infection
Routine testing of hemodialysis patients for HIV infection for infection control purposes is not necessary or recommended. However, patients with risk factors for HIV infection should be tested so that, if infected, they can receive proper medical care and counseling regarding preventing transmission of the virus (201 ).
Infection control precautions recommended for all hemodialysis patients (see Recommended Practices at a Glance) are sufficient to prevent HIV transmission between patients. HIV-infected patients do not have to be isolated from other patients or dialyzed separately on dedicated machines. In addition, they can participate in dialyzer reuse programs. Because HIV is not transmitted efficiently through occupational exposures, reprocessing dialyzers from HIV-positive patients should not place staff members at increased risk for infection.
# Prevention and Management of Bacterial Infections
Follow published guidelines for judicious use of antimicrobials, particularly vancomycin, to reduce selection for antimicrobial-resistant pathogens (202 ). Infection control precautions recommended for all hemodialysis patients (see Recommended Practices at a Glance) are adequate to prevent transmission for most patients infected or colonized with pathogenic bacteria, including antimicrobial-resistant strains. However, additional infection control precautions should be considered for treatment of patients who might be at increased risk for transmitting pathogenic bacteria. Such patients include those with either a) an infected skin wound with drainage that is not contained by dressings (the drainage does not have to be culture positive for VRE, MRSA, or any specific pathogen) or b) fecal incontinence or diarrhea uncontrolled with personal hygiene measures. For these patients, consider using the following additional precautions: a) staff members treating the patient should wear a separate gown over their usual clothing and remove the gown when finished caring for the patient and b) dialyze the patient at a station with as few adjacent stations as possible (e.g., at the end or corner of the unit).
# SURVEILLANCE FOR INFECTIONS AND OTHER ADVERSE EVENTS
Develop and maintain a separate centralized record-keeping system (e.g., log book or electronic file) to record the results of patients' vaccination status, serologic testing results for viral hepatitis (including ALT), episodes of bacteremia or loss of the vascular access caused by infection (including date of onset, site of infection, genus and species of the infecting organism, and selected antimicrobial susceptibility results),* and adverse events (e.g., blood leaks and spills, dialysis machine malfunctions). Designate a staff person to promptly review the results of routine testing each time such testing is performed and periodically review recorded episodes of bacteremia or vascular access infections. Specify a procedure for actions required when changes occur in test results or in the frequency of episodes of bacteremias or vascular access loss because of infection. Maintain records for each patient that include the location of the dialysis station and machine number used for each dialysis session and the names of staff members who connect and disconnect the patient to and from a machine.
# INFECTION CONTROL TRAINING AND EDUCATION
Training and education is recommended for both staff members and patients (or their family care givers). Training should be appropriate to the cognitive level of the staff member, patient, or family member, and rationales should be provided for appropriate infection control behaviors and techniques to increase compliance. Regulations and recommendations regarding infection control training for health-care workers in general, and dialysis personnel in particular, have been previously published (180,(203)(204)(205). The following recommendations are intended to highlight and augment the earlier recommendations.
• Training and education for all employees at risk for occupational exposure to blood should be provided at least annually, given to new employees before they begin working in the unit, and documented. At a minimum, they should include information on the following topics:
-proper hand hygiene technique;
-proper use of protective equipment;
-modes of transmission for bloodborne viruses, pathogenic bacteria, and other microorganisms as appropriate;
-infection control practices recommended for hemodialysis units and how they differ from Standard Precautions recommended for other health-care settings;
-proper handling and delivery of patient medications;
-rationale for segregating HBsAg-positive patients with a separate room, machine, instruments, supplies, medications, and staff members;
-proper infection control techniques for initiation, care, and maintenance of access sites;
-housekeeping to minimize transmission of microorganisms, including proper methods to clean and disinfect equipment and environmental surfaces; and -centralized record keeping to monitor and prevent complications, including routine serologic testing results for HBV and HCV, hepatitis B vaccine status, episodes of bacteremia and loss of access caused by infection, and other adverse events. Records of surveillance for water and dialysate quality should also be maintained.
• Training and education of patients (or family members for patients unable to be responsible for their own care) regarding infection control practices should be given on admission to dialysis and at least annually thereafter and should address the following topics:
-personal hygiene and hand washing technique;
-patient responsibility for proper care of the access and recognition of signs of infection, which should be reviewed each time the patient has a change in access type; and -recommended vaccinations (206 ).
# FUTURE DIRECTIONS
Infection control strategies that prevent and control HBV infection among hemodialysis patients are well-established. Areas that need additional research include determining the ideal hepatitis B vaccine dosage regimen for pre-and postdialysis pediatric patients and for predialysis adult patients, as well as the optimal timing for follow-up testing and administration of booster doses among vaccine responders. In addition, further studies are needed to clarify the specific factors responsible for transmission of HCV among hemodialysis patients and to evaluate the effect of the current recommendations on prevention and control of HCV infection in this setting. Many areas related to bacterial infections in chronic hemodialysis patients need additional information. Studies are needed on the prevalence and epidemiology of bacterial infections among chronic hemodialysis patients and the patient care practices (e.g., those related to vascular access care and puncture) that would be most useful in preventing bacterial infections. Because of the prominent role of dialysis patients in the epidemic of antimicrobial resistance, researchers need to learn more regarding optimal strategies to ensure judicious use of antimicrobials in these patients. Additional topics for future research include determining the frequency of transmission of pathogenic bacteria in the dialysis unit and whether additional precautions are necessary to prevent such transmission.
This document is available on the Internet at <http://www.cdc.gov/hepatitis>. Copies also can be obtained by using the order form at this Internet site or by writing the Hepatitis Branch, Mailstop G37, CDC, Atlanta, GA 30333.
#
The following CDC staff members prepared this report:
#
vaccine to ensure that protective levels of antibody are maintained. No routine followup testing is necessary for patients who are positive for both anti-HBs and anti-HBc.
HBV-immune patients can undergo dialysis in the same area as HBsAg-positive patients, or they can serve as a geographic buffer between HBsAg-positive and HBVsusceptible patients. Staff members can be assigned to care for both infected and immune patients on the same shift.
Isolated Anti-HBc-Positive Patients. Patients who test positive for isolated anti-HBc (i.e., those who are anti-HBc positive, HBsAg negative, and anti-HBs negative) should be retested on a separate serum sample for total anti-HBc, and if positive, for IgM anti-HBc. The following guidelines should be used for interpretation and follow-up:
• If total anti-HBc is negative, consider patient susceptible, and follow recommendations for vaccination.
• If total anti-HBc is positive and IgM anti-HBc is negative, follow recommendations for vaccination.
-If anti-HBs is <10 mIU/mL even after revaccination, test for HBV DNA.
-If HBV DNA is negative, consider patient susceptible (i.e., the anti-HBc result is a false positive), and test monthly for HBsAg.
-If HBV DNA is positive, consider patient as having past infection or "low-level" chronic infection (i.e., the anti-HBc result is a true positive); no further testing is necessary.
-Isolation is not necessary because HBsAg is not detectable.
• If both total and IgM anti-HBc are positive, consider patient recently infected and test for anti-HBs in 4-6 months; no further routine testing is necessary.
-Isolation is not necessary because HBsAg is not detectable.
# Prevention and Management of HCV Infection
HCV transmission within the dialysis environment can be prevented by strict adherence to infection control precautions recommended for all hemodialysis patients (see Recommended Practices at a Glance). Although isolation of HCV-infected patients is not recommended, routine testing for ALT and anti-HCV is important for monitoring transmission within centers and ensuring that appropriate precautions are being properly and consistently used.
HCV-Negative Patients. Monthly ALT testing will facilitate timely detection of new infections and provide a pattern from which to determine when exposure or infection might have occurred. In the absence of unexplained ALT elevations, testing for anti-HCV every 6 months should be sufficient to monitor the occurrence of new HCV infections. If unexplained ALT elevations are observed in patients who are anti-HCV negative, repeat anti-HCV testing is warranted. If unexplained ALT elevations persist in patients who repeatedly test anti-HCV negative, testing for HCV RNA should be considered.
Anti-HCV Seroconversions. Report anti-HCV-positive seroconversions to the local health department as required by law or regulation. When a seroconversion occurs, review all other patients' routine laboratory test results to identify additional cases. Perform additional testing as indicated later in this section. Investigate potential sources
# ACCREDITATION
# Continuing Medical Education (CME). CDC is accredited by the Accreditation Council for Continuing Medical Education
(ACCME) to provide continuing medical education for physicians. CDC designates this educational activity for a maximum of 2 hours in category 1 credit towards the AMA Physician's Recognition Award. Each physician should claim only those hours of credit that he/she actually spent in the educational activity.
# Continuing Education Unit (CEU). CDC has been approved as an authorized provider of continuing education and training programs by the International Association for Continuing Education and Training and awards 0.2 hour Continuing Education Units (CEUs).
# Continuing Nursing Education (CNE).
This activity for 2.2 contact hours is provided by CDC, which is accredited as a provider of continuing education in nursing by the American Nurses Credentialing Center's Commission on Accreditation.
# CE-2 MMWR
April 27, 2001
# GOAL AND OBJECTIVES
This MMWR provides recommendations regarding the prevention of bloodborne virus and bacterial infections in hemodialysis settings. These recommendations were prepared by CDC staff members after consultation with staff members from other federal agencies and specialists in the field. The goal of this report is to serve as a resource for health-care professionals, public health officials, and organizations involved in the care of patients receiving hemodialysis. Upon completion of this continuing education activity, the reader should be able to describe the recommendations for a) preventing bloodborne virus infections in hemodialysis settings, b) preventing bacterial infections in hemodialysis settings, c) developing and maintaining surveillance systems for infections and other adverse events, and d) developing training and education programs.
To receive continuing education credit, please answer all of the following questions.
# Detach or Photocopy
# Signature Date I Completed Exam
# MMWR
The Morbidity and Mortality Weekly Report (MMWR) Series is prepared by the Centers for Disease Control and Prevention (CDC) and is available free of charge in electronic format and on a paid subscription basis for paper copy. To receive an electronic copy on Friday of each week, send an e-mail message to [email protected]. The body content should read SUBscribe mmwr-toc. Electronic copy also is available from CDC's World-Wide Web server at http://www.cdc.gov/mmwr/ or from CDC's file transfer protocol server at ftp://ftp.cdc.gov/pub/Publications/mmwr/. To subscribe for paper copy, contact Superintendent of Documents, U.S. Government PrintingOffice, Washington, DC 20402; telephone (202) 512-1800.
Data in the weekly MMWR are provisional, based on weekly reports to CDC by state health departments. The reporting week concludes at close of business on Friday; compiled data on a national basis are officially released to the public on the following Friday. Address inquiries about the MMWR Series, including material to be considered for publication, to: Editor, MMWR Series, Mailstop C-08, CDC, 1600 Clifton Rd., N.E., Atlanta, GA 30333; telephone (888) 232-3228.
All material in the MMWR Series is in the public domain and may be used and reprinted without permission; citation as to source, however, is appreciated.
# IU.S. Government Printing Office: 2001-633-173/48222 Region IV
| None | None |
332b309c80a0f3b833619fcf65ed45c271835812 | cdc | None | The Occupational Safety and Health Act of 1970 emphasizes the need for standards to protect the health and safety of workers exposed to an ever-increasing number of potential hazards at their workplace. To provide relevant data from which valid criteria and effective standards can be deduced, the National Institute for Occupational Safety and Health has projected a formal system of research, with priorities determined on the basis of specified indices. It is intended to present successive reports as research and epidemiologic studies are completed and sampling and analytical methods are developed. Criteria and standards will be reviewed periodically to ensure continuing protection of the worker. I am pleased to acknowledge the contributions to this report on sulfur dioxide by members of my staff, the valuable and constructive comments presented by the Review Consultants on Sulfur Dioxide, the ad hoc committees of the American Academy of Occupational Medicine and the American Conference of Governmental Industrial Hygienists, by Robert B. O'Connor, M.D., NIOSH consultant in occupational medicine, and by William A. Burgess, NIOSH consultant on respiratory protection. The NIOSH recommendations for standards are not necessarily a consensus of all the consultants and professional societies that reviewed this criteria document on sulfur dioxide. Lists of the NIOSH Review Committee members and of the Review Consultants appear on the following pages.# I. RECOMMENDATIONS FOR
Sufficient technology exists to permit compliance with the recommended standard. The standard will be subject to review and will be revised as necessary.
"Exposure to sulfur dioxide" means exposure to a concentration of sulfur dioxide equal to or above one-half the recommended workroom environmental standard. Exposures at lower environmental concentrations will not require adherence to the following sections. Procedures for identification of exposure areas can be accomplished by time-weighted average (TWA) determinations by methods described in Appendices I and II or by any method shown to be equivalent in accuracy, precision, and sensitivity to the methods specified.
If "exposure" to other chemicals also occurs, for example from arsenic, then provisions of any applicable standard for the other chemicals shall also be followed.
# Section 1 -Environmental (Workplace Air) (a) Concentration
Occupational exposure to sulfur dioxide shall be controlled so that workers shall not be exposed to sulfur dioxide at a concentration greater than 2 parts per million parts of air (5 milligrams per cubic meter of air) determined as a time-weighted average exposure for an 8-hour work day.
# (b) Sampling, Calibration, and Analysis
Procedures for sampling, calibration of equipment, and analysis of environmental samples shall be as provided in Appendix I or by any method shown to be equivalent in accuracy, precision, and sensitivity to the method specified.
Section 2 -Medical (a) Comprehensive preplacement and annual medical examinations shall be provided for all workers subject to "exposure to sulfur dioxide."
The examination shall be directed toward but not limited to the eyes and the cardiopulmonary system; particular attention shall be focused on complaints of mucous membrane irritation and cough. An evaluation of the advisability of a worker's using negative-or positive-pressure respirators shall also be made. (a)
# Respiratory Protection
Engineering controls shall be used wherever feasible to maintain sulfur dioxide concentrations below the prescribed limit. Appropriate respirators shall be provided and used when a variance has been granted to allow respirators as a means of control of exposure to routine operations and while the application is pending. Administrative controls should also be used to reduce exposure. Respirators shall also be provided and used for nonroutine operations (occasional brief exposures above the TWA of 2 ppm and for emergencies); however, for these instances a variance is not required but the requirements set forth below continue to apply.
Appropriate respirators as described in Table 1-1 shall only be used pursuant to the following requirements:
(1) For the purpose of determining the type of respirator to be used, the employer shall measure the atmospheric concentration of sulfur dioxide in the workplace when the initial application for variance is made and thereafter whenever process, worksite, climate, or control changes occur which are likely to Increase the sulfur dioxide concentration. This requirement shall not apply when only atmospheresupplying positive pressure respirators are used. The employer shall ensure that no worker is being exposed to sulfur dioxide in excess of the standard either because of improper respirator selection, fit, use, or maintenance.
The respirator and cartridge or canister used shall be of the appropriate class, as determined on the basis of exposure to sulfur dioxide gas.
The employer shall provide respirators in accordance with Table 1-1 below and shall ensure that the employee uses the respirator provided.
(5) Respiratory protective devices described in (6) Respirators specified for use in higher concentrations of sulfur dioxide are permitted in atmospheres of lower concentrations.
Employees shall be given instruction on the use of respirators assigned to them, cleaning of the respirators, and how to test for leakage.
(8) Wherever bulk sulfur dioxide is handled, emergency and escape-type respirators shall be made readily available for each worker. (2) Type C supplied air respirator, demand type (negative pressure), with quarter or half mask facepiece.
# Less than or
(1) Gas mask with chin style canister equal to lOOx for acid gases.
(2) Gas mask with front or back mounted chest type canister for acid gases.
(3) Type C supplied air respirator, demand (negative pressure); pressure-demand; or continuous flow type with full facepiece.
# Greater than lOOx
# Emergency (No concentration limit)
(4) Self-contained breathing apparatus in demand mode (negative pressure) with full facepiece.
(1) Self-contained breathing apparatus in pressure-demand mode (positive pressure).
(2) Combination supplied air respirator, pressure-demand type, with auxiliary self-contained air supply.
(1) Self-contained breathing apparatus in pressure-demand mode (positive pressure)
(2) Combination supplied air respirator, pressure-demand type, with auxiliary self-contained air supply.
# Evacuation or escape
(1) Self-contained breathing apparatus (No concentration in demand or p_ '.ssure-demand mode limit) (negative or positive pressure).
(2) Gas mask with acid gas chest canister, and mouthpiece respirator. (2) Chemical safety goggles-cup-type or rubber-framed goggles, equipped with approved impact-resistant glass or plastic lenses, shall be worn whenever there is danger of eye contact, such as working with pipelines, valves, etc, which might leak and spurt liquid sulfur dioxide.
(3) Spectacle-type safety goggles-metal or plastic rim safety spectacles with unperforated side shields, or suitable all-plastic safety goggles may be used where continuous eye protection is desirable.
If use of this type of eye protection is mandatory, prescription lenses shall be provided for those employees who need them.
(4) Face shield-plastic shields with forehead protection may be worn in place of or in addition to goggles.
# (c) Work Clothing
(1) Work clothing should be changed at least twice a week or more frequently if required.
(2) Sulfur dioxide-wetted clothing, unless impervious, shall be removed promptly. (2)
Each container of sulfur dioxide shall be examined for leaks upon its arrival or upon filling and shall be reexamined periodically at least every 3 months.
(3) Prior to transferring sulfur dioxide from a storage container, an inspection shall be conducted to detect any gas leaks in the transport system (eg, cylinder seal with gas regulator, regulator apparatus, regulator seal with transport conduits, conduit system, etc).
(4) Cylinders of sulfur dioxide shall be secured so they cannot be damaged during transport or use.
# (b) Emergency Procedures
(1) Procedures for emergencies shall be established to meet foreseeable events. The irritant and choking properties of sulfur dioxide provide warning of overexposure and evacuation from the area should begin as soon as possible.
(2) Appropriate respirators shall be available for wear during evacuation.
(3) Where there is the possibility of sulfur dioxide contact on the eyes or skin, drench-type showers, eye-wash fountains, and cleansing facilities should be installed and maintained to provide prompt, immediate access by the workers.
# (c) Exhaust Systems and Enclosure
Exhaust ventilation and enclosure processes shall be used wherever practicable to control workplace concentrations. Systems shall be designed and maintained to prevent the accumulation or recirculation of sulfur dioxide into the workroom.
In addition, necessary measures shall be taken to ensure that discharge outdoors will not produce a health hazard to humans, animals, or plants.
# (d) General Housekeeping
Emphasis shall be placed upon cleanup, inspection and repair of equipment and leaks, and proper storage of materials. In the case of intense exposures, even though they occurred frequently, there was believed to be no evidence of damage of a serious or a permanent type. It was surprising that the high frequency of symptoms of respiratory disease was the greatest' in the age groups under 50 where employment exposure time had been shortest. According to the author, the most likely explanation was that because respiratory disease was rare in the younger age groups, the effect of small external insults was easier to detect than in the older age groups where respiratory disease from other causes was more common and small additions would be less noticeable.
# Anderson
In Later, the patient was exposed in a chamber to 10 ppm sulfur dioxide for 30 minutes.
On the following day, lesions again appeared but were weaker than had been previously experienced. The eruption disappeared the following night.
Another chamber exposure to 40 ppm sulfur dioxide for 10 minutes was given, after which the patient was permitted to breathe fresh air for an unspecified period and then returned to the chamber for another 10 minutes.
On the following day, an eruption again developed which was more severe than to the 10 ppm exposure. Regression of the lesions followed in approximately 2 days. It thus seems that these 2 reported cases were due to a systemic allergic reaction.
In There is far less time lag than that experienced with laboratory analytical results. Rapid detecting units are valuable for determining whether a hazardous condition exists at a given location at a given time so that workers may be evacuated or suitable protective devices provided. In addition, industrial operators and process engineers need inexpensive and rapid tools for day-to-day evaluation of the atmospheric levels in a work area.
The accuracy of detector tubes is limited; at best they give only an indication of the contaminant concentration. In evaluating measurements performed with detector tubes, interferences, difficulty of endpoint readings, and possible calibration inaccuracies must all be considered.
# (d)
# Accuracy and Precision
At 2.5 ppm, the accuracy is 5% with a relative standard deviation of 4%. At 25 ppm, the accuracy and relative standard deviation can be improved to about 1%.
# (e) Advantages and Disadvantages
The samples are easily collected and conveniently shipped to the laboratory for analysis in glass vials.
The sulfuric acid formed is stable and nonvolatile, making this manner of collection of sulfur dioxide desirable.
The analysis is relatively rapid and simple.
Spillage from the impingers is possible and could be hazardous if spilled into molten metal.
# (f) Apparatus
(1) Absorber-glass midget impingers.
(2) Personal sampling pump with flowmeter capable of sampling at a rate of 1-2 liters/minute.
(3) 37 mm mixed cellulose ester filter, 0.8 micron nominal pore size.
(4) Necessary glassware.
( If a specific item of information is inapplicable, the initials "n.a." (not applicable) should be inserted. (1) Toxic level for total compound or mixture, relevant symptoms of exposure, skin and eye irritation properties, principal routes of absorption, effects of chronic (long-term) exposure, and emergency and first-aid procedures.
(g) Section VI. Reactivity Data.
(1) Chemical stability, incompatibility, hazardous decomposition products, and hazardous polymerization.
(h) Section VII. Spill or Leak Procedures.
(1) Detailed procedures to be followed with emphasis on precautions to be taken in cleaning up and safe disposal of materials leaked or spilled. This includes proper labeling and disposal of containers holding residues, contaminated absorbents, etc.
(i) Section VIII. Special Protection Information. | The Occupational Safety and Health Act of 1970 emphasizes the need for standards to protect the health and safety of workers exposed to an ever-increasing number of potential hazards at their workplace. To provide relevant data from which valid criteria and effective standards can be deduced, the National Institute for Occupational Safety and Health has projected a formal system of research, with priorities determined on the basis of specified indices. It is intended to present successive reports as research and epidemiologic studies are completed and sampling and analytical methods are developed. Criteria and standards will be reviewed periodically to ensure continuing protection of the worker. I am pleased to acknowledge the contributions to this report on sulfur dioxide by members of my staff, the valuable and constructive comments presented by the Review Consultants on Sulfur Dioxide, the ad hoc committees of the American Academy of Occupational Medicine and the American Conference of Governmental Industrial Hygienists, by Robert B. O'Connor, M.D., NIOSH consultant in occupational medicine, and by William A. Burgess, NIOSH consultant on respiratory protection. The NIOSH recommendations for standards are not necessarily a consensus of all the consultants and professional societies that reviewed this criteria document on sulfur dioxide. Lists of the NIOSH Review Committee members and of the Review Consultants appear on the following pages.# I. RECOMMENDATIONS FOR
Sufficient technology exists to permit compliance with the recommended standard. The standard will be subject to review and will be revised as necessary.
"Exposure to sulfur dioxide" means exposure to a concentration of sulfur dioxide equal to or above one-half the recommended workroom environmental standard. Exposures at lower environmental concentrations will not require adherence to the following sections. Procedures for identification of exposure areas can be accomplished by time-weighted average (TWA) determinations by methods described in Appendices I and II or by any method shown to be equivalent in accuracy, precision, and sensitivity to the methods specified.
If "exposure" to other chemicals also occurs, for example from arsenic, then provisions of any applicable standard for the other chemicals shall also be followed.
# Section 1 -Environmental (Workplace Air) (a) Concentration
Occupational exposure to sulfur dioxide shall be controlled so that workers shall not be exposed to sulfur dioxide at a concentration greater than 2 parts per million parts of air (5 milligrams per cubic meter of air) determined as a time-weighted average exposure for an 8-hour work day.
# (b) Sampling, Calibration, and Analysis
Procedures for sampling, calibration of equipment, and analysis of environmental samples shall be as provided in Appendix I or by any method shown to be equivalent in accuracy, precision, and sensitivity to the method specified.
Section 2 -Medical (a) Comprehensive preplacement and annual medical examinations shall be provided for all workers subject to "exposure to sulfur dioxide."
The examination shall be directed toward but not limited to the eyes and the cardiopulmonary system; particular attention shall be focused on complaints of mucous membrane irritation and cough. An evaluation of the advisability of a worker's using negative-or positive-pressure respirators shall also be made. (a)
# Respiratory Protection
Engineering controls shall be used wherever feasible to maintain sulfur dioxide concentrations below the prescribed limit. Appropriate respirators shall be provided and used when a variance has been granted to allow respirators as a means of control of exposure to routine operations and while the application is pending. Administrative controls should also be used to reduce exposure. Respirators shall also be provided and used for nonroutine operations (occasional brief exposures above the TWA of 2 ppm and for emergencies); however, for these instances a variance is not required but the requirements set forth below continue to apply.
Appropriate respirators as described in Table 1-1 shall only be used pursuant to the following requirements:
(1) For the purpose of determining the type of respirator to be used, the employer shall measure the atmospheric concentration of sulfur dioxide in the workplace when the initial application for variance is made and thereafter whenever process, worksite, climate, or control changes occur which are likely to Increase the sulfur dioxide concentration. This requirement shall not apply when only atmospheresupplying positive pressure respirators are used. The employer shall ensure that no worker is being exposed to sulfur dioxide in excess of the standard either because of improper respirator selection, fit, use, or maintenance.
(2)
The respirator and cartridge or canister used shall be of the appropriate class, as determined on the basis of exposure to sulfur dioxide gas.
( (4)
The employer shall provide respirators in accordance with Table 1-1 below and shall ensure that the employee uses the respirator provided.
(5) Respiratory protective devices described in (6) Respirators specified for use in higher concentrations of sulfur dioxide are permitted in atmospheres of lower concentrations.
Employees shall be given instruction on the use of respirators assigned to them, cleaning of the respirators, and how to test for leakage.
(8) Wherever bulk sulfur dioxide is handled, emergency and escape-type respirators shall be made readily available for each worker. (2) Type C supplied air respirator, demand type (negative pressure), with quarter or half mask facepiece.
# Less than or
(1) Gas mask with chin style canister equal to lOOx for acid gases.
(2) Gas mask with front or back mounted chest type canister for acid gases.
(3) Type C supplied air respirator, demand (negative pressure); pressure-demand; or continuous flow type with full facepiece.
# Greater than lOOx
# Emergency (No concentration limit)
(4) Self-contained breathing apparatus in demand mode (negative pressure) with full facepiece.
(1) Self-contained breathing apparatus in pressure-demand mode (positive pressure).
(2) Combination supplied air respirator, pressure-demand type, with auxiliary self-contained air supply.
(1) Self-contained breathing apparatus in pressure-demand mode (positive pressure)
(2) Combination supplied air respirator, pressure-demand type, with auxiliary self-contained air supply.
# Evacuation or escape
(1) Self-contained breathing apparatus (No concentration in demand or p_ '.ssure-demand mode limit) (negative or positive pressure).
(2) Gas mask with acid gas chest canister, and mouthpiece respirator. (2) Chemical safety goggles-cup-type or rubber-framed goggles, equipped with approved impact-resistant glass or plastic lenses, shall be worn whenever there is danger of eye contact, such as working with pipelines, valves, etc, which might leak and spurt liquid sulfur dioxide.
(3) Spectacle-type safety goggles-metal or plastic rim safety spectacles with unperforated side shields, or suitable all-plastic safety goggles may be used where continuous eye protection is desirable.
If use of this type of eye protection is mandatory, prescription lenses shall be provided for those employees who need them.
(4) Face shield-plastic shields with forehead protection may be worn in place of or in addition to goggles.
# (c) Work Clothing
(1) Work clothing should be changed at least twice a week or more frequently if required.
(2) Sulfur dioxide-wetted clothing, unless impervious, shall be removed promptly. (2)
Each container of sulfur dioxide shall be examined for leaks upon its arrival or upon filling and shall be reexamined periodically at least every 3 months.
(3) Prior to transferring sulfur dioxide from a storage container, an inspection shall be conducted to detect any gas leaks in the transport system (eg, cylinder seal with gas regulator, regulator apparatus, regulator seal with transport conduits, conduit system, etc).
(4) Cylinders of sulfur dioxide shall be secured so they cannot be damaged during transport or use.
# (b) Emergency Procedures
(1) Procedures for emergencies shall be established to meet foreseeable events. The irritant and choking properties of sulfur dioxide provide warning of overexposure and evacuation from the area should begin as soon as possible.
(2) Appropriate respirators shall be available for wear during evacuation.
(3) Where there is the possibility of sulfur dioxide contact on the eyes or skin, drench-type showers, eye-wash fountains, and cleansing facilities should be installed and maintained to provide prompt, immediate access by the workers.
# (c) Exhaust Systems and Enclosure
Exhaust ventilation and enclosure processes shall be used wherever practicable to control workplace concentrations. Systems shall be designed and maintained to prevent the accumulation or recirculation of sulfur dioxide into the workroom.
In addition, necessary measures shall be taken to ensure that discharge outdoors will not produce a health hazard to humans, animals, or plants.
# (d) General Housekeeping
Emphasis shall be placed upon cleanup, inspection and repair of equipment and leaks, and proper storage of materials. In the case of intense exposures, even though they occurred frequently, there was believed to be no evidence of damage of a serious or a permanent type. It was surprising that the high frequency of symptoms of respiratory disease was the greatest' in the age groups under 50 where employment exposure time had been shortest. According to the author, [18] the most likely explanation was that because respiratory disease was rare in the younger age groups, the effect of small external insults was easier to detect than in the older age groups where respiratory disease from other causes was more common and small additions would be less noticeable.
# Anderson
In Later, the patient was exposed in a chamber to 10 ppm sulfur dioxide for 30 minutes.
On the following day, lesions again appeared but were weaker than had been previously experienced. The eruption disappeared the following night.
Another chamber exposure to 40 ppm sulfur dioxide for 10 minutes was given, after which the patient was permitted to breathe fresh air for an unspecified period and then returned to the chamber for another 10 minutes.
On the following day, an eruption again developed which was more severe than to the 10 ppm exposure. Regression of the lesions followed in approximately 2 days. It thus seems that these 2 reported cases were due to a systemic allergic reaction.
In There is far less time lag than that experienced with laboratory analytical results. Rapid detecting units are valuable for determining whether a hazardous condition exists at a given location at a given time so that workers may be evacuated or suitable protective devices provided. In addition, industrial operators and process engineers need inexpensive and rapid tools for day-to-day evaluation of the atmospheric levels in a work area.
The accuracy of detector tubes is limited; at best they give only an indication of the contaminant concentration. In evaluating measurements performed with detector tubes, interferences, difficulty of endpoint readings, and possible calibration inaccuracies must all be considered.
# (d)
# Accuracy and Precision
At 2.5 ppm, the accuracy is 5% with a relative standard deviation of 4%. At 25 ppm, the accuracy and relative standard deviation can be improved to about 1%.
# (e) Advantages and Disadvantages
The samples are easily collected and conveniently shipped to the laboratory for analysis in glass vials.
The sulfuric acid formed is stable and nonvolatile, making this manner of collection of sulfur dioxide desirable.
The analysis is relatively rapid and simple.
Spillage from the impingers is possible and could be hazardous if spilled into molten metal.
# (f) Apparatus
(1) Absorber-glass midget impingers.
(2) Personal sampling pump with flowmeter capable of sampling at a rate of 1-2 liters/minute.
(3) 37 mm mixed cellulose ester filter, 0.8 micron nominal pore size.
(4) Necessary glassware.
( If a specific item of information is inapplicable, the initials "n.a." (not applicable) should be inserted. (1) Toxic level for total compound or mixture, relevant symptoms of exposure, skin and eye irritation properties, principal routes of absorption, effects of chronic (long-term) exposure, and emergency and first-aid procedures.
(g) Section VI. Reactivity Data.
(1) Chemical stability, incompatibility, hazardous decomposition products, and hazardous polymerization.
(h) Section VII. Spill or Leak Procedures.
(1) Detailed procedures to be followed with emphasis on precautions to be taken in cleaning up and safe disposal of materials leaked or spilled. This includes proper labeling and disposal of containers holding residues, contaminated absorbents, etc.
(i) Section VIII. Special Protection Information.
( | None | None |
c74dc8c097cb69db36287353e5e371e22197812f | cdc | None | depar depar depar depar department of health and human ser tment of health and human ser tment of health and human ser tment of health and human ser tment of health and human services vices vices vices vices# Nonfatal Motor-Vehicle Animal Crash-Related Injuries -United States, 2001-2002
In 2000, an estimated 6.1 million light-vehicle (e.g., passenger cars, sport utility vehicles, vans, and pickup trucks) crashes on U.S. roadways were reported to police (1). Of these reported crashes, 247,000 (4.0%) involved incidents in which the motor vehicle (MV) directly hit an animal on the roadway (1). Each year, an estimated 200 human deaths result from crashes involving animals (i.e., deaths from a direct MV animal collision or from a crash in which a driver tried to avoid an animal and ran off the roadway) (2). To characterize nonfatal injuries from these incidents, CDC analyzed data from the National Electronic Injury Surveillance System-All Injury Program (NEISS-AIP). This report summarizes the results of that analysis, which indicated that, during 2001-2002, an estimated 26,647 MV occupants per year were involved in crashes from encounters with animals (predominantly deer) in a roadway and treated for nonfatal injuries in U.S. hospital emergency departments (EDs). Cost-effective measures targeting both drivers (e.g., speed reduction and early warnings) and animals (e.g., fencing and underpasses) are needed to reduce injuries associated with MV collisions involving animals.
NEISS-AIP is operated by the Consumer Product Safety Commission and collects data about initial visits for all types and causes of injuries treated in U.S. EDs (3). NEISS-AIP data are drawn from a nationally representative subsample of 66 of 100 NEISS-AIP hospitals selected as a stratified probability sample of hospitals in the United States and its territories with a minimum of six beds and a 24-hour ED. NEISS-AIP provides data on approximately 500,000 injuryand consumer product-related ED cases each year. Data for each case include a comment variable that contains additional information about the circumstances of the injury.
Each case was assigned a sample weight on the basis of the inverse probability of selection; these weights were summed to provide national estimates of MV animal crash-related injuries. Confidence intervals (CIs) were calculated by using a direct variance estimation procedure that accounted for the sample weights and complex sample design. Rates were calculated by using 2001 and 2002 U.S. Census bridged-race population estimates from the National Center for Health Statistics (4).
Data used in this study were obtained from medical records of 676 ED patients treated for nonfatal injuries incurred while driving or riding in a light vehicle and encountering an animal in the roadway. This report focuses on the majority of these patients, who encountered larger animals (e.g., deer, moose, elk, bear, horses, or cattle) entering the roadway. Smaller animals (e.g., dogs, cats, squirrels, raccoons, and possums) were included only in the overall national estimate. No information was obtained on type of vehicle. MV animal crashes were defined as those involving direct collision with an animal on a roadway or those occurring on or off the roadway as a result of trying to avoid hitting the animal. These cases were identified by using a brief narrative captured in the NEISS-AIP database that described the circumstances of the injury incident. An additional 79 patients injured as motorcyclists involved in MV-animal crashes were excluded from this study. During 2001During -2002, an estimated 26,647 (9.3 per 100,000 population; 95% CI = 6.7-11.9) persons were treated annually in U.S. EDs for MV animal crash-related injuries, of which 22,498 (84.8%) were MV occupants in crashes involving larger animals (Table 1). The highest MV large animal crashrelated injury rate (21.1 per 100,000 population) occurred among persons aged 15-24 years (Table 1). The age distribution of those injured in MV large animal crashes was different from those injured during all other types of MV trafficrelated crashes (p<0.03); most of this difference was attributed to an overrepresentation of persons aged 15-24 years (p<0.0001) and an underrepresentation of children aged 0-14 years (p<0.0001) (Figure). Among injured persons aged 15-24 years, 48.9% were driving the vehicle. The MV large animal crash-related injury rate was similar for males and females (Table 1). Approximately 6% of those treated in U.S. EDs required hospitalization for their injuries.
MV large animal crash-related injuries were mostly strains/ sprains (36.5%) and contusions/abrasions (33.9%) and involved the head/face (28.1%), neck (22.7%), and upper trunk (15.3%) (Table 2). The majority (94.5%) of the neck injuries were strains and sprains, and 62.5% of head/face injuries were contusions, abrasions, or lacerations. Persons injured during MV large animal crashes were treated more often during October and November than other months. Deer were the most common large animals involved in these incidents (86.9%). Approximately half (54.4%) of these crashes involved a direct collision with the animal, and the remainder (44.8%) resulted from the driver trying to avoid hitting the animal. Of those incidents in which the animal was avoided, the crash most commonly involved an MV leaving the roadway (29.0%); an MV hitting a tree, pole, or guardrail (21.4%); or an MV rollover (17.3%) (Table 2). Editorial Note: Nationally, nonfatal MV animal crashrelated injuries account for <1.0% of approximately three million MV occupants treated in U.S. EDs annually (5). Direct MV animal crashes represent nearly 4.0% of an estimated 6.1 million light-vehicle crashes reported to police in the United States (1). However, in rural areas with large deer populations, MV animal crashes and associated occupant deaths and injuries, wildlife loss, and property damage are important concerns. For instance, in Wisconsin, MV deer crashes accounted for nearly 16% of all statewide police-reported MV crashes in 2002 (6).
National estimates reported from this study are consistent with state MV animal crash data reported to police. In this study, the majority of MV occupant injuries resulted from encounters between the MV and deer; however, 12% of those injured resulted from MV crashes involving large domesticated animals (e.g., horses and cattle). MV occupant injuries can occur because of a direct MV collision with the large animal or from swerving or maneuvering to avoid a collision with the animal. In this study, 63.8% of younger drivers swerved to avoid the animal, resulting in an MV crash and subsequent injury. Similar to other MV occupant injuries from crashes that occur on U.S. highways, a majority of the injuries were neck sprains/strains, and contusions/abrasions to the head and face. One fourth of MV animal crash-related injuries were treated in October and November at the height of the fall deer hunting, mating, and migration season (7). MV animal crashes are more likely to occur in the early morning hours and especially at dusk, when deer are actively moving about and likely to cross the road in rural areas (6)(7)(8). The findings of this report are subject to at least three limitations. First, although the risk for MV animal crash-related injury can vary among states and local areas, NEISS-AIP is designed to provide only national estimates and does not provide regional, state, or local estimates or estimates by urban and rural categories. Second, because of the small number of cases reported, this study excluded motorcyclists, who are known to be at higher risk for injury in crashes (6). Finally, NEISS-AIP only provides data on injured persons treated in hospital EDs.
Prevention efforts have focused on warning signs to alert drivers to animal crossings, speed restrictions, roadway fencing and underpasses/overpasses aimed at directing animals toward safe passage, roadside clearing, roadside mirrors and reflectors (i.e., to deflect headlight beams toward the sides of the road to alert deer), and reduction of deer populations through recreational hunting (7,9). Evaluation studies have been conducted to assess the cost and effectiveness of these methods, but the results are inconsistent (10). Interventions with some supportive evidence (e.g., fences combined with underpasses or overpasses) also are among the most expensive to build and maintain.
Primary prevention of MV animal crashes can be accomplished by keeping large animals, especially deer, from entering the roadway or by providing drivers with more time to react to a potentially dangerous situation. The same behaviors that are recommended to help prevent crashes in general are relevant for MV animal crashes. Driving within speed limits, staying alert and reducing distracted and drowsy driving, and eliminating alcohol-impaired driving will give drivers, particularly teenagers and younger adults, more time to react and avoid collisions. Prevention of injury if a crash occurs can be accomplished by the universal use of proper restraints, including safety belts, child safety seats, and booster seats.
# Transmission of Hepatitis B Virus in Correctional Facilities -Georgia, January 1999-June 2002
Incarcerated persons have a disproportionate burden of infectious diseases (1), including hepatitis B virus (HBV) infection. Among U.S. adult prison inmates, the overall prevalence of current or previous HBV infection ranges from 13% to 47%. The prevalence of chronic HBV infection among inmates is approximately 1.0%-3.7%, two to six times the prevalence among adults in the general U.S. population (1). Incarcerated persons can acquire HBV infection in the community or in correctional settings (1). This report summarizes the results of 1) an analysis of hepatitis B cases among Georgia inmates reported to the Georgia Department of Human Resources, Division of Public Health (DPH) during January 1999-June 2002, including a retrospective investigation of cases reported during January 2001-June 2002; and 2) a prevalence survey conducted in prison intake centers during February-March 2003. These efforts identified cases of acute hepatitis B in multiple Georgia prisons and documented evidence of ongoing transmission of HBV in the state correctional system. The findings underscore the need for hepatitis B vaccination programs in correctional facilities.
The Georgia correctional system houses approximately 45,000 inmates in 68 correctional facilities; approximately 16,000 new inmates are admitted each year and processed through one of five intake centers. The correctional system does not routinely screen inmates for HBV infection, and diagnostic testing is left to the judgment of individual physicians. In August 2000, in response to two hepatitis B Online know what matters. e asy.
MMWR Online makes it possible for you to access vital public health reports and news as soon as CDC publishes them. Get the information you want, when you need it, from a trusted source.
Visit cdc.gov/mmwr and stay current on important public health topics -the easy way.
-utbreaks at one Georgia correctional facility (2,3), DPH began to monitor reports of acute hepatitis B cases among inmates at all Georgia correctional facilities, as determined by the inmates' addresses on laboratory reports.
A case of acute HBV infection was defined as a positive serologic test for IgM antibodies to hepatitis B core antigen (IgM anti-HBc) on at least one occasion and at least one additional supporting finding (e.g., compatible symptoms, liver enzyme elevation, or another positive hepatitis B serologic test), received by DPH during January 1999-June 2002. Cases reported during January 2001-June 2002 were confirmed by retrospective review of the inmate's medical and laboratory records. The date of diagnosis of acute HBV infection was defined as the date that alanine aminotransferase (ALT) or aspartate aminotransferase (AST) levels were elevated at least two times greater than the upper limit of normal in conjunction with a positive test for IgM anti-HBc. When ALT or AST levels were not available, the date of the blood draw with a positive IgM anti-HBc result was used as the approximate date of diagnosis.
Incarceration histories of inmates with acute HBV infections reported during January 2001-June 2002 were reviewed to identify inmate locations and number of transfers between correctional facilities before illness onset. Persons with asymp-tomatic and symptomatic cases were considered to have been infected while incarcerated if they were in prison or jail during the 12 months or 6 months, respectively, before illness onset.
A prevalence survey to assess the HBV infection status of prisoners on entry was conducted at three Georgia prison intake centers for males and one intake center for females during February-March 2003. Consenting inmates underwent HBV serologic testing; all inmates at intake when the survey was conducted were offered hepatitis B vaccine.
During January 1999-June 2002, a total of 92 cases of acute HBV infection were identified, of which 57 (62%) were reported during January 2001-June 2002 and included in the retrospective investigation (Figure). Among the 57 inmates with HBV infection, the median age was 34 years (range: 18-59 years); 52 (91%) were male, and 35 (61%) were non-Hispanic blacks. Ten (18%) had symptoms that included jaundice, abdominal pain, fever, and vomiting. Seven (12%) subsequently were determined to have chronic infections. The chronic infection status of four inmates was not assessed.
Among the 57 inmates included in the retrospective investigation, the most frequently reported reason for HBV testing was the presence of symptoms or elevated liver enzymes (21 cases ). Other reasons included reported characteristics and behaviors that might be associated with HBV transmission (e.g., tattoos or unprotected sex contacts) (14 ), serologic testing performed as part of initial medical evaluation (13 ), and being positive for human immunodeficiency virus (five ). Prison staff reported counseling and providing medical follow-up for 52 (91%) of the 57 inmates.
The 57 cases were reported from 27 prisons and four probation detention centers in Georgia, with a mean of 1.8 cases per facility and a range of one to three cases for the 30 facilities that were not involved in the previously recognized outbreaks (2,3). The 57 inmates had been incarcerated for a median of 2.2 years (range: 0-23.7 years) before illness onset and had been transferred 1.4 times on average (median: one time; range: one to seven times) during the 12 months before diagnosis. The majority of HBV infections (41 ) were acquired in prison. Of the remaining 16 cases, 13 (81%) occurred in persons who had been in prison or jail for 1-6 months before receiving a diagnosis. The remaining three (19%) inmates were asymptomatic and had been in prison or jail for 10-11 months before receiving a diagnosis.
As of August 2002, the seven inmates who had chronic infections had been transferred among prison facilities 13 times during the cumulative 89 months of incarceration that followed their diagnosis, resulting in a mean of 1.8 transfers per person-year of incarceration (median: two transfers; range: zero to five transfers). Three inmates with chronic infection were released from prison.
Of 546 inmates surveyed at intake during February-March 2003, a total of 489 (90%) consented to serologic testing, and 428 (78%) consented to hepatitis B vaccination. Of the 489 inmates tested, three (0.6%) had acute HBV infections, four (0.8%) had chronic infections, 64 (13%) had evidence of resolved infections, and 374 (76%) were susceptible to HBV infection. Two of three inmates with acute infection had spent 5.5-11.0 months in jail before intake. Editorial Note: HBV is a bloodborne pathogen, transmitted by percutaneous or permucosal exposure to infectious blood or body fluids. The prevalence of chronic infection is higher among prison inmates (1.0%-3.7%) than among the general U.S. population (0.5%) (1), reflecting an overrepresentation of persons entering prison who are at high risk for HBV infection (e.g., injection-drug users and those with reported histories of multiple sex partners). The prevalence of chronic infection among the intake population in this report (0.8%) suggests that high-risk behaviors practiced within the community before incarceration might not account entirely for the burden of HBV infection in correctional facilities. Although studies are limited, transmission of HBV infection within correctional settings has been documented, with incidence ranging from 0.8% to 3.8% per year (2,(4)(5)(6).
The retrospective investigation described in this report identified an increase in HBV infections in Georgia correctional facilities, beginning in January 2001. This increase likely was related to multiple factors, including enhanced surveillance and increased diagnostic testing by correctional medical staff. Changes in diagnostic practices might have occurred because of increased awareness of hepatitis B among medical staff after outbreaks at a Georgia correctional facility in June 2000 and again in June 2001. Nonetheless, the number of reported cases probably underestimates the extent of HBV transmission in the correctional system because the majority of persons with acute HBV infection are asymptomatic and investigations of single cases are not conducted routinely. In the first previous outbreak, one symptomatic patient reported to DPH was associated with a cluster of 11 acute cases, and four chronic HBV infections were identified (2).
The majority of inmates with identified acute HBV infections were housed in multiple Georgia correctional facilities and were infected during their incarceration, suggesting widespread ongoing transmission in multiple facilities. Inmates infected with HBV were transferred frequently among facilities. Thus, potential sources of HBV transmission were distributed throughout the prison system.
In the Georgia correctional system, approximately one third of inmates are released each year (7). Inmates who become chronically infected and subsequently are released represent potential sources of infection for others in the community. In addition, susceptible inmates who are released continue to be at increased risk for HBV infection (1). The majority of inmates in the intake survey were susceptible to HBV infection and consented to vaccination, suggesting that vaccination efforts in correctional facilities might effectively capture susceptible, high-risk populations.
Although data are lacking regarding the overall burden of HBV infection in correctional systems, the ongoing transmission demonstrated in Georgia prisons might be occurring in other states, where similar conditions are likely to exist. All inmates who receive a medical evaluation should be vaccinated to prevent HBV infection (1). However, the majority of state correctional systems in the United States, including the Georgia system, do not have hepatitis B vaccination programs (1). Implementation of such programs in correctional settings nationwide could result in a considerable reduction in the hepatitis B-associated disease burden, not only by eliminating transmission among the incarcerated population, but also by reducing transmission in the community (8).
# Hepatitis B Vaccination of Inmates in Correctional Facilities -Texas, 2000-2002
In December 2002, approximately 2.2 million persons were incarcerated in the United States (1); an estimated 8 million were released to the community that year (2). In 2001, approximately 22,000 acute hepatitis B cases and 78,000 new hepatitis B virus (HBV) infections occurred in the United States (3); an estimated 29% of these cases were in persons who had been incarcerated previously (4). The majority of HBV infections among incarcerated persons are acquired in the community; however, infection also is transmitted within correctional settings (2). Hepatitis B vaccination of incarcerated persons is recommended to prevent transmission in correctional facilities and in previously incarcerated persons on their return to the community (2). In May 2000, the Texas Department of Criminal Justice (TDCJ), which oversees custody of state jail and prison inmates, implemented a hepatitis B vaccination program. To determine hepatitis B vaccination rates of inmates during 2000-2002, TDCJ reviewed charts of inmates released during a 3-day period for documentation of vaccination. This report summarizes the results of that study, which indicated that rates of vaccine acceptance and vaccine series completion among inmates were high. Establishing hepatitis B vaccination programs in prisons and jails can prevent a substantial proportion of HBV infections among adults in the outside community.
During 2000-2002, TDCJ housed approximately 151,000 inmates in 105 adult facilities, including prisons (median sentence of inmates: 9 years; range: 2-99 years) and jails (median sentence of inmates: 1.3 years; range: 3 months-2 years). Approximately 40,000 new offenders enter these facilities annually, and an estimated 1% of inmates are transferred between facilities daily (5,6). In 1999, state funds were appropriated for hepatitis B vaccination of all inmates in jails and prisons.
Before implementation of the vaccination program, a costeffectiveness model was developed that estimated the cost effectiveness of prevaccination testing for immunity to HBV infection among inmates. Stored serum specimens from 889 inmates incarcerated during 1998-1999 were tested for antibodies to hepatitis B core antigen (anti-HBc); HBV prevalence was 18%. The model estimated that at a threshold prevalence of 25%, the cost of a program with prevaccination testing was equivalent to that of vaccination without testing; at lower prevalence, prevaccination testing would not be cost effective (Figure). On the basis of these findings, all of the estimated 40,000 entering inmates were offered vaccine without prevaccination testing.
Entering inmates were offered the first hepatitis B vaccine dose at the time of admission. Persons who were already incarcerated were offered the first dose at the time of their annual health evaluation, which occurred on their anniversary month of incarceration. After vaccination of incarcerated persons, only newly admitted inmates were offered vaccine.
Vaccine was administered on a 0-, 2-, and 4-month schedule. An electronic pharmacy auto-renewal system was used to send second and third vaccine doses to the appropriate facility for each inmate. Health-care workers also recorded vaccine dose administration in each inmate's medical record, enabling inmates to complete the vaccination series despite frequent transfers within the system.
In February 2002, TDCJ evaluated vaccine acceptance and series completion rates. Charts of 232 prison inmates and 211 jail inmates released during a 3-day period were audited for receipt of hepatitis B vaccine; 426 (96%) inmates with no record of previous vaccination or HBV infection were considered to be eligible for vaccination. Lack of documentation of a vaccination encounter was interpreted as a failure to offer vaccine, and only a signed informed refusal form was counted as a vaccination refusal.
Hepatitis B vaccine was offered to 319 (75%) of 426 inmates. Prison inmates were more likely to be offered vaccine (185/220 ) than jail inmates (134/206 ) (p<0.001), which might be related to higher inmate turnover and lack of staff contact time in jails (Table ). However, acceptance of the first vaccine dose was higher among jail inmates (114/134 ) than among prison inmates (134/185 ) (p = 0.005).
Among 125 prison and 99 jail inmates who began vaccination and were incarcerated for >4 months, the 3-dose completion rate was 96% and 54%, respectively. In December 2002, the hepatitis B vaccination program was suspended because of a lack of funds. Editorial Note: Evaluation of the TDCJ hepatitis B vaccination program demonstrated that high vaccine coverage could be achieved for inmates in a state correctional system. Incarceration provides an opportunity to vaccinate persons at high risk typically not served by prevention services in the public or private sectors, and vaccination of incarcerated populations is cost effective (7).
The findings in this report illustrate the need to tailor a program to a particular facility. Completion of the vaccine series is a more feasible goal for long-term facilities; shortterm facilities should initiate the vaccine series, supply an immunization record and, where feasible, provide information at discharge about facilities offering the remaining vaccine doses. Vaccination also can be completed if the person returns to a correctional institution.
Prevaccination testing to detect existing immunity can eliminate the cost of revaccinating persons who were vaccinated previously or infected. TDCJ's decision not to perform prevaccination testing was based on a model that included the costs of testing and vaccination and the series completion rate. The model assumed that all inmates who received the first vaccine dose would return for subsequent doses; if attrition caused by release was included in the model, prevaccination testing would only be cost effective if the prevalence of immunity was higher. Changes in prevalence of immunity to HBV infection or costs (e.g., vaccine, labor, and testing) also would change the cost effectiveness of prevaccination testing. In particular, immunity to HBV infection in young adults is changing rapidly within most communities because of an increase in vaccinated adolescents. If adequate immunization records are not available for inmates, periodic monitoring of the prevalence of immunity to HBV infection using a serologic marker to detect both infection (i.e., anti-HBc) and immunization (i.e., antibodies to hepatitis B surface antigen) will help corrections officials determine when prevaccination testing might reduce costs (2). The findings in this report are subject to at least two limitations. First, inmates with shorter sentences are more likely to be discharged and might be overrepresented by the sampling. Because inmates with short sentences might not have been incarcerated long enough to complete the vaccination series, more inmates might have completed the vaccination series than this study demonstrated. Second, lack of long-term follow-up precludes evaluation of the eventual series completion by jail inmates, who might have accessed additional doses outside the correctional system or during subsequent incarcerations.
# FIGURE. Cost effectiveness of prevaccination testing for immunity to hepatitis B virus (HBV) infection among jail and prison inmates -Texas
Hepatitis B vaccination of inmates in state correctional facilities is feasible if resources are available to purchase and administer vaccine. In 2000, a survey of state correctional facility medical directors indicated that the majority of prison systems would vaccinate inmates if resources were available (8). Although hepatitis B vaccination of inmates has been recommended since the vaccine first became available in 1982 ( 9), only five states (Hawaii, Michigan, New Mexico, Vermont, and Wisconsin) vaccinate inmates routinely (D. Burnett, M.D., Wisconsin Department of Corrections and F. Pullara, M.D., New Mexico Department of Corrections, personal communications, 2004) (8). Collaborations between public health and corrections authorities at the state and local level are essential to overcome barriers to vaccination program implementation.
# Tuberculosis Associated with Blocking Agents Against Tumor Necrosis Factor-Alpha -California, 2002-2003
The Food and Drug Administration (FDA) has determined that tuberculosis (TB) disease is a potential adverse reaction from treatment with the tumor necrosis factor-alpha (TNF-α) antagonists infliximab (Remicade ® ), etanercept (Enbrel ® ), and adalimumab (Humira ® )*; the three products are labeled accordingly (1,2). These products work by blocking TNF-α, an inflammatory cytokine, and are approved for treating rheumatoid arthritis and other selected autoimmune diseases. TNF-α is associated with the immunology and pathophysiology of certain infectious diseases, notably TB; blocking TNF-α can allow TB disease to emerge from latent Mycobacterium tuberculosis infection. In 2002, a California county health department reported three cases of TB disease occurring in association with infliximab therapy. This report summarizes those cases and nine subsequently reported cases and provides interim recommendations for TB prevention and management in recipients of these blocking agents. Healthcare providers should take steps to prevent TB in immunocompromised patients and remain vigilant for TB as a cause of unexplained febrile illness.
# Case Reports
Case 1. In January 2002, a U.S.-born man aged 55 years with rheumatoid arthritis had pulmonary TB disease diagnosed 17 months after starting infliximab therapy. In 1995, he had a positive tuberculin skin test (TST) and reportedly took isoniazid for 12 months; however, his adherence to therapy was questionable. During September 2000-January 2002, he received 13 infusions of infliximab, and his arthritic symptoms decreased. However, in January he had fever and weight loss. Four weeks later, a supraclavicular lymph node became enlarged, and a chest radiograph revealed a rightupper-lobe lung cavity with a nodular infiltrate. M. tuberculosis was isolated from sputum and lymph node specimens, and his condition improved with anti-TB medications. In July 2002, he again lost weight. He had smoked cigarettes for many years and was found to have lung cancer; he died in November 2002.
Case 2. A woman aged 64 years with rheumatoid arthritis had pulmonary and pericardial TB disease diagnosed in June 2002. She had begun infliximab therapy in September 2001 and received 7 doses before onset of fever and weight loss in April 2002. Her chest radiograph revealed a large pericardial effusion and a right-upper-lobe lung infiltrate. M. tuberculosis resistant to isoniazid, rifampin, pyrazinamide, and ethambutol was isolated from sputum and pericardial fluid. The patient was born in the Philippines, where TB often is drug resistant (3). In 1999, she was exposed to a person with drugsusceptible TB in the United States and subsequently had two TSTs with negative results in 2000; however, she was taking prednisone for her arthritis at the time of the TSTs. After 12 months of therapy with second-line anti-TB medications, her medical condition has improved. Case 3. A U.S.-born woman aged 54 years was exposed to contagious TB in 1996; she had a positive TST result during the contact investigation but was not treated for latent TB infection (LTBI). The patient has Crohn's disease and received infliximab in February 2001 and June 2002. Two weeks after her second infusion, but 16 months after her first infusion, she sought care for cough, fever, and abdominal pain. Her chest radiograph revealed upper-lobe lung nodules with a pleural effusion, and sputum specimens yielded M. tuberculosis. She started standard, four-drug anti-TB therapy but experienced gastrointestinal intolerance. Isoniazid was discontinued, and she was free of TB disease after treatment with rifampin, pyrazinamide, and ethambutol.
# Additional Reports
In 2003, the state of California Department of Health Services asked local jurisdictions to report TB cases associated with TNF-α antagonists since January 2002. As of September 2003, nine additional reports had been received, for a Eleven of the patients had at least one risk factor for LTBI (e.g., born in countries where TB is prevalent or contact with a person with TB disease). Eight were taking other immunosuppressive therapies at the time of their TB diagnoses. Three patients underwent a medical history for TB risk factors before beginning therapy with a TNF-α antagonist. In addition to the patient in case 1, a second patient died (from cardiomyopathy) while being treated for TB disease.
Editorial Note: As of January 2004, FDA's adverse-event reporting system had received several hundred reports, mostly from outside the United States, of TB disease in patients who received TNF-α antagonists. Manufacturers of these products are required to report known cases, but reporting is voluntary for others. The majority of the cases probably represent progression of LTBI to TB disease, although the contribution of newly acquired M. tuberculosis infection to the total number of reports is unknown (1). Reports have included atypical presentations, extrapulmonary and disseminated disease, and deaths (1,4,5).
In California, after the initial three reports, nine additional cases of TB disease were reported during January 2002-August 2003 in patients taking TNF-α antagonists. Although reporting of TB cases is mandatory in California, reporting the association with TNF-α antagonists was voluntary, and an underestimate might have resulted.
Eight of the 12 patients in California were born in countries where TB is prevalent. In certain instances, physicians had not screened for risk factors for M. tuberculosis infection or tested their patients for infection before beginning therapy with TNF-α antagonists. In other instances, testing was performed, but LTBI was not diagnosed, possibly because of cutaneous anergy. Many patients who receive TNF-α antagonists already are receiving other immunosuppressive therapies, and certain conditions such as rheumatoid arthritis also can decrease sensitivity to tuberculin; therefore, TST results at the time of initiating TNF-α antagonist therapy might be falsely negative. Some experts advocate treating for presumed LTBI when a candidate for TNF-α antagonists has risk factors for M. tuberculosis infection but a negative TST result (4,5).
TNF-α, an inflammatory cytokine expressed by activated macrophages, T-cells, and other immune cells, plays a crucial role in the host response against M. tuberculosis and other intracellular pathogens. Infliximab and adalimumab are monoclonal antibodies; etanercept is a dimeric soluble form of the TNF-α receptor. All three products are approved for the treatment of patients with rheumatoid arthritis. Infliximab also is approved for Crohn's disease, and etanercept is approved for specific other arthritides and for psoriasis. Use of these agents has been associated with other life-threatening infectious diseases besides TB, including candidiasis, histoplasmosis, aspergillosis, and listeriosis (1). TNF-α antagonists often are used in conjunction with other immunosuppressive therapies, particularly glucocorticoids and methotrexate. Whether the increased rates of TB or other infectious diseases are caused by interactions among these therapies is unknown.
Diagnosing LTBI in candidates for TNF-α antagonist therapy is challenging (Box). For patients who undergo treatment for LTBI, the optimal time for starting TNF-α antagonist therapy is undetermined. Some experts advocate postponing therapy until LTBI treatment is complete. However, this delay might be impractical (4,6). The risk for TB relapse in patients previously cured of TB disease and subsequently treated with TNF-α antagonists is unknown.
# BOX. Recommendations for screening, diagnosis, and treatment of latent TB infection (LTBI) and tuberculosis (TB)
in patients administered or scheduled to receive tumor necrosis factor-alpha (TNF-α α α α α) antagonists If active TB disease develops during TNF-α antagonist therapy, the TNF-α antagonist should be discontinued, at least until the anti-TB regimen has been started and the patient's condition has improved. The optimal time for resuming TNF-α antagonist therapy is undetermined. Outcomes with other immunosuppressive agents during the treatment of TB disease have been variable. Use of glucocorticosteroids during the treatment of TB disease is considered safe (7), and studies of TB disease in organ transplant recipients suggest that survival is not decreased by the use of cyclosporine or azathioprine (8). Etanercept, administered in a phase-1 clinical trial along with a standard initial anti-TB regimen, did not delay the resolution of TB disease markers in a group of patients coinfected with human immunodeficiency virus in comparison with historical controls; adverse effects were not detected (9). However, use of anti-T-cell agents in transplant recipients with TB disease is associated with increased mortality; whether this increased mortality is because of the suppression of immune response or the dysfunction of the transplanted organ is unclear (8).
7 0 Illinois 0 1 1 2 0 Iowa 1 2 0 3 1 Michigan 1 0 0 1 0 Missouri 1 0 0 1 0 Nebraska 0 1 0 1 0 Nevada 2 0 0 2 0 New Mexico 1 4 0 5 0 New York 2 1 0 3 0 North Dakota 0 1 0 1 0 Ohio 1 0 0 1 1 Pennsylvania 1 0 0 1 0 South Dakota 1 8 0 9 0 Texas 2 1 0 3 1 Wyoming 0 1 0 1 0
Practitioners who prescribe TNF-α antagonists should educate their patients about the symptoms of TB disease, with added emphasis on extrapulmonary symptoms, which can include fever, malaise, or development of a mass. A patient with symptoms should undergo diagnostic testing for TB. In addition to following local reporting requirements, healthcare providers should report TB cases associated with TNF-α antagonists to FDA's Medwatch system (available at http:// www.fda.gov/medwatch).
Ongoing clinical trials are using both approved and experimental TNF-α antagonists in the treatment of additional conditions (4). Novel therapies that inhibit other related inflammatory cytokines are under development. As the use of these blocking agents expands, associated cases of TB might increase. Vigilance for TB in association with these agents is critical to early recognition and successful treatment.
# West Nile Virus Activity -United
States, July 28-August 3, 2004 and Nevada) and in two wild hatchling birds from Ohio. Three seropositive sentinel horses were reported from Puerto Rico. A total of 1,486 WNV-positive mosquito pools have been reported from 24 states (Arizona, Arkansas, California, Colorado, Connecticut, Georgia, Illinois, Indiana, Kansas, Louisiana, Michigan, Mississippi, Missouri, Nebraska, Nevada, New Jersey, New Mexico, Ohio, Pennsylvania, South Dakota, Tennessee, Texas, Utah, and Virginia).
Additional information about national WNV activity is available from CDC at / westnile/index.htm and at .
# Notice to Readers
# Final 2003 Reports of Notifiable Diseases
The -
- - - - Idaho - - - - - - W y o . - - - - - 2 Colo. N N - - - 621 N . M e x . - - - - 1 4 A r i z . - - - - 5 7 Utah - - - - - - N e v . - 1 - - - 2 PACIFIC - - - - - 2 Wash. - - - - - - Oreg. - - - - - - Calif. - - - - - 2 Alaska - - - - - - H a w a i i - - - - - - Guam - - - - - - P . R . - - - - - - V . I . - - - - - - Amer. Samoa - - - - - - C.N.
# MMWR 697
- No measles cases were reported for the current 4-week period yielding a ratio for week 30 of zero (0). † Ratio of current 4-week total to mean of 15 4-week totals (from previous, comparable, and subsequent 4-week periods for the past 5 years). The point where the hatched area begins is based on the mean and two standard deviations of these 4-week totals. | depar depar depar depar department of health and human ser tment of health and human ser tment of health and human ser tment of health and human ser tment of health and human services vices vices vices vices# Nonfatal Motor-Vehicle Animal Crash-Related Injuries -United States, 2001-2002
In 2000, an estimated 6.1 million light-vehicle (e.g., passenger cars, sport utility vehicles, vans, and pickup trucks) crashes on U.S. roadways were reported to police (1). Of these reported crashes, 247,000 (4.0%) involved incidents in which the motor vehicle (MV) directly hit an animal on the roadway (1). Each year, an estimated 200 human deaths result from crashes involving animals (i.e., deaths from a direct MV animal collision or from a crash in which a driver tried to avoid an animal and ran off the roadway) (2). To characterize nonfatal injuries from these incidents, CDC analyzed data from the National Electronic Injury Surveillance System-All Injury Program (NEISS-AIP). This report summarizes the results of that analysis, which indicated that, during 2001-2002, an estimated 26,647 MV occupants per year were involved in crashes from encounters with animals (predominantly deer) in a roadway and treated for nonfatal injuries in U.S. hospital emergency departments (EDs). Cost-effective measures targeting both drivers (e.g., speed reduction and early warnings) and animals (e.g., fencing and underpasses) are needed to reduce injuries associated with MV collisions involving animals.
NEISS-AIP is operated by the Consumer Product Safety Commission and collects data about initial visits for all types and causes of injuries treated in U.S. EDs (3). NEISS-AIP data are drawn from a nationally representative subsample of 66 of 100 NEISS-AIP hospitals selected as a stratified probability sample of hospitals in the United States and its territories with a minimum of six beds and a 24-hour ED. NEISS-AIP provides data on approximately 500,000 injuryand consumer product-related ED cases each year. Data for each case include a comment variable that contains additional information about the circumstances of the injury.
Each case was assigned a sample weight on the basis of the inverse probability of selection; these weights were summed to provide national estimates of MV animal crash-related injuries. Confidence intervals (CIs) were calculated by using a direct variance estimation procedure that accounted for the sample weights and complex sample design. Rates were calculated by using 2001 and 2002 U.S. Census bridged-race population estimates from the National Center for Health Statistics (4).
Data used in this study were obtained from medical records of 676 ED patients treated for nonfatal injuries incurred while driving or riding in a light vehicle and encountering an animal in the roadway. This report focuses on the majority of these patients, who encountered larger animals (e.g., deer, moose, elk, bear, horses, or cattle) entering the roadway. Smaller animals (e.g., dogs, cats, squirrels, raccoons, and possums) were included only in the overall national estimate. No information was obtained on type of vehicle. MV animal crashes were defined as those involving direct collision with an animal on a roadway or those occurring on or off the roadway as a result of trying to avoid hitting the animal. These cases were identified by using a brief narrative captured in the NEISS-AIP database that described the circumstances of the injury incident. An additional 79 patients injured as motorcyclists involved in MV-animal crashes were excluded from this study. During 2001During -2002, an estimated 26,647 (9.3 per 100,000 population; 95% CI = 6.7-11.9) persons were treated annually in U.S. EDs for MV animal crash-related injuries, of which 22,498 (84.8%) were MV occupants in crashes involving larger animals (Table 1). The highest MV large animal crashrelated injury rate (21.1 per 100,000 population) occurred among persons aged 15-24 years (Table 1). The age distribution of those injured in MV large animal crashes was different from those injured during all other types of MV trafficrelated crashes (p<0.03); most of this difference was attributed to an overrepresentation of persons aged 15-24 years (p<0.0001) and an underrepresentation of children aged 0-14 years (p<0.0001) (Figure). Among injured persons aged 15-24 years, 48.9% were driving the vehicle. The MV large animal crash-related injury rate was similar for males and females (Table 1). Approximately 6% of those treated in U.S. EDs required hospitalization for their injuries.
MV large animal crash-related injuries were mostly strains/ sprains (36.5%) and contusions/abrasions (33.9%) and involved the head/face (28.1%), neck (22.7%), and upper trunk (15.3%) (Table 2). The majority (94.5%) of the neck injuries were strains and sprains, and 62.5% of head/face injuries were contusions, abrasions, or lacerations. Persons injured during MV large animal crashes were treated more often during October and November than other months. Deer were the most common large animals involved in these incidents (86.9%). Approximately half (54.4%) of these crashes involved a direct collision with the animal, and the remainder (44.8%) resulted from the driver trying to avoid hitting the animal. Of those incidents in which the animal was avoided, the crash most commonly involved an MV leaving the roadway (29.0%); an MV hitting a tree, pole, or guardrail (21.4%); or an MV rollover (17.3%) (Table 2). Editorial Note: Nationally, nonfatal MV animal crashrelated injuries account for <1.0% of approximately three million MV occupants treated in U.S. EDs annually (5). Direct MV animal crashes represent nearly 4.0% of an estimated 6.1 million light-vehicle crashes reported to police in the United States (1). However, in rural areas with large deer populations, MV animal crashes and associated occupant deaths and injuries, wildlife loss, and property damage are important concerns. For instance, in Wisconsin, MV deer crashes accounted for nearly 16% of all statewide police-reported MV crashes in 2002 (6).
National estimates reported from this study are consistent with state MV animal crash data reported to police. In this study, the majority of MV occupant injuries resulted from encounters between the MV and deer; however, 12% of those injured resulted from MV crashes involving large domesticated animals (e.g., horses and cattle). MV occupant injuries can occur because of a direct MV collision with the large animal or from swerving or maneuvering to avoid a collision with the animal. In this study, 63.8% of younger drivers swerved to avoid the animal, resulting in an MV crash and subsequent injury. Similar to other MV occupant injuries from crashes that occur on U.S. highways, a majority of the injuries were neck sprains/strains, and contusions/abrasions to the head and face. One fourth of MV animal crash-related injuries were treated in October and November at the height of the fall deer hunting, mating, and migration season (7). MV animal crashes are more likely to occur in the early morning hours and especially at dusk, when deer are actively moving about and likely to cross the road in rural areas (6)(7)(8). The findings of this report are subject to at least three limitations. First, although the risk for MV animal crash-related injury can vary among states and local areas, NEISS-AIP is designed to provide only national estimates and does not provide regional, state, or local estimates or estimates by urban and rural categories. Second, because of the small number of cases reported, this study excluded motorcyclists, who are known to be at higher risk for injury in crashes (6). Finally, NEISS-AIP only provides data on injured persons treated in hospital EDs.
Prevention efforts have focused on warning signs to alert drivers to animal crossings, speed restrictions, roadway fencing and underpasses/overpasses aimed at directing animals toward safe passage, roadside clearing, roadside mirrors and reflectors (i.e., to deflect headlight beams toward the sides of the road to alert deer), and reduction of deer populations through recreational hunting (7,9). Evaluation studies have been conducted to assess the cost and effectiveness of these methods, but the results are inconsistent (10). Interventions with some supportive evidence (e.g., fences combined with underpasses or overpasses) also are among the most expensive to build and maintain.
Primary prevention of MV animal crashes can be accomplished by keeping large animals, especially deer, from entering the roadway or by providing drivers with more time to react to a potentially dangerous situation. The same behaviors that are recommended to help prevent crashes in general are relevant for MV animal crashes. Driving within speed limits, staying alert and reducing distracted and drowsy driving, and eliminating alcohol-impaired driving will give drivers, particularly teenagers and younger adults, more time to react and avoid collisions. Prevention of injury if a crash occurs can be accomplished by the universal use of proper restraints, including safety belts, child safety seats, and booster seats.
# Transmission of Hepatitis B Virus in Correctional Facilities -Georgia, January 1999-June 2002
Incarcerated persons have a disproportionate burden of infectious diseases (1), including hepatitis B virus (HBV) infection. Among U.S. adult prison inmates, the overall prevalence of current or previous HBV infection ranges from 13% to 47%. The prevalence of chronic HBV infection among inmates is approximately 1.0%-3.7%, two to six times the prevalence among adults in the general U.S. population (1). Incarcerated persons can acquire HBV infection in the community or in correctional settings (1). This report summarizes the results of 1) an analysis of hepatitis B cases among Georgia inmates reported to the Georgia Department of Human Resources, Division of Public Health (DPH) during January 1999-June 2002, including a retrospective investigation of cases reported during January 2001-June 2002; and 2) a prevalence survey conducted in prison intake centers during February-March 2003. These efforts identified cases of acute hepatitis B in multiple Georgia prisons and documented evidence of ongoing transmission of HBV in the state correctional system. The findings underscore the need for hepatitis B vaccination programs in correctional facilities.
The Georgia correctional system houses approximately 45,000 inmates in 68 correctional facilities; approximately 16,000 new inmates are admitted each year and processed through one of five intake centers. The correctional system does not routinely screen inmates for HBV infection, and diagnostic testing is left to the judgment of individual physicians. In August 2000, in response to two hepatitis B Online know what matters. e asy.
MMWR Online makes it possible for you to access vital public health reports and news as soon as CDC publishes them. Get the information you want, when you need it, from a trusted source.
Visit cdc.gov/mmwr and stay current on important public health topics -the easy way.
outbreaks at one Georgia correctional facility (2,3), DPH began to monitor reports of acute hepatitis B cases among inmates at all Georgia correctional facilities, as determined by the inmates' addresses on laboratory reports.
A case of acute HBV infection was defined as a positive serologic test for IgM antibodies to hepatitis B core antigen (IgM anti-HBc) on at least one occasion and at least one additional supporting finding (e.g., compatible symptoms, liver enzyme elevation, or another positive hepatitis B serologic test), received by DPH during January 1999-June 2002. Cases reported during January 2001-June 2002 were confirmed by retrospective review of the inmate's medical and laboratory records. The date of diagnosis of acute HBV infection was defined as the date that alanine aminotransferase (ALT) or aspartate aminotransferase (AST) levels were elevated at least two times greater than the upper limit of normal in conjunction with a positive test for IgM anti-HBc. When ALT or AST levels were not available, the date of the blood draw with a positive IgM anti-HBc result was used as the approximate date of diagnosis.
Incarceration histories of inmates with acute HBV infections reported during January 2001-June 2002 were reviewed to identify inmate locations and number of transfers between correctional facilities before illness onset. Persons with asymp-tomatic and symptomatic cases were considered to have been infected while incarcerated if they were in prison or jail during the 12 months or 6 months, respectively, before illness onset.
A prevalence survey to assess the HBV infection status of prisoners on entry was conducted at three Georgia prison intake centers for males and one intake center for females during February-March 2003. Consenting inmates underwent HBV serologic testing; all inmates at intake when the survey was conducted were offered hepatitis B vaccine.
During January 1999-June 2002, a total of 92 cases of acute HBV infection were identified, of which 57 (62%) were reported during January 2001-June 2002 and included in the retrospective investigation (Figure). Among the 57 inmates with HBV infection, the median age was 34 years (range: 18-59 years); 52 (91%) were male, and 35 (61%) were non-Hispanic blacks. Ten (18%) had symptoms that included jaundice, abdominal pain, fever, and vomiting. Seven (12%) subsequently were determined to have chronic infections. The chronic infection status of four inmates was not assessed.
Among the 57 inmates included in the retrospective investigation, the most frequently reported reason for HBV testing was the presence of symptoms or elevated liver enzymes (21 cases [37%]). Other reasons included reported characteristics and behaviors that might be associated with HBV transmission (e.g., tattoos or unprotected sex contacts) (14 [24%]), serologic testing performed as part of initial medical evaluation (13 [23%]), and being positive for human immunodeficiency virus (five [9%]). Prison staff reported counseling and providing medical follow-up for 52 (91%) of the 57 inmates.
The 57 cases were reported from 27 prisons and four probation detention centers in Georgia, with a mean of 1.8 cases per facility and a range of one to three cases for the 30 facilities that were not involved in the previously recognized outbreaks (2,3). The 57 inmates had been incarcerated for a median of 2.2 years (range: 0-23.7 years) before illness onset and had been transferred 1.4 times on average (median: one time; range: one to seven times) during the 12 months before diagnosis. The majority of HBV infections (41 [72%]) were acquired in prison. Of the remaining 16 cases, 13 (81%) occurred in persons who had been in prison or jail for 1-6 months before receiving a diagnosis. The remaining three (19%) inmates were asymptomatic and had been in prison or jail for 10-11 months before receiving a diagnosis.
As of August 2002, the seven inmates who had chronic infections had been transferred among prison facilities 13 times during the cumulative 89 months of incarceration that followed their diagnosis, resulting in a mean of 1.8 transfers per person-year of incarceration (median: two transfers; range: zero to five transfers). Three inmates with chronic infection were released from prison.
Of 546 inmates surveyed at intake during February-March 2003, a total of 489 (90%) consented to serologic testing, and 428 (78%) consented to hepatitis B vaccination. Of the 489 inmates tested, three (0.6%) had acute HBV infections, four (0.8%) had chronic infections, 64 (13%) had evidence of resolved infections, and 374 (76%) were susceptible to HBV infection. Two of three inmates with acute infection had spent 5.5-11.0 months in jail before intake. Editorial Note: HBV is a bloodborne pathogen, transmitted by percutaneous or permucosal exposure to infectious blood or body fluids. The prevalence of chronic infection is higher among prison inmates (1.0%-3.7%) than among the general U.S. population (0.5%) (1), reflecting an overrepresentation of persons entering prison who are at high risk for HBV infection (e.g., injection-drug users and those with reported histories of multiple sex partners). The prevalence of chronic infection among the intake population in this report (0.8%) suggests that high-risk behaviors practiced within the community before incarceration might not account entirely for the burden of HBV infection in correctional facilities. Although studies are limited, transmission of HBV infection within correctional settings has been documented, with incidence ranging from 0.8% to 3.8% per year (2,(4)(5)(6).
The retrospective investigation described in this report identified an increase in HBV infections in Georgia correctional facilities, beginning in January 2001. This increase likely was related to multiple factors, including enhanced surveillance and increased diagnostic testing by correctional medical staff. Changes in diagnostic practices might have occurred because of increased awareness of hepatitis B among medical staff after outbreaks at a Georgia correctional facility in June 2000 and again in June 2001. Nonetheless, the number of reported cases probably underestimates the extent of HBV transmission in the correctional system because the majority of persons with acute HBV infection are asymptomatic and investigations of single cases are not conducted routinely. In the first previous outbreak, one symptomatic patient reported to DPH was associated with a cluster of 11 acute cases, and four chronic HBV infections were identified (2).
The majority of inmates with identified acute HBV infections were housed in multiple Georgia correctional facilities and were infected during their incarceration, suggesting widespread ongoing transmission in multiple facilities. Inmates infected with HBV were transferred frequently among facilities. Thus, potential sources of HBV transmission were distributed throughout the prison system.
In the Georgia correctional system, approximately one third of inmates are released each year (7). Inmates who become chronically infected and subsequently are released represent potential sources of infection for others in the community. In addition, susceptible inmates who are released continue to be at increased risk for HBV infection (1). The majority of inmates in the intake survey were susceptible to HBV infection and consented to vaccination, suggesting that vaccination efforts in correctional facilities might effectively capture susceptible, high-risk populations.
Although data are lacking regarding the overall burden of HBV infection in correctional systems, the ongoing transmission demonstrated in Georgia prisons might be occurring in other states, where similar conditions are likely to exist. All inmates who receive a medical evaluation should be vaccinated to prevent HBV infection (1). However, the majority of state correctional systems in the United States, including the Georgia system, do not have hepatitis B vaccination programs (1). Implementation of such programs in correctional settings nationwide could result in a considerable reduction in the hepatitis B-associated disease burden, not only by eliminating transmission among the incarcerated population, but also by reducing transmission in the community (8).
# Hepatitis B Vaccination of Inmates in Correctional Facilities -Texas, 2000-2002
In December 2002, approximately 2.2 million persons were incarcerated in the United States (1); an estimated 8 million were released to the community that year (2). In 2001, approximately 22,000 acute hepatitis B cases and 78,000 new hepatitis B virus (HBV) infections occurred in the United States (3); an estimated 29% of these cases were in persons who had been incarcerated previously (4). The majority of HBV infections among incarcerated persons are acquired in the community; however, infection also is transmitted within correctional settings (2). Hepatitis B vaccination of incarcerated persons is recommended to prevent transmission in correctional facilities and in previously incarcerated persons on their return to the community (2). In May 2000, the Texas Department of Criminal Justice (TDCJ), which oversees custody of state jail and prison inmates, implemented a hepatitis B vaccination program. To determine hepatitis B vaccination rates of inmates during 2000-2002, TDCJ reviewed charts of inmates released during a 3-day period for documentation of vaccination. This report summarizes the results of that study, which indicated that rates of vaccine acceptance and vaccine series completion among inmates were high. Establishing hepatitis B vaccination programs in prisons and jails can prevent a substantial proportion of HBV infections among adults in the outside community.
During 2000-2002, TDCJ housed approximately 151,000 inmates in 105 adult facilities, including prisons (median sentence of inmates: 9 years; range: 2-99 years) and jails (median sentence of inmates: 1.3 years; range: 3 months-2 years). Approximately 40,000 new offenders enter these facilities annually, and an estimated 1% of inmates are transferred between facilities daily (5,6). In 1999, state funds were appropriated for hepatitis B vaccination of all inmates in jails and prisons.
Before implementation of the vaccination program, a costeffectiveness model was developed that estimated the cost effectiveness of prevaccination testing for immunity to HBV infection among inmates. Stored serum specimens from 889 inmates incarcerated during 1998-1999 were tested for antibodies to hepatitis B core antigen (anti-HBc); HBV prevalence was 18%. The model estimated that at a threshold prevalence of 25%, the cost of a program with prevaccination testing was equivalent to that of vaccination without testing; at lower prevalence, prevaccination testing would not be cost effective (Figure). On the basis of these findings, all of the estimated 40,000 entering inmates were offered vaccine without prevaccination testing.
Entering inmates were offered the first hepatitis B vaccine dose at the time of admission. Persons who were already incarcerated were offered the first dose at the time of their annual health evaluation, which occurred on their anniversary month of incarceration. After vaccination of incarcerated persons, only newly admitted inmates were offered vaccine.
Vaccine was administered on a 0-, 2-, and 4-month schedule. An electronic pharmacy auto-renewal system was used to send second and third vaccine doses to the appropriate facility for each inmate. Health-care workers also recorded vaccine dose administration in each inmate's medical record, enabling inmates to complete the vaccination series despite frequent transfers within the system.
In February 2002, TDCJ evaluated vaccine acceptance and series completion rates. Charts of 232 prison inmates and 211 jail inmates released during a 3-day period were audited for receipt of hepatitis B vaccine; 426 (96%) inmates with no record of previous vaccination or HBV infection were considered to be eligible for vaccination. Lack of documentation of a vaccination encounter was interpreted as a failure to offer vaccine, and only a signed informed refusal form was counted as a vaccination refusal.
Hepatitis B vaccine was offered to 319 (75%) of 426 inmates. Prison inmates were more likely to be offered vaccine (185/220 [84%]) than jail inmates (134/206 [65%]) (p<0.001), which might be related to higher inmate turnover and lack of staff contact time in jails (Table ). However, acceptance of the first vaccine dose was higher among jail inmates (114/134 [85%]) than among prison inmates (134/185 [72%]) (p = 0.005).
Among 125 prison and 99 jail inmates who began vaccination and were incarcerated for >4 months, the 3-dose completion rate was 96% and 54%, respectively. In December 2002, the hepatitis B vaccination program was suspended because of a lack of funds. Editorial Note: Evaluation of the TDCJ hepatitis B vaccination program demonstrated that high vaccine coverage could be achieved for inmates in a state correctional system. Incarceration provides an opportunity to vaccinate persons at high risk typically not served by prevention services in the public or private sectors, and vaccination of incarcerated populations is cost effective (7).
The findings in this report illustrate the need to tailor a program to a particular facility. Completion of the vaccine series is a more feasible goal for long-term facilities; shortterm facilities should initiate the vaccine series, supply an immunization record and, where feasible, provide information at discharge about facilities offering the remaining vaccine doses. Vaccination also can be completed if the person returns to a correctional institution.
Prevaccination testing to detect existing immunity can eliminate the cost of revaccinating persons who were vaccinated previously or infected. TDCJ's decision not to perform prevaccination testing was based on a model that included the costs of testing and vaccination and the series completion rate. The model assumed that all inmates who received the first vaccine dose would return for subsequent doses; if attrition caused by release was included in the model, prevaccination testing would only be cost effective if the prevalence of immunity was higher. Changes in prevalence of immunity to HBV infection or costs (e.g., vaccine, labor, and testing) also would change the cost effectiveness of prevaccination testing. In particular, immunity to HBV infection in young adults is changing rapidly within most communities because of an increase in vaccinated adolescents. If adequate immunization records are not available for inmates, periodic monitoring of the prevalence of immunity to HBV infection using a serologic marker to detect both infection (i.e., anti-HBc) and immunization (i.e., antibodies to hepatitis B surface antigen) will help corrections officials determine when prevaccination testing might reduce costs (2). The findings in this report are subject to at least two limitations. First, inmates with shorter sentences are more likely to be discharged and might be overrepresented by the sampling. Because inmates with short sentences might not have been incarcerated long enough to complete the vaccination series, more inmates might have completed the vaccination series than this study demonstrated. Second, lack of long-term follow-up precludes evaluation of the eventual series completion by jail inmates, who might have accessed additional doses outside the correctional system or during subsequent incarcerations.
# FIGURE. Cost effectiveness of prevaccination testing for immunity to hepatitis B virus (HBV) infection among jail and prison inmates -Texas
Hepatitis B vaccination of inmates in state correctional facilities is feasible if resources are available to purchase and administer vaccine. In 2000, a survey of state correctional facility medical directors indicated that the majority of prison systems would vaccinate inmates if resources were available (8). Although hepatitis B vaccination of inmates has been recommended since the vaccine first became available in 1982 ( 9), only five states (Hawaii, Michigan, New Mexico, Vermont, and Wisconsin) vaccinate inmates routinely (D. Burnett, M.D., Wisconsin Department of Corrections and F. Pullara, M.D., New Mexico Department of Corrections, personal communications, 2004) (8). Collaborations between public health and corrections authorities at the state and local level are essential to overcome barriers to vaccination program implementation.
# Tuberculosis Associated with Blocking Agents Against Tumor Necrosis Factor-Alpha -California, 2002-2003
The Food and Drug Administration (FDA) has determined that tuberculosis (TB) disease is a potential adverse reaction from treatment with the tumor necrosis factor-alpha (TNF-α) antagonists infliximab (Remicade ® ), etanercept (Enbrel ® ), and adalimumab (Humira ® )*; the three products are labeled accordingly (1,2). These products work by blocking TNF-α, an inflammatory cytokine, and are approved for treating rheumatoid arthritis and other selected autoimmune diseases. TNF-α is associated with the immunology and pathophysiology of certain infectious diseases, notably TB; blocking TNF-α can allow TB disease to emerge from latent Mycobacterium tuberculosis infection. In 2002, a California county health department reported three cases of TB disease occurring in association with infliximab therapy. This report summarizes those cases and nine subsequently reported cases and provides interim recommendations for TB prevention and management in recipients of these blocking agents. Healthcare providers should take steps to prevent TB in immunocompromised patients and remain vigilant for TB as a cause of unexplained febrile illness.
# Case Reports
Case 1. In January 2002, a U.S.-born man aged 55 years with rheumatoid arthritis had pulmonary TB disease diagnosed 17 months after starting infliximab therapy. In 1995, he had a positive tuberculin skin test (TST) and reportedly took isoniazid for 12 months; however, his adherence to therapy was questionable. During September 2000-January 2002, he received 13 infusions of infliximab, and his arthritic symptoms decreased. However, in January he had fever and weight loss. Four weeks later, a supraclavicular lymph node became enlarged, and a chest radiograph revealed a rightupper-lobe lung cavity with a nodular infiltrate. M. tuberculosis was isolated from sputum and lymph node specimens, and his condition improved with anti-TB medications. In July 2002, he again lost weight. He had smoked cigarettes for many years and was found to have lung cancer; he died in November 2002.
Case 2. A woman aged 64 years with rheumatoid arthritis had pulmonary and pericardial TB disease diagnosed in June 2002. She had begun infliximab therapy in September 2001 and received 7 doses before onset of fever and weight loss in April 2002. Her chest radiograph revealed a large pericardial effusion and a right-upper-lobe lung infiltrate. M. tuberculosis resistant to isoniazid, rifampin, pyrazinamide, and ethambutol was isolated from sputum and pericardial fluid. The patient was born in the Philippines, where TB often is drug resistant (3). In 1999, she was exposed to a person with drugsusceptible TB in the United States and subsequently had two TSTs with negative results in 2000; however, she was taking prednisone for her arthritis at the time of the TSTs. After 12 months of therapy with second-line anti-TB medications, her medical condition has improved. Case 3. A U.S.-born woman aged 54 years was exposed to contagious TB in 1996; she had a positive TST result during the contact investigation but was not treated for latent TB infection (LTBI). The patient has Crohn's disease and received infliximab in February 2001 and June 2002. Two weeks after her second infusion, but 16 months after her first infusion, she sought care for cough, fever, and abdominal pain. Her chest radiograph revealed upper-lobe lung nodules with a pleural effusion, and sputum specimens yielded M. tuberculosis. She started standard, four-drug anti-TB therapy but experienced gastrointestinal intolerance. Isoniazid was discontinued, and she was free of TB disease after treatment with rifampin, pyrazinamide, and ethambutol.
# Additional Reports
In 2003, the state of California Department of Health Services asked local jurisdictions to report TB cases associated with TNF-α antagonists since January 2002. As of September 2003, nine additional reports had been received, for a Eleven of the patients had at least one risk factor for LTBI (e.g., born in countries where TB is prevalent or contact with a person with TB disease). Eight were taking other immunosuppressive therapies at the time of their TB diagnoses. Three patients underwent a medical history for TB risk factors before beginning therapy with a TNF-α antagonist. In addition to the patient in case 1, a second patient died (from cardiomyopathy) while being treated for TB disease.
Editorial Note: As of January 2004, FDA's adverse-event reporting system had received several hundred reports, mostly from outside the United States, of TB disease in patients who received TNF-α antagonists. Manufacturers of these products are required to report known cases, but reporting is voluntary for others. The majority of the cases probably represent progression of LTBI to TB disease, although the contribution of newly acquired M. tuberculosis infection to the total number of reports is unknown (1). Reports have included atypical presentations, extrapulmonary and disseminated disease, and deaths (1,4,5).
In California, after the initial three reports, nine additional cases of TB disease were reported during January 2002-August 2003 in patients taking TNF-α antagonists. Although reporting of TB cases is mandatory in California, reporting the association with TNF-α antagonists was voluntary, and an underestimate might have resulted.
Eight of the 12 patients in California were born in countries where TB is prevalent. In certain instances, physicians had not screened for risk factors for M. tuberculosis infection or tested their patients for infection before beginning therapy with TNF-α antagonists. In other instances, testing was performed, but LTBI was not diagnosed, possibly because of cutaneous anergy. Many patients who receive TNF-α antagonists already are receiving other immunosuppressive therapies, and certain conditions such as rheumatoid arthritis also can decrease sensitivity to tuberculin; therefore, TST results at the time of initiating TNF-α antagonist therapy might be falsely negative. Some experts advocate treating for presumed LTBI when a candidate for TNF-α antagonists has risk factors for M. tuberculosis infection but a negative TST result (4,5).
TNF-α, an inflammatory cytokine expressed by activated macrophages, T-cells, and other immune cells, plays a crucial role in the host response against M. tuberculosis and other intracellular pathogens. Infliximab and adalimumab are monoclonal antibodies; etanercept is a dimeric soluble form of the TNF-α receptor. All three products are approved for the treatment of patients with rheumatoid arthritis. Infliximab also is approved for Crohn's disease, and etanercept is approved for specific other arthritides and for psoriasis. Use of these agents has been associated with other life-threatening infectious diseases besides TB, including candidiasis, histoplasmosis, aspergillosis, and listeriosis (1). TNF-α antagonists often are used in conjunction with other immunosuppressive therapies, particularly glucocorticoids and methotrexate. Whether the increased rates of TB or other infectious diseases are caused by interactions among these therapies is unknown.
Diagnosing LTBI in candidates for TNF-α antagonist therapy is challenging (Box). For patients who undergo treatment for LTBI, the optimal time for starting TNF-α antagonist therapy is undetermined. Some experts advocate postponing therapy until LTBI treatment is complete. However, this delay might be impractical (4,6). The risk for TB relapse in patients previously cured of TB disease and subsequently treated with TNF-α antagonists is unknown.
# BOX. Recommendations for screening, diagnosis, and treatment of latent TB infection (LTBI) and tuberculosis (TB)
in patients administered or scheduled to receive tumor necrosis factor-alpha (TNF-α α α α α) antagonists If active TB disease develops during TNF-α antagonist therapy, the TNF-α antagonist should be discontinued, at least until the anti-TB regimen has been started and the patient's condition has improved. The optimal time for resuming TNF-α antagonist therapy is undetermined. Outcomes with other immunosuppressive agents during the treatment of TB disease have been variable. Use of glucocorticosteroids during the treatment of TB disease is considered safe (7), and studies of TB disease in organ transplant recipients suggest that survival is not decreased by the use of cyclosporine or azathioprine (8). Etanercept, administered in a phase-1 clinical trial along with a standard initial anti-TB regimen, did not delay the resolution of TB disease markers in a group of patients coinfected with human immunodeficiency virus in comparison with historical controls; adverse effects were not detected (9). However, use of anti-T-cell agents in transplant recipients with TB disease is associated with increased mortality; whether this increased mortality is because of the suppression of immune response or the dysfunction of the transplanted organ is unclear (8).
7 0 Illinois 0 1 1 2 0 Iowa 1 2 0 3 1 Michigan 1 0 0 1 0 Missouri 1 0 0 1 0 Nebraska 0 1 0 1 0 Nevada 2 0 0 2 0 New Mexico 1 4 0 5 0 New York 2 1 0 3 0 North Dakota 0 1 0 1 0 Ohio 1 0 0 1 1 Pennsylvania 1 0 0 1 0 South Dakota 1 8 0 9 0 Texas 2 1 0 3 1 Wyoming 0 1 0 1 0
Practitioners who prescribe TNF-α antagonists should educate their patients about the symptoms of TB disease, with added emphasis on extrapulmonary symptoms, which can include fever, malaise, or development of a mass. A patient with symptoms should undergo diagnostic testing for TB. In addition to following local reporting requirements, healthcare providers should report TB cases associated with TNF-α antagonists to FDA's Medwatch system (available at http:// www.fda.gov/medwatch).
Ongoing clinical trials are using both approved and experimental TNF-α antagonists in the treatment of additional conditions (4). Novel therapies that inhibit other related inflammatory cytokines are under development. As the use of these blocking agents expands, associated cases of TB might increase. Vigilance for TB in association with these agents is critical to early recognition and successful treatment.
# West Nile Virus Activity -United
States, July 28-August 3, 2004 and Nevada) and in two wild hatchling birds from Ohio. Three seropositive sentinel horses were reported from Puerto Rico. A total of 1,486 WNV-positive mosquito pools have been reported from 24 states (Arizona, Arkansas, California, Colorado, Connecticut, Georgia, Illinois, Indiana, Kansas, Louisiana, Michigan, Mississippi, Missouri, Nebraska, Nevada, New Jersey, New Mexico, Ohio, Pennsylvania, South Dakota, Tennessee, Texas, Utah, and Virginia).
Additional information about national WNV activity is available from CDC at http://www.cdc.gov/ncidod/dvbid/ westnile/index.htm and at http://westnilemaps.usgs.gov.
# Notice to Readers
# Final 2003 Reports of Notifiable Diseases
The -
- - - - Idaho - - - - - - W y o . - - - - - 2 Colo. N N - - - 621 N . M e x . - - - - 1 4 A r i z . - - - - 5 7 Utah - - - - - - N e v . - 1 - - - 2 PACIFIC - - - - - 2 Wash. - - - - - - Oreg. - - - - - - Calif. - - - - - 2 Alaska - - - - - - H a w a i i - - - - - - Guam - - - - - - P . R . - - - - - - V . I . - - - - - - Amer. Samoa - - - - - - C.N.
# MMWR 697
* No measles cases were reported for the current 4-week period yielding a ratio for week 30 of zero (0). † Ratio of current 4-week total to mean of 15 4-week totals (from previous, comparable, and subsequent 4-week periods for the past 5 years). The point where the hatched area begins is based on the mean and two standard deviations of these 4-week totals. | None | None |
03a530eb595e6bdf2b8c8de5f0b45d014f20d4bd | cdc | None | CDC ILI surveillance case definition: fever (≥100ºF ), plus cough, sore throat, or both in the absence of another known cause of illness. Vol. 58 / No. 37 MMWR 1031 - By real-time reverse transcription-polymerase chain reaction assay; all patients tested negative for seasonal influenza. † Remel Xpect Flu A&B test (Remel Products, Lenexa, Kansas). TABLE. Performance of a rapid influenza detection test (RIDT)- in patients with suspected and confirmed † 2009 pandemic influenza A (H1N1) virus infection, by clinical syndrome consistent with CDC-defined influenza-like illness (ILI) § -Connecticut, 2009 rRT-PCR positive rRT-PCR negative Total RIDT positive RIDT negative RIDT positive RIDT negative Sensitivity % Specificity % PPV ¶ % NPV % Overall 63 23 26 2 12 47 86 92 32 CDC-defined ILI 48 19 21 1 7 48 88 95 25 No CDC-defined ILI 15 4 5 1 5 44 83 80 50 - Remel Xpect Flu A&B test (Remel Products, Lenexa, Kansas). † By real-time reverse transcription-polymerase chain reaction (rRT-PCR); all patients tested negative for seasonal influenza. § CDC ILI surveillance case definition: fever (≥100°F ) plus cough, sore throat, or both in the absence of another known cause of illness. ¶ Positive predictive value. Negative predictive value.#
During May 2009, a few weeks after 2009 pandemic influenza A (H1N1) infection was first detected in the United States (1), outbreaks among students from two schools were detected in Greenwich, Connecticut. Staff members from Greenwich Hospital and the Connecticut Department of Public Health collected data on symptoms for 63 patients and submitted nasopharyngeal washings for testing using a rapid influenza diagnostic test (RIDT) for influenza A and B and real-time reverse transcription-polymerase chain reaction (rRT-PCR) assay, thereby affording an opportunity to assess the field performance of the RIDT. A total of 49 patients had infections with pandemic influenza A (H1N1) confirmed by rRT-PCR. This report summarizes the findings from this performance assessment, which indicated that, compared with rRT-PCR, the sensitivity of the RIDT for detecting infection in patients with 2009 pandemic influenza A (H1N1) was 47%, and the specificity was 86%. Sensitivity and specificity did not vary substantially by the presence or absence of CDC-defined influenza-like illness (ILI) or by time from symptom onset to specimen acquisition. In this group of patients, although positive RIDT results performed well in predicting confirmed infection with pandemic H1N1 virus (positive predictive value: 92%), negative tests did not accurately predict the absence of infection (negative predictive value: 32%). These results affirm recent CDC recommendations against using negative RIDT results for management of patients with possible 2009 pandemic influenza A (H1N1) infection (2).
During April 29-May 1, 2009, 78 students from a private school (school A) near Greenwich, Connecticut, participated in a class trip to Pennsylvania. Several students became sick with a respiratory illness. Because infection with 2009 pandemic influenza A (H1N1) was suspected, upon returning home, 11 of the students, a sibling, and two other students went to the Greenwich Hospital for outpatient influenza testing and treatment.
During May 18-20, 133 students and eight teachers from a public school (school B) in Greenwich traveled to a camp in Connecticut. Among these students, 36 visited the camp infirmary with fever, headache, or fatigue. The Greenwich Health Department asked physicians at the hospital to assist with testing the students for pandemic H1N1. A total of 67 students and staff from school B became ill, and 49 of these patients went to the hospital for influenza testing.
A total of 63 patients (14 students from school A and 49 students and staff from school B) were tested for influenza at the hospital. A standard symptom survey was completed by a physician for each patient after which a nasopharyngeal washing was performed by an experienced respiratory therapist trained in the procedure. All samples were placed in viral transport media and sent to the Connecticut Department of Public Health laboratory for influenza virus detection by rRT-PCR. Rapid screening for influenza A and B was performed concurrently at the hospital laboratory using the Remel Xpect Flu A&B test (Remel Products, Lenexa, Kansas) according to manufacturer's instructions (3). Although the number of ill persons who eventually received antiviral therapy is unknown, all nasopharyngeal washings were obtained before initiation of therapy.
Of the 63 patients tested by RIDT, 49 patients, 11 (79%) from school A and 38 (78%) from school B, were found to have 2009 pandemic influenza A (H1N1) infection by rRT-PCR (Figure). Of the 49 patients with confirmed infection, 23 (47%) tested positive (eight from school A and 15 from school B) and 26 (53%) tested negative for 2009 pandemic influenza A (H1N1) by RIDT. Among 11 patients with positive rRT-PCR tests from school A and 38 from school B, the numbers of positive RIDT tests were 8 (73%) and 15 (39%) respectively.
Among the 14 patient samples from both schools that tested negative by rRT-PCR, three were from students at school A, and 11 were from school B. Of the 14 rRT-PCR negative specimens, two tested positive by RIDT (one from school A and one from school B). The overall sensitivity of the RIDT was 23 of 49 (47%), and the specificity was 12 of 14 (86%). The positive predictive value was 23 of 25 (92%), and the negative predictive value was 12 of 38 (32%).
The schools did not differ significantly with respect to percentage of patients with confirmed pandemic H1N1 by rRT-PCR, severity of symptoms, interval between the onset of symptoms and collection of specimens for testing, or overall RIDT positivity rate. Among all the patients tested by RIDT, no significant differences between true positives and false negatives were seen with respect to ILI.- In RIDT positive and RIDT negative patients with pandemic H1N1, the median interval from symptom onset to specimen collection was 36 hours. Of the 34 patients with washings obtained ≤36 hours from the onset of symptoms, 16 (47%) were RIDT positive; of the 15 patients with washings collected after 36 hours of symptoms, seven (47%) were positive. RIDT test performance was assessed for patients with and without CDC-defined ILI (Table ). The sensitivity and specificity were approximately the same for the two groups (48% versus 44% and 88% versus 83%, respectively). Editorial Note: When cases of 2009 pandemic influenza A (H1N1) began appearing in the United States in April 2009, several RIDTs had been in common use in the United States as point-of-care tests for seasonal influenza, but the performance of these tests in patients infected with 2009 pandemic influenza A (H1N1) virus was unknown. CDC has since reported varying sensitivities of RIDTs in retrospective analyses of rRT-PCR positive respiratory samples, from 40%-69%. In these analyses, RIDT sensitivity was positively associated with the titer of virus in the sample (4).
The analysis in this report of pandemic H1N1 cases at two schools determined that the RIDT used detected less than half the cases confirmed by rRT-PCR. The low sensitivity and low negative predictive value of the test during these outbreaks highlight the limitations of using this test alone to establish diagnosis and aid clinical management. These results affirm current recommendations not to use negative RIDT results to rule out pandemic H1N1 or to make infection control decisions (2). Rapid tests differ in their sensitivity and specificity for detecting seasonal influenza in respiratory specimens but generally have low to moderate sensitivity compared with viral culture or rRT-PCR. Previous RIDT studies have described the performance of the QuickVue Influenza A+B test (Quidel Corporation, San Diego, California) for detecting seasonal influenza in three different populations during 2008. Sensitivity when compared with rRT-PCR was low for all populations (median: 27%; range: 19%-32%) (5).
The RIDT used in the current study has a reported sensitivity of 92.5% and a specificity of 100% for the diagnosis of seasonal influenza A by nasopharyngeal wash (3). This investigation yielded much lower sensitivity (47%) and specificity (86%) in patients having confirmed infection with 2009 pandemic influenza A (H1N1) virus.
The findings in this report are comparable to recently reported observations of low performance of RIDTs in patients with pandemic H1N1. In a report of hospitalized patients in California, rapid antigen test results were positive in 67% of cases of pandemic H1N1 tested (6). In an assessment of rapid testing compared with rRT-PCR conducted on 6,090 patient samples from the New York City area, the sensitivity and specificity for the detection of 2009 pandemic influenza A (H1N1) virus by rapid antigen testing, using the BinaxNOW Influenza A&B test (Binax, Inc., Scarborough, Maine) and the 3M Rapid Detection Flu A+B test (3M, St. Paul, Minnesota) were 17.8% and 93.6% respectively (7). A recent report from the Naval Health Research Center described screening 3,066 clinical samples from service personal with influenza-like illness; of those screened, 767 rapid test results by QuickVue Influenza A+B test were available for comparison with rRT-PCR results (8). Of 39 patients with pandemic H1N1, 20 were RIDT positive, with a 51% sensitivity; for seasonal influenza A the sensitivity was 63% for H1N1 and 31% for H3N2. Specificity was 99% for all three subtypes when compared with rRT-PCR.
The results of these studies and the findings in this report affirm that a negative result for this rapid test does not rule out 2009 pandemic influenza A (H1N1) virus infection in an individual with symptoms consistent with influenza. Factors that might decrease the performance of rapid influenza antigen tests include improper specimen collection, not testing the recommended clinical sample (e.g., nasal versus nasopharyngeal swab), quality of the specimen, prolonged time from illness onset to specimen collection (because viral shedding decreases over time), and improper handling and storage of the specimen before testing. The reason for the suboptimal detection of 2009 pandemic influenza A (H1N1) by the RIDT used in this study was not specifically determined but did not appear to be related to differences in the interval (median: 36 hours for both groups) from onset of symptoms to specimen collection or to the severity of symptoms. As with all screening tests, the positive and negative predictive values of RIDTs are dependent on the prevalence of the disease in the population.
The findings in this report are subject to at least one limitation. The assessment involved a limited number of patients from two small outbreaks. The results should be viewed in this context. In other field situations (e.g., with other disease prevalences, collection and transport methods, or using other RIDTs), RIDTs might have different performance characteristics.
RIDTs can be an important tool for patient care during the normal influenza season because they usually provide results within 30 minutes. In addition, these tests can be used to make decisions about isolating or cohorting patients in health-care settings and recommending or restricting patient movements in outpatient settings. They might be especially important for hospitals limited by the expense of rRT-PCR and in identifying influenza during outbreaks in defined patient groups, such as those in schools or nursing homes. However, if used for management of patients with possible pandemic H1N1 virus infection, false-negative test reports might result in inappropriate exposure of susceptible persons to infected patients. Additional large studies to better characterize the performance of RIDTs for detection of infection in patients with pandemic H1N1 virus and improvements in rapid testing for pandemic H1N1 are needed.
# Anaplasmosis and Ehrlichiosis -Maine, 2008
Anaplasmosis and ehrlichiosis are rickettsial tickborne diseases that have had at least a twofold increase in prevalence in the United States since 2000 (1,2). Despite similar clinical presentations, the causative organisms are carried by different ticks with distinct geographic and ecologic associations (3). Surveillance efforts are complicated by ambiguous terminology and serologic testing with antibody cross-reactivity. Although anaplasmosis historically has been reported in Maine, ehrlichiosis has been reported infrequently. During 2007-2008, the number of physician-reported anaplasmosis cases nearly doubled in Maine, and ehrlichiosis cases increased more than fourfold. To examine this increase, the Maine Department of Health and Human Services (MDHHS) analyzed available data on tick burden and physician-reported cases of anaplasmosis and ehrlichiosis during 2000-2008. This report describes the results of that analysis, which indicated that Ixodes scapularis (the tick vector for Anaplasma phagocytophilum) was broadly distributed in Maine, whereas Amblyomma americanum (the tick vector for Erhlichia chaffeenisis) was scarce. Moreover, 95% of physician-reported ehrlichiosis cases lacked a concurrent serologic assessment to exclude anaplasmosis, suggesting that antibody cross-reactivity might have resulted in misclassification. In 2008, Maine modified case classification to enhance specificity; ehrlichiosis cases that lack a concurrent test for anaplasmosis are now classified as suspect rather than probable and therefore are not included in national surveillance summaries. The accuracy of case classification and surveillance can be improved by educating health-care providers regarding 1) the expected geographic distribution of tick vectors and 2) recommendations for confirmatory testing to distinguish between the causative organisms of anaplasmosis and ehrlichiosis.
In Maine, laboratories electronically report positive anaplasmosis and ehrlichiosis results to the health department (referred to as physician reported). Field epidemiology personnel follow up positive results by interviewing physicians and patients and by obtaining clinical, laboratory, and epidemiologic information required to complete the CDC tickborne rickettsial disease case report form.- MDHHS conducted a review of available data on tick burden in the state and reviewed the clinical and public health surveillance data for physician-reported human ehrlichiosis and anaplasmosis during 2000-2008. Maine classified cases according to Council of State and Territorial Epidemiologists (CSTE) case definition † with the exception that the 2008 cases were classified according to a modified ehrlichiosis case definition that had increased specificity.
# Tick Surveillance Data
During 2000-2008, the Vector Borne Disease Laboratory of the Maine Medical Center Research Institute conducted active surveillance of ticks in Maine (through flagging and trapping) and passive surveillance (through receipt of ticks submitted by state residents through the mail) (4). A total of 5,089 I. scapularis were collected, but only 15 A. americanum ticks were detected. All life stages of I. scapularis (larvae, nymphs, and adults) were identified; the tick distribution increased and expanded along the southern coastline and up the river valleys, corresponding to areas of increasing settlement of human populations in this geographic distribution. During 2007-2008, Maine residents submitted 1,968 I. scapularis and only six A. americanum. The surveillance results suggested that A. americanum, the ehrlichiosis vector, had only a sparse and sporadic distribution in Maine.
# Human Anaplasmosis Surveillance Data
During 2000-2008, a total of 45 cases of anaplasmosis cases were reported in Maine. Fifteen (33%) cases were confirmed, 30 (67%) were probable, and no suspect cases were reported (Tables 1 and 2). Among the 15 confirmed cases, three (20%) patients were diagnosed by demonstration in paired sera of a fourfold or greater increase in antibodies to A. phagocytophilum in acute versus convalescent samples; 12 (80%) patients were diagnosed by polmerase chain reaction (PCR) detection of A. phagocytophilum DNA, including two patients who also had positive single A. phagocytophilum serologic test. Among the 30 probable cases, 23 (77%) patients were diagnosed only by a single test for antibodies to A. phagocytophilum, including one (3%) patient who also had detection of morulae consistent with A. phagocytophilum on a blood smear. Seven (23%) patients were tested for antibodies to both A. phagocytophilum and E. chaffeensis, and all showed higher antibody titers to A. phagocytophilum. The median patient age among all confirmed and probable cases was 57 years (range: 21-89 years); 28 patients (62%) were males. Seventeen (38%) patients were hospitalized, and one (2%) patient died from renal failure relating to infection. Two (4%) patients were diagnosed with concurrent Lyme disease, and two (4%) with concurrent babesiosis. Reported anaplasmosis cases occurred during April-December; 30 (67%) of 45 patients had onset dates during May-September. Anaplasmosis was reported in six (38%) of 16 counties; the majority occurred in southern coastal Maine. One patient with confirmed anaplasmosis had traveled to New York, an anaplasmosis-endemic state, during the preceding month.
# MMWR September 25, 2009
Human Ehrlichiosis Surveillance Data
During 2000-2008, a total of cases of ehrlichiosis were reported in Maine (Tables 1 and 2). The single confirmed case, which was diagnosed by PCR, occurred in a male aged 58 years who worked as an interstate truck driver; therefore, outof-state exposure to E. chaffeensis was possible. An additional 19 ehrlichiosis cases were reported during this same period (including six cases reported during 2005-2007 and 13 cases reported during 2008). All 19 cases were diagnosed by a single positive Ehrlichia serologic assay, and none had accompanying serologic tests to exclude anaplasmosis. Although all 13 cases reported in 2008 would have met the CSTE case definition for probable ehrlichiosis, beginning in that year, Maine had adopted a modified ehrlichiosis case definition to increase specificity; therefore, these 13 case were classified as suspect. Ten of the 20 cases were in persons who had either concurrent Lyme disease (seven persons) or babesiosis (three persons), which, like Anaplasma, are transmitted by I. scapularis.
# Classification of Ehrlichiosis Cases
Based on the lack of evidence for a sustained tick vector population in the state, lack of travel history among patients, and the cross-reactive serologic tests for ehrlichiosis and anaplasmosis, MDHHS implemented a new ehrlichiosis case classification strategy using a modified CSTE case definition in 2008 (5). Probable ehrlichiosis cases were defined as clinically compatible with one positive immunoglobulin G (IgG) serologic result for E. chaffeensis and either a concurrent lower titer serologic test for A. phagocytophilum or visualization of intracytoplasmic morulae in peripheral monocytes or macrophages. For cases having serologic reactivity to both agents, the higher antibody level was used to identify the most likely infection (5). Ehrlichiosis reports that did not meet this new more stringent probable case definition (i.e., those that were only tested for ehrlichiosis) were classified as suspect cases, which are excluded from national notifiable disease surveillance summaries.
Editorial Note: The findings in this report underscore that the use of cross-reactive serologic assays, which test for ehrlichiosis alone in anaplasmosis-endemic areas, can result in an inaccurately high ehrlichiosis incidence and contribute to underrecognition of actual anaplasmosis cases. Serologic assays for A. phagocytophilum and E. chaffeensis have >50% cross reactiv-ity; thus, differentiating between ehrlichiosis or anaplasmosis based on single serologic assay is not possible (6)(7)(8). In 2008, Maine classified 13 ehrlichiosis cases as suspect because they more likely represent infection with A. phagocytophilum given that tick data did not support a sustained ehrlichiosis vector in the state and confirmatory laboratory testing and supporting travel history for ehrlichiosis infection were lacking. The likelihood these suspect cases are anaplasmosis cases is further supported by the fact that 54% of suspect ehrlichiosis cases occurred in persons who had either concurrent Lyme disease or babesiosis, which, like Anaplasma, are transmitted by I. scapularis. Whether the emergence of anaplasmosis in Maine and nationwide is an actual increase in incidence or an increase in awareness and testing is unclear. Reports of anaplasmosis have increased threefold (from 351 cases in 2000 to 1,053 cases in 2008), and reports of ehrlichiosis have increased more than fourfold (from 200 cases in 2000 to approximately 800 cases in 2008) (1; CDC, unpublished data, 2009). Most cases of ehrlichiosis have been reported from the southern and south-central United States, corresponding to the geographic distribution of the tick vector, A. americanum. However, during 2008-2009, a concerning trend of increased ehrlichiosis case reports from some northern-area states, including Maine, has been noted (CDC, unpublished data, 2009). Possible explanations for this increase include expanding geographic ranges of the tick vector A. americanum or misclassification of cases.
Anaplasmosis, referred to as human granulocytic anaplasmosis, is caused by A. phagocytophilum. Before a taxonomic reorganization in 2001, this organism was called Ehrlichia phagocytophilum, and the infection was described as human granulocytic ehrlichiosis. I. scapularis (the black-legged tick), the vector for anaplasmosis, is reported commonly from northern and northeastern states. Ehrlichiosis, known as human monocytic ehrlichiosis, is caused by E. chaffeensis and is transmitted by A. americanum (the lone star tick). E. chaffeensis is commonly reported in the southern and south-central states, where the vector is common. Both anaplasmosis and ehrlichiosis are nationally notifiable diseases. In Maine, the vector A. americanum responsible for transmission of E. chaffeensis is not endemic. Conversely, A. phagocytophilum DNA has been detected in 16% of 94 I. scapularis ticks tested in 2008 (9). The fact that 95% of physician-reported ehrlichiosis cases lacked a concurrent serologic assessment to exclude anaplasmosis supports the likelihood that antibody cross-reactivity could have resulted in misclassification. One factor contributing to this misclassification might have been confusion among physicians regarding the recent change in terminology for A. phagocytophilum infection (from human granulocytic ehrlichiosis to anaplasmosis) and a lack of understanding of appropriate testing strategies. Since taxonomic changes were adopted in 2001, the term "anaplasmosis" has gradually replaced the term "human granulocytic ehrlichiosis" to describe human infections with A. phagocytophilum. However, some medical references and commercial test names still use the term "ehrlichiosis," which might cause confusion among physicians regarding the selection of appropriate diagnostic tests.
Health-care providers should assess clinical and ecologic features and, as indicated, include concurrent confirmatory testing for both anaplasmosis and ehrlichiosis or other tickborne diseases when evaluating patients with suspected tickborne illness. Compared with anaplasmosis patients, ehrlichiosis patients might have a higher potential for severe or fatal outcome, and a higher proportion (up to 30%) of ehrlichiosis patients have rash; thus, these diagnostic clues also can prompt physicians to request concurrent testing for ehrlichiosis (3). If serologic testing is selected to evaluate patients, serology should include 1) concurrent testing for both A. phagocytophilum and E. chaffeensis and 2) testing of paired acute and convalescent sera whenever possible. PCR is considered a confirmatory test and is the recommended diagnostic tool preferred over serology because it can differentiate between the two infections (4,10). Patients with suspected anaplasmosis or ehrlichiosis should be treated promptly with doxycycline, without regard to initial serologic test results, because antibodies in the first week of illness frequently are not detected. § Seven patients were tested for antibodies to both A. phagocytophilum and E. chaffeensis concurrently, and all showed higher antibody titers to A. phagocytophilum. ¶ Diagnosed by demonstration in paired sera of a fourfold or greater increase in antibodies to A. phagocytophilum in acute versus convalescent samples. Polymerase chain reaction. † † Visualization of intracytoplasmic morulae in granulocytes for anaplasmosis or peripheral monocytes or macrophages for ehrlichiosis.
# MMWR September 25, 2009
# Progress Toward Measles Control -African Region, 2001-2008
In 2001, the countries of the World Health Organization (WHO) African Region (AFR) became part of a global initiative with a goal of reducing the number of measles deaths by 50% by 2005, compared with 1999. Recommended strategies for measles mortality reduction included 1) increasing rou-increasing routine coverage for the first dose of measles-containing vaccine (MCV1) for all children, 2) providing a second opportunity for measles vaccination through supplemental immunization activities (SIAs), 3) improving measles case management, and 4) establishing case-based surveillance with laboratory confirmation of all suspected measles cases (1). Before introduction of MCV throughout AFR, approximately 1 million measles cases had been reported each year in the early 1980s (2). After strengthening measles-control activities, annual reported cases declined to an estimated 300,000-580,000 during the 1990s. (3,4). However, inaccuracies in reported vaccination coverage exist, surveillance is suboptimal, and measles outbreaks continue to occur in AFR countries. Further progress in measles control will require full implementation of recommended strategies, including validation of vaccination coverage.
Since the 1980s, AFR countries have reported measles vaccination coverage and the number of measles cases each year to the WHO African Regional Office (AFRO), using the WHO and United Nations Children's Fund (UNICEF) Joint Reporting Form. These data are collected through administrative reports from routine vaccination programs and SIAs and routine surveillance systems that provide aggregated case counts based on clinical diagnosis. Estimates of routine coverage with MCV1 are based on review of coverage data from administrative records, surveys, national reports, and consultation with local and regional experts. Coverage achieved during nationwide SIAs against measles are reported on the basis of the reported number of doses administered, divided by the target population.
In 1999, as part of the measles mortality reduction strategy, case-based surveillance with laboratory testing for all suspected measles cases was introduced with support from WHO AFRO. A suspected measles case is defined as 1) any person with generalized maculo-papular rash and fever plus cough or coryza or conjunctivitis or 2) any person in whom a clinician suspects measles. Each suspected measles case should be reported using an individual case-investigation form, and a blood specimen should be collected and sent to the laboratory for measles-specific immunoglobulin M testing. Laboratory confirmation of individual cases is discontinued after an outbreak has been confirmed as measles. An outbreak is confirmed when three or more measles laboratory-confirmed cases are detected in a health facility or district in 1 month; subsequent cases are confirmed by epidemiologic link. An epidemiologic link is defined as a suspected measles case that did not have a specimen collected for laboratory testing and is linked in person, place, and time to a laboratory-confirmed case (i.e., in a patient living in the same district or an adjacent district with a patient with laboratory-confirmed measles where a likelihood of transmission and onset of rash in the two patients within 30 days of each other exists) (5). Case-based surveillance data from AFR countries are shared regularly with WHO AFRO. Data quality is monitored using annualized performance indicators that include the 1) percentage of districts reporting one or more suspected case with a blood specimen (target: >80%) and 2) nonmeasles febrile rash illness rate (target: >2 cases per 100,000).
# Routine Vaccination Activities
In AFR, MCV1 is administered through routine services to children at age 9 months. According to WHO and UNICEF estimates, AFR MCV1 coverage increased from 57% in 2001 to 73% in 2008 (Figure). In 2008, among the 46 AFR countries,- three (7%) had MCV1 coverage of <60%, 13 (28%) had coverage of 60%-69%, 11 (24%) had coverage of 70-79%, 10 (22%) had coverage of 80-89%, and nine (20%) had coverage of ≥90% (Table 1
# SIA Results
SIAs provide a second opportunity for measles immunization to all children, including those not vaccinated with MCV1 and those previously vaccinated; approximately 15% of children vaccinated with a single dose at age 9 months will not develop immunity to measles. The SIA strategy generally consists of a one-time catch-up SIA, targeted to a wide age range, which aims to reduce susceptibility to measles in the population. This is followed by periodic follow-up SIAs targeting children born since the last SIA, thus reducing the accumulation of susceptible children in new birth cohorts.
Before 2000, seven (15%) AFR countries (Botswana, Lesotho, Malawi, Namibia, South Africa, Swaziland, and Zimbabwe) had completed a catch-up SIA, and Namibia and South Africa had completed a follow-up SIA (6). By the end of 2008, 43 AFR countries (all except Algeria, Mauritius, and Seychelles) had completed a catch-up SIA, and all but Comoros and Guinea-Bissau had completed at least one follow-up SIA (Table 2
# Measles Surveillance
By December 2008, all AFR countries except Algeria, Comoros, Guinea Bissau, Mauritius, Sao Tome & Principe, and Seychelles had established measles case-based surveillance in accordance with the WHO AFRO measles surveillance guidelines (5). In 2008, of the 40 countries with case-based surveillance, 21 (53%) met the target of >80% of districts reporting one or more suspected cases; 24 (60%) had a nonmeasles febrile rash illness rate of >2 cases per 100,000 popula->2 cases per 100,000 popula-population; and 16 (40%) met both targets. However, despite this progress, vaccination coverage reports remain imprecise, disease surveillance remains suboptimal, and outbreaks continue to occur, even in countries that reported implementation of all recommended components of the measles strategy. Available mathematical models likely overes-. Available mathematical models likely overestimate the disease burden and underreporting of measles cases is common, even with high-performing surveillance systems; therefore, caution is recommended when drawing comparisons between reported incidence of measles and estimates of measles deaths generated from models.
# Monitoring Measles Incidence
SIAs are recommended to provide a second opportunity for immunization and increase the likelihood of vaccinating hard-to-reach children. SIA coverage usually is estimated by an administrative method relying on the reported number of vaccine doses administered and available target population denominator data, both of which often are imprecise. For example, during 2001-2008, several countries reported vac-, several countries reported vaccinating >100% of children targets in SIAs. Improved methods for determining the actual target population size for SIAs are needed; reported coverage also should be routinely validated by independent surveys. In addition, detailed field investigations of outbreaks should be undertaken to identify post-SIA risk factors for measles, and help refine vaccination strategies.
The findings in this report are subject to at least two limitations. First, a change in measles surveillance methods might result in underestimates or overestimates of the disease burden over time. For example, in 1999, AFR countries routinely (6). Second, although the case definition for suspected measles remained the same, the change in measles reporting practices might have led to either underreporting, because of the additional resources needed to complete individual case investigations and collect blood samples, or overreporting because of overall efforts to strengthen measles surveillance.
In light of progress made toward reducing measles deaths, a more advanced goal was proposed recently for the region with several recommendations to improve vaccination coverage and surveillance performance. The AFR measles technical advisory group met in May 2008 and recommended that AFR countries aim to meet the following targets by 2012: 1) reducing estimated measles deaths by 98%, compared with 2000 estimates; 2) reducing measles incidence to 80% in all districts; 4) achieving >95% SIA coverage in all districts; and 5) attaining two primary measles surveillance performance indicator targets (a nonmeasles febrile rash illness rate of >2 cases per 100,000 population per year and one or more suspected measles case investigated with blood specimen in >80% of districts per year); and 6) routine reporting from all districts (10). The group also recommended that AFR countries consider introduction of MCV2 in the routine vaccination schedule if MCV1 coverage of >80% has been achieved and maintained for ≥3 consecutive years and at least one of the two primary measles surveillance indicator targets has been achieved and maintained for at least 2 years. For countries adopting a 2-dose routine measles vaccination schedule, continued follow-up SIAs were recommended for all new birth cohorts every 3-5 years until national MCV2 coverage of ≥90% is sustained for at least 2 years (10).
# Updated Recommendation from the Advisory Committee on Immunization Practices (ACIP) for Revaccination of Persons at Prolonged Increased Risk for Meningococcal Disease
The Advisory Committee on Immunization Practices (ACIP) recommends quadrivalent meningococcal conjugate vaccine, (MCV4) (Menactra, Sanofi Pasteur, Swiftwater, Pennsylvania) for all persons aged 11-18 years and for persons aged 2-55 years at increased risk for meningococcal disease (1-3). MCV4 is licensed as a single dose. Because of the high risk for meningococcal disease among certain groups and limited data on duration of protection, at its June 2009 meeting ACIP recommended that persons previously vaccinated with either MCV4 or MPSV4 (Menomune, Sanofi Pasteur) who are at prolonged increased risk for meningococcal disease should be revaccinated with MCV4. Persons who previously were vaccinated at age ≥7 years and are at prolonged increased risk should be revaccinated 5 years after their previous meningococcal vaccine, and persons who previously were vaccinated at ages 2-6 years and are at prolonged increased risk should be revaccinated 3 years after their previous meningococcal vaccine. Persons at prolonged increased risk for meningococcal disease include 1) persons with increased susceptibility such as persistent complement component deficiencies (e.g., C3, properdin, Factor D, and late complement component deficiencies), 2) persons with anatomic or functional asplenia, and 3) persons who have prolonged exposure (e.g., microbiologists routinely working with Neisseria meningitidis, or travelers to or residents of countries where meningococcal disease is hyperendemic or epidemic). This report provides the rationale for the new recommendation and updates and replaces previous recommendations for revaccination with MCV4.
ACIP's Meningococcal Vaccine Work Group reviewed data on the risk for meningococcal disease, antibody titer decline, and the safety and immunogenicity of revaccination with MCV4 at 3 years and 5 years after the first dose of MCV4 or MPSV4 (2,3). Persons with prolonged increased risk for meningococcal disease have increased susceptibility to the disease or ongoing increased risk for exposure to N. meningitidis, higher levels of serum bactericidal antibody (SBA) against N. meningitidis can provide these groups increased protection against disease. SBA is a measure of the ability of sera to kill a strain of N. meningitidis in the presence of complement. In clinical trials, a baby rabbit SBA titer of 1:128 was used as a conservative correlate of protection (1). Small subsets of subjects from the MCV4 prelicensure clinical trial were revaccinated 3 years (n = 76) and 5 years (n = 134) after receiving MCV4. Of 71 persons aged 11-18 years at primary vaccination who had been vaccinated with MCV4 3 years previously, 75% and 86% had SBA titers greater than 1:128 for serogroups C and Y, respectively, before revaccination. Of 108 persons aged 2-10 years at primary vaccination who had been vaccinated with MCV4 5 years previously, 55% and 94% had SBA titers greater than 1:128 for serogroups C and Y, respectively, before revaccination. All persons revaccinated with MCV4 in these studies achieved SBA titers greater than 1:128 for serogroups C and Y. Approximately 50%-70% of persons in both the previously vaccinated (n = 210) and vaccine naive groups (n = 323) reported mild to moderate local and systemic adverse events after revaccination (or initial vaccination) with MCV4. However, no serious adverse events were reported in either group (Sanofi Pasteur, unpublished data, 2009).
On the basis of these data, expert opinion of the workgroup members, and feedback from partner organizations, the workgroup proposed that persons at prolonged increased risk for meningococcal disease be revaccinated with MCV4. ACIP approved this proposal at its June 24, 2009, meeting. Persons who previously were vaccinated at age ≥7 years and are at prolonged increased risk should be revaccinated 5 years after their previous meningococcal vaccine. Persons who previously were vaccinated at ages 2-6 years and are at prolonged increased risk should be revaccinated 3 years after their previous meningococcal vaccine. Persons who remain in one of these increased risk groups indefinitely should continue to be revaccinated at 5-year intervals.
Although the duration of protection from MCV4 is unknown, most entering college students will have received MCV4 within the preceding 4 years. Because of the limited period of increased risk, ACIP currently does not recommend that college freshmen living in dormitories who were previously vaccinated with MCV4 be revaccinated. However, college freshmen living in dormitories who were vaccinated with MPSV4 ≥5 years previously are recommended to be vaccinated with MCV4. Information regarding MCV4 and other recommendations for persons aged 2-55 years (2,3), including a routine recommendation for vaccination with MCV4 in persons aged 11-18 years (4), has been published previously.
# Announcement
World Heart Day -September 27, 2009
Each year, approximately 17 million persons die from cardiovascular disease, mainly heart disease and stroke, making it the world's leading cause of death (1). Controlling certain risk factors, such as high blood pressure, high cholesterol, diabetes, obesity, tobacco use, and physical inactivity, can help prevent heart disease and stroke.
In 2000, the World Heart Federation, a nongovernmental organization based in Geneva, Switzerland, created the annual World Heart Day campaign to increase public awareness of the threat of heart disease and stroke. The theme of the 2009 World Heart Day is "Work with Heart -A Workplace That Encourages Healthy Habits Can Reduce Heart Disease and Stroke." Promoting physical activity and healthful eating and discouraging tobacco use around the workplace are simple ways to foster health in the workplace. Activities organized by members and partners of the World Heart Federation will include public talks, concerts, and sporting events. The national member organizations in the United States are the American College of Cardiology and the American Heart Association.
CDC funds heart disease and stroke prevention programs in 41 states and the District of Columbia. Additional information about these programs is available at / state_program/index.htm. Information about World Heart Day and the World Heart Federation is available at . world-heart-federation.org/what-we-do/world-heart-day.
# Announcement
# NHANES 50th Anniversary and Conference
The 50th anniversary of the National Health and Nutrition Examination Survey (NHANES) will be celebrated on September 29, 2009, at a conference at the National Center for Health Statistics in Hyattsville, Maryland. Collaborating agencies, data users, and program and field staff members will share their perspectives on the survey.
# NHANES began in 1959 as the National Health Examination
Survey. NHANES data come from household interviews and standardized examinations and laboratory testing of a sample of the nation's civilian, noninstitutionalized population. NHANES has expanded since the survey's inception to include a nutritional component now conducted in collaboration with the U.S. Department of Agriculture and measures of environmental exposure with the National Center for Environmental Health.
NHANES has long been a primary source of data on the nation's health. NHANES findings were used to set the goals and track the progress in reducing cholesterol levels, the prevalence of high blood pressure, and the risks of blood lead exposure in the United States. NHANES documented the rise in obesity and diabetes and produced the first populationbased estimates of human immunodeficiency virus infection and osteoporosis. NHANES data also are used for the growth charts by which pediatricians and parents check children's growth and development.
A hallmark of NHANES is its partnerships with other CDC programs, the National Institutes of Health, other U.S. Department of Health and Human Services programs, and other government agencies to collect data needed for public health policies and practice. Additional information about the NHANES 50th anniversary is available at / nchs/nhanes/nhanes50th.htm. The course includes a review of the fundamentals of descriptive epidemiology and biostatistics, measures of association, normal and binomial distributions, confounding, statistical tests, stratification, logistic regression models, and computer programs as used in epidemiology.
# Announcement
# Epidemiology in Action
The prerequisite is an introductory course in epidemiology, such as Epidemiology in Action or the International Course in Applied Epidemiology. Tuition will be charged. The application deadline is December 1, 2009, or until all slots have been filled. 1971-1974, 1976-1980, 1988-1994, 1999-2000, 2001-2002, 2003-2004, 2005-2006 1971-1974, 1976-1980, 1988-1994, 1999-2000, 2001-2002, 2003-2004, 2005-2006 Survey period Average total cholesterol (mg/dL) 1959-1962 1971-1974 1976-1980 1988-1994 Men - Incidence data for reporting year 2009 is provisional, whereas data for 2004 through 2008 are finalized. † Calculated by summing the incidence counts for the current week, the 2 weeks preceding the current week, and the 2 weeks following the current week, for a total of 5 preceding years. The total sum of incident cases is then divided by 25 weeks. Additional information is available at . § Not reportable in all states. Data from states where the condition is not reportable are excluded from this | CDC ILI surveillance case definition: fever (≥100ºF [≥37.8ºC]), plus cough, sore throat, or both in the absence of another known cause of illness. Vol. 58 / No. 37 MMWR 1031 * By real-time reverse transcription-polymerase chain reaction assay; all patients tested negative for seasonal influenza. † Remel Xpect Flu A&B test (Remel Products, Lenexa, Kansas). TABLE. Performance of a rapid influenza detection test (RIDT)* in patients with suspected and confirmed † 2009 pandemic influenza A (H1N1) virus infection, by clinical syndrome consistent with CDC-defined influenza-like illness (ILI) § -Connecticut, 2009 rRT-PCR positive rRT-PCR negative Total RIDT positive RIDT negative RIDT positive RIDT negative Sensitivity % Specificity % PPV ¶ % NPV** % Overall 63 23 26 2 12 47 86 92 32 CDC-defined ILI** 48 19 21 1 7 48 88 95 25 No CDC-defined ILI 15 4 5 1 5 44 83 80 50 * Remel Xpect Flu A&B test (Remel Products, Lenexa, Kansas). † By real-time reverse transcription-polymerase chain reaction (rRT-PCR); all patients tested negative for seasonal influenza. § CDC ILI surveillance case definition: fever (≥100°F [≥37.8°C]) plus cough, sore throat, or both in the absence of another known cause of illness. ¶ Positive predictive value. ** Negative predictive value.#
During May 2009, a few weeks after 2009 pandemic influenza A (H1N1) infection was first detected in the United States (1), outbreaks among students from two schools were detected in Greenwich, Connecticut. Staff members from Greenwich Hospital and the Connecticut Department of Public Health collected data on symptoms for 63 patients and submitted nasopharyngeal washings for testing using a rapid influenza diagnostic test (RIDT) for influenza A and B and real-time reverse transcription-polymerase chain reaction (rRT-PCR) assay, thereby affording an opportunity to assess the field performance of the RIDT. A total of 49 patients had infections with pandemic influenza A (H1N1) confirmed by rRT-PCR. This report summarizes the findings from this performance assessment, which indicated that, compared with rRT-PCR, the sensitivity of the RIDT for detecting infection in patients with 2009 pandemic influenza A (H1N1) was 47%, and the specificity was 86%. Sensitivity and specificity did not vary substantially by the presence or absence of CDC-defined influenza-like illness (ILI) or by time from symptom onset to specimen acquisition. In this group of patients, although positive RIDT results performed well in predicting confirmed infection with pandemic H1N1 virus (positive predictive value: 92%), negative tests did not accurately predict the absence of infection (negative predictive value: 32%). These results affirm recent CDC recommendations against using negative RIDT results for management of patients with possible 2009 pandemic influenza A (H1N1) infection (2).
During April 29-May 1, 2009, 78 students from a private school (school A) near Greenwich, Connecticut, participated in a class trip to Pennsylvania. Several students became sick with a respiratory illness. Because infection with 2009 pandemic influenza A (H1N1) was suspected, upon returning home, 11 of the students, a sibling, and two other students went to the Greenwich Hospital for outpatient influenza testing and treatment.
During May 18-20, 133 students and eight teachers from a public school (school B) in Greenwich traveled to a camp in Connecticut. Among these students, 36 visited the camp infirmary with fever, headache, or fatigue. The Greenwich Health Department asked physicians at the hospital to assist with testing the students for pandemic H1N1. A total of 67 students and staff from school B became ill, and 49 of these patients went to the hospital for influenza testing.
A total of 63 patients (14 students from school A and 49 students and staff from school B) were tested for influenza at the hospital. A standard symptom survey was completed by a physician for each patient after which a nasopharyngeal washing was performed by an experienced respiratory therapist trained in the procedure. All samples were placed in viral transport media and sent to the Connecticut Department of Public Health laboratory for influenza virus detection by rRT-PCR. Rapid screening for influenza A and B was performed concurrently at the hospital laboratory using the Remel Xpect Flu A&B test (Remel Products, Lenexa, Kansas) according to manufacturer's instructions (3). Although the number of ill persons who eventually received antiviral therapy is unknown, all nasopharyngeal washings were obtained before initiation of therapy.
Of the 63 patients tested by RIDT, 49 patients, 11 (79%) from school A and 38 (78%) from school B, were found to have 2009 pandemic influenza A (H1N1) infection by rRT-PCR (Figure). Of the 49 patients with confirmed infection, 23 (47%) tested positive (eight from school A and 15 from school B) and 26 (53%) tested negative for 2009 pandemic influenza A (H1N1) by RIDT. Among 11 patients with positive rRT-PCR tests from school A and 38 from school B, the numbers of positive RIDT tests were 8 (73%) and 15 (39%) respectively.
Among the 14 patient samples from both schools that tested negative by rRT-PCR, three were from students at school A, and 11 were from school B. Of the 14 rRT-PCR negative specimens, two tested positive by RIDT (one from school A and one from school B). The overall sensitivity of the RIDT was 23 of 49 (47%), and the specificity was 12 of 14 (86%). The positive predictive value was 23 of 25 (92%), and the negative predictive value was 12 of 38 (32%).
The schools did not differ significantly with respect to percentage of patients with confirmed pandemic H1N1 by rRT-PCR, severity of symptoms, interval between the onset of symptoms and collection of specimens for testing, or overall RIDT positivity rate. Among all the patients tested by RIDT, no significant differences between true positives and false negatives were seen with respect to ILI.* In RIDT positive and RIDT negative patients with pandemic H1N1, the median interval from symptom onset to specimen collection was 36 hours. Of the 34 patients with washings obtained ≤36 hours from the onset of symptoms, 16 (47%) were RIDT positive; of the 15 patients with washings collected after 36 hours of symptoms, seven (47%) were positive. RIDT test performance was assessed for patients with and without CDC-defined ILI (Table ). The sensitivity and specificity were approximately the same for the two groups (48% versus 44% and 88% versus 83%, respectively). Editorial Note: When cases of 2009 pandemic influenza A (H1N1) began appearing in the United States in April 2009, several RIDTs had been in common use in the United States as point-of-care tests for seasonal influenza, but the performance of these tests in patients infected with 2009 pandemic influenza A (H1N1) virus was unknown. CDC has since reported varying sensitivities of RIDTs in retrospective analyses of rRT-PCR positive respiratory samples, from 40%-69%. In these analyses, RIDT sensitivity was positively associated with the titer of virus in the sample (4).
The analysis in this report of pandemic H1N1 cases at two schools determined that the RIDT used detected less than half the cases confirmed by rRT-PCR. The low sensitivity and low negative predictive value of the test during these outbreaks highlight the limitations of using this test alone to establish diagnosis and aid clinical management. These results affirm current recommendations not to use negative RIDT results to rule out pandemic H1N1 or to make infection control decisions (2). Rapid tests differ in their sensitivity and specificity for detecting seasonal influenza in respiratory specimens but generally have low to moderate sensitivity compared with viral culture or rRT-PCR. Previous RIDT studies have described the performance of the QuickVue Influenza A+B test (Quidel Corporation, San Diego, California) for detecting seasonal influenza in three different populations during 2008. Sensitivity when compared with rRT-PCR was low for all populations (median: 27%; range: 19%-32%) (5).
The RIDT used in the current study has a reported sensitivity of 92.5% and a specificity of 100% for the diagnosis of seasonal influenza A by nasopharyngeal wash (3). This investigation yielded much lower sensitivity (47%) and specificity (86%) in patients having confirmed infection with 2009 pandemic influenza A (H1N1) virus.
The findings in this report are comparable to recently reported observations of low performance of RIDTs in patients with pandemic H1N1. In a report of hospitalized patients in California, rapid antigen test results were positive in 67% of cases of pandemic H1N1 tested (6). In an assessment of rapid testing compared with rRT-PCR conducted on 6,090 patient samples from the New York City area, the sensitivity and specificity for the detection of 2009 pandemic influenza A (H1N1) virus by rapid antigen testing, using the BinaxNOW Influenza A&B test (Binax, Inc., Scarborough, Maine) and the 3M Rapid Detection Flu A+B test (3M, St. Paul, Minnesota) were 17.8% and 93.6% respectively (7). A recent report from the Naval Health Research Center described screening 3,066 clinical samples from service personal with influenza-like illness; of those screened, 767 rapid test results by QuickVue Influenza A+B test were available for comparison with rRT-PCR results (8). Of 39 patients with pandemic H1N1, 20 were RIDT positive, with a 51% sensitivity; for seasonal influenza A the sensitivity was 63% for H1N1 and 31% for H3N2. Specificity was 99% for all three subtypes when compared with rRT-PCR.
The results of these studies and the findings in this report affirm that a negative result for this rapid test does not rule out 2009 pandemic influenza A (H1N1) virus infection in an individual with symptoms consistent with influenza. Factors that might decrease the performance of rapid influenza antigen tests include improper specimen collection, not testing the recommended clinical sample (e.g., nasal versus nasopharyngeal swab), quality of the specimen, prolonged time from illness onset to specimen collection (because viral shedding decreases over time), and improper handling and storage of the specimen before testing. The reason for the suboptimal detection of 2009 pandemic influenza A (H1N1) by the RIDT used in this study was not specifically determined but did not appear to be related to differences in the interval (median: 36 hours for both groups) from onset of symptoms to specimen collection or to the severity of symptoms. As with all screening tests, the positive and negative predictive values of RIDTs are dependent on the prevalence of the disease in the population.
The findings in this report are subject to at least one limitation. The assessment involved a limited number of patients from two small outbreaks. The results should be viewed in this context. In other field situations (e.g., with other disease prevalences, collection and transport methods, or using other RIDTs), RIDTs might have different performance characteristics.
RIDTs can be an important tool for patient care during the normal influenza season because they usually provide results within 30 minutes. In addition, these tests can be used to make decisions about isolating or cohorting patients in health-care settings and recommending or restricting patient movements in outpatient settings. They might be especially important for hospitals limited by the expense of rRT-PCR and in identifying influenza during outbreaks in defined patient groups, such as those in schools or nursing homes. However, if used for management of patients with possible pandemic H1N1 virus infection, false-negative test reports might result in inappropriate exposure of susceptible persons to infected patients. Additional large studies to better characterize the performance of RIDTs for detection of infection in patients with pandemic H1N1 virus and improvements in rapid testing for pandemic H1N1 are needed.
# Anaplasmosis and Ehrlichiosis -Maine, 2008
Anaplasmosis and ehrlichiosis are rickettsial tickborne diseases that have had at least a twofold increase in prevalence in the United States since 2000 (1,2). Despite similar clinical presentations, the causative organisms are carried by different ticks with distinct geographic and ecologic associations (3). Surveillance efforts are complicated by ambiguous terminology and serologic testing with antibody cross-reactivity. Although anaplasmosis historically has been reported in Maine, ehrlichiosis has been reported infrequently. During 2007-2008, the number of physician-reported anaplasmosis cases nearly doubled in Maine, and ehrlichiosis cases increased more than fourfold. To examine this increase, the Maine Department of Health and Human Services (MDHHS) analyzed available data on tick burden and physician-reported cases of anaplasmosis and ehrlichiosis during 2000-2008. This report describes the results of that analysis, which indicated that Ixodes scapularis (the tick vector for Anaplasma phagocytophilum) was broadly distributed in Maine, whereas Amblyomma americanum (the tick vector for Erhlichia chaffeenisis) was scarce. Moreover, 95% of physician-reported ehrlichiosis cases lacked a concurrent serologic assessment to exclude anaplasmosis, suggesting that antibody cross-reactivity might have resulted in misclassification. In 2008, Maine modified case classification to enhance specificity; ehrlichiosis cases that lack a concurrent test for anaplasmosis are now classified as suspect rather than probable and therefore are not included in national surveillance summaries. The accuracy of case classification and surveillance can be improved by educating health-care providers regarding 1) the expected geographic distribution of tick vectors and 2) recommendations for confirmatory testing to distinguish between the causative organisms of anaplasmosis and ehrlichiosis.
In Maine, laboratories electronically report positive anaplasmosis and ehrlichiosis results to the health department (referred to as physician reported). Field epidemiology personnel follow up positive results by interviewing physicians and patients and by obtaining clinical, laboratory, and epidemiologic information required to complete the CDC tickborne rickettsial disease case report form.* MDHHS conducted a review of available data on tick burden in the state and reviewed the clinical and public health surveillance data for physician-reported human ehrlichiosis and anaplasmosis during 2000-2008. Maine classified cases according to Council of State and Territorial Epidemiologists (CSTE) case definition † with the exception that the 2008 cases were classified according to a modified ehrlichiosis case definition that had increased specificity.
# Tick Surveillance Data
During 2000-2008, the Vector Borne Disease Laboratory of the Maine Medical Center Research Institute conducted active surveillance of ticks in Maine (through flagging and trapping) and passive surveillance (through receipt of ticks submitted by state residents through the mail) (4). A total of 5,089 I. scapularis were collected, but only 15 A. americanum ticks were detected. All life stages of I. scapularis (larvae, nymphs, and adults) were identified; the tick distribution increased and expanded along the southern coastline and up the river valleys, corresponding to areas of increasing settlement of human populations in this geographic distribution. During 2007-2008, Maine residents submitted 1,968 I. scapularis and only six A. americanum. The surveillance results suggested that A. americanum, the ehrlichiosis vector, had only a sparse and sporadic distribution in Maine.
# Human Anaplasmosis Surveillance Data
During 2000-2008, a total of 45 cases of anaplasmosis cases were reported in Maine. Fifteen (33%) cases were confirmed, 30 (67%) were probable, and no suspect cases were reported (Tables 1 and 2). Among the 15 confirmed cases, three (20%) patients were diagnosed by demonstration in paired sera of a fourfold or greater increase in antibodies to A. phagocytophilum in acute versus convalescent samples; 12 (80%) patients were diagnosed by polmerase chain reaction (PCR) detection of A. phagocytophilum DNA, including two patients who also had positive single A. phagocytophilum serologic test. Among the 30 probable cases, 23 (77%) patients were diagnosed only by a single test for antibodies to A. phagocytophilum, including one (3%) patient who also had detection of morulae consistent with A. phagocytophilum on a blood smear. Seven (23%) patients were tested for antibodies to both A. phagocytophilum and E. chaffeensis, and all showed higher antibody titers to A. phagocytophilum. The median patient age among all confirmed and probable cases was 57 years (range: 21-89 years); 28 patients (62%) were males. Seventeen (38%) patients were hospitalized, and one (2%) patient died from renal failure relating to infection. Two (4%) patients were diagnosed with concurrent Lyme disease, and two (4%) with concurrent babesiosis. Reported anaplasmosis cases occurred during April-December; 30 (67%) of 45 patients had onset dates during May-September. Anaplasmosis was reported in six (38%) of 16 counties; the majority occurred in southern coastal Maine. One patient with confirmed anaplasmosis had traveled to New York, an anaplasmosis-endemic state, during the preceding month.
# MMWR September 25, 2009
Human Ehrlichiosis Surveillance Data
During 2000-2008, a total of cases of ehrlichiosis were reported in Maine (Tables 1 and 2). The single confirmed case, which was diagnosed by PCR, occurred in a male aged 58 years who worked as an interstate truck driver; therefore, outof-state exposure to E. chaffeensis was possible. An additional 19 ehrlichiosis cases were reported during this same period (including six cases reported during 2005-2007 and 13 cases reported during 2008). All 19 cases were diagnosed by a single positive Ehrlichia serologic assay, and none had accompanying serologic tests to exclude anaplasmosis. Although all 13 cases reported in 2008 would have met the CSTE case definition for probable ehrlichiosis, beginning in that year, Maine had adopted a modified ehrlichiosis case definition to increase specificity; therefore, these 13 case were classified as suspect. Ten of the 20 cases were in persons who had either concurrent Lyme disease (seven persons) or babesiosis (three persons), which, like Anaplasma, are transmitted by I. scapularis.
# Classification of Ehrlichiosis Cases
Based on the lack of evidence for a sustained tick vector population in the state, lack of travel history among patients, and the cross-reactive serologic tests for ehrlichiosis and anaplasmosis, MDHHS implemented a new ehrlichiosis case classification strategy using a modified CSTE case definition in 2008 (5). Probable ehrlichiosis cases were defined as clinically compatible with one positive immunoglobulin G (IgG) serologic result for E. chaffeensis and either a concurrent lower titer serologic test for A. phagocytophilum or visualization of intracytoplasmic morulae in peripheral monocytes or macrophages. For cases having serologic reactivity to both agents, the higher antibody level was used to identify the most likely infection (5). Ehrlichiosis reports that did not meet this new more stringent probable case definition (i.e., those that were only tested for ehrlichiosis) were classified as suspect cases, which are excluded from national notifiable disease surveillance summaries.
Editorial Note: The findings in this report underscore that the use of cross-reactive serologic assays, which test for ehrlichiosis alone in anaplasmosis-endemic areas, can result in an inaccurately high ehrlichiosis incidence and contribute to underrecognition of actual anaplasmosis cases. Serologic assays for A. phagocytophilum and E. chaffeensis have >50% cross reactiv-ity; thus, differentiating between ehrlichiosis or anaplasmosis based on single serologic assay is not possible (6)(7)(8). In 2008, Maine classified 13 ehrlichiosis cases as suspect because they more likely represent infection with A. phagocytophilum given that tick data did not support a sustained ehrlichiosis vector in the state and confirmatory laboratory testing and supporting travel history for ehrlichiosis infection were lacking. The likelihood these suspect cases are anaplasmosis cases is further supported by the fact that 54% of suspect ehrlichiosis cases occurred in persons who had either concurrent Lyme disease or babesiosis, which, like Anaplasma, are transmitted by I. scapularis. Whether the emergence of anaplasmosis in Maine and nationwide is an actual increase in incidence or an increase in awareness and testing is unclear. Reports of anaplasmosis have increased threefold (from 351 cases in 2000 to 1,053 cases in 2008), and reports of ehrlichiosis have increased more than fourfold (from 200 cases in 2000 to approximately 800 cases in 2008) (1; CDC, unpublished data, 2009). Most cases of ehrlichiosis have been reported from the southern and south-central United States, corresponding to the geographic distribution of the tick vector, A. americanum. However, during 2008-2009, a concerning trend of increased ehrlichiosis case reports from some northern-area states, including Maine, has been noted (CDC, unpublished data, 2009). Possible explanations for this increase include expanding geographic ranges of the tick vector A. americanum or misclassification of cases.
Anaplasmosis, referred to as human granulocytic anaplasmosis, is caused by A. phagocytophilum. Before a taxonomic reorganization in 2001, this organism was called Ehrlichia phagocytophilum, and the infection was described as human granulocytic ehrlichiosis. I. scapularis (the black-legged tick), the vector for anaplasmosis, is reported commonly from northern and northeastern states. Ehrlichiosis, known as human monocytic ehrlichiosis, is caused by E. chaffeensis and is transmitted by A. americanum (the lone star tick). E. chaffeensis is commonly reported in the southern and south-central states, where the vector is common. Both anaplasmosis and ehrlichiosis are nationally notifiable diseases. In Maine, the vector A. americanum responsible for transmission of E. chaffeensis is not endemic. Conversely, A. phagocytophilum DNA has been detected in 16% of 94 I. scapularis ticks tested in 2008 (9). The fact that 95% of physician-reported ehrlichiosis cases lacked a concurrent serologic assessment to exclude anaplasmosis supports the likelihood that antibody cross-reactivity could have resulted in misclassification. One factor contributing to this misclassification might have been confusion among physicians regarding the recent change in terminology for A. phagocytophilum infection (from human granulocytic ehrlichiosis to anaplasmosis) and a lack of understanding of appropriate testing strategies. Since taxonomic changes were adopted in 2001, the term "anaplasmosis" has gradually replaced the term "human granulocytic ehrlichiosis" to describe human infections with A. phagocytophilum. However, some medical references and commercial test names still use the term "ehrlichiosis," which might cause confusion among physicians regarding the selection of appropriate diagnostic tests.
Health-care providers should assess clinical and ecologic features and, as indicated, include concurrent confirmatory testing for both anaplasmosis and ehrlichiosis or other tickborne diseases when evaluating patients with suspected tickborne illness. Compared with anaplasmosis patients, ehrlichiosis patients might have a higher potential for severe or fatal outcome, and a higher proportion (up to 30%) of ehrlichiosis patients have rash; thus, these diagnostic clues also can prompt physicians to request concurrent testing for ehrlichiosis (3). If serologic testing is selected to evaluate patients, serology should include 1) concurrent testing for both A. phagocytophilum and E. chaffeensis and 2) testing of paired acute and convalescent sera whenever possible. PCR is considered a confirmatory test and is the recommended diagnostic tool preferred over serology because it can differentiate between the two infections (4,10). Patients with suspected anaplasmosis or ehrlichiosis should be treated promptly with doxycycline, without regard to initial serologic test results, because antibodies in the first week of illness frequently are not detected. § Seven patients were tested for antibodies to both A. phagocytophilum and E. chaffeensis concurrently, and all showed higher antibody titers to A. phagocytophilum. ¶ Diagnosed by demonstration in paired sera of a fourfold or greater increase in antibodies to A. phagocytophilum in acute versus convalescent samples. ** Polymerase chain reaction. † † Visualization of intracytoplasmic morulae in granulocytes for anaplasmosis or peripheral monocytes or macrophages for ehrlichiosis.
# MMWR September 25, 2009
# Progress Toward Measles Control -African Region, 2001-2008
In 2001, the countries of the World Health Organization (WHO) African Region (AFR) became part of a global initiative with a goal of reducing the number of measles deaths by 50% by 2005, compared with 1999. Recommended strategies for measles mortality reduction included 1) increasing rou-increasing routine coverage for the first dose of measles-containing vaccine (MCV1) for all children, 2) providing a second opportunity for measles vaccination through supplemental immunization activities (SIAs), 3) improving measles case management, and 4) establishing case-based surveillance with laboratory confirmation of all suspected measles cases (1). Before introduction of MCV throughout AFR, approximately 1 million measles cases had been reported each year in the early 1980s (2). After strengthening measles-control activities, annual reported cases declined to an estimated 300,000-580,000 during the 1990s. (3,4). However, inaccuracies in reported vaccination coverage exist, surveillance is suboptimal, and measles outbreaks continue to occur in AFR countries. Further progress in measles control will require full implementation of recommended strategies, including validation of vaccination coverage.
Since the 1980s, AFR countries have reported measles vaccination coverage and the number of measles cases each year to the WHO African Regional Office (AFRO), using the WHO and United Nations Children's Fund (UNICEF) Joint Reporting Form. These data are collected through administrative reports from routine vaccination programs and SIAs and routine surveillance systems that provide aggregated case counts based on clinical diagnosis. Estimates of routine coverage with MCV1 are based on review of coverage data from administrative records, surveys, national reports, and consultation with local and regional experts. Coverage achieved during nationwide SIAs against measles are reported on the basis of the reported number of doses administered, divided by the target population.
In 1999, as part of the measles mortality reduction strategy, case-based surveillance with laboratory testing for all suspected measles cases was introduced with support from WHO AFRO. A suspected measles case is defined as 1) any person with generalized maculo-papular rash and fever plus cough or coryza or conjunctivitis or 2) any person in whom a clinician suspects measles. Each suspected measles case should be reported using an individual case-investigation form, and a blood specimen should be collected and sent to the laboratory for measles-specific immunoglobulin M testing. Laboratory confirmation of individual cases is discontinued after an outbreak has been confirmed as measles. An outbreak is confirmed when three or more measles laboratory-confirmed cases are detected in a health facility or district in 1 month; subsequent cases are confirmed by epidemiologic link. An epidemiologic link is defined as a suspected measles case that did not have a specimen collected for laboratory testing and is linked in person, place, and time to a laboratory-confirmed case (i.e., in a patient living in the same district or an adjacent district with a patient with laboratory-confirmed measles where a likelihood of transmission and onset of rash in the two patients within 30 days of each other exists) (5). Case-based surveillance data from AFR countries are shared regularly with WHO AFRO. Data quality is monitored using annualized performance indicators that include the 1) percentage of districts reporting one or more suspected case with a blood specimen (target: >80%) and 2) nonmeasles febrile rash illness rate (target: >2 cases per 100,000).
# Routine Vaccination Activities
In AFR, MCV1 is administered through routine services to children at age 9 months. According to WHO and UNICEF estimates, AFR MCV1 coverage increased from 57% in 2001 to 73% in 2008 (Figure). In 2008, among the 46 AFR countries,* three (7%) had MCV1 coverage of <60%, 13 (28%) had coverage of 60%-69%, 11 (24%) had coverage of 70-79%, 10 (22%) had coverage of 80-89%, and nine (20%) had coverage of ≥90% (Table 1
# SIA Results
SIAs provide a second opportunity for measles immunization to all children, including those not vaccinated with MCV1 and those previously vaccinated; approximately 15% of children vaccinated with a single dose at age 9 months will not develop immunity to measles. The SIA strategy generally consists of a one-time catch-up SIA, targeted to a wide age range, which aims to reduce susceptibility to measles in the population. This is followed by periodic follow-up SIAs targeting children born since the last SIA, thus reducing the accumulation of susceptible children in new birth cohorts.
Before 2000, seven (15%) AFR countries (Botswana, Lesotho, Malawi, Namibia, South Africa, Swaziland, and Zimbabwe) had completed a catch-up SIA, and Namibia and South Africa had completed a follow-up SIA (6). By the end of 2008, 43 AFR countries (all except Algeria, Mauritius, and Seychelles) had completed a catch-up SIA, and all but Comoros and Guinea-Bissau had completed at least one follow-up SIA (Table 2
# Measles Surveillance
By December 2008, all AFR countries except Algeria, Comoros, Guinea Bissau, Mauritius, Sao Tome & Principe, and Seychelles had established measles case-based surveillance in accordance with the WHO AFRO measles surveillance guidelines (5). In 2008, of the 40 countries with case-based surveillance, 21 (53%) met the target of >80% of districts reporting one or more suspected cases; 24 (60%) had a nonmeasles febrile rash illness rate of >2 cases per 100,000 popula->2 cases per 100,000 popula-population; and 16 (40%) met both targets. However, despite this progress, vaccination coverage reports remain imprecise, disease surveillance remains suboptimal, and outbreaks continue to occur, even in countries that reported implementation of all recommended components of the measles strategy. Available mathematical models likely overes-. Available mathematical models likely overestimate the disease burden and underreporting of measles cases is common, even with high-performing surveillance systems; therefore, caution is recommended when drawing comparisons between reported incidence of measles and estimates of measles deaths generated from models.
# Monitoring Measles Incidence
SIAs are recommended to provide a second opportunity for immunization and increase the likelihood of vaccinating hard-to-reach children. SIA coverage usually is estimated by an administrative method relying on the reported number of vaccine doses administered and available target population denominator data, both of which often are imprecise. For example, during 2001-2008, several countries reported vac-, several countries reported vaccinating >100% of children targets in SIAs. Improved methods for determining the actual target population size for SIAs are needed; reported coverage also should be routinely validated by independent surveys. In addition, detailed field investigations of outbreaks should be undertaken to identify post-SIA risk factors for measles, and help refine vaccination strategies.
The findings in this report are subject to at least two limitations. First, a change in measles surveillance methods might result in underestimates or overestimates of the disease burden over time. For example, in 1999, AFR countries routinely (6). Second, although the case definition for suspected measles remained the same, the change in measles reporting practices might have led to either underreporting, because of the additional resources needed to complete individual case investigations and collect blood samples, or overreporting because of overall efforts to strengthen measles surveillance.
In light of progress made toward reducing measles deaths, a more advanced goal was proposed recently for the region with several recommendations to improve vaccination coverage and surveillance performance. The AFR measles technical advisory group met in May 2008 and recommended that AFR countries aim to meet the following targets by 2012: 1) reducing estimated measles deaths by 98%, compared with 2000 estimates; 2) reducing measles incidence to < 5 cases per 1 million population per year; 3) achieving ≥90% routine MCV1 coverage nationwide and >80% in all districts; 4) achieving >95% SIA coverage in all districts; and 5) attaining two primary measles surveillance performance indicator targets (a nonmeasles febrile rash illness rate of >2 cases per 100,000 population per year and one or more suspected measles case investigated with blood specimen in >80% of districts per year); and 6) routine reporting from all districts (10). The group also recommended that AFR countries consider introduction of MCV2 in the routine vaccination schedule if MCV1 coverage of >80% has been achieved and maintained for ≥3 consecutive years and at least one of the two primary measles surveillance indicator targets has been achieved and maintained for at least 2 years. For countries adopting a 2-dose routine measles vaccination schedule, continued follow-up SIAs were recommended for all new birth cohorts every 3-5 years until national MCV2 coverage of ≥90% is sustained for at least 2 years (10).
# Updated Recommendation from the Advisory Committee on Immunization Practices (ACIP) for Revaccination of Persons at Prolonged Increased Risk for Meningococcal Disease
The Advisory Committee on Immunization Practices (ACIP) recommends quadrivalent meningococcal conjugate vaccine, (MCV4) (Menactra, Sanofi Pasteur, Swiftwater, Pennsylvania) for all persons aged 11-18 years and for persons aged 2-55 years at increased risk for meningococcal disease (1-3). MCV4 is licensed as a single dose. Because of the high risk for meningococcal disease among certain groups and limited data on duration of protection, at its June 2009 meeting ACIP recommended that persons previously vaccinated with either MCV4 or MPSV4 (Menomune, Sanofi Pasteur) who are at prolonged increased risk for meningococcal disease should be revaccinated with MCV4. Persons who previously were vaccinated at age ≥7 years and are at prolonged increased risk should be revaccinated 5 years after their previous meningococcal vaccine, and persons who previously were vaccinated at ages 2-6 years and are at prolonged increased risk should be revaccinated 3 years after their previous meningococcal vaccine. Persons at prolonged increased risk for meningococcal disease include 1) persons with increased susceptibility such as persistent complement component deficiencies (e.g., C3, properdin, Factor D, and late complement component deficiencies), 2) persons with anatomic or functional asplenia, and 3) persons who have prolonged exposure (e.g., microbiologists routinely working with Neisseria meningitidis, or travelers to or residents of countries where meningococcal disease is hyperendemic or epidemic). This report provides the rationale for the new recommendation and updates and replaces previous recommendations for revaccination with MCV4.
ACIP's Meningococcal Vaccine Work Group reviewed data on the risk for meningococcal disease, antibody titer decline, and the safety and immunogenicity of revaccination with MCV4 at 3 years and 5 years after the first dose of MCV4 or MPSV4 (2,3). Persons with prolonged increased risk for meningococcal disease have increased susceptibility to the disease or ongoing increased risk for exposure to N. meningitidis, higher levels of serum bactericidal antibody (SBA) against N. meningitidis can provide these groups increased protection against disease. SBA is a measure of the ability of sera to kill a strain of N. meningitidis in the presence of complement. In clinical trials, a baby rabbit SBA titer of 1:128 was used as a conservative correlate of protection (1). Small subsets of subjects from the MCV4 prelicensure clinical trial were revaccinated 3 years (n = 76) and 5 years (n = 134) after receiving MCV4. Of 71 persons aged 11-18 years at primary vaccination who had been vaccinated with MCV4 3 years previously, 75% and 86% had SBA titers greater than 1:128 for serogroups C and Y, respectively, before revaccination. Of 108 persons aged 2-10 years at primary vaccination who had been vaccinated with MCV4 5 years previously, 55% and 94% had SBA titers greater than 1:128 for serogroups C and Y, respectively, before revaccination. All persons revaccinated with MCV4 in these studies achieved SBA titers greater than 1:128 for serogroups C and Y. Approximately 50%-70% of persons in both the previously vaccinated (n = 210) and vaccine naive groups (n = 323) reported mild to moderate local and systemic adverse events after revaccination (or initial vaccination) with MCV4. However, no serious adverse events were reported in either group (Sanofi Pasteur, unpublished data, 2009).
On the basis of these data, expert opinion of the workgroup members, and feedback from partner organizations, the workgroup proposed that persons at prolonged increased risk for meningococcal disease be revaccinated with MCV4. ACIP approved this proposal at its June 24, 2009, meeting. Persons who previously were vaccinated at age ≥7 years and are at prolonged increased risk should be revaccinated 5 years after their previous meningococcal vaccine. Persons who previously were vaccinated at ages 2-6 years and are at prolonged increased risk should be revaccinated 3 years after their previous meningococcal vaccine. Persons who remain in one of these increased risk groups indefinitely should continue to be revaccinated at 5-year intervals.
Although the duration of protection from MCV4 is unknown, most entering college students will have received MCV4 within the preceding 4 years. Because of the limited period of increased risk, ACIP currently does not recommend that college freshmen living in dormitories who were previously vaccinated with MCV4 be revaccinated. However, college freshmen living in dormitories who were vaccinated with MPSV4 ≥5 years previously are recommended to be vaccinated with MCV4. Information regarding MCV4 and other recommendations for persons aged 2-55 years (2,3), including a routine recommendation for vaccination with MCV4 in persons aged 11-18 years (4), has been published previously.
# Announcement
World Heart Day -September 27, 2009
Each year, approximately 17 million persons die from cardiovascular disease, mainly heart disease and stroke, making it the world's leading cause of death (1). Controlling certain risk factors, such as high blood pressure, high cholesterol, diabetes, obesity, tobacco use, and physical inactivity, can help prevent heart disease and stroke.
In 2000, the World Heart Federation, a nongovernmental organization based in Geneva, Switzerland, created the annual World Heart Day campaign to increase public awareness of the threat of heart disease and stroke. The theme of the 2009 World Heart Day is "Work with Heart -A Workplace That Encourages Healthy Habits Can Reduce Heart Disease and Stroke." Promoting physical activity and healthful eating and discouraging tobacco use around the workplace are simple ways to foster health in the workplace. Activities organized by members and partners of the World Heart Federation will include public talks, concerts, and sporting events. The national member organizations in the United States are the American College of Cardiology and the American Heart Association.
CDC funds heart disease and stroke prevention programs in 41 states and the District of Columbia. Additional information about these programs is available at http://www.cdc.gov/dhdsp/ state_program/index.htm. Information about World Heart Day and the World Heart Federation is available at http://www. world-heart-federation.org/what-we-do/world-heart-day.
# Announcement
# NHANES 50th Anniversary and Conference
The 50th anniversary of the National Health and Nutrition Examination Survey (NHANES) will be celebrated on September 29, 2009, at a conference at the National Center for Health Statistics in Hyattsville, Maryland. Collaborating agencies, data users, and program and field staff members will share their perspectives on the survey.
# NHANES began in 1959 as the National Health Examination
Survey. NHANES data come from household interviews and standardized examinations and laboratory testing of a sample of the nation's civilian, noninstitutionalized population. NHANES has expanded since the survey's inception to include a nutritional component now conducted in collaboration with the U.S. Department of Agriculture and measures of environmental exposure with the National Center for Environmental Health.
NHANES has long been a primary source of data on the nation's health. NHANES findings were used to set the goals and track the progress in reducing cholesterol levels, the prevalence of high blood pressure, and the risks of blood lead exposure in the United States. NHANES documented the rise in obesity and diabetes and produced the first populationbased estimates of human immunodeficiency virus infection and osteoporosis. NHANES data also are used for the growth charts by which pediatricians and parents check children's growth and development.
A hallmark of NHANES is its partnerships with other CDC programs, the National Institutes of Health, other U.S. Department of Health and Human Services programs, and other government agencies to collect data needed for public health policies and practice. Additional information about the NHANES 50th anniversary is available at http://www.cdc.gov/ nchs/nhanes/nhanes50th.htm. The course includes a review of the fundamentals of descriptive epidemiology and biostatistics, measures of association, normal and binomial distributions, confounding, statistical tests, stratification, logistic regression models, and computer programs as used in epidemiology.
# Announcement
# Epidemiology in Action
The prerequisite is an introductory course in epidemiology, such as Epidemiology in Action or the International Course in Applied Epidemiology. Tuition will be charged. The application deadline is December 1, 2009, or until all slots have been filled. 1971-1974, 1976-1980, 1988-1994, 1999-2000, 2001-2002, 2003-2004, 2005-2006 1971-1974, 1976-1980, 1988-1994, 1999-2000, 2001-2002, 2003-2004, 2005-2006 Survey period Average total cholesterol (mg/dL) 1959-1962 1971-1974 1976-1980 1988-1994 Men * Incidence data for reporting year 2009 is provisional, whereas data for 2004 through 2008 are finalized. † Calculated by summing the incidence counts for the current week, the 2 weeks preceding the current week, and the 2 weeks following the current week, for a total of 5 preceding years. The total sum of incident cases is then divided by 25 weeks. Additional information is available at http://www.cdc.gov/epo/dphsi/phs/files/5yearweeklyaverage.pdf. § Not reportable in all states. Data from states where the condition is not reportable are excluded from this
# Acknowledgment
The findings in this report are based, in part, on data provided by the Westchester County Dept of Health, New Rochelle, New York.
# Acknowledgments
This report is based, in part, on contributions by K Bisgard, DVM, Office of Workforce and Career Development, CDC.
# MMWR
September 25, 2009 in the United States, most of which have populations of >100,000. A death is reported by the place of its occurrence and by the week that the death certificate was filed. Fetal deaths are not included. † Pneumonia and influenza. § Because of changes in reporting methods in this Pennsylvania city, these numbers are partial counts for the current week. Complete counts will be available in 4 to 6 weeks. ¶ Total includes unknown ages. | None | None |
48c6eb4a0c41b4f6dd95afaea11db1e2b676102d | cdc | None | Revisions to the May 1, 2014, version of the guidelines include key updates to several existing sections and the addition of two new tables. Significant updates are highlighted throughout the document.#
- There are now five Recommended regimens for antiretroviral therapy (ART)-naive patients-four integrase strand transfer inhibitor (INSTI)-based regimens and one ritonavir-boosted protease inhibitor (PI/r)-based regimen, as listed below:
# INSTI-Based Regimens:
- Dolutegravir/abacavir/lamivudine (DTG/ABC/3TC)-only for patients who are HLA-B*5701 negative (AI)
- DTG plus tenofovir disoproxil fumarate/emtricitabine (TDF/FTC) (AI)
- Elvitegravir/cobicistat/TDF/FTC (EVG/c/TDF/FTC)-only for patients with pre-ART CrCl >70 mL/min (AI)
- Raltegravir (RAL) plus TDF/FTC (AI) PI/r-Based Regimen:
- Darunavir/ritonavir (DRV/r) plus TDF/FTC (AI)
- Two regimens previously classified as Recommended regimens have been moved to the Alternative regimens category, with the rationale stated below:
- Atazanavir/ritonavir (ATV/r) plus TDF/FTC (BI)-Based on the results of a large comparative clinical trial showing a greater rate of discontinuation with ATV/r plus TDF/FTC because of toxicities when compared to (DRV/r or RAL) plus TDF/FTC
- Efavirenz/TDF/FTC (EFV/TDF/FTC) (BI)-Based on concerns about the tolerability of EFV in clinical trials and practice, especially the high rate of central nervous system (CNS)-related toxicities and a possible association with suicidality
- Three regimens (ATV/r plus ABC/3TC, EFV plus ABC/3TC, and rilpivirine/TDF/FTC) that were previously listed as Recommended regimens for baseline HIV RNA 200 cells/mm 3 are now in the Alternative or Other category, with the same caveat about limiting their use in these populations.
- Two regimens that use fewer than two nucleoside reverse transcriptase inhibitors (DRV/r plus RAL and lopinavir/ritonavir plus 3TC) are now listed among the Other regimens, with the caveat that their use would be limited to those patients who cannot take either TDF or ABC.
- Coformulations of atazanavir (ATV) and darunavir (DRV) with the pharmacokinetic (PK) enhancer cobicistat (COBI) have been added to the Alternative regimen options.
# Virologic Failure
The following key updates have been made to this section:
- The Management of Virologic Failure in Different Clinical Scenarios subsection has been expanded to provide guidance on the management of patients failing first and second ART regimens.
- A new subsection on Isolated CNS Virologic Failure and New Onset Neurologic Symptoms has been added.
- The Suboptimal Immunologic Response Despite Viral Suppression subsection has been moved from this section to become a stand-alone section (see below). Antiretroviral therapy (ART) for the treatment of HIV infection has improved steadily since the advent of potent combination therapy in 1996. New drugs that offer new mechanisms of action, improvements in potency and activity even against multidrug-resistant viruses, dosing convenience, and tolerability have been approved. ART has dramatically reduced HIV-associated morbidity and mortality and has transformed HIV disease into a chronic, manageable condition. In addition, effective treatment of HIV-infected individuals with ART is highly effective at preventing transmission to sexual partners. 1 However, less than one-third of HIV-infected individuals in the United States have suppressed viral loads, 2 which is mostly a result of undiagnosed HIV infection and failure to link or retain diagnosed patients in care. Despite remarkable improvements in HIV treatment and prevention, economic and social barriers that result in continued morbidity, mortality, and new HIV infections persist.
# Table of Contents
# Management of the
# List of Tables
The Department of Health and Human Services (HHS) Panel on Antiretroviral Guidelines for Adults and Adolescents (the Panel) is a working group of the Office of AIDS Research Advisory Council (OARAC). The primary goal of the Panel is to provide HIV care practitioners with recommendations based on current knowledge of antiretroviral (ARV) drugs used to treat adults and adolescents with HIV infection in the United States. The Panel reviews new evidence and updates recommendations in these guidelines when needed. The Panel's primary areas of attention have included baseline assessment, treatment goals, indications for initiation of ART, choice of the initial regimen for ART-naive patients, drugs or combinations to avoid, management of adverse effects and drug interactions, management of treatment failure, and special ART-related considerations in specific patient populations. For recommendations related to pre-exposure HIV prophylaxis (PrEP) for HIV-uninfected persons, please refer to recommendations from the Centers for Disease Control and Prevention (CDC). 3,4 These guidelines generally represent the state of knowledge regarding the use of ARV agents. However, because the science of HIV evolves rapidly, the availability of new agents and new clinical data may change therapeutic options and preferences. Information included in these guidelines may not be consistent with approved labeling for the particular products or indications in question, and the use of the terms "safe" and "effective" may not be synonymous with the Food and Drug Administration (FDA)-defined legal standards for product approval. The Panel frequently updates the guidelines (current and archived versions of the guidelines are available on the AIDSinfo website at ). However, the guidelines cannot always be updated apace with the rapid evolution of new data in the field of HIV and cannot offer guidance on care for all patients. Clinicians should exercise clinical judgment in management decisions tailored to unique patient circumstances.
The Panel recognizes the importance of clinical research in generating evidence to address unanswered questions related to the optimal safety and efficacy of ART. The Panel encourages both the development of protocols and patient participation in well-designed, Institutional Review Board (IRB)-approved clinical trials.
# Basis for Recommendations
Recommendations in these guidelines are based upon scientific evidence and expert opinion. Each recommended statement includes a letter (A, B, or C) that represents the strength of the recommendation and with a Roman numeral (I, II, or III) that represents the quality of the evidence that supports the recommendation (see Table 2).
# Table 2. Rating Scheme for Recommendations
# HIV Expertise in Clinical Care
Many studies have demonstrated that outcomes achieved in HIV-infected outpatients are better when care is delivered by a clinician with HIV expertise, which reflects the complexity of HIV infection and its treatment. Thus, appropriate training and experience, as well as ongoing continuing education, are important components of optimal care. Primary care providers without HIV experience, such as those who provide service in rural or underserved areas, should identify experts in their regions who will be available for consultation when needed.
Baseline Evaluation (Last updated May 1, 2014; last reviewed May 1, 2014)
Every HIV-infected patient entering into care should have a complete medical history, physical examination, and laboratory evaluation and should be counseled regarding the implications of HIV infection. The goals of the initial evaluation are to confirm the diagnosis of HIV infection, obtain appropriate baseline historical and laboratory data, ensure patient understanding about HIV infection and its transmission, and to initiate care as recommended in HIV primary care guidelines 1 and guidelines for prevention and treatment of HIV-associated opportunistic infections. 2 The initial evaluation also should include introductory discussion on the benefits of antiretroviral therapy (ART) for the patient's health and to prevent HIV transmission. Baseline information then can be used to define management goals and plans. In the case of previously treated patients who present for an initial evaluation with a new health care provider, it is critical to obtain a complete antiretroviral (ARV) history (including drug-resistance testing results, if available), preferably through the review of past medical records. Newly diagnosed patients should also be asked about any prior use of ARV agents for prevention of HIV infection.
The following laboratory tests performed during initial patient visits can be used to stage HIV disease and to assist in the selection of ARV drug regimens:
- HIV antibody testing (if prior documentation is not available or if HIV RNA is below the assay's limit of detection) (AI);
- CD4 T-cell count (CD4 count) (AI);
- Plasma HIV RNA (viral load) (AI);
- Complete blood count, chemistry profile, transaminase levels, blood urea nitrogen (BUN), and creatinine, urinalysis, and serologies for hepatitis A, B, and C viruses (AIII);
- Fasting blood glucose and serum lipids (AIII); and
- Genotypic resistance testing at entry into care, regardless of whether ART will be initiated immediately (AII). For patients who have HIV RNA levels <500 to 1,000 copies/mL, viral amplification for resistance testing may not always be successful (BII).
In addition, other tests (including screening tests for sexually transmitted infections and tests for determining the risk of opportunistic infections and need for prophylaxis) should be performed as recommended in HIV primary care and opportunistic infections guidelines. 1,2 Patients living with HIV infection often must cope with many social, psychiatric, and medical issues that are best addressed through a patient-centered, multi-disciplinary approach to the disease. The baseline evaluation should include an evaluation of the patient's readiness for ART, including an assessment of high-risk behaviors, substance abuse, social support, mental illness, comorbidities, economic factors (e.g., unstable housing), medical insurance status and adequacy of coverage, and other factors that are known to impair adherence to ART and increase the risk of HIV transmission. Once evaluated, these factors should be managed accordingly.
The baseline evaluation should also include a discussion of risk reduction and disclosure to sexual and/or needle sharing partners, especially with untreated patients who are still at high risk of HIV transmission. √ HIV RNA (viral load) and CD4 T lymphocyte (CD4) cell count are the two surrogate markers of antiretroviral treatment (ART) responses and HIV disease progression that have been used for decades to manage and monitor HIV infection.
During
Viral load is a marker of response to ART. A patient's pre-ART viral load level and the magnitude of viral load decline after initiation of ART provide prognostic information about the probability of disease progression. 1 The key goal of ART is to achieve and maintain durable viral suppression. Thus, the most important use of the viral load is to monitor the effectiveness of therapy after initiation of ART.
Measurement of CD4 count is particularly useful before initiation of ART. The CD4 cell count provides information on the overall immune function of an HIV-infected patient. The measurement is critical in establishing thresholds for the initiation and discontinuation of opportunistic infection (OI) prophylaxis and in assessing the urgency to initiate ART.
The management of HIV-infected patients has changed substantially with the availability of newer, more potent, and less toxic antiretroviral (ARV) agents. In the United States, ART is now recommended for all HIV-infected patients regardless of their viral load or CD4 count. In the past, clinical practice, which was supported by treatment guidelines, was generally to monitor both CD4 cell count and viral load concurrently. However, because most HIV-infected patients in care now receive ART, the rationale for frequent CD4 monitoring is weaker. The roles and usefulness of these two tests in clinical practice are discussed in the following sections.
# Plasma HIV-1 RNA (Viral Load) Monitoring
Viral load is the most important indicator of initial and sustained response to ART (AI) and should be measured in all HIV-infected patients at entry into care (AIII), at initiation of therapy (AIII), and on a regular basis thereafter. For those patients who choose to delay therapy, repeat viral load testing while not on ART is optional (CIII). Pre-treatment viral load level is also an important factor in the selection of an initial ARV regimen because several currently approved ARV drugs or regimens have been associated with poorer responses in patients with high baseline viral load (see What to Start). Commercially available HIV-1 RNA assays do not detect HIV-2 viral load. For further discussion on HIV-2 RNA monitoring in patients with HIV-1/HIV-2 co-infection or HIV-2 mono-infection, see HIV-2 Infection.
Several systematic reviews of data from clinical trials involving thousands of participants have established that decreases in viral load following initiation of ART are associated with reduced risk of progression to AIDS or death. Thus, viral load testing is an established surrogate marker for treatment response. 4 The minimal change in viral load considered to be statistically significant (2 standard deviations) is a three-fold change (equivalent to a 0.5 log 10 copies/mL change). Optimal viral suppression is defined generally as a viral load persistently below the level of detection (HIV RNA 200 copies/mL-a threshold that eliminates most cases of apparent viremia caused by viral load blips or assay variability 10 (see Virologic Failure and Suboptimal Immunologic Response).
Individuals who are adherent to their ARV regimens and do not harbor resistance mutations to the component drugs can generally achieve viral suppression 8 to 24 weeks after ART initiation; rarely, in some patients it Downloaded from on 9/16/2015
Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents C-6 may take longer. Recommendations on the frequency of viral load monitoring are summarized below:
- After initiation of ART or modification of therapy because of virologic failure. Plasma viral load should be measured before initiation of ART and within 2 to 4 weeks but no later than 8 weeks after treatment initiation or modification (AIII). The purpose of the measurements is to confirm an adequate initial virologic response to ART, indicating appropriate regimen selection and patient adherence to therapy. Repeat viral load measurement should be performed at 4-to 8-week intervals until the level falls below the assay's limit of detection (BIII).
- In virologically suppressed patients in whom ART was modified because of drug toxicity or for regimen simplification. Viral load measurement should be performed within 4 to 8 weeks after changing therapy (AIII). The purpose of viral load monitoring at this point is to confirm the effectiveness of the new regimen.
- In patients on a stable, suppressive ARV regimen. Viral load should be repeated every 3 to 4 months (AIII) or as clinically indicated to confirm continuous viral suppression. Clinicians may extend the interval to 6 months for adherent patients whose viral load has been suppressed for more than 2 years and whose clinical and immunologic status is stable (AIII).
- In patients with suboptimal response. The frequency of viral load monitoring will depend on clinical circumstances, such as adherence and availability of further treatment options. In addition to viral load monitoring, a number of additional factors, such as patient adherence to prescribed medications, suboptimal drug exposure, or drug interactions, should be assessed. Patients who fail to achieve viral suppression should undergo resistance testing to aid in the selection of an alternative regimen (see Drug-Resistance Testing and Virologic Failure and Suboptimal Immunologic Response sections).
# CD4 Count Monitoring
The CD4 count is the most important laboratory indicator of immune function in HIV-infected patients. It is also the strongest predictor of subsequent disease progression and survival according to findings from clinical trials and cohort studies. 11,12 CD4 counts are highly variable; a significant change (2 standard deviations) between 2 tests is approximately a 30% change in the absolute count, or an increase or decrease in CD4 percentage by 3 percentage points. Monitoring of lymphocyte subsets other than CD4 (e.g., CD8, CD19) has not proven clinically useful, is more expensive, and is not routinely recommended (BIII).
# Use of CD4 Count for Initial Assessment
CD4 count should be measured in all patients at entry into care (AI). It is the key factor in determining the need to initiate OI prophylaxis (see the Adult Opportunistic Infection Guidelines) 13 and the urgency to initiate ART (AI) (see the Initiating Antiretroviral Therapy in Antiretroviral-Naive Patients section of these guidelines). Although most OIs occur in patients with CD4 counts <200 cells/mm 3 , some OIs can occur in patients with higher CD4 counts. 14
# Use of CD4 Count for Monitoring Therapeutic Response
The CD4 count is used to assess a patient's immunologic response to ART. It is also used to determine whether prophylaxis for OIs can be discontinued (see the Adult Opportunistic Infection Guidelines) 13 . For most patients on therapy, an adequate response is defined as an increase in CD4 count in the range of 50 to 150 cells/mm 3 during the first year of ART, generally with an accelerated response in the first 3 months of treatment. Subsequent increases average approximately 50 to 100 cells/mm 3 per year until a steady state level is reached. 15 Patients who initiate therapy with a low CD4 count 16 or at an older age 17 may have a blunted increase in their counts despite virologic suppression.
The CD4 count response to ART varies widely, but a poor CD4 response in a patient with viral suppression is rarely an indication for modifying an ARV regimen. In patients with consistently suppressed viral loads who have already experienced ART-related immune reconstitution, the CD4 count provides limited information.
Frequent testing is unnecessary because the results rarely lead to a change in clinical management. One retrospective study found that declines in CD4 count to 300 cells/mm 3 . 18 Similarly, the ARTEMIS trial found that CD4 monitoring had no clinical benefit in patients who had suppressed viral loads and CD4 counts >200 cells/mm 3 after 48 weeks of therapy. 19 Furthermore, the risk of Pneumocystis jirovecii pneumonia is extremely low in patients on suppressive ART who have CD4 counts between 100 and 200 cells/mm 3 . 20 Although uncommon, CD4 count declines can occur in a small percentage of virologically suppressed patients and may be associated with adverse clinical outcomes such as cardiovascular disease, malignancy, and death. 21 An analysis of costs associated with CD4 monitoring in the United States estimated that reducing CD4 monitoring in treated patients from every 6 months to every 12 months could result in annual savings of approximately $10 million. 22 For the patient on a suppressive regimen whose CD4 count has consistently ranged between 300 and 500 cells/ mm 3 for at least 2 years, the Panel recommends CD4 monitoring on an annual basis (BII). Continued CD4 monitoring for virologically suppressed patients whose CD4 counts have been consistently >500 cells/mm 3 for at least 2 years may be considered optional (CIII). The CD4 count should be monitored more frequently, as clinically indicated, when there are changes in a patient's clinical status that may decrease CD4 count and thus prompt OI prophylaxis. Examples of such changes include the appearance of new HIV-associated clinical symptoms or initiation of treatment known to reduce CD4 cell count (e.g., interferon, chronic corticosteroids, or anti-neoplastic agents) (AIII). In patients who fail to maintain viral suppression while on ART, the Panel recommends CD4 count monitoring every 3 to 6 months (AIII) (see Virologic Failure and Suboptimal Immunologic Response section).
# Factors that Affect Absolute CD4 Count
The absolute CD4 count is a calculated value based on the total white blood cell (WBC) count and the percentages of total and CD4+ T lymphocytes. This absolute number may fluctuate in individuals or may be influenced by factors that may affect the total WBC count and lymphocyte percentages, such as use of bone marrow-suppressive medications or the presence of acute infections. Splenectomy 23,24 or co-infection with human T-lymphotropic virus type I (HTLV-1) 25 may cause misleadingly elevated CD4 counts. Alpha-interferon may reduce the absolute CD4 count without changing the CD4 percentage. 26 In all these settings, CD4 percentage remains stable and may be a more appropriate parameter to assess a patient's immune function.
# Clinical Scenario Viral Load Monitoring CD4 Count Monitoring
Before initiating ART At entry into care (AIII)
If ART initiation is deferred, repeat before initiating ART (AIII).
In patients not initiating ART, repeat testing is optional (CIII).
# At entry into care (AI)
If ART is deferred, every 3 to 6 months (AIII).
b
After initiating ART Preferably within 2 to 4 weeks (and no later than 8 weeks) after initiation of ART (AIII); thereafter, every 4 to 8 weeks until viral load suppressed (BIII).
# months after initiation of ART (AIII)
After modifying ART because of drug toxicities or for regimen simplification in a patient with viral suppression 4 to 8 weeks after modification of ART to confirm effectiveness of new regimen (AIII).
Monitor according to prior CD4 count and duration on ART, as outlined below.
After modifying ART because of virologic failure
Preferably within 2 to 4 weeks (and no later than 8 weeks) after modification (AIII); thereafter, every 4 to 8 weeks until viral load suppressed (BIII). If viral suppression is not possible, repeat viral load every 3 months or more frequently if indicated (AIII).
# Every 3 to 6 months (AI)
During the first 2 years of ART Every 3 to 4 months (AIII) Every 3 to 6 months a (BII)
After 2 years of ART (VL consistently suppressed, CD4 consistently 300-500 cells/mm 3 ) Can extend to every 6 months for patients with consistent viral suppression for ≥2 years (AIII).
# Every 12 months (BII)
After 2 years of ART (VL consistently suppressed, CD4 consistently >500 cells/ mm 3 )
Optional (CIII)
While on ART with detectable viremia (VL repeatedly >200 copies/mL) a Monitoring of lymphocyte subsets other than CD4 (e.g., CD8, CD19) has not proven clinically useful, adds to costs, and is not routinely recommended (BIII).
Every
b Some experts may repeat CD4 count every 3 months in patients with low baseline CD4 count (300 cells/mm 3 ). c The following are examples of clinically indicated scenarios: changes in a patient's clinical status that may decrease CD4 count and thus prompt initiation of prophylaxis for opportunistic infections (OI), such as new HIV-associated symptoms, or initiation of treatment with medications which are known to reduce CD4 cell count.
Drug-Resistance Testing (Last updated May 1, 2014; last reviewed May 1, 2014)
# Genotypic and Phenotypic Resistance Assays
Genotypic and phenotypic resistance assays are used to assess viral strains and inform selection of treatment strategies. Standard assays provide information on resistance to nucleoside reverse transcriptase inhibitors (NRTIs), non-nucleoside reverse transcriptase inhibitors (NNRTIs), and protease inhibitors (PIs). Testing for integrase and fusion inhibitor resistance can also be ordered separately from several commercial laboratories.
Co-receptor tropism assays should be performed whenever the use of a CCR5 antagonist is being considered. Phenotypic co-receptor tropism assays have been used in clinical practice. A genotypic assay to predict coreceptor use is now commercially available (see Co-receptor Tropism Assays).
# Genotypic Assays
Genotypic assays detect drug-resistance mutations present in relevant viral genes. Most genotypic assays involve sequencing of the RT and PR genes to detect mutations that are known to confer drug resistance. Genotypic assays that assess mutations in the integrase and gp41 (envelope) genes are also commercially available. Genotypic assays can be performed rapidly and results are available within 1 to 2 weeks of sample collection. Interpretation of test results requires knowledge of the mutations selected by different antiretroviral (ARV) drugs and of the potential for cross resistance to other drugs conferred by certain mutations. The International AIDS Society-USA (IAS-USA) maintains an updated list of significant resistance-associated mutations in the RT, PR, integrase, and envelope genes (see
# Panel's Recommendations
- HIV drug-resistance testing is recommended in persons with HIV infection at entry into care regardless of whether antiretroviral therapy (ART) will be initiated immediately or deferred (AII). If therapy is deferred, repeat testing should be considered at the time of ART initiation (CIII).
- Genotypic testing is recommended as the preferred resistance testing to guide therapy in antiretroviral (ARV)-naive patients (AIII).
- Standard genotypic drug-resistance testing in ARV-naive persons involves testing for mutations in the reverse transcriptase (RT) and protease (PR) genes. If transmitted integrase strand transfer inhibitor (INSTI) resistance is a concern, providers may wish to supplement standard genotypic resistance testing with an INSTI genotype test (CIII).
- HIV drug-resistance testing should be performed to assist in the selection of active drugs when changing ARV regimens in persons with virologic failure and HIV RNA levels >1,000 copies/mL (AI). In persons with HIV RNA levels >500 but <1,000 copies/mL, testing may be unsuccessful but should still be considered (BII).
- Drug-resistance testing should also be performed when managing suboptimal viral load reduction (AII).
- In persons failing INSTI-based regimens, genotypic testing for INSTI resistance should be performed to determine whether to include a drug from this class in subsequent regimens (AII).
- Drug-resistance testing in the setting of virologic failure should be performed while the person is taking prescribed ARV drugs or, if not possible, within 4 weeks after discontinuing therapy (AII). If greater than 4 weeks has lapsed since the ARVs were discontinued, resistance testing may still provide useful information to guide therapy, recognizing that previously selected resistance mutations can be missed (CIII).
- Genotypic testing is recommended as the preferred resistance testing to guide therapy in patients with suboptimal virologic responses or virologic failure while on first or second regimens (AII).
- The addition of phenotypic to genotypic testing is generally preferred for persons with known or suspected complex drug-resistance mutation patterns, particularly to protease inhibitors (PIs) (BIII).
- Genotypic resistance testing is recommended for all pregnant women before initiation of ART (AIII) and for those entering pregnancy with detectable HIV RNA levels while on therapy (AI) (see the Perinatal Treatment Guidelines for more detailed discussion). ). 1 The Stanford University HIV Drug Resistance Database () also provides helpful guidance for interpreting genotypic resistance test results. Various tools to assist the provider in interpreting genotypic test results are now available. Clinical trials have demonstrated that consultation with specialists in HIV drug resistance improves virologic outcomes. 6 Clinicians are thus encouraged to consult a specialist to facilitate interpretation of genotypic test results and design of an optimal new regimen.
# Rating of Recommendations
# Phenotypic Assays
Phenotypic assays measure the ability of a virus to grow in different concentrations of ARV drugs. RT and PR gene sequences and, more recently, integrase and envelope sequences derived from patient plasma HIV RNA are inserted into the backbone of a laboratory clone of HIV or used to generate pseudotyped viruses that express the patient-derived HIV genes of interest. Replication of these viruses at different drug concentrations is monitored by expression of a reporter gene and is compared with replication of a reference HIV strain. The drug concentration that inhibits viral replication by 50% (i.e., the median inhibitory concentration ) is calculated, and the ratio of the IC 50 of test and reference viruses is reported as the fold increase in IC 50 (i.e., fold resistance).
Automated phenotypic assays that can produce results in 2 to 3 weeks are commercially available, but they cost more to perform than genotypic assays. In addition, interpretation of phenotypic assay results is complicated by incomplete information regarding the specific resistance level (i.e., fold increase in IC 50 ) that is associated with drug failure, although clinically significant fold increase cutoffs are now available for some drugs. Again, consultation with a specialist to interpret test results can be helpful.
Further limitations of both genotypic and phenotypic assays include lack of uniform quality assurance testing for all available assays, relatively high cost, and insensitivity to minor viral species. Despite being present, drug-resistant viruses that constitute less than 10% to 20% of the circulating virus population will probably not be detected by commercially available assays. This limitation is important because after drugs exerting selective pressure on drug-resistant populations are discontinued, a wild-type virus often re-emerges as the predominant population in the plasma. As a consequence, the proportion of virus with resistance mutations decreases to below the 10% to 20% threshold. In the case of some drugs, this reversion to predominantly wild-type virus can occur in the first 4 to 6 weeks after the drugs are discontinued. Prospective clinical studies have shown that despite this plasma reversion, re-initiation of the same ARV agents (or those sharing similar resistance pathways) is usually associated with early drug failure, and that the virus present at failure is derived from previously archived resistant virus. 15 Therefore, resistance testing is of greatest value when performed before or within 4 weeks after drugs are discontinued (AII). Because resistant virus may persist in the plasma of some patients for longer periods of time, resistance testing done 4 to 6 weeks after discontinuation of drugs may still detect mutations. However, the absence of detectable resistance in such patients must be interpreted with caution when designing subsequent ARV regimens.
# Use of Resistance Assays in Clinical Practice (See Table 5)
# Use of Resistance Assays in Determining Initial Treatment
Transmission of drug-resistant HIV strains is well documented and associated with suboptimal virologic response to initial antiretroviral therapy (ART). The likelihood that a patient will acquire drug-resistant virus is related to the prevalence of drug resistance in HIV-infected persons engaging in high-risk behaviors in the community. In the United States and Europe, recent studies suggest that the risk that transmitted virus will be resistant to at least one ARV drug is in the range of 6% to 16%. Up to 8%, but generally less than 5% of transmitted viruses will exhibit resistance to drugs from more than one class. 24, If the decision is made to initiate therapy in a person with early HIV infection, resistance testing at baseline can guide regimen selection to optimize virologic response. Therefore, resistance testing in this situation is recommended (AII). A genotypic assay is preferred for this purpose (AIII). In this setting, treatment initiation should not be delayed pending resistance testing results. Once results are obtained, the treatment regimen can be modified if warranted (see Acute and Recent HIV Infection). In the absence of therapy, resistant viruses may decline over time to less than the detection limit of standard resistance tests, but when therapy is eventually initiated, resistant viruses even at a low level may still increase the risk of treatment failure. Therefore, if therapy is deferred, resistance testing should still be done during acute HIV infection (AIII). In this situation, the genotypic resistance test result may be kept on record until the patient is to be started on ART. Repeat resistance testing at the time treatment is started should be considered because it is possible for a patient to acquire drug-resistant virus (i.e., superinfection) between entry into care and initiation of ART (CIII).
Performing drug-resistance testing before ART initiation in patients with chronic HIV infection is less straightforward. The rate at which transmitted resistance-associated mutations revert to wild-type virus has not been completely delineated, but mutations present at the time of HIV transmission are more stable than those selected under drug pressure. It is often possible to detect resistance-associated mutations in viruses that were transmitted several years earlier. No prospective trial has addressed whether drug-resistance testing before initiation of therapy confers benefit in this population. However, data from several, but not all, studies suggest that virologic responses in persons with baseline resistance mutations are suboptimal. In addition, a cost-effectiveness analysis of early genotypic resistance testing suggests that baseline testing in this population should be performed. 38 Therefore, resistance testing in chronically infected persons is recommended at the time of entry into HIV care (AII). Although no definitive prospective data exist to support the choice of one type of resistance testing over another, genotypic testing is generally preferred in this situation because of lower cost, more rapid turnaround time, the assay's ability to detect mixtures of wild-type and resistant virus, and the relative ease of interpreting test results (AIII). If therapy is deferred, repeat testing soon before initiation of ART should be considered because the patient may have acquired drug-resistant virus (i.e., superinfection) (CIII).
Standard genotypic drug-resistance testing in ARV-naive persons involves testing for mutations in the RT and PR genes. Although transmission of integrase strand transfer inhibitor (INSTI)-resistant virus has rarely been reported, as use of INSTIs increases, the potential for transmission of INSTI-resistant virus may also increase. Therefore, when INSTI resistance is suspected, providers may wish to supplement standard baseline genotypic resistance testing with genotypic testing for resistance to this class of drugs (CIII).
# Use of Resistance Assays in the Event of Virologic Failure
Resistance assays are useful in guiding treatment decisions for patients who experience virologic failure while on ART. Several prospective studies assessed the utility of resistance testing to guide ARV drug selection in patients with virologic failure. These studies involved genotypic assays, phenotypic assays, or both. 6, In general, these studies found that changes in therapy that were informed by resistance testing results produced better early virologic response to salvage regimens than regimen changes guided only by clinical judgment.
In addition, one observational cohort study found that performance of genotypic drug-resistance testing in ART-experienced patients with detectable plasma HIV RNA was independently associated with improved survival. 46 Thus, resistance testing is recommended as a tool in selecting active drugs when changing ARV regimens because of virologic failure in persons with HIV RNA >1,000 copies/mL (AI) (see Virologic Failure and Suboptimal Immunologic Response). In persons with HIV RNA >500 copies/mL but <1,000 copies/mL, testing may be unsuccessful but should still be considered (BII). Drug-resistance testing in persons with a plasma viral load <500 copies/mL is not usually recommended because resistance assays cannot be consistently performed given low HIV RNA levels (AIII).
Resistance testing also can help guide treatment decisions for patients with suboptimal viral load reduction (AII). Virologic failure in the setting of combination ART is, for certain patients, associated with resistance to only one component of the regimen. In this situation, substituting individual drugs in a failing regimen may be a possible option, but this concept will require clinical validation (see Virologic Failure and Suboptimal Immunologic Response).
In patients who are on a failing first or second ARV drug regimen and experiencing virologic failure or suboptimal viral load reduction, genotypic testing is generally preferred for resistance testing (AII). This is based on the fact that, when compared with phenotypic testing, genotypic testing costs less to perform, has a faster turnaround time, and greater sensitivity for detecting mixtures of wild-type and resistant virus. In addition, observations show that the assays are comparable predictors of virologic response to subsequent ART regimens. 50 Addition of phenotypic to genotypic testing is generally preferred for persons with known or suspected complex drug-resistance mutation patterns, particularly to PIs (BIII).
In patients failing INSTI-based regimens, testing for INSTI resistance should be performed to determine whether to include drugs from this class in subsequent regimens (AII); genotypic testing is preferred for this purpose.
When the use of a CCR5 antagonist is being considered, a co-receptor tropism assay should be performed (AI). Phenotypic co-receptor tropism assays have been used in clinical practice. A genotypic assay to predict co-receptor use is now commercially available and is less expensive than phenotypic assays. Evaluation of genotypic assays is ongoing, but current data suggest that such testing should be considered as an alternative assay. The same principles regarding testing for co-receptor use also apply to testing when patients exhibit virologic failure on a CCR5 antagonist. 51 Resistance to CCR5 antagonists in the absence of detectable CXCR4-using virus has been reported, but such resistance is uncommon (see Co-receptor Tropism Assays).
# Use of Resistance Assays in Pregnant Women
In pregnant women, the goal of ART is to maximally reduce plasma HIV RNA to provide optimal maternal therapy and to prevent perinatal transmission of HIV. Genotypic resistance testing is recommended for all pregnant women before initiation of therapy (AIII) and for those entering pregnancy with detectable HIV RNA levels while on therapy (AI). Phenotypic testing in those found to have complex drug-resistance mutation patterns, particularly to PIs, may provide additional information (BIII). Optimal prevention of perinatal transmission may require initiation of ART pending resistance testing results. Once the results are available, the ARV regimen can be changed as needed.
# Clinical Setting/Recommendation Rationale
# Drug-resistance assay recommended
In acute HIV infection: Drug-resistance testing is recommended regardless of whether antiretroviral therapy (ART) is initiated immediately or deferred (AII). A genotypic assay is generally preferred (AIII).
If ART is initiated immediately, drug-resistance testing can determine whether drug-resistant virus was transmitted. Test results will help in the design of initial regimens or to modify or change regimens if results are obtained after treatment initiation.
Genotypic testing is preferred to phenotypic testing because of lower cost, faster turnaround time, and greater sensitivity for detecting mixtures of wild-type and resistant virus.
If ART is deferred, repeat resistance testing should be considered at the time therapy is initiated (CIII). A genotypic assay generally is preferred (AIII).
If ART is deferred, testing should still be performed because of the greater likelihood that transmitted resistance-associated mutations will be detected earlier in the course of HIV infection.
Results of resistance testing may be important when treatment is initiated. Repeat testing at the time ART is initiated should be considered because the patient may have acquired a drugresistant virus (i.e., superinfection).
In ART-naive patients with chronic HIV infection: Drug-resistance testing is recommended at entry into HIV care, regardless of whether therapy is initiated immediately or deferred (AII). A genotypic assay is generally preferred (AIII).
If therapy is deferred, repeat resistance testing should be considered before initiation of ART (CIII). A genotypic assay is generally preferred (AIII).
If an INSTI is considered for an ART-naive patient and transmitted INSTI resistance is a concern, providers may supplement standard resistance testing with a specific INSTI genotypic resistance assay (CIII).
If use of a CCR5 antagonist is being considered, a co-receptor tropism assay should be performed (AI) (see Co-receptor Tropism Assays)
Transmitted HIV with baseline resistance to at least 1 drug is seen in 6% to 16% of patients, and suboptimal virologic responses may be seen in patients with baseline resistant mutations. Some drug-resistance mutations can remain detectable for years in untreated, chronically infected patients.
Repeat testing before initiation of ART should be considered because the patient may have acquired a drug-resistant virus (i.e., a superinfection).
Genotypic testing is preferred to phenotypic testing because of lower cost, faster turnaround time, and greater sensitivity for detecting mixtures of wild-type and resistant virus.
Standard genotypic drug-resistance assays test only for mutations in the RT and PR genes.
(see Co-receptor Tropism Assays)
In patients with virologic failure: Drug-resistance testing is recommended in patients on combination ART with HIV RNA levels >1,000 copies/mL (AI). In patients with HIV RNA levels >500 copies/mL but <1,000 copies/mL, testing may not be successful but should still be considered (BII).
A standard genotypic resistance assay is generally preferred for patients experiencing virologic failure on their first or second regimens (AII).
In patients failing INSTI-based regimens, genotypic testing for INSTI resistance should be performed to determine whether to include drugs from this class in subsequent regimens (AII).
If use of a CCR5 antagonist is being considered, a co-receptor tropism assay should be performed (AI) (see Co-receptor Tropism Assays).
Addition of phenotypic assay to genotypic assay is generally preferred in patients with known or suspected complex drug-resistance patterns, particularly to protease inhibitors (PIs) (BIII).
Testing can help determine the role of resistance in drug failure and maximize the clinician's ability to select active drugs for the new regimen. Drug-resistance testing should be performed while the patient is taking prescribed ARV drugs or, if not possible, within 4 weeks after discontinuing therapy.
Genotypic testing is preferred to phenotypic testing because of lower cost, faster turnaround time, and greater sensitivity for detecting mixtures of wild-type and resistant HIV.
Standard genotypic drug-resistance assays test only for mutations in the RT and PR genes.
Phenotypic testing can provide additional useful information in patients with complex drug-resistance mutation patterns, particularly to PIs.
# Clinical Setting/Recommendation Rationale
# Drug-resistance assay recommended
In patients with suboptimal suppression of viral load: Drugresistance testing is recommended in patients with suboptimal suppression of viral load after initiation of ART (AII).
Testing can help determine the role of resistance and thus assist the clinician in identifying the number of active drugs available for a new regimen.
In HIV-infected pregnant women: Genotypic resistance testing is recommended for all pregnant women before initiation of ART (AIII) and for those entering pregnancy with detectable HIV RNA levels while on therapy (AI).
The goal of ART in HIV-infected pregnant women is to achieve maximal viral suppression for treatment of maternal HIV infection and for prevention of perinatal transmission of HIV. Genotypic resistance testing will assist the clinician in selecting the optimal regimen for the patient.
# Drug-resistance assay not usually recommended
After therapy is discontinued: Drug-resistance testing is not usually recommended more than 4 weeks after discontinuation of ARV drugs (BIII).
Drug-resistance mutations may become minor species in the absence of selective drug pressure, and available assays may not detect minor drug-resistant species. If testing is performed in this setting, the detection of drug resistance may be of value; however, the absence of resistance does not rule out the presence of minor drug-resistant species.
In patients with low HIV RNA levels: Drug-resistance testing is not usually recommended in patients with a plasma viral load <500 copies/mL (AIII).
Resistance assays cannot be consistently performed given low HIV RNA levels. HIV enters cells by a complex process that involves sequential attachment to the CD4 receptor followed by binding to either the CCR5 or CXCR4 molecules and fusion of the viral and cellular membranes. 1 CCR5 coreceptor antagonists prevent HIV entry into target cells by binding to the CCR5 receptors. 2 Phenotypic and, to a lesser degree, genotypic assays have been developed that can determine or predict the co-receptor tropism (i.e., CCR5, CXCR4, or both) of the patient's dominant virus population. An older generation assay (Trofile, Monogram Biosciences, Inc., South San Francisco, CA) was used to screen patients who were participating in clinical trials that led to the approval of maraviroc (MVC), the only CCR5 antagonist currently available. The assay has been improved and is now available with enhanced sensitivity. In addition, a genotypic assay to predict co-receptor usage is now commercially available.
During acute/recent infection, the vast majority of patients harbor a CCR5-utilizing virus (R5 virus), which suggests that the R5 variant is preferentially transmitted. Viruses in many untreated patients eventually exhibit a shift in co-receptor tropism from CCR5 usage to either CXCR4 or both CCR5 and CXCR4 tropism (i.e., dual-or mixed-tropic; D/M-tropic). This shift is temporally associated with a more rapid decline in CD4 T-cell counts, 3,4 but whether this tropism shift is a cause or a consequence of progressive immunodeficiency remains undetermined. 1 Antiretroviral (ARV)-treated patients with extensive drug resistance are more likely to harbor X4-or D/M-tropic variants than untreated patients with comparable CD4 counts. 5 The prevalence of X4-or D/M-tropic variants increases to more than 50% in treated patients who have CD4 counts <100 cells/mm 3 . 5,6
# Phenotypic Assays
Phenotypic assays characterize the co-receptor usage of plasma-derived virus. These assays involve the generation of laboratory viruses that express patient-derived envelope proteins (i.e., gp120 and gp41). These pseudoviruses, which are replication-defective, are used to infect target cell lines that express either CCR5 or CXCR4. 7,8 Using the Trofile assay, the co-receptor tropism of the patient-derived virus is confirmed by testing the susceptibility of the virus to specific CCR5 or CXCR4 inhibitors in vitro. This assay takes about 2 weeks to perform and requires a plasma HIV RNA level ≥1,000 copies/mL.
The performance characteristics of these assays have evolved. Most, if not all, patients enrolled in premarketing clinical trials of MVC and other CCR5 antagonists were screened with an earlier, less sensitive version of the Trofile assay. 8 This earlier assay failed to routinely detect low levels of CXCR4-utilizing variants. As a consequence, some patients enrolled in these clinical trials harbored low levels of CXCR4utilizing virus at baseline that were below the assay limit of detection and exhibited rapid virologic failure after initiation of a CCR5 antagonist. 9 The assay has been revised and is now able to detect lower levels of CXCR4-utlizing viruses. In vitro, the assay can detect CXCR4-utilizing clones with 100% sensitivity when those clones represent 0.3% or more of the virus population. 10 Although this more sensitive assay has had limited use in prospective clinical trials, it is now the only one that is commercially available. For unclear
# Panel's Recommendations
- A co-receptor tropism assay should be performed whenever the use of a CCR5 co-receptor antagonist is being considered (AI).
- Co-receptor tropism testing is also recommended for patients who exhibit virologic failure on a CCR5 antagonist (BIII).
- A phenotypic tropism assay is preferred to determine HIV-1 co-receptor usage (AI).
- A genotypic tropism assay should be considered as an alternative test to predict HIV-1 co-receptor usage (BII). The ABC HSR is a multiorgan clinical syndrome typically seen within the initial 6 weeks of ABC treatment. This reaction has been reported in 5%-8% of patients participating in clinical trials when using clinical criteria for the diagnosis, and it is the major reason for early discontinuation of ABC. Discontinuing ABC usually promptly reverses HSR, whereas subsequent rechallenge can cause a rapid, severe, and even lifethreatening recurrence. 1 Studies that evaluated demographic risk factors for ABC HSR have shown racial background as a risk factor, with white patients generally having a higher risk (5%-8%) than black patients (2%-3%). Several groups reported a highly significant association between ABC HSR and the presence of the major histocompatibility complex (MHC) class I allele HLA-B*5701. Because the clinical criteria used for ABC HSR are overly sensitive and may lead to false-positive ABC HSR diagnoses, an ABC skin patch test (SPT) was developed as a research tool to immunologically confirm ABC HSR. 4 A positive ABC SPT is an ABC-specific delayed HSR that results in redness and swelling at the skin site of application. All ABC SPT-positive patients studied were also positive for the HLA-B*5701 allele. 5 The ABC SPT could be falsely negative for some patients with ABC HSR and, at this point, is not recommended for use as a clinical tool. The PREDICT-1 study randomized patients before starting ABC either to be prospectively screened for HLA-B*5701 (with HLA-B*5701-positive patients not offered ABC) or to standard of care at the time of the study (i.e., no HLA screening, with all patients receiving ABC). 6 The overall HLA-B*5701 prevalence in this predominately white population was 5.6%. In this cohort, screening for HLA-B*5701 eliminated immunologic ABC HSR (defined as ABC SPT positive) compared with standard of care (0% vs. 2.7%), yielding a 100% negative predictive value with respect to SPT and significantly decreasing the rate of clinically suspected ABC HSR (3.4% vs. 7.8%). The SHAPE study corroborated the low rate of immunologically validated ABC HSR in black patients and confirmed the utility of HLA-B*5701 screening for the risk of ABC HSR (100% sensitivity in black and white populations). 7 On the basis of the results of these studies, the Panel recommends screening for HLA-B*5701 before starting patients on an ABC-containing regimen (AI). HLA-B*5701-positive patients should not be prescribed ABC (AI), and the positive status should be recorded as an ABC allergy in the patient's medical record (AII). HLA-B*5701 testing is needed only once in a patient's lifetime; thus, efforts to carefully record and maintain the test result and to educate the patient about its implications are important. The specificity of the HLA-B*5701 test in predicting ABC HSR is lower than the sensitivity (i.e., 33%-50% of HLA-B*5701-positive patients would likely not develop confirmed ABC HSR if exposed to ABC). HLA-B*5701 should not be used as a substitute for clinical judgment or pharmacovigilance, because a negative HLA-B*5701 result does not absolutely rule out the possibility of some form of ABC HSR. When HLA-B*5701 screening is not
# Rating of Recommendations
# Panel's Recommendations
- The Panel recommends screening for HLA-B*5701 before starting patients on an abacavir (ABC)-containing regimen to reduce the risk of hypersensitivity reaction (HSR) (AI).
- HLA-B*5701-positive patients should not be prescribed ABC (AI).
- The positive status should be recorded as an ABC allergy in the patient's medical record (AII).
- When HLA-B*5701 screening is not readily available, it remains reasonable to initiate ABC with appropriate clinical counseling and monitoring for any signs of HSR (CIII). Eradication of HIV infection cannot be achieved with available antiretroviral (ARV) regimens even when new, potent drugs are added to a regimen that is already suppressing plasma viral load below the limits of detection of commercially available assays. 1 This is chiefly because the pool of latently infected CD4 T cells is established during the earliest stages of acute HIV infection 2 and persists with a long half-life, despite prolonged suppression of plasma viremia. Therefore the primary goals for initiating antiretroviral therapy (ART) are to:
# Rating of Recommendations
- reduce HIV-associated morbidity and prolong the duration and quality of survival,
- restore and preserve immunologic function,
- maximally and durably suppress plasma HIV viral load (see Plasma HIV RNA Testing), and
- prevent HIV transmission.
ART has reduced HIV-related morbidity and mortality and has reduced perinatal 12 and behavior-associated transmission of HIV. HIV suppression with ART may also decrease inflammation and immune activation thought to contribute to higher rates of cardiovascular and other end-organ damage reported in HIV-infected cohorts. (See Initiating Antiretroviral Therapy.) Maximal and durable suppression of plasma viremia delays or prevents the selection of drug-resistance mutations, preserves CD4 T-cell numbers, and confers substantial clinical benefits, all of which are important treatment goals. Achieving viral suppression requires the use of ARV regimens with at least two, and preferably three, active drugs from two or more drug classes. Baseline resistance testing and patient characteristics should guide design of the specific regimen. (See What to Start: Initial Combination Regimens for the Antiretroviral-Naive Patient.) When initial suppression is not achieved or is lost, rapidly changing to a new regimen with at least two active drugs is required. (See Virologic Failure and Suboptimal Immunologic Response.) The increasing number of drugs and drug classes makes viral suppression below detection limits an appropriate goal in all patients.
Viral load reduction to below limits of assay detection in an ART-naive patient usually occurs within the first 12-24 weeks of therapy. Predictors of virologic success include:
- high potency of ARV regimen,
- excellent adherence to treatment regimen, 20 - low baseline viremia, 21 - higher baseline CD4 count (>200 cells/mm 3 ), 22 and
- rapid reduction of viremia in response to treatment. 21,23 Successful outcomes are usually observed, although adherence difficulties may lower the success rate in clinical practice to below the 90% rate commonly seen in clinical trials. 24
# Strategies to Achieve Treatment Goals
Achieving treatment goals requires a balance of sometimes competing considerations, outlined below. Providers and patients must work together to define individualized strategies to achieve treatment goals.
# Selection of Initial Combination Regimen
Several preferred and alternative ARV regimens are recommended for use. (See What to Start.) Many of these regimens have comparable efficacy but vary to some degree in dosing frequency and symmetry, pill
# Introduction
Without treatment, most HIV-infected individuals will eventually develop progressive immunosuppression, as evident by CD4 T lymphocyte (CD4) cell depletion, leading to AIDS-defining illnesses and premature death. The primary goal of ART is to prevent HIV-associated morbidity and mortality. This goal is best accomplished by using effective ART to maximally inhibit HIV replication so that plasma HIV RNA (viral load) remains below levels detectable by commercially available assays. Durable viral suppression improves immune function and overall quality of life, lowers the risk of both AIDS-defining and non-AIDS-defining complications, and prolongs life.
Furthermore, high plasma HIV RNA is a major risk factor for HIV transmission, and effective antiretroviral therapy (ART) can reduce viremia and transmission of HIV to sexual partners by more than 96%. 1,2 Modelling studies suggest that expanded use of ART may result in lower incidence and, eventually, prevalence of HIV on a community or population level. 3 Thus, a secondary goal of ART is to reduce the risk of HIV transmission.
Historically, HIV-infected individuals have had low CD4 counts at presentation to care. 4 However, there have been concerted efforts to increase testing of at-risk patients and to link these patients to medical care before they have advanced HIV disease. Deferring ART until CD4 count declines put an individual at risk of AIDSdefining conditions has been associated with higher risk of morbidity and mortality (as discussed below). Furthermore, the magnitude of CD4 recovery is directly correlated with CD4 count at ART initiation. Consequently, many individuals who start treatment with CD4 counts 500 cells/mm 3 after up to 6 years on ART. 5 The recommendation to initiate ART in individuals with high CD4 cell counts-whose short-term risk for death and development of AIDS-defining illness is low 6,7 -is based on growing evidence that untreated HIV infection or uncontrolled viremia is associated with development of non-AIDS-defining diseases, including cardiovascular disease (CVD), kidney disease, liver disease, neurologic complications, and malignancies. Furthermore, newer ART regimens are more effective, more convenient, and better tolerated than regimens used in the past.
# Panel's Recommendations
- Antiretroviral therapy (ART) is recommended for all HIV-infected individuals to reduce the risk of disease progression.
The strength of and evidence for this recommendation vary by pretreatment CD4 T lymphocyte (CD4) cell count: CD4 count 500 cells/mm 3 (BIII).
- ART is also recommended for HIV-infected individuals to prevent of transmission of HIV.
The strength of and evidence for this recommendation vary by transmission risks: perinatal transmission (AI); heterosexual transmission (AI); other transmission risk groups (AIII).
- Patients starting ART should be willing and able to commit to treatment and understand the benefits and risks of therapy and the importance of adherence (AIII). Patients may choose to postpone therapy, and providers, on a case-by-case basis, may elect to defer therapy on the basis of clinical and/or psychosocial factors. Regardless of CD4 count, the decision to initiate ART should always include consideration of a patient's comorbid conditions, his or her willingness and readiness to initiate therapy, and available resources. In settings where there are insufficient resources to initiate ART in all patients, treatment should be prioritized for patients with the following clinical conditions: pregnancy; CD4 count <200 cells/mm 3 or history of an AIDS-defining illness including HIV-associated dementia, HIV-associated nephropathy (HIVAN), or hepatitis B virus (HBV); and acute HIV infection.
# Rating of Recommendations
Tempering the enthusiasm to treat all patients regardless of CD4 count is the absence of randomized trial data that demonstrate a definitive clinical benefit of ART in patients with higher CD4 counts (e.g., >350 cells/ mm 3 ) and mixed results from observational cohort studies as to the definitive benefits of early ART (i.e., when CD4 count >500 cells/mm 3 ). For some asymptomatic patients, the potential risks of short-or long-term drug-related complications and non-adherence to long-term therapy may offset possible benefits of earlier initiation of therapy. An ongoing randomized controlled trial evaluating the role of immediate versus delayed ART in patients with CD4 counts >500 cells/mm 3 (see Strategic Timing of Antiretroviral Treatment (START); ClinicalTrials.gov identifier NCT00867048) should help to further define the role of ART in this patient population.
The known and potential benefits and limitations of ART in general, and in different patient populations are discussed below.
# Benefits of Antiretroviral Therapy
# Reduction in Mortality and/or AIDS-Related Morbidity According to Pretreatment CD4 Cell Count
Patients with a History of an AIDS-Defining Illness or CD4 Count 200 cells/mm 3 ) with later treatment (i.e., initiated at CD4 count 200 cells/mm 3 . CIPRA HT-001, a randomized clinical trial conducted in Haiti, enrolled 816 participants without AIDS. Participants were randomized to start ART with CD4 counts in the 200 to 350 cells/mm 3 range or to defer treatment until their CD4 counts dropped to <200 cells/mm 3 or they developed an AIDS-defining condition. The study was terminated when an interim analysis showed a survival benefit in the early treatment arm. When compared with participants who began ART with CD4 counts in the 200 to 350 cells/mm 3 range, patients who deferred therapy had a higher mortality rate (23 versus 6 deaths; hazard ratio = 4.0; 95% confidence interval , 1.6-9.8) and a higher rate of incident tuberculosis (TB) (HR = 2.0; 95% CI, 1.2-3.6). 17 Collectively, these studies support the Panel's recommendation that ART should be initiated in patients with a history of an AIDS-defining illness or with a CD4 count <350 cells/mm 3 (AI).
# Patients with CD4 Counts Between 350 and 500 cells/mm 3
Data supporting initiation of ART in patients with CD4 counts ranging from 350 cells/mm 3 to 500 cells/mm 3 are from large observational studies conducted in North America, Europe, and Australia and from secondary analysis of randomized controlled trials. Findings from the observational studies were analyzed using advanced statistical methods that minimize the bias and confounding that arise when observational data are used to address the question of when to start ART. However, unmeasured confounders for which adjustment was not possible may have influenced the analysis.
Among the cohort studies analyzed, the ART Cohort Collaboration (ART-CC) included 45,691 patients from 18 cohort studies conducted primarily in North America and Europe. Data from ART-CC showed that the rate of progression to AIDS and/or death was higher in participants who delayed ART initiation until their CD4 counts fell to 251 to 350 cells/mm 3 than in those who initiated ART at CD4 count level of 351 to 450 cells/mm 3 (risk ratio: 1.28; 95% CI, 1.04-1.57). 13 When analysis of the data was restricted to mortality alone, the difference between the 2 strategies was weaker and not statistically significant (risk ratio: 1.13; 95% CI, 0.80-1.60).
The NA-ACCORD cohort evaluated patients regardless whether they had started therapy. The 6,278 patients who deferred therapy until their CD4 counts fell to 500 cells/mm 3 that declined to <500 cells/mm 3 . 16 The study estimated that delaying initiation of ART until CD4 count fell to <350 cells/mm 3 was associated with a greater risk of AIDS-defining illness or death than initiating ART with CD4 count between 350 cells/mm 3 and 500 cells/mm 3 (HR: 1.38; 95% CI, 1.23-1.56). However, there was no difference in mortality between the 2 groups (HR: 1.01; 95% CI, 0.84-1.22).
The CASCADE cohort included 5,527 ART-naive patients with CD4 counts in the 350 to 499 cells/mm 3 range. Compared with patients who deferred therapy until their CD4 counts fell to 350 cells/mm 3 were randomized to continuous ART or to treatment interruption until their CD4 counts fell to <250 cells/mm 3 . In the subgroup of 249 participants who were ART naive at enrollment (median CD4 count: 437 cells/mm 3 ), those who deferred ART until their CD4 counts dropped to <250 cells/mm 3 had a greater risk of serious AIDS-and non-AIDS-related events than those who initiated therapy immediately (7 vs. 2 events; HR: 4.6; 95% CI, 1.0-22.2). 20 HPTN 052 was a large multi-continent randomized trial that examined whether treatment of HIV-infected individuals reduces transmission to their uninfected sexual partners. 2 A secondary objective of the study was to determine whether ART reduces clinical events in the HIV-infected participants. This trial enrolled 1,763 HIV infected participants with CD4 counts between 350 and 550 cells/mm 3 and their HIV uninfected partners. The infected participants were randomized to initiate ART immediately or to delay initiation until they had 2 consecutive CD4 counts <250 cells/mm 3 . At a median follow-up of 2.1 years, there were 57 primary events in the early therapy arm versus 77 events in the delayed therapy arm (HR: 0.73; 95% CI, 0.52-1.03). The most frequent event was tuberculosis (17 cases in the early therapy arm and 34 cases in the delayed therapy arm); deaths were relatively rare (11 cases in the early therapy arm and 15 cases in the delayed therapy arm). 21,22 Collectively, these studies suggest that initiating ART in patients with CD4 counts between 350 and 500 cells/mm 3 reduces HIV-related disease progression; whether there is a corresponding reduction in mortality is unclear. This benefit supports the Panel's recommendation that ART should be initiated in patients with CD4 counts 350 to 500 cells/mm 3 (AII). Recent evidence demonstrating the public health benefit of earlier initiation of ART in reducing HIV transmission further supports the strength of this recommendation (see Prevention of Sexual Transmission).
Patients with CD4 Counts >500 cells/mm 3 An analysis of the risks of HIV-associated disease progression in ART-naive patients with CD4 cell counts >500 cells/mm 3 is difficult because only a small proportion of individuals present for clinical care with CD4 cell counts at this level. 4,23 However, studies have demonstrated a gradient of increased risk of AIDS and death when ART is initiated at lower CD4 cell count levels and have provided no evidence of a safe CD4 count level. 6,24,25 To date, questions regarding the risks and benefits of starting ART in patients with CD4 cell counts >500 cells/mm 3 as compared to deferring initiation until CD4 cell counts are lower have not yet been answered in a definitive randomized clinical trial. Evidence supporting early initiation comes from an observational study. The NA-ACCORD study observed patients who started ART with CD4 counts >500 cells/mm 3 or after their CD4 counts dropped below this threshold. The adjusted mortality rates were significantly higher in the 6,935 patients who deferred therapy until their CD4 counts fell to 500 cells/mm 3 (risk ratio: 1.94; 95% CI, 1.37-2.79). 18 In contrast, in an analysis of the ART-CC cohort, 13 the rate of progression to AIDS/death associated with deferral of therapy until CD4 counts fell to the 351 to 450 cells/mm 3 range was similar to the rate with initiation of therapy with CD4 counts in the 451 to 550 cells/mm 3 range (HR: 0.99; 95% CI, 0.76-1.29). The analysis showed no significant difference in rate of death in the immediate and deferred therapy groups (HR: 0.93; 95% CI, 0.60-1.44). In the CASCADE Collaboration, 19 among the 5,162 patients with CD4 counts in the 500 to 799 cells/mm 3 range, compared with patients who deferred therapy, those who started ART immediately did not experience a significant reduction in the composite outcome of progression to AIDS/death (HR: 1.10; 95% CI, 0.67-1.79) or death (HR: 1.02; 95% CI, 0.49-2.12).
Although not a clinical endpoint study, a recent clinical trial (Setpoint Study) randomized patients within 6 months of HIV seroconversion to receive either immediate ART for 36 weeks or deferred treatment. More than 57% of the study participants had CD4 counts >500 cells/mm 3 . The deferred treatment group had a statistically higher risk of meeting study defined ART initiation criteria than the immediate treatment group.
The study was halted early, showing that the time from diagnosis of early infection and the need for initiation of ART was shorter than anticipated in the deferral therapy group. Fully half of the participants in the deferral group met the criteria for treatment initiation by week 72. 26 Another recent study provides evidence that early treatment enhances recovery of CD4 counts to levels >900 cells/mm 3 . 27 Among individuals who were identified during primary infection, those who initiated ART within 4 months after the estimated date of infection were more likely to have CD4 cell recovery and had a faster rate of recovery than those initiating ART at 4 to 12 months or >12 months after the estimated date of infection. However, even among participants who started ART earlier, those who initiated ART with lower CD4 counts were less likely to have CD4 cell recovery and had a lower rate of recovery than those who initiated ART with higher CD4 counts.
With a better understanding of the pathogenesis of HIV infection, the growing awareness that untreated HIV infection increases the risk of many non-AIDS-defining diseases (as discussed below), and the benefit of ART in reducing transmission of HIV, the Panel recommends initiation of ART in patients with CD4 counts >500 cells/mm 3 (BIII).
When discussing initiation of ART at high CD4 cell counts (>500 cells/mm 3 ), clinicians should inform patients that data on the clinical benefit of starting treatment at such levels are not conclusive, especially for patients with very high CD4 counts. Clinicians should also inform patients that viral suppression from effective ART can reduce the risk of sexual transmission. Lastly, patients should be informed that untreated HIV infection will eventually lead to immunological deterioration and increased risk of clinical disease and death. Therefore, if therapy is not initiated, continued monitoring and close follow-up are necessary.
Further ongoing research (both randomized clinical trials and cohort studies) to assess the short-and longterm clinical and public health benefits and cost effectiveness of starting therapy at higher CD4 counts is needed. Findings from such research will provide further evidence to help the Panel make future recommendations.
# Effects of Viral Replication on HIV-Related Morbidity
Since the mid-1990s, it has been known that measures of viral replication predict HIV disease progression. Among untreated HIV-infected individuals, time to clinical progression and mortality is fastest in those with higher viral loads. 28 This finding is confirmed across the spectrum of HIV-infected patient populations, such as injection drug users (IDUs), 29 women, 30 and individuals with hemophilia. 31 Several studies have shown the prognostic value of pre-treatment viral load for predicting post-therapy response. 32,33 Once therapy has been initiated, failure to achieve viral suppression and viral load at the time of treatment failure 37 are predictive of clinical disease progression.
More recent studies have examined the impact of ongoing viral replication for both longer durations and at higher CD4 cell counts. Using viremia copy-years, a novel metric for quantifying viral load over time, the Centers for AIDS Research Network of Integrated Clinical Systems (CNICS) cohort found that cumulative exposure to replicating virus is independently associated with mortality. Using viremia copy-years, the HR for mortality was 1.81 per log 10 copy-year/mL (95% CI, 1.51-2.18), which was the only viral load-related variable that retained statistical significance in the multivariable model (HR 1.44 per log 10 copy-year/mL; 95% CI, 1.07-1.94). These findings support the concept that unchecked viral replication, which occurs in the absence of effective ART, is a factor in disease progression and death independent of CD4 count. 38 The EuroSIDA collaboration evaluated HIV-infected individuals with CD4 counts >350 cells/mm 3 segregated by three viral load strata (<500 copies/mL, 500-9,999 copies/mL, and ≥10,000 copies/mL) to determine the impact of viral load on rates of fatal and nonfatal AIDS-related and non-AIDS-related events.
The lower viral load stratum included more participants on ART (92%) than the middle (62%) and high (31%) viral load strata. After adjustment for age, region, and ART, the rates of non-AIDS events were 61% (P = 0.001) and 66% (P = 0.004) higher in participants with viral loads 500 to 9,999 copies/mL and >10,000 copies/mL, respectively, than in individuals with viral loads 350 cells/mm 3 . 39 Collectively, these data show that the harm of ongoing viral replication affects both untreated patients and those who are on ART but remain viremic. The harm of ongoing viral replication in patients on ART is compounded by the risk of emergence of drug-resistant virus. Therefore, all patients on ART should be carefully monitored and counseled on the importance of adherence to therapy.
# Effects of Antiretroviral Therapy on HIV-Related Morbidity
HIV-associated immune deficiency, the direct effects of HIV on end organs, and the indirect effects of HIVassociated inflammation on these organs all likely contribute to HIV-related morbidity and mortality. In general, the available data demonstrate the following:
- Untreated HIV infection (ongoing viral replication) may have negative effects at all stages of infection.
- Earlier treatment may prevent the damage associated with HIV replication during early stages of infection.
- ART is beneficial even when initiated later in infection; however, later therapy may not repair damage associated with viral replication during early stages of infection.
- Sustaining viral suppression and maintaining higher CD4 count levels, mostly as a result of effective combination ART, may delay, prevent, or reverse some non-AIDS-defining complications, such as HIVassociated kidney disease, liver disease, CVD, neurologic complications, and malignancies, as discussed below.
# HIV-Associated Nephropathy
HIVAN is the most common cause of chronic kidney disease in HIV-infected individuals that may lead to end-stage kidney disease. 40 HIVAN is almost exclusively seen in black patients and can occur at any CD4 count. Ongoing viral replication appears to be directly involved in renal injury; 41 HIVAN is extremely uncommon in virologically suppressed patients. 42 ART in patients with HIVAN has been associated with both preserved renal function and prolonged survival. Therefore, regardless of CD4 count, ART should be started in all patients with HIVAN at the earliest sign of renal dysfunction (AII).
# Coinfection with Hepatitis B Virus and/or Hepatitis C Virus
HIV infection is associated with more rapid progression of viral hepatitis-related liver disease, including cirrhosis, end-stage liver disease, hepatocellular carcinoma, and fatal hepatic failure. 46 48 The pathogenesis of accelerated liver disease in HIV-infected patients has not been fully elucidated, but HIV-related immunodeficiency and a direct interaction between HIV and hepatic stellate and Kupffer cells have been implicated. In individuals co-infected with HBV and/or hepatitis C virus (HCV), ART may attenuate liver disease progression by preserving or restoring immune function and reducing HIV-related immune activation and inflammation. Antiretroviral (ARV) drugs active against both HIV and HBV (such as tenofovir disoproxil fumarate , lamivudine , and emtricitabine ) also may prevent development of significant liver disease by directly suppressing HBV replication. 56,57 Although ARV drugs do not inhibit HCV replication directly, HCV treatment outcomes typically improve when HIV replication is controlled or CD4 counts increase. 58 In one prospective cohort, after controlling for liver and HIV disease stage, HCV coinfected patients receiving ART were approximately 66% less likely to experience end-stage liver disease, hepatocellular carcinoma, and fatal hepatic failure than patients not receiving ART. 59 While some studies have shown that chronic viral hepatitis increases the risk of ART-induced liver injury, the majority of coinfected persons do not develop clinically significant liver injury and the rate of hepatotoxicity may be greater in persons with more advanced HIV disease. Collectively, these data suggest that earlier treatment of HIV infection in persons coinfected with HBV (and likely HCV) may reduce the risk of liver disease progression. ART is recommended for patients coinfected with HBV, and the ART regimen should include drugs with activity against both HIV and HBV (AII) (also see Hepatitis B Virus/HIV Coinfection). ART is also recommended for most patients coinfected with HCV (BII), including those with high CD4 counts and those with cirrhosis. This recommendation is based on findings from retrospective and prospective cohort studies that indicated that the receipt of ART is associated with slower progression of hepatic fibrosis and reduced risk of liver disease outcomes. 59, Combined treatment of HIV and HCV can be complicated by large pill burden, drug interactions, and overlapping toxicities; however, the complexity of treatment depends on the HCV regimen selected. ART should be considered for HIV/HCV-coinfected patients regardless of CD4 cell count. However, for patients with CD4 counts >500 cells/mm 3 and also infected with HCV genotype 1, if treatment is to include an HCV protease inhibitor, some clinicians may choose to defer ART until HCV treatment is completed (also see HIV/Hepatitis C Virus Co-Infection).
# Cardiovascular Disease
In HIV-infected patients, CVD is a major cause of morbidity and mortality, accounting for one-third of serious non-AIDS conditions and at least 10% of deaths. A number of studies have found that, over time, HIV-infected persons are at greater risk for CVD events than age-matched uninfected individuals.
Persons living with HIV infection have higher rates of established CVD risk factors, particularly smoking and dyslipidemia, than HIV-uninfected individuals. In the Data Collection on Adverse Events of Anti-HIV Drugs (D:A:D) cohort study such factors, including age, male gender, obesity, smoking, family history of CVD, diabetes, and dyslipidemia, were each independently associated with risk of myocardial infarction (MI). 69 This study also found that the risk of CVD was greater with exposure to some ARV drugs, including certain PIs (ritonavir-boosted lopinavir and ritonavir-boosted fosamprenavir) and abacavir, than with exposure to other ARV drugs. 69,70 In terms of preventing the progression to CVD events, it has not been determined whether delaying ART initiation is preferable to immediate treatment. In the meta-analysis mentioned above, the risk of CVD in HIV-infected individuals was 1.5 times higher in those treated with ART than in those not treated with ART. 63 These analyses were limited by concern that the treated individuals may have been infected for longer periods of time and had prior episodes of untreated HIV disease, as well as the fact that the untreated people were at higher risk for competing events, including death. Furthermore, there is evidence that untreated HIV infection may also be associated with an increased risk of CVD. In the SMART study, the risk of cardiovascular events was greater in participants randomized to CD4-guided treatment interruption than in participants who received continuous ART. 71 In other studies, ART resulted in marked improvement in parameters associated with CVD, including markers of inflammation (such as interleukin 6 ), immune dysfunction (e.g., T cell activation, T cell senescence), monocyte activation (e.g., IL-6, soluble CD14 and CD163), hyper-coagulation (e.g., D-dimers) and, most importantly, endothelial dysfunction. 72,73 Low nadir and/or proximal on-therapy CD4 cell count has been linked to CVD (MI and/or stroke), suggesting that low CD4 count might result in increased risk of CVD.
Collectively, the increased risk of cardiovascular events with treatment interruption, the effects of ART on markers of inflammation and endothelial dysfunction, and the association between CVD and CD4 cell depletion suggest that early control of HIV replication with ART can be used as a strategy to reduce risk of CVD, particularly if drugs with potential cardiovascular toxicity are avoided. However, no study has demonstrated that initiation of ART prevents CVD. Therefore, a role for early ART in preventing CVD remains to be established. For HIV-infected individuals with a significant risk of CVD, as assessed by medical history and estimated risk calculations, risk of CVD should be considered when selecting a specific ART regimen.
# Malignancies
HIV-infected individuals are at increased risk for developing several cancers and human papilloma virus (HPV)-related pre-malignant intraepithelial neoplasia. 77,78 Increased rates of Kaposi sarcoma and non-Hodgkin lymphoma in patients with advanced HIV infection have been noted since early in the AIDS epidemic, and, together with cervical cancer, both diseases have been defined as AIDS-defining malignancies (ADMs) for public health surveillance purposes. HIV infection and associated immunosuppression increase the risk of several cancers identified as non-AIDS-defining malignancies (NADMs). Importantly, the incidence of lung, anal, oropharyngeal, liver and skin cancers, Hodgkin lymphoma, and melanoma, is higher in HIV-infected individuals than in matched HIV-uninfected controls, and the burden of these NADMs continued to increase in the United States between 1996 and 2007. 82 Incidental cancers that occur in HIV-infected individuals are becoming more common, which is due to the aging of the HIV population rather than to HIV-associated risks of malignancies. These cancers are also sometimes considered NADMs. Most cancers with increased incidence are either virally related (i.e., Hodgkin lymphoma, anal cancer, liver cancer) or smoking related (lung cancer), although HIV remains an independent risk factor for the later. 83 Large cohort studies enrolling mainly patients receiving ART have reported a consistent link between low CD4 counts (500 cells/mm 3 , patients with CD4 counts <500 cells/mm 3 had a statistically significant relative risk of all cancers evaluated (except for anal carcinoma). The study also showed an increased risk of anal cancer based on extent of time with CD4 counts <200 cells/mm 3 , and that, regardless of CD4 count, ART has a protective effect for HIV-associated malignancies. 84 This potential effect of HIV-associated immunodeficiency is striking particularly with regard to cancers and premalignant diseases associated with chronic viral infections such as HBV, HCV, HPV, Epstein-Barr virus, and human herpes virus-8. 88,89 For some cancers, risk is related to HIV viremia. Cumulative HIV viremia, independent of other factors, is associated with increased risk of non-Hodgkin lymphoma and other ADM. 87,90 In the SMART study, 91 patients randomized to the drug conservation arm (ART interruption with re-initiation if CD4 count fell to <250 cells/mm 3 ) had a higher incidence of ADM but not NADM, although increased NADM was noted in non-smokers in the drug-conservation arm.
From the early 1990s through 2000, incidence rates for many cancers occurring with advanced immunosuppression, including Kaposi sarcoma, diffuse large B-cell lymphoma, and primary central nervous system (CNS) lymphoma, declined markedly in HIV-infected individuals in the United States, with more gradual declines noted after 2000. 92 However, for other ADMs and NADMs, such as Burkitt lymphoma, Hodgkin lymphoma, cervical cancer, and anal cancer, similar reductions in incidence have not been observed. 92,93 Declines in competing causes of mortality (e.g., opportunistic infections ) and concurrent cancer risk factors such as smoking or aging of HIV-infected cohorts, may confound a full assessment of the relative impact of ART on cancer prevention for NADMs. 82,94 Additionally, data from the era of potent combination ART suggest that overall survival in HIV-infected patients who develop ADMs or NADMs also depends on immune status as measured by CD4 count. 85,95,96 For non-Hodgkin lymphoma, data from the Center for AIDS Research Network of Integrated Clinical Systems Cohort shows that across CD4 strata, the level of HIV viremia 6 months after the diagnosis of lymphoma (including Hodgkin lymphoma) is associated with an increased risk of death. 95 Together this evidence suggests that initiating ART to suppress HIV replication, maximize immune reconstitution, and maintain CD4 counts at levels >350 to 500 cells/mm 3 reduces the overall incidence of ADMs and may reduce the risk of some NADMs as well. The effect of ART on cancer incidence and mortality in patients with cancer 95,97 is likely to be heterogeneous across various cancer types.
# Neurological Complications
In the untreated HIV-infected patient, CNS involvement is a nearly universal facet of systemic HIV infection as evident by detection of HIV RNA in cerebrospinal fluid (CSF). The CNS is an important target of ART, not only to treat neurologically symptomatic infection but also to prevent later development of virusrelated brain injury, which can range from severe and debilitating encephalopathy to milder and more insidious cognitive and motor dysfunction. Like systemic infection, CNS virus populations and the character of CNS infection can evolve within individual patients. Characteristically during the earliest phases of systemic infection, CSF viral isolates are similar to those found in blood and likely reflect transfer of blood populations across CNS barriers in T lymphocytes. 105 Over time CSF isolates may exhibit increasing compartmentalization that reflect divergence from the predominant blood populations, a transformation most notable in patients with frank HIV encephalitis presenting with HIV-associated dementia (HAD). 106 Combination ART usually reduces CSF HIV RNA to below the level of detection, 99,107 largely preventing this development, and consequently, reducing the incidence of severe HIV-related brain disease in virologically suppressed patients. Hence, prevention of HAD is among the arguments for early ART, although the CD4 threshold for treatment to prevent this disorder is not established. Additionally, treatment of patients presenting with HAD-usually seen in the context of late HIV presentation-can arrest and variably reverse neurological abnormalities; 111 therefore, the diagnosis of HAD is an indication for rapid initiation of ART (AI).
With the successful control of HAD with ART, attention has shifted to milder forms of neurocognitive impairment in HIV infection, largely recognized by reduced neuropsychological test performance. 104,112 These milder forms of impairment are categorized in two groups: asymptomatic neurocognitive impairment and mild neurocognitive disorder. Although patients with either form exhibit the same degree of impairment on neuropsychological tests (<1 SD below normative performance in two neurocognitive domains), they differ as to the absence or presence of symptoms or mild functional impairment in everyday activities. 103 Even after exclusion of confounding conditions, the prevalence of these milder forms of neurocognitive impairment appears to be substantial, including in treated patients with plasma viral suppression. 104,112 Less certain is the extent to which these impairments are the consequence of earlier mild or subclinical brain injury sustained before ART initiation, or alternatively, reflect ongoing injury despite ART and plasma viral suppression. Association of these milder deficits with nadir CD4 count may favor the role of earlier injury, 100, providing further argument for early treatment.
Peripheral neuropathies are a second category of important HIV-associated neurological disease. 116 In the early decades of the discovery of HIV infection and the use of some nucleoside analogs, painful distal sensory neuropathy was particularly common and a difficult problem that did not respond to ART. 117 Although some reports suggest that the incidence of this HIV-associated neuropathy remains high, clinical experience suggests that the condition mainly affects patients with longer duration of HIV infection who initiated ART late in the course of the disease. 118 There appears to be a reduced incidence of neuropathies as more patients begin treatment at earlier stages of HIV infection.
Overall, effective ART may be beneficial in preventing and treating symptomatic and subclinical CNS HIV infection and the CNS and peripheral nervous system consequences of infection.
# Age and Treatment-Related Immune Reconstitution
Also see HIV and the Older Patient.
The CD4 cell response to ART is an important predictor of short-and long-term morbidity and mortality. In most, but not all studies, treatment initiation at an older age has been associated with a less robust CD4 count response; starting therapy at a younger age may result in better immunologic and perhaps clinical outcomes. 4,
# Persistent Inflammation and Immunodeficiency During Antiretroviral Therapy
Untreated HIV infection is associated with chronic inflammation, as defined by the frequency of activated T cells and monocyte/macrophages and levels of a number of pro-inflammatory cytokines (e.g., IL-6, CRP, soluble CD14). Effective ART decreases levels of most of these inflammatory markers, but the effect is often incomplete, with levels in many of those on ART remaining higher than those observed in age-matched uninfected adults. 123,124 Chronic inflammation during both untreated and treated disease is strongly associated with risk of non-AIDS defining morbidity and all-cause mortality. Because HIV replication contributes to this inflammatory state through both direct and indirect mechanisms, earlier use of ART to blunt this process may be beneficial. However, there are no data showing that ART-mediated changes in any inflammatory biomarker are associated with reduced morbidity and mortality.
Immune function as defined by the peripheral CD4 cell count is also an important determinant of health.
Although effective ART results in a sustained and beneficial increase in CD4 cell counts, this effect is often incomplete. Patients who delay therapy to the point of advanced immunodeficiency may require several years of ART to normalize their peripheral CD4 cell counts, 129 and some patients may never achieve a normal level. 130 A lower CD4 count on therapy is associated with higher risk of developing cancer, liver disease, cardiovascular disease and death. 14 In some studies a history of low CD4 counts is associated with risk of morbidity and mortality during subsequent effective therapy. 131,132 Collectively, these observations support earlier use of ART. Treatment decreases the level of inflammation, which may be associated with reduced short-term risk of AIDS-and non-AIDS-related morbidity and mortality. 125,133,134 ART also prevents progressive loss of CD4 cells, thus reducing risk of immunodeficiency and its related complications. Some studies have shown that a patient's pre-therapy CD4 cell count nadir is predictive of the degree of residual inflammation and/or T-cell dysfunction during ART. 123,135,136 Thus, earlier ART may result in less residual immunological perturbations during treatment, which theoretically may result in reduced risk of disease during the decades that a patient requires ART (CIII).
# Antiretroviral Therapy for Prevention of HIV Transmission
# Prevention of Perinatal Transmission
Effective ART reduces transmission of HIV. The most dramatic and well-established example of this effect is the use of ART in pregnant women to prevent perinatal transmission of HIV. Effective suppression of HIV replication, as reflected in plasma HIV RNA, is a key determinant in reducing perinatal transmission. In the setting of ART initiation before 28 weeks' gestation and an HIV RNA level <50 copies/mL near delivery, use of combination ART during pregnancy has reduced the rate of perinatal transmission of HIV from approximately 20% to 30% to 0.1% to 0.5%. 137,138 Thus, use of combination ART drug regimens is recommended for all HIV-infected pregnant women (AI). Following delivery, in the absence of breastfeeding, considerations regarding continuation of the ARV regimen for maternal therapeutic indications are the same as those regarding ART for other non-pregnant individuals. For detailed recommendations, see the Perinatal Guidelines. 139
# Prevention of Sexual Transmission
A number of investigations, including biological, ecological and epidemiological studies and one randomized clinical trial, provide strong support for the premise that treatment of the HIV-infected individual can significantly reduce sexual transmission of HIV. Lower plasma HIV RNA levels are associated with decreases in the concentration of the virus in genital secretions. 140,141 Studies of HIV-serodiscordant heterosexual couples have demonstrated a relationship between level of plasma viremia and risk of transmission of HIV-when plasma HIV RNA levels are lower, transmission events are less common. 1, A study conducted in KwaZulu-Natal, South Africa, used geospatial techniques to assess the relationship between ART use and HIV incidence in an observational cohort of more than 16,000 study participants living in many different communities. 146 After adjustment for sexual behavior and prevalent HIV cases, each percentage point increase in ART coverage of HIV-infected persons lowered the HIV infection risk in a community by 1.7%.
Most significantly, the multi-continental HPTN 052 trial enrolled 1,763 HIV-serodiscordant couples in which the HIV-infected partner was ART naive with a CD4 count of 350 to 550 cells/mm 3 at enrollment to compare the effect of immediate ART versus delayed therapy (not started until CD4 count <250 cells/mm 3 ) on HIV transmission to the HIV-infected partner. 2 At study entry, 97% of the participants were in heterosexual monogamous relationships. All study participants were counseled on behavioral modification and condom use. Twenty-eight linked HIV transmission events were identified during the study period, but only 1 event occurred in the early therapy arm. This 96% reduction in transmission associated with early ART was statistically significant (HR 0.04; 95% CI, 0.01-0.27; P <0.001). These results show that early ART is more effective at preventing transmission of HIV than all other behavioral and biomedical prevention interventions studied. This study, as well as other observational studies and modeling analyses showing a decreased rate of HIV transmission among serodiscordant heterosexual couples following the introduction of ART, demonstrate that suppression of viremia in ART-adherent patients with no concomitant sexually transmitted diseases (STDs) substantially reduces the risk of transmission of HIV. 3,144,145, HPTN 052 was conducted in heterosexual couples and not in populations at risk of transmission via homosexual exposure or needle sharing. In addition, in this clinical trial, adherence to ART was well supported and near complete. However, the prevention benefits of effective ART observed in HPTN 052 can reasonably be presumed to apply broadly. Therefore, the Panel recommends that ART be offered to patients who are at risk of transmitting HIV to sexual partners (the strength of this recommendation varies according to mode of sexual transmission: AI for heterosexual transmission and AIII for male-to-male and other modes of sexual transmission). Clinicians should discuss with patients the potential individual and public health benefits of therapy and the need for adherence to the prescribed regimen and counsel patients that ART is not a substitute for condom use and behavioral modification and that ART does not protect against other STDs (see Preventing Secondary Transmission of HIV).
# Concerns Regarding Earlier Initiation of Therapy
Despite increasing evidence showing the benefits of earlier initiation of ART, four areas of concern remain as reasons for deferral of HIV therapy.
# ARV Drug Toxicities Have an Adverse Effect on Quality of Life and Adherence
Earlier initiation of ART extends exposure to ARV agents by several years. The D:A:D study found an increased incidence of CVD associated with cumulative exposure to some drugs in the nucleoside reverse transcriptase inhibitor and protease inhibitor (PI) drug classes. 69,150 Renal and bone health are also of concern. Aging coupled with long term use of tenofovir may increase risk of significant renal dysfunction. In the SMART study, compared with interruption or deferral of therapy, continuous exposure to ART was associated with significantly greater loss of bone density. 71 There may be unknown complications related to cumulative use of ARV drugs for many decades. A list of known ARV-associated toxicities can be found in Adverse Effects of Antiretroviral Agents.
ART frequently improves quality of life for symptomatic patients. However, some side effects of ART may impair quality of life for some patients, especially those who are asymptomatic at initiation of therapy and at low risk of AIDS events. For example, efavirenz can cause neurocognitive or psychiatric side effects and PIs have been associated with gastrointestinal side effects. As noted above, some therapies may increase the risk of CVD. Patients who find that the inconvenience of taking medication every day outweighs the overall benefit of early ART may choose to delay therapy.
# ARV Non-Adherence May Have an Impact on Virologic Response.
At any CD4 count, adherence to therapy is essential to achieve viral suppression and prevent emergence of drug-resistance mutations. Several clinical, behavioral, and social factors associated with poor adherence, such as untreated major psychiatric disorders, active substance abuse, unfavorable social circumstances, patient concerns about side effects, and poor adherence to clinic visits, have been identified. Clinicians should identify areas where additional intervention is needed to improve adherence both before and after initiation of therapy. Some strategies to improve adherence are discussed in Adherence to Antiretroviral Therapy.
# Earlier Development of Resistance may Reduce Future Therapeutic Options.
Non-adherence and subsequent virologic failure may promote emergence of drug resistance mutations and limit subsequent treatment options. Despite concerns about the development of resistance to ARV drugs, the evidence thus far indicates that resistance occurs more frequently in individuals who initiate therapy later in the course of infection than in those who initiate ART earlier. 154 Furthermore, recent data have indicated a slight increase in the prevalence of 2-drug class resistance from 2000 to 2005. 155 Cost may be a Barrier to Early Initiation of Therapy.
In resource-rich countries, the cost of ART exceeds $10,000 per year (see Cost Considerations and Antiretroviral Therapy). Several modeling studies support the cost effectiveness of HIV therapy initiated soon after diagnosis. One study reported that the annual cost of care is 2.5 times higher for patients with CD4 counts 350 cells/mm 3 . 159 Much of the health care expenditure in patients with advanced infection is from non-ARV drugs and hospitalization. However, there are no comparisons of the cost of earlier ART initiation (i.e., CD4 count 350-500 cells/mm 3 ) versus later initiation (i.e., CD4 count >500 cells/ mm 3 ). As generic formulations for more ARV drugs become available in the next several years, the cost of ART may decline. However, despite any significant cost savings, decisions regarding which ARVs to select for system-wide HIV programs must be based on rigorous costeffectiveness assessments (see Cost section). 160
# Conditions Favoring More Urgent Initiation of Therapy
Several conditions increase the urgency for therapy, including:
- Pregnancy (AI). Clinicians should refer to the Perinatal Guidelines for more detailed recommendations on the management of HIV-infected pregnant women. 139
- AIDS-defining conditions, including HAD (AI)
- Acute OIs (see discussion below)
- Lower CD4 counts (e.g., <200 cells/mm 3 ) (AI)
- HIVAN (AII)
- Acute/Early Infection (BII). See more discussion in the Acute/Early Infection section.
- HIV/HBV coinfection (AII)
- HIV/HCV coinfection (BII)
- Rapidly declining CD4 counts (e.g., >100 cells/mm 3 decrease per year) (AIII)
- Higher viral loads (e.g., >100,000 copies/mL) (BII)
# Acute Opportunistic Infections
In patients who have opportunistic diseases for which no effective therapy exists (e.g., cryptosporidiosis, microsporidiosis, progressive multifocal leukoencephalopathy), but in whom ART may improve outcomes by improving immune responses, treatment should be started as soon as possible (AIII). For patients with mild to moderate cutaneous Kaposi's sarcoma (KS), prompt initiation of ART alone without chemotherapy has been associated with improvement of the KS lesions, even though initial transient progression of KS lesion as a manifestation of immune reconstitution inflammatory syndrome (IRIS) can also occur. 161 In the setting of some OIs, such as cryptococcal meningitis, for which immediate therapy may increase the risk of serious immune reconstitution inflammatory syndrome (IRIS), a short delay before initiating ART may be warranted. In the setting of other OIs, such as Pneumocystis jirovecii pneumonia, early initiation of ART is associated with increased survival; 10 therefore, therapy should not be delayed (AI).
In patients who have active TB, initiating ART during treatment for TB confers a significant survival advantage; therefore, ART should be initiated as recommended in Mycobacterium Tuberculosis Disease with HIV Coinfection.
Clinicians should refer to the Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents 161 for more detailed discussion on when to initiate ART in the setting of a specific OI.
# Conditions Where Deferral of Therapy May be Considered
Some patients and their clinicians may decide to defer therapy on the basis of clinical or personal circumstances. Deferring therapy for the reasons discussed below may be reasonable in patients with high CD4 counts (e.g., >500 cells/mm 3 ), but deferring therapy in patients with much lower CD4 counts (e.g., <200 cells/mm 3 ) should be considered only in rare situations and should be undertaken with close clinical follow-up. Briefly delaying therapy to allow a patient more time to prepare for lifelong treatment may be considered.
# When There are Significant Barriers to Adherence
Also see Adherence to Antiretroviral Therapy.
In patients with higher CD4 counts who are at risk of poor adherence, it may be prudent to defer treatment while addressing the barriers to adherence. However, in patients with conditions that require urgent initiation of ART (see above), therapy should be started while simultaneously addressing the barriers to adherence.
Several methods are available to assess adherence. When the most feasible measure of adherence is selfreport, this assessment should be completed at each clinic visit using one of the available reliable and valid instruments. 170,171 If other objective measures (e.g., pharmacy refill data, pill count) are available, these methods should be used to assess adherence at each follow-up visit. Continual assessment and counseling allow the clinician to intervene early to address barriers to adherence occurring at any point during treatment (see Adherence to Antiretroviral Therapy).
# Presence of Comorbidities that Complicate or Prohibit Antiretroviral Therapy
Deferral of ART may be considered when either the treatment or manifestations of other medical conditions may complicate the treatment of HIV infection or vice versa. Examples include:
- Surgery that may result in an extended interruption of ART
- Treatment with medications that have clinically significant drug interactions with ART and for which alternative medications are not available
In each of these circumstances, the assumption is that the situation is temporary and that ART will be initiated after the conflicting condition has resolved.
There are some less common situations that preclude ART at any time while CD4 counts remain high. In particular, such situations include that of patients who have a poor prognosis because of a concomitant medical condition and are not expected to gain survival or quality-of-life benefits from ART. Examples include patients with incurable non-HIV-related malignancies or end-stage liver disease who are not being considered for liver transplantation. In this setting, deciding to forgo ART may be easier in patients with higher CD4 counts who are likely asymptomatic for HIV and in whom ART is unlikely to prolong survival. However, it should be noted that ART may improve outcomes, including survival, in patients with some HIV-associated malignancies (e.g., lymphoma, Kaposi sarcoma) and in patients with liver disease due to chronic HBV or HCV.
# Long-term Non-Progressors and Elite HIV Controllers
A small subset of HIV-infected individuals (~3% to 5%) can maintain normal CD4 counts for many years without treatment (long-term non-progressors), and an even smaller subset (~1%) can maintain low to undetectable HIV RNA levels for years (elite controllers). 175,176 Although there is significant overlap in these clinical phenotypes, many long-term non-progressors have detectable viremia and some controllers progress immunologically and clinically despite having no detectable viremia.
There are limited data on how to manage these individuals. Given potential harm associated with uncontrolled HIV replication, many of the preceding arguments for early therapy likely apply to nonprogressors who have consistently detectable viremia (i.e., HIV RNA >200 to 1000 copies/mL). Given that ongoing HIV replication occurs even in controllers, ART is also recommended for those rare controllers with evidence of disease progression, as defined by declining CD4 counts or development of HIV-related complications (AII). The Panel has no recommendations on managing controllers with high CD4 counts, although the fact that ART reduces the level of inflammation in this setting suggests that treatment may be beneficial. 177
# The Need for Early Diagnosis of HIV
Fundamental to the earlier initiation of ART recommended in these guidelines is the assumption that patients will be diagnosed early in the course of HIV infection, making earlier initiation of therapy an option. Unfortunately, most HIV-infections are diagnosed at later stages of disease, although in recent years, HIV is increasingly being detected earlier. 4 Despite the recommendations for routine, opt-out HIV screening in the health care setting regardless of perceptions about a patient's risk of infection, 182 the median CD4 count of newly diagnosed patients remains below 350 cells/mm 3 , although this number is increasing. 4 Diagnosis of HIV infection is delayed more often in nonwhites, IDUs, and older patients than in other populations, and many individuals in these groups develop AIDS-defining illnesses within 1 year of diagnosis. Therefore, to ensure that the current treatment guidelines have maximum impact, routine HIV screening per current CDC recommendations is essential. It is also critical that all newly diagnosed patients are educated about HIV disease and linked to care for full evaluation, follow-up, and management. Once patients are in care, focused effort is required to retain them in the health care system so that both the infected individuals and their sexual partners can fully benefit from early diagnosis and treatment.
# Conclusion
The current recommendations are based on growing evidence supporting earlier initiation of ART and the lack of demonstrable harm in starting therapy earlier. The strength of each recommendation varies according to the quality and availability of existing evidence supporting the recommendation. In addition to the benefit of earlier initiation of therapy for the health of the HIV-infected individual, the reduction in sexual transmission to HIV-uninfected individuals provides further reason for earlier initiation of ART. The Panel will continue to monitor and assess the results of ongoing and planned randomized clinical trials and observational studies, which will provide information to guide future Panel recommendations.
# Introduction
More than 25 antiretroviral (ARV) drugs in 6 mechanistic classes are Food and Drug Administration (FDA) approved for treatment of HIV infection. These six classes include the nucleoside/nucleotide reverse transcriptase inhibitors (NRTIs), non-nucleoside reverse transcriptase inhibitors (NNRTIs), protease inhibitors (PIs), a fusion inhibitor (FI), a CCR5 antagonist, and integrase strand transfer inhibitors (INSTIs).
In addition, two drugs (pharmacokinetic enhancers or boosters) are used solely to improve the pharmacokinetic profiles of some ARV drugs (e.g., PIs and the INSTI elvitegravir ).
The initial ARV regimen for a treatment-naive patient generally consists of two NRTIs, usually abacavir plus lamivudine (ABC/3TC) or tenofovir disoproxil fumarate plus emtricitabine (TDF/FTC), plus a drug from one of three drug classes: an INSTI, an NNRTI, or a PK-enhanced PI. As shown in clinical trials and by retrospective evaluation of cohorts of patients in clinical care, this strategy for initial treatment has resulted in HIV RNA decreases and CD4 T lymphocyte (CD4) cell increases in most patients.
# Data Used for Making Recommendations
The Panel on Antiretroviral Guidelines for Adults and Adolescents (the Panel)'s recommendations are primarily based on clinical trial data published in peer-reviewed journals and data prepared by manufacturers for FDA review. In select cases, the Panel considers data presented in abstract format at major scientific meetings. The Panel's first criterion for selection of evidence on which to base recommendations is published information from a randomized, prospective clinical trial with an adequate sample size that demonstrates that an ARV regimen has shown high rates of viral suppression, increased CD4 cell count, and has a favorable
# Panel's Recommendations
- An antiretroviral regimen for a treatment-naive patient generally consists of two nucleoside reverse transcriptase inhibitors in combination with a third active antiretroviral drug from one of three drug classes: an integrase strand transfer inhibitor, a nonnucleoside reverse transcriptase inhibitor, or a protease inhibitor with a pharmacokinetic enhancer (cobicistat or ritonavir).
- - On the basis of individual patient characteristics and needs, an Alternative regimen or; less frequently, an Other regimen; may in some instances be the optimal regimen for a patient. A list of Alternative and Other regimens can be found in Table 6.
- Given the large number of excellent options for initial therapy, selection of a regimen for a particular patient should be guided by factors such as virologic efficacy, toxicity, pill burden, dosing frequency, drug-drug interaction potential, resistance testing results, comorbid conditions, and cost. Table 7 provides guidance on choosing an antiretroviral regimen based on selected clinical case scenarios. Table 8 highlights the advantages and disadvantages of different components in a regimen.
# Rating of Recommendations: A = Strong; B = Moderate; C = Optional
# Rating of Evidence: I = Data from randomized controlled trials; II = Data from well-designed nonrandomized trials or observational cohort studies with long-term clinical outcomes; III = Expert Opinion
a Lamivudine may substitute for emtricitabine or vice versa.
Downloaded from on 9/16/2015
Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents F-2 safety profile. Comparative clinical trials of initial treatments generally show no significant differences in HIV-related clinical endpoints or survival. Thus, assessment of regimen efficacy and safety are primarily based on surrogate marker endpoints (especially rates of HIV RNA suppression) and the incidence and severity of adverse events. When developing recommendations, the Panel also considers post-marketing safety data, observational cohort data published in peer-reviewed publications, and the experience of clinicians and community members who are actively engaged in patient care.
The Panel reviewed the available data to arrive at Recommended, Alternative, or Other regimens, as specified in Table 6. Each of the regimens listed in Table 6 has shown potent virologic efficacy as measured by the proportion of participants in comparative clinical trials able to achieve and maintain viral suppression.
Recommended regimens are those studied in randomized controlled trials and shown to have optimal and durable virologic efficacy, favorable tolerability and toxicity profiles, and ease of use. Alternative regimens are those that are effective but have potential disadvantages, limitations for use in certain patient population, or less supporting data than Recommended regimens. In certain situations, depending on individual patient characteristics and needs, an Alternative regimen may actually be the optimal regimen for a specific patient. Some regimens are classified as Other regimens because, compared with Recommended or Alternative regimens, they have reduced virologic activity, limited supporting data from large comparative clinical trials, or other factors such as greater toxicities, higher pill burden, drug interaction potential, or limitations for use in certain patient populations.
In addition to Table 6, a number of tables presented below and at the end of the guidelines provide clinicians with guidance on selecting and prescribing an optimal regimen for an individual patient. Table 7 lists specific case scenarios to guide regimen selection for patients with common clinical conditions. Table 8 lists the potential advantages and disadvantages of the components used in Recommended and Alternative regimens. Table 9 lists agents or regimens not recommended for initial treatment. Appendix B, Tables 1-6 lists characteristics of individual ARV agents, such as formulations, dosing recommendations, PKs, and common adverse effects. Appendix B, Table 7 provides ARV dosing recommendations for patients who have renal or hepatic insufficiency.
# Changes Since the Last Revision of the Guidelines
Since the last revision of these guidelines, new data from clinical trials and cohort studies, as well as experience in clinical practice, have prompted significant changes to the list of Recommended, Alternative, and Other regimens for treatment-naive patients (Table 6). Among these changes, the following deserve emphasis:
- There are now five Recommended regimens for antiretroviral therapy (ART)-naive patients: four INSTIbased regimens and one ritonavir-boosted PI (PI/r)-based regimen.
- Results from a large comparative clinical trial comparing atazanavir/ritonavir (ATV/r) plus TDF/FTC to darunavir/ritonavir (DRV/r) or raltegravir (RAL) plus TDF/FTC showed a greater rate of toxicitiesrelated discontinuation in the ATV/r arm. 4 Therefore, ATV/r plus TDF/FTC has been moved from the Recommended to the Alternative category.
- The Panel has also moved EFV/TDF/FTC from the Recommended to the Alternative category because of concerns about the tolerability of efavirenz (EFV) in clinical trials and practice, especially the high rate of central nervous system (CNS) related toxicities, and a possible association with suicidality observed in one analysis of four clinical trials. 5 - Regimens that were previously listed as Recommended for patients with baseline HIV RNA 200 cells/mm 3 are now in the Alternative or Other category, with the same caveat to limit their use to patients with the cited HIV RNA and CD4 levels.
- Two regimens that use fewer than two NRTIs (DRV/r plus RAL and lopinavir/ritonavir plus 3TC) are listed among the Other regimens, with the caveat that their use be limited to patients who cannot take either TDF or ABC.
Downloaded from on 9/16/2015
Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents F-3
- Coformulations of ATV and DRV with the PK enhancer cobicistat (COBI) have been added to the Alternative regimen options. An ARV regimen generally consists of two NRTIs (one of which is FTC or 3TC) plus an INSTI, NNRTI, or PKenhanced PI. Selection of a regimen should be individualized on the basis of virologic efficacy, potential adverse effects, pill burden, dosing frequency, drug-drug interaction potential, a patient's resistance test results and comorbid conditions, and cost. Table 7 lists specific case scenarios to guide regimen selection for patients with common clinical conditions. For more detailed recommendations on ARV choices and dosing in HIV-infected pregnant women, refer to the latest perinatal guidelines available at .
# Recommended Regimen Options
(Drug classes and regimens within each class are arranged in alphabetical order.)
INSTI-Based Regimens:
- DTG/ABC/3TC a -only for patients who are HLA-B*5701 negative (AI)
- DTG plus TDF/FTC a (AI)
- EVG/c/TDF/FTC-only for patients with pre-treatment estimated CrCl ≥70 mL/min (AI)
- RAL plus TDF/FTC a (AI)
PI-Based Regimens:
- DRV/r plus TDF/FTC a (AI)
# Alternative Regimen Options
(Drug classes and regimens within each class are arranged in alphabetical order.)
Regimens that are effective and tolerable, but that have potential disadvantages when compared with the recommended regimens listed above, have limitations for use in certain patient population, or have less supporting data from randomized clinical trials. An alternative regimen may be the preferred regimen for some patients.
# NNRTI-Based Regimens:
- EFV/TDF/FTC a (BI)
- RPV/TDF/FTC a -only for patients with pre-treatment HIV RNA 200 cells/mm 3 (BI) PI-Based Regimens:
- ATV/c plus TDF/FTC a -only for patients with pre-treatment estimated CrCl ≥70 mL/min (BI)
- ATV/r plus TDF/FTC a (BI)
# Other Regimen Options
(Drugs classes and regimens within each class are arranged in alphabetical order.)
Regimens that, in comparison with Recommended and Alternative regimens, may have reduced virologic activity, limited supporting data from large comparative clinical trials, or other factors such as greater toxicities, higher pill burden, drug interaction potential, or limitations for use in certain patient populations.
# INSTI-Based Regimen:
- RAL plus ABC/3TC a -only for patients who are HLA-B*5701 negative (CII) NNRTI-Based Regimen:
- EFV plus ABC/3TC a -only for patients who are HLA-B*5701 negative and with pre-treatment HIV RNA <100,000 copies/mL (CI)
PI-Based Regimens:
- (ATV/c or ATV/r) plus ABC/3TC a -only for patients who are HLA-B*5701 negative and with pre-treatment HIV RNA <100,000 copies/mL (CIII for ATV/c and CI for ATV/r)
- LPV/r (once b or twice daily) plus ABC/3TC a -only for patients who are HLA-B*5701 negative (CI)
- LPV/r (once b or twice daily) plus TDF/FTC a (CI)
Other Regimens When TDF or ABC Cannot be Used:
- DRV/r plus RAL-only for patients with pre-treatment HIV RNA 200 cells/mm 3 (CI)
- LPV/r (twice daily) plus 3TC (twice daily) (CI) In some situations, an NNRTI-based regimen may be a better choice for a particular patient. Table 7 provides guidance on regimen selection based on various patient-and regimenspecific characteristics.
# Rating of Recommendations
# Other Regimen Options
Regimens that, in comparison with Recommended and Alternative regimens, may have reduced virologic activity, limited supporting data from large comparative clinical trials, or other factors such as greater toxicities, higher pill burden, drug interaction potential, or limitations for use in certain patient populations.
# Factors to Consider When Selecting an Initial Regimen
When selecting a regimen for an individual patient, a number of patient and regimen specific characteristics should be considered, with the goal of providing a potent, safe, tolerable, and easy to adhere to regimen for the patient in order to achieve sustained virologic control. Some of the factors can be grouped into the following categories: This table is designed to guide clinicians in choosing an initial ARV regimen according to various patient and regimen characteristics and specific clinical scenarios. When more than one scenario applies to a patient, clinicians should review considerations for each relevant scenario and use their clinical judgment to select the most appropriate regimen. This table is intended to guide the initial choice of regimen. However, if a patient is doing well on a particular regimen, it is not necessary to switch to another regimen based on the scenarios outlined in this table.
Please see Table 8 for additional information regarding the advantages and disadvantages of particular ARV medications.
# Pre-ART Characteristics
CD4 count <200 cells/mm 3 Do Not Use the Following Regimens:
# ART Specific Characteristics
One pill once daily regimen desired ART Options Include:
- DTG/ABC/3TC
- EFV/TDF/FTC
- EVG/c/TDF/FTC
- RPV/TDF/FTC (if HIV RNA 200/mm 3 )
# Available as fixed-dose combination tablets
Food effects Regimens that Should be Taken with Food:
- ATV/r or ATV/c-based regimens
# HCV treatment required
Refer to recommendations in the HIV/HCV co-infection section.
# TB infection
If Rifampin is Used:
- EFV-based regimens have the least drugdrug interactions.
- If RAL is used, increase RAL dose to 800 mg BID.
- Use DTG at 50 mg BID dose only in patients without selected INSTI mutations (refer to product label).
If using a PI-based regimen, rifabutin should be used in place of rifampin in the TB regimen.
# Choosing Between an Integrase Strand Transfer Inhibitor-, A Non-Nucleoside Reverse Transcriptase Inhibitor-, or A Protease Inhibitor-Based Regimen
The choice between an INSTI, NNRTI, or PI as the third drug in an initial ARV regimen should be guided by the regimen's efficacy, genetic barrier to resistance, adverse effects profile, and convenience; the patient's comorbidities; and concomitant medications and the potential for drug-drug interactions (See Tables 7 and 8 showed that ATV/r had a higher rate of adverse effect-associated drug discontinuation with than the comparators (DRV/r and RAL). Thus, despite these favorable attributes, based on the above considerations, EFV-, RPV-, and ATV/r-containing regimens are no longer Recommended Regimens as initial therapy in all patients, and are listed as Alternatives. However, based on individual patient characteristics, some Alternative regimens may actually be the optimal regimen for some patients. Furthermore, patients who are doing well on EFV-, RPV-, and ATV/r-containing regimens should not necessarily be switched to other agents.
# Choosing Among Different Drugs from an Antiretroviral Drug Class
The sections below provides clinicians with comparisons of different currently recommended ARV drugs within a drug class, including information related to the safety and virologic efficacy of different drugs based on clinical trial results and/or post-marketing data, special considerations to take into account, and the rationales for the Panel's recommendations.
# Dual-Nucleoside Reverse Transcriptase Inhibitor Options A Part of Initial Combination Therapy
# Summary
TDF/FTC and ABC/3TC are NRTI combinations commonly used for initial therapy. Table 6 provides recommendations and ratings for the individual regimens. These recommendations are based on the virologic potency and durability, short-and long-term toxicity, and dosing convenience of these drugs.
# Clinical Trials Comparing Abacavir/Lamivudine to Tenofovir/Emtricitabine
Several randomized controlled trials in ART-naive participants compared ABC/3TC to TDF/FTC, each with the same or a different third ARV drug (also see discussion in the DTG section). 10 - The ACTG 5202 study, a randomized controlled trial in more than 1,800 participants, evaluated the efficacy and safety of ABC/3TC and TDF/FTC when each used in combination with either EFV or ATV/r.
- Treatment randomization was stratified on the basis of a screening HIV RNA level <100,000 copies/mL or ≥100,000 copies/mL. HLA B*5701 testing was not required before study entry.
- A Data Safety Monitoring Board recommended early termination of the ≥100,000 copies/mL stratification group because of a significantly shorter time to study-defined virologic failure in the ABC/3TC arm than in the TDF/FTC arm. 7 This difference in time to virologic failure between the arms was observed regardless of whether the third active drug was EFV or ATV/r.
- There was no difference between ABC/3TC and TDF/FTC in time to virologic failure for participants who had plasma HIV RNA <100,000 copies/mL at screening. 11 - The ASSERT study compared open label ABC/3TC with TDF/FTC in 385 HLA B*5701-negative, ARTnaive patients; all participants also received EFV. The primary study endpoint was renal safety of the regimens. At week 48, the proportion of participants with HIV RNA <50 copies/mL was lower among ABC/3TC-treated participants than among TDF/FTC-treated participants. 8 - In the HEAT study, 688 participants received ABC/3TC or TDF/FTC in combination with once-daily LPV/r. Virologic efficacy was similar in the two study arms. In a subgroup analysis of patients with baseline HIV RNA ≥100,000 copies/mL, the proportion of participants who achieved HIV RNA <50 copies/mL at 96 weeks did not differ between the two regimens. 9
# Dual-Nucleoside Reverse Transcriptase Inhibitor Choices
Note: In alphabetical order.
# Abacavir/Lamivudine
ABC plus 3TC has been studied in combination with EFV, several PIs, and DTG in ART-naive patients. 10, Adverse Effects:
Hypersensitivity Reactions:
- Clinically suspected hypersensitivity reactions (HSRs) were observed in 5% to 8% of individuals who started ABC in clinical trials conducted before the use of HLA-B*5701 testing. The risk of HSRs is highly associated with the presence of the HLA-B*5701 allele. 15,16 Cardiovascular Risk:
- An association between ABC use and myocardial infarction (MI) was first reported in the D:A:D study. This large, multinational observational study group found that recent (within 6 months) or current use of ABC was associated with an increased risk of MI, particularly in participants with pre-existing cardiac risk factors. 17,18 - Since the D:A:D report, several studies have evaluated the relationship between ABC therapy and cardiovascular events. Some studies have found an association; others, including an FDA metaanalysis of 26 randomized clinical trials that evaluated ABC, have not. - No consensus has been reached on the association between ABC use and MI risk or the mechanism for such an association.
Other Factors and Considerations:
- ABC/3TC is available as a co-formulated tablet and as a coformulated single-tablet regimen with DTG.
- ABC and 3TC are available separately in generic tablet formulations. - ABC does not cause renal dysfunction and is an option for TDF in patients with underlying renal dysfunction or who are at risk for renal effects. No dosage adjustment is required in patients with renal dysfunction.
Panel's Recommendations:
- ABC should only be prescribed for patients who are HLA B*5701 negative.
- On the basis of clinical trial safety and efficacy data, experience in clinical practice, and the availability of ABC/3TC as a component of co-formulated products, the Panel classifies ABC/3TC plus DTG as a Recommended regimen (AI) (see discussion regarding DTG in this section regarding the clinical efficacy data for ABC/3TC plus DTG) .
- ABC/3TC use with EFV, ATV/r, or ATV/c is only recommended for patients with pre-treatment HIV RNA <100,000 copies/mL.
- ABC/3TC is a part of several Alternative or Other regimens when combined with another ARV drug. See Table 6 for more detailed recommendations on use of ABC/3TC with other drugs.
- ABC should be used with caution or avoided in patients with known high cardiovascular risk.
# Tenofovir/Emtricitabine
TDF, with either 3TC or FTC, has been studied in combination with EFV, RPV, several boosted PIs, EVG/c, RAL, and DTG in randomized clinical trials. Adverse Effects:
- New onset or worsening renal impairment has been associated with TDF use. 38,39 Risk factors may include advanced HIV disease; longer treatment history; low body weight, especially in females; 40 and pre-existing renal impairment. 41 - Concomitant use of a PK-enhanced regimen (with a PI or EVG) can increase TDF concentrations; studies have suggested a greater risk of renal dysfunction when TDF is used in these regimens. 39, - While initiation of all NRTI-containing regimens has been associated with a decrease in bone mineral density (BMD), the loss of BMD is greater with TDF-containing regimens. For example, in two randomized studies comparing TDF/FTC with ABC/3TC, participants receiving TDF/FTC experienced a significantly greater decline in bone mineral density than ABC/3TC-treated participants. 47,48 Following an early decline after ART initiation, BMD generally stabilizes.
- Cases of osteomalacia associated with proximal renal tubulopathy have been reported with the use of TDF. 49 Other Factors and Considerations:
- TDF/FTC is available in fixed-dose drug combinations with EFV, EVG/c, and RPV, allowing the regimens to be administered as a single pill, given once daily.
- Renal function, urine glucose, and urine protein should be assessed before initiating treatment with TDF and periodically during treatment (see Laboratory Monitoring section). In patients who have pre-existing renal insufficiency (CrCl <60 mL/min), 50 TDF should generally be avoided. If TDF is used, dosage adjustment is required if the patient's CrCl falls below 50 mL/min (see Appendix B, Table 7 for dosage recommendations).
- Both TDF and FTC are active against HBV. In patients with HIV/HBV coinfection, TDF/FTC should be used as the NRTI pair of the ART regimen because the drugs have activity against both viruses (also see HIV/HBV Coinfection section). - The FLAMINGO study, a randomized open-label clinical trial, compared DTG 50 mg once daily to DRV/r 800 mg/100 mg once daily, each in combination with investigator-selected ABC/3TC or TDF/FTC. At week 48, DTG was superior to DRV/r because of the higher rate of discontinuation in the DRV/r arm. 6,52 The difference in response rates favoring DTG was greater in patients with pre-treatment HIV RNA levels >100,000 copies/mL. At week 96, DTG remained superior to DRV/r. 53 Adverse Effects:
- DTG is generally well tolerated. The most common adverse reactions of moderate to severe intensity with an incidence ≥2% in the clinical trials were insomnia and headache. Cases of hypersensitivity reactions were reported in <1% of trial participants.
Other Factors and Considerations:
- In treatment-naive patients, DTG is given once daily, with or without food. - DTG decreases tubular secretion of creatinine without affecting glomerular function, with increases in serum creatinine observed within the first 4 weeks of treatment (mean increase in serum creatinine was 0.11 mg/dL after 48 weeks).
- DTG has few drug interactions. DTG increases metformin levels approximately two-fold; close monitoring for metformin adverse effects is advisable. Rifampin decreases DTG levels, therefore, an increase in dosing of DTG to 50 mg twice daily is required.
- DTG absorption may be reduced when the ARV is coadministered with polyvalent cations (see Drug Interaction section). DTG should be taken at least 2 hours before or 6 hours after cation-containing antacids or laxatives. Alternatively, DTG and supplements containing calcium or iron can be taken simultaneously with food.
- Treatment-emergent mutations that confer DTG resistance have not been reported in patients receiving DTG for initial therapy, which suggests that DTG has a higher genetic barrier to resistance than other INSTIs.
Panel's Recommendation:
- On the basis of clinical trial data, the Panel categorizes DTG in combination with either ABC/3TC or TDF/FTC as a Recommended regimen in ART-naive patients (AI).
# Elvitegravir
EVG is available as a component of a four-drug, fixed-dose combination product containing EVG, COBI, TDF, and FTC (EVG/c/TDF/FTC). COBI is a specific, potent CYP3A inhibitor that has no activity against HIV. It acts as a PK enhancer of EVG, which allows for once daily dosing of the combination.
Efficacy in Clinical Trials:
The efficacy of EVG/c/TDF/FTC in ARV-naive participants has been evaluated in two randomized, doubleblind active-controlled trials.
- At 144 weeks, EVG/c/TDF/FTC was non-inferior to fixed-dose EFV/TDF/FTC. 54 - EVG/c/TDF/FTC was also found to be non-inferior to a combination containing ATV/r plus TDF/FTC. 55 Adverse Effects:
- The most common adverse events reported with EVG/c/TDF/FTC were diarrhea, nausea, upper respiratory infection, and headache. 54,55 Other Factors and Considerations:
- EVG is metabolized primarily by CYP3A enzymes; as a result, CYP3A inducers or inhibitors may alter EVG concentrations.
- Because COBI inhibits CYP3A, it interacts with a number of medications that are metabolized by this enzyme (see Drug-Drug Interactions section). 56 - EVG plasma concentrations are lower when the ARV is administered simultaneously with polyvalent cation-containing antacids or supplements (see Drug Interaction section). Separate EVG/cobi/TDF/FTC and polyvalent antacid administration by at least 2 hours; administer polyvalent cation-containing supplements at least 2 hours before or 6 hours after EVG dosing.
- COBI inhibits active tubular secretion of creatinine, resulting in increases in serum creatinine and a reduction in estimated CrCl without reducing glomerular function. 57 Patients with a confirmed increase in serum creatinine greater than 0.4 mg/dL from baseline while taking EVG/c/TDF/FTC should be closely monitored and evaluated for evidence of TDF-related proximal renal tubulopathy. 46 - EVG/c/TDF/FTC is not recommended for patients with pre-treatment estimated CrCl <70 mL/min. 46 - At the time of virologic failure, INSTI-associated mutations were detected in some EVG/c/TDF/FTCtreated patients whose therapy failed. 54,55 These mutations conferred cross-resistance to RAL, with most retaining susceptibility to DTG.
Panel's Recommendation:
- On the basis of the above factors, the Panel classifies EVG/c/FTC/TDF as a Recommended regimen in ART-naive patients (AI).
# Raltegravir
RAL was the first INSTI approved for use in both ARV-naive and ARV-experienced patients.
Efficacy in Clinical Trials:
The efficacy of RAL (with either TDF/FTC or ABC/3TC) as initial therapy has been evaluated in two randomized, double-blinded, controlled clinical trials, and a third open-label randomized trial.
- STARTMRK compared RAL 400 mg twice daily to EFV 600 mg once daily, each in combination with TDF/FTC. RAL was non-inferior to EFV at 48 weeks. 33 RAL was superior to EFV at 4 and 5 years, 36,58 in part because of more frequent discontinuations due to adverse events in the EFV group than in the RAL group.
- The SPRING-2 trial compared DTG 50 mg once daily to RAL 400 mg twice daily, each in combination with investigator-selected ABC/3TC or TDF/FTC. At week 96, DTG was non-inferior to RAL.
- The SPRING-2 trial also provided non-randomized data on the efficacy of RAL plus ABC/3TC. In this trial, 164 participants (39 and 125 with baseline viral loads ≥100,000 copies/mL and <100,000 copies/mL, respectively) received RAL in combination with ABC/3TC. After 96 weeks, there was no difference in virologic response between the ABC/3TC and TDF/FTC groups when RAL was given as the third drug. 37 - ACTG A5257, a large randomized open-label trial, compared 3 NNRTI-sparing regimens containing RAL, ATV/r, or DRV/r, each given with TDF/FTC. At week 96, all 3 regimens had similar virologic efficacy, but RAL was superior to both ATV/r and DRV/r for the combined endpoints of virologic efficacy and tolerability. Lipids increased more in participants in the PI/r arms than in the RAL arm, and bone mineral density decreased to a greater extent in participants in the PI/r arms than in participants in the RAL arm. 4 Adverse Effects:
- RAL use has been associated with creatine kinase elevations. Myositis and rhabdomyolysis have been reported.
- Rare cases of severe skin reactions and systemic hypersensitivity reactions in patients who received RAL have been reported during post-marketing surveillance. 59 Other Factors and Considerations:
- RAL must be administered twice daily-a potential disadvantage when comparing RAL-based treatment with other Recommended regimens.
- Coadministration of RAL with aluminum and/or magnesium-containing antacids can reduce absorption of RAL and is not recommended. Raltegravir may be coadministered with calcium carbonate-containing antacids. Polyvalent cation-containing supplements may also reduce absorption of RAL; thus, RAL should be given at least 2 hours before or 6 hours after cation-containing supplements.
- RAL has a lower genetic barrier to resistance than RTV-boosted PIs and DTG.
Panel's Recommendations:
- On the basis of these data and long-term clinical experience with RAL, the Panel considers RAL plus TDF/FTC as a Recommended regimen in ARV-naive patients (AI).
# Efavirenz
EFV is an NNRTI approved for use in combination with 2-NRTIs for ART-naive patients.
# Efficacy in Clinical Trials:
Large randomized, controlled trials and cohort studies in ART-naive patients have demonstrated potent and durable viral suppression in patients treated with EFV plus two NRTIs. In clinical trials, EFV-based regimens in ART-naive patients have demonstrated superiority or non-inferiority to several comparator regimens.
- In ACTG 5142, EFV was superior to LPV/r, although drug resistance was more common after EFV failure than after LPV/r failure. 63 - In the 2NN study, compared to EFV, NVP did not meet non-inferiority criteria. 64 - In ACTG 5202, EFV was comparable to ATV/r when each was given with either TDF/FTC or ABC/3TC. 65 - In the ECHO and THRIVE studies, EFV was non-inferior to RPV, with less virologic failure but more discontinuations due to adverse events. The virologic advantage of EFV was most notable in participants with pre-ART viral loads >100,000 copies/mL, and NRTI and NNRTI resistance was more frequent with RPV failure. 66 - In the GS 102 study, EFV/TDF/FTC was non-inferior to EVG/c/TDF/FTC. 54 More recently, some regimens have demonstrated superiority to EFV, based primarily on fewer discontinuations because of adverse events:
- In the SINGLE trial, a DTG-based regimen was superior to EFV at the primary endpoint of viral suppression at Week 48. 10 - In the STARTMRK trial, RAL was non-inferior to EFV at 48 weeks. 33 5 years, 36,58 in part because of more frequent discontinuations due to adverse events in the EFV group than in the RAL group.
- In the open-label STaR trial, participants with baseline viral loads ≤100,000 copies/mL had higher rates of treatment success on RPV than on EFV. 67 A recent multinational randomized placebo-controlled trial compared two once daily doses of EFV (combined with TDF/FTC): EFV 600 mg (standard dose) versus EFV 400 mg (reduced dose). At 48 weeks, EFV 400 mg was non-inferior to EFV 600 mg for rate of viral suppression. 68 Study drug-related adverse events were less frequent in the EFV 400 mg group than in the 600 mg group. Although there were fewer self-reported CNS events in the 400 mg group, the two groups had similar rates of psychiatric events. Unlike the 600 mg dose of EFV, the 400 mg dose is not approved for initial treatment and is not co-formulated as a component of a single pill regimen.
Adverse Effects:
- EFV can cause CNS side effects, such as abnormal dreams, dizziness, headache, and depression, which resolve over a period of days to weeks in most patients. However, more subtle, long-term neuropsychiatric effects can occur. A recent analysis of 4 AIDS Clinical Trial Group (ACTG) comparative trials showed a higher rate of suicidality (i.e., reported suicidal ideation or attempted or completed suicide) among EFV-treated patients than among patients taking comparator regimens. 5 This association, however, was not found in analyses of two large observational cohorts. 69,70 - EFV may cause elevation in LDL cholesterol and triglycerides.
Other Factors and Considerations:
- EFV is formulated both as a single-drug tablet and in a fixed-dose combination tablet of EFV/TDF/FTC that allows for once daily dosing.
- EFV is a substrate of CYP3A4 and an inducer of CYP3A4 and 2D6 and therefore may potentially interact with other drugs using the same pathways.
- EFV has been associated with CNS birth defects in non-human primates, and cases of neural tube defects have been reported after first trimester exposure in humans. 71 Alternative regimens should be considered in women who are planning to become pregnant or who are sexually active and not using effective contraception. Because the risk of neural tube defects is restricted to the first 5 to 6 weeks of pregnancy, before pregnancy is usually recognized, a suppressive EFV-based regimen can be continued in pregnant women who present for antenatal care in the first trimester, or may be initiated after the first trimester (see Perinatal Guidelines).
Panel's Recommendations:
- Given the availability of regimens with fewer treatment-limiting adverse events with non-inferior or superior efficacy, the Panel classifies EFV/TDF/FTC as an Alternative regimen for ART-naive patients (BI).
- Given virologic and pharmacogenetic parameters that limit its use in some patients, the Panel recommends EFV with ABC/3TC as an Other regimen, and only for patients with a pre-ART viral load <100,000 copies/mL and negative HLA B*5701 status (see discussion in ABC/3TC section) (CI).
- EFV at a reduced dose has not been studied in the U.S. population. The Panel cannot recommend use of reduced dose EFV until further data to support its use in the U.S. population are available.
# Rilpivirine
RPV is an NNRTI approved for use in combination with NRTIs for ART-naive patients with pre-treatment viral loads <100,000 copies/mL.
# Efficacy in Clinical Trials:
Two Phase 3 randomized, double-blinded clinical trials, ECHO and THRIVE, compared RPV and EFV, each combined with 2 NRTIs. 66 At 96 weeks, the following findings were reported:
- RPV was non-inferior to EFV overall.
- Among participants with a pre-ART viral load >100,000 copies/mL, more RPV-treated than EFV-treated participants experienced virologic failure. Moreover, in this subgroup of participants with virologic failure, NNRTI and NRTI resistance was more frequently identified in those treated with RPV.
- Among the RPV-treated participants, the rate of virologic failure was greater in those with pre-treatment CD4 counts <200 cells/mm 3 than in those with CD4 counts ≥200 cells/mm 3 .
STaR, a Phase 3b, open-label study, compared the fixed-dose combinations of RPV/TDF/FTC and EFV/TDF/FTC in 786 treatment-naive patients. At 96 weeks, the following key findings were reported: 67 - RPV was non-inferior to EFV overall.
- RPV was superior to EFV in patients with pre-ART viral loads ≤100,000 copies/mL and non-inferior in those with pre-ART viral loads >100,000 copies/mL. In patients with pre-ART viral loads >500,000 copies/mL., virologic failure was more common in RPV-treated patients than in EFV-treated patients.
- At 48 weeks, NRTI and NNRTI resistance occurred in 2% and 1% of RPVand EFV-treated patients, respectively, with viral loads ≤100,000; in 5% and 0% of RPVand EFV-treated patients, respectively, with viral loads 100,000 to 500,000; and in 19% and 4% of RPVand EFV-treated patients, respectively, with viral loads >500,000 copies/mL.
Adverse Effects:
- RPV is generally well tolerated. In the ECHO, THRIVE, and STaR trials, fewer CNS adverse events (e.g., abnormal dreams, dizziness, psychiatric side effects), skin rash, and dyslipidemia were reported in the RPV arms than the EFV arms, and fewer patients in the RPV arms discontinued therapy due to adverse events.
Other Factors and Considerations:
- RPV is formulated both as a single-drug tablet and in a fixed-dose combination tablet with TDF/FTC. Among available single pill regimens, it is the smallest tablet.
- RPV/TDF/FTC is given as a once daily regimen, and must be administered with a meal (at least 400 kcal).
- The oral drug absorption of RPV can be significantly reduced in the presence of acid-lowering agents. RPV is contraindicated in patients who are receiving proton pump inhibitors, and should be used with caution in those receiving H2 antagonists or antacids (see Drug Interaction section for dosing recommendations).
- RPV is primarily metabolized in the liver by CYP3A enzyme; its plasma concentration may be affected in the presence of CYP3A inhibitors or inducers (see Drug Interaction section).
- At higher than the approved dose of 25 mg, RPV may cause QTc interval prolongation. RPV should be used with caution when coadministered with a drug known to increase the risk of Torsades de Pointes.
Panel's Recommendations:
- Given the availability of other effective regimens that do not have virologic and immunologic prerequisites to initiate treatment, the Panel recommends RPV/TDF/FTC as an Alternative regimen.
- Use of RPV with TDF/FTC should be limited to ART-naive patients with pre-treatment viral load 200 cells/mm 3 (BI).
- Data on RPV with ABC/3TC are insufficient to consider recommending this regimen as a Recommended, Alternative, or Other regimen. 8 and Appendix B, Table 3.
A number of metabolic abnormalities, including dyslipidemia and insulin resistance, have been associated with PI use. The currently available PIs differ in their propensity to cause these metabolic complications, which also depends on the dose of RTV used as a pharmacokinetic enhancing agent. Two large observational cohort studies suggest that LPV/r, IDV, FPV, or FPV/r may be associated with increased rates of MI or stroke. 18,24 This association was not seen with ATV. 74 Because of the limited number of patients receiving DRV/r, this boosted-PI was not included in the analysis of the two studies.
Recommended PIs for use in ART-naive patients should have proven virologic efficacy, once daily dosing, a low pill count, and good tolerability. On the basis of these criteria, the Panel considers once-daily DRV/r plus TDF/FTC as a Recommended PI. In a large, randomized controlled trial comparing DRV/r, ATV/r, and RAL, all in combination with TDF/FTC, all three regimens achieved similar virologic suppression rates; however, the proportion of patients who discontinued their assigned treatment because of adverse effects was greater in the in the ATV/r arm than in the other two arms. 4 Because of its higher rate of adverse effects, the Panel now classifies ATV/r plus TDF/FTC as an Alternative regimen (BI). ATV/c-and DRV/c-based regimens are considered Alternative PI regimens for the reasons detailed below.
LPV/r has twice the daily dose of RTV as other PI/r and is associated with more metabolic complications and gastrointestinal side effects than PK-enhanced ATV or DRV. LPV/r remains as an Other PI/r because it is currently the only PI co-formulated with RTV and it has extensive experience in clinical trials and practice. Compared to other PIs, FPV/r, unboosted ATV, and SQV/r have disadvantages such as greater pill burden, lower efficacy, or increased toxicity, and thus are no longer included as an option for initial therapy. Nonetheless, patients who are doing well on regimens containing these PIs should not necessarily be switched to other agents.
# Recommended Protease Inhibitor-Based Regimen
# Darunavir/Ritonavir
Efficacy in Clinical Trials:
- The ARTEMIS study compared DRV/r (800/100 mg once daily) with LPV/r (800/200 mg once daily or 400/100 mg twice daily), both in combination with TDF/FTC, in a randomized, open-label, non-inferiority trial. DRV/r was non-inferior to LPV/r at week 48, 31 and superior at week 192. 75 Among participants with baseline HIV RNA levels >100,000 copies/mL, virologic response rates were lower in the LPV/r arm than in the DRV/r arm.
- The FLAMINGO study compared DRV/r with DTG, each in combination with two NRTIs, in 488 ARTnaive participants. The rate of virologic suppression at week 48 was significantly greater among those who received DTG than in those who received DRV/r, largely because of more drug discontinuations in the DRV/r group. 6 - A small retrospective study that followed participants for 48 weeks suggested that DRV/r plus ABC/3TC may be effective in treatment-naive patients. 76 - The ACTG A5257 study showed similar virologic efficacy for DRV/r, ATV/r, and RAL, but more participants in the ATV/r group discontinued randomized treatment because of adverse events. 4 Adverse Effects:
- In the ARTEMIS Study, grades 2 to 4 adverse events, primarily diarrhea, were seen less frequently in DRV/r recipients than in LPV/r recipients.
- Patients starting DRV/r may develop a skin rash, which is usually mild-to-moderately severe and selflimited. Treatment discontinuation is necessary on rare occasions when severe rash with fever or elevated transaminases occur.
Other Factors and Considerations:
- DRV/r is administered once daily with food in treatment-naive patients.
- DRV has a sulfonamide moiety, and should be used with caution in patients with severe sulfonamide allergies. In clinical trials, the incidence and severity of rash were similar in participants who did or did not have a history of sulfonamide allergy. Most patients with sulfonamide allergy are able to tolerate DRV.
- DRV/r is a potent CYP3A4 inhibitor, and may lead to significant interactions with other medications metabolized through this same pathway (see Drug Interactions section).
Panel's Recommendation:
- On the basis of efficacy and safety data from clinical trials and clinical experience, the Panel classifies DRV/r with TDF/FTC as a Recommended regimen (AI). DRV/r with ABC/3TC is considered an Alternative regimen because there are fewer studies to support its use (BII).
# Alternative Protease Inhibitor-Based Regimens
# Atazanavir/Ritonavir or Atazanavir/Cobicistat
Efficacy in Clinical Trials:
- The CASTLE study compared once-daily ATV/r (300/100 mg) with twice-daily LPV/r (400/100 mg), each in combination with TDF/FTC. In this open-label, non-inferiority study, the 2 regimens showed similar virologic and CD4 responses at 48 weeks 30 and at 96 weeks. 77 - The ACTG A5202 study compared open-label ATV/r and EFV, each given in combination with placebocontrolled TDF/FTC or ABC/3TC. Efficacy was similar in the ATV/r and EFV groups. 65 In a separate analysis, women assigned to ATV/r were found to have a higher risk of virologic failure than women assigned to EFV or men assigned to ATV/r. 78 - In a study comparing ATV/r plus TDF/FTC to EVG/c/TDF/FTC, virologic suppression rates through 144 weeks were similar in the two groups. 55 - ACTG A5257, a large randomized open-label trial, compared ATV/r with DRV/r or RAL, each given with TDF/FTC. At week 96, all 3 regimens had similar virologic efficacy. However, a significantly higher proportion of patients in the ATV/r arm discontinued randomized treatment because of adverse events, mostly for elevated indirect bilirubin/jaundice or gastrointestinal toxicities. Lipid changes in participants in the ATV/r and DRV/r arms were similar. Bone mineral density decreased to a greater extent in participants in the ATV/r and DRV/r arms than in participants in the RAL arm. 4 - The Gilead Study 114 enrolled 692 treatment-naive patients. All patients received TDF/FTC and ATV, and were randomized to receive either RTV or COBI as PK enhancers. Both RTV and COBI were given as a separate pill with matching placebos. At 48 weeks, similar percentages of patients achieved virologic suppression, had adverse events, and changes in serum creatinine and indirect bilirubin levels. 79 Adverse Effects:
- The main adverse effect associated with ATV/c or ATV/r is reversible indirect hyperbilirubinemia, with or without jaundice or scleral icterus, but without concomitant hepatic transaminase elevations.
- Nephrolithiasis, nephrotoxicity, 83 and cholelithiasis 84 have also been reported in patients who received ATV, with or without RTV.
- Both ATV/c and ATV/r can cause gastrointestinal side effects including diarrhea.
Other Factors and Considerations:
- ATV/c and ATV/r are dosed once daily and with food.
- ATV requires acidic gastric pH for dissolution. As a result, concomitant use of drugs that raise gastric pH (e.g., antacids, H2 antagonists, and particularly PPIs) may impair absorption of ATV. Table 19a provides recommendations for use of ATV/c or ATV/r with these agents.
- ATV/c and ATV/r are potent CYP3A4 inhibitors and may have significant interactions with other medications metabolized through this same pathway (see Drug Interaction section).
- ATV/c coadministered with TDF/FTC is not recommended for patients with CrCl <70 mL/min.
Panel's Recommendations:
- On the basis of clinical trial safety and efficacy data, the Panel classifies ATV/r and ATV/c plus TDF/FTC as Alternative regimens for ART-naive patients regardless of pre-treatment HIV RNA (BI).
- Because of an inferior virologic response seen in patients with a high baseline viral load, the Panel recommends ATV/r or ATV/c plus ABC/3TC as Other regimens. Use of the regimens should be limited to patients with pre-ART HIV RNA <100,000 copies/mL (CI).
- As noted earlier, ATV/c plus TDF/FTC is not recommended for patients with CrCl <70 mL/min.
# Darunavir/Cobicistat
A combination of (DRV 800 mg with COBI 150 mg) is bioequivalent to (DRV 800 mg with RTV 100 mg) in healthy volunteers. 85 Efficacy in Clinical Trial:
- In a single arm trial of treatment-naive (94%) and treatment-experienced (6%) patients, the coformulated DRV/c 800 mg/150 mg tablet was evaluated in combination with investigator-selected NRTI/NtRTI (99% of participants were given TDF/FTC). At week 48, 81% of participants achieved HIV RNA <50 copies/ml; 5% of participants discontinued treatment because of adverse events. 86 Adverse Effects:
- In the single arm trial, the most common treatment emergent adverse events were diarrhea, nausea, and headache.
Other Factors:
- (DRV 800 mg and COBI 150 mg) is available as a co-formulated tablet.
- Coadministration with TDF is not recommended in patients with CrCl <70 mL/min.
Panel's Recommendation:
- On the basis of the bioequivalence study and the single arm trial, the Panel recommends DRV/c plus TDF/FTC (BII) and DRV/c plus ABC/3TC (BIII) as Alternative Regimens for ART-naive patients.
- As noted earlier, DRV/c plus TDF/FTC is not recommended for patients with CrCl <70 mL/min.
# Other Protease Inhibitor-Based Regimens
# Lopinavir/Ritonavir
Efficacy in Clinical Trials:
- A 7-year follow-up study of LPV/r and 2 NRTIs showed sustained virologic suppression in patients who were maintained on the originally assigned regimen. 87 - Results of clinical trials that compared LPV/r with ATV/r and DRV/r are discussed above, demonstrating more favorable safety and tolerability of ATV/r and DRV/r.
- In the ACTG 5142 study, at 96 weeks, a smaller proportion of patients who received LPV/r plus 2 NRTIs achieved viral suppression (HIV RNA <50 copies/mL) than those who received EFV plus 2 NRTIs. However, the CD4 cell response was greater with LPV/r, and there was less drug resistance associated with virologic failure. 63 - In the GARDEL study, patients were randomized to 3TC or a 2 NRTI combination, with all study participants receiving LPV/r. The results demonstrated non-inferiority of the two strategies. 88 Adverse Effects:
- In addition to diarrhea, major adverse effects of LPV/r include insulin resistance and hyperlipidemia, especially hypertriglyceridemia; these require pharmacologic management in some patients.
- In the D:A:D and French observational cohorts, cumulative use of LPV/r was associated with a slightly increased risk of MI. 18,24 - In another D:A:D study, LPV/r use was also reported as an independent predictor of chronic renal impairment. 83 Other Factors and Considerations:
- LPV/r must be boosted with 200 mg/day of RTV and is associated with higher rates of GI side effects and hyperlipidemia than ATV/r and DRV/r, both of which are boosted with 100 mg/day of RTV.
- LPV/r can be given once or twice daily.
- Once-daily dosing should not be used in pregnant women, especially during the third trimester, when LPV levels are expected to decline (see Perinatal Guidelines).
- LPV/r is currently the only available PI co-formulated with RTV. Panel's Recommendation:
- On the basis of greater potential for adverse events and higher RTV dose and pill burden than ATV/r and DRV/r, the Panel recommends LPV/r plus TDF/FTC or LPV/r plus ABC/3TC as Other regimens (CI).
# Other Antiretroviral Regimens for Initial Therapy When Abacavir or Tenofovir Cannot Be Used
All currently Recommended and Alternative regimens consist of two NRTIs plus a third active drug. This strategy, however, may not be possible or optimal in all patients. In some situations it may be necessary to avoid both TDF and ABC, such as in the case of a patient with pre-existing renal disease who is HLA B*5701 positive or at high risk of cardiovascular disease.
Based on these concerns, several clinical studies have evaluated strategies using initial regimens that avoid 2 NRTIs or the NRTI drug class altogether. Many of these studies were not fully powered to permit comparisons, and regimens from these studies will not be discussed further. However, there are now sufficient data on two regimens (DRV/r plus RAL and LPV/r plus 3TC) to warrant including them as options when ABC or TDF cannot be used.
# Darunavir/Ritonavir plus Raltegravir
In the NEAT/ANRS 143 study, 805 treatment-naive participants were randomized to receive either twicedaily RAL or once-daily TDF/FTC, both with DRV/r (800 mg/100 mg once daily). At week 96, DRV/r plus RAL was non-inferior to DRV/r plus TDF/FTC based on the primary endpoint of proportion of patients with virologic or clinical failure. Among those with baseline CD4 cell count 100,000 copies/mL were also seen in two smaller studies of DRV/r plus RAL. 90,91 On the basis of these study results, the Panel recommends that DRV/r plus RAL be considered for use only in patients with HIV RNA 200/mm 3 , and only in those patients who cannot take either TDF or ABC (CI).
# Lopinavir/Ritonavir plus Lamivudine
In the GARDEL study, 426 ART-naive patients were randomized to receive twice-daily LPV/r plus either open-label 3TC (twice daily) or two NRTIs selected by the study investigators. At 48 weeks, a similar number of patients in each arm had HIV RNA <50 copies/mL, meeting the study's non-inferiority criteria.
The LPV/r plus 3TC regimen was better tolerated than the LPV/r plus 2 NRTI regimen. 88 An important limitation of the GARDEL study is the use of LPV/r, twice daily dosing, and relatively high pill burden (total of 6 tablets per day). LPV/r is not considered a Recommended or Alternative initial PI because of its unfavorable adverse event and pill burden characteristics as compared to pharmacokinetically enhanced ATV and DRV. Given the above limitations, the Panel recommends that LPV/r plus 3TC be considered for use only in patients who cannot take either TDF or ABC (CI).
In summary, the aggregate results from these two fully powered studies with NRTI-limiting regimens demonstrate that these initial strategies have significant deficiencies as compared to standard-of-care treatment approaches, in particular, disadvantages related to pill burden or dosing frequency. In addition, there are concerns about the virologic efficacy of DRV/r plus RAL in patients with high viral loads or low CD4 cell counts. The Panel only recommend LPV/r plus 3TC or DRV/r plus RAL for initial therapy when both TDF and ABC are contraindicated. Other less well-tested NRTI-limiting combinations are not recommended. 18 and 19a) Some antiretroviral (ARV) regimens or components are not generally recommended because of suboptimal antiviral potency, unacceptable toxicities, or pharmacologic concerns. These are summarized below.
Key
# Antiretroviral Regimens Not Recommended
Monotherapy with nucleoside reverse transcriptase inhibitor (NRTI). Single-NRTI therapy does not demonstrate potent and sustained antiviral activity and should not be used (AII). For prevention of motherto-child transmission (PMTCT), zidovudine (ZDV) monotherapy is not recommended but might be considered in certain unusual circumstances in women with HIV RNA <1,000 copies/mL, although the use of a potent combination regimen is preferred. (See Perinatal Guidelines, 1 available at .)
Single-drug treatment regimens with a ritonavir (RTV)-boosted protease inhibitor (PI), either lopinavir (LPV), 2 atazanavir (ATV), 3 or darunavir (DRV) are under investigation with mixed results, and cannot be recommended outside of a clinical trial at this time.
Dual-NRTI regimens. These regimens are not recommended because they have not demonstrated potent and sustained antiviral activity compared with triple-drug combination regimens (AI). 6 Triple-NRTI regimens. In general, triple-NRTI regimens other than abacavir/lamivudine/zidovudine (ABC/3TC/ZDV) (BI) and possibly lamivudine/zidovudine + tenofovir (3TC/ZDV + TDF) (BII) should not be used because of suboptimal virologic activity or lack of data (AI).
# Antiretroviral Components Not Recommended
Atazanavir (ATV) + indinavir (IDV). Both of these PIs can cause Grade 3 to 4 hyperbilirubinemia and jaundice. Additive adverse effects may be possible when these agents are used concomitantly. Therefore, these two PIs are not recommended for combined use (AIII).
# Didanosine (ddI) + stavudine (d4T).
The combined use of ddI and d4T as a dual-NRTI backbone can result in a high incidence of toxicities, particularly peripheral neuropathy, pancreatitis, and lactic acidosis. This combination has been implicated in the deaths of several HIV-infected pregnant women secondary to severe lactic acidosis with or without hepatic steatosis and pancreatitis. 14 Therefore, the combined use of ddI and d4T is not recommended (AII).
# Didanosine (ddI) + tenofovir (TDF).
Use of ddI + TDF may increase ddI concentrations 15 and serious ddIassociated toxicities including pancreatitis and lactic acidosis. These toxicities may be lessened by ddI dose reduction. The use of this combination has also been associated with immunologic nonresponse or CD4 cell decline despite viral suppression, high rates of early virologic failure, and rapid selection of resistance mutations. Because of these adverse outcomes, this dual-NRTI combination is not generally recommended (AII). Clinicians caring for patients who are clinically stable on regimens containing ddI + TDF should consider altering the NRTIs to avoid this combination.
Two-non-nucleoside reverse transcriptase inhibitor (2-NNRTI) combinations. In the 2NN trial, ARVnaive participants were randomized to receive once-or twice-daily nevirapine (NVP) versus efavirenz (EFV) versus EFV plus NVP, all combined with d4T and 3TC. 23 A higher frequency of clinical adverse events that led to treatment discontinuation was reported in participants randomized to the two-NNRTI arm. Both EFV and NVP may induce metabolism of etravirine (ETR), which leads to reduction in ETR drug exposure. 24 Based on these findings, the Panel does not recommend using two NNRTIs in combination in any regimen (AI).
Efavirenz (EFV) in first trimester of pregnancy and in women with significant childbearing potential.
EFV use was associated with significant teratogenic effects in nonhuman primates at drug exposures similar to those representing human exposure. Several cases of congenital anomalies have been reported after early human gestational exposure to EFV. EFV should be avoided in pregnancy, particularly during the first trimester, and in women of childbearing potential who are trying to conceive or who are not using effective and consistent contraception (AIII). If no other ARV options are available for the woman who is pregnant or at risk of becoming pregnant, the provider should consult with a clinician who has expertise in both HIV infection and pregnancy. (See Perinatal Guidelines, 1 available at .)
Emtricitabine (FTC) + lamivudine (3TC). Both of these drugs have similar resistance profiles and have minimal additive antiviral activity. Inhibition of intracellular phosphorylation may occur in vivo, as seen with other dual-cytidine analog combinations. 27 These two agents should not be used as a dual-NRTI combination (AIII).
Etravirine (ETR) + unboosted PI. ETR may induce the metabolism and significantly reduce the drug exposure of unboosted PIs. Appropriate doses of the PIs have not been established 24 (AII).
# Etravirine (ETR) + ritonavir (RTV)-boosted atazanavir (ATV) or fosamprenavir (FPV).
ETR may alter the concentrations of these PIs. Appropriate doses of the PIs have not been established 24 (AII).
# Etravirine (ETR) + ritonavir (RTV)-boosted tipranavir (TPV).
RTV-boosted TPV significantly reduces ETR concentrations. These drugs should not be coadministered 24 (AII).
Nevirapine (NVP) initiated in ARV-naive women with CD4 counts >250 cells/mm 3 or in ARV-naive men with CD4 counts >400 cells/mm 3 . Greater risk of symptomatic hepatic events, including serious and life-threatening events, has been observed in these patient groups. NVP should not be initiated in these patients (BI) unless the benefit clearly outweighs the risk. Patients who experience CD4 count increases to levels above these thresholds as a result of antiretroviral therapy (ART) can be safely switched to NVP. 31 Unboosted darunavir (DRV), saquinavir (SQV), or tipranavir (TPV). The virologic benefit of these PIs has been demonstrated only when they were used with concomitant RTV. Therefore, use of these agents as part of a combination regimen without RTV is not recommended (AII).
# Stavudine (d4T) + zidovudine (ZDV).
These two NRTIs should not be used in combination because of antagonism demonstrated in vitro 32 and in vivo 33 (AII).
# 2-NNRTI combination (AI)
- When EFV combined with NVP, higher incidence of clinical adverse events seen when compared with either EFV-or NVP-based regimen.
- Both EFV and NVP may induce metabolism and may lead to reductions in ETR exposure; thus, they should not be used in combination with ETR. Antiretroviral (ARV) regimens currently recommended for initial therapy of HIV-infected patients have a high likelihood of achieving and maintaining plasma HIV RNA levels below the lower limits of detection (LLOD) of currently used assays (see What to Start). Patients on antiretroviral therapy (ART) who do not achieve this treatment goal or who experience virologic rebound often develop resistance mutations to one or more components of their regimen. Based on surveillance data for HIV patients in care in selected cities in the United States in 2009, an estimated 89% of the patients were receiving ART, of whom 72% had viral loads <200 copies/mL. 1 Many patients with detectable viral loads are non-adherent to treatment. Depending on their treatment histories, some of these patients may have minimal or no drug resistance; others may have extensive resistance. Managing patients with extensive resistance is complex and usually requires consultation with an HIV expert. This section of the guidelines defines virologic failure in patients on ART and discusses strategies to manage these individuals.
# Virologic Response Definitions
The following definitions are used in this section to describe the different levels of virologic response to ART.
# Panel's Recommendations
- Assessing and managing a patient experiencing failure of antiretroviral therapy (ART) is complex. Expert advice is critical and should be sought.
- Evaluation of virologic failure should include an assessment of adherence, drug-drug or drug-food interactions, drug tolerability, HIV RNA and CD4 T lymphocyte (CD4) cell count trends over time, treatment history, and prior and current drug-resistance testing results.
- Drug-resistance testing should be performed while the patient is taking the failing antiretroviral (ARV) regimen (AI) or within 4 weeks of treatment discontinuation (AII). Even if more than 4 weeks have elapsed since ARVs were discontinued, resistance testingalthough it may not detect previously selected resistance mutations-can still provide useful information to guide therapy (CIII).
- The goal of treatment for ART-experienced patients with drug resistance who are experiencing virologic failure is to establish virologic suppression (i.e., HIV RNA below the lower limits of detection of currently used assays) (AI).
- A new regimen should include at least two, and preferably three, fully active agents (AI). A fully active agent is one that is expected to have uncompromised activity on the basis of the patient's treatment history and drug-resistance testing results and/or the drug's novel mechanism of action.
- In general, adding a single ARV agent to a virologically failing regimen is not recommended because this may risk the development of resistance to all drugs in the regimen (BII).
- For some highly ART-experienced patients, maximal virologic suppression is not possible. In this case, ART should be continued (AI) with regimens designed to minimize toxicity, preserve CD4 cell counts, and delay clinical progression.
- When it is not possible to construct a viable suppressive regimen for a patient with multidrug resistant HIV, the clinician should consider enrolling the patient in a clinical trial of investigational agents or contacting pharmaceutical companies that may have investigational agents available.
- Discontinuing or briefly interrupting therapy may lead to a rapid increase in HIV RNA and a decrease in CD4 cell count and increases the risk of clinical progression. Therefore, this strategy is not recommended in the setting of virologic failure (AI). Virologic suppression: A confirmed HIV RNA level below the LLOD of available assays Virologic failure: The inability to achieve or maintain suppression of viral replication to an HIV RNA level <200 copies/mL Incomplete virologic response: Two consecutive plasma HIV RNA levels ≥200 copies/mL after 24 weeks on an ARV regimen in a patient who has not yet had documented virologic suppression on this regimen. A patient's baseline HIV RNA level may affect the time course of response, and some regimens will take longer than others to suppress HIV RNA levels.
# Rating of Recommendations
Virologic rebound: Confirmed HIV RNA ≥200 copies/mL after virologic suppression Virologic blip: After virologic suppression, an isolated detectable HIV RNA level that is followed by a return to virologic suppression
# ART Treatment Goals and Virologic Responses
The goal of ART is to suppress HIV replication to a level below which drug-resistance mutations do not emerge. Although not conclusive, the evidence suggests that selection of drug-resistance mutations does not occur in patients with HIV RNA levels persistently suppressed to below the LLOD of current assays. 2 Viremia "blips"-defined by viral suppression followed by an isolated detectable HIV RNA level and subsequent return to undetectable levels-are not usually associated with subsequent virologic failure. 3 In contrast, there is controversy regarding the clinical implications of persistent HIV RNA levels between the LLOD and 200 copies/mL. 7 Two other retrospective studies also support the supposition that virologic rebound is more likely to occur in patients with viral loads >200 copies/mL than in those with low-level viremia between 50 to 199 copies/mL. 8,9 However, other studies have suggested that viremia at this low level (500 copies/mL. 14 Therefore, persistent plasma HIV RNA levels ≥200 copies/mL should be considered virologic failure.
# Causes of Virologic Failure
Virologic failure can occur for many reasons. Data from patient cohorts in the earlier era of combination ART suggested that suboptimal adherence and drug intolerance/toxicity accounted for 28% to 40% of virologic failure and regimen discontinuations. 15,16 Presence of pre-existing (transmitted) drug resistance may also be the cause of virologic failure. 17 Virologic failure may be associated with both patient-and regimenrelated factors, as listed below:
# Management of Patients with Virologic Failure
# Assessment of Virologic Failure
If virologic failure is suspected or confirmed, a thorough assessment that includes consideration of the factors listed in the Causes of Virologic Failure section above is indicated. Often the causes of virologic failure can be identified, but in some cases, the causes are not obvious. It is important to distinguish among the causes of virologic failure because the approaches to subsequent therapy differ. The following potential causes of virologic failure should be explored in depth:
- Suboptimal Adherence. Assess the patient's adherence to the regimen. Identify and address the underlying cause(s) for incomplete adherence (e.g., drug intolerance, difficulty accessing medications, depression, active substance abuse) and, if possible, simplify the regimen (e.g., decrease pill count or dosing frequency). (See Adherence.)
- Medication Intolerance. Assess the patient's tolerance of the current regimen and the severity and duration of side effects, keeping in mind that even minor side effects can affect adherence. Management strategies to address intolerance in the absence of drug resistance may include:
- Symptomatic treatment (e.g., antiemetics, antidiarrheals)
- A switch from one ARV in a regimen to another agent in the same drug class (see the Adverse Effects section) - A switch from one drug class to another class (e.g., from a non-nucleoside reverse transcriptase inhibitor to a protease inhibitor or an integrase strand transfer inhibitor ), if necessary (see the Adverse Effects section)
- Pharmacokinetic Issues
- Review food requirement for each medication, and assess whether the patient adheres to the requirement. - Review the patient's recent history of gastrointestinal symptoms such as vomiting or diarrhea that may result in short-term malabsorption. - Review concomitant medications and dietary supplements for possible adverse drug-drug interactions (consult the Drug Interactions section and tables for common interactions) and, if possible, make appropriate substitutions for ARV agents and/or concomitant medications. - Consider therapeutic drug monitoring if pharmacokinetic drug-drug interactions or impaired drug absorption leading to decreased ARV exposure is suspected (see also Exposure-Response
Relationship and Therapeutic Drug Monitoring).
- Suspected Drug Resistance. Perform resistance testing while the patient is still taking the failing regimen or within 4 weeks of regimen discontinuation if the patient's plasma HIV RNA level is >1,000 copies/mL (AI), and possibly even if between 500 to 1,000 copies/mL (BII). (See Drug-Resistance Testing.) In some patients, resistance testing should be considered even after treatment interruptions of more than 4 weeks, recognizing that the lack of evidence of resistance in this setting does not exclude the possibility that resistance mutations may be present at low levels (CIII). Evaluate the extent of drug resistance, taking into account the patient's past treatment history and prior resistance-test results. Drug resistance is cumulative; thus, all prior treatment history and resistance test results should be considered when evaluating resistance. Genotypic or phenotypic testing provides information relevant for selecting nucleoside reverse transcriptase inhibitors (NRTIs), NNRTIs, PIs, and INSTIs. Additional drug-resistance tests for patients experiencing failure on a fusion inhibitor (AII) and viral tropism tests for patients experiencing failure on a CCR5 antagonist (BIII) are also available. (See Drug-Resistance Testing.)
# Approach to Patients with Confirmed Virologic Failure
Once virologic failure is confirmed, every effort should be made to assess whether suboptimal adherence and drug-drug or drug-food interactions may be contributing to the inadequate virologic response to ART. If virologic failure persists after these issues have been adequately addressed, resistance testing should be performed, and the regimen should be changed as soon as possible to avoid progressive accumulation of resistance mutations. 18 In addition, several studies have shown that virologic responses to new regimens are greater in individuals with lower HIV RNA levels 10,19 and/or higher CD4 cell counts at the time of regimen changes. 10,19 Discontinuing or briefly interrupting therapy in a patient with viremia may lead to a rapid increase in HIV RNA and a decrease in CD4 cell count and increases the risk of clinical progression; 20,21 therefore, this strategy is not recommended (AI). See Discontinuation or Interruption of Antiretroviral Therapy.
Ideally, a new ARV regimen should contain at least two, and preferably three, fully active drugs whose predicted activity is based on the patient's drug treatment history, resistance testing, or the mechanistic action of a new drug class (AI). 10, Despite drug resistance, some ARV drugs (e.g., NRTIs) may contribute partial ARV activity to a regimen, 21 while other agents (e.g., enfuvirtide , NNRTIs, the INSTI raltegravir ) likely will not. Using a "new" drug that a patient has never used previously does not ensure that the drug will be fully active; there is potential for cross-resistance, particularly among drugs from the same class. In addition, archived drug-resistance mutations may not be detected by standard drug-resistance tests, particularly if testing is performed when the patient is not taking the drug in question. Therefore, both treatment history and prior and current drug-resistance test results must be considered when designing a new regimen. When designing a new ART regimen, drug potency and viral susceptibility are more important factors to consider than the number of component drugs.
In general, patients who receive at least three active drugs, selected based on a review of the patient's treatment history and past and most current drug-resistance test results, experience better and more sustained virologic response than those receiving fewer active drugs in the regimen. 23,24,26,27,35,36 However, there are increasing data in treatment-naive and treatment-experienced patients showing that an active pharmacokinetically enhanced PI plus one other active drug or several partially active drugs will effectively reduce viral load in most patients. Active drugs are ARVs that, based on resistance test results and treatment history, are expected to have antiviral activity equivalent to that seen when there is no resistance to the specific drugs; ARVs with partial activity are those predicted to reduce HIV RNA but to a lesser extent than when there is no underlying drug resistance. The activity of a given drug must be uniquely defined for each patient. Active drugs may be newer members of existing drug classes that are active against HIV isolates that are resistant to older drugs in the same classes (e.g., etravirine , darunavir and tipranavir, and dolutegravir ) An active drug may also be one with unique mechanisms of action (e.g., the fusion inhibitor T20, the CCR5 antagonist maraviroc in patients with no detectable CXCR4-using virus).
In the presence of certain drug resistance mutations, some ARVs such as DTG, ritonavir-boosted DRV, and ritonavir-boosted lopinavir (LPV/r) need to be given twice daily instead of once daily to achieve higher drug concentrations necessary to be active against the less sensitive virus. 41,42 Addressing Detectable Viral Load in Different Clinical Situations
- HIV RNA above the LLOD and <200 copies/mL. Confirm that levels remain above the LLOD and assess adherence, drug-drug interactions (including those with over-the-counter products and supplements), and drug-food interactions. Patients with HIV RNA typically below the LLOD with transient increases in HIV RNA (i.e., blips) do not require a change in treatment (AII). 5 Although there is no consensus on how to manage patients with persistent HIV RNA levels above the LLOD and <200 copies/mL, the risk of emerging resistance is believed to be relatively low. Therefore, these patients should maintain on their current regimens and have HIV RNA levels monitored at least every 3 months to assess the need for changes in ART in the future (AIII).
- HIV RNA ≥200 and 500 copies/mL. 8,9 Persistent plasma HIV RNA levels in the 200 to 1,000 copies/mL range should be considered as virologic failure, and resistance testing should be attempted, particularly if HIV RNA >500 copies/mL. When resistance testing can successfully be performed and no resistance is detected, manage the patient as outlined below in the section on HIV RNA >1,000 copies/mL and no drug resistance identified. If drug resistance is detected, manage the patient as outlined below in the section on HIV RNA >1,000 copies/mL and drug resistance identified. When resistance testing cannot be performed because of low-level viremia, the decision whether to empirically change ARVs should be made on a case-by-case basis.
- HIV RNA >1,000 copies/mL and no drug resistance identified. This scenario is almost always associated with suboptimal adherence. Conduct a thorough assessment to determine the level of adherence and identify any drug-drug and drug-food interactions. Consider the timing of the drugresistance test (e.g., was the patient mostly or completely ART-non-adherent for more than 4 weeks before testing). If the current regimen is well tolerated and there are no significant drug-drug or drugfood interactions, it is reasonable to resume the same regimen. If the agents are poorly tolerated or there are important drug-drug or drug-food interactions, consider changing the regimen. Two to four weeks after treatment is resumed or started, repeat viral load testing; if viral load remains >500 copies/mL, perform genotypic testing to determine whether a resistant viral strain emerges (CIII).
- HIV RNA >1,000 copies/mL and drug resistance identified. The availability of newer ARVs, including some with new mechanisms of action, makes it possible to suppress HIV RNA levels to below the LLOD in most of these patients. The options in this setting depend on the extent of drug resistance present and are addressed in the clinical scenarios outlined below.
# Management of Virologic Failure in Different Clinical Scenarios
First Regimen Failure
- Failing an NNRTI plus NRTI regimen. Patients failing an NNRTI-based regimen often have viral resistance to the NNRTI, with or without lamivudine (3TC) and emtricitabine (FTC) resistance. Although several options are available for these patients, several studies have explored the activity of a pharmacokinetically boosted PI with NRTIs or an INSTI. Two of the studies found that regimens containing a ritonavir-boosted PI (PI/r) combined with NRTIs were as active as regimens containing the PI/r combined with RAL. 43,45 Two studies also demonstrated higher rates of virologic suppression with use of a PI/r plus NRTIs than with a PI/r alone. 44,45 On the basis of these studies, even patients with NRTI resistance can often be treated with a pharmacokinetically boosted PI plus NRTIs or RAL (AI). Although LPV/r was used in these studies, it is likely that other pharmacokinetically boosted PIs would behave similarly. Although data are limited, the second-generation NNRTI ETR or the other INSTIs (i.e., elvitegravir or DTG) combined with a pharmacokinetically boosted PI may also be options in this setting.
- Failing a pharmacokinetically boosted PI plus NRTI regimen. In this scenario, most patients will have either no resistance or resistance limited to 3TC and FTC. 46,47 Failure in this setting is often attributed to poor adherence, drug-drug interactions, or drug-food interactions. A systematic review of multiple randomized trials of PI/r first-line failure showed that maintaining the same regimen, presumably with efforts to enhance adherence, is as effective as changing to new regimens with or without drugs from new classes. 48 In this setting, resistance testing should be performed along with an assessment of overall adherence and tolerability of the regimen. If the regimen is well tolerated and there are no concerns regarding drug-drug or drug-food interactions, the regimen can be continued with adherence support and viral monitoring. Alternatively, if poor tolerability or interactions may be contributing to virologic failure, the regimen can be modified to include a different pharmacokinetically boosted PI plus NRTIs-even if not all of the NRTIs are fully active-or to a new non-PI-based regimen that includes more than two fully active agents (AII).
# Second-Line Regimen Failure and Beyond
- Drug resistance with treatment options allowing for full virologic suppression. Depending on treatment history and drug-resistance data, one can predict whether or not to have a fully active pharmacokinetically boosted PI to include in future regimens. For example, those who have no documented PI resistance and previously have never been treated with an unboosted PI are likely to harbor virus that is fully susceptible to ARVs in the PI class. In this setting, viral suppression should be achievable using a pharmacokinetically boosted PI combined with either NRTIs or an INSTI-provided the virus is susceptible to the INSTI. If a fully susceptible pharmacokinetically boosted PI is not an option, the new regimen should include at least two, and preferably three, fully active agents, if possible. Drugs to be included in the regimen should be selected based on the likelihood that they will be active as determined by the patient's treatment history, past and present drug-resistance testing, and tropism testing if a CCR5 antagonist is being considered.
- Multidrug resistance without treatment options allowing for full virologic suppression. Use of currently available ARVs has resulted in a dramatic decline in the number of patients who have few treatment options because of multi-class drug resistance. 50,51 Despite this progress, there remain patients who have experienced toxicities and/or developed resistance to all or most currently available drugs. If maximal virologic suppression cannot be achieved, the goals of ART will be to preserve immunologic function, prevent clinical progression, and minimize increasing resistance to drug classes that may eventually include new drugs that may be important for future regimens. Consensus on the optimal management of these patients is lacking. If resistance to NNRTIs, T20, EVG or RAL are identified, there is rarely a reason to continue these drugs, as there is little evidence that keeping them in the regimen helps delay disease progression (BII). Moreover, continuing these drugs, in particular INSTIs, may allow for further increasing resistance and within-class cross resistance that may limit future treatment options. It should be noted that even partial virologic suppression of HIV RNA to >0.5 log 10 copies/mL from baseline correlates with clinical benefits. 50,52 Cohort studies provide evidence that continuing therapy, even in the presence of viremia and the absence of CD4 count increases, reduces the risk of disease progression. 53 Other cohort studies suggest continued immunologic and clinical benefits with even modest reductions in HIV RNA levels. 54,55 However, all these potential benefits must be balanced with the ongoing risk of accumulating additional resistance mutations. In general, adding a single fully active ARV to the regimen is not recommended because of the risk of rapid development of resistance (BII).
Patients with ongoing viremia who lack sufficient treatment options to construct a fully suppressive regimen may be candidates for research studies or expanded access programs or may qualify for single-patient access of an investigational new drug as specified in Food and Drug Administration regulations: . Information about these programs may also be available from the sponsoring pharmaceutical manufacturer.
- Previously treated patient with suspected drug resistance who need care but present with limited information (i.e., incomplete or no self-reported history, medical records, or resistance-testing results). Every effort should be made to obtain the patient's medical records and prior drug-resistance testing results; however, this may not always be possible. One strategy is to restart the most recent ARV regimen and assess drug resistance in 2 to 4 weeks to guide selection of the next regimen. Another strategy is to start two or three drugs predicted to be active on the basis of the patient's treatment history.
# Isolated Central Nervous System (CNS) Virologic Failure and New Onset Neurologic Symptoms
Presentation with new-onset CNS signs and symptoms has been reported as a rare form of virologic failure. These patients present with new, usually subacute, neurological symptoms associated with breakthrough of HIV infection within the CNS compartment despite plasma HIV RNA suppression. 56,57 Clinical evaluation frequently shows abnormalities on MRI brain imaging and abnormal cerebrospinal fluid (CSF) findings with characteristic lymphocytic pleocytosis. When available, measurement of CSF HIV RNA shows higher concentrations in the CSF than in plasma, and in most patients, evidence of drug-resistant CSF virus. Drugresistance testing of HIV in CSF, if available, can be used to guide changes in the treatment regimen according to principles outlined above for plasma HIV RNA resistance (CIII). In these patients it may be useful to consider CNS pharmacokinetics in drug selection (CIII). If CSF HIV resistance testing is not available, the regimen may be changed based on the patient's treatment history or on predicted drug penetration into the CNS 58-60 (CIII). This "neurosymptomatic" CNS viral escape should be distinguished from: (1) other CNS infections that can induce a transient increase in CSF HIV RNA (e.g., herpes zoster 61 ), (2) incidental detection of asymptomatic mild CSF HIV RNA elevation likely equivalent to plasma blips, 62 or (3) relatively common chronic, usually mild, neurocognitive impairment in HIV-infected patients without evidence of CNS viral breakthrough. 63 None of these latter conditions currently warrant a change in ART. 64
# Summary
In summary, the management of treatment-experienced patients with virologic failure often requires expert advice to construct virologically suppressive regimens. Before modifying a regimen, it is critical to carefully evaluate the cause(s) of virologic failure, including incomplete adherence, poor tolerability, and drug and food interactions, as well as review HIV RNA and CD4 cell count changes over time, treatment history, and drug-resistance test results. If HIV RNA suppression is not possible with currently approved agents, consider use of investigational agents through participation in clinical trials or expanded/single-patient access programs. If virologic suppression is still not achievable, the choice of regimens should focus on minimizing toxicity and preserving treatment options while maintaining CD4 cell counts to delay clinical progression.
# Poor CD4 Cell Recovery and Persistent Inflammation Despite Viral Suppression (Last updated April 8, 2015; last reviewed April 8, 2015)
Despite marked improvements in antiretroviral treatment (ART), morbidity and mortality in HIV-infected individuals continues to be greater than in the general population, particularly when ART is delayed until advanced disease stages. These morbidities include cardiovascular disease, many non-AIDS cancers, non-AIDS infections, chronic obstructive pulmonary disease, osteoporosis, type II diabetes, thromboembolic disease, liver disease, renal disease, neurocognitive dysfunction, and frailty. 1 Although health-related behaviors and toxicities of antiretroviral (ARV) drugs may also contribute to the increased risk of illness and death, poor CD4 T lymphocyte (CD4) cell recovery, persistent immune activation, and inflammation likely also contribute to the risk.
# Poor CD4 Cell Recovery
As long as ART-mediated viral suppression is maintained, peripheral blood CD4 cell counts in most HIVinfected individuals will continue to increase for at least a decade. The rate of CD4 cell recovery is typically most rapid in the first 3 months of suppressive ART, followed by more gradual increases over time. If ARTmediated viral suppression is maintained, most individuals will eventually recover CD4 counts in the normal range (>500 cells /mm 3 ); however, approximately 15% to 20% of individuals who initiate ART at very low CD4 counts (<200 cells/mm 3 ) may plateau at abnormally low CD4 cell counts. Early initiation of ART in recently HIV-infected individuals likely provides the best opportunity for maximal CD4 cell recovery. 6 Persistently low CD4 cell counts despite ART-mediated viral suppression are associated with increased risk of morbidity and mortality. For example, HIV-infected individuals with CD4 counts <200 cells/mm 3 despite at least 3 years of suppressive ART had a 2.6-fold greater risk of mortality than those with higher CD4 cell counts. 7 Lower CD4 cell counts during ART-mediated viral suppression are associated with an increased risk
- Morbidity and mortality from several AIDS and non-AIDS conditions are increased in HIV-infected individuals despite antiretroviral therapy (ART)-mediated viral suppression, and are predicted by persistently low CD4 T lymphocyte (CD4) cell counts and/or persistent immune activation.
- ART intensification by adding antiretroviral (ARV) drugs to a suppressive ART regimen does not consistently improve CD4 cell recovery or reduce immune activation and is not recommended (AI).
- In individuals with viral suppression, switching ARV drug classes does not consistently improve CD4 cell recovery or reduce immune activation and is not recommended (BIII).
- No interventions designed to increase CD4 cell counts and/or decrease immune activation are recommended at this time (in particular, interleukin-2 is not recommended ) because none has been proven to decrease morbidity or mortality during ARTmediated viral suppression.
- Monitoring markers of immune activation and inflammation is not recommended because no immunologically targeted intervention has proven to improve the health of individuals with abnormally high biomarker levels, and many markers that predict morbidity and mortality fluctuate widely in individuals (AII).
- Because there are no proven interventions to improve CD4 cell recovery and/or inflammation, efforts should focus on addressing modifiable risk factors for chronic disease (e.g., encouraging smoking cessation, a healthy diet, and exercise; treating hypertension, hyperlipidemia) (AII). of non-AIDS morbidity and mortality, including cardiovascular disease, 12 osteoporosis and fractures, 13 liver disease, 14 and infection-related cancers. 15 The prognostic importance of higher CD4 cell counts likely spans all ranges of CD4 cell counts, though incremental benefits are harder to discern once CD4 counts increase to >500 cells/mm 3 . 16 Individuals with poor CD4 cell recovery should be evaluated for modifiable causes of CD4 cell lymphopenia. Concomitant medications should be reviewed, with a focus on those known to decrease white blood cells or, specifically, CD4 cells (e.g., cancer chemotherapy, interferon, zidovudine, 17 or the combination of tenofovir disoproxil fumarate (TDF) and didanosine (ddI). 18,19 If possible, these drugs should be substituted for or discontinued. Untreated coinfections (e.g., HCV, HIV-2) and serious medical conditions (e.g., malignancy) should also be considered as possible causes of CD4 lymphopenia, particularly in individuals with consistently declining CD4 cell counts (and percentages) and/or in those with CD4 counts consistently below 100 cells/mm 3 . In many cases, no obvious cause for suboptimal immunologic response can be identified.
# Rating of Recommendations
Despite strong evidence linking low CD4 cell counts and increased morbidity during ART-mediated viral suppression, no adjunctive therapies that increase CD4 cell count beyond levels achievable with ART alone have been proven to decrease morbidity or mortality. Adding ARV drugs to an already suppressive ART regimen does not improve CD4 cell recovery, and does not reduce morbidity or mortality. Therefore, ART intensification is not recommended as a strategy to improve CD4 cell recovery (AI). In individuals maintaining viral suppression, switching ARV drug classes in a suppressive regimen also does not consistently improve CD4 cell recovery and is not recommended (BIII). 26 Two large clinical trials, powered to assess impact on clinical endpoints (AIDS and death), evaluated the role of interleukin-2, an immunebased therapy, in improving CD4 cell recovery. Interleukin-2 adjunctive therapy resulted in CD4 cell count increases but with no observable clinical benefit. Therefore, interleukin-2 is not recommended (AI). 27 Other immune-based therapies that increase CD4 cell counts (e.g., growth hormone, interleukin-7) are under investigation. However, none of the therapies have been evaluated in clinical endpoint trials; therefore, whether any of these approaches will offer clinical benefit is unclear. Currently, such immune-based therapies should not be used except in the context of a clinical trial.
# Persistent Immune Activation and Inflammation
Although poor CD4 cell recovery likely contributes to morbidity and mortality during ART-mediated viral suppression, there is increasing focus on persistent immune activation and inflammation as potentially independent mediators of risk. HIV infection results in heightened systemic immune activation and inflammation, effects that are evident during acute infection, persist throughout chronic untreated infection, and predict more rapid CD4 cell decline and progression to AIDS and death, independent of plasma HIV RNA levels. 28 Although immune activation declines with suppressive ART, it often persists at abnormal levels in many HIV-infected individuals maintaining long-term ART-mediated viral suppression-even in those with CD4 cell recovery to normal levels. 29,30 Immune activation and inflammatory markers (e.g., IL-6, D-dimer, hs-CRP) also predict mortality and non-AIDS morbidity during ART-mediated viral suppression, including cardiovascular and thromboembolic events, cancer, neurocognitive dysfunction, and frailty. 28 Although individuals with poor CD4 cell recovery (i.e., counts persistently 500 cells/mm 3 , there is evidence that immune activation and inflammation contribute to morbidity and mortality. 33 Thus, innate immune activation and inflammation are potentially important targets for future interventions.
Although the drivers of persistent immune activation during ART are not completely understood, HIV persistence, coinfections, and microbial translocation likely play important roles. 28 Interventions to reduce each of these presumed drivers are currently being investigated. Importantly, adding ARV drugs to an already suppressive ART regimen (ART intensification) does not consistently improve immune activation. 25 Although some studies have suggested that switching an ART regimen to one with a more favorable lipid profile may improve some markers of immune activation and inflammation, 34,35 these studies have limitations and results are not consistent across markers and among studies. Thus, at this time, ART modification cannot be recommended as a strategy to reduce immune activation (BIII). Other commonly used medications with anti-inflammatory properties (e.g., statins, aspirin) are being studied, and preliminary evidence suggests that some may reduce immune activation in treated HIV infection. 36,37 However, because no intervention specifically targeting immune activation or inflammation has been studied in a clinical outcomes trial in treated HIV infection, no interventions to reduce immune activation are recommended at this time.
In the absence of proven interventions, there is currently no clear rationale to monitor levels of immune activation and inflammation in treated HIV infection. Furthermore, many of the inflammatory markers that predict morbidity and mortality fluctuate significantly in HIV-infected individuals. Thus, clinical monitoring with immune activation or inflammatory markers is not currently recommended (AII). The focus of care to reduce chronic non-AIDS morbidity and mortality should be on maintaining ART-mediated viral suppression and addressing strategies to reduce risk factors (e.g., smoking cessation, healthy diet, and exercise) and managing chronic comorbidities such as hypertension, hyperlipidemia, and diabetes (AII).
# Regimen Switching In the Setting of Virologic Suppression (Last updated May 1, 2014; last reviewed May 1, 2014)
With use of currently available antiretroviral therapy (ART), most HIV-infected patients are able to achieve sustained HIV viral suppression. Furthermore, advances in treatment and better understanding about drug resistance make it possible to consider switching an effective regimen to an alternative regimen in some situations (see below). When contemplating such a switch, clinicians must consider several key principles to maintain viral suppression while addressing concerns with the current treatment.
Reasons to Consider Regimen Switching in the Setting of Viral Suppression:
- To simplify the regimen by reducing pill burden and dosing frequency to improve adherence
- To enhance tolerability and decrease short-or long-term toxicity (see Adverse Effects section)
- To change food or fluid requirements
- To avoid parenteral administration
- To minimize or address drug interaction concerns (see Drug Interactions section)
- To allow for optimal use of ART during pregnancy or should pregnancy occur (see Perinatal Guidelines) 1
- To reduce costs (see Cost section)
# Principles and Strategies of Regimen Switching
The cardinal principle of regimen switching is to maintain viral suppression without jeopardizing future treatment options. If a regimen switch results in virologic failure with emergence of new resistance mutations, the patient may require more complex, difficult to follow, or expensive regimens. Principles for successful regimen switching are highlighted below:
- It is critical to review a patient's full antiretroviral (ARV) history (including virologic responses, resistance test results, and past adverse events) before any treatment switch.
- Once a particular resistance mutation has been selected, it is generally archived in the HIV reservoir and is likely to reappear under the appropriate selective drug pressure, even if not detected in the most recent resistance test. If resistance data are unavailable, resistance may often be inferred from a patient's treatment history. For example, a clinician should assume that patients who have failed a cytosine analogue (e.g., a lamivudine (3TC)-or emtricitabine (FTC)-containing regimen), likely have the M184V substitution, even if the substitution is not documented. The same assumption of resistance may also apply to patients with documented failure to an non-nucleoside reverse transcriptase inhibitor (NNRTI)or an integrase strand transfer inhibitors (INSTI)-based regimen because these drugs generally have a lower barrier to resistance. If there is uncertainty about prior resistance, it is generally not advisable to switch a suppressive ARV regimen unless the new regimen is likely to be as active against resistant virus as the suppressive regimen.
- Consultation with an HIV specialist is recommended when considering a regimen switch for a patient with a history of resistance to one or more drug classes.
- Switching from a ritonavir (RTV)-boosted protease inhibitor (PI) regimen to a regimen composed of drugs with a lower barrier to resistance generally maintains viral suppression provided there is no resistance to the other components of the regimen. However, such switches should be avoided if there is any doubt about the activity of the other agents in the regimen.
- Within-class switches prompted by adverse events usually maintain viral suppression provided that there is no drug resistance to the other ARV agents in the same drug class.
- In the absence of any likely drug resistance, switching from complex regimens, parenteral drug (i.e., enfuvirtide), or drugs known now to be more toxic (e.g., zidovudine, stavudine, or didanosine) or with higher pill burden or dosing frequency to simpler regimens (e.g., from a regimen including ritonavirboosted saquinavir to one including ritonavir-boosted darunavir ) or to ARVs in a new drug class (e.g., an INSTI) generally results in similar or improved adherence, continued viral suppression and possibly improved quality of life.
- More intensive monitoring of tolerability, viral suppression, adherence, and laboratory changes is recommended during the first 3 months after a regimen switch.
# Alternative Switch Strategies for Patients with Virologic Suppression
# RTV-Boosted PI Monotherapy
The strategy of switching virologically suppressed patients without PI resistance from one ART regimen to RTV-boosted PI monotherapy has been studied. The rationale for this strategy is to avoid nucleoside reverse transcriptase inhibitor (NRTI) toxicities and decrease costs, while taking advantage of the high barrier to resistance of RTV-boosted PIs. RTV-boosted PI monotherapy maintains virologic suppression in most patients, but at slightly lower rates than standard therapy that includes 2 NRTIs. 2,3 Low-level viremia, generally without the emergence of PI resistance, appears to be more common with monotherapy. In most studies, resumption of NRTIs in patients experiencing low level viral rebound has led to re-suppression.
No clinical trials comparing available RTV-boosted PI monotherapy regimens have been conducted. Findings from an observational study suggest that the rate of treatment failure is higher in patients on RTV-boosted atazanavir (ATV/r) than in those on RTV-boosted lopinavir (LPV/r) or DRV/r. 4 Another pilot study reported early viral rebound with use of ATV/r monotherapy. 5 There are rare reports of central nervous system virologic escape, sometimes with clinical symptoms, in patients on RTV-boosted PI monotherapy. 6,7 On the basis of the results from these studies, RTV-boosted PI monotherapy should generally be avoided.
Other strategies to avoid use of NRTIs (i.e., use of a RTV-boosted PI plus a NNRTI, an INSTI, or maraviroc ) are also being studied, but data on these strategies are limited.
# Switching from a Ritonavir-Boosted Protease Inhibitor to Unboosted Atazanavir
Several clinical studies have evaluated switching a RTV-boosted PI to unboosted atazanavir (ATV) in virologically suppressed patients without NRTI resistance. Two comparative clinical trials reported that ATV/r and ATV, both in combination with 2 NRTIs (mostly ABC/3TC), demonstrated comparable levels of virologic suppression and a similar lack of treatment-emergent resistance. The benefits of the unboosted ATV regimen included a slightly improved lipid profile and a lower incidence of hyperbilirubinemia. 8,9 An additional study of 296 patients with virologic suppression on tenofovir disoproxil fumarate (TDF)/FTC plus ATV/r showed that patients switched to ABC/3TC plus ATV maintained viral suppression and showed improvements in certain bone and renal biomarkers. 10 The results of these and other non-comparative studies suggest that a regimen of ABC/3TC plus ATV can be considered in virologically suppressed patients, especially in those who have adverse effects from TDF or RTV.
# Switching to Maraviroc
Co-receptor usage in virologically suppressed patients can be determined from proviral DNA obtained from peripheral blood mononuclear cells. Individuals found to have R5-tropic virus by this technique could potentially have a component of their regimens switched to MVC. 11,12 However, although the use of MVC after DNA tropism testing has potential, this strategy cannot be recommended until more data from larger clinical studies are available (see Tropism Testing section).
# De-intensification
De-intensification of a standard RTV-boosted PI regimen from three to two active drugs (e.g., to a boosted PI plus one NRTI, 13 a boosted PI plus an INSTI, 14,15 or an NNRTI such as etravirine 15 or the CCR5 antagonist MVC 12 ) may be more effective virologically than RTV-boosted PI monotherapy, but, thus far, comparative data on this approach are limited. In general, switching a regimen -even in a patient without known drug resistance-from an effective three-drug regimen to a two-drug regimen has not been validated and is not recommended.
# Monitoring After Treatment Changes
Patients should be evaluated more closely for several months after a treatment switch (i.e., a clinic visit or phone call 1 to 2 weeks after the change and a viral load test to check for rebound viremia 4 to 8 weeks after the switch). The goal of the intensive monitoring is to assess medication tolerance and conduct targeted laboratory testing if the patient had pre-existing laboratory abnormalities or there are potential concerns with the new regimen. For example, if lipid abnormalities were present and/or were a reason for the ARV change or are a concern with the new regimen, fasting cholesterol subsets and triglycerides should be assessed within 3 months after the change in therapy. Absent any specific complaints, laboratory abnormalities, or evidence of viral rebound at this 3-month visit, clinical and laboratory monitoring of the patient may resume on a regularly scheduled basis (see Laboratory Testing section).
# Exposure-Response Relationship and Therapeutic Drug Monitoring (TDM) for Antiretroviral Agents (Last updated April 8, 2015; last reviewed April 8, 2015)
Knowledge about the relationship between a drug's systemic exposure (or concentration) and responses (beneficial and/or adverse) is key in selecting the dose of a drug, in understanding why patients may respond differently to the same drug and dose, and in designing strategies to optimize drug response and tolerability.
Therapeutic drug monitoring (TDM) is a strategy used to guide dosing of certain antiarrhythmics, anticonvulsants, antineoplastics, and antimicrobial agents by using measured drug concentrations to improve the likelihood of the desired therapeutic and safety outcomes. Drugs suitable for TDM are characterized by a known exposure-response relationship and a therapeutic range of concentrations. The therapeutic range is a range of concentrations established through clinical investigations that are associated with a greater likelihood of achieving the desired therapeutic response and/or reducing the frequency of drug-associated adverse reactions.
Several antiretroviral (ARV) agents meet most of the characteristics of agents suitable for a TDM strategy. 1 Specifically, some ARVs have considerable interpatient variability in drug concentrations; other ARVs have known drug concentrations associated with efficacy and/or toxicity; and in the case of other drugs, data from small prospective studies have demonstrated that TDM improved virologic response and/or decreased the incidence of concentration-related drug toxicities. 2,3 TDM for ARV agents, however, is not recommended for routine use in the management of HIVinfected adults (BII). This recommendation is based on multiple factors that limit the routine use of TDM in HIV-infected patients. These limiting factors include lack of prospective studies that demonstrate routine use of TDM improves clinical outcomes, uncertain therapeutic thresholds for most ARV agents, great intra-and inter-patient variability in drug concentrations achieved, and a lack of commercial laboratories to perform real time quantitation of ARV concentrations.
# Scenarios for Consideration of Therapeutic Drug Monitoring
Although routine use of TDM is not recommended, in some scenarios, ARV concentration data may be useful in patient management. In these cases, assistance from a clinical pharmacologist or a clinical pharmacist to interpret the concentration data may be advisable. These scenarios include the following:
- Suspect clinically significant drug-drug or drug-food interactions that may result in reduced efficacy or increased dose-related toxicities;
- Changes in pathophysiologic states that may impair gastrointestinal, hepatic, or renal function, thereby potentially altering drug absorption, distribution, metabolism, or elimination;
- Among pregnant women who have risk factors for virologic failure (e.g., those not achieving viral suppression during earlier stage of pregnancy)-during the later stages of pregnancy, physiologic changes may result in reduced drug exposure and thus further increase the risk of virologic failure;
# Panel's Recommendations
- Therapeutic drug monitoring for antiretroviral agents is not recommended for routine use in the management of HIV-infected patients (BII).
- TDM may be considered in selected clinical scenarios, as discussed in the text below. - Heavily pretreated patients experiencing virologic failure and who may have viral isolates with reduced susceptibility to ARVs;
# Rating of Recommendations
- Use of alternative dosing regimens and ARV combinations for which safety and efficacy have not been established in clinical trials;
- Concentration-dependent, drug-associated toxicities; and
- Lack of expected virologic response in medication-adherent patients.
# Resources for Therapeutic Drug Monitoring Target Concentrations
Most TDM-proposed target concentrations for ARVs focus on a minimum concentration (C min ) (i.e., the plasma concentration at the end of a dosing interval before the next ARV dose). A summary of population average ARV C min can be found in a review on the role of ARV-related TDM. 2 Population average C min for newer ARVs can be found in the Food and Drug Administration-approved product labels.
Guidelines for the collection of blood samples and other practical suggestions related to TDM can be found in a position paper by the Adult AIDS Clinical Trials Group Pharmacology Committee. 4
# Challenges and Considerations in Using Drug Concentrations to Guide Therapy
There are several challenges and considerations for implementation of TDM in the clinical setting. Use of TDM to monitor ARV concentrations in a patient requires the following:
- quantification of the concentration of the drug, usually in plasma or serum;
- determination of the patient's pharmacokinetic characteristics;
- integration of information on patient adherence;
- interpretation of the drug concentrations; and
- adjustment of the drug dose to achieve concentrations within the therapeutic range, if necessary.
A final caveat to the use of measured drug concentrations in patient management is a general one-drug concentration information cannot be used alone; it must be integrated with other clinical information, including the patient's ARV history and adherence before the TDM result. In addition, as knowledge of associations between ARV concentrations and virologic response evolves, clinicians who use a TDM strategy for patient management should evaluate the most up-to-date information regarding the exposure-response relationship of the tested ARV agent. Discontinuation of antiretroviral therapy (ART) may result in viral rebound, immune decompensation, and clinical progression. Thus, planned interruptions of ART are not generally recommended. However, unplanned interruption of ART may occur under certain circumstances as discussed below.
# Short-Term Therapy Interruptions
Reasons for short-term interruption (days to weeks) of ART vary and may include drug toxicity; intercurrent illnesses that preclude oral intake, such as gastroenteritis or pancreatitis; surgical procedures; or interrupted access to drugs. Stopping ART for a short time (i.e., less than 1 to 2 days) because of a medical/surgical procedure can usually be done by holding all drugs in the regimen. Recommendations for some other scenarios are listed below:
# Unanticipated Short-Term Therapy Interruption
When a Patient Experiences a Severe or Life-Threatening Toxicity or Unexpected Inability to Take Oral Medications:
- All components of the drug regimen should be stopped simultaneously, regardless of drug half-life.
# Planned Short-Term Therapy Interruption (Up to 2 Weeks)
When All Regimen Components Have Similar Half-Lives and Do Not Require Food for Proper Absorption:
- All drugs may be given with a sip of water, if allowed; otherwise, all drugs should be stopped simultaneously. All discontinued regimen components should be restarted simultaneously.
# When All Regimen Components have Similar Half-Lives and Require Food for Adequate Absorption, and the
Patient Cannot Take Anything by Mouth for a Short Time:
- Temporary discontinuation of all drug components is indicated. The regimen should be restarted as soon as the patient can resume oral intake.
# When the ARV Regimen Contains Drugs with Different Half-Lives:
- Stopping all drugs simultaneously may result in functional monotherapy with the drug with the longest half-life (typically a non-nucleoside reverse transcriptase inhibitor ), which may increase the risk of selection of NNRTI-resistant mutations. Some experts recommend stopping the NNRTI first and the other ARV drugs 2 to 4 weeks later. Alternatively, the NNRTI may be replaced with a ritonavir (or cobicistat)-boosted protease inhibitor (PI/r or PI/c) for 4 weeks. The optimal time sequence for staggered discontinuation of regimen components, or replacement of the NNRTI with a PI/r (or PI/c), has not been determined.
# Planned Long-Term Therapy Interruptions
Planned long-term therapy interruptions are not recommended outside of controlled clinical trials (AI). Several research studies are evaluating approaches to a functional (virological control in the absence of therapy) or sterilizing (virus eradication) cure of HIV infection. Currently, the only way to reliably test the effectiveness of these strategies may be to interrupt ART and closely monitor viral rebound over time in the setting of a clinical trial. a Early infection represents either acute or recent infection.
Definitions: Acute HIV-1 infection is the phase of HIV-1 disease immediately after infection that is characterized by an initial burst of viremia; although, anti-HIV-1 antibodies are undetectable, HIV-1 RNA or p24 antigen are present. Recent infection generally is considered the phase up to 6 months after infection during which anti-HIV-1 antibodies are detectable. Throughout this section, the term "early HIV-1 infection" is used to refer to either acute or recent HIV-1 infection.
An estimated 40% to 90% of patients with acute HIV-1 infection will experience symptoms of acute retroviral syndrome, such as fever, lymphadenopathy, pharyngitis, skin rash, myalgias/arthralgias, and other symptoms. However, because the self-limiting symptoms are similar to those of many other viral infections, such as influenza and infectious mononucleosis, primary care clinicians often do not recognize acute HIV-1 infection. Acute infection can also be asymptomatic. Table 11 provides practitioners with guidance to recognize, diagnose, and manage acute HIV-1 infection.
# Diagnosing Acute HIV Infection
Health care providers should maintain a high level of suspicion of acute HIV-1 infection in patients who have a compatible clinical syndrome-especially in those who report recent high-risk behavior (see Table 11). 7 Patients may not always disclose or admit to high-risk behaviors or perceive that their behaviors put them at risk for HIV-1 acquisition. Thus, even in the absence of reported high-risk behaviors, signs and symptoms
# Panel's Recommendations
- Antiretroviral therapy (ART) is recommended for all individuals with HIV-1 infection and should be offered to those with early a HIV-1 infection (BII), although definitive data to confirm whether this approach will result in long-term virologic, immunologic, or clinical benefits are lacking.
- All pregnant women with early HIV-1 infection should start ART as soon as possible to prevent perinatal transmission of HIV-1 (AI).
- If treatment is initiated in a patient with early HIV-1 infection, the goal is to suppress plasma HIV-1 RNA to undetectable levels (AIII).
- In patients with early HIV-1 infection in whom therapy is initiated, testing for plasma HIV-1 RNA levels, CD4 T lymphocyte counts, and toxicity monitoring should be performed as described for patients with chronic HIV-1 infection (AII).
- Genotypic drug resistance testing should be performed before initiation of ART to guide the selection of the regimen (AII). If therapy is deferred, genotypic resistance testing should still be performed because the results will be useful in selecting a regimen with the greatest potential for achieving optimal virologic response once therapy is initiated (AII).
- In patients without transmitted drug resistant virus, therapy should be initiated with one of the combination regimens that is recommended for patients with chronic HIV-1 infection (see What to Start) (AIII).
- ART can be initiated before drug resistance test results are available. Because resistance to pharmacokinetically enhanced protease inhibitors emerges slowly and clinically significant transmitted resistance to protease inhibitors is uncommon, these drugs and 2 nucleoside reverse transcriptase inhibitors should be used in this setting (AIII).
- Patients starting ART should be willing and able to commit to treatment and should understand the possible benefits and risks of therapy and the importance of adherence (AIII). Patients may choose to postpone therapy, and providers, on a case-by-case basis, may elect to defer therapy because of clinical and/or psychosocial factors. consistent with acute retroviral syndrome should motivate consideration of a diagnosis of acute HIV-1 infection.
# Rating of Recommendations
Acute HIV-1 infection is usually defined as detectable HIV-1 RNA or p24 antigen in serum or plasma in the setting of a negative or indeterminate HIV-1 antibody test result. 7,8 Combination immunoassays that detect HIV-1 and HIV-2 antibodies and HIV-1 p24 antigen are now approved by the Food and Drug Administration (FDA), and the most recent Centers for Disease Control and Prevention testing algorithm recommends them as the preferred assay to use for HIV screening, including for possible acute HIV-1 infection. Specimens that are reactive on this initial assay should be tested with an immunoassay that differentiates HIV-1 and HIV-2 antibodies. 9 Specimens that are reactive on the initial assay and have either negative or indeterminate antibody differentiation test results should undergo testing using an FDA-approved quantitative or qualitative HIV-1 RNA test; a negative HIV-1 RNA test result indicates that the original Ag/Ab test result was a false positive. Detection of HIV-1 RNA indicates that acute HIV-1 infection is highly likely, 9 and that antiretroviral therapy (ART) may be warranted (see Treatment for Early HIV-1 Infection). HIV-1 infection should be confirmed by subsequent testing to document HIV antibody seroconversion.
Some health care facilities may still be following HIV testing algorithms that recommend initial testing with an assay that only tests for the presence of HIV antibody. In such settings, when acute HIV-1 infection is suspected in a patient with a negative or indeterminate HIV antibody result, a quantitative or qualitative FDA-approved HIV-1 RNA test should be performed (AII). A presumptive diagnosis of acute HIV-1 infection can be made on the basis of a negative or indeterminate HIV antibody test result and a positive HIV-1 RNA test result, in which case, ART may be warranted (see Treatment for Early HIV-1 Infection).
Providers should be aware that a low-positive quantitative HIV-1 RNA level (e.g., 100,000 copies/mL). 5,6 Therefore, when a low-positive quantitative HIV-1 RNA result is obtained, the HIV-1 RNA test should be repeated using a different specimen from the same patient. 6 In this setting, the diagnosis of HIV-1 infection should be confirmed by subsequent documentation of HIV antibody seroconversion (see Table 11).
# Treating Early HIV-1 Infection
Clinical trial data regarding the treatment of early HIV-1 infection is limited. Many patients who enrolled in studies to assess the role of ART in early HIV-1 infection (outlined below) were identified as trial participants because they presented with signs or symptoms of acute infection. With the introduction of HIV screening tests that include assays for HIV-1 RNA or p24 antigen and wider HIV screening in healthcare systems, the number of asymptomatic patients identified with early infection may increase. The natural history of HIV-1 disease in these patients may differ from that in individuals with symptomatic infections, thus further studies on the impact of ART on the natural history of asymptomatic acute HIV-1 infection are needed. The initial burst of high level viremia in infected individuals usually declines shortly after acute infection (e.g., within 2 months); however, a rationale for treatment during recent infection (e.g., 2-6 months after infection) remains, because during this transition period the immune system may not yet have maximally contained viral replication in the lymphoid tissue. 10 Several trials have addressed the question of the long-term benefit of potent treatment regimens initiated during early HIV-1 infection. The potential benefits and risks of treating HIV-1 during this stage of disease are discussed below.
# Potential Benefits of Treatment During Early HIV-1 Infection
Preliminary data indicate that treatment of early HIV-1 infection with combination ART improves laboratory markers of disease progression. The data, though limited, indicate that treatment of early HIV-1 infection may also reduce the severity of acute disease; lower the viral set point, which can affect the rate of disease progression if therapy is stopped; reduce the size of the viral reservoir; 19 and decrease the rate of viral mutation by suppressing viral replication and preserving immune function. 20 Because early HIV-1 infection is often associated with high viral loads and increased infectiousness, 21 and ART use by HIV-1-infected individuals reduces transmission to serodiscordant sexual partners, 22 treatment during early HIV-1 infection is expected to substantially reduce the risk of HIV-1 transmission. In addition, although data are limited and the clinical relevance unclear, the profound loss of gastrointestinal lymphoid tissue that occurs during the first weeks of infection may be mitigated by initiating ART during early HIV-1 infection. 23,24 Many of the potential benefits described above may be more likely to occur with treatment of acute infection, but they also may occur if treatment is initiated during recent HIV-1 infection.
# Potential Risks of Treatment During Early HIV-1 Infection
The potential disadvantages of initiating therapy during early HIV-1 infection include more prolonged exposure to ART without a known long-term clinical benefit. This prolonged exposure to ART could result in drug toxicities, development of drug resistance if the patient is non-adherent to the regimen, and adverse effects on the patient's quality of life due to earlier initiation of lifelong therapy that requires strict adherence.
# Clinical Trial Data on Treatment During Early Infection
Several randomized controlled trials have studied the effect of ART during acute and recent infection to assess whether initiating early therapy would allow patients to stop treatment and still maintain lower viral loads and higher CD4 T lymphocyte (CD4) counts while off ART for prolonged periods of time. This objective was of interest when these studies were initiated but is now less relevant because treatment is recommended for virtually all HIV-1-infected patients and treatment interruptions are not recommended (see Initiating Antiretroviral Therapy in Treatment-Naive Patients).
The Setpoint Study (ACTG A5217 Study) randomized patients with recent but not acute HIV-1 infection to either defer therapy or immediately initiate ART for 36 weeks and then stop treatment. 16 The primary study end point was a composite of meeting criteria for ART or re-initiation of ART and viral load results at week 72 in both groups and at week 36 in the deferred treatment group. The study was stopped prematurely by the Data and Safety Monitoring Board because of an apparent benefit associated with early therapy that was driven mostly by the greater proportion of participants meeting the criteria for ART initiation in the deferred treatment group (50%) than in the immediate treatment group (10%). Nearly half of the patients in the deferred treatment group needed to start therapy during the first year of study enrollment.
The Randomized Primo-SHM Trial randomized patients with acute (~70%) or recent (~30%) infection to either defer ART or undergo treatment for 24 or 60 weeks and then stop. 17 Significantly lower viral loads were observed 36 weeks after treatment interruption in the patients who had been treated early. These patients also took longer to reach a CD4 count threshold of <350 cells/mm 3 for restarting ART. The median time to starting treatment was 0.7 years for the deferred therapy group and 3.0 and 1.8 years for the 24-and 60-week treatment arms, respectively. The time to reaching a CD4 count of <500 cells/mm 3 was only 0.5 years in the deferred group.
The SPARTAC Trial included patients with acute and recent infection randomized to either defer therapy or received ART for 12 or 48 weeks and then stop. 18 In this trial, the time to reach CD4 <350 cells/mm 3 or initiate therapy was significantly longer in the group treated for 48 weeks than in the deferred treatment group or the group treated for 12 weeks. However, no difference was observed between the participants who received 12 weeks of ART and those who deferred treatment during early infection.
The strategies tested in these studies are of limited relevance today given that treatment interruption is not recommended. The study results may not fully reflect the natural history of HIV-1 disease in persons with asymptomatic acute infection because most patients in these trials were enrolled on the basis of identified early symptomatic HIV-1 infections. Nevertheless, the results do demonstrate that some immunologic and virologic benefits may be associated with the treatment of early HIV-1 infection. Moreover, all the findings suggest, at least in the population recruited for these studies, that the time to initiating ART after identification of early infection is quite short when the threshold for ART initiation is 350 CD4 cells/mm 3 , and nonexistent when therapy is advised for all individuals regardless of CD4 cell count as currently recommended in these guidelines. These observations must be balanced with the risks of early treatment, risks that are largely the same as those when therapy is initiated in chronically infected asymptomatic patients with high CD4 counts. Consequently, the health care provider and the patient should be fully aware that the rationale for initiating therapy during early HIV-1 infection is based on theoretical benefits and the extrapolation of data from the strategy trials outlined above. These potential benefits must be weighed against the risks. For these reasons, and because ART is currently recommended for all HIV-1-infected patients (see Initiating Antiretroviral Therapy in Treatment Naive Patients), ART should be offered to all patients with early HIV-1 infection (BII). However, patients must be willing and able to commit to treatment, and providers, on a case-by-case basis, may elect to defer therapy for clinical and/or psychosocial reasons. Providers also should consider enrolling patients with early HIV-1 infection in clinical studies to further evaluate the natural history of this stage of HIV-1 infection and to further define the role of ART in this setting. Providers can obtain information regarding such trials at www.clinicaltrials.gov or from local HIV treatment experts.
# Treating Early HIV-1 Infection During Pregnancy
Because early HIV-1 infection is associated with a high risk of perinatal transmission, all HIV-1-infected pregnant women should start combination ART as soon as possible to prevent perinatal transmission of HIV-1 (AI). 25
# Treatment Regimen for Early HIV-1 Infection
Data from the United States and Europe demonstrate that transmitted virus may be resistant to at least 1 antiretroviral drug in 6% to 16% of patients. In one study, 21% of isolates from patients with acute HIV-1 infection demonstrated resistance to at least 1 drug. 29 Therefore, before initiating ART in a person with early HIV-1 infection, genotypic antiretroviral (ARV) drug resistance testing should be performed to guide selection of a regimen (AII). If the decision is made to initiate therapy during early infection, especially in the setting of acute infection, treatment initiation should not be delayed pending resistance testing results.
Once results are available, the treatment regimen can be modified if warranted. If therapy is deferred, resistance testing still should be performed because the results will help guide selection of a regimen that has the greatest potential to optimize virologic response once therapy is initiated (AII).
The goal of therapy during early HIV-1 infection is to suppress plasma HIV-1 RNA to undetectable levels (AIII). Because data are insufficient to draw firm conclusions regarding specific drug combinations to use in this stage of HIV-1 infection, ART should be initiated with one of the combination regimens recommended for patients with chronic infection (AIII) (see What to Start). If therapy is started before the results of drug resistance testing are available, a pharmacologically boosted protease inhibitor (PI) should be used because resistance to these agents emerges slowly and clinically significant transmitted resistance is uncommon (AIII).
If available, the results of ARV drug resistance testing or the ARV resistance pattern of the source person's virus should be used to guide selection of the ARV regimen. Given the increasing use of daily tenofovir disoproxil fumarate/emtricitabine (TDF/FTC) for pre-exposure prophylaxis (PrEP) in HIV-negative individuals, early infection may be diagnosed in some patients while they are taking TDF/FTC as PrEP. In this setting, resistance testing should be performed; however, because PI resistance is unlikely, use of a pharmacologically boosted PI and TDF/FTC remains a reasonable option pending resistance testing results (see What to Start).
# Patient Follow-Up
Testing for plasma HIV-1 RNA levels, CD4 cell counts, and toxicity monitoring should be performed as described in Laboratory Testing for Initial Assessment and Monitoring While on Antiretroviral Therapy (i.e.,
HIV-1 RNA at initiation of therapy, after 2 to 8 weeks, then every 4 to 8 weeks until viral suppression, and thereafter, every 3 to 4 months) (AII).
# Duration of Therapy for Early HIV-1 Infection
The optimal duration of therapy for patients with early HIV-1 infection is unknown. Recent studies of early HIV-1 infection have evaluated starting and then stopping treatment as a potential strategy. Although these studies showed some benefits associated with this strategy, a large randomized controlled trial of patients with chronic HIV-1 infection found that treatment interruption was harmful in terms of increased risk of AIDS and non-AIDS events, 33 and that the strategy was associated with increased markers of inflammation, immune activation, and coagulation. 34 For these reasons and the potential benefit of ART in reducing the risk of HIV-1 transmission, the Panel does not recommend discontinuation of ART in patients treated for early HIV-1 infection (AIII).
# Table 11. Identifying, Diagnosing, and Managing Acute and Recent HIV-1 Infection
Suspicion of Acute HIV-1 Infection:
- Acute HIV-1 infection should be considered in individuals with signs or symptoms of acute HIV-1 infection and recent (within 2 to 6 weeks) high risk of exposure to HIV-1
.a
- Signs, symptoms, or laboratory findings may include but are not limited to one or more of the following: fever, lymphadenopathy, skin rash, myalgia/arthralgia, headache, diarrhea, oral ulcers, leucopenia, thrombocytopenia, transaminase elevation.
- High-risk exposures include sexual contact with an HIV-1-infected person or a person at risk of HIV-1 infection, sharing injection drug use paraphernalia, or contact of mucous membranes or breaks in skin with potentially infectious fluids.
- Differential diagnosis: The differential diagnosis of patients presenting with HIV-1 infection may include but is not limited to viral illnesses such as Epstein-Barr virus (EBV) and non-EBV (e.g., cytomegalovirus) infectious mononucleosis syndromes, influenza, viral hepatitis, streptococcal infection, or syphilis.
Evaluation/Diagnosis of Acute HIV-1 Infection:
- Acute HIV-1 infection is defined as detectable HIV-1 RNA or p24 antigen (the antigen used in currently available HIV antigen/antibody combination assays) in the setting of a negative or indeterminate HIV-1 antibody test result.
- A reactive HIV antibody test result or Ag/Ab combination test result must be followed by supplemental confirmatory testing.
- A negative or indeterminate HIV-1 antibody test result in a person with a reactive Ag/Ab test result or in whom acute HIV-1 infection is suspected requires assessment of plasma HIV-1 RNA to diagnose acute HIV-1 infection.
- A positive result on an FDA-approved quantitative or qualitative plasma HIV-1 RNA test in the setting of a negative or indeterminate antibody test result is consistent with acute HIV-1 infection.
Considerations for ART During Early HIV-1 Infection:
- All pregnant women with early HIV-1 infection should begin taking combination ART as soon as possible to prevent perinatal transmission of HIV-1 (AI).
- Treatment for early HIV-1 infection should be offered to all non-pregnant individuals (BII).
- The risks of ART during early HIV-1 infection are largely the same as those when ART is initiated in chronically infected asymptomatic patients with high CD4 counts.
- If therapy is initiated, the goal should be sustained plasma virologic suppression (AIII).
a In some settings, behaviors that increase the risk of HIV-1 infection may not be recognized or perceived as risky by the health care provider or the patient or both. Thus, even in the absence of reported high-risk behaviors, symptoms and signs consistent with acute retroviral syndrome should motivate consideration of a diagnosis of acute HIV-1 infection. Older children and adolescents now make up the largest percentage of HIV-infected children cared for at pediatric HIV clinics in the United States. The Centers for Disease Control and Prevention (CDC) estimates that 26% of the approximately 50,000 new HIV infections diagnosed in 2010 were among youth 13 to 24 years of age. In this age group, 57% of the infections were among young black/African Americans and 75% among young men who have sex with men (MSM). 1 Among youth living with HIV infection in 2010, CDC estimates that almost 60% had undiagnosed infections and were unaware they were HIV-infected. 2 Recent trends in HIV/AIDS prevalence reveal that the disproportionate burden of AIDS among racial minorities is even greater among minority youth 13 to 24 years of age (64% to 66% of cases) than among those older than 24 years (48% of cases). 3 Furthermore, trends for all HIV diagnoses among adolescents and young adults in 46 states and 5 U.S. dependent areas from 2007 to 2010 decreased or remained stable for all transmission categories except among young MSM. HIV-infected adolescents represent a heterogeneous group in terms of sociodemographics, mode of HIV infection, sexual and substance abuse history, clinical and immunologic status, psychosocial development, and readiness to adhere to medications. Many of these factors may influence decisions concerning when to start antiretroviral therapy (ART) and what antiretroviral (ARV) medications to use.
Most adolescents who acquire HIV are infected through sexual risk behaviors. Many of them are recently infected and unaware of their HIV infection status. Thus, many are in an early stage of HIV infection, which makes them ideal candidates for early interventions, such as prevention counseling and linkage to and engagement in care. 4 High grade viremia was reported among a cohort of youth identified as HIV-infected by adolescent HIV specialty clinics in 15 major metropolitan U.S. cities. The mean HIV viral load for the cohort was 94,398 copies/ml; 30% of the youth were not successfully linked to care. 5 A study among HIV-infected adolescents and young adults presenting for care identified primary genotypic resistance mutations to ARV medications in up to 18% of the evaluable sample of recently infected youth, as determined by the detuned antibody testing assay strategy that defined recent infection as occurring within 180 days of testing. 6 Recently, substantial multiclass resistance was noted in a cohort of behaviorally-infected, treatment-naive youth who were screened for an ARV treatment trial. 7 As these youth were naive to all ART, this reflects transmission of resistant virus. This transmission dynamic reflects that a substantial proportion of youth's sexual partners are likely older and may be more ART experienced; thus, awareness of the importance of baseline resistance testing among recently infected youth naive to ART is imperative.
A limited but increasing number of HIV-infected adolescents are long-term survivors of HIV infection acquired perinatally or in infancy through blood products. Such adolescents are usually heavily ART experienced and may have a unique clinical course that differs from that of adolescents infected later in life. 8 Those adolescents infected perinatally or in infancy were often started on ART early in life with mono or dual therapy regimens resulting in incomplete viral suppression and emergence of resistance. If these heavily ART-experienced adolescents harbor resistant virus, optimal ARV regimens should be selected on the basis of the same guiding principles used for heavily ART-experienced adults (see Virologic Failure and Suboptimal Immunologic Response).
Adolescents are developmentally at a difficult crossroad. Their needs for autonomy and independence and their evolving decisional capacity intersect and compete with their concrete thinking processes, risk-taking behaviors, preoccupation with self-image, and need to fit in with their peers. This makes it challenging to attract and sustain adolescents' focus on maintaining their health, particularly for those with chronic illnesses. These challenges are not specific to any particular transmission mode or stage of disease. Thus, irrespective of disease duration or mode of HIV transmission, every effort must be made to engage and maintain adolescents in care so they can improve and maintain their health for the long term. Adolescents may seek care in several settings including pediatric-focused HIV clinics, adolescent/young adult clinics, and adult-focused clinics. 9 Regardless of the setting, expertise in caring for adolescents is critical to creating a Downloaded from on 9/16/2015
Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents I-9
supportive environment for engaging youth in care. 9,10
# Antiretroviral Therapy Considerations in Adolescents
Adult guidelines for ART are usually appropriate for postpubertal adolescents because the clinical course of HIV infection in adolescents who were infected sexually or through injection drug use during adolescence is more similar to that in adults than that in children. Adult guidelines can also be useful for postpubertal youth who were perinatally infected. These patients often have treatment challenges associated with the long-term use of ART that mirror those of ART-experienced adults, such as extensive resistance, complex regimens, and adverse drug effects.
Dosage of medications for HIV infection and opportunistic infections should be prescribed according to Tanner staging of puberty and not solely on the basis of age. 11,12 Adolescents in early puberty (i.e., Tanner Stages I and II) should be administered doses on pediatric schedules, whereas those in late puberty (i.e., Tanner Stage V) should follow adult dosing schedules. However, Tanner stage and age are not necessarily directly predictive of drug pharmacokinetics. Because puberty may be delayed in children who were infected with HIV perinatally, 13 continued use of pediatric doses in puberty-delayed adolescents can result in medication doses that are higher than the usual adult doses. Because data are not available to predict optimal medication doses for each ARV medication for this group of children, issues such as toxicity, pill or liquid volume burden, adherence, and virologic and immunologic parameters should be considered in determining when to transition from pediatric to adult doses. Youth who are in their growth spurt period (i.e., Tanner Stage III in females and Tanner Stage IV in males) and following adult or pediatric dosing guidelines and adolescents who have transitioned from pediatric to adult doses should be closely monitored for medication efficacy and toxicity. Therapeutic drug monitoring can be considered in each of these selected circumstances to help guide therapy decisions. Pharmacokinetic studies of drugs in youth are needed to better define appropriate dosing. For a more detailed discussion, see Guidelines for the Use of Antiretroviral Agents in Pediatric HIV Infection. 14
# Adherence Concerns in Adolescents
HIV-infected adolescents are especially vulnerable to specific adherence problems on the basis of their psychosocial and cognitive developmental trajectory. Comprehensive systems of care are required to serve both the medical and psychosocial needs of HIV-infected adolescents, who are frequently inexperienced with health care systems and who lack health insurance. Recent studies in adolescents infected through risk behaviors and in adolescents infected through perinatal transmission demonstrate that many adolescents in both groups face numerous barriers to adherence. Compared with adults, these youth have lower rates of viral suppression and higher rates of virologic rebound and loss to follow up. 18 Many HIV-infected adolescents face challenges in adhering to medical regimens for reasons that include:
- Denial and fear of their HIV infection;
- Misinformation;
- Distrust of the medical establishment;
- Fear and lack of belief in the effectiveness of medications;
- Low self-esteem;
- Unstructured and chaotic lifestyles;
- Mood disorders and other mental illness;
- Lack of familial and social support;
- Absence of or inconsistent access to care or health insurance; and
- Risk of inadvertent parental disclosure of the youth's HIV infection status if parental health insurance is used.
In selecting treatment regimens for adolescents, clinicians must balance the goal of prescribing a maximally potent ART regimen with realistic assessment of existing and potential support systems to facilitate adherence. Adolescents benefit from reminder systems (e.g., beepers, timers, and pill boxes) that are stylish and/or inconspicuous. 19 In a recent randomized controlled study among non-adherent youth 15 to 24 years of age, youth who received cell phone medication reminders demonstrated significantly higher adherence and lower viral loads than youth who did not receive the reminder calls. 20 It is important to make medication adherence as user friendly and the least stigmatizing possible for the older child or adolescent. The concrete thought processes of adolescents make it difficult for them to take medications when they are asymptomatic, particularly if the medications have side effects. Adherence to complex regimens is particularly challenging at a time of life when adolescents do not want to be different from their peers. Directly observed therapy may be considered for selected HIV-infected adolescents such as those with mental illness.
# Difficult Adherence Problems
Because adolescence is characterized by rapid changes in physical maturation, cognitive processes, and life style, predicting long-term adherence in an adolescent can be very challenging. The ability of youth to adhere to therapy needs to be considered as part of therapeutic decision making concerning the risks and benefits of starting treatment. Erratic adherence may result in the loss of future regimens because of the development of resistance mutations. Clinicians who care for HIV-infected adolescents frequently manage youth who, while needing therapy, pose significant concerns regarding their ability to adhere to therapy. In these cases, alternative considerations to initiation of therapy can be the following:
1. A short-term deferral of treatment until adherence is more likely or while adherence-related problems are aggressively addressed;
2. An adherence testing period in which a placebo (e.g., vitamin pill) is administered; and
3. The avoidance of any regimens with low genetic resistance barriers.
Such decisions are ideally individualized to each patient and should be made carefully in context with the individual's clinical status. For a more detailed discussion on specific therapy and adherence issues for HIVinfected adolescents, see Guidelines for Use of Antiretroviral Agents in Pediatric HIV Infection. 14
# Special Considerations in Adolescents
Sexually transmitted infections (STIs), in particular human papilloma virus (HPV), should also be addressed in all adolescents. In young MSM, screening for STIs may require sampling from several body sites because oropharyngeal, rectal, and urethral infections may be present in this population. 29 For a more detailed discussion on STIs, see the most recent CDC guidelines 30 and the adult and pediatric opportunistic infection treatment guidelines on HPV among HIV-infected adolescents. 31,32 Family planning counseling, including a discussion of the risks of perinatal transmission of HIV and methods to reduce risks, should be provided to all youth. Providing gynecologic care for HIV-infected female adolescents is especially important. Contraception, including the interaction of specific ARV drugs with hormonal contraceptives, and the potential for pregnancy also may alter choices of ART. As an example, efavirenz (EFV) should be used with caution in females of childbearing age and should only be prescribed after intensive counseling and education about the potential effects on the fetus, the need for close monitoring-including periodic pregnancy testing-and a commitment on the part of the teen to use effective contraception. For a more detailed discussion, see HIV-Infected Women and the Perinatal Guidelines. 33
# Transitioning Care
Given lifelong infection with HIV and the need for treatment through several stages of growth and development, HIV care programs and providers need flexibility to appropriately transition care for HIVinfected children, adolescents, and young adults. A successful transition requires an awareness of some fundamental differences between many adolescent and adult HIV care models. In most adolescent HIV clinics, care is more teen-centered and multidisciplinary, with primary care highly integrated into HIV care.
Teen services, such as sexual and reproductive health, substance abuse treatment, mental health, treatment education, and adherence counseling are all found in one clinic setting. In contrast, some adult HIV clinics may rely more on referral of the patient to separate subspecialty care settings, such as gynecology.
Transitioning the care of an emerging young adult includes considerations of areas such as medical insurance; the adolescent's degree of independence/autonomy and decisional capacity; patient confidentiality; and informed consent. Also, adult clinic settings tend to be larger and can easily intimidate younger, less motivated patients. As an additional complication to this transition, HIV-infected adolescents belong to two epidemiologically distinct subgroups:
1. Those perinatally infected-who would likely have more disease burden history, complications, and chronicity; less functional autonomy; greater need for ART; and higher mortality risk-and 2. Those more recently infected because of high-risk behaviors.
Thus, these subgroups have unique biomedical and psychosocial considerations and needs.
To maximize the likelihood of a successful transition, interventions to facilitate transition are best implemented early on. 34 These include the following:
- Developing an individualized transition plan to address comprehensive care needs including medical, psychosocial and financial aspects of transitioning;
- Optimizing provider communication between adolescent and adult clinics;
- Identifying adult care providers willing to care for adolescents and young adults;
- Addressing patient/family resistance caused by lack of information, stigma or disclosure concerns, and differences in practice styles;
- Preparing youth for life skills development, including counseling them on the appropriate use of a primary care provider and appointment management, the importance of prompt symptom recognition and reporting, and the importance of self-efficacy in managing medications, insurance, and entitlements;
- Identifying an optimal clinic model for a given setting (i.e., simultaneous transition of mental health and/or case management versus a gradual phase-in);
- Implementing ongoing evaluation to measure the success of a selected model;
- Engaging in regular multidisciplinary case conferences between adult and adolescent care providers;
- Implementing interventions that may be associated with improved outcomes, such as support groups and mental health consultation;
- Incorporating a family planning component into clinical care; and
- Educating HIV care teams and staff about transitioning.
Discussions regarding transition should begin early and before the actual transition process. 35 Attention to these key areas will likely improve adherence to appointments and avert the potential for a youth to fall through the cracks, as it is commonly referred to in adolescent medicine. For a more detailed discussion on specific topics on transitioning care for adolescents and young adults, see /.
# Treatment Challenges of HIV-Infected Illicit Drug Users
Injection drug use is the second most common mode of HIV transmission in the United States. In addition, noninjection illicit drug use may facilitate sexual transmission of HIV. Injection and noninjection illicit drugs include the following: heroin, cocaine, marijuana, and club drugs (i.e., methamphetamine, ketamine, gammahydroxybutyrate , and amyl nitrate ). The most commonly used illicit drugs associated with HIV infection are heroin and stimulants (e.g., cocaine and amphetamines); however, the use of club drugs has increased substantially in the past several years and is common among individuals who have HIV infection or who are at risk of HIV infection. The association between club drugs and high-risk sexual behavior in men who have sex with men (MSM) is strongest for methamphetamine and amyl nitrate; this association is less consistent with the other club drugs. 1 Illicit drug use has been associated with depression and anxiety, either as part of the withdrawal process or as a consequence of repeated use. This is particularly relevant in the treatment of HIV infection because depression is one of the strongest predictors of poor adherence and poor treatment outcomes. 2 Treatment of HIV disease in illicit drug users can be successful but HIV-infected illicit drug users present special treatment challenges. These challenges may include the following: (1) an array of complicating comorbid medical and mental health conditions; (2) limited access to HIV care; (3) inadequate adherence to therapy; (4) medication side effects and toxicities; (5) the need for substance abuse treatment; and (6) drug interactions that can complicate HIV treatment. 3 Underlying health problems in injection and noninjection drug users result in increased morbidity and mortality, either independent of or accentuated by HIV disease. Many of these problems are the consequence of prior exposures to infectious pathogens from nonsterile needle and syringe use. Such problems can include hepatitis B or C virus infection, tuberculosis (TB), skin and soft tissue infections, recurrent bacterial pneumonia, and endocarditis. Other morbidities such as alteration in levels of consciousness and neurologic and renal disease are not uncommon. Furthermore, these comorbidities are associated with a higher risk of drug overdoses in illicit drug users with HIV disease than in HIV-uninfected illicit drug users, due in part to respiratory, hepatic, and neurological impairments associated with HIV infection. 4 Successful HIV therapy for illicit drug users often depends on clinicians becoming familiar with and managing these comorbid conditions and providing overdose prevention support.
Illicit drug users have less access to HIV care and are less likely to receive antiretroviral therapy (ART) than other populations. Factors associated with low rates of ART use among illicit drug users include active drug use, younger age, female gender, suboptimal health care, recent incarceration, lack of access to rehabilitation programs, and health care providers' lack of expertise in HIV treatment. The typically unstable, chaotic life patterns of many illicit drug users; the powerful pull of addictive substances; and common misperceptions about the dangers, impact, and benefits of ART all contribute to decreased adherence. 7 The chronic and relapsing nature of substance abuse as a biologic and medical disease, compounded by the high rate of mental illness that antedates and/or is exacerbated by illicit substance use, additionally complicate the relationship between health care workers and illicit drug users. The first step in provision of care and treatment for these individuals is to recognize the existence of a substance abuse problem. It is often obvious that the problem exists, but some patients may hide these problem behaviors from clinicians. Assessment of a patient for substance abuse should be part of routine medical history taking and should be done in a professional, straightforward, and nonjudgmental manner.
# Treatment Efficacy in HIV-Infected Illicit Drug Use Populations
Although illicit drug users are underrepresented in HIV therapy clinical trials, available data indicate that efficacy of ART in illicit drug users-when they are not actively using drugs-is similar to that seen in other populations. 10 Furthermore, therapeutic failure in this population generally correlates with the degree that drug use disrupts daily activities rather than with drug use per se. 11 Providers need to remain attentive to the possible impact of disruptions caused by drug use on the patient both before and while receiving ART. Although many illicit drug users can sufficiently control their drug use for long enough time to benefit from care, substance abuse treatment is often necessary for successful HIV management.
Close collaboration with substance abuse treatment programs and proper support and attention to this population's special multidisciplinary needs are critical components of successful HIV treatment. Essential to this end are accommodating, flexible, community-based HIV care sites that are characterized by familiarity with and nonjudgmental expertise in management of drug users' wide array of needs and in development of effective strategies to promote medication adherence. 9 These strategies should include, if available, the use of adherence support mechanisms such as modified directly observed therapy (mDOT), which has shown promise in this population. 12
# Antiretroviral Agents and Opioid Substitution Therapy
Compared with noninjection drug users receiving ART, injection drug users (IDUs) receiving ART are more likely to experience an increased frequency of side effects and toxicities of ART. Although not systematically studied, this is likely because underlying hepatic, renal, neurologic, psychiatric, gastrointestinal (GI), and hematologic disorders are highly prevalent among IDUs. These comorbid conditions should be considered when selecting antiretroviral (ARV) agents in this population. Opioid substitution therapies such as methadone and buprenorphine/naloxone and extended-release naltrexone are commonly used for management of opioid dependence in HIV-infected patients.
Methadone and Antiretroviral Therapy. Methadone, an orally administered, long-acting opioid agonist, is the most common pharmacologic treatment for opioid addiction. Its use is associated with decreased heroin use, decreased needle sharing, and improved quality of life. Because of its opioid-induced effects on gastric emptying and the metabolism of cytochrome P (CYP) 450 isoenzymes 2B6, 3A4, and 2D6, pharmacologic effects and interactions with ARV agents may commonly occur. 13 These may diminish the effectiveness of either or both therapies by causing opioid withdrawal or overdose, increased methadone toxicity, and/or decreased ARV efficacy. Efavirenz (EFV), nevirapine (NVP), and lopinavir/ritonavir (LPV/r) have been associated with significant decreases in methadone levels. Patients and substance abuse treatment facilities should be informed of the likelihood of this interaction. The clinical effect is usually seen after 7 days of coadministration and may be managed by increasing the methadone dosage, usually in 5-mg to 10-mg increments daily until the desired effect is achieved.
Buprenorphine and Antiretroviral Therapy. Buprenorphine, a partial µ-opioid agonist, is administrated sublingually and is often coformulated with naloxone. It is increasingly used for opioid dependence treatment. Compared with methadone, buprenorphine has a lower risk of respiratory depression and overdose. This allows physicians in primary care to prescribe buprenorphine for the treatment of opioid dependency. The flexibility of the primary care setting can be of significant value to opioid-addicted HIVinfected patients who require ART because it enables one physician or program to provide both medical and substance abuse services. Limited information is currently available about interactions between buprenorphine and ARV agents. Findings from available studies show that the drug interaction profile of buprenorphine is more favorable than that of methadone.
Naltrexone and Antiretroviral Therapy. A once-monthly extended-release intramuscular formulation of naltrexone was recently approved for prevention of relapse in patients who have undergone an opioid detoxification program. Naltrexone is also indicated for treatment of alcohol dependency. Naltrexone is not metabolized via the CYP450 enzyme system and is not expected to interact with protease inhibitors (PIs) or non-nucleoside reverse transcriptase inhibitors (NNRTIs). 15 Currently available pharmacokinetic (PK) interaction data that clinicians can use as a guide for managing patients receiving ART and methadone or buprenorphine can be found in Tables 19a-d. Particular attention is needed concerning communication between HIV care providers and drug treatment programs regarding additive drug toxicities and drug interactions resulting in opiate withdrawal or excess.
Methylenedioxymethamphetamine (MDMA), GHB, ketamine, and methamphetamine all have the potential to interact with ARV agents because all are metabolized, at least in part, by the CYP450 system. Overdoses secondary to interactions between the party drugs (i.e., MDMA or GHB) and PI-based ART have been reported. 16
# Summary
It is usually possible over time to support most active drug users such that acceptable adherence levels with ARV agents can be achieved. Providers must work to combine all available resources to stabilize an active drug user in preparation for ART. This should include identification of concurrent medical and psychiatric illnesses, drug treatment and needle and syringe exchange programs, strategies to reduce highrisk sexual behavior, and harm-reduction strategies. A history of drug use alone is insufficient reason to withhold ART because individuals with a history of prior drug use have adherence rates similar to those who do not abuse drugs.
Important considerations in the selection of successful regimens and the provision of appropriate patient monitoring in this population include need for supportive clinical sites; linkage to substance abuse treatment; and awareness of the interactions between illicit drugs and ARV agents, including the increased risk of side effects and toxicities. Simple regimens should be considered to enhance medication adherence. Preference should be given to ARV agents that have a lower risk of hepatic and neuropsychiatric side effects, simple dosing schedules, and minimal interaction with methadone. This section provides discussion of some basic principles and unique considerations to follow when caring for HIV-infected women, including during pregnancy. Clinicians who provide care for pregnant women should consult the current Perinatal Guidelines 1 for more in-depth discussion and management assistance. Additional guidance on the management of HIV-infected women can be found at .
# Gender Considerations in Antiretroviral Therapy
In general, studies to date have not shown gender differences in virologic responses to antritretroviral therapy (ART), but a number of studies have suggested that gender may influence the frequency, presentation, and severity of selected antiretroviral (ARV)-related adverse events. 5 Although data are limited, evidence also exists that pharmacokinetics for some ARV drugs may differ between men and women, possibly because of variations between men and women in factors such as body weight, plasma volume, gastric emptying time, plasma protein levels, cytochrome P (CYP) 450 activity, drug transporter function, and excretion activity. Adverse Effects:
- Nevirapine (NVP)-associated hepatotoxicity: NVP has been associated with an increased risk of symptomatic, potentially fatal, and often rash-associated liver toxicity in ARV-naive individuals; women with higher CD4 counts (>250 cells/mm 3 ) or elevated baseline transaminase levels appear to be at greatest risk. It is generally recommended that NVP not be prescribed to ARV-naive women who have CD4 counts >250 cells/mm 3 unless there is no other alternative and the benefit from NVP outweighs the risk of hepatotoxicity (AI).
# Panel's Recommendations
- The indications for initiation of antiretroviral therapy (ART) and the goals of treatment are the same for HIV-infected women as for other HIV-infected adults and adolescents (AI).
- Women taking antiretroviral (ARV) drugs that have significant pharmacokinetic interactions with oral contraceptives should use an additional or alternative contraceptive method to prevent unintended pregnancy (AIII).
- In pregnant women, an additional goal of therapy is prevention of perinatal transmission of HIV, with a goal of maximal viral suppression to reduce the risk of transmission of HIV to the fetus and newborn (AI).
- When selecting an ARV combination regimen for a pregnant woman, clinicians should consider the known safety, efficacy, and pharmacokinetic data on use during pregnancy for each agent (AIII).
- Women of childbearing potential should undergo pregnancy testing before initiation of efavirenz (EFV) and receive counseling about the potential risk to the fetus and desirability of avoiding pregnancy while on EFV-based regimens (AIII).
- Alternative regimens that do not include EFV should be strongly considered in women who are planning to become pregnant or sexually active and not using effective contraception, assuming these alternative regimens are acceptable to the provider and are not thought to compromise the woman's health (BIII).
- Because the risk of neural tube defects is restricted to the first 5 to 6 weeks of pregnancy and pregnancy is rarely recognized before 4 to 6 weeks of pregnancy, EFV can be continued in pregnant women receiving an EFV-based regimen who present for antenatal care in the first trimester, provided the regimen produces virologic suppression (CIII).
- When designing a regimen for a pregnant woman, clinicians should consult the most current Health and Human Services (HHS) Perinatal Guidelines (AIII). - Lactic acidosis: There is a female predominance in the increased incidence of symptomatic and even fatal lactic acidosis associated with prolonged exposure to nucleoside reverse transcriptase inhibitors (NRTIs). Lactic acidosis is most common with stavudine (d4T), didanosine (ddI), and zidovudine (ZDV) but it can occur with other NRTIs. 13 - Metabolic complications: A few studies have compared women and men in terms of metabolic complications associated with ARV use. Compared with HIV-infected men, HIV-infected women are more likely to experience increases in central fat with ART and are less likely to have triglyceride elevations on treatment. 14,15 Women have an increased risk of osteopenia/osteoporosis, particularly after menopause, and this risk is exacerbated by HIV and ART. 16,17 At the present time, none of these differences requires women-specific recommendations regarding treatment or monitoring.
# Rating of Recommendations
# Women of Childbearing Potential
All women of childbearing potential should be offered pre-conception counseling and care as a component of routine primary medical care. Counseling should include discussion of special considerations pertaining to ARV use when trying to conceive and during pregnancy (see Perinatal Guidelines 1 ). Safe sexual practices, reproductive desires and options for conception, HIV status of sexual partner(s), and use of effective contraception to prevent unintended pregnancy should be discussed. An HIV-infected woman who wishes to conceive with an HIV-uninfected male partner should be informed of options to prevent sexual transmission of HIV while attempting conception. Interventions include initiation of maximally suppressive ART, which significantly decreases the risk of sexual transmission (see Preventing Secondary Transmission of HIV), and artificial insemination, including the option to self-inseminate with the partner's sperm during the periovulatory period 18 (for more extensive discussion on this topic, see the Reproductive Options for HIV-Concordant and Serodiscordant Couples section of the Perinatal Guidelines. 1 Efavirenz (EFV) is teratogenic in non-human primates. Women of childbearing potential should undergo pregnancy testing before initiation of EFV and receive counseling about the potential risk to the fetus and desirability of avoiding pregnancy while on EFV-based regimens (AIII). Alternative regimens that do not include EFV should be strongly considered in women who are planning to become pregnant or who are sexually active and not using effective contraception, assuming these alternative regimens are acceptable to the provider and are not thought to compromise the woman's health (BIII). The most vulnerable period in fetal organogenesis is early in gestation, before pregnancy is recognized.
# Hormonal Contraception
Safe and effective reproductive health and family planning services to reduce unintended pregnancy and perinatal transmission of HIV are an essential component of care for HIV-infected women of childbearing age. Counseling about reproductive issues should be provided on an ongoing basis.
Providers should be aware of potential interactions between ARV drugs and hormonal contraceptives that could lower contraceptive efficacy. Several protease inhibitors (PIs) and non-nucleoside reverse transcriptase inhibitors (NNRTIs) have drug interactions with combined oral contraceptives (COCs). Interactions include either a decrease or an increase in blood levels of ethinyl estradiol, norethindrone, or norgestimate (see Tables 20a and 20b), which potentially decreases contraceptive efficacy or increases estrogen-or progestinrelated adverse effects (e.g., thromboembolism). Small studies of HIV-infected women receiving injectable depot-medroxyprogesterone acetate (DMPA) while on ART showed no significant interactions between DMPA and EFV, NVP, nelfinavir (NFV), or NRTI drugs. Contraceptive failure of the etonogestrel implant in two patients on EFV-based therapy has been reported and a study has shown EFV may decrease plasma progestin concentrations of COCs containing ethinyl estradiol and norgestimate. 22,23 Several RTVboosted PIs decrease oral contraceptive estradiol levels. 24,25 A small study from Malawi showed that NVP use did not significantly affect estradiol or progestin levels in HIV-infected women. 26 Overall, data are relatively limited and the clinical implications of these findings are unclear. The magnitudes of change in drug levels that may reduce contraceptive efficacy or increase adverse effects are unknown. Concerns about pharmacokinetic interactions between oral and implant hormonal contraceptives and ARVs should not prevent clinicians from prescribing hormonal contraceptives for women on ART if that is their preferred contraceptive method. However, when women wish to use hormonal contraceptives and drug interactions with ARVs are known, additional or alternative contraceptive methods may be recommended (see drug interaction Tables 19a, 19b, and 19d and Perinatal Guidelines 1 ). Consistent use of male or female condoms to prevent transmission of HIV and protect against other sexually transmitted diseases (STDs) is recommended for all HIV-infected women and their partners, regardless of contraceptive use.
The data on the association between hormonal contraception and the risk of acquisition of HIV are conflicting. 27 A retrospective secondary analysis of two studies of serodiscordant couples in Africa in which the HIV-infected partner was not receiving ART found that women using hormonal contraception (the vast majority using injectable DMPA) had a twofold increased risk of acquiring HIV (for HIV-infected male/HIVuninfected female couples) or transmitting HIV (HIV-infected female/HIV-uninfected male couples). HIV-infected women using hormonal contraception had higher genital HIV RNA concentrations than did women not using hormonal contraceptives. 28 Oral contraceptive use was not significantly associated with transmission of HIV; however, the number of women using oral contraceptives in this study was insufficient to adequately assess risk. It is important to note that not all studies have supported a link between hormonal contraception and transmission or acquisition of HIV and that the individuals in this study were not receiving ART. Further research is needed to definitively determine if hormonal contraceptive use is an independent risk factor for acquisition and transmission of HIV, particularly in the setting of ART. 27,29 Intrauterine devices (IUDs) appear to be a safe and effective contraceptive option for HIV-infected women. Although studies have focused primarily on non-hormone-containing IUDs (e.g., copper IUD), several small studies have also found levonorgestrel-releasing IUDs to be safe and not associated with increased genital tract shedding of HIV. 31,34,35
# Pregnant Women
Clinicians should review the Perinatal Guidelines 1 for a detailed discussion of the management of HIVinfected pregnant women. The use of combination ARV regimens is recommended for all HIV-infected pregnant women, regardless of virologic, immunologic, or clinical parameters (AI). Pregnant HIV-infected women should be counseled regarding the known benefits and risks of ARV use during pregnancy to the woman, fetus, and newborn. A woman's decision regarding ARV use should be respected. Coercive and punitive approaches undermine provider-patient trust and could discourage women from seeking prenatal care and adopting health care behaviors that optimize maternal, fetal, and neonatal well-being.
# Prevention of Perinatal Transmission of HIV.
The use of ARVs and the resultant reduction of HIV RNA levels decrease perinatal transmission of HIV. The goal of ARV use is to achieve maximal and sustained suppression of HIV RNA levels during pregnancy.
As in non-pregnant individuals, genotypic resistance testing is recommended for all pregnant women before ARV initiation (AIII) and for pregnant women with detectable HIV RNA levels while on therapy (AI).
Optimal prevention of perinatal transmission may require initiation of ARV drugs before results of resistance testing are available. If results demonstrate the presence of significant mutation(s) that may confer resistance to the prescribed ARV regimen, the regimen should be modified.
Long-term follow-up is recommended for all infants born to women who have received ARVs during pregnancy, regardless of the infant's HIV status (see the Perinatal Guidelines 1 ).
Regimen Considerations. Pregnancy should not preclude the use of optimal drug regimens. Because recommendations on ARVs to use for treatment of HIV-infected pregnant women are subject to unique considerations, recommendations specific to the timing of therapy initiation and the choice of ARVs for pregnant women may differ from those for non-pregnant individuals. These considerations include the following:
- Potential changes in pharmacokinetics and, thus, dosing requirements, which result from physiologic changes associated with pregnancy;
- potential ARV-associated adverse effects in pregnant women and the woman's ability to adhere to a particular regimen during pregnancy; and
- potential short-and long-term effects of the ARV on the fetus and newborn, which are unknown for many drugs.
Combination drug regimens are considered the standard of care in pregnancy, both for the treatment of HIV infection and for the prevention of perinatal transmission of HIV. Because the risk of neural tube defects is restricted to the first 5 to 6 weeks of pregnancy and pregnancy is rarely recognized before 4 to 6 weeks of pregnancy, and unnecessary changes in ARV drugs during pregnancy may be associated with loss of viral control and increased risk of perinatal transmission, EFV can be continued in pregnant women receiving an EFV-based regimen who present for antenatal care in the first trimester, provided the regimen produces virologic suppression (CIII). Detailed recommendations on ARV choice in pregnancy are discussed in detail in the Perinatal Guidelines (see Perinatal Guidelines 1 ).
Intravenous (IV) zidovudine (ZDV) infusion to the mother during labor is recommended if maternal HIV RNA is ≥400 copies/mL (or with unknown HIV RNA levels) near delivery, regardless of antepartum regimen or mode of delivery (AI). Consideration can be given to omitting IV ZDV infusion during labor for HIVinfected women receiving combination ART regimens who have HIV RNA <400 copies/mL near delivery (BII); however, the combination ART should continue to be administered during labor.
Clinicians who are treating HIV-infected pregnant women are strongly encouraged to report cases of prenatal exposure to ARVs (either administered alone or in combinations) to the Antiretroviral Pregnancy Registry (). The registry collects observational data regarding exposure to Food and Drug Administration-approved ARV drugs during pregnancy for the purpose of assessing potential teratogenicity. For more information regarding selection and use of ART during pregnancy, refer to the Perinatal Guidelines. 1
# Postpartum Management
Following delivery, clinical, immunologic, and virologic follow-up should continue as recommended for non-pregnant adults and adolescents. Because maternal ART reduces but does not eliminate the risk of transmission of HIV in breast milk and postnatal transmission can occur despite maternal ART, women should also be counseled to avoid breastfeeding. 1 HIV-infected women should avoid pre-mastication of food fed to their infants because the practice has been associated with transmission of HIV from mother to child. 39 Considerations regarding continuation of ART for maternal therapeutic indications are the same as those for ART use in other non-pregnant individuals. For more information regarding postpartum discontinuation of ART, refer to the Perinatal Guidelines. 1 Several studies have demonstrated that adherence to ART may worsen in the postpartum period. Clinicians caring for women postpartum who are receiving ART should specifically address adherence, including an evaluation of specific facilitators and barriers to adherence. Clinicians may consider an intervention to improve adherence (see Adherence to Antiretroviral Therapy).
# Clinical Course of HIV-2 Infection
Compared to HIV-1 infection, the clinical course of HIV-2 infection is generally characterized by a longer asymptomatic stage, lower plasma HIV-2 viral loads, and lower mortality rate. 1,2 However, HIV-2 infection can also progress to AIDS over time. Concomitant HIV-1 and HIV-2 infection may occur and should be considered in patients from areas with a high prevalence of HIV-2.
# Diagnosis of HIV-2 Infection
In the appropriate epidemiologic setting, HIV-2 infection should be suspected in patients with clinical conditions suggestive of HIV infection but with atypical serologic results (e.g., a positive screening assay with an indeterminate HIV-1 Western blotf 3 The possibility of HIV-2 infection should also be considered in the appropriate epidemiologic setting in patients with serologically confirmed HIV infection but low or undetectable HIV-1 RNA levels or in those with declining CD4 T lymphocyte (CD4) cell counts despite apparent virologic suppression on antiretroviral therapy (ART).
The 2014 Centers for Disease Control and Prevention guidelines for HIV diagnostic testing 4 recommend initial HIV testing using an HIV-1/HIV-2 antigen/antibody combination immunoassay and subsequent testing using an HIV-1/HIV-2 antibody differentiation immunoassay. The Multispot HIV-1/HIV-2 Rapid Test (Bio-Rad Laboratories) is Food and Drug Administration approved for differentiating HIV-1 from HIV-2 infection. Commercially available HIV-1 viral load assays do not reliably detect or quantify HIV-2. 5,6 Quantitative HIV-2 plasma RNA viral load testing has recently become available for clinical care at the University of Washington
# Summary of HIV-2 Infection
- Compared to HIV-1 infection, the clinical course of HIV-2 infection is generally characterized by a longer asymptomatic stage, lower plasma HIV-2 RNA levels, and lower mortality; however, progression to AIDS does occur.
- There have been no randomized trials addressing the question of when to start antiretroviral therapy or the choice of initial or second-line therapy for HIV-2 infection; thus, the optimal treatment strategy has not been defined.
- Although the optimal CD4 T lymphocyte (CD4) cell count threshold for initiating antiretroviral therapy in HIV-2 infection is unknown, therapy should be started before there is clinical progression.
- HIV-2 is intrinsically resistant to non-nucleoside reverse transcriptase inhibitors and to enfuvirtide; thus, these drugs should not be included in an antiretroviral regimen for an HIV-2 infected patient.
- Pending more definitive data on outcomes in an antiretroviral therapy -naive patient who has HIV-2 mono-infection or HIV-1/HIV-2 dual infection and requires treatment, an initial antiretroviral therapy regimen for these patients should include two nucleoside reverse transcriptase inhibitors plus an HIV-2 active boosted protease inhibitor or integrase strand transfer inhibitors.
- A few laboratories now offer quantitative plasma HIV-2 RNA testing for clinical care (see section text).
- Monitoring of HIV-2 RNA levels, CD4 cell counts, and clinical improvements can be used to assess treatment response, as is recommended for HIV-1 infection.
- Resistance-associated viral mutations to nucleoside reverse transcriptase inhibitors, protease inhibitors, and/or integrase strand transfer inhibitors may develop in HIV-2 infected patients while on therapy. However, no validated HIV-2 genotypic or phenotypic antiretroviral resistance assays are available for clinical use.
- In the event of virologic, immunologic, or clinical failure, second-line treatment should be instituted in consultation with an expert in HIV-2 management.
() 7 and the New York State Department of Health (). 8 However, it is important to note that approximately one-quarter to one-third of HIV-2-infected patients without ART will have HIV-2 RNA levels below the limits of detection; some of these patients will have clinical progression and CD4 cell count decline. No validated HIV-2 genotypic or phenotypic antiretroviral (ARV) resistance assays are available for clinical use.
# Treatment of HIV-2 Infection
To date, no randomized trials addressing the question of when to start ART or the choice of initial or secondline therapy for HIV-2 infection have been completed; 9 thus, the optimal treatment strategy has not been defined. Three clinical trials to assess first-line ART for HIV-2 infection are currently underway; 2 are enrolling patients with CD4 counts 200 and ≤600 cells/mm 3 (NCT02150993). Although the optimal CD4 cell count threshold for initiating ART in HIV-2 infection is unknown, therapy should be started before there is clinical progression.
HIV-2 is intrinsically resistant to non-nucleoside reverse transcriptase inhibitors (NNRTI) 10 and to enfuvirtide (T20). 11 Data from in vitro studies suggest that HIV-2 is sensitive to the currently available nucleoside reverse transcriptase inhibitors (NRTIs), although with a lower barrier to resistance than HIV-1. 12,13 Darunavir (DRV), lopinavir (LPV), and saquinavir (SQV) are more active against HIV-2 than other approved protease inhibitors (PIs); one of these boosted PIs should be used if a PI-based regimen is used. Other PIs should be avoided because of their lack of ARV activity and high failure rates. The integrase strand transfer inhibitors (INSTIs) raltegravir (RAL), elvitegravir (EVG), and dolutegravir (DTG) have potent activity against HIV-2. The CCR5 antagonist maraviroc (MVC) appears active against some HIV-2 isolates; 22 however, no approved assays to determine HIV-2 co-receptor tropism exist and HIV-2 is known to use many other minor co-receptors in addition to CCR5 and CXCR4. 23 Several small studies suggest poor responses in HIV-2 infected individuals treated with some ARV regimens including dual-NRTI regimens; regimens containing NNRTI plus 2NRTIs; and some unboosted PI-based regimens including nelfinavir (NFV) or indinavir (IDV) plus zidovudine (ZDV) and lamivudine (3TC); and atazanavir (ATV)-based regimens. 9, Clinical data on the effectiveness of triple-NRTI regimens are conflicting. 28,29 In general, HIV-2 active, boosted PI-containing regimens have resulted in more favorable virologic and immunologic responses than 2 or 3-NRTI-based regimens. However, CD4 cell recovery on therapy are generally poorer than that observed for HIV-1. INSTI-based regimens may also have favorable treatment responses. 34,35 A recent large systematic review of ART for HIV-2-infected patients (n = 17 studies, 976 HIV-2 infected patients) was unable to conclude which specific regimens are preferred. 36 Resistance-associated viral mutations to NRTIs, PIs and/or INSTIs commonly develop in HIV-2 infected patients while on therapy. 24,29,41 Currently, HIV-2 transmitted drug resistance appears rare. 42 In one small study, DTG was found to have activity as a second-line INSTI in some HIV-2 patients with extensive ARV experience and RAL resistance. 43 Genotypic algorithms used to predict drug resistance in HIV-1 may not be applicable to HIV-2, because pathways and mutational patterns leading to resistance may differ between the HIV types. 13,29,44 Some groups have recommended specific preferred and alternative regimens for initial therapy of HIV-2 infection; Effective antiretroviral therapy (ART) has increased survival in HIV-infected individuals, resulting in an increasing number of older individuals living with HIV infection. In the United States, approximately 30% of people currently living with HIV/AIDS are age 50 years or older and trends suggest that the proportion of older persons living with HIV/AIDS will increase steadily. 1 Care of HIV-infected patients increasingly will involve adults 60 to 80 years of age, a population for which data from clinical trials or pharmacokinetic studies are very limited.
There are several distinct areas of concern regarding the association between age and HIV disease. 2 First, older HIV-infected patients may suffer from aging-related comorbid illnesses that can complicate the management of HIV infection, as outlined in detail below. Second, HIV disease may affect the biology of aging, possibly resulting in early manifestations of many clinical syndromes generally associated with advanced age. Third, reduced mucosal and immunologic defenses (such as post-menopausal atrophic vaginitis) and changes in risk behaviors (for example, decrease in condom use because of less concern about pregnancy and increased use of erectile dysfunction drugs) in older adults could lead to increased risk of acquisition and transmission of HIV. Finally, because older adults generally are perceived to be at low risk of HIV infection, screening for HIV in this population remains low. For these reasons, HIV infection in many older adults may not be diagnosed until late in the disease process. This section focuses on HIV diagnosis and treatment considerations in the older HIV-infected patient.
# HIV Diagnosis and Prevention
Even though many older individuals are engaged in risk behaviors associated with acquisition of HIV, they may be perceived to be at low risk of infection and, as a result, they are less likely to be tested for HIV than younger persons. 5 According to one U.S. survey, 71% of men and 51% of women age 60 years and older continue to be sexually active, 6 with less concern about the possibility of pregnancy contributing to less condom use. Another national survey reported that among individuals age 50 years or older, condoms were not used during most recent intercourse with 91% of casual partners or 70% of new partners. 7 In addition, results from a CDC survey 8 show that in 2008 only 35% of adults age 45 to 64 years had ever been tested for HIV infection despite the 2006 CDC recommendation that individuals age 13 to 64 years be tested at least once and more often if sexually active. 9 Clinicians must be attuned to the possibility of HIV infection in older patients, including those older than 64 years of age who, based on CDC recommendations, would not
# Key Considerations When Caring for Older HIV-Infected Patients
- Antiretroviral therapy (ART) is recommended in patients >50 years of age, regardless of CD4 cell count (BIII), because the risk of non-AIDS related complications may increase and the immunologic response to ART may be reduced in older HIV-infected patients.
- ART-associated adverse events may occur more frequently in older HIV-infected adults than in younger HIV-infected individuals. Therefore, the bone, kidney, metabolic, cardiovascular, and liver health of older HIV-infected adults should be monitored closely.
- The increased risk of drug-drug interactions between antiretroviral (ARV) drugs and other medications commonly used in older HIVinfected patients should be assessed regularly, especially when starting or switching ART and concomitant medications.
- HIV experts and primary care providers should work together to optimize the medical care of older HIV-infected patients with complex comorbidities.
- Counseling to prevent secondary transmission of HIV remains an important aspect of the care of the older HIV-infected patient. be screened for HIV. Furthermore, sexual history taking, risk-reduction counseling, and screening for sexually transmitted diseases (STDs) (if indicated), are important components of general health care for HIVinfected and -uninfected older patients.
# Rating of Recommendations
Failure to consider a diagnosis of HIV in older persons likely contributes to later disease presentation and initiation of ART. 10 One surveillance report showed that the proportion of patients who progressed to AIDS within 1 year of diagnosis was greater among patients >60 years of age (52%) than among patients younger than 25 years (16%). 1 When individuals >50 years of age present with severe illnesses, AIDS-related opportunistic infections (OIs) need to be considered in the differential diagnosis of the illness.
# Initiating Antiretroviral Therapy
Concerns about decreased immune recovery and increased risk of serious non-AIDS events are factors that favor initiating ART in patients >50 years of age regardless of CD4 cell count (BIII). (See Initiating Antiretroviral Therapy in Treatment-Naive Patients.) Data that would favor use of any one of the Panel's recommended initial ART regimens (see What to Start) on the basis of age are not available. The choice of regimen should be informed by a comprehensive review of the patient's other medical conditions and medications. A noteworthy limitation of currently available information is lack of data on the long-term safety of specific antiretroviral (ARV) drugs in older patients, such as use of tenofovir disoproxil fumarate (TDF) in older patients with declining renal function. The recommendations on how frequently to monitor parameters of ART effectiveness and safety for adults age >50 years are similar to those for the general HIV-infected population; however, the recommendations for older adults focus particularly on the adverse events of ART pertaining to renal, liver, cardiovascular, metabolic, and bone health (see Table 15).
# HIV, Aging, and Antiretroviral Therapy
The efficacy, pharmacokinetics, adverse effects, and drug interaction potentials of ART in the older adult have not been studied systematically. There is no evidence that the virologic response to ART is different in older patients than in younger patients. However, CD4 T-cell recovery after starting ART generally is less robust in older patients than in younger patients. This observation suggests that starting ART at a younger age will result in better immunologic and possibly clinical outcomes.
Hepatic metabolism and renal elimination are the major routes of drug clearance, including the clearance of ARV drugs. Both liver and kidney function may decrease with age, which may result in impaired drug elimination and drug accumulation. 15 Current ARV drug doses are based on pharmacokinetic and pharmacodynamic data derived from studies conducted in subjects with normal organ function. Most clinical trials include only a small proportion of study participants >50 years of age. Whether drug accumulation in the older patient may lead to greater incidence and severity of adverse effects than seen in younger patients is unknown.
HIV-infected patients with aging-associated comorbidities may require additional pharmacologic intervention, making therapeutic management increasingly complex. In addition to taking medications to manage HIV infection and comorbid conditions, many older HIV-infected patients also are taking medications to ameliorate discomfort (e.g., pain medications, sedatives) or to manage adverse effects of medications (e.g., anti-emetics). They also may self-medicate with over-the-counter medicines or supplements. In the HIV-negative population, polypharmacy is a major cause of iatrogenic problems in geriatric patients. 16 This may be the result of medication errors (by prescribers or patients), nonadherence, additive drug toxicities, and drug-drug interactions. Older HIV-infected patients probably are at an even greater risk of polypharmacy and its attendant adverse consequences than younger HIV-infected or similarly aged HIV-uninfected patients.
Drug-drug interactions are common with ART and easily can be overlooked by prescribers. 17 The available drug interaction information on ARV agents is derived primarily from pharmacokinetic studies performed in a small number of relatively young, HIV-uninfected subjects with normal organ function (see ). Data from these studies provide clinicians with a basis to assess whether a significant interaction may exist. However, the magnitude of the interaction may be different in older HIV-infected patients than in younger HIV-infected patients.
Nonadherence is the most common cause of treatment failure. Complex dosing requirements, high pill burden, inability to access medications because of cost or availability, limited health literacy including lack of numeracy skills, misunderstanding of instructions, depression, and neurocognitive impairment are among the key reasons for nonadherence. 18 Although many of these factors likely will be more prevalent in an aging HIV-infected population, some data suggest that older HIV-infected patients may be more adherent to ART than younger HIV-infected patients. Clinicians should assess adherence regularly to identify any factors, such as neurocognitive deficits, that may make adherence a challenge. One or more interventions such as discontinuation of unnecessary medications; regimen simplification; or use of adherence tools, including pillboxes, daily calendars, and evidence-based behavioral approaches may be necessary to facilitate medication adherence (see Adherence to Antiretroviral Therapy).
# Non-AIDS HIV-Related Complications and other Comorbidities
With the reduction in AIDS-related morbidity and mortality observed with effective use of ART, non-AIDS conditions constitute an increasing proportion of serious illnesses in ART-treated HIV-infected populations. Heart disease and cancer are the leading causes of death in older Americans. 25 Similarly, for HIV-infected patients on ART, non-AIDS events such as heart disease, liver disease, and cancer have emerged as major causes of morbidity and mortality. Neurocognitive impairment, already a major health problem in aging patients, may be exacerbated by the effect of HIV infection on the brain. 26 That the presence of multiple non-AIDS comorbidities coupled with the immunologic effects of HIV infection could add to the disease burden of an aging HIV-infected person is a concern. At present, primary care recommendations are the same for HIV-infected and HIV-uninfected adults and focus on identifying and managing risks of conditions such as heart, liver, and renal disease; cancer; and bone demineralization.
# Discontinuing Antiretroviral Therapy in Older Patients
Important issues to discuss with aging HIV-infected patients are living wills, advance directives, and longterm care planning including financial concerns. Health care cost sharing (e.g., co-pays, out-of-pocket costs), loss of employment, and other financial-related factors can cause interruptions in treatment. Clinic systems can minimize loss of treatment by helping patients maintain access to insurance.
For the severely debilitated or terminally ill HIV-infected patient, adding palliative care medications, while perhaps beneficial, further increases the complexity and risk of negative drug interactions. For such patients, a balanced consideration of both the expected benefits of ART and the toxicities and negative quality-of-life effects of ART is needed.
Few data exist on the use of ART in severely debilitated patients with chronic, severe, or non-AIDS terminal conditions. Withdrawal of ART usually results in rebound viremia and a decline in CD4 cell count. Acute retroviral syndrome after abrupt discontinuation of ART has been reported. In very debilitated patients, if there are no significant adverse reactions to ART, most clinicians would continue therapy. In cases where ART negatively affects quality of life, the decision to continue therapy should be made together with the patient and/or family members after a discussion on the risks and benefits of continuing or withdrawing ART.
# Conclusion
HIV infection may increase the risk of many major health conditions experienced by aging adults and possibly accelerate the aging process. 35 As HIV-infected adults age, their health problems become increasingly complex, placing additional demands on the health care system. This adds to the concern that outpatient clinics providing HIV care in the United States share the same financial problems as other chronic disease and primary care clinics and that reimbursement for care is not sufficient to maintain care at a sustainable level. 36 Continued involvement of HIV experts in the care of older HIV-infected patients is warranted. However, given that the current shortage of primary care providers and geriatricians is projected to continue, current HIV providers will need to adapt to the shifting need for expertise in geriatrics through continuing education and ongoing assessment of the evolving health needs of aging HIV-infected patients. 37 The aging of the HIV-infected population also signals a need for more information on long-term safety and efficacy of ARV drugs in older patients.
- Some ARV agents can cause increases in transaminase levels. The rate and magnitude of these increases are higher with HBV coinfection. The etiology and consequences of these changes in liver function tests are unclear because continuation of ART may be accompanied by resolution of the changes. Nevertheless, some experts suspend the implicated agent(s) when the serum alanine transferase (ALT) level is increased to 5-10 times the upper limit of normal. However, in HIV/HBV-coinfected persons, increases in transaminase levels can herald hepatitis B e antigen (HBeAg) seroconversion due to immune reconstitution, so the cause of the elevations should be investigated prior to the decision to discontinue medications. In persons with transaminase increases, HBeAg seroconversion should be evaluated by testing for HBeAg and anti-HBe as well as HBV DNA levels.
# Recommendations for HBV/HIV-Coinfected Patients
- All patients with chronic HBV should be advised to abstain from alcohol, assessed for immunity to hepatitis A virus (HAV) infection (anti-HAV antibody total) and vaccinated if nonimmune, advised on methods to prevent HBV transmission (methods that do not differ from those to prevent HIV transmission), and evaluated for the severity of HBV infection as outlined in the Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents. 14 - Prior to intiation of ART, all persons who test positive for HBsAg should be tested for HBV DNA using a quantitative assay to determine the level of HBV replication (AIII). Persons with chronic HBV infection already receiving ART active against HBV should undergo quantitative HBV DNA testing every 6-12 months to determine the effectiveness of therapy in suppressing HBV replication. The goal of HBV therapy with NRTIs is to prevent liver disease complications by sustained suppression of HBV replication to the lowest achievable level.
If not yet on therapy and HBV or HIV treatment is needed: In persons without HIV infection, the recommended anti-HBV drugs for the treatment of persons naive to HBV therapy are TDF and entecavir. In HIV-infected patients, however, only TDF can be considered part of the ARV regimen; entecavir has weak anti-HIV activity and must not be considered part of an ARV regimen. In addition, only TDF is fully active for the treatment of persons with known or suspected 3TC-resistant HBV infection. To avoid selection of HBV-resistant variants, when possible, these agents should not be used as the only agent with anti-HBV activity in an ARV regimen (AIII).
Preferred regimen. The combination of TDF + FTC or TDF + 3TC should be used as the NRTI backbone of a fully suppressive ARV regimen and for the treatment of HBV infection (AII). Alternative regimens. If TDF cannot safely be used, entecavir should be used in addition to a fully suppressive ARV regimen (AII); importantly, entecavir should not be considered to be a part of the ARV regimen 20 (BII). Due to a partially overlapping HBV-resistance pathway, it is not known if the combination of entectavir + 3TC or FTC will provide additional virologic or clinical benefit compared with entecavir alone. In persons with known or suspected 3TC-resistant HBV infection, the entecavir dose should be increased from 0.5 mg/day to 1 mg/day. However, entecavir resistance may emerge rapidly in patients with 3TC-resistant HBV infection. Therefore, entecavir should be used with caution in such patients with frequent monitoring (~ every 3 months) of the HBV DNA level to detect viral breakthrough. Other HBV treatment regimens include peginterferon alfa monotherapy or adefovir in combination with 3TC or FTC or telbivudine in addition to a fully suppressive ARV regimen; 17, however, data on these regimens in persons with HIV/HBV coinfection are limited (BII). Due to safety concerns, peginterferon alfa should not be used in HIV/HBV-coinfected persons with cirrhosis.
- Need to discontinue medications active against HBV: The patient's clinical course should be monitored with frequent liver function tests. The use of adefovir dipivoxil, entecavir, or telbivudine to prevent flares, especially in patients with marginal hepatic reserve such as persons with compensated or decompensated cirrhosis, can be considered. 8 These alternative HBV regimens should only be used in addition to a fully suppressive ARV regimen.
- Need to change ART because of HIV resistance: If the patient has adequate HBV suppression, the ARV drugs active against HBV should be continued for HBV treatment in combination with other suitable ARV agents to achieve HIV suppression (AIII).
infected patients, the combined use of either boceprevir or telaprevir with PegIFN/RBV was associated with higher rates of SVR than use of PegIFN/RBV alone. However, combined use of these drugs was associated with a large pill burden, increased dosing frequency, and adverse effects. Subsequently approved DAA agents in the same class and in newer classes that are used with or without RBV have higher SVR rates, reduced pill burden, less frequent dosing, fewer side effects, and shorter durations of therapy. 14, Therefore, the combination of boceprevir or telaprevir and PegIFN/RBV is no longer recommended, and has been replaced by newer combination regimens. Additional guidance on the treatment and management of HCV in HIV-infected and uninfected adults can be found at /. 20
# Assessment of HIV/Hepatitis C Virus Coinfection
- All HIV-infected patients should be screened for HCV infection using sensitive immunoassays licensed for detection of antibody to HCV in blood. 21 At risk HCV-seronegative patients should undergo repeat testing annually. HCV-seropositive patients should be tested for HCV RNA using a sensitive quantitative assay to confirm the presence of active infection. 22,23 Patients who test HCV RNA-positive should undergo HCV genotyping and liver disease staging as recommended by the most updated HCV guidelines (see /).
- Patients with HIV/HCV coinfection should be counseled to avoid consuming alcohol and to use appropriate precautions to prevent transmission of HIV and/or HCV to others. HIV/HCV-coinfected patients who are susceptible to hepatitis A virus (HAV) or hepatitis B virus (HBV) infection should be vaccinated against these viruses.
- All patients with HIV/HCV coinfection should be evaluated for HCV therapy.
# Antiretroviral Therapy in HIV/Hepatitis C Virus Coinfection
When to Start Antiretroviral Therapy
The rate of liver disease (liver fibrosis) progression is accelerated in HIV/HCV-coinfected patients, particularly in individuals with low CD4 counts (≤350 cells/mm 3 ). Data largely from retrospective cohort studies are inconsistent regarding the effect of ART on the natural history of HCV disease; 6,24,25 however, some studies suggest that ART may slow the progression of liver disease by preserving or restoring immune function and by reducing HIV-related immune activation and inflammation. Therefore, ART should be initiated in most HIV/HCV-coinfected patients, regardless of CD4 count (BII). However, in HIV treatmentnaive patients with CD4 counts >500 cells/mm 3 , some clinicians may choose to defer ART until HCV treatment is completed to avoid drug-drug interactions (CIII). Compared to patients with CD4 counts >350 cells/mm 3 , those with CD4 counts <200 had lower HCV treatment response rates and higher rates of toxicity due to PegIFN/RBV. 29 Data regarding HCV treatment response to combination therapy with DAA agents in those with advanced immunosuppression is lacking. For patients with lower CD4 counts (e.g., <200 cells/mm 3 ), ART should be initiated promptly (AI) and HCV therapy may be delayed until the patient is stable on HIV treatment (CIII). 23,
# Antiretroviral Drugs to Start and Avoid
Initial ARV combination regimens recommended for most HIV treatment-naive patients with HCV are the same as those recommended for patients without HCV infection. Special considerations for ARV selection in HIV/HCV-coinfected patients include the folllowing:
- When both HIV and HCV treatments are indicated, the ARV regimen should be selected with special considerations of potential drug-drug interactions (see Table 12) and overlapping toxicities with the HCV treatment regimen.
- Cirrhotic patients should be carefully evaluated by an expert in advanced liver disease for signs of liver decompensation according to the Child-Turcotte-Pugh classification system. This assessment is necessary because hepatically metabolized ARV and HCV DAA drugs may be contraindicated or require dose modification in patients with Child-Pugh class B and C disease (see Appendix B, Table 7).
# Hepatotoxicity
Drug-induced liver injury (DILI) following the initiation of ART is more common in HIV/HCV-coinfected patients than in those with HIV monoinfection. The greatest risk of DILI may be observed in coinfected individuals with advanced liver disease (e.g., cirrhosis, end-stage liver disease). 33 Eradication of HCV infection with treatment may decrease the likelihood of ARV-associated DILI. 34 - Given the substantial heterogeneity in patient populations and drug regimens, comparison of DILI incidence rates for individual ARV agents across clinical trials is difficult. The incidence of significant elevations in liver enzyme levels (more than 5 times the upper limit of the normal laboratory reference range) is low with currently recommended ART regimens. Hypersensitivity (or allergic) reactions associated with rash and elevations in liver enzymes can occur with certain ARVs. Alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels should be monitored 2 to 8 weeks after initiation of ART and every 3 to 6 months thereafter. Mild to moderate fluctuations in ALT and/or AST are typical in individuals with chronic HCV infection. In the absence of signs and/or symptoms of liver disease or increases in bilirubin, these fluctuations do not warrant interruption of ART. Patients with significant ALT and/or AST elevation should be careful evaluated for signs and symptoms of liver insufficiency and for alternative causes of liver injury (e.g., acute HAV or HBV infection, hepatobiliary disease, or alcoholic hepatitis). Short-term interruption of the ART regimen or of the specific drug suspected of causing the DILI may be required. 35
# Concurrent Treatment of HIV and Hepatitis C Virus Infection
Concurrent treatment of HIV and HCV is feasible but may be complicated by pill burden, drug-drug interactions, and toxicities. In this context, the stage of HCV disease should be assessed to determine the medical need for HCV treatment and inform decision making on when to start HCV. Additional guidance on the treatment and management of HCV in HIV-infected and uninfected adults can be found at /. If the decision is to treat HCV, the ART regimen may need to be modified before HCV treatment is initiated to reduce the potential for drug-drug interactions and/or toxicities that may develop during the period of concurrent HIV and HCV treatment. (See Table 12 for recommendations on the concomitant use of selected drugs for treatment of HCV and HIV infection.) In patients with suppressed plasma HIV RNA and modified ART, HIV RNA should be measured within 4 to 8 weeks after changing HIV therapy to confirm the effectiveness of the new regimen. After completion of HCV treatment, the modified ART regimen should be continued for at least 2 weeks before reinitiating the original regimen. Continued use of the modified regimen is necessary because of the prolonged half-life of some HCV drugs and the potential risk of drug-drug interactions if a prior HIV regimen is resumed soon after HCV treatment is completed.
# Drug-Drug Interaction
Considerations for the concurrent use of ART and recommended HCV agents (per /) are discussed below. Table 12 provides recommendations on the concomitant use of selected drugs for treatment of HCV and HIV infection.
- Sofosbuvir is an HCV NS5B nucleotide polymerase inhibitors that is not metabolized by the cytochrome P450 enzyme system and, therefore, can be used in combination with most ARV drugs. Sofosbuvir is a substrate of p-glycoprotein (P-gp). P-gp inducers, such as tipranavir (TPV), may decrease sofosbuvir plasma concentrations and should not be co-administered with sofosbuvir. No other clinicially significant pharmocokinetic intractions between sofosbuvir and ARVs have been identified. Drug-drug interaction studies in healthy volunteers did not find any significant interaction between sofosbuvir and darunavir/ritonavir (DRV/r), efavirenz (EFV), rilpivirine (RPV), raltegravir (RAL), tenofovir disoproxil fumarate (TDF), or emtricitabine (FTC). 36 See Table 12 for recommendations on the concomitant use of selected drugs for treatment of HCV and HIV infection.
- Ledipasvir is an HCV NS5A inhibitor and is part of a fixed-dose drug combination of sofosbuvir and ledipasvir. 37 Similar to sofosbuvir, ledipasvir is not metabolized by the cytochrome P450 system (CYP) of enzymes and is a substrate for P-gp. Ledipasvir is an inhibitor of the drug transporters P-gp and breast cancer resistance protein (BCRP) and may increase intestinal absorption of coadministered substrates for these transporters. The use of P-gp inducers is not recommended with ledipasivir/sofosbuvir. The coadministration of ledipasvir/sofosbuvir and ARV regimens containing TDF is associated with increased exposure to TDF, especially when TDF is taken with an HIV PI boosted with either RTV or cobicistat (COBI) (see Table 12 for recommendations on the concomitant use of selected drugs for treatment of HCV and HIV infection). In some patients, alternative HCV or ARV drugs should be considered to avoid increases in TDF exposures. If the drugs are co-administered, the patient should be monitored for potential TDF-associated renal injury by assessing measurements of renal function (i.e., estimated creatinine clearance, serum phosphorus, urine glucose, and urine protein) before HCV treatment initiation and periodically during treatment.
- The fixed-dose drug combination of ombitasvir (a NS5A inhibitor), paritaprevir (an HCV PI), and RTV (a pharmacokinetic enhancer) is co-packaged and used in combination with dasabuvir, an NS5B inhibitor. 38 Paritaprevir is a substrate and inhibitor of the CYP3A4 enzymes and therefore may have significant interactions with certain ARVs that are metabolized by, or may induce or inhibit the same pathways. Dasabuvir is primarily metabolized by the CYP2C8 enzymes. Furthermore, ombitasvir, paritaprevir, and dasabuvir are inhibitors of UGT1A1 and also substrates of P-gp and BCRP. Paritaprevir is also a substrate and inhibitor of OATP1B1/3. Coadministration with drugs that are substrates or inhibitors of these enzymes and drug transporters may result in increased plasma concentrations of either the coadministered drug or the HCV drugs. Given that several CYP enzymes and drug transporters are involved in the metabolism of dasabuvir, ombitasvir, paritaprevir, and RTV, complex drug-drug interactions are likely. Therefore clinicians need to consider all coadministered drugs for potential drugdrug interactions. No significant drug-drug interactions have been found when dasabuvir, ombitasvir, paritaprevir, and RTV are used in conjunction with ATV or RAL. When either RTV or COBI is used in conjunction with ATV, the boosting agent should be discontinued during HCV therapy and ATV should be taken in the morning at the same time as ombitasvir, paritaprevir/r, and dasabuvir. RTV or COBI should be restarted after completion of HCV treatment. See Table 12 for other recommendations for concomitmant use of HCV drugs with ARVs. HIV-infected patients not on ART should be placed on an alternative HCV regimen because RTV has activity against HIV.
- Simeprevir is a HCV NS3/4A PI that has been studied in HIV/HCV-coinfected patients. 39 Simeprevir is a substrate and inhibitor of CYP3A4 and P gp enzymes, and therefore may have significant interactions with certain ARVs that are metabolized by the same pathways. Simeprevir is also an inhibitor of the drug transporter OATP1B1/3. On the basis of drug-drug interaction studies in healthy volunteers, simeprevir can be coadministered with RAL, DTG, RPV, and TDF. 40 However, coadministration of simeprevir with EFV, ETR, HIV PIs, COBI, or EVG/c/TDF/FTC is not recommended. (See Table 12 for recommendations on the concomitant use of selected drugs for treatment of HCV and HIV infection.)
Given that the treatment of HCV is rapidly evolving, this section will be updated when new HCV drugs are approved that may have an impact on the treatment of HIV. For guidance on the treatment of HCV infection, refer to /. individuals without HIV (AI). Treatment of drug-susceptible TB disease should include a standard regimen that consists of isoniazid (INH) + a rifamycin (rifampin or rifabutin) + pyrazinamide + ethambutol given for 2 months, followed by INH + a rifamycin for 4 to 7 months. 4 The Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents 4 include a more complete discussion of the diagnosis and treatment of TB disease in HIV-infected patients.
All patients with HIV/TB disease should be treated with ART (AI). Important issues related to the use of ART in patients with active TB disease include: (1) when to start ART, (2) significant pharmacokinetic drugdrug interactions between rifamycins and some antiretroviral (ARV) agents, (3) the additive toxicities associated with concomitant ARV and TB drug use, ( 4) the development of TB-associated IRIS after ART initiation, and ( 5) the need for treatment support including DOT and the integration of HIV and TB care and treatment.
# Antiretroviral Therapy in Patients with Active Tuberculosis
# Patients Diagnosed with Tuberculosis While Receiving Antiretroviral Therapy
When TB is diagnosed in a patient receiving ART, the patient's ARV regimen should be assessed with particular attention to potential pharmacokinetic interactions with rifamycins (discussed below). The patient's regimen may need to be modified to permit use of the optimal TB treatment regimen (see for dosing recommendations).
# Patients Not Yet Receiving Antiretroviral Therapy
Until recently, when to start ART in patients with active TB has been a subject of debate. Survival is improved when ART is started early following initiation of TB therapy, but a delay in initiating ART often was favored because of the potential complications of high pill burden, additive toxicities, drug interactions, adherence, and the potential for development of IRIS.Recent studies primarily conducted in resource-limited settings, including three randomized controlled trials, have helped clarify the question of when to start ART in patients with active TB. The SAPiT study conducted in South Africa convincingly demonstrated that starting ART during rather than after concluding treatment for TB can significantly reduce mortality. In this study, ambulatory HIV-infected patients with smear-positive TB and CD4 counts <500 cells/mm 3 were randomized to one of three treatment arms: integrated therapy with ART initiated either during the first 4 weeks of TB therapy or after the first 8 weeks of TB treatment (i.e., during the continuation phase of TB therapy) or sequential therapy with ART initiated after the conclusion of standard TB therapy. The median CD4 cell count of participants at study entry was 150 cells/mm 3 . The sequential therapy arm was stopped when an early analysis demonstrated that the mortality rate in the combined two integrated arms was 56% lower than the rate in the sequential therapy arm. Treatment was continued in the two integrated arms until study completion. 5 With the completion of SAPiT and 2 other randomized controlled trials, CAMELIA and STRIDE, the question on the optimal time to initiate ART during TB therapy has been addressed. Findings from these trials now serve as the basis for the Panel's recommendations on when to start ART in patients with active TB.
In the final analysis of the SAPiT trial, there were no differences in rates of AIDS or death between the 2 integrated arms of the study (patients who started ART within 4 weeks after initiating TB treatment vs. those who started ART at 8-12 weeks ). However, in patients with baseline CD4 counts <50 cells/mm 3 (17% of the study population), the rate of AIDS or death was lower in the earlier therapy group than in the later therapy group (8.5 vs. 26.3 cases per 100 person-years, a strong trend favoring the earlier treatment arm, P = 0.06). For all patients, regardless of CD4 cell count, earlier therapy was associated with a higher incidence of IRIS and of adverse events that required a switch in ARV drugs than later therapy. Two deaths were attributed to IRIS. 6 In the CAMELIA study, which was conducted in Cambodia 7 , patients who had CD4 counts <200 cells/mm 3 were randomized to initiate ART at 2 weeks or 8 weeks after initiation of TB treatment. Study participants had advanced HIV disease, with a median entry CD4 count of 25 cells/mm 3 ; low BMIs (median = 16.8 kg/m 2 ), Karnofsky scores (87% <70), and hemoglobin levels (median = 8.7 g/dl); and high rates of disseminated TB disease. Compared with therapy initiated at 8 weeks, ART initiated at 2 weeks resulted in a 38% reduction in mortality (P = 0.006). A significant reduction in mortality was seen in patients with CD4 counts ≤50 cells/mm 3 and in patients with CD4 counts 51 to 200 cells/mm 3 . Overall, 6 deaths associated with TB-IRIS were reported.
The ACTG 5221 (STRIDE) trial, a multinational study conducted at 28 sites, randomized ART-naive patients with confirmed or probable TB and CD4 counts <250 cells/mm 3 to earlier (<2 weeks) or later (8-12 weeks) ART. 8 At study entry, the participants' median CD4 count was 77 cells/mm 3 . The rates of mortality and AIDS diagnoses were not different between the earlier and later arms, although higher rates of IRIS were seen in the earlier arm. However, a significant reduction in AIDS or death was seen in the subset of patients with CD4 counts <50 cells/mm 3 who were randomized to the earlier ART arm (P = 0.02).
In each of these 3 studies, IRIS was more common in patients initiating ART earlier than in patients starting ART later, but the syndrome was infrequently associated with mortality. Collectively these 3 trials demonstrate that in patients with active TB and with very low CD4 cell counts (i.e., <50 cells/mm 3 ), early initiation of ART can reduce mortality and AIDS progression, albeit at the risk of increased IRIS. These findings strongly favor initiation of ART within the first 2 weeks of TB treatment in patients with CD4 cell counts <50 cells/mm 3 (AI).
The question of when to start ART in patients with CD4 counts ≥50 cells/mm 3 is also informed by these studies. The STRIDE and SAPiT studies-in which the patients with CD4 cell counts ≥50 cells/mm 3 were relatively healthy and with reasonable Karnofsky scores (note the SAPiT study excluded patients with Karnofsky scores 500 cells/mm 3 ).
However, the CAMELIA study, which included more patients who were severely ill than the STRIDE and SAPiT studies, showed that early initiation of ART improved survival both in patients with CD4 counts ≤50 cells/mm 3 and in patients with CD4 counts from 51 to 200 cells/mm 3 . In a multivariate analysis, age >40 years, low BMI (1.25 x the upper limit of normal ), disseminated and MDR TB were independently associated with poor survival; whereas in a univariate analysis, hemoglobin <10g/dl also was associated with poor survival.
Thus, recently published results from the three clinical trials are complementary in defining the need for ART and use of CD4 count and clinical status to inform decisions on the optimal time to initiate ART in patients with HIV and TB disease. Earlier initiation of ART within 2 to 4 weeks of TB treatment should be strongly considered for patients with CD4 cell counts from 50 to 200 cells/mm 3 who have evidence of clinical disease of major severity as indicated by clinical evaluation, low Karnofsky score, low BMI, low hemoglobin, low albumin, or organ system dysfunction (BI). Initiation of ART within 2 to 4 weeks also should be considered for patients with CD4 counts >200 cells/mm 3 who present with evidence of severe disease (BIII).
Of additional importance, each of the above studies demonstrated excellent responses to ART, with 90% and >95% of participants achieving suppressed viremia (HIV RNA <400 copies/mL) at 12 months in the SAPiT and CAMELIA studies, respectively, and 74% of participants at 2 years in the STRIDE study.
Mortality rates in patients with MDR or XDR TB and HIV coinfection are very high. 9 Retrospective case control studies and case series provide growing evidence of better outcomes associated with receipt of ART in such coinfected patients, 10 but the optimal timing for initiation of ART is unknown. However, given the high rates and rapid mortality, most experts recommend that ART be initiated within 2 to 4 weeks after confirmation of the diagnosis of drug resistance and initiation of second-line TB therapy (BIII).
All HIV-infected pregnant women with active TB should be started on ART as early as feasible, both for maternal health and to prevent perinatal transmission of HIV (AIII). The choice of ART should be based on efficacy and safety in pregnancy and take into account potential drug-drug interactions between ARVs and rifamycins (see Perinatal Guidelines for more detailed discussions). 11 TB meningitis often is associated with severe complications and high mortality rate. In a randomized study conducted in Vietnam, patients were randomized to immediate ART or to therapy deferred until 2 months after initiation of TB treatment. A higher rate of severe (Grade 4) adverse events was seen in patients who received immediate ART than in those who deferred therapy (80.3% vs. 69.1%, respectively; P = 0.04). 12 In this study 59.8% of the immediate ART patients and 55.5% of the delayed ART patients died within 9 months. However, in the United States, where patients may be more closely monitored and treated for severe adverse events such as central nervous system (CNS) IRIS, many experts feel that ART should be initiated as for other HIV/TB-coinfected patients (CIII).
# Drug Interaction Considerations
A rifamycin is a crucial component in treatment of drug-sensitive TB. However, both rifampin and rifabutin are inducers of the hepatic cytochrome P (CYP) 450 and uridine diphosphate gluconyltransferase (UGT) 1A1 enzymes and are associated with significant interactions with most ARV agents including all PIs, nonnucleoside reverse transcriptase inhibitors (NNRTIs), maraviroc (MVC), and raltegravir (RAL). Rifampin is a potent enzyme inducer, leading to accelerated drug clearance and significant reduction in ARV drug exposure. Despite these interactions, some observational studies suggest that good virologic, immunologic, and clinical outcomes may be achieved with standard doses of efavirenz (EFV) and, to a lesser extent, nevirapine (NVP) when combined with rifampin. However, rifampin is not recommended in combination with all PIs and the NNRTIs etravirine (ETR) and rilpivirine (RPV). When rifampin is used with MVC or RAL, increased dosage of the ARV is generally recommended. Rifabutin, a weaker enzyme inducer, is an alternative to rifampin. Because rifabutin is a substrate of the CYP 450 enzyme system, its metabolism may be affected by the NNRTI or PI. Tables 18,19a,19b,19d,and 19e outline the magnitude of these interactions and provide dosing recommendations when rifamycins and selected ARV drugs are used concomitantly. After determining the drugs and doses to use, clinicians should monitor patients closely to assure good control of both TB and HIV infections. Suboptimal HIV suppression or suboptimal response to TB treatment should prompt assessment of drug adherence, subtherapeutic drug levels (consider therapeutic drug monitoring ), and acquired drug resistance.
Rifapentine is a long-acting rifamycin that can be given once weekly with INH for the treatment of active or latent TB infection. Similar to rifampin and rifabutin, rifapentine is also a CYP3A4 inducer. No systematic study has been performed to assess the magnitude of the enzyme induction effect of rifapentine on the metabolism of ARV drugs and other concomitant drugs. Significant enzyme induction can result in reduced ARV drug exposure, which may compromise virologic efficacy. Rifapentine is not recommended for treatment of latent or active TB infection in patients receiving ART, unless given in the context of a clinical trial (AIII).
# Anti-Tuberculosis/Antiretroviral Drug Toxicities
ARV agents and TB drugs, particularly INH, rifamycin, and pyrazinamide, can cause drug-induced hepatitis. These first-line TB drugs should be used for treatment of active TB disease, even with coadministration of other potentially hepatotoxic drugs or when baseline liver disease is present (AIII). Patients receiving potentially hepatotoxic drugs should be monitored frequently for clinical symptoms and signs of hepatitis and have laboratory monitoring for hepatotoxicity. Peripheral neuropathy can occur with administration of INH, didanosine (ddI), or stavudine (d4T) or may be a manifestation of HIV infection. All patients receiving INH also should receive supplemental pyridoxine to reduce peripheral neuropathy. Patients should be monitored closely for signs of drug-related toxicities and receive alternative ARVs to ddI or d4T.
# Immune Reconstitution Inflammatory Syndrome with Tuberculosis and Antiretroviral Agents
IRIS occurs in two forms: unmasking and paradoxical. The mechanism of the syndrome is the same for both forms: restoration of immune competence by administration of ART, resulting in an exuberant host response to TB bacilli and/or antigens. Unmasking IRIS refers to the initial clinical manifestations of active TB that occurs soon after ART is started. Paradoxical IRIS refers to the worsening of TB clinical symptoms after ART is started in patients who are receiving TB treatment. Severity of IRIS ranges from mild to severe to life threatening. IRIS has been reported in 8% to more than 40% of patients starting ART after TB is diagnosed, although the incidence depends on the definition of IRIS and the intensity of monitoring. Predictors of IRIS include CD4 count <50 cells/mm 3 ; higher on-ART CD4 counts; high pre-ART and lower on-ART HIV viral loads; severity of TB disease, especially high pathogen burden; and less than 30-day interval between initiation of TB and HIV treatments. Most IRIS in HIV/TB disease occurs within 3 months of the start of TB treatment. Delaying initiation of ART for 2 to 8 weeks may reduce the incidence and severity of IRIS. However, this possible advantage of delayed ART must be weighed against the potential benefit of earlier ART in improving immune function and preventing progression of HIV disease and mortality.
Patients with mild or moderately severe IRIS can be managed symptomatically or treated with nonsteroidal anti-inflammatory agents. Patients with more severe IRIS can be treated successfully with corticosteroids. A recent randomized, placebo-controlled trial demonstrated benefit of corticosteroids in the management of IRIS symptoms (as measured by decreasing days of hospitalization and Karnofsky performance score) without adverse consequences. 23 In the presence of IRIS, neither TB therapy nor ART should be stopped because both therapies are necessary for the long-term health of the patient (AIII).
# Immune Reconstitution with Antiretroviral Therapy: Conversion to Positive Tuberculin Skin Test and Interferon-Gamma Release Assay
Immune reconstitution with ART may result in unmasking LTBI (i.e., conversion of a previously negative tuberculin skin test to a positive TST or a positive interferon-gamma release assay for Mycobacterium tuberculosis-specific proteins). A positive IGRA, similar to a positive TST, is indicative of LTBI in the absence of evidence of active TB disease. 24 Because treatment for LTBI is indicated in the absence of evidence of active TB disease, clinicians should be aware of this phenomenon. Patients with a negative TST or IGRA and advanced HIV disease (i.e., CD4 count 200 cells/mm 3 (BII). 25
# Limitations to Treatment Safety and Efficacy
Adherence to Antiretroviral Therapy (Last updated May 1, 2014; last reviewed May 1, 2014)
Strict adherence to antiretroviral therapy (ART) is key to sustained HIV suppression, reduced risk of drug resistance, improved overall health, quality of life, and survival, 1,2 as well as decreased risk of HIV transmission. 3 Conversely, poor adherence is the major cause of therapeutic failure. Achieving adherence to ART is a critical determinant of long-term outcome in HIV infected patients. For many chronic diseases, such as diabetes or hypertension, drug regimens remain effective even after treatment is resumed following a period of interruption. In the case of HIV infection, however, loss of virologic control as a consequence of non-adherence to ART may lead to emergence of drug resistance and loss of future treatment options. Many patients initiating ART or already on therapy are able to maintain consistent levels of adherence with resultant viral suppression, CD4+ T-lymphocyte (CD4) count recovery, and improved clinical outcomes. Others, however, have poor adherence from the outset of ART and/or experience periodic lapses in adherence over the lifelong course of treatment. Identifying those with adherence-related challenges that require attention and implementing appropriate strategies to enhance adherence are essential roles for all members of the treatment team.
Recent data underscore the importance of conceptualizing treatment adherence broadly to include early engagement in care and sustained retention in care. The concept of an HIV "treatment cascade" has been used to describe the process of HIV testing, linkage to care, initiation of effective ART, adherence to treatment, and retention in care. The U.S. Centers for Disease Control and Prevention estimates that only 36% of the people living with HIV in the United States are prescribed ART and that among these individuals, only 76% have suppressed viral loads. 4 Thus, to achieve optimal clinical outcomes and to realize the potential public health benefit of treatment as prevention, attention to each step in the treatment cascade is critical. 5 Therefore, provider skill and involvement to retain patients in care and help them achieve high levels of medication adherence are crucial.
This section provides updated guidance on assessing and monitoring adherence and outlines strategies to help patients maintain high levels of adherence.
# Factors Associated with Adherence Success and Failure
Adherence to ART can be influenced by a number of factors, including the patient's social situation and clinical condition; the prescribed regimen; and the patient-provider relationship. 6 It is critical that each patient receives and understands information about HIV disease including the goals of therapy (achieving and maintaining viral suppression, decreasing HIV-associated morbidity and mortality, and preventing sexual transmission of HIV), the prescribed regimen (including dosing schedule and potential side effects), the importance of strict adherence to ART, and the potential for the development of drug resistance as a consequence of suboptimal adherence. However, information alone is not sufficent to assure high levels of adherence; patients must also be positively motivated to initiate and maintain therapy.
From a patient perspective, nonadherence is often a consequence of one or more behavioral, structural, and psychosocial barriers (e.g., depression and other mental illnesses, neurocognitive impairment, low health literacy, low levels of social support, stressful life events, high levels of alcohol consumption and active substance use, homelessness, poverty, nondisclosure of HIV serostatus, denial, stigma, and inconsistent access to medications). Furthermore, patient age may affect adherence. For example, some adolescent and young adult HIV patients, in particular, have substantial challenges in achieving levels of adherence necessary for successful therapeutic outcomes (see HIV-Infected Adolescents section). 10,11 In additon, failure to adopt practices that facilitate adherence, such as linking medication taking to daily activities or using a medication reminder system or a pill organizer, is also associated with treatment failure. 12 Characteristics of one or more components of the prescribed regimen can affect adherence. Simple, oncedaily regimens, 13 including those with low pill burden, without a food requirement, and few side effects or toxicities, are associated with higher levels of adherence. 14,15 Many currently available ARV regimens are much easier to take and better tolerated than older regimens. Studies have shown that patients taking oncedaily regimens have higher rates of adherence than those taking twice-daily dosing regimens. 15 However, data to support or refute the superiority of fixed-dose combination product of 1-pill versus 3-pills (of individual drug products), once-daily regimens-as might be required for the use of some soon-to-beavailable generic-based ARV regimens-are limited.
Characteristics of the clinical setting can also have important structural influences on the success or failure of medication adherence. Settings that provide comprehensive multidisciplinary care (e.g., with case managers, pharmacists, social workers, psychiatric care providers) are often more successful in supporting patients' complex needs, including their medication adherence-related needs. Further, specific settings, such as prisons and other institutional settings, may thwart or support medication adherence. Drug abuse treatment programs are often best suited to address substance use that may confound adherence and may offer services, such as directly observed therapy, that promote adherence.
Finally, a patient-provider relationship that enhances patient trust through non-judgmental and supportive care and use of motivational strategies can positively influence medication adherence.
# Routine Monitoring of Adherence and Retention in Care
Although there is no gold standard for assessing adherence, 1 properly implemented validated tools and assessment strategies can prove valuable in most clinical settings. Viral load suppression is one of the most reliable indicators of adherence and can be used as positive reinforcement to encourage continuous adherence.
When patients initiating ART fail to achieve viral suppression by 24 weeks of treatment, the possibility of suboptimal adherence and other factors must be assessed. Similarly, treatment failure as measured by detectable viral load during chronic care is most likely the result of non-adherence. Patient self-report, the most frequently used method for evaluating medication adherence, remains a useful tool for assessing adherence over time. However, self-reports must be properly and carefully assessed as patients may overestimate adherence. While carefully assessed patient self report of high-level adherence to ART has been associated with favorable viral load responses, 16,17 patient admission of suboptimal adherence is highly correlated with poor therapeutic response. The reliability of self report often depends on how the clinican elicits the information. It is most reliable when ascertained in a simple, nonjudgmental, routine, and structured format that normalizes less-than-perfect adherence and minimizes socially desirable or "white coat adherence" responses. Some patients may selectively adhere to components of a regimen believed to have the fewest side effects or the lowest dosing frequency or pill burden. To allow patients to more accurately disclose lapses in adherence, some experts suggest that providers inquire about the number of missed doses during a defined time period rather than directly asking "Are you taking your medicines?" Others advocate simply asking patients to rate their adherence during the last 4 weeks on a 5-or 6-point Likert scale. 18,19 Regardless of how obtained, patient selfreport, in contrast to other measures of adherence, allows for immediate patient-provider discussion to identify reasons for missed doses and to explore corrective strategies.
Other measures of adherence include pharmacy records and pill counts. Pharmacy records can be valuable when medications are obtained exclusively from a single source so that refills can be traced. Pill counts are commonly used but can be altered by patients. Other methods of assessing adherence include the use of therapeutic drug monitoring and electronic measurement devices (e.g., MEMS bottle caps and dispensing systems). However, these methods are costly and are usually done primarily in research settings.
# Interventions to Improve Adherence and Retention in Care
A continuum of ART adherence support services is necessary to meet individual patient needs. All health care team members, including physicians, physician assistants, nurse practitioners, nurse midwives, nurses, pharmacists, medication managers, and social workers play integral roles in successful adherence programs. 17, Effective adherence interventions vary in modality and duration, and by clinical setting, provider, and patient. There are many options that can be customized to suit a range of needs and settings (see Table 13).
An increasing number of interventions have proven effective in improving adherence to ART. For descriptions of the interventions, see: . 23 Clinicians should provide all patients with a basic level of adherence-related information and support. Before writing the first prescription(s) for patients initiating or reinitiating ART, clinicians should assess the patient's adherence readiness. Clinicians should evaluate patients' knowledge about HIV disease, treatment, and prevention and provide basic information about ART, viral load and CD4 count and the expected outcome of ART based on these parameters, the importance of strict adherence to ART, and the consequences of nonadherence. In addition, clinicians should assess patients' motivation to successfully adhere to ART and identify and support facilitating factors and address potential barriers to adherence. Finally, clinicians should be assured that patients have the necessary medication taking skills to follow the regimen as prescribed.
Given the wide array of treatment options, individualizing treatment with patient involvement in decision making is the cornerstone of treatment planning and therapeutic success. The first principle of successful treatment is to design an understandable plan to which the patient can commit. 24,25 It is important to consider the patient's daily schedule; patient tolerance of pill number, size and frequency; and any issues affecting absorption (e.g., use of acid reducing therapy and food requirements). With the patient's input, a medication choice and administration schedule should be tailored to his/her routine daily activities. If necessary, soliciting help from family members may also improve adherence. Patients who are naive to ART should understand that their first regimen usually offers the best chance for taking a simple regimen that affords long-term treatment success and prevention of drug resistance. Establishing a trusting patient-provider relationship over time and maintaining good communication will help to improve adherence and long-term outcomes. Medication taking can also be enhanced by the use of pill organizers and medication reminder aids (e.g., alarm clock, pager, calendar).
Positive reinforcement can greatly help patients maintain high levels of adherence. This technique to foster adherence includes informing patients of their low or suppressed HIV viral load levels and increases in CD4 cell counts. Motivational interviewing has also been used with some successes. Recognizing high levels of adherence with incentives and rewards can facilitate treatment success in some patients. Adherence-contingent reward incentives such as meal tickets, grocery bags, lotto tickets, and cash have been used in the treatment of HIV and other chronic diseases. The effectiveness of using cash incentives to promote HIV testing, entry to care, and adherence to ART is currently being studied in the multi-site HPTN 065 trial. Other effective interventions include nurse home visits, a five-session group intervention, pager messaging, and couples or family-based interventions. To maintain high levels of adherence in some patients, it is critically important to provide substance abuse therapy and to strengthen social support. Directly observed therapy (DOT) has been effective in providing ART to active drug users 26 but not to patients in a general clinic population. 27 To determine whether additional adherence or retention interventions are warranted, assessments should be done at each clinical encounter and should be the responsibility of the entire health care team. Routine monitoring of HIV viral load, pharmacy records, and indicators that measure retention in care are useful to determine if more intense efforts are needed to improve adherence. Patients with a history of non-adherence to ART are at risk for poor adherence when re-starting therapy with the same or new drugs. Special attention should be given to identify and address any reason for previous poor adherence. Preferential use of ritonavirboosted protease inhibitor-(PI/r)-based ART, which has a higher barrier to the development of resistance than other treatment options, should be considered if poor adherence is predicted.
The critical elements of adherence go hand in hand with linkage-to-care and retention in care. A recently released guideline provides a number of strategies to improve entry and retention in care and adherence to therapy for HIV infected patients. 5 As with adherence monitoring, research advances offer many options for systematic monitoring of retention in care that may be used in accordance with local resources and standards.
The options include surveillance of visit adherence, gaps in care, and the number of visits during a specified period of time. 28
# Conclusion
Adherence to ART is central to therapeutic success. Given the many available assessment strategies and interventions, the challenge for the treatment team is to select the techniques that best fit each patient and patient population, and, according to available resources, the treatment setting. In addition to maintaining high levels of medication adherence, attention to effective linkage to care, engagement in care, and retention in care is critical for successful treatment outcomes. To foster treatment success, there are interventions to support each step in the cascade of care, as well as guidance on systematic monitoring of each step in the cascade. 5
# Strategies Examples
Use a multidisciplinary team approach.
Provide an accessible, trustworthy health care team.
- Nonjudgmental providers, nurses, social workers, pharmacists, and medication managers Strengthen early linkage to care and retention in care.
- Encourage healthcare team participation in linkage to and retention in care.
Assess patient readiness to start ART.
Evaluate patient's knowledge about HIV disease, prevention and treatment and, on the basis of the assessment, provide HIV-related information.
- Considering the patient's current knowledge base, provide information about HIV, including the natural history of the disease, HIV viral load and CD4 count and expected clinical outcomes according to these parameters, and therapeutic and prevention consequences of non-adherence.
Identify facilitators, potential barriers to adherence, and necessary medication management skills before starting ART medication.
- Assess patient's cognitive competence and impairment.
- Assess behavioral and psychosocial challenges including depression, mental illnesses, levels of social support, high levels of alcohol consumption and active substance use, non-disclosure of HIV serostatus and stigma.
- Identify and address language and literacy barriers.
- Assess beliefs, perceptions, and expectations about taking ART (e.g., impact on health, side effects, disclosure issues, consequences of non-adherence).
- Ask about medication taking skills and foreseeable challenges with adherence (e.g., past difficulty keeping appointments, adverse effects from previous medications, issues managing other chronic medications, need for medication reminders and organizers).
- Assess structural issues including unstable housing, lack of income, unpredictable daily schedule, lack of prescription drug coverage, lack of continuous access to medications.
Provide needed resources.
- Provide or refer for mental health and/or substance abuse treatment.
- Provide resources to obtain prescription drug coverage, stable housing, social support, and income and food security.
# Strategies Examples
Involve the patient in ARV regimen selection.
- Review regimen potency, potential side effects, dosing frequency, pill burden, storage requirements, food requirements, and consequences of nonadherence.
- Assess daily activities and tailor regimen to predictable and routine daily events.
- Consider preferential use of PI/r-based ART if poor adherence is predicted.
- Consider use of fixed-dose combination formulation.
- Assess if cost/co-payment for drugs can affect access to medications and adherence.
Assess adherence at every clinic visit.
- Monitor viral load as a strong biologic measure of adherence.
- Use a simple behavioral rating scale.
- Employ a structured format that normalizes or assumes less-than-perfect adherence and minimizes socially desirable or "white coat adherence" responses.
- Ensure that other members of the health care team also assess adherence.
Use positive reinforcement to foster adherence success.
- Inform patients of low or non-detectable levels of HIV viral load and increases in CD4 cell counts.
- When needed, consider providing incentives and rewards for achieving high levels of adherence and treatment success.
Identify the type of and reasons for nonadherence. - Failure to fill the prescription(s)
- Failure to understand dosing instructions - Use adherence-related tools to complement education and counseling interventions (e.g., pill boxes, dose planners, reminder devices).
- Use community resources to support adherence (e.g., visiting nurses, community workers, family, peer advocates).
- Use patient prescription assistance programs.
- Use motivational interviews.
# Strategies Examples
Systematically monitor retention in care.
- Record and follow up on missed visits.
On the basis of any problems identified through systematic monitoring, consider options to enhance retention in care given resources available.
- Provide outreach for those patients who drop out of care.
- Use peer or paraprofessional treatment navigators.
- Employ incentives to encourage clinic attendance or recognize positive clinical outcomes resulting from good adherence.
- Arrange for directly observed therapy (if feasible).
Key to Acronyms: ART = antiretroviral therapy; CD4 = CD4 T lymphocyte; PI = protease inhibitor; PI/r = ritonavir-boosted protease inhibitor
# Switching Antiretroviral Therapy Because of Adverse Effects
Most patients do not experience treatment-limiting ART-associated toxicities; however, some patients do, and in these cases, ART must be modified. ART-associated adverse events can range from acute and potentially life threatening to chronic and insidious. Acute life-threatening events (e.g., acute hypersensitivity reaction due to ABC, lactic acidosis due to stavudine and didanosine , liver and/or severe cutaneous toxicities due to NVP) usually require the immediate discontinuation of all ARV drugs and re-initiation of an alternative regimen without overlapping toxicity. Non-life threatening toxicities (e.g., urolithiasis with atazanavir , renal tubulopathy with tenofovir ) can usually be managed by substituting another ARV agent for the presumed causative agent without interruption of ART. Other, chronic, non-life threatening adverse events (e.g., dyslipidemia) can be addressed either by switching the potentially causative agent for another agent or by managing the adverse event with additional pharmacological or nonpharmacological interventions. Management strategies must be individualized for each patient.
Switching from an effective ARV regimen to a new regimen must be done carefully and only when the potential benefits of the change outweigh the potential complications of altering treatment. The fundamental principle of regimen switching is to maintain viral suppression. When selecting a new agent or regimen, providers should be aware that resistance mutations selected for, regardless of whether previously or currently identified by genotypic resistance testing, are archived in HIV reservoirs, and even if absent from subsequent resistance test results, may reappear under selective pressure. It is critical that providers review the following before implementing any treatment switch:
- the patient's medical and complete ARV history including prior virologic responses to ART;
- resistance test results;
- viral tropism (when maraviroc is being considered);
- HLA B*5701 status (when ABC is being considered);
- co-morbidities;
- adherence history;
- prior intolerances to any medications; and
- concomitant medications and supplements and their potential for drug interactions with ARVs.
Patient acceptance of new food or dosing requirements must also be assessed. In some cases, medication costs may also be a factor to consider before switching treatment. Signs and symptoms of ART-associated adverse events may mimic those of comorbidities, adverse effects of concomitant medications, or HIV infection itself. Therefore, concurrent with ascribing a particular clinical event to ART, alternative causes for the event should be investigated. In the case of a severe adverse event, it may be necessary to discontinue or switch ARVs pending the outcome of such an investigation. For the first few months after an ART switch, the patient should be closely monitored for any new adverse events. The patient's viral load should also be monitored to assure continued viral suppression. greater scale. One analysis suggests the possibility of saving approximately $900 million nationally in the first year of switching from a branded fixed-dose combination product to a three-pill regimen containing generic efavirenz. 3 In summary, understanding HIV and ART-related costs in the United States is complicated because of the wide variability in medical coverage, accessibility, and expenses across regions, insurance plans, and pharmacies. In an effort to retain excellent clinical outcomes in an environment of cost-containment strategies, providers should remain informed of current insurance and payment structures, ART costs (see Table 16 below for estimates of drugs' average wholesale prices), discounts among preferred pharmacies, and available generic ART options. Providers should work with patients and their case managers and social workers to understand their patients' particular pharmacy benefit plans and potential financial barriers to filling their prescriptions. Additionally, providers should familiarize themselves with ARV affordability resources (such as ADAP and pharmaceutical company patient assistance programs for patients who qualify) and refer patients to such assistance if needed. Pharmacokinetic (PK) drug-drug interactions between antiretroviral (ARV) drugs and concomitant medications are common, and may lead to increased or decreased drug exposure. In some instances, changes in drug exposure may increase toxicities or affect therapeutic responses. When prescribing or switching one or more drugs in an ARV regimen, clinicians must consider the potential for drug-drug interactions-both those that affect ARVs and those that ARVs affect on other drugs a patient is taking. A thorough review of concomitant medications in consultation with a clinician with expertise in ARV pharmacology can help in designing a regimen that minimizes undesirable interactions. Recommendations for managing a particular drug interaction may differ depending on whether a new ARV is being initiated in a patient on a stable concomitant medication or a new concomitant medication is being initiated in a patient on a stable ARV regimen. The magnitude and significance of interactions are difficult to predict when several drugs with competing metabolic pathways are prescribed concomitantly. When prescribing interacting drugs is necessary, clinicians should be vigilant in monitoring for therapeutic efficacy and/or concentration-related toxicities.
# Mechanisms of Pharmacokinetic Interactions
PK interactions may occur during absorption, metabolism, or elimination of the ARV and/or the interacting drugs.
The most common mechanisms of interactions are described below and listed for each ARV drug in Table 17.
# Pharmacokinetic Interactions Affecting Drug Absorption
The extent of oral absorption of drugs can be affected by the following mechanisms:
- Acid reducing agents, such as proton pump inhibitors, H2 antagonists, or antacids, can reduce the absorption of ARVs that require gastric acidity for optimal absorption (i.e., atazanavir and rilpivirine ).
- Products that contain polyvalent cations, such as aluminum, calcium, magnesium-containing antacids, supplements, or iron products, can bind to integrase inhibitors (INSTI) and reduce absorption of these ARV agents.
- Drugs that induce or inhibit the enzyme CYP3A4 or efflux transporter p-glycoprotein in the intestines may reduce or promote the absorption of other drugs.
# Pharmacokinetic Interactions Affecting Hepatic Metabolism
Two major enzyme systems are most frequently responsible for clinically significant drug interactions.
1. The cytochrome P450 enzyme system is responsible for the metabolism of many drugs, including the non-nucleoside reverse transcriptase inhibitors (NNRTI), protease inhibitors (PI), CCR5 antagonist maraviroc (MVC), and the INSTI elvitegravir (EVG). Cytochrome P450 3A4 (CYP3A4) is the most common enzyme responsible for drug metabolism, though multiple enzymes may be involved in the metabolism of a drug. ARVs and concomitant medications may be inducers, inhibitors, and/or substrates of these enzymes.
2. The uridine diphosphate (UDP)-glucuronosyltransferase (UGT) 1A1 enzyme is the primary enzyme responsible for the metabolism of the INSTIs dolutegravir (DTG) and raltegravir (RAL). Drugs that induce or inhibit the UGT enzyme can affect the PKs of these INSTIs.
# Pharmacokinetic Enhancers (Boosters)
PK enhancing is a strategy used to increase exposure of an ARV by concomitantly administering a drug that inhibits the enzymes that metabolize the ARV. Currently in clinical practice, two agents are used as PK enhancers: ritonavir (RTV) and cobicistat (COBI). Both of these agents are potent inhibitors of the CYP3A4 enzyme, resulting in higher drug exposures of the coadministered ARV metabolized by this pathway.
Importantly, RTV and COBI may have different effects on other CYP or UGT metabolizing enzymes and drug transporters. Complex or unknown mechanisms of PK-based interactions preclude extrapolation of RTV drug interactions to certain COBI interactions, such as interactions with warfarin, phenytoin, voriconazole, oral contraceptives, certain HMG-CoA reductase inhibitors (or statins), and other drugs.
# Other Mechanisms of Pharmacokinetic Interactions
Knowledge of drug transporters is evolving, elucidating additional drug interaction mechanisms. For example, DTG decreases the renal clearance of metformin by inhibiting organic anion transporters in renal tubular cells. Similar transporters aid hepatic, renal, and biliary clearance of drugs and may be susceptible to drug interactions. ARVs and concomitant medications may be inducers, inhibitors, and/or substrates of these drug transporters.
Tables 18-20b provide information on known or suspected drug interactions between ARV agents and commonly prescribed medications based on published PK data or information from product labels. The tables provide general guidance on drugs that should not be coadministered and recommendations for dose modifications or alternative therapy. - Start with tadalafil 5-mg dose and do not exceed a single dose of 10 mg every 72 hours. Monitor for adverse effects of tadalafil.
# For Treatment of PAH
In patients on a PI >7 days:
- Start with tadalafil 20 mg once daily and increase to 40 mg once daily based on tolerability.
In patients on tadalafil who require a PI:
- Stop tadalafil ≥24 hours before PI initiation. 7 days after PI initiation restart tadalafil at 20 mg once daily, and increase to 40 mg once daily based on tolerability.
In patients switching between COBI and RTV:
- Maintain tadalafil dose.
For Treatment of Benign Prostatic Hyperplasia:
- Maximum recommended daily dose is 2.5 mg per day. For treatment of gout flares:
- Colchicine 0.6 mg for 1 dose, followed by 0.3 mg 1 hour later. Do not repeat dose for at least 3 days.
For prophylaxis of gout flares:
- If original dose was colchicine 0.6 mg BID, decrease to colchicine 0.3 mg once daily. If regimen was 0.6 mg once daily, decrease to 0.3 mg every other day.
For treatment of Familial Mediterranean Fever:
- Do not exceed colchicine 0.6 mg once daily or 0.3 mg BID. Despite substantial advances in prevention and treatment of HIV infection in the United States, the rate of new infections has remained stable. Although earlier prevention interventions mainly were behavioral, recent data demonstrate the strong impact of antiretroviral therapy (ART) on secondary HIV transmission. The most effective strategy to stem the spread of HIV will probably be a combination of behavioral, biological, and pharmacological interventions. 3
# Sedative/Hypnotics
# Prevention Counseling
Counseling and related behavioral interventions for those living with HIV infection can reduce behaviors associated with secondary transmission of HIV. Each patient encounter offers the clinician an opportunity to reinforce HIV prevention messages, but multiple studies show that prevention counseling is frequently neglected in clinical practice. Although delivering effective prevention interventions in a busy practice setting may be challenging, clinicians should be aware that patients often look to their providers for messages about HIV prevention. Multiple approaches to prevention counseling are available, including formal guidance from the Centers for Disease Control and Prevention (CDC) for incorporating HIV prevention into medical care settings. Such interventions have been demonstrated to be effective in changing sexual risk behavior and can reinforce self-directed behavior change early after diagnosis. 9 CDC has identified several prevention interventions for individuals infected with HIV that meet stringent criteria for efficacy and scientific rigor (). The following three interventions have proven effective in treatment settings and can be delivered by providers as brief messages during clinic visits:
- Partnership for Health (),
- Options (),
- Positive Choice ().
In addition, CDC's "Prevention Is Care" campaign () helps providers (and members of a multidisciplinary care team) integrate simple methods to prevent transmission by HIV-infected individuals into routine care. These prevention interventions are designed to reduce the risk of secondary HIV transmission through sexual contact. The interventions are designed generally for implementation at the community or group level, but some can be adapted and administered in clinical settings by a multidisciplinary care team.
# Need for Screening for High-Risk Behaviors
The primary care visit provides an opportunity to screen patients for ongoing high-risk drug and sexual behaviors for transmitting HIV infection. Routine screening and symptom-directed testing for and treatment of sexually transmitted diseases (STDs), as recommended by CDC, 10 remain essential adjuncts to prevention counseling. Genital ulcers may facilitate HIV transmission and STDs may increase HIV viral load in plasma and genital secretions. 7, They also provide objective evidence of unprotected sexual activity, which should prompt prevention counseling.
The contribution of substance and alcohol use to HIV risk behaviors and transmission has been well established in multiple populations; therefore, effective counseling for injection and noninjection drug users is essential to prevent HIV transmission. Identifying the substance(s) of use is important because HIV prevalence, transmission risk, risk behaviors, transmission rates, and potential for pharmacologic intervention all vary according to the type of substance used. Risk-reduction strategies for injection drug users (IDUs), in addition to condom use, include needle exchange and instructions on cleaning drug paraphernalia. Evidence supporting the efficacy of interventions to reduce injection drug use risk behavior also exists. Interventions include both behavioral strategies 22 and opiate substitution treatment with methadone or buprenorphine. No successful pharmacologic interventions have been found for cocaine and methamphetamine users; cognitive and behavioral interventions demonstrate the greatest effect on reducing the risk behaviors of these users. Given the significant impact of cocaine and methamphetamine on sexual risk behavior, reinforcement of sexual risk-reduction strategies is important. 28 Antiretroviral Therapy as Prevention ART can play an important role in preventing HIV transmission. Lower levels of plasma HIV RNA have been associated with decreases in the concentration of virus in genital secretions. Observational studies have demonstrated the association between low serum or genital HIV RNA and a decreased rate of HIV transmission among serodiscordant heterosexual couples. 29, Ecological studies of communities with relatively high concentrations of men who have sex with men (MSM) and IDUs suggest increased use of ART is associated with decreased community viral load and reduced rates of new HIV diagnoses. These data suggest that the risk of HIV transmission is low when an individual's viral load is below 400 copies/mL, 35,38 but the threshold below which transmission of the virus becomes impossible is unknown. Furthermore, to be effective at preventing transmission it is assumed that: (1) ART is capable of durably and continuously suppressing viremia; (2) adherence to an effective ARV regimen is high; and (3) there is an absence of a concomitant STD. Importantly, detection of HIV RNA in genital secretions has been documented in individuals with controlled plasma HIV RNA and data describing a differential in concentration of most ARV drugs in the blood and genital compartments exist. 30,39 At least one case of HIV transmission from a patient with suppressed plasma viral load to a monogamous uninfected sexual partner has been reported. 40 In the HPTN 052 trial in HIV-discordant couples, the HIV-infected partners who were ART naive and had CD4 counts between 350 and 550 cells/mm 3 were randomized to initiate or delay ART. In this study, those who initiated ART had a 96% reduction in HIV transmission to the uninfected partners. 3 Almost all of the participants were in heterosexual relationships, all participants received risk-reduction counseling, and the absolute number of transmission events was low: 1 among ART initiators and 27 among ART delayers. Over the course of the study virologic failure rates were less than 5%, a value much lower than generally seen in individuals taking ART for their own health. These low virologic failure rates suggest high levels of adherence to ART in the study, which may have been facilitated by the frequency of study follow-up (study visits were monthly) and by participants' sense of obligation to protect their uninfected partners. Therefore, caution is indicated when interpreting the extent to which ART for the HIV-infected partner protects seronegative partners in contexts where adherence and, thus, rates of continuous viral suppression, may be lower. Furthermore, for HIV-infected MSM and IDUs, biological and observational data suggest suppressive ART also should protect against transmission, but the actual extent of protection has not been established.
Rates of HIV risk behaviors can increase coincidently with the availability of potent combination ART, in some cases almost doubling compared with rates in the era prior to highly effective therapy. 9 A meta-analysis demonstrated that the prevalence of unprotected sex acts was increased in HIV-infected individuals who believed that receiving ART or having a suppressed viral load protected against transmitting HIV. 41 Attitudinal shifts away from safer sexual practices since the availability of potent ART underscore the role of provider-initiated HIV prevention counseling. With wider recognition that effective treatment decreases the risk of HIV transmission, it is particularly important for providers to help patients understand that a sustained viral load below the limits of detection will dramatically reduce but does not absolutely assure the absence of HIV in the genital and blood compartments and, hence, the inability to transmit HIV to others. Maximal suppression of viremia not only depends on the potency of the ARV regimen used but also on the patient's adherence to prescribed therapy. Suboptimal adherence can lead to viremia that not only harms the patient but also increases his/her risk of transmitting HIV (including drug-resistant strains) via sex or needle sharing. Screening for and treating behavioral conditions that can impact adherence, such as depression and alcohol and substance use, improve overall health and reduce the risk of secondary transmission.
# Summary
Consistent and effective use of ART resulting in a sustained reduction in viral load in conjunction with consistent condom usage, safer sex and drug use practices, and detection and treatment of STDs are essential tools for prevention of sexual and blood-borne transmission of HIV. Given these important considerations, medical visits provide a vital opportunity to reinforce HIV prevention messages, discuss sex-and drugrelated risk behaviors, diagnose and treat intercurrent STDs, review the importance of medication adherence, and foster open communication between provider and patient.
(e.g., renal, cardiac, hepatic, or neurologic complications), development of drug resistance, and the need for chemoprophylaxis against opportunistic infections as a result of CD4 decline. Patients should be counseled about the need for close clinical and laboratory monitoring during therapy interruptions. Approximately 5%-10% of HIV-infected persons also have chronic HBV infection, defined as testing positive for HBsAg for more than 6 months. 1 The progression of chronic HBV to cirrhosis, end-stage liver disease, and/or hepatocellular carcinoma is more rapid in HIV-infected persons than in persons with chronic HBV alone. 2 Conversely, chronic HBV does not substantially alter the progression of HIV infection and does not influence HIV suppression or CD4 cell responses following ART initiation. However, several liverassociated complications that are ascribed to flares in HBV activity, discontinuation of dually active ARVs, or toxicity of ARVs can affect the treatment of HIV in patients with HBV coinfection. These include the following:
# Considerations for Antiretroviral Use in Patients with Coinfections
- FTC, 3TC, and TDF are approved ARVs that also have antiviral activity against HBV. Discontinuation of these drugs may potentially cause serious hepatocellular damage resulting from reactivation of HBV. 8 - Entecavir has activity against HIV; its use for HBV treatment without ART in patients with dual infection may result in the selection of the M184V mutation that confers HIV resistance to 3TC and FTC. Therefore, entecavir must be used in addition to a fully suppressive ARV regimen when used in HIV/HBV-coinfected patients (AII). 9 - 3TC-resistant HBV is observed in approximately 40% of patients after 2 years on 3TC for chronic HBV and in approximately 90% of patients after 4 years when 3TC is used as the only active drug for HBV in coinfected patients. Therefore, 3TC or FTC should be used in combination with other anti-HBV drugs (AII). 10 Panel's Recommendations
- Prior to initiation of antiretroviral therapy (ART), all patients who test positive for hepatitis B surface antigen (HBsAg) should be tested for hepatitis B virus (HBV) DNA using a quantitative assay to determine the level of HBV replication (AIII).
- Because emtricitabine (FTC), lamivudine (3TC), and tenofovir (TDF) have activity against both HIV and HBV, if HBV or HIV treatment is needed, ART should be initiated with the combination of TDF + FTC or TDF + 3TC as the nucleoside reverse transcriptase inhibitor (NRTI) backbone of a fully suppressive antiretroviral (ARV) regimen (AI).
- If HBV treatment is needed and TDF cannot safely be used, the alternative recommended HBV therapy is entecavir in addition to a fully suppressive ARV regimen (BI). Other HBV treatment regimens include peginterferon alfa monotherapy or adefovir in combination with 3TC or FTC or telbivudine in addition to a fully suppressive ARV regimen (BII).
- Entecavir has activity against HIV; its use for HBV treatment without ART in patients with dual infection may result in the selection of the M184V mutation that confers HIV resistance to 3TC and FTC. Therefore, entecavir must be used in addition to a fully suppressive ARV regimen when used in HIV/HBV-coinfected patients (AII).
- Discontinuation of agents with anti-HBV activity may cause serious hepatocellular damage resulting from reactivation of HBV; patients should be advised against self-discontinuation and carefully monitored during interruptions in HBV treatment (AII).
- If ART needs to be modified due to HIV virologic failure and the patient has adequate HBV suppression, the ARV drugs active against HBV should be continued for HBV treatment in combination with other suitable ARV agents to achieve HIV suppression (AIII). The management of hepatitis C virus (HCV)-infected patients is rapidly evolving. Data suggest that HIV/HCV-coinfected patients treated with all-oral HCV regimens have sustained virologic response rates comparable to those of HCV-monoinfected patients. The purpose of this section is to discuss hepatic safety and drug-drug interaction issues related to HIV/HCV coinfection and the concomitant use of antiretroviral (ARV) agents and HCV drugs. For specific guidance on HCV treatment, please refer to /.
# Rating of Recommendations
Among patients with chronic HCV infection, approximately one-third progress to cirrhosis, at a median time of less than 20 years. 1,2 The rate of progression increases with older age, alcoholism, male sex, and HIV infection. A meta-analysis found that HIV/HCV-coinfected patients had a three fold greater risk of progression to cirrhosis or decompensated liver disease than HCV-monoinfected patients. 5 The risk of progression is even greater in HIV/HCV-coinfected patients with low CD4 T lymphocyte (CD4) cell counts.
Although antiretroviral therapy (ART) appears to slow the rate of HCV disease progression in HIV/HCVcoinfected patients, several studies have demonstrated that the rate continues to exceed that observed in those without HIV infection. 7,8 Whether HCV infection accelerates HIV progression, as measured by AIDS-related opportunistic infections (OIs) or death, 9 is unclear. Although some older ARV drugs that are no longer commonly used have been associated with higher rates of hepatotoxicity in patients with chronic HCV infection, 10,11 newer ARV agents currently in use appear to be less hepatotoxic.
For more than a decade, the mainstay of treatment for HCV infection was a combination regimen of peginterferon and ribavirin (PegIFN/RBV), but this regimen was associated with a poor rate of sustained virologic response (SVR), especially in HIV/HCV-coinfected patients. Rapid advances in HCV drug development led to the discovery of new classes of direct acting antiviral (DAA) agents that target the HCV replication cycle. These new agents, when used with or without PegIFN and RBV, have been shown to achieve high SVR rates. The first DAA agents approved for the treatment of HCV infection in combination with PegIFN/RBV were the HCV protease inhibitors (PI), boceprevir and telaprevir. In HCV genotype 1
# Panel Recommendations
- All HIV-infected patients should be screened for hepatitis C virus infection (HCV). Patients at high risk of HCV infection should be screened annually and whenever HCV infection is suspected.
- Antiretroviral therapy may slow the progression of liver disease by preserving or restoring immune function and reducing HIV-related immune activation and inflammation. For most HIV/HCV-coinfected patients, including those with cirrhosis, the benefits of antiretroviral therapy outweigh concerns regarding drug-induced liver injury. Therefore, antiretroviral therapy should be initiated in most HIV/HCV-coinfected patients, regardless of CD4 T lymphocyte (CD4) cell count (BII).
- Initial antiretroviral therapy combination regimens recommended for most HIV/HCV-coinfected patients are the same as those recommended for individuals without HCV infection. However, when treatment for both HIV and HCV is indicated, the antiretroviral regimen should be selected with special considerations of potential drug-drug interactions and overlapping toxicities with the HCV treatment regimen (see discussion in the text below and in Table 12).
- Combined treatment of HIV and HCV can be complicated by drug-drug interactions, increased pill burden, and toxicities. Although antiretroviral therapy should be initiated for most HIV/HCV-coinfected patients regardless of CD4 cell count, in antiretroviral therapynaive patients with CD4 counts >500 cells/mm 3 some clinicians may choose to defer antiretroviral therapy until HCV treatment is completed (CIII).
- In patients with lower CD4 counts (e.g., <200 cells/mm 3 ), antiretroviral therapy should be initiated promptly (AI) and HCV therapy may be delayed until the patient is stable on HIV treatment (CIII).
# Rating of Recommendations
# Treatment of Active Tuberculosis in HIV-Infected Patients
HIV infection significantly increases the risk of progression from latent to active TB disease. The CD4 cell count influences both the frequency and severity of active TB disease. Active TB also negatively affects HIV disease. It may be associated with a higher HIV viral load and more rapid progression of HIV disease. 3 Active pulmonary or extrapulmonary TB disease requires prompt initiation of TB treatment. The treatment of active TB disease in HIV-infected patients should follow the general principles guiding treatment for Panel's Recommendations - The principles for treatment of active tuberculosis (TB) disease in HIV-infected patients are the same as those for HIV-uninfected patients (AI).
- All HIV-infected patients with diagnosed active TB should be started on TB treatment immediately (AI).
- All HIV-infected patients with diagnosed active TB should be treated with antiretroviral therapy (ART) (AI).
- In patients with CD4 counts <50 cells/mm 3 , ART should be initiated within 2 weeks of starting TB treatment (AI).
- In patients with CD4 counts ≥50 cells/mm 3 who present with clinical disease of major severity as indicated by clinical evaluation (including low Karnofsky score, low body mass index , low hemoglobin, low albumin, organ system dysfunction, or extent of disease), ART should be initiated within 2 to 4 weeks of starting TB treatment. The strength of this recommendation varies on the basis of CD4 cell count:
- CD4 count 50 to 200 cells/mm 3 (BI)
- CD4 count >200 cells/mm 3 (BIII)
- In patients with CD4 counts ≥50 cells/mm 3 who do not have severe clinical disease, ART can be delayed beyond 2 to 4 weeks of starting TB therapy but should be started within 8 to 12 weeks of TB therapy initiation. The strength of this recommendation also varies on the basis of CD4 cell count:
- CD4 count 50 to 500 cells/mm 3 (AI)
- CD4 count >500 cells/mm 3 (BIII)
- In all HIV-infected pregnant women with active TB, ART should be started as early as feasible, both for maternal health and for prevention of mother-to-child transmission (PMTCT) of HIV (AIII).
- In HIV-infected patients with documented multidrug-resistant (MDR) and extensively drug-resistant (XDR) TB, ART should be initiated within 2 to 4 weeks of confirmation of TB drug resistance and initiation of second-line TB therapy (BIII).
- Despite pharmacokinetic drug interactions, a rifamycin (rifampin or rifabutin) should be included in TB regimens for patients receiving ART, with dosage adjustment if necessary (AII).
- Rifabutin is the preferred rifamycin to use in HIV-infected patients with active TB disease on a protease inhibitor (PI)-based regimen because the risk of substantial drug interactions with PIs is lower with rifabutin than with rifampin (AII).
- Coadministration of rifampin and PIs (with or without ritonavir boosting) is not recommended (AII).
- Rifapentine (RPT) is NOT recommended in HIV-infected patients receiving ART for treatment of latent TB infection (LTBI) or active TB, unless in the context of a clinical trial (AIII).
- Immune reconstitution inflammatory syndrome (IRIS) may occur after initiation of ART. Both ART and TB treatment should be continued while managing IRIS (AIII).
- Treatment support, which can include directly observed therapy (DOT) of TB treatment, is strongly recommended for HIV-infected patients with active TB disease (AII).
# Rating of Recommendations
# Caring for Patients with HIV and Tuberculosis
Close collaboration among clinicians, health care institutions, and public health programs involved in the diagnosis and treatment of HIV-infected patients with active TB disease is necessary in order to integrate care and improve medication adherence and TB treatment completion rates, reduce drug toxicities, and maximize HIV outcomes. HIV-infected patients with active TB disease should receive treatment support, including adherence counseling and DOT, corresponding to their needs (AII). ART simplification or use of coformulated fixed-dose combinations also may help to improve drug adherence.
Adverse Effects of Antiretroviral Agents (Last updated April 8, 2015; last reviewed April 8,
Adverse effects have been reported with the use of all antiretroviral (ARV) drugs and are among the most common reasons cited for switching or discontinuing therapy and for medication non-adherence. 1 Fortunately, newer ARV regimens are less toxic than regimens used in the past. Generally less than 10% of antiretroviral therapy (ART)-naive patients enrolled in randomized trials have treatment-limiting adverse events. However, because most clinical trials have a relatively short follow-up duration, the longer term complications of ART can be underestimated. In the Swiss Cohort study during a median of 6 years of follow-up, the presence of laboratory adverse events probably or certainly related to ART was associated with higher rates of mortality, which highlights the importance of monitoring for adverse events in overall patient management. 2 Several factors may predispose individuals to adverse effects of ARV medications. For example, compared with men, women (especially ART-naive women with CD4 T lymphocyte cell counts >250 cells/mm 3 ) seem to have a higher propensity to develop Stevens-Johnson syndrome, rashes, and hepatotoxicity from nevirapine (NVP) and have higher rates of lactic acidosis due to nucleoside reverse transcriptase inhibitors. Other factors may also contribute to the development of adverse events:
- Concomitant use of medications with overlapping and additive toxicities;
- Comorbid conditions that increase the risk of or exacerbate adverse effects (e.g., alcoholism 9 or coinfection with viral hepatitis increases the risk of hepatotoxicity);
- Drug-drug interactions that may lead to an increase in drug toxicities (e.g., interactions that result from concomitant use of statins with protease inhibitors); or
- Genetic factors that predispose patients to abacavir (ABC) hypersensitivity reaction. 13,14 The therapeutic goals of ART are to safely achieve and maintain viral suppression and improve immune function. To accomplish these goals, the clinician must consider the toxicity potential of an ARV regimen, as well as the individual patient's underlying conditions, concomitant medications, and prior history of drug intolerances. In addition, it should be appreciated that, in general, the overall benefits of ART outweigh its risks and that some non-AIDS related conditions (e.g., anemia, cardiovascular disease, renal impairment) may be more likely in the absence of ART. 15,16 Information on the adverse events of ARVs is outlined in several tables in the guidelines. Table 14 provides clinicians with a list of the most common and/or severe known ARV-associated adverse events for each drug class. The most common adverse effects of individual ARV agents are summarized in Appendix B, Tables 1-6. Although antiretroviral therapy (ART) is expensive (see Table 16 below), the cost-effectiveness of ART has been demonstrated in analyses of older 1 and newer regimens, 2,3 as well as for treatment-experienced patients with drug-resistant HIV. 4 Given the recommendations for immediate initiation of lifelong treatment and the increasing number of patients taking ART, the Panel now introduces cost-related issues pertaining to medication adherence and cost-containment strategies, as discussed below.
# Costs as They Relate to Adherence from a Patient Perspective
Cost sharing: Cost sharing is where the patient is responsible for some of the medication cost burden (usually accomplished via co-payments, co-insurance, or deductibles); these costs are often higher for branded medications than for generic medications. In one comprehensive review, increased patient cost sharing resulted in decreased medical adherence and more frequent drug discontinuation; for patients with chronic diseases, increased cost sharing was also associated with increased use of the medical system. 5 Conversely, co-payment reductions, such as those that might be used to incentivize prescribing of generic drugs, have been associated with improved adherence in patients with chronic diseases. 6 Whereas costsharing disproportionately affects low income patients, resources (e.g., the Ryan White AIDS Drug Assistance Program ) are available to assist eligible patients with co-pays and deductibles. Given the clear association between out-of-pocket costs for patients with chronic diseases and the ability of those patients to pay for and adhere to medications, clinicians should minimize patients' out-of-pocket drug-related expenses whenever possible.
Prior authorizations: As a cost-containment strategy, some programs require that clinicians obtain prior authorizations or permission before prescribing newer or more costly treatments rather than older or less expensive drugs. Although there are data demonstrating that prior authorizations do reduce spending, several studies have also shown that prior authorizations result in fewer prescriptions filled and increased nonadherence. Prior authorizations in HIV care specifically have been reported to cost over $40 each in provider personnel time (a hidden cost) and have substantially reduced timely access to medications. 10
Generic ART: The impact of the availability of generic antiretroviral (ARV) drugs on selection of ART in the United States is unknown. Because U.S. patent laws currently limit the co-formulation of some generic alternatives to branded drugs, generic options may result in increased pill burden. To the extent that pill burden, rather than drug frequency, results in reduced adherence, generic ART could lead to decreased costs but at the potential expense of worsening virologic suppression rates and poorer clinical outcomes. 11,12 Furthermore, prescribing the individual, less-expensive generic components of a branded co-formulated product rather than the branded product itself could, under some insurance plans, lead to higher copays-an out-of-pocket cost increase that may reduce medication adherence.
# Potential Cost Containment Strategies from a Societal Perspective
Given resource constraints, it is important to maximize the use of resources without sacrificing clinical outcomes. Evidence-based revisions to these guidelines recommend tailored laboratory monitoring for patients with long-term virologic suppression on ART as one possible way to provide overall cost savings. Data suggest that continued CD4 monitoring yields no clinical benefit for patients whose viral loads are suppressed and CD4 counts exceed 200 cells/mm 3 after 48 weeks of therapy. 13 A reduction in laboratory use from biannual to annual CD4 monitoring could save ~$10 million per year in the United States 14 (see the Laboratory Monitoring section). Although this is a small proportion of the overall costs associated with HIV care, such a strategy could reduce patients' personal expenses if they have deductibles for laboratory tests. The present and future availability of generic formulations of certain ARV drugs, despite the potential caveats of increased pill burden and reduced adherence, offers other money-saving possibilities on a much b Certain listed drugs are contraindicated on the basis of theoretical considerations. Thus, drugs with narrow therapeutic indices and suspected metabolic involvement with CYP450 3A, 2D6, or unknown pathways are included in this table. Actual interactions may or may not occur in patients.
c HCV agents listed include only those that are commercially available at the publication of these guidelines.
d HIV-infected patients who received rifapentine as part of a treatment regimen for TB had a higher rate of TB relapse and acquired rifamycin resistance than those treated with other rifamycin-based regimens. Therefore an alternative agent to rifapentine is recommended for TB treatment.
e Use of oral midazolam is contraindicated. Single-dose parenteral midazolam can be used with caution and can be given in a monitored situation for procedural sedation. f The manufacturer of cisapride has a limited-access protocol for patients who meet specific clinical eligibility criteria.
g A high rate of Grade 4 serum transaminase elevation was seen when a higher dose of RTV was added to LPV/r or SQV or when double-dose LPV/r was used with rifampin to compensate for rifampin's induction effect; therefore, these dosing strategies should not be used.
Suggested alternatives to:
- Lovastatin, simvastatin: Fluvastatin, pitavastatin, and pravastatin (except for pravastatin with DRV/r) have the least potential for drug-drug interactions (see Table 19a). Use atorvastatin and rosuvastatin with caution; start with the lowest possible dose and titrate based on tolerance and lipid-lowering efficacy.
- Rifampin: Rifabutin (with dosage adjustment, see Tables 19a and 19b This table provides known or predicted information regarding PK interactions between PIs and non-ARV drugs. When information is available, interactions for specific pharmacologically-boosted (with either RTV or COBI) and unboosted PIs are listed separately. The term "All PIs" refers to both unboosted and pharmacologically-boosted PI products. For interactions between ARV agents and for dosing recommendations, refer to Tables 19c, 20a, and 20b.
# H2 Receptor Antagonists
# ATV (unboosted)
↓ ATV H2 receptor antagonist single dose should not exceed a dose equivalent to famotidine 20 mg and the total daily dose should not exceed a dose equivalent to famotidine 20 mg BID in ART-naive patients.
Give ATV at least 2 hours before and at least 10 hours after the H2 receptor antagonist.
ATV/c, ATV/r ↓ ATV H2 receptor antagonist dose should not exceed a dose equivalent to famotidine 40 mg BID in ART-naive patients or 20 mg BID in ARTexperienced patients.
Give ATV 300 mg plus COBI 150 mg or RTV 100 mg simultaneously with and/or ≥10 hours after the dose of H2 receptor antagonist. - Start quetiapine at the lowest dose and titrate up as needed.
Monitor for quetiapine effectiveness and adverse effects.
Starting a PI in a patient receiving a stable dose of quetiapine:
- Reduce quetiapine dose to 1/6 of the original dose. Closely monitor for quetiapine effectiveness and adverse effects. For Treatment of Gout Flares:
- Colchicine 0.6 mg x 1 dose, followed by 0.3 mg 1 hour later. Do not repeat dose for at least 3 days.
With FPV without RTV:
- 1.2 mg x 1 dose and no repeat dose for at least 3 days For Prophylaxis of Gout Flares:
- Colchicine 0.3 mg once daily or every other day
With FPV without RTV:
- Colchicine 0.3 mg BID or 0.6 mg once daily or 0.3 mg once daily For Treatment of Familial Mediterranean Fever:
- Do not exceed colchicine 0.6 mg once daily or 0.3 mg BID.
With FPV without RTV:
- Do not exceed 1.2 mg once daily or 0.6 mg BID.
Do not coadminister in patients with hepatic or renal impairment.
# Salmeterol
All PIs ↑ salmeterol possible Do not coadminister because of potential increased risk of salmeterol-associated cardiovascular events.
a DHA is an active metabolite of artemether. a Approved dose for RPV is 25 mg once daily. Most PK interaction studies were performed using 75 to 150 mg per dose.
b Norbuprenorphine is an active metabolite of buprenorphine.
c R-methadone is the active form of methadone. The Panel has carefully reviewed recent results from clinical trials in HIV therapy and considered how they inform appropriate care guidelines. The Panel appreciates that HIV care is highly complex and rapidly evolving. Guidelines are never fixed and must always be individualized. Where possible, the Panel has based recommendations on the best evidence from prospective trials with defined endpoints. When such evidence does not yet exist, the Panel attempted to reflect reasonable options in its conclusions.
# Key to
HIV care requires, as always, partnerships and open communication. The provider can make recommendations most likely to lead to positive outcomes only if the patient's own point of view and social context are well known. Guidelines are only a starting point for medical decision making. They can identify some of the boundaries of high-quality care but cannot substitute for sound judgment.
As further research is conducted and reported, guidelines will be modified. The Panel anticipates continued progress in the simplicity of regimens, improved potency and barrier to resistance, and reduced toxicity. The Panel hopes the guidelines are useful and is committed to their continued adjustment and improvement. Ziagen:
- 300 mg tablet - 20 mg/mL oral solution Ziagen:
- 300 mg BID, or
- 600 mg once daily
- Take without regard to meals.
# Metabolized by alcohol dehydrogenase and glucuronyl transferase
Renal excretion of metabolites: 82% Dosage adjustment for ABC is recommended in patients with hepatic insufficiency (see Appendix B, Table 7).
1.5 hours/ 12-26 hours
- HSRs: Patients who test positive for HLA-B*5701 are at highest risk. HLA screening should be done before initiation of ABC.
- For patients with history of HSR, re-challenge is not recommended.
- Symptoms of HSR may include fever, rash, nausea, vomiting, diarrhea, abdominal pain, malaise, fatigue, or respiratory symptoms such as sore throat, cough, or shortness of breath.
- Some cohort studies suggest increased risk of MI with recent or current use of ABC, but this risk is not substantiated in other studies. - 125, 200, 250, and 400 mg capsules Videx:
- 10 mg/mL oral solution Body Weight ≥60 kg:
- 400 mg once daily With TDF:
- 250 mg once daily Body Weight <60 kg:
- 250 mg once daily With TDF:
- 200 mg once daily Take 1/2 hour before or 2 hours after a meal.
Note: Preferred dosing with oral solution is BID (total daily dose divided into 2 doses).
# Renal excretion: 50%
Dosage adjustment in patients with renal insufficiency is recommended (see Appendix B, Table 7). Epivir:
- 150 and 300 mg tablets
- 10 mg/mL oral solution Epivir:
- 150 mg BID, or
- 300 mg once daily
- Take without regard to meals.
# Renal excretion: 70%
Dosage adjustment in patients with renal insufficiency is recommended (see Appendix B, Table 7). - 300 mg once daily, or
- 7.5 level scoops once daily (dosing scoop dispensed with each prescription; one level scoop contains 1 g of oral powder).
- Take without regard to meals.
Mix oral powder with 2-4 ounces of a soft food that does not require chewing (e.g., applesauce, yogurt). Do not mix oral powder with liquid.
Renal excretion is primary route of elimination.
Dosage adjustment in patients with renal insufficiency is recommended (see Appendix B, Table 7). Retrovir:
- 100 mg capsule - 300 mg tablet (only available as generic)
- 10 mg/mL intravenous solution
- 10 mg/mL oral solution Retrovir:
- 300 mg BID, or
- 200 mg TID
- Take without regard to meals.
# Metabolized to GAZT
Renal excretion of GAZT Dosage adjustment in patients with renal insufficiency is recommended (see Appendix B, Table 7). - (ZDV 300 mg plus 3TC 150 mg plus ABC 300 mg) tablet
Trizivir:
- 1 tablet BID
- Take without regard to meals.
a For dosage adjustment in renal or hepatic insufficiency, see Appendix B, Table 7.
b Also see Table 14. Sustiva:
# Key to
- 50 and 200 mg capsules
- 600 mg tablet Sustiva:
- 600 mg once daily, at or before bedtime
- Take on an empty stomach to reduce side effects. - 1 tablet once daily
- Take with a meal.
a For dosage adjustment in renal or hepatic insufficiency, see Appendix B, Table 7.
b Also see Table 14.
c Rare cases of Stevens-Johnson syndrome have been reported with most NNRTIs; the highest incidence of rash was seen with NVP.
d Adverse events can include dizziness, somnolence, insomnia, abnormal dreams, depression, suicidality (suicide, suicide attempt or ideation), confusion, abnormal thinking, impaired concentration, amnesia, agitation, depersonalization, hallucinations, and euphoria. Approximately 50% of patients receiving EFV may experience any of these symptoms. Symptoms usually subside spontaneously after 2 to 4 weeks but may necessitate discontinuation of EFV in a small percentage of patients. 7.
# Key to
b Also see Table 14. a For dosage adjustment in hepatic insufficiency, see Appendix, Table 7.
b Also see Table 14. a For dosage adjustment in hepatic insufficiency, see Appendix, Table 7.
# Key to
b Also see Table 14. Child-Pugh Score 5-9:
# Key to
- 700 mg BID Child-Pugh Score 10-15:
- 350 mg BID PI-Naive or PI-Experienced Patients:
Child-Pugh Score 5-6:
- (700 mg BID plus RTV 100 mg) once daily
Child-Pugh Score 7-9:
- (450 mg BID plus RTV 100 mg) once daily
Child-Pugh Score 10-15:
- (300 mg BID plus RTV 100 mg) once daily - No dosage adjustment Moderate-to-severe hepatic impairment:
- Do not use.
# Ritonavir (RTV) Norvir
As a PI-Boosting Agent:
- 100-400 mg per day
No dosage adjustment necessary. Refer to recommendations for the primary PI.
# Saquinavir (SQV) Invirase
(SQV 1000 mg plus RTV 100 mg) PO BID No dosage adjustment necessary. Mild-to-Moderate Hepatic Impairment:
- Use with caution.
Severe Hepatic Impairment: a Refer to Appendix B, Tables 1 | Revisions to the May 1, 2014, version of the guidelines include key updates to several existing sections and the addition of two new tables. Significant updates are highlighted throughout the document.#
• There are now five Recommended regimens for antiretroviral therapy (ART)-naive patients-four integrase strand transfer inhibitor (INSTI)-based regimens and one ritonavir-boosted protease inhibitor (PI/r)-based regimen, as listed below:
# INSTI-Based Regimens:
• Dolutegravir/abacavir/lamivudine (DTG/ABC/3TC)-only for patients who are HLA-B*5701 negative (AI)
• DTG plus tenofovir disoproxil fumarate/emtricitabine (TDF/FTC) (AI)
• Elvitegravir/cobicistat/TDF/FTC (EVG/c/TDF/FTC)-only for patients with pre-ART CrCl >70 mL/min (AI)
• Raltegravir (RAL) plus TDF/FTC (AI) PI/r-Based Regimen:
• Darunavir/ritonavir (DRV/r) plus TDF/FTC (AI)
• Two regimens previously classified as Recommended regimens have been moved to the Alternative regimens category, with the rationale stated below:
• Atazanavir/ritonavir (ATV/r) plus TDF/FTC (BI)-Based on the results of a large comparative clinical trial showing a greater rate of discontinuation with ATV/r plus TDF/FTC because of toxicities when compared to (DRV/r or RAL) plus TDF/FTC
• Efavirenz/TDF/FTC (EFV/TDF/FTC) (BI)-Based on concerns about the tolerability of EFV in clinical trials and practice, especially the high rate of central nervous system (CNS)-related toxicities and a possible association with suicidality
• Three regimens (ATV/r plus ABC/3TC, EFV plus ABC/3TC, and rilpivirine/TDF/FTC) that were previously listed as Recommended regimens for baseline HIV RNA <100,000 copies/mL or CD4 T lymphocyte (CD4) count >200 cells/mm 3 are now in the Alternative or Other category, with the same caveat about limiting their use in these populations.
• Two regimens that use fewer than two nucleoside reverse transcriptase inhibitors (DRV/r plus RAL and lopinavir/ritonavir plus 3TC) are now listed among the Other regimens, with the caveat that their use would be limited to those patients who cannot take either TDF or ABC.
• Coformulations of atazanavir (ATV) and darunavir (DRV) with the pharmacokinetic (PK) enhancer cobicistat (COBI) have been added to the Alternative regimen options.
# Virologic Failure
The following key updates have been made to this section:
• The Management of Virologic Failure in Different Clinical Scenarios subsection has been expanded to provide guidance on the management of patients failing first and second ART regimens.
• A new subsection on Isolated CNS Virologic Failure and New Onset Neurologic Symptoms has been added.
• The Suboptimal Immunologic Response Despite Viral Suppression subsection has been moved from this section to become a stand-alone section (see below). Antiretroviral therapy (ART) for the treatment of HIV infection has improved steadily since the advent of potent combination therapy in 1996. New drugs that offer new mechanisms of action, improvements in potency and activity even against multidrug-resistant viruses, dosing convenience, and tolerability have been approved. ART has dramatically reduced HIV-associated morbidity and mortality and has transformed HIV disease into a chronic, manageable condition. In addition, effective treatment of HIV-infected individuals with ART is highly effective at preventing transmission to sexual partners. 1 However, less than one-third of HIV-infected individuals in the United States have suppressed viral loads, 2 which is mostly a result of undiagnosed HIV infection and failure to link or retain diagnosed patients in care. Despite remarkable improvements in HIV treatment and prevention, economic and social barriers that result in continued morbidity, mortality, and new HIV infections persist.
# Table of Contents
# Management of the
# List of Tables
The Department of Health and Human Services (HHS) Panel on Antiretroviral Guidelines for Adults and Adolescents (the Panel) is a working group of the Office of AIDS Research Advisory Council (OARAC). The primary goal of the Panel is to provide HIV care practitioners with recommendations based on current knowledge of antiretroviral (ARV) drugs used to treat adults and adolescents with HIV infection in the United States. The Panel reviews new evidence and updates recommendations in these guidelines when needed. The Panel's primary areas of attention have included baseline assessment, treatment goals, indications for initiation of ART, choice of the initial regimen for ART-naive patients, drugs or combinations to avoid, management of adverse effects and drug interactions, management of treatment failure, and special ART-related considerations in specific patient populations. For recommendations related to pre-exposure HIV prophylaxis (PrEP) for HIV-uninfected persons, please refer to recommendations from the Centers for Disease Control and Prevention (CDC). 3,4 These guidelines generally represent the state of knowledge regarding the use of ARV agents. However, because the science of HIV evolves rapidly, the availability of new agents and new clinical data may change therapeutic options and preferences. Information included in these guidelines may not be consistent with approved labeling for the particular products or indications in question, and the use of the terms "safe" and "effective" may not be synonymous with the Food and Drug Administration (FDA)-defined legal standards for product approval. The Panel frequently updates the guidelines (current and archived versions of the guidelines are available on the AIDSinfo website at http://www.aidsinfo.nih.gov). However, the guidelines cannot always be updated apace with the rapid evolution of new data in the field of HIV and cannot offer guidance on care for all patients. Clinicians should exercise clinical judgment in management decisions tailored to unique patient circumstances.
The Panel recognizes the importance of clinical research in generating evidence to address unanswered questions related to the optimal safety and efficacy of ART. The Panel encourages both the development of protocols and patient participation in well-designed, Institutional Review Board (IRB)-approved clinical trials.
# Basis for Recommendations
Recommendations in these guidelines are based upon scientific evidence and expert opinion. Each recommended statement includes a letter (A, B, or C) that represents the strength of the recommendation and with a Roman numeral (I, II, or III) that represents the quality of the evidence that supports the recommendation (see Table 2).
# Table 2. Rating Scheme for Recommendations
# HIV Expertise in Clinical Care
Many studies have demonstrated that outcomes achieved in HIV-infected outpatients are better when care is delivered by a clinician with HIV expertise, [5][6][7][8][9][10] which reflects the complexity of HIV infection and its treatment. Thus, appropriate training and experience, as well as ongoing continuing education, are important components of optimal care. Primary care providers without HIV experience, such as those who provide service in rural or underserved areas, should identify experts in their regions who will be available for consultation when needed.
Baseline Evaluation (Last updated May 1, 2014; last reviewed May 1, 2014)
Every HIV-infected patient entering into care should have a complete medical history, physical examination, and laboratory evaluation and should be counseled regarding the implications of HIV infection. The goals of the initial evaluation are to confirm the diagnosis of HIV infection, obtain appropriate baseline historical and laboratory data, ensure patient understanding about HIV infection and its transmission, and to initiate care as recommended in HIV primary care guidelines 1 and guidelines for prevention and treatment of HIV-associated opportunistic infections. 2 The initial evaluation also should include introductory discussion on the benefits of antiretroviral therapy (ART) for the patient's health and to prevent HIV transmission. Baseline information then can be used to define management goals and plans. In the case of previously treated patients who present for an initial evaluation with a new health care provider, it is critical to obtain a complete antiretroviral (ARV) history (including drug-resistance testing results, if available), preferably through the review of past medical records. Newly diagnosed patients should also be asked about any prior use of ARV agents for prevention of HIV infection.
The following laboratory tests performed during initial patient visits can be used to stage HIV disease and to assist in the selection of ARV drug regimens:
• HIV antibody testing (if prior documentation is not available or if HIV RNA is below the assay's limit of detection) (AI);
• CD4 T-cell count (CD4 count) (AI);
• Plasma HIV RNA (viral load) (AI);
• Complete blood count, chemistry profile, transaminase levels, blood urea nitrogen (BUN), and creatinine, urinalysis, and serologies for hepatitis A, B, and C viruses (AIII);
• Fasting blood glucose and serum lipids (AIII); and
• Genotypic resistance testing at entry into care, regardless of whether ART will be initiated immediately (AII). For patients who have HIV RNA levels <500 to 1,000 copies/mL, viral amplification for resistance testing may not always be successful (BII).
In addition, other tests (including screening tests for sexually transmitted infections and tests for determining the risk of opportunistic infections and need for prophylaxis) should be performed as recommended in HIV primary care and opportunistic infections guidelines. 1,2 Patients living with HIV infection often must cope with many social, psychiatric, and medical issues that are best addressed through a patient-centered, multi-disciplinary approach to the disease. The baseline evaluation should include an evaluation of the patient's readiness for ART, including an assessment of high-risk behaviors, substance abuse, social support, mental illness, comorbidities, economic factors (e.g., unstable housing), medical insurance status and adequacy of coverage, and other factors that are known to impair adherence to ART and increase the risk of HIV transmission. Once evaluated, these factors should be managed accordingly.
The baseline evaluation should also include a discussion of risk reduction and disclosure to sexual and/or needle sharing partners, especially with untreated patients who are still at high risk of HIV transmission. √ HIV RNA (viral load) and CD4 T lymphocyte (CD4) cell count are the two surrogate markers of antiretroviral treatment (ART) responses and HIV disease progression that have been used for decades to manage and monitor HIV infection.
During
Viral load is a marker of response to ART. A patient's pre-ART viral load level and the magnitude of viral load decline after initiation of ART provide prognostic information about the probability of disease progression. 1 The key goal of ART is to achieve and maintain durable viral suppression. Thus, the most important use of the viral load is to monitor the effectiveness of therapy after initiation of ART.
Measurement of CD4 count is particularly useful before initiation of ART. The CD4 cell count provides information on the overall immune function of an HIV-infected patient. The measurement is critical in establishing thresholds for the initiation and discontinuation of opportunistic infection (OI) prophylaxis and in assessing the urgency to initiate ART.
The management of HIV-infected patients has changed substantially with the availability of newer, more potent, and less toxic antiretroviral (ARV) agents. In the United States, ART is now recommended for all HIV-infected patients regardless of their viral load or CD4 count. In the past, clinical practice, which was supported by treatment guidelines, was generally to monitor both CD4 cell count and viral load concurrently. However, because most HIV-infected patients in care now receive ART, the rationale for frequent CD4 monitoring is weaker. The roles and usefulness of these two tests in clinical practice are discussed in the following sections.
# Plasma HIV-1 RNA (Viral Load) Monitoring
Viral load is the most important indicator of initial and sustained response to ART (AI) and should be measured in all HIV-infected patients at entry into care (AIII), at initiation of therapy (AIII), and on a regular basis thereafter. For those patients who choose to delay therapy, repeat viral load testing while not on ART is optional (CIII). Pre-treatment viral load level is also an important factor in the selection of an initial ARV regimen because several currently approved ARV drugs or regimens have been associated with poorer responses in patients with high baseline viral load (see What to Start). Commercially available HIV-1 RNA assays do not detect HIV-2 viral load. For further discussion on HIV-2 RNA monitoring in patients with HIV-1/HIV-2 co-infection or HIV-2 mono-infection, see HIV-2 Infection.
Several systematic reviews of data from clinical trials involving thousands of participants have established that decreases in viral load following initiation of ART are associated with reduced risk of progression to AIDS or death. [1][2][3] Thus, viral load testing is an established surrogate marker for treatment response. 4 The minimal change in viral load considered to be statistically significant (2 standard deviations) is a three-fold change (equivalent to a 0.5 log 10 copies/mL change). Optimal viral suppression is defined generally as a viral load persistently below the level of detection (HIV RNA <20 to 75 copies/mL, depending on the assay used). However, isolated blips (viral loads transiently detectable at low levels, typically HIV RNA <400 copies/mL) are not uncommon in successfully treated patients and are not predictive of virologic failure. 5 Furthermore, the data on the association between persistently low level but quantifiable viremia (HIV RNA <200 copies/mL) and virologic failure is conflicting. One recent study showed an increased risk of subsequent failure at this level of viremia; however, the association was not observed in other studies. [6][7][8][9] These guidelines and the AIDS Clinical Trials Group (ACTG) now define virologic failure as a confirmed viral load >200 copies/mL-a threshold that eliminates most cases of apparent viremia caused by viral load blips or assay variability 10 (see Virologic Failure and Suboptimal Immunologic Response).
Individuals who are adherent to their ARV regimens and do not harbor resistance mutations to the component drugs can generally achieve viral suppression 8 to 24 weeks after ART initiation; rarely, in some patients it Downloaded from http://aidsinfo.nih.gov/guidelines on 9/16/2015
Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents C-6 may take longer. Recommendations on the frequency of viral load monitoring are summarized below:
• After initiation of ART or modification of therapy because of virologic failure. Plasma viral load should be measured before initiation of ART and within 2 to 4 weeks but no later than 8 weeks after treatment initiation or modification (AIII). The purpose of the measurements is to confirm an adequate initial virologic response to ART, indicating appropriate regimen selection and patient adherence to therapy. Repeat viral load measurement should be performed at 4-to 8-week intervals until the level falls below the assay's limit of detection (BIII).
• In virologically suppressed patients in whom ART was modified because of drug toxicity or for regimen simplification. Viral load measurement should be performed within 4 to 8 weeks after changing therapy (AIII). The purpose of viral load monitoring at this point is to confirm the effectiveness of the new regimen.
• In patients on a stable, suppressive ARV regimen. Viral load should be repeated every 3 to 4 months (AIII) or as clinically indicated to confirm continuous viral suppression. Clinicians may extend the interval to 6 months for adherent patients whose viral load has been suppressed for more than 2 years and whose clinical and immunologic status is stable (AIII).
• In patients with suboptimal response. The frequency of viral load monitoring will depend on clinical circumstances, such as adherence and availability of further treatment options. In addition to viral load monitoring, a number of additional factors, such as patient adherence to prescribed medications, suboptimal drug exposure, or drug interactions, should be assessed. Patients who fail to achieve viral suppression should undergo resistance testing to aid in the selection of an alternative regimen (see Drug-Resistance Testing and Virologic Failure and Suboptimal Immunologic Response sections).
# CD4 Count Monitoring
The CD4 count is the most important laboratory indicator of immune function in HIV-infected patients. It is also the strongest predictor of subsequent disease progression and survival according to findings from clinical trials and cohort studies. 11,12 CD4 counts are highly variable; a significant change (2 standard deviations) between 2 tests is approximately a 30% change in the absolute count, or an increase or decrease in CD4 percentage by 3 percentage points. Monitoring of lymphocyte subsets other than CD4 (e.g., CD8, CD19) has not proven clinically useful, is more expensive, and is not routinely recommended (BIII).
# Use of CD4 Count for Initial Assessment
CD4 count should be measured in all patients at entry into care (AI). It is the key factor in determining the need to initiate OI prophylaxis (see the Adult Opportunistic Infection Guidelines) 13 and the urgency to initiate ART (AI) (see the Initiating Antiretroviral Therapy in Antiretroviral-Naive Patients section of these guidelines). Although most OIs occur in patients with CD4 counts <200 cells/mm 3 , some OIs can occur in patients with higher CD4 counts. 14
# Use of CD4 Count for Monitoring Therapeutic Response
The CD4 count is used to assess a patient's immunologic response to ART. It is also used to determine whether prophylaxis for OIs can be discontinued (see the Adult Opportunistic Infection Guidelines) 13 . For most patients on therapy, an adequate response is defined as an increase in CD4 count in the range of 50 to 150 cells/mm 3 during the first year of ART, generally with an accelerated response in the first 3 months of treatment. Subsequent increases average approximately 50 to 100 cells/mm 3 per year until a steady state level is reached. 15 Patients who initiate therapy with a low CD4 count 16 or at an older age 17 may have a blunted increase in their counts despite virologic suppression.
The CD4 count response to ART varies widely, but a poor CD4 response in a patient with viral suppression is rarely an indication for modifying an ARV regimen. In patients with consistently suppressed viral loads who have already experienced ART-related immune reconstitution, the CD4 count provides limited information.
Frequent testing is unnecessary because the results rarely lead to a change in clinical management. One retrospective study found that declines in CD4 count to <200 cells/mm 3 are rare in patients with viral suppression and CD4 counts >300 cells/mm 3 . 18 Similarly, the ARTEMIS trial found that CD4 monitoring had no clinical benefit in patients who had suppressed viral loads and CD4 counts >200 cells/mm 3 after 48 weeks of therapy. 19 Furthermore, the risk of Pneumocystis jirovecii pneumonia is extremely low in patients on suppressive ART who have CD4 counts between 100 and 200 cells/mm 3 . 20 Although uncommon, CD4 count declines can occur in a small percentage of virologically suppressed patients and may be associated with adverse clinical outcomes such as cardiovascular disease, malignancy, and death. 21 An analysis of costs associated with CD4 monitoring in the United States estimated that reducing CD4 monitoring in treated patients from every 6 months to every 12 months could result in annual savings of approximately $10 million. 22 For the patient on a suppressive regimen whose CD4 count has consistently ranged between 300 and 500 cells/ mm 3 for at least 2 years, the Panel recommends CD4 monitoring on an annual basis (BII). Continued CD4 monitoring for virologically suppressed patients whose CD4 counts have been consistently >500 cells/mm 3 for at least 2 years may be considered optional (CIII). The CD4 count should be monitored more frequently, as clinically indicated, when there are changes in a patient's clinical status that may decrease CD4 count and thus prompt OI prophylaxis. Examples of such changes include the appearance of new HIV-associated clinical symptoms or initiation of treatment known to reduce CD4 cell count (e.g., interferon, chronic corticosteroids, or anti-neoplastic agents) (AIII). In patients who fail to maintain viral suppression while on ART, the Panel recommends CD4 count monitoring every 3 to 6 months (AIII) (see Virologic Failure and Suboptimal Immunologic Response section).
# Factors that Affect Absolute CD4 Count
The absolute CD4 count is a calculated value based on the total white blood cell (WBC) count and the percentages of total and CD4+ T lymphocytes. This absolute number may fluctuate in individuals or may be influenced by factors that may affect the total WBC count and lymphocyte percentages, such as use of bone marrow-suppressive medications or the presence of acute infections. Splenectomy 23,24 or co-infection with human T-lymphotropic virus type I (HTLV-1) 25 may cause misleadingly elevated CD4 counts. Alpha-interferon may reduce the absolute CD4 count without changing the CD4 percentage. 26 In all these settings, CD4 percentage remains stable and may be a more appropriate parameter to assess a patient's immune function.
# Clinical Scenario Viral Load Monitoring CD4 Count Monitoring
Before initiating ART At entry into care (AIII)
If ART initiation is deferred, repeat before initiating ART (AIII).
In patients not initiating ART, repeat testing is optional (CIII).
# At entry into care (AI)
If ART is deferred, every 3 to 6 months (AIII).
b
After initiating ART Preferably within 2 to 4 weeks (and no later than 8 weeks) after initiation of ART (AIII); thereafter, every 4 to 8 weeks until viral load suppressed (BIII).
# months after initiation of ART (AIII)
After modifying ART because of drug toxicities or for regimen simplification in a patient with viral suppression 4 to 8 weeks after modification of ART to confirm effectiveness of new regimen (AIII).
Monitor according to prior CD4 count and duration on ART, as outlined below.
After modifying ART because of virologic failure
Preferably within 2 to 4 weeks (and no later than 8 weeks) after modification (AIII); thereafter, every 4 to 8 weeks until viral load suppressed (BIII). If viral suppression is not possible, repeat viral load every 3 months or more frequently if indicated (AIII).
# Every 3 to 6 months (AI)
During the first 2 years of ART Every 3 to 4 months (AIII) Every 3 to 6 months a (BII)
After 2 years of ART (VL consistently suppressed, CD4 consistently 300-500 cells/mm 3 ) Can extend to every 6 months for patients with consistent viral suppression for ≥2 years (AIII).
# Every 12 months (BII)
After 2 years of ART (VL consistently suppressed, CD4 consistently >500 cells/ mm 3 )
Optional (CIII)
While on ART with detectable viremia (VL repeatedly >200 copies/mL) a Monitoring of lymphocyte subsets other than CD4 (e.g., CD8, CD19) has not proven clinically useful, adds to costs, and is not routinely recommended (BIII).
Every
b Some experts may repeat CD4 count every 3 months in patients with low baseline CD4 count (<200-300 cells/mm 3 ) before ART but every 6 months in those who initiated ART at higher CD4 cell count (e.g., >300 cells/mm 3 ). c The following are examples of clinically indicated scenarios: changes in a patient's clinical status that may decrease CD4 count and thus prompt initiation of prophylaxis for opportunistic infections (OI), such as new HIV-associated symptoms, or initiation of treatment with medications which are known to reduce CD4 cell count.
Drug-Resistance Testing (Last updated May 1, 2014; last reviewed May 1, 2014)
# Genotypic and Phenotypic Resistance Assays
Genotypic and phenotypic resistance assays are used to assess viral strains and inform selection of treatment strategies. Standard assays provide information on resistance to nucleoside reverse transcriptase inhibitors (NRTIs), non-nucleoside reverse transcriptase inhibitors (NNRTIs), and protease inhibitors (PIs). Testing for integrase and fusion inhibitor resistance can also be ordered separately from several commercial laboratories.
Co-receptor tropism assays should be performed whenever the use of a CCR5 antagonist is being considered. Phenotypic co-receptor tropism assays have been used in clinical practice. A genotypic assay to predict coreceptor use is now commercially available (see Co-receptor Tropism Assays).
# Genotypic Assays
Genotypic assays detect drug-resistance mutations present in relevant viral genes. Most genotypic assays involve sequencing of the RT and PR genes to detect mutations that are known to confer drug resistance. Genotypic assays that assess mutations in the integrase and gp41 (envelope) genes are also commercially available. Genotypic assays can be performed rapidly and results are available within 1 to 2 weeks of sample collection. Interpretation of test results requires knowledge of the mutations selected by different antiretroviral (ARV) drugs and of the potential for cross resistance to other drugs conferred by certain mutations. The International AIDS Society-USA (IAS-USA) maintains an updated list of significant resistance-associated mutations in the RT, PR, integrase, and envelope genes (see
# Panel's Recommendations
• HIV drug-resistance testing is recommended in persons with HIV infection at entry into care regardless of whether antiretroviral therapy (ART) will be initiated immediately or deferred (AII). If therapy is deferred, repeat testing should be considered at the time of ART initiation (CIII).
• Genotypic testing is recommended as the preferred resistance testing to guide therapy in antiretroviral (ARV)-naive patients (AIII).
• Standard genotypic drug-resistance testing in ARV-naive persons involves testing for mutations in the reverse transcriptase (RT) and protease (PR) genes. If transmitted integrase strand transfer inhibitor (INSTI) resistance is a concern, providers may wish to supplement standard genotypic resistance testing with an INSTI genotype test (CIII).
• HIV drug-resistance testing should be performed to assist in the selection of active drugs when changing ARV regimens in persons with virologic failure and HIV RNA levels >1,000 copies/mL (AI). In persons with HIV RNA levels >500 but <1,000 copies/mL, testing may be unsuccessful but should still be considered (BII).
• Drug-resistance testing should also be performed when managing suboptimal viral load reduction (AII).
• In persons failing INSTI-based regimens, genotypic testing for INSTI resistance should be performed to determine whether to include a drug from this class in subsequent regimens (AII).
• Drug-resistance testing in the setting of virologic failure should be performed while the person is taking prescribed ARV drugs or, if not possible, within 4 weeks after discontinuing therapy (AII). If greater than 4 weeks has lapsed since the ARVs were discontinued, resistance testing may still provide useful information to guide therapy, recognizing that previously selected resistance mutations can be missed (CIII).
• Genotypic testing is recommended as the preferred resistance testing to guide therapy in patients with suboptimal virologic responses or virologic failure while on first or second regimens (AII).
• The addition of phenotypic to genotypic testing is generally preferred for persons with known or suspected complex drug-resistance mutation patterns, particularly to protease inhibitors (PIs) (BIII).
• Genotypic resistance testing is recommended for all pregnant women before initiation of ART (AIII) and for those entering pregnancy with detectable HIV RNA levels while on therapy (AI) (see the Perinatal Treatment Guidelines for more detailed discussion). http://www.iasusa.org/resistance_mutations). 1 The Stanford University HIV Drug Resistance Database (http://hivdb.stanford.edu) also provides helpful guidance for interpreting genotypic resistance test results. Various tools to assist the provider in interpreting genotypic test results are now available. [2][3][4][5] Clinical trials have demonstrated that consultation with specialists in HIV drug resistance improves virologic outcomes. 6 Clinicians are thus encouraged to consult a specialist to facilitate interpretation of genotypic test results and design of an optimal new regimen.
# Rating of Recommendations
# Phenotypic Assays
Phenotypic assays measure the ability of a virus to grow in different concentrations of ARV drugs. RT and PR gene sequences and, more recently, integrase and envelope sequences derived from patient plasma HIV RNA are inserted into the backbone of a laboratory clone of HIV or used to generate pseudotyped viruses that express the patient-derived HIV genes of interest. Replication of these viruses at different drug concentrations is monitored by expression of a reporter gene and is compared with replication of a reference HIV strain. The drug concentration that inhibits viral replication by 50% (i.e., the median inhibitory concentration [IC 50 ]) is calculated, and the ratio of the IC 50 of test and reference viruses is reported as the fold increase in IC 50 (i.e., fold resistance).
Automated phenotypic assays that can produce results in 2 to 3 weeks are commercially available, but they cost more to perform than genotypic assays. In addition, interpretation of phenotypic assay results is complicated by incomplete information regarding the specific resistance level (i.e., fold increase in IC 50 ) that is associated with drug failure, although clinically significant fold increase cutoffs are now available for some drugs. [7][8][9][10][11] Again, consultation with a specialist to interpret test results can be helpful.
Further limitations of both genotypic and phenotypic assays include lack of uniform quality assurance testing for all available assays, relatively high cost, and insensitivity to minor viral species. Despite being present, drug-resistant viruses that constitute less than 10% to 20% of the circulating virus population will probably not be detected by commercially available assays. This limitation is important because after drugs exerting selective pressure on drug-resistant populations are discontinued, a wild-type virus often re-emerges as the predominant population in the plasma. As a consequence, the proportion of virus with resistance mutations decreases to below the 10% to 20% threshold. [12][13][14] In the case of some drugs, this reversion to predominantly wild-type virus can occur in the first 4 to 6 weeks after the drugs are discontinued. Prospective clinical studies have shown that despite this plasma reversion, re-initiation of the same ARV agents (or those sharing similar resistance pathways) is usually associated with early drug failure, and that the virus present at failure is derived from previously archived resistant virus. 15 Therefore, resistance testing is of greatest value when performed before or within 4 weeks after drugs are discontinued (AII). Because resistant virus may persist in the plasma of some patients for longer periods of time, resistance testing done 4 to 6 weeks after discontinuation of drugs may still detect mutations. However, the absence of detectable resistance in such patients must be interpreted with caution when designing subsequent ARV regimens.
# Use of Resistance Assays in Clinical Practice (See Table 5)
# Use of Resistance Assays in Determining Initial Treatment
Transmission of drug-resistant HIV strains is well documented and associated with suboptimal virologic response to initial antiretroviral therapy (ART). [16][17][18][19] The likelihood that a patient will acquire drug-resistant virus is related to the prevalence of drug resistance in HIV-infected persons engaging in high-risk behaviors in the community. In the United States and Europe, recent studies suggest that the risk that transmitted virus will be resistant to at least one ARV drug is in the range of 6% to 16%. [20][21][22][23][24][25] Up to 8%, but generally less than 5% of transmitted viruses will exhibit resistance to drugs from more than one class. 24,[26][27][28] If the decision is made to initiate therapy in a person with early HIV infection, resistance testing at baseline can guide regimen selection to optimize virologic response. Therefore, resistance testing in this situation is recommended (AII). A genotypic assay is preferred for this purpose (AIII). In this setting, treatment initiation should not be delayed pending resistance testing results. Once results are obtained, the treatment regimen can be modified if warranted (see Acute and Recent HIV Infection). In the absence of therapy, resistant viruses may decline over time to less than the detection limit of standard resistance tests, but when therapy is eventually initiated, resistant viruses even at a low level may still increase the risk of treatment failure. [29][30][31] Therefore, if therapy is deferred, resistance testing should still be done during acute HIV infection (AIII). In this situation, the genotypic resistance test result may be kept on record until the patient is to be started on ART. Repeat resistance testing at the time treatment is started should be considered because it is possible for a patient to acquire drug-resistant virus (i.e., superinfection) between entry into care and initiation of ART (CIII).
Performing drug-resistance testing before ART initiation in patients with chronic HIV infection is less straightforward. The rate at which transmitted resistance-associated mutations revert to wild-type virus has not been completely delineated, but mutations present at the time of HIV transmission are more stable than those selected under drug pressure. It is often possible to detect resistance-associated mutations in viruses that were transmitted several years earlier. [32][33][34] No prospective trial has addressed whether drug-resistance testing before initiation of therapy confers benefit in this population. However, data from several, but not all, studies suggest that virologic responses in persons with baseline resistance mutations are suboptimal. [16][17][18][19][35][36][37] In addition, a cost-effectiveness analysis of early genotypic resistance testing suggests that baseline testing in this population should be performed. 38 Therefore, resistance testing in chronically infected persons is recommended at the time of entry into HIV care (AII). Although no definitive prospective data exist to support the choice of one type of resistance testing over another, genotypic testing is generally preferred in this situation because of lower cost, more rapid turnaround time, the assay's ability to detect mixtures of wild-type and resistant virus, and the relative ease of interpreting test results (AIII). If therapy is deferred, repeat testing soon before initiation of ART should be considered because the patient may have acquired drug-resistant virus (i.e., superinfection) (CIII).
Standard genotypic drug-resistance testing in ARV-naive persons involves testing for mutations in the RT and PR genes. Although transmission of integrase strand transfer inhibitor (INSTI)-resistant virus has rarely been reported, as use of INSTIs increases, the potential for transmission of INSTI-resistant virus may also increase. Therefore, when INSTI resistance is suspected, providers may wish to supplement standard baseline genotypic resistance testing with genotypic testing for resistance to this class of drugs (CIII).
# Use of Resistance Assays in the Event of Virologic Failure
Resistance assays are useful in guiding treatment decisions for patients who experience virologic failure while on ART. Several prospective studies assessed the utility of resistance testing to guide ARV drug selection in patients with virologic failure. These studies involved genotypic assays, phenotypic assays, or both. 6,[39][40][41][42][43][44][45] In general, these studies found that changes in therapy that were informed by resistance testing results produced better early virologic response to salvage regimens than regimen changes guided only by clinical judgment.
In addition, one observational cohort study found that performance of genotypic drug-resistance testing in ART-experienced patients with detectable plasma HIV RNA was independently associated with improved survival. 46 Thus, resistance testing is recommended as a tool in selecting active drugs when changing ARV regimens because of virologic failure in persons with HIV RNA >1,000 copies/mL (AI) (see Virologic Failure and Suboptimal Immunologic Response). In persons with HIV RNA >500 copies/mL but <1,000 copies/mL, testing may be unsuccessful but should still be considered (BII). Drug-resistance testing in persons with a plasma viral load <500 copies/mL is not usually recommended because resistance assays cannot be consistently performed given low HIV RNA levels (AIII).
Resistance testing also can help guide treatment decisions for patients with suboptimal viral load reduction (AII). Virologic failure in the setting of combination ART is, for certain patients, associated with resistance to only one component of the regimen. [47][48][49] In this situation, substituting individual drugs in a failing regimen may be a possible option, but this concept will require clinical validation (see Virologic Failure and Suboptimal Immunologic Response).
In patients who are on a failing first or second ARV drug regimen and experiencing virologic failure or suboptimal viral load reduction, genotypic testing is generally preferred for resistance testing (AII). This is based on the fact that, when compared with phenotypic testing, genotypic testing costs less to perform, has a faster turnaround time, and greater sensitivity for detecting mixtures of wild-type and resistant virus. In addition, observations show that the assays are comparable predictors of virologic response to subsequent ART regimens. 50 Addition of phenotypic to genotypic testing is generally preferred for persons with known or suspected complex drug-resistance mutation patterns, particularly to PIs (BIII).
In patients failing INSTI-based regimens, testing for INSTI resistance should be performed to determine whether to include drugs from this class in subsequent regimens (AII); genotypic testing is preferred for this purpose.
When the use of a CCR5 antagonist is being considered, a co-receptor tropism assay should be performed (AI). Phenotypic co-receptor tropism assays have been used in clinical practice. A genotypic assay to predict co-receptor use is now commercially available and is less expensive than phenotypic assays. Evaluation of genotypic assays is ongoing, but current data suggest that such testing should be considered as an alternative assay. The same principles regarding testing for co-receptor use also apply to testing when patients exhibit virologic failure on a CCR5 antagonist. 51 Resistance to CCR5 antagonists in the absence of detectable CXCR4-using virus has been reported, but such resistance is uncommon (see Co-receptor Tropism Assays).
# Use of Resistance Assays in Pregnant Women
In pregnant women, the goal of ART is to maximally reduce plasma HIV RNA to provide optimal maternal therapy and to prevent perinatal transmission of HIV. Genotypic resistance testing is recommended for all pregnant women before initiation of therapy (AIII) and for those entering pregnancy with detectable HIV RNA levels while on therapy (AI). Phenotypic testing in those found to have complex drug-resistance mutation patterns, particularly to PIs, may provide additional information (BIII). Optimal prevention of perinatal transmission may require initiation of ART pending resistance testing results. Once the results are available, the ARV regimen can be changed as needed.
# Clinical Setting/Recommendation Rationale
# Drug-resistance assay recommended
In acute HIV infection: Drug-resistance testing is recommended regardless of whether antiretroviral therapy (ART) is initiated immediately or deferred (AII). A genotypic assay is generally preferred (AIII).
If ART is initiated immediately, drug-resistance testing can determine whether drug-resistant virus was transmitted. Test results will help in the design of initial regimens or to modify or change regimens if results are obtained after treatment initiation.
Genotypic testing is preferred to phenotypic testing because of lower cost, faster turnaround time, and greater sensitivity for detecting mixtures of wild-type and resistant virus.
If ART is deferred, repeat resistance testing should be considered at the time therapy is initiated (CIII). A genotypic assay generally is preferred (AIII).
If ART is deferred, testing should still be performed because of the greater likelihood that transmitted resistance-associated mutations will be detected earlier in the course of HIV infection.
Results of resistance testing may be important when treatment is initiated. Repeat testing at the time ART is initiated should be considered because the patient may have acquired a drugresistant virus (i.e., superinfection).
In ART-naive patients with chronic HIV infection: Drug-resistance testing is recommended at entry into HIV care, regardless of whether therapy is initiated immediately or deferred (AII). A genotypic assay is generally preferred (AIII).
If therapy is deferred, repeat resistance testing should be considered before initiation of ART (CIII). A genotypic assay is generally preferred (AIII).
If an INSTI is considered for an ART-naive patient and transmitted INSTI resistance is a concern, providers may supplement standard resistance testing with a specific INSTI genotypic resistance assay (CIII).
If use of a CCR5 antagonist is being considered, a co-receptor tropism assay should be performed (AI) (see Co-receptor Tropism Assays)
Transmitted HIV with baseline resistance to at least 1 drug is seen in 6% to 16% of patients, and suboptimal virologic responses may be seen in patients with baseline resistant mutations. Some drug-resistance mutations can remain detectable for years in untreated, chronically infected patients.
Repeat testing before initiation of ART should be considered because the patient may have acquired a drug-resistant virus (i.e., a superinfection).
Genotypic testing is preferred to phenotypic testing because of lower cost, faster turnaround time, and greater sensitivity for detecting mixtures of wild-type and resistant virus.
Standard genotypic drug-resistance assays test only for mutations in the RT and PR genes.
(see Co-receptor Tropism Assays)
In patients with virologic failure: Drug-resistance testing is recommended in patients on combination ART with HIV RNA levels >1,000 copies/mL (AI). In patients with HIV RNA levels >500 copies/mL but <1,000 copies/mL, testing may not be successful but should still be considered (BII).
A standard genotypic resistance assay is generally preferred for patients experiencing virologic failure on their first or second regimens (AII).
In patients failing INSTI-based regimens, genotypic testing for INSTI resistance should be performed to determine whether to include drugs from this class in subsequent regimens (AII).
If use of a CCR5 antagonist is being considered, a co-receptor tropism assay should be performed (AI) (see Co-receptor Tropism Assays).
Addition of phenotypic assay to genotypic assay is generally preferred in patients with known or suspected complex drug-resistance patterns, particularly to protease inhibitors (PIs) (BIII).
Testing can help determine the role of resistance in drug failure and maximize the clinician's ability to select active drugs for the new regimen. Drug-resistance testing should be performed while the patient is taking prescribed ARV drugs or, if not possible, within 4 weeks after discontinuing therapy.
Genotypic testing is preferred to phenotypic testing because of lower cost, faster turnaround time, and greater sensitivity for detecting mixtures of wild-type and resistant HIV.
Standard genotypic drug-resistance assays test only for mutations in the RT and PR genes.
Phenotypic testing can provide additional useful information in patients with complex drug-resistance mutation patterns, particularly to PIs.
# Clinical Setting/Recommendation Rationale
# Drug-resistance assay recommended
In patients with suboptimal suppression of viral load: Drugresistance testing is recommended in patients with suboptimal suppression of viral load after initiation of ART (AII).
Testing can help determine the role of resistance and thus assist the clinician in identifying the number of active drugs available for a new regimen.
In HIV-infected pregnant women: Genotypic resistance testing is recommended for all pregnant women before initiation of ART (AIII) and for those entering pregnancy with detectable HIV RNA levels while on therapy (AI).
The goal of ART in HIV-infected pregnant women is to achieve maximal viral suppression for treatment of maternal HIV infection and for prevention of perinatal transmission of HIV. Genotypic resistance testing will assist the clinician in selecting the optimal regimen for the patient.
# Drug-resistance assay not usually recommended
After therapy is discontinued: Drug-resistance testing is not usually recommended more than 4 weeks after discontinuation of ARV drugs (BIII).
Drug-resistance mutations may become minor species in the absence of selective drug pressure, and available assays may not detect minor drug-resistant species. If testing is performed in this setting, the detection of drug resistance may be of value; however, the absence of resistance does not rule out the presence of minor drug-resistant species.
In patients with low HIV RNA levels: Drug-resistance testing is not usually recommended in patients with a plasma viral load <500 copies/mL (AIII).
Resistance assays cannot be consistently performed given low HIV RNA levels. HIV enters cells by a complex process that involves sequential attachment to the CD4 receptor followed by binding to either the CCR5 or CXCR4 molecules and fusion of the viral and cellular membranes. 1 CCR5 coreceptor antagonists prevent HIV entry into target cells by binding to the CCR5 receptors. 2 Phenotypic and, to a lesser degree, genotypic assays have been developed that can determine or predict the co-receptor tropism (i.e., CCR5, CXCR4, or both) of the patient's dominant virus population. An older generation assay (Trofile, Monogram Biosciences, Inc., South San Francisco, CA) was used to screen patients who were participating in clinical trials that led to the approval of maraviroc (MVC), the only CCR5 antagonist currently available. The assay has been improved and is now available with enhanced sensitivity. In addition, a genotypic assay to predict co-receptor usage is now commercially available.
During acute/recent infection, the vast majority of patients harbor a CCR5-utilizing virus (R5 virus), which suggests that the R5 variant is preferentially transmitted. Viruses in many untreated patients eventually exhibit a shift in co-receptor tropism from CCR5 usage to either CXCR4 or both CCR5 and CXCR4 tropism (i.e., dual-or mixed-tropic; D/M-tropic). This shift is temporally associated with a more rapid decline in CD4 T-cell counts, 3,4 but whether this tropism shift is a cause or a consequence of progressive immunodeficiency remains undetermined. 1 Antiretroviral (ARV)-treated patients with extensive drug resistance are more likely to harbor X4-or D/M-tropic variants than untreated patients with comparable CD4 counts. 5 The prevalence of X4-or D/M-tropic variants increases to more than 50% in treated patients who have CD4 counts <100 cells/mm 3 . 5,6
# Phenotypic Assays
Phenotypic assays characterize the co-receptor usage of plasma-derived virus. These assays involve the generation of laboratory viruses that express patient-derived envelope proteins (i.e., gp120 and gp41). These pseudoviruses, which are replication-defective, are used to infect target cell lines that express either CCR5 or CXCR4. 7,8 Using the Trofile assay, the co-receptor tropism of the patient-derived virus is confirmed by testing the susceptibility of the virus to specific CCR5 or CXCR4 inhibitors in vitro. This assay takes about 2 weeks to perform and requires a plasma HIV RNA level ≥1,000 copies/mL.
The performance characteristics of these assays have evolved. Most, if not all, patients enrolled in premarketing clinical trials of MVC and other CCR5 antagonists were screened with an earlier, less sensitive version of the Trofile assay. 8 This earlier assay failed to routinely detect low levels of CXCR4-utilizing variants. As a consequence, some patients enrolled in these clinical trials harbored low levels of CXCR4utilizing virus at baseline that were below the assay limit of detection and exhibited rapid virologic failure after initiation of a CCR5 antagonist. 9 The assay has been revised and is now able to detect lower levels of CXCR4-utlizing viruses. In vitro, the assay can detect CXCR4-utilizing clones with 100% sensitivity when those clones represent 0.3% or more of the virus population. 10 Although this more sensitive assay has had limited use in prospective clinical trials, it is now the only one that is commercially available. For unclear
# Panel's Recommendations
• A co-receptor tropism assay should be performed whenever the use of a CCR5 co-receptor antagonist is being considered (AI).
• Co-receptor tropism testing is also recommended for patients who exhibit virologic failure on a CCR5 antagonist (BIII).
• A phenotypic tropism assay is preferred to determine HIV-1 co-receptor usage (AI).
• A genotypic tropism assay should be considered as an alternative test to predict HIV-1 co-receptor usage (BII). The ABC HSR is a multiorgan clinical syndrome typically seen within the initial 6 weeks of ABC treatment. This reaction has been reported in 5%-8% of patients participating in clinical trials when using clinical criteria for the diagnosis, and it is the major reason for early discontinuation of ABC. Discontinuing ABC usually promptly reverses HSR, whereas subsequent rechallenge can cause a rapid, severe, and even lifethreatening recurrence. 1 Studies that evaluated demographic risk factors for ABC HSR have shown racial background as a risk factor, with white patients generally having a higher risk (5%-8%) than black patients (2%-3%). Several groups reported a highly significant association between ABC HSR and the presence of the major histocompatibility complex (MHC) class I allele HLA-B*5701. [2][3] Because the clinical criteria used for ABC HSR are overly sensitive and may lead to false-positive ABC HSR diagnoses, an ABC skin patch test (SPT) was developed as a research tool to immunologically confirm ABC HSR. 4 A positive ABC SPT is an ABC-specific delayed HSR that results in redness and swelling at the skin site of application. All ABC SPT-positive patients studied were also positive for the HLA-B*5701 allele. 5 The ABC SPT could be falsely negative for some patients with ABC HSR and, at this point, is not recommended for use as a clinical tool. The PREDICT-1 study randomized patients before starting ABC either to be prospectively screened for HLA-B*5701 (with HLA-B*5701-positive patients not offered ABC) or to standard of care at the time of the study (i.e., no HLA screening, with all patients receiving ABC). 6 The overall HLA-B*5701 prevalence in this predominately white population was 5.6%. In this cohort, screening for HLA-B*5701 eliminated immunologic ABC HSR (defined as ABC SPT positive) compared with standard of care (0% vs. 2.7%), yielding a 100% negative predictive value with respect to SPT and significantly decreasing the rate of clinically suspected ABC HSR (3.4% vs. 7.8%). The SHAPE study corroborated the low rate of immunologically validated ABC HSR in black patients and confirmed the utility of HLA-B*5701 screening for the risk of ABC HSR (100% sensitivity in black and white populations). 7 On the basis of the results of these studies, the Panel recommends screening for HLA-B*5701 before starting patients on an ABC-containing regimen (AI). HLA-B*5701-positive patients should not be prescribed ABC (AI), and the positive status should be recorded as an ABC allergy in the patient's medical record (AII). HLA-B*5701 testing is needed only once in a patient's lifetime; thus, efforts to carefully record and maintain the test result and to educate the patient about its implications are important. The specificity of the HLA-B*5701 test in predicting ABC HSR is lower than the sensitivity (i.e., 33%-50% of HLA-B*5701-positive patients would likely not develop confirmed ABC HSR if exposed to ABC). HLA-B*5701 should not be used as a substitute for clinical judgment or pharmacovigilance, because a negative HLA-B*5701 result does not absolutely rule out the possibility of some form of ABC HSR. When HLA-B*5701 screening is not
# Rating of Recommendations
# Panel's Recommendations
• The Panel recommends screening for HLA-B*5701 before starting patients on an abacavir (ABC)-containing regimen to reduce the risk of hypersensitivity reaction (HSR) (AI).
• HLA-B*5701-positive patients should not be prescribed ABC (AI).
• The positive status should be recorded as an ABC allergy in the patient's medical record (AII).
• When HLA-B*5701 screening is not readily available, it remains reasonable to initiate ABC with appropriate clinical counseling and monitoring for any signs of HSR (CIII). Eradication of HIV infection cannot be achieved with available antiretroviral (ARV) regimens even when new, potent drugs are added to a regimen that is already suppressing plasma viral load below the limits of detection of commercially available assays. 1 This is chiefly because the pool of latently infected CD4 T cells is established during the earliest stages of acute HIV infection 2 and persists with a long half-life, despite prolonged suppression of plasma viremia. [3][4][5][6][7] Therefore the primary goals for initiating antiretroviral therapy (ART) are to:
# Rating of Recommendations
• reduce HIV-associated morbidity and prolong the duration and quality of survival,
• restore and preserve immunologic function,
• maximally and durably suppress plasma HIV viral load (see Plasma HIV RNA Testing), and
• prevent HIV transmission.
ART has reduced HIV-related morbidity and mortality [8][9][10][11] and has reduced perinatal 12 and behavior-associated transmission of HIV. [13][14][15][16][17] HIV suppression with ART may also decrease inflammation and immune activation thought to contribute to higher rates of cardiovascular and other end-organ damage reported in HIV-infected cohorts. (See Initiating Antiretroviral Therapy.) Maximal and durable suppression of plasma viremia delays or prevents the selection of drug-resistance mutations, preserves CD4 T-cell numbers, and confers substantial clinical benefits, all of which are important treatment goals. [18][19] Achieving viral suppression requires the use of ARV regimens with at least two, and preferably three, active drugs from two or more drug classes. Baseline resistance testing and patient characteristics should guide design of the specific regimen. (See What to Start: Initial Combination Regimens for the Antiretroviral-Naive Patient.) When initial suppression is not achieved or is lost, rapidly changing to a new regimen with at least two active drugs is required. (See Virologic Failure and Suboptimal Immunologic Response.) The increasing number of drugs and drug classes makes viral suppression below detection limits an appropriate goal in all patients.
Viral load reduction to below limits of assay detection in an ART-naive patient usually occurs within the first 12-24 weeks of therapy. Predictors of virologic success include:
• high potency of ARV regimen,
• excellent adherence to treatment regimen, 20 • low baseline viremia, 21 • higher baseline CD4 count (>200 cells/mm 3 ), 22 and
• rapid reduction of viremia in response to treatment. 21,23 Successful outcomes are usually observed, although adherence difficulties may lower the success rate in clinical practice to below the 90% rate commonly seen in clinical trials. 24
# Strategies to Achieve Treatment Goals
Achieving treatment goals requires a balance of sometimes competing considerations, outlined below. Providers and patients must work together to define individualized strategies to achieve treatment goals.
# Selection of Initial Combination Regimen
Several preferred and alternative ARV regimens are recommended for use. (See What to Start.) Many of these regimens have comparable efficacy but vary to some degree in dosing frequency and symmetry, pill
# Introduction
Without treatment, most HIV-infected individuals will eventually develop progressive immunosuppression, as evident by CD4 T lymphocyte (CD4) cell depletion, leading to AIDS-defining illnesses and premature death. The primary goal of ART is to prevent HIV-associated morbidity and mortality. This goal is best accomplished by using effective ART to maximally inhibit HIV replication so that plasma HIV RNA (viral load) remains below levels detectable by commercially available assays. Durable viral suppression improves immune function and overall quality of life, lowers the risk of both AIDS-defining and non-AIDS-defining complications, and prolongs life.
Furthermore, high plasma HIV RNA is a major risk factor for HIV transmission, and effective antiretroviral therapy (ART) can reduce viremia and transmission of HIV to sexual partners by more than 96%. 1,2 Modelling studies suggest that expanded use of ART may result in lower incidence and, eventually, prevalence of HIV on a community or population level. 3 Thus, a secondary goal of ART is to reduce the risk of HIV transmission.
Historically, HIV-infected individuals have had low CD4 counts at presentation to care. 4 However, there have been concerted efforts to increase testing of at-risk patients and to link these patients to medical care before they have advanced HIV disease. Deferring ART until CD4 count declines put an individual at risk of AIDSdefining conditions has been associated with higher risk of morbidity and mortality (as discussed below). Furthermore, the magnitude of CD4 recovery is directly correlated with CD4 count at ART initiation. Consequently, many individuals who start treatment with CD4 counts <350 cells/mm 3 never achieve counts >500 cells/mm 3 after up to 6 years on ART. 5 The recommendation to initiate ART in individuals with high CD4 cell counts-whose short-term risk for death and development of AIDS-defining illness is low 6,7 -is based on growing evidence that untreated HIV infection or uncontrolled viremia is associated with development of non-AIDS-defining diseases, including cardiovascular disease (CVD), kidney disease, liver disease, neurologic complications, and malignancies. Furthermore, newer ART regimens are more effective, more convenient, and better tolerated than regimens used in the past.
# Panel's Recommendations
• Antiretroviral therapy (ART) is recommended for all HIV-infected individuals to reduce the risk of disease progression.
The strength of and evidence for this recommendation vary by pretreatment CD4 T lymphocyte (CD4) cell count: CD4 count <350 cells/mm 3 (AI); CD4 count 350 to 500 cells/mm 3 (AII); CD4 count >500 cells/mm 3 (BIII).
• ART is also recommended for HIV-infected individuals to prevent of transmission of HIV.
The strength of and evidence for this recommendation vary by transmission risks: perinatal transmission (AI); heterosexual transmission (AI); other transmission risk groups (AIII).
• Patients starting ART should be willing and able to commit to treatment and understand the benefits and risks of therapy and the importance of adherence (AIII). Patients may choose to postpone therapy, and providers, on a case-by-case basis, may elect to defer therapy on the basis of clinical and/or psychosocial factors. Regardless of CD4 count, the decision to initiate ART should always include consideration of a patient's comorbid conditions, his or her willingness and readiness to initiate therapy, and available resources. In settings where there are insufficient resources to initiate ART in all patients, treatment should be prioritized for patients with the following clinical conditions: pregnancy; CD4 count <200 cells/mm 3 or history of an AIDS-defining illness including HIV-associated dementia, HIV-associated nephropathy (HIVAN), or hepatitis B virus (HBV); and acute HIV infection.
# Rating of Recommendations
Tempering the enthusiasm to treat all patients regardless of CD4 count is the absence of randomized trial data that demonstrate a definitive clinical benefit of ART in patients with higher CD4 counts (e.g., >350 cells/ mm 3 ) and mixed results from observational cohort studies as to the definitive benefits of early ART (i.e., when CD4 count >500 cells/mm 3 ). For some asymptomatic patients, the potential risks of short-or long-term drug-related complications and non-adherence to long-term therapy may offset possible benefits of earlier initiation of therapy. An ongoing randomized controlled trial evaluating the role of immediate versus delayed ART in patients with CD4 counts >500 cells/mm 3 (see Strategic Timing of Antiretroviral Treatment (START); ClinicalTrials.gov identifier NCT00867048) should help to further define the role of ART in this patient population.
The known and potential benefits and limitations of ART in general, and in different patient populations are discussed below.
# Benefits of Antiretroviral Therapy
# Reduction in Mortality and/or AIDS-Related Morbidity According to Pretreatment CD4 Cell Count
Patients with a History of an AIDS-Defining Illness or CD4 Count <350 cells/mm 3 HIV-infected patients with CD4 counts <200 cells/mm 3 are at higher risk of opportunistic diseases, non-AIDS morbidity, and death than HIV-infected patients with higher CD4 counts. Randomized controlled trials in patients with CD4 counts <200 cells/mm 3 and/or a history of an AIDS-defining condition provide strong evidence that ART improves survival and delays disease progression in these patients. [8][9][10] Long-term data from multiple observational cohort studies comparing earlier ART (i.e., initiated at CD4 count >200 cells/mm 3 ) with later treatment (i.e., initiated at CD4 count <200 cells/mm 3 ) have also provided strong support for these findings. [11][12][13][14][15][16] Few large, randomized controlled trials address when to start therapy in patients with CD4 counts >200 cells/mm 3 . CIPRA HT-001, a randomized clinical trial conducted in Haiti, enrolled 816 participants without AIDS. Participants were randomized to start ART with CD4 counts in the 200 to 350 cells/mm 3 range or to defer treatment until their CD4 counts dropped to <200 cells/mm 3 or they developed an AIDS-defining condition. The study was terminated when an interim analysis showed a survival benefit in the early treatment arm. When compared with participants who began ART with CD4 counts in the 200 to 350 cells/mm 3 range, patients who deferred therapy had a higher mortality rate (23 versus 6 deaths; hazard ratio [HR] = 4.0; 95% confidence interval [CI], 1.6-9.8) and a higher rate of incident tuberculosis (TB) (HR = 2.0; 95% CI, 1.2-3.6). 17 Collectively, these studies support the Panel's recommendation that ART should be initiated in patients with a history of an AIDS-defining illness or with a CD4 count <350 cells/mm 3 (AI).
# Patients with CD4 Counts Between 350 and 500 cells/mm 3
Data supporting initiation of ART in patients with CD4 counts ranging from 350 cells/mm 3 to 500 cells/mm 3 are from large observational studies conducted in North America, Europe, and Australia and from secondary analysis of randomized controlled trials. Findings from the observational studies were analyzed using advanced statistical methods that minimize the bias and confounding that arise when observational data are used to address the question of when to start ART. However, unmeasured confounders for which adjustment was not possible may have influenced the analysis.
Among the cohort studies analyzed, the ART Cohort Collaboration (ART-CC) included 45,691 patients from 18 cohort studies conducted primarily in North America and Europe. Data from ART-CC showed that the rate of progression to AIDS and/or death was higher in participants who delayed ART initiation until their CD4 counts fell to 251 to 350 cells/mm 3 than in those who initiated ART at CD4 count level of 351 to 450 cells/mm 3 (risk ratio: 1.28; 95% CI, 1.04-1.57). 13 When analysis of the data was restricted to mortality alone, the difference between the 2 strategies was weaker and not statistically significant (risk ratio: 1.13; 95% CI, 0.80-1.60).
The NA-ACCORD cohort evaluated patients regardless whether they had started therapy. The 6,278 patients who deferred therapy until their CD4 counts fell to <350 cells/mm 3 had a greater risk of death than the 2,084 patients who initiated therapy with CD4 counts between 351 cells/mm 3 and 500 cells/mm 3 (risk ratio: 1.69; 95% CI, 1.26-2.26) after adjustment for other factors that differed between these 2 groups. 18 The HIV-CAUSAL cohort evaluated 8,392 ART-naive patients with initial CD4 counts >500 cells/mm 3 that declined to <500 cells/mm 3 . 16 The study estimated that delaying initiation of ART until CD4 count fell to <350 cells/mm 3 was associated with a greater risk of AIDS-defining illness or death than initiating ART with CD4 count between 350 cells/mm 3 and 500 cells/mm 3 (HR: 1.38; 95% CI, 1.23-1.56). However, there was no difference in mortality between the 2 groups (HR: 1.01; 95% CI, 0.84-1.22).
The CASCADE cohort included 5,527 ART-naive patients with CD4 counts in the 350 to 499 cells/mm 3 range. Compared with patients who deferred therapy until their CD4 counts fell to <350 cells/mm 3 , patients who started ART immediately had a marginally lower risk of AIDS-defining illness or death (HR: 0.75; 95% CI, 0.49-1.14) and a lower risk of death (HR: 0.51; 95% CI,98 0.33-0.80). 19 Randomized data showing clinical evidence that supports ART for patients with higher CD4 cell counts came from two studies. In the SMART trial, HIV-infected participants with CD4 counts >350 cells/mm 3 were randomized to continuous ART or to treatment interruption until their CD4 counts fell to <250 cells/mm 3 . In the subgroup of 249 participants who were ART naive at enrollment (median CD4 count: 437 cells/mm 3 ), those who deferred ART until their CD4 counts dropped to <250 cells/mm 3 had a greater risk of serious AIDS-and non-AIDS-related events than those who initiated therapy immediately (7 vs. 2 events; HR: 4.6; 95% CI, 1.0-22.2). 20 HPTN 052 was a large multi-continent randomized trial that examined whether treatment of HIV-infected individuals reduces transmission to their uninfected sexual partners. 2 A secondary objective of the study was to determine whether ART reduces clinical events in the HIV-infected participants. This trial enrolled 1,763 HIV infected participants with CD4 counts between 350 and 550 cells/mm 3 and their HIV uninfected partners. The infected participants were randomized to initiate ART immediately or to delay initiation until they had 2 consecutive CD4 counts <250 cells/mm 3 . At a median follow-up of 2.1 years, there were 57 primary events in the early therapy arm versus 77 events in the delayed therapy arm (HR: 0.73; 95% CI, 0.52-1.03). The most frequent event was tuberculosis (17 cases in the early therapy arm and 34 cases in the delayed therapy arm); deaths were relatively rare (11 cases in the early therapy arm and 15 cases in the delayed therapy arm). 21,22 Collectively, these studies suggest that initiating ART in patients with CD4 counts between 350 and 500 cells/mm 3 reduces HIV-related disease progression; whether there is a corresponding reduction in mortality is unclear. This benefit supports the Panel's recommendation that ART should be initiated in patients with CD4 counts 350 to 500 cells/mm 3 (AII). Recent evidence demonstrating the public health benefit of earlier initiation of ART in reducing HIV transmission further supports the strength of this recommendation (see Prevention of Sexual Transmission).
Patients with CD4 Counts >500 cells/mm 3 An analysis of the risks of HIV-associated disease progression in ART-naive patients with CD4 cell counts >500 cells/mm 3 is difficult because only a small proportion of individuals present for clinical care with CD4 cell counts at this level. 4,23 However, studies have demonstrated a gradient of increased risk of AIDS and death when ART is initiated at lower CD4 cell count levels and have provided no evidence of a safe CD4 count level. 6,24,25 To date, questions regarding the risks and benefits of starting ART in patients with CD4 cell counts >500 cells/mm 3 as compared to deferring initiation until CD4 cell counts are lower have not yet been answered in a definitive randomized clinical trial. Evidence supporting early initiation comes from an observational study. The NA-ACCORD study observed patients who started ART with CD4 counts >500 cells/mm 3 or after their CD4 counts dropped below this threshold. The adjusted mortality rates were significantly higher in the 6,935 patients who deferred therapy until their CD4 counts fell to <500 cells/mm 3 than in the 2,200 patients who started therapy with CD4 counts >500 cells/mm 3 (risk ratio: 1.94; 95% CI, 1.37-2.79). 18 In contrast, in an analysis of the ART-CC cohort, 13 the rate of progression to AIDS/death associated with deferral of therapy until CD4 counts fell to the 351 to 450 cells/mm 3 range was similar to the rate with initiation of therapy with CD4 counts in the 451 to 550 cells/mm 3 range (HR: 0.99; 95% CI, 0.76-1.29). The analysis showed no significant difference in rate of death in the immediate and deferred therapy groups (HR: 0.93; 95% CI, 0.60-1.44). In the CASCADE Collaboration, 19 among the 5,162 patients with CD4 counts in the 500 to 799 cells/mm 3 range, compared with patients who deferred therapy, those who started ART immediately did not experience a significant reduction in the composite outcome of progression to AIDS/death (HR: 1.10; 95% CI, 0.67-1.79) or death (HR: 1.02; 95% CI, 0.49-2.12).
Although not a clinical endpoint study, a recent clinical trial (Setpoint Study) randomized patients within 6 months of HIV seroconversion to receive either immediate ART for 36 weeks or deferred treatment. More than 57% of the study participants had CD4 counts >500 cells/mm 3 . The deferred treatment group had a statistically higher risk of meeting study defined ART initiation criteria than the immediate treatment group.
The study was halted early, showing that the time from diagnosis of early infection and the need for initiation of ART was shorter than anticipated in the deferral therapy group. Fully half of the participants in the deferral group met the criteria for treatment initiation by week 72. 26 Another recent study provides evidence that early treatment enhances recovery of CD4 counts to levels >900 cells/mm 3 . 27 Among individuals who were identified during primary infection, those who initiated ART within 4 months after the estimated date of infection were more likely to have CD4 cell recovery and had a faster rate of recovery than those initiating ART at 4 to 12 months or >12 months after the estimated date of infection. However, even among participants who started ART earlier, those who initiated ART with lower CD4 counts were less likely to have CD4 cell recovery and had a lower rate of recovery than those who initiated ART with higher CD4 counts.
With a better understanding of the pathogenesis of HIV infection, the growing awareness that untreated HIV infection increases the risk of many non-AIDS-defining diseases (as discussed below), and the benefit of ART in reducing transmission of HIV, the Panel recommends initiation of ART in patients with CD4 counts >500 cells/mm 3 (BIII).
When discussing initiation of ART at high CD4 cell counts (>500 cells/mm 3 ), clinicians should inform patients that data on the clinical benefit of starting treatment at such levels are not conclusive, especially for patients with very high CD4 counts. Clinicians should also inform patients that viral suppression from effective ART can reduce the risk of sexual transmission. Lastly, patients should be informed that untreated HIV infection will eventually lead to immunological deterioration and increased risk of clinical disease and death. Therefore, if therapy is not initiated, continued monitoring and close follow-up are necessary.
Further ongoing research (both randomized clinical trials and cohort studies) to assess the short-and longterm clinical and public health benefits and cost effectiveness of starting therapy at higher CD4 counts is needed. Findings from such research will provide further evidence to help the Panel make future recommendations.
# Effects of Viral Replication on HIV-Related Morbidity
Since the mid-1990s, it has been known that measures of viral replication predict HIV disease progression. Among untreated HIV-infected individuals, time to clinical progression and mortality is fastest in those with higher viral loads. 28 This finding is confirmed across the spectrum of HIV-infected patient populations, such as injection drug users (IDUs), 29 women, 30 and individuals with hemophilia. 31 Several studies have shown the prognostic value of pre-treatment viral load for predicting post-therapy response. 32,33 Once therapy has been initiated, failure to achieve viral suppression [34][35][36] and viral load at the time of treatment failure 37 are predictive of clinical disease progression.
More recent studies have examined the impact of ongoing viral replication for both longer durations and at higher CD4 cell counts. Using viremia copy-years, a novel metric for quantifying viral load over time, the Centers for AIDS Research Network of Integrated Clinical Systems (CNICS) cohort found that cumulative exposure to replicating virus is independently associated with mortality. Using viremia copy-years, the HR for mortality was 1.81 per log 10 copy-year/mL (95% CI, 1.51-2.18), which was the only viral load-related variable that retained statistical significance in the multivariable model (HR 1.44 per log 10 copy-year/mL; 95% CI, 1.07-1.94). These findings support the concept that unchecked viral replication, which occurs in the absence of effective ART, is a factor in disease progression and death independent of CD4 count. 38 The EuroSIDA collaboration evaluated HIV-infected individuals with CD4 counts >350 cells/mm 3 segregated by three viral load strata (<500 copies/mL, 500-9,999 copies/mL, and ≥10,000 copies/mL) to determine the impact of viral load on rates of fatal and nonfatal AIDS-related and non-AIDS-related events.
The lower viral load stratum included more participants on ART (92%) than the middle (62%) and high (31%) viral load strata. After adjustment for age, region, and ART, the rates of non-AIDS events were 61% (P = 0.001) and 66% (P = 0.004) higher in participants with viral loads 500 to 9,999 copies/mL and >10,000 copies/mL, respectively, than in individuals with viral loads <500 copies/mL. These data further confirm that unchecked viral replication is associated with adverse clinical outcomes in individuals with CD4 counts >350 cells/mm 3 . 39 Collectively, these data show that the harm of ongoing viral replication affects both untreated patients and those who are on ART but remain viremic. The harm of ongoing viral replication in patients on ART is compounded by the risk of emergence of drug-resistant virus. Therefore, all patients on ART should be carefully monitored and counseled on the importance of adherence to therapy.
# Effects of Antiretroviral Therapy on HIV-Related Morbidity
HIV-associated immune deficiency, the direct effects of HIV on end organs, and the indirect effects of HIVassociated inflammation on these organs all likely contribute to HIV-related morbidity and mortality. In general, the available data demonstrate the following:
• Untreated HIV infection (ongoing viral replication) may have negative effects at all stages of infection.
• Earlier treatment may prevent the damage associated with HIV replication during early stages of infection.
• ART is beneficial even when initiated later in infection; however, later therapy may not repair damage associated with viral replication during early stages of infection.
• Sustaining viral suppression and maintaining higher CD4 count levels, mostly as a result of effective combination ART, may delay, prevent, or reverse some non-AIDS-defining complications, such as HIVassociated kidney disease, liver disease, CVD, neurologic complications, and malignancies, as discussed below.
# HIV-Associated Nephropathy
HIVAN is the most common cause of chronic kidney disease in HIV-infected individuals that may lead to end-stage kidney disease. 40 HIVAN is almost exclusively seen in black patients and can occur at any CD4 count. Ongoing viral replication appears to be directly involved in renal injury; 41 HIVAN is extremely uncommon in virologically suppressed patients. 42 ART in patients with HIVAN has been associated with both preserved renal function and prolonged survival. [43][44][45] Therefore, regardless of CD4 count, ART should be started in all patients with HIVAN at the earliest sign of renal dysfunction (AII).
# Coinfection with Hepatitis B Virus and/or Hepatitis C Virus
HIV infection is associated with more rapid progression of viral hepatitis-related liver disease, including cirrhosis, end-stage liver disease, hepatocellular carcinoma, and fatal hepatic failure. 46 48 The pathogenesis of accelerated liver disease in HIV-infected patients has not been fully elucidated, but HIV-related immunodeficiency and a direct interaction between HIV and hepatic stellate and Kupffer cells have been implicated. [49][50][51][52] In individuals co-infected with HBV and/or hepatitis C virus (HCV), ART may attenuate liver disease progression by preserving or restoring immune function and reducing HIV-related immune activation and inflammation. [53][54][55] Antiretroviral (ARV) drugs active against both HIV and HBV (such as tenofovir disoproxil fumarate [TDF], lamivudine [3TC], and emtricitabine [FTC]) also may prevent development of significant liver disease by directly suppressing HBV replication. 56,57 Although ARV drugs do not inhibit HCV replication directly, HCV treatment outcomes typically improve when HIV replication is controlled or CD4 counts increase. 58 In one prospective cohort, after controlling for liver and HIV disease stage, HCV coinfected patients receiving ART were approximately 66% less likely to experience end-stage liver disease, hepatocellular carcinoma, and fatal hepatic failure than patients not receiving ART. 59 While some studies have shown that chronic viral hepatitis increases the risk of ART-induced liver injury, the majority of coinfected persons do not develop clinically significant liver injury [60][61][62] and the rate of hepatotoxicity may be greater in persons with more advanced HIV disease. Collectively, these data suggest that earlier treatment of HIV infection in persons coinfected with HBV (and likely HCV) may reduce the risk of liver disease progression. ART is recommended for patients coinfected with HBV, and the ART regimen should include drugs with activity against both HIV and HBV (AII) (also see Hepatitis B Virus/HIV Coinfection). ART is also recommended for most patients coinfected with HCV (BII), including those with high CD4 counts and those with cirrhosis. This recommendation is based on findings from retrospective and prospective cohort studies that indicated that the receipt of ART is associated with slower progression of hepatic fibrosis and reduced risk of liver disease outcomes. 59,[63][64][65] Combined treatment of HIV and HCV can be complicated by large pill burden, drug interactions, and overlapping toxicities; however, the complexity of treatment depends on the HCV regimen selected. ART should be considered for HIV/HCV-coinfected patients regardless of CD4 cell count. However, for patients with CD4 counts >500 cells/mm 3 and also infected with HCV genotype 1, if treatment is to include an HCV protease inhibitor, some clinicians may choose to defer ART until HCV treatment is completed (also see HIV/Hepatitis C Virus Co-Infection).
# Cardiovascular Disease
In HIV-infected patients, CVD is a major cause of morbidity and mortality, accounting for one-third of serious non-AIDS conditions and at least 10% of deaths. [66][67][68] A number of studies have found that, over time, HIV-infected persons are at greater risk for CVD events than age-matched uninfected individuals.
Persons living with HIV infection have higher rates of established CVD risk factors, particularly smoking and dyslipidemia, than HIV-uninfected individuals. In the Data Collection on Adverse Events of Anti-HIV Drugs (D:A:D) cohort study such factors, including age, male gender, obesity, smoking, family history of CVD, diabetes, and dyslipidemia, were each independently associated with risk of myocardial infarction (MI). 69 This study also found that the risk of CVD was greater with exposure to some ARV drugs, including certain PIs (ritonavir-boosted lopinavir and ritonavir-boosted fosamprenavir) and abacavir, than with exposure to other ARV drugs. 69,70 In terms of preventing the progression to CVD events, it has not been determined whether delaying ART initiation is preferable to immediate treatment. In the meta-analysis mentioned above, the risk of CVD in HIV-infected individuals was 1.5 times higher in those treated with ART than in those not treated with ART. 63 These analyses were limited by concern that the treated individuals may have been infected for longer periods of time and had prior episodes of untreated HIV disease, as well as the fact that the untreated people were at higher risk for competing events, including death. Furthermore, there is evidence that untreated HIV infection may also be associated with an increased risk of CVD. In the SMART study, the risk of cardiovascular events was greater in participants randomized to CD4-guided treatment interruption than in participants who received continuous ART. 71 In other studies, ART resulted in marked improvement in parameters associated with CVD, including markers of inflammation (such as interleukin 6 [IL-6]), immune dysfunction (e.g., T cell activation, T cell senescence), monocyte activation (e.g., IL-6, soluble CD14 and CD163), hyper-coagulation (e.g., D-dimers) and, most importantly, endothelial dysfunction. 72,73 Low nadir and/or proximal on-therapy CD4 cell count has been linked to CVD (MI and/or stroke), [74][75][76] suggesting that low CD4 count might result in increased risk of CVD.
Collectively, the increased risk of cardiovascular events with treatment interruption, the effects of ART on markers of inflammation and endothelial dysfunction, and the association between CVD and CD4 cell depletion suggest that early control of HIV replication with ART can be used as a strategy to reduce risk of CVD, particularly if drugs with potential cardiovascular toxicity are avoided. However, no study has demonstrated that initiation of ART prevents CVD. Therefore, a role for early ART in preventing CVD remains to be established. For HIV-infected individuals with a significant risk of CVD, as assessed by medical history and estimated risk calculations, risk of CVD should be considered when selecting a specific ART regimen.
# Malignancies
HIV-infected individuals are at increased risk for developing several cancers and human papilloma virus (HPV)-related pre-malignant intraepithelial neoplasia. 77,78 Increased rates of Kaposi sarcoma and non-Hodgkin lymphoma in patients with advanced HIV infection have been noted since early in the AIDS epidemic, and, together with cervical cancer, both diseases have been defined as AIDS-defining malignancies (ADMs) for public health surveillance purposes. HIV infection and associated immunosuppression increase the risk of several cancers identified as non-AIDS-defining malignancies (NADMs). Importantly, the incidence of lung, anal, oropharyngeal, liver and skin cancers, Hodgkin lymphoma, and melanoma, is higher in HIV-infected individuals than in matched HIV-uninfected controls, [79][80][81] and the burden of these NADMs continued to increase in the United States between 1996 and 2007. 82 Incidental cancers that occur in HIV-infected individuals are becoming more common, which is due to the aging of the HIV population rather than to HIV-associated risks of malignancies. These cancers are also sometimes considered NADMs. Most cancers with increased incidence are either virally related (i.e., Hodgkin lymphoma, anal cancer, liver cancer) or smoking related (lung cancer), although HIV remains an independent risk factor for the later. 83 Large cohort studies enrolling mainly patients receiving ART have reported a consistent link between low CD4 counts (<350 to 500 cells/mm 3 ) and the risk of ADMs and/or NADMs. 14,76,[84][85][86][87] The ANRS C04 Study demonstrated that, in contrast to patients with CD4 counts >500 cells/mm 3 , patients with CD4 counts <500 cells/mm 3 had a statistically significant relative risk of all cancers evaluated (except for anal carcinoma). The study also showed an increased risk of anal cancer based on extent of time with CD4 counts <200 cells/mm 3 , and that, regardless of CD4 count, ART has a protective effect for HIV-associated malignancies. 84 This potential effect of HIV-associated immunodeficiency is striking particularly with regard to cancers and premalignant diseases associated with chronic viral infections such as HBV, HCV, HPV, Epstein-Barr virus, and human herpes virus-8. 88,89 For some cancers, risk is related to HIV viremia. Cumulative HIV viremia, independent of other factors, is associated with increased risk of non-Hodgkin lymphoma and other ADM. 87,90 In the SMART study, 91 patients randomized to the drug conservation arm (ART interruption with re-initiation if CD4 count fell to <250 cells/mm 3 ) had a higher incidence of ADM but not NADM, although increased NADM was noted in non-smokers in the drug-conservation arm.
From the early 1990s through 2000, incidence rates for many cancers occurring with advanced immunosuppression, including Kaposi sarcoma, diffuse large B-cell lymphoma, and primary central nervous system (CNS) lymphoma, declined markedly in HIV-infected individuals in the United States, with more gradual declines noted after 2000. 92 However, for other ADMs and NADMs, such as Burkitt lymphoma, Hodgkin lymphoma, cervical cancer, and anal cancer, similar reductions in incidence have not been observed. 92,93 Declines in competing causes of mortality (e.g., opportunistic infections [OIs]) and concurrent cancer risk factors such as smoking or aging of HIV-infected cohorts, may confound a full assessment of the relative impact of ART on cancer prevention for NADMs. 82,94 Additionally, data from the era of potent combination ART suggest that overall survival in HIV-infected patients who develop ADMs or NADMs also depends on immune status as measured by CD4 count. 85,95,96 For non-Hodgkin lymphoma, data from the Center for AIDS Research Network of Integrated Clinical Systems Cohort shows that across CD4 strata, the level of HIV viremia 6 months after the diagnosis of lymphoma (including Hodgkin lymphoma) is associated with an increased risk of death. 95 Together this evidence suggests that initiating ART to suppress HIV replication, maximize immune reconstitution, and maintain CD4 counts at levels >350 to 500 cells/mm 3 reduces the overall incidence of ADMs and may reduce the risk of some NADMs as well. The effect of ART on cancer incidence and mortality in patients with cancer 95,97 is likely to be heterogeneous across various cancer types.
# Neurological Complications
In the untreated HIV-infected patient, CNS involvement is a nearly universal facet of systemic HIV infection as evident by detection of HIV RNA in cerebrospinal fluid (CSF). [98][99][100][101] The CNS is an important target of ART, not only to treat neurologically symptomatic infection but also to prevent later development of virusrelated brain injury, which can range from severe and debilitating encephalopathy to milder and more insidious cognitive and motor dysfunction. [102][103][104] Like systemic infection, CNS virus populations and the character of CNS infection can evolve within individual patients. Characteristically during the earliest phases of systemic infection, CSF viral isolates are similar to those found in blood and likely reflect transfer of blood populations across CNS barriers in T lymphocytes. 105 Over time CSF isolates may exhibit increasing compartmentalization that reflect divergence from the predominant blood populations, a transformation most notable in patients with frank HIV encephalitis presenting with HIV-associated dementia (HAD). 106 Combination ART usually reduces CSF HIV RNA to below the level of detection, 99,107 largely preventing this development, and consequently, reducing the incidence of severe HIV-related brain disease in virologically suppressed patients. [108][109][110] Hence, prevention of HAD is among the arguments for early ART, although the CD4 threshold for treatment to prevent this disorder is not established. Additionally, treatment of patients presenting with HAD-usually seen in the context of late HIV presentation-can arrest and variably reverse neurological abnormalities; 111 therefore, the diagnosis of HAD is an indication for rapid initiation of ART (AI).
With the successful control of HAD with ART, attention has shifted to milder forms of neurocognitive impairment in HIV infection, largely recognized by reduced neuropsychological test performance. 104,112 These milder forms of impairment are categorized in two groups: asymptomatic neurocognitive impairment and mild neurocognitive disorder. Although patients with either form exhibit the same degree of impairment on neuropsychological tests (<1 SD below normative performance in two neurocognitive domains), they differ as to the absence or presence of symptoms or mild functional impairment in everyday activities. 103 Even after exclusion of confounding conditions, the prevalence of these milder forms of neurocognitive impairment appears to be substantial, including in treated patients with plasma viral suppression. 104,112 Less certain is the extent to which these impairments are the consequence of earlier mild or subclinical brain injury sustained before ART initiation, or alternatively, reflect ongoing injury despite ART and plasma viral suppression. Association of these milder deficits with nadir CD4 count may favor the role of earlier injury, 100,[113][114][115] providing further argument for early treatment.
Peripheral neuropathies are a second category of important HIV-associated neurological disease. 116 In the early decades of the discovery of HIV infection and the use of some nucleoside analogs, painful distal sensory neuropathy was particularly common and a difficult problem that did not respond to ART. 117 Although some reports suggest that the incidence of this HIV-associated neuropathy remains high, clinical experience suggests that the condition mainly affects patients with longer duration of HIV infection who initiated ART late in the course of the disease. 118 There appears to be a reduced incidence of neuropathies as more patients begin treatment at earlier stages of HIV infection.
Overall, effective ART may be beneficial in preventing and treating symptomatic and subclinical CNS HIV infection and the CNS and peripheral nervous system consequences of infection.
# Age and Treatment-Related Immune Reconstitution
Also see HIV and the Older Patient.
The CD4 cell response to ART is an important predictor of short-and long-term morbidity and mortality. In most, but not all studies, treatment initiation at an older age has been associated with a less robust CD4 count response; starting therapy at a younger age may result in better immunologic and perhaps clinical outcomes. 4,[119][120][121][122]
# Persistent Inflammation and Immunodeficiency During Antiretroviral Therapy
Untreated HIV infection is associated with chronic inflammation, as defined by the frequency of activated T cells and monocyte/macrophages and levels of a number of pro-inflammatory cytokines (e.g., IL-6, CRP, soluble CD14). Effective ART decreases levels of most of these inflammatory markers, but the effect is often incomplete, with levels in many of those on ART remaining higher than those observed in age-matched uninfected adults. 123,124 Chronic inflammation during both untreated and treated disease is strongly associated with risk of non-AIDS defining morbidity and all-cause mortality. [125][126][127][128] Because HIV replication contributes to this inflammatory state through both direct and indirect mechanisms, earlier use of ART to blunt this process may be beneficial. However, there are no data showing that ART-mediated changes in any inflammatory biomarker are associated with reduced morbidity and mortality.
Immune function as defined by the peripheral CD4 cell count is also an important determinant of health.
Although effective ART results in a sustained and beneficial increase in CD4 cell counts, this effect is often incomplete. Patients who delay therapy to the point of advanced immunodeficiency may require several years of ART to normalize their peripheral CD4 cell counts, 129 and some patients may never achieve a normal level. 130 A lower CD4 count on therapy is associated with higher risk of developing cancer, liver disease, cardiovascular disease and death. 14 In some studies a history of low CD4 counts is associated with risk of morbidity and mortality during subsequent effective therapy. 131,132 Collectively, these observations support earlier use of ART. Treatment decreases the level of inflammation, which may be associated with reduced short-term risk of AIDS-and non-AIDS-related morbidity and mortality. 125,133,134 ART also prevents progressive loss of CD4 cells, thus reducing risk of immunodeficiency and its related complications. Some studies have shown that a patient's pre-therapy CD4 cell count nadir is predictive of the degree of residual inflammation and/or T-cell dysfunction during ART. 123,135,136 Thus, earlier ART may result in less residual immunological perturbations during treatment, which theoretically may result in reduced risk of disease during the decades that a patient requires ART (CIII).
# Antiretroviral Therapy for Prevention of HIV Transmission
# Prevention of Perinatal Transmission
Effective ART reduces transmission of HIV. The most dramatic and well-established example of this effect is the use of ART in pregnant women to prevent perinatal transmission of HIV. Effective suppression of HIV replication, as reflected in plasma HIV RNA, is a key determinant in reducing perinatal transmission. In the setting of ART initiation before 28 weeks' gestation and an HIV RNA level <50 copies/mL near delivery, use of combination ART during pregnancy has reduced the rate of perinatal transmission of HIV from approximately 20% to 30% to 0.1% to 0.5%. 137,138 Thus, use of combination ART drug regimens is recommended for all HIV-infected pregnant women (AI). Following delivery, in the absence of breastfeeding, considerations regarding continuation of the ARV regimen for maternal therapeutic indications are the same as those regarding ART for other non-pregnant individuals. For detailed recommendations, see the Perinatal Guidelines. 139
# Prevention of Sexual Transmission
A number of investigations, including biological, ecological and epidemiological studies and one randomized clinical trial, provide strong support for the premise that treatment of the HIV-infected individual can significantly reduce sexual transmission of HIV. Lower plasma HIV RNA levels are associated with decreases in the concentration of the virus in genital secretions. 140,141 Studies of HIV-serodiscordant heterosexual couples have demonstrated a relationship between level of plasma viremia and risk of transmission of HIV-when plasma HIV RNA levels are lower, transmission events are less common. 1,[142][143][144][145] A study conducted in KwaZulu-Natal, South Africa, used geospatial techniques to assess the relationship between ART use and HIV incidence in an observational cohort of more than 16,000 study participants living in many different communities. 146 After adjustment for sexual behavior and prevalent HIV cases, each percentage point increase in ART coverage of HIV-infected persons lowered the HIV infection risk in a community by 1.7%.
Most significantly, the multi-continental HPTN 052 trial enrolled 1,763 HIV-serodiscordant couples in which the HIV-infected partner was ART naive with a CD4 count of 350 to 550 cells/mm 3 at enrollment to compare the effect of immediate ART versus delayed therapy (not started until CD4 count <250 cells/mm 3 ) on HIV transmission to the HIV-infected partner. 2 At study entry, 97% of the participants were in heterosexual monogamous relationships. All study participants were counseled on behavioral modification and condom use. Twenty-eight linked HIV transmission events were identified during the study period, but only 1 event occurred in the early therapy arm. This 96% reduction in transmission associated with early ART was statistically significant (HR 0.04; 95% CI, 0.01-0.27; P <0.001). These results show that early ART is more effective at preventing transmission of HIV than all other behavioral and biomedical prevention interventions studied. This study, as well as other observational studies and modeling analyses showing a decreased rate of HIV transmission among serodiscordant heterosexual couples following the introduction of ART, demonstrate that suppression of viremia in ART-adherent patients with no concomitant sexually transmitted diseases (STDs) substantially reduces the risk of transmission of HIV. 3,144,145,[147][148][149] HPTN 052 was conducted in heterosexual couples and not in populations at risk of transmission via homosexual exposure or needle sharing. In addition, in this clinical trial, adherence to ART was well supported and near complete. However, the prevention benefits of effective ART observed in HPTN 052 can reasonably be presumed to apply broadly. Therefore, the Panel recommends that ART be offered to patients who are at risk of transmitting HIV to sexual partners (the strength of this recommendation varies according to mode of sexual transmission: AI for heterosexual transmission and AIII for male-to-male and other modes of sexual transmission). Clinicians should discuss with patients the potential individual and public health benefits of therapy and the need for adherence to the prescribed regimen and counsel patients that ART is not a substitute for condom use and behavioral modification and that ART does not protect against other STDs (see Preventing Secondary Transmission of HIV).
# Concerns Regarding Earlier Initiation of Therapy
Despite increasing evidence showing the benefits of earlier initiation of ART, four areas of concern remain as reasons for deferral of HIV therapy.
# ARV Drug Toxicities Have an Adverse Effect on Quality of Life and Adherence
Earlier initiation of ART extends exposure to ARV agents by several years. The D:A:D study found an increased incidence of CVD associated with cumulative exposure to some drugs in the nucleoside reverse transcriptase inhibitor and protease inhibitor (PI) drug classes. 69,150 Renal and bone health are also of concern. Aging coupled with long term use of tenofovir may increase risk of significant renal dysfunction. [151][152][153] In the SMART study, compared with interruption or deferral of therapy, continuous exposure to ART was associated with significantly greater loss of bone density. 71 There may be unknown complications related to cumulative use of ARV drugs for many decades. A list of known ARV-associated toxicities can be found in Adverse Effects of Antiretroviral Agents.
ART frequently improves quality of life for symptomatic patients. However, some side effects of ART may impair quality of life for some patients, especially those who are asymptomatic at initiation of therapy and at low risk of AIDS events. For example, efavirenz can cause neurocognitive or psychiatric side effects and PIs have been associated with gastrointestinal side effects. As noted above, some therapies may increase the risk of CVD. Patients who find that the inconvenience of taking medication every day outweighs the overall benefit of early ART may choose to delay therapy.
# ARV Non-Adherence May Have an Impact on Virologic Response.
At any CD4 count, adherence to therapy is essential to achieve viral suppression and prevent emergence of drug-resistance mutations. Several clinical, behavioral, and social factors associated with poor adherence, such as untreated major psychiatric disorders, active substance abuse, unfavorable social circumstances, patient concerns about side effects, and poor adherence to clinic visits, have been identified. Clinicians should identify areas where additional intervention is needed to improve adherence both before and after initiation of therapy. Some strategies to improve adherence are discussed in Adherence to Antiretroviral Therapy.
# Earlier Development of Resistance may Reduce Future Therapeutic Options.
Non-adherence and subsequent virologic failure may promote emergence of drug resistance mutations and limit subsequent treatment options. Despite concerns about the development of resistance to ARV drugs, the evidence thus far indicates that resistance occurs more frequently in individuals who initiate therapy later in the course of infection than in those who initiate ART earlier. 154 Furthermore, recent data have indicated a slight increase in the prevalence of 2-drug class resistance from 2000 to 2005. 155 Cost may be a Barrier to Early Initiation of Therapy.
In resource-rich countries, the cost of ART exceeds $10,000 per year (see Cost Considerations and Antiretroviral Therapy). Several modeling studies support the cost effectiveness of HIV therapy initiated soon after diagnosis. [156][157][158] One study reported that the annual cost of care is 2.5 times higher for patients with CD4 counts <50 cells/mm 3 than for patients with CD4 counts >350 cells/mm 3 . 159 Much of the health care expenditure in patients with advanced infection is from non-ARV drugs and hospitalization. However, there are no comparisons of the cost of earlier ART initiation (i.e., CD4 count 350-500 cells/mm 3 ) versus later initiation (i.e., CD4 count >500 cells/ mm 3 ). As generic formulations for more ARV drugs become available in the next several years, the cost of ART may decline. However, despite any significant cost savings, decisions regarding which ARVs to select for system-wide HIV programs must be based on rigorous costeffectiveness assessments (see Cost section). 160
# Conditions Favoring More Urgent Initiation of Therapy
Several conditions increase the urgency for therapy, including:
• Pregnancy (AI). Clinicians should refer to the Perinatal Guidelines for more detailed recommendations on the management of HIV-infected pregnant women. 139
• AIDS-defining conditions, including HAD (AI)
• Acute OIs (see discussion below)
• Lower CD4 counts (e.g., <200 cells/mm 3 ) (AI)
• HIVAN (AII)
• Acute/Early Infection (BII). See more discussion in the Acute/Early Infection section.
• HIV/HBV coinfection (AII)
• HIV/HCV coinfection (BII)
• Rapidly declining CD4 counts (e.g., >100 cells/mm 3 decrease per year) (AIII)
• Higher viral loads (e.g., >100,000 copies/mL) (BII)
# Acute Opportunistic Infections
In patients who have opportunistic diseases for which no effective therapy exists (e.g., cryptosporidiosis, microsporidiosis, progressive multifocal leukoencephalopathy), but in whom ART may improve outcomes by improving immune responses, treatment should be started as soon as possible (AIII). For patients with mild to moderate cutaneous Kaposi's sarcoma (KS), prompt initiation of ART alone without chemotherapy has been associated with improvement of the KS lesions, even though initial transient progression of KS lesion as a manifestation of immune reconstitution inflammatory syndrome (IRIS) can also occur. 161 In the setting of some OIs, such as cryptococcal meningitis, for which immediate therapy may increase the risk of serious immune reconstitution inflammatory syndrome (IRIS), a short delay before initiating ART may be warranted. [162][163][164] In the setting of other OIs, such as Pneumocystis jirovecii pneumonia, early initiation of ART is associated with increased survival; 10 therefore, therapy should not be delayed (AI).
In patients who have active TB, initiating ART during treatment for TB confers a significant survival advantage; [165][166][167][168][169] therefore, ART should be initiated as recommended in Mycobacterium Tuberculosis Disease with HIV Coinfection.
Clinicians should refer to the Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents 161 for more detailed discussion on when to initiate ART in the setting of a specific OI.
# Conditions Where Deferral of Therapy May be Considered
Some patients and their clinicians may decide to defer therapy on the basis of clinical or personal circumstances. Deferring therapy for the reasons discussed below may be reasonable in patients with high CD4 counts (e.g., >500 cells/mm 3 ), but deferring therapy in patients with much lower CD4 counts (e.g., <200 cells/mm 3 ) should be considered only in rare situations and should be undertaken with close clinical follow-up. Briefly delaying therapy to allow a patient more time to prepare for lifelong treatment may be considered.
# When There are Significant Barriers to Adherence
Also see Adherence to Antiretroviral Therapy.
In patients with higher CD4 counts who are at risk of poor adherence, it may be prudent to defer treatment while addressing the barriers to adherence. However, in patients with conditions that require urgent initiation of ART (see above), therapy should be started while simultaneously addressing the barriers to adherence.
Several methods are available to assess adherence. When the most feasible measure of adherence is selfreport, this assessment should be completed at each clinic visit using one of the available reliable and valid instruments. 170,171 If other objective measures (e.g., pharmacy refill data, pill count) are available, these methods should be used to assess adherence at each follow-up visit. [172][173][174] Continual assessment and counseling allow the clinician to intervene early to address barriers to adherence occurring at any point during treatment (see Adherence to Antiretroviral Therapy).
# Presence of Comorbidities that Complicate or Prohibit Antiretroviral Therapy
Deferral of ART may be considered when either the treatment or manifestations of other medical conditions may complicate the treatment of HIV infection or vice versa. Examples include:
• Surgery that may result in an extended interruption of ART
• Treatment with medications that have clinically significant drug interactions with ART and for which alternative medications are not available
In each of these circumstances, the assumption is that the situation is temporary and that ART will be initiated after the conflicting condition has resolved.
There are some less common situations that preclude ART at any time while CD4 counts remain high. In particular, such situations include that of patients who have a poor prognosis because of a concomitant medical condition and are not expected to gain survival or quality-of-life benefits from ART. Examples include patients with incurable non-HIV-related malignancies or end-stage liver disease who are not being considered for liver transplantation. In this setting, deciding to forgo ART may be easier in patients with higher CD4 counts who are likely asymptomatic for HIV and in whom ART is unlikely to prolong survival. However, it should be noted that ART may improve outcomes, including survival, in patients with some HIV-associated malignancies (e.g., lymphoma, Kaposi sarcoma) and in patients with liver disease due to chronic HBV or HCV.
# Long-term Non-Progressors and Elite HIV Controllers
A small subset of HIV-infected individuals (~3% to 5%) can maintain normal CD4 counts for many years without treatment (long-term non-progressors), and an even smaller subset (~1%) can maintain low to undetectable HIV RNA levels for years (elite controllers). 175,176 Although there is significant overlap in these clinical phenotypes, many long-term non-progressors have detectable viremia and some controllers progress immunologically and clinically despite having no detectable viremia.
There are limited data on how to manage these individuals. Given potential harm associated with uncontrolled HIV replication, many of the preceding arguments for early therapy likely apply to nonprogressors who have consistently detectable viremia (i.e., HIV RNA >200 to 1000 copies/mL). Given that ongoing HIV replication occurs even in controllers, ART is also recommended for those rare controllers with evidence of disease progression, as defined by declining CD4 counts or development of HIV-related complications (AII). The Panel has no recommendations on managing controllers with high CD4 counts, although the fact that ART reduces the level of inflammation in this setting suggests that treatment may be beneficial. 177
# The Need for Early Diagnosis of HIV
Fundamental to the earlier initiation of ART recommended in these guidelines is the assumption that patients will be diagnosed early in the course of HIV infection, making earlier initiation of therapy an option. Unfortunately, most HIV-infections are diagnosed at later stages of disease, [178][179][180][181] although in recent years, HIV is increasingly being detected earlier. 4 Despite the recommendations for routine, opt-out HIV screening in the health care setting regardless of perceptions about a patient's risk of infection, 182 the median CD4 count of newly diagnosed patients remains below 350 cells/mm 3 , although this number is increasing. 4 Diagnosis of HIV infection is delayed more often in nonwhites, IDUs, and older patients than in other populations, and many individuals in these groups develop AIDS-defining illnesses within 1 year of diagnosis. [178][179][180][181] Therefore, to ensure that the current treatment guidelines have maximum impact, routine HIV screening per current CDC recommendations is essential. It is also critical that all newly diagnosed patients are educated about HIV disease and linked to care for full evaluation, follow-up, and management. Once patients are in care, focused effort is required to retain them in the health care system so that both the infected individuals and their sexual partners can fully benefit from early diagnosis and treatment.
# Conclusion
The current recommendations are based on growing evidence supporting earlier initiation of ART and the lack of demonstrable harm in starting therapy earlier. The strength of each recommendation varies according to the quality and availability of existing evidence supporting the recommendation. In addition to the benefit of earlier initiation of therapy for the health of the HIV-infected individual, the reduction in sexual transmission to HIV-uninfected individuals provides further reason for earlier initiation of ART. The Panel will continue to monitor and assess the results of ongoing and planned randomized clinical trials and observational studies, which will provide information to guide future Panel recommendations.
# Introduction
More than 25 antiretroviral (ARV) drugs in 6 mechanistic classes are Food and Drug Administration (FDA) approved for treatment of HIV infection. These six classes include the nucleoside/nucleotide reverse transcriptase inhibitors (NRTIs), non-nucleoside reverse transcriptase inhibitors (NNRTIs), protease inhibitors (PIs), a fusion inhibitor (FI), a CCR5 antagonist, and integrase strand transfer inhibitors (INSTIs).
In addition, two drugs (pharmacokinetic [PK] enhancers or boosters) are used solely to improve the pharmacokinetic profiles of some ARV drugs (e.g., PIs and the INSTI elvitegravir [EVG]).
The initial ARV regimen for a treatment-naive patient generally consists of two NRTIs, usually abacavir plus lamivudine (ABC/3TC) or tenofovir disoproxil fumarate plus emtricitabine (TDF/FTC), plus a drug from one of three drug classes: an INSTI, an NNRTI, or a PK-enhanced PI. As shown in clinical trials and by retrospective evaluation of cohorts of patients in clinical care, this strategy for initial treatment has resulted in HIV RNA decreases and CD4 T lymphocyte (CD4) cell increases in most patients. [1][2][3]
# Data Used for Making Recommendations
The Panel on Antiretroviral Guidelines for Adults and Adolescents (the Panel)'s recommendations are primarily based on clinical trial data published in peer-reviewed journals and data prepared by manufacturers for FDA review. In select cases, the Panel considers data presented in abstract format at major scientific meetings. The Panel's first criterion for selection of evidence on which to base recommendations is published information from a randomized, prospective clinical trial with an adequate sample size that demonstrates that an ARV regimen has shown high rates of viral suppression, increased CD4 cell count, and has a favorable
# Panel's Recommendations
• An antiretroviral regimen for a treatment-naive patient generally consists of two nucleoside reverse transcriptase inhibitors in combination with a third active antiretroviral drug from one of three drug classes: an integrase strand transfer inhibitor, a nonnucleoside reverse transcriptase inhibitor, or a protease inhibitor with a pharmacokinetic enhancer (cobicistat or ritonavir).
• • On the basis of individual patient characteristics and needs, an Alternative regimen or; less frequently, an Other regimen; may in some instances be the optimal regimen for a patient. A list of Alternative and Other regimens can be found in Table 6.
• Given the large number of excellent options for initial therapy, selection of a regimen for a particular patient should be guided by factors such as virologic efficacy, toxicity, pill burden, dosing frequency, drug-drug interaction potential, resistance testing results, comorbid conditions, and cost. Table 7 provides guidance on choosing an antiretroviral regimen based on selected clinical case scenarios. Table 8 highlights the advantages and disadvantages of different components in a regimen.
# Rating of Recommendations: A = Strong; B = Moderate; C = Optional
# Rating of Evidence: I = Data from randomized controlled trials; II = Data from well-designed nonrandomized trials or observational cohort studies with long-term clinical outcomes; III = Expert Opinion
a Lamivudine may substitute for emtricitabine or vice versa.
Downloaded from http://aidsinfo.nih.gov/guidelines on 9/16/2015
Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents F-2 safety profile. Comparative clinical trials of initial treatments generally show no significant differences in HIV-related clinical endpoints or survival. Thus, assessment of regimen efficacy and safety are primarily based on surrogate marker endpoints (especially rates of HIV RNA suppression) and the incidence and severity of adverse events. When developing recommendations, the Panel also considers post-marketing safety data, observational cohort data published in peer-reviewed publications, and the experience of clinicians and community members who are actively engaged in patient care.
The Panel reviewed the available data to arrive at Recommended, Alternative, or Other regimens, as specified in Table 6. Each of the regimens listed in Table 6 has shown potent virologic efficacy as measured by the proportion of participants in comparative clinical trials able to achieve and maintain viral suppression.
Recommended regimens are those studied in randomized controlled trials and shown to have optimal and durable virologic efficacy, favorable tolerability and toxicity profiles, and ease of use. Alternative regimens are those that are effective but have potential disadvantages, limitations for use in certain patient population, or less supporting data than Recommended regimens. In certain situations, depending on individual patient characteristics and needs, an Alternative regimen may actually be the optimal regimen for a specific patient. Some regimens are classified as Other regimens because, compared with Recommended or Alternative regimens, they have reduced virologic activity, limited supporting data from large comparative clinical trials, or other factors such as greater toxicities, higher pill burden, drug interaction potential, or limitations for use in certain patient populations.
In addition to Table 6, a number of tables presented below and at the end of the guidelines provide clinicians with guidance on selecting and prescribing an optimal regimen for an individual patient. Table 7 lists specific case scenarios to guide regimen selection for patients with common clinical conditions. Table 8 lists the potential advantages and disadvantages of the components used in Recommended and Alternative regimens. Table 9 lists agents or regimens not recommended for initial treatment. Appendix B, Tables 1-6 lists characteristics of individual ARV agents, such as formulations, dosing recommendations, PKs, and common adverse effects. Appendix B, Table 7 provides ARV dosing recommendations for patients who have renal or hepatic insufficiency.
# Changes Since the Last Revision of the Guidelines
Since the last revision of these guidelines, new data from clinical trials and cohort studies, as well as experience in clinical practice, have prompted significant changes to the list of Recommended, Alternative, and Other regimens for treatment-naive patients (Table 6). Among these changes, the following deserve emphasis:
• There are now five Recommended regimens for antiretroviral therapy (ART)-naive patients: four INSTIbased regimens and one ritonavir-boosted PI (PI/r)-based regimen.
• Results from a large comparative clinical trial comparing atazanavir/ritonavir (ATV/r) plus TDF/FTC to darunavir/ritonavir (DRV/r) or raltegravir (RAL) plus TDF/FTC showed a greater rate of toxicitiesrelated discontinuation in the ATV/r arm. 4 Therefore, ATV/r plus TDF/FTC has been moved from the Recommended to the Alternative category.
• The Panel has also moved EFV/TDF/FTC from the Recommended to the Alternative category because of concerns about the tolerability of efavirenz (EFV) in clinical trials and practice, especially the high rate of central nervous system (CNS) related toxicities, and a possible association with suicidality observed in one analysis of four clinical trials. 5 • Regimens that were previously listed as Recommended for patients with baseline HIV RNA <100,000 copies/mL or CD4 count >200 cells/mm 3 are now in the Alternative or Other category, with the same caveat to limit their use to patients with the cited HIV RNA and CD4 levels.
• Two regimens that use fewer than two NRTIs (DRV/r plus RAL and lopinavir/ritonavir [LPV/r] plus 3TC) are listed among the Other regimens, with the caveat that their use be limited to patients who cannot take either TDF or ABC.
Downloaded from http://aidsinfo.nih.gov/guidelines on 9/16/2015
Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents F-3
• Coformulations of ATV and DRV with the PK enhancer cobicistat (COBI) have been added to the Alternative regimen options. An ARV regimen generally consists of two NRTIs (one of which is FTC or 3TC) plus an INSTI, NNRTI, or PKenhanced PI. Selection of a regimen should be individualized on the basis of virologic efficacy, potential adverse effects, pill burden, dosing frequency, drug-drug interaction potential, a patient's resistance test results and comorbid conditions, and cost. Table 7 lists specific case scenarios to guide regimen selection for patients with common clinical conditions. For more detailed recommendations on ARV choices and dosing in HIV-infected pregnant women, refer to the latest perinatal guidelines available at http://aidsinfo.nih.gov/guidelines.
# Recommended Regimen Options
(Drug classes and regimens within each class are arranged in alphabetical order.)
INSTI-Based Regimens:
• DTG/ABC/3TC a -only for patients who are HLA-B*5701 negative (AI)
• DTG plus TDF/FTC a (AI)
• EVG/c/TDF/FTC-only for patients with pre-treatment estimated CrCl ≥70 mL/min (AI)
• RAL plus TDF/FTC a (AI)
PI-Based Regimens:
• DRV/r plus TDF/FTC a (AI)
# Alternative Regimen Options
(Drug classes and regimens within each class are arranged in alphabetical order.)
Regimens that are effective and tolerable, but that have potential disadvantages when compared with the recommended regimens listed above, have limitations for use in certain patient population, or have less supporting data from randomized clinical trials. An alternative regimen may be the preferred regimen for some patients.
# NNRTI-Based Regimens:
• EFV/TDF/FTC a (BI)
• RPV/TDF/FTC a -only for patients with pre-treatment HIV RNA <100,000 copies/mL and CD4 cell count >200 cells/mm 3 (BI) PI-Based Regimens:
• ATV/c plus TDF/FTC a -only for patients with pre-treatment estimated CrCl ≥70 mL/min (BI)
• ATV/r plus TDF/FTC a (BI)
# Other Regimen Options
(Drugs classes and regimens within each class are arranged in alphabetical order.)
Regimens that, in comparison with Recommended and Alternative regimens, may have reduced virologic activity, limited supporting data from large comparative clinical trials, or other factors such as greater toxicities, higher pill burden, drug interaction potential, or limitations for use in certain patient populations.
# INSTI-Based Regimen:
• RAL plus ABC/3TC a -only for patients who are HLA-B*5701 negative (CII) NNRTI-Based Regimen:
• EFV plus ABC/3TC a -only for patients who are HLA-B*5701 negative and with pre-treatment HIV RNA <100,000 copies/mL (CI)
PI-Based Regimens:
• (ATV/c or ATV/r) plus ABC/3TC a -only for patients who are HLA-B*5701 negative and with pre-treatment HIV RNA <100,000 copies/mL (CIII for ATV/c and CI for ATV/r)
• LPV/r (once b or twice daily) plus ABC/3TC a -only for patients who are HLA-B*5701 negative (CI)
• LPV/r (once b or twice daily) plus TDF/FTC a (CI)
Other Regimens When TDF or ABC Cannot be Used:
• DRV/r plus RAL-only for patients with pre-treatment HIV RNA <100,000 copies/mL and CD4 cell count >200 cells/mm 3 (CI)
• LPV/r (twice daily) plus 3TC (twice daily) (CI) In some situations, an NNRTI-based regimen may be a better choice for a particular patient. Table 7 provides guidance on regimen selection based on various patient-and regimenspecific characteristics.
# Rating of Recommendations
# Other Regimen Options
Regimens that, in comparison with Recommended and Alternative regimens, may have reduced virologic activity, limited supporting data from large comparative clinical trials, or other factors such as greater toxicities, higher pill burden, drug interaction potential, or limitations for use in certain patient populations.
# Factors to Consider When Selecting an Initial Regimen
When selecting a regimen for an individual patient, a number of patient and regimen specific characteristics should be considered, with the goal of providing a potent, safe, tolerable, and easy to adhere to regimen for the patient in order to achieve sustained virologic control. Some of the factors can be grouped into the following categories: This table is designed to guide clinicians in choosing an initial ARV regimen according to various patient and regimen characteristics and specific clinical scenarios. When more than one scenario applies to a patient, clinicians should review considerations for each relevant scenario and use their clinical judgment to select the most appropriate regimen. This table is intended to guide the initial choice of regimen. However, if a patient is doing well on a particular regimen, it is not necessary to switch to another regimen based on the scenarios outlined in this table.
Please see Table 8 for additional information regarding the advantages and disadvantages of particular ARV medications.
# Pre-ART Characteristics
CD4 count <200 cells/mm 3 Do Not Use the Following Regimens:
•
# ART Specific Characteristics
One pill once daily regimen desired ART Options Include:
• DTG/ABC/3TC
• EFV/TDF/FTC
• EVG/c/TDF/FTC
• RPV/TDF/FTC (if HIV RNA <100,000 copies/mL and CD4 count >200/mm 3 )
# Available as fixed-dose combination tablets
Food effects Regimens that Should be Taken with Food:
• ATV/r or ATV/c-based regimens
# HCV treatment required
Refer to recommendations in the HIV/HCV co-infection section.
# TB infection
If Rifampin is Used:
• EFV-based regimens have the least drugdrug interactions.
• If RAL is used, increase RAL dose to 800 mg BID.
• Use DTG at 50 mg BID dose only in patients without selected INSTI mutations (refer to product label).
If using a PI-based regimen, rifabutin should be used in place of rifampin in the TB regimen.
•
# Choosing Between an Integrase Strand Transfer Inhibitor-, A Non-Nucleoside Reverse Transcriptase Inhibitor-, or A Protease Inhibitor-Based Regimen
The choice between an INSTI, NNRTI, or PI as the third drug in an initial ARV regimen should be guided by the regimen's efficacy, genetic barrier to resistance, adverse effects profile, and convenience; the patient's comorbidities; and concomitant medications and the potential for drug-drug interactions (See Tables 7 and 8 showed that ATV/r had a higher rate of adverse effect-associated drug discontinuation with than the comparators (DRV/r and RAL). Thus, despite these favorable attributes, based on the above considerations, EFV-, RPV-, and ATV/r-containing regimens are no longer Recommended Regimens as initial therapy in all patients, and are listed as Alternatives. However, based on individual patient characteristics, some Alternative regimens may actually be the optimal regimen for some patients. Furthermore, patients who are doing well on EFV-, RPV-, and ATV/r-containing regimens should not necessarily be switched to other agents.
# Choosing Among Different Drugs from an Antiretroviral Drug Class
The sections below provides clinicians with comparisons of different currently recommended ARV drugs within a drug class, including information related to the safety and virologic efficacy of different drugs based on clinical trial results and/or post-marketing data, special considerations to take into account, and the rationales for the Panel's recommendations.
# Dual-Nucleoside Reverse Transcriptase Inhibitor Options A Part of Initial Combination Therapy
# Summary
TDF/FTC and ABC/3TC are NRTI combinations commonly used for initial therapy. Table 6 provides recommendations and ratings for the individual regimens. These recommendations are based on the virologic potency and durability, short-and long-term toxicity, and dosing convenience of these drugs.
# Clinical Trials Comparing Abacavir/Lamivudine to Tenofovir/Emtricitabine
Several randomized controlled trials in ART-naive participants compared ABC/3TC to TDF/FTC, each with the same [7][8][9] or a different third ARV drug (also see discussion in the DTG section). 10 • The ACTG 5202 study, a randomized controlled trial in more than 1,800 participants, evaluated the efficacy and safety of ABC/3TC and TDF/FTC when each used in combination with either EFV or ATV/r.
• Treatment randomization was stratified on the basis of a screening HIV RNA level <100,000 copies/mL or ≥100,000 copies/mL. HLA B*5701 testing was not required before study entry.
• A Data Safety Monitoring Board recommended early termination of the ≥100,000 copies/mL stratification group because of a significantly shorter time to study-defined virologic failure in the ABC/3TC arm than in the TDF/FTC arm. 7 This difference in time to virologic failure between the arms was observed regardless of whether the third active drug was EFV or ATV/r.
• There was no difference between ABC/3TC and TDF/FTC in time to virologic failure for participants who had plasma HIV RNA <100,000 copies/mL at screening. 11 • The ASSERT study compared open label ABC/3TC with TDF/FTC in 385 HLA B*5701-negative, ARTnaive patients; all participants also received EFV. The primary study endpoint was renal safety of the regimens. At week 48, the proportion of participants with HIV RNA <50 copies/mL was lower among ABC/3TC-treated participants than among TDF/FTC-treated participants. 8 • In the HEAT study, 688 participants received ABC/3TC or TDF/FTC in combination with once-daily LPV/r. Virologic efficacy was similar in the two study arms. In a subgroup analysis of patients with baseline HIV RNA ≥100,000 copies/mL, the proportion of participants who achieved HIV RNA <50 copies/mL at 96 weeks did not differ between the two regimens. 9
# Dual-Nucleoside Reverse Transcriptase Inhibitor Choices
Note: In alphabetical order.
# Abacavir/Lamivudine
ABC plus 3TC has been studied in combination with EFV, several PIs, and DTG in ART-naive patients. 10,[12][13][14] Adverse Effects:
Hypersensitivity Reactions:
• Clinically suspected hypersensitivity reactions (HSRs) were observed in 5% to 8% of individuals who started ABC in clinical trials conducted before the use of HLA-B*5701 testing. The risk of HSRs is highly associated with the presence of the HLA-B*5701 allele. 15,16 Cardiovascular Risk:
• An association between ABC use and myocardial infarction (MI) was first reported in the D:A:D study. This large, multinational observational study group found that recent (within 6 months) or current use of ABC was associated with an increased risk of MI, particularly in participants with pre-existing cardiac risk factors. 17,18 • Since the D:A:D report, several studies have evaluated the relationship between ABC therapy and cardiovascular events. Some studies have found an association; [19][20][21][22] others, including an FDA metaanalysis of 26 randomized clinical trials that evaluated ABC, have not. [23][24][25][26][27] • No consensus has been reached on the association between ABC use and MI risk or the mechanism for such an association.
Other Factors and Considerations:
• ABC/3TC is available as a co-formulated tablet and as a coformulated single-tablet regimen with DTG.
• ABC and 3TC are available separately in generic tablet formulations. • ABC does not cause renal dysfunction and is an option for TDF in patients with underlying renal dysfunction or who are at risk for renal effects. No dosage adjustment is required in patients with renal dysfunction.
Panel's Recommendations:
• ABC should only be prescribed for patients who are HLA B*5701 negative.
• On the basis of clinical trial safety and efficacy data, experience in clinical practice, and the availability of ABC/3TC as a component of co-formulated products, the Panel classifies ABC/3TC plus DTG as a Recommended regimen (AI) (see discussion regarding DTG in this section regarding the clinical efficacy data for ABC/3TC plus DTG) .
• ABC/3TC use with EFV, ATV/r, or ATV/c is only recommended for patients with pre-treatment HIV RNA <100,000 copies/mL.
• ABC/3TC is a part of several Alternative or Other regimens when combined with another ARV drug. See Table 6 for more detailed recommendations on use of ABC/3TC with other drugs.
• ABC should be used with caution or avoided in patients with known high cardiovascular risk.
# Tenofovir/Emtricitabine
TDF, with either 3TC or FTC, has been studied in combination with EFV, RPV, several boosted PIs, EVG/c, RAL, and DTG in randomized clinical trials. [28][29][30][31][32][33][34][35][36][37] Adverse Effects:
• New onset or worsening renal impairment has been associated with TDF use. 38,39 Risk factors may include advanced HIV disease; longer treatment history; low body weight, especially in females; 40 and pre-existing renal impairment. 41 • Concomitant use of a PK-enhanced regimen (with a PI or EVG) can increase TDF concentrations; studies have suggested a greater risk of renal dysfunction when TDF is used in these regimens. 39,[42][43][44][45][46] • While initiation of all NRTI-containing regimens has been associated with a decrease in bone mineral density (BMD), the loss of BMD is greater with TDF-containing regimens. For example, in two randomized studies comparing TDF/FTC with ABC/3TC, participants receiving TDF/FTC experienced a significantly greater decline in bone mineral density than ABC/3TC-treated participants. 47,48 Following an early decline after ART initiation, BMD generally stabilizes.
• Cases of osteomalacia associated with proximal renal tubulopathy have been reported with the use of TDF. 49 Other Factors and Considerations:
• TDF/FTC is available in fixed-dose drug combinations with EFV, EVG/c, and RPV, allowing the regimens to be administered as a single pill, given once daily.
• Renal function, urine glucose, and urine protein should be assessed before initiating treatment with TDF and periodically during treatment (see Laboratory Monitoring section). In patients who have pre-existing renal insufficiency (CrCl <60 mL/min), 50 TDF should generally be avoided. If TDF is used, dosage adjustment is required if the patient's CrCl falls below 50 mL/min (see Appendix B, Table 7 for dosage recommendations).
• Both TDF and FTC are active against HBV. In patients with HIV/HBV coinfection, TDF/FTC should be used as the NRTI pair of the ART regimen because the drugs have activity against both viruses (also see HIV/HBV Coinfection section). • The FLAMINGO study, a randomized open-label clinical trial, compared DTG 50 mg once daily to DRV/r 800 mg/100 mg once daily, each in combination with investigator-selected ABC/3TC or TDF/FTC. At week 48, DTG was superior to DRV/r because of the higher rate of discontinuation in the DRV/r arm. 6,52 The difference in response rates favoring DTG was greater in patients with pre-treatment HIV RNA levels >100,000 copies/mL. At week 96, DTG remained superior to DRV/r. 53 Adverse Effects:
• DTG is generally well tolerated. The most common adverse reactions of moderate to severe intensity with an incidence ≥2% in the clinical trials were insomnia and headache. Cases of hypersensitivity reactions were reported in <1% of trial participants.
Other Factors and Considerations:
• In treatment-naive patients, DTG is given once daily, with or without food. • DTG decreases tubular secretion of creatinine without affecting glomerular function, with increases in serum creatinine observed within the first 4 weeks of treatment (mean increase in serum creatinine was 0.11 mg/dL after 48 weeks).
• DTG has few drug interactions. DTG increases metformin levels approximately two-fold; close monitoring for metformin adverse effects is advisable. Rifampin decreases DTG levels, therefore, an increase in dosing of DTG to 50 mg twice daily is required.
• DTG absorption may be reduced when the ARV is coadministered with polyvalent cations (see Drug Interaction section). DTG should be taken at least 2 hours before or 6 hours after cation-containing antacids or laxatives. Alternatively, DTG and supplements containing calcium or iron can be taken simultaneously with food.
• Treatment-emergent mutations that confer DTG resistance have not been reported in patients receiving DTG for initial therapy, which suggests that DTG has a higher genetic barrier to resistance than other INSTIs.
Panel's Recommendation:
• On the basis of clinical trial data, the Panel categorizes DTG in combination with either ABC/3TC or TDF/FTC as a Recommended regimen in ART-naive patients (AI).
# Elvitegravir
EVG is available as a component of a four-drug, fixed-dose combination product containing EVG, COBI, TDF, and FTC (EVG/c/TDF/FTC). COBI is a specific, potent CYP3A inhibitor that has no activity against HIV. It acts as a PK enhancer of EVG, which allows for once daily dosing of the combination.
Efficacy in Clinical Trials:
The efficacy of EVG/c/TDF/FTC in ARV-naive participants has been evaluated in two randomized, doubleblind active-controlled trials.
• At 144 weeks, EVG/c/TDF/FTC was non-inferior to fixed-dose EFV/TDF/FTC. 54 • EVG/c/TDF/FTC was also found to be non-inferior to a combination containing ATV/r plus TDF/FTC. 55 Adverse Effects:
• The most common adverse events reported with EVG/c/TDF/FTC were diarrhea, nausea, upper respiratory infection, and headache. 54,55 Other Factors and Considerations:
• EVG is metabolized primarily by CYP3A enzymes; as a result, CYP3A inducers or inhibitors may alter EVG concentrations.
• Because COBI inhibits CYP3A, it interacts with a number of medications that are metabolized by this enzyme (see Drug-Drug Interactions section). 56 • EVG plasma concentrations are lower when the ARV is administered simultaneously with polyvalent cation-containing antacids or supplements (see Drug Interaction section). Separate EVG/cobi/TDF/FTC and polyvalent antacid administration by at least 2 hours; administer polyvalent cation-containing supplements at least 2 hours before or 6 hours after EVG dosing.
• COBI inhibits active tubular secretion of creatinine, resulting in increases in serum creatinine and a reduction in estimated CrCl without reducing glomerular function. 57 Patients with a confirmed increase in serum creatinine greater than 0.4 mg/dL from baseline while taking EVG/c/TDF/FTC should be closely monitored and evaluated for evidence of TDF-related proximal renal tubulopathy. 46 • EVG/c/TDF/FTC is not recommended for patients with pre-treatment estimated CrCl <70 mL/min. 46 • At the time of virologic failure, INSTI-associated mutations were detected in some EVG/c/TDF/FTCtreated patients whose therapy failed. 54,55 These mutations conferred cross-resistance to RAL, with most retaining susceptibility to DTG.
Panel's Recommendation:
• On the basis of the above factors, the Panel classifies EVG/c/FTC/TDF as a Recommended regimen in ART-naive patients (AI).
# Raltegravir
RAL was the first INSTI approved for use in both ARV-naive and ARV-experienced patients.
Efficacy in Clinical Trials:
The efficacy of RAL (with either TDF/FTC or ABC/3TC) as initial therapy has been evaluated in two randomized, double-blinded, controlled clinical trials, and a third open-label randomized trial.
• STARTMRK compared RAL 400 mg twice daily to EFV 600 mg once daily, each in combination with TDF/FTC. RAL was non-inferior to EFV at 48 weeks. 33 RAL was superior to EFV at 4 and 5 years, 36,58 in part because of more frequent discontinuations due to adverse events in the EFV group than in the RAL group.
• The SPRING-2 trial compared DTG 50 mg once daily to RAL 400 mg twice daily, each in combination with investigator-selected ABC/3TC or TDF/FTC. At week 96, DTG was non-inferior to RAL.
• The SPRING-2 trial also provided non-randomized data on the efficacy of RAL plus ABC/3TC. In this trial, 164 participants (39 and 125 with baseline viral loads ≥100,000 copies/mL and <100,000 copies/mL, respectively) received RAL in combination with ABC/3TC. After 96 weeks, there was no difference in virologic response between the ABC/3TC and TDF/FTC groups when RAL was given as the third drug. 37 • ACTG A5257, a large randomized open-label trial, compared 3 NNRTI-sparing regimens containing RAL, ATV/r, or DRV/r, each given with TDF/FTC. At week 96, all 3 regimens had similar virologic efficacy, but RAL was superior to both ATV/r and DRV/r for the combined endpoints of virologic efficacy and tolerability. Lipids increased more in participants in the PI/r arms than in the RAL arm, and bone mineral density decreased to a greater extent in participants in the PI/r arms than in participants in the RAL arm. 4 Adverse Effects:
• RAL use has been associated with creatine kinase elevations. Myositis and rhabdomyolysis have been reported.
• Rare cases of severe skin reactions and systemic hypersensitivity reactions in patients who received RAL have been reported during post-marketing surveillance. 59 Other Factors and Considerations:
• RAL must be administered twice daily-a potential disadvantage when comparing RAL-based treatment with other Recommended regimens.
• Coadministration of RAL with aluminum and/or magnesium-containing antacids can reduce absorption of RAL and is not recommended. Raltegravir may be coadministered with calcium carbonate-containing antacids. Polyvalent cation-containing supplements may also reduce absorption of RAL; thus, RAL should be given at least 2 hours before or 6 hours after cation-containing supplements.
• RAL has a lower genetic barrier to resistance than RTV-boosted PIs and DTG.
Panel's Recommendations:
• On the basis of these data and long-term clinical experience with RAL, the Panel considers RAL plus TDF/FTC as a Recommended regimen in ARV-naive patients (AI).
# Efavirenz
EFV is an NNRTI approved for use in combination with 2-NRTIs for ART-naive patients.
# Efficacy in Clinical Trials:
Large randomized, controlled trials and cohort studies in ART-naive patients have demonstrated potent and durable viral suppression in patients treated with EFV plus two NRTIs. In clinical trials, EFV-based regimens in ART-naive patients have demonstrated superiority or non-inferiority to several comparator regimens.
• In ACTG 5142, EFV was superior to LPV/r, although drug resistance was more common after EFV failure than after LPV/r failure. 63 • In the 2NN study, compared to EFV, NVP did not meet non-inferiority criteria. 64 • In ACTG 5202, EFV was comparable to ATV/r when each was given with either TDF/FTC or ABC/3TC. 65 • In the ECHO and THRIVE studies, EFV was non-inferior to RPV, with less virologic failure but more discontinuations due to adverse events. The virologic advantage of EFV was most notable in participants with pre-ART viral loads >100,000 copies/mL, and NRTI and NNRTI resistance was more frequent with RPV failure. 66 • In the GS 102 study, EFV/TDF/FTC was non-inferior to EVG/c/TDF/FTC. 54 More recently, some regimens have demonstrated superiority to EFV, based primarily on fewer discontinuations because of adverse events:
• In the SINGLE trial, a DTG-based regimen was superior to EFV at the primary endpoint of viral suppression at Week 48. 10 • In the STARTMRK trial, RAL was non-inferior to EFV at 48 weeks. 33 5 years, 36,58 in part because of more frequent discontinuations due to adverse events in the EFV group than in the RAL group.
• In the open-label STaR trial, participants with baseline viral loads ≤100,000 copies/mL had higher rates of treatment success on RPV than on EFV. 67 A recent multinational randomized placebo-controlled trial compared two once daily doses of EFV (combined with TDF/FTC): EFV 600 mg (standard dose) versus EFV 400 mg (reduced dose). At 48 weeks, EFV 400 mg was non-inferior to EFV 600 mg for rate of viral suppression. 68 Study drug-related adverse events were less frequent in the EFV 400 mg group than in the 600 mg group. Although there were fewer self-reported CNS events in the 400 mg group, the two groups had similar rates of psychiatric events. Unlike the 600 mg dose of EFV, the 400 mg dose is not approved for initial treatment and is not co-formulated as a component of a single pill regimen.
Adverse Effects:
• EFV can cause CNS side effects, such as abnormal dreams, dizziness, headache, and depression, which resolve over a period of days to weeks in most patients. However, more subtle, long-term neuropsychiatric effects can occur. A recent analysis of 4 AIDS Clinical Trial Group (ACTG) comparative trials showed a higher rate of suicidality (i.e., reported suicidal ideation or attempted or completed suicide) among EFV-treated patients than among patients taking comparator regimens. 5 This association, however, was not found in analyses of two large observational cohorts. 69,70 • EFV may cause elevation in LDL cholesterol and triglycerides.
Other Factors and Considerations:
• EFV is formulated both as a single-drug tablet and in a fixed-dose combination tablet of EFV/TDF/FTC that allows for once daily dosing.
• EFV is a substrate of CYP3A4 and an inducer of CYP3A4 and 2D6 and therefore may potentially interact with other drugs using the same pathways.
• EFV has been associated with CNS birth defects in non-human primates, and cases of neural tube defects have been reported after first trimester exposure in humans. 71 Alternative regimens should be considered in women who are planning to become pregnant or who are sexually active and not using effective contraception. Because the risk of neural tube defects is restricted to the first 5 to 6 weeks of pregnancy, before pregnancy is usually recognized, a suppressive EFV-based regimen can be continued in pregnant women who present for antenatal care in the first trimester, or may be initiated after the first trimester (see Perinatal Guidelines).
Panel's Recommendations:
• Given the availability of regimens with fewer treatment-limiting adverse events with non-inferior or superior efficacy, the Panel classifies EFV/TDF/FTC as an Alternative regimen for ART-naive patients (BI).
• Given virologic and pharmacogenetic parameters that limit its use in some patients, the Panel recommends EFV with ABC/3TC as an Other regimen, and only for patients with a pre-ART viral load <100,000 copies/mL and negative HLA B*5701 status (see discussion in ABC/3TC section) (CI).
• EFV at a reduced dose has not been studied in the U.S. population. The Panel cannot recommend use of reduced dose EFV until further data to support its use in the U.S. population are available.
# Rilpivirine
RPV is an NNRTI approved for use in combination with NRTIs for ART-naive patients with pre-treatment viral loads <100,000 copies/mL.
# Efficacy in Clinical Trials:
Two Phase 3 randomized, double-blinded clinical trials, ECHO and THRIVE, compared RPV and EFV, each combined with 2 NRTIs. 66 At 96 weeks, the following findings were reported:
• RPV was non-inferior to EFV overall.
• Among participants with a pre-ART viral load >100,000 copies/mL, more RPV-treated than EFV-treated participants experienced virologic failure. Moreover, in this subgroup of participants with virologic failure, NNRTI and NRTI resistance was more frequently identified in those treated with RPV.
• Among the RPV-treated participants, the rate of virologic failure was greater in those with pre-treatment CD4 counts <200 cells/mm 3 than in those with CD4 counts ≥200 cells/mm 3 .
STaR, a Phase 3b, open-label study, compared the fixed-dose combinations of RPV/TDF/FTC and EFV/TDF/FTC in 786 treatment-naive patients. At 96 weeks, the following key findings were reported: 67 • RPV was non-inferior to EFV overall.
• RPV was superior to EFV in patients with pre-ART viral loads ≤100,000 copies/mL and non-inferior in those with pre-ART viral loads >100,000 copies/mL. In patients with pre-ART viral loads >500,000 copies/mL., virologic failure was more common in RPV-treated patients than in EFV-treated patients.
• At 48 weeks, NRTI and NNRTI resistance occurred in 2% and 1% of RPVand EFV-treated patients, respectively, with viral loads ≤100,000; in 5% and 0% of RPVand EFV-treated patients, respectively, with viral loads 100,000 to 500,000; and in 19% and 4% of RPVand EFV-treated patients, respectively, with viral loads >500,000 copies/mL.
Adverse Effects:
• RPV is generally well tolerated. In the ECHO, THRIVE, and STaR trials, fewer CNS adverse events (e.g., abnormal dreams, dizziness, psychiatric side effects), skin rash, and dyslipidemia were reported in the RPV arms than the EFV arms, and fewer patients in the RPV arms discontinued therapy due to adverse events.
Other Factors and Considerations:
• RPV is formulated both as a single-drug tablet and in a fixed-dose combination tablet with TDF/FTC. Among available single pill regimens, it is the smallest tablet.
• RPV/TDF/FTC is given as a once daily regimen, and must be administered with a meal (at least 400 kcal).
• The oral drug absorption of RPV can be significantly reduced in the presence of acid-lowering agents. RPV is contraindicated in patients who are receiving proton pump inhibitors, and should be used with caution in those receiving H2 antagonists or antacids (see Drug Interaction section for dosing recommendations).
• RPV is primarily metabolized in the liver by CYP3A enzyme; its plasma concentration may be affected in the presence of CYP3A inhibitors or inducers (see Drug Interaction section).
• At higher than the approved dose of 25 mg, RPV may cause QTc interval prolongation. RPV should be used with caution when coadministered with a drug known to increase the risk of Torsades de Pointes.
Panel's Recommendations:
• Given the availability of other effective regimens that do not have virologic and immunologic prerequisites to initiate treatment, the Panel recommends RPV/TDF/FTC as an Alternative regimen.
• Use of RPV with TDF/FTC should be limited to ART-naive patients with pre-treatment viral load <100,000 copies/mL and CD4 count >200 cells/mm 3 (BI).
• Data on RPV with ABC/3TC are insufficient to consider recommending this regimen as a Recommended, Alternative, or Other regimen. 8 and Appendix B, Table 3.
A number of metabolic abnormalities, including dyslipidemia and insulin resistance, have been associated with PI use. The currently available PIs differ in their propensity to cause these metabolic complications, which also depends on the dose of RTV used as a pharmacokinetic enhancing agent. Two large observational cohort studies suggest that LPV/r, IDV, FPV, or FPV/r may be associated with increased rates of MI or stroke. 18,24 This association was not seen with ATV. 74 Because of the limited number of patients receiving DRV/r, this boosted-PI was not included in the analysis of the two studies.
Recommended PIs for use in ART-naive patients should have proven virologic efficacy, once daily dosing, a low pill count, and good tolerability. On the basis of these criteria, the Panel considers once-daily DRV/r plus TDF/FTC as a Recommended PI. In a large, randomized controlled trial comparing DRV/r, ATV/r, and RAL, all in combination with TDF/FTC, all three regimens achieved similar virologic suppression rates; however, the proportion of patients who discontinued their assigned treatment because of adverse effects was greater in the in the ATV/r arm than in the other two arms. 4 Because of its higher rate of adverse effects, the Panel now classifies ATV/r plus TDF/FTC as an Alternative regimen (BI). ATV/c-and DRV/c-based regimens are considered Alternative PI regimens for the reasons detailed below.
LPV/r has twice the daily dose of RTV as other PI/r and is associated with more metabolic complications and gastrointestinal side effects than PK-enhanced ATV or DRV. LPV/r remains as an Other PI/r because it is currently the only PI co-formulated with RTV and it has extensive experience in clinical trials and practice. Compared to other PIs, FPV/r, unboosted ATV, and SQV/r have disadvantages such as greater pill burden, lower efficacy, or increased toxicity, and thus are no longer included as an option for initial therapy. Nonetheless, patients who are doing well on regimens containing these PIs should not necessarily be switched to other agents.
# Recommended Protease Inhibitor-Based Regimen
# Darunavir/Ritonavir
Efficacy in Clinical Trials:
• The ARTEMIS study compared DRV/r (800/100 mg once daily) with LPV/r (800/200 mg once daily or 400/100 mg twice daily), both in combination with TDF/FTC, in a randomized, open-label, non-inferiority trial. DRV/r was non-inferior to LPV/r at week 48, 31 and superior at week 192. 75 Among participants with baseline HIV RNA levels >100,000 copies/mL, virologic response rates were lower in the LPV/r arm than in the DRV/r arm.
• The FLAMINGO study compared DRV/r with DTG, each in combination with two NRTIs, in 488 ARTnaive participants. The rate of virologic suppression at week 48 was significantly greater among those who received DTG than in those who received DRV/r, largely because of more drug discontinuations in the DRV/r group. 6 • A small retrospective study that followed participants for 48 weeks suggested that DRV/r plus ABC/3TC may be effective in treatment-naive patients. 76 • The ACTG A5257 study showed similar virologic efficacy for DRV/r, ATV/r, and RAL, but more participants in the ATV/r group discontinued randomized treatment because of adverse events. 4 Adverse Effects:
• In the ARTEMIS Study, grades 2 to 4 adverse events, primarily diarrhea, were seen less frequently in DRV/r recipients than in LPV/r recipients.
• Patients starting DRV/r may develop a skin rash, which is usually mild-to-moderately severe and selflimited. Treatment discontinuation is necessary on rare occasions when severe rash with fever or elevated transaminases occur.
Other Factors and Considerations:
• DRV/r is administered once daily with food in treatment-naive patients.
• DRV has a sulfonamide moiety, and should be used with caution in patients with severe sulfonamide allergies. In clinical trials, the incidence and severity of rash were similar in participants who did or did not have a history of sulfonamide allergy. Most patients with sulfonamide allergy are able to tolerate DRV.
• DRV/r is a potent CYP3A4 inhibitor, and may lead to significant interactions with other medications metabolized through this same pathway (see Drug Interactions section).
Panel's Recommendation:
• On the basis of efficacy and safety data from clinical trials and clinical experience, the Panel classifies DRV/r with TDF/FTC as a Recommended regimen (AI). DRV/r with ABC/3TC is considered an Alternative regimen because there are fewer studies to support its use (BII).
# Alternative Protease Inhibitor-Based Regimens
# Atazanavir/Ritonavir or Atazanavir/Cobicistat
Efficacy in Clinical Trials:
• The CASTLE study compared once-daily ATV/r (300/100 mg) with twice-daily LPV/r (400/100 mg), each in combination with TDF/FTC. In this open-label, non-inferiority study, the 2 regimens showed similar virologic and CD4 responses at 48 weeks 30 and at 96 weeks. 77 • The ACTG A5202 study compared open-label ATV/r and EFV, each given in combination with placebocontrolled TDF/FTC or ABC/3TC. Efficacy was similar in the ATV/r and EFV groups. 65 In a separate analysis, women assigned to ATV/r were found to have a higher risk of virologic failure than women assigned to EFV or men assigned to ATV/r. 78 • In a study comparing ATV/r plus TDF/FTC to EVG/c/TDF/FTC, virologic suppression rates through 144 weeks were similar in the two groups. 55 • ACTG A5257, a large randomized open-label trial, compared ATV/r with DRV/r or RAL, each given with TDF/FTC. At week 96, all 3 regimens had similar virologic efficacy. However, a significantly higher proportion of patients in the ATV/r arm discontinued randomized treatment because of adverse events, mostly for elevated indirect bilirubin/jaundice or gastrointestinal toxicities. Lipid changes in participants in the ATV/r and DRV/r arms were similar. Bone mineral density decreased to a greater extent in participants in the ATV/r and DRV/r arms than in participants in the RAL arm. 4 • The Gilead Study 114 enrolled 692 treatment-naive patients. All patients received TDF/FTC and ATV, and were randomized to receive either RTV or COBI as PK enhancers. Both RTV and COBI were given as a separate pill with matching placebos. At 48 weeks, similar percentages of patients achieved virologic suppression, had adverse events, and changes in serum creatinine and indirect bilirubin levels. 79 Adverse Effects:
• The main adverse effect associated with ATV/c or ATV/r is reversible indirect hyperbilirubinemia, with or without jaundice or scleral icterus, but without concomitant hepatic transaminase elevations.
• Nephrolithiasis, [80][81][82] nephrotoxicity, 83 and cholelithiasis 84 have also been reported in patients who received ATV, with or without RTV.
• Both ATV/c and ATV/r can cause gastrointestinal side effects including diarrhea.
Other Factors and Considerations:
• ATV/c and ATV/r are dosed once daily and with food.
• ATV requires acidic gastric pH for dissolution. As a result, concomitant use of drugs that raise gastric pH (e.g., antacids, H2 antagonists, and particularly PPIs) may impair absorption of ATV. Table 19a provides recommendations for use of ATV/c or ATV/r with these agents.
• ATV/c and ATV/r are potent CYP3A4 inhibitors and may have significant interactions with other medications metabolized through this same pathway (see Drug Interaction section).
• ATV/c coadministered with TDF/FTC is not recommended for patients with CrCl <70 mL/min.
Panel's Recommendations:
• On the basis of clinical trial safety and efficacy data, the Panel classifies ATV/r and ATV/c plus TDF/FTC as Alternative regimens for ART-naive patients regardless of pre-treatment HIV RNA (BI).
• Because of an inferior virologic response seen in patients with a high baseline viral load, the Panel recommends ATV/r or ATV/c plus ABC/3TC as Other regimens. Use of the regimens should be limited to patients with pre-ART HIV RNA <100,000 copies/mL (CI).
• As noted earlier, ATV/c plus TDF/FTC is not recommended for patients with CrCl <70 mL/min.
# Darunavir/Cobicistat
A combination of (DRV 800 mg with COBI 150 mg) is bioequivalent to (DRV 800 mg with RTV 100 mg) in healthy volunteers. 85 Efficacy in Clinical Trial:
• In a single arm trial of treatment-naive (94%) and treatment-experienced (6%) patients, the coformulated DRV/c 800 mg/150 mg tablet was evaluated in combination with investigator-selected NRTI/NtRTI (99% of participants were given TDF/FTC). At week 48, 81% of participants achieved HIV RNA <50 copies/ml; 5% of participants discontinued treatment because of adverse events. 86 Adverse Effects:
• In the single arm trial, the most common treatment emergent adverse events were diarrhea, nausea, and headache.
Other Factors:
• (DRV 800 mg and COBI 150 mg) is available as a co-formulated tablet.
• Coadministration with TDF is not recommended in patients with CrCl <70 mL/min.
Panel's Recommendation:
• On the basis of the bioequivalence study and the single arm trial, the Panel recommends DRV/c plus TDF/FTC (BII) and DRV/c plus ABC/3TC (BIII) as Alternative Regimens for ART-naive patients.
• As noted earlier, DRV/c plus TDF/FTC is not recommended for patients with CrCl <70 mL/min.
# Other Protease Inhibitor-Based Regimens
# Lopinavir/Ritonavir
Efficacy in Clinical Trials:
• A 7-year follow-up study of LPV/r and 2 NRTIs showed sustained virologic suppression in patients who were maintained on the originally assigned regimen. 87 • Results of clinical trials that compared LPV/r with ATV/r and DRV/r are discussed above, demonstrating more favorable safety and tolerability of ATV/r and DRV/r.
• In the ACTG 5142 study, at 96 weeks, a smaller proportion of patients who received LPV/r plus 2 NRTIs achieved viral suppression (HIV RNA <50 copies/mL) than those who received EFV plus 2 NRTIs. However, the CD4 cell response was greater with LPV/r, and there was less drug resistance associated with virologic failure. 63 • In the GARDEL study, patients were randomized to 3TC or a 2 NRTI combination, with all study participants receiving LPV/r. The results demonstrated non-inferiority of the two strategies. 88 Adverse Effects:
• In addition to diarrhea, major adverse effects of LPV/r include insulin resistance and hyperlipidemia, especially hypertriglyceridemia; these require pharmacologic management in some patients.
• In the D:A:D and French observational cohorts, cumulative use of LPV/r was associated with a slightly increased risk of MI. 18,24 • In another D:A:D study, LPV/r use was also reported as an independent predictor of chronic renal impairment. 83 Other Factors and Considerations:
• LPV/r must be boosted with 200 mg/day of RTV and is associated with higher rates of GI side effects and hyperlipidemia than ATV/r and DRV/r, both of which are boosted with 100 mg/day of RTV.
• LPV/r can be given once or twice daily.
• Once-daily dosing should not be used in pregnant women, especially during the third trimester, when LPV levels are expected to decline (see Perinatal Guidelines).
• LPV/r is currently the only available PI co-formulated with RTV. Panel's Recommendation:
• On the basis of greater potential for adverse events and higher RTV dose and pill burden than ATV/r and DRV/r, the Panel recommends LPV/r plus TDF/FTC or LPV/r plus ABC/3TC as Other regimens (CI).
# Other Antiretroviral Regimens for Initial Therapy When Abacavir or Tenofovir Cannot Be Used
All currently Recommended and Alternative regimens consist of two NRTIs plus a third active drug. This strategy, however, may not be possible or optimal in all patients. In some situations it may be necessary to avoid both TDF and ABC, such as in the case of a patient with pre-existing renal disease who is HLA B*5701 positive or at high risk of cardiovascular disease.
Based on these concerns, several clinical studies have evaluated strategies using initial regimens that avoid 2 NRTIs or the NRTI drug class altogether. Many of these studies were not fully powered to permit comparisons, and regimens from these studies will not be discussed further. However, there are now sufficient data on two regimens (DRV/r plus RAL and LPV/r plus 3TC) to warrant including them as options when ABC or TDF cannot be used.
# Darunavir/Ritonavir plus Raltegravir
In the NEAT/ANRS 143 study, 805 treatment-naive participants were randomized to receive either twicedaily RAL or once-daily TDF/FTC, both with DRV/r (800 mg/100 mg once daily). At week 96, DRV/r plus RAL was non-inferior to DRV/r plus TDF/FTC based on the primary endpoint of proportion of patients with virologic or clinical failure. Among those with baseline CD4 cell count <200/mm 3 , however, there were more failures in the two-drug arm; a trend towards more failure was also observed for those with pre-treatment HIV RNA ≥100,000 copies/mL. 89 High rates of virologic failure in patients with HIV RNA >100,000 copies/mL were also seen in two smaller studies of DRV/r plus RAL. 90,91 On the basis of these study results, the Panel recommends that DRV/r plus RAL be considered for use only in patients with HIV RNA <100,000 copies/uL and CD4 cell counts >200/mm 3 , and only in those patients who cannot take either TDF or ABC (CI).
# Lopinavir/Ritonavir plus Lamivudine
In the GARDEL study, 426 ART-naive patients were randomized to receive twice-daily LPV/r plus either open-label 3TC (twice daily) or two NRTIs selected by the study investigators. At 48 weeks, a similar number of patients in each arm had HIV RNA <50 copies/mL, meeting the study's non-inferiority criteria.
The LPV/r plus 3TC regimen was better tolerated than the LPV/r plus 2 NRTI regimen. 88 An important limitation of the GARDEL study is the use of LPV/r, twice daily dosing, and relatively high pill burden (total of 6 tablets per day). LPV/r is not considered a Recommended or Alternative initial PI because of its unfavorable adverse event and pill burden characteristics as compared to pharmacokinetically enhanced ATV and DRV. Given the above limitations, the Panel recommends that LPV/r plus 3TC be considered for use only in patients who cannot take either TDF or ABC (CI).
In summary, the aggregate results from these two fully powered studies with NRTI-limiting regimens demonstrate that these initial strategies have significant deficiencies as compared to standard-of-care treatment approaches, in particular, disadvantages related to pill burden or dosing frequency. In addition, there are concerns about the virologic efficacy of DRV/r plus RAL in patients with high viral loads or low CD4 cell counts. The Panel only recommend LPV/r plus 3TC or DRV/r plus RAL for initial therapy when both TDF and ABC are contraindicated. Other less well-tested NRTI-limiting combinations are not recommended. 18 and 19a) Some antiretroviral (ARV) regimens or components are not generally recommended because of suboptimal antiviral potency, unacceptable toxicities, or pharmacologic concerns. These are summarized below.
Key
# Antiretroviral Regimens Not Recommended
Monotherapy with nucleoside reverse transcriptase inhibitor (NRTI). Single-NRTI therapy does not demonstrate potent and sustained antiviral activity and should not be used (AII). For prevention of motherto-child transmission (PMTCT), zidovudine (ZDV) monotherapy is not recommended but might be considered in certain unusual circumstances in women with HIV RNA <1,000 copies/mL, although the use of a potent combination regimen is preferred. (See Perinatal Guidelines, 1 available at http://aidsinfo.nih.gov.)
Single-drug treatment regimens with a ritonavir (RTV)-boosted protease inhibitor (PI), either lopinavir (LPV), 2 atazanavir (ATV), 3 or darunavir (DRV) [4][5] are under investigation with mixed results, and cannot be recommended outside of a clinical trial at this time.
Dual-NRTI regimens. These regimens are not recommended because they have not demonstrated potent and sustained antiviral activity compared with triple-drug combination regimens (AI). 6 Triple-NRTI regimens. In general, triple-NRTI regimens other than abacavir/lamivudine/zidovudine (ABC/3TC/ZDV) (BI) and possibly lamivudine/zidovudine + tenofovir (3TC/ZDV + TDF) (BII) should not be used because of suboptimal virologic activity [7][8][9] or lack of data (AI).
# Antiretroviral Components Not Recommended
Atazanavir (ATV) + indinavir (IDV). Both of these PIs can cause Grade 3 to 4 hyperbilirubinemia and jaundice. Additive adverse effects may be possible when these agents are used concomitantly. Therefore, these two PIs are not recommended for combined use (AIII).
# Didanosine (ddI) + stavudine (d4T).
The combined use of ddI and d4T as a dual-NRTI backbone can result in a high incidence of toxicities, particularly peripheral neuropathy, pancreatitis, and lactic acidosis. [10][11][12][13] This combination has been implicated in the deaths of several HIV-infected pregnant women secondary to severe lactic acidosis with or without hepatic steatosis and pancreatitis. 14 Therefore, the combined use of ddI and d4T is not recommended (AII).
# Didanosine (ddI) + tenofovir (TDF).
Use of ddI + TDF may increase ddI concentrations 15 and serious ddIassociated toxicities including pancreatitis and lactic acidosis. [16][17] These toxicities may be lessened by ddI dose reduction. The use of this combination has also been associated with immunologic nonresponse or CD4 cell decline despite viral suppression, [18][19] high rates of early virologic failure, [20][21] and rapid selection of resistance mutations. [20][21][22] Because of these adverse outcomes, this dual-NRTI combination is not generally recommended (AII). Clinicians caring for patients who are clinically stable on regimens containing ddI + TDF should consider altering the NRTIs to avoid this combination.
Two-non-nucleoside reverse transcriptase inhibitor (2-NNRTI) combinations. In the 2NN trial, ARVnaive participants were randomized to receive once-or twice-daily nevirapine (NVP) versus efavirenz (EFV) versus EFV plus NVP, all combined with d4T and 3TC. 23 A higher frequency of clinical adverse events that led to treatment discontinuation was reported in participants randomized to the two-NNRTI arm. Both EFV and NVP may induce metabolism of etravirine (ETR), which leads to reduction in ETR drug exposure. 24 Based on these findings, the Panel does not recommend using two NNRTIs in combination in any regimen (AI).
Efavirenz (EFV) in first trimester of pregnancy and in women with significant childbearing potential.
EFV use was associated with significant teratogenic effects in nonhuman primates at drug exposures similar to those representing human exposure. Several cases of congenital anomalies have been reported after early human gestational exposure to EFV. [25][26] EFV should be avoided in pregnancy, particularly during the first trimester, and in women of childbearing potential who are trying to conceive or who are not using effective and consistent contraception (AIII). If no other ARV options are available for the woman who is pregnant or at risk of becoming pregnant, the provider should consult with a clinician who has expertise in both HIV infection and pregnancy. (See Perinatal Guidelines, 1 available at http://aidsinfo.nih.gov.)
Emtricitabine (FTC) + lamivudine (3TC). Both of these drugs have similar resistance profiles and have minimal additive antiviral activity. Inhibition of intracellular phosphorylation may occur in vivo, as seen with other dual-cytidine analog combinations. 27 These two agents should not be used as a dual-NRTI combination (AIII).
Etravirine (ETR) + unboosted PI. ETR may induce the metabolism and significantly reduce the drug exposure of unboosted PIs. Appropriate doses of the PIs have not been established 24 (AII).
# Etravirine (ETR) + ritonavir (RTV)-boosted atazanavir (ATV) or fosamprenavir (FPV).
ETR may alter the concentrations of these PIs. Appropriate doses of the PIs have not been established 24 (AII).
# Etravirine (ETR) + ritonavir (RTV)-boosted tipranavir (TPV).
RTV-boosted TPV significantly reduces ETR concentrations. These drugs should not be coadministered 24 (AII).
Nevirapine (NVP) initiated in ARV-naive women with CD4 counts >250 cells/mm 3 or in ARV-naive men with CD4 counts >400 cells/mm 3 . Greater risk of symptomatic hepatic events, including serious and life-threatening events, has been observed in these patient groups. NVP should not be initiated in these patients (BI) unless the benefit clearly outweighs the risk. [28][29][30] Patients who experience CD4 count increases to levels above these thresholds as a result of antiretroviral therapy (ART) can be safely switched to NVP. 31 Unboosted darunavir (DRV), saquinavir (SQV), or tipranavir (TPV). The virologic benefit of these PIs has been demonstrated only when they were used with concomitant RTV. Therefore, use of these agents as part of a combination regimen without RTV is not recommended (AII).
# Stavudine (d4T) + zidovudine (ZDV).
These two NRTIs should not be used in combination because of antagonism demonstrated in vitro 32 and in vivo 33 (AII).
# 2-NNRTI combination (AI)
• When EFV combined with NVP, higher incidence of clinical adverse events seen when compared with either EFV-or NVP-based regimen.
• Both EFV and NVP may induce metabolism and may lead to reductions in ETR exposure; thus, they should not be used in combination with ETR. Antiretroviral (ARV) regimens currently recommended for initial therapy of HIV-infected patients have a high likelihood of achieving and maintaining plasma HIV RNA levels below the lower limits of detection (LLOD) of currently used assays (see What to Start). Patients on antiretroviral therapy (ART) who do not achieve this treatment goal or who experience virologic rebound often develop resistance mutations to one or more components of their regimen. Based on surveillance data for HIV patients in care in selected cities in the United States in 2009, an estimated 89% of the patients were receiving ART, of whom 72% had viral loads <200 copies/mL. 1 Many patients with detectable viral loads are non-adherent to treatment. Depending on their treatment histories, some of these patients may have minimal or no drug resistance; others may have extensive resistance. Managing patients with extensive resistance is complex and usually requires consultation with an HIV expert. This section of the guidelines defines virologic failure in patients on ART and discusses strategies to manage these individuals.
# Virologic Response Definitions
The following definitions are used in this section to describe the different levels of virologic response to ART.
# Panel's Recommendations
• Assessing and managing a patient experiencing failure of antiretroviral therapy (ART) is complex. Expert advice is critical and should be sought.
• Evaluation of virologic failure should include an assessment of adherence, drug-drug or drug-food interactions, drug tolerability, HIV RNA and CD4 T lymphocyte (CD4) cell count trends over time, treatment history, and prior and current drug-resistance testing results.
• Drug-resistance testing should be performed while the patient is taking the failing antiretroviral (ARV) regimen (AI) or within 4 weeks of treatment discontinuation (AII). Even if more than 4 weeks have elapsed since ARVs were discontinued, resistance testingalthough it may not detect previously selected resistance mutations-can still provide useful information to guide therapy (CIII).
• The goal of treatment for ART-experienced patients with drug resistance who are experiencing virologic failure is to establish virologic suppression (i.e., HIV RNA below the lower limits of detection of currently used assays) (AI).
• A new regimen should include at least two, and preferably three, fully active agents (AI). A fully active agent is one that is expected to have uncompromised activity on the basis of the patient's treatment history and drug-resistance testing results and/or the drug's novel mechanism of action.
• In general, adding a single ARV agent to a virologically failing regimen is not recommended because this may risk the development of resistance to all drugs in the regimen (BII).
• For some highly ART-experienced patients, maximal virologic suppression is not possible. In this case, ART should be continued (AI) with regimens designed to minimize toxicity, preserve CD4 cell counts, and delay clinical progression.
• When it is not possible to construct a viable suppressive regimen for a patient with multidrug resistant HIV, the clinician should consider enrolling the patient in a clinical trial of investigational agents or contacting pharmaceutical companies that may have investigational agents available.
• Discontinuing or briefly interrupting therapy may lead to a rapid increase in HIV RNA and a decrease in CD4 cell count and increases the risk of clinical progression. Therefore, this strategy is not recommended in the setting of virologic failure (AI). Virologic suppression: A confirmed HIV RNA level below the LLOD of available assays Virologic failure: The inability to achieve or maintain suppression of viral replication to an HIV RNA level <200 copies/mL Incomplete virologic response: Two consecutive plasma HIV RNA levels ≥200 copies/mL after 24 weeks on an ARV regimen in a patient who has not yet had documented virologic suppression on this regimen. A patient's baseline HIV RNA level may affect the time course of response, and some regimens will take longer than others to suppress HIV RNA levels.
# Rating of Recommendations
Virologic rebound: Confirmed HIV RNA ≥200 copies/mL after virologic suppression Virologic blip: After virologic suppression, an isolated detectable HIV RNA level that is followed by a return to virologic suppression
# ART Treatment Goals and Virologic Responses
The goal of ART is to suppress HIV replication to a level below which drug-resistance mutations do not emerge. Although not conclusive, the evidence suggests that selection of drug-resistance mutations does not occur in patients with HIV RNA levels persistently suppressed to below the LLOD of current assays. 2 Viremia "blips"-defined by viral suppression followed by an isolated detectable HIV RNA level and subsequent return to undetectable levels-are not usually associated with subsequent virologic failure. 3 In contrast, there is controversy regarding the clinical implications of persistent HIV RNA levels between the LLOD and <200 copies/mL in patients on ART. Furthermore, viremia at this threshold is detected with some frequency by commonly used real-time polymerase chain reaction (PCR) assays, which are more sensitive than PCR-based viral load platforms used in the past. [4][5][6] Findings from a large retrospective analysis showed that, as a threshold for virologic failure, HIV RNA levels of 200 copies/mL and <50 copies/mL had the same predictive value for subsequent rebound to >200 copies/mL. 7 Two other retrospective studies also support the supposition that virologic rebound is more likely to occur in patients with viral loads >200 copies/mL than in those with low-level viremia between 50 to 199 copies/mL. 8,9 However, other studies have suggested that viremia at this low level (<200 copies/mL) can be predictive of progressive viral rebound 10,11 and can be associated with the evolution of drug resistance. 12 Persistent HIV RNA levels ≥200 copies/mL are often associated with evidence of viral evolution and accumulation of drug-resistance mutations. 13 This association is particularly common when HIV RNA levels are >500 copies/mL. 14 Therefore, persistent plasma HIV RNA levels ≥200 copies/mL should be considered virologic failure.
# Causes of Virologic Failure
Virologic failure can occur for many reasons. Data from patient cohorts in the earlier era of combination ART suggested that suboptimal adherence and drug intolerance/toxicity accounted for 28% to 40% of virologic failure and regimen discontinuations. 15,16 Presence of pre-existing (transmitted) drug resistance may also be the cause of virologic failure. 17 Virologic failure may be associated with both patient-and regimenrelated factors, as listed below:
•
# Management of Patients with Virologic Failure
# Assessment of Virologic Failure
If virologic failure is suspected or confirmed, a thorough assessment that includes consideration of the factors listed in the Causes of Virologic Failure section above is indicated. Often the causes of virologic failure can be identified, but in some cases, the causes are not obvious. It is important to distinguish among the causes of virologic failure because the approaches to subsequent therapy differ. The following potential causes of virologic failure should be explored in depth:
• Suboptimal Adherence. Assess the patient's adherence to the regimen. Identify and address the underlying cause(s) for incomplete adherence (e.g., drug intolerance, difficulty accessing medications, depression, active substance abuse) and, if possible, simplify the regimen (e.g., decrease pill count or dosing frequency). (See Adherence.)
• Medication Intolerance. Assess the patient's tolerance of the current regimen and the severity and duration of side effects, keeping in mind that even minor side effects can affect adherence. Management strategies to address intolerance in the absence of drug resistance may include:
• Symptomatic treatment (e.g., antiemetics, antidiarrheals)
• A switch from one ARV in a regimen to another agent in the same drug class (see the Adverse Effects section) • A switch from one drug class to another class (e.g., from a non-nucleoside reverse transcriptase inhibitor [NNRTI] to a protease inhibitor [PI] or an integrase strand transfer inhibitor [INSTI]), if necessary (see the Adverse Effects section)
• Pharmacokinetic Issues
• Review food requirement for each medication, and assess whether the patient adheres to the requirement. • Review the patient's recent history of gastrointestinal symptoms such as vomiting or diarrhea that may result in short-term malabsorption. • Review concomitant medications and dietary supplements for possible adverse drug-drug interactions (consult the Drug Interactions section and tables for common interactions) and, if possible, make appropriate substitutions for ARV agents and/or concomitant medications. • Consider therapeutic drug monitoring if pharmacokinetic drug-drug interactions or impaired drug absorption leading to decreased ARV exposure is suspected (see also Exposure-Response
Relationship and Therapeutic Drug Monitoring).
• Suspected Drug Resistance. Perform resistance testing while the patient is still taking the failing regimen or within 4 weeks of regimen discontinuation if the patient's plasma HIV RNA level is >1,000 copies/mL (AI), and possibly even if between 500 to 1,000 copies/mL (BII). (See Drug-Resistance Testing.) In some patients, resistance testing should be considered even after treatment interruptions of more than 4 weeks, recognizing that the lack of evidence of resistance in this setting does not exclude the possibility that resistance mutations may be present at low levels (CIII). Evaluate the extent of drug resistance, taking into account the patient's past treatment history and prior resistance-test results. Drug resistance is cumulative; thus, all prior treatment history and resistance test results should be considered when evaluating resistance. Genotypic or phenotypic testing provides information relevant for selecting nucleoside reverse transcriptase inhibitors (NRTIs), NNRTIs, PIs, and INSTIs. Additional drug-resistance tests for patients experiencing failure on a fusion inhibitor (AII) and viral tropism tests for patients experiencing failure on a CCR5 antagonist (BIII) are also available. (See Drug-Resistance Testing.)
# Approach to Patients with Confirmed Virologic Failure
Once virologic failure is confirmed, every effort should be made to assess whether suboptimal adherence and drug-drug or drug-food interactions may be contributing to the inadequate virologic response to ART. If virologic failure persists after these issues have been adequately addressed, resistance testing should be performed, and the regimen should be changed as soon as possible to avoid progressive accumulation of resistance mutations. 18 In addition, several studies have shown that virologic responses to new regimens are greater in individuals with lower HIV RNA levels 10,19 and/or higher CD4 cell counts at the time of regimen changes. 10,19 Discontinuing or briefly interrupting therapy in a patient with viremia may lead to a rapid increase in HIV RNA and a decrease in CD4 cell count and increases the risk of clinical progression; 20,21 therefore, this strategy is not recommended (AI). See Discontinuation or Interruption of Antiretroviral Therapy.
Ideally, a new ARV regimen should contain at least two, and preferably three, fully active drugs whose predicted activity is based on the patient's drug treatment history, resistance testing, or the mechanistic action of a new drug class (AI). 10,[22][23][24][25][26][27][28][29][30][31] Despite drug resistance, some ARV drugs (e.g., NRTIs) may contribute partial ARV activity to a regimen, 21 while other agents (e.g., enfuvirtide [T20], NNRTIs, the INSTI raltegravir [RAL]) likely will not. [32][33][34] Using a "new" drug that a patient has never used previously does not ensure that the drug will be fully active; there is potential for cross-resistance, particularly among drugs from the same class. In addition, archived drug-resistance mutations may not be detected by standard drug-resistance tests, particularly if testing is performed when the patient is not taking the drug in question. Therefore, both treatment history and prior and current drug-resistance test results must be considered when designing a new regimen. When designing a new ART regimen, drug potency and viral susceptibility are more important factors to consider than the number of component drugs.
In general, patients who receive at least three active drugs, selected based on a review of the patient's treatment history and past and most current drug-resistance test results, experience better and more sustained virologic response than those receiving fewer active drugs in the regimen. 23,24,26,27,35,36 However, there are increasing data in treatment-naive and treatment-experienced patients showing that an active pharmacokinetically enhanced PI plus one other active drug or several partially active drugs will effectively reduce viral load in most patients. [37][38][39][40] Active drugs are ARVs that, based on resistance test results and treatment history, are expected to have antiviral activity equivalent to that seen when there is no resistance to the specific drugs; ARVs with partial activity are those predicted to reduce HIV RNA but to a lesser extent than when there is no underlying drug resistance. The activity of a given drug must be uniquely defined for each patient. Active drugs may be newer members of existing drug classes that are active against HIV isolates that are resistant to older drugs in the same classes (e.g., etravirine [ETR], darunavir [DRV] and tipranavir, and dolutegravir [DTG]) An active drug may also be one with unique mechanisms of action (e.g., the fusion inhibitor T20, the CCR5 antagonist maraviroc in patients with no detectable CXCR4-using virus).
In the presence of certain drug resistance mutations, some ARVs such as DTG, ritonavir-boosted DRV, and ritonavir-boosted lopinavir (LPV/r) need to be given twice daily instead of once daily to achieve higher drug concentrations necessary to be active against the less sensitive virus. 41,42 Addressing Detectable Viral Load in Different Clinical Situations
• HIV RNA above the LLOD and <200 copies/mL. Confirm that levels remain above the LLOD and assess adherence, drug-drug interactions (including those with over-the-counter products and supplements), and drug-food interactions. Patients with HIV RNA typically below the LLOD with transient increases in HIV RNA (i.e., blips) do not require a change in treatment (AII). 5 Although there is no consensus on how to manage patients with persistent HIV RNA levels above the LLOD and <200 copies/mL, the risk of emerging resistance is believed to be relatively low. Therefore, these patients should maintain on their current regimens and have HIV RNA levels monitored at least every 3 months to assess the need for changes in ART in the future (AIII).
• HIV RNA ≥200 and <1,000 copies/mL. Confirm that HIV RNA levels remain in this range and assess adherence and potential drug-drug interactions (including those with over-the-counter products and supplements) and drug-food interactions. In contrast to patients with HIV RNA levels persistently <200 copies/mL, those with levels persistently ≥200 copies/mL often develop drug resistance, particularly with HIV RNA levels >500 copies/mL. 8,9 Persistent plasma HIV RNA levels in the 200 to 1,000 copies/mL range should be considered as virologic failure, and resistance testing should be attempted, particularly if HIV RNA >500 copies/mL. When resistance testing can successfully be performed and no resistance is detected, manage the patient as outlined below in the section on HIV RNA >1,000 copies/mL and no drug resistance identified. If drug resistance is detected, manage the patient as outlined below in the section on HIV RNA >1,000 copies/mL and drug resistance identified. When resistance testing cannot be performed because of low-level viremia, the decision whether to empirically change ARVs should be made on a case-by-case basis.
• HIV RNA >1,000 copies/mL and no drug resistance identified. This scenario is almost always associated with suboptimal adherence. Conduct a thorough assessment to determine the level of adherence and identify any drug-drug and drug-food interactions. Consider the timing of the drugresistance test (e.g., was the patient mostly or completely ART-non-adherent for more than 4 weeks before testing). If the current regimen is well tolerated and there are no significant drug-drug or drugfood interactions, it is reasonable to resume the same regimen. If the agents are poorly tolerated or there are important drug-drug or drug-food interactions, consider changing the regimen. Two to four weeks after treatment is resumed or started, repeat viral load testing; if viral load remains >500 copies/mL, perform genotypic testing to determine whether a resistant viral strain emerges (CIII).
• HIV RNA >1,000 copies/mL and drug resistance identified. The availability of newer ARVs, including some with new mechanisms of action, makes it possible to suppress HIV RNA levels to below the LLOD in most of these patients. The options in this setting depend on the extent of drug resistance present and are addressed in the clinical scenarios outlined below.
# Management of Virologic Failure in Different Clinical Scenarios
First Regimen Failure
• Failing an NNRTI plus NRTI regimen. Patients failing an NNRTI-based regimen often have viral resistance to the NNRTI, with or without lamivudine (3TC) and emtricitabine (FTC) resistance. Although several options are available for these patients, several studies have explored the activity of a pharmacokinetically boosted PI with NRTIs or an INSTI. [43][44][45] Two of the studies found that regimens containing a ritonavir-boosted PI (PI/r) combined with NRTIs were as active as regimens containing the PI/r combined with RAL. 43,45 Two studies also demonstrated higher rates of virologic suppression with use of a PI/r plus NRTIs than with a PI/r alone. 44,45 On the basis of these studies, even patients with NRTI resistance can often be treated with a pharmacokinetically boosted PI plus NRTIs or RAL (AI). Although LPV/r was used in these studies, it is likely that other pharmacokinetically boosted PIs would behave similarly. Although data are limited, the second-generation NNRTI ETR or the other INSTIs (i.e., elvitegravir [EVG] or DTG) combined with a pharmacokinetically boosted PI may also be options in this setting.
• Failing a pharmacokinetically boosted PI plus NRTI regimen. In this scenario, most patients will have either no resistance or resistance limited to 3TC and FTC. 46,47 Failure in this setting is often attributed to poor adherence, drug-drug interactions, or drug-food interactions. A systematic review of multiple randomized trials of PI/r first-line failure showed that maintaining the same regimen, presumably with efforts to enhance adherence, is as effective as changing to new regimens with or without drugs from new classes. 48 In this setting, resistance testing should be performed along with an assessment of overall adherence and tolerability of the regimen. If the regimen is well tolerated and there are no concerns regarding drug-drug or drug-food interactions, the regimen can be continued with adherence support and viral monitoring. Alternatively, if poor tolerability or interactions may be contributing to virologic failure, the regimen can be modified to include a different pharmacokinetically boosted PI plus NRTIs-even if not all of the NRTIs are fully active-or to a new non-PI-based regimen that includes more than two fully active agents (AII).
•
# Second-Line Regimen Failure and Beyond
• Drug resistance with treatment options allowing for full virologic suppression. Depending on treatment history and drug-resistance data, one can predict whether or not to have a fully active pharmacokinetically boosted PI to include in future regimens. For example, those who have no documented PI resistance and previously have never been treated with an unboosted PI are likely to harbor virus that is fully susceptible to ARVs in the PI class. In this setting, viral suppression should be achievable using a pharmacokinetically boosted PI combined with either NRTIs or an INSTI-provided the virus is susceptible to the INSTI. If a fully susceptible pharmacokinetically boosted PI is not an option, the new regimen should include at least two, and preferably three, fully active agents, if possible. Drugs to be included in the regimen should be selected based on the likelihood that they will be active as determined by the patient's treatment history, past and present drug-resistance testing, and tropism testing if a CCR5 antagonist is being considered.
• Multidrug resistance without treatment options allowing for full virologic suppression. Use of currently available ARVs has resulted in a dramatic decline in the number of patients who have few treatment options because of multi-class drug resistance. 50,51 Despite this progress, there remain patients who have experienced toxicities and/or developed resistance to all or most currently available drugs. If maximal virologic suppression cannot be achieved, the goals of ART will be to preserve immunologic function, prevent clinical progression, and minimize increasing resistance to drug classes that may eventually include new drugs that may be important for future regimens. Consensus on the optimal management of these patients is lacking. If resistance to NNRTIs, T20, EVG or RAL are identified, there is rarely a reason to continue these drugs, as there is little evidence that keeping them in the regimen helps delay disease progression (BII). Moreover, continuing these drugs, in particular INSTIs, may allow for further increasing resistance and within-class cross resistance that may limit future treatment options. It should be noted that even partial virologic suppression of HIV RNA to >0.5 log 10 copies/mL from baseline correlates with clinical benefits. 50,52 Cohort studies provide evidence that continuing therapy, even in the presence of viremia and the absence of CD4 count increases, reduces the risk of disease progression. 53 Other cohort studies suggest continued immunologic and clinical benefits with even modest reductions in HIV RNA levels. 54,55 However, all these potential benefits must be balanced with the ongoing risk of accumulating additional resistance mutations. In general, adding a single fully active ARV to the regimen is not recommended because of the risk of rapid development of resistance (BII).
Patients with ongoing viremia who lack sufficient treatment options to construct a fully suppressive regimen may be candidates for research studies or expanded access programs or may qualify for single-patient access of an investigational new drug as specified in Food and Drug Administration regulations: http://www.fda.gov/AboutFDA/CentersOffices/OfficeofMedicalProductsandTobacco/CDER/ucm163982.htm. Information about these programs may also be available from the sponsoring pharmaceutical manufacturer.
• Previously treated patient with suspected drug resistance who need care but present with limited information (i.e., incomplete or no self-reported history, medical records, or resistance-testing results). Every effort should be made to obtain the patient's medical records and prior drug-resistance testing results; however, this may not always be possible. One strategy is to restart the most recent ARV regimen and assess drug resistance in 2 to 4 weeks to guide selection of the next regimen. Another strategy is to start two or three drugs predicted to be active on the basis of the patient's treatment history.
# Isolated Central Nervous System (CNS) Virologic Failure and New Onset Neurologic Symptoms
Presentation with new-onset CNS signs and symptoms has been reported as a rare form of virologic failure. These patients present with new, usually subacute, neurological symptoms associated with breakthrough of HIV infection within the CNS compartment despite plasma HIV RNA suppression. 56,57 Clinical evaluation frequently shows abnormalities on MRI brain imaging and abnormal cerebrospinal fluid (CSF) findings with characteristic lymphocytic pleocytosis. When available, measurement of CSF HIV RNA shows higher concentrations in the CSF than in plasma, and in most patients, evidence of drug-resistant CSF virus. Drugresistance testing of HIV in CSF, if available, can be used to guide changes in the treatment regimen according to principles outlined above for plasma HIV RNA resistance (CIII). In these patients it may be useful to consider CNS pharmacokinetics in drug selection (CIII). If CSF HIV resistance testing is not available, the regimen may be changed based on the patient's treatment history or on predicted drug penetration into the CNS 58-60 (CIII). This "neurosymptomatic" CNS viral escape should be distinguished from: (1) other CNS infections that can induce a transient increase in CSF HIV RNA (e.g., herpes zoster 61 ), (2) incidental detection of asymptomatic mild CSF HIV RNA elevation likely equivalent to plasma blips, 62 or (3) relatively common chronic, usually mild, neurocognitive impairment in HIV-infected patients without evidence of CNS viral breakthrough. 63 None of these latter conditions currently warrant a change in ART. 64
# Summary
In summary, the management of treatment-experienced patients with virologic failure often requires expert advice to construct virologically suppressive regimens. Before modifying a regimen, it is critical to carefully evaluate the cause(s) of virologic failure, including incomplete adherence, poor tolerability, and drug and food interactions, as well as review HIV RNA and CD4 cell count changes over time, treatment history, and drug-resistance test results. If HIV RNA suppression is not possible with currently approved agents, consider use of investigational agents through participation in clinical trials or expanded/single-patient access programs. If virologic suppression is still not achievable, the choice of regimens should focus on minimizing toxicity and preserving treatment options while maintaining CD4 cell counts to delay clinical progression.
# Poor CD4 Cell Recovery and Persistent Inflammation Despite Viral Suppression (Last updated April 8, 2015; last reviewed April 8, 2015)
Despite marked improvements in antiretroviral treatment (ART), morbidity and mortality in HIV-infected individuals continues to be greater than in the general population, particularly when ART is delayed until advanced disease stages. These morbidities include cardiovascular disease, many non-AIDS cancers, non-AIDS infections, chronic obstructive pulmonary disease, osteoporosis, type II diabetes, thromboembolic disease, liver disease, renal disease, neurocognitive dysfunction, and frailty. 1 Although health-related behaviors and toxicities of antiretroviral (ARV) drugs may also contribute to the increased risk of illness and death, poor CD4 T lymphocyte (CD4) cell recovery, persistent immune activation, and inflammation likely also contribute to the risk.
# Poor CD4 Cell Recovery
As long as ART-mediated viral suppression is maintained, peripheral blood CD4 cell counts in most HIVinfected individuals will continue to increase for at least a decade. The rate of CD4 cell recovery is typically most rapid in the first 3 months of suppressive ART, followed by more gradual increases over time. [2][3][4] If ARTmediated viral suppression is maintained, most individuals will eventually recover CD4 counts in the normal range (>500 cells /mm 3 ); however, approximately 15% to 20% of individuals who initiate ART at very low CD4 counts (<200 cells/mm 3 ) may plateau at abnormally low CD4 cell counts. [3][4][5] Early initiation of ART in recently HIV-infected individuals likely provides the best opportunity for maximal CD4 cell recovery. 6 Persistently low CD4 cell counts despite ART-mediated viral suppression are associated with increased risk of morbidity and mortality. For example, HIV-infected individuals with CD4 counts <200 cells/mm 3 despite at least 3 years of suppressive ART had a 2.6-fold greater risk of mortality than those with higher CD4 cell counts. 7 Lower CD4 cell counts during ART-mediated viral suppression are associated with an increased risk
• Morbidity and mortality from several AIDS and non-AIDS conditions are increased in HIV-infected individuals despite antiretroviral therapy (ART)-mediated viral suppression, and are predicted by persistently low CD4 T lymphocyte (CD4) cell counts and/or persistent immune activation.
• ART intensification by adding antiretroviral (ARV) drugs to a suppressive ART regimen does not consistently improve CD4 cell recovery or reduce immune activation and is not recommended (AI).
• In individuals with viral suppression, switching ARV drug classes does not consistently improve CD4 cell recovery or reduce immune activation and is not recommended (BIII).
• No interventions designed to increase CD4 cell counts and/or decrease immune activation are recommended at this time (in particular, interleukin-2 is not recommended [AI]) because none has been proven to decrease morbidity or mortality during ARTmediated viral suppression.
• Monitoring markers of immune activation and inflammation is not recommended because no immunologically targeted intervention has proven to improve the health of individuals with abnormally high biomarker levels, and many markers that predict morbidity and mortality fluctuate widely in individuals (AII).
• Because there are no proven interventions to improve CD4 cell recovery and/or inflammation, efforts should focus on addressing modifiable risk factors for chronic disease (e.g., encouraging smoking cessation, a healthy diet, and exercise; treating hypertension, hyperlipidemia) (AII). of non-AIDS morbidity and mortality, [8][9][10][11] including cardiovascular disease, 12 osteoporosis and fractures, 13 liver disease, 14 and infection-related cancers. 15 The prognostic importance of higher CD4 cell counts likely spans all ranges of CD4 cell counts, though incremental benefits are harder to discern once CD4 counts increase to >500 cells/mm 3 . 16 Individuals with poor CD4 cell recovery should be evaluated for modifiable causes of CD4 cell lymphopenia. Concomitant medications should be reviewed, with a focus on those known to decrease white blood cells or, specifically, CD4 cells (e.g., cancer chemotherapy, interferon, zidovudine, 17 or the combination of tenofovir disoproxil fumarate (TDF) and didanosine (ddI). 18,19 If possible, these drugs should be substituted for or discontinued. Untreated coinfections (e.g., HCV, HIV-2) and serious medical conditions (e.g., malignancy) should also be considered as possible causes of CD4 lymphopenia, particularly in individuals with consistently declining CD4 cell counts (and percentages) and/or in those with CD4 counts consistently below 100 cells/mm 3 . In many cases, no obvious cause for suboptimal immunologic response can be identified.
# Rating of Recommendations
Despite strong evidence linking low CD4 cell counts and increased morbidity during ART-mediated viral suppression, no adjunctive therapies that increase CD4 cell count beyond levels achievable with ART alone have been proven to decrease morbidity or mortality. Adding ARV drugs to an already suppressive ART regimen does not improve CD4 cell recovery, [20][21][22][23][24][25] and does not reduce morbidity or mortality. Therefore, ART intensification is not recommended as a strategy to improve CD4 cell recovery (AI). In individuals maintaining viral suppression, switching ARV drug classes in a suppressive regimen also does not consistently improve CD4 cell recovery and is not recommended (BIII). 26 Two large clinical trials, powered to assess impact on clinical endpoints (AIDS and death), evaluated the role of interleukin-2, an immunebased therapy, in improving CD4 cell recovery. Interleukin-2 adjunctive therapy resulted in CD4 cell count increases but with no observable clinical benefit. Therefore, interleukin-2 is not recommended (AI). 27 Other immune-based therapies that increase CD4 cell counts (e.g., growth hormone, interleukin-7) are under investigation. However, none of the therapies have been evaluated in clinical endpoint trials; therefore, whether any of these approaches will offer clinical benefit is unclear. Currently, such immune-based therapies should not be used except in the context of a clinical trial.
# Persistent Immune Activation and Inflammation
Although poor CD4 cell recovery likely contributes to morbidity and mortality during ART-mediated viral suppression, there is increasing focus on persistent immune activation and inflammation as potentially independent mediators of risk. HIV infection results in heightened systemic immune activation and inflammation, effects that are evident during acute infection, persist throughout chronic untreated infection, and predict more rapid CD4 cell decline and progression to AIDS and death, independent of plasma HIV RNA levels. 28 Although immune activation declines with suppressive ART, it often persists at abnormal levels in many HIV-infected individuals maintaining long-term ART-mediated viral suppression-even in those with CD4 cell recovery to normal levels. 29,30 Immune activation and inflammatory markers (e.g., IL-6, D-dimer, hs-CRP) also predict mortality and non-AIDS morbidity during ART-mediated viral suppression, including cardiovascular and thromboembolic events, cancer, neurocognitive dysfunction, and frailty. 28 Although individuals with poor CD4 cell recovery (i.e., counts persistently <350 cells/mm 3 ) tend to have greater immune activation and inflammation than those with greater recovery, 29 the relationship between innate immune activation and inflammation and morbidity/mortality is largely independent of CD4 cell count. 31,32 Even in individuals with CD4 counts >500 cells/mm 3 , there is evidence that immune activation and inflammation contribute to morbidity and mortality. 33 Thus, innate immune activation and inflammation are potentially important targets for future interventions.
Although the drivers of persistent immune activation during ART are not completely understood, HIV persistence, coinfections, and microbial translocation likely play important roles. 28 Interventions to reduce each of these presumed drivers are currently being investigated. Importantly, adding ARV drugs to an already suppressive ART regimen (ART intensification) does not consistently improve immune activation. [20][21][22][23]25 Although some studies have suggested that switching an ART regimen to one with a more favorable lipid profile may improve some markers of immune activation and inflammation, 34,35 these studies have limitations and results are not consistent across markers and among studies. Thus, at this time, ART modification cannot be recommended as a strategy to reduce immune activation (BIII). Other commonly used medications with anti-inflammatory properties (e.g., statins, aspirin) are being studied, and preliminary evidence suggests that some may reduce immune activation in treated HIV infection. 36,37 However, because no intervention specifically targeting immune activation or inflammation has been studied in a clinical outcomes trial in treated HIV infection, no interventions to reduce immune activation are recommended at this time.
In the absence of proven interventions, there is currently no clear rationale to monitor levels of immune activation and inflammation in treated HIV infection. Furthermore, many of the inflammatory markers that predict morbidity and mortality fluctuate significantly in HIV-infected individuals. Thus, clinical monitoring with immune activation or inflammatory markers is not currently recommended (AII). The focus of care to reduce chronic non-AIDS morbidity and mortality should be on maintaining ART-mediated viral suppression and addressing strategies to reduce risk factors (e.g., smoking cessation, healthy diet, and exercise) and managing chronic comorbidities such as hypertension, hyperlipidemia, and diabetes (AII).
# Regimen Switching In the Setting of Virologic Suppression (Last updated May 1, 2014; last reviewed May 1, 2014)
With use of currently available antiretroviral therapy (ART), most HIV-infected patients are able to achieve sustained HIV viral suppression. Furthermore, advances in treatment and better understanding about drug resistance make it possible to consider switching an effective regimen to an alternative regimen in some situations (see below). When contemplating such a switch, clinicians must consider several key principles to maintain viral suppression while addressing concerns with the current treatment.
Reasons to Consider Regimen Switching in the Setting of Viral Suppression:
• To simplify the regimen by reducing pill burden and dosing frequency to improve adherence
• To enhance tolerability and decrease short-or long-term toxicity (see Adverse Effects section)
• To change food or fluid requirements
• To avoid parenteral administration
• To minimize or address drug interaction concerns (see Drug Interactions section)
• To allow for optimal use of ART during pregnancy or should pregnancy occur (see Perinatal Guidelines) 1
• To reduce costs (see Cost section)
# Principles and Strategies of Regimen Switching
The cardinal principle of regimen switching is to maintain viral suppression without jeopardizing future treatment options. If a regimen switch results in virologic failure with emergence of new resistance mutations, the patient may require more complex, difficult to follow, or expensive regimens. Principles for successful regimen switching are highlighted below:
• It is critical to review a patient's full antiretroviral (ARV) history (including virologic responses, resistance test results, and past adverse events) before any treatment switch.
• Once a particular resistance mutation has been selected, it is generally archived in the HIV reservoir and is likely to reappear under the appropriate selective drug pressure, even if not detected in the most recent resistance test. If resistance data are unavailable, resistance may often be inferred from a patient's treatment history. For example, a clinician should assume that patients who have failed a cytosine analogue (e.g., a lamivudine (3TC)-or emtricitabine (FTC)-containing regimen), likely have the M184V substitution, even if the substitution is not documented. The same assumption of resistance may also apply to patients with documented failure to an non-nucleoside reverse transcriptase inhibitor (NNRTI)or an integrase strand transfer inhibitors (INSTI)-based regimen because these drugs generally have a lower barrier to resistance. If there is uncertainty about prior resistance, it is generally not advisable to switch a suppressive ARV regimen unless the new regimen is likely to be as active against resistant virus as the suppressive regimen.
• Consultation with an HIV specialist is recommended when considering a regimen switch for a patient with a history of resistance to one or more drug classes.
• Switching from a ritonavir (RTV)-boosted protease inhibitor (PI) regimen to a regimen composed of drugs with a lower barrier to resistance generally maintains viral suppression provided there is no resistance to the other components of the regimen. However, such switches should be avoided if there is any doubt about the activity of the other agents in the regimen.
• Within-class switches prompted by adverse events usually maintain viral suppression provided that there is no drug resistance to the other ARV agents in the same drug class.
• In the absence of any likely drug resistance, switching from complex regimens, parenteral drug (i.e., enfuvirtide), or drugs known now to be more toxic (e.g., zidovudine, stavudine, or didanosine) or with higher pill burden or dosing frequency to simpler regimens (e.g., from a regimen including ritonavirboosted saquinavir [SQV/r] to one including ritonavir-boosted darunavir [DRV/r]) or to ARVs in a new drug class (e.g., an INSTI) generally results in similar or improved adherence, continued viral suppression and possibly improved quality of life.
• More intensive monitoring of tolerability, viral suppression, adherence, and laboratory changes is recommended during the first 3 months after a regimen switch.
# Alternative Switch Strategies for Patients with Virologic Suppression
# RTV-Boosted PI Monotherapy
The strategy of switching virologically suppressed patients without PI resistance from one ART regimen to RTV-boosted PI monotherapy has been studied. The rationale for this strategy is to avoid nucleoside reverse transcriptase inhibitor (NRTI) toxicities and decrease costs, while taking advantage of the high barrier to resistance of RTV-boosted PIs. RTV-boosted PI monotherapy maintains virologic suppression in most patients, but at slightly lower rates than standard therapy that includes 2 NRTIs. 2,3 Low-level viremia, generally without the emergence of PI resistance, appears to be more common with monotherapy. In most studies, resumption of NRTIs in patients experiencing low level viral rebound has led to re-suppression.
No clinical trials comparing available RTV-boosted PI monotherapy regimens have been conducted. Findings from an observational study suggest that the rate of treatment failure is higher in patients on RTV-boosted atazanavir (ATV/r) than in those on RTV-boosted lopinavir (LPV/r) or DRV/r. 4 Another pilot study reported early viral rebound with use of ATV/r monotherapy. 5 There are rare reports of central nervous system virologic escape, sometimes with clinical symptoms, in patients on RTV-boosted PI monotherapy. 6,7 On the basis of the results from these studies, RTV-boosted PI monotherapy should generally be avoided.
Other strategies to avoid use of NRTIs (i.e., use of a RTV-boosted PI plus a NNRTI, an INSTI, or maraviroc [MVC]) are also being studied, but data on these strategies are limited.
# Switching from a Ritonavir-Boosted Protease Inhibitor to Unboosted Atazanavir
Several clinical studies have evaluated switching a RTV-boosted PI to unboosted atazanavir (ATV) in virologically suppressed patients without NRTI resistance. Two comparative clinical trials reported that ATV/r and ATV, both in combination with 2 NRTIs (mostly ABC/3TC), demonstrated comparable levels of virologic suppression and a similar lack of treatment-emergent resistance. The benefits of the unboosted ATV regimen included a slightly improved lipid profile and a lower incidence of hyperbilirubinemia. 8,9 An additional study of 296 patients with virologic suppression on tenofovir disoproxil fumarate (TDF)/FTC plus ATV/r showed that patients switched to ABC/3TC plus ATV maintained viral suppression and showed improvements in certain bone and renal biomarkers. 10 The results of these and other non-comparative studies suggest that a regimen of ABC/3TC plus ATV can be considered in virologically suppressed patients, especially in those who have adverse effects from TDF or RTV.
# Switching to Maraviroc
Co-receptor usage in virologically suppressed patients can be determined from proviral DNA obtained from peripheral blood mononuclear cells. Individuals found to have R5-tropic virus by this technique could potentially have a component of their regimens switched to MVC. 11,12 However, although the use of MVC after DNA tropism testing has potential, this strategy cannot be recommended until more data from larger clinical studies are available (see Tropism Testing section).
# De-intensification
De-intensification of a standard RTV-boosted PI regimen from three to two active drugs (e.g., to a boosted PI plus one NRTI, 13 a boosted PI plus an INSTI, 14,15 or an NNRTI such as etravirine 15 or the CCR5 antagonist MVC 12 ) may be more effective virologically than RTV-boosted PI monotherapy, but, thus far, comparative data on this approach are limited. In general, switching a regimen -even in a patient without known drug resistance-from an effective three-drug regimen to a two-drug regimen has not been validated and is not recommended.
# Monitoring After Treatment Changes
Patients should be evaluated more closely for several months after a treatment switch (i.e., a clinic visit or phone call 1 to 2 weeks after the change and a viral load test to check for rebound viremia 4 to 8 weeks after the switch). The goal of the intensive monitoring is to assess medication tolerance and conduct targeted laboratory testing if the patient had pre-existing laboratory abnormalities or there are potential concerns with the new regimen. For example, if lipid abnormalities were present and/or were a reason for the ARV change or are a concern with the new regimen, fasting cholesterol subsets and triglycerides should be assessed within 3 months after the change in therapy. Absent any specific complaints, laboratory abnormalities, or evidence of viral rebound at this 3-month visit, clinical and laboratory monitoring of the patient may resume on a regularly scheduled basis (see Laboratory Testing section).
# Exposure-Response Relationship and Therapeutic Drug Monitoring (TDM) for Antiretroviral Agents (Last updated April 8, 2015; last reviewed April 8, 2015)
Knowledge about the relationship between a drug's systemic exposure (or concentration) and responses (beneficial and/or adverse) is key in selecting the dose of a drug, in understanding why patients may respond differently to the same drug and dose, and in designing strategies to optimize drug response and tolerability.
Therapeutic drug monitoring (TDM) is a strategy used to guide dosing of certain antiarrhythmics, anticonvulsants, antineoplastics, and antimicrobial agents by using measured drug concentrations to improve the likelihood of the desired therapeutic and safety outcomes. Drugs suitable for TDM are characterized by a known exposure-response relationship and a therapeutic range of concentrations. The therapeutic range is a range of concentrations established through clinical investigations that are associated with a greater likelihood of achieving the desired therapeutic response and/or reducing the frequency of drug-associated adverse reactions.
Several antiretroviral (ARV) agents meet most of the characteristics of agents suitable for a TDM strategy. 1 Specifically, some ARVs have considerable interpatient variability in drug concentrations; other ARVs have known drug concentrations associated with efficacy and/or toxicity; and in the case of other drugs, data from small prospective studies have demonstrated that TDM improved virologic response and/or decreased the incidence of concentration-related drug toxicities. 2,3 TDM for ARV agents, however, is not recommended for routine use in the management of HIVinfected adults (BII). This recommendation is based on multiple factors that limit the routine use of TDM in HIV-infected patients. These limiting factors include lack of prospective studies that demonstrate routine use of TDM improves clinical outcomes, uncertain therapeutic thresholds for most ARV agents, great intra-and inter-patient variability in drug concentrations achieved, and a lack of commercial laboratories to perform real time quantitation of ARV concentrations. [2][3][4][5]
# Scenarios for Consideration of Therapeutic Drug Monitoring
Although routine use of TDM is not recommended, in some scenarios, ARV concentration data may be useful in patient management. In these cases, assistance from a clinical pharmacologist or a clinical pharmacist to interpret the concentration data may be advisable. These scenarios include the following:
• Suspect clinically significant drug-drug or drug-food interactions that may result in reduced efficacy or increased dose-related toxicities;
• Changes in pathophysiologic states that may impair gastrointestinal, hepatic, or renal function, thereby potentially altering drug absorption, distribution, metabolism, or elimination;
• Among pregnant women who have risk factors for virologic failure (e.g., those not achieving viral suppression during earlier stage of pregnancy)-during the later stages of pregnancy, physiologic changes may result in reduced drug exposure and thus further increase the risk of virologic failure;
# Panel's Recommendations
• Therapeutic drug monitoring for antiretroviral agents is not recommended for routine use in the management of HIV-infected patients (BII).
• TDM may be considered in selected clinical scenarios, as discussed in the text below. • Heavily pretreated patients experiencing virologic failure and who may have viral isolates with reduced susceptibility to ARVs;
# Rating of Recommendations
• Use of alternative dosing regimens and ARV combinations for which safety and efficacy have not been established in clinical trials;
• Concentration-dependent, drug-associated toxicities; and
• Lack of expected virologic response in medication-adherent patients.
# Resources for Therapeutic Drug Monitoring Target Concentrations
Most TDM-proposed target concentrations for ARVs focus on a minimum concentration (C min ) (i.e., the plasma concentration at the end of a dosing interval before the next ARV dose). A summary of population average ARV C min can be found in a review on the role of ARV-related TDM. 2 Population average C min for newer ARVs can be found in the Food and Drug Administration-approved product labels.
Guidelines for the collection of blood samples and other practical suggestions related to TDM can be found in a position paper by the Adult AIDS Clinical Trials Group Pharmacology Committee. 4
# Challenges and Considerations in Using Drug Concentrations to Guide Therapy
There are several challenges and considerations for implementation of TDM in the clinical setting. Use of TDM to monitor ARV concentrations in a patient requires the following:
• quantification of the concentration of the drug, usually in plasma or serum;
• determination of the patient's pharmacokinetic characteristics;
• integration of information on patient adherence;
• interpretation of the drug concentrations; and
• adjustment of the drug dose to achieve concentrations within the therapeutic range, if necessary.
A final caveat to the use of measured drug concentrations in patient management is a general one-drug concentration information cannot be used alone; it must be integrated with other clinical information, including the patient's ARV history and adherence before the TDM result. In addition, as knowledge of associations between ARV concentrations and virologic response evolves, clinicians who use a TDM strategy for patient management should evaluate the most up-to-date information regarding the exposure-response relationship of the tested ARV agent. Discontinuation of antiretroviral therapy (ART) may result in viral rebound, immune decompensation, and clinical progression. [1][2][3][4][5] Thus, planned interruptions of ART are not generally recommended. However, unplanned interruption of ART may occur under certain circumstances as discussed below.
# Short-Term Therapy Interruptions
Reasons for short-term interruption (days to weeks) of ART vary and may include drug toxicity; intercurrent illnesses that preclude oral intake, such as gastroenteritis or pancreatitis; surgical procedures; or interrupted access to drugs. Stopping ART for a short time (i.e., less than 1 to 2 days) because of a medical/surgical procedure can usually be done by holding all drugs in the regimen. Recommendations for some other scenarios are listed below:
# Unanticipated Short-Term Therapy Interruption
When a Patient Experiences a Severe or Life-Threatening Toxicity or Unexpected Inability to Take Oral Medications:
• All components of the drug regimen should be stopped simultaneously, regardless of drug half-life.
# Planned Short-Term Therapy Interruption (Up to 2 Weeks)
When All Regimen Components Have Similar Half-Lives and Do Not Require Food for Proper Absorption:
• All drugs may be given with a sip of water, if allowed; otherwise, all drugs should be stopped simultaneously. All discontinued regimen components should be restarted simultaneously.
# When All Regimen Components have Similar Half-Lives and Require Food for Adequate Absorption, and the
Patient Cannot Take Anything by Mouth for a Short Time:
• Temporary discontinuation of all drug components is indicated. The regimen should be restarted as soon as the patient can resume oral intake.
# When the ARV Regimen Contains Drugs with Different Half-Lives:
• Stopping all drugs simultaneously may result in functional monotherapy with the drug with the longest half-life (typically a non-nucleoside reverse transcriptase inhibitor [NNRTI]), which may increase the risk of selection of NNRTI-resistant mutations. Some experts recommend stopping the NNRTI first and the other ARV drugs 2 to 4 weeks later. Alternatively, the NNRTI may be replaced with a ritonavir (or cobicistat)-boosted protease inhibitor (PI/r or PI/c) for 4 weeks. The optimal time sequence for staggered discontinuation of regimen components, or replacement of the NNRTI with a PI/r (or PI/c), has not been determined.
# Planned Long-Term Therapy Interruptions
Planned long-term therapy interruptions are not recommended outside of controlled clinical trials (AI). Several research studies are evaluating approaches to a functional (virological control in the absence of therapy) or sterilizing (virus eradication) cure of HIV infection. Currently, the only way to reliably test the effectiveness of these strategies may be to interrupt ART and closely monitor viral rebound over time in the setting of a clinical trial. a Early infection represents either acute or recent infection.
Definitions: Acute HIV-1 infection is the phase of HIV-1 disease immediately after infection that is characterized by an initial burst of viremia; although, anti-HIV-1 antibodies are undetectable, HIV-1 RNA or p24 antigen are present. Recent infection generally is considered the phase up to 6 months after infection during which anti-HIV-1 antibodies are detectable. Throughout this section, the term "early HIV-1 infection" is used to refer to either acute or recent HIV-1 infection.
An estimated 40% to 90% of patients with acute HIV-1 infection will experience symptoms of acute retroviral syndrome, such as fever, lymphadenopathy, pharyngitis, skin rash, myalgias/arthralgias, and other symptoms. [1][2][3][4][5][6] However, because the self-limiting symptoms are similar to those of many other viral infections, such as influenza and infectious mononucleosis, primary care clinicians often do not recognize acute HIV-1 infection. Acute infection can also be asymptomatic. Table 11 provides practitioners with guidance to recognize, diagnose, and manage acute HIV-1 infection.
# Diagnosing Acute HIV Infection
Health care providers should maintain a high level of suspicion of acute HIV-1 infection in patients who have a compatible clinical syndrome-especially in those who report recent high-risk behavior (see Table 11). 7 Patients may not always disclose or admit to high-risk behaviors or perceive that their behaviors put them at risk for HIV-1 acquisition. Thus, even in the absence of reported high-risk behaviors, signs and symptoms
# Panel's Recommendations
• Antiretroviral therapy (ART) is recommended for all individuals with HIV-1 infection and should be offered to those with early a HIV-1 infection (BII), although definitive data to confirm whether this approach will result in long-term virologic, immunologic, or clinical benefits are lacking.
• All pregnant women with early HIV-1 infection should start ART as soon as possible to prevent perinatal transmission of HIV-1 (AI).
• If treatment is initiated in a patient with early HIV-1 infection, the goal is to suppress plasma HIV-1 RNA to undetectable levels (AIII).
• In patients with early HIV-1 infection in whom therapy is initiated, testing for plasma HIV-1 RNA levels, CD4 T lymphocyte counts, and toxicity monitoring should be performed as described for patients with chronic HIV-1 infection (AII).
• Genotypic drug resistance testing should be performed before initiation of ART to guide the selection of the regimen (AII). If therapy is deferred, genotypic resistance testing should still be performed because the results will be useful in selecting a regimen with the greatest potential for achieving optimal virologic response once therapy is initiated (AII).
• In patients without transmitted drug resistant virus, therapy should be initiated with one of the combination regimens that is recommended for patients with chronic HIV-1 infection (see What to Start) (AIII).
• ART can be initiated before drug resistance test results are available. Because resistance to pharmacokinetically enhanced protease inhibitors emerges slowly and clinically significant transmitted resistance to protease inhibitors is uncommon, these drugs and 2 nucleoside reverse transcriptase inhibitors should be used in this setting (AIII).
• Patients starting ART should be willing and able to commit to treatment and should understand the possible benefits and risks of therapy and the importance of adherence (AIII). Patients may choose to postpone therapy, and providers, on a case-by-case basis, may elect to defer therapy because of clinical and/or psychosocial factors. consistent with acute retroviral syndrome should motivate consideration of a diagnosis of acute HIV-1 infection.
# Rating of Recommendations
Acute HIV-1 infection is usually defined as detectable HIV-1 RNA or p24 antigen in serum or plasma in the setting of a negative or indeterminate HIV-1 antibody test result. 7,8 Combination immunoassays that detect HIV-1 and HIV-2 antibodies and HIV-1 p24 antigen are now approved by the Food and Drug Administration (FDA), and the most recent Centers for Disease Control and Prevention testing algorithm recommends them as the preferred assay to use for HIV screening, including for possible acute HIV-1 infection. Specimens that are reactive on this initial assay should be tested with an immunoassay that differentiates HIV-1 and HIV-2 antibodies. 9 Specimens that are reactive on the initial assay and have either negative or indeterminate antibody differentiation test results should undergo testing using an FDA-approved quantitative or qualitative HIV-1 RNA test; a negative HIV-1 RNA test result indicates that the original Ag/Ab test result was a false positive. Detection of HIV-1 RNA indicates that acute HIV-1 infection is highly likely, 9 and that antiretroviral therapy (ART) may be warranted (see Treatment for Early HIV-1 Infection). HIV-1 infection should be confirmed by subsequent testing to document HIV antibody seroconversion.
Some health care facilities may still be following HIV testing algorithms that recommend initial testing with an assay that only tests for the presence of HIV antibody. In such settings, when acute HIV-1 infection is suspected in a patient with a negative or indeterminate HIV antibody result, a quantitative or qualitative FDA-approved HIV-1 RNA test should be performed (AII). A presumptive diagnosis of acute HIV-1 infection can be made on the basis of a negative or indeterminate HIV antibody test result and a positive HIV-1 RNA test result, in which case, ART may be warranted (see Treatment for Early HIV-1 Infection).
Providers should be aware that a low-positive quantitative HIV-1 RNA level (e.g., <10,000 copies/mL) may represent a false-positive result because HIV-1 RNA levels in acute infection are generally very high (e.g., >100,000 copies/mL). 5,6 Therefore, when a low-positive quantitative HIV-1 RNA result is obtained, the HIV-1 RNA test should be repeated using a different specimen from the same patient. 6 In this setting, the diagnosis of HIV-1 infection should be confirmed by subsequent documentation of HIV antibody seroconversion (see Table 11).
# Treating Early HIV-1 Infection
Clinical trial data regarding the treatment of early HIV-1 infection is limited. Many patients who enrolled in studies to assess the role of ART in early HIV-1 infection (outlined below) were identified as trial participants because they presented with signs or symptoms of acute infection. With the introduction of HIV screening tests that include assays for HIV-1 RNA or p24 antigen and wider HIV screening in healthcare systems, the number of asymptomatic patients identified with early infection may increase. The natural history of HIV-1 disease in these patients may differ from that in individuals with symptomatic infections, thus further studies on the impact of ART on the natural history of asymptomatic acute HIV-1 infection are needed. The initial burst of high level viremia in infected individuals usually declines shortly after acute infection (e.g., within 2 months); however, a rationale for treatment during recent infection (e.g., 2-6 months after infection) remains, because during this transition period the immune system may not yet have maximally contained viral replication in the lymphoid tissue. 10 Several trials have addressed the question of the long-term benefit of potent treatment regimens initiated during early HIV-1 infection. The potential benefits and risks of treating HIV-1 during this stage of disease are discussed below.
# Potential Benefits of Treatment During Early HIV-1 Infection
Preliminary data indicate that treatment of early HIV-1 infection with combination ART improves laboratory markers of disease progression. [11][12][13][14][15] The data, though limited, indicate that treatment of early HIV-1 infection may also reduce the severity of acute disease; lower the viral set point, [16][17][18] which can affect the rate of disease progression if therapy is stopped; reduce the size of the viral reservoir; 19 and decrease the rate of viral mutation by suppressing viral replication and preserving immune function. 20 Because early HIV-1 infection is often associated with high viral loads and increased infectiousness, 21 and ART use by HIV-1-infected individuals reduces transmission to serodiscordant sexual partners, 22 treatment during early HIV-1 infection is expected to substantially reduce the risk of HIV-1 transmission. In addition, although data are limited and the clinical relevance unclear, the profound loss of gastrointestinal lymphoid tissue that occurs during the first weeks of infection may be mitigated by initiating ART during early HIV-1 infection. 23,24 Many of the potential benefits described above may be more likely to occur with treatment of acute infection, but they also may occur if treatment is initiated during recent HIV-1 infection.
# Potential Risks of Treatment During Early HIV-1 Infection
The potential disadvantages of initiating therapy during early HIV-1 infection include more prolonged exposure to ART without a known long-term clinical benefit. This prolonged exposure to ART could result in drug toxicities, development of drug resistance if the patient is non-adherent to the regimen, and adverse effects on the patient's quality of life due to earlier initiation of lifelong therapy that requires strict adherence.
# Clinical Trial Data on Treatment During Early Infection
Several randomized controlled trials have studied the effect of ART during acute and recent infection to assess whether initiating early therapy would allow patients to stop treatment and still maintain lower viral loads and higher CD4 T lymphocyte (CD4) counts while off ART for prolonged periods of time. This objective was of interest when these studies were initiated but is now less relevant because treatment is recommended for virtually all HIV-1-infected patients and treatment interruptions are not recommended (see Initiating Antiretroviral Therapy in Treatment-Naive Patients).
The Setpoint Study (ACTG A5217 Study) randomized patients with recent but not acute HIV-1 infection to either defer therapy or immediately initiate ART for 36 weeks and then stop treatment. 16 The primary study end point was a composite of meeting criteria for ART or re-initiation of ART and viral load results at week 72 in both groups and at week 36 in the deferred treatment group. The study was stopped prematurely by the Data and Safety Monitoring Board because of an apparent benefit associated with early therapy that was driven mostly by the greater proportion of participants meeting the criteria for ART initiation in the deferred treatment group (50%) than in the immediate treatment group (10%). Nearly half of the patients in the deferred treatment group needed to start therapy during the first year of study enrollment.
The Randomized Primo-SHM Trial randomized patients with acute (~70%) or recent (~30%) infection to either defer ART or undergo treatment for 24 or 60 weeks and then stop. 17 Significantly lower viral loads were observed 36 weeks after treatment interruption in the patients who had been treated early. These patients also took longer to reach a CD4 count threshold of <350 cells/mm 3 for restarting ART. The median time to starting treatment was 0.7 years for the deferred therapy group and 3.0 and 1.8 years for the 24-and 60-week treatment arms, respectively. The time to reaching a CD4 count of <500 cells/mm 3 was only 0.5 years in the deferred group.
The SPARTAC Trial included patients with acute and recent infection randomized to either defer therapy or received ART for 12 or 48 weeks and then stop. 18 In this trial, the time to reach CD4 <350 cells/mm 3 or initiate therapy was significantly longer in the group treated for 48 weeks than in the deferred treatment group or the group treated for 12 weeks. However, no difference was observed between the participants who received 12 weeks of ART and those who deferred treatment during early infection.
The strategies tested in these studies are of limited relevance today given that treatment interruption is not recommended. The study results may not fully reflect the natural history of HIV-1 disease in persons with asymptomatic acute infection because most patients in these trials were enrolled on the basis of identified early symptomatic HIV-1 infections. Nevertheless, the results do demonstrate that some immunologic and virologic benefits may be associated with the treatment of early HIV-1 infection. Moreover, all the findings suggest, at least in the population recruited for these studies, that the time to initiating ART after identification of early infection is quite short when the threshold for ART initiation is 350 CD4 cells/mm 3 , and nonexistent when therapy is advised for all individuals regardless of CD4 cell count as currently recommended in these guidelines. These observations must be balanced with the risks of early treatment, risks that are largely the same as those when therapy is initiated in chronically infected asymptomatic patients with high CD4 counts. Consequently, the health care provider and the patient should be fully aware that the rationale for initiating therapy during early HIV-1 infection is based on theoretical benefits and the extrapolation of data from the strategy trials outlined above. These potential benefits must be weighed against the risks. For these reasons, and because ART is currently recommended for all HIV-1-infected patients (see Initiating Antiretroviral Therapy in Treatment Naive Patients), ART should be offered to all patients with early HIV-1 infection (BII). However, patients must be willing and able to commit to treatment, and providers, on a case-by-case basis, may elect to defer therapy for clinical and/or psychosocial reasons. Providers also should consider enrolling patients with early HIV-1 infection in clinical studies to further evaluate the natural history of this stage of HIV-1 infection and to further define the role of ART in this setting. Providers can obtain information regarding such trials at www.clinicaltrials.gov or from local HIV treatment experts.
# Treating Early HIV-1 Infection During Pregnancy
Because early HIV-1 infection is associated with a high risk of perinatal transmission, all HIV-1-infected pregnant women should start combination ART as soon as possible to prevent perinatal transmission of HIV-1 (AI). 25
# Treatment Regimen for Early HIV-1 Infection
Data from the United States and Europe demonstrate that transmitted virus may be resistant to at least 1 antiretroviral drug in 6% to 16% of patients. [26][27][28] In one study, 21% of isolates from patients with acute HIV-1 infection demonstrated resistance to at least 1 drug. 29 Therefore, before initiating ART in a person with early HIV-1 infection, genotypic antiretroviral (ARV) drug resistance testing should be performed to guide selection of a regimen (AII). If the decision is made to initiate therapy during early infection, especially in the setting of acute infection, treatment initiation should not be delayed pending resistance testing results.
Once results are available, the treatment regimen can be modified if warranted. If therapy is deferred, resistance testing still should be performed because the results will help guide selection of a regimen that has the greatest potential to optimize virologic response once therapy is initiated (AII).
The goal of therapy during early HIV-1 infection is to suppress plasma HIV-1 RNA to undetectable levels (AIII). Because data are insufficient to draw firm conclusions regarding specific drug combinations to use in this stage of HIV-1 infection, ART should be initiated with one of the combination regimens recommended for patients with chronic infection (AIII) (see What to Start). If therapy is started before the results of drug resistance testing are available, a pharmacologically boosted protease inhibitor (PI) should be used because resistance to these agents emerges slowly and clinically significant transmitted resistance is uncommon (AIII).
If available, the results of ARV drug resistance testing or the ARV resistance pattern of the source person's virus should be used to guide selection of the ARV regimen. Given the increasing use of daily tenofovir disoproxil fumarate/emtricitabine (TDF/FTC) for pre-exposure prophylaxis (PrEP) in HIV-negative individuals, [30][31][32] early infection may be diagnosed in some patients while they are taking TDF/FTC as PrEP. In this setting, resistance testing should be performed; however, because PI resistance is unlikely, use of a pharmacologically boosted PI and TDF/FTC remains a reasonable option pending resistance testing results (see What to Start).
# Patient Follow-Up
Testing for plasma HIV-1 RNA levels, CD4 cell counts, and toxicity monitoring should be performed as described in Laboratory Testing for Initial Assessment and Monitoring While on Antiretroviral Therapy (i.e.,
HIV-1 RNA at initiation of therapy, after 2 to 8 weeks, then every 4 to 8 weeks until viral suppression, and thereafter, every 3 to 4 months) (AII).
# Duration of Therapy for Early HIV-1 Infection
The optimal duration of therapy for patients with early HIV-1 infection is unknown. Recent studies of early HIV-1 infection have evaluated starting and then stopping treatment as a potential strategy. [16][17][18] Although these studies showed some benefits associated with this strategy, a large randomized controlled trial of patients with chronic HIV-1 infection found that treatment interruption was harmful in terms of increased risk of AIDS and non-AIDS events, 33 and that the strategy was associated with increased markers of inflammation, immune activation, and coagulation. 34 For these reasons and the potential benefit of ART in reducing the risk of HIV-1 transmission, the Panel does not recommend discontinuation of ART in patients treated for early HIV-1 infection (AIII).
# Table 11. Identifying, Diagnosing, and Managing Acute and Recent HIV-1 Infection
Suspicion of Acute HIV-1 Infection:
• Acute HIV-1 infection should be considered in individuals with signs or symptoms of acute HIV-1 infection and recent (within 2 to 6 weeks) high risk of exposure to HIV-1
.a
• Signs, symptoms, or laboratory findings may include but are not limited to one or more of the following: fever, lymphadenopathy, skin rash, myalgia/arthralgia, headache, diarrhea, oral ulcers, leucopenia, thrombocytopenia, transaminase elevation.
• High-risk exposures include sexual contact with an HIV-1-infected person or a person at risk of HIV-1 infection, sharing injection drug use paraphernalia, or contact of mucous membranes or breaks in skin with potentially infectious fluids.
• Differential diagnosis: The differential diagnosis of patients presenting with HIV-1 infection may include but is not limited to viral illnesses such as Epstein-Barr virus (EBV) and non-EBV (e.g., cytomegalovirus) infectious mononucleosis syndromes, influenza, viral hepatitis, streptococcal infection, or syphilis.
Evaluation/Diagnosis of Acute HIV-1 Infection:
• Acute HIV-1 infection is defined as detectable HIV-1 RNA or p24 antigen (the antigen used in currently available HIV antigen/antibody [Ag/Ab] combination assays) in the setting of a negative or indeterminate HIV-1 antibody test result.
• A reactive HIV antibody test result or Ag/Ab combination test result must be followed by supplemental confirmatory testing.
• A negative or indeterminate HIV-1 antibody test result in a person with a reactive Ag/Ab test result or in whom acute HIV-1 infection is suspected requires assessment of plasma HIV-1 RNA to diagnose acute HIV-1 infection.
• A positive result on an FDA-approved quantitative or qualitative plasma HIV-1 RNA test in the setting of a negative or indeterminate antibody test result is consistent with acute HIV-1 infection.
Considerations for ART During Early HIV-1 Infection:
• All pregnant women with early HIV-1 infection should begin taking combination ART as soon as possible to prevent perinatal transmission of HIV-1 (AI).
• Treatment for early HIV-1 infection should be offered to all non-pregnant individuals (BII).
• The risks of ART during early HIV-1 infection are largely the same as those when ART is initiated in chronically infected asymptomatic patients with high CD4 counts.
• If therapy is initiated, the goal should be sustained plasma virologic suppression (AIII).
a In some settings, behaviors that increase the risk of HIV-1 infection may not be recognized or perceived as risky by the health care provider or the patient or both. Thus, even in the absence of reported high-risk behaviors, symptoms and signs consistent with acute retroviral syndrome should motivate consideration of a diagnosis of acute HIV-1 infection. Older children and adolescents now make up the largest percentage of HIV-infected children cared for at pediatric HIV clinics in the United States. The Centers for Disease Control and Prevention (CDC) estimates that 26% of the approximately 50,000 new HIV infections diagnosed in 2010 were among youth 13 to 24 years of age. In this age group, 57% of the infections were among young black/African Americans and 75% among young men who have sex with men (MSM). 1 Among youth living with HIV infection in 2010, CDC estimates that almost 60% had undiagnosed infections and were unaware they were HIV-infected. 2 Recent trends in HIV/AIDS prevalence reveal that the disproportionate burden of AIDS among racial minorities is even greater among minority youth 13 to 24 years of age (64% to 66% of cases) than among those older than 24 years (48% of cases). 3 Furthermore, trends for all HIV diagnoses among adolescents and young adults in 46 states and 5 U.S. dependent areas from 2007 to 2010 decreased or remained stable for all transmission categories except among young MSM. HIV-infected adolescents represent a heterogeneous group in terms of sociodemographics, mode of HIV infection, sexual and substance abuse history, clinical and immunologic status, psychosocial development, and readiness to adhere to medications. Many of these factors may influence decisions concerning when to start antiretroviral therapy (ART) and what antiretroviral (ARV) medications to use.
Most adolescents who acquire HIV are infected through sexual risk behaviors. Many of them are recently infected and unaware of their HIV infection status. Thus, many are in an early stage of HIV infection, which makes them ideal candidates for early interventions, such as prevention counseling and linkage to and engagement in care. 4 High grade viremia was reported among a cohort of youth identified as HIV-infected by adolescent HIV specialty clinics in 15 major metropolitan U.S. cities. The mean HIV viral load for the cohort was 94,398 copies/ml; 30% of the youth were not successfully linked to care. 5 A study among HIV-infected adolescents and young adults presenting for care identified primary genotypic resistance mutations to ARV medications in up to 18% of the evaluable sample of recently infected youth, as determined by the detuned antibody testing assay strategy that defined recent infection as occurring within 180 days of testing. 6 Recently, substantial multiclass resistance was noted in a cohort of behaviorally-infected, treatment-naive youth who were screened for an ARV treatment trial. 7 As these youth were naive to all ART, this reflects transmission of resistant virus. This transmission dynamic reflects that a substantial proportion of youth's sexual partners are likely older and may be more ART experienced; thus, awareness of the importance of baseline resistance testing among recently infected youth naive to ART is imperative.
A limited but increasing number of HIV-infected adolescents are long-term survivors of HIV infection acquired perinatally or in infancy through blood products. Such adolescents are usually heavily ART experienced and may have a unique clinical course that differs from that of adolescents infected later in life. 8 Those adolescents infected perinatally or in infancy were often started on ART early in life with mono or dual therapy regimens resulting in incomplete viral suppression and emergence of resistance. If these heavily ART-experienced adolescents harbor resistant virus, optimal ARV regimens should be selected on the basis of the same guiding principles used for heavily ART-experienced adults (see Virologic Failure and Suboptimal Immunologic Response).
Adolescents are developmentally at a difficult crossroad. Their needs for autonomy and independence and their evolving decisional capacity intersect and compete with their concrete thinking processes, risk-taking behaviors, preoccupation with self-image, and need to fit in with their peers. This makes it challenging to attract and sustain adolescents' focus on maintaining their health, particularly for those with chronic illnesses. These challenges are not specific to any particular transmission mode or stage of disease. Thus, irrespective of disease duration or mode of HIV transmission, every effort must be made to engage and maintain adolescents in care so they can improve and maintain their health for the long term. Adolescents may seek care in several settings including pediatric-focused HIV clinics, adolescent/young adult clinics, and adult-focused clinics. 9 Regardless of the setting, expertise in caring for adolescents is critical to creating a Downloaded from http://aidsinfo.nih.gov/guidelines on 9/16/2015
Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents I-9
supportive environment for engaging youth in care. 9,10
# Antiretroviral Therapy Considerations in Adolescents
Adult guidelines for ART are usually appropriate for postpubertal adolescents because the clinical course of HIV infection in adolescents who were infected sexually or through injection drug use during adolescence is more similar to that in adults than that in children. Adult guidelines can also be useful for postpubertal youth who were perinatally infected. These patients often have treatment challenges associated with the long-term use of ART that mirror those of ART-experienced adults, such as extensive resistance, complex regimens, and adverse drug effects.
Dosage of medications for HIV infection and opportunistic infections should be prescribed according to Tanner staging of puberty and not solely on the basis of age. 11,12 Adolescents in early puberty (i.e., Tanner Stages I and II) should be administered doses on pediatric schedules, whereas those in late puberty (i.e., Tanner Stage V) should follow adult dosing schedules. However, Tanner stage and age are not necessarily directly predictive of drug pharmacokinetics. Because puberty may be delayed in children who were infected with HIV perinatally, 13 continued use of pediatric doses in puberty-delayed adolescents can result in medication doses that are higher than the usual adult doses. Because data are not available to predict optimal medication doses for each ARV medication for this group of children, issues such as toxicity, pill or liquid volume burden, adherence, and virologic and immunologic parameters should be considered in determining when to transition from pediatric to adult doses. Youth who are in their growth spurt period (i.e., Tanner Stage III in females and Tanner Stage IV in males) and following adult or pediatric dosing guidelines and adolescents who have transitioned from pediatric to adult doses should be closely monitored for medication efficacy and toxicity. Therapeutic drug monitoring can be considered in each of these selected circumstances to help guide therapy decisions. Pharmacokinetic studies of drugs in youth are needed to better define appropriate dosing. For a more detailed discussion, see Guidelines for the Use of Antiretroviral Agents in Pediatric HIV Infection. 14
# Adherence Concerns in Adolescents
HIV-infected adolescents are especially vulnerable to specific adherence problems on the basis of their psychosocial and cognitive developmental trajectory. Comprehensive systems of care are required to serve both the medical and psychosocial needs of HIV-infected adolescents, who are frequently inexperienced with health care systems and who lack health insurance. Recent studies in adolescents infected through risk behaviors and in adolescents infected through perinatal transmission demonstrate that many adolescents in both groups face numerous barriers to adherence. [15][16][17] Compared with adults, these youth have lower rates of viral suppression and higher rates of virologic rebound and loss to follow up. 18 Many HIV-infected adolescents face challenges in adhering to medical regimens for reasons that include:
• Denial and fear of their HIV infection;
• Misinformation;
• Distrust of the medical establishment;
• Fear and lack of belief in the effectiveness of medications;
• Low self-esteem;
• Unstructured and chaotic lifestyles;
• Mood disorders and other mental illness;
• Lack of familial and social support;
• Absence of or inconsistent access to care or health insurance; and
• Risk of inadvertent parental disclosure of the youth's HIV infection status if parental health insurance is used.
In selecting treatment regimens for adolescents, clinicians must balance the goal of prescribing a maximally potent ART regimen with realistic assessment of existing and potential support systems to facilitate adherence. Adolescents benefit from reminder systems (e.g., beepers, timers, and pill boxes) that are stylish and/or inconspicuous. 19 In a recent randomized controlled study among non-adherent youth 15 to 24 years of age, youth who received cell phone medication reminders demonstrated significantly higher adherence and lower viral loads than youth who did not receive the reminder calls. 20 It is important to make medication adherence as user friendly and the least stigmatizing possible for the older child or adolescent. The concrete thought processes of adolescents make it difficult for them to take medications when they are asymptomatic, particularly if the medications have side effects. Adherence to complex regimens is particularly challenging at a time of life when adolescents do not want to be different from their peers. [21][22][23] Directly observed therapy may be considered for selected HIV-infected adolescents such as those with mental illness. [24][25][26][27][28]
# Difficult Adherence Problems
Because adolescence is characterized by rapid changes in physical maturation, cognitive processes, and life style, predicting long-term adherence in an adolescent can be very challenging. The ability of youth to adhere to therapy needs to be considered as part of therapeutic decision making concerning the risks and benefits of starting treatment. Erratic adherence may result in the loss of future regimens because of the development of resistance mutations. Clinicians who care for HIV-infected adolescents frequently manage youth who, while needing therapy, pose significant concerns regarding their ability to adhere to therapy. In these cases, alternative considerations to initiation of therapy can be the following:
1. A short-term deferral of treatment until adherence is more likely or while adherence-related problems are aggressively addressed;
2. An adherence testing period in which a placebo (e.g., vitamin pill) is administered; and
3. The avoidance of any regimens with low genetic resistance barriers.
Such decisions are ideally individualized to each patient and should be made carefully in context with the individual's clinical status. For a more detailed discussion on specific therapy and adherence issues for HIVinfected adolescents, see Guidelines for Use of Antiretroviral Agents in Pediatric HIV Infection. 14
# Special Considerations in Adolescents
Sexually transmitted infections (STIs), in particular human papilloma virus (HPV), should also be addressed in all adolescents. In young MSM, screening for STIs may require sampling from several body sites because oropharyngeal, rectal, and urethral infections may be present in this population. 29 For a more detailed discussion on STIs, see the most recent CDC guidelines 30 and the adult and pediatric opportunistic infection treatment guidelines on HPV among HIV-infected adolescents. 31,32 Family planning counseling, including a discussion of the risks of perinatal transmission of HIV and methods to reduce risks, should be provided to all youth. Providing gynecologic care for HIV-infected female adolescents is especially important. Contraception, including the interaction of specific ARV drugs with hormonal contraceptives, and the potential for pregnancy also may alter choices of ART. As an example, efavirenz (EFV) should be used with caution in females of childbearing age and should only be prescribed after intensive counseling and education about the potential effects on the fetus, the need for close monitoring-including periodic pregnancy testing-and a commitment on the part of the teen to use effective contraception. For a more detailed discussion, see HIV-Infected Women and the Perinatal Guidelines. 33
# Transitioning Care
Given lifelong infection with HIV and the need for treatment through several stages of growth and development, HIV care programs and providers need flexibility to appropriately transition care for HIVinfected children, adolescents, and young adults. A successful transition requires an awareness of some fundamental differences between many adolescent and adult HIV care models. In most adolescent HIV clinics, care is more teen-centered and multidisciplinary, with primary care highly integrated into HIV care.
Teen services, such as sexual and reproductive health, substance abuse treatment, mental health, treatment education, and adherence counseling are all found in one clinic setting. In contrast, some adult HIV clinics may rely more on referral of the patient to separate subspecialty care settings, such as gynecology.
Transitioning the care of an emerging young adult includes considerations of areas such as medical insurance; the adolescent's degree of independence/autonomy and decisional capacity; patient confidentiality; and informed consent. Also, adult clinic settings tend to be larger and can easily intimidate younger, less motivated patients. As an additional complication to this transition, HIV-infected adolescents belong to two epidemiologically distinct subgroups:
1. Those perinatally infected-who would likely have more disease burden history, complications, and chronicity; less functional autonomy; greater need for ART; and higher mortality risk-and 2. Those more recently infected because of high-risk behaviors.
Thus, these subgroups have unique biomedical and psychosocial considerations and needs.
To maximize the likelihood of a successful transition, interventions to facilitate transition are best implemented early on. 34 These include the following:
• Developing an individualized transition plan to address comprehensive care needs including medical, psychosocial and financial aspects of transitioning;
• Optimizing provider communication between adolescent and adult clinics;
• Identifying adult care providers willing to care for adolescents and young adults;
• Addressing patient/family resistance caused by lack of information, stigma or disclosure concerns, and differences in practice styles;
• Preparing youth for life skills development, including counseling them on the appropriate use of a primary care provider and appointment management, the importance of prompt symptom recognition and reporting, and the importance of self-efficacy in managing medications, insurance, and entitlements;
• Identifying an optimal clinic model for a given setting (i.e., simultaneous transition of mental health and/or case management versus a gradual phase-in);
• Implementing ongoing evaluation to measure the success of a selected model;
• Engaging in regular multidisciplinary case conferences between adult and adolescent care providers;
• Implementing interventions that may be associated with improved outcomes, such as support groups and mental health consultation;
• Incorporating a family planning component into clinical care; and
• Educating HIV care teams and staff about transitioning.
Discussions regarding transition should begin early and before the actual transition process. 35 Attention to these key areas will likely improve adherence to appointments and avert the potential for a youth to fall through the cracks, as it is commonly referred to in adolescent medicine. For a more detailed discussion on specific topics on transitioning care for adolescents and young adults, see http://www.hivguidelines.org/clinicalguidelines/adolescents/transitioning-hiv-infected-adolescents-into-adult-care/.
# Treatment Challenges of HIV-Infected Illicit Drug Users
Injection drug use is the second most common mode of HIV transmission in the United States. In addition, noninjection illicit drug use may facilitate sexual transmission of HIV. Injection and noninjection illicit drugs include the following: heroin, cocaine, marijuana, and club drugs (i.e., methamphetamine, ketamine, gammahydroxybutyrate [GHB], and amyl nitrate [i.e., poppers]). The most commonly used illicit drugs associated with HIV infection are heroin and stimulants (e.g., cocaine and amphetamines); however, the use of club drugs has increased substantially in the past several years and is common among individuals who have HIV infection or who are at risk of HIV infection. The association between club drugs and high-risk sexual behavior in men who have sex with men (MSM) is strongest for methamphetamine and amyl nitrate; this association is less consistent with the other club drugs. 1 Illicit drug use has been associated with depression and anxiety, either as part of the withdrawal process or as a consequence of repeated use. This is particularly relevant in the treatment of HIV infection because depression is one of the strongest predictors of poor adherence and poor treatment outcomes. 2 Treatment of HIV disease in illicit drug users can be successful but HIV-infected illicit drug users present special treatment challenges. These challenges may include the following: (1) an array of complicating comorbid medical and mental health conditions; (2) limited access to HIV care; (3) inadequate adherence to therapy; (4) medication side effects and toxicities; (5) the need for substance abuse treatment; and (6) drug interactions that can complicate HIV treatment. 3 Underlying health problems in injection and noninjection drug users result in increased morbidity and mortality, either independent of or accentuated by HIV disease. Many of these problems are the consequence of prior exposures to infectious pathogens from nonsterile needle and syringe use. Such problems can include hepatitis B or C virus infection, tuberculosis (TB), skin and soft tissue infections, recurrent bacterial pneumonia, and endocarditis. Other morbidities such as alteration in levels of consciousness and neurologic and renal disease are not uncommon. Furthermore, these comorbidities are associated with a higher risk of drug overdoses in illicit drug users with HIV disease than in HIV-uninfected illicit drug users, due in part to respiratory, hepatic, and neurological impairments associated with HIV infection. 4 Successful HIV therapy for illicit drug users often depends on clinicians becoming familiar with and managing these comorbid conditions and providing overdose prevention support.
Illicit drug users have less access to HIV care and are less likely to receive antiretroviral therapy (ART) than other populations. [5][6] Factors associated with low rates of ART use among illicit drug users include active drug use, younger age, female gender, suboptimal health care, recent incarceration, lack of access to rehabilitation programs, and health care providers' lack of expertise in HIV treatment. [5][6] The typically unstable, chaotic life patterns of many illicit drug users; the powerful pull of addictive substances; and common misperceptions about the dangers, impact, and benefits of ART all contribute to decreased adherence. 7 The chronic and relapsing nature of substance abuse as a biologic and medical disease, compounded by the high rate of mental illness that antedates and/or is exacerbated by illicit substance use, additionally complicate the relationship between health care workers and illicit drug users. [8][9] The first step in provision of care and treatment for these individuals is to recognize the existence of a substance abuse problem. It is often obvious that the problem exists, but some patients may hide these problem behaviors from clinicians. Assessment of a patient for substance abuse should be part of routine medical history taking and should be done in a professional, straightforward, and nonjudgmental manner.
# Treatment Efficacy in HIV-Infected Illicit Drug Use Populations
Although illicit drug users are underrepresented in HIV therapy clinical trials, available data indicate that efficacy of ART in illicit drug users-when they are not actively using drugs-is similar to that seen in other populations. 10 Furthermore, therapeutic failure in this population generally correlates with the degree that drug use disrupts daily activities rather than with drug use per se. 11 Providers need to remain attentive to the possible impact of disruptions caused by drug use on the patient both before and while receiving ART. Although many illicit drug users can sufficiently control their drug use for long enough time to benefit from care, substance abuse treatment is often necessary for successful HIV management.
Close collaboration with substance abuse treatment programs and proper support and attention to this population's special multidisciplinary needs are critical components of successful HIV treatment. Essential to this end are accommodating, flexible, community-based HIV care sites that are characterized by familiarity with and nonjudgmental expertise in management of drug users' wide array of needs and in development of effective strategies to promote medication adherence. 9 These strategies should include, if available, the use of adherence support mechanisms such as modified directly observed therapy (mDOT), which has shown promise in this population. 12
# Antiretroviral Agents and Opioid Substitution Therapy
Compared with noninjection drug users receiving ART, injection drug users (IDUs) receiving ART are more likely to experience an increased frequency of side effects and toxicities of ART. Although not systematically studied, this is likely because underlying hepatic, renal, neurologic, psychiatric, gastrointestinal (GI), and hematologic disorders are highly prevalent among IDUs. These comorbid conditions should be considered when selecting antiretroviral (ARV) agents in this population. Opioid substitution therapies such as methadone and buprenorphine/naloxone and extended-release naltrexone are commonly used for management of opioid dependence in HIV-infected patients.
Methadone and Antiretroviral Therapy. Methadone, an orally administered, long-acting opioid agonist, is the most common pharmacologic treatment for opioid addiction. Its use is associated with decreased heroin use, decreased needle sharing, and improved quality of life. Because of its opioid-induced effects on gastric emptying and the metabolism of cytochrome P (CYP) 450 isoenzymes 2B6, 3A4, and 2D6, pharmacologic effects and interactions with ARV agents may commonly occur. 13 These may diminish the effectiveness of either or both therapies by causing opioid withdrawal or overdose, increased methadone toxicity, and/or decreased ARV efficacy. Efavirenz (EFV), nevirapine (NVP), and lopinavir/ritonavir (LPV/r) have been associated with significant decreases in methadone levels. Patients and substance abuse treatment facilities should be informed of the likelihood of this interaction. The clinical effect is usually seen after 7 days of coadministration and may be managed by increasing the methadone dosage, usually in 5-mg to 10-mg increments daily until the desired effect is achieved.
Buprenorphine and Antiretroviral Therapy. Buprenorphine, a partial µ-opioid agonist, is administrated sublingually and is often coformulated with naloxone. It is increasingly used for opioid dependence treatment. Compared with methadone, buprenorphine has a lower risk of respiratory depression and overdose. This allows physicians in primary care to prescribe buprenorphine for the treatment of opioid dependency. The flexibility of the primary care setting can be of significant value to opioid-addicted HIVinfected patients who require ART because it enables one physician or program to provide both medical and substance abuse services. Limited information is currently available about interactions between buprenorphine and ARV agents. [13][14] Findings from available studies show that the drug interaction profile of buprenorphine is more favorable than that of methadone.
Naltrexone and Antiretroviral Therapy. A once-monthly extended-release intramuscular formulation of naltrexone was recently approved for prevention of relapse in patients who have undergone an opioid detoxification program. Naltrexone is also indicated for treatment of alcohol dependency. Naltrexone is not metabolized via the CYP450 enzyme system and is not expected to interact with protease inhibitors (PIs) or non-nucleoside reverse transcriptase inhibitors (NNRTIs). 15 Currently available pharmacokinetic (PK) interaction data that clinicians can use as a guide for managing patients receiving ART and methadone or buprenorphine can be found in Tables 19a-d. Particular attention is needed concerning communication between HIV care providers and drug treatment programs regarding additive drug toxicities and drug interactions resulting in opiate withdrawal or excess.
Methylenedioxymethamphetamine (MDMA), GHB, ketamine, and methamphetamine all have the potential to interact with ARV agents because all are metabolized, at least in part, by the CYP450 system. Overdoses secondary to interactions between the party drugs (i.e., MDMA or GHB) and PI-based ART have been reported. 16
# Summary
It is usually possible over time to support most active drug users such that acceptable adherence levels with ARV agents can be achieved. [17][18] Providers must work to combine all available resources to stabilize an active drug user in preparation for ART. This should include identification of concurrent medical and psychiatric illnesses, drug treatment and needle and syringe exchange programs, strategies to reduce highrisk sexual behavior, and harm-reduction strategies. A history of drug use alone is insufficient reason to withhold ART because individuals with a history of prior drug use have adherence rates similar to those who do not abuse drugs.
Important considerations in the selection of successful regimens and the provision of appropriate patient monitoring in this population include need for supportive clinical sites; linkage to substance abuse treatment; and awareness of the interactions between illicit drugs and ARV agents, including the increased risk of side effects and toxicities. Simple regimens should be considered to enhance medication adherence. Preference should be given to ARV agents that have a lower risk of hepatic and neuropsychiatric side effects, simple dosing schedules, and minimal interaction with methadone. This section provides discussion of some basic principles and unique considerations to follow when caring for HIV-infected women, including during pregnancy. Clinicians who provide care for pregnant women should consult the current Perinatal Guidelines 1 for more in-depth discussion and management assistance. Additional guidance on the management of HIV-infected women can be found at http://hab.hrsa.gov/deliverhivaidscare/clinicalguide11.
# Gender Considerations in Antiretroviral Therapy
In general, studies to date have not shown gender differences in virologic responses to antritretroviral therapy (ART), [2][3][4] but a number of studies have suggested that gender may influence the frequency, presentation, and severity of selected antiretroviral (ARV)-related adverse events. 5 Although data are limited, evidence also exists that pharmacokinetics for some ARV drugs may differ between men and women, possibly because of variations between men and women in factors such as body weight, plasma volume, gastric emptying time, plasma protein levels, cytochrome P (CYP) 450 activity, drug transporter function, and excretion activity. [6][7][8] Adverse Effects:
• Nevirapine (NVP)-associated hepatotoxicity: NVP has been associated with an increased risk of symptomatic, potentially fatal, and often rash-associated liver toxicity in ARV-naive individuals; women with higher CD4 counts (>250 cells/mm 3 ) or elevated baseline transaminase levels appear to be at greatest risk. [9][10][11][12] It is generally recommended that NVP not be prescribed to ARV-naive women who have CD4 counts >250 cells/mm 3 unless there is no other alternative and the benefit from NVP outweighs the risk of hepatotoxicity (AI).
# Panel's Recommendations
• The indications for initiation of antiretroviral therapy (ART) and the goals of treatment are the same for HIV-infected women as for other HIV-infected adults and adolescents (AI).
• Women taking antiretroviral (ARV) drugs that have significant pharmacokinetic interactions with oral contraceptives should use an additional or alternative contraceptive method to prevent unintended pregnancy (AIII).
• In pregnant women, an additional goal of therapy is prevention of perinatal transmission of HIV, with a goal of maximal viral suppression to reduce the risk of transmission of HIV to the fetus and newborn (AI).
• When selecting an ARV combination regimen for a pregnant woman, clinicians should consider the known safety, efficacy, and pharmacokinetic data on use during pregnancy for each agent (AIII).
• Women of childbearing potential should undergo pregnancy testing before initiation of efavirenz (EFV) and receive counseling about the potential risk to the fetus and desirability of avoiding pregnancy while on EFV-based regimens (AIII).
• Alternative regimens that do not include EFV should be strongly considered in women who are planning to become pregnant or sexually active and not using effective contraception, assuming these alternative regimens are acceptable to the provider and are not thought to compromise the woman's health (BIII).
• Because the risk of neural tube defects is restricted to the first 5 to 6 weeks of pregnancy and pregnancy is rarely recognized before 4 to 6 weeks of pregnancy, EFV can be continued in pregnant women receiving an EFV-based regimen who present for antenatal care in the first trimester, provided the regimen produces virologic suppression (CIII).
• When designing a regimen for a pregnant woman, clinicians should consult the most current Health and Human Services (HHS) Perinatal Guidelines (AIII). • Lactic acidosis: There is a female predominance in the increased incidence of symptomatic and even fatal lactic acidosis associated with prolonged exposure to nucleoside reverse transcriptase inhibitors (NRTIs). Lactic acidosis is most common with stavudine (d4T), didanosine (ddI), and zidovudine (ZDV) but it can occur with other NRTIs. 13 • Metabolic complications: A few studies have compared women and men in terms of metabolic complications associated with ARV use. Compared with HIV-infected men, HIV-infected women are more likely to experience increases in central fat with ART and are less likely to have triglyceride elevations on treatment. 14,15 Women have an increased risk of osteopenia/osteoporosis, particularly after menopause, and this risk is exacerbated by HIV and ART. 16,17 At the present time, none of these differences requires women-specific recommendations regarding treatment or monitoring.
# Rating of Recommendations
# Women of Childbearing Potential
All women of childbearing potential should be offered pre-conception counseling and care as a component of routine primary medical care. Counseling should include discussion of special considerations pertaining to ARV use when trying to conceive and during pregnancy (see Perinatal Guidelines 1 ). Safe sexual practices, reproductive desires and options for conception, HIV status of sexual partner(s), and use of effective contraception to prevent unintended pregnancy should be discussed. An HIV-infected woman who wishes to conceive with an HIV-uninfected male partner should be informed of options to prevent sexual transmission of HIV while attempting conception. Interventions include initiation of maximally suppressive ART, which significantly decreases the risk of sexual transmission (see Preventing Secondary Transmission of HIV), and artificial insemination, including the option to self-inseminate with the partner's sperm during the periovulatory period 18 (for more extensive discussion on this topic, see the Reproductive Options for HIV-Concordant and Serodiscordant Couples section of the Perinatal Guidelines. 1 Efavirenz (EFV) is teratogenic in non-human primates. Women of childbearing potential should undergo pregnancy testing before initiation of EFV and receive counseling about the potential risk to the fetus and desirability of avoiding pregnancy while on EFV-based regimens (AIII). Alternative regimens that do not include EFV should be strongly considered in women who are planning to become pregnant or who are sexually active and not using effective contraception, assuming these alternative regimens are acceptable to the provider and are not thought to compromise the woman's health (BIII). The most vulnerable period in fetal organogenesis is early in gestation, before pregnancy is recognized.
# Hormonal Contraception
Safe and effective reproductive health and family planning services to reduce unintended pregnancy and perinatal transmission of HIV are an essential component of care for HIV-infected women of childbearing age. Counseling about reproductive issues should be provided on an ongoing basis.
Providers should be aware of potential interactions between ARV drugs and hormonal contraceptives that could lower contraceptive efficacy. Several protease inhibitors (PIs) and non-nucleoside reverse transcriptase inhibitors (NNRTIs) have drug interactions with combined oral contraceptives (COCs). Interactions include either a decrease or an increase in blood levels of ethinyl estradiol, norethindrone, or norgestimate (see Tables 20a and 20b), which potentially decreases contraceptive efficacy or increases estrogen-or progestinrelated adverse effects (e.g., thromboembolism). Small studies of HIV-infected women receiving injectable depot-medroxyprogesterone acetate (DMPA) while on ART showed no significant interactions between DMPA and EFV, NVP, nelfinavir (NFV), or NRTI drugs. [19][20][21] Contraceptive failure of the etonogestrel implant in two patients on EFV-based therapy has been reported and a study has shown EFV may decrease plasma progestin concentrations of COCs containing ethinyl estradiol and norgestimate. 22,23 Several RTVboosted PIs decrease oral contraceptive estradiol levels. 24,25 A small study from Malawi showed that NVP use did not significantly affect estradiol or progestin levels in HIV-infected women. 26 Overall, data are relatively limited and the clinical implications of these findings are unclear. The magnitudes of change in drug levels that may reduce contraceptive efficacy or increase adverse effects are unknown. Concerns about pharmacokinetic interactions between oral and implant hormonal contraceptives and ARVs should not prevent clinicians from prescribing hormonal contraceptives for women on ART if that is their preferred contraceptive method. However, when women wish to use hormonal contraceptives and drug interactions with ARVs are known, additional or alternative contraceptive methods may be recommended (see drug interaction Tables 19a, 19b, and 19d and Perinatal Guidelines 1 ). Consistent use of male or female condoms to prevent transmission of HIV and protect against other sexually transmitted diseases (STDs) is recommended for all HIV-infected women and their partners, regardless of contraceptive use.
The data on the association between hormonal contraception and the risk of acquisition of HIV are conflicting. 27 A retrospective secondary analysis of two studies of serodiscordant couples in Africa in which the HIV-infected partner was not receiving ART found that women using hormonal contraception (the vast majority using injectable DMPA) had a twofold increased risk of acquiring HIV (for HIV-infected male/HIVuninfected female couples) or transmitting HIV (HIV-infected female/HIV-uninfected male couples). HIV-infected women using hormonal contraception had higher genital HIV RNA concentrations than did women not using hormonal contraceptives. 28 Oral contraceptive use was not significantly associated with transmission of HIV; however, the number of women using oral contraceptives in this study was insufficient to adequately assess risk. It is important to note that not all studies have supported a link between hormonal contraception and transmission or acquisition of HIV and that the individuals in this study were not receiving ART. Further research is needed to definitively determine if hormonal contraceptive use is an independent risk factor for acquisition and transmission of HIV, particularly in the setting of ART. 27,29 Intrauterine devices (IUDs) appear to be a safe and effective contraceptive option for HIV-infected women. [30][31][32][33] Although studies have focused primarily on non-hormone-containing IUDs (e.g., copper IUD), several small studies have also found levonorgestrel-releasing IUDs to be safe and not associated with increased genital tract shedding of HIV. 31,34,35
# Pregnant Women
Clinicians should review the Perinatal Guidelines 1 for a detailed discussion of the management of HIVinfected pregnant women. The use of combination ARV regimens is recommended for all HIV-infected pregnant women, regardless of virologic, immunologic, or clinical parameters (AI). Pregnant HIV-infected women should be counseled regarding the known benefits and risks of ARV use during pregnancy to the woman, fetus, and newborn. A woman's decision regarding ARV use should be respected. Coercive and punitive approaches undermine provider-patient trust and could discourage women from seeking prenatal care and adopting health care behaviors that optimize maternal, fetal, and neonatal well-being.
# Prevention of Perinatal Transmission of HIV.
The use of ARVs and the resultant reduction of HIV RNA levels decrease perinatal transmission of HIV. [36][37][38] The goal of ARV use is to achieve maximal and sustained suppression of HIV RNA levels during pregnancy.
As in non-pregnant individuals, genotypic resistance testing is recommended for all pregnant women before ARV initiation (AIII) and for pregnant women with detectable HIV RNA levels while on therapy (AI).
Optimal prevention of perinatal transmission may require initiation of ARV drugs before results of resistance testing are available. If results demonstrate the presence of significant mutation(s) that may confer resistance to the prescribed ARV regimen, the regimen should be modified.
Long-term follow-up is recommended for all infants born to women who have received ARVs during pregnancy, regardless of the infant's HIV status (see the Perinatal Guidelines 1 ).
Regimen Considerations. Pregnancy should not preclude the use of optimal drug regimens. Because recommendations on ARVs to use for treatment of HIV-infected pregnant women are subject to unique considerations, recommendations specific to the timing of therapy initiation and the choice of ARVs for pregnant women may differ from those for non-pregnant individuals. These considerations include the following:
• Potential changes in pharmacokinetics and, thus, dosing requirements, which result from physiologic changes associated with pregnancy;
• potential ARV-associated adverse effects in pregnant women and the woman's ability to adhere to a particular regimen during pregnancy; and
• potential short-and long-term effects of the ARV on the fetus and newborn, which are unknown for many drugs.
Combination drug regimens are considered the standard of care in pregnancy, both for the treatment of HIV infection and for the prevention of perinatal transmission of HIV. Because the risk of neural tube defects is restricted to the first 5 to 6 weeks of pregnancy and pregnancy is rarely recognized before 4 to 6 weeks of pregnancy, and unnecessary changes in ARV drugs during pregnancy may be associated with loss of viral control and increased risk of perinatal transmission, EFV can be continued in pregnant women receiving an EFV-based regimen who present for antenatal care in the first trimester, provided the regimen produces virologic suppression (CIII). Detailed recommendations on ARV choice in pregnancy are discussed in detail in the Perinatal Guidelines (see Perinatal Guidelines 1 ).
Intravenous (IV) zidovudine (ZDV) infusion to the mother during labor is recommended if maternal HIV RNA is ≥400 copies/mL (or with unknown HIV RNA levels) near delivery, regardless of antepartum regimen or mode of delivery (AI). Consideration can be given to omitting IV ZDV infusion during labor for HIVinfected women receiving combination ART regimens who have HIV RNA <400 copies/mL near delivery (BII); however, the combination ART should continue to be administered during labor.
Clinicians who are treating HIV-infected pregnant women are strongly encouraged to report cases of prenatal exposure to ARVs (either administered alone or in combinations) to the Antiretroviral Pregnancy Registry (http://www.apregistry.com). The registry collects observational data regarding exposure to Food and Drug Administration-approved ARV drugs during pregnancy for the purpose of assessing potential teratogenicity. For more information regarding selection and use of ART during pregnancy, refer to the Perinatal Guidelines. 1
# Postpartum Management
Following delivery, clinical, immunologic, and virologic follow-up should continue as recommended for non-pregnant adults and adolescents. Because maternal ART reduces but does not eliminate the risk of transmission of HIV in breast milk and postnatal transmission can occur despite maternal ART, women should also be counseled to avoid breastfeeding. 1 HIV-infected women should avoid pre-mastication of food fed to their infants because the practice has been associated with transmission of HIV from mother to child. 39 Considerations regarding continuation of ART for maternal therapeutic indications are the same as those for ART use in other non-pregnant individuals. For more information regarding postpartum discontinuation of ART, refer to the Perinatal Guidelines. 1 Several studies have demonstrated that adherence to ART may worsen in the postpartum period. [40][41][42][43][44] Clinicians caring for women postpartum who are receiving ART should specifically address adherence, including an evaluation of specific facilitators and barriers to adherence. Clinicians may consider an intervention to improve adherence (see Adherence to Antiretroviral Therapy).
# Clinical Course of HIV-2 Infection
Compared to HIV-1 infection, the clinical course of HIV-2 infection is generally characterized by a longer asymptomatic stage, lower plasma HIV-2 viral loads, and lower mortality rate. 1,2 However, HIV-2 infection can also progress to AIDS over time. Concomitant HIV-1 and HIV-2 infection may occur and should be considered in patients from areas with a high prevalence of HIV-2.
# Diagnosis of HIV-2 Infection
In the appropriate epidemiologic setting, HIV-2 infection should be suspected in patients with clinical conditions suggestive of HIV infection but with atypical serologic results (e.g., a positive screening assay with an indeterminate HIV-1 Western blotf 3 The possibility of HIV-2 infection should also be considered in the appropriate epidemiologic setting in patients with serologically confirmed HIV infection but low or undetectable HIV-1 RNA levels or in those with declining CD4 T lymphocyte (CD4) cell counts despite apparent virologic suppression on antiretroviral therapy (ART).
The 2014 Centers for Disease Control and Prevention guidelines for HIV diagnostic testing 4 recommend initial HIV testing using an HIV-1/HIV-2 antigen/antibody combination immunoassay and subsequent testing using an HIV-1/HIV-2 antibody differentiation immunoassay. The Multispot HIV-1/HIV-2 Rapid Test (Bio-Rad Laboratories) is Food and Drug Administration approved for differentiating HIV-1 from HIV-2 infection. Commercially available HIV-1 viral load assays do not reliably detect or quantify HIV-2. 5,6 Quantitative HIV-2 plasma RNA viral load testing has recently become available for clinical care at the University of Washington
# Summary of HIV-2 Infection
• Compared to HIV-1 infection, the clinical course of HIV-2 infection is generally characterized by a longer asymptomatic stage, lower plasma HIV-2 RNA levels, and lower mortality; however, progression to AIDS does occur.
• There have been no randomized trials addressing the question of when to start antiretroviral therapy or the choice of initial or second-line therapy for HIV-2 infection; thus, the optimal treatment strategy has not been defined.
• Although the optimal CD4 T lymphocyte (CD4) cell count threshold for initiating antiretroviral therapy in HIV-2 infection is unknown, therapy should be started before there is clinical progression.
• HIV-2 is intrinsically resistant to non-nucleoside reverse transcriptase inhibitors and to enfuvirtide; thus, these drugs should not be included in an antiretroviral regimen for an HIV-2 infected patient.
• Pending more definitive data on outcomes in an antiretroviral therapy -naive patient who has HIV-2 mono-infection or HIV-1/HIV-2 dual infection and requires treatment, an initial antiretroviral therapy regimen for these patients should include two nucleoside reverse transcriptase inhibitors plus an HIV-2 active boosted protease inhibitor or integrase strand transfer inhibitors.
• A few laboratories now offer quantitative plasma HIV-2 RNA testing for clinical care (see section text).
• Monitoring of HIV-2 RNA levels, CD4 cell counts, and clinical improvements can be used to assess treatment response, as is recommended for HIV-1 infection.
• Resistance-associated viral mutations to nucleoside reverse transcriptase inhibitors, protease inhibitors, and/or integrase strand transfer inhibitors may develop in HIV-2 infected patients while on therapy. However, no validated HIV-2 genotypic or phenotypic antiretroviral resistance assays are available for clinical use.
• In the event of virologic, immunologic, or clinical failure, second-line treatment should be instituted in consultation with an expert in HIV-2 management.
(http://depts.washington.edu/labweb/AboutLM/Contact.htm) 7 and the New York State Department of Health (http://www.wadsworth.org/divisions/infdis/hiv/Diagnostic_HIV_Testing_Services.html). 8 However, it is important to note that approximately one-quarter to one-third of HIV-2-infected patients without ART will have HIV-2 RNA levels below the limits of detection; some of these patients will have clinical progression and CD4 cell count decline. No validated HIV-2 genotypic or phenotypic antiretroviral (ARV) resistance assays are available for clinical use.
# Treatment of HIV-2 Infection
To date, no randomized trials addressing the question of when to start ART or the choice of initial or secondline therapy for HIV-2 infection have been completed; 9 thus, the optimal treatment strategy has not been defined. Three clinical trials to assess first-line ART for HIV-2 infection are currently underway; 2 are enrolling patients with CD4 counts <500 cells/mm 3 (NCT016058090 and NCT02180438) and 1 is enrolling patients with CD4 count >200 and ≤600 cells/mm 3 (NCT02150993). Although the optimal CD4 cell count threshold for initiating ART in HIV-2 infection is unknown, therapy should be started before there is clinical progression.
HIV-2 is intrinsically resistant to non-nucleoside reverse transcriptase inhibitors (NNRTI) 10 and to enfuvirtide (T20). 11 Data from in vitro studies suggest that HIV-2 is sensitive to the currently available nucleoside reverse transcriptase inhibitors (NRTIs), although with a lower barrier to resistance than HIV-1. 12,13 Darunavir (DRV), lopinavir (LPV), and saquinavir (SQV) are more active against HIV-2 than other approved protease inhibitors (PIs); [14][15][16][17] one of these boosted PIs should be used if a PI-based regimen is used. Other PIs should be avoided because of their lack of ARV activity and high failure rates. The integrase strand transfer inhibitors (INSTIs) raltegravir (RAL), elvitegravir (EVG), and dolutegravir (DTG) have potent activity against HIV-2. [18][19][20][21] The CCR5 antagonist maraviroc (MVC) appears active against some HIV-2 isolates; 22 however, no approved assays to determine HIV-2 co-receptor tropism exist and HIV-2 is known to use many other minor co-receptors in addition to CCR5 and CXCR4. 23 Several small studies suggest poor responses in HIV-2 infected individuals treated with some ARV regimens including dual-NRTI regimens; regimens containing NNRTI plus 2NRTIs; and some unboosted PI-based regimens including nelfinavir (NFV) or indinavir (IDV) plus zidovudine (ZDV) and lamivudine (3TC); and atazanavir (ATV)-based regimens. 9,[24][25][26][27] Clinical data on the effectiveness of triple-NRTI regimens are conflicting. 28,29 In general, HIV-2 active, boosted PI-containing regimens have resulted in more favorable virologic and immunologic responses than 2 or 3-NRTI-based regimens. [29][30][31] However, CD4 cell recovery on therapy are generally poorer than that observed for HIV-1. [31][32][33] INSTI-based regimens may also have favorable treatment responses. 34,35 A recent large systematic review of ART for HIV-2-infected patients (n = 17 studies, 976 HIV-2 infected patients) was unable to conclude which specific regimens are preferred. 36 Resistance-associated viral mutations to NRTIs, PIs and/or INSTIs commonly develop in HIV-2 infected patients while on therapy. 24,29,[37][38][39][40]41 Currently, HIV-2 transmitted drug resistance appears rare. 42 In one small study, DTG was found to have activity as a second-line INSTI in some HIV-2 patients with extensive ARV experience and RAL resistance. 43 Genotypic algorithms used to predict drug resistance in HIV-1 may not be applicable to HIV-2, because pathways and mutational patterns leading to resistance may differ between the HIV types. 13,29,44 Some groups have recommended specific preferred and alternative regimens for initial therapy of HIV-2 infection; [45][46][47][48] Effective antiretroviral therapy (ART) has increased survival in HIV-infected individuals, resulting in an increasing number of older individuals living with HIV infection. In the United States, approximately 30% of people currently living with HIV/AIDS are age 50 years or older and trends suggest that the proportion of older persons living with HIV/AIDS will increase steadily. 1 Care of HIV-infected patients increasingly will involve adults 60 to 80 years of age, a population for which data from clinical trials or pharmacokinetic studies are very limited.
There are several distinct areas of concern regarding the association between age and HIV disease. 2 First, older HIV-infected patients may suffer from aging-related comorbid illnesses that can complicate the management of HIV infection, as outlined in detail below. Second, HIV disease may affect the biology of aging, possibly resulting in early manifestations of many clinical syndromes generally associated with advanced age. Third, reduced mucosal and immunologic defenses (such as post-menopausal atrophic vaginitis) and changes in risk behaviors (for example, decrease in condom use because of less concern about pregnancy and increased use of erectile dysfunction drugs) in older adults could lead to increased risk of acquisition and transmission of HIV. [3][4] Finally, because older adults generally are perceived to be at low risk of HIV infection, screening for HIV in this population remains low. For these reasons, HIV infection in many older adults may not be diagnosed until late in the disease process. This section focuses on HIV diagnosis and treatment considerations in the older HIV-infected patient.
# HIV Diagnosis and Prevention
Even though many older individuals are engaged in risk behaviors associated with acquisition of HIV, they may be perceived to be at low risk of infection and, as a result, they are less likely to be tested for HIV than younger persons. 5 According to one U.S. survey, 71% of men and 51% of women age 60 years and older continue to be sexually active, 6 with less concern about the possibility of pregnancy contributing to less condom use. Another national survey reported that among individuals age 50 years or older, condoms were not used during most recent intercourse with 91% of casual partners or 70% of new partners. 7 In addition, results from a CDC survey 8 show that in 2008 only 35% of adults age 45 to 64 years had ever been tested for HIV infection despite the 2006 CDC recommendation that individuals age 13 to 64 years be tested at least once and more often if sexually active. 9 Clinicians must be attuned to the possibility of HIV infection in older patients, including those older than 64 years of age who, based on CDC recommendations, would not
# Key Considerations When Caring for Older HIV-Infected Patients
• Antiretroviral therapy (ART) is recommended in patients >50 years of age, regardless of CD4 cell count (BIII), because the risk of non-AIDS related complications may increase and the immunologic response to ART may be reduced in older HIV-infected patients.
• ART-associated adverse events may occur more frequently in older HIV-infected adults than in younger HIV-infected individuals. Therefore, the bone, kidney, metabolic, cardiovascular, and liver health of older HIV-infected adults should be monitored closely.
• The increased risk of drug-drug interactions between antiretroviral (ARV) drugs and other medications commonly used in older HIVinfected patients should be assessed regularly, especially when starting or switching ART and concomitant medications.
• HIV experts and primary care providers should work together to optimize the medical care of older HIV-infected patients with complex comorbidities.
• Counseling to prevent secondary transmission of HIV remains an important aspect of the care of the older HIV-infected patient. be screened for HIV. Furthermore, sexual history taking, risk-reduction counseling, and screening for sexually transmitted diseases (STDs) (if indicated), are important components of general health care for HIVinfected and -uninfected older patients.
# Rating of Recommendations
Failure to consider a diagnosis of HIV in older persons likely contributes to later disease presentation and initiation of ART. 10 One surveillance report showed that the proportion of patients who progressed to AIDS within 1 year of diagnosis was greater among patients >60 years of age (52%) than among patients younger than 25 years (16%). 1 When individuals >50 years of age present with severe illnesses, AIDS-related opportunistic infections (OIs) need to be considered in the differential diagnosis of the illness.
# Initiating Antiretroviral Therapy
Concerns about decreased immune recovery and increased risk of serious non-AIDS events are factors that favor initiating ART in patients >50 years of age regardless of CD4 cell count (BIII). (See Initiating Antiretroviral Therapy in Treatment-Naive Patients.) Data that would favor use of any one of the Panel's recommended initial ART regimens (see What to Start) on the basis of age are not available. The choice of regimen should be informed by a comprehensive review of the patient's other medical conditions and medications. A noteworthy limitation of currently available information is lack of data on the long-term safety of specific antiretroviral (ARV) drugs in older patients, such as use of tenofovir disoproxil fumarate (TDF) in older patients with declining renal function. The recommendations on how frequently to monitor parameters of ART effectiveness and safety for adults age >50 years are similar to those for the general HIV-infected population; however, the recommendations for older adults focus particularly on the adverse events of ART pertaining to renal, liver, cardiovascular, metabolic, and bone health (see Table 15).
# HIV, Aging, and Antiretroviral Therapy
The efficacy, pharmacokinetics, adverse effects, and drug interaction potentials of ART in the older adult have not been studied systematically. There is no evidence that the virologic response to ART is different in older patients than in younger patients. However, CD4 T-cell recovery after starting ART generally is less robust in older patients than in younger patients. [11][12][13][14] This observation suggests that starting ART at a younger age will result in better immunologic and possibly clinical outcomes.
Hepatic metabolism and renal elimination are the major routes of drug clearance, including the clearance of ARV drugs. Both liver and kidney function may decrease with age, which may result in impaired drug elimination and drug accumulation. 15 Current ARV drug doses are based on pharmacokinetic and pharmacodynamic data derived from studies conducted in subjects with normal organ function. Most clinical trials include only a small proportion of study participants >50 years of age. Whether drug accumulation in the older patient may lead to greater incidence and severity of adverse effects than seen in younger patients is unknown.
HIV-infected patients with aging-associated comorbidities may require additional pharmacologic intervention, making therapeutic management increasingly complex. In addition to taking medications to manage HIV infection and comorbid conditions, many older HIV-infected patients also are taking medications to ameliorate discomfort (e.g., pain medications, sedatives) or to manage adverse effects of medications (e.g., anti-emetics). They also may self-medicate with over-the-counter medicines or supplements. In the HIV-negative population, polypharmacy is a major cause of iatrogenic problems in geriatric patients. 16 This may be the result of medication errors (by prescribers or patients), nonadherence, additive drug toxicities, and drug-drug interactions. Older HIV-infected patients probably are at an even greater risk of polypharmacy and its attendant adverse consequences than younger HIV-infected or similarly aged HIV-uninfected patients.
Drug-drug interactions are common with ART and easily can be overlooked by prescribers. 17 The available drug interaction information on ARV agents is derived primarily from pharmacokinetic studies performed in a small number of relatively young, HIV-uninfected subjects with normal organ function (see ). Data from these studies provide clinicians with a basis to assess whether a significant interaction may exist. However, the magnitude of the interaction may be different in older HIV-infected patients than in younger HIV-infected patients.
Nonadherence is the most common cause of treatment failure. Complex dosing requirements, high pill burden, inability to access medications because of cost or availability, limited health literacy including lack of numeracy skills, misunderstanding of instructions, depression, and neurocognitive impairment are among the key reasons for nonadherence. 18 Although many of these factors likely will be more prevalent in an aging HIV-infected population, some data suggest that older HIV-infected patients may be more adherent to ART than younger HIV-infected patients. [19][20][21] Clinicians should assess adherence regularly to identify any factors, such as neurocognitive deficits, that may make adherence a challenge. One or more interventions such as discontinuation of unnecessary medications; regimen simplification; or use of adherence tools, including pillboxes, daily calendars, and evidence-based behavioral approaches may be necessary to facilitate medication adherence (see Adherence to Antiretroviral Therapy).
# Non-AIDS HIV-Related Complications and other Comorbidities
With the reduction in AIDS-related morbidity and mortality observed with effective use of ART, non-AIDS conditions constitute an increasing proportion of serious illnesses in ART-treated HIV-infected populations. [22][23][24] Heart disease and cancer are the leading causes of death in older Americans. 25 Similarly, for HIV-infected patients on ART, non-AIDS events such as heart disease, liver disease, and cancer have emerged as major causes of morbidity and mortality. Neurocognitive impairment, already a major health problem in aging patients, may be exacerbated by the effect of HIV infection on the brain. 26 That the presence of multiple non-AIDS comorbidities coupled with the immunologic effects of HIV infection could add to the disease burden of an aging HIV-infected person is a concern. [27][28][29] At present, primary care recommendations are the same for HIV-infected and HIV-uninfected adults and focus on identifying and managing risks of conditions such as heart, liver, and renal disease; cancer; and bone demineralization. [30][31][32]
# Discontinuing Antiretroviral Therapy in Older Patients
Important issues to discuss with aging HIV-infected patients are living wills, advance directives, and longterm care planning including financial concerns. Health care cost sharing (e.g., co-pays, out-of-pocket costs), loss of employment, and other financial-related factors can cause interruptions in treatment. Clinic systems can minimize loss of treatment by helping patients maintain access to insurance.
For the severely debilitated or terminally ill HIV-infected patient, adding palliative care medications, while perhaps beneficial, further increases the complexity and risk of negative drug interactions. For such patients, a balanced consideration of both the expected benefits of ART and the toxicities and negative quality-of-life effects of ART is needed.
Few data exist on the use of ART in severely debilitated patients with chronic, severe, or non-AIDS terminal conditions. [33][34] Withdrawal of ART usually results in rebound viremia and a decline in CD4 cell count. Acute retroviral syndrome after abrupt discontinuation of ART has been reported. In very debilitated patients, if there are no significant adverse reactions to ART, most clinicians would continue therapy. In cases where ART negatively affects quality of life, the decision to continue therapy should be made together with the patient and/or family members after a discussion on the risks and benefits of continuing or withdrawing ART.
# Conclusion
HIV infection may increase the risk of many major health conditions experienced by aging adults and possibly accelerate the aging process. 35 As HIV-infected adults age, their health problems become increasingly complex, placing additional demands on the health care system. This adds to the concern that outpatient clinics providing HIV care in the United States share the same financial problems as other chronic disease and primary care clinics and that reimbursement for care is not sufficient to maintain care at a sustainable level. 36 Continued involvement of HIV experts in the care of older HIV-infected patients is warranted. However, given that the current shortage of primary care providers and geriatricians is projected to continue, current HIV providers will need to adapt to the shifting need for expertise in geriatrics through continuing education and ongoing assessment of the evolving health needs of aging HIV-infected patients. 37 The aging of the HIV-infected population also signals a need for more information on long-term safety and efficacy of ARV drugs in older patients.
• Some ARV agents can cause increases in transaminase levels. The rate and magnitude of these increases are higher with HBV coinfection. [12][13] The etiology and consequences of these changes in liver function tests are unclear because continuation of ART may be accompanied by resolution of the changes. Nevertheless, some experts suspend the implicated agent(s) when the serum alanine transferase (ALT) level is increased to 5-10 times the upper limit of normal. However, in HIV/HBV-coinfected persons, increases in transaminase levels can herald hepatitis B e antigen (HBeAg) seroconversion due to immune reconstitution, so the cause of the elevations should be investigated prior to the decision to discontinue medications. In persons with transaminase increases, HBeAg seroconversion should be evaluated by testing for HBeAg and anti-HBe as well as HBV DNA levels.
# Recommendations for HBV/HIV-Coinfected Patients
• All patients with chronic HBV should be advised to abstain from alcohol, assessed for immunity to hepatitis A virus (HAV) infection (anti-HAV antibody total) and vaccinated if nonimmune, advised on methods to prevent HBV transmission (methods that do not differ from those to prevent HIV transmission), and evaluated for the severity of HBV infection as outlined in the Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents. 14 • Prior to intiation of ART, all persons who test positive for HBsAg should be tested for HBV DNA using a quantitative assay to determine the level of HBV replication (AIII). Persons with chronic HBV infection already receiving ART active against HBV should undergo quantitative HBV DNA testing every 6-12 months to determine the effectiveness of therapy in suppressing HBV replication. The goal of HBV therapy with NRTIs is to prevent liver disease complications by sustained suppression of HBV replication to the lowest achievable level.
•
If not yet on therapy and HBV or HIV treatment is needed: In persons without HIV infection, the recommended anti-HBV drugs for the treatment of persons naive to HBV therapy are TDF and entecavir. [15][16] In HIV-infected patients, however, only TDF can be considered part of the ARV regimen; entecavir has weak anti-HIV activity and must not be considered part of an ARV regimen. In addition, only TDF is fully active for the treatment of persons with known or suspected 3TC-resistant HBV infection. To avoid selection of HBV-resistant variants, when possible, these agents should not be used as the only agent with anti-HBV activity in an ARV regimen (AIII).
Preferred regimen. The combination of TDF + FTC or TDF + 3TC should be used as the NRTI backbone of a fully suppressive ARV regimen and for the treatment of HBV infection (AII). [17][18][19] Alternative regimens. If TDF cannot safely be used, entecavir should be used in addition to a fully suppressive ARV regimen (AII); importantly, entecavir should not be considered to be a part of the ARV regimen 20 (BII). Due to a partially overlapping HBV-resistance pathway, it is not known if the combination of entectavir + 3TC or FTC will provide additional virologic or clinical benefit compared with entecavir alone. In persons with known or suspected 3TC-resistant HBV infection, the entecavir dose should be increased from 0.5 mg/day to 1 mg/day. However, entecavir resistance may emerge rapidly in patients with 3TC-resistant HBV infection. Therefore, entecavir should be used with caution in such patients with frequent monitoring (~ every 3 months) of the HBV DNA level to detect viral breakthrough. Other HBV treatment regimens include peginterferon alfa monotherapy or adefovir in combination with 3TC or FTC or telbivudine in addition to a fully suppressive ARV regimen; 17,[21][22] however, data on these regimens in persons with HIV/HBV coinfection are limited (BII). Due to safety concerns, peginterferon alfa should not be used in HIV/HBV-coinfected persons with cirrhosis.
• Need to discontinue medications active against HBV: The patient's clinical course should be monitored with frequent liver function tests. The use of adefovir dipivoxil, entecavir, or telbivudine to prevent flares, especially in patients with marginal hepatic reserve such as persons with compensated or decompensated cirrhosis, can be considered. 8 These alternative HBV regimens should only be used in addition to a fully suppressive ARV regimen.
• Need to change ART because of HIV resistance: If the patient has adequate HBV suppression, the ARV drugs active against HBV should be continued for HBV treatment in combination with other suitable ARV agents to achieve HIV suppression (AIII).
infected patients, the combined use of either boceprevir or telaprevir with PegIFN/RBV was associated with higher rates of SVR than use of PegIFN/RBV alone. [12][13][14][15] However, combined use of these drugs was associated with a large pill burden, increased dosing frequency, and adverse effects. Subsequently approved DAA agents in the same class and in newer classes that are used with or without RBV have higher SVR rates, reduced pill burden, less frequent dosing, fewer side effects, and shorter durations of therapy. 14,[16][17][18][19] Therefore, the combination of boceprevir or telaprevir and PegIFN/RBV is no longer recommended, and has been replaced by newer combination regimens. Additional guidance on the treatment and management of HCV in HIV-infected and uninfected adults can be found at http://www.hcvguidelines.org/. 20
# Assessment of HIV/Hepatitis C Virus Coinfection
• All HIV-infected patients should be screened for HCV infection using sensitive immunoassays licensed for detection of antibody to HCV in blood. 21 At risk HCV-seronegative patients should undergo repeat testing annually. HCV-seropositive patients should be tested for HCV RNA using a sensitive quantitative assay to confirm the presence of active infection. 22,23 Patients who test HCV RNA-positive should undergo HCV genotyping and liver disease staging as recommended by the most updated HCV guidelines (see http://www.hcvguidelines.org/).
• Patients with HIV/HCV coinfection should be counseled to avoid consuming alcohol and to use appropriate precautions to prevent transmission of HIV and/or HCV to others. HIV/HCV-coinfected patients who are susceptible to hepatitis A virus (HAV) or hepatitis B virus (HBV) infection should be vaccinated against these viruses.
• All patients with HIV/HCV coinfection should be evaluated for HCV therapy.
# Antiretroviral Therapy in HIV/Hepatitis C Virus Coinfection
When to Start Antiretroviral Therapy
The rate of liver disease (liver fibrosis) progression is accelerated in HIV/HCV-coinfected patients, particularly in individuals with low CD4 counts (≤350 cells/mm 3 ). Data largely from retrospective cohort studies are inconsistent regarding the effect of ART on the natural history of HCV disease; 6,24,25 however, some studies suggest that ART may slow the progression of liver disease by preserving or restoring immune function and by reducing HIV-related immune activation and inflammation. [26][27][28] Therefore, ART should be initiated in most HIV/HCV-coinfected patients, regardless of CD4 count (BII). However, in HIV treatmentnaive patients with CD4 counts >500 cells/mm 3 , some clinicians may choose to defer ART until HCV treatment is completed to avoid drug-drug interactions (CIII). Compared to patients with CD4 counts >350 cells/mm 3 , those with CD4 counts <200 had lower HCV treatment response rates and higher rates of toxicity due to PegIFN/RBV. 29 Data regarding HCV treatment response to combination therapy with DAA agents in those with advanced immunosuppression is lacking. For patients with lower CD4 counts (e.g., <200 cells/mm 3 ), ART should be initiated promptly (AI) and HCV therapy may be delayed until the patient is stable on HIV treatment (CIII). 23,[30][31][32]
# Antiretroviral Drugs to Start and Avoid
Initial ARV combination regimens recommended for most HIV treatment-naive patients with HCV are the same as those recommended for patients without HCV infection. Special considerations for ARV selection in HIV/HCV-coinfected patients include the folllowing:
• When both HIV and HCV treatments are indicated, the ARV regimen should be selected with special considerations of potential drug-drug interactions (see Table 12) and overlapping toxicities with the HCV treatment regimen.
• Cirrhotic patients should be carefully evaluated by an expert in advanced liver disease for signs of liver decompensation according to the Child-Turcotte-Pugh classification system. This assessment is necessary because hepatically metabolized ARV and HCV DAA drugs may be contraindicated or require dose modification in patients with Child-Pugh class B and C disease (see Appendix B, Table 7).
# Hepatotoxicity
Drug-induced liver injury (DILI) following the initiation of ART is more common in HIV/HCV-coinfected patients than in those with HIV monoinfection. The greatest risk of DILI may be observed in coinfected individuals with advanced liver disease (e.g., cirrhosis, end-stage liver disease). 33 Eradication of HCV infection with treatment may decrease the likelihood of ARV-associated DILI. 34 • Given the substantial heterogeneity in patient populations and drug regimens, comparison of DILI incidence rates for individual ARV agents across clinical trials is difficult. The incidence of significant elevations in liver enzyme levels (more than 5 times the upper limit of the normal laboratory reference range) is low with currently recommended ART regimens. Hypersensitivity (or allergic) reactions associated with rash and elevations in liver enzymes can occur with certain ARVs. Alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels should be monitored 2 to 8 weeks after initiation of ART and every 3 to 6 months thereafter. Mild to moderate fluctuations in ALT and/or AST are typical in individuals with chronic HCV infection. In the absence of signs and/or symptoms of liver disease or increases in bilirubin, these fluctuations do not warrant interruption of ART. Patients with significant ALT and/or AST elevation should be careful evaluated for signs and symptoms of liver insufficiency and for alternative causes of liver injury (e.g., acute HAV or HBV infection, hepatobiliary disease, or alcoholic hepatitis). Short-term interruption of the ART regimen or of the specific drug suspected of causing the DILI may be required. 35
# Concurrent Treatment of HIV and Hepatitis C Virus Infection
Concurrent treatment of HIV and HCV is feasible but may be complicated by pill burden, drug-drug interactions, and toxicities. In this context, the stage of HCV disease should be assessed to determine the medical need for HCV treatment and inform decision making on when to start HCV. Additional guidance on the treatment and management of HCV in HIV-infected and uninfected adults can be found at http://www.hcvguidelines.org/. If the decision is to treat HCV, the ART regimen may need to be modified before HCV treatment is initiated to reduce the potential for drug-drug interactions and/or toxicities that may develop during the period of concurrent HIV and HCV treatment. (See Table 12 for recommendations on the concomitant use of selected drugs for treatment of HCV and HIV infection.) In patients with suppressed plasma HIV RNA and modified ART, HIV RNA should be measured within 4 to 8 weeks after changing HIV therapy to confirm the effectiveness of the new regimen. After completion of HCV treatment, the modified ART regimen should be continued for at least 2 weeks before reinitiating the original regimen. Continued use of the modified regimen is necessary because of the prolonged half-life of some HCV drugs and the potential risk of drug-drug interactions if a prior HIV regimen is resumed soon after HCV treatment is completed.
# Drug-Drug Interaction
Considerations for the concurrent use of ART and recommended HCV agents (per http://hcvguidelines.org/) are discussed below. Table 12 provides recommendations on the concomitant use of selected drugs for treatment of HCV and HIV infection.
• Sofosbuvir is an HCV NS5B nucleotide polymerase inhibitors that is not metabolized by the cytochrome P450 enzyme system and, therefore, can be used in combination with most ARV drugs. Sofosbuvir is a substrate of p-glycoprotein (P-gp). P-gp inducers, such as tipranavir (TPV), may decrease sofosbuvir plasma concentrations and should not be co-administered with sofosbuvir. No other clinicially significant pharmocokinetic intractions between sofosbuvir and ARVs have been identified. Drug-drug interaction studies in healthy volunteers did not find any significant interaction between sofosbuvir and darunavir/ritonavir (DRV/r), efavirenz (EFV), rilpivirine (RPV), raltegravir (RAL), tenofovir disoproxil fumarate (TDF), or emtricitabine (FTC). 36 See Table 12 for recommendations on the concomitant use of selected drugs for treatment of HCV and HIV infection.
• Ledipasvir is an HCV NS5A inhibitor and is part of a fixed-dose drug combination of sofosbuvir and ledipasvir. 37 Similar to sofosbuvir, ledipasvir is not metabolized by the cytochrome P450 system (CYP) of enzymes and is a substrate for P-gp. Ledipasvir is an inhibitor of the drug transporters P-gp and breast cancer resistance protein (BCRP) and may increase intestinal absorption of coadministered substrates for these transporters. The use of P-gp inducers is not recommended with ledipasivir/sofosbuvir. The coadministration of ledipasvir/sofosbuvir and ARV regimens containing TDF is associated with increased exposure to TDF, especially when TDF is taken with an HIV PI boosted with either RTV or cobicistat (COBI) (see Table 12 for recommendations on the concomitant use of selected drugs for treatment of HCV and HIV infection). In some patients, alternative HCV or ARV drugs should be considered to avoid increases in TDF exposures. If the drugs are co-administered, the patient should be monitored for potential TDF-associated renal injury by assessing measurements of renal function (i.e., estimated creatinine clearance, serum phosphorus, urine glucose, and urine protein) before HCV treatment initiation and periodically during treatment.
• The fixed-dose drug combination of ombitasvir (a NS5A inhibitor), paritaprevir (an HCV PI), and RTV (a pharmacokinetic enhancer) is co-packaged and used in combination with dasabuvir, an NS5B inhibitor. 38 Paritaprevir is a substrate and inhibitor of the CYP3A4 enzymes and therefore may have significant interactions with certain ARVs that are metabolized by, or may induce or inhibit the same pathways. Dasabuvir is primarily metabolized by the CYP2C8 enzymes. Furthermore, ombitasvir, paritaprevir, and dasabuvir are inhibitors of UGT1A1 and also substrates of P-gp and BCRP. Paritaprevir is also a substrate and inhibitor of OATP1B1/3. Coadministration with drugs that are substrates or inhibitors of these enzymes and drug transporters may result in increased plasma concentrations of either the coadministered drug or the HCV drugs. Given that several CYP enzymes and drug transporters are involved in the metabolism of dasabuvir, ombitasvir, paritaprevir, and RTV, complex drug-drug interactions are likely. Therefore clinicians need to consider all coadministered drugs for potential drugdrug interactions. No significant drug-drug interactions have been found when dasabuvir, ombitasvir, paritaprevir, and RTV are used in conjunction with ATV or RAL. When either RTV or COBI is used in conjunction with ATV, the boosting agent should be discontinued during HCV therapy and ATV should be taken in the morning at the same time as ombitasvir, paritaprevir/r, and dasabuvir. RTV or COBI should be restarted after completion of HCV treatment. See Table 12 for other recommendations for concomitmant use of HCV drugs with ARVs. HIV-infected patients not on ART should be placed on an alternative HCV regimen because RTV has activity against HIV.
• Simeprevir is a HCV NS3/4A PI that has been studied in HIV/HCV-coinfected patients. 39 Simeprevir is a substrate and inhibitor of CYP3A4 and P gp enzymes, and therefore may have significant interactions with certain ARVs that are metabolized by the same pathways. Simeprevir is also an inhibitor of the drug transporter OATP1B1/3. On the basis of drug-drug interaction studies in healthy volunteers, simeprevir can be coadministered with RAL, DTG, RPV, and TDF. 40 However, coadministration of simeprevir with EFV, ETR, HIV PIs, COBI, or EVG/c/TDF/FTC is not recommended. (See Table 12 for recommendations on the concomitant use of selected drugs for treatment of HCV and HIV infection.)
Given that the treatment of HCV is rapidly evolving, this section will be updated when new HCV drugs are approved that may have an impact on the treatment of HIV. For guidance on the treatment of HCV infection, refer to http://www.hcvguidelines.org/. individuals without HIV (AI). Treatment of drug-susceptible TB disease should include a standard regimen that consists of isoniazid (INH) + a rifamycin (rifampin or rifabutin) + pyrazinamide + ethambutol given for 2 months, followed by INH + a rifamycin for 4 to 7 months. 4 The Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents 4 include a more complete discussion of the diagnosis and treatment of TB disease in HIV-infected patients.
All patients with HIV/TB disease should be treated with ART (AI). Important issues related to the use of ART in patients with active TB disease include: (1) when to start ART, (2) significant pharmacokinetic drugdrug interactions between rifamycins and some antiretroviral (ARV) agents, (3) the additive toxicities associated with concomitant ARV and TB drug use, ( 4) the development of TB-associated IRIS after ART initiation, and ( 5) the need for treatment support including DOT and the integration of HIV and TB care and treatment.
# Antiretroviral Therapy in Patients with Active Tuberculosis
# Patients Diagnosed with Tuberculosis While Receiving Antiretroviral Therapy
When TB is diagnosed in a patient receiving ART, the patient's ARV regimen should be assessed with particular attention to potential pharmacokinetic interactions with rifamycins (discussed below). The patient's regimen may need to be modified to permit use of the optimal TB treatment regimen (see for dosing recommendations).
# Patients Not Yet Receiving Antiretroviral Therapy
Until recently, when to start ART in patients with active TB has been a subject of debate. Survival is improved when ART is started early following initiation of TB therapy, but a delay in initiating ART often was favored because of the potential complications of high pill burden, additive toxicities, drug interactions, adherence, and the potential for development of IRIS.Recent studies primarily conducted in resource-limited settings, including three randomized controlled trials, have helped clarify the question of when to start ART in patients with active TB. [5][6][7][8] The SAPiT study conducted in South Africa convincingly demonstrated that starting ART during rather than after concluding treatment for TB can significantly reduce mortality. In this study, ambulatory HIV-infected patients with smear-positive TB and CD4 counts <500 cells/mm 3 were randomized to one of three treatment arms: integrated therapy with ART initiated either during the first 4 weeks of TB therapy or after the first 8 weeks of TB treatment (i.e., during the continuation phase of TB therapy) or sequential therapy with ART initiated after the conclusion of standard TB therapy. The median CD4 cell count of participants at study entry was 150 cells/mm 3 . The sequential therapy arm was stopped when an early analysis demonstrated that the mortality rate in the combined two integrated arms was 56% lower than the rate in the sequential therapy arm. Treatment was continued in the two integrated arms until study completion. 5 With the completion of SAPiT and 2 other randomized controlled trials, CAMELIA and STRIDE, the question on the optimal time to initiate ART during TB therapy has been addressed. Findings from these trials now serve as the basis for the Panel's recommendations on when to start ART in patients with active TB.
In the final analysis of the SAPiT trial, there were no differences in rates of AIDS or death between the 2 integrated arms of the study (patients who started ART within 4 weeks after initiating TB treatment vs. those who started ART at 8-12 weeks [i.e., within 4 weeks after completing the intensive phase of TB treatment]). However, in patients with baseline CD4 counts <50 cells/mm 3 (17% of the study population), the rate of AIDS or death was lower in the earlier therapy group than in the later therapy group (8.5 vs. 26.3 cases per 100 person-years, a strong trend favoring the earlier treatment arm, P = 0.06). For all patients, regardless of CD4 cell count, earlier therapy was associated with a higher incidence of IRIS and of adverse events that required a switch in ARV drugs than later therapy. Two deaths were attributed to IRIS. 6 In the CAMELIA study, which was conducted in Cambodia 7 , patients who had CD4 counts <200 cells/mm 3 were randomized to initiate ART at 2 weeks or 8 weeks after initiation of TB treatment. Study participants had advanced HIV disease, with a median entry CD4 count of 25 cells/mm 3 ; low BMIs (median = 16.8 kg/m 2 ), Karnofsky scores (87% <70), and hemoglobin levels (median = 8.7 g/dl); and high rates of disseminated TB disease. Compared with therapy initiated at 8 weeks, ART initiated at 2 weeks resulted in a 38% reduction in mortality (P = 0.006). A significant reduction in mortality was seen in patients with CD4 counts ≤50 cells/mm 3 and in patients with CD4 counts 51 to 200 cells/mm 3 . Overall, 6 deaths associated with TB-IRIS were reported.
The ACTG 5221 (STRIDE) trial, a multinational study conducted at 28 sites, randomized ART-naive patients with confirmed or probable TB and CD4 counts <250 cells/mm 3 to earlier (<2 weeks) or later (8-12 weeks) ART. 8 At study entry, the participants' median CD4 count was 77 cells/mm 3 . The rates of mortality and AIDS diagnoses were not different between the earlier and later arms, although higher rates of IRIS were seen in the earlier arm. However, a significant reduction in AIDS or death was seen in the subset of patients with CD4 counts <50 cells/mm 3 who were randomized to the earlier ART arm (P = 0.02).
In each of these 3 studies, IRIS was more common in patients initiating ART earlier than in patients starting ART later, but the syndrome was infrequently associated with mortality. Collectively these 3 trials demonstrate that in patients with active TB and with very low CD4 cell counts (i.e., <50 cells/mm 3 ), early initiation of ART can reduce mortality and AIDS progression, albeit at the risk of increased IRIS. These findings strongly favor initiation of ART within the first 2 weeks of TB treatment in patients with CD4 cell counts <50 cells/mm 3 (AI).
The question of when to start ART in patients with CD4 counts ≥50 cells/mm 3 is also informed by these studies. The STRIDE and SAPiT studies-in which the patients with CD4 cell counts ≥50 cells/mm 3 were relatively healthy and with reasonable Karnofsky scores (note the SAPiT study excluded patients with Karnofsky scores <70) and BMIs-demonstrated that ART initiation in these patients can be delayed until 8 to 12 weeks after initiation of TB therapy (AI for CD4 counts 51-500 cells/mm 3 and BIII for CD4 counts >500 cells/mm 3 ).
However, the CAMELIA study, which included more patients who were severely ill than the STRIDE and SAPiT studies, showed that early initiation of ART improved survival both in patients with CD4 counts ≤50 cells/mm 3 and in patients with CD4 counts from 51 to 200 cells/mm 3 . In a multivariate analysis, age >40 years, low BMI (<16), low Karnofsky score (<40), elevated aspartate aminotransferase (AST) level (>1.25 x the upper limit of normal [ULN]), disseminated and MDR TB were independently associated with poor survival; whereas in a univariate analysis, hemoglobin <10g/dl also was associated with poor survival.
Thus, recently published results from the three clinical trials are complementary in defining the need for ART and use of CD4 count and clinical status to inform decisions on the optimal time to initiate ART in patients with HIV and TB disease. Earlier initiation of ART within 2 to 4 weeks of TB treatment should be strongly considered for patients with CD4 cell counts from 50 to 200 cells/mm 3 who have evidence of clinical disease of major severity as indicated by clinical evaluation, low Karnofsky score, low BMI, low hemoglobin, low albumin, or organ system dysfunction (BI). Initiation of ART within 2 to 4 weeks also should be considered for patients with CD4 counts >200 cells/mm 3 who present with evidence of severe disease (BIII).
Of additional importance, each of the above studies demonstrated excellent responses to ART, with 90% and >95% of participants achieving suppressed viremia (HIV RNA <400 copies/mL) at 12 months in the SAPiT and CAMELIA studies, respectively, and 74% of participants at 2 years in the STRIDE study.
Mortality rates in patients with MDR or XDR TB and HIV coinfection are very high. 9 Retrospective case control studies and case series provide growing evidence of better outcomes associated with receipt of ART in such coinfected patients, 10 but the optimal timing for initiation of ART is unknown. However, given the high rates and rapid mortality, most experts recommend that ART be initiated within 2 to 4 weeks after confirmation of the diagnosis of drug resistance and initiation of second-line TB therapy (BIII).
All HIV-infected pregnant women with active TB should be started on ART as early as feasible, both for maternal health and to prevent perinatal transmission of HIV (AIII). The choice of ART should be based on efficacy and safety in pregnancy and take into account potential drug-drug interactions between ARVs and rifamycins (see Perinatal Guidelines for more detailed discussions). 11 TB meningitis often is associated with severe complications and high mortality rate. In a randomized study conducted in Vietnam, patients were randomized to immediate ART or to therapy deferred until 2 months after initiation of TB treatment. A higher rate of severe (Grade 4) adverse events was seen in patients who received immediate ART than in those who deferred therapy (80.3% vs. 69.1%, respectively; P = 0.04). 12 In this study 59.8% of the immediate ART patients and 55.5% of the delayed ART patients died within 9 months. However, in the United States, where patients may be more closely monitored and treated for severe adverse events such as central nervous system (CNS) IRIS, many experts feel that ART should be initiated as for other HIV/TB-coinfected patients (CIII).
# Drug Interaction Considerations
A rifamycin is a crucial component in treatment of drug-sensitive TB. However, both rifampin and rifabutin are inducers of the hepatic cytochrome P (CYP) 450 and uridine diphosphate gluconyltransferase (UGT) 1A1 enzymes and are associated with significant interactions with most ARV agents including all PIs, nonnucleoside reverse transcriptase inhibitors (NNRTIs), maraviroc (MVC), and raltegravir (RAL). Rifampin is a potent enzyme inducer, leading to accelerated drug clearance and significant reduction in ARV drug exposure. Despite these interactions, some observational studies suggest that good virologic, immunologic, and clinical outcomes may be achieved with standard doses of efavirenz (EFV) [13][14] and, to a lesser extent, nevirapine (NVP) [15][16] when combined with rifampin. However, rifampin is not recommended in combination with all PIs and the NNRTIs etravirine (ETR) and rilpivirine (RPV). When rifampin is used with MVC or RAL, increased dosage of the ARV is generally recommended. Rifabutin, a weaker enzyme inducer, is an alternative to rifampin. Because rifabutin is a substrate of the CYP 450 enzyme system, its metabolism may be affected by the NNRTI or PI. Tables 18,19a,19b,19d,and 19e outline the magnitude of these interactions and provide dosing recommendations when rifamycins and selected ARV drugs are used concomitantly. After determining the drugs and doses to use, clinicians should monitor patients closely to assure good control of both TB and HIV infections. Suboptimal HIV suppression or suboptimal response to TB treatment should prompt assessment of drug adherence, subtherapeutic drug levels (consider therapeutic drug monitoring [TDM]), and acquired drug resistance.
Rifapentine is a long-acting rifamycin that can be given once weekly with INH for the treatment of active or latent TB infection. Similar to rifampin and rifabutin, rifapentine is also a CYP3A4 inducer. No systematic study has been performed to assess the magnitude of the enzyme induction effect of rifapentine on the metabolism of ARV drugs and other concomitant drugs. Significant enzyme induction can result in reduced ARV drug exposure, which may compromise virologic efficacy. Rifapentine is not recommended for treatment of latent or active TB infection in patients receiving ART, unless given in the context of a clinical trial (AIII).
# Anti-Tuberculosis/Antiretroviral Drug Toxicities
ARV agents and TB drugs, particularly INH, rifamycin, and pyrazinamide, can cause drug-induced hepatitis. These first-line TB drugs should be used for treatment of active TB disease, even with coadministration of other potentially hepatotoxic drugs or when baseline liver disease is present (AIII). Patients receiving potentially hepatotoxic drugs should be monitored frequently for clinical symptoms and signs of hepatitis and have laboratory monitoring for hepatotoxicity. Peripheral neuropathy can occur with administration of INH, didanosine (ddI), or stavudine (d4T) or may be a manifestation of HIV infection. All patients receiving INH also should receive supplemental pyridoxine to reduce peripheral neuropathy. Patients should be monitored closely for signs of drug-related toxicities and receive alternative ARVs to ddI or d4T.
# Immune Reconstitution Inflammatory Syndrome with Tuberculosis and Antiretroviral Agents
IRIS occurs in two forms: unmasking and paradoxical. The mechanism of the syndrome is the same for both forms: restoration of immune competence by administration of ART, resulting in an exuberant host response to TB bacilli and/or antigens. Unmasking IRIS refers to the initial clinical manifestations of active TB that occurs soon after ART is started. Paradoxical IRIS refers to the worsening of TB clinical symptoms after ART is started in patients who are receiving TB treatment. Severity of IRIS ranges from mild to severe to life threatening. IRIS has been reported in 8% to more than 40% of patients starting ART after TB is diagnosed, although the incidence depends on the definition of IRIS and the intensity of monitoring. [17][18] Predictors of IRIS include CD4 count <50 cells/mm 3 ; higher on-ART CD4 counts; high pre-ART and lower on-ART HIV viral loads; severity of TB disease, especially high pathogen burden; and less than 30-day interval between initiation of TB and HIV treatments. [19][20][21][22] Most IRIS in HIV/TB disease occurs within 3 months of the start of TB treatment. Delaying initiation of ART for 2 to 8 weeks may reduce the incidence and severity of IRIS. However, this possible advantage of delayed ART must be weighed against the potential benefit of earlier ART in improving immune function and preventing progression of HIV disease and mortality.
Patients with mild or moderately severe IRIS can be managed symptomatically or treated with nonsteroidal anti-inflammatory agents. Patients with more severe IRIS can be treated successfully with corticosteroids. A recent randomized, placebo-controlled trial demonstrated benefit of corticosteroids in the management of IRIS symptoms (as measured by decreasing days of hospitalization and Karnofsky performance score) without adverse consequences. 23 In the presence of IRIS, neither TB therapy nor ART should be stopped because both therapies are necessary for the long-term health of the patient (AIII).
# Immune Reconstitution with Antiretroviral Therapy: Conversion to Positive Tuberculin Skin Test and Interferon-Gamma Release Assay
Immune reconstitution with ART may result in unmasking LTBI (i.e., conversion of a previously negative tuberculin skin test [TST] to a positive TST or a positive interferon-gamma [IFN-γ] release assay [IGRA] for Mycobacterium tuberculosis-specific proteins). A positive IGRA, similar to a positive TST, is indicative of LTBI in the absence of evidence of active TB disease. 24 Because treatment for LTBI is indicated in the absence of evidence of active TB disease, clinicians should be aware of this phenomenon. Patients with a negative TST or IGRA and advanced HIV disease (i.e., CD4 count <200 cells/mm 3 ) should have a repeat TST or IGRA after initiation of ART and CD4 count increase to >200 cells/mm 3 (BII). 25
# Limitations to Treatment Safety and Efficacy
Adherence to Antiretroviral Therapy (Last updated May 1, 2014; last reviewed May 1, 2014)
Strict adherence to antiretroviral therapy (ART) is key to sustained HIV suppression, reduced risk of drug resistance, improved overall health, quality of life, and survival, 1,2 as well as decreased risk of HIV transmission. 3 Conversely, poor adherence is the major cause of therapeutic failure. Achieving adherence to ART is a critical determinant of long-term outcome in HIV infected patients. For many chronic diseases, such as diabetes or hypertension, drug regimens remain effective even after treatment is resumed following a period of interruption. In the case of HIV infection, however, loss of virologic control as a consequence of non-adherence to ART may lead to emergence of drug resistance and loss of future treatment options. Many patients initiating ART or already on therapy are able to maintain consistent levels of adherence with resultant viral suppression, CD4+ T-lymphocyte (CD4) count recovery, and improved clinical outcomes. Others, however, have poor adherence from the outset of ART and/or experience periodic lapses in adherence over the lifelong course of treatment. Identifying those with adherence-related challenges that require attention and implementing appropriate strategies to enhance adherence are essential roles for all members of the treatment team.
Recent data underscore the importance of conceptualizing treatment adherence broadly to include early engagement in care and sustained retention in care. The concept of an HIV "treatment cascade" has been used to describe the process of HIV testing, linkage to care, initiation of effective ART, adherence to treatment, and retention in care. The U.S. Centers for Disease Control and Prevention estimates that only 36% of the people living with HIV in the United States are prescribed ART and that among these individuals, only 76% have suppressed viral loads. 4 Thus, to achieve optimal clinical outcomes and to realize the potential public health benefit of treatment as prevention, attention to each step in the treatment cascade is critical. 5 Therefore, provider skill and involvement to retain patients in care and help them achieve high levels of medication adherence are crucial.
This section provides updated guidance on assessing and monitoring adherence and outlines strategies to help patients maintain high levels of adherence.
# Factors Associated with Adherence Success and Failure
Adherence to ART can be influenced by a number of factors, including the patient's social situation and clinical condition; the prescribed regimen; and the patient-provider relationship. 6 It is critical that each patient receives and understands information about HIV disease including the goals of therapy (achieving and maintaining viral suppression, decreasing HIV-associated morbidity and mortality, and preventing sexual transmission of HIV), the prescribed regimen (including dosing schedule and potential side effects), the importance of strict adherence to ART, and the potential for the development of drug resistance as a consequence of suboptimal adherence. However, information alone is not sufficent to assure high levels of adherence; patients must also be positively motivated to initiate and maintain therapy.
From a patient perspective, nonadherence is often a consequence of one or more behavioral, structural, and psychosocial barriers (e.g., depression and other mental illnesses, neurocognitive impairment, low health literacy, low levels of social support, stressful life events, high levels of alcohol consumption and active substance use, homelessness, poverty, nondisclosure of HIV serostatus, denial, stigma, and inconsistent access to medications). [7][8][9] Furthermore, patient age may affect adherence. For example, some adolescent and young adult HIV patients, in particular, have substantial challenges in achieving levels of adherence necessary for successful therapeutic outcomes (see HIV-Infected Adolescents section). 10,11 In additon, failure to adopt practices that facilitate adherence, such as linking medication taking to daily activities or using a medication reminder system or a pill organizer, is also associated with treatment failure. 12 Characteristics of one or more components of the prescribed regimen can affect adherence. Simple, oncedaily regimens, 13 including those with low pill burden, without a food requirement, and few side effects or toxicities, are associated with higher levels of adherence. 14,15 Many currently available ARV regimens are much easier to take and better tolerated than older regimens. Studies have shown that patients taking oncedaily regimens have higher rates of adherence than those taking twice-daily dosing regimens. 15 However, data to support or refute the superiority of fixed-dose combination product of 1-pill versus 3-pills (of individual drug products), once-daily regimens-as might be required for the use of some soon-to-beavailable generic-based ARV regimens-are limited.
Characteristics of the clinical setting can also have important structural influences on the success or failure of medication adherence. Settings that provide comprehensive multidisciplinary care (e.g., with case managers, pharmacists, social workers, psychiatric care providers) are often more successful in supporting patients' complex needs, including their medication adherence-related needs. Further, specific settings, such as prisons and other institutional settings, may thwart or support medication adherence. Drug abuse treatment programs are often best suited to address substance use that may confound adherence and may offer services, such as directly observed therapy, that promote adherence.
Finally, a patient-provider relationship that enhances patient trust through non-judgmental and supportive care and use of motivational strategies can positively influence medication adherence.
# Routine Monitoring of Adherence and Retention in Care
Although there is no gold standard for assessing adherence, 1 properly implemented validated tools and assessment strategies can prove valuable in most clinical settings. Viral load suppression is one of the most reliable indicators of adherence and can be used as positive reinforcement to encourage continuous adherence.
When patients initiating ART fail to achieve viral suppression by 24 weeks of treatment, the possibility of suboptimal adherence and other factors must be assessed. Similarly, treatment failure as measured by detectable viral load during chronic care is most likely the result of non-adherence. Patient self-report, the most frequently used method for evaluating medication adherence, remains a useful tool for assessing adherence over time. However, self-reports must be properly and carefully assessed as patients may overestimate adherence. While carefully assessed patient self report of high-level adherence to ART has been associated with favorable viral load responses, 16,17 patient admission of suboptimal adherence is highly correlated with poor therapeutic response. The reliability of self report often depends on how the clinican elicits the information. It is most reliable when ascertained in a simple, nonjudgmental, routine, and structured format that normalizes less-than-perfect adherence and minimizes socially desirable or "white coat adherence" responses. Some patients may selectively adhere to components of a regimen believed to have the fewest side effects or the lowest dosing frequency or pill burden. To allow patients to more accurately disclose lapses in adherence, some experts suggest that providers inquire about the number of missed doses during a defined time period rather than directly asking "Are you taking your medicines?" Others advocate simply asking patients to rate their adherence during the last 4 weeks on a 5-or 6-point Likert scale. 18,19 Regardless of how obtained, patient selfreport, in contrast to other measures of adherence, allows for immediate patient-provider discussion to identify reasons for missed doses and to explore corrective strategies.
Other measures of adherence include pharmacy records and pill counts. Pharmacy records can be valuable when medications are obtained exclusively from a single source so that refills can be traced. Pill counts are commonly used but can be altered by patients. Other methods of assessing adherence include the use of therapeutic drug monitoring and electronic measurement devices (e.g., MEMS bottle caps and dispensing systems). However, these methods are costly and are usually done primarily in research settings.
# Interventions to Improve Adherence and Retention in Care
A continuum of ART adherence support services is necessary to meet individual patient needs. All health care team members, including physicians, physician assistants, nurse practitioners, nurse midwives, nurses, pharmacists, medication managers, and social workers play integral roles in successful adherence programs. 17,[20][21][22] Effective adherence interventions vary in modality and duration, and by clinical setting, provider, and patient. There are many options that can be customized to suit a range of needs and settings (see Table 13).
An increasing number of interventions have proven effective in improving adherence to ART. For descriptions of the interventions, see: http://www.cdc.gov/hiv/topics/research/prs/ma-good-evidenceinterventions.htm. 23 Clinicians should provide all patients with a basic level of adherence-related information and support. Before writing the first prescription(s) for patients initiating or reinitiating ART, clinicians should assess the patient's adherence readiness. Clinicians should evaluate patients' knowledge about HIV disease, treatment, and prevention and provide basic information about ART, viral load and CD4 count and the expected outcome of ART based on these parameters, the importance of strict adherence to ART, and the consequences of nonadherence. In addition, clinicians should assess patients' motivation to successfully adhere to ART and identify and support facilitating factors and address potential barriers to adherence. Finally, clinicians should be assured that patients have the necessary medication taking skills to follow the regimen as prescribed.
Given the wide array of treatment options, individualizing treatment with patient involvement in decision making is the cornerstone of treatment planning and therapeutic success. The first principle of successful treatment is to design an understandable plan to which the patient can commit. 24,25 It is important to consider the patient's daily schedule; patient tolerance of pill number, size and frequency; and any issues affecting absorption (e.g., use of acid reducing therapy and food requirements). With the patient's input, a medication choice and administration schedule should be tailored to his/her routine daily activities. If necessary, soliciting help from family members may also improve adherence. Patients who are naive to ART should understand that their first regimen usually offers the best chance for taking a simple regimen that affords long-term treatment success and prevention of drug resistance. Establishing a trusting patient-provider relationship over time and maintaining good communication will help to improve adherence and long-term outcomes. Medication taking can also be enhanced by the use of pill organizers and medication reminder aids (e.g., alarm clock, pager, calendar).
Positive reinforcement can greatly help patients maintain high levels of adherence. This technique to foster adherence includes informing patients of their low or suppressed HIV viral load levels and increases in CD4 cell counts. Motivational interviewing has also been used with some successes. Recognizing high levels of adherence with incentives and rewards can facilitate treatment success in some patients. Adherence-contingent reward incentives such as meal tickets, grocery bags, lotto tickets, and cash have been used in the treatment of HIV and other chronic diseases. The effectiveness of using cash incentives to promote HIV testing, entry to care, and adherence to ART is currently being studied in the multi-site HPTN 065 trial. Other effective interventions include nurse home visits, a five-session group intervention, pager messaging, and couples or family-based interventions. To maintain high levels of adherence in some patients, it is critically important to provide substance abuse therapy and to strengthen social support. Directly observed therapy (DOT) has been effective in providing ART to active drug users 26 but not to patients in a general clinic population. 27 To determine whether additional adherence or retention interventions are warranted, assessments should be done at each clinical encounter and should be the responsibility of the entire health care team. Routine monitoring of HIV viral load, pharmacy records, and indicators that measure retention in care are useful to determine if more intense efforts are needed to improve adherence. Patients with a history of non-adherence to ART are at risk for poor adherence when re-starting therapy with the same or new drugs. Special attention should be given to identify and address any reason for previous poor adherence. Preferential use of ritonavirboosted protease inhibitor-(PI/r)-based ART, which has a higher barrier to the development of resistance than other treatment options, should be considered if poor adherence is predicted.
The critical elements of adherence go hand in hand with linkage-to-care and retention in care. A recently released guideline provides a number of strategies to improve entry and retention in care and adherence to therapy for HIV infected patients. 5 As with adherence monitoring, research advances offer many options for systematic monitoring of retention in care that may be used in accordance with local resources and standards.
The options include surveillance of visit adherence, gaps in care, and the number of visits during a specified period of time. 28
# Conclusion
Adherence to ART is central to therapeutic success. Given the many available assessment strategies and interventions, the challenge for the treatment team is to select the techniques that best fit each patient and patient population, and, according to available resources, the treatment setting. In addition to maintaining high levels of medication adherence, attention to effective linkage to care, engagement in care, and retention in care is critical for successful treatment outcomes. To foster treatment success, there are interventions to support each step in the cascade of care, as well as guidance on systematic monitoring of each step in the cascade. 5
# Strategies Examples
Use a multidisciplinary team approach.
Provide an accessible, trustworthy health care team.
• Nonjudgmental providers, nurses, social workers, pharmacists, and medication managers Strengthen early linkage to care and retention in care.
• Encourage healthcare team participation in linkage to and retention in care.
Assess patient readiness to start ART.
Evaluate patient's knowledge about HIV disease, prevention and treatment and, on the basis of the assessment, provide HIV-related information.
• Considering the patient's current knowledge base, provide information about HIV, including the natural history of the disease, HIV viral load and CD4 count and expected clinical outcomes according to these parameters, and therapeutic and prevention consequences of non-adherence.
Identify facilitators, potential barriers to adherence, and necessary medication management skills before starting ART medication.
• Assess patient's cognitive competence and impairment.
• Assess behavioral and psychosocial challenges including depression, mental illnesses, levels of social support, high levels of alcohol consumption and active substance use, non-disclosure of HIV serostatus and stigma.
• Identify and address language and literacy barriers.
• Assess beliefs, perceptions, and expectations about taking ART (e.g., impact on health, side effects, disclosure issues, consequences of non-adherence).
• Ask about medication taking skills and foreseeable challenges with adherence (e.g., past difficulty keeping appointments, adverse effects from previous medications, issues managing other chronic medications, need for medication reminders and organizers).
• Assess structural issues including unstable housing, lack of income, unpredictable daily schedule, lack of prescription drug coverage, lack of continuous access to medications.
Provide needed resources.
• Provide or refer for mental health and/or substance abuse treatment.
• Provide resources to obtain prescription drug coverage, stable housing, social support, and income and food security.
# Strategies Examples
Involve the patient in ARV regimen selection.
• Review regimen potency, potential side effects, dosing frequency, pill burden, storage requirements, food requirements, and consequences of nonadherence.
• Assess daily activities and tailor regimen to predictable and routine daily events.
• Consider preferential use of PI/r-based ART if poor adherence is predicted.
• Consider use of fixed-dose combination formulation.
• Assess if cost/co-payment for drugs can affect access to medications and adherence.
Assess adherence at every clinic visit.
• Monitor viral load as a strong biologic measure of adherence.
• Use a simple behavioral rating scale.
• Employ a structured format that normalizes or assumes less-than-perfect adherence and minimizes socially desirable or "white coat adherence" responses.
• Ensure that other members of the health care team also assess adherence.
Use positive reinforcement to foster adherence success.
• Inform patients of low or non-detectable levels of HIV viral load and increases in CD4 cell counts.
• When needed, consider providing incentives and rewards for achieving high levels of adherence and treatment success.
Identify the type of and reasons for nonadherence. • Failure to fill the prescription(s)
• Failure to understand dosing instructions • Use adherence-related tools to complement education and counseling interventions (e.g., pill boxes, dose planners, reminder devices).
• Use community resources to support adherence (e.g., visiting nurses, community workers, family, peer advocates).
• Use patient prescription assistance programs.
• Use motivational interviews.
# Strategies Examples
Systematically monitor retention in care.
• Record and follow up on missed visits.
On the basis of any problems identified through systematic monitoring, consider options to enhance retention in care given resources available.
• Provide outreach for those patients who drop out of care.
• Use peer or paraprofessional treatment navigators.
• Employ incentives to encourage clinic attendance or recognize positive clinical outcomes resulting from good adherence.
• Arrange for directly observed therapy (if feasible).
Key to Acronyms: ART = antiretroviral therapy; CD4 = CD4 T lymphocyte; PI = protease inhibitor; PI/r = ritonavir-boosted protease inhibitor
# Switching Antiretroviral Therapy Because of Adverse Effects
Most patients do not experience treatment-limiting ART-associated toxicities; however, some patients do, and in these cases, ART must be modified. ART-associated adverse events can range from acute and potentially life threatening to chronic and insidious. Acute life-threatening events (e.g., acute hypersensitivity reaction due to ABC, lactic acidosis due to stavudine [d4T] and didanosine [ddI], liver and/or severe cutaneous toxicities due to NVP) usually require the immediate discontinuation of all ARV drugs and re-initiation of an alternative regimen without overlapping toxicity. Non-life threatening toxicities (e.g., urolithiasis with atazanavir [ATV], renal tubulopathy with tenofovir [TDF]) can usually be managed by substituting another ARV agent for the presumed causative agent without interruption of ART. Other, chronic, non-life threatening adverse events (e.g., dyslipidemia) can be addressed either by switching the potentially causative agent for another agent or by managing the adverse event with additional pharmacological or nonpharmacological interventions. Management strategies must be individualized for each patient.
Switching from an effective ARV regimen to a new regimen must be done carefully and only when the potential benefits of the change outweigh the potential complications of altering treatment. The fundamental principle of regimen switching is to maintain viral suppression. When selecting a new agent or regimen, providers should be aware that resistance mutations selected for, regardless of whether previously or currently identified by genotypic resistance testing, are archived in HIV reservoirs, and even if absent from subsequent resistance test results, may reappear under selective pressure. It is critical that providers review the following before implementing any treatment switch:
• the patient's medical and complete ARV history including prior virologic responses to ART;
• resistance test results;
• viral tropism (when maraviroc [MVC] is being considered);
• HLA B*5701 status (when ABC is being considered);
• co-morbidities;
• adherence history;
• prior intolerances to any medications; and
• concomitant medications and supplements and their potential for drug interactions with ARVs.
Patient acceptance of new food or dosing requirements must also be assessed. In some cases, medication costs may also be a factor to consider before switching treatment. Signs and symptoms of ART-associated adverse events may mimic those of comorbidities, adverse effects of concomitant medications, or HIV infection itself. Therefore, concurrent with ascribing a particular clinical event to ART, alternative causes for the event should be investigated. In the case of a severe adverse event, it may be necessary to discontinue or switch ARVs pending the outcome of such an investigation. For the first few months after an ART switch, the patient should be closely monitored for any new adverse events. The patient's viral load should also be monitored to assure continued viral suppression. greater scale. One analysis suggests the possibility of saving approximately $900 million nationally in the first year of switching from a branded fixed-dose combination product to a three-pill regimen containing generic efavirenz. 3 In summary, understanding HIV and ART-related costs in the United States is complicated because of the wide variability in medical coverage, accessibility, and expenses across regions, insurance plans, and pharmacies. In an effort to retain excellent clinical outcomes in an environment of cost-containment strategies, providers should remain informed of current insurance and payment structures, ART costs (see Table 16 below for estimates of drugs' average wholesale prices), discounts among preferred pharmacies, and available generic ART options. Providers should work with patients and their case managers and social workers to understand their patients' particular pharmacy benefit plans and potential financial barriers to filling their prescriptions. Additionally, providers should familiarize themselves with ARV affordability resources (such as ADAP and pharmaceutical company patient assistance programs for patients who qualify) and refer patients to such assistance if needed. Pharmacokinetic (PK) drug-drug interactions between antiretroviral (ARV) drugs and concomitant medications are common, and may lead to increased or decreased drug exposure. In some instances, changes in drug exposure may increase toxicities or affect therapeutic responses. When prescribing or switching one or more drugs in an ARV regimen, clinicians must consider the potential for drug-drug interactions-both those that affect ARVs and those that ARVs affect on other drugs a patient is taking. A thorough review of concomitant medications in consultation with a clinician with expertise in ARV pharmacology can help in designing a regimen that minimizes undesirable interactions. Recommendations for managing a particular drug interaction may differ depending on whether a new ARV is being initiated in a patient on a stable concomitant medication or a new concomitant medication is being initiated in a patient on a stable ARV regimen. The magnitude and significance of interactions are difficult to predict when several drugs with competing metabolic pathways are prescribed concomitantly. When prescribing interacting drugs is necessary, clinicians should be vigilant in monitoring for therapeutic efficacy and/or concentration-related toxicities.
# Mechanisms of Pharmacokinetic Interactions
PK interactions may occur during absorption, metabolism, or elimination of the ARV and/or the interacting drugs.
The most common mechanisms of interactions are described below and listed for each ARV drug in Table 17.
# Pharmacokinetic Interactions Affecting Drug Absorption
The extent of oral absorption of drugs can be affected by the following mechanisms:
• Acid reducing agents, such as proton pump inhibitors, H2 antagonists, or antacids, can reduce the absorption of ARVs that require gastric acidity for optimal absorption (i.e., atazanavir [ATV] and rilpivirine [RPV]).
• Products that contain polyvalent cations, such as aluminum, calcium, magnesium-containing antacids, supplements, or iron products, can bind to integrase inhibitors (INSTI) and reduce absorption of these ARV agents.
• Drugs that induce or inhibit the enzyme CYP3A4 or efflux transporter p-glycoprotein in the intestines may reduce or promote the absorption of other drugs.
# Pharmacokinetic Interactions Affecting Hepatic Metabolism
Two major enzyme systems are most frequently responsible for clinically significant drug interactions.
1. The cytochrome P450 enzyme system is responsible for the metabolism of many drugs, including the non-nucleoside reverse transcriptase inhibitors (NNRTI), protease inhibitors (PI), CCR5 antagonist maraviroc (MVC), and the INSTI elvitegravir (EVG). Cytochrome P450 3A4 (CYP3A4) is the most common enzyme responsible for drug metabolism, though multiple enzymes may be involved in the metabolism of a drug. ARVs and concomitant medications may be inducers, inhibitors, and/or substrates of these enzymes.
2. The uridine diphosphate (UDP)-glucuronosyltransferase (UGT) 1A1 enzyme is the primary enzyme responsible for the metabolism of the INSTIs dolutegravir (DTG) and raltegravir (RAL). Drugs that induce or inhibit the UGT enzyme can affect the PKs of these INSTIs.
# Pharmacokinetic Enhancers (Boosters)
PK enhancing is a strategy used to increase exposure of an ARV by concomitantly administering a drug that inhibits the enzymes that metabolize the ARV. Currently in clinical practice, two agents are used as PK enhancers: ritonavir (RTV) and cobicistat (COBI). Both of these agents are potent inhibitors of the CYP3A4 enzyme, resulting in higher drug exposures of the coadministered ARV metabolized by this pathway.
Importantly, RTV and COBI may have different effects on other CYP or UGT metabolizing enzymes and drug transporters. Complex or unknown mechanisms of PK-based interactions preclude extrapolation of RTV drug interactions to certain COBI interactions, such as interactions with warfarin, phenytoin, voriconazole, oral contraceptives, certain HMG-CoA reductase inhibitors (or statins), and other drugs.
# Other Mechanisms of Pharmacokinetic Interactions
Knowledge of drug transporters is evolving, elucidating additional drug interaction mechanisms. For example, DTG decreases the renal clearance of metformin by inhibiting organic anion transporters in renal tubular cells. Similar transporters aid hepatic, renal, and biliary clearance of drugs and may be susceptible to drug interactions. ARVs and concomitant medications may be inducers, inhibitors, and/or substrates of these drug transporters.
Tables 18-20b provide information on known or suspected drug interactions between ARV agents and commonly prescribed medications based on published PK data or information from product labels. The tables provide general guidance on drugs that should not be coadministered and recommendations for dose modifications or alternative therapy. • Start with tadalafil 5-mg dose and do not exceed a single dose of 10 mg every 72 hours. Monitor for adverse effects of tadalafil.
# For Treatment of PAH
In patients on a PI >7 days:
• Start with tadalafil 20 mg once daily and increase to 40 mg once daily based on tolerability.
In patients on tadalafil who require a PI:
• Stop tadalafil ≥24 hours before PI initiation. 7 days after PI initiation restart tadalafil at 20 mg once daily, and increase to 40 mg once daily based on tolerability.
In patients switching between COBI and RTV:
• Maintain tadalafil dose.
For Treatment of Benign Prostatic Hyperplasia:
• Maximum recommended daily dose is 2.5 mg per day. For treatment of gout flares:
• Colchicine 0.6 mg for 1 dose, followed by 0.3 mg 1 hour later. Do not repeat dose for at least 3 days.
For prophylaxis of gout flares:
• If original dose was colchicine 0.6 mg BID, decrease to colchicine 0.3 mg once daily. If regimen was 0.6 mg once daily, decrease to 0.3 mg every other day.
For treatment of Familial Mediterranean Fever:
• Do not exceed colchicine 0.6 mg once daily or 0.3 mg BID. Despite substantial advances in prevention and treatment of HIV infection in the United States, the rate of new infections has remained stable. [1][2] Although earlier prevention interventions mainly were behavioral, recent data demonstrate the strong impact of antiretroviral therapy (ART) on secondary HIV transmission. The most effective strategy to stem the spread of HIV will probably be a combination of behavioral, biological, and pharmacological interventions. 3
# Sedative/Hypnotics
# Prevention Counseling
Counseling and related behavioral interventions for those living with HIV infection can reduce behaviors associated with secondary transmission of HIV. Each patient encounter offers the clinician an opportunity to reinforce HIV prevention messages, but multiple studies show that prevention counseling is frequently neglected in clinical practice. [4][5] Although delivering effective prevention interventions in a busy practice setting may be challenging, clinicians should be aware that patients often look to their providers for messages about HIV prevention. Multiple approaches to prevention counseling are available, including formal guidance from the Centers for Disease Control and Prevention (CDC) for incorporating HIV prevention into medical care settings. Such interventions have been demonstrated to be effective in changing sexual risk behavior [6][7][8] and can reinforce self-directed behavior change early after diagnosis. 9 CDC has identified several prevention interventions for individuals infected with HIV that meet stringent criteria for efficacy and scientific rigor (http://www.cdc.gov/hiv/topics/research/prs/index.htm). The following three interventions have proven effective in treatment settings and can be delivered by providers as brief messages during clinic visits:
• Partnership for Health (http://effectiveinterventions.org/en/Interventions/PfH.aspx),
• Options (http://www.cdc.gov/hiv/topics/research/prs/resources/factsheets/options.htm),
• Positive Choice (http://www.cdc.gov/hiv/topics/research/prs/resources/factsheets/positive-choice.htm).
In addition, CDC's "Prevention Is Care" campaign (http://www.actagainstaids.org/provider/pic/index.html) helps providers (and members of a multidisciplinary care team) integrate simple methods to prevent transmission by HIV-infected individuals into routine care. These prevention interventions are designed to reduce the risk of secondary HIV transmission through sexual contact. The interventions are designed generally for implementation at the community or group level, but some can be adapted and administered in clinical settings by a multidisciplinary care team.
# Need for Screening for High-Risk Behaviors
The primary care visit provides an opportunity to screen patients for ongoing high-risk drug and sexual behaviors for transmitting HIV infection. Routine screening and symptom-directed testing for and treatment of sexually transmitted diseases (STDs), as recommended by CDC, 10 remain essential adjuncts to prevention counseling. Genital ulcers may facilitate HIV transmission and STDs may increase HIV viral load in plasma and genital secretions. 7,[11][12][13] They also provide objective evidence of unprotected sexual activity, which should prompt prevention counseling.
The contribution of substance and alcohol use to HIV risk behaviors and transmission has been well established in multiple populations; [14][15][16][17][18] therefore, effective counseling for injection and noninjection drug users is essential to prevent HIV transmission. Identifying the substance(s) of use is important because HIV prevalence, transmission risk, risk behaviors, transmission rates, and potential for pharmacologic intervention all vary according to the type of substance used. [19][20][21] Risk-reduction strategies for injection drug users (IDUs), in addition to condom use, include needle exchange and instructions on cleaning drug paraphernalia. Evidence supporting the efficacy of interventions to reduce injection drug use risk behavior also exists. Interventions include both behavioral strategies [14][15]22 and opiate substitution treatment with methadone or buprenorphine. [23][24] No successful pharmacologic interventions have been found for cocaine and methamphetamine users; cognitive and behavioral interventions demonstrate the greatest effect on reducing the risk behaviors of these users. [25][26][27] Given the significant impact of cocaine and methamphetamine on sexual risk behavior, reinforcement of sexual risk-reduction strategies is important. [14][15][16][17][18]28 Antiretroviral Therapy as Prevention ART can play an important role in preventing HIV transmission. Lower levels of plasma HIV RNA have been associated with decreases in the concentration of virus in genital secretions. [29][30][31][32] Observational studies have demonstrated the association between low serum or genital HIV RNA and a decreased rate of HIV transmission among serodiscordant heterosexual couples. 29,[33][34] Ecological studies of communities with relatively high concentrations of men who have sex with men (MSM) and IDUs suggest increased use of ART is associated with decreased community viral load and reduced rates of new HIV diagnoses. [35][36][37] These data suggest that the risk of HIV transmission is low when an individual's viral load is below 400 copies/mL, 35,38 but the threshold below which transmission of the virus becomes impossible is unknown. Furthermore, to be effective at preventing transmission it is assumed that: (1) ART is capable of durably and continuously suppressing viremia; (2) adherence to an effective ARV regimen is high; and (3) there is an absence of a concomitant STD. Importantly, detection of HIV RNA in genital secretions has been documented in individuals with controlled plasma HIV RNA and data describing a differential in concentration of most ARV drugs in the blood and genital compartments exist. 30,39 At least one case of HIV transmission from a patient with suppressed plasma viral load to a monogamous uninfected sexual partner has been reported. 40 In the HPTN 052 trial in HIV-discordant couples, the HIV-infected partners who were ART naive and had CD4 counts between 350 and 550 cells/mm 3 were randomized to initiate or delay ART. In this study, those who initiated ART had a 96% reduction in HIV transmission to the uninfected partners. 3 Almost all of the participants were in heterosexual relationships, all participants received risk-reduction counseling, and the absolute number of transmission events was low: 1 among ART initiators and 27 among ART delayers. Over the course of the study virologic failure rates were less than 5%, a value much lower than generally seen in individuals taking ART for their own health. These low virologic failure rates suggest high levels of adherence to ART in the study, which may have been facilitated by the frequency of study follow-up (study visits were monthly) and by participants' sense of obligation to protect their uninfected partners. Therefore, caution is indicated when interpreting the extent to which ART for the HIV-infected partner protects seronegative partners in contexts where adherence and, thus, rates of continuous viral suppression, may be lower. Furthermore, for HIV-infected MSM and IDUs, biological and observational data suggest suppressive ART also should protect against transmission, but the actual extent of protection has not been established.
Rates of HIV risk behaviors can increase coincidently with the availability of potent combination ART, in some cases almost doubling compared with rates in the era prior to highly effective therapy. 9 A meta-analysis demonstrated that the prevalence of unprotected sex acts was increased in HIV-infected individuals who believed that receiving ART or having a suppressed viral load protected against transmitting HIV. 41 Attitudinal shifts away from safer sexual practices since the availability of potent ART underscore the role of provider-initiated HIV prevention counseling. With wider recognition that effective treatment decreases the risk of HIV transmission, it is particularly important for providers to help patients understand that a sustained viral load below the limits of detection will dramatically reduce but does not absolutely assure the absence of HIV in the genital and blood compartments and, hence, the inability to transmit HIV to others. [41][42] Maximal suppression of viremia not only depends on the potency of the ARV regimen used but also on the patient's adherence to prescribed therapy. Suboptimal adherence can lead to viremia that not only harms the patient but also increases his/her risk of transmitting HIV (including drug-resistant strains) via sex or needle sharing. Screening for and treating behavioral conditions that can impact adherence, such as depression and alcohol and substance use, improve overall health and reduce the risk of secondary transmission.
# Summary
Consistent and effective use of ART resulting in a sustained reduction in viral load in conjunction with consistent condom usage, safer sex and drug use practices, and detection and treatment of STDs are essential tools for prevention of sexual and blood-borne transmission of HIV. Given these important considerations, medical visits provide a vital opportunity to reinforce HIV prevention messages, discuss sex-and drugrelated risk behaviors, diagnose and treat intercurrent STDs, review the importance of medication adherence, and foster open communication between provider and patient.
#
(e.g., renal, cardiac, hepatic, or neurologic complications), development of drug resistance, and the need for chemoprophylaxis against opportunistic infections as a result of CD4 decline. Patients should be counseled about the need for close clinical and laboratory monitoring during therapy interruptions. Approximately 5%-10% of HIV-infected persons also have chronic HBV infection, defined as testing positive for HBsAg for more than 6 months. 1 The progression of chronic HBV to cirrhosis, end-stage liver disease, and/or hepatocellular carcinoma is more rapid in HIV-infected persons than in persons with chronic HBV alone. 2 Conversely, chronic HBV does not substantially alter the progression of HIV infection and does not influence HIV suppression or CD4 cell responses following ART initiation. [3][4] However, several liverassociated complications that are ascribed to flares in HBV activity, discontinuation of dually active ARVs, or toxicity of ARVs can affect the treatment of HIV in patients with HBV coinfection. [5][6][7] These include the following:
# Considerations for Antiretroviral Use in Patients with Coinfections
• FTC, 3TC, and TDF are approved ARVs that also have antiviral activity against HBV. Discontinuation of these drugs may potentially cause serious hepatocellular damage resulting from reactivation of HBV. 8 • Entecavir has activity against HIV; its use for HBV treatment without ART in patients with dual infection may result in the selection of the M184V mutation that confers HIV resistance to 3TC and FTC. Therefore, entecavir must be used in addition to a fully suppressive ARV regimen when used in HIV/HBV-coinfected patients (AII). 9 • 3TC-resistant HBV is observed in approximately 40% of patients after 2 years on 3TC for chronic HBV and in approximately 90% of patients after 4 years when 3TC is used as the only active drug for HBV in coinfected patients. Therefore, 3TC or FTC should be used in combination with other anti-HBV drugs (AII). 10 Panel's Recommendations
• Prior to initiation of antiretroviral therapy (ART), all patients who test positive for hepatitis B surface antigen (HBsAg) should be tested for hepatitis B virus (HBV) DNA using a quantitative assay to determine the level of HBV replication (AIII).
• Because emtricitabine (FTC), lamivudine (3TC), and tenofovir (TDF) have activity against both HIV and HBV, if HBV or HIV treatment is needed, ART should be initiated with the combination of TDF + FTC or TDF + 3TC as the nucleoside reverse transcriptase inhibitor (NRTI) backbone of a fully suppressive antiretroviral (ARV) regimen (AI).
• If HBV treatment is needed and TDF cannot safely be used, the alternative recommended HBV therapy is entecavir in addition to a fully suppressive ARV regimen (BI). Other HBV treatment regimens include peginterferon alfa monotherapy or adefovir in combination with 3TC or FTC or telbivudine in addition to a fully suppressive ARV regimen (BII).
• Entecavir has activity against HIV; its use for HBV treatment without ART in patients with dual infection may result in the selection of the M184V mutation that confers HIV resistance to 3TC and FTC. Therefore, entecavir must be used in addition to a fully suppressive ARV regimen when used in HIV/HBV-coinfected patients (AII).
• Discontinuation of agents with anti-HBV activity may cause serious hepatocellular damage resulting from reactivation of HBV; patients should be advised against self-discontinuation and carefully monitored during interruptions in HBV treatment (AII).
• If ART needs to be modified due to HIV virologic failure and the patient has adequate HBV suppression, the ARV drugs active against HBV should be continued for HBV treatment in combination with other suitable ARV agents to achieve HIV suppression (AIII). The management of hepatitis C virus (HCV)-infected patients is rapidly evolving. Data suggest that HIV/HCV-coinfected patients treated with all-oral HCV regimens have sustained virologic response rates comparable to those of HCV-monoinfected patients. The purpose of this section is to discuss hepatic safety and drug-drug interaction issues related to HIV/HCV coinfection and the concomitant use of antiretroviral (ARV) agents and HCV drugs. For specific guidance on HCV treatment, please refer to http://www.hcvguidelines.org/.
# Rating of Recommendations
Among patients with chronic HCV infection, approximately one-third progress to cirrhosis, at a median time of less than 20 years. 1,2 The rate of progression increases with older age, alcoholism, male sex, and HIV infection. [3][4][5][6] A meta-analysis found that HIV/HCV-coinfected patients had a three fold greater risk of progression to cirrhosis or decompensated liver disease than HCV-monoinfected patients. 5 The risk of progression is even greater in HIV/HCV-coinfected patients with low CD4 T lymphocyte (CD4) cell counts.
Although antiretroviral therapy (ART) appears to slow the rate of HCV disease progression in HIV/HCVcoinfected patients, several studies have demonstrated that the rate continues to exceed that observed in those without HIV infection. 7,8 Whether HCV infection accelerates HIV progression, as measured by AIDS-related opportunistic infections (OIs) or death, 9 is unclear. Although some older ARV drugs that are no longer commonly used have been associated with higher rates of hepatotoxicity in patients with chronic HCV infection, 10,11 newer ARV agents currently in use appear to be less hepatotoxic.
For more than a decade, the mainstay of treatment for HCV infection was a combination regimen of peginterferon and ribavirin (PegIFN/RBV), but this regimen was associated with a poor rate of sustained virologic response (SVR), especially in HIV/HCV-coinfected patients. Rapid advances in HCV drug development led to the discovery of new classes of direct acting antiviral (DAA) agents that target the HCV replication cycle. These new agents, when used with or without PegIFN and RBV, have been shown to achieve high SVR rates. The first DAA agents approved for the treatment of HCV infection in combination with PegIFN/RBV were the HCV protease inhibitors (PI), boceprevir and telaprevir. In HCV genotype 1
# Panel Recommendations
• All HIV-infected patients should be screened for hepatitis C virus infection (HCV). Patients at high risk of HCV infection should be screened annually and whenever HCV infection is suspected.
• Antiretroviral therapy may slow the progression of liver disease by preserving or restoring immune function and reducing HIV-related immune activation and inflammation. For most HIV/HCV-coinfected patients, including those with cirrhosis, the benefits of antiretroviral therapy outweigh concerns regarding drug-induced liver injury. Therefore, antiretroviral therapy should be initiated in most HIV/HCV-coinfected patients, regardless of CD4 T lymphocyte (CD4) cell count (BII).
• Initial antiretroviral therapy combination regimens recommended for most HIV/HCV-coinfected patients are the same as those recommended for individuals without HCV infection. However, when treatment for both HIV and HCV is indicated, the antiretroviral regimen should be selected with special considerations of potential drug-drug interactions and overlapping toxicities with the HCV treatment regimen (see discussion in the text below and in Table 12).
• Combined treatment of HIV and HCV can be complicated by drug-drug interactions, increased pill burden, and toxicities. Although antiretroviral therapy should be initiated for most HIV/HCV-coinfected patients regardless of CD4 cell count, in antiretroviral therapynaive patients with CD4 counts >500 cells/mm 3 some clinicians may choose to defer antiretroviral therapy until HCV treatment is completed (CIII).
• In patients with lower CD4 counts (e.g., <200 cells/mm 3 ), antiretroviral therapy should be initiated promptly (AI) and HCV therapy may be delayed until the patient is stable on HIV treatment (CIII).
# Rating of Recommendations
# Treatment of Active Tuberculosis in HIV-Infected Patients
HIV infection significantly increases the risk of progression from latent to active TB disease. The CD4 cell count influences both the frequency and severity of active TB disease. [1][2] Active TB also negatively affects HIV disease. It may be associated with a higher HIV viral load and more rapid progression of HIV disease. 3 Active pulmonary or extrapulmonary TB disease requires prompt initiation of TB treatment. The treatment of active TB disease in HIV-infected patients should follow the general principles guiding treatment for Panel's Recommendations • The principles for treatment of active tuberculosis (TB) disease in HIV-infected patients are the same as those for HIV-uninfected patients (AI).
• All HIV-infected patients with diagnosed active TB should be started on TB treatment immediately (AI).
• All HIV-infected patients with diagnosed active TB should be treated with antiretroviral therapy (ART) (AI).
• In patients with CD4 counts <50 cells/mm 3 , ART should be initiated within 2 weeks of starting TB treatment (AI).
• In patients with CD4 counts ≥50 cells/mm 3 who present with clinical disease of major severity as indicated by clinical evaluation (including low Karnofsky score, low body mass index [BMI], low hemoglobin, low albumin, organ system dysfunction, or extent of disease), ART should be initiated within 2 to 4 weeks of starting TB treatment. The strength of this recommendation varies on the basis of CD4 cell count:
• CD4 count 50 to 200 cells/mm 3 (BI)
• CD4 count >200 cells/mm 3 (BIII)
• In patients with CD4 counts ≥50 cells/mm 3 who do not have severe clinical disease, ART can be delayed beyond 2 to 4 weeks of starting TB therapy but should be started within 8 to 12 weeks of TB therapy initiation. The strength of this recommendation also varies on the basis of CD4 cell count:
• CD4 count 50 to 500 cells/mm 3 (AI)
• CD4 count >500 cells/mm 3 (BIII)
• In all HIV-infected pregnant women with active TB, ART should be started as early as feasible, both for maternal health and for prevention of mother-to-child transmission (PMTCT) of HIV (AIII).
• In HIV-infected patients with documented multidrug-resistant (MDR) and extensively drug-resistant (XDR) TB, ART should be initiated within 2 to 4 weeks of confirmation of TB drug resistance and initiation of second-line TB therapy (BIII).
• Despite pharmacokinetic drug interactions, a rifamycin (rifampin or rifabutin) should be included in TB regimens for patients receiving ART, with dosage adjustment if necessary (AII).
• Rifabutin is the preferred rifamycin to use in HIV-infected patients with active TB disease on a protease inhibitor (PI)-based regimen because the risk of substantial drug interactions with PIs is lower with rifabutin than with rifampin (AII).
• Coadministration of rifampin and PIs (with or without ritonavir [RTV] boosting) is not recommended (AII).
• Rifapentine (RPT) is NOT recommended in HIV-infected patients receiving ART for treatment of latent TB infection (LTBI) or active TB, unless in the context of a clinical trial (AIII).
• Immune reconstitution inflammatory syndrome (IRIS) may occur after initiation of ART. Both ART and TB treatment should be continued while managing IRIS (AIII).
• Treatment support, which can include directly observed therapy (DOT) of TB treatment, is strongly recommended for HIV-infected patients with active TB disease (AII).
# Rating of Recommendations
# Caring for Patients with HIV and Tuberculosis
Close collaboration among clinicians, health care institutions, and public health programs involved in the diagnosis and treatment of HIV-infected patients with active TB disease is necessary in order to integrate care and improve medication adherence and TB treatment completion rates, reduce drug toxicities, and maximize HIV outcomes. HIV-infected patients with active TB disease should receive treatment support, including adherence counseling and DOT, corresponding to their needs (AII). ART simplification or use of coformulated fixed-dose combinations also may help to improve drug adherence.
Adverse Effects of Antiretroviral Agents (Last updated April 8, 2015; last reviewed April 8,
# 2015)
Adverse effects have been reported with the use of all antiretroviral (ARV) drugs and are among the most common reasons cited for switching or discontinuing therapy and for medication non-adherence. 1 Fortunately, newer ARV regimens are less toxic than regimens used in the past. Generally less than 10% of antiretroviral therapy (ART)-naive patients enrolled in randomized trials have treatment-limiting adverse events. However, because most clinical trials have a relatively short follow-up duration, the longer term complications of ART can be underestimated. In the Swiss Cohort study during a median of 6 years of follow-up, the presence of laboratory adverse events probably or certainly related to ART was associated with higher rates of mortality, which highlights the importance of monitoring for adverse events in overall patient management. 2 Several factors may predispose individuals to adverse effects of ARV medications. For example, compared with men, women (especially ART-naive women with CD4 T lymphocyte cell counts >250 cells/mm 3 ) seem to have a higher propensity to develop Stevens-Johnson syndrome, rashes, and hepatotoxicity from nevirapine (NVP) [3][4][5] and have higher rates of lactic acidosis due to nucleoside reverse transcriptase inhibitors. [6][7][8] Other factors may also contribute to the development of adverse events:
• Concomitant use of medications with overlapping and additive toxicities;
• Comorbid conditions that increase the risk of or exacerbate adverse effects (e.g., alcoholism 9 or coinfection with viral hepatitis [10][11][12] increases the risk of hepatotoxicity);
• Drug-drug interactions that may lead to an increase in drug toxicities (e.g., interactions that result from concomitant use of statins with protease inhibitors); or
• Genetic factors that predispose patients to abacavir (ABC) hypersensitivity reaction. 13,14 The therapeutic goals of ART are to safely achieve and maintain viral suppression and improve immune function. To accomplish these goals, the clinician must consider the toxicity potential of an ARV regimen, as well as the individual patient's underlying conditions, concomitant medications, and prior history of drug intolerances. In addition, it should be appreciated that, in general, the overall benefits of ART outweigh its risks and that some non-AIDS related conditions (e.g., anemia, cardiovascular disease, renal impairment) may be more likely in the absence of ART. 15,16 Information on the adverse events of ARVs is outlined in several tables in the guidelines. Table 14 provides clinicians with a list of the most common and/or severe known ARV-associated adverse events for each drug class. The most common adverse effects of individual ARV agents are summarized in Appendix B, Tables 1-6. Although antiretroviral therapy (ART) is expensive (see Table 16 below), the cost-effectiveness of ART has been demonstrated in analyses of older 1 and newer regimens, 2,3 as well as for treatment-experienced patients with drug-resistant HIV. 4 Given the recommendations for immediate initiation of lifelong treatment and the increasing number of patients taking ART, the Panel now introduces cost-related issues pertaining to medication adherence and cost-containment strategies, as discussed below.
# Costs as They Relate to Adherence from a Patient Perspective
Cost sharing: Cost sharing is where the patient is responsible for some of the medication cost burden (usually accomplished via co-payments, co-insurance, or deductibles); these costs are often higher for branded medications than for generic medications. In one comprehensive review, increased patient cost sharing resulted in decreased medical adherence and more frequent drug discontinuation; for patients with chronic diseases, increased cost sharing was also associated with increased use of the medical system. 5 Conversely, co-payment reductions, such as those that might be used to incentivize prescribing of generic drugs, have been associated with improved adherence in patients with chronic diseases. 6 Whereas costsharing disproportionately affects low income patients, resources (e.g., the Ryan White AIDS Drug Assistance Program [ADAP]) are available to assist eligible patients with co-pays and deductibles. Given the clear association between out-of-pocket costs for patients with chronic diseases and the ability of those patients to pay for and adhere to medications, clinicians should minimize patients' out-of-pocket drug-related expenses whenever possible.
Prior authorizations: As a cost-containment strategy, some programs require that clinicians obtain prior authorizations or permission before prescribing newer or more costly treatments rather than older or less expensive drugs. Although there are data demonstrating that prior authorizations do reduce spending, several studies have also shown that prior authorizations result in fewer prescriptions filled and increased nonadherence. [7][8][9] Prior authorizations in HIV care specifically have been reported to cost over $40 each in provider personnel time (a hidden cost) and have substantially reduced timely access to medications. 10
Generic ART: The impact of the availability of generic antiretroviral (ARV) drugs on selection of ART in the United States is unknown. Because U.S. patent laws currently limit the co-formulation of some generic alternatives to branded drugs, generic options may result in increased pill burden. To the extent that pill burden, rather than drug frequency, results in reduced adherence, generic ART could lead to decreased costs but at the potential expense of worsening virologic suppression rates and poorer clinical outcomes. 11,12 Furthermore, prescribing the individual, less-expensive generic components of a branded co-formulated product rather than the branded product itself could, under some insurance plans, lead to higher copays-an out-of-pocket cost increase that may reduce medication adherence.
# Potential Cost Containment Strategies from a Societal Perspective
Given resource constraints, it is important to maximize the use of resources without sacrificing clinical outcomes. Evidence-based revisions to these guidelines recommend tailored laboratory monitoring for patients with long-term virologic suppression on ART as one possible way to provide overall cost savings. Data suggest that continued CD4 monitoring yields no clinical benefit for patients whose viral loads are suppressed and CD4 counts exceed 200 cells/mm 3 after 48 weeks of therapy. 13 A reduction in laboratory use from biannual to annual CD4 monitoring could save ~$10 million per year in the United States 14 (see the Laboratory Monitoring section). Although this is a small proportion of the overall costs associated with HIV care, such a strategy could reduce patients' personal expenses if they have deductibles for laboratory tests. The present and future availability of generic formulations of certain ARV drugs, despite the potential caveats of increased pill burden and reduced adherence, offers other money-saving possibilities on a much b Certain listed drugs are contraindicated on the basis of theoretical considerations. Thus, drugs with narrow therapeutic indices and suspected metabolic involvement with CYP450 3A, 2D6, or unknown pathways are included in this table. Actual interactions may or may not occur in patients.
c HCV agents listed include only those that are commercially available at the publication of these guidelines.
d HIV-infected patients who received rifapentine as part of a treatment regimen for TB had a higher rate of TB relapse and acquired rifamycin resistance than those treated with other rifamycin-based regimens. Therefore an alternative agent to rifapentine is recommended for TB treatment.
e Use of oral midazolam is contraindicated. Single-dose parenteral midazolam can be used with caution and can be given in a monitored situation for procedural sedation. f The manufacturer of cisapride has a limited-access protocol for patients who meet specific clinical eligibility criteria.
g A high rate of Grade 4 serum transaminase elevation was seen when a higher dose of RTV was added to LPV/r or SQV or when double-dose LPV/r was used with rifampin to compensate for rifampin's induction effect; therefore, these dosing strategies should not be used.
Suggested alternatives to:
• Lovastatin, simvastatin: Fluvastatin, pitavastatin, and pravastatin (except for pravastatin with DRV/r) have the least potential for drug-drug interactions (see Table 19a). Use atorvastatin and rosuvastatin with caution; start with the lowest possible dose and titrate based on tolerance and lipid-lowering efficacy.
• Rifampin: Rifabutin (with dosage adjustment, see Tables 19a and 19b This table provides known or predicted information regarding PK interactions between PIs and non-ARV drugs. When information is available, interactions for specific pharmacologically-boosted (with either RTV or COBI) and unboosted PIs are listed separately. The term "All PIs" refers to both unboosted and pharmacologically-boosted PI products. For interactions between ARV agents and for dosing recommendations, refer to Tables 19c, 20a, and 20b.
# H2 Receptor Antagonists
# ATV (unboosted)
↓ ATV H2 receptor antagonist single dose should not exceed a dose equivalent to famotidine 20 mg and the total daily dose should not exceed a dose equivalent to famotidine 20 mg BID in ART-naive patients.
Give ATV at least 2 hours before and at least 10 hours after the H2 receptor antagonist.
ATV/c, ATV/r ↓ ATV H2 receptor antagonist dose should not exceed a dose equivalent to famotidine 40 mg BID in ART-naive patients or 20 mg BID in ARTexperienced patients.
Give ATV 300 mg plus COBI 150 mg or RTV 100 mg simultaneously with and/or ≥10 hours after the dose of H2 receptor antagonist. • Start quetiapine at the lowest dose and titrate up as needed.
Monitor for quetiapine effectiveness and adverse effects.
Starting a PI in a patient receiving a stable dose of quetiapine:
• Reduce quetiapine dose to 1/6 of the original dose. Closely monitor for quetiapine effectiveness and adverse effects. For Treatment of Gout Flares:
• Colchicine 0.6 mg x 1 dose, followed by 0.3 mg 1 hour later. Do not repeat dose for at least 3 days.
With FPV without RTV:
• 1.2 mg x 1 dose and no repeat dose for at least 3 days For Prophylaxis of Gout Flares:
• Colchicine 0.3 mg once daily or every other day
With FPV without RTV:
• Colchicine 0.3 mg BID or 0.6 mg once daily or 0.3 mg once daily For Treatment of Familial Mediterranean Fever:
• Do not exceed colchicine 0.6 mg once daily or 0.3 mg BID.
With FPV without RTV:
• Do not exceed 1.2 mg once daily or 0.6 mg BID.
Do not coadminister in patients with hepatic or renal impairment.
# Salmeterol
All PIs ↑ salmeterol possible Do not coadminister because of potential increased risk of salmeterol-associated cardiovascular events.
a DHA is an active metabolite of artemether. a Approved dose for RPV is 25 mg once daily. Most PK interaction studies were performed using 75 to 150 mg per dose.
b Norbuprenorphine is an active metabolite of buprenorphine.
c R-methadone is the active form of methadone. The Panel has carefully reviewed recent results from clinical trials in HIV therapy and considered how they inform appropriate care guidelines. The Panel appreciates that HIV care is highly complex and rapidly evolving. Guidelines are never fixed and must always be individualized. Where possible, the Panel has based recommendations on the best evidence from prospective trials with defined endpoints. When such evidence does not yet exist, the Panel attempted to reflect reasonable options in its conclusions.
# Key to
HIV care requires, as always, partnerships and open communication. The provider can make recommendations most likely to lead to positive outcomes only if the patient's own point of view and social context are well known. Guidelines are only a starting point for medical decision making. They can identify some of the boundaries of high-quality care but cannot substitute for sound judgment.
As further research is conducted and reported, guidelines will be modified. The Panel anticipates continued progress in the simplicity of regimens, improved potency and barrier to resistance, and reduced toxicity. The Panel hopes the guidelines are useful and is committed to their continued adjustment and improvement. Ziagen:
• 300 mg tablet • 20 mg/mL oral solution Ziagen:
• 300 mg BID, or
• 600 mg once daily
• Take without regard to meals.
# Metabolized by alcohol dehydrogenase and glucuronyl transferase
Renal excretion of metabolites: 82% Dosage adjustment for ABC is recommended in patients with hepatic insufficiency (see Appendix B, Table 7).
1.5 hours/ 12-26 hours
• HSRs: Patients who test positive for HLA-B*5701 are at highest risk. HLA screening should be done before initiation of ABC.
• For patients with history of HSR, re-challenge is not recommended.
• Symptoms of HSR may include fever, rash, nausea, vomiting, diarrhea, abdominal pain, malaise, fatigue, or respiratory symptoms such as sore throat, cough, or shortness of breath.
• Some cohort studies suggest increased risk of MI with recent or current use of ABC, but this risk is not substantiated in other studies. • 125, 200, 250, and 400 mg capsules Videx:
• 10 mg/mL oral solution Body Weight ≥60 kg:
• 400 mg once daily With TDF:
• 250 mg once daily Body Weight <60 kg:
• 250 mg once daily With TDF:
• 200 mg once daily Take 1/2 hour before or 2 hours after a meal.
Note: Preferred dosing with oral solution is BID (total daily dose divided into 2 doses).
# Renal excretion: 50%
Dosage adjustment in patients with renal insufficiency is recommended (see Appendix B, Table 7). Epivir:
• 150 and 300 mg tablets
• 10 mg/mL oral solution Epivir:
• 150 mg BID, or
• 300 mg once daily
• Take without regard to meals.
# Renal excretion: 70%
Dosage adjustment in patients with renal insufficiency is recommended (see Appendix B, Table 7). • 300 mg once daily, or
• 7.5 level scoops once daily (dosing scoop dispensed with each prescription; one level scoop contains 1 g of oral powder).
• Take without regard to meals.
Mix oral powder with 2-4 ounces of a soft food that does not require chewing (e.g., applesauce, yogurt). Do not mix oral powder with liquid.
Renal excretion is primary route of elimination.
Dosage adjustment in patients with renal insufficiency is recommended (see Appendix B, Table 7). Retrovir:
• 100 mg capsule • 300 mg tablet (only available as generic)
• 10 mg/mL intravenous solution
• 10 mg/mL oral solution Retrovir:
• 300 mg BID, or
• 200 mg TID
• Take without regard to meals.
# Metabolized to GAZT
Renal excretion of GAZT Dosage adjustment in patients with renal insufficiency is recommended (see Appendix B, Table 7). • (ZDV 300 mg plus 3TC 150 mg plus ABC 300 mg) tablet
Trizivir:
• 1 tablet BID
• Take without regard to meals.
a For dosage adjustment in renal or hepatic insufficiency, see Appendix B, Table 7.
b Also see Table 14. Sustiva:
# Key to
• 50 and 200 mg capsules
• 600 mg tablet Sustiva:
• 600 mg once daily, at or before bedtime
• Take on an empty stomach to reduce side effects. • 1 tablet once daily
• Take with a meal.
a For dosage adjustment in renal or hepatic insufficiency, see Appendix B, Table 7.
b Also see Table 14.
c Rare cases of Stevens-Johnson syndrome have been reported with most NNRTIs; the highest incidence of rash was seen with NVP.
d Adverse events can include dizziness, somnolence, insomnia, abnormal dreams, depression, suicidality (suicide, suicide attempt or ideation), confusion, abnormal thinking, impaired concentration, amnesia, agitation, depersonalization, hallucinations, and euphoria. Approximately 50% of patients receiving EFV may experience any of these symptoms. Symptoms usually subside spontaneously after 2 to 4 weeks but may necessitate discontinuation of EFV in a small percentage of patients. 7.
# Key to
b Also see Table 14. a For dosage adjustment in hepatic insufficiency, see Appendix, Table 7.
b Also see Table 14. a For dosage adjustment in hepatic insufficiency, see Appendix, Table 7.
# Key to
b Also see Table 14. Child-Pugh Score 5-9:
# Key to
• 700 mg BID Child-Pugh Score 10-15:
• 350 mg BID PI-Naive or PI-Experienced Patients:
Child-Pugh Score 5-6:
• (700 mg BID plus RTV 100 mg) once daily
Child-Pugh Score 7-9:
• (450 mg BID plus RTV 100 mg) once daily
Child-Pugh Score 10-15:
• (300 mg BID plus RTV 100 mg) once daily • No dosage adjustment Moderate-to-severe hepatic impairment:
• Do not use.
# Ritonavir (RTV) Norvir
As a PI-Boosting Agent:
• 100-400 mg per day
No dosage adjustment necessary. Refer to recommendations for the primary PI.
# Saquinavir (SQV) Invirase
(SQV 1000 mg plus RTV 100 mg) PO BID No dosage adjustment necessary. Mild-to-Moderate Hepatic Impairment:
• Use with caution.
Severe Hepatic Impairment: a Refer to Appendix B, Tables 1
• | None | None |
442c7905b70a37b10ded8f4dbaaaa89538a837af | cdc | None | This document examines the occupational health problems associated with the use of vibrating tools (including both hand-held vibrating tools and stationary tools that transmit vibration through a workpiece), and it provides criteria for reducing the risk of developing vibration-induced health problems. The major health problems associated with the use of vibrating tools are signs and symptoms of peripheral vascular and peripheral neural disorders of the fingers and hands. These signs and symptoms include numbness, pain, and blanching of the fingers. This composite of vibration-induced signs and symptoms is referred to as hand-arm vibration syndrome (HAVS), sometimes called Raynaud's phenomenon of oc cupational origin, or vibration white finger disease. In the United States, an estimated 1.45 million workers use vibrating tools. The prevalence of HAVS in a worker population that has used vibrating tools ranges from 6% to 100%, with an average of about 50%. The development of HAVS depends on many factors, including the level of acceleration (vibration energy) produced by the tool, the length of time the tool is used each day, the cumulative number of months or years the worker has used the tool, and the ergonomics of tool use. The tools most commonly associated with HAVS are powered hammers, chisels, chain saws, sanders, grinders, riveters, breakers, drills, compac tors, sharpeners, and shapers.# FOREWORD
The purpose of the Occupational Safety and Health Act of 1970 (Public Law 91-596) is to assure safe and healthful working conditions for eveiy working person and to preserve our human resources by providing medical and other criteria that will assure, insofar as practicable, that no worker will suffer diminished health, functional capacity, or life expectancy as a result of his or her work experience. The Act authorizes the National Institute for Occupational Safety and Health (NIOSH) to develop and recommend occupa tional safety and health standards and to develop criteria for improving them. By this means, NIOSH communicates these criteria to regulatory agencies (including the Occupational Safety and Health Administration and the Mine Safety and Health Administration) and others in the community of occupational safety and health.
Criteria documents provide the basis for the occupational safety and health standards sought by Congress. These documents generally contain a critical review of the scientific and technical information available on the prevalence of hazards, the existence of safety and health risks, and the adequacy of control methods. NIOSH distributes these documents to health professionals in academic institutions, industry, organized labor, public interest groups, and other government agencies. This criteria document examines the occupational health problems associated with the use of vibrating tools and provides criteria for reducing the risk of developing vibration-induced health problems. In this document, the term "vibrating tools" includes both hand-held vibrating tools and stationary tools that transmit vibration through a workpiece. The major health problems associated with the use of vibrating tools are signs and symptoms of peripheral vascular and peripheral neural disorders of the fingers and hands. These signs and symptoms include numbness, pain, and blanching of the fingers, and loss of finger dexterity. This composite of vibration-induced signs and symptoms is referred to as hand-arm vibration syndrome (HAVS).
On the basis of the 1983 National Occupational Exposure Survey, an estimated 1.45 million U.S. workers use vibrating tools. The prevalence of HAVS in workers who use such tools is reported to range from 6% to 100%, with an average of approximately 50%. Primary Raynaud's disease, whose signs and symptoms resemble those of HAVS, has been reported to occur in an estimated 5% of the general population. This percentage is consistent with the number of unexposed comparison workers who report such symptoms in studies of HAVS.
HAVS is a chronic progressive disorder with a latency period that may vary from a few months to several years. The development of HAVS in a population of workers and the length of the latency period depend on many interacting factors, including vibration level produced by the tool, hours of tool use per day, environmental conditions, type and design of the tool, manner in which the tool is held, vibration spectrum produced by the tool, vibration tolerance of the worker, and tobacco and drug use by the worker.
Because of the complex interactions among these and other factors, the general lack of epidemiologic and clinical data, and the uncertainty associated with some vibration meas urements, it is not currently possible to establish meaningful dose-response relationships. Thus it is not possible to establish a specific recommended exposure limit (REL) that will protect workers against the development of HAVS in all occupational situations. However, the problem of HAVS is too serious and pervasive to delay measures for correcting it.
NIOSH has therefore recommended a standard for exposure to hand-arm vibration that includes no specific exposure limit but does include engineering controls, good work practices, use of protective clothing and equipment, worker training programs, administra tive controls such as limited daily use time, and medical monitoring and surveillance. Frequency-unweighted measurements of acceleration are also recommended since they provide simpler, more appropriate means for assessing the health risk of using vibrating tools at all frequencies. A cornerstone of this standard is the requirement for medical monitoring of all vibration-exposed workers to identify the first signs and symptoms of HAVS and to remove such workers from the job until they are free of all vibration-related symptoms.
Implementation of this standard will protect users of vibrating tools from the debilitating effects of HAVS. NIOSH also anticipates that this criteria document will stimulate research and development in all areas relating to hand-arm vibration. Future research may provide new and more effective methods for reducing occupational exposure to vibration.
When appropriate data become available to develop a specific REL for vibration exposures, NIOSH will revise its recommended standard. Until then, adherence to the standard described in this criteria document should prevent or greatly reduce the potential for vibration-exposed workers to develop the painful and disabling HAVS.
NIOSH takes sole responsibility for the conclusions and recommendations presented in this document. All reviewers' comments are being sent with this document to the Occupational Safety and Health Administration (OSHA) and the Mine Safety and Healjh-Administration (MSHA) for consideration in standard setting. The prevalence and severity of HAVS usually increase as the acceleration level and duration of use increase. HAVS is a chronic, progressive disorder with a latency period that may vary from a few months to several years. The early stages of HAVS are usually reversible if further exposure to vibration is reduced or eliminated; but treatment is usually ineffective for the advanced stages of HAVS, and the disorder may progress to loss of effective hand function and necrosis of the fingers. Prevention is therefore critical. Adherence to the exposure controls recommended in this document should prevent or greatly reduce the potential for vibration-exposed workers to develop HAVS.
# IV-9
Hand-arm vibration acceleration levels ranked from highest to lowest for studies listed in Table IV -8
# . 64 I Glossary
Harmonic: A frequency that is an integral multiple of some fundamental or base fre quency.
Hertz: A unit of frequency (cycles per second). Impedance: The ratio of a harmonic excitation of a system to its response; ratio of ap plied force to resulting velocity. Impedance, mechanical: Ratio of applied vibratory force to the resulting velocity.
Incidence: Number of new cases of a disease or condition reported in a population over a given period.
Jerk: Time rate of acceleration change. Joule: A unit of energy equal to the amount of work done when a point is displaced 1 m by the application of a force of 1 N. A unit of energy equal to 107 ergs, or about 0.738 foot pounds. Latency: The time interval between the application of force or stimulus and the ap pearance of a response.
Mass: Quantity of matter; the inertial resistance of a body to acceleration.
Mass, dynamic: Ratio of applied force to resulting acceleration.
Modulus, dynamic: Ratio of stress to strain; stress required to produce a unit of strain.
Newton: Force required to accelerate a 1-kg mass 1 m/sec2 (100,000 dynes).
# Oscillation:
The variation in the position of an object over time in reference to its start ing point. Oscillation, period of: Time required for an oscillation to be completed. Power, spectral density: The mean square value of energy per unit of time passed through a given frequency range. Prevalence: Number of current cases (old and new) of a disease or condition in a popula tion at a given point in time (point prevalence) or during a given period (period prevalence).
# Radians:
The angle subtended at the center of a circle by an arc equal in length to a radius of the circle.
xv i
# Glossary
Resonance : The tendency of a body to act in concert with an externally generated vibra tion to amplify the impinging vibration; the amplification of an oscillation of a system by a force wave or oscillation of exactly equal period or frequency. Root mean square: The square root of the arithmetic mean of the squares of a series of numbers.
# Stiffness:
The ratio of force or torque to the resulting change in displacement of an elas tic body.
# Spectrum, vibration:
The distribution of frequencies that describes the frequencies that are present in a vibrating system.
# Transfer function:
The mathematical relation between the input into a system and the response.
# Transmissibility:
The ratio of vibration output divided by the input as a function of fre quency.
# Velocity:
The first derivative of displacement with respect to time (m/sec). Vibration: The oscillation or periodic motion of a rigid or elastic body from a position of equilibrium.
Vibration, random: An oscillatory motion in which the acceleration varies over time in a nonperiodic manner; a vibration whose magnitude is not precisely predictable for any point in time.
# I. RECOMMENDATIONS FOR A STANDARD
The National Institute for Occupational Safety and Health (NIOSH) recommends that worker exposure to vibration from the use of vibrating tools be controlled by compliance with all recommendations given in Chapter I of this document. Adherence to these recommendations should prevent or greatly reduce the risk of incurring hand-artn vibra tion syndrome (HAVS) in workers who use vibrating tools. In this document, the term "vibrating tools" includes both hand-held vibrating tools and stationary tools that transmit vibration through a workpiece. An estimated 5% of the general population may develop primary Raynaud's disease (whose signs and symptoms resemble those of HAVS) without exposure to vibration. The recommendations are designed to prevent workers who use vibrating tools from developing the signs and symptoms of Stage 1 HAVS during a working lifetime.
# SECTION 1. VIBRATION EXPOSURE
HAVS has been observed in workers who have used vibrating tools that transmit vibration energy to the hands and arms over a wide range of acceleration levels. The level of acceleration produced by a tool is influenced by many factors, including tool type and weight, operating speed, ergonomics of tool use, environmental conditions, antivibration materials used, etc. (see Chapter HI, D and Chapter VII). Thus NIOSH cannot currently establish a specific quantitative exposure limit that will eliminate the risk of developing HAVS in all workers exposed to hand-transmitted vibration from all types of vibrating tools. NIOSH therefore recommends that exposure to hand-arm vibration be reduced to the lowest feasible acceleration levels and exposure times by adhering to the requirements presented in Section 4, Control of Vibration.
# SECTION 2. EXPOSURE MONITORING
The epidemiologic and clinical evidence reviewed in Chapter IV supports the conclusion that a linear relationship exists between the acceleration exposure dose (level of acceleration and years of exposure) and the time of onset and severity of HAVS. Data on the vibration acceleration level produced by the vibrating tools are needed for the design of tools and work strategies that will help prevent and control HAVS at the earliest possible stage.
The components of the hand-transmitted vibration that shall be measured are (a) acceleration (m/sec or g), (b) frequency (Hz), and (c) duration of exposure (min/day or hr/day).
# Hand-Arm Vibration
(a) Vibration acceleration shall be measured in the three orthogonal basicentric axes at the point on the tool where the vibration enters the hand or as close as possible to that point. The basicentric axis of greatest acceleration may be used to calculate acceleration levels. The magnitude of acceleration shall be measured using an accelerometer with sufficient dynamic range to cover the acceleration band of 1 to 1,000 m/sec2. The mass of the accelerometer shall be small enough that it does not affect the vibration amplitude being measured (<5 grams if possible). The vibration measuring system shall be calibrated in accordance with appropriate standards based on National Bureau of Standards procedures. The accelerometer(s) shall be attached to the vibrating source as described in Chapter HI, B, Methods of Measuring Hand-Transmitted Vibration.
(b) The frequency-unweighted acceleration shall be expressed in m/sec (ims) of the 1/3-octave-band center frequencies from 6.3 to 5,000 Hz.
(c) The vibration measurement system shall have a uniform response integrated over 1/3-octave-band center frequencies of 6.3 to 5,000 Hz. All measurements and analyses of the vibration acceleration and frequency shall be performed by trained technical personnel.
(d) The vibration characteristics (acceleration and frequency spectrum) for each tool shall be measured at the time the tool is first put into use and at annual intervals thereafter. The vibration shall be measured when the tool is operating under full power and actual or simulated conditions of use.
(e) The time the tool is in use shall be determined by measuring actual operating time over a workday; these measurements can then be used to calculate average daily vibration acceleration exposures. The total daily vibration acceleration exposure shall be converted to a normalized 4-hr acceleration amplitude in m/sec2 (frequency unweighted) (see Chapter III, Equation 13).
(f) A hand-held vibration meter may be used for screening or monitoring purposes to determine the approximate acceleration levels being produced by the vibrating system. However, proper mounting of such an acceleration measuring device onto the vibrating tool is critical (see Chapter HI, B).
# SECTION 3. MEDICAL MONITORING (a) General
(1) The employer shall provide a health monitoring program for all workers occupa tionally exposed to hand-arm vibration from the use of vibrating tools.
(2) The employer shall ensure that all medical examinations and procedures are per-formed by or under the direction of a licensed physician with special training and experience in occupational health problems. Board certification in occupational medicine is one way to demonstrate such training and experience.
(3) The employer or physician shall (a) counsel all workers who use tobacco about its possible role in augmenting the harmful effects of vibrating tools, and (b) encourage these workers to stop using tobacco.
# (b) Preplacement Medical Examinations
At a minimum, a preplacement medical examination shall be conducted for each worker who will use vibrating tools on the job. The baseline data obtained from these examinations are for comparison with the data derived from the periodic medical examinations. The examination shall include the following:
(1) A comprehensive work history with special emphasis on present or past use of vibrating tools during work or hobby activities
(2) A medical history, including relevant information on any peripheral vascular, peripheral neural, or musculoskeletal complaints (3) A comprehensive physical examination with special attention to peripheral vas cular and peripheral neural integrity, grip strength, muscle force, and signs and symptoms of the disorders listed in Table IV-1 (4) An assessment of the use of substances that influence normal vascular and neural function, which include certain prescription drugs, alcohol, tobacco, and illicit sub stances.
# (c) Periodic Medical Examinations
(1) Periodic medical examinations shall be made available at least annually to all workers who use vibrating tools on the job. The periodic medical examination shall include all those items specified in Chapter 1, Section 3b, and any other items considered relevant by the examining physician. If circumstances warrant (e.g., an increase in job-related vibration exposure, or a change in health status), the medical examination shall be offered at shorter intervals at the discretion of the attending physician.
(2) The peripheral neural and peripheral vascular signs and symptoms noted during the examination shall be reported in conformance with the classification presented in Tables IV-4 and IV-5.
# (d) Medical Removal
Any worker occupationally exposed to hand-transmitted vibration who develops peripheral I Hand-Arm Vibration neural or peripheral vascular signs and symptoms of Stage 2 HAVS or above on the Stockholm Workshop classification described in Tables IV-4 and IV-5 shall not be exposed to further hand-arm vibration until his or her signs and symptoms have improved sufficiently that they no longer meet the criteria for Stage 1 HAVS.
If the attending physician recommends that a worker be removed from a job requiring the use of vibrating tools, the employer shall ensure tfiat the worker retains all earnings, seniority, and other employment rights and benefits.
# (e) Information for Health Care Professionals
The employer shall furnish the following information to the health care professional responsible for the medical monitoring program:
- A copy of this criteria document
- A description of the worker's duties and activities as they relate to vibration exposure
- An estimate of the worker's daily exposure to vibration and years of exposure
- A list of basic types of vibrating tools used
- A list of the acceleration levels produced by the tools - A description of antivibration protective clothing and antivibration tool designs in use
- A list of all tasks that involve vibrating tools and workpieces and that require strong hand grip force
- Relevant information from previous work and medical histories and medical examinations
- A description of the special features of the task and the way in which this task is performed
- A description of the environmental conditions at the work site (ambient tempera ture, humidity, wind velocity, rain, snow, etc.)
E a
# I. Recommendations for a Standard (f) Written Report and Opinion
The employer shall receive the following information from the attending health care professional:
- An opinion as to the worker's ability to use vibrating tools
- Any recommended limitations to on-the-job exposure
- Any limitation to the worker's ability to use any required protective equipment or clothing
- With the worker's written consent, information about any condition requiring treatment or special consideration Engineering and work practice controls shall be used to reduce hand-transmitted vibration exposure to the lowest feasible level. These controls shall also be supplemented by other control strategies such as the use of antivibration clothing, mittens, gloves, and equipment, and by worker training programs in the proper handling of the vibrating tools.
# (b) Engineering Controls
(1) The vibration acceleration level shall be controlled by reducing the vibration energy produced by the vibrating tool to the lowest level consistent with optimal operations and/or by changing the process to reduce the requirement for using the tool.
(2) The power and weight of the tool shall be optimized to levels that minimize vibration but still permit the work to be efficiently performed.
(3) The tool manufacturers shall furnish data on the vibration acceleration and frequency characteristics of their tools as measured by a standard test protocol of simulated operation.
# (c) Work Practices
In addition to all possible engineering controls, work shall be modified to minimize vibration exposure. Work modification approaches include but are not limited to the following procedures:
Hand-Arm Vibration
- Reducing the number of hours a worker uses a vibrating tool during the workday
- Reducing the number of days per week the vibrating tool is used
- Arranging work tasks so that vibrating and nonvibrating tools can be used alternately, and assuring that the nonvibrating tools do not introduce other musculoskeletal stress factors
- Scheduling maintenance breaks as necessary to ensure that tools are sharp, lubricated, and tuned
- Selecting tools that produce the least amount of vibration consistent with satis factory performance of the task
- Designing the work task and workplace to incorporate ergonomic principles to minimize vibration stress
- Reducing the grip force on the tool handle and the force applied at the tool/workpiece interface in a manner consistent with safety and performance
- Restricting the use of piecework and incentive pay
# (d) Protective Clothing and Equipment
Protective clothing and equipment shall be used where feasible to reduce the level of the vibration energy transmitted to the hand and arm. Some approaches to protecting the worker with clothing and equipment are The following data shall be furnished by the manufacturer of vibrating tools and antivibra tion equipment:
(a) All hand-held tools that produce vibration shall carry a label stating the frequen cy-unweighted acceleration level (m/sec2) produced by the tool during normal opera tion.
(b) The manufacturer of antivibration equipment, clothing, and hand gear shall provide information on the vibration-damping characteristics of each type of an tivibration item produced for sale.
# SECTION 6. RECORDKEEPING (a) Maintaining Records
For all workers who are occupationally exposed to vibrating tools, the employer shall establish and maintain a record of the following:
- Type, model, and manufacturer of the vibrating tools used In accordance with the requirements of 29 CFR 1910.20(d), Preservation of Records, the employer shall retain the records described in Chapter I of this document for at least the following periods:
(1) Thirty years for exposure monitoring records (2) The duration of employment plus 30 years for medical monitoring and surveil lance records and other records described in Chapter I of this document (c) Availability of Records
(1) In accordance with 29 CFR 1910.20, Access to Employee Exposure and Medical Records, the employer shall, upon request, allow examination and copying of ex posure monitoring records by a worker, a former worker, or anyone having the specific written consent of the worker or former worker.
(2) Any medical records that are required by this recommended standard shall be provided, upon request, for examination and copying to the worker, the former worker, or anyone having the specific written consent of the worker or former worker.
# (d) Transfer of Records
The employer shall comply with the requirements for the transfer of records as specified in 29 CFR 1910.20(h), Transfer of Records.
*Code of Federal Regulations. See CFR in references.
# II. INTRODUCTION
For more than three-quarters of a century, workers who operated vibrating tools- on the job have reported complaints resembling the signs and symptoms of primary Raynaud ' s disease. The major complaints were episodic numbness and tingling of the fingers, episodic blanch ing of the fingers, with pain occurring mainly in response to cold exposure and on return of circulation, and reduction in grip strength and finger dexterity. These signs and symptoms increased in number and severity as the exposure to vibration (acceleration intensity and duration of exposure) increased. In a worker population that has used vibrating tools, the prevalence of HAVS ranges from 6% to 100%, with an average of about 50%. The development of HAVS depends on many factors such as the level of acceleration (vibration energy) produced by the tool, the length of time the tool is used each day, the cumulative number of hours, months, and years the worker has used the tool, and the ergonomics of tool use. Minimum daily exposures for several hours each day for months or years are usually required before the first signs and symptoms appear.
HAVS is a chronic disorder with a latency period of a few months to several years. The early stages of HAVS are usually reversible if further exposure to vibration is reduced or eliminated, but advanced stages are progressive. However, treatment is usually ineffective for the advanced stages of HAVS, and the disorder can progress to loss of effective hand function and necrosis of the fingers.
*In this document, the term "vibrating tools" includes both hand-held vibrating tools and stationary tools that transmit vibration through a workpiece.
a
# II. Introduction
In recognition of the health and safety hazards of vibration exposure, NIOSH published Current Intelligence Bulletin 38, Vibration Syndrome . This Current Intel ligence Bulletin emphasized the magnitude of the problem and the seriousness of the health and safety aspects of vibration exposure. The publication was designed to alert management, labor organizations, workers, health specialists, and engineers to the need for recognition, assessment, and control of the problem in industries where vibrating tools are used.
This criteria document presents criteria, techniques, and procedures for the assessment, evaluation, and control of HAVS. Engineering controls, work practices, administrative procedures, medical supervision, worker training, ergonomic design of the tools and the task, and other procedures can be implemented to effectively reduce the risk of developing HAVS.
# I. RECOMMENDATIONS FOR A STANDARD
The National Institute for Occupational Safety and Health (NIOSH) recommends that worker exposure to vibration from the use of vibrating tools be controlled by compliance with all recommendations given in Chapter I of this document. Adherence to these recommendations should prevent or greatly reduce the risk of incurring hand-arm vibra tion syndrome (HAVS) in workers who use vibrating tools. In this document, the term "vibrating tools" includes both hand-held vibrating tools and stationary tools that transmit vibration through a workpiece. An estimated 5% of the general population may develop primary Raynaud's disease (whose signs and symptoms resemble those of HAVS) without exposure to vibration. The recommendations are designed to prevent workers who use vibrating tools from developing the signs and symptoms of Stage 1 HAVS during a working lifetime.
# SECTION 1. VIBRATION EXPOSURE
HAVS has been observed in workers who have used vibrating tools that transmit vibration energy to the hands and arms over a wide range of acceleration levels. The level of acceleration produced by a tool is influenced by many factors, including tool type and weight, operating speed, ergonomics of tool use, environmental conditions, antivibration materials used, etc. (see Chapter HI, D and Chapter VII). Thus NIOSH cannot currently establish a specific quantitative exposure limit that will eliminate the risk of developing HAVS in all workers exposed to hand-transmitted vibration from all types of vibrating tools. NIOSH therefore recommends that exposure to hand-arm vibration be reduced to the lowest feasible acceleration levels and exposure times by adhering to the requirements presented in Section 4, Control of Vibration.
# SECTION 2. EXPOSURE MONITORING
The epidemiologic and clinical evidence reviewed in Chapter IV supports the conclusion that a linear relationship exists between the acceleration exposure dose (level of acceleration and years of exposure) and the time of onset and severity of HAVS. Data on the vibration acceleration level produced by the vibrating tools are needed for the design of tools and work strategies that will help prevent and control HAVS at the earliest possible stage.
The components of the hand-transmitted vibration that shall be measured are (a) acceleration (m/sec or g), (b) frequency (Hz), and (c) duration of exposure (min/day or hr/day).
# Hand-Arm Vibration
(a) Vibration acceleration shall be measured in the three orthogonal basicentric axes at the point on the tool where the vibration enters the hand or as close as possible to that point. The basicentric axis of greatest acceleration may be used to calculate acceleration levels. The magnitude of acceleration shall be measured using an accelerometer with sufficient dynamic range to cover the acceleration band of 1 to 1,000 m/sec2. The mass of the accelerometer shall be small enough that it does not affect the vibration amplitude being measured (<5 grams if possible). The vibration measuring system shall be calibrated in accordance with appropriate standards based on National Bureau of Standards procedures. The accelerometer(s) shall be attached to the vibrating source as described in Chapter HI, B, Methods of Measuring Hand-Transmitted Vibration.
(b) The frequency-unweighted acceleration shall be expressed in m/sec (rms) of the 1/3-octave-band center frequencies from 6.3 to 5,000 Hz.
(c) The vibration measurement system shall have a uniform response integrated over 1/3-octave-band center frequencies of 6.3 to 5,000 Hz. All measurements and analyses of the vibration acceleration and frequency shall be performed by trained technical personnel.
(d) The vibration characteristics (acceleration and frequency spectrum) for each tool shall be measured at the time the tool is first put into use and at annual intervals thereafter. The vibration shall be measured when the tool is operating under full power and actual or simulated conditions of use.
(e) The time the tool is in use shall be determined by measuring actual operating time over a workday; these measurements can then be used to calculate average daily vibration acceleration exposures. The total daily vibration acceleration exposure shall be converted to a normalized 4-hr acceleration amplitude in m/sec2 (frequency unweighted) (see Chapter III, Equation 13).
(f) A hand-held vibration meter may be used for screening or monitoring purposes to determine the approximate acceleration levels being produced by the vibrating system. However, proper mounting of such an acceleration measuring device onto the vibrating tool is critical (see Chapter HI, B).
# SECTION 3. MEDICAL MONITORING (a) General
(1) The employer shall provide a health monitoring program for all workers occupa tionally exposed to hand-arm vibration from the use of vibrating tools.
(2) The employer shall ensure that all medical examinations and procedures are per-formed by or under the direction of a licensed physician with special training and experience in occupational health problems. Board certification in occupational medicine is one way to demonstrate such training and experience.
(3) The employer or physician shall (a) counsel all workers who use tobacco about its possible role in augmenting the harmful effects of vibrating tools, and (b) encourage these workers to stop using tobacco.
# (b) Preplacement Medical Examinations
At a minimum, a preplacement medical examination shall be conducted for each worker who will use vibrating tools on the job. The baseline data obtained from these examinations are for comparison with the data derived from the periodic medical examinations. The examination shall include the following:
(1) A comprehensive work history with special emphasis on present or past use of vibrating tools during work or hobby activities
(2) A medical history, including relevant information on any peripheral vascular, peripheral neural, or musculoskeletal complaints (3) A comprehensive physical examination with special attention to peripheral vas cular and peripheral neural integrity, grip strength, muscle force, and signs and symptoms of the disorders listed in Table IV-1 (4) An assessment of the use of substances that influence normal vascular and neural function, which include certain prescription drugs, alcohol, tobacco, and illicit sub stances.
# (c) Periodic Medical Examinations
(1) Periodic medical examinations shall be made available at least annually to all workers who use vibrating tools on the job. The periodic medical examination shall include all those items specified in Chapter 1, Section 3b, and any other items considered relevant by the examining physician. If circumstances warrant (e.g., an increase in job-related vibration exposure, or a change in health status), the medical examination shall be offered at shorter intervals at the discretion of the attending physician.
(2) The peripheral neural and peripheral vascular signs and symptoms noted during the examination shall be reported in conformance with the classification presented in Tables IV-4 and IV-5.
# (d) Medical Removal
Any worker occupationally exposed to hand-transmitted vibration who develops peripheral I Hand-Arm Vibration neural or peripheral vascular signs and symptoms of Stage 2 HAVS or above on the Stockholm Woikshop classification described in Tables IV-4 and IV-5 shall not be exposed to further hand-arm vibration until his or her signs and symptoms have improved sufficiently that they no longer meet the criteria for Stage 1 HAVS.
If the attending physician recommends that a worker be removed from a job requiring the use of vibrating tools, the employer shall ensure tfiat the worker retains all earnings, seniority, and other employment rights and benefits.
# (e) Information for Health Care Professionals
The employer shall furnish the following information to the health care professional responsible for the medical monitoring program:
- A copy of this criteria document
- A description of the worker's duties and activities as they relate to vibration exposure
- An estimate of the worker's daily exposure to vibration and years of exposure - A list of basic types of vibrating tools used
- A list of the acceleration levels produced by the tools - A description of antivibration protective clothing and antivibration tool designs in use
- A list of all tasks that involve vibrating tools and workpieces and that require strong hand grip force - Relevant information from previous work and medical histories and medical examinations
- A description of the special features of the task and the way in which this task is performed
- A description of the environmental conditions at the work site (ambient tempera ture, humidity, wind velocity, rain, snow, etc.)
E a
# I. Recommendations for a Standard (f) Written Report and Opinion
The employer shall receive the following information from the attending health care professional:
- An opinion as to the worker's ability to use vibrating tools
- Any recommended limitations to on-the-job exposure
- Any limitation to the worker's ability to use any required protective equipment or clothing
- With the worker's written consent, information about any condition requiring treatment or special consideration Engineering and work practice controls shall be used to reduce hand-transmitted vibration exposure to the lowest feasible level. These controls shall also be supplemented by other control strategies such as the use of antivibration clothing, mittens, gloves, and equipment, and by worker training programs in the proper handling of the vibrating tools.
# (b) Engineering Controls
(1) The vibration acceleration level shall be controlled by reducing the vibration energy produced by the vibrating tool to the lowest level consistent with optimal operations and/or by changing the process to reduce the requirement for using the tool.
(2) The power and weight of the tool shall be optimized to levels that minimize vibration but still permit the work to be efficiently performed.
(3) The tool manufacturers shall furnish data on the vibration acceleration and frequency characteristics of their tools as measured by a standard test protocol of simulated operation.
# (c) Work Practices
In addition to all possible engineering controls, work shall be modified to minimize vibration exposure. Work modification approaches include but are not limited to the following procedures:
Hand-Arm Vibration
- Reducing the number of hours a worker uses a vibrating tool during the workday The following data shall be furnished by the manufacturer of vibrating tools and antivibra tion equipment:
(a) All hand-held tools that produce vibration shall carry a label stating the frequen cy-unweighted acceleration level (m/sec2) produced by the tool during normal opera tion.
(b) The manufacturer of antivibration equipment, clothing, and hand gear shall provide information on the vibration-damping characteristics of each type of an tivibration item produced for sale.
# SECTION 6. RECORDKEEPING (a) Maintaining Records
For all workers who are occupationally exposed to vibrating tools, the employer shall establish and maintain a record of the following:
- Type, model, and manufacturer of the vibrating tools used In accordance with the requirements of 29 CFR 1910.20(d), Preservation of Records, the employer shall retain the records described in Chapter I of this document for at least the following periods:
(1) Thirty years for exposure monitoring records (2) The duration of employment plus 30 years for medical monitoring and surveil lance records and other records described in Chapter I of this document (1) In accordance with 29 CFR 1910.20, Access to Employee Exposure and Medical Records, the employer shall, upon request, allow examination and copying of ex posure monitoring records by a worker, a former worker, or anyone having the specific written consent of the worker or former worker.
(2) Any medical records that are required by this recommended standard shall be provided, upon request, for examination and copying to the worker, the former worker, or anyone having the specific written consent of the worker or former worker.
# (d) Transfer of Records
The employer shall comply with the requirements for the transfer of records as specified in 29 CFR 1910.20(h), Transfer of Records.
*Code of Federal Regulations. See CFR in references.
# II. INTRODUCTION
For more than three-quarters of a century, workers who operated vibrating tools- on the job have reported complaints resembling the signs and symptoms of primary Raynaud ' s disease. The major complaints were episodic numbness and tingling of the fingers, episodic blanch ing of the fingers, with pain occurring mainly in response to cold exposure and on return of circulation, and reduction in grip strength and finger dexterity. These signs and symptoms increased in number and severity as the exposure to vibration (acceleration intensity and duration of exposure) increased. In a worker population that has used vibrating tools, the prevalence of HAVS ranges from 6% to 100%, with an average of about 50%. The development of HAVS depends on many factors such as the level of acceleration (vibration energy) produced by the tool, the length of time the tool is used each day, the cumulative number of hours, months, and years the worker has used the tool, and the ergonomics of tool use. Minimum daily exposures for several hours each day for months or years are usually required before the first signs and symptoms appear.
HAVS is a chronic disorder with a latency period of a few months to several years. The early stages of HAVS are usually reversible if further exposure to vibration is reduced or eliminated, but advanced stages are progressive. However, treatment is usually ineffective for the advanced stages of HAVS, and the disorder can progress to loss of effective hand function and necrosis of the fingers.
a
# II. Introduction
In recognition of the health and safety hazards of vibration exposure, NIOSH published Current Intelligence Bulletin 38, Vibration Syndrome . This Current Intel ligence Bulletin emphasized the magnitude of the problem and the seriousness of the health and safety aspects of vibration exposure. The publication was designed to alert management, labor organizations, workers, health specialists, and engineers to the need for recognition, assessment, and control of the problem in industries where vibrating tools are used. Three components of a vibrating system are (1) mass, ( 2) elasticity, and ( 3) damping. The kinetic energy of the system is a function of the mass and motion of the system. The potential energy of the system is a function of the mass and elasticity of the system. When a system vibrates, the energy in the system alternately changes back and forth between kinetic and potential energy. In the absence of any mechanism to take energy out of the system, a system will theoretically vibrate forever once it begins to vibrate. Damping is the mechanism that transforms the kinetic and potential energy into heat and thereby takes energy out of a vibrating system. Thus if no energy is directed into a vibrating system to keep it in motion, the damping that is present will dissipate the initial energy in the system and all motion will stop. The human hand-arm system contains mass, elasticity, and damping and can be visualized as a series of masses coimected by elastic and damping elements. When the values for any two of the parameters are known for any single frequency, the values for the other two can be calculated. When the motion is harmonic, the displace ment
[X(t)\ is X(t) = X sin((ût) (1)
where X is the peak displacement amplitude in meters, Of) is the angular frequency of oscillation in radians/sec, and t is the time in seconds The angular frequency can be expressed as <d = 2 n f or f = - where n is a constant equal to 3.1416, and /is frequency (cycles/second, or hertz ). The frequency if) represents the number of complete cycles of oscillations an object makes in 1 sec. For example, if an object undergoes 10 complete cycles of oscillation in 1 sec, it has a frequency of 10 cycles/sec, or 10 Hz. The period of oscillation is where t is seconds. The period of oscillation represents the time it takes an object to complete one cycle of oscillation.
The velocity of an object refers to the time rate of change of displacement and represents the first derivative of the displacement function given above (Equation 1). Velocity is expressed as indicating that velocity leads displacement by a phase of 90*.
The acceleration of an object refers to the time rate of change of velocity and represents the second derivative with respect to time of the displacement function, or
v(t) = = (ûXcos((ût) (4
where toX is the peak velocity (m/sec). Velocity can be written as
v(t) = (oX sin (oef + ~ ) (5) = -(û2X sin(cùt)( 6) 9 2
where © X is the peak acceleration amplitude (m/sec ). Acceleration can be written ait) = (ù2X sin((ût + k ) (
I
# III. Vibration as a Hazard
indicating that acceleration leads velocity by a phase of 90- and displacement by a phase of 180*.
When a vibrating system acts in concert with externally applied vibration so that certain vibration frequencies impinging on the system are amplified, the frequencies at which maximum amplification occurs are referred to as resonances or natural frequencies. In the case of hand-arm vibration, a fundamental resonance is thought to occur between 100 and 200 Hz .
# Mechanical Impedance
When a vibrating stimulus is applied to a human, a mechanical structure, or another system, a motion results at the same frequency as the stimulus at the point of application and at other points in the system. The mechanical impedance of the system to which the stimulus is applied can be used to describe the dynamic characteristics and the motion of the vibrating system. Mechanical impedance is defined as the ratio of the applied vibrating force divided by the resulting velocity , or
z m (8)
Mechanical impedance is measured as a function of the frequency of the applied force. When both the applied force and resulting velocity are measured at the point of contact between the applied force and the vibrating system, the impedance is referred to as the "driving point mechanical impedance." When the resulting velocity is measured at a point on the system other than the point where the force is applied, the impedance is referred to as the "transfer mechanical impedance." Mechanical impedance measurements have been extensively used in human vibration to determine resonance, stiffness, damping, and other dynamic characteristics of the human body. Impedance is a measure of the total dynamic opposition the human body offers to the movement imparted by the vibration stimulus and can reflect body resonances without interfering with normal body function. Mechanical impedance measurements are noninvasive measurements that can be used to determine the dynamic properties of the body or different parts of the body such as the hand and arm.
Instead of velocity system dynamics in opposition (mechanical impedance) to movement, vibration can be viewed as a form of movement or dynamic compliance. The dynamic compliance is defined as the ratio of the displacement divided by the driving force , or
D (°» -J m
# Hand-Arm Vibration
Human response to vibration depends on several factors: Vibration is a vector quantity (i.e., it has a magnitude and direction). Thus nearly all of the variables above must be extended to multiple axes, depending on the nature of the vibration that is being examined.
As specified by the International Organization for Standardization (ISO) , the vibration produced by the tool or the vibration transmitted to the hand should be measured in the three orthogonal basicentric or biodynamic directions specified in interaction between the hands and a vibrating tool is influenced by many factors, which should be reported in detail when assessing the magnitude of the hand-transmitted vibration . These factors include - The type and condition of the tool being used - The acceleration and the frequency spectrum produced by the tool under normal operating conditions
- The magnitude and direction of sustained forces applied through the hands to the tool or the workpiece (e.g., gripping force, axial thrust force, rotational moments)
- The orientation and posture of the hands, arms, and body during work (specifically, the angles of the wrists, elbows, and shoulder joints)
- The parts of the hands that are in direct contact with vibrating surfaces
- Types and sizes of the surfaces in contact with the hands
- The work practices used
- The total number of years the worker has used vibrating tools on any job
- Climatic conditions such as the ambient temperature and humidity and the temperatures of hand-held surfaces of the tool or workpiece
The following information should be reported when assessing the duration of hand-trans mitted vibration exposure :
- The duration of vibration exposure per working day and the total exposure time in hours, months, and years
- The pattern of exposure within a period of time and its association with the working method (e.g., the length and frequency of scheduled and unscheduled work and rest periods, the intermittence of vibration during the work period, whether the vibrating tool is laid aside or held during rest breaks)
Hand-Amt Vibration
# B. METHODS OF MEASURING HAND-TRANSMITTED VIBRATION
# Measurement of Acceleration
The three parameters that describe the amplitude of vibration as a function of frequency are (1) displacement, ( 2) velocity, and ( 3) acceleration. However, vibration is generally specified in terms of acceleration for the following reasons:
a. The velocity and displacement can be obtained from the measurement of accelera tion. b. A large variety of accelerometers are commercially available.
c. The amplitude of acceleration at the higher frequencies is substantially higher than either displacement or velocity and, therefore, is easier to measure.
When acceleration is measured with an accelerometer, the velocity can be obtained by electronically integrating the acceleration signal over time. The displacement can be obtained by electronically integrating the acceleration signal a second time. Electronic integration tends to reduce or minimize noise introduced into the measurements.
# Accelerometers
Piezoelectric accelerometers are usually used to measure the amplitude of vibration as sociated with hand-transmitted vibration. These accelerometers can be designed to measure vibration within the frequency range of 1 to 50,000 Hz. When vibration impinges on a piezoelectric accelerometer, it moves a small mass against the face of a crystal element. The crystal element produces an electrical voltage proportional to the compression of the mass against the crystal. This voltage is proportional to the acceleration. Because the voltage produced is often very small and loss in signal can easily occur over a long cable connecting an accelerometer to a corresponding instrument, a charge amplifier is used in conjunction with the accelerometer. This amplifier overcomes signal loss problems by measuring changes in the electrical charge (or capacitance) of the crystal caused by vibration. Because the crystal charge simultaneously varies with the voltage signal, a measure of acceleration is obtained. With some accelerometers, the charge amplifier is an external device (i.e., the charge signal from the accelerometer is directed to an external amplifier that converts the charge signal to a corresponding amplified voltage signal proportional to vibration amplitude). With other accelerometers, the circuitry for converting the charge signal to a voltage signal is an integral part of the accelerometer. For these, a voltage signal from the accelerometer is directed to a voltage amplifier that generates an amplified voltage signal proportional to vibration amplitude.
When vibration is measured, it is necessary to specify whether the vibration is being measured on an impact-or nonimpact-type tool. Impact tools include chipping hammers, scalers, pneumatic riveting hammers, pneumatic nailers, jack hammers, and any other tool that generates impulse vibration signals that dominate the vibration spectrum. Nonimpact tools include chain saws, nibblers, pneumatic wrenches, grinders, routers, circular saws, reciprocating saws, and other similar tools. To measure vibration amplitudes of impact tools, specially designed shock accelerometers or ordinary accelerometers with mechanical filters must be used. These accelerometers, which are commercially available, can withstand repeated high-level, high-crest-factor acceleration pulses. If regular accelerometers are used when impact vibration is present, serious errors can be introduced into the vibration measurements . These errors are associated with DC shifts within the accelerometer that seriously distort the low-frequency vibration amplitudes being measured. Shock accelerometers can be used to measure both impact and nonimpact vibration, but nonshock accelerometers can be used to measure nonimpact vibration only.
Although shock accelerometers can withstand exceptionally high impulse acceleration levels, they usually have very low voltage or charge sensitivities. In the case of impact vibration, the vibration amplitudes are sufficiently high that generally no signal-to-noise problem is associated with the recording or measuring instrumentation used to record and analyze the vibration signal. In the case of nonimpulse vibration, the vibration amplitudes can be so low that the acceleration signals are near the lower sensitivity of the recording or measuring instrumentation being used. For these cases, it is necessary to use accelerometers that have substantially higher voltage or charge sensitivities.
The accelerometer should not affect the vibration amplitudes that are being measured. Large accelerometers can cause "mass-loading" on die surface to which they are mounted. That is, the mass of the accelerometer is sufficiently large compared with the mass of the object to which it is attached that the vibration signal being measured is significantly distorted. Many commercially available, light-weight accelerometers weigh 5 grams or less. The smallest accelerometer that can be used for a specific application should be chosen. The total weight of the accelerometer assembly (weight of multiple accelerometers, if more than one is used, plus accelerometer mounting block) should not exceed 20 grams in most cases. Accelerometers weighing less than 20 grams may be required for measuring vibration on small, lightweight tools.
Because vibration is a vector quantity, it is necessary to make vibration measurements in the three orthogonal axes. These axes should always be oriented in the manner specified in Figure HI-2. The vibration measurements in die three axes should always be made at or as near as feasible to the surfaces of the vibrating hand-held tool or workpiece where the maximum vibration energy enters the hands. Figures III-3 through IH-6 show suggested accelerometer mounting locations for chain saws, chipping hammers, and horizontal and vertical grinders . The vibration in the three basicentric orthogonal axes may be measured with a specially designed triaxial accelerometer (a commercially available multiple accelerometer block that measures vibration in three axes) or by three regular accelerometers that are oriented along the three orthogonal basicentric axes (Fig ure IH-3) that are attached to a small metal cubic block. The accelerometers should be attached directly to the vibrating surface, and the accelerometer and accelerometer-mounting configuration should be selected so that they do not distort the vibration measurements. More detailed information on procedures associated with the mounting of accelerometers can be found in Hempstock and O'Connor , , Wasserman et al. , and Wasserman .
# Vibration Frequencies
Many vibration frequencies found in the workplace and other environments contribute to the total vibration measured. In the case of hand-transmitted vibration, the frequency range of importance designated by the International Organization for Standardization (ISO) is 5.6 to about 1,400 Hz . However, many types of tools produce vibration up to 5,000 to 10,000 Hz. Measured vibration data can be separated into its constituent parts by using a Fourier spectrum analysis. Mathematically, this can be expressed as where through a" and b\ through bn define the amplitude of each of the corresponding vibration frequencies coi through©« present in a given frequency spectrum. The combined sine and cosine terms give the actual vibration frequency components comprising the spectrum in the frequency range of interest and in their corresponding phases. The vibration spectrum is the frequency "finger print" of the vibration present in a given situation. Spectra are usually derived by means of computer analysis and graphically displayed as follows: a. The horizontal axis represents frequency (Hz). is not necessary to determine specific vibration frequencies at which these amplitudes exist. When this is the case, vibration amplitudes are measured using 1/3-octave-band filters.
/(f) =
In many cases when measurements are made to determine whether a particular level of vibration is within acceptable limits specified by a standard or regulation, using a single number to express the vibration stress is desirable. With respect to hand-transmitted vibration, the frequency-weighted acceleration level in m/sec2 is the single-number variable used by the American National Standards Institute (ANSI) , the ISO , the American Conference of Governmental Industrial Hygienists (ACGIH) , and the British Standards Institution (BSI) . The frequencyweighted acceleration may be obtained by passing the signal through a frequency-weighting filter.
# General Considerations Associated with Vibration Measurements
The duration of vibration signals associated with many vibrating hand-held tools or workpieces is relatively short. Thus to measure the vibration spectra or the 1/3-octave-band center frequency vibration acceleration associated with these signals, real-time analyzers must be used. These analyzers measure or compute the vibration amplitudes at all frequen cies simultaneously. The dynamic range of these analyzers should be as large as possible over the frequency range of 5 to 5,000 Hz.
To analyze vibration signals, the signals must first be recorded and then played back through the recording device to an analyzer. This procedure is usually necessary when multiaxis acceleration measurements are being made relative to both hands at the same time. The recording device is usually a multichannel FM tape recorder or a multichannel analog-todigital board that directs the recorded signals into a computer.
When high-peak acceleration signals associated with percussive tools are being analyzed, precautions must be taken to ensure that no part of the measuring, recording, or analyzing system is overloaded. To avoid overload, one of the following may be used:
- A commercially available shock accelerometer with a low voltage or charge sensitivity
- An electronic low-pass filter with an upper cut-off frequency above 5,000 Hz placed between the accelerometer voltage or charge amplifier and the recording device or analyzer
- A mechanical low-pass filter with a linear transfer function between 5 and 5,000 Hz placed between the accelerometer and the tool or workpiece !
# Hand-Arm Vibration
The acceleration signals associated with hand-transmitted vibration vary with time. Thus when measuring acceleration, it is always necessary to obtain values that are averaged over time. The acceleration is measured and reported as the root mean square {rms) value of acceleration [d(rms)\ i*1 m/sec2. The mis value of acceleration is
The value of T in Equation 11 must be long enough to be representative of the task associated with the use of the tool being investigated. Also, T should be sufficiently long to ensure reasonable statistical accuracy of the data .
During a vibration measurement, the tool or workpiece should be operated in a manner that is representative of its everyday use. The measured vibration signals in each of the three basicentric orthogonal axes of vibration should be reported as rms acceleration in each of the 1/3-octave-band center frequencies.
# C. GUIDELINES FOR ASSESSING VIBRATION AMPLITUDES
Most assessments of vibration amplitudes are based on vibration measurements of the dominant, single-axis vibration directed into the hand .
That is, the largest of the rms acceleration amplitudes along the three orthogonal basicentric axes shown in Figure HI-2 may be used for assessing exposure to hand-transmitted vibration.
Recommendations of the ISO, ANSI, and BSI are derived from studies associated with such tools as chain saws, pneumatic chipping hammers, and hand-held grinders. The level of vibration exposure associated with these tools is characterized not only by the vibration of the tool, but also by the type of coupling that exists between the tool and the hands of the tool operator (e.g., tight grip or axial thrust force), and the length of time the tool is used without interruption. Most studies assume good coupling exists between the tool and hands. Many of the assessment guidelines are based on time-averaged, frequency-weighted rms acceleration levels. Most of the studies indicate that regular daily vibration exposures do not exceed 4 hr per regular 8-hr workday .
where a(t) is the instantaneous amplitude of acceleration, and T is the period of time over which a(t) is averaged.
The overall time-averaged intensity of exposure to hand-transmitted vibration varies with such factors as the tool operator's work assignments, work practices, intermittence of exposure to vibration, and length of rest periods between vibration exposures. Thus when measuring vibration to assess the effects of exposure to hand-transmitted vibration, the estimates of total daily exposure should be based on representative vibration measure ments for all of the different operating conditions (e.g., using more than one type of tool) associated with the operator's total work assignments over an 8-hr workday. This approach will usually result in several different sets of 1/3-octave-band center frequencies with different nns acceleration amplitudes for each of the different operating conditions. The total daily time-averaged rms acceleration for each 1/3-octave-band can be obtained from
a t(rms) r=i Vz (12
where a(rms)i ^ the component of rms acceleration with a time duration of T( for the i(fi operating condition
n T, = £ T> r= l
Many of the assessments and recommendations are based on an actual tool use of 4 hr over an 8-hr workday. If the value of Tt in Equation 12 is other than 4 hr, the total daily rms acceleration amplitude can be converted to an equivalent 4-hr acceleration amplitude by Equation 13 :
\r m s ) = Tt 4 Vi X a(rms) ^hrs) (13
where at{rms) (7y0is the rms value of acceleration given by Equation 12, and Tt is tne total daily exposure time. The acceleration associated with vibration in the three basicentric orthogonal directions in Figure III-2 can be obtained from the following equation:
I Hand-Arm Vibration r 2 2 2 " 1â
xyz (rms) = \_ax{ms) + ay{rms) + dz(rms) J ( 14)
where ax(rms)iS ^ie rms va'ue °f acceleration in the x direction, ay(rms) *s rms value °f acceleration in the y direction, and az(rms) *s rms value °f acceleration in the z direction. When comparing measured tool vibration acceleration levels with recommended limits, the comparison should be made using the acceleration level measured in the dominant basicentric axis.
# D. FACTORS THAT INFLUENCE VIBRATION AMPLITUDES
# Effects of Tool Type
Several factors influence the vibration levels produced by vibrating tools. The first is whether or not it is an impact tool. Vibration acceleration levels related to impact tools are generally higher than vibration levels associated with nonimpact tools. When ap propriate elastomer or similar materials isolate the vibration-generating parts of tools from contact with the hands, the vibration acceleration levels are usually reduced.
# Effects of Tool Operation
Other factors that affect the vibration acceleration levels of tools are associated with the ergonomics of operating the tool and related tool design. For example, a chipping hammer works by means of a reciprocating piston actuated by fluctuating pressure pulses. The vibration is generated by the repeated impact of the piston on the end of the chisel inserted into the hammer and the subsequent impact of the chisel on the workpiece. The fundamental vibration frequency is associated with the repetition rate at which the piston strikes the chisel. There is a vibration frequency at multiple harmonics of the primary repetition rate of the tool. The weight of the hammer also influences the vibration acceleration amplitudes directed into the hand. For similar operations, the heavier hammers appear to direct lower vibration levels into the hand at the tool handle. More of the vibration energy generated by the heavier tools goes into moving the tool mass, leaving less energy directed into the hand at the handle. However, increasing the tool weight may increase the grip force required to use the tool and thus increase vibration transmission to the hand. Increased tool weight could also increase stress on the wrist, elbow, and/or shoulder, which in turn could result in musculoskeletal disorders such as carpal tunnel syndrome (CTS).
Imbalance and repetitive impulses are the primary causes of vibration in chain saws and other tools using gasoline engines as the driving mechanism. Imbalance is associated with the rotating and reciprocating masses of the engine. The primary vibration frequency is directly related to the operating speed of the engine. Repetitive impulses are associated with the motion of the chain on the guide bar and the explosions of the gas-air mixture in the engine. The hand-transmitted vibration associated with these vibration mechanisms can be significantly reduced by properly designing and placing elastomer vibration-isolation pads between the engine and the chain saw handles.
The vibration associated with grinders and similar tools is related to the unbalanced rotating mass of the grinder and to the interaction between die grinder wheel, cup or pad, and the workpiece. If the grinder is well maintained, the vibration associated with the unbalanced rotating mass of the grinder is usually not a problem. The condition of the grinder wheel or cup, however, has a very significant effect on the vibration amplitudes produced. If the wheel or cup is well dressed andkept "in round," the vibration associated with the interaction of the wheel or cup with the workpiece will be at a minimum. If the wheel or cup is not periodically "dressed" during use, it can become "out-of-round" and very rough. This substantially increases the vibration acceleration of a poorly maintained grinder compared with a new grinder .
# Effects of Tool Maintenance
Poor maintenance of vibrating tools significantly influences the vibration acceleration amplitudes that are generated. For example, the vibration acceleration of poorly maintained grinders may be many times higher than the corresponding vibration acceleration of new grinders. Part of the difference can be associated with poorly dressed grinding wheels. As was mentioned above, the use of elastomer vibration-isolation pads in chain saws can be very effective in reducing chain saw vibration directed into the hand. However, these pads must be inspected and replaced periodically.
# Effects of Work Cycle and Work Conditions
The work cycles, work conditions, and work incentives significantly affect the timeaveraged vibration acceleration level associated with many tools. For example, a major use of chipping hammers is for cleaning castings in foundries. In some foundries, the workers clean castings on a piecework basis-the more castings cleaned, the more wages earned. For these situations, the chipping hammers are generally operated at full throttle for periods of up to 4 hr or more in an 8-hr workday .
Another use of chipping hammers is to fonn propeller blades. For this situation, the chipping hammers are operated at 1/2 to 3/4 throttle for periods of up to 3 hr over an 8-hr workday . Typically, grinders are used for an additional 2.5 to 3 hr during the workday. The time-averaged vibration acceleration at the handle of the chipping hammer was 10 to 14 m/sec2 for the hammer operated at 1/2 to 3/4 throttle versus 50 to 190 m/sec2 for the hammer operated at full throttle . The total time-averaged rms acceleration amplitudes depend on the duration of use and corresponding acceleration associated with the chipping hammer and the grinder.
# Hand-Arm Vibration
# Effects of Coupling between Hand and Tool
Another factor that can influence the transmission of vibration energy produced by vibrating tools is the coupling that exists between the tool and the hands of the operator. Even though the degree of coupling between the hand and a vibrating tool affects the amount of vibration energy transmitted to the hand from the tool, it will not have much effect on the measured vibration acceleration amplitudes produced by the tool. The reason is that the vibrating mass of the tool in contact with the hand is usually much greater than the total effective mass of the hand that is coupled to the tool. In some situations (e.g., electrically driven engraving tools, small riveting guns, and the light-weight handles of small, antivibration hobby chain saws), the mass of the hand may be of the same order of magnitude as the mass of the vibrating tool. For these situations, the degree of coupling between the hand and the tool will have an effect on the vibration acceleration amplitudes measured on the tool.
# E. VIBRATION RESPONSE CHARACTERISTICS OF THE HAND
# Factors Influencing the Vibration Response Characteristics of the Hand
Several factors influence the vibration response characteristics of the hand. These include the following:
- Grip force exerted by the hand around the tool handle - Axial or static force exerted by the hand on the tool - Size of vibrating surface in contact with the hand - Body position associated with using the hand tool - Clothing and gloves worn Of these factors, the effects of grip and axial force are the most important, followed by body position and gloves .
Although it has been demonstrated that the presence of vibration-related disorders affect an individual's subjective response to and perception of vibration directed into the hand, these disorders do not have a measurable effect on the vibration-response characteristics of the hand . Radwin et al. reported that vibration can affect the way operators hold and use tools, which is then reflected in altered work performance and injury risk. With increased vibration, grip force on the tool handle is increased, and tactile sensitivity is decreased.
# V
III. Vibration as a Hazard
# Energy Directed into the Hands
Many vibration assessment guidelines are based on 1/3-octave-band, center-frequencyweighted rms acceleration levels. However, acceleration levels alone do not necessarily represent a true measure of the energy that is directed into the hand. To obtain this information, the coupling between the tool handle must be considered along with the acceleration levels. This can be accomplished by attaching a specially designed fixture to the handle of a vibration tool to measure grip force (coupling) as well as acceleration. A second method is to use the results of acceleration measurements on a tool handle in conjunction with dynamic compliance .
If the vibration directed into the hand is harmonic in nature or can be broken down into harmonic components, it can be shown that the amplitude of the energy dissipated (ED) in the hand and aim as a result of damping or other dissipative mechanisms is
E d = & L s M < P l ( 1 5 ) 2co4
Vf where co is the frequency in units of radians/second, X is the measured amplitude of acceleration (m/sec ) at (0, Vf is the dynamic compliance (m/N), and is the radians.
Similarly, the energy (E$) that is stored in the hand as kinetic and potential energy, and is consequently transferred back and forth between the hand and vibrating tool handle, is presented by Brammer and Taylor , , and Wasserman et al. as follows:
ES = - 2cf W (16
2(0 Vf
Also of interest is the time rate of change of energy or power transmitted to the hand. The power (WO is
a 1I7 X sin (<D) Vv = ------- or W = (0 Ed (17) 2co Vf
# Hand-Arm Vibration
The power transmitted to the hand and arm is related to the energy that is dissipated in the hand and arm.
# Mathematical Models of the Hand and Arm
The hand-arm system is a very complicated, continuous, nonhomogeneous system that consists of skin, muscle, bone, etc. An accurate model must take all of these components into account. Many investigators have developed models of the hand and arm . Mechanical impedance or dynamic compliance data or both were used as the basis for developing many of these vibration models. The parameters of many of the models can be related to the physiology of the hand and arm. However, there is no general agreement about which parts of the hand and arm should be described by a model. For example, work reported by Suggs and Mishoe and Wood and Suggs supports the idea that the mass elements of a model should represent the respective masses of the fingers, hand, arm, etc. However, the work reported by Reynolds and Keith , Reynolds and Falkenburg , and Wasserman et al. supports the idea that the mass elements of a model should represent the components of dermis and epidermis of the skin, sub cutaneous tissue, and muscle tissue in the area of the hand that is in direct contact with a vibrating surface. Most models imply that (1) vibration energy directed into the hand at frequencies below 80 Hz is transmitted to and can be perceived in the arm, and ( 2) vibration energy directed into the hand at frequencies above 100 Hz is generally local to the area of the hand in contact with a vibrating surface. These implications are confirmed by vibration transmissibility tests in the hand and arm.
# E
# IV. BIOLOGIC EFFECTS A. HAND-ARM VIBRATION SYNDROME (HAVS)
HAVS comprises a composite of pathophysiologic signs and symptoms that develop over time in workers who use hand-held vibrating tools. Many of the signs and symptoms of HAVS are also seen in other clinical entities such as primary Raynaud's disease, occlusive vascular disease, traumatic injury of hands, proximal vasculature compression, peripheral neuropathies, carpal tunnel syndrome, etc. . The factors listed in Table IV-1 must be considered in differential diagnoses for HAVS.
# B. PATHOPHYSIOLOGY OF HAVS
The development of HAVS is a gradual progressive process that may involve years of exposure to hand-arm vibration . Some of the etiologic aspects of HAVS have been reviewed by Pyykko and Starck , and Taylor . A requisite for diagnosis of occupational HAVS is a history of occupational use of vibrating tools such as drills, chipping hammers, grinders, concrete vibrators and levelers, polishers, swagging tools, shoe pound-up tools, caulking tools, fettling tools, clinching and flanging tools, burring tools, rock drills, chain saws, jackhammers, riveting hammers, bucking bars, and jackleg hammers.
In primary Raynaud's disease, the signs, symptoms, and involvements are usually symmetri cal (same areas of both hands involved), whereas in secondary Raynaud's disorders, including HAVS, the involvement is usually asymmetrical . Presently, however, no single test is available that will reliably distinguish HAVS from other secondary Raynaud's disorders .
The classification of the clinical stages of signs and symptoms of HAVS most widely used in the past is the one suggested by Taylor and Pelmear . This classification assumes two major pathophysiologic consequences of using vibrating tools: peripheral neural and peripheral vascular involvements. This classification does not specifically distinguish the peripheral neural and peripheral vascular progressive changes as separate entities (Table IV -2).
A revision of the Taylor-Pelmear classification of the stages of HAVS has been proposed by Taylor . This revised classification takes into account the concept
Hand-Arm Vibration Taylor and Pelmear .
Hand-Arm Vibration that the peripheral neural and the peripheral vascular involvements in HAVS may be distinct entities and that the disabilities related to each may progress independently of the other. The revision also recognizes that the tactile sensory deficits can and should be measured and considered independently of the vasospastic episodes (Table IV-3).
At the 1986 Stockholm Workshop, a new staging classification of vibration-induced signs and symptoms was introduced Gemneet al. 1987;Taylor 1987;Taylor 1989]. The Stockholm Workshop staging classification of the peripheral-neural and the peripheral-vascular pathophysiologic effects of hand-ann vibration exposure are considered separately, thus reflecting the concept that they are two clinical entities. In addition, a system is provided for a semiquantitative expression of the extent of the involvement of each finger on each hand. This system provides a mechanism for a quantitative clinical estimate and description of the involvement. The stagings as presented at the Stockholm Workshop are shown in Tables IV-4 and IV-5. It was suggested at the Workshop that this staging classification be used in all future hand-arm vibration studies. A standard staging classifica tion will enhance the comparability of the data.
The signs and symptoms and their time sequence in appearance indicate that vibration affects several components of hand and arm function . HAVS may involve, separately or in combination, the (1) peripheral neural system, (2) peripheral vascular system, ( 3) muscles of the hands and arms, ( 4) bones and joints of the hands and arms, and ( 5) central nervous system.
The Russian and Japanese 3) musculoskeletal, and ( 4) brain stem and neuro psychiatric. The degree of impairment ranges from no change (-), to minimal change (+), to extensive involvement (++++). The possible involvement of the central autonomic nervous system in HAVS was the subject for an international symposium in 1983 .
A classification for staging the severity of vibration-induced HAVS, including some functional changes, has been proposed in Japan .
The major features of the classification are summarized in Table IV Occasional attacks that affect only the tips of one or more fingers 2Occasional attacks that affect the distal and middle (rarely also proximal) phalanges of one or more fingers 3
Frequent attacks affecting all phalanges of most fingers 4As in stage 3, with trophic skin changes in the finger tips ♦Adapted from . 'The Stage is determined separately for each hand. . 'The sensorineural stage is determined separately for each hand. - Use of tobacco, some drugs, and some chemicals Taylor and Brammer and Brammer have categorized the factors as physical, biodynamic, and individual (Table IV-7). These factors may vary extensively in amount and combinations from one exposure situation to another and from day to day when using the same tool . Knowledge of HAVS is based mainly on retrospective epidemiologic studies or clinical examinations and comparisons between workers who use and do not use vibrating tools, and who do or do not have symptoms of HAVS. Lack of objective data from controlled laboratory investigations limits the accuracy of any dose-response or risk factor predictions. Taylor [1988Taylor [ ,1989, in reviewing the biological effects of hand-arm vibration, pointed out some of the information gaps in the understanding of the mechanisms involved in the neurological, vascular, and musculoskeletal damage.
# Peripheral Neural Effects
The early symptoms frequently experienced by workers exposed to hand-arm vibration include intermittent attacks of tingling and/or numbness of the fingers with or without pain . On continued exposure, the attacks may become more frequent and the symptoms more severe with decreased tactile sensitivity, decreased temperature sensitivity, and decreased manual dexterity and grip strength .
The mechanisms involved in the observed peripheral neural changes have not been fully described. In workers who have been exposed to hand-arm vibration on the job and who have developed intermittent peripheral neural symptoms (numbness, tingling, pain, loss of sensitivity), the increased vibration perception threshold may reflect the functional disturb ance of the peripheral nerves, of the sensory nerve endings, or of the mechanoreceptors, including the Pacinian corpuscles . Harada and Matsumota suggested that the peripheral neural effects are a pathophysiologic entity separate from and independent of the circulatory disturbances. This suggestion was based on neural and Brammer . vascular tests of workers not exposed to vibration, workers who used vibrating tools but had no symptoms, and workers who used vibrating tools and had symptoms of HAVS. Workers with neurophysiologic symptoms compatible with hand-arm vibration syndrome have a decreased sensory nerve conduction velocity from the fingers to the wrist . These findings are consistent with the concept of a direct pathophysiologic effect of vibration on the peripheral nerves and nerve endings.
On the basis of a study of 245 vibration-exposed subjects with a history of nerve symptoms or evidence of neural injury, Lukas and Lukas and Kuzel concluded that the peripheral neural lesions may result from causes other than the direct effect of vibration. Nerve conduction velocity measurements of the fast motor and sensory fibers of the median and ulnar nerves frequently indicated that only one of the nerves tested was involved. In individuals using hand-held vibrating tools, both nerves would be expected to be affected. The authors also observed that conduction velocities in the distal portion of the sensory and motor fibers of the median and ulnar nerves were significantly reduced in the patients with symptoms of vasoneurosis as compared with the patients without vasospastic symptoms. The author concluded that the peripheral neural damage was secondary to the complex damage to the vascular, joint, and muscular systems of the arms and hands (multifactorial). Juntunen et al. found that nerve conduction velocity was slower and motor nerve latency longer in the patients with vibration syndrome who had neurologic signs of polyneuropathy. The authors stated that these findings provided evidence of a wider neural involvement than just the peripheral nerves.
On the basis of an analysis of data from forest workers, Farkkila et al. suggested that a large part of the previously diagnosed vibration neuropathies belong to the category of carpal tunnel syndrome (CTS), which is the most common entrapment neuropathy among forest workers. Brammer et al. evaluated the degradation of vibrotactile and spatial-tactile perception in workers who used hand-held vibrating tools. The vibrotactile perception threshold values in workers with HAVS Stage 1,2, or 3 of the Taylor and Pelmear classification exceeded the values of workers with no vibration exposure by more than 2 standard deviations. On the spatial-tactile resolution test , the workers with vibration syndrome had values exceeding the controls by 2 to 4 standard deviations. Brammer et al. concluded that the neurological signs and symptoms in workers with chronic hand-arm vibration exposure involve both the peripheral nerve fibers and the mechanoreceptors.
Several types of neurophysiologic structures in the skin of the fingers are involved in the sense of touch . The different structures function (fire) in response to different mechanical stimuli. The Pacinian corpuscles, the quick-adapting receptors, and the two types of slow-adapting receptors are the most important mechanoreceptors in the skin that are involved in the sense of touch . For the sense of touch as measured by the sharp edges of the aesthesiometer (tactospatial), the slow-acting Type I receptors were more sensitive than the Pacinian corpuscles, the quick-acting receptors, or the slow-acting Type II receptors. Brammer et al. reported a decrease in the vibrotactile sensitivity that reflected the threshold of the Pacinian corpuscles.
In a biopsy study of 60 fingers with HAVS, Takeuchi et al. reported a decreased number of axon cylinders and a destruction of the myelin sheath in 90% of the cases. Such histopathologic deterioration could provide the basis for the sensory changes.
Researchers in this field agree that exposure to hand-arm vibration will eventually result in peripheral neural impairment with sensory loss, numbness, and decreased sensory and motor nerve conduction velocities but that the cause-effect mechanisms are not clear . Taylor summarized the state of knowledge as follows: "It is not known whether vibration directly injures the peripheral nerves thereby causing numbness and subsequently sensory loss, or whether the para-anesthesia of the hands is secondary to the vascular constriction of the blood vessels causing ischemia... in the nerve-end organs." Lundborg et al. investigated the value of the vibrotactile sense test in assessing vibration-related neuropathies. The vibration sensation threshold for individuals who had not used vibrating tools was constant at vibration frequencies from 8 to 250 Hz. At 500 Hz, the sensation threshold was higher. For workers who used vibrating tools and had symptoms ranging from intermittent numbness to constant numbness and pain, the vibration sensation threshold increased progressively with higher vibration frequencies. The abnormalities in the vibrogram (sensation threshold) correlated not only with numbness and pain, but also with the occurrence of white finger. The authors concluded that the numbness resulted from a change in the intraneural vascular function. The finger blanching and pain and the numbness all reflect a common peripheral vascular disorder.
# Peripheral Vascular Effects
The earliest signs of peripheral vascular changes in HAVS are the episodic attacks of fingertip blanching. These initial attacks of ischemia usually occur during cold exposure . With the continued exposure to vibration, the frequency and severity of the episodes of white finger increase until the blanching extends to the base of the fingers and may occur even in warm weather. The time between the first use of vibrating tools and the first appearance of episodic finger blanching (vasospasms) is designated as the latent interval. The latent interval appears to vary with the vibration intensity, as well as with other factors such as the type, model, unique individual characteristics of the tool, material on which the tool is used, tool maintenance, operating speed, operating technique, user characteristics, hand-grip force, push force, hand and arm posture, work/rest regimen, air temperature and moisture, protective hand gear, and clothing .
In one of the early reports, the peripheral vascular symptoms of HAVS were considered to be only a nuisance . However, for the individual worker, the effects may seriously interfere with work . Laroche reported that 10 out of 13 patients with HAVS had to change jobs because of the disabling effects of the disorder.
Although the phenomenon of the vasospastic episodes (sequence of events) has been described and accepted, basic underlying pathophysiologic mechanisms are not understood.
# Hand-Arm Vibration
Nonetheless several have been proposed. The present concepts are built on data derived mainly from epidemiologic and clinical studies.
The sequence of events in the progression of the episodes of blanching appear to involve (1) bouts of digital arterial spasms that become progressively more frequent and prolonged, (2) arterial hypertrophy with an increase in the medial muscular layer of the arterial wall, (3) perivascular fibrosis with increased collagen fonnation, and (4) increased vasoconstric tor sensitivity. The hypertrophy of the arterial smooth muscle may progress until the arterial lumen is partially or completely obliterated . Biopsies on 60 fingers from 30 patients with HAVS revealed increased thickening of the muscular layer that was severe in 82% and moderate in 15% when compared with 7 biopsies on 3 control subjects. Perivascular fibrosis was found frequently and was severe in 55% and moderate in 37%. Intimal thickening was minimal in 35% and moderate in 7% of the HAVS workers . Okada et al. in animal experiments observed that vibration resulted in intimal changes in the small arterioles with minimal medial changes. Similar findings were reported by Inaba et al. .
Several etiologic theories have been postulated to account for the observed pathophysiologic changes in the digital arteries, but no single theory can account for all the changes. The mechanisms that could help explain the events seen in HAVS include (1) direct effects of vibration on the digital arteries, (2) effects on the peripheral sensory aspects of the sympathetic nervous control of the peripheral circulation, (3) central neural control, (4) hypersensitivity to chemical mediators (prostaglandins, serotonin, and noradrenalin), and (5) some combination of the above . The use of tobacco has been reported to be an additional risk factor in the development of HAVS in workers who operate noise-producing, hand-held vibrating tools . Ekenvall and Lindblad measured the levels of nicotine and cotinine in the blood of 111 tobacco users and nontobacco users who did or did not have HAVS as determined by the digital systolic blood pressure after finger cooling. Blood nicotine concentrations in ng/ml were 0.8 in nontobacco users, 14.5 in cigarette smokers, 10.8 in snuff users, and 16.3 in users of other tobacco products; the cotinine levels were 0.7,196, 252, and 210 ng/ml, respectively. When the 111 workers were grouped according to the Taylor- Pelmear stages of HAVS, the blood levels of cotinine in ng/ml were 5.7 for stages 0T and 0V, 8.7 for Stages 1 and 2, and 11.8 for Stages 3 and 4; the cotinine levels were 124, 117, and 171, respectively. The digital systolic blood pressure (as a percent of the arm systolic pressure during finger cooling at 15"C) was significantly lower in the tobacco users: 52% for nonusers, 29% for smokers, and 45% for snuff users. On the basis of their study results and a survey of the relevant literature, the authors concluded that "habitual use of tobacco aggravates the symptoms of VWF disease and has a direct effect on the results of a cold provocation test in this disease" .
Obi iterative histopathologic changes reported in biopsies and arteriograms of the peripheral arterioles in some workers with HAVS appear convincing. But whether these changes are relevant histopathologic factors concerned with episodic finger blanching has been ques tioned on the basis of physiologic blood flow studies . Using venous occlusion plethysmography before and after induced vasodilation, these authors observed that the maximum blood flow after vasodilation was similar in the control subjects who were not exposed to hand-arm vibration and in vibration-exposed workers with advanced symptoms of HAVS. They reasoned that if the vessel lumen were narrowed by occlusive muscle hypertrophy, then blood flow would not be normal when maximum vasodilation was induced. Arteriograms were not taken; consequently, evidence of whether these subjects actually had arterial occlusion was lacking.
Regardless of the mechanisms involved in episodic finger blanching, the primary response concerns the digital arteries. During ischemic attacks, arterial blood flow to the affected segments of the fingers is reduced or completely shut off by contraction of the smooth muscles in the medial arterial wall. The episodic arterial muscle contractions could reflect an increased sympathetic nervous activity or an increased sensitivity of the arterial muscula ture (vasomotor tone) to local factors (chemical mediators including prostaglandins, serotonin, and noradrenalin) .
The episodic ischemic attacks could be inappropriate pathophysiologic vascular responses to the vibration forces transmitted to the hands of the workers using vibrating tools. The medial muscle hypertrophy could be a histopathologic response to the sustained contraction of the vascular muscles. Any intimal changes could be a direct response to the vibration or a response to some changes in the blood chemistry . If the sympathetic nerve supply to the digital arteries is cut at the stellate ganglion, episodic blanching of the fingers induced by cold will return after an initial dilation of the digital arteries, which could last 3 to 4 months. This would imply that local chemical mediators may be at least partially involved.
A series of studies on workers with or without exposure to vibration and vibration-exposed workers with or without HAVS indicated that the finger vasospasm in the vibration-exposed group is the result of chronic stimulation of the mechanoreceptors in the fingers by the vibration. The receptors then serve as the sensory receptor link to the sympathetic nervous system with the effectors being the smooth muscle of the medial layer of the finger arterioles .
Although the findings in these studies support the concept that the vibration sensory receptors contribute to HAVS by initiating excessive afferent impulses in the sympathetic reflex involving the peripheral vascular musculature, the exact etiologic (pathophysiologic) mechanisms are not fully known . Generally, in experimental studies when the hand is stimulated by vibration, a vasoconstriction occurs in the fingers. In workers who have not used vibrating tools, the vasoconstriction response to vibration stimuli was mild (about 10% have a strong response). Among workers who have used vibrating tools occupationally, about 40% exhibited a strong vasoconstrictive response, and 40% had a mild response similar to that of the controls . This suggests that chronic vibration stimulation increases the sensitivity of the mechanoreceptors to the vibration stimuli and increases the level of afferent impulses to the central nervous system with resulting increased reflex-sympathetic vasoconstriction. The prolonged contraction of the vascular muscles could result in the hypertrophy of the medial musculature and increased narrowing of the vessel lumen .
# Skeletal Muscle Force and Muscle Fatigue
The subjective complaints of deterioration of hand grip force and muscle strength in workers using vibrating tools have been mentioned in many of the studies of HAVS. This aspect of HAVS has received specific emphasis in studies in Japan and in Finland . Among Japanese chain saw operators with more than 2,000 hr of chain saw use, about 28% reported symptoms of decreased grip force and muscle strength. These symptoms were reported by 20% of Finnish chain saw operators with more than 5,000 hr of chain saw use.
The Finnish group measured maximum grip strength and rate of development of muscle fatigue with or without acute vibration exposure under controlled laboratory conditions. Lumberjacks with or without symptoms of diminished grip force and with or without symptoms of HAVS were compared with a control group who had no occupational vibration exposure. In the group of lumberjacks with HAVS, some experienced only episodes of white finger without ever experiencing decreased grip force; some reported finger numbness without decreased grip force; and some experienced decreased grip force and white finger and/or finger numbness.
The data indicated the following relationships:
- Grip force was reduced in lumberjacks throughout the entire muscle fatigue curve when the hand was exposed to vibration.
- Grip force was reduced more in workers who reported numbness, reduced muscle strength, or muscle pains.
- Acute vibration exposures reduced grip force more in those with symptoms than in those without symptoms of white finger.
- Reduced muscle strength was present in lumberjacks with 5,000 or more hours of total chain saw operating time.
- Muscle force was reduced and the prevalence of symptoms increased when total exposure times exceeded 5,000 hr.
- Lumberjacks with white finger used a stronger grip force when using the chain saws than did those who did not have white finger.
- A dose-rcsponse relationship seemed to exist between diminished muscle force and vibration exposure.
- Grip strength decreased as a function of age in vibration-exposed and unexposed groups.
- Muscle strength fatigue curve for the chain saw operators was similar to that of unexposed workers.
- Muscle strength for controls and for chain saw operators was the same when the hand was not exposed to vibration.
- Muscle strength of the controls was similar to that of the lumberjacks who had no symptoms of white finger.
The pathophysiologic mechanisms involved in the reduced muscle strength aspect of HAVS are not clear. Some of the possibilities include neurogenic muscle dysfunctions, direct mechanical effect on the muscle fibers, biochemical alterations in the muscle intracellular substances, and neuropathies. Whatever the mechanism(s) involved, diminished grip force can progress to the point of significant occupational disability .
# Bone Cysts
Degenerative changes in the bones of the fingers and wrists of workers using vibrating hand-held tools have been reported . The changes observed were mainly cysts, vacuoles, and areas of décalcification. It is clear, however, that bone cysts were not observed as being specific to HAVS . Kumlin et al. found that 7 of 35 lumberjacks (20%) studied showed radiographic presence of cysts and vacuoles in the metacarpal bones or the phalanges or both. These seven lumbeijacks had used chain saws for 10 years or more and had one or more subjective symptoms typical of HAVS.
Radiographs of the hands were specifically included in a British health survey of occupa tional chain saw operators . The objective of this investigation was the association, if any, between the presence of wrist and hand bone cysts and the occupational exposure to hand-arm vibration. X-rays of the hands were taken of 165 lumberjacks and 162 controls (manual laborers in the same environment as the lumberjacks). Each X-ray was read independently by three radiologists. Based on positive findings by two or more of the three readers, the incidence of vacuoles was 44% in the lumberjacks versus 33% in the controls. The difference between the incidence of vacuoles in lumberjacks and in other workers who did not use vibrating tools was not statistically significant.
In a 1977-78 study of Italian shipyard workers, 169 caulkers who worked with vibrating tools were compared with 60 welders and electricians who were not exposed to hand-arm vibration . Only the workers who used hand-held vibrating tools were X-rayed. In the caulkers, 51% exhibited HAVS in Stages 1 and 2 of the Taylor and Pelmear classification. Only 7% of the control group showed similar signs and symptoms. Bone cysts, vacuoles, or both were reported in the hand/wrist bones of 31% of the caulkers. No X-ray data from controls were available for comparison. This is similar to the incidence of bone cysts-vacuoles that reported in lumberjacks and controls not exposed to vibration.
A NIOSH study compared 205 foundry and shipyard chipping and grinding workers with 63 manual workers in the same industries who did not use vibrating tools .
The frequency, location, and size of cysts and vacuoles in the hand and wrist bones as inicated on X-rays were compared. The films were read independently by two radiologists. The vibration-exposed and the control workers showed no statistical dif ferences in frequency, location, or size of cysts and vacuoles. This study, with its adequate control group, supports the concept of that cysts and vacuoles occur in the hand and wrist bones of workers performing manual work but that these changes are not necessarily vibration related. The presence of bone cysts in workers exposed to vibration is therefore not a useful, objective diagnostic criterion for HAVS.
Gemne and Saraste surveyed the literature (125 published articles) to evaluate the evidence for and against radiological demonstrable effects of vibration on the bones and joints of the arm and hand. The authors concluded that the evidence does not support a "causal relationship between vibration exposure and the formation of bone cysts and vacuoles."
# Central Nervous System
The inclusion of the central nervous system in the hand-arm vibration syndrome has been postulated by USSR and Japanese researchers . The etiology of the "systemic effects" involves the concept that hand-arm vibration can impair central nervous system function through damage to the autonomic centers in the brain [Matoba et al. 1975a[Matoba et al. , 1975b.
The symptomatology alleged to be associated with vibration-induced central nervous system disturbances includes anxiety, depression, insomnia, headache, palmar sweating, vertigo, irritability, emotional instability, etc. , in summarizing the conclusions from an international symposium on hand-arm vibration and the central nervous system, stated that the present data do not support the hypothesis that exposure to hand-arm vibration may cause damage to the autonomic centers in the brain. In a study of 78 HAVS patients, Taylor et al. found no evidence to support an involvement of the central nervous system in HAVS.
# Other Responses
Several other responses, whose significance in the identification and description of HAVS is unclear at present, may have some diagnostic value. These include the following: a. In comparing the grip strength of nonvibration-and vibration-exposed workers, Miyashita et al. observed that grip strength progressively decreased as the total vibration exposure time increased: 52.5 kg grip strength in controls; 46.5 kg (-11.5%) in workers with up to 2,500 hr of total vibration exposure time; 40.1 kg (-24%) in wokers with more than 7,500 hr. Because of the wide differences in grip strengths among people, individual previbration-exposure values would be needed for grip strength to be a reliable diagnostic tool.
b. In the same control and exposure groups, sarcoplasmic enzyme levels (aldolase , creatinine phosphokinase , and lactic dehydrogenase ) in the exposure group increased over controls: 6% and 30% for ALD, 23% and 20% for CPK, 15% and 13% for LDH for 7,500 hr of vibrating tool use, respectively . Adrenaline and noradrenalin in the urine of the exposed group were also measured and, when expressed as ng/mg creatinine, increased over control values by 260% and 269% for adrenaline, and 12% and 11% for noradrenalin for vibration exposures up to 4,000 hr and longer than 12,000 hr, respectively. Whether these changes are a general stress response or are specific to vibration stress remains to be proved.
c. It has been suggested that whole blood viscosity may play a role in HAVS and might be a useful tool in diagnosing HAVS between attacks. Whole blood viscosity in workers with HAVS was reported to be statistically significantly higher than in workers without HAVS (p<0.01) . However, Inaba et al. found no change in blood viscosity, hematocrit, cholesterol, and high density lipoproteins in vibration-exposed animals.
d. Okada et al. postulated a possible role of enhanced peripheral vasoconstriction caused by the exaggerated response of alpha adrenergic receptors in the arterial smooth muscles during attacks of white finger in workers with HAVS. These authors reported that during the cold provocation test (CPT), the plasma level of cyclic guanosine 3', 5'monophosphate (cyclic GMP) was increased to 170% over pretest levels in workers with HAVS. The cyclic GMP levels did not increase in control subjects during the CPT. Without the CPT, the control and HAVS subjects had similar levels of cyclic GMP.
Phentolamine administered before and during the CPT and atropine injected subcutaneously immediately before the CPT inhibited the plasma rise in cyclic GMP during the CPT. The authors suggested that in individuals with HAVS, the increase in endogenous noradrenalin was enough to cause a significant increase in cyclic GMP in response to cold exposure (the CPT). This increased cyclic GMP response could result in an enhanced alpha-adrenergic response and a peripheral vasoconstriction.
e. An increased digital blood vessel reactivity to cold was reported by Bovenzi . Brown et al. measured radial digital artery blood flow in workers with and without HAVS before and after 20 min of chipping hammer use. Blood flow was measured by a 20-MHz, pulsed, ultrasonic Doppler velocimeter. Digital artery blood flow rate following the 20-min use of the chipping hammer increased substantially in the HAVS group, but there was little change in the control group. Pre-exposure flow rates were approximately equal in the control group and those with Stage 2 HAVS. The authors suggest that the 20-MHz Doppler velocimeter might be a valuable indicator tool for studying HAVS pathology.
# C. EPIDEMIOLOGIC STUDIES
Epidemiologic studies of workers using hand-held vibrating tools have been conducted in Europe, North America, and Asia. Workers using gasoline-powered chain saws in forestry have been studied most frequendy, followed by studies of workers using pneumatic chipping hammers in foundries, shipyards, and quarries, and pneumatic jack-leg drills in mining. These have been cross-sectional studies except for a few longitudinal studies of chain sawyers in the United Kingdom, Finland, and Japan. Cross-sectional studies examine a group of workers using hand-held vibrating tools in an industry at one particular time to determine the proportion of workers with HAVS (i.e., the prevalence of HAVS). Lon gitudinal studies of HAVS examine a group of workers at more than one point in time. The prevalence of HAVS is usually expressed as the prevalence of specific symptoms of HAVS such as vascular or neurologic symptoms. Sometimes studies report the latency of HAVS symptoms, the years of exposure to hand-arm vibration from the tool, and the hand-arm vibration acceleration level of the tool. The latency of a HAVS symptom is defined as the time from first use of a tool to the first appearance of the symptom. in the form given in the cited article. A method of standardization (presented in Appendix A) was applied to the acceleration measurements of hand-arm vibration if they were reported in a study. This method of standardization makes the measurements comparable with each other.
# Cross-Sectional Studies of HAVS
The prevalence of vascular symptoms of HAVS in Table IV-8 ranged from 6% to 100%.
To evaluate the relative significance of these prevalence values, they must be compared with the background rate of vascular symptoms among worker populations that have not been exposed to hand-arm vibration. Nineteen of the studies reported the prevalence of vascular symptoms among a group of control workers who had not been exposed to hand-arm vibration and had worked at the same site as the exposed workers . The prevalence of vascular symptoms among these 19groups of control workers ranged from 0% to 14% with a mean prevalence of 5.4% and a median of 4%.
Most of the studies listed in Table IV-8 had prevalence rates of vascular symptoms that were well above background rates. More than half of the studies had HAVS prevalence rates that were greater than 40%. Epidemiologic studies of HAVS clearly confirm an association between vascular symptoms and exposure to hand-arm vibration from hand-held vibrating tools and workpieces. These studies also provide clues to HAVS prevention. A study showing a relatively low prevalence of vascular symptoms or a relatively long latency of vascular symptoms may provide such clues. In addition, some of the studies in Table IV-8 had tool vibration measurements taken at the time of the cross-sectional medical evaluations, and these studies indicate the exposure-response relationship between HAVS and hand-arm vibration.
Nine of the studies in Table IV -8 |Taylor et al. 1975a;Iwata et al. 1980;Behrens et al. 1982Behrens et al. , 1984Moon et al. 1982;Futatsuka 1984;Harkonen et al. 1984;Walker et al. 1985;Zeng-Shun et al. 1986] reported prevalence rates of vascular symptoms among the exposed workers that were nearly within range of the prevalence rates for the control group (i.e., from 0%to 14%). The study by Iwata etal. found an 8% prevalence of vascular symptoms among chain saw operators. A control group was not included in this study. The low prevalence rate may have been due to the high proportion (75%) of chain saw operators in this study who had less than 10 years of exposure to hand-arm vibration from chain saws, or it may have been that the use of antivibration chain saws by 1980 reduced exposure. Although the authors did not report the latency of vascular symptoms for this group of chain saw operators, the average latency for other studies of chain saw operators in Table IV-8 ranged from 4 to 13 years. Thus the group of chain saw operators in the study by Iwata et al. probably had not experienced sufficient exposure for all cases of HAVS (with vascular symptoms) to manifest themselves. Harkonen et al. observed the relatively low 18% prevalence of vascular symptoms of among a group of chain saw operators. A control or reference group of peat bog workers were examined and were found to have a 3% prevalence of vascular symptoms. The authors reported that the difference in prevalence between the exposed and control groups was statistically significant (pcO.OOl).
In the study of workers using gasoline-powered brush saws, Futatsuka reported a 6% prevalence of vascular symptoms, the lowest reported prevalence in Table IV-8. No control group was examined in this study. Among the exposed group, the mean duration of exposure to brush sawing was 7 years and the mean latency of vascular symptoms was 6.4 years.
Because the mean exposure time was greater than the mean latency, the prevalence of vascular symptoms in this group of brush saw operators would not be likely to increase appreciably with further exposure. The author reported some factors that probably con tributed to the low prevalence of vascular symptoms in these brush saw operators. Workers used the brush saws for 4 to 5 months a year, during the warmer season of May to September. Also, since 1970, the use of the brush saw was limited to 2 to 3 hr/day. Before that date, workers were using the brush saws up to 6 hr/day. The effect of limiting the number of hours of brush saw use per day was revealed in the difference between the prevalence of vascular symptoms in workers who started using the brush saws in 1961 and 1962 (12% peak prevalence from 1961 to 1980) and workers who started in 1969 and 1970 (0% prevalence from 1969 to 1980).
A relatively low prevalence of vascular symptoms among chipping and grinding workers was reported by Behrens et al. . In this group of chipping hammer and grinder operators, the prevalence would probably increase over time because the mean exposure time (12 years) was less than the mean latency for vascular symptoms (17 years).
Four other studies in Table IV-8 showed relatively low prevalence rates of vascular symptoms .
All of these studies reported the prevalence of vascular symptoms in a control group of workers. The study of pedestal grinders by Taylor et al. found an 11% prevalence in the exposed group and 4% in the control group. The authors did not compare the prevalence statistically. Also, the authors did not report a mean exposure time for this group of pedestal grinders, although the mean latency of vascular symptoms was reported as 14 years. In the study by Moon et al. , the prevalence of vascular symptoms among anthracite miners using pneumatic rock drills was 13%, whereas the prevalence in the control group was 0.9%. The statistical comparison of prevalence rates was significant (p<0.05). Similarly, Zeng-Shunet al. reported that the prevalence of vascular symptoms among TV. Biologic Effects railroad woikers using riveters, chipping hammers, and grinders was 13%, whereas the control group prevalence was 1.6% (pcO.OOl).
The Walker et al. study of workers in the gas industry who used pavement breakers is the only study in Table IV-8 in which the difference in prevalence between the exposed and control groups was not statistically significant. The prevalence rates of vascular symptoms in the workers using pavement breakers and the workers not exposed to hand-arm vibration were both 10%. After adjustment for differences in the ages of the exposed and control groups, the age-adjusted prevalence was 12% in the exposed group and 10% in the control group. This comparison was not statistically significant. The authors did not report the latency of vascular symptoms, but the prevalence of vascular symptoms among workers using the pavement breakers for 1 to 5 years was 9%, whereas the prevalence in workers using the pavement breakers more than 20 years was 18%. Two factors may have contributed to the nonsignificant and relatively low prevalence of vascular symptoms in this group of pavement breaker operators. First, the average latency of vascular symptoms may have been longer than latencies recorded for exposures to other tool types because the prevalence among the exposed workers did not increase much above that of the control group until the exposed workers had more than 20 years of exposure. Second, the prevalence of vascular symptoms in the control group was relatively high (10% prevalence in this control group compared with a mean prevalence of 5.4% in 19 control groups from Table IV -8).
A recent survey of workers who used impact power tools indicated a prevalence rate of 29% for numbness and tingling of the fingers and 17% for white finger. The workers used the impact tools for an average of 23% of the workday. Frequency-weighted acceleration levels exceeded 12 m/sec2 for all measurements, and they averaged approximately 24 m/sec2 for chipping hammers and rammers. The mean cumulative exposure for each worker over a working lifetime was nearly 4,000 hr. The 17%-to 29%-prevalence of signs and symptoms of HAVS occurred even though the daily tool use time was only about 2 hr .
Forty-four studies listed in Table IV-8 included some information about the latency of vascular symptoms among exposed workers. Thirty-three of these 44 studies reported the mean latency of vascular symptoms. These 33 mean latencies ranged from 0.7 to 17 years, with a mean value of 6.3 years. When compared with the range and mean values of the 33 mean latencies, four studies found a 13-year mean latency for vascular symptoms among 18 (out of 20 total) workers using pneumatic chipping hammers at a granite quarry. Despite the relatively long latency, the prevalence of vascular symptoms was 72% (13/18). The high I Hand-Arm Vibration prevalence is expected because the mean duration of exposure (20 years) for the workers was greater than the mean latency. For the 18 quarry workers, the individual latencies varied from 0 to 27 years. A latency of 0 years may indicate that this quarry worker had vascular symptoms before starting to use the chipping hammer at this quarry. The next four lowest latencies for individual workers were 2,4, 7, and 7 years. Thus the individual variation in onset of vascular symptoms shows that all workers in this group could not be protected by limiting the years of exposure.
In a study of shipyard workers using chipping and grinding tools .
The Pelmear et al. study of hand grinders found a 13.7-year mean latency of vascular symptoms, and the Taylor et al. study of pedestal grinders found a 14-year mean latency. Neither of these studies reported the range of latencies or individual latency values. The mean exposure time (19 years) for workers using hand grinders in a foundry was greater than the mean latency (13.7 years), which resulted in a substantial 35% prevalence of vascular symptoms. Workers using pedestal grinders in a foundry had an 11% prevalence (and a 14-year mean latency), but the authors did not report the average years of exposure. As a result, die relationship between the latency, the years of exposure, and prevalence in this group of workers is not known.
Vibration measurements were reported for 23 of the studies listed in Table IV-8. These 23 studies are ranked in Table IV-9, in descending order, from highest to lowest hand-arm vibration acceleration level. The prevalence of vascular symptoms, the tool type, and the publication reference are also repeated in Table IV-9. The 23 hand-arm vibration accelera tion levels in Table IV-9 range from 10 to 2,014 m/sec2, and the mean and median values were, respectively, 312 and 195 m/sec . The relationship between the hand-arm vibration acceleration level and the prevalence of vascular symptoms for these 23 studies was tested for linearity by calculating a correlation coefficient. The correlation coefficient was 0.67 and was statistically significant at the 1% level (p<0.01). Thus the prevalence of vascular symptoms tends to increase as the hand-arm vibration acceleration level increases for these 23 studies.
In general, the studies in Table IV-9 that showed hand-arm vibration acceleration levels greater than the median acceleration level for these 23 studies (195 m/sec2) also showed prevalence rates of vascular symptoms greater than 40%. Only the Bovenzi et al. study deviated from this trend. Also, in general, the studies in Table IV-9 with acceleration levels less than or equal to the median acceleration level had prevalence rates of less than Taylor et al. 1984Oliver et al. 1979Taylor et al. 1981Bentley et al. 1982Agate et al. 1946Agate 1949Matsumoto et al. 1979Chatterjee et al. 1978Robert et al. 1977Matsumoto et al. 1977, 1979Behrens et al. 1984Wasserman et al. 1984Bovenzi et al. 1980Walker et al. 1985Pelmearetal. 1975Taylor et al. 1975cStarck et al. 1983Iwata 1968 (continued) See footnotes at end of table. (Iwata ; Pelmear et al. ; Starck et al. ;and Brubaker et al. ) did not follow this trend.
In the Bovenzi et al. study of shipyard workers using chipping hammers and grinders, the hand-arm vibration acceleration level was 205 m/sec and the prevalence of vascular symptoms was 31%. The authors did not report the latency of vascular symptoms for those shipyard workers with symptoms. They did report that the mean duration of exposure to hand-arm vibration was 7.3 years for the 169 shipyard workers studied, and that 46% had been exposed for 5 years or less and 44% for 6 to 10 years. Also, in this study, the mean duration years of exposure for shipyard workers with vascular symptoms was 10.2 years, whereas the mean duration of exposure for shipyard workers without vascular symptoms was 6.1 years. Thus at least 46% of the shipyard workers studied had been exposed for fewer years (i.e., <6) than the mean years of exposure for workers with vascular symptoms (approximately 10 years). These results indirectly indicate that the prevalence of vascular symptoms in the group of shipyard workers studied by Bovenzi et al. would probably increase over time and with further exposure.
Two other studies in Table IV-9 that deviate from the trend of a linear relationship between hand-arm vibration acceleration levels and prevalence of vascular symptoms are the pedestal grinder studies of Pelmear et al. and Starck et al. . For both of these studies, the prevalence of vascular symptoms was exceptionally high (96% for Pelmear et al. and 100% for Starck et al. ). The authors for both of these studies attributed the high prevalence rates to the use of zirconium wheels on the pedestal grinding machines because the prevalence of vascular symptoms increased markedly in their study groups when wheels of "softer" material were replaced by "harder" zirconium wheels. The Taylor et al. study of pedestal grinders in Table IV-9 reported a relatively low prevalence (11%), an average acceleration level of 100 m/sec2, and the use of "soft" wheels on the pedestal grinding machines. The only other study of pedestal grinders in Table IV-9 (by Agate et al. ) did not specify the type of wheels used. Brubaker et al. found that 45% of hard rock miners using jack-leg drills had vascular symptoms but that the hand-arm vibration acceleration level for the jack-leg drills was frequency weighted at 20 m/sec2, a relatively low acceleration level. Acceleration levels for jack-leg drills were reported for four other studies in Table IV-9; the levels were all greater than 100 m/sec2, and for three of these studies, the levels were greater than 300 m/sec2. Brubaker et al. measured the jack-leg drills "under actual drilling conditions at the mine sites according to guidelines specified in ISO 5349." The authors pointed out that ISO 5349 suggests that 50% of the workers exposed to a frequency-weighted vibration level of 20 m/sec2 will develop vascular symptoms after a 3-to 5-year exposure. Therefore, a 45% prevalence of vascular symptoms may not be unexpected for this group of workers. Brubaker et al. did not compare their measurements of jack-leg drills to those of other investigators and thereby offered no explanation for the relatively low acceleration levels they reported.
# I
# Hand-Arm Vibration
5349 suggests that 50% of the workers exposed to a frequency-weighted vibration level of 20 m/sec2 will develop vascular symptoms after a 3-to 5-year exposure time. Therefore, a 45% prevalence of vascular symptoms may not be unexpected for this group of workers. Brubaker et al. did not compare their measurements of jack-leg drills to those of other investigators and thereby offered no explanation for the relatively low acceleration levels they reported.
The study by Iwata shows a similar result to that of Brubaker et al. . For workers using jack-leg drills, Iwata found a relatively high prevalence of vascular symptoms (72%) but a below-average hand-arm acceleration level (121 m/sec2). Iwata's study was reported earlier than the other studies of jack-leg drills in Table IV-9. He could not compare his hand-arm vibration measurements with other studies of jack-leg drills, and he did not perform the measurements according to international standards recommended during the late 1960s.
# Longitudinal Studies of HA VS
Longitudinal studies of workers exposed to hand-arm vibration demonstrate the effect that lowering the acceleration level of a hand-held vibrating tool has on the prevalence of HA VS. Three longitudinal studies have been conducted; all of them concern forestry workers using gasoline-powered chain saws. Tables IV-10, IV-11, and IV-12 summarize the longitudinal studies of chain saw operators in the United Kingdom, Finland, and Japan, respectively. Neither a longitudinal nor a cross-sectional study of chain saw operators has been done in the United States.
Gasoline-powered chain saws in the 1950s were large and difficult to maneuver, and their use was limited to 1 to 2 hr per day. In the 1960s, technical improvements in the design of chain saws allowed their use to be extended to 4 to 6 hr per day. By the early 1970s, initial reports of HAVS among chain saw operators were made public. In the early 1970s, chain saws were redesigned to lower the vibration acceleration levels. These saws are called antivibration chain saws. By the 1980s, the prevalence of HAVS among chain saw operators had been reduced.
Table IV-10 presents a summary of the longitudinal studies of antivibration chain saw operators in the United Kingdom reported by Taylor and co-workers (Taylor et al. 1974(Taylor et al. , 1975a(Taylor et al. , 1975b(Taylor et al. , 1975c(Taylor et al. , 1977Riddle and Taylor 1982]. An original group of 46 forestry workers using gasoline-engine-powered chain saws was followed from 1970 to at least 1981. In 1970, the prevalence of vascular symptoms in this group was 85%. Antivibration chain saws were introduced in 1973, and by 1975, 73% of the 44 remaining chain saw operators had vascular symptoms. In 1981,28 of the original 46 chain saw operators were still working in forestry, and 46% of these workers had vascular symptoms. Taylor and co-workers noted that some workers had recovered and no longer had vascular symptoms after the introduction of antivibration chain saws. Also in 1981,18 chain saw operators who had worked exclusively with antivibration chain saws [1974,1975a, 1975b, 1975c, 1977 Pyykko et al. [1978Pyykko et al. [ , 1982bPyykko et al. [ , 1986b. *Hand-arm. Denotes data not available from articles cited. Hand-Arm Vibration were examined and were found to have a 17% prevalence of vascular symptoms.
Hand-arm vibration acceleration levels for chain saws measured before the introduction of antivibration designs ranged from 150 to 350 m/sec2, whereas antivibration chain saws ranged from 15 to 50 m/sec .
Pyykko and co-workers . Forestry workers employed by the Japanese government in national forests have been examined on a regular basis since 1965, and results of these examinations have been reported through 1980. Chain saw operators in this study were grouped according to the year when they first began using a chain saw (see Table IV -12). The peak prevalence of vascular symptoms for chain saw operators who began chain saw use in 1958 and 1959 was 63%. For chain saws measured in 1966 (the earliest year measurements were available), the vibration acceleration level ranged from 111 to 304 m/sec2. The peak prevalence for chain saw operators who began chain saw use in 1968 and 1969 was 22%. For nonantivibration chain saws measured in 1970, acceleration levels ranged from 49 to 105 m/sec . The peak prevalence for chain saw operators who began working in 1974 and 1975, after the introduction of antivibration chain saws, was only 2%. For antivibration chain saws measured in 1975, acceleration levels ranged from 10 to 33 m/sec2.
The Japanese government in the early 1970s began restricting the number of hours per day that chain saws could be operated. Between 1970 and1975, chain saw use was limited to 2 hr/day for the national forestry operations. Futatsuka andUeno reported that of the 185 chain saw operators who began using chain saws in 1972 and 1973, only 3 (2%) had vascular symptoms as of 1980 (not shown in Table IV -12). These chain saw operators had been exposed for at least 7 years, a period of time greater than the 6.4-year mean latency of vascular symptoms for the entire study population (see Table IV-12).
# Summary of Epidemiologic Studies of HAVS
Epidemiologic studies of workers using hand-held vibrating tools show a strong association between exposure to hand-ami vibration and vascular symptoms of HAVS or Raynaud's phenomenon. Only 9 of the cross-sectional studies presented in Table IV-8 had relatively
I a
# IV. Biologic Effects
low prevalence rates of vascular symptoms (i.e., less than 20%) compared with prevalence rates of vascular symptoms in 19 control groups. In five of these nine studies, the prevalence of vascular symptoms in the exposed group of workers was compared with the prevalence in a control group. In four of these five studies, the prevalence was significantly higher in the exposed group than in the control group even though the prevalence of vascular symptoms in the exposed group was relatively low.
The study with the lowest prevalence of vascular symptoms (6%) in Table IV-8 was the only one of the eight studies with relatively low prevalence rates that offered a plausible reason for the low prevalence. In this study of brush saw workers, the use of the brush saw was restricted to 4 to 5 months/year during the summer season and to 2 to 3 hr/day. The conditions of using the brush saw in this study seemed to produce a very low prevalence despite a hand-arm vibration acceleration level of 59 m/sec2. The study in Table IV-9 with die lowest frequency-weighted acceleration level (10 m/sec2) reported a prevalence of vascular symptoms (25%) among workers using pneumatic drills, riveters, shavers, and bucking bars that was four times greater than that reported by Futatsuka although the frequency-weighted acceleration level (10 m/sec2) was less. The vibration frequencies produced by the tools used in the Engstrom and Dandanell study were much higher (up to 10,000 Hz) than those reported by Futatsuka .
Twenty-three studies from Table IV-8 included measurements of hand-arm vibration acceleration levels. These studies showed a statistically significant linear relationship between increasing exposure to hand-arm vibration and increasing prevalence of vascular symptoms of HAVS. Even though this relationship could be demonstrated statistically, only 3 of the 6 studies reporting the lowest acceleration levels (i.e., less than or equal to 60 m/sec ) among these 23 studies (see Table IV-9) also reported relatively low prevalence of vascular symptoms (i.e., less than 20%). The relationship between hand-arm vibration exposure and the prevalence of vascular symptoms of HAVS among these 23 studies was more consistent for those with higher acceleration levels than for those with lower levels.
The longitudinal studies of chain saw operators were able to demonstrate an appreciable decrease in the prevalence of vascular symptoms after the introduction of the antivibra tion chain saw. The lower acceleration level of the antivibration chain saw apparently contributed to the decrease, although the amount of decrease varied from study to study. Riddle and Taylor reported a 17% prevalence among 18 workers exclusively using antivibration chain saws; Pyykko et al. reported a 2% prevalence in 185 workers who started using chain saws in the mid-1970s when antivibration chain saws were introduced. The exceptionally low prevalence in Japanese chain saw operators could reflect the requirement that they do not operate chain saws for more than 2 hr/day [Saito 1987J.
- Laboratory/Hospital Tests Vascular Assessment Doppler (peripheral segmental blood flow and pressure in arms) Digital plethysmography (at rest and following cold stress) Digital systolic pressure (plethysmography with local cooling, and whole body cooling as well if necessary) Cold provocation test (immersion of digits and hands with recording of digital temperatures)
# Neurologic Assessment
EMG (to record median and ulnar sensory and motor nerve conductivity)
# Hematologic Assessment
Total and differential, sedimentation rate, blood viscosity, uric acid, rheumatoid factor, antinuclear antibodies, cryoglobulins, serum protein electrophoresis
# U rinalysis
Proteinuria, glycosuria
# X-rays
Cervical spine and ribs (to exclude costoclavicular syndrome)
Olsen conducted a comparative study of diagnostic tests for vibration white finger.
In the four tests used, various aspects of finger blood flow and finger blood pressure were measured. The study concluded that the finger color test may be as valuable as finger systolic blood pressure for diagnostic purposes. The diagnostic values of some of the tests are discussed below.
# Cold Provocation Test (CPT)
Two generic variations of the CPT have been used in studying HAVS. The versions vary mainly in the length of exposure to the stimulus, the temperature of the cold stimulus, and the responses measured. The subject must be in thermal balance before the test. This is achieved by having the subject rest for about 30 minutes in a room with air temperatures from 21- to 24*C (70- to 75*F).
# I
# Hand-Arm Vibration a. Short Exposure
In the short exposure version of the CPT, the hand is immersed up to the wrist in ice water for 1 to 3 minutes. Blood flow in the fingers of the opposite hand can be measured by plethysmography before, during, and after immersion. The most important measurements involve the reduction in blood flow during cold exposure and the recovery of blood flow following immersion. Finger rewarming time after a short (3-minute) immersion in water at 10°C (SOT) was 1.4 minutes for the control subjects and 2.9 minutes for workers with HAVS (p = <0.01). Excluded from the HAVS group were those whose finger temperature did not rise to 30*C during body heating at a room temperature of 40° to 45'C (104- to 113'F) for 15 minutes . Niioka et al. found that the finger skin rewarming time after a CPT could distinguish between HAVS patients and controls with a false discrimina tion of 6%, a sensitivity of 80%, and a specificity of 100%.
# b. Long Exposure
In the long exposure CPT, after the subject has achieved thermal equilibrium in a thermal neutral room, the arm up to the elbow or shoulder is immersed in water at 10° to 15'C (50' to 59°F) for a period of 10 to 15 minutes. After the hand and arm have been removed from the cold water and dried, the time is measured for the finger skin to regain its color and/or temperature (indicating vasodilation and resumption of blood flow). Skin temperature below control values, 5 and 10 minutes after a 10-minute cold exposure, gave a correct diagnosis in 80% to 90% of workers with HAVS and workers without HAVS who had more than 5,000 hr of chain saw use . However, finger-skin temperature response did not distinguish between subjects who did not use vibrating tools, those with Raynaud's disease, and those with less than 5,000 hr of saw use .
The response of finger-skin temperature to cold exposure in nonsymptomatic, vibration-ex posed and unexposed workers was reported by Scheffer and Dupuis for laboratory and field studies. The test conditions (5°C air temperature, vibration acceleration of 6.3 m/sec2 , grip force of 15 N, and push force on the tool of 40 N) all contributed to the skin temperature response. The authors suggest that improved protection against cold (e.g., heated tool handles) could be an effective preventive technique.
The response of finger systolic blood pressure (FSBP) to finger cooling has been used to measure changes in peripheral vascular response to cooling in vibration-exposed workers. Olsen et al. and Olsen and Nielsen reported that FSBP changes predict 60% to 85% of workers with vibration white finger even when the history of HAVS is not known.
Their subjects, however, had vibration white finger, Stage 2 to 3 . In less severe cases of HAVS (Stage 1), neither FSBP nor peripheral blood flow measurements were very sensitive. During field conditions, however, measuring FSBP is easier than measuring blood flow . The fingernail compression test may also be used. The occurrence of spastic vasospasm and pain in the finger is noted.
IV. Biologic Effects Hack et al. compared responses on the cold provocation test and reactive hyperemia with the history of vibration-induced white finger in workers with no symptoms, symptoms of tingling and numbness, and symptoms of HAVS. The tests distinguished between groups, but only about 60% of the subjects fell into the correct staging category.
Bovenzi reported that the skin temperature recovery time following finger cooling was significantly prolonged in workers with HAVS, indicating that the workers with HAVS had a more severe and prolonged vasoconstrictive response to the cold provocation test. Gemne et al. found the finger blood flow at vasodilatation (finger arterial inflow) after occlusion was less in the group with HAVS than in a reference group without HAVS.
Peripheral resistance was also higher in the HAVS group. The authors suggested that the increased peripheral resistance in the HAVS group may be due to a local defect in the vessels with a reduction in flow and intramural pressure.
Ameklon-Nobin et al. reported that the FSBP, the ratio of the finger systolic blood pressure to the arm systolic blood pressure (FSBP/ASBP), and finger skin temperature measured before and after vasodilatation by body warming are altered in vibration-ex posed workers. Finger skin temperature and FSBP were lower in the workers with HAVS both before and after vasodilatation. Digital rewarming time was markedly slower in the vibration-exposed individuals. These studies suggest that measuring the finger skin temperature and FSBP before and after finger cooling and after finger rewarming could be useful diagnostic tests.
Bovenzi suggested that the finger systolic blood pressure response with finger cooling and ischemia may be a useful objective test for vascular hyperactivity in subjects with HAVS. In Ills study, the test had a sensitivity to increased arterial tone of 100% and a specificity (negative test without HAVS) of 87%.
# Plethysmography
Finger plethysmography, a technique used for measuring finger blood flow, is based on the fact that with each heart contraction, the volume of the fingers increases. This change in finger volume can be measured with a photocell or strain gauge. In practice, the photocell plethysmograph is used more frequently than the strain gauge. The instrumentation for a photocell plethysmograph and the test conditions that can be used in field and laboratory studies have recently been published . Finger plethysmography, after local cooling, has been recommended as an objective test for HAVS . Vibration instead of cold water may be used as the stimulus. Standardization of the test procedure and strict adherence to the test protocol are of utmost importance if the results from different studies are to be compared.
Hand-Arm Vibration
# Aesthesiometry
One of the tests of peripheral neural changes is the finger tip two-point and depth discrim ination tests. A version of the test instrumentation has been described . As with other semiobjective tests, standardization of the instrumenta tion and strict adherence to the test protocol are very important (e.g., small differences in the pressure applied by the finger tip against the grooves will change the detection point sensitivity). The results of the tests can be used to support a diagnosis of advanced HAVS (Stages 2 or 3), but because of the number of false-positive and false-negative results, the test data should not be used to override other data and the examining physician's judgment . Data obtained using the improved test correlated significantly with the clinical staging of HAVS in workers with Stage 2 and above . For individual diagnostic purposes, however, the test lacked sufficient discriminatory power. Haines and Chong reviewed the literature in which peripheral neurological tests were used to assess the acute and chronic effects of exposure to hand-arm vibration. The peripheral neurological tests demonstrated their usefulness in epidemiologic studies.
Arteriography Ashe et al. , Ashe and Williams , and Takeuchi et al. , utilizing finger biopsy material, observed extensive damage to the digital arterial walls with narrowing of the lumen in the fingers of workers with HAVS. These findings led to the concept that hand arteriography might be a useful tool for the diagnosis of HAVS . The procedure does, however, require an intraarterial injection of a dye and, therefore, is an invasive procedure.
The data reported by James and Galloway indicate that almost all of the workers who had symptoms of HAVS showed digital artery occlusion that was partial or nearly complete.
Their control data were limited to three nonvibration-exposed individuals (members of the observation team) who showed little evidence of digital artery narrowing or occlusion. Takeuchi et al. reported medial muscular hypertrophy and intima fibrosis in the digital arteries of vibrating tool users. Okada et al. observed thickening of the intima of finger arteries in workers who used vibrating tools. Inaba et al. 11988] reported a thickening of the intima in animals subjected to vibration. Intimal thickening appears to be part of the arterial pathological changes.
I IV. Biologic Effects
# Grip Force
Hand and finger grip force can be easily measured with a strain gauge or a simple spring resistance dynamometer. Several types of measurements can be made. These include (1) maximum grip force, ( 2) fatigue curve while producing maximum grip force, and
(3) fatigue curve during rhythmic contraction-relaxations. These measurements can be made both before and after a work period, or before and after exposure to vibration .
Because maximum grip force appears to be reduced, and strength fatigue is faster in workers who have used vibrating tools for several years (and may or may not have symptoms of HAVS), a simple grip strength measurement (hand dynamometer) can have some diagnostic usefulness. However, as pointed out earlier, normal standard values for grip strength and grip fatigue indicate a wide inter-and intra-individual variability, which make comparisons difficult to interpret.
# Nerve Conduction
A decrease in motor and sensory peripheral nerve maximum conduction velocity in the median and ulnar nerves has been reported in workers with histories of occupational hand-vibration-exposure . Maximum conduction velocity of the ulnar or median nerves can be determined by electrical stimulation of the nerves at a designated point and by recording the time for a motor response to occur. The time required for the nerve impulse to travel the distance between the two points can also be calculated . In a group of vibration-exposed workers who had complaints and symptoms of HAVS, about 50% showed conduction velocity reduction , Sakurai and Matoba also reported a decreased motor nerve conduction velocity (MCV) and sensory nerve conduction velocity (SCV) in workers who used vibrating tools. Chatterjee et al. (1978) found that in rock drillers, the SCV in the median nerve was reduced but the MCV was not. Latency, duration, and amplitude of the sensory action potential were also significantly changed in the rock drillers. Brammer and Pyykko analyzed the electroneurographic data from 23 studies of workers who used hand-held vibrating tools. After control of the data for polyneuropathy and the effects of hard manual work, a neuropathy remained that involved mainly the sensory nerves in the hands. This sensory neuropathy could be distinguished from compression neuropathies (carpal tunnel syndrome) by measuring the nerve conduction velocity. Araki et al. reported that the distribution of sensory nerve conduction velocities (median nerve) was altered and the magnitude of the sensory nerve conduction velocities was significantly slowed in chain saw operators. Farkkila et al. , in a neurological study of 186 forestry chain saw operators (average usage time 16,600 hr) and 31 nonvibration-exposed workers, found that the disturbance of the ulnar and median MCV and distal latency (DL) did not correlate significantly with the history of HAVS or numbness of the hands. However, a significant correlation was reported between vibrotactile detection thresholds and MCV and DL of the median and ulnar nerves.
# Sensory Acuity
Some of the common tests of finger tip sensory acuity may assist the physician in diagnosing HAVS. These include (1) cotton wool test (light touch), ( 2) hot and cold probes (tempera ture), ( 3) pin prick (pain), and ( 4) tuning fork (vibrotactile). A decrease in sensitivity may indicate peripheral neural changes. Taylor et al. reported that stage assessment of HAVS, based on medical examination and history of exposure, did not correlate well with tests of sensory loss, loss of pain, and temperature discrimination. Sensory acuity tests cannot be used as positive indicators of HAVS . Ekenvall et al. reported that the temperature neutral zone was increased from about 5°C (9*F) in controls to 10'C (18'F) in 17 vibration-exposed workers with neurological symptoms of HAVS. The vibration threshold was also nearly doubled in the vibration-exposed group as compared with controls.
# E. TREATMENT
Several recent studies reported on hospitalized patients with different stages of HAVS who received various types of therapeutic treatment. The effectiveness of the various treatments was analyzed and evaluated. Because multiple treatments were used in all the studies, direct evaluation of the effectiveness of any single treatment is not possible. Matoba and Sakurai described their experiences in treating 500 male workers with HAVS over a 10-year period. The workers had used vibrating tools for an average of 10.5 years, and all exhibited mild to severe symptoms and signs of HAVS. All treatments were given in a hospital, with an average hospital stay of 105 days. Treatment consisted of physiobalneotherapy (water bath), alone or with one or more drugs, nerve blocking, and/or surgical therapy, along with education and training.
Recognizing that an evaluation of the relative effectiveness of all the various combinations of treatment is not possible, the researchers nevertheless selected a group of 60 inpatients matched for age and vibration exposure. Some of the patients received only physiobal neotherapy (group P), whereas the others received physiobalneotherapy plus vasodilating drugs (group D) over a 6-week period. Subjective and laboratory signs improved about 30% to 40% in group P and 60% to 80% in group D . The authors concluded that physiobalneotherapy is the key treatment but that drug therapy, vasodilators, and calcium channel blockers can accelerate improvement in the circulatory, neural, and motor problems present in HAVS. Improvement was not as good in patients with severe HAVS as in those with lesser stages of involvement.
a
# IV. Biologic Effects
Bielski [19881 reported the benefits derived from balneological treatment of 824 chain saw operators who had peripheral vascular symptoms of HAVS (Stage not specified). Thermog raphy and plethysmography tests indicated statistically relevant improvement in 91% of the patients treated with a brine bath at 34*C (93.2'F) for 20 minutes a day for 24 days. The improvement persisted for at least 6 months after treatment even though the workers were again using chain saws. The author suggested that workers who use chain saws should undergo a 2 to 3 week annual treatment with balneotherapy to reverse and prevent the progression of HAVS. The vibration level produced by the chain saws used was not reported.
Nasu reported that the use of defibrinogenating drugs in the treatment of HAVS patients provided both subjective and objective improvement. With treatment, statisti cally significant improvement was observed in the finger-skin temperature, the amplitude of the finger plethysmogram, and the nail compression test before and after cold provocation. The subjective feeling of warmth after treatment was reported by all but 5 of the 118 patients studied. The beneficial effects of the treatment did not appear to be permanent but "reaggravation ranged usually from several months to more than a year" after treatment was stopped. The author also reported (without substantiating data) that the addition of alpha 1 blocker (bunazosin hydrochloride) had a better effect than the defibrinogenating drug alone.
The results obtained from treatment trials must be interpreted with caution because (1) with the present state of knowledge, the extent of spontaneous (without treatment) reversal of HAVS when vibration stimulus is withdrawn is unknown, (2) in many studies control populations given hospital treatment and therapy are not included, and (3) there is doubt about the accuracy of assessment of subjects in the absence of proven objective tests. Subjective improvement without objective tests is not acceptable.
# F. REVERSIBILITY
The British and Canadian groups have emphasized prevention over treatment as the better approach to the control of HAVS . Olsen and Nielsen reported data from a 5-year study of three groups of forestry workers examined in 1978 and again in 1983. Group A (n=13) had no subjective symptoms in 1978 and continued sawing until 1983; group B (n=12) had no symptoms in I Hand-Arm Vibration 1978 and stopped sawing; group C (n=12) had symptoms of HAVS in 1978 but did not stop using chain saws. FSBP was measured with a CPT in 1978and again in 1983 groups had increased response to the cold provocation when compared to 20 nonvibration-exposed controls. From 1978 to 1983, the vasoconstriction response to the CPT increased in group A (p0.10), and improved in group C (p<0.05). Antivibration saws were used between 1978 and 1983. In group A, the use of antivibration saws did not prevent further increase in hyperactivity; the improvement of workers in group C (who had HAVS) may have been due to a shift from regular to antivibration saws in 1978. The data suggest that while the use of antivibration saws will not entirely prevent the development of HAVS, it may reduce the occurrence and progress of the disorder.
A 3-year followup study of 55 forestry workers with HAVS was conducted by Ekenvall and Carlsson to determine the effect of cessation of working with vibrating tools on subjective symptoms and FSBP during finger cooling. The group on first examination included 14 with Stage 1 Taylor-Pelmear symptoms, 25 with Stage 2, and 16 with Stages 3 and 4. Of the 15 workers who continued outdoor work with vibrating tools during the 3-year followup period, none showed any improvement of symptoms (8 showed no change and 7 showed increased subjective impairment). Of the 32 who did not use vibrating tools during the 3-year followup study, 8 showed improvement, 19 showed no change, and 5 showed increased impairment. The subjective improvement reported in this study could not be confirmed by CPT. On the other hand, this study showed an increased reactivity to cold in the impaired group. Thus the CPT appears to provide objective confirmation of the deterioration.
Other studies have indicated that the signs and symptoms of HAVS may be reduced or reversed in some chain saw operators, chippers, and grinders when the worker is no longer exposed to vibration .
# I
# V. BASIS FOR THE RECOMMENDED STANDARD
The NIOSH recommendations for control of hand-arm vibration are based on review and analysis of (1) epidemiologic data derived from field investigations, ( 2) data from clinical examinations of workers who have used vibrating tools, and (3) data derived from laboratory studies. Chapters HI and IV contain reviews of the published data on which this recom mended standard is based. HA VS is a chronic, progressive disorder that normally requires months or years of vibration exposure to manifest itself. The quantitative relationship between the magnitude of the vibration exposure and the latency and severity of the disorder is not precisely known.
# A. PREVALENCE OF HAVS
Several hundred published epidemiologic and clinical studies have reported the development of HAVS in workers who used vibrating tools. In the epidemiologic studies summarized in Table IV-8, the prevalence of the vascular symptoms of HAVS ranged from 6% to 100%, with more than half of the studies showing a prevalence rate greater than 40%.
Vascular symptoms were reported in 0% to 14% of control workers who did not use vibration-producing tools, with a median prevalence of 4%. In all studies that compared workers who did with those who did not use vibrating tools, the prevalence of vascular symptoms was always higher in the vibration-exposed group.
The epidemiologic and clinical data support the conclusion that healthy workers who use vibrating tools can be protected from developing the disabling effects of HAVS. Protection can be provided by medical monitoring of the workers, engineering controls to reduce the vibration levels produced by the tools, work practices such as limited daily use time of vibrating tools and ergonomic design of tools and work methods, protective clothing and equipment, and worker training programs in the proper handling and maintenance of vibrating tools and in recognition of the early symptoms of HAVS.
# B. RATIONALE FOR FREQUENCY-UNWEIGHTED ACCELERATION MEASUREMENTS
The 1/3-octave-band center-frequency weighting of the acceleration has been used pre viously to express the magnitude of the vibration exposure. However, on the basis of recently published data cited in this section, NIOSH proposes the use of the frequency-un weighted acceleration. The frequency-weighted acceleration concept assumes that the harmful effects of 1/3-octave-band center-frequency accelerations are independent of fire-I Hand-Arm Vibration quency between 6.3 and 16 Hz but progressively decrease with higher frequencies between and 1,500 Hz. The frequency-unweighted concept assumes that the magnitude of pathophysiologic effects from exposure to vibration are proportional to the acceleration and are frequency independent at all frequencies.
The rationale for frequency weighting is based primarily on the data reported by Miwa and Dandanell and Engstrom reported vibration acceleration levels and frequencies produced by riveting hammers, bucking bars, rivet shavers, and drills used in the aircraft industry. Most of the acceleration occurred at frequencies above 400 Hz (up to 10,000 Hz). If the ISO frequency-weighting criteria were applied, most of the higher frequency acceleration would be excluded from the exposure assessment. At frequencies below 400 Hz, the frequency-weighted acceleration was only about 10 m/sec2 for the riveting hammer and bucking bar. At frequencies between 400 and 10,000 Hz, the frequency-weighted acceleration was 2 m/sec2 for drills, 5 m/sec2 for rivet shavers, and 6 to 10 m/sec2 for riveting hammers and bucking bars. In the absence of frequency weighting, the acceleration was about 100 m/sec2 at frequencies between 100 and 10,000 Hz.
Riveting hammers and bucking bars were used not more than 15 minutes per working day, with a total daily exposure to vibrating tools of not more than 30 minutes. Of the 288 workers studied, the authors reported that 59 showed finger blanching; of those with more than 10 years of exposure, 50% had HAVS. This prevalence of HAVS far exceeded that expected from exposures at 10 m/sec2 (frequency weighted) for similar years of exposure and 30 minutes of daily use time. The authors suggested that frequency weighting would have grossly underestimated the health impact of the high-frequency vibration acceleration produced by these vibrating tools.
The data from experimental studies of Nohara et al. also call into question the assumption that pathophysiologic effects of vibration acceleration are frequency-inde pendent at 16 Hz or below and frequency-dependent above 16 Hz. The test group consisted of five healthy, 25-to 31 -year-old males who were nonsmokers and had never used vibrating tools. For the 1-hr test periods at 1-to 4-day intervals, subjects grasped with the left hand a 40-mm- (1.6-in.-) diameter handle that was fixed to a vibrating plate. A constant acceleration of 50 m/sec2 at randomized frequencies of 30, 60,120, 240, and 960 Hz was applied to the plate during the test period. For control values, the subjects grasped the handle for 1 hr without vibration. Physiologic parameters measured were finger blood flow, finger skin temperature, and peripheral motor nerve conduction velocity of the ulnar and median nerves. The data were analyzed by NIOSH and are summarized in Table V- Nohara et al. . fMotor nerve conduction velocity.
§Without vibration (control). After-vibration exposure value is higher than before-vibration value.
The following generalizations can be made based on the data summarized in Table V-l at a fixed vibration acceleration of 50 m/sec2:
- None of the physiologic functions measured showed a consistent change in function with vibration frequency.
# I
Hand-Amt Vibration
- Each physiologic function had one or more vibration frequencies at which the physiologic effects were greatest.
- The frequencies at which the maximum effects occurred were different for the various physiologic functions.
- The maximum effects occurred at the lowest exposure frequency (30 Hz) for only one function (peripheral blood flow).
- Maximum change occurred in skin temperature at 240 and 480 Hz, in blood flow at 30 Hz, and in MCV at 120 Hz.
- Grasping the handle for 1 hr without vibration (control) also resulted in changes in the physiologic functions measured. Nohara et al. concluded that the peripheral nervous system was affected most at the lower frequencies and the circulatory system was affected significantly at both the lower and the higher frequencies. The data from the study do not support the assumption that frequencies above 16 Hz have progressively less harmful effects than the lower frequencies.
The Nohara study has the following obvious shortcomings: only a small number of subjects were tested, exposures were not repeated at any of the frequencies, and each exposure was limited to 1 hr per test session. Starck and Pekkarinen compared the observed and predicted prevalence and latency periods of HAVS among workers using different types of vibrating tools. For operators of chain saws that produce relatively low-frequency and low-impulse vibrations, the predicted and observed values were in good agreement when acceleration was calculated according to the ISO 5349 frequency weighting . However, for pedestal grinders, stone workers, shipyard workers, and platers whose tools produced higher impulses and frequen cies, the comparisons were less consistent. Frequency weighting of the acceleration in accordance with ISO 5349 did not appear to adequately reflect the harmful effects of tools that produced higher-frequency and higher-impulse vibrations.
The data reported by Hyvarinen et al. suggest no constant frequency relationships on the threshold acceleration levels required for the production of finger vasospasms in lumberjacks who had a "history of traumatic vasospastic disease." The frequency of 125 Hz was more effective in producing finger vasospasms than higher or lower frequencies. These data suggest that acceleration frequency weightings throughout the entire vibrationfrequency spectrum produced by vibrating tools may underestimate the potential risk to workers exposed at higher vibration frequencies. The degree of intimal thickening observed Brammer . 9 in experimental animals subjected to either 30 or480 Hz at 50 m/sec was comparable .
Literature surveys by Brammer [1982aBrammer [ , 1982b suggest that the minimal vibration accelera tion level required to produce a sensation of vibration and a pulseless vasospasm does not consistently increase as the vibration frequency is increased. For the production of vasospasm, the minimum vibration acceleration required did not vary with vibration frequencies between 31.5 and 2,000 Hz, and the minimum vibration acceleration required to produce vibration sensation was independent of frequency between 31.5 and 500 Hz. The minimum vibration acceleration levels required to produce vasospasm and sensation at frequencies of 31.5 to 2,000 Hz are given in Table
V-2.
Because of the lack of objective, experimentally derived data, it is not possible to quantita tively convert the health impact of frequency-weighted accelerations to frequency-unweighted accelerations. However, some semiquantitative conversions are possible. Frequency weighting that is done by reducing the input of the higher frequencies (especially above 400 Hz) decreases the total acceleration energy calculated for the vibrating tool. The frequency-weighted acceleration will therefore underestimate the total energy produced by the vibrating system. Frequency-unweighted acceleration calculated over the entire fre quency range of the tool will be higher than the frequency-weighted acceleration, but it is a more complete representation of the energy actually produced.
The rationale for recommending the use of frequency-unweighted acceleration is supported by the following information:
1. Data from epidemiologic, clinical, and laboratory studies suggest that the hazardous effects of vibration exposure are frequency independent. 2. Exposure measurements based on frequency-unweighted acceleration have the advantage of simplifying the measurement of vibration acceleration levels of vibrating tools used in industry. 3. The prevalence of HA VS among users of high-frequency (up to 10,000 Hz) vibrating tools was 50% with 10 years of exposure at a frequency-weighted acceleration of about 10 m/sec2 for about 30 minutes per day of actual tool use . The frequency-weighted acceleration level grossly underestimated the HAVS-producing effect of the high-frequency vibration exposure.
# C. 4-HR-PER-DAY USE TIME
All of the guidelines, standards, and published studies of the harmful effects of vibration exposure accept a time-dose relationship between total vibration exposure and the develop ment of HAVS. The exposure dose can be expressed as m/sec2 normalized for 4 hr, 8 hr, or any other amount of tool use time per day. If the acceleration level is expressed by all researchers as a time-corrected, 4-hr/day equivalent, comparisons of data from different studies would be easier. The ISO and ANSI [19861 guidelines recommend using a 4-hr energy equivalent acceleration expressed in m/sec . The time (hr/day) and dose (acceleration in m/sec2) energy equivalents are plotted as a log-log function. In these relationships it is assumed that the daily exposure time required to produce symptoms is inversely proportional to the square of the acceleration and is independent of the vibration characteristics of the tool. Thus if the vibration level is reduced by one-half, the exposure time may be doubled. The total daily time of actual tool use has not usually been reported, but in most industries it does not exceed 4/hr day.
# D. DOSE-RESPONSE RELATIONSHIP
HAVS is a chronic disorder with a latency period between the first exposures and the appearance of the first signs and symptoms. The latency period may vary from a few months to several years, depending on many interacting factors. Among the more important factors that determine the clinical profile of HAVS are As a result of the complexity of the confounding interactions between these factors and the lack of experimentally derived objective data, dose-response relationships cannot be estab lished with precision. Establishing a reliable, valid, minimal dose-risk level would require quantitative data not presently available. , Brammer . The predicted minimum (frequency-weighted) ac celeration (m/sec2) required to produce Stage 1 HAVS (finger blanching) has been reported to be 1 to 2.9 by Brammer , 1 to 2.1 by Miura et al. , and <4.7 by .
The data on the pathogenesis of HAVS are not sufficient to establish an REL that would ensure that healthy workers who use vibrating tools would not develop signs and symptoms of HAVS. Because such an REL cannot be justified on the basis of present dose-response data, the prevention and control of HAVS as an occupationally-induced disorder must be based on other considerations. The approach to controlling HAVS must be through (1) medical monitoring to recognize the first signs and symptoms of developing HAVS, (2) medical removal of workers who exhibit signs and symptoms of Stage 2 HAVS,(3) engineering controls to minimize the level of vibration produced by tools, (4) establishment of a work regimen to reduce exposure to a feasible minimum, (5) ergonomic design of tools and workplaces, ( 6) training of workers to recognize and report early signs of HAVS, and ( 7) supervision to ensure optimal tool maintenance and use.
# E. CONCLUSIONS
# Setting a Standard
HAVS is a chronic disorder with a latency period varying from a few months to several years. The latency is believed to depend on many interacting factors, including vibration level produced by the tool, hours of tool use per day, environmental conditions, type and design of the tool, manner in which the tool is held, vibration spectrum produced by the tool, vibration "tolerance" of the worker, and tobacco and drug use by die worker. Because of the complex interactions among diese and other factors and the general lack of objective data, it is not currently possible to establish meaningful dose-response relationships. Thus it is not possible to establish a specific REL that will protect all workers against the development of HAVS in all occupational situations. However, the problem of HAVS is too serious and pervasive to delay measures for correcting it. NIOSH has therefore recommended a standard for exposure to hand-arm vibration that includes no specific exposure limit but does include medical monitoring and surveillance, engineering controls, good work practices, use of protective clothing and equipment, worker training programs, and administrative controls such as limited daily use time. If this standard is implemented, it will protect workers who use vibrating tools from the debilitating effects of HAVS. NIOSH also anticipates that this criteria document will stimulate research and development in all areas relating to hand-arm vibration.
# Use of Frequency-Unweighted Acceleration Measurements
The 1/3-octave-band, center-frequency-weighted acceleration historically has been used to express the magnitude of vibration acceleration levels. The frequency-weighted accelera tion concept assumes that the harmful effects of vibration are independent of frequencies between 6.3 and 16 Hz but that the effects progressively decrease with higher frequencies between 16 and 1,500 Hz. On the basis of data published in recent studies, however, NIOSH has concluded that the use of the frequency-unweighted acceleration is a more appropriate means of assessing the health risk to exposed workers. Although the major consensus standaids-setting organizations currently recommend the frequency-weighted acceleration levels, NIOSH believes that this measurement grossly underestimates the HAVS-producing effects from tools that vibrate at high frequencies. Exposure measurements based on frequency-unweighted acceleration provide the additional benefit of simplifying the meas urements because the acceleration data produced by the accelerometer is frequency un weighted.
# Medical Monitoring
Medical monitoring of workers who use vibrating hand tools is a vital component of any standard for preventing or controlling HAVS. The medical monitoring program must include (1) a preplacement medical examination with special emphasis on peripheral vascular and neural factors, (2) yearly or more frequent exams designed to detect HAVS in a V. Basis for the Recommended Standard its early and reversible stages, and ( 3) an open channel of communication with the workers to ensure that the early symptoms are promptly reported.
# Medical Removal
NIOSH recommends that workers who develop Stage 2 HAVS be removed from further exposure to vibration until they are free of signs and symptoms of HAVS. If HAVS is permitted to progress beyond Stage 2 by the continued use of vibrating tools, the effects can become irreversible. A provision for medical removal could be controversial, but it would provide a powerful incentive for the employer to implement the engineering and administra tive controls necessary to reduce the worker's risk of developing HAVS.
# VI. OTHER STANDARDS AND RECOMMENDATIONS
Recommendations and guidelines for permissible worker exposure to hand-arm vibration have been formulated or are in the process of being formulated in several countries, including the USSR, Czechoslovakia, Finland, Sweden, Australia, United Kingdom, Japan, Poland, and the United States. Even though the problems of objectively diagnosing HAVS, measuring the input parameters of vibration energy transmitted to the hand and arm, and establishing reliable dose-response relations are formidable, some agreement has been reached in establishing vibration exposure criteria . The major national and international guidelines, standards, and recommendations reviewed in this chapter suggest that vibration exposure be expressed as acceleration in m/sec2 over die vibration spectrum of 1/3-octave-band center frequencies of 6.3 to 1,250 Hz. The acceleration limit is standardized to 4 hr of actual tool use time per day. However, objective and subjective tests that are required for the diagnosis of HAVS, its stage of progression, and medical removal of affected workers are not stressed.
# American National Standards Institute (ANSI)
The American National Standards Institute's Guide fo r the Measurement and Evaluation o f Human Exposure to Vibration Transmitted to the Hand (S3.34-1986) was prepared by a working group of the Acoustical Society of America . This guide is more comprehensive than either the ISO Guideline 5349 or the ACGIH TLV. The major features of the ANSI guide include (1) methods for the measurement of vibration and analysis of the data, and (2) procedures for reporting worker exposure. The goal of this document is to reduce worker exposure to hand-arm vibration and thereby reduce the probability of incurring HAVS. Special features include (1) a discussion of the factors that may influence the probability of occurrence or die severity of the pathophysiologic effects of vibration, The ISO Guidelines fo r the Measurement and the Assessment o f Human Exposure to Hand-Transmitted Vibration emphasizes standardized procedures for measuring and assessing the levels of hand-arm vibration to which the worker may be exposed when using various vibrating tools. It does not specify the limits for safe exposure in terms of acceleration and daily exposure, nor does it specify the risk of health impairment for different operations and tools. The document presents guidance "to protect the majority of workers against serious health impairment and to assist in the development of hand-operated tools the use of which will reduce the risk of disorders in workers caused by vibration."
The ISO guidelines lack a description of (1) the clinical features of hand-arm vibration syndrome and ( 2) objective tests and procedures for diagnosing HAVS. Appendix A of the ISO guidelines presents exposure time in years for different percentiles of population groups exposed to various levels of frequency-weighted acceleration (m/sec2) before finger blanch ing occurs. However, finger blanching is only one aspect of HAVS and usually is not the first to occur.
The ISO document points out its shortcomings and gives precautions about the use of their guidelines. The procedures and techniques for measurement, assessment, and expression of the vibration intensity are similar to the approaches used in other vibration guidelines.
Of special interest is Appendix B, which contains recommendations for medical preventive measures, engineering control methods, administrative approaches, and worker training. Appendices A and B are not part of the official standard; thus the ISO guide does not include a recommended numerical exposure limit. . This publication presents guidelines for whole-body, hand-arm, and low-frequency vibration exposures and is not an official standard. These guidelines take into consideration vibration characteristics, health effects, sources, control methods, medical monitoring, measurements, and prevention. The presentation reviews the state of the art and does not introduce new data or new concepts. Specific details are not given for measuring the vibration of hand-held tools. The acceptable weighted acceleration levels cited (in m/sec2) are based on the draft version of ISO Guideline 5349 . A frequency-weighted, 4-hr exposure limit of 1 m/sec is suggested.
The document provides an informative summary of the measurement of vibration, the effects of vibration on the body, and useful procedures for controlling or preventing the effects. However, the guidelines are directed more to trade union personnel than to those responsible for the measurement, assessment, and control of HAVS.
# USSR
The 1972 USSR State Standard (Gost Standard 17770-72) is a revision of earlier state standards and sanitary standards . Some of the pertinent features of the standard are as follows:
- Limits are for octave bands of 8 to 2,000 Hz.
- Procedures are given for measuring the vibration levels of tools.
- Hand-held vibrating tools should not weigh more than 22 pounds (10 kg).
- Force exerted on the tool should not exceed 44 pounds (20 kg).
- Preemployment and yearly medical examinations should be given for those working at vibration levels exceeding 20% of the limit.
- Actual maximum daily use time for vibrating tools should be 5 to 6 hr.
- Working environment temperatures should be above 16"C (60*F); rewarming facilities should be required when they are below 16'C.
- Gloves are required to prevent hand cooling.
- If IIAVS symptoms occur, the worker should be transferred to work that does not involve vibration exposure.
- Prophylactic measures are suggested (e.g., massage, exercise, vitamins, and ultraviolet radiation).
The limits for vibration exposure for vibrating tools were 2 m/sec at 10 Hz to 50 m/sec at 2,000 Hz. Vibration disease from the use of vibrating tools covered by this standard includes whole-body complaints, as well as peripheral neural, vascular, and muscular symptoms. Hand-Arm Vibration
# United Kingdom
The 1987 British Standard Guide to the Measurement and Evaluation o f Human Exposure to Vibration Transmitted to the Hand "provides guidance on measuring and evaluation of hand-transmitted vibration exposure ... a uniform method for measur ing and reporting hand-transmitted vibration." The sections on characterization of handtransmitted vibration, measurement of hand-transmitted vibration, and characterization of vibration exposure cover the same areas as ANSI 53.34 and ISO Guideline 5349 (frequency-weighted acceleration and frequency cutoff at 1,250 Hz 1/3-octave-band center frequencies). Of special interest and value are Appendices A and B, which contain discussions of the dose-effect relationship for hand-transmitted vibration and the guideline for preventive procedures. However, those discussions are included as appendices and are not considered to be part of the standard. No numerical recommended exposure limits are given. A particularly important guideline presented in Appendix A indicates that with "a tool having a frequency weighted vibration magnitude of about 4 m/sec2 rms, used regularly for 4 hours a day, there may be an occurrence of symptoms of (finger) blanching in about 10% of the vibration-exposed population after about 8 years."
# Japan
Early Japanese guidelines for permissible vibration exposure levels are derived from both field and laboratory data and are based on the concept of "no complaint" and "complaints by 50%" of the subjects [Miwa 1967[Miwa ,1968a[Miwa , 1968b. The Miwa curves for "tolerance limits" and "unpleasant limits" were frequency dependent with acceleration levels of 17.8 m/sec2 for "tolerance limit" and 3.2 m/sec2 for "unpleasant limit" at 20 Hz. In 1970, the Japanese Association of Industrial Health (JAIH) proposed limits for exposure to hand-held vibrating tools. The limits were for "intolerable levels" of vibration for 10 to 400 minutes daily at octave bands of 8 to 250 Hz. Permissible acceleration levels for 400 minutes of exposure ranged from about 1.5 m/sec2 below 16 Hz to 35 m/sec2 at 250 Hz; and for 30 minutes of daily exposure, permissible acceleration levels were about 6.5 m/sec below 16 Hz and 100rn/sec2 at 250 Hz. The limits based on "intolerable levels," although not strictly comparable with ISO guidelines, appear to be higher than the levels recommended in ISO Guideline 5349, which are based on the development of HAVS in vibrating tool users.
# Czechoslovakia
The official 1977 Czechoslovakian Guide evolved through a series of revisions, including the 1967 Hygiene Regulation #33 of the Czechoslovakian Ministry of Health . The 1967 regulation is for vibration octave bands ranging from 8 to 500 Hz, and it is based on 2-hr daily exposures. If daily exposures are less than 2 hr for either uninterrupted or regularly interrupted exposure patterns, correction factors in permissible acceleration levels are provided. The guide states that when exposures exceed these limits, protective measures are required. At frequencies below 20 Hz, permissible acceleration levels are constant but are exposure-time dependent.
# I
# VI. Other Standards and Recommendations
The exposure limits in the 1977 Guide are similar to but not exactly the same as those in ISO Guideline 5349. The frequency range and the frequency weighting are similar; however, for exposure time above 1 hr, the vibration limits are lower than those in ISO Guideline 5349.
# Sweden
Efforts in Sweden to establish guidelines for vibration exposure control have been directed mainly to chain saws and their use . The earlier studies led to the conclusion that vibrations in the frequency range of 50 to 500 Hz were important in producing hand-arm injuries. Two vibration exposure limits were suggested-the "injury risk limit" and the "occupational injury limit." Below the injury risk limit, there was no danger of vibrationinduced injury, whereas above the occupational injury limit, there was a definite risk of injury. Between the two limits, the risk of injury depended on exposure duration. Short exposures above the occupational injury limit were considered to have minimal risk . The SFS 1977: 1166 Labor Safety Board Ordinance concerning the use of vibrating tools has revised directions that became valid January 1,1987, as Ordinance AFS1986:7, "Vibration from Hand-Held Tools" . The manufacturers, suppliers, and purchasers of Swedish equipment are all held responsible for ensuring that the equipment is constructed to produce the least possible amount of vibration. The worker must be infonned of the risks of using vibrating tools, and medical examinations must be furnished at no cost to the workers.
In 1973, the Swedish Board of Occupational Safety and Health set a limit of 50 N as the maximum permissible vibration force. Studies by Axelsson indicated that a 50-N force measured in a laboratory would correspond to 90 to 100 m/sec2 rms measured on chain saws held by an operator (this equivalent may change with the grip force applied by the operator); 90 m/sec2 is the 1-to 2-hr exposure at 500 Hz given in ISO Guideline 5349.
# Poland
In 1986, Poland published proposed maximum pennissible intensity values for hand-arm vibration exposures . In general, the document followed the draft version of ISO Guideline 5349 . The measurement of vibration and the analysis procedure follow the ISO guidelines. The Polish guidelines are based on 8 hr of daily use of the vibrating tools.
The maximum permissible acceleration levels at various vibration frequencies for an 8-hr day of tool use are presented. For 1/3-octave-band center frequencies, the permissible acceleration levels in m/sec2 are listed as 1 m/sec2 at 20 Hz, 2 m/sec2 at 40 Hz, 4 m/sec2 at 80 Hz, 8 m/sec2 at 160 Hz, 16 m/sec2 at 320 Hz, 32 rn/sec2 at 640 Hz, and 50 m/sec2 at 1,000 Hz. This represents another method of vibration frequency weighting of acceleration level. For the frequency range of 5.6 to 1,400 Hz, the frequency-weighted maximum permissible acceleration level for an 8-hr daily tool use is 1.4 m/sec . For a 4-hr tool use,
The major emphasis for worker protection from HAVS should be directed toward preven tion. After the disorder has progressed beyond Stage 2 of the Stockholm classification, procedures designed to reverse the process are usually not effective. Because the develop ment of HAVS is dose related, effective control procedures should be directed to (1) reduc ing the intensity (acceleration) of the vibration, ( 2) reducing die exposure duration, ( 3) identifying the early signs and symptoms, and ( 4) identifying vibration-sensitive in dividuals. Control strategies include (1) exposure monitoring, ( 2) engineering controls, (3) work practices, ( 4) ergonomic considerations, ( 5) protective clothing and equipment, ( 6) worker training, and ( 7) medical monitoring.
# A. EXPOSURE MONITORING
Any effective control procedure requires objective data on the degree of hazard to which the worker is exposed. For the use of vibrating tools, these needed data are the vibration acceleration expressed in m/sec2 rms measured in the three basicentric coordinates (or the coordinate with the highest acceleration), and the time in minutes per day that the tool is actually in use (scheduled or nonscheduled rest breaks are not included as exposure time).
The acceleration measurements should be made as described in Chapter III, B.l and B.2.
# B. ENGINEERING CONTROLS
The major engineering approaches to the elimination or reduction of the vibration accelera tion level exposure are (1) reduction at the source, (2) reduction of transmission, and (3) process modification.
# Reduction at the Source
The acceleration level usually increases with an increase in the speed at which the tool is operated (e.g., a chain saw operating at two-thirds throttle produces significantly less vibration energy than one operating at full throttle). A tool designed to operate at a reduced speed while providing adequate power for the job could be beneficial. The relationship between the weight of the tool and the power needed to drive the tool will also influence the amount of vibration produced. The reciprocating gasoline engine used to power some tools is a major source of vibration. A rotary gasoline engine or an electric motor as a power source may be a successful alternative, provided it meets the operational I Hand-Arm Vibration requirements. If several tools are available that serve the same function, the tool producing the lowest acceleration should be chosen.
How well the tool is maintained will influence the level of vibration during operation. A sharp chisel or saw chain, a flat-dressed grinding wheel, and a finely tuned engine will reduce the vibration level. To maintain the optimal level of tool maintenance, the operating personnel must be adequately trained in maintenance procedures and be aware of the need for maintenance. A scheduled maintenance program should be established.
# Reduction of Transmission
The vibration energy produced by the vibrating tool must be transmitted to the operator's hands or arms to produce a harmful effect. Any strategy that reduces the transmission from tool to hand will help prevent HA VS. Several types of energy-damping materials have been used to cover the handles of the tools or have been incorporated into the fingers and palms of hand gear with varying degrees of success. Some materials will reduce vibration transmissions at low-frequencies, and others may reduce those at higher frequencies. Damping materials in handwear are usually more effective for the higher frequencies. However, coverings on the tool handles or glove fingers and palms may interfere with the ability to control the tool during operation and thus may lead to reduced production or increased risk of accidents. Rens et al. reported that cotton or leather gloves used for protection against trauma, chemicals, and temperature provide little or no protection against vibration and may even increase the transmission of the vibration.
Another approach to reducing vibration transmission is the use of offset handles, springloaded handles, and shock-adsorbing exhaust mechanisms. Again, the operating efficiency at the tool/work-surface interface would have to be considered. A decrease in the vibration transmission level must not be offset by an increase in the time needed to complete the task.
# Process Modification
An ergonomic analysis of the entire industrial process is recommended to determine whether changes in some aspects of the process could reduce or eliminate the need for vibrating tools. For example, introducing a different casting process in a foundry might result in smoother castings and might therefore reduce or eliminate the need for grinders or power chisels. Using mechanical aids such as chucks and clamps to hold the piece being worked on can reduce the time and the intensity of the vibration exposure. Introducing automation and robots (e.g., robots used for spot welding to replace hand-held riveting guns) could reduce the need for workers to use vibrating tools. Where the size of the trees and the terrain are suitable, automated logging machines can reduce the need for chain saws to fell and debranch trees. Substituting alternative materials (e.g., plastics for cast metal) might reduce or eliminate the need for grinding or chipping operations.
Where the process produces such extreme vibration forces that they cannot be adequately controlled by any means, complete abandonment of the process may be the only feasible solution. Although such a situation may never occur, the possibility must be kept in mind.
# C. WORK PRACTICES
Because the pathophysiologic effects of using vibrating tools are related to vibration intensity and use time, the total daily, weekly, and yearly exposure time and the daily exposure schedule are important factors in preventing workers from developing HAVS. The epidemiologic data and clinical experiences discussed in Chapter IV suggest some practical and acceptable work practices that can be implemented to reduce the health impact of using vibrating tools. Saito studied the effects of limited tool use time on the presence of HAVS in 155 chain saw operators between 1978 and 1983. Each year the operators were medically examined. Skin temperature, vibratory threshold, recovery of nail bed color after compres sion, and pain sense were measured before a 10-min exposure of the hand to cold water (10°C) and 5 and 10 min after exposure. The results of 6 years of observation suggest that limiting chain saw use time can help prevent the occurrence of HAVS. The suggested chain saw use schedule was as follows: The daily duration of exposure can be regulated by the length of the workday or by introducing exposure/nonexposure cycles of varying lengths throughout the usual workday. Most exposures are not continuous throughout the workday but consist of actual tool operation of varying lengths of time interposed with scheduled and nonscheduled periods when the tool is not in operation. The large number of possible combinations of work/rest cycle schedules permit choosing one that will best fit the requirements of most industries. air temperature of 23.9'C (75*F) has about 1 do of insulation value. Clothing that is 1/4-in. thick provides about 1 clo of insulation. The insulation value of clothing under minimal airflow conditions is not a function of fiber or fabric type but depends on the amount of air trapped between the fabric layers or between the fibers.
If the clothing is not adequate to prevent a negative body heat balance, the circulatory system will respond with a peripheral vasoconstriction, particularly of the fingers and toes. Thus exposure to cold air may precipitate an attack of white finger, especially in susceptible individuals with HAVS. For a discussion of cold weather clothing, see Horvath , Goldman , Belding , Newburgh , ACGIH , andNIOSH .
Besides the insulation value of the clothing andhandwear, the following other factors should be considered for cold weather operations:
- In the presence of rain or snow, a water-repellent outer clothing layer should be used. - Handgear should be kept diy. If the handgear becomes wet, a change to dry gear should be made and the wet articles should be dried before being used again.
- In cold conditions (<0°C or 32*F) when wind velocities are greater than 0.5 mile/hr (0.8 km/hr), air-impermeable coverings for hands and torso should be provided. Wind barriers to reduce airflow over the body surface can effectively change the rate of heat loss.
- Warm-up breaks may be required even when the air temperature is above freezing.
A work/warm-up schedule for a 4-hr shift is presented in the TLV on cold stress proposed by the ACGIH . Because the blood circulation of the fingers is especially sensitive to even short exposures to cold, responding by acute vasoconstriction and reduced blood flow, constant vigilance must be exercised to protect the fingers from cold exposure when using vibrating tools. Exposing the hands to cold can cause a vasoconstriction even though the body as a whole is in thermal balance and the torso skin temperature is normal. Warm-up facilities may range from portable handwarmers to whole-body warming shelters.
- Battery-powered, electrically heated handgear is, in some situations, a viable solution to cold-induced vasoconstriction of the fingers.
# F. WORKER TRAINING
Because of the wide range in tolerance to vibration within a group of workers, it is imperative that each worker be instructed in the recognition of early symptoms of HAVS and in the cause and prevention of HAVS. - Role of tool maintenance and vibration production
- Ergonomic aspects of tool use, including the influence of handgrip force, pressure exerted at the tool/workpiece interface, manner in which the tool is held, body posture, etc.
- Need and procedures for keeping the body and hands warm and dry
- Use of protective clothing and equipment
- Work/rest schedules to control exposure duration
- Informing supervisor about any abnormal functioning of the tools
- Possible aggravation of HAVS from smoking and use of some drugs
The training should be provided to each new worker and repeated at intervals for each worker using vibrating tools to ensure continued worker awareness of the potential problems.
Because the earliest signs and symptoms of HAVS are periodic numbness or tingling of the fingers, or episodic blanching of the fingertips, the worker will be the first to recognize that something unusual is occurring. A trained worker can recognize the disorder at the early stages, when further progression can be prevented or reversed.
# G. MEDICAL MONITORING
Medical monitoring of workers using vibrating tools should be a primary approach to HAVS prevention and control, but it presents some difficulties because there is no specific clinical or medical test to objectively diagnose or assess the presence of HAVS. HAVS, as the name suggests, is a composite of signs and symptoms. The medical monitoring program should consist of (1) a preplacement medical examination with special attention to peripheral vascular and neural factors, (2) yearly or more frequent examinations designed to elicit responses that may be related to early HAVS, and ( 3) continued communication with the workers to ensure that early signs and symptoms are reported. Regardless of the signs and symptoms present, a diagnosis of HAVS is not justified without an occupational history of the use of vibrating tools.
# Preplacement Baseline Medical Examinations
The primary purpose of the preplacement medical examination is to identify (1) any worker who has HAVS from previous vibration exposures, (2) workers who have primary Raynaud's disease, ( 3) workers who have other disorders with signs and symptoms similar to HAVS (e.g., peripheral vascular or neural disease), ( 4) workers who are on medications or drugs that may have peripheral vascular or neural effects and ( 5) baseline data for comparison with subsequent examinations. The preplacement medical examination should be structured to elicit information pertinent to these points.
Specific screening tests considered useful in the diagnosis of HAVS are listed in Chapter IV, D (Screening and Diagnostic Tests). At aminimum, the preplacement medical examina tion should include tests or questions to identify the following:
- Peripheral neural status-light touch, pain, temperature, two-point discrimination, depth perception, vibrotactile sensitivity level
- Peripheral vascular status-finger blood flow response to the cold and cold provocation test with before, during, and after plethysmography conducted under standardized conditions
- Presence of carpal tunnel syndrome, tennis elbow, or other work-related cumula tive trauma disorders of the hand or arm
- Old injuries that could have peripheral vascular or neural effects (cold injury, bums, trauma, etc.)
- Primary Raynaud's disease, and its history - Other disorders that may have similar peripheral vascular or neural signs and symptoms (polyneuritis, occlusive vascular disease, thromboangiitis, chemical intoxication)
- Use of therapeutic and/or other drugs that have peripheral vascular or neural effects (including alcohol and tobacco) a
# VII. Methods for Worker Protection
- Anatomical abnormalities that may interfere with the safe use of the vibrating tools
- Presence of cold sensitivity and previous cold injuries
- History of past use of vibrating tools (including type of tool and duration of use)
- Age, sex, race, body weight, and other demographic data that may be relevant to differences in peripheral neural and vascular function and cold sensitivity
- Baseline measurements of vibrotactile threshold, grip force, muscle strength, etc.
# Periodic Medical Examinations
Periodic medical examinations for workers exposed to vibration from vibrating tools should be offered on a yearly basis or more frequently for affected workers on the recommendation of the responsible physician. The periodic medical examination should emphasize tests and questions that will elicit information on the early signs and symptoms of HAVS or the progress of its severity.
The periodic medical examination should include
- Review of worker health complaints
- Review and updating of the data derived from the preplacement examination
- Repetition of tests and procedures directed to peripheral vascular and neural functions and symptoms
- Assessment of peripheral vascular and neurological signs and symptoms, aesthesiometric and vibrotactile test results, grip strength, and presence of musculo skeletal symptomatology to establish whether HAVS has developed to Stage 1 or has progressed further
# Medical Surveillance
To ensure that the control practices provide adequate protection to workers exposed to hand-transmitted vibration, the responsible health professional can use the workplace exposure data, periodic medical data, and the interview history to determine any significant changes within a worker or group of workers since the previous examination. These events may include complaints of episodic numbness, tingling, or cold-induced white fingers; changes in grip strength and muscle force; and pain in the hands, arms, and shoulders. The events may lead the physician to suspect overexposure of the work population or a change in an individual's health status or susceptibility. The occurrence of these sentinel health events (SHEs) could signal a breakdown of or inadequacy of the vibration exposure control systems established at the workplace.
# H. RECORDS AND RECORDKEEPING
Records of the data obtained from the following measurements are required to establish adequate control procedures: (1) updated acceleration and frequency characteristics of the vibrating tools used, ( 2) hours per day the worker operates the tool, ( 3) intraday exposure pattern, ( 4) years of operating the tool, ( 5) nonoccupational exposure to hand-arm vibration, ( 6) exposure year in which HAVS symptoms first appeared, ( 7) stage assessment of HAVS, ( 8) environmental conditions at the workplace, including air temperature, wind speed, and humidity, ( 9) type of personal protective clothing and equipment used, (10) results of preplacement and periodic medical examinations, (11) change in medical status between medical examinations, and ( 12) worker training programs.
The records on vibration exposure levels and times and medical status should be retained in accordance with the requirements of 29 CFR 1910.20(d). HAVS should be considered a reportable occupation-related disorder.
Guidelines and recommendations for the control and prevention of HAVS are based mainly on clinical experiences and retrospective epidemiologic studies. These experiences and studies are limited, however, because no two industrial situations are exactly alike. Measur ing methods and results may vary greatly from one work site to another. In addition, no controlled laboratory studies on the production of HAVS in human subjects have been, or ethically should be, conducted. Progress in knowledge about HAVS control will depend on epidemiologic and clinical data carefully collected under standardized situations of in dustrial use.
# A. DOSE-RESPONSE
To make the data from different epidemiological studies comparable, a minimum list of factors required from all investigators would include all those factors known to have a significant influence on the development of HAVS. If data on those factors were collected in every study, data from several studies could be grouped to increase the number of observations and increase the reliability of the risk predictions. Some of the factors that are known to have a dose-response effect and that must be routinely included are (1) vibration measurement techniques and instruments (for acceleration, frequency, and exposure time), ( 2) work history of previous use of vibrating tools, (3) medical signs and symptoms of peripheral neural, vascular, and muscular complaints, ( 4) environmental conditions such as temperature, wind, and moisture, and ( 5) ergonomics of how the task is performed (tool/workpiece force interface, grip force on tool, arm and body posture, manner in which the tool is held and used, tool maintenance, and type of tool). Other factors that may influence the development of HAVS must be searched for and included.
# B. CLINICAL TESTS AND STOCKHOLM STAGES
All clinicians and researchers should now use the Stockholm classification to determine the stage of vascular and neurological symptoms from the patient's history so that studies may be compared. In addition, internationally accepted objective tests should be conducted and the results should be correlated with the Stockholm stages to assist parties involved in litigation and compensation.
Objective methods for evaluating and determining the stage are also needed to correctly estimate improvement or deterioration with and without (a) further hand-ann vibration exposure, (b) therapy or surgical intervention, and (c) a combination of these factors.
# I
# Hand-Arm Vibration
# C. IDENTIFICATION OF VIBRATION-INTOLERANT WORKERS
Identifying vibration-intolerant workers and strictly limiting their exposure before signs and symptoms of I4AVS develop would be an effective preventive procedure. Presently, complaints and symptoms of peripheral neural, vascular, and/or muscular involvement must first appear before vibration intervention procedures are indicated. No currently available set of medical or padiophysiologic measures can be used al one to predict, with an acceptable degree of reliability, those workers who are especially sensitive to the effects of toolproduced vibration and who are at high risk of developing HAVS as a result of using vibrating tools.
# D. ENGINEERING MODIFICATION OF TOOLS
During the past decade, considerable success has been achieved with the engineering approach to reducing the vibration level of some powered tools and workpieces. Greater improvement is needed, however, to make the various types of vibrating tools acceptable for routine use. Engineering modification may be directed to the design of the tool or to the design of the task. Reducing tool vibration to acceptable levels during optimum operating conditions will lower the worker's risk of developing HAVS.
# E. ERGONOMICS OF THE WORK TASK
Several important ergonomic factors that affect the impact of die vibrating tool on normal hand-ann function are (1) the grip force exerted on the tool handle to hold and control the tool, (2) the muscular force required at the tool/workpiece interface to do the work, and (3) the amount of flexion, abduction, and rotation at the wrist, elbow, and shoulder joints required to guide the tool properly. A change in bench height, workpiece orientation, and muscular forces required to do the job may reduce the pathophysiologic consequences of the vibration exposure task. This aspect of the HAVS problem has not received much research attention, even though it has a vast potential for significantly reducing HAVS.
# F. EXPOSURE SCHEDULE
Adhering to an optimum exposure/nonexposure schedule during the workday can be a successful approach to hazard control. This concept is known from studying other hazards and is recognized in the ISO Guide 5349, ACGIH TLV, ANSI Standard S3.34, BSI Standard 6842, and other guidelines for HAVS control . The vibration exposure data on which the concept is based, however, are mainly extrapolations and best estimates. The common denominator in these guidelines and recommendations is usually "minutes of exposure per day." The question is whether the health effects of exposure to a constant level of vibration are the same for 120 continuous minutes of exposure in an 8-hr day as they are for 120 minutes of noncontinuous exposure (that is, eight 15-minute periods of exposure, each followed by 45 minutes of nonexposure).
# I VIII. Research Needs
# G. PROTECTIVE DEVICES
Protective devices can be inserted between the tool producing the vibration and the tissue of the hand where the transmitted vibration energy is absorbed. The protection may be applied to the handles of the tool, or it may be incorporated into handgear worn by the tool operator. The amount of vibration that will be absorbed will be influenced by the vibration force (acceleration) or the vibration frequency (hertz). Data are available on the transmission and damping characteristics of some materials. However, for a large number of materials, there are no available data on which to base a choice of vibration-reducing material suited to the vibration characteristics of a particular vibrating tool or class of tools. New concepts for antivibration and damping devices and materials need to be explored. Until such data are available, specific recommendations for the type and amount of protective material cannot be made.
# H. ETIOLOGY AND PATHOGENESIS OF HA VS
Although it is well established that the use of vibrating tools is associated with the development of HAVS, it has not been fully explained how the vibration energy causes organ, tissue, and cellular changes and damage. A rational approach to the prevention and treatment of HAVS will require fundamental data on the mechanisms involved in changes in the arteries, muscles, nerves, connective tissue, and tendons associated with HAVS. New therapeutic or prophylactic drugs need to be explored.
# I. EXPOSURE MONITORING
With the instrumentation available today, measurement of the acceleration and frequency of the vibration produced by a tool is not a simple task. A dosimeter-type instrument that could be attached to the worker or the tool and that could provide an integrated acceleration level over time would do much to ease the burden of conducting vibration testing. Because vibration frequencies above 1,400 Hz are produced by some vibrating tools (up to 10,000 Hz), accelerometers need a window wide enough to capture these high frequencies.
A pressing need exists for investigators to evaluate the health effects from both frequencyweighted and -unweighted acceleration measurements over the extended frequency range. Particular attention should be paid to the high-frequency component for the possible pathophysiological effects on the hand structure components.
# J. HAVS RECOGNITION TRAINING PROGRAM
H AVS differs from many other occupationally-induced health disorders in that an acceptable risk/exposure factor cannot be set. This dictates a secondary prevention approach requiring that early signs and symptoms be recognized by the attending health professional and by the exposed worker to prevent progression of the disorder and to minimize morbidity. Most health professionals are not adequately trained or experienced to detect the early signs and symptoms of HAVS. To ensure that HAVS will be recognized and diagnosed at an early, reversible stage, a refresher course and self-instruction aids should be developed for interested physicians.
# K. OBJECTIVE TESTS
A pressing research need is the development of laboratory and clinical tests for objec tively identifying the signs and symptoms of the early stages of HAVS. The tests must be both sensitive and specific. To be clinically practical, they must be easy to perform and noninvasive, and they must not require esoteric equipment. n
# Hand-Arm Vibration
HAVS was found among workers exposed to hand-arm vibration in all of the epidemiologic studies cited, regardless of the level of vibration exposure. These studies therefore provide no basis for determining an exposure level at which no cases of HAVS would occur. However, the studies do provide ample evidence that the use of vibrationproducing, hand-held tools is associated with the development of HAVS.
# D. SCREENING AND DIAGNOSTIC TESTS
The signs and symptoms characteristic of HAVS are also observed individually or in various combinations in some other disorders. No single sign or symptom is specific to HAVS alone. This introduces uncertainties and difficulties in the classification and diagnosis of HAVS. Regardless of the complaints and symptoms presented by an individual, a diagnosis of HAVS is not justified unless a history of using vibrating tools is present . Several tests can be used to help substantiate a clinical diagnosis of HAVS. Hand-Arm Vibration it would be 2.8 m/sec . In Table 2 of the Polish document, correction factors are listed for the actual use time in each hr that is less than 60 minutes.
The document does not include a discussion of health effects, diagnosis, treatment, or control procedures.
# I
# Hand-Arm Vibration
Types of exposure schedules that are applicable include the following:
- Alternating work tasks involving a vibrating tool with some other task that does not involve exposure to vibration (on hourly or daily basis)
- Limiting daily use of vibrating tools as much as possible if acceleration is high
- Limiting use of vibrating tools to 1 or 2 days a week
- Scheduling sufficiently long rest periods each hour to reduce the time-weighted acceleration levels
# D. ERGONOMIC CONSIDERATIONS
The amount of the tool-produced vibration that is transmitted to the hands and arms of the operator is influenced by (1) the grip force with which the tool is held, and ( 2) the force applied by the operator holding the tool against the workpiece Matoba 1986, Farkkila 1978J. The tool should be held as loosely as safe tool control and operating requirements permit. The force applied to hold the tool against the workpiece should be minimal. The weight of the tool should be used to help provide the required tool/workpiece interface pressure for optimal working speed and efficiency. Moisture at the hand/tool interface (sweat or liquids) may require the worker to exert greater grip force to control the tool. A slip-resistant interface surface is desirable.
Another important ergonomic factor is the position of the body while operating the tool. The angle of the wrists, elbows, and shoulders during tool operation will influence the level of stress exerted on the joints and tendons and the incidence of such problems as tendinitis, carpal tunnel syndrome, tennis elbow, painful shoulders, and HAVS.
An ergonomic analysis of how the work is done is important. Such an analysis can determine the operating practices that may require modification to minimize health problems.
# E. PROTECTIVE CLOTHING AND EQUIPMENT
Two generic types of protective clothing and equipment may be used to provide protection against the effects of vibration. These include (1) those that reduce transmission of vibration energy to the hand and (2) those that protect against exposure to cold and trauma.
Various types of vibration-damping materials have been incorporated into gloves and mittens to protect the user of vibrating tools. If these are sufficiently successful as energy dampers, this approach could be very acceptable. For most tasks involving vibrating tools, hand gear of some type is used for protection against trauma and cold. Presently, the major K a VII. Methods for Worker Protection problem is finding energy-damping materials that (1) provide adequate damping with minimal thickness so that the dexterity required for safe and efficient tool operation will not be reduced, and ( 2) have adequate damping characteristics over the vibration frequency spectrum associated with HAVS. Although several materials are available, an optimal, all-purpose material is not available.
Acute episodes of white finger, especially in the early stages of HAVS, are frequently triggered by exposure of the hands or body to cold. Thermal protection by adequate body clothing and handgear to prevent hand or central body cooling might reduce the frequency of the attacks. However, protecting the hands and body in cold weather is a complex problem that depends on many interacting factors such as
where a0 is the reference acceleration value, and a is the measurement value.
In the cases where only mechanical displacement was given, the following formula was used,
# Speak | This document examines the occupational health problems associated with the use of vibrating tools (including both hand-held vibrating tools and stationary tools that transmit vibration through a workpiece), and it provides criteria for reducing the risk of developing vibration-induced health problems. The major health problems associated with the use of vibrating tools are signs and symptoms of peripheral vascular and peripheral neural disorders of the fingers and hands. These signs and symptoms include numbness, pain, and blanching of the fingers. This composite of vibration-induced signs and symptoms is referred to as hand-arm vibration syndrome (HAVS), sometimes called Raynaud's phenomenon of oc cupational origin, or vibration white finger disease. In the United States, an estimated 1.45 million workers use vibrating tools. The prevalence of HAVS in a worker population that has used vibrating tools ranges from 6% to 100%, with an average of about 50%. The development of HAVS depends on many factors, including the level of acceleration (vibration energy) produced by the tool, the length of time the tool is used each day, the cumulative number of months or years the worker has used the tool, and the ergonomics of tool use. The tools most commonly associated with HAVS are powered hammers, chisels, chain saws, sanders, grinders, riveters, breakers, drills, compac tors, sharpeners, and shapers.# FOREWORD
The purpose of the Occupational Safety and Health Act of 1970 (Public Law 91-596) is to assure safe and healthful working conditions for eveiy working person and to preserve our human resources by providing medical and other criteria that will assure, insofar as practicable, that no worker will suffer diminished health, functional capacity, or life expectancy as a result of his or her work experience. The Act authorizes the National Institute for Occupational Safety and Health (NIOSH) to develop and recommend occupa tional safety and health standards and to develop criteria for improving them. By this means, NIOSH communicates these criteria to regulatory agencies (including the Occupational Safety and Health Administration and the Mine Safety and Health Administration) and others in the community of occupational safety and health.
Criteria documents provide the basis for the occupational safety and health standards sought by Congress. These documents generally contain a critical review of the scientific and technical information available on the prevalence of hazards, the existence of safety and health risks, and the adequacy of control methods. NIOSH distributes these documents to health professionals in academic institutions, industry, organized labor, public interest groups, and other government agencies. This criteria document examines the occupational health problems associated with the use of vibrating tools and provides criteria for reducing the risk of developing vibration-induced health problems. In this document, the term "vibrating tools" includes both hand-held vibrating tools and stationary tools that transmit vibration through a workpiece. The major health problems associated with the use of vibrating tools are signs and symptoms of peripheral vascular and peripheral neural disorders of the fingers and hands. These signs and symptoms include numbness, pain, and blanching of the fingers, and loss of finger dexterity. This composite of vibration-induced signs and symptoms is referred to as hand-arm vibration syndrome (HAVS).
On the basis of the 1983 National Occupational Exposure Survey, an estimated 1.45 million U.S. workers use vibrating tools. The prevalence of HAVS in workers who use such tools is reported to range from 6% to 100%, with an average of approximately 50%. Primary Raynaud's disease, whose signs and symptoms resemble those of HAVS, has been reported to occur in an estimated 5% of the general population. This percentage is consistent with the number of unexposed comparison workers who report such symptoms in studies of HAVS.
HAVS is a chronic progressive disorder with a latency period that may vary from a few months to several years. The development of HAVS in a population of workers and the length of the latency period depend on many interacting factors, including vibration level produced by the tool, hours of tool use per day, environmental conditions, type and design of the tool, manner in which the tool is held, vibration spectrum produced by the tool, vibration tolerance of the worker, and tobacco and drug use by the worker.
Because of the complex interactions among these and other factors, the general lack of epidemiologic and clinical data, and the uncertainty associated with some vibration meas urements, it is not currently possible to establish meaningful dose-response relationships. Thus it is not possible to establish a specific recommended exposure limit (REL) that will protect workers against the development of HAVS in all occupational situations. However, the problem of HAVS is too serious and pervasive to delay measures for correcting it.
NIOSH has therefore recommended a standard for exposure to hand-arm vibration that includes no specific exposure limit but does include engineering controls, good work practices, use of protective clothing and equipment, worker training programs, administra tive controls such as limited daily use time, and medical monitoring and surveillance. Frequency-unweighted measurements of acceleration are also recommended since they provide simpler, more appropriate means for assessing the health risk of using vibrating tools at all frequencies. A cornerstone of this standard is the requirement for medical monitoring of all vibration-exposed workers to identify the first signs and symptoms of HAVS and to remove such workers from the job until they are free of all vibration-related symptoms.
Implementation of this standard will protect users of vibrating tools from the debilitating effects of HAVS. NIOSH also anticipates that this criteria document will stimulate research and development in all areas relating to hand-arm vibration. Future research may provide new and more effective methods for reducing occupational exposure to vibration.
When appropriate data become available to develop a specific REL for vibration exposures, NIOSH will revise its recommended standard. Until then, adherence to the standard described in this criteria document should prevent or greatly reduce the potential for vibration-exposed workers to develop the painful and disabling HAVS.
NIOSH takes sole responsibility for the conclusions and recommendations presented in this document. All reviewers' comments are being sent with this document to the Occupational Safety and Health Administration (OSHA) and the Mine Safety and Healjh-Administration (MSHA) for consideration in standard setting. The prevalence and severity of HAVS usually increase as the acceleration level and duration of use increase. HAVS is a chronic, progressive disorder with a latency period that may vary from a few months to several years. The early stages of HAVS are usually reversible if further exposure to vibration is reduced or eliminated; but treatment is usually ineffective for the advanced stages of HAVS, and the disorder may progress to loss of effective hand function and necrosis of the fingers. Prevention is therefore critical. Adherence to the exposure controls recommended in this document should prevent or greatly reduce the potential for vibration-exposed workers to develop HAVS.
# IV-9
Hand-arm vibration acceleration levels ranked from highest to lowest for studies listed in Table IV -8
# . 64 I Glossary
Harmonic: A frequency that is an integral multiple of some fundamental or base fre quency.
Hertz: A unit of frequency (cycles per second). Impedance: The ratio of a harmonic excitation of a system to its response; ratio of ap plied force to resulting velocity. Impedance, mechanical: Ratio of applied vibratory force to the resulting velocity.
Incidence: Number of new cases of a disease or condition reported in a population over a given period.
Jerk: Time rate of acceleration change. Joule: A unit of energy equal to the amount of work done when a point is displaced 1 m by the application of a force of 1 N. A unit of energy equal to 107 ergs, or about 0.738 foot pounds. Latency: The time interval between the application of force or stimulus and the ap pearance of a response.
Mass: Quantity of matter; the inertial resistance of a body to acceleration.
Mass, dynamic: Ratio of applied force to resulting acceleration.
Modulus, dynamic: Ratio of stress to strain; stress required to produce a unit of strain.
Newton: Force required to accelerate a 1-kg mass 1 m/sec2 (100,000 dynes).
# Oscillation:
The variation in the position of an object over time in reference to its start ing point. Oscillation, period of: Time required for an oscillation to be completed. Power, spectral density: The mean square value of energy per unit of time passed through a given frequency range. Prevalence: Number of current cases (old and new) of a disease or condition in a popula tion at a given point in time (point prevalence) or during a given period (period prevalence).
# Radians:
The angle subtended at the center of a circle by an arc equal in length to a radius of the circle.
xv i
# Glossary
Resonance : The tendency of a body to act in concert with an externally generated vibra tion to amplify the impinging vibration; the amplification of an oscillation of a system by a force wave or oscillation of exactly equal period or frequency. Root mean square: The square root of the arithmetic mean of the squares of a series of numbers.
# Stiffness:
The ratio of force or torque to the resulting change in displacement of an elas tic body.
# Spectrum, vibration:
The distribution of frequencies that describes the frequencies that are present in a vibrating system.
# Transfer function:
The mathematical relation between the input into a system and the response.
# Transmissibility:
The ratio of vibration output divided by the input as a function of fre quency.
# Velocity:
The first derivative of displacement with respect to time (m/sec). Vibration: The oscillation or periodic motion of a rigid or elastic body from a position of equilibrium.
Vibration, random: An oscillatory motion in which the acceleration varies over time in a nonperiodic manner; a vibration whose magnitude is not precisely predictable for any point in time.
# I. RECOMMENDATIONS FOR A STANDARD
The National Institute for Occupational Safety and Health (NIOSH) recommends that worker exposure to vibration from the use of vibrating tools be controlled by compliance with all recommendations given in Chapter I of this document. Adherence to these recommendations should prevent or greatly reduce the risk of incurring hand-artn vibra tion syndrome (HAVS) in workers who use vibrating tools. In this document, the term "vibrating tools" includes both hand-held vibrating tools and stationary tools that transmit vibration through a workpiece. An estimated 5% of the general population may develop primary Raynaud's disease (whose signs and symptoms resemble those of HAVS) without exposure to vibration. The recommendations are designed to prevent workers who use vibrating tools from developing the signs and symptoms of Stage 1 HAVS during a working lifetime.
# SECTION 1. VIBRATION EXPOSURE
HAVS has been observed in workers who have used vibrating tools that transmit vibration energy to the hands and arms over a wide range of acceleration levels. The level of acceleration produced by a tool is influenced by many factors, including tool type and weight, operating speed, ergonomics of tool use, environmental conditions, antivibration materials used, etc. (see Chapter HI, D and Chapter VII). Thus NIOSH cannot currently establish a specific quantitative exposure limit that will eliminate the risk of developing HAVS in all workers exposed to hand-transmitted vibration from all types of vibrating tools. NIOSH therefore recommends that exposure to hand-arm vibration be reduced to the lowest feasible acceleration levels and exposure times by adhering to the requirements presented in Section 4, Control of Vibration.
# SECTION 2. EXPOSURE MONITORING
The epidemiologic and clinical evidence reviewed in Chapter IV supports the conclusion that a linear relationship exists between the acceleration exposure dose (level of acceleration and years of exposure) and the time of onset and severity of HAVS. Data on the vibration acceleration level produced by the vibrating tools are needed for the design of tools and work strategies that will help prevent and control HAVS at the earliest possible stage.
The components of the hand-transmitted vibration that shall be measured are (a) acceleration (m/sec or g), (b) frequency (Hz), and (c) duration of exposure (min/day or hr/day).
# Hand-Arm Vibration
(a) Vibration acceleration shall be measured in the three orthogonal basicentric axes at the point on the tool where the vibration enters the hand or as close as possible to that point. The basicentric axis of greatest acceleration may be used to calculate acceleration levels. The magnitude of acceleration shall be measured using an accelerometer with sufficient dynamic range to cover the acceleration band of 1 to 1,000 m/sec2. The mass of the accelerometer shall be small enough that it does not affect the vibration amplitude being measured (<5 grams if possible). The vibration measuring system shall be calibrated in accordance with appropriate standards based on National Bureau of Standards procedures. The accelerometer(s) shall be attached to the vibrating source as described in Chapter HI, B, Methods of Measuring Hand-Transmitted Vibration.
(b) The frequency-unweighted acceleration shall be expressed in m/sec (ims) of the 1/3-octave-band center frequencies from 6.3 to 5,000 Hz.
(c) The vibration measurement system shall have a uniform response integrated over 1/3-octave-band center frequencies of 6.3 to 5,000 Hz. All measurements and analyses of the vibration acceleration and frequency shall be performed by trained technical personnel.
(d) The vibration characteristics (acceleration and frequency spectrum) for each tool shall be measured at the time the tool is first put into use and at annual intervals thereafter. The vibration shall be measured when the tool is operating under full power and actual or simulated conditions of use.
(e) The time the tool is in use shall be determined by measuring actual operating time over a workday; these measurements can then be used to calculate average daily vibration acceleration exposures. The total daily vibration acceleration exposure shall be converted to a normalized 4-hr acceleration amplitude in m/sec2 (frequency unweighted) (see Chapter III, Equation 13).
(f) A hand-held vibration meter may be used for screening or monitoring purposes to determine the approximate acceleration levels being produced by the vibrating system. However, proper mounting of such an acceleration measuring device onto the vibrating tool is critical (see Chapter HI, B).
# SECTION 3. MEDICAL MONITORING (a) General
(1) The employer shall provide a health monitoring program for all workers occupa tionally exposed to hand-arm vibration from the use of vibrating tools.
(2) The employer shall ensure that all medical examinations and procedures are per-formed by or under the direction of a licensed physician with special training and experience in occupational health problems. Board certification in occupational medicine is one way to demonstrate such training and experience.
(3) The employer or physician shall (a) counsel all workers who use tobacco about its possible role in augmenting the harmful effects of vibrating tools, and (b) encourage these workers to stop using tobacco.
# (b) Preplacement Medical Examinations
At a minimum, a preplacement medical examination shall be conducted for each worker who will use vibrating tools on the job. The baseline data obtained from these examinations are for comparison with the data derived from the periodic medical examinations. The examination shall include the following:
(1) A comprehensive work history with special emphasis on present or past use of vibrating tools during work or hobby activities
(2) A medical history, including relevant information on any peripheral vascular, peripheral neural, or musculoskeletal complaints (3) A comprehensive physical examination with special attention to peripheral vas cular and peripheral neural integrity, grip strength, muscle force, and signs and symptoms of the disorders listed in Table IV-1 (4) An assessment of the use of substances that influence normal vascular and neural function, which include certain prescription drugs, alcohol, tobacco, and illicit sub stances.
# (c) Periodic Medical Examinations
(1) Periodic medical examinations shall be made available at least annually to all workers who use vibrating tools on the job. The periodic medical examination shall include all those items specified in Chapter 1, Section 3b, and any other items considered relevant by the examining physician. If circumstances warrant (e.g., an increase in job-related vibration exposure, or a change in health status), the medical examination shall be offered at shorter intervals at the discretion of the attending physician.
(2) The peripheral neural and peripheral vascular signs and symptoms noted during the examination shall be reported in conformance with the classification presented in Tables IV-4 and IV-5.
# (d) Medical Removal
Any worker occupationally exposed to hand-transmitted vibration who develops peripheral I Hand-Arm Vibration neural or peripheral vascular signs and symptoms of Stage 2 HAVS or above on the Stockholm Workshop classification described in Tables IV-4 and IV-5 shall not be exposed to further hand-arm vibration until his or her signs and symptoms have improved sufficiently that they no longer meet the criteria for Stage 1 HAVS.
If the attending physician recommends that a worker be removed from a job requiring the use of vibrating tools, the employer shall ensure tfiat the worker retains all earnings, seniority, and other employment rights and benefits.
# (e) Information for Health Care Professionals
The employer shall furnish the following information to the health care professional responsible for the medical monitoring program:
• A copy of this criteria document
• A description of the worker's duties and activities as they relate to vibration exposure
• An estimate of the worker's daily exposure to vibration and years of exposure
• A list of basic types of vibrating tools used
• A list of the acceleration levels produced by the tools • A description of antivibration protective clothing and antivibration tool designs in use
• A list of all tasks that involve vibrating tools and workpieces and that require strong hand grip force
• Relevant information from previous work and medical histories and medical examinations
• A description of the special features of the task and the way in which this task is performed
• A description of the environmental conditions at the work site (ambient tempera ture, humidity, wind velocity, rain, snow, etc.)
E a
# I. Recommendations for a Standard (f) Written Report and Opinion
The employer shall receive the following information from the attending health care professional:
• An opinion as to the worker's ability to use vibrating tools
• Any recommended limitations to on-the-job exposure
• Any limitation to the worker's ability to use any required protective equipment or clothing
• With the worker's written consent, information about any condition requiring treatment or special consideration Engineering and work practice controls shall be used to reduce hand-transmitted vibration exposure to the lowest feasible level. These controls shall also be supplemented by other control strategies such as the use of antivibration clothing, mittens, gloves, and equipment, and by worker training programs in the proper handling of the vibrating tools.
# (b) Engineering Controls
(1) The vibration acceleration level shall be controlled by reducing the vibration energy produced by the vibrating tool to the lowest level consistent with optimal operations and/or by changing the process to reduce the requirement for using the tool.
(2) The power and weight of the tool shall be optimized to levels that minimize vibration but still permit the work to be efficiently performed.
(3) The tool manufacturers shall furnish data on the vibration acceleration and frequency characteristics of their tools as measured by a standard test protocol of simulated operation.
# (c) Work Practices
In addition to all possible engineering controls, work shall be modified to minimize vibration exposure. Work modification approaches include but are not limited to the following procedures:
Hand-Arm Vibration
• Reducing the number of hours a worker uses a vibrating tool during the workday
• Reducing the number of days per week the vibrating tool is used
• Arranging work tasks so that vibrating and nonvibrating tools can be used alternately, and assuring that the nonvibrating tools do not introduce other musculoskeletal stress factors
• Scheduling maintenance breaks as necessary to ensure that tools are sharp, lubricated, and tuned
• Selecting tools that produce the least amount of vibration consistent with satis factory performance of the task
• Designing the work task and workplace to incorporate ergonomic principles to minimize vibration stress
• Reducing the grip force on the tool handle and the force applied at the tool/workpiece interface in a manner consistent with safety and performance
• Restricting the use of piecework and incentive pay
# (d) Protective Clothing and Equipment
Protective clothing and equipment shall be used where feasible to reduce the level of the vibration energy transmitted to the hand and arm. Some approaches to protecting the worker with clothing and equipment are The following data shall be furnished by the manufacturer of vibrating tools and antivibra tion equipment:
(a) All hand-held tools that produce vibration shall carry a label stating the frequen cy-unweighted acceleration level (m/sec2) produced by the tool during normal opera tion.
(b) The manufacturer of antivibration equipment, clothing, and hand gear shall provide information on the vibration-damping characteristics of each type of an tivibration item produced for sale.
# SECTION 6. RECORDKEEPING (a) Maintaining Records
For all workers who are occupationally exposed to vibrating tools, the employer shall establish and maintain a record of the following:
• Type, model, and manufacturer of the vibrating tools used In accordance with the requirements of 29 CFR 1910.20(d), Preservation of Records, the employer shall retain the records described in Chapter I of this document for at least the following periods:
(1) Thirty years for exposure monitoring records (2) The duration of employment plus 30 years for medical monitoring and surveil lance records and other records described in Chapter I of this document (c) Availability of Records
(1) In accordance with 29 CFR 1910.20, Access to Employee Exposure and Medical Records, the employer shall, upon request, allow examination and copying of ex posure monitoring records by a worker, a former worker, or anyone having the specific written consent of the worker or former worker.
(2) Any medical records that are required by this recommended standard shall be provided, upon request, for examination and copying to the worker, the former worker, or anyone having the specific written consent of the worker or former worker.
# (d) Transfer of Records
The employer shall comply with the requirements for the transfer of records as specified in 29 CFR 1910.20(h), Transfer of Records.
*Code of Federal Regulations. See CFR in references.
# II. INTRODUCTION
For more than three-quarters of a century, workers who operated vibrating tools* on the job have reported complaints resembling the signs and symptoms of primary Raynaud ' s disease. The major complaints were episodic numbness and tingling of the fingers, episodic blanch ing of the fingers, with pain occurring mainly in response to cold exposure and on return of circulation, and reduction in grip strength and finger dexterity. These signs and symptoms increased in number and severity as the exposure to vibration (acceleration intensity and duration of exposure) increased. In a worker population that has used vibrating tools, the prevalence of HAVS ranges from 6% to 100%, with an average of about 50%. The development of HAVS depends on many factors such as the level of acceleration (vibration energy) produced by the tool, the length of time the tool is used each day, the cumulative number of hours, months, and years the worker has used the tool, and the ergonomics of tool use. Minimum daily exposures for several hours each day for months or years are usually required before the first signs and symptoms appear.
HAVS is a chronic disorder with a latency period of a few months to several years. The early stages of HAVS are usually reversible if further exposure to vibration is reduced or eliminated, but advanced stages are progressive. However, treatment is usually ineffective for the advanced stages of HAVS, and the disorder can progress to loss of effective hand function and necrosis of the fingers.
*In this document, the term "vibrating tools" includes both hand-held vibrating tools and stationary tools that transmit vibration through a workpiece.
a
# II. Introduction
In recognition of the health and safety hazards of vibration exposure, NIOSH published Current Intelligence Bulletin 38, Vibration Syndrome [NIOSH 1983a]. This Current Intel ligence Bulletin emphasized the magnitude of the problem and the seriousness of the health and safety aspects of vibration exposure. The publication was designed to alert management, labor organizations, workers, health specialists, and engineers to the need for recognition, assessment, and control of the problem in industries where vibrating tools are used.
This criteria document presents criteria, techniques, and procedures for the assessment, evaluation, and control of HAVS. Engineering controls, work practices, administrative procedures, medical supervision, worker training, ergonomic design of the tools and the task, and other procedures can be implemented to effectively reduce the risk of developing HAVS.
# I. RECOMMENDATIONS FOR A STANDARD
The National Institute for Occupational Safety and Health (NIOSH) recommends that worker exposure to vibration from the use of vibrating tools be controlled by compliance with all recommendations given in Chapter I of this document. Adherence to these recommendations should prevent or greatly reduce the risk of incurring hand-arm vibra tion syndrome (HAVS) in workers who use vibrating tools. In this document, the term "vibrating tools" includes both hand-held vibrating tools and stationary tools that transmit vibration through a workpiece. An estimated 5% of the general population may develop primary Raynaud's disease (whose signs and symptoms resemble those of HAVS) without exposure to vibration. The recommendations are designed to prevent workers who use vibrating tools from developing the signs and symptoms of Stage 1 HAVS during a working lifetime.
# SECTION 1. VIBRATION EXPOSURE
HAVS has been observed in workers who have used vibrating tools that transmit vibration energy to the hands and arms over a wide range of acceleration levels. The level of acceleration produced by a tool is influenced by many factors, including tool type and weight, operating speed, ergonomics of tool use, environmental conditions, antivibration materials used, etc. (see Chapter HI, D and Chapter VII). Thus NIOSH cannot currently establish a specific quantitative exposure limit that will eliminate the risk of developing HAVS in all workers exposed to hand-transmitted vibration from all types of vibrating tools. NIOSH therefore recommends that exposure to hand-arm vibration be reduced to the lowest feasible acceleration levels and exposure times by adhering to the requirements presented in Section 4, Control of Vibration.
# SECTION 2. EXPOSURE MONITORING
The epidemiologic and clinical evidence reviewed in Chapter IV supports the conclusion that a linear relationship exists between the acceleration exposure dose (level of acceleration and years of exposure) and the time of onset and severity of HAVS. Data on the vibration acceleration level produced by the vibrating tools are needed for the design of tools and work strategies that will help prevent and control HAVS at the earliest possible stage.
The components of the hand-transmitted vibration that shall be measured are (a) acceleration (m/sec or g), (b) frequency (Hz), and (c) duration of exposure (min/day or hr/day).
# Hand-Arm Vibration
(a) Vibration acceleration shall be measured in the three orthogonal basicentric axes at the point on the tool where the vibration enters the hand or as close as possible to that point. The basicentric axis of greatest acceleration may be used to calculate acceleration levels. The magnitude of acceleration shall be measured using an accelerometer with sufficient dynamic range to cover the acceleration band of 1 to 1,000 m/sec2. The mass of the accelerometer shall be small enough that it does not affect the vibration amplitude being measured (<5 grams if possible). The vibration measuring system shall be calibrated in accordance with appropriate standards based on National Bureau of Standards procedures. The accelerometer(s) shall be attached to the vibrating source as described in Chapter HI, B, Methods of Measuring Hand-Transmitted Vibration.
(b) The frequency-unweighted acceleration shall be expressed in m/sec (rms) of the 1/3-octave-band center frequencies from 6.3 to 5,000 Hz.
(c) The vibration measurement system shall have a uniform response integrated over 1/3-octave-band center frequencies of 6.3 to 5,000 Hz. All measurements and analyses of the vibration acceleration and frequency shall be performed by trained technical personnel.
(d) The vibration characteristics (acceleration and frequency spectrum) for each tool shall be measured at the time the tool is first put into use and at annual intervals thereafter. The vibration shall be measured when the tool is operating under full power and actual or simulated conditions of use.
(e) The time the tool is in use shall be determined by measuring actual operating time over a workday; these measurements can then be used to calculate average daily vibration acceleration exposures. The total daily vibration acceleration exposure shall be converted to a normalized 4-hr acceleration amplitude in m/sec2 (frequency unweighted) (see Chapter III, Equation 13).
(f) A hand-held vibration meter may be used for screening or monitoring purposes to determine the approximate acceleration levels being produced by the vibrating system. However, proper mounting of such an acceleration measuring device onto the vibrating tool is critical (see Chapter HI, B).
# SECTION 3. MEDICAL MONITORING (a) General
(1) The employer shall provide a health monitoring program for all workers occupa tionally exposed to hand-arm vibration from the use of vibrating tools.
(2) The employer shall ensure that all medical examinations and procedures are per-formed by or under the direction of a licensed physician with special training and experience in occupational health problems. Board certification in occupational medicine is one way to demonstrate such training and experience.
(3) The employer or physician shall (a) counsel all workers who use tobacco about its possible role in augmenting the harmful effects of vibrating tools, and (b) encourage these workers to stop using tobacco.
# (b) Preplacement Medical Examinations
At a minimum, a preplacement medical examination shall be conducted for each worker who will use vibrating tools on the job. The baseline data obtained from these examinations are for comparison with the data derived from the periodic medical examinations. The examination shall include the following:
(1) A comprehensive work history with special emphasis on present or past use of vibrating tools during work or hobby activities
(2) A medical history, including relevant information on any peripheral vascular, peripheral neural, or musculoskeletal complaints (3) A comprehensive physical examination with special attention to peripheral vas cular and peripheral neural integrity, grip strength, muscle force, and signs and symptoms of the disorders listed in Table IV-1 (4) An assessment of the use of substances that influence normal vascular and neural function, which include certain prescription drugs, alcohol, tobacco, and illicit sub stances.
# (c) Periodic Medical Examinations
(1) Periodic medical examinations shall be made available at least annually to all workers who use vibrating tools on the job. The periodic medical examination shall include all those items specified in Chapter 1, Section 3b, and any other items considered relevant by the examining physician. If circumstances warrant (e.g., an increase in job-related vibration exposure, or a change in health status), the medical examination shall be offered at shorter intervals at the discretion of the attending physician.
(2) The peripheral neural and peripheral vascular signs and symptoms noted during the examination shall be reported in conformance with the classification presented in Tables IV-4 and IV-5.
# (d) Medical Removal
Any worker occupationally exposed to hand-transmitted vibration who develops peripheral I Hand-Arm Vibration neural or peripheral vascular signs and symptoms of Stage 2 HAVS or above on the Stockholm Woikshop classification described in Tables IV-4 and IV-5 shall not be exposed to further hand-arm vibration until his or her signs and symptoms have improved sufficiently that they no longer meet the criteria for Stage 1 HAVS.
If the attending physician recommends that a worker be removed from a job requiring the use of vibrating tools, the employer shall ensure tfiat the worker retains all earnings, seniority, and other employment rights and benefits.
# (e) Information for Health Care Professionals
The employer shall furnish the following information to the health care professional responsible for the medical monitoring program:
• A copy of this criteria document
• A description of the worker's duties and activities as they relate to vibration exposure
• An estimate of the worker's daily exposure to vibration and years of exposure • A list of basic types of vibrating tools used
• A list of the acceleration levels produced by the tools • A description of antivibration protective clothing and antivibration tool designs in use
• A list of all tasks that involve vibrating tools and workpieces and that require strong hand grip force • Relevant information from previous work and medical histories and medical examinations
• A description of the special features of the task and the way in which this task is performed
• A description of the environmental conditions at the work site (ambient tempera ture, humidity, wind velocity, rain, snow, etc.)
E a
# I. Recommendations for a Standard (f) Written Report and Opinion
The employer shall receive the following information from the attending health care professional:
• An opinion as to the worker's ability to use vibrating tools
• Any recommended limitations to on-the-job exposure
• Any limitation to the worker's ability to use any required protective equipment or clothing
• With the worker's written consent, information about any condition requiring treatment or special consideration Engineering and work practice controls shall be used to reduce hand-transmitted vibration exposure to the lowest feasible level. These controls shall also be supplemented by other control strategies such as the use of antivibration clothing, mittens, gloves, and equipment, and by worker training programs in the proper handling of the vibrating tools.
# (b) Engineering Controls
(1) The vibration acceleration level shall be controlled by reducing the vibration energy produced by the vibrating tool to the lowest level consistent with optimal operations and/or by changing the process to reduce the requirement for using the tool.
(2) The power and weight of the tool shall be optimized to levels that minimize vibration but still permit the work to be efficiently performed.
(3) The tool manufacturers shall furnish data on the vibration acceleration and frequency characteristics of their tools as measured by a standard test protocol of simulated operation.
# (c) Work Practices
In addition to all possible engineering controls, work shall be modified to minimize vibration exposure. Work modification approaches include but are not limited to the following procedures:
Hand-Arm Vibration
• Reducing the number of hours a worker uses a vibrating tool during the workday The following data shall be furnished by the manufacturer of vibrating tools and antivibra tion equipment:
(a) All hand-held tools that produce vibration shall carry a label stating the frequen cy-unweighted acceleration level (m/sec2) produced by the tool during normal opera tion.
(b) The manufacturer of antivibration equipment, clothing, and hand gear shall provide information on the vibration-damping characteristics of each type of an tivibration item produced for sale.
# SECTION 6. RECORDKEEPING (a) Maintaining Records
For all workers who are occupationally exposed to vibrating tools, the employer shall establish and maintain a record of the following:
• Type, model, and manufacturer of the vibrating tools used In accordance with the requirements of 29 CFR 1910.20(d), Preservation of Records, the employer shall retain the records described in Chapter I of this document for at least the following periods:
(1) Thirty years for exposure monitoring records (2) The duration of employment plus 30 years for medical monitoring and surveil lance records and other records described in Chapter I of this document (1) In accordance with 29 CFR 1910.20, Access to Employee Exposure and Medical Records, the employer shall, upon request, allow examination and copying of ex posure monitoring records by a worker, a former worker, or anyone having the specific written consent of the worker or former worker.
(2) Any medical records that are required by this recommended standard shall be provided, upon request, for examination and copying to the worker, the former worker, or anyone having the specific written consent of the worker or former worker.
# (d) Transfer of Records
The employer shall comply with the requirements for the transfer of records as specified in 29 CFR 1910.20(h), Transfer of Records.
*Code of Federal Regulations. See CFR in references.
# II. INTRODUCTION
For more than three-quarters of a century, workers who operated vibrating tools* on the job have reported complaints resembling the signs and symptoms of primary Raynaud ' s disease. The major complaints were episodic numbness and tingling of the fingers, episodic blanch ing of the fingers, with pain occurring mainly in response to cold exposure and on return of circulation, and reduction in grip strength and finger dexterity. These signs and symptoms increased in number and severity as the exposure to vibration (acceleration intensity and duration of exposure) increased. In a worker population that has used vibrating tools, the prevalence of HAVS ranges from 6% to 100%, with an average of about 50%. The development of HAVS depends on many factors such as the level of acceleration (vibration energy) produced by the tool, the length of time the tool is used each day, the cumulative number of hours, months, and years the worker has used the tool, and the ergonomics of tool use. Minimum daily exposures for several hours each day for months or years are usually required before the first signs and symptoms appear.
HAVS is a chronic disorder with a latency period of a few months to several years. The early stages of HAVS are usually reversible if further exposure to vibration is reduced or eliminated, but advanced stages are progressive. However, treatment is usually ineffective for the advanced stages of HAVS, and the disorder can progress to loss of effective hand function and necrosis of the fingers.
a
# II. Introduction
In recognition of the health and safety hazards of vibration exposure, NIOSH published Current Intelligence Bulletin 38, Vibration Syndrome [NIOSH 1983a]. This Current Intel ligence Bulletin emphasized the magnitude of the problem and the seriousness of the health and safety aspects of vibration exposure. The publication was designed to alert management, labor organizations, workers, health specialists, and engineers to the need for recognition, assessment, and control of the problem in industries where vibrating tools are used. Three components of a vibrating system are (1) mass, ( 2) elasticity, and ( 3) damping. The kinetic energy of the system is a function of the mass and motion of the system. The potential energy of the system is a function of the mass and elasticity of the system. When a system vibrates, the energy in the system alternately changes back and forth between kinetic and potential energy. In the absence of any mechanism to take energy out of the system, a system will theoretically vibrate forever once it begins to vibrate. Damping is the mechanism that transforms the kinetic and potential energy into heat and thereby takes energy out of a vibrating system. Thus if no energy is directed into a vibrating system to keep it in motion, the damping that is present will dissipate the initial energy in the system and all motion will stop. The human hand-arm system contains mass, elasticity, and damping and can be visualized as a series of masses coimected by elastic and damping elements. When the values for any two of the parameters are known for any single frequency, the values for the other two can be calculated. When the motion is harmonic, the displace ment
[X(t)\ is X(t) = X sin((ût) (1)
where X is the peak displacement amplitude in meters, Of) is the angular frequency of oscillation in radians/sec, and t is the time in seconds The angular frequency can be expressed as <d = 2 n f or f = - where n is a constant equal to 3.1416, and /is frequency (cycles/second, or hertz [Hz]). The frequency if) represents the number of complete cycles of oscillations an object makes in 1 sec. For example, if an object undergoes 10 complete cycles of oscillation in 1 sec, it has a frequency of 10 cycles/sec, or 10 Hz. The period of oscillation is where t is seconds. The period of oscillation represents the time it takes an object to complete one cycle of oscillation.
The velocity of an object refers to the time rate of change of displacement and represents the first derivative of the displacement function given above (Equation 1). Velocity [v(t)] is expressed as indicating that velocity leads displacement by a phase of 90*.
The acceleration [a( t)] of an object refers to the time rate of change of velocity and represents the second derivative with respect to time of the displacement function, or
v(t) = = (ûXcos((ût) (4
)
where toX is the peak velocity (m/sec). Velocity can be written as
v(t) = (oX sin (oef + ~ ) (5) = -(û2X sin(cùt)( 6) 9 2
where © X is the peak acceleration amplitude (m/sec ). Acceleration can be written ait) = (ù2X sin((ût + k ) (
I
# III. Vibration as a Hazard
indicating that acceleration leads velocity by a phase of 90* and displacement by a phase of 180*.
When a vibrating system acts in concert with externally applied vibration so that certain vibration frequencies impinging on the system are amplified, the frequencies at which maximum amplification occurs are referred to as resonances or natural frequencies. In the case of hand-arm vibration, a fundamental resonance is thought to occur between 100 and 200 Hz [Wasserman 1988].
# Mechanical Impedance
When a vibrating stimulus is applied to a human, a mechanical structure, or another system, a motion results at the same frequency as the stimulus at the point of application and at other points in the system. The mechanical impedance of the system to which the stimulus is applied can be used to describe the dynamic characteristics and the motion of the vibrating system. Mechanical impedance [Z(co)] is defined as the ratio of the applied vibrating force [F(co)] divided by the resulting velocity [v((o)], or
z <" > ■ m (8)
Mechanical impedance is measured as a function of the frequency of the applied force. When both the applied force and resulting velocity are measured at the point of contact between the applied force and the vibrating system, the impedance is referred to as the "driving point mechanical impedance." When the resulting velocity is measured at a point on the system other than the point where the force is applied, the impedance is referred to as the "transfer mechanical impedance." Mechanical impedance measurements have been extensively used in human vibration to determine resonance, stiffness, damping, and other dynamic characteristics of the human body. Impedance is a measure of the total dynamic opposition the human body offers to the movement imparted by the vibration stimulus and can reflect body resonances without interfering with normal body function. Mechanical impedance measurements are noninvasive measurements that can be used to determine the dynamic properties of the body or different parts of the body such as the hand and arm.
Instead of velocity system dynamics in opposition (mechanical impedance) to movement, vibration can be viewed as a form of movement or dynamic compliance. The dynamic compliance [£>(©)] is defined as the ratio of the displacement [X(co)] divided by the driving force [F(co)], or
D (°» -J m <9>
# Hand-Arm Vibration
Human response to vibration depends on several factors: Vibration is a vector quantity (i.e., it has a magnitude and direction). Thus nearly all of the variables above must be extended to multiple axes, depending on the nature of the vibration that is being examined.
As specified by the International Organization for Standardization (ISO) [ISO 1986], the vibration produced by the tool or the vibration transmitted to the hand should be measured in the three orthogonal basicentric or biodynamic directions specified in interaction between the hands and a vibrating tool is influenced by many factors, which should be reported in detail when assessing the magnitude of the hand-transmitted vibration [Brammer and Taylor 1982;Starck and Pyykko 1986;Wasserman et al. 1977;Taylor 1974;ANSI 1986;ISO 1986]. These factors include • The type and condition of the tool being used • The acceleration and the frequency spectrum produced by the tool under normal operating conditions
• The magnitude and direction of sustained forces applied through the hands to the tool or the workpiece (e.g., gripping force, axial thrust force, rotational moments)
• The orientation and posture of the hands, arms, and body during work (specifically, the angles of the wrists, elbows, and shoulder joints)
• The parts of the hands that are in direct contact with vibrating surfaces
• Types and sizes of the surfaces in contact with the hands
• The work practices used
• The total number of years the worker has used vibrating tools on any job
• Climatic conditions such as the ambient temperature and humidity and the temperatures of hand-held surfaces of the tool or workpiece
The following information should be reported when assessing the duration of hand-trans mitted vibration exposure [ANSI 1986;ISO 1986]:
• The duration of vibration exposure per working day and the total exposure time in hours, months, and years
• The pattern of exposure within a period of time and its association with the working method (e.g., the length and frequency of scheduled and unscheduled work and rest periods, the intermittence of vibration during the work period, whether the vibrating tool is laid aside or held during rest breaks)
Hand-Amt Vibration
# B. METHODS OF MEASURING HAND-TRANSMITTED VIBRATION
# Measurement of Acceleration
The three parameters that describe the amplitude of vibration as a function of frequency are (1) displacement, ( 2) velocity, and ( 3) acceleration. However, vibration is generally specified in terms of acceleration for the following reasons:
a. The velocity and displacement can be obtained from the measurement of accelera tion. b. A large variety of accelerometers are commercially available.
c. The amplitude of acceleration at the higher frequencies is substantially higher than either displacement or velocity and, therefore, is easier to measure.
When acceleration is measured with an accelerometer, the velocity can be obtained by electronically integrating the acceleration signal over time. The displacement can be obtained by electronically integrating the acceleration signal a second time. Electronic integration tends to reduce or minimize noise introduced into the measurements.
# Accelerometers
Piezoelectric accelerometers are usually used to measure the amplitude of vibration as sociated with hand-transmitted vibration. These accelerometers can be designed to measure vibration within the frequency range of 1 to 50,000 Hz. When vibration impinges on a piezoelectric accelerometer, it moves a small mass against the face of a crystal element. The crystal element produces an electrical voltage proportional to the compression of the mass against the crystal. This voltage is proportional to the acceleration. Because the voltage produced is often very small and loss in signal can easily occur over a long cable connecting an accelerometer to a corresponding instrument, a charge amplifier is used in conjunction with the accelerometer. This amplifier overcomes signal loss problems by measuring changes in the electrical charge (or capacitance) of the crystal caused by vibration. Because the crystal charge simultaneously varies with the voltage signal, a measure of acceleration is obtained. With some accelerometers, the charge amplifier is an external device (i.e., the charge signal from the accelerometer is directed to an external amplifier that converts the charge signal to a corresponding amplified voltage signal proportional to vibration amplitude). With other accelerometers, the circuitry for converting the charge signal to a voltage signal is an integral part of the accelerometer. For these, a voltage signal from the accelerometer is directed to a voltage amplifier that generates an amplified voltage signal proportional to vibration amplitude.
When vibration is measured, it is necessary to specify whether the vibration is being measured on an impact-or nonimpact-type tool. Impact tools include chipping hammers, scalers, pneumatic riveting hammers, pneumatic nailers, jack hammers, and any other tool that generates impulse vibration signals that dominate the vibration spectrum. Nonimpact tools include chain saws, nibblers, pneumatic wrenches, grinders, routers, circular saws, reciprocating saws, and other similar tools. To measure vibration amplitudes of impact tools, specially designed shock accelerometers or ordinary accelerometers with mechanical filters must be used. These accelerometers, which are commercially available, can withstand repeated high-level, high-crest-factor acceleration pulses. If regular accelerometers are used when impact vibration is present, serious errors can be introduced into the vibration measurements [Wasserman et al. 1977;Wasserman, etal. 1981]. These errors are associated with DC shifts within the accelerometer that seriously distort the low-frequency vibration amplitudes being measured. Shock accelerometers can be used to measure both impact and nonimpact vibration, but nonshock accelerometers can be used to measure nonimpact vibration only.
Although shock accelerometers can withstand exceptionally high impulse acceleration levels, they usually have very low voltage or charge sensitivities. In the case of impact vibration, the vibration amplitudes are sufficiently high that generally no signal-to-noise problem is associated with the recording or measuring instrumentation used to record and analyze the vibration signal. In the case of nonimpulse vibration, the vibration amplitudes can be so low that the acceleration signals are near the lower sensitivity of the recording or measuring instrumentation being used. For these cases, it is necessary to use accelerometers that have substantially higher voltage or charge sensitivities.
The accelerometer should not affect the vibration amplitudes that are being measured. Large accelerometers can cause "mass-loading" on die surface to which they are mounted. That is, the mass of the accelerometer is sufficiently large compared with the mass of the object to which it is attached that the vibration signal being measured is significantly distorted. Many commercially available, light-weight accelerometers weigh 5 grams or less. The smallest accelerometer that can be used for a specific application should be chosen. The total weight of the accelerometer assembly (weight of multiple accelerometers, if more than one is used, plus accelerometer mounting block) should not exceed 20 grams in most cases. Accelerometers weighing less than 20 grams may be required for measuring vibration on small, lightweight tools.
Because vibration is a vector quantity, it is necessary to make vibration measurements in the three orthogonal axes. These axes should always be oriented in the manner specified in Figure HI-2. The vibration measurements in die three axes should always be made at or as near as feasible to the surfaces of the vibrating hand-held tool or workpiece where the maximum vibration energy enters the hands. Figures III-3 through IH-6 show suggested accelerometer mounting locations for chain saws, chipping hammers, and horizontal and vertical grinders [Wasserman et al. 1981]. The vibration in the three basicentric orthogonal axes may be measured with a specially designed triaxial accelerometer (a commercially available multiple accelerometer block that measures vibration in three axes) or by three regular accelerometers that are oriented along the three orthogonal basicentric axes (Fig ure IH-3) that are attached to a small metal cubic block. The accelerometers should be attached directly to the vibrating surface, and the accelerometer and accelerometer-mounting configuration should be selected so that they do not distort the vibration measurements. More detailed information on procedures associated with the mounting of accelerometers can be found in Hempstock and O'Connor [1977], , Wasserman et al. [1981], and Wasserman [1987].
# Vibration Frequencies
Many vibration frequencies found in the workplace and other environments contribute to the total vibration measured. In the case of hand-transmitted vibration, the frequency range of importance designated by the International Organization for Standardization (ISO) is 5.6 to about 1,400 Hz [ISO 1986]. However, many types of tools produce vibration up to 5,000 to 10,000 Hz. Measured vibration data can be separated into its constituent parts by using a Fourier spectrum analysis. Mathematically, this can be expressed as where through a" and b\ through bn define the amplitude of each of the corresponding vibration frequencies coi through©« present in a given frequency spectrum. The combined sine and cosine terms give the actual vibration frequency components comprising the spectrum in the frequency range of interest and in their corresponding phases. The vibration spectrum is the frequency "finger print" of the vibration present in a given situation. Spectra are usually derived by means of computer analysis and graphically displayed as follows: a. The horizontal axis represents frequency (Hz). is not necessary to determine specific vibration frequencies at which these amplitudes exist. When this is the case, vibration amplitudes are measured using 1/3-octave-band filters.
/(f) =
In many cases when measurements are made to determine whether a particular level of vibration is within acceptable limits specified by a standard or regulation, using a single number to express the vibration stress is desirable. With respect to hand-transmitted vibration, the frequency-weighted acceleration level in m/sec2 is the single-number variable used by the American National Standards Institute (ANSI) [ANSI 1986], the ISO [ISO 1986], the American Conference of Governmental Industrial Hygienists (ACGIH) [ACGIH 1988], and the British Standards Institution (BSI) [BSI 1987]. The frequencyweighted acceleration may be obtained by passing the signal through a frequency-weighting filter.
# General Considerations Associated with Vibration Measurements
The duration of vibration signals associated with many vibrating hand-held tools or workpieces is relatively short. Thus to measure the vibration spectra or the 1/3-octave-band center frequency vibration acceleration associated with these signals, real-time analyzers must be used. These analyzers measure or compute the vibration amplitudes at all frequen cies simultaneously. The dynamic range of these analyzers should be as large as possible over the frequency range of 5 to 5,000 Hz.
To analyze vibration signals, the signals must first be recorded and then played back through the recording device to an analyzer. This procedure is usually necessary when multiaxis acceleration measurements are being made relative to both hands at the same time. The recording device is usually a multichannel FM tape recorder or a multichannel analog-todigital board that directs the recorded signals into a computer.
When high-peak acceleration signals associated with percussive tools are being analyzed, precautions must be taken to ensure that no part of the measuring, recording, or analyzing system is overloaded. To avoid overload, one of the following may be used:
• A commercially available shock accelerometer with a low voltage or charge sensitivity
• An electronic low-pass filter with an upper cut-off frequency above 5,000 Hz placed between the accelerometer voltage or charge amplifier and the recording device or analyzer
• A mechanical low-pass filter with a linear transfer function between 5 and 5,000 Hz placed between the accelerometer and the tool or workpiece !
# Hand-Arm Vibration
The acceleration signals associated with hand-transmitted vibration vary with time. Thus when measuring acceleration, it is always necessary to obtain values that are averaged over time. The acceleration is measured and reported as the root mean square {rms) value of acceleration [d(rms)\ i*1 m/sec2. The mis value of acceleration is
The value of T in Equation 11 must be long enough to be representative of the task associated with the use of the tool being investigated. Also, T should be sufficiently long to ensure reasonable statistical accuracy of the data [Hempstock and O'Connor 1977;ANSI 1986;ISO 1986].
During a vibration measurement, the tool or workpiece should be operated in a manner that is representative of its everyday use. The measured vibration signals in each of the three basicentric orthogonal axes of vibration should be reported as rms acceleration in each of the 1/3-octave-band center frequencies.
# C. GUIDELINES FOR ASSESSING VIBRATION AMPLITUDES
Most assessments of vibration amplitudes are based on vibration measurements of the dominant, single-axis vibration directed into the hand [ISO 1986;ANSI 1986;BSI 1987].
That is, the largest of the rms acceleration amplitudes along the three orthogonal basicentric axes shown in Figure HI-2 may be used for assessing exposure to hand-transmitted vibration.
Recommendations of the ISO, ANSI, and BSI are derived from studies associated with such tools as chain saws, pneumatic chipping hammers, and hand-held grinders. The level of vibration exposure associated with these tools is characterized not only by the vibration of the tool, but also by the type of coupling that exists between the tool and the hands of the tool operator (e.g., tight grip or axial thrust force), and the length of time the tool is used without interruption. Most studies assume good coupling exists between the tool and hands. Many of the assessment guidelines are based on time-averaged, frequency-weighted rms acceleration levels. Most of the studies indicate that regular daily vibration exposures do not exceed 4 hr per regular 8-hr workday [Brammer and Taylor 1982;Starck and Pyykko 1986;ANSI 1986;ISO 1986].
where a(t) is the instantaneous amplitude of acceleration, and T is the period of time over which a(t) is averaged.
The overall time-averaged intensity of exposure to hand-transmitted vibration varies with such factors as the tool operator's work assignments, work practices, intermittence of exposure to vibration, and length of rest periods between vibration exposures. Thus when measuring vibration to assess the effects of exposure to hand-transmitted vibration, the estimates of total daily exposure should be based on representative vibration measure ments for all of the different operating conditions (e.g., using more than one type of tool) associated with the operator's total work assignments over an 8-hr workday. This approach will usually result in several different sets of 1/3-octave-band center frequencies with different nns acceleration amplitudes for each of the different operating conditions. The total daily time-averaged rms acceleration [cif(rmiS)] for each 1/3-octave-band can be obtained from
a t(rms) r=i Vz (12
)
where a(rms)i ^ the component of rms acceleration with a time duration of T( for the i(fi operating condition
n T, = £ T> r= l
Many of the assessments and recommendations are based on an actual tool use of 4 hr over an 8-hr workday. If the value of Tt in Equation 12 is other than 4 hr, the total daily rms acceleration amplitude can be converted to an equivalent 4-hr acceleration amplitude [at{rms)(4 /j)] by Equation 13 [ANSI 1986;ISO 1986;Wasserman 1987]:
\r m s ) = Tt 4 Vi X a(rms) ^hrs) (13
)
where at{rms) (7y0is the rms value of acceleration given by Equation 12, and Tt is tne total daily exposure time. The acceleration associated with vibration in the three basicentric orthogonal directions in Figure III-2 can be obtained from the following equation:
I Hand-Arm Vibration r 2 2 2 " 1â
xyz (rms) = \_ax{ms) + ay{rms) + dz(rms) J ( 14)
where ax(rms)iS ^ie rms va'ue °f acceleration in the x direction, ay(rms) *s rms value °f acceleration in the y direction, and az(rms) *s rms value °f acceleration in the z direction. When comparing measured tool vibration acceleration levels with recommended limits, the comparison should be made using the acceleration level measured in the dominant basicentric axis.
# D. FACTORS THAT INFLUENCE VIBRATION AMPLITUDES
# Effects of Tool Type
Several factors influence the vibration levels produced by vibrating tools. The first is whether or not it is an impact tool. Vibration acceleration levels related to impact tools are generally higher than vibration levels associated with nonimpact tools. When ap propriate elastomer or similar materials isolate the vibration-generating parts of tools from contact with the hands, the vibration acceleration levels are usually reduced.
# Effects of Tool Operation
Other factors that affect the vibration acceleration levels of tools are associated with the ergonomics of operating the tool and related tool design. For example, a chipping hammer works by means of a reciprocating piston actuated by fluctuating pressure pulses. The vibration is generated by the repeated impact of the piston on the end of the chisel inserted into the hammer and the subsequent impact of the chisel on the workpiece. The fundamental vibration frequency is associated with the repetition rate at which the piston strikes the chisel. There is a vibration frequency at multiple harmonics of the primary repetition rate of the tool. The weight of the hammer also influences the vibration acceleration amplitudes directed into the hand. For similar operations, the heavier hammers appear to direct lower vibration levels into the hand at the tool handle. More of the vibration energy generated by the heavier tools goes into moving the tool mass, leaving less energy directed into the hand at the handle. However, increasing the tool weight may increase the grip force required to use the tool and thus increase vibration transmission to the hand. Increased tool weight could also increase stress on the wrist, elbow, and/or shoulder, which in turn could result in musculoskeletal disorders such as carpal tunnel syndrome (CTS).
Imbalance and repetitive impulses are the primary causes of vibration in chain saws and other tools using gasoline engines as the driving mechanism. Imbalance is associated with the rotating and reciprocating masses of the engine. The primary vibration frequency is directly related to the operating speed of the engine. Repetitive impulses are associated with the motion of the chain on the guide bar and the explosions of the gas-air mixture in the engine. The hand-transmitted vibration associated with these vibration mechanisms can be significantly reduced by properly designing and placing elastomer vibration-isolation pads between the engine and the chain saw handles.
The vibration associated with grinders and similar tools is related to the unbalanced rotating mass of the grinder and to the interaction between die grinder wheel, cup or pad, and the workpiece. If the grinder is well maintained, the vibration associated with the unbalanced rotating mass of the grinder is usually not a problem. The condition of the grinder wheel or cup, however, has a very significant effect on the vibration amplitudes produced. If the wheel or cup is well dressed andkept "in round," the vibration associated with the interaction of the wheel or cup with the workpiece will be at a minimum. If the wheel or cup is not periodically "dressed" during use, it can become "out-of-round" and very rough. This substantially increases the vibration acceleration of a poorly maintained grinder compared with a new grinder [NIOSH 1984].
# Effects of Tool Maintenance
Poor maintenance of vibrating tools significantly influences the vibration acceleration amplitudes that are generated. For example, the vibration acceleration of poorly maintained grinders may be many times higher than the corresponding vibration acceleration of new grinders. Part of the difference can be associated with poorly dressed grinding wheels. As was mentioned above, the use of elastomer vibration-isolation pads in chain saws can be very effective in reducing chain saw vibration directed into the hand. However, these pads must be inspected and replaced periodically.
# Effects of Work Cycle and Work Conditions
The work cycles, work conditions, and work incentives significantly affect the timeaveraged vibration acceleration level associated with many tools. For example, a major use of chipping hammers is for cleaning castings in foundries. In some foundries, the workers clean castings on a piecework basis-the more castings cleaned, the more wages earned. For these situations, the chipping hammers are generally operated at full throttle for periods of up to 4 hr or more in an 8-hr workday [Brammer and Taylor 1982].
Another use of chipping hammers is to fonn propeller blades. For this situation, the chipping hammers are operated at 1/2 to 3/4 throttle for periods of up to 3 hr over an 8-hr workday [Brammer and Taylor 1982]. Typically, grinders are used for an additional 2.5 to 3 hr during the workday. The time-averaged vibration acceleration at the handle of the chipping hammer was 10 to 14 m/sec2 for the hammer operated at 1/2 to 3/4 throttle versus 50 to 190 m/sec2 for the hammer operated at full throttle [NIOSH 1981]. The total time-averaged rms acceleration amplitudes depend on the duration of use and corresponding acceleration associated with the chipping hammer and the grinder.
# Hand-Arm Vibration
# Effects of Coupling between Hand and Tool
Another factor that can influence the transmission of vibration energy produced by vibrating tools is the coupling that exists between the tool and the hands of the operator. Even though the degree of coupling between the hand and a vibrating tool affects the amount of vibration energy transmitted to the hand from the tool, it will not have much effect on the measured vibration acceleration amplitudes produced by the tool. The reason is that the vibrating mass of the tool in contact with the hand is usually much greater than the total effective mass of the hand that is coupled to the tool. In some situations (e.g., electrically driven engraving tools, small riveting guns, and the light-weight handles of small, antivibration hobby chain saws), the mass of the hand may be of the same order of magnitude as the mass of the vibrating tool. For these situations, the degree of coupling between the hand and the tool will have an effect on the vibration acceleration amplitudes measured on the tool.
# E. VIBRATION RESPONSE CHARACTERISTICS OF THE HAND
# Factors Influencing the Vibration Response Characteristics of the Hand
Several factors influence the vibration response characteristics of the hand. These include the following:
• Grip force exerted by the hand around the tool handle • Axial or static force exerted by the hand on the tool • Size of vibrating surface in contact with the hand • Body position associated with using the hand tool • Clothing and gloves worn Of these factors, the effects of grip and axial force are the most important, followed by body position and gloves [Griffin et al. 1982;Goel and Rim 1987].
Although it has been demonstrated that the presence of vibration-related disorders affect an individual's subjective response to and perception of vibration directed into the hand, these disorders do not have a measurable effect on the vibration-response characteristics of the hand [Wasserman et al. 1981]. Radwin et al. [1987] reported that vibration can affect the way operators hold and use tools, which is then reflected in altered work performance and injury risk. With increased vibration, grip force on the tool handle is increased, and tactile sensitivity is decreased.
# V
III. Vibration as a Hazard
# Energy Directed into the Hands
Many vibration assessment guidelines are based on 1/3-octave-band, center-frequencyweighted rms acceleration levels. However, acceleration levels alone do not necessarily represent a true measure of the energy that is directed into the hand. To obtain this information, the coupling between the tool handle must be considered along with the acceleration levels. This can be accomplished by attaching a specially designed fixture to the handle of a vibration tool to measure grip force (coupling) as well as acceleration. A second method is to use the results of acceleration measurements on a tool handle in conjunction with dynamic compliance [Brammer and Taylor 1982;Wasserman et al. 1981].
If the vibration directed into the hand is harmonic in nature or can be broken down into harmonic components, it can be shown that the amplitude of the energy dissipated (ED) in the hand and aim as a result of damping or other dissipative mechanisms is
E d = & L s M < P l ( 1 5 ) 2co4
Vf where co is the frequency in units of radians/second, X is the measured amplitude of acceleration (m/sec ) at (0, Vf is the dynamic compliance (m/N), and is the radians.
Similarly, the energy (E$) that is stored in the hand as kinetic and potential energy, and is consequently transferred back and forth between the hand and vibrating tool handle, is presented by Brammer and Taylor [1982], , and Wasserman et al. [1981] as follows:
ES = * 2cf W (16
)
2(0 Vf
Also of interest is the time rate of change of energy or power transmitted to the hand. The power (WO is
a 1I7 X sin (<D) Vv = ------- or W = (0 Ed (17) 2co Vf
# Hand-Arm Vibration
The power transmitted to the hand and arm is related to the energy that is dissipated in the hand and arm.
# Mathematical Models of the Hand and Arm
The hand-arm system is a very complicated, continuous, nonhomogeneous system that consists of skin, muscle, bone, etc. An accurate model must take all of these components into account. Many investigators have developed models of the hand and arm [Brammer and Taylor 1982;Meltzer et al. 1980;Mishoe and Suggs 1977;Miwa 1968a;Reynolds and Keith 1977;Wassennan et al. 1977;Reynolds and Falkenberg 1984;Starck and Pyykko 1986]. Mechanical impedance or dynamic compliance data or both were used as the basis for developing many of these vibration models. The parameters of many of the models can be related to the physiology of the hand and arm. However, there is no general agreement about which parts of the hand and arm should be described by a model. For example, work reported by Suggs and Mishoe [1977] and Wood and Suggs [1977] supports the idea that the mass elements of a model should represent the respective masses of the fingers, hand, arm, etc. However, the work reported by Reynolds and Keith [1977], Reynolds and Falkenburg [1984], and Wasserman et al. [1977] supports the idea that the mass elements of a model should represent the components of dermis and epidermis of the skin, sub cutaneous tissue, and muscle tissue in the area of the hand that is in direct contact with a vibrating surface. Most models imply that (1) vibration energy directed into the hand at frequencies below 80 Hz is transmitted to and can be perceived in the arm, and ( 2) vibration energy directed into the hand at frequencies above 100 Hz is generally local to the area of the hand in contact with a vibrating surface. These implications are confirmed by vibration transmissibility tests in the hand and arm.
# E
# IV. BIOLOGIC EFFECTS A. HAND-ARM VIBRATION SYNDROME (HAVS)
HAVS comprises a composite of pathophysiologic signs and symptoms that develop over time in workers who use hand-held vibrating tools. Many of the signs and symptoms of HAVS are also seen in other clinical entities such as primary Raynaud's disease, occlusive vascular disease, traumatic injury of hands, proximal vasculature compression, peripheral neuropathies, carpal tunnel syndrome, etc. [Taylor 1989;Taylor andPelmear 1975;Taylor and Brammer 1982;Pyykko and Starck 1986;Wasserman 1987]. The factors listed in Table IV-1 [NIOSH 1983a] must be considered in differential diagnoses for HAVS.
# B. PATHOPHYSIOLOGY OF HAVS
The development of HAVS is a gradual progressive process that may involve years of exposure to hand-arm vibration [NIOSH 1983a]. Some of the etiologic aspects of HAVS have been reviewed by Pyykko and Starck [1986], and Taylor [1988]. A requisite for diagnosis of occupational HAVS is a history of occupational use of vibrating tools such as drills, chipping hammers, grinders, concrete vibrators and levelers, polishers, swagging tools, shoe pound-up tools, caulking tools, fettling tools, clinching and flanging tools, burring tools, rock drills, chain saws, jackhammers, riveting hammers, bucking bars, and jackleg hammers.
In primary Raynaud's disease, the signs, symptoms, and involvements are usually symmetri cal (same areas of both hands involved), whereas in secondary Raynaud's disorders, including HAVS, the involvement is usually asymmetrical [NIOSH 1983a]. Presently, however, no single test is available that will reliably distinguish HAVS from other secondary Raynaud's disorders [NIOSH 1983a;NIOSH 1984;Gemne 1982;Brammer et al. 1986;Pyykko 1986].
The classification of the clinical stages of signs and symptoms of HAVS most widely used in the past is the one suggested by Taylor and Pelmear [1975]. This classification assumes two major pathophysiologic consequences of using vibrating tools: peripheral neural and peripheral vascular involvements. This classification does not specifically distinguish the peripheral neural and peripheral vascular progressive changes as separate entities (Table IV -2).
A revision of the Taylor-Pelmear classification of the stages of HAVS has been proposed by Taylor [Brammer et al. 1986]. This revised classification takes into account the concept
Hand-Arm Vibration Taylor and Pelmear [1975].
Hand-Arm Vibration that the peripheral neural and the peripheral vascular involvements in HAVS may be distinct entities and that the disabilities related to each may progress independently of the other. The revision also recognizes that the tactile sensory deficits can and should be measured and considered independently of the vasospastic episodes (Table IV-3).
At the 1986 Stockholm Workshop, a new staging classification of vibration-induced signs and symptoms was introduced Gemneet al. 1987;Taylor 1987;Taylor 1989]. The Stockholm Workshop staging classification of the peripheral-neural and the peripheral-vascular pathophysiologic effects of hand-ann vibration exposure are considered separately, thus reflecting the concept that they are two clinical entities. In addition, a system is provided for a semiquantitative expression of the extent of the involvement of each finger on each hand. This system provides a mechanism for a quantitative clinical estimate and description of the involvement. The stagings as presented at the Stockholm Workshop are shown in Tables IV-4 and IV-5. It was suggested at the Workshop that this staging classification be used in all future hand-arm vibration studies. A standard staging classifica tion will enhance the comparability of the data.
The signs and symptoms and their time sequence in appearance indicate that vibration affects several components of hand and arm function [Taylor and Brammer 1982;Farkkila et al. 1982;Pyykko et al. 1982aPyykko et al. , 1982bFutatsuka and Ueno 1985;Farkkila 1986]. HAVS may involve, separately or in combination, the (1) peripheral neural system, (2) peripheral vascular system, ( 3) muscles of the hands and arms, ( 4) bones and joints of the hands and arms, and ( 5) central nervous system.
The Russian and Japanese [Griffin 1980;Habu 1984] 3) musculoskeletal, and ( 4) brain stem and neuro psychiatric. The degree of impairment ranges from no change (-), to minimal change (+), to extensive involvement (++++). The possible involvement of the central autonomic nervous system in HAVS was the subject for an international symposium in 1983 [Gemne and Taylor 1983].
A classification for staging the severity of vibration-induced HAVS, including some functional changes, has been proposed in Japan [Okada 1983;Okada and Suzuki 1982].
The major features of the classification are summarized in Table IV Occasional attacks that affect only the tips of one or more fingers 2Occasional attacks that affect the distal and middle (rarely also proximal) phalanges of one or more fingers 3
Frequent attacks affecting all phalanges of most fingers 4As in stage 3, with trophic skin changes in the finger tips ♦Adapted from . 'The Stage is determined separately for each hand. . 'The sensorineural stage is determined separately for each hand. • Use of tobacco, some drugs, and some chemicals Taylor and Brammer [1982] and Brammer [1984] have categorized the factors as physical, biodynamic, and individual (Table IV-7). These factors may vary extensively in amount and combinations from one exposure situation to another and from day to day when using the same tool [Brammer 1984]. Knowledge of HAVS is based mainly on retrospective epidemiologic studies or clinical examinations and comparisons between workers who use and do not use vibrating tools, and who do or do not have symptoms of HAVS. Lack of objective data from controlled laboratory investigations limits the accuracy of any dose-response or risk factor predictions. Taylor [1988Taylor [ ,1989, in reviewing the biological effects of hand-arm vibration, pointed out some of the information gaps in the understanding of the mechanisms involved in the neurological, vascular, and musculoskeletal damage.
# Peripheral Neural Effects
The early symptoms frequently experienced by workers exposed to hand-arm vibration include intermittent attacks of tingling and/or numbness of the fingers with or without pain [Brammer 1984;Taylor and Brammer 1982;Brammer and Taylor 1982;Taylor 1982a;Taylor 1982b;Vines 1984;Pyykko 1986]. On continued exposure, the attacks may become more frequent and the symptoms more severe with decreased tactile sensitivity, decreased temperature sensitivity, and decreased manual dexterity and grip strength [Taylor and Brammer 1982;Brammer et al. 1986;NIOSH 1983a;Farkkilaet al. 1982;Brammer 1984].
The mechanisms involved in the observed peripheral neural changes have not been fully described. In workers who have been exposed to hand-arm vibration on the job and who have developed intermittent peripheral neural symptoms (numbness, tingling, pain, loss of sensitivity), the increased vibration perception threshold may reflect the functional disturb ance of the peripheral nerves, of the sensory nerve endings, or of the mechanoreceptors, including the Pacinian corpuscles [Lundstrom 1986]. Harada and Matsumota [1982] suggested that the peripheral neural effects are a pathophysiologic entity separate from and independent of the circulatory disturbances. This suggestion was based on neural and Brammer [1982J andBrammer [1984]. vascular tests of workers not exposed to vibration, workers who used vibrating tools but had no symptoms, and workers who used vibrating tools and had symptoms of HAVS. Workers with neurophysiologic symptoms compatible with hand-arm vibration syndrome have a decreased sensory nerve conduction velocity from the fingers to the wrist [Alaranta and Seppalainen 1977;Sakurai and Matoba 1986]. These findings are consistent with the concept of a direct pathophysiologic effect of vibration on the peripheral nerves and nerve endings.
On the basis of a study of 245 vibration-exposed subjects with a history of nerve symptoms or evidence of neural injury, Lukas [1982] and Lukas and Kuzel [1971] concluded that the peripheral neural lesions may result from causes other than the direct effect of vibration. Nerve conduction velocity measurements of the fast motor and sensory fibers of the median and ulnar nerves frequently indicated that only one of the nerves tested was involved. In individuals using hand-held vibrating tools, both nerves would be expected to be affected. The authors also observed that conduction velocities in the distal portion of the sensory and motor fibers of the median and ulnar nerves were significantly reduced in the patients with symptoms of vasoneurosis as compared with the patients without vasospastic symptoms. The author concluded that the peripheral neural damage was secondary to the complex damage to the vascular, joint, and muscular systems of the arms and hands (multifactorial). Juntunen et al. [1983] found that nerve conduction velocity was slower and motor nerve latency longer in the patients with vibration syndrome who had neurologic signs of polyneuropathy. The authors stated that these findings provided evidence of a wider neural involvement than just the peripheral nerves.
On the basis of an analysis of data from forest workers, Farkkila et al. [1988] suggested that a large part of the previously diagnosed vibration neuropathies belong to the category of carpal tunnel syndrome (CTS), which is the most common entrapment neuropathy among forest workers. Brammer et al. [1986] evaluated the degradation of vibrotactile and spatial-tactile perception in workers who used hand-held vibrating tools. The vibrotactile perception threshold values in workers with HAVS Stage 1,2, or 3 of the Taylor and Pelmear classification exceeded the values of workers with no vibration exposure by more than 2 standard deviations. On the spatial-tactile resolution test [Carlson et al. 1984], the workers with vibration syndrome had values exceeding the controls by 2 to 4 standard deviations. Brammer et al. [1986] concluded that the neurological signs and symptoms in workers with chronic hand-arm vibration exposure involve both the peripheral nerve fibers and the mechanoreceptors.
Several types of neurophysiologic structures in the skin of the fingers are involved in the sense of touch [Vallbo and Johansson 1984]. The different structures function (fire) in response to different mechanical stimuli. The Pacinian corpuscles, the quick-adapting receptors, and the two types of slow-adapting receptors are the most important mechanoreceptors in the skin that are involved in the sense of touch [Lundstrom 1986]. For the sense of touch as measured by the sharp edges of the aesthesiometer (tactospatial), the slow-acting Type I receptors were more sensitive than the Pacinian corpuscles, the quick-acting receptors, or the slow-acting Type II receptors. Brammer et al. [1986] reported a decrease in the vibrotactile sensitivity that reflected the threshold of the Pacinian corpuscles.
In a biopsy study of 60 fingers with HAVS, Takeuchi et al. [1986] reported a decreased number of axon cylinders and a destruction of the myelin sheath in 90% of the cases. Such histopathologic deterioration could provide the basis for the sensory changes.
Researchers in this field agree that exposure to hand-arm vibration will eventually result in peripheral neural impairment with sensory loss, numbness, and decreased sensory and motor nerve conduction velocities but that the cause-effect mechanisms are not clear [Brammer 1986;Taylor and Brammer 1982;Brammer and Taylor 1982;Pyykko 1986;Ekenvall et al. 1986;Lundstrom 1986;Sarakiet al. 1988;Radwinet al. 1987]. Taylor [1982a] summarized the state of knowledge as follows: "It is not known whether vibration directly injures the peripheral nerves thereby causing numbness and subsequently sensory loss, or whether the para-anesthesia of the hands is secondary to the vascular constriction of the blood vessels causing ischemia... in the nerve-end organs." Lundborg et al. [1987] investigated the value of the vibrotactile sense test in assessing vibration-related neuropathies. The vibration sensation threshold for individuals who had not used vibrating tools was constant at vibration frequencies from 8 to 250 Hz. At 500 Hz, the sensation threshold was higher. For workers who used vibrating tools and had symptoms ranging from intermittent numbness to constant numbness and pain, the vibration sensation threshold increased progressively with higher vibration frequencies. The abnormalities in the vibrogram (sensation threshold) correlated not only with numbness and pain, but also with the occurrence of white finger. The authors concluded that the numbness resulted from a change in the intraneural vascular function. The finger blanching and pain and the numbness all reflect a common peripheral vascular disorder.
# Peripheral Vascular Effects
The earliest signs of peripheral vascular changes in HAVS are the episodic attacks of fingertip blanching. These initial attacks of ischemia usually occur during cold exposure [Taylor and Brammer 1982;Brammer 1984;Pyykko 1986;Wasserman 1987]. With the continued exposure to vibration, the frequency and severity of the episodes of white finger increase until the blanching extends to the base of the fingers and may occur even in warm weather. The time between the first use of vibrating tools and the first appearance of episodic finger blanching (vasospasms) is designated as the latent interval. The latent interval appears to vary with the vibration intensity, as well as with other factors such as the type, model, unique individual characteristics of the tool, material on which the tool is used, tool maintenance, operating speed, operating technique, user characteristics, hand-grip force, push force, hand and arm posture, work/rest regimen, air temperature and moisture, protective hand gear, and clothing [Taylor and Brammer 1982;Brammer 1984].
In one of the early reports, the peripheral vascular symptoms of HAVS were considered to be only a nuisance [Pecora et al. I960]. However, for the individual worker, the effects may seriously interfere with work [Taylor et al. 1977;Pyykko 1986]. Laroche [1976] reported that 10 out of 13 patients with HAVS had to change jobs because of the disabling effects of the disorder.
Although the phenomenon of the vasospastic episodes (sequence of events) has been described and accepted, basic underlying pathophysiologic mechanisms are not understood.
# Hand-Arm Vibration
Nonetheless several have been proposed. The present concepts are built on data derived mainly from epidemiologic and clinical studies.
The sequence of events in the progression of the episodes of blanching appear to involve (1) bouts of digital arterial spasms that become progressively more frequent and prolonged, (2) arterial hypertrophy with an increase in the medial muscular layer of the arterial wall, (3) perivascular fibrosis with increased collagen fonnation, and (4) increased vasoconstric tor sensitivity. The hypertrophy of the arterial smooth muscle may progress until the arterial lumen is partially or completely obliterated [Ashe et al. 1962[Ashe et al. , 1964Pyykko et al. 1982a;Brammer and Taylor 1982;Brammer 1984;Wegelius 1972;Takeuchi et al. 1986]. Biopsies on 60 fingers from 30 patients with HAVS revealed increased thickening of the muscular layer that was severe in 82% and moderate in 15% when compared with 7 biopsies on 3 control subjects. Perivascular fibrosis was found frequently and was severe in 55% and moderate in 37%. Intimal thickening was minimal in 35% and moderate in 7% of the HAVS workers [Takeuchi et al. 1986]. Okada et al. [1987a] in animal experiments observed that vibration resulted in intimal changes in the small arterioles with minimal medial changes. Similar findings were reported by Inaba et al. [1988].
Several etiologic theories have been postulated to account for the observed pathophysiologic changes in the digital arteries, but no single theory can account for all the changes. The mechanisms that could help explain the events seen in HAVS include (1) direct effects of vibration on the digital arteries, (2) effects on the peripheral sensory aspects of the sympathetic nervous control of the peripheral circulation, (3) central neural control, (4) hypersensitivity to chemical mediators (prostaglandins, serotonin, and noradrenalin), and (5) some combination of the above [Brammer 1984;Taylor and Brammer 1982;Azuma and Ohhashi 1982;Gemne et al. 1986]. The use of tobacco has been reported to be an additional risk factor in the development of HAVS in workers who operate noise-producing, hand-held vibrating tools [Miyakita et al. 1987;Bovenzi 1986;Ekenvall and Lindblad 1989]. Ekenvall and Lindblad [1989] measured the levels of nicotine and cotinine in the blood of 111 tobacco users and nontobacco users who did or did not have HAVS as determined by the digital systolic blood pressure after finger cooling. Blood nicotine concentrations in ng/ml were 0.8 in nontobacco users, 14.5 in cigarette smokers, 10.8 in snuff users, and 16.3 in users of other tobacco products; the cotinine levels were 0.7,196, 252, and 210 ng/ml, respectively. When the 111 workers were grouped according to the Taylor* Pelmear stages of HAVS, the blood levels of cotinine in ng/ml were 5.7 for stages 0T and 0V, 8.7 for Stages 1 and 2, and 11.8 for Stages 3 and 4; the cotinine levels were 124, 117, and 171, respectively. The digital systolic blood pressure (as a percent of the arm systolic pressure during finger cooling at 15"C) was significantly lower in the tobacco users: 52% for nonusers, 29% for smokers, and 45% for snuff users. On the basis of their study results and a survey of the relevant literature, the authors concluded that "habitual use of tobacco aggravates the symptoms of VWF disease and has a direct effect on the results of a cold provocation test in this disease" [Ekenvall and Lindblad 1989].
Obi iterative histopathologic changes reported in biopsies and arteriograms of the peripheral arterioles in some workers with HAVS appear convincing. But whether these changes are relevant histopathologic factors concerned with episodic finger blanching has been ques tioned on the basis of physiologic blood flow studies . Using venous occlusion plethysmography before and after induced vasodilation, these authors observed that the maximum blood flow after vasodilation was similar in the control subjects who were not exposed to hand-arm vibration and in vibration-exposed workers with advanced symptoms of HAVS. They reasoned that if the vessel lumen were narrowed by occlusive muscle hypertrophy, then blood flow would not be normal when maximum vasodilation was induced. Arteriograms were not taken; consequently, evidence of whether these subjects actually had arterial occlusion was lacking.
Regardless of the mechanisms involved in episodic finger blanching, the primary response concerns the digital arteries. During ischemic attacks, arterial blood flow to the affected segments of the fingers is reduced or completely shut off by contraction of the smooth muscles in the medial arterial wall. The episodic arterial muscle contractions could reflect an increased sympathetic nervous activity or an increased sensitivity of the arterial muscula ture (vasomotor tone) to local factors (chemical mediators including prostaglandins, serotonin, and noradrenalin) [Brammer 1984;Azuma and Ohhashi 1982;Bovenzi 1986J. Repeated contractions of the arterial muscles could lead to muscle hypertrophy. Gradual occlusion of the arterial lumen could result from intimal thickening. Stimulation of the vascular smooth muscle by adrenergic nerves constricts the digital artery lumen. Vasodila tion occurs passively in the absence of vasoconstrictive action [Taylor and Brammer 1982].
The episodic ischemic attacks could be inappropriate pathophysiologic vascular responses to the vibration forces transmitted to the hands of the workers using vibrating tools. The medial muscle hypertrophy could be a histopathologic response to the sustained contraction of the vascular muscles. Any intimal changes could be a direct response to the vibration or a response to some changes in the blood chemistry [Taylor and Brammer 1982;Brammer 1984]. If the sympathetic nerve supply to the digital arteries is cut at the stellate ganglion, episodic blanching of the fingers induced by cold will return after an initial dilation of the digital arteries, which could last 3 to 4 months. This would imply that local chemical mediators may be at least partially involved.
A series of studies on workers with or without exposure to vibration and vibration-exposed workers with or without HAVS indicated that the finger vasospasm in the vibration-exposed group is the result of chronic stimulation of the mechanoreceptors in the fingers by the vibration. The receptors then serve as the sensory receptor link to the sympathetic nervous system with the effectors being the smooth muscle of the medial layer of the finger arterioles [Hyvarinen et al. 1973;Pyykko 1974b;Farkkila et al. 1985;Farkkila and Pyykko 1979;Pyykko et al. 1982a;Koradecka 1977].
Although the findings in these studies support the concept that the vibration sensory receptors contribute to HAVS by initiating excessive afferent impulses in the sympathetic reflex involving the peripheral vascular musculature, the exact etiologic (pathophysiologic) mechanisms are not fully known [Pyykko et al. 1982a]. Generally, in experimental studies when the hand is stimulated by vibration, a vasoconstriction occurs in the fingers. In workers who have not used vibrating tools, the vasoconstriction response to vibration stimuli was mild (about 10% have a strong response). Among workers who have used vibrating tools occupationally, about 40% exhibited a strong vasoconstrictive response, and 40% had a mild response similar to that of the controls [Pyykko et al. 1982a]. This suggests that chronic vibration stimulation increases the sensitivity of the mechanoreceptors to the vibration stimuli and increases the level of afferent impulses to the central nervous system with resulting increased reflex-sympathetic vasoconstriction. The prolonged contraction of the vascular muscles could result in the hypertrophy of the medial musculature and increased narrowing of the vessel lumen [Ashe et al. 1962;Ashe and Williams 1964;Takeuchi et al. 1986].
# Skeletal Muscle Force and Muscle Fatigue
The subjective complaints of deterioration of hand grip force and muscle strength in workers using vibrating tools have been mentioned in many of the studies of HAVS. This aspect of HAVS has received specific emphasis in studies in Japan [Miyashita et al. 1983] and in Finland [Farkkila et al. 1982;Farkkila et al. 1980;Farkkila et al. 1979;Farkkila 1978]. Among Japanese chain saw operators with more than 2,000 hr of chain saw use, about 28% reported symptoms of decreased grip force and muscle strength. These symptoms were reported by 20% of Finnish chain saw operators with more than 5,000 hr of chain saw use.
The Finnish group measured maximum grip strength and rate of development of muscle fatigue with or without acute vibration exposure under controlled laboratory conditions. Lumberjacks with or without symptoms of diminished grip force and with or without symptoms of HAVS were compared with a control group who had no occupational vibration exposure. In the group of lumberjacks with HAVS, some experienced only episodes of white finger without ever experiencing decreased grip force; some reported finger numbness without decreased grip force; and some experienced decreased grip force and white finger and/or finger numbness.
The data indicated the following relationships:
• Grip force was reduced in lumberjacks throughout the entire muscle fatigue curve when the hand was exposed to vibration.
• Grip force was reduced more in workers who reported numbness, reduced muscle strength, or muscle pains.
• Acute vibration exposures reduced grip force more in those with symptoms than in those without symptoms of white finger.
• Reduced muscle strength was present in lumberjacks with 5,000 or more hours of total chain saw operating time.
• Muscle force was reduced and the prevalence of symptoms increased when total exposure times exceeded 5,000 hr.
• Lumberjacks with white finger used a stronger grip force when using the chain saws than did those who did not have white finger.
• A dose-rcsponse relationship seemed to exist between diminished muscle force and vibration exposure.
• Grip strength decreased as a function of age in vibration-exposed and unexposed groups.
• Muscle strength fatigue curve for the chain saw operators was similar to that of unexposed workers.
• Muscle strength for controls and for chain saw operators was the same when the hand was not exposed to vibration.
• Muscle strength of the controls was similar to that of the lumberjacks who had no symptoms of white finger.
The pathophysiologic mechanisms involved in the reduced muscle strength aspect of HAVS are not clear. Some of the possibilities include neurogenic muscle dysfunctions, direct mechanical effect on the muscle fibers, biochemical alterations in the muscle intracellular substances, and neuropathies. Whatever the mechanism(s) involved, diminished grip force can progress to the point of significant occupational disability [Faikkila et al. 1982].
# Bone Cysts
Degenerative changes in the bones of the fingers and wrists of workers using vibrating hand-held tools have been reported [McLaren and Camb 1937;Wilson et al. 1967]. The changes observed were mainly cysts, vacuoles, and areas of décalcification. It is clear, however, that bone cysts were not observed as being specific to HAVS [Casciu et al. 1968;Kumlin et al. 1971]. Kumlin et al. [1973] found that 7 of 35 lumberjacks (20%) studied showed radiographic presence of cysts and vacuoles in the metacarpal bones or the phalanges or both. These seven lumbeijacks had used chain saws for 10 years or more and had one or more subjective symptoms typical of HAVS.
Radiographs of the hands were specifically included in a British health survey of occupa tional chain saw operators . The objective of this investigation was the association, if any, between the presence of wrist and hand bone cysts and the occupational exposure to hand-arm vibration. X-rays of the hands were taken of 165 lumberjacks and 162 controls (manual laborers in the same environment as the lumberjacks). Each X-ray was read independently by three radiologists. Based on positive findings by two or more of the three readers, the incidence of vacuoles was 44% in the lumberjacks versus 33% in the controls. The difference between the incidence of vacuoles in lumberjacks and in other workers who did not use vibrating tools was not statistically significant.
In a 1977-78 study of Italian shipyard workers, 169 caulkers who worked with vibrating tools were compared with 60 welders and electricians who were not exposed to hand-arm vibration [Bovenzi et al. 1980]. Only the workers who used hand-held vibrating tools were X-rayed. In the caulkers, 51% exhibited HAVS in Stages 1 and 2 of the Taylor and Pelmear classification. Only 7% of the control group showed similar signs and symptoms. Bone cysts, vacuoles, or both were reported in the hand/wrist bones of 31% of the caulkers. No X-ray data from controls were available for comparison. This is similar to the incidence of bone cysts-vacuoles that reported in lumberjacks and controls not exposed to vibration.
A NIOSH study compared 205 foundry and shipyard chipping and grinding workers with 63 manual workers in the same industries who did not use vibrating tools [NIOSH 1984].
The frequency, location, and size of cysts and vacuoles in the hand and wrist bones as inicated on X-rays were compared. The films were read independently by two radiologists. The vibration-exposed and the control workers showed no statistical dif ferences in frequency, location, or size of cysts and vacuoles. This study, with its adequate control group, supports the concept of that cysts and vacuoles occur in the hand and wrist bones of workers performing manual work but that these changes are not necessarily vibration related. The presence of bone cysts in workers exposed to vibration is therefore not a useful, objective diagnostic criterion for HAVS.
Gemne and Saraste [1987] surveyed the literature (125 published articles) to evaluate the evidence for and against radiological demonstrable effects of vibration on the bones and joints of the arm and hand. The authors concluded that the evidence does not support a "causal relationship between vibration exposure and the formation of bone cysts and vacuoles."
# Central Nervous System
The inclusion of the central nervous system in the hand-arm vibration syndrome has been postulated by USSR and Japanese researchers [Griffin 1980;Matoba et al. 1975aMatoba et al. , 1975bHabu 1984]. The etiology of the "systemic effects" involves the concept that hand-arm vibration can impair central nervous system function through damage to the autonomic centers in the brain [Matoba et al. 1975a[Matoba et al. , 1975b.
The symptomatology alleged to be associated with vibration-induced central nervous system disturbances includes anxiety, depression, insomnia, headache, palmar sweating, vertigo, irritability, emotional instability, etc. [Habu 1984J. These signs and symptoms, derived from I a IV. Biologic Effects statements made by the subjects being examined, usually have not been objectively assessed and are not specific to a single stressor such as vibration. Gemne and Taylor [1983], in summarizing the conclusions from an international symposium on hand-arm vibration and the central nervous system, stated that the present data do not support the hypothesis that exposure to hand-arm vibration may cause damage to the autonomic centers in the brain. In a study of 78 HAVS patients, Taylor et al. [1986] found no evidence to support an involvement of the central nervous system in HAVS.
# Other Responses
Several other responses, whose significance in the identification and description of HAVS is unclear at present, may have some diagnostic value. These include the following: a. In comparing the grip strength of nonvibration-and vibration-exposed workers, Miyashita et al. [1983] observed that grip strength progressively decreased as the total vibration exposure time increased: 52.5 kg grip strength in controls; 46.5 kg (-11.5%) in workers with up to 2,500 hr of total vibration exposure time; 40.1 kg (-24%) in wokers with more than 7,500 hr. Because of the wide differences in grip strengths among people, individual previbration-exposure values would be needed for grip strength to be a reliable diagnostic tool.
b. In the same control and exposure groups, sarcoplasmic enzyme levels (aldolase [ALD], creatinine phosphokinase [CPK], and lactic dehydrogenase [LDH]) in the exposure group increased over controls: 6% and 30% for ALD, 23% and 20% for CPK, 15% and 13% for LDH for <2,500 and >7,500 hr of vibrating tool use, respectively [Miyashita et al. 1983]. Adrenaline and noradrenalin in the urine of the exposed group were also measured and, when expressed as ng/mg creatinine, increased over control values by 260% and 269% for adrenaline, and 12% and 11% for noradrenalin for vibration exposures up to 4,000 hr and longer than 12,000 hr, respectively. Whether these changes are a general stress response or are specific to vibration stress remains to be proved.
c. It has been suggested that whole blood viscosity may play a role in HAVS and might be a useful tool in diagnosing HAVS between attacks. Whole blood viscosity in workers with HAVS was reported to be statistically significantly higher than in workers without HAVS (p<0.01) [Okada et al. 1982;Okada et al. 1987b]. However, Inaba et al. [1988] found no change in blood viscosity, hematocrit, cholesterol, and high density lipoproteins in vibration-exposed animals.
d. Okada et al. [1983] postulated a possible role of enhanced peripheral vasoconstriction caused by the exaggerated response of alpha adrenergic receptors in the arterial smooth muscles during attacks of white finger in workers with HAVS. These authors reported that during the cold provocation test (CPT), the plasma level of cyclic guanosine 3', 5'monophosphate (cyclic GMP) was increased to 170% over pretest levels in workers with HAVS. The cyclic GMP levels did not increase in control subjects during the CPT. Without the CPT, the control and HAVS subjects had similar levels of cyclic GMP.
Phentolamine administered before and during the CPT and atropine injected subcutaneously immediately before the CPT inhibited the plasma rise in cyclic GMP during the CPT. The authors suggested that in individuals with HAVS, the increase in endogenous noradrenalin was enough to cause a significant increase in cyclic GMP in response to cold exposure (the CPT). This increased cyclic GMP response could result in an enhanced alpha-adrenergic response and a peripheral vasoconstriction.
e. An increased digital blood vessel reactivity to cold was reported by Bovenzi [1986]. Brown et al. [1988] measured radial digital artery blood flow in workers with and without HAVS before and after 20 min of chipping hammer use. Blood flow was measured by a 20-MHz, pulsed, ultrasonic Doppler velocimeter. Digital artery blood flow rate following the 20-min use of the chipping hammer increased substantially in the HAVS group, but there was little change in the control group. Pre-exposure flow rates were approximately equal in the control group and those with Stage 2 HAVS. The authors suggest that the 20-MHz Doppler velocimeter might be a valuable indicator tool for studying HAVS pathology.
# C. EPIDEMIOLOGIC STUDIES
Epidemiologic studies of workers using hand-held vibrating tools have been conducted in Europe, North America, and Asia. Workers using gasoline-powered chain saws in forestry have been studied most frequendy, followed by studies of workers using pneumatic chipping hammers in foundries, shipyards, and quarries, and pneumatic jack-leg drills in mining. These have been cross-sectional studies except for a few longitudinal studies of chain sawyers in the United Kingdom, Finland, and Japan. Cross-sectional studies examine a group of workers using hand-held vibrating tools in an industry at one particular time to determine the proportion of workers with HAVS (i.e., the prevalence of HAVS). Lon gitudinal studies of HAVS examine a group of workers at more than one point in time. The prevalence of HAVS is usually expressed as the prevalence of specific symptoms of HAVS such as vascular or neurologic symptoms. Sometimes studies report the latency of HAVS symptoms, the years of exposure to hand-arm vibration from the tool, and the hand-arm vibration acceleration level of the tool. The latency of a HAVS symptom is defined as the time from first use of a tool to the first appearance of the symptom. in the form given in the cited article. A method of standardization (presented in Appendix A) was applied to the acceleration measurements of hand-arm vibration if they were reported in a study. This method of standardization makes the measurements comparable with each other.
# Cross-Sectional Studies of HAVS
The prevalence of vascular symptoms of HAVS in Table IV-8 ranged from 6% to 100%.
To evaluate the relative significance of these prevalence values, they must be compared with the background rate of vascular symptoms among worker populations that have not been exposed to hand-arm vibration. Nineteen of the studies reported the prevalence of vascular symptoms among a group of control workers who had not been exposed to hand-arm vibration and had worked at the same site as the exposed workers [Allingham and Firth 1972;Hellstrom and Andersen 1972;Taylor et al. 1974;Pelmear et al. 1975;Taylor et al. 1975a;Matsumoto et al. 1977;Chatterjee et al. 1978;Bovenzi et al. 1980;Matsumoto et al. 1981;Moon et al. 1982;Patri et al. 1982;Pelnar et al. 1982;Theriault et al. 1982;Brubaker et al. 1983;Behrens et al. 1984;Harkonen et al. 1984;Walker et al. 1985;Brubaker et al. 1986;Zeng-Shun et al. 1986]. The prevalence of vascular symptoms among these 19groups of control workers ranged from 0% to 14% with a mean prevalence of 5.4% and a median of 4%.
Most of the studies listed in Table IV-8 had prevalence rates of vascular symptoms that were well above background rates. More than half of the studies had HAVS prevalence rates that were greater than 40%. Epidemiologic studies of HAVS clearly confirm an association between vascular symptoms and exposure to hand-arm vibration from hand-held vibrating tools and workpieces. These studies also provide clues to HAVS prevention. A study showing a relatively low prevalence of vascular symptoms or a relatively long latency of vascular symptoms may provide such clues. In addition, some of the studies in Table IV-8 had tool vibration measurements taken at the time of the cross-sectional medical evaluations, and these studies indicate the exposure-response relationship between HAVS and hand-arm vibration.
Nine of the studies in Table IV -8 |Taylor et al. 1975a;Iwata et al. 1980;Behrens et al. 1982Behrens et al. , 1984Moon et al. 1982;Futatsuka 1984;Harkonen et al. 1984;Walker et al. 1985;Zeng-Shun et al. 1986] reported prevalence rates of vascular symptoms among the exposed workers that were nearly within range of the prevalence rates for the control group (i.e., from 0%to 14%). The study by Iwata etal. [1980] found an 8% prevalence of vascular symptoms among chain saw operators. A control group was not included in this study. The low prevalence rate may have been due to the high proportion (75%) of chain saw operators in this study who had less than 10 years of exposure to hand-arm vibration from chain saws, or it may have been that the use of antivibration chain saws by 1980 reduced exposure. Although the authors did not report the latency of vascular symptoms for this group of chain saw operators, the average latency for other studies of chain saw operators in Table IV-8 ranged from 4 to 13 years. Thus the group of chain saw operators in the study by Iwata et al. [1980] probably had not experienced sufficient exposure for all cases of HAVS (with vascular symptoms) to manifest themselves. Harkonen et al. [1984] observed the relatively low 18% prevalence of vascular symptoms of among a group of chain saw operators. A control or reference group of peat bog workers were examined and were found to have a 3% prevalence of vascular symptoms. The authors reported that the difference in prevalence between the exposed and control groups was statistically significant (pcO.OOl).
In the study of workers using gasoline-powered brush saws, Futatsuka [1984] reported a 6% prevalence of vascular symptoms, the lowest reported prevalence in Table IV-8. No control group was examined in this study. Among the exposed group, the mean duration of exposure to brush sawing was 7 years and the mean latency of vascular symptoms was 6.4 years.
Because the mean exposure time was greater than the mean latency, the prevalence of vascular symptoms in this group of brush saw operators would not be likely to increase appreciably with further exposure. The author reported some factors that probably con tributed to the low prevalence of vascular symptoms in these brush saw operators. Workers used the brush saws for 4 to 5 months a year, during the warmer season of May to September. Also, since 1970, the use of the brush saw was limited to 2 to 3 hr/day. Before that date, workers were using the brush saws up to 6 hr/day. The effect of limiting the number of hours of brush saw use per day was revealed in the difference between the prevalence of vascular symptoms in workers who started using the brush saws in 1961 and 1962 (12% peak prevalence from 1961 to 1980) and workers who started in 1969 and 1970 (0% prevalence from 1969 to 1980).
A relatively low prevalence of vascular symptoms among chipping and grinding workers was reported by Behrens et al. [1982Behrens et al. [ , 1984. In this study of workers using pneumatic chipping hammers and grinders at a shipyard, the prevalence of vascular symptoms was 19%. A control group working at the shipyard was included in this study, and the prevalence of vascular symptoms in the control group was 0%. The difference in prevalence rates between the exposed and control groups was statistically significant (p<0.0001) [Wasserman et al. 1982]. In this group of chipping hammer and grinder operators, the prevalence would probably increase over time because the mean exposure time (12 years) was less than the mean latency for vascular symptoms (17 years).
Four other studies in Table IV-8 showed relatively low prevalence rates of vascular symptoms [Taylor etal. 1975a;Moon etal. 1982;Walker etal. 1985;Zeng-Shunetal. 1986].
All of these studies reported the prevalence of vascular symptoms in a control group of workers. The study of pedestal grinders by Taylor et al. [1975a] found an 11% prevalence in the exposed group and 4% in the control group. The authors did not compare the prevalence statistically. Also, the authors did not report a mean exposure time for this group of pedestal grinders, although the mean latency of vascular symptoms was reported as 14 years. In the study by Moon et al. [1982], the prevalence of vascular symptoms among anthracite miners using pneumatic rock drills was 13%, whereas the prevalence in the control group was 0.9%. The statistical comparison of prevalence rates was significant (p<0.05). Similarly, Zeng-Shunet al. [1986] reported that the prevalence of vascular symptoms among TV. Biologic Effects railroad woikers using riveters, chipping hammers, and grinders was 13%, whereas the control group prevalence was 1.6% (pcO.OOl).
The Walker et al. [1985] study of workers in the gas industry who used pavement breakers is the only study in Table IV-8 in which the difference in prevalence between the exposed and control groups was not statistically significant. The prevalence rates of vascular symptoms in the workers using pavement breakers and the workers not exposed to hand-arm vibration were both 10%. After adjustment for differences in the ages of the exposed and control groups, the age-adjusted prevalence was 12% in the exposed group and 10% in the control group. This comparison was not statistically significant. The authors did not report the latency of vascular symptoms, but the prevalence of vascular symptoms among workers using the pavement breakers for 1 to 5 years was 9%, whereas the prevalence in workers using the pavement breakers more than 20 years was 18%. Two factors may have contributed to the nonsignificant and relatively low prevalence of vascular symptoms in this group of pavement breaker operators. First, the average latency of vascular symptoms may have been longer than latencies recorded for exposures to other tool types because the prevalence among the exposed workers did not increase much above that of the control group until the exposed workers had more than 20 years of exposure. Second, the prevalence of vascular symptoms in the control group was relatively high (10% prevalence in this control group compared with a mean prevalence of 5.4% in 19 control groups from Table IV -8).
A recent survey of workers who used impact power tools indicated a prevalence rate of 29% for numbness and tingling of the fingers and 17% for white finger. The workers used the impact tools for an average of 23% of the workday. Frequency-weighted acceleration levels exceeded 12 m/sec2 for all measurements, and they averaged approximately 24 m/sec2 for chipping hammers and rammers. The mean cumulative exposure for each worker over a working lifetime was nearly 4,000 hr. The 17%-to 29%-prevalence of signs and symptoms of HAVS occurred even though the daily tool use time was only about 2 hr [Musson et al. 1989].
Forty-four studies listed in Table IV-8 included some information about the latency of vascular symptoms among exposed workers. Thirty-three of these 44 studies reported the mean latency of vascular symptoms. These 33 mean latencies ranged from 0.7 to 17 years, with a mean value of 6.3 years. When compared with the range and mean values of the 33 mean latencies, four studies [Pelmear et al. 1975;Taylor et al. 1975a;Olsen and Nielsen 1979;Behrens et al. 1982Behrens et al. ,1984 reported relatively long mean latencies. A relatively long latency of vascular symptoms suggests the possibility that some workers may never show vascular symptoms. Olsen and Nielsen [1979] found a 13-year mean latency for vascular symptoms among 18 (out of 20 total) workers using pneumatic chipping hammers at a granite quarry. Despite the relatively long latency, the prevalence of vascular symptoms was 72% (13/18). The high I Hand-Arm Vibration prevalence is expected because the mean duration of exposure (20 years) for the workers was greater than the mean latency. For the 18 quarry workers, the individual latencies varied from 0 to 27 years. A latency of 0 years may indicate that this quarry worker had vascular symptoms before starting to use the chipping hammer at this quarry. The next four lowest latencies for individual workers were 2,4, 7, and 7 years. Thus the individual variation in onset of vascular symptoms shows that all workers in this group could not be protected by limiting the years of exposure.
In a study of shipyard workers using chipping and grinding tools [Behrens et al. 1982[Behrens et al. ,1984, the mean latency of vascular symptoms was 17 years, with a range of 4 to 35 years. Eleven shipyard workers had vascular symptoms, and 5 of these 11 workers had latencies of less than 10 years. At the high end of the range, 2 of the 11 workers had latencies greater than 30 years. Therefore, the mean latency was relatively long among these shipyard workers because of the wide variation in individual latencies, as was also shown in the study by Olsen and Nielsen [1979].
The Pelmear et al. [1975] study of hand grinders found a 13.7-year mean latency of vascular symptoms, and the Taylor et al. [1975a] study of pedestal grinders found a 14-year mean latency. Neither of these studies reported the range of latencies or individual latency values. The mean exposure time (19 years) for workers using hand grinders in a foundry [Pelmear et al. 1975] was greater than the mean latency (13.7 years), which resulted in a substantial 35% prevalence of vascular symptoms. Workers using pedestal grinders in a foundry [Taylor et al. J 975a] had an 11% prevalence (and a 14-year mean latency), but the authors did not report the average years of exposure. As a result, die relationship between the latency, the years of exposure, and prevalence in this group of workers is not known.
Vibration measurements were reported for 23 of the studies listed in Table IV-8. These 23 studies are ranked in Table IV-9, in descending order, from highest to lowest hand-arm vibration acceleration level. The prevalence of vascular symptoms, the tool type, and the publication reference are also repeated in Table IV-9. The 23 hand-arm vibration accelera tion levels in Table IV-9 range from 10 to 2,014 m/sec2, and the mean and median values were, respectively, 312 and 195 m/sec . The relationship between the hand-arm vibration acceleration level and the prevalence of vascular symptoms for these 23 studies was tested for linearity by calculating a correlation coefficient. The correlation coefficient was 0.67 and was statistically significant at the 1% level (p<0.01). Thus the prevalence of vascular symptoms tends to increase as the hand-arm vibration acceleration level increases for these 23 studies.
In general, the studies in Table IV-9 that showed hand-arm vibration acceleration levels greater than the median acceleration level for these 23 studies (195 m/sec2) also showed prevalence rates of vascular symptoms greater than 40%. Only the Bovenzi et al. [1980] study deviated from this trend. Also, in general, the studies in Table IV-9 with acceleration levels less than or equal to the median acceleration level had prevalence rates of less than Taylor et al. 1984Oliver et al. 1979Taylor et al. 1981Bentley et al. 1982Agate et al. 1946Agate 1949Matsumoto et al. 1979Chatterjee et al. 1978Robert et al. 1977Matsumoto et al. 1977, 1979Behrens et al. 1984Wasserman et al. 1984Bovenzi et al. 1980Walker et al. 1985Pelmearetal. 1975Taylor et al. 1975cStarck et al. 1983Iwata 1968 (continued) See footnotes at end of table. (Iwata [1968]; Pelmear et al. [1975]; Starck et al. [1983];and Brubaker et al. [1986]) did not follow this trend.
In the Bovenzi et al. [ 1980] study of shipyard workers using chipping hammers and grinders, the hand-arm vibration acceleration level was 205 m/sec and the prevalence of vascular symptoms was 31%. The authors did not report the latency of vascular symptoms for those shipyard workers with symptoms. They did report that the mean duration of exposure to hand-arm vibration was 7.3 years for the 169 shipyard workers studied, and that 46% had been exposed for 5 years or less and 44% for 6 to 10 years. Also, in this study, the mean duration years of exposure for shipyard workers with vascular symptoms was 10.2 years, whereas the mean duration of exposure for shipyard workers without vascular symptoms was 6.1 years. Thus at least 46% of the shipyard workers studied had been exposed for fewer years (i.e., <6) than the mean years of exposure for workers with vascular symptoms (approximately 10 years). These results indirectly indicate that the prevalence of vascular symptoms in the group of shipyard workers studied by Bovenzi et al. [1980] would probably increase over time and with further exposure.
Two other studies in Table IV-9 that deviate from the trend of a linear relationship between hand-arm vibration acceleration levels and prevalence of vascular symptoms are the pedestal grinder studies of Pelmear et al. [1975] and Starck et al. [1983]. For both of these studies, the prevalence of vascular symptoms was exceptionally high (96% for Pelmear et al. [1975] and 100% for Starck et al. [1983]). The authors for both of these studies attributed the high prevalence rates to the use of zirconium wheels on the pedestal grinding machines because the prevalence of vascular symptoms increased markedly in their study groups when wheels of "softer" material were replaced by "harder" zirconium wheels. The Taylor et al. [1975a] study of pedestal grinders in Table IV-9 reported a relatively low prevalence (11%), an average acceleration level of 100 m/sec2, and the use of "soft" wheels on the pedestal grinding machines. The only other study of pedestal grinders in Table IV-9 (by Agate et al. [1946]) did not specify the type of wheels used. Brubaker et al. [1986] found that 45% of hard rock miners using jack-leg drills had vascular symptoms but that the hand-arm vibration acceleration level for the jack-leg drills was frequency weighted at 20 m/sec2, a relatively low acceleration level. Acceleration levels for jack-leg drills were reported for four other studies in Table IV-9; the levels were all greater than 100 m/sec2, and for three of these studies, the levels were greater than 300 m/sec2. Brubaker et al. [1986] measured the jack-leg drills "under actual drilling conditions at the mine sites according to guidelines specified in ISO 5349." The authors pointed out that ISO 5349 [ISO 1986] suggests that 50% of the workers exposed to a frequency-weighted vibration level of 20 m/sec2 will develop vascular symptoms after a 3-to 5-year exposure. Therefore, a 45% prevalence of vascular symptoms may not be unexpected for this group of workers. Brubaker et al. [1986] did not compare their measurements of jack-leg drills to those of other investigators and thereby offered no explanation for the relatively low acceleration levels they reported.
# I
# Hand-Arm Vibration
5349 [ISO 1986] suggests that 50% of the workers exposed to a frequency-weighted vibration level of 20 m/sec2 will develop vascular symptoms after a 3-to 5-year exposure time. Therefore, a 45% prevalence of vascular symptoms may not be unexpected for this group of workers. Brubaker et al. [1986] did not compare their measurements of jack-leg drills to those of other investigators and thereby offered no explanation for the relatively low acceleration levels they reported.
The study by Iwata [1968] shows a similar result to that of Brubaker et al. [1986]. For workers using jack-leg drills, Iwata [1968] found a relatively high prevalence of vascular symptoms (72%) but a below-average hand-arm acceleration level (121 m/sec2). Iwata's study [1968] was reported earlier than the other studies of jack-leg drills in Table IV-9. He could not compare his hand-arm vibration measurements with other studies of jack-leg drills, and he did not perform the measurements according to international standards recommended during the late 1960s.
# Longitudinal Studies of HA VS
Longitudinal studies of workers exposed to hand-arm vibration demonstrate the effect that lowering the acceleration level of a hand-held vibrating tool has on the prevalence of HA VS. Three longitudinal studies have been conducted; all of them concern forestry workers using gasoline-powered chain saws. Tables IV-10, IV-11, and IV-12 summarize the longitudinal studies of chain saw operators in the United Kingdom, Finland, and Japan, respectively. Neither a longitudinal nor a cross-sectional study of chain saw operators has been done in the United States.
Gasoline-powered chain saws in the 1950s were large and difficult to maneuver, and their use was limited to 1 to 2 hr per day. In the 1960s, technical improvements in the design of chain saws allowed their use to be extended to 4 to 6 hr per day. By the early 1970s, initial reports of HAVS among chain saw operators were made public. In the early 1970s, chain saws were redesigned to lower the vibration acceleration levels. These saws are called antivibration chain saws. By the 1980s, the prevalence of HAVS among chain saw operators had been reduced.
Table IV-10 presents a summary of the longitudinal studies of antivibration chain saw operators in the United Kingdom reported by Taylor and co-workers (Taylor et al. 1974(Taylor et al. , 1975a(Taylor et al. , 1975b(Taylor et al. , 1975c(Taylor et al. , 1977Riddle and Taylor 1982]. An original group of 46 forestry workers using gasoline-engine-powered chain saws was followed from 1970 to at least 1981. In 1970, the prevalence of vascular symptoms in this group was 85%. Antivibration chain saws were introduced in 1973, and by 1975, 73% of the 44 remaining chain saw operators had vascular symptoms. In 1981,28 of the original 46 chain saw operators were still working in forestry, and 46% of these workers had vascular symptoms. Taylor and co-workers [Riddle and Taylor 1982] noted that some workers had recovered and no longer had vascular symptoms after the introduction of antivibration chain saws. Also in 1981,18 chain saw operators who had worked exclusively with antivibration chain saws [1974,1975a, 1975b, 1975c, 1977 Pyykko et al. [1978Pyykko et al. [ , 1982bPyykko et al. [ , 1986b. *Hand-arm. Denotes data not available from articles cited. Hand-Arm Vibration were examined and were found to have a 17% prevalence of vascular symptoms.
Hand-arm vibration acceleration levels for chain saws measured before the introduction of antivibration designs ranged from 150 to 350 m/sec2, whereas antivibration chain saws ranged from 15 to 50 m/sec .
Pyykko and co-workers [Pyykko 1974aand Pyykko et al. 1978, 1986b in Finland followed 66 forestry workers using gasoline-powered chain saws from 1972 until 1983 (see Table IV -11). The prevalence of vascular symptoms in this group was 34% in 1972 and reached apeak of 38% in 1975. Antivibration chain saws were introduced in the mid-1970s, and the prevalence of vascular symptoms in the study group of 66 chain saw operators had decreased to 5% by 1983. Hand-arm vibration acceleration levels on chain saws measured A longitudinal study of forestry workers using gasoline-engine-powered chain saws in Japan was conducted by Futatsuka andUeno [1985, 1986]. Forestry workers employed by the Japanese government in national forests have been examined on a regular basis since 1965, and results of these examinations have been reported through 1980. Chain saw operators in this study were grouped according to the year when they first began using a chain saw (see Table IV -12). The peak prevalence of vascular symptoms for chain saw operators who began chain saw use in 1958 and 1959 was 63%. For chain saws measured in 1966 (the earliest year measurements were available), the vibration acceleration level ranged from 111 to 304 m/sec2. The peak prevalence for chain saw operators who began chain saw use in 1968 and 1969 was 22%. For nonantivibration chain saws measured in 1970, acceleration levels ranged from 49 to 105 m/sec . The peak prevalence for chain saw operators who began working in 1974 and 1975, after the introduction of antivibration chain saws, was only 2%. For antivibration chain saws measured in 1975, acceleration levels ranged from 10 to 33 m/sec2.
The Japanese government in the early 1970s began restricting the number of hours per day that chain saws could be operated. Between 1970 and1975, chain saw use was limited to 2 hr/day for the national forestry operations. Futatsuka andUeno [1985,1986] reported that of the 185 chain saw operators who began using chain saws in 1972 and 1973, only 3 (2%) had vascular symptoms as of 1980 (not shown in Table IV -12). These chain saw operators had been exposed for at least 7 years, a period of time greater than the 6.4-year mean latency of vascular symptoms for the entire study population (see Table IV-12).
# Summary of Epidemiologic Studies of HAVS
Epidemiologic studies of workers using hand-held vibrating tools show a strong association between exposure to hand-ami vibration and vascular symptoms of HAVS or Raynaud's phenomenon. Only 9 of the cross-sectional studies presented in Table IV-8 had relatively
I a
# IV. Biologic Effects
low prevalence rates of vascular symptoms (i.e., less than 20%) compared with prevalence rates of vascular symptoms in 19 control groups. In five of these nine studies, the prevalence of vascular symptoms in the exposed group of workers was compared with the prevalence in a control group. In four of these five studies, the prevalence was significantly higher in the exposed group than in the control group even though the prevalence of vascular symptoms in the exposed group was relatively low.
The study [Futatsuka 1984] with the lowest prevalence of vascular symptoms (6%) in Table IV-8 was the only one of the eight studies with relatively low prevalence rates that offered a plausible reason for the low prevalence. In this study of brush saw workers, the use of the brush saw was restricted to 4 to 5 months/year during the summer season and to 2 to 3 hr/day. The conditions of using the brush saw in this study [Futatsuka 1984] seemed to produce a very low prevalence despite a hand-arm vibration acceleration level of 59 m/sec2. The study in Table IV-9 with die lowest frequency-weighted acceleration level (10 m/sec2) [Engstrom and Dandanell 1986] reported a prevalence of vascular symptoms (25%) among workers using pneumatic drills, riveters, shavers, and bucking bars that was four times greater than that reported by Futatsuka [1984] although the frequency-weighted acceleration level (10 m/sec2) was less. The vibration frequencies produced by the tools used in the Engstrom and Dandanell [1986] study were much higher (up to 10,000 Hz) than those reported by Futatsuka [1984].
Twenty-three studies from Table IV-8 included measurements of hand-arm vibration acceleration levels. These studies showed a statistically significant linear relationship between increasing exposure to hand-arm vibration and increasing prevalence of vascular symptoms of HAVS. Even though this relationship could be demonstrated statistically, only 3 of the 6 studies reporting the lowest acceleration levels (i.e., less than or equal to 60 m/sec ) among these 23 studies (see Table IV-9) also reported relatively low prevalence of vascular symptoms (i.e., less than 20%). The relationship between hand-arm vibration exposure and the prevalence of vascular symptoms of HAVS among these 23 studies was more consistent for those with higher acceleration levels than for those with lower levels.
The longitudinal studies of chain saw operators were able to demonstrate an appreciable decrease in the prevalence of vascular symptoms after the introduction of the antivibra tion chain saw. The lower acceleration level of the antivibration chain saw apparently contributed to the decrease, although the amount of decrease varied from study to study. Riddle and Taylor [ 1982] reported a 17% prevalence among 18 workers exclusively using antivibration chain saws; Pyykko et al. [1986bJ reported a 5% prevalence for 66 workers in 1983 who had used antivibration chain saws since the mid-1970s;and Futatsuka and Ueno [1985] reported a 2% prevalence in 185 workers who started using chain saws in the mid-1970s when antivibration chain saws were introduced. The exceptionally low prevalence in Japanese chain saw operators [Futatsuka and Ueno 1985] could reflect the requirement that they do not operate chain saws for more than 2 hr/day [Saito 1987J.
• Laboratory/Hospital Tests Vascular Assessment Doppler (peripheral segmental blood flow and pressure in arms) Digital plethysmography (at rest and following cold stress) Digital systolic pressure (plethysmography with local cooling, and whole body cooling as well if necessary) Cold provocation test (immersion of digits and hands with recording of digital temperatures)
# Neurologic Assessment
EMG (to record median and ulnar sensory and motor nerve conductivity)
# Hematologic Assessment
Total and differential, sedimentation rate, blood viscosity, uric acid, rheumatoid factor, antinuclear antibodies, cryoglobulins, serum protein electrophoresis
# U rinalysis
Proteinuria, glycosuria
# X-rays
Cervical spine and ribs (to exclude costoclavicular syndrome)
Olsen [1988] conducted a comparative study of diagnostic tests for vibration white finger.
In the four tests used, various aspects of finger blood flow and finger blood pressure were measured. The study concluded that the finger color test may be as valuable as finger systolic blood pressure for diagnostic purposes. The diagnostic values of some of the tests are discussed below.
# Cold Provocation Test (CPT)
Two generic variations of the CPT have been used in studying HAVS. The versions vary mainly in the length of exposure to the stimulus, the temperature of the cold stimulus, and the responses measured. The subject must be in thermal balance before the test. This is achieved by having the subject rest for about 30 minutes in a room with air temperatures from 21* to 24*C (70* to 75*F).
# I
# Hand-Arm Vibration a. Short Exposure
In the short exposure version of the CPT, the hand is immersed up to the wrist in ice water for 1 to 3 minutes. Blood flow in the fingers of the opposite hand can be measured by plethysmography before, during, and after immersion. The most important measurements involve the reduction in blood flow during cold exposure and the recovery of blood flow following immersion. Finger rewarming time after a short (3-minute) immersion in water at 10°C (SOT) was 1.4 minutes for the control subjects and 2.9 minutes for workers with HAVS (p = <0.01). Excluded from the HAVS group were those whose finger temperature did not rise to 30*C during body heating at a room temperature of 40° to 45'C (104* to 113'F) for 15 minutes [Welsh 1986]. Niioka et al. [1986] found that the finger skin rewarming time after a CPT could distinguish between HAVS patients and controls with a false discrimina tion of 6%, a sensitivity of 80%, and a specificity of 100%.
# b. Long Exposure
In the long exposure CPT, after the subject has achieved thermal equilibrium in a thermal neutral room, the arm up to the elbow or shoulder is immersed in water at 10° to 15'C (50' to 59°F) for a period of 10 to 15 minutes. After the hand and arm have been removed from the cold water and dried, the time is measured for the finger skin to regain its color and/or temperature (indicating vasodilation and resumption of blood flow). Skin temperature below control values, 5 and 10 minutes after a 10-minute cold exposure, gave a correct diagnosis in 80% to 90% of workers with HAVS and workers without HAVS who had more than 5,000 hr of chain saw use [Kurumatani et al. 1986;Welsh 1986;Niioka et al. 1986]. However, finger-skin temperature response did not distinguish between subjects who did not use vibrating tools, those with Raynaud's disease, and those with less than 5,000 hr of saw use [Welsh 1986;Kurumatani et al. 1986;Niioka et al. 1986].
The response of finger-skin temperature to cold exposure in nonsymptomatic, vibration-ex posed and unexposed workers was reported by Scheffer and Dupuis [1989] for laboratory and field studies. The test conditions (5°C air temperature, vibration acceleration of 6.3 m/sec2 [frequency-weighted], grip force of 15 N, and push force on the tool of 40 N) all contributed to the skin temperature response. The authors suggest that improved protection against cold (e.g., heated tool handles) could be an effective preventive technique.
The response of finger systolic blood pressure (FSBP) to finger cooling has been used to measure changes in peripheral vascular response to cooling in vibration-exposed workers. Olsen et al. [1981] and Olsen and Nielsen [1979] reported that FSBP changes predict 60% to 85% of workers with vibration white finger even when the history of HAVS is not known.
Their subjects, however, had vibration white finger, Stage 2 to 3 [Taylor and Pelmear classification]. In less severe cases of HAVS (Stage 1), neither FSBP nor peripheral blood flow measurements were very sensitive. During field conditions, however, measuring FSBP is easier than measuring blood flow [Pyykko et al. 1986a]. The fingernail compression test may also be used. The occurrence of spastic vasospasm and pain in the finger is noted.
IV. Biologic Effects Hack et al. [1986] compared responses on the cold provocation test and reactive hyperemia with the history of vibration-induced white finger in workers with no symptoms, symptoms of tingling and numbness, and symptoms of HAVS. The tests distinguished between groups, but only about 60% of the subjects fell into the correct staging category.
Bovenzi [1986] reported that the skin temperature recovery time following finger cooling was significantly prolonged in workers with HAVS, indicating that the workers with HAVS had a more severe and prolonged vasoconstrictive response to the cold provocation test. Gemne et al. [1986] found the finger blood flow at vasodilatation (finger arterial inflow) after occlusion was less in the group with HAVS than in a reference group without HAVS.
Peripheral resistance was also higher in the HAVS group. The authors suggested that the increased peripheral resistance in the HAVS group may be due to a local defect in the vessels with a reduction in flow and intramural pressure.
Ameklon-Nobin et al. [1987] reported that the FSBP, the ratio of the finger systolic blood pressure to the arm systolic blood pressure (FSBP/ASBP), and finger skin temperature measured before and after vasodilatation by body warming are altered in vibration-ex posed workers. Finger skin temperature and FSBP were lower in the workers with HAVS both before and after vasodilatation. Digital rewarming time was markedly slower in the vibration-exposed individuals. These studies suggest that measuring the finger skin temperature and FSBP before and after finger cooling and after finger rewarming could be useful diagnostic tests.
Bovenzi [1988] suggested that the finger systolic blood pressure response with finger cooling and ischemia may be a useful objective test for vascular hyperactivity in subjects with HAVS. In Ills study, the test had a sensitivity to increased arterial tone of 100% and a specificity (negative test without HAVS) of 87%.
# Plethysmography
Finger plethysmography, a technique used for measuring finger blood flow, is based on the fact that with each heart contraction, the volume of the fingers increases. This change in finger volume can be measured with a photocell or strain gauge. In practice, the photocell plethysmograph is used more frequently than the strain gauge. The instrumentation for a photocell plethysmograph and the test conditions that can be used in field and laboratory studies have recently been published [Samueloff et al. 1984;Samueloff et al. 1981]. Finger plethysmography, after local cooling, has been recommended as an objective test for HAVS [Pelnar 1986]. Vibration instead of cold water may be used as the stimulus. Standardization of the test procedure and strict adherence to the test protocol are of utmost importance if the results from different studies are to be compared.
Hand-Arm Vibration
# Aesthesiometry
One of the tests of peripheral neural changes is the finger tip two-point and depth discrim ination tests. A version of the test instrumentation has been described [Carlson et al. 1979;Carlson et al. 1984]. As with other semiobjective tests, standardization of the instrumenta tion and strict adherence to the test protocol are very important (e.g., small differences in the pressure applied by the finger tip against the grooves will change the detection point sensitivity). The results of the tests can be used to support a diagnosis of advanced HAVS (Stages 2 or 3), but because of the number of false-positive and false-negative results, the test data should not be used to override other data and the examining physician's judgment [Carlson et al. 1984;Sivayoganathan et al. 1982]. Data obtained using the improved test correlated significantly with the clinical staging of HAVS in workers with Stage 2 and above [Taylor et al. 1986]. For individual diagnostic purposes, however, the test lacked sufficient discriminatory power. Haines and Chong [1987] reviewed the literature in which peripheral neurological tests were used to assess the acute and chronic effects of exposure to hand-arm vibration. The peripheral neurological tests demonstrated their usefulness in epidemiologic studies.
# 4.
Arteriography Ashe et al. [1962], Ashe and Williams [1964], and Takeuchi et al. [1986], utilizing finger biopsy material, observed extensive damage to the digital arterial walls with narrowing of the lumen in the fingers of workers with HAVS. These findings led to the concept that hand arteriography might be a useful tool for the diagnosis of HAVS [Wegelius 1972;Zweifler 1977;James and Galloway 1975;Takeuchi et al. 1986]. The procedure does, however, require an intraarterial injection of a dye and, therefore, is an invasive procedure.
The data reported by James and Galloway [1975] indicate that almost all of the workers who had symptoms of HAVS showed digital artery occlusion that was partial or nearly complete.
Their control data were limited to three nonvibration-exposed individuals (members of the observation team) who showed little evidence of digital artery narrowing or occlusion. Takeuchi et al. [1986] reported medial muscular hypertrophy and intima fibrosis in the digital arteries of vibrating tool users. Okada et al. [1987a] observed thickening of the intima of finger arteries in workers who used vibrating tools. Inaba et al. 11988] reported a thickening of the intima in animals subjected to vibration. Intimal thickening appears to be part of the arterial pathological changes.
I IV. Biologic Effects
# Grip Force
Hand and finger grip force can be easily measured with a strain gauge or a simple spring resistance dynamometer. Several types of measurements can be made. These include (1) maximum grip force, ( 2) fatigue curve while producing maximum grip force, and
(3) fatigue curve during rhythmic contraction-relaxations. These measurements can be made both before and after a work period, or before and after exposure to vibration [Farkkila et al. 1982].
Because maximum grip force appears to be reduced, and strength fatigue is faster in workers who have used vibrating tools for several years (and may or may not have symptoms of HAVS), a simple grip strength measurement (hand dynamometer) can have some diagnostic usefulness. However, as pointed out earlier, normal standard values for grip strength and grip fatigue indicate a wide inter-and intra-individual variability, which make comparisons difficult to interpret.
# Nerve Conduction
A decrease in motor and sensory peripheral nerve maximum conduction velocity in the median and ulnar nerves has been reported in workers with histories of occupational hand-vibration-exposure [Lukas 1982;Seppalainen 1972;Sakurai and Matoba 1986]. Maximum conduction velocity of the ulnar or median nerves can be determined by electrical stimulation of the nerves at a designated point and by recording the time for a motor response to occur. The time required for the nerve impulse to travel the distance between the two points can also be calculated [Seppalainen 1972]. In a group of vibration-exposed workers who had complaints and symptoms of HAVS, about 50% showed conduction velocity reduction [Lukas 1982], Sakurai and Matoba [1986] also reported a decreased motor nerve conduction velocity (MCV) and sensory nerve conduction velocity (SCV) in workers who used vibrating tools. Chatterjee et al. (1978) found that in rock drillers, the SCV in the median nerve was reduced but the MCV was not. Latency, duration, and amplitude of the sensory action potential were also significantly changed in the rock drillers. Brammer and Pyykko [1987] analyzed the electroneurographic data from 23 studies of workers who used hand-held vibrating tools. After control of the data for polyneuropathy and the effects of hard manual work, a neuropathy remained that involved mainly the sensory nerves in the hands. This sensory neuropathy could be distinguished from compression neuropathies (carpal tunnel syndrome) by measuring the nerve conduction velocity. Araki et al. [1988] reported that the distribution of sensory nerve conduction velocities (median nerve) was altered and the magnitude of the sensory nerve conduction velocities was significantly slowed in chain saw operators. Farkkila et al. [1988], in a neurological study of 186 forestry chain saw operators (average usage time 16,600 hr) and 31 nonvibration-exposed workers, found that the disturbance of the ulnar and median MCV and distal latency (DL) did not correlate significantly with the history of HAVS or numbness of the hands. However, a significant correlation was reported between vibrotactile detection thresholds and MCV and DL of the median and ulnar nerves.
# Sensory Acuity
Some of the common tests of finger tip sensory acuity may assist the physician in diagnosing HAVS. These include (1) cotton wool test (light touch), ( 2) hot and cold probes (tempera ture), ( 3) pin prick (pain), and ( 4) tuning fork (vibrotactile). A decrease in sensitivity may indicate peripheral neural changes. Taylor et al. [1986] reported that stage assessment of HAVS, based on medical examination and history of exposure, did not correlate well with tests of sensory loss, loss of pain, and temperature discrimination. Sensory acuity tests cannot be used as positive indicators of HAVS [Harada and Matsumoto 1982]. Ekenvall et al. [1986] reported that the temperature neutral zone was increased from about 5°C (9*F) in controls to 10'C (18'F) in 17 vibration-exposed workers with neurological symptoms of HAVS. The vibration threshold was also nearly doubled in the vibration-exposed group as compared with controls.
# E. TREATMENT
Several recent studies reported on hospitalized patients with different stages of HAVS who received various types of therapeutic treatment. The effectiveness of the various treatments was analyzed and evaluated. Because multiple treatments were used in all the studies, direct evaluation of the effectiveness of any single treatment is not possible. Matoba and Sakurai [1986] described their experiences in treating 500 male workers with HAVS over a 10-year period. The workers had used vibrating tools for an average of 10.5 years, and all exhibited mild to severe symptoms and signs of HAVS. All treatments were given in a hospital, with an average hospital stay of 105 days. Treatment consisted of physiobalneotherapy (water bath), alone or with one or more drugs, nerve blocking, and/or surgical therapy, along with education and training.
Recognizing that an evaluation of the relative effectiveness of all the various combinations of treatment is not possible, the researchers nevertheless selected a group of 60 inpatients matched for age and vibration exposure. Some of the patients received only physiobal neotherapy (group P), whereas the others received physiobalneotherapy plus vasodilating drugs (group D) over a 6-week period. Subjective and laboratory signs improved about 30% to 40% in group P and 60% to 80% in group D [Matoba and Sakurai 1986]. The authors concluded that physiobalneotherapy is the key treatment but that drug therapy, vasodilators, and calcium channel blockers can accelerate improvement in the circulatory, neural, and motor problems present in HAVS. Improvement was not as good in patients with severe HAVS as in those with lesser stages of involvement.
a
# IV. Biologic Effects
Bielski [19881 reported the benefits derived from balneological treatment of 824 chain saw operators who had peripheral vascular symptoms of HAVS (Stage not specified). Thermog raphy and plethysmography tests indicated statistically relevant improvement in 91% of the patients treated with a brine bath at 34*C (93.2'F) for 20 minutes a day for 24 days. The improvement persisted for at least 6 months after treatment even though the workers were again using chain saws. The author suggested that workers who use chain saws should undergo a 2 to 3 week annual treatment with balneotherapy to reverse and prevent the progression of HAVS. The vibration level produced by the chain saws used was not reported.
Nasu [1986] reported that the use of defibrinogenating drugs in the treatment of HAVS patients provided both subjective and objective improvement. With treatment, statisti cally significant improvement was observed in the finger-skin temperature, the amplitude of the finger plethysmogram, and the nail compression test before and after cold provocation. The subjective feeling of warmth after treatment was reported by all but 5 of the 118 patients studied. The beneficial effects of the treatment did not appear to be permanent but "reaggravation ranged usually from several months to more than a year" after treatment was stopped. The author also reported (without substantiating data) that the addition of alpha 1 blocker (bunazosin hydrochloride) had a better effect than the defibrinogenating drug alone.
The results obtained from treatment trials must be interpreted with caution because (1) with the present state of knowledge, the extent of spontaneous (without treatment) reversal of HAVS when vibration stimulus is withdrawn is unknown, (2) in many studies control populations given hospital treatment and therapy are not included, and (3) there is doubt about the accuracy of assessment of subjects in the absence of proven objective tests. Subjective improvement without objective tests is not acceptable.
# F. REVERSIBILITY
The British and Canadian groups have emphasized prevention over treatment as the better approach to the control of HAVS [Brammer 1984;Taylor and Brammer 1982;Taylor 1982aTaylor , 1982b. If HAVS has not progressed beyond the Taylor-Pelmear Stage 2, the signs and symptoms tend to disappear with time if no further exposure to vibration is permitted or if the exposure level (acceleration and time) is sufficiendy reduced. For workers with Stages 3 and 4 vibration syndrome, no tested regimen of treatment has resulted in a significant reversal of HAVS signs and symptoms. Therapy is essentially palliative [Brammer 1984;Taylor and Brammer 1982]. Olsen and Nielsen [1988] reported data from a 5-year study of three groups of forestry workers examined in 1978 and again in 1983. Group A (n=13) had no subjective symptoms in 1978 and continued sawing until 1983; group B (n=12) had no symptoms in I Hand-Arm Vibration 1978 and stopped sawing; group C (n=12) had symptoms of HAVS in 1978 but did not stop using chain saws. FSBP was measured with a CPT in 1978and again in 1983 groups had increased response to the cold provocation when compared to 20 nonvibration-exposed controls. From 1978 to 1983, the vasoconstriction response to the CPT increased in group A (p<0.05), was unchanged in group B (p>0.10), and improved in group C (p<0.05). Antivibration saws were used between 1978 and 1983. In group A, the use of antivibration saws did not prevent further increase in hyperactivity; the improvement of workers in group C (who had HAVS) may have been due to a shift from regular to antivibration saws in 1978. The data suggest that while the use of antivibration saws will not entirely prevent the development of HAVS, it may reduce the occurrence and progress of the disorder.
A 3-year followup study of 55 forestry workers with HAVS was conducted by Ekenvall and Carlsson [1987] to determine the effect of cessation of working with vibrating tools on subjective symptoms and FSBP during finger cooling. The group on first examination included 14 with Stage 1 Taylor-Pelmear symptoms, 25 with Stage 2, and 16 with Stages 3 and 4. Of the 15 workers who continued outdoor work with vibrating tools during the 3-year followup period, none showed any improvement of symptoms (8 showed no change and 7 showed increased subjective impairment). Of the 32 who did not use vibrating tools during the 3-year followup study, 8 showed improvement, 19 showed no change, and 5 showed increased impairment. The subjective improvement reported in this study could not be confirmed by CPT. On the other hand, this study showed an increased reactivity to cold in the impaired group. Thus the CPT appears to provide objective confirmation of the deterioration.
Other studies have indicated that the signs and symptoms of HAVS may be reduced or reversed in some chain saw operators, chippers, and grinders when the worker is no longer exposed to vibration [Riddle and Taylor 1982;Hursh 1982].
# I
# V. BASIS FOR THE RECOMMENDED STANDARD
The NIOSH recommendations for control of hand-arm vibration are based on review and analysis of (1) epidemiologic data derived from field investigations, ( 2) data from clinical examinations of workers who have used vibrating tools, and (3) data derived from laboratory studies. Chapters HI and IV contain reviews of the published data on which this recom mended standard is based. HA VS is a chronic, progressive disorder that normally requires months or years of vibration exposure to manifest itself. The quantitative relationship between the magnitude of the vibration exposure and the latency and severity of the disorder is not precisely known.
# A. PREVALENCE OF HAVS
Several hundred published epidemiologic and clinical studies have reported the development of HAVS in workers who used vibrating tools. In the epidemiologic studies summarized in Table IV-8, the prevalence of the vascular symptoms of HAVS ranged from 6% to 100%, with more than half of the studies showing a prevalence rate greater than 40%.
Vascular symptoms were reported in 0% to 14% of control workers who did not use vibration-producing tools, with a median prevalence of 4%. In all studies that compared workers who did with those who did not use vibrating tools, the prevalence of vascular symptoms was always higher in the vibration-exposed group.
The epidemiologic and clinical data support the conclusion that healthy workers who use vibrating tools can be protected from developing the disabling effects of HAVS. Protection can be provided by medical monitoring of the workers, engineering controls to reduce the vibration levels produced by the tools, work practices such as limited daily use time of vibrating tools and ergonomic design of tools and work methods, protective clothing and equipment, and worker training programs in the proper handling and maintenance of vibrating tools and in recognition of the early symptoms of HAVS.
# B. RATIONALE FOR FREQUENCY-UNWEIGHTED ACCELERATION MEASUREMENTS
The 1/3-octave-band center-frequency weighting of the acceleration has been used pre viously to express the magnitude of the vibration exposure. However, on the basis of recently published data cited in this section, NIOSH proposes the use of the frequency-un weighted acceleration. The frequency-weighted acceleration concept assumes that the harmful effects of 1/3-octave-band center-frequency accelerations are independent of fire-I Hand-Arm Vibration quency between 6.3 and 16 Hz but progressively decrease with higher frequencies between and 1,500 Hz. The frequency-unweighted concept assumes that the magnitude of pathophysiologic effects from exposure to vibration are proportional to the acceleration and are frequency independent at all frequencies.
The rationale for frequency weighting is based primarily on the data reported by Miwa [1967Miwa [ , 1968aMiwa [ , 1968b. From these studies, data were obtained on the levels of acceleration that subjects identified as "tolerance limit" or "unpleasant" sensations when they pressed a hand on aplate that was vibrating at a frequency of 10,20,30,60,100, or 300 Hz. The acceleration level required for the subjective sensation of "tolerance" and "unpleasant" limits increased progressively with vibration frequency above 16 Hz. These psychophysically derived test data were not analyzed to determine the correlation between frequency and acceleration and the development of clinical or pathophysiologic signs and symptoms of HAVS. The investigators assumed that the subjective degree of "intolerance" would be related to injury. Data from some epidemiologic and laboratory studies support the concept that the pathophysiologic effects of vibration are mainly frequency independent. Engstrom and Dandanell [1986] and Dandanell and Engstrom [1986] reported vibration acceleration levels and frequencies produced by riveting hammers, bucking bars, rivet shavers, and drills used in the aircraft industry. Most of the acceleration occurred at frequencies above 400 Hz (up to 10,000 Hz). If the ISO [1986] frequency-weighting criteria were applied, most of the higher frequency acceleration would be excluded from the exposure assessment. At frequencies below 400 Hz, the frequency-weighted acceleration was only about 10 m/sec2 for the riveting hammer and bucking bar. At frequencies between 400 and 10,000 Hz, the frequency-weighted acceleration was 2 m/sec2 for drills, 5 m/sec2 for rivet shavers, and 6 to 10 m/sec2 for riveting hammers and bucking bars. In the absence of frequency weighting, the acceleration was about 100 m/sec2 at frequencies between 100 and 10,000 Hz.
Riveting hammers and bucking bars were used not more than 15 minutes per working day, with a total daily exposure to vibrating tools of not more than 30 minutes. Of the 288 workers studied, the authors reported that 59 showed finger blanching; of those with more than 10 years of exposure, 50% had HAVS. This prevalence of HAVS far exceeded that expected from exposures at 10 m/sec2 (frequency weighted) for similar years of exposure and 30 minutes of daily use time. The authors suggested that frequency weighting would have grossly underestimated the health impact of the high-frequency vibration acceleration produced by these vibrating tools.
The data from experimental studies of Nohara et al. [1986] also call into question the assumption that pathophysiologic effects of vibration acceleration are frequency-inde pendent at 16 Hz or below and frequency-dependent above 16 Hz. The test group consisted of five healthy, 25-to 31 -year-old males who were nonsmokers and had never used vibrating tools. For the 1-hr test periods at 1-to 4-day intervals, subjects grasped with the left hand a 40-mm- (1.6-in.-) diameter handle that was fixed to a vibrating plate. A constant acceleration of 50 m/sec2 at randomized frequencies of 30, 60,120, 240, and 960 Hz was applied to the plate during the test period. For control values, the subjects grasped the handle for 1 hr without vibration. Physiologic parameters measured were finger blood flow, finger skin temperature, and peripheral motor nerve conduction velocity of the ulnar and median nerves. The data were analyzed by NIOSH and are summarized in Table V- Nohara et al. [1986]. fMotor nerve conduction velocity.
§Without vibration (control). **After-vibration exposure value is higher than before-vibration value.
The following generalizations can be made based on the data summarized in Table V-l at a fixed vibration acceleration of 50 m/sec2:
• None of the physiologic functions measured showed a consistent change in function with vibration frequency.
# I
Hand-Amt Vibration
• Each physiologic function had one or more vibration frequencies at which the physiologic effects were greatest.
• The frequencies at which the maximum effects occurred were different for the various physiologic functions.
• The maximum effects occurred at the lowest exposure frequency (30 Hz) for only one function (peripheral blood flow).
• Maximum change occurred in skin temperature at 240 and 480 Hz, in blood flow at 30 Hz, and in MCV at 120 Hz.
• Grasping the handle for 1 hr without vibration (control) also resulted in changes in the physiologic functions measured. Nohara et al. [1986] concluded that the peripheral nervous system was affected most at the lower frequencies and the circulatory system was affected significantly at both the lower and the higher frequencies. The data from the study do not support the assumption that frequencies above 16 Hz have progressively less harmful effects than the lower frequencies.
The Nohara study has the following obvious shortcomings: only a small number of subjects were tested, exposures were not repeated at any of the frequencies, and each exposure was limited to 1 hr per test session. Starck and Pekkarinen [1988] compared the observed and predicted prevalence and latency periods of HAVS among workers using different types of vibrating tools. For operators of chain saws that produce relatively low-frequency and low-impulse vibrations, the predicted and observed values were in good agreement when acceleration was calculated according to the ISO 5349 frequency weighting [ISO 1986]. However, for pedestal grinders, stone workers, shipyard workers, and platers whose tools produced higher impulses and frequen cies, the comparisons were less consistent. Frequency weighting of the acceleration in accordance with ISO 5349 did not appear to adequately reflect the harmful effects of tools that produced higher-frequency and higher-impulse vibrations.
The data reported by Hyvarinen et al. [1973] suggest no constant frequency relationships on the threshold acceleration levels required for the production of finger vasospasms in lumberjacks who had a "history of traumatic vasospastic disease." The frequency of 125 Hz was more effective in producing finger vasospasms than higher or lower frequencies. These data suggest that acceleration frequency weightings throughout the entire vibrationfrequency spectrum produced by vibrating tools may underestimate the potential risk to workers exposed at higher vibration frequencies. The degree of intimal thickening observed Brammer [1982a]. 9 in experimental animals subjected to either 30 or480 Hz at 50 m/sec was comparable [Inaba et al. 1988].
Literature surveys by Brammer [1982aBrammer [ , 1982b suggest that the minimal vibration accelera tion level required to produce a sensation of vibration and a pulseless vasospasm does not consistently increase as the vibration frequency is increased. For the production of vasospasm, the minimum vibration acceleration required did not vary with vibration frequencies between 31.5 and 2,000 Hz, and the minimum vibration acceleration required to produce vibration sensation was independent of frequency between 31.5 and 500 Hz. The minimum vibration acceleration levels required to produce vasospasm and sensation at frequencies of 31.5 to 2,000 Hz are given in Table
V-2.
Because of the lack of objective, experimentally derived data, it is not possible to quantita tively convert the health impact of frequency-weighted accelerations to frequency-unweighted accelerations. However, some semiquantitative conversions are possible. Frequency weighting that is done by reducing the input of the higher frequencies (especially above 400 Hz) decreases the total acceleration energy calculated for the vibrating tool. The frequency-weighted acceleration will therefore underestimate the total energy produced by the vibrating system. Frequency-unweighted acceleration calculated over the entire fre quency range of the tool will be higher than the frequency-weighted acceleration, but it is a more complete representation of the energy actually produced.
The rationale for recommending the use of frequency-unweighted acceleration is supported by the following information:
1. Data from epidemiologic, clinical, and laboratory studies suggest that the hazardous effects of vibration exposure are frequency independent. 2. Exposure measurements based on frequency-unweighted acceleration have the advantage of simplifying the measurement of vibration acceleration levels of vibrating tools used in industry. 3. The prevalence of HA VS among users of high-frequency (up to 10,000 Hz) vibrating tools was 50% with 10 years of exposure at a frequency-weighted acceleration of about 10 m/sec2 for about 30 minutes per day of actual tool use [Dandanell and Engstrom 1986]. The frequency-weighted acceleration level grossly underestimated the HAVS-producing effect of the high-frequency vibration exposure.
# C. 4-HR-PER-DAY USE TIME
All of the guidelines, standards, and published studies of the harmful effects of vibration exposure accept a time-dose relationship between total vibration exposure and the develop ment of HAVS. The exposure dose can be expressed as m/sec2 normalized for 4 hr, 8 hr, or any other amount of tool use time per day. If the acceleration level is expressed by all researchers as a time-corrected, 4-hr/day equivalent, comparisons of data from different studies would be easier. The ISO [1986] and ANSI [19861 guidelines recommend using a 4-hr energy equivalent acceleration expressed in m/sec . The time (hr/day) and dose (acceleration in m/sec2) energy equivalents are plotted as a log-log function. In these relationships it is assumed that the daily exposure time required to produce symptoms is inversely proportional to the square of the acceleration and is independent of the vibration characteristics of the tool. Thus if the vibration level is reduced by one-half, the exposure time may be doubled. The total daily time of actual tool use has not usually been reported, but in most industries it does not exceed 4/hr day.
# D. DOSE-RESPONSE RELATIONSHIP
HAVS is a chronic disorder with a latency period between the first exposures and the appearance of the first signs and symptoms. The latency period may vary from a few months to several years, depending on many interacting factors. Among the more important factors that determine the clinical profile of HAVS are As a result of the complexity of the confounding interactions between these factors and the lack of experimentally derived objective data, dose-response relationships cannot be estab lished with precision. Establishing a reliable, valid, minimal dose-risk level would require quantitative data not presently available. , Brammer [1982a analyzed the epidemiologic data derived from several reports that contained data on the vibration level produced by the tool used (frequencyweighted m/sec2), daily tool use (hr/day), and the latency period (years of tool use) preceding the first appearance of vascular symptoms. The analysis was presented as percentiles of population that would be expected to have Stage 1 HAVS as a function of acceleration (frequency-weighted) and years of tool use. Based on extrapolations of these analyses, predictions are that 5% of the workers who use vibrating tools will develop early Stage 1 HAVS in <2 years at 10 m/sec2, in 5 years at 4 m/sec2, in 10 years at 2 m/sec2, and in >20 years at 1 m/sec2 [Brammer 1982a]. The predicted minimum (frequency-weighted) ac celeration (m/sec2) required to produce Stage 1 HAVS (finger blanching) has been reported to be 1 to 2.9 by Brammer [1982a], 1 to 2.1 by Miura et al. [1959], and <4.7 by .
The data on the pathogenesis of HAVS are not sufficient to establish an REL that would ensure that healthy workers who use vibrating tools would not develop signs and symptoms of HAVS. Because such an REL cannot be justified on the basis of present dose-response data, the prevention and control of HAVS as an occupationally-induced disorder must be based on other considerations. The approach to controlling HAVS must be through (1) medical monitoring to recognize the first signs and symptoms of developing HAVS, (2) medical removal of workers who exhibit signs and symptoms of Stage 2 HAVS,(3) engineering controls to minimize the level of vibration produced by tools, (4) establishment of a work regimen to reduce exposure to a feasible minimum, (5) ergonomic design of tools and workplaces, ( 6) training of workers to recognize and report early signs of HAVS, and ( 7) supervision to ensure optimal tool maintenance and use.
# E. CONCLUSIONS
# Setting a Standard
HAVS is a chronic disorder with a latency period varying from a few months to several years. The latency is believed to depend on many interacting factors, including vibration level produced by the tool, hours of tool use per day, environmental conditions, type and design of the tool, manner in which the tool is held, vibration spectrum produced by the tool, vibration "tolerance" of the worker, and tobacco and drug use by die worker. Because of the complex interactions among diese and other factors and the general lack of objective data, it is not currently possible to establish meaningful dose-response relationships. Thus it is not possible to establish a specific REL that will protect all workers against the development of HAVS in all occupational situations. However, the problem of HAVS is too serious and pervasive to delay measures for correcting it. NIOSH has therefore recommended a standard for exposure to hand-arm vibration that includes no specific exposure limit but does include medical monitoring and surveillance, engineering controls, good work practices, use of protective clothing and equipment, worker training programs, and administrative controls such as limited daily use time. If this standard is implemented, it will protect workers who use vibrating tools from the debilitating effects of HAVS. NIOSH also anticipates that this criteria document will stimulate research and development in all areas relating to hand-arm vibration.
# Use of Frequency-Unweighted Acceleration Measurements
The 1/3-octave-band, center-frequency-weighted acceleration historically has been used to express the magnitude of vibration acceleration levels. The frequency-weighted accelera tion concept assumes that the harmful effects of vibration are independent of frequencies between 6.3 and 16 Hz but that the effects progressively decrease with higher frequencies between 16 and 1,500 Hz. On the basis of data published in recent studies, however, NIOSH has concluded that the use of the frequency-unweighted acceleration is a more appropriate means of assessing the health risk to exposed workers. Although the major consensus standaids-setting organizations currently recommend the frequency-weighted acceleration levels, NIOSH believes that this measurement grossly underestimates the HAVS-producing effects from tools that vibrate at high frequencies. Exposure measurements based on frequency-unweighted acceleration provide the additional benefit of simplifying the meas urements because the acceleration data produced by the accelerometer is frequency un weighted.
# Medical Monitoring
Medical monitoring of workers who use vibrating hand tools is a vital component of any standard for preventing or controlling HAVS. The medical monitoring program must include (1) a preplacement medical examination with special emphasis on peripheral vascular and neural factors, (2) yearly or more frequent exams designed to detect HAVS in a V. Basis for the Recommended Standard its early and reversible stages, and ( 3) an open channel of communication with the workers to ensure that the early symptoms are promptly reported.
# Medical Removal
NIOSH recommends that workers who develop Stage 2 HAVS be removed from further exposure to vibration until they are free of signs and symptoms of HAVS. If HAVS is permitted to progress beyond Stage 2 by the continued use of vibrating tools, the effects can become irreversible. A provision for medical removal could be controversial, but it would provide a powerful incentive for the employer to implement the engineering and administra tive controls necessary to reduce the worker's risk of developing HAVS.
# VI. OTHER STANDARDS AND RECOMMENDATIONS
Recommendations and guidelines for permissible worker exposure to hand-arm vibration have been formulated or are in the process of being formulated in several countries, including the USSR, Czechoslovakia, Finland, Sweden, Australia, United Kingdom, Japan, Poland, and the United States. Even though the problems of objectively diagnosing HAVS, measuring the input parameters of vibration energy transmitted to the hand and arm, and establishing reliable dose-response relations are formidable, some agreement has been reached in establishing vibration exposure criteria [Griffin 1980]. The major national and international guidelines, standards, and recommendations reviewed in this chapter suggest that vibration exposure be expressed as acceleration in m/sec2 over die vibration spectrum of 1/3-octave-band center frequencies of 6.3 to 1,250 Hz. The acceleration limit is standardized to 4 hr of actual tool use time per day. However, objective and subjective tests that are required for the diagnosis of HAVS, its stage of progression, and medical removal of affected workers are not stressed.
# American National Standards Institute (ANSI)
The American National Standards Institute's Guide fo r the Measurement and Evaluation o f Human Exposure to Vibration Transmitted to the Hand (S3.34-1986) was prepared by a working group of the Acoustical Society of America [ANSI 1986]. This guide is more comprehensive than either the ISO Guideline 5349 or the ACGIH TLV. The major features of the ANSI guide include (1) methods for the measurement of vibration and analysis of the data, and (2) procedures for reporting worker exposure. The goal of this document is to reduce worker exposure to hand-arm vibration and thereby reduce the probability of incurring HAVS. Special features include (1) a discussion of the factors that may influence the probability of occurrence or die severity of the pathophysiologic effects of vibration, The ISO Guidelines fo r the Measurement and the Assessment o f Human Exposure to Hand-Transmitted Vibration [ISO 1986] emphasizes standardized procedures for measuring and assessing the levels of hand-arm vibration to which the worker may be exposed when using various vibrating tools. It does not specify the limits for safe exposure in terms of acceleration and daily exposure, nor does it specify the risk of health impairment for different operations and tools. The document presents guidance "to protect the majority of workers against serious health impairment and to assist in the development of hand-operated tools the use of which will reduce the risk of disorders in workers caused by vibration."
The ISO guidelines lack a description of (1) the clinical features of hand-arm vibration syndrome and ( 2) objective tests and procedures for diagnosing HAVS. Appendix A of the ISO guidelines presents exposure time in years for different percentiles of population groups exposed to various levels of frequency-weighted acceleration (m/sec2) before finger blanch ing occurs. However, finger blanching is only one aspect of HAVS and usually is not the first to occur.
The ISO document points out its shortcomings and gives precautions about the use of their guidelines. The procedures and techniques for measurement, assessment, and expression of the vibration intensity are similar to the approaches used in other vibration guidelines.
Of special interest is Appendix B, which contains recommendations for medical preventive measures, engineering control methods, administrative approaches, and worker training. Appendices A and B are not part of the official standard; thus the ISO guide does not include a recommended numerical exposure limit. [ACTU-VTHC 1982]. This publication presents guidelines for whole-body, hand-arm, and low-frequency vibration exposures and is not an official standard. These guidelines take into consideration vibration characteristics, health effects, sources, control methods, medical monitoring, measurements, and prevention. The presentation reviews the state of the art and does not introduce new data or new concepts. Specific details are not given for measuring the vibration of hand-held tools. The acceptable weighted acceleration levels cited (in m/sec2) are based on the draft version of ISO Guideline 5349 [ISO 1986]. A frequency-weighted, 4-hr exposure limit of 1 m/sec is suggested.
The document provides an informative summary of the measurement of vibration, the effects of vibration on the body, and useful procedures for controlling or preventing the effects. However, the guidelines are directed more to trade union personnel than to those responsible for the measurement, assessment, and control of HAVS.
# USSR
The 1972 USSR State Standard (Gost Standard 17770-72) is a revision of earlier state standards and sanitary standards [Griffin 1980]. Some of the pertinent features of the standard are as follows:
• Limits are for octave bands of 8 to 2,000 Hz.
• Procedures are given for measuring the vibration levels of tools.
• Hand-held vibrating tools should not weigh more than 22 pounds (10 kg).
• Force exerted on the tool should not exceed 44 pounds (20 kg).
• Preemployment and yearly medical examinations should be given for those working at vibration levels exceeding 20% of the limit.
• Actual maximum daily use time for vibrating tools should be 5 to 6 hr.
• Working environment temperatures should be above 16"C (60*F); rewarming facilities should be required when they are below 16'C.
• Gloves are required to prevent hand cooling.
• If IIAVS symptoms occur, the worker should be transferred to work that does not involve vibration exposure.
• Prophylactic measures are suggested (e.g., massage, exercise, vitamins, and ultraviolet radiation).
The limits for vibration exposure for vibrating tools were 2 m/sec at 10 Hz to 50 m/sec at 2,000 Hz. Vibration disease from the use of vibrating tools covered by this standard includes whole-body complaints, as well as peripheral neural, vascular, and muscular symptoms. Hand-Arm Vibration
# United Kingdom
The 1987 British Standard Guide to the Measurement and Evaluation o f Human Exposure to Vibration Transmitted to the Hand [BSI 1987] "provides guidance on measuring and evaluation of hand-transmitted vibration exposure ... [and] a uniform method for measur ing and reporting hand-transmitted vibration." The sections on characterization of handtransmitted vibration, measurement of hand-transmitted vibration, and characterization of vibration exposure cover the same areas as ANSI 53.34 [ANSI 1986] and ISO Guideline 5349 [ISO 1986] (frequency-weighted acceleration and frequency cutoff at 1,250 Hz 1/3-octave-band center frequencies). Of special interest and value are Appendices A and B, which contain discussions of the dose-effect relationship for hand-transmitted vibration and the guideline for preventive procedures. However, those discussions are included as appendices and are not considered to be part of the standard. No numerical recommended exposure limits are given. A particularly important guideline presented in Appendix A indicates that with "a tool having a frequency weighted vibration magnitude of about 4 m/sec2 rms, used regularly for 4 hours a day, there may be an occurrence of symptoms of (finger) blanching in about 10% of the vibration-exposed population after about 8 years."
# Japan
Early Japanese guidelines for permissible vibration exposure levels are derived from both field and laboratory data and are based on the concept of "no complaint" and "complaints by 50%" of the subjects [Miwa 1967[Miwa ,1968a[Miwa , 1968b. The Miwa curves for "tolerance limits" and "unpleasant limits" were frequency dependent with acceleration levels of 17.8 m/sec2 for "tolerance limit" and 3.2 m/sec2 for "unpleasant limit" at 20 Hz. In 1970, the Japanese Association of Industrial Health (JAIH) proposed limits for exposure to hand-held vibrating tools. The limits were for "intolerable levels" of vibration for 10 to 400 minutes daily at octave bands of 8 to 250 Hz. Permissible acceleration levels for 400 minutes of exposure ranged from about 1.5 m/sec2 below 16 Hz to 35 m/sec2 at 250 Hz; and for 30 minutes of daily exposure, permissible acceleration levels were about 6.5 m/sec below 16 Hz and 100rn/sec2 at 250 Hz. The limits based on "intolerable levels," although not strictly comparable with ISO guidelines, appear to be higher than the levels recommended in ISO Guideline 5349, which are based on the development of HAVS in vibrating tool users.
# Czechoslovakia
The official 1977 Czechoslovakian Guide evolved through a series of revisions, including the 1967 Hygiene Regulation #33 of the Czechoslovakian Ministry of Health [Griffin 1980]. The 1967 regulation is for vibration octave bands ranging from 8 to 500 Hz, and it is based on 2-hr daily exposures. If daily exposures are less than 2 hr for either uninterrupted or regularly interrupted exposure patterns, correction factors in permissible acceleration levels are provided. The guide states that when exposures exceed these limits, protective measures are required. At frequencies below 20 Hz, permissible acceleration levels are constant but are exposure-time dependent.
# I
# VI. Other Standards and Recommendations
The exposure limits in the 1977 Guide are similar to but not exactly the same as those in ISO Guideline 5349. The frequency range and the frequency weighting are similar; however, for exposure time above 1 hr, the vibration limits are lower than those in ISO Guideline 5349.
# Sweden
Efforts in Sweden to establish guidelines for vibration exposure control have been directed mainly to chain saws and their use [Griffin 1980]. The earlier studies led to the conclusion that vibrations in the frequency range of 50 to 500 Hz were important in producing hand-arm injuries. Two vibration exposure limits were suggested-the "injury risk limit" and the "occupational injury limit." Below the injury risk limit, there was no danger of vibrationinduced injury, whereas above the occupational injury limit, there was a definite risk of injury. Between the two limits, the risk of injury depended on exposure duration. Short exposures above the occupational injury limit were considered to have minimal risk [Axelsson 1977]. The SFS 1977: 1166 Labor Safety Board Ordinance concerning the use of vibrating tools has revised directions that became valid January 1,1987, as Ordinance AFS1986:7, "Vibration from Hand-Held Tools" [Danielson 1986]. The manufacturers, suppliers, and purchasers of Swedish equipment are all held responsible for ensuring that the equipment is constructed to produce the least possible amount of vibration. The worker must be infonned of the risks of using vibrating tools, and medical examinations must be furnished at no cost to the workers.
In 1973, the Swedish Board of Occupational Safety and Health set a limit of 50 N as the maximum permissible vibration force. Studies by Axelsson [1977] indicated that a 50-N force measured in a laboratory would correspond to 90 to 100 m/sec2 rms measured on chain saws held by an operator (this equivalent may change with the grip force applied by the operator); 90 m/sec2 is the 1-to 2-hr exposure at 500 Hz given in ISO Guideline 5349.
# Poland
In 1986, Poland published proposed maximum pennissible intensity values for hand-arm vibration exposures [Biuletyn Zeszyt 1986]. In general, the document followed the draft version of ISO Guideline 5349 [ISO 1986]. The measurement of vibration and the analysis procedure follow the ISO guidelines. The Polish guidelines are based on 8 hr of daily use of the vibrating tools.
The maximum permissible acceleration levels at various vibration frequencies for an 8-hr day of tool use are presented. For 1/3-octave-band center frequencies, the permissible acceleration levels in m/sec2 are listed as 1 m/sec2 at 20 Hz, 2 m/sec2 at 40 Hz, 4 m/sec2 at 80 Hz, 8 m/sec2 at 160 Hz, 16 m/sec2 at 320 Hz, 32 rn/sec2 at 640 Hz, and 50 m/sec2 at 1,000 Hz. This represents another method of vibration frequency weighting of acceleration level. For the frequency range of 5.6 to 1,400 Hz, the frequency-weighted maximum permissible acceleration level for an 8-hr daily tool use is 1.4 m/sec . For a 4-hr tool use,
The major emphasis for worker protection from HAVS should be directed toward preven tion. After the disorder has progressed beyond Stage 2 of the Stockholm classification, procedures designed to reverse the process are usually not effective. Because the develop ment of HAVS is dose related, effective control procedures should be directed to (1) reduc ing the intensity (acceleration) of the vibration, ( 2) reducing die exposure duration, ( 3) identifying the early signs and symptoms, and ( 4) identifying vibration-sensitive in dividuals. Control strategies include (1) exposure monitoring, ( 2) engineering controls, (3) work practices, ( 4) ergonomic considerations, ( 5) protective clothing and equipment, ( 6) worker training, and ( 7) medical monitoring.
# A. EXPOSURE MONITORING
Any effective control procedure requires objective data on the degree of hazard to which the worker is exposed. For the use of vibrating tools, these needed data are the vibration acceleration expressed in m/sec2 rms measured in the three basicentric coordinates (or the coordinate with the highest acceleration), and the time in minutes per day that the tool is actually in use (scheduled or nonscheduled rest breaks are not included as exposure time).
The acceleration measurements should be made as described in Chapter III, B.l and B.2.
# B. ENGINEERING CONTROLS
The major engineering approaches to the elimination or reduction of the vibration accelera tion level exposure are (1) reduction at the source, (2) reduction of transmission, and (3) process modification.
# Reduction at the Source
The acceleration level usually increases with an increase in the speed at which the tool is operated (e.g., a chain saw operating at two-thirds throttle produces significantly less vibration energy [acceleration] than one operating at full throttle). A tool designed to operate at a reduced speed while providing adequate power for the job could be beneficial. The relationship between the weight of the tool and the power needed to drive the tool will also influence the amount of vibration produced. The reciprocating gasoline engine used to power some tools is a major source of vibration. A rotary gasoline engine or an electric motor as a power source may be a successful alternative, provided it meets the operational I Hand-Arm Vibration requirements. If several tools are available that serve the same function, the tool producing the lowest acceleration should be chosen.
How well the tool is maintained will influence the level of vibration during operation. A sharp chisel or saw chain, a flat-dressed grinding wheel, and a finely tuned engine will reduce the vibration level. To maintain the optimal level of tool maintenance, the operating personnel must be adequately trained in maintenance procedures and be aware of the need for maintenance. A scheduled maintenance program should be established.
# Reduction of Transmission
The vibration energy produced by the vibrating tool must be transmitted to the operator's hands or arms to produce a harmful effect. Any strategy that reduces the transmission from tool to hand will help prevent HA VS. Several types of energy-damping materials have been used to cover the handles of the tools or have been incorporated into the fingers and palms of hand gear with varying degrees of success. Some materials will reduce vibration transmissions at low-frequencies, and others may reduce those at higher frequencies. Damping materials in handwear are usually more effective for the higher frequencies. However, coverings on the tool handles or glove fingers and palms may interfere with the ability to control the tool during operation and thus may lead to reduced production or increased risk of accidents. Rens et al. [1987] reported that cotton or leather gloves used for protection against trauma, chemicals, and temperature provide little or no protection against vibration and may even increase the transmission of the vibration.
Another approach to reducing vibration transmission is the use of offset handles, springloaded handles, and shock-adsorbing exhaust mechanisms. Again, the operating efficiency at the tool/work-surface interface would have to be considered. A decrease in the vibration transmission level must not be offset by an increase in the time needed to complete the task.
# Process Modification
An ergonomic analysis of the entire industrial process is recommended to determine whether changes in some aspects of the process could reduce or eliminate the need for vibrating tools. For example, introducing a different casting process in a foundry might result in smoother castings and might therefore reduce or eliminate the need for grinders or power chisels. Using mechanical aids such as chucks and clamps to hold the piece being worked on can reduce the time and the intensity of the vibration exposure. Introducing automation and robots (e.g., robots used for spot welding to replace hand-held riveting guns) could reduce the need for workers to use vibrating tools. Where the size of the trees and the terrain are suitable, automated logging machines can reduce the need for chain saws to fell and debranch trees. Substituting alternative materials (e.g., plastics for cast metal) might reduce or eliminate the need for grinding or chipping operations.
Where the process produces such extreme vibration forces that they cannot be adequately controlled by any means, complete abandonment of the process may be the only feasible solution. Although such a situation may never occur, the possibility must be kept in mind.
# C. WORK PRACTICES
Because the pathophysiologic effects of using vibrating tools are related to vibration intensity and use time, the total daily, weekly, and yearly exposure time and the daily exposure schedule are important factors in preventing workers from developing HAVS. The epidemiologic data and clinical experiences discussed in Chapter IV suggest some practical and acceptable work practices that can be implemented to reduce the health impact of using vibrating tools. Saito [1987] studied the effects of limited tool use time on the presence of HAVS in 155 chain saw operators between 1978 and 1983. Each year the operators were medically examined. Skin temperature, vibratory threshold, recovery of nail bed color after compres sion, and pain sense were measured before a 10-min exposure of the hand to cold water (10°C) and 5 and 10 min after exposure. The results of 6 years of observation suggest that limiting chain saw use time can help prevent the occurrence of HAVS. The suggested chain saw use schedule was as follows: The daily duration of exposure can be regulated by the length of the workday or by introducing exposure/nonexposure cycles of varying lengths throughout the usual workday. Most exposures are not continuous throughout the workday but consist of actual tool operation of varying lengths of time interposed with scheduled and nonscheduled periods when the tool is not in operation. The large number of possible combinations of work/rest cycle schedules permit choosing one that will best fit the requirements of most industries. air temperature of 23.9'C (75*F) has about 1 do of insulation value. Clothing that is 1/4-in. thick provides about 1 clo of insulation. The insulation value of clothing under minimal airflow conditions is not a function of fiber or fabric type but depends on the amount of air trapped between the fabric layers or between the fibers.
If the clothing is not adequate to prevent a negative body heat balance, the circulatory system will respond with a peripheral vasoconstriction, particularly of the fingers and toes. Thus exposure to cold air may precipitate an attack of white finger, especially in susceptible individuals with HAVS. For a discussion of cold weather clothing, see Horvath [1985], Goldman [1973], Belding [1973], Newburgh [1949], ACGIH [1988], andNIOSH [1986].
Besides the insulation value of the clothing andhandwear, the following other factors should be considered for cold weather operations:
• In the presence of rain or snow, a water-repellent outer clothing layer should be used. • Handgear should be kept diy. If the handgear becomes wet, a change to dry gear should be made and the wet articles should be dried before being used again.
• In cold conditions (<0°C or 32*F) when wind velocities are greater than 0.5 mile/hr (0.8 km/hr), air-impermeable coverings for hands and torso should be provided. Wind barriers to reduce airflow over the body surface can effectively change the rate of heat loss.
• Warm-up breaks may be required even when the air temperature is above freezing.
A work/warm-up schedule for a 4-hr shift is presented in the TLV on cold stress proposed by the ACGIH [1988]. Because the blood circulation of the fingers is especially sensitive to even short exposures to cold, responding by acute vasoconstriction and reduced blood flow, constant vigilance must be exercised to protect the fingers from cold exposure when using vibrating tools. Exposing the hands to cold can cause a vasoconstriction even though the body as a whole is in thermal balance and the torso skin temperature is normal. Warm-up facilities may range from portable handwarmers to whole-body warming shelters.
• Battery-powered, electrically heated handgear is, in some situations, a viable solution to cold-induced vasoconstriction of the fingers.
# F. WORKER TRAINING
Because of the wide range in tolerance to vibration within a group of workers, it is imperative that each worker be instructed in the recognition of early symptoms of HAVS and in the cause and prevention of HAVS. • Role of tool maintenance and vibration production
• Ergonomic aspects of tool use, including the influence of handgrip force, pressure exerted at the tool/workpiece interface, manner in which the tool is held, body posture, etc.
• Need and procedures for keeping the body and hands warm and dry
• Use of protective clothing and equipment
• Work/rest schedules to control exposure duration
• Informing supervisor about any abnormal functioning of the tools
• Possible aggravation of HAVS from smoking and use of some drugs
The training should be provided to each new worker and repeated at intervals for each worker using vibrating tools to ensure continued worker awareness of the potential problems.
Because the earliest signs and symptoms of HAVS are periodic numbness or tingling of the fingers, or episodic blanching of the fingertips, the worker will be the first to recognize that something unusual is occurring. A trained worker can recognize the disorder at the early stages, when further progression can be prevented or reversed.
# G. MEDICAL MONITORING
Medical monitoring of workers using vibrating tools should be a primary approach to HAVS prevention and control, but it presents some difficulties because there is no specific clinical or medical test to objectively diagnose or assess the presence of HAVS. HAVS, as the name suggests, is a composite of signs and symptoms. The medical monitoring program should consist of (1) a preplacement medical examination with special attention to peripheral vascular and neural factors, (2) yearly or more frequent examinations designed to elicit responses that may be related to early HAVS, and ( 3) continued communication with the workers to ensure that early signs and symptoms are reported. Regardless of the signs and symptoms present, a diagnosis of HAVS is not justified without an occupational history of the use of vibrating tools.
# Preplacement Baseline Medical Examinations
The primary purpose of the preplacement medical examination is to identify (1) any worker who has HAVS from previous vibration exposures, (2) workers who have primary Raynaud's disease, ( 3) workers who have other disorders with signs and symptoms similar to HAVS (e.g., peripheral vascular or neural disease), ( 4) workers who are on medications or drugs that may have peripheral vascular or neural effects and ( 5) baseline data for comparison with subsequent examinations. The preplacement medical examination should be structured to elicit information pertinent to these points.
Specific screening tests considered useful in the diagnosis of HAVS are listed in Chapter IV, D (Screening and Diagnostic Tests). At aminimum, the preplacement medical examina tion should include tests or questions to identify the following:
• Peripheral neural status-light touch, pain, temperature, two-point discrimination, depth perception, vibrotactile sensitivity level
• Peripheral vascular status-finger blood flow response to the cold and cold provocation test with before, during, and after plethysmography conducted under standardized conditions
• Presence of carpal tunnel syndrome, tennis elbow, or other work-related cumula tive trauma disorders of the hand or arm
• Old injuries that could have peripheral vascular or neural effects (cold injury, bums, trauma, etc.)
• Primary Raynaud's disease, and its history • Other disorders that may have similar peripheral vascular or neural signs and symptoms (polyneuritis, occlusive vascular disease, thromboangiitis, chemical intoxication)
• Use of therapeutic and/or other drugs that have peripheral vascular or neural effects (including alcohol and tobacco) a
# VII. Methods for Worker Protection
• Anatomical abnormalities that may interfere with the safe use of the vibrating tools
• Presence of cold sensitivity and previous cold injuries
• History of past use of vibrating tools (including type of tool and duration of use)
• Age, sex, race, body weight, and other demographic data that may be relevant to differences in peripheral neural and vascular function and cold sensitivity
• Baseline measurements of vibrotactile threshold, grip force, muscle strength, etc.
# Periodic Medical Examinations
Periodic medical examinations for workers exposed to vibration from vibrating tools should be offered on a yearly basis or more frequently for affected workers on the recommendation of the responsible physician. The periodic medical examination should emphasize tests and questions that will elicit information on the early signs and symptoms of HAVS or the progress of its severity.
The periodic medical examination should include
• Review of worker health complaints
• Review and updating of the data derived from the preplacement examination
• Repetition of tests and procedures directed to peripheral vascular and neural functions and symptoms
• Assessment of peripheral vascular and neurological signs and symptoms, aesthesiometric and vibrotactile test results, grip strength, and presence of musculo skeletal symptomatology to establish whether HAVS has developed to Stage 1 or has progressed further
# Medical Surveillance
To ensure that the control practices provide adequate protection to workers exposed to hand-transmitted vibration, the responsible health professional can use the workplace exposure data, periodic medical data, and the interview history to determine any significant changes within a worker or group of workers since the previous examination. These events may include complaints of episodic numbness, tingling, or cold-induced white fingers; changes in grip strength and muscle force; and pain in the hands, arms, and shoulders. The events may lead the physician to suspect overexposure of the work population or a change in an individual's health status or susceptibility. The occurrence of these sentinel health events (SHEs) could signal a breakdown of or inadequacy of the vibration exposure control systems established at the workplace.
# H. RECORDS AND RECORDKEEPING
Records of the data obtained from the following measurements are required to establish adequate control procedures: (1) updated acceleration and frequency characteristics of the vibrating tools used, ( 2) hours per day the worker operates the tool, ( 3) intraday exposure pattern, ( 4) years of operating the tool, ( 5) nonoccupational exposure to hand-arm vibration, ( 6) exposure year in which HAVS symptoms first appeared, ( 7) stage assessment of HAVS, ( 8) environmental conditions at the workplace, including air temperature, wind speed, and humidity, ( 9) type of personal protective clothing and equipment used, (10) results of preplacement and periodic medical examinations, (11) change in medical status between medical examinations, and ( 12) worker training programs.
The records on vibration exposure levels and times and medical status should be retained in accordance with the requirements of 29 CFR 1910.20(d). HAVS should be considered a reportable occupation-related disorder.
Guidelines and recommendations for the control and prevention of HAVS are based mainly on clinical experiences and retrospective epidemiologic studies. These experiences and studies are limited, however, because no two industrial situations are exactly alike. Measur ing methods and results may vary greatly from one work site to another. In addition, no controlled laboratory studies on the production of HAVS in human subjects have been, or ethically should be, conducted. Progress in knowledge about HAVS control will depend on epidemiologic and clinical data carefully collected under standardized situations of in dustrial use.
# A. DOSE-RESPONSE
To make the data from different epidemiological studies comparable, a minimum list of factors required from all investigators would include all those factors known to have a significant influence on the development of HAVS. If data on those factors were collected in every study, data from several studies could be grouped to increase the number of observations and increase the reliability of the risk predictions. Some of the factors that are known to have a dose-response effect and that must be routinely included are (1) vibration measurement techniques and instruments (for acceleration, frequency, and exposure time), ( 2) work history of previous use of vibrating tools, (3) medical signs and symptoms of peripheral neural, vascular, and muscular complaints, ( 4) environmental conditions such as temperature, wind, and moisture, and ( 5) ergonomics of how the task is performed (tool/workpiece force interface, grip force on tool, arm and body posture, manner in which the tool is held and used, tool maintenance, and type of tool). Other factors that may influence the development of HAVS must be searched for and included.
# B. CLINICAL TESTS AND STOCKHOLM STAGES
All clinicians and researchers should now use the Stockholm classification to determine the stage of vascular and neurological symptoms from the patient's history so that studies may be compared. In addition, internationally accepted objective tests should be conducted and the results should be correlated with the Stockholm stages to assist parties involved in litigation and compensation.
Objective methods for evaluating and determining the stage are also needed to correctly estimate improvement or deterioration with and without (a) further hand-ann vibration exposure, (b) therapy or surgical intervention, and (c) a combination of these factors.
# I
# Hand-Arm Vibration
# C. IDENTIFICATION OF VIBRATION-INTOLERANT WORKERS
Identifying vibration-intolerant workers and strictly limiting their exposure before signs and symptoms of I4AVS develop would be an effective preventive procedure. Presently, complaints and symptoms of peripheral neural, vascular, and/or muscular involvement must first appear before vibration intervention procedures are indicated. No currently available set of medical or padiophysiologic measures can be used al one to predict, with an acceptable degree of reliability, those workers who are especially sensitive to the effects of toolproduced vibration and who are at high risk of developing HAVS as a result of using vibrating tools.
# D. ENGINEERING MODIFICATION OF TOOLS
During the past decade, considerable success has been achieved with the engineering approach to reducing the vibration level of some powered tools and workpieces. Greater improvement is needed, however, to make the various types of vibrating tools acceptable for routine use. Engineering modification may be directed to the design of the tool or to the design of the task. Reducing tool vibration to acceptable levels during optimum operating conditions will lower the worker's risk of developing HAVS.
# E. ERGONOMICS OF THE WORK TASK
Several important ergonomic factors that affect the impact of die vibrating tool on normal hand-ann function are (1) the grip force exerted on the tool handle to hold and control the tool, (2) the muscular force required at the tool/workpiece interface to do the work, and (3) the amount of flexion, abduction, and rotation at the wrist, elbow, and shoulder joints required to guide the tool properly. A change in bench height, workpiece orientation, and muscular forces required to do the job may reduce the pathophysiologic consequences of the vibration exposure task. This aspect of the HAVS problem has not received much research attention, even though it has a vast potential for significantly reducing HAVS.
# F. EXPOSURE SCHEDULE
Adhering to an optimum exposure/nonexposure schedule during the workday can be a successful approach to hazard control. This concept is known from studying other hazards and is recognized in the ISO Guide 5349, ACGIH TLV, ANSI Standard S3.34, BSI Standard 6842, and other guidelines for HAVS control [ISO 1986;ACGIH 1988;ANSI 1986;BSI 1987]. The vibration exposure data on which the concept is based, however, are mainly extrapolations and best estimates. The common denominator in these guidelines and recommendations is usually "minutes of exposure per day." The question is whether the health effects of exposure to a constant level of vibration are the same for 120 continuous minutes of exposure in an 8-hr day as they are for 120 minutes of noncontinuous exposure (that is, eight 15-minute periods of exposure, each followed by 45 minutes of nonexposure).
# I VIII. Research Needs
# G. PROTECTIVE DEVICES
Protective devices can be inserted between the tool producing the vibration and the tissue of the hand where the transmitted vibration energy is absorbed. The protection may be applied to the handles of the tool, or it may be incorporated into handgear worn by the tool operator. The amount of vibration that will be absorbed will be influenced by the vibration force (acceleration) or the vibration frequency (hertz). Data are available on the transmission and damping characteristics of some materials. However, for a large number of materials, there are no available data on which to base a choice of vibration-reducing material suited to the vibration characteristics of a particular vibrating tool or class of tools. New concepts for antivibration and damping devices and materials need to be explored. Until such data are available, specific recommendations for the type and amount of protective material cannot be made.
# H. ETIOLOGY AND PATHOGENESIS OF HA VS
Although it is well established that the use of vibrating tools is associated with the development of HAVS, it has not been fully explained how the vibration energy causes organ, tissue, and cellular changes and damage. A rational approach to the prevention and treatment of HAVS will require fundamental data on the mechanisms involved in changes in the arteries, muscles, nerves, connective tissue, and tendons associated with HAVS. New therapeutic or prophylactic drugs need to be explored.
# I. EXPOSURE MONITORING
With the instrumentation available today, measurement of the acceleration and frequency of the vibration produced by a tool is not a simple task. A dosimeter-type instrument that could be attached to the worker or the tool and that could provide an integrated acceleration level over time would do much to ease the burden of conducting vibration testing. Because vibration frequencies above 1,400 Hz are produced by some vibrating tools (up to 10,000 Hz), accelerometers need a window wide enough to capture these high frequencies.
A pressing need exists for investigators to evaluate the health effects from both frequencyweighted and -unweighted acceleration measurements over the extended frequency range. Particular attention should be paid to the high-frequency component for the possible pathophysiological effects on the hand structure components.
# J. HAVS RECOGNITION TRAINING PROGRAM
H AVS differs from many other occupationally-induced health disorders in that an acceptable risk/exposure factor cannot be set. This dictates a secondary prevention approach requiring that early signs and symptoms be recognized by the attending health professional and by the exposed worker to prevent progression of the disorder and to minimize morbidity. Most health professionals are not adequately trained or experienced to detect the early signs and symptoms of HAVS. To ensure that HAVS will be recognized and diagnosed at an early, reversible stage, a refresher course and self-instruction aids should be developed for interested physicians.
# K. OBJECTIVE TESTS
A pressing research need is the development of laboratory and clinical tests for objec tively identifying the signs and symptoms of the early stages of HAVS. The tests must be both sensitive and specific. To be clinically practical, they must be easy to perform and noninvasive, and they must not require esoteric equipment. n
# Hand-Arm Vibration
HAVS was found among workers exposed to hand-arm vibration in all of the epidemiologic studies cited, regardless of the level of vibration exposure. These studies therefore provide no basis for determining an exposure level at which no cases of HAVS would occur. However, the studies do provide ample evidence that the use of vibrationproducing, hand-held tools is associated with the development of HAVS.
# D. SCREENING AND DIAGNOSTIC TESTS
The signs and symptoms characteristic of HAVS are also observed individually or in various combinations in some other disorders. No single sign or symptom is specific to HAVS alone. This introduces uncertainties and difficulties in the classification and diagnosis of HAVS. Regardless of the complaints and symptoms presented by an individual, a diagnosis of HAVS is not justified unless a history of using vibrating tools is present [Taylor 1982a[Taylor , 1982bGemne 1982;NIOSH 1984;Pyykko and Starck 1986;Matoba and Sakurai 1987;Faikkila 1987]. Several tests can be used to help substantiate a clinical diagnosis of HAVS. Hand-Arm Vibration it would be 2.8 m/sec . In Table 2 of the Polish document, correction factors are listed for the actual use time in each hr that is less than 60 minutes.
The document does not include a discussion of health effects, diagnosis, treatment, or control procedures.
# <2
# I
# Hand-Arm Vibration
Types of exposure schedules that are applicable include the following:
• Alternating work tasks involving a vibrating tool with some other task that does not involve exposure to vibration (on hourly or daily basis)
• Limiting daily use of vibrating tools as much as possible if acceleration is high
• Limiting use of vibrating tools to 1 or 2 days a week
• Scheduling sufficiently long rest periods each hour to reduce the time-weighted acceleration levels
# D. ERGONOMIC CONSIDERATIONS
The amount of the tool-produced vibration that is transmitted to the hands and arms of the operator is influenced by (1) the grip force with which the tool is held, and ( 2) the force applied by the operator holding the tool against the workpiece Matoba 1986, Farkkila 1978J. The tool should be held as loosely as safe tool control and operating requirements permit. The force applied to hold the tool against the workpiece should be minimal. The weight of the tool should be used to help provide the required tool/workpiece interface pressure for optimal working speed and efficiency. Moisture at the hand/tool interface (sweat or liquids) may require the worker to exert greater grip force to control the tool. A slip-resistant interface surface is desirable.
Another important ergonomic factor is the position of the body while operating the tool. The angle of the wrists, elbows, and shoulders during tool operation will influence the level of stress exerted on the joints and tendons and the incidence of such problems as tendinitis, carpal tunnel syndrome, tennis elbow, painful shoulders, and HAVS.
An ergonomic analysis of how the work is done is important. Such an analysis can determine the operating practices that may require modification to minimize health problems.
# E. PROTECTIVE CLOTHING AND EQUIPMENT
Two generic types of protective clothing and equipment may be used to provide protection against the effects of vibration. These include (1) those that reduce transmission of vibration energy to the hand and (2) those that protect against exposure to cold and trauma.
Various types of vibration-damping materials have been incorporated into gloves and mittens to protect the user of vibrating tools. If these are sufficiently successful as energy dampers, this approach could be very acceptable. For most tasks involving vibrating tools, hand gear of some type is used for protection against trauma and cold. Presently, the major K a VII. Methods for Worker Protection problem is finding energy-damping materials that (1) provide adequate damping with minimal thickness so that the dexterity required for safe and efficient tool operation will not be reduced, and ( 2) have adequate damping characteristics over the vibration frequency spectrum associated with HAVS. Although several materials are available, an optimal, all-purpose material is not available.
Acute episodes of white finger, especially in the early stages of HAVS, are frequently triggered by exposure of the hands or body to cold. Thermal protection by adequate body clothing and handgear to prevent hand or central body cooling might reduce the frequency of the attacks. However, protecting the hands and body in cold weather is a complex problem that depends on many interacting factors such as
where a0 is the reference acceleration value, and a is the measurement value.
In the cases where only mechanical displacement was given, the following formula was used,
# Speak
| None | None |
a90ea2f33aa6ad3e68e67781c1b36b25ca512b23 | cdc | None | # I. RECOMMENDATIONS FOR A NOISE STANDARD
The National Institute for Occupational Safety and Health (NIOSH) recommends that employee exposure to noise in the workplace be controlled by requiring compliance with the standard set forth in the following sections. Control of employee exposure to the occupational limits stated and adherence to the precautionary procedures prescribed will improve the protection of the working population from incurring noise induced hearing loss that could impair their abilities to understand everyday speech.
Such control and adherence at the workplace is believed sufficiently effective to reduce also the possibility of other forms of occupational Injury and illness related to noise. This standard is amenable to techniques that are valid, reproducible, and presently available. It will le reviewed and revised as additional information becomes available.
# Section 1 -Applicability
The provisions of this standard are applicable to occupational noise exposures at places of employment and are intended to apply for all noise even though additional controls may be necessary for certain specific types of noise, such as some impact and impulsive noise. For the purposes of this standard the noise exposure is determined for an 8-hour workday.
# Section 2 -Definitions
As used in this standard, the term: (a) "Administrative control" means any procedure that limits daily exposure to noise by control of the work schedule. (b) "Audiogram" means a graph or table obtained from an audiometric examination showing hearing level as a function of frequency.
1-1 (c) "Baseline audiogram" means an audiogram obtained from an audio metric examination that is preceded by a period of at least 14 hours of quiet.
(e) "Audiometer setting" means a setting on an audiometer corres ponding to a specific combination of hearing level and sound frequency.
(f) "Daily Noise Dose" means that value for D derived from the equation:
D -£ L + Sl + + £2.
# Ti T2 Tn
where Cl, C2 . . . , Cn are the actual durations of exposure for an employee at the various noise levels, Tl, T2, . . . , Tn are the respective duration limits obtained from Figure 1-1 and D is the Daily Noise Dose.
(g) "dBA -Slow" means the unit of measurement of sound level indicated by a sound level meter conforming as a minimum requirement to the American National Standard Specification for Sound Level Meters, ANSI SI.4 (1971) Type S2A, when used for A-weighted sound level, slow response.
(h) "Engineering control" means any procedure other than administrative control that reduces the sound level either at the source of the noise or in the hearing zone of the employees.
(i) "Hearing level" means the amount, in decibels, by which the threshold of audibility for an ear differs from a standard audiometric threshold.
1-2 (j) "Environmental noise level" means the noise level in dBA-Slow as measured in accord with Section 3(c).
(k) "Effective noise level" means (1) for employees not wearing ear protectors, the environmental noise level; (2) for employees wearing ear protectors, the result of subtracting the dBA reduction, R, for the ear protectors (determined as specified in Appendix A) from the measured environmental noise level. Effective noise level is expressed in units oi dBA-Slow.
(1) "Noise exposure" means a combination of effective noise level and exposure duration. (1) Occupational noise exposure shall be controlled so that no worker shall be exposed in excess of the limit described as line B in The Indicated duration limits which exceed 8 hours are to be used only for purposes of computing Daily Noise Dose and are not to be regarded as defining noise exposure limits for work days which exceed 8 hours.
employment is believed necessary to permit the Department of Labor to conduct an extensive feasibility study.
(iii) At no time shall any worker be exposed to effective noise levels exceeding 115 dBA-Slow.
(c) Measurements (i) Compliance with the permitted daily noise exposures defined by Section 3(b) shall be determined on the basis of measurements made with a sound level meter conforming as a minimum to the requirement of the American National Standard Specification for Sound Level Meters, SI.4 (1971)
Type S2A, and set to use an A-weighted slow response.
(ii) All measurements shall be made with the sound level meter at a position which most closely approximates the noise levels at the head position of the employee during normal operations.
(iii) An acoustical calibrator accurate within plus or minus one decibel shall be used to calibrate the sound level meter on each day that noise measurements are taken. (i) A baseline audiogram for each employee who is initially assigned or reassigned to work subject to conditions stated in (a) of this section shall be taken within 30 days of assignment to such employment, in the sixth year of such employment, and once every sixth year thereafter. It is recognized that some delay in implementation of this requirement may be necessary for employers with a small work force.
# 1-5 (ii)
A baseline audiogram should be taken for each employee presently assigned to work subject to conditions stated in (a) of this section at the time of effective date of this regulation, in the sixth year, and once every sixth year thereafter.
(iii)
In addition an audiogram, not necessarily baseline, for all exposed employees should be taken every second year.
(c) Each audiogram shall contain (1) employee's name or identifying number,
(2) employee's job location, (3) significant aural medical history of the employee, (4) the examiner's name and signature, (5) the date and time of test, (6) serial number of the audiometer, and (7) last exposure to high level noise: number of hours since exposure; type of exposure; and noise level, if known.
(d) Each employee's audiogram shall be examined to determine whether it indicates for either ear any threshold shift (higher threshold), that equals or exceeds 10 dB at 500, 1000, 2000, or 3000 Hz, or 15 dB at 4000 or 6000 Hz as evidenced by a comparison of that audiogram with the employee's most recent baseline audiogram and with his initial baseline audiogram as corrected to his current age by the method described in Appendix B. If either comparison indicates a shift as described above:
(i) refer the employee for appropriate medical evaluation, (ii) if the employee needs personal protective equipment or devices, insure that he has the appropriate effective equipment and that he is instructed in the proper use and care of the equipment, and
(iii) if the audiogram was not a baseline audiogram, take a baseline audiogram within sixty days.
(e) Audiometric tests shall be pure tone, air-conduction, hearing threshold examinations, with test frequencies including 500, 1000, 2000, 3000, 4000, and 6000 Hz and shall be taken separately for the right and left ears.
# 1-6 (i)
The tests shall be conducted in a room whose ambient noise levels conform to all requirements except that part concerning octave bands whose center frequencies are less than 250 Hz of the American National Standard Criteria for Background Noise in Audiometer Rooms, ANSI S3.1 (1960 R-1971), when measured by equipment conforming to American National Standard Specification for Sound Level Meters, ANSI SI.4 (1971) Type 2 and American National Standard Specification for Octave, Half-Octave, and Third-Octave Band Filter Sets, ANSI SI.11 (1966, R-1971).
(ii)
The tests shall be administered using an audiometer which conforms to the requirements for limited range pure tone audiometers prescribed by the American National Standards Specifications for Audiometers, ANSI S3. 6 (1969), and which is of the discrete frequency type. If a pulsed tone audiometer is used, the on-time of the tone shall be at least 200 milliseconds. The instrument used in the testing shall be either a manual audiometer, or a self-recording audiometer which is subject to the following additional restrictions:
(1) The chart upon which the audiogram is traced shall have printed lines at positions corresponding to all multiples of 10 dB hearing level within the intensity range spanned by the audiometer. The lines shall be equally spaced and shall be separated by at least 1/4 inch.
Additional graduations are optional. The pen which traces the audiogram shall have a fine point so that the tracing shall not exceed 2 dB in width.
(2) It shall be possible to disable the stylus drive 1-7 mechanism so that the stylus can be manually set at the 10-dB graduation lines for calibration purposes.
The slewing rate for the audiometer attenuator shall be 6 dB/sec or less except that an initial slewing rate greater than 6 dli/sec is permitted at the beginning of each new test frequency, but only until the second subject response.
(A) The audiometer shall remain at each required test frequency for 30 seconds (+ 3 seconds). The audiogram shall be clearly marked at each change of frequency and the actual frequency change of the audiometer shall not deviate from the frequency boundaries marked on the audiogram by more than + 3 seconds.
(5) If an audiogram fails to pass the following criteria, the subject shall be retested:
At each test frequency it must be possible to place a horizontal line segment parallel to the time axis on the audiogram, such that the audiometric tracing crosses the line segment at least six times at that test frequency.
# (iv)
The audiometer shall be maintained in calibration in accordance with the provisions of Appendix C. If noise exposures to which employees could be exposed exceed the limits specified, personal protective equipment (i.e., ear protectors) shall be provided by the employer to be used in conjunction with an audiometric testing program, as specified in Section 4, subject to the f oJlowing requirements:
(i) The use of personal protective equipment to prevent occupational noise exposure of the employer in excess of the prescribed limits is authorized only until engineering and administrative controls and procedures can be implemented to maintain the occupational noise exposures within prescribed limits.
(ii) Any ear protector used by an employee shall reduce the effective noise level to which he is exposed so that his noise exposure is within the limits prescribed in Section 3(b).
(iii) Insert -type ear protectors shall be fitted by a person trained In this procedure.
(iv) Inspection procedures to assure proper Issuance, main tenance, and use of personal protective equipment shall be established by the employer.
# 1-9 (b)
The employer shall provide training In the proper care and use of all personal protective equipment.
Section 8 -Apprisal of Employees of Hazards from Noise Each worker exposed to noise shall be apprised of all hazards, relevant symptoms, and proper conditions and precautions for working in noisy areas.
The information shall be kept on file and readily accessible to the worker at all places of employment where the noise levels equal or exceed the limits prescribed in Section 3 (b).
# Section 9 -Monitoring & Recordkeeping Requirements
(a) Employers will be required to maintain records of:
(i) environmental exposure monitoring for a period of 10 years, (ii) all audiograms for a period of 20 years.
(iii) all audiometric calibration data for a period of 20 years.
(b) When exposure times of less than 8 hours/day are required in a specific work area or ear protection is used to meet the exposure limits, records of the method of control shall be maintained.
Appendix A -Determination of dBA Reduction R for Ear Protectors 1. The pure tone attenuation vs. frequency characteristics of the ear protector (normally supplied by the manufacturer) shall have been determined
In accordance with the American National Standard for Measurement of the Real-Ear Attenuation of Ear Protectors at Threshold, ANSI Z24. 22 (1957). The "-10.0" correction term is to account for possible noise spectrum irregularities and noise leakage which might be caused by long hair, safety glasses, head movement, or various other factors.
# Let
3. If the octave band levels of the noise are not known, then the dBA reduction R may be computed simply as R --10 log S -3.0 where S antilog (-0.1 X Qj) + antilog (-0.1 X Q2)
- antilog (-0.1 X Q3) + antilog (-0.1 X Q4) + antilog (-0.1 X Q5) + antilog (-0.1 X Q6) + antilog (-0.1 X Q7)
This calculation is approximate, and is based upon the assumption that the octave band levels are equal. For most types of noise it will give results close to those obtained by the more accurate method of (2) above. (1) Set audiometer to 70 dB hearing threshold level and measure sound pressure levels of test tones using an NBS-9A-type coupler, for both earphones and at all test frequencies.
(2) At 1000 Hz, for both earphones measure the earphone decibel levels of the audiometer for 10 dB settings in the range 70 to 10 dB hearing threshold level. This measurement may be made acoustically with a 9A coupler, or electrically at the earphone terminals.
(3) Measure the test tone frequencies with the audiometer set at 70 dB hearing threshold level, for one earphone only.
(4) In making the measurements in (1) -( 3) above the accuracy of the calibrating equipment shall be sufficient to prove that the audiometer is within the tolerances permitted by ANSI S3.6-1969.
(5) A careful listening test, more extensive than that required in the biological calibration, shall be made in order to ensure that the audiometer displays no evidence of distortion, unwanted sound, or other technical problems.
(6) General function of the audiometer shall be checked, particularly in the case of a self-recording audiometer.
(7) All observed deviations from required performance shall be corrected.
C. An exhaustive calibration shall be performed at least every five years. This shall include testing at all settings for both earphones.
The test results must prove unequivocally that the audiometer meets for the following parameters the specific requirements stated in the applicable sections of ANSI-S. as noted in parenthesis.
(1) Accuracy of decibel level settings of test tones (Sections 4.1 .4. 1 and 4.1 .4.3).
(2) Accuracy of test tone frequencies (Section 4.1.2).
(3) Harmonic distortion of test tones (Section 4.1.3).
(4) Tone-envelope characteristics, i.e., rise and decay times, overshoot, "off" level (Section 4.5).
(5) Sound from second earphone (Section 4.4.2).
(6) Sound from test earphone (Section 4.4.1). ation. In the case of periodic sound pressures, the interval must be an integral number of periods or an interval that is long compared to a period.
# III-l
Frequency -The frequency of a function periodic in time is the reciprocal of the primitive period. The unit is the cycle per unit time and must be specified. The unit cycle per second is commonly called Hertz (Hz).
Level -In acoustics, the level of a quantity is the logarithm of the ratio of that quantity to a reference quantity of the same kind. The base of the logarithm, the reference quantity, and the kind of level must be specified.
Noise -(1) Noise is any undesired sound; and, by extension, noise is any unwanted disturbance within a useful frequency band, such as undesired electric waves in a transmission channel or device. (2) Noise is an erratic, intermittent, or statistically random oscillation. Since the definitions of noise are not mutually exclusive, it is usually necessary to depend upon context for the distinction.
Noise Level -(1) Noise level is the level of noise, the type of which must be indicated by further modifier or context. The physical quantity measured (e.g., voltage), the reference quantity, the instrument used, and the bandwidth or other weighting characteristic must be indicated.
(2) For airborne sound, unless specified to the contrary, noise level is the weighted sound pressure level called sound level; the weighting must be indicated.
Oscillation -Oscillation is the variation, usually with time, of the magnitude of a quantity with respect to a specified reference when the magnitude is alternately greater and smaller than the reference.
Period -The period of a periodic quantity is the smallest increment of the independent variable for which the function repeats Itself.
# III-2
Periodic Quantity -A periodic quantity is an oscillating quantity whose values recur for certain increments of the independent variable.
# Sound -(1)
Sound is an oscillation in pressure, stress, particle displacement, particle velocity, etc., in a medium with internal forces (e.g., elastic, viscous), or the superimposition of such propagated oscilla tions. (2) Sound is an auditory sensation evoked by the oscillation described above.
Sound Absorption -Sound absorption is the change of sound energy into some other form, usually heat, in passing through a medium or on striking a surface.
Sound Level (SL) -Sound level is a weighted sound pressure level, obtained by the use of metering characteristics and the weightings A,B, or C as specified in the American National Standard Specification for Sound Level Meters, ANSI-S1.4-1971. The weighting employed must be stated.
Sound Pressure -The sound pressure at a point is the total instanta neous pressure at that point in the presence of a sound wave minus the static pressure at that point.
Sound Pressure Level (SPL) -The sound pressure level, in decibels, of a sound is 20 times the logarithm to the base 10 of the ratio of the pressure of this sound to the reference pressure. The reference pressure must be stated. The following reference pressure is in common use for measurements concerned with hearing and with sound in air and liquids: 2 X 10 N/M^. Unless otherwise explicitly stated, it is to be understood that the sound pressure is the effective (rms) sound pressure.
# III-4
# Response of the Ear
Upon inspection of the definition of sound pressure level, it is evident that there is no reference to frequency. In actuality, the ear does not show equal response to all frequencies, and in fact, it is more sensitive to the middle frequencies than to the low or high ones. Studies have been made which determine the sound pressure levels of simple tones at various frequencies which sound just as loud to an observer as a 1000 Hz tone of a particular SPL. The results of such comparisons are given as equal loudness curves in Figure 1 . The number of each curve, loudness level in phons. is the SPL of the 1000 Hz tone used for comparison in 3 determining the curve.
# Measurement Scales
These equal loudness contours have been taken into account in the standardization of several frequency weighting networks which are included on most sound measuring equipment. The frequency characteristics of these networks are given in Figure 2. The A scale corresponds approximately to the 40-phon equal loudness contour, the B-scale corresponds to 70-phons, and the C-scale corresponds to the 100-phon contour. With these weighting networks, which modify sound pressure level to approximate the ear's response, the term to be used is sound level, and the weighting used must always be stated. (?'The A-sound level is 36 dB" or "86 dBA" are appropriate ex--5 2 pressions.) The reference pressure is 2 X 10 N/M ).
The A scale is commonly used in measuring noise to evaluate its effect on people, and the A-weighted sound level is considered an adequate number to indicate or rate the hazard of a certain noise. Explanation of these measurements is given in Part IV.
# III-5
# Correction of Original Baseline Audiograms for Age
To determine whether there has been a significant change in an employee's hearing due to noise exposure by comparing an audiogram taken since the original baseline audiogram with that audiogram it la necessary to make a correction for difference in age.
The best way to make this correction is to use data from a non-noise exposed group from the same area tested in the same manner as the group under consideration. Quite often this is not possible; therefore, It Is necessary to establish an age correction that can be used universally. The data from these four studies with respect to differences in hearing level from age 20 are quite similar. However, the greater changes apparent
In the National Health Survey data at the upper frequencies could be expected because this population was not screened for significant noise exposure.
# III-6
Thus, to provide a uniform correction, tables B-l and B-2 (Appendix B) derived from the NIOSH data, will be used as specified in the standard.
# Conversion of Octave Band Levels to dBA Levels
When the octave-band sound pressure levels of a noise have been measured it is often desirable to compute the A-weighted sound pressure level from them. This can be done as follows:
1. From each octave band level, subtract (or add) the A-weighting correction value shown in Table III. corresponding to the frequency of the octave band. This method is quite accurate although it does involve some approximation.
# Calculation of dBA Reduction R for an Ear Protector
Calculation of dBA reduction R for ear protectors can be done as follows:
1. When the octave band levels of the noise are known: If the dB attenuation levels of the ear protector were known for each octave band, then the dBA reduction of the ear protector could be determined by subtracting these attenuation levels from the original octave band noise levels, and then calculating the dBA level of the resulting attenuated octave band levels using the method described in the previous section. One would then subtract this dBA level from the original dBA level to obtain the dBA reduction.
# III-7
However, the American National Standard for Measurement of Real-Ear Attenuation of Ear Protectors at Threshold, ANSI Z24. 22 (1957), prescribes pure-tone tests at 125, 250, 500, 1000, 2000, 3000, 4000, 6000, and 8000 Hz.
We shall also assume that the 4000 Hz octave band attenuation level can be obtained by averaging the pure tone attenuation levels at 3000 and 4000 Hz, and that the 8000 Hz octave band attenuation level can be obtained by averaging the pure tone attenuation levels at 6000 and 8000 Hz.
This method has been formulated concisely in Appendix A of the Recommended Noise Standard, also including a factor of 10 which is to be subtracted to account for possible noise spectrum irregularities and noise leakage which might be caused by long hair, safety glasses, head movement, or various other factors. It ignores noise in the 31.5 Hz, and 16,000 Hz bands, but these rarely contribute substantially to the dBA level.
When the octave band levels are not known it is assumed that the noise has a uniform "pink" spectrum, i.e., equal levels in each octave band.
This type of noise is representative of "average" occupational noise, and the error introduced by making this approximation is usually small. The assumption results in a simplified formula for calculation, as presented in Appendix A of the recommended Noise Standard. It is recommended, however, that the more exact method described in (1 ) above be used whenever octave band noise levels are available.
# IV. REVIEW OF EFFECTS OF NOISE ON MAN
Exposures to noise levels found at the workplace, particularly in mechanized Industries, are likely to be the most Intense and sustained of any experienced In dally living. As such, they represent the severest form of acoustic insult to man and therein pose the greatest harm to human function. Real or alleged effects of occupational noise exposures include the following:
-Temporary and permanent losses in hearing sensitivity.
-Physical and psychological disorders.
-Interference with speech communications or the reception of other wanted sounds.
-Disruption of job performance.
These different listed effects of noise can be classified in various ways. For example, the first two effects can be treated in the context of health or medical problems owing to their underlying biological basis.
That is, noise-induced hearing loss, as will be described later, involves damage to the cell structures of the hearing organ, and physical or psychological disorders due to noise presume alterations in normal physiologic or nervous system responses. In contrast, the remaining two effects, interference with sound reception and performance loss, are deemed annoyance or economic problems since they involve no pathology or physical dysfunction to the organism.
The aforementioned noise effects can also be classified as "auditory"
and "extra-auditory" in nature. In this regard, hearing loss and speech interference caused by noise are deemed auditory effects since they both involve disturbance to the hearing organ and/or its functional processes.
# IV-1
Noise effects on physical and psychological health states ¡md/or performance represent extra-auditory effects in that they extend beyond or are apart from auditory experience per se.
The intent of this part is to summarize current knowledge of these various adverse effects of noise as it relates to occupational noise conditions, and to establish their importance relative to needs for noise control in industry.
# Hearing Loss
The ear is the organ structure of the body especially adapted and most responsive to the pressure changes underlying airborne sounds or noise. Anatomically, it is divided into three subdivisions -the outer, middle, and inner ear. Some key structures within these subdivisions are shown in Figures 3 and 4 structures by high level sounds subjects them to shearing forces or other mechanical stresses that may jar them loose from their supporting cells or otherwise damage them.1 Another is that constant intense sound stimula tion forces the hair cell receptors to high metabolic levels that cannot be maintained. As a result, the metabolic processes essential for cellular life become exhausted or poisoned, leading to the death of the cells
12 involved.
# IV-3
Since direct observation of the cell structures of the intact ear on a live human is impossible, injury to these parts are inferred from audio grams which show losses in threshold hearing levels for certain pure tone frequencies relative to some reference value. Such losses, when due to noise, may be of a temporary or permanent nature. Temporary hearing loss, more usually called temporary threshold shift or TTS, can be produced by brief exposures to high level sound and shows recovery following a period of time in quiet. Figure 6 describes an example of TTS caused by a twohour exposure in the laboratory to a broad-band noise of fairly high level (103 dBA). In this instance an audiogram was taken on the listener just before and at various times after the cessation of the noise exposure.
Differences between pre-and post-exposure threshold levels for the specified test frequencies display the amount of TTS induced by the noise.
TTS is greatest immediately after exposure and progressively diminishes with increasing time in the quiet, reflecting ear recovery from the apparent noise overstimulation .
As a general rule, a noise capable of causing significant TTS with brief exposures is probably capable of causing significant permanent losses in hearing, given prolonged or recurrent exposures. In fact, some limited evidence from animal studies suggests the presence of minor hair cell damage even in those ears showing complete recovery from noise-induced temporary threshold shift. 13 In any case, daily exposures to TTS-producing noises for several hours per day for months or years would pose a risk of permanent hearing loss. That is, the ear is not likely to recover completely with recurrent exposures of this type. Rather, only partial recovery may occur IV-4 in due course with new resting thresholds established, poorer than those found at the beginning of the overall noise experience. This residual loss is indicative of permanent hearing damage. Figure 7 describes these permanent losses in one group of employees as a function of their years of exposure to workplace noise levels appoximating the level used 14 in the TTS example above.
The TTS component in the losses evident in these hearing data was eliminated by allowing sufficient time after the workshift ended before taking audiograms on the worker group. Deductions have also been made in the hearing levels to remove those hearing changes related to aging (i.e., presbycusis).
Figure 7 indicates that the most significant noise-induced hearing losses occur first in the high frequency range, most prominently at 4,000 cycles per second or Hertz (Hz). Decreased sensitivity to these high frequency sounds may go unnoticed by the listener since they are relatively unimportant to speech reception. With increasing exposure years, however, the losses grow and also broaden to involve other frequencies which are more critical to speech reception, namely, those in the range 500 to 3,000
Hz. In actuality, in the United States, generally accepted procedures for rating hearing handicap for speech consider losses only at frequencies 500, 1000, and 2000 Hz on the audiogram.^ Controversy centers around the need to include 3000 Hz in these judgments since consonant discrimination may depend on hearing sensitivity for sounds higher than 2000
The pattern of permanent hearing loss shown in Figure 8 seems typical of noise-induced hearing damage as revealed in noise and hearing surveys in assorted industries (see Table IV). Why high frequency hearing, parti cularly around 4000 Hz, shows most vulnerability to noise is not altogether IV-5 clear. One possible explanation is that the resonant frequency of the ear canal is in region 2000 -5000 Hz which, in effect, adds strength to corres-19 20 ponding frequencies in an incoming noise signal. - Complicating evaluations of hearing loss due to industrial noise are a number of factors. First, hearing sensitivity normally decreases with age, and these losses (presbycusis) are quite similar to those caused by excessive noise, i.e., differentially greater losses at the higher fre- Other causes of hearing loss besides noise and age include use of 23 drugs, illness and disease processes, blows on the head. Special audio metric procedures are sometimes necessary to diagnose a given case of hearing loss in order to determine the likelihood that it may have been caused by excessive noise rather than other agents.
Even when there is clear audiometric evidence of noise-induced hearing loss, questions may be raised as to whether such damage was produced entirely by workplace noise. It is apparent that off-job noise conditions, particularly in recreation, can pose some risk of hearing change by themselves or can 24 exacerbate the acoustic insult associated with the job situation.
# IV-6
While indicating the need for close appraisal of audiometric results, the aforementioned complicating factors should not be construed as minimizing the seriousness of noise and hearing loss problems in industry. As will be noted in subsequent section, noise surveys in assorted manufacturing, construction, mining, transportation and farm operations indicate exposure conditions potentially harmful to millions of workers. Indeed, the popula tion at risk with regards to noise-induced hearing loss may be greater than any other hazard in the work environment. Audiometric data already col lected on samples of employees in many of the jobs surveyed above for excessive noise show them to have poorer hearing relative to other groups of workers not so exposed. Composite reviews of published occupational Obviously, the rate and number of such impact sounds constituting an exposure period are also factors in making hazard judgments for these types of sounds.
Noise and hearing surveys in industry dealing with these types of exposure conditions are just beginning. Most permanent hearing loss data reflooting impulse noise hazards have been based on military studies involving gunfire.
# IV-9
Physical and Psychological Disturbances Aside from hearing loss, noise may trigger changes in cardiovascular, 35 37-39 endocrine, neurologic, and other physiologic functions, - all of which are suggestive of a general stress reaction. These physiologic changes are produced typically by intense sounds of sudden onset, but can also occur under sustained high level or even moderately strong noise conditions.
Whether repeated noise induced reactions of this type can ultimately degrade one's physical and mental health is still uncertain. For example, the aforementioned physiologic changes tend to subside with recurrent exposures to the same sounds, suggesting adaptation and presumably no health difficulty. These observations, however, may not have been conducted over a sufficiently long time period to judge the possible long-term cost 40 of this adaptation to the health of the organism.
There are some reports which show that prolonged exposure to high level noise may lead to physiologic disorders in animals. For example, Anthony and Ackerman reported that guinea pigs presented with intense siren-type noises for fairly long periods of time eventually revealed endocrine and metabolic deficits which reduced their ability to cope with 41 the noise stress.
Additional siren exposure here resulted in gastro intestinal ailments, cardiovascular disease and even tissue damage in the kidneys and liver. Reproductive dysfunction and reduced resistance to infectious disease have also been reported in animals subjected to recurrent 42 43 or prolonged high level noise conditions. '
The results of these studies have not been without criticism.in some instances, they have lacked for certain controls, e.g., handling of test animals in noise but not non-noise groups, or not differentiating the groups. Also, rodents have often been used as subjects, and these animals are known to have special IV-10 susceptibility to the effects of certain sounds. Furthermore, the sound levels used in many of these experiments have usually been well above those normally encountered by man even in the noisiest environmental situations.
With regard to human exposures, there are Indications in the foreign literature which suggest that routine exposures to intense industrial noise might lead to chronic physical disturbances. A German study, for example revealed a higher incidence of circulatory and neurologic irregularities among steel workers in noisy jobs as compared with other worker groups in 44 less noisy plant areas.
Neurological examinations of Italian weavers exposed daily to intense noise showed their reflexes to be hyperactive, and in a few cases, electroencephalography traced a pattern of desynchron-25 ization similar to that seen in personality disorders.
A study in the Russian literature showed workers in noisy ball-bearing and steel plants to have a relatively greater prevalence of cardiovascular irregularities 45 such as bradycardia.
Complaints of fatigue, irritability, and social conflicts in many noise exposed workers have also been reported in connection 25 44 with several of the investigations just noted. '
The fact that those who work in high noise levels show greater medical difficulties than those who work under quieter conditions is not conclusive evidence that noise is the crucial causal factor. In each case, it is possible that the differences in the specified health parameters may be explained by other factors such as age, other environmental contaminants, work load and job habits. In any case, replication of these findings seems indicated with attempts being made to statistically isolate and better control factors that could confound possible noise effects on a variety of health indicators.
# IV-11
Concern may be raised as to whether excessive noise poses any added hazards to persons with preexisting health problems. That is, losses in performance may occur when the noise appears and also when it disappears.
Apparently, change in noise levels is the degrading factor. Of interest here is that sound levels required to cause notable performance changes may exceed hearing conservation limits for routine workday exposure. Thus, noise standards for safeguarding hearing could also offset possible noise 38 effects on job efficiency.
More moderate levels of noise may actually benefit task performance relative to quiet conditions. The presence of such noise may provide for a more uniform acoustic background, masking stray sounds which could be otherwise audible in a quiet work area and cause distraction. Also on the positive side, pulsating-type sounds may pace or drive performance and, in effect, reduce fatigue on tasks that are trying. The rhythm component in music may serve this purpose too.^"- Not all performance capacities suffer equally from the disruptive effects of noise. In fact, noise may aid performance on simple, wellpracticed or repetitive tasks through causing increased arousal in an otherwise boring job. There are indications in fact, that only those tasks which require unremitting attention (e.g., vigilance in machine monitoring, product inspection) or which place extreme mental demands on IV-14 the employee (short-term high-memory loads) may be most vulnerable to the degrading effects of n o i s e .^ In short, tasks which by themselves tax the total capacity of the Individual do not permit any accommodation to noise and consequently show loss. In some Instances, noise seems more Inclined to disturb the quality rather than the quantity of work. That Is, noise might not change work output, but may cause more errors. Along these lines, performance under noise may be subject to worker fluctuations, with periods of poor performance being Interwoven with periods of heightened 56 effort.
These performance swings, when averaged across the total work session, may yield little or no overall performance decrement.
Individual differences are quite commonly found In investigations of noise effects on performance. Attitudes toward noise are a basic factor in this variance. A recent laboratory study found subjects sensing that they had no control over randomly occurring noise intrusions to perform 57 poorer than those who could terminate such sounds.
Personality factors also seem to underlie performance variations in noise. Tense, anxious persons, as defined by personality inventories and certain physiologic indicators, seemed less able to cope with certain laboratory tasks as 58 compared with those who were more relaxed.
The importance of attitude factors in noise-performance studies is even more evident in field investigations. For example» morale and egoinvolvement in one's job can override stresses imposed by noise.Other employees dissatisfied with their job situations can use noise as a "scape goat" for poor performance. It should be mentioned, too, that through a process of self-selection, only the more noise tolerant employees probably stay at a noisy job. The more noise sensitive persons would remove themselves from these situations. Measures of absenteeism and labor turnover could IV-15 reflect the latter occurrences, but could be difficult to relate causally to noise.
The numerous factors that can influence noise effects on performance make for highly qualified conclusions and conservative predictions. Generally speaking, intense sounds» preferably impulsive» and a taxing task performed by a tense person offer the combination of conditions most likely to display a noise-induced decrement in performance.
# Cumulative Effect
This discussion has separately treated different adverse effects of noise that may result from occupational exposures. It is unrealistic, however, to conceive of employees In their everyday job routines experiencing one form of noise disturbance to the exclusion of the others. Indeed, one's daily encounters with workplace noise may degrade hearing, mask reception of desired sounds, heighten emotions and physiologic activity, disrupt con centration , or otherwise hinder job efficiency or safety. The collective impact of these noise effects clearly poses a significant challenge to the employee's health, productivity, and well-being.
The establishment of noise exposure limits for safeguarding the employee's hearing will in the main prevent the occurrence of the worst physical defect that noise can have in humans. Adherence to these limits may also have other benefits. Specifically, physical and psychological disturbances from occupational noise exposures will be less likely to arise under more controlled exposure conditions. Of course, the question remains as to whether excessive noise by itself can cause physical and mental disorders.
Nevertheless, noise levels which meet hearing conservation requirements may also be within limits that do not cause losses in job performance.
# IV-16
# V. PROCEDURES FOR REDUCING EXPOSURES
The information in this part (1) is not an attempt to present exact figures as to how many employees are exposed to hazardous noise levels; rather it substantiates that noise is Indeed a common occupational hazard which could affect a large number of employees. The companies were asked to answer the following question: "How many of your employeees are located In areas where noise levels are 90 dBA or above?" When this question was asked in August 1971, the recommended level for an 8-hour exposure limit was still 90 dBA, however, it can be assumed that a greater population is at risk. In interpreting the answers to the question stated in the preceding paragraph and the results which appear in Table VI the following points must also be considered:
V-l 1. The answers from this question cannot be used to determine how many employees are incurring hazardous noise exposures because information concerned with length of exposure time and the exact level of the exposure is not available.
2. The 341 plants volunteered this information, and the information is based upon their own noise level evaluations.
# Many other plants involved in the questionnaire survey could not
-r did not answer the question.
4. The table does not contain information concerned with the 4,511,000 transportation workers, the 3,502,000 construction workers, the 626,000 miners, or the 4,746,000 agricultural w orkers.
The projected numbers of employees located in areas of noise 90 dBA F. Use sharp and properly shaped cutting and drilling tools.
# Substitution of Machines
A. Substitute belt drives for gears.
# Vibration Dampening
A. Increase mass.
B. Increase stiffness.
C. Use rubber or plastic linings to dampen noise.
D. Improve supports.
# Reduction of Solid-Borne Transmission
A. Flexible mounts for motors and other types of machinery.
B. Flexible hose in pipes or electrical conduits.
C. Flexible coupling on shafts.
# . Reduction of Noise Caused by Fluid Flow
A. Install or replace intake and exhaust mufflers on internal combustion engines and compressors.
# Isolate Noise Source
A. Construct sound reduction enclosures around equipment or parts of equipment.
# Isolate Operator
A. Provide a relatively sound-proof enclosure for the operator or attendant of one or more machines.
# V-4
Of the items listed above, the preferred procedures for reducing environmental noise are those which are directed at reducing the noise at its source (Items 1-7). Generally, these procedures have proven to be far more efficient in terms of actual noise reduction than the procedure listed as Item 8 . Furthermore, source noise controls provide protection for both the operators of the equipment as well as workers in the immediate exposure environment.
# Administrative Controls
Another effective approach to reducing the hazard of excessive noise exposure is to limit the dally amount of exposure which each employee receives, by means of strict control of the work schedule.
The following are several methods suggested by the Department of Labor "1. Arrange work schedules so that employees working the major portion of a day at or very close to the criteria limit are not exposed to higher noise levels.
2. Ensure that employees who have reached the upper limit of duration for a high noise level, work the remainder of the day in an en vironment with a noise level well below criteria limit.
3. Where the man-hours required for a job exceed the permissible time for one man in one day for the existing sound level, divide the work among two, three, or as many men as are needed, either successively or together, to keep individual noise exposure within permissible time limits.
4. If less than full-time operation of a noisy machine is needed, arrange to run it a portion of each day, rather than all day for part of the week.
V-5
Perform occasional high level noise producing operations at night or at other times when a minimum number of employees will be exposed."
When personnel are rotated, extreme care must be taken to insure that no single employee is exposed to a high level noise for a period longer than is allowed by the noise exposure limits.
# V-6
VI.
# DEVELOPMENT OF THE STANDARD
Attempts at limiting human exposure to noise have been based on damage risk criteria. The purpose of such criteria is to define maximum permissible levels of noise for stated durations which, if not exceeded, would result in an acceptably small effect on hearing levels over a working lifetime of exposure.
Previous 1. Measurement of spectral distribution (Noise Spectrum).
2. Determination of the temporal characteristics of exposure (Noise Duration).
# Identification of a protection goal (Biologic Response).
In the discussion which follows, selected damage risk criteria listed in As may be seen from this figure, although the DRC differ in estimates of safe sound pressure level per octave, they all weight the spectrum similarly.
The second major Impetus for measurement of noise based on octave band analysis came from research which indicated that, at least for most audio metric frequencies, the amount of threshold shift observed (either temporary or permanent) was closely related to the frequency or spectrum of the stimulus. Results of "stimulation deafness" (temporary threshold shift) studies indicated that for pure tone stimuli the maximum shift in hearing appears to be about one-half octave above the frequency of total Prior to 1956 damage risk criteria set as a goal for protection (see Protection Goal), the prevention of hearing loss at all frequencies. This necessitated assessment of the noise at each octave band. After this time, VI-3 however, much more qualified protection goals were established (usually pro tection of loss in the so-called "speech frequencies") such that only knowledge of the sound pressure in certain critical octave bands (not to" be confused with aural critical bands) was required In order to assess the risk of noise exposure to hearing. This approach characterized the damage risk criteria developed by the Air Force in 1956, The American Academy of Ophthalmology and Otolaryngology in 1957, the International Standards Organ ization in 1961, and the American Academy of Ophthalmology and Otolaryngology in its revision of the 1957 criteria in 1964 (see Table IX).
The procedure for rating noise hazards by this mehtod consists of measuring the octave band levels in the critical octaves, and then comparing the measured levels with damage risk contours. This is best exemplified by the use of the "Noise Rating" curves developed by the International 80 Standards Organization.
The octave band levels of the noise are measured and then compared with the noise rating curve (Figure 9). The highest curve which is exceeded by the level of these bands yields the noise rating number (N). For this particular scheme, a noise rating of 85 was suggested as the protection criterion.
# The Use of A-weighted Sound Level
Since the publishing of the first Intersociety "Guidelines for Noise 81 Exposure Control," a relatively new approach, A-weighted sound level measurement, has become a popular measure for assessing overall noise hazard. As stated in Part III, the weighting on the A-scale approximates the 40-phon equal loudness contour (Figure 8). Use of the A-weighting is thought, therefore, to insure the rating of noises in a reasonably similar manner as would the human ear.
# VI-4
Several studies have been conducted In order to evaluate the efficacy of using A-weighted sound levels In rating hazardous exposures to noise.
82 In a study of 580 Industrial noises, Botsford showed that the A-weighted sound level Indicated the hazard to hearing as accurately as did limits expressed as octave band sound pressure levels in 80% of the cases and was slightly more conservative than octave band measures in 16% of the noises. Passchier-Vermeer2^ found that, except In one noise condition, sound level In d BA was as accurate as Nose Rating (NR) in estimating noise 83 induced hearing loss. In a study of hearing loss in 759 subjects, Robinson concluded that the error incurred from using dBA in predicting hearing level was within + 2 dB, even for noises ranging in slope from + 4 dB/ 84 octave to -5 dB/octave. A recent study found that even though dBA perhaps discounted too much low frequency energy, in all cases but one it predicted TTS2 resulting from exposures to noises of different spectra (slopes of -6 dB/octave, 0 dB/octave, and 6 dB/octave) as well as or better than other noise rating schemes which employed spectral measurements in octave-bands.
As a result of its simplicity and accuracy in rating hazard to hearing, the A-weighted sound level was adopted as the measure for assessing noise exposure by the American Conference of Governmental Industrial Hygienlsts
# VI-5
In keeping with the several precedents which have been established for its use in rating the hazard resulting from industrial noise exposure, and because it has been shown to be a reasonably accurate measure of such hazard, the A-welghted sound level measurement has been recommended for use in rating noise hazard in the Recommended Standard.
# Protection Goal
The limit of noise exposure that is established ultimately depends upon the degree of hearing which is to be protected and the number of persons in an exposed population to be protected. If a very strict protection criterion is contemplated such that no person exposed to noise will develop hearing loss at any frequency, the maximum permissible noise level governing a daily, or near daily, exposure would be quite low. Conversely, if the protection goal were to permit a certain amount of hearing loss in a small percentage of workers over a working lifetime, then the permissible exposure level would be raised accordingly. For example, Figure 10 formula whereby the ability to hear everyday speech was estimated by multi plying the hearing levels at 500, 1000, and 2000 Hz by 0.8 and then computing the average over these three frequencies. The major contribution of this formula was the introduction of the concept that hearing loss for speech could be estimated by the average hearing levels at what has now become known as the "speech frequencies"-500, 1000, and 2000 Hz.
The American Medical Association in 1947 recommended that hearing loss for speech be determined by the pure tone hearing losses at 500, 1000, 2000, and 4000 Hz. The four frequencies were given a weighting in accordance with what was presumed to be the importance of each frequency in hearing for speech (i.e., 15% at 500 Hz, 30% at 1000 Hz, 40% at 2000 Hz, and 15%
at 4000 H z ) . This guideline further suggested that hearing loss for speech does not begin until the weighted average hearing loss equaled 10 dB, and total loss for speech hearing occurred when the loss at 500 Hz reached 90 dB or the losses at the other 3 frequencies reached 95 dB.
In a later article which reviewed the assumptions In computing hearing 94 loss for speech, the AM A made the following observations and recommendations:
The 1947 formula was inadequate for calculating hearing loss for speech in sensorineural hearing loss. (This is particularly interesting in that the method used today for computing hearing loss for speech, developed by the AAOO in 1959 and accepted by the AMA in 1961, eliminated the most VI-9 sensitive indicator of sensorineural hearing loss (i.e., losses at 4000 Hz.))
(2) Everyday communication should be the basis for evaluation of hearing disability. "Ideally, hearing impairment should be evaluated in terms of ability to hear everyday speech under everyday conditions. The ability to hear sentences and to repeat them correctly in a quiet environment is taken as satisfactory evidence for correct hearing of everyday speech. Because of present limitation of speech audiometry, the hearing loss for speech is estimated from measurements made with a pure tone audiometer. For this estimate, the simple average of the hearing levels at the 3 frequencies 500, 1000, and 2000 cps is recommended.
V I -10 "In order to evaluate the hearing impairment, it must be recognized that the range of impairment is not nearly so wide as the audiometric range of human hearing. Audiometric zero, which is presumably the average normal threshold level is not the point at which Impairment 1. The basis of hearing impairment should be not only the ability to hear speech, but also the ability to understand speech.
# The ability to hear sentences and repeat them correctly in quiet
is not satisfactory evidence of adequate hearing for speech communication under everyday conditions. 2) above, the ability to understand speech under everyday conditions is best predicted on the basis of the hearing levels at VI-11 1000, 2000, and 3000 He.
# From (1) and (
The point at which the average of hearing losses in the stated three frequency range of 1000 -3000 Hz begins to have a detrimental effect oil the ability to understand speech is 25 dB re ANSI (1969).
With reference to the determination of hearing impairment (1. above), the dbility to "hear" speech, measured in terms of the lowest intensity at which a listener can barely identify speech materials, provides little information concerning communication difficulties under everyday con-QQ ditions. As Sataloff states, "It implies the presence of obvious difficulties in hearing speech. Actually, the difficulty mofe often lies not so much in 'hearing' speech as in 'understanding' it." Furthermore, Davis and S i l v e r m a n^ observed that "... a man with severe high-tone nerve deafness (as is seen in occupational noise induced hearing loss), will always fall to hear certain sounds and will never make a perfect articulation score. On the other hand, the same man may hear some words, the easy low-frequency words, as well as anyone else does. He may have a normal threshold for speech."
This issue is further clarified if one compares the "typical" clinical picture of a person having a conductive hearing loss versus a person having A sensorineural hearing loss resulting from noise exposure. Both cases would be expected to have elevated speech reception thresholds (a measure of hearing for speech); however, in the case of the conductive loss, speech discrimination (measure of understanding) would be approximately the same as that iot a person having normal hearing, provided that the presentation level ift sufficiently above the speech reception threshold level. The person with occupational hearing loss (sensorineural), on the other hand, would have VI-12 relatively poor discrimination scores, and the effect of raising the pre sentation level to higher levels often serves to reduce the articulation 100 score (see example in Figure 11). In applying the AAOO-AMA formula to the cases shown in Figure 11 it is possible that both would be rated identically in terms of hearing impairment, yet the sensorineural case has much more difficulty in understanding speech than does the conductive case.
It is apparent, therefore, that the formula applied to compute hearing impairment should consider discrimination ability and that the pure tone frequencies used in the formula should be highly correlated with this latter function.
With reference to speech communication under everyday conditions (see
100Z. Furthermore, everyday speech rarely takes the form of complete sentence communications; thus, the number of speech cues available for 88 accurate speech perception under everyday conditions is greatly reduced.
From this discussion, it may be concluded that an appropriate predicting scheme for determination of hearing impairment must include some consideration VI-13 for an actual daily communication environment rather than some optimum condition as suggested by the AAOO -AMA.
With reference to predicting ability to understand speech on the basis of heavy levels at the pure tone average at 1000. 2000. and 3000 Hz (point 3 above), results of several studies indicate that hearing levels at these three frequencies predict hearing loss for speech under mild conditions of distortion better than the three frequency average at 500, 1000, and 2000. In chinchillas. However, they cautioned that their findings were only applicable to continous exposures and not to intermittent exposures.
Variables that are germane to Interrupted exposures but do not play a significant role in limiting hazard from short-term continuous exposures further complicate the problem of how the ear responds and integrates noise over time. One such variable is the "acoustic" or "middle ear" reflex.
When the ear is exposed to loud noise, the middle ear muscles contract, thus altering the impedance of the middle ear. This reflex, which serves to attenuate the noise reaching the inner ear, adapts out or disappears quickly if the noise is continuous and relatively unchanging over time.
However, if the noise level varies considerably or is interrupted on a regular or irregular basis, then the reflex is sustained.
A second variable which plays an important role in reducing the hazard of interrupted noises relative to short-term continuous noises concerns the off-time of the exposure cycles. Depending upon the over-all level of the noise and the nature of the relationship between on-time and off-time, a considerable reduction in the degree of temporary hearing threshold shift may be observed.
To date, the only empirical data available on permanent hearing losses resulting from intermittent exposures comes from a study of iron ore miners conducted by Sataloff et a l .^^ Their findings indicated that intermittent noises had to be some 15 dB more intense than continuous noises to cause the same additional hearing impairment in men ages 30 to 50 years. Although this 113 VI-18 evidence confirms Che general notion that intermittent exposures are less hazardous than continuous steady-state exposures of the same duration and noise level, the applicability of this rule to other schedules of intermittency must await further investigation.
Since 1960, several damage risk criteria have been proposed to limit 82,107,115 exposure to intermittent noise.
For the most part, these criteria, like the rules for assessing Intermittent noise exposure discussed below, have been based predominantly upon evidence collected from studies of temporary threshold shift.
At least three different rules have been proposed in order to assess the hazard of exposures to intermittent noise. The first of these rules, 28 developed by Ward et al.
was called the "on-fraction" rule. This rule states that the amount of temporary threshold shift resulting from a given intermittent exposure can be determined on the basis of noise level and average on-fractlon (the time the noise is on divided by the total duration of exposure). This procedure assumes that levels below 75 dB SPL are not hazardous to hearing; thus, the amount of on-time is taken as the total time the noise is above 75 dB SPL. In a critical test of the on-fraction rule, Selters and Ward^1 found that this rule was invalid when the regular on-off times exceeded two minutes.
For burst durations longer than two minutes, a second rule has been The essential feature of this approach is that residual TTS is translated into exposure time.
One of the crucial assumptions of the "exposure-equivalent" rule is that the course of recovery from TTS is Independent of the type of noise 33 that produce the TTS. In a recent article, Ward has presented data that question the validity of this assumption. It appears that intermittent exposure to high level, high frequency noise causes a considerable delay in the recovery of TTS relative to intermittent low frequency exposures.
A third approach in determining hazard from interrupted noise has been to determine the total on-time of the noise, regardless of how the noise bursts are distributed in time, and to consider the intermittent exposure in terms of an equivalent continuous exposure. This approach attempts to take into consideration the reduced hazard of interrupted noise by adjusting the rule which relates noise level and exposure duration.
Although possibly not as scientifically rigorous as the previously mentioned procedures, the "equivalent continuous" rule is not constrained by the assumption concerning the regularity of exposure cycles which is basic to the other rules.
# VI-20
Intermittent noise exposure criteria based upon the first and/or second rules include those developed by Glorig, Ward, and N i x o n , 113 CHABA 107 82 Working Group 46, and Botsford. Botsford's i n t e m i t t e n c y criteria reflect a simplification and consolidation of the CHABA continuous exposure, long-burst intermittent, and short-burst intermittent contours into one general figure relating dBA level, total on-time (noise level above 89 d B A ) , and number of exposure cycles (see Figure 13). The limits of intermittent exposure expressed in these contours (shown in Table X) 27 have recently been adopted by the Second Intersociety Committee. Similar limits have been adopted as part of a revision of the German document con-116 cerned with assessment of industrial noise in working areas.
Recent research designed to investigate the efficacy of the limits proposed In Table X have generally shown that the limits do not acburately predict risk to hearing, at least so far as temporary threshold shift is concerned. In a laboratory study11^ designed to evaluate selected exposure conditions from Table X» it was found that (1) the table shows concen trations of noise exposure within an eight-hour workday than can cause excessive amounts of temporary threshold shift and (2) the conditions did not yield equal effects on hearing, thus not affording equal protection.
Conversely in a study of forestry employees It was found that although the noise exposures were rated as hazardous according to Table X, the audiometric results indicated that the exposures did not pose a risk to hearing.
Considerably more data must be collected to evaluate present criteria which attempt to designate safe levels of exposure to Intermittent noise. on the other hand, suggested that the "off" level was frequently dependent. For example, the safe level of exposure for the octave band 300 -600 Hz was seen to be 89 dB SPL, whereas It was approximately 85 dB SPL for octave band 1200 -2400 Hz.
Recently, Botsford®^ computed a dBA equivalent from the octave band damage risk criteria developed by CHABA. The results of this computation suggested that the "off level" based upon one-third octave or octave band sound pressure level will, in many cases, be below the level designated by Botsford (particularly in the case of strong narrow band components in the noise). Both the CHABA and Botsford criteria do not appear to be in accord with the intended meaning of a safe intermittent level in that present data suggest that there is a significant increase in the proportion of the popu lation having hearing impairment in those groups exposed to continuous noise VI-22 levels at and slightly below 85 dBA as compared with a non-noise exposed population.
Two lines of evidence suggest that the lower limit of Interrupted exposure is considerably below the levels mentioned above. In a review of XI.
The audiometric van used for the hearing tests was capable of testing six individuals at one time. All employees were tested before the beginning of their work shift, and, due to scheduling problems, the number of employees in a test session ranged from one to six. When less than six employees were present at a testing session, an attempt was made to randomize the assign ment of audiometers. It was also necessary to use headphones with otocups to properly shield the employees from the possible effects of interference caused from hearing the other test tones in the van. However, it was found from the results of two independent studies in the NIOSH laboratory that there was no significant difference in measured thresholds between headphones fitted with otocups and those fitted with standard MX-41/Ar type ear cushions.
Before data analysis could be done, it was necessary to check the calibration data accumulated during the respective survey. Calibration of the audiometeres used to take the audiograms was usually performed before and after each survey. The data were corrected where necessary to the appropriate values given in the American National Standard Specifications for Audiometers, ANSI S 3 .6 (1969).
Used for purposes of data analysis were the three-frequency averages mentioned above In the definitions of hearing impairment. HLI (0.5, 1, 2)
and HLI (1,2,3) are used to denote these averages performed over both ears. (HLI stands for "hearing level index.")
# VI-25
The samples were grouped Into age and experience ranges to assure equal numbers per cell and a consistent spread of the data across the various dBA levels.
The following lists the steps made in the data analysis:
1. Hearing level indices for 87 and 94 dBA noise exposed individuals were grouped into 31 samples for three-way cross-classification with respect to dBA level, age group, and experience group. The data were transformed by taking natural logarithms, and the resulting variances of log HLI (0.5, 1, 2)
and log HLI (1, 2, 3) were computed for each sample. For each of the two dBA levels, Bartlett's tests for homogeneity of variances were performed over all age and experience combinations. Separate tests were performed for HLI (0. 5, 1, 2) and HLI (1, 2, 3) average noise Indices. Of the four Bartlett's tests, three showed no suggestion of nonhomogeneity of variance, but the fourth was significant at the 0.05 prbbability level. However, only one atypical variance was found within the "nonhomogeneous" group, and this was believed to be caused by an improbable combination of purely random variations and not indicative of a real elevation of variability for the cell in question. Thus, the conclusions were that variability of log HLI (0.5, 1, 2) and log HLI (1, 2, 3) for replicate subjects was stable over all cells defined by the crosa-clasalfication.
2. Fifth-degrfee orthogonal polynomial regression curves were fitted to log HLI v s . dBA for each age and experience cell using data for all dBA levels. Significance tests for nullity of regression coefficients were performed. For most of the curves which exhibited any significant trend, a straight line fitted the data within the limits of unexplained variability.
# VI-26
In several cases, fourth or fifth degree coefficients showed significance, but examination of the plotted points revealed these to be artifacts due to clustering of the dBA levels for those plots, i.e., too few levels of the independent variable so that the polynomial tended to "fit the random errors."
3. Histograms of pooled deviations of log HLI values from the respective regression lines for H L I (0.5, 1, 2) and HLI (1,2,3) were constructed by fitting normal distribution curves. Chi-square goodness-of-fit tests were performed. The tests revealed that the log HLI deviations from the means were normally distributed over the full range of variability to a very significant degree of approximation as shown in Figures 14 and 15 Means were found to be zero, and pooled variances were calculated for use in later stages of the analysis.
4. Regression lines for different age groups within an experiencelevel were tested for parallelism, and in every case, the lines were found to be parallel within the limits of error in the slope estimates. Pooled slopes were calculated, and the intercepts were revised to reflect the small differences between the separate and pooled slopes. Families of parallel lines were plotted. Tests for coincidence of sets of parallel lines were then made by the method of covariance analysis. This revealed significant difference at the 0 .0 1 probability level in all cases.
5. Regression lines for different experience levels within an age group were not found to be parallel, and, for each age group, the intercepts were compared by means of Student's t-tests. The "intercepts" were defined as ordinates of the regression lines at a dBA of 79, which represented the control group exposed to less than 80 dBA. These regression lines were found to be significantly different families of nonparallel lines from common intercepts.
VI-27 6.
For each age and experience combination, the normal distribution of pooled variation in replicate subjects was distributed about the re gression line with its zero mean centered at the ordinate of the line.
This model was then used to calculate a predicted percentage of subjects whose hearing levels exceeded a "fence". Thus, such percentages could be tabulated as a function of dBA for each age and experience category.
Furthermore, risk values were then derived as the percentage difference between employees exposed to noise levels 80 dBA or greater and those exposed to less than 80 dBA (Table XII and XIII).
This analysis indicates that the 85 dBA-Slow noise limit for an eighthour day, in conjunction with the medical program prescribed in the standard, will improve the protection of the working population from hearing loss that could impair their abilities to understand everyday speech. The reliability of the analysis is evidenced by homogeneity of the variance and normality of the population distributions. In other words, the evaluation is repeatable and is representative of a random sample. Thus, the Intersociety analysis differs from that of NIOSH in several characteristics: use of one ear only, nonseparation of experience groups, use of SIL in noise levels, and use of a dissimilar composite population.
Some of these characteristics tend to produce lower risk values and con siderably more uncertainty than the NIOSH analysis, as evidenced in Table VII-3.
Another study whose analysis determined risk is published In ISO 90 Reconmendation R1999 (1971).
This analysis differs from the NIOSH analysis VI-30 in three ways. The first is that only the right ear was used. The second is that no separation of age groups into work experience groups was done. The third is that no screening for otological abnormalities was done in the ISO study. On the other hand, the entire sample of data used in this analysis is homogeneous in that all members of the sample 126 were taken from one comprehensive examination.
The lack of otological screening has some effect on incidence of hearing impairment for both the noise exposed and the non-noise exposed groups, but, when risk is calculated by subtracting the two incidences, the effect is essentially cancelled. Thus
# OCTAVE BAN D SPL R E 2x10 N/M
75 150 300 600 1200 2400 4800 9600 The hearing levels of the heavy earth equipment operators were found to be significantly higher than the non noise exposed groups. The paper bag workers had higher hearing levels but not as high as the earth equipment operators. The airport ramp personnel, however, had the lowest hearing levels, probably due to the intermittency of their ex posures .
# APPROX. SCALE 8PIRAL SANGLiÖN
# INNER
# CONT I N U A T I O N (6) O F T A B L E IX | # I. RECOMMENDATIONS FOR A NOISE STANDARD
The National Institute for Occupational Safety and Health (NIOSH) recommends that employee exposure to noise in the workplace be controlled by requiring compliance with the standard set forth in the following sections. Control of employee exposure to the occupational limits stated and adherence to the precautionary procedures prescribed will improve the protection of the working population from incurring noise induced hearing loss that could impair their abilities to understand everyday speech.
Such control and adherence at the workplace is believed sufficiently effective to reduce also the possibility of other forms of occupational Injury and illness related to noise. This standard is amenable to techniques that are valid, reproducible, and presently available. It will le reviewed and revised as additional information becomes available.
# Section 1 -Applicability
The provisions of this standard are applicable to occupational noise exposures at places of employment and are intended to apply for all noise even though additional controls may be necessary for certain specific types of noise, such as some impact and impulsive noise. For the purposes of this standard the noise exposure is determined for an 8-hour workday.
# Section 2 -Definitions
As used in this standard, the term: (a) "Administrative control" means any procedure that limits daily exposure to noise by control of the work schedule. (b) "Audiogram" means a graph or table obtained from an audiometric examination showing hearing level as a function of frequency.
1-1 (c) "Baseline audiogram" means an audiogram obtained from an audio metric examination that is preceded by a period of at least 14 hours of quiet.
(e) "Audiometer setting" means a setting on an audiometer corres ponding to a specific combination of hearing level and sound frequency.
(f) "Daily Noise Dose" means that value for D derived from the equation:
D -£ L + Sl + + £2.
# Ti T2 Tn
where Cl, C2 . . . , Cn are the actual durations of exposure for an employee at the various noise levels, Tl, T2, . . . , Tn are the respective duration limits obtained from Figure 1-1 and D is the Daily Noise Dose.
(g) "dBA -Slow" means the unit of measurement of sound level indicated by a sound level meter conforming as a minimum requirement to the American National Standard Specification for Sound Level Meters, ANSI SI.4 (1971) Type S2A, when used for A-weighted sound level, slow response.
(h) "Engineering control" means any procedure other than administrative control that reduces the sound level either at the source of the noise or in the hearing zone of the employees.
(i) "Hearing level" means the amount, in decibels, by which the threshold of audibility for an ear differs from a standard audiometric threshold.
1-2 (j) "Environmental noise level" means the noise level in dBA-Slow as measured in accord with Section 3(c).
(k) "Effective noise level" means (1) for employees not wearing ear protectors, the environmental noise level; (2) for employees wearing ear protectors, the result of subtracting the dBA reduction, R, for the ear protectors (determined as specified in Appendix A) from the measured environmental noise level. Effective noise level is expressed in units oi dBA-Slow.
(1) "Noise exposure" means a combination of effective noise level and exposure duration. (1) Occupational noise exposure shall be controlled so that no worker shall be exposed in excess of the limit described as line B in The Indicated duration limits which exceed 8 hours are to be used only for purposes of computing Daily Noise Dose and are not to be regarded as defining noise exposure limits for work days which exceed 8 hours.
# 1-4
employment is believed necessary to permit the Department of Labor to conduct an extensive feasibility study.
(iii) At no time shall any worker be exposed to effective noise levels exceeding 115 dBA-Slow.
(c) Measurements (i) Compliance with the permitted daily noise exposures defined by Section 3(b) shall be determined on the basis of measurements made with a sound level meter conforming as a minimum to the requirement of the American National Standard Specification for Sound Level Meters, SI.4 (1971)
Type S2A, and set to use an A-weighted slow response.
(ii) All measurements shall be made with the sound level meter at a position which most closely approximates the noise levels at the head position of the employee during normal operations.
(iii) An acoustical calibrator accurate within plus or minus one decibel shall be used to calibrate the sound level meter on each day that noise measurements are taken. (i) A baseline audiogram for each employee who is initially assigned or reassigned to work subject to conditions stated in (a) of this section shall be taken within 30 days of assignment to such employment, in the sixth year of such employment, and once every sixth year thereafter. It is recognized that some delay in implementation of this requirement may be necessary for employers with a small work force.
# 1-5 (ii)
A baseline audiogram should be taken for each employee presently assigned to work subject to conditions stated in (a) of this section at the time of effective date of this regulation, in the sixth year, and once every sixth year thereafter.
(iii)
In addition an audiogram, not necessarily baseline, for all exposed employees should be taken every second year.
(c) Each audiogram shall contain (1) employee's name or identifying number,
(2) employee's job location, (3) significant aural medical history of the employee, (4) the examiner's name and signature, (5) the date and time of test, (6) serial number of the audiometer, and (7) last exposure to high level noise: number of hours since exposure; type of exposure; and noise level, if known.
(d) Each employee's audiogram shall be examined to determine whether it indicates for either ear any threshold shift (higher threshold), that equals or exceeds 10 dB at 500, 1000, 2000, or 3000 Hz, or 15 dB at 4000 or 6000 Hz as evidenced by a comparison of that audiogram with the employee's most recent baseline audiogram and with his initial baseline audiogram as corrected to his current age by the method described in Appendix B. If either comparison indicates a shift as described above:
(i) refer the employee for appropriate medical evaluation, (ii) if the employee needs personal protective equipment or devices, insure that he has the appropriate effective equipment and that he is instructed in the proper use and care of the equipment, and
(iii) if the audiogram was not a baseline audiogram, take a baseline audiogram within sixty days.
(e) Audiometric tests shall be pure tone, air-conduction, hearing threshold examinations, with test frequencies including 500, 1000, 2000, 3000, 4000, and 6000 Hz and shall be taken separately for the right and left ears.
# 1-6 (i)
The tests shall be conducted in a room whose ambient noise levels conform to all requirements except that part concerning octave bands whose center frequencies are less than 250 Hz of the American National Standard Criteria for Background Noise in Audiometer Rooms, ANSI S3.1 (1960 R-1971), when measured by equipment conforming to American National Standard Specification for Sound Level Meters, ANSI SI.4 (1971) Type 2 and American National Standard Specification for Octave, Half-Octave, and Third-Octave Band Filter Sets, ANSI SI.11 (1966, R-1971).
(ii)
The tests shall be administered using an audiometer which conforms to the requirements for limited range pure tone audiometers prescribed by the American National Standards Specifications for Audiometers, ANSI S3. 6 (1969), and which is of the discrete frequency type. If a pulsed tone audiometer is used, the on-time of the tone shall be at least 200 milliseconds. The instrument used in the testing shall be either a manual audiometer, or a self-recording audiometer which is subject to the following additional restrictions:
(1) The chart upon which the audiogram is traced shall have printed lines at positions corresponding to all multiples of 10 dB hearing level within the intensity range spanned by the audiometer. The lines shall be equally spaced and shall be separated by at least 1/4 inch.
Additional graduations are optional. The pen which traces the audiogram shall have a fine point so that the tracing shall not exceed 2 dB in width.
(2) It shall be possible to disable the stylus drive 1-7 mechanism so that the stylus can be manually set at the 10-dB graduation lines for calibration purposes.
(3)
The slewing rate for the audiometer attenuator shall be 6 dB/sec or less except that an initial slewing rate greater than 6 dli/sec is permitted at the beginning of each new test frequency, but only until the second subject response.
(A) The audiometer shall remain at each required test frequency for 30 seconds (+ 3 seconds). The audiogram shall be clearly marked at each change of frequency and the actual frequency change of the audiometer shall not deviate from the frequency boundaries marked on the audiogram by more than + 3 seconds.
(5) If an audiogram fails to pass the following criteria, the subject shall be retested:
At each test frequency it must be possible to place a horizontal line segment parallel to the time axis on the audiogram, such that the audiometric tracing crosses the line segment at least six times at that test frequency.
# (iv)
The audiometer shall be maintained in calibration in accordance with the provisions of Appendix C. If noise exposures to which employees could be exposed exceed the limits specified, personal protective equipment (i.e., ear protectors) shall be provided by the employer to be used in conjunction with an audiometric testing program, as specified in Section 4, subject to the f oJlowing requirements:
(i) The use of personal protective equipment to prevent occupational noise exposure of the employer in excess of the prescribed limits is authorized only until engineering and administrative controls and procedures can be implemented to maintain the occupational noise exposures within prescribed limits.
(ii) Any ear protector used by an employee shall reduce the effective noise level to which he is exposed so that his noise exposure is within the limits prescribed in Section 3(b).
(iii) Insert -type ear protectors shall be fitted by a person trained In this procedure.
(iv) Inspection procedures to assure proper Issuance, main tenance, and use of personal protective equipment shall be established by the employer.
# 1-9 (b)
The employer shall provide training In the proper care and use of all personal protective equipment.
Section 8 -Apprisal of Employees of Hazards from Noise Each worker exposed to noise shall be apprised of all hazards, relevant symptoms, and proper conditions and precautions for working in noisy areas.
The information shall be kept on file and readily accessible to the worker at all places of employment where the noise levels equal or exceed the limits prescribed in Section 3 (b).
# Section 9 -Monitoring & Recordkeeping Requirements
(a) Employers will be required to maintain records of:
(i) environmental exposure monitoring for a period of 10 years, (ii) all audiograms for a period of 20 years.
(iii) all audiometric calibration data for a period of 20 years.
(b) When exposure times of less than 8 hours/day are required in a specific work area or ear protection is used to meet the exposure limits, records of the method of control shall be maintained.
# 1-10
Appendix A -Determination of dBA Reduction R for Ear Protectors 1. The pure tone attenuation vs. frequency characteristics of the ear protector (normally supplied by the manufacturer) shall have been determined
In accordance with the American National Standard for Measurement of the Real-Ear Attenuation of Ear Protectors at Threshold, ANSI Z24. 22 (1957). The "-10.0" correction term is to account for possible noise spectrum irregularities and noise leakage which might be caused by long hair, safety glasses, head movement, or various other factors.
# Let
3. If the octave band levels of the noise are not known, then the dBA reduction R may be computed simply as R --10 log S -3.0 where S ■ antilog (-0.1 X Qj) + antilog (-0.1 X Q2)
+ antilog (-0.1 X Q3) + antilog (-0.1 X Q4) + antilog (-0.1 X Q5) + antilog (-0.1 X Q6) + antilog (-0.1 X Q7)
This calculation is approximate, and is based upon the assumption that the octave band levels are equal. For most types of noise it will give results close to those obtained by the more accurate method of (2) above. (1) Set audiometer to 70 dB hearing threshold level and measure sound pressure levels of test tones using an NBS-9A-type coupler, for both earphones and at all test frequencies.
(2) At 1000 Hz, for both earphones measure the earphone decibel levels of the audiometer for 10 dB settings in the range 70 to 10 dB hearing threshold level. This measurement may be made acoustically with a 9A coupler, or electrically at the earphone terminals.
# 1-18
(3) Measure the test tone frequencies with the audiometer set at 70 dB hearing threshold level, for one earphone only.
(4) In making the measurements in (1) -( 3) above the accuracy of the calibrating equipment shall be sufficient to prove that the audiometer is within the tolerances permitted by ANSI S3.6-1969.
(5) A careful listening test, more extensive than that required in the biological calibration, shall be made in order to ensure that the audiometer displays no evidence of distortion, unwanted sound, or other technical problems.
(6) General function of the audiometer shall be checked, particularly in the case of a self-recording audiometer.
(7) All observed deviations from required performance shall be corrected.
C. An exhaustive calibration shall be performed at least every five years. This shall include testing at all settings for both earphones.
The test results must prove unequivocally that the audiometer meets for the following parameters the specific requirements stated in the applicable sections of ANSI-S. as noted in parenthesis.
(1) Accuracy of decibel level settings of test tones (Sections 4.1 .4. 1 and 4.1 .4.3).
(2) Accuracy of test tone frequencies (Section 4.1.2).
(3) Harmonic distortion of test tones (Section 4.1.3).
(4) Tone-envelope characteristics, i.e., rise and decay times, overshoot, "off" level (Section 4.5).
(5) Sound from second earphone (Section 4.4.2).
(6) Sound from test earphone (Section 4.4.1). ation. In the case of periodic sound pressures, the interval must be an integral number of periods or an interval that is long compared to a period.
# III-l
Frequency -The frequency of a function periodic in time is the reciprocal of the primitive period. The unit is the cycle per unit time and must be specified. The unit cycle per second is commonly called Hertz (Hz).
Level -In acoustics, the level of a quantity is the logarithm of the ratio of that quantity to a reference quantity of the same kind. The base of the logarithm, the reference quantity, and the kind of level must be specified.
Noise -(1) Noise is any undesired sound; and, by extension, noise is any unwanted disturbance within a useful frequency band, such as undesired electric waves in a transmission channel or device. (2) Noise is an erratic, intermittent, or statistically random oscillation. Since the definitions of noise are not mutually exclusive, it is usually necessary to depend upon context for the distinction.
Noise Level -(1) Noise level is the level of noise, the type of which must be indicated by further modifier or context. The physical quantity measured (e.g., voltage), the reference quantity, the instrument used, and the bandwidth or other weighting characteristic must be indicated.
(2) For airborne sound, unless specified to the contrary, noise level is the weighted sound pressure level called sound level; the weighting must be indicated.
Oscillation -Oscillation is the variation, usually with time, of the magnitude of a quantity with respect to a specified reference when the magnitude is alternately greater and smaller than the reference.
Period -The period of a periodic quantity is the smallest increment of the independent variable for which the function repeats Itself.
# III-2
Periodic Quantity -A periodic quantity is an oscillating quantity whose values recur for certain increments of the independent variable.
# Sound -(1)
Sound is an oscillation in pressure, stress, particle displacement, particle velocity, etc., in a medium with internal forces (e.g., elastic, viscous), or the superimposition of such propagated oscilla tions. (2) Sound is an auditory sensation evoked by the oscillation described above.
Sound Absorption -Sound absorption is the change of sound energy into some other form, usually heat, in passing through a medium or on striking a surface.
Sound Level (SL) -Sound level is a weighted sound pressure level, obtained by the use of metering characteristics and the weightings A,B, or C as specified in the American National Standard Specification for Sound Level Meters, ANSI-S1.4-1971. The weighting employed must be stated.
Sound Pressure -The sound pressure at a point is the total instanta neous pressure at that point in the presence of a sound wave minus the static pressure at that point.
Sound Pressure Level (SPL) -The sound pressure level, in decibels, of a sound is 20 times the logarithm to the base 10 of the ratio of the pressure of this sound to the reference pressure. The reference pressure must be stated. The following reference pressure is in common use for measurements concerned with hearing and with sound in air and liquids: 2 X 10 N/M^. Unless otherwise explicitly stated, it is to be understood that the sound pressure is the effective (rms) sound pressure.
# III-4
# Response of the Ear
Upon inspection of the definition of sound pressure level, it is evident that there is no reference to frequency. In actuality, the ear does not show equal response to all frequencies, and in fact, it is more sensitive to the middle frequencies than to the low or high ones. Studies have been made which determine the sound pressure levels of simple tones at various frequencies which sound just as loud to an observer as a 1000 Hz tone of a particular SPL. The results of such comparisons are given as equal loudness curves in Figure 1 . The number of each curve, loudness level in phons. is the SPL of the 1000 Hz tone used for comparison in 3 determining the curve.
# Measurement Scales
These equal loudness contours have been taken into account in the standardization of several frequency weighting networks which are included on most sound measuring equipment. The frequency characteristics of these networks are given in Figure 2. The A scale corresponds approximately to the 40-phon equal loudness contour, the B-scale corresponds to 70-phons, and the C-scale corresponds to the 100-phon contour. With these weighting networks, which modify sound pressure level to approximate the ear's response, the term to be used is sound level, and the weighting used must always be stated. (?'The A-sound level is 36 dB" or "86 dBA" are appropriate ex--5 2 pressions.) The reference pressure is 2 X 10 N/M ).
The A scale is commonly used in measuring noise to evaluate its effect on people, and the A-weighted sound level is considered an adequate number to indicate or rate the hazard of a certain noise. Explanation of these measurements is given in Part IV.
# III-5
# Correction of Original Baseline Audiograms for Age
To determine whether there has been a significant change in an employee's hearing due to noise exposure by comparing an audiogram taken since the original baseline audiogram with that audiogram it la necessary to make a correction for difference in age.
The best way to make this correction is to use data from a non-noise exposed group from the same area tested in the same manner as the group under consideration. Quite often this is not possible; therefore, It Is necessary to establish an age correction that can be used universally. The data from these four studies with respect to differences in hearing level from age 20 are quite similar. However, the greater changes apparent
In the National Health Survey data at the upper frequencies could be expected because this population was not screened for significant noise exposure.
# III-6
Thus, to provide a uniform correction, tables B-l and B-2 (Appendix B) derived from the NIOSH data, will be used as specified in the standard.
# Conversion of Octave Band Levels to dBA Levels
When the octave-band sound pressure levels of a noise have been measured it is often desirable to compute the A-weighted sound pressure level from them. This can be done as follows:
1. From each octave band level, subtract (or add) the A-weighting correction value shown in Table III. corresponding to the frequency of the octave band. This method is quite accurate although it does involve some approximation.
# Calculation of dBA Reduction R for an Ear Protector
Calculation of dBA reduction R for ear protectors can be done as follows:
1. When the octave band levels of the noise are known: If the dB attenuation levels of the ear protector were known for each octave band, then the dBA reduction of the ear protector could be determined by subtracting these attenuation levels from the original octave band noise levels, and then calculating the dBA level of the resulting attenuated octave band levels using the method described in the previous section. One would then subtract this dBA level from the original dBA level to obtain the dBA reduction.
# III-7
However, the American National Standard for Measurement of Real-Ear Attenuation of Ear Protectors at Threshold, ANSI Z24. 22 (1957), prescribes pure-tone tests at 125, 250, 500, 1000, 2000, 3000, 4000, 6000, and 8000 Hz.
We shall also assume that the 4000 Hz octave band attenuation level can be obtained by averaging the pure tone attenuation levels at 3000 and 4000 Hz, and that the 8000 Hz octave band attenuation level can be obtained by averaging the pure tone attenuation levels at 6000 and 8000 Hz.
This method has been formulated concisely in Appendix A of the Recommended Noise Standard, also including a factor of 10 which is to be subtracted to account for possible noise spectrum irregularities and noise leakage which might be caused by long hair, safety glasses, head movement, or various other factors. It ignores noise in the 31.5 Hz, and 16,000 Hz bands, but these rarely contribute substantially to the dBA level.
# 2.
When the octave band levels are not known it is assumed that the noise has a uniform "pink" spectrum, i.e., equal levels in each octave band.
This type of noise is representative of "average" occupational noise, and the error introduced by making this approximation is usually small. The assumption results in a simplified formula for calculation, as presented in Appendix A of the recommended Noise Standard. It is recommended, however, that the more exact method described in (1 ) above be used whenever octave band noise levels are available.
# IV. REVIEW OF EFFECTS OF NOISE ON MAN
Exposures to noise levels found at the workplace, particularly in mechanized Industries, are likely to be the most Intense and sustained of any experienced In dally living. As such, they represent the severest form of acoustic insult to man and therein pose the greatest harm to human function. Real or alleged effects of occupational noise exposures include the following:
-Temporary and permanent losses in hearing sensitivity.
-Physical and psychological disorders.
-Interference with speech communications or the reception of other wanted sounds.
-Disruption of job performance.
These different listed effects of noise can be classified in various ways. For example, the first two effects can be treated in the context of health or medical problems owing to their underlying biological basis.
That is, noise-induced hearing loss, as will be described later, involves damage to the cell structures of the hearing organ, and physical or psychological disorders due to noise presume alterations in normal physiologic or nervous system responses. In contrast, the remaining two effects, interference with sound reception and performance loss, are deemed annoyance or economic problems since they involve no pathology or physical dysfunction to the organism.
The aforementioned noise effects can also be classified as "auditory"
and "extra-auditory" in nature. In this regard, hearing loss and speech interference caused by noise are deemed auditory effects since they both involve disturbance to the hearing organ and/or its functional processes.
# IV-1
Noise effects on physical and psychological health states ¡md/or performance represent extra-auditory effects in that they extend beyond or are apart from auditory experience per se.
The intent of this part is to summarize current knowledge of these various adverse effects of noise as it relates to occupational noise conditions, and to establish their importance relative to needs for noise control in industry.
# Hearing Loss
The ear is the organ structure of the body especially adapted and most responsive to the pressure changes underlying airborne sounds or noise. Anatomically, it is divided into three subdivisions -the outer, middle, and inner ear. Some key structures within these subdivisions are shown in Figures 3 and 4 structures by high level sounds subjects them to shearing forces or other mechanical stresses that may jar them loose from their supporting cells or otherwise damage them.1** Another is that constant intense sound stimula tion forces the hair cell receptors to high metabolic levels that cannot be maintained. As a result, the metabolic processes essential for cellular life become exhausted or poisoned, leading to the death of the cells
< i ^ u >12 involved.
# IV-3
Since direct observation of the cell structures of the intact ear on a live human is impossible, injury to these parts are inferred from audio grams which show losses in threshold hearing levels for certain pure tone frequencies relative to some reference value. Such losses, when due to noise, may be of a temporary or permanent nature. Temporary hearing loss, more usually called temporary threshold shift or TTS, can be produced by brief exposures to high level sound and shows recovery following a period of time in quiet. Figure 6 describes an example of TTS caused by a twohour exposure in the laboratory to a broad-band noise of fairly high level (103 dBA). In this instance an audiogram was taken on the listener just before and at various times after the cessation of the noise exposure.
Differences between pre-and post-exposure threshold levels for the specified test frequencies display the amount of TTS induced by the noise.
TTS is greatest immediately after exposure and progressively diminishes with increasing time in the quiet, reflecting ear recovery from the apparent noise overstimulation .
As a general rule, a noise capable of causing significant TTS with brief exposures is probably capable of causing significant permanent losses in hearing, given prolonged or recurrent exposures. In fact, some limited evidence from animal studies suggests the presence of minor hair cell damage even in those ears showing complete recovery from noise-induced temporary threshold shift. 13 In any case, daily exposures to TTS-producing noises for several hours per day for months or years would pose a risk of permanent hearing loss. That is, the ear is not likely to recover completely with recurrent exposures of this type. Rather, only partial recovery may occur IV-4 in due course with new resting thresholds established, poorer than those found at the beginning of the overall noise experience. This residual loss is indicative of permanent hearing damage. Figure 7 describes these permanent losses in one group of employees as a function of their years of exposure to workplace noise levels appoximating the level used 14 in the TTS example above.
The TTS component in the losses evident in these hearing data was eliminated by allowing sufficient time after the workshift ended before taking audiograms on the worker group. Deductions have also been made in the hearing levels to remove those hearing changes related to aging (i.e., presbycusis).
Figure 7 indicates that the most significant noise-induced hearing losses occur first in the high frequency range, most prominently at 4,000 cycles per second or Hertz (Hz). Decreased sensitivity to these high frequency sounds may go unnoticed by the listener since they are relatively unimportant to speech reception. With increasing exposure years, however, the losses grow and also broaden to involve other frequencies which are more critical to speech reception, namely, those in the range 500 to 3,000
Hz. In actuality, in the United States, generally accepted procedures for rating hearing handicap for speech consider losses only at frequencies 500, 1000, and 2000 Hz on the audiogram.^ Controversy centers around the need to include 3000 Hz in these judgments since consonant discrimination may depend on hearing sensitivity for sounds higher than 2000
The pattern of permanent hearing loss shown in Figure 8 seems typical of noise-induced hearing damage as revealed in noise and hearing surveys in assorted industries (see Table IV). Why high frequency hearing, parti cularly around 4000 Hz, shows most vulnerability to noise is not altogether IV-5 clear. One possible explanation is that the resonant frequency of the ear canal is in region 2000 -5000 Hz which, in effect, adds strength to corres-19 20 ponding frequencies in an incoming noise signal. * Complicating evaluations of hearing loss due to industrial noise are a number of factors. First, hearing sensitivity normally decreases with age, and these losses (presbycusis) are quite similar to those caused by excessive noise, i.e., differentially greater losses at the higher fre- Other causes of hearing loss besides noise and age include use of 23 drugs, illness and disease processes, blows on the head. Special audio metric procedures are sometimes necessary to diagnose a given case of hearing loss in order to determine the likelihood that it may have been caused by excessive noise rather than other agents.
Even when there is clear audiometric evidence of noise-induced hearing loss, questions may be raised as to whether such damage was produced entirely by workplace noise. It is apparent that off-job noise conditions, particularly in recreation, can pose some risk of hearing change by themselves or can 24 exacerbate the acoustic insult associated with the job situation.
# IV-6
While indicating the need for close appraisal of audiometric results, the aforementioned complicating factors should not be construed as minimizing the seriousness of noise and hearing loss problems in industry. As will be noted in subsequent section, noise surveys in assorted manufacturing, construction, mining, transportation and farm operations indicate exposure conditions potentially harmful to millions of workers. Indeed, the popula tion at risk with regards to noise-induced hearing loss may be greater than any other hazard in the work environment. Audiometric data already col lected on samples of employees in many of the jobs surveyed above for excessive noise show them to have poorer hearing relative to other groups of workers not so exposed. Composite reviews of published occupational Obviously, the rate and number of such impact sounds constituting an exposure period are also factors in making hazard judgments for these types of sounds.
Noise and hearing surveys in industry dealing with these types of exposure conditions are just beginning. Most permanent hearing loss data reflooting impulse noise hazards have been based on military studies involving gunfire.
# IV-9
Physical and Psychological Disturbances Aside from hearing loss, noise may trigger changes in cardiovascular, 35 37-39 endocrine, neurologic, and other physiologic functions, * all of which are suggestive of a general stress reaction. These physiologic changes are produced typically by intense sounds of sudden onset, but can also occur under sustained high level or even moderately strong noise conditions.
Whether repeated noise induced reactions of this type can ultimately degrade one's physical and mental health is still uncertain. For example, the aforementioned physiologic changes tend to subside with recurrent exposures to the same sounds, suggesting adaptation and presumably no health difficulty. These observations, however, may not have been conducted over a sufficiently long time period to judge the possible long-term cost 40 of this adaptation to the health of the organism.
There are some reports which show that prolonged exposure to high level noise may lead to physiologic disorders in animals. For example, Anthony and Ackerman reported that guinea pigs presented with intense siren-type noises for fairly long periods of time eventually revealed endocrine and metabolic deficits which reduced their ability to cope with 41 the noise stress.
Additional siren exposure here resulted in gastro intestinal ailments, cardiovascular disease and even tissue damage in the kidneys and liver. Reproductive dysfunction and reduced resistance to infectious disease have also been reported in animals subjected to recurrent 42 43 or prolonged high level noise conditions. '
The results of these studies have not been without criticism.in some instances, they have lacked for certain controls, e.g., handling of test animals in noise but not non-noise groups, or not differentiating the groups. Also, rodents have often been used as subjects, and these animals are known to have special IV-10 susceptibility to the effects of certain sounds. Furthermore, the sound levels used in many of these experiments have usually been well above those normally encountered by man even in the noisiest environmental situations.
With regard to human exposures, there are Indications in the foreign literature which suggest that routine exposures to intense industrial noise might lead to chronic physical disturbances. A German study, for example revealed a higher incidence of circulatory and neurologic irregularities among steel workers in noisy jobs as compared with other worker groups in 44 less noisy plant areas.
Neurological examinations of Italian weavers exposed daily to intense noise showed their reflexes to be hyperactive, and in a few cases, electroencephalography traced a pattern of desynchron-25 ization similar to that seen in personality disorders.
A study in the Russian literature showed workers in noisy ball-bearing and steel plants to have a relatively greater prevalence of cardiovascular irregularities 45 such as bradycardia.
Complaints of fatigue, irritability, and social conflicts in many noise exposed workers have also been reported in connection 25 44 with several of the investigations just noted. '
The fact that those who work in high noise levels show greater medical difficulties than those who work under quieter conditions is not conclusive evidence that noise is the crucial causal factor. In each case, it is possible that the differences in the specified health parameters may be explained by other factors such as age, other environmental contaminants, work load and job habits. In any case, replication of these findings seems indicated with attempts being made to statistically isolate and better control factors that could confound possible noise effects on a variety of health indicators.
# IV-11
Concern may be raised as to whether excessive noise poses any added hazards to persons with preexisting health problems. That is, losses in performance may occur when the noise appears and also when it disappears.
Apparently, change in noise levels is the degrading factor. Of interest here is that sound levels required to cause notable performance changes may exceed hearing conservation limits for routine workday exposure. Thus, noise standards for safeguarding hearing could also offset possible noise 38 effects on job efficiency.
More moderate levels of noise may actually benefit task performance relative to quiet conditions. The presence of such noise may provide for a more uniform acoustic background, masking stray sounds which could be otherwise audible in a quiet work area and cause distraction. Also on the positive side, pulsating-type sounds may pace or drive performance and, in effect, reduce fatigue on tasks that are trying. The rhythm component in music may serve this purpose too.^"* Not all performance capacities suffer equally from the disruptive effects of noise. In fact, noise may aid performance on simple, wellpracticed or repetitive tasks through causing increased arousal in an otherwise boring job. There are indications in fact, that only those tasks which require unremitting attention (e.g., vigilance in machine monitoring, product inspection) or which place extreme mental demands on IV-14 the employee (short-term high-memory loads) may be most vulnerable to the degrading effects of n o i s e .^ In short, tasks which by themselves tax the total capacity of the Individual do not permit any accommodation to noise and consequently show loss. In some Instances, noise seems more Inclined to disturb the quality rather than the quantity of work. That Is, noise might not change work output, but may cause more errors. Along these lines, performance under noise may be subject to worker fluctuations, with periods of poor performance being Interwoven with periods of heightened 56 effort.
These performance swings, when averaged across the total work session, may yield little or no overall performance decrement.
Individual differences are quite commonly found In investigations of noise effects on performance. Attitudes toward noise are a basic factor in this variance. A recent laboratory study found subjects sensing that they had no control over randomly occurring noise intrusions to perform 57 poorer than those who could terminate such sounds.
Personality factors also seem to underlie performance variations in noise. Tense, anxious persons, as defined by personality inventories and certain physiologic indicators, seemed less able to cope with certain laboratory tasks as 58 compared with those who were more relaxed.
The importance of attitude factors in noise-performance studies is even more evident in field investigations. For example» morale and egoinvolvement in one's job can override stresses imposed by noise.Other employees dissatisfied with their job situations can use noise as a "scape goat" for poor performance. It should be mentioned, too, that through a process of self-selection, only the more noise tolerant employees probably stay at a noisy job. The more noise sensitive persons would remove themselves from these situations. Measures of absenteeism and labor turnover could IV-15 reflect the latter occurrences, but could be difficult to relate causally to noise.
The numerous factors that can influence noise effects on performance make for highly qualified conclusions and conservative predictions. Generally speaking, intense sounds» preferably impulsive» and a taxing task performed by a tense person offer the combination of conditions most likely to display a noise-induced decrement in performance.
# Cumulative Effect
This discussion has separately treated different adverse effects of noise that may result from occupational exposures. It is unrealistic, however, to conceive of employees In their everyday job routines experiencing one form of noise disturbance to the exclusion of the others. Indeed, one's daily encounters with workplace noise may degrade hearing, mask reception of desired sounds, heighten emotions and physiologic activity, disrupt con centration , or otherwise hinder job efficiency or safety. The collective impact of these noise effects clearly poses a significant challenge to the employee's health, productivity, and well-being.
The establishment of noise exposure limits for safeguarding the employee's hearing will in the main prevent the occurrence of the worst physical defect that noise can have in humans. Adherence to these limits may also have other benefits. Specifically, physical and psychological disturbances from occupational noise exposures will be less likely to arise under more controlled exposure conditions. Of course, the question remains as to whether excessive noise by itself can cause physical and mental disorders.
Nevertheless, noise levels which meet hearing conservation requirements may also be within limits that do not cause losses in job performance.
# IV-16
# V. PROCEDURES FOR REDUCING EXPOSURES
The information in this part (1) is not an attempt to present exact figures as to how many employees are exposed to hazardous noise levels; rather it substantiates that noise is Indeed a common occupational hazard which could affect a large number of employees. The companies were asked to answer the following question: "How many of your employeees are located In areas where noise levels are 90 dBA or above?" When this question was asked in August 1971, the recommended level for an 8-hour exposure limit was still 90 dBA, however, it can be assumed that a greater population is at risk. In interpreting the answers to the question stated in the preceding paragraph and the results which appear in Table VI the following points must also be considered:
V-l 1. The answers from this question cannot be used to determine how many employees are incurring hazardous noise exposures because information concerned with length of exposure time and the exact level of the exposure is not available.
2. The 341 plants volunteered this information, and the information is based upon their own noise level evaluations.
# Many other plants involved in the questionnaire survey could not
or did not answer the question.
4. The table does not contain information concerned with the 4,511,000 transportation workers, the 3,502,000 construction workers, the 626,000 miners, or the 4,746,000 agricultural w orkers.
The projected numbers of employees located in areas of noise 90 dBA F. Use sharp and properly shaped cutting and drilling tools.
# Substitution of Machines
A. Substitute belt drives for gears.
# Vibration Dampening
A. Increase mass.
B. Increase stiffness.
C. Use rubber or plastic linings to dampen noise.
D. Improve supports.
# Reduction of Solid-Borne Transmission
A. Flexible mounts for motors and other types of machinery.
B. Flexible hose in pipes or electrical conduits.
C. Flexible coupling on shafts.
# . Reduction of Noise Caused by Fluid Flow
A. Install or replace intake and exhaust mufflers on internal combustion engines and compressors.
# Isolate Noise Source
A. Construct sound reduction enclosures around equipment or parts of equipment.
# Isolate Operator
A. Provide a relatively sound-proof enclosure for the operator or attendant of one or more machines.
# V-4
Of the items listed above, the preferred procedures for reducing environmental noise are those which are directed at reducing the noise at its source (Items 1-7). Generally, these procedures have proven to be far more efficient in terms of actual noise reduction than the procedure listed as Item 8 . Furthermore, source noise controls provide protection for both the operators of the equipment as well as workers in the immediate exposure environment.
# Administrative Controls
Another effective approach to reducing the hazard of excessive noise exposure is to limit the dally amount of exposure which each employee receives, by means of strict control of the work schedule.
The following are several methods suggested by the Department of Labor "1. Arrange work schedules so that employees working the major portion of a day at or very close to the criteria limit are not exposed to higher noise levels.
2. Ensure that employees who have reached the upper limit of duration for a high noise level, work the remainder of the day in an en vironment with a noise level well below criteria limit.
3. Where the man-hours required for a job exceed the permissible time for one man in one day for the existing sound level, divide the work among two, three, or as many men as are needed, either successively or together, to keep individual noise exposure within permissible time limits.
4. If less than full-time operation of a noisy machine is needed, arrange to run it a portion of each day, rather than all day for part of the week.
V-5
# 5.
Perform occasional high level noise producing operations at night or at other times when a minimum number of employees will be exposed."
When personnel are rotated, extreme care must be taken to insure that no single employee is exposed to a high level noise for a period longer than is allowed by the noise exposure limits.
# V-6
VI.
# DEVELOPMENT OF THE STANDARD
Attempts at limiting human exposure to noise have been based on damage risk criteria. The purpose of such criteria is to define maximum permissible levels of noise for stated durations which, if not exceeded, would result in an acceptably small effect on hearing levels over a working lifetime of exposure.
Previous 1. Measurement of spectral distribution (Noise Spectrum).
2. Determination of the temporal characteristics of exposure (Noise Duration).
# Identification of a protection goal (Biologic Response).
In the discussion which follows, selected damage risk criteria listed in As may be seen from this figure, although the DRC differ in estimates of safe sound pressure level per octave, they all weight the spectrum similarly.
The second major Impetus for measurement of noise based on octave band analysis came from research which indicated that, at least for most audio metric frequencies, the amount of threshold shift observed (either temporary or permanent) was closely related to the frequency or spectrum of the stimulus. Results of "stimulation deafness" (temporary threshold shift) studies indicated that for pure tone stimuli the maximum shift in hearing appears to be about one-half octave above the frequency of total Prior to 1956 damage risk criteria set as a goal for protection (see Protection Goal), the prevention of hearing loss at all frequencies. This necessitated assessment of the noise at each octave band. After this time, VI-3 however, much more qualified protection goals were established (usually pro tection of loss in the so-called "speech frequencies") such that only knowledge of the sound pressure in certain critical octave bands (not to" be confused with aural critical bands) was required In order to assess the risk of noise exposure to hearing. This approach characterized the damage risk criteria developed by the Air Force in 1956, The American Academy of Ophthalmology and Otolaryngology in 1957, the International Standards Organ ization in 1961, and the American Academy of Ophthalmology and Otolaryngology in its revision of the 1957 criteria in 1964 (see Table IX).
The procedure for rating noise hazards by this mehtod consists of measuring the octave band levels in the critical octaves, and then comparing the measured levels with damage risk contours. This is best exemplified by the use of the "Noise Rating" curves developed by the International 80 Standards Organization.
The octave band levels of the noise are measured and then compared with the noise rating curve (Figure 9). The highest curve which is exceeded by the level of these bands yields the noise rating number (N). For this particular scheme, a noise rating of 85 was suggested as the protection criterion.
# The Use of A-weighted Sound Level
Since the publishing of the first Intersociety "Guidelines for Noise 81 Exposure Control," a relatively new approach, A-weighted sound level measurement, has become a popular measure for assessing overall noise hazard. As stated in Part III, the weighting on the A-scale approximates the 40-phon equal loudness contour (Figure 8). Use of the A-weighting is thought, therefore, to insure the rating of noises in a reasonably similar manner as would the human ear.
# VI-4
Several studies have been conducted In order to evaluate the efficacy of using A-weighted sound levels In rating hazardous exposures to noise.
82 In a study of 580 Industrial noises, Botsford showed that the A-weighted sound level Indicated the hazard to hearing as accurately as did limits expressed as octave band sound pressure levels in 80% of the cases and was slightly more conservative than octave band measures in 16% of the noises. Passchier-Vermeer2^ found that, except In one noise condition, sound level In d BA was as accurate as Nose Rating (NR) in estimating noise 83 induced hearing loss. In a study of hearing loss in 759 subjects, Robinson concluded that the error incurred from using dBA in predicting hearing level was within + 2 dB, even for noises ranging in slope from + 4 dB/ 84 octave to -5 dB/octave. A recent study found that even though dBA perhaps discounted too much low frequency energy, in all cases but one it predicted TTS2 resulting from exposures to noises of different spectra (slopes of -6 dB/octave, 0 dB/octave, and 6 dB/octave) as well as or better than other noise rating schemes which employed spectral measurements in octave-bands.
As a result of its simplicity and accuracy in rating hazard to hearing, the A-weighted sound level was adopted as the measure for assessing noise exposure by the American Conference of Governmental Industrial Hygienlsts
# VI-5
In keeping with the several precedents which have been established for its use in rating the hazard resulting from industrial noise exposure, and because it has been shown to be a reasonably accurate measure of such hazard, the A-welghted sound level measurement has been recommended for use in rating noise hazard in the Recommended Standard.
# Protection Goal
The limit of noise exposure that is established ultimately depends upon the degree of hearing which is to be protected and the number of persons in an exposed population to be protected. If a very strict protection criterion is contemplated such that no person exposed to noise will develop hearing loss at any frequency, the maximum permissible noise level governing a daily, or near daily, exposure would be quite low. Conversely, if the protection goal were to permit a certain amount of hearing loss in a small percentage of workers over a working lifetime, then the permissible exposure level would be raised accordingly. For example, Figure 10 formula whereby the ability to hear everyday speech was estimated by multi plying the hearing levels at 500, 1000, and 2000 Hz by 0.8 and then computing the average over these three frequencies. The major contribution of this formula was the introduction of the concept that hearing loss for speech could be estimated by the average hearing levels at what has now become known as the "speech frequencies"-500, 1000, and 2000 Hz.
# 93
The American Medical Association in 1947 recommended that hearing loss for speech be determined by the pure tone hearing losses at 500, 1000, 2000, and 4000 Hz. The four frequencies were given a weighting in accordance with what was presumed to be the importance of each frequency in hearing for speech (i.e., 15% at 500 Hz, 30% at 1000 Hz, 40% at 2000 Hz, and 15%
at 4000 H z ) . This guideline further suggested that hearing loss for speech does not begin until the weighted average hearing loss equaled 10 dB, and total loss for speech hearing occurred when the loss at 500 Hz reached 90 dB or the losses at the other 3 frequencies reached 95 dB.
In a later article which reviewed the assumptions In computing hearing 94 loss for speech, the AM A made the following observations and recommendations:
(1)
The 1947 formula was inadequate for calculating hearing loss for speech in sensorineural hearing loss. (This is particularly interesting in that the method used today for computing hearing loss for speech, developed by the AAOO in 1959 and accepted by the AMA in 1961, eliminated the most VI-9 sensitive indicator of sensorineural hearing loss (i.e., losses at 4000 Hz.))
(2) Everyday communication should be the basis for evaluation of hearing disability. "Ideally, hearing impairment should be evaluated in terms of ability to hear everyday speech under everyday conditions. The ability to hear sentences and to repeat them correctly in a quiet environment is taken as satisfactory evidence for correct hearing of everyday speech. Because of present limitation of speech audiometry, the hearing loss for speech is estimated from measurements made with a pure tone audiometer. For this estimate, the simple average of the hearing levels at the 3 frequencies 500, 1000, and 2000 cps is recommended.
V I -10 "In order to evaluate the hearing impairment, it must be recognized that the range of impairment is not nearly so wide as the audiometric range of human hearing. Audiometric zero, which is presumably the average normal threshold level is not the point at which Impairment 1. The basis of hearing impairment should be not only the ability to hear speech, but also the ability to understand speech.
# The ability to hear sentences and repeat them correctly in quiet
is not satisfactory evidence of adequate hearing for speech communication under everyday conditions. 2) above, the ability to understand speech under everyday conditions is best predicted on the basis of the hearing levels at VI-11 1000, 2000, and 3000 He.
# From (1) and (
# 4.
The point at which the average of hearing losses in the stated three frequency range of 1000 -3000 Hz begins to have a detrimental effect oil the ability to understand speech is 25 dB re ANSI (1969).
With reference to the determination of hearing impairment (1. above), the dbility to "hear" speech, measured in terms of the lowest intensity at which a listener can barely identify speech materials, provides little information concerning communication difficulties under everyday con-QQ ditions. As Sataloff states, "It [occupational deafness] implies the presence of obvious difficulties in hearing speech. Actually, the difficulty mofe often lies not so much in 'hearing' speech as in 'understanding' it." Furthermore, Davis and S i l v e r m a n^ observed that "... a man with severe high-tone nerve deafness (as is seen in occupational noise induced hearing loss), will always fall to hear certain sounds and will never make a perfect articulation score. On the other hand, the same man may hear some words, the easy low-frequency words, as well as anyone else does. He may have a normal threshold for speech."
This issue is further clarified if one compares the "typical" clinical picture of a person having a conductive hearing loss versus a person having A sensorineural hearing loss resulting from noise exposure. Both cases would be expected to have elevated speech reception thresholds (a measure of hearing for speech); however, in the case of the conductive loss, speech discrimination (measure of understanding) would be approximately the same as that iot a person having normal hearing, provided that the presentation level ift sufficiently above the speech reception threshold level. The person with occupational hearing loss (sensorineural), on the other hand, would have VI-12 relatively poor discrimination scores, and the effect of raising the pre sentation level to higher levels often serves to reduce the articulation 100 score (see example in Figure 11). In applying the AAOO-AMA formula to the cases shown in Figure 11 it is possible that both would be rated identically in terms of hearing impairment, yet the sensorineural case has much more difficulty in understanding speech than does the conductive case.
It is apparent, therefore, that the formula applied to compute hearing impairment should consider discrimination ability and that the pure tone frequencies used in the formula should be highly correlated with this latter function.
With reference to speech communication under everyday conditions (see
# 101
100Z. Furthermore, everyday speech rarely takes the form of complete sentence communications; thus, the number of speech cues available for 88 accurate speech perception under everyday conditions is greatly reduced.
From this discussion, it may be concluded that an appropriate predicting scheme for determination of hearing impairment must include some consideration VI-13 for an actual daily communication environment rather than some optimum condition as suggested by the AAOO -AMA.
With reference to predicting ability to understand speech on the basis of heavy levels at the pure tone average at 1000. 2000. and 3000 Hz (point 3 above), results of several studies indicate that hearing levels at these three frequencies predict hearing loss for speech under mild conditions of distortion better than the three frequency average at 500, 1000, and 2000. In chinchillas. However, they cautioned that their findings were only applicable to continous exposures and not to intermittent exposures.
Variables that are germane to Interrupted exposures but do not play a significant role in limiting hazard from short-term continuous exposures further complicate the problem of how the ear responds and integrates noise over time. One such variable is the "acoustic" or "middle ear" reflex.
When the ear is exposed to loud noise, the middle ear muscles contract, thus altering the impedance of the middle ear. This reflex, which serves to attenuate the noise reaching the inner ear, adapts out or disappears quickly if the noise is continuous and relatively unchanging over time.
However, if the noise level varies considerably or is interrupted on a regular or irregular basis, then the reflex is sustained.
A second variable which plays an important role in reducing the hazard of interrupted noises relative to short-term continuous noises concerns the off-time of the exposure cycles. Depending upon the over-all level of the noise and the nature of the relationship between on-time and off-time, a considerable reduction in the degree of temporary hearing threshold shift may be observed.
To date, the only empirical data available on permanent hearing losses resulting from intermittent exposures comes from a study of iron ore miners conducted by Sataloff et a l .^^ Their findings indicated that intermittent noises had to be some 15 dB more intense than continuous noises to cause the same additional hearing impairment in men ages 30 to 50 years. Although this 113 VI-18 evidence confirms Che general notion that intermittent exposures are less hazardous than continuous steady-state exposures of the same duration and noise level, the applicability of this rule to other schedules of intermittency must await further investigation.
Since 1960, several damage risk criteria have been proposed to limit 82,107,115 exposure to intermittent noise.
For the most part, these criteria, like the rules for assessing Intermittent noise exposure discussed below, have been based predominantly upon evidence collected from studies of temporary threshold shift.
At least three different rules have been proposed in order to assess the hazard of exposures to intermittent noise. The first of these rules, 28 developed by Ward et al.
was called the "on-fraction" rule. This rule states that the amount of temporary threshold shift resulting from a given intermittent exposure can be determined on the basis of noise level and average on-fractlon (the time the noise is on divided by the total duration of exposure). This procedure assumes that levels below 75 dB SPL are not hazardous to hearing; thus, the amount of on-time is taken as the total time the noise is above 75 dB SPL. In a critical test of the on-fraction rule, Selters and Ward^1 found that this rule was invalid when the regular on-off times exceeded two minutes.
For burst durations longer than two minutes, a second rule has been The essential feature of this approach is that residual TTS is translated into exposure time.
One of the crucial assumptions of the "exposure-equivalent" rule is that the course of recovery from TTS is Independent of the type of noise 33 that produce the TTS. In a recent article, Ward has presented data that question the validity of this assumption. It appears that intermittent exposure to high level, high frequency noise causes a considerable delay in the recovery of TTS relative to intermittent low frequency exposures.
A third approach in determining hazard from interrupted noise has been to determine the total on-time of the noise, regardless of how the noise bursts are distributed in time, and to consider the intermittent exposure in terms of an equivalent continuous exposure. This approach attempts to take into consideration the reduced hazard of interrupted noise by adjusting the rule which relates noise level and exposure duration.
Although possibly not as scientifically rigorous as the previously mentioned procedures, the "equivalent continuous" rule is not constrained by the assumption concerning the regularity of exposure cycles which is basic to the other rules.
# VI-20
Intermittent noise exposure criteria based upon the first and/or second rules include those developed by Glorig, Ward, and N i x o n , 113 CHABA 107 82 Working Group 46, and Botsford. Botsford's i n t e m i t t e n c y criteria reflect a simplification and consolidation of the CHABA continuous exposure, long-burst intermittent, and short-burst intermittent contours into one general figure relating dBA level, total on-time (noise level above 89 d B A ) , and number of exposure cycles (see Figure 13). The limits of intermittent exposure expressed in these contours (shown in Table X) 27 have recently been adopted by the Second Intersociety Committee. Similar limits have been adopted as part of a revision of the German document con-116 cerned with assessment of industrial noise in working areas.
Recent research designed to investigate the efficacy of the limits proposed In Table X have generally shown that the limits do not acburately predict risk to hearing, at least so far as temporary threshold shift is concerned. In a laboratory study11^ designed to evaluate selected exposure conditions from Table X» it was found that (1) the table shows concen trations of noise exposure within an eight-hour workday than can cause excessive amounts of temporary threshold shift and (2) the conditions did not yield equal effects on hearing, thus not affording equal protection.
# 118
Conversely in a study of forestry employees It was found that although the noise exposures were rated as hazardous according to Table X, the audiometric results indicated that the exposures did not pose a risk to hearing.
Considerably more data must be collected to evaluate present criteria which attempt to designate safe levels of exposure to Intermittent noise. on the other hand, suggested that the "off" level was frequently dependent. For example, the safe level of exposure for the octave band 300 -600 Hz was seen to be 89 dB SPL, whereas It was approximately 85 dB SPL for octave band 1200 -2400 Hz.
Recently, Botsford®^ computed a dBA equivalent from the octave band damage risk criteria developed by CHABA. The results of this computation suggested that the "off level" based upon one-third octave or octave band sound pressure level will, in many cases, be below the level designated by Botsford (particularly in the case of strong narrow band components in the noise). Both the CHABA and Botsford criteria do not appear to be in accord with the intended meaning of a safe intermittent level in that present data suggest that there is a significant increase in the proportion of the popu lation having hearing impairment in those groups exposed to continuous noise VI-22 levels at and slightly below 85 dBA as compared with a non-noise exposed population.
Two lines of evidence suggest that the lower limit of Interrupted exposure is considerably below the levels mentioned above. In a review of XI.
The audiometric van used for the hearing tests was capable of testing six individuals at one time. All employees were tested before the beginning of their work shift, and, due to scheduling problems, the number of employees in a test session ranged from one to six. When less than six employees were present at a testing session, an attempt was made to randomize the assign ment of audiometers. It was also necessary to use headphones with otocups to properly shield the employees from the possible effects of interference caused from hearing the other test tones in the van. However, it was found from the results of two independent studies in the NIOSH laboratory that there was no significant difference in measured thresholds between headphones fitted with otocups and those fitted with standard MX-41/Ar type ear cushions.
Before data analysis could be done, it was necessary to check the calibration data accumulated during the respective survey. Calibration of the audiometeres used to take the audiograms was usually performed before and after each survey. The data were corrected where necessary to the appropriate values given in the American National Standard Specifications for Audiometers, ANSI S 3 .6 (1969).
Used for purposes of data analysis were the three-frequency averages mentioned above In the definitions of hearing impairment. HLI (0.5, 1, 2)
and HLI (1,2,3) are used to denote these averages performed over both ears. (HLI stands for "hearing level index.")
# VI-25
The samples were grouped Into age and experience ranges to assure equal numbers per cell and a consistent spread of the data across the various dBA levels.
The following lists the steps made in the data analysis:
1. Hearing level indices for 87 and 94 dBA noise exposed individuals were grouped into 31 samples for three-way cross-classification with respect to dBA level, age group, and experience group. The data were transformed by taking natural logarithms, and the resulting variances of log HLI (0.5, 1, 2)
and log HLI (1, 2, 3) were computed for each sample. For each of the two dBA levels, Bartlett's tests for homogeneity of variances were performed over all age and experience combinations. Separate tests were performed for HLI (0. 5, 1, 2) and HLI (1, 2, 3) average noise Indices. Of the four Bartlett's tests, three showed no suggestion of nonhomogeneity of variance, but the fourth was significant at the 0.05 prbbability level. However, only one atypical variance was found within the "nonhomogeneous" group, and this was believed to be caused by an improbable combination of purely random variations and not indicative of a real elevation of variability for the cell in question. Thus, the conclusions were that variability of log HLI (0.5, 1, 2) and log HLI (1, 2, 3) for replicate subjects was stable over all cells defined by the crosa-clasalfication.
2. Fifth-degrfee orthogonal polynomial regression curves were fitted to log HLI v s . dBA for each age and experience cell using data for all dBA levels. Significance tests for nullity of regression coefficients were performed. For most of the curves which exhibited any significant trend, a straight line fitted the data within the limits of unexplained variability.
# VI-26
In several cases, fourth or fifth degree coefficients showed significance, but examination of the plotted points revealed these to be artifacts due to clustering of the dBA levels for those plots, i.e., too few levels of the independent variable so that the polynomial tended to "fit the random errors."
3. Histograms of pooled deviations of log HLI values from the respective regression lines for H L I (0.5, 1, 2) and HLI (1,2,3) were constructed by fitting normal distribution curves. Chi-square goodness-of-fit tests were performed. The tests revealed that the log HLI deviations from the means were normally distributed over the full range of variability to a very significant degree of approximation as shown in Figures 14 and 15 Means were found to be zero, and pooled variances were calculated for use in later stages of the analysis.
4. Regression lines for different age groups within an experiencelevel were tested for parallelism, and in every case, the lines were found to be parallel within the limits of error in the slope estimates. Pooled slopes were calculated, and the intercepts were revised to reflect the small differences between the separate and pooled slopes. Families of parallel lines were plotted. Tests for coincidence of sets of parallel lines were then made by the method of covariance analysis. This revealed significant difference at the 0 .0 1 probability level in all cases.
5. Regression lines for different experience levels within an age group were not found to be parallel, and, for each age group, the intercepts were compared by means of Student's t-tests. The "intercepts" were defined as ordinates of the regression lines at a dBA of 79, which represented the control group exposed to less than 80 dBA. These regression lines were found to be significantly different families of nonparallel lines from common intercepts.
VI-27 6.
For each age and experience combination, the normal distribution of pooled variation in replicate subjects was distributed about the re gression line with its zero mean centered at the ordinate of the line.
This model was then used to calculate a predicted percentage of subjects whose hearing levels exceeded a "fence". Thus, such percentages could be tabulated as a function of dBA for each age and experience category.
Furthermore, risk values were then derived as the percentage difference between employees exposed to noise levels 80 dBA or greater and those exposed to less than 80 dBA (Table XII and XIII).
This analysis indicates that the 85 dBA-Slow noise limit for an eighthour day, in conjunction with the medical program prescribed in the standard, will improve the protection of the working population from hearing loss that could impair their abilities to understand everyday speech. The reliability of the analysis is evidenced by homogeneity of the variance and normality of the population distributions. In other words, the evaluation is repeatable and is representative of a random sample. Thus, the Intersociety analysis differs from that of NIOSH in several characteristics: use of one ear only, nonseparation of experience groups, use of SIL in noise levels, and use of a dissimilar composite population.
Some of these characteristics tend to produce lower risk values and con siderably more uncertainty than the NIOSH analysis, as evidenced in Table VII-3.
Another study whose analysis determined risk is published In ISO 90 Reconmendation R1999 (1971).
This analysis differs from the NIOSH analysis VI-30 in three ways. The first is that only the right ear was used. The second is that no separation of age groups into work experience groups was done. The third is that no screening for otological abnormalities was done in the ISO study. On the other hand, the entire sample of data used in this analysis is homogeneous in that all members of the sample 126 were taken from one comprehensive examination.
The lack of otological screening has some effect on incidence of hearing impairment for both the noise exposed and the non-noise exposed groups, but, when risk is calculated by subtracting the two incidences, the effect is essentially cancelled. Thus
# OCTAVE BAN D SPL R E 2x10 N/M
75 150 300 600 1200 2400 4800 9600 The hearing levels of the heavy earth equipment operators were found to be significantly higher than the non noise exposed groups. The paper bag workers had higher hearing levels but not as high as the earth equipment operators. The airport ramp personnel, however, had the lowest hearing levels, probably due to the intermittency of their ex posures .
# APPROX. SCALE 8PIRAL SANGLiÖN
# INNER
# CONT I N U A T I O N (6) O F T A B L E IX
| None | None |
e37483d33b89138556f4c9ccc39757e2093e79dc | cdc | None | These recommendations represent the first statement by the Advisory Committee on Immunization Practices (ACIP) on the use of live, attenuated varicella virus vaccine-VARIVAX ® -manufactured by Merck and Company, Inc. and licensed in March 1995 for use in healthy persons ≥12 months of age. In addition to presenting information regarding vaccine, this statement updates previous recommendations concerning the use of varicella zoster immune globulin (VZIG) as prophylaxis against varicella ( MMWR 1984;33:84-90,95-100).# INTRODUCTION
Varicella (i.e., chickenpox) is a highly contagious disease caused by varicella zoster virus (VZV). Secondary attack rates for this virus may reach 90% for susceptible household contacts. VZV causes a systemic infection that usually results in lifetime immunity. In otherwise healthy persons, clinical illness after reexposure is rare; such illness is more likely to occur among immunocompromised persons. However, as with other viral diseases, reexposure to wild-type varicella often leads to reinfection that boosts antibody titers without causing clinical illness or detectable viremia. VZV remains dormant in sensory-nerve ganglia and may be reactivated at a later time causing herpes zoster (i.e., shingles)-a painful vesicular rash usually appearing in a dermatomal distribution of one or two sensory-nerve roots.
Among children, varicella is usually a self-limited disease that lasts 4-5 days and is characterized by fever, malaise, and a generalized vesicular rash typically consisting of 250-500 lesions. Adolescents, adults, and immunocompromised persons usually have more severe disease and are at higher risk for complications. Primary subclinical infection with VZV is rare for persons of all ages.
# EPIDEMIOLOGY OF VARICELLA
# General
VZV is transmitted from person to person by a) direct contact, droplet, or aerosol from vesicular fluid of skin lesions or b) secretions from the respiratory tract. The virus enters the host through the upper-respiratory tract.
The average incubation period for varicella is 14-16 days; however, this period can range from 10 to 21 days. The period of contagiousness of infected persons is estimated to begin 1-2 days before the onset of rash and end when all lesions are crusted, which is usually 4-5 days after onset of rash. Persons who have progressive varicella may be contagious longer, presumably because their immune response is depressed, which allows viral replication to persist.
Because varicella develops in nearly all persons who live in the United States, the incidence is estimated to approximate the birth cohort. Data from the National Health Interview Survey (NHIS) for the period 1980-1990 indicated that an estimated 3.7 million cases occur annually (annual incidence rate: 1,498 cases per 100,000 population) (CDC, unpublished data). Varicella is not a nationally notifiable disease, and surveillance data are limited. In 1994, only 28 states, the District of Columbia, and New York City reported cases to CDC's National Notifiable Disease Surveillance System (NNDSS), and reporting within states was incomplete. Reporting efficiency is only an estimated 4%-5%.
Age-specific incidence data were derived from NHIS for the period 1980-1990 (CDC, unpublished data). An estimated 33% of cases occurred in preschool-age children (i.e., children 1-4 years of age ), and 44% occurred in school-age children (i.e., children 5-9 years of age ) (Figure 1). More than 90% of cases occurred in persons 49 years of age. Epidemiologic and serologic studies confirm that >90% of adults are immune to VZV (CDC, unpublished data;1 ). Rates of immunity may be lower for adults who were raised in certain tropical or subtropical areas (e.g., Puerto Rico) (2 ).
Otherwise healthy children and adolescents (i.e., persons <15 years of age) comprise the largest proportion (80%) of an estimated 9,300 annual varicella-related hospitalizations. However, the rate of complications is substantially higher for persons ≥15 years of age and for infants (i.e., children <1 year of age). The most common complications of varicella, which can result in hospitalization, are bacterial infections of skin lesions, pneumonia, dehydration, encephalitis, and hepatitis. Since the association between Reye syndrome and aspirin use was identified, Reye syndrome, which was once considered a common complication resulting from varicella infection, now rarely occurs (3,4 ).
The mean annual number of persons who died in the United States as a result of complications of varicella decreased from 106 persons during 1973-1979 57 persons during 1982-1986. This decrease may have resulted from a) the substantial reduction in cases of Reye syndrome, b) the availability of acyclovir, c) the selective use of varicella zoster immune globulin (VZIG), and d) improvements in supportive care. However, during 1987-1992, the mean annual number of varicella-related deaths increased to 94 persons; the cause of this increase is unknown. The case-fatality rate is lower for children and adolescents 1-14 years of age than for infants (0.75 cases per 100,000 children and 6.23 cases per 100,000 infants). Among persons ≥15 years of age, the risk for death increases with age, from 2.7 per 100,000 among persons 15-19 years of age to 25.2 per 100,000 among persons 30-49 years of age (CDC, unpublished data). Although the varicella-related mortality rate among children generally is low, during periods of increased varicella incidence, the circulation of virulent strains of group A streptococci (which are more likely to cause invasive, fatal infections) can result in an unusually high number of hospitalizations and deaths among children (5,6 ).
to
# Prenatal and Perinatal Exposure
Although prenatal infection is uncommon because most women of childbearing age are immune to VZV (7 ), varicella in pregnant women is associated with a risk for VZV transmission to the fetus or newborn. Intrauterine VZV infection may result in congenital varicella syndrome, clinical varicella (during the newborn period), or clinical zoster (during infancy or early childhood) (8)(9)(10)(11)(12)(13)(14)(15)(16)(17). Infants who are prenatally exposed to VZV, even if asymptomatic, may have measurable varicella-specific IgM antibody during the newborn period, have persistent varicella-specific IgG immunity after 1 year of age without a history of postnatal varicella, or demonstrate positive lymphocyte transformation in response to VZV antigen (8 ).
Congenital varicella syndrome, first recognized in 1947 (11 ), can occur among infants born to mothers infected during the first half of pregnancy and may be manifested by low birthweight, cutaneous scarring, limb hypoplasia, microcephaly, cortical atrophy, chorioretinitis, cataracts, and other anomalies. Aggregate results from prospective studies (8,(13)(14)(15) indicate that congenital varicella syndrome developed in four (0.7%) of 564 infants born to mothers who had varicella during the first trimester of pregnancy. In a prospective study conducted in the United Kingdom and West Germany from 1980 to 1993, a higher risk for congenital varicella syndrome was observed when maternal infection occurred during 13-20 weeks' gestation than when infection occurred from conception through 12 weeks' gestation (2% versus 0.4%, respectively) (14 ). In this same population, herpes zoster developed during infancy or early childhood in four (0.8%) of 477 infants who were exposed to VZV during 13-24 weeks' gestation and six (1.7%) of 345 infants who were exposed during 25-36 weeks' gestation.
The onset of varicella in pregnant women from 5 days before to 2 days after delivery results in severe varicella infection in an estimated 17%-30% of their newborn infants. These infants are exposed to VZV without sufficient maternal antibody to lessen the severity of disease. The risk for death among neonates has been estimated to be 31% among those infants whose mothers had onset of rash 0-4 days before giving birth (16 ). This estimated risk was based on a limited number of infant deaths and may be inflated because some cases resulted from selective reporting and occurred before neonatal intensive care was available. When cases were reevaluated, several infants had been at higher risk for death because of low birthweight. In at least one case, another cause of death had been probable (17 ). Although the risk for death among neonates who do not receive VZIG intervention is likely substantially lower than was previously estimated, VZIG has had a salutary effect on neonatal disease. For example, although only 21 neonatal deaths were reported in the United Kingdom during a 20-year period before VZIG was available, the proportion of deaths among neonates infected with varicella decreased from 7% to none after routine use of VZIG (18 ).
# Nosocomial Transmission
Nosocomial transmission of VZV is well recognized (19)(20)(21)(22)(23)(24)(25)(26)(27)(28)(29), and guidelines for the prevention of nosocomial VZV infection previously have been published (30 ). Guidelines concerning infection control for hospital personnel are being developed (CDC, unpublished data). Sources of nosocomial exposure have included patients, hospital staff, and visitors (e.g., the children of hospital employees) who are infected with varicella or herpes zoster. In hospitals, airborne transmission of VZV has been demonstrated when varicella has occurred in susceptible persons who have had no direct contact with the index case-patient (31)(32)(33)(34)(35).
Although severe varicella disease and complications can occur in all susceptible, hospitalized patients, certain conditions are associated with higher risk. Patients at high risk for severe disease and complications include a) premature infants born to susceptible mothers, b) infants who are born at <28 weeks' gestation or who weigh ≤1,000 g (regardless of maternal immune status), and c) immunocompromised persons of all ages-including persons who are undergoing immunosuppressive therapy, have malignant disease, and are immunodeficient.
Strategies for managing clusters of VZV infection in hospitals have included isolating patients who have varicella and susceptible patients who have been exposed to the virus; controlling air flow; using rapid serologic testing; furloughing or screening exposed, susceptible personnel daily for skin lesions, fever, and systemic symptoms; and temporarily reassigning susceptible personnel to locations remote from patientcare areas (36)(37)(38)(39)(40)(41)(42)(43). Appropriate isolation of hospitalized patients who have confirmed or suspected VZV infection can reduce the risk for transmission to personnel. Only personnel who are immune to varicella should care for these patients. If susceptible personnel are exposed to varicella, they are potentially infective 10-21 days after exposure and are often furloughed, usually at substantial cost. The use of VZIG following exposure can be costly, does not necessarily prevent varicella, and may prolong the incubation period by ≥1 week, thus extending the time during which personnel should not work in patient areas.
# Herpes Zoster
Following varicella, VZV persists in a latent form in sensory-nerve ganglia without any clinical manifestation. The latent virus can be reactivated, causing herpes zoster. Approximately 15% of the population will experience herpes zoster during their lifetimes (44 ). Herpes zoster develops most frequently among immunocompromised persons and the elderly. Disseminated herpes zoster with generalized skin eruptions and central nervous system, pulmonary, hepatic, and pancreatic involvement is more likely to occur in immunocompromised persons than in the general population. VZV can be transmitted from the lesions of patients who have herpes zoster to susceptible contacts, although the likelihood of transmission of VZV from herpes zoster is much less than that from primary varicella. Transmission of VZV from patients who have herpes zoster results in primary varicella in susceptible contacts.
# VARICELLA ANTIBODY TESTING
A reliable history of varicella is a valid measure of immunity. Because the rash is distinctive and subclinical cases rarely occur, most parents know if their child has had varicella. A negative history of varicella substantiated by a parent may be more accurate than a self-reported negative history given by an adult. Data from one study indicated that the attack rate following household exposure in parents who reported themselves as being susceptible was 5%; however, among children whose parents reported them as being susceptible, the attack rate was 87%. In children with positive histories, the attack rate was 7% (45 ).
Serologic tests have been used to assess the accuracy of reported histories of varicella (1,26,42,46,47 ). In adults, a positive history of varicella is highly predictive of serologic immunity (97%-99% of persons are seropositive); however, the majority of adults who have negative or uncertain histories are also seropositive (71%-93%).
The appropriateness of a laboratory test to detect antibody to VZV depends on the purpose for obtaining the information; tests differ in their ability to detect antibody acquired from natural varicella versus antibody acquired from vaccination-levels of which are lower than those following natural infection. Likewise, tests that rapidly assess the susceptibility of persons at high risk who are exposed to varicella differ from those used in serologic surveys. Certain tests require equipment or techniques that are not appropriate for general diagnostic laboratories. Thus, the criteria for selection of an antibody-detection assay include test sensitivity and specificity, the length of time required to obtain results, and availability of the assay.
Many methods have been used to detect antibody to VZV, including complement fixation (CF), indirect fluorescent antibody (IFA), fluorescent antibody to membrane antigen (FAMA), neutralization (N), indirect hemagglutination (IHA), immune adherence hemagglutination (IAHA), radioimmunoassay (RIA), latex agglutination (LA), and enzyme-linked immunosorbent assay (ELISA) (48)(49)(50)(51)(52)(53)(54)(55)(56)(57)(58)(59)(60). IFA, FAMA, N, and RIA are sensitive tests, but they are time consuming and have requirements that make them unsuitable for use in general diagnostic laboratories. The CF test has been widely used but is the least sensitive test; antibody may diminish to levels undetectable by CF several months after natural varicella infection. RIA and ELISA are equal in sensitivity; both tests are tenfold more sensitive than IFA and twentyfold more sensitive than CF (54 ). ELISA tests, which are commercially available, range in sensitivity from 86% to 97% and range in specificity from 82% to 99% in detecting antibody after natural varicella infection. A highly sensitive gpELISA using purified viral glycoproteins as antigens has been used in clinical trials for the large-scale testing of immunogenicity of varicella virus vaccine, but it is not commercially available (58 ). A commercially available LA test using latex particles coated with VZV glycoprotein antigens can be completed in 15 minutes and does not require special equipment (59 ). The sensitivity and specificity of the LA test are comparable to those of FAMA in detecting antibody response following natural varicella infection, but the LA test is less sensitive in detecting antibody following vaccination; for both purposes, the LA test generally is more sensitive than commercial ELISAs. The LA test has detected antibody for up to 11 years after varicella vaccination (60 ).
# ACYCLOVIR FOR THE TREATMENT AND PREVENTION OF VARICELLA
Acyclovir is a synthetic nucleoside analog that inhibits replication of human herpes viruses, including VZV. Intravenous acyclovir has been available since the early 1980s for use in immunocompromised persons who have varicella and, when administered within 24 hours of onset of rash, has been effective in reducing the morbidity and mortality associated with varicella (61)(62)(63).
In 1992, the Food and Drug Administration (FDA) approved the use of oral acyclovir for the treatment of varicella in otherwise healthy children. Approval was based on placebo-controlled, double-blind studies (64)(65) that indicated that beneficial clinical effects occurred (i.e., a decrease in the number of days in which new lesions appeared, the duration of fever, and the severity of cutaneous and systemic signs and symptoms) when acyclovir was administered within 24 hours of onset of rash. No serious adverse events occurred during the period of drug administration. Acyclovir did not decrease transmission of varicella or reduce the duration of absence from school. The rate of complications from varicella is low for healthy children. Data from these studies could not determine whether acyclovir had a significant effect on this rate because too few complications occurred. In these studies, antibody titers following infection in children receiving acyclovir were not substantially different from titers of children in the control group (64,65 ). Clinical trials among adolescents and adults (66)(67)(68) have indicated that acyclovir is safe and effective in reducing the duration and severity of clinical illness if the drug is administered within 24 hours of the onset of rash.
The Committee on Infectious Disease of the American Academy of Pediatrics (AAP) published a statement on the use of acyclovir (69 ). The Committee did not consider the administration of acyclovir to healthy children to be beneficial enough to justify routine administration to such children; however, the Committee acknowledged that certain circumstances may justify the minimal clinical benefit. Complications and more severe varicella may occur in adolescents and adults or in secondary casepatients who live in the households of infected children; therefore, AAP considered such situations appropriate for the use of this drug.
The safety of systemic acyclovir therapy among pregnant women has not been established. Although studies involving animals have not indicated teratogenic effects, adequate, well-controlled studies among pregnant women have not been conducted. Acyclovir is classified as Category C in the FDA use-in-pregnancy rating (i.e., risk cannot be ruled out, but potential benefits may justify the possible risk) (Burroughs Wellcome Company, Zovirax™ package insert). AAP does not recommend oral acyclovir for pregnant women; however, in instances of serious, viral-mediated complications (e.g., pneumonia), AAP stated that intravenous acyclovir should be considered. Burroughs Wellcome Company maintains the Acyclovir in Pregnancy Registry to monitor the maternal-fetal outcomes of pregnant women who are administered systemic acyclovir. The registry is a collaborative effort of Burroughs Wellcome Company, CDC, and academic epidemiologists.- Two nucleoside analogs, acyclovir and famciclovir, have been approved by FDA for treating herpes zoster. If administered within 72 hours of rash onset, acyclovir has accelerated the rate of cutaneous healing and has reduced the severity of acute necrosis in adults who have herpes zoster (70 ). Oral famciclovir, when administered during the same period of time, has similar efficacy (71 ).
The prophylactic use of acyclovir in susceptible children following household exposure to varicella recently has been studied. These studies indicated fewer and less severe cases among children administered acyclovir than among children in the control group. Data from one study indicated that varicella developed in 16% of children treated with acyclovir during the second week after exposure compared with 100% of children in the control group (72 ). In another study, 85% of children who were treated during the first week after exposure seroconverted (a fourfold or greater increase in antibody in convalescent sera), as did 79% of those treated during the second week after exposure (73 ). Seroconversion in the absence of clinical disease occurred more frequently in children who received acyclovir during the second week after exposure (73%) than among those who received acyclovir during the first week after exposure (9%). Thus, although acyclovir appeared to prevent or modify clinical disease in most cases, some children remained susceptible. Serologic testing is required to distinguish those children with subclinical disease who seroconverted from those children who were not infected (74 ).
Postexposure use of acyclovir may be a less costly alternative to the use of VZIG in some susceptible persons. However, before such a strategy could be considered, additional data are needed concerning the prophylactic use of acyclovir in healthy and immunocompromised persons in all age groups.
# LIVE, ATTENUATED VARICELLA VIRUS VACCINE
The varicella virus vaccine licensed in the United States is composed of the Oka strain of live, attenuated VZV. The Oka strain was isolated in Japan (75 ) in the early 1970s from vesicular fluid in a healthy child who had natural varicella and was attenuated through sequential propagation in cultures of human embryonic lung cells, embryonic guinea-pig cells, and human diploid cells (WI-38). The virus in the Oka/ Merck vaccine has undergone further passage through human diploid-cell cultures (MRC-5) for a total of 31 passages. Varicella virus vaccine was first licensed for use among high-risk children in several European countries in 1984, in Japan in 1986, and in Korea in 1988. In Japan and Korea, licensure was extended to healthy children in 1989; no concerns about vaccine safety have been identified after the administration of >2 million doses in these countries.
Varicella virus vaccine is lyophilized, and when reconstituted as directed in the package insert and stored at room temperature for 30 minutes, the vaccine contains >1,350 plaque forming units (PFUs) of Oka/Merck VZV in each 0.5-mL dose. Each 0.5-mL dose also contains 12.5 mg of hydrolyzed gelatin, trace amounts of neomycin and fetal bovine serum, 25 mg of sucrose, and trace residual components of MRC-5 cells (including DNA and protein). The vaccine does not contain preservatives. Since 1981, a total of 9,454 healthy children and 1,648 healthy adolescents and adults have received several formulations of the Oka/Merck vaccine as part of clinical trials conducted in the United States (76)(77)(78)(79)(80)(81)(82)(83). The occurrence of serious adverse events has been minimal (see Vaccine-Associated Adverse Events). Antibody responses have been measured by gpELISA.
# Immunogenicity
The seroconversion rate (gpELISA >0.3 U) after one dose of vaccine among 6,889 susceptible children 12 months-12 years of age was demonstrated to be 97%; 76% of these children achieved antibody titers of gpELISA ≥5 U (Merck and Company, Inc., unpublished data). Persistence of antibody (i.e., IgG >5 by FAMA) measured yearly for 4 years after vaccination was consistently high (i.e., >90%) in children vaccinated at 12, 13, 14, 15, 16-23, 24-36, or 48-144 months of age, although the numbers of children tested decreased considerably as the length of time since vaccination increased. Six years after vaccination at ages ranging from 1 to 12 years, 35 children had no decrease in antibody titers (84 ). In Japan, antibodies to VZV were present in 97% of children 7-10 years after vaccination, and titers were comparable to those in children who had natural varicella infection 7-10 years earlier (85 ). A subsequent 20-year follow-up study revealed that antibody levels were higher than those observed 10 years earlier (86 ). These higher levels might have resulted from asymptomatic boosting of vaccine-induced immunity by exposure to wild-type VZV, because <20% of children in Japan were vaccinated during 1991-1993.
Among persons ≥13 years of age, 78% of vaccinees seroconverted after the first dose of varicella virus vaccine, and 99% seroconverted after a second dose, which was administered 4-8 weeks later (Merck and Company, Inc., unpublished data); the proportion of vaccinees who seroconverted did not differ by age. Detectable antibody levels have persisted for at least 1 year in 97% of adolescents and adults who were administered two doses of vaccine 4-8 weeks apart.
# Efficacy and Breakthrough Infections
In clinical trials, the vaccine has proven to be effective for >10 years in preventing varicella. However, breakthrough infections (i.e., cases of varicella that occur in some vaccinated persons following exposure to wild-type virus) can occur, usually resulting in mild illness.
In a double-blind, placebo-controlled trial using vaccine that contained 17,430 PFUs, efficacy among children 1-14 years of age was 100% after the first varicella season and 96% after the second season. On the basis of a long-term evaluation of a subset of vaccinees whose vaccination status was revealed after the second year following vaccination, efficacy was an estimated 95% after 7 years (77 ). A controlled efficacy trial was not conducted for adults.
Data from all trials in which vaccinees of all ages were actively followed for up to 9 years indicated that varicella developed in <1%-4.4% of vaccinees per year, depending on vaccine lot and time interval since vaccination (Merck and Company, Inc., unpublished data). Active and passive surveillance data collected during 6 years of follow-up have indicated that each year, varicella developed in 2.1%-3.6% of the 4,142 children who received earlier lots of vaccine containing 1,000-1,625 PFUs of attenuated virus. Natural varicella attack rates in children 1-9 years of age are an estimated 8.3%-9.1%; thus, these data represent an estimated 67% (range: 57%-77%) decrease from the total number of expected cases. For up to 3 years of follow-up, varicella developed in 0.2%-1% of 1,164 children who received the current vaccine containing 2,900-9,000 PFUs per year, representing an average 93% decrease from expected rates. The attack rate after household exposure for a subset of 259 persons who received early lots of vaccine decreased by 77% compared with the expected attack rate for unvaccinated persons (attack rate: 20% and 87%, respectively) (45,64 ; Merck and Company, Inc., unpublished data). In these clinical trials, varicella subsequently developed in substantially fewer children who had postvaccination gpELISA titers of ≥5 U varicella than those children who had postvaccination gpELISA titers of <5 U.
Varicella is substantially less severe among vaccinated persons than unvaccinated persons, who usually have fever and several hundred vesicular lesions (87 ). For vaccinees in whom varicella has developed, the median number of skin lesions has been <50 (88,89; Merck and Company, Inc., unpublished data). In addition, most vaccinees have been afebrile, have had fewer vesicular lesions, and have had shorter duration of illness than unvaccinated persons. Illnesses associated with vaccine failure are attenuated and have not increased in severity during the 7-10 years of follow-up study.
The rate of disease transmission from vaccinees in whom varicella develops is low for children but has not been studied in adults. In 10 different trials conducted from 1981 through 1989 involving 2,141 vaccinated children, breakthrough infections occurred in 78 vaccinated children during the 1-8 year follow-up period of active surveillance, resulting in secondary transmission to 11 (12.2%) of their 90 vaccinated siblings (89 ). Illness was mild in both index and secondary case-patients. Transmission to a susceptible mother from a vaccinated child in whom breakthrough disease occurred also has been reported (Merck and Company, Inc., unpublished data).
Varicella virus vaccine provides 70%-90% protection against infection and 95% protection against severe disease for 7-10 years after vaccination. Data are insufficient to evaluate the extent of the protection provided by varicella vaccination against serious complications from varicella (e.g., bacterial infections of skin lesions, pneumonia, and encephalitis) in persons of all ages. However, serious complications are anticipated to be reduced, because data indicate attenuation of common manifestations of disease in vaccinees.
Current data concerning vaccine efficacy and persistence of antibody in vaccinees are based on research that has been conducted when natural VZV infection has been highly prevalent and has not been affected by wide use of the vaccine. Thus, the extent to which the protection provided by vaccination has been increased by boosting from exposure to natural virus and whether longer term immunity may wane as the circulation of natural VZV decreases are unknown.
# Transmission of Vaccine Virus
Available data suggest that healthy children are unlikely to transmit vaccine virus to susceptible contacts, but that risk for transmission from vaccinees who are immunocompromised is higher and may be associated with occurrence of rash following vaccination. Risk for transmission of vaccine virus was assessed in siblings of vaccinated children who received placebo themselves (76 ). During the 8 weeks following vaccination, six (1%) of 439 placebo recipients seroconverted without rash; their vaccinated siblings also had no rash. Among three of the six children who seroconverted, serologic data suggested that the preparations administered to the assigned vaccine and placebo recipients were mistakenly switched. In addition, varicella developed in three other placebo recipients during months of high varicella incidence (i.e., from December through June); one recipient had had an exposure to natural varicella at school. In another study, no evidence of transmission of vaccine virus was found after vaccinating 37 healthy siblings of 30 immunocompromised children (90 ). None of the immunocompromised children had rash or demonstrated evidence of humoral or cell-mediated immune responses.
Higher risk for transmission of vaccine virus has been documented among children who have both rash following vaccination and leukemia. Data from one study indicated that varicella virus vaccine infection occurred in 15 (17%) of 88 exposed, healthy siblings of leukemic vaccine recipients; mild rash developed in 11 siblings (91 ). In one family, tertiary transmission to a second healthy sibling occurred, with rash developing 18 days after rash onset in the secondary case-patient and 33 days after rash onset in the leukemic child. Both healthy siblings had mild rash (i.e., 11 and 40 lesions, respectively), and vaccine virus was isolated from all three case-patients.
These data suggest that healthy, vaccinated persons have a minimal risk for transmitting vaccine virus to their contacts; this risk may be higher in vaccinees in whom a varicella-like rash develops following vaccination. In clinical trials, nonlocalized rash developed in 3.8% of children and 5.5% of adolescents and adults (median: five lesions) after the first injection and 0.9% of adolescents and adults after the second injection.
# Herpes Zoster Following Vaccination
The incidence of herpes zoster after varicella vaccination among otherwise healthy children is approximately 18 per 100,000 person years of follow-up (Merck and Company, Inc., unpublished data). A population-based study indicated that the incidence of herpes zoster after natural varicella infection among healthy children was 77 per 100,000 person years. However, these two rates should be compared cautiously, because the latter rate was based on a larger pediatric population that was monitored for a longer period of time than were the vaccinees (92,93 ). One case of herpes zoster has been reported among adult vaccinees, resulting in an incidence of 12.8 per 100,000 person years. Although unknown, the rate of herpes zoster in unvaccinated adults is expected to be higher than that in adult vaccinees. All of the vaccinees' illnesses were mild and without complications. Wild-type virus was identified in one vaccinated child and one vaccinated adult by using restriction endonuclease analysis in cultures from vesicles, which suggests that some herpes zoster cases in vaccinees may result from antecedent natural varicella infection (Merck and Company, Inc., unpublished data;94 ).
# Vaccine as Postexposure Prophylaxis
No data exist regarding postexposure efficacy of the current varicella virus vaccine. Postexposure prophylaxis of children using previous formulations of varicella virus vaccine has been conducted in two controlled studies. In Japan ( 95) and the United States (79 ), protective efficacy was ≥90% when children were vaccinated within 3 days of exposure.
# Cost Benefit of Vaccine
A recent cost-effectiveness study (96 ) was performed using current estimates of morbidity and mortality (CDC, unpublished data), mathematical modeling of the projected impact of vaccination (97 ), and current direct and indirect costs. Unlike a previous study published in 1985 (98 ), the recent analysis accounted for potential changes in the frequency and severity of varicella-related complications resulting from expected changes in the epidemiology and age distribution of varicella following widespread use of varicella virus vaccine. Additional efficacy data for 1985-1993 were available, and empiric data on medical utilization and costs of work-loss resulting from varicella were used. The results of this study, which were determined using an estimated cost of $35 per dose of vaccine and $5 for vaccine administration, indicated a savings of $5.40 for each dollar spent on routine vaccination of preschool-age children when direct and indirect costs were considered. When only direct medical costs were considered, the benefit-cost ratio was 0.90:1. Benefit-cost ratios were only slightly lower when lower estimates of the short-term and long-term effectiveness of the vaccine were used.
# DISTRIBUTION, HANDLING, AND STORAGE OF VACCINE
To maintain potency, the lyophilized vaccine must be stored frozen at an average temperature of ≤5 F (≤-15 C). Household freezers manufactured since the mid-1980s are designed to maintain temperatures from -4 F (-20 C) to 5 F (-15 C). When tested, VARIVAX ® has remained stable in frost-free refrigerators. Refrigerators with ice compartments that are either not tightly enclosed or enclosed with unsealed, uninsulated doors (e.g., small, dormitory-style refrigerators) may not meet temperature requirements. Regardless of the type of freezer, providers should check the adequacy of their freezer by verifying its temperature before obtaining vaccine.
The diluent should be stored separately either at room temperature or in the refrigerator. The vaccine should be reconstituted according to the directions in the package insert and only with the diluent supplied with the vaccine, which does not contain preservative or other antiviral substances that could inactivate the vaccine virus. Once reconstituted, the vaccine should be used immediately to minimize loss of potency. The vaccine should be discarded if not used within 30 minutes after reconstitution.
# Handling of Vaccine Within a Clinic and for Clinics That do not Have Adequate Facilities to Store Vaccine
When an immunization session is being held at a site distant from the freezer in which the vaccine is stored, the needed number of vaccine vials for the immunization session should be stored in a suitable container (i.e., the original shipping container or a comparable container with a properly fitting lid) with an adequate quantity of dry ice (i.e., a minimum of 6 lbs/box), so that dry ice would remain if any unreconstituted vaccine must be returned to the freezer. Dry ice, when placed in a suitable container, will maintain a temperature of 5 F (-15 C) or colder.
When optimal handling conditions are not feasible because of the location of the freezer storage area or concern for security of the room where vaccines are administered within a clinic, or when vaccine must be transported to a clinic site distant from the freezer-storage area, minimal potency can be maintained if varicella virus vaccine is stored continuously for up to 72 hours at temperatures of 36-46 F (2-8 C). This vaccine should be discarded if not used within 72 hours of placing it into storage.*
# Minimizing Wastage of Vaccine
Vaccine wastage can be minimized by accurately determining the number of doses needed for clinics that do not have adequate freezer-storage facilities. To ensure maximal vaccine potency, smaller shipments of vaccine should be ordered more frequently-preferably at least once every 3 months. Vaccine lots with a longer expiration period (i.e., >12 months to expiration) should be selected for use in clinics that do not have adequate facilities to store vaccine.
# Transfer of Vaccine Between Clinic Sites
When transferring vaccine between clinic sites is required (e.g., when supply must be adjusted), the vaccine should be packed in the manufacturer's shipping container or a container with comparable insulating qualities using appropriate quantities of dry ice (e.g., a minimum of 6 lbs/box). Residual dry ice should be available at the receiving site. If dry ice is not available, the vaccine should be discarded unless a temperature recorder has been included in the transport box; if the temperature has been ≤36-46 F (≤2-8 C) for up to 72 hours, the vaccine can be used within 72 hours of removal from the freezer-storage area.
# RECOMMENDATIONS FOR THE USE OF VARICELLA VIRUS VACCINE
# Persons <13 Years of Age
Varicella virus vaccine has been approved for use among healthy children 12 months-12 years of age. Children in this age group should receive one 0.5-mL dose of vaccine subcutaneously.
Children who have a reliable history of varicella are considered immune, and those who do not have such a history or who have an uncertain history of varicella are considered susceptible. Serologic testing of children before vaccination is not warranted because a) most children 12 months-12 years of age who do not have a clinical history of varicella are susceptible and b) the vaccine is well tolerated in seropositive persons.
12-18 Months of Age. All children should be routinely vaccinated at 12-18 months of age. Varicella virus vaccine may be administered to all children at this ageregardless of a history of varicella; however, vaccination is not necessary for children who have reliable histories of varicella. Varicella virus vaccine preferably should be administered routinely to children at the same time as measles-mumps-rubella (MMR) vaccine. Varicella virus vaccine is safe and effective in healthy children ≥12 months of age when administered at the same time as MMR vaccine at separate sites and with separate syringes or when administered separately ≥30 days apart. The number and types of adverse events in children who have received VARIVAX ® and MMR concurrently have not differed from those in children who have been administered the vaccines at different visits (Merck and Company, Inc., unpublished data). Data concerning the effect of simultaneous administration of VARIVAX ® with various *For information regarding use of vaccine inadvertently exposed to conditions not addressed in these guidelines, inquiries should be directed to Merck and Company, Inc. (telephone: (800)-9-VARIVAX).
combinations of MMR-, diphtheria and tetanus toxoids and pertussis (DTP)-, and Haemophilus influenzae type b (Hib)-containing vaccines have not yet been published. However, data regarding simultaneous administration of an investigational quadrivalent vaccine containing varicella (MMRII V™) with diphtheria and tetanus toxoids and acellular pertussis (DTaP) and Hib vaccines suggest that no notable interactions exist between varicella and any other vaccines that are routinely administered to young children (e.g., measles, mumps, rubella, diphtheria, tetanus, pertussis, and Haemophilus influenzae type b vaccines). Furthermore, the simultaneous administration of most widely used live, attenuated and inactivated vaccines has not resulted in impaired antibody response or an increased rate of adverse events. Therefore, varicella virus vaccine may be administered simultaneously with all of the vaccines recommended for children 12-18 months of age. Simultaneous administration is particularly important when health-care providers anticipate that, because of certain factors (e.g., previously missed vaccination opportunities), a child may not return for subsequent vaccination.
19 Months-12 Years of Age. Varicella vaccine is recommended for all susceptible children by their 13th birthday. After 12 years of age, natural varicella is more severe and complications are more frequent. Recently, ACIP recommended establishing a routine immunization visit at 11-12 years of age to review immunization status and to administer necessary vaccinations (99 ). Although vaccine may be administered at any time after 18 months of age, varicella virus vaccine should be administered to susceptible children during this routine visit.
# Persons ≥13 Years of Age
Varicella vaccine is approved for use among healthy adolescents and adults. Because natural VZV infection can be severe in older adolescents and adults, varicella immunity is desirable in these age groups. Persons ≥13 years of age should be administered two 0.5-mL doses of vaccine, subcutaneously, 4-8 weeks apart. If >8 weeks elapse following the first dose, the second dose can be administered without restarting the schedule.
Persons ≥13 years of age who have reliable histories of varicella are considered immune. Those who do not have such histories are considered susceptible and can be tested to determine immune status or can be vaccinated without testing. Because 71%-93% of adults who do not have a reliable history of varicella are actually immune (1,26,42,46,47 ), serologic testing before vaccination is likely to be cost effective for both adults and adolescents (100 ).
Adolescents and adults should be assessed for varicella immune status, and those who are susceptible should be vaccinated. Priority should be given to vaccination of susceptible adolescents and adults who are at high risk for exposure and for transmitting disease; specific assessment efforts are targeted to these persons (Box 1).
# Health-Care Workers*
All susceptible health-care workers should ensure that they are immune to varicella. In health-care institutions, serologic screening of personnel who have a negative or uncertain history of varicella is likely to be cost effective.
*The recommendations for health-care workers were prepared jointly by ACIP and the Hospital Infection Control Practices Advisory Committee.
Routine testing for varicella immunity after two doses of vaccine is not necessary for the management of vaccinated health-care workers who may be exposed to varicella, because 99% of persons are seropositive after the second dose. Seroconversion, however, does not always result in full protection against disease. Testing vaccinees for seropositivity immediately after exposure to VZV is a potentially effective strategy for identifying persons who remain at risk for varicella. Prompt serologic results may be obtained using the LA test. Varicella is unlikely to develop in persons who have detectable antibody; persons who do not have such antibody can be retested in 5-6 days to determine if an anamnestic response is present, in which case development of disease is unlikely. Persons who remain susceptible may be furloughed. Alternatively, persons can be monitored daily to determine clinical status and then furloughed at the onset of manifestations of varicella. Institutional guidelines are needed for the management of exposed vaccinees who do not have detectable antibody and for persons who develop clinical varicella.
More information is needed concerning the risk for transmission of vaccine virus from vaccinees in whom varicella-like rash develops following vaccination. On the basis of available data, the risk appears to be minimal, and the benefits of vaccinating susceptible health-care workers outweigh this potential risk. As a safeguard, institutions may wish to consider precautions for personnel in whom rash develops not pregnant-but who may become pregnant in the future-will reduce the risk for VZV transmission to the fetus. Varicella immunity may be ascertained at any routine health-care visit or in any setting in which vaccination history may be reviewed (e.g., upon college entry). Women should be asked if they are pregnant and advised to avoid pregnancy for 1 month following each dose of vaccine. d) International travelers. Vaccination should be considered for international travelers who do not have evidence of immunity to VZV (e.g., serologic tests), especially if the traveler expects to have close personal contact with local populations, because varicella is endemic in most countries.
- Vaccination of other susceptible adolescents and adults is desirable and may be offered during routine health-care visits.
# BOX 1. Vaccination of persons ≥13 years of age
following vaccination and for other vaccinated personnel who will have contact with susceptible persons at high risk for serious complications. Vaccination should be considered for unvaccinated health-care workers who are exposed to varicella and whose immunity is not documented. However, because the protective effects of postexposure vaccination are unknown, persons vaccinated after an exposure should be managed in the manner recommended for unvaccinated persons.
# Household Contacts of Immunocompromised Persons
Immunocompromised persons are at high risk for serious varicella infections. Disseminated disease occurs in approximately 30% of such persons who have primary infection. Vaccination of household contacts provides protection for immunocompromised persons by decreasing the likelihood that wild-type varicella virus will be introduced into the household. Vaccination of household contacts of immunocompromised persons theoretically may pose a minimal risk of transmission of vaccine virus to immunocompromised persons, although in one study, no evidence of transmission of vaccine virus was found after vaccinating 37 healthy siblings of 30 children with malignancy. Available data indicate that disease caused by vaccine virus in immunocompromised persons is milder than wild-type disease and can be treated with acyclovir. More information is needed concerning the risk for transmission of the vaccine virus from both vaccinees who have and who do not have varicella-like rash following vaccination. On the basis of available data, the benefits of vaccinating susceptible household contacts of immunocompromised persons outweigh the potential risk for transmission of vaccine virus to immunocompromised contacts.
# VACCINE-ASSOCIATED ADVERSE EVENTS
Varicella virus vaccine has been well tolerated when administered to >11,000 healthy children, adolescents, and adults during clinical trials. Inadvertent vaccination of persons immune to varicella has not resulted in an increase in adverse events. In a double-blind, placebo-controlled study of 914 healthy, susceptible children and adolescents (76 ), pain and redness at the injection site were the only adverse events that occurred significantly more often (p<0.05) in vaccine recipients than in placebo recipients.
# Persons 12 Months-12 Years of Age
In uncontrolled clinical trials of approximately 8,900 healthy children (Merck and Company, Inc., package insert) who were administered one dose of vaccine and then monitored for up to 42 days, 14.7% developed fever (i.e., oral temperature ≥102 F ); these febrile episodes occurred throughout the 42-day period and were usually associated with intercurrent illness. A total of 19.3% of vaccine recipients had complaints regarding the injection site (e.g., pain/soreness, swelling, erythema, rash, pruritus, hematoma, induration, and stiffness), 3.4% had a mild, varicella-like rash at the injection site consisting of a median number of two lesions and occurring at a peak of 8-19 days postvaccination, and 3.8% had a nonlocalized, varicella-like rash consisting of a median number of five lesions and occurring at a peak of 5-26 days postvaccination. Febrile seizures following vaccination occurred in <0.1% of children; a causal relationship has not been established.
# Persons ≥13 Years of Age
In uncontrolled trials of persons ≥13 years of age, approximately 1,600 vaccinees who received one dose and 955 who received two doses of varicella vaccine were monitored for 42 days for adverse events (Merck and Company, Inc., package insert). After the first and second doses, 10.2% and 9.5% of vaccinees, respectively, developed fever (i.e., oral temperature ≥100 F ); these febrile episodes occurred throughout the 42-day period and were usually associated with intercurrent illness. After one and two doses, 24.4% and 32.5% of vaccinees, respectively, had complaints regarding the injection site (e.g., soreness, swelling, erythema, rash, pruritus, hematoma, pyrexia, induration, and numbness); a varicella-like rash at the injection site consisting of a median number of two lesions and occurring at a peak of 6-20 days and 0-6 days postvaccination, respectively, developed in 3% and 1% of vaccinees, respectively; and a nonlocalized rash consisting of a median number of five lesions developed in 5.5% and 0.9% of vaccinees, respectively, and occurred at a peak of 7-21 days and 0-23 days postvaccination, respectively.
# Postlicensure Adverse Vaccine Events
During the first 12 months following vaccine licensure, more than 2.3 million doses of vaccine were distributed in the United States. The Vaccine Adverse Events Reporting System (VAERS) and the vaccine manufacturer have received a limited number of reports of serious medical events occurring within 6 weeks after varicella virus vaccination, including encephalitis (n=4), ataxia (n=7), and erythema multiforme (n=10). Three cases of anaphylaxis have occurred within 10 minutes of vaccination. A causal relationship between the vaccine and these events has not been determined. Potential delayed or underreporting of events to VAERS may have occurred. Physicians and health-care providers are encouraged to report any suspected adverse events that occur after varicella virus vaccination (see Reporting of Adverse Events). Postmarketing surveillance for adverse events will be ongoing.
# Reporting of Adverse Events
The National Vaccine Injury Act of 1986 (101 ) requires physicians and other healthcare providers who administer vaccines to maintain permanent immunization records and to report occurrences of adverse events for selected vaccines. Although the Act currently does not apply to varicella virus vaccine, the same recording and reporting requirements should be followed. Serious adverse events (i.e., all events requiring medical attention), regardless of whether they are suspected to have been caused by varicella virus vaccine, should be reported to VAERS. VAERS forms and instructions are available in the FDA Drug Bulletin and the Physicians' Desk Reference or by calling the 24-hour VAERS information recording (telephone: 822-7967).
# CONTRAINDICATIONS AND PRECAUTIONS
# Allergy to Vaccine Components
The administration of live varicella virus vaccine rarely results in hypersensitivity. The information in the package insert should be carefully reviewed before vaccine is administered; vaccination is contraindicated for persons who have a history of anaphylactic reaction to any component of the vaccine, including gelatin. Varicella virus vaccine does not contain preservatives or egg protein-substances that have caused hypersensitive reactions to other vaccines. Varicella virus vaccine should not be administered to persons who have a history of anaphylactic reaction to neomycin. Neomycin allergy is usually manifested as a contact dermatitis, which is a delayedtype immune response rather than anaphylaxis. For persons who experience such a response, the adverse reaction, if any, would be an erythematous, pruritic nodule or papule present 48-96 hours after vaccination. A history of contact dermatitis to neomycin is not a contraindication to receiving varicella virus vaccine.
# Illness
Vaccination of persons who have severe illness should be postponed until recovery. The decision to delay vaccination depends on the severity of symptoms and on the etiology of the disease. Vaccine can be administered to susceptible children who have mild illnesses with or without low-grade fever (e.g., diarrhea or upperrespiratory infection) (102 ). Studies suggest that failure to vaccinate children with minor illnesses can impede vaccination efforts (103 ).
Although no data exist regarding whether either varicella or live varicella virus vaccine exacerbates tuberculosis, vaccination is not recommended for persons who have untreated, active tuberculosis. Tuberculin skin testing, however, is not a prerequisite for varicella vaccination.
# Altered Immunity
Varicella virus vaccine is not licensed for use in persons who have any malignant condition, including blood dyscrasias, leukemia, lymphomas of any type, or other malignant neoplasms affecting the bone marrow or lymphatic systems. However, vaccine is available to any physician free of charge from the manufacturer- through a research protocol (104 ) for use in patients who have acute lymphoblastic leukemia (ALL) who a) are 12 months-17 years of age, b) have disease that has been in remission for at least 12 continuous months, c) have a negative history of varicella disease, d) have a peripheral blood-lymphocyte count of >700 cells/mm 3 , and e) have a platelet count of >100,000 cells/mm 3 within 24 hours of vaccination. The vaccine is well tolerated, immunogenic, and protective in children who meet these criteria (105)(106)(107)(108)(109)(110). The most common reaction to the vaccine in patients who have ALL is a mild to moderate varicella-like rash (i.e., two to 200 lesions), which occurs in approximately 5% of children who have completed their chemotherapy before vaccination and 40% of vaccinees on maintenance chemotherapy (106 ).
Varicella virus vaccine should not be administered to persons who have primary or acquired immunodeficiency, including immunosuppression associated with acquired immunodeficiency syndrome (AIDS) or other clinical manifestations of human immunodeficiency virus (HIV) infections, cellular immunodeficiencies, hypogammaglobulinemia, and dysgammaglobulinemia. The use of varicella virus vaccine in persons who are infected with HIV has not been studied; therefore, vaccination of these persons is not recommended, although routine screening for HIV before *The physician must provide information requested in the protocol, and the protocol and consent form for the study must be approved by the institution's Investigational Review Board. vaccination also is not recommended. The use of varicella virus vaccine in HIVinfected children is being investigated. If inadvertent vaccination of HIV-infected persons results in clinical disease, the use of acyclovir may modify the severity of disease.
Varicella virus vaccine should not be administered to persons who have a family history of congenital or hereditary immunodeficiency in first-degree relatives (e.g., parents and siblings) unless the immune competence of the potential vaccine recipient has been clinically substantiated or verified by a laboratory.
Varicella virus vaccine should not be administered to persons receiving immunosuppressive therapy-except children who have ALL in remission, as previously described. Such persons are more susceptible to infections than healthy persons. Administration of live, attenuated varicella virus vaccine can result in a more extensive vaccine-associated rash or disseminated disease in persons receiving immunosuppressive doses of corticosteroids (111 ). This contraindication does not apply to persons who are receiving corticosteroid-replacement therapy.
# Children Who Have Conditions That Require Steroid Therapy
No data have been published concerning whether susceptible children receiving only inhaled doses of steroids can be vaccinated safely. However, most experts concur, on the basis of clinical experience, that vaccination of these children is safe. Susceptible children who are receiving systemic steroids for certain conditions (e.g., asthma) and who are not otherwise immunocompromised can be vaccinated if they are receiving <2 mg/kg of body weight or a total of 20 mg/day of prednisone or its equivalent. Antibody status should be assessed 6 weeks postvaccination, and children who have not seroconverted should be revaccinated. Some experts suggest withholding steroids for 2-3 weeks following vaccination when possible. Data from one study conducted in Japan indicated that children taking steroids for nephrosis were vaccinated safely when the steroids were suspended for 1-2 weeks before vaccination, although no serious reactions occurred among children vaccinated when steroid therapy was not suspended (112 ). Children who are receiving high doses of systemic steroids (i.e., ≥2 mg/kg prednisone) for ≥2 weeks may be vaccinated after steroid therapy has been discontinued for at least 3 months in accordance with the general recommendations for the use of live-virus vaccines (113 ); however, withholding steroids for at least 1 month before varicella vaccination is probably sufficient.
# Exposure of Immunocompromised Persons to Vaccinees
Healthy persons in whom varicella-like rash develops following vaccination appear to have a minimal risk for transmission of vaccine virus to their close contacts (e.g., family members). Seroconversion has been documented in healthy siblings of healthy vaccinees in whom rash did not develop, although such an occurrence is rare (76 ). Vaccinees in whom vaccine-related rash develops, particularly health-care workers and household contacts of immunocompromised persons, should avoid contact with susceptible persons who are at high risk for severe complications. If a susceptible, immunocompromised person is inadvertently exposed to a person who has a vaccine-related rash, VZIG need not be administered because disease associated with this type of transmission is expected to be mild.
# Recent Administration of Blood, Plasma, or Immune Globulin
Although passively acquired antibody is known to interfere with response to measles and rubella vaccines (114 ), the effect of the administration of immune globulin (IG) on the response to varicella virus vaccine is unknown. The duration of interference with the response to measles vaccination depends on the dosage and ranges from 3-11 months. Because of the potential inhibition of the response to varicella vaccination by passively transferred antibodies, varicella virus vaccine should not be administered for at least 5 months after administration of blood (except washed red blood cells), plasma, IG, or VZIG (113 ). In addition, IG and VZIG should not be administered for 3 weeks after vaccination unless the benefits exceed those of vaccination. In such cases, the vaccinee should either be revaccinated 5 months later or tested for immunity 6 months later and then revaccinated if seronegative.
# Use of Salicylates
No adverse events associated with the use of salicylates after varicella vaccination have been reported. However, the vaccine manufacturer recommends that vaccine recipients avoid using salicylates for 6 weeks after receiving varicella virus vaccine because of the association between aspirin use and Reye syndrome following varicella. Vaccination with subsequent close monitoring should be considered for children who have rheumatoid arthritis or other conditions requiring theraputic aspirin because the risk for serious complications associated with aspirin is likely to be greater in children in whom natural varicella disease develops than in children who receive the vaccine containing attenuated VZV. No association has been documented between Reye syndrome and analgesics or antipyretics that do not contain salicylic acid.
# Pregnancy
The effects of the varicella virus vaccine on the fetus are unknown; therefore, pregnant women should not be vaccinated. Nonpregnant women who are vaccinated should avoid becoming pregnant for 1 month following each injection. For susceptible persons, having a pregnant household member is not a contraindication to vaccination.
If a pregnant woman is vaccinated or becomes pregnant within 1 month of vaccination, she should be counseled about potential effects on the fetus. Wild-type varicella poses only a very small risk to the fetus (see Prenatal and Perinatal Exposure). Because the virulence of the attenuated virus used in the vaccine is less than that of the wild-type virus, the risk to the fetus, if any, should be even lower. In most circumstances, the decision to terminate a pregnancy should not be based on whether vaccine was administered during pregnancy. The manufacturer, in collaboration with CDC, has established the VARIVAX ® Pregnancy Registry to monitor the maternal-fetal outcomes of pregnant women who are inadvertently administered varicella virus vaccine 3 months before or at any time during pregnancy (telephone: 986-8999) (115 ).
# Nursing Mothers
Whether attenuated vaccine VZV is excreted in human milk and, if so, whether the infant could be infected are not known. Most live vaccines have not been demonstrated to be secreted in breast milk. Attenuated rubella vaccine virus has been detected in breast milk but has produced only asymptomatic infection in the nursing infant. Therefore, varicella virus vaccine may be considered for a nursing mother.
# USE OF VZIG FOR POSTEXPOSURE PROPHYLAXIS
Studies conducted in 1969 indicated that zoster immune globulin (ZIG) (prepared from patients recovering from herpes zoster) prevented clinical varicella in susceptible, healthy children if administered within 72 hours of exposure (116 ). ZIG also lowered attack rates among immunocompromised persons if administered no later than 96 hours after exposure (116 ).
VZIG (prepared from plasma obtained from healthy, volunteer blood donors who are identified by routine screening to have high antibody titers to VZV) became available in 1978. Both serologic and clinical evaluations have demonstrated that the product is equivalent to ZIG in preventing or modifying clinical illness in susceptible, immunocompromised persons who are exposed to varicella. VZIG is a sterile, 10%-18% solution of the globulin fraction of human plasma, primarily immunoglobulin G (IgG) in 0.3 M glycine as a stabilizer and 1:10,000 thimerosal as a preservative. VZIG is prepared by using Cohn cold ethanol precipitation, which eliminates hepatitis B virus, HIV, and other known infectious agents from the product. VZIG prepared using an additional viral-inactivation step (the solvent detergent treatment) has recently become available.
# Supply
VZIG is produced by the United States Biologics Laboratories (Massachusetts) and is distributed by American Red Cross regional distribution centers and service areas (Appendix). In Massachusetts, VZIG is distributed by the Massachusetts Department of Public Health.
# Administration
VZIG provides maximum benefit when administered as soon as possible after the presumed exposure, but it may be effective if administered as late as 96 hours after exposure. The effectiveness of VZIG when administered 96 hours after initial exposure has not been evaluated. VZIG is not recommended for vaccinated persons who were previously seropositive and found to be seronegative following exposure because such persons would be expected to have a mild case; no further benefit would be gained by administering VZIG.
VZIG has not been proven to be useful in treating clinical varicella or herpes zoster or in preventing disseminated zoster and is not recommended for such use. The duration of protection that is provided after administration of VZIG is unknown, but protection should last at least one half-life of the IG (i.e., approximately 3 weeks). Susceptible persons at high risk for whom varicella vaccination is contraindicated and who are again exposed ≥3 weeks after a dose of VZIG should receive another full dose of VZIG.
# Dosage
VZIG is supplied in two different dosages-the 125-U vial and the 625-U vial. The recommended dose is 125 U/10 kg (22 lbs) of body weight, up to a maximum of 625 U. The minimum dose is 125 U; fractional doses are not recommended. VZIG administration has not been evaluated as a prophylactic measure in healthy or immunocompromised adults. Therefore, the appropriate dose for prophylaxis in adults cannot be calculated. However, 625 U should be sufficient to modify or prevent infection in healthy adults. Higher doses may be necessary for immunocompromised adults.
VZIG should be administered intramuscularly as directed by the manufacturer. VZIG should never be administered intravenously.
# Indications for the Use of VZIG
The decision to administer VZIG to a person exposed to varicella should be based on a) whether the patient is susceptible (either by having a negative history of varicella or by lacking documentation of vaccination), b) whether the exposure is likely to result in infection, and c) whether the patient is at greater risk for complications than the general population. VZIG is costly (i.e., approximately $90 per 125-U vial or $400 for persons >40 kg body weight) and only provides temporary protection. The long-term effects of VZIG on immunity and on the occurrence of herpes zoster are unknown.
For immunocompromised persons, an accurate history of varicella should be obtained before determining immune status and whether to administer VZIG. Immunocompromised persons who do not have histories of disease, but who have low levels of antibody detected by the most sensitive assays, have contracted varicella. Presumably, the low levels of antibody in most of these patients were passively acquired from recent transfusions of blood, blood derivatives, or blood products containing antibody.
Both healthy and immunocompromised children and adults who have positive histories of varicella (except for bone-marrow transplant recipients) can be considered immune (see Recommendations for the Use of Varicella Virus Vaccine). However, varicella may develop in some infants after exposure despite the presence of detectable antibody, although in most circumstances such illness is less severe than the illness occurring in infants who do not have detectable antibody. Therefore, sensitive assays may not be useful in assessing whether clinical disease will develop in neonates or young infants exposed to varicella.
The association between positive histories of varicella in bone-marrow donors and susceptibility to varicella in recipients following transplants has not been adequately studied. Thus, persons who receive bone-marrow transplants should be considered susceptible-regardless of prior history of varicella or varicella vaccination in themselves or in their donors. Bone-marrow recipients in whom varicella or herpes zoster develops following transplantation should subsequently be considered immune.
# Types of Exposure
Several types of exposure can place susceptible persons at risk for varicella. Direct contact exposure is defined as >1 hour of direct contact with an infectious person while indoors; substantial exposure for hospital contacts consists of sharing the same hospital room with an infectious patient or prolonged, direct, face-to-face contact with an infectious person (e.g., health-care workers). Brief contacts with an infectious person (e.g., contact with x-ray technicians or housekeeping personnel) are less likely to result in VZV transmission than are more prolonged contacts.
Persons with continuous exposure to household members who have varicella are at greatest risk for infection. Varicella develops in approximately 90% of susceptible household contacts. Following household exposure, attack rates among immunocompromised children administered VZIG are 33%-50%. Data are not available for immunocompromised, susceptible persons who were not administered VZIG. The risk for varicella following close contact (e.g., contact with playmates) or hospital exposure is approximately 20% of the risk occurring from household exposure.
The attack rate in healthy neonates who are exposed in utero within 5 days of delivery and administered VZIG after birth is 30%-40%, which is not substantially different from rates reported for neonates who are similarly exposed but not treated with VZIG. However, the occurrence of complications and fatal outcomes is substantially lower for neonates who are treated with VZIG than for those who are not.
# RECOMMENDATIONS FOR THE USE OF VZIG
# Persons <13 Years of Age
Immunocompromised children. VZIG primarily is used for passive immunization of susceptible, immunocompromised children after substantial exposure to varicella or herpes zoster-including children who a) have primary and acquired immunedeficiency disorders, b) have neoplastic diseases, and c) are receiving immunosuppressive treatment.
Data are limited regarding whether routine therapy with intravenous IG yields the persistence of a sufficient amount of passively acquired VZV antibody to protect susceptible, immunocompromised persons who become exposed to VZV. Data from one study indicated that three of 17 HIV-infected children in whom varicella developed were receiving regular intravenous IG and had detectable antibody against varicella (117 ). One of the three children had been treated with VZIG after two previous exposures to varicella that did not result in disease but was not administered VZIG after an unrecognized exposure, which resulted in varicella. To ensure protection against severe disease, immunocompromised persons receiving intravenous IG should be administered VZIG if exposed to wild-type VZV.
Neonates whose mothers become infected with varicella shortly before delivery. VZIG is indicated for neonates whose mothers have signs and symptoms of varicella within 5 days before and 2 days after delivery. VZIG is probably not necessary for neonates whose mothers have signs and symptoms of varicella >5 days before delivery, because those infants should be protected from severe varicella by transplacentally acquired maternal antibody. No evidence exists suggesting that infants born to mothers in whom varicella develops >48 hours after delivery are at increased risk for serious complications (e.g., pneumonia or death).
Postnatal exposure of neonates. Transmission of varicella in the hospital nursery is rare because most neonates are protected by maternal antibody. Premature infants who have substantial postnatal exposure should be evaluated on an individual basis. The risk for complications of postnatally acquired varicella in premature infants is unknown. Because the immune systems of premature infants may be compromised, administration of VZIG to those who are exposed and born to susceptible mothers may be prudent. These infants should be considered at risk for as long as they are hospitalized. Premature infants who are <28 weeks' gestation or who weigh ≤1,000 g at birth who are exposed to VZV should receive VZIG, regardless of maternal history, because such infants may not have acquired maternal antibody. Most premature infants of ≥28 weeks' gestation born to immune mothers have enough acquired maternal antibody to protect them from severe disease and complications.
Although infants are at higher risk for serious and fatal complications than are older children, the risk for healthy, full-term infants who develop varicella following postnatal exposure is substantially less than for infants whose mothers were infected 5 days before to 2 days after delivery. VZIG is not recommended for healthy, full-term infants who are exposed postnatally, even if their mothers have no history of varicella infection.
# Persons ≥13 Years of Age
Rates of complications and death for immunocompromised adolescents and adults in whom varicella develops are higher than those for healthy adolescents and adults. To prevent complications, immunocompromised persons who are considered susceptible and who have had substantial exposure to varicella should receive VZIG. The rationale for the use of VZIG among adolescent and adult patients routinely treated with intravenous IG (IVIG) is equivalent to that for the use of VZIG among immunocompromised children (see Immunocompromised Children).
Varicella is usually more severe in otherwise healthy adolescents or adults than in healthy children. The decision to administer VZIG to susceptible, healthy adolescents and adults should be made on an individual basis. The objective of using VZIG among healthy adolescents and adults is to modify, rather than to prevent, illness with the hope of inducing lifetime immunity. When deciding whether to administer VZIG, clinicians should consider the patients' health status, the type of exposure, and the likelihood of previous varicella infection. Adults who were older siblings in large families or whose children have had varicella likely are immune. If, after careful evaluation, a healthy, unvaccinated adolescent or adult who has had substantial exposure is determined as being susceptible, VZIG can be considered. If varicella is prevented through the use of VZIG, vaccination should be offered later. As the use of varicella virus vaccine becomes widespread, the demand for VZIG should decrease.
Pregnant women. Pregnant women should be evaluated in the same manner as other adults; however, because such women are at higher risk for severe varicella and complications (8,13,118 ), VZIG should be strongly considered for susceptible pregnant women who have been exposed. Administration of VZIG to susceptible, pregnant women has not been found to prevent viremia, fetal infection, congenital varicella syndrome, or neonatal varicella. Thus, the primary indication for VZIG in pregnant women is to prevent complications of varicella in the mother, rather than to protect the fetus. VZIG may extend the incubation period of the virus from 10-21 days to ≥28 days. Neonates born to mothers who have signs and symptoms of varicella within 5 days preceding or 2 days after delivery should receive VZIG-regardless of whether the mother received VZIG.
Hospital personnel. Varicella virus vaccine is recommended for all susceptible hospital personnel; widespread use of the vaccine should limit the need for VZIG in this setting. If exposed, hospital personnel who have negative or uncertain histories of varicella and no history of vaccination should be evaluated in the same manner as other adults. In addition, types of exposure and histories of prior exposure to patients with varicella should be considered before administration of VZIG. Serologic testing also may help in assessing whether to administer VZIG and in determining whether work restrictions are necessary during the incubation period. In general, the same control measures apply-regardless of whether susceptible personnel or patients receive VZIG. Because VZIG can prolong the incubation period of the virus, the period of removal from direct patient contact should be extended at least 1 week.
# VZIG-ASSOCIATED ADVERSE EVENTS AND PRECAUTIONS
The most frequent adverse reaction following VZIG administration is local discomfort at the injection site. Pain, redness, and swelling occur at the injection site in approximately 1% of persons. Less frequent adverse events include gastrointestinal symptoms, malaise, headache, rash, and respiratory symptoms, which occur in approximately 0.2% of recipients. Severe events, such as angioneurotic edema and anaphylactic shock, are rare (i.e., occurring in approximately <0.1% of recipients).
VZIG may be indicated for patients who have severe thrombocytopenia or any other coagulation disorder that would ordinarily be a contraindication to intramuscular injections. In this circumstance, the expected benefits of administering this biologic usually outweigh the risks.
# FUTURE CONCERNS
As the use of varicella virus vaccine increases, the epidemiologic features of the disease are expected to change. The circulation of wild-type VZV is not currently affected by the use of the vaccine. Under present conditions, antibody to varicella has been demonstrated to persist for 6-10 years following vaccination in children; however, the extent to which longer-term immunity may wane is unknown. The importance of immunologic boosting following exogenous reexposure to VZV to the long-term persistence of both humoral and cell-mediated immunity to varicella is unknown. The significance of the loss of natural boosting in relation to the incidence of herpes zoster in persons who were vaccinated or exposed to wild-type virus is also unknown. Increased antibody levels have been observed in vaccinees following exposure to natural varicella; however, opportunities for immunologic boosting will be greatly reduced with widespread use of the vaccine. Revaccination 4-6 years after initial vaccination also has resulted in a boost in antibody levels. In addition, the changes in epidemiology of varicella resulting from the widespread use of vaccine in younger children are expected to decrease the circulation of wild-type virus and may establish a population of older children who were neither vaccinated nor exposed to wild-type virus, eventually resulting in a population of adults who are susceptible to varicella. School requirements for varicella immunization are possible mechanisms to ultimately prevent an increase in the population of susceptible adults. To foster more rapid control of varicella and achieve high immunity levels, state legislatures may consider including varicella vaccination in their requirements for entry into school and Head Start or day care programs. Before instituting these or other such requirements, the distribution of and access to varicella virus vaccine should be determined as adequate to accomplish universal vaccination of those children subjected to the requirements.
The need for any changes in vaccine use will be determined by both postmarketing surveillance (conducted by the manufacturer of the vaccine) and ongoing surveillance (conducted by CDC). Presently, only 4%-5% of expected cases of varicella are reported annually to NNDSS. Enhanced surveillance, focused on improvement in the proportion of cases reported and the type of information obtained (including vaccination status), is needed to monitor the impact of vaccination on the incidence of varicella, the age distribution and other demographic features of infected persons, and the associated morbidity and mortality. Several active-surveillance sites have been established to provide this information until the widespread use of the vaccine reduces incidence to a manageable level and varicella becomes a nationally reportable disease.
# Summary of Recommendations for Varicella Vaccination PERSONS <13 YEARS OF AGE
- Persons of this age group should receive one 0.5-mL dose of vaccine subcutaneously.
- Children who have not been vaccinated previously and who lack a reliable history of varicella infection are considered susceptible.
# 12-18 Months of Age
- All children should be routinely vaccinated at 12-18 months of age. Varicella virus vaccine may be administered to all children at this age regardless of prior history of varicella; however, vaccination is not necessary for children who have reliable histories of varicella.
19 Months-12 Years of Age - Varicella vaccine is recommended for immunization of all susceptible children by the 13th birthday.
- Varicella virus vaccine should be administered to susceptible children during the routine immunization visit at 11-12 years of age but may be administered at any time during childhood.
# PERSONS ≥13 YEARS OF AGE
- Persons in this age group should be administered two 0.5-mL doses of vaccine, subcutaneously, 4-8 weeks apart.
- Vaccination is recommended for susceptible persons who have close contact with persons at high risk for serious complications (e.g., health-care workers and family contacts of immunocompromised persons).
- Vaccination should be considered for susceptible persons in the following groups who are at high risk for exposure: a) Persons who live or work in environments in which transmission of VZV is likely (e.g., teachers of young children, day-care employees, and residents and staff in institutional settings). b) Persons who live or work in environments in which varicella transmission can occur (e.g., college students, inmates and staff of correctional institutions, and military personnel). c) Nonpregnant women of childbearing age. Vaccination of women who are not pregnant-but who may become pregnant in the future-will reduce the risk for VZV transmission to the fetus. Varicella immunity may be ascertained at any routine health-care visit or in any setting in which vaccination history may be reviewed (e.g., upon college entry). Women should be asked if they are pregnant and advised to avoid pregnancy for 1 month following each dose of vaccine. | These recommendations represent the first statement by the Advisory Committee on Immunization Practices (ACIP) on the use of live, attenuated varicella virus vaccine-VARIVAX ® -manufactured by Merck and Company, Inc. and licensed in March 1995 for use in healthy persons ≥12 months of age. In addition to presenting information regarding vaccine, this statement updates previous recommendations concerning the use of varicella zoster immune globulin (VZIG) as prophylaxis against varicella ( MMWR 1984;33:84-90,95-100).# INTRODUCTION
Varicella (i.e., chickenpox) is a highly contagious disease caused by varicella zoster virus (VZV). Secondary attack rates for this virus may reach 90% for susceptible household contacts. VZV causes a systemic infection that usually results in lifetime immunity. In otherwise healthy persons, clinical illness after reexposure is rare; such illness is more likely to occur among immunocompromised persons. However, as with other viral diseases, reexposure to wild-type varicella often leads to reinfection that boosts antibody titers without causing clinical illness or detectable viremia. VZV remains dormant in sensory-nerve ganglia and may be reactivated at a later time causing herpes zoster (i.e., shingles)-a painful vesicular rash usually appearing in a dermatomal distribution of one or two sensory-nerve roots.
Among children, varicella is usually a self-limited disease that lasts 4-5 days and is characterized by fever, malaise, and a generalized vesicular rash typically consisting of 250-500 lesions. Adolescents, adults, and immunocompromised persons usually have more severe disease and are at higher risk for complications. Primary subclinical infection with VZV is rare for persons of all ages.
# EPIDEMIOLOGY OF VARICELLA
# General
VZV is transmitted from person to person by a) direct contact, droplet, or aerosol from vesicular fluid of skin lesions or b) secretions from the respiratory tract. The virus enters the host through the upper-respiratory tract.
The average incubation period for varicella is 14-16 days; however, this period can range from 10 to 21 days. The period of contagiousness of infected persons is estimated to begin 1-2 days before the onset of rash and end when all lesions are crusted, which is usually 4-5 days after onset of rash. Persons who have progressive varicella may be contagious longer, presumably because their immune response is depressed, which allows viral replication to persist.
Because varicella develops in nearly all persons who live in the United States, the incidence is estimated to approximate the birth cohort. Data from the National Health Interview Survey (NHIS) for the period 1980-1990 indicated that an estimated 3.7 million cases occur annually (annual incidence rate: 1,498 cases per 100,000 population) (CDC, unpublished data). Varicella is not a nationally notifiable disease, and surveillance data are limited. In 1994, only 28 states, the District of Columbia, and New York City reported cases to CDC's National Notifiable Disease Surveillance System (NNDSS), and reporting within states was incomplete. Reporting efficiency is only an estimated 4%-5%.
Age-specific incidence data were derived from NHIS for the period 1980-1990 (CDC, unpublished data). An estimated 33% of cases occurred in preschool-age children (i.e., children 1-4 years of age [annual incidence rate: 82.8 cases per 1,000 children]), and 44% occurred in school-age children (i.e., children 5-9 years of age [annual incidence rate: 91.1 cases per 1,000 children]) (Figure 1). More than 90% of cases occurred in persons <15 years of age, and few cases occurred in persons >49 years of age. Epidemiologic and serologic studies confirm that >90% of adults are immune to VZV (CDC, unpublished data;1 ). Rates of immunity may be lower for adults who were raised in certain tropical or subtropical areas (e.g., Puerto Rico) (2 ).
Otherwise healthy children and adolescents (i.e., persons <15 years of age) comprise the largest proportion (80%) of an estimated 9,300 annual varicella-related hospitalizations. However, the rate of complications is substantially higher for persons ≥15 years of age and for infants (i.e., children <1 year of age). The most common complications of varicella, which can result in hospitalization, are bacterial infections of skin lesions, pneumonia, dehydration, encephalitis, and hepatitis. Since the association between Reye syndrome and aspirin use was identified, Reye syndrome, which was once considered a common complication resulting from varicella infection, now rarely occurs (3,4 ).
The mean annual number of persons who died in the United States as a result of complications of varicella decreased from 106 persons during 1973-1979 57 persons during 1982-1986. This decrease may have resulted from a) the substantial reduction in cases of Reye syndrome, b) the availability of acyclovir, c) the selective use of varicella zoster immune globulin (VZIG), and d) improvements in supportive care. However, during 1987-1992, the mean annual number of varicella-related deaths increased to 94 persons; the cause of this increase is unknown. The case-fatality rate is lower for children and adolescents 1-14 years of age than for infants (0.75 cases per 100,000 children and 6.23 cases per 100,000 infants). Among persons ≥15 years of age, the risk for death increases with age, from 2.7 per 100,000 among persons 15-19 years of age to 25.2 per 100,000 among persons 30-49 years of age (CDC, unpublished data). Although the varicella-related mortality rate among children generally is low, during periods of increased varicella incidence, the circulation of virulent strains of group A streptococci (which are more likely to cause invasive, fatal infections) can result in an unusually high number of hospitalizations and deaths among children (5,6 ).
to
# Prenatal and Perinatal Exposure
Although prenatal infection is uncommon because most women of childbearing age are immune to VZV (7 ), varicella in pregnant women is associated with a risk for VZV transmission to the fetus or newborn. Intrauterine VZV infection may result in congenital varicella syndrome, clinical varicella (during the newborn period), or clinical zoster (during infancy or early childhood) (8)(9)(10)(11)(12)(13)(14)(15)(16)(17). Infants who are prenatally exposed to VZV, even if asymptomatic, may have measurable varicella-specific IgM antibody during the newborn period, have persistent varicella-specific IgG immunity after 1 year of age without a history of postnatal varicella, or demonstrate positive lymphocyte transformation in response to VZV antigen (8 ).
Congenital varicella syndrome, first recognized in 1947 (11 ), can occur among infants born to mothers infected during the first half of pregnancy and may be manifested by low birthweight, cutaneous scarring, limb hypoplasia, microcephaly, cortical atrophy, chorioretinitis, cataracts, and other anomalies. Aggregate results from prospective studies (8,(13)(14)(15) indicate that congenital varicella syndrome developed in four (0.7%) of 564 infants born to mothers who had varicella during the first trimester of pregnancy. In a prospective study conducted in the United Kingdom and West Germany from 1980 to 1993, a higher risk for congenital varicella syndrome was observed when maternal infection occurred during 13-20 weeks' gestation than when infection occurred from conception through 12 weeks' gestation (2% versus 0.4%, respectively) (14 ). In this same population, herpes zoster developed during infancy or early childhood in four (0.8%) of 477 infants who were exposed to VZV during 13-24 weeks' gestation and six (1.7%) of 345 infants who were exposed during 25-36 weeks' gestation.
The onset of varicella in pregnant women from 5 days before to 2 days after delivery results in severe varicella infection in an estimated 17%-30% of their newborn infants. These infants are exposed to VZV without sufficient maternal antibody to lessen the severity of disease. The risk for death among neonates has been estimated to be 31% among those infants whose mothers had onset of rash 0-4 days before giving birth (16 ). This estimated risk was based on a limited number of infant deaths and may be inflated because some cases resulted from selective reporting and occurred before neonatal intensive care was available. When cases were reevaluated, several infants had been at higher risk for death because of low birthweight. In at least one case, another cause of death had been probable (17 ). Although the risk for death among neonates who do not receive VZIG intervention is likely substantially lower than was previously estimated, VZIG has had a salutary effect on neonatal disease. For example, although only 21 neonatal deaths were reported in the United Kingdom during a 20-year period before VZIG was available, the proportion of deaths among neonates infected with varicella decreased from 7% to none after routine use of VZIG (18 ).
# Nosocomial Transmission
Nosocomial transmission of VZV is well recognized (19)(20)(21)(22)(23)(24)(25)(26)(27)(28)(29), and guidelines for the prevention of nosocomial VZV infection previously have been published (30 ). Guidelines concerning infection control for hospital personnel are being developed (CDC, unpublished data). Sources of nosocomial exposure have included patients, hospital staff, and visitors (e.g., the children of hospital employees) who are infected with varicella or herpes zoster. In hospitals, airborne transmission of VZV has been demonstrated when varicella has occurred in susceptible persons who have had no direct contact with the index case-patient (31)(32)(33)(34)(35).
Although severe varicella disease and complications can occur in all susceptible, hospitalized patients, certain conditions are associated with higher risk. Patients at high risk for severe disease and complications include a) premature infants born to susceptible mothers, b) infants who are born at <28 weeks' gestation or who weigh ≤1,000 g (regardless of maternal immune status), and c) immunocompromised persons of all ages-including persons who are undergoing immunosuppressive therapy, have malignant disease, and are immunodeficient.
Strategies for managing clusters of VZV infection in hospitals have included isolating patients who have varicella and susceptible patients who have been exposed to the virus; controlling air flow; using rapid serologic testing; furloughing or screening exposed, susceptible personnel daily for skin lesions, fever, and systemic symptoms; and temporarily reassigning susceptible personnel to locations remote from patientcare areas (36)(37)(38)(39)(40)(41)(42)(43). Appropriate isolation of hospitalized patients who have confirmed or suspected VZV infection can reduce the risk for transmission to personnel. Only personnel who are immune to varicella should care for these patients. If susceptible personnel are exposed to varicella, they are potentially infective 10-21 days after exposure and are often furloughed, usually at substantial cost. The use of VZIG following exposure can be costly, does not necessarily prevent varicella, and may prolong the incubation period by ≥1 week, thus extending the time during which personnel should not work in patient areas.
# Herpes Zoster
Following varicella, VZV persists in a latent form in sensory-nerve ganglia without any clinical manifestation. The latent virus can be reactivated, causing herpes zoster. Approximately 15% of the population will experience herpes zoster during their lifetimes (44 ). Herpes zoster develops most frequently among immunocompromised persons and the elderly. Disseminated herpes zoster with generalized skin eruptions and central nervous system, pulmonary, hepatic, and pancreatic involvement is more likely to occur in immunocompromised persons than in the general population. VZV can be transmitted from the lesions of patients who have herpes zoster to susceptible contacts, although the likelihood of transmission of VZV from herpes zoster is much less than that from primary varicella. Transmission of VZV from patients who have herpes zoster results in primary varicella in susceptible contacts.
# VARICELLA ANTIBODY TESTING
A reliable history of varicella is a valid measure of immunity. Because the rash is distinctive and subclinical cases rarely occur, most parents know if their child has had varicella. A negative history of varicella substantiated by a parent may be more accurate than a self-reported negative history given by an adult. Data from one study indicated that the attack rate following household exposure in parents who reported themselves as being susceptible was 5%; however, among children whose parents reported them as being susceptible, the attack rate was 87%. In children with positive histories, the attack rate was 7% (45 ).
Serologic tests have been used to assess the accuracy of reported histories of varicella (1,26,42,46,47 ). In adults, a positive history of varicella is highly predictive of serologic immunity (97%-99% of persons are seropositive); however, the majority of adults who have negative or uncertain histories are also seropositive (71%-93%).
The appropriateness of a laboratory test to detect antibody to VZV depends on the purpose for obtaining the information; tests differ in their ability to detect antibody acquired from natural varicella versus antibody acquired from vaccination-levels of which are lower than those following natural infection. Likewise, tests that rapidly assess the susceptibility of persons at high risk who are exposed to varicella differ from those used in serologic surveys. Certain tests require equipment or techniques that are not appropriate for general diagnostic laboratories. Thus, the criteria for selection of an antibody-detection assay include test sensitivity and specificity, the length of time required to obtain results, and availability of the assay.
Many methods have been used to detect antibody to VZV, including complement fixation (CF), indirect fluorescent antibody (IFA), fluorescent antibody to membrane antigen (FAMA), neutralization (N), indirect hemagglutination (IHA), immune adherence hemagglutination (IAHA), radioimmunoassay (RIA), latex agglutination (LA), and enzyme-linked immunosorbent assay (ELISA) (48)(49)(50)(51)(52)(53)(54)(55)(56)(57)(58)(59)(60). IFA, FAMA, N, and RIA are sensitive tests, but they are time consuming and have requirements that make them unsuitable for use in general diagnostic laboratories. The CF test has been widely used but is the least sensitive test; antibody may diminish to levels undetectable by CF several months after natural varicella infection. RIA and ELISA are equal in sensitivity; both tests are tenfold more sensitive than IFA and twentyfold more sensitive than CF (54 ). ELISA tests, which are commercially available, range in sensitivity from 86% to 97% and range in specificity from 82% to 99% in detecting antibody after natural varicella infection. A highly sensitive gpELISA using purified viral glycoproteins as antigens has been used in clinical trials for the large-scale testing of immunogenicity of varicella virus vaccine, but it is not commercially available (58 ). A commercially available LA test using latex particles coated with VZV glycoprotein antigens can be completed in 15 minutes and does not require special equipment (59 ). The sensitivity and specificity of the LA test are comparable to those of FAMA in detecting antibody response following natural varicella infection, but the LA test is less sensitive in detecting antibody following vaccination; for both purposes, the LA test generally is more sensitive than commercial ELISAs. The LA test has detected antibody for up to 11 years after varicella vaccination (60 ).
# ACYCLOVIR FOR THE TREATMENT AND PREVENTION OF VARICELLA
Acyclovir is a synthetic nucleoside analog that inhibits replication of human herpes viruses, including VZV. Intravenous acyclovir has been available since the early 1980s for use in immunocompromised persons who have varicella and, when administered within 24 hours of onset of rash, has been effective in reducing the morbidity and mortality associated with varicella (61)(62)(63).
In 1992, the Food and Drug Administration (FDA) approved the use of oral acyclovir for the treatment of varicella in otherwise healthy children. Approval was based on placebo-controlled, double-blind studies (64)(65) that indicated that beneficial clinical effects occurred (i.e., a decrease in the number of days in which new lesions appeared, the duration of fever, and the severity of cutaneous and systemic signs and symptoms) when acyclovir was administered within 24 hours of onset of rash. No serious adverse events occurred during the period of drug administration. Acyclovir did not decrease transmission of varicella or reduce the duration of absence from school. The rate of complications from varicella is low for healthy children. Data from these studies could not determine whether acyclovir had a significant effect on this rate because too few complications occurred. In these studies, antibody titers following infection in children receiving acyclovir were not substantially different from titers of children in the control group (64,65 ). Clinical trials among adolescents and adults (66)(67)(68) have indicated that acyclovir is safe and effective in reducing the duration and severity of clinical illness if the drug is administered within 24 hours of the onset of rash.
The Committee on Infectious Disease of the American Academy of Pediatrics (AAP) published a statement on the use of acyclovir (69 ). The Committee did not consider the administration of acyclovir to healthy children to be beneficial enough to justify routine administration to such children; however, the Committee acknowledged that certain circumstances may justify the minimal clinical benefit. Complications and more severe varicella may occur in adolescents and adults or in secondary casepatients who live in the households of infected children; therefore, AAP considered such situations appropriate for the use of this drug.
The safety of systemic acyclovir therapy among pregnant women has not been established. Although studies involving animals have not indicated teratogenic effects, adequate, well-controlled studies among pregnant women have not been conducted. Acyclovir is classified as Category C in the FDA use-in-pregnancy rating (i.e., risk cannot be ruled out, but potential benefits may justify the possible risk) (Burroughs Wellcome Company, Zovirax™ package insert). AAP does not recommend oral acyclovir for pregnant women; however, in instances of serious, viral-mediated complications (e.g., pneumonia), AAP stated that intravenous acyclovir should be considered. Burroughs Wellcome Company maintains the Acyclovir in Pregnancy Registry to monitor the maternal-fetal outcomes of pregnant women who are administered systemic acyclovir. The registry is a collaborative effort of Burroughs Wellcome Company, CDC, and academic epidemiologists.* Two nucleoside analogs, acyclovir and famciclovir, have been approved by FDA for treating herpes zoster. If administered within 72 hours of rash onset, acyclovir has accelerated the rate of cutaneous healing and has reduced the severity of acute necrosis in adults who have herpes zoster (70 ). Oral famciclovir, when administered during the same period of time, has similar efficacy (71 ).
The prophylactic use of acyclovir in susceptible children following household exposure to varicella recently has been studied. These studies indicated fewer and less severe cases among children administered acyclovir than among children in the control group. Data from one study indicated that varicella developed in 16% of children treated with acyclovir during the second week after exposure compared with 100% of children in the control group (72 ). In another study, 85% of children who were treated during the first week after exposure seroconverted (a fourfold or greater increase in antibody in convalescent sera), as did 79% of those treated during the second week after exposure (73 ). Seroconversion in the absence of clinical disease occurred more frequently in children who received acyclovir during the second week after exposure (73%) than among those who received acyclovir during the first week after exposure (9%). Thus, although acyclovir appeared to prevent or modify clinical disease in most cases, some children remained susceptible. Serologic testing is required to distinguish those children with subclinical disease who seroconverted from those children who were not infected (74 ).
Postexposure use of acyclovir may be a less costly alternative to the use of VZIG in some susceptible persons. However, before such a strategy could be considered, additional data are needed concerning the prophylactic use of acyclovir in healthy and immunocompromised persons in all age groups.
# LIVE, ATTENUATED VARICELLA VIRUS VACCINE
The varicella virus vaccine licensed in the United States is composed of the Oka strain of live, attenuated VZV. The Oka strain was isolated in Japan (75 ) in the early 1970s from vesicular fluid in a healthy child who had natural varicella and was attenuated through sequential propagation in cultures of human embryonic lung cells, embryonic guinea-pig cells, and human diploid cells (WI-38). The virus in the Oka/ Merck vaccine has undergone further passage through human diploid-cell cultures (MRC-5) for a total of 31 passages. Varicella virus vaccine was first licensed for use among high-risk children in several European countries in 1984, in Japan in 1986, and in Korea in 1988. In Japan and Korea, licensure was extended to healthy children in 1989; no concerns about vaccine safety have been identified after the administration of >2 million doses in these countries.
Varicella virus vaccine is lyophilized, and when reconstituted as directed in the package insert and stored at room temperature for 30 minutes, the vaccine contains >1,350 plaque forming units (PFUs) of Oka/Merck VZV in each 0.5-mL dose. Each 0.5-mL dose also contains 12.5 mg of hydrolyzed gelatin, trace amounts of neomycin and fetal bovine serum, 25 mg of sucrose, and trace residual components of MRC-5 cells (including DNA and protein). The vaccine does not contain preservatives. Since 1981, a total of 9,454 healthy children and 1,648 healthy adolescents and adults have received several formulations of the Oka/Merck vaccine as part of clinical trials conducted in the United States (76)(77)(78)(79)(80)(81)(82)(83). The occurrence of serious adverse events has been minimal (see Vaccine-Associated Adverse Events). Antibody responses have been measured by gpELISA.
# Immunogenicity
The seroconversion rate (gpELISA >0.3 U) after one dose of vaccine among 6,889 susceptible children 12 months-12 years of age was demonstrated to be 97%; 76% of these children achieved antibody titers of gpELISA ≥5 U (Merck and Company, Inc., unpublished data). Persistence of antibody (i.e., IgG >5 by FAMA) measured yearly for 4 years after vaccination was consistently high (i.e., >90%) in children vaccinated at 12, 13, 14, 15, 16-23, 24-36, or 48-144 months of age, although the numbers of children tested decreased considerably as the length of time since vaccination increased. Six years after vaccination at ages ranging from 1 to 12 years, 35 children had no decrease in antibody titers (84 ). In Japan, antibodies to VZV were present in 97% of children 7-10 years after vaccination, and titers were comparable to those in children who had natural varicella infection 7-10 years earlier (85 ). A subsequent 20-year follow-up study revealed that antibody levels were higher than those observed 10 years earlier (86 ). These higher levels might have resulted from asymptomatic boosting of vaccine-induced immunity by exposure to wild-type VZV, because <20% of children in Japan were vaccinated during 1991-1993.
Among persons ≥13 years of age, 78% of vaccinees seroconverted after the first dose of varicella virus vaccine, and 99% seroconverted after a second dose, which was administered 4-8 weeks later (Merck and Company, Inc., unpublished data); the proportion of vaccinees who seroconverted did not differ by age. Detectable antibody levels have persisted for at least 1 year in 97% of adolescents and adults who were administered two doses of vaccine 4-8 weeks apart.
# Efficacy and Breakthrough Infections
In clinical trials, the vaccine has proven to be effective for >10 years in preventing varicella. However, breakthrough infections (i.e., cases of varicella that occur in some vaccinated persons following exposure to wild-type virus) can occur, usually resulting in mild illness.
In a double-blind, placebo-controlled trial using vaccine that contained 17,430 PFUs, efficacy among children 1-14 years of age was 100% after the first varicella season and 96% after the second season. On the basis of a long-term evaluation of a subset of vaccinees whose vaccination status was revealed after the second year following vaccination, efficacy was an estimated 95% after 7 years (77 ). A controlled efficacy trial was not conducted for adults.
Data from all trials in which vaccinees of all ages were actively followed for up to 9 years indicated that varicella developed in <1%-4.4% of vaccinees per year, depending on vaccine lot and time interval since vaccination (Merck and Company, Inc., unpublished data). Active and passive surveillance data collected during 6 years of follow-up have indicated that each year, varicella developed in 2.1%-3.6% of the 4,142 children who received earlier lots of vaccine containing 1,000-1,625 PFUs of attenuated virus. Natural varicella attack rates in children 1-9 years of age are an estimated 8.3%-9.1%; thus, these data represent an estimated 67% (range: 57%-77%) decrease from the total number of expected cases. For up to 3 years of follow-up, varicella developed in 0.2%-1% of 1,164 children who received the current vaccine containing 2,900-9,000 PFUs per year, representing an average 93% decrease from expected rates. The attack rate after household exposure for a subset of 259 persons who received early lots of vaccine decreased by 77% compared with the expected attack rate for unvaccinated persons (attack rate: 20% and 87%, respectively) (45,64 ; Merck and Company, Inc., unpublished data). In these clinical trials, varicella subsequently developed in substantially fewer children who had postvaccination gpELISA titers of ≥5 U varicella than those children who had postvaccination gpELISA titers of <5 U.
Varicella is substantially less severe among vaccinated persons than unvaccinated persons, who usually have fever and several hundred vesicular lesions (87 ). For vaccinees in whom varicella has developed, the median number of skin lesions has been <50 (88,89; Merck and Company, Inc., unpublished data). In addition, most vaccinees have been afebrile, have had fewer vesicular lesions, and have had shorter duration of illness than unvaccinated persons. Illnesses associated with vaccine failure are attenuated and have not increased in severity during the 7-10 years of follow-up study.
The rate of disease transmission from vaccinees in whom varicella develops is low for children but has not been studied in adults. In 10 different trials conducted from 1981 through 1989 involving 2,141 vaccinated children, breakthrough infections occurred in 78 vaccinated children during the 1-8 year follow-up period of active surveillance, resulting in secondary transmission to 11 (12.2%) of their 90 vaccinated siblings (89 ). Illness was mild in both index and secondary case-patients. Transmission to a susceptible mother from a vaccinated child in whom breakthrough disease occurred also has been reported (Merck and Company, Inc., unpublished data).
Varicella virus vaccine provides 70%-90% protection against infection and 95% protection against severe disease for 7-10 years after vaccination. Data are insufficient to evaluate the extent of the protection provided by varicella vaccination against serious complications from varicella (e.g., bacterial infections of skin lesions, pneumonia, and encephalitis) in persons of all ages. However, serious complications are anticipated to be reduced, because data indicate attenuation of common manifestations of disease in vaccinees.
Current data concerning vaccine efficacy and persistence of antibody in vaccinees are based on research that has been conducted when natural VZV infection has been highly prevalent and has not been affected by wide use of the vaccine. Thus, the extent to which the protection provided by vaccination has been increased by boosting from exposure to natural virus and whether longer term immunity may wane as the circulation of natural VZV decreases are unknown.
# Transmission of Vaccine Virus
Available data suggest that healthy children are unlikely to transmit vaccine virus to susceptible contacts, but that risk for transmission from vaccinees who are immunocompromised is higher and may be associated with occurrence of rash following vaccination. Risk for transmission of vaccine virus was assessed in siblings of vaccinated children who received placebo themselves (76 ). During the 8 weeks following vaccination, six (1%) of 439 placebo recipients seroconverted without rash; their vaccinated siblings also had no rash. Among three of the six children who seroconverted, serologic data suggested that the preparations administered to the assigned vaccine and placebo recipients were mistakenly switched. In addition, varicella developed in three other placebo recipients during months of high varicella incidence (i.e., from December through June); one recipient had had an exposure to natural varicella at school. In another study, no evidence of transmission of vaccine virus was found after vaccinating 37 healthy siblings of 30 immunocompromised children (90 ). None of the immunocompromised children had rash or demonstrated evidence of humoral or cell-mediated immune responses.
Higher risk for transmission of vaccine virus has been documented among children who have both rash following vaccination and leukemia. Data from one study indicated that varicella virus vaccine infection occurred in 15 (17%) of 88 exposed, healthy siblings of leukemic vaccine recipients; mild rash developed in 11 siblings (91 ). In one family, tertiary transmission to a second healthy sibling occurred, with rash developing 18 days after rash onset in the secondary case-patient and 33 days after rash onset in the leukemic child. Both healthy siblings had mild rash (i.e., 11 and 40 lesions, respectively), and vaccine virus was isolated from all three case-patients.
These data suggest that healthy, vaccinated persons have a minimal risk for transmitting vaccine virus to their contacts; this risk may be higher in vaccinees in whom a varicella-like rash develops following vaccination. In clinical trials, nonlocalized rash developed in 3.8% of children and 5.5% of adolescents and adults (median: five lesions) after the first injection and 0.9% of adolescents and adults after the second injection.
# Herpes Zoster Following Vaccination
The incidence of herpes zoster after varicella vaccination among otherwise healthy children is approximately 18 per 100,000 person years of follow-up (Merck and Company, Inc., unpublished data). A population-based study indicated that the incidence of herpes zoster after natural varicella infection among healthy children was 77 per 100,000 person years. However, these two rates should be compared cautiously, because the latter rate was based on a larger pediatric population that was monitored for a longer period of time than were the vaccinees (92,93 ). One case of herpes zoster has been reported among adult vaccinees, resulting in an incidence of 12.8 per 100,000 person years. Although unknown, the rate of herpes zoster in unvaccinated adults is expected to be higher than that in adult vaccinees. All of the vaccinees' illnesses were mild and without complications. Wild-type virus was identified in one vaccinated child and one vaccinated adult by using restriction endonuclease analysis in cultures from vesicles, which suggests that some herpes zoster cases in vaccinees may result from antecedent natural varicella infection (Merck and Company, Inc., unpublished data;94 ).
# Vaccine as Postexposure Prophylaxis
No data exist regarding postexposure efficacy of the current varicella virus vaccine. Postexposure prophylaxis of children using previous formulations of varicella virus vaccine has been conducted in two controlled studies. In Japan ( 95) and the United States (79 ), protective efficacy was ≥90% when children were vaccinated within 3 days of exposure.
# Cost Benefit of Vaccine
A recent cost-effectiveness study (96 ) was performed using current estimates of morbidity and mortality (CDC, unpublished data), mathematical modeling of the projected impact of vaccination (97 ), and current direct and indirect costs. Unlike a previous study published in 1985 (98 ), the recent analysis accounted for potential changes in the frequency and severity of varicella-related complications resulting from expected changes in the epidemiology and age distribution of varicella following widespread use of varicella virus vaccine. Additional efficacy data for 1985-1993 were available, and empiric data on medical utilization and costs of work-loss resulting from varicella were used. The results of this study, which were determined using an estimated cost of $35 per dose of vaccine and $5 for vaccine administration, indicated a savings of $5.40 for each dollar spent on routine vaccination of preschool-age children when direct and indirect costs were considered. When only direct medical costs were considered, the benefit-cost ratio was 0.90:1. Benefit-cost ratios were only slightly lower when lower estimates of the short-term and long-term effectiveness of the vaccine were used.
# DISTRIBUTION, HANDLING, AND STORAGE OF VACCINE
To maintain potency, the lyophilized vaccine must be stored frozen at an average temperature of ≤5 F (≤-15 C). Household freezers manufactured since the mid-1980s are designed to maintain temperatures from -4 F (-20 C) to 5 F (-15 C). When tested, VARIVAX ® has remained stable in frost-free refrigerators. Refrigerators with ice compartments that are either not tightly enclosed or enclosed with unsealed, uninsulated doors (e.g., small, dormitory-style refrigerators) may not meet temperature requirements. Regardless of the type of freezer, providers should check the adequacy of their freezer by verifying its temperature before obtaining vaccine.
The diluent should be stored separately either at room temperature or in the refrigerator. The vaccine should be reconstituted according to the directions in the package insert and only with the diluent supplied with the vaccine, which does not contain preservative or other antiviral substances that could inactivate the vaccine virus. Once reconstituted, the vaccine should be used immediately to minimize loss of potency. The vaccine should be discarded if not used within 30 minutes after reconstitution.
# Handling of Vaccine Within a Clinic and for Clinics That do not Have Adequate Facilities to Store Vaccine
When an immunization session is being held at a site distant from the freezer in which the vaccine is stored, the needed number of vaccine vials for the immunization session should be stored in a suitable container (i.e., the original shipping container or a comparable container with a properly fitting lid) with an adequate quantity of dry ice (i.e., a minimum of 6 lbs/box), so that dry ice would remain if any unreconstituted vaccine must be returned to the freezer. Dry ice, when placed in a suitable container, will maintain a temperature of 5 F (-15 C) or colder.
When optimal handling conditions are not feasible because of the location of the freezer storage area or concern for security of the room where vaccines are administered within a clinic, or when vaccine must be transported to a clinic site distant from the freezer-storage area, minimal potency can be maintained if varicella virus vaccine is stored continuously for up to 72 hours at temperatures of 36-46 F (2-8 C). This vaccine should be discarded if not used within 72 hours of placing it into storage.*
# Minimizing Wastage of Vaccine
Vaccine wastage can be minimized by accurately determining the number of doses needed for clinics that do not have adequate freezer-storage facilities. To ensure maximal vaccine potency, smaller shipments of vaccine should be ordered more frequently-preferably at least once every 3 months. Vaccine lots with a longer expiration period (i.e., >12 months to expiration) should be selected for use in clinics that do not have adequate facilities to store vaccine.
# Transfer of Vaccine Between Clinic Sites
When transferring vaccine between clinic sites is required (e.g., when supply must be adjusted), the vaccine should be packed in the manufacturer's shipping container or a container with comparable insulating qualities using appropriate quantities of dry ice (e.g., a minimum of 6 lbs/box). Residual dry ice should be available at the receiving site. If dry ice is not available, the vaccine should be discarded unless a temperature recorder has been included in the transport box; if the temperature has been ≤36-46 F (≤2-8 C) for up to 72 hours, the vaccine can be used within 72 hours of removal from the freezer-storage area.
# RECOMMENDATIONS FOR THE USE OF VARICELLA VIRUS VACCINE
# Persons <13 Years of Age
Varicella virus vaccine has been approved for use among healthy children 12 months-12 years of age. Children in this age group should receive one 0.5-mL dose of vaccine subcutaneously.
Children who have a reliable history of varicella are considered immune, and those who do not have such a history or who have an uncertain history of varicella are considered susceptible. Serologic testing of children before vaccination is not warranted because a) most children 12 months-12 years of age who do not have a clinical history of varicella are susceptible and b) the vaccine is well tolerated in seropositive persons.
12-18 Months of Age. All children should be routinely vaccinated at 12-18 months of age. Varicella virus vaccine may be administered to all children at this ageregardless of a history of varicella; however, vaccination is not necessary for children who have reliable histories of varicella. Varicella virus vaccine preferably should be administered routinely to children at the same time as measles-mumps-rubella (MMR) vaccine. Varicella virus vaccine is safe and effective in healthy children ≥12 months of age when administered at the same time as MMR vaccine at separate sites and with separate syringes or when administered separately ≥30 days apart. The number and types of adverse events in children who have received VARIVAX ® and MMR concurrently have not differed from those in children who have been administered the vaccines at different visits (Merck and Company, Inc., unpublished data). Data concerning the effect of simultaneous administration of VARIVAX ® with various *For information regarding use of vaccine inadvertently exposed to conditions not addressed in these guidelines, inquiries should be directed to Merck and Company, Inc. (telephone: (800)-9-VARIVAX).
combinations of MMR-, diphtheria and tetanus toxoids and pertussis (DTP)-, and Haemophilus influenzae type b (Hib)-containing vaccines have not yet been published. However, data regarding simultaneous administration of an investigational quadrivalent vaccine containing varicella (MMRII V™) with diphtheria and tetanus toxoids and acellular pertussis (DTaP) and Hib vaccines suggest that no notable interactions exist between varicella and any other vaccines that are routinely administered to young children (e.g., measles, mumps, rubella, diphtheria, tetanus, pertussis, and Haemophilus influenzae type b vaccines). Furthermore, the simultaneous administration of most widely used live, attenuated and inactivated vaccines has not resulted in impaired antibody response or an increased rate of adverse events. Therefore, varicella virus vaccine may be administered simultaneously with all of the vaccines recommended for children 12-18 months of age. Simultaneous administration is particularly important when health-care providers anticipate that, because of certain factors (e.g., previously missed vaccination opportunities), a child may not return for subsequent vaccination.
19 Months-12 Years of Age. Varicella vaccine is recommended for all susceptible children by their 13th birthday. After 12 years of age, natural varicella is more severe and complications are more frequent. Recently, ACIP recommended establishing a routine immunization visit at 11-12 years of age to review immunization status and to administer necessary vaccinations (99 ). Although vaccine may be administered at any time after 18 months of age, varicella virus vaccine should be administered to susceptible children during this routine visit.
# Persons ≥13 Years of Age
Varicella vaccine is approved for use among healthy adolescents and adults. Because natural VZV infection can be severe in older adolescents and adults, varicella immunity is desirable in these age groups. Persons ≥13 years of age should be administered two 0.5-mL doses of vaccine, subcutaneously, 4-8 weeks apart. If >8 weeks elapse following the first dose, the second dose can be administered without restarting the schedule.
Persons ≥13 years of age who have reliable histories of varicella are considered immune. Those who do not have such histories are considered susceptible and can be tested to determine immune status or can be vaccinated without testing. Because 71%-93% of adults who do not have a reliable history of varicella are actually immune (1,26,42,46,47 ), serologic testing before vaccination is likely to be cost effective for both adults and adolescents (100 ).
Adolescents and adults should be assessed for varicella immune status, and those who are susceptible should be vaccinated. Priority should be given to vaccination of susceptible adolescents and adults who are at high risk for exposure and for transmitting disease; specific assessment efforts are targeted to these persons (Box 1).
# Health-Care Workers*
All susceptible health-care workers should ensure that they are immune to varicella. In health-care institutions, serologic screening of personnel who have a negative or uncertain history of varicella is likely to be cost effective.
*The recommendations for health-care workers were prepared jointly by ACIP and the Hospital Infection Control Practices Advisory Committee.
Routine testing for varicella immunity after two doses of vaccine is not necessary for the management of vaccinated health-care workers who may be exposed to varicella, because 99% of persons are seropositive after the second dose. Seroconversion, however, does not always result in full protection against disease. Testing vaccinees for seropositivity immediately after exposure to VZV is a potentially effective strategy for identifying persons who remain at risk for varicella. Prompt serologic results may be obtained using the LA test. Varicella is unlikely to develop in persons who have detectable antibody; persons who do not have such antibody can be retested in 5-6 days to determine if an anamnestic response is present, in which case development of disease is unlikely. Persons who remain susceptible may be furloughed. Alternatively, persons can be monitored daily to determine clinical status and then furloughed at the onset of manifestations of varicella. Institutional guidelines are needed for the management of exposed vaccinees who do not have detectable antibody and for persons who develop clinical varicella.
More information is needed concerning the risk for transmission of vaccine virus from vaccinees in whom varicella-like rash develops following vaccination. On the basis of available data, the risk appears to be minimal, and the benefits of vaccinating susceptible health-care workers outweigh this potential risk. As a safeguard, institutions may wish to consider precautions for personnel in whom rash develops not pregnant-but who may become pregnant in the future-will reduce the risk for VZV transmission to the fetus. Varicella immunity may be ascertained at any routine health-care visit or in any setting in which vaccination history may be reviewed (e.g., upon college entry). Women should be asked if they are pregnant and advised to avoid pregnancy for 1 month following each dose of vaccine. d) International travelers. Vaccination should be considered for international travelers who do not have evidence of immunity to VZV (e.g., serologic tests), especially if the traveler expects to have close personal contact with local populations, because varicella is endemic in most countries.
• Vaccination of other susceptible adolescents and adults is desirable and may be offered during routine health-care visits.
# BOX 1. Vaccination of persons ≥13 years of age
following vaccination and for other vaccinated personnel who will have contact with susceptible persons at high risk for serious complications. Vaccination should be considered for unvaccinated health-care workers who are exposed to varicella and whose immunity is not documented. However, because the protective effects of postexposure vaccination are unknown, persons vaccinated after an exposure should be managed in the manner recommended for unvaccinated persons.
# Household Contacts of Immunocompromised Persons
Immunocompromised persons are at high risk for serious varicella infections. Disseminated disease occurs in approximately 30% of such persons who have primary infection. Vaccination of household contacts provides protection for immunocompromised persons by decreasing the likelihood that wild-type varicella virus will be introduced into the household. Vaccination of household contacts of immunocompromised persons theoretically may pose a minimal risk of transmission of vaccine virus to immunocompromised persons, although in one study, no evidence of transmission of vaccine virus was found after vaccinating 37 healthy siblings of 30 children with malignancy. Available data indicate that disease caused by vaccine virus in immunocompromised persons is milder than wild-type disease and can be treated with acyclovir. More information is needed concerning the risk for transmission of the vaccine virus from both vaccinees who have and who do not have varicella-like rash following vaccination. On the basis of available data, the benefits of vaccinating susceptible household contacts of immunocompromised persons outweigh the potential risk for transmission of vaccine virus to immunocompromised contacts.
# VACCINE-ASSOCIATED ADVERSE EVENTS
Varicella virus vaccine has been well tolerated when administered to >11,000 healthy children, adolescents, and adults during clinical trials. Inadvertent vaccination of persons immune to varicella has not resulted in an increase in adverse events. In a double-blind, placebo-controlled study of 914 healthy, susceptible children and adolescents (76 ), pain and redness at the injection site were the only adverse events that occurred significantly more often (p<0.05) in vaccine recipients than in placebo recipients.
# Persons 12 Months-12 Years of Age
In uncontrolled clinical trials of approximately 8,900 healthy children (Merck and Company, Inc., package insert) who were administered one dose of vaccine and then monitored for up to 42 days, 14.7% developed fever (i.e., oral temperature ≥102 F [≥39 C]); these febrile episodes occurred throughout the 42-day period and were usually associated with intercurrent illness. A total of 19.3% of vaccine recipients had complaints regarding the injection site (e.g., pain/soreness, swelling, erythema, rash, pruritus, hematoma, induration, and stiffness), 3.4% had a mild, varicella-like rash at the injection site consisting of a median number of two lesions and occurring at a peak of 8-19 days postvaccination, and 3.8% had a nonlocalized, varicella-like rash consisting of a median number of five lesions and occurring at a peak of 5-26 days postvaccination. Febrile seizures following vaccination occurred in <0.1% of children; a causal relationship has not been established.
# Persons ≥13 Years of Age
In uncontrolled trials of persons ≥13 years of age, approximately 1,600 vaccinees who received one dose and 955 who received two doses of varicella vaccine were monitored for 42 days for adverse events (Merck and Company, Inc., package insert). After the first and second doses, 10.2% and 9.5% of vaccinees, respectively, developed fever (i.e., oral temperature ≥100 F [37.7 C]); these febrile episodes occurred throughout the 42-day period and were usually associated with intercurrent illness. After one and two doses, 24.4% and 32.5% of vaccinees, respectively, had complaints regarding the injection site (e.g., soreness, swelling, erythema, rash, pruritus, hematoma, pyrexia, induration, and numbness); a varicella-like rash at the injection site consisting of a median number of two lesions and occurring at a peak of 6-20 days and 0-6 days postvaccination, respectively, developed in 3% and 1% of vaccinees, respectively; and a nonlocalized rash consisting of a median number of five lesions developed in 5.5% and 0.9% of vaccinees, respectively, and occurred at a peak of 7-21 days and 0-23 days postvaccination, respectively.
# Postlicensure Adverse Vaccine Events
During the first 12 months following vaccine licensure, more than 2.3 million doses of vaccine were distributed in the United States. The Vaccine Adverse Events Reporting System (VAERS) and the vaccine manufacturer have received a limited number of reports of serious medical events occurring within 6 weeks after varicella virus vaccination, including encephalitis (n=4), ataxia (n=7), and erythema multiforme (n=10). Three cases of anaphylaxis have occurred within 10 minutes of vaccination. A causal relationship between the vaccine and these events has not been determined. Potential delayed or underreporting of events to VAERS may have occurred. Physicians and health-care providers are encouraged to report any suspected adverse events that occur after varicella virus vaccination (see Reporting of Adverse Events). Postmarketing surveillance for adverse events will be ongoing.
# Reporting of Adverse Events
The National Vaccine Injury Act of 1986 (101 ) requires physicians and other healthcare providers who administer vaccines to maintain permanent immunization records and to report occurrences of adverse events for selected vaccines. Although the Act currently does not apply to varicella virus vaccine, the same recording and reporting requirements should be followed. Serious adverse events (i.e., all events requiring medical attention), regardless of whether they are suspected to have been caused by varicella virus vaccine, should be reported to VAERS. VAERS forms and instructions are available in the FDA Drug Bulletin and the Physicians' Desk Reference or by calling the 24-hour VAERS information recording (telephone: [800] 822-7967).
# CONTRAINDICATIONS AND PRECAUTIONS
# Allergy to Vaccine Components
The administration of live varicella virus vaccine rarely results in hypersensitivity. The information in the package insert should be carefully reviewed before vaccine is administered; vaccination is contraindicated for persons who have a history of anaphylactic reaction to any component of the vaccine, including gelatin. Varicella virus vaccine does not contain preservatives or egg protein-substances that have caused hypersensitive reactions to other vaccines. Varicella virus vaccine should not be administered to persons who have a history of anaphylactic reaction to neomycin. Neomycin allergy is usually manifested as a contact dermatitis, which is a delayedtype immune response rather than anaphylaxis. For persons who experience such a response, the adverse reaction, if any, would be an erythematous, pruritic nodule or papule present 48-96 hours after vaccination. A history of contact dermatitis to neomycin is not a contraindication to receiving varicella virus vaccine.
# Illness
Vaccination of persons who have severe illness should be postponed until recovery. The decision to delay vaccination depends on the severity of symptoms and on the etiology of the disease. Vaccine can be administered to susceptible children who have mild illnesses with or without low-grade fever (e.g., diarrhea or upperrespiratory infection) (102 ). Studies suggest that failure to vaccinate children with minor illnesses can impede vaccination efforts (103 ).
Although no data exist regarding whether either varicella or live varicella virus vaccine exacerbates tuberculosis, vaccination is not recommended for persons who have untreated, active tuberculosis. Tuberculin skin testing, however, is not a prerequisite for varicella vaccination.
# Altered Immunity
Varicella virus vaccine is not licensed for use in persons who have any malignant condition, including blood dyscrasias, leukemia, lymphomas of any type, or other malignant neoplasms affecting the bone marrow or lymphatic systems. However, vaccine is available to any physician free of charge from the manufacturer* through a research protocol (104 ) for use in patients who have acute lymphoblastic leukemia (ALL) who a) are 12 months-17 years of age, b) have disease that has been in remission for at least 12 continuous months, c) have a negative history of varicella disease, d) have a peripheral blood-lymphocyte count of >700 cells/mm 3 , and e) have a platelet count of >100,000 cells/mm 3 within 24 hours of vaccination. The vaccine is well tolerated, immunogenic, and protective in children who meet these criteria (105)(106)(107)(108)(109)(110). The most common reaction to the vaccine in patients who have ALL is a mild to moderate varicella-like rash (i.e., two to 200 lesions), which occurs in approximately 5% of children who have completed their chemotherapy before vaccination and 40% of vaccinees on maintenance chemotherapy (106 ).
Varicella virus vaccine should not be administered to persons who have primary or acquired immunodeficiency, including immunosuppression associated with acquired immunodeficiency syndrome (AIDS) or other clinical manifestations of human immunodeficiency virus (HIV) infections, cellular immunodeficiencies, hypogammaglobulinemia, and dysgammaglobulinemia. The use of varicella virus vaccine in persons who are infected with HIV has not been studied; therefore, vaccination of these persons is not recommended, although routine screening for HIV before *The physician must provide information requested in the protocol, and the protocol and consent form for the study must be approved by the institution's Investigational Review Board. vaccination also is not recommended. The use of varicella virus vaccine in HIVinfected children is being investigated. If inadvertent vaccination of HIV-infected persons results in clinical disease, the use of acyclovir may modify the severity of disease.
Varicella virus vaccine should not be administered to persons who have a family history of congenital or hereditary immunodeficiency in first-degree relatives (e.g., parents and siblings) unless the immune competence of the potential vaccine recipient has been clinically substantiated or verified by a laboratory.
Varicella virus vaccine should not be administered to persons receiving immunosuppressive therapy-except children who have ALL in remission, as previously described. Such persons are more susceptible to infections than healthy persons. Administration of live, attenuated varicella virus vaccine can result in a more extensive vaccine-associated rash or disseminated disease in persons receiving immunosuppressive doses of corticosteroids (111 ). This contraindication does not apply to persons who are receiving corticosteroid-replacement therapy.
# Children Who Have Conditions That Require Steroid Therapy
No data have been published concerning whether susceptible children receiving only inhaled doses of steroids can be vaccinated safely. However, most experts concur, on the basis of clinical experience, that vaccination of these children is safe. Susceptible children who are receiving systemic steroids for certain conditions (e.g., asthma) and who are not otherwise immunocompromised can be vaccinated if they are receiving <2 mg/kg of body weight or a total of 20 mg/day of prednisone or its equivalent. Antibody status should be assessed 6 weeks postvaccination, and children who have not seroconverted should be revaccinated. Some experts suggest withholding steroids for 2-3 weeks following vaccination when possible. Data from one study conducted in Japan indicated that children taking steroids for nephrosis were vaccinated safely when the steroids were suspended for 1-2 weeks before vaccination, although no serious reactions occurred among children vaccinated when steroid therapy was not suspended (112 ). Children who are receiving high doses of systemic steroids (i.e., ≥2 mg/kg prednisone) for ≥2 weeks may be vaccinated after steroid therapy has been discontinued for at least 3 months in accordance with the general recommendations for the use of live-virus vaccines (113 ); however, withholding steroids for at least 1 month before varicella vaccination is probably sufficient.
# Exposure of Immunocompromised Persons to Vaccinees
Healthy persons in whom varicella-like rash develops following vaccination appear to have a minimal risk for transmission of vaccine virus to their close contacts (e.g., family members). Seroconversion has been documented in healthy siblings of healthy vaccinees in whom rash did not develop, although such an occurrence is rare (76 ). Vaccinees in whom vaccine-related rash develops, particularly health-care workers and household contacts of immunocompromised persons, should avoid contact with susceptible persons who are at high risk for severe complications. If a susceptible, immunocompromised person is inadvertently exposed to a person who has a vaccine-related rash, VZIG need not be administered because disease associated with this type of transmission is expected to be mild.
# Recent Administration of Blood, Plasma, or Immune Globulin
Although passively acquired antibody is known to interfere with response to measles and rubella vaccines (114 ), the effect of the administration of immune globulin (IG) on the response to varicella virus vaccine is unknown. The duration of interference with the response to measles vaccination depends on the dosage and ranges from 3-11 months. Because of the potential inhibition of the response to varicella vaccination by passively transferred antibodies, varicella virus vaccine should not be administered for at least 5 months after administration of blood (except washed red blood cells), plasma, IG, or VZIG (113 ). In addition, IG and VZIG should not be administered for 3 weeks after vaccination unless the benefits exceed those of vaccination. In such cases, the vaccinee should either be revaccinated 5 months later or tested for immunity 6 months later and then revaccinated if seronegative.
# Use of Salicylates
No adverse events associated with the use of salicylates after varicella vaccination have been reported. However, the vaccine manufacturer recommends that vaccine recipients avoid using salicylates for 6 weeks after receiving varicella virus vaccine because of the association between aspirin use and Reye syndrome following varicella. Vaccination with subsequent close monitoring should be considered for children who have rheumatoid arthritis or other conditions requiring theraputic aspirin because the risk for serious complications associated with aspirin is likely to be greater in children in whom natural varicella disease develops than in children who receive the vaccine containing attenuated VZV. No association has been documented between Reye syndrome and analgesics or antipyretics that do not contain salicylic acid.
# Pregnancy
The effects of the varicella virus vaccine on the fetus are unknown; therefore, pregnant women should not be vaccinated. Nonpregnant women who are vaccinated should avoid becoming pregnant for 1 month following each injection. For susceptible persons, having a pregnant household member is not a contraindication to vaccination.
If a pregnant woman is vaccinated or becomes pregnant within 1 month of vaccination, she should be counseled about potential effects on the fetus. Wild-type varicella poses only a very small risk to the fetus (see Prenatal and Perinatal Exposure). Because the virulence of the attenuated virus used in the vaccine is less than that of the wild-type virus, the risk to the fetus, if any, should be even lower. In most circumstances, the decision to terminate a pregnancy should not be based on whether vaccine was administered during pregnancy. The manufacturer, in collaboration with CDC, has established the VARIVAX ® Pregnancy Registry to monitor the maternal-fetal outcomes of pregnant women who are inadvertently administered varicella virus vaccine 3 months before or at any time during pregnancy (telephone: [800] 986-8999) (115 ).
# Nursing Mothers
Whether attenuated vaccine VZV is excreted in human milk and, if so, whether the infant could be infected are not known. Most live vaccines have not been demonstrated to be secreted in breast milk. Attenuated rubella vaccine virus has been detected in breast milk but has produced only asymptomatic infection in the nursing infant. Therefore, varicella virus vaccine may be considered for a nursing mother.
# USE OF VZIG FOR POSTEXPOSURE PROPHYLAXIS
Studies conducted in 1969 indicated that zoster immune globulin (ZIG) (prepared from patients recovering from herpes zoster) prevented clinical varicella in susceptible, healthy children if administered within 72 hours of exposure (116 ). ZIG also lowered attack rates among immunocompromised persons if administered no later than 96 hours after exposure (116 ).
VZIG (prepared from plasma obtained from healthy, volunteer blood donors who are identified by routine screening to have high antibody titers to VZV) became available in 1978. Both serologic and clinical evaluations have demonstrated that the product is equivalent to ZIG in preventing or modifying clinical illness in susceptible, immunocompromised persons who are exposed to varicella. VZIG is a sterile, 10%-18% solution of the globulin fraction of human plasma, primarily immunoglobulin G (IgG) in 0.3 M glycine as a stabilizer and 1:10,000 thimerosal as a preservative. VZIG is prepared by using Cohn cold ethanol precipitation, which eliminates hepatitis B virus, HIV, and other known infectious agents from the product. VZIG prepared using an additional viral-inactivation step (the solvent detergent treatment) has recently become available.
# Supply
VZIG is produced by the United States Biologics Laboratories (Massachusetts) and is distributed by American Red Cross regional distribution centers and service areas (Appendix). In Massachusetts, VZIG is distributed by the Massachusetts Department of Public Health.
# Administration
VZIG provides maximum benefit when administered as soon as possible after the presumed exposure, but it may be effective if administered as late as 96 hours after exposure. The effectiveness of VZIG when administered 96 hours after initial exposure has not been evaluated. VZIG is not recommended for vaccinated persons who were previously seropositive and found to be seronegative following exposure because such persons would be expected to have a mild case; no further benefit would be gained by administering VZIG.
VZIG has not been proven to be useful in treating clinical varicella or herpes zoster or in preventing disseminated zoster and is not recommended for such use. The duration of protection that is provided after administration of VZIG is unknown, but protection should last at least one half-life of the IG (i.e., approximately 3 weeks). Susceptible persons at high risk for whom varicella vaccination is contraindicated and who are again exposed ≥3 weeks after a dose of VZIG should receive another full dose of VZIG.
# Dosage
VZIG is supplied in two different dosages-the 125-U vial and the 625-U vial. The recommended dose is 125 U/10 kg (22 lbs) of body weight, up to a maximum of 625 U. The minimum dose is 125 U; fractional doses are not recommended. VZIG administration has not been evaluated as a prophylactic measure in healthy or immunocompromised adults. Therefore, the appropriate dose for prophylaxis in adults cannot be calculated. However, 625 U should be sufficient to modify or prevent infection in healthy adults. Higher doses may be necessary for immunocompromised adults.
VZIG should be administered intramuscularly as directed by the manufacturer. VZIG should never be administered intravenously.
# Indications for the Use of VZIG
The decision to administer VZIG to a person exposed to varicella should be based on a) whether the patient is susceptible (either by having a negative history of varicella or by lacking documentation of vaccination), b) whether the exposure is likely to result in infection, and c) whether the patient is at greater risk for complications than the general population. VZIG is costly (i.e., approximately $90 per 125-U vial or $400 for persons >40 kg [88 lbs] body weight) and only provides temporary protection. The long-term effects of VZIG on immunity and on the occurrence of herpes zoster are unknown.
For immunocompromised persons, an accurate history of varicella should be obtained before determining immune status and whether to administer VZIG. Immunocompromised persons who do not have histories of disease, but who have low levels of antibody detected by the most sensitive assays, have contracted varicella. Presumably, the low levels of antibody in most of these patients were passively acquired from recent transfusions of blood, blood derivatives, or blood products containing antibody.
Both healthy and immunocompromised children and adults who have positive histories of varicella (except for bone-marrow transplant recipients) can be considered immune (see Recommendations for the Use of Varicella Virus Vaccine). However, varicella may develop in some infants after exposure despite the presence of detectable antibody, although in most circumstances such illness is less severe than the illness occurring in infants who do not have detectable antibody. Therefore, sensitive assays may not be useful in assessing whether clinical disease will develop in neonates or young infants exposed to varicella.
The association between positive histories of varicella in bone-marrow donors and susceptibility to varicella in recipients following transplants has not been adequately studied. Thus, persons who receive bone-marrow transplants should be considered susceptible-regardless of prior history of varicella or varicella vaccination in themselves or in their donors. Bone-marrow recipients in whom varicella or herpes zoster develops following transplantation should subsequently be considered immune.
# Types of Exposure
Several types of exposure can place susceptible persons at risk for varicella. Direct contact exposure is defined as >1 hour of direct contact with an infectious person while indoors; substantial exposure for hospital contacts consists of sharing the same hospital room with an infectious patient or prolonged, direct, face-to-face contact with an infectious person (e.g., health-care workers). Brief contacts with an infectious person (e.g., contact with x-ray technicians or housekeeping personnel) are less likely to result in VZV transmission than are more prolonged contacts.
Persons with continuous exposure to household members who have varicella are at greatest risk for infection. Varicella develops in approximately 90% of susceptible household contacts. Following household exposure, attack rates among immunocompromised children administered VZIG are 33%-50%. Data are not available for immunocompromised, susceptible persons who were not administered VZIG. The risk for varicella following close contact (e.g., contact with playmates) or hospital exposure is approximately 20% of the risk occurring from household exposure.
The attack rate in healthy neonates who are exposed in utero within 5 days of delivery and administered VZIG after birth is 30%-40%, which is not substantially different from rates reported for neonates who are similarly exposed but not treated with VZIG. However, the occurrence of complications and fatal outcomes is substantially lower for neonates who are treated with VZIG than for those who are not.
# RECOMMENDATIONS FOR THE USE OF VZIG
# Persons <13 Years of Age
Immunocompromised children. VZIG primarily is used for passive immunization of susceptible, immunocompromised children after substantial exposure to varicella or herpes zoster-including children who a) have primary and acquired immunedeficiency disorders, b) have neoplastic diseases, and c) are receiving immunosuppressive treatment.
Data are limited regarding whether routine therapy with intravenous IG yields the persistence of a sufficient amount of passively acquired VZV antibody to protect susceptible, immunocompromised persons who become exposed to VZV. Data from one study indicated that three of 17 HIV-infected children in whom varicella developed were receiving regular intravenous IG and had detectable antibody against varicella (117 ). One of the three children had been treated with VZIG after two previous exposures to varicella that did not result in disease but was not administered VZIG after an unrecognized exposure, which resulted in varicella. To ensure protection against severe disease, immunocompromised persons receiving intravenous IG should be administered VZIG if exposed to wild-type VZV.
Neonates whose mothers become infected with varicella shortly before delivery. VZIG is indicated for neonates whose mothers have signs and symptoms of varicella within 5 days before and 2 days after delivery. VZIG is probably not necessary for neonates whose mothers have signs and symptoms of varicella >5 days before delivery, because those infants should be protected from severe varicella by transplacentally acquired maternal antibody. No evidence exists suggesting that infants born to mothers in whom varicella develops >48 hours after delivery are at increased risk for serious complications (e.g., pneumonia or death).
Postnatal exposure of neonates. Transmission of varicella in the hospital nursery is rare because most neonates are protected by maternal antibody. Premature infants who have substantial postnatal exposure should be evaluated on an individual basis. The risk for complications of postnatally acquired varicella in premature infants is unknown. Because the immune systems of premature infants may be compromised, administration of VZIG to those who are exposed and born to susceptible mothers may be prudent. These infants should be considered at risk for as long as they are hospitalized. Premature infants who are <28 weeks' gestation or who weigh ≤1,000 g at birth who are exposed to VZV should receive VZIG, regardless of maternal history, because such infants may not have acquired maternal antibody. Most premature infants of ≥28 weeks' gestation born to immune mothers have enough acquired maternal antibody to protect them from severe disease and complications.
Although infants are at higher risk for serious and fatal complications than are older children, the risk for healthy, full-term infants who develop varicella following postnatal exposure is substantially less than for infants whose mothers were infected 5 days before to 2 days after delivery. VZIG is not recommended for healthy, full-term infants who are exposed postnatally, even if their mothers have no history of varicella infection.
# Persons ≥13 Years of Age
Rates of complications and death for immunocompromised adolescents and adults in whom varicella develops are higher than those for healthy adolescents and adults. To prevent complications, immunocompromised persons who are considered susceptible and who have had substantial exposure to varicella should receive VZIG. The rationale for the use of VZIG among adolescent and adult patients routinely treated with intravenous IG (IVIG) is equivalent to that for the use of VZIG among immunocompromised children (see Immunocompromised Children).
Varicella is usually more severe in otherwise healthy adolescents or adults than in healthy children. The decision to administer VZIG to susceptible, healthy adolescents and adults should be made on an individual basis. The objective of using VZIG among healthy adolescents and adults is to modify, rather than to prevent, illness with the hope of inducing lifetime immunity. When deciding whether to administer VZIG, clinicians should consider the patients' health status, the type of exposure, and the likelihood of previous varicella infection. Adults who were older siblings in large families or whose children have had varicella likely are immune. If, after careful evaluation, a healthy, unvaccinated adolescent or adult who has had substantial exposure is determined as being susceptible, VZIG can be considered. If varicella is prevented through the use of VZIG, vaccination should be offered later. As the use of varicella virus vaccine becomes widespread, the demand for VZIG should decrease.
Pregnant women. Pregnant women should be evaluated in the same manner as other adults; however, because such women are at higher risk for severe varicella and complications (8,13,118 ), VZIG should be strongly considered for susceptible pregnant women who have been exposed. Administration of VZIG to susceptible, pregnant women has not been found to prevent viremia, fetal infection, congenital varicella syndrome, or neonatal varicella. Thus, the primary indication for VZIG in pregnant women is to prevent complications of varicella in the mother, rather than to protect the fetus. VZIG may extend the incubation period of the virus from 10-21 days to ≥28 days. Neonates born to mothers who have signs and symptoms of varicella within 5 days preceding or 2 days after delivery should receive VZIG-regardless of whether the mother received VZIG.
Hospital personnel. Varicella virus vaccine is recommended for all susceptible hospital personnel; widespread use of the vaccine should limit the need for VZIG in this setting. If exposed, hospital personnel who have negative or uncertain histories of varicella and no history of vaccination should be evaluated in the same manner as other adults. In addition, types of exposure and histories of prior exposure to patients with varicella should be considered before administration of VZIG. Serologic testing also may help in assessing whether to administer VZIG and in determining whether work restrictions are necessary during the incubation period. In general, the same control measures apply-regardless of whether susceptible personnel or patients receive VZIG. Because VZIG can prolong the incubation period of the virus, the period of removal from direct patient contact should be extended at least 1 week.
# VZIG-ASSOCIATED ADVERSE EVENTS AND PRECAUTIONS
The most frequent adverse reaction following VZIG administration is local discomfort at the injection site. Pain, redness, and swelling occur at the injection site in approximately 1% of persons. Less frequent adverse events include gastrointestinal symptoms, malaise, headache, rash, and respiratory symptoms, which occur in approximately 0.2% of recipients. Severe events, such as angioneurotic edema and anaphylactic shock, are rare (i.e., occurring in approximately <0.1% of recipients).
VZIG may be indicated for patients who have severe thrombocytopenia or any other coagulation disorder that would ordinarily be a contraindication to intramuscular injections. In this circumstance, the expected benefits of administering this biologic usually outweigh the risks.
# FUTURE CONCERNS
As the use of varicella virus vaccine increases, the epidemiologic features of the disease are expected to change. The circulation of wild-type VZV is not currently affected by the use of the vaccine. Under present conditions, antibody to varicella has been demonstrated to persist for 6-10 years following vaccination in children; however, the extent to which longer-term immunity may wane is unknown. The importance of immunologic boosting following exogenous reexposure to VZV to the long-term persistence of both humoral and cell-mediated immunity to varicella is unknown. The significance of the loss of natural boosting in relation to the incidence of herpes zoster in persons who were vaccinated or exposed to wild-type virus is also unknown. Increased antibody levels have been observed in vaccinees following exposure to natural varicella; however, opportunities for immunologic boosting will be greatly reduced with widespread use of the vaccine. Revaccination 4-6 years after initial vaccination also has resulted in a boost in antibody levels. In addition, the changes in epidemiology of varicella resulting from the widespread use of vaccine in younger children are expected to decrease the circulation of wild-type virus and may establish a population of older children who were neither vaccinated nor exposed to wild-type virus, eventually resulting in a population of adults who are susceptible to varicella. School requirements for varicella immunization are possible mechanisms to ultimately prevent an increase in the population of susceptible adults. To foster more rapid control of varicella and achieve high immunity levels, state legislatures may consider including varicella vaccination in their requirements for entry into school and Head Start or day care programs. Before instituting these or other such requirements, the distribution of and access to varicella virus vaccine should be determined as adequate to accomplish universal vaccination of those children subjected to the requirements.
The need for any changes in vaccine use will be determined by both postmarketing surveillance (conducted by the manufacturer of the vaccine) and ongoing surveillance (conducted by CDC). Presently, only 4%-5% of expected cases of varicella are reported annually to NNDSS. Enhanced surveillance, focused on improvement in the proportion of cases reported and the type of information obtained (including vaccination status), is needed to monitor the impact of vaccination on the incidence of varicella, the age distribution and other demographic features of infected persons, and the associated morbidity and mortality. Several active-surveillance sites have been established to provide this information until the widespread use of the vaccine reduces incidence to a manageable level and varicella becomes a nationally reportable disease.
# Summary of Recommendations for Varicella Vaccination PERSONS <13 YEARS OF AGE
• Persons of this age group should receive one 0.5-mL dose of vaccine subcutaneously.
• Children who have not been vaccinated previously and who lack a reliable history of varicella infection are considered susceptible.
# 12-18 Months of Age
• All children should be routinely vaccinated at 12-18 months of age. Varicella virus vaccine may be administered to all children at this age regardless of prior history of varicella; however, vaccination is not necessary for children who have reliable histories of varicella.
19 Months-12 Years of Age • Varicella vaccine is recommended for immunization of all susceptible children by the 13th birthday.
• Varicella virus vaccine should be administered to susceptible children during the routine immunization visit at 11-12 years of age but may be administered at any time during childhood.
# PERSONS ≥13 YEARS OF AGE
• Persons in this age group should be administered two 0.5-mL doses of vaccine, subcutaneously, 4-8 weeks apart.
• Vaccination is recommended for susceptible persons who have close contact with persons at high risk for serious complications (e.g., health-care workers and family contacts of immunocompromised persons).
• Vaccination should be considered for susceptible persons in the following groups who are at high risk for exposure: a) Persons who live or work in environments in which transmission of VZV is likely (e.g., teachers of young children, day-care employees, and residents and staff in institutional settings). b) Persons who live or work in environments in which varicella transmission can occur (e.g., college students, inmates and staff of correctional institutions, and military personnel). c) Nonpregnant women of childbearing age. Vaccination of women who are not pregnant-but who may become pregnant in the future-will reduce the risk for VZV transmission to the fetus. Varicella immunity may be ascertained at any routine health-care visit or in any setting in which vaccination history may be reviewed (e.g., upon college entry). Women should be asked if they are pregnant and advised to avoid pregnancy for 1 month following each dose of vaccine.
# Acknowledgment
The authors thank the following former members of the Advisory Committee on Immunization Practices and the associated liaison groups who were members of the Varicella Working Group
# Summary of Recommendations for Varicella
Vaccination -Continued d) International travelers. Vaccination should be considered for international travelers who do not have evidence of immunity to VZV (e.g., serologic tests), especially if the traveler expects to have close personal contact with local populations, because varicella is endemic in most countries.
• Vaccination of other susceptible adolescents and adults is desirable and may be offered during routine health-care visits. | None | None |
8b8a0df1a3d37ae59f20497dec6ad1620faa7cdb | cdc | None | AGE GROUP 19-21 years 22-26 years 27-49 years 50-59 years 60-64 years ≥ 65 years Influenza *,2 Tetanus, diphtheria, pertussis (Td/Tdap) *,3 Varicella *,4 Human papillomavirus (HPV) Female *,5 Human papillomavirus (HPV) Male *,5 Zoster 6 Measles, mumps, rubella (MMR) *,7 Pneumococcal 13-valent conjugate (PCV13) *,8 Pneumococcal 23-valent polysaccharide (PPSV23) 8 Hepatitis A *,9 Hepatitis B *,10 Meningococcal 4-valent conjugate (MenACWY) or polysaccharide (MPSV4) *,11 Meningococcal B (MenB) 11 Haemophilus influenzae type b (Hib) *,12 *Covered by the Vaccine Injury Compensation Program 3 doses 1 or 3 doses depending on indication 2 or 3 doses depending on vaccine 1 or more doses depending on indication 2 or 3 doses depending on vaccine 1 dose 1 or 2 doses depending on indication 1 dose 3 doses 2 doses Substitute Tdap for Td once, then Td booster every 10 yrs 1 dose annually Recommended for all persons who meet the age requirement, lack documentation of vaccination, or lack evidence of past infection; zoster vaccine is recommended regardless of past episode of zoster Recommended for persons with a risk factor (medical, occupational, lifestyle, or other indication) No recommendationNote: These recommendations must be read with the footnotes that follow containing number of doses, intervals between doses, and other important information.#
Report all clinically significant postvaccination reactions to the Vaccine Adverse Event Reporting System (VAERS). Reporting forms and instructions on filing a VAERS report are available at www.vaers.hhs.gov or by telephone, 800-822-7967.
Information on how to file a Vaccine Injury Compensation Program claim is available at www.hrsa.gov/vaccinecompensation or by telephone, 800-338-2382. To file a claim for vaccine injury, contact the U.S. Court of Federal Claims, 717 Madison Place, N.W., Washington, D.C. 20005;telephone, 202-357-6400.
Additional information about the vaccines in this schedule, extent of available data, and contraindications for vaccination is also available at www.cdc.gov/vaccines or from the CDC-INFO Contact Center at 800-CDC- in English and Spanish, 8:00 a.m. -8:00 p.m. Eastern Time, Monday -Friday, excluding holidays.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services.
The recommendations in this schedule were approved by the Centers for Disease Control and Prevention's (CDC) Advisory Committee on Immunization Practices (ACIP), the American Academy of Family Physicians (AAFP), the America College of Physicians (ACP), the American College of Obstetricians and Gynecologists (ACOG) and the American College of Nurse-Midwives (ACNM).
# VACCINE INDICATION Pregnancy
Immunocompromising conditions (excluding HIV infection) 4,6,7,8,13 HIV infection CD4+ count (cells/μL) 4,6,7,8,13 Influenza *,2 Tetanus, diphtheria, pertussis (Td/Tdap) *,3
Varicella *,4 Human papillomavirus (HPV) Female *,5 Human papillomavirus (HPV) Male *,5 Zoster 6
Measles, mumps, rubella (MMR) *,7 Pneumococcal 13-valent conjugate (PCV13) *,8 Pneumococcal polysaccharide (PPSV23) 8 Hepatitis A *,9 Hepatitis B *,10 Meningococcal 4-valent conjugate (MenACWY) or polysaccharide (MPSV4) *,11 Meningococcal B (MenB) 11
Haemophilus influenzae type b (Hib) *,12 These schedules indicate the recommended age groups and medical indications for which administration of currently licensed vaccines is commonly recommended for adults aged ≥19 years, as of February 2016. For all vaccines being recommended on the Adult Immunization Schedule: a vaccine series does not need to be restarted, regardless of the time that has elapsed between doses. Licensed combination vaccines may be used whenever any components of the combination are indicated and when the vaccine's other components are not contraindicated. For detailed recommendations on all vaccines, including those used primarily for travelers or that are issued during the year, consult the manufacturers' package inserts and the complete statements from the Advisory Committee on Immunization Practices (www.cdc.gov/vaccines/hcp/acip-recs/index.html). Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services.
# dose 3 doses post-HSCT recipients only
Recommended for all persons who meet the age requirement, lack documentation of vaccination, or lack evidence of past infection; zoster vaccine is recommended regardless of past episode of zoster vaccine status is unknown should receive a dose of Tdap followed by tetanus and diphtheria toxoids (Td) booster doses every 10 years thereafter. Tdap can be administered regardless of interval since the most recent tetanus or diphtheriatoxoid-containing vaccine. - Adults with an unknown or incomplete history of completing a 3-dose primary vaccination series with Td-containing vaccines should begin or complete a primary vaccination series including a Tdap dose. - For unvaccinated adults, administer the first 2 doses at least 4 weeks apart and the third dose 6-12 months after the second. - For incompletely vaccinated (i.e., less than 3 doses) adults, administer remaining doses. - Refer to the ACIP statement for recommendations for administering Td/Tdap as prophylaxis in wound management (see footnote 1).
# Varicella vaccination
- All adults without evidence of immunity to varicella (as defined below) should receive 2 doses of single-antigen varicella vaccine or a second dose if they have received only 1 dose. - Vaccination should be emphasized for those who have close contact with persons at high risk for severe disease (e.g., health care personnel and family contacts of persons with immunocompromising conditions) or are at high risk for exposure or transmission (e.g., teachers; child care employees; residents and staff members of institutional settings, including correctional institutions; college students; military personnel; adolescents and adults living in households with children; nonpregnant women of childbearing age; and international travelers). - Pregnant women should be assessed for evidence of varicella immunity. Women who do not have evidence of immunity should receive the first dose of varicella vaccine upon completion or termination of pregnancy and before discharge from the health care facility. The second dose should be administered 4-8 weeks after the first dose. - Evidence of immunity to varicella in adults includes any of the following: -documentation of 2 doses of varicella vaccine at least 4 weeks apart; -U.S.-born before 1980, except health care personnel and pregnant women; -history of varicella based on diagnosis or verification of varicella disease by a health care provider; -history of herpes zoster based on diagnosis or verification of herpes zoster disease by a health care provider; or laboratory evidence of immunity or laboratory confirmation of disease.
# Human papillomavirus (HPV) vaccination
- Three HPV vaccines are licensed for use in females (bivalent HPV vaccine , quadrivalent HPV vaccine , and 9-valent HPV vaccine ) and two HPV vaccines are licensed for use in males (4vHPV and 9vHPV). - For females, 2vHPV, 4vHPV, or 9vHPV is recommended in a 3-dose series for routine vaccination at age 11 or 12 years and for those aged 13 through 26 years, if not previously vaccinated. - For males, 4vHPV or 9vHPV is recommended in a 3-dose series for routine vaccination at age 11 or 12 years and for those aged 13 through 21 years, if not previously vaccinated. Males aged 22 through 26 years may be vaccinated. - HPV vaccination is recommended for men who have sex with men through age 26 years who did not get any or all doses when they were younger. - Vaccination is recommended for immunocompromised persons (including those with HIV infection) through age 26 years who did not get any or all doses when they were younger. - A complete HPV vaccination series consists of 3 doses. The second dose should be administered 4-8 weeks (minimum interval of 4 weeks) after the first dose; the third dose should be administered 24 weeks after the first dose and 16 weeks after the second dose (minimum interval of 12 weeks).
- HPV vaccines are not recommended for use in pregnant women. However, pregnancy testing is not needed before vaccination. If a woman is found to be pregnant after initiating the vaccination series, no intervention is needed; the remainder of the 3-dose series should be delayed until completion or termination of pregnancy.
# Zoster vaccination
- A single dose of zoster vaccine is recommended for adults aged ≥60 years regardless of whether they report a prior episode of herpes zoster. Although the vaccine is licensed by the U.S. Food and Drug Administration for use among and can be administered to persons aged ≥50 years, ACIP recommends that vaccination begin at age 60 years. - Persons aged ≥60 years with chronic medical conditions may be vaccinated unless their condition constitutes a contraindication, such as pregnancy or severe immunodeficiency.
# Measles, mumps, rubella (MMR) vaccination
- Adults born before 1957 are generally considered immune to measles and mumps.
All adults born in 1957 or later should have documentation of 1 or more doses of MMR vaccine unless they have a medical contraindication to the vaccine or laboratory evidence of immunity to each of the three diseases. Documentation of provider-diagnosed disease is not considered acceptable evidence of immunity for measles, mumps, or rubella. heart failure and cardiomyopathies, excluding hypertension), chronic lung disease (including chronic obstructive lung disease, emphysema, and asthma), chronic liver disease (including cirrhosis), alcoholism, or diabetes mellitus, or who smoke cigarettes: administer PPSV23. At age ≥65 years, administer PCV13 at least 1 year after PPSV23, followed by another dose of PPSV23 at least 1 year after PCV13 and at least 5 years after the last dose of PPSV23. - Routine pneumococcal vaccination is not recommended for American Indian/ Alaska Native or other adults unless they have an indication as above; however, public health authorities may consider recommending the use of pneumococcal vaccines for American Indians/Alaska Natives or other adults who live in areas with increased risk for invasive pneumococcal disease.
# Hepatitis A vaccination
- Vaccinate any person seeking protection from hepatitis A virus (HAV) infection and persons with any of the following indications:
men who have sex with men; -persons who use injection or noninjection illicit drugs; -persons working with HAV-infected primates or with HAV in a research laboratory setting; -persons with chronic liver disease and persons who receive clotting factor concentrates; -persons traveling to or working in countries that have high or intermediate endemicity of hepatitis A (see footnote 1); and unvaccinated persons who anticipate close personal contact (e.g., household or regular babysitting) with an international adoptee during the first 60 days after arrival in the United States from a country with high or intermediate endemicity of hepatitis A (see footnote 1). The first dose of the 2-dose hepatitis A vaccine series should be administered as soon as adoption is planned, ideally 2 or more weeks before the arrival of the adoptee. - Single-antigen vaccine formulations should be administered in a 2-dose schedule at either 0 and 6-12 months (Havrix), or 0 and 6-18 months (Vaqta). If the combined hepatitis A and hepatitis B vaccine (Twinrix) is used, administer 3 doses at 0, 1, and 6 months; alternatively, a 4-dose schedule may be used, administered on days 0, 7, and 21-30 followed by a booster dose at 12 months.
# Hepatitis B vaccination
- Vaccinate any person seeking protection from hepatitis B virus (HBV) infection and persons with any of the following indications:
sexually active persons who are not in a long-term, mutually monogamous relationship (e.g., persons with more than 1 sex partner during the previous 6 months); persons seeking evaluation or treatment for a sexually transmitted disease (STD); current or recent injection drug users; and men who have sex with men; -health care personnel and public safety workers who are potentially exposed to blood or other infectious body fluids; -persons who are aged <60 years with diabetes as soon as feasible after diagnosis; persons with diabetes who are aged ≥60 years at the discretion of the treating clinician based on the likelihood of acquiring HBV infection, including the risk posed by an increased need for assisted blood glucose monitoring in long-term care facilities, the likelihood of experiencing chronic sequelae if infected with HBV, and the likelihood of immune response to vaccination; -persons with end-stage renal disease (including patients receiving hemodialysis), persons with HIV infection, and persons with chronic liver disease; -household contacts and sex partners of hepatitis B surface antigenpositive persons, clients and staff members of institutions for persons with developmental disabilities, and international travelers to regions with high or intermediate levels of endemic HBV infection (see footnote 1); and all adults in the following settings: STD treatment facilities, HIV testing and treatment facilities, facilities providing drug abuse treatment and prevention services, health care settings targeting services to injection drug users or men who have sex with men, correctional facilities, end-stage renal disease programs and facilities for chronic hemodialysis patients, and institutions and nonresidential day care facilities for persons with developmental disabilities. - Administer missing doses to complete a 3-dose series of hepatitis B vaccine to those persons not vaccinated or not completely vaccinated. The second dose should be administered at least 1 month after the first dose; the third dose should be administered at least 2 months after the second dose (and at least 4 months after the first dose). If the combined hepatitis A and hepatitis B vaccine (Twinrix) is used, give 3 doses at 0, 1, and 6 months; alternatively, a 4-dose Twinrix schedule may be used, administered on days 0, 7, and 21-30, followed by a booster dose at 12 months. - Adult patients receiving hemodialysis or with other immunocompromising conditions should receive 1 dose of 40 mcg/mL (Recombivax HB) administered on a 3-dose schedule at 0, 1, and 6 months or 2 doses of 20 mcg/mL (Engerix-B) administered simultaneously on a 4-dose schedule at 0, 1, 2, and 6 months.
# Meningococcal vaccination
- - First-year college students aged ≤21 years who live in residence halls: administer a single dose of MenACWY vaccine if they have not received a dose on or after their 16 th birthday. - Young adults aged 16 through 23 years (preferred age range is 16 through 18 years): may be vaccinated with a series of MenB vaccine to provide short-term protection against most strains of serogroup B meningococcal disease.
# Haemophilus influenzae type b (Hib) vaccination
- One dose of Hib vaccine should be administered to persons who have anatomical or functional asplenia or sickle cell disease or are undergoing elective splenectomy if they have not previously received Hib vaccine. Hib vaccination 14 or more days before splenectomy is suggested. - Recipients of a hematopoietic stem cell transplant (HSCT) should be vaccinated with a 3-dose regimen 6-12 months after a successful transplant, regardless of vaccination history; at least 4 weeks should separate doses. - Hib vaccine is not recommended for adults with HIV infection since their risk for Hib infection is low.
# Immunocompromising conditions
- Inactivated vaccines (e.g., pneumococcal, meningococcal, and inactivated influenza vaccines) generally are acceptable and live vaccines generally should be avoided in persons with immune deficiencies or immunocompromising conditions. Information on specific conditions is available at www.cdc.gov/ vaccines/hcp/acip-recs/index.html. | AGE GROUP 19-21 years 22-26 years 27-49 years 50-59 years 60-64 years ≥ 65 years Influenza *,2 Tetanus, diphtheria, pertussis (Td/Tdap) *,3 Varicella *,4 Human papillomavirus (HPV) Female *,5 Human papillomavirus (HPV) Male *,5 Zoster 6 Measles, mumps, rubella (MMR) *,7 Pneumococcal 13-valent conjugate (PCV13) *,8 Pneumococcal 23-valent polysaccharide (PPSV23) 8 Hepatitis A *,9 Hepatitis B *,10 Meningococcal 4-valent conjugate (MenACWY) or polysaccharide (MPSV4) *,11 Meningococcal B (MenB) 11 Haemophilus influenzae type b (Hib) *,12 *Covered by the Vaccine Injury Compensation Program 3 doses 1 or 3 doses depending on indication 2 or 3 doses depending on vaccine 1 or more doses depending on indication 2 or 3 doses depending on vaccine 1 dose 1 or 2 doses depending on indication 1 dose 3 doses 2 doses Substitute Tdap for Td once, then Td booster every 10 yrs 1 dose annually Recommended for all persons who meet the age requirement, lack documentation of vaccination, or lack evidence of past infection; zoster vaccine is recommended regardless of past episode of zoster Recommended for persons with a risk factor (medical, occupational, lifestyle, or other indication) No recommendationNote: These recommendations must be read with the footnotes that follow containing number of doses, intervals between doses, and other important information.#
Report all clinically significant postvaccination reactions to the Vaccine Adverse Event Reporting System (VAERS). Reporting forms and instructions on filing a VAERS report are available at www.vaers.hhs.gov or by telephone, 800-822-7967.
Information on how to file a Vaccine Injury Compensation Program claim is available at www.hrsa.gov/vaccinecompensation or by telephone, 800-338-2382. To file a claim for vaccine injury, contact the U.S. Court of Federal Claims, 717 Madison Place, N.W., Washington, D.C. 20005;telephone, 202-357-6400.
Additional information about the vaccines in this schedule, extent of available data, and contraindications for vaccination is also available at www.cdc.gov/vaccines or from the CDC-INFO Contact Center at 800-CDC- in English and Spanish, 8:00 a.m. -8:00 p.m. Eastern Time, Monday -Friday, excluding holidays.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services.
The recommendations in this schedule were approved by the Centers for Disease Control and Prevention's (CDC) Advisory Committee on Immunization Practices (ACIP), the American Academy of Family Physicians (AAFP), the America College of Physicians (ACP), the American College of Obstetricians and Gynecologists (ACOG) and the American College of Nurse-Midwives (ACNM).
# VACCINE INDICATION Pregnancy
Immunocompromising conditions (excluding HIV infection) 4,6,7,8,13 HIV infection CD4+ count (cells/μL) 4,6,7,8,13 Influenza *,2 Tetanus, diphtheria, pertussis (Td/Tdap) *,3
Varicella *,4 Human papillomavirus (HPV) Female *,5 Human papillomavirus (HPV) Male *,5 Zoster 6
Measles, mumps, rubella (MMR) *,7 Pneumococcal 13-valent conjugate (PCV13) *,8 Pneumococcal polysaccharide (PPSV23) 8 Hepatitis A *,9 Hepatitis B *,10 Meningococcal 4-valent conjugate (MenACWY) or polysaccharide (MPSV4) *,11 Meningococcal B (MenB) 11
Haemophilus influenzae type b (Hib) *,12 These schedules indicate the recommended age groups and medical indications for which administration of currently licensed vaccines is commonly recommended for adults aged ≥19 years, as of February 2016. For all vaccines being recommended on the Adult Immunization Schedule: a vaccine series does not need to be restarted, regardless of the time that has elapsed between doses. Licensed combination vaccines may be used whenever any components of the combination are indicated and when the vaccine's other components are not contraindicated. For detailed recommendations on all vaccines, including those used primarily for travelers or that are issued during the year, consult the manufacturers' package inserts and the complete statements from the Advisory Committee on Immunization Practices (www.cdc.gov/vaccines/hcp/acip-recs/index.html). Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services.
# dose 3 doses post-HSCT recipients only
Recommended for all persons who meet the age requirement, lack documentation of vaccination, or lack evidence of past infection; zoster vaccine is recommended regardless of past episode of zoster vaccine status is unknown should receive a dose of Tdap followed by tetanus and diphtheria toxoids (Td) booster doses every 10 years thereafter. Tdap can be administered regardless of interval since the most recent tetanus or diphtheriatoxoid-containing vaccine. • Adults with an unknown or incomplete history of completing a 3-dose primary vaccination series with Td-containing vaccines should begin or complete a primary vaccination series including a Tdap dose. • For unvaccinated adults, administer the first 2 doses at least 4 weeks apart and the third dose 6-12 months after the second. • For incompletely vaccinated (i.e., less than 3 doses) adults, administer remaining doses. • Refer to the ACIP statement for recommendations for administering Td/Tdap as prophylaxis in wound management (see footnote 1).
# Varicella vaccination
• All adults without evidence of immunity to varicella (as defined below) should receive 2 doses of single-antigen varicella vaccine or a second dose if they have received only 1 dose. • Vaccination should be emphasized for those who have close contact with persons at high risk for severe disease (e.g., health care personnel and family contacts of persons with immunocompromising conditions) or are at high risk for exposure or transmission (e.g., teachers; child care employees; residents and staff members of institutional settings, including correctional institutions; college students; military personnel; adolescents and adults living in households with children; nonpregnant women of childbearing age; and international travelers). • Pregnant women should be assessed for evidence of varicella immunity. Women who do not have evidence of immunity should receive the first dose of varicella vaccine upon completion or termination of pregnancy and before discharge from the health care facility. The second dose should be administered 4-8 weeks after the first dose. • Evidence of immunity to varicella in adults includes any of the following: -documentation of 2 doses of varicella vaccine at least 4 weeks apart; -U.S.-born before 1980, except health care personnel and pregnant women; -history of varicella based on diagnosis or verification of varicella disease by a health care provider; -history of herpes zoster based on diagnosis or verification of herpes zoster disease by a health care provider; or laboratory evidence of immunity or laboratory confirmation of disease.
# Human papillomavirus (HPV) vaccination
• Three HPV vaccines are licensed for use in females (bivalent HPV vaccine [2vHPV], quadrivalent HPV vaccine [4vHPV], and 9-valent HPV vaccine [9vHPV]) and two HPV vaccines are licensed for use in males (4vHPV and 9vHPV). • For females, 2vHPV, 4vHPV, or 9vHPV is recommended in a 3-dose series for routine vaccination at age 11 or 12 years and for those aged 13 through 26 years, if not previously vaccinated. • For males, 4vHPV or 9vHPV is recommended in a 3-dose series for routine vaccination at age 11 or 12 years and for those aged 13 through 21 years, if not previously vaccinated. Males aged 22 through 26 years may be vaccinated. • HPV vaccination is recommended for men who have sex with men through age 26 years who did not get any or all doses when they were younger. • Vaccination is recommended for immunocompromised persons (including those with HIV infection) through age 26 years who did not get any or all doses when they were younger. • A complete HPV vaccination series consists of 3 doses. The second dose should be administered 4-8 weeks (minimum interval of 4 weeks) after the first dose; the third dose should be administered 24 weeks after the first dose and 16 weeks after the second dose (minimum interval of 12 weeks).
• HPV vaccines are not recommended for use in pregnant women. However, pregnancy testing is not needed before vaccination. If a woman is found to be pregnant after initiating the vaccination series, no intervention is needed; the remainder of the 3-dose series should be delayed until completion or termination of pregnancy.
# Zoster vaccination
• A single dose of zoster vaccine is recommended for adults aged ≥60 years regardless of whether they report a prior episode of herpes zoster. Although the vaccine is licensed by the U.S. Food and Drug Administration for use among and can be administered to persons aged ≥50 years, ACIP recommends that vaccination begin at age 60 years. • Persons aged ≥60 years with chronic medical conditions may be vaccinated unless their condition constitutes a contraindication, such as pregnancy or severe immunodeficiency.
# Measles, mumps, rubella (MMR) vaccination
• Adults born before 1957 are generally considered immune to measles and mumps.
All adults born in 1957 or later should have documentation of 1 or more doses of MMR vaccine unless they have a medical contraindication to the vaccine or laboratory evidence of immunity to each of the three diseases. Documentation of provider-diagnosed disease is not considered acceptable evidence of immunity for measles, mumps, or rubella. heart failure and cardiomyopathies, excluding hypertension), chronic lung disease (including chronic obstructive lung disease, emphysema, and asthma), chronic liver disease (including cirrhosis), alcoholism, or diabetes mellitus, or who smoke cigarettes: administer PPSV23. At age ≥65 years, administer PCV13 at least 1 year after PPSV23, followed by another dose of PPSV23 at least 1 year after PCV13 and at least 5 years after the last dose of PPSV23. • Routine pneumococcal vaccination is not recommended for American Indian/ Alaska Native or other adults unless they have an indication as above; however, public health authorities may consider recommending the use of pneumococcal vaccines for American Indians/Alaska Natives or other adults who live in areas with increased risk for invasive pneumococcal disease.
# Hepatitis A vaccination
• Vaccinate any person seeking protection from hepatitis A virus (HAV) infection and persons with any of the following indications:
men who have sex with men; -persons who use injection or noninjection illicit drugs; -persons working with HAV-infected primates or with HAV in a research laboratory setting; -persons with chronic liver disease and persons who receive clotting factor concentrates; -persons traveling to or working in countries that have high or intermediate endemicity of hepatitis A (see footnote 1); and unvaccinated persons who anticipate close personal contact (e.g., household or regular babysitting) with an international adoptee during the first 60 days after arrival in the United States from a country with high or intermediate endemicity of hepatitis A (see footnote 1). The first dose of the 2-dose hepatitis A vaccine series should be administered as soon as adoption is planned, ideally 2 or more weeks before the arrival of the adoptee. • Single-antigen vaccine formulations should be administered in a 2-dose schedule at either 0 and 6-12 months (Havrix), or 0 and 6-18 months (Vaqta). If the combined hepatitis A and hepatitis B vaccine (Twinrix) is used, administer 3 doses at 0, 1, and 6 months; alternatively, a 4-dose schedule may be used, administered on days 0, 7, and 21-30 followed by a booster dose at 12 months.
# Hepatitis B vaccination
• Vaccinate any person seeking protection from hepatitis B virus (HBV) infection and persons with any of the following indications:
sexually active persons who are not in a long-term, mutually monogamous relationship (e.g., persons with more than 1 sex partner during the previous 6 months); persons seeking evaluation or treatment for a sexually transmitted disease (STD); current or recent injection drug users; and men who have sex with men; -health care personnel and public safety workers who are potentially exposed to blood or other infectious body fluids; -persons who are aged <60 years with diabetes as soon as feasible after diagnosis; persons with diabetes who are aged ≥60 years at the discretion of the treating clinician based on the likelihood of acquiring HBV infection, including the risk posed by an increased need for assisted blood glucose monitoring in long-term care facilities, the likelihood of experiencing chronic sequelae if infected with HBV, and the likelihood of immune response to vaccination; -persons with end-stage renal disease (including patients receiving hemodialysis), persons with HIV infection, and persons with chronic liver disease; -household contacts and sex partners of hepatitis B surface antigenpositive persons, clients and staff members of institutions for persons with developmental disabilities, and international travelers to regions with high or intermediate levels of endemic HBV infection (see footnote 1); and all adults in the following settings: STD treatment facilities, HIV testing and treatment facilities, facilities providing drug abuse treatment and prevention services, health care settings targeting services to injection drug users or men who have sex with men, correctional facilities, end-stage renal disease programs and facilities for chronic hemodialysis patients, and institutions and nonresidential day care facilities for persons with developmental disabilities. • Administer missing doses to complete a 3-dose series of hepatitis B vaccine to those persons not vaccinated or not completely vaccinated. The second dose should be administered at least 1 month after the first dose; the third dose should be administered at least 2 months after the second dose (and at least 4 months after the first dose). If the combined hepatitis A and hepatitis B vaccine (Twinrix) is used, give 3 doses at 0, 1, and 6 months; alternatively, a 4-dose Twinrix schedule may be used, administered on days 0, 7, and 21-30, followed by a booster dose at 12 months. • Adult patients receiving hemodialysis or with other immunocompromising conditions should receive 1 dose of 40 mcg/mL (Recombivax HB) administered on a 3-dose schedule at 0, 1, and 6 months or 2 doses of 20 mcg/mL (Engerix-B) administered simultaneously on a 4-dose schedule at 0, 1, 2, and 6 months.
# Meningococcal vaccination
• • First-year college students aged ≤21 years who live in residence halls: administer a single dose of MenACWY vaccine if they have not received a dose on or after their 16 th birthday. • Young adults aged 16 through 23 years (preferred age range is 16 through 18 years): may be vaccinated with a series of MenB vaccine to provide short-term protection against most strains of serogroup B meningococcal disease.
# Haemophilus influenzae type b (Hib) vaccination
• One dose of Hib vaccine should be administered to persons who have anatomical or functional asplenia or sickle cell disease or are undergoing elective splenectomy if they have not previously received Hib vaccine. Hib vaccination 14 or more days before splenectomy is suggested. • Recipients of a hematopoietic stem cell transplant (HSCT) should be vaccinated with a 3-dose regimen 6-12 months after a successful transplant, regardless of vaccination history; at least 4 weeks should separate doses. • Hib vaccine is not recommended for adults with HIV infection since their risk for Hib infection is low.
# Immunocompromising conditions
• Inactivated vaccines (e.g., pneumococcal, meningococcal, and inactivated influenza vaccines) generally are acceptable and live vaccines generally should be avoided in persons with immune deficiencies or immunocompromising conditions. Information on specific conditions is available at www.cdc.gov/ vaccines/hcp/acip-recs/index.html. | None | None |
46834bdbafc386ce39ecd4c7df631cd18bec5540 | cdc | None | Division of Criteria Documentation and Standards Development, National Institute for Occupational Safety and Health, had primary responsibility for the development of the criteria and recommended standard for Nitroglycerin and Ethylene Glycol Dinitrate. Anthony E. Romero of this Division served as criteria manager. SRI International developed the basic information for consideration by NIOSH staff and consultants under contract CDC-99-74-31. The Division review of this document was provided by J.#
(e) Employees who may be occupationally exposed to NG or EGDN shall be counseled by the physician so that each is aware that headache, dizziness, palpitations, and nausea are symptoms of overexposure, that these symptoms usually become worse when alcohol is used, and that some of these symptoms may disappear with continued exposure as tolerance develops.
Employees shall be warned that symptoms, such as headache, palpitations, and chest pain, can occur, particularly on weekends, on holidays, or at the beginning of the workweek, as a result of interruption of exposure to NG or EGDN. They shall be advised to consult a physician promptly if they experience such symptoms.
# If respiratory protection is required in accordance with
To determine the type of respirator to be used, the employer shall measure the concentration of airborne NG or EGDN in the workplace initially and thereafter whenever control, process, operation, worksite, or climatic changes occur that are likely to increase the concentration of these compounds in the air of the workplace.
(2) The employer shall ensure that no employee is exposed to NG or EGDN at concentrations above the recommended limit because of improper respirator selection, fit, use, or maintenance.
# (b) Ignition Sources and Detonation Hazards
The danger of explosion in buildings where NG or EGDN is manufactured or handled shall be minimized by compliance with the following provisions:
(1) Facilities should consist of detached units, with explosion-venting systems if possible.
(2) Each unit shall be subdivided by fire-and pressureresistant walls to restrict hazardous areas.
(3) The amount of NG or EGDN present in any building shall not exceed the amount being processed at any one time.
Motor-driven portable equipment, internal combustion engines, and vehicles shall not be used unless they have been approved for use in an explosive atmosphere.
# (c) Regulated Areas
Access to buildings in which NG or EGDN is manufactured or handled in liquid form or in explosive mixtures such as dynamite shall be regulated to comply with the following provisions:
(1) Access shall be restricted to authorized persons.
(2) For each such building, a limit shall be established for the number of persons who may be present, based on the minimum number necessary for efficient performance of the operation. This limit shall be posted outside the building. A log of persons entering the building should be kept in some secure location outside the building. (1) Entry into confined spaces, such as tanks, pits, or vessels, that may contain NG or EGDN shall be controlled by a permit system. Permits shall be signed by an authorized representative of the employer certifying that preventive and protective measures have been followed.
Confined spaces that have contained NG or EGDN shall be cleaned with water and purged with air. They shall be tested for NG or EGDN and other contaminants and for oxygen and inspected for compliance with these requirements prior to each entry. Adequate ventilation shall be maintained while workers are within the confined space. (2) Containers of NG or EGDN shall be kept tightly closed at all times when not in use and shall be stored in a manner that will minimize the risk of spills.
(3) Only properly informed, trained, and equipped personnel shall be involved in storing, loading and unloading, or processing liquid NG, EGDN, or explosive mixtures containing these compounds. NG and EGDN are absorbed through the lungs and the skin. Absorption through the skin is usually the major route of exposure for workers who have direct dermal contact with NG or EGDN. Thus, work practices designed to limit skin absorption of these compounds should be followed carefully.
The recommended standard for NG, EGDN, or a mixture of these two compounds is based on their effects on the cardiovascular system. The initial physiologic effect of exposure to these compounds is dilatation of the blood vessels, and the initial signs and symptoms of exposure include headache, dizziness, nausea, palpitations, and decreases in systolic, diastolic, and pulse pressures. These signs and symptoms tend to disappear after 3-4 days of repeated exposure, probably as the result of compensatory vasoconstriction. After a brief period of withdrawal from exposure, eg, a weekend, workers may develop angina pectoris. Some workers exposed to
The death was attributed to a cause other than cardiovascular disease (not specified). The AEHA concluded that only two of the seven deaths that occurred in workers employed at the Badger plant should be classified as "sudden," but their criteria may have been too stringent.
# Concentrations of airborne NG in the
# Adapted from a report of the Army Environmental Hygiene Agency
Based on three to five blood pressure readings, the AEHA concluded that there were no consistent changes in blood pressure or pulse rate, although the data were not included in the report.
The AEHA concluded that "withdrawal from chronic NG exposure could precipitate chest pain and in some instances sudden death."
The report stated that the findings from this study were not sufficient to show, however, that workplace exposure to NG can cause, or contribute to, the development of coronary artery disease.
The AEHA survey of the health of workers exposed to NG at the Badger He speculated that the "trinitrate grouping" in both of these compounds behaved as a hapten that elicited the immunologic response, although evidence supporting this idea was not provided. The possibility that cross-sensitivity also had a role in causing the rash was suggested by the authors as well.
A The results indicated that dogs apparently developed tolerance to NG, although no explanation was provided for the mechanism of action.
To determine whether short-term exposure to NG had a lasting effect on tolerance, the ED 25-mmHg was determined 7 days after the initial blood pressure measurement for three dogs that had been pretreated with 20 mg/kg In untreated bacteria, the frequency of mutation was about 0. The recommended sampling method, using a Tenax GC tube and a personal sampling pump, is described in detail in Appendix I.
The siting of magazines must conform to the requirements of the American
Each new employee should be thoroughly informed about the process, hazards, personal protective equipment, and emergency procedures.
In addition, the signs and symptoms of intoxication by the nitroesters, workers when they were no longer exposed to NG but that some signs of heart disease remained. By reviewing death certificates from a county in Sweden, Hogstedt and Axelson found that N G :EGDN dynamite workers were more likely to die from heart disease than were other men in the same county.
Twenty-one deaths from heart disease occurred in men who had been employed at the dynamite plant for 1 year or more; 4 occurred in workers who were actively employed, but the other 17 occurred in men who had not worked at the plant for months or years. "safety solvent," or "aliphatic hydrocarbon" when the specific name is known.
The "%" may be the approximate percentage by weight or volume (indicate basis) which each hazardous ingredient of the mixture bears to the whole mixture. This may be indicated as a range or maximum amount, ie, "10-40% vol" or "10% max wt" to avoid disclosure of trade secrets. | Division of Criteria Documentation and Standards Development, National Institute for Occupational Safety and Health, had primary responsibility for the development of the criteria and recommended standard for Nitroglycerin and Ethylene Glycol Dinitrate. Anthony E. Romero of this Division served as criteria manager. SRI International developed the basic information for consideration by NIOSH staff and consultants under contract CDC-99-74-31. The Division review of this document was provided by J.#
(e) Employees who may be occupationally exposed to NG or EGDN shall be counseled by the physician so that each is aware that headache, dizziness, palpitations, and nausea are symptoms of overexposure, that these symptoms usually become worse when alcohol is used, and that some of these symptoms may disappear with continued exposure as tolerance develops.
Employees shall be warned that symptoms, such as headache, palpitations, and chest pain, can occur, particularly on weekends, on holidays, or at the beginning of the workweek, as a result of interruption of exposure to NG or EGDN. They shall be advised to consult a physician promptly if they experience such symptoms.
# If respiratory protection is required in accordance with
To determine the type of respirator to be used, the employer shall measure the concentration of airborne NG or EGDN in the workplace initially and thereafter whenever control, process, operation, worksite, or climatic changes occur that are likely to increase the concentration of these compounds in the air of the workplace.
(2) The employer shall ensure that no employee is exposed to NG or EGDN at concentrations above the recommended limit because of improper respirator selection, fit, use, or maintenance.
# (b) Ignition Sources and Detonation Hazards
The danger of explosion in buildings where NG or EGDN is manufactured or handled shall be minimized by compliance with the following provisions:
(1) Facilities should consist of detached units, with explosion-venting systems if possible.
(2) Each unit shall be subdivided by fire-and pressureresistant walls to restrict hazardous areas.
(3) The amount of NG or EGDN present in any building shall not exceed the amount being processed at any one time.
Motor-driven portable equipment, internal combustion engines, and vehicles shall not be used unless they have been approved for use in an explosive atmosphere.
# (c) Regulated Areas
Access to buildings in which NG or EGDN is manufactured or handled in liquid form or in explosive mixtures such as dynamite shall be regulated to comply with the following provisions:
(1) Access shall be restricted to authorized persons.
(2) For each such building, a limit shall be established for the number of persons who may be present, based on the minimum number necessary for efficient performance of the operation. This limit shall be posted outside the building. A log of persons entering the building should be kept in some secure location outside the building. (1) Entry into confined spaces, such as tanks, pits, or vessels, that may contain NG or EGDN shall be controlled by a permit system. Permits shall be signed by an authorized representative of the employer certifying that preventive and protective measures have been followed.
(2)
Confined spaces that have contained NG or EGDN shall be cleaned with water and purged with air. They shall be tested for NG or EGDN and other contaminants and for oxygen and inspected for compliance with these requirements prior to each entry. Adequate ventilation shall be maintained while workers are within the confined space. (2) Containers of NG or EGDN shall be kept tightly closed at all times when not in use and shall be stored in a manner that will minimize the risk of spills.
(3) Only properly informed, trained, and equipped personnel shall be involved in storing, loading and unloading, or processing liquid NG, EGDN, or explosive mixtures containing these compounds. NG and EGDN are absorbed through the lungs and the skin. Absorption through the skin is usually the major route of exposure for workers who have direct dermal contact with NG or EGDN. Thus, work practices designed to limit skin absorption of these compounds should be followed carefully.
The recommended standard for NG, EGDN, or a mixture of these two compounds is based on their effects on the cardiovascular system. The initial physiologic effect of exposure to these compounds is dilatation of the blood vessels, and the initial signs and symptoms of exposure include headache, dizziness, nausea, palpitations, and decreases in systolic, diastolic, and pulse pressures. These signs and symptoms tend to disappear after 3-4 days of repeated exposure, probably as the result of compensatory vasoconstriction. After a brief period of withdrawal from exposure, eg, a weekend, workers may develop angina pectoris. Some workers exposed to
# 1968.
The death was attributed to a cause other than cardiovascular disease (not specified). The AEHA concluded that only two of the seven deaths that occurred in workers employed at the Badger plant should be classified as "sudden," but their criteria may have been too stringent.
# Concentrations of airborne NG in the
# Adapted from a report of the Army Environmental Hygiene Agency [36]
Based on three to five blood pressure readings, the AEHA concluded that there were no consistent changes in blood pressure or pulse rate, although the data were not included in the report.
The AEHA concluded that "withdrawal from chronic NG exposure could precipitate chest pain and in some instances sudden death."
The report stated that the findings from this study were not sufficient to show, however, that workplace exposure to NG can cause, or contribute to, the development of coronary artery disease.
The AEHA survey of the health of workers exposed to NG at the Badger He speculated that the "trinitrate grouping" in both of these compounds behaved as a hapten that elicited the immunologic response, although evidence supporting this idea was not provided. The possibility that cross-sensitivity also had a role in causing the rash was suggested by the authors as well.
A The results indicated that dogs apparently developed tolerance to NG, although no explanation was provided for the mechanism of action.
To determine whether short-term exposure to NG had a lasting effect on tolerance, the ED 25-mmHg was determined 7 days after the initial blood pressure measurement for three dogs that had been pretreated with 20 mg/kg In untreated bacteria, the frequency of mutation was about 0. The recommended sampling method, using a Tenax GC tube and a personal sampling pump, is described in detail in Appendix I.
# 147
The siting of magazines must conform to the requirements of the American
#
Each new employee should be thoroughly informed about the process, hazards, personal protective equipment, and emergency procedures.
In addition, the signs and symptoms of intoxication by the nitroesters, workers when they were no longer exposed to NG but that some signs of heart disease remained. By reviewing death certificates from a county in Sweden, Hogstedt and Axelson [75] found that N G :EGDN dynamite workers were more likely to die from heart disease than were other men in the same county.
Twenty-one deaths from heart disease occurred in men who had been employed at the dynamite plant for 1 year or more; 4 occurred in workers who were actively employed, but the other 17 occurred in men who had not worked at the plant for months or years. "safety solvent," or "aliphatic hydrocarbon" when the specific name is known.
The "%" may be the approximate percentage by weight or volume (indicate basis) which each hazardous ingredient of the mixture bears to the whole mixture. This may be indicated as a range or maximum amount, ie, "10-40% vol" or "10% max wt" to avoid disclosure of trade secrets. | None | None |
fd7659fc55e872e3fd3167f36432c5fe26e6b698 | cdc | None | depar depar depar depar department of health and human ser tment of health and human ser tment of health and human ser tment of health and human ser tment of health and human services vices vices vices vices# Introduction
Physicians and other health-care providers play a critical role in preventing and treating sexually transmitted diseases (STDs). These guidelines for the treatment of STDs are intended to assist with that effort. Although these guidelines emphasize treatment, prevention strategies and diagnostic recommendations also are discussed.
# Methods
This report was produced through a multistage process. Beginning in 2004, CDC personnel and professionals knowledgeable in the field of STDs systematically reviewed evidence, including published abstracts and peer-reviewed journal articles concerning each of the major STDs, focusing on information that had become available since publication of the Sexually Transmitted Diseases Treatment Guidelines, 2002 (1). Background papers were written and tables of evidence were constructed summarizing the type of study (e.g., randomized controlled trial or case series), study population and setting, treatments or other interventions, outcome measures assessed, reported findings, and weaknesses and biases in study design and analysis. A draft document was developed on the basis of the reviews.
In April 2005, CDC staff members and invited consultants assembled in Atlanta, Georgia, for a 3-day meeting to present the key questions regarding STD treatment that emerged from the evidence-based reviews and the information available to answer those questions. When relevant, the questions focused on four principal outcomes of STD therapy for each individual disease: 1) microbiologic cure, 2) alleviation of signs and symptoms, 3) prevention of sequelae, and 4) prevention of transmission. Cost-effectiveness and other advantages (e.g., single-dose formulations and directly observed therapy of specific regimens) also were discussed. The consultants then assessed whether the questions identified were relevant, ranked them in order of priority, and attempted to arrive at answers using the available evidence. In addition, the consultants evaluated the quality of evidence supporting the answers on the basis of the number, type, and quality of the studies.
In several areas, the process diverged from that previously described. The sections on hepatitis B virus (HBV) and hepatitis A virus (HAV) infections are based on previously or recently approved recommendations (2)(3)(4) of the Advisory Committee on Immunization Practices. The recommendations for STD screening during pregnancy were developed after CDC staff reviewed the recommendations from other knowledgeable groups.
Throughout this report, the evidence used as the basis for specific recommendations is discussed briefly. More comprehensive, annotated discussions of such evidence will appear in background papers that will be published in a supplement issue of Clinical Infectious Diseases. When more than one therapeutic regimen is recommended, the sequence is in alphabetical order unless the choices for therapy are prioritized based on efficacy, convenience, or cost. For STDs with more than one recommended treatment regimen, it can be assumed that all regimens have similar efficacy and similar rates of intolerance or toxicity, unless otherwise specified. Persons treating STDs should use recommended regimens primarily; alternative regimens can be considered in instances of substantial drug allergy or other contraindications to the recommended regimens.
These recommendations were developed in consultation with public and private sector professionals knowledgeable in the treatment of persons with STDs (see Consultants list). The recommendations are applicable to various patient-care settings, including family planning clinics, private physicians' offices, managed care organizations, and other primary-care facilities.
These recommendations are meant to serve as a source of clinical guidance: health-care providers should always consider the individual clinical circumstances of each person in the context of local disease prevalence. These guidelines focus on the treatment and counseling of individual persons and do not address other community services and interventions that are important in STD/human immunodeficiency virus (HIV) prevention.
# Clinical Prevention Guidance
The prevention and control of STDs are based on the following five major strategies: 1) education and counseling of persons at risk on ways to avoid STDs through changes in sexual behaviors; 2) identification of asymptomatically infected persons and of symptomatic persons unlikely to seek diagnostic and treatment services; 3) effective diagnosis and treatment of infected persons; 4) evaluation, treatment, and counseling of sex partners of persons who are infected with an STD; and 5) preexposure vaccination of persons at risk for vaccine-preventable STD.
Primary prevention of STD begins with changing the sexual behaviors that place persons at risk for infection. Health-care providers have a unique opportunity to provide education and counseling to their patients. As part of the clinical interview, health-care providers should routinely and regularly obtain sexual histories from their patients and address management of risk reduction as indicated in this report. Guid-ance in obtaining a sexual history is available in Contraceptive Technology, 18th edition (5) and in the curriculum provided by CDC's STD/HIV Prevention Training Centers (http:// www.stdhivpreventiontraining.org). Counseling skills, characterized by respect, compassion, and a nonjudgmental attitude toward all patients, are essential to obtaining a thorough sexual history and to delivering prevention messages effectively. Key techniques that can be effective in facilitating rapport with patients include the use of 1) open-ended questions (e.g., "Tell me about any new sex partners you've had since your last visit" and "what's your experience with using condoms been like?"), 2) understandable language ("have you ever had a sore or scab on your penis?"), and 3) normalizing language ("some of my patients have difficulty using a condom with every sex act. How is it for you?"). One approach to eliciting information concerning five key areas of interest has been summarized.
The Five Ps: Partners, Prevention of Pregnancy, Protection from STDs, Practices, Past History of STDs 1. Partners - "Do you have sex with men, women, or both?"
- "In the past 2 months, how many partners have you had sex with?" - "In the past 12 months, how many partners have you had sex with?" 2. Prevention of pregnancy - "Are you or your partner trying to get pregnant?" If no, "What are you doing to prevent pregnancy?" 3. Protection from STDs - "What do you do to protect yourself from STDs and HIV?" 4. Practices - "To understand your risks for STDs, I need to understand the kind of sex you have had recently." - "Have you had vaginal sex, meaning 'penis in vagina sex'"? - If yes, "Do you use condoms: never, sometimes, or always?" - "Have you had anal sex, meaning 'penis in rectum/anus sex'"? - If yes, "Do you use condoms: never, sometimes, or always?" - "Have you had oral sex, meaning 'mouth on penis/ vagina'"? For condom answers - If "never:" "Why don't you use condoms?" - If "sometimes": "In what situations or with whom, do you not use condoms?" 5. Past history of STDs - "Have you ever had an STD?"
- "Have any of your partners had an STD?" Additional questions to identify HIV and hepatitis risk - "Have you or any of your partners ever injected drugs?
- "Have any of your partners exchanged money or drugs for sex?" - "Is there anything else about your sexual practices that I need to know about?" Patients should be reassured that treatment will be provided regardless of individual circumstances (e.g., ability to pay, citizenship or immigration status, language spoken, or specific sex practices). Many patients seeking treatment or screening for a particular STD should be evaluated for all common STDs; even so, all patients should be informed concerning all the STDs for which they are being tested and if testing for a common STD (e.g., genital herpes) is not being performed.
# STD/HIV Prevention Counseling
Effective delivery of prevention messages requires that providers integrate communication of general risk reduction messages that are relevant to the client (i.e., client-centered counseling) and education regarding specific actions that can reduce the risk for STD/HIV transmission (e.g., abstinence, condom use, limiting the number of sex partners, modifying sexual behaviors, and vaccination). Each of these specific actions is discussed separately in this report.
- Interactive counseling approaches directed at a patient's personal risk, the situations in which risk occurs, and the use of goal-setting strategies are effective in STD/HIV prevention (6). One such approach, client-centered STD/ HIV prevention counseling, involves tailoring a discussion of risk reduction to the patient's individual situation. Client-centered counseling can have a beneficial effect on the likelihood of patients using risk-reduction practices and can reduce the risk for future acquisition of an STD. One effective client-centered approach is Project RESPECT, which demonstrated that a brief counseling intervention was associated with a reduced frequency of STD/HIV risk-related behaviors and with a lowered acquisition of STDs (7,8). Practice models based on Project RESPECT have been successfully implemented in clinicbased settings. Other approaches use motivational interviewing to move clients toward achievable risk reduction goals. CDC provides additional information on these and other effective behavioral interventions at http:// effectiveinterventions.org. - Interactive counseling can be used effectively by all healthcare providers or can be conducted by specially trained counselors. The quality of counseling is best ensured when providers receive basic training in prevention counseling methods and skill-building approaches, periodic observation of counseling with immediate feedback by persons with expertise in the counseling approach, periodic counselor and/or patient satisfaction evaluations, and availability of expert assistance or referral for challenging situations. Training in client-centered counseling is available through the CDC STD/HIV Prevention Training Centers (). Prevention counseling is most effective if provided in a nonjudgmental manner appropriate to the patient's culture, language, sex, sexual orientation, age, and developmental level. In addition to individual prevention counseling, some videos and large group presentations provide explicit information concerning how to use condoms correctly. These have been effective in reducing the occurrence of additional STDs among persons at high risk, including STD clinic patients and adolescents.
Because the incidence of some STDs, notably syphilis, has increased in HIV-infected persons, the use of client-centered STD counseling for HIV-infected persons has received strong emphasis from public health agencies and organizations. Consensus guidelines issued by CDC, the Health Resources and Services Administration, the HIV Medicine Association of the Infectious Diseases Society of America, and the National Institutes of Health emphasize that STD/HIV risk assessment, STD screening, and client-centered risk reduction counseling should be provided routinely to HIV-infected persons (9). Several specific methods have been designed for the HIV care setting (10)(11)(12). Additional information regarding these approaches is available at .
The most reliable way to avoid transmission of STDs is to abstain from sex (i.e., oral, vaginal, or anal sex) or to be in a long-term, mutually monogamous relationship with an uninfected partner. Counseling that encourages abstinence from sexual intercourse is crucial for persons who are being treated for an STD (or whose partners are undergoing treatment) and for persons who want to avoid the possible consequences of sex completely (e.g., STD/HIV and unintended pregnancy). A more comprehensive discussion of abstinence is available in Contraceptive Technology, 18th edition (5). For persons embarking on a mutually monogamous relationship, screening for common STDs before initiating sex might reduce the risk for future transmission of asymptomatic STDs.
# Preexposure Vaccination
Preexposure vaccination is one of the most effective methods for preventing transmission of some STDs. For example, because HBV infection is frequently sexually transmitted, hepatitis B vaccination is recommended for all unvaccinated, uninfected persons being evaluated for an STD. In addition, hepatitis A vaccine is licensed and is recommended for men who have sex with men (MSM) and illicit drug users (i.e., both injecting and noninjecting). Specific details regarding hepatitis A and B vaccination are available at http:// www.cdc.gov/hepatitis. A quadrivalent vaccine against human papillomavirus (HPV types 6,11,16,18) is now available and licensed for females aged 9-26 years. Vaccine trials for other STDs are being conducted.
# Male Condoms
When used consistently and correctly, male latex condoms are highly effective in preventing the sexual transmission of HIV infection (i.e., HIV-negative partners in heterosexual serodiscordant relationships in which condoms were consistently used were 80% less likely to become HIV-infected compared with persons in similar relationships in which condoms were not used) and can reduce the risk for other STDs, including chlamydia, gonorrhea, and trichomoniasis, and might reduce the risk of women developing pelvic inflammatory disease (PID) (13,14). Condom use might reduce the risk for transmission of herpes simplex virus-2 (HSV-2), although data for this effect are more limited (15,16). Condom use might reduce the risk for HPV-associated diseases (e.g., genital warts and cervical cancer ) and mitigate the adverse consequences of infection with HPV, as their use has been associated with higher rates of regression of cervical intraepithelial neoplasia (CIN) and clearance of HPV infection in women (18), and with regression of HPV-associated penile lesions in men (19). A limited number of prospective studies have demonstrated a protective effect of condoms on the acquisition of genital HPV; one recent prospective study among newly sexually active college women demonstrated that consistent condom use was associated with a 70% reduction in risk for HPV transmission (20).
Condoms are regulated as medical devices and are subject to random sampling and testing by the Food and Drug Administration (FDA). Each latex condom manufactured in the United States is tested electronically for holes before packaging. Rates of condom breakage during sexual intercourse and withdrawal are approximately two broken condoms per 100 condoms used in the United States. The failure of condoms to protect against STD transmission or unintended pregnancy usually results from inconsistent or incorrect use rather than condom breakage.
Male condoms made of materials other than latex are available in the United States. Although they have had higher breakage and slippage rates when compared with latex condoms and are usually more costly, the pregnancy rates among women whose partners use these condoms are similar to latex condoms. Two general categories of nonlatex condoms exist. The first type is made of polyurethane or other synthetic material and provides protection against STD/HIV and pregnancy equal to that of latex condoms. These can be substituted for persons with latex allergy. The second type is natural membrane condoms (frequently called "natural" condoms or, incorrectly, lambskin condoms). These condoms are usually made from lamb cecum and can have pores up to 1500 nm in diameter. Whereas these pores do not allow the passage of sperm, they are more than 10 times the diameter of HIV and more than 25 times that of HBV. Moreover, laboratory studies demonstrate that viral STD transmission can occur with natural membrane condoms. Using natural membrane condoms for protection against STDs is not recommended.
Patients should be advised that condoms must be used consistently and correctly to be effective in preventing STDs, and they should be instructed in the correct use of condoms. The following recommendations ensure the proper use of male condoms:
- Use a new condom with each sex act (e.g., oral, vaginal, and anal). - Carefully handle the condom to avoid damaging it with fingernails, teeth, or other sharp objects. - Put the condom on after the penis is erect and before any genital, oral, or anal contact with the partner. - Use only water-based lubricants (e.g., K-Y Jelly™, Astroglide™, AquaLube™, and glycerin) with latex condoms. Oil-based lubricants (e.g., petroleum jelly, shortening, mineral oil, massage oils, body lotions, and cooking oil) can weaken latex. - Ensure adequate lubrication during vaginal and anal sex, which might require the use of exogenous water-based lubricants. - To prevent the condom from slipping off, hold the condom firmly against the base of the penis during withdrawal, and withdraw while the penis is still erect.
# Female Condoms
Laboratory studies indicate that the female condom (Reality™), which consists of a lubricated polyurethane sheath with a ring on each end that is inserted into the vagina, is an effective mechanical barrier to viruses, including HIV, and to semen (21). A limited number of clinical studies have evalu-ated the efficacy of female condoms in providing protection from STDs, including HIV (22). If used consistently and correctly, the female condom might substantially reduce the risk for STDs. When a male condom cannot be used properly, sex partners should consider using a female condom. Female condoms are costly compared with male condoms. The female condom also has been used for STD/HIV protection during receptive anal intercourse (23). Whereas it might provide some protection in this setting, its efficacy is undefined.
# Vaginal Spermicides and Diaphragms
Vaginal spermicides containing nonoxynol-9 (N-9) are not effective in preventing cervical gonorrhea, chlamydia, or HIV infection (24). Furthermore, frequent use of spermicides containing N-9 has been associated with disruption of the genital epithelium, which might be associated with an increased risk for HIV transmission. Therefore, N-9 is not recommended for STD/HIV prevention. In case-control and crosssectional studies, diaphragm use has been demonstrated to protect against cervical gonorrhea, chlamydia, and trichomoniasis; a randomized controlled trial will be conducted. On the basis of all available evidence, diaphragms should not be relied on as the sole source of protection against HIV infection. Diaphragm and spermicide use have been associated with an increased risk for bacterial urinary tract infections in women.
# Condoms and N-9 Vaginal Spermicides
Condoms lubricated with spermicides are no more effective than other lubricated condoms in protecting against the transmission of HIV and other STDs, and those that are lubricated with N-9 pose the concerns that have been previously discussed. Use of condoms lubricated with N-9 is not recommended for STD/HIV prevention because spermicidecoated condoms cost more, have a shorter shelf-life than other lubricated condoms, and have been associated with urinary tract infection in young women.
# Rectal Use of N-9 Spermicides
Recent studies indicate that N-9 might increase the risk for HIV transmission during vaginal intercourse (24). Although similar studies have not been conducted among men who use N-9 spermicide during anal intercourse with other men, N-9 can damage the cells lining the rectum, which might provide a portal of entry for HIV and other sexually transmissible agents. Therefore, N-9 should not be used as a microbicide or lubricant during anal intercourse.
# Nonbarrier Contraception, Surgical Sterilization, and Hysterectomy
Sexually active women who are not at risk for pregnancy might incorrectly perceive themselves to be at no risk for STDs, including HIV infection. Contraceptive methods that are not mechanical barriers offer no protection against HIV or other STDs. Women who use hormonal contraception (e.g., oral contraceptives, Norplant™, and Depo-Provera™), have intrauterine devices (IUD), have been surgically sterilized, or have had hysterectomies should be counseled regarding the use of condoms and the risk for STDs, including HIV infection.
# Emergency Contraception (EC)
Emergency use of oral contraceptive pills containing levonorgesterol alone reduces the risk for pregnancy after unprotected intercourse by 89%. Pills containing a combination of ethinyl estradiol and either norgestrel or levonorgestrel can be used and reduce the risk for pregnancy by 75%. Emergency insertion of a copper IUD also is highly effective, reducing the risk by as much as 99%. EC with oral contraceptive pills should be initiated as soon as possible after unprotected intercourse and definitely within 120 hours (i.e., 5 days). The only medical contraindication to provision of EC is current pregnancy.
Providers who manage persons at risk for STDs should counsel women concerning the option for EC, if indicated, and provide it in a timely fashion if desired by the woman. Plan B (two 750 mcg levonorgestrel tablets) has been approved by FDA and is available in the United States for the prevention of unintended pregnancy. Additional information on EC is available in Contraceptive Technology, 18th edition (5), or at / contraceptionresources.
# Postexposure Prophylaxis (PEP) for HIV
Guidelines for the use of PEP aimed at preventing HIV acquisition as a result of sexual exposure are available and are discussed in this report (see Sexual Assault and STDs).
# Partner Management
Partner notification, previously referred to as "contact tracing" but recently included in the broader category of partner services, is the process by which providers or public health authorities learn from persons with STDs about their sex partners and help to arrange for the evaluation and treatment of sex partners. Providers can seek this information and help to arrange for evaluation and treatment of sex partners, either directly or with assistance from state and local health departments. The intensity of partner services and the specific STDs for which they are offered vary among providers, agencies, and geographic areas. Ideally, such services should be accompanied by health counseling and might include referral of patients and their partners for other services, whenever appropriate.
In general, whether partner notification effectively decreases exposure to STDs and whether it changes the incidence and prevalence of STDs in a community are uncertain. The paucity of supporting evidence regarding the effectiveness of partner notification has spurred the exploration of alternative approaches. One such approach is to place partner notification in a larger context by making interventions in the sexual and social networks in which persons are exposed to STDs. Prospective evaluations incorporating assessment of venues, community structure, and social and sexual, contacts in conjunction with partner notification of efforts are promising in terms of increasing case-finding and warrant further exploration. The scope of such efforts probably precludes individual clinician efforts to use network-based approaches, but STDcontrol programs might find them useful.
Many persons individually benefit from partner notification. When partners are treated, index patients have reduced risk for reinfection. At a population level, partner notification can disrupt networks of STD transmission and reduce disease incidence. Therefore, providers should encourage their patients with STDs to notify their sex partners and urge them to seek medical evaluation and treatment, regardless of whether assistance is available from health agencies. When medical evaluation, counseling, and treatment of partners cannot be done because of the particular circumstances of a patient or partner or because of resource limitations, other partner management options can be considered. One option is patientdelivered therapy, a form of expedited partner therapy (EPT) in which partners of infected patients are treated without previous medical evaluation or prevention counseling (http:// www.cdc.gov/std/treatment/EPTFinalReport2006.pdf ). The evidence supporting patient-delivered therapy is based on three clinical trials that included heterosexual men and women with chlamydia or gonorrhea. The strength of the supporting evidence differed by STD and by the sex of the index case when reinfection of the index case was the measured outcome (25)(26)(27). Despite this variation, patient-delivered therapy (i.e., via medications or prescriptions) can prevent reinfection of index case and has been associated with a higher likelihood of partner notification, compared with unassisted patient referral of partners. Medications and prescriptions for patient-delivered therapy should be accompanied by treatment instructions, appropriate warnings about taking medications if pregnant, general health counseling, and advice that partners should seek personal medical evaluations, particularly women with symptoms of STDs or PID. Existing data suggest that EPT has a limited role in partner management for trichomoniasis (28). No data support its use in the routine management of syphilis. There is no experience with expedited partner therapy for gonorrhea or chlamydia infection among MSM. Currently, EPT is not feasible in many settings because of operational barriers, including the lack of clear legal status of EPT in some states.
# Reporting and Confidentiality
The accurate and timely reporting of STDs is integrally important for assessing morbidity trends, targeting limited resources, and assisting local health authorities in partner notification and treatment. STD/HIV and acquired immunodeficiency syndrome (AIDS) cases should be reported in accordance with state and local statutory requirements. Syphilis, gonorrhea, chlamydia, chanroid, HIV infection, and AIDS are reportable diseases in every state. The requirements for reporting other STDs differ by state, and clinicians should be familiar with state and local reporting requirements.
Reporting can be provider-and/or laboratory-based. Clinicians who are unsure of state and local reporting requirements should seek advice from state or local health departments or STD programs. STD and HIV reports are kept strictly confidential. In the majority of jurisdictions, such reports are protected by statute from subpoena. Before public health representatives conduct a follow-up of a positive STDtest result, they should consult the patient's health-care provider to verify the diagnosis and treatment.
# Special Populations Pregnant Women
Intrauterine or perinatally transmitted STDs can have severely debilitating effects on pregnant women, their partners, and their fetuses. All pregnant women and their sex partners should be asked about STDs, counseled about the possibility of perinatal infections, and ensured access to treatment, if needed.
# Recommended Screening Tests
- All pregnant women in the United States should be tested for HIV infection as early in pregnancy as possible. Testing should be conducted after the woman is notified that she will be tested for HIV as part of the routine panel of prenatal tests, unless she declines the test (i.e., opt-out screening). For women who decline HIV testing, providers should address their objections, and where appropriate, continue to strongly encourage testing. Women who decline testing because they have had a previous negative HIV test should be informed of the importance of retesting during each pregnancy. Testing pregnant women is vital not only to maintain the health of the patient but also because interventions (i.e., antiretroviral and obstetrical) are available that can reduce perinatal transmission of HIV. Retesting in the third trimester (i.e., preferably before 36 weeks' gestation) is recommended for women at high risk for acquiring HIV infection (i.e., women who use illicit drugs, have STDs during pregnancy, have multiple sex partners during pregnancy, or have HIV-infected partners). Rapid HIV testing should be performed on women in labor with undocumented HIV status. If a rapid HIV test result is positive, antiretroviral prophylaxis (with consent) should be administered without waiting for the results of the confirmatory test. - A serologic test for syphilis should be performed on all pregnant women at the first prenatal visit. In populations in which use of prenatal care is not optimal, rapid plasma reagin (RPR) card test screening (and treatment, if that test is reactive) should be performed at the time a pregnancy is confirmed. Women who are at high risk for syphilis, live in areas of high syphilis morbidity, are previously untested, or have positive serology in the first trimester should be screened again early in the third trimester (28 weeks' gestation) and at delivery. Some states require all women to be screened at delivery. Infants should not be discharged from the hospital unless the syphilis serologic status of the mother has been determined at least one time during pregnancy and preferably again at delivery. Any woman who delivers a stillborn infant should be tested for syphilis. - All pregnant women should be routinely tested for hepatitis B surface antigen (HBsAg) during an early prenatal visit (e.g., first trimester) in each pregnancy, even if they have been previously vaccinated or tested. Women who were not screened prenatally, those who engage in behaviors that put them at high risk for infection (e.g., more than one sex partner in the previous 6 months, evaluation or treatment for an STD, recent or current injectingdrug use, and HBsAg-positive sex partner), and those with clinical hepatitis should be retested at the time of admission to the hospital for delivery. Women at risk for HBV infection also should be vaccinated. To avoid misinterpreting a transient positive HBsAg result during the 21 days after vaccination, HBsAg testing should be performed before the vaccination. - All laboratories that conduct HBsAg tests should use an HBsAg test that is FDA-cleared and should perform testing according to the manufacturer's labeling, including testing of initially reactive specimens with a licensed neutralizing confirmatory test. When pregnant women are tested for HBsAg at the time of admission for delivery, shortened testing protocols may be used, and initially reactive results should prompt expedited administration of immunoprophylaxis to infants.
- All pregnant women should be routinely tested for Chlamydia trachomatis (see Chlamydia Infections, Diagnostic Considerations) at the first prenatal visit. Women aged <25 years and those at increased risk for chlamydia (i.e., women who have a new or more than one sex partner) also should be retested during the third trimester to prevent maternal postnatal complications and chlamydial infection in the infant. Screening during the first trimester might prevent the adverse effects of chlamydia during pregnancy, but supportive evidence for this is lacking. If screening is performed only during the first trimester, a longer period exists for acquiring infection before delivery. - All pregnant women at risk for gonorrhea or living in an area in which the prevalence of Neisseria gonorrhoeae is high should be tested at the first prenatal visit for N. gonorrhoeae. (See Gonococcal Infections, Diagnostic Considerations). A repeat test should be performed during the third trimester for those at continued risk. - All pregnant women at high risk for hepatitis C infection should be tested for hepatitis C antibodies (see Hepatitis C, Diagnostic Considerations) at the first prenatal visit. Women at high risk include those with a history of injecting-drug use and those with a history of blood transfusion or organ transplantion before 1992. - Evaluation for bacterial vaginosis (BV) might be conducted during the first prenatal visit for asymptomatic patients who are at high risk for preterm labor (e.g., those who have a history of a previous preterm delivery). Evidence does not support routine testing for BV. - A Papanicolaou (Pap) smear should be obtained at the first prenatal visit if none has been documented during the preceding year.
# Other Concerns
- Women who are HBsAg positive should be reported to the local and/or state health department to ensure that they are entered into a case-management system and that timely and appropriate prophylaxis is provided for their infants. Information concerning the pregnant woman's HBsAg status should be provided to the hospital in which delivery is planned and to the health-care provider who will care for the newborn. In addition, household and sex contacts of women who are HBsAg positive should be vaccinated. - Women who are HBsAg positive should be provided with, or referred for, appropriate counseling and medical management. Pregnant women who are HBsAg positive pregnant women should receive information regarding hepatitis B that addresses -modes of transmission;
MMWR August 4, 2006
-perinatal concerns (e.g., breastfeeding is not contraindicated); -prevention of HBV transmission, including the importance of postexposure prophylaxis for the newborn infant and hepatitis B vaccination for household contacts and sex partners; and -evaluation for and treatment of chronic HBV infection. - No treatment is available for HCV-infected pregnant women. However, all women with HCV infection should receive appropriate counseling and supportive care as needed (see Hepatitis C, Prevention). No vaccine is available to prevent HCV transmission. - In the absence of lesions during the third trimester, routine serial cultures for HSV are not indicated for women who have a history of recurrent genital herpes. Prophylactic cesarean section is not indicated for women who do not have active genital lesions at the time of delivery.
In addition, insufficient evidence exists to recommend routine HSV-2 serologic screening among previously undiagnosed women during pregnancy, nor does sufficient evidence exist to recommend routine antiviral suppressive therapy late in gestation for all HSV-2 positive women. - The presence of genital warts is not an indication for cesarean section. - Not enough evidence exists to recommend routine screening for Trichomonas vaginalis in asymptomatic pregnant women. For a more detailed discussion of STD testing and treatment among pregnant women and other infections not transmitted sexually, refer to the following references: Guide to Clinical Preventive Services (29); Guidelines for Perinatal Care (30) (41).
These sources are not entirely consistent in their recommendations. For example, the Guide to Clinical Preventive Services recommends screening of patients at high risk for chlamydia but indicates that the optimal timing for screening is uncertain. The Guidelines for Perinatal Care recommends that pregnant women at high risk for chlamydia be screened for infection during the first prenatal care visit and during the third trimester. Recommendations to screen pregnant women for STDs are based on disease severity and sequelae, prevalence in the population, costs, medicolegal considerations (e.g., state laws), and other factors. The screening recommendations in this report are broader (i.e., if followed, more women will be screened for more STDs than would be screened by following other recommendations) and are compatible with other CDC guidelines.
# Adolescents
The rates of many STDs are highest among adolescents. For example, the reported rates of chlamydia and gonorrhea are highest among females aged 15-19 years, and many persons acquire HPV infection during their adolescent years. Among adolescents with acute HBV infection, the most commonly reported risk factors are having sexual contact with a chronically infected person or with multiple sex partners, or reporting their sexual preference as homosexual. As part of a comprehensive strategy to eliminate HBV transmission in the United States, ACIP has recommended that all children and adolescents be administered HBV vaccine (2).
Younger adolescents (i.e., persons aged <15 years) who are sexually active are at particular risk for STDs, especially youth in detention facilities, STD clinic patients, male homosexuals, and injecting-drug users (IDUs). Adolescents are at higher risk for STDs because they frequently have unprotected intercourse, are biologically more susceptible to infection, are engaged in sexual partnerships frequently of limited duration, and face multiple obstacles to using health care. Several of these issues can be addressed by clinicians who provide services to adolescents. Clinicians can address adolescents' lack of knowledge and awareness regarding the risks and consequences of STDs by offering guidance concerning healthy sexual behavior and, therefore, prevent the establishment of patterns of behavior that can undermine sexual health.
With a few exceptions, all adolescents in the United States can legally consent to the confidential diagnosis and treatment of STDs. In all 50 states and the District of Columbia, medical care for STDs can be provided to adolescents without parental consent or knowledge. In addition, in the ma-jority of states, adolescents can consent to HIV counseling and testing. Consent laws for vaccination of adolescents differ by state. Several states consider provision of vaccine similar to treatment of STDs and provide vaccination services without parental consent. Because of the crucial importance of confidentially, health-care providers should follow policies that provide confidentiality and comply with state laws for STD services.
Despite the prevalence of STDs among adolescents, providers frequently fail to inquire about sexual behavior, assess risk for STDs, provide counseling on risk reduction, and screen for asymptomatic infection during clinical encounters. The style and content of counseling and health education on these sensitive subjects should be adapted for adolescents. Discussions should be appropriate for the patient's developmental level and should be aimed at identifying risky behaviors (e.g., sex and drug-use behaviors). Careful, nonjudgmental, and thorough counseling are particularly vital for adolescents who might not acknowledge that they engage in high-risk behaviors.
# Children
Management of children who have STDs requires close cooperation between clinicians, laboratorians, and childprotection authorities. Official investigations, when indicated, should be initiated promptly. Some diseases (e.g., gonorrhea, syphilis, and chlamydia), if acquired after the neonatal period, are virtually 100% indicative of sexual contact. For other diseases (e.g., HPV infection and vaginitis), the association with sexual contact is not as clear (see Sexual Assault and STDs).
# MSM
Some MSM are at high risk for HIV infection and other viral and bacterial STDs. The frequency of unsafe sexual practices and the reported rates of bacterial STDs and incident HIV infection have declined substantially in MSM from the 1980s through the mid-1990s. However, during the previous 10 years, increased rates of infectious syphilis, gonorrhea, and chlamydial infection and of higher rates of unsafe sexual behaviors have been documented among MSM in the United States and virtually all industrialized countries. The effect of these behavioral changes on HIV transmission has not been ascertained, but preliminary data suggest that the incidence of HIV infection might be increasing among some MSM. These adverse trends probably are related to changing attitudes concerning HIV infection because of the effects of improved HIV/AIDS therapy on quality of life and survival, changing patterns of substance abuse, demographic shifts in MSM populations, and changes in sex partner networks resulting from new venues for partner acquisition.
Clinicians should assess the risks of STDs for all male patients, including a routine inquiry about the sex of patients' sex partners. MSM, including those with HIV infection, should routinely undergo nonjudgmental STD/HIV risk assessment and client-centered prevention counseling to reduce the likelihood of acquiring or transmitting HIV or other STDs. Clinicians should be familiar with local community resources available to assist MSM at high risk in facilitating behavioral change. Clinicians also should routinely ask sexually active MSM about symptoms consistent with common STDs, including urethral discharge, dysuria, genital and perianal ulcers, regional lymphadenopathy, skin rash, and anorectal symptoms consistent with proctitis. Clinicians also should maintain a low threshold for diagnostic testing of symptomatic patients.
Routine laboratory screening for common STDs is indicated for all sexually active MSM. The following screening recommendations are based on preliminary data (42,43). These tests should be performed at least annually for sexually active MSM, including men with or without established HIV infection:
- HIV serology, if HIV negative or not tested within the previous year; - syphilis serology; - a test for urethral infection with N. gonorrhoeae and C. trachomatis in men who have had insertive intercourse- during the preceding year; - a test for rectal infection † with N. gonorrhoeae and C. trachomatis in men who have had receptive anal intercourse- during the preceding year; - a test for pharyngeal infection † with N. gonorrhoeae in men who have acknowledged participation in receptive oral intercourse- during the preceding year; testing for C. trachomatis pharyngeal infection is not recommended. In addition, some specialists would consider type-specific serologic tests for HSV-2, if infection status is unknown. Routine testing for anal cytologic abnormalities or anal HPV infection is not recommended until more data are available on the reliability of screening methods, the safety of and response to treatment, and programmatic considerations.
More frequent STD screening (i.e., at 3-6 month intervals) is indicated for MSM who have multiple or anonymous partners, have sex in conjunction with illicit drug use, use methamphetamine, or whose sex partners participate in these activities.
Vaccination against hepatitis A and B is recommended for all MSM in whom previous infection or immunization cannot be documented. Preimmunization serologic testing might be considered to reduce the cost of vaccinating MSM who are already immune to these infections, but this testing should not be delay vaccination. Vaccinating persons who are immune to HAV or HBV infection because of previous infection or vaccination does not increase the risk for vaccine-related adverse events (see Hepatitis B, Prevaccination Antibody Screening).
# Women Who Have Sex with Women (WSW)
Few data are available on the risk of STDs conferred by sex between women, but transmission risk probably varies by the specific STD and sexual practice (e.g., oral-genital sex, vaginal or anal sex using hands, fingers, or penetrative sex items, and oral-anal sex) (44,45). Practices involving digitalvaginal or digital-anal contact, particularly with shared penetrative sex items, present a possible means for transmission of infected cervicovaginal secretions. This possibility is most directly supported by reports of metronidazole-resistant trichomoniasis and genotype-concordant HIV transmitted sexually between women who reported these behaviors and by the high prevalence of BV among monogamous WSW. Transmission of HPV can occur with skin-to-skin or skin-tomucosa contact, which can occur during sex between women. HPV deoxyribonucleic acid (DNA) has been detected through polymerase chain reaction (PCR)-based methods from the cervix, vagina, and vulva in 13%-30% of WSW, and highand low-grade squamous intraepithelial lesions (SIL) have been detected on Pap tests in WSW who reported no previous sex with men (46). However, the majority of self-identified WSW (53%-99%) have had sex with men and might continue this practice (47). Therefore, all women should undergo Pap test screening using current national guidelines, regardless of sexual preference or sexual practices.
HSV-2 genital transmission between female sex partners is probably inefficient, but the relatively frequent practice of orogenital sex among WSW might place them at higher risk for genital infection with HSV-1. This hypothesis is supported by the recognized association between HSV-1 seropositivity and previous number of female partners among WSW. Transmission of syphilis between female sex partners, probably through oral sex, has been reported. Although the rate of transmission of C. trachomatis between women is unknown, WSW who also have sex with men are at risk and should undergo routine screening according to guidelines.
# HIV Infection: Detection, Counseling, and Referral
Infection with HIV produces a spectrum of disease that progresses from a clinically latent or asymptomatic state to AIDS as a late manifestation. The pace of disease progression varies. In untreated patients, the time between infection with HIV and the development of AIDS ranges from a few months to as long as 17 years (median: 10 years). The majority of adults and adolescents infected with HIV remain symptomfree for extended periods, but viral replication is active during all stages of infection and increases substantially as the immune system deteriorates. In the absence of treatment, AIDS will develop eventually in nearly all HIV-infected persons.
Improvements in antiretroviral therapy and increasing awareness among both patients and health-care providers of the risk factors associated with HIV transmission have led to more testing for HIV and earlier diagnosis, frequently before symptoms develop. However, the conditions of nearly 40% of persons who acquire HIV infection continue to be diagnosed late, within 1 year of acquiring AIDS. Prompt diagnosis of HIV infection is essential for multiple reasons. Treatments are available that slow the decline of immune system function; use of these therapies has been associated with substantial declines in HIV-associated morbidity and mortality in recent years. HIV-infected persons who have altered immune function are at increased risk for infections for which preventive measures are available (e.g., Pneumocystis jiroveci pneumonia, toxoplasma encephalitis , disseminated Mycobacterium avium complex disease, tuberculosis , and bacterial pneumonia). Because of its effect on the immune system, HIV affects the diagnosis, evaluation, treatment, and follow-up of multiple other diseases and might affect the efficacy of antimicrobial therapy for some STDs. Finally, the early diagnosis of HIV enables health-care providers to counsel infected patients, refer them to various support services, and help prevent HIV transmission to others. Acutely infected persons might have elevated HIV viral loads and, therefore, might be more likely to transmit HIV to their partners (48,49).
Proper management of HIV infection involves a complex array of behavioral, psychosocial, and medical services. Although some services might not be available in STD treatment facilities. Therefore, referral to a health-care provider or facility experienced in caring for HIV-infected patients is advised. Providers working in STD-treatment facilities should be knowledgeable about the options for referral available in their communities. While receiving care in STD-treatment facilities, HIV-infected patients should be educated about HIV infection and the various options available for support services and HIV care.
A detailed discussion of the multiple, complex services required for management of HIV infection is beyond the scope of this section; however, this information is available in other published resources (6,9,50,51). In subsequent sections, this report provides information regarding diagnostic testing for HIV infection, counseling patients who have HIV infection, referral of patients for support services, including medical care, and the management of sex and injecting-drug partners in STD-treatment facilities. In addition, the report discusses HIV infection during pregnancy and in infants and children.
# Detection of HIV Infection: Screening and Diagnostic Testing
All persons who seek evaluation and treatment for STDs should be screened for HIV infection. Screening should be routine, regardless of whether the patient is known or suspected to have specific behavioral risks for HIV infection.
# Consent and Pretest Information
HIV screening should be voluntary and conducted only with the patient's knowledge and understanding that testing is planned. Persons should be informed orally or in writing that HIV testing will be performed unless they decline (i.e., opt-out screening). Oral or written communications should include an explanation of positive and negative test results, and patients should be offered an opportunity to ask questions and to decline testing.
# Prevention Counseling
Prevention counseling does not need to be explicitly linked to the HIV-testing process. However, some patients might be more likely to think about HIV and consider their risks when undergoing an HIV test. HIV testing might present an ideal opportunity to provide or arrange for prevention counseling to assist with behavior changes that can reduce risk for acquiring HIV infection. Prevention counseling should be offered and encouraged in all health-care facilities serving patients at high risk and in those (e.g., STD clinics) where information on HIV-risk behaviors is routinely elicited.
# Diagnostic Testing
HIV infection usually is diagnosed by tests for antibodies against HIV-1. Some combination tests also detect antibodies against HIV-2 (i.e., HIV-1/2). Antibody testing begins with a sensitive screening test (e.g., the enzyme immunoassay or rapid test). The advent of HIV rapid testing has enabled clinicians to make a substantially accurate presumptive diagnosis of HIV-1 infection within half an hour. This testing can facilitate the identification of the more than 250,000 persons living with undiagnosed HIV in the United States. Reactive screening tests must be confirmed by a supplemental test (e.g., the Western blot ) or an immunofluorescence assay (IFA) (52). If confirmed by a supplemental test, a positive antibody test result indicates that a person is infected with HIV and is capable of transmitting the virus to others. HIV antibody is detectable in at least 95% of patients within 3 months after infection. Although a negative antibody test result usually indicates that a person is not infected, antibody tests cannot exclude recent infection.
The majority of HIV infections in the United States are caused by HIV-1. However, HIV-2 infection should be suspected in persons who have epidemiologic risk factors, including being from West Africa (where HIV-2 is endemic) or have sex partners from endemic areas, have sex partners known to be infected with HIV-2, or have received a blood transfusion or nonsterile injection in a West African country. HIV-2 testing also is indicated when clinical evidence of HIV exists but tests for HIV-1 antibodies or HIV-1 viral load are not positive, or when HIV-1 WB results include the unusual indeterminate pattern of gag (p55, p24, p17) plus pol (p66, p51, p31) bands in the absence of env (gp160, gp120, gp41) bands.
Health-care providers should be knowledgeable about the symptoms and signs of acute retroviral syndrome, which is characterized by fever, malaise, lymphadenopathy, and skin rash. This syndrome frequently occurs in the first few weeks after HIV infection, before antibody test results become positive. Suspicion of acute retroviral syndrome should prompt nucleic acid testing (HIV plasma ribonucleic acid ) to detect the presence of HIV, although not all nucleic acid tests are approved for diagnostic purposes; a positive HIV nucleic acid test should be confirmed by subsequent antibody testing to document seroconversion (using standard methods, EIA, and WB). Acutely infected patients might be highly contagious because of increased plasma and genital HIV RNA concentrations and might be continuing to engage in risky behaviors (48,49). Current guidelines suggest that persons with recently acquired HIV infection might benefit from antiretroviral drugs and be candidates for clinical trials (53,54). Therefore, patients with acute HIV infection should be referred immediately to an HIV clinical care provider.
Diagnosis of HIV infection should prompt efforts to reduce the risk behavior that resulted in HIV infection and could result in transmission of HIV to others (55)
# Counseling for Patients with HIV Infection and Referral to Support Services
Persons can be expected to be distressed when first informed of a positive HIV test result. Such persons face multiple major adaptive challenges, including 1) accepting the possibility of a shortened life span, 2) coping with the reactions of others to a stigmatizing illness, 3) developing and adopting strategies for maintaining physical and emotional health, and 4) initiating changes in behavior to prevent HIV transmission to others. Many persons will require assistance with making reproductive choices, gaining access to health services, confronting possible employment or housing discrimination, and coping with changes in personal relationships. Therefore, behavioral and psychosocial services are an integral part of health care for HIV-infected persons. Such services should be available on site or through referral when HIV infection is diagnosed. A comprehensive discussion of specific recommendations is available in the Guidelines for HIV Counseling, Testing, and Referral and Revised Recommendations for HIV Screening of Pregnant Women (6). Innovative and successful interventions to decrease risk taking by HIV-infected patients have been developed for diverse populations (12).
Practice settings for offering HIV care differ depending on local resources and needs. Primary care providers and outpatient facilities should ensure that appropriate resources are available for each patient to avoid fragmentation of care. Although a single source that is capable of providing comprehensive care for all stages of HIV infection is preferred, the limited availability of such resources frequently results in the need to coordinate care among medical and social service providers in different locations. Providers should avoid long delays between diagnosis of HIV infection and access to additional medical and psychosocial services. The use of HIV rapid testing can help avoid unnecessary delays.
Recently identified HIV infection might not have been recently acquired. Persons newly diagnosed with HIV might be at any stage of infection. Therefore, health-care providers should be alert for symptoms or signs that suggest advanced HIV infection (e.g., fever, weight loss, diarrhea, cough, shortness of breath, and oral candidiasis). The presence of any of these symptoms should prompt urgent referral for specialty medical care. Similarly, providers should be alert for signs of psychologic distress and be prepared to refer patients accordingly.
Diagnosis of HIV infection reinforces the need to counsel patients regarding high-risk behaviors because the consequences of such behaviors include the risk for acquiring additional STDs and for transmitting HIV (and other STDs) to other persons. Such attention to behaviors in HIV-infected persons is consistent with national strategies for HIV prevention (55). Providers should refer patients for prevention counseling and risk-reduction support concerning high-risk behaviors (e.g., substance abuse and high-risk sexual behaviors). In multiple recent studies, researchers have developed successful prevention interventions for different HIV-infected populations that can be adapted to individuals (56,57).
Persons with newly diagnosed HIV infection who receive care in the STD treatment setting should be educated concerning what to expect as they enter medical care for HIV infection (51). In nonemergent situations, the initial evaluation of HIV-positive patients usually includes the following:
- a detailed medical history, including sexual and substance abuse history; vaccination history; previous STDs; and specific HIV-related symptoms or diagnoses; - a physical examination, including a gynecologic examination for women; - testing for N. gonorrhoeae and C. trachomatis (and for women, a Pap test and wet mount examination of vaginal secretions);
- complete blood and platelet counts and blood chemistry profile; - toxoplasma antibody test;
- tests for antibodies to HCV; testing for previous or present HAV or HBV infection is recommended if determined to be cost-effective before considering vaccination (see Hepatitis A and Hepatitis B); - syphilis serology; - a CD4 T-lymphocyte analysis and determination of HIV plasma viral load; - a tuberculin skin test (sometimes referred to as a purified protein derivative); - a urinalysis; and - a chest radiograph. Some specialists recommend type-specific testing for HSV-2 if herpes infection status is unknown. A first dose of hepatitis A and/or hepatitis B vaccination for previously unvaccinated persons for whom vaccine is recommended (see Hepatitis A and Hepatitis B) should be administered at this first visit.
In subsequent visits, when the results of laboratory and skin tests are available, antiretroviral therapy may be offered, if indicated, after initial antiretroviral resistance testing is performed (53) and specific prophylactic medications are administered to reduce the incidence of opportunistic infections (e.g., Pneumocystis jiroveci pneumonia, TE, disseminated MAC infection, and TB) (50). The vaccination series for hepatitis A and/or B should be offered for those in whom vaccination is recommended. Influenza vaccination should be offered annually, and pneumococcal vaccination should be given if it has not been administered in the previous 5 years (50,51).
Providers should be alert to the possibility of new or recurrent STDs and should treat such conditions aggressively. The occurrence of an STD in an HIV-infected person is an indication of high-risk behavior and should prompt referral for counseling. Because many STDs are asymptomatic, routine screening for curable STDs (e.g., syphilis, gonorrhea, and chlamydia) should be performed at least yearly for sexually active persons. Women should be screened for cervical cancer precursor lesions by annual Pap smears. More frequent STD screening might be appropriate depending on individual risk behaviors, the local epidemiology of STDs, and whether incident STDs are detected by screening or by the presence of symptoms.
Newly diagnosed HIV-infected persons should receive or be referred for a thorough psychosocial evaluation, including ascertainment of behavioral factors indicating risk for transmitting HIV. Patients might require referral for specific behavioral intervention (e.g., a substance abuse program), mental health disorders (e.g., depression), or emotional distress. They might require assistance with securing and maintaining employment and housing. Women should be counseled or appropriately referred regarding reproductive choices and contraceptive options. Patients with multiple psychosocial problems might be candidates for comprehensive riskreduction counseling and services (8).
The following are specific recommendations for HIV counseling and referral:
- (11,12). Involvement of nongovernment organizations and community-based organizations might complement such efforts in the clinical setting.
# Management of Sex Partners and Injecting-Drug Partners
Clinicians evaluating HIV-infected persons should collect information to determine whether any partners should be notified concerning possible exposure to HIV (6). When referring to persons who are infected with HIV, the term "partner" includes not only sex partners but also IDUs who share syringes or other injection equipment. The rationale for partner notification is that the early diagnosis and treatment of HIV infection in these partners might reduce morbidity and provides the opportunity to encourage risk-reducing behaviors. Partner notification for HIV infection should be confidential and depends on the voluntary cooperation of the patient. Specific guidance regarding spousal notification may vary by jurisdiction.
Two complementary notification processes, patient referral and provider referral, can be used to identify partners. With patient referral, patients directly inform their partners of their exposure to HIV infection. With provider referral, trained health department personnel locate partners on the basis of the names, descriptions, and addresses provided by the patient. During the notification process, the confidentiality of patients is protected; their names are not revealed to partners who are notified. Many state and local health departments provide these services.
The following are specific recommendations for implementing partner-notification procedures:
- HIV-infected patients should be encouraged to notify their partners and to refer them for counseling and testing. If requested by the patient, health-care providers should assist in this process, either directly or by referral to health department partner-notification programs. - If patients are unwilling to notify their partners or if they cannot ensure that their partners will seek counseling, physicians or health department personnel should use confidential partner notification procedures. - Partners who are contacted within 72 hours of a highrisk sexual or injecting-drug exposure to an HIV-infected partner, which involves exposure to genital secretions and/ or blood, should be offered PEP with combination antiretroviral therapy to complete a 28-day course (58).
# Special Considerations
Pregnancy. All pregnant women in the United States should be tested for HIV infection as early during pregnancy as possible. Testing should occur after the patient is notified that she will be tested for HIV as part of the routine panel of prenatal tests, unless she declines (i.e., opt-out screening) (30)(31)(32). For women who decline, providers should continue to strongly encourage testing and address concerns that pose obstacles to testing. Women who decline testing because they have had a previous negative HIV test should be informed of the importance of retesting during each pregnancy. Testing pregnant women is particularly important, not only to maintain the health of the patient, but also because interventions (i.e., antiretroviral and obstetrical) can reduce the risk of perinatal transmission of HIV.
After pregnant women have been identified as being HIVinfected, they should be educated about the risk of perinatal infection. Evidence indicates that, in the absence of antiretroviral and other interventions, 15%-25% of infants born to HIV-infected mothers will become infected with HIV; such evidence also indicates that an additional 12%-14% will become infected during breastfeeding where HIV-infected women breastfeed their infants into the second year of life (59,60).
The risk of perinatal HIV transmission can be reduced substantially to <2% through the use of antiretroviral regimens and obstetrical interventions (i.e., zidovudine or nevirapine and elective cesarean section at 38 weeks of pregnancy) and by avoiding breastfeeding (61). Pregnant women who are HIV infected should be counseled concerning their options (either on-site or by referral), given appropriate antenatal treatment, and advised not to breastfeed their infants (for women living in the United States, where infant formula is readily available and can be safely prepared).
HIV Infection Among Infants and Children. Diagnosis of HIV infection in a pregnant woman indicates the need to consider whether other children of the woman might be infected. Infants and young children with HIV infection differ from adults and adolescents with respect to the diagnosis, clinical presentation, and management of HIV disease. For example, because maternal HIV antibody passes through the placenta, antibody tests for HIV are expected to be positive in the sera of both infected and uninfected infants born to seropositive mothers. A definitive determination of HIV infection for an infant aged <18 months is usually based on HIV nucleic acid testing. Management of infants, children, and adolescents who are known or suspected to be infected with HIV requires referral to physicians familiar with the manifestations and treatment of pediatric HIV infection (50,51,62).
# Diseases Characterized by Genital Ulcers
# Management of Patients Who Have Genital Ulcers
In the United States, the majority of young, sexually active patients who have genital ulcers have either genital herpes, syphilis, or chancroid. The frequency of each condition differs by geographic area and patient population; however, genital herpes is the most prevalent of these diseases. More than one of these diseases can be present in a patient who has genital ulcers. All three of these diseases has been associated with an increased risk for HIV infection. Not all genital ulcers are caused by sexually transmitted infections.
A diagnosis based only on the patient's medical history and physical examination frequently is inaccurate. Therefore, all patients who have genital ulcers should be evaluated with a serologic test for syphilis and a diagnostic evaluation for genital herpes; in settings where chancroid is prevalent, a test for Haemophilus ducreyi should also be performed. Specific tests for evaluation of genital ulcers include 1) syphilis serology and either darkfield examination or direct immunofluorescence test for T. pallidum; 2) culture or antigen test for HSV; and 3) culture for H. ducreyi.
No FDA-cleared PCR test for these organisms is available in the United States; however, such testing can be performed by clinical laboratories that have developed their own tests and conducted a Clinical Laboratory Improvement Amendment (CLIA) verification study. Type-specific serology for HSV-2 might be helpful in identifying persons with genital herpes (see Genital Herpes, Type-Specific Serologic Tests). Biopsy of genital ulcers might be helpful in identifying the cause of ulcers that are unusual or that do not respond to initial therapy. HIV testing should be performed on all patients who have genital ulcers caused by T. pallidum or H. ducreyi, and should be strongly considered for those who have genital ulcers caused by HSV (see Diagnostic Considerations, sections, Syphilis, Chancroid, and Genital Herpes Simplex Virus).
Health-care providers frequently must treat patients before test results are available because early treatment decreases the possibility of ongoing transmission and because successful treatment of genital herpes depends on prompt initiation of therapy. The clinician should treat for the diagnosis considered most likely, on the basis of clinical presentation and epidemiologic circumstances. In some instances, treatment must be initiated for additional conditions because of diagnostic uncertainty. Even after complete diagnostic evaluation, at least 25% of patients who have genital ulcers have no laboratoryconfirmed diagnosis.
# Chancroid
In the United States, chancroid usually occurs in discrete outbreaks, although the disease is endemic in some areas. Chancroid is a cofactor for HIV transmission, as are genital herpes and syphilis; high rates of HIV infection among patients who have chancroid occur in the United States and other countries. Approximately 10% of persons who have chancroid that was acquired in the United States are coinfected with T. pallidum or HSV; this percentage is higher in persons who have acquired chancroid outside the United States.
A definitive diagnosis of chancroid requires the identification of H. ducreyi on special culture media that is not widely available from commercial sources; even when these media are used, sensitivity is <80%. No FDA-cleared PCR test for H. ducreyi is available in the United States, but such testing can be performed by clinical laboratories that have developed their own PCR test and conducted a CLIA verification study.
The combination of a painful genital ulcer and tender suppurative inguinal adenopathy suggests the diagnosis of chancroid. A probable diagnosis of chancroid, for both clinical and surveillance purposes, can be made if all of the following criteria are met: 1) the patient has one or more painful genital ulcers; 2) the patient has no evidence of T. pallidum infection by darkfield examination of ulcer exudate or by a serologic test for syphilis performed at least 7 days after onset of ulcers; 3) the clinical presentation, appearance of genital ulcers and, if present, regional lymphadenopathy are typical for chancroid; and 4) a test for HSV performed on the ulcer exudate is negative.
# Treatment
Successful treatment for chancroid cures the infection, resolves the clinical symptoms, and prevents transmission to others. In advanced cases, scarring can result, despite successful therapy.
# Recommended Regimens
# Other Management Considerations
Male patients who are uncircumcised and patients with HIV infection do not respond as well to treatment as those who are circumcised or HIV negative. Patients should be tested for HIV infection at the time chancroid is diagnosed. Patients should be retested for syphilis and HIV 3 months after the diagnosis of chancroid, if the initial test results were negative.
# Follow-Up
Patients should be reexamined 3-7 days after initiation of therapy. If treatment is successful, ulcers usually improve symptomatically within 3 days and objectively within 7 days after therapy. If no clinical improvement is evident, the clinician must consider whether 1) the diagnosis is correct, 2) the patient is coinfected with another STD, 3) the patient is infected with HIV, 4) the treatment was not used as instructed, or 5) the H. ducreyi strain causing the infection is resistant to the prescribed antimicrobial. The time required for complete healing depends on the size of the ulcer; large ulcers might require >2 weeks. In addition, healing is slower for some uncircumcised men who have ulcers under the foreskin. Clinical resolution of fluctuant lymphadenopathy is slower than resolution for ulcers and might require needle aspiration or incision and drainage. Although needle aspiration of chancroid buboes is a simple procedure, incision and drainage might be preferred because of a reduced need for repeat drainage procedures.
# Management of Sex Partners
Sex partners of patients who have chancroid should be examined and treated, regardless of whether symptoms of the disease are present, if they had sexual contact with the patient during the 10 days preceding the patient's onset of symptoms.
# Special Considerations
# Pregnancy
The safety and efficacy of azithromycin for pregnant and lactating women have not been established. Ciprofloxacin is contraindicated during pregnancy and lactation. No adverse effects of chancroid on pregnancy outcome have been reported.
# HIV Infection
HIV-infected patients who have chancroid should be monitored closely because, as a group, these patients are more likely to experience treatment failure and to have ulcers that heal more slowly. HIV-infected patients might require longer courses of therapy than those recommended for HIVnegative patients, and treatment failures can occur with any regimen. Because evidence is limited concerning the therapeutic efficacy of the recommended ceftriaxone and azithromycin regimens in HIV-infected patients, these regimens should be used for such patients only if follow-up can be ensured. Some specialists prefer the erythromycin 7-day regimen for treating HIV-infected persons.
# Genital HSV Infections
Genital herpes is a chronic, life-long viral infection. Two types of HSV have been identified, HSV-1 and HSV-2. The majority of cases of recurrent genital herpes are caused by HSV-2 although HSV-1 might become more common as a cause of first episode genital herpes. At least 50 million persons in the United States have genital HSV infection.
The majority of persons infected with HSV-2 have not been diagnosed with genital herpes. Many such persons have mild or unrecognized infections but shed virus intermittently in the genital tract. The majority of genital herpes infections are transmitted by persons unaware that they have the infection or who are asymptomatic when transmission occurs.
# Diagnosis of HSV Infection
The clinical diagnosis of genital herpes is both insensitive and nonspecific. The classical painful multiple vesicular or ulcerative lesions are absent in many infected persons. Up to 50% of first-episode cases of genital herpes are caused by HSV-1 (63), but recurrences and subclinical shedding are much less frequent for genital HSV-1 infection than genital HSV-2 infection (64,65). Therefore, whether genital herpes is caused by HSV-1 or HSV-2 influences prognosis and coun-seling. Therefore, the clinical diagnosis of genital herpes should be confirmed by laboratory testing (66). Both virologic and type-specific serologic tests for HSV should be available in clinical settings that provide care for patients with STDs or those at risk for STDs.
# Virologic Tests
Isolation of HSV in cell culture is the preferred virologic test for patients who seek medical treatment for genital ulcers or other mucocutaneous lesions. However, the sensitivity of culture is low, especially for recurrent lesions, and declines rapidly as lesions begin to heal. PCR assays for HSV DNA are more sensitive and have been used instead of viral culture (67,68); however, PCR tests are not FDA-cleared for testing of genital specimens. PCR is the test of choice for detecting HSV in spinal fluid for diagnosis of HSV infection of the central nervous system (CNS). Viral culture isolates should be typed to determine if HSV-1 or HSV-2 is the cause of the infection. Lack of HSV detection (i.e., culture or PCR) does not indicate a lack of HSV infection, as viral shedding is intermittent. The use of cytologic detection of cellular changes of HSV infection is an insensitive and nonspecific method of diagnosis, both for genital lesions (i.e., Tzanck preparation) and for cervical Pap smears and should not be relied upon.
# Type-Specific Serologic Tests
Both type-specific and nontype-specific antibodies to HSV develop during the first several weeks after infection and persist indefinitely. Accurate type-specific HSV serologic assays are based on the HSV-specific glycoprotein G2 (HSV-2) and glycoprotein G1 (HSV-1). Such assays first became commercially available in 1999, but older assays that do not accurately distinguish HSV-1 from HSV-2 antibody (despite claims to the contrary) remain on the market. Therefore, the serologic type-specific glycoprotein G (gG)-based assays should be specifically requested when serology is performed (69)(70)(71).
The FDA-cleared glycoprotein G-based type-specific assays include the laboratory-based assays HerpeSelect™-1 enzymelinked immunosorbent assay (ELISA) immunoglobulin G (IgG) or HerpeSelect™-2 ELISA IgG and HerpeSelect™ 1 and 2 Immunoblot IgG (Focus Technology, Inc., Herndon, Virginia), and HSV-2 ELISA (Trinity Biotech USA, Berkeley Heights, New Jersey). Two other assays, Biokit HSV-2 and SureVue HSV-2 (Biokit USA, Lexington, Massachusetts, and Fisher Scientific, Pittsburgh, Pennsylvania, respectively), are point-of-care tests that provide results for HSV-2 antibodies from capillary blood or serum during a clinic visit. The sensitivities of these glycoprotein G type-specific tests for the detection of HSV-2 antibody vary from 80%-98%, and false-negative results might be more frequent at early stages of infection. The specificities of these assays are >96%. Falsepositive results can occur, especially in patients with a low likelihood of HSV infection. Repeat or confirmatory testing might be indicated in some settings, especially if recent acquisition of genital herpes is suspected.
Because nearly all HSV-2 infections are sexually acquired, the presence of type-specific HSV-2 antibody implies anogenital infection and education and counseling appropriate for persons with genital herpes should be provided. The presence of HSV-1 antibody alone is more difficult to interpret. The majority of persons with HSV-1 antibody have oral HSV infection acquired during childhood, which might be asymptomatic. However, acquisition of genital HSV-1 appears to be increasing, and genital HSV-1 also might be asymptomatic. Lack of symptoms in an HSV-1 seropositive person does not distinguish anogenital from orolabial or cutaneous infection. Persons with HSV-1 infection, regardless of site of infection, remain at risk for HSV-2 acquisition.
Type-specific HSV serologic assays might be useful in the following scenarios: 1) recurrent genital symptoms or atypical symptoms with negative HSV cultures; 2) a clinical diagnosis of genital herpes without laboratory confirmation; and 3) a partner with genital herpes. Some specialists believe that HSV serologic testing should be included in a comprehensive evaluation for STDs among persons with multiple sex partners, HIV infection, and among MSM at increased risk for HIV acquisition. Screening for HSV-1 or HSV-2 in the general population is not indicated.
# Principles of Management of Genital Herpes
Antiviral chemotherapy offers clinical benefits to the majority of symptomatic patients and is the mainstay of management. Counseling regarding the natural history of genital herpes, sexual and perinatal transmission, and methods to reduce transmission is integral to clinical management.
Systemic antiviral drugs can partially control the signs and symptoms of herpes episodes when used to treat first clinical and recurrent episodes, or when used as daily suppressive therapy. However, these drugs neither eradicate latent virus nor affect the risk, frequency, or severity of recurrences after the drug is discontinued. Randomized trials have indicated that three antiviral medications provide clinical benefit for genital herpes: acyclovir, valacyclovir, and famciclovir (72)(73)(74)(75)(76)(77)(78)(79)(80). Valacyclovir is the valine ester of acyclovir and has enhanced absorption after oral administration. Famciclovir also has high oral bioavailability. Topical therapy with antiviral drugs offers minimal clinical benefit, and its use is discouraged.
# First Clinical Episode of Genital Herpes
Many persons with first-episode herpes have mild clinical manifestations but later develop severe or prolonged symptoms. Therefore, patients with initial genital herpes should receive antiviral therapy.
# Recommended Regimens*
Acyclovir 400 mg orally three times a day for 7-10 days OR Acyclovir 200 mg orally five times a day for 7-10 days OR Famciclovir 250 mg orally three times a day for 7-10 days OR Valacyclovir 1 g orally twice a day for 7-10 days
# Established HSV-2 infection
The majority of patients with symptomatic, first-episode genital HSV-2 infection subsequently experience recurrent episodes of genital lesions; recurrences are less frequent after initial genital HSV-1 infection. Intermittent asymptomatic shedding occurs in persons with genital HSV-2 infection, even in those with longstanding or clinically silent infection. Antiviral therapy for recurrent genital herpes can be administered either episodically to ameliorate or shorten the duration of lesions or continuously as suppressive therapy to reduce the frequency of recurrences. Many persons, including those with mild or infrequent recurrent outbreaks, benefit from antiviral therapy; therefore, options for treatment should be discussed. Some persons might prefer suppressive therapy, which has the additional advantage of decreasing the risk of genital HSV-2 transmission to susceptible partners (81).
# Suppressive Therapy for Recurrent Genital Herpes
Suppressive therapy reduces the frequency of genital herpes recurrences by 70%-80% in patients who have frequent recurrences (i.e., >6 recurrences per year), and many patients report no symptomatic outbreaks. Treatment also is effective in patients with less frequent recurrences. Safety and efficacy have been documented among patients receiving daily therapy with acyclovir for as long as 6 years and with valacyclovir or famciclovir for 1 year. Quality of life frequently is improved in patients with frequent recurrences who receive suppressive therapy, compared with episodic treatment.
The frequency of recurrent genital herpes outbreaks diminishes over time in many patients, and the patient's psychological adjustment to the disease might change. Therefore, periodically during suppressive treatment (e.g., once a year), providers should discuss the need to continue therapy with the patient. Daily treatment with valacyclovir 500 mg daily decreases the rate of HSV-2 transmission in discordant, heterosexual couples in which the source partner has a history of genital HSV-2 infection (82). Such couples should be encouraged to consider suppressive antiviral therapy as part of a strategy to prevent transmission, in addition to consistent condom use and avoidance of sexual activity during recurrences. Suppressive antiviral therapy probably reduces transmission when used by persons who have multiple partners (including MSM) and by those who are HSV-2 seropositive without a history of genital herpes.
# Recommended Regimens
Acyclovir 400 mg orally twice a day OR Famiciclovir 250 mg orally twice a day OR Valacyclovir 500 mg orally once a day OR Valacyclovir 1.0 g orally once a day Valacyclovir 500 mg once a day might be less effective than other valacyclovir or acyclovir dosing regimens in patients who have very frequent recurrences (i.e., >10 episodes per year). Several studies have compared valacyclovir or famciclovir with acyclovir. The results of these studies suggest that valacyclovir and famciclovir are comparable to acyclovir in clinical outcome (74,78,79,83). Ease of administration and cost also are important considerations for prolonged treatment.
# Episodic Therapy for Recurrent Genital Herpes
Effective episodic treatment of recurrent herpes requires initiation of therapy within 1 day of lesion onset or during the prodrome that precedes some outbreaks. The patient should be provided with a supply of drug or a prescription for the medication with instructions to initiate treatment immediately when symptoms begin.
# Recommended Regimens
Acyclovir 400 mg orally three times a day for 5 days OR Acyclovir 800 mg orally twice a day for 5 days OR Acyclovir 800 mg orally three times a day for 2 days OR Famciclovir 125 mg orally twice daily for 5 days OR Famciclovir 1000 mg orally twice daily for 1 day OR Valacyclovir 500 mg orally twice a day for 3 days OR Valacyclovir 1.0 g orally once a day for 5 days
# Severe Disease
Intravenous (IV) acyclovir therapy should be provided for patients who have severe HSV disease or complications that necessitate hospitalization (e.g., disseminated infection, pneumonitis, or hepatitis) or CNS complications (e.g., meningitis or encephalitis). The recommended regimen is acyclovir 5-10 mg/kg body weight IV every 8 hours for 2-7 days or until clinical improvement is observed, followed by oral antiviral therapy to complete at least 10 days of total therapy.
# Counseling
Counseling of infected persons and their sex partners is critical to the management of genital herpes. The goal of counseling is to 1) help patients cope with the infection and 2) prevent sexual and perinatal transmission (8). Although initial counseling can be provided at the first visit, many patients benefit from learning about the chronic aspects of the disease after the acute illness subsides. Multiple resources, including websites ( and ) and printed materials are available to assist patients, their partners, and clinicians in counseling.
HSV-infected persons might express anxiety concerning genital herpes that does not reflect the actual clinical severity of their disease; the psychological effect of HSV infection frequently is substantial. Common concerns regarding genital herpes include the severity of initial clinical manifestations, recurrent episodes, sexual relationships and transmission to sex partners, and ability to bear healthy children. The misconception that HSV causes cancer should be dispelled. The psychological effect of a serologic diagnosis of HSV-2 infection in a person with asymptomatic or unrecognized genital herpes appears small and transient (84).
The following recommendations apply to counseling of persons with HSV infection:
- Persons who have genital herpes should be educated concerning the natural history of the disease, with emphasis on the potential for recurrent episodes, asymptomatic viral shedding, and the attendant risks of sexual transmission. - Persons experiencing a first episode of genital herpes should be advised that suppressive therapy is available and is effective in preventing symptomatic recurrent episodes and that episodic therapy sometimes is useful in shortening the duration of recurrent episodes.
# Management of Sex Partners
The sex partners of patients who have genital herpes can benefit from evaluation and counseling. Symptomatic sex partners should be evaluated and treated in the same manner as patients who have genital lesions. Asymptomatic sex partners of patients who have genital herpes should be questioned concerning histories of genital lesions and offered type-specific serologic testing for HSV infection.
# Special Considerations
# Allergy, Intolerance, and Adverse Reactions
Allergic and other adverse reactions to acyclovir, valacyclovir, and famciclovir are rare. Desensitization to acyclovir has been described (85).
# HIV Infection
Immunocompromised patients might have prolonged or severe episodes of genital, perianal, or oral herpes. Lesions caused by HSV are common among HIV-infected patients and might be severe, painful, and atypical. HSV shedding is increased in HIV-infected persons. Whereas antiretroviral therapy reduces the severity and frequency of symptomatic genital herpes, frequent subclinical shedding still occurs (86). Suppressive or episodic therapy with oral antiviral agents is effective in decreasing the clinical manifestations of HSV among HIV-positive persons (87)(88)(89). HIV-infected persons are likely to be more contagious for HSV; the extent to which suppressive antiviral therapy will decrease HSV transmission from this population is unknown. Some specialists suggest that HSV type-specific serologies be offered to HIV-positive persons during their initial evaluation, and that suppressive antiviral therapy be considered in those who have HSV-2 infection.
# Recommended Regimens for Daily Suppressive Therapy in Persons Infected with HIV
Acyclovir 400-800 mg orally twice to three times a day OR Famciclovir 500 mg orally twice a day OR Valacyclovir 500 mg orally twice a day
# Recommended Regimens for Episodic Infection in Persons Infected with HIV
Acyclovir 400 mg orally three times a day for 5-10 days OR Famiciclovir 500 mg orally twice a day for 5-10 days OR Valacyclovir 1.0 grams orally twice a day for 5-10 days Acyclovir, valacyclovir, and famciclovir are safe for use in immunocompromised patients in the doses recommended for treatment of genital herpes. For severe HSV disease, initiating therapy with acyclovir 5-10 mg/kg body weight IV every 8 hours might be necessary.
If lesions persist or recur in a patient receiving antiviral treatment, HSV resistance should be suspected and a viral isolate should be obtained for sensitivity testing (90). Such patients should be managed in consultation with an HIV specialist, and alternate therapy should be administered. All acyclovir-resistant strains are resistant to valacyclovir, and the majority are resistant to famciclovir. Foscarnet, 40 mg/kg body weight IV every 8 hours until clinical resolution is attained, is frequently effective for treatment of acyclovir-resistant genital herpes. Topical cidofovir gel 1% applied to the lesions once daily for 5 consecutive days also might be effective. This preparation is not commercially available and must be compounded at a pharmacy.
# Genital Herpes in Pregnancy
The majority of mothers of infants who acquire neonatal herpes lack histories of clinically evident genital herpes. The risk for transmission to the neonate from an infected mother is high (30%-50%) among women who acquire genital herpes near the time of delivery and is low (<1%) among women with histories of recurrent herpes at term or who acquire genital HSV during the first half of pregnancy. However, because recurrent genital herpes is much more common than initial HSV infection during pregnancy, the proportion of neonatal HSV infections acquired from mothers with recurrent herpes is substantial. Prevention of neonatal herpes depends both on preventing acquisition of genital HSV infection during late pregnancy and avoiding exposure of the infant to herpetic lesions during delivery.
Women without known genital herpes should be counseled to avoid intercourse during the third trimester with partners known or suspected of having genital herpes. In addition, pregnant women without known orolabial herpes should be advised to avoid receptive oral sex during the third trimester with partners known or suspected to have orolabial herpes. Some specialists believe that type-specific serologic tests are useful to identify pregnant women at risk for HSV infection and to guide counseling regarding the risk for acquiring genital herpes during pregnancy. Such testing should be offered to women without genital herpes whose sex partner has HSV infection. The effectiveness of antiviral therapy to decrease the risk for HSV transmission to pregnant women has not been studied.
All pregnant women should be asked whether they have a history of genital herpes. At the onset of labor, all women should be questioned carefully about symptoms of genital herpes, including prodromal symptoms, and all women should be examined carefully for herpetic lesions. Women without symptoms or signs of genital herpes or its prodrome can deliver vaginally. The majority of specialists recommend that women with recurrent genital herpetic lesions at the onset of labor deliver by cesarean section to prevent neonatal herpes. However, cesarean section does not completely eliminate the risk for HSV transmission to the infant.
The safety of systemic acyclovir, valacyclovir, and famciclovir therapy in pregnant women has not been definitively established. Available data do not indicate an increased risk for major birth defects compared with the general population in women treated with acyclovir during the first trimester (91). These findings provide some assurance to women who have had prenatal exposure to acyclovir. The experience with prenatal exposure to valacyclovir and famciclovir is too limited to provide useful information on pregnancy outcomes. Acyclovir may be administered orally to pregnant women with first episode genital herpes or severe recurrent herpes and should be administered IV to pregnant women with severe HSV infection. Acyclovir treatment late in pregnancy reduces the frequency of cesarean sections among women who have recurrent genital herpes by diminishing the frequency of recurrences at term, and many specialists recommend such treatment (92)(93)(94). No data support the use of antiviral therapy among HSV seropositive women without a history of genital herpes. The risk for herpes is high in infants of women who acquire genital HSV during late pregnancy; such women should be managed in consultation with an infectious diseases specialist. Some specialists recommend acyclovir therapy in this circumstance, some recommend routine cesarean section to reduce the risk for neonatal herpes, and others recommend both.
# Neonatal Herpes
Infants exposed to HSV during birth, as documented by maternal virologic testing or presumed by observation of maternal lesions, should be followed carefully in consultation with a specialist. Some specialists recommend that such infants undergo surveillance cultures of mucosal surfaces to detect HSV infection before development of clinical signs of neonatal herpes. In addition, some specialists recommend the use of acyclovir for infants born to women who acquired HSV near term because the risk for neonatal herpes is high for these infants. All infants who have neonatal herpes should be promptly evaluated and treated with systemic acyclovir. The recommended regimen for infants treated for known or suspected neonatal herpes is acyclovir 20 mg/kg body weight IV every 8 hours for 21 days for disseminated and CNS disease or for 14 days for disease limited to the skin and mucous membranes.
# Granuloma Inguinale (Donovanosis)
Granuloma inguinale is a genital ulcerative disease caused by the intracellular gram-negative bacterium Klebsiella granulomatis (formerly known as Calymmatobacterium granulomatis). The disease occurs rarely in the United States, although it is endemic in some tropical and developing areas, including India; Papua, New Guinea; central Australia; and southern Africa. Clinically, the disease is commonly characterized as painless, progressive ulcerative lesions without regional lymphadenopathy. The lesions are highly vascular (i.e., beefy red appearance) and bleed easily on contact. However, the clinical presentation also can include hypertrophic, necrotic, or sclerotic variants. The causative organism is difficult to culture, and diagnosis requires visualization of dark-staining Donovan bodies on tissue crush preparation or biopsy. No FDA-cleared PCR tests for the detection of K. granulomatis DNA exist, but such an assay might be useful if a CLIA verification study has been conducted. The lesions might develop secondary bacterial infection or can coexist with other sexually transmitted pathogens.
# Treatment
A limited number of studies on Donovanosis treatment have been published. Treatment halts progression of lesions, although prolonged therapy is usually required to permit granulation and reepithelialization of the ulcers. Healing typically proceeds inward from the ulcer margins. Relapse can occur 6-18 months after apparently effective therapy. Several antimicrobial regimens have been effective, but a limited number of controlled trials have been published (95).
# Recommended Regimen
Doxycycline 100 mg orally twice a day for at least 3 weeks and until all lesions have completely healed
# Alternative Regimens
Azithromycin 1 g orally once per week for at least 3 weeks and until all lesions have completely healed OR Ciprofloxacin 750 mg orally twice a day for at least 3 weeks and until all lesions have completely healed OR Erythromycin base 500 mg orally four times a day for at least 3 weeks and until all lesions have completely healed OR Trimethoprim-sulfamethoxazole one double-strength (160 mg/800 mg) tablet orally twice a day for at least 3 weeks and until all lesions have completely healed Therapy should be continued at least 3 weeks and until all lesions have completely healed. Some specialists recommend the addition of an aminoglycoside (e.g., gentamicin 1 mg/kg IV every 8 hours) to these regimens if improvement is not evident within the first few days of therapy.
# Follow-Up
Patients should be followed clinically until signs and symptoms have resolved.
# Management of Sex Partners
Persons who have had sexual contact with a patient who has granuloma inguinale within the 60 days before onset of the patient's symptoms should be examined and offered therapy. However, the value of empiric therapy in the absence of clinical signs and symptoms has not been established.
# Special Considerations
# Pregnancy
Pregnancy is a relative contraindication to the use of sulfonamides. Pregnant and lactating women should be treated with the erythromycin regimen, and consideration should be given to the addition of a parenteral aminoglycoside (e.g., gentamicin). Azithromycin might prove useful for treating granuloma inguinale during pregnancy, but published data are lacking. Doxycycline and ciprofloxacin are contraindicated in pregnant women.
# HIV Infection
Persons with both granuloma inguinale and HIV infection should receive the same regimens as those who are HIV negative. Consideration should be given to the addition of a parenteral aminoglycoside (e.g., gentamicin).
# Lymphogranuloma Venereum
Lymphogranuloma venereum (LGV) is caused by C. trachomatis serovars L1, L2, or L3 (96). The most common clinical manifestation of LGV among heterosexuals is tender inguinal and/or femoral lymphadenopathy that is typically unilateral. A self-limited genital ulcer or papule sometimes occurs at the site of inoculation. However, by the time patients seek care, the lesions might have disappeared. Rectal exposure in women or MSM might result in proctocolitis (including mucoid and/or hemorrhagic rectal discharge, anal pain, constipation, fever, and/or tenesmus).
LGV is an invasive, systemic infection, and if it is not treated early, LGV proctocolitis might lead to chronic, colorectal fistulas and strictures. Genital and colorectal LGV lesions might also develop secondary bacterial infection or might be coinfected with other sexually and nonsexually transmitted pathogens.
Diagnosis is based on clinical suspicion, epidemiologic information, and the exclusion of other etiologies (of proctocolitis, inguinal lymphadenopathy, or genital or rectal ulcers), along with C. trachomatis testing, if available.
Genital and lymph node specimens (i.e., lesion swab or bubo aspirate) may be tested for C. trachomatis by culture, direct immunofluorescence, or nucleic acid detection. Nucleic acid amplification tests (NAAT) for C. trachomatis are not FDAcleared for testing rectal specimens. Additional procedures (e.g., genotyping) are required for differentiating LGV from non-LGV C. trachomatis but are not widely available.
Chlamydia serology (complement fixation titers >1:64) can support the diagnosis in the appropriate clinical context. Comparative data between types of serologic tests are lacking, and the diagnostic utility of serologic methods other than complement fixation and some microimmunofluorescence procedures has not been established. Serologic test interpretation for LGV is not standardized, tests have not been validated for clinical proctitis presentations, and C. trachomatis serovar-specific serologic tests are not widely available.
In the absence of specific LGV diagnostic testing, patients with a clinical syndrome consistent with LGV, including proctocolitis or genital ulcer disease with lymphadenopathy, should be treated for LGV as described in this report.
# Treatment
Treatment cures infection and prevents ongoing tissue damage, although tissue reaction to the injection can result in scarring. Buboes might require aspiration through intact skin or incision and drainage to prevent the formation of inguinal/ femoral ulcerations. Doxycycline is the preferred treatment.
# Recommended Regimen
# Doxycycline 100 mg orally twice a day for 21 days
# Alternative Regimen
Erythromycin base 500 mg orally four times a day for 21 days Some STD specialists believe that azithromycin 1.0 g orally once weekly for 3 weeks is probably effective, although clinical data are lacking.
# Follow-Up
Patients should be followed clinically until signs and symptoms have resolved.
# Management of Sex Partners
Persons who have had sexual contact with a patient who has LGV within the 60 days before onset of the patient's symptoms should be examined, tested for urethral or cervical chlamydial infection, and treated with a standard chlamydia regimen (azithromycin 1 gm orally x 1 or doxycycline 100 mg orally twice a day for 7 days). The optimum contact interval is unknown; some specialists use longer contact intervals.
# Special Considerations
# Pregnancy
Pregnant and lactating women should be treated with erythromycin. Azithromycin might prove useful for treatment of LGV in pregnancy, but no published data are available regarding its safety and efficacy. Doxycycline is contraindicated in pregnant women.
# HIV Infection
Persons with both LGV and HIV infection should receive the same regimens as those who are HIV negative. Prolonged therapy might be required, and delay in resolution of symptoms might occur.
# Syphilis General Principles
# Background
Syphilis is a systemic disease caused by T. pallidum. Patients who have syphilis might seek treatment for signs or symptoms of primary infection (i.e., ulcer or chancre at the infection site), secondary infection (i.e., manifestations that include, but are not limited to, skin rash, mucocutaneous lesions, and lymphadenopathy), or tertiary infection (e.g., cardiac or ophthalmic manifestations, auditory abnormalities, or gummatous lesions). Latent infections (i.e., those lacking clinical manifestations) are detected by serologic testing. Latent syphilis acquired within the preceding year is referred to as early latent syphilis; all other cases of latent syphilis are either late latent syphilis or latent syphilis of unknown duration. Treatment for both late latent syphilis and tertiary syphilis theoretically might require a longer duration of therapy because organisms are dividing more slowly; however, the validity of this concept has not been assessed.
# Diagnostic Considerations and Use of Serologic Tests
Darkfield examinations and direct fluorescent antibody (DFA) tests of lesion exudate or tissue are the definitive methods for diagnosing early syphilis. A presumptive diagnosis is possible with the use of two types of serologic tests: 1) nontreponemal tests (e.g., Venereal Disease Research Laboratory and RPR) and 2) treponemal tests (e.g., fluorescent treponemal antibody absorbed and T. pallidum particle agglutination ). The use of only one type of serologic test is insufficient for diagnosis because false-positive nontreponemal test results are sometimes associated with various medical conditions unrelated to syphilis.
Nontreponemal test antibody titers usually correlate with disease activity, and results should be reported quantitatively. A fourfold change in titer, equivalent to a change of two dilutions (e.g., from 1:16-1:4 or from 1:8-1:32), is considered necessary to demonstrate a clinically significant difference between two nontreponemal test results that were obtained using the same serologic test. Sequential serologic tests in individual patients should be performed by using the same testing method (e.g., VDRL or RPR), preferably by the same laboratory. The VDRL and RPR are equally valid assays, but quantitative results from the two tests cannot be compared directly because RPR titers frequently are slightly higher than VDRL titers. Nontreponemal tests usually become nonreactive with time after treatment; however, in some patients, nontreponemal antibodies can persist at a low titer for a long period of time, sometimes for the life of the patient. This response is referred to as the serofast reaction.
The majority of patients who have reactive treponemal tests will have reactive tests for the remainder of their lives, regardless of treatment or disease activity. However, 15%-25% of patients treated during the primary stage revert to being serologically nonreactive after 2-3 years (97). Treponemal test antibody titers do not correlate with disease activity and should not be used to assess treatment response.
Some clinical laboratories and blood banks have begun to screen samples using treponemal EIA tests (98). This strategy will identify both persons with previous treatment and persons with untreated or incompletely treated syphilis. Falsepositive results can occur, particularly among populations with a low prevalence of syphilis.
Persons with a positive treponemal screening test should have a standard nontreponemal test with titer to guide patient management decisions. If the nontreponemal test is negative, then a different treponemal test should be performed to confirm the results of the initial test. If a second trepomenal test is positive, treatment decisions should be discussed in consultation with a specialist. Some HIV-infected patients can have atypical serologic test results (i.e., unusually high, unusually low, or fluctuating titers). For such patients, when serologic tests do not correspond with clinical syndromes suggestive of early syphilis, use of other tests (e.g., biopsy and direct microscopy) should be considered. However, for the majority of HIV-infected patients, serologic tests are accurate and reliable for the diagnosis of syphilis and for following the response to treatment.
No single test can be used to diagnose neurosyphilis. The VDRL-cerebrospinal fluid (CSF) is highly specific, but it is insensitive. The majority of other tests are both insensitive and nonspecific and must be interpreted in relation to other test results and the clinical assessment. Therefore, the diagno-sis of neurosyphilis usually depends on various combinations of reactive serologic test results, CSF cell count or protein, or a reactive VDRL-CSF with or without clinical manifestations. The CSF leukocyte count usually is elevated (>5 white blood cell count /mm 3 ) in patients with neurosyphilis; this count also is a sensitive measure of the effectiveness of therapy. The VDRL-CSF is the standard serologic test for CSF, and when reactive in the absence of substantial contamination of CSF with blood, it is considered diagnostic of neurosyphilis. However, the VDRL-CSF might be nonreactive even when neurosyphilis is present. Some specialists recommend performing an FTA-ABS test on CSF. The CSF FTA-ABS is less specific (i.e., yields more false-positive results) for neurosyphilis than the VDRL-CSF, but the test is highly sensitive. Therefore, some specialists believe that a negative CSF FTA-ABS test excludes neurosyphilis.
# Treatment
Penicillin G, administered parenterally, is the preferred drug for treatment of all stages of syphilis. The preparation(s) used (i.e., benzathine, aqueous procaine, or aqueous crystalline), the dosage, and the length of treatment depend on the stage and clinical manifestations of the disease. However, neither combinations of benzathine penicillin and procaine penicillin nor oral penicillin preparations are considered appropriate for the treatment of syphilis. Reports have indicated that inappropriate use of combination benzathine-procaine penicillin (Bicillin C-R ® ) instead of the standard benzathine penicillin product widely used in the United States (Bicillin L-A ® ) has occurred. Practitioners, pharmacists, and purchasing agents should be aware of the similar names of these two products and avoid use of the inappropriate combination therapy agent for treating syphilis (99).
The efficacy of penicillin for the treatment of syphilis was well established through clinical experience even before the value of randomized controlled clinical trials was recognized. Therefore, nearly all the recommendations for the treatment of syphilis are based on the opinions of persons knowledgeable about STDs and are reinforced by case series, clinical trials, and 50 years of clinical experience.
Parenteral penicillin G is the only therapy with documented efficacy for syphilis during pregnancy. Pregnant women with syphilis in any stage who report penicillin allergy should be desensitized and treated with penicillin. Skin testing for penicillin allergy might be useful in pregnant women; such testing also is useful in other patients (see Management of Patients Who Have a History of Penicillin Allergy).
The Jarisch-Herxheimer reaction is an acute febrile reaction frequently accompanied by headache, myalgia, and other symptoms that usually occur within the first 24 hours after any therapy for syphilis. Patients should be informed about this possible adverse reaction. The Jarisch-Herxheimer reaction occurs most frequently among patients who have early syphilis. Antipyretics may be used, but they have not been proven to prevent this reaction. The Jarisch-Herxheimer reaction might induce early labor or cause fetal distress in pregnant women, but this should not prevent or delay therapy (see Syphilis During Pregnancy).
# Management of Sex Partners
Sexual transmission of T. pallidum occurs only when mucocutaneous syphilitic lesions are present; such manifestations are uncommon after the first year of infection. However, persons exposed sexually to a patient who has syphilis in any stage should be evaluated clinically and serologically and treated with a recommended regimen, according to the following recommendations:
- Persons who were exposed within the 90 days preceding the diagnosis of primary, secondary, or early latent syphilis in a sex partner might be infected even if seronegative; therefore, such persons should be treated presumptively. - Persons who were exposed >90 days before the diagnosis of primary, secondary, or early latent syphilis in a sex partner should be treated presumptively if serologic test results are not available immediately and the opportunity for follow-up is uncertain. - For purposes of partner notification and presumptive treatment of exposed sex partners, patients with syphilis of unknown duration who have high nontreponemal serologic test titers (i.e., >1:32) can be assumed to have early syphilis. However, serologic titers should not be used to differentiate early from late latent syphilis for the purpose of determining treatment (see Latent Syphilis, Treatment). - Long-term sex partners of patients who have latent syphilis should be evaluated clinically and serologically for syphilis and treated on the basis of the evaluation findings. For identification of at-risk sexual partners, the periods before treatment are 1) 3 months plus duration of symptoms for primary syphilis, 2) 6 months plus duration of symptoms for secondary syphilis, and 3) 1 year for early latent syphilis.
# Primary and Secondary Syphilis
# Treatment
Parenteral penicillin G has been used effectively for more than 50 years to achieve clinical resolution (i.e., healing of lesions and prevention of sexual transmission) and to prevent late sequelae. However, no comparative trials have been adequately conducted to guide the selection of an optimal penicillin regimen (i.e., the dose, duration, and preparation). Substantially fewer data are available for nonpenicillin regimens.
# Recommended Regimen for Adults*
Benzathine penicillin G 2.4 million units IM in a single dose - Recommendations for treating HIV-infected persons and pregnant women for syphilis have been discussed in this report (see Syphilis, Special considerations and Syphilis in Pregnancy).
# Recommended Regimen for Children
After the newborn period (aged >1 month), children with syphilis should have a CSF examination to detect asymptomatic neurosyphilis, and birth and maternal medical records should be reviewed to assess whether such children have congenital or acquired syphilis (see Congenital Syphilis). Children with acquired primary or secondary syphilis should be evaluated (e.g., through consultation with child-protection services) (see Sexual Assault or Abuse of Children) and treated by using the following pediatric regimen.
Benzathine penicillin G 50,000 units/kg IM, up to the adult dose of 2.4 million units in a single dose
# Other Management Considerations
All patients who have syphilis should be tested for HIV infection. In geographic areas in which the prevalence of HIV is high, patients who have primary syphilis should be retested for HIV after 3 months if the first HIV test result was negative.
Patients who have syphilis and symptoms or signs suggesting neurologic disease (e.g., meningitis) or ophthalmic disease (e.g., uveitis, iritis, neuroretinitis, or optic neuritis) should have an evaluation that includes CSF analysis and ocular slitlamp examination. Treatment should be guided by the results of this evaluation.
Invasion of CSF by T. pallidum accompanied by CSF abnormalities is common among adults who have primary or secondary syphilis. However, neurosyphilis develops in only a limited number of patients after treatment with the penicillin regimens recommended for primary and secondary syphilis. Therefore, unless clinical signs or symptoms of neurologic or ophthalmic involvement are present, CSF analysis is not recommended for routine evaluation of patients who have primary or secondary syphilis.
# Follow-Up
Treatment failure can occur with any regimen. However, assessing response to treatment frequently is difficult, and definitive criteria for cure or failure have not been established. Nontreponemal test titers might decline more slowly for persons who previously had syphilis. Patients should be reexamined clinically and serologically 6 months and 12 months after treatment; more frequent evaluation might be prudent if follow-up is uncertain.
Patients who have signs or symptoms that persist or recur or who have a sustained fourfold increase in nontreponemal test titer (i.e., compared with the maximum or baseline titer at the time of treatment) probably failed treatment or were reinfected. These patients should be retreated and reevaluated for HIV infection. Because treatment failure usually cannot be reliably distinguished from reinfection with T. pallidum, a CSF analysis also should be performed. Clinical trial data have demonstrated that 15% of patients with early syphilis treated with the recommended therapy will not achieve a two dilution decline in nontreponemal titer used to define response at 1 year after treatment (100).
Failure of nontreponemal test titers to decline fourfold within 6 months after therapy for primary or secondary syphilis might be indicative of probable treatment failure. Persons for whom titers remain serofast should be reevaluated for HIV infection. Optimal management of such patients is unclear. At a minimum, these patients should receive additional clinical and serologic follow-up. HIV-infected patients should be evaluated more frequently (i.e., at 3-month intervals instead of 6-month intervals). If additional follow-up cannot be ensured, re-treatment is recommended. Because treatment failure might be the result of unrecognized CNS infection, many specialists recommend CSF examination in such situations.
For retreatment, the majority of STD specialists recommend administering weekly injections of benzathine penicillin G 2.4 million units IM for 3 weeks, unless CSF examination indicates that neurosyphilis is present. In rare instances, serologic titers do not decline despite a negative CSF examination and a repeated course of therapy. Additional therapy or repeated CSF examinations are not warranted in these circumstances.
# Management of Sex Partners
See General Principles, Management of Sex Partners.
# Special Considerations
Penicillin Allergy. Data to support the use of alternatives to penicillin in the treatment of early syphilis are limited. However, several therapies might be effective in nonpregnant, penicillin-allergic patients who have primary or secondary syphilis. Doxycycline (100 mg orally twice daily for 14 days) and tetracycline (500 mg four times daily for 14 days) are regimens that have been used for many years. Compliance is likely to be better with doxycycline than tetracycline because tetracycline can cause gastrointestinal side effects. Although limited clinical studies, along with biologic and pharmacologic evidence, suggest that ceftriaxone is effective for treating early syphilis, the optimal dose and duration of ceftriaxone therapy have not been defined. Some specialists recommend 1 g daily either IM or IV for 8-10 days. Some patients who are allergic to penicillin also might be allergic to ceftriaxone; in these circumstances, use of an alternative agent might be required. Preliminary data suggest that azithromycin might be effective as a single oral dose of 2 g (101,102). However, several cases of azithromycin treatment failure have been reported, and resistance to azithromycin has been documented in several geographic areas (103). Close follow-up of persons receiving alternative therapies is essential. The use of any of these therapies in HIV-infected persons has not been wellstudied; therefore, the use of doxycycline, ceftriaxone, and azithromycin among such persons must be undertaken with caution.
Patients with penicillin allergy whose compliance with therapy or follow-up cannot be ensured should be desensitized and treated with benzathine penicillin. Skin testing for penicillin allergy might be useful in some circumstances in which the reagents and expertise are available to perform the test adequately (see Management of Patients Who Have a History of Penicillin Allergy).
Pregnancy. Pregnant patients who are allergic to penicillin should be desensitized and treated with penicillin (see Management of Patients Who Have a History of Penicillin Allergy and Syphilis During Pregnancy).
HIV Infection. See Syphilis Among HIV-Infected Persons.
# Latent Syphilis
Latent syphilis is defined as syphilis characterized by seroreactivity without other evidence of disease. Patients who have latent syphilis and who acquired syphilis within the preceding year are classified as having early latent syphilis. Patients' conditions can be diagnosed as early latent syphilis if, within the year preceding the evaluation, they had 1) a documented seroconversion or fourfold or greater increase in titer of a nontreponemal test; 2) unequivocal symptoms of primary or secondary syphilis; 3) a sex partner documented to have primary, secondary, or early latent syphilis; or 4) reactive nontreponemal and treponemal tests from a person whose only possible exposure occurred within the previous 12 months. Nontreponemal serologic titers usually are higher during early latent syphilis than late latent syphilis. However, early latent syphilis cannot be reliably distinguished from late latent syphilis solely on the basis of nontreponemal titers. All patients with latent syphilis should have careful examination of all accessible mucosal surfaces (i.e., the oral cavity, the perineum in women, and perianal area, underneath the foreskin in uncircumcised men) to evaluate for internal mucosal lesions. All patients who have syphilis should be tested for HIV infection.
# MMWR August 4, 2006
# Treatment
Treatment of latent syphilis usually does not affect transmission and is intended to prevent late complications. Although clinical experience supports the effectiveness of penicillin in achieving this goal, limited evidence is available for guidance in choosing specific regimens.
The following regimens are recommended for penicillin nonallergic patients who have normal CSF examinations (if performed).
# Recommended Regimens for Adults
# Early Latent Syphilis
Benzathine penicillin G 2.4 million units IM in a single dose Late Latent Syphilis or Latent Syphilis of Unknown Duration Benzathine penicillin G 7.2 million units total, administered as 3 doses of 2.4 million units IM each at 1week intervals
After the newborn period, children with syphilis should have a CSF examination to exclude neurosyphilis. In addition, birth and maternal medical records should be reviewed to assess whether children have congenital or acquired syphilis (see Congenital Syphilis). Older children with acquired latent syphilis should be evaluated as described for adults and treated using the following pediatric regimens (see Sexual Assault or Abuse of Children). These regimens are for penicillin nonallergic children who have acquired syphilis and who have normal CSF examination results.
# Recommended Regimens for Children
# Early Latent Syphilis
Benzathine penicillin G 50,000 units/kg IM, up to the adult dose of 2.4 million units in a single dose Late Latent Syphilis or Latent Syphilis of Unknown Duration Benzathine penicillin G 50,000 units/kg IM, up to the adult dose of 2.4 million units, administered as 3 doses at 1-week intervals (total 150,000 units/kg up to the adult total dose of 7.2 million units)
# Other Management Considerations
All persons who have latent syphilis should be evaluated clinically for evidence of tertiary disease (e.g., aortitis and gumma) and syphilitic ocular disease (e.g., iritis and uveitis). Patients who have syphilis and who demonstrate any of the following criteria should have a prompt CSF examination:
- neurologic or ophthalmic signs or symptoms,
- evidence of active tertiary syphilis (e.g., aortitis and gumma), - treatment failure, or - HIV infection with late latent syphilis or syphilis of unknown duration. If dictated by circumstances and patient preferences, a CSF examination may be performed for patients who do not meet these criteria. Some specialists recommend performing a CSF examination on all patients who have latent syphilis and a nontreponemal serologic test of >1:32 or if the patient is HIVinfected with a serum CD4 count <350 (104). However, the likelihood of neurosyphilis in this circumstance is unknown. If a CSF examination is performed and the results indicate abnormalities consistent with neurosyphilis, the patient should be treated for neurosyphilis (see Neurosyphilis).
If a patient misses a dose of penicillin in a course of weekly therapy for late syphilis, the appropriate course of action is unclear. Pharmacologic considerations suggest that an interval of 10-14 days between doses of benzathine penicillin for late syphilis or latent syphilis of unknown duration might be acceptable before restarting the sequence of injections. Missed doses are not acceptable for pregnant patients receiving therapy for late latent syphilis; pregnant women who miss any dose of therapy must repeat the full course of therapy.
Follow-Up. Quantitative nontreponemal serologic tests should be repeated at 6, 12, and 24 months. Patients with a normal CSF examination should be re-treated for latent syphilis if 1) titers increase fourfold, 2) an initially high titer (>1:32) fails to decline at least fourfold (i.e., two dilutions) within 12-24 months of therapy, or 3) signs or symptoms attributable to syphilis develop. In rare instances, despite a negative CSF examination and a repeated course of therapy, serologic titers might still not decline. In these circumstances, the need for additional therapy or repeated CSF examinations is unclear.
Management of Sex Partners. See General Principles, Management of Sex Partners.
# Special Considerations
Penicillin Allergy. The effectiveness of alternatives to penicillin in the treatment of latent syphilis has not been welldocumented. Nonpregnant patients allergic to penicillin who have clearly defined early latent syphilis should respond to therapies recommended as alternatives to penicillin for the treatment of primary and secondary syphilis (see Primary and Secondary Syphilis, Treatment). The only acceptable alternatives for the treatment of late latent syphilis or latent syphilis of unknown duration are doxycycline (100 mg orally twice daily) or tetracycline (500 mg orally four times daily), both for 28 days. These therapies should be used only in conjunc-tion with close serologic and clinical follow-up. Limited clinical studies, along with biologic and pharmacologic evidence, suggest that ceftriaxone might be effective for treating late latent syphilis or syphilis of unknown duration (105). However, the optimal dose and duration of ceftriaxone therapy have not been defined, and treatment decisions should be discussed in consultation with a specialist. Some patients who are allergic to penicillin also might be allergic to ceftriaxone; in these circumstances, use of an alternative agent might be required. The efficacy of these alternative regimens in HIVinfected persons has not been well-studied and, therefore, must be considered with caution.
Pregnancy. Pregnant patients who are allergic to penicillin should be desensitized and treated with penicillin (see Management of Patients Who Have a History of Penicillin Allergy and Syphilis During Pregnancy).
HIV Infection. See Syphilis Among HIV-Infected Persons.
# Tertiary Syphilis
Tertiary syphilis refers to gumma and cardiovascular syphilis but not to all neurosyphilis. Patients who are not allergic to penicillin and have no evidence of neurosyphilis should be treated with the following regimen.
# Recommended Regimen
Benzathine penicillin G 7.2 million units total, administered as 3 doses of 2.4 million units IM each at 1week intervals
# Other Management Considerations
Patients who have symptomatic late syphilis should be given a CSF examination before therapy is initiated. Some providers treat all patients who have cardiovascular syphilis with a neurosyphilis regimen. The complete management of patients who have cardiovascular or gummatous syphilis is beyond the scope of these guidelines. These patients should be managed in consultation with an infectious diseases specialist.
Follow-Up. Limited information is available concerning clinical response and follow-up of patients who have tertiary syphilis.
Management of Sex Partners. See General Principles, Management of Sex Partners.
# Special Considerations
Penicillin Allergy. Patients allergic to penicillin should be treated according to treatment regimens recommended for late latent syphilis.
Pregnancy. Pregnant patients who are allergic to penicillin should be desensitized, if necessary, and treated with penicillin (see Management of Patients Who Have a History of Penicillin Allergy and Syphilis During Pregnancy).
HIV Infection. See Syphilis Among HIV-Infected Persons.
# Neurosyphilis
# Treatment
CNS involvement can occur during any stage of syphilis. A patient who has clinical evidence of neurologic involvement with syphilis (e.g., cognitive dysfunction, motor or sensory deficits, ophthalmic or auditory symptoms, cranial nerve palsies, and symptoms or signs of meningitis) should have a CSF examination.
Syphilitic uveitis or other ocular manifestations frequently are associated with neurosyphilis; patients with these symptoms should be treated according to the recommendations for patients with neurosyphilis. A CSF examination should be performed for all such patients to identify those with abnormalities that require follow-up CSF examinations to assess treatment response.
Patients who have neurosyphilis or syphilitic eye disease (e.g., uveitis, neuroretinitis, and optic neuritis) should be treated with the following regimen.
# Recommended Regimen
Aqueous crystalline penicillin G 18-24 million units per day, administered as 3-4 million units IV every 4 hours or continuous infusion, for 10-14 days
If compliance with therapy can be ensured, patients may be treated with the following alternative regimen.
# Alternative Regimen
Procaine penicillin 2.4 million units IM once daily PLUS Probenecid 500 mg orally four times a day, both for 10-14 days
The durations of the recommended and alternative regimens for neurosyphilis are shorter than that of the regimen used for late syphilis in the absence of neurosyphilis. Therefore, some specialists administer benzathine penicillin, 2.4 million units IM once per week for up to 3 weeks after completion of these neurosyphilis treatment regimens to provide a comparable total duration of therapy.
# Other Management Considerations
Other considerations in the management of patients who have neurosyphilis are as follows:
- All patients who have syphilis should be tested for HIV.
- Many specialists recommend treating patients who have evidence of auditory disease caused by syphilis in the same manner as patients who have neurosyphilis, regardless of CSF examination results. Although systemic steroids are used frequently as adjunctive therapy for otologic syphilis, such drugs have not been proven beneficial. Follow-Up. If CSF pleocytosis was present initially, a CSF examination should be repeated every 6 months until the cell count is normal. Follow-up CSF examinations also can be used to evaluate changes in the VDRL-CSF or CSF protein after therapy; however, changes in these two parameters occur more slowly than cell counts, and persistent abnormalities might be less important. If the cell count has not decreased after 6 months or if the CSF is not normal after 2 years, retreatment should be considered. Recent data on HIV-infected persons with neurosyphilis suggest that CSF abnormalities might persist for extended periods in these persons, and close clinical follow-up is warranted (105,106).
Management of Sex Partners. See General Principles, Management of Sex Partners.
# Special Considerations
Penicillin Allergy. Ceftriaxone can be used as an alternative treatment for patients with neurosyphilis, although the possibility of cross-reactivity between this agent and penicillin exists. Some specialists recommend ceftriaxone 2 g daily either IM or IV for 10-14 days. Other regimens have not been adequately evaluated for treatment of neurosyphilis. Therefore, if concern exists regarding the safety of ceftriaxone for a patient with neurosyphilis, the patient should obtain skin testing to confirm penicillin allergy and, if necessary, be desensitized and managed in consultation with a specialist.
Pregnancy. Pregnant patients who are allergic to penicillin should be desensitized, if necessary, and treated with penicillin (see Syphilis During Pregnancy).
HIV Infection. See Syphilis Among HIV-Infected Patients.
# Syphilis Among HIV-Infected Persons
# Diagnostic Considerations
Unusual serologic responses have been observed among HIV-infected persons who have syphilis. The majority of reports have involved serologic titers that were higher than expected, but false-negative serologic test results and delayed appearance of seroreactivity also have been reported. However, unusual serologic responses are uncommon, and the majority of specialists believe that both treponemal and nontreponemal serologic tests for syphilis can be interpreted in the usual manner for the majority of patients who are coinfected with T. pallidum and HIV.
When clinical findings are suggestive of syphilis but serologic tests are nonreactive or their interpretation is unclear, alternative tests (e.g., biopsy of a lesion, darkfield examination, or DFA staining of lesion material) might be useful for diagnosis. Neurosyphilis should be considered in the differential diagnosis of neurologic disease in HIV-infected persons.
# Treatment
Compared with HIV-negative patients, HIV-positive patients who have early syphilis might be at increased risk for neurologic complications and might have higher rates of treatment failure with currently recommended regimens. The magnitude of these risks is not defined precisely but is likely minimal. No treatment regimens for syphilis have been demonstrated to be more effective in preventing neurosyphilis in HIV-infected patients than the syphilis regimens recommended for HIV-negative patients (100). Careful follow-up after therapy is essential.
# Primary and Secondary Syphilis Among HIV-Infected Persons
# Treatment
Treatment with benzathine penicillin G, 2.4 million units IM in a single dose is recommended. Some specialists recommend additional treatments (e.g., benzathine penicillin G administered at 1-week intervals for 3 weeks, as recommended for late syphilis) in addition to benzathine penicillin G 2.4 million units IM.
# Other Management Considerations
Because CSF abnormalities (e.g., mononuclear pleocytosis and elevated protein levels) are common in patients with early syphilis and in persons with HIV infection, the clinical and prognostic significance of such CSF abnormalities in HIVinfected persons with primary or secondary syphilis is unknown. Although the majority of HIV-infected persons respond appropriately to standard benzathine penicillin therapy, some specialists recommend intensified therapy when CNS syphilis is suspected in these persons. Therefore, some specialists recommend CSF examination before treatment of HIV-infected persons with early syphilis, with follow-up CSF examination conducted after treatment in persons with initial abnormalities.
Follow-Up. HIV-infected persons should be evaluated clinically and serologically for treatment failure at 3, 6, 9, 12, and 24 months after therapy. Although of unproven benefit, some specialists recommend a CSF examination 6 months after therapy.
HIV-infected persons who meet the criteria for treatment failure (i.e., signs or symptoms that persist or recur or persons who have fourfold increase in nontreponemal test titer) should be managed in the same manner as HIV-negative patients (i.e., a CSF examination and re-treatment). CSF examination and re-treatment also should be strongly considered for persons whose nontreponemal test titers do not decrease fourfold within 6-12 months of therapy. The majority of specialists would re-treat patients with benzathine penicillin G administered as 3 doses of 2.4 million units IM each at weekly intervals, if CSF examinations are normal.
# Special Considerations
Penicillin Allergy. Penicillin-allergic patients who have primary or secondary syphilis and HIV infection should be managed according to the recommendations for penicillin-allergic, HIV-negative patients. The use of alternatives to penicillin has not been well studied in HIV-infected patients.
# Latent Syphilis Among HIV-Infected Persons
# Diagnostic Considerations
HIV-infected patients who have early latent syphilis should be managed and treated according to the recommendations for HIV-negative patients who have primary and secondary syphilis. HIV-infected patients who have either late latent syphilis or syphilis of unknown duration should have a CSF examination before treatment.
# Treatment
Patients with late latent syphilis or syphilis of unknown duration and a normal CSF examination can be treated with benzathine penicillin G, at weekly doses of 2.4 million units for 3 weeks. Patients who have CSF consistent with neurosyphilis should be treated and managed as patients who have neurosyphilis (see Neurosyphilis).
Follow-Up. Patients should be evaluated clinically and serologically at 6, 12, 18, and 24 months after therapy. If, at any time, clinical symptoms develop or nontreponemal titers rise fourfold, a repeat CSF examination should be performed and treatment administered accordingly. If during 12-24 months the nontreponemal titer does not decline fourfold, the CSF examination should be repeated and treatment administered accordingly.
# Special Considerations
Penicillin Allergy. The efficacy of alternative nonpenicillin regimens in HIV-infected persons has not been well studied. Patients with penicillin allergy whose compliance with therapy or follow-up cannot be ensured should be desensitized and treated with penicillin (see Management of Patients Who Have a History of Penicillin Allergy). These therapies should be used only in conjunction with close serologic and clinical follow-up. Limited clinical studies, along with biologic and pharmacologic evidence, suggest that ceftriaxone might be effective (105). However, optimal dose and duration of ceftriaxone therapy have not been defined.
# Syphilis During Pregnancy
All women should be screened serologically for syphilis during the early stages of pregnancy. The majority of states mandate screening at the first prenatal visit for all women. Antepartum screening by nontreponemal antibody testing is typical, but in some settings, treponemal antibody testing is being used. Pregnant women with reactive treponemal screening tests should have confirmatory testing with nontreponemal tests with titers. In populations in which use of prenatal care is not optimal, RPR-card test screening and treatment (i.e., if the RPR-card test is reactive) should be performed at the time a pregnancy is diagnosed. For communities and populations in which the prevalence of syphilis is high or for patients at high risk, serologic testing should be performed twice during the third trimester, at 28 to 32 weeks' gestation and at delivery. Any woman who delivers a stillborn infant after 20 weeks' gestation should be tested for syphilis. No infant should leave the hospital without the maternal serologic status having been determined at least once during pregnancy.
# Diagnostic Considerations
Seropositive pregnant women should be considered infected unless an adequate treatment history is documented clearly in the medical records and sequential serologic antibody titers have declined. Serofast low antibody titers might not require treatment; however, persistent higher titer antibody tests might indicate reinfection and require treatment.
# Treatment
Penicillin is effective for preventing maternal transmission to the fetus and for treating fetal infection. Evidence is insufficient to determine specific, recommended penicillin regimens that are optimal (107).
# Recommended Regimen
Treatment during pregnancy should be the penicillin regimen appropriate for the stage of syphilis.
# Other Management Considerations
Some specialists recommend additional therapy for pregnant women in some settings (e.g., a second dose of benzathine penicillin 2.4 million units IM administered 1 week after the initial dose for women who have primary, secondary, or early latent syphilis). During the second half of pregnancy, syphilis management may be facilitated by a sonographic fetal evaluation for congenital syphilis, but this evaluation should not delay therapy. Sonographic signs of fetal or placental syphilis (i.e., hepatomegaly, ascites, hydrops, or a thickened placenta) indicate a greater risk for fetal treatment failure (108); such cases should be managed in consultation with obstetric spe-cialists. Evidence is insufficient to recommend specific regimens for these situations.
Women treated for syphilis during the second half of pregnancy are at risk for premature labor and/or fetal distress, if the treatment precipitates the Jarisch-Herxheimer reaction. These women should be advised to seek obstetric attention after treatment, if they notice any contractions or decrease in fetal movements. Stillbirth is a rare complication of treatment, but concern for this complication should not delay necessary treatment. All patients who have syphilis should be offered testing for HIV infection.
Follow-Up. Coordinated prenatal care and treatment followup are vital. Serologic titers should be repeated at 28-32 weeks' gestation, at delivery, and following the recommendations for the stage of disease. Serologic titers can be checked monthly in women at high risk for reinfection or in geographic areas in which the prevalence of syphilis is high. The clinical and antibody response should be appropriate for the stage of disease. The majority of women will deliver before their serologic response to treatment can be assessed definitively. Inadequate maternal treatment is likely if delivery occurs within 30 days of therapy, if clinical signs of infection are present at delivery, or if the maternal antibody titer is fourfold higher than the pretreatment titer.
Management of Sex Partners. See General Principles, Management of Sex Partners.
# Special Considerations
Penicillin Allergy. For treatment of syphilis during pregnancy, no proven alternatives to penicillin exist. Pregnant women who have a history of penicillin allergy should be desensitized and treated with penicillin. Skin testing might be helpful (see Management of Patients Who Have a History of Penicillin Allergy).
Tetracycline and doxycycline usually are not used during pregnancy. Erythromycin should not be used because it does not reliably cure an infected fetus. Data are insufficient to recommend azithromycin or ceftriaxone for treatment of maternal infection and prevention of congenital syphilis.
HIV Infection. Placental inflammation from congenital infection might increase the risk for perinatal transmission of HIV. All HIV-infected women should be evaluated for infectious syphilis and treated. Data are insufficient to recommend a specific regimen (see Syphilis Among HIV-Infected Patients).
# Congenital Syphilis
Effective prevention and detection of congenital syphilis depends on the identification of syphilis in pregnant women and, therefore, on the routine serologic screening of pregnant women during the first prenatal visit. In communities and populations in which the risk for congenital syphilis is high, serologic testing and a sexual history also should be obtained at 28 weeks' gestation and at delivery. Moreover, as part of the management of pregnant women who have syphilis, information concerning treatment of sex partners should be obtained to assess the risk for reinfection. All pregnant women who have syphilis should be tested for HIV infection. Routine screening of newborn sera or umbilical cord blood is not recommended. Serologic testing of the mother's serum is preferred rather than testing of the infant's serum because the serologic tests performed on infant serum can be nonreactive if the mother's serologic test result is of low titer or was infected late in pregnancy (see Diagnostic Considerations and Use of Serologic Tests). No infant or mother should leave the hospital unless the maternal serologic status has been documented at least once during pregnancy, and at delivery in communities and populations in which the risk for congenital syphilis is high.
# Evaluation and Treatment of Infants During the First Month of Life
The diagnosis of congenital syphilis is complicated by the transplacental transfer of maternal nontreponemal and treponemal IgG antibodies to the fetus. This transfer of antibodies makes the interpretation of reactive serologic tests for syphilis in infants difficult. Treatment decisions frequently must be made on the basis of 1) identification of syphilis in the mother; 2) adequacy of maternal treatment; 3) presence of clinical, laboratory, or radiographic evidence of syphilis in the infant; and 4) comparison of maternal (at delivery) and infant nontreponemal serologic titers by using the same test and preferably the same laboratory.
All infants born to mothers who have reactive nontreponemal and treponemal test results should be evaluated with a quantitative nontreponemal serologic test (RPR or VDRL) performed on infant serum because umbilical cord blood can become contaminated with maternal blood and could yield a false-positive result. Conducting a treponemal test (i.e., TP-PA or FTA-ABS) on a newborn's serum is not necessary. No commercially available immunoglobulin (IgM) test can be recommended.
All infants born to women who have reactive serologic tests for syphilis should be examined thoroughly for evidence of congenital syphilis (e.g., nonimmune hydrops, jaundice, hepatosplenomegaly, rhinitis, skin rash, and/or pseudoparalysis of an extremity). Pathologic examination of the placenta or umbilical cord by using specific fluorescent antitreponemal antibody staining is suggested. Darkfield microscopic exami-nation or DFA staining of suspicious lesions or body fluids (e.g., nasal discharge) also should be performed.
The following scenarios describe the evaluation and treatment of infants for congenital syphilis: Scenario 1. Infants with proven or highly probable disease and 1. an abnormal physical examination that is consistent with congenital syphilis, 2. a serum quantitative nontreponemal serologic titer that is fourfold higher than the mother's titer, § or 3. a positive darkfield or fluorescent antibody test of body fluid(s).
# Recommended Evaluation
- CSF analysis for VDRL, cell count, and protein ¶ - Complete blood count (CBC) and differential and platelet count - Other tests as clinically indicated (e.g., long-bone radiographs, chest radiograph, liver-function tests, cranial ultrasound, ophthalmologic examination, and auditory brainstem response)
# Recommended Regimens
Aqueous crystalline penicillin G 100,000-150,000 units/kg/day, administered as 50,000 units/kg/dose IV every 12 hours during the first 7 days of life and every 8 hours thereafter for a total of 10 days OR Procaine penicillin G 50,000 units/kg/dose IM in a single daily dose for 10 days If >1 day of therapy is missed, the entire course should be restarted. Data are insufficient regarding the use of other antimicrobial agents (e.g., ampicillin). When possible, a full 10day course of penicillin is preferred, even if ampicillin was initially provided for possible sepsis. The use of agents other than penicillin requires close serologic follow-up to assess adequacy of therapy. In all other situations, the maternal history of infection with T. pallidum and treatment for syphilis must be considered when evaluating and treating the infant.
# Scenario 2. Infants who have a normal physical examination and a serum quantitive
nontreponemal serologic titer the same or less than fourfold the maternal titer and the 1. mother was not treated, inadequately treated, or has no documentation of having received treatment; 2. mother was treated with erythromycin or other nonpenicillin regimen; or 3. mother received treatment <4 weeks before delivery.
# Recommended Evaluation
- CSF analysis for VDRL, cell count, and protein - CBC and differential and platelet count - Long-bone radiographs A complete evaluation is not necessary if 10 days of parenteral therapy is administered. However, such evaluations might be useful; a lumbar puncture might document CSF abnormalities that would prompt close follow-up. Other tests (e.g., CBC, platelet count, and bone radiographs) may be performed to further support a diagnosis of congenital syphilis. If a single dose of benzathine penicillin G is used, then the infant must be fully evaluated (i.e., through CSF examination, long-bone radiographs, and CBC with platelets), the full evaluation must be normal, and follow-up must be certain. If any part of the infant's evaluation is abnormal or not performed or if the CSF analysis is rendered uninterpretable because of contamination with blood, then a 10-day course of penicillin is required. † †
# Recommended Regimens
Aqueous crystalline penicillin G 100,000-150,000 units/kg/day, administered as 50,000 units/kg/dose IV every 12 hours during the first 7 days of life and every 8 hours thereafter for a total of 10 days OR Procaine penicillin G 50,000 units/kg/dose IM in a single daily dose for 10 days OR Benzathine penicillin G 50,000 units/kg/dose IM in a single dose Some specialists prefer the 10 days of parenteral therapy if the mother has untreated early syphilis at delivery. § The absence of a fourfold or greater titer for an infant does not exclude congenital syphilis. ¶ CSF test results obtained during the neonatal period can be difficult to interpret; normal values differ by gestational age and are higher in preterm infants. Values as high as 25 white blood cells (WBCs)/mm 3 and/or protein of 150 mg/dL might occur among normal neonates; some specialists, however, recommend that lower values (i.e., 5 WBCs/mm 3 and protein of 40 mg/dL) be considered the upper limits of normal. Other causes of elevated values should be considered when an infant is being evaluated for congenital syphilis.
A woman treated with a regimen other than those recommended in these guidelines for treatment should be considered untreated. † † If the infant's nontreponemal test is nonreactive and the likelihood of the infant being infected is low, certain specialists recommend no evaluation but treatment of the infant with a single IM dose of benzathine penicillin G 50,000 units/kg for possible incubating syphilis, after which the infant should receive close serologic follow-up.
# Scenario 3. Infants who have a normal physical examination and a serum quantitative nontreponemal serologic titer
the same or less than fourfold the maternal titer and the 1. mother was treated during pregnancy, treatment was appropriate for the stage of infection, and treatment was administered >4 weeks before delivery; and 2. mother has no evidence of reinfection or relapse.
# Recommended Evaluation
No evaluation is required.
# Recommended Regimen
Benzathine penicillin G 50,000 units/kg/dose IM in a single dose § § Scenario 4. Infants who have a normal physical examination and a serum quantitative nontreponemal serologic titer the same or less than fourfold the maternal titer and the 1. mother's treatment was adequate before pregnancy, and 2. mother's nontreponemal serologic titer remained low and stable before and during pregnancy and at delivery (VDRL <1:2; RPR <1:4).
# Recommended Evaluation
No evaluation is required.
# Recommended Regimen
No treatment is required; however, some specialists would treat with benzathine penicillin G 50,000 units/kg as a single IM injection, particularly if follow-up is uncertain.
# Evaluation and Treatment of Older Infants and Children
Children who are identified as having reactive serologic tests for syphilis after the neonatal period (i.e., aged >1 month) should have maternal serology and records reviewed to assess whether the child has congenital or acquired syphilis (see Primary and Secondary Syphilis and Latent Syphilis, Sexual Assault or Abuse of Children). Any child at risk for congenital syphilis should receive a full evaluation and testing for HIV infection.
# Recommended Evaluation
- CSF analysis for VDRL, cell count, and protein - CBC, differential, and platelet count - Other tests as clinically indicated (e.g., long-bone radiographs, chest radiograph, liver function tests, abdominal ultrasound, ophthalmologic examination, and auditory brain stem response)
# Recommended Regimen
Aqueous crystalline penicillin G 200,000-300,000 units/kg/day IV, administered as 50,000 units/kg every 4-6 hours for 10 days
If the child has no clinical manifestations of disease, the CSF examination is normal, and the CSF VDRL test result is negative, some specialists would treat with up to 3 weekly doses of benzathine penicillin G, 50,000 U/kg IM.
Any child who is suspected of having congenital syphilis or who has neurologic involvement should be treated with aqueous penicillin G. Some specialists also suggest giving these patients a single dose of benzathine penicillin G, 50,000 units/ kg IM after the 10-day course of IV aqueous penicillin. This treatment also would be adequate for children who might have other treponemal infections.
# Follow-Up
All seroreactive infants (or infants whose mothers were seroreactive at delivery) should receive careful follow-up examinations and serologic testing (i.e., a nontreponemal test) every 2-3 months until the test becomes nonreactive or the titer has decreased fourfold. Nontreponemal antibody titers should decline by age 3 months and should be nonreactive by age 6 months if the infant was not infected (i.e., if the reactive test result was caused by passive transfer of maternal IgG antibody) or was infected but adequately treated. The serologic response after therapy might be slower for infants treated after the neonatal period. If these titers are stable or increase after age 6-12 months, the child should be evaluated (e.g., given a CSF examination) and treated with a 10-day course of parenteral penicillin G.
Treponemal tests should not be used to evaluate treatment response because the results for an infected child can remain positive despite effective therapy. Passively transferred maternal treponemal antibodies can be present in an infant until age 15 months. A reactive treponemal test after age 18 months is diagnostic of congenital syphilis. If the nontreponemal test is nonreactive at this time, no further evaluation or treatment is necessary. If the nontreponemal test is reactive at age 18 months, the infant should be fully (re)evaluated and treated for congenital syphilis. § § Some specialists would not treat the infant but would provide close serologic follow-up in those whose mother's nontreponemal titers decreased fourfold after appropriate therapy for early syphilis or remained stable or low for late syphilis.
Infants whose initial CSF evaluations are abnormal should undergo a repeat lumbar puncture approximately every 6 months until the results are normal. A reactive CSF VDRL test or abnormal CSF indices that cannot be attributed to other ongoing illness requires re-treatment for possible neurosyphilis.
Follow-up of children treated for congenital syphilis after the newborn period should be conducted as is recommended for neonates.
# Special Considerations
# Penicillin Allergy
Infants and children who require treatment for syphilis but who have a history of penicillin allergy or develop an allergic reaction presumed secondary to penicillin should be desensitized, if necessary, and then treated with penicillin (see Management of Patients With a History of Penicillin Allergy). Data are insufficient regarding the use of other antimicrobial agents (e.g., ceftriaxone); if a nonpenicillin agent is used, close serologic and CSF follow-up are indicated.
# HIV Infection
Evidence is insufficient to determine whether infants who have congenital syphilis and whose mothers are coinfected with HIV require different evaluation, therapy, or follow-up for syphilis than is recommended for all infants.
# Penicillin Shortage
During periods when the availability of penicillin is compromised, the following is recommended (see http:// www.cdc.gov/nchstp/dstd/penicillinG.htm):
1. For infants with clinical evidence of congenital syphilis (Scenario 1), check local sources for aqueous crystalline penicillin G (potassium or sodium). If IV penicillin G is limited, substitute some or all daily doses with procaine penicillin G (50,000 U/kg/dose IM a day in a single daily dose for 10 days). If aqueous or procaine penicillin G is not available, ceftriaxone (in doses according to age and weight) may be considered with careful clinical and serologic follow-up. Ceftriaxone must be used with caution in infants with jaundice. For infants aged >30 days, use 75 mg/kg IV/IM a day in a single daily dose for 10-14 days; however, dose adjustment might be necessary based on birthweight. For older infants, the dose should be 100 mg/kg a day in a single daily dose. Studies that strongly support ceftriaxone for the treatment of congenital syphilis have not been conducted. Therefore, ceftriaxone should be used in consultation with a specialist in the treatment of infants with congenital syphilis. Manage-ment may include a repeat CSF examination at age 6 months if the initial examination was abnormal.
# Management of Patients Who Have a History of Penicillin Allergy
No proven alternatives to penicillin are available for treating neurosyphilis, congenital syphilis, or syphilis in pregnant women. Penicillin also is recommended for use, whenever possible, in HIV-infected patients. Of the adult U.S. population, 3%-10% have experienced an immunoglobulin E (IgE) mediated allergic response to penicillin such as urticaria, angioedema, or anaphylaxis (i.e., upper airway obstruction, bronchospasm, or hypotension). Re-administration of penicillin to these patients can cause severe, immediate reactions. Because anaphylactic reactions to penicillin can be fatal, every effort should be made to avoid administering penicillin to penicillin-allergic patients, unless they undergo acute desensitization to eliminate anaphylactic sensitivity.
An estimated 10% of persons who report a history of severe allergic reactions to penicillin remain allergic. With the passage of time, the majority of persons who have had a severe reaction to penicillin stop expressing penicillin-specific IgE. These persons can be treated safely with penicillin. The results of many investigations indicate that skin testing with the major and minor determinants of penicillin can reliably identify persons at high risk for penicillin reactions. Although these reagents are easily generated and have been available for >30 years, only benzylpenicilloyl poly-L-lysine (Pre-Pen ® ) and penicillin G have been available commercially. Testing with only the major determinant and penicillin G identifies an estimated 90%-97% of the currently allergic patients. However, because skin testing without the minor determinants would still miss 3%-10% of allergic patients and because serious or fatal reactions can occur among these minor-determinant-positive patients, specialists suggest exercising caution when the full battery of skin-test reagents is not available (Box 1). An additional challenge has occurred with the recent unavailability of Pre-Pen ® ; however, plans for future availability of this product have been made, as well as a companion minor determinant mixture.
# Major
# Recommendations
If the full battery of skin-test reagents is available, including the major and minor determinants (see Penicillin Allergy Skin Testing), patients who report a history of penicillin reaction and who are skin-test negative can receive conventional penicillin therapy. Skin-test-positive patients should be desensitized.
If the full battery of skin-test reagents, including the minor determinants, is not available, the patient should be skin tested using benzylpenicilloyl poly-L-lysine (i.e., the major determinant) and penicillin G. Patients who have positive test results should be desensitized. Some specialists suggest that persons who have negative test results should be regarded as probably allergic and should be desensitized. Others suggest that those with negative skin-test results can be test-dosed gradually with oral penicillin in a monitored setting in which treatment for anaphylactic reaction can be provided.
If the major determinant (Pre-Pen ® ) is not available for skin testing, all patients with a history suggesting IgE mediated reactions (anaphylaxis, angioedema, bronchospasm, or urticaria) to penicillin should be desensitized in a hospital setting. In patients with reactions not likely to be IgE mediated, outpatient oral desensitization or monitored test doses may be considered.
# Penicillin Allergy Skin Testing
Patients at high risk for anaphylaxis, including those who 1) have a history of penicillin-related anaphylaxis, asthma, or other diseases that would make anaphylaxis more dangerous or 2) are being treated with beta-adrenergic blocking agents should be tested with 100-fold dilutions of the full-strength skin-test reagents before being tested with full-strength reagents. In these situations, patients should be tested in a monitored setting in which treatment for an anaphylactic reaction is available. If possible, the patient should not have taken antihistamines recently (e.g., chlorpheniramine maleate or terfenadine during the preceding 24 hours, diphenhydramine HCl or hydroxyzine during the preceding 4 days, or astemizole during the preceding 3 weeks).
# Procedures
Dilute the antigens either 1) 100-fold for preliminary testing if the patient has had a life-threatening reaction to penicillin or 2) 10-fold if the patient has had another type of immediate, generalized reaction to penicillin within the preceding year.
# Epicutaneous (Prick) Tests
Duplicate drops of skin-test reagent are placed on the volar surface of the forearm. The underlying epidermis is pierced with a 26-gauge needle without drawing blood.
An epicutaneous test is positive if the average wheal diameter after 15 minutes is 4 mm larger than that of negative controls; otherwise, the test is negative. The histamine controls should be positive to ensure that results are not falsely negative because of the effect of antihistaminic drugs.
# Intradermal Test
If epicutaneous tests are negative, duplicate 0.02-mL intradermal injections of negative control and antigen solutions are made into the volar surface of the forearm by using a 26or 27-gauge needle on a syringe. The diameters of the wheals induced by the injections should be recorded. An intradermal test is positive if the average wheal diameter 15 minutes after injection is >2 mm larger than the initial wheal size and also is >2 mm larger than the negative controls. Otherwise, the tests are negative.
# Desensitization
Patients who have a positive skin test to one of the penicillin determinants can be desensitized (Table 1). This is a straightforward, relatively safe procedure that can be performed orally or IV. Although the two approaches have not been compared, oral desensitization is regarded as safer and easier to perform. Patients should be desensitized in a hospital setting because serious IgE-mediated allergic reactions can occur. Desensitization usually can be completed in approximately 4 hours, after which the first dose of penicillin is administered. After desensitization, patients must be maintained on penicillin continuously for the duration of the course of therapy.
# Diseases Characterized by Urethritis and Cervicitis
# Management of Male Patients Who Have Urethritis
Urethritis, as characterized by urethral inflammation, can result from infectious and noninfectious conditions. Symptoms, if present, include discharge of mucopurulent or purulent material, dysuria, or urethral pruritus. Asymptomatic infections are common. N. gonorrhoeae and C. trachomatis are clinically important infectious causes of urethritis. If clinicbased diagnostic tools (Gram stain microscopy) are not available, patients should be treated for both gonorrhea and chlamydia. Further testing to determine the specific etiology is recommended because both chlamydia and gonorrhea are reportable to state health departments, and a specific diagnosis might enhance partner notification and improve compliance with treatment, especially in exposed partners. Culture, nucleic acid hybridization tests, and nucleic acid amplification tests are available for the detection of both N. gonorrhoeae and C. trachomatis. Culture and hybridization tests require urethral swab specimens, whereas amplification tests can be performed on urine specimens. Because of their higher sensitivity, amplification tests are preferred for the detection of C. trachomatis.
# Etiology
Several organisms can cause infectious urethritis. The presence of Gram-negative intracellular diplococci (GNID) on urethral smear is indicative of gonorrhea infection, which is frequently accompanied by chlamydial infection. Nongonoccocal urethritis (NGU) is diagnosed when microscopy indicates inflammation without GNID. C. trachomatis is a frequent cause of NGU (i.e., 15%-55% of cases); however, the prevalence varies by age group, with lower prevalence among older men. The proportion of NGU cases caused by chlamydia has been declining gradually. Complications of NGU among men infected with C. trachomatis include epididymitis, prostatitis, and Reiter's syndrome. Documentation of chlamydia infection is essential because of the need for partner referral for evaluation and treatment.
The etiology of the majority of cases of nonchlamydial NGU is unknown. Ureaplasma urealyticum and Mycoplasma genitalium have been implicated as etiologic agents of NGU in some studies; however, detection of these organisms is frequently difficult (109)(110)(111). T. vaginalis, HSV, and adenovirus might also cause NGU (112)(113)(114). Diagnostic and treatment procedures for these organisms are reserved for situations in which these infections are suspected (e.g., contact with trichomoniasis and genital lesions or severe dysuria and meatitis, which might suggest genital herpes) or when NGU is not responsive to therapy. Enteric bacteria have been identified as an uncommon cause of NGU and might be associated with insertive anal sex.
# Confirmed Urethritis
Clinicians should document that urethritis is present. Urethritis can be documented on the basis of any of the following signs or laboratory tests:
- Mucopurulent or purulent discharge.
- Gram stain of urethral secretions demonstrating >5 WBC per oil immersion field. The Gram stain is the preferred rapid diagnostic test for evaluating urethritis. It is highly sensitive and specific for documenting both urethritis and the presence or absence of gonococcal infection. Gonococcal infection is established by documenting the presence of WBC containing GNID, or - Positive leukocyte esterase test on first-void urine or microscopic examination of first-void urine sediment demonstrating >10 WBC per high power field. If none of these criteria are present, treatment should be deferred, and the patient should be tested for N. gonorrhoeae and C. trachomatis and followed closely if test results are negative. If the results demonstrate infection with either N. gonorrhoeae or C. trachomatis, the appropriate treatment should be given and sex partners referred for evaluation and treatment.
Empiric treatment of symptoms without documentation of urethritis is recommended only for patients at high risk for infection who are unlikely to return for a follow-up evaluation. Such patients should be treated for gonorrhea and chlamydia. Partners of patients treated empirically should be evaluated and treated.
# Management of Patients Who Have Nongonococcal Urethritis Diagnosis
All patients who have confirmed or suspected urethritis should be tested for gonorrhea and chlamydia. Testing for chlamydia is strongly recommended because of the increased utility and availability of highly sensitive and specific testing methods and because a specific diagnosis might enhance partner notification and improve compliance with treatment, especially in the exposed partner.
# Treatment
Treatment should be initiated as soon as possible after diagnosis. Azithromycin and doxycycline are highly effective for chlamydial urethritis; however, infections with M. genitalium may respond better to azithromycin (115). Single-dose regimens have the advantage of improved compliance and directly observed treatment. To improve compliance, ideally the medication should be provided in the clinic or health-care provider's office.
# Recommended Regimens
Azithromycin 1 g orally in a single dose OR Doxycycline 100 mg orally twice a day for 7 days
# Alternative Regimens
Erythromycin base 500 mg orally four times a day for 7 days OR Erythromycin ethylsuccinate 800 mg orally four times a day for 7 days OR Ofloxacin 300 mg orally twice a day for 7 days OR Levofloxacin 500 mg orally once daily for 7 days
# Follow-Up for Patients Who Have Urethritis
Patients should be instructed to return for evaluation if symptoms persist or recur after completion of therapy. Symptoms alone, without documentation of signs or laboratory evidence of urethral inflammation, are not a sufficient basis for retreatment. Patients should be instructed to abstain from sexual intercourse until 7 days after therapy is initiated, provided their symptoms have resolved and their sex partners have been adequately treated. Persistence of pain, discomfort, and irritative voiding symptoms beyond 3 months should alert the clinician to the possibility of chronic prostatitis/chronic pelvic pain syndrome in men. Persons whose conditions have been diagnosed as a new STD should receive testing for other STDs, including syphilis and HIV.
# Partner Referral
Persons with NGU should refer for evaluation and treatment all sex partners within the preceding 60 days. Because a specific diagnosis might facilitate partner referral, testing for gonorrhea and chlamydia is encouraged.
# Recurrent and Persistent Urethritis
Objective signs of urethritis should be present before initiation of antimicrobial therapy. In persons who have persistent symptoms after treatment without objective signs of urethritis, the value of extending the duration of antimicrobials has not been demonstrated. Persons who have persistent or recurrent urethritis can be re-treated with the initial regimen if they did not comply with the treatment regimen or if they were reexposed to an untreated sex partner. Otherwise, a T. vaginalis culture should be performed using an intraurethral swab or a first-void urine specimen (112). Some cases of recurrent urethritis after doxycycline treatment might be caused by tetracycline-resistant U. urealyticum. Urologic examinations usually do not reveal a specific etiology. Approximately 50% of men with chronic nonbacterial prostatitis/chronic pelvic pain syndrome have evidence of urethral inflammation without any identifiable microbial pathogens. If the pa-tient was compliant with the initial regimen and reexposure can be excluded, the following regimen is recommended.
# Recommended Regimens
Metronidazole 2 g orally in a single dose OR Tinidazole 2 g orally in a single dose PLUS Azithromycin 1 g orally in a single dose (if not used for initial episode)
# Special Considerations HIV Infection
Gonococcal urethritis, chlamydial urethritis, and nongonococcal, nonchlamydial urethritis might facilitate HIV transmission. Patients who have NGU and also are infected with HIV should receive the same treatment regimen as those who are HIV negative.
# Management of Patients Who Have Cervicitis
Two major diagnostic signs characterize cervicitis: 1) a purulent or mucopurulent endocervical exudate visible in the endocervical canal or on an endocervical swab specimen (commonly referred to as "mucopurulent cervicitis" or cervicitis), and 2) sustained endocervical bleeding easily induced by gentle passage of a cotton swab through the cervical os. Either or both signs might be present. Cervicitis frequently is asymptomatic, but some women complain of an abnormal vaginal discharge and intermenstrual vaginal bleeding (e.g., after sexual intercourse). A finding of leukorrhea (>10 WBC per high power field on microscopic examination of vaginal fluid) has been associated with chlamydial and gonococcal infection of the cervix. In the absence of inflammatory vaginitis, leukorrhea might be a sensitive indicator of cervical inflammation with a high negative predictive value (116). Although some specialists consider an increased number of polymorphonuclear leukocytes on endocervical Gram stain as being useful in the diagnosis of cervicitis, this criterion has not been standardized. In addition, it has a low positive-predictive value (PPV) for infection with C. trachomatis and N. gonorrhoeae and is not available in the majority of clinical settings. Finally, although the presence of GNID on Gram stain of endocervical fluid is specific for the diagnosis of gonococcal cervical infection, it is insensitive because it is observed in only 50% of women with this infection.
# Etiology
When an etiologic organism is isolated in the setting of cervicitis, it is typically C. trachomatis or N. gonorrhoeae. Cervicitis also can accompany trichomoniasis and genital herpes (especially primary HSV-2 infection). However, in the majority of cases of cervicitis, no organism is isolated, especially in women at relatively low risk for recent acquisition of these STDs (for example, women aged >30 years). Limited data indicate that infection with M. genitalium and BV as well as frequent douching might cause cervicitis (117)(118)(119). For reasons that are unclear, cervicitis can persist despite repeated courses of antimicrobial therapy. Because the majority of persistent cases of cervicitis are not caused by relapse or reinfection with C. trachomatis or N. gonorrhoeae, other determinants (e.g., persistent abnormality of vaginal flora, douching or exposure to chemical irritants, or idiopathic inflammation in the zone of ectopy) might be involved.
# Diagnosis
Because cervicitis might be a sign of upper genital tract infection (endometritis), women who seek medical treatment for a new episode of cervicitis should be assessed for signs of PID and should be tested for C. trachomatis and for N. gonorrhoeae with the most sensitive and specific test available, NAAT. Women with cervicitis also should be evaluated for the presence of BV and trichomoniasis, and these conditions should be treated, if present. Because the sensitivity of microscopy to detect T. vaginalis is relatively low (approximately 50%), symptomatic women with cervicitis and negative microscopy for trichomonads should receive further testing (i.e., culture or antigen-based detection). Although HSV-2 infection has been associated with cervicitis, the utility of specific testing (i.e., culture or serologic testing) for HSV-2 in this setting is unclear. Standardized diagnostic tests for M. genitalium are not commercially available.
NAAT for C. trachomatis and N. gonorrhoeae are preferred for the diagnostic evaluation of cervicitis and can be performed on either cervical or urine samples. A finding of >10 WBC in vaginal fluid, in the absence of trichomoniasis, might indicate endocervical inflammation caused specifically by C. trachomatis or N. gonorrhoeae (116,120,121).
# Treatment
Several factors should affect the decision to provide presumptive therapy for cervicitis or to await the results of diagnostic tests. Treatment with antibiotics for C. trachomatis should be provided in women at increased risk for this common STD (age 5%) in the patient population (young age and facility prevalence).
Concomitant trichomoniasis or symptomatic BV should also be treated if detected. For women in whom any component of (or all) presumptive therapy is deferred, the results of sensitive tests for C. trachomatis and N. gonorrhoeae (e.g., nucleic acid amplification tests) should determine the need for treatment subsequent to the initial evaluation.
# Recommended Regimens for Presumptive Treatment*
Azithromycin 1 g orally in a single dose OR Doxycycline 100 mg orally twice a day for 7 days - Consider concurrent treatment for gonococcal infection if prevalence of gonorrhea is high in the patient population under assessment.
# Recurrent and Persistent Cervicitis
Women with persistent cervicitis should be reevaluated for possible reexposure to an STD, and her vaginal flora should be reassessed. If relapse and/or reinfection with a specific STD has been excluded, BV is not present, and sex partners have been evaluated and treated, management options for persistent cervicitis are undefined. For such women, the value of repeated or prolonged administration of antibiotic therapy for persistent symptomatic cervicitis is unknown. Women who receive such a course should return after treatment so that a determination can be made regarding whether cervicitis has resolved. In women with persistent symptoms that are clearly attributable to cervicitis, ablative therapy may be considered by a gynecologic specialist.
# Follow-Up
Follow-up should be conducted as recommended for the infections for which a woman is treated. If symptoms persist, women should be instructed to return for reevaluation.
# Management of Sex Partners
Management of sex partners of women treated for cervicitis should be appropriate for the identified or suspected STD. Partners should be notified and examined if chlamydia, gonorrhea, or trichomoniasis was identified or suspected in the index patient and treated for the STDs for which the index patient received treatment. To avoid re-infection, patients and their sex partners should abstain from sexual intercourse until therapy is completed (i.e., 7 days after a single-dose regimen or after completion of a 7-day regimen).
# Special Considerations
# HIV Infection
Patients who have cervicitis and also are infected with HIV should receive the same treatment regimen as those who are HIV negative. Treatment of cervicitis in HIV-infected women is vital because cervicitis increases cervical HIV shedding. Treatment of cervicitis in HIV-infected women reduces HIV shedding from the cervix and might reduce HIV transmission to susceptible sex partners (122).
# Chlamydial Infections Chlamydial Infections in Adolescents and Adults
In the United States, chlamydial genital infection is the most frequently reported infectious disease, and the prevalence is highest in persons aged <25 years (123). Several important sequelae can result from C. trachomatis infection in women; the most serious of these include PID, ectopic pregnancy, and infertility. Some women who have uncomplicated cervical infection already have subclinical upper reproductive tract infection.
Asymptomatic infection is common among both men and women, and to detect chlamydial infections health-care providers frequently rely on screening tests. Annual screening of all sexually active women aged <25 years is recommended (124), as is screening of older women with risk factors (e.g., those who have a new sex partner or multiple sex partners). The benefits of C. trachomatis screening in women have been demonstrated in areas where screening programs have reduced both the prevalence of infection and rates of PID (125,126). Evidence is insufficient to recommend routine screening for C. trachomatis in sexually active young men, based on feasibility, efficacy, and cost-effectiveness. However, screening of sexually active young men should be considered in clinical settings with a high prevalence of chlamydia (e.g., adolescent clinics, correctional facilities, and STD clinics). An appropriate sexual risk assessment should be conducted for all persons and might indicate more frequent screening for some women or certain men.
# Diagnostic Considerations
C. trachomatis urogenital infection in women can be diagnosed by testing urine or swab specimens collected from the endocervix or vagina. Diagnosis of C. trachomatis urethral infection in men can be made by testing a urethral swab or urine specimen. Rectal C. trachomatis infections in persons that engage in receptive anal intercourse can be diagnosed by testing a rectal swab specimen. Culture, direct immunofluorescence, EIA, nucleic acid hybridization tests, and NAATs are available for the detection of C. trachomatis on endocervical and male urethral swab specimens (127). NAATs are the most sensitive tests for these specimens and are FDA-cleared for use with urine, and some tests are cleared for use with vaginal swab specimens. The majority of tests, including NAAT and nucleic acid hybridization tests, are not FDAcleared for use with rectal swab specimens, and chlamydia culture is not widely available for this purpose. Some noncommercial laboratories have initiated NAAT of rectal swab specimens after establishing the performance of the test to meet CLIA requirements. Patients' whose condition has been diagnosed as chlamydia also should be tested for other STDs.
# Treatment
Treating infected patients prevents transmission to sex partners. In addition, treating pregnant women usually prevents transmission of C. trachomatis to infants during birth. Treatment of sex partners helps to prevent reinfection of the index patient and infection of other partners.
Coinfection with C. trachomatis frequently occurs among patients who have gonococcal infection; therefore, presumptive treatment of such patients for chlamydia is appropriate (see Gonococcal Infection, Dual Therapy for Gonococcal and Chlamydial Infections). The following recommended treatment regimens and alternative regimens cure infection and usually relieve symptoms.
# Recommended Regimens
Azithromycin 1 g orally in a single dose OR Doxycycline 100 mg orally twice a day for 7 days
# Alternative Regimens
Erythromycin base 500 mg orally four times a day for 7 days OR Erythromycin ethylsuccinate 800 mg orally four times a day for 7 days OR Ofloxacin 300 mg orally twice a day for 7 days OR Levofloxacin 500 mg orally once daily for 7 days A recent meta-analysis of 12 randomized clinical trials of azithromycin versus doxycycline for the treatment of genital chlamydial infection demonstrated that the treatments were equally efficacious, with microbial cure rates of 97% and 98%, respectively (128). These studies were conducted primarily in populations in which follow-up was encouraged, adherence to a 7-day regimen was effective, and culture or EIA (rather than the more sensitive NAAT was used for determining microbiological outcome. Azithromycin should always be available to treat patients for whom compliance with multiday dosing is in question.
In populations that have erratic health-care-seeking behavior, poor treatment compliance, or unpredictable follow-up, azithromycin might be more cost-effective because it enables the provision of a single-dose of directly observed therapy. However, doxycycline costs less than azithromycin and has no higher risk for adverse events (128). Erythromycin might be less efficacious than either azithromycin or doxycycline, mainly because of the frequent occurrence of gastrointestinal side effects that discourage compliance. Ofloxacin and levofloxacin are effective treatment alternatives but are more expensive and offer no advantage in the dosage regimen. Other quinolones either are not reliably effective against chlamydial infection or have not been evaluated adequately.
To maximize compliance with recommended therapies, medications for chlamydial infections should be dispensed on site, and the first dose should be directly observed. To minimize transmission, persons treated for chlamydia should be instructed to abstain from sexual intercourse for 7 days after single-dose therapy or until completion of a 7-day regimen. To minimize the risk for reinfection, patients also should be instructed to abstain from sexual intercourse until all of their sex partners are treated.
# Follow-up
Except in pregnant women, test-of-cure (repeat testing 3-4 weeks after completing therapy) is not recommended for persons treated with the recommended or alterative regimens, unless therapeutic compliance is in question, symptoms persist, or reinfection is suspected. Moreover, the validity of chlamydial diagnostic testing at <3 weeks after completion of therapy (to identify patients who did not respond to therapy) has not been established. False-negative results might occur because of persistent infections involving limited numbers of chlamydial organisms. In addition, NAAT conducted at <3 weeks after completion of therapy in persons who were treated successfully could yield false-positive results because of the continued presence of dead organisms.
A high prevalence of C. trachomatis infection is observed in women who were treated for chlamydial infection in the preceding several months (129,130). The majority of posttreatment infections result from reinfection, frequently occurring because the patient's sex partners were not treated or because the patient resumed sex with a new partner infected with C. trachomatis. Repeat infections confer an elevated risk for PID and other complications when compared with the initial infection. Therefore, recently infected women are a major pri-ority for repeat testing for C. trachomatis. Clinicians and health-care agencies should consider advising all women with chlamydial infection to be retested approximately 3 months after treatment. Providers also are strongly encouraged to retest all women treated for chlamydial infection whenever they next seek medical care within the following 3-12 months, regardless of whether the patient believes that her sex partners were treated. Recognizing that retesting is distinct from a testof-cure, as discussed in this report, is vital. Limited evidence is available on the benefit of retesting for chlamydia in men previously infected; however, some specialists suggest retesting men approximately 3 months after treatment.
# Management of Sex Partners
Patients should be instructed to refer their sex partners for evaluation, testing, and treatment. The following recommendations on exposure intervals are based on limited evaluation. Sex partners should be evaluated, tested, and treated if they had sexual contact with the patient during the 60 days preceding onset of symptoms in the patient or diagnosis of chlamydia. The most recent sex partner should be evaluated and treated, even if the time of the last sexual contact was >60 days before symptom onset or diagnosis.
If concerns exist that sex partners will not seek evaluation and treatment, or if other management strategies are impractical or unsuccessful, then delivery of antibiotic therapy (either a prescription or medication) by heterosexual male or female patients to their partners might be an option (see Partner Management). Limited studies to date have demonstrated a trend toward a decrease in rates of persistent or recurrent chlamydia with this approach compared with standard partner referral (25,27). Male patients must inform female partners of their infection and be given accompanying written materials about the importance of seeking evaluation for PID (especially if symptomatic). Patient-delivered partner therapy is not routinely recommended for MSM because of a high risk for coexisting infections, especially undiagnosed HIV infection, in their partners.
Patients should be instructed to abstain from sexual intercourse until they and their sex partners have completed treatment. Abstinence should be continued until 7 days after a single-dose regimen or after completion of a 7-day regimen. Timely treatment of sex partners is essential for decreasing the risk for reinfecting the index patient.
# Special Considerations
Pregnancy. Doxycycline, ofloxacin, and levofloxacin are contraindicated in pregnant women. However, clinical experience and studies suggest that azithromycin is safe and effective (131)(132)(133). Repeat testing (preferably by NAAT) 3 weeks after completion of therapy with the following regimens is recommended for all pregnant women to ensure therapeutic cure, considering the sequelae that might occur in the mother and neonate if the infection persists. The frequent gastrointestinal side effects associated with erythromycin might discourage patient compliance with the alternative regimens.
# Recommended Regimens
Azithromycin 1 g orally in a single dose OR Amoxicillin 500 mg orally three times a day for 7 days
# Alternative Regimens
Erythromycin base 500 mg orally four times a day for 7 days OR Erythromycin base 250 mg orally four times a day for 14 days OR Erythromycin ethylsuccinate 800 mg orally four times a day for 7 days OR Erythromycin ethylsuccinate 400 mg orally four times a day for 14 days Erythromycin estolate is contraindicated during pregnancy because of drug-related hepatotoxicity. The lower dose 14day erythromycin regimens may be considered if gastrointestinal tolerance is a concern.
HIV Infection. Patients who have chlamydial infection and also are infected with HIV should receive the same treatment regimen as those who are HIV negative.
# Chlamydial Infections Among Infants
Prenatal screening of pregnant women can prevent chlamydial infection among neonates. Pregnant women aged <25 years are at high risk for infection. Local or regional prevalence surveys of chlamydial infection can be conducted to confirm the utility of using these recommendations in particular settings.
C. trachomatis infection of neonates results from perinatal exposure to the mother's infected cervix. Neonatal ocular prophylaxis with silver nitrate solution or antibiotic ointments does not prevent perinatal transmission of C. trachomatis from mother to infant. However, ocular prophylaxis with those agents does prevent gonococcal ophthalmia and, therefore, should be continued (see Ophthalmia Neonatorum Prophylaxis).
Initial C. trachomatis perinatal infection involves the mucous membranes of the eye, oropharynx, urogenital tract, and rectum and might be asymptomatic in these locations.
C. trachomatis infection in neonates is most frequently recognized by conjunctivitis that develops 5-12 days after birth. C. trachomatis also can cause a subacute, afebrile pneumonia with onset at ages 1-3 months. C. trachomatis has been the most frequent identifiable infectious cause of ophthalmia neonatorum, but perinatal chlamydial infections, including opthalmia and pneumonia, are detected less frequently because of the institution of widespread prenatal screening and treatment of pregnant women.
# Ophthalmia Neonatorum Caused by C. trachomatis
A chlamydial etiology should be considered for all infants aged <30 days who have conjunctivitis, especially if the mother has a history of untreated chlamydia infection.
# Diagnostic Considerations
Sensitive and specific methods used to diagnose chlamydial ophthalmia in the neonate include both tissue culture and nonculture tests (e.g., DFA tests, EIA, and NAAT). The majority of nonculture tests are not FDA-cleared for the detection of chlamydia from conjunctival swabs, and clinical laboratories must verify the procedure according to CLIA regulations. Specimens must contain conjunctival cells, not exudate alone. Specimens for culture isolation and nonculture tests should be obtained from the everted eyelid using a dacrontipped swab or the swab specified by the manufacturer's test kit. A specific diagnosis of C. trachomatis infection confirms the need for treatment not only for the neonate but also for the mother and her sex partner(s). Ocular exudate from infants being evaluated for chlamydial conjunctivitis also should be tested for N. gonorrhoeae.
# Recommended Regimen
Erythromycin base or ethylsuccinate 50 mg/kg/day orally divided into 4 doses daily for 14 days ¶ ¶, * Topical antibiotic therapy alone is inadequate for treatment of chlamydial infection and is unnecessary when systemic treatment is administered.
# Follow-Up
The efficacy of erythromycin treatment is approximately 80%; a second course of therapy might be required and, there-fore, follow-up of infants is recommended to determine whether initial treatment was effective. The possibility of concomitant chlamydial pneumonia should be considered.
# Management of Mothers and Their Sex Partners
The mothers of infants who have chlamydial infection and the sex partners of these women should be evaluated and treated (see Chlamydial Infection in Adolescents and Adults).
# Infant Pneumonia Caused by C. trachomatis
Characteristic signs of chlamydial pneumonia in infants include 1) a repetitive staccato cough with tachypnea and 2) hyperinflation and bilateral diffuse infiltrates on a chest radiograph. Wheezing is rare, and infants are typically afebrile. Peripheral eosinophilia (>400 cells/mm 3 ) occurs frequently. Because clinical presentations differ, initial treatment and diagnostic tests should include C. trachomatis for all infants aged 1-3 months who possibly have pneumonia (especially with untreated maternal chlamydial infection).
# Diagnostic Considerations
Specimens for chlamydial testing should be collected from the nasopharynx. Tissue culture is the definitive standard for chlamydial pneumonia. Nonculture tests (e.g., EIA, DFA, and NAAT) can be used, although nonculture tests of nasopharyngeal specimens have a lower sensitivity and specificity than nonculture tests of ocular specimens. DFA is the only FDAcleared test for the detection of C. trachomatis from nasopharyngeal specimens. Tracheal aspirates and lung biopsy specimens, if collected, should be tested for C. trachomatis.
Because of the delay in obtaining test results for chlamydia, the decision to provide treatment for C. trachomatis pneumonia must frequently be based on clinical and radiologic findings. The results of tests for chlamydial infection assist in the management of an infant's illness and determine the need for treating the mother and her sex partner(s).
# Recommended Regimen
Erythromycin base or ethylsuccinate 50 mg/kg/day orally divided into 4 doses daily for 14 days
# Follow-Up
The effectiveness of erythromycin in treating pneumonia caused by C. trachomatis is approximately 80%; a second course of therapy might be required. Follow-up of infants is recommended to determine whether the pneumonia has resolved. Some infants with chlamydial pneumonia have abnormal pulmonary function tests later in childhood. ¶ ¶ An association between oral erythromycin and infantile hypertrophic pyloric stenosis has been reported in infants aged <6 weeks who were treated with this drug. Infants treated with erythromycin should be followed for signs and symptoms of idiopathic hypertrophic pyloric stenosis (IHPS). * Data on use of other macrolides (e.g., azithromycin and clarithromycin) for the treatment of neonatal chlamydia infection are limited. The results of one study involving a limited number of patients suggest that a short course of azithromycin, 20 mg/kg/day orally, 1 dose daily for 3 days, may be effective.
# Management of Mothers and Their Sex Partners
Mothers of infants who have chlamydia pneumonia and the sex partners of these women should be evaluated and treated according to the recommended treatment of adults for chlamydial infections (see Chlamydial Infection in Adolescents and Adults).
# Infants Born to Mothers Who Have Chlamydial Infection
Infants born to mothers who have untreated chlamydia are at high risk for infection; however, prophylatic antibiotic treatment is not indicated, and the efficacy of such treatment is unknown. Infants should be monitored to ensure appropriate treatment if symptoms develop.
# Chlamydial Infections Among Children
Sexual abuse must be considered a cause of chlamydial infection in preadolescent children, although perinatally transmitted C. trachomatis infection of the nasopharynx, urogenital tract, and rectum might persist for >1 year (see Sexual Assault or Abuse of Children).
# Diagnostic Considerations
Nonculture, nonamplified probe tests for chlamydia (EIA, DFA) should not be used because of the possibility of falsepositive test results. With respiratory tract specimens, falsepositive results can occur because of cross-reaction of test reagents with C. pneumoniae; with genital and anal specimens, false-positive results might occur because of cross-reaction with fecal flora.
# Recommended Regimens for Children Who Weigh <45 kg
Erythromycin base or ethylsuccinate 50 mg/kg/day orally divided into 4 doses daily for 14 days
# Recommended Regimen for Children Who Weigh >45 kg but Who Are Aged <8 Years
Azithromycin 1 g orally in a single dose
# Recommended Regimens for Children Aged >8 years
Azithromycin 1 g orally in a single dose OR Doxycycline 100 mg orally twice a day for 7 days
# Other Management Considerations
See Sexual Assault or Abuse of Children. Follow-Up. Follow-up cultures are necessary to ensure that treatment has been effective.
# Gonococcal Infections Gonococcal Infections in Adolescents and Adults
In the United States, an estimated 600,000 new N. gonorrhoeae infections occur each year (123). Gonorrhea is the second most commonly reported bacterial STD. The majority of urethral infections caused by N. gonorrhoeae among men produce symptoms that cause them to seek curative treatment soon enough to prevent serious sequelae, but treatment might not be soon enough to prevent transmission to others. Among women, several infections do not produce recognizable symptoms until complications (e.g., PID) have occurred. Both symptomatic and asymptomatic cases of PID can result in tubal scarring that can lead to infertility or ectopic pregnancy.
Because gonococcal infections among women frequently are asymptomatic, an essential component of gonorrhea control in the United States continues to be the screening of women at high risk for STDs. The U.S. Preventive Services Task Force (USPSTF) recommends that clinicians screen all sexually active women, including those who are pregnant, for gonorrhea infection if they are at increased risk. Women aged <25 years are at highest risk for gonorrhea infection. Other risk factors for gonorrhea include a previous gonorrhea infection, other sexually transmitted infections, new or multiple sex partners, inconsistent condom use, commercial sex work, and drug use. The prevalence of gonorrhea infection varies widely among communities and patient populations. The USPSTF does not recommend screening for gonorrhea in men and women who are at low risk for infection (134).
# Diagnostic Considerations
Because of high specificity (>99%) and sensitivity (>95%), a Gram stain of a male urethral specimen that demonstrates polymorphonuclear leukocytes with intracellular Gramnegative diplococci can be considered diagnostic for infection with N. gonorrhoeae in symptomatic men. However, because of lower sensitivity, a negative Gram stain should not be considered sufficient for ruling out infection in asymptomatic men. In addition, Gram stain of endocervical specimens, pharyngeal, or rectal specimens also are not sufficient to detect infection and, therefore, are not recommended. Specific testing for N. gonorrhoeae is recommended because of the increased utility and availability of highly sensitive and specific testing methods and because a specific diagnosis might enhance partner notification.
Specific diagnosis of infection with N. gonorrhoeae may be performed by testing endocervical, vaginal, male urethral, or urine specimens. Culture, nucleic acid hybridization tests, and NAAT are available for the detection of genitourinary infection with N. gonorrhoeae (127). Culture and nucleic acid hybridization tests require female endocervical or male urethral swab specimens. NAAT offer the widest range of testing specimen types because they are FDA-cleared for use with endocervical swabs, vaginal swabs, male urethral swabs, and female and male urine. However, product inserts for each NAAT vendor must be carefully examined to assess current indications because FDA-cleared specimen types might vary. In general, culture is the most widely available option for the diagnosis of infection with N. gonorrhoeae in nongenital sites (e.g., rectum and pharynx). Nonculture tests are not FDAcleared for use in the rectum and pharynx. Some NAATs have the potential to cross-react with nongonococcal Neisseria and related organisms that are commonly found in the throat. Some noncommercial laboratories have initiated NAAT of rectal and pharyngeal swab specimens after establishing the performance of the test to meet CLIA requirements.
Because nonculture tests cannot provide antimicrobial susceptibility results, in cases of persistent gonococcal infection after treatment, clinicians should perform both culture and antimicrobial susceptibility testing.
All patients tested for gonorrhea should be tested for other STDs, including chlamydia, syphilis, and HIV.
# Dual Therapy for Gonococcal and Chlamydial Infections
Patients infected with N. gonorrhoeae frequently are coinfected with C. trachomatis; this finding has led to the recommendation that patients treated for gonococcal infection also be treated routinely with a regimen that is effective against uncomplicated genital C. trachomatis infection (135). Because the majority of gonococci in the United States are susceptible to doxycycline and azithromycin, routine cotreatment might also hinder the development of antimicrobial-resistant N. gonorrhoeae.
Because of the high sensitivity of NAATs for chlamydial infection, patients with a negative chlamydial NAAT result at the time of treatment for gonorrhea do not need to be treated for chlamydia as well. However, if chlamydial test results are not available or if a non-NAAT was negative for chlamydia, patients should be treated for both gonorrhea and chlamydia.
# Quinolone-Resistant N. gonorrhoeae (QRNG)
QRNG continues to spread, making the treatment of gonorrhea with quinolones such as ciprofloxacin inadvisable in many areas and populations (136). Resistance to ciprofloxacin usually indicates resistance to other quinolones as well. QRNG is common in parts of Europe, the Middle East, Asia, and the Pacific. In the United States, QRNG is becoming increasingly common. Previously, CDC had advised that quinolones not be used in California and Hawaii because of the high prevalence of QRNG in these areas (137). The prevalence of QRNG has increased in other areas of the United States, which has resulted in changes in recommended treatment regimens by other states and local areas. QRNG prevalence will continue to increase, and quinolones will eventually not be advisable for the treatment of gonorrhea. The CDC website () or state health departments can provide the most current information. In 2004, of 6,322 isolates collected by CDC's Gonococcal Isolate Surveillance Project (GISP), 6.8% were resistant to ciprofloxacin (minimum inhibitory concentrations >1.0 µg/mL). Excluding isolates from California and Hawaii, 3.6% of isolates were QRNG. QRNG was more common among MSM than among heterosexual men (23.9% versus 2.9%). In 2004, QRNG among heterosexual men outside of California and Hawaii was 1.4% (138).
Quinolones should not be used for the treatment of gonorrhea among MSM (139) or in areas with increased QRNG prevalence in the United States (e.g., California and Hawaii) or for infections acquired while traveling abroad. Because oral alternatives to quinolones are limited, quinolones may continue to be used for heterosexual men and women in areas and populations not known to have elevated levels of resistance. Clinicians should obtain information on the sexual behavior and recent travel history (including histories from sex partners) of persons to be treated for gonorrhea to ensure appropriate antibiotic therapy.
Resistance of N. gonorrhoeae to fluoroquinolones and other antimicrobials is expected to continue to spread; therefore, state and local surveillance for antimicrobial resistance is crucial for guiding local therapy recommendations. GISP, which samples approximately 3% of all U.S. men who have gonococcal infections, is a mainstay of surveillance. However, surveillance by clinicians also is critical. Clinicians who have diagnosed N. gonorrhoeae infection in a person who was previously treated with a recommended regimen and who probably has not been reexposed should perform culture and susceptibility testing of relevant clinical specimens and report the case to the local health department. To maximize compliance with recommended therapies, medications for gonococcal infections should be dispensed on site.
# Uncomplicated Gonococcal Infections of the Cervix, Urethra, and Rectum
# Recommended Regimens*
Ceftriaxone in a single injection of 125 mg provides sustained, high bactericidal levels in the blood. Extensive clinical experience indicates that ceftriaxone is safe and effective for the treatment of uncomplicated gonorrhea at all anatomic sites, curing 98.9% of uncomplicated urogenital and anorectal infections in published clinical trials (140).
Cefixime has an antimicrobial spectrum similar to that of ceftriaxone, but the 400 mg oral dose does not provide as high, nor as sustained, a bactericidal level as that provided by the 125 mg dose of ceftriaxone. In published clinical trials, the 400 mg dose cured 97.4% of uncomplicated urogenital and anorectal gonococcal infections (140). The advantage of cefixime is that it can be administered orally. Updates on the availability of cefixime are available from CDC or state health departments.
Ciprofloxacin is no longer universally effective against N. gonorrhoeae in the United States (138). However, ciprofloxacin is safe, inexpensive, and can be administered orally. In published clinical trials of uncomplicated urogenital and anorectal infections in the absence of QRNG, a dose of 500 mg of ciprofloxacin provides sustained bactericidal levels with cure rates of 99.8% (140). If QRNG is suspected, ceftriaxone IM or cefixime PO (by mouth) should be used. If neither of these regimens are feasible options, then one of the alternative nonquinolone regimens in this report should be considered.
Similar to ciprofloxacin, ofloxacin is no longer universally effective against N. gonorrhoeae in the United States. The 400 mg oral dose of ofloxacin has been effective for treatment of uncomplicated urogenital and anorectal infections; in clinical trials, 98.6% of infections were cured (140). Levofloxacin, the active l-isomer of ofloxacin, can be used in place of ofloxacin as a single dose of 250 mg.
# Alternative Regimens
Spectinomycin 2 g in a single IM dose OR Single-dose cephalosporin regimens OR Single-dose quinolone regimens Several other antimicrobials are active against N. gonorrhoeae, but none have substantial advantages over the recommended regimens. Spectinomycin is expensive and must be injected; however, it has been effective in published clinical trials, curing 98.2% of uncomplicated urogenital and anorectal gonococcal infections (140). Spectinomycin is useful for the treatment of patients who cannot tolerate cephalosporins and quinolones.
Single-dose cephalosporin regimens (other than ceftriaxone 125 mg IM and cefixime 400 mg orally) that are safe and highly effective against uncomplicated urogenital and anorectal gonococcal infections include ceftizoxime (500 mg, administered IM), cefoxitin (2 g, administered IM with probenecid 1 g orally), and cefotaxime (500 mg, administered IM). None of the injectable cephalosporins offer any advantage over ceftriaxone.
Single-dose quinolone regimens include gatifloxacin 400 mg orally, norfloxacin 800 mg orally, and lomefloxacin 400 mg orally. These regimens appear to be safe and effective for the treatment of uncomplicated gonorrhea, but data regarding their use are limited. None of the regimens appear to offer any advantage over ciprofloxacin, ofloxacin, or levofloxacin, and they are not effective against QRNG. Some evidence suggests that cefpodoxime and cefuroxime axetil 1 g orally might be additional oral alternatives in the treatment of uncomplicated urogenital gonorrhea; additional information on alternative oral regimens are available at . Cefpodoxime proxetil 200 mg PO is less active against N. gonorrhoeae than cefixime and also does not quite meet the minimum efficacy criteria (demonstrated efficacy with lower 95% confidence interval of >95% in summed clinical trials) with cure rates, 96.5% (CI = 94.8%-98.9%) for urogenital and rectal infection; efficacy in treating pharyngeal infection is unsatisfactory, 78.9% (CI = 54.5%-94%). Clinical studies are being conducted to assess whether cefpodoxime 400 mg PO is an acceptable oral alternative. Treatment with cefuroxime axetil 1 g PO does not quite meet the minimum efficacy criteria for urogenital and rectal infection (95.9%; CI = 94.5%-97.3%) and, its efficacy in treating pharyngeal infection is unacceptable (56.9%; CI = 42.2%-70.7%).
Azithromycin 2 g orally is effective against uncomplicated gonococcal infection but is expensive and causes gastrointestinal distress and is not recommended for treatment of gonorrhea. Although azithromycin 1 g theoretically meets alternative regimen criteria, it is not recommended because of concerns regarding the possible rapid emergence of antimicrobial resistance. N. gonorrhoeae in the United States is not adequately susceptible to penicillins, tetracyclines, and macrolides (e.g., erythromycin) for these antimicrobials to be recommended.
# Uncomplicated Gonococcal Infections of the Pharynx
Gonococcal infections of the pharynx are more difficult to eradicate than infections at urogenital and anorectal sites. Few antimicrobial regimens can reliably cure >90% of gonococcal pharyngeal infections. Although chlamydial coinfection of the pharynx is unusual, coinfection at genital sites sometimes occurs. Therefore, treatment for both gonorrhea and chlamydia is recommended.
# Recommended Regimens
# Recommended Regimens for MSM or Heterosexuals with a History of Recent Travel
Ceftriaxone 125 mg IM in a single dose
# PLUS TREATMENT FOR CHLAMYDIA IN CHLAMY-DIAL INFECTION IS NOT RULED OUT
# Follow-Up
Patients who have uncomplicated gonorrhea and who are treated with any of the recommended or alternative regimens do not need a test of cure. Patients who have symptoms that persist after treatment should be evaluated by culture for N. gonorrhoeae, and any gonococci isolated should be tested for antimicrobial susceptibility. Persistent urethritis, cervicitis, or proctitis also might be caused by C. trachomatis or other organisms.
A high prevalence of N. gonorrhoeae infection is observed in patients who have had gonorrhea in the preceding several months (141,142). The majority of infections identified after treatment with one of the recommended regimens result from reinfection rather than treatment failure, indicating a need for improved patient education and referral of sex partners. Clinicians should consider advising all patients with gonorrhea to be retested 3 months after treatment. If patients do not seek medical care for retesting in 3 months, providers are encouraged to test these patients whenever they next seek medical care within the following 12 months, regardless of whether the patient believes that their sex partners were treated. Retesting is distinct from test of cure to detect therapeutic failure, which is not recommended.
# Management of Sex Partners
Effective clinical management of patients with treatable STDs requires treatment of the patients' recent sex partners to prevent reinfection and curtail further transmission. Patients should be instructed to refer their sex partners for evaluation and treatment. Sex partners of patients with N. gonorrhoeae infection whose last sexual contact with the patient was within 60 days before onset of symptoms or diagnosis of infection in the patient should be evaluated and treated for N. gonorrhoeae and C. trachomatis infections. If a patient's last sexual intercourse was >60 days before onset of symptoms or diagnosis, the patient's most recent sex partner should be treated. Patients should be instructed to avoid sexual intercourse until therapy is completed and until they and their sex partners no longer have symptoms.
For patients with gonorrhea whose partners' treatment cannot be ensured or is unlikely, delivery of antibiotic therapy (i.e., either a prescription or medication) by heterosexual male or female patients to their partners is an option (see Partner Management). Use of this approach (25,27) should always be accompanied by efforts to educate partners about symptoms and to encourage partners to seek clinical evaluation. Male patients must inform female partners of their infection and be given accompanying materials about the importance of seeking medical evaluation for PID (especially if symptomatic). Possible undertreatment of PID in female partners and possible missed opportunities to diagnose other STDs are of concern and have not been evaluated in comparisons with patient-delivered therapy and partner referral. Patient-delivered therapy for patients with gonorrhea should routinely include treatment for chlamydia. This approach should not be considered a routine partner management strategy in MSM because of the high risk of coexisting undiagnosed STDs or HIV infection.
# Special Considerations Allergy, Intolerance, and Adverse Reactions
Persons who cannot tolerate cephalosporins or quinolones should be treated with spectinomycin. Because spectinomycin is unreliable (52% effective) against pharyngeal infections, patients who have suspected or known pharyngeal infection should have a pharyngeal culture 3-5 days after treatment to verify eradication of infection.
# Pregnancy
Pregnant women should not be treated with quinolones or tetracyclines. Those infected with N. gonorrhoeae should be treated with a recommended or alternate cephalosporin. Women who cannot tolerate a cephalosporin should be administered a single 2-g dose of spectinomycin IM. Either azithromycin or amoxicillin is recommended for treatment of presumptive or diagnosed C. trachomatis infection during pregnancy (see Chlamydial Infections).
# Administration of Quinolones to Adolescents
Fluoroquinolones have not been recommended for persons aged 45 kg can be treated with any regimen recommended for adults (See Gonococcal Infections).
# HIV Infection
Patients who have gonococcal infection and also are infected with HIV should receive the same treatment regimen as those who are HIV negative.
# Gonococcal Conjunctivitis
In the only published study of the treatment of gonococcal conjunctivitis among U.S. adults, all 12 study participants responded to a single 1-g IM injection of ceftriaxone (144). The following recommendation reflects the opinions of consultants knowledgeable in the field of STDs.
# Recommended Regimen
Ceftriaxone 1 g IM in a single dose Consider lavage of the infected eye with saline solution once.
# Management of Sex Partners
Patients should be instructed to refer their sex partners for evaluation and treatment (see Gonococcal Infections, Management of Sex Partners).
# Disseminated Gonococcal Infection (DGI)
DGI results from gonococcal bacteremia. DGI frequently results in petechial or pustular acral skin lesions, asymmetrical arthralgia, tenosynovitis, or septic arthritis. The infection is complicated occasionally by perihepatitis and rarely by endocarditis or meningitis. Some strains of N. gonorrhoeae that cause DGI may cause minimal genital inflammation.
No studies on the treatment of DGI among adults have been published since publication of the last CDC STD treatment guidelines publication. DGI treatment recommendations reflect the opinions of consultants. No treatment failures have been reported with the recommended regimens.
# Treatment
Hospitalization is recommended for initial therapy, especially for patients who might not comply with treatment, for those in whom diagnosis is uncertain, and for those who have purulent synovial effusions or other complications. Patients should be examined for clinical evidence of endocarditis and meningitis. Patients treated for DGI should be treated presumptively for concurrent C. trachomatis infection, unless appropriate testing excludes this infection. All of the preceding regimens should be continued for 24-48 hours after improvement begins, at which time therapy may be switched to one of the following regimens to complete at least 1 week of antimicrobial therapy.
# Recommended Regimen
Cefixime 400 mg orally twice daily OR Ciprofloxacin 500 mg orally twice daily- OR Ofloxacin 400 mg orally twice daily- OR Levofloxacin 500 mg orally once daily- - Quinolones should not be used for infections in MSM or in those with a history of recent foreign travel or partners' travel, infections acquired in California or Hawaii, or infections acquired in other areas with increased QRNG prevalence.
# Management of Sex Partners
Gonococcal infection frequently is asymptomatic in sex partners of patients who have DGI. As with uncomplicated gonococcal infections, patients should be instructed to refer their sex partners for evaluation and treatment (see Gonococcal Infection, Management of Sex Partners).
# Gonococcal Meningitis and Endocarditis
# Recommended Regimen
# Ceftriaxone 1-2 g IV every 12 hours
Therapy for meningitis should be continued for 10-14 days; therapy for endocarditis should be continued for at least 4 weeks. Treatment of complicated DGI should be undertaken in consultation with a specialist.
# Management of Sex Partners
Patients should be instructed to refer their sex partners for evaluation and treatment (see Gonococcal Infection, Management of Sex Partners).
# Gonococcal Infections Among Infants
Gonococcal infection among infants usually results from exposure to infected cervical exudate at birth. It is usually an acute illness that manifests 2-5 days after birth. The prevalence of infection among infants depends on the prevalence of infection among pregnant women, whether pregnant women are screened for gonorrhea, and whether newborns receive ophthalmia prophylaxis. The most severe manifestations of N. gonorrhoeae infection in newborns are ophthalmia neonatorum and sepsis, which can include arthritis and meningitis. Less severe manifestations include rhinitis, vaginitis, urethritis, and reinfection at sites of fetal monitoring.
# Ophthalmia Neonatorum Caused by N. gonorrhoeae
In the United States, although N. gonorrhoeae causes ophthalmia neonatorum less frequently than C. trachomatis and nonsexually transmitted agents, identifying and treating this infection is especially important because ophthalmia neonatorum can result in perforation of the globe of the eye and blindness.
# Diagnostic Considerations
Infants at increased risk for gonococcal ophthalmia are those who do not receive ophthalmia prophylaxis and those whose mothers have had no prenatal care or whose mothers have a history of STDs or substance abuse. Gonococcal ophthalmia is strongly suspected when intracellular gram-negative diplococci are identified in conjunctival exudate, justifying presumptive treatment for gonorrhea after appropriate cultures for N. gonorrhoeae are obtained. Appropriate chlamydial testing should be done simultaneously. Presumptive treatment for N. gonorrhoeae might be indicated for newborns who are at increased risk for gonococcal ophthalmia and who have conjunctivitis but do not have gonococci in a Gram-stained smear of conjunctival exudate.
In all cases of neonatal conjunctivitis, conjunctival exudates should be cultured for N. gonorrhoeae and tested for antibiotic susceptibility before a definitive diagnosis is made. A definitive diagnosis is vital because of the public health and social consequences of a diagnosis of gonorrhea. Nongonococcal causes of neonatal ophthalmia include Moraxella catarrhalis and other Neisseria species that are indistinguishable from N. gonorrhoeae on Gram-stained smear but can be differentiated in the microbiology laboratory.
# Recommended Regimen
Ceftriaxone 25-50 mg/kg IV or IM in a single dose, not to exceed 125 mg Topical antibiotic therapy alone is inadequate and is unnecessary if systemic treatment is administered.
# Other Management Considerations
Simultaneous infection with C. trachomatis should be considered when a patient does not improve after treatment. Both mother and infant should be tested for chlamydial infection at the same time that gonorrhea testing is conducted (see Ophthalmia Neonatorum Caused by C. trachomatis). Ceftriaxone should be administered cautiously to hyperbilirubinemic infants, especially those born prematurely.
# Follow-Up
Infants who have gonococcal ophthalmia should be hospitalized and evaluated for signs of disseminated infection (e.g., sepsis, arthritis, and meningitis). One dose of ceftriaxone is adequate therapy for gonococcal conjunctivitis.
# MMWR August 4, 2006
# Management of Mothers and Their Sex Partners
The mothers of infants who have gonococcal infection and the mothers' sex partners should be evaluated and treated according to the recommendations for treating gonococcal infections in adults (see Gonococcal Infections in Adolescents and Adults).
# DGI and Gonococcal Scalp Abscesses in Newborns
Sepsis, arthritis, and meningitis (or any combination of these conditions) are rare complications of neonatal gonococcal infection. Localized gonococcal infection of the scalp can result from fetal monitoring through scalp electrodes. Detection of gonococcal infection in neonates who have sepsis, arthritis, meningitis, or scalp abscesses requires cultures of blood, CSF, and joint aspirate on chocolate agar. Specimens obtained from the conjunctiva, vagina, oropharynx, and rectum that are cultured on gonococcal selective medium are useful for identifying the primary site(s) of infection, especially if inflammation is present. Positive Gram-stained smears of exudate, CSF, or joint aspirate provide a presumptive basis for initiating treatment for N. gonorrhoeae. Diagnoses based on Gram-stained smears or presumptive identification of cultures should be confirmed with definitive tests on culture isolates.
# Recommended Regimens
Ceftriaxone 25-50 mg/kg/day IV or IM in a single daily dose for 7 days, with a duration of 10-14 days, if meningitis is documented OR Cefotaxime 25 mg/kg IV or IM every 12 hours for 7 days, with a duration of 10-14 days, if meningitis is documented
# Prophylactic Treatment for Infants Whose Mothers Have Gonococcal Infection
Infants born to mothers who have untreated gonorrhea are at high risk for infection.
# Recommended Regimen in the Absence of Signs of Gonococcal Infection
Ceftriaxone 25-50 mg/kg IV or IM, not to exceed 125 mg, in a single dose
# Other Management Considerations
Both mother and infant should be tested for chlamydial infection.
# Follow-Up
Follow-up examination is not required.
# Management of Mothers and Their Sex Partners
The mothers of infants who have gonococcal infection and the mothers' sex partners should be evaluated and treated according to the recommendations for treatment of gonococcal infections in adults (see Gonococcal Infections).
# Gonococcal Infections Among Children
Sexual abuse is the most frequent cause of gonococcal infection in pre-adolescent children (see Sexual Assault or Abuse of Children). Vaginitis is the most common manifestation of gonococcal infection in preadolescent girls. PID after vaginal infection is probably less common in children than among adults. Among sexually abused children, anorectal and pharyngeal infections with N. gonorrhoeae are common and frequently asymptomatic.
# Diagnostic Considerations
Because of the legal implications of a diagnosis of N. gonorrhoeae infection in a child, only standard culture procedures for the isolation of N. gonorrhoeae should be used for children. Nonculture gonococcal tests for gonococci (e.g., Gram-stained smear, nucleic acid hybridization tests, EIA, and NAAT) should not be used without standard culture; none of these tests have been approved by FDA for use with specimens obtained from the oropharynx, rectum, or genital tract of children. Specimens from the vagina, urethra, pharynx, or rectum should be streaked onto selective media for isolation of N. gonorrhoeae, and all presumptive isolates of N. gonorrhoeae should be identified definitively by at least two tests that involve different principles (e.g., biochemical, enzyme substrate, or serologic). Isolates should be preserved to enable additional or repeated testing.
# Recommended Regimens for Children Who Weigh >45 kg
Treat with one of the regimens recommended for adults (see Gonococcal Infections)
Fluoroquinolones have not been recommended for persons aged <18 years because they have damaged articular cartilage in young animals. However, no such joint damage clearly attributable to quinolone therapy has been observed in children, even in those receiving multiple-dose regimens.
# Recommended Regimens for Children Who Weigh <45 kg and Who Have Uncomplicated Gonococcal Vulvovaginitis, Cervicitis, Urethritis, Pharyngitis, or Proctitis
Ceftriaxone 125 mg IM in a single dose
# Alternative Regimen
Spectinomycin 40 mg/kg (maximum dose: 2 g) IM in a single dose may be used, but this therapy is unreliable for treatment of pharyngeal infections. Some specialists use cefixime to treat gonococcal infections in children because it can be administered orally; however, no reports have been published concerning the safety or effectiveness of cefixime used for this purpose.
# Recommended Regimen for Children Who Weigh <45 kg and Who Have Bacteremia or Arthritis
Ceftriaxone 50 mg/kg (maximum dose: 1 g) IM or IV in a single dose daily for 7 days
# Recommended Regimen for Children Who Weigh >45 kg and Who Have Bacteremia or Arthritis
Ceftriaxone 50 mg/kg IM or IV in a single dose daily for 7 days
# Follow-Up
Follow-up cultures are unnecessary if ceftriaxone is used. If spectinomycin is used to treat pharyngitis, a follow-up culture is necessary to ensure that treatment was effective.
# Other Management Considerations
Only parenteral cephalosporins are recommended for use in children. Ceftriaxone is approved for all gonococcal infections in children; cefotaxime is approved for gonococcal ophthalmia only. Oral cephalosporins used for treatment of gonococcal infections in children have not been adequately evaluated.
All children who have gonococcal infections should be evaluated for coinfection with syphilis and C. trachomatis. (For a discussion of concerns regarding sexual assault, refer to Sexual Assault or Abuse of Children).
# Ophthalmia Neonatorum Prophylaxis
To prevent gonococcal ophthalmia neonatorum, a prophylactic agent should be instilled into the eyes of all newborn infants; this procedure is required by law in the majority of states. All of the recommended prophylactic regimens in this section prevent gonococcal ophthalmia. However, the efficacy of these preparations in preventing chlamydial ophthalmia is less clear, and they do not eliminate nasopharyngeal colonization by C. trachomatis. The diagnosis and treatment of gonococcal and chlamydial infections in pregnant women is the best method for preventing neonatal gonococcal and chlamydial disease. Not all women, however, receive prenatal care. Ocular prophylaxis is warranted because it can prevent sight-threatening gonococcal ophthalmia and because it is safe, easy to administer, and inexpensive.
# Prophylaxis
# Recommended Regimens
Erythromycin (0.5%) ophthalmic ointment in a single application OR Tetracycline ophthalmic ointment (1%) in a single application
One of these recommended preparations should be instilled into both eyes of every neonate as soon as possible after delivery. If prophylaxis is delayed (i.e., not administered in the delivery room), a monitoring system should be established to ensure that all infants receive prophylaxis. All infants should be administered ocular prophylaxis, regardless of whether they are delivered vaginally or by cesarean section. Single-use tubes or ampules are preferable to multiple-use tubes. Bacitracin is not effective. Use of povidone iodine has not been studied adequately.
# Diseases Characterized by Vaginal Discharge
# Management of Patients Who Have Vaginal Infections
Vaginitis is usually characterized by a vaginal discharge and/ or vulvar itching and irritation, and a vaginal odor might be present. The three diseases most frequently associated with vaginal discharge are BV (replacement of the normal vaginal flora by an overgrowth of anaerobic microorganisms, mycoplasmas, and Gardnerella vaginalis), trichomoniasis (T. vaginalis), and candidiasis (usually caused by Candida albicans). Cervicitis can sometimes cause a vaginal discharge. Although vulvovaginal candidiasis (VVC) usually is not transmitted sexually, it is included in this section because it is frequently diagnosed in women being evaluated for STDs.
Various diagnostic methods are available to identify the etiology of an abnormal vaginal discharge. Laboratory testing fails to identify the cause of vaginitis in a minority of women. The cause of vaginal symptoms usually can be determined by pH and microscopic examination of fresh samples of the discharge. The pH of the vaginal secretions can be determined by narrow-range pH paper; an elevated pH (i.e., >4.5) is common with BV or trichomoniasis but might not be highly specific. Discharge can be further examined by diluting one sample in one to two drops of 0.9% normal saline solution on one slide and a second sample in 10% potassium hydroxide (KOH) solution. An amine odor detected immediately after applying KOH suggests BV. Cover slips are placed on the slides, and they are examined under a microscope at lowand high-dry power. Motile T. vaginalis or clue cells (epithelial cells with borders obscured by small bacteria), which are characteristic of BV, usually are identified easily in the saline specimen. WBCs without evidence of trichomonads or yeast are usually suggestive of cervicitis (see Cervicitis). The yeast or pseudohyphae of Candida species are more easily identified in the KOH specimen. However, the absence of trichomonads or pseudohyphae does not rule out these infections because several studies have demonstrated the presence of these pathogens by culture or PCR after a negative microscopic examination. The presence of objective signs of vulvar inflammation in the absence of vaginal pathogens, along with a minimal amount of discharge, suggests the possibility of mechanical, chemical, allergic, or other noninfectious irritation of the vulva. Culture for T. vaginalis is more sensitive than microscopic examination. In settings where microscopy is not available, alternative point-of-care tests may be used to diagnose vaginitis.
# Bacterial Vaginosis
BV is a polymicrobial clinical syndrome resulting from replacement of the normal H2O2-producing Lactobacillus sp. in the vagina with high concentrations of anaerobic bacteria (e.g., Prevotella sp. and Mobiluncus sp.), G. vaginalis, and Mycoplasma hominis. BV is the most prevalent cause of vaginal discharge or malodor; however, more than 50% of women with BV are asymptomatic. The cause of the microbial alteration is not fully understood. BV is associated with having multiple sex partners, a new sex partner, douching, and lack of vaginal lactobacilli; whether BV results from acquisition of a sexually transmitted pathogen is unclear. Women who have never been sexually active are rarely affected. Treatment of male sex partners has not been beneficial in preventing the recurrence of BV.
# Diagnostic Considerations
BV can be diagnosed by the use of clinical criteria or Gram stain. Clinical criteria require three of the following symptoms or signs:
- homogeneous, thin, white discharge that smoothly coats the vaginal walls; - presence of clue cells on microscopic examination; - pH of vaginal fluid >4.5; and - a fishy odor of vaginal discharge before or after addition of 10% KOH (i.e., the whiff test).
When a Gram stain is used, determining the relative concentration of lactobacilli (long Gram-positive rods), Gramnegative and Gram-variable rods and cocci (i.e., G. vaginalis, Prevotella, Porphyromonas, and peptostreptococci), and curved Gram-negative rods (Mobiluncus) characteristic of BV is considered the gold standard laboratory method for diagnosing BV. Culture of G. vaginalis is not recommended as a diagnostic tool because it is not specific. However, a DNA probebased test for high concentrations of G. vaginalis (Affirm TM VP III, Becton Dickinson, Sparks, Maryland) might have clinical utility. Cervical Pap tests have no clinical utility for the diagnosis of BV because of low sensitivity. Other commercially available tests that might be useful for the diagnosis of BV include a card test for the detection of elevated pH and trimethylamine (QuickVue Advance Quidel, San Diego, California) and prolineaminopeptidase (Pip Activity TestCard TM , Quidel, San Diego, California).
# Treatment
The established benefits of therapy for BV in nonpregnant women are to 1) relieve vaginal symptoms and signs of infection and 2) reduce the risk for infectious complications after abortion or hysterectomy. Other potential benefits might include a reduction in risk for other infections (e.g., HIV and other STDs). All women who have symptomatic disease require treatment.
BV during pregnancy is associated with adverse pregnancy outcomes, including premature rupture of the membranes, preterm labor, preterm birth, intraamniotic infection, and postpartum endometritis. The established benefit of therapy for BV in pregnant women is to relieve vaginal symptoms and signs of infection. Additional potential benefits of therapy include 1) reducing the risk for infectious complications associated with BV during pregnancy and 2) reducing the risk for other infections (e.g., other STDs or HIV). The results of several investigations indicate that treatment of pregnant women with BV who are at high risk for preterm delivery (i.e., those who previously delivered a premature infant) might reduce the risk for prematurity (145)(146)(147). Therefore, clinicians should consider evaluation and treatment of high-risk pregnant women with asymptomatic BV.
The bacterial flora that characterizes BV have been recovered from the endometria and salpinges of women who have PID. BV has been associated with endometritis, PID, and vaginal cuff cellulitis after invasive procedures, including endometrial biopsy, hysterectomy, hysterosalpingography, placement of an IUD, cesarean section, and uterine curettage. The results of two randomized controlled trials have indicated that treatment of BV with metronidazole substantially reduced postabortion PID (148,149). Three trials that evaluated the use of anaerobic antimicrobial coverage (i.e., metronidazole) for routine operative prophylaxis before abortion and seven trials that evaluated this additional coverage for women undergoing hysterectomy demonstrated a substantial reduction in postoperative infectious complications (148)(149)(150)(151)(152)(153)(154)(155)(156). Because of the increased risk for postoperative infectious complications associated with BV, some specialists suggest that before performing surgical abortion or hysterectomy, providers should screen for and treat women with BV in addition to providing routine prophylaxis. However, more information is needed before recommending treatment of asymptomatic BV before other invasive procedures.
# Recommended Regimens
Metronidazole 500 mg orally twice a day for 7 days OR Metronidazole gel, 0.75%, one full applicator (5 g) intravaginally, once a day for 5 days OR Clindamycin cream, 2%, one full applicator (5 g) intravaginally at bedtime for 7 days
Patients should be advised to avoid consuming alcohol during treatment with metronidazole and for 24 hours thereafter. Clindamycin cream is oil-based and might weaken latex condoms and diaphragms for 5 days after use. Refer to clindamycin product labeling for additional information. Topical clindamycin preparations should not be used in the second half of pregnancy.
The recommended metronidazole regimens are equally efficacious. One randomized trial evaluated the clinical equivalency of intravaginal metronidazole gel 0.75% once daily versus twice daily and demonstrated similar cure rates 1 month after therapy (157).
# Alternative Regimens
Clindamycin 300 mg orally twice a day for 7 days OR Clindamycin ovules 100 mg intravaginally once at bedtime for 3 days Metronidazole 2 g single-dose therapy has the lowest efficacy for BV and is no longer a recommended or alternative regimen. FDA has cleared metronidazole 750 mg extended release tablets once daily for 7 days and a single dose of clindamycin intravaginal cream. Limited data have been published that compares the clinical or microbiologic equivalencies of these regimens with other regimens. Cure rates do not differ between intravaginal clindamycin cream and ovules (158).
Several studies have evaluated the clinical and microbiologic efficacy of using lactobacillus intravaginal suppositories to restore normal flora and treat BV. However, no currently available lactobacillus suppository was determined to be better than placebo 1 month after therapy for either clinical or microbiologic cure. No data support the use of douching for treatment or relief of symptoms.
# Follow-Up
Follow-up visits are unnecessary if symptoms resolve. Because recurrence of BV is not unusual, women should be advised to return for additional therapy if symptoms recur. A treatment regimen different from the original regimen may be used to treat recurrent disease. However, women with multiple recurrences should be managed in consultation with a specialist. One randomized trial for persistent BV indicated that metronidazole gel 0.75% twice per week for 6 months after completion of a recommended regimen was effective in maintaining a clinical cure for 6 months (159).
# Management of Sex Partners
The results of clinical trials indicate that a woman's response to therapy and the likelihood of relapse or recurrence are not affected by treatment of her sex partner(s). Therefore, routine treatment of sex partners is not recommended.
# Special Considerations
# Allergy or Intolerance to the Recommended Therapy
Intravaginal clindamycin cream is preferred in case of allergy or intolerance to metronidazole. Intravaginal metronidazole gel can be considered for patients who do not tolerate systemic metronidazole, but patients allergic to oral metronidazole should not be administered intravaginal metronidazole.
# Pregnancy
All pregnant women who have symptomatic disease require treatment. BV has been associated with adverse pregnancy outcomes (e.g., premature rupture of the membranes, chorioamnionitis, preterm labor, preterm birth, intraamniotic infection, postpartum endometritis, and postcesarean wound infection). Some specialists prefer using systemic therapy to treat possible subclinical upper genital tract infections.
Treatment of BV in asymptomatic pregnant women at high risk for preterm delivery (i.e., those who have previously delivered a premature infant) with a recommended oral regimen has reduced preterm delivery in three of four randomized controlled trials (145,146,160,161); some specialists recommend screening and oral treatment of these women. However, the optimal treatment regimens have not been established.
Screening (if conducted) and treatment should be performed during the first prenatal visit.
Two trials that evaluated the efficacy of metronidazole during pregnancy used the 250-mg regimen (145,146). However, some specialists suggest using a regimen of 500 mg twice daily in pregnant women. One small trial demonstrated that treatment with oral metronidazole 500 mg twice daily was equally effective as metronidazole gel, with cure rates of 70% (162). These regimens were not effective in reducing preterm birth in any group of women. Multiple studies and metaanalyses have not demonstrated an association between metronidazole use during pregnancy and teratogenic or mutagenic effects in newborns (164)(165)(166).
# Recommended Regimens for Pregnant Women
Metronidazole 500 mg orally twice a day for 7 days OR Metronidazole 250 mg orally three times a day for 7 days OR Clindamycin 300 mg orally twice a day for 7 days Whether treatment of asymptomatic pregnant women with BV who are at low risk for preterm delivery reduces adverse outcomes of pregnancy is unclear. One trial in which oral clindamycin was used demonstrated a reduction in spontaneous preterm birth (147). Several trials have evaluated the use of intravaginal clindamycin during pregnancy to reduce preterm birth and treat asymptomatic BV. One trial in which women were treated before 20 weeks' gestation demonstrated a reduction in preterm birth (166). In three other trials, intravaginal clindamycin cream was administered at 16-32 weeks' gestation, and an increase in adverse events (e.g., low birthweight and neonatal infections) was observed in newborns (167)(168)(169). Therefore, intravaginal clindamycin cream should only be used during the first half of pregnancy.
# Follow-Up of Pregnant Women
Treatment of BV in asymptomatic pregnant women who are at high risk for preterm delivery might prevent adverse pregnancy outcomes. Therefore, a follow-up evaluation 1 month after completion of treatment should be considered to evaluate whether therapy was effective.
# HIV Infection
Patients who have BV and also are infected with HIV should receive the same treatment regimen as those who are HIV negative. BV appears to be more persistent in HIV-positive women.
# Trichomoniasis
Trichomoniasis is caused by the protozoan T. vaginalis. Some men who are infected with T. vaginalis might not have symptoms; others have NGU. Many infected women have symptoms characterized by a diffuse, malodorous, yellow-green vaginal discharge with vulvar irritation. However, some women have minimal or no symptoms.
Diagnosis of vaginal trichomoniasis is usually performed by microscopy of vaginal secretions, but this method has a sensitivity of only approximately 60%-70% and requires immediate evaluation of wet preparation slide for optimal results. Other FDA-cleared tests for trichomoniasis in women include OSOM Trichomonas Rapid Test (Genzyme Diagnostics, Cambridge, Massachusetts), an immunochromatographic capillary flow dipstick technology, and the Affirm™ VP III (Becton Dickenson, San Jose, California), a nucleic acid probe test that evaluates for T. vaginalis, G. vaginalis, and C. albicans. These tests are both performed on vaginal secretions and have a sensitivity >83% and a specificity >97%. Both tests are pointof-care diagnostics. The results of the OSOM Trichomonas Rapid Test are available in approximately 10 minutes, and results of the Affirm™ VP III are available within 45 minutes. Although these tests tend to be more sensitive than vaginal wet preparation, false positives might occur especially in low prevalence populations. Culture is the most sensitive and specific commercially available method of diagnosis. In women in whom trichomoniasis is suspected but not confirmed by microscopy, vaginal secretions should be cultured for T. vaginalis.
In men, wet preparation is insensitive, and culture testing of urethral swab, urine, and semen is required for optimal sensitivity. No FDA-cleared PCR test for T. vaginalis is available in the United States, but such testing might be available from commercial laboratories that have developed their own PCR tests.
# Recommended Regimens
Metronidazole 2 g orally in a single dose OR Tinidazole 2 g orally in a single dose
# Alternative Regimen
Metronidazole 500 mg orally twice a day for 7 days Patients should be advised to avoid consuming alcohol during treatment with metronidazole or tinidazole. Abstinence from alcohol use should continue for 24 hours after completion of metronidazole or 72 hours after completion of tinidazole.
The nitroimidazoles comprise the only class of drugs useful for the oral or parenteral therapy of trichomoniasis. Of these drugs, metronidazole and tinidazole are available in the United States and are cleared by the FDA for the treatment of trichomoniasis. In randomized clinical trials, the recommended metronidazole regimens have resulted in cure rates of approximately 90%-95%, and the recommended tinidazole regimen has resulted in cure rates of approximately 86%-100%. The appropriate treatment of sex partners might increase these reported rates. Randomized controlled trials comparing single 2 g doses of metronidazole and tinidazole suggest that tinidazole is equivalent to, or superior to, metronidazole in achieving parasitologic cure and resolution of symptoms (170). Treatment of patients and sex partners results in relief of symptoms, microbiologic cure, and reduction of transmission.
Metronidazole gel is considerably less efficacious for the treatment of trichomoniasis (<50%) than oral preparations of metronidazole. Topically applied antimicrobials (e.g., metronidazole gel) are unlikely to achieve therapeutic levels in the urethra or perivaginal glands; therefore, use of the gel is not recommended. Several other topically applied antimicrobials occasionally have been used for treatment of trichomoniasis; however, these preparations probably do not have greater efficacy than metronidazole gel.
# Follow-Up
Follow-up is unnecessary for men and women who become asymptomatic after treatment or who are initially asymptomatic. Some strains of T. vaginalis can have diminished susceptibility to metronidazole; however, infections caused by the majority of these organisms respond to tinidazole or higher doses of metronidazole. Low-level metronidazole resistance has been identified in 2%-5% of cases of vaginal trichomoniasis. High-level resistance is rare. Tinidazole has a longer serum half-life and reaches higher levels in genitourinary tissues than metronidazole. In addition, many T. vaginalis isolates have lower minimum inhibitory concentrations (MICs) to tinidazole than metronidazole.
If treatment failure occurs with metronidazole 2 g single dose and reinfection is excluded, the patient can be treated with metronidazole 500 mg orally twice daily for 7 days or tinidazole 2 g single dose. For patients failing either of these regimens, clinicians should consider treatment with tinidazole or metronidazole at 2 g orally for 5 days. If these therapies are not effective, further management should be discussed with a specialist. The consultation should ideally include determination of the susceptibility of T. vaginalis to metronidazole and tinidazole. Consultation and T. vaginalis susceptibility testing is available from CDC (telephone: 770-488-4115; website: ).
# Management of Sex Partners
Sex partners of patients with T. vaginalis should be treated. Patients should be instructed to avoid sex until they and their sex partners are cured (i.e., when therapy has been completed and patient and partner(s) are asymptomatic).
# Special Considerations
# Allergy, Intolerance, and Adverse Reactions
Metronidazole and tinidazole are both nitroimidazoles. Patients with an immediate-type allergy to a nitroimidazole can be managed by metronidazole desensitization in consultation with a specialist (171,172). Topical therapy with drugs other than nitroimidazoles can be attempted, but cure rates are low (<50%).
# Pregnancy
Vaginal trichomoniasis has been associated with adverse pregnancy outcomes, particularly premature rupture of membranes, preterm delivery, and low birthweight. However, data do not suggest that metronidazole treatment results in a reduction in perinatal morbidity. Although some trials suggest the possibility of increased prematurity or low birthweight after metronidazole treatment, limitations of the studies prevent definitive conclusions regarding risks of treatment (173,174). Treatment of T. vaginalis might relieve symptoms of vaginal discharge in pregnant women and might prevent respiratory or genital infection of the newborn and further sexual transmission. Clinicians should counsel patients regarding the potential risks and benefits of treatment. Some specialists would defer therapy in asymptomatic pregnant women until after 37 weeks' gestation. In addition, these pregnant women should be provided careful counseling regarding condom use and the continued risk of sexual transmission.
Women may be treated with 2 g of metronidazole in a single dose. Metronidazole is pregnancy category B (animal studies have revealed no evidence of harm to the fetus, but no adequate, well-controlled studies among pregnant women have been conducted). Multiple studies and meta-analyses have not demonstrated a consistent association between metronidazole use during pregnancy and teratogenic or mutagenic effects in infants (163)(164)(165). Tinidazole is pregnancy category C (animal studies have demonstrated an adverse event, and no adequate, well-controlled studies in pregnant women have been conducted), and its safety in pregnant women has not been well-evaluated.
In lactating women who are administered metronidazole, withholding breastfeeding during treatment and for 12-24 hours after the last dose will reduce the exposure of metronidazole to the infant. While using tinidazole, interruption of breastfeeding is recommended during treatment and for 3 days after the last dose.
# HIV Infection
Patients who have trichomoniasis and also are infected with HIV should receive the same treatment regimen as those who are HIV negative. The incidence, persistence, and recurrence of trichomoniasis in HIV-infected women are not correlated with immune status.
# Vulvovaginal Candidiasis
VVC usually is caused by C. albicans but occasionally is caused by other Candida sp. or yeasts. Typical symptoms of VVC include pruritus, vaginal soreness, dyspareunia, external dysuria, and abnormal vaginal discharge. None of these symptoms is specific for VVC. An estimated 75% of women will have at least one episode of VVC, and 40%-45% will have two or more episodes. On the basis of clinical presentation, microbiology, host factors, and response to therapy, VVC can be classified as either uncomplicated or complicated (Box 2). Approximately 10%-20% of women will have complicated VVC, suggesting diagnostic and therapeutic considerations.
# Uncomplicated VVC
# Diagnostic Considerations in Uncomplicated VVC
A diagnosis of Candida vaginitis is suggested clinically by the presence of external dysuria and vulvar pruritus, pain, swelling, and redness. Signs include vulvar edema, fissures, excoriations, or thick curdy vaginal discharge. The diagnosis can be made in a woman who has signs and symptoms of vaginitis when either 1) a wet preparation (saline, 10% KOH) or Gram stain of vaginal discharge demonstrates yeasts or pseudohyphae or 2) a culture or other test yields a positive result for a yeast species. Candida vaginitis is associated with a normal vaginal pH (<4.5). Use of 10% KOH in wet preparations improves the visualization of yeast and mycelia by disrupting cellular material that might obscure the yeast or pseudohyphae. Examination of a wet mount with KOH preparation should be performed for all women with symptoms or signs of VVC, and women with a positive result should receive treatment. For those with negative wet mounts, vaginal cultures for Candida should be considered for those with any sign or multiple symptoms. If Candida cultures cannot be done, empiric treatment can be considered for symptomatic women with any sign of VVC on examination when the wet mount is negative. Identifying Candida by culture in the absence of symptoms or signs is not an indication for treatment because approximately 10%-20% of women harbor Candida sp. and other yeasts in the vagina. VVC can occur concomitantly with STDs. The majority of healthy women with uncomplicated VVC have no identifiable precipitating factors.
# Treatment
Short-course topical formulations (i.e., single dose and regimens of 1-3 days) effectively treat uncomplicated VVC. The topically applied azole drugs are more effective than nystatin. Treatment with azoles results in relief of symptoms and negative cultures in 80%-90% of patients who complete therapy.
# Recommended Regimens
# Intravaginal Agents:
Butoconazole 2% cream 5 g intravaginally for 3 days- OR Butoconazole 2% cream 5 g (Butaconazole1-sustained release), single intravaginal application OR Clotrimazole 1% cream 5 g intravaginally for 7-14 days- OR Clotrimazole 100 mg vaginal tablet for 7 days OR Clotrimazole 100 mg vaginal tablet, two tablets for 3 days OR Miconazole 2% cream 5 g intravaginally for 7 days- OR The creams and suppositories in this regimen are oil-based and might weaken latex condoms and diaphragms. Refer to condom product labeling for further information.
Intravaginal preparations of butaconazole, clotrimazole, miconazole, and tioconazole are available over-the-counter (OTC). Women whose condition has previously been diagnosed with VVC are not necessarily more likely to be able to diagnose themselves; therefore, any woman whose symptoms persist after using an OTC preparation, or who has a recurrence of symptoms within 2 months, should be evaluated with office-based testing. Unnecessary or inappropriate use of OTC preparations is common and can lead to a delay in the treatment of other vulvovaginitis etiologies, which can result in adverse clinical outcomes.
# Follow-Up
Patients should be instructed to return for follow-up visits only if symptoms persist or recur within 2 months of onset of initial symptoms.
# Management of Sex Partners
VVC is not usually acquired through sexual intercourse; treatment of sex partners is not recommended but may be considered in women who have recurrent infection. A minority of male sex partners might have balanitis, which is characterized by erythematous areas on the glans of the penis in conjunction with pruritus or irritation. These men benefit from treatment with topical antifungal agents to relieve symptoms.
# Special Considerations
# Allergy, Intolerance, and Adverse Reactions
Topical agents usually cause no systemic side effects, although local burning or irritation might occur. Oral agents occasionally cause nausea, abdominal pain, and headache. Therapy with the oral azoles has been associated rarely with abnormal elevations of liver enzymes. Clinically important interactions can occur when these oral agents are administered with other drugs, including astemizole, calcium channel antagonists, cisapride, coumadin, cyclosporin A, oral hypoglycemic agents, phenytoin, protease inhibitors, tacrolimus, terfenadine, theophylline, trimetrexate, and rifampin.
# Complicated VVC
# Recurrent Vulvovaginal Candidiasis (RVVC)
RVVC, usually defined as four or more episodes of symptomatic VVC in 1 year, affects a small percentage of women (<5%). The pathogenesis of RVVC is poorly understood, and the majority of women with RVVC have no apparent predisposing or underlying conditions. Vaginal cultures should be obtained from patients with RVVC to confirm the clinical diagnosis and to identify unusual species, including nonalbicans species, particularly Candida glabrata (C. glabrata does not form pseudohyphae or hyphae and is not easily recognized on microscopy). C. glabrata and other nonalbicans Candidia species are observed in 10%-20% of patients with RVVC. Conventional antimycotic therapies are not as effective against these species as against C. albicans.
# Treatment
Each individual episode of RVVC caused by C. albicans responds well to short duration oral or topical azole therapy. However, to maintain clinical and mycologic control, some specialists recommend a longer duration of initial therapy (e.g., 7-14 days of topical therapy or a 100 mg, 150 mg, or 200 mg oral dose of fluconazole every third day for a total of 3 doses (day 1, 4, and 7) to attempt mycologic remission before initiating a maintenance antifungal regimen.
# Maintenance Regimens
Oral fluconazole (i.e., 100-mg, 150-mg, or 200-mg dose) weekly for 6 months is the first line of treatment. If this regimen is not feasible, some specialists recommend topical clotrimazole 200 mg twice a week, clotrimazole (500-mg dose vaginal suppositories once weekly), or other topical treatments used intermittently.
Suppressive maintenance antifungal therapies are effective in reducing RVVC. However, 30%-50% of women will have recurrent disease after maintenance therapy is discontinued. Routine treatment of sex partners is controversial. C. albicans azole resistance is rare in vaginal isolates, and susceptibility testing is usually not warranted for individual treatment guidance.
# Severe VVC
Severe vulvovaginitis (i.e., extensive vulvar erythema, edema, excoriation, and fissure formation) is associated with lower clinical response rates in patients treated with short courses of topical or oral therapy. Either 7-14 days of topical azole or 150 mg of fluconazole in two sequential doses (second dose 72 hours after initial dose) is recommended.
# Nonalbicans VVC
The optimal treatment of nonalbicans VVC remains unknown. Options include longer duration of therapy (7-14 days) with a nonfluconazole azole drug (oral or topical) as first-line therapy. If recurrence occurs, 600 mg of boric acid in a gelatin capsule is recommended, administered vaginally once daily for 2 weeks. This regimen has clinical and mycologic eradication rates of approximately 70% (175). If symptoms recur, referral to a specialist is advised.
# Compromised Host
Women with underlying debilitating medical conditions (e.g., those with uncontrolled diabetes or those receiving corticosteroid treatment) do not respond as well to short-term therapies. Efforts to correct modifiable conditions should be made, and more prolonged (i.e., 7-14 days) conventional antimycotic treatment is necessary.
# Pregnancy
VVC frequently occurs during pregnancy. Only topical azole therapies, applied for 7 days, are recommended for use among pregnant women.
# HIV Infection
The incidence of VVC in HIV-infected women is unknown. Vaginal Candida colonization rates among HIV-infected women are higher than among those for seronegative women with similar demographic characteristics and high-risk behaviors, and the colonization rates correlate with increasing severity of immunosuppression. Symptomatic VVC is more frequent in seropositive women and similarly correlates with severity of immunodeficiency. In addition, among HIV-infected women, systemic azole exposure is associated with the isolation of nonalbicans Candida species from the vagina.
Based on available data, therapy for VVC in HIV-infected women should not differ from that for seronegative women. Although long-term prophylactic therapy with fluconazole at a dose of 200 mg weekly has been effective in reducing C. albicans colonization and symptomatic VVC (176), this regimen is not recommended for routine primary prophylaxis in HIV-infected women in the absence of recurrent VVC (50). Given the frequency at which RVVC occurs in the immmunocompetent healthy population, the occurrence of RVVC should not be considered an indication for HIV testing.
# Pelvic Inflammatory Disease
PID comprises a spectrum of inflammatory disorders of the upper female genital tract, including any combination of endometritis, salpingitis, tubo-ovarian abscess, and pelvic peritonitis. Sexually transmitted organisms, especially N. gonorrhoeae and C. trachomatis, are implicated in many cases; however, microorganisms that comprise the vaginal flora (e.g., anaerobes, G. vaginalis, Haemophilus influenzae, enteric Gram-negative rods, and Streptococcus agalactiae) also have been associated with PID. In addition, cytomegalovirus (CMV), M. hominis, U. urealyticum, and M. genitalium might be associated with some cases of PID. All women who are diagnosed with acute PID should be tested for N. gonorrhoeae and C. trachomatis and should be screened for HIV infection.
# Diagnostic Considerations
Acute PID is difficult to diagnose because of the wide variation in the symptoms and signs. Many women with PID have subtle or mild symptoms. Delay in diagnosis and treatment probably contributes to inflammatory sequelae in the upper reproductive tract. Laparoscopy can be used to obtain a more accurate diagnosis of salpingitis and a more complete bacteriologic diagnosis. However, this diagnostic tool frequently is not readily available, and its use is not easy to justify when symptoms are mild or vague. Moreover, laparoscopy will not detect endometritis and might not detect subtle inflammation of the fallopian tubes. Consequently, a diagnosis of PID usually is based on clinical findings.
The clinical diagnosis of acute PID is imprecise (177,178). Data indicate that a clinical diagnosis of symptomatic PID has a positive predictive value (PPV) for salpingitis of 65%-90% compared with laparoscopy. The PPV of a clinical diagnosis of acute PID depends on the epidemiologic characteristics of the population, with higher PPVs among sexually active young women (particularly adolescents), among patients attending STD clinics, or in other settings where the rates of gonorrhea or chlamydia are high. In all settings, however, no single historical, physical, or laboratory finding is both sensitive and specific for the diagnosis of acute PID (i.e., can be used both to detect all cases of PID and to exclude all women without PID). Combinations of diagnostic findings that improve either sensitivity (i.e., detect more women who have PID) or specificity (i.e., exclude more women who do not have PID) do so only at the expense of the other. For example, requiring two or more findings excludes more women who do not have PID but also reduces the number of women with PID who are identified.
Many episodes of PID go unrecognized. Although some cases are asymptomatic, others are not diagnosed because the patient or the health-care provider fails to recognize the implications of mild or nonspecific symptoms or signs (e.g., abnormal bleeding, dyspareunia, and vaginal discharge). Because of the difficulty of diagnosis and the potential for damage to the reproductive health of women, even by apparently mild or subclinical PID, health-care providers should maintain a low threshold for the diagnosis of PID.
The optimal treatment regimen and long-term outcome of early treatment of women with asymptomatic or subclinical PID are unknown. The following recommendations for diagnosing PID are intended to help health-care providers recognize when PID should be suspected and when they need to obtain additional information to increase diagnostic certainty. Diagnosis and management of other common causes of lower abdominal pain (e.g., ectopic pregnancy, acute appendicitis, and functional pain) are unlikely to be impaired by initiating empiric antimicrobial therapy for PID.
Empiric treatment of PID should be initiated in sexually active young women and other women at risk for STDs if they are experiencing pelvic or lower abdominal pain, if no cause for the illness other than PID can be identified, and if one or more of the following minimum criteria are present on pelvic examination:
- cervical motion tenderness OR uterine tenderness OR adnexal tenderness. The requirement that all three minimum criteria be present before the initiation of empiric treatment could result in insufficient sensitivity for the diagnosis of PID. The presence of signs of lower genital tract inflammation, in addition to one of the three minimum criteria, increases the specificity of diagnosis. In deciding upon the initiation of empiric treatment, clinicians should also consider the risk profile of the patient for STDs.
More elaborate diagnostic evaluation frequently is needed because incorrect diagnosis and management might cause unnecessary morbidity. These additional criteria may be used to enhance the specificity of the minimum criteria. The following additional criteria can be used to enhance the specificity of the minimum criteria and support a diagnosis of PID:
- oral temperature >101°F (>38.3°C),
- abnormal cervical or vaginal mucopurulent discharge, - presence of abundant numbers of WBC on saline microscopy of vaginal secretions, - elevated erythrocyte sedimentation rate, - elevated C-reactive protein, and - laboratory documentation of cervical infection with N. gonorrhoeae or C. trachomatis. The majority of women with PID have either mucopurulent cervical discharge or evidence of WBC on a microscopic evaluation of a saline preparation of vaginal fluid. If the cervical discharge appears normal and no WBCs are observed on the wet prep of vaginal fluid, the diagnosis of PID is unlikely, and alternative causes of pain should be investigated. A wet prep of vaginal fluid offers the ability to detect the presence of concomitant infections (e.g., bacterial vaginosis and trichomoniasis).
The most specific criteria for diagnosing PID include the following:
- endometrial biopsy with histopathologic evidence of endometritis; - transvaginal sonography or magnetic resonance imaging techniques showing thickened, fluid-filled tubes with or without free pelvic fluid or tubo-ovarian complex, or doppler studies suggesting pelvic infection (e.g., tubal hyperemia); and - laparoscopic abnormalities consistent with PID. A diagnostic evaluation that includes some of these more extensive studies might be warranted in some cases. Endometrial biopsy is warranted in women undergoing laparoscopy who do not have visual evidence of salpingitis, as some women with PID have endometritis alone.
# Treatment
PID treatment regimens must provide empiric, broad spectrum coverage of likely pathogens. Several antimicrobial regimens have been effective in achieving clinical and microbiologic cure in randomized clinical trials with shortterm follow-up. However, only a limited number of investigations have assessed and compared these regimens with regard to elimination of infection in the endometrium and fallopian tubes or determined the incidence of long-term complications (e.g., tubal infertility and ectopic pregnancy) after antimicrobial regimens (179,180).
All treatment regimens should be effective against N. gonorrhoeae and C. trachomatis because negative endocer- vical screening for these organisms does not rule out upper reproductive tract infection. The need to eradicate anaerobes from women who have PID has not been determined definitively. Anaerobic bacteria have been isolated from the upper reproductive tract of women who have PID, and data from in vitro studies have revealed that some anaerobes (e.g., Bacteroides fragilis) can cause tubal and epithelial destruction. In addition, BV also is present in many women who have PID (181).Until treatment regimens that do not adequately cover these microbes have been demonstrated to prevent long-term sequelae (e.g., infertility and ectopic pregnancy) as successfully as the regimens that are effective against these microbes, the use of regimens with anaerobic activity should be considered. Treatment should be initiated as soon as the presumptive diagnosis has been made because prevention of long-term sequelae is dependent on immediate administration of appropriate antibiotics. When selecting a treatment regimen, health-care providers should consider availability, cost, patient acceptance, and antimicrobial susceptibility. Some specialists have recommended that all patients with PID be hospitalized so that bed rest and supervised treatment with parenteral antibiotics can be initiated. However, in women with PID of mild or moderate clinical severity, outpatient therapy can provide short-and long-term clinical outcomes similar to inpatient therapy. Limited data support the use of outpatient therapy in women with more severe clinical presentations. The decision of whether hospitalization is necessary should be based on the discretion of the health-care provider.
The following criteria for hospitalization are suggested:
- surgical emergencies (e.g., appendicitis) cannot be excluded; - the patient is pregnant; - the patient does not respond clinically to oral antimicrobial therapy; - the patient is unable to follow or tolerate an outpatient oral regimen; - the patient has severe illness, nausea and vomiting, or high fever; and - the patient has a tubo-ovarian abscess. Many practitioners have preferred to hospitalize adolescent women whose condition is diagnosed as acute PID. No evidence is available suggesting that adolescents benefit from hospitalization for treatment of PID. Younger women with mild-to-moderate acute PID have similar outcomes with either outpatient therapy or inpatient therapy. Further, clinical response to outpatient treatment is similar among younger and older women. The decision to hospitalize adolescents with acute PID should be based on the same criteria used for older women. Whether women in their later reproductive years benefit from hospitalization for treatment of PID also is unclear, although women aged >35 years who are hospitalized with PID are more likely than younger women to have a complicated clinical course.
# Parenteral Treatment
For women with PID of mild or moderate severity, parenteral and oral therapy appears to have similar clinical efficacy. Many randomized trials have demonstrated the efficacy of both parenteral and oral regimens (180,182,183). In the majority of clinical trials, parenteral treatment for at least 48 hours has been used after the patient has demonstrated substantial clinical improvement. Clinical experience should guide decisions regarding transition to oral therapy, which usually can be initiated within 24 hours of clinical improvement. The majority of clinicians recommend at least 24 hours of direct inpatient observation for patients who have tuboovarian abscesses.
# Recommended Parenteral Regimen A
Cefotetan 2 g IV every 12 hours OR Cefoxitin 2 g IV every 6 hours PLUS Doxycycline 100 mg orally or IV every 12 hours Because of the pain associated with infusion, doxycycline should be administered orally when possible, even when the patient is hospitalized. Oral and IV administration of doxycycline provide similar bioavailability.
Parenteral therapy may be discontinued 24 hours after a patient improves clinically, and oral therapy with doxycycline (100 mg twice a day) should continue to complete 14 days of therapy. When tubo-ovarian abscess is present, many healthcare providers use clindamycin or metronidazole with doxycycline for continued therapy, rather than doxycycline alone, because it provides more effective anaerobic coverage.
Clinical data are limited regarding the use of other secondor third-generation cephalosporins (e.g., ceftizoxime, cefotaxime, and ceftriaxone), which also might be effective therapy for PID and may replace cefotetan or cefoxitin. However, these cephalosporins are less active than cefotetan or cefoxitin against anaerobic bacteria.
# Recommmended Parenteral Regimen B
Clindamycin 900 mg IV every 8 hours PLUS Gentamicin loading dose IV or IM (2 mg/kg of body weight), followed by a maintenance dose (1.5 mg/kg) every 8 hours. Single daily dosing may be substituted.
Although use of a single daily dose of gentamicin has not been evaluated for the treatment of PID, it is efficacious in analogous situations. Parenteral therapy can be discontinued 24 hours after a patient improves clinically; continuing oral therapy should consist of doxycycline 100 mg orally twice a day or clindamycin 450 mg orally four times a day to complete a total of 14 days of therapy. When tubo-ovarian abscess is present, many health-care providers use clindamycin for continued therapy, rather than doxycycline, because clindamycin provides more effective anaerobic coverage.
# Alternative Parenteral Regimens
Limited data support the use of other parenteral regimens, but the following three regimens have been investigated in at least one clinical trial, and they have broad spectrum coverage. IV ofloxacin has been investigated as a single agent; however, because of concerns regarding its spectum, metronidazole may be included in the regimen. Levofloxacin is as effective as ofloxacin and may be substituted; its single daily dosing makes it advantageous from a compliance perspective. One trial demonstrated high short-term clinical cure rates with azithromycin, either alone for 1 week (at least one IV dose followed by oral therapy) or with a 12-day course of metronidazole (184). Ampicillin/sulbactam plus doxycycline is effective coverage against C. trachomatis, N. gonorrhoeae, and anaerobes and for patients who have tubo-ovarian abscess.
# Oral Treatment
Oral therapy can be considered for women with mild-tomoderately severe acute PID, as the clinical outcomes among women treated with oral therapy are similar to those treated with parenteral therapy. The following regimens provide coverage against the frequent etiologic agents of PID. Patients who do not respond to oral therapy within 72 hours should be reevaluated to confirm the diagnosis and should be administered parenteral therapy on either an outpatient or inpatient basis.
# Recommended Regimen A
Levofloxacin 500 mg orally once daily for 14 days- OR Ofloxacin 400 mg orally twice daily for 14 days- WITH OR WITHOUT Metronidazole 500 mg orally twice a day for 14 days - Quinolones should not be used in persons with a history of recent foreign travel or partners' travel, infections acquired in California or Hawaii, or infections acquired in other areas with increased QRNG prevalence.
Oral ofloxacin has been investigated as a single agent in two clinical trials, and it is effective against both N. gonorrhoeae and C. trachomatis (185,186). Despite the results of these trials, lack of anaerobic coverage with ofloxacin is a concern; the addition of metronidazole to the treatment regimen provides this coverage. Levofloxacin is as effective as ofloxacin and may be substituted. Azithromycin has been demonstrated in one randomized trial to be an effective regimen for acute PID (184). The addition of metronidazole should be considered, as anaerobic organisms are suspected in the etiology of the majority of PID cases. Metronidazole will also treat BV, which frequently is associated with PID.
# Regimen B
Ceftriaxone 250 mg IM in a single dose PLUS Doxycycline 100 mg orally twice a day for 14 days WITH OR WITHOUT Metronidazole 500 mg orally twice a day for 14 days OR Cefoxitin 2 g IM in a single dose and Probenecid, 1 g orally administered concurrently in a single dose PLUS Doxycycline 100 mg orally twice a day for 14 days WITH OR WITHOUT Metronidazole 500 mg orally twice a day for 14 days
# OR
Other parenteral third-generation cephalosporin (e.g., ceftizoxime or cefotaxime) PLUS Doxycycline 100 mg orally twice a day for 14 days WITH OR WITHOUT Metronidazole 500 mg orally twice a day for 14 days
The optimal choice of a cephalosporin for Regimen B is unclear; although cefoxitin has better anaerobic coverage, ceftriaxone has better coverage against N. gonorrhoeae. Clinical trials have demonstrated that a single dose of cefoxitin is effective in obtaining short-term clinical response in women who have PID. However, the theoretical limitations in cefoxitin's coverage of anaerobes might require the addition of metronidazole to the treatment regimen (182). Metronidazole also will effectively treat BV, which is frequently associated with PID. No data have been published regarding the use of oral cephalosporins for the treatment of PID. Limited data suggest that the combination of oral metronidazole and doxycycline after primary parenteral therapy is safe and effective (187).
# Alternative Oral Regimens
Although information regarding other outpatient regimens is limited, one other regimen has undergone at least one clinical trial and has broad spectrum coverage. Amoxicillin/clavulanic acid and doxycycline was effective in obtaining short-term clinical response in a single clinical trial; however, gastrointestinal symptoms might limit compliance with this regimen.
# Follow-Up
Patients should demonstrate substantial clinical improvement (e.g., defervescence; reduction in direct or rebound abdominal tenderness; and reduction in uterine, adnexal, and cervical motion tenderness) within 3 days after initiation of therapy. Patients who do not improve within this period usually require hospitalization, additional diagnostic tests, and surgical intervention.
If no clinical improvement has occurred within 72 hours after outpatient oral or parenteral therapy (using the criteria for clinical improvement described previously), an examination should be performed. Subsequent hospitalization, parenteral therapy, and diagnostic evaluation, including the consideration of diagnostic laparoscopy for alternative diagnoses, are recommended in women without clinical improvement. Some specialists also recommend rescreening for C. trachomatis and N. gonorrhoeae 4-6 weeks after therapy is completed in women with documented infection with these pathogens. All women diagnosed with acute PID should be offered HIV testing.
# Management of Sex Partners
Male sex partners of women with PID should be examined and treated if they had sexual contact with the patient during the 60 days preceding the patient's onset of symptoms. Evaluation and treatment are imperative because of the risk for reinfection of the patient and the strong likelihood of urethral gonococcal or chlamydial infection in the sex partner. Male partners of women who have PID caused by C. trachomatis and/or N. gonorrhoeae frequently are asymptomatic.
Sex partners should be treated empirically with regimens effective against both of these infections, regardless of the etiology of PID or pathogens isolated from the infected woman. Even in clinical settings in which only women are treated, arrangements should be made to provide care for male sex partners of women who have PID. When providing care for male sex partners is not feasible, health-care providers should ensure that sex partners are referred for appropriate treatment.
# Prevention
Prevention of chlamydial infection by screening and treating high-risk women reduces the incidence of PID (125). Theoretically, the majority of cases of PID can be prevented by screening all women or those determined to be at high risk (based on age or other factors) by using DNA amplification on cervical specimens (in women receiving pelvic examinations) and on urine specimens (in women not undergoing examinations). Although BV is associated with PID, whether the incidence of PID can be reduced by identifying and treating women with BV is unclear (181).
# Special Considerations
Pregnancy. Because of the high risk for maternal morbidity and preterm delivery, pregnant women who have suspected PID should be hospitalized and treated with parenteral antibiotics.
HIV Infection. Differences in the clinical manifestations of PID between HIV-infected women and HIV-negative women have not been well-delineated. In previous observational studies, HIV-infected women with PID were more likely to require surgical intervention. More comprehensive observational and controlled studies (published since the 2002 STD Treatment Guidelines) have demonstrated that HIV-infected women with PID had similar symptoms when compared with uninfected controls (125,(188)(189)(190). They were more likely to have a tubo-ovarian abscess but responded equally well to standard parenteral and oral antibiotic regimens when compared with HIV-negative women. The microbiologic findings for HIV-positive and HIV-negative women were similar, except HIV-infected women had higher rates of concomitant M. hominis, candida, streptococcal, and HPV infections and HPV-related cytologic abnormalities. Whether the management of immunodeficient HIV-infected women with PID requires more aggressive interventions (e.g., hospitalization or parenteral antimicrobial regimens) has not been determined.
IUD. Intrauterine contraceptive devices are becoming a popular contraceptive choice for women. Both levonorgestreland copper-containing devices are marketed in the United States. The risk of PID associated with IUD use is primarily confined to the first 3 weeks after insertion and is uncommon thereafter (191). Given the popularity of IUDs, practitioners might encounter PID in IUD users. No evidence suggests that IUDs should be removed in women diagnosed with acute PID. However, caution should be exercised if the IUD remains in place, and close clinical follow-up is mandatory. The rate of treatment failure and recurrent PID in women continuing to use an IUD is unknown. No data exist on antibiotic selection and treatment outcomes according to type of IUD (e.g., copper or levonorgestrel).
# Epididymitis
Acute epididymitis is a clinical syndrome consisting of pain, swelling, and inflammation of the epididymis of <6 weeks. Chronic epididymitis is characterized by a 3-month or longer history of symptoms of discomfort and/or pain in the scrotum, testicle, or epididymis that is localized on clinical examination. Chronic epididymitis has been subcategorized into inflammatory chronic epididymitis, obstructive chronic epididymitis, and chronic epididymalgia (192).
Among sexually active men aged 35 years, sexually transmitted epididymitis is uncommon. However, bacteriuria secondary to obstructive urinary disease is relatively common. In this group, nonsexually transmitted epididymitis is associated with urinary-tract instrumentation or surgery, systemic disease, or immunosuppression.
Although the majority of patients can be treated on an outpatient basis, hospitalization should be considered when severe pain suggests other diagnoses (e.g., torsion, testicular infarction, or abscess) or when patients are febrile or might be noncompliant with an antimicrobial regimen.
# Diagnostic Considerations
Men who have acute epididymitis typically have unilateral testicular pain and tenderness; hydrocele and palpable swelling of the epididymis usually are present. Although the inflammation and swelling usually begin in the tail of the epididymis, they can spread to involve the rest of the epididymis and testicle. The spermatic cord is usually tender and swollen.Testicular torsion, a surgical emergency, should be considered in all cases, but it occurs more frequently among adolescents and in men without evidence of inflammation or infection. Emergency testing for torsion might be indicated when the onset of pain is sudden, pain is severe, or the test results available during the initial examination do not support a diagnosis of urethritis or urinary-tract infection. If the diagnosis is questionable, a specialist should be consulted immediately because testicular viability might be compromised. Radionuclide scanning of the scrotum is the most accurate radiologic method of diagnosis, although it is not routinely available. Color duplex doppler ultrasonography has a sensitivity of 70% and a specificity of 88% in diagnosing acute epididymitis.
The evaluation of men for epididymitis should include one of the following:
- Gram stain of urethral secretions demonstrating >5 WBC per oil immersion field. The Gram stain is the preferred rapid diagnostic test for evaluating urethritis. It is highly sensitive and specific for documenting both urethritis and the presence or absence of gonococcal infection. Gonococcal infection is established by documenting the presence of WBC containing intracellular Gram-negative diplococci on urethral Gram stain. - Positive leukocyte esterase test on first-void urine or microscopic examination of first-void urine sediment demonstrating >10 WBC per high power field. Culture, nucleic acid hybridization tests, and nucleic acid amplification tests are available for the detection of both N. gonorrhoeae and C. trachomatis. Culture and nucleic acid hybridization tests require urethral swab specimens, whereas amplification tests can be performed on urine specimens. Because of their higher sensitivity, amplification tests are preferred for the detection of C. trachomatis. Depending on the risk, patients whose conditions have been diagnosed as a new STD should receive testing for other STDs.
# Treatment
Empiric therapy is indicated before laboratory test results are available. The goals of treatment of acute epididymitis caused by C. trachomatis or N. gonorrhoeae are 1) microbiologic cure of infection, 2) improvement of signs and symptoms, 3) prevention of transmission to others, and 4) a decrease in potential complications (e.g., infertility or chronic pain). As an adjunct to therapy, bed rest, scrotal elevation, and analgesics are recommended until fever and local inflammation have subsided.
# Recommended Regimens
# For acute epididymitis most likely caused by gonococcal or chlamydial infection:
Ceftriaxone 250 mg IM in a single dose PLUS Doxycycline 100 mg orally twice a day for 10 days
# For acute epididymitis most likely caused by enteric
-rganisms or for patients allergic to cephalosporins and/or tetracyclines: Ofloxacin 300 mg orally twice a day for 10 days OR Levofloxacin 500 mg orally once daily for 10 days
# Follow-Up
Failure to improve within 3 days of the initiation of treatment requires reevaluation of both the diagnosis and therapy. Swelling and tenderness that persist after completion of antimicrobial therapy should be evaluated comprehensively. The differential diagnosis includes tumor, abscess, infarction, testicular cancer, TB, and fungal epididymitis.
# Management of Sex Partners
Patients who have acute epididymitis, confirmed or suspected to be caused by N. gonorrhoeae or C. trachomatis, should be instructed to refer sex partners for evaluation and treatment if their contact with the index patient was within the 60 days preceding onset of the patient's symptoms.
Patients should be instructed to avoid sexual intercourse until they and their sex partners are cured (i.e., until therapy is completed and patient and partners no longer have symptoms).
# Special Considerations
# HIV Infection
Patients who have uncomplicated acute epididymitis and also are infected with HIV should receive the same treatment regimen as those who are HIV negative. Fungi and mycobacteria, however, are more likely to cause acute epididymitis in immunosuppressed patients than in immunocompetent patients.
# HPV Infection
More than 100 types of HPV exist; more than 30 types can infect the genital area. The majority of HPV infections are asymptomatic, unrecognized, or subclinical. Genital HPV infection is common and usually self-limited. Genital HPV infection occurs more frequently than visible genital warts among both men and women and cervical cell changes among women.
Genital HPV infection can cause genital warts, usually associated with HPV types 6 or 11. Other HPV types that in-fect the anogenital region (e.g., high-risk HPV types 16, 18, 31, 33, and 35) are strongly associated with cervical neoplasia. Persistent infection with high-risk types of HPV is the most important risk factor for cervical neoplasia.
# HPV Tests
A definitive diagnosis of HPV infection is based on detection of viral nucleic acid (i.e., DNA or RNA) or capsid protein. Tests that detect several types of HPV DNA in cells scraped from the cervix are available and might be useful in the triage of women with atypical squamous cells of undetermined significance (ASC-US) or in screening women aged >30 years in conjunction with the Pap test (see Cervical Cancer Screening for Women Who Attend STD Clinics or Have a History of of STDs). Women determined to have HPV infection on such testing should be counseled that HPV infection is common, infection is frequently transmitted between partners, and that infection usually goes away on its own. If any Pap test or biopsy abnormalities have been observed, further evaluation is recommended. Screening women or men with the HPV test, outside of the above recommendations for use of the test with cervical cancer screening, is not recommended.
# Treatment
In the absence of genital warts or cervical SIL, treatment is not recommended for subclinical genital HPV infection, whether it is diagnosed by colposcopy, biopsy, acetic acid application, or through the detection of HPV by laboratory tests. Genital HPV infection frequently goes away on its own, and no therapy has been identified that can eradicate infection. In the presence of coexistent SIL, management should be based on histopathologic findings.
# Genital Warts
HPV types 6 or 11 are commonly found before, or at the time of, detection of genital warts; however, the use of HPV testing for genital wart diagnosis is not recommended.
Genital warts are usually flat, papular, or pedunculated growths on the genital mucosa. Diagnosis of genital warts is made by visual inspection and may be confirmed by biopsy, although biopsy is needed only under certain circumstances (e.g., if the diagnosis is uncertain; the lesions do not respond to standard therapy; the disease worsens during therapy; the patient is immunocompromised; or warts are pigmented, indurated, fixed, bleeding, or ulcerated). No data support the use of HPV nucleic acid tests in the routine diagnosis or management of visible genital warts.
The application of 3%-5% acetic acid usually turns HPVinfected genital mucosal tissue to a whitish color. However, acetic acid application is not a specific test for HPV infection, and the specificity and sensitivity of this procedure for screening have not been defined. Therefore, the routine use of this procedure for screening to detect HPV infection is not recommended. However, some clinicians, who are experienced in the management of genital warts, have determined that this test is useful for identifying flat genital warts.
In addition to the external genitalia (i.e., penis, vulva, scrotum, perineum, and perianal skin), genital warts can occur on the uterine cervix and in the vagina, urethra, anus, and mouth. Intra-anal warts are observed predominantly in patients who have had receptive anal intercourse; these warts are distinct from perianal warts, which can occur in men and women who do not have a history of anal sex. In addition to the genital area, HPV types 6 and 11 have been associated with conjunctival, nasal, oral, and laryngeal warts. Genital warts are usually asymptomatic, but depending on the size and anatomic location, genital warts can be painful, friable, or pruritic.
HPV types 16, 18, 31, 33, and 35 are found occasionally in visible genital warts and have been associated with external genital (i.e., vulvar, penile, and anal) squamous intraepithelial neoplasia (i.e., squamous cell carcinoma in situ, bowenoid papulosis, Erythroplasia of Queyrat, or Bowen's disease of the genitalia). These HPV types also have been associated with vaginal, anal, and CIN and anogenital and some head and neck squamous cell carcinomas. Patients who have visible genital warts are frequently infected simultaneously with multiple HPV types.
# Treatment
The primary goal of treating visible genital warts is the removal of the warts. In the majority of patients, treatment can induce wart-free periods. If left untreated, visible genital warts might resolve on their own, remain unchanged, or increase in size or number. Treatment possibly reduces, but does not eliminate, HPV infection. Existing data indicate that currently available therapies for genital warts might reduce, but probably do not eradicate, HPV infectivity. Whether the reduction in HPV viral DNA, resulting from treatment, impacts future transmission remains unclear. No evidence indicates that the presence of genital warts or their treatment is associated with the development of cervical cancer.
# Regimens
Treatment of genital warts should be guided by the preference of the patient, the available resources, and the experience of the health-care provider. No definitive evidence suggests that any of the available treatments are superior to any other and no single treatment is ideal for all patients or all warts. The use of locally developed and monitored treatment algorithms has been associated with improved clinical outcomes and should be encouraged. Because of uncertainty regarding the effect of treatment on future transmission of HPV and the possibility of spontaneous resolution, an acceptable alternative for some persons is to forego treatment and wait for spontaneous resolution.
The majority of patients have <10 genital warts, with a total wart area of 0.5-1.0 cm 2 . These warts respond to various treatment modalities. Factors that might influence selection of treatment include wart size, wart number, anatomic site of wart, wart morphology, patient preference, cost of treatment, convenience, adverse effects, and provider experience. Factors that might affect response to therapy include the presence of immunosuppression and compliance with therapy. The majority of patients require a course of therapy rather than a single treatment. In general, warts located on moist surfaces or in intertriginous areas respond better to topical treatment than do warts on drier surfaces.
The treatment modality should be changed if a patient has not improved substantially. The majority of genital warts respond within 3 months of therapy. The response to treatment and its side effects should be evaluated throughout the course of therapy.
Complications occur rarely if treatments for warts are employed properly. Patients should be warned that persistent hypopigmentation or hyperpigmentation occurs commonly with ablative modalities. Depressed or hypertrophic scars are uncommon but can occur, especially if the patient has had insufficient time to heal between treatments. Rarely, treatment can result in disabling chronic pain syndromes (e.g., vulvodynia or analdynia, and hyperesthesia of the treatment site) or, in the case of rectal warts, painful defecation or fistulas. A limited number of case reports of severe systemic effects from podophyllin resin and interferon have been documented.
Treatment regimens are classified into patient-applied and provider-applied modalities. Patient-applied modalities are preferred by some patients because they can be administered in the privacy of the patient's home. To use patient-applied modalities effectively, compliance with the treatment regimen is important along with the ability to identify and reach all genital warts.
# MMWR August 4, 2006
# Recommended Regimens for External Genital Warts
Patient-Applied: Podofilox 0.5% solution or gel. Patients should apply podofilox solution with a cotton swab, or podofilox gel with a finger, to visible genital warts twice a day for 3 days, followed by 4 days of no therapy. This cycle may be repeated, as necessary, for up to four cycles.
The total wart area treated should not exceed 10 cm 2 , and the total volume of podofilox should be limited to 0.5 mL per day. If possible, the health-care provider should apply the initial treatment to demonstrate the proper application technique and identify which warts should be treated. The safety of podofilox during pregnancy has not been established. OR Imiquimod 5% cream. Patients should apply imiquimod cream once daily at bedtime, three times a week for up to 16 weeks. The treatment area should be washed with soap and water 6-10 hours after the application. The safety of imiquimod during pregnancy has not been established.
# Provider-Administered:
Cryotherapy with liquid nitrogen or cryoprobe. Repeat applications every 1-2 weeks. OR Podophyllin resin 10%-25% in a compound tincture of benzoin. A small amount should be applied to each wart and allowed to air dry. The treatment can be repeated weekly, if necessary. To avoid the possibility of complications associated with systemic absorption and toxicity, two important guidelines should be followed: 1) application should be limited to <0.5 mL of podophyllin or an area of <10 cm 2 of warts per session, and 2) no open lesions or wounds should exist in the area to which treatment is administered. Some specialists suggest that the preparation should be thoroughly washed off 1-4 hours after application to reduce local irritation. The safety of podophyllin during pregnancy has not been established. OR Trichloroacetic acid (TCA) or Bichloroacetic acid (BCA) 80%-90%. A small amount should be applied only to the warts and allowed to dry, at which time a white "frosting" develops. If an excess amount of acid is applied, the treated area should be powdered with talc, sodium bicarbonate (i.e., baking soda), or liquid soap preparations to remove unreacted acid. This treatment can be repeated weekly, if necessary.
# OR Surgical removal either by tangential scissor excision, tangential shave excision, curettage, or electrosurgery
# Alternative Regimens
Intralesional interferon OR Laser surgery Podofilox 0.5% solution or gel, an antimitotic drug that destroys warts, is relatively inexpensive, easy to use, safe, and self-applied by patients. The majority of patients experience mild-to-moderate pain or local irritation after treatment. Imiquimod is a topically active immune enhancer that stimulates production of interferon and other cytokines. Local inflammatory reactions are common with the use of imiquimod; these reactions include redness and irritation and are usually mild to moderate. Traditionally, follow-up visits are not required for patients using self-administered therapy. However, follow-up might be useful several weeks into therapy to determine the appropriateness of medication use and the response to treatment.
Cryotherapy destroys warts by thermal-induced cytolysis. Health-care providers must be trained on the proper use of this therapy because over-and undertreatment might result in complications or low efficacy. Pain after application of the liquid nitrogen, followed by necrosis and sometimes blistering, is common. Local anesthesia (topical or injected) might facilitate therapy if warts are present in many areas or if the area of warts is large.
Podophyllin resin, which contains several compounds, including antimitotic podophyllin lignans, is another treatment option. The resin is most frequently compounded at 10%-25% in a tincture of benzoin. However, podophyllin resin preparations differ in the concentration of active components and contaminants. The shelf life and stability of podophyllin preparations are unknown. A thin layer of podophyllin resin must be applied to the warts and allowed to air dry before the treated area comes into contact with clothing; overapplication or failure to air dry can result in local irritation caused by spread of the compound to adjacent areas.
Both TCA and BCA are caustic agents that destroy warts by chemical coagulation of proteins. Although these preparations are widely used, they have not been investigated thoroughly. TCA solutions have a low viscosity comparable with that of water and can spread rapidly if applied excessively; therefore, they can damage adjacent tissues. Both TCA and BCA should be applied sparingly and allowed to dry before the patient sits or stands. If pain is intense, the acid can be neutralized with soap or sodium bicarbonate.
Surgical therapy has the advantage of usually eliminating warts at a single visit. However, such therapy requires substantial clinical training, additional equipment, and a longer office visit. After local anesthesia is applied, the visible genital warts can be physically destroyed by electrocautery, in which case no additional hemostasis is required. Care must be taken to control the depth of electrocautery to prevent scarring. Alternatively, the warts can be removed either by tangential excision with a pair of fine scissors or a scalpel or by curettage. Because the majority of warts are exophytic, this procedure can be accomplished with a resulting wound that only extends into the upper dermis. Hemostasis can be achieved with an electrocautery unit or a chemical styptic (e.g., an aluminum chloride solution). Suturing is neither required nor indicated in the majority of cases if surgical removal is performed properly. Surgical therapy is most beneficial for patients who have a large number or area of genital warts. Carbon dioxide laser and surgery might be useful in the management of extensive warts or intraurethral warts, particularly for those patients who have not responded to other treatments.
Interferons, both natural or recombinant, have been used for the treatment of genital warts. They have been administered systemically (i.e., subcutaneously at a distant site or IM) and intralesionally (i.e., injected into the warts). Systemic interferon is not effective. The efficacy and recurrence rates of intralesional interferon are comparable to other treatment modalities. Administration of intralesional interferon is associated with stinging, burning, and pain at the injection site. Interferon is probably effective because of its antiviral and/or immunostimulating effects. Interferon therapy is not recommended as a primary modality because of inconvenient routes of administration, frequent office visits, and the association between its use and a high frequency of systemic adverse effects.
Because of the shortcomings associated with all available treatments, some clinics employ combination therapy (i.e., the simultaneous use of two or more modalities on the same wart at the same time). No data support the use of more than one therapy at a time to improve efficacy of treatment, and some specialists believe that combining modalities might increase complications.
# Recommended Regimens for Cervical Warts
For women who have exophytic cervical warts, high-grade SIL must be excluded before treatment is initiated.
Management of exophytic cervical warts should include consultation with a specialist.
# Recommended Regimens for Vaginal Warts
Cryotherapy with liquid nitrogen. The use of a cryoprobe in the vagina is not recommended because of the risk for vaginal perforation and fistula formation. OR TCA or BCA 80%-90% applied to warts. A small amount should be applied only to warts and allowed to dry, at which time a white "frosting" develops. If an excess amount of acid is applied, the treated area should be powdered with talc, sodium bicarbonate, or liquid soap preparations to remove unreacted acid. This treatment can be repeated weekly, if necessary.
# Recommended Regimens for Urethral Meatus Warts
Cryotherapy with liquid nitrogen OR Podophyllin 10%-25% in compound tincture of benzoin. The treatment area must be dry before contact with normal mucosa. This treatment can be repeated weekly, if necessary. The safety of podophyllin during pregnancy has not been established.
Although data evaluating the use of podofilox and imiquimod for the treatment of distal meatal warts are limited, some specialists recommend their use in some patients.
# Recommended Regimens for Anal Warts
Cryotherapy with liquid nitrogen OR TCA or BCA 80%-90% applied to warts. A small amount should be applied only to warts and allowed to dry, at which time a white "frosting" develops. If an excess amount of acid is applied, the treated area should be powdered with talc, sodium bicarbonate, or liquid soap preparations to remove unreacted acid. This treatment can be repeated weekly, if necessary.
# OR Surgical removal
Warts on the rectal mucosa should be managed in consultation with a specialist. Many persons with warts on the anal mucosa also have warts on the rectal mucosa, so persons with anal warts can benefit from an inspection of the rectal mucosa by digital examination or anoscopy.
# Counseling Genital HPV Infection
Education and counseling are vital aspects of managing patients with genital warts. Patients can be educated through patient education materials, including pamphlets, hotlines, and websites ( or / std/hpv).
Attempts should be made to convey the following key messages:
- Genital HPV infection is common among sexually active adults. The majority of sexually active adults will have it at some point in their lives, although the majority of them will never know because the infection usually has no symptoms and clears on its own. - Genital HPV infection is usually sexually transmitted.
The incubation period (i.e., the interval between initial exposure and established infection or disease) is variable, and determining the timing and source of infection is frequently difficult. Within ongoing sexual relationships, sex partners usually are infected by the time of the patient's diagnosis, although they might have no symptoms or signs of infection. - No recommended uses of the HPV test to diagnose HPV infection in sex partners have been established. HPV infection is commonly transmitted to partners but usually goes away on its own.
# Genital Warts
- Genital warts are caused by specific types of HPV infection. The types that cause genital warts are different from the types that cause cervical and other anogenital cancers. - Persons can possibly have infection with the types of HPV that cause genital warts but never develop symptoms. Why some persons with genital HPV infection develop warts and others do not is unclear. Immunity probably plays a key role. - The natural history of genital warts is usually benign, but recurrence of genital warts within the first several months after treatment is common. Treatment for genital warts can reduce HPV infection, but whether the treatment results in a reduction in risk for transmission of HPV to sex partners is unclear. The duration of infectivity after wart treatment is unknown. - Condoms might reduce the risk for HPV-associated diseases (e.g., genital warts and cervical cancer). Consistent condom use also may reduce the risk for genital HPV (18). HPV infection can occur in areas that are not covered or protected by a condom (e.g., scrotum, vulva, or perianus). - The presence of genital warts is not an indication for HPV testing, a change in the frequency of Pap tests, or cervical colposcopy. - HPV testing is not indicated for partners of persons with genital warts.
# Follow-Up
After visible genital warts have cleared, a follow-up evaluation might be helpful. Patients should be cautioned to watch for recurrences, which occur most frequently during the first 3 months. External genital warts can be difficult to identify, so it might be useful for patients to have a follow-up evaluation 3 months after treatment. Earlier follow-up visits also might be useful for some patients to document the absence of warts, to monitor for or treat complications of therapy, and to provide an additional opportunity for patient education and counseling. Women should be counseled to undergo regular Pap screening as recommended for women without genital warts.
# Management of Sex Partners
Examination of sex partners is not necessary for the management of genital warts because no data indicate that reinfection plays a role in recurrences. In addition, providing treatment for genital warts solely for the purpose of preventing future transmission cannot be recommended because the value of treatment in reducing infectivity is unknown. However, sex partners of patients who have genital warts might benefit from counseling and examination to assess the presence of genital warts and other STDs. The counseling of sex partners provides an opportunity for these partners to 1) learn that HPV infection is common and probably shared between partners and 2) receive STD evaluation and screening and Pap screening if they are female. Female sex partners of patients who have genital warts should be reminded that cytologic screening for cervical cancer is recommended for all sexually active women.
# Special Considerations Pregnancy
Imiquimod, podophyllin, and podofilox should not be used during pregnancy. However, because genital warts can proliferate and become friable during pregnancy, many specialists advocate their removal during pregnancy. HPV types 6 and 11 can cause respiratory papillomatosis in infants and children. The route of transmission (i.e., transplacental, perinatal, or postnatal) is not completely understood. Whether cesarean section prevents respiratory papillomatosis in infants and children is unclear; therefore, cesarean delivery should not be performed solely to prevent transmission of HPV infection to the newborn. Cesarean delivery might be indicated for women with genital warts if the pelvic outlet is obstructed or if vaginal delivery would result in excessive bleeding. Pregnant women with genital warts should be counseled concerning the low risk for warts on the larynx (recurrent respiratory papillomatosis) in their infants or children (193). No controlled studies have suggested that cesarean section prevents this condition.
# HIV Infection
No data suggest that treatment modalities for external genital warts should be different in the setting of HIV-infection. However, persons who are immunosuppressed because of HIV or other reasons might have larger or more numerous warts, might not respond as well as immunocompetent persons to therapy for genital warts, and might have more frequent recurrences after treatment (194,195). Squamous cell carcinomas arising in or resembling genital warts might occur more frequently among immunosuppressed persons, therefore, requiring biopsy for confirmation of diagnosis. Because of the increased incidence of anal cancer in HIV-infected homosexual men, screening for anal SIL by cytology in this population is recommended by some specialists. However, evidence is limited concerning the natural history of anal intraepithelial neoplasias, the reliability of screening methods, the safety and response to treatments, and the programmatic considerations that would support this screening approach. Until additional data are generated on screening for anal SIL, this screening approach cannot be recommended.
# Squamous Cell Carcinoma in Situ
Patients in whom squamous cell carcinoma in situ of the genitalia is diagnosed should be referred to a specialist for treatment. Ablative modalities usually are effective, but careful follow-up is essential. The risk for these lesions leading to invasive squamous cell carcinoma of the external genitalia in immunocompetent patients is unknown but is probably low. Female partners of male patients who have squamous cell carcinoma in situ are at high risk for cervical abnormalities.
# Cervical Cancer Screening for Women Who Attend STD Clinics or Have a History of STDs
Women with a history of STDs might be at increased risk for cervical cancer, and women attending STD clinics might have other risk factors that place them at even greater risk. Prevalence studies indicate that precursor lesions for cervical cancer occur approximately five times more frequently among women attending STD clinics than among women attending family planning clinics (196). Cervical cancer screening using the Pap test is an effective, low-cost screening test for preventing invasive cervical cancer. Recommendations for cervical cancer screening intervals vary in the United States, but the American Cancer Society and American College of Obstetri-cians and Gynecologists guidelines recommend annual screening for women aged 21-30 years and then every 2-3 years for women aged >30 years if three consecutive annual Pap tests are negative (197,198).
# Recommendations
During the appointment in which a pelvic examination for STD screening is performed, the health-care provider should inquire about the result of the patient's most recent Pap test and discuss the following information with the patient:
# Follow-Up
STD clinics offering cervical cancer screening are encouraged to use cytopathology laboratories that report results by using the Bethesda System of classification (199). † † † If the † † † The Bethesda System for Reporting Cervical/Vaginal Cytologic Results uses the terms "low-grade SIL" and "high-grade SIL" for abnormal results (199). If repeat Pap tests are used to follow ASC-US results, a test should be performed every 6 months until 3 negative results are noted before the women returns to cervical cancer screening at a normal interval for age. If subsequent Pap tests demonstrate progression to SIL, follow-up should be conducted according to ASCCP Consensus Guidelines (i.e., frequent colposcopy and directed cervical biopsy). If specific infections other than HPV are identified, the patient might need to have a repeat Pap test after appropriate treatment for those infections. In the majority of instances, even in the presence of some severe infections, Pap tests will be reported as satisfactory for evaluation, so they may be read and final reports produced without the necessity to treat and repeat the Pap test. When repeating the Pap test is necessary because of an unsatisfactory for interpretation report, the repeat test must be interpreted by the laboratory as satisfactory and also be negative before returning the woman to Pap tests at regularly scheduled intervals.
A third strategy for managing patients with ASC-US Pap test results involves testing for HPV DNA. Whereas conducting HPV testing in some STD clinics might not be possible or appropriate because of inadequate resources, such testing might be appropriate in other public health clinic settings. Only one FDA-cleared test exists, the Digene Hybrid Capture II. The HPV DNA test may be performed by 1) co-collecting a specimen; 2) using a supplied swab at the time of the Pap test, if conventional cytology is used; 3) reflex testing, if liquid-based cytology is used and enough residual material is available in the cytology test vial; or 4) scheduling a separate follow-up appointment when the Pap test report results are known. If the high-risk HPV DNA test is positive, women are referred immediately for colposcopy, and if indicated, directed cervical biopsy. Because many public health clinics, including the majority of STD clinics, cannot provide clinical follow-up of abnormal Pap tests, women with Pap tests demonstrating low or high grade SIL or ASC-US usually need a referral to other local health-care providers or clinics for colposcopy and biopsy. Clinics and health-care providers who offer Pap test screening services but cannot provide appropriate colposcopic follow-up of abnormal Pap tests should arrange referral to health-care facilities in which 1) a patient will be promptly evaluated and treated and 2) the results of the evaluation will be reported to the referring clinic or healthcare provider. Clinics and health-care providers should develop protocols that identify women who miss follow-up appointments so that these women can be located and scheduled for needed studies and management, and they should reevaluate such protocols routinely. Pap test results, type and location of follow-up appointments, and results of follow-up appointments should be clearly documented in the clinic record. The establishment of colposcopy and biopsy services in local health departments, especially in circumstances in which referrals are difficult and follow-up is unlikely, should be considered if resources are available.
# Other Management Considerations
Other considerations in performing Pap tests include the following:
# Special Considerations
# Pregnancy
Pregnant women should have a Pap test as part of routine prenatal care. A cytobrush and an Ayers spatula might be used for obtaining Pap tests in pregnant women.
# HIV Infection
Several studies have documented an increased prevalence of SIL in HIV-infected women (200,201). The following recommendations for Pap test screening among HIV-infected women are consistent with other guidelines published by the U.S. Department of Health and Human Services (50) and are based partially on the opinions of professionals knowledgeable about the care and management of cervical cancer and HIV infection in women.
After obtaining a complete history of previous cervical disease, HIV-infected women should be provided a comprehen-sive gynecologic examination, including a pelvic examination and Pap test, as part of their initial evaluation. A Pap test should be obtained twice in the first year after diagnosis of HIV infection and, if the results are normal, annually thereafter. If the results of the Pap test are abnormal, care should be provided according to the ASCCP Consensus Guidelines for Management of Abnormal Cervical Cytology (198). Women with cytological reports of ASC-US, low or high-grade SIL or squamous cell carcinoma, regardless of CD4+ count or antiretroviral treatment status, should undergo colposcopy and directed biopsy. Colposcopy and biopsy are not indicated in HIV-positive women with negative Pap test reports.
# Vaccine Preventable STDs
Some STDs can be effectively prevented through preexposure vaccination. Vaccines are under development or are undergoing clinical trials for certain STDs, including HIV and HSV. However, the only vaccines currently available are for prevention of HAV, HBV, and HPV infection. Vaccination efforts focus largely on integrating the use of these available vaccines into STD prevention and treatment activities.
Every person being evaluated or treated for an STD, who is not already vaccinated, should receive hepatitis B vaccination. In addition, some persons (e.g., MSM and illegal-drug users) should receive hepatitis A vaccination.
# Hepatitis A
Hepatitis A, caused by infection with HAV, has an incubation period of approximately 28 days (range: 15-50 days). HAV replicates in the liver and is shed in high concentrations in feces from 2 weeks before to 1 week after the onset of clinical illness. HAV infection produces a self-limited disease that does not result in chronic infection or chronic liver disease. However, 10%-15% of patients might experience a relapse of symptoms during the 6 months after acute illness. Acute liver failure from hepatitis A is rare (overall case-fatality rate: 0.5%). The risk for symptomatic infection is directly related to age, with >80% of adults having symptoms compatible with acute viral hepatitis and the majority of children having either asymptomatic or unrecognized infection. Antibody produced in response to HAV infection persists for life and confers protection against reinfection.
HAV infection is primarily transmitted by the fecal-oral route, by either person-to-person contact, or through consumption of contaminated food or water. Although viremia occurs early in infection and can persist for several weeks after onset of symptoms, bloodborne transmission of HAV is uncommon. HAV occasionally might be detected in saliva in † 0 months represents the timing of the initial dose; subsequent numbers represent the months after the initial dose. § Hepatitis A vaccine, inactivated, GlaxoSmithKline Biologicals. This vaccine also is licensed for a 3-dose series in children aged 1-18 years, with 360 EL.U., 0.5-mL doses at 0, 1, and 6-12 months. ¶ Hepatitis A vaccine, inactivated, Merck & Co., Inc.
experimentally infected animals, but transmission by saliva has not been demonstrated.
In the United States, nearly half of all reported hepatitis A cases have no specific risk factor identified. Among adults with identified risk factors, the majority of cases are among MSM, persons who use illegal drugs, and international travelers (202). Because transmission of HAV during sexual activity probably occurs because of fecal-oral contact, measures typically used to prevent the transmission of other STDs (e.g., use of condoms) do not prevent HAV transmission. In addition, efforts to promote good personal hygiene have not been successful in interrupting outbreaks of hepatitis A. Vaccination is the most effective means of preventing HAV transmission among persons at risk for infection, many of whom might seek services in STD clinics.
# Diagnosis
The diagnosis of hepatitis A cannot be made on clinical grounds alone and requires serologic testing. The presence of IgM antibody to HAV is diagnostic of acute HAV infection. A positive test for total anti-HAV indicates immunity to HAV infection but does not differentiate current from previous HAV infection. Although usually not sensitive enough to detect the low level of protective antibody after vaccination, anti-HAV tests might be positive after hepatitis A vaccination.
# Treatment
Patients with acute hepatitis A usually require only supportive care, with no restrictions in diet or activity. Hospitalization might be necessary for patients who become dehydrated because of nausea and vomiting and is critical for patients with signs or symptoms of acute liver failure. Medications that might cause liver damage or are metabolized by the liver should be used with caution among persons with hepatitis A.
# Prevention
Two products are available for the prevention of HAV infection: hepatitis A vaccine (Table 2) and immune globulin (Ig) for IM administration. Hepatitis A vaccines are prepared from formalin-inactivated, cell-culture-derived HAV and have been available in the United States since 1995, initially for persons aged >2 years. In 2005, the vaccines were approved by FDA for persons aged >12 months. Administered IM in a 2-dose series, these vaccines induce protective antibody levels in virtually all adults. By 1 month after the first dose, 94%-100% of adults have protective antibody levels; 100% of adults develop protective antibody after a second dose. In randomized controlled trials, the equivalent of 1 dose of hepatitis A vaccine administered before exposure has been 94%-100% effective in preventing clinical hepatitis A (3). Kinetic models of antibody decline indicate that protective levels of antibody persist for at least 20 years.
A combined hepatitis A and hepatitis B vaccine have been developed and licensed for use as a 3-dose series in adults aged >18 years (see Table 3, Hepatitis B). When administered IM on a 0-, 1-, and 6-month schedule, the vaccine has equivalent immunogenicity to that of the monovalent vaccines.
- Hepatitis A vaccine is available for eligible children and adolescents aged 85% effective in preventing HAV infections.
# Preexposure Immunization
Persons in the following groups who are likely to be treated in STD clinic settings should be offered hepatitis A vaccine: 1) all MSM; 2) illegal drug users (both injecting and noninjecting drugs); and 3) persons with CLD, including persons with chronic HBV and HCV infection who have evidence of CLD.
# Prevaccination Serologic Testing for Susceptibility
Approximately one third of the U.S. population has serologic evidence of previous HAV infection, which increases directly with age and reaches 75% among persons aged >70 years. Screening for HAV infection might be cost-effective in
# Postexposure Prophylaxis
Previously unvaccinated persons exposed to HAV (e.g., through household or sexual contact or by sharing illegal drugs with a person who has hepatitis A) should be administered a single IM dose of Ig (0.02 mL/kg) as soon as possible but not >2 weeks after exposure. Persons who have had 1 dose of hepatitis A vaccine at least 1 month before exposure to HAV do not need Ig. If hepatitis A vaccine is recommended for a person receiving Ig, it can be administered simultaneously at a separate anatomic injection site. The use of hepatitis A vaccine alone is not recommended for PEP.
# Special Considerations
Limited data indicate that vaccination of persons with CLD and of HIV-infected persons results in lower seroprotection rates and antibody concentrations (50). In HIV-infected persons, antibody response might be directly related to CD4+ levels.
# Hepatitis B
Hepatitis B is caused by infection with HBV. The incubation period from the time of exposure to onset of symptoms is 6 weeks to 6 months. HBV is found in highest concentrations in blood and in lower concentrations in other body fluids (e.g., semen, vaginal secretions, and wound exudates). HBV infection can be self-limited or chronic. In adults, only approximately half of newly acquired HBV infections are symptomatic, and approximately 1% of reported cases result in acute liver failure and death. Risk for chronic infection is inversely related to age at infection: approximately 90% of infected infants and 30% of infected children aged <5 years become chronically infected, compared with 2%-6% of adults. Among persons with chronic HBV infection, the risk for premature death from cirrhosis or hepatocellular carcinoma (HCC) is 15%-25%.
HBV is efficiently transmitted by percutaneous or mucous membrane exposure to infectious blood or body fluids that contain blood. The primary risk factors that have been associated with infection among adolescents and adults are unprotected sex with an infected partner, unprotected sex with more than one partner, MSM, history of other STDs, and illegal injecting-drug use.
CDC's national strategy to eliminate transmission of HBV infection includes 1) prevention of perinatal infection through routine screening of all pregnant women for HBsAg and immunoprophylaxis of infants born to HBsAg-positive mothers and infants born to mothers with unknown HBsAg status, 2) routine infant vaccination, 3) vaccination of previously unvaccinated children and adolescents through age 18 years, and 4) vaccination of previously unvaccinated adults at in- creased risk for infection (2,4). High vaccination coverage rates, with subsequent declines in acute hepatitis B incidence, have been achieved among infants and adolescents (2,203,204). In contrast, vaccination coverage among the majority of high-risk adult groups (e.g., persons with more than one sex partner in the previous 6 months, MSM, and IDUs) have remained low, and the majority of new infections occur in these high-risk groups (4,(205)(206)(207). STD clinics and other settings that provide services targeted to high-risk adults are ideal sites in which to provide hepatitis B vaccination to adults at risk for HBV infection. All unvaccinated adults seeking services in these settings should be assumed to be at risk for hepatitis B and should receive hepatitis B vaccination.
# Diagnosis
Diagnosis of acute or chronic HBV infection requires serologic testing (Table 4). HBsAg is present in both acute and chronic infection. The presence of IgM antibody to hepatitis B core antigen (IgM anti-HBc) is diagnostic of acute or recently acquired HBV infection. Antibody to HBsAg (anti-HBs) is produced after a resolved infection and is the only HBV antibody marker present after immunization. The presence of HBsAg and total anti-HBc, with a negative test for IgM anti-HBc, indicates chronic HBV infection. The presence of anti-HBc alone might indicate a false-positive result or acute, resolved, or chronic infection.
# Treatment
No specific therapy is available for persons with acute hepatitis B; treatment is supportive. Persons with chronic HBV infection should be referred for evaluation to a physician experienced in the management of CLD. Therapeutic agents approved by FDA for treatment of chronic hepatitis B can achieve sustained suppression of HBV replication and remission of liver disease in some persons. In addition, patients with chronic hepatitis B might benefit from screening to detect HCC at an early stage.
# Prevention
Two products have been approved for hepatitis B prevention: hepatitis B immune globulin (HBIG) and hepatitis B vaccine. HBIG provides temporary (i.e., 3-6 months) protection from HBV infection and is typically used as PEP either as an adjunct to hepatitis B vaccination in previously unvaccinated persons or alone in persons who have not responded to vaccination. HBIG is prepared from plasma known to contain high concentrations of anti-HBs. The recommended dose of HBIG is 0.06 mL/kg.
Hepatitis B vaccine contains HBsAg produced in yeast by recombinant DNA technology and provides protection from HBV infection when used for both preexposure immunization and PEP. The two available monovalent hepatitis B vaccines for use in adolescents and adults are Recombivax HB ® (Merck and Co., Inc., Whitehouse Station, New Jersey) and Engerix-B ® (GlaxoSmithKline Biologicals, Pittsburgh, Pennsylvania). A combination vaccine (hepatitis A and hepatitis B) for use in adults, Twinrix ® (GlaxoSmithKline Biologicals, Pittsburgh, Pennsylvania), also is available. The recommended HBV dose varies by product and age of recipient (Table 3).
When selecting a hepatitis B vaccination schedule, the health-care provider should consider the need to achieve completion of the vaccine series. Approved adolescent and adult schedules for both monovalent hepatitis B vaccine (i.e., Engerix-B ® and Recombivax HB ® ) include the following: 0, 1, and 6 months; 0, 1, and 4 months; and 0, 2, and 4 months. A 4-dose schedule of Engerix-B ® at 0, 1, 2, and 12 months is licensed for all age groups. A 2-dose schedule of Recombivax HB ® adult formulation (10 µg) is licensed for adolescents aged 11-15 years. When scheduled to receive the second dose, adolescents aged >15 years should be switched to a 3-dose series, with doses 2 and 3 consisting of the pediatric formulation (5 µg) administered on an appropriate schedule. Twinrix ® may be administered to persons aged >18 years at risk for both HAV and HBV infections at 0, 1, and 6 months.
Hepatitis B vaccine should be administered IM in the deltoid muscle and may be administered simultaneously with other vaccines. For adolescents and adults, the needle length should be 1-2 inches, depending on the recipient's weight (1 inch for females weighing 120 kg and females >100 kg). A 22-to 25-gauge needle is recommended. If the vaccine series is interrupted after the first or second dose of vaccine, the missed dose should be administered as soon as possible. The series does not need to be restarted after a missed dose.
In adolescents and healthy adults aged 10 mIU/mL) after the first vaccine dose, 75% after the second, and >90% after the third. Vaccine-induced immune memory has been demonstrated to persist for at least 15-20 years. Periodic testing to determine antibody levels in immunocompetent persons is not necessary, and booster doses of vaccine are not recommended.
Hepatitis B vaccination is generally well-tolerated by the majority of recipients. Pain at the injection site and low-grade fever are reported by a minority of recipients. Evidence for a causal association between receipt of hepatitis B vaccination and anaphylaxis exists, which is estimated to occur in 1 of 1.1 million doses of vaccine administered among children and adolescents; no deaths have been reported after anaphylaxis. Vaccine is contraindicated in persons with a history of anaphylaxis after a previous dose of hepatitis B vaccine and in persons with a known anaphylactic reaction to any vaccine component. No evidence for a causal association has been demonstrated for other adverse events reported after administration of hepatitis B vaccine.
# Preexposure Vaccination
Hepatitis B vaccination is recommended for all unvaccinated adolescents, all unvaccinated adults at risk for HBV infection, and all adults seeking protection from HBV infection. For adults, acknowledgement of a specific risk factor is not a requirement for vaccination.
Hepatitis B vaccine should be routinely offered to all unvaccinated persons attending STD clinics and to all unvaccinated persons seeking treatment for STDs in other settings. Other settings where all unvaccinated adults should be assumed to be at risk for hepatitis B and should receive hepatitis B vaccination include correctional facilities, facilities providing drug abuse treatment and prevention services, health-care settings serving MSM, and HIV testing and treatment facilities. All persons who receive clinical services in these settings should be offered hepatitis B vaccine, unless they have a reliable vaccination history (i.e., a written, dated record of each dose of a complete series). In all settings, vaccination should be initiated even though completion of the vaccine series might not be ensured.
# Prevaccination Antibody Screening
Prevaccination serologic testing for susceptibility may be considered to reduce the cost of vaccinating adult populations that have an expected high prevalence of HBV infection (i.e., >20%-30%) (e.g., IDUs and MSM ). In addition, prevaccination testing for susceptibility is recommended for unvaccinated household, sexual, and needle-sharing contacts of HBsAg-positive persons.
Anti-HBc is the test of choice for prevaccination testing; persons who are anti-HBc-positive should be tested for HBsAg. If persons are determined to be HBsAg negative, no further action is required. If persons are determined to be HBsAg positive, the person should be referred for medical follow-up, including counseling and evaluation for antiviral treatment (see Management of HBsAg-Positive Persons). In addition, all household members, sex partners, and needlesharing partners of HBsAg-positive persons should be vaccinated.
Serologic testing should not be a barrier to vaccination of susceptible persons, especially in populations that are difficult to access. In the majority of situations, the first vaccine dose should be administered immediately after collection of the blood sample for serologic testing. Vaccination of persons who are immune to HBV infection because of current or previous infection or vaccination does not increase the risk for adverse events.
# Postvaccination Testing for Serologic Response
Serologic testing for immunity is not necessary after routine vaccination of adolescents or adults. Testing after vaccination is recommended for persons whose subsequent clinical management depends on knowledge of their immune status (e.g., health-care workers or public safety workers at high risk for continued percutaneous or mucosal exposure to blood or body fluids). In addition, testing is recommended for 1) HIVinfected persons and other immunocompromised persons to determine the need for revaccination and the type of followup testing; and 2) sex and needle-sharing partners of HBsAgpositive persons to determine the need for revaccination and for other methods to protect themselves from HBV infection.
If indicated, testing should be performed 1-2 months after administration of the last dose of the vaccine series by using a method that allows determination of a protective level of anti-HBs (>10 mIU/mL). Persons determined to have anti-HBs levels of <10 mIU/mL after the primary vaccine series should be revaccinated with a 3-dose series, followed by anti-HBs testing 1-2 months after the third dose. Persons who do not respond to revaccination should be tested for HBsAg. If HBsAg positive, the person should receive appropriate management (see Management of HBsAg-Positive Persons); if HBsAg negative, the person should be considered suscep-tible to HBV infection and counseled concerning precautions to prevent HBV infection and the need for HBIG PEP for any known exposure (see PEP).
# Postexposure Prophylaxis
Both passive-active PEP with HBIG and hepatitis B vaccination and active PEP with hepatitis B vaccination alone have been demonstrated to be highly effective in preventing transmission after exposure to HBV (2). HBIG alone also has been demonstrated to be effective in preventing HBV transmission, but with the availability of hepatitis B vaccine, HBIG typically is used as an adjunct to vaccination.
Exposure to HBsAg-Positive Source. Unvaccinated persons or persons known not to have responded to a complete hepatitis B vaccine series should receive both HBIG and hepatitis vaccine as soon as possible (preferably <24 hours) after a discrete, identifiable exposure to blood or body fluids that contain blood from an HBsAg-positive source (Table 5). Hepatitis B vaccine should be administered simultaneously with HBIG in a separate injection site, and the vaccine series should be completed by using the age-appropriate vaccine dose and schedule (Table 3). Exposed persons who are in the process of being vaccinated but who have not completed the vaccine series should receive the appropriate dose of HBIG (i.e., 0.06 mL/kg) and should complete the vaccine series. Exposed persons who are known to have responded to vaccination are considered protected and need no further vaccine doses. Persons who have written documentation of a complete hepatitis B vaccine series and who did not receive post-vaccination testing should receive a single vaccine booster dose. Alternatively, these persons can be managed according to guidelines for management of persons with occupational exposure to blood or body fluids that contain blood (207).
Exposure to Source with Unknown HBsAg Status. Unvaccinated persons who have a discrete, identifiable exposure to blood or body fluids containing blood from a source with unknown HBsAg status should receive the hepatitis B vaccine series, with the first dose initiated as soon as possible after exposure (preferably within 24 hours) and the series completed by using the age-appropriate dose and schedule. Exposed persons who are not fully vaccinated should complete the vaccine series. Exposed persons with written documentation of a complete hepatitis B vaccine series require no further treatment.
# Special Considerations
Pregnancy. All pregnant women receiving STD services should be tested for HBsAg, regardless of whether they have been previously tested or vaccinated. All HBsAg-positive pregnant women should be reported to state and local perinatal hepatitis B prevention programs. HBsAg-negative pregnant women seeking STD treatment who have not been previously vaccinated should receive hepatitis B vaccination. Additional information regarding management of HBsAg-positive pregnant women and their infants is available at http:// www.cdc.gov/mmwr/PDF/rr/rr5416.pdf.
HIV Infection. HIV infection can impair the response to hepatitis B vaccination. HIV-infected persons should be tested for anti-HBs 1-2 months after the third vaccine dose (see Postvaccination Testing for Serologic Response). Modified dosing regimens, including a doubling of the standard antigen dose and administration of additional doses, might increase the response rate.
# Management of HBsAg-Positive Persons
This section provides recommendations for management of all HBsAg-positive persons. Additional recommendations for management of HBsAg-positive persons who are coinfected with HIV are available at / mmwr/preview/mmwrhtml/rr5315a1.htm.
# Hepatitis C
Hepatitis C virus (HCV) infection is the most common chronic bloodborne infection in the United States; approximately 2.7 million persons are chronically infected (204). Although HCV is not efficiently transmitted sexually, persons at risk for infection through injection-drug use might seek care in STD treatment facilities, HIV counseling and testing facilities, correctional facilities, drug treatment facilities, and other public health settings where STD and HIV prevention and control services are available.
Persons newly infected with HCV typically are either asymptomatic or have a mild clinical illness. HCV RNA can be detected in blood within 1-3 weeks after exposure. The average time from exposure to antibody to HCV (anti-HCV) seroconversion is 8-9 weeks, and anti-HCV can be detected in >97% of persons by 6 months after exposure. Chronic HCV infection develops in 60%-85% of HCV-infected persons; 60%-70% of chronically infected persons have evidence of active liver disease. The majority of infected persons might not be aware of their infection because they are not clinically ill. However, infected persons serve as a source of transmission to others and are at risk for CLD or other HCV-related chronic diseases for decades after infection.
HCV is most efficiently transmitted through large or repeated percutaneous exposure to infected blood (e.g., through transfusion of blood from unscreened donors or through use of injecting drugs), although less efficient, occupational, perinatal, and sexual exposures also can result in transmission of HCV.
The role of sexual activity in the transmission of HCV has been controversial. Case-control studies have reported an association between acquiring HCV infection and exposure to a sex contact with HCV infection or exposure to multiple sex partners. Surveillance data also indicate that 15%-20% of persons reported with acute HCV infection have a history of sexual exposure in the absence of other risk factors (204,208). Case reports of acute HCV infection among HIV-positive MSM who deny injecting-drug use have indicated that this occurrence is frequently associated with other STDs (e.g., syphilis) (209,210). In contrast, a low prevalence (average: 1.5%) of HCV infection has been demonstrated in studies of long-term spouses of patients with chronic HCV infection who had no other risk factors for infection, and multiple published studies have demonstrated the prevalence of HCV infection among MSM who have not reported a history of injecting-drug use to be no higher than that of heterosexuals (211)(212)(213). Because sexual transmission of bloodborne viruses is more efficient among homosexual men compared with heterosexual men and women, the reason that HCV infection rates are not substantially higher among MSM compared with heterosexuals is unclear. Overall, these findings indicate that sexual transmission of HCV is possible but inefficient. Additional data are needed to determine whether sexual transmission of HCV might be increased in the context of HIV infection or other STDs.
# Diagnosis and Treatment
Anti-HCV testing is recommended for routine screening of asymptomatic persons based on their risk for infection or based on a recognized exposure (see Hepatitis C, Prevention). For such persons, testing for HCV infection should include the use of an FDA-cleared test for antibody to HCV (i.e., immunoassay, EIA, or enhanced chemiluminescence assay and, if recommended, a supplemental antibody test) (214).
Persons counseled and tested for HCV infection and determined to be anti-HCV positive should be evaluated (by referral or consultation, if appropriate) for presence of active infection, presence or development of CLD, and for possible treatment. Reverse transcriptase polymerase chain reaction to detect HCV RNA may be used to confirm the diagnosis of current HCV infection, and an elevated alanine aminotransferase (ALT) level is biochemical evidence of CLD. Combination therapy with pegylated interferon and ribavirin is the treatment of choice for patients with chronic hepatitis C. Because of advances in the field of antiviral therapy for acute and chronic hepatitis C, clinicians should consult with specialists knowledgeable about management of hepatitis C infection.
# Prevention
No vaccine for hepatitis C is available, and prophylaxis with immune globulin is not effective in preventing HCV infection after exposure. Reducing the burden of HCV infection and disease in the United States requires implementation of both primary and secondary prevention activities (208). Primary prevention reduces or eliminates HCV transmission; secondary prevention activities reduce liver and other chronic diseases in HCV-infected persons by identifying them and providing appropriate medical management and antiviral therapy, if appropriate.
Persons seeking care in STD clinics or other primary-care settings should be screened to identify those who should be offered HCV counseling and testing. In STD clinics and other settings that serve large numbers of persons at high risk for bloodborne infections (e.g., correctional settings), the major risk factor for which to screen for HCV infection is injection of illegal drugs. In addition, for clinical management issues, all persons with HIV infection should also be offered HCV counseling and testing. Other risk factors for which routine HCV testing is recommended include persons
- who had a blood transfusion or solid organ transplant before July 1992, - who received clotting factor concentrates produced before 1987, - who have been on long-term dialysis, and - those with signs and symptoms of liver disease (e.g., abnormal ALT). Persons who test positive for anti-HCV (see Diagnosis and Treatment) should be provided information regarding 1) how to protect their liver from further harm, 2) how to prevent transmission to others, and 3) the need for medical evaluation for CLD and possible treatment.
- To protect their liver from further harm, HCV-positive persons should be advised to avoid alcohol and taking any new medicines (including OTC and herbals) without checking with their doctor. - To reduce the risk for transmission to others, HCVpositive persons should be advised to 1) not donate blood, body organs, other tissue, or semen; 2) not share any personal items that might have blood on them (e.g., toothbrushes and razors); and 3) cover cuts and sores on the skin to keep from spreading infectious blood or secretions. HCV-positive persons with one long-term, steady sex partner do not need to change their sexual practices. They should discuss the low but present risk for transmission with their partner and discuss the need for counseling and testing. HCV-positive women do not need to avoid pregnancy or breastfeeding. - HCV-positive persons should be evaluated (by referral or consultation, if appropriate) for presence of development of CLD, including assessment of liver function tests, assessment for severity of liver disease and possible treatment, and determination of the need for hepatitis A and B vaccination. Persons who test negative for anti-HCV who had an exposure previously should be reassured that they are not infected.
# Regardless of test results, persons who use or inject illegal drugs should be counseled to
- stop using and injecting drugs;
- enter and complete substance abuse treatment, including relapse prevention; - take the following steps to reduce personal and public health risks, if they continue to inject drugs: -never reuse or share syringes, water, or drug preparation equipment; -use only syringes obtained from a reliable source (e.g., pharmacies); -use a new, sterile syringe to prepare and inject drugs; -if possible, use sterile water to prepare drugs; otherwise, use clean water from a reliable source (e.g., fresh tap water); -use a new or disinfected container ("cooker") and a new filter ("cotton") to prepare drugs; -clean the injection site before injection with a new alcohol swab; -safely dispose of syringes after one use; and -get vaccinated for hepatitis A and B.
# Postexposure Follow-Up
No PEP has been demonstrated to be effective against HCV. Testing to determine whether HCV infection has developed is recommended for health-care workers after percutaneous or permucosal exposures to HCV-positive blood and for children born to HCV-positive women.
# Special Considerations
# Pregnancy
Routine testing for HCV infection is not recommended for all pregnant women. Pregnant women with a known risk factor for HCV infection should be offered counseling and testing. Patients should be advised that approximately five of every 100 infants born to HCV-infected woman become infected. This infection occurs predominantly during or near delivery, and no treatment or delivery method is known to decrease this risk. The risk is increased by the presence of maternal HCV viremia at delivery and also is greater (2-3 times) if the woman is coinfected with HIV. Breastfeeding does not appear to transmit HCV, although HCV-positive mothers should consider abstaining from breastfeeding if their nipples are cracked or bleeding. Infants born to HCV-positive mothers should be tested for HCV infection and, if positive, evaluated for the presence of CLD.
# HIV Infection
Because of the high prevalence of HIV/HCV coinfection and because of critical clinical management issues for coinfected persons, all HIV-infected persons should be tested for HCV. Because a small percentage of coinfected persons fail to acquire HCV antibodies, HCV RNA should be tested in HIV-positive persons with unexplained liver disease who are anti-HCV negative. The course of liver disease is more rapid in HIV/HCV coinfected persons, and the risk for cirrhosis is nearly twice that in persons with HCV infection alone. Treatment of HCV in coinfected persons might improve tolerance to highly active antiretroviral therapy (HAART) for HIV infection because of the increased risk for hepatotoxicity from HAART with HCV infection. However, anti-HCV treatment in coinfected persons is still investigational, and based on ongoing clinical trials, more data are needed to determine the best regimens.
# Proctitis, Proctocolitis, and Enteritis
Sexually transmitted gastrointestinal syndromes include proctitis, proctocolitis, and enteritis. Evaluation for these syndromes should include appropriate diagnostic procedures (e.g., anoscopy or sigmoidoscopy, stool examination, and culture).
Proctitis is inflammation of the rectum (i.e., the distal 10-12 cm) that might be associated with anorectal pain, tenesmus, or rectal discharge. N. gonorrhoeae, C. trachomatis (including LGV serovars), T. pallidum, and HSV are the most common sexually transmitted pathogens involved. In patients coinfected with HIV, herpes proctitis might be especially severe. Proctitis occurs predominantly among persons who participate in receptive anal intercourse.
Proctocolitis is associated with symptoms of proctitis and diarrhea or abdominal cramps and inflammation of the colonic mucosa, extending to 12 cm above the anus. Fecal leukocytes might be detected on stool examination, depending on the pathogen. Pathogenic organisms include Campylobacter sp., Shigella sp., Entamoeba histolytica, and, rarely, LGV serovars of C. trachomatis. CMV or other opportunistic agents might be involved in immunosuppressed HIV-infected patients. Proctocolitis can be acquired by the oral route or by oral-anal contact, depending on the pathogen.
Enteritis usually results in diarrhea and abdominal cramping without signs of proctitis or proctocolitis; it occurs among persons whose sexual practices include oral-anal contact. In otherwise healthy persons, Giardia lamblia is most frequently implicated. When outbreaks of gastrointestinal illness occur among social or sexual networks of MSM, clinicians should consider sexual transmission as a mode of spread and provide counseling accordingly. Among HIV-infected patients, gastrointestinal illness can be caused by other infections that usually are not sexually transmitted, including CMV, Mycobacterium avium-intracellulare, Salmonella sp., Campylobacter sp., Shigella sp., Cryptosporidium, Microsporidium, and Isospora. Multiple stool examinations might be necessary to detect Giardia, and special stool preparations are required to diagnose cryptosporidiosis and microsporidiosis. In addition, enteritis might be directly caused by HIV infection.
When laboratory diagnostic capabilities are available, treatment decisions should be based on the specific diagnosis. Diagnostic and treatment recommendations for all enteric infections are beyond the scope of these guidelines.
# Treatment
Acute proctitis of recent onset among persons who have recently practiced receptive anal intercourse is usually sexually acquired (215,216). Such patients should be examined by anoscopy and should be evaluated for infection with HSV, N. gonorrhoeae, C. trachomatis, and T. pallidum. If an anorectal exudate is detected on examination or if polymorphonuclear leukocytes are detected on a Gram-stained smear of anorectal secretions, the following therapy may be prescribed while awaiting additional laboratory tests.
# Recommended Regimen
Ceftriaxone 125 mg IM (or another agent effective against rectal and genital gonorrhea) PLUS Doxycycline 100 mg orally twice a day for 7 days Patients with suspected or documented herpes proctitis should be managed in the same manner as those with genital herpes (see Genital HSV Infections). If painful perianal ulcers are present or mucosal ulcers are detected on anoscopy, presumptive therapy should include a regimen for treating genital herpes. In addition, LGV proctitis and proctocolitis also should be considered. Appropriate diagnostic testing for LGV should be conducted in accordance with state or federal guidelines, and doxycycline therapy should be administered 100 mg orally twice daily for 3 weeks.
# Follow-Up
Follow-up should be based on specific etiology and severity of clinical symptoms. Reinfection might be difficult to distinguish from treatment failure.
# Management of Sex Partners
Partners of patients with sexually transmitted enteric infections should be evaluated for any diseases diagnosed in the index patient.
# Ectoparasitic Infections Pediculosis Pubis
Patients who have pediculosis pubis (i.e., pubic lice) usually seek medical attention because of pruritus or because they notice lice or nits on their pubic hair. Pediculosis pubis is usually transmitted by sexual contact.
# Recommended Regimens
Permethrin 1% cream rinse applied to affected areas and washed off after 10 minutes OR Pyrethrins with piperonyl butoxide applied to the affected area and washed off after 10 minutes
# Alternative Regimens
Malathion 0.5% lotion applied for 8-12 hours and washed off OR Ivermectin 250 ug/kg repeated in 2 weeks Reported resistance to pediculcides has been increasing and is widespread. Malathion may be used when treatment failure is believed to have occurred because of resistance (217). The odor and long duration of application for malathion make it a less attractive alternative than the recommended pediculcides. Ivermectin has been successfully used to treat lice but has only been evaluated in small studies.
Lindane is not recommended as first-line therapy because of toxicity. It should only be used as an alternative because of inability to tolerate other therapies or if other therapies have failed. Lindane toxicity, as indicated by seizure and aplastic anemia, has not been reported when treatment was limited to the recommended 4-minute period. Permethrin has less potential for toxicity than lindane.
# Other Management Considerations
The recommended regimens should not be applied to the eyes. Pediculosis of the eyelashes should be treated by applying occlusive ophthalmic ointment to the eyelid margins twice a day for 10 days. Bedding and clothing should be decontaminated (i.e., machine-washed, machine-dried using the heat cycle, or dry cleaned) or removed from body contact for at least 72 hours. Fumigation of living areas is not necessary.
Patients with pediculosis pubis should be evaluated for other STDs.
# Follow-Up
Patients should be evaluated after 1 week if symptoms persist. Re-treatment might be necessary if lice are found or if eggs are observed at the hair-skin junction. Patients who do not respond to one of the recommended regimens should be re-treated with an alternative regimen.
# Management of Sex Partners
Sex partners within the previous month should be treated. Patients should avoid sexual contact with their sex partner(s) until patients and partners have been treated and reevaluated to rule out persistent disease.
# Special Considerations
# Pregnancy
Pregnant and lactating women should be treated with either permethrin or pyrethrins with piperonyl butoxide; lindane is contraindicated in pregnancy.
# HIV Infection
Patients who have pediculosis pubis and also are infected with HIV should receive the same treatment regimen as those who are HIV negative.
# Scabies
The predominant symptom of scabies is pruritus. Sensitization to Sarcoptes scabiei occurs before pruritus begins. The first time a person is infested with S. scabiei, sensitization takes up to several weeks to develop. However, pruritus might occur within 24 hours after a subsequent reinfestation. Scabies in adults frequently is sexually acquired, although scabies in children usually is not.
# Recommended Regimens
Permethrin cream (5%) applied to all areas of the body from the neck down and washed off after 8-14 hours OR Ivermectin 200ug/kg orally, repeated in 2 weeks Alternative Regimens Lindane (1%) 1 oz. of lotion or 30 g of cream applied in a thin layer to all areas of the body from the neck down and thoroughly washed off after 8 hours Lindane is not recommended as first-line therapy because of toxicity. It should only be used as an alternative if the patient cannot tolerate other therapies or if other therapies have failed.
Lindane should not be used immediately after a bath or shower, and it should not be used by persons who have extensive dermatitis, women who are pregnant or lactating, or children aged <2 years. Lindane resistance has been reported in some areas of the world, including parts of the United States. Seizures have occurred when lindane was applied after a bath or used by patients who had extensive dermatitis. Aplastic anemia after lindane use also has been reported.
Permethrin is effective and safe and less expensive than ivermectin. One study demonstrated increased mortality among elderly, debilitated persons who received ivermectin, but this observation has not been confirmed in subsequent reports (218).
# Other Management Considerations
Bedding and clothing should be decontaminated (i.e., either machine-washed, machine-dried using the hot cycle, or dry cleaned) or removed from body contact for at least 72 hours. Fumigation of living areas is unnecessary.
# Crusted Scabies
Crusted scabies (i.e., Norwegian scabies) is an aggressive infestation that usually occurs in immunodeficient, debilitated, or malnourished persons. Patients who are receiving systemic or potent topical glucocorticoids, organ transplant recipients, mentally retarded or physically incapacitated persons, HIV-infected or human T-lymphotrophic virus-1infected persons, and persons with various hematologic malignancies are at risk for developing crusted scabies. Crusted scabies is associated with greater transmissibility than scabies. No controlled therapeutic studies for crusted scabies have been conducted, and the appropriate treatment remains unclear. Substantial treatment failure might occur with a single topical scabicide or with oral ivermectin treatment. Some specialists recommend combined treatment with a topical scabicide and oral ivermectin or repeated treatments with ivermectin 200 ug/kg on days 1, 15, and 29. Lindane should be avoided because of the risks for neurotoxicity with heavy applications or denuded skin. Patient's fingernails should be closely trimmed to reduce injury from excessive scratching.
# Follow-Up
Patients should be informed that the rash and pruritus of scabies might persist for up to 2 weeks after treatment. Symptoms or signs that persist for >2 weeks can be attributed to several factors. Treatment failure might be caused by resistance to medication or by faulty application of topical scabicides. Patients with crusted scabies might have poor penetration into thick scaly skin and harbor mites in these difficult-to-penetrate layers. Particular attention must be given to the fingernails of these patients. Reinfection from family members or fomites might occur in the absence of appropriate contact treatment and washing of bedding and clothing. Even when treatment is successful and reinfection is avoided, symptoms can persist or worsen as a result of allergic dermatitis. Finally, household mites can cause symptoms to persist as a result of crossreactivity between antigens. Some special-ists recommend re-treatment after 1-2 weeks for patients who are still symptomatic; others recommend re-treatment only if live mites are observed. Patients who do not respond to the recommended treatment should be re-treated with an alternative regimen.
# Management of Sex Partners and Household Contacts
Both sexual and close personal or household contacts within the preceding month should be examined and treated.
# Management of Outbreaks in Communities, Nursing Homes, and Other Institutional Settings
Scabies epidemics frequently occur in nursing homes, hospitals, residential facilities, and other communities. Control of an epidemic can only be achieved by treatment of the entire population at risk. Ivermectin can be considered in this setting, especially if treatment with topical scabicides fails. Epidemics should be managed in consultation with a specialist.
# Special Considerations
# Infants, Young Children, and Pregnant or Lactating Women
Infants, young children, and pregnant or lactating women should not be treated with lindane. They can be treated with permethrin.
Ivermectin is not recommended for pregnant or lactating patients. The safety of ivermectin in children who weigh <15 kg has not been determined.
# HIV Infection
Patients who have uncomplicated scabies and also are infected with HIV should receive the same treatment regimens as those who are HIV negative. HIV-infected patients and others who are immunosuppressed are at increased risk for crusted scabies. Ivermectin has been reported to be useful in small, noncontrolled studies. Such patients should be managed in consultation with a specialist.
# Sexual Assault and STDs
# Adults and Adolescents
The recommendations in this report are limited to the identification, prophylaxis, and treatment of sexually transmitted infections and conditions commonly identified in the management of such infections. The documentation of findings, collection of nonmicrobiologic specimens for forensic purposes, and the management of potential pregnancy or physical and psychological trauma are beyond the scope of this report. Examinations of survivors of sexual assault should be conducted by an experienced clinician in a way that minimizes further trauma to the survivor. The decision to obtain genital or other specimens for STD diagnosis should be made on an individual basis. Care systems for survivors should be designed to ensure continuity (including timely review of test results), support adherence, and monitor for adverse reactions to any therapeutic or prophylactic regimens prescribed at initial examination. Laws in all 50 states strictly limit the evidentiary use of a survivor's previous sexual history, including evidence of previously acquired STDs, as part of an effort to undermine the credibility of the survivor's testimony. Evidentiary privilege against revealing any aspect of the examination or treatment is enforced in the majority of states. In unanticipated, exceptional situations, STD diagnoses may later be accessed, and the survivor and clinician may opt to defer testing for this reason. However, collection of specimens at initial examination for laboratory STD diagnosis gives the survivor and clinician the option to defer empiric prophylactic antimicrobial treatment. Among sexually active adults, the identification of sexually transmitted infection after an assault might be more important for the psychological and medical management of the patient than for legal purposes because the infection could have been acquired before the assault.
Trichomoniasis, BV, gonorrhea, and chlamydial infection are the most frequently diagnosed infections among women who have been sexually assaulted. Because the prevalence of these infections is high among sexually active women, their presence after an assault does not necessarily signify acquisition during the assault. A postassault examination is, however, an opportunity to identify or prevent sexually transmitted infections, regardless of whether they were acquired during an assault. Chlamydial and gonococcal infections in women are of particular concern because of the possibility of ascending infection. In addition, HBV infection might be prevented by postexposure administration of hepatitis B vaccine. Reproductive-aged female survivors should be evaluated for pregnancy, if appropriate.
# Evaluation for Sexually Transmitted Infections Initial Examination
An initial examination should include the following procedures:
- Testing for N. gonorrhoeae and C. trachomatis from specimens collected from any sites of penetration or attempted penetration.
# Follow-Up Examinations
After the initial postassault examination, follow-up examinations provide an opportunity to 1) detect new infections acquired during or after the assault; 2) complete hepatitis B immunization, if indicated; 3) complete counseling and treatment for other STDs; and 4) monitor side effects and adherence to postexposure prophylactic medication, if prescribed.
Examination for STDs should be repeated within 1-2 weeks of the assault. Because infectious agents acquired through assault might not have produced sufficient concentrations of organisms to result in positive test results at the initial examination, testing should be repeated during the follow-up visit, unless prophylactic treatment was provided. If treatment was provided, testing should be conducted only if the survivor reports having symptoms. If treatment was not provided, follow-up examination should be conducted within 1 week to ensure that results of positive tests can be discussed promptly with the survivor and that treatment is provided. Serologic tests for syphilis and HIV infection should be repeated 6 weeks, 3 months, and 6 months after the assault if initial test results were negative and infection in the assailant could not be ruled out (see Sexual Assaults, Risk for Acquiring HIV Infection).
# Prophylaxis
Many specialists recommend routine preventive therapy after a sexual assault because follow-up of survivors of sexual assault can be difficult. The following prophylactic regimen is suggested as preventive therapy:
- Postexposure hepatitis B vaccination, without HBIG, should adequately protect against HBV infection. Hepatitis B vaccination should be administered to sexual assault victims at the time of the initial examination if they have not been previously vaccinated. Follow-up doses of vaccine should be administered 1-2 and 4-6 months after the first dose. - An empiric antimicrobial regimen for chlamydia, gonorrhea, trichomonas, and BV. - EC should be offered if the postassault could result in pregnancy in the survivor.
# MMWR August 4, 2006
# Recommended Regimens
Ceftriaxone 125 mg IM in a single dose PLUS Metronidazole 2 g orally in a single dose PLUS Azithromycin 1 g orally in a single dose OR Doxycycline 100 mg orally twice a day for 7 days For patients requiring alternative treatments, refer to the sections in this report relevant to the specific agent. The efficacy of these regimens in preventing infections after sexual assault has not been evaluated. Clinicians should counsel patients regarding the possible benefits and toxicities associated with these treatment regimens; gastrointestinal side effects can occur with this combination. Providers might also consider anti-emetic medications, particularly if EC also is provided.
# Other Management Considerations
At the initial examination and, if indicated, at follow-up examinations, patients should be counseled regarding 1) symptoms of STDs and the need for immediate examination if symptoms occur and 2) abstinence from sexual intercourse until STD prophylactic treatment is completed.
# Risk for Acquiring HIV Infection
HIV seroconversion has occurred in persons whose only known risk factor was sexual assault or sexual abuse, but the frequency of this occurrence is probably low. In consensual sex, the risk for HIV transmission from vaginal intercourse is 0.1%-0.2% and for receptive rectal intercourse, 0.5%-3% (219). The risk for HIV transmission from oral sex is substantially lower. Specific circumstances of an assault might increase risk for HIV transmission (e.g., trauma, including bleeding) with vaginal, anal, or oral penetration; site of exposure to ejaculate; viral load in ejaculate; and the presence of an STD or genital lesions in the assailant or survivor.
Children might be at higher risk for transmission because child sexual abuse is frequently associated with multiple episodes of assault and might result in mucosal trauma (see Sexual Assault or Abuse of Children).
Postexposure therapy with zidovudine was associated with a reduced risk for acquiring HIV in a study of health-care workers who had percutaneous exposures to HIV-infected blood (220). On the basis of these results and the results of animal studies, PEP has been recommended for health-care workers who have occupational exposures to HIV (207). These findings have been extrapolated to other types of HIV exposure, including sexual assault (58). If HIV exposure has occurred, initiation of PEP as soon as possible after the exposure likely increases benefit. Although a definitive statement of benefit cannot be made regarding PEP after sexual assault, the possibility of HIV exposure from the assault should be assessed at the time of the postassault examination. The possible benefit of PEP in preventing HIV infection also should be discussed with the assault survivor if risk exists for HIV exposure from the assault.
The likelihood of the assailant having HIV, any exposure characteristics that might increase the risk for HIV transmission, the time elapsed after the event, as well as potential benefits and risks the PEP are all factors that will impact the medical recommendation for PEP and impact the assault survivor's acceptance of that recommendation (58). Determination of assailant's HIV status at the time of the assault examination will usually be impossible. Therefore, the healthcare provider should assess any available information concerning HIV-risk behaviors of the assailant(s) (e.g., a man who has sex with other men and injecting-drug or crack cocaine use), local epidemiology of HIV/AIDS, and exposure characteristics of the assault. When an assailant's HIV status is unknown, factors that should be considered in determining whether an increased risk for HIV transmission exists include 1) whether vaginal or anal penetration occurred; 2) whether ejaculation occurred on mucous membranes; 3) whether multiple assailants were involved; 4) whether mucosal lesions are present in the assailant or survivor; and 5) other characteristics of the assault, survivor, or assailant that might increase risk for HIV transmission.
If PEP is offered, the following information should be discussed with the patient: 1) the unproven benefit and known toxicities of antiretrovirals; 2) the close follow-up that will be necessary; 3) the benefit of adherence to recommended dosing; and 4) the necessity of early initiation of PEP to optimize potential benefits (as soon as possible after and up to 72 hours after the assault). Providers should emphasize that PEP appears to be well-tolerated in both adults and children and that severe adverse effects are rare. Clinical management of the survivor should be implemented according to the following guidelines (58). Specialist consultation on PEP regimens is recommended if HIV exposure during the assault was possible and if PEP is being considered. The sooner PEP is initiated after the exposure, the higher the likelihood that it will prevent HIV transmission, if HIV exposure occurred; however, distress after an assault also might prevent the survivor from accurately weighing exposure risks and benefits of PEP and making an informed decision to start PEP. If use of PEP is judged to be warranted, the survivor should be offered a 3-5-day supply of PEP with a follow-up visit scheduled for additional counseling after several days.
# Sexual Assault or Abuse of Children
Recommendations in this report are limited to the identification and treatment of STDs. Management of the psychosocial aspects of the sexual assault or abuse of children is beyond the scope of these recommendations.
The identification of sexually transmissible agents in children beyond the neonatal period suggests sexual abuse. The significance of the identification of a sexually transmitted agent in such children as evidence of possible child sexual abuse varies by pathogen. Postnatally acquired gonorrhea; syphilis; and nontransfusion, nonperinatally acquired HIV are usually diagnostic of sexual abuse. Sexual abuse should be suspected when genital herpes is diagnosed. The investigation of sexual abuse among children who possibly have an infection that might have been sexually transmitted should be conducted in compliance with recommendations by clinicians who have experience and training in all elements of the evaluation of child abuse, neglect, and assault. The social importance of infection that might have been acquired sexually and the recommended action regarding reporting of suspected child sexual abuse varies by the specific organism (Table 6). In all cases in which a sexually transmitted infection has been diagnosed in a child, efforts should be made to detect evidence of sexual abuse, including conducting diagnostic testing for other commonly occurring sexually transmitted infections (221).
The general rule that sexually transmissible infections beyond the neonatal period are evidence of sexual abuse has exceptions. For example, rectal or genital infection with C. trachomatis among young children might be the result of perinatally acquired infection and has, in some cases, persisted for as long as 2-3 years. Genital warts have been diagnosed in children who have been sexually abused, but also in children who have no other evidence of sexual abuse. BV has been diagnosed in children who have been abused, but its presence alone does not prove sexual abuse. The majority of HBV infections in children result from household exposure to persons who have chronic HBV infection.
The possibility of sexual abuse should be strongly considered if no conclusive explanation for nonsexual transmission of a sexually transmitted infection can be identified. When the only evidence of sexual abuse is the isolation of an organism or the detection of antibodies to a sexually transmissible agent, findings should be confirmed and the implications considered carefully.
# Evaluation for Sexually Transmitted Infections
Examinations of children for sexual assault or abuse should be conducted in a manner designed to minimize pain and trauma to the child. Collection of vaginal specimens in prepubertal children can be very uncomfortable and should be performed by an experienced clinician to avoid psychological § § § Assistance with postexposure prophylaxis decisions can be obtained by calling the National Clinician's Post-Exposure Prophylaxis Hotline (PEPLine), telephone: 888-448-4911. and physical trauma to the child. The decision to obtain genital or other specimens from a child to conduct an STD evaluation must be made on an individual basis. The following situations involve a high risk for STDs and constitute a strong indication for testing:
- The child has or has had symptoms or signs of an STD or of an infection that can be sexually transmitted, even in the absence of suspicion of sexual abuse. Among the signs that are associated with a confirmed STD diagnosis are vaginal discharge or pain, genital itching or odor, urinary symptoms, and genital ulcers or lesions. - A suspected assailant is known to have an STD or to be at high risk for STDs (e.g., has multiple sex partners or a history of STDs). - A sibling or another child or adult in the household or child's immediate environment has an STD. - The patient or parent requests testing.
- Evidence of genital, oral, or anal penetration or ejaculation is present. If a child has symptoms, signs, or evidence of an infection that might be sexually transmitted, the child should be tested for other common STDs before the initiation of any treatment that could interfere with the diagnosis of those other STDs. Because of the legal and psychosocial consequences of a false-positive diagnosis, only tests with high specificities should be used. The potential benefit to the child of a reliable diagnosis of an STD justifies deferring presumptive treatment until specimens for highly specific tests are obtained by providers with experience in the evaluation of sexually abused and assaulted children.
The scheduling of an examination should depend on the history of assault or abuse. If the initial exposure was recent, the infectious agents acquired through the exposure might not have produced sufficient concentrations of organisms to result in positive test results. A follow-up visit approximately 2 weeks after the most recent sexual exposure may include a repeat physical examination and collection of additional specimens. To allow sufficient time for antibodies to develop, another follow-up visit approximately 12 weeks after the most recent sexual exposure might be necessary to collect sera. A single examination might be sufficient if the child was abused for an extended period and if the last suspected episode of abuse occurred substantially before the child received medical evaluation.
The following recommendations for scheduling examinations serve as a general guide. The exact timing and nature of follow-up examinations should be determined on an individual basis and should be performed to minimize the possibility for psychological trauma and social stigma. Compliance with follow-up appointments might be improved when law enforcement personnel or child protective services are involved.
# Initial and 2-Week Follow-Up Examinations
During the initial examination and 2-week follow-up examination (if indicated), the following should be performed:
- Visual inspection of the genital, perianal, and oral areas for genital discharge, odor, bleeding, irritation, warts, and ulcerative lesions. The clinical manifestations of some STDs are different in children than in adults. For example, typical vesicular lesions might not be present in the presence of HSV infection. Because this infection is suspicious for sexual abuse, specimens should be obtained from all vesicular or ulcerative genital or perianal lesions compatible with genital herpes and then sent for viral culture. - Specimen collection for culture for N. gonorrhoeae from the pharynx and anus in both boys and girls, the vagina in girls, and the urethra in boys. Cervical specimens are not recommended for prepubertal girls. For boys with a urethral discharge, a meatal specimen discharge is an adequate substitute for an intraurethral swab specimen. Only standard culture systems for the isolation of N. gonorrhoeae should be used. All presumptive isolates of N. gonorrhoeae should be confirmed by at least two tests that involve different principles (i.e., biochemical, enzyme substrate, serologic, or nucleic acid hybridization test methods).
Isolates and specimens should be retained or preserved in case additional or repeated testing is needed. Gram stains are inadequate to evaluate prepubertal children for gonorrhea and should not be used to diagnose or exclude gonorrhea. - Cultures for C. trachomatis from specimens collected from the anus in both boys and girls and from the vagina in girls. Some data suggest that the likelihood of recovering C. trachomatis from the urethra of prepubertal boys is too low to justify the trauma involved in obtaining an intraurethral specimen. However, a meatal specimen should be obtained if urethral discharge is present. Pharyngeal specimens for C. trachomatis are not recommended for children of either sex because the yield is low, perinatally acquired infection might persist beyond infancy, and culture systems in some laboratories do not distinguish between C. trachomatis and C. pneumoniae. HIV infection has been reported in children whose only known risk factor was sexual abuse. Serologic testing for HIV infection should be considered for abused children. The decision to test for HIV infection should be made on a case-bycase basis, depending on the likelihood of infection among assailant(s). Data are insufficient concerning the efficacy and safety of PEP among both children and adults. However, antiretroviral treatment is well-tolerated by infants and children with and without HIV infection. In addition, children who receive such treatment have a minimal risk for serious adverse reactions because of the short period recommended for prophylaxis (58,62). In considering whether to offer antiretroviral PEP, health-care providers should consider whether the child can be treated soon after the sexual exposure (i.e., within 72 hours), the likelihood that the assailant is at risk for HIV infection, and the likelihood of high compliance with the prophylactic regimen. The potential benefit of treating a sexually abused child should be weighed against the risk for adverse reactions. If antiretroviral PEP is being considered, a professional specializing in HIV-infected children should be consulted.
# Recommendations for HIV-Related Postexposure Assessment of Children within 72 Hours of Sexual Assault
- Review HIV/AIDS local epidemiology and assess risk for HIV infection in the assailant.
- Evaluate circumstances of assault that might affect risk for HIV transmission. - Consult with a specialist in treating HIV-infected children if PEP is considered. - If the child appears to be at risk for HIV transmission from the assault, discuss PEP with the caregiver(s), including its toxicity and unknown efficacy. - If caregivers choose for the child to receive antiretroviral PEP (58,62,222), provide enough medication to last until the return visit at 3-7 days after the initial assessment, at which time the child should be reevaluated and tolerance of medication should be assessed; dosages should not exceed those for adults. - Perform HIV antibody test at original assessment, 6 weeks, 3 months, and 6 months.
# Follow-Up Examination After Assault
In circumstances in which transmission of syphilis, HIV, or hepatitis B is a concern but baseline tests are negative, an examination approximately 6 weeks, 3 months, and 6 months after the last suspected sexual exposure is recommended to allow time for antibodies to infectious agents to develop. In addition, results of HBsAg testing must be interpreted carefully, because HBV can be transmitted nonsexually. Decisions regarding which tests should be performed must be made on an individual basis.
# Presumptive Treatment
The risk of a child acquiring an STD as a result of sexual abuse or assault has not been well studied. Presumptive treatment for children who have been sexually assaulted or abused is not recommended because 1) the incidence of the majority of STDs in children is low after abuse/assault, 2) prepubertal girls appear to be at lower risk for ascending infection than adolescent or adult women, and 3) regular follow-up of children usually can be ensured. However, some children or their parent(s) or guardian(s) might be concerned about the possibility of infection with an STD, even if the risk is perceived to be low by the health-care provider. Such concerns might be an appropriate indication for presumptive treatment in some settings and may be considered after all specimens for diagnostic tests relevant to the investigation have been collected.
# Reporting
U.S. states and territories have laws that require the reporting of child abuse. Although the exact requirements differ by state, if a health-care provider has reasonable cause to suspect child abuse, a report must be made. Health-care providers should contact their state or local child-protection service agency regarding child-abuse reporting requirements in their states.
§ Pediatric formulation administered on a 3-dose schedule; higher doses might be more immunogenic, but no specific recommendations have been made. ¶ Not applicable. Adult formulation administered on a 2-dose schedule. † † Dialysis formulation administered on a 3-dose schedule at 0, 1, and 6 months. § § Two 1.0-mL doses of the adult formulation administered at one site on a 4-dose schedule at 0, 1, 2, and 6 months.
populations where the prevalence of infection is likely to be high (e.g., persons aged >40 years and persons born in areas of high HAV endemicity). The potential cost-savings of testing should be weighed against the cost and the likelihood that testing will interfere with initiating vaccination. Vaccination of a person who is already immune is not harmful.
# Postvaccination Serologic Testing
Postvaccination serologic testing is not indicated because the majority of persons respond to the vaccine. In addition, the commercially available serologic test is not sensitive enough to detect the low, but protective, levels of antibody produced by vaccination.
# Recommendations for Postexposure Assessment of Adolescent and Adult Survivors Within 72 hours of Sexual Assault § § §
- Assess risk for HIV infection in the assailant.
- Evaluate characteristics of the assault event that might increase risk for HIV transmission. - Consult with a specialist in HIV treatment, if PEP is being considered. - If the survivor appears to be at risk for HIV transmission from the assault, discuss antiretroviral prophylaxis, including toxicity and lack of proven benefit. - If the survivor chooses to start antiretroviral PEP (58), provide enough medication to last until the next return visit; reevaluate the survivor 3-7 days after initial assessment and assess tolerance of medications. - If PEP is started, perform CBC and serum chemistry at baseline (initiation of PEP should not be delayed, pending results). - Perform HIV antibody test at original assessment; repeat at 6 weeks, 3 months, and 6 months.
# Terms and Abbreviations Used in This Report | depar depar depar depar department of health and human ser tment of health and human ser tment of health and human ser tment of health and human ser tment of health and human services vices vices vices vices# Introduction
Physicians and other health-care providers play a critical role in preventing and treating sexually transmitted diseases (STDs). These guidelines for the treatment of STDs are intended to assist with that effort. Although these guidelines emphasize treatment, prevention strategies and diagnostic recommendations also are discussed.
# Methods
This report was produced through a multistage process. Beginning in 2004, CDC personnel and professionals knowledgeable in the field of STDs systematically reviewed evidence, including published abstracts and peer-reviewed journal articles concerning each of the major STDs, focusing on information that had become available since publication of the Sexually Transmitted Diseases Treatment Guidelines, 2002 (1). Background papers were written and tables of evidence were constructed summarizing the type of study (e.g., randomized controlled trial or case series), study population and setting, treatments or other interventions, outcome measures assessed, reported findings, and weaknesses and biases in study design and analysis. A draft document was developed on the basis of the reviews.
In April 2005, CDC staff members and invited consultants assembled in Atlanta, Georgia, for a 3-day meeting to present the key questions regarding STD treatment that emerged from the evidence-based reviews and the information available to answer those questions. When relevant, the questions focused on four principal outcomes of STD therapy for each individual disease: 1) microbiologic cure, 2) alleviation of signs and symptoms, 3) prevention of sequelae, and 4) prevention of transmission. Cost-effectiveness and other advantages (e.g., single-dose formulations and directly observed therapy of specific regimens) also were discussed. The consultants then assessed whether the questions identified were relevant, ranked them in order of priority, and attempted to arrive at answers using the available evidence. In addition, the consultants evaluated the quality of evidence supporting the answers on the basis of the number, type, and quality of the studies.
In several areas, the process diverged from that previously described. The sections on hepatitis B virus (HBV) and hepatitis A virus (HAV) infections are based on previously or recently approved recommendations (2)(3)(4) of the Advisory Committee on Immunization Practices. The recommendations for STD screening during pregnancy were developed after CDC staff reviewed the recommendations from other knowledgeable groups.
Throughout this report, the evidence used as the basis for specific recommendations is discussed briefly. More comprehensive, annotated discussions of such evidence will appear in background papers that will be published in a supplement issue of Clinical Infectious Diseases. When more than one therapeutic regimen is recommended, the sequence is in alphabetical order unless the choices for therapy are prioritized based on efficacy, convenience, or cost. For STDs with more than one recommended treatment regimen, it can be assumed that all regimens have similar efficacy and similar rates of intolerance or toxicity, unless otherwise specified. Persons treating STDs should use recommended regimens primarily; alternative regimens can be considered in instances of substantial drug allergy or other contraindications to the recommended regimens.
These recommendations were developed in consultation with public and private sector professionals knowledgeable in the treatment of persons with STDs (see Consultants list). The recommendations are applicable to various patient-care settings, including family planning clinics, private physicians' offices, managed care organizations, and other primary-care facilities.
These recommendations are meant to serve as a source of clinical guidance: health-care providers should always consider the individual clinical circumstances of each person in the context of local disease prevalence. These guidelines focus on the treatment and counseling of individual persons and do not address other community services and interventions that are important in STD/human immunodeficiency virus (HIV) prevention.
# Clinical Prevention Guidance
The prevention and control of STDs are based on the following five major strategies: 1) education and counseling of persons at risk on ways to avoid STDs through changes in sexual behaviors; 2) identification of asymptomatically infected persons and of symptomatic persons unlikely to seek diagnostic and treatment services; 3) effective diagnosis and treatment of infected persons; 4) evaluation, treatment, and counseling of sex partners of persons who are infected with an STD; and 5) preexposure vaccination of persons at risk for vaccine-preventable STD.
Primary prevention of STD begins with changing the sexual behaviors that place persons at risk for infection. Health-care providers have a unique opportunity to provide education and counseling to their patients. As part of the clinical interview, health-care providers should routinely and regularly obtain sexual histories from their patients and address management of risk reduction as indicated in this report. Guid-ance in obtaining a sexual history is available in Contraceptive Technology, 18th edition (5) and in the curriculum provided by CDC's STD/HIV Prevention Training Centers (http:// www.stdhivpreventiontraining.org). Counseling skills, characterized by respect, compassion, and a nonjudgmental attitude toward all patients, are essential to obtaining a thorough sexual history and to delivering prevention messages effectively. Key techniques that can be effective in facilitating rapport with patients include the use of 1) open-ended questions (e.g., "Tell me about any new sex partners you've had since your last visit" and "what's your experience with using condoms been like?"), 2) understandable language ("have you ever had a sore or scab on your penis?"), and 3) normalizing language ("some of my patients have difficulty using a condom with every sex act. How is it for you?"). One approach to eliciting information concerning five key areas of interest has been summarized.
The Five Ps: Partners, Prevention of Pregnancy, Protection from STDs, Practices, Past History of STDs 1. Partners • "Do you have sex with men, women, or both?"
• "In the past 2 months, how many partners have you had sex with?" • "In the past 12 months, how many partners have you had sex with?" 2. Prevention of pregnancy • "Are you or your partner trying to get pregnant?" If no, "What are you doing to prevent pregnancy?" 3. Protection from STDs • "What do you do to protect yourself from STDs and HIV?" 4. Practices • "To understand your risks for STDs, I need to understand the kind of sex you have had recently." • "Have you had vaginal sex, meaning 'penis in vagina sex'"? • If yes, "Do you use condoms: never, sometimes, or always?" • "Have you had anal sex, meaning 'penis in rectum/anus sex'"? • If yes, "Do you use condoms: never, sometimes, or always?" • "Have you had oral sex, meaning 'mouth on penis/ vagina'"? For condom answers • If "never:" "Why don't you use condoms?" • If "sometimes": "In what situations or with whom, do you not use condoms?" 5. Past history of STDs • "Have you ever had an STD?"
• "Have any of your partners had an STD?" Additional questions to identify HIV and hepatitis risk • "Have you or any of your partners ever injected drugs?
• "Have any of your partners exchanged money or drugs for sex?" • "Is there anything else about your sexual practices that I need to know about?" Patients should be reassured that treatment will be provided regardless of individual circumstances (e.g., ability to pay, citizenship or immigration status, language spoken, or specific sex practices). Many patients seeking treatment or screening for a particular STD should be evaluated for all common STDs; even so, all patients should be informed concerning all the STDs for which they are being tested and if testing for a common STD (e.g., genital herpes) is not being performed.
# STD/HIV Prevention Counseling
Effective delivery of prevention messages requires that providers integrate communication of general risk reduction messages that are relevant to the client (i.e., client-centered counseling) and education regarding specific actions that can reduce the risk for STD/HIV transmission (e.g., abstinence, condom use, limiting the number of sex partners, modifying sexual behaviors, and vaccination). Each of these specific actions is discussed separately in this report.
• Interactive counseling approaches directed at a patient's personal risk, the situations in which risk occurs, and the use of goal-setting strategies are effective in STD/HIV prevention (6). One such approach, client-centered STD/ HIV prevention counseling, involves tailoring a discussion of risk reduction to the patient's individual situation. Client-centered counseling can have a beneficial effect on the likelihood of patients using risk-reduction practices and can reduce the risk for future acquisition of an STD. One effective client-centered approach is Project RESPECT, which demonstrated that a brief counseling intervention was associated with a reduced frequency of STD/HIV risk-related behaviors and with a lowered acquisition of STDs (7,8). Practice models based on Project RESPECT have been successfully implemented in clinicbased settings. Other approaches use motivational interviewing to move clients toward achievable risk reduction goals. CDC provides additional information on these and other effective behavioral interventions at http:// effectiveinterventions.org. • Interactive counseling can be used effectively by all healthcare providers or can be conducted by specially trained counselors. The quality of counseling is best ensured when providers receive basic training in prevention counseling methods and skill-building approaches, periodic observation of counseling with immediate feedback by persons with expertise in the counseling approach, periodic counselor and/or patient satisfaction evaluations, and availability of expert assistance or referral for challenging situations. Training in client-centered counseling is available through the CDC STD/HIV Prevention Training Centers (http://www.stdhivpreventiontraining.org). Prevention counseling is most effective if provided in a nonjudgmental manner appropriate to the patient's culture, language, sex, sexual orientation, age, and developmental level. In addition to individual prevention counseling, some videos and large group presentations provide explicit information concerning how to use condoms correctly. These have been effective in reducing the occurrence of additional STDs among persons at high risk, including STD clinic patients and adolescents.
Because the incidence of some STDs, notably syphilis, has increased in HIV-infected persons, the use of client-centered STD counseling for HIV-infected persons has received strong emphasis from public health agencies and organizations. Consensus guidelines issued by CDC, the Health Resources and Services Administration, the HIV Medicine Association of the Infectious Diseases Society of America, and the National Institutes of Health emphasize that STD/HIV risk assessment, STD screening, and client-centered risk reduction counseling should be provided routinely to HIV-infected persons (9). Several specific methods have been designed for the HIV care setting (10)(11)(12). Additional information regarding these approaches is available at http://effectiveinterventions.org.
The most reliable way to avoid transmission of STDs is to abstain from sex (i.e., oral, vaginal, or anal sex) or to be in a long-term, mutually monogamous relationship with an uninfected partner. Counseling that encourages abstinence from sexual intercourse is crucial for persons who are being treated for an STD (or whose partners are undergoing treatment) and for persons who want to avoid the possible consequences of sex completely (e.g., STD/HIV and unintended pregnancy). A more comprehensive discussion of abstinence is available in Contraceptive Technology, 18th edition (5). For persons embarking on a mutually monogamous relationship, screening for common STDs before initiating sex might reduce the risk for future transmission of asymptomatic STDs.
# Preexposure Vaccination
Preexposure vaccination is one of the most effective methods for preventing transmission of some STDs. For example, because HBV infection is frequently sexually transmitted, hepatitis B vaccination is recommended for all unvaccinated, uninfected persons being evaluated for an STD. In addition, hepatitis A vaccine is licensed and is recommended for men who have sex with men (MSM) and illicit drug users (i.e., both injecting and noninjecting). Specific details regarding hepatitis A and B vaccination are available at http:// www.cdc.gov/hepatitis. A quadrivalent vaccine against human papillomavirus (HPV types 6,11,16,18) is now available and licensed for females aged 9-26 years. Vaccine trials for other STDs are being conducted.
# Male Condoms
When used consistently and correctly, male latex condoms are highly effective in preventing the sexual transmission of HIV infection (i.e., HIV-negative partners in heterosexual serodiscordant relationships in which condoms were consistently used were 80% less likely to become HIV-infected compared with persons in similar relationships in which condoms were not used) and can reduce the risk for other STDs, including chlamydia, gonorrhea, and trichomoniasis, and might reduce the risk of women developing pelvic inflammatory disease (PID) (13,14). Condom use might reduce the risk for transmission of herpes simplex virus-2 (HSV-2), although data for this effect are more limited (15,16). Condom use might reduce the risk for HPV-associated diseases (e.g., genital warts and cervical cancer [17]) and mitigate the adverse consequences of infection with HPV, as their use has been associated with higher rates of regression of cervical intraepithelial neoplasia (CIN) and clearance of HPV infection in women (18), and with regression of HPV-associated penile lesions in men (19). A limited number of prospective studies have demonstrated a protective effect of condoms on the acquisition of genital HPV; one recent prospective study among newly sexually active college women demonstrated that consistent condom use was associated with a 70% reduction in risk for HPV transmission (20).
Condoms are regulated as medical devices and are subject to random sampling and testing by the Food and Drug Administration (FDA). Each latex condom manufactured in the United States is tested electronically for holes before packaging. Rates of condom breakage during sexual intercourse and withdrawal are approximately two broken condoms per 100 condoms used in the United States. The failure of condoms to protect against STD transmission or unintended pregnancy usually results from inconsistent or incorrect use rather than condom breakage.
Male condoms made of materials other than latex are available in the United States. Although they have had higher breakage and slippage rates when compared with latex condoms and are usually more costly, the pregnancy rates among women whose partners use these condoms are similar to latex condoms. Two general categories of nonlatex condoms exist. The first type is made of polyurethane or other synthetic material and provides protection against STD/HIV and pregnancy equal to that of latex condoms. These can be substituted for persons with latex allergy. The second type is natural membrane condoms (frequently called "natural" condoms or, incorrectly, lambskin condoms). These condoms are usually made from lamb cecum and can have pores up to 1500 nm in diameter. Whereas these pores do not allow the passage of sperm, they are more than 10 times the diameter of HIV and more than 25 times that of HBV. Moreover, laboratory studies demonstrate that viral STD transmission can occur with natural membrane condoms. Using natural membrane condoms for protection against STDs is not recommended.
Patients should be advised that condoms must be used consistently and correctly to be effective in preventing STDs, and they should be instructed in the correct use of condoms. The following recommendations ensure the proper use of male condoms:
• Use a new condom with each sex act (e.g., oral, vaginal, and anal). • Carefully handle the condom to avoid damaging it with fingernails, teeth, or other sharp objects. • Put the condom on after the penis is erect and before any genital, oral, or anal contact with the partner. • Use only water-based lubricants (e.g., K-Y Jelly™, Astroglide™, AquaLube™, and glycerin) with latex condoms. Oil-based lubricants (e.g., petroleum jelly, shortening, mineral oil, massage oils, body lotions, and cooking oil) can weaken latex. • Ensure adequate lubrication during vaginal and anal sex, which might require the use of exogenous water-based lubricants. • To prevent the condom from slipping off, hold the condom firmly against the base of the penis during withdrawal, and withdraw while the penis is still erect.
# Female Condoms
Laboratory studies indicate that the female condom (Reality™), which consists of a lubricated polyurethane sheath with a ring on each end that is inserted into the vagina, is an effective mechanical barrier to viruses, including HIV, and to semen (21). A limited number of clinical studies have evalu-ated the efficacy of female condoms in providing protection from STDs, including HIV (22). If used consistently and correctly, the female condom might substantially reduce the risk for STDs. When a male condom cannot be used properly, sex partners should consider using a female condom. Female condoms are costly compared with male condoms. The female condom also has been used for STD/HIV protection during receptive anal intercourse (23). Whereas it might provide some protection in this setting, its efficacy is undefined.
# Vaginal Spermicides and Diaphragms
Vaginal spermicides containing nonoxynol-9 (N-9) are not effective in preventing cervical gonorrhea, chlamydia, or HIV infection (24). Furthermore, frequent use of spermicides containing N-9 has been associated with disruption of the genital epithelium, which might be associated with an increased risk for HIV transmission. Therefore, N-9 is not recommended for STD/HIV prevention. In case-control and crosssectional studies, diaphragm use has been demonstrated to protect against cervical gonorrhea, chlamydia, and trichomoniasis; a randomized controlled trial will be conducted. On the basis of all available evidence, diaphragms should not be relied on as the sole source of protection against HIV infection. Diaphragm and spermicide use have been associated with an increased risk for bacterial urinary tract infections in women.
# Condoms and N-9 Vaginal Spermicides
Condoms lubricated with spermicides are no more effective than other lubricated condoms in protecting against the transmission of HIV and other STDs, and those that are lubricated with N-9 pose the concerns that have been previously discussed. Use of condoms lubricated with N-9 is not recommended for STD/HIV prevention because spermicidecoated condoms cost more, have a shorter shelf-life than other lubricated condoms, and have been associated with urinary tract infection in young women.
# Rectal Use of N-9 Spermicides
Recent studies indicate that N-9 might increase the risk for HIV transmission during vaginal intercourse (24). Although similar studies have not been conducted among men who use N-9 spermicide during anal intercourse with other men, N-9 can damage the cells lining the rectum, which might provide a portal of entry for HIV and other sexually transmissible agents. Therefore, N-9 should not be used as a microbicide or lubricant during anal intercourse.
# Nonbarrier Contraception, Surgical Sterilization, and Hysterectomy
Sexually active women who are not at risk for pregnancy might incorrectly perceive themselves to be at no risk for STDs, including HIV infection. Contraceptive methods that are not mechanical barriers offer no protection against HIV or other STDs. Women who use hormonal contraception (e.g., oral contraceptives, Norplant™, and Depo-Provera™), have intrauterine devices (IUD), have been surgically sterilized, or have had hysterectomies should be counseled regarding the use of condoms and the risk for STDs, including HIV infection.
# Emergency Contraception (EC)
Emergency use of oral contraceptive pills containing levonorgesterol alone reduces the risk for pregnancy after unprotected intercourse by 89%. Pills containing a combination of ethinyl estradiol and either norgestrel or levonorgestrel can be used and reduce the risk for pregnancy by 75%. Emergency insertion of a copper IUD also is highly effective, reducing the risk by as much as 99%. EC with oral contraceptive pills should be initiated as soon as possible after unprotected intercourse and definitely within 120 hours (i.e., 5 days). The only medical contraindication to provision of EC is current pregnancy.
Providers who manage persons at risk for STDs should counsel women concerning the option for EC, if indicated, and provide it in a timely fashion if desired by the woman. Plan B (two 750 mcg levonorgestrel tablets) has been approved by FDA and is available in the United States for the prevention of unintended pregnancy. Additional information on EC is available in Contraceptive Technology, 18th edition (5), or at http://www.arhp.org/healthcareproviders/resources/ contraceptionresources.
# Postexposure Prophylaxis (PEP) for HIV
Guidelines for the use of PEP aimed at preventing HIV acquisition as a result of sexual exposure are available and are discussed in this report (see Sexual Assault and STDs).
# Partner Management
Partner notification, previously referred to as "contact tracing" but recently included in the broader category of partner services, is the process by which providers or public health authorities learn from persons with STDs about their sex partners and help to arrange for the evaluation and treatment of sex partners. Providers can seek this information and help to arrange for evaluation and treatment of sex partners, either directly or with assistance from state and local health departments. The intensity of partner services and the specific STDs for which they are offered vary among providers, agencies, and geographic areas. Ideally, such services should be accompanied by health counseling and might include referral of patients and their partners for other services, whenever appropriate.
In general, whether partner notification effectively decreases exposure to STDs and whether it changes the incidence and prevalence of STDs in a community are uncertain. The paucity of supporting evidence regarding the effectiveness of partner notification has spurred the exploration of alternative approaches. One such approach is to place partner notification in a larger context by making interventions in the sexual and social networks in which persons are exposed to STDs. Prospective evaluations incorporating assessment of venues, community structure, and social and sexual, contacts in conjunction with partner notification of efforts are promising in terms of increasing case-finding and warrant further exploration. The scope of such efforts probably precludes individual clinician efforts to use network-based approaches, but STDcontrol programs might find them useful.
Many persons individually benefit from partner notification. When partners are treated, index patients have reduced risk for reinfection. At a population level, partner notification can disrupt networks of STD transmission and reduce disease incidence. Therefore, providers should encourage their patients with STDs to notify their sex partners and urge them to seek medical evaluation and treatment, regardless of whether assistance is available from health agencies. When medical evaluation, counseling, and treatment of partners cannot be done because of the particular circumstances of a patient or partner or because of resource limitations, other partner management options can be considered. One option is patientdelivered therapy, a form of expedited partner therapy (EPT) in which partners of infected patients are treated without previous medical evaluation or prevention counseling (http:// www.cdc.gov/std/treatment/EPTFinalReport2006.pdf ). The evidence supporting patient-delivered therapy is based on three clinical trials that included heterosexual men and women with chlamydia or gonorrhea. The strength of the supporting evidence differed by STD and by the sex of the index case when reinfection of the index case was the measured outcome (25)(26)(27). Despite this variation, patient-delivered therapy (i.e., via medications or prescriptions) can prevent reinfection of index case and has been associated with a higher likelihood of partner notification, compared with unassisted patient referral of partners. Medications and prescriptions for patient-delivered therapy should be accompanied by treatment instructions, appropriate warnings about taking medications if pregnant, general health counseling, and advice that partners should seek personal medical evaluations, particularly women with symptoms of STDs or PID. Existing data suggest that EPT has a limited role in partner management for trichomoniasis (28). No data support its use in the routine management of syphilis. There is no experience with expedited partner therapy for gonorrhea or chlamydia infection among MSM. Currently, EPT is not feasible in many settings because of operational barriers, including the lack of clear legal status of EPT in some states.
# Reporting and Confidentiality
The accurate and timely reporting of STDs is integrally important for assessing morbidity trends, targeting limited resources, and assisting local health authorities in partner notification and treatment. STD/HIV and acquired immunodeficiency syndrome (AIDS) cases should be reported in accordance with state and local statutory requirements. Syphilis, gonorrhea, chlamydia, chanroid, HIV infection, and AIDS are reportable diseases in every state. The requirements for reporting other STDs differ by state, and clinicians should be familiar with state and local reporting requirements.
Reporting can be provider-and/or laboratory-based. Clinicians who are unsure of state and local reporting requirements should seek advice from state or local health departments or STD programs. STD and HIV reports are kept strictly confidential. In the majority of jurisdictions, such reports are protected by statute from subpoena. Before public health representatives conduct a follow-up of a positive STDtest result, they should consult the patient's health-care provider to verify the diagnosis and treatment.
# Special Populations Pregnant Women
Intrauterine or perinatally transmitted STDs can have severely debilitating effects on pregnant women, their partners, and their fetuses. All pregnant women and their sex partners should be asked about STDs, counseled about the possibility of perinatal infections, and ensured access to treatment, if needed.
# Recommended Screening Tests
• All pregnant women in the United States should be tested for HIV infection as early in pregnancy as possible. Testing should be conducted after the woman is notified that she will be tested for HIV as part of the routine panel of prenatal tests, unless she declines the test (i.e., opt-out screening). For women who decline HIV testing, providers should address their objections, and where appropriate, continue to strongly encourage testing. Women who decline testing because they have had a previous negative HIV test should be informed of the importance of retesting during each pregnancy. Testing pregnant women is vital not only to maintain the health of the patient but also because interventions (i.e., antiretroviral and obstetrical) are available that can reduce perinatal transmission of HIV. Retesting in the third trimester (i.e., preferably before 36 weeks' gestation) is recommended for women at high risk for acquiring HIV infection (i.e., women who use illicit drugs, have STDs during pregnancy, have multiple sex partners during pregnancy, or have HIV-infected partners). Rapid HIV testing should be performed on women in labor with undocumented HIV status. If a rapid HIV test result is positive, antiretroviral prophylaxis (with consent) should be administered without waiting for the results of the confirmatory test. • A serologic test for syphilis should be performed on all pregnant women at the first prenatal visit. In populations in which use of prenatal care is not optimal, rapid plasma reagin (RPR) card test screening (and treatment, if that test is reactive) should be performed at the time a pregnancy is confirmed. Women who are at high risk for syphilis, live in areas of high syphilis morbidity, are previously untested, or have positive serology in the first trimester should be screened again early in the third trimester (28 weeks' gestation) and at delivery. Some states require all women to be screened at delivery. Infants should not be discharged from the hospital unless the syphilis serologic status of the mother has been determined at least one time during pregnancy and preferably again at delivery. Any woman who delivers a stillborn infant should be tested for syphilis. • All pregnant women should be routinely tested for hepatitis B surface antigen (HBsAg) during an early prenatal visit (e.g., first trimester) in each pregnancy, even if they have been previously vaccinated or tested. Women who were not screened prenatally, those who engage in behaviors that put them at high risk for infection (e.g., more than one sex partner in the previous 6 months, evaluation or treatment for an STD, recent or current injectingdrug use, and HBsAg-positive sex partner), and those with clinical hepatitis should be retested at the time of admission to the hospital for delivery. Women at risk for HBV infection also should be vaccinated. To avoid misinterpreting a transient positive HBsAg result during the 21 days after vaccination, HBsAg testing should be performed before the vaccination. • All laboratories that conduct HBsAg tests should use an HBsAg test that is FDA-cleared and should perform testing according to the manufacturer's labeling, including testing of initially reactive specimens with a licensed neutralizing confirmatory test. When pregnant women are tested for HBsAg at the time of admission for delivery, shortened testing protocols may be used, and initially reactive results should prompt expedited administration of immunoprophylaxis to infants.
• All pregnant women should be routinely tested for Chlamydia trachomatis (see Chlamydia Infections, Diagnostic Considerations) at the first prenatal visit. Women aged <25 years and those at increased risk for chlamydia (i.e., women who have a new or more than one sex partner) also should be retested during the third trimester to prevent maternal postnatal complications and chlamydial infection in the infant. Screening during the first trimester might prevent the adverse effects of chlamydia during pregnancy, but supportive evidence for this is lacking. If screening is performed only during the first trimester, a longer period exists for acquiring infection before delivery. • All pregnant women at risk for gonorrhea or living in an area in which the prevalence of Neisseria gonorrhoeae is high should be tested at the first prenatal visit for N. gonorrhoeae. (See Gonococcal Infections, Diagnostic Considerations). A repeat test should be performed during the third trimester for those at continued risk. • All pregnant women at high risk for hepatitis C infection should be tested for hepatitis C antibodies (see Hepatitis C, Diagnostic Considerations) at the first prenatal visit. Women at high risk include those with a history of injecting-drug use and those with a history of blood transfusion or organ transplantion before 1992. • Evaluation for bacterial vaginosis (BV) might be conducted during the first prenatal visit for asymptomatic patients who are at high risk for preterm labor (e.g., those who have a history of a previous preterm delivery). Evidence does not support routine testing for BV. • A Papanicolaou (Pap) smear should be obtained at the first prenatal visit if none has been documented during the preceding year.
# Other Concerns
• Women who are HBsAg positive should be reported to the local and/or state health department to ensure that they are entered into a case-management system and that timely and appropriate prophylaxis is provided for their infants. Information concerning the pregnant woman's HBsAg status should be provided to the hospital in which delivery is planned and to the health-care provider who will care for the newborn. In addition, household and sex contacts of women who are HBsAg positive should be vaccinated. • Women who are HBsAg positive should be provided with, or referred for, appropriate counseling and medical management. Pregnant women who are HBsAg positive pregnant women should receive information regarding hepatitis B that addresses -modes of transmission;
MMWR August 4, 2006
-perinatal concerns (e.g., breastfeeding is not contraindicated); -prevention of HBV transmission, including the importance of postexposure prophylaxis for the newborn infant and hepatitis B vaccination for household contacts and sex partners; and -evaluation for and treatment of chronic HBV infection. • No treatment is available for HCV-infected pregnant women. However, all women with HCV infection should receive appropriate counseling and supportive care as needed (see Hepatitis C, Prevention). No vaccine is available to prevent HCV transmission. • In the absence of lesions during the third trimester, routine serial cultures for HSV are not indicated for women who have a history of recurrent genital herpes. Prophylactic cesarean section is not indicated for women who do not have active genital lesions at the time of delivery.
In addition, insufficient evidence exists to recommend routine HSV-2 serologic screening among previously undiagnosed women during pregnancy, nor does sufficient evidence exist to recommend routine antiviral suppressive therapy late in gestation for all HSV-2 positive women. • The presence of genital warts is not an indication for cesarean section. • Not enough evidence exists to recommend routine screening for Trichomonas vaginalis in asymptomatic pregnant women. For a more detailed discussion of STD testing and treatment among pregnant women and other infections not transmitted sexually, refer to the following references: Guide to Clinical Preventive Services (29); Guidelines for Perinatal Care (30) (41).
These sources are not entirely consistent in their recommendations. For example, the Guide to Clinical Preventive Services recommends screening of patients at high risk for chlamydia but indicates that the optimal timing for screening is uncertain. The Guidelines for Perinatal Care recommends that pregnant women at high risk for chlamydia be screened for infection during the first prenatal care visit and during the third trimester. Recommendations to screen pregnant women for STDs are based on disease severity and sequelae, prevalence in the population, costs, medicolegal considerations (e.g., state laws), and other factors. The screening recommendations in this report are broader (i.e., if followed, more women will be screened for more STDs than would be screened by following other recommendations) and are compatible with other CDC guidelines.
# Adolescents
The rates of many STDs are highest among adolescents. For example, the reported rates of chlamydia and gonorrhea are highest among females aged 15-19 years, and many persons acquire HPV infection during their adolescent years. Among adolescents with acute HBV infection, the most commonly reported risk factors are having sexual contact with a chronically infected person or with multiple sex partners, or reporting their sexual preference as homosexual. As part of a comprehensive strategy to eliminate HBV transmission in the United States, ACIP has recommended that all children and adolescents be administered HBV vaccine (2).
Younger adolescents (i.e., persons aged <15 years) who are sexually active are at particular risk for STDs, especially youth in detention facilities, STD clinic patients, male homosexuals, and injecting-drug users (IDUs). Adolescents are at higher risk for STDs because they frequently have unprotected intercourse, are biologically more susceptible to infection, are engaged in sexual partnerships frequently of limited duration, and face multiple obstacles to using health care. Several of these issues can be addressed by clinicians who provide services to adolescents. Clinicians can address adolescents' lack of knowledge and awareness regarding the risks and consequences of STDs by offering guidance concerning healthy sexual behavior and, therefore, prevent the establishment of patterns of behavior that can undermine sexual health.
With a few exceptions, all adolescents in the United States can legally consent to the confidential diagnosis and treatment of STDs. In all 50 states and the District of Columbia, medical care for STDs can be provided to adolescents without parental consent or knowledge. In addition, in the ma-jority of states, adolescents can consent to HIV counseling and testing. Consent laws for vaccination of adolescents differ by state. Several states consider provision of vaccine similar to treatment of STDs and provide vaccination services without parental consent. Because of the crucial importance of confidentially, health-care providers should follow policies that provide confidentiality and comply with state laws for STD services.
Despite the prevalence of STDs among adolescents, providers frequently fail to inquire about sexual behavior, assess risk for STDs, provide counseling on risk reduction, and screen for asymptomatic infection during clinical encounters. The style and content of counseling and health education on these sensitive subjects should be adapted for adolescents. Discussions should be appropriate for the patient's developmental level and should be aimed at identifying risky behaviors (e.g., sex and drug-use behaviors). Careful, nonjudgmental, and thorough counseling are particularly vital for adolescents who might not acknowledge that they engage in high-risk behaviors.
# Children
Management of children who have STDs requires close cooperation between clinicians, laboratorians, and childprotection authorities. Official investigations, when indicated, should be initiated promptly. Some diseases (e.g., gonorrhea, syphilis, and chlamydia), if acquired after the neonatal period, are virtually 100% indicative of sexual contact. For other diseases (e.g., HPV infection and vaginitis), the association with sexual contact is not as clear (see Sexual Assault and STDs).
# MSM
Some MSM are at high risk for HIV infection and other viral and bacterial STDs. The frequency of unsafe sexual practices and the reported rates of bacterial STDs and incident HIV infection have declined substantially in MSM from the 1980s through the mid-1990s. However, during the previous 10 years, increased rates of infectious syphilis, gonorrhea, and chlamydial infection and of higher rates of unsafe sexual behaviors have been documented among MSM in the United States and virtually all industrialized countries. The effect of these behavioral changes on HIV transmission has not been ascertained, but preliminary data suggest that the incidence of HIV infection might be increasing among some MSM. These adverse trends probably are related to changing attitudes concerning HIV infection because of the effects of improved HIV/AIDS therapy on quality of life and survival, changing patterns of substance abuse, demographic shifts in MSM populations, and changes in sex partner networks resulting from new venues for partner acquisition.
Clinicians should assess the risks of STDs for all male patients, including a routine inquiry about the sex of patients' sex partners. MSM, including those with HIV infection, should routinely undergo nonjudgmental STD/HIV risk assessment and client-centered prevention counseling to reduce the likelihood of acquiring or transmitting HIV or other STDs. Clinicians should be familiar with local community resources available to assist MSM at high risk in facilitating behavioral change. Clinicians also should routinely ask sexually active MSM about symptoms consistent with common STDs, including urethral discharge, dysuria, genital and perianal ulcers, regional lymphadenopathy, skin rash, and anorectal symptoms consistent with proctitis. Clinicians also should maintain a low threshold for diagnostic testing of symptomatic patients.
Routine laboratory screening for common STDs is indicated for all sexually active MSM. The following screening recommendations are based on preliminary data (42,43). These tests should be performed at least annually for sexually active MSM, including men with or without established HIV infection:
• HIV serology, if HIV negative or not tested within the previous year; • syphilis serology; • a test for urethral infection with N. gonorrhoeae and C. trachomatis in men who have had insertive intercourse* during the preceding year; • a test for rectal infection † with N. gonorrhoeae and C. trachomatis in men who have had receptive anal intercourse* during the preceding year; • a test for pharyngeal infection † with N. gonorrhoeae in men who have acknowledged participation in receptive oral intercourse* during the preceding year; testing for C. trachomatis pharyngeal infection is not recommended. In addition, some specialists would consider type-specific serologic tests for HSV-2, if infection status is unknown. Routine testing for anal cytologic abnormalities or anal HPV infection is not recommended until more data are available on the reliability of screening methods, the safety of and response to treatment, and programmatic considerations.
More frequent STD screening (i.e., at 3-6 month intervals) is indicated for MSM who have multiple or anonymous partners, have sex in conjunction with illicit drug use, use methamphetamine, or whose sex partners participate in these activities.
Vaccination against hepatitis A and B is recommended for all MSM in whom previous infection or immunization cannot be documented. Preimmunization serologic testing might be considered to reduce the cost of vaccinating MSM who are already immune to these infections, but this testing should not be delay vaccination. Vaccinating persons who are immune to HAV or HBV infection because of previous infection or vaccination does not increase the risk for vaccine-related adverse events (see Hepatitis B, Prevaccination Antibody Screening).
# Women Who Have Sex with Women (WSW)
Few data are available on the risk of STDs conferred by sex between women, but transmission risk probably varies by the specific STD and sexual practice (e.g., oral-genital sex, vaginal or anal sex using hands, fingers, or penetrative sex items, and oral-anal sex) (44,45). Practices involving digitalvaginal or digital-anal contact, particularly with shared penetrative sex items, present a possible means for transmission of infected cervicovaginal secretions. This possibility is most directly supported by reports of metronidazole-resistant trichomoniasis and genotype-concordant HIV transmitted sexually between women who reported these behaviors and by the high prevalence of BV among monogamous WSW. Transmission of HPV can occur with skin-to-skin or skin-tomucosa contact, which can occur during sex between women. HPV deoxyribonucleic acid (DNA) has been detected through polymerase chain reaction (PCR)-based methods from the cervix, vagina, and vulva in 13%-30% of WSW, and highand low-grade squamous intraepithelial lesions (SIL) have been detected on Pap tests in WSW who reported no previous sex with men (46). However, the majority of self-identified WSW (53%-99%) have had sex with men and might continue this practice (47). Therefore, all women should undergo Pap test screening using current national guidelines, regardless of sexual preference or sexual practices.
HSV-2 genital transmission between female sex partners is probably inefficient, but the relatively frequent practice of orogenital sex among WSW might place them at higher risk for genital infection with HSV-1. This hypothesis is supported by the recognized association between HSV-1 seropositivity and previous number of female partners among WSW. Transmission of syphilis between female sex partners, probably through oral sex, has been reported. Although the rate of transmission of C. trachomatis between women is unknown, WSW who also have sex with men are at risk and should undergo routine screening according to guidelines.
# HIV Infection: Detection, Counseling, and Referral
Infection with HIV produces a spectrum of disease that progresses from a clinically latent or asymptomatic state to AIDS as a late manifestation. The pace of disease progression varies. In untreated patients, the time between infection with HIV and the development of AIDS ranges from a few months to as long as 17 years (median: 10 years). The majority of adults and adolescents infected with HIV remain symptomfree for extended periods, but viral replication is active during all stages of infection and increases substantially as the immune system deteriorates. In the absence of treatment, AIDS will develop eventually in nearly all HIV-infected persons.
Improvements in antiretroviral therapy and increasing awareness among both patients and health-care providers of the risk factors associated with HIV transmission have led to more testing for HIV and earlier diagnosis, frequently before symptoms develop. However, the conditions of nearly 40% of persons who acquire HIV infection continue to be diagnosed late, within 1 year of acquiring AIDS. Prompt diagnosis of HIV infection is essential for multiple reasons. Treatments are available that slow the decline of immune system function; use of these therapies has been associated with substantial declines in HIV-associated morbidity and mortality in recent years. HIV-infected persons who have altered immune function are at increased risk for infections for which preventive measures are available (e.g., Pneumocystis jiroveci pneumonia, toxoplasma encephalitis [TE], disseminated Mycobacterium avium complex [MAC] disease, tuberculosis [TB], and bacterial pneumonia). Because of its effect on the immune system, HIV affects the diagnosis, evaluation, treatment, and follow-up of multiple other diseases and might affect the efficacy of antimicrobial therapy for some STDs. Finally, the early diagnosis of HIV enables health-care providers to counsel infected patients, refer them to various support services, and help prevent HIV transmission to others. Acutely infected persons might have elevated HIV viral loads and, therefore, might be more likely to transmit HIV to their partners (48,49).
Proper management of HIV infection involves a complex array of behavioral, psychosocial, and medical services. Although some services might not be available in STD treatment facilities. Therefore, referral to a health-care provider or facility experienced in caring for HIV-infected patients is advised. Providers working in STD-treatment facilities should be knowledgeable about the options for referral available in their communities. While receiving care in STD-treatment facilities, HIV-infected patients should be educated about HIV infection and the various options available for support services and HIV care.
A detailed discussion of the multiple, complex services required for management of HIV infection is beyond the scope of this section; however, this information is available in other published resources (6,9,50,51). In subsequent sections, this report provides information regarding diagnostic testing for HIV infection, counseling patients who have HIV infection, referral of patients for support services, including medical care, and the management of sex and injecting-drug partners in STD-treatment facilities. In addition, the report discusses HIV infection during pregnancy and in infants and children.
# Detection of HIV Infection: Screening and Diagnostic Testing
All persons who seek evaluation and treatment for STDs should be screened for HIV infection. Screening should be routine, regardless of whether the patient is known or suspected to have specific behavioral risks for HIV infection.
# Consent and Pretest Information
HIV screening should be voluntary and conducted only with the patient's knowledge and understanding that testing is planned. Persons should be informed orally or in writing that HIV testing will be performed unless they decline (i.e., opt-out screening). Oral or written communications should include an explanation of positive and negative test results, and patients should be offered an opportunity to ask questions and to decline testing.
# Prevention Counseling
Prevention counseling does not need to be explicitly linked to the HIV-testing process. However, some patients might be more likely to think about HIV and consider their risks when undergoing an HIV test. HIV testing might present an ideal opportunity to provide or arrange for prevention counseling to assist with behavior changes that can reduce risk for acquiring HIV infection. Prevention counseling should be offered and encouraged in all health-care facilities serving patients at high risk and in those (e.g., STD clinics) where information on HIV-risk behaviors is routinely elicited.
# Diagnostic Testing
HIV infection usually is diagnosed by tests for antibodies against HIV-1. Some combination tests also detect antibodies against HIV-2 (i.e., HIV-1/2). Antibody testing begins with a sensitive screening test (e.g., the enzyme immunoassay [EIA] or rapid test). The advent of HIV rapid testing has enabled clinicians to make a substantially accurate presumptive diagnosis of HIV-1 infection within half an hour. This testing can facilitate the identification of the more than 250,000 persons living with undiagnosed HIV in the United States. Reactive screening tests must be confirmed by a supplemental test (e.g., the Western blot [WB]) or an immunofluorescence assay (IFA) (52). If confirmed by a supplemental test, a positive antibody test result indicates that a person is infected with HIV and is capable of transmitting the virus to others. HIV antibody is detectable in at least 95% of patients within 3 months after infection. Although a negative antibody test result usually indicates that a person is not infected, antibody tests cannot exclude recent infection.
The majority of HIV infections in the United States are caused by HIV-1. However, HIV-2 infection should be suspected in persons who have epidemiologic risk factors, including being from West Africa (where HIV-2 is endemic) or have sex partners from endemic areas, have sex partners known to be infected with HIV-2, or have received a blood transfusion or nonsterile injection in a West African country. HIV-2 testing also is indicated when clinical evidence of HIV exists but tests for HIV-1 antibodies or HIV-1 viral load are not positive, or when HIV-1 WB results include the unusual indeterminate pattern of gag (p55, p24, p17) plus pol (p66, p51, p31) bands in the absence of env (gp160, gp120, gp41) bands.
Health-care providers should be knowledgeable about the symptoms and signs of acute retroviral syndrome, which is characterized by fever, malaise, lymphadenopathy, and skin rash. This syndrome frequently occurs in the first few weeks after HIV infection, before antibody test results become positive. Suspicion of acute retroviral syndrome should prompt nucleic acid testing (HIV plasma ribonucleic acid [RNA]) to detect the presence of HIV, although not all nucleic acid tests are approved for diagnostic purposes; a positive HIV nucleic acid test should be confirmed by subsequent antibody testing to document seroconversion (using standard methods, EIA, and WB). Acutely infected patients might be highly contagious because of increased plasma and genital HIV RNA concentrations and might be continuing to engage in risky behaviors (48,49). Current guidelines suggest that persons with recently acquired HIV infection might benefit from antiretroviral drugs and be candidates for clinical trials (53,54). Therefore, patients with acute HIV infection should be referred immediately to an HIV clinical care provider.
Diagnosis of HIV infection should prompt efforts to reduce the risk behavior that resulted in HIV infection and could result in transmission of HIV to others (55)
# Counseling for Patients with HIV Infection and Referral to Support Services
Persons can be expected to be distressed when first informed of a positive HIV test result. Such persons face multiple major adaptive challenges, including 1) accepting the possibility of a shortened life span, 2) coping with the reactions of others to a stigmatizing illness, 3) developing and adopting strategies for maintaining physical and emotional health, and 4) initiating changes in behavior to prevent HIV transmission to others. Many persons will require assistance with making reproductive choices, gaining access to health services, confronting possible employment or housing discrimination, and coping with changes in personal relationships. Therefore, behavioral and psychosocial services are an integral part of health care for HIV-infected persons. Such services should be available on site or through referral when HIV infection is diagnosed. A comprehensive discussion of specific recommendations is available in the Guidelines for HIV Counseling, Testing, and Referral and Revised Recommendations for HIV Screening of Pregnant Women (6). Innovative and successful interventions to decrease risk taking by HIV-infected patients have been developed for diverse populations (12).
Practice settings for offering HIV care differ depending on local resources and needs. Primary care providers and outpatient facilities should ensure that appropriate resources are available for each patient to avoid fragmentation of care. Although a single source that is capable of providing comprehensive care for all stages of HIV infection is preferred, the limited availability of such resources frequently results in the need to coordinate care among medical and social service providers in different locations. Providers should avoid long delays between diagnosis of HIV infection and access to additional medical and psychosocial services. The use of HIV rapid testing can help avoid unnecessary delays.
Recently identified HIV infection might not have been recently acquired. Persons newly diagnosed with HIV might be at any stage of infection. Therefore, health-care providers should be alert for symptoms or signs that suggest advanced HIV infection (e.g., fever, weight loss, diarrhea, cough, shortness of breath, and oral candidiasis). The presence of any of these symptoms should prompt urgent referral for specialty medical care. Similarly, providers should be alert for signs of psychologic distress and be prepared to refer patients accordingly.
Diagnosis of HIV infection reinforces the need to counsel patients regarding high-risk behaviors because the consequences of such behaviors include the risk for acquiring additional STDs and for transmitting HIV (and other STDs) to other persons. Such attention to behaviors in HIV-infected persons is consistent with national strategies for HIV prevention (55). Providers should refer patients for prevention counseling and risk-reduction support concerning high-risk behaviors (e.g., substance abuse and high-risk sexual behaviors). In multiple recent studies, researchers have developed successful prevention interventions for different HIV-infected populations that can be adapted to individuals (56,57).
Persons with newly diagnosed HIV infection who receive care in the STD treatment setting should be educated concerning what to expect as they enter medical care for HIV infection (51). In nonemergent situations, the initial evaluation of HIV-positive patients usually includes the following:
• a detailed medical history, including sexual and substance abuse history; vaccination history; previous STDs; and specific HIV-related symptoms or diagnoses; • a physical examination, including a gynecologic examination for women; • testing for N. gonorrhoeae and C. trachomatis (and for women, a Pap test and wet mount examination of vaginal secretions);
• complete blood and platelet counts and blood chemistry profile; • toxoplasma antibody test;
• tests for antibodies to HCV; testing for previous or present HAV or HBV infection is recommended if determined to be cost-effective before considering vaccination (see Hepatitis A and Hepatitis B); • syphilis serology; • a CD4 T-lymphocyte analysis and determination of HIV plasma viral load; • a tuberculin skin test (sometimes referred to as a purified protein derivative); • a urinalysis; and • a chest radiograph. Some specialists recommend type-specific testing for HSV-2 if herpes infection status is unknown. A first dose of hepatitis A and/or hepatitis B vaccination for previously unvaccinated persons for whom vaccine is recommended (see Hepatitis A and Hepatitis B) should be administered at this first visit.
In subsequent visits, when the results of laboratory and skin tests are available, antiretroviral therapy may be offered, if indicated, after initial antiretroviral resistance testing is performed (53) and specific prophylactic medications are administered to reduce the incidence of opportunistic infections (e.g., Pneumocystis jiroveci pneumonia, TE, disseminated MAC infection, and TB) (50). The vaccination series for hepatitis A and/or B should be offered for those in whom vaccination is recommended. Influenza vaccination should be offered annually, and pneumococcal vaccination should be given if it has not been administered in the previous 5 years (50,51).
Providers should be alert to the possibility of new or recurrent STDs and should treat such conditions aggressively. The occurrence of an STD in an HIV-infected person is an indication of high-risk behavior and should prompt referral for counseling. Because many STDs are asymptomatic, routine screening for curable STDs (e.g., syphilis, gonorrhea, and chlamydia) should be performed at least yearly for sexually active persons. Women should be screened for cervical cancer precursor lesions by annual Pap smears. More frequent STD screening might be appropriate depending on individual risk behaviors, the local epidemiology of STDs, and whether incident STDs are detected by screening or by the presence of symptoms.
Newly diagnosed HIV-infected persons should receive or be referred for a thorough psychosocial evaluation, including ascertainment of behavioral factors indicating risk for transmitting HIV. Patients might require referral for specific behavioral intervention (e.g., a substance abuse program), mental health disorders (e.g., depression), or emotional distress. They might require assistance with securing and maintaining employment and housing. Women should be counseled or appropriately referred regarding reproductive choices and contraceptive options. Patients with multiple psychosocial problems might be candidates for comprehensive riskreduction counseling and services (8).
The following are specific recommendations for HIV counseling and referral:
• (11,12). Involvement of nongovernment organizations and community-based organizations might complement such efforts in the clinical setting.
# Management of Sex Partners and Injecting-Drug Partners
Clinicians evaluating HIV-infected persons should collect information to determine whether any partners should be notified concerning possible exposure to HIV (6). When referring to persons who are infected with HIV, the term "partner" includes not only sex partners but also IDUs who share syringes or other injection equipment. The rationale for partner notification is that the early diagnosis and treatment of HIV infection in these partners might reduce morbidity and provides the opportunity to encourage risk-reducing behaviors. Partner notification for HIV infection should be confidential and depends on the voluntary cooperation of the patient. Specific guidance regarding spousal notification may vary by jurisdiction.
Two complementary notification processes, patient referral and provider referral, can be used to identify partners. With patient referral, patients directly inform their partners of their exposure to HIV infection. With provider referral, trained health department personnel locate partners on the basis of the names, descriptions, and addresses provided by the patient. During the notification process, the confidentiality of patients is protected; their names are not revealed to partners who are notified. Many state and local health departments provide these services.
The following are specific recommendations for implementing partner-notification procedures:
• HIV-infected patients should be encouraged to notify their partners and to refer them for counseling and testing. If requested by the patient, health-care providers should assist in this process, either directly or by referral to health department partner-notification programs. • If patients are unwilling to notify their partners or if they cannot ensure that their partners will seek counseling, physicians or health department personnel should use confidential partner notification procedures. • Partners who are contacted within 72 hours of a highrisk sexual or injecting-drug exposure to an HIV-infected partner, which involves exposure to genital secretions and/ or blood, should be offered PEP with combination antiretroviral therapy to complete a 28-day course (58).
# Special Considerations
Pregnancy. All pregnant women in the United States should be tested for HIV infection as early during pregnancy as possible. Testing should occur after the patient is notified that she will be tested for HIV as part of the routine panel of prenatal tests, unless she declines (i.e., opt-out screening) (30)(31)(32). For women who decline, providers should continue to strongly encourage testing and address concerns that pose obstacles to testing. Women who decline testing because they have had a previous negative HIV test should be informed of the importance of retesting during each pregnancy. Testing pregnant women is particularly important, not only to maintain the health of the patient, but also because interventions (i.e., antiretroviral and obstetrical) can reduce the risk of perinatal transmission of HIV.
After pregnant women have been identified as being HIVinfected, they should be educated about the risk of perinatal infection. Evidence indicates that, in the absence of antiretroviral and other interventions, 15%-25% of infants born to HIV-infected mothers will become infected with HIV; such evidence also indicates that an additional 12%-14% will become infected during breastfeeding where HIV-infected women breastfeed their infants into the second year of life (59,60).
The risk of perinatal HIV transmission can be reduced substantially to <2% through the use of antiretroviral regimens and obstetrical interventions (i.e., zidovudine or nevirapine and elective cesarean section at 38 weeks of pregnancy) and by avoiding breastfeeding (61). Pregnant women who are HIV infected should be counseled concerning their options (either on-site or by referral), given appropriate antenatal treatment, and advised not to breastfeed their infants (for women living in the United States, where infant formula is readily available and can be safely prepared).
HIV Infection Among Infants and Children. Diagnosis of HIV infection in a pregnant woman indicates the need to consider whether other children of the woman might be infected. Infants and young children with HIV infection differ from adults and adolescents with respect to the diagnosis, clinical presentation, and management of HIV disease. For example, because maternal HIV antibody passes through the placenta, antibody tests for HIV are expected to be positive in the sera of both infected and uninfected infants born to seropositive mothers. A definitive determination of HIV infection for an infant aged <18 months is usually based on HIV nucleic acid testing. Management of infants, children, and adolescents who are known or suspected to be infected with HIV requires referral to physicians familiar with the manifestations and treatment of pediatric HIV infection (50,51,62).
# Diseases Characterized by Genital Ulcers
# Management of Patients Who Have Genital Ulcers
In the United States, the majority of young, sexually active patients who have genital ulcers have either genital herpes, syphilis, or chancroid. The frequency of each condition differs by geographic area and patient population; however, genital herpes is the most prevalent of these diseases. More than one of these diseases can be present in a patient who has genital ulcers. All three of these diseases has been associated with an increased risk for HIV infection. Not all genital ulcers are caused by sexually transmitted infections.
A diagnosis based only on the patient's medical history and physical examination frequently is inaccurate. Therefore, all patients who have genital ulcers should be evaluated with a serologic test for syphilis and a diagnostic evaluation for genital herpes; in settings where chancroid is prevalent, a test for Haemophilus ducreyi should also be performed. Specific tests for evaluation of genital ulcers include 1) syphilis serology and either darkfield examination or direct immunofluorescence test for T. pallidum; 2) culture or antigen test for HSV; and 3) culture for H. ducreyi.
No FDA-cleared PCR test for these organisms is available in the United States; however, such testing can be performed by clinical laboratories that have developed their own tests and conducted a Clinical Laboratory Improvement Amendment (CLIA) verification study. Type-specific serology for HSV-2 might be helpful in identifying persons with genital herpes (see Genital Herpes, Type-Specific Serologic Tests). Biopsy of genital ulcers might be helpful in identifying the cause of ulcers that are unusual or that do not respond to initial therapy. HIV testing should be performed on all patients who have genital ulcers caused by T. pallidum or H. ducreyi, and should be strongly considered for those who have genital ulcers caused by HSV (see Diagnostic Considerations, sections, Syphilis, Chancroid, and Genital Herpes Simplex Virus).
Health-care providers frequently must treat patients before test results are available because early treatment decreases the possibility of ongoing transmission and because successful treatment of genital herpes depends on prompt initiation of therapy. The clinician should treat for the diagnosis considered most likely, on the basis of clinical presentation and epidemiologic circumstances. In some instances, treatment must be initiated for additional conditions because of diagnostic uncertainty. Even after complete diagnostic evaluation, at least 25% of patients who have genital ulcers have no laboratoryconfirmed diagnosis.
# Chancroid
In the United States, chancroid usually occurs in discrete outbreaks, although the disease is endemic in some areas. Chancroid is a cofactor for HIV transmission, as are genital herpes and syphilis; high rates of HIV infection among patients who have chancroid occur in the United States and other countries. Approximately 10% of persons who have chancroid that was acquired in the United States are coinfected with T. pallidum or HSV; this percentage is higher in persons who have acquired chancroid outside the United States.
A definitive diagnosis of chancroid requires the identification of H. ducreyi on special culture media that is not widely available from commercial sources; even when these media are used, sensitivity is <80%. No FDA-cleared PCR test for H. ducreyi is available in the United States, but such testing can be performed by clinical laboratories that have developed their own PCR test and conducted a CLIA verification study.
The combination of a painful genital ulcer and tender suppurative inguinal adenopathy suggests the diagnosis of chancroid. A probable diagnosis of chancroid, for both clinical and surveillance purposes, can be made if all of the following criteria are met: 1) the patient has one or more painful genital ulcers; 2) the patient has no evidence of T. pallidum infection by darkfield examination of ulcer exudate or by a serologic test for syphilis performed at least 7 days after onset of ulcers; 3) the clinical presentation, appearance of genital ulcers and, if present, regional lymphadenopathy are typical for chancroid; and 4) a test for HSV performed on the ulcer exudate is negative.
# Treatment
Successful treatment for chancroid cures the infection, resolves the clinical symptoms, and prevents transmission to others. In advanced cases, scarring can result, despite successful therapy.
# Recommended Regimens
# Other Management Considerations
Male patients who are uncircumcised and patients with HIV infection do not respond as well to treatment as those who are circumcised or HIV negative. Patients should be tested for HIV infection at the time chancroid is diagnosed. Patients should be retested for syphilis and HIV 3 months after the diagnosis of chancroid, if the initial test results were negative.
# Follow-Up
Patients should be reexamined 3-7 days after initiation of therapy. If treatment is successful, ulcers usually improve symptomatically within 3 days and objectively within 7 days after therapy. If no clinical improvement is evident, the clinician must consider whether 1) the diagnosis is correct, 2) the patient is coinfected with another STD, 3) the patient is infected with HIV, 4) the treatment was not used as instructed, or 5) the H. ducreyi strain causing the infection is resistant to the prescribed antimicrobial. The time required for complete healing depends on the size of the ulcer; large ulcers might require >2 weeks. In addition, healing is slower for some uncircumcised men who have ulcers under the foreskin. Clinical resolution of fluctuant lymphadenopathy is slower than resolution for ulcers and might require needle aspiration or incision and drainage. Although needle aspiration of chancroid buboes is a simple procedure, incision and drainage might be preferred because of a reduced need for repeat drainage procedures.
# Management of Sex Partners
Sex partners of patients who have chancroid should be examined and treated, regardless of whether symptoms of the disease are present, if they had sexual contact with the patient during the 10 days preceding the patient's onset of symptoms.
# Special Considerations
# Pregnancy
The safety and efficacy of azithromycin for pregnant and lactating women have not been established. Ciprofloxacin is contraindicated during pregnancy and lactation. No adverse effects of chancroid on pregnancy outcome have been reported.
# HIV Infection
HIV-infected patients who have chancroid should be monitored closely because, as a group, these patients are more likely to experience treatment failure and to have ulcers that heal more slowly. HIV-infected patients might require longer courses of therapy than those recommended for HIVnegative patients, and treatment failures can occur with any regimen. Because evidence is limited concerning the therapeutic efficacy of the recommended ceftriaxone and azithromycin regimens in HIV-infected patients, these regimens should be used for such patients only if follow-up can be ensured. Some specialists prefer the erythromycin 7-day regimen for treating HIV-infected persons.
# Genital HSV Infections
Genital herpes is a chronic, life-long viral infection. Two types of HSV have been identified, HSV-1 and HSV-2. The majority of cases of recurrent genital herpes are caused by HSV-2 although HSV-1 might become more common as a cause of first episode genital herpes. At least 50 million persons in the United States have genital HSV infection.
The majority of persons infected with HSV-2 have not been diagnosed with genital herpes. Many such persons have mild or unrecognized infections but shed virus intermittently in the genital tract. The majority of genital herpes infections are transmitted by persons unaware that they have the infection or who are asymptomatic when transmission occurs.
# Diagnosis of HSV Infection
The clinical diagnosis of genital herpes is both insensitive and nonspecific. The classical painful multiple vesicular or ulcerative lesions are absent in many infected persons. Up to 50% of first-episode cases of genital herpes are caused by HSV-1 (63), but recurrences and subclinical shedding are much less frequent for genital HSV-1 infection than genital HSV-2 infection (64,65). Therefore, whether genital herpes is caused by HSV-1 or HSV-2 influences prognosis and coun-seling. Therefore, the clinical diagnosis of genital herpes should be confirmed by laboratory testing (66). Both virologic and type-specific serologic tests for HSV should be available in clinical settings that provide care for patients with STDs or those at risk for STDs.
# Virologic Tests
Isolation of HSV in cell culture is the preferred virologic test for patients who seek medical treatment for genital ulcers or other mucocutaneous lesions. However, the sensitivity of culture is low, especially for recurrent lesions, and declines rapidly as lesions begin to heal. PCR assays for HSV DNA are more sensitive and have been used instead of viral culture (67,68); however, PCR tests are not FDA-cleared for testing of genital specimens. PCR is the test of choice for detecting HSV in spinal fluid for diagnosis of HSV infection of the central nervous system (CNS). Viral culture isolates should be typed to determine if HSV-1 or HSV-2 is the cause of the infection. Lack of HSV detection (i.e., culture or PCR) does not indicate a lack of HSV infection, as viral shedding is intermittent. The use of cytologic detection of cellular changes of HSV infection is an insensitive and nonspecific method of diagnosis, both for genital lesions (i.e., Tzanck preparation) and for cervical Pap smears and should not be relied upon.
# Type-Specific Serologic Tests
Both type-specific and nontype-specific antibodies to HSV develop during the first several weeks after infection and persist indefinitely. Accurate type-specific HSV serologic assays are based on the HSV-specific glycoprotein G2 (HSV-2) and glycoprotein G1 (HSV-1). Such assays first became commercially available in 1999, but older assays that do not accurately distinguish HSV-1 from HSV-2 antibody (despite claims to the contrary) remain on the market. Therefore, the serologic type-specific glycoprotein G (gG)-based assays should be specifically requested when serology is performed (69)(70)(71).
The FDA-cleared glycoprotein G-based type-specific assays include the laboratory-based assays HerpeSelect™-1 enzymelinked immunosorbent assay (ELISA) immunoglobulin G (IgG) or HerpeSelect™-2 ELISA IgG and HerpeSelect™ 1 and 2 Immunoblot IgG (Focus Technology, Inc., Herndon, Virginia), and HSV-2 ELISA (Trinity Biotech USA, Berkeley Heights, New Jersey). Two other assays, Biokit HSV-2 and SureVue HSV-2 (Biokit USA, Lexington, Massachusetts, and Fisher Scientific, Pittsburgh, Pennsylvania, respectively), are point-of-care tests that provide results for HSV-2 antibodies from capillary blood or serum during a clinic visit. The sensitivities of these glycoprotein G type-specific tests for the detection of HSV-2 antibody vary from 80%-98%, and false-negative results might be more frequent at early stages of infection. The specificities of these assays are >96%. Falsepositive results can occur, especially in patients with a low likelihood of HSV infection. Repeat or confirmatory testing might be indicated in some settings, especially if recent acquisition of genital herpes is suspected.
Because nearly all HSV-2 infections are sexually acquired, the presence of type-specific HSV-2 antibody implies anogenital infection and education and counseling appropriate for persons with genital herpes should be provided. The presence of HSV-1 antibody alone is more difficult to interpret. The majority of persons with HSV-1 antibody have oral HSV infection acquired during childhood, which might be asymptomatic. However, acquisition of genital HSV-1 appears to be increasing, and genital HSV-1 also might be asymptomatic. Lack of symptoms in an HSV-1 seropositive person does not distinguish anogenital from orolabial or cutaneous infection. Persons with HSV-1 infection, regardless of site of infection, remain at risk for HSV-2 acquisition.
Type-specific HSV serologic assays might be useful in the following scenarios: 1) recurrent genital symptoms or atypical symptoms with negative HSV cultures; 2) a clinical diagnosis of genital herpes without laboratory confirmation; and 3) a partner with genital herpes. Some specialists believe that HSV serologic testing should be included in a comprehensive evaluation for STDs among persons with multiple sex partners, HIV infection, and among MSM at increased risk for HIV acquisition. Screening for HSV-1 or HSV-2 in the general population is not indicated.
# Principles of Management of Genital Herpes
Antiviral chemotherapy offers clinical benefits to the majority of symptomatic patients and is the mainstay of management. Counseling regarding the natural history of genital herpes, sexual and perinatal transmission, and methods to reduce transmission is integral to clinical management.
Systemic antiviral drugs can partially control the signs and symptoms of herpes episodes when used to treat first clinical and recurrent episodes, or when used as daily suppressive therapy. However, these drugs neither eradicate latent virus nor affect the risk, frequency, or severity of recurrences after the drug is discontinued. Randomized trials have indicated that three antiviral medications provide clinical benefit for genital herpes: acyclovir, valacyclovir, and famciclovir (72)(73)(74)(75)(76)(77)(78)(79)(80). Valacyclovir is the valine ester of acyclovir and has enhanced absorption after oral administration. Famciclovir also has high oral bioavailability. Topical therapy with antiviral drugs offers minimal clinical benefit, and its use is discouraged.
# First Clinical Episode of Genital Herpes
Many persons with first-episode herpes have mild clinical manifestations but later develop severe or prolonged symptoms. Therefore, patients with initial genital herpes should receive antiviral therapy.
# Recommended Regimens*
Acyclovir 400 mg orally three times a day for 7-10 days OR Acyclovir 200 mg orally five times a day for 7-10 days OR Famciclovir 250 mg orally three times a day for 7-10 days OR Valacyclovir 1 g orally twice a day for 7-10 days
# Established HSV-2 infection
The majority of patients with symptomatic, first-episode genital HSV-2 infection subsequently experience recurrent episodes of genital lesions; recurrences are less frequent after initial genital HSV-1 infection. Intermittent asymptomatic shedding occurs in persons with genital HSV-2 infection, even in those with longstanding or clinically silent infection. Antiviral therapy for recurrent genital herpes can be administered either episodically to ameliorate or shorten the duration of lesions or continuously as suppressive therapy to reduce the frequency of recurrences. Many persons, including those with mild or infrequent recurrent outbreaks, benefit from antiviral therapy; therefore, options for treatment should be discussed. Some persons might prefer suppressive therapy, which has the additional advantage of decreasing the risk of genital HSV-2 transmission to susceptible partners (81).
# Suppressive Therapy for Recurrent Genital Herpes
Suppressive therapy reduces the frequency of genital herpes recurrences by 70%-80% in patients who have frequent recurrences (i.e., >6 recurrences per year), and many patients report no symptomatic outbreaks. Treatment also is effective in patients with less frequent recurrences. Safety and efficacy have been documented among patients receiving daily therapy with acyclovir for as long as 6 years and with valacyclovir or famciclovir for 1 year. Quality of life frequently is improved in patients with frequent recurrences who receive suppressive therapy, compared with episodic treatment.
The frequency of recurrent genital herpes outbreaks diminishes over time in many patients, and the patient's psychological adjustment to the disease might change. Therefore, periodically during suppressive treatment (e.g., once a year), providers should discuss the need to continue therapy with the patient. Daily treatment with valacyclovir 500 mg daily decreases the rate of HSV-2 transmission in discordant, heterosexual couples in which the source partner has a history of genital HSV-2 infection (82). Such couples should be encouraged to consider suppressive antiviral therapy as part of a strategy to prevent transmission, in addition to consistent condom use and avoidance of sexual activity during recurrences. Suppressive antiviral therapy probably reduces transmission when used by persons who have multiple partners (including MSM) and by those who are HSV-2 seropositive without a history of genital herpes.
# Recommended Regimens
Acyclovir 400 mg orally twice a day OR Famiciclovir 250 mg orally twice a day OR Valacyclovir 500 mg orally once a day OR Valacyclovir 1.0 g orally once a day Valacyclovir 500 mg once a day might be less effective than other valacyclovir or acyclovir dosing regimens in patients who have very frequent recurrences (i.e., >10 episodes per year). Several studies have compared valacyclovir or famciclovir with acyclovir. The results of these studies suggest that valacyclovir and famciclovir are comparable to acyclovir in clinical outcome (74,78,79,83). Ease of administration and cost also are important considerations for prolonged treatment.
# Episodic Therapy for Recurrent Genital Herpes
Effective episodic treatment of recurrent herpes requires initiation of therapy within 1 day of lesion onset or during the prodrome that precedes some outbreaks. The patient should be provided with a supply of drug or a prescription for the medication with instructions to initiate treatment immediately when symptoms begin.
# Recommended Regimens
Acyclovir 400 mg orally three times a day for 5 days OR Acyclovir 800 mg orally twice a day for 5 days OR Acyclovir 800 mg orally three times a day for 2 days OR Famciclovir 125 mg orally twice daily for 5 days OR Famciclovir 1000 mg orally twice daily for 1 day OR Valacyclovir 500 mg orally twice a day for 3 days OR Valacyclovir 1.0 g orally once a day for 5 days
# Severe Disease
Intravenous (IV) acyclovir therapy should be provided for patients who have severe HSV disease or complications that necessitate hospitalization (e.g., disseminated infection, pneumonitis, or hepatitis) or CNS complications (e.g., meningitis or encephalitis). The recommended regimen is acyclovir 5-10 mg/kg body weight IV every 8 hours for 2-7 days or until clinical improvement is observed, followed by oral antiviral therapy to complete at least 10 days of total therapy.
# Counseling
Counseling of infected persons and their sex partners is critical to the management of genital herpes. The goal of counseling is to 1) help patients cope with the infection and 2) prevent sexual and perinatal transmission (8). Although initial counseling can be provided at the first visit, many patients benefit from learning about the chronic aspects of the disease after the acute illness subsides. Multiple resources, including websites (http://www.ashastd.org and http://www.ihmf.org) and printed materials are available to assist patients, their partners, and clinicians in counseling.
HSV-infected persons might express anxiety concerning genital herpes that does not reflect the actual clinical severity of their disease; the psychological effect of HSV infection frequently is substantial. Common concerns regarding genital herpes include the severity of initial clinical manifestations, recurrent episodes, sexual relationships and transmission to sex partners, and ability to bear healthy children. The misconception that HSV causes cancer should be dispelled. The psychological effect of a serologic diagnosis of HSV-2 infection in a person with asymptomatic or unrecognized genital herpes appears small and transient (84).
The following recommendations apply to counseling of persons with HSV infection:
• Persons who have genital herpes should be educated concerning the natural history of the disease, with emphasis on the potential for recurrent episodes, asymptomatic viral shedding, and the attendant risks of sexual transmission. • Persons experiencing a first episode of genital herpes should be advised that suppressive therapy is available and is effective in preventing symptomatic recurrent episodes and that episodic therapy sometimes is useful in shortening the duration of recurrent episodes.
# Management of Sex Partners
The sex partners of patients who have genital herpes can benefit from evaluation and counseling. Symptomatic sex partners should be evaluated and treated in the same manner as patients who have genital lesions. Asymptomatic sex partners of patients who have genital herpes should be questioned concerning histories of genital lesions and offered type-specific serologic testing for HSV infection.
# Special Considerations
# Allergy, Intolerance, and Adverse Reactions
Allergic and other adverse reactions to acyclovir, valacyclovir, and famciclovir are rare. Desensitization to acyclovir has been described (85).
# HIV Infection
Immunocompromised patients might have prolonged or severe episodes of genital, perianal, or oral herpes. Lesions caused by HSV are common among HIV-infected patients and might be severe, painful, and atypical. HSV shedding is increased in HIV-infected persons. Whereas antiretroviral therapy reduces the severity and frequency of symptomatic genital herpes, frequent subclinical shedding still occurs (86). Suppressive or episodic therapy with oral antiviral agents is effective in decreasing the clinical manifestations of HSV among HIV-positive persons (87)(88)(89). HIV-infected persons are likely to be more contagious for HSV; the extent to which suppressive antiviral therapy will decrease HSV transmission from this population is unknown. Some specialists suggest that HSV type-specific serologies be offered to HIV-positive persons during their initial evaluation, and that suppressive antiviral therapy be considered in those who have HSV-2 infection.
# Recommended Regimens for Daily Suppressive Therapy in Persons Infected with HIV
Acyclovir 400-800 mg orally twice to three times a day OR Famciclovir 500 mg orally twice a day OR Valacyclovir 500 mg orally twice a day
# Recommended Regimens for Episodic Infection in Persons Infected with HIV
Acyclovir 400 mg orally three times a day for 5-10 days OR Famiciclovir 500 mg orally twice a day for 5-10 days OR Valacyclovir 1.0 grams orally twice a day for 5-10 days Acyclovir, valacyclovir, and famciclovir are safe for use in immunocompromised patients in the doses recommended for treatment of genital herpes. For severe HSV disease, initiating therapy with acyclovir 5-10 mg/kg body weight IV every 8 hours might be necessary.
If lesions persist or recur in a patient receiving antiviral treatment, HSV resistance should be suspected and a viral isolate should be obtained for sensitivity testing (90). Such patients should be managed in consultation with an HIV specialist, and alternate therapy should be administered. All acyclovir-resistant strains are resistant to valacyclovir, and the majority are resistant to famciclovir. Foscarnet, 40 mg/kg body weight IV every 8 hours until clinical resolution is attained, is frequently effective for treatment of acyclovir-resistant genital herpes. Topical cidofovir gel 1% applied to the lesions once daily for 5 consecutive days also might be effective. This preparation is not commercially available and must be compounded at a pharmacy.
# Genital Herpes in Pregnancy
The majority of mothers of infants who acquire neonatal herpes lack histories of clinically evident genital herpes. The risk for transmission to the neonate from an infected mother is high (30%-50%) among women who acquire genital herpes near the time of delivery and is low (<1%) among women with histories of recurrent herpes at term or who acquire genital HSV during the first half of pregnancy. However, because recurrent genital herpes is much more common than initial HSV infection during pregnancy, the proportion of neonatal HSV infections acquired from mothers with recurrent herpes is substantial. Prevention of neonatal herpes depends both on preventing acquisition of genital HSV infection during late pregnancy and avoiding exposure of the infant to herpetic lesions during delivery.
Women without known genital herpes should be counseled to avoid intercourse during the third trimester with partners known or suspected of having genital herpes. In addition, pregnant women without known orolabial herpes should be advised to avoid receptive oral sex during the third trimester with partners known or suspected to have orolabial herpes. Some specialists believe that type-specific serologic tests are useful to identify pregnant women at risk for HSV infection and to guide counseling regarding the risk for acquiring genital herpes during pregnancy. Such testing should be offered to women without genital herpes whose sex partner has HSV infection. The effectiveness of antiviral therapy to decrease the risk for HSV transmission to pregnant women has not been studied.
All pregnant women should be asked whether they have a history of genital herpes. At the onset of labor, all women should be questioned carefully about symptoms of genital herpes, including prodromal symptoms, and all women should be examined carefully for herpetic lesions. Women without symptoms or signs of genital herpes or its prodrome can deliver vaginally. The majority of specialists recommend that women with recurrent genital herpetic lesions at the onset of labor deliver by cesarean section to prevent neonatal herpes. However, cesarean section does not completely eliminate the risk for HSV transmission to the infant.
The safety of systemic acyclovir, valacyclovir, and famciclovir therapy in pregnant women has not been definitively established. Available data do not indicate an increased risk for major birth defects compared with the general population in women treated with acyclovir during the first trimester (91). These findings provide some assurance to women who have had prenatal exposure to acyclovir. The experience with prenatal exposure to valacyclovir and famciclovir is too limited to provide useful information on pregnancy outcomes. Acyclovir may be administered orally to pregnant women with first episode genital herpes or severe recurrent herpes and should be administered IV to pregnant women with severe HSV infection. Acyclovir treatment late in pregnancy reduces the frequency of cesarean sections among women who have recurrent genital herpes by diminishing the frequency of recurrences at term, and many specialists recommend such treatment (92)(93)(94). No data support the use of antiviral therapy among HSV seropositive women without a history of genital herpes. The risk for herpes is high in infants of women who acquire genital HSV during late pregnancy; such women should be managed in consultation with an infectious diseases specialist. Some specialists recommend acyclovir therapy in this circumstance, some recommend routine cesarean section to reduce the risk for neonatal herpes, and others recommend both.
# Neonatal Herpes
Infants exposed to HSV during birth, as documented by maternal virologic testing or presumed by observation of maternal lesions, should be followed carefully in consultation with a specialist. Some specialists recommend that such infants undergo surveillance cultures of mucosal surfaces to detect HSV infection before development of clinical signs of neonatal herpes. In addition, some specialists recommend the use of acyclovir for infants born to women who acquired HSV near term because the risk for neonatal herpes is high for these infants. All infants who have neonatal herpes should be promptly evaluated and treated with systemic acyclovir. The recommended regimen for infants treated for known or suspected neonatal herpes is acyclovir 20 mg/kg body weight IV every 8 hours for 21 days for disseminated and CNS disease or for 14 days for disease limited to the skin and mucous membranes.
# Granuloma Inguinale (Donovanosis)
Granuloma inguinale is a genital ulcerative disease caused by the intracellular gram-negative bacterium Klebsiella granulomatis (formerly known as Calymmatobacterium granulomatis). The disease occurs rarely in the United States, although it is endemic in some tropical and developing areas, including India; Papua, New Guinea; central Australia; and southern Africa. Clinically, the disease is commonly characterized as painless, progressive ulcerative lesions without regional lymphadenopathy. The lesions are highly vascular (i.e., beefy red appearance) and bleed easily on contact. However, the clinical presentation also can include hypertrophic, necrotic, or sclerotic variants. The causative organism is difficult to culture, and diagnosis requires visualization of dark-staining Donovan bodies on tissue crush preparation or biopsy. No FDA-cleared PCR tests for the detection of K. granulomatis DNA exist, but such an assay might be useful if a CLIA verification study has been conducted. The lesions might develop secondary bacterial infection or can coexist with other sexually transmitted pathogens.
# Treatment
A limited number of studies on Donovanosis treatment have been published. Treatment halts progression of lesions, although prolonged therapy is usually required to permit granulation and reepithelialization of the ulcers. Healing typically proceeds inward from the ulcer margins. Relapse can occur 6-18 months after apparently effective therapy. Several antimicrobial regimens have been effective, but a limited number of controlled trials have been published (95).
# Recommended Regimen
Doxycycline 100 mg orally twice a day for at least 3 weeks and until all lesions have completely healed
# Alternative Regimens
Azithromycin 1 g orally once per week for at least 3 weeks and until all lesions have completely healed OR Ciprofloxacin 750 mg orally twice a day for at least 3 weeks and until all lesions have completely healed OR Erythromycin base 500 mg orally four times a day for at least 3 weeks and until all lesions have completely healed OR Trimethoprim-sulfamethoxazole one double-strength (160 mg/800 mg) tablet orally twice a day for at least 3 weeks and until all lesions have completely healed Therapy should be continued at least 3 weeks and until all lesions have completely healed. Some specialists recommend the addition of an aminoglycoside (e.g., gentamicin 1 mg/kg IV every 8 hours) to these regimens if improvement is not evident within the first few days of therapy.
# Follow-Up
Patients should be followed clinically until signs and symptoms have resolved.
# Management of Sex Partners
Persons who have had sexual contact with a patient who has granuloma inguinale within the 60 days before onset of the patient's symptoms should be examined and offered therapy. However, the value of empiric therapy in the absence of clinical signs and symptoms has not been established.
# Special Considerations
# Pregnancy
Pregnancy is a relative contraindication to the use of sulfonamides. Pregnant and lactating women should be treated with the erythromycin regimen, and consideration should be given to the addition of a parenteral aminoglycoside (e.g., gentamicin). Azithromycin might prove useful for treating granuloma inguinale during pregnancy, but published data are lacking. Doxycycline and ciprofloxacin are contraindicated in pregnant women.
# HIV Infection
Persons with both granuloma inguinale and HIV infection should receive the same regimens as those who are HIV negative. Consideration should be given to the addition of a parenteral aminoglycoside (e.g., gentamicin).
# Lymphogranuloma Venereum
Lymphogranuloma venereum (LGV) is caused by C. trachomatis serovars L1, L2, or L3 (96). The most common clinical manifestation of LGV among heterosexuals is tender inguinal and/or femoral lymphadenopathy that is typically unilateral. A self-limited genital ulcer or papule sometimes occurs at the site of inoculation. However, by the time patients seek care, the lesions might have disappeared. Rectal exposure in women or MSM might result in proctocolitis (including mucoid and/or hemorrhagic rectal discharge, anal pain, constipation, fever, and/or tenesmus).
LGV is an invasive, systemic infection, and if it is not treated early, LGV proctocolitis might lead to chronic, colorectal fistulas and strictures. Genital and colorectal LGV lesions might also develop secondary bacterial infection or might be coinfected with other sexually and nonsexually transmitted pathogens.
Diagnosis is based on clinical suspicion, epidemiologic information, and the exclusion of other etiologies (of proctocolitis, inguinal lymphadenopathy, or genital or rectal ulcers), along with C. trachomatis testing, if available.
Genital and lymph node specimens (i.e., lesion swab or bubo aspirate) may be tested for C. trachomatis by culture, direct immunofluorescence, or nucleic acid detection. Nucleic acid amplification tests (NAAT) for C. trachomatis are not FDAcleared for testing rectal specimens. Additional procedures (e.g., genotyping) are required for differentiating LGV from non-LGV C. trachomatis but are not widely available.
Chlamydia serology (complement fixation titers >1:64) can support the diagnosis in the appropriate clinical context. Comparative data between types of serologic tests are lacking, and the diagnostic utility of serologic methods other than complement fixation and some microimmunofluorescence procedures has not been established. Serologic test interpretation for LGV is not standardized, tests have not been validated for clinical proctitis presentations, and C. trachomatis serovar-specific serologic tests are not widely available.
In the absence of specific LGV diagnostic testing, patients with a clinical syndrome consistent with LGV, including proctocolitis or genital ulcer disease with lymphadenopathy, should be treated for LGV as described in this report.
# Treatment
Treatment cures infection and prevents ongoing tissue damage, although tissue reaction to the injection can result in scarring. Buboes might require aspiration through intact skin or incision and drainage to prevent the formation of inguinal/ femoral ulcerations. Doxycycline is the preferred treatment.
# Recommended Regimen
# Doxycycline 100 mg orally twice a day for 21 days
# Alternative Regimen
Erythromycin base 500 mg orally four times a day for 21 days Some STD specialists believe that azithromycin 1.0 g orally once weekly for 3 weeks is probably effective, although clinical data are lacking.
# Follow-Up
Patients should be followed clinically until signs and symptoms have resolved.
# Management of Sex Partners
Persons who have had sexual contact with a patient who has LGV within the 60 days before onset of the patient's symptoms should be examined, tested for urethral or cervical chlamydial infection, and treated with a standard chlamydia regimen (azithromycin 1 gm orally x 1 or doxycycline 100 mg orally twice a day for 7 days). The optimum contact interval is unknown; some specialists use longer contact intervals.
# Special Considerations
# Pregnancy
Pregnant and lactating women should be treated with erythromycin. Azithromycin might prove useful for treatment of LGV in pregnancy, but no published data are available regarding its safety and efficacy. Doxycycline is contraindicated in pregnant women.
# HIV Infection
Persons with both LGV and HIV infection should receive the same regimens as those who are HIV negative. Prolonged therapy might be required, and delay in resolution of symptoms might occur.
# Syphilis General Principles
# Background
Syphilis is a systemic disease caused by T. pallidum. Patients who have syphilis might seek treatment for signs or symptoms of primary infection (i.e., ulcer or chancre at the infection site), secondary infection (i.e., manifestations that include, but are not limited to, skin rash, mucocutaneous lesions, and lymphadenopathy), or tertiary infection (e.g., cardiac or ophthalmic manifestations, auditory abnormalities, or gummatous lesions). Latent infections (i.e., those lacking clinical manifestations) are detected by serologic testing. Latent syphilis acquired within the preceding year is referred to as early latent syphilis; all other cases of latent syphilis are either late latent syphilis or latent syphilis of unknown duration. Treatment for both late latent syphilis and tertiary syphilis theoretically might require a longer duration of therapy because organisms are dividing more slowly; however, the validity of this concept has not been assessed.
# Diagnostic Considerations and Use of Serologic Tests
Darkfield examinations and direct fluorescent antibody (DFA) tests of lesion exudate or tissue are the definitive methods for diagnosing early syphilis. A presumptive diagnosis is possible with the use of two types of serologic tests: 1) nontreponemal tests (e.g., Venereal Disease Research Laboratory [VDRL] and RPR) and 2) treponemal tests (e.g., fluorescent treponemal antibody absorbed [FTA-ABS] and T. pallidum particle agglutination [TP-PA]). The use of only one type of serologic test is insufficient for diagnosis because false-positive nontreponemal test results are sometimes associated with various medical conditions unrelated to syphilis.
Nontreponemal test antibody titers usually correlate with disease activity, and results should be reported quantitatively. A fourfold change in titer, equivalent to a change of two dilutions (e.g., from 1:16-1:4 or from 1:8-1:32), is considered necessary to demonstrate a clinically significant difference between two nontreponemal test results that were obtained using the same serologic test. Sequential serologic tests in individual patients should be performed by using the same testing method (e.g., VDRL or RPR), preferably by the same laboratory. The VDRL and RPR are equally valid assays, but quantitative results from the two tests cannot be compared directly because RPR titers frequently are slightly higher than VDRL titers. Nontreponemal tests usually become nonreactive with time after treatment; however, in some patients, nontreponemal antibodies can persist at a low titer for a long period of time, sometimes for the life of the patient. This response is referred to as the serofast reaction.
The majority of patients who have reactive treponemal tests will have reactive tests for the remainder of their lives, regardless of treatment or disease activity. However, 15%-25% of patients treated during the primary stage revert to being serologically nonreactive after 2-3 years (97). Treponemal test antibody titers do not correlate with disease activity and should not be used to assess treatment response.
Some clinical laboratories and blood banks have begun to screen samples using treponemal EIA tests (98). This strategy will identify both persons with previous treatment and persons with untreated or incompletely treated syphilis. Falsepositive results can occur, particularly among populations with a low prevalence of syphilis.
Persons with a positive treponemal screening test should have a standard nontreponemal test with titer to guide patient management decisions. If the nontreponemal test is negative, then a different treponemal test should be performed to confirm the results of the initial test. If a second trepomenal test is positive, treatment decisions should be discussed in consultation with a specialist. Some HIV-infected patients can have atypical serologic test results (i.e., unusually high, unusually low, or fluctuating titers). For such patients, when serologic tests do not correspond with clinical syndromes suggestive of early syphilis, use of other tests (e.g., biopsy and direct microscopy) should be considered. However, for the majority of HIV-infected patients, serologic tests are accurate and reliable for the diagnosis of syphilis and for following the response to treatment.
No single test can be used to diagnose neurosyphilis. The VDRL-cerebrospinal fluid (CSF) is highly specific, but it is insensitive. The majority of other tests are both insensitive and nonspecific and must be interpreted in relation to other test results and the clinical assessment. Therefore, the diagno-sis of neurosyphilis usually depends on various combinations of reactive serologic test results, CSF cell count or protein, or a reactive VDRL-CSF with or without clinical manifestations. The CSF leukocyte count usually is elevated (>5 white blood cell count [WBC]/mm 3 ) in patients with neurosyphilis; this count also is a sensitive measure of the effectiveness of therapy. The VDRL-CSF is the standard serologic test for CSF, and when reactive in the absence of substantial contamination of CSF with blood, it is considered diagnostic of neurosyphilis. However, the VDRL-CSF might be nonreactive even when neurosyphilis is present. Some specialists recommend performing an FTA-ABS test on CSF. The CSF FTA-ABS is less specific (i.e., yields more false-positive results) for neurosyphilis than the VDRL-CSF, but the test is highly sensitive. Therefore, some specialists believe that a negative CSF FTA-ABS test excludes neurosyphilis.
# Treatment
Penicillin G, administered parenterally, is the preferred drug for treatment of all stages of syphilis. The preparation(s) used (i.e., benzathine, aqueous procaine, or aqueous crystalline), the dosage, and the length of treatment depend on the stage and clinical manifestations of the disease. However, neither combinations of benzathine penicillin and procaine penicillin nor oral penicillin preparations are considered appropriate for the treatment of syphilis. Reports have indicated that inappropriate use of combination benzathine-procaine penicillin (Bicillin C-R ® ) instead of the standard benzathine penicillin product widely used in the United States (Bicillin L-A ® ) has occurred. Practitioners, pharmacists, and purchasing agents should be aware of the similar names of these two products and avoid use of the inappropriate combination therapy agent for treating syphilis (99).
The efficacy of penicillin for the treatment of syphilis was well established through clinical experience even before the value of randomized controlled clinical trials was recognized. Therefore, nearly all the recommendations for the treatment of syphilis are based on the opinions of persons knowledgeable about STDs and are reinforced by case series, clinical trials, and 50 years of clinical experience.
Parenteral penicillin G is the only therapy with documented efficacy for syphilis during pregnancy. Pregnant women with syphilis in any stage who report penicillin allergy should be desensitized and treated with penicillin. Skin testing for penicillin allergy might be useful in pregnant women; such testing also is useful in other patients (see Management of Patients Who Have a History of Penicillin Allergy).
The Jarisch-Herxheimer reaction is an acute febrile reaction frequently accompanied by headache, myalgia, and other symptoms that usually occur within the first 24 hours after any therapy for syphilis. Patients should be informed about this possible adverse reaction. The Jarisch-Herxheimer reaction occurs most frequently among patients who have early syphilis. Antipyretics may be used, but they have not been proven to prevent this reaction. The Jarisch-Herxheimer reaction might induce early labor or cause fetal distress in pregnant women, but this should not prevent or delay therapy (see Syphilis During Pregnancy).
# Management of Sex Partners
Sexual transmission of T. pallidum occurs only when mucocutaneous syphilitic lesions are present; such manifestations are uncommon after the first year of infection. However, persons exposed sexually to a patient who has syphilis in any stage should be evaluated clinically and serologically and treated with a recommended regimen, according to the following recommendations:
• Persons who were exposed within the 90 days preceding the diagnosis of primary, secondary, or early latent syphilis in a sex partner might be infected even if seronegative; therefore, such persons should be treated presumptively. • Persons who were exposed >90 days before the diagnosis of primary, secondary, or early latent syphilis in a sex partner should be treated presumptively if serologic test results are not available immediately and the opportunity for follow-up is uncertain. • For purposes of partner notification and presumptive treatment of exposed sex partners, patients with syphilis of unknown duration who have high nontreponemal serologic test titers (i.e., >1:32) can be assumed to have early syphilis. However, serologic titers should not be used to differentiate early from late latent syphilis for the purpose of determining treatment (see Latent Syphilis, Treatment). • Long-term sex partners of patients who have latent syphilis should be evaluated clinically and serologically for syphilis and treated on the basis of the evaluation findings. For identification of at-risk sexual partners, the periods before treatment are 1) 3 months plus duration of symptoms for primary syphilis, 2) 6 months plus duration of symptoms for secondary syphilis, and 3) 1 year for early latent syphilis.
# Primary and Secondary Syphilis
# Treatment
Parenteral penicillin G has been used effectively for more than 50 years to achieve clinical resolution (i.e., healing of lesions and prevention of sexual transmission) and to prevent late sequelae. However, no comparative trials have been adequately conducted to guide the selection of an optimal penicillin regimen (i.e., the dose, duration, and preparation). Substantially fewer data are available for nonpenicillin regimens.
# Recommended Regimen for Adults*
Benzathine penicillin G 2.4 million units IM in a single dose * Recommendations for treating HIV-infected persons and pregnant women for syphilis have been discussed in this report (see Syphilis, Special considerations and Syphilis in Pregnancy).
# Recommended Regimen for Children
After the newborn period (aged >1 month), children with syphilis should have a CSF examination to detect asymptomatic neurosyphilis, and birth and maternal medical records should be reviewed to assess whether such children have congenital or acquired syphilis (see Congenital Syphilis). Children with acquired primary or secondary syphilis should be evaluated (e.g., through consultation with child-protection services) (see Sexual Assault or Abuse of Children) and treated by using the following pediatric regimen.
Benzathine penicillin G 50,000 units/kg IM, up to the adult dose of 2.4 million units in a single dose
# Other Management Considerations
All patients who have syphilis should be tested for HIV infection. In geographic areas in which the prevalence of HIV is high, patients who have primary syphilis should be retested for HIV after 3 months if the first HIV test result was negative.
Patients who have syphilis and symptoms or signs suggesting neurologic disease (e.g., meningitis) or ophthalmic disease (e.g., uveitis, iritis, neuroretinitis, or optic neuritis) should have an evaluation that includes CSF analysis and ocular slitlamp examination. Treatment should be guided by the results of this evaluation.
Invasion of CSF by T. pallidum accompanied by CSF abnormalities is common among adults who have primary or secondary syphilis. However, neurosyphilis develops in only a limited number of patients after treatment with the penicillin regimens recommended for primary and secondary syphilis. Therefore, unless clinical signs or symptoms of neurologic or ophthalmic involvement are present, CSF analysis is not recommended for routine evaluation of patients who have primary or secondary syphilis.
# Follow-Up
Treatment failure can occur with any regimen. However, assessing response to treatment frequently is difficult, and definitive criteria for cure or failure have not been established. Nontreponemal test titers might decline more slowly for persons who previously had syphilis. Patients should be reexamined clinically and serologically 6 months and 12 months after treatment; more frequent evaluation might be prudent if follow-up is uncertain.
Patients who have signs or symptoms that persist or recur or who have a sustained fourfold increase in nontreponemal test titer (i.e., compared with the maximum or baseline titer at the time of treatment) probably failed treatment or were reinfected. These patients should be retreated and reevaluated for HIV infection. Because treatment failure usually cannot be reliably distinguished from reinfection with T. pallidum, a CSF analysis also should be performed. Clinical trial data have demonstrated that 15% of patients with early syphilis treated with the recommended therapy will not achieve a two dilution decline in nontreponemal titer used to define response at 1 year after treatment (100).
Failure of nontreponemal test titers to decline fourfold within 6 months after therapy for primary or secondary syphilis might be indicative of probable treatment failure. Persons for whom titers remain serofast should be reevaluated for HIV infection. Optimal management of such patients is unclear. At a minimum, these patients should receive additional clinical and serologic follow-up. HIV-infected patients should be evaluated more frequently (i.e., at 3-month intervals instead of 6-month intervals). If additional follow-up cannot be ensured, re-treatment is recommended. Because treatment failure might be the result of unrecognized CNS infection, many specialists recommend CSF examination in such situations.
For retreatment, the majority of STD specialists recommend administering weekly injections of benzathine penicillin G 2.4 million units IM for 3 weeks, unless CSF examination indicates that neurosyphilis is present. In rare instances, serologic titers do not decline despite a negative CSF examination and a repeated course of therapy. Additional therapy or repeated CSF examinations are not warranted in these circumstances.
# Management of Sex Partners
See General Principles, Management of Sex Partners.
# Special Considerations
Penicillin Allergy. Data to support the use of alternatives to penicillin in the treatment of early syphilis are limited. However, several therapies might be effective in nonpregnant, penicillin-allergic patients who have primary or secondary syphilis. Doxycycline (100 mg orally twice daily for 14 days) and tetracycline (500 mg four times daily for 14 days) are regimens that have been used for many years. Compliance is likely to be better with doxycycline than tetracycline because tetracycline can cause gastrointestinal side effects. Although limited clinical studies, along with biologic and pharmacologic evidence, suggest that ceftriaxone is effective for treating early syphilis, the optimal dose and duration of ceftriaxone therapy have not been defined. Some specialists recommend 1 g daily either IM or IV for 8-10 days. Some patients who are allergic to penicillin also might be allergic to ceftriaxone; in these circumstances, use of an alternative agent might be required. Preliminary data suggest that azithromycin might be effective as a single oral dose of 2 g (101,102). However, several cases of azithromycin treatment failure have been reported, and resistance to azithromycin has been documented in several geographic areas (103). Close follow-up of persons receiving alternative therapies is essential. The use of any of these therapies in HIV-infected persons has not been wellstudied; therefore, the use of doxycycline, ceftriaxone, and azithromycin among such persons must be undertaken with caution.
Patients with penicillin allergy whose compliance with therapy or follow-up cannot be ensured should be desensitized and treated with benzathine penicillin. Skin testing for penicillin allergy might be useful in some circumstances in which the reagents and expertise are available to perform the test adequately (see Management of Patients Who Have a History of Penicillin Allergy).
Pregnancy. Pregnant patients who are allergic to penicillin should be desensitized and treated with penicillin (see Management of Patients Who Have a History of Penicillin Allergy and Syphilis During Pregnancy).
HIV Infection. See Syphilis Among HIV-Infected Persons.
# Latent Syphilis
Latent syphilis is defined as syphilis characterized by seroreactivity without other evidence of disease. Patients who have latent syphilis and who acquired syphilis within the preceding year are classified as having early latent syphilis. Patients' conditions can be diagnosed as early latent syphilis if, within the year preceding the evaluation, they had 1) a documented seroconversion or fourfold or greater increase in titer of a nontreponemal test; 2) unequivocal symptoms of primary or secondary syphilis; 3) a sex partner documented to have primary, secondary, or early latent syphilis; or 4) reactive nontreponemal and treponemal tests from a person whose only possible exposure occurred within the previous 12 months. Nontreponemal serologic titers usually are higher during early latent syphilis than late latent syphilis. However, early latent syphilis cannot be reliably distinguished from late latent syphilis solely on the basis of nontreponemal titers. All patients with latent syphilis should have careful examination of all accessible mucosal surfaces (i.e., the oral cavity, the perineum in women, and perianal area, underneath the foreskin in uncircumcised men) to evaluate for internal mucosal lesions. All patients who have syphilis should be tested for HIV infection.
# MMWR August 4, 2006
# Treatment
Treatment of latent syphilis usually does not affect transmission and is intended to prevent late complications. Although clinical experience supports the effectiveness of penicillin in achieving this goal, limited evidence is available for guidance in choosing specific regimens.
The following regimens are recommended for penicillin nonallergic patients who have normal CSF examinations (if performed).
# Recommended Regimens for Adults
# Early Latent Syphilis
Benzathine penicillin G 2.4 million units IM in a single dose Late Latent Syphilis or Latent Syphilis of Unknown Duration Benzathine penicillin G 7.2 million units total, administered as 3 doses of 2.4 million units IM each at 1week intervals
After the newborn period, children with syphilis should have a CSF examination to exclude neurosyphilis. In addition, birth and maternal medical records should be reviewed to assess whether children have congenital or acquired syphilis (see Congenital Syphilis). Older children with acquired latent syphilis should be evaluated as described for adults and treated using the following pediatric regimens (see Sexual Assault or Abuse of Children). These regimens are for penicillin nonallergic children who have acquired syphilis and who have normal CSF examination results.
# Recommended Regimens for Children
# Early Latent Syphilis
Benzathine penicillin G 50,000 units/kg IM, up to the adult dose of 2.4 million units in a single dose Late Latent Syphilis or Latent Syphilis of Unknown Duration Benzathine penicillin G 50,000 units/kg IM, up to the adult dose of 2.4 million units, administered as 3 doses at 1-week intervals (total 150,000 units/kg up to the adult total dose of 7.2 million units)
# Other Management Considerations
All persons who have latent syphilis should be evaluated clinically for evidence of tertiary disease (e.g., aortitis and gumma) and syphilitic ocular disease (e.g., iritis and uveitis). Patients who have syphilis and who demonstrate any of the following criteria should have a prompt CSF examination:
• neurologic or ophthalmic signs or symptoms,
• evidence of active tertiary syphilis (e.g., aortitis and gumma), • treatment failure, or • HIV infection with late latent syphilis or syphilis of unknown duration. If dictated by circumstances and patient preferences, a CSF examination may be performed for patients who do not meet these criteria. Some specialists recommend performing a CSF examination on all patients who have latent syphilis and a nontreponemal serologic test of >1:32 or if the patient is HIVinfected with a serum CD4 count <350 (104). However, the likelihood of neurosyphilis in this circumstance is unknown. If a CSF examination is performed and the results indicate abnormalities consistent with neurosyphilis, the patient should be treated for neurosyphilis (see Neurosyphilis).
If a patient misses a dose of penicillin in a course of weekly therapy for late syphilis, the appropriate course of action is unclear. Pharmacologic considerations suggest that an interval of 10-14 days between doses of benzathine penicillin for late syphilis or latent syphilis of unknown duration might be acceptable before restarting the sequence of injections. Missed doses are not acceptable for pregnant patients receiving therapy for late latent syphilis; pregnant women who miss any dose of therapy must repeat the full course of therapy.
Follow-Up. Quantitative nontreponemal serologic tests should be repeated at 6, 12, and 24 months. Patients with a normal CSF examination should be re-treated for latent syphilis if 1) titers increase fourfold, 2) an initially high titer (>1:32) fails to decline at least fourfold (i.e., two dilutions) within 12-24 months of therapy, or 3) signs or symptoms attributable to syphilis develop. In rare instances, despite a negative CSF examination and a repeated course of therapy, serologic titers might still not decline. In these circumstances, the need for additional therapy or repeated CSF examinations is unclear.
Management of Sex Partners. See General Principles, Management of Sex Partners.
# Special Considerations
Penicillin Allergy. The effectiveness of alternatives to penicillin in the treatment of latent syphilis has not been welldocumented. Nonpregnant patients allergic to penicillin who have clearly defined early latent syphilis should respond to therapies recommended as alternatives to penicillin for the treatment of primary and secondary syphilis (see Primary and Secondary Syphilis, Treatment). The only acceptable alternatives for the treatment of late latent syphilis or latent syphilis of unknown duration are doxycycline (100 mg orally twice daily) or tetracycline (500 mg orally four times daily), both for 28 days. These therapies should be used only in conjunc-tion with close serologic and clinical follow-up. Limited clinical studies, along with biologic and pharmacologic evidence, suggest that ceftriaxone might be effective for treating late latent syphilis or syphilis of unknown duration (105). However, the optimal dose and duration of ceftriaxone therapy have not been defined, and treatment decisions should be discussed in consultation with a specialist. Some patients who are allergic to penicillin also might be allergic to ceftriaxone; in these circumstances, use of an alternative agent might be required. The efficacy of these alternative regimens in HIVinfected persons has not been well-studied and, therefore, must be considered with caution.
Pregnancy. Pregnant patients who are allergic to penicillin should be desensitized and treated with penicillin (see Management of Patients Who Have a History of Penicillin Allergy and Syphilis During Pregnancy).
HIV Infection. See Syphilis Among HIV-Infected Persons.
# Tertiary Syphilis
Tertiary syphilis refers to gumma and cardiovascular syphilis but not to all neurosyphilis. Patients who are not allergic to penicillin and have no evidence of neurosyphilis should be treated with the following regimen.
# Recommended Regimen
Benzathine penicillin G 7.2 million units total, administered as 3 doses of 2.4 million units IM each at 1week intervals
# Other Management Considerations
Patients who have symptomatic late syphilis should be given a CSF examination before therapy is initiated. Some providers treat all patients who have cardiovascular syphilis with a neurosyphilis regimen. The complete management of patients who have cardiovascular or gummatous syphilis is beyond the scope of these guidelines. These patients should be managed in consultation with an infectious diseases specialist.
Follow-Up. Limited information is available concerning clinical response and follow-up of patients who have tertiary syphilis.
Management of Sex Partners. See General Principles, Management of Sex Partners.
# Special Considerations
Penicillin Allergy. Patients allergic to penicillin should be treated according to treatment regimens recommended for late latent syphilis.
Pregnancy. Pregnant patients who are allergic to penicillin should be desensitized, if necessary, and treated with penicillin (see Management of Patients Who Have a History of Penicillin Allergy and Syphilis During Pregnancy).
HIV Infection. See Syphilis Among HIV-Infected Persons.
# Neurosyphilis
# Treatment
CNS involvement can occur during any stage of syphilis. A patient who has clinical evidence of neurologic involvement with syphilis (e.g., cognitive dysfunction, motor or sensory deficits, ophthalmic or auditory symptoms, cranial nerve palsies, and symptoms or signs of meningitis) should have a CSF examination.
Syphilitic uveitis or other ocular manifestations frequently are associated with neurosyphilis; patients with these symptoms should be treated according to the recommendations for patients with neurosyphilis. A CSF examination should be performed for all such patients to identify those with abnormalities that require follow-up CSF examinations to assess treatment response.
Patients who have neurosyphilis or syphilitic eye disease (e.g., uveitis, neuroretinitis, and optic neuritis) should be treated with the following regimen.
# Recommended Regimen
Aqueous crystalline penicillin G 18-24 million units per day, administered as 3-4 million units IV every 4 hours or continuous infusion, for 10-14 days
If compliance with therapy can be ensured, patients may be treated with the following alternative regimen.
# Alternative Regimen
Procaine penicillin 2.4 million units IM once daily PLUS Probenecid 500 mg orally four times a day, both for 10-14 days
The durations of the recommended and alternative regimens for neurosyphilis are shorter than that of the regimen used for late syphilis in the absence of neurosyphilis. Therefore, some specialists administer benzathine penicillin, 2.4 million units IM once per week for up to 3 weeks after completion of these neurosyphilis treatment regimens to provide a comparable total duration of therapy.
# Other Management Considerations
Other considerations in the management of patients who have neurosyphilis are as follows:
• All patients who have syphilis should be tested for HIV.
• Many specialists recommend treating patients who have evidence of auditory disease caused by syphilis in the same manner as patients who have neurosyphilis, regardless of CSF examination results. Although systemic steroids are used frequently as adjunctive therapy for otologic syphilis, such drugs have not been proven beneficial. Follow-Up. If CSF pleocytosis was present initially, a CSF examination should be repeated every 6 months until the cell count is normal. Follow-up CSF examinations also can be used to evaluate changes in the VDRL-CSF or CSF protein after therapy; however, changes in these two parameters occur more slowly than cell counts, and persistent abnormalities might be less important. If the cell count has not decreased after 6 months or if the CSF is not normal after 2 years, retreatment should be considered. Recent data on HIV-infected persons with neurosyphilis suggest that CSF abnormalities might persist for extended periods in these persons, and close clinical follow-up is warranted (105,106).
Management of Sex Partners. See General Principles, Management of Sex Partners.
# Special Considerations
Penicillin Allergy. Ceftriaxone can be used as an alternative treatment for patients with neurosyphilis, although the possibility of cross-reactivity between this agent and penicillin exists. Some specialists recommend ceftriaxone 2 g daily either IM or IV for 10-14 days. Other regimens have not been adequately evaluated for treatment of neurosyphilis. Therefore, if concern exists regarding the safety of ceftriaxone for a patient with neurosyphilis, the patient should obtain skin testing to confirm penicillin allergy and, if necessary, be desensitized and managed in consultation with a specialist.
Pregnancy. Pregnant patients who are allergic to penicillin should be desensitized, if necessary, and treated with penicillin (see Syphilis During Pregnancy).
HIV Infection. See Syphilis Among HIV-Infected Patients.
# Syphilis Among HIV-Infected Persons
# Diagnostic Considerations
Unusual serologic responses have been observed among HIV-infected persons who have syphilis. The majority of reports have involved serologic titers that were higher than expected, but false-negative serologic test results and delayed appearance of seroreactivity also have been reported. However, unusual serologic responses are uncommon, and the majority of specialists believe that both treponemal and nontreponemal serologic tests for syphilis can be interpreted in the usual manner for the majority of patients who are coinfected with T. pallidum and HIV.
When clinical findings are suggestive of syphilis but serologic tests are nonreactive or their interpretation is unclear, alternative tests (e.g., biopsy of a lesion, darkfield examination, or DFA staining of lesion material) might be useful for diagnosis. Neurosyphilis should be considered in the differential diagnosis of neurologic disease in HIV-infected persons.
# Treatment
Compared with HIV-negative patients, HIV-positive patients who have early syphilis might be at increased risk for neurologic complications and might have higher rates of treatment failure with currently recommended regimens. The magnitude of these risks is not defined precisely but is likely minimal. No treatment regimens for syphilis have been demonstrated to be more effective in preventing neurosyphilis in HIV-infected patients than the syphilis regimens recommended for HIV-negative patients (100). Careful follow-up after therapy is essential.
# Primary and Secondary Syphilis Among HIV-Infected Persons
# Treatment
Treatment with benzathine penicillin G, 2.4 million units IM in a single dose is recommended. Some specialists recommend additional treatments (e.g., benzathine penicillin G administered at 1-week intervals for 3 weeks, as recommended for late syphilis) in addition to benzathine penicillin G 2.4 million units IM.
# Other Management Considerations
Because CSF abnormalities (e.g., mononuclear pleocytosis and elevated protein levels) are common in patients with early syphilis and in persons with HIV infection, the clinical and prognostic significance of such CSF abnormalities in HIVinfected persons with primary or secondary syphilis is unknown. Although the majority of HIV-infected persons respond appropriately to standard benzathine penicillin therapy, some specialists recommend intensified therapy when CNS syphilis is suspected in these persons. Therefore, some specialists recommend CSF examination before treatment of HIV-infected persons with early syphilis, with follow-up CSF examination conducted after treatment in persons with initial abnormalities.
Follow-Up. HIV-infected persons should be evaluated clinically and serologically for treatment failure at 3, 6, 9, 12, and 24 months after therapy. Although of unproven benefit, some specialists recommend a CSF examination 6 months after therapy.
HIV-infected persons who meet the criteria for treatment failure (i.e., signs or symptoms that persist or recur or persons who have fourfold increase in nontreponemal test titer) should be managed in the same manner as HIV-negative patients (i.e., a CSF examination and re-treatment). CSF examination and re-treatment also should be strongly considered for persons whose nontreponemal test titers do not decrease fourfold within 6-12 months of therapy. The majority of specialists would re-treat patients with benzathine penicillin G administered as 3 doses of 2.4 million units IM each at weekly intervals, if CSF examinations are normal.
# Special Considerations
Penicillin Allergy. Penicillin-allergic patients who have primary or secondary syphilis and HIV infection should be managed according to the recommendations for penicillin-allergic, HIV-negative patients. The use of alternatives to penicillin has not been well studied in HIV-infected patients.
# Latent Syphilis Among HIV-Infected Persons
# Diagnostic Considerations
HIV-infected patients who have early latent syphilis should be managed and treated according to the recommendations for HIV-negative patients who have primary and secondary syphilis. HIV-infected patients who have either late latent syphilis or syphilis of unknown duration should have a CSF examination before treatment.
# Treatment
Patients with late latent syphilis or syphilis of unknown duration and a normal CSF examination can be treated with benzathine penicillin G, at weekly doses of 2.4 million units for 3 weeks. Patients who have CSF consistent with neurosyphilis should be treated and managed as patients who have neurosyphilis (see Neurosyphilis).
Follow-Up. Patients should be evaluated clinically and serologically at 6, 12, 18, and 24 months after therapy. If, at any time, clinical symptoms develop or nontreponemal titers rise fourfold, a repeat CSF examination should be performed and treatment administered accordingly. If during 12-24 months the nontreponemal titer does not decline fourfold, the CSF examination should be repeated and treatment administered accordingly.
# Special Considerations
Penicillin Allergy. The efficacy of alternative nonpenicillin regimens in HIV-infected persons has not been well studied. Patients with penicillin allergy whose compliance with therapy or follow-up cannot be ensured should be desensitized and treated with penicillin (see Management of Patients Who Have a History of Penicillin Allergy). These therapies should be used only in conjunction with close serologic and clinical follow-up. Limited clinical studies, along with biologic and pharmacologic evidence, suggest that ceftriaxone might be effective (105). However, optimal dose and duration of ceftriaxone therapy have not been defined.
# Syphilis During Pregnancy
All women should be screened serologically for syphilis during the early stages of pregnancy. The majority of states mandate screening at the first prenatal visit for all women. Antepartum screening by nontreponemal antibody testing is typical, but in some settings, treponemal antibody testing is being used. Pregnant women with reactive treponemal screening tests should have confirmatory testing with nontreponemal tests with titers. In populations in which use of prenatal care is not optimal, RPR-card test screening and treatment (i.e., if the RPR-card test is reactive) should be performed at the time a pregnancy is diagnosed. For communities and populations in which the prevalence of syphilis is high or for patients at high risk, serologic testing should be performed twice during the third trimester, at 28 to 32 weeks' gestation and at delivery. Any woman who delivers a stillborn infant after 20 weeks' gestation should be tested for syphilis. No infant should leave the hospital without the maternal serologic status having been determined at least once during pregnancy.
# Diagnostic Considerations
Seropositive pregnant women should be considered infected unless an adequate treatment history is documented clearly in the medical records and sequential serologic antibody titers have declined. Serofast low antibody titers might not require treatment; however, persistent higher titer antibody tests might indicate reinfection and require treatment.
# Treatment
Penicillin is effective for preventing maternal transmission to the fetus and for treating fetal infection. Evidence is insufficient to determine specific, recommended penicillin regimens that are optimal (107).
# Recommended Regimen
Treatment during pregnancy should be the penicillin regimen appropriate for the stage of syphilis.
# Other Management Considerations
Some specialists recommend additional therapy for pregnant women in some settings (e.g., a second dose of benzathine penicillin 2.4 million units IM administered 1 week after the initial dose for women who have primary, secondary, or early latent syphilis). During the second half of pregnancy, syphilis management may be facilitated by a sonographic fetal evaluation for congenital syphilis, but this evaluation should not delay therapy. Sonographic signs of fetal or placental syphilis (i.e., hepatomegaly, ascites, hydrops, or a thickened placenta) indicate a greater risk for fetal treatment failure (108); such cases should be managed in consultation with obstetric spe-cialists. Evidence is insufficient to recommend specific regimens for these situations.
Women treated for syphilis during the second half of pregnancy are at risk for premature labor and/or fetal distress, if the treatment precipitates the Jarisch-Herxheimer reaction. These women should be advised to seek obstetric attention after treatment, if they notice any contractions or decrease in fetal movements. Stillbirth is a rare complication of treatment, but concern for this complication should not delay necessary treatment. All patients who have syphilis should be offered testing for HIV infection.
Follow-Up. Coordinated prenatal care and treatment followup are vital. Serologic titers should be repeated at 28-32 weeks' gestation, at delivery, and following the recommendations for the stage of disease. Serologic titers can be checked monthly in women at high risk for reinfection or in geographic areas in which the prevalence of syphilis is high. The clinical and antibody response should be appropriate for the stage of disease. The majority of women will deliver before their serologic response to treatment can be assessed definitively. Inadequate maternal treatment is likely if delivery occurs within 30 days of therapy, if clinical signs of infection are present at delivery, or if the maternal antibody titer is fourfold higher than the pretreatment titer.
Management of Sex Partners. See General Principles, Management of Sex Partners.
# Special Considerations
Penicillin Allergy. For treatment of syphilis during pregnancy, no proven alternatives to penicillin exist. Pregnant women who have a history of penicillin allergy should be desensitized and treated with penicillin. Skin testing might be helpful (see Management of Patients Who Have a History of Penicillin Allergy).
Tetracycline and doxycycline usually are not used during pregnancy. Erythromycin should not be used because it does not reliably cure an infected fetus. Data are insufficient to recommend azithromycin or ceftriaxone for treatment of maternal infection and prevention of congenital syphilis.
HIV Infection. Placental inflammation from congenital infection might increase the risk for perinatal transmission of HIV. All HIV-infected women should be evaluated for infectious syphilis and treated. Data are insufficient to recommend a specific regimen (see Syphilis Among HIV-Infected Patients).
# Congenital Syphilis
Effective prevention and detection of congenital syphilis depends on the identification of syphilis in pregnant women and, therefore, on the routine serologic screening of pregnant women during the first prenatal visit. In communities and populations in which the risk for congenital syphilis is high, serologic testing and a sexual history also should be obtained at 28 weeks' gestation and at delivery. Moreover, as part of the management of pregnant women who have syphilis, information concerning treatment of sex partners should be obtained to assess the risk for reinfection. All pregnant women who have syphilis should be tested for HIV infection. Routine screening of newborn sera or umbilical cord blood is not recommended. Serologic testing of the mother's serum is preferred rather than testing of the infant's serum because the serologic tests performed on infant serum can be nonreactive if the mother's serologic test result is of low titer or was infected late in pregnancy (see Diagnostic Considerations and Use of Serologic Tests). No infant or mother should leave the hospital unless the maternal serologic status has been documented at least once during pregnancy, and at delivery in communities and populations in which the risk for congenital syphilis is high.
# Evaluation and Treatment of Infants During the First Month of Life
The diagnosis of congenital syphilis is complicated by the transplacental transfer of maternal nontreponemal and treponemal IgG antibodies to the fetus. This transfer of antibodies makes the interpretation of reactive serologic tests for syphilis in infants difficult. Treatment decisions frequently must be made on the basis of 1) identification of syphilis in the mother; 2) adequacy of maternal treatment; 3) presence of clinical, laboratory, or radiographic evidence of syphilis in the infant; and 4) comparison of maternal (at delivery) and infant nontreponemal serologic titers by using the same test and preferably the same laboratory.
All infants born to mothers who have reactive nontreponemal and treponemal test results should be evaluated with a quantitative nontreponemal serologic test (RPR or VDRL) performed on infant serum because umbilical cord blood can become contaminated with maternal blood and could yield a false-positive result. Conducting a treponemal test (i.e., TP-PA or FTA-ABS) on a newborn's serum is not necessary. No commercially available immunoglobulin (IgM) test can be recommended.
All infants born to women who have reactive serologic tests for syphilis should be examined thoroughly for evidence of congenital syphilis (e.g., nonimmune hydrops, jaundice, hepatosplenomegaly, rhinitis, skin rash, and/or pseudoparalysis of an extremity). Pathologic examination of the placenta or umbilical cord by using specific fluorescent antitreponemal antibody staining is suggested. Darkfield microscopic exami-nation or DFA staining of suspicious lesions or body fluids (e.g., nasal discharge) also should be performed.
The following scenarios describe the evaluation and treatment of infants for congenital syphilis: Scenario 1. Infants with proven or highly probable disease and 1. an abnormal physical examination that is consistent with congenital syphilis, 2. a serum quantitative nontreponemal serologic titer that is fourfold higher than the mother's titer, § or 3. a positive darkfield or fluorescent antibody test of body fluid(s).
# Recommended Evaluation
• CSF analysis for VDRL, cell count, and protein ¶ • Complete blood count (CBC) and differential and platelet count • Other tests as clinically indicated (e.g., long-bone radiographs, chest radiograph, liver-function tests, cranial ultrasound, ophthalmologic examination, and auditory brainstem response)
# Recommended Regimens
Aqueous crystalline penicillin G 100,000-150,000 units/kg/day, administered as 50,000 units/kg/dose IV every 12 hours during the first 7 days of life and every 8 hours thereafter for a total of 10 days OR Procaine penicillin G 50,000 units/kg/dose IM in a single daily dose for 10 days If >1 day of therapy is missed, the entire course should be restarted. Data are insufficient regarding the use of other antimicrobial agents (e.g., ampicillin). When possible, a full 10day course of penicillin is preferred, even if ampicillin was initially provided for possible sepsis. The use of agents other than penicillin requires close serologic follow-up to assess adequacy of therapy. In all other situations, the maternal history of infection with T. pallidum and treatment for syphilis must be considered when evaluating and treating the infant.
# Scenario 2. Infants who have a normal physical examination and a serum quantitive
nontreponemal serologic titer the same or less than fourfold the maternal titer and the 1. mother was not treated, inadequately treated, or has no documentation of having received treatment; 2. mother was treated with erythromycin or other nonpenicillin regimen;** or 3. mother received treatment <4 weeks before delivery.
# Recommended Evaluation
• CSF analysis for VDRL, cell count, and protein • CBC and differential and platelet count • Long-bone radiographs A complete evaluation is not necessary if 10 days of parenteral therapy is administered. However, such evaluations might be useful; a lumbar puncture might document CSF abnormalities that would prompt close follow-up. Other tests (e.g., CBC, platelet count, and bone radiographs) may be performed to further support a diagnosis of congenital syphilis. If a single dose of benzathine penicillin G is used, then the infant must be fully evaluated (i.e., through CSF examination, long-bone radiographs, and CBC with platelets), the full evaluation must be normal, and follow-up must be certain. If any part of the infant's evaluation is abnormal or not performed or if the CSF analysis is rendered uninterpretable because of contamination with blood, then a 10-day course of penicillin is required. † †
# Recommended Regimens
Aqueous crystalline penicillin G 100,000-150,000 units/kg/day, administered as 50,000 units/kg/dose IV every 12 hours during the first 7 days of life and every 8 hours thereafter for a total of 10 days OR Procaine penicillin G 50,000 units/kg/dose IM in a single daily dose for 10 days OR Benzathine penicillin G 50,000 units/kg/dose IM in a single dose Some specialists prefer the 10 days of parenteral therapy if the mother has untreated early syphilis at delivery. § The absence of a fourfold or greater titer for an infant does not exclude congenital syphilis. ¶ CSF test results obtained during the neonatal period can be difficult to interpret; normal values differ by gestational age and are higher in preterm infants. Values as high as 25 white blood cells (WBCs)/mm 3 and/or protein of 150 mg/dL might occur among normal neonates; some specialists, however, recommend that lower values (i.e., 5 WBCs/mm 3 and protein of 40 mg/dL) be considered the upper limits of normal. Other causes of elevated values should be considered when an infant is being evaluated for congenital syphilis.
** A woman treated with a regimen other than those recommended in these guidelines for treatment should be considered untreated. † † If the infant's nontreponemal test is nonreactive and the likelihood of the infant being infected is low, certain specialists recommend no evaluation but treatment of the infant with a single IM dose of benzathine penicillin G 50,000 units/kg for possible incubating syphilis, after which the infant should receive close serologic follow-up.
# Scenario 3. Infants who have a normal physical examination and a serum quantitative nontreponemal serologic titer
the same or less than fourfold the maternal titer and the 1. mother was treated during pregnancy, treatment was appropriate for the stage of infection, and treatment was administered >4 weeks before delivery; and 2. mother has no evidence of reinfection or relapse.
# Recommended Evaluation
No evaluation is required.
# Recommended Regimen
Benzathine penicillin G 50,000 units/kg/dose IM in a single dose § § Scenario 4. Infants who have a normal physical examination and a serum quantitative nontreponemal serologic titer the same or less than fourfold the maternal titer and the 1. mother's treatment was adequate before pregnancy, and 2. mother's nontreponemal serologic titer remained low and stable before and during pregnancy and at delivery (VDRL <1:2; RPR <1:4).
# Recommended Evaluation
No evaluation is required.
# Recommended Regimen
No treatment is required; however, some specialists would treat with benzathine penicillin G 50,000 units/kg as a single IM injection, particularly if follow-up is uncertain.
# Evaluation and Treatment of Older Infants and Children
Children who are identified as having reactive serologic tests for syphilis after the neonatal period (i.e., aged >1 month) should have maternal serology and records reviewed to assess whether the child has congenital or acquired syphilis (see Primary and Secondary Syphilis and Latent Syphilis, Sexual Assault or Abuse of Children). Any child at risk for congenital syphilis should receive a full evaluation and testing for HIV infection.
# Recommended Evaluation
• CSF analysis for VDRL, cell count, and protein • CBC, differential, and platelet count • Other tests as clinically indicated (e.g., long-bone radiographs, chest radiograph, liver function tests, abdominal ultrasound, ophthalmologic examination, and auditory brain stem response)
# Recommended Regimen
Aqueous crystalline penicillin G 200,000-300,000 units/kg/day IV, administered as 50,000 units/kg every 4-6 hours for 10 days
If the child has no clinical manifestations of disease, the CSF examination is normal, and the CSF VDRL test result is negative, some specialists would treat with up to 3 weekly doses of benzathine penicillin G, 50,000 U/kg IM.
Any child who is suspected of having congenital syphilis or who has neurologic involvement should be treated with aqueous penicillin G. Some specialists also suggest giving these patients a single dose of benzathine penicillin G, 50,000 units/ kg IM after the 10-day course of IV aqueous penicillin. This treatment also would be adequate for children who might have other treponemal infections.
# Follow-Up
All seroreactive infants (or infants whose mothers were seroreactive at delivery) should receive careful follow-up examinations and serologic testing (i.e., a nontreponemal test) every 2-3 months until the test becomes nonreactive or the titer has decreased fourfold. Nontreponemal antibody titers should decline by age 3 months and should be nonreactive by age 6 months if the infant was not infected (i.e., if the reactive test result was caused by passive transfer of maternal IgG antibody) or was infected but adequately treated. The serologic response after therapy might be slower for infants treated after the neonatal period. If these titers are stable or increase after age 6-12 months, the child should be evaluated (e.g., given a CSF examination) and treated with a 10-day course of parenteral penicillin G.
Treponemal tests should not be used to evaluate treatment response because the results for an infected child can remain positive despite effective therapy. Passively transferred maternal treponemal antibodies can be present in an infant until age 15 months. A reactive treponemal test after age 18 months is diagnostic of congenital syphilis. If the nontreponemal test is nonreactive at this time, no further evaluation or treatment is necessary. If the nontreponemal test is reactive at age 18 months, the infant should be fully (re)evaluated and treated for congenital syphilis. § § Some specialists would not treat the infant but would provide close serologic follow-up in those whose mother's nontreponemal titers decreased fourfold after appropriate therapy for early syphilis or remained stable or low for late syphilis.
Infants whose initial CSF evaluations are abnormal should undergo a repeat lumbar puncture approximately every 6 months until the results are normal. A reactive CSF VDRL test or abnormal CSF indices that cannot be attributed to other ongoing illness requires re-treatment for possible neurosyphilis.
Follow-up of children treated for congenital syphilis after the newborn period should be conducted as is recommended for neonates.
# Special Considerations
# Penicillin Allergy
Infants and children who require treatment for syphilis but who have a history of penicillin allergy or develop an allergic reaction presumed secondary to penicillin should be desensitized, if necessary, and then treated with penicillin (see Management of Patients With a History of Penicillin Allergy). Data are insufficient regarding the use of other antimicrobial agents (e.g., ceftriaxone); if a nonpenicillin agent is used, close serologic and CSF follow-up are indicated.
# HIV Infection
Evidence is insufficient to determine whether infants who have congenital syphilis and whose mothers are coinfected with HIV require different evaluation, therapy, or follow-up for syphilis than is recommended for all infants.
# Penicillin Shortage
During periods when the availability of penicillin is compromised, the following is recommended (see http:// www.cdc.gov/nchstp/dstd/penicillinG.htm):
1. For infants with clinical evidence of congenital syphilis (Scenario 1), check local sources for aqueous crystalline penicillin G (potassium or sodium). If IV penicillin G is limited, substitute some or all daily doses with procaine penicillin G (50,000 U/kg/dose IM a day in a single daily dose for 10 days). If aqueous or procaine penicillin G is not available, ceftriaxone (in doses according to age and weight) may be considered with careful clinical and serologic follow-up. Ceftriaxone must be used with caution in infants with jaundice. For infants aged >30 days, use 75 mg/kg IV/IM a day in a single daily dose for 10-14 days; however, dose adjustment might be necessary based on birthweight. For older infants, the dose should be 100 mg/kg a day in a single daily dose. Studies that strongly support ceftriaxone for the treatment of congenital syphilis have not been conducted. Therefore, ceftriaxone should be used in consultation with a specialist in the treatment of infants with congenital syphilis. Manage-ment may include a repeat CSF examination at age 6 months if the initial examination was abnormal.
# Management of Patients Who Have a History of Penicillin Allergy
No proven alternatives to penicillin are available for treating neurosyphilis, congenital syphilis, or syphilis in pregnant women. Penicillin also is recommended for use, whenever possible, in HIV-infected patients. Of the adult U.S. population, 3%-10% have experienced an immunoglobulin E (IgE) mediated allergic response to penicillin such as urticaria, angioedema, or anaphylaxis (i.e., upper airway obstruction, bronchospasm, or hypotension). Re-administration of penicillin to these patients can cause severe, immediate reactions. Because anaphylactic reactions to penicillin can be fatal, every effort should be made to avoid administering penicillin to penicillin-allergic patients, unless they undergo acute desensitization to eliminate anaphylactic sensitivity.
An estimated 10% of persons who report a history of severe allergic reactions to penicillin remain allergic. With the passage of time, the majority of persons who have had a severe reaction to penicillin stop expressing penicillin-specific IgE. These persons can be treated safely with penicillin. The results of many investigations indicate that skin testing with the major and minor determinants of penicillin can reliably identify persons at high risk for penicillin reactions. Although these reagents are easily generated and have been available for >30 years, only benzylpenicilloyl poly-L-lysine (Pre-Pen ® [i.e., the major determinant]) and penicillin G have been available commercially. Testing with only the major determinant and penicillin G identifies an estimated 90%-97% of the currently allergic patients. However, because skin testing without the minor determinants would still miss 3%-10% of allergic patients and because serious or fatal reactions can occur among these minor-determinant-positive patients, specialists suggest exercising caution when the full battery of skin-test reagents is not available (Box 1). An additional challenge has occurred with the recent unavailability of Pre-Pen ® ; however, plans for future availability of this product have been made, as well as a companion minor determinant mixture.
# Major
# Recommendations
If the full battery of skin-test reagents is available, including the major and minor determinants (see Penicillin Allergy Skin Testing), patients who report a history of penicillin reaction and who are skin-test negative can receive conventional penicillin therapy. Skin-test-positive patients should be desensitized.
If the full battery of skin-test reagents, including the minor determinants, is not available, the patient should be skin tested using benzylpenicilloyl poly-L-lysine (i.e., the major determinant) and penicillin G. Patients who have positive test results should be desensitized. Some specialists suggest that persons who have negative test results should be regarded as probably allergic and should be desensitized. Others suggest that those with negative skin-test results can be test-dosed gradually with oral penicillin in a monitored setting in which treatment for anaphylactic reaction can be provided.
If the major determinant (Pre-Pen ® ) is not available for skin testing, all patients with a history suggesting IgE mediated reactions (anaphylaxis, angioedema, bronchospasm, or urticaria) to penicillin should be desensitized in a hospital setting. In patients with reactions not likely to be IgE mediated, outpatient oral desensitization or monitored test doses may be considered.
# Penicillin Allergy Skin Testing
Patients at high risk for anaphylaxis, including those who 1) have a history of penicillin-related anaphylaxis, asthma, or other diseases that would make anaphylaxis more dangerous or 2) are being treated with beta-adrenergic blocking agents should be tested with 100-fold dilutions of the full-strength skin-test reagents before being tested with full-strength reagents. In these situations, patients should be tested in a monitored setting in which treatment for an anaphylactic reaction is available. If possible, the patient should not have taken antihistamines recently (e.g., chlorpheniramine maleate or terfenadine during the preceding 24 hours, diphenhydramine HCl or hydroxyzine during the preceding 4 days, or astemizole during the preceding 3 weeks).
# Procedures
Dilute the antigens either 1) 100-fold for preliminary testing if the patient has had a life-threatening reaction to penicillin or 2) 10-fold if the patient has had another type of immediate, generalized reaction to penicillin within the preceding year.
# Epicutaneous (Prick) Tests
Duplicate drops of skin-test reagent are placed on the volar surface of the forearm. The underlying epidermis is pierced with a 26-gauge needle without drawing blood.
An epicutaneous test is positive if the average wheal diameter after 15 minutes is 4 mm larger than that of negative controls; otherwise, the test is negative. The histamine controls should be positive to ensure that results are not falsely negative because of the effect of antihistaminic drugs.
# Intradermal Test
If epicutaneous tests are negative, duplicate 0.02-mL intradermal injections of negative control and antigen solutions are made into the volar surface of the forearm by using a 26or 27-gauge needle on a syringe. The diameters of the wheals induced by the injections should be recorded. An intradermal test is positive if the average wheal diameter 15 minutes after injection is >2 mm larger than the initial wheal size and also is >2 mm larger than the negative controls. Otherwise, the tests are negative.
# Desensitization
Patients who have a positive skin test to one of the penicillin determinants can be desensitized (Table 1). This is a straightforward, relatively safe procedure that can be performed orally or IV. Although the two approaches have not been compared, oral desensitization is regarded as safer and easier to perform. Patients should be desensitized in a hospital setting because serious IgE-mediated allergic reactions can occur. Desensitization usually can be completed in approximately 4 hours, after which the first dose of penicillin is administered. After desensitization, patients must be maintained on penicillin continuously for the duration of the course of therapy.
# Diseases Characterized by Urethritis and Cervicitis
# Management of Male Patients Who Have Urethritis
Urethritis, as characterized by urethral inflammation, can result from infectious and noninfectious conditions. Symptoms, if present, include discharge of mucopurulent or purulent material, dysuria, or urethral pruritus. Asymptomatic infections are common. N. gonorrhoeae and C. trachomatis are clinically important infectious causes of urethritis. If clinicbased diagnostic tools (Gram stain microscopy) are not available, patients should be treated for both gonorrhea and chlamydia. Further testing to determine the specific etiology is recommended because both chlamydia and gonorrhea are reportable to state health departments, and a specific diagnosis might enhance partner notification and improve compliance with treatment, especially in exposed partners. Culture, nucleic acid hybridization tests, and nucleic acid amplification tests are available for the detection of both N. gonorrhoeae and C. trachomatis. Culture and hybridization tests require urethral swab specimens, whereas amplification tests can be performed on urine specimens. Because of their higher sensitivity, amplification tests are preferred for the detection of C. trachomatis.
# Etiology
Several organisms can cause infectious urethritis. The presence of Gram-negative intracellular diplococci (GNID) on urethral smear is indicative of gonorrhea infection, which is frequently accompanied by chlamydial infection. Nongonoccocal urethritis (NGU) is diagnosed when microscopy indicates inflammation without GNID. C. trachomatis is a frequent cause of NGU (i.e., 15%-55% of cases); however, the prevalence varies by age group, with lower prevalence among older men. The proportion of NGU cases caused by chlamydia has been declining gradually. Complications of NGU among men infected with C. trachomatis include epididymitis, prostatitis, and Reiter's syndrome. Documentation of chlamydia infection is essential because of the need for partner referral for evaluation and treatment.
The etiology of the majority of cases of nonchlamydial NGU is unknown. Ureaplasma urealyticum and Mycoplasma genitalium have been implicated as etiologic agents of NGU in some studies; however, detection of these organisms is frequently difficult (109)(110)(111). T. vaginalis, HSV, and adenovirus might also cause NGU (112)(113)(114). Diagnostic and treatment procedures for these organisms are reserved for situations in which these infections are suspected (e.g., contact with trichomoniasis and genital lesions or severe dysuria and meatitis, which might suggest genital herpes) or when NGU is not responsive to therapy. Enteric bacteria have been identified as an uncommon cause of NGU and might be associated with insertive anal sex.
# Confirmed Urethritis
Clinicians should document that urethritis is present. Urethritis can be documented on the basis of any of the following signs or laboratory tests:
• Mucopurulent or purulent discharge.
• Gram stain of urethral secretions demonstrating >5 WBC per oil immersion field. The Gram stain is the preferred rapid diagnostic test for evaluating urethritis. It is highly sensitive and specific for documenting both urethritis and the presence or absence of gonococcal infection. Gonococcal infection is established by documenting the presence of WBC containing GNID, or • Positive leukocyte esterase test on first-void urine or microscopic examination of first-void urine sediment demonstrating >10 WBC per high power field. If none of these criteria are present, treatment should be deferred, and the patient should be tested for N. gonorrhoeae and C. trachomatis and followed closely if test results are negative. If the results demonstrate infection with either N. gonorrhoeae or C. trachomatis, the appropriate treatment should be given and sex partners referred for evaluation and treatment.
Empiric treatment of symptoms without documentation of urethritis is recommended only for patients at high risk for infection who are unlikely to return for a follow-up evaluation. Such patients should be treated for gonorrhea and chlamydia. Partners of patients treated empirically should be evaluated and treated.
# Management of Patients Who Have Nongonococcal Urethritis Diagnosis
All patients who have confirmed or suspected urethritis should be tested for gonorrhea and chlamydia. Testing for chlamydia is strongly recommended because of the increased utility and availability of highly sensitive and specific testing methods and because a specific diagnosis might enhance partner notification and improve compliance with treatment, especially in the exposed partner.
# Treatment
Treatment should be initiated as soon as possible after diagnosis. Azithromycin and doxycycline are highly effective for chlamydial urethritis; however, infections with M. genitalium may respond better to azithromycin (115). Single-dose regimens have the advantage of improved compliance and directly observed treatment. To improve compliance, ideally the medication should be provided in the clinic or health-care provider's office.
# Recommended Regimens
Azithromycin 1 g orally in a single dose OR Doxycycline 100 mg orally twice a day for 7 days
# Alternative Regimens
Erythromycin base 500 mg orally four times a day for 7 days OR Erythromycin ethylsuccinate 800 mg orally four times a day for 7 days OR Ofloxacin 300 mg orally twice a day for 7 days OR Levofloxacin 500 mg orally once daily for 7 days
# Follow-Up for Patients Who Have Urethritis
Patients should be instructed to return for evaluation if symptoms persist or recur after completion of therapy. Symptoms alone, without documentation of signs or laboratory evidence of urethral inflammation, are not a sufficient basis for retreatment. Patients should be instructed to abstain from sexual intercourse until 7 days after therapy is initiated, provided their symptoms have resolved and their sex partners have been adequately treated. Persistence of pain, discomfort, and irritative voiding symptoms beyond 3 months should alert the clinician to the possibility of chronic prostatitis/chronic pelvic pain syndrome in men. Persons whose conditions have been diagnosed as a new STD should receive testing for other STDs, including syphilis and HIV.
# Partner Referral
Persons with NGU should refer for evaluation and treatment all sex partners within the preceding 60 days. Because a specific diagnosis might facilitate partner referral, testing for gonorrhea and chlamydia is encouraged.
# Recurrent and Persistent Urethritis
Objective signs of urethritis should be present before initiation of antimicrobial therapy. In persons who have persistent symptoms after treatment without objective signs of urethritis, the value of extending the duration of antimicrobials has not been demonstrated. Persons who have persistent or recurrent urethritis can be re-treated with the initial regimen if they did not comply with the treatment regimen or if they were reexposed to an untreated sex partner. Otherwise, a T. vaginalis culture should be performed using an intraurethral swab or a first-void urine specimen (112). Some cases of recurrent urethritis after doxycycline treatment might be caused by tetracycline-resistant U. urealyticum. Urologic examinations usually do not reveal a specific etiology. Approximately 50% of men with chronic nonbacterial prostatitis/chronic pelvic pain syndrome have evidence of urethral inflammation without any identifiable microbial pathogens. If the pa-tient was compliant with the initial regimen and reexposure can be excluded, the following regimen is recommended.
# Recommended Regimens
Metronidazole 2 g orally in a single dose OR Tinidazole 2 g orally in a single dose PLUS Azithromycin 1 g orally in a single dose (if not used for initial episode)
# Special Considerations HIV Infection
Gonococcal urethritis, chlamydial urethritis, and nongonococcal, nonchlamydial urethritis might facilitate HIV transmission. Patients who have NGU and also are infected with HIV should receive the same treatment regimen as those who are HIV negative.
# Management of Patients Who Have Cervicitis
Two major diagnostic signs characterize cervicitis: 1) a purulent or mucopurulent endocervical exudate visible in the endocervical canal or on an endocervical swab specimen (commonly referred to as "mucopurulent cervicitis" or cervicitis), and 2) sustained endocervical bleeding easily induced by gentle passage of a cotton swab through the cervical os. Either or both signs might be present. Cervicitis frequently is asymptomatic, but some women complain of an abnormal vaginal discharge and intermenstrual vaginal bleeding (e.g., after sexual intercourse). A finding of leukorrhea (>10 WBC per high power field on microscopic examination of vaginal fluid) has been associated with chlamydial and gonococcal infection of the cervix. In the absence of inflammatory vaginitis, leukorrhea might be a sensitive indicator of cervical inflammation with a high negative predictive value (116). Although some specialists consider an increased number of polymorphonuclear leukocytes on endocervical Gram stain as being useful in the diagnosis of cervicitis, this criterion has not been standardized. In addition, it has a low positive-predictive value (PPV) for infection with C. trachomatis and N. gonorrhoeae and is not available in the majority of clinical settings. Finally, although the presence of GNID on Gram stain of endocervical fluid is specific for the diagnosis of gonococcal cervical infection, it is insensitive because it is observed in only 50% of women with this infection.
# Etiology
When an etiologic organism is isolated in the setting of cervicitis, it is typically C. trachomatis or N. gonorrhoeae. Cervicitis also can accompany trichomoniasis and genital herpes (especially primary HSV-2 infection). However, in the majority of cases of cervicitis, no organism is isolated, especially in women at relatively low risk for recent acquisition of these STDs (for example, women aged >30 years). Limited data indicate that infection with M. genitalium and BV as well as frequent douching might cause cervicitis (117)(118)(119). For reasons that are unclear, cervicitis can persist despite repeated courses of antimicrobial therapy. Because the majority of persistent cases of cervicitis are not caused by relapse or reinfection with C. trachomatis or N. gonorrhoeae, other determinants (e.g., persistent abnormality of vaginal flora, douching or exposure to chemical irritants, or idiopathic inflammation in the zone of ectopy) might be involved.
# Diagnosis
Because cervicitis might be a sign of upper genital tract infection (endometritis), women who seek medical treatment for a new episode of cervicitis should be assessed for signs of PID and should be tested for C. trachomatis and for N. gonorrhoeae with the most sensitive and specific test available, NAAT. Women with cervicitis also should be evaluated for the presence of BV and trichomoniasis, and these conditions should be treated, if present. Because the sensitivity of microscopy to detect T. vaginalis is relatively low (approximately 50%), symptomatic women with cervicitis and negative microscopy for trichomonads should receive further testing (i.e., culture or antigen-based detection). Although HSV-2 infection has been associated with cervicitis, the utility of specific testing (i.e., culture or serologic testing) for HSV-2 in this setting is unclear. Standardized diagnostic tests for M. genitalium are not commercially available.
NAAT for C. trachomatis and N. gonorrhoeae are preferred for the diagnostic evaluation of cervicitis and can be performed on either cervical or urine samples. A finding of >10 WBC in vaginal fluid, in the absence of trichomoniasis, might indicate endocervical inflammation caused specifically by C. trachomatis or N. gonorrhoeae (116,120,121).
# Treatment
Several factors should affect the decision to provide presumptive therapy for cervicitis or to await the results of diagnostic tests. Treatment with antibiotics for C. trachomatis should be provided in women at increased risk for this common STD (age <25 years, new or multiple sex partners, and unprotected sex), especially if follow-up cannot be ensured and if a relatively insensitive diagnostic test (not a NAAT) is used. Concurrent therapy for N. gonorrhoeae is indicated if the prevalence of this infection is high (>5%) in the patient population (young age and facility prevalence).
Concomitant trichomoniasis or symptomatic BV should also be treated if detected. For women in whom any component of (or all) presumptive therapy is deferred, the results of sensitive tests for C. trachomatis and N. gonorrhoeae (e.g., nucleic acid amplification tests) should determine the need for treatment subsequent to the initial evaluation.
# Recommended Regimens for Presumptive Treatment*
Azithromycin 1 g orally in a single dose OR Doxycycline 100 mg orally twice a day for 7 days * Consider concurrent treatment for gonococcal infection if prevalence of gonorrhea is high in the patient population under assessment.
# Recurrent and Persistent Cervicitis
Women with persistent cervicitis should be reevaluated for possible reexposure to an STD, and her vaginal flora should be reassessed. If relapse and/or reinfection with a specific STD has been excluded, BV is not present, and sex partners have been evaluated and treated, management options for persistent cervicitis are undefined. For such women, the value of repeated or prolonged administration of antibiotic therapy for persistent symptomatic cervicitis is unknown. Women who receive such a course should return after treatment so that a determination can be made regarding whether cervicitis has resolved. In women with persistent symptoms that are clearly attributable to cervicitis, ablative therapy may be considered by a gynecologic specialist.
# Follow-Up
Follow-up should be conducted as recommended for the infections for which a woman is treated. If symptoms persist, women should be instructed to return for reevaluation.
# Management of Sex Partners
Management of sex partners of women treated for cervicitis should be appropriate for the identified or suspected STD. Partners should be notified and examined if chlamydia, gonorrhea, or trichomoniasis was identified or suspected in the index patient and treated for the STDs for which the index patient received treatment. To avoid re-infection, patients and their sex partners should abstain from sexual intercourse until therapy is completed (i.e., 7 days after a single-dose regimen or after completion of a 7-day regimen).
# Special Considerations
# HIV Infection
Patients who have cervicitis and also are infected with HIV should receive the same treatment regimen as those who are HIV negative. Treatment of cervicitis in HIV-infected women is vital because cervicitis increases cervical HIV shedding. Treatment of cervicitis in HIV-infected women reduces HIV shedding from the cervix and might reduce HIV transmission to susceptible sex partners (122).
# Chlamydial Infections Chlamydial Infections in Adolescents and Adults
In the United States, chlamydial genital infection is the most frequently reported infectious disease, and the prevalence is highest in persons aged <25 years (123). Several important sequelae can result from C. trachomatis infection in women; the most serious of these include PID, ectopic pregnancy, and infertility. Some women who have uncomplicated cervical infection already have subclinical upper reproductive tract infection.
Asymptomatic infection is common among both men and women, and to detect chlamydial infections health-care providers frequently rely on screening tests. Annual screening of all sexually active women aged <25 years is recommended (124), as is screening of older women with risk factors (e.g., those who have a new sex partner or multiple sex partners). The benefits of C. trachomatis screening in women have been demonstrated in areas where screening programs have reduced both the prevalence of infection and rates of PID (125,126). Evidence is insufficient to recommend routine screening for C. trachomatis in sexually active young men, based on feasibility, efficacy, and cost-effectiveness. However, screening of sexually active young men should be considered in clinical settings with a high prevalence of chlamydia (e.g., adolescent clinics, correctional facilities, and STD clinics). An appropriate sexual risk assessment should be conducted for all persons and might indicate more frequent screening for some women or certain men.
# Diagnostic Considerations
C. trachomatis urogenital infection in women can be diagnosed by testing urine or swab specimens collected from the endocervix or vagina. Diagnosis of C. trachomatis urethral infection in men can be made by testing a urethral swab or urine specimen. Rectal C. trachomatis infections in persons that engage in receptive anal intercourse can be diagnosed by testing a rectal swab specimen. Culture, direct immunofluorescence, EIA, nucleic acid hybridization tests, and NAATs are available for the detection of C. trachomatis on endocervical and male urethral swab specimens (127). NAATs are the most sensitive tests for these specimens and are FDA-cleared for use with urine, and some tests are cleared for use with vaginal swab specimens. The majority of tests, including NAAT and nucleic acid hybridization tests, are not FDAcleared for use with rectal swab specimens, and chlamydia culture is not widely available for this purpose. Some noncommercial laboratories have initiated NAAT of rectal swab specimens after establishing the performance of the test to meet CLIA requirements. Patients' whose condition has been diagnosed as chlamydia also should be tested for other STDs.
# Treatment
Treating infected patients prevents transmission to sex partners. In addition, treating pregnant women usually prevents transmission of C. trachomatis to infants during birth. Treatment of sex partners helps to prevent reinfection of the index patient and infection of other partners.
Coinfection with C. trachomatis frequently occurs among patients who have gonococcal infection; therefore, presumptive treatment of such patients for chlamydia is appropriate (see Gonococcal Infection, Dual Therapy for Gonococcal and Chlamydial Infections). The following recommended treatment regimens and alternative regimens cure infection and usually relieve symptoms.
# Recommended Regimens
Azithromycin 1 g orally in a single dose OR Doxycycline 100 mg orally twice a day for 7 days
# Alternative Regimens
Erythromycin base 500 mg orally four times a day for 7 days OR Erythromycin ethylsuccinate 800 mg orally four times a day for 7 days OR Ofloxacin 300 mg orally twice a day for 7 days OR Levofloxacin 500 mg orally once daily for 7 days A recent meta-analysis of 12 randomized clinical trials of azithromycin versus doxycycline for the treatment of genital chlamydial infection demonstrated that the treatments were equally efficacious, with microbial cure rates of 97% and 98%, respectively (128). These studies were conducted primarily in populations in which follow-up was encouraged, adherence to a 7-day regimen was effective, and culture or EIA (rather than the more sensitive NAAT was used for determining microbiological outcome. Azithromycin should always be available to treat patients for whom compliance with multiday dosing is in question.
In populations that have erratic health-care-seeking behavior, poor treatment compliance, or unpredictable follow-up, azithromycin might be more cost-effective because it enables the provision of a single-dose of directly observed therapy. However, doxycycline costs less than azithromycin and has no higher risk for adverse events (128). Erythromycin might be less efficacious than either azithromycin or doxycycline, mainly because of the frequent occurrence of gastrointestinal side effects that discourage compliance. Ofloxacin and levofloxacin are effective treatment alternatives but are more expensive and offer no advantage in the dosage regimen. Other quinolones either are not reliably effective against chlamydial infection or have not been evaluated adequately.
To maximize compliance with recommended therapies, medications for chlamydial infections should be dispensed on site, and the first dose should be directly observed. To minimize transmission, persons treated for chlamydia should be instructed to abstain from sexual intercourse for 7 days after single-dose therapy or until completion of a 7-day regimen. To minimize the risk for reinfection, patients also should be instructed to abstain from sexual intercourse until all of their sex partners are treated.
# Follow-up
Except in pregnant women, test-of-cure (repeat testing 3-4 weeks after completing therapy) is not recommended for persons treated with the recommended or alterative regimens, unless therapeutic compliance is in question, symptoms persist, or reinfection is suspected. Moreover, the validity of chlamydial diagnostic testing at <3 weeks after completion of therapy (to identify patients who did not respond to therapy) has not been established. False-negative results might occur because of persistent infections involving limited numbers of chlamydial organisms. In addition, NAAT conducted at <3 weeks after completion of therapy in persons who were treated successfully could yield false-positive results because of the continued presence of dead organisms.
A high prevalence of C. trachomatis infection is observed in women who were treated for chlamydial infection in the preceding several months (129,130). The majority of posttreatment infections result from reinfection, frequently occurring because the patient's sex partners were not treated or because the patient resumed sex with a new partner infected with C. trachomatis. Repeat infections confer an elevated risk for PID and other complications when compared with the initial infection. Therefore, recently infected women are a major pri-ority for repeat testing for C. trachomatis. Clinicians and health-care agencies should consider advising all women with chlamydial infection to be retested approximately 3 months after treatment. Providers also are strongly encouraged to retest all women treated for chlamydial infection whenever they next seek medical care within the following 3-12 months, regardless of whether the patient believes that her sex partners were treated. Recognizing that retesting is distinct from a testof-cure, as discussed in this report, is vital. Limited evidence is available on the benefit of retesting for chlamydia in men previously infected; however, some specialists suggest retesting men approximately 3 months after treatment.
# Management of Sex Partners
Patients should be instructed to refer their sex partners for evaluation, testing, and treatment. The following recommendations on exposure intervals are based on limited evaluation. Sex partners should be evaluated, tested, and treated if they had sexual contact with the patient during the 60 days preceding onset of symptoms in the patient or diagnosis of chlamydia. The most recent sex partner should be evaluated and treated, even if the time of the last sexual contact was >60 days before symptom onset or diagnosis.
If concerns exist that sex partners will not seek evaluation and treatment, or if other management strategies are impractical or unsuccessful, then delivery of antibiotic therapy (either a prescription or medication) by heterosexual male or female patients to their partners might be an option (see Partner Management). Limited studies to date have demonstrated a trend toward a decrease in rates of persistent or recurrent chlamydia with this approach compared with standard partner referral (25,27). Male patients must inform female partners of their infection and be given accompanying written materials about the importance of seeking evaluation for PID (especially if symptomatic). Patient-delivered partner therapy is not routinely recommended for MSM because of a high risk for coexisting infections, especially undiagnosed HIV infection, in their partners.
Patients should be instructed to abstain from sexual intercourse until they and their sex partners have completed treatment. Abstinence should be continued until 7 days after a single-dose regimen or after completion of a 7-day regimen. Timely treatment of sex partners is essential for decreasing the risk for reinfecting the index patient.
# Special Considerations
Pregnancy. Doxycycline, ofloxacin, and levofloxacin are contraindicated in pregnant women. However, clinical experience and studies suggest that azithromycin is safe and effective (131)(132)(133). Repeat testing (preferably by NAAT) 3 weeks after completion of therapy with the following regimens is recommended for all pregnant women to ensure therapeutic cure, considering the sequelae that might occur in the mother and neonate if the infection persists. The frequent gastrointestinal side effects associated with erythromycin might discourage patient compliance with the alternative regimens.
# Recommended Regimens
Azithromycin 1 g orally in a single dose OR Amoxicillin 500 mg orally three times a day for 7 days
# Alternative Regimens
Erythromycin base 500 mg orally four times a day for 7 days OR Erythromycin base 250 mg orally four times a day for 14 days OR Erythromycin ethylsuccinate 800 mg orally four times a day for 7 days OR Erythromycin ethylsuccinate 400 mg orally four times a day for 14 days Erythromycin estolate is contraindicated during pregnancy because of drug-related hepatotoxicity. The lower dose 14day erythromycin regimens may be considered if gastrointestinal tolerance is a concern.
HIV Infection. Patients who have chlamydial infection and also are infected with HIV should receive the same treatment regimen as those who are HIV negative.
# Chlamydial Infections Among Infants
Prenatal screening of pregnant women can prevent chlamydial infection among neonates. Pregnant women aged <25 years are at high risk for infection. Local or regional prevalence surveys of chlamydial infection can be conducted to confirm the utility of using these recommendations in particular settings.
C. trachomatis infection of neonates results from perinatal exposure to the mother's infected cervix. Neonatal ocular prophylaxis with silver nitrate solution or antibiotic ointments does not prevent perinatal transmission of C. trachomatis from mother to infant. However, ocular prophylaxis with those agents does prevent gonococcal ophthalmia and, therefore, should be continued (see Ophthalmia Neonatorum Prophylaxis).
Initial C. trachomatis perinatal infection involves the mucous membranes of the eye, oropharynx, urogenital tract, and rectum and might be asymptomatic in these locations.
C. trachomatis infection in neonates is most frequently recognized by conjunctivitis that develops 5-12 days after birth. C. trachomatis also can cause a subacute, afebrile pneumonia with onset at ages 1-3 months. C. trachomatis has been the most frequent identifiable infectious cause of ophthalmia neonatorum, but perinatal chlamydial infections, including opthalmia and pneumonia, are detected less frequently because of the institution of widespread prenatal screening and treatment of pregnant women.
# Ophthalmia Neonatorum Caused by C. trachomatis
A chlamydial etiology should be considered for all infants aged <30 days who have conjunctivitis, especially if the mother has a history of untreated chlamydia infection.
# Diagnostic Considerations
Sensitive and specific methods used to diagnose chlamydial ophthalmia in the neonate include both tissue culture and nonculture tests (e.g., DFA tests, EIA, and NAAT). The majority of nonculture tests are not FDA-cleared for the detection of chlamydia from conjunctival swabs, and clinical laboratories must verify the procedure according to CLIA regulations. Specimens must contain conjunctival cells, not exudate alone. Specimens for culture isolation and nonculture tests should be obtained from the everted eyelid using a dacrontipped swab or the swab specified by the manufacturer's test kit. A specific diagnosis of C. trachomatis infection confirms the need for treatment not only for the neonate but also for the mother and her sex partner(s). Ocular exudate from infants being evaluated for chlamydial conjunctivitis also should be tested for N. gonorrhoeae.
# Recommended Regimen
Erythromycin base or ethylsuccinate 50 mg/kg/day orally divided into 4 doses daily for 14 days ¶ ¶, *** Topical antibiotic therapy alone is inadequate for treatment of chlamydial infection and is unnecessary when systemic treatment is administered.
# Follow-Up
The efficacy of erythromycin treatment is approximately 80%; a second course of therapy might be required and, there-fore, follow-up of infants is recommended to determine whether initial treatment was effective. The possibility of concomitant chlamydial pneumonia should be considered.
# Management of Mothers and Their Sex Partners
The mothers of infants who have chlamydial infection and the sex partners of these women should be evaluated and treated (see Chlamydial Infection in Adolescents and Adults).
# Infant Pneumonia Caused by C. trachomatis
Characteristic signs of chlamydial pneumonia in infants include 1) a repetitive staccato cough with tachypnea and 2) hyperinflation and bilateral diffuse infiltrates on a chest radiograph. Wheezing is rare, and infants are typically afebrile. Peripheral eosinophilia (>400 cells/mm 3 ) occurs frequently. Because clinical presentations differ, initial treatment and diagnostic tests should include C. trachomatis for all infants aged 1-3 months who possibly have pneumonia (especially with untreated maternal chlamydial infection).
# Diagnostic Considerations
Specimens for chlamydial testing should be collected from the nasopharynx. Tissue culture is the definitive standard for chlamydial pneumonia. Nonculture tests (e.g., EIA, DFA, and NAAT) can be used, although nonculture tests of nasopharyngeal specimens have a lower sensitivity and specificity than nonculture tests of ocular specimens. DFA is the only FDAcleared test for the detection of C. trachomatis from nasopharyngeal specimens. Tracheal aspirates and lung biopsy specimens, if collected, should be tested for C. trachomatis.
Because of the delay in obtaining test results for chlamydia, the decision to provide treatment for C. trachomatis pneumonia must frequently be based on clinical and radiologic findings. The results of tests for chlamydial infection assist in the management of an infant's illness and determine the need for treating the mother and her sex partner(s).
# Recommended Regimen
Erythromycin base or ethylsuccinate 50 mg/kg/day orally divided into 4 doses daily for 14 days
# Follow-Up
The effectiveness of erythromycin in treating pneumonia caused by C. trachomatis is approximately 80%; a second course of therapy might be required. Follow-up of infants is recommended to determine whether the pneumonia has resolved. Some infants with chlamydial pneumonia have abnormal pulmonary function tests later in childhood. ¶ ¶ An association between oral erythromycin and infantile hypertrophic pyloric stenosis has been reported in infants aged <6 weeks who were treated with this drug. Infants treated with erythromycin should be followed for signs and symptoms of idiopathic hypertrophic pyloric stenosis (IHPS). *** Data on use of other macrolides (e.g., azithromycin and clarithromycin) for the treatment of neonatal chlamydia infection are limited. The results of one study involving a limited number of patients suggest that a short course of azithromycin, 20 mg/kg/day orally, 1 dose daily for 3 days, may be effective.
# Management of Mothers and Their Sex Partners
Mothers of infants who have chlamydia pneumonia and the sex partners of these women should be evaluated and treated according to the recommended treatment of adults for chlamydial infections (see Chlamydial Infection in Adolescents and Adults).
# Infants Born to Mothers Who Have Chlamydial Infection
Infants born to mothers who have untreated chlamydia are at high risk for infection; however, prophylatic antibiotic treatment is not indicated, and the efficacy of such treatment is unknown. Infants should be monitored to ensure appropriate treatment if symptoms develop.
# Chlamydial Infections Among Children
Sexual abuse must be considered a cause of chlamydial infection in preadolescent children, although perinatally transmitted C. trachomatis infection of the nasopharynx, urogenital tract, and rectum might persist for >1 year (see Sexual Assault or Abuse of Children).
# Diagnostic Considerations
Nonculture, nonamplified probe tests for chlamydia (EIA, DFA) should not be used because of the possibility of falsepositive test results. With respiratory tract specimens, falsepositive results can occur because of cross-reaction of test reagents with C. pneumoniae; with genital and anal specimens, false-positive results might occur because of cross-reaction with fecal flora.
# Recommended Regimens for Children Who Weigh <45 kg
Erythromycin base or ethylsuccinate 50 mg/kg/day orally divided into 4 doses daily for 14 days
# Recommended Regimen for Children Who Weigh >45 kg but Who Are Aged <8 Years
Azithromycin 1 g orally in a single dose
# Recommended Regimens for Children Aged >8 years
Azithromycin 1 g orally in a single dose OR Doxycycline 100 mg orally twice a day for 7 days
# Other Management Considerations
See Sexual Assault or Abuse of Children. Follow-Up. Follow-up cultures are necessary to ensure that treatment has been effective.
# Gonococcal Infections Gonococcal Infections in Adolescents and Adults
In the United States, an estimated 600,000 new N. gonorrhoeae infections occur each year (123). Gonorrhea is the second most commonly reported bacterial STD. The majority of urethral infections caused by N. gonorrhoeae among men produce symptoms that cause them to seek curative treatment soon enough to prevent serious sequelae, but treatment might not be soon enough to prevent transmission to others. Among women, several infections do not produce recognizable symptoms until complications (e.g., PID) have occurred. Both symptomatic and asymptomatic cases of PID can result in tubal scarring that can lead to infertility or ectopic pregnancy.
Because gonococcal infections among women frequently are asymptomatic, an essential component of gonorrhea control in the United States continues to be the screening of women at high risk for STDs. The U.S. Preventive Services Task Force (USPSTF) recommends that clinicians screen all sexually active women, including those who are pregnant, for gonorrhea infection if they are at increased risk. Women aged <25 years are at highest risk for gonorrhea infection. Other risk factors for gonorrhea include a previous gonorrhea infection, other sexually transmitted infections, new or multiple sex partners, inconsistent condom use, commercial sex work, and drug use. The prevalence of gonorrhea infection varies widely among communities and patient populations. The USPSTF does not recommend screening for gonorrhea in men and women who are at low risk for infection (134).
# Diagnostic Considerations
Because of high specificity (>99%) and sensitivity (>95%), a Gram stain of a male urethral specimen that demonstrates polymorphonuclear leukocytes with intracellular Gramnegative diplococci can be considered diagnostic for infection with N. gonorrhoeae in symptomatic men. However, because of lower sensitivity, a negative Gram stain should not be considered sufficient for ruling out infection in asymptomatic men. In addition, Gram stain of endocervical specimens, pharyngeal, or rectal specimens also are not sufficient to detect infection and, therefore, are not recommended. Specific testing for N. gonorrhoeae is recommended because of the increased utility and availability of highly sensitive and specific testing methods and because a specific diagnosis might enhance partner notification.
Specific diagnosis of infection with N. gonorrhoeae may be performed by testing endocervical, vaginal, male urethral, or urine specimens. Culture, nucleic acid hybridization tests, and NAAT are available for the detection of genitourinary infection with N. gonorrhoeae (127). Culture and nucleic acid hybridization tests require female endocervical or male urethral swab specimens. NAAT offer the widest range of testing specimen types because they are FDA-cleared for use with endocervical swabs, vaginal swabs, male urethral swabs, and female and male urine. However, product inserts for each NAAT vendor must be carefully examined to assess current indications because FDA-cleared specimen types might vary. In general, culture is the most widely available option for the diagnosis of infection with N. gonorrhoeae in nongenital sites (e.g., rectum and pharynx). Nonculture tests are not FDAcleared for use in the rectum and pharynx. Some NAATs have the potential to cross-react with nongonococcal Neisseria and related organisms that are commonly found in the throat. Some noncommercial laboratories have initiated NAAT of rectal and pharyngeal swab specimens after establishing the performance of the test to meet CLIA requirements.
Because nonculture tests cannot provide antimicrobial susceptibility results, in cases of persistent gonococcal infection after treatment, clinicians should perform both culture and antimicrobial susceptibility testing.
All patients tested for gonorrhea should be tested for other STDs, including chlamydia, syphilis, and HIV.
# Dual Therapy for Gonococcal and Chlamydial Infections
Patients infected with N. gonorrhoeae frequently are coinfected with C. trachomatis; this finding has led to the recommendation that patients treated for gonococcal infection also be treated routinely with a regimen that is effective against uncomplicated genital C. trachomatis infection (135). Because the majority of gonococci in the United States are susceptible to doxycycline and azithromycin, routine cotreatment might also hinder the development of antimicrobial-resistant N. gonorrhoeae.
Because of the high sensitivity of NAATs for chlamydial infection, patients with a negative chlamydial NAAT result at the time of treatment for gonorrhea do not need to be treated for chlamydia as well. However, if chlamydial test results are not available or if a non-NAAT was negative for chlamydia, patients should be treated for both gonorrhea and chlamydia.
# Quinolone-Resistant N. gonorrhoeae (QRNG)
QRNG continues to spread, making the treatment of gonorrhea with quinolones such as ciprofloxacin inadvisable in many areas and populations (136). Resistance to ciprofloxacin usually indicates resistance to other quinolones as well. QRNG is common in parts of Europe, the Middle East, Asia, and the Pacific. In the United States, QRNG is becoming increasingly common. Previously, CDC had advised that quinolones not be used in California and Hawaii because of the high prevalence of QRNG in these areas (137). The prevalence of QRNG has increased in other areas of the United States, which has resulted in changes in recommended treatment regimens by other states and local areas. QRNG prevalence will continue to increase, and quinolones will eventually not be advisable for the treatment of gonorrhea. The CDC website (http://www.cdc.gov/std/gisp) or state health departments can provide the most current information. In 2004, of 6,322 isolates collected by CDC's Gonococcal Isolate Surveillance Project (GISP), 6.8% were resistant to ciprofloxacin (minimum inhibitory concentrations [MICs] >1.0 µg/mL). Excluding isolates from California and Hawaii, 3.6% of isolates were QRNG. QRNG was more common among MSM than among heterosexual men (23.9% versus 2.9%). In 2004, QRNG among heterosexual men outside of California and Hawaii was 1.4% (138).
Quinolones should not be used for the treatment of gonorrhea among MSM (139) or in areas with increased QRNG prevalence in the United States (e.g., California and Hawaii) or for infections acquired while traveling abroad. Because oral alternatives to quinolones are limited, quinolones may continue to be used for heterosexual men and women in areas and populations not known to have elevated levels of resistance. Clinicians should obtain information on the sexual behavior and recent travel history (including histories from sex partners) of persons to be treated for gonorrhea to ensure appropriate antibiotic therapy.
Resistance of N. gonorrhoeae to fluoroquinolones and other antimicrobials is expected to continue to spread; therefore, state and local surveillance for antimicrobial resistance is crucial for guiding local therapy recommendations. GISP, which samples approximately 3% of all U.S. men who have gonococcal infections, is a mainstay of surveillance. However, surveillance by clinicians also is critical. Clinicians who have diagnosed N. gonorrhoeae infection in a person who was previously treated with a recommended regimen and who probably has not been reexposed should perform culture and susceptibility testing of relevant clinical specimens and report the case to the local health department. To maximize compliance with recommended therapies, medications for gonococcal infections should be dispensed on site.
# Uncomplicated Gonococcal Infections of the Cervix, Urethra, and Rectum
# Recommended Regimens*
Ceftriaxone in a single injection of 125 mg provides sustained, high bactericidal levels in the blood. Extensive clinical experience indicates that ceftriaxone is safe and effective for the treatment of uncomplicated gonorrhea at all anatomic sites, curing 98.9% of uncomplicated urogenital and anorectal infections in published clinical trials (140).
Cefixime has an antimicrobial spectrum similar to that of ceftriaxone, but the 400 mg oral dose does not provide as high, nor as sustained, a bactericidal level as that provided by the 125 mg dose of ceftriaxone. In published clinical trials, the 400 mg dose cured 97.4% of uncomplicated urogenital and anorectal gonococcal infections (140). The advantage of cefixime is that it can be administered orally. Updates on the availability of cefixime are available from CDC or state health departments.
Ciprofloxacin is no longer universally effective against N. gonorrhoeae in the United States (138). However, ciprofloxacin is safe, inexpensive, and can be administered orally. In published clinical trials of uncomplicated urogenital and anorectal infections in the absence of QRNG, a dose of 500 mg of ciprofloxacin provides sustained bactericidal levels with cure rates of 99.8% (140). If QRNG is suspected, ceftriaxone IM or cefixime PO (by mouth) should be used. If neither of these regimens are feasible options, then one of the alternative nonquinolone regimens in this report should be considered.
Similar to ciprofloxacin, ofloxacin is no longer universally effective against N. gonorrhoeae in the United States. The 400 mg oral dose of ofloxacin has been effective for treatment of uncomplicated urogenital and anorectal infections; in clinical trials, 98.6% of infections were cured (140). Levofloxacin, the active l-isomer of ofloxacin, can be used in place of ofloxacin as a single dose of 250 mg.
# Alternative Regimens
Spectinomycin 2 g in a single IM dose OR Single-dose cephalosporin regimens OR Single-dose quinolone regimens Several other antimicrobials are active against N. gonorrhoeae, but none have substantial advantages over the recommended regimens. Spectinomycin is expensive and must be injected; however, it has been effective in published clinical trials, curing 98.2% of uncomplicated urogenital and anorectal gonococcal infections (140). Spectinomycin is useful for the treatment of patients who cannot tolerate cephalosporins and quinolones.
Single-dose cephalosporin regimens (other than ceftriaxone 125 mg IM and cefixime 400 mg orally) that are safe and highly effective against uncomplicated urogenital and anorectal gonococcal infections include ceftizoxime (500 mg, administered IM), cefoxitin (2 g, administered IM with probenecid 1 g orally), and cefotaxime (500 mg, administered IM). None of the injectable cephalosporins offer any advantage over ceftriaxone.
Single-dose quinolone regimens include gatifloxacin 400 mg orally, norfloxacin 800 mg orally, and lomefloxacin 400 mg orally. These regimens appear to be safe and effective for the treatment of uncomplicated gonorrhea, but data regarding their use are limited. None of the regimens appear to offer any advantage over ciprofloxacin, ofloxacin, or levofloxacin, and they are not effective against QRNG. Some evidence suggests that cefpodoxime and cefuroxime axetil 1 g orally might be additional oral alternatives in the treatment of uncomplicated urogenital gonorrhea; additional information on alternative oral regimens are available at http://www.cdc.gov/std. Cefpodoxime proxetil 200 mg PO is less active against N. gonorrhoeae than cefixime and also does not quite meet the minimum efficacy criteria (demonstrated efficacy with lower 95% confidence interval [CI] of >95% in summed clinical trials) with cure rates, 96.5% (CI = 94.8%-98.9%) for urogenital and rectal infection; efficacy in treating pharyngeal infection is unsatisfactory, 78.9% (CI = 54.5%-94%). Clinical studies are being conducted to assess whether cefpodoxime 400 mg PO is an acceptable oral alternative. Treatment with cefuroxime axetil 1 g PO does not quite meet the minimum efficacy criteria for urogenital and rectal infection (95.9%; CI = 94.5%-97.3%) and, its efficacy in treating pharyngeal infection is unacceptable (56.9%; CI = 42.2%-70.7%).
Azithromycin 2 g orally is effective against uncomplicated gonococcal infection but is expensive and causes gastrointestinal distress and is not recommended for treatment of gonorrhea. Although azithromycin 1 g theoretically meets alternative regimen criteria, it is not recommended because of concerns regarding the possible rapid emergence of antimicrobial resistance. N. gonorrhoeae in the United States is not adequately susceptible to penicillins, tetracyclines, and macrolides (e.g., erythromycin) for these antimicrobials to be recommended.
# Uncomplicated Gonococcal Infections of the Pharynx
Gonococcal infections of the pharynx are more difficult to eradicate than infections at urogenital and anorectal sites. Few antimicrobial regimens can reliably cure >90% of gonococcal pharyngeal infections. Although chlamydial coinfection of the pharynx is unusual, coinfection at genital sites sometimes occurs. Therefore, treatment for both gonorrhea and chlamydia is recommended.
# Recommended Regimens
# Recommended Regimens for MSM or Heterosexuals with a History of Recent Travel
Ceftriaxone 125 mg IM in a single dose
# PLUS TREATMENT FOR CHLAMYDIA IN CHLAMY-DIAL INFECTION IS NOT RULED OUT
# Follow-Up
Patients who have uncomplicated gonorrhea and who are treated with any of the recommended or alternative regimens do not need a test of cure. Patients who have symptoms that persist after treatment should be evaluated by culture for N. gonorrhoeae, and any gonococci isolated should be tested for antimicrobial susceptibility. Persistent urethritis, cervicitis, or proctitis also might be caused by C. trachomatis or other organisms.
A high prevalence of N. gonorrhoeae infection is observed in patients who have had gonorrhea in the preceding several months (141,142). The majority of infections identified after treatment with one of the recommended regimens result from reinfection rather than treatment failure, indicating a need for improved patient education and referral of sex partners. Clinicians should consider advising all patients with gonorrhea to be retested 3 months after treatment. If patients do not seek medical care for retesting in 3 months, providers are encouraged to test these patients whenever they next seek medical care within the following 12 months, regardless of whether the patient believes that their sex partners were treated. Retesting is distinct from test of cure to detect therapeutic failure, which is not recommended.
# Management of Sex Partners
Effective clinical management of patients with treatable STDs requires treatment of the patients' recent sex partners to prevent reinfection and curtail further transmission. Patients should be instructed to refer their sex partners for evaluation and treatment. Sex partners of patients with N. gonorrhoeae infection whose last sexual contact with the patient was within 60 days before onset of symptoms or diagnosis of infection in the patient should be evaluated and treated for N. gonorrhoeae and C. trachomatis infections. If a patient's last sexual intercourse was >60 days before onset of symptoms or diagnosis, the patient's most recent sex partner should be treated. Patients should be instructed to avoid sexual intercourse until therapy is completed and until they and their sex partners no longer have symptoms.
For patients with gonorrhea whose partners' treatment cannot be ensured or is unlikely, delivery of antibiotic therapy (i.e., either a prescription or medication) by heterosexual male or female patients to their partners is an option (see Partner Management). Use of this approach (25,27) should always be accompanied by efforts to educate partners about symptoms and to encourage partners to seek clinical evaluation. Male patients must inform female partners of their infection and be given accompanying materials about the importance of seeking medical evaluation for PID (especially if symptomatic). Possible undertreatment of PID in female partners and possible missed opportunities to diagnose other STDs are of concern and have not been evaluated in comparisons with patient-delivered therapy and partner referral. Patient-delivered therapy for patients with gonorrhea should routinely include treatment for chlamydia. This approach should not be considered a routine partner management strategy in MSM because of the high risk of coexisting undiagnosed STDs or HIV infection.
# Special Considerations Allergy, Intolerance, and Adverse Reactions
Persons who cannot tolerate cephalosporins or quinolones should be treated with spectinomycin. Because spectinomycin is unreliable (52% effective) against pharyngeal infections, patients who have suspected or known pharyngeal infection should have a pharyngeal culture 3-5 days after treatment to verify eradication of infection.
# Pregnancy
Pregnant women should not be treated with quinolones or tetracyclines. Those infected with N. gonorrhoeae should be treated with a recommended or alternate cephalosporin. Women who cannot tolerate a cephalosporin should be administered a single 2-g dose of spectinomycin IM. Either azithromycin or amoxicillin is recommended for treatment of presumptive or diagnosed C. trachomatis infection during pregnancy (see Chlamydial Infections).
# Administration of Quinolones to Adolescents
Fluoroquinolones have not been recommended for persons aged <18 years because studies have indicated that they can damage articular cartilage in some young animals. However, no joint damage attributable to quinolone therapy has been observed in children treated with prolonged ciprofloxacin regimens (143). Therefore, children who weigh >45 kg can be treated with any regimen recommended for adults (See Gonococcal Infections).
# HIV Infection
Patients who have gonococcal infection and also are infected with HIV should receive the same treatment regimen as those who are HIV negative.
# Gonococcal Conjunctivitis
In the only published study of the treatment of gonococcal conjunctivitis among U.S. adults, all 12 study participants responded to a single 1-g IM injection of ceftriaxone (144). The following recommendation reflects the opinions of consultants knowledgeable in the field of STDs.
# Recommended Regimen
Ceftriaxone 1 g IM in a single dose Consider lavage of the infected eye with saline solution once.
# Management of Sex Partners
Patients should be instructed to refer their sex partners for evaluation and treatment (see Gonococcal Infections, Management of Sex Partners).
# Disseminated Gonococcal Infection (DGI)
DGI results from gonococcal bacteremia. DGI frequently results in petechial or pustular acral skin lesions, asymmetrical arthralgia, tenosynovitis, or septic arthritis. The infection is complicated occasionally by perihepatitis and rarely by endocarditis or meningitis. Some strains of N. gonorrhoeae that cause DGI may cause minimal genital inflammation.
No studies on the treatment of DGI among adults have been published since publication of the last CDC STD treatment guidelines publication. DGI treatment recommendations reflect the opinions of consultants. No treatment failures have been reported with the recommended regimens.
# Treatment
Hospitalization is recommended for initial therapy, especially for patients who might not comply with treatment, for those in whom diagnosis is uncertain, and for those who have purulent synovial effusions or other complications. Patients should be examined for clinical evidence of endocarditis and meningitis. Patients treated for DGI should be treated presumptively for concurrent C. trachomatis infection, unless appropriate testing excludes this infection. All of the preceding regimens should be continued for 24-48 hours after improvement begins, at which time therapy may be switched to one of the following regimens to complete at least 1 week of antimicrobial therapy.
# Recommended Regimen
Cefixime 400 mg orally twice daily OR Ciprofloxacin 500 mg orally twice daily* OR Ofloxacin 400 mg orally twice daily* OR Levofloxacin 500 mg orally once daily* * Quinolones should not be used for infections in MSM or in those with a history of recent foreign travel or partners' travel, infections acquired in California or Hawaii, or infections acquired in other areas with increased QRNG prevalence.
# Management of Sex Partners
Gonococcal infection frequently is asymptomatic in sex partners of patients who have DGI. As with uncomplicated gonococcal infections, patients should be instructed to refer their sex partners for evaluation and treatment (see Gonococcal Infection, Management of Sex Partners).
# Gonococcal Meningitis and Endocarditis
# Recommended Regimen
# Ceftriaxone 1-2 g IV every 12 hours
Therapy for meningitis should be continued for 10-14 days; therapy for endocarditis should be continued for at least 4 weeks. Treatment of complicated DGI should be undertaken in consultation with a specialist.
# Management of Sex Partners
Patients should be instructed to refer their sex partners for evaluation and treatment (see Gonococcal Infection, Management of Sex Partners).
# Gonococcal Infections Among Infants
Gonococcal infection among infants usually results from exposure to infected cervical exudate at birth. It is usually an acute illness that manifests 2-5 days after birth. The prevalence of infection among infants depends on the prevalence of infection among pregnant women, whether pregnant women are screened for gonorrhea, and whether newborns receive ophthalmia prophylaxis. The most severe manifestations of N. gonorrhoeae infection in newborns are ophthalmia neonatorum and sepsis, which can include arthritis and meningitis. Less severe manifestations include rhinitis, vaginitis, urethritis, and reinfection at sites of fetal monitoring.
# Ophthalmia Neonatorum Caused by N. gonorrhoeae
In the United States, although N. gonorrhoeae causes ophthalmia neonatorum less frequently than C. trachomatis and nonsexually transmitted agents, identifying and treating this infection is especially important because ophthalmia neonatorum can result in perforation of the globe of the eye and blindness.
# Diagnostic Considerations
Infants at increased risk for gonococcal ophthalmia are those who do not receive ophthalmia prophylaxis and those whose mothers have had no prenatal care or whose mothers have a history of STDs or substance abuse. Gonococcal ophthalmia is strongly suspected when intracellular gram-negative diplococci are identified in conjunctival exudate, justifying presumptive treatment for gonorrhea after appropriate cultures for N. gonorrhoeae are obtained. Appropriate chlamydial testing should be done simultaneously. Presumptive treatment for N. gonorrhoeae might be indicated for newborns who are at increased risk for gonococcal ophthalmia and who have conjunctivitis but do not have gonococci in a Gram-stained smear of conjunctival exudate.
In all cases of neonatal conjunctivitis, conjunctival exudates should be cultured for N. gonorrhoeae and tested for antibiotic susceptibility before a definitive diagnosis is made. A definitive diagnosis is vital because of the public health and social consequences of a diagnosis of gonorrhea. Nongonococcal causes of neonatal ophthalmia include Moraxella catarrhalis and other Neisseria species that are indistinguishable from N. gonorrhoeae on Gram-stained smear but can be differentiated in the microbiology laboratory.
# Recommended Regimen
Ceftriaxone 25-50 mg/kg IV or IM in a single dose, not to exceed 125 mg Topical antibiotic therapy alone is inadequate and is unnecessary if systemic treatment is administered.
# Other Management Considerations
Simultaneous infection with C. trachomatis should be considered when a patient does not improve after treatment. Both mother and infant should be tested for chlamydial infection at the same time that gonorrhea testing is conducted (see Ophthalmia Neonatorum Caused by C. trachomatis). Ceftriaxone should be administered cautiously to hyperbilirubinemic infants, especially those born prematurely.
# Follow-Up
Infants who have gonococcal ophthalmia should be hospitalized and evaluated for signs of disseminated infection (e.g., sepsis, arthritis, and meningitis). One dose of ceftriaxone is adequate therapy for gonococcal conjunctivitis.
# MMWR August 4, 2006
# Management of Mothers and Their Sex Partners
The mothers of infants who have gonococcal infection and the mothers' sex partners should be evaluated and treated according to the recommendations for treating gonococcal infections in adults (see Gonococcal Infections in Adolescents and Adults).
# DGI and Gonococcal Scalp Abscesses in Newborns
Sepsis, arthritis, and meningitis (or any combination of these conditions) are rare complications of neonatal gonococcal infection. Localized gonococcal infection of the scalp can result from fetal monitoring through scalp electrodes. Detection of gonococcal infection in neonates who have sepsis, arthritis, meningitis, or scalp abscesses requires cultures of blood, CSF, and joint aspirate on chocolate agar. Specimens obtained from the conjunctiva, vagina, oropharynx, and rectum that are cultured on gonococcal selective medium are useful for identifying the primary site(s) of infection, especially if inflammation is present. Positive Gram-stained smears of exudate, CSF, or joint aspirate provide a presumptive basis for initiating treatment for N. gonorrhoeae. Diagnoses based on Gram-stained smears or presumptive identification of cultures should be confirmed with definitive tests on culture isolates.
# Recommended Regimens
Ceftriaxone 25-50 mg/kg/day IV or IM in a single daily dose for 7 days, with a duration of 10-14 days, if meningitis is documented OR Cefotaxime 25 mg/kg IV or IM every 12 hours for 7 days, with a duration of 10-14 days, if meningitis is documented
# Prophylactic Treatment for Infants Whose Mothers Have Gonococcal Infection
Infants born to mothers who have untreated gonorrhea are at high risk for infection.
# Recommended Regimen in the Absence of Signs of Gonococcal Infection
Ceftriaxone 25-50 mg/kg IV or IM, not to exceed 125 mg, in a single dose
# Other Management Considerations
Both mother and infant should be tested for chlamydial infection.
# Follow-Up
Follow-up examination is not required.
# Management of Mothers and Their Sex Partners
The mothers of infants who have gonococcal infection and the mothers' sex partners should be evaluated and treated according to the recommendations for treatment of gonococcal infections in adults (see Gonococcal Infections).
# Gonococcal Infections Among Children
Sexual abuse is the most frequent cause of gonococcal infection in pre-adolescent children (see Sexual Assault or Abuse of Children). Vaginitis is the most common manifestation of gonococcal infection in preadolescent girls. PID after vaginal infection is probably less common in children than among adults. Among sexually abused children, anorectal and pharyngeal infections with N. gonorrhoeae are common and frequently asymptomatic.
# Diagnostic Considerations
Because of the legal implications of a diagnosis of N. gonorrhoeae infection in a child, only standard culture procedures for the isolation of N. gonorrhoeae should be used for children. Nonculture gonococcal tests for gonococci (e.g., Gram-stained smear, nucleic acid hybridization tests, EIA, and NAAT) should not be used without standard culture; none of these tests have been approved by FDA for use with specimens obtained from the oropharynx, rectum, or genital tract of children. Specimens from the vagina, urethra, pharynx, or rectum should be streaked onto selective media for isolation of N. gonorrhoeae, and all presumptive isolates of N. gonorrhoeae should be identified definitively by at least two tests that involve different principles (e.g., biochemical, enzyme substrate, or serologic). Isolates should be preserved to enable additional or repeated testing.
# Recommended Regimens for Children Who Weigh >45 kg
Treat with one of the regimens recommended for adults (see Gonococcal Infections)
Fluoroquinolones have not been recommended for persons aged <18 years because they have damaged articular cartilage in young animals. However, no such joint damage clearly attributable to quinolone therapy has been observed in children, even in those receiving multiple-dose regimens.
# Recommended Regimens for Children Who Weigh <45 kg and Who Have Uncomplicated Gonococcal Vulvovaginitis, Cervicitis, Urethritis, Pharyngitis, or Proctitis
Ceftriaxone 125 mg IM in a single dose
# Alternative Regimen
Spectinomycin 40 mg/kg (maximum dose: 2 g) IM in a single dose may be used, but this therapy is unreliable for treatment of pharyngeal infections. Some specialists use cefixime to treat gonococcal infections in children because it can be administered orally; however, no reports have been published concerning the safety or effectiveness of cefixime used for this purpose.
# Recommended Regimen for Children Who Weigh <45 kg and Who Have Bacteremia or Arthritis
Ceftriaxone 50 mg/kg (maximum dose: 1 g) IM or IV in a single dose daily for 7 days
# Recommended Regimen for Children Who Weigh >45 kg and Who Have Bacteremia or Arthritis
Ceftriaxone 50 mg/kg IM or IV in a single dose daily for 7 days
# Follow-Up
Follow-up cultures are unnecessary if ceftriaxone is used. If spectinomycin is used to treat pharyngitis, a follow-up culture is necessary to ensure that treatment was effective.
# Other Management Considerations
Only parenteral cephalosporins are recommended for use in children. Ceftriaxone is approved for all gonococcal infections in children; cefotaxime is approved for gonococcal ophthalmia only. Oral cephalosporins used for treatment of gonococcal infections in children have not been adequately evaluated.
All children who have gonococcal infections should be evaluated for coinfection with syphilis and C. trachomatis. (For a discussion of concerns regarding sexual assault, refer to Sexual Assault or Abuse of Children).
# Ophthalmia Neonatorum Prophylaxis
To prevent gonococcal ophthalmia neonatorum, a prophylactic agent should be instilled into the eyes of all newborn infants; this procedure is required by law in the majority of states. All of the recommended prophylactic regimens in this section prevent gonococcal ophthalmia. However, the efficacy of these preparations in preventing chlamydial ophthalmia is less clear, and they do not eliminate nasopharyngeal colonization by C. trachomatis. The diagnosis and treatment of gonococcal and chlamydial infections in pregnant women is the best method for preventing neonatal gonococcal and chlamydial disease. Not all women, however, receive prenatal care. Ocular prophylaxis is warranted because it can prevent sight-threatening gonococcal ophthalmia and because it is safe, easy to administer, and inexpensive.
# Prophylaxis
# Recommended Regimens
Erythromycin (0.5%) ophthalmic ointment in a single application OR Tetracycline ophthalmic ointment (1%) in a single application
One of these recommended preparations should be instilled into both eyes of every neonate as soon as possible after delivery. If prophylaxis is delayed (i.e., not administered in the delivery room), a monitoring system should be established to ensure that all infants receive prophylaxis. All infants should be administered ocular prophylaxis, regardless of whether they are delivered vaginally or by cesarean section. Single-use tubes or ampules are preferable to multiple-use tubes. Bacitracin is not effective. Use of povidone iodine has not been studied adequately.
# Diseases Characterized by Vaginal Discharge
# Management of Patients Who Have Vaginal Infections
Vaginitis is usually characterized by a vaginal discharge and/ or vulvar itching and irritation, and a vaginal odor might be present. The three diseases most frequently associated with vaginal discharge are BV (replacement of the normal vaginal flora by an overgrowth of anaerobic microorganisms, mycoplasmas, and Gardnerella vaginalis), trichomoniasis (T. vaginalis), and candidiasis (usually caused by Candida albicans). Cervicitis can sometimes cause a vaginal discharge. Although vulvovaginal candidiasis (VVC) usually is not transmitted sexually, it is included in this section because it is frequently diagnosed in women being evaluated for STDs.
Various diagnostic methods are available to identify the etiology of an abnormal vaginal discharge. Laboratory testing fails to identify the cause of vaginitis in a minority of women. The cause of vaginal symptoms usually can be determined by pH and microscopic examination of fresh samples of the discharge. The pH of the vaginal secretions can be determined by narrow-range pH paper; an elevated pH (i.e., >4.5) is common with BV or trichomoniasis but might not be highly specific. Discharge can be further examined by diluting one sample in one to two drops of 0.9% normal saline solution on one slide and a second sample in 10% potassium hydroxide (KOH) solution. An amine odor detected immediately after applying KOH suggests BV. Cover slips are placed on the slides, and they are examined under a microscope at lowand high-dry power. Motile T. vaginalis or clue cells (epithelial cells with borders obscured by small bacteria), which are characteristic of BV, usually are identified easily in the saline specimen. WBCs without evidence of trichomonads or yeast are usually suggestive of cervicitis (see Cervicitis). The yeast or pseudohyphae of Candida species are more easily identified in the KOH specimen. However, the absence of trichomonads or pseudohyphae does not rule out these infections because several studies have demonstrated the presence of these pathogens by culture or PCR after a negative microscopic examination. The presence of objective signs of vulvar inflammation in the absence of vaginal pathogens, along with a minimal amount of discharge, suggests the possibility of mechanical, chemical, allergic, or other noninfectious irritation of the vulva. Culture for T. vaginalis is more sensitive than microscopic examination. In settings where microscopy is not available, alternative point-of-care tests may be used to diagnose vaginitis.
# Bacterial Vaginosis
BV is a polymicrobial clinical syndrome resulting from replacement of the normal H2O2-producing Lactobacillus sp. in the vagina with high concentrations of anaerobic bacteria (e.g., Prevotella sp. and Mobiluncus sp.), G. vaginalis, and Mycoplasma hominis. BV is the most prevalent cause of vaginal discharge or malodor; however, more than 50% of women with BV are asymptomatic. The cause of the microbial alteration is not fully understood. BV is associated with having multiple sex partners, a new sex partner, douching, and lack of vaginal lactobacilli; whether BV results from acquisition of a sexually transmitted pathogen is unclear. Women who have never been sexually active are rarely affected. Treatment of male sex partners has not been beneficial in preventing the recurrence of BV.
# Diagnostic Considerations
BV can be diagnosed by the use of clinical criteria or Gram stain. Clinical criteria require three of the following symptoms or signs:
• homogeneous, thin, white discharge that smoothly coats the vaginal walls; • presence of clue cells on microscopic examination; • pH of vaginal fluid >4.5; and • a fishy odor of vaginal discharge before or after addition of 10% KOH (i.e., the whiff test).
When a Gram stain is used, determining the relative concentration of lactobacilli (long Gram-positive rods), Gramnegative and Gram-variable rods and cocci (i.e., G. vaginalis, Prevotella, Porphyromonas, and peptostreptococci), and curved Gram-negative rods (Mobiluncus) characteristic of BV is considered the gold standard laboratory method for diagnosing BV. Culture of G. vaginalis is not recommended as a diagnostic tool because it is not specific. However, a DNA probebased test for high concentrations of G. vaginalis (Affirm TM VP III, Becton Dickinson, Sparks, Maryland) might have clinical utility. Cervical Pap tests have no clinical utility for the diagnosis of BV because of low sensitivity. Other commercially available tests that might be useful for the diagnosis of BV include a card test for the detection of elevated pH and trimethylamine (QuickVue Advance Quidel, San Diego, California) and prolineaminopeptidase (Pip Activity TestCard TM , Quidel, San Diego, California).
# Treatment
The established benefits of therapy for BV in nonpregnant women are to 1) relieve vaginal symptoms and signs of infection and 2) reduce the risk for infectious complications after abortion or hysterectomy. Other potential benefits might include a reduction in risk for other infections (e.g., HIV and other STDs). All women who have symptomatic disease require treatment.
BV during pregnancy is associated with adverse pregnancy outcomes, including premature rupture of the membranes, preterm labor, preterm birth, intraamniotic infection, and postpartum endometritis. The established benefit of therapy for BV in pregnant women is to relieve vaginal symptoms and signs of infection. Additional potential benefits of therapy include 1) reducing the risk for infectious complications associated with BV during pregnancy and 2) reducing the risk for other infections (e.g., other STDs or HIV). The results of several investigations indicate that treatment of pregnant women with BV who are at high risk for preterm delivery (i.e., those who previously delivered a premature infant) might reduce the risk for prematurity (145)(146)(147). Therefore, clinicians should consider evaluation and treatment of high-risk pregnant women with asymptomatic BV.
The bacterial flora that characterizes BV have been recovered from the endometria and salpinges of women who have PID. BV has been associated with endometritis, PID, and vaginal cuff cellulitis after invasive procedures, including endometrial biopsy, hysterectomy, hysterosalpingography, placement of an IUD, cesarean section, and uterine curettage. The results of two randomized controlled trials have indicated that treatment of BV with metronidazole substantially reduced postabortion PID (148,149). Three trials that evaluated the use of anaerobic antimicrobial coverage (i.e., metronidazole) for routine operative prophylaxis before abortion and seven trials that evaluated this additional coverage for women undergoing hysterectomy demonstrated a substantial reduction in postoperative infectious complications (148)(149)(150)(151)(152)(153)(154)(155)(156). Because of the increased risk for postoperative infectious complications associated with BV, some specialists suggest that before performing surgical abortion or hysterectomy, providers should screen for and treat women with BV in addition to providing routine prophylaxis. However, more information is needed before recommending treatment of asymptomatic BV before other invasive procedures.
# Recommended Regimens
Metronidazole 500 mg orally twice a day for 7 days OR Metronidazole gel, 0.75%, one full applicator (5 g) intravaginally, once a day for 5 days OR Clindamycin cream, 2%, one full applicator (5 g) intravaginally at bedtime for 7 days
Patients should be advised to avoid consuming alcohol during treatment with metronidazole and for 24 hours thereafter. Clindamycin cream is oil-based and might weaken latex condoms and diaphragms for 5 days after use. Refer to clindamycin product labeling for additional information. Topical clindamycin preparations should not be used in the second half of pregnancy.
The recommended metronidazole regimens are equally efficacious. One randomized trial evaluated the clinical equivalency of intravaginal metronidazole gel 0.75% once daily versus twice daily and demonstrated similar cure rates 1 month after therapy (157).
# Alternative Regimens
Clindamycin 300 mg orally twice a day for 7 days OR Clindamycin ovules 100 mg intravaginally once at bedtime for 3 days Metronidazole 2 g single-dose therapy has the lowest efficacy for BV and is no longer a recommended or alternative regimen. FDA has cleared metronidazole 750 mg extended release tablets once daily for 7 days and a single dose of clindamycin intravaginal cream. Limited data have been published that compares the clinical or microbiologic equivalencies of these regimens with other regimens. Cure rates do not differ between intravaginal clindamycin cream and ovules (158).
Several studies have evaluated the clinical and microbiologic efficacy of using lactobacillus intravaginal suppositories to restore normal flora and treat BV. However, no currently available lactobacillus suppository was determined to be better than placebo 1 month after therapy for either clinical or microbiologic cure. No data support the use of douching for treatment or relief of symptoms.
# Follow-Up
Follow-up visits are unnecessary if symptoms resolve. Because recurrence of BV is not unusual, women should be advised to return for additional therapy if symptoms recur. A treatment regimen different from the original regimen may be used to treat recurrent disease. However, women with multiple recurrences should be managed in consultation with a specialist. One randomized trial for persistent BV indicated that metronidazole gel 0.75% twice per week for 6 months after completion of a recommended regimen was effective in maintaining a clinical cure for 6 months (159).
# Management of Sex Partners
The results of clinical trials indicate that a woman's response to therapy and the likelihood of relapse or recurrence are not affected by treatment of her sex partner(s). Therefore, routine treatment of sex partners is not recommended.
# Special Considerations
# Allergy or Intolerance to the Recommended Therapy
Intravaginal clindamycin cream is preferred in case of allergy or intolerance to metronidazole. Intravaginal metronidazole gel can be considered for patients who do not tolerate systemic metronidazole, but patients allergic to oral metronidazole should not be administered intravaginal metronidazole.
# Pregnancy
All pregnant women who have symptomatic disease require treatment. BV has been associated with adverse pregnancy outcomes (e.g., premature rupture of the membranes, chorioamnionitis, preterm labor, preterm birth, intraamniotic infection, postpartum endometritis, and postcesarean wound infection). Some specialists prefer using systemic therapy to treat possible subclinical upper genital tract infections.
Treatment of BV in asymptomatic pregnant women at high risk for preterm delivery (i.e., those who have previously delivered a premature infant) with a recommended oral regimen has reduced preterm delivery in three of four randomized controlled trials (145,146,160,161); some specialists recommend screening and oral treatment of these women. However, the optimal treatment regimens have not been established.
Screening (if conducted) and treatment should be performed during the first prenatal visit.
Two trials that evaluated the efficacy of metronidazole during pregnancy used the 250-mg regimen (145,146). However, some specialists suggest using a regimen of 500 mg twice daily in pregnant women. One small trial demonstrated that treatment with oral metronidazole 500 mg twice daily was equally effective as metronidazole gel, with cure rates of 70% (162). These regimens were not effective in reducing preterm birth in any group of women. Multiple studies and metaanalyses have not demonstrated an association between metronidazole use during pregnancy and teratogenic or mutagenic effects in newborns (164)(165)(166).
# Recommended Regimens for Pregnant Women
Metronidazole 500 mg orally twice a day for 7 days OR Metronidazole 250 mg orally three times a day for 7 days OR Clindamycin 300 mg orally twice a day for 7 days Whether treatment of asymptomatic pregnant women with BV who are at low risk for preterm delivery reduces adverse outcomes of pregnancy is unclear. One trial in which oral clindamycin was used demonstrated a reduction in spontaneous preterm birth (147). Several trials have evaluated the use of intravaginal clindamycin during pregnancy to reduce preterm birth and treat asymptomatic BV. One trial in which women were treated before 20 weeks' gestation demonstrated a reduction in preterm birth (166). In three other trials, intravaginal clindamycin cream was administered at 16-32 weeks' gestation, and an increase in adverse events (e.g., low birthweight and neonatal infections) was observed in newborns (167)(168)(169). Therefore, intravaginal clindamycin cream should only be used during the first half of pregnancy.
# Follow-Up of Pregnant Women
Treatment of BV in asymptomatic pregnant women who are at high risk for preterm delivery might prevent adverse pregnancy outcomes. Therefore, a follow-up evaluation 1 month after completion of treatment should be considered to evaluate whether therapy was effective.
# HIV Infection
Patients who have BV and also are infected with HIV should receive the same treatment regimen as those who are HIV negative. BV appears to be more persistent in HIV-positive women.
# Trichomoniasis
Trichomoniasis is caused by the protozoan T. vaginalis. Some men who are infected with T. vaginalis might not have symptoms; others have NGU. Many infected women have symptoms characterized by a diffuse, malodorous, yellow-green vaginal discharge with vulvar irritation. However, some women have minimal or no symptoms.
Diagnosis of vaginal trichomoniasis is usually performed by microscopy of vaginal secretions, but this method has a sensitivity of only approximately 60%-70% and requires immediate evaluation of wet preparation slide for optimal results. Other FDA-cleared tests for trichomoniasis in women include OSOM Trichomonas Rapid Test (Genzyme Diagnostics, Cambridge, Massachusetts), an immunochromatographic capillary flow dipstick technology, and the Affirm™ VP III (Becton Dickenson, San Jose, California), a nucleic acid probe test that evaluates for T. vaginalis, G. vaginalis, and C. albicans. These tests are both performed on vaginal secretions and have a sensitivity >83% and a specificity >97%. Both tests are pointof-care diagnostics. The results of the OSOM Trichomonas Rapid Test are available in approximately 10 minutes, and results of the Affirm™ VP III are available within 45 minutes. Although these tests tend to be more sensitive than vaginal wet preparation, false positives might occur especially in low prevalence populations. Culture is the most sensitive and specific commercially available method of diagnosis. In women in whom trichomoniasis is suspected but not confirmed by microscopy, vaginal secretions should be cultured for T. vaginalis.
In men, wet preparation is insensitive, and culture testing of urethral swab, urine, and semen is required for optimal sensitivity. No FDA-cleared PCR test for T. vaginalis is available in the United States, but such testing might be available from commercial laboratories that have developed their own PCR tests.
# Recommended Regimens
Metronidazole 2 g orally in a single dose OR Tinidazole 2 g orally in a single dose
# Alternative Regimen
Metronidazole 500 mg orally twice a day for 7 days Patients should be advised to avoid consuming alcohol during treatment with metronidazole or tinidazole. Abstinence from alcohol use should continue for 24 hours after completion of metronidazole or 72 hours after completion of tinidazole.
The nitroimidazoles comprise the only class of drugs useful for the oral or parenteral therapy of trichomoniasis. Of these drugs, metronidazole and tinidazole are available in the United States and are cleared by the FDA for the treatment of trichomoniasis. In randomized clinical trials, the recommended metronidazole regimens have resulted in cure rates of approximately 90%-95%, and the recommended tinidazole regimen has resulted in cure rates of approximately 86%-100%. The appropriate treatment of sex partners might increase these reported rates. Randomized controlled trials comparing single 2 g doses of metronidazole and tinidazole suggest that tinidazole is equivalent to, or superior to, metronidazole in achieving parasitologic cure and resolution of symptoms (170). Treatment of patients and sex partners results in relief of symptoms, microbiologic cure, and reduction of transmission.
Metronidazole gel is considerably less efficacious for the treatment of trichomoniasis (<50%) than oral preparations of metronidazole. Topically applied antimicrobials (e.g., metronidazole gel) are unlikely to achieve therapeutic levels in the urethra or perivaginal glands; therefore, use of the gel is not recommended. Several other topically applied antimicrobials occasionally have been used for treatment of trichomoniasis; however, these preparations probably do not have greater efficacy than metronidazole gel.
# Follow-Up
Follow-up is unnecessary for men and women who become asymptomatic after treatment or who are initially asymptomatic. Some strains of T. vaginalis can have diminished susceptibility to metronidazole; however, infections caused by the majority of these organisms respond to tinidazole or higher doses of metronidazole. Low-level metronidazole resistance has been identified in 2%-5% of cases of vaginal trichomoniasis. High-level resistance is rare. Tinidazole has a longer serum half-life and reaches higher levels in genitourinary tissues than metronidazole. In addition, many T. vaginalis isolates have lower minimum inhibitory concentrations (MICs) to tinidazole than metronidazole.
If treatment failure occurs with metronidazole 2 g single dose and reinfection is excluded, the patient can be treated with metronidazole 500 mg orally twice daily for 7 days or tinidazole 2 g single dose. For patients failing either of these regimens, clinicians should consider treatment with tinidazole or metronidazole at 2 g orally for 5 days. If these therapies are not effective, further management should be discussed with a specialist. The consultation should ideally include determination of the susceptibility of T. vaginalis to metronidazole and tinidazole. Consultation and T. vaginalis susceptibility testing is available from CDC (telephone: 770-488-4115; website: http://www.cdc.gov/std).
# Management of Sex Partners
Sex partners of patients with T. vaginalis should be treated. Patients should be instructed to avoid sex until they and their sex partners are cured (i.e., when therapy has been completed and patient and partner(s) are asymptomatic).
# Special Considerations
# Allergy, Intolerance, and Adverse Reactions
Metronidazole and tinidazole are both nitroimidazoles. Patients with an immediate-type allergy to a nitroimidazole can be managed by metronidazole desensitization in consultation with a specialist (171,172). Topical therapy with drugs other than nitroimidazoles can be attempted, but cure rates are low (<50%).
# Pregnancy
Vaginal trichomoniasis has been associated with adverse pregnancy outcomes, particularly premature rupture of membranes, preterm delivery, and low birthweight. However, data do not suggest that metronidazole treatment results in a reduction in perinatal morbidity. Although some trials suggest the possibility of increased prematurity or low birthweight after metronidazole treatment, limitations of the studies prevent definitive conclusions regarding risks of treatment (173,174). Treatment of T. vaginalis might relieve symptoms of vaginal discharge in pregnant women and might prevent respiratory or genital infection of the newborn and further sexual transmission. Clinicians should counsel patients regarding the potential risks and benefits of treatment. Some specialists would defer therapy in asymptomatic pregnant women until after 37 weeks' gestation. In addition, these pregnant women should be provided careful counseling regarding condom use and the continued risk of sexual transmission.
Women may be treated with 2 g of metronidazole in a single dose. Metronidazole is pregnancy category B (animal studies have revealed no evidence of harm to the fetus, but no adequate, well-controlled studies among pregnant women have been conducted). Multiple studies and meta-analyses have not demonstrated a consistent association between metronidazole use during pregnancy and teratogenic or mutagenic effects in infants (163)(164)(165). Tinidazole is pregnancy category C (animal studies have demonstrated an adverse event, and no adequate, well-controlled studies in pregnant women have been conducted), and its safety in pregnant women has not been well-evaluated.
In lactating women who are administered metronidazole, withholding breastfeeding during treatment and for 12-24 hours after the last dose will reduce the exposure of metronidazole to the infant. While using tinidazole, interruption of breastfeeding is recommended during treatment and for 3 days after the last dose.
# HIV Infection
Patients who have trichomoniasis and also are infected with HIV should receive the same treatment regimen as those who are HIV negative. The incidence, persistence, and recurrence of trichomoniasis in HIV-infected women are not correlated with immune status.
# Vulvovaginal Candidiasis
VVC usually is caused by C. albicans but occasionally is caused by other Candida sp. or yeasts. Typical symptoms of VVC include pruritus, vaginal soreness, dyspareunia, external dysuria, and abnormal vaginal discharge. None of these symptoms is specific for VVC. An estimated 75% of women will have at least one episode of VVC, and 40%-45% will have two or more episodes. On the basis of clinical presentation, microbiology, host factors, and response to therapy, VVC can be classified as either uncomplicated or complicated (Box 2). Approximately 10%-20% of women will have complicated VVC, suggesting diagnostic and therapeutic considerations.
# Uncomplicated VVC
# Diagnostic Considerations in Uncomplicated VVC
A diagnosis of Candida vaginitis is suggested clinically by the presence of external dysuria and vulvar pruritus, pain, swelling, and redness. Signs include vulvar edema, fissures, excoriations, or thick curdy vaginal discharge. The diagnosis can be made in a woman who has signs and symptoms of vaginitis when either 1) a wet preparation (saline, 10% KOH) or Gram stain of vaginal discharge demonstrates yeasts or pseudohyphae or 2) a culture or other test yields a positive result for a yeast species. Candida vaginitis is associated with a normal vaginal pH (<4.5). Use of 10% KOH in wet preparations improves the visualization of yeast and mycelia by disrupting cellular material that might obscure the yeast or pseudohyphae. Examination of a wet mount with KOH preparation should be performed for all women with symptoms or signs of VVC, and women with a positive result should receive treatment. For those with negative wet mounts, vaginal cultures for Candida should be considered for those with any sign or multiple symptoms. If Candida cultures cannot be done, empiric treatment can be considered for symptomatic women with any sign of VVC on examination when the wet mount is negative. Identifying Candida by culture in the absence of symptoms or signs is not an indication for treatment because approximately 10%-20% of women harbor Candida sp. and other yeasts in the vagina. VVC can occur concomitantly with STDs. The majority of healthy women with uncomplicated VVC have no identifiable precipitating factors.
# Treatment
Short-course topical formulations (i.e., single dose and regimens of 1-3 days) effectively treat uncomplicated VVC. The topically applied azole drugs are more effective than nystatin. Treatment with azoles results in relief of symptoms and negative cultures in 80%-90% of patients who complete therapy.
# Recommended Regimens
# Intravaginal Agents:
Butoconazole 2% cream 5 g intravaginally for 3 days* OR Butoconazole 2% cream 5 g (Butaconazole1-sustained release), single intravaginal application OR Clotrimazole 1% cream 5 g intravaginally for 7-14 days* OR Clotrimazole 100 mg vaginal tablet for 7 days OR Clotrimazole 100 mg vaginal tablet, two tablets for 3 days OR Miconazole 2% cream 5 g intravaginally for 7 days* OR The creams and suppositories in this regimen are oil-based and might weaken latex condoms and diaphragms. Refer to condom product labeling for further information.
Intravaginal preparations of butaconazole, clotrimazole, miconazole, and tioconazole are available over-the-counter (OTC). Women whose condition has previously been diagnosed with VVC are not necessarily more likely to be able to diagnose themselves; therefore, any woman whose symptoms persist after using an OTC preparation, or who has a recurrence of symptoms within 2 months, should be evaluated with office-based testing. Unnecessary or inappropriate use of OTC preparations is common and can lead to a delay in the treatment of other vulvovaginitis etiologies, which can result in adverse clinical outcomes.
# Follow-Up
Patients should be instructed to return for follow-up visits only if symptoms persist or recur within 2 months of onset of initial symptoms.
# Management of Sex Partners
VVC is not usually acquired through sexual intercourse; treatment of sex partners is not recommended but may be considered in women who have recurrent infection. A minority of male sex partners might have balanitis, which is characterized by erythematous areas on the glans of the penis in conjunction with pruritus or irritation. These men benefit from treatment with topical antifungal agents to relieve symptoms.
# Special Considerations
# Allergy, Intolerance, and Adverse Reactions
Topical agents usually cause no systemic side effects, although local burning or irritation might occur. Oral agents occasionally cause nausea, abdominal pain, and headache. Therapy with the oral azoles has been associated rarely with abnormal elevations of liver enzymes. Clinically important interactions can occur when these oral agents are administered with other drugs, including astemizole, calcium channel antagonists, cisapride, coumadin, cyclosporin A, oral hypoglycemic agents, phenytoin, protease inhibitors, tacrolimus, terfenadine, theophylline, trimetrexate, and rifampin.
# Complicated VVC
# Recurrent Vulvovaginal Candidiasis (RVVC)
RVVC, usually defined as four or more episodes of symptomatic VVC in 1 year, affects a small percentage of women (<5%). The pathogenesis of RVVC is poorly understood, and the majority of women with RVVC have no apparent predisposing or underlying conditions. Vaginal cultures should be obtained from patients with RVVC to confirm the clinical diagnosis and to identify unusual species, including nonalbicans species, particularly Candida glabrata (C. glabrata does not form pseudohyphae or hyphae and is not easily recognized on microscopy). C. glabrata and other nonalbicans Candidia species are observed in 10%-20% of patients with RVVC. Conventional antimycotic therapies are not as effective against these species as against C. albicans.
# Treatment
Each individual episode of RVVC caused by C. albicans responds well to short duration oral or topical azole therapy. However, to maintain clinical and mycologic control, some specialists recommend a longer duration of initial therapy (e.g., 7-14 days of topical therapy or a 100 mg, 150 mg, or 200 mg oral dose of fluconazole every third day for a total of 3 doses (day 1, 4, and 7) to attempt mycologic remission before initiating a maintenance antifungal regimen.
# Maintenance Regimens
Oral fluconazole (i.e., 100-mg, 150-mg, or 200-mg dose) weekly for 6 months is the first line of treatment. If this regimen is not feasible, some specialists recommend topical clotrimazole 200 mg twice a week, clotrimazole (500-mg dose vaginal suppositories once weekly), or other topical treatments used intermittently.
Suppressive maintenance antifungal therapies are effective in reducing RVVC. However, 30%-50% of women will have recurrent disease after maintenance therapy is discontinued. Routine treatment of sex partners is controversial. C. albicans azole resistance is rare in vaginal isolates, and susceptibility testing is usually not warranted for individual treatment guidance.
# Severe VVC
Severe vulvovaginitis (i.e., extensive vulvar erythema, edema, excoriation, and fissure formation) is associated with lower clinical response rates in patients treated with short courses of topical or oral therapy. Either 7-14 days of topical azole or 150 mg of fluconazole in two sequential doses (second dose 72 hours after initial dose) is recommended.
# Nonalbicans VVC
The optimal treatment of nonalbicans VVC remains unknown. Options include longer duration of therapy (7-14 days) with a nonfluconazole azole drug (oral or topical) as first-line therapy. If recurrence occurs, 600 mg of boric acid in a gelatin capsule is recommended, administered vaginally once daily for 2 weeks. This regimen has clinical and mycologic eradication rates of approximately 70% (175). If symptoms recur, referral to a specialist is advised.
# Compromised Host
Women with underlying debilitating medical conditions (e.g., those with uncontrolled diabetes or those receiving corticosteroid treatment) do not respond as well to short-term therapies. Efforts to correct modifiable conditions should be made, and more prolonged (i.e., 7-14 days) conventional antimycotic treatment is necessary.
# Pregnancy
VVC frequently occurs during pregnancy. Only topical azole therapies, applied for 7 days, are recommended for use among pregnant women.
# HIV Infection
The incidence of VVC in HIV-infected women is unknown. Vaginal Candida colonization rates among HIV-infected women are higher than among those for seronegative women with similar demographic characteristics and high-risk behaviors, and the colonization rates correlate with increasing severity of immunosuppression. Symptomatic VVC is more frequent in seropositive women and similarly correlates with severity of immunodeficiency. In addition, among HIV-infected women, systemic azole exposure is associated with the isolation of nonalbicans Candida species from the vagina.
Based on available data, therapy for VVC in HIV-infected women should not differ from that for seronegative women. Although long-term prophylactic therapy with fluconazole at a dose of 200 mg weekly has been effective in reducing C. albicans colonization and symptomatic VVC (176), this regimen is not recommended for routine primary prophylaxis in HIV-infected women in the absence of recurrent VVC (50). Given the frequency at which RVVC occurs in the immmunocompetent healthy population, the occurrence of RVVC should not be considered an indication for HIV testing.
# Pelvic Inflammatory Disease
PID comprises a spectrum of inflammatory disorders of the upper female genital tract, including any combination of endometritis, salpingitis, tubo-ovarian abscess, and pelvic peritonitis. Sexually transmitted organisms, especially N. gonorrhoeae and C. trachomatis, are implicated in many cases; however, microorganisms that comprise the vaginal flora (e.g., anaerobes, G. vaginalis, Haemophilus influenzae, enteric Gram-negative rods, and Streptococcus agalactiae) also have been associated with PID. In addition, cytomegalovirus (CMV), M. hominis, U. urealyticum, and M. genitalium might be associated with some cases of PID. All women who are diagnosed with acute PID should be tested for N. gonorrhoeae and C. trachomatis and should be screened for HIV infection.
# Diagnostic Considerations
Acute PID is difficult to diagnose because of the wide variation in the symptoms and signs. Many women with PID have subtle or mild symptoms. Delay in diagnosis and treatment probably contributes to inflammatory sequelae in the upper reproductive tract. Laparoscopy can be used to obtain a more accurate diagnosis of salpingitis and a more complete bacteriologic diagnosis. However, this diagnostic tool frequently is not readily available, and its use is not easy to justify when symptoms are mild or vague. Moreover, laparoscopy will not detect endometritis and might not detect subtle inflammation of the fallopian tubes. Consequently, a diagnosis of PID usually is based on clinical findings.
The clinical diagnosis of acute PID is imprecise (177,178). Data indicate that a clinical diagnosis of symptomatic PID has a positive predictive value (PPV) for salpingitis of 65%-90% compared with laparoscopy. The PPV of a clinical diagnosis of acute PID depends on the epidemiologic characteristics of the population, with higher PPVs among sexually active young women (particularly adolescents), among patients attending STD clinics, or in other settings where the rates of gonorrhea or chlamydia are high. In all settings, however, no single historical, physical, or laboratory finding is both sensitive and specific for the diagnosis of acute PID (i.e., can be used both to detect all cases of PID and to exclude all women without PID). Combinations of diagnostic findings that improve either sensitivity (i.e., detect more women who have PID) or specificity (i.e., exclude more women who do not have PID) do so only at the expense of the other. For example, requiring two or more findings excludes more women who do not have PID but also reduces the number of women with PID who are identified.
Many episodes of PID go unrecognized. Although some cases are asymptomatic, others are not diagnosed because the patient or the health-care provider fails to recognize the implications of mild or nonspecific symptoms or signs (e.g., abnormal bleeding, dyspareunia, and vaginal discharge). Because of the difficulty of diagnosis and the potential for damage to the reproductive health of women, even by apparently mild or subclinical PID, health-care providers should maintain a low threshold for the diagnosis of PID.
The optimal treatment regimen and long-term outcome of early treatment of women with asymptomatic or subclinical PID are unknown. The following recommendations for diagnosing PID are intended to help health-care providers recognize when PID should be suspected and when they need to obtain additional information to increase diagnostic certainty. Diagnosis and management of other common causes of lower abdominal pain (e.g., ectopic pregnancy, acute appendicitis, and functional pain) are unlikely to be impaired by initiating empiric antimicrobial therapy for PID.
Empiric treatment of PID should be initiated in sexually active young women and other women at risk for STDs if they are experiencing pelvic or lower abdominal pain, if no cause for the illness other than PID can be identified, and if one or more of the following minimum criteria are present on pelvic examination:
• cervical motion tenderness OR uterine tenderness OR adnexal tenderness. The requirement that all three minimum criteria be present before the initiation of empiric treatment could result in insufficient sensitivity for the diagnosis of PID. The presence of signs of lower genital tract inflammation, in addition to one of the three minimum criteria, increases the specificity of diagnosis. In deciding upon the initiation of empiric treatment, clinicians should also consider the risk profile of the patient for STDs.
More elaborate diagnostic evaluation frequently is needed because incorrect diagnosis and management might cause unnecessary morbidity. These additional criteria may be used to enhance the specificity of the minimum criteria. The following additional criteria can be used to enhance the specificity of the minimum criteria and support a diagnosis of PID:
• oral temperature >101°F (>38.3°C),
• abnormal cervical or vaginal mucopurulent discharge, • presence of abundant numbers of WBC on saline microscopy of vaginal secretions, • elevated erythrocyte sedimentation rate, • elevated C-reactive protein, and • laboratory documentation of cervical infection with N. gonorrhoeae or C. trachomatis. The majority of women with PID have either mucopurulent cervical discharge or evidence of WBC on a microscopic evaluation of a saline preparation of vaginal fluid. If the cervical discharge appears normal and no WBCs are observed on the wet prep of vaginal fluid, the diagnosis of PID is unlikely, and alternative causes of pain should be investigated. A wet prep of vaginal fluid offers the ability to detect the presence of concomitant infections (e.g., bacterial vaginosis and trichomoniasis).
The most specific criteria for diagnosing PID include the following:
• endometrial biopsy with histopathologic evidence of endometritis; • transvaginal sonography or magnetic resonance imaging techniques showing thickened, fluid-filled tubes with or without free pelvic fluid or tubo-ovarian complex, or doppler studies suggesting pelvic infection (e.g., tubal hyperemia); and • laparoscopic abnormalities consistent with PID. A diagnostic evaluation that includes some of these more extensive studies might be warranted in some cases. Endometrial biopsy is warranted in women undergoing laparoscopy who do not have visual evidence of salpingitis, as some women with PID have endometritis alone.
# Treatment
PID treatment regimens must provide empiric, broad spectrum coverage of likely pathogens. Several antimicrobial regimens have been effective in achieving clinical and microbiologic cure in randomized clinical trials with shortterm follow-up. However, only a limited number of investigations have assessed and compared these regimens with regard to elimination of infection in the endometrium and fallopian tubes or determined the incidence of long-term complications (e.g., tubal infertility and ectopic pregnancy) after antimicrobial regimens (179,180).
All treatment regimens should be effective against N. gonorrhoeae and C. trachomatis because negative endocer- vical screening for these organisms does not rule out upper reproductive tract infection. The need to eradicate anaerobes from women who have PID has not been determined definitively. Anaerobic bacteria have been isolated from the upper reproductive tract of women who have PID, and data from in vitro studies have revealed that some anaerobes (e.g., Bacteroides fragilis) can cause tubal and epithelial destruction. In addition, BV also is present in many women who have PID (181).Until treatment regimens that do not adequately cover these microbes have been demonstrated to prevent long-term sequelae (e.g., infertility and ectopic pregnancy) as successfully as the regimens that are effective against these microbes, the use of regimens with anaerobic activity should be considered. Treatment should be initiated as soon as the presumptive diagnosis has been made because prevention of long-term sequelae is dependent on immediate administration of appropriate antibiotics. When selecting a treatment regimen, health-care providers should consider availability, cost, patient acceptance, and antimicrobial susceptibility. Some specialists have recommended that all patients with PID be hospitalized so that bed rest and supervised treatment with parenteral antibiotics can be initiated. However, in women with PID of mild or moderate clinical severity, outpatient therapy can provide short-and long-term clinical outcomes similar to inpatient therapy. Limited data support the use of outpatient therapy in women with more severe clinical presentations. The decision of whether hospitalization is necessary should be based on the discretion of the health-care provider.
The following criteria for hospitalization are suggested:
• surgical emergencies (e.g., appendicitis) cannot be excluded; • the patient is pregnant; • the patient does not respond clinically to oral antimicrobial therapy; • the patient is unable to follow or tolerate an outpatient oral regimen; • the patient has severe illness, nausea and vomiting, or high fever; and • the patient has a tubo-ovarian abscess. Many practitioners have preferred to hospitalize adolescent women whose condition is diagnosed as acute PID. No evidence is available suggesting that adolescents benefit from hospitalization for treatment of PID. Younger women with mild-to-moderate acute PID have similar outcomes with either outpatient therapy or inpatient therapy. Further, clinical response to outpatient treatment is similar among younger and older women. The decision to hospitalize adolescents with acute PID should be based on the same criteria used for older women. Whether women in their later reproductive years benefit from hospitalization for treatment of PID also is unclear, although women aged >35 years who are hospitalized with PID are more likely than younger women to have a complicated clinical course.
# Parenteral Treatment
For women with PID of mild or moderate severity, parenteral and oral therapy appears to have similar clinical efficacy. Many randomized trials have demonstrated the efficacy of both parenteral and oral regimens (180,182,183). In the majority of clinical trials, parenteral treatment for at least 48 hours has been used after the patient has demonstrated substantial clinical improvement. Clinical experience should guide decisions regarding transition to oral therapy, which usually can be initiated within 24 hours of clinical improvement. The majority of clinicians recommend at least 24 hours of direct inpatient observation for patients who have tuboovarian abscesses.
# Recommended Parenteral Regimen A
Cefotetan 2 g IV every 12 hours OR Cefoxitin 2 g IV every 6 hours PLUS Doxycycline 100 mg orally or IV every 12 hours Because of the pain associated with infusion, doxycycline should be administered orally when possible, even when the patient is hospitalized. Oral and IV administration of doxycycline provide similar bioavailability.
Parenteral therapy may be discontinued 24 hours after a patient improves clinically, and oral therapy with doxycycline (100 mg twice a day) should continue to complete 14 days of therapy. When tubo-ovarian abscess is present, many healthcare providers use clindamycin or metronidazole with doxycycline for continued therapy, rather than doxycycline alone, because it provides more effective anaerobic coverage.
Clinical data are limited regarding the use of other secondor third-generation cephalosporins (e.g., ceftizoxime, cefotaxime, and ceftriaxone), which also might be effective therapy for PID and may replace cefotetan or cefoxitin. However, these cephalosporins are less active than cefotetan or cefoxitin against anaerobic bacteria.
# Recommmended Parenteral Regimen B
Clindamycin 900 mg IV every 8 hours PLUS Gentamicin loading dose IV or IM (2 mg/kg of body weight), followed by a maintenance dose (1.5 mg/kg) every 8 hours. Single daily dosing may be substituted.
Although use of a single daily dose of gentamicin has not been evaluated for the treatment of PID, it is efficacious in analogous situations. Parenteral therapy can be discontinued 24 hours after a patient improves clinically; continuing oral therapy should consist of doxycycline 100 mg orally twice a day or clindamycin 450 mg orally four times a day to complete a total of 14 days of therapy. When tubo-ovarian abscess is present, many health-care providers use clindamycin for continued therapy, rather than doxycycline, because clindamycin provides more effective anaerobic coverage.
# Alternative Parenteral Regimens
Limited data support the use of other parenteral regimens, but the following three regimens have been investigated in at least one clinical trial, and they have broad spectrum coverage. IV ofloxacin has been investigated as a single agent; however, because of concerns regarding its spectum, metronidazole may be included in the regimen. Levofloxacin is as effective as ofloxacin and may be substituted; its single daily dosing makes it advantageous from a compliance perspective. One trial demonstrated high short-term clinical cure rates with azithromycin, either alone for 1 week (at least one IV dose followed by oral therapy) or with a 12-day course of metronidazole (184). Ampicillin/sulbactam plus doxycycline is effective coverage against C. trachomatis, N. gonorrhoeae, and anaerobes and for patients who have tubo-ovarian abscess.
# Oral Treatment
Oral therapy can be considered for women with mild-tomoderately severe acute PID, as the clinical outcomes among women treated with oral therapy are similar to those treated with parenteral therapy. The following regimens provide coverage against the frequent etiologic agents of PID. Patients who do not respond to oral therapy within 72 hours should be reevaluated to confirm the diagnosis and should be administered parenteral therapy on either an outpatient or inpatient basis.
# Recommended Regimen A
Levofloxacin 500 mg orally once daily for 14 days* OR Ofloxacin 400 mg orally twice daily for 14 days* WITH OR WITHOUT Metronidazole 500 mg orally twice a day for 14 days * Quinolones should not be used in persons with a history of recent foreign travel or partners' travel, infections acquired in California or Hawaii, or infections acquired in other areas with increased QRNG prevalence.
Oral ofloxacin has been investigated as a single agent in two clinical trials, and it is effective against both N. gonorrhoeae and C. trachomatis (185,186). Despite the results of these trials, lack of anaerobic coverage with ofloxacin is a concern; the addition of metronidazole to the treatment regimen provides this coverage. Levofloxacin is as effective as ofloxacin and may be substituted. Azithromycin has been demonstrated in one randomized trial to be an effective regimen for acute PID (184). The addition of metronidazole should be considered, as anaerobic organisms are suspected in the etiology of the majority of PID cases. Metronidazole will also treat BV, which frequently is associated with PID.
# Regimen B
Ceftriaxone 250 mg IM in a single dose PLUS Doxycycline 100 mg orally twice a day for 14 days WITH OR WITHOUT Metronidazole 500 mg orally twice a day for 14 days OR Cefoxitin 2 g IM in a single dose and Probenecid, 1 g orally administered concurrently in a single dose PLUS Doxycycline 100 mg orally twice a day for 14 days WITH OR WITHOUT Metronidazole 500 mg orally twice a day for 14 days
# OR
Other parenteral third-generation cephalosporin (e.g., ceftizoxime or cefotaxime) PLUS Doxycycline 100 mg orally twice a day for 14 days WITH OR WITHOUT Metronidazole 500 mg orally twice a day for 14 days
The optimal choice of a cephalosporin for Regimen B is unclear; although cefoxitin has better anaerobic coverage, ceftriaxone has better coverage against N. gonorrhoeae. Clinical trials have demonstrated that a single dose of cefoxitin is effective in obtaining short-term clinical response in women who have PID. However, the theoretical limitations in cefoxitin's coverage of anaerobes might require the addition of metronidazole to the treatment regimen (182). Metronidazole also will effectively treat BV, which is frequently associated with PID. No data have been published regarding the use of oral cephalosporins for the treatment of PID. Limited data suggest that the combination of oral metronidazole and doxycycline after primary parenteral therapy is safe and effective (187).
# Alternative Oral Regimens
Although information regarding other outpatient regimens is limited, one other regimen has undergone at least one clinical trial and has broad spectrum coverage. Amoxicillin/clavulanic acid and doxycycline was effective in obtaining short-term clinical response in a single clinical trial; however, gastrointestinal symptoms might limit compliance with this regimen.
# Follow-Up
Patients should demonstrate substantial clinical improvement (e.g., defervescence; reduction in direct or rebound abdominal tenderness; and reduction in uterine, adnexal, and cervical motion tenderness) within 3 days after initiation of therapy. Patients who do not improve within this period usually require hospitalization, additional diagnostic tests, and surgical intervention.
If no clinical improvement has occurred within 72 hours after outpatient oral or parenteral therapy (using the criteria for clinical improvement described previously), an examination should be performed. Subsequent hospitalization, parenteral therapy, and diagnostic evaluation, including the consideration of diagnostic laparoscopy for alternative diagnoses, are recommended in women without clinical improvement. Some specialists also recommend rescreening for C. trachomatis and N. gonorrhoeae 4-6 weeks after therapy is completed in women with documented infection with these pathogens. All women diagnosed with acute PID should be offered HIV testing.
# Management of Sex Partners
Male sex partners of women with PID should be examined and treated if they had sexual contact with the patient during the 60 days preceding the patient's onset of symptoms. Evaluation and treatment are imperative because of the risk for reinfection of the patient and the strong likelihood of urethral gonococcal or chlamydial infection in the sex partner. Male partners of women who have PID caused by C. trachomatis and/or N. gonorrhoeae frequently are asymptomatic.
Sex partners should be treated empirically with regimens effective against both of these infections, regardless of the etiology of PID or pathogens isolated from the infected woman. Even in clinical settings in which only women are treated, arrangements should be made to provide care for male sex partners of women who have PID. When providing care for male sex partners is not feasible, health-care providers should ensure that sex partners are referred for appropriate treatment.
# Prevention
Prevention of chlamydial infection by screening and treating high-risk women reduces the incidence of PID (125). Theoretically, the majority of cases of PID can be prevented by screening all women or those determined to be at high risk (based on age or other factors) by using DNA amplification on cervical specimens (in women receiving pelvic examinations) and on urine specimens (in women not undergoing examinations). Although BV is associated with PID, whether the incidence of PID can be reduced by identifying and treating women with BV is unclear (181).
# Special Considerations
Pregnancy. Because of the high risk for maternal morbidity and preterm delivery, pregnant women who have suspected PID should be hospitalized and treated with parenteral antibiotics.
HIV Infection. Differences in the clinical manifestations of PID between HIV-infected women and HIV-negative women have not been well-delineated. In previous observational studies, HIV-infected women with PID were more likely to require surgical intervention. More comprehensive observational and controlled studies (published since the 2002 STD Treatment Guidelines) have demonstrated that HIV-infected women with PID had similar symptoms when compared with uninfected controls (125,(188)(189)(190). They were more likely to have a tubo-ovarian abscess but responded equally well to standard parenteral and oral antibiotic regimens when compared with HIV-negative women. The microbiologic findings for HIV-positive and HIV-negative women were similar, except HIV-infected women had higher rates of concomitant M. hominis, candida, streptococcal, and HPV infections and HPV-related cytologic abnormalities. Whether the management of immunodeficient HIV-infected women with PID requires more aggressive interventions (e.g., hospitalization or parenteral antimicrobial regimens) has not been determined.
IUD. Intrauterine contraceptive devices are becoming a popular contraceptive choice for women. Both levonorgestreland copper-containing devices are marketed in the United States. The risk of PID associated with IUD use is primarily confined to the first 3 weeks after insertion and is uncommon thereafter (191). Given the popularity of IUDs, practitioners might encounter PID in IUD users. No evidence suggests that IUDs should be removed in women diagnosed with acute PID. However, caution should be exercised if the IUD remains in place, and close clinical follow-up is mandatory. The rate of treatment failure and recurrent PID in women continuing to use an IUD is unknown. No data exist on antibiotic selection and treatment outcomes according to type of IUD (e.g., copper or levonorgestrel).
# Epididymitis
Acute epididymitis is a clinical syndrome consisting of pain, swelling, and inflammation of the epididymis of <6 weeks. Chronic epididymitis is characterized by a 3-month or longer history of symptoms of discomfort and/or pain in the scrotum, testicle, or epididymis that is localized on clinical examination. Chronic epididymitis has been subcategorized into inflammatory chronic epididymitis, obstructive chronic epididymitis, and chronic epididymalgia (192).
Among sexually active men aged <35 years, acute epididymitis is most frequently caused by C. trachomatis or N. gonorrhoeae. Acute epididymitis caused by sexually transmitted enteric organisms (e.g., Escherichia coli) also occurs among men who are the insertive partner during anal intercourse. Sexually transmitted acute epididymitis usually is accompanied by urethritis, which frequently is asymptomatic and is usually never accompanied by bacteriuria. In men aged >35 years, sexually transmitted epididymitis is uncommon. However, bacteriuria secondary to obstructive urinary disease is relatively common. In this group, nonsexually transmitted epididymitis is associated with urinary-tract instrumentation or surgery, systemic disease, or immunosuppression.
Although the majority of patients can be treated on an outpatient basis, hospitalization should be considered when severe pain suggests other diagnoses (e.g., torsion, testicular infarction, or abscess) or when patients are febrile or might be noncompliant with an antimicrobial regimen.
# Diagnostic Considerations
Men who have acute epididymitis typically have unilateral testicular pain and tenderness; hydrocele and palpable swelling of the epididymis usually are present. Although the inflammation and swelling usually begin in the tail of the epididymis, they can spread to involve the rest of the epididymis and testicle. The spermatic cord is usually tender and swollen.Testicular torsion, a surgical emergency, should be considered in all cases, but it occurs more frequently among adolescents and in men without evidence of inflammation or infection. Emergency testing for torsion might be indicated when the onset of pain is sudden, pain is severe, or the test results available during the initial examination do not support a diagnosis of urethritis or urinary-tract infection. If the diagnosis is questionable, a specialist should be consulted immediately because testicular viability might be compromised. Radionuclide scanning of the scrotum is the most accurate radiologic method of diagnosis, although it is not routinely available. Color duplex doppler ultrasonography has a sensitivity of 70% and a specificity of 88% in diagnosing acute epididymitis.
The evaluation of men for epididymitis should include one of the following:
• Gram stain of urethral secretions demonstrating >5 WBC per oil immersion field. The Gram stain is the preferred rapid diagnostic test for evaluating urethritis. It is highly sensitive and specific for documenting both urethritis and the presence or absence of gonococcal infection. Gonococcal infection is established by documenting the presence of WBC containing intracellular Gram-negative diplococci on urethral Gram stain. • Positive leukocyte esterase test on first-void urine or microscopic examination of first-void urine sediment demonstrating >10 WBC per high power field. Culture, nucleic acid hybridization tests, and nucleic acid amplification tests are available for the detection of both N. gonorrhoeae and C. trachomatis. Culture and nucleic acid hybridization tests require urethral swab specimens, whereas amplification tests can be performed on urine specimens. Because of their higher sensitivity, amplification tests are preferred for the detection of C. trachomatis. Depending on the risk, patients whose conditions have been diagnosed as a new STD should receive testing for other STDs.
# Treatment
Empiric therapy is indicated before laboratory test results are available. The goals of treatment of acute epididymitis caused by C. trachomatis or N. gonorrhoeae are 1) microbiologic cure of infection, 2) improvement of signs and symptoms, 3) prevention of transmission to others, and 4) a decrease in potential complications (e.g., infertility or chronic pain). As an adjunct to therapy, bed rest, scrotal elevation, and analgesics are recommended until fever and local inflammation have subsided.
# Recommended Regimens
# For acute epididymitis most likely caused by gonococcal or chlamydial infection:
Ceftriaxone 250 mg IM in a single dose PLUS Doxycycline 100 mg orally twice a day for 10 days
# For acute epididymitis most likely caused by enteric
organisms or for patients allergic to cephalosporins and/or tetracyclines: Ofloxacin 300 mg orally twice a day for 10 days OR Levofloxacin 500 mg orally once daily for 10 days
# Follow-Up
Failure to improve within 3 days of the initiation of treatment requires reevaluation of both the diagnosis and therapy. Swelling and tenderness that persist after completion of antimicrobial therapy should be evaluated comprehensively. The differential diagnosis includes tumor, abscess, infarction, testicular cancer, TB, and fungal epididymitis.
# Management of Sex Partners
Patients who have acute epididymitis, confirmed or suspected to be caused by N. gonorrhoeae or C. trachomatis, should be instructed to refer sex partners for evaluation and treatment if their contact with the index patient was within the 60 days preceding onset of the patient's symptoms.
Patients should be instructed to avoid sexual intercourse until they and their sex partners are cured (i.e., until therapy is completed and patient and partners no longer have symptoms).
# Special Considerations
# HIV Infection
Patients who have uncomplicated acute epididymitis and also are infected with HIV should receive the same treatment regimen as those who are HIV negative. Fungi and mycobacteria, however, are more likely to cause acute epididymitis in immunosuppressed patients than in immunocompetent patients.
# HPV Infection
More than 100 types of HPV exist; more than 30 types can infect the genital area. The majority of HPV infections are asymptomatic, unrecognized, or subclinical. Genital HPV infection is common and usually self-limited. Genital HPV infection occurs more frequently than visible genital warts among both men and women and cervical cell changes among women.
Genital HPV infection can cause genital warts, usually associated with HPV types 6 or 11. Other HPV types that in-fect the anogenital region (e.g., high-risk HPV types 16, 18, 31, 33, and 35) are strongly associated with cervical neoplasia. Persistent infection with high-risk types of HPV is the most important risk factor for cervical neoplasia.
# HPV Tests
A definitive diagnosis of HPV infection is based on detection of viral nucleic acid (i.e., DNA or RNA) or capsid protein. Tests that detect several types of HPV DNA in cells scraped from the cervix are available and might be useful in the triage of women with atypical squamous cells of undetermined significance (ASC-US) or in screening women aged >30 years in conjunction with the Pap test (see Cervical Cancer Screening for Women Who Attend STD Clinics or Have a History of of STDs). Women determined to have HPV infection on such testing should be counseled that HPV infection is common, infection is frequently transmitted between partners, and that infection usually goes away on its own. If any Pap test or biopsy abnormalities have been observed, further evaluation is recommended. Screening women or men with the HPV test, outside of the above recommendations for use of the test with cervical cancer screening, is not recommended.
# Treatment
In the absence of genital warts or cervical SIL, treatment is not recommended for subclinical genital HPV infection, whether it is diagnosed by colposcopy, biopsy, acetic acid application, or through the detection of HPV by laboratory tests. Genital HPV infection frequently goes away on its own, and no therapy has been identified that can eradicate infection. In the presence of coexistent SIL, management should be based on histopathologic findings.
# Genital Warts
HPV types 6 or 11 are commonly found before, or at the time of, detection of genital warts; however, the use of HPV testing for genital wart diagnosis is not recommended.
Genital warts are usually flat, papular, or pedunculated growths on the genital mucosa. Diagnosis of genital warts is made by visual inspection and may be confirmed by biopsy, although biopsy is needed only under certain circumstances (e.g., if the diagnosis is uncertain; the lesions do not respond to standard therapy; the disease worsens during therapy; the patient is immunocompromised; or warts are pigmented, indurated, fixed, bleeding, or ulcerated). No data support the use of HPV nucleic acid tests in the routine diagnosis or management of visible genital warts.
The application of 3%-5% acetic acid usually turns HPVinfected genital mucosal tissue to a whitish color. However, acetic acid application is not a specific test for HPV infection, and the specificity and sensitivity of this procedure for screening have not been defined. Therefore, the routine use of this procedure for screening to detect HPV infection is not recommended. However, some clinicians, who are experienced in the management of genital warts, have determined that this test is useful for identifying flat genital warts.
In addition to the external genitalia (i.e., penis, vulva, scrotum, perineum, and perianal skin), genital warts can occur on the uterine cervix and in the vagina, urethra, anus, and mouth. Intra-anal warts are observed predominantly in patients who have had receptive anal intercourse; these warts are distinct from perianal warts, which can occur in men and women who do not have a history of anal sex. In addition to the genital area, HPV types 6 and 11 have been associated with conjunctival, nasal, oral, and laryngeal warts. Genital warts are usually asymptomatic, but depending on the size and anatomic location, genital warts can be painful, friable, or pruritic.
HPV types 16, 18, 31, 33, and 35 are found occasionally in visible genital warts and have been associated with external genital (i.e., vulvar, penile, and anal) squamous intraepithelial neoplasia (i.e., squamous cell carcinoma in situ, bowenoid papulosis, Erythroplasia of Queyrat, or Bowen's disease of the genitalia). These HPV types also have been associated with vaginal, anal, and CIN and anogenital and some head and neck squamous cell carcinomas. Patients who have visible genital warts are frequently infected simultaneously with multiple HPV types.
# Treatment
The primary goal of treating visible genital warts is the removal of the warts. In the majority of patients, treatment can induce wart-free periods. If left untreated, visible genital warts might resolve on their own, remain unchanged, or increase in size or number. Treatment possibly reduces, but does not eliminate, HPV infection. Existing data indicate that currently available therapies for genital warts might reduce, but probably do not eradicate, HPV infectivity. Whether the reduction in HPV viral DNA, resulting from treatment, impacts future transmission remains unclear. No evidence indicates that the presence of genital warts or their treatment is associated with the development of cervical cancer.
# Regimens
Treatment of genital warts should be guided by the preference of the patient, the available resources, and the experience of the health-care provider. No definitive evidence suggests that any of the available treatments are superior to any other and no single treatment is ideal for all patients or all warts. The use of locally developed and monitored treatment algorithms has been associated with improved clinical outcomes and should be encouraged. Because of uncertainty regarding the effect of treatment on future transmission of HPV and the possibility of spontaneous resolution, an acceptable alternative for some persons is to forego treatment and wait for spontaneous resolution.
The majority of patients have <10 genital warts, with a total wart area of 0.5-1.0 cm 2 . These warts respond to various treatment modalities. Factors that might influence selection of treatment include wart size, wart number, anatomic site of wart, wart morphology, patient preference, cost of treatment, convenience, adverse effects, and provider experience. Factors that might affect response to therapy include the presence of immunosuppression and compliance with therapy. The majority of patients require a course of therapy rather than a single treatment. In general, warts located on moist surfaces or in intertriginous areas respond better to topical treatment than do warts on drier surfaces.
The treatment modality should be changed if a patient has not improved substantially. The majority of genital warts respond within 3 months of therapy. The response to treatment and its side effects should be evaluated throughout the course of therapy.
Complications occur rarely if treatments for warts are employed properly. Patients should be warned that persistent hypopigmentation or hyperpigmentation occurs commonly with ablative modalities. Depressed or hypertrophic scars are uncommon but can occur, especially if the patient has had insufficient time to heal between treatments. Rarely, treatment can result in disabling chronic pain syndromes (e.g., vulvodynia or analdynia, and hyperesthesia of the treatment site) or, in the case of rectal warts, painful defecation or fistulas. A limited number of case reports of severe systemic effects from podophyllin resin and interferon have been documented.
Treatment regimens are classified into patient-applied and provider-applied modalities. Patient-applied modalities are preferred by some patients because they can be administered in the privacy of the patient's home. To use patient-applied modalities effectively, compliance with the treatment regimen is important along with the ability to identify and reach all genital warts.
# MMWR August 4, 2006
# Recommended Regimens for External Genital Warts
Patient-Applied: Podofilox 0.5% solution or gel. Patients should apply podofilox solution with a cotton swab, or podofilox gel with a finger, to visible genital warts twice a day for 3 days, followed by 4 days of no therapy. This cycle may be repeated, as necessary, for up to four cycles.
The total wart area treated should not exceed 10 cm 2 , and the total volume of podofilox should be limited to 0.5 mL per day. If possible, the health-care provider should apply the initial treatment to demonstrate the proper application technique and identify which warts should be treated. The safety of podofilox during pregnancy has not been established. OR Imiquimod 5% cream. Patients should apply imiquimod cream once daily at bedtime, three times a week for up to 16 weeks. The treatment area should be washed with soap and water 6-10 hours after the application. The safety of imiquimod during pregnancy has not been established.
# Provider-Administered:
Cryotherapy with liquid nitrogen or cryoprobe. Repeat applications every 1-2 weeks. OR Podophyllin resin 10%-25% in a compound tincture of benzoin. A small amount should be applied to each wart and allowed to air dry. The treatment can be repeated weekly, if necessary. To avoid the possibility of complications associated with systemic absorption and toxicity, two important guidelines should be followed: 1) application should be limited to <0.5 mL of podophyllin or an area of <10 cm 2 of warts per session, and 2) no open lesions or wounds should exist in the area to which treatment is administered. Some specialists suggest that the preparation should be thoroughly washed off 1-4 hours after application to reduce local irritation. The safety of podophyllin during pregnancy has not been established. OR Trichloroacetic acid (TCA) or Bichloroacetic acid (BCA) 80%-90%. A small amount should be applied only to the warts and allowed to dry, at which time a white "frosting" develops. If an excess amount of acid is applied, the treated area should be powdered with talc, sodium bicarbonate (i.e., baking soda), or liquid soap preparations to remove unreacted acid. This treatment can be repeated weekly, if necessary.
# OR Surgical removal either by tangential scissor excision, tangential shave excision, curettage, or electrosurgery
# Alternative Regimens
Intralesional interferon OR Laser surgery Podofilox 0.5% solution or gel, an antimitotic drug that destroys warts, is relatively inexpensive, easy to use, safe, and self-applied by patients. The majority of patients experience mild-to-moderate pain or local irritation after treatment. Imiquimod is a topically active immune enhancer that stimulates production of interferon and other cytokines. Local inflammatory reactions are common with the use of imiquimod; these reactions include redness and irritation and are usually mild to moderate. Traditionally, follow-up visits are not required for patients using self-administered therapy. However, follow-up might be useful several weeks into therapy to determine the appropriateness of medication use and the response to treatment.
Cryotherapy destroys warts by thermal-induced cytolysis. Health-care providers must be trained on the proper use of this therapy because over-and undertreatment might result in complications or low efficacy. Pain after application of the liquid nitrogen, followed by necrosis and sometimes blistering, is common. Local anesthesia (topical or injected) might facilitate therapy if warts are present in many areas or if the area of warts is large.
Podophyllin resin, which contains several compounds, including antimitotic podophyllin lignans, is another treatment option. The resin is most frequently compounded at 10%-25% in a tincture of benzoin. However, podophyllin resin preparations differ in the concentration of active components and contaminants. The shelf life and stability of podophyllin preparations are unknown. A thin layer of podophyllin resin must be applied to the warts and allowed to air dry before the treated area comes into contact with clothing; overapplication or failure to air dry can result in local irritation caused by spread of the compound to adjacent areas.
Both TCA and BCA are caustic agents that destroy warts by chemical coagulation of proteins. Although these preparations are widely used, they have not been investigated thoroughly. TCA solutions have a low viscosity comparable with that of water and can spread rapidly if applied excessively; therefore, they can damage adjacent tissues. Both TCA and BCA should be applied sparingly and allowed to dry before the patient sits or stands. If pain is intense, the acid can be neutralized with soap or sodium bicarbonate.
Surgical therapy has the advantage of usually eliminating warts at a single visit. However, such therapy requires substantial clinical training, additional equipment, and a longer office visit. After local anesthesia is applied, the visible genital warts can be physically destroyed by electrocautery, in which case no additional hemostasis is required. Care must be taken to control the depth of electrocautery to prevent scarring. Alternatively, the warts can be removed either by tangential excision with a pair of fine scissors or a scalpel or by curettage. Because the majority of warts are exophytic, this procedure can be accomplished with a resulting wound that only extends into the upper dermis. Hemostasis can be achieved with an electrocautery unit or a chemical styptic (e.g., an aluminum chloride solution). Suturing is neither required nor indicated in the majority of cases if surgical removal is performed properly. Surgical therapy is most beneficial for patients who have a large number or area of genital warts. Carbon dioxide laser and surgery might be useful in the management of extensive warts or intraurethral warts, particularly for those patients who have not responded to other treatments.
Interferons, both natural or recombinant, have been used for the treatment of genital warts. They have been administered systemically (i.e., subcutaneously at a distant site or IM) and intralesionally (i.e., injected into the warts). Systemic interferon is not effective. The efficacy and recurrence rates of intralesional interferon are comparable to other treatment modalities. Administration of intralesional interferon is associated with stinging, burning, and pain at the injection site. Interferon is probably effective because of its antiviral and/or immunostimulating effects. Interferon therapy is not recommended as a primary modality because of inconvenient routes of administration, frequent office visits, and the association between its use and a high frequency of systemic adverse effects.
Because of the shortcomings associated with all available treatments, some clinics employ combination therapy (i.e., the simultaneous use of two or more modalities on the same wart at the same time). No data support the use of more than one therapy at a time to improve efficacy of treatment, and some specialists believe that combining modalities might increase complications.
# Recommended Regimens for Cervical Warts
For women who have exophytic cervical warts, high-grade SIL must be excluded before treatment is initiated.
Management of exophytic cervical warts should include consultation with a specialist.
# Recommended Regimens for Vaginal Warts
Cryotherapy with liquid nitrogen. The use of a cryoprobe in the vagina is not recommended because of the risk for vaginal perforation and fistula formation. OR TCA or BCA 80%-90% applied to warts. A small amount should be applied only to warts and allowed to dry, at which time a white "frosting" develops. If an excess amount of acid is applied, the treated area should be powdered with talc, sodium bicarbonate, or liquid soap preparations to remove unreacted acid. This treatment can be repeated weekly, if necessary.
# Recommended Regimens for Urethral Meatus Warts
Cryotherapy with liquid nitrogen OR Podophyllin 10%-25% in compound tincture of benzoin. The treatment area must be dry before contact with normal mucosa. This treatment can be repeated weekly, if necessary. The safety of podophyllin during pregnancy has not been established.
Although data evaluating the use of podofilox and imiquimod for the treatment of distal meatal warts are limited, some specialists recommend their use in some patients.
# Recommended Regimens for Anal Warts
Cryotherapy with liquid nitrogen OR TCA or BCA 80%-90% applied to warts. A small amount should be applied only to warts and allowed to dry, at which time a white "frosting" develops. If an excess amount of acid is applied, the treated area should be powdered with talc, sodium bicarbonate, or liquid soap preparations to remove unreacted acid. This treatment can be repeated weekly, if necessary.
# OR Surgical removal
Warts on the rectal mucosa should be managed in consultation with a specialist. Many persons with warts on the anal mucosa also have warts on the rectal mucosa, so persons with anal warts can benefit from an inspection of the rectal mucosa by digital examination or anoscopy.
# Counseling Genital HPV Infection
Education and counseling are vital aspects of managing patients with genital warts. Patients can be educated through patient education materials, including pamphlets, hotlines, and websites (http://www.ashastd.org or http://www.cdc.gov/ std/hpv).
Attempts should be made to convey the following key messages:
• Genital HPV infection is common among sexually active adults. The majority of sexually active adults will have it at some point in their lives, although the majority of them will never know because the infection usually has no symptoms and clears on its own. • Genital HPV infection is usually sexually transmitted.
The incubation period (i.e., the interval between initial exposure and established infection or disease) is variable, and determining the timing and source of infection is frequently difficult. Within ongoing sexual relationships, sex partners usually are infected by the time of the patient's diagnosis, although they might have no symptoms or signs of infection. • No recommended uses of the HPV test to diagnose HPV infection in sex partners have been established. HPV infection is commonly transmitted to partners but usually goes away on its own.
# Genital Warts
• Genital warts are caused by specific types of HPV infection. The types that cause genital warts are different from the types that cause cervical and other anogenital cancers. • Persons can possibly have infection with the types of HPV that cause genital warts but never develop symptoms. Why some persons with genital HPV infection develop warts and others do not is unclear. Immunity probably plays a key role. • The natural history of genital warts is usually benign, but recurrence of genital warts within the first several months after treatment is common. Treatment for genital warts can reduce HPV infection, but whether the treatment results in a reduction in risk for transmission of HPV to sex partners is unclear. The duration of infectivity after wart treatment is unknown. • Condoms might reduce the risk for HPV-associated diseases (e.g., genital warts and cervical cancer). Consistent condom use also may reduce the risk for genital HPV (18). HPV infection can occur in areas that are not covered or protected by a condom (e.g., scrotum, vulva, or perianus). • The presence of genital warts is not an indication for HPV testing, a change in the frequency of Pap tests, or cervical colposcopy. • HPV testing is not indicated for partners of persons with genital warts.
# Follow-Up
After visible genital warts have cleared, a follow-up evaluation might be helpful. Patients should be cautioned to watch for recurrences, which occur most frequently during the first 3 months. External genital warts can be difficult to identify, so it might be useful for patients to have a follow-up evaluation 3 months after treatment. Earlier follow-up visits also might be useful for some patients to document the absence of warts, to monitor for or treat complications of therapy, and to provide an additional opportunity for patient education and counseling. Women should be counseled to undergo regular Pap screening as recommended for women without genital warts.
# Management of Sex Partners
Examination of sex partners is not necessary for the management of genital warts because no data indicate that reinfection plays a role in recurrences. In addition, providing treatment for genital warts solely for the purpose of preventing future transmission cannot be recommended because the value of treatment in reducing infectivity is unknown. However, sex partners of patients who have genital warts might benefit from counseling and examination to assess the presence of genital warts and other STDs. The counseling of sex partners provides an opportunity for these partners to 1) learn that HPV infection is common and probably shared between partners and 2) receive STD evaluation and screening and Pap screening if they are female. Female sex partners of patients who have genital warts should be reminded that cytologic screening for cervical cancer is recommended for all sexually active women.
# Special Considerations Pregnancy
Imiquimod, podophyllin, and podofilox should not be used during pregnancy. However, because genital warts can proliferate and become friable during pregnancy, many specialists advocate their removal during pregnancy. HPV types 6 and 11 can cause respiratory papillomatosis in infants and children. The route of transmission (i.e., transplacental, perinatal, or postnatal) is not completely understood. Whether cesarean section prevents respiratory papillomatosis in infants and children is unclear; therefore, cesarean delivery should not be performed solely to prevent transmission of HPV infection to the newborn. Cesarean delivery might be indicated for women with genital warts if the pelvic outlet is obstructed or if vaginal delivery would result in excessive bleeding. Pregnant women with genital warts should be counseled concerning the low risk for warts on the larynx (recurrent respiratory papillomatosis) in their infants or children (193). No controlled studies have suggested that cesarean section prevents this condition.
# HIV Infection
No data suggest that treatment modalities for external genital warts should be different in the setting of HIV-infection. However, persons who are immunosuppressed because of HIV or other reasons might have larger or more numerous warts, might not respond as well as immunocompetent persons to therapy for genital warts, and might have more frequent recurrences after treatment (194,195). Squamous cell carcinomas arising in or resembling genital warts might occur more frequently among immunosuppressed persons, therefore, requiring biopsy for confirmation of diagnosis. Because of the increased incidence of anal cancer in HIV-infected homosexual men, screening for anal SIL by cytology in this population is recommended by some specialists. However, evidence is limited concerning the natural history of anal intraepithelial neoplasias, the reliability of screening methods, the safety and response to treatments, and the programmatic considerations that would support this screening approach. Until additional data are generated on screening for anal SIL, this screening approach cannot be recommended.
# Squamous Cell Carcinoma in Situ
Patients in whom squamous cell carcinoma in situ of the genitalia is diagnosed should be referred to a specialist for treatment. Ablative modalities usually are effective, but careful follow-up is essential. The risk for these lesions leading to invasive squamous cell carcinoma of the external genitalia in immunocompetent patients is unknown but is probably low. Female partners of male patients who have squamous cell carcinoma in situ are at high risk for cervical abnormalities.
# Cervical Cancer Screening for Women Who Attend STD Clinics or Have a History of STDs
Women with a history of STDs might be at increased risk for cervical cancer, and women attending STD clinics might have other risk factors that place them at even greater risk. Prevalence studies indicate that precursor lesions for cervical cancer occur approximately five times more frequently among women attending STD clinics than among women attending family planning clinics (196). Cervical cancer screening using the Pap test is an effective, low-cost screening test for preventing invasive cervical cancer. Recommendations for cervical cancer screening intervals vary in the United States, but the American Cancer Society and American College of Obstetri-cians and Gynecologists guidelines recommend annual screening for women aged 21-30 years and then every 2-3 years for women aged >30 years if three consecutive annual Pap tests are negative (197,198).
# Recommendations
During the appointment in which a pelvic examination for STD screening is performed, the health-care provider should inquire about the result of the patient's most recent Pap test and discuss the following information with the patient:
•
# Follow-Up
STD clinics offering cervical cancer screening are encouraged to use cytopathology laboratories that report results by using the Bethesda System of classification (199). † † † If the † † † The Bethesda System for Reporting Cervical/Vaginal Cytologic Results uses the terms "low-grade SIL" and "high-grade SIL" for abnormal results (199). If repeat Pap tests are used to follow ASC-US results, a test should be performed every 6 months until 3 negative results are noted before the women returns to cervical cancer screening at a normal interval for age. If subsequent Pap tests demonstrate progression to SIL, follow-up should be conducted according to ASCCP Consensus Guidelines (i.e., frequent colposcopy and directed cervical biopsy). If specific infections other than HPV are identified, the patient might need to have a repeat Pap test after appropriate treatment for those infections. In the majority of instances, even in the presence of some severe infections, Pap tests will be reported as satisfactory for evaluation, so they may be read and final reports produced without the necessity to treat and repeat the Pap test. When repeating the Pap test is necessary because of an unsatisfactory for interpretation report, the repeat test must be interpreted by the laboratory as satisfactory and also be negative before returning the woman to Pap tests at regularly scheduled intervals.
A third strategy for managing patients with ASC-US Pap test results involves testing for HPV DNA. Whereas conducting HPV testing in some STD clinics might not be possible or appropriate because of inadequate resources, such testing might be appropriate in other public health clinic settings. Only one FDA-cleared test exists, the Digene Hybrid Capture II. The HPV DNA test may be performed by 1) co-collecting a specimen; 2) using a supplied swab at the time of the Pap test, if conventional cytology is used; 3) reflex testing, if liquid-based cytology is used and enough residual material is available in the cytology test vial; or 4) scheduling a separate follow-up appointment when the Pap test report results are known. If the high-risk HPV DNA test is positive, women are referred immediately for colposcopy, and if indicated, directed cervical biopsy. Because many public health clinics, including the majority of STD clinics, cannot provide clinical follow-up of abnormal Pap tests, women with Pap tests demonstrating low or high grade SIL or ASC-US usually need a referral to other local health-care providers or clinics for colposcopy and biopsy. Clinics and health-care providers who offer Pap test screening services but cannot provide appropriate colposcopic follow-up of abnormal Pap tests should arrange referral to health-care facilities in which 1) a patient will be promptly evaluated and treated and 2) the results of the evaluation will be reported to the referring clinic or healthcare provider. Clinics and health-care providers should develop protocols that identify women who miss follow-up appointments so that these women can be located and scheduled for needed studies and management, and they should reevaluate such protocols routinely. Pap test results, type and location of follow-up appointments, and results of follow-up appointments should be clearly documented in the clinic record. The establishment of colposcopy and biopsy services in local health departments, especially in circumstances in which referrals are difficult and follow-up is unlikely, should be considered if resources are available.
# Other Management Considerations
Other considerations in performing Pap tests include the following:
•
# Special Considerations
# Pregnancy
Pregnant women should have a Pap test as part of routine prenatal care. A cytobrush and an Ayers spatula might be used for obtaining Pap tests in pregnant women.
# HIV Infection
Several studies have documented an increased prevalence of SIL in HIV-infected women (200,201). The following recommendations for Pap test screening among HIV-infected women are consistent with other guidelines published by the U.S. Department of Health and Human Services (50) and are based partially on the opinions of professionals knowledgeable about the care and management of cervical cancer and HIV infection in women.
After obtaining a complete history of previous cervical disease, HIV-infected women should be provided a comprehen-sive gynecologic examination, including a pelvic examination and Pap test, as part of their initial evaluation. A Pap test should be obtained twice in the first year after diagnosis of HIV infection and, if the results are normal, annually thereafter. If the results of the Pap test are abnormal, care should be provided according to the ASCCP Consensus Guidelines for Management of Abnormal Cervical Cytology (198). Women with cytological reports of ASC-US, low or high-grade SIL or squamous cell carcinoma, regardless of CD4+ count or antiretroviral treatment status, should undergo colposcopy and directed biopsy. Colposcopy and biopsy are not indicated in HIV-positive women with negative Pap test reports.
# Vaccine Preventable STDs
Some STDs can be effectively prevented through preexposure vaccination. Vaccines are under development or are undergoing clinical trials for certain STDs, including HIV and HSV. However, the only vaccines currently available are for prevention of HAV, HBV, and HPV infection. Vaccination efforts focus largely on integrating the use of these available vaccines into STD prevention and treatment activities.
Every person being evaluated or treated for an STD, who is not already vaccinated, should receive hepatitis B vaccination. In addition, some persons (e.g., MSM and illegal-drug users) should receive hepatitis A vaccination.
# Hepatitis A
Hepatitis A, caused by infection with HAV, has an incubation period of approximately 28 days (range: 15-50 days). HAV replicates in the liver and is shed in high concentrations in feces from 2 weeks before to 1 week after the onset of clinical illness. HAV infection produces a self-limited disease that does not result in chronic infection or chronic liver disease. However, 10%-15% of patients might experience a relapse of symptoms during the 6 months after acute illness. Acute liver failure from hepatitis A is rare (overall case-fatality rate: 0.5%). The risk for symptomatic infection is directly related to age, with >80% of adults having symptoms compatible with acute viral hepatitis and the majority of children having either asymptomatic or unrecognized infection. Antibody produced in response to HAV infection persists for life and confers protection against reinfection.
HAV infection is primarily transmitted by the fecal-oral route, by either person-to-person contact, or through consumption of contaminated food or water. Although viremia occurs early in infection and can persist for several weeks after onset of symptoms, bloodborne transmission of HAV is uncommon. HAV occasionally might be detected in saliva in † 0 months represents the timing of the initial dose; subsequent numbers represent the months after the initial dose. § Hepatitis A vaccine, inactivated, GlaxoSmithKline Biologicals. This vaccine also is licensed for a 3-dose series in children aged 1-18 years, with 360 EL.U., 0.5-mL doses at 0, 1, and 6-12 months. ¶ Hepatitis A vaccine, inactivated, Merck & Co., Inc.
experimentally infected animals, but transmission by saliva has not been demonstrated.
In the United States, nearly half of all reported hepatitis A cases have no specific risk factor identified. Among adults with identified risk factors, the majority of cases are among MSM, persons who use illegal drugs, and international travelers (202). Because transmission of HAV during sexual activity probably occurs because of fecal-oral contact, measures typically used to prevent the transmission of other STDs (e.g., use of condoms) do not prevent HAV transmission. In addition, efforts to promote good personal hygiene have not been successful in interrupting outbreaks of hepatitis A. Vaccination is the most effective means of preventing HAV transmission among persons at risk for infection, many of whom might seek services in STD clinics.
# Diagnosis
The diagnosis of hepatitis A cannot be made on clinical grounds alone and requires serologic testing. The presence of IgM antibody to HAV is diagnostic of acute HAV infection. A positive test for total anti-HAV indicates immunity to HAV infection but does not differentiate current from previous HAV infection. Although usually not sensitive enough to detect the low level of protective antibody after vaccination, anti-HAV tests might be positive after hepatitis A vaccination.
# Treatment
Patients with acute hepatitis A usually require only supportive care, with no restrictions in diet or activity. Hospitalization might be necessary for patients who become dehydrated because of nausea and vomiting and is critical for patients with signs or symptoms of acute liver failure. Medications that might cause liver damage or are metabolized by the liver should be used with caution among persons with hepatitis A.
# Prevention
Two products are available for the prevention of HAV infection: hepatitis A vaccine (Table 2) and immune globulin (Ig) for IM administration. Hepatitis A vaccines are prepared from formalin-inactivated, cell-culture-derived HAV and have been available in the United States since 1995, initially for persons aged >2 years. In 2005, the vaccines were approved by FDA for persons aged >12 months. Administered IM in a 2-dose series, these vaccines induce protective antibody levels in virtually all adults. By 1 month after the first dose, 94%-100% of adults have protective antibody levels; 100% of adults develop protective antibody after a second dose. In randomized controlled trials, the equivalent of 1 dose of hepatitis A vaccine administered before exposure has been 94%-100% effective in preventing clinical hepatitis A (3). Kinetic models of antibody decline indicate that protective levels of antibody persist for at least 20 years.
A combined hepatitis A and hepatitis B vaccine have been developed and licensed for use as a 3-dose series in adults aged >18 years (see Table 3, Hepatitis B). When administered IM on a 0-, 1-, and 6-month schedule, the vaccine has equivalent immunogenicity to that of the monovalent vaccines.
• Hepatitis A vaccine is available for eligible children and adolescents aged <19 years through the Vaccines for Children program (telephone: 800-232-2522). • Ig is a sterile solution of concentrated immunoglobulins prepared from pooled human plasma processed by cold ethanol fractionation. In the United States, Ig is produced only from plasma that has tested negative for hepatitis B surface antigen, antibodies to HIV and HCV, and HCV RNA. In addition, the process used to manufacture Ig inactivates viruses (e.g., HBV, HCV, and HIV). When administered IM before or within 2 weeks after exposure to HAV, Ig is >85% effective in preventing HAV infections.
# Preexposure Immunization
Persons in the following groups who are likely to be treated in STD clinic settings should be offered hepatitis A vaccine: 1) all MSM; 2) illegal drug users (both injecting and noninjecting drugs); and 3) persons with CLD, including persons with chronic HBV and HCV infection who have evidence of CLD.
# Prevaccination Serologic Testing for Susceptibility
Approximately one third of the U.S. population has serologic evidence of previous HAV infection, which increases directly with age and reaches 75% among persons aged >70 years. Screening for HAV infection might be cost-effective in
# Postexposure Prophylaxis
Previously unvaccinated persons exposed to HAV (e.g., through household or sexual contact or by sharing illegal drugs with a person who has hepatitis A) should be administered a single IM dose of Ig (0.02 mL/kg) as soon as possible but not >2 weeks after exposure. Persons who have had 1 dose of hepatitis A vaccine at least 1 month before exposure to HAV do not need Ig. If hepatitis A vaccine is recommended for a person receiving Ig, it can be administered simultaneously at a separate anatomic injection site. The use of hepatitis A vaccine alone is not recommended for PEP.
# Special Considerations
Limited data indicate that vaccination of persons with CLD and of HIV-infected persons results in lower seroprotection rates and antibody concentrations (50). In HIV-infected persons, antibody response might be directly related to CD4+ levels.
# Hepatitis B
Hepatitis B is caused by infection with HBV. The incubation period from the time of exposure to onset of symptoms is 6 weeks to 6 months. HBV is found in highest concentrations in blood and in lower concentrations in other body fluids (e.g., semen, vaginal secretions, and wound exudates). HBV infection can be self-limited or chronic. In adults, only approximately half of newly acquired HBV infections are symptomatic, and approximately 1% of reported cases result in acute liver failure and death. Risk for chronic infection is inversely related to age at infection: approximately 90% of infected infants and 30% of infected children aged <5 years become chronically infected, compared with 2%-6% of adults. Among persons with chronic HBV infection, the risk for premature death from cirrhosis or hepatocellular carcinoma (HCC) is 15%-25%.
HBV is efficiently transmitted by percutaneous or mucous membrane exposure to infectious blood or body fluids that contain blood. The primary risk factors that have been associated with infection among adolescents and adults are unprotected sex with an infected partner, unprotected sex with more than one partner, MSM, history of other STDs, and illegal injecting-drug use.
CDC's national strategy to eliminate transmission of HBV infection includes 1) prevention of perinatal infection through routine screening of all pregnant women for HBsAg and immunoprophylaxis of infants born to HBsAg-positive mothers and infants born to mothers with unknown HBsAg status, 2) routine infant vaccination, 3) vaccination of previously unvaccinated children and adolescents through age 18 years, and 4) vaccination of previously unvaccinated adults at in- creased risk for infection (2,4). High vaccination coverage rates, with subsequent declines in acute hepatitis B incidence, have been achieved among infants and adolescents (2,203,204). In contrast, vaccination coverage among the majority of high-risk adult groups (e.g., persons with more than one sex partner in the previous 6 months, MSM, and IDUs) have remained low, and the majority of new infections occur in these high-risk groups (4,(205)(206)(207). STD clinics and other settings that provide services targeted to high-risk adults are ideal sites in which to provide hepatitis B vaccination to adults at risk for HBV infection. All unvaccinated adults seeking services in these settings should be assumed to be at risk for hepatitis B and should receive hepatitis B vaccination.
# Diagnosis
Diagnosis of acute or chronic HBV infection requires serologic testing (Table 4). HBsAg is present in both acute and chronic infection. The presence of IgM antibody to hepatitis B core antigen (IgM anti-HBc) is diagnostic of acute or recently acquired HBV infection. Antibody to HBsAg (anti-HBs) is produced after a resolved infection and is the only HBV antibody marker present after immunization. The presence of HBsAg and total anti-HBc, with a negative test for IgM anti-HBc, indicates chronic HBV infection. The presence of anti-HBc alone might indicate a false-positive result or acute, resolved, or chronic infection.
# Treatment
No specific therapy is available for persons with acute hepatitis B; treatment is supportive. Persons with chronic HBV infection should be referred for evaluation to a physician experienced in the management of CLD. Therapeutic agents approved by FDA for treatment of chronic hepatitis B can achieve sustained suppression of HBV replication and remission of liver disease in some persons. In addition, patients with chronic hepatitis B might benefit from screening to detect HCC at an early stage.
# Prevention
Two products have been approved for hepatitis B prevention: hepatitis B immune globulin (HBIG) and hepatitis B vaccine. HBIG provides temporary (i.e., 3-6 months) protection from HBV infection and is typically used as PEP either as an adjunct to hepatitis B vaccination in previously unvaccinated persons or alone in persons who have not responded to vaccination. HBIG is prepared from plasma known to contain high concentrations of anti-HBs. The recommended dose of HBIG is 0.06 mL/kg.
Hepatitis B vaccine contains HBsAg produced in yeast by recombinant DNA technology and provides protection from HBV infection when used for both preexposure immunization and PEP. The two available monovalent hepatitis B vaccines for use in adolescents and adults are Recombivax HB ® (Merck and Co., Inc., Whitehouse Station, New Jersey) and Engerix-B ® (GlaxoSmithKline Biologicals, Pittsburgh, Pennsylvania). A combination vaccine (hepatitis A and hepatitis B) for use in adults, Twinrix ® (GlaxoSmithKline Biologicals, Pittsburgh, Pennsylvania), also is available. The recommended HBV dose varies by product and age of recipient (Table 3).
When selecting a hepatitis B vaccination schedule, the health-care provider should consider the need to achieve completion of the vaccine series. Approved adolescent and adult schedules for both monovalent hepatitis B vaccine (i.e., Engerix-B ® and Recombivax HB ® ) include the following: 0, 1, and 6 months; 0, 1, and 4 months; and 0, 2, and 4 months. A 4-dose schedule of Engerix-B ® at 0, 1, 2, and 12 months is licensed for all age groups. A 2-dose schedule of Recombivax HB ® adult formulation (10 µg) is licensed for adolescents aged 11-15 years. When scheduled to receive the second dose, adolescents aged >15 years should be switched to a 3-dose series, with doses 2 and 3 consisting of the pediatric formulation (5 µg) administered on an appropriate schedule. Twinrix ® may be administered to persons aged >18 years at risk for both HAV and HBV infections at 0, 1, and 6 months.
Hepatitis B vaccine should be administered IM in the deltoid muscle and may be administered simultaneously with other vaccines. For adolescents and adults, the needle length should be 1-2 inches, depending on the recipient's weight (1 inch for females weighing <70 kg), 1.5 inches for males weighing <120 kg; and 2 inches for males weighing >120 kg and females >100 kg). A 22-to 25-gauge needle is recommended. If the vaccine series is interrupted after the first or second dose of vaccine, the missed dose should be administered as soon as possible. The series does not need to be restarted after a missed dose.
In adolescents and healthy adults aged <40 years, approximately 30%-55% acquire a protective antibody response (anti-HBs >10 mIU/mL) after the first vaccine dose, 75% after the second, and >90% after the third. Vaccine-induced immune memory has been demonstrated to persist for at least 15-20 years. Periodic testing to determine antibody levels in immunocompetent persons is not necessary, and booster doses of vaccine are not recommended.
Hepatitis B vaccination is generally well-tolerated by the majority of recipients. Pain at the injection site and low-grade fever are reported by a minority of recipients. Evidence for a causal association between receipt of hepatitis B vaccination and anaphylaxis exists, which is estimated to occur in 1 of 1.1 million doses of vaccine administered among children and adolescents; no deaths have been reported after anaphylaxis. Vaccine is contraindicated in persons with a history of anaphylaxis after a previous dose of hepatitis B vaccine and in persons with a known anaphylactic reaction to any vaccine component. No evidence for a causal association has been demonstrated for other adverse events reported after administration of hepatitis B vaccine.
# Preexposure Vaccination
Hepatitis B vaccination is recommended for all unvaccinated adolescents, all unvaccinated adults at risk for HBV infection, and all adults seeking protection from HBV infection. For adults, acknowledgement of a specific risk factor is not a requirement for vaccination.
Hepatitis B vaccine should be routinely offered to all unvaccinated persons attending STD clinics and to all unvaccinated persons seeking treatment for STDs in other settings. Other settings where all unvaccinated adults should be assumed to be at risk for hepatitis B and should receive hepatitis B vaccination include correctional facilities, facilities providing drug abuse treatment and prevention services, health-care settings serving MSM, and HIV testing and treatment facilities. All persons who receive clinical services in these settings should be offered hepatitis B vaccine, unless they have a reliable vaccination history (i.e., a written, dated record of each dose of a complete series). In all settings, vaccination should be initiated even though completion of the vaccine series might not be ensured.
# Prevaccination Antibody Screening
Prevaccination serologic testing for susceptibility may be considered to reduce the cost of vaccinating adult populations that have an expected high prevalence of HBV infection (i.e., >20%-30%) (e.g., IDUs and MSM [especially in older age groups]). In addition, prevaccination testing for susceptibility is recommended for unvaccinated household, sexual, and needle-sharing contacts of HBsAg-positive persons.
Anti-HBc is the test of choice for prevaccination testing; persons who are anti-HBc-positive should be tested for HBsAg. If persons are determined to be HBsAg negative, no further action is required. If persons are determined to be HBsAg positive, the person should be referred for medical follow-up, including counseling and evaluation for antiviral treatment (see Management of HBsAg-Positive Persons). In addition, all household members, sex partners, and needlesharing partners of HBsAg-positive persons should be vaccinated.
Serologic testing should not be a barrier to vaccination of susceptible persons, especially in populations that are difficult to access. In the majority of situations, the first vaccine dose should be administered immediately after collection of the blood sample for serologic testing. Vaccination of persons who are immune to HBV infection because of current or previous infection or vaccination does not increase the risk for adverse events.
# Postvaccination Testing for Serologic Response
Serologic testing for immunity is not necessary after routine vaccination of adolescents or adults. Testing after vaccination is recommended for persons whose subsequent clinical management depends on knowledge of their immune status (e.g., health-care workers or public safety workers at high risk for continued percutaneous or mucosal exposure to blood or body fluids). In addition, testing is recommended for 1) HIVinfected persons and other immunocompromised persons to determine the need for revaccination and the type of followup testing; and 2) sex and needle-sharing partners of HBsAgpositive persons to determine the need for revaccination and for other methods to protect themselves from HBV infection.
If indicated, testing should be performed 1-2 months after administration of the last dose of the vaccine series by using a method that allows determination of a protective level of anti-HBs (>10 mIU/mL). Persons determined to have anti-HBs levels of <10 mIU/mL after the primary vaccine series should be revaccinated with a 3-dose series, followed by anti-HBs testing 1-2 months after the third dose. Persons who do not respond to revaccination should be tested for HBsAg. If HBsAg positive, the person should receive appropriate management (see Management of HBsAg-Positive Persons); if HBsAg negative, the person should be considered suscep-tible to HBV infection and counseled concerning precautions to prevent HBV infection and the need for HBIG PEP for any known exposure (see PEP).
# Postexposure Prophylaxis
Both passive-active PEP with HBIG and hepatitis B vaccination and active PEP with hepatitis B vaccination alone have been demonstrated to be highly effective in preventing transmission after exposure to HBV (2). HBIG alone also has been demonstrated to be effective in preventing HBV transmission, but with the availability of hepatitis B vaccine, HBIG typically is used as an adjunct to vaccination.
Exposure to HBsAg-Positive Source. Unvaccinated persons or persons known not to have responded to a complete hepatitis B vaccine series should receive both HBIG and hepatitis vaccine as soon as possible (preferably <24 hours) after a discrete, identifiable exposure to blood or body fluids that contain blood from an HBsAg-positive source (Table 5). Hepatitis B vaccine should be administered simultaneously with HBIG in a separate injection site, and the vaccine series should be completed by using the age-appropriate vaccine dose and schedule (Table 3). Exposed persons who are in the process of being vaccinated but who have not completed the vaccine series should receive the appropriate dose of HBIG (i.e., 0.06 mL/kg) and should complete the vaccine series. Exposed persons who are known to have responded to vaccination are considered protected and need no further vaccine doses. Persons who have written documentation of a complete hepatitis B vaccine series and who did not receive post-vaccination testing should receive a single vaccine booster dose. Alternatively, these persons can be managed according to guidelines for management of persons with occupational exposure to blood or body fluids that contain blood (207).
Exposure to Source with Unknown HBsAg Status. Unvaccinated persons who have a discrete, identifiable exposure to blood or body fluids containing blood from a source with unknown HBsAg status should receive the hepatitis B vaccine series, with the first dose initiated as soon as possible after exposure (preferably within 24 hours) and the series completed by using the age-appropriate dose and schedule. Exposed persons who are not fully vaccinated should complete the vaccine series. Exposed persons with written documentation of a complete hepatitis B vaccine series require no further treatment.
# Special Considerations
Pregnancy. All pregnant women receiving STD services should be tested for HBsAg, regardless of whether they have been previously tested or vaccinated. All HBsAg-positive pregnant women should be reported to state and local perinatal hepatitis B prevention programs. HBsAg-negative pregnant women seeking STD treatment who have not been previously vaccinated should receive hepatitis B vaccination. Additional information regarding management of HBsAg-positive pregnant women and their infants is available at http:// www.cdc.gov/mmwr/PDF/rr/rr5416.pdf.
HIV Infection. HIV infection can impair the response to hepatitis B vaccination. HIV-infected persons should be tested for anti-HBs 1-2 months after the third vaccine dose (see Postvaccination Testing for Serologic Response). Modified dosing regimens, including a doubling of the standard antigen dose and administration of additional doses, might increase the response rate.
# Management of HBsAg-Positive Persons
This section provides recommendations for management of all HBsAg-positive persons. Additional recommendations for management of HBsAg-positive persons who are coinfected with HIV are available at http://www.cdc.gov/ mmwr/preview/mmwrhtml/rr5315a1.htm.
•
# Hepatitis C
Hepatitis C virus (HCV) infection is the most common chronic bloodborne infection in the United States; approximately 2.7 million persons are chronically infected (204). Although HCV is not efficiently transmitted sexually, persons at risk for infection through injection-drug use might seek care in STD treatment facilities, HIV counseling and testing facilities, correctional facilities, drug treatment facilities, and other public health settings where STD and HIV prevention and control services are available.
Persons newly infected with HCV typically are either asymptomatic or have a mild clinical illness. HCV RNA can be detected in blood within 1-3 weeks after exposure. The average time from exposure to antibody to HCV (anti-HCV) seroconversion is 8-9 weeks, and anti-HCV can be detected in >97% of persons by 6 months after exposure. Chronic HCV infection develops in 60%-85% of HCV-infected persons; 60%-70% of chronically infected persons have evidence of active liver disease. The majority of infected persons might not be aware of their infection because they are not clinically ill. However, infected persons serve as a source of transmission to others and are at risk for CLD or other HCV-related chronic diseases for decades after infection.
HCV is most efficiently transmitted through large or repeated percutaneous exposure to infected blood (e.g., through transfusion of blood from unscreened donors or through use of injecting drugs), although less efficient, occupational, perinatal, and sexual exposures also can result in transmission of HCV.
The role of sexual activity in the transmission of HCV has been controversial. Case-control studies have reported an association between acquiring HCV infection and exposure to a sex contact with HCV infection or exposure to multiple sex partners. Surveillance data also indicate that 15%-20% of persons reported with acute HCV infection have a history of sexual exposure in the absence of other risk factors (204,208). Case reports of acute HCV infection among HIV-positive MSM who deny injecting-drug use have indicated that this occurrence is frequently associated with other STDs (e.g., syphilis) (209,210). In contrast, a low prevalence (average: 1.5%) of HCV infection has been demonstrated in studies of long-term spouses of patients with chronic HCV infection who had no other risk factors for infection, and multiple published studies have demonstrated the prevalence of HCV infection among MSM who have not reported a history of injecting-drug use to be no higher than that of heterosexuals (211)(212)(213). Because sexual transmission of bloodborne viruses is more efficient among homosexual men compared with heterosexual men and women, the reason that HCV infection rates are not substantially higher among MSM compared with heterosexuals is unclear. Overall, these findings indicate that sexual transmission of HCV is possible but inefficient. Additional data are needed to determine whether sexual transmission of HCV might be increased in the context of HIV infection or other STDs.
# Diagnosis and Treatment
Anti-HCV testing is recommended for routine screening of asymptomatic persons based on their risk for infection or based on a recognized exposure (see Hepatitis C, Prevention). For such persons, testing for HCV infection should include the use of an FDA-cleared test for antibody to HCV (i.e., immunoassay, EIA, or enhanced chemiluminescence assay and, if recommended, a supplemental antibody test) (214).
Persons counseled and tested for HCV infection and determined to be anti-HCV positive should be evaluated (by referral or consultation, if appropriate) for presence of active infection, presence or development of CLD, and for possible treatment. Reverse transcriptase polymerase chain reaction to detect HCV RNA may be used to confirm the diagnosis of current HCV infection, and an elevated alanine aminotransferase (ALT) level is biochemical evidence of CLD. Combination therapy with pegylated interferon and ribavirin is the treatment of choice for patients with chronic hepatitis C. Because of advances in the field of antiviral therapy for acute and chronic hepatitis C, clinicians should consult with specialists knowledgeable about management of hepatitis C infection.
# Prevention
No vaccine for hepatitis C is available, and prophylaxis with immune globulin is not effective in preventing HCV infection after exposure. Reducing the burden of HCV infection and disease in the United States requires implementation of both primary and secondary prevention activities (208). Primary prevention reduces or eliminates HCV transmission; secondary prevention activities reduce liver and other chronic diseases in HCV-infected persons by identifying them and providing appropriate medical management and antiviral therapy, if appropriate.
Persons seeking care in STD clinics or other primary-care settings should be screened to identify those who should be offered HCV counseling and testing. In STD clinics and other settings that serve large numbers of persons at high risk for bloodborne infections (e.g., correctional settings), the major risk factor for which to screen for HCV infection is injection of illegal drugs. In addition, for clinical management issues, all persons with HIV infection should also be offered HCV counseling and testing. Other risk factors for which routine HCV testing is recommended include persons
• who had a blood transfusion or solid organ transplant before July 1992, • who received clotting factor concentrates produced before 1987, • who have been on long-term dialysis, and • those with signs and symptoms of liver disease (e.g., abnormal ALT). Persons who test positive for anti-HCV (see Diagnosis and Treatment) should be provided information regarding 1) how to protect their liver from further harm, 2) how to prevent transmission to others, and 3) the need for medical evaluation for CLD and possible treatment.
• To protect their liver from further harm, HCV-positive persons should be advised to avoid alcohol and taking any new medicines (including OTC and herbals) without checking with their doctor. • To reduce the risk for transmission to others, HCVpositive persons should be advised to 1) not donate blood, body organs, other tissue, or semen; 2) not share any personal items that might have blood on them (e.g., toothbrushes and razors); and 3) cover cuts and sores on the skin to keep from spreading infectious blood or secretions. HCV-positive persons with one long-term, steady sex partner do not need to change their sexual practices. They should discuss the low but present risk for transmission with their partner and discuss the need for counseling and testing. HCV-positive women do not need to avoid pregnancy or breastfeeding. • HCV-positive persons should be evaluated (by referral or consultation, if appropriate) for presence of development of CLD, including assessment of liver function tests, assessment for severity of liver disease and possible treatment, and determination of the need for hepatitis A and B vaccination. Persons who test negative for anti-HCV who had an exposure previously should be reassured that they are not infected.
# Regardless of test results, persons who use or inject illegal drugs should be counseled to
• stop using and injecting drugs;
• enter and complete substance abuse treatment, including relapse prevention; • take the following steps to reduce personal and public health risks, if they continue to inject drugs: -never reuse or share syringes, water, or drug preparation equipment; -use only syringes obtained from a reliable source (e.g., pharmacies); -use a new, sterile syringe to prepare and inject drugs; -if possible, use sterile water to prepare drugs; otherwise, use clean water from a reliable source (e.g., fresh tap water); -use a new or disinfected container ("cooker") and a new filter ("cotton") to prepare drugs; -clean the injection site before injection with a new alcohol swab; -safely dispose of syringes after one use; and -get vaccinated for hepatitis A and B.
# Postexposure Follow-Up
No PEP has been demonstrated to be effective against HCV. Testing to determine whether HCV infection has developed is recommended for health-care workers after percutaneous or permucosal exposures to HCV-positive blood and for children born to HCV-positive women.
# Special Considerations
# Pregnancy
Routine testing for HCV infection is not recommended for all pregnant women. Pregnant women with a known risk factor for HCV infection should be offered counseling and testing. Patients should be advised that approximately five of every 100 infants born to HCV-infected woman become infected. This infection occurs predominantly during or near delivery, and no treatment or delivery method is known to decrease this risk. The risk is increased by the presence of maternal HCV viremia at delivery and also is greater (2-3 times) if the woman is coinfected with HIV. Breastfeeding does not appear to transmit HCV, although HCV-positive mothers should consider abstaining from breastfeeding if their nipples are cracked or bleeding. Infants born to HCV-positive mothers should be tested for HCV infection and, if positive, evaluated for the presence of CLD.
# HIV Infection
Because of the high prevalence of HIV/HCV coinfection and because of critical clinical management issues for coinfected persons, all HIV-infected persons should be tested for HCV. Because a small percentage of coinfected persons fail to acquire HCV antibodies, HCV RNA should be tested in HIV-positive persons with unexplained liver disease who are anti-HCV negative. The course of liver disease is more rapid in HIV/HCV coinfected persons, and the risk for cirrhosis is nearly twice that in persons with HCV infection alone. Treatment of HCV in coinfected persons might improve tolerance to highly active antiretroviral therapy (HAART) for HIV infection because of the increased risk for hepatotoxicity from HAART with HCV infection. However, anti-HCV treatment in coinfected persons is still investigational, and based on ongoing clinical trials, more data are needed to determine the best regimens.
# Proctitis, Proctocolitis, and Enteritis
Sexually transmitted gastrointestinal syndromes include proctitis, proctocolitis, and enteritis. Evaluation for these syndromes should include appropriate diagnostic procedures (e.g., anoscopy or sigmoidoscopy, stool examination, and culture).
Proctitis is inflammation of the rectum (i.e., the distal 10-12 cm) that might be associated with anorectal pain, tenesmus, or rectal discharge. N. gonorrhoeae, C. trachomatis (including LGV serovars), T. pallidum, and HSV are the most common sexually transmitted pathogens involved. In patients coinfected with HIV, herpes proctitis might be especially severe. Proctitis occurs predominantly among persons who participate in receptive anal intercourse.
Proctocolitis is associated with symptoms of proctitis and diarrhea or abdominal cramps and inflammation of the colonic mucosa, extending to 12 cm above the anus. Fecal leukocytes might be detected on stool examination, depending on the pathogen. Pathogenic organisms include Campylobacter sp., Shigella sp., Entamoeba histolytica, and, rarely, LGV serovars of C. trachomatis. CMV or other opportunistic agents might be involved in immunosuppressed HIV-infected patients. Proctocolitis can be acquired by the oral route or by oral-anal contact, depending on the pathogen.
Enteritis usually results in diarrhea and abdominal cramping without signs of proctitis or proctocolitis; it occurs among persons whose sexual practices include oral-anal contact. In otherwise healthy persons, Giardia lamblia is most frequently implicated. When outbreaks of gastrointestinal illness occur among social or sexual networks of MSM, clinicians should consider sexual transmission as a mode of spread and provide counseling accordingly. Among HIV-infected patients, gastrointestinal illness can be caused by other infections that usually are not sexually transmitted, including CMV, Mycobacterium avium-intracellulare, Salmonella sp., Campylobacter sp., Shigella sp., Cryptosporidium, Microsporidium, and Isospora. Multiple stool examinations might be necessary to detect Giardia, and special stool preparations are required to diagnose cryptosporidiosis and microsporidiosis. In addition, enteritis might be directly caused by HIV infection.
When laboratory diagnostic capabilities are available, treatment decisions should be based on the specific diagnosis. Diagnostic and treatment recommendations for all enteric infections are beyond the scope of these guidelines.
# Treatment
Acute proctitis of recent onset among persons who have recently practiced receptive anal intercourse is usually sexually acquired (215,216). Such patients should be examined by anoscopy and should be evaluated for infection with HSV, N. gonorrhoeae, C. trachomatis, and T. pallidum. If an anorectal exudate is detected on examination or if polymorphonuclear leukocytes are detected on a Gram-stained smear of anorectal secretions, the following therapy may be prescribed while awaiting additional laboratory tests.
# Recommended Regimen
Ceftriaxone 125 mg IM (or another agent effective against rectal and genital gonorrhea) PLUS Doxycycline 100 mg orally twice a day for 7 days Patients with suspected or documented herpes proctitis should be managed in the same manner as those with genital herpes (see Genital HSV Infections). If painful perianal ulcers are present or mucosal ulcers are detected on anoscopy, presumptive therapy should include a regimen for treating genital herpes. In addition, LGV proctitis and proctocolitis also should be considered. Appropriate diagnostic testing for LGV should be conducted in accordance with state or federal guidelines, and doxycycline therapy should be administered 100 mg orally twice daily for 3 weeks.
# Follow-Up
Follow-up should be based on specific etiology and severity of clinical symptoms. Reinfection might be difficult to distinguish from treatment failure.
# Management of Sex Partners
Partners of patients with sexually transmitted enteric infections should be evaluated for any diseases diagnosed in the index patient.
# Ectoparasitic Infections Pediculosis Pubis
Patients who have pediculosis pubis (i.e., pubic lice) usually seek medical attention because of pruritus or because they notice lice or nits on their pubic hair. Pediculosis pubis is usually transmitted by sexual contact.
# Recommended Regimens
Permethrin 1% cream rinse applied to affected areas and washed off after 10 minutes OR Pyrethrins with piperonyl butoxide applied to the affected area and washed off after 10 minutes
# Alternative Regimens
Malathion 0.5% lotion applied for 8-12 hours and washed off OR Ivermectin 250 ug/kg repeated in 2 weeks Reported resistance to pediculcides has been increasing and is widespread. Malathion may be used when treatment failure is believed to have occurred because of resistance (217). The odor and long duration of application for malathion make it a less attractive alternative than the recommended pediculcides. Ivermectin has been successfully used to treat lice but has only been evaluated in small studies.
Lindane is not recommended as first-line therapy because of toxicity. It should only be used as an alternative because of inability to tolerate other therapies or if other therapies have failed. Lindane toxicity, as indicated by seizure and aplastic anemia, has not been reported when treatment was limited to the recommended 4-minute period. Permethrin has less potential for toxicity than lindane.
# Other Management Considerations
The recommended regimens should not be applied to the eyes. Pediculosis of the eyelashes should be treated by applying occlusive ophthalmic ointment to the eyelid margins twice a day for 10 days. Bedding and clothing should be decontaminated (i.e., machine-washed, machine-dried using the heat cycle, or dry cleaned) or removed from body contact for at least 72 hours. Fumigation of living areas is not necessary.
Patients with pediculosis pubis should be evaluated for other STDs.
# Follow-Up
Patients should be evaluated after 1 week if symptoms persist. Re-treatment might be necessary if lice are found or if eggs are observed at the hair-skin junction. Patients who do not respond to one of the recommended regimens should be re-treated with an alternative regimen.
# Management of Sex Partners
Sex partners within the previous month should be treated. Patients should avoid sexual contact with their sex partner(s) until patients and partners have been treated and reevaluated to rule out persistent disease.
# Special Considerations
# Pregnancy
Pregnant and lactating women should be treated with either permethrin or pyrethrins with piperonyl butoxide; lindane is contraindicated in pregnancy.
# HIV Infection
Patients who have pediculosis pubis and also are infected with HIV should receive the same treatment regimen as those who are HIV negative.
# Scabies
The predominant symptom of scabies is pruritus. Sensitization to Sarcoptes scabiei occurs before pruritus begins. The first time a person is infested with S. scabiei, sensitization takes up to several weeks to develop. However, pruritus might occur within 24 hours after a subsequent reinfestation. Scabies in adults frequently is sexually acquired, although scabies in children usually is not.
# Recommended Regimens
Permethrin cream (5%) applied to all areas of the body from the neck down and washed off after 8-14 hours OR Ivermectin 200ug/kg orally, repeated in 2 weeks Alternative Regimens Lindane (1%) 1 oz. of lotion or 30 g of cream applied in a thin layer to all areas of the body from the neck down and thoroughly washed off after 8 hours Lindane is not recommended as first-line therapy because of toxicity. It should only be used as an alternative if the patient cannot tolerate other therapies or if other therapies have failed.
Lindane should not be used immediately after a bath or shower, and it should not be used by persons who have extensive dermatitis, women who are pregnant or lactating, or children aged <2 years. Lindane resistance has been reported in some areas of the world, including parts of the United States. Seizures have occurred when lindane was applied after a bath or used by patients who had extensive dermatitis. Aplastic anemia after lindane use also has been reported.
Permethrin is effective and safe and less expensive than ivermectin. One study demonstrated increased mortality among elderly, debilitated persons who received ivermectin, but this observation has not been confirmed in subsequent reports (218).
# Other Management Considerations
Bedding and clothing should be decontaminated (i.e., either machine-washed, machine-dried using the hot cycle, or dry cleaned) or removed from body contact for at least 72 hours. Fumigation of living areas is unnecessary.
# Crusted Scabies
Crusted scabies (i.e., Norwegian scabies) is an aggressive infestation that usually occurs in immunodeficient, debilitated, or malnourished persons. Patients who are receiving systemic or potent topical glucocorticoids, organ transplant recipients, mentally retarded or physically incapacitated persons, HIV-infected or human T-lymphotrophic virus-1infected persons, and persons with various hematologic malignancies are at risk for developing crusted scabies. Crusted scabies is associated with greater transmissibility than scabies. No controlled therapeutic studies for crusted scabies have been conducted, and the appropriate treatment remains unclear. Substantial treatment failure might occur with a single topical scabicide or with oral ivermectin treatment. Some specialists recommend combined treatment with a topical scabicide and oral ivermectin or repeated treatments with ivermectin 200 ug/kg on days 1, 15, and 29. Lindane should be avoided because of the risks for neurotoxicity with heavy applications or denuded skin. Patient's fingernails should be closely trimmed to reduce injury from excessive scratching.
# Follow-Up
Patients should be informed that the rash and pruritus of scabies might persist for up to 2 weeks after treatment. Symptoms or signs that persist for >2 weeks can be attributed to several factors. Treatment failure might be caused by resistance to medication or by faulty application of topical scabicides. Patients with crusted scabies might have poor penetration into thick scaly skin and harbor mites in these difficult-to-penetrate layers. Particular attention must be given to the fingernails of these patients. Reinfection from family members or fomites might occur in the absence of appropriate contact treatment and washing of bedding and clothing. Even when treatment is successful and reinfection is avoided, symptoms can persist or worsen as a result of allergic dermatitis. Finally, household mites can cause symptoms to persist as a result of crossreactivity between antigens. Some special-ists recommend re-treatment after 1-2 weeks for patients who are still symptomatic; others recommend re-treatment only if live mites are observed. Patients who do not respond to the recommended treatment should be re-treated with an alternative regimen.
# Management of Sex Partners and Household Contacts
Both sexual and close personal or household contacts within the preceding month should be examined and treated.
# Management of Outbreaks in Communities, Nursing Homes, and Other Institutional Settings
Scabies epidemics frequently occur in nursing homes, hospitals, residential facilities, and other communities. Control of an epidemic can only be achieved by treatment of the entire population at risk. Ivermectin can be considered in this setting, especially if treatment with topical scabicides fails. Epidemics should be managed in consultation with a specialist.
# Special Considerations
# Infants, Young Children, and Pregnant or Lactating Women
Infants, young children, and pregnant or lactating women should not be treated with lindane. They can be treated with permethrin.
Ivermectin is not recommended for pregnant or lactating patients. The safety of ivermectin in children who weigh <15 kg has not been determined.
# HIV Infection
Patients who have uncomplicated scabies and also are infected with HIV should receive the same treatment regimens as those who are HIV negative. HIV-infected patients and others who are immunosuppressed are at increased risk for crusted scabies. Ivermectin has been reported to be useful in small, noncontrolled studies. Such patients should be managed in consultation with a specialist.
# Sexual Assault and STDs
# Adults and Adolescents
The recommendations in this report are limited to the identification, prophylaxis, and treatment of sexually transmitted infections and conditions commonly identified in the management of such infections. The documentation of findings, collection of nonmicrobiologic specimens for forensic purposes, and the management of potential pregnancy or physical and psychological trauma are beyond the scope of this report. Examinations of survivors of sexual assault should be conducted by an experienced clinician in a way that minimizes further trauma to the survivor. The decision to obtain genital or other specimens for STD diagnosis should be made on an individual basis. Care systems for survivors should be designed to ensure continuity (including timely review of test results), support adherence, and monitor for adverse reactions to any therapeutic or prophylactic regimens prescribed at initial examination. Laws in all 50 states strictly limit the evidentiary use of a survivor's previous sexual history, including evidence of previously acquired STDs, as part of an effort to undermine the credibility of the survivor's testimony. Evidentiary privilege against revealing any aspect of the examination or treatment is enforced in the majority of states. In unanticipated, exceptional situations, STD diagnoses may later be accessed, and the survivor and clinician may opt to defer testing for this reason. However, collection of specimens at initial examination for laboratory STD diagnosis gives the survivor and clinician the option to defer empiric prophylactic antimicrobial treatment. Among sexually active adults, the identification of sexually transmitted infection after an assault might be more important for the psychological and medical management of the patient than for legal purposes because the infection could have been acquired before the assault.
Trichomoniasis, BV, gonorrhea, and chlamydial infection are the most frequently diagnosed infections among women who have been sexually assaulted. Because the prevalence of these infections is high among sexually active women, their presence after an assault does not necessarily signify acquisition during the assault. A postassault examination is, however, an opportunity to identify or prevent sexually transmitted infections, regardless of whether they were acquired during an assault. Chlamydial and gonococcal infections in women are of particular concern because of the possibility of ascending infection. In addition, HBV infection might be prevented by postexposure administration of hepatitis B vaccine. Reproductive-aged female survivors should be evaluated for pregnancy, if appropriate.
# Evaluation for Sexually Transmitted Infections Initial Examination
An initial examination should include the following procedures:
• Testing for N. gonorrhoeae and C. trachomatis from specimens collected from any sites of penetration or attempted penetration.
# Follow-Up Examinations
After the initial postassault examination, follow-up examinations provide an opportunity to 1) detect new infections acquired during or after the assault; 2) complete hepatitis B immunization, if indicated; 3) complete counseling and treatment for other STDs; and 4) monitor side effects and adherence to postexposure prophylactic medication, if prescribed.
Examination for STDs should be repeated within 1-2 weeks of the assault. Because infectious agents acquired through assault might not have produced sufficient concentrations of organisms to result in positive test results at the initial examination, testing should be repeated during the follow-up visit, unless prophylactic treatment was provided. If treatment was provided, testing should be conducted only if the survivor reports having symptoms. If treatment was not provided, follow-up examination should be conducted within 1 week to ensure that results of positive tests can be discussed promptly with the survivor and that treatment is provided. Serologic tests for syphilis and HIV infection should be repeated 6 weeks, 3 months, and 6 months after the assault if initial test results were negative and infection in the assailant could not be ruled out (see Sexual Assaults, Risk for Acquiring HIV Infection).
# Prophylaxis
Many specialists recommend routine preventive therapy after a sexual assault because follow-up of survivors of sexual assault can be difficult. The following prophylactic regimen is suggested as preventive therapy:
• Postexposure hepatitis B vaccination, without HBIG, should adequately protect against HBV infection. Hepatitis B vaccination should be administered to sexual assault victims at the time of the initial examination if they have not been previously vaccinated. Follow-up doses of vaccine should be administered 1-2 and 4-6 months after the first dose. • An empiric antimicrobial regimen for chlamydia, gonorrhea, trichomonas, and BV. • EC should be offered if the postassault could result in pregnancy in the survivor.
# MMWR August 4, 2006
# Recommended Regimens
Ceftriaxone 125 mg IM in a single dose PLUS Metronidazole 2 g orally in a single dose PLUS Azithromycin 1 g orally in a single dose OR Doxycycline 100 mg orally twice a day for 7 days For patients requiring alternative treatments, refer to the sections in this report relevant to the specific agent. The efficacy of these regimens in preventing infections after sexual assault has not been evaluated. Clinicians should counsel patients regarding the possible benefits and toxicities associated with these treatment regimens; gastrointestinal side effects can occur with this combination. Providers might also consider anti-emetic medications, particularly if EC also is provided.
# Other Management Considerations
At the initial examination and, if indicated, at follow-up examinations, patients should be counseled regarding 1) symptoms of STDs and the need for immediate examination if symptoms occur and 2) abstinence from sexual intercourse until STD prophylactic treatment is completed.
# Risk for Acquiring HIV Infection
HIV seroconversion has occurred in persons whose only known risk factor was sexual assault or sexual abuse, but the frequency of this occurrence is probably low. In consensual sex, the risk for HIV transmission from vaginal intercourse is 0.1%-0.2% and for receptive rectal intercourse, 0.5%-3% (219). The risk for HIV transmission from oral sex is substantially lower. Specific circumstances of an assault might increase risk for HIV transmission (e.g., trauma, including bleeding) with vaginal, anal, or oral penetration; site of exposure to ejaculate; viral load in ejaculate; and the presence of an STD or genital lesions in the assailant or survivor.
Children might be at higher risk for transmission because child sexual abuse is frequently associated with multiple episodes of assault and might result in mucosal trauma (see Sexual Assault or Abuse of Children).
Postexposure therapy with zidovudine was associated with a reduced risk for acquiring HIV in a study of health-care workers who had percutaneous exposures to HIV-infected blood (220). On the basis of these results and the results of animal studies, PEP has been recommended for health-care workers who have occupational exposures to HIV (207). These findings have been extrapolated to other types of HIV exposure, including sexual assault (58). If HIV exposure has occurred, initiation of PEP as soon as possible after the exposure likely increases benefit. Although a definitive statement of benefit cannot be made regarding PEP after sexual assault, the possibility of HIV exposure from the assault should be assessed at the time of the postassault examination. The possible benefit of PEP in preventing HIV infection also should be discussed with the assault survivor if risk exists for HIV exposure from the assault.
The likelihood of the assailant having HIV, any exposure characteristics that might increase the risk for HIV transmission, the time elapsed after the event, as well as potential benefits and risks the PEP are all factors that will impact the medical recommendation for PEP and impact the assault survivor's acceptance of that recommendation (58). Determination of assailant's HIV status at the time of the assault examination will usually be impossible. Therefore, the healthcare provider should assess any available information concerning HIV-risk behaviors of the assailant(s) (e.g., a man who has sex with other men and injecting-drug or crack cocaine use), local epidemiology of HIV/AIDS, and exposure characteristics of the assault. When an assailant's HIV status is unknown, factors that should be considered in determining whether an increased risk for HIV transmission exists include 1) whether vaginal or anal penetration occurred; 2) whether ejaculation occurred on mucous membranes; 3) whether multiple assailants were involved; 4) whether mucosal lesions are present in the assailant or survivor; and 5) other characteristics of the assault, survivor, or assailant that might increase risk for HIV transmission.
If PEP is offered, the following information should be discussed with the patient: 1) the unproven benefit and known toxicities of antiretrovirals; 2) the close follow-up that will be necessary; 3) the benefit of adherence to recommended dosing; and 4) the necessity of early initiation of PEP to optimize potential benefits (as soon as possible after and up to 72 hours after the assault). Providers should emphasize that PEP appears to be well-tolerated in both adults and children and that severe adverse effects are rare. Clinical management of the survivor should be implemented according to the following guidelines (58). Specialist consultation on PEP regimens is recommended if HIV exposure during the assault was possible and if PEP is being considered. The sooner PEP is initiated after the exposure, the higher the likelihood that it will prevent HIV transmission, if HIV exposure occurred; however, distress after an assault also might prevent the survivor from accurately weighing exposure risks and benefits of PEP and making an informed decision to start PEP. If use of PEP is judged to be warranted, the survivor should be offered a 3-5-day supply of PEP with a follow-up visit scheduled for additional counseling after several days.
# Sexual Assault or Abuse of Children
Recommendations in this report are limited to the identification and treatment of STDs. Management of the psychosocial aspects of the sexual assault or abuse of children is beyond the scope of these recommendations.
The identification of sexually transmissible agents in children beyond the neonatal period suggests sexual abuse. The significance of the identification of a sexually transmitted agent in such children as evidence of possible child sexual abuse varies by pathogen. Postnatally acquired gonorrhea; syphilis; and nontransfusion, nonperinatally acquired HIV are usually diagnostic of sexual abuse. Sexual abuse should be suspected when genital herpes is diagnosed. The investigation of sexual abuse among children who possibly have an infection that might have been sexually transmitted should be conducted in compliance with recommendations by clinicians who have experience and training in all elements of the evaluation of child abuse, neglect, and assault. The social importance of infection that might have been acquired sexually and the recommended action regarding reporting of suspected child sexual abuse varies by the specific organism (Table 6). In all cases in which a sexually transmitted infection has been diagnosed in a child, efforts should be made to detect evidence of sexual abuse, including conducting diagnostic testing for other commonly occurring sexually transmitted infections (221).
The general rule that sexually transmissible infections beyond the neonatal period are evidence of sexual abuse has exceptions. For example, rectal or genital infection with C. trachomatis among young children might be the result of perinatally acquired infection and has, in some cases, persisted for as long as 2-3 years. Genital warts have been diagnosed in children who have been sexually abused, but also in children who have no other evidence of sexual abuse. BV has been diagnosed in children who have been abused, but its presence alone does not prove sexual abuse. The majority of HBV infections in children result from household exposure to persons who have chronic HBV infection.
The possibility of sexual abuse should be strongly considered if no conclusive explanation for nonsexual transmission of a sexually transmitted infection can be identified. When the only evidence of sexual abuse is the isolation of an organism or the detection of antibodies to a sexually transmissible agent, findings should be confirmed and the implications considered carefully.
# Evaluation for Sexually Transmitted Infections
Examinations of children for sexual assault or abuse should be conducted in a manner designed to minimize pain and trauma to the child. Collection of vaginal specimens in prepubertal children can be very uncomfortable and should be performed by an experienced clinician to avoid psychological § § § Assistance with postexposure prophylaxis decisions can be obtained by calling the National Clinician's Post-Exposure Prophylaxis Hotline (PEPLine), telephone: 888-448-4911. and physical trauma to the child. The decision to obtain genital or other specimens from a child to conduct an STD evaluation must be made on an individual basis. The following situations involve a high risk for STDs and constitute a strong indication for testing:
• The child has or has had symptoms or signs of an STD or of an infection that can be sexually transmitted, even in the absence of suspicion of sexual abuse. Among the signs that are associated with a confirmed STD diagnosis are vaginal discharge or pain, genital itching or odor, urinary symptoms, and genital ulcers or lesions. • A suspected assailant is known to have an STD or to be at high risk for STDs (e.g., has multiple sex partners or a history of STDs). • A sibling or another child or adult in the household or child's immediate environment has an STD. • The patient or parent requests testing.
• Evidence of genital, oral, or anal penetration or ejaculation is present. If a child has symptoms, signs, or evidence of an infection that might be sexually transmitted, the child should be tested for other common STDs before the initiation of any treatment that could interfere with the diagnosis of those other STDs. Because of the legal and psychosocial consequences of a false-positive diagnosis, only tests with high specificities should be used. The potential benefit to the child of a reliable diagnosis of an STD justifies deferring presumptive treatment until specimens for highly specific tests are obtained by providers with experience in the evaluation of sexually abused and assaulted children.
The scheduling of an examination should depend on the history of assault or abuse. If the initial exposure was recent, the infectious agents acquired through the exposure might not have produced sufficient concentrations of organisms to result in positive test results. A follow-up visit approximately 2 weeks after the most recent sexual exposure may include a repeat physical examination and collection of additional specimens. To allow sufficient time for antibodies to develop, another follow-up visit approximately 12 weeks after the most recent sexual exposure might be necessary to collect sera. A single examination might be sufficient if the child was abused for an extended period and if the last suspected episode of abuse occurred substantially before the child received medical evaluation.
The following recommendations for scheduling examinations serve as a general guide. The exact timing and nature of follow-up examinations should be determined on an individual basis and should be performed to minimize the possibility for psychological trauma and social stigma. Compliance with follow-up appointments might be improved when law enforcement personnel or child protective services are involved.
# Initial and 2-Week Follow-Up Examinations
During the initial examination and 2-week follow-up examination (if indicated), the following should be performed:
• Visual inspection of the genital, perianal, and oral areas for genital discharge, odor, bleeding, irritation, warts, and ulcerative lesions. The clinical manifestations of some STDs are different in children than in adults. For example, typical vesicular lesions might not be present in the presence of HSV infection. Because this infection is suspicious for sexual abuse, specimens should be obtained from all vesicular or ulcerative genital or perianal lesions compatible with genital herpes and then sent for viral culture. • Specimen collection for culture for N. gonorrhoeae from the pharynx and anus in both boys and girls, the vagina in girls, and the urethra in boys. Cervical specimens are not recommended for prepubertal girls. For boys with a urethral discharge, a meatal specimen discharge is an adequate substitute for an intraurethral swab specimen. Only standard culture systems for the isolation of N. gonorrhoeae should be used. All presumptive isolates of N. gonorrhoeae should be confirmed by at least two tests that involve different principles (i.e., biochemical, enzyme substrate, serologic, or nucleic acid hybridization test methods).
Isolates and specimens should be retained or preserved in case additional or repeated testing is needed. Gram stains are inadequate to evaluate prepubertal children for gonorrhea and should not be used to diagnose or exclude gonorrhea. • Cultures for C. trachomatis from specimens collected from the anus in both boys and girls and from the vagina in girls. Some data suggest that the likelihood of recovering C. trachomatis from the urethra of prepubertal boys is too low to justify the trauma involved in obtaining an intraurethral specimen. However, a meatal specimen should be obtained if urethral discharge is present. Pharyngeal specimens for C. trachomatis are not recommended for children of either sex because the yield is low, perinatally acquired infection might persist beyond infancy, and culture systems in some laboratories do not distinguish between C. trachomatis and C. pneumoniae. HIV infection has been reported in children whose only known risk factor was sexual abuse. Serologic testing for HIV infection should be considered for abused children. The decision to test for HIV infection should be made on a case-bycase basis, depending on the likelihood of infection among assailant(s). Data are insufficient concerning the efficacy and safety of PEP among both children and adults. However, antiretroviral treatment is well-tolerated by infants and children with and without HIV infection. In addition, children who receive such treatment have a minimal risk for serious adverse reactions because of the short period recommended for prophylaxis (58,62). In considering whether to offer antiretroviral PEP, health-care providers should consider whether the child can be treated soon after the sexual exposure (i.e., within 72 hours), the likelihood that the assailant is at risk for HIV infection, and the likelihood of high compliance with the prophylactic regimen. The potential benefit of treating a sexually abused child should be weighed against the risk for adverse reactions. If antiretroviral PEP is being considered, a professional specializing in HIV-infected children should be consulted.
# Recommendations for HIV-Related Postexposure Assessment of Children within 72 Hours of Sexual Assault
• Review HIV/AIDS local epidemiology and assess risk for HIV infection in the assailant.
• Evaluate circumstances of assault that might affect risk for HIV transmission. • Consult with a specialist in treating HIV-infected children if PEP is considered. • If the child appears to be at risk for HIV transmission from the assault, discuss PEP with the caregiver(s), including its toxicity and unknown efficacy. • If caregivers choose for the child to receive antiretroviral PEP (58,62,222), provide enough medication to last until the return visit at 3-7 days after the initial assessment, at which time the child should be reevaluated and tolerance of medication should be assessed; dosages should not exceed those for adults. • Perform HIV antibody test at original assessment, 6 weeks, 3 months, and 6 months.
# Follow-Up Examination After Assault
In circumstances in which transmission of syphilis, HIV, or hepatitis B is a concern but baseline tests are negative, an examination approximately 6 weeks, 3 months, and 6 months after the last suspected sexual exposure is recommended to allow time for antibodies to infectious agents to develop. In addition, results of HBsAg testing must be interpreted carefully, because HBV can be transmitted nonsexually. Decisions regarding which tests should be performed must be made on an individual basis.
# Presumptive Treatment
The risk of a child acquiring an STD as a result of sexual abuse or assault has not been well studied. Presumptive treatment for children who have been sexually assaulted or abused is not recommended because 1) the incidence of the majority of STDs in children is low after abuse/assault, 2) prepubertal girls appear to be at lower risk for ascending infection than adolescent or adult women, and 3) regular follow-up of children usually can be ensured. However, some children or their parent(s) or guardian(s) might be concerned about the possibility of infection with an STD, even if the risk is perceived to be low by the health-care provider. Such concerns might be an appropriate indication for presumptive treatment in some settings and may be considered after all specimens for diagnostic tests relevant to the investigation have been collected.
# Reporting
U.S. states and territories have laws that require the reporting of child abuse. Although the exact requirements differ by state, if a health-care provider has reasonable cause to suspect child abuse, a report must be made. Health-care providers should contact their state or local child-protection service agency regarding child-abuse reporting requirements in their states.
#
§ Pediatric formulation administered on a 3-dose schedule; higher doses might be more immunogenic, but no specific recommendations have been made. ¶ Not applicable. ** Adult formulation administered on a 2-dose schedule. † † Dialysis formulation administered on a 3-dose schedule at 0, 1, and 6 months. § § Two 1.0-mL doses of the adult formulation administered at one site on a 4-dose schedule at 0, 1, 2, and 6 months.
populations where the prevalence of infection is likely to be high (e.g., persons aged >40 years and persons born in areas of high HAV endemicity). The potential cost-savings of testing should be weighed against the cost and the likelihood that testing will interfere with initiating vaccination. Vaccination of a person who is already immune is not harmful.
# Postvaccination Serologic Testing
Postvaccination serologic testing is not indicated because the majority of persons respond to the vaccine. In addition, the commercially available serologic test is not sensitive enough to detect the low, but protective, levels of antibody produced by vaccination.
# Recommendations for Postexposure Assessment of Adolescent and Adult Survivors Within 72 hours of Sexual Assault § § §
• Assess risk for HIV infection in the assailant.
• Evaluate characteristics of the assault event that might increase risk for HIV transmission. • Consult with a specialist in HIV treatment, if PEP is being considered. • If the survivor appears to be at risk for HIV transmission from the assault, discuss antiretroviral prophylaxis, including toxicity and lack of proven benefit. • If the survivor chooses to start antiretroviral PEP (58), provide enough medication to last until the next return visit; reevaluate the survivor 3-7 days after initial assessment and assess tolerance of medications. • If PEP is started, perform CBC and serum chemistry at baseline (initiation of PEP should not be delayed, pending results). • Perform HIV antibody test at original assessment; repeat at 6 weeks, 3 months, and 6 months.
# Terms and Abbreviations Used in This Report
| None | None |
055b178ee2275005d93ff491f6b5e95e66c76339 | cdc | None | These policy guidelines for the prevention and control o f Chlamydia trachomatis infections were established after careful deliberation by a group of experts# and sta ff of the Centers for Disease Control (CDC) .' Commentary received after preliminary documents were circulated among a large group o f physicians was also considered Certain aspects o f these guidelines represent the best judgment o f experts. The guidelines should not be construed as rules, but rather as a source o f guidance within the United States. This is particularly true for topics that are based on limited data.# Background
Infections caused by Chlamydia trachomatis are now recognized as the most prevalent-and are among the most damaging -of all sexually transmitted diseases (STD) seen in the United States today (/). An estimated 3-4 million Americans suffer from a chlamydial infection each year (2). Men, women, and infants are affected, but women bear an inordinate burden because of their increased risk for adverse reproductive consequences. While C. trachomatis infection is currently not a reportable disease on a national level in the United States, data obtained from metropolitan STD clinics suggest sharp increases in inci dence in the period 1975-1983 (/). In England and Wales, where nongonococcal urethritis (about half the cases of which are caused by C. trachomatis) is a reportable disease, the inci dence has nearly doubled in the last decade ( 1).
Chlamydiae are unique microorganisms whose specific properties have been delineated largely in the last tw o decades. Although they are classified as bacteria, they share properties with viruses and bacteria. Like viruses, chlamydiae grow only intracellularly. For this reason, culture of Chlamydia has been difficult because expensive cell-culture methods similar to those used to recover viruses are required. Unlike viruses, however, chlamydiae contain both deoxyribonucleic acid (DNA) and ribonucleic acid (RNA), divide by binary fission, and have cell walls similar to those of gram-negative bacteria.
The wider availability of laboratory diagnostic tests for Chlamydia has opened the door to further exploration of the broad spectrum of disease caused by this organism C. trachomatis is now recognized as the causative agent for a diverse group of genital and neonatal infections, including many that were previously considered to be of unknown cause ( 1,3,4) (Table 1).
C. trachomatis causes approximately 50% of the reported cases of nongonococcal urethri tis (NGU) among men. This STD has an estimated incidence 2.5 times that of gonococcal urethritis ( 1 ). Chlamydia is also responsible for approximately 50% of the estimated 500,000 cases of acute epididymitis seen each year in the United States (2)
Even more important are chlamydial infections among women. Most of these infections are asymptomatic, but C. trachomatis also plays an important role in causing mucopurulent cervicitis (MPC) (5), acute pelvic inflammatory disease (PID) (6), and maternal and infant in fections during pregnancy and following delivery (7). Chlamydia accounts fo r one-quarter to one-half of the 1 million recognized cases of PID in the United States each year. These infec tions, in addition to C. trachomatis infections of the fallopian tube not clinically recognized as PID, contribute significantly to the increasing number of women who experience ectopic pregnancy or involuntary infertility. Besides its association with mucopurulent cervicitis and PID, Chlamydia plays an important role in the urethral syndrome (dysuria-pyuria syndrome) and in perihepatitis or Fitz-Hugh-Curtis syndrome ( 1,8).
Maternal infection during pregnancy has been associated with postpartum endometritis and in some studies with an increased perinatal mortality; the latter relationship requires fur ther study. Infants with infected mothers can acquire a chlamydial infection at birth from con tact with infected cervicovaginal secretions. Each year more than 155,000 infants are born to Chlamydia-infected mothers. These newborns are at high risk of developing inclusion con junctivitis and pneumonia and are at slightly elevated risk of having otitis media and bronchi olitis. In fact, Chlamydia is the most common cause of neonatal eye infections and of afebrile interstitial pneumonia in infants < 6 months of age.
Enormous cost is associated with chlamydial infections. Each year, more than $1 billion in direct and indirect costs are expended on these infections in the United States. Many of these Trachoma, the leading cause of preventable blindness in the world, is also caused by C h la m y d ia but has been excluded because it is not generally sexually transmitted, tA rrow indicates direction of transmission of infection.
Question mark indicates that a relationship has not been firm ly established.
Associated with lymphogranuloma venereum. costs result from the management of women with PID and its complications (9) and from the management of infants hospitalized with chlamydial pneumonia. This estimated cost does not reflect the human suffering experienced by those with chlamydial disease. Further growth in the economic burden of chlamydial infections will occur as these infections become more prevalent.
To reduce the morbidity and subsequent complications associated with C. trachomatis in fection in the United States, effective prevention and control strategies must be implemented. Comprehensive guidelines for the formulation of such control programs, as well as diagnostic and therapeutic approaches to infected individuals, are provided in this document. These policy guidelines were established after careful deliberation by an invited panel of experts in collaboration with staff of the Division of Sexually Transmitted Diseases, CDC.
# R isk A s s e s s m e n t
Establishing a profile fo r patients at increased risk of having a genital infection caused by C. trachomatis can be based on multiple criteria.
# Individual Characteristics and Practices
Age, number of sex partners, socioeconomic status, and sexual preference are predictors of C. trachomatis infection. Genital infection rates appear to be inversely related to age and posi tively correlated with number of sex partners. Sexually active women < 20 years of age have chlamydial infection rates 2-3 times higher than those for women ^ 20 years of age, and the rates for women ages 20-29 are considerably higher than those for women ^ 30 years of age (/, 10). Similarly, the rates of urethral infection among teenage males are higher than those for adults (11). Risk of infection increases with the number of sex partners (12,13).
In some studies, lower socioeconomic status and ethnicity have been correlated with an i creased risk of chlamydial infections (10-12). The prevalence of urethral chlamyd.al .nfect.on among homosexual men is approximately one-third the prevalence among heterosexual men (11,14), but 4%-8% of homosexual men seen in STD clinics have rectal chlamydial infection.
# Clinical Syndromes
Several clinical syndromes are associated with C. trachomatis infection. Some are more clearly defined than others, and their prevalence and manifestations differ depending on the population studied. Nevertheless, these conditions often provide the most suitable basis for initiating treatment, especially if complete bacteriologic evaluation is not possible or while the practitioner awaits the results of specific laboratory tests. However, it cannot be overempha sized that most women with cervical chlamydial infection, most homosexual men with rectal chlamydial infection, and as many as 30% of heterosexual men with chlamydial urethritis have few or no symptoms. These asymptomatic infections can sometimes be recognized by physical examination or by increased numbers of leukocytes on a Gram stain of infected secretions.
Three Chlamydia-associated syndromes- are common among women: (1) MPC, (2) ureth ral syndrome or urethritis, and (3) PID. C. trachomatis has been isolated from 30% to 50% of women examined who have mucopurulent endocervical exudate (5). Similarly, C. trachomatis *For a m ore com plete description o f syndromes, see section on Treatment Regimens, pages 65S-67S.
# 56S MM W R
A u g u st 23,1985 has been isolated from female patients with acute dysuria, particularly those with pyuria and a negative Gram stain of unspun urine (8). Among women with PID, the Chlamydia recovery rate is approximately 25%-50% with optimal technique, but serologic data suggest that as many as 50% of acute PID cases may be associated with C. trachomatis. Two Ch/amydia-assoc\aXe6 syndromes are common among men: nongonococcal urethritis (NGU) and acute epididymo-orchitis. C. trachomatis has been consistently isolated from up to 50% of men with NGU. Likewise, investigators have cultured C. trachomatis from 30% to 50% of patients with acute epididymitis and have demonstrated the organism to be the lead ing known cause of epididymitis among men < 35 years of age ( 1 ).
# Contact with an STD Patient
Individuals with a history of sexual exposure to persons with a chlamydial or gonococcal infection are themselves at high risk for chlamydial infection. Approximately 70% and 36%, re spectively, of female sex partners of men with confirmed chlamydial urethritis or confirmed gonococcal urethritis have Chlamydia isolated from the endocervical tract. Of all the women whose sex partners are reported to have NGU, 30%-40% harbor cervical chlamydial infection. Of men who are the sex partners of women with confirmed chlamydial MPC or PID, 25%-50% have Chlamydia isolated from the urethra. Many of these contacts are asymptomatic.
# Coexistence of Chlamydial Infection with Other STD
Approximately 1 5%-30% of heterosexual men with gonococcal urethritis have simultane ous urethral infection caused by C. trachomatis [1,15,16). An even higher proportion (25/o-50%) of women with Neisseria gonorrhoeae infection also have C. trachomatis infec tion of the cervix ( 1,15-1 7). Women who have other STD such as trichomoniasis and bacte rial vaginosis are also at increased risk of having chlamydial infection.
# Method of Contraception
Persons who use barrier methods of contraception (condom, diaphragm, diaphragm and foam) are at reduced risk for chlamydial infection relative to those who do not use any form of contraception (12). In contrast, women who use oral contraceptives have been reported to have a higher prevalence of cervical infection with C. trachomatis than women who do not use oral contraceptives ( 18). Use of intrauterine devices has not yet been investigated for its effect on rates of C. trachomatis infection.
# Pregnancy
In the United States, the prevalence of reported cervical chlamydial infection among preg nant women has varied from 2% to 37%, with most studies reporting infection rates of ap proximately 8%-12% (7 ,13,19). In general, infection has been most prevalent in the youngest age group; among unmarried women; and among inner-city, lower socioeconomic-status women.
# Health-Care Facility
Various types of health-care facilities will report different expected infection rates among women attendees. Not surprisingly, STD clinics report the highest rates of C. trachomatis in fection (an average of 20%-30% of all patients tested) (1,15). The next highest isolation rates are reported from clinics for adolescent patients (8%-26%) ( 13 ,2 0-23) and from family plan ning clinics (6%-23%) (10). Insufficient data are available to estimate expected rates in private practices, community health centers, and hospital emergency rooms.
# Lab o rato ry M etho d s
The absence of an inexpensive, simple, and reliable diagnostic test for chlamydial infection has limited control efforts. Historically, time-consuming and expensive tissue-culture tech niques have been required to definitively diagnose most C. trachomatis infections. Cytology was also available, but is only of comparable sensitivity to tissue culture in diagnosing new born conjunctivitis. In recent years antigen detection methods have offered a cost-effective al ternative to culture. Serologic methods are available, but remain principally a research tool.
Despite these encouraging improvements in diagnostic capability, current tests are not ideal. They are relatively difficult to perform, require considerable experience, and have limited application. Active investigation of new diagnostic methods for C. trachomatis continues, and antigen and antibody detection systems are improving rapidly. In such a dynamic environ ment, recommendations for the specific diagnostic methods discussed below must be flexible and should be revised as better methods become available.
# Culture
Tissue culture is presently the "gold standard" for laboratory diagnosis. Although pub lished methods are fairly standard (4), in practice many laboratories introduce variations that alter the sensitivity and specificity of the test. Rigorous adherence to standard methodology is strongly encouraged.
Two major components are needed to culture for C. trachomatis: (1) a cell-culture system * " t i -II lin o r \ f r h n i r o ic and (2) a method to identify inclusions growing in cell culture. The cell line of choice is
u ih j \*_/ a i i i c t i i u u tu 1U 0 111117 ,, ------ v , _ _ 1 1 ,, _,,
McCoy. Alternatively, a particular strain of HeLa cells (HeLa 229)
) can e us ally restricted to research laboratories. Specimen material is centnfuged o ,^2 5 H n cu ttio n 1 hour and then incubated for 2-3 days in medium containing cycloh«jm de can take place in individual vials with cover slips at their ase- °r ^ dictated by the plastic microtiter plates (26). The choice between t ese slightly more sensitive number of specimens a laboratory has to process; the vial ^e,hod2 S'^n 7 exDenslve and less susceptible to cross-contamination, but is more time consu usually used FA For identification, either iodine stain or fluorescent antibody (FA) sta.n " ' " £^, 2 stain offers the advantages of higher sensitivity and shorter processing i res'one requires a fluorescence microscope. The standard method for 10 ine s ainin blind passage, which increases the processing time to 4-6 days. In microtiter p a es' s ® ing without passage appears equivalent to iodine staining with one blind passage e most sensitive culture method currently available involves using cycloheximide treated McCoy cells in vials in the presence of fluorescent monoclonal antibodies.
Compared with other diagnostic tests for C. trachomatis, the major advantage of tissue culture is its specificity. With this method, the organism can also be positively identified or saved for other marker studies such as immunotyping. Thus, culture is clearly the method of choice for research studies. Determining the sensitivity and specificity of the culture has not been possible since it is the reference standard for other methods; however, it is estimated that culture has a sensitivity of 80%-90%, and a specificity of 100% (28).
Culture also has several disadvantages: (1) the cost and complexity of laboratory require ments can be prohibitive; (2) specimens can be kept at 4 C for only up to 24 hours (preferably 12) before processing, or frozen at -70 C if they cannot be inoculated within 24 hours;
(3) specimens must be placed in specially prepared transport media; and (4) the cell monolay er may be contaminated with other bacteria or viruses, particularly in vaginal or rectal specimens.
# 58S
# MMWR
A u g u s t 23, 1985
# Cytologic Methods
Cytologic identification of chlamydial infections-the only method available in the period 1909-1957-is an examination of epithelial cell scrapings (e.g., conjunctival, cervical, ureth ral) on a stained smear. A modified Giemsa stain is most often used, although W right's and other standard tissue stains can be used. Infection is identified by visualizing characteristic intracytoplasmic inclusions. Alternatively, cell scrapings can be examined using FA stains (4).
The advantage of cytologic examination is clearly the simplicity of the process, particularly if light microscopy is used. The disadvantage is the poor sensitivity fo r diagnosing chlamydial infections other than neonatal conjunctivitis, for which the sensitivity of cytology compared with culture is 95%. The sensitivity of cytologic methods in identifying chlamydial adult con junctivitis is 45% for Giemsa and 85% for FA. In tests for cervical infection, the tw o stains have sensitivities of only 40% and 65%, respectively, and for urethral infection, 15% and 60% (28). Moreover, these upper levels of sensitivity can only be obtained with good specimens (many epithelial cells) and an experienced observer.
Thus, standard cytology is of little practical value as a diagnostic aid fo r genital chlamydial infection. However, tw o recent studies (29,30) suggest that the inflammatory pattern on Papanicolaou-stained cervical smears may be useful when it is used as a screening test to select patients for confirmation of infection by culture or monoclonal antibody tests, but the Papanicolaou method used alone is not satisfactory for diagnosing chlamydial infection.
# Antigen Detection
To date, two methods of antigen detection are available: (1) FA examination of a direct smear and (2) enzyme immunoassay (EIA). One example of each method is presently available commercially,- and both have undergone considerable evaluation.
However, continued revision of these tests takes place even after they become available commercially. Consequently, initial published data on efficacy may be outdated, so the most recent references should be used. Other antigen detection tests are expected to be available soon.
D irect-Sm ear FA Test (31) With this procedure, specimen material is obtained by swab and applied directly to a slide, which is fixed and then incubated with fluorescein-conjugated monoclonal antibody before being examined under a fluorescence microscope. Total processing time is usually 3 0 -4 0 min utes. Critical steps include (1) obtaining a satisfactory specimen and preparing a satisfactory smear (this can be checked before or after staining), (2) drying the specimen properly before fixing it, (3) using a high-quality fluorescence microscope, and (4) obtaining and maintaining an experienced microscopist who can recognize elementary bodies and artifacts.
Compared with culture, the sensitivity of the direct smear test is ^ 90% in most published studies, and the specificity is ^ 98%. The positive predictive value of this test has ranged from approximately 80% in populations with a Chlamydia prevalence of 10% to 95% in popu lations with a prevalence of 30% (32). Lower sensitivities and specificities are often encoun tered in situations in which specimens are less than optimal or individuals reading the slides are relatively inexperienced. In these instances, assessment of the proficiency of laboratory techniques is essential. This can be accomplished by comparing results with those obtained with tissue culture or by exchanging slides with a central reference laboratory that does proficiency testing. K
The major advantages of the direct smear test are (1) the uncomplicated transport and storage of specimens, (2) rapid processing time compared with that required for other meth ods (33), (3) a high specificity, and (4) the ability to check on adequacy of specimen collec tion (i.e., cells on the slide). Disadvantages of the method are (1) the requirement for precise specimen collection, (2) the need for high-quality fluorescence microscope equipment, (3) the need for an experienced microscopist, and (4) the relatively labor-intensive nature of the process.
# Enzym e Im m un o a ssa y (34)
This test measures antigen-antibody reactions through an enzyme-linked immunoabsorbent assay (ELISA) and requires a spectrophotometer. Processing time for specimens is ap proximately 4 hours.
Questions continue to be raised about the reliability of available ElAs for C. trachomatis. The sensitivity of the test has varied from 67% to 90%, the specificity from 92% to 97%, and the positive predictive value from 32% to 87%, depending on the population studied (35). Much of the observed disparity has been attributed to variable sensitivity of the tissue culture systems against which the EIA has been compared.
The advantages of the EIA are (1) the uncomplicated transport and storage of specimens, (2) the objective method of measurement in the laboratory, which involves standard equip ment and does not depend upon a specially trained observer, and (3) the ability to test large numbers of specimens at a time.
The disadvantages are that (1) the adequacy of the specimen cannot be checked and ( 2) th e test cannot be performed while the patient is waiting (although this is also true for the dir smear test if no fluorescence microscope is available).
It is not known whether either method of antigen detection can be use or specime sites other than the eyes and genitals (e.g., pharynx).
# Serology
Currently, Chlamydia serology has little value in routine clinical management and basically remains a research tool. Although some serologic tests are commercially available, they have not been shown to be useful in routine diagnosis.
There are tw o standard methods-complement fixation and microimmunofluorescence (MIF) (35). ELISA tests have been developed, but none are recommended for wide use (36,37). The only valid clinical uses of serologic tests are in infant pneumonia, where specific immunoglobulin M (IgM) MIF serology, when available, is the diagnostic test of choice; and in occasional cases of suspected lymphogranuloma venereum (LGV). The difficulties in prepar ing the antigen and conducting the test restrict the use of the test to a limited number of re search laboratories.
# Diagnostic Considerations
The value of rapid diagnostic tests for detecting C. trachomatis infection depends primari-V on the prevalence of disease in the population tested and the availability of other tests For ow-r.sk groups, the predictive value of a positive test is lower than for high-prevalence popu lations, even if the test is highly sensitive and specific. For example, in a population with a 5% 60S MMWR A u g u st 23,1985 prevalence, a rapid test with a 95% specificity and sensitivity will have a predictive value posi tive of 50% (meaning that there is only a 50% chance that an individual who is diagnosed as having disease actually has it). In situations in which an increase in the predictive value of a positive test is desired, in order to lower risks of incorrectly labeling persons as having STD, positive screening tests can be confirmed by culture, or culture methods can be used for screening (with an accompanying rise in cost). As new tests become available, physicians, hospital and commercial laboratorians, and public health program directors must be aware of the sensitivity, specificity, and predictive value of such tests when determining whether to use them in specific situations.
As more laboratories begin to do diagnostic testing for Chlamydia, laboratory quality con trol assumes increasing importance. Each laboratory should verify the accuracy of test meth ods other than culture by periodically comparing results with those obtained using cultures. Such comparisons are particularly important when the laboratory implements a new test method. Laboratories that do cell-culture isolation of Chlamydia should run appropriate posi tive and negative controls to verify sensitivity of the cell cultures being used and should peri odically evaluate the effectiveness of transport systems. Regional reference laboratories should be established for verification of culture results or evaluation of unexpected or discrep ant results. Proficiency testing programs should be developed for culture and other test meth ods so that laboratories can evaluate their methods using unknown specimens.
# Patient Management H igh-Risk Groups
High-risk groups should be defined using demographic profiles and the estimated or estab lished prevalence of chlamydial infection in a particular community or patient population. Al though the criteria described under Risk Assessment can be used as a guide to establishing a high-risk profile, local determinants of risk are more precise and should be identified if possi ble. Local data also provide more accurate baseline prevalences, against which the success of prevention and control strategies can be measured.
When culture results are available, they should be used in decisions concerning appropriate therapy. However, undiagnosed patients who fit an established high-risk profile should also be offered treatment, unless local or individual circumstances dictate otherwise. Patients in the following groups should immediately receive a regimen that includes effective treatment against C. trachomatis infection.
# Symptomatic Syndromes Associated with Chlamydia
# Asymptomatic Contacts of Syndromes Associated with Chlamydia
Individuals exposed through sexual contact with patients who have any of the above symptomatic syndromes (within 30 days of the onset of their symptoms or clinical evaluation) should be evaluated for STD and treated for presumptive chlamydial infection.
# Gonococcal Infection
Women with confirmed N. gonorrhoeae infection of the endocervix, heterosexual men with diagnosed gonococcal infection of the urethra, and sex partners of members of both of these groups of patients should be treated with an antimicrobial regimen that is effective against both N. gonorrhoeae and C. trachomatis infection.
# Screening
Selective screening to detect asymptomatic infection is an essential component of a suc cessful control program. Whenever possible, criteria for routine screening should be based on local determinants of risk. An appropriate diagnostic method must be selected. Diagnostic considerations for current tests/methods are discussed above. The following guidelines are provided to assist in determining which test to use.
# Screening Criteria
_ . A .. .
No single individual characteristic or practice (see p. 55S), is in itself a su icien cri erion to define which persons should be screened. However, a composite of in i v i ua a c °rs _ conjunction with a community factor such as type of health-care aci ity see ' help to maximize yield from screening. Consequently, available evidence ea s o mendation that the priorities for routine screening shown below be used.
# STD Clinic
1. Individuals attending STD clinics who otherwise would not be offered antichlamydial treatment should be screened first. (The screening of asymptomatic, high-risk women should be accorded the highest priority. In general, the screening of heterosexual men should have a higher priority than screening homosexual men.) 2. Individuals with symptomatic syndromes associated with Chlamydia should be screened next. (Screening of women should be accorded higher priority than screening of men.)
# Oth er High -Risk Health -Care Faci/it y
Health-care facilities other than STD clinics may also have a high prevalence of chlamydial infections. In particular, many adolescent and family planning clinics are categorized as highrisk centers, but a wide disparity in rates of chlamydial infection may be observed in different populations." Facilities that serve high-risk populations should follow the order of screening priority for STD clinics above; those serving undetermined or low-risk populations should follow the priority below for Undetermined/Low-Risk Health-Care Facility.
Undetermined/Low-Risk Health-Care Facility 1. Persons in urban settings who are younger, have lower socioeconomic status, and have multiple sex partners, and who otherwise would not be offered antichlamydial treatment, should be screened first. (In this category of high-risk patients, women should be accorded highest priority for screening.) 2. Individuals with symptomatic syndromes associated with Chlamydia should also be screened. (Screening of women should be accorded higher priority than screening of men.)
# Diagnostic Method
Culture and two different antigen detection tests are currently the only diagnostic methods acceptable for screening for Chlamydia infection. Culture remains the most accurate method, but is costly and takes at least 2-3 days before results are available. Antigen detection tests have emerged as reasonable alternatives, but questions remain about their reliability for lowprevalence populations. Following are guidelines fo r the use of diagnostic tests in screening.
1 Culture, based upon availability, is the preferred method for routine screening. 2. Direct smear using fluorescent antibody (DFA) is the most thoroughly evaluated alterna tive to culture. However, optimal results with the currently marketed test have been achieved for high-risk women and symptomatic men by very experienced research laboratories. For other populations, test results obtained by less experienced technolo gists may not be as reliable. Consequently, DFA results should be compared periodically with those obtained through culturing. 3. Enzyme immunoassays have not been as completely evaluated as the DFA tests. The currently marketed test probably is less sensitive and specific than DFA, but the quality of results is also less likely to depend on the level of experience of laboratory personnel.
It is important that regional reference laboratories be available to monitor the perfor mance of these and other new antigen detection tests and to advise about appropriate applications and quality control problems.
# Recommendation
Screening is suggested at th e firs t p renatal visit fo r th e fo llo w in g g ro u p s o f pregnant w o m e n :
1. Adolescents (< 20 years of age)
MMWR 63S
2. Unmarried women 3. Married women who may be at high risk because of multiple sex partners or a history of other STD Screening of pregnant women who fall into any of these high-risk categories in inner-city hospitals is particularly important because of the high prevalence of asymptomatic infections among the patients served by these facilities.
# Neonates
# Ophthalmia Prophylaxis
None of the presently recommended approaches for prophylaxis against gonococcal and chlamydial ophthalmia neonatorum is completely effective. Silver nitrate is effective in prevent ing gonococcal infections but does not prevent chlamydial disease and frequently causes chemical conjunctivitis. Erythromycin is effective in preventing both gonococcal and chlamy dial ophthalmia and does not cause chemical conjunctivitis, but the topical use of this drug does not prevent nasopharyngeal chlamydial infection or pneumonia. Furthermore, eryth romycin prophylaxis is considerably more expensive than silver nitrate prophylaxis. Tetracy cline ointment has not been as extensively evaluated as has erythromycin but appears to be as effective. Whichever type of prophylaxis is used should be implemented no later than 1 hour after birth -preferably immediately after delivery since delayed application may reduce efficacy.
# Recommendation
Erythromycin (0.5%) ophthalmic ointment, tetracycline (1%) ointment, or silver nitrate should be instilled into the eyes of all neonates as soon as possible after delivery and never later than 1 hour after birth. Single-use tubes or ampules are preferable to multiple-use tubes.
# Neonatal Infection
Eighteen to fifty percent of infants born to infected mothers will have conjunctivitis be tween 1 and 3 weeks after birth (7). The symptoms are often mild, and the disease may be missed unless looked for carefully. Though considerable morbidity results acutely from the severe form of this disease, it is self-limited and does not appear to result in loss of vision. Three to eighteen percent of infants born to infected mothers will develop chlamydial pneumonia/bronchiolitis, usually at 1 -4 months of age (7). In most cases this is a mild disease, but it can be severe and require hospitalization.
# Recommendation
Screening for neonatal infection is not indicated. Newborns with conjunctivitis and afebrile pneumonia/bronchiolitis should have specimens culture-tested for C. trachomatis and be appropriately treated as recommended below. If cultures are positive, mothers (and their sex partners) of the infected children should also be treated.
# 64S
# MMWR
A u g u st 23,1985 Treatment Regimens
# CONFIRMED INFECTIONS
# Uncomplicated Urethral, Endocervical, or Rectal Infection in Adults
# Drug Regimens of Choice
Tetracycline hydrochloride (HCI): 500 mg, by mouth, 4 times a day fo r 7 days.
# OR
Doxycycline hyclate: 100 mg, by mouth, 2 times a day for 7 days.
# Alternative Regimens
(for patients for whom tetracyclines are contraindicated or not tolerated) Erythromycin base or stearate: 500 mg, by mouth, 4 times a day fo r 7 days, or eryth romycin ethyl succinate: 800 mg, by mouth, 4 times a day for 7 days.
Sulfonamides are also active against C. trachomatis. Although optimal dosages of sulfona mides for chlamydial infection have not been defined, sulfamethoxazole, 1 g by mouth, twice a day for 10 days, is probably effective.
# Follow-Up
When taken as directed, the tetracycline and erythromycin regimens listed above are highly effective (> 95% cure rates). No tetracycline-resistant Chlamydia has been described. Post-treatment cultures are not advisable if laboratory resources are limited. A positive p o s t treatment culture is more likely to represent noncompliance with treatment, failure to trea t sex partners, or laboratory error than resistance to the antibiotic. Patients who do have posi tive post-treatment cultures should be treated again according to one of the above regim ens.
# Management of Sex Partners
All persons sexually exposed to C. trachomatis infection (within 30 days after their sex partner develops symptoms or has a positive clinical evaluation) should be examined for STD and promptly treated for C. trachomatis with one of the above regimens. This group includes sex partners of individuals with sexually acquired chlamydial infection, mothers of infected newborns, and the sex partners of these mothers.
# Urogenital Infections during Pregnancy
# Drug Regimen of Choice
Erythromycin base: 500 mg, by mouth, 4 times a day for 7 days, or erythromycin ethyl succinate: 800 mg, by mouth, 4 times a day for 7 days.
Erythromycin stearate in appropriate doses may also be effective, but has not been ade quately studied.
# MMWR
# 65S
# Alternative Regimen
(for female patients who cannot tolerate the above regimen, a decreased daily dose is recommended) Erythromycin base: 250 mg, by mouth, 4 times a day for 14 days.
The optimal dose and duration of antibiotic therapy for pregnant women have not been es tablished. Currently, there are no completely acceptable alternative regimens for female pa tients who are allergic to erythromycin or otherwise cannot tolerate erythromycin. In the case of proven treatment failure, the patient should be re-treated with erythromycin according to either of the dosage schedules outlined above.
# Established Conjunctivitis of the Newborn*
# Drug Regimen of Choice
Oral erythromycin syrup: 50 mg/kg body weight/day in 4 divided doses for 14 days.
There is no indication that topical therapy provides additional benefit. If inclusion conjunc tivitis recurs after therapy, erythromycin treatment should be reinstituted for an additional 1 -2 weeks.
# Pneumonia among Infants
# Drug Regimen of Choice
Oral erythromycin syrup: 50 mg/kg/day in 4 divided doses for 14 days.
# CHLAM
# YDIA-ASSOCIATED SYNDROM ES
# Nongonococcal Urethritis
NGU can be diagnosed for a male patient if tests for N. gonorrhoeae are negative and the patient has objective evidence of urethritis. Objective evidence of urethritis includes a visibly abnormal discharge, pyuria defined as > 10 polymorphonuclear leukocytes (PMN) per high dry field in the sediment of a first-voided urine specimen, or > 4 PMN per oil immersion field in a Gram-stained urethral smear. Approximately 50% of the cases of urethritis not associated with N. gonorrhoeae are caused by C. trachomatis. NGU requires prompt antimicrobial treat ment of the patient and evaluation and treatment of any sex partners.
# Drug Regimens of Choice
Tetracycline HCI: 500 mg, by mouth, 4 times a day for 7 days. Alternative Regimen (for patients for whom tetracyclines are contraindicated or not tolerated) Erythromycin base or stearate: 500 mg, by mouth, 4 times a day fo r 7 days, or eryth romycin ethyl succinate: 800 mg, by mouth, 4 times a day for 7 days.
Sulfonamides are not suitable for treatment fo r clinical syndromes when Chlamydia cul tures are not performed, since they may not be effective against Ureap/asma urea/yticum and other organisms that cause nonchlamydial genital infection.
# Management of Sex Partners
All persons who are sex partners of patients with NGU (within last 30 days) should be examined for STD and treated promptly with one of the above regimens.
# Follow-Up
Patients should be advised to return for follow-up medical care if symptoms persist or recur.
# Mucopurulent Cervicitis*
The presence of mucopurulent endocervical exudate often reflects cervicitis due to chlamydial and/or gonococcal infection. If N. gonorrhoeae is found on Gram stain or culture of endocervical or urethral discharge, a treatment regimen effective against both gonococcal and chlamydial infection should be used. When only chlamydial infection is proven or suspect ed, therapy should consist of one of the regimens below.
# Drug Regimens of Choice
Tetracycline HCI: 500 mg, by mouth, 4 times a day for 7 days.
OR Doxycycline: 100 mg, by mouth, twice a day for 7 days.
# Alternative Regimens
(for patients for whom tetracyclines are contraindicated or not tolerated) Erythromycin base or stearate: 500 mg, by mouth, 4 times a day fo r 7 days, or eryth romycin ethyl succinate: 800 mg, by mouth, 4 times a day for 7 days.
# Management of Sex Partners
Men exposed to women with MPC attributed to chlamydial infection should be evaluated for STD and treated with one of the above regimens. If N. gonorrhoeae is found, treatment should be with a regimen effective against uncomplicated gonococcal and chlamydial infection.
-Criteria for presumptive diagnosis include (1) m u c o p u ru le n t s e c re tio n from the endocervix, which is usually yellow or green when viewed on a white cotton-tipped swab (positive swab test); (2) ^ 10 p o ly m orp h o n ucle a r le u k o c y te s per microscopic oil immersion field (X 1,000) in a Gram-stained smear of en docervical secretions; and (3) c e rv ic itis , determined by cervical friability (bleeding when the first swab culture is taken) and/or by erythema or edema within a zone of cervical ectopy. Acute PID refers to the acute clinical syndrome attributed to the ascending spread of mi croorganisms, unrelated to pregnancy or surgery, from the vagina and endocervix to the endo metrium, fallopian tubes, and/or contiguous structures. Clinical findings for most patients with PID include lower abdominal tenderness, adnexal tenderness, and pain induced by lateral motion of the uterine cervix. Many cases of PID are caused by more than one organism. Causative agents include C. trachomatis, N. g o n anaerobic bac oides and gram-positive cocci), and facultative gram-negative rods (such as Actinom yces israelii, and Mycoplasma horn inis.
These agents cannot usually be differentiated in individual patients. Consequently, treat ment regimens should be used that are active against the broadest range of the pathogens. CDC has already published comprehensive guidelines regarding criteria for hospitalization, rationale for selection of antimicrobials, and general treatment regimens for the major patho gens associated with PID (39): Below are examples of specific combinations of regimens for optimal coverage for C. trachomatis and for adequate coverage for the other common causa tive agents.
# Inpatient Treatment
Doxycycline: 100 g, intravenous (IV), 2 times a day.
# PLUS
Cefoxitin: 2.0 g, IV, 4 times a day. Continue drugs IV for at least 4 days and at least 48 hoursa*®r^a p T - C°nt'nUe doxycycline 100 mg, by mouth, 2 times a day, to complete 10-V
# Ambulatory Treatment
Cefoxitin: 2.0 g, intramuscular (IM), OR amoxicillin: 3.0 g, by mouth, OR ar"P 3.5 g, by mouth, OR aqueous procaine penicillin G: 4.8 million units, IM, at 2 sites (eac along with probenecid: 1.0 g, by mouth), OR ceftriaxone: 250 mg, IM FOLLOWED BY Doxycycline: 100 mg, by mouth, 2 times a day for 10-14 days.
Tetracycline HCI 500 mg, by mouth, 4 times a day, can also be used, but is less active against certain anaerobes and requires more frequent doses; both factors represent draw backs in treatment of PID.
# Management o f Sex Partners
All persons who are sex partners of patients with PID (within the 30 days prior to onset of their symptoms or positive clinical evaluation) should be examined for STD and treated promptly with a regimen effective against uncomplicated gonococcal and chlamydial infection.
A CDC update of these Guidelines is in press.
# 68S
# MMWR
A u g u st 23, 1985
# Follow-Up
All patients treated as outpatients should be clinically reevaluated in 4 8 -7 2 hours. Those not responding favorably should be hospitalized. Patients should also be reevaluated after they complete treatment.
# Intrauterine Device
The intrauterine device (IUD) is a risk factor for the development of PID. Although the exact effect removing an IUD has on the response of acute salpingitis to antimicrobial therapy and on the risk of recurrent salpingitis is unknown, it is recommended that the IUD be removed as soon as possible after antimicrobial therapy has been initiated. When an IUD is removed, contraceptive counseling is necessary.
# Acute Epididymo-Orchitis
Acute epididymo-orchitis has two forms: (1) a sexually transmitted form usually associat ed with urethritis and commonly caused by C. trachomatis and/or N. gonorrhoeae and (2) a nonsexually transmitted form associated with urinary tract infections caused by Enterobacteriaceae or other nonsexually transmitted uropathogens. Urine should be examined by Gram stain and culture to exclude bacteruria in all patients, including those with urethritis. An impor tant part of the differential diagnoses is testicular torsion, a surgical emergency.
Sexually transmitted epididymo-orchitis usually affects young adults and is associated with presence of clinical or subclinical urethritis, absence of underlying genitourinary patholo gy, and absence of gram-negative rods on Gram stain of urine.
# Drug Regimens of Choice
Amoxicillin: 3.0 g, by mouth, OR ampicillin: 3.5 g, by mouth, OR aqueous procaine peni cillin G: 4.8 million units, IM at 2 sites (each along with probenicid. 1.0 g, by mouth), OR spectinomycin: 2.0 g, IM, OR ceftriaxone: 250 mg, IM
# FOLLOWED B Y
Tetracycline HCI: 500 mg, by mouth, 4 times a day for 10 days.
# OR
Doxycycline: 100 mg, by mouth, 2 times a day for 10 days.
# Alternative Regimens
(for patients for whom tetracyclines are contraindicated or not tolerated) Erythromycin base or stearate: 500 mg, by mouth, 4 times a day fo r 7 days, or eryth romycin ethyl succinate . 800 mg, by mouth, 4 times a day for 7 days.
# Management of Sex Partners
Sex partners of patients with sexually transmitted acute epididymo-orchitis (diagnosed within 30 days of exposure) should be examined for STD and promptly treated with a regimen effective against uncomplicated gonococcal and chlamydial infection.
# MMWR
# 69S
# Fo llow -U p
Failure to improve within 3 days requires reevaluation of diagnosis/therapy and considera tion fo r hospitalization.
# Patient Education
# Patient Counseling
The effective management of chlamydial infection includes counseling of patients. Such counseling should be designed to influence specific behavior that will contribute to successful therapy, disease intervention, and prevention. Patient handouts designed for easy comprehen sion are an efficient way of conveying basic information. These messages should be rein forced by practitioners through discussions with patients that are tailored to the individual and provide an opportunity for questions.
# Recommendation
Practitioners should provide counseling to patients regarding their disease, its treatment, and the overall responsibility of the patient in the process. Information conveyed to patients should at least include:
1 Instructions for taking medication, including the dosage, timing, and length of the regimen. Patients must clearly understand that they must continue to take medication according to schedule, despite abatement of symp toms. 2. Advice regarding follow-up for side effects or other difficulty with medica tion, continued or worsened symptoms, and test of cure, if indicated. Suggestion to abstain from sexual activity until medication is completed by both patient and partner. If this is not possible, patients should be en couraged to use condoms until treatment is completed. Suggestion to cease sexual activity immediately if the same or other STD symptoms recur, and to return to the practitioner/clinic with the steady sex partner. 5. Suggestion to regularly use barrier methods, particularly condoms, to pre vent chlamydial infection and other STD.
# Sex Partner Referral
The sex partners of patients with chlamydial infection should be referred for medical care through the efforts of individual patients, or through a disease intervention specialist (DIS) Al though the latter process is time-consuming, it may be very effective. However, locating and referring sex partners through a DIS is clearly not feasible for all patients with chlamydial in fection and the C/?/aA7?yc//3-associated syndromes discussed above. First priority for interviewing/counseling efforts by a DIS should be given to patients with proven chlamydial infection. The contract method of sex partner referral should be used, with the patient assuming referral responsibility whenever possible. The referral of sex partners by the patient is a more practical approach in terms of human resources, but the effectiveness of this practice has not been evaluated among Chlamydia patients. Nevertheless, attempts must be made to capitalize on patients' knowledge of and persuasiveness with their own sex partners.
# Recommendation
Patients with chlamydial infection should be encouraged to refer all persons with whom they had sexual encounters in the 30 days prior to onset of their symptoms or clinical evaluation. (Approximately 94% of sex partners to NGU pa tients brought to treatment have been exposed within 30 days.)
# Prevention
Of all possible Chlamydia control approaches, successfully preventing the initial infection remains the most effective. Education of the public and of health professionals is essential for prevention at all three levels (primary, secondary, tertiary), especially in the absence of an ef fective vaccine.
# Professional Training/Education
Providers of health care can play a leading role in reducing the incidence of C. trachomatis infection and its complications. Timely diagnosis and appropriate treatment of chlamydial in fection by practitioners will prevent further transmission and minimize the risk that the infect ed individual will have adverse consequences. Additionally, clinicians are in a position to in fluence a patient to avoid behavior likely to result in transmitting disease or in being reinfected. STD education for health-care professionals should promote the following:
1 Recognizing Ch/amydia-assoc\aXe6 syndromes and high-risk patients. 2. Following recommended STD treatment guidelines. 3. Reporting cases promptly and completely. 4. Counseling patients to refer all sex partners for medical evaluation, to take all medica tion as prescribed, and to modify their behavior so as to reduce the risk of future infection.
# Recommendation
1. Professional recognition should be enhanced by incorporating knowledge about chlamydial infection into education and training programs fo r physi cians, nurses, laboratory personnel, and allied health professionals (such as physician assistants). 2. Organizations for health professionals, academic centers, colleges, and societies should be encouraged to formally support the chlamydial preven tion and control efforts by (a) providing appropriate continuing medical/ professional education courses about chlamydial infections at national/regional/local meetings and (b) encouraging health-professional journalsespecially official organizational p u b lications-to publish chlamydial policy guidelines and clinical reviews and research papers on Chlamydia and as sociated infections.
# MMWR
# 71S
Public Education/Health Promotion Education of the public is necessary to provide a high level of awareness of chlamydial in fections (and other STD) and to influence people to know and communicate about the preven tion, recognition, and treatment for Chlamydia; to support control efforts; and to reduce their personal risk of acquiring or transmitting a chlamydial infection. Accumulating evidence sug gests that public education can influence individuals to reduce their risk of acquiring an STD by changing sexual practices.
One such practice that should be encouraged is the use of barrier methods of contracep tion. Barrier methods of contraception (condoms and diaphragms) are known to provide pro tection against Chlamydia infection and other STD when used properly. The effectiveness of spermicides in preventing Chlamydia infection has not been determined. However, spermi cides do not enhance infection and do achieve some measure of protection when used in con junction with a diaphragm or condom.
# Recommendation
Disseminate the following information to the public: 1. Risks of chlamydial infection associated with sexual activity, especially when multiple partners are involved. 2. Role of barrier methods of contraception for personal prophylaxis to pre vent chlamydial infection and other STD.
# Surveillance
A fundamental requisite for control and prevention of chlamydial infection is a national sur veillance system, since it provides quantitative estimates of incidence and prevalence, a basis for determining secular trends, and a tool for evaluating control efforts. Current methods for diagnosis now permit the establishment of a multitiered, multifocal disease surveillance system. The tiers are local, state, and national. The foci include subgroups at special risk, clini cal syndromes of particular importance, and the general population.
A national surveillance system will require state reporting laws and/or regulations to pro vide the necessary support for prevention activities. Reporting laws promote and legitimize the involvement of public health authorities in assuring adequate individual patient management-including referral of sex partners-and may facilitate other activities such as screening and education. Moreover, case reporting provides a uniform basis for describing the extent and trpnH nf Hicoaco
# 72S
# MMWR
A u g u st 23,1985 Prevention and control activities for chlamydial infections have been proposed in this document, although the inadequacies in current diagnostic methods are acknowledged. In particular, patient management, including sex partner referral, is recommended for selected C h la m y d ia -associated clinical diagnoses (not dependent on the results of a laboratory test for C h la m y d ia ). Similarly, case reporting should include selected clinically diagnosed conditions associated with C h la m y d ia infection in addition to laboratory-diagnosed C h la m y d ia infection. Pending development of nationwide laboratory capability for identifying C h la m y d ia , condi tions should be selected that will best serve as indices fo r chlamydial infection, and that repre sent important public health problems in their own right. Reporting of clinically diagnosed conditions should augment rather than replace reporting of laboratory-diagnosed problems, since continuing efforts to develop a national laboratory capability will greatly enhance oppor tunities for ongoing improvements in patient management and public health interventions.
Although a national surveillance system should be based on case reporting, additional ap proaches, involving classical statistical methods, should be utilized, at least at the national level, to provide extent and trend estimates less vulnerable to the biases inherent in estimates based on case reports.
# Recommendation
#No absolute criteria exist for defining the clinical syndromes of NGU and PID/AS, but a constellation of signs and symptoms may be suggestive. For NGU, these include a patient with dysuria, white cells on Gram stain of urethral smears, and/or frank urethral discharge, in the presence of negative tests for gonorrhea. PID/AS is more protean in its manifestations, and the diagnosis ultimately rests on the judg ment of the attending clinician. Usual features include a combination of (1) lower abdominal pain, (2) adnexal tenderness, (3) adnexal mass, (4) pain on cervical motion, (5) mucopurulent discharge, and (6) temperature elevation. No single combination is pathognomonic. | These policy guidelines for the prevention and control o f Chlamydia trachomatis infections were established after careful deliberation by a group of experts# and sta ff of the Centers for Disease Control (CDC) .' Commentary received after preliminary documents were circulated among a large group o f physicians was also considered Certain aspects o f these guidelines represent the best judgment o f experts. The guidelines should not be construed as rules, but rather as a source o f guidance within the United States. This is particularly true for topics that are based on limited data.# Background
Infections caused by Chlamydia trachomatis are now recognized as the most prevalent-and are among the most damaging -of all sexually transmitted diseases (STD) seen in the United States today (/). An estimated 3-4 million Americans suffer from a chlamydial infection each year (2). Men, women, and infants are affected, but women bear an inordinate burden because of their increased risk for adverse reproductive consequences. While C. trachomatis infection is currently not a reportable disease on a national level in the United States, data obtained from metropolitan STD clinics suggest sharp increases in inci dence in the period 1975-1983 (/). In England and Wales, where nongonococcal urethritis (about half the cases of which are caused by C. trachomatis) is a reportable disease, the inci dence has nearly doubled in the last decade ( 1).
Chlamydiae are unique microorganisms whose specific properties have been delineated largely in the last tw o decades. Although they are classified as bacteria, they share properties with viruses and bacteria. Like viruses, chlamydiae grow only intracellularly. For this reason, culture of Chlamydia has been difficult because expensive cell-culture methods similar to those used to recover viruses are required. Unlike viruses, however, chlamydiae contain both deoxyribonucleic acid (DNA) and ribonucleic acid (RNA), divide by binary fission, and have cell walls similar to those of gram-negative bacteria.
The wider availability of laboratory diagnostic tests for Chlamydia has opened the door to further exploration of the broad spectrum of disease caused by this organism C. trachomatis is now recognized as the causative agent for a diverse group of genital and neonatal infections, including many that were previously considered to be of unknown cause ( 1,3,4) (Table 1).
C. trachomatis causes approximately 50% of the reported cases of nongonococcal urethri tis (NGU) among men. This STD has an estimated incidence 2.5 times that of gonococcal urethritis ( 1 ). Chlamydia is also responsible for approximately 50% of the estimated 500,000 cases of acute epididymitis seen each year in the United States (2)
Even more important are chlamydial infections among women. Most of these infections are asymptomatic, but C. trachomatis also plays an important role in causing mucopurulent cervicitis (MPC) (5), acute pelvic inflammatory disease (PID) (6), and maternal and infant in fections during pregnancy and following delivery (7). Chlamydia accounts fo r one-quarter to one-half of the 1 million recognized cases of PID in the United States each year. These infec tions, in addition to C. trachomatis infections of the fallopian tube not clinically recognized as PID, contribute significantly to the increasing number of women who experience ectopic pregnancy or involuntary infertility. Besides its association with mucopurulent cervicitis and PID, Chlamydia plays an important role in the urethral syndrome (dysuria-pyuria syndrome) and in perihepatitis or Fitz-Hugh-Curtis syndrome ( 1,8).
Maternal infection during pregnancy has been associated with postpartum endometritis and in some studies with an increased perinatal mortality; the latter relationship requires fur ther study. Infants with infected mothers can acquire a chlamydial infection at birth from con tact with infected cervicovaginal secretions. Each year more than 155,000 infants are born to Chlamydia-infected mothers. These newborns are at high risk of developing inclusion con junctivitis and pneumonia and are at slightly elevated risk of having otitis media and bronchi olitis. In fact, Chlamydia is the most common cause of neonatal eye infections and of afebrile interstitial pneumonia in infants < 6 months of age.
Enormous cost is associated with chlamydial infections. Each year, more than $1 billion in direct and indirect costs are expended on these infections in the United States. Many of these Trachoma, the leading cause of preventable blindness in the world, is also caused by C h la m y d ia but has been excluded because it is not generally sexually transmitted, tA rrow indicates direction of transmission of infection.
Question mark indicates that a relationship has not been firm ly established.
Associated with lymphogranuloma venereum. costs result from the management of women with PID and its complications (9) and from the management of infants hospitalized with chlamydial pneumonia. This estimated cost does not reflect the human suffering experienced by those with chlamydial disease. Further growth in the economic burden of chlamydial infections will occur as these infections become more prevalent.
To reduce the morbidity and subsequent complications associated with C. trachomatis in fection in the United States, effective prevention and control strategies must be implemented. Comprehensive guidelines for the formulation of such control programs, as well as diagnostic and therapeutic approaches to infected individuals, are provided in this document. These policy guidelines were established after careful deliberation by an invited panel of experts in collaboration with staff of the Division of Sexually Transmitted Diseases, CDC.
# R isk A s s e s s m e n t
Establishing a profile fo r patients at increased risk of having a genital infection caused by C. trachomatis can be based on multiple criteria.
# Individual Characteristics and Practices
Age, number of sex partners, socioeconomic status, and sexual preference are predictors of C. trachomatis infection. Genital infection rates appear to be inversely related to age and posi tively correlated with number of sex partners. Sexually active women < 20 years of age have chlamydial infection rates 2-3 times higher than those for women ^ 20 years of age, and the rates for women ages 20-29 are considerably higher than those for women ^ 30 years of age (/, 10). Similarly, the rates of urethral infection among teenage males are higher than those for adults (11). Risk of infection increases with the number of sex partners (12,13).
In some studies, lower socioeconomic status and ethnicity have been correlated with an i creased risk of chlamydial infections (10-12). The prevalence of urethral chlamyd.al .nfect.on among homosexual men is approximately one-third the prevalence among heterosexual men (11,14), but 4%-8% of homosexual men seen in STD clinics have rectal chlamydial infection.
# Clinical Syndromes
Several clinical syndromes are associated with C. trachomatis infection. Some are more clearly defined than others, and their prevalence and manifestations differ depending on the population studied. Nevertheless, these conditions often provide the most suitable basis for initiating treatment, especially if complete bacteriologic evaluation is not possible or while the practitioner awaits the results of specific laboratory tests. However, it cannot be overempha sized that most women with cervical chlamydial infection, most homosexual men with rectal chlamydial infection, and as many as 30% of heterosexual men with chlamydial urethritis have few or no symptoms. These asymptomatic infections can sometimes be recognized by physical examination or by increased numbers of leukocytes on a Gram stain of infected secretions.
Three Chlamydia-associated syndromes* are common among women: (1) MPC, (2) ureth ral syndrome or urethritis, and (3) PID. C. trachomatis has been isolated from 30% to 50% of women examined who have mucopurulent endocervical exudate (5). Similarly, C. trachomatis *For a m ore com plete description o f syndromes, see section on Treatment Regimens, pages 65S-67S.
# 56S MM W R
A u g u st 23,1985 has been isolated from female patients with acute dysuria, particularly those with pyuria and a negative Gram stain of unspun urine (8). Among women with PID, the Chlamydia recovery rate is approximately 25%-50% with optimal technique, but serologic data suggest that as many as 50% of acute PID cases may be associated with C. trachomatis. Two Ch/amydia-assoc\aXe6 syndromes are common among men: nongonococcal urethritis (NGU) and acute epididymo-orchitis. C. trachomatis has been consistently isolated from up to 50% of men with NGU. Likewise, investigators have cultured C. trachomatis from 30% to 50% of patients with acute epididymitis and have demonstrated the organism to be the lead ing known cause of epididymitis among men < 35 years of age ( 1 ).
# Contact with an STD Patient
Individuals with a history of sexual exposure to persons with a chlamydial or gonococcal infection are themselves at high risk for chlamydial infection. Approximately 70% and 36%, re spectively, of female sex partners of men with confirmed chlamydial urethritis or confirmed gonococcal urethritis have Chlamydia isolated from the endocervical tract. Of all the women whose sex partners are reported to have NGU, 30%-40% harbor cervical chlamydial infection. Of men who are the sex partners of women with confirmed chlamydial MPC or PID, 25%-50% have Chlamydia isolated from the urethra. Many of these contacts are asymptomatic.
# Coexistence of Chlamydial Infection with Other STD
Approximately 1 5%-30% of heterosexual men with gonococcal urethritis have simultane ous urethral infection caused by C. trachomatis [1,15,16). An even higher proportion (25/o-50%) of women with Neisseria gonorrhoeae infection also have C. trachomatis infec tion of the cervix ( 1,15-1 7). Women who have other STD such as trichomoniasis and bacte rial vaginosis are also at increased risk of having chlamydial infection.
# Method of Contraception
Persons who use barrier methods of contraception (condom, diaphragm, diaphragm and foam) are at reduced risk for chlamydial infection relative to those who do not use any form of contraception (12). In contrast, women who use oral contraceptives have been reported to have a higher prevalence of cervical infection with C. trachomatis than women who do not use oral contraceptives ( 18). Use of intrauterine devices has not yet been investigated for its effect on rates of C. trachomatis infection.
# Pregnancy
In the United States, the prevalence of reported cervical chlamydial infection among preg nant women has varied from 2% to 37%, with most studies reporting infection rates of ap proximately 8%-12% (7 ,13,19). In general, infection has been most prevalent in the youngest age group; among unmarried women; and among inner-city, lower socioeconomic-status women.
# Health-Care Facility
Various types of health-care facilities will report different expected infection rates among women attendees. Not surprisingly, STD clinics report the highest rates of C. trachomatis in fection (an average of 20%-30% of all patients tested) (1,15). The next highest isolation rates are reported from clinics for adolescent patients (8%-26%) ( 13 ,2 0-23) and from family plan ning clinics (6%-23%) (10). Insufficient data are available to estimate expected rates in private practices, community health centers, and hospital emergency rooms.
# Lab o rato ry M etho d s
The absence of an inexpensive, simple, and reliable diagnostic test for chlamydial infection has limited control efforts. Historically, time-consuming and expensive tissue-culture tech niques have been required to definitively diagnose most C. trachomatis infections. Cytology was also available, but is only of comparable sensitivity to tissue culture in diagnosing new born conjunctivitis. In recent years antigen detection methods have offered a cost-effective al ternative to culture. Serologic methods are available, but remain principally a research tool.
Despite these encouraging improvements in diagnostic capability, current tests are not ideal. They are relatively difficult to perform, require considerable experience, and have limited application. Active investigation of new diagnostic methods for C. trachomatis continues, and antigen and antibody detection systems are improving rapidly. In such a dynamic environ ment, recommendations for the specific diagnostic methods discussed below must be flexible and should be revised as better methods become available.
# Culture
Tissue culture is presently the "gold standard" for laboratory diagnosis. Although pub lished methods are fairly standard (4), in practice many laboratories introduce variations that alter the sensitivity and specificity of the test. Rigorous adherence to standard methodology is strongly encouraged.
Two major components are needed to culture for C. trachomatis: (1) a cell-culture system *■ " t i -II lin o r \ f r h n i r o ic and (2) a method to identify inclusions growing in cell culture. The cell line of choice is
u ih j \*_/ a i i i c t i i u u tu 1U 0 111117 ,, ------ v , _ _ 1 1 ■ ,, _,,
McCoy. Alternatively, a particular strain of HeLa cells (HeLa 229)
) can e us ally restricted to research laboratories. Specimen material is centnfuged o ,^2 5 H n cu ttio n 1 hour and then incubated for 2-3 days in medium containing cycloh«jm de can take place in individual vials with cover slips at their ase* °r ^ dictated by the plastic microtiter plates (26). The choice between t ese slightly more sensitive number of specimens a laboratory has to process; the vial ^e,hod2 S'^n 7 exDenslve and less susceptible to cross-contamination, but is more time consu usually used FA For identification, either iodine stain or fluorescent antibody (FA) sta.n " ' " £^, 2 stain offers the advantages of higher sensitivity and shorter processing i res'one requires a fluorescence microscope. The standard method for 10 ine s ainin blind passage, which increases the processing time to 4-6 days. In microtiter p a es' s ® ing without passage appears equivalent to iodine staining with one blind passage e most sensitive culture method currently available involves using cycloheximide treated McCoy cells in vials in the presence of fluorescent monoclonal antibodies.
Compared with other diagnostic tests for C. trachomatis, the major advantage of tissue culture is its specificity. With this method, the organism can also be positively identified or saved for other marker studies such as immunotyping. Thus, culture is clearly the method of choice for research studies. Determining the sensitivity and specificity of the culture has not been possible since it is the reference standard for other methods; however, it is estimated that culture has a sensitivity of 80%-90%, and a specificity of 100% (28).
Culture also has several disadvantages: (1) the cost and complexity of laboratory require ments can be prohibitive; (2) specimens can be kept at 4 C for only up to 24 hours (preferably 12) before processing, or frozen at -70 C if they cannot be inoculated within 24 hours;
(3) specimens must be placed in specially prepared transport media; and (4) the cell monolay er may be contaminated with other bacteria or viruses, particularly in vaginal or rectal specimens.
# 58S
# MMWR
A u g u s t 23, 1985
# Cytologic Methods
Cytologic identification of chlamydial infections-the only method available in the period 1909-1957-is an examination of epithelial cell scrapings (e.g., conjunctival, cervical, ureth ral) on a stained smear. A modified Giemsa stain is most often used, although W right's and other standard tissue stains can be used. Infection is identified by visualizing characteristic intracytoplasmic inclusions. Alternatively, cell scrapings can be examined using FA stains (4).
The advantage of cytologic examination is clearly the simplicity of the process, particularly if light microscopy is used. The disadvantage is the poor sensitivity fo r diagnosing chlamydial infections other than neonatal conjunctivitis, for which the sensitivity of cytology compared with culture is 95%. The sensitivity of cytologic methods in identifying chlamydial adult con junctivitis is 45% for Giemsa and 85% for FA. In tests for cervical infection, the tw o stains have sensitivities of only 40% and 65%, respectively, and for urethral infection, 15% and 60% (28). Moreover, these upper levels of sensitivity can only be obtained with good specimens (many epithelial cells) and an experienced observer.
Thus, standard cytology is of little practical value as a diagnostic aid fo r genital chlamydial infection. However, tw o recent studies (29,30) suggest that the inflammatory pattern on Papanicolaou-stained cervical smears may be useful when it is used as a screening test to select patients for confirmation of infection by culture or monoclonal antibody tests, but the Papanicolaou method used alone is not satisfactory for diagnosing chlamydial infection.
# Antigen Detection
To date, two methods of antigen detection are available: (1) FA examination of a direct smear and (2) enzyme immunoassay (EIA). One example of each method is presently available commercially,* and both have undergone considerable evaluation.
However, continued revision of these tests takes place even after they become available commercially. Consequently, initial published data on efficacy may be outdated, so the most recent references should be used. Other antigen detection tests are expected to be available soon.
D irect-Sm ear FA Test (31) With this procedure, specimen material is obtained by swab and applied directly to a slide, which is fixed and then incubated with fluorescein-conjugated monoclonal antibody before being examined under a fluorescence microscope. Total processing time is usually 3 0 -4 0 min utes. Critical steps include (1) obtaining a satisfactory specimen and preparing a satisfactory smear (this can be checked before or after staining), (2) drying the specimen properly before fixing it, (3) using a high-quality fluorescence microscope, and (4) obtaining and maintaining an experienced microscopist who can recognize elementary bodies and artifacts.
Compared with culture, the sensitivity of the direct smear test is ^ 90% in most published studies, and the specificity is ^ 98%. The positive predictive value of this test has ranged from approximately 80% in populations with a Chlamydia prevalence of 10% to 95% in popu lations with a prevalence of 30% (32). Lower sensitivities and specificities are often encoun tered in situations in which specimens are less than optimal or individuals reading the slides are relatively inexperienced. In these instances, assessment of the proficiency of laboratory techniques is essential. This can be accomplished by comparing results with those obtained with tissue culture or by exchanging slides with a central reference laboratory that does proficiency testing. K
The major advantages of the direct smear test are (1) the uncomplicated transport and storage of specimens, (2) rapid processing time compared with that required for other meth ods (33), (3) a high specificity, and (4) the ability to check on adequacy of specimen collec tion (i.e., cells on the slide). Disadvantages of the method are (1) the requirement for precise specimen collection, (2) the need for high-quality fluorescence microscope equipment, (3) the need for an experienced microscopist, and (4) the relatively labor-intensive nature of the process.
# Enzym e Im m un o a ssa y (34)
This test measures antigen-antibody reactions through an enzyme-linked immunoabsorbent assay (ELISA) and requires a spectrophotometer. Processing time for specimens is ap proximately 4 hours.
Questions continue to be raised about the reliability of available ElAs for C. trachomatis. The sensitivity of the test has varied from 67% to 90%, the specificity from 92% to 97%, and the positive predictive value from 32% to 87%, depending on the population studied (35). Much of the observed disparity has been attributed to variable sensitivity of the tissue culture systems against which the EIA has been compared.
The advantages of the EIA are (1) the uncomplicated transport and storage of specimens, (2) the objective method of measurement in the laboratory, which involves standard equip ment and does not depend upon a specially trained observer, and (3) the ability to test large numbers of specimens at a time.
The disadvantages are that (1) the adequacy of the specimen cannot be checked and ( 2) th e test cannot be performed while the patient is waiting (although this is also true for the dir smear test if no fluorescence microscope is available).
It is not known whether either method of antigen detection can be use or specime sites other than the eyes and genitals (e.g., pharynx).
# Serology
Currently, Chlamydia serology has little value in routine clinical management and basically remains a research tool. Although some serologic tests are commercially available, they have not been shown to be useful in routine diagnosis.
There are tw o standard methods-complement fixation and microimmunofluorescence (MIF) (35). ELISA tests have been developed, but none are recommended for wide use (36,37). The only valid clinical uses of serologic tests are in infant pneumonia, where specific immunoglobulin M (IgM) MIF serology, when available, is the diagnostic test of choice; and in occasional cases of suspected lymphogranuloma venereum (LGV). The difficulties in prepar ing the antigen and conducting the test restrict the use of the test to a limited number of re search laboratories.
# Diagnostic Considerations
The value of rapid diagnostic tests for detecting C. trachomatis infection depends primari-V on the prevalence of disease in the population tested and the availability of other tests For ow-r.sk groups, the predictive value of a positive test is lower than for high-prevalence popu lations, even if the test is highly sensitive and specific. For example, in a population with a 5% 60S MMWR A u g u st 23,1985 prevalence, a rapid test with a 95% specificity and sensitivity will have a predictive value posi tive of 50% (meaning that there is only a 50% chance that an individual who is diagnosed as having disease actually has it). In situations in which an increase in the predictive value of a positive test is desired, in order to lower risks of incorrectly labeling persons as having STD, positive screening tests can be confirmed by culture, or culture methods can be used for screening (with an accompanying rise in cost). As new tests become available, physicians, hospital and commercial laboratorians, and public health program directors must be aware of the sensitivity, specificity, and predictive value of such tests when determining whether to use them in specific situations.
As more laboratories begin to do diagnostic testing for Chlamydia, laboratory quality con trol assumes increasing importance. Each laboratory should verify the accuracy of test meth ods other than culture by periodically comparing results with those obtained using cultures. Such comparisons are particularly important when the laboratory implements a new test method. Laboratories that do cell-culture isolation of Chlamydia should run appropriate posi tive and negative controls to verify sensitivity of the cell cultures being used and should peri odically evaluate the effectiveness of transport systems. Regional reference laboratories should be established for verification of culture results or evaluation of unexpected or discrep ant results. Proficiency testing programs should be developed for culture and other test meth ods so that laboratories can evaluate their methods using unknown specimens.
# Patient Management H igh-Risk Groups
High-risk groups should be defined using demographic profiles and the estimated or estab lished prevalence of chlamydial infection in a particular community or patient population. Al though the criteria described under Risk Assessment can be used as a guide to establishing a high-risk profile, local determinants of risk are more precise and should be identified if possi ble. Local data also provide more accurate baseline prevalences, against which the success of prevention and control strategies can be measured.
When culture results are available, they should be used in decisions concerning appropriate therapy. However, undiagnosed patients who fit an established high-risk profile should also be offered treatment, unless local or individual circumstances dictate otherwise. Patients in the following groups should immediately receive a regimen that includes effective treatment against C. trachomatis infection.
# Symptomatic Syndromes Associated with Chlamydia
# Asymptomatic Contacts of Syndromes Associated with Chlamydia
Individuals exposed through sexual contact with patients who have any of the above symptomatic syndromes (within 30 days of the onset of their symptoms or clinical evaluation) should be evaluated for STD and treated for presumptive chlamydial infection.
# Gonococcal Infection
Women with confirmed N. gonorrhoeae infection of the endocervix, heterosexual men with diagnosed gonococcal infection of the urethra, and sex partners of members of both of these groups of patients should be treated with an antimicrobial regimen that is effective against both N. gonorrhoeae and C. trachomatis infection.
# Screening
Selective screening to detect asymptomatic infection is an essential component of a suc cessful control program. Whenever possible, criteria for routine screening should be based on local determinants of risk. An appropriate diagnostic method must be selected. Diagnostic considerations for current tests/methods are discussed above. The following guidelines are provided to assist in determining which test to use.
# Screening Criteria
_ . A .. .
No single individual characteristic or practice (see p. 55S), is in itself a su icien cri erion to define which persons should be screened. However, a composite of in i v i ua a c °rs _ conjunction with a community factor such as type of health-care aci ity see ' help to maximize yield from screening. Consequently, available evidence ea s o mendation that the priorities for routine screening shown below be used.
# STD Clinic
1. Individuals attending STD clinics who otherwise would not be offered antichlamydial treatment should be screened first. (The screening of asymptomatic, high-risk women should be accorded the highest priority. In general, the screening of heterosexual men should have a higher priority than screening homosexual men.) 2. Individuals with symptomatic syndromes associated with Chlamydia should be screened next. (Screening of women should be accorded higher priority than screening of men.)
# Oth er High -Risk Health -Care Faci/it y
Health-care facilities other than STD clinics may also have a high prevalence of chlamydial infections. In particular, many adolescent and family planning clinics are categorized as highrisk centers, but a wide disparity in rates of chlamydial infection may be observed in different populations." Facilities that serve high-risk populations should follow the order of screening priority for STD clinics above; those serving undetermined or low-risk populations should follow the priority below for Undetermined/Low-Risk Health-Care Facility.
Undetermined/Low-Risk Health-Care Facility 1. Persons in urban settings who are younger, have lower socioeconomic status, and have multiple sex partners, and who otherwise would not be offered antichlamydial treatment, should be screened first. (In this category of high-risk patients, women should be accorded highest priority for screening.) 2. Individuals with symptomatic syndromes associated with Chlamydia should also be screened. (Screening of women should be accorded higher priority than screening of men.)
# Diagnostic Method
Culture and two different antigen detection tests are currently the only diagnostic methods acceptable for screening for Chlamydia infection. Culture remains the most accurate method, but is costly and takes at least 2-3 days before results are available. Antigen detection tests have emerged as reasonable alternatives, but questions remain about their reliability for lowprevalence populations. Following are guidelines fo r the use of diagnostic tests in screening.
1 Culture, based upon availability, is the preferred method for routine screening. 2. Direct smear using fluorescent antibody (DFA) is the most thoroughly evaluated alterna tive to culture. However, optimal results with the currently marketed test have been achieved for high-risk women and symptomatic men by very experienced research laboratories. For other populations, test results obtained by less experienced technolo gists may not be as reliable. Consequently, DFA results should be compared periodically with those obtained through culturing. 3. Enzyme immunoassays have not been as completely evaluated as the DFA tests. The currently marketed test probably is less sensitive and specific than DFA, but the quality of results is also less likely to depend on the level of experience of laboratory personnel.
It is important that regional reference laboratories be available to monitor the perfor mance of these and other new antigen detection tests and to advise about appropriate applications and quality control problems.
# Recommendation
Screening is suggested at th e firs t p renatal visit fo r th e fo llo w in g g ro u p s o f pregnant w o m e n :
1. Adolescents (< 20 years of age)
MMWR 63S
2. Unmarried women 3. Married women who may be at high risk because of multiple sex partners or a history of other STD Screening of pregnant women who fall into any of these high-risk categories in inner-city hospitals is particularly important because of the high prevalence of asymptomatic infections among the patients served by these facilities.
# Neonates
# Ophthalmia Prophylaxis
None of the presently recommended approaches for prophylaxis against gonococcal and chlamydial ophthalmia neonatorum is completely effective. Silver nitrate is effective in prevent ing gonococcal infections but does not prevent chlamydial disease and frequently causes chemical conjunctivitis. Erythromycin is effective in preventing both gonococcal and chlamy dial ophthalmia and does not cause chemical conjunctivitis, but the topical use of this drug does not prevent nasopharyngeal chlamydial infection or pneumonia. Furthermore, eryth romycin prophylaxis is considerably more expensive than silver nitrate prophylaxis. Tetracy cline ointment has not been as extensively evaluated as has erythromycin but appears to be as effective. Whichever type of prophylaxis is used should be implemented no later than 1 hour after birth -preferably immediately after delivery since delayed application may reduce efficacy.
# Recommendation
Erythromycin (0.5%) ophthalmic ointment, tetracycline (1%) ointment, or silver nitrate should be instilled into the eyes of all neonates as soon as possible after delivery and never later than 1 hour after birth. Single-use tubes or ampules are preferable to multiple-use tubes.
# Neonatal Infection
Eighteen to fifty percent of infants born to infected mothers will have conjunctivitis be tween 1 and 3 weeks after birth (7). The symptoms are often mild, and the disease may be missed unless looked for carefully. Though considerable morbidity results acutely from the severe form of this disease, it is self-limited and does not appear to result in loss of vision. Three to eighteen percent of infants born to infected mothers will develop chlamydial pneumonia/bronchiolitis, usually at 1 -4 months of age (7). In most cases this is a mild disease, but it can be severe and require hospitalization.
# Recommendation
Screening for neonatal infection is not indicated. Newborns with conjunctivitis and afebrile pneumonia/bronchiolitis should have specimens culture-tested for C. trachomatis and be appropriately treated as recommended below. If cultures are positive, mothers (and their sex partners) of the infected children should also be treated.
# 64S
# MMWR
A u g u st 23,1985 Treatment Regimens
# CONFIRMED INFECTIONS
# Uncomplicated Urethral, Endocervical, or Rectal Infection in Adults
# Drug Regimens of Choice
Tetracycline hydrochloride (HCI): 500 mg, by mouth, 4 times a day fo r 7 days.
# OR
Doxycycline hyclate: 100 mg, by mouth, 2 times a day for 7 days.
# Alternative Regimens
(for patients for whom tetracyclines are contraindicated or not tolerated) Erythromycin base or stearate: 500 mg, by mouth, 4 times a day fo r 7 days, or eryth romycin ethyl succinate: 800 mg, by mouth, 4 times a day for 7 days.
Sulfonamides are also active against C. trachomatis. Although optimal dosages of sulfona mides for chlamydial infection have not been defined, sulfamethoxazole, 1 g by mouth, twice a day for 10 days, is probably effective.
# Follow-Up
When taken as directed, the tetracycline and erythromycin regimens listed above are highly effective (> 95% cure rates). No tetracycline-resistant Chlamydia has been described. Post-treatment cultures are not advisable if laboratory resources are limited. A positive p o s t treatment culture is more likely to represent noncompliance with treatment, failure to trea t sex partners, or laboratory error than resistance to the antibiotic. Patients who do have posi tive post-treatment cultures should be treated again according to one of the above regim ens.
# Management of Sex Partners
All persons sexually exposed to C. trachomatis infection (within 30 days after their sex partner develops symptoms or has a positive clinical evaluation) should be examined for STD and promptly treated for C. trachomatis with one of the above regimens. This group includes sex partners of individuals with sexually acquired chlamydial infection, mothers of infected newborns, and the sex partners of these mothers.
# Urogenital Infections during Pregnancy
# Drug Regimen of Choice
Erythromycin base: 500 mg, by mouth, 4 times a day for 7 days, or erythromycin ethyl succinate: 800 mg, by mouth, 4 times a day for 7 days.
Erythromycin stearate in appropriate doses may also be effective, but has not been ade quately studied.
# MMWR
# 65S
# Alternative Regimen
(for female patients who cannot tolerate the above regimen, a decreased daily dose is recommended) Erythromycin base: 250 mg, by mouth, 4 times a day for 14 days.
The optimal dose and duration of antibiotic therapy for pregnant women have not been es tablished. Currently, there are no completely acceptable alternative regimens for female pa tients who are allergic to erythromycin or otherwise cannot tolerate erythromycin. In the case of proven treatment failure, the patient should be re-treated with erythromycin according to either of the dosage schedules outlined above.
# Established Conjunctivitis of the Newborn*
# Drug Regimen of Choice
Oral erythromycin syrup: 50 mg/kg body weight/day in 4 divided doses for 14 days.
There is no indication that topical therapy provides additional benefit. If inclusion conjunc tivitis recurs after therapy, erythromycin treatment should be reinstituted for an additional 1 -2 weeks.
# Pneumonia among Infants
# Drug Regimen of Choice
Oral erythromycin syrup: 50 mg/kg/day in 4 divided doses for 14 days.
# CHLAM
# YDIA-ASSOCIATED SYNDROM ES
# Nongonococcal Urethritis
NGU can be diagnosed for a male patient if tests for N. gonorrhoeae are negative and the patient has objective evidence of urethritis. Objective evidence of urethritis includes a visibly abnormal discharge, pyuria defined as > 10 polymorphonuclear leukocytes (PMN) per high dry field in the sediment of a first-voided urine specimen, or > 4 PMN per oil immersion field in a Gram-stained urethral smear. Approximately 50% of the cases of urethritis not associated with N. gonorrhoeae are caused by C. trachomatis. NGU requires prompt antimicrobial treat ment of the patient and evaluation and treatment of any sex partners.
# Drug Regimens of Choice
Tetracycline HCI: 500 mg, by mouth, 4 times a day for 7 days. Alternative Regimen (for patients for whom tetracyclines are contraindicated or not tolerated) Erythromycin base or stearate: 500 mg, by mouth, 4 times a day fo r 7 days, or eryth romycin ethyl succinate: 800 mg, by mouth, 4 times a day for 7 days.
Sulfonamides are not suitable for treatment fo r clinical syndromes when Chlamydia cul tures are not performed, since they may not be effective against Ureap/asma urea/yticum and other organisms that cause nonchlamydial genital infection.
# Management of Sex Partners
All persons who are sex partners of patients with NGU (within last 30 days) should be examined for STD and treated promptly with one of the above regimens.
# Follow-Up
Patients should be advised to return for follow-up medical care if symptoms persist or recur.
# Mucopurulent Cervicitis*
The presence of mucopurulent endocervical exudate often reflects cervicitis due to chlamydial and/or gonococcal infection. If N. gonorrhoeae is found on Gram stain or culture of endocervical or urethral discharge, a treatment regimen effective against both gonococcal and chlamydial infection should be used. When only chlamydial infection is proven or suspect ed, therapy should consist of one of the regimens below.
# Drug Regimens of Choice
Tetracycline HCI: 500 mg, by mouth, 4 times a day for 7 days.
OR Doxycycline: 100 mg, by mouth, twice a day for 7 days.
# Alternative Regimens
(for patients for whom tetracyclines are contraindicated or not tolerated) Erythromycin base or stearate: 500 mg, by mouth, 4 times a day fo r 7 days, or eryth romycin ethyl succinate: 800 mg, by mouth, 4 times a day for 7 days.
# Management of Sex Partners
Men exposed to women with MPC attributed to chlamydial infection should be evaluated for STD and treated with one of the above regimens. If N. gonorrhoeae is found, treatment should be with a regimen effective against uncomplicated gonococcal and chlamydial infection.
•Criteria for presumptive diagnosis include (1) m u c o p u ru le n t s e c re tio n from the endocervix, which is usually yellow or green when viewed on a white cotton-tipped swab (positive swab test); (2) ^ 10 p o ly m orp h o n ucle a r le u k o c y te s per microscopic oil immersion field (X 1,000) in a Gram-stained smear of en docervical secretions; and (3) c e rv ic itis , determined by cervical friability (bleeding when the first swab culture is taken) and/or by erythema or edema within a zone of cervical ectopy. Acute PID refers to the acute clinical syndrome attributed to the ascending spread of mi croorganisms, unrelated to pregnancy or surgery, from the vagina and endocervix to the endo metrium, fallopian tubes, and/or contiguous structures. Clinical findings for most patients with PID include lower abdominal tenderness, adnexal tenderness, and pain induced by lateral motion of the uterine cervix. Many cases of PID are caused by more than one organism. Causative agents include C. trachomatis, N. g o n anaerobic bac oides and gram-positive cocci), and facultative gram-negative rods (such as Actinom yces israelii, and Mycoplasma horn inis.
These agents cannot usually be differentiated in individual patients. Consequently, treat ment regimens should be used that are active against the broadest range of the pathogens. CDC has already published comprehensive guidelines regarding criteria for hospitalization, rationale for selection of antimicrobials, and general treatment regimens for the major patho gens associated with PID (39): Below are examples of specific combinations of regimens for optimal coverage for C. trachomatis and for adequate coverage for the other common causa tive agents.
# Inpatient Treatment
Doxycycline: 100 g, intravenous (IV), 2 times a day.
# PLUS
Cefoxitin: 2.0 g, IV, 4 times a day. Continue drugs IV for at least 4 days and at least 48 hoursa*®r^a p T * C°nt'nUe doxycycline 100 mg, by mouth, 2 times a day, to complete 10-V
# Ambulatory Treatment
Cefoxitin: 2.0 g, intramuscular (IM), OR amoxicillin: 3.0 g, by mouth, OR ar"P 3.5 g, by mouth, OR aqueous procaine penicillin G: 4.8 million units, IM, at 2 sites (eac along with probenecid: 1.0 g, by mouth), OR ceftriaxone: 250 mg, IM FOLLOWED BY Doxycycline: 100 mg, by mouth, 2 times a day for 10-14 days.
Tetracycline HCI 500 mg, by mouth, 4 times a day, can also be used, but is less active against certain anaerobes and requires more frequent doses; both factors represent draw backs in treatment of PID.
# Management o f Sex Partners
All persons who are sex partners of patients with PID (within the 30 days prior to onset of their symptoms or positive clinical evaluation) should be examined for STD and treated promptly with a regimen effective against uncomplicated gonococcal and chlamydial infection.
A CDC update of these Guidelines is in press.
# 68S
# MMWR
A u g u st 23, 1985
# Follow-Up
All patients treated as outpatients should be clinically reevaluated in 4 8 -7 2 hours. Those not responding favorably should be hospitalized. Patients should also be reevaluated after they complete treatment.
# Intrauterine Device
The intrauterine device (IUD) is a risk factor for the development of PID. Although the exact effect removing an IUD has on the response of acute salpingitis to antimicrobial therapy and on the risk of recurrent salpingitis is unknown, it is recommended that the IUD be removed as soon as possible after antimicrobial therapy has been initiated. When an IUD is removed, contraceptive counseling is necessary.
# Acute Epididymo-Orchitis
Acute epididymo-orchitis has two forms: (1) a sexually transmitted form usually associat ed with urethritis and commonly caused by C. trachomatis and/or N. gonorrhoeae and (2) a nonsexually transmitted form associated with urinary tract infections caused by Enterobacteriaceae or other nonsexually transmitted uropathogens. Urine should be examined by Gram stain and culture to exclude bacteruria in all patients, including those with urethritis. An impor tant part of the differential diagnoses is testicular torsion, a surgical emergency.
Sexually transmitted epididymo-orchitis usually affects young adults and is associated with presence of clinical or subclinical urethritis, absence of underlying genitourinary patholo gy, and absence of gram-negative rods on Gram stain of urine.
# Drug Regimens of Choice
Amoxicillin: 3.0 g, by mouth, OR ampicillin: 3.5 g, by mouth, OR aqueous procaine peni cillin G: 4.8 million units, IM at 2 sites (each along with probenicid. 1.0 g, by mouth), OR spectinomycin: 2.0 g, IM, OR ceftriaxone: 250 mg, IM
# FOLLOWED B Y
Tetracycline HCI: 500 mg, by mouth, 4 times a day for 10 days.
# OR
Doxycycline: 100 mg, by mouth, 2 times a day for 10 days.
# Alternative Regimens
(for patients for whom tetracyclines are contraindicated or not tolerated) Erythromycin base or stearate: 500 mg, by mouth, 4 times a day fo r 7 days, or eryth romycin ethyl succinate . 800 mg, by mouth, 4 times a day for 7 days.
# Management of Sex Partners
Sex partners of patients with sexually transmitted acute epididymo-orchitis (diagnosed within 30 days of exposure) should be examined for STD and promptly treated with a regimen effective against uncomplicated gonococcal and chlamydial infection.
# MMWR
# 69S
# Fo llow -U p
Failure to improve within 3 days requires reevaluation of diagnosis/therapy and considera tion fo r hospitalization.
# Patient Education
# Patient Counseling
The effective management of chlamydial infection includes counseling of patients. Such counseling should be designed to influence specific behavior that will contribute to successful therapy, disease intervention, and prevention. Patient handouts designed for easy comprehen sion are an efficient way of conveying basic information. These messages should be rein forced by practitioners through discussions with patients that are tailored to the individual and provide an opportunity for questions.
# Recommendation
Practitioners should provide counseling to patients regarding their disease, its treatment, and the overall responsibility of the patient in the process. Information conveyed to patients should at least include:
1 Instructions for taking medication, including the dosage, timing, and length of the regimen. Patients must clearly understand that they must continue to take medication according to schedule, despite abatement of symp toms. 2. Advice regarding follow-up for side effects or other difficulty with medica tion, continued or worsened symptoms, and test of cure, if indicated. Suggestion to abstain from sexual activity until medication is completed by both patient and partner. If this is not possible, patients should be en couraged to use condoms until treatment is completed. Suggestion to cease sexual activity immediately if the same or other STD symptoms recur, and to return to the practitioner/clinic with the steady sex partner. 5. Suggestion to regularly use barrier methods, particularly condoms, to pre vent chlamydial infection and other STD.
# 3.
# 4.
# Sex Partner Referral
The sex partners of patients with chlamydial infection should be referred for medical care through the efforts of individual patients, or through a disease intervention specialist (DIS) Al though the latter process is time-consuming, it may be very effective. However, locating and referring sex partners through a DIS is clearly not feasible for all patients with chlamydial in fection and the C/?/aA7?yc//3-associated syndromes discussed above. First priority for interviewing/counseling efforts by a DIS should be given to patients with proven chlamydial infection. The contract method of sex partner referral should be used, with the patient assuming referral responsibility whenever possible. The referral of sex partners by the patient is a more practical approach in terms of human resources, but the effectiveness of this practice has not been evaluated among Chlamydia patients. Nevertheless, attempts must be made to capitalize on patients' knowledge of and persuasiveness with their own sex partners.
# Recommendation
Patients with chlamydial infection should be encouraged to refer all persons with whom they had sexual encounters in the 30 days prior to onset of their symptoms or clinical evaluation. (Approximately 94% of sex partners to NGU pa tients brought to treatment have been exposed within 30 days.)
# Prevention
Of all possible Chlamydia control approaches, successfully preventing the initial infection remains the most effective. Education of the public and of health professionals is essential for prevention at all three levels (primary, secondary, tertiary), especially in the absence of an ef fective vaccine.
# Professional Training/Education
Providers of health care can play a leading role in reducing the incidence of C. trachomatis infection and its complications. Timely diagnosis and appropriate treatment of chlamydial in fection by practitioners will prevent further transmission and minimize the risk that the infect ed individual will have adverse consequences. Additionally, clinicians are in a position to in fluence a patient to avoid behavior likely to result in transmitting disease or in being reinfected. STD education for health-care professionals should promote the following:
1 Recognizing Ch/amydia-assoc\aXe6 syndromes and high-risk patients. 2. Following recommended STD treatment guidelines. 3. Reporting cases promptly and completely. 4. Counseling patients to refer all sex partners for medical evaluation, to take all medica tion as prescribed, and to modify their behavior so as to reduce the risk of future infection.
# Recommendation
1. Professional recognition should be enhanced by incorporating knowledge about chlamydial infection into education and training programs fo r physi cians, nurses, laboratory personnel, and allied health professionals (such as physician assistants). 2. Organizations for health professionals, academic centers, colleges, and societies should be encouraged to formally support the chlamydial preven tion and control efforts by (a) providing appropriate continuing medical/ professional education courses about chlamydial infections at national/regional/local meetings and (b) encouraging health-professional journalsespecially official organizational p u b lications-to publish chlamydial policy guidelines and clinical reviews and research papers on Chlamydia and as sociated infections.
# MMWR
# 71S
Public Education/Health Promotion Education of the public is necessary to provide a high level of awareness of chlamydial in fections (and other STD) and to influence people to know and communicate about the preven tion, recognition, and treatment for Chlamydia; to support control efforts; and to reduce their personal risk of acquiring or transmitting a chlamydial infection. Accumulating evidence sug gests that public education can influence individuals to reduce their risk of acquiring an STD by changing sexual practices.
One such practice that should be encouraged is the use of barrier methods of contracep tion. Barrier methods of contraception (condoms and diaphragms) are known to provide pro tection against Chlamydia infection and other STD when used properly. The effectiveness of spermicides in preventing Chlamydia infection has not been determined. However, spermi cides do not enhance infection and do achieve some measure of protection when used in con junction with a diaphragm or condom.
# Recommendation
Disseminate the following information to the public: 1. Risks of chlamydial infection associated with sexual activity, especially when multiple partners are involved. 2. Role of barrier methods of contraception for personal prophylaxis to pre vent chlamydial infection and other STD.
# Surveillance
A fundamental requisite for control and prevention of chlamydial infection is a national sur veillance system, since it provides quantitative estimates of incidence and prevalence, a basis for determining secular trends, and a tool for evaluating control efforts. Current methods for diagnosis now permit the establishment of a multitiered, multifocal disease surveillance system. The tiers are local, state, and national. The foci include subgroups at special risk, clini cal syndromes of particular importance, and the general population.
A national surveillance system will require state reporting laws and/or regulations to pro vide the necessary support for prevention activities. Reporting laws promote and legitimize the involvement of public health authorities in assuring adequate individual patient management-including referral of sex partners-and may facilitate other activities such as screening and education. Moreover, case reporting provides a uniform basis for describing the extent and trpnH nf Hicoaco
# 72S
# MMWR
A u g u st 23,1985 Prevention and control activities for chlamydial infections have been proposed in this document, although the inadequacies in current diagnostic methods are acknowledged. In particular, patient management, including sex partner referral, is recommended for selected C h la m y d ia -associated clinical diagnoses (not dependent on the results of a laboratory test for C h la m y d ia ). Similarly, case reporting should include selected clinically diagnosed conditions associated with C h la m y d ia infection in addition to laboratory-diagnosed C h la m y d ia infection. Pending development of nationwide laboratory capability for identifying C h la m y d ia , condi tions should be selected that will best serve as indices fo r chlamydial infection, and that repre sent important public health problems in their own right. Reporting of clinically diagnosed conditions should augment rather than replace reporting of laboratory-diagnosed problems, since continuing efforts to develop a national laboratory capability will greatly enhance oppor tunities for ongoing improvements in patient management and public health interventions.
Although a national surveillance system should be based on case reporting, additional ap proaches, involving classical statistical methods, should be utilized, at least at the national level, to provide extent and trend estimates less vulnerable to the biases inherent in estimates based on case reports.
# Recommendation
#
#No absolute criteria exist for defining the clinical syndromes of NGU and PID/AS, but a constellation of signs and symptoms may be suggestive. For NGU, these include a patient with dysuria, white cells on Gram stain of urethral smears, and/or frank urethral discharge, in the presence of negative tests for gonorrhea. PID/AS is more protean in its manifestations, and the diagnosis ultimately rests on the judg ment of the attending clinician. Usual features include a combination of (1) lower abdominal pain, (2) adnexal tenderness, (3) adnexal mass, (4) pain on cervical motion, (5) mucopurulent discharge, and (6) temperature elevation. No single combination is pathognomonic. | None | None |
1be8b645ef1a848509fb10e4d2f445706019e46c | cdc | None | Tickborne rickettsial diseases (TBRD) continue to cause severe illness and death in otherwise healthy adults and children, despite the availability of low cost, effective antimicrobial therapy. The greatest challenge to clinicians is the difficult diagnostic dilemma posed by these infections early in their clinical course, when antibiotic therapy is most effective. Early signs and symptoms of these illnesses are notoriously nonspecific or mimic benign viral illnesses, making diagnosis difficult. In October 2004, CDC's Viral and Rickettsial Zoonoses Branch, in consultation with 11 clinical and academic specialists of Rocky Mountain spotted fever, human granulocytotropic anaplasmosis, and human monocytotropic ehrlichiosis, developed guidelines to address the need for a consolidated source for the diagnosis and management of TBRD. The preparers focused on the practical aspects of epidemiology, clinical assessment, treatment, and laboratory diagnosis of TBRD. This report will assist clinicians and other health-care and public health professionals to 1) recognize epidemiologic features and clinical manifestations of TBRD, 2) develop a differential diagnosis that includes and ranks TBRD, 3) understand that the recommendations for doxycycline are the treatment of choice for both adults and children, 4) understand that early empiric antibiotic therapy can prevent severe morbidity and death, and 5) report suspect or confirmed cases of TBRD to local public health authorities to assist them with control measures and public health education efforts. The reported incidence of these diseases has increased during the previous decade. Despite the availability of lowcost and effective antibiotic therapy, which may be used empirically for suspected cases, TBRD continue to cause severe illness and death in otherwise healthy adults and children. The greatest challenge to clinicians is diagnosing these infections early in their clinical course, when antibiotic therapy is most effective (2,3). The majority of patients with TBRD seek medical care within 2-4 days of onset of illness (4-7). In general, these patients are first evaluated by family practitioners, pediatricians, internists, emergency department (ED) physicians, or physician extenders. Early signs and symptoms of these illnesses are notoriously nonspecific, or they might mimic benign viral illnesses, making diagnosis difficult. For example, even in areas where awareness of RMSF is high, approximately 60%-75% of patients with this TBRD receive an alternate MMWR# Introduction
Tickborne rickettsial diseases (TBRD) are clinically similar, yet epidemiologically and etiologically distinct illnesses. In the United States, these diseases include 1) Rocky Mountain spotted fever (RMSF), 2) human monocytotropic (or monocytic) ehrlichiosis (HME), 3) human granulocytotropic (or granulocytic) anaplasmosis (HGA, formerly known as human granulocytotropic ehrlichiosis or HGE) (1), 4) Ehrlichia ewingii infection, and 5) other emerging TBRD. diagnosis on their first visit for medical care (8,9). Moreover, the earlier patients seek care in the course of their illness, the more likely an alternate diagnosis will be made (4). The lack of a specific initial syndrome, however, does not imply that the course of these diseases will be benign.
In October 2004, to address the need for a consolidated resource for the diagnosis and management of TBRD, CDC's Viral and Rickettsial Zoonoses Branch collaborated with 11 clinical and academic specialists of RMSF, HGA, and HME. These external contributors were invited by CDC subject matter specialists to participate among clinicians and researchers in the field of TBRD, based on direct working interactions related to case consultation and recognized expertise from peer-reviewed publications. In December 2004, the framework of this report was developed by CDC's Viral and Rickettsial Zoonoses Branch, based on a summary of the peer-reviewed published reports on the epidemiology and clinical aspects of TBRD. External contributors further developed recommendations for the diagnosis and treatment of TBRD based on their clinical research and experience. All work group collaborators reviewed and provided input and approved the final content of this report.
The primary goal of this report is to provide primary care physicians and physician extenders with practical information to assist with the diagnosis and care of patients with TBRD. This report provides a framework for recognizing suggestive symptoms, considering likely alternative diagnoses, eliciting relevant history, requesting appropriate diagnostic tests, and initiating prompt, effective treatment. Information in this guide is designed to assist clinicians to - recognize common epidemiologic situations and clinical manifestations of TBRD; - obtain appropriate history and diagnostic tests for TBRD; - develop a differential diagnosis that includes and ranks TBRD; - make treatment decisions based on epidemiologic and clinical evidence; - recognize that doxycycline is the treatment of choice for both adults and children; - recognize that early and empiric antibiotic therapy can prevent severe morbidity or death; - identify the availability, limitations, and utility of confirmatory laboratory assays; - recognize potential severe manifestations of TBRD; and - report suspected and confirmed cases to appropriate public health authorities to assist with control measures and public health education efforts.
This report also provides resources on TBRD for healthcare and public health professionals. Clinical cases are included for self-evaluation and to reinforce the information presented in this guide. Additional information concerning TBRD in this report is available from medical specialists, various medical societies, CDC, and state and local health authorities.
# Epidemiology of TBRD
RMSF, HME, and HGA are tickborne zoonoses caused by Rickettsia rickettsii, Ehrlichia chaffeensis, and Anaplasma phagocytophilum, respectively. These pathogens are maintained in natural cycles involving wild mammals and hard-bodied (ixodid) ticks. The epidemiologies of these diseases reflect the geographic distribution and seasonal activities of the vectors and reservoirs and the human behaviors that place persons at risk for tick attachment and subsequent infection. Selected epidemiologic and clinical features of TBRD have been summarized (Table 1). RMSF, HME, and HGA are reported each month of the year in the United States, although 90%-93% of reported cases occur during April-September (6,(10)(11)(12), coincident with peak levels of tick feeding activity on humans. Travelers outside of the United States might also be exposed to other tick vectors in other countries that transmit related agents that result in disease after they return to the United States.
Males appear to be at higher risk for infection with all TBRD, possibly because of greater recreational or occupational exposures to tick habitats. Although previous studies have indicated that the highest incidences of RMSF have occurred in children aged 70 and 60-69 years, respectively (14). The higher frequency of disease reporting in adults might reflect greater susceptibility to recognizable disease rather than higher infection rates. Two recent cross-sectional studies in the southeastern and south central United States- have indicated that up to 22% of children have serologic evidence of previous exposure to antigens of both E. chaffeensis (15) and R. rickettsii (16), suggesting that rickettsial and ehrlichial infection might be more common than previously recognized.
# RMSF
In the United States, R. rickettsii is transmitted to humans by several tick species. However, the species that transmit R. rickettsii most frequently include the American dog tick (Dermacentor variabilis; Figure 1) in the eastern, central, and Pacific coastal United States and the Rocky Mountain wood tick (Dermacentor andersoni; Figure 2) in the western United States. In 2005, the brown dog tick (Rhipicephalus sanguineus; Figure 3), a vector of RMSF in Mexico (17), was implicated as a vector of this disease in a confined geographic area in Arizona (18). The cayenne tick (Amblyomma cajennense; Figure 4) is a common vector for RMSF in Central and South America, and its range extends into the United States in Texas (19). During 1997-2002, the estimated average annual incidence of RMSF, based on passive surveillance, was 2.2 cases per million persons. More than half (56%) of reported cases of RMSF were from only five states: North Carolina, South Carolina, Tennessee, Oklahoma, and Arkansas (CDC, unpublished data, 2005). However, cases have been reported from each of the contiguous 48 states, except Vermont and Maine (10,11). Average reported annual incidence of RMSF per 1 million population, based on cases reported to CDC during 1997-2002, has been reported (Figure 5). Incidence varies considerably by geographic area. RMSF is also (17,19,20). Household clusters of disease and hyperendemic foci of infected ticks have been reported (3,21). Dogs are susceptible to RMSF, and they might frequently develop the disease concurrently with other household members in an endemic focus (22,23).
# HME
E. chaffeensis is transmitted to humans by the lone star tick, A. americanum (Figure 6), and possibly other ticks. The white-tailed deer is a major host of all stages of lone star ticks and is an important natural reservoir for E. chaffeensis. Natural infections of coyotes, dogs, and goats
# FIGURE 2. An adult female Dermacentor andersoni (Rocky Mountain wood tick)
Photo/CDC have been documented. The lone star tick is among the most commonly encountered ticks in the southeastern United States, with range extensions into areas of the South Central and New England states (Figure 7). Cases of HME are most commonly reported to CDC from Missouri, Oklahoma, Tennessee, Arkansas, and Maryland, although the disease is found throughout the range of the lone star tick. The average reported annual incidence of HME was 0.7 cases per million population, but incidence varied by state, based on cases reported to CDC from 2001 to 2002 (Figure 8). In a prospective study among febrile patients with a history of a recent tick bite in central North Carolina, the incidence of ehrlichial infection was approximately twice that of RMSF (24). The reported incidence probably represents an underestimate of the true burden of disease in areas where E. chaffeensis is endemic (24,25). Clusters of HME have been reported, suggesting that foci of ticks infected with E. chaffeensis do occur (21,26).
# HGA
The blacklegged tick (Ixodes scapularis; Figure 9) is the vector of A. phagocytophilum in New England and North Central United States, whereas the western blacklegged tick (Ixodes pacificus; Figure 10) is the principal vector in northern California. Deer, elk, and wild rodents are thought to be reservoirs. HGA is more frequently reported than HME, resulting in an average reported annual incidence of 1.6 cases per million during 2001-2002. States that reported the highest incidence during this period were Rhode Island (36.5 cases per million), Minnesota (12.3 cases per million), Connecticut (8.1 cases per million), New York (2.3 cases per million), and Maryland (1.6 cases per million) (Figure 11). HGA has been identified as a substantial cause of unexplained fever during the tick season in Wisconsin (27). Evidence suggests that the incidence of HGA in Wisconsin might be much higher than that in Minnesota (7). Because these Ixodes species ticks also transmit Borrelia burgdorferi (the causative agent of Lyme disease) and various Babesia species (agents of human babesiosis), the preponderance of cases of HGA occur in the same states that report high incidences of Lyme disease and human babesiosis. Simultaneous infection with A. phagocytophilum and B. burgdorferi has been reported (28), and discerning such a mixed infection is vital because it might affect antimicrobial choice. For example, amoxicillin can be used to treat early stage Lyme disease, but it is not effective for HGA.
# Ehrlichia ewingii Infection
Amblyomma americanum also is the principal vector of the ehrlichial pathogen, E. ewingii. (29,30). E. ewingii infections in dogs or ticks also have been described in these states and in Arkansas, Texas, Florida, Georgia, Mississippi, North Carolina, and Virginia, suggesting that human infections with this pathogen might be expected to occur throughout the range of the lone star tick (31,32).
The following is a summary of the salient epidemiologic features of TBRD:
- Occurrence is seasonal, with the majority of illness onset during warmer spring and summer months, but cases might develop throughout the year. - RMSF has been reported in all of the contiguous 48 states, except Vermont and Maine. - RMSF and HME are most commonly reported in the southeastern and south central United States. - HGA is reported most frequently in New England, the north central states, and in focal areas along the West Coast.
# Pathogen Tropisms and Clinical Presentation
R. rickettsii, E. chaffeensis, E. ewingii, and A. phagocytophilum have specific and distinct cell tropisms. R. rickettsii infects endothelial cells and more rarely infects underlying smooth muscle cells, where rickettsiae multiply freely in the cytoplasm. The rickettsiae cause a small-vessel vasculitis, resulting in a maculopapular or petechial rash in the majority of patients. Vasculitis occurring in organs (e.g., the brain or lungs) can result in life-threatening complications. R. rickettsii does not stain with the majority of routine histopathologic stains and is not detected by blood smear evaluation because of limited numbers of circulating bacteria. Ehrlichioses and anaplasmosis are characterized by infection of leukocytes, where the causative agents multiply in cytoplasmic membrane-bound vacuoles as microcolonies called morulae. E. chaffeensis most frequently infects monocytes, whereas A. phagocytophilum and E. ewingii demonstrate a predilection for granulocytes. Morulae may be stained with conventional Wright or Giemsa stains and are occasionally observed in leukocytes in smears of peripheral blood, buffy coat preparations, or cerebrospinal fluid. In this context, a routine blood smear can provide a presumptive clue for early diagnosis; however, the visualization of morulae still requires confirmatory testing for Ehrlichia or Anaplasma species by serology, polymerase chain reaction (PCR), or immunostaining methods (33). The demonstration of morulae is also not sensitive, and a case of ehrlichiosis or anaplasmosis might be missed if the diagnosis relies solely on detection of morulae on blood smears. Although the diagnostic sensitivity of a blood smear is greater for HGA than for HME, blood smears might only be positive in up to 60% of patients with HGA (34).
The following is a summary of salient features of pathogen tropisms:
- R. rickettsii infects endothelial cells, causing vasculitis, which leads to rash and life-threatening damage to the brain, lungs, and other viscera. - R. rickettsii is not evident in blood smears, and these bacteria and do not stain with the majority of conventional stains. - Ehrlichia and Anaplasma species infect monocytes or granulocytes, respectively, and morulae might occasionally be observed on peripheral blood smears by using routine stains.
# Clues from the Clinical History
A thorough clinical history that elicits recent tick exposure, specific recreational or occupational exposures to tickinfested habitats, recent travel to areas where TBRD might be endemic, or similar illnesses in family members, coworkers, or pet dogs can provide critical information that can be used to make a presumptive diagnosis of TBRD and help guide subsequent therapeutic actions. However, the absence of certain features does not exclude a diagnosis of TBRD. These features include 1) history of tick bite or exposure, 2) recent travel to areas endemic for TBRD, and 3) similar illness in family members, coworkers, or pets.
# History of Tick Bite or Exposure
A detailed medical history might reveal activities that suggest potential exposure to ticks. Outdoor activities during April-September, particularly in areas with high uncut grass, weeds, and low brush can increase the risk for tick bites (35). These activities include recreational pursuits (e.g., camping, hiking, fishing, hunting, gardening, and walking dogs) as well as occupational activities that involve persons being in brushy or grassy areas that might be inhabited by ticks. Vegetation that borders roads, trails, yards, or fields also are potential areas that might be inhabited by ticks. In endemic areas (where the agents causing TBRD are present at all times), even adults or children who play in grassy areas in their backyard are at risk. Queries concerning frequency of contact with family pets, especially dogs, and findings of tick attachment to animals or removal can be useful. The majority of patients will not recall or recognize an attached tick because the location of the tick might be obscure; the bite is typically painless; and bites from smaller immature stages of ticks (e.g., nymphs are approximately 1-2 mm or the size of the head of a pin; Figure 12) might not be readily detected but might still result in infection. A specific history of a tick bite within 14 days of illness onset is typically only reported in 60% of RMSF cases (10,11) and has been reported in only 68% of ehrlichiosis cases (6). Therefore, the absence of definite tick attachment should never dissuade a physician from considering the diagnosis of a TBRD. Finally, certain patients do not specifically recall tick exposure but might describe other pruritic, erythematous, or ulcerated cutaneous lesions that they call a mosquito bite, spider bite, chigger bite, or bug bite, which can be indistinguishable from an actual tick bite.
# Recent Travel to Areas Endemic for TBRD
Clinicians in areas of the United States where the incidence of TBRD is historically low are typically at a disadvantage in distinguishing these diseases among multiple other infectious and noninfectious syndromes that they resemble. Because TBRD are typically sporadic, identifying these infections requires high clinical acumen, especially in an environment in which TBRD have not previously been recognized as occurring frequently.
Knowledge of the epidemiology of these illnesses, including regions of the country with a high incidence (number of reported cases per million persons per year) of TBRD (e.g., south Atlantic, north central, and south central and New England states), is important. A history of recent travel from an endemic area of TBRD (e.g., within 2 weeks preceding illness), especially if the patient had participated in an outdoor activity, might support a suspicion of tickborne illness. Physicians should also consider the possibility that changes in tick vector range can influence the distribution of TBRD. In addition, in 2004, a total of 13 cases of RMSF occurred in eastern Arizona, a state in which the disease was previously rarely diagnosed (18).
Clinicians should also consider that TBRD occur worldwide and might have epidemiologic, seasonal, and clinical features distinct from those observed in the United States. International travel to destinations (e.g., southern Mediterranean, Central and South America, Africa, Asia, and the Middle East) might result in tick vector exposure, particularly if the patient participated in rural or outdoor activities. For example, African tick-bite fever (ATBF), an increasingly reported travel-related rickettsiosis caused by R. africae, has an estimated incidence of 4%-5.3% among international travelers to sub-Saharan Africa and has been identified in clusters of infection among group travelers (e.g., game hunters, safari tourists , and humanitarian workers; 37). A related rickettsial organism, R. conorii, endemic in the Mediterranean basin, Middle East, and parts of Africa and the Indian subcontinent causes Mediterranean spotted fever (MSF; 38). ATBF and MSF are characterized by fever, malaise, headache, and myalgia, which are typical symptoms for other TBRD. However, a distinguishing clinical feature of both travel-related diseases is the development of one or more eschars (a dark, scab-like plaque overlying a shallow ulcer with surrounding erythema or scaling) at the site of tick attachment that is noted coincident with or shortly after the onset of fever in 30%-50% of patients (36,39).
# Emerging TBRD
Similarly, considering TBRD as a diagnosis is essential because of new, previously unrecognized rickettsial pathogens that have been observed in tick vectors in the United States. For example, in 2002, R. parkeri was identified as a new cause of spotted fever rickettsiosis in a patient living in the southeastern coastal United States (40). This agent is present in A. maculatum (the Gulf Coast tick; Figure 13), which is found in the southeastern United States. A clinical presentation, similar to ATBF and MSF (i.e., fever, headache, eschars, and regional lymphadenopathy), was observed in a patient with no substantial travel history (Figure 14). The diagnosis of spotted fever rickettsiosis was confirmed by using rickettsial culture from an eschar skin biopsy and serologic and molecular methods (40). Other spotted fever group rickettsiae might also cause mild febrile illness in certain persons exposed to ticks in highly endemic areas (41). The common observation of antibodies to rickettsiae and ehrlichiae in persons and dogs might indicate expo-sure to other rickettsial agents of varying pathogenicity (15,16,24).
# Similar Illness in Family Members, Coworkers, or Pets
Clinicians might be inclined to offer diagnoses of a communicable viral infection when more than one family member is affected by an illness. However, clustering of certain TBRD is a well-recognized epidemiologic phenomenon and might occur after exposure to natural foci of infected ticks. Temporally and geographically related clusters occurring among family members, coworkers, or persons frequenting a particular common area have been observed. These clusters include family clusters of RMSF (3), clusters of ehrlichiosis among residents of a golfing community (26), and soldiers on field maneuvers (21). Common exposures to tick-infested habitats or outdoor activities might place certain or all members of a family or group, including pet dogs, at risk for TBRD. Concurrent infections with R. rickettsii and Ehrlichia species also have been observed in humans and dogs (22,24,29). Therefore, clinicians should query patients concerning similar illnesses among family members, close coworkers, or community residents, and even among household dogs.
The following is a summary of salient features of clues from the clinical history:
- A detailed history of recent recreational or occupational activities might reveal potential exposure to ticks. - Exposure can occur in the patient's backyard or neighborhood. - Familiarity with TBRD epidemiology will be helpful when querying patients regarding recent travel to endemic areas (domestic and international; 38,39). - Clustering of certain TBRD is well-recognized and has been reported among family members, coworkers, and other defined groups.
# Clinical Assessment
# Signs and Symptoms
The early signs and symptoms of HME, HGA, RMSF, and E. ewingii infection might resemble nonspecific findings of other infectious and noninfectious diseases. The majority of patients with TBRD visit a physician during the first 2-4 days of illness, after an incubation period of approximately 5-10 days after a tick bite (5). Patients with HGA might seek medical care later (4-8 days after fever onset) (7). Substantial overlap occurs in the initial clinical presentation of the three diseases. Initial symptoms commonly include a sudden onset of fever, chills, and headache, commonly associated with malaise and myalgia. In adults, photophobia might be observed. Headache is nearly always reported by adults who seek medical care and can be severe. Patients also might report nausea, vomiting, and anorexia early in the course of their illness, especially with RMSF (35) and HME in children. Diarrhea might occasionally occur. Other frequently observed signs and symptoms in children with either RMSF or HME are abdominal pain, altered mental status, and conjunctival injection. Abdominal pain might be severe enough to mimic appendicitis or other causes of acute abdominal pain (42). Certain findings described in medical textbooks are less commonly observed by clinicians and include bilateral periorbital edema, edema of the dorsum of hands and feet, and calf pain and tenderness. Because the signs and symptoms that persons have when they first seek medical care are nonspecific, clinicians frequently must incorporate clues from the clinical and epidemiologic history and consider other features (e.g., the presence of rash or abnormalities of routine laboratory tests).
In RMSF, a rash typically appears 2-4 days after onset of fever; however, the majority of patients will seek medical care before this period. For adults and children with RMSF, rash frequently occurs earlier in children than in adults (43) and is eventually observed in approximately 90% of children. The exanthem typically begins as small, blanching, pink macules on the ankles, wrists, or forearms that evolve to maculopapules (Figure 15). In half of cases, the rash might evolve to petechiae over the next several days of illness. The classic centripetal spread of rash is typically not noticed by the patient and might be difficult to elicit from the clinical history. The rash can expand to involve the entire body, including the palms and soles, but its presence on the face is usually limited. Discerning the rash in darker-skinned persons might be difficult. The classic spotted or generalized petechial rash of RMSF is usually not apparent until the fifth or sixth day of the illness and signifies progression of the disease, although the progression is considerably variable (Figure 16). Patients with petechial rash are often severely ill, and although fever and organ dysfunction might resolve quickly with treatment, complete recovery can take longer to occur. The rash progression of RMSF includes several critical exceptions and considerations.
- A rash on the palms and soles is not pathognomonic and might occur in illnesses caused by drug hypersensitivity reactions, infective endocarditis, and a diverse group of other agents, including Treponema pallidum, Neisseria meningitidis, Streptobacillus moniliformis, E. chaffeensis, and certain enteroviruses. - The rash might be evanescent or localized to a particular region of the body.
- A rash might be completely absent or atypical in up to 20% of RMSF cases (4,43,44). Rash is observed in approximately one third of all patients with HME (although rash is described in up to 66% of children) and is rare in patients with HGA or E. ewingii infection (45,46). For children with HME and a rash, distinguishing the condition from RMSF might be difficult. Rash patterns occasionally associated with HME vary in character from petechial or maculopapular (Figure 17; 47) to diffuse erythema (48) and typically occur later in the course of disease (median: 5 days after onset; 6).The rash patterns might involve the extremities, trunk, face or, rarely, the palms and soles (49).
In certain cases, patients with RMSF or ehrlichiosis might seek medical attention for a febrile illness that mimics viral meningoencephalitis. Focal neurologic deficits, including cranial or peripheral motor nerve paralysis or sudden transient deafness, might also be observed (50).
# Differential Diagnosis of Febrile Patients with Rash
The differential diagnosis of febrile patients with rash is broad. The onset of TBRD is frequently rapid, and the majority of patients experience high fever, shaking chills, severe headache, and generalized myalgias, in contrast to other tickborne diseases (e.g., Lyme disease). Tickborne viral fevers (e.g., Colorado tick fever) infrequently cause rash but should be included in the differential diagnoses of TBRD, particularly when leukopenia and thrombocytopenia are present in a patient who has recently traveled to the western United States. Clinically, TBRD might be essentially indistinguishable from the majority of viral infections, particularly those in children. The dermatologic classification of the rash, its distribution, pattern of progression and timing relative to onset of fever, and other systemic signs provide clues that help the clinician rule out other exanthemata. Maculopapular rashes might occur in association with multiple condi-tions, including human herpesvirus 6 infection (i.e., roseola), human parvovirus B19, enteroviral infection (e.g., coxsackievirus and echovirus), Epstein-Barr virus infection, disseminated gonococcal infection, Mycoplasma pneumoniae infection, leptospirosis, secondary syphilis, Kawasaki disease, thrombotic thrombocytopenic purpura (TTP), drug reactions, and immune complex-mediated illness (51). A petechial rash can occur in association with meningococcal infection, enteroviral infection, immune thrombocytopenic purpura, and after group A streptococcal pharyngitis. R. rickettsii infection is noted for causing a rash on the soles and palms, although this distribution typically occurs late in RMSF and in only half of cases, whereas in the majority of other bacterial or viral infections rash has not been observed. Initially, clinicians might experience difficulty distinguishing N. meningitidis infection from RMSF because both can begin as a maculopapular rash and progress to a petechial rash, but the rash and other clinical features progress more rapidly in meningococcemia than in RMSF. Selected infectious causes and features of maculopapular and petechial rash illnesses have been reported (Table 2). Other exanthematous diseases that can occasionally be confused with TBRD include toxic-shock syndrome, erythema multiforme, and Stevens-Johnson syndrome.
# Laboratory Findings
Obtaining a complete blood cell count (CBC), comprehensive metabolic panel, and examination of peripheral blood smear are essential when considering a diagnosis of TBRD. The total white blood cell (WBC) count is typically normal in patients with RMSF, but increased numbers of immature bands are generally observed. Thrombocytopenia, mild elevations in hepatic transaminases, and hyponatremia might be observed with RMSF (35), whereas leukopenia (up to 53% of patients), thrombocytopenia (up to 94% of patients), and modest elevations of liver transaminase levels are particularly suggestive of HME and HGA (52,53). An inverse relation has been reported between the mean WBC and platelet count and the probability that HGA is the cause of nonspecific fever (53). Blood smears might be useful in identifying patients with HGA (34) or E. ewingii infection. Nonspecific changes in the concentrations of routine laboratory parameters that have been observed for patients infected with E. chaffeensis (52) or A. phagocytophilum have been reported (53; Table 3).
Cerebrospinal fluid (CSF) analysis might be a useful adjunct to laboratory diagnosis of TBRD. When CSF is evaluated in patients with RMSF or HME, a pleocytosis (usually <100 cells/microliter) is typically observed (with either a polymorphonuclear or lymphocytic predominance), whereas CSF evaluated in E. ewingii infection is characterized by a neutrophilic pleocytosis (29). Moderately elevated protein (100-200 mg/dL) and normal glucose levels also are commonly observed in patients with RMSF (54,55).
A Gram stain indicating gram-negative diplococci, very low glucose (i.e., <20-30 mg/dL), or neutrophilic pleocytosis is more suggestive of meningococcal meningitis. Clinicians should distinguish TBRD-related CNS involvement from other infections (e.g., N. meningitidis); however, in the majority of patients, reliably distinguishing between RMSF, HME, and meningococcal infection based on laboratory testing is difficult (unless a pathogen is cultured). Therefore, empiric treatment for both TBRD and meningococcemia is necessary for ill patients with fever and rash and for patients in whom neither disease can be ruled out.
The following is a summary of salient clinical assessment features:
- Early clinical presentations of HME, HGA, RMSF, and E. ewingii infection include fever, headache, myalgia, and malaise and are difficult to distinguish from other infectious and noninfectious diseases.
- Patients with RMSF typically do not have a spotted or petechial rash when they initially seek medical care during the first 2-4 days of illness. - A CBC, metabolic panel, and peripheral blood smear examination are helpful in developing both a differential diagnosis and treatment approach to TBRD. - CSF analysis might reveal neutrophilic or lymphocytic pleocytosis and elevated protein but might not reliably distinguish TBRD and meningococcal disease, necessitating empiric antibiotic therapy for both conditions when indicated. - Leukopenia, thrombocytopenia, mild hyponatremia, and mildly elevated hepatic transaminase levels are common and particularly useful clinical features of TBRD, although the absence of these features does not exclude a diagnosis of TBRD. - Infrequent features of TBRD include severe abdominal pain and meningoencephalitis. - Rash is observed frequently in RMSF, occasionally in HME, and rarely in HGA or E. ewingii infection.
# Treatment and Management
An assessment of clinical signs and symptoms, along with laboratory diagnostic tests and a thorough clinical history, will help guide clinicians in developing a differential diagnosis and treatment plan. At least 50% of patients with TBRD might need to be hospitalized. Patients with evidence of organ dysfunction and severe thrombocytopenia, mental status changes, and the need for supportive therapy should be hospitalized. Essential considerations include social factors, the likelihood that the patient can and will take oral medications, and existing comorbidities. For example, a patient who appears well, has acute febrile illness and an unrevealing history and physical examination, and whose laboratory indices are within normal limits might warrant a "wait and watch" approach for 24 hours with reassessment if the patient fails to improve. If laboratory testing of a patient with a history compatible with TBRD reveals leukopenia or thrombocytopenia, or metabolic abnormalities, the clinician should consider obtaining blood cultures for other likely pathogens and specific laboratory tests and initiating empiric oral antimicrobial therapy that will effectively treat TBRD. Certain patients with TBRD can be treated on an outpatient basis with oral medication, particularly if a reliable caregiver is available in the home and the patient is compliant with follow-up medical care. When other diagnoses are under consideration, empiric treatment for these conditions can be incorporated into the therapeutic plan. For example, for a patient's con-dition in which meningococcal disease cannot be ruled out, intramuscular ceftriaxone should be administered in addition to oral doxycycline to provide activity against possible meningococcal infection, pending culture results. Inpatient observation and assessment of the blood cultures after 24 hours of incubation should be considered for such patients. A critical step is for clinicians to keep in close contact with patients who are treated in the outpatient setting to ensure that they are responding to therapy as expected.
Appropriate antibiotic treatment should be initiated immediately when a clinician suspects that the diagnosis could be RMSF, HME, HGA, or E. ewingii infection, based on clinical, laboratory, or epidemiologic findings. Delay in treatment can lead to severe disease and fatal outcome for TBRD (2)(3)(4). Because each of the agents causing TBRD is susceptible to tetracycline-class antibiotics, these drugs, particularly doxycycline, are considered the therapy of choice in nearly all clinical situations. Fever typically subsides within 24-48 hours after treatment when the patient receives doxycycline or another tetracycline during the first 4-5 days of illness. If a patient fails to respond to early treatment with a tetracycline antibiotic (i.e., within 48 hours), this response might be an indication that their condition is not a TBRD. Severely ill patients might require longer periods before clinical improvement is noted, especially if they have multiple organ dysfunction. Doxycycline is the drug of choice for treatment of all TBRD in children and adults. This drug is bacteriostatic in its activity against rickettsial organisms. The recommended dose is 100 mg per dose administered twice daily (orally or intravenously) for adults or 2.2 mg/kg body weight per dose administered twice daily (orally or intravenously) for children weighing <100 lbs. (45.4 kg). Intravenous therapy is frequently indicated for hospitalized patients, and oral therapy is acceptable for patients considered to be early in the disease and who can be managed as outpatients. Oral therapy also can be used for inpatients who are not vomiting or obtunded. The optimal duration of therapy has not been established, but current recommendations for RMSF and HME are for treatment for at least 3 days after the fever subsides and until evidence of clinical improvement is noted, which is typically for a minimum total course of 5-7 days. Severe or complicated disease might require longer treatment courses. Patients with HGA should be treated with doxycycline for 10-14 days to provide appropriate length of therapy for possible incubating coinfection with Lyme disease (45).
The use of tetracyclines to treat children with TBRD is no longer a subject of controversy (56)(57)(58). Concerns regarding dental staining after tetracycline therapy have been based primarily on studies conducted during the 1960s that involved children receiving multiple courses of the drug for recurrent otitis media (59,60). The propensity of tetracyclines to bind calcium can lead to darkening of the teeth if the antibiotic is ingested during the period of tooth crown formation. More recent studies in 1971 and 1998, however, have demonstrated that although multiple exposures to tetracycline increase the risk for tooth staining, limited use of this drug in children during the first 6-7 years of life has a negligible effect on the color of permanent incisors (56,57). Beyond ages 6-7 years, the risk for tetracycline staining is of minimal consequence because visible tooth formation is complete. Moreover, a prospective study of children treated with doxycycline for RMSF demonstrated that these children did not have substantial discoloration of permanent teeth compared with those who had never received the drug (56). Because TBRD can be life-threatening and limited courses of therapy with tetracycline-class antibiotics do not pose a substantial risk for tooth staining, the American Academy of Pediatrics Committee on Infectious Diseases revised its recommendations in 1997 and has identified doxycycline as the drug of choice for treating presumed or confirmed RMSF and ehrlichial infections in children of any age (61,62).
Chloramphenicol is an alternative drug that has been used to treat RMSF (50); however, this drug is associated with various side effects and might require monitoring of blood indices. Chloramphenicol is no longer available in the oral form in the United States. Moreover, epidemiologic studies in which CDC case report data have been used suggested that patients with RMSF treated with chloramphenicol have a higher risk of dying than persons who received a tetracycline (11,63). In vitro evidence also indicates that chloramphenicol might not be an effective antibiotic for HME or HGA (64,65). Clinicians who suspect a TBRD and are considering empiric antibiotic therapy before laboratory confirmation should be aware that doxycycline provides therapeutic coverage for RMSF, HME, HGA, and E. ewingii infection.
Tetracyclines are generally contraindicated for use in pregnant women because of risks associated with malformation of teeth and bones in the fetus and hepatotoxicity and pancreatitis in the mother (66). However, tetracycline has been used successfully to treat HME in pregnant women (67), and the use of tetracyclines might be warranted during pregnancy in life-threatening situations where clinical suspicion of TBRD is high. Whereas chloramphenicol is typically the preferred treatment for RMSF during pregnancy, care must be used when administering chloramphenicol late during the third trimester of pregnancy because of risks associated with grey baby syndrome (66). Substantially limited clinical data exist that support the use of other antimicrobials during pregnancy, although rifampin has been used successfully in several pregnant women with HGA (68). In vitro studies have demonstrated that rifamycins provide effective activity against Ehrlichia and Anaplasma species (64,65), and therapy with rifampin may be considered for patients with HGA who are unsuited for tetracycline treatment because of pregnancy or a history of drug allergy (45). Clinicians should use caution, however, in ensuring that RMSF can be ruled out because the clinical presentations of RMSF and anaplasmosis are similar, and the comparative effectiveness of rifampin and doxycycline is unknown at this time.
Because certain patients with TBRD might initially receive an alternative diagnosis, they might be empirically treated with antibiotics inactive against rickettsiae, including penicillins, cephalosporins, aminoglycosides, erythromycin, or sulfonamides. This situation presents both diagnostic and therapeutic challenges. In certain cases, patients treated with beta-lactam antibiotics or sulfacontaining drugs are mistakenly thought to have drug eruptions when they later manifest a rash (66), further postponing a correct diagnosis and appropriate treatment. Because the physician might conclude that the prescribed treatment will take time to work, a delay in obtaining critical additional laboratory or clinical information also might be a result. In addition, sulfa-containing antimicrobials have been associated with increased severity of TBRD, although whether disease severity is directly related to the use of sulfa-containing drugs or the delayed administration of more effective antimicrobials is not clear. Cases of severe ehrlichiosis complicated by acute respiratory distress syndrome have been associated with the use of trimethoprim-sulfamethoxazole (69,70).
In addition, clinicians should note the overlap between early symptoms of invasive meningococcal infection and TBRD. These conditions are difficult to distinguish early in the course of illness. In patients for whom both conditions are included in the initial differential diagnoses, after performing blood cultures and a lumbar puncture, empirically treating for both diseases is appropriate. This treatment can be accomplished by adding an appropriate parenteral penicillin or cephalosporin that has activity against N. meningitidis to doxycycline therapy.
Preventive antibiotic therapy for rickettsial infection is not indicated for patients who have had recent tick bites and are not ill. Limited numbers of ticks in areas where tickborne diseases are endemic are infected with pathogenic rickettsiae. Approximately 1%-3% of vector ticks are infected with spotted fever group rickettsiae (71). How- ever, less than 1% of these rickettsiae usually have been confirmed to be R. rickettsii (72,73). Approximately 5%-15% of lone star ticks are infected with E. chaffeensis (47), and 10%-50% of I. scapularis ticks are reported to be infected with A. phagocytophilum (74,75) in endemic areas. Therefore, the risk for such infection after a tick bite is low. Moreover, for RMSF, preventive therapy has been demonstrated to delay but not prevent the onset of symptoms (76).
The following is a summary of salient features of treatment and management:
- Clinical history, symptoms, and physical and laboratory findings should guide the clinician's approach to patient management and treatment. - Not all patients with TBRD will require hospitalization.
- Clinicians may consider a wait and watch approach for 24-48 hours for patients early in the course of illness and who have nonsupporting history, nonspecific clinical signs, and normal laboratory findings. - Doxycycline is the drug of choice for the treatment of presumptive or confirmed TBRD in both adults and children. - Limited courses of tetracycline-class antibiotics (e.g., doxycycline) do not pose a substantial threat of tooth staining in children. - Tetracyclines typically are contraindicated for use during pregnancy but might be warranted in lifethreatening situations where clinical suspicion of TBRD is high. - Delay in treatment can lead to severe disease and fatal outcome of TBRD. - In evaluating for TBRD, when early invasive meningococcal infection cannot be ruled out, providing treatment for both conditions by adding an antimicrobial that has activity against N. meningitidis is appropriate. - Prophylactic use of antibotics after a tick bite is not recommended.
# Considerations for Management of Patients with Severe Manifestations of TBRD
A substantial number of patients with TBRD require hospitalization (6,7,10). Severe manifestations of TBRD might include prolonged fever, renal failure, disseminated intravascular coagulopathy (DIC), hemophagocytic syndrome, meningoencephalitis, and acute respiratory distress syndrome. A notable exception is that HGA has not been associated with meningoencephalitis.
RMSF is frequently a severe illness, and patients commonly require hospitalization. Up to 20% of untreated cases and 5% of treated cases have fatal outcome, making RMSF the most commonly fatal rickettsial disease in the United States (5,10). However, assessment of passive reporting of RMSF-associated death has suggested that only one third of fatal cases of RMSF were reported to CDC during 1983-1998 (77). Therefore, the actual case-fatality rate of RMSF might be closer to 5%-10%. Host factors associated with severe or fatal RMSF include advanced age, male gender, black race, chronic alcohol abuse, and glucose-6-phosphatedehydrogenase (G6PD) deficiency (50). Deficiency of G6PD is a sex-linked genetic condition affecting approximately 12% of the U.S. black male population; deficiency of this enzyme is associated with a high proportion of fulminant cases of RMSF (50,78). Fulminant cases follow a clinical course that is fatal within 5 days of onset. Longterm health effects persisting for >1 year after acute RMSF infection include partial paralysis of the lower extremities; gangrene requiring amputation of fingers, toes, arms, or legs; hearing loss; blindness; loss of bowel or bladder control; movement disorders; and speech disorders (79). These complications are observed most frequently in persons recovering from severe, life-threatening disease, often after lengthy hospitalizations. Digital necrosis in a patient occurring late in the course of RMSF has been illustrated (Figure 18).
Similarly, HME and HGA can cause serious or fatal disease as well, although at lower rates than are observed for RMSF. At least 50% of patients with HGA and HME are hospitalized to rule out other potentially life-threatening conditions and to manage the illness (34,47). Clinical indications for admission might include immunocompromised state, pain management (i.e., headache and myalgias), mental confusion, cough, infiltrate in chest radiograph, abnormal spinal fluid findings, or specific acute organ failure. Approximately 3% of HME patients and less than 1% of HGA patients with symptoms severe enough to seek medical attention will die from the infection (25,34,47). The severity of ehrlichiosis might be related, in part, to the immune status of the patient. Persons with compromised immune systems caused by immunosuppressive therapies (e.g., corticosteroids or cancer chemotherapy), human immunodeficiency virus (HIV) infection, organ transplantation, or splenectomy appear to develop more severe disease from E. chaffeenis infection, and case-fatality rates for these persons are characteristically higher than casefatality rates reported for the general population (30). Although the case fatality rate for HGA (0.5%-1.0%) is lower than that for HME, notable complications, including respiratory failure, a toxic-shock-like syndrome, rhabdomyolysis, pancreatitis, acute renal failure, and invasive infections caused by opportunistic viral or fungal agents can occur, especially among patients who have co-morbid illnesses or who are actively immunosuppressed (45). In addition, advanced patient age and delay in diagnosis and the onset of specific antibiotic therapy are predictors of a more severe course of HGA (53).
Management of severely ill patients with TBRD should include careful assessment of fluid and electrolyte balance. Vasopressors and rigorous fluid management might be needed, especially when the illness is complicated by renal failure or hypotension. Patients might have pulmonary infiltrates because of vasculitis that are erroneously thought to be caused by cardiac failure or pneumonia. Seizures might require aggressive treatment, and arrhythmias (e.g., atrial fibrillation or flutter) will frequently respond to treatment of the patient's underlying disease. Consultation with an intensivist or an infectious disease subspecialist might be helpful in managing these complications.
The following is a summary of salient features of severe manifestations:
- TBRD can be life-threatening.
- Severe manifestations of TBRD include prolonged fever, renal failure, myocarditis, meningoencephalitis, hypotension, acute respiratory distress syndrome, and multiple organ failure.
# Confirmatory Diagnostic Tests
Rickettsial infections pose difficult diagnostic challenges to both clinicians and laboratorians. Rapid confirmatory assays are not commonly available to guide treatment decisions of acutely ill patients. However, confirmatory assays provide the physician with vital information that retrospectively validates the accuracy of the clinical diagnosis. Laboratory confirmation of infection is also vital to understanding the epidemiology and public health impact of TBRD.
Several laboratory methods are available to diagnose TBRD. However, they vary in the time required to obtain results and in the type of information they provide the clinician. Therefore, treatment decisions should be based on epidemiologic and clinical clues and should never be delayed while waiting for laboratory confirmation of a diagnosis. Similarly, test results should be interpreted in the context of the patient's illness and the epidemiologic setting. Misuse of specialized tests for patients with a low probability of the disease and in areas with a low prevalence of disease might result in confusion. A fundamental understanding of the signs, symptoms, and epidemiology of the disease is critical in guiding requests for tests and interpretation of test results for ehrlichioses, anaplasmosis, and RMSF. Studies have suggested that antibiotic therapy might diminish the development of convalescent antibodies in RMSF (CDC, unpublished data, 2005). However, the degree to which doxycycline might cause this occurrence is uncertain. If molecular or culture diagnostic methods are conducted, obtaining blood for testing before antibiotics are administered is essential to obtain the best results.
# Blood-Smear Microscopy
Microscopic examination of blood smears stained with eosin-azure type dyes (e.g., Wright-Giemsa stain) might reveal morulae in the cytoplasm of infected circulating leukocytes (1%-20%) of patients with HME and 20%-80% of patients with HGA (45,47) during the first week of infection, which is highly suggestive of ehrlichial or anaplasma infection. However, blood smear examination is insensitive and should be performed by an experienced microscopist. In addition, a negative blood smear examination should not dissuade the caregiver from initiating treatment with doxycycline if the clinical presentation and routine laboratory findings support the diagnosis of ehrlichiosis or anaplasmosis. Blood smear examination is not useful for diagnosis of RMSF.
# Serologic Testing
Serologic assays for RMSF, HME, and HGA are commonly available through multiple commercial and state public health laboratories. Serologic evaluations are commonly conducted by using the indirect immunofluorescence antibody (IFA) assay. Antibodies in the serum bind to fixed antigens on a slide and are detected by a fluorescein-labeled conjugate. Although IFA remains the principle diagnostic tool for the diagnosis of rickettsial and ehrlichial infections, no standardized antigens, conjugates, or agreement on what consti-tutes a positive result among the various laboratories providing these tests exist. Individual laboratories should be consulted regarding their test threshold levels. Enzyme-linked immunosorbent assay (ELISA) is becoming a more frequently used assay. Similar to IFA, the accuracy of ELISA depends on the laboratory conducting the test, the quality and specificity of the antigen, and the threshold levels at which a positive result is considered. Available ELISA tests are qualitative and cannot be used effectively to monitor increases or decreases in antibody titer.
The sensitivity of the IFA assay is substantially dependent on the timing of collection of the sample. Early in any TBRD, a majority of serologic tests will be negative. Clinical illness nearly always precedes laboratory diagnosis by any method. As the illness progresses to 7-10 days, the sensitivity of IFA serology increases. The IFA is estimated to be 94%-100% sensitive after 14 days, and that sensitivity is increased if paired samples are tested (80). The IFA is considered to be the gold standard of serologic testing for rickettsial diseases, and other serologic tests have not been developed that surpass the sensitivity and specificity of these assays. Testing two sequential serum or plasma samples together to demonstrate a rising IgG or IgM antibody level is essential to confirm acute infection. Paired serum specimens taken early (i.e., acute) and later (i.e., convalescent) in the disease course represent the preferred specimens for evaluation. Typically, these specimens should be taken at least 2-3 weeks apart to examine for a four-fold or greater increase in antibody titer (33).
The majority of patients demonstrate increased IgM or IgG titers by the second week of the illness (patients infected with certain imported rickettsiae might not demonstrate increased titers until 4 weeks after illness onset). However, patients might lack diagnostic IgG and IgM antibody titers in the first 7 days of illness, a period when the majority of patients initially seek medical care and laboratory testing is performed. The duration of time that antibodies will persist after recovery from the infection is variable. In certain persons, high titers of antibodies against A. phagocytophilum have been observed for 3½ years after the acute illness (81). For RMSF, IgG and IgM titers increase concurrently by the second week of illness, and IgM antibodies wane after 3-4 months, whereas IgG titers persist for 7-8 months (82). The majority of commercial reference laboratories conduct testing for IgG and IgM antibodies.
Cross-reactivity of antigens results in antibody responses that are typically group-specific, but not necessarily species-specific, after infections with these pathogens. For example, serologic tests that detect antibodies reactive with R. rickettsii might have resulted from previous infections with other spotted fever group rickettsial species. Similarly, antibodies reactive with E. chaffeensis or A. phagocytophilum occasionally react with the other ehrlichial species, which might impede epidemiologic distinction between the ehrlichial infections (83). Most patients with E. ewingii infections develop antibodies that react with E. chaffeensis antigens. Little cross-reactivity of Rickettsia with Ehrlichia or Anaplasma species exists. Certain serologically confirmed cases of infection thought to be RMSF, HME, or HGA might represent infections with the other agent or with another antigenically related species. The predominance of non-R. rickettsii species in tick vectors collected in RMSFendemic areas suggests that related organisms of undetermined pathogenicity might play a role in human illness (84). This occurrence is especially true for persons who are infected with rickettsial organisms from endemic areas outside of the United States.
# Nucleic Acid Detection
Amplification of specific DNA by PCR provides a rapid method for detecting TBRD infections. These tests are available from CDC, certain state health laboratories, and a limited number of research and commercial laboratories (Box). Conventional PCR tests have no specified standard, and diagnostic sensitivity and specificity might vary among individual assays (80). Doxycyline treatment, in particular, can also decrease the sensitivity of PCR (45). In studies of A. phagocytophilum infection, PCR was estimated as 60%-70% sensitive (53), and for diagnosis of infection with E. chaffeensis, PCR was estimated to be 52%-56% sensitive (25) to 87% sensitive (85). For RMSF, PCR is probably more useful for detecting the etiologic agent in a skin biopsy or autopsy tissue specimen than it is in an acute blood sample because, typically, low numbers of rickettsiae circulate in the blood in the absence of advanced disease or fulminant infection (18). PCR testing of skin biopsies alone does not offer ideal sensitivity, and a negative result does not exclude the diagnosis because of focality of vessel involvement. Laboratory confirmation of RMSF in the acute stage is improved when PCR is used in conjunction with IHC staining. PCR of whole blood specimens is more useful for confirming HME, HGA, and E. ewingii infection because of the tropism of these pathogens for circulating WBC. However, no optimal time frame has been established that is ideal for sample collection to ensure the highest sensitivity for diagnosing ehrlichioses or anaplasmosis. New techniques (e.g., real-time PCR) might offer the advantages of speed, reproducibility, quantitative
# IHC Staining
Another approach to diagnosing TBRD is immunohistochemical (IHC) staining of antigens in formalin-fixed, paraffin-embedded biopsy or autopsy tissues. This test can be particularly useful to diagnose fatal TBRD in those patients for whom diagnostic levels of antibodies have not developed before death. For patients with a rash, IHC or immunofluorescence staining of a skin biopsy can be a critical diagnostic technique for RMSF. Immunostaining of skin biopsy specimens has been reported to be 100% specific and 70% sensitive in diagnosing RMSF (35). This method has been used to diagnose fatal and nonfatal cases of RMSF (18,(87)(88)(89). Because rickettsiae might be focally distributed in tissue, this test might not always detect the agent. Autopsy tissues also are appropriate for evaluation and include the liver, spleen, lung, heart, kidney, and brain. The IHC method is most useful in documenting the presence of organisms in patients before initiation of antibiotic therapy or within the first 48 hours after antibiotic therapy has been initiated. IHC techniques also are available for diagnosing cases of ehrlichioses and anaplasmosis from bone marrow biopsies and tissue obtained at autopsy of fatal cases, including the spleen, lymph nodes, liver, and lung (90)(91)(92). Immunostaining for spotted fever group rickettsiae, E. chaffeensis, and A. phagocytophilum is offered by CDC and certain university-based hospitals and commercial laboratories in the United States (Box).
# Culture
Because the agents that cause TBRD are obligate intracellular pathogens, they must be isolated by using cell culture techniques that are typically more labor-intensive and timeconsuming than serologic, molecular, or IHC assays. Theoretically, any laboratory capable of performing routine viral isolations might have the expertise to isolate these pathogens. However, R. rickettsii is classified as a Biosafety Level-3 (BSL-3) agent, and attempts to isolate this agent should be made only in laboratories equipped to handle BSL-3 pathogens (93). Laboratories attempting culture of R. rickettsii bacteria need to comply completely with federal regulations (42 C.F.R. ) regarding the registration and use of select agents (93). As a result, culture is rarely used for diagnosis, and other methods (e.g., serology, PCR, or immunostaining) are used to confirm infection.
The following is a summary of salient features of diagnostic testing:
- Blood smear microscopy might reveal presence of morulae in infected leukocytes, which is highly suggestive of HGA or, less commonly, HME. Tickborne illness characterized by acute onset of fever and possible headache, malaise, myalgia, and nausea/vomiting or neurologic signs. A macular or maculopapular rash is reported in the majority of patients and is frequently observed on the palms and soles.
# Clinical description
Tickborne illness characterized by acute onset of fever, headache, myalgia, and possible malaise. Nausea, vomiting, or rash might be observed in certain cases. Clinical laboratory findings might include thrombocytopenia, leukopenia, and possibly elevated liver enzymes. Intracytoplasmic morulae might be visible in the leukocytes of certain patients.
# Laboratory criteria
# HME
# HGA Unspecified ehrlichiosis
Serologic evidence of 4-fold change in serum antibody titer against Rickettsia rickettsii antigens between paired serum samples, as determined by IFA § or ELISA ¶ ; or demonstration of R. rickettsii antigen in a clinical specimen by IHC methods; or detection of R. rickettsii DNA in a clinical specimen by PCR assay; or isolation of R. rickettsii from a clinical specimen in cell culture.
# Case classification
Probable case: Identified in a person with a clinically compatible illness with either a single positive IFA titer (based on cutoff titers established by the laboratory performing the test) or the visualization of morulae in leukocytes.
Confirmed case: Identified in a person with a clinically compatible illness that is laboratory confirmed by a 4-fold change in serum antibody titer, as determined by IFA or ELISA or positive PCR or positive IHC, or isolation in culture.
- Whole blood specimens might be useful for a PCR confirmation of HME, HGA, and E. ewingii infection; however, a negative result does not rule out the diagnosis.
# Surveillance and Reporting
National reporting requirements are determined collaboratively by the Council of State and Territorial Epidemiologists and CDC. RMSF, anaplasmosis, and all forms of ehrlichiosis are nationally notifiable diseases. RMSF became nationally notifiable in 1989 and anaplasmosis and ehrlichiosis, in 1998. When health-care providers identify a potential case of TBRD, they should notify the local health department. The local health department, in cooperation with the state health department, can assist the healthcare provider in obtaining appropriate diagnostic testing to confirm the diagnosis. All confirmed or probable cases of RMSF, HME, HGA, and E. ewingii infection should be reported to the state health department. The case defini-tions for confirmed and probable cases of RMSF, HME, and HGA have been reported (Table 4; 33,94). Each state health department compiles case reports and submits them to CDC, where data are compared and disseminated via the MMWR Weekly and annual Surveillance Summaries.
Since 1981, CDC has collected and analyzed surveillance data on RMSF by using two complementary systems. States submit reports electronically via the National Electronic Telecommunications System for Surveillance (NETSS) as part of the National Notifiable Disease Surveillance System. NETSS reports capture diagnosis, date of onset, and basic demographic and geographic data related to the case. In addition, physicians are encouraged to complete a standardized case report form (CRF; Appendix) and forward it to the state health department, where it is compiled with similar reports and forwarded to CDC. The CRF summarizes demographic, epidemiologic, and outcome data that are not reported in NETSS. Data collected on the CRF are useful in summarizing the epidemiologic characteristics of tion per application. Products with DEET concentrations as low as 10% and those containing 25%-35% concentrations are considered optimal. No evidence exists that concentrations >50% are more efficacious or provide longer duration of protection (95). The American Academy of Pediatrics has recommended that DEET concentrations no greater than 20%-30% should be used for children (96). Products containing permethrin (e.g., permanone) can be used to treat outer clothing (e.g., shirts and pants) and should not be applied to skin. Permethrin is available commercially as a spray-on preparation. It should be applied evenly to outer clothing, according to label directions in a wellventilated area. Clothing should be allowed to completely dry before being worn. Pre-treated clothing is available and remains effective for multiple launderings. The use of DEET and permethrin should be considered by persons who enter heavily infested tick habitats where the risk for being bitten is high and the potential for TBRD infection exists.
Adults entering wooded or grassy areas should inspect themselves and their children frequently for ticks. Because several hours might elapse before ticks attach and inject pathogens, frequent checks increase the likelihood of finding ticks before they transmit an infectious agent. The duration of tick attachment necessary to transmit rickettsial organisms is substantially variable and has been reported to be as little as 2-10 hours (97) to 10-20 hours (98) for R. rickettsii. Limited data exist regarding the interval of transmission after tick attachment for A. phagocytophilum, but animal studies indicate that 24-48 hours might elapse before pathogen transmission (99,100). No comparable data exists for E. chaffeensis. Sites where ticks commonly attach include, but are not limited to, the scalp, waist, armpits, groin, and under socks and the beltline. Pets should also be checked for ticks because they can carry ticks back to their homes and human companions. Regular application of ectoparasite control on pets helps to reduce the risk for human exposure to ticks.
If an attached tick is found, it should be removed by grasping with tweezers or fine-tipped forceps close to the skin and gently pulling with constant pressure. Folk remedies, including gasoline, kerosene, petroleum jelly, fingernail polish, or lit matches should never be used to extract ticks (101). Removing the tick with bare hands should be avoided because fluids containing infectious organisms might be present in the tick's body and at the wound site. Ticks that have been removed should not be crushed between the fingers to prevent contamination, and hands should be washed to avoid potential conjunctival inoculation. The bite wound should then be disinfected. disease and focusing on prevention and treatment. This process includes examining lesser understood aspects of these conditions (e.g., the role of immunosuppression as a risk factor for disease; the prevalence of severe outcomes of infection, including death; and hospitalization trends). In 2001, the form was expanded to include reporting of other common TBRD, including HGA and HME, in addition to RMSF.
A surveillance system is critical for studying the changing epidemiology of TBRD and for developing effective prevention strategies and public health education programs. The detection of a cluster of RMSF cases in a region of Arizona where the disease was not known to occur and subsequent prevention and control initiatives underscore the vital role of surveillance and reporting in protecting the public's health. By the end of 2004, the highest number of RMSF cases was reported to CDC (n = 1,514), suggesting potential increased activity. However, underreporting of TBRD is probably common.
The following is a summary of salient features of surveillance and reporting:
- RMSF, HME, HGA, and other ehrlichioses are reportable diseases in the United States. - Physicians who identify a potential case of TBRD should notify the local health department, which can assist with obtaining diagnostic testing to confirm the diagnosis. - Surveillance and reporting of TBRD are key components of public health education and disease prevention efforts.
# Prevention
No licensed vaccines for TBRD exist. Avoiding tick bites and promptly removing attached ticks remain the best disease prevention strategies. Persons should limit their exposure to tick-infested habitats, including wooded or grassy areas. Persons should walk on cleared trails and avoid brushing against tall grass and other vegetation. This practice is particularly essential during periods of peak tick activity (i.e., late spring and summer) but should be observed, regardless of the season. Protective clothing, including a hat, long-sleeved shirts, pants, socks, and closed-toe shoes are helpful in preventing ticks from reaching the skin and attaching. Wearing light-colored clothing is preferred because crawling ticks can be seen easily.
Various over-the-counter products containing DEET (N,N-diethyl-m-toluamide) are available for application on exposed skin and clothing to repel ticks. The higher the concentration of DEET, the longer the duration of protec-The following is a summary of salient features of prevention: - Avoid tick bites, which is key to the prevention of TBRD. - Limit exposure to tick habitats, including grassy and wooded areas. - Inspect the body carefully for ticks after being in a tick habitat. - Remove attached ticks immediately by grasping with tweezers close to skin and pulling gently with steady pressure.
# TBRD Cases
The following TBRD cases were observed in health-care settings. Information from the cases can be used to reinforce medical management information related to TBRD (3,22,102) and are intended to illustrate certain common pitfalls in the diagnosis and treatment of TBRD. The case reports include a description of the case and salient features that can be considered when dealing with a potential case of TBRD.
# Case 1
In June 2001, a girl aged 5 years was taken to an ED in Missouri with a 3-day history of intermittent fever, headache, mild nausea, and a sore throat. On physical examination, the patient had a fever of 105°F (40.6 º C) and a maculopapular rash on her legs, including the soles of her feet.
- What should be included in the differential diagnosis? Possible causes of fever and rash in this child include meningococcemia, RMSF, HME, enteroviral infections, Kawasaki disease, drug reactions, and streptococcal disease with exanthem.
# What additional information would assist with the diagnosis?
Determine how long the rash has been present and when and where it appeared relative to onset of fever. The parent should be queried concerning medication use, immunocompromising conditions, and recent activities that could have led to animal exposures (including dogs), sick contacts, recent travel, outdoor activities (e.g., hiking, camping, and playing in brushy areas or backyard), and real or potential tick exposures.
The parent noticed the rash, which began on the arms and legs, on the same day that the child was taken to the ED. They did not own a dog, and no history of recent travel out of the local area and no history of a tick bite were noted, although the parent said that ticks were in the area around their house.
# What laboratory tests might be useful?
A CBC, comprehensive metabolic panel, blood culture, and a rapid Streptococcus pharyngitis screen should be performed. An acute serum should be obtained for IgG and IgM antibodies to R. rickettsii, E. chaffeensis, and A. phagocytophilum, but subsequent management of the patient should not depend on results. PCR for E. chaffeensis and A. phagocytophilum using EDTA whole blood might be useful if these tests are available from a reference laboratory.
Laboratory results included a WBC count of 8,800 x 10 9 cells/L (normal: 4.5-11.0 x 10 9 cells/L), with 5% bands (normal: 0%-5%), 70% neutrophils (normal: 45%-75%), 17% lymphocytes (normal: 16%-46%), and 8% monocytes (normal: 4%-11%). The platelet count was 50 x 10 9 cells/L (normal: 150-350 x 10 9 cells/L). Serology results were not available for 3 days.
# How does this information assist with the diagnosis?
The time of year for these clinical signs should raise suspicion for TBRD. A normal WBC is frequently observed in patients with viral infections and with RMSF. Patients with RMSF will commonly develop moderate to severe thrombocytopenia as the disease progresses, although a normal platelet count is frequently observed early in the course of illness. If serologic results are not immediately available, the clinician should not be dissuaded from initiating therapy if it is clinically indicated.
# What actions, including treatment, should be taken?
On the basis of history, clinical signs, geographic location, and time of year, suspicion of a TBRD is reasonable. An appropriate course of action would include treatment with doxycycline (2.2 mg/kg body weight administered orally twice daily for a minimum of 5 days) and close follow-up to ascertain clinical response to therapy while continuing to rule out other possible causes. Appropriate antimicrobial therapy for other suspected etiologies should be considered until they can be reasonably excluded. For example, certain experts recommend administering an intramuscular dose of ceftriaxone, pending blood culture results, because meningococcal disease cannot be reliably distinguished from TBRD on clinical grounds alone. Convalescent-phase serology for RMSF, HGA, and HME should be performed 2-4 weeks later to confirm the diagnosis.
- What preventive measures can the patient and her family take to prevent infection in the future?
The most effective preventive measure is to 1) limit exposure to ticks during peak periods of activity (prima-rily April-September), 2) inspect body and clothing thoroughly for ticks after being in wooded or grassy areas, 3) remove attached ticks immediately by grasping with tweezers or forceps close to the skin and pulling gently with steady pressure, and 4) apply insect repellant (e.g., DEET) when exposure to grassy or wooded areas is anticipated. Case 1 synopsis. This patient's clinical history suggested exposure to ticks, although no definitive indication of a tick bite was reported. Ticks are small (particularly in their nymphal and larval stages), and bites frequently go unnoticed because ticks might attach in places that are difficult to observe (e.g., the scalp, axillae, and inguinal regions). Up to 40% of patients with RMSF report no history of a tick bite (10,11). Therefore, the clinician should not be dissuaded from making a diagnosis of RMSF when no report of a tick bite is made. The clinical signs and laboratory values and a history that are compatible with tick exposure should guide the diagnosis and therapeutic actions. Serum samples collected on days 7 and 35 of illness demonstrated rising IgG antibody titers to R. rickettsii at 32 and 2,048, respectively.
# Case 2
In mid-August 2003, a male child aged 14 months was taken to a community health clinic in Arizona after 1 day of fever 103.7°F (39.8°C). On physical examination, the child had a maculopapular rash that involved his palms and soles. On auscultation, abnormal breath sounds were detected in the right lower lung. The parent stated that they had not traveled out of the local area recently. No one else in the family was ill, and the child was up-to-date on vaccinations. Chest radiographic evaluation revealed a possible right lower lobe infiltrate. On the basis of clinical and radiographic findings, pneumonia and roseola infantum were diagnosed. The child was administered an intramuscular injection of ceftriaxone and sent home with a prescription for oral amoxicillin/clavulanate.
The next day, the child was taken back to the clinic with vomiting and rash that was petechial. His fever was 105.7°F (41°C). He was admitted to the hospital, and antibiotic treatment for pneumonia was continued. On day 3 of hospitalization, the child developed DIC. Remarkable laboratory findings included: WBC count, 16.2 x 10 9 cells/L (normal: 4.5-11.0 x 10 9 cells/L); platelet count, 46 x 10 9 platelets/L (normal: 150-350 x 10 9 cells/L); aspartate aminotransferase (AST), 291 U/L (normal: 10-40 U/L); and alanine aminotransferase (ALT), 99 U/L (normal: 10-55 U/L). The child's condition worsened, and 7 days after the onset of illness, he died of pulmonary hemorrhage.
# Case 2 synopsis.
A serum sample collected 5 days before the child's death tested negative by IFA for IgM and IgG antibodies reactive with R. rickettsii. However, R. rickettsii DNA was detected in serum by PCR assay. RMSF can have a rapid course; 50% of RMSF deaths occur within 9 days of illness onset (10,11). IgM and IgG antibodies are typically not detectable before the second week of illness; therefore, serology will be not useful in diagnosing the infection in its earliest stages. Fever and rash in a young child can be caused by various enteroviruses, human herpesvirus 6, N. meningitidis, measles virus, R. rickettsii, and E. chaffeensis, among other agents. Common causes of bacterial pneumonia in a child this age might include Streptococcus pneumoniae, Staphylococcus aureus, Streptococcus pyogenes, and, less commonly, M. pneumoniae. Although this child lived in an area where RMSF is not common (e.g., Arizona), the diagnosis should not be excluded because of geography. Although RMSF is more common in the south central and south Atlantic states, it should be considered endemic throughout the contiguous United States (10). TBRD are seldom treated with the appropriate antibiotic, unless they are suspected. In this context, the majority of broad spectrum antimicrobials, including penicillins, cephalosporins, aminoglycosides, erythromycin, and sulfa-containing drugs are not effective against rickettsiae, ehrlichiae, or anaplasmae.
# Case 3
In early June 1996, a man aged 52 years who was HIVseropositive sought medical care at a hospital in Florida. He had a 4-day history of fever, headache, myalgias, nausea, and vomiting. The patient had been previously healthy, with no known previous opportunistic infections. An absolute CD4+ lymphocyte count of 164 cells/µl was documented 2 months before this visit. Physical examination revealed an acutely ill man; the patient had a fever of 103.5 º F (39.7 º C) and experienced dizziness and low blood pressure when he stood up (orthostatic hypotension). He reported that 2 weeks before admission, he had been bitten by a tick while hiking in central Georgia.
A CBC and chemistry panel and, because of the history of a tick bite, serologic tests for E. chaffeensis were ordered. Remarkable laboratory findings included hemoglobin 11.5 g/dL (normal: 13-18 g/dL); WBC count, 2.0 x 10 9 cells/L (normal: 4.5-11.0 x 10 9 cells/L), with 66% neutrophils (normal: 45%-75%), 18% bands (normal: 0%-5%), 8% lymphocytes (normal: 16%-46%), and 8% monocytes (normal: 4%-11%); and platelet count, 16 x 10 9 cells/L (normal: 150-350 x 10 9 cells/L). Peripheral blood smears revealed ehrlichial morulae in 2.5% of all leukocytes, including monocytes, lymphocytes, atypical On the basis of laboratory and clinical findings, a diagnosis of HME was made, and intravenous doxycycline (100 mg every 12 hours) was initiated. Despite doxycycline therapy, the patient remained febrile, severely thrombocytopenic, and continued to have elevated liver enzymes. He developed right lower lobe pneumonia and renal failure and died 6 days after hospitalization.
Case 3 synopsis. Patient sera obtained on days 1 and 5 of hospitalization were negative for IgG and IgM antibodies reactive with E. chaffeensis. However, the correct diagnosis was revealed on admission by a finding of morulae in leukocytes, and this diagnosis was subsequently confirmed when E. chaffeensis DNA was detected by using PCR in whole blood specimens from the patient, and the agent was isolated in cell culture. HME can be a severe disease, particularly in immunosuppressed persons. HME does not commonly cause rash in adults; therefore, history of tick exposure and characteristic leukopenia and thrombocytopenia were most useful in arriving at a diagnosis. Although morulae were observed in the patient's peripheral blood, microscopy is generally insensitive, and morulae are reported to be observed in only 1%-20% of patients with HME (45,47). Therefore, a diagnosis of HME would need to be confirmed by PCR, serology, or immunostaining, or culture isolation.
# Case 4
In mid-May 1999, a female aged 69 years went to her physician in upstate New York. She had a 3-day history of nausea, vomiting, fatigue, and fever. She said that her dog had died 2 days earlier after a brief illness characterized by signs similar to her own. Physical examination revealed no abnormalities. Her temperature was 100.4 º F (38 º C).
- What should be included in the differential diagnosis? Possible diagnoses that should be considered include viral syndrome, foodborne illness, and urinary tract infection.
# What additional information would assist with the diagnosis?
Patient should be queried regarding other signs and symptoms, recent activities and travel, exposure to other ill persons, foods consumed, and contact with ticks. The patient had no other symptoms to report and reported no unusual activities or recent travel.
# What diagnostic tests, if any, are needed?
Because the patient's symptoms were nonspecific, a CBC should be ordered. Results will not be available until the next day.
On the basis of the signs present when the patient first went to her physician, she was diagnosed with gastroenteritis and instructed to return within 24-48 hours, if her symptoms did not improve. The patient would be contacted regarding her laboratory test results. The next day, the patient returned with continued fever and changes in mental status. Her temperature remained at 100.4 º F (38 º C), but she was notably confused and lethargic. Her physical examination was unremarkable and did not reveal the presence of a rash.
Laboratory tests obtained on the previous day revealed a WBC count of 3.8 x 10 9 cells/L (normal: 4.5-11.0 x 10 9 cells/L); a platelet count of 99 x 10 9 cells/L (normal: 150-350 x 10 9 cells/L); and a hemoglobin concentration of 12.7 g/dL (normal: 12-16 g/dL).
# How does this information assist with the diagnosis?
On the basis of the patient's thrombocytopenia, leukopenia, and worsening clinical condition, encephalitis and sepsis should be included in the differential diagnosis.
# What actions, including treatment, should be taken?
On the basis of presenting signs and laboratory tests, the patient was hospitalized and intravenous levofloxacin therapy was initiated for fever of unknown cause. Blood, urine, and stool cultures were ordered as well as serologic assays for B. burgdorferi, E. chaffeensis, and A. phagocytophilum, and PCR for E. chaffeensis and A. phagocytophilum.
The patient's temperature returned to normal within 48 hours, her nausea and vomiting resolved, and her blood counts returned to normal. She was discharged after 3 days. Blood, urine, and stool cultures revealed no specific pathogens, and serologic assays were negative for antibodies reactive with B. burgdorferi, E. chaffeensis, and A. phagocytophilum. Case 4 synopsis. IHC staining of tissues from the patient's dog, submitted by the veterinarian to CDC, demonstrated abundant spotted fever group rickettsial antigens, and rickettsiae were identified within and around blood vessels in multiple tissues, including brain and testes. The cause of the dog's illness was identified as RMSF. This information was communicated to the patient's physician. When the physician contacted the patient, she reported that her fatigue and headache had persisted after discharge from the hospital. The patient was treated with oral doxycycline, and all symptoms resolved within 1 week. Subsequent testing of the patient's sera for early and late convalescent-phase antibody titer confirmed a diagnosis of RMSF. Titers of IgM and IgG antibodies were 1,024 and 512, respectively, on day 17 and declined to 256 and 256, respectively, on day 89 after ill-ness onset. The patient did not recall a tick bite and had not seen or removed ticks from her dog, although her dog roamed freely in wooded areas before its illness. Dogs can serve as sentinels for RMSF in human populations, and infections in canines have been associated with increased risk for infection in their owners (22).
# Case 5
In May 2001, a man aged 38 years sought medical attention in Tennessee with complaints of headache, fever, sore throat, and vomiting. He was treated 3 days previously by his primary care physician who diagnosed pneumonia and prescribed azithromycin and levofloxacin, but his fevers persisted. He was taken to the ED by his wife, and she said that he had new onset of confusion. He had no pets or animal exposures. He worked as a construction manager and was frequently outdoors in wooded areas but did not recall a tick bite.
- What should be included in the differential diagnosis?
The initial signs and symptoms were nonspecific, but the patient's confused state raised concern for possible involvement of the CNS. During the summer months, the differential diagnosis included viral meningitis (particularly enteroviral), arboviral meningoencephalitis (West Nile virus and others), TTP, and TBRD. Bacterial meningitis and herpes simplex virus (HSV) encephalitis do not have confined seasonality but also could cause this presentation. Sepsis and other multisystem illnesses are associated with encephalopathy, however, so the differential diagnosis remained broad.
The patient had an oral temperature of 103.4°F (39.7 º C); blood pressure, 100/60 mmHg; and heart rate, 120 beats/minute. The skin examination revealed diffuse erythema with a several scabs on the lower legs. Examination of the abdomen revealed moderate epigastric tenderness with deep palpation but no rebound tenderness or organomegaly. Neurologic examination was nonfocal, except for altered mentation (i.e., Glasgow coma score: 13).
Laboratory testing revealed the following: WBC, 11.9 x 10 9 cells/L (normal: 4.5-11.0 x 10 9 cells/L); 84% segmented neutrophils (normal: 45%-75%); 8% band neutrophils (normal: 0%-5%); 3% lymphocytes (normal: 16%-46%); 5% monocytes (normal: 4%-11%); platelets, 50 x 10 9 cells/L (normal: 150-350 x 10 9 cells/L); total bilirubin, 3.5 mg/dL (normal: 0-1.0 mg/dL); AST, 439 U/L (normal: 10-40 U/L); ALT, 471 U/L (normal: 10-55 U/L); and alkaline phosphatase, 236 U/L (normal: 45-115 U/L). Lumbar puncture revealed a WBC of 0, RBC of 1 with normal glucose of 55 mg/dL and normal protein of 20 mg/dL. Creatinine was elevated at 3.9 mg/dL (normal: 0.6-1.5 mg/dL). Computed tomography scan of the head did not demonstrate an acute abnormality.
- How does the physical examination and laboratory information change the differential diagnosis? Because of the normal lumbar puncture, meningitis (i.e., viral or bacterial) was a less likely diagnosis. However, examination of the CSF might be unremarkable in patients with encephalitis. The presence of thrombocytopenia and elevated transaminases was suggestive of TBRD. Additional considerations included acute cholecystitis, sepsis (possibly associated with DIC), toxic-shock syndrome (rash with multiple organ failure), and TTP (i.e., acute renal failure with fever, altered mental status, and thrombocytopenia).
- What additional tests should be performed? Appropriate diagnostic studies should include blood culture, serologic testing for RMSF and HME (and PCR for these if available), prothrombin time and partial thromboplastin time, examination of the peripheral blood smear (with particular attention for schistocytes or intracellular morulae), and ultrasound of the gallbladder to evaluate for inflammation.
The coagulation studies were within normal limits, and no schistocytes or morulae were observed on smear. Abdominal ultrasound revealed a normal gallbladder but mild splenomegaly. Therapy was initiated with ceftriaxone and vancomycin. Approximately 6 hours later, the patient developed seizures, and acyclovir and doxycycline were added to the course of medicine to effectively treat herpesvirus infection and TBRD. A magnetic resonance imaging scan of the brain was normal, and electroencephalography revealed nonspecific slowing. Antibodies to R. rickettsii and E. chaffeensis were not detected in acute sera. HSV PCR on CSF was negative. Blood cultures did not grow bacteria. The patient defervesced, and mental status normalized over the next 3 days. Case 5 synopsis. Serum obtained 31 days after the initial signs and symptoms contained no antibodies to R. rickettsii but had an IgG titer of 256 to E. chaffeensis, retrospectively confirming the diagnosis of HME. Whereas headache is a nearly universal complaint among patients with HME, altered sensorium might be observed in up to 20% of cases (6). Other CNS manifestations include seizures, meningismus, cranial nerve palsies, focal weakness, and coma. A lymphocytic pleocytosis can be observed in the CSF in approximately 50% of patients with HME who undergo lumbar puncture (103). Neutrophilic pleocytosis can be observed early in the course of the illness. March 31, 2006 Neuroimaging studies are usually normal or nonspecific. TBRD should be included in the differential diagnosis of patients presenting with clinical evidence of CNS infection or CSF findings suggestive of aseptic meningitis.
# Case 6
In July 1994, a man aged 44 years went to see his physician in central Minnesota. He complained of a 1-week history of fever, chills, generalized myalgias, and right temporomandibular joint pain. When he became ill, he treated himself empirically with ampicillin, which was available at home, for 2 days. Because the patient experienced no clinical improvement, he sought medical care. The patient worked outdoors and was frequently in wooded areas. Fourteen days before he went to his physician, he removed two deer ticks that had been attached to his skin for an unknown period.
Physical examination findings. The patient had a lowgrade fever of 100.6 º F (38.1 º C). Examination of heart, lungs, and abdomen were normal. No lymphadenopathy, hepatosplenomegaly, or skin rash were noted. Cardiovascular, pulmonary, gastrointestinal, or neurological symptoms were not present. Overall, physical examination was unremarkable, except for fever.
Laboratory findings. No laboratory evaluations were performed during the visit. A presumptive diagnosis of acute Lyme disease was made, and empirical treatment with amoxicillin and probenecid was initiated; a 1-week followup visit was scheduled. Five days after the outpatient visit, the patient died suddenly at home. He had complained of shortness of breath the day before his death.
Case 6 synopsis. Histopathologic examination of the patient's heart revealed widespread transmural myocarditis with neutrophilic and lymphocytic infiltrates. Postmortem serum specimens were evaluated initially for presumptive carditis as a result of B. burgdorferi infection. Serum titers of IgG and IgM antibodies to B. burgdorferi were not detected by ELISA and western blotting. PCR assays of serum and whole blood for B. burgdorferi also were negative. However, antibody titers to A. phagocytophilum (formerly known as E. equi) were significantly elevated at titer >256 by IFA methods. Detection of DNA extracted by PCR from whole blood and positive IHC staining of cardiac tissue confirmed a diagnosis of anaplasmosis. Although infection with A. phagocytophilum was demonstrated in this case, the pathogenesis of the associated carditis was less clear (104).
The diagnosis of HGA can be difficult because of the nonspecific nature of the febrile illness frequently observed when the patient first seeks medical care. In regions where both Lyme disease and HGA are known to occur, distinguishing between the diseases in the early stages of illness might be difficult. Because treatment should be initiated before a definitive diagnosis is made, selection of an antimicrobial effective against both rickettsial organisms and B. burgdorferi (e.g., doxycycline) is recommended. This case also underscores the importance of close follow-up of patients treated for TBRD on an outpatient basis. Because these diseases can rapidly progress, clinicians should emphasize to patients the need to return for reevaluation if substantial improvement is not observed within 24-48 hours of initiation of treatment.
# Conclusion
TBRD continue to cause severe illness and death in otherwise healthy adults and children, despite the availability of low cost, effective antimicrobial therapy. The greatest challenge to clinicians is the difficult diagnostic dilemma posed by these infections early in their clinical course when antibiotic therapy is most effective.
Early clinical presentations of HME, HGA, RMSF, and E. ewingii infection include fever, headache, myalgia, and malaise and are difficult to distinguish from other infectious and noninfectious diseases. Rash is observed frequently in RMSF, occasionally in HME, and rarely in HGA. TBRD tend to occur seasonally, with the majority of cases occurring during the warmer spring and summer months. However, cases might develop year-round. A detailed history of recent recreational or occupational activities might reveal potential exposure to ticks, although the absence of a history of a recent tick bite should not dissuade clinicians from considering a diagnosis of TBRD.
TBRD can be life-threatening. Severe manifestations of TBRD include prolonged fever, renal failure, myocarditis, meningoencephalitis, hypotension, acute respiratory distress syndrome, and multiple organ failure. Patients usually do not have diagnostic serum antibody levels during the first week of illness; therefore, an inability to detect antibodies (IgG or IgM) in acute-phase serum does not exclude TBRD. Health-care providers should not delay treatment while waiting for a diagnosis; rather, they should empirically provide treatment if they suspect TBRD. Doxycycline is the drug of choice for the treatment of presumptive or confirmed TBRD in both adults and children.
Examination of paired serum samples obtained during acute illness and 2-3 weeks later that demonstrate a rise in antibody titer is the most appropriate approach to confirm TBRD. Physicians who identify a potential case of TBRD should notify the local health department, which can assist with obtaining diagnostic testing to confirm the diagnosis.
No licensed vaccines for TBRD are available. Avoiding tick bites and promptly removing attached ticks remain the best disease prevention strategies. | Tickborne rickettsial diseases (TBRD) continue to cause severe illness and death in otherwise healthy adults and children, despite the availability of low cost, effective antimicrobial therapy. The greatest challenge to clinicians is the difficult diagnostic dilemma posed by these infections early in their clinical course, when antibiotic therapy is most effective. Early signs and symptoms of these illnesses are notoriously nonspecific or mimic benign viral illnesses, making diagnosis difficult. In October 2004, CDC's Viral and Rickettsial Zoonoses Branch, in consultation with 11 clinical and academic specialists of Rocky Mountain spotted fever, human granulocytotropic anaplasmosis, and human monocytotropic ehrlichiosis, developed guidelines to address the need for a consolidated source for the diagnosis and management of TBRD. The preparers focused on the practical aspects of epidemiology, clinical assessment, treatment, and laboratory diagnosis of TBRD. This report will assist clinicians and other health-care and public health professionals to 1) recognize epidemiologic features and clinical manifestations of TBRD, 2) develop a differential diagnosis that includes and ranks TBRD, 3) understand that the recommendations for doxycycline are the treatment of choice for both adults and children, 4) understand that early empiric antibiotic therapy can prevent severe morbidity and death, and 5) report suspect or confirmed cases of TBRD to local public health authorities to assist them with control measures and public health education efforts. The reported incidence of these diseases has increased during the previous decade. Despite the availability of lowcost and effective antibiotic therapy, which may be used empirically for suspected cases, TBRD continue to cause severe illness and death in otherwise healthy adults and children. The greatest challenge to clinicians is diagnosing these infections early in their clinical course, when antibiotic therapy is most effective (2,3). The majority of patients with TBRD seek medical care within 2-4 days of onset of illness (4-7). In general, these patients are first evaluated by family practitioners, pediatricians, internists, emergency department (ED) physicians, or physician extenders. Early signs and symptoms of these illnesses are notoriously nonspecific, or they might mimic benign viral illnesses, making diagnosis difficult. For example, even in areas where awareness of RMSF is high, approximately 60%-75% of patients with this TBRD receive an alternate MMWR# Introduction
Tickborne rickettsial diseases (TBRD) are clinically similar, yet epidemiologically and etiologically distinct illnesses. In the United States, these diseases include 1) Rocky Mountain spotted fever (RMSF), 2) human monocytotropic (or monocytic) ehrlichiosis (HME), 3) human granulocytotropic (or granulocytic) anaplasmosis (HGA, formerly known as human granulocytotropic ehrlichiosis or HGE) (1), 4) Ehrlichia ewingii infection, and 5) other emerging TBRD. diagnosis on their first visit for medical care (8,9). Moreover, the earlier patients seek care in the course of their illness, the more likely an alternate diagnosis will be made (4). The lack of a specific initial syndrome, however, does not imply that the course of these diseases will be benign.
In October 2004, to address the need for a consolidated resource for the diagnosis and management of TBRD, CDC's Viral and Rickettsial Zoonoses Branch collaborated with 11 clinical and academic specialists of RMSF, HGA, and HME. These external contributors were invited by CDC subject matter specialists to participate among clinicians and researchers in the field of TBRD, based on direct working interactions related to case consultation and recognized expertise from peer-reviewed publications. In December 2004, the framework of this report was developed by CDC's Viral and Rickettsial Zoonoses Branch, based on a summary of the peer-reviewed published reports on the epidemiology and clinical aspects of TBRD. External contributors further developed recommendations for the diagnosis and treatment of TBRD based on their clinical research and experience. All work group collaborators reviewed and provided input and approved the final content of this report.
The primary goal of this report is to provide primary care physicians and physician extenders with practical information to assist with the diagnosis and care of patients with TBRD. This report provides a framework for recognizing suggestive symptoms, considering likely alternative diagnoses, eliciting relevant history, requesting appropriate diagnostic tests, and initiating prompt, effective treatment. Information in this guide is designed to assist clinicians to • recognize common epidemiologic situations and clinical manifestations of TBRD; • obtain appropriate history and diagnostic tests for TBRD; • develop a differential diagnosis that includes and ranks TBRD; • make treatment decisions based on epidemiologic and clinical evidence; • recognize that doxycycline is the treatment of choice for both adults and children; • recognize that early and empiric antibiotic therapy can prevent severe morbidity or death; • identify the availability, limitations, and utility of confirmatory laboratory assays; • recognize potential severe manifestations of TBRD; and • report suspected and confirmed cases to appropriate public health authorities to assist with control measures and public health education efforts.
This report also provides resources on TBRD for healthcare and public health professionals. Clinical cases are included for self-evaluation and to reinforce the information presented in this guide. Additional information concerning TBRD in this report is available from medical specialists, various medical societies, CDC, and state and local health authorities.
# Epidemiology of TBRD
RMSF, HME, and HGA are tickborne zoonoses caused by Rickettsia rickettsii, Ehrlichia chaffeensis, and Anaplasma phagocytophilum, respectively. These pathogens are maintained in natural cycles involving wild mammals and hard-bodied (ixodid) ticks. The epidemiologies of these diseases reflect the geographic distribution and seasonal activities of the vectors and reservoirs and the human behaviors that place persons at risk for tick attachment and subsequent infection. Selected epidemiologic and clinical features of TBRD have been summarized (Table 1). RMSF, HME, and HGA are reported each month of the year in the United States, although 90%-93% of reported cases occur during April-September (6,(10)(11)(12), coincident with peak levels of tick feeding activity on humans. Travelers outside of the United States might also be exposed to other tick vectors in other countries that transmit related agents that result in disease after they return to the United States.
Males appear to be at higher risk for infection with all TBRD, possibly because of greater recreational or occupational exposures to tick habitats. Although previous studies have indicated that the highest incidences of RMSF have occurred in children aged <10 years, surveillance during 2003 demonstrates a higher age-specific incidence for RMSF among persons aged 40-64 years, compared with other age groups (13). For HME and HGA, the highest age-specific incidences occurred among persons aged >70 and 60-69 years, respectively (14). The higher frequency of disease reporting in adults might reflect greater susceptibility to recognizable disease rather than higher infection rates. Two recent cross-sectional studies in the southeastern and south central United States* have indicated that up to 22% of children have serologic evidence of previous exposure to antigens of both E. chaffeensis (15) and R. rickettsii (16), suggesting that rickettsial and ehrlichial infection might be more common than previously recognized.
# RMSF
In the United States, R. rickettsii is transmitted to humans by several tick species. However, the species that transmit R. rickettsii most frequently include the American dog tick (Dermacentor variabilis; Figure 1) in the eastern, central, and Pacific coastal United States and the Rocky Mountain wood tick (Dermacentor andersoni; Figure 2) in the western United States. In 2005, the brown dog tick (Rhipicephalus sanguineus; Figure 3), a vector of RMSF in Mexico (17), was implicated as a vector of this disease in a confined geographic area in Arizona (18). The cayenne tick (Amblyomma cajennense; Figure 4) is a common vector for RMSF in Central and South America, and its range extends into the United States in Texas (19). During 1997-2002, the estimated average annual incidence of RMSF, based on passive surveillance, was 2.2 cases per million persons. More than half (56%) of reported cases of RMSF were from only five states: North Carolina, South Carolina, Tennessee, Oklahoma, and Arkansas (CDC, unpublished data, 2005). However, cases have been reported from each of the contiguous 48 states, except Vermont and Maine (10,11). Average reported annual incidence of RMSF per 1 million population, based on cases reported to CDC during 1997-2002, has been reported (Figure 5). Incidence varies considerably by geographic area. RMSF is also (17,19,20). Household clusters of disease and hyperendemic foci of infected ticks have been reported (3,21). Dogs are susceptible to RMSF, and they might frequently develop the disease concurrently with other household members in an endemic focus (22,23).
# HME
E. chaffeensis is transmitted to humans by the lone star tick, A. americanum (Figure 6), and possibly other ticks. The white-tailed deer is a major host of all stages of lone star ticks and is an important natural reservoir for E. chaffeensis. Natural infections of coyotes, dogs, and goats
# FIGURE 2. An adult female Dermacentor andersoni (Rocky Mountain wood tick)
Photo/CDC have been documented. The lone star tick is among the most commonly encountered ticks in the southeastern United States, with range extensions into areas of the South Central and New England states (Figure 7). Cases of HME are most commonly reported to CDC from Missouri, Oklahoma, Tennessee, Arkansas, and Maryland, although the disease is found throughout the range of the lone star tick. The average reported annual incidence of HME was 0.7 cases per million population, but incidence varied by state, based on cases reported to CDC from 2001 to 2002 (Figure 8). In a prospective study among febrile patients with a history of a recent tick bite in central North Carolina, the incidence of ehrlichial infection was approximately twice that of RMSF (24). The reported incidence probably represents an underestimate of the true burden of disease in areas where E. chaffeensis is endemic (24,25). Clusters of HME have been reported, suggesting that foci of ticks infected with E. chaffeensis do occur (21,26).
# HGA
The blacklegged tick (Ixodes scapularis; Figure 9) is the vector of A. phagocytophilum in New England and North Central United States, whereas the western blacklegged tick (Ixodes pacificus; Figure 10) is the principal vector in northern California. Deer, elk, and wild rodents are thought to be reservoirs. HGA is more frequently reported than HME, resulting in an average reported annual incidence of 1.6 cases per million during 2001-2002. States that reported the highest incidence during this period were Rhode Island (36.5 cases per million), Minnesota (12.3 cases per million), Connecticut (8.1 cases per million), New York (2.3 cases per million), and Maryland (1.6 cases per million) (Figure 11). HGA has been identified as a substantial cause of unexplained fever during the tick season in Wisconsin (27). Evidence suggests that the incidence of HGA in Wisconsin might be much higher than that in Minnesota (7). Because these Ixodes species ticks also transmit Borrelia burgdorferi (the causative agent of Lyme disease) and various Babesia species (agents of human babesiosis), the preponderance of cases of HGA occur in the same states that report high incidences of Lyme disease and human babesiosis. Simultaneous infection with A. phagocytophilum and B. burgdorferi has been reported (28), and discerning such a mixed infection is vital because it might affect antimicrobial choice. For example, amoxicillin can be used to treat early stage Lyme disease, but it is not effective for HGA.
# Ehrlichia ewingii Infection
Amblyomma americanum also is the principal vector of the ehrlichial pathogen, E. ewingii. (29,30). E. ewingii infections in dogs or ticks also have been described in these states and in Arkansas, Texas, Florida, Georgia, Mississippi, North Carolina, and Virginia, suggesting that human infections with this pathogen might be expected to occur throughout the range of the lone star tick (31,32).
The following is a summary of the salient epidemiologic features of TBRD:
• Occurrence is seasonal, with the majority of illness onset during warmer spring and summer months, but cases might develop throughout the year. • RMSF has been reported in all of the contiguous 48 states, except Vermont and Maine. • RMSF and HME are most commonly reported in the southeastern and south central United States. • HGA is reported most frequently in New England, the north central states, and in focal areas along the West Coast.
# Pathogen Tropisms and Clinical Presentation
R. rickettsii, E. chaffeensis, E. ewingii, and A. phagocytophilum have specific and distinct cell tropisms. R. rickettsii infects endothelial cells and more rarely infects underlying smooth muscle cells, where rickettsiae multiply freely in the cytoplasm. The rickettsiae cause a small-vessel vasculitis, resulting in a maculopapular or petechial rash in the majority of patients. Vasculitis occurring in organs (e.g., the brain or lungs) can result in life-threatening complications. R. rickettsii does not stain with the majority of routine histopathologic stains and is not detected by blood smear evaluation because of limited numbers of circulating bacteria. Ehrlichioses and anaplasmosis are characterized by infection of leukocytes, where the causative agents multiply in cytoplasmic membrane-bound vacuoles as microcolonies called morulae. E. chaffeensis most frequently infects monocytes, whereas A. phagocytophilum and E. ewingii demonstrate a predilection for granulocytes. Morulae may be stained with conventional Wright or Giemsa stains and are occasionally observed in leukocytes in smears of peripheral blood, buffy coat preparations, or cerebrospinal fluid. In this context, a routine blood smear can provide a presumptive clue for early diagnosis; however, the visualization of morulae still requires confirmatory testing for Ehrlichia or Anaplasma species by serology, polymerase chain reaction (PCR), or immunostaining methods (33). The demonstration of morulae is also not sensitive, and a case of ehrlichiosis or anaplasmosis might be missed if the diagnosis relies solely on detection of morulae on blood smears. Although the diagnostic sensitivity of a blood smear is greater for HGA than for HME, blood smears might only be positive in up to 60% of patients with HGA (34).
The following is a summary of salient features of pathogen tropisms:
• R. rickettsii infects endothelial cells, causing vasculitis, which leads to rash and life-threatening damage to the brain, lungs, and other viscera. • R. rickettsii is not evident in blood smears, and these bacteria and do not stain with the majority of conventional stains. • Ehrlichia and Anaplasma species infect monocytes or granulocytes, respectively, and morulae might occasionally be observed on peripheral blood smears by using routine stains.
# Clues from the Clinical History
A thorough clinical history that elicits recent tick exposure, specific recreational or occupational exposures to tickinfested habitats, recent travel to areas where TBRD might be endemic, or similar illnesses in family members, coworkers, or pet dogs can provide critical information that can be used to make a presumptive diagnosis of TBRD and help guide subsequent therapeutic actions. However, the absence of certain features does not exclude a diagnosis of TBRD. These features include 1) history of tick bite or exposure, 2) recent travel to areas endemic for TBRD, and 3) similar illness in family members, coworkers, or pets.
# History of Tick Bite or Exposure
A detailed medical history might reveal activities that suggest potential exposure to ticks. Outdoor activities during April-September, particularly in areas with high uncut grass, weeds, and low brush can increase the risk for tick bites (35). These activities include recreational pursuits (e.g., camping, hiking, fishing, hunting, gardening, and walking dogs) as well as occupational activities that involve persons being in brushy or grassy areas that might be inhabited by ticks. Vegetation that borders roads, trails, yards, or fields also are potential areas that might be inhabited by ticks. In endemic areas (where the agents causing TBRD are present at all times), even adults or children who play in grassy areas in their backyard are at risk. Queries concerning frequency of contact with family pets, especially dogs, and findings of tick attachment to animals or removal can be useful. The majority of patients will not recall or recognize an attached tick because the location of the tick might be obscure; the bite is typically painless; and bites from smaller immature stages of ticks (e.g., nymphs are approximately 1-2 mm or the size of the head of a pin; Figure 12) might not be readily detected but might still result in infection. A specific history of a tick bite within 14 days of illness onset is typically only reported in 60% of RMSF cases (10,11) and has been reported in only 68% of ehrlichiosis cases (6). Therefore, the absence of definite tick attachment should never dissuade a physician from considering the diagnosis of a TBRD. Finally, certain patients do not specifically recall tick exposure but might describe other pruritic, erythematous, or ulcerated cutaneous lesions that they call a mosquito bite, spider bite, chigger bite, or bug bite, which can be indistinguishable from an actual tick bite.
# Recent Travel to Areas Endemic for TBRD
Clinicians in areas of the United States where the incidence of TBRD is historically low are typically at a disadvantage in distinguishing these diseases among multiple other infectious and noninfectious syndromes that they resemble. Because TBRD are typically sporadic, identifying these infections requires high clinical acumen, especially in an environment in which TBRD have not previously been recognized as occurring frequently.
Knowledge of the epidemiology of these illnesses, including regions of the country with a high incidence (number of reported cases per million persons per year) of TBRD (e.g., south Atlantic, north central, and south central and New England states), is important. A history of recent travel from an endemic area of TBRD (e.g., within 2 weeks preceding illness), especially if the patient had participated in an outdoor activity, might support a suspicion of tickborne illness. Physicians should also consider the possibility that changes in tick vector range can influence the distribution of TBRD. In addition, in 2004, a total of 13 cases of RMSF occurred in eastern Arizona, a state in which the disease was previously rarely diagnosed (18).
Clinicians should also consider that TBRD occur worldwide and might have epidemiologic, seasonal, and clinical features distinct from those observed in the United States. International travel to destinations (e.g., southern Mediterranean, Central and South America, Africa, Asia, and the Middle East) might result in tick vector exposure, particularly if the patient participated in rural or outdoor activities. For example, African tick-bite fever (ATBF), an increasingly reported travel-related rickettsiosis caused by R. africae, has an estimated incidence of 4%-5.3% among international travelers to sub-Saharan Africa and has been identified in clusters of infection among group travelers (e.g., game hunters, safari tourists [36], and humanitarian workers; 37). A related rickettsial organism, R. conorii, endemic in the Mediterranean basin, Middle East, and parts of Africa and the Indian subcontinent causes Mediterranean spotted fever (MSF; 38). ATBF and MSF are characterized by fever, malaise, headache, and myalgia, which are typical symptoms for other TBRD. However, a distinguishing clinical feature of both travel-related diseases is the development of one or more eschars (a dark, scab-like plaque overlying a shallow ulcer with surrounding erythema or scaling) at the site of tick attachment that is noted coincident with or shortly after the onset of fever in 30%-50% of patients (36,39).
# Emerging TBRD
Similarly, considering TBRD as a diagnosis is essential because of new, previously unrecognized rickettsial pathogens that have been observed in tick vectors in the United States. For example, in 2002, R. parkeri was identified as a new cause of spotted fever rickettsiosis in a patient living in the southeastern coastal United States (40). This agent is present in A. maculatum (the Gulf Coast tick; Figure 13), which is found in the southeastern United States. A clinical presentation, similar to ATBF and MSF (i.e., fever, headache, eschars, and regional lymphadenopathy), was observed in a patient with no substantial travel history (Figure 14). The diagnosis of spotted fever rickettsiosis was confirmed by using rickettsial culture from an eschar skin biopsy and serologic and molecular methods (40). Other spotted fever group rickettsiae might also cause mild febrile illness in certain persons exposed to ticks in highly endemic areas (41). The common observation of antibodies to rickettsiae and ehrlichiae in persons and dogs might indicate expo-sure to other rickettsial agents of varying pathogenicity (15,16,24).
# Similar Illness in Family Members, Coworkers, or Pets
Clinicians might be inclined to offer diagnoses of a communicable viral infection when more than one family member is affected by an illness. However, clustering of certain TBRD is a well-recognized epidemiologic phenomenon and might occur after exposure to natural foci of infected ticks. Temporally and geographically related clusters occurring among family members, coworkers, or persons frequenting a particular common area have been observed. These clusters include family clusters of RMSF (3), clusters of ehrlichiosis among residents of a golfing community (26), and soldiers on field maneuvers (21). Common exposures to tick-infested habitats or outdoor activities might place certain or all members of a family or group, including pet dogs, at risk for TBRD. Concurrent infections with R. rickettsii and Ehrlichia species also have been observed in humans and dogs (22,24,29). Therefore, clinicians should query patients concerning similar illnesses among family members, close coworkers, or community residents, and even among household dogs.
The following is a summary of salient features of clues from the clinical history:
• A detailed history of recent recreational or occupational activities might reveal potential exposure to ticks. • Exposure can occur in the patient's backyard or neighborhood. • Familiarity with TBRD epidemiology will be helpful when querying patients regarding recent travel to endemic areas (domestic and international; 38,39). • Clustering of certain TBRD is well-recognized and has been reported among family members, coworkers, and other defined groups.
# Clinical Assessment
# Signs and Symptoms
The early signs and symptoms of HME, HGA, RMSF, and E. ewingii infection might resemble nonspecific findings of other infectious and noninfectious diseases. The majority of patients with TBRD visit a physician during the first 2-4 days of illness, after an incubation period of approximately 5-10 days after a tick bite (5). Patients with HGA might seek medical care later (4-8 days after fever onset) (7). Substantial overlap occurs in the initial clinical presentation of the three diseases. Initial symptoms commonly include a sudden onset of fever, chills, and headache, commonly associated with malaise and myalgia. In adults, photophobia might be observed. Headache is nearly always reported by adults who seek medical care and can be severe. Patients also might report nausea, vomiting, and anorexia early in the course of their illness, especially with RMSF (35) and HME in children. Diarrhea might occasionally occur. Other frequently observed signs and symptoms in children with either RMSF or HME are abdominal pain, altered mental status, and conjunctival injection. Abdominal pain might be severe enough to mimic appendicitis or other causes of acute abdominal pain (42). Certain findings described in medical textbooks are less commonly observed by clinicians and include bilateral periorbital edema, edema of the dorsum of hands and feet, and calf pain and tenderness. Because the signs and symptoms that persons have when they first seek medical care are nonspecific, clinicians frequently must incorporate clues from the clinical and epidemiologic history and consider other features (e.g., the presence of rash or abnormalities of routine laboratory tests).
In RMSF, a rash typically appears 2-4 days after onset of fever; however, the majority of patients will seek medical care before this period. For adults and children with RMSF, rash frequently occurs earlier in children than in adults (43) and is eventually observed in approximately 90% of children. The exanthem typically begins as small, blanching, pink macules on the ankles, wrists, or forearms that evolve to maculopapules (Figure 15). In half of cases, the rash might evolve to petechiae over the next several days of illness. The classic centripetal spread of rash is typically not noticed by the patient and might be difficult to elicit from the clinical history. The rash can expand to involve the entire body, including the palms and soles, but its presence on the face is usually limited. Discerning the rash in darker-skinned persons might be difficult. The classic spotted or generalized petechial rash of RMSF is usually not apparent until the fifth or sixth day of the illness and signifies progression of the disease, although the progression is considerably variable (Figure 16). Patients with petechial rash are often severely ill, and although fever and organ dysfunction might resolve quickly with treatment, complete recovery can take longer to occur. The rash progression of RMSF includes several critical exceptions and considerations.
• A rash on the palms and soles is not pathognomonic and might occur in illnesses caused by drug hypersensitivity reactions, infective endocarditis, and a diverse group of other agents, including Treponema pallidum, Neisseria meningitidis, Streptobacillus moniliformis, E. chaffeensis, and certain enteroviruses. • The rash might be evanescent or localized to a particular region of the body.
• A rash might be completely absent or atypical in up to 20% of RMSF cases (4,43,44). Rash is observed in approximately one third of all patients with HME (although rash is described in up to 66% of children) and is rare in patients with HGA or E. ewingii infection (45,46). For children with HME and a rash, distinguishing the condition from RMSF might be difficult. Rash patterns occasionally associated with HME vary in character from petechial or maculopapular (Figure 17; 47) to diffuse erythema (48) and typically occur later in the course of disease (median: 5 days after onset; 6).The rash patterns might involve the extremities, trunk, face or, rarely, the palms and soles (49).
In certain cases, patients with RMSF or ehrlichiosis might seek medical attention for a febrile illness that mimics viral meningoencephalitis. Focal neurologic deficits, including cranial or peripheral motor nerve paralysis or sudden transient deafness, might also be observed (50).
# Differential Diagnosis of Febrile Patients with Rash
The differential diagnosis of febrile patients with rash is broad. The onset of TBRD is frequently rapid, and the majority of patients experience high fever, shaking chills, severe headache, and generalized myalgias, in contrast to other tickborne diseases (e.g., Lyme disease). Tickborne viral fevers (e.g., Colorado tick fever) infrequently cause rash but should be included in the differential diagnoses of TBRD, particularly when leukopenia and thrombocytopenia are present in a patient who has recently traveled to the western United States. Clinically, TBRD might be essentially indistinguishable from the majority of viral infections, particularly those in children. The dermatologic classification of the rash, its distribution, pattern of progression and timing relative to onset of fever, and other systemic signs provide clues that help the clinician rule out other exanthemata. Maculopapular rashes might occur in association with multiple condi-tions, including human herpesvirus 6 infection (i.e., roseola), human parvovirus B19, enteroviral infection (e.g., coxsackievirus and echovirus), Epstein-Barr virus infection, disseminated gonococcal infection, Mycoplasma pneumoniae infection, leptospirosis, secondary syphilis, Kawasaki disease, thrombotic thrombocytopenic purpura (TTP), drug reactions, and immune complex-mediated illness (51). A petechial rash can occur in association with meningococcal infection, enteroviral infection, immune thrombocytopenic purpura, and after group A streptococcal pharyngitis. R. rickettsii infection is noted for causing a rash on the soles and palms, although this distribution typically occurs late in RMSF and in only half of cases, whereas in the majority of other bacterial or viral infections rash has not been observed. Initially, clinicians might experience difficulty distinguishing N. meningitidis infection from RMSF because both can begin as a maculopapular rash and progress to a petechial rash, but the rash and other clinical features progress more rapidly in meningococcemia than in RMSF. Selected infectious causes and features of maculopapular and petechial rash illnesses have been reported (Table 2). Other exanthematous diseases that can occasionally be confused with TBRD include toxic-shock syndrome, erythema multiforme, and Stevens-Johnson syndrome.
# Laboratory Findings
Obtaining a complete blood cell count (CBC), comprehensive metabolic panel, and examination of peripheral blood smear are essential when considering a diagnosis of TBRD. The total white blood cell (WBC) count is typically normal in patients with RMSF, but increased numbers of immature bands are generally observed. Thrombocytopenia, mild elevations in hepatic transaminases, and hyponatremia might be observed with RMSF (35), whereas leukopenia (up to 53% of patients), thrombocytopenia (up to 94% of patients), and modest elevations of liver transaminase levels are particularly suggestive of HME and HGA (52,53). An inverse relation has been reported between the mean WBC and platelet count and the probability that HGA is the cause of nonspecific fever (53). Blood smears might be useful in identifying patients with HGA (34) or E. ewingii infection. Nonspecific changes in the concentrations of routine laboratory parameters that have been observed for patients infected with E. chaffeensis (52) or A. phagocytophilum have been reported (53; Table 3).
Cerebrospinal fluid (CSF) analysis might be a useful adjunct to laboratory diagnosis of TBRD. When CSF is evaluated in patients with RMSF or HME, a pleocytosis (usually <100 cells/microliter) is typically observed (with either a polymorphonuclear or lymphocytic predominance), whereas CSF evaluated in E. ewingii infection is characterized by a neutrophilic pleocytosis (29). Moderately elevated protein (100-200 mg/dL) and normal glucose levels also are commonly observed in patients with RMSF (54,55).
A Gram stain indicating gram-negative diplococci, very low glucose (i.e., <20-30 mg/dL), or neutrophilic pleocytosis is more suggestive of meningococcal meningitis. Clinicians should distinguish TBRD-related CNS involvement from other infections (e.g., N. meningitidis); however, in the majority of patients, reliably distinguishing between RMSF, HME, and meningococcal infection based on laboratory testing is difficult (unless a pathogen is cultured). Therefore, empiric treatment for both TBRD and meningococcemia is necessary for ill patients with fever and rash and for patients in whom neither disease can be ruled out.
The following is a summary of salient clinical assessment features:
• Early clinical presentations of HME, HGA, RMSF, and E. ewingii infection include fever, headache, myalgia, and malaise and are difficult to distinguish from other infectious and noninfectious diseases.
• Patients with RMSF typically do not have a spotted or petechial rash when they initially seek medical care during the first 2-4 days of illness. • A CBC, metabolic panel, and peripheral blood smear examination are helpful in developing both a differential diagnosis and treatment approach to TBRD. • CSF analysis might reveal neutrophilic or lymphocytic pleocytosis and elevated protein but might not reliably distinguish TBRD and meningococcal disease, necessitating empiric antibiotic therapy for both conditions when indicated. • Leukopenia, thrombocytopenia, mild hyponatremia, and mildly elevated hepatic transaminase levels are common and particularly useful clinical features of TBRD, although the absence of these features does not exclude a diagnosis of TBRD. • Infrequent features of TBRD include severe abdominal pain and meningoencephalitis. • Rash is observed frequently in RMSF, occasionally in HME, and rarely in HGA or E. ewingii infection.
# Treatment and Management
An assessment of clinical signs and symptoms, along with laboratory diagnostic tests and a thorough clinical history, will help guide clinicians in developing a differential diagnosis and treatment plan. At least 50% of patients with TBRD might need to be hospitalized. Patients with evidence of organ dysfunction and severe thrombocytopenia, mental status changes, and the need for supportive therapy should be hospitalized. Essential considerations include social factors, the likelihood that the patient can and will take oral medications, and existing comorbidities. For example, a patient who appears well, has acute febrile illness and an unrevealing history and physical examination, and whose laboratory indices are within normal limits might warrant a "wait and watch" approach for 24 hours with reassessment if the patient fails to improve. If laboratory testing of a patient with a history compatible with TBRD reveals leukopenia or thrombocytopenia, or metabolic abnormalities, the clinician should consider obtaining blood cultures for other likely pathogens and specific laboratory tests and initiating empiric oral antimicrobial therapy that will effectively treat TBRD. Certain patients with TBRD can be treated on an outpatient basis with oral medication, particularly if a reliable caregiver is available in the home and the patient is compliant with follow-up medical care. When other diagnoses are under consideration, empiric treatment for these conditions can be incorporated into the therapeutic plan. For example, for a patient's con-dition in which meningococcal disease cannot be ruled out, intramuscular ceftriaxone should be administered in addition to oral doxycycline to provide activity against possible meningococcal infection, pending culture results. Inpatient observation and assessment of the blood cultures after 24 hours of incubation should be considered for such patients. A critical step is for clinicians to keep in close contact with patients who are treated in the outpatient setting to ensure that they are responding to therapy as expected.
Appropriate antibiotic treatment should be initiated immediately when a clinician suspects that the diagnosis could be RMSF, HME, HGA, or E. ewingii infection, based on clinical, laboratory, or epidemiologic findings. Delay in treatment can lead to severe disease and fatal outcome for TBRD (2)(3)(4). Because each of the agents causing TBRD is susceptible to tetracycline-class antibiotics, these drugs, particularly doxycycline, are considered the therapy of choice in nearly all clinical situations. Fever typically subsides within 24-48 hours after treatment when the patient receives doxycycline or another tetracycline during the first 4-5 days of illness. If a patient fails to respond to early treatment with a tetracycline antibiotic (i.e., within 48 hours), this response might be an indication that their condition is not a TBRD. Severely ill patients might require longer periods before clinical improvement is noted, especially if they have multiple organ dysfunction. Doxycycline is the drug of choice for treatment of all TBRD in children and adults. This drug is bacteriostatic in its activity against rickettsial organisms. The recommended dose is 100 mg per dose administered twice daily (orally or intravenously) for adults or 2.2 mg/kg body weight per dose administered twice daily (orally or intravenously) for children weighing <100 lbs. (45.4 kg). Intravenous therapy is frequently indicated for hospitalized patients, and oral therapy is acceptable for patients considered to be early in the disease and who can be managed as outpatients. Oral therapy also can be used for inpatients who are not vomiting or obtunded. The optimal duration of therapy has not been established, but current recommendations for RMSF and HME are for treatment for at least 3 days after the fever subsides and until evidence of clinical improvement is noted, which is typically for a minimum total course of 5-7 days. Severe or complicated disease might require longer treatment courses. Patients with HGA should be treated with doxycycline for 10-14 days to provide appropriate length of therapy for possible incubating coinfection with Lyme disease (45).
The use of tetracyclines to treat children with TBRD is no longer a subject of controversy (56)(57)(58). Concerns regarding dental staining after tetracycline therapy have been based primarily on studies conducted during the 1960s that involved children receiving multiple courses of the drug for recurrent otitis media (59,60). The propensity of tetracyclines to bind calcium can lead to darkening of the teeth if the antibiotic is ingested during the period of tooth crown formation. More recent studies in 1971 and 1998, however, have demonstrated that although multiple exposures to tetracycline increase the risk for tooth staining, limited use of this drug in children during the first 6-7 years of life has a negligible effect on the color of permanent incisors (56,57). Beyond ages 6-7 years, the risk for tetracycline staining is of minimal consequence because visible tooth formation is complete. Moreover, a prospective study of children treated with doxycycline for RMSF demonstrated that these children did not have substantial discoloration of permanent teeth compared with those who had never received the drug (56). Because TBRD can be life-threatening and limited courses of therapy with tetracycline-class antibiotics do not pose a substantial risk for tooth staining, the American Academy of Pediatrics Committee on Infectious Diseases revised its recommendations in 1997 and has identified doxycycline as the drug of choice for treating presumed or confirmed RMSF and ehrlichial infections in children of any age (61,62).
Chloramphenicol is an alternative drug that has been used to treat RMSF (50); however, this drug is associated with various side effects and might require monitoring of blood indices. Chloramphenicol is no longer available in the oral form in the United States. Moreover, epidemiologic studies in which CDC case report data have been used suggested that patients with RMSF treated with chloramphenicol have a higher risk of dying than persons who received a tetracycline (11,63). In vitro evidence also indicates that chloramphenicol might not be an effective antibiotic for HME or HGA (64,65). Clinicians who suspect a TBRD and are considering empiric antibiotic therapy before laboratory confirmation should be aware that doxycycline provides therapeutic coverage for RMSF, HME, HGA, and E. ewingii infection.
Tetracyclines are generally contraindicated for use in pregnant women because of risks associated with malformation of teeth and bones in the fetus and hepatotoxicity and pancreatitis in the mother (66). However, tetracycline has been used successfully to treat HME in pregnant women (67), and the use of tetracyclines might be warranted during pregnancy in life-threatening situations where clinical suspicion of TBRD is high. Whereas chloramphenicol is typically the preferred treatment for RMSF during pregnancy, care must be used when administering chloramphenicol late during the third trimester of pregnancy because of risks associated with grey baby syndrome (66). Substantially limited clinical data exist that support the use of other antimicrobials during pregnancy, although rifampin has been used successfully in several pregnant women with HGA (68). In vitro studies have demonstrated that rifamycins provide effective activity against Ehrlichia and Anaplasma species (64,65), and therapy with rifampin may be considered for patients with HGA who are unsuited for tetracycline treatment because of pregnancy or a history of drug allergy (45). Clinicians should use caution, however, in ensuring that RMSF can be ruled out because the clinical presentations of RMSF and anaplasmosis are similar, and the comparative effectiveness of rifampin and doxycycline is unknown at this time.
Because certain patients with TBRD might initially receive an alternative diagnosis, they might be empirically treated with antibiotics inactive against rickettsiae, including penicillins, cephalosporins, aminoglycosides, erythromycin, or sulfonamides. This situation presents both diagnostic and therapeutic challenges. In certain cases, patients treated with beta-lactam antibiotics or sulfacontaining drugs are mistakenly thought to have drug eruptions when they later manifest a rash (66), further postponing a correct diagnosis and appropriate treatment. Because the physician might conclude that the prescribed treatment will take time to work, a delay in obtaining critical additional laboratory or clinical information also might be a result. In addition, sulfa-containing antimicrobials have been associated with increased severity of TBRD, although whether disease severity is directly related to the use of sulfa-containing drugs or the delayed administration of more effective antimicrobials is not clear. Cases of severe ehrlichiosis complicated by acute respiratory distress syndrome have been associated with the use of trimethoprim-sulfamethoxazole (69,70).
In addition, clinicians should note the overlap between early symptoms of invasive meningococcal infection and TBRD. These conditions are difficult to distinguish early in the course of illness. In patients for whom both conditions are included in the initial differential diagnoses, after performing blood cultures and a lumbar puncture, empirically treating for both diseases is appropriate. This treatment can be accomplished by adding an appropriate parenteral penicillin or cephalosporin that has activity against N. meningitidis to doxycycline therapy.
Preventive antibiotic therapy for rickettsial infection is not indicated for patients who have had recent tick bites and are not ill. Limited numbers of ticks in areas where tickborne diseases are endemic are infected with pathogenic rickettsiae. Approximately 1%-3% of vector ticks are infected with spotted fever group rickettsiae (71). How- ever, less than 1% of these rickettsiae usually have been confirmed to be R. rickettsii (72,73). Approximately 5%-15% of lone star ticks are infected with E. chaffeensis (47), and 10%-50% of I. scapularis ticks are reported to be infected with A. phagocytophilum (74,75) in endemic areas. Therefore, the risk for such infection after a tick bite is low. Moreover, for RMSF, preventive therapy has been demonstrated to delay but not prevent the onset of symptoms (76).
The following is a summary of salient features of treatment and management:
• Clinical history, symptoms, and physical and laboratory findings should guide the clinician's approach to patient management and treatment. • Not all patients with TBRD will require hospitalization.
• Clinicians may consider a wait and watch approach for 24-48 hours for patients early in the course of illness and who have nonsupporting history, nonspecific clinical signs, and normal laboratory findings. • Doxycycline is the drug of choice for the treatment of presumptive or confirmed TBRD in both adults and children. • Limited courses of tetracycline-class antibiotics (e.g., doxycycline) do not pose a substantial threat of tooth staining in children. • Tetracyclines typically are contraindicated for use during pregnancy but might be warranted in lifethreatening situations where clinical suspicion of TBRD is high. • Delay in treatment can lead to severe disease and fatal outcome of TBRD. • In evaluating for TBRD, when early invasive meningococcal infection cannot be ruled out, providing treatment for both conditions by adding an antimicrobial that has activity against N. meningitidis is appropriate. • Prophylactic use of antibotics after a tick bite is not recommended.
# Considerations for Management of Patients with Severe Manifestations of TBRD
A substantial number of patients with TBRD require hospitalization (6,7,10). Severe manifestations of TBRD might include prolonged fever, renal failure, disseminated intravascular coagulopathy (DIC), hemophagocytic syndrome, meningoencephalitis, and acute respiratory distress syndrome. A notable exception is that HGA has not been associated with meningoencephalitis.
RMSF is frequently a severe illness, and patients commonly require hospitalization. Up to 20% of untreated cases and 5% of treated cases have fatal outcome, making RMSF the most commonly fatal rickettsial disease in the United States (5,10). However, assessment of passive reporting of RMSF-associated death has suggested that only one third of fatal cases of RMSF were reported to CDC during 1983-1998 (77). Therefore, the actual case-fatality rate of RMSF might be closer to 5%-10%. Host factors associated with severe or fatal RMSF include advanced age, male gender, black race, chronic alcohol abuse, and glucose-6-phosphatedehydrogenase (G6PD) deficiency (50). Deficiency of G6PD is a sex-linked genetic condition affecting approximately 12% of the U.S. black male population; deficiency of this enzyme is associated with a high proportion of fulminant cases of RMSF (50,78). Fulminant cases follow a clinical course that is fatal within 5 days of onset. Longterm health effects persisting for >1 year after acute RMSF infection include partial paralysis of the lower extremities; gangrene requiring amputation of fingers, toes, arms, or legs; hearing loss; blindness; loss of bowel or bladder control; movement disorders; and speech disorders (79). These complications are observed most frequently in persons recovering from severe, life-threatening disease, often after lengthy hospitalizations. Digital necrosis in a patient occurring late in the course of RMSF has been illustrated (Figure 18).
Similarly, HME and HGA can cause serious or fatal disease as well, although at lower rates than are observed for RMSF. At least 50% of patients with HGA and HME are hospitalized to rule out other potentially life-threatening conditions and to manage the illness (34,47). Clinical indications for admission might include immunocompromised state, pain management (i.e., headache and myalgias), mental confusion, cough, infiltrate in chest radiograph, abnormal spinal fluid findings, or specific acute organ failure. Approximately 3% of HME patients and less than 1% of HGA patients with symptoms severe enough to seek medical attention will die from the infection (25,34,47). The severity of ehrlichiosis might be related, in part, to the immune status of the patient. Persons with compromised immune systems caused by immunosuppressive therapies (e.g., corticosteroids or cancer chemotherapy), human immunodeficiency virus (HIV) infection, organ transplantation, or splenectomy appear to develop more severe disease from E. chaffeenis infection, and case-fatality rates for these persons are characteristically higher than casefatality rates reported for the general population (30). Although the case fatality rate for HGA (0.5%-1.0%) is lower than that for HME, notable complications, including respiratory failure, a toxic-shock-like syndrome, rhabdomyolysis, pancreatitis, acute renal failure, and invasive infections caused by opportunistic viral or fungal agents can occur, especially among patients who have co-morbid illnesses or who are actively immunosuppressed (45). In addition, advanced patient age and delay in diagnosis and the onset of specific antibiotic therapy are predictors of a more severe course of HGA (53).
Management of severely ill patients with TBRD should include careful assessment of fluid and electrolyte balance. Vasopressors and rigorous fluid management might be needed, especially when the illness is complicated by renal failure or hypotension. Patients might have pulmonary infiltrates because of vasculitis that are erroneously thought to be caused by cardiac failure or pneumonia. Seizures might require aggressive treatment, and arrhythmias (e.g., atrial fibrillation or flutter) will frequently respond to treatment of the patient's underlying disease. Consultation with an intensivist or an infectious disease subspecialist might be helpful in managing these complications.
The following is a summary of salient features of severe manifestations:
• TBRD can be life-threatening.
• Severe manifestations of TBRD include prolonged fever, renal failure, myocarditis, meningoencephalitis, hypotension, acute respiratory distress syndrome, and multiple organ failure.
# Confirmatory Diagnostic Tests
Rickettsial infections pose difficult diagnostic challenges to both clinicians and laboratorians. Rapid confirmatory assays are not commonly available to guide treatment decisions of acutely ill patients. However, confirmatory assays provide the physician with vital information that retrospectively validates the accuracy of the clinical diagnosis. Laboratory confirmation of infection is also vital to understanding the epidemiology and public health impact of TBRD.
Several laboratory methods are available to diagnose TBRD. However, they vary in the time required to obtain results and in the type of information they provide the clinician. Therefore, treatment decisions should be based on epidemiologic and clinical clues and should never be delayed while waiting for laboratory confirmation of a diagnosis. Similarly, test results should be interpreted in the context of the patient's illness and the epidemiologic setting. Misuse of specialized tests for patients with a low probability of the disease and in areas with a low prevalence of disease might result in confusion. A fundamental understanding of the signs, symptoms, and epidemiology of the disease is critical in guiding requests for tests and interpretation of test results for ehrlichioses, anaplasmosis, and RMSF. Studies have suggested that antibiotic therapy might diminish the development of convalescent antibodies in RMSF (CDC, unpublished data, 2005). However, the degree to which doxycycline might cause this occurrence is uncertain. If molecular or culture diagnostic methods are conducted, obtaining blood for testing before antibiotics are administered is essential to obtain the best results.
# Blood-Smear Microscopy
Microscopic examination of blood smears stained with eosin-azure type dyes (e.g., Wright-Giemsa stain) might reveal morulae in the cytoplasm of infected circulating leukocytes (1%-20%) of patients with HME and 20%-80% of patients with HGA (45,47) during the first week of infection, which is highly suggestive of ehrlichial or anaplasma infection. However, blood smear examination is insensitive and should be performed by an experienced microscopist. In addition, a negative blood smear examination should not dissuade the caregiver from initiating treatment with doxycycline if the clinical presentation and routine laboratory findings support the diagnosis of ehrlichiosis or anaplasmosis. Blood smear examination is not useful for diagnosis of RMSF.
# Serologic Testing
Serologic assays for RMSF, HME, and HGA are commonly available through multiple commercial and state public health laboratories. Serologic evaluations are commonly conducted by using the indirect immunofluorescence antibody (IFA) assay. Antibodies in the serum bind to fixed antigens on a slide and are detected by a fluorescein-labeled conjugate. Although IFA remains the principle diagnostic tool for the diagnosis of rickettsial and ehrlichial infections, no standardized antigens, conjugates, or agreement on what consti-tutes a positive result among the various laboratories providing these tests exist. Individual laboratories should be consulted regarding their test threshold levels. Enzyme-linked immunosorbent assay (ELISA) is becoming a more frequently used assay. Similar to IFA, the accuracy of ELISA depends on the laboratory conducting the test, the quality and specificity of the antigen, and the threshold levels at which a positive result is considered. Available ELISA tests are qualitative and cannot be used effectively to monitor increases or decreases in antibody titer.
The sensitivity of the IFA assay is substantially dependent on the timing of collection of the sample. Early in any TBRD, a majority of serologic tests will be negative. Clinical illness nearly always precedes laboratory diagnosis by any method. As the illness progresses to 7-10 days, the sensitivity of IFA serology increases. The IFA is estimated to be 94%-100% sensitive after 14 days, and that sensitivity is increased if paired samples are tested (80). The IFA is considered to be the gold standard of serologic testing for rickettsial diseases, and other serologic tests have not been developed that surpass the sensitivity and specificity of these assays. Testing two sequential serum or plasma samples together to demonstrate a rising IgG or IgM antibody level is essential to confirm acute infection. Paired serum specimens taken early (i.e., acute) and later (i.e., convalescent) in the disease course represent the preferred specimens for evaluation. Typically, these specimens should be taken at least 2-3 weeks apart to examine for a four-fold or greater increase in antibody titer (33).
The majority of patients demonstrate increased IgM or IgG titers by the second week of the illness (patients infected with certain imported rickettsiae might not demonstrate increased titers until 4 weeks after illness onset). However, patients might lack diagnostic IgG and IgM antibody titers in the first 7 days of illness, a period when the majority of patients initially seek medical care and laboratory testing is performed. The duration of time that antibodies will persist after recovery from the infection is variable. In certain persons, high titers of antibodies against A. phagocytophilum have been observed for 3½ years after the acute illness (81). For RMSF, IgG and IgM titers increase concurrently by the second week of illness, and IgM antibodies wane after 3-4 months, whereas IgG titers persist for 7-8 months (82). The majority of commercial reference laboratories conduct testing for IgG and IgM antibodies.
Cross-reactivity of antigens results in antibody responses that are typically group-specific, but not necessarily species-specific, after infections with these pathogens. For example, serologic tests that detect antibodies reactive with R. rickettsii might have resulted from previous infections with other spotted fever group rickettsial species. Similarly, antibodies reactive with E. chaffeensis or A. phagocytophilum occasionally react with the other ehrlichial species, which might impede epidemiologic distinction between the ehrlichial infections (83). Most patients with E. ewingii infections develop antibodies that react with E. chaffeensis antigens. Little cross-reactivity of Rickettsia with Ehrlichia or Anaplasma species exists. Certain serologically confirmed cases of infection thought to be RMSF, HME, or HGA might represent infections with the other agent or with another antigenically related species. The predominance of non-R. rickettsii species in tick vectors collected in RMSFendemic areas suggests that related organisms of undetermined pathogenicity might play a role in human illness (84). This occurrence is especially true for persons who are infected with rickettsial organisms from endemic areas outside of the United States.
# Nucleic Acid Detection
Amplification of specific DNA by PCR provides a rapid method for detecting TBRD infections. These tests are available from CDC, certain state health laboratories, and a limited number of research and commercial laboratories (Box). Conventional PCR tests have no specified standard, and diagnostic sensitivity and specificity might vary among individual assays (80). Doxycyline treatment, in particular, can also decrease the sensitivity of PCR (45). In studies of A. phagocytophilum infection, PCR was estimated as 60%-70% sensitive (53), and for diagnosis of infection with E. chaffeensis, PCR was estimated to be 52%-56% sensitive (25) to 87% sensitive (85). For RMSF, PCR is probably more useful for detecting the etiologic agent in a skin biopsy or autopsy tissue specimen than it is in an acute blood sample because, typically, low numbers of rickettsiae circulate in the blood in the absence of advanced disease or fulminant infection (18). PCR testing of skin biopsies alone does not offer ideal sensitivity, and a negative result does not exclude the diagnosis because of focality of vessel involvement. Laboratory confirmation of RMSF in the acute stage is improved when PCR is used in conjunction with IHC staining. PCR of whole blood specimens is more useful for confirming HME, HGA, and E. ewingii infection because of the tropism of these pathogens for circulating WBC. However, no optimal time frame has been established that is ideal for sample collection to ensure the highest sensitivity for diagnosing ehrlichioses or anaplasmosis. New techniques (e.g., real-time PCR) might offer the advantages of speed, reproducibility, quantitative
# IHC Staining
Another approach to diagnosing TBRD is immunohistochemical (IHC) staining of antigens in formalin-fixed, paraffin-embedded biopsy or autopsy tissues. This test can be particularly useful to diagnose fatal TBRD in those patients for whom diagnostic levels of antibodies have not developed before death. For patients with a rash, IHC or immunofluorescence staining of a skin biopsy can be a critical diagnostic technique for RMSF. Immunostaining of skin biopsy specimens has been reported to be 100% specific and 70% sensitive in diagnosing RMSF (35). This method has been used to diagnose fatal and nonfatal cases of RMSF (18,(87)(88)(89). Because rickettsiae might be focally distributed in tissue, this test might not always detect the agent. Autopsy tissues also are appropriate for evaluation and include the liver, spleen, lung, heart, kidney, and brain. The IHC method is most useful in documenting the presence of organisms in patients before initiation of antibiotic therapy or within the first 48 hours after antibiotic therapy has been initiated. IHC techniques also are available for diagnosing cases of ehrlichioses and anaplasmosis from bone marrow biopsies and tissue obtained at autopsy of fatal cases, including the spleen, lymph nodes, liver, and lung (90)(91)(92). Immunostaining for spotted fever group rickettsiae, E. chaffeensis, and A. phagocytophilum is offered by CDC and certain university-based hospitals and commercial laboratories in the United States (Box).
# Culture
Because the agents that cause TBRD are obligate intracellular pathogens, they must be isolated by using cell culture techniques that are typically more labor-intensive and timeconsuming than serologic, molecular, or IHC assays. Theoretically, any laboratory capable of performing routine viral isolations might have the expertise to isolate these pathogens. However, R. rickettsii is classified as a Biosafety Level-3 (BSL-3) agent, and attempts to isolate this agent should be made only in laboratories equipped to handle BSL-3 pathogens (93). Laboratories attempting culture of R. rickettsii bacteria need to comply completely with federal regulations (42 C.F.R. [2004]) regarding the registration and use of select agents (93). As a result, culture is rarely used for diagnosis, and other methods (e.g., serology, PCR, or immunostaining) are used to confirm infection.
The following is a summary of salient features of diagnostic testing:
• Blood smear microscopy might reveal presence of morulae in infected leukocytes, which is highly suggestive of HGA or, less commonly, HME. Tickborne illness characterized by acute onset of fever and possible headache, malaise, myalgia, and nausea/vomiting or neurologic signs. A macular or maculopapular rash is reported in the majority of patients and is frequently observed on the palms and soles.
# Clinical description
Tickborne illness characterized by acute onset of fever, headache, myalgia, and possible malaise. Nausea, vomiting, or rash might be observed in certain cases. Clinical laboratory findings might include thrombocytopenia, leukopenia, and possibly elevated liver enzymes. Intracytoplasmic morulae might be visible in the leukocytes of certain patients.
# Laboratory criteria
# HME
# HGA Unspecified ehrlichiosis
Serologic evidence of 4-fold change in serum antibody titer against Rickettsia rickettsii antigens between paired serum samples, as determined by IFA § or ELISA ¶ ; or demonstration of R. rickettsii antigen in a clinical specimen by IHC** methods; or detection of R. rickettsii DNA in a clinical specimen by PCR assay; or isolation of R. rickettsii from a clinical specimen in cell culture.
# Case classification
Probable case: Identified in a person with a clinically compatible illness with either a single positive IFA titer (based on cutoff titers established by the laboratory performing the test) or the visualization of morulae in leukocytes.
Confirmed case: Identified in a person with a clinically compatible illness that is laboratory confirmed by a 4-fold change in serum antibody titer, as determined by IFA or ELISA or positive PCR or positive IHC, or isolation in culture.
• Whole blood specimens might be useful for a PCR confirmation of HME, HGA, and E. ewingii infection; however, a negative result does not rule out the diagnosis.
# Surveillance and Reporting
National reporting requirements are determined collaboratively by the Council of State and Territorial Epidemiologists and CDC. RMSF, anaplasmosis, and all forms of ehrlichiosis are nationally notifiable diseases. RMSF became nationally notifiable in 1989 and anaplasmosis and ehrlichiosis, in 1998. When health-care providers identify a potential case of TBRD, they should notify the local health department. The local health department, in cooperation with the state health department, can assist the healthcare provider in obtaining appropriate diagnostic testing to confirm the diagnosis. All confirmed or probable cases of RMSF, HME, HGA, and E. ewingii infection should be reported to the state health department. The case defini-tions for confirmed and probable cases of RMSF, HME, and HGA have been reported (Table 4; 33,94). Each state health department compiles case reports and submits them to CDC, where data are compared and disseminated via the MMWR Weekly and annual Surveillance Summaries.
Since 1981, CDC has collected and analyzed surveillance data on RMSF by using two complementary systems. States submit reports electronically via the National Electronic Telecommunications System for Surveillance (NETSS) as part of the National Notifiable Disease Surveillance System. NETSS reports capture diagnosis, date of onset, and basic demographic and geographic data related to the case. In addition, physicians are encouraged to complete a standardized case report form (CRF; Appendix) and forward it to the state health department, where it is compiled with similar reports and forwarded to CDC. The CRF summarizes demographic, epidemiologic, and outcome data that are not reported in NETSS. Data collected on the CRF are useful in summarizing the epidemiologic characteristics of tion per application. Products with DEET concentrations as low as 10% and those containing 25%-35% concentrations are considered optimal. No evidence exists that concentrations >50% are more efficacious or provide longer duration of protection (95). The American Academy of Pediatrics has recommended that DEET concentrations no greater than 20%-30% should be used for children (96). Products containing permethrin (e.g., permanone) can be used to treat outer clothing (e.g., shirts and pants) and should not be applied to skin. Permethrin is available commercially as a spray-on preparation. It should be applied evenly to outer clothing, according to label directions in a wellventilated area. Clothing should be allowed to completely dry before being worn. Pre-treated clothing is available and remains effective for multiple launderings. The use of DEET and permethrin should be considered by persons who enter heavily infested tick habitats where the risk for being bitten is high and the potential for TBRD infection exists.
Adults entering wooded or grassy areas should inspect themselves and their children frequently for ticks. Because several hours might elapse before ticks attach and inject pathogens, frequent checks increase the likelihood of finding ticks before they transmit an infectious agent. The duration of tick attachment necessary to transmit rickettsial organisms is substantially variable and has been reported to be as little as 2-10 hours (97) to 10-20 hours (98) for R. rickettsii. Limited data exist regarding the interval of transmission after tick attachment for A. phagocytophilum, but animal studies indicate that 24-48 hours might elapse before pathogen transmission (99,100). No comparable data exists for E. chaffeensis. Sites where ticks commonly attach include, but are not limited to, the scalp, waist, armpits, groin, and under socks and the beltline. Pets should also be checked for ticks because they can carry ticks back to their homes and human companions. Regular application of ectoparasite control on pets helps to reduce the risk for human exposure to ticks.
If an attached tick is found, it should be removed by grasping with tweezers or fine-tipped forceps close to the skin and gently pulling with constant pressure. Folk remedies, including gasoline, kerosene, petroleum jelly, fingernail polish, or lit matches should never be used to extract ticks (101). Removing the tick with bare hands should be avoided because fluids containing infectious organisms might be present in the tick's body and at the wound site. Ticks that have been removed should not be crushed between the fingers to prevent contamination, and hands should be washed to avoid potential conjunctival inoculation. The bite wound should then be disinfected. disease and focusing on prevention and treatment. This process includes examining lesser understood aspects of these conditions (e.g., the role of immunosuppression as a risk factor for disease; the prevalence of severe outcomes of infection, including death; and hospitalization trends). In 2001, the form was expanded to include reporting of other common TBRD, including HGA and HME, in addition to RMSF.
A surveillance system is critical for studying the changing epidemiology of TBRD and for developing effective prevention strategies and public health education programs. The detection of a cluster of RMSF cases in a region of Arizona where the disease was not known to occur and subsequent prevention and control initiatives underscore the vital role of surveillance and reporting in protecting the public's health. By the end of 2004, the highest number of RMSF cases was reported to CDC (n = 1,514), suggesting potential increased activity. However, underreporting of TBRD is probably common.
The following is a summary of salient features of surveillance and reporting:
• RMSF, HME, HGA, and other ehrlichioses are reportable diseases in the United States. • Physicians who identify a potential case of TBRD should notify the local health department, which can assist with obtaining diagnostic testing to confirm the diagnosis. • Surveillance and reporting of TBRD are key components of public health education and disease prevention efforts.
# Prevention
No licensed vaccines for TBRD exist. Avoiding tick bites and promptly removing attached ticks remain the best disease prevention strategies. Persons should limit their exposure to tick-infested habitats, including wooded or grassy areas. Persons should walk on cleared trails and avoid brushing against tall grass and other vegetation. This practice is particularly essential during periods of peak tick activity (i.e., late spring and summer) but should be observed, regardless of the season. Protective clothing, including a hat, long-sleeved shirts, pants, socks, and closed-toe shoes are helpful in preventing ticks from reaching the skin and attaching. Wearing light-colored clothing is preferred because crawling ticks can be seen easily.
Various over-the-counter products containing DEET (N,N-diethyl-m-toluamide) are available for application on exposed skin and clothing to repel ticks. The higher the concentration of DEET, the longer the duration of protec-The following is a summary of salient features of prevention: • Avoid tick bites, which is key to the prevention of TBRD. • Limit exposure to tick habitats, including grassy and wooded areas. • Inspect the body carefully for ticks after being in a tick habitat. • Remove attached ticks immediately by grasping with tweezers close to skin and pulling gently with steady pressure.
# TBRD Cases
The following TBRD cases were observed in health-care settings. Information from the cases can be used to reinforce medical management information related to TBRD (3,22,102) and are intended to illustrate certain common pitfalls in the diagnosis and treatment of TBRD. The case reports include a description of the case and salient features that can be considered when dealing with a potential case of TBRD.
# Case 1
In June 2001, a girl aged 5 years was taken to an ED in Missouri with a 3-day history of intermittent fever, headache, mild nausea, and a sore throat. On physical examination, the patient had a fever of 105°F (40.6 º C) and a maculopapular rash on her legs, including the soles of her feet.
• What should be included in the differential diagnosis? Possible causes of fever and rash in this child include meningococcemia, RMSF, HME, enteroviral infections, Kawasaki disease, drug reactions, and streptococcal disease with exanthem.
# • What additional information would assist with the diagnosis?
Determine how long the rash has been present and when and where it appeared relative to onset of fever. The parent should be queried concerning medication use, immunocompromising conditions, and recent activities that could have led to animal exposures (including dogs), sick contacts, recent travel, outdoor activities (e.g., hiking, camping, and playing in brushy areas or backyard), and real or potential tick exposures.
The parent noticed the rash, which began on the arms and legs, on the same day that the child was taken to the ED. They did not own a dog, and no history of recent travel out of the local area and no history of a tick bite were noted, although the parent said that ticks were in the area around their house.
# • What laboratory tests might be useful?
A CBC, comprehensive metabolic panel, blood culture, and a rapid Streptococcus pharyngitis screen should be performed. An acute serum should be obtained for IgG and IgM antibodies to R. rickettsii, E. chaffeensis, and A. phagocytophilum, but subsequent management of the patient should not depend on results. PCR for E. chaffeensis and A. phagocytophilum using EDTA whole blood might be useful if these tests are available from a reference laboratory.
Laboratory results included a WBC count of 8,800 x 10 9 cells/L (normal: 4.5-11.0 x 10 9 cells/L), with 5% bands (normal: 0%-5%), 70% neutrophils (normal: 45%-75%), 17% lymphocytes (normal: 16%-46%), and 8% monocytes (normal: 4%-11%). The platelet count was 50 x 10 9 cells/L (normal: 150-350 x 10 9 cells/L). Serology results were not available for 3 days.
# • How does this information assist with the diagnosis?
The time of year for these clinical signs should raise suspicion for TBRD. A normal WBC is frequently observed in patients with viral infections and with RMSF. Patients with RMSF will commonly develop moderate to severe thrombocytopenia as the disease progresses, although a normal platelet count is frequently observed early in the course of illness. If serologic results are not immediately available, the clinician should not be dissuaded from initiating therapy if it is clinically indicated.
# • What actions, including treatment, should be taken?
On the basis of history, clinical signs, geographic location, and time of year, suspicion of a TBRD is reasonable. An appropriate course of action would include treatment with doxycycline (2.2 mg/kg body weight administered orally twice daily for a minimum of 5 days) and close follow-up to ascertain clinical response to therapy while continuing to rule out other possible causes. Appropriate antimicrobial therapy for other suspected etiologies should be considered until they can be reasonably excluded. For example, certain experts recommend administering an intramuscular dose of ceftriaxone, pending blood culture results, because meningococcal disease cannot be reliably distinguished from TBRD on clinical grounds alone. Convalescent-phase serology for RMSF, HGA, and HME should be performed 2-4 weeks later to confirm the diagnosis.
• What preventive measures can the patient and her family take to prevent infection in the future?
The most effective preventive measure is to 1) limit exposure to ticks during peak periods of activity (prima-rily April-September), 2) inspect body and clothing thoroughly for ticks after being in wooded or grassy areas, 3) remove attached ticks immediately by grasping with tweezers or forceps close to the skin and pulling gently with steady pressure, and 4) apply insect repellant (e.g., DEET) when exposure to grassy or wooded areas is anticipated. Case 1 synopsis. This patient's clinical history suggested exposure to ticks, although no definitive indication of a tick bite was reported. Ticks are small (particularly in their nymphal and larval stages), and bites frequently go unnoticed because ticks might attach in places that are difficult to observe (e.g., the scalp, axillae, and inguinal regions). Up to 40% of patients with RMSF report no history of a tick bite (10,11). Therefore, the clinician should not be dissuaded from making a diagnosis of RMSF when no report of a tick bite is made. The clinical signs and laboratory values and a history that are compatible with tick exposure should guide the diagnosis and therapeutic actions. Serum samples collected on days 7 and 35 of illness demonstrated rising IgG antibody titers to R. rickettsii at 32 and 2,048, respectively.
# Case 2
In mid-August 2003, a male child aged 14 months was taken to a community health clinic in Arizona after 1 day of fever 103.7°F (39.8°C). On physical examination, the child had a maculopapular rash that involved his palms and soles. On auscultation, abnormal breath sounds were detected in the right lower lung. The parent stated that they had not traveled out of the local area recently. No one else in the family was ill, and the child was up-to-date on vaccinations. Chest radiographic evaluation revealed a possible right lower lobe infiltrate. On the basis of clinical and radiographic findings, pneumonia and roseola infantum were diagnosed. The child was administered an intramuscular injection of ceftriaxone and sent home with a prescription for oral amoxicillin/clavulanate.
The next day, the child was taken back to the clinic with vomiting and rash that was petechial. His fever was 105.7°F (41°C). He was admitted to the hospital, and antibiotic treatment for pneumonia was continued. On day 3 of hospitalization, the child developed DIC. Remarkable laboratory findings included: WBC count, 16.2 x 10 9 cells/L (normal: 4.5-11.0 x 10 9 cells/L); platelet count, 46 x 10 9 platelets/L (normal: 150-350 x 10 9 cells/L); aspartate aminotransferase (AST), 291 U/L (normal: 10-40 U/L); and alanine aminotransferase (ALT), 99 U/L (normal: 10-55 U/L). The child's condition worsened, and 7 days after the onset of illness, he died of pulmonary hemorrhage.
# Case 2 synopsis.
A serum sample collected 5 days before the child's death tested negative by IFA for IgM and IgG antibodies reactive with R. rickettsii. However, R. rickettsii DNA was detected in serum by PCR assay. RMSF can have a rapid course; 50% of RMSF deaths occur within 9 days of illness onset (10,11). IgM and IgG antibodies are typically not detectable before the second week of illness; therefore, serology will be not useful in diagnosing the infection in its earliest stages. Fever and rash in a young child can be caused by various enteroviruses, human herpesvirus 6, N. meningitidis, measles virus, R. rickettsii, and E. chaffeensis, among other agents. Common causes of bacterial pneumonia in a child this age might include Streptococcus pneumoniae, Staphylococcus aureus, Streptococcus pyogenes, and, less commonly, M. pneumoniae. Although this child lived in an area where RMSF is not common (e.g., Arizona), the diagnosis should not be excluded because of geography. Although RMSF is more common in the south central and south Atlantic states, it should be considered endemic throughout the contiguous United States (10). TBRD are seldom treated with the appropriate antibiotic, unless they are suspected. In this context, the majority of broad spectrum antimicrobials, including penicillins, cephalosporins, aminoglycosides, erythromycin, and sulfa-containing drugs are not effective against rickettsiae, ehrlichiae, or anaplasmae.
# Case 3
In early June 1996, a man aged 52 years who was HIVseropositive sought medical care at a hospital in Florida. He had a 4-day history of fever, headache, myalgias, nausea, and vomiting. The patient had been previously healthy, with no known previous opportunistic infections. An absolute CD4+ lymphocyte count of 164 cells/µl was documented 2 months before this visit. Physical examination revealed an acutely ill man; the patient had a fever of 103.5 º F (39.7 º C) and experienced dizziness and low blood pressure when he stood up (orthostatic hypotension). He reported that 2 weeks before admission, he had been bitten by a tick while hiking in central Georgia.
A CBC and chemistry panel and, because of the history of a tick bite, serologic tests for E. chaffeensis were ordered. Remarkable laboratory findings included hemoglobin 11.5 g/dL (normal: 13-18 g/dL); WBC count, 2.0 x 10 9 cells/L (normal: 4.5-11.0 x 10 9 cells/L), with 66% neutrophils (normal: 45%-75%), 18% bands (normal: 0%-5%), 8% lymphocytes (normal: 16%-46%), and 8% monocytes (normal: 4%-11%); and platelet count, 16 x 10 9 cells/L (normal: 150-350 x 10 9 cells/L). Peripheral blood smears revealed ehrlichial morulae in 2.5% of all leukocytes, including monocytes, lymphocytes, atypical On the basis of laboratory and clinical findings, a diagnosis of HME was made, and intravenous doxycycline (100 mg every 12 hours) was initiated. Despite doxycycline therapy, the patient remained febrile, severely thrombocytopenic, and continued to have elevated liver enzymes. He developed right lower lobe pneumonia and renal failure and died 6 days after hospitalization.
Case 3 synopsis. Patient sera obtained on days 1 and 5 of hospitalization were negative for IgG and IgM antibodies reactive with E. chaffeensis. However, the correct diagnosis was revealed on admission by a finding of morulae in leukocytes, and this diagnosis was subsequently confirmed when E. chaffeensis DNA was detected by using PCR in whole blood specimens from the patient, and the agent was isolated in cell culture. HME can be a severe disease, particularly in immunosuppressed persons. HME does not commonly cause rash in adults; therefore, history of tick exposure and characteristic leukopenia and thrombocytopenia were most useful in arriving at a diagnosis. Although morulae were observed in the patient's peripheral blood, microscopy is generally insensitive, and morulae are reported to be observed in only 1%-20% of patients with HME (45,47). Therefore, a diagnosis of HME would need to be confirmed by PCR, serology, or immunostaining, or culture isolation.
# Case 4
In mid-May 1999, a female aged 69 years went to her physician in upstate New York. She had a 3-day history of nausea, vomiting, fatigue, and fever. She said that her dog had died 2 days earlier after a brief illness characterized by signs similar to her own. Physical examination revealed no abnormalities. Her temperature was 100.4 º F (38 º C).
• What should be included in the differential diagnosis? Possible diagnoses that should be considered include viral syndrome, foodborne illness, and urinary tract infection.
# • What additional information would assist with the diagnosis?
Patient should be queried regarding other signs and symptoms, recent activities and travel, exposure to other ill persons, foods consumed, and contact with ticks. The patient had no other symptoms to report and reported no unusual activities or recent travel.
# • What diagnostic tests, if any, are needed?
Because the patient's symptoms were nonspecific, a CBC should be ordered. Results will not be available until the next day.
On the basis of the signs present when the patient first went to her physician, she was diagnosed with gastroenteritis and instructed to return within 24-48 hours, if her symptoms did not improve. The patient would be contacted regarding her laboratory test results. The next day, the patient returned with continued fever and changes in mental status. Her temperature remained at 100.4 º F (38 º C), but she was notably confused and lethargic. Her physical examination was unremarkable and did not reveal the presence of a rash.
Laboratory tests obtained on the previous day revealed a WBC count of 3.8 x 10 9 cells/L (normal: 4.5-11.0 x 10 9 cells/L); a platelet count of 99 x 10 9 cells/L (normal: 150-350 x 10 9 cells/L); and a hemoglobin concentration of 12.7 g/dL (normal: 12-16 g/dL).
# • How does this information assist with the diagnosis?
On the basis of the patient's thrombocytopenia, leukopenia, and worsening clinical condition, encephalitis and sepsis should be included in the differential diagnosis.
# • What actions, including treatment, should be taken?
On the basis of presenting signs and laboratory tests, the patient was hospitalized and intravenous levofloxacin therapy was initiated for fever of unknown cause. Blood, urine, and stool cultures were ordered as well as serologic assays for B. burgdorferi, E. chaffeensis, and A. phagocytophilum, and PCR for E. chaffeensis and A. phagocytophilum.
The patient's temperature returned to normal within 48 hours, her nausea and vomiting resolved, and her blood counts returned to normal. She was discharged after 3 days. Blood, urine, and stool cultures revealed no specific pathogens, and serologic assays were negative for antibodies reactive with B. burgdorferi, E. chaffeensis, and A. phagocytophilum. Case 4 synopsis. IHC staining of tissues from the patient's dog, submitted by the veterinarian to CDC, demonstrated abundant spotted fever group rickettsial antigens, and rickettsiae were identified within and around blood vessels in multiple tissues, including brain and testes. The cause of the dog's illness was identified as RMSF. This information was communicated to the patient's physician. When the physician contacted the patient, she reported that her fatigue and headache had persisted after discharge from the hospital. The patient was treated with oral doxycycline, and all symptoms resolved within 1 week. Subsequent testing of the patient's sera for early and late convalescent-phase antibody titer confirmed a diagnosis of RMSF. Titers of IgM and IgG antibodies were 1,024 and 512, respectively, on day 17 and declined to 256 and 256, respectively, on day 89 after ill-ness onset. The patient did not recall a tick bite and had not seen or removed ticks from her dog, although her dog roamed freely in wooded areas before its illness. Dogs can serve as sentinels for RMSF in human populations, and infections in canines have been associated with increased risk for infection in their owners (22).
# Case 5
In May 2001, a man aged 38 years sought medical attention in Tennessee with complaints of headache, fever, sore throat, and vomiting. He was treated 3 days previously by his primary care physician who diagnosed pneumonia and prescribed azithromycin and levofloxacin, but his fevers persisted. He was taken to the ED by his wife, and she said that he had new onset of confusion. He had no pets or animal exposures. He worked as a construction manager and was frequently outdoors in wooded areas but did not recall a tick bite.
• What should be included in the differential diagnosis?
The initial signs and symptoms were nonspecific, but the patient's confused state raised concern for possible involvement of the CNS. During the summer months, the differential diagnosis included viral meningitis (particularly enteroviral), arboviral meningoencephalitis (West Nile virus and others), TTP, and TBRD. Bacterial meningitis and herpes simplex virus (HSV) encephalitis do not have confined seasonality but also could cause this presentation. Sepsis and other multisystem illnesses are associated with encephalopathy, however, so the differential diagnosis remained broad.
The patient had an oral temperature of 103.4°F (39.7 º C); blood pressure, 100/60 mmHg; and heart rate, 120 beats/minute. The skin examination revealed diffuse erythema with a several scabs on the lower legs. Examination of the abdomen revealed moderate epigastric tenderness with deep palpation but no rebound tenderness or organomegaly. Neurologic examination was nonfocal, except for altered mentation (i.e., Glasgow coma score: 13).
Laboratory testing revealed the following: WBC, 11.9 x 10 9 cells/L (normal: 4.5-11.0 x 10 9 cells/L); 84% segmented neutrophils (normal: 45%-75%); 8% band neutrophils (normal: 0%-5%); 3% lymphocytes (normal: 16%-46%); 5% monocytes (normal: 4%-11%); platelets, 50 x 10 9 cells/L (normal: 150-350 x 10 9 cells/L); total bilirubin, 3.5 mg/dL (normal: 0-1.0 mg/dL); AST, 439 U/L (normal: 10-40 U/L); ALT, 471 U/L (normal: 10-55 U/L); and alkaline phosphatase, 236 U/L (normal: 45-115 U/L). Lumbar puncture revealed a WBC of 0, RBC of 1 with normal glucose of 55 mg/dL and normal protein of 20 mg/dL. Creatinine was elevated at 3.9 mg/dL (normal: 0.6-1.5 mg/dL). Computed tomography scan of the head did not demonstrate an acute abnormality.
• How does the physical examination and laboratory information change the differential diagnosis? Because of the normal lumbar puncture, meningitis (i.e., viral or bacterial) was a less likely diagnosis. However, examination of the CSF might be unremarkable in patients with encephalitis. The presence of thrombocytopenia and elevated transaminases was suggestive of TBRD. Additional considerations included acute cholecystitis, sepsis (possibly associated with DIC), toxic-shock syndrome (rash with multiple organ failure), and TTP (i.e., acute renal failure with fever, altered mental status, and thrombocytopenia).
• What additional tests should be performed? Appropriate diagnostic studies should include blood culture, serologic testing for RMSF and HME (and PCR for these if available), prothrombin time and partial thromboplastin time, examination of the peripheral blood smear (with particular attention for schistocytes or intracellular morulae), and ultrasound of the gallbladder to evaluate for inflammation.
The coagulation studies were within normal limits, and no schistocytes or morulae were observed on smear. Abdominal ultrasound revealed a normal gallbladder but mild splenomegaly. Therapy was initiated with ceftriaxone and vancomycin. Approximately 6 hours later, the patient developed seizures, and acyclovir and doxycycline were added to the course of medicine to effectively treat herpesvirus infection and TBRD. A magnetic resonance imaging scan of the brain was normal, and electroencephalography revealed nonspecific slowing. Antibodies to R. rickettsii and E. chaffeensis were not detected in acute sera. HSV PCR on CSF was negative. Blood cultures did not grow bacteria. The patient defervesced, and mental status normalized over the next 3 days. Case 5 synopsis. Serum obtained 31 days after the initial signs and symptoms contained no antibodies to R. rickettsii but had an IgG titer of 256 to E. chaffeensis, retrospectively confirming the diagnosis of HME. Whereas headache is a nearly universal complaint among patients with HME, altered sensorium might be observed in up to 20% of cases (6). Other CNS manifestations include seizures, meningismus, cranial nerve palsies, focal weakness, and coma. A lymphocytic pleocytosis can be observed in the CSF in approximately 50% of patients with HME who undergo lumbar puncture (103). Neutrophilic pleocytosis can be observed early in the course of the illness. March 31, 2006 Neuroimaging studies are usually normal or nonspecific. TBRD should be included in the differential diagnosis of patients presenting with clinical evidence of CNS infection or CSF findings suggestive of aseptic meningitis.
# Case 6
In July 1994, a man aged 44 years went to see his physician in central Minnesota. He complained of a 1-week history of fever, chills, generalized myalgias, and right temporomandibular joint pain. When he became ill, he treated himself empirically with ampicillin, which was available at home, for 2 days. Because the patient experienced no clinical improvement, he sought medical care. The patient worked outdoors and was frequently in wooded areas. Fourteen days before he went to his physician, he removed two deer ticks that had been attached to his skin for an unknown period.
Physical examination findings. The patient had a lowgrade fever of 100.6 º F (38.1 º C). Examination of heart, lungs, and abdomen were normal. No lymphadenopathy, hepatosplenomegaly, or skin rash were noted. Cardiovascular, pulmonary, gastrointestinal, or neurological symptoms were not present. Overall, physical examination was unremarkable, except for fever.
Laboratory findings. No laboratory evaluations were performed during the visit. A presumptive diagnosis of acute Lyme disease was made, and empirical treatment with amoxicillin and probenecid was initiated; a 1-week followup visit was scheduled. Five days after the outpatient visit, the patient died suddenly at home. He had complained of shortness of breath the day before his death.
Case 6 synopsis. Histopathologic examination of the patient's heart revealed widespread transmural myocarditis with neutrophilic and lymphocytic infiltrates. Postmortem serum specimens were evaluated initially for presumptive carditis as a result of B. burgdorferi infection. Serum titers of IgG and IgM antibodies to B. burgdorferi were not detected by ELISA and western blotting. PCR assays of serum and whole blood for B. burgdorferi also were negative. However, antibody titers to A. phagocytophilum (formerly known as E. equi) were significantly elevated at titer >256 by IFA methods. Detection of DNA extracted by PCR from whole blood and positive IHC staining of cardiac tissue confirmed a diagnosis of anaplasmosis. Although infection with A. phagocytophilum was demonstrated in this case, the pathogenesis of the associated carditis was less clear (104).
The diagnosis of HGA can be difficult because of the nonspecific nature of the febrile illness frequently observed when the patient first seeks medical care. In regions where both Lyme disease and HGA are known to occur, distinguishing between the diseases in the early stages of illness might be difficult. Because treatment should be initiated before a definitive diagnosis is made, selection of an antimicrobial effective against both rickettsial organisms and B. burgdorferi (e.g., doxycycline) is recommended. This case also underscores the importance of close follow-up of patients treated for TBRD on an outpatient basis. Because these diseases can rapidly progress, clinicians should emphasize to patients the need to return for reevaluation if substantial improvement is not observed within 24-48 hours of initiation of treatment.
# Conclusion
TBRD continue to cause severe illness and death in otherwise healthy adults and children, despite the availability of low cost, effective antimicrobial therapy. The greatest challenge to clinicians is the difficult diagnostic dilemma posed by these infections early in their clinical course when antibiotic therapy is most effective.
Early clinical presentations of HME, HGA, RMSF, and E. ewingii infection include fever, headache, myalgia, and malaise and are difficult to distinguish from other infectious and noninfectious diseases. Rash is observed frequently in RMSF, occasionally in HME, and rarely in HGA. TBRD tend to occur seasonally, with the majority of cases occurring during the warmer spring and summer months. However, cases might develop year-round. A detailed history of recent recreational or occupational activities might reveal potential exposure to ticks, although the absence of a history of a recent tick bite should not dissuade clinicians from considering a diagnosis of TBRD.
TBRD can be life-threatening. Severe manifestations of TBRD include prolonged fever, renal failure, myocarditis, meningoencephalitis, hypotension, acute respiratory distress syndrome, and multiple organ failure. Patients usually do not have diagnostic serum antibody levels during the first week of illness; therefore, an inability to detect antibodies (IgG or IgM) in acute-phase serum does not exclude TBRD. Health-care providers should not delay treatment while waiting for a diagnosis; rather, they should empirically provide treatment if they suspect TBRD. Doxycycline is the drug of choice for the treatment of presumptive or confirmed TBRD in both adults and children.
Examination of paired serum samples obtained during acute illness and 2-3 weeks later that demonstrate a rise in antibody titer is the most appropriate approach to confirm TBRD. Physicians who identify a potential case of TBRD should notify the local health department, which can assist with obtaining diagnostic testing to confirm the diagnosis.
No licensed vaccines for TBRD are available. Avoiding tick bites and promptly removing attached ticks remain the best disease prevention strategies.
# Acknowledgments
The preparers acknowledge Jim Gathany, CDC, for the tick photographs and Karoyle Colbert, CDC, for creating the tick distribution map.
# Appendix Tickborne Rickettsial Disease Case Report Form
CDC is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians. CDC designates this educational activity for a maximum of 2.0 hours in category 1 credit toward the AMA Physician's Recognition Award. Each physician should claim only those hours of credit that he/she actually spent in the educational activity.
# Continuing Education Unit (CEU)
. CDC has been approved as an authorized provider of continuing education and training programs by the International Association for Continuing Education and Training. CDC will award 0.2 continuing education units to participants who successfully complete this activity.
# Continuing Nursing Education (CNE)
. This activity for 2.4 contact hours is provided by CDC, which is accredited as a provider of continuing education in nursing by the American Nurses Credentialing Center's Commission on Accreditation.
# Goal and Objectives
This report provides practical information on the diagnosis, treatment, and reporting of tickborne rickettsial diseases (TBRD). This report represents a collaborative effort by a work group comprised of general practitioners, adult and pediatric infectious disease specialists, clinical laboratorians, and epidemiologists from clinical practice, academic centers, and CDC. The goal of this report is to present a framework to assist clinicians in recognizing the symptoms of TBRD, obtaining appropriate diagnostic tests, and initiating prompt and effective treatment. Upon completion of this educational activity, the reader should be able to 1) describe common epidemiologic manifestations of TBRD; 2) describe common clinical manifestations of TBRD; 3) list a differential diagnosis that ranks TBRD; 4) identify treatment decisions based on epidemiologic clues; 5) identify treatment decisions based on clinical clues; 6) identify the utility of confirmatory laboratory assay for TBRD; and 7) identify doxcycline treatment for patients with suspected TBRD.
To receive continuing education credit, please answer all of the following questions.
# Treatment of TBRD using doxycycline should only be initiated after laboratory confirmation of infection is obtained.
A. True. B. False. | None | None |
4f435b86b1b10a9afd501f830e583c46b0ed55b6 | cdc | None | All clinically significant postvaccination reactions should be reported to the Vaccine Adverse Event Reporting System (VAERS). Reporting forms and instructions on filing a VAERS report are available at www.vaers.hhs.gov or by telephone, 800-822-7967. Additional details regarding ACIP recommendations for each of the vaccines listed in the schedule can be found at www.cdc.gov/vaccines/hcp/acip-recs/index.html.#
Report all clinically significant postvaccination reactions to the Vaccine Adverse Event Reporting System (VAERS). Reporting forms and instructions on filing a VAERS report are available at www.vaers.hhs.gov or by telephone, 800-822-7967.
Information on how to file a Vaccine Injury Compensation Program claim is available at www.hrsa.gov/vaccinecompensation or by telephone, 800-338-2382. To file a claim for vaccine injury, contact the U.S. Court of Federal Claims, 717 Madison Place, N.W., Washington, D.C. 20005; telephone, 202-357-6400.
Additional information about the vaccines in this schedule, extent of available data, and contraindications for vaccination is also available at www.cdc.gov/vaccines or from the CDC-INFO Contact Center at 800-CDC-INFO (800-232-4636) in English and Spanish, 8:00 a.m. -8:00 p.m. Eastern Time, Monday -Friday, excluding holidays.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services.
The recommendations in this schedule were approved by the Centers for Disease Control and Prevention's (CDC) Advisory Committee on Immunization Practices (ACIP), the American Academy of Family Physicians (AAFP), the America College of Physicians (ACP), American College of Obstetricians and Gynecologists (ACOG) and American College of Nurse-Midwives (ACNM). Tetanus, diphtheria, pertussis (Td/Tdap) *, 3 Varicella *,4 Human papillomavirus (HPV) Female *,5 Human papillomavirus (HPV) Male *,5
Zoster 6 Measles, mumps, rubella (MMR) *,7 Pneumococcal 13-valent conjugate (PCV13) *,8 Pneumococcal polysaccharide (PPSV23) 8
Meningococcal *,9 Hepatitis A *,10 Hepatitis B *,11 Haemophilus influenzae type b (Hib) *,12 These schedules indicate the recommended age groups and medical indications for which administration of currently licensed vaccines is commonly recommended for adults ages 19 years and older, as of February 1, 2015. For all vaccines being recommended on the Adult Immunization Schedule: a vaccine series does not need to be restarted, regardless of the time that has elapsed between doses. Licensed combination vaccines may be used whenever any components of the combination are indicated and when the vaccine's other components are not contraindicated. For detailed recommendations on all vaccines, including those used primarily for travelers or that are issued during the year, consult the manufacturers' package inserts and the complete statements from the Advisory Committee on Immunization Practices (www.cdc.gov/vaccines/hcp/acip-recs/index.html). Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services.
# post-HSCT recipients only
For all persons in this category who meet the age requirements and who lack documentation of vaccination or have no evidence of previous infection; zoster vaccine recommended regardless of prior episode of zoster Recommended if some other risk factor is present (e.g., on the basis of medical, occupational, lifestyle, or other indications)
# Tetanus, diphtheria, and acellular pertussis (Td/Tdap) vaccination
- Administer 1 dose of Tdap vaccine to pregnant women during each pregnancy (preferably during 27 to 36 weeks' gestation) regardless of interval since prior Td or Tdap vaccination. - Persons aged 11 years or older who have not received Tdap vaccine or for whom vaccine status is unknown should receive a dose of Tdap followed by tetanus and diphtheria toxoids (Td) booster doses every 10 years thereafter. Tdap can be administered regardless of interval since the most recent tetanus or diphtheria-toxoid containing vaccine.
- Adults with an unknown or incomplete history of completing a 3-dose primary vaccination series with Td-containing vaccines should begin or complete a primary vaccination series including a Tdap dose. - For unvaccinated adults, administer the first 2 doses at least 4 weeks apart and the third dose 6 to 12 months after the second. - For incompletely vaccinated (i.e., less than 3 doses) adults, administer remaining doses. - Refer to the ACIP statement for recommendations for administering Td/Tdap as prophylaxis in wound management (see footnote 1).
# Varicella vaccination
- All adults without evidence of immunity to varicella (as defined below) should receive 2 doses of single-antigen varicella vaccine or a second dose if they have received only 1 dose. - Vaccination should be emphasized for those who have close contact with persons at high risk for severe disease (e.g., health care personnel and family contacts of persons with immunocompromising conditions) or are at high risk for exposure or transmission (e.g., teachers; child care employees; residents and staff members of institutional settings, including correctional institutions; college students; military personnel; adolescents and adults living in households with children; nonpregnant women of childbearing age; and international travelers). - Pregnant women should be assessed for evidence of varicella immunity. Women who do not have evidence of immunity should receive the first dose of varicella vaccine upon completion or termination of pregnancy and before discharge from the health care facility. The second dose should be administered 4 to 8 weeks after the first dose.
- Evidence of immunity to varicella in adults includes any of the following: -documentation of 2 doses of varicella vaccine at least 4 weeks apart; -U.S.-born before 1980, except health care personnel and pregnant women; -history of varicella based on diagnosis or verification of varicella disease by a health care provider; -history of herpes zoster based on diagnosis or verification of herpes zoster disease by a health care provider; or laboratory evidence of immunity or laboratory confirmation of disease.
# Human papillomavirus (HPV) vaccination
- Two vaccines are licensed for use in females, bivalent HPV vaccine (HPV2) and quadrivalent HPV vaccine (HPV4), and one HPV vaccine for use in males (HPV4). - For females, either HPV4 or HPV2 is recommended in a 3-dose series for routine vaccination at age 11 or 12 years and for those aged 13 through 26 years, if not previously vaccinated.
- For males, HPV4 is recommended in a 3-dose series for routine vaccination at age 11 or 12 years and for those aged 13 through 21 years, if not previously vaccinated. Males aged 22 through 26 years may be vaccinated. - HPV4 is recommended for men who have sex with men through age 26 years for those who did not get any or all doses when they were younger. - Vaccination is recommended for immunocompromised persons (including those with HIV infection) through age 26 years for those who did not get any or all doses when they were younger. - A complete series for either HPV4 or HPV2 consists of 3 doses. The second dose should be administered 4 to 8 weeks (minimum interval of 4 weeks) after the first dose; the third dose should be administered 24 weeks after the first dose and 16 weeks after the second dose (minimum interval of at least 12 weeks). - HPV vaccines are not recommended for use in pregnant women. However, pregnancy testing is not needed before vaccination. If a woman is found to be pregnant after initiating the vaccination series, no intervention is needed; the remainder of the 3-dose series should be delayed until completion or termination of pregnancy.
# Zoster vaccination
- A single dose of zoster vaccine is recommended for adults aged 60 years or older regardless of whether they report a prior episode of herpes zoster.
Although the vaccine is licensed by the U.S. Food and Drug Administration for use among and can be administered to persons aged 50 years or older, ACIP recommends that vaccination begin at age 60 years. - Persons aged 60 years or older with chronic medical conditions may be vaccinated unless their condition constitutes a contraindication, such as pregnancy or severe immunodeficiency.
# Measles, mumps, rubella (MMR) vaccination
- Adults born before 1957 are generally considered immune to measles and mumps. All adults born in 1957 or later should have documentation of 1 or more doses of MMR vaccine unless they have a medical contraindication to the vaccine or laboratory evidence of immunity to each of the three diseases. Documentation of provider-diagnosed disease is not considered acceptable evidence of immunity for measles, mumps, or rubella.
# Measles component:
- A routine second dose of MMR vaccine, administered a minimum of 28 days after the first dose, is recommended for adults who:
are students in postsecondary educational institutions, -work in a health care facility, or plan to travel internationally. - Persons who received inactivated (killed) measles vaccine or measles vaccine of unknown type during 1963-1967 should be revaccinated with 2 doses of MMR vaccine.
# Mumps component:
- A routine second dose of MMR vaccine, administered a minimum of 28 days after the first dose, is recommended for adults who:
are students in a postsecondary educational institution, -work in a health care facility, or plan to travel internationally. - Persons vaccinated before 1979 with either killed mumps vaccine or mumps vaccine of unknown type who are at high risk for mumps infection (e.g., persons who are working in a health care facility) should be considered for revaccination with 2 doses of MMR vaccine.
# Rubella component:
- For women of childbearing age, regardless of birth year, rubella immunity should be determined. If there is no evidence of immunity, women who are not pregnant should be vaccinated. Pregnant women who do not have evidence of immunity should receive MMR vaccine upon completion or termination of pregnancy and before discharge from the health care facility.
Health care personnel born before 1957:
- For unvaccinated health care personnel born before 1957 who lack laboratory evidence of measles, mumps, and/or rubella immunity or laboratory confirmation of disease, health care facilities should consider vaccinating personnel with 2 doses of MMR vaccine at the appropriate interval for measles and mumps or 1 dose of MMR vaccine for rubella.
# Pneumococcal (13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine ) vaccination
- General information -When indicated, only a single dose of PCV13 is recommended for adults.
-No additional dose of PPSV23 is indicated for adults vaccinated with PPSV23 at or after age 65 years. and treatment facilities, facilities providing drug abuse treatment and prevention services, health care settings targeting services to injection drug users or men who have sex with men, correctional facilities, end-stage renal disease programs and facilities for chronic hemodialysis patients, and institutions and nonresidential day care facilities for persons with developmental disabilities. - Administer missing doses to complete a 3-dose series of hepatitis B vaccine to those persons not vaccinated or not completely vaccinated. The second dose should be administered 1 month after the first dose; the third dose should be given at least 2 months after the second dose (and at least 4 months after the first dose). If the combined hepatitis A and hepatitis B vaccine (Twinrix) is used, give 3 doses at 0, 1, and 6 months; alternatively, a 4-dose Twinrix schedule, administered on days 0, 7, and 21 to 30 followed by a booster dose at month 12 may be used. - Adult patients receiving hemodialysis or with other immunocompromising conditions should receive 1 dose of 40 mcg/mL (Recombivax HB) administered on a 3-dose schedule at 0, 1, and 6 months or 2 doses of 20 mcg/mL (Engerix-B) administered simultaneously on a 4-dose schedule at 0, 1, 2, and 6 months.
# Haemophilus influenzae type b (Hib) vaccination
- One dose of Hib vaccine should be administered to persons who have anatomical or functional asplenia or sickle cell disease or are undergoing elective splenectomy if they have not previously received Hib vaccine. Hib vaccination 14 or more days before splenectomy is suggested. - Recipients of a hematopoietic stem cell transplant (HSCT) should be vaccinated with a 3-dose regimen 6 to 12 months after a successful transplant, regardless of vaccination history; at least 4 weeks should separate doses. - Hib vaccine is not recommended for adults with HIV infection since their risk for Hib infection is low.
# Immunocompromising conditions
- Inactivated vaccines generally are acceptable (e.g., pneumococcal, meningococcal, and inactivated influenza vaccine) and live vaccines generally are avoided in persons with immune deficiencies or immunocompromising conditions. Information on specific conditions is available at www.cdc.gov/vaccines/hcp/acip-recs/index.html.
# Vaccine Contraindications Precautions
Influenza, inactivated (IIV) 2 - Severe allergic reaction (e.g., anaphylaxis) after previous dose of any influenza vaccine; or to a vaccine component, including egg protein
- Moderate or severe acute illness with or without fever - History of Guillain-Barré Syndrome within 6 weeks of previous influenza vaccination - Adults who experience only hives with exposure to eggs may receive RIV or, with additional safety precautions, IIV 2 Influenza, recombinant (RIV)
- Severe allergic reaction (e.g., anaphylaxis) after previous dose of RIV or to a vaccine component. RIV does not contain any egg protein 2
- Moderate or severe acute illness with or without fever - History of Guillain-Barré Syndrome within 6 weeks of previous influenza vaccination Influenza, live attenuated (LAIV) 2,3 - Severe allergic reaction (e.g., anaphylaxis) to any component of the vaccine, or to a previous dose of any influenza vaccine - In addition, ACIP recommends that LAIV not be used in the following populations:
pregnant women immunosuppressed adults adults with egg allergy of any severity adults who have taken influenza antiviral medications (amantadine, rimantadine, zanamivir, or oseltamivir) within the previous 48 hours; avoid use of these antiviral drugs for 14 days after vaccination hours before vaccination; avoid use of these antiviral drugs for 14 days after vaccination Measles, mumps, rubella (MMR) 3 - Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine component - Known severe immunodeficiency (e.g., from hematologic and solid tumors, receipt of chemotherapy, congenital immunodeficiency, or long-term immunosuppressive therapy, 4 or patients with HIV infection who are severely immunocompromised) - Pregnancy
- Moderate or severe acute illness with or without fever - Recent (within 11 months) receipt of antibody-containing blood product (specific interval depends on product) 5 - History of thrombocytopenia or thrombocytopenic purpura - Need for tuberculin skin testing 6 Pneumococcal conjugate (PCV13) - Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine component, including to any vaccine containing diphtheria toxoid | All clinically significant postvaccination reactions should be reported to the Vaccine Adverse Event Reporting System (VAERS). Reporting forms and instructions on filing a VAERS report are available at www.vaers.hhs.gov or by telephone, 800-822-7967. Additional details regarding ACIP recommendations for each of the vaccines listed in the schedule can be found at www.cdc.gov/vaccines/hcp/acip-recs/index.html.#
Report all clinically significant postvaccination reactions to the Vaccine Adverse Event Reporting System (VAERS). Reporting forms and instructions on filing a VAERS report are available at www.vaers.hhs.gov or by telephone, 800-822-7967.
Information on how to file a Vaccine Injury Compensation Program claim is available at www.hrsa.gov/vaccinecompensation or by telephone, 800-338-2382. To file a claim for vaccine injury, contact the U.S. Court of Federal Claims, 717 Madison Place, N.W., Washington, D.C. 20005; telephone, 202-357-6400.
Additional information about the vaccines in this schedule, extent of available data, and contraindications for vaccination is also available at www.cdc.gov/vaccines or from the CDC-INFO Contact Center at 800-CDC-INFO (800-232-4636) in English and Spanish, 8:00 a.m. -8:00 p.m. Eastern Time, Monday -Friday, excluding holidays.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services.
The recommendations in this schedule were approved by the Centers for Disease Control and Prevention's (CDC) Advisory Committee on Immunization Practices (ACIP), the American Academy of Family Physicians (AAFP), the America College of Physicians (ACP), American College of Obstetricians and Gynecologists (ACOG) and American College of Nurse-Midwives (ACNM). Tetanus, diphtheria, pertussis (Td/Tdap) *, 3 Varicella *,4 Human papillomavirus (HPV) Female *,5 Human papillomavirus (HPV) Male *,5
Zoster 6 Measles, mumps, rubella (MMR) *,7 Pneumococcal 13-valent conjugate (PCV13) *,8 Pneumococcal polysaccharide (PPSV23) 8
Meningococcal *,9 Hepatitis A *,10 Hepatitis B *,11 Haemophilus influenzae type b (Hib) *,12 These schedules indicate the recommended age groups and medical indications for which administration of currently licensed vaccines is commonly recommended for adults ages 19 years and older, as of February 1, 2015. For all vaccines being recommended on the Adult Immunization Schedule: a vaccine series does not need to be restarted, regardless of the time that has elapsed between doses. Licensed combination vaccines may be used whenever any components of the combination are indicated and when the vaccine's other components are not contraindicated. For detailed recommendations on all vaccines, including those used primarily for travelers or that are issued during the year, consult the manufacturers' package inserts and the complete statements from the Advisory Committee on Immunization Practices (www.cdc.gov/vaccines/hcp/acip-recs/index.html). Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services.
# post-HSCT recipients only
For all persons in this category who meet the age requirements and who lack documentation of vaccination or have no evidence of previous infection; zoster vaccine recommended regardless of prior episode of zoster Recommended if some other risk factor is present (e.g., on the basis of medical, occupational, lifestyle, or other indications)
# Tetanus, diphtheria, and acellular pertussis (Td/Tdap) vaccination
• Administer 1 dose of Tdap vaccine to pregnant women during each pregnancy (preferably during 27 to 36 weeks' gestation) regardless of interval since prior Td or Tdap vaccination. • Persons aged 11 years or older who have not received Tdap vaccine or for whom vaccine status is unknown should receive a dose of Tdap followed by tetanus and diphtheria toxoids (Td) booster doses every 10 years thereafter. Tdap can be administered regardless of interval since the most recent tetanus or diphtheria-toxoid containing vaccine.
• Adults with an unknown or incomplete history of completing a 3-dose primary vaccination series with Td-containing vaccines should begin or complete a primary vaccination series including a Tdap dose. • For unvaccinated adults, administer the first 2 doses at least 4 weeks apart and the third dose 6 to 12 months after the second. • For incompletely vaccinated (i.e., less than 3 doses) adults, administer remaining doses. • Refer to the ACIP statement for recommendations for administering Td/Tdap as prophylaxis in wound management (see footnote 1).
# Varicella vaccination
• All adults without evidence of immunity to varicella (as defined below) should receive 2 doses of single-antigen varicella vaccine or a second dose if they have received only 1 dose. • Vaccination should be emphasized for those who have close contact with persons at high risk for severe disease (e.g., health care personnel and family contacts of persons with immunocompromising conditions) or are at high risk for exposure or transmission (e.g., teachers; child care employees; residents and staff members of institutional settings, including correctional institutions; college students; military personnel; adolescents and adults living in households with children; nonpregnant women of childbearing age; and international travelers). • Pregnant women should be assessed for evidence of varicella immunity. Women who do not have evidence of immunity should receive the first dose of varicella vaccine upon completion or termination of pregnancy and before discharge from the health care facility. The second dose should be administered 4 to 8 weeks after the first dose.
• Evidence of immunity to varicella in adults includes any of the following: -documentation of 2 doses of varicella vaccine at least 4 weeks apart; -U.S.-born before 1980, except health care personnel and pregnant women; -history of varicella based on diagnosis or verification of varicella disease by a health care provider; -history of herpes zoster based on diagnosis or verification of herpes zoster disease by a health care provider; or laboratory evidence of immunity or laboratory confirmation of disease.
# Human papillomavirus (HPV) vaccination
• Two vaccines are licensed for use in females, bivalent HPV vaccine (HPV2) and quadrivalent HPV vaccine (HPV4), and one HPV vaccine for use in males (HPV4). • For females, either HPV4 or HPV2 is recommended in a 3-dose series for routine vaccination at age 11 or 12 years and for those aged 13 through 26 years, if not previously vaccinated.
• For males, HPV4 is recommended in a 3-dose series for routine vaccination at age 11 or 12 years and for those aged 13 through 21 years, if not previously vaccinated. Males aged 22 through 26 years may be vaccinated. • HPV4 is recommended for men who have sex with men through age 26 years for those who did not get any or all doses when they were younger. • Vaccination is recommended for immunocompromised persons (including those with HIV infection) through age 26 years for those who did not get any or all doses when they were younger. • A complete series for either HPV4 or HPV2 consists of 3 doses. The second dose should be administered 4 to 8 weeks (minimum interval of 4 weeks) after the first dose; the third dose should be administered 24 weeks after the first dose and 16 weeks after the second dose (minimum interval of at least 12 weeks). • HPV vaccines are not recommended for use in pregnant women. However, pregnancy testing is not needed before vaccination. If a woman is found to be pregnant after initiating the vaccination series, no intervention is needed; the remainder of the 3-dose series should be delayed until completion or termination of pregnancy.
# Zoster vaccination
• A single dose of zoster vaccine is recommended for adults aged 60 years or older regardless of whether they report a prior episode of herpes zoster.
Although the vaccine is licensed by the U.S. Food and Drug Administration for use among and can be administered to persons aged 50 years or older, ACIP recommends that vaccination begin at age 60 years. • Persons aged 60 years or older with chronic medical conditions may be vaccinated unless their condition constitutes a contraindication, such as pregnancy or severe immunodeficiency.
# Measles, mumps, rubella (MMR) vaccination
• Adults born before 1957 are generally considered immune to measles and mumps. All adults born in 1957 or later should have documentation of 1 or more doses of MMR vaccine unless they have a medical contraindication to the vaccine or laboratory evidence of immunity to each of the three diseases. Documentation of provider-diagnosed disease is not considered acceptable evidence of immunity for measles, mumps, or rubella.
# Measles component:
• A routine second dose of MMR vaccine, administered a minimum of 28 days after the first dose, is recommended for adults who:
are students in postsecondary educational institutions, -work in a health care facility, or plan to travel internationally. • Persons who received inactivated (killed) measles vaccine or measles vaccine of unknown type during 1963-1967 should be revaccinated with 2 doses of MMR vaccine.
# Mumps component:
• A routine second dose of MMR vaccine, administered a minimum of 28 days after the first dose, is recommended for adults who:
are students in a postsecondary educational institution, -work in a health care facility, or plan to travel internationally. • Persons vaccinated before 1979 with either killed mumps vaccine or mumps vaccine of unknown type who are at high risk for mumps infection (e.g., persons who are working in a health care facility) should be considered for revaccination with 2 doses of MMR vaccine.
# Rubella component:
• For women of childbearing age, regardless of birth year, rubella immunity should be determined. If there is no evidence of immunity, women who are not pregnant should be vaccinated. Pregnant women who do not have evidence of immunity should receive MMR vaccine upon completion or termination of pregnancy and before discharge from the health care facility.
Health care personnel born before 1957:
• For unvaccinated health care personnel born before 1957 who lack laboratory evidence of measles, mumps, and/or rubella immunity or laboratory confirmation of disease, health care facilities should consider vaccinating personnel with 2 doses of MMR vaccine at the appropriate interval for measles and mumps or 1 dose of MMR vaccine for rubella.
# Pneumococcal (13-valent pneumococcal conjugate vaccine [PCV13] and 23-valent pneumococcal polysaccharide vaccine [PPSV23]) vaccination
• General information -When indicated, only a single dose of PCV13 is recommended for adults.
-No additional dose of PPSV23 is indicated for adults vaccinated with PPSV23 at or after age 65 years. and treatment facilities, facilities providing drug abuse treatment and prevention services, health care settings targeting services to injection drug users or men who have sex with men, correctional facilities, end-stage renal disease programs and facilities for chronic hemodialysis patients, and institutions and nonresidential day care facilities for persons with developmental disabilities. • Administer missing doses to complete a 3-dose series of hepatitis B vaccine to those persons not vaccinated or not completely vaccinated. The second dose should be administered 1 month after the first dose; the third dose should be given at least 2 months after the second dose (and at least 4 months after the first dose). If the combined hepatitis A and hepatitis B vaccine (Twinrix) is used, give 3 doses at 0, 1, and 6 months; alternatively, a 4-dose Twinrix schedule, administered on days 0, 7, and 21 to 30 followed by a booster dose at month 12 may be used. • Adult patients receiving hemodialysis or with other immunocompromising conditions should receive 1 dose of 40 mcg/mL (Recombivax HB) administered on a 3-dose schedule at 0, 1, and 6 months or 2 doses of 20 mcg/mL (Engerix-B) administered simultaneously on a 4-dose schedule at 0, 1, 2, and 6 months.
# Haemophilus influenzae type b (Hib) vaccination
• One dose of Hib vaccine should be administered to persons who have anatomical or functional asplenia or sickle cell disease or are undergoing elective splenectomy if they have not previously received Hib vaccine. Hib vaccination 14 or more days before splenectomy is suggested. • Recipients of a hematopoietic stem cell transplant (HSCT) should be vaccinated with a 3-dose regimen 6 to 12 months after a successful transplant, regardless of vaccination history; at least 4 weeks should separate doses. • Hib vaccine is not recommended for adults with HIV infection since their risk for Hib infection is low.
# Immunocompromising conditions
• Inactivated vaccines generally are acceptable (e.g., pneumococcal, meningococcal, and inactivated influenza vaccine) and live vaccines generally are avoided in persons with immune deficiencies or immunocompromising conditions. Information on specific conditions is available at www.cdc.gov/vaccines/hcp/acip-recs/index.html.
# Vaccine Contraindications Precautions
Influenza, inactivated (IIV) 2 • Severe allergic reaction (e.g., anaphylaxis) after previous dose of any influenza vaccine; or to a vaccine component, including egg protein
• Moderate or severe acute illness with or without fever • History of Guillain-Barré Syndrome within 6 weeks of previous influenza vaccination • Adults who experience only hives with exposure to eggs may receive RIV or, with additional safety precautions, IIV 2 Influenza, recombinant (RIV)
• Severe allergic reaction (e.g., anaphylaxis) after previous dose of RIV or to a vaccine component. RIV does not contain any egg protein 2
• Moderate or severe acute illness with or without fever • History of Guillain-Barré Syndrome within 6 weeks of previous influenza vaccination Influenza, live attenuated (LAIV) 2,3 • Severe allergic reaction (e.g., anaphylaxis) to any component of the vaccine, or to a previous dose of any influenza vaccine • In addition, ACIP recommends that LAIV not be used in the following populations:
pregnant women immunosuppressed adults adults with egg allergy of any severity adults who have taken influenza antiviral medications (amantadine, rimantadine, zanamivir, or oseltamivir) within the previous 48 hours; avoid use of these antiviral drugs for 14 days after vaccination hours before vaccination; avoid use of these antiviral drugs for 14 days after vaccination Measles, mumps, rubella (MMR) 3 • Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine component • Known severe immunodeficiency (e.g., from hematologic and solid tumors, receipt of chemotherapy, congenital immunodeficiency, or long-term immunosuppressive therapy, 4 or patients with HIV infection who are severely immunocompromised) • Pregnancy
• Moderate or severe acute illness with or without fever • Recent (within 11 months) receipt of antibody-containing blood product (specific interval depends on product) 5 • History of thrombocytopenia or thrombocytopenic purpura • Need for tuberculin skin testing 6 Pneumococcal conjugate (PCV13) • Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a vaccine component, including to any vaccine containing diphtheria toxoid | None | None |
e01de8eb753d9704b308d9e603d62ba799e88bab | cdc | None | Hepatitis B virus (HBV) causes acute and chronic infection ofthe liver leading to substantial morbidity and mortality. In the United States, since 1996, a total of 29 outbreaks of HBV infection in one or multiple long-term-care (LTC) facilities, including nursing homes and assisted-living facilities, were reported to CDC; ofthese, 25 involved adults with diabetes receiving assisted blood glucose monitoring (1; CDC, unpublished data, 2011). These outbreaks prompted the Hepatitis Vaccines Work Group o f the Advisory Committee on Immunization Practices (ACIP) to evaluate the risk for HBV infection among all adults with diagnosed diabetes. The Work Group reviewed HBV infection-related morbidity and mortality and the effectiveness o f implementing infection prevention and control measures. The strength o f scientific evi dence regarding protection was evaluated using the Grading o f Recommendations, Assessment, Development, and Evaluation (GRADE) methodology,- and safety, values, and cost-effectiveness were incorporated into a recommendation using the GRADE system. Based on the Work Group findings, on October 25, 2011, ACIP recommended that all previously unvaccinated adults aged 19 through 59 years with diabetes mellitus (type 1 and type 2) be vaccinated against hepatitis B as soon as possible after a diagnosis o f diabetes is made (recommendation category A). Data on the risk for hepatitis B among adults aged >60 years are less robust. Therefore, ACIP recommended that unvaccinated adults aged >60 years with diabetes may be vaccinated at the discretion ofthe treating clinician after assessing their risk and the likelihood ofan adequate immune response to vaccination (recommendation category B). This report summarizes these recommendations and provides the rationale used by ACIP to inform their decision making.# Risk for HBV Infection
An estimate o f the risk for HBV infection for adults with diabetes living in LTC facilities was not available; continuing outbreaks suggest that it might be substantial. T he population - Recommendation category A: a recommendation that applies to all persons in an age or risk-based group. Recommendation category B: a recommendation for individual clinical decision making. Evidence type 1: randomized controlled trials, or overwhelming evidence from observational studies. Evidence type 2: randomized controlled trials with important limitations, or exceptionally strong evidence from observational studies. Evidence type 3: observational studies, or randomized controlled trials with notable limitations.
# M orbidity and M ortality
The severity ofacute HBV infection among adults ranges from asymptomatic to fulminant hepatitis. National viral hepatitis surveillance data indicate that of the 3,371 acute HBV infec tions reported in 2009, 47% of the 2,126 infections for which information was available resulted in hospitalization, and 1% o f the 1,900 infections for which information was available were fatal (3). Data from EIP for the period 2009-2010 indicated a higher case-fatality rate among acute HBV-infected persons with diagnosed diabetes compared with those without diabetes, although the difference was not statistically significant (5% versus 2%, p=0.127) (2). Acute HBV infection progresses to chronic infection in approximately 5% of otherwise healthy adults (4), but is believed to be greater among older adults with diabetes (5). In the United States, an estimated 700,000 to 1.4 million persons are infected with HBV (3). Because chronic HBV infection can persist for decades, persons with chronic HBV infection are the reservoir for continuing HBV transmission. Chronic HBV infec tion is associated with high morbidity and mortality, leading to cirrhosis and liver cancer in >15% o f affected adults (5).
Diabetes is associated with nonalcoholic fatty liver disease, includ ing its most severe form, nonalcoholic steatohepatitis. A study o f veterans without HBV infection indicated that adults with diabetes have approximately twice the risk for chronic nonalcoholic liver disease and hepatocellular carcinoma as those without diabetes (6).
# Infection Control
HBV is highly infectious and environmentally stable (5); HBV can be transmitted by medical equipment that is contaminated with blood that is not visible to the unaided eye. Percutaneous exposures to HBV occur as a result o f assisted m onitoring o f blood glucose (7) and other procedures involving instruments or parenteral treatments shared between persons. Lapses in infection control during assisted blood glucose monitoring that have led to HBV transmission include multipatient use of finger stick devices designed for single-patient use and inadequate disinfection and cleaning o f blood glucose monitors between patients. Breaches have been documented in various settings, including LTC facilities, hospitals, community health centers, ambulatory surgical centers, private offices, homes, and health fairs (7; C D C , unpublished data, 2011). Initiatives are ongoing to encourage improvement in the design and labeling o f devices used in diabetes monitoring and care, and for greater oversight and training o f staff responsible for providing diabetes care.'f' Infection control guidelines for safe blood glucose monitoring have been available since 1990, and guidelines targeting LTC settings were published in 2005 (8). Since 1982, hepatitis B vaccination has been recommended for health-care personnel, including personnel exposed to blood in LTC settings, in con junction with meticulous attention to infection control practice (5,8). In addition, a recommendation for hepatitis B vaccination exists for persons beginning hemodialysis (5).
# Hepatitis B Vaccine
Two single-antigen recom binant hepatitis B vaccines, R ecom bivax H B (M erck & C o., Inc.) and Engerix-B (GlaxoSmithKline Biologicals), and one com bination hepa titis A and hepatitis B vaccine, Twinrix (GlaxoSmithKline Biologicals), are available in the United States. Hepatitis B vac cines have been used in the United States since 1982. Extensive data support their safety in all age groups (5).
Hepatitis B vaccination usually consists o f 3 doses o f vac cine administered intramuscularly at 0, 1, and 6 months; other schedules are available. At younger ages, the immune response tô A dditional inform ation available at ww.cdc.gov/injectionsafety/ meetings/stickingwsafety52010.html.
vaccine is similar among adults with and without diabetes. The proportion of adults who achieve seroprotection (>10 mIU/mL antibody to hepatitis B surface antigen ) after receipt o f the 3-dose vaccine series decreases with age, obesity, smoking, immunosuppression, and comorbid conditions including diabetes. W hen the antibody responses among older adults with and with out diabetes are compared, the response might be reduced among those with diabetes. A synthesis of available literature suggests a protective response is achieved after completion of the hepatitis B vaccine series in >90%, 80%, 65%, and 70 years, respectively (CDC, unpublished data, 2011). Revaccination with 1-3 additional doses ofhepatitis B vaccine safely increases the proportion ofadults who achieve a protective level o f anti-HBs (>10 mIU/mL) (5). The duration o f protection against symptomatic and chronic HBV infection lasts >22 years among healthy vaccine responders ( 9); duration o f immunity among persons with diabetes is unknown.
# Cost-Effectiveness
The Hepatitis Vaccines W ork Group developed economic models that yielded age-stratified calculations (base case) o f the incremental cost per quality-adjusted life-year (QALY) saved based on vaccinating adults with diabetes against hepatitis B. § The estimated cost per QALY saved was $75,100 for persons aged 20 through 59 years but increased substantially with increasing age. From a lifetime perspective, a one-time vaccination program consisting o f a 3-dose series of hepatitis B vaccine, covering 10% o f unvaccinated U.S. adults with diagnosed diabetes aged 20 through 59 years (or approximately 528,047 persons) would be expected to prevent 4271 HBV infections, 467 hospitalizations, 256 chronic cases, 33 cases o f hepatocellular carcinoma, 13 liver transplants, and 130 deaths. Postvaccination serologic testing and revaccination would add considerable cost, with limited increase in disease protection (CDC, unpublished data, 2011).
# ACIP Recommendations
O n the basis ofavailable information about HBV risk, morbid ity and mortality, available vaccines, age at diagnosis o f diabetes, and cost-effectiveness, ACIP recommends the following: § T he Charter of ACIP states that, when considering recommendations for use of a vaccine, ACIP members' deliberations should include consideration of vaccine efficacy as well as cost-benefit and risk-benefit analyses. N o predefined threshold for cost-effectiveness is considered. To ensure that economic data presented to the C om m ittee and its W orking G roups are uniform in presentation, understandable, and of the highest quality, lead economists and the Health Economics Research Group at C D C developed Guidance fo r Health Economics Studies Presented to the Advisory Committee on Immunization Practices (ACIP), available at . htm . T he guidance specifically mandates technical review of any economic study that is presented to ACIP
- Hepatitis B vaccination should be administered to unvaccinated adults with diabetes mellitus who are aged 19 through 59 years (recommendation category A; evidence type 2). - H epatitis B vaccination may be adm inistered at the discretion o f the treating clinician to unvaccinated adults w ith d ia b e te s m e llitu s w ho are aged >60 years (recommendation category B; evidence type 2).
# Remarks
Continued efforts are needed to increase adherence to rec omm ended infection control practice. Shared use o f bloodcontam inated equipm ent increases the risk for exposure to bloodborne pathogens, including hepatitis C virus, hum an immunodeficiency virus, and HBV, which is highly infectious.
A dm inistration o f the hepatitis B vaccine series should be completed as soon as feasible after diabetes is diagnosed. Available data do not confirm an advantage to any specific hepatitis B vaccine, dosage, or approved schedule for adults with diabetes. No serologic testing or additional hepatitis B vaccination is recommended for adults who received a com plete series o f hepatitis B vaccinations at any time in the past.
T he hepatitis B vaccination series can be given safely to persons o f any age, but current hepatitis B vaccines are less efficacious and less cost-effective among older adults. Evidence for the extent o f increased risk for acute HBV infection among persons with diabetes who are aged >60 years is less strong than for younger persons w ith diabetes. In 2008, the median age of diabetes diagnosis was 53 years; two thirds o f adult diabetes diagnoses were made before age 60 years.D ecisions to vaccinate adults with diabetes who are aged >60 years o f age should incorporate consideration o f the patient's likelihood o f acquiring HBV infection, including the risk posed by an increased need for assisted blood-glucose m onitoring in LTC facilities, the likelihood o f experiencing chronic sequelae if infected with HBV, and the declining immunologic responses to vaccines that are associated with frailty, a geriatric syndrome characterized by decreased physiologic reserve and increased vulnerability, leading to early m ortality in older adults (10).
Hepatitis B vaccine may be administered during health-care visits scheduled for other purposes as long as minimum intervals between doses are observed; there is no maximum interval between doses that makes the hepatitis B vaccination series ineffective. | Hepatitis B virus (HBV) causes acute and chronic infection ofthe liver leading to substantial morbidity and mortality. In the United States, since 1996, a total of 29 outbreaks of HBV infection in one or multiple long-term-care (LTC) facilities, including nursing homes and assisted-living facilities, were reported to CDC; ofthese, 25 involved adults with diabetes receiving assisted blood glucose monitoring (1; CDC, unpublished data, 2011). These outbreaks prompted the Hepatitis Vaccines Work Group o f the Advisory Committee on Immunization Practices (ACIP) to evaluate the risk for HBV infection among all adults with diagnosed diabetes. The Work Group reviewed HBV infection-related morbidity and mortality and the effectiveness o f implementing infection prevention and control measures. The strength o f scientific evi dence regarding protection was evaluated using the Grading o f Recommendations, Assessment, Development, and Evaluation (GRADE) methodology,* and safety, values, and cost-effectiveness were incorporated into a recommendation using the GRADE system. Based on the Work Group findings, on October 25, 2011, ACIP recommended that all previously unvaccinated adults aged 19 through 59 years with diabetes mellitus (type 1 and type 2) be vaccinated against hepatitis B as soon as possible after a diagnosis o f diabetes is made (recommendation category A). Data on the risk for hepatitis B among adults aged >60 years are less robust. Therefore, ACIP recommended that unvaccinated adults aged >60 years with diabetes may be vaccinated at the discretion ofthe treating clinician after assessing their risk and the likelihood ofan adequate immune response to vaccination (recommendation category B). This report summarizes these recommendations and provides the rationale used by ACIP to inform their decision making.# Risk for HBV Infection
An estimate o f the risk for HBV infection for adults with diabetes living in LTC facilities was not available; continuing outbreaks suggest that it might be substantial. T he population * Recommendation category A: a recommendation that applies to all persons in an age or risk-based group. Recommendation category B: a recommendation for individual clinical decision making. Evidence type 1: randomized controlled trials, or overwhelming evidence from observational studies. Evidence type 2: randomized controlled trials with important limitations, or exceptionally strong evidence from observational studies. Evidence type 3: observational studies, or randomized controlled trials with notable limitations.
# M orbidity and M ortality
The severity ofacute HBV infection among adults ranges from asymptomatic to fulminant hepatitis. National viral hepatitis surveillance data indicate that of the 3,371 acute HBV infec tions reported in 2009, 47% of the 2,126 infections for which information was available resulted in hospitalization, and 1% o f the 1,900 infections for which information was available were fatal (3). Data from EIP for the period 2009-2010 indicated a higher case-fatality rate among acute HBV-infected persons with diagnosed diabetes compared with those without diabetes, although the difference was not statistically significant (5% versus 2%, p=0.127) (2). Acute HBV infection progresses to chronic infection in approximately 5% of otherwise healthy adults (4), but is believed to be greater among older adults with diabetes (5). In the United States, an estimated 700,000 to 1.4 million persons are infected with HBV (3). Because chronic HBV infection can persist for decades, persons with chronic HBV infection are the reservoir for continuing HBV transmission. Chronic HBV infec tion is associated with high morbidity and mortality, leading to cirrhosis and liver cancer in >15% o f affected adults (5).
Diabetes is associated with nonalcoholic fatty liver disease, includ ing its most severe form, nonalcoholic steatohepatitis. A study o f veterans without HBV infection indicated that adults with diabetes have approximately twice the risk for chronic nonalcoholic liver disease and hepatocellular carcinoma as those without diabetes (6).
# Infection Control
HBV is highly infectious and environmentally stable (5); HBV can be transmitted by medical equipment that is contaminated with blood that is not visible to the unaided eye. Percutaneous exposures to HBV occur as a result o f assisted m onitoring o f blood glucose (7) and other procedures involving instruments or parenteral treatments shared between persons. Lapses in infection control during assisted blood glucose monitoring that have led to HBV transmission include multipatient use of finger stick devices designed for single-patient use and inadequate disinfection and cleaning o f blood glucose monitors between patients. Breaches have been documented in various settings, including LTC facilities, hospitals, community health centers, ambulatory surgical centers, private offices, homes, and health fairs (7; C D C , unpublished data, 2011). Initiatives are ongoing to encourage improvement in the design and labeling o f devices used in diabetes monitoring and care, and for greater oversight and training o f staff responsible for providing diabetes care.'f' Infection control guidelines for safe blood glucose monitoring have been available since 1990, and guidelines targeting LTC settings were published in 2005 (8). Since 1982, hepatitis B vaccination has been recommended for health-care personnel, including personnel exposed to blood in LTC settings, in con junction with meticulous attention to infection control practice (5,8). In addition, a recommendation for hepatitis B vaccination exists for persons beginning hemodialysis (5).
# Hepatitis B Vaccine
Two single-antigen recom binant hepatitis B vaccines, R ecom bivax H B (M erck & C o., Inc.) and Engerix-B (GlaxoSmithKline Biologicals), and one com bination hepa titis A and hepatitis B vaccine, Twinrix (GlaxoSmithKline Biologicals), are available in the United States. Hepatitis B vac cines have been used in the United States since 1982. Extensive data support their safety in all age groups (5).
Hepatitis B vaccination usually consists o f 3 doses o f vac cine administered intramuscularly at 0, 1, and 6 months; other schedules are available. At younger ages, the immune response tô A dditional inform ation available at http://w ww.cdc.gov/injectionsafety/ meetings/stickingwsafety52010.html.
vaccine is similar among adults with and without diabetes. The proportion of adults who achieve seroprotection (>10 mIU/mL antibody to hepatitis B surface antigen [anti-HBs]) after receipt o f the 3-dose vaccine series decreases with age, obesity, smoking, immunosuppression, and comorbid conditions including diabetes. W hen the antibody responses among older adults with and with out diabetes are compared, the response might be reduced among those with diabetes. A synthesis of available literature suggests a protective response is achieved after completion of the hepatitis B vaccine series in >90%, 80%, 65%, and <40% of adults with diabetes lacking comorbid conditions aged <40 years, 41 through 59 years, 60 through 69 years, and >70 years, respectively (CDC, unpublished data, 2011). Revaccination with 1-3 additional doses ofhepatitis B vaccine safely increases the proportion ofadults who achieve a protective level o f anti-HBs (>10 mIU/mL) (5). The duration o f protection against symptomatic and chronic HBV infection lasts >22 years among healthy vaccine responders ( 9); duration o f immunity among persons with diabetes is unknown.
# Cost-Effectiveness
The Hepatitis Vaccines W ork Group developed economic models that yielded age-stratified calculations (base case) o f the incremental cost per quality-adjusted life-year (QALY) saved based on vaccinating adults with diabetes against hepatitis B. § The estimated cost per QALY saved was $75,100 for persons aged 20 through 59 years but increased substantially with increasing age. From a lifetime perspective, a one-time vaccination program consisting o f a 3-dose series of hepatitis B vaccine, covering 10% o f unvaccinated U.S. adults with diagnosed diabetes aged 20 through 59 years (or approximately 528,047 persons) would be expected to prevent 4271 HBV infections, 467 hospitalizations, 256 chronic cases, 33 cases o f hepatocellular carcinoma, 13 liver transplants, and 130 deaths. Postvaccination serologic testing and revaccination would add considerable cost, with limited increase in disease protection (CDC, unpublished data, 2011).
# ACIP Recommendations
O n the basis ofavailable information about HBV risk, morbid ity and mortality, available vaccines, age at diagnosis o f diabetes, and cost-effectiveness, ACIP recommends the following: § T he Charter of ACIP states that, when considering recommendations for use of a vaccine, ACIP members' deliberations should include consideration of vaccine efficacy as well as cost-benefit and risk-benefit analyses. N o predefined threshold for cost-effectiveness is considered. To ensure that economic data presented to the C om m ittee and its W orking G roups are uniform in presentation, understandable, and of the highest quality, lead economists and the Health Economics Research Group at C D C developed Guidance fo r Health Economics Studies Presented to the Advisory Committee on Immunization Practices (ACIP), available at http://www.cdc.gov/vaccines/recs/acip/economic-studies. htm . T he guidance specifically mandates technical review of any economic study that is presented to ACIP
• Hepatitis B vaccination should be administered to unvaccinated adults with diabetes mellitus who are aged 19 through 59 years (recommendation category A; evidence type 2). • H epatitis B vaccination may be adm inistered at the discretion o f the treating clinician to unvaccinated adults w ith d ia b e te s m e llitu s w ho are aged >60 years (recommendation category B; evidence type 2).
# Remarks
Continued efforts are needed to increase adherence to rec omm ended infection control practice. Shared use o f bloodcontam inated equipm ent increases the risk for exposure to bloodborne pathogens, including hepatitis C virus, hum an immunodeficiency virus, and HBV, which is highly infectious.
A dm inistration o f the hepatitis B vaccine series should be completed as soon as feasible after diabetes is diagnosed. Available data do not confirm an advantage to any specific hepatitis B vaccine, dosage, or approved schedule for adults with diabetes. No serologic testing or additional hepatitis B vaccination is recommended for adults who received a com plete series o f hepatitis B vaccinations at any time in the past.
T he hepatitis B vaccination series can be given safely to persons o f any age, but current hepatitis B vaccines are less efficacious and less cost-effective among older adults. Evidence for the extent o f increased risk for acute HBV infection among persons with diabetes who are aged >60 years is less strong than for younger persons w ith diabetes. In 2008, the median age of diabetes diagnosis was 53 years; two thirds o f adult diabetes diagnoses were made before age 60 years.D ecisions to vaccinate adults with diabetes who are aged >60 years o f age should incorporate consideration o f the patient's likelihood o f acquiring HBV infection, including the risk posed by an increased need for assisted blood-glucose m onitoring in LTC facilities, the likelihood o f experiencing chronic sequelae if infected with HBV, and the declining immunologic responses to vaccines that are associated with frailty, a geriatric syndrome characterized by decreased physiologic reserve and increased vulnerability, leading to early m ortality in older adults (10).
Hepatitis B vaccine may be administered during health-care visits scheduled for other purposes as long as minimum intervals between doses are observed; there is no maximum interval between doses that makes the hepatitis B vaccination series ineffective. | None | None |
f64b0a4301cf3dc787e355e47cabf319efea221f | cdc | None | depar depar depar depar department of health and human ser tment of health and human ser tment of health and human ser tment of health and human ser tment of health and human services vices vices vices vices# Introduction
Pertussis is an acute and prolonged infectious cough illness caused by Bordetella pertussis, a fastidious gram-negative coccobacillus. Pertussis results in substantial morbidity among adults and adolescents whose immunity to past childhood vaccination or B. pertussis infection might have waned and who have not received booster immunization for pertussis with adult tetanus, reduced diphtheria, and acellular pertussis (Tdap) vaccine (1,2). In 2004, women aged 15-39 years accounted for 97% of all live births in the United States (3). During 2000-2006, a total of 103,940 cases of pertussis were reported to CDC's National Notifiable Diseases Surveillance System (NNDSS); 27,759 (27%) of these cases occurred among persons aged 15-39 years (CDC, unpublished data, 2007). Parents with pertussis, including new mothers, are the identified source of B. pertussis infection in >25% of pertussis cases in early infancy, when rates for complications and fatalities are highest (4)(5)(6)(7)(8). Infants aged <12 months accounted for 145 (93%) of 156 pertussis-related deaths reported to CDC for (CDC, unpublished data, 2007. Decennial booster vaccination with adult tetanus toxoid and reduced diphtheria toxoid (Td) vaccine has been largely responsible for reducing the average annual number of tetanus and respiratory diphtheria cases reported during 2000-2006 to 31 and less than one, respectively. In contrast, the average annual number of pertussis cases was 14,849 during the same period (9-15;CDC, unpublished data, 2007).
In 2005, two Tdap vaccines were licensed in the United States: ADACEL ® (sanofi pasteur, Swiftwater, Pennsylvania) for use in persons aged 11-64 years (16) and BOOSTRIX ® (GlaxoSmithKline Biologicals, Rixensart, Belgium) for persons aged 10-18 years (17) (Table 1). Both vaccines are licensed for single-dose administration. Acellular pertussis vaccines formulated with tetanus and diphtheria toxoids also are available for adults and adolescents in other countries, including an increasing number of European countries (e.g., France, Austria, and Germany), Canada, and Australia (18)(19)(20). No vaccine containing acellular pertussis antigens without tetanus and diphtheria toxoids is available in the United States.
Vaccinating adults and adolescents using Tdap reduces the burden of pertussis among vaccine recipients and might prevent transmission of B. pertussis to infants (1,2). Statements and recommendations by CDC's Advisory Committee for Immunization Practices (ACIP) regarding use of Tdap by adults, including health-care personnel, and adolescents (Table 2) provide background information on pertussis and extensive discussion regarding the safety and immunogenicity of Tdap in prelicensure trials. These recommendations encourage adult and adolescent women of childbearing age to receive Tdap at a routine health assessment before conception to prevent the morbidity of pertussis that could occur during pregnancy and encourage use of Tdap among adults and adolescents who anticipate contact with an infant aged <12 months both for personal protection and to reduce the risk for transmitting B. pertussis to the infants (1,2).
In 2006, ACIP recommended routine administration of Tdap for postpartum women who were not vaccinated previously with Tdap to provide personal protection and reduce the risk for transmitting pertussis to their infants (1,2) . After careful consideration, in June 2006, ACIP voted to reaffirm its recommendation for use of Td in pregnant women who have urgent indication for tetanus toxoid or diphtheria toxoid vaccination to prevent maternal or neonatal tetanus, or to prevent diphtheria. Pregnant women not vaccinated previously with Tdap will receive a measure of protection against pertus-sis by ensuring that children in the household are up-to-date with recommended doses of pediatric diphtheria and tetanus toxoids and acellular pertussis vaccine (DTaP)- (21)(22)(23) and that adult and adolescent household contacts have received a dose of Tdap (Table 2) (1,2). Health-care providers can monitor pregnant women who have not received a dose of Tdap for exposures to pertussis or to respiratory illness consistent with pertussis, and they can administer antimicrobials for postexposure prophylaxis or treatment of pertussis, if needed, to reduce the risk for transmitting pertussis to their infants.
This report provides the background and rationale for routine administration of Tdap in postpartum women who were not vaccinated previously with Tdap and for maintaining the previous recommendation for use of Td in pregnant women if indicated. The safety and efficacy of using Tdap in pregnant women has not been demonstrated, and Tdap is not recommended for use in pregnant women in any country. No evidence exists of excess morbidity or any fatality among pregnant women ascribed to pertussis. No evidence exists demonstrating whether
- Tdap in pregnant women harms the fetus or increases risk for adverse pregnancy outcomes, - transplacental antibody induced by Tdap administered during pregnancy will protect infants against pertussis, or - Tdap-induced transplacental maternal antibody will have a negative impact on an infant's protective immune response to later-administered routine pediatric DTaP or to conjugate vaccines containing tetanus toxoid or diphtheria toxoid. This report discusses certain situations in which health-care providers might choose to administer Tdap to a pregnant woman. Health-care providers should weigh the theoretical risks and benefits before choosing to administer Tdap vaccine to a pregnant woman.
# Methods
During June 2006, ACIP evaluated the limited evidence available concerning safety, immunogenicity, and pregnancy outcomes after administration of Tdap; evidence from historic use of pertussis, tetanus, and diphtheria vaccines in pregnant women; and the potential effects of transplacental maternal antibody on the infant's immune response to active immunization with pediatric diphtheria and tetanus toxoids and whole-cell pertussis (DTP) or DTaP vaccines, or to con-jugate vaccines containing tetanus toxoid or diphtheria toxoid. The evaluation included a synthesis of information from scientific literature published in English, unpublished sources of information, consultations, analyses, and extensive discussion by an ACIP working group † during . The working group comprised persons with expertise in pertussis, tetanus, and diphtheria; obstetrics and gynecology; pediatrics, family practice, internal medicine, immunology, public health, and vaccine regulation; and liaison members from partner organizations.
The workgroup considered multiple diverse views on the adequacy of evidence needed to form a recommendation for use of Tdap in pregnant and postpartum women. A minority view held that available data from nonpregnant women and men, and experience with the use of Td in pregnant women to prevent neonatal and maternal tetanus, were sufficient to support a recommendation for the safe use of Tdap in pregnant women for individual protection from pertussis. The majority view, while acknowledging the desirability of preventing pertussis in pregnant women and the substantial body of information demonstrating the usefulness of Td to prevent maternal and neonatal tetanus, held that the evidence was insufficient at this time to support a recommendation for routine administration of Tdap in pregnant women. The specific issues for pertussis differ from those for tetanus and diphtheria. Important among these is the limited understanding of immunity and correlates of protection for pertussis. In addition, data supporting the safety of vaccinating pregnant women with Tdap to prevent pertussis are scarce for women, their fetuses, and pregnancy outcomes. Whether transplacental maternal antibody exerts an inhibitory or other effect on the infant-protective immune response to active immunization with pediatric DTaP or conjugate vaccines containing tetanus toxoid or diphtheria toxoid has not been studied. Protection against infant pertussis through Tdap-induced transplacental maternal antibody has not been demonstrated. Until additional information is available, the majority view of the working group held that Tdap administered to women in the immediate postpartum period, in addition to ensuring pertussis vaccination of close contacts, would likely provide a measure of protection for mother and infant. - Td recommended during pregnancy, † † or - Tdap-postpartum before leaving hospital or birthing center instead of Td during pregnancy, if sufficient tetanus and diphtheria protection is likely until delivery Tdap, ideally administered at least 2 wks before contact with the infant; interval as short as 2 yrs suggested ¶ Tdap-postpartum before leaving hospital or birthing center; interval as short as 2 yrs ¶ † † ; pregnant women should be advised of symptoms of pertussis and the benefits of treatment and early prophylaxis for household contacts exposed to pertussis Td for urgent protection during pregnancy † † ; Tdap postpartum before leaving hospital or birthing center Td when indicated for pregnant women † † § § 1 dose Td during pregnancy followed by dose 2 Td >4 wks later † † and dose 3 as Tdap 6-12 mos later (postpartum) - ACIP recommends routine vaccination with tetanus and diphtheria toxoids every 10 years to boost tetanus and diphtheria protection. In 2006, ACIP recommended that adults and adolescents who have not been vaccinated previously with tetanus and reduced diphtheria toxoids and acellular pertussis (Tdap), including persons with a history of pertussis, receive a dose of Tdap to boost pertussis protection in addition to tetanus and diphtheria protection. Tdap is licensed for single-dose administration. In persons who have received Tdap, tetanus and reduced diphtheria toxoids (Td) vaccine should be administered when subsequent decennial booster vaccination is indicated for tetanus or diphtheria protection. † For adults and adolescents, tetanus and diphtheria toxoids-containing vaccines include tetanus toxoid (TT), Tdap, and Td; for infants and children, tetanus toxoid and diphtheria toxoids-containing vaccines include pediatric diphtheria and tetanus toxoids and whole-cell pertussis (DTP), pediatric diphtheria and tetanus toxoids and acellular pertussis (DTaP), pediatric diphtheria and tetanus toxoids and acellular pertussis, inactivated poliovirus and hepatitis B (DTaP-IPV-Hep B), and pediatric diphtheria and tetanus toxoids (DT). § During 2000-2006, U.S. adolescents aged 10-19 years had the highest incidence of reported pertussis outside of infancy (CDC, unpublished data, 2008). For this reason, a catch-up dose of Tdap is recommended for adolescents aged 11-18 years to add protection against pertussis if they have received Td but not Tdap. For catch-up Tdap, an interval of at least 5 years from the most recent tetanus and/or diphtheria toxoids-containing vaccine is encouraged to reduce the risk for local and systemic reactions that could result when concentration of tetanus and/or diphtheria antitoxin is high. An interval less than 5 years after Td may be used, particularly when the benefit of providing pertussis protection is likely to be increased. Adolescents who have received a childhood series of pediatric DTP or DTaP and Td or Tdap are protected against tetanus and diphtheria. ¶ A shorter interval may be used. Limited evidence informs the risk of local and systemic reactions after Tdap at intervals of 5 years have elapsed since the previous Td. Persons who have completed the 3-dose primary tetanus vaccination series and have received a tetanus toxoid-containing vaccine within the preceding 5 years are protected against tetanus and do not require a tetanus toxoidcontaining vaccine as part of wound management. Pertussis is transmitted from person to person via large respiratory droplets generated by coughing or sneezing; early reports suggested that B. pertussis can be recovered from dried mucus for up to 3 days (28,30). Pertussis is highly infectious, with attack rates among exposed, nonimmune household contacts as high as 80%-90% (29,37,38). The most infectious periods are the catarrhal and early paroxysmal phases (28). Untreated patients, particularly infants, remain infectious for 6 weeks or longer (29). Among older children and adults with previous vaccination or infection, the infectious period typically is <21 days (29).
Routine
In a Canadian study conducted in 1999, a source was identified in 60%-70% of adults and adolescents with pertussis. Among adults aged 18-39 years, the source was a person in the household in 25%-44% of cases or at work or school in 17%-25% of cases. Among adolescents aged 12-17 years, the source was a person in the household in 9% of cases and a friend or person at school or work in 51% of cases (39).
# Pertussis During Pregnancy
Case reports suggest that the morbidity of pertussis is not increased among pregnant women compared with nonpregnant women. In a general medical practice during 1979-1980, four pregnant women had onset of cough during the 12th, 14th, 14th, and 36th week of gestation and cough that lasted 36, 6, 8, and 6 weeks, respectively; two women had vomiting after coughing and worsening cough paroxysms at night; and one woman developed hemoptysis and subconjunctival hemorrhage after repeated and forceful coughing paroxysms (40). A 1993 case report described a pregnant woman who was hospitalized 6 days before delivery for severe paroxysms and posttussive emesis (41). In a series of 32 women who had pertussis during pregnancy or at term, the illness was characterized as "a very tiresome disease"; no obstetric complication was reported, and no infant was premature (42). No pertussis-related deaths have been reported in pregnant women. The source of pertussis in infected pregnant women has not been examined systematically.
Reports of fetal morbidity among pregnant women with pertussis are rare, and no causal relationship with abnormal fetal development, fetal morbidity, or adverse outcome of pregnancy has been confirmed. One fetus of a mother who had severe paroxysmal coughing early in pregnancy had an extradural hematoma that was identified by ultrasonography and magnetic resonance at 31 weeks' gestation; studies had been normal at 12 and 22 weeks' gestation (43). Another fetus of a mother who had pertussis during the first trimester had prenatal diagnosis of laryngotracheal obstruction (44).
# Infantile Pertussis
Infants aged <12 months typically have the most severe pertussis, often requiring hospitalization for respiratory or other complications (Table 3) (8,(45)(46)(47)(48)(49). The risk for pertussis death or severe pertussis is highest among infants in the first 6 months of life and remains elevated until infants have received 1-2 doses of pediatric DTaP (8,50,51). During 2000-2006, the average annual incidence of pertussis among infants aged <6 months was 111 cases per 100,000 population; for infants aged 6-11 months, incidence was 19 cases per 100,000 population (CDC, unpublished data, 2007).
Complications and deaths from infant pertussis have been characterized by necrotizing bronchiolitis (52) and high rates of primary or secondary pneumonia and/or coinfection with bacterial and viral pathogens (8,28,47,53). Since 1993, pulmonary hypertension has been increasingly recognized among fatal infant cases (47,52,(54)(55)(56)(57)(58). The majority of all infant deaths have occurred among unvaccinated infants (47,53,58;CDC, unpublished data, 2007). Hispanic infants and infants born at estimated gestational age <37 weeks or with low birth weight have comprised a larger proportion of pertussis deaths than would have been expected on the basis of population estimates (47,53,58). Compared with the prevaccine era, during 2000-2006, the proportion of reported pertussis deaths among infants aged <3 months increased from 37% to 83% (Figure 1) (38,47;CDC, unpublished data, 2007).
Since the 1970s, parents, especially mothers, have been identified as the most important source of infant pertussis; however, a source has been identified in only 30%-60% of cases investigated (5)(6)(7)34,38,42,48,(59)(60)(61)(62)(63)(64)(65)(66)(67)(68). One or more household contact with pertussis is the source of pertussis in approximately 75% of cases among infants aged <6 months for whom the source is identified. A parent is implicated in approximately 25% of cases in infants, including the mother in 16%-19% of cases. A sibling is implicated as the source of transmission in <10% of cases (5,7,34).
Mathematical modeling evaluating different vaccine strategies for the United States has suggested that pertussis vaccination of 90% of household contacts (children, adolescents, and adults) of newborns, in addition to pertussis vaccination of 75% of adolescents generally in the population, might prevent approximately 75% of pertussis cases among infants aged 0-23 months (69). Another model estimated vaccination of both parents of an infant before discharge from the hospital could prevent 38% of infant cases and deaths (70). However, the efficacy of these strategies in practice has not been evaluated.
# Disease Burden
Although pertussis is a nationally notifiable disease in the United States (71), data on the pregnancy status of women with pertussis have not been collected. However, the burden of pertussis among pregnant women is likely to be similar to the burden among other adults in the population. Pertussis reports typically demonstrate increases in activity every 3-4 years (72); aside from these cycles of activity, the number of reported cases of pertussis in the United States has increased gradually since 1976. During 2004-2005, more than 25,000 cases were reported per year (Figure 2 (CDC unpublished data, 2007). Prospective and serologic studies suggest that pertussis infection and reinfection are underrecognized among adults and adolescents (29,(73)(74)(75). The pertussis burden is believed to be substantially more than the number of reported cases; approximately 600,000 cases are estimated to occur annually just among adults (1,34,76).
# Transmission in Obstetric and Neonatal Health-Care Settings
Health-care personnel can transmit B. pertussis in health-care settings if pertussis has not been considered by hospital staff (1,77,78). Outbreaks have been documented in prenatal and postnatal clinics (79,80), maternity wards (51,62,(81)(82)(83), neonatal nurseries, and neonatal intensive-care services (62,81,(84)(85)(86)(87)(88)(89)(90). Ongoing transmission is facilitated by delay in isolation and treatment of patients and in prophylaxis of contacts and by inconsistent use of face or nose and mouth protection (1,85,87,91). Unprotected exposures to pertussis in health-care settings can result in labor-intensive, disruptive, and costly investigations and control measures, particularly when the number of contacts is substantial (80,92). Pertussis transmitted to health-care personnel or patients can result in substantial morbidity (and on rare occasions in fatal disease) among hospitalized infants (79,80,(85)(86)(87)(88)93,94).
Health-care personnel who have not been vaccinated with Tdap (Table 2) can be an important source of pertussis and pertussis outbreaks in obstetric and neonatal settings. A wide range of health-care disciplines have been implicated, including physicians, resident physicians, and students (80,82,85,95); nurses and nurse midwives (51,81,85,87,(96)(97)(98); and aides, medical assistants, and educators (1,51,78,79,81,82,85,87). Pregnant and postpartum women with unrecognized pertussis and visitors to prenatal, obstetric, and neonatal units, including fathers and other close relatives, pose a substantial 1938-1940 1990-1999 2000-2006 Age (mos)
Percentage risk for transmission to infants, pregnant women, and healthcare personnel and have been associated with outbreaks in these settings (6,41,62,80,81,(84)(85)(86)93,98). Early recognition and treatment of pertussis in pregnant and postpartum women and prophylaxis of household contacts who visit health-care settings is critical to prevent continuing transmission. Antimicrobial treatment for women who have pertussis near term or at delivery and prophylaxis for their newborns and household contacts are effective in preventing further transmission (42,99).
# Diagnosis
The diagnosis of pertussis is complicated by the limitations of currently available diagnostic tests. The only pertussis diagnostic tests that are accepted to confirm a case for purposes of national reporting are culture and polymerase chain reaction (PCR) (when the clinical case definition also is met) (100; Box 1). Multiple factors affect the sensitivity, specificity, and interpretation of diagnostic tests for pertussis (101,102).
# Culture
Culture to isolate B. pertussis is essential for identifying the organism early in the course of disease (103) and for antimicrobial susceptibility testing, if indicated. Isolation of B. pertussis by culture is 100% specific; for optimal yield, culture requires specimens that contain nasopharyngeal cells obtained by aspirate or nasopharyngeal swab and special medium for growth. The sensitivity of culture early in pertussis varies (range: 30%-60%) (103)(104)(105). Outside of infancy, the yield of B. pertussis declines to 1%-3% in specimens taken in the third week of cough illness or later, after starting antimicrobial treatment, or in a patient who was vaccinated previously (106,107). B. pertussis can be isolated in culture as early as 72 hours after plating but requires 1-2 weeks before a result can definitively be called negative (108).
# Polymerase Chain Reaction
DNA amplification (e.g., PCR) to detect B. pertussis has increased sensitivity and more rapid turnaround time (109)(110)(111). When symptoms of classic pertussis are present (e.g., >2 weeks of paroxysmal cough), PCR can be two to three times more likely than culture to detect B. pertussis in a known positive sample (101,103,112,113). As with culture, the PCR result is affected by the technique used to collect the specimen; a poorly taken nasopharyngeal swab is more likely to be negative by both culture and PCR. PCR is less affected than culture by antimicrobial therapy because the organism does not need to be viable for the test to be positive. Adults and adolescents who have specimens taken later in the course of illness, who have started antibiotic treatment, or who were vaccinated previously tend to have PCR-positive, culture-negative test results (103,114).
Although PCR testing for pertussis has been available for nearly 20 years (115), no U.S. Food and Drug Administration (FDA)-licensed PCR test kit is available. The analytical sensitivity, accuracy, and quality control of PCR-based B. pertussis tests vary widely among laboratories. PCR assays used by the majority of laboratories amplify a single gene sequence, typically within the insertion sequence IS481. Both false-positive and false-negative results have been reported with these assays; reported outbreaks of respiratory illness mistakenly attributed to pertussis have resulted in unnecessary investigation and treatment, and unnecessary chemoprophylaxis of contacts (112,(116)(117)(118)(119). Using more than one genetic target and consensus interpretation criteria for PCR diagnosis of pertussis (120,121) has been suggested as a way to provide increased assurance of specificity (122) and to allow discrimination between Bordetella species.
# Other Diagnostic Tests
Direct fluorescent antibody (DFA) tests provide rapid results (within hours), but sensitivity (10%-50%) is less than with culture (123). With use of monoclonal reagents, the specificity of DFA should be >90%. However, interpretation of the test is subjective, and, when interpreted by an inexperienced microbiologist, the specificity can be lower (110). Diagnosis of pertussis by serology requires a substantial change in titer for pertussis antigens (typically fourfold) from acute (4 weeks after the acute sample). The results typically become available too late in the course of the illness to be useful clinically. Singlesample serologic tests for antipertussis toxin (anti-PT) IgG have been developed for research purposes; sera must be col-lected at least 2 weeks after the onset of symptoms (124). Pertussis serology assays using commercial reagents are available, but these assays are not validated clinically and do not differentiate between recent and remote infection and vaccination (125,126). No serologic assay is licensed by FDA for routine diagnostic use in the United States.
# Postexposure Prophylaxis and Treatment
A macrolide (erythromycin, azithromycin, or clarithromycin) is the preferred antimicrobial for postexposure prophylaxis and treatment of pertussis (127). Antimicrobial treatment administered in the early (catarrhal) phase of the illness can modify the severity of the symptoms (36,128,129). An antimicrobial generally does not modify the severity or the course of the illness after paroxysmal cough is established but is used to eliminate B. pertussis and halt transmission (36,(127)(128)(129). Without use of an effective antimicrobial, B. pertussis can be recovered for 6 weeks or longer from infant patients and for 21 days or longer from adult and adolescent patients. Detailed recommendations, indications, and schedules for postexposure antimicrobial prophylaxis and treatment of pertussis have been published previously (127).
Pregnant women with pertussis near term and other household contacts with pertussis are an important source of pertussis for newborn infants (6,41,42,62,64,99). Antimicrobial treatment and prophylaxis are effective in preventing transmission of pertussis to neonates. A macrolide is administered to a woman with pertussis that is acquired late in pregnancy or shortly before delivery, her household contacts, and the neonate. Early recognition of pertussis in a pregnant woman is necessary to ensure the effectiveness of this approach (42,99).
Pregnancy is not a contraindication for use of erythromycin, azithromycin, or clarithromycin. Erythromycin and azithromycin are listed as FDA Category B drugs, and clarithromycin is listed as a Category C drug (130)(131)(132). Macrolides can interact with a variety of other therapeutic agents, precluding concurrent use. Although macrolides can have gastrointestional side effects (e.g., nausea and vomiting), serious side effects (e.g., hepatic dysfunction or pseudomembranous colitis) are rare (127). Infants aged <1 month who receive erythromycin are at increased risk for infantile hypertrophic pyloric stenosis (83,(133)(134)(135)(136). For this reason, and because azithromycin is associated with fewer adverse effects than erythromycin, azithromycin is the preferred antimicrobial for prophylaxis of neonates exposed to pertussis (127). Infantile hypertrophic pyloric stenosis has been reported in two preterm infants who received azithromycin for postexposure prophylaxis (137) between infantile hypertrophic pyloric stenosis and azithromycin has not been established.
# Immunity to Pertussis
The mechanisms of protection against pertussis are incompletely understood. On the basis of studies in animals and humans, both humoral and cellular immunity are believed to play a complementary role (138)(139)(140)(141)(142)(143). The protection that results from B. pertussis infection or pertussis vaccines persists for an estimated 5-10 years or more. Protection wanes over time, leaving persons susceptible to infection or reinfection (4,75,(144)(145)(146)(147)(148)(149)(150).
# Humoral Immunity to Pertussis Vaccine Antigens
Immune responses to B. pertussis can be directed variably against a range of pertussis toxins and antigens. No level of antibody, presence of specific antibodies, or antibody profile has been accepted universally as a quantifiable serologic measure of protection (139,141,(151)(152)(153)(154)(155)(156)(157)(158). Studies of parenterally administered immune globulins for postexposure prophylaxis (159,160) or for treatment of pertussis (28,(161)(162)(163)(164)(165) report mixed results and do not clarify the role of passive antibodies in prevention or treatment of pertussis. By extrapolation, these results do not help predict the role of transplacental maternal antibodies in infant protection.
Pertussis toxin (PT), previously called lymphocytosis promoting factor (LPF), is considered one of the most important of a range of clinically relevant toxins and virulence factors of B. pertussis (including pertactin or 69-kDa protein , fimbriae types 2 and 3 , filamentous hemagglutinin ) (140,142,152,157,(166)(167)(168)(169). Detoxified PT is a component of all pertussis vaccines. The preventive efficacy of a pediatric DTaP vaccine containing detoxified PT as the only immunizing antigen was 71% (95% confidence interval = 63%-78%) against classical pertussis (170). However, the contribution to protection by anti-PT varied in analyses of the humoral immune responses to specific vaccine antigens when evaluated in two household studies. Elevated concentrations of anti-PRN and anti-FIM were associated most closely with protection in these (152,157) and other studies (171). Evidence of added protection from anti-FHA has been mixed (152,156,157,172,173).
# Cellular Immunity to Pertussis Vaccine Antigens
Cell-mediated immune mechanisms clear B. pertussis from within macrophages and other cells (52,139,(174)(175)(176)(177). In addition to humoral immune responses, B. pertussis antigens in acellular pertussis vaccines induce cell-mediated immune responses (178) after primary immunization with pediatric DTaP among infants (158,179), after booster vaccination among children (140,141,149), and after booster vaccination with reduced pertussis antigen content vaccines among adolescents (178,(180)(181)(182)(183) and adults (183,184). Protection is maintained among children whose antibody levels drop below the level of detection over time (185) suggesting that cell-mediated immunity is an important component of protection. Cell-mediated immune responses remain measurable substantially longer than antibodies to the same antigens, particularly PT, and the cell-mediated immune responses to initial doses of pertussis vaccines are believed to correlate better with long-term immunity than antibody responses (140,141,149,158,178,180,181,183,185).
# Prevalence of Pertussis-Specific Antibodies: Pregnant Women and their Infants
Although the importance of antipertussis activity in sera relative to protection remains uncertain, studies conducted since the 1930s have determined the prevalence of antipertussis activity in sera from mothers and infants using multiple assays (Tables 4-8) (37,154,(186)(187)(188)(189)(190)(191)(192)(193)(194)(195)(196)(197)(198)(199). Detectable pertussisspecific antibodies have been identified in unvaccinated women without a history of pertussis (28,187,190,192), women with a past history of pertussis (28,187,190,192), women who likely received whole-cell pertussis vaccine during childhood (195,196,(198)(199)(200), and women with a recent history of pertussis (99). With the exception of women with recent pertussis, the majority of pregnant women have low geometric mean concentrations (GMCs) of anti-PT and antibodies to other pertussis antigens (Tables 4-8) (159), consistent with generally low concentrations of antipertussis antibodies among adults surveyed in the general population (147,(201)(202)(203)(204)(205). GMCs of pertussis-specific antibodies among pregnant women typically have been low regardless of age, as demonstrated in a predominantly (80%) African-American population reported in 2005 (199). A 2006 study of pregnant Hispanics found lower GMCs among adolescents than among women aged >20 years (198).
The efficiency of maternal-fetal transfer of IgG antibodies to pertussis-specific antigens varies; the majority of investigators report similar antigen-specific concentrations in cord or neonatal infant sera and in maternal sera measured late in pregnancy or at delivery (195)(196)(197)(198)(199)(200), but higher concentrations in cord or neonatal sera than in maternal sera have been reported, which might indicate active transport in certain settings (Tables 7 and 8) (195,197,199). In a 2005 survey of mothers and their infants, anti-PT, anti-FHA, and anti-PRN were detected in maternal sera from 35%, 95%, and 80% of women, respectively, and in cord sera from 45%, 93%, and May 30, 2008 ¶ Infants were all of "premature" birth, and their specimens were obtained at age 2-9 wks. Infant cells were obtained at age 6-29 days (median age of immunized and nonimmunized infant groups was 10 and 11 days, respectively). The opsonic titer was calculated as the product of an arbitrary factor: 0, 1, 3, 8, and 12, respectively, for 0, 0-5, 6-20, 21-40, and >41 organisms per cell. The sum of the products defined the "opsonic titer" as "negative to weak"(0-50), "weak to moderate" (51-100), "moderate to strong" , and "strong" . 81% of infants, respectively (199). Among 17 infants studied in 1990, the half-life of transplacental maternal antibody was 36.3 days for anti-PT, 40.3 days for anti-FHA, and 55.0 days for pertussis agglutinins (195). Transplacental maternal antibody was not detectable or was negligible in the majority of infants by age 6-8 weeks (195,197) or by age 4 months (195), consistent with the results of early studies (186). By contrast, in a study of 23 unvaccinated Swedish infants whose mothers had pertussis late in pregnancy, five infants had neutralizing antibody detectable as long as 14 months and detectable anti-PT for 5 months or longer (99).
# Kinetics of Pertussis Booster Vaccination in Nonpregnant Adults and Adolescents
The majority of adults and adolescents have had exposure to B. pertussis, pertussis antigen-containing vaccines, or both, and they will have a booster response to vaccination with pertussis antigens (184,206). A rise in antibodies is measurable by 7 days after vaccination (207), and GMCs reach near-peak levels by 2 weeks after booster vaccination (207)(208)(209)(210). Antibody concentrations decline rapidly in the first few months following vaccination, after which the rate of decline slows (157,181,209,211). Anti-PT levels decline more rapidly than anti-PRN or anti-FHA levels. Among adults who received a booster dose of an acellular pertussis vaccine without tetanus or diphtheria toxoids, concentrations of IgG anti-PT and anti-PRN declined 58% and 39%, respectively, after 6 months. By 18 months after vaccination, concentrations declined 73% and 56%, respectively (209).
# Vaccinating Pregnant Women against Pertussis Tdap
No prelicensure studies were conducted with Tdap in pregnant women. In 2005, to increase understanding of the safety of Tdap in relationship to pregnancy, both Tdap manufacturers established registries to solicit voluntary reports of pregnant women who received Tdap during pregnancy or who received Tdap and were determined subsequently to be pregnant (212,213). The main utility of the registries is to signal the possibility and nature of any risk (214). All women who are vaccinated with Tdap at any time during pregnancy should be reported to the registry as early as possible during the preg-nancy. Information from pregnancy registries differs from surveillance reports, which are used to evaluate outcomes among women when an adverse outcome of pregnancy already might have occurred (e.g., an infant born with a birth defect) (214).
As of December 31, 2007, GlaxoSmithKline had received five reports of pregnancy exposure to BOOSTRIX ® within 28 days before conception or during any trimester of pregnancy, including two in the first trimester, one in the second trimester, and two during an unknown trimester. Among the two first-trimester exposures, one subject delivered a normal infant at 33 weeks' gestation, and one subject was lost to followup. Of the remaining exposures, information on the outcome of two pregnancies was not yet available, and one subject was lost to follow-up (GlaxoSmithKline, unreported data, 2008).
As of November 23, 2007, sanofi pasteur had received 107 spontaneous reports and 47 reports from postlicensing surveillance studies of exposure to ADACEL ® during pregnancy. For these 154 reports, pregnancy outcomes were 68 live infants (including 64 term deliveries [one with a congenital (215,216). Pregnancy was not an exclusion criterion for Tdap; 24 health-care personnel who received Tdap identified themselves as pregnant at the time of vaccination. Among 2,676 (59%) survey respondents, 1,792 (67%) received Tdap at an interval of >2 years after their most recent dose of Td; 17 of these respondents identified themselves as pregnant. Adverse reactions reported by the 17 pregnant women were compared with reactions reported by 472 nonpregnant female personnel aged 18-44 years. The frequencies of injection-site pain, redness, and swelling of moderate to severe intensity were not greater among the pregnant women than among the nonpregnant women. Three of the pregnant women reported feeling "feverish" after receiving Tdap. None of the 17 pregnant women reported seeking nonroutine medical attention for the adverse reaction (215,216). Among the pregnant women vaccinated with Tdap, results of the outcome of pregnancy were known for 10 women; no pregnancy resulted in premature birth or abnormality in the infant when assessed shortly after birth (Elizabeth A. Talbot, Dartmouth College, Lebanon, New Hampshire, personal communication, 2007).
# Whole-Cell Pertussis Vaccine
Five clinical trials conducted during the 1930s and 1940s evaluated vaccinating pregnant women with whole-cell per-May 30, 2008 tussis vaccine as a strategy to increase the levels of maternal pertussis-specific antibodies transferred to their infants via the placenta (Table 9) (186,189,190,192,193,217). The protective efficacy of the vaccine against pertussis in the women was not a consideration. Whole-cell pertussis vaccine was prepared from sterile extracts of killed B. pertussis. To maximize the passive transfer of maternal antibody, pregnant women were vaccinated with 2-6 doses at 1-to 2-week intervals during the third trimester.
Local reactions to vaccination in the pregnant women were common, some of which were severe. Systemic reactions were uncommon, adverse pregnancy outcomes were not reported (Table 9) (190,192,193,217).
The majority of women had substantial rise in titer to B. pertussis antigens in postvaccination sera compared with prevaccine titers (Tables 4-6) (186,189,190,192,193,217). Neither history of pertussis (190,192) nor preexisting titers of antibodies in the women correlated with maternal titers after vaccination (193). The majority of infant antibody titers were lower than (186) or similar to maternal titers (37,150,186,187,(189)(190)(191)(192)(193). Infant titers exceeded maternal titers in certain cases although higher titers might have been within the range of assay variation (37,(186)(187)(188)(189)(190)(191)193).
In subsets of infants in two studies, the duration of detectable transplacental pertussis antibodies was followed among unvaccinated infants (186,217). The mothers in both studies had received 3 doses of whole-cell pertussis vaccine during the third trimester. The mean of the agglutinin titers among infants in one study dropped from 1:160 § at birth to 1:80 at age 2 months; titers no longer were measurable at "a few months of age" (186). Of 36 infants with high agglutinin titers at birth in the other study, 16 (44%) had titers of >1:300 at age 3 months. None of 9 infants followed to age 6 months had a titer of 1:300 (217).
# Infant Protection by Transplacental Maternal Antibody
The role of transplacental maternal antibody in infant protection against pertussis remains uncertain. Prevaccine era observations concluded that infants have no "congenital immunity" and are susceptible to pertussis from the "day of birth," with the possible exception of an infant whose mother had pertussis during pregnancy (35,189,190,192,193,219). Transplacental maternal antibodies might explain the smaller proportion of infant pertussis deaths observed in the first month of life compared with the second and third months of life (Figure 1) (35,45). An alternative explanation might be that parents avoid exposing newborn infants to ill contacts (99,219).
Two retrospective surveys were conducted after early vaccine trials in pregnant women to assess infant protection (217,220). In one survey conducted during the 1940s, a subset of 100 (59%) of 170 women who received 6 doses of wholecell pertussis vaccine during the third trimester and 100 women who were not vaccinated were questioned regarding pertussis in their infants during the first year of life. During the first 6 months of life, eight exposures (three of which were "close exposures") and no cases of pertussis were reported among infants whose mothers had been vaccinated, and six exposures and three cases of infant pertussis were reported among infants whose mothers had not been vaccinated. From age 6-11 months, two cases of infant pertussis were reported in each group (220). In a second survey by the same investigators, a subset of 66 (62%) of 106 women who received 3 doses of whole-cell pertussis vaccine during the third trimester reported two exposures and no case of pertussis among their infants during the first 6 months of life (217). The results of these surveys suggested that high concentration of transplacental pertussis antibodies might provide a degree of infant protection against pertussis in the first 6 months of life (217,220).
# Inhibitory Effect of Transplacental Maternal Antibody on Infant Immunization
Transplacental maternal antibodies to pertussis antigens can interfere with the infant's response to active immunization with the pertussis components of pediatric DTP and pediatric DTaP (221). A proposed mechanism for the interference with pertussis and other vaccine antigens is maternal antibody binding to vaccine antigens, masking the vaccine antigens from the infant's B cells. Infant antigen-presenting cells also might take up maternal antibody-vaccine antigen complexes stimulating selective T-cell responses without humoral immune responses to the vaccine antigens (221)(222)(223). The concentrations and specificities of the maternal antibodies for vaccine-antigen epitopes contributes to the degree of interference (221,(223)(224)(225). The inhibitory effect of transplacental maternal antibody can be detectable for a few weeks or for more than 1 year (221,222,(224)(225)(226)(227)(228). As transplacental maternal antibody declines over time, a threshold is reached when the infant's immune system responds to vaccine antigens in subsequent doses. In theory, the threshold concentration of residual maternal antibody could be lower than the concentration of antibody needed for infant protection, but this concentration is not known for pertussis. In this setting, a theoretical window of "relative susceptibility" exists for the infant until the infant mounts a humoral immune response to a subsequent dose of vaccine (222,229).
# Interference with Pertussis Responses to Pediatric DTP
Substantially lower concentrations of infant IgG anti-PT result after 3 doses of pediatric DTP among infants with "high" (variably defined) prevaccination levels of maternal IgG anti-PT, than among infants with "low" or no measurable prevaccination level of maternal IgG anti-PT (195,(230)(231)(232)(233). The post-dose 3 concentrations of infant anti-PT in one study were 28% or 56% lower with each doubling of the concentration of transplacental maternal anti-PT, respectively, for the two DTP products studied (p <0.05) (233). The reductions in post-dose 3 concentrations also were significant for anti-FIM (18% lower) and agglutinins (15% lower) for one DTP product, and for anti-FHA (16% lower) for the other DTP product, with each doubling of the concentration of the specific transplacental maternal antibodies (p <0.05) (233).
# Interference with Pertussis Responses to Pediatric DTaP
Transplacental maternal IgG anti-PT might interfere less with infant responses after 3 doses of pediatric DTaP than § Titers of >1:320 have been reported to correlate with protection in some studies (218).
after pediatric DTP (195,196,230,233). The percentage decrease in post-dose 3 infant antibody response with each doubling of the concentration of maternal antibodies was 3% for anti-PT (not statistically significant), but was 13% for anti-PRN, 17% for anti-FIM, 10% for agglutinins, and 8% for anti-FHA (all statistically significant; p <0.05) when results from several DTaP products were combined in one study (233). The difference between interference by maternal antibody with infant responses to DTP and DTaP might result from the higher content of pertussis-specific antigens in pediatric DTaP than in pediatric DTP relative to the concentration of transplacental maternal antibody (159,222). In addition, the maternal antibodies induced by the mothers' childhood DTP vaccinations might have less specificity for the pertussis vaccine antigens in acellular pertussis vaccines (222,(234)(235)(236).
# Noninterference with Pertussis Cellular Immune Responses to Pediatric DTP or DTaP
Infants who have relatively poor humoral immune responses to active immunization with whole-cell or acellular pertussis vaccine in the presence of inhibitory concentrations of transplacental maternal antibody have evidence of T-cell priming for booster (anamestic) responses (158,237). Protection against pertussis in T-cell primed infants in the absence of specific humoral antibodies has not been established (158,(238)(239)(240)(241).
# Lactation
Existing data do not provide evidence that human colostral pertussis antibodies contribute to infant protection, although pertussis-specific antibodies present in the mother are found in colostral milk (186,190,242). Protection studies in animal models suggest human and animal colostral-derived pertussis antibodies can protect animals when the antibodies are absorbed or injected parenterally (243)(244)(245); however, the relevance of these studies for human infants is uncertain (190,246,247). Human breast milk antibodies do not enter the human neonatal circulation from the intestine in substantial amounts. In contrast, infant pigs, horses, ruminants, dogs, and cats acquire the majority of neonatal protection through intestinal uptake of colostral antibodies (245,(248)(249)(250). Maternal antibodies in human milk do not interfere with the infant immune response to pediatric vaccines (23).
# Tetanus
Tetanus is caused by Clostridium tetani spores, which are ubiquitous in the environment. Spores enter the body through disrupted skin or mucus membranes. When inoculated into oxygen-poor sites (e.g., necrotic tissue or wounds), C. tetani spores germinate to vegetative bacilli that elaborate tetanospasmin, a potent neurotoxin. More than 80% of cases of tetanus are of the generalized syndrome; the remaining cases are localized or cephalic. Persons with generalized cases typically have trismus (lockjaw), followed by rigidity and painful contractions of the skeletal muscles that can impair respiratory function. Glottic spasm, respiratory failure, and autonomic instability can result in death. The onset of tetanus typically is within 7 days of the injury (range: 0-112 days) The course of tetanus is up to 4 weeks or longer, followed by a prolonged period of convalescence (251,252).
# Obstetric and Neonatal Tetanus
Obstetric tetanus is defined as tetanus during pregnancy or with onset within 6 weeks after the termination of pregnancy (253). Obstetric tetanus occurs after contamination of wounds or abrasions during pregnancy or after unclean deliveries or abortions. In a review covering 1941-1990, an estimated 65%-80% of cases of obstetric tetanus occurred in the puerperal or postpartum period; the majority of the other cases occurred after surgical or spontaneous abortions (254).
Obstetric tetanus has the highest mortality when the incubation period is short and respiratory complications are present (255). Cases can be complicated by gram-negative sepsis (256). Case-fatality rates vary (range: 16%->50%); higher fatality rates are reported from places where access to medical intensive care is limited (255,257,258). Case-fatality rates historically have been higher for postabortal than for postpartum obstetric tetanus (254).
Neonatal tetanus (tetanus neonatorum) is associated with contamination of the umbilical stump. In nearly all cases of infant tetanus, onset occurs in the first month of life. Symptoms commonly begin at 3-14 days of life and are characterized by increasing irritability and difficulty feeding. Signs of neonatal tetanus are similar to tetanus in older age groups. Case-fatality rates vary (range: 10%-100%) (252,259). Infants who survive can have residual neurologic injury (e.g., cerebral palsy and psychomotor retardation) (252).
# Burden
Tetanus is a nationally notifiable disease in the United States (260). In 2006, a total of 41 cases were reported. No cases occurred among women aged 15-19 years or those aged 30-39 years. One case occurred among women aged 20-29 years, and three cases occurred among women aged 40-49 years. None of the women died. During 1972-2006, case reporting forms did not collect information regarding pregnancy; however, no case of obstetric tetanus was identified among more than 1,000 reports to NNDSS (CDC, unpublished data, 2006). In 1999, tetanus-specific coding became available in CDC's mortality database; no case of tetanusassociated obstetric death was reported through 2005, the most recent year for which data are available (CDC, unpublished data, 2008).
During the 1950s, approximately 100 neonatal tetanus deaths were reported annually in the United States, and neonates comprised more than one third of tetanus deaths in all age groups (261,262). During 1972During -2006, the cumulative number of reported neonatal tetanus cases decreased to 32; the most recent cases were reported in 1989, 1995, 1998, and 2001 (263). Among these 32 neonatal cases, 27 (84%) births occurred in a nonhospital setting; 30 of 31 mothers with available history reported never having received a dose of tetanus toxoid vaccine (264-266;CDC, unpublished data, 2006).
# Diagnosis and Treatment
The diagnosis of tetanus is clinical and is supported by a compatible setting, immunization history, and exclusion of other possible diseases. Anaerobic cultures of tissues or aspirates for C. tetani typically are not positive. Low or undetectable levels of serum antitoxin at the time of onset are compatible with the diagnosis of tetanus, but higher levels of antitoxin do not exclude the diagnosis (252,267). Electromyography might aid in the diagnosis of certain cases (268). Postpartum eclampsia, which typically occurs within the first few days after delivery, was the most important disease in the differential diagnosis in community-based studies (254).
Treatment of tetanus is directed at neutralizing unbound toxin with administration of human tetanus immune globulin, removing the source of infection through debridement, and use of an antimicrobial (e.g., metronidazole). The control of rigidity and spasms, attendant respiratory and autonomic dysfunction and their complications, and maintaining nutrition require careful and sustained attention that is best provided in intensive-care settings with specialty consultation (251,252,269).
# Immunity to Tetanus
The level of antitoxin that protects against obstetric and neonatal tetanus can vary with the wound characteristics, the degree of contamination, the specificity of the antitoxin, and the type of assay employed to measure the antitoxin level (270). The minimum level of antitoxin correlating with protection is 0.01 IU/mL as measured by in vivo neutralization assay. An antitoxin concentration at >0.1 IU/mL is the preferred correlate of protection based on the results of other assays (e.g., enzyme-linked immunoabsorbant assay ), and because higher concentrations of antitoxin might be necessary to protect in certain circumstances (252,270). The serum level of tetanus antitoxin achieved in response to vaccination is determined by the number of doses of tetanus toxoid, the type of tetanus toxoid administered (adjuvanted toxoid, which is more immunogenic, has replaced fluid toxoid), the interval since the most recent dose, and individual variation in the response to vaccination (270).
# Deferring Td During Pregnancy to Substitute Tdap in the Immediate Postpartum Period
Ensuring maternal and neonatal tetanus protection as part of prenatal care is a priority for women who are due for a recommended decennial tetanus and diphtheria toxoids booster dose. For women who have not received a dose of Tdap previously, administering Td during pregnancy, followed in a few months by Tdap postpartum, theoretically could increase the risk or severity of adverse reaction, which typically is local. Moderate to severe local reactions have been associated with high levels of tetanus and diphtheria antitoxin (see Interval Between Td and Tdap). In these women, deferring the Td booster during pregnancy to substitute Tdap in the immediate postpartum period may be considered to boost protection against pertussis as well as tetanus and diphtheria. The majority of women of childbearing age who have lived in the United States since infancy or childhood have received 4-5 infant and childhood doses of tetanus toxoid with pediatric DTP or DTaP and >1 booster dose of Td (or tetanus toxoid without diphtheria toxoid ) in accordance with national recommendations (1,2,271). The recommended schedule of vaccination to prevent tetanus is intended to maintain levels of antitoxin considerably higher than the minimum level required for protection against the majority of cases of tetanus, including protection among persons with intrinsically lower responses to vaccination (1,2,252,(271)(272)(273).
In 2004, women aged 15-39 years accounted for 97% of all births in the United States (3). Data from a populationbased serosurvey conducted nationwide in the United States during 1988-1994 documented tetanus antitoxin concentrations at >0.15 IU/mL among >80% of women aged 12-39 years (274,275). The proportion of women with antitoxin at >0.15 IU/mL declined with increasing age to 62% among women aged 40-49 years (274,275). Slightly lower prevalence of this titer was found among women aged 20-59 years who were not born in the United States (276). A 1999-2000 study evaluated 2,134 adult patients in an emergency department for wound management and measurement of their antitoxin titer (277). Antitoxin concentrations of >0.15 IU/mL were present among 1,051 (95%) of 1,106 adults aged 18-39 years. Among adults of all ages studied, approximately 95% of those with up-to-date vaccination histories and approximately 86% of those whose vaccinations were not up-to-date had antitoxin titers >0.15 IU/mL. The rates of a protective titer were lower for immigrants, persons with less education, and persons aged >70 years (277). Limitations of these studies are that one study did not report any connection between vaccination histories and antitoxin concentrations (274)(275)(276), and the other study included subjects who might not be representative of the U.S. population (277). However, when combined with the small number of tetanus cases among women of childbearing age in the United States, these studies suggest that when pregnant women have previously received the recommended schedule of tetanus and diphtheria toxoids vaccinations, a routine decennial Td booster during pregnancy typically can be deferred so Tdap can be substituted at delivery or before discharge from the hospital or birthing center.
# Vaccinating to Prevent Obstetric and Neonatal Tetanus
Success in preventing obstetric and neonatal tetanus relies on antitoxin being present at delivery (254). In countries where access to childhood vaccines is limited, neonatal tetanus constitutes a major cause of infant mortality; during 1978-1985, an estimated 800,000 neonatal tetanus deaths occurred annually worldwide (278). In 1974, worldwide elimination of neonatal tetanus (less than one case per 1,000 live births) through vaccine initiatives became a major focus of the Expanded Program of Immunization of the World Health Organization (WHO) (259,279). The initiative promoted clean deliveries and tetanus toxoid vaccination for pregnant women. Nonpregnant women of childbearing age also were targeted for at least 3 doses of tetanus toxoid vaccine in supplemental immunization activities.
The strategy of targeting pregnant women for vaccination to prevent neonatal tetanus was based on reports published in the 1960s concerning two vaccine trials that demonstrated that >2 doses of tetanus toxoid administered during pregnancy were >95% effective in preventing neonatal tetanus (Table 10) (280,281). Subsequent studies confirmed that 3 doses of aluminum phosphate-adjuvanted tetanus toxoid (rather than fluid toxoid) administered during pregnancy induced antitoxin levels that would protect the mother and prevent neonatal tetanus for >10 years. Adjuvanted vaccine also lowered the rates of local reactions in pregnant women (282)(283)(284).
Although the burden of obstetric tetanus has not been characterized as well as the burden of neonatal tetanus, the annual worldwide burden of obstetric tetanus deaths has been esti-mated at 15,000-30,000, accounting for approximately 5% of all maternal deaths in the 1990s (254,259). In April 2006, WHO's Strategic Advisory Group of Experts (SAGE) reported on the success of the maternal and neonatal tetanus elimination initiatives and the plan to transition from vaccination goals for women of childbearing age to universal tetanus control, to be achieved through sustained high coverage with pediatric DTP starting in infancy and childhood and booster doses to prevent tetanus throughout life (259,285,286).
# Safety of Tetanus Vaccination During Pregnancy
No evidence suggests that adverse outcomes for a mother or fetus increase after tetanus toxoid is administered to a pregnant woman (1,2,23). Tetanus toxoid administered during any trimester of pregnancy was evaluated for association with congenital abnormalities at birth during 1980-1994 in Budapest, Hungary. The rate of tetanus toxoid vaccination among 21,563 mothers of infants with congenital abnormalities was not significantly different than the rate of tetanus toxoid vaccination among 35,727 mothers of infants who were normal (0.12% and 0.09%, respectively; p = 0.39) (287). In a similar study conducted in nine countries in South America starting in 1977, approximately one half of the women had received tetanus toxoid during the first trimester of pregnancy. The rate of early tetanus toxoid vaccination among the mothers of 34,293 newborns with congenital malformations (9.2 per 1,000 mothers) was not substantially different than the rate among the mothers of 34,477 newborns who were normal (7.6 per 1,000 mothers) (288).
# Infant Protection by Transplacental Maternal Antibody
Tetanus toxoid is one of the most immunogenic protein antigens in any vaccine. Administration of 2 doses of tetanus toxoid to pregnant women at least 4-6 weeks before delivery stimulates antitoxin that protects the mother and readily crosses the placenta, thereby protecting the newborn against tetanus when the risk is highest (289). Pregnant women who receive a booster dose of tetanus toxoid have a measurable immune response within 5 days and a peak response in <2 weeks. The response to vaccination might be slower after a first (primary) dose or when the interval after the most recent booster dose is long (252,272). Placental transport of maternal IgG antitoxin is efficient; cord blood levels generally are similar to maternal levels (290,291). After the neonatal period, the infant is at little risk for tetanus until becoming self-mobile, typically at an age when sustained protection has been induced by 3 infant doses of pediatric DTP or DTaP (252).
# Inhibitory Effect of Transplacental Maternal Antibody on Infant Immunization
Transplacental maternal tetanus antitoxin can interfere with the infant response to active immunization after up to 3 doses of tetanus toxoid (e.g., in pediatric DTP, DTaP, or DT) (222,230,(292)(293)(294)(295)(296)(297). Certain studies (296,297), but not all (298), indicate that antitoxin inhibits the response to tetanus toxoid after vaccination with Haemophilus influenzae type b polysaccharide conjugated to tetanus toxoid. An ageaccelerated schedule results in further decrease in infant responses in the presence of maternal antitoxin (295). When levels of transplacental maternal antitoxin wane sufficiently, infants respond to subsequent doses of vaccine (229,293,294,(299)(300)(301). T-cell priming for a booster response is not substantially affected by maternal antitoxin (222,302,303). Typically, infants respond to the second dose of tetanus toxoid-containing vaccine with a protective level of antitoxin, even when the initial levels of maternal antitoxin are high; 3 doses of tetanus toxoid are required to achieve antitoxin concentrations that persist above protective levels (292,304).
# Lactation
No substantial difference in the infant immune response to tetanus toxoid (in DTP) has been identified with consumption of human milk compared with consumption of cow milk (305).
# Diphtheria
Respiratory diphtheria is an acute, severe infection caused by strains of Corynebacterium diphtheriae that produce diphtheria toxin. Rarely, toxin-producing strains of C. ulcerans cause a diphtheria-like illness (306). Respiratory diphtheria is characterized by a grayish-colored adherent membrane on the pharynx, palate, or nasal mucosa that can obstruct the airway with fatal outcome. The disease can be complicated by toxinmediated cardiac, neurologic, or renal dysfunction. Casefatality rates are >10% (307,308).
# Obstetric and Neonatal Diphtheria
Respiratory diphtheria (309)(310)(311)(312) or vulvovaginal infection (313,314) can occur during any trimester of pregnancy, at term, or in the postpartum period. The mortality rate of obstetric respiratory diphtheria is high (estimated at 50%) without infusion of diphtheria antitoxin, even with tracheostomy or intubation, and is accompanied by fetal loss or premature birth in approximately one third of survivors. Early treatment with serum diphtheria antitoxin improves survival and pregnancy outcomes, although complications of the disease might require prolonged supportive care (309)(310)(311)(312). Postpartum women with respiratory diphtheria can transmit C. diphtheriae to their neonates (310).
# Burden
Respiratory diphtheria is a nationally notifiable disease in the United States. Rare cases occur in the United States after infection with diphtheria toxin-producing strains of C. diphtheriae or other corynebacteria (315,316). During 1998-2006, seven cases of respiratory diphtheria were reported to CDC. The most recent culture-confirmed adult case of respiratory diphtheria caused by C. diphtheriae was reported in 2000, and an adult case of respiratory diphtheria caused by C. ulcerans was reported in 2005 (306). The risk for diphtheria can be increased during travel to areas in which diphtheria is endemic; a list of these areas is available at . gov/travel/default.aspx. Diphtheria also can be acquired from persons with imported cases or from carriers (i.e., asymptomatic persons who are colonized with toxin-producing C. diphtheriae) (315,316).
# MMWR May 30, 2008
# Diagnosis and Treatment
The diagnosis of diphtheria is confirmed by isolation of C. diphtheriae in culture of the adherent membrane and by testing the isolate for toxin production (317). The mainstay of treatment in respiratory diphtheria is early administration of diphtheria antitoxin (equine), which is available to physicians in the United States from CDC through an FDA-Investigational New Drug protocol (24-hour telephone, 770-488-7100). Additional information is available at . No human-derived serum diphtheria antitoxin is available. Antibiotics are administered to limit transmission and to prevent continuing production of diphtheria toxin (318). Prompt reporting of suspect cases, investigation, culture, and antimicrobial prophylaxis of contacts and immunization of the affected community (317,318) is of critical importance. Because respiratory diphtheria does not always confer protection against future illness, patients should complete active immunization with diphtheria toxoid after recovery (286).
# Diphtheria Immunity
Protection against respiratory diphtheria is predominantly from IgG antibody to diphtheria toxin (antitoxin) induced after infection with toxin-producing C. diphtheriae or after vaccination with diphtheria toxoid. In areas with little or no endemic exposure to toxin-producing C. diphtheriae, periodic vaccination is required to maintain immunity (237,286,307,(319)(320)(321). Although the immune responses to infection and vaccination vary, antitoxin concentrations of >0.1 IU/mL typically are considered protective. Concentrations of 0.01 IU/mL-0.1 IU/mL might provide protection against severe disease; concentrations <0.01 IU/mL do not protect against diphtheria (286,307,322).
# Td Booster During Pregnancy for Diphtheria Protection
Data from a national population-based serosurvey conducted during 1988-1994 that evaluated the prevalence of immunity to diphtheria (defined as a diphtheria antitoxin concentration of >0.1 IU/mL) among women in the United States determined immunity to diphtheria to be lower than immunity to tetanus (see Tetanus: Deferring Td During Pregnancy to Substitute Tdap in the Immediate Postpartum Period). The prevalence of immunity to diphtheria decreased with increasing age (77% among women aged 12-19 years, 74% among women aged 20-29 years, 65% among women aged 30-39 years, and 40 years) and with birth outside the United States or less formal education (274,276).
# Vaccinating Pregnant Women, Infant Protection by Transplacental Antibody
Diphtheria toxoid vaccine trials conducted among pregnant women in the 1940s demonstrated quantitative increases in diphtheria antitoxin after the women were vaccinated. Maternal antitoxin was transferred efficiently to the fetus (217,226,320,323,324). Several studies indicate transplacental maternal antitoxin provides newborn infants with protection against diphtheria at birth if their mother is immune (226,250,321,325).
# Safety
The safety of diphtheria toxoid (without tetanus toxoid) vaccination in pregnant women was examined during the 1970s (326). After diphtheria toxoid was administered during the first 4 months of pregnancy, 75 mother-child pairs were followed for malformations until the child reached age 7 years. Although the number of vaccinated pregnant women studied was small, the risk for malformations in their children was lower than the risk among children in a much larger group of mother-child pairs in which the women were not vaccinated with diphtheria toxoid during pregnancy (survival-and race-standardized relative risk: 0.88) (327).
# Inhibitory Effect of Transplacental Maternal Antibody on Infant Immunization
Transplacental maternal diphtheria antitoxin concentrations of 3 infant doses of high-content diphtheria toxoid vaccine when maternal antitoxin concentrations are >1.0 IU/mL in cord sera (225,229,292,299,321,329,331,332). When infants receive subsequent doses of diphtheria toxoid, the responses are rapid, often within 2 weeks (330), suggesting that T-cell priming occurs in the absence of an infant antibody response to previous doses of vaccine (229,237,324,329,330).
# Lactation
Consumption of human milk does not affect the infant immune response to diphtheria toxoid-containing vaccines (292,332). Ingestion of colostrum from an immune mother does not result in an increase in the concentration of diphtheria antitoxin in infant sera (250).
# Adult and Adolescent Acellular Pertussis Combined with Tetanus and Reduced Diphtheria Toxoids (Tdap) Vaccines and Tetanus and Reduced Diphtheria Toxoids (Td) Vaccines
Both Tdap vaccines used in the United States (ADACEL ® and BOOSTRIX ® ) were licensed on the basis of clinical trials in the United States demonstrating immunogenicity not inferior to that of U.S.-licensed Td (333,334) and the pertussis components of pediatric DTaP made by the same manufacturer and an acceptable safety profile (212,213). Adsorbed Td products for adults and adolescents have been licensed in the United States since the 1950s (335). Components of these and other diphtheria and tetanus toxoids-containing vaccines have been listed (Table 1) and are available at . gov/cber/vaccines.htm.
In prelicensure trials, data on local and systemic adverse events were collected using standard diaries for the day of vaccination and the next 14 consecutive days (212,213,(336)(337)(338). The efficacies of the tetanus toxoid and the diphtheria toxoid components of Tdap were inferred from the immunogenicity of the antigens in Tdap compared with Td using established serologic correlates of protection in sera obtained before and approximately 1 month after vaccination. Because no wellaccepted serologic or laboratory correlate of protection is available for pertussis, the efficacy of the pertussis components of Tdap was inferred using a serologic bridge (comparison) to the immune response to vaccine antigens among infants who received 3 doses of pediatric DTaP (made by the same manufacturer) during clinical efficacy trials for pertussis during the 1990s (339). The efficacy against pertussis of an acellular pertussis vaccine without tetanus and diphtheria toxoids was 92% (CI = 32%-99%) for adults and adolescents in a randomized, controlled trial (340); these results were not considered in the evaluation of Tdap for licensure in the United States.
Selected results from the prelicensure trials are summarized below. Additional information can be found in previous ACIP statements discussing use of Tdap among adults and adolescents and in the package labels of the specific products (1,2,212,213).
# ADACEL ®
ADACEL ® contains the same tetanus toxoid, diphtheria toxoid, and five pertussis antigens as those in DAPTACEL ® (pediatric DTaP, also made by sanofi pasteur), but ADACEL ® is formulated with reduced quantities of diphtheria toxoid and detoxified PT. Prelicensure trials in the United States evaluated the immunogenicity and the safety of ADACEL ® among adults aged 18-64 years and among adolescents aged 11-17 years, randomized to receive a single dose of ADACEL ® or a single dose of Td made by the same manufacturer (Table 1) (1,2,212,333). Pregnant women were excluded.
# Immunogenicity
Tetanus and Diphtheria Toxoids. The rates of seroprotection and booster response for both antitetanus and antidiphtheria among adults and adolescents who received a single dose of ADACEL ® were noninferior to rates among those who received Td. Nearly all (>99%) subjects in the ADACEL ® and Td groups achieved seroprotective antitetanus levels (>0.1 IU/mL), and >94% of adults and >99% of adolescents achieved seroprotective antidiphtheria levels (>0.1 IU/mL) in ADACEL ® and Td groups (212,341).
Pertussis Antigens. The efficacy of the pertussis components was inferred by comparing the immune responses (GMCs) of adults and adolescents vaccinated with a single dose of ADACEL ® to those of infants vaccinated with 3 doses of DAPTACEL ® in a Swedish vaccine efficacy trial (338,342). The efficacy of 3 doses of pediatric DAPTACEL ® against WHO-defined pertussis (>21 days of paroxysmal cough with confirmation of B. pertussis infection by culture or serologic testing, or an epidemiologic link to a household member with culture-confirmed pertussis) was 85% (CI = 80%-89%) (338,342). The GMCs of anti-PT, anti-FHA, anti-PRN, and anti-FIM among adults and adolescents after a single dose of ADACEL ® were noninferior to those of infants after 3 doses of DAPTACEL. ® The prespecified criteria for booster responses also were met (1,2,212,336,341).
# Safety
The safety of ADACEL ® was evaluated in four clinical studies with data from 2,448 adults aged 18-64 years and 3,393 adolescents aged 11-17 years (212).
Immediate Events. No anaphylaxis was reported. Five adults reported an immediate event within 30 minutes of vaccination (four persons for ADACEL ® and one person for Td); three of these five events were classified as nervous system disorders (hypoesthesia/paresthesia). Eleven adolescents reported an immediate event (six persons for ADACEL ® and five persons for Td); these events included dizziness, syncope, or vasovagal reactions in addi-May 30, 2008 tion to pain and erythema at the injection site. All events resolved without sequelae (338,341,343).
Solicited Local and Systemic Adverse Events. Rates of erythema and swelling (Figures 3 and 4), or systemic (headache, generalized body aches, and tiredness ) adverse events reported to occur during 0-14 days following vaccination with Td or Tdap were similar (1,2,212,338,341). Fever >100.4°F (>38°C) was reported with the same frequency by adults vaccinated with Td and with Tdap (Figure 3) (212); the rate of any fever reported by adolescents vaccinated with Tdap (5%) was higher than the rate for those vaccinated with Td (3%) but met the noninferiority criterion (Figure 4) (212,341). No case of whole-arm swelling was reported (341).
Serious Adverse Events. Among adults, serious adverse events (e.g., appendicitis) within 6 months after vaccination were reported for 33 (2%) of 1,752 persons in the ADACEL ® group and for 11 (2%) of 573 persons in the Td group (338,341). Two serious adverse events in ADACEL ® recipients were neuropathic and were assessed by the investigators as possibly related to vaccination. In both cases, the symptoms resolved completely over several days (1,212,338,341,343). Among adolescents, serious adverse events within 6 months after vaccination were reported for 11 (1%) of 1,184 persons in the ADACEL ® group and for eight (1%) of 792 persons in the Td group. All events were reported by investigators to be unrelated to the study vaccine (341). No physician-diagnosed Arthus reaction (see Important Local Reactions) or case of Guillain-Barré syndrome (see Neurologic and Systemic Events) was reported (1).
# Simultaneous Administration of Tdap with Other Vaccines
Trivalent Inactivated Influenza Vaccine. The safety and immunogenicity of ADACEL ® co-administered with trivalent inactivated influenza vaccine ( Fluzone, ® sanofi pasteur, Swiftwater, Pennsylvania) were evaluated in nonpregnant adults aged 19-64 years randomized to simultaneous administration in different arms (n = 359), or to TIV administered first, followed by ADACEL ® 4-6 weeks later (n = 361). Rates of fever and injection site erythema and swelling were similar following ADACEL ® administered concurrently with TIV or separately. Pain at the ADACEL ® injection site occurred more frequently after simultaneous administration than after separate administration (67% and 61%, respectively) (338). Immunogenicity criteria were met with the following exceptions: the GMC of anti-PRN was lower in the simultaneous group than in the sequential group (338,344), and the tetanus booster response rates were lower after simultaneous administration than after sequential administration (79% and 83%, respectively). However, more than 98% of subjects in both groups achieved seroprotective levels (>0.1 IU/mL) of tetanus antitoxin (338,344).
Hepatitis B Vaccine. The safety and immunogenicity of ADACEL ® administered with hepatitis B (Hep B) vaccine (Recombivax HB, ® Merck and Co., White House Station, New Jersey) were evaluated among nonpregnant adolescents Td] was 10.7% whereas the noninferiority criterion was <10%). † The rate of "any" fever was higher after Tdap than after Td (p<0.05); however, the noninferiority criterion was met for Tdap. aged 11-14 years randomized to simultaneous administration (n = 206) or to ADACEL ® administered first, followed by hepatitis B vaccine 4-6 weeks later (n = 204). Rates of solicited erythema and swelling at the ADACEL ® injection site were higher in the simultaneous group than in the sequential group, and noninferiority was not achieved (1,338). No interference was observed in the immune responses to any of the vaccine antigens when ADACEL ® and hepatitis B vaccine were administered concurrently or separately (212).
# BOOSTRIX ®
BOOSTRIX ® contains the same tetanus toxoid, diphtheria toxoid, and three pertussis antigens as those in INFANRIX ® (pediatric DTaP, also made by GlaxoSmithKline), but BOOSTRIX ® is formulated with reduced quantities of antigens. Prelicensure trials conducted in the United States evaluated the immunogenicity and safety of BOOSTRIX ® among adolescents aged 10-18 years (213,337), randomized to receive a single dose of BOOSTRIX ® or a single dose of Td (Massachusetts Public Health Biologic Laboratory, Mattapan, Massachusetts) (Table 1) (213,334,337). Pregnant adolescents were excluded.
# Immunogenicity
Tetanus and Diphtheria Toxoids. The rates of seroprotection and booster response for both antitetanus and antidiphtheria among adolescents who received a single dose of BOOSTRIX ® were noninferior to those who received Td. All adolescents had seroprotective antitetanus levels (>0.1 IU/mL); >99% of adolescents had seroprotective antidiphtheria levels (>0.1 IU/mL) (1,213,336).
Pertussis Antigens. The efficacy of the pertussis components was inferred by comparing the immune responses of adolescents vaccinated with a single dose of BOOSTRIX ® with the immune responses of infants vaccinated with 3 doses of INFANRIX ® in a German vaccine efficacy trial (213, 336,345). The efficacy of 3 doses of pediatric INFANRIX ® against WHO-defined pertussis was 89% (CI = 77%-95%) (213,345). The GMCs of anti-PT, anti-FHA, and anti-PRN after a single dose of BOOSTRIX ® were noninferior to those of infants after 3 doses of INFANRIX. ® The prespecified criteria for booster responses also were met (1,213,336,337).
# Safety
A total of 3,080 adolescents aged 10-18 years received BOOSTRIX ® in the primary safety study (213). No immediate events (i.e., those occurring within 30 minutes of vaccination) were reported (1,213,336,337).
# Solicited Local and Systemic Adverse Events.
No substantial differences were observed between the BOOSTRIX ® and Td recipients in the rates of solicited local (redness, swelling, and increase in arm circumference above baseline) (Figure 5) or systemic (headache, fatigue, gastrointestinal systemic events, fever >100.4°F ) adverse events (1,213,336,337). No case of whole-arm swelling was reported (1).
Serious Adverse Events. Serious adverse events within 6 months after vaccination were reported among 14 (0.4%) of 3,005 adolescents vaccinated with BOOSTRIX ® and two (0.2%) of 1,003 adolescents vaccinated with Td. All events were reported by the investigators to be unrelated to the study vaccine (213,336,337,346). No physician-diagnosed Arthus reaction or case of Guillain-Barré syndrome was reported (1,213,337,346).
# Pregnant Women Vaccinated with Tdap
Pregnant women were excluded from prelicensure trials of Tdap. The outcome of pregnancy among six women who were administered ADACEL ® inadvertently during or within 1 month of conception was a healthy full-term infant (n = 3), a preterm infant (n = 1), or a miscarriage (n = 2). No infant was born with a congenital anomaly (sanofi-pasteur, unreported data, 2007). Two pregnancies occurred in BOOSTRIX ® recipients >4 months postvaccination; one subject experienced a spontaneous abortion within the first trimester, and the other subject delivered a healthy infant (337).
# Regulatory Considerations for Tdap in Pregnant Women
As with the majority of vaccines, Tdap is labeled pregnancy category C. This designation indicates that no adequate and well-controlled studies have been conducted with the vaccine in pregnant women to determine the product's safety (347,348).
# Safety Considerations for Adult and Adolescent Use of Td or Tdap
Prelicensure studies in nonpregnant adults and adolescents evaluated the safety of Tdap with respect to local and systemic adverse events (212,213). The sample sizes were insufficient to detect rare adverse events. Enrollment criteria excluded persons who were pregnant; had received vaccines containing tetanus toxoid, diphtheria toxoid, or pertussis components more recently than either the preceding 5 years for ADACEL ® (212) or the preceding 10 years for BOOSTRIX ® (213); or had certain neurologic conditions or events (336)(337)(338)341,346). Safety data are being collected by the Vaccine Adverse Event Reporting System (VAERS), and postlicensure studies continue to monitor for potential adverse reactions following widespread use of Tdap in adults and adolescents (16,17). Registries have been established by both Tdap manufacturers for reporting women vaccinated with Tdap during pregnancy.
# Interval between Td and Tdap
ACIP has made several recommendations for intervals between tetanus toxoid-and diphtheria toxoid-containing vaccines that balance the benefits of protection against the risks of moderate and severe local reactions. Moderate and severe local reactions, including Arthus reaction, are associated with frequent dosing at short intervals and larger doses of toxoid. High antitoxin levels are more likely to result when the interval between doses is short and the number of doses increases (349)(350)(351)(352)(353)(354). High preexisting antibody titers to tetanus or diphtheria toxoids also are associated with increased rates and severity of local reactions to booster doses in adults (349,(354)(355)(356).
ACIP recommends a 10-year interval for routine administration of Td (e.g., decennial Td booster), and a 5-year interval for Td when indicated for wounds management (1,2,357). Administering Td more often than every 10 years (5 years for certain nonclean, nonminor wounds) is not necessary to provide protection against tetanus or diphtheria; however, administering a single dose of Tdap at an interval shorter than 5 years after Td could provide a health benefit by adding protection against pertussis (Table 2) (1,2). When Tdap is administered to add protection against pertussis, ACIP encourages an interval of >5 years between the most recent Td and the Tdap dose for adolescents because they might receive other recommended vaccines containing tetanus or diphtheria toxoids (including quadrivalent meningococcal conjugate vaccine ) (2). An interval as short as 2 years is recommended between the most recent Td and the single dose of Tdap for health-care personnel with direct patient contact, and a 2-year interval between the most recent Td and Tdap is suggested for adults in close contact with infants (1). ACIP allows for a shorter interval between the most recent Td and administration of Tdap in certain circumstances that might require urgent protection (1,2).
Several studies have suggested that an interval as short as 2 years between Td and a single dose of Tdap is acceptably safe. Three studies conducted among Canadian children and adolescents evaluated the safety of Tdap (ADACEL ® ) at an interval shorter than 5 years after Td or after pediatric DTP or DTaP (358)(359)(360). The largest was an open-label study of 7,001 students aged 7-19 years. Rates of local reactions were not increased among students who had received the most recent of 5 pediatric DTP or DTaP doses, or a Td dose, >2 years before Tdap, compared with >10 years before Tdap (358). The other Canadian studies demonstrated similar safety when Tdap was administered at an interval of <5 years after the previous tetanus toxoid-and diphtheria toxoid-containing vaccine (359,360).
Adverse reactions after Tdap (ADACEL ® ) administered at an interval of 2 years (n = 1,792) or 2 years after the most recent dose of Td; causality was not assessed. The events were a case of Guillain-Barré syndrome (not requiring hospitalization) with onset 11 days after Tdap, a case of anaphylaxis-like reaction with onset 6 days after Tdap, and a case of eosinophilic nephritis with onset 6 days after Tdap in a health-care worker with a history of a renal transplant (215,216).
# Important Local Reactions Arthus Reaction
Arthus reaction (type III hypersensitivity reaction) can occur after tetanus toxoid-or diphtheria toxoid-containing vaccines (354,357,362-366;CDC, unpublished data, 2005). Arthus reaction is a local vasculitis with deposition of immune complexes and activation of complement; it occurs in the setting of high local concentration of vaccine antigens and high circulating antibody concentration (354,362,363,367). The reaction is characterized by severe pain, swelling, induration, edema, and hemorrhage, and occasionally by local necrosis. Vaccine-related arthus reaction typically resolves without sequelae. The onset of symptoms and signs is 4-12 hours after vaccination, compared with anaphylaxis (immediate type I hypersensitivity reaction), which has onset within minutes after vaccination. ACIP recommends that persons who experience an Arthus reaction after administration of a tetanus toxoid-containing vaccine not receive Td or other tetanus toxoid-containing vaccine more frequently than every 10 years, even for tetanus prophylaxis as part of wound management (1,357).
# Extensive Limb Swelling
Extensive limb swelling reactions have been reported to VAERS following administration of Td (368,369) and are described following dose 4 or dose 5 of pediatric DTaP (23,208,368,(370)(371)(372)(373). Extensive limb swelling after pediatric DTaP resolves without complication within 4-7 days (370), and is not considered a precaution or contraindication for Tdap (23).
# Neurologic and Systemic Events Pertussis Components
Concerns regarding a possible role of pertussis vaccine components in causing neurologic reactions or exacerbating underlying neurologic conditions in infants and children are long-standing (29,374). In 1991, the Institute of Medicine (IOM) concluded that evidence favored acceptance of a causal relation between pediatric DTP vaccine and acute encephalopathy (365). A subsequent retrospective analysis of >2 million children in the United States did not demonstrate that pediatric DTP was associated with an increased risk for encephalopathy after vaccination (375). Active surveillance in Canada during 1993-2002 also failed to identify any acute encephalopathy cases causally related to whole-cell or acellular pertussis vaccines among a population administered 6.5 million doses of pertussis-containing vaccines (376). Results of one recent investigation suggested that some acute encepha-lopathies attributed previously to pertussis-containing vaccines could be the result of genetically determined epileptic encephalopathies related to mutations in the sodium channel gene SCN1A (377,378). A history of encephalopathy (e.g., coma or prolonged seizures) not attributable to an identifiable cause within 7 days of administration of a vaccine with pertussis components remains a contraindication for Tdap (but not Td) in adults and adolescents.
The possibility that Tdap would complicate neurologic evaluation of chronic progressive neurologic disorders that are stable in adults (e.g., dementia) is of limited clinical concern and does not constitute a reason to delay administration of Tdap (1). Unstable or evolving neurologic conditions (e.g., cerebrovascular events or acute encephalopathic conditions) would be reason to delay administration of Tdap until the condition has stabilized (1). Among adolescents who have progressive or uncontrolled underlying neurologic disease, concerns regarding administering Tdap must be weighed against the morbidity from pertussis, which could be severe (2). ACIP does not consider a history of well-controlled seizures or a family history of seizures (febrile or afebrile) or other neurologic disorder to be a contraindication or precaution to vaccination with pertussis components (22).
# Tetanus Toxoid Component
ACIP considers Guillain-Barré syndrome within 6 weeks after receipt of a tetanus toxoid-containing vaccine to be a precaution (see Precautions and Reasons to Defer Td or Tdap) for administration of subsequent tetanus toxoid-containing vaccines (23). Although IOM concluded that evidence favored acceptance of a causal relation between tetanus toxoidcontaining vaccines and Guillain-Barré syndrome on the basis of a single well-documented case (365,379), subsequent analysis of data from both adult and pediatric populations failed to demonstrate an association (380). As of January 29, 2007, eight patients with Guillain-Barré syndrome temporally associated with receipt of Tdap or of Tdap administered on the same day with other vaccines had been reported to VAERS. The onsets were not clustered by the interval since vaccination or by a single pattern of vaccine exposure (361).
ACIP does not consider a history of brachial neuritis to be a precaution or contraindication for administration of tetanus toxoid-containing vaccines (23,381). IOM concluded that evidence from case reports and uncontrolled studies involving tetanus toxoid-containing vaccines did favor a causal relation between tetanus toxoid-containing vaccines and brachial neuritis (365); however, brachial neuritis typically is self-limited (23,381). Brachial neuritis is a compensable event through the Vaccine Injury Compensation Program (VICP) (365).
# MMWR May 30, 2008
# Economic Considerations
No study has evaluated the disease morbidity and societal costs associated with pertussis among pregnant women or modeled the cost benefit or cost effectiveness of a Tdap strategy that includes vaccination of pregnant women. The morbidity and societal cost of pertussis in adults is substantial (1,2). A retrospective assessment of medical costs of confirmed pertussis in 936 adults in Massachusetts during 1998-2000, and a prospective assessment of nonmedical costs in 203 adults during 2001-2003 (31) indicated that the mean medical and nonmedical cost per case was $326 and $447, respectively, for a societal cost of $773. If the cost of antimicrobials to treat contacts and the cost of personal time were included, the societal cost could be as high as $1,952 per adult case (31).
Cost-benefit and cost-effectiveness analyses of adult Tdap vaccination have varied in their results (382,383). When discrepancies in the models were addressed, an adult Tdap vaccination program was cost-effective when incidence of pertussis exceeded 120 cases per 100,000 population, using a benchmark of $50,000 per quality-adjusted life year saved (384)(385)(386). After adjusting for the severity of the illness at high disease incidence, little effect was observed on the overall cost effectiveness of a vaccination program. Similar results were obtained when program costs and benefits were analyzed over the lifetime of the adult cohort for decennial booster strategies (1,387).
# Implementing Tdap Preconception Assessments
Administering a dose of Tdap during routine wellness visits of adult and adolescent women of childbearing age, if indicated, is the most effective programmatic strategy to ensure that women are protected against pertussis in addition to tetanus and diphtheria and minimizes any theoretical effect of vaccination on infant immune responses should the woman become pregnant (see Immunity to Pertussis and Kinetics of Pertussis Booster Vaccination in Nonpregnant Adults and Adolescents) (1,(388)(389)(390)(391)(392). Because Tdap contains only toxoids and purified bacterial components, women who receive Tdap do not need to wait after vaccination to become pregnant (23). Assessments provide repeated opportunities for documenting the history of past doses of Td (or TT) and any serious adverse reactions to tetanus, diphtheria, and pertussis vaccines. To access and maintain immunization records, statebased immunization information systems (IIS) are increasingly becoming available to clinicians and public health officials. These confidential, computerized information systems, which consolidate vaccination data from multiple health-care providers, can generate reminder and recall notifications, assist with vaccine management and adverse events reporting, and capture lifespan vaccination histories (393). Additional guidance regarding administration of vaccines during routine assessments, record keeping, vaccine storage, and related topics has been published previously (23).
# Prenatal Visits: Deferring Td During Pregnancy to Substitute Tdap in the Immediate Postpartum Period
In 2004, a total of 96% of pregnant women started prenatal care in the first or second trimester (394). Prenatal visits provide additional opportunities for assessing the history of past vaccination with Tdap, Td, or TT and any serious adverse reactions to tetanus, diphtheria, and pertussis vaccines. Women who have not received a previous dose of Tdap can be advised that ACIP recommends Tdap postpartum before discharge from the hospital or birthing center to provide personal protection and reduce the risk for transmitting pertussis to their infants.
Health-care providers can monitor pregnant women for respiratory illness consistent with pertussis or for recent exposure to pertussis, either to themselves or to family members, and prescribe a macrolide antimicrobial for treatment of pertussis or postexposure prophylaxis, if indicated. Women and their partners should receive counseling regarding the severity of infant pertussis and ACIP's recommendation for a single dose of Tdap for adults and adolescents who anticipate contact with an infant (1,2). In a 2005 national survey of obstetricians, 72% of respondents affirmed the belief that obstetricians, pediatricians, adult primary care providers, and public health providers share responsibility to promote administration of Tdap for adults who anticipate contact with an infant, including fathers and close relatives (395). Ideally, health-care providers delivering prenatal care will encourage persons likely to have contact with an infant, including child care providers, to receive Tdap first.
When pregnant women who have not received Tdap have indications for tetanus or diphtheria booster protection (>10 years since the most recent Td), ACIP recommends receipt of Td during pregnancy (Table 2). ACIP has developed criteria for safely deferring administration of Td until delivery among women who have received past tetanus toxoidcontaining vaccinations, so the majority of these women can substitute Tdap in the immediate postpartum period for Td during pregnancy (see Deferring Td During Pregnancy to Substitute Tdap in the Immediate Postpartum Period). When the history of tetanus toxoid vaccination for the women is uncertain or lacking, health-care providers can determine the con-centration of tetanus antitoxin to ensure protective concentrations of tetanus antitoxin (>0.1 IU/mL by ELISA). Because diphtheria is rare in the United States, serologic screening for diphtheria antitoxin typically is not necessary. A woman who anticipates travel to an area in which diphtheria is endemic can improve protection against diphtheria by receiving a booster dose of Td during pregnancy or a dose of Tdap postpartum. Serologic screening to establish immunity to pertussis is not useful.
In special situations in which a pregnant woman has increased risk for tetanus, diphtheria, or pertussis, ACIP acknowledges that health-care providers may choose to administer Tdap instead of Td during pregnancy to add protection against pertussis, after discussing the theoretical benefits and risks for her, her fetus, and the pregnancy outcome with the woman before vaccination (see Considerations for Use of Tdap in Pregnant Women in Special Situations). Data to inform this decision are scarce. No theoretical risk for harm to the mother or fetus exists from Tdap, and administration of Tdap in the pregnant woman might provide a degree of early protection to the infant against pertussis. However, a theoretical risk for the infant is that the dose of Tdap in pregnancy might not result in early protection against pertussis or could increase transplacental pertussis-specific antibodies to levels that would have a negative effect on the infant's response to immunization with pediatric DTaP or with conjugate vaccines containing tetanus toxoid or diphtheria toxoid (e.g., Haemophilus influenzae type b pneumococcal conjugate vaccine) (222). Health-care providers who choose to vaccinate pregnant women with Tdap are encouraged to report such administration to the manufacturers' pregnancy registry.
# Postpartum Tdap
In 2004, a reported 99% of live births in the United States occurred in a hospital. Of out-of-hospital live births, 27% occurred at a free-standing birthing center and 65% at a residence (394). In these settings, attendants can implement protocols to ensure that postpartum women who have not received Tdap previously receive it before discharge. They also can encourage previously unvaccinated adults and adolescents who anticipate contact with an infant to receive Tdap. Tdap vaccination of the women and potential contacts before discharge rather than at a follow-up visit has the advantage of decreasing the time when new mothers and contacts of the newborns could acquire and transmit pertussis to the infants (1,2). Standing orders for postpartum Tdap vaccination before discharge have successfully raised vaccination rates to more than 80% of eligible women (396). Although obtaining a history of the most recent Td vaccination was anticipated to be a barrier to postpartum vaccination with Tdap, in practice it was not identified as a barrier (395,396).
Vaccination of parents and household contacts of premature infants has been advocated to ensure that such persons receive Tdap (397). Premature and low birth weight infants are at increased risk for severe and complicated pertussis. The case-fatality rate for pertussis is increased compared with term infants, and premature infants might respond less well than term infants to initial doses of DTaP vaccine because of comorbidities or treatments (e.g., dexamethasone) (47,53,(398)(399)(400)(401)(402)(403).
Parents should be reminded of other measures to protect infants from pertussis. To the extent feasible, parents can limit infant exposures to persons who have respiratory illness until they are determined to be noninfectious (99,219,321). When pertussis exposure occurs, antimicrobial prophylaxis of exposed contacts can be effective in preventing transmission of pertussis (42,99,404,405). Ensuring that infants begin the pediatric DTaP vaccination series at the recommended chronologic age of 6-8 weeks is critical to protection and reducing the severity of pertussis (8,45,397,406). Administration of 2 or 3 doses of pediatric DTP or DTaP can prevent hospitalization for pertussis and its complications (5,8,(407)(408)(409).
# Recommendations
Recommendations for routine use of Td and Tdap among women of childbearing age who might become pregnant have been published previously (1,2) and have been summarized (Table 2). Women are encouraged to receive a single dose of Tdap either as ADACEL ® (adults and adolescents aged 11-64 years) or as BOOSTRIX ® (adolescents aged 11-18 years) before conception (e.g., during routine wellness visits) if they have not already received Tdap. Recommendations for adults and adolescents who anticipate or have household contact with an infant aged <12 months also have been published previously (1,2) and summarized (Table 2). The dose of Tdap will provide active booster immunization against tetanus, diphtheria, and pertussis and will replace the next dose of Td according to routine recommendations. A single preconception dose of Tdap will prevent pertussis, reduce morbidity associated with pertussis, and might prevent exposing persons at increased risk for pertussis and its complications, including infants. The risk for pertussis death and severe pertussis is highest among infants in the first months of life and remains elevated until an infant has received 1-2 doses of pediatric DTaP (8,45,47).
The following sections present recommendations for use of Td and Tdap among pregnant and postpartum women, including routine vaccination, contraindications, precautions, and special situations. As with most inactivated vaccines and toxoids, pregnancy is not a contraindication for use of Tdap. Although the safety and immunogenicity of Tdap is expected to be similar in pregnant and nonpregnant women, few data on the safety of Tdap for women, fetuses, and pregnancy outcomes are available, and no information is available on the immunogenicity of Tdap in pregnant women. Vaccinating pregnant women with a single dose of Tdap might provide a degree of protection against pertussis to the infant in early life through transplacental maternal antibody, but evidence supporting this hypothesis is lacking. A concern is the unknown effect of potential interference by maternal antibody on the ability of the infant to mount an adequate immune response when the infant receives pediatric DTaP or conjugate vaccines containing tetanus toxoid or diphtheria toxoid.
In special situations, administration of Tdap during pregnancy might be warranted for pregnant women who were not vaccinated previously with Tdap. Health-care providers who choose to administer Tdap to pregnant women should discuss with the women the potential risks and benefits of immunization including the lack of data on Tdap administered during pregnancy or its unknown effects on active immunization of their infant. The following recommendations are intended to provide guidance to clinicians until additional information is available.
# Routine Tdap Vaccination
# 1-A. Recommendations for Use of Postpartum Tdap
For women who have not received Tdap previously (including women who are breastfeeding), Tdap is recommended as soon as feasible in the immediate postpartum period to protect the women from pertussis and reduce the risk for exposing their infants to pertussis. The postpartum Tdap should be administered before discharge from the hospital or birthing center. If Tdap cannot be administered at or before discharge, the dose should be administered as soon as feasible thereafter. Elevated levels of pertussis antibodies in the mother are likely within 1-2 weeks after vaccination.
Although an interval of 10 years since receipt of the most recent Td dose is recommended for the next routine Td booster, to reduce the risk for women exposing their infants to pertussis, an interval as short as 2 years between the most recent Td and administering Tdap ¶ is suggested for postpartum women.
The safety of such an interval is supported by three Canadian studies among adolescents and by a study among nonpregnant adult health-care personnel (215,(358)(359)(360), an interval shorter than 2 years may be used (see Postpartum Tdap When <2 Years Have Elapsed Since the Most Recent Td). In this setting, the benefit of Tdap to protect against pertussis typically outweighs the risk for local and systemic reactions after vaccination. Routine postpartum Tdap recommendations are supported by evidence from randomized controlled clinical trials, nonrandomized open-label trials and a retrospective survey, observational studies, and expert opinion (Box 2).
# 1-B. Dosage and Administration
The dose of Tdap or, if indicated, the dose of Td is 0.5 mL, administered intramuscularly (IM), preferably into the deltoid muscle.
# 1-C. Simultaneous Vaccination with Tdap and Other Vaccines
If two or more vaccines are indicated, they typically should be administered during the same visit (i.e., simultaneous vaccination). Each vaccine should be administered using a separate syringe at a different anatomic site. Certain experts recommend administering no more than two injections per muscle, separated by at least one inch. Administering all indicated vaccines during a single visit increases the likelihood that pregnant and postpartum women will receive recommended vaccinations (23).
# 1-D. Interchangeable Use of Tdap Vaccines
A single dose of ADACEL ® may be used for adults aged 19-64 years, and a single dose of either ADACEL ® or BOOSTRIX ® may be used for adolescents aged 11-18 years, regardless of the type or manufacturer of pediatric DTP or pediatric DTaP used for childhood vaccination.
# 1-E. Preventing Adverse Events
Attention to proper immunization technique, including use of an appropriate needle length and standard routes of administration (i.e., IM for Td and Tdap) might minimize the risk for adverse events. Guidance for administration of vaccines is available (23).
Syncope can occur after vaccination and might be more common among young adults and adolescents than among other age groups. Syncope rarely has resulted in serious injury (23,(410)(411)(412). Vaccine providers should strongly consider observing patients for 15 minutes after they are vaccinated (23,412). If syncope occurs, patients should be observed until symptoms resolve. ¶ An interval of 5 years since the most recent tetanus and diphtheria toxoidscontaining vaccine is encouraged for routine vaccination of adolescents who are not pregnant (2).
# 1-F. Inadvertent Administration of Pediatric DTaP, BOOSTRIX ® Tdap, or Purified Protein Derivative (PPD)
The potential for administration errors involving tetanus toxoid-containing vaccines (413) and other vaccines is welldocumented (414)(415)(416). Pediatric DTaP and pediatric diphtheria toxoid and tetanus toxoid vaccine (DT) formulations indicated for use in children aged 6 weeks-6 years should not be administered to adults or adolescents; these vaccines can be associated with more severe local reactions than adult formulations (350,417). Packaging of adult and adolescent Tdap vaccines, pediatric DTaP, and purified protein derivative (PPD) might appear similar. Only one formulation of Tdap, ADACEL, ® is licensed and recommended for adults aged 19-64 years. Both formulations of Tdap (BOOSTRIX ® and ADACEL ® ) are licensed and recommended for adolescents aged 11-18 years. Providers should review product labels before administering these vaccines. If pediatric DTaP is administered inadvertently to an adult or adolescent, or if BOOSTRIX ® is administered inadvertently to an adult aged >19 years, the dose should be counted as the Tdap dose, and the person should not receive an additional dose of Tdap. Adults or adolescents who receive PPD instead of Tdap should receive a dose of Tdap.
# 1-G. Record Keeping
Health-care providers who administer vaccines to adults and adolescents are required to keep permanent vaccination records of vaccines covered under the National Childhood Vaccine Injury Compensation Act. ACIP has recommended that this practice include all vaccines (23). Encouraging adults and adolescents to maintain a personal vaccination record is important to minimize administration of unnecessary vaccinations. Ideally, the personal vaccine record will document the type of the vaccine, manufacturer, anatomic site, route, and date of administration, and the name of the administering facility (23).
# Contraindications and Precautions for Use of Td and Tdap
# 2-A. Contraindications
The following conditions are contraindications for Td or Tdap:
- Td and Tdap are contraindicated for persons with a history of serious allergic reaction (i.e., anaphylaxis) to any component of the vaccine. Because of the importance of tetanus vaccination, persons with a history of anaphylaxis to components included in any Td or Tdap vaccines should be referred to an allergist to determine whether they have a specific allergy to tetanus toxoid and whether they can safely receive TT vaccination. - Tdap (but not Td) is contraindicated for adults and adolescents with a history of encephalopathy (e.g., coma or prolonged seizures) not attributable to an identifiable cause within 7 days of administration of a vaccine with pertussis components. This contraindication is for the pertussis components, and these persons should receive Td instead of Tdap.
# 2-B. Precautions and Reasons to Defer Td or Tdap
A precaution is a condition in a vaccine recipient that might increase the risk for a serious adverse reaction (23)
# 2-C. Conditions Under Which Td or Tdap May Be Administered If Otherwise Indicated
The following conditions are not contraindications or precautions for Td or Tdap:
- stable neurologic disorder, including well-controlled seizures, a history of a seizure disorder that has resolved, or cerebral palsy; - brachial neuritis after a previous dose of tetanus toxoidor diphtheria toxoid-containing vaccine; - a history of an extensive limb swelling reaction that was not an Arthus hypersensitivity reaction after pediatric DTP or DTaP or after Td; - immunosuppression, including persons with human immunodeficiency virus (HIV) (the immunogenicity of Tdap in persons with immunosuppression has not been studied and could be suboptimal); - breastfeeding; - intercurrent minor illness; and - use of antimicrobials. Latex allergies other than anaphylactic allergies (e.g., a history of contact allergy to latex gloves) are not a contraindication or precaution to Tdap (417). The tip and rubber plunger of the BOOSTRIX ® needleless syringe contain latex. The BOOSTRIX ® single dose vial and ADACEL ® preparations contain no latex. Certain Td products contain latex. The package inserts should be consulted for details (Table 1).
# Special Situations
# 3-A. Deferring Td during Pregnancy to Substitute Tdap in the Immediate Postpartum Period
Tetanus and diphtheria booster vaccination is recommended for pregnant women if >10 years have elapsed since the previous Td vaccination (1,2). To add protection against pertussis, health-care providers may defer the Td vaccination during pregnancy to substitute Tdap as soon as feasible postpartum if the woman is likely to have sufficient tetanus and diphtheria protection until delivery.
Sufficient tetanus protection is likely if:
- a pregnant woman aged 1 Td booster dose during adolescence or as an adult (a primary series consisting of 3 doses of Td (or TT) administered during adolescence or as an adult substitutes for the childhood series of immunization), - a pregnant woman aged >31 years has received a complete childhood series of immunization (4-5 doses of pediatric DTP, DTaP, and/or DT) and >2 Td booster doses, - a primary series consisting of 3 doses of Td (or TT) was administered during adolescence or as an adult substitute for the childhood series of immunization, or - a pregnant woman has a protective level of serum tetanus antitoxin (>0.1 IU/mL by ELISA). A woman should receive Td during pregnancy if she - does not have sufficient tetanus immunity to protect against maternal and neonatal tetanus, or - requires urgent booster protection against diphtheria (e.g., for travel to an area in which diphtheria is endemic † † ). Alternatively, health-care providers may choose to administer Tdap instead of Td during pregnancy (see Considerations for Use of Tdap in Pregnant Women in Special Situations).
# 3-B. Postpartum Tdap When <2 Years Have Elapsed Since the Most Recent Td
Certain postpartum women (e.g., those who have received Td or TT within 2 years of the immediate postpartum period) might benefit from Tdap for pertussis protection. Few subjects have been evaluated to determine the risk for adverse local and systemic reactions after Tdap at intervals <2 years Women who have had a 3-dose series as TT instead of Td will likely have protection against tetanus but might not be protected against diphtheria.
A protective titer of diphtheria antitoxin is >0.1 IU/mL by ELISA. † † A list of areas in which diphtheria is endemic is available at www.cdc.gov/ travel/diseases/dtp.htm.
since the most recent Td (or other tetanus toxoid-or diphtheria toxoid-containing vaccine) (215). After obtaining a history to exclude women with moderate or severe adverse reactions following previous doses, health-care providers may choose to administer Tdap in postpartum women who received tetanus toxoid-or diphtheria toxoid-containing vaccine § § <2 years previously (see Precautions and Reasons to Defer Td and Tdap). Health-care providers should encourage vaccination of household and child care provider contacts of infants aged <12 months for protection against pertussis, according to current recommendations (Table 2) (1,2). Women should be advised of the symptoms of pertussis and the effectiveness of early antimicrobial prophylaxis for themselves, their infant, and members of their household, if pertussis is suspected (127).
# 3-C. History of Pertussis
Postpartum women who have a history of pertussis should receive Tdap according to the routine recommendation (see Recommendations for Use of Postpartum Tdap). This practice is preferred because the duration of protection induced by pertussis is unknown (waning might begin as early as 5-10 years after infection) (4), and a diagnosis of pertussis often is not reliably confirmed. Administering pertussis vaccine to persons with a history of pertussis presents no theoretical safety concern.
# 3-D. Considerations for Use of Tdap in Pregnant Women in Special Situations
ACIP recommends administration of Td for booster protection against tetanus and diphtheria in pregnant women. However, health-care providers may choose to administer Tdap instead of Td during pregnancy to add protection against pertussis in special situations. In these situations, the pregnant woman should be informed of the lack of data confirming the safety and immunogenicity of Tdap in pregnant women, the unknown potential for early protection of the infant against pertussis by transplacental maternal antibodies, and the possible adverse effect of maternal antibodies on the ability of the infant to mount an adequate immune response to antigens in pediatric DTaP or conjugate vaccines containing tetanus toxoid or diphtheria toxoid.
Special situations in which Tdap might be used might include instances when - a pregnant woman has insufficient tetanus or diphtheria protection until delivery, or - a pregnant woman is at increased risk for pertussis. Persons at increased risk for pertussis might include adolescents aged 11-18 years, health-care personnel, and women employed in institutions in which a pertussis outbreak is occurring or living in a community in which a pertussis outbreak is occurring.
Adverse pregnancy outcomes are most common in the first trimester (418). To minimize the perception of an association of vaccine with an adverse outcome, vaccinating with tetanus toxoid-containing vaccines during the second or third trimester is preferred.
Because information on the use of Tdap in pregnant women is lacking, both manufacturers of Tdap have established a pregnancy registry. Health-care providers are encouraged to report vaccination of pregnant women with Tdap, regardless of trimester, to the appropriate manufacturer's registry. For ADACEL, ® vaccination should be reported to sanofi pasteur, telephone 1-800-822-2463 (1-800-VACCINE), and for BOOSTRIX, ® vaccination should be reported to GlaxoSmithKline Biologicals, telephone 1-888-825-5249.
# 3-E. Tetanus Prophylaxis for Wound Management
ACIP has recommended administering tetanus toxoidcontaining vaccine and tetanus immune globulin (TIG) as part of standard wound management to prevent tetanus (Table 11) (357). A Td booster might be recommended for wound management in pregnant women if 5 years or more have elapsed since the previous Td (1,2). Health-care providers may choose to substitute Tdap for Td during pregnancy in these women (see Considerations for Use of Tdap in Pregnant Women in Special Situations). For pregnant women vaccinated previously with Tdap, Td should be used if a tetanus toxoid-containing vaccine is indicated for wound care. Pregnant women who have completed the 3-dose primary tetanus vaccination series and have received a tetanus toxoid-containing vaccine within the preceding 5 years are protected against tetanus and do not require a tetanus toxoid-containing vaccine as part of wound management.
To avoid unnecessary vaccination, health-care providers should attempt to determine whether the woman has completed the 3-dose primary tetanus vaccination series. Pregnant women with unknown or uncertain previous tetanus vaccination histories should be considered to have had no prior tetanus toxoid-containing vaccine and they should complete a 3-dose primary series of immunization to prevent maternal and neonatal tetanus (see Pregnant Women with Unknown § § Tetanus toxoid-and/or diphtheria toxoid-containing vaccines include pediatric DTP, DTaP, DT, other pediatric combination vaccines including any of these components (e.g., pediatric DTaP-inactivated poliovirus vaccine-Hep B and pediatric DTaP-Haemophilus influenzae type b), and adult and adolescent Td, Tdap, and TT). MCV4 contains diphtheria toxoid but not tetanus toxoid (2).
# MMWR May 30, 2008
-r Incomplete Tetanus Vaccination). Pregnant women who have not completed the primary series might require tetanus toxoid and passive vaccination with TIG at the time of wound management (Table 11). When both TIG and a tetanus toxoid-containing vaccine are indicated, each product should be administered using a separate syringe at different anatomic sites. Pregnant women with a history of Arthus reaction after a previous dose of a tetanus toxoid-containing vaccine should not receive a tetanus toxoid-containing vaccine until 10 years or more after the most recent dose, even if they have a wound that is neither clean nor minor. If the Arthus reaction was associated with a vaccine that contained diphtheria toxoid without tetanus toxoid (e.g., MCV4), deferring Td or Tdap might leave the pregnant women inadequately protected against tetanus, and TT should be administered (see Precautions and Reasons to Defer Td or Tdap). In all circumstances, the decision to administer TIG is based on the primary vaccination history for tetanus (Table 11).
# 3-F. Pregnant Women with Unknown or Incomplete Tetanus Vaccination
Pregnant women who never have been vaccinated against tetanus (i.e., have received no dose of pediatric DTP, DTaP, or DT or of adult Td or TT) should receive a series of three vaccinations containing tetanus and diphtheria toxoids starting during pregnancy to ensure protection against maternal and neonatal tetanus. A primary series consists of a first dose administered as soon as feasible, a second dose at least 4 weeks later, and a third dose 6 calendar months after the second dose. If feasible, pregnant women who have received fewer than 3 doses of tetanus toxoid-containing vaccine should complete the 3-dose primary series during pregnancy. Td is preferred for the doses during pregnancy. Health-care providers may choose to substitute a single dose of Tdap for 1 dose of Td during pregnancy and complete the series with Td. In such cases, the women should be informed of the lack of data on safety, immunogenicity, and pregnancy outcomes for pregnant women who receive Tdap (see Considerations for Use of Tdap in Pregnant Women in Special Situations).
# Reporting Adverse Events after Vaccination
As with any newly licensed vaccine, surveillance for rare adverse events associated with administration of Tdap is important for assessing its safety in large-scale use. The National Childhood Vaccine Injury Act of 1986 requires health-care providers to report specific adverse events that follow tetanus, diphtheria, or pertussis vaccination. A table of reportable events following vaccination is available from VAERS at . All clinically significant adverse events should be reported to VAERS even if causal relation to vaccination is not certain. VAERS reporting forms and information are available electronically at or by telephone, 1-800-822-7967. To promote better timeliness and quality of safety data, providers are encouraged to report electronically by using web-based reporting ().
# Vaccine Injury Compensation Program
VICP is a system established by the National Childhood Vaccine Injury Act of 1986 that enables compensation to be paid on behalf of a person thought to have been injured or died as a result of receiving a vaccine covered by the program. Anyone receiving a covered vaccine, regardless of age, can file - For example, wounds contaminated with dirt, feces, soil, and saliva; puncture wounds; avulsions; and wounds resulting from missiles, crushing, burns, and frostbite. † Adult tetanus and diphtheria toxoids vaccine (Td) is preferred to tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine (Tdap) for pregnant women who have never received Tdap. Tdap is preferred to Td for nonpregnant adults and adolescents who have never received Tdap. In special situations, use of Tdap during pregnancy might be warranted. Health-care providers who choose to administer Tdap during pregnancy should discuss with the women the lack of evidence of safety and effectiveness for the mother, fetus, pregnancy outcome, and the lack of evidence of the effectiveness of transplacental maternal antibodies to provide early pertussis protection to the infant. In addition, no study has examined the effectiveness of transplacental pertussis antibodies induced by Tdap on the adequacy of the infant immune response to pediatric DTaP and conjugate vaccines containing tetanus toxoid or diphtheria toxoid. Because adverse outcomes of pregnancy are most common in the first trimester, vaccinating pregnant women with Tdap during the second or third trimester is preferred to minimize the perception of an association of Tdap with an adverse outcome, unless vaccine is needed urgently. Td is preferred to tetanus toxoid vaccine (TT) for adults who received Tdap previously or who require tetanus protection when Tdap is not available. If TT and tetanus immune globulin (TIG) are both used, tetanus toxoid adsorbed rather than tetanus toxoid (fluid vaccine) should be administered.
a petition under VICP. The program is intended as an alternative to civil litigation under the traditional tort system because negligence need not be proven.
The Act establishes 1) a vaccine injury table that lists the vaccines covered by the program; 2) the injuries, disabilities, and conditions (including death) for which compensation might be paid without proof of causation; and 3) the period after vaccination during which the first symptom or substantial aggravation of the injury must appear. Persons might be compensated for an injury listed in the table or one that can be demonstrated to result from administration of a listed vaccine. All tetanus toxoid-containing vaccines and vaccines with pertussis components (e.g., Tdap, Td, and pediatric DTaP) are covered under the Act. Additional information regarding the program is available at compensation or by telephone, 1-800-338-2382.
# Areas for Future Research
Interest in vaccinating pregnant women to prevent infant pertussis declined in the late 1940s when whole-cell vaccine trials demonstrated pertussis-specific antibodies in as many as 75% of infants vaccinated starting at birth or in the first few months of life (38,186,188,218,237) and infant and childhood vaccination was adopted as the primary national strategy for protection against childhood diseases (419,420). Aside from initiatives to eliminate neonatal tetanus and more recently to prevent influenza during pregnancy, limited attention has been focused on vaccinating pregnant women as a strategy to prevent disease in the women and their infants during the first few months of life (290,(421)(422)(423)(424)(425)(426)(427)(428)(429)(430). A major barrier to conducting vaccine trials in pregnant women is the potential liability from expected adverse pregnancy outcomes that might be related temporally to vaccination (388,431,432). However, the high morbidity and mortality of certain infections that affect pregnant women and neonates warrant renewed consideration of the strategy of vaccinating pregnant women.
Ensuring the safety of vaccination for mother and fetus and for pregnancy outcomes is a public health priority. In addition, important considerations include understanding whether a degree of protection might be achieved for the mother and for her newborn by vaccinating during pregnancy, whether maternal vaccination would be required with each pregnancy to achieve these benefits (if any), and whether change in the levels of transplacental maternal antibody might affect infant responses to routine vaccination (159,222,224,228). Because few vaccines are currently recommended for pregnant women (e.g., Td and influenza), the effects of the transplacental maternal antibodies on the subsequent infant responses to rou-tine vaccination with the same antigens are not known for most vaccines. Change in the levels of transplacental antibody can affect infant susceptibility to disease at a population level. For example, a decrease over time in the level of transplacental maternal antibody from women who were immunized with measles vaccine during childhood (rather than by measles disease) resulted in susceptibility to measles among their infants at an earlier age, and to the decision to recommend infant measles vaccination at age 12 months rather than age 15-18 months in the United States (228,433,434).
Major gaps exist in the knowledge of how best to prevent pertussis in early infancy. These include 1) the safety of pertussis vaccines for pregnant women, their fetuses, and pregnancy outcomes; 2) the immunogenicity of acellular pertussis vaccines in pregnant women and transplacental maternal antibodies with respect to the timing of immunization during pregnancy; 3) the degree and duration of protection against pertussis in early infancy through transplacental maternal antibodies; and 4) the effects of transplacental maternal antibodies (induced by pertussis, DTP, DTaP, and/or Tdap) on the infant responses to active immunization with pediatric DTaP and conjugate vaccines containing tetanus toxoid or diphtheria toxoid (159,222,234,235,435). To understand the range of options for protecting women and infants from pertussis, studies are needed to determine the safety and any benefits of accelerated infant pertussis vaccination schedules or dosing (e.g., pertussis vaccination starting at birth or employing acellular vaccines that do not contain diphtheria toxoid and tetanus toxoid) (221,436,437). Alternative infant vaccination strategies examined independently or in conjunction with vaccinating pregnant women will determine the most effective and practical approaches to reduce the morbidity and mortality of pertussis.
Alternatively, health-care providers may choose to administer Tdap instead of Td during pregnancy (see Considerations for Use of Tdap in Pregnant Women in Special Situations).
# Postpartum Tdap When <2 Years Have Elapsed Since the Most Recent Dose of Td
Health-care providers should obtain a history of adverse reaction after previous doses of vaccines containing tetanus and diphtheria toxoids. Limited information is available concerning the risk for local and systemic reactions after Tdap at intervals of <2 years. Providers may choose to administer Tdap to these women postpartum for protection against pertussis after excluding a history of moderate to severe adverse reactions following previous tetanus and diphtheria-toxoidscontaining vaccines.
Health-care providers should encourage vaccination of household and child care provider contacts of infants aged <12 months. Women should be advised of the symptoms of pertussis and the effectiveness of early antimicrobial prophylaxis, if pertussis is suspected.
# Considerations for Use of Tdap in Pregnant Women in Special Situations
ACIP recommends that Td be administered when booster protection is indicated during pregnancy. Health-care providers may choose to administer Tdap instead of Td during pregnancy to add protection against pertussis in situations when Td cannot be delayed until delivery or when the risk for pertussis is increased. In such cases, the women should be informed of the lack of data on safety, immunogenicity, and pregnancy outcomes for pregnant women who receive Tdap. Whether administration of Tdap to pregnant women results in protection of the infant against pertussis through transplacental maternal antibodies is unknown. Maternal antibodies might interfere with the infant's immune response to infant doses of DTaP or conjugate vaccines containing tetanus toxoid or diphtheria toxoid.
If Tdap is administered, the second or third trimester is preferred unless protection is needed urgently. Providers are encouraged to report Tdap administrations regardless of trimester to the appropriate manufacturers' pregnancy registry: for ADACEL, ® to sanofi pasteur, telephone 1-800-822-2463 (1-800-VACCINE) and for BOOSTRIX, ® to GlaxoSmithKline Biologicals, telephone 1-888-825-5249.
# Tetanus Prophylaxis for Wound Management
ACIP recommends administration of a Td booster for wound management in pregnant women in certain situations if >5 years have elapsed since the previous Td. Health-care providers may choose to administer Tdap instead of Td during pregnancy to add protection against pertussis in these situations. In such cases, the women should be informed of the lack of data on safety, immunogenicity, and pregnancy outcomes for pregnant women who receive Tdap (see Considerations for Use of Tdap in Pregnant Women in Special Situations).
# Pregnant Women with Unknown or Incomplete Vaccination
Pregnant women who have not received 3 doses of a vaccine containing tetanus and diphtheria toxoids should complete a series of three vaccinations, including 2 doses of Td during pregnancy, to ensure protection against maternal and neonatal tetanus. The preferred schedule in pregnant women is 2 doses of Td separated by 4 weeks and 1 dose of Tdap administered 6 months after the second dose (postpartum). Health-care providers may choose to substitute a single dose of Tdap for a dose of Td during pregnancy. In such cases, the women should be informed of the lack of data on safety, immunogenicity, and pregnancy outcomes for pregnant women who receive Tdap (see Considerations for Use of Tdap in Pregnant Women in Special Situations).
# Reporting Adverse Events after Vaccination
All clinically significant adverse events should be reported to VAERS even if a causal relation to vaccination is uncertain. VAERS reporting forms and information are available at or by telephone, 1-800-822-7967. Providers are encouraged to report adverse events electronically at . | depar depar depar depar department of health and human ser tment of health and human ser tment of health and human ser tment of health and human ser tment of health and human services vices vices vices vices# Introduction
Pertussis is an acute and prolonged infectious cough illness caused by Bordetella pertussis, a fastidious gram-negative coccobacillus. Pertussis results in substantial morbidity among adults and adolescents whose immunity to past childhood vaccination or B. pertussis infection might have waned and who have not received booster immunization for pertussis with adult tetanus, reduced diphtheria, and acellular pertussis (Tdap) vaccine (1,2). In 2004, women aged 15-39 years accounted for 97% of all live births in the United States (3). During 2000-2006, a total of 103,940 cases of pertussis were reported to CDC's National Notifiable Diseases Surveillance System (NNDSS); 27,759 (27%) of these cases occurred among persons aged 15-39 years (CDC, unpublished data, 2007). Parents with pertussis, including new mothers, are the identified source of B. pertussis infection in >25% of pertussis cases in early infancy, when rates for complications and fatalities are highest (4)(5)(6)(7)(8). Infants aged <12 months accounted for 145 (93%) of 156 pertussis-related deaths reported to CDC for (CDC, unpublished data, 2007. Decennial booster vaccination with adult tetanus toxoid and reduced diphtheria toxoid (Td) vaccine has been largely responsible for reducing the average annual number of tetanus and respiratory diphtheria cases reported during 2000-2006 to 31 and less than one, respectively. In contrast, the average annual number of pertussis cases was 14,849 during the same period (9-15;CDC, unpublished data, 2007).
In 2005, two Tdap vaccines were licensed in the United States: ADACEL ® (sanofi pasteur, Swiftwater, Pennsylvania) for use in persons aged 11-64 years (16) and BOOSTRIX ® (GlaxoSmithKline Biologicals, Rixensart, Belgium) for persons aged 10-18 years (17) (Table 1). Both vaccines are licensed for single-dose administration. Acellular pertussis vaccines formulated with tetanus and diphtheria toxoids also are available for adults and adolescents in other countries, including an increasing number of European countries (e.g., France, Austria, and Germany), Canada, and Australia (18)(19)(20). No vaccine containing acellular pertussis antigens without tetanus and diphtheria toxoids is available in the United States.
Vaccinating adults and adolescents using Tdap reduces the burden of pertussis among vaccine recipients and might prevent transmission of B. pertussis to infants (1,2). Statements and recommendations by CDC's Advisory Committee for Immunization Practices (ACIP) regarding use of Tdap by adults, including health-care personnel, and adolescents (Table 2) provide background information on pertussis and extensive discussion regarding the safety and immunogenicity of Tdap in prelicensure trials. These recommendations encourage adult and adolescent women of childbearing age to receive Tdap at a routine health assessment before conception to prevent the morbidity of pertussis that could occur during pregnancy and encourage use of Tdap among adults and adolescents who anticipate contact with an infant aged <12 months both for personal protection and to reduce the risk for transmitting B. pertussis to the infants (1,2).
In 2006, ACIP recommended routine administration of Tdap for postpartum women who were not vaccinated previously with Tdap to provide personal protection and reduce the risk for transmitting pertussis to their infants (1,2) . After careful consideration, in June 2006, ACIP voted to reaffirm its recommendation for use of Td in pregnant women who have urgent indication for tetanus toxoid or diphtheria toxoid vaccination to prevent maternal or neonatal tetanus, or to prevent diphtheria. Pregnant women not vaccinated previously with Tdap will receive a measure of protection against pertus-sis by ensuring that children in the household are up-to-date with recommended doses of pediatric diphtheria and tetanus toxoids and acellular pertussis vaccine (DTaP)* (21)(22)(23) and that adult and adolescent household contacts have received a dose of Tdap (Table 2) (1,2). Health-care providers can monitor pregnant women who have not received a dose of Tdap for exposures to pertussis or to respiratory illness consistent with pertussis, and they can administer antimicrobials for postexposure prophylaxis or treatment of pertussis, if needed, to reduce the risk for transmitting pertussis to their infants.
This report provides the background and rationale for routine administration of Tdap in postpartum women who were not vaccinated previously with Tdap and for maintaining the previous recommendation for use of Td in pregnant women if indicated. The safety and efficacy of using Tdap in pregnant women has not been demonstrated, and Tdap is not recommended for use in pregnant women in any country. No evidence exists of excess morbidity or any fatality among pregnant women ascribed to pertussis. No evidence exists demonstrating whether
• Tdap in pregnant women harms the fetus or increases risk for adverse pregnancy outcomes, • transplacental antibody induced by Tdap administered during pregnancy will protect infants against pertussis, or • Tdap-induced transplacental maternal antibody will have a negative impact on an infant's protective immune response to later-administered routine pediatric DTaP or to conjugate vaccines containing tetanus toxoid or diphtheria toxoid. This report discusses certain situations in which health-care providers might choose to administer Tdap to a pregnant woman. Health-care providers should weigh the theoretical risks and benefits before choosing to administer Tdap vaccine to a pregnant woman.
# Methods
During June 2006, ACIP evaluated the limited evidence available concerning safety, immunogenicity, and pregnancy outcomes after administration of Tdap; evidence from historic use of pertussis, tetanus, and diphtheria vaccines in pregnant women; and the potential effects of transplacental maternal antibody on the infant's immune response to active immunization with pediatric diphtheria and tetanus toxoids and whole-cell pertussis (DTP) or DTaP vaccines, or to con-jugate vaccines containing tetanus toxoid or diphtheria toxoid. The evaluation included a synthesis of information from scientific literature published in English, unpublished sources of information, consultations, analyses, and extensive discussion by an ACIP working group † during [2005][2006]. The working group comprised persons with expertise in pertussis, tetanus, and diphtheria; obstetrics and gynecology; pediatrics, family practice, internal medicine, immunology, public health, and vaccine regulation; and liaison members from partner organizations.
The workgroup considered multiple diverse views on the adequacy of evidence needed to form a recommendation for use of Tdap in pregnant and postpartum women. A minority view held that available data from nonpregnant women and men, and experience with the use of Td in pregnant women to prevent neonatal and maternal tetanus, were sufficient to support a recommendation for the safe use of Tdap in pregnant women for individual protection from pertussis. The majority view, while acknowledging the desirability of preventing pertussis in pregnant women and the substantial body of information demonstrating the usefulness of Td to prevent maternal and neonatal tetanus, held that the evidence was insufficient at this time to support a recommendation for routine administration of Tdap in pregnant women. The specific issues for pertussis differ from those for tetanus and diphtheria. Important among these is the limited understanding of immunity and correlates of protection for pertussis. In addition, data supporting the safety of vaccinating pregnant women with Tdap to prevent pertussis are scarce for women, their fetuses, and pregnancy outcomes. Whether transplacental maternal antibody exerts an inhibitory or other effect on the infant-protective immune response to active immunization with pediatric DTaP or conjugate vaccines containing tetanus toxoid or diphtheria toxoid has not been studied. Protection against infant pertussis through Tdap-induced transplacental maternal antibody has not been demonstrated. Until additional information is available, the majority view of the working group held that Tdap administered to women in the immediate postpartum period, in addition to ensuring pertussis vaccination of close contacts, would likely provide a measure of protection for mother and infant. • Td recommended during pregnancy, † † or • Tdap-postpartum before leaving hospital or birthing center instead of Td during pregnancy, if sufficient tetanus and diphtheria protection is likely until delivery Tdap, ideally administered at least 2 wks before contact with the infant; interval as short as 2 yrs suggested ¶ Tdap-postpartum before leaving hospital or birthing center; interval as short as 2 yrs ¶ ** † † ; pregnant women should be advised of symptoms of pertussis and the benefits of treatment and early prophylaxis for household contacts exposed to pertussis Td for urgent protection during pregnancy † † ; Tdap postpartum before leaving hospital or birthing center Td when indicated for pregnant women † † § § 1 dose Td during pregnancy followed by dose 2 Td >4 wks later † † and dose 3 as Tdap 6-12 mos later (postpartum) * ACIP recommends routine vaccination with tetanus and diphtheria toxoids every 10 years to boost tetanus and diphtheria protection. In 2006, ACIP recommended that adults and adolescents who have not been vaccinated previously with tetanus and reduced diphtheria toxoids and acellular pertussis (Tdap), including persons with a history of pertussis, receive a dose of Tdap to boost pertussis protection in addition to tetanus and diphtheria protection. Tdap is licensed for single-dose administration. In persons who have received Tdap, tetanus and reduced diphtheria toxoids (Td) vaccine should be administered when subsequent decennial booster vaccination is indicated for tetanus or diphtheria protection. † For adults and adolescents, tetanus and diphtheria toxoids-containing vaccines include tetanus toxoid (TT), Tdap, and Td; for infants and children, tetanus toxoid and diphtheria toxoids-containing vaccines include pediatric diphtheria and tetanus toxoids and whole-cell pertussis (DTP), pediatric diphtheria and tetanus toxoids and acellular pertussis (DTaP), pediatric diphtheria and tetanus toxoids and acellular pertussis, inactivated poliovirus and hepatitis B (DTaP-IPV-Hep B), and pediatric diphtheria and tetanus toxoids (DT). § During 2000-2006, U.S. adolescents aged 10-19 years had the highest incidence of reported pertussis outside of infancy (CDC, unpublished data, 2008). For this reason, a catch-up dose of Tdap is recommended for adolescents aged 11-18 years to add protection against pertussis if they have received Td but not Tdap. For catch-up Tdap, an interval of at least 5 years from the most recent tetanus and/or diphtheria toxoids-containing vaccine is encouraged to reduce the risk for local and systemic reactions that could result when concentration of tetanus and/or diphtheria antitoxin is high. An interval less than 5 years after Td may be used, particularly when the benefit of providing pertussis protection is likely to be increased. Adolescents who have received a childhood series of pediatric DTP or DTaP and Td or Tdap are protected against tetanus and diphtheria. ¶ A shorter interval may be used. ** Limited evidence informs the risk of local and systemic reactions after Tdap at intervals of <2 years. Higher rates of local and systemic reactions and more severe reactions can occur with high preexisting serum titers of tetanus or diphtheria antitoxin. Providers may choose to administer Tdap in postpartum women who received a tetanus toxoid-and/or diphtheria toxoid-containing vaccine (e.g., Td or TT) less than 2 years previously if the women have no history of serious adverse reaction after the most recent dose of tetanus and/or diphtheria toxoid-containing vaccine. † † In special situations, a dose of Tdap might be warranted during pregnancy. Health-care providers who choose to administer Tdap to pregnant women should discuss with the women the lack of evidence of safety and effectiveness for the mother, fetus, pregnancy outcome, and effectiveness of transplacental maternal antibodies to provide early pertussis protection to the infant. These women should be informed that no study has examined the effectiveness of transplacental pertussis antibodies induced by Tdap on the adequacy of the infant immune response to pediatric DTaP and conjugate vaccines containing tetanus toxoid or diphtheria toxoid. Because adverse outcomes of pregnancy are most common in the first trimester, vaccinating these pregnant women with Tdap during the second or third trimester is preferred to minimize the perception of an association of Tdap with an adverse outcome, unless vaccine is needed urgently. § § A Td booster might be recommended for wound management if >5 years have elapsed since the previous Td. Persons who have completed the 3-dose primary tetanus vaccination series and have received a tetanus toxoid-containing vaccine within the preceding 5 years are protected against tetanus and do not require a tetanus toxoidcontaining vaccine as part of wound management. Pertussis is transmitted from person to person via large respiratory droplets generated by coughing or sneezing; early reports suggested that B. pertussis can be recovered from dried mucus for up to 3 days (28,30). Pertussis is highly infectious, with attack rates among exposed, nonimmune household contacts as high as 80%-90% (29,37,38). The most infectious periods are the catarrhal and early paroxysmal phases (28). Untreated patients, particularly infants, remain infectious for 6 weeks or longer (29). Among older children and adults with previous vaccination or infection, the infectious period typically is <21 days (29).
Routine
In a Canadian study conducted in 1999, a source was identified in 60%-70% of adults and adolescents with pertussis. Among adults aged 18-39 years, the source was a person in the household in 25%-44% of cases or at work or school in 17%-25% of cases. Among adolescents aged 12-17 years, the source was a person in the household in 9% of cases and a friend or person at school or work in 51% of cases (39).
# Pertussis During Pregnancy
Case reports suggest that the morbidity of pertussis is not increased among pregnant women compared with nonpregnant women. In a general medical practice during 1979-1980, four pregnant women had onset of cough during the 12th, 14th, 14th, and 36th week of gestation and cough that lasted 36, 6, 8, and 6 weeks, respectively; two women had vomiting after coughing and worsening cough paroxysms at night; and one woman developed hemoptysis and subconjunctival hemorrhage after repeated and forceful coughing paroxysms (40). A 1993 case report described a pregnant woman who was hospitalized 6 days before delivery for severe paroxysms and posttussive emesis (41). In a series of 32 women who had pertussis during pregnancy or at term, the illness was characterized as "a very tiresome disease"; no obstetric complication was reported, and no infant was premature (42). No pertussis-related deaths have been reported in pregnant women. The source of pertussis in infected pregnant women has not been examined systematically.
Reports of fetal morbidity among pregnant women with pertussis are rare, and no causal relationship with abnormal fetal development, fetal morbidity, or adverse outcome of pregnancy has been confirmed. One fetus of a mother who had severe paroxysmal coughing early in pregnancy had an extradural hematoma that was identified by ultrasonography and magnetic resonance at 31 weeks' gestation; studies had been normal at 12 and 22 weeks' gestation (43). Another fetus of a mother who had pertussis during the first trimester had prenatal diagnosis of laryngotracheal obstruction (44).
# Infantile Pertussis
Infants aged <12 months typically have the most severe pertussis, often requiring hospitalization for respiratory or other complications (Table 3) (8,(45)(46)(47)(48)(49). The risk for pertussis death or severe pertussis is highest among infants in the first 6 months of life and remains elevated until infants have received 1-2 doses of pediatric DTaP (8,50,51). During 2000-2006, the average annual incidence of pertussis among infants aged <6 months was 111 cases per 100,000 population; for infants aged 6-11 months, incidence was 19 cases per 100,000 population (CDC, unpublished data, 2007).
Complications and deaths from infant pertussis have been characterized by necrotizing bronchiolitis (52) and high rates of primary or secondary pneumonia and/or coinfection with bacterial and viral pathogens (8,28,47,53). Since 1993, pulmonary hypertension has been increasingly recognized among fatal infant cases (47,52,(54)(55)(56)(57)(58). The majority of all infant deaths have occurred among unvaccinated infants (47,53,58;CDC, unpublished data, 2007). Hispanic infants and infants born at estimated gestational age <37 weeks or with low birth weight have comprised a larger proportion of pertussis deaths than would have been expected on the basis of population estimates (47,53,58). Compared with the prevaccine era, during 2000-2006, the proportion of reported pertussis deaths among infants aged <3 months increased from 37% to 83% (Figure 1) (38,47;CDC, unpublished data, 2007).
Since the 1970s, parents, especially mothers, have been identified as the most important source of infant pertussis; however, a source has been identified in only 30%-60% of cases investigated (5)(6)(7)34,38,42,48,(59)(60)(61)(62)(63)(64)(65)(66)(67)(68). One or more household contact with pertussis is the source of pertussis in approximately 75% of cases among infants aged <6 months for whom the source is identified. A parent is implicated in approximately 25% of cases in infants, including the mother in 16%-19% of cases. A sibling is implicated as the source of transmission in <10% of cases (5,7,34).
Mathematical modeling evaluating different vaccine strategies for the United States has suggested that pertussis vaccination of 90% of household contacts (children, adolescents, and adults) of newborns, in addition to pertussis vaccination of 75% of adolescents generally in the population, might prevent approximately 75% of pertussis cases among infants aged 0-23 months (69). Another model estimated vaccination of both parents of an infant before discharge from the hospital could prevent 38% of infant cases and deaths (70). However, the efficacy of these strategies in practice has not been evaluated.
# Disease Burden
Although pertussis is a nationally notifiable disease in the United States (71), data on the pregnancy status of women with pertussis have not been collected. However, the burden of pertussis among pregnant women is likely to be similar to the burden among other adults in the population. Pertussis reports typically demonstrate increases in activity every 3-4 years (72); aside from these cycles of activity, the number of reported cases of pertussis in the United States has increased gradually since 1976. During 2004-2005, more than 25,000 cases were reported per year (Figure 2 (CDC unpublished data, 2007). Prospective and serologic studies suggest that pertussis infection and reinfection are underrecognized among adults and adolescents (29,(73)(74)(75). The pertussis burden is believed to be substantially more than the number of reported cases; approximately 600,000 cases are estimated to occur annually just among adults (1,34,76).
# Transmission in Obstetric and Neonatal Health-Care Settings
Health-care personnel can transmit B. pertussis in health-care settings if pertussis has not been considered by hospital staff (1,77,78). Outbreaks have been documented in prenatal and postnatal clinics (79,80), maternity wards (51,62,(81)(82)(83), neonatal nurseries, and neonatal intensive-care services (62,81,(84)(85)(86)(87)(88)(89)(90). Ongoing transmission is facilitated by delay in isolation and treatment of patients and in prophylaxis of contacts and by inconsistent use of face or nose and mouth protection (1,85,87,91). Unprotected exposures to pertussis in health-care settings can result in labor-intensive, disruptive, and costly investigations and control measures, particularly when the number of contacts is substantial (80,92). Pertussis transmitted to health-care personnel or patients can result in substantial morbidity (and on rare occasions in fatal disease) among hospitalized infants (79,80,(85)(86)(87)(88)93,94).
Health-care personnel who have not been vaccinated with Tdap (Table 2) can be an important source of pertussis and pertussis outbreaks in obstetric and neonatal settings. A wide range of health-care disciplines have been implicated, including physicians, resident physicians, and students (80,82,85,95); nurses and nurse midwives (51,81,85,87,(96)(97)(98); and aides, medical assistants, and educators (1,51,78,79,81,82,85,87). Pregnant and postpartum women with unrecognized pertussis and visitors to prenatal, obstetric, and neonatal units, including fathers and other close relatives, pose a substantial 1938-1940 1990-1999 2000-2006 Age (mos)
Percentage risk for transmission to infants, pregnant women, and healthcare personnel and have been associated with outbreaks in these settings (6,41,62,80,81,(84)(85)(86)93,98). Early recognition and treatment of pertussis in pregnant and postpartum women and prophylaxis of household contacts who visit health-care settings is critical to prevent continuing transmission. Antimicrobial treatment for women who have pertussis near term or at delivery and prophylaxis for their newborns and household contacts are effective in preventing further transmission (42,99).
# Diagnosis
The diagnosis of pertussis is complicated by the limitations of currently available diagnostic tests. The only pertussis diagnostic tests that are accepted to confirm a case for purposes of national reporting are culture and polymerase chain reaction (PCR) (when the clinical case definition also is met) (100; Box 1). Multiple factors affect the sensitivity, specificity, and interpretation of diagnostic tests for pertussis (101,102).
# Culture
Culture to isolate B. pertussis is essential for identifying the organism early in the course of disease (103) and for antimicrobial susceptibility testing, if indicated. Isolation of B. pertussis by culture is 100% specific; for optimal yield, culture requires specimens that contain nasopharyngeal cells obtained by aspirate or nasopharyngeal swab and special medium for growth. The sensitivity of culture early in pertussis varies (range: 30%-60%) (103)(104)(105). Outside of infancy, the yield of B. pertussis declines to 1%-3% in specimens taken in the third week of cough illness or later, after starting antimicrobial treatment, or in a patient who was vaccinated previously (106,107). B. pertussis can be isolated in culture as early as 72 hours after plating but requires 1-2 weeks before a result can definitively be called negative (108).
# Polymerase Chain Reaction
DNA amplification (e.g., PCR) to detect B. pertussis has increased sensitivity and more rapid turnaround time (109)(110)(111). When symptoms of classic pertussis are present (e.g., >2 weeks of paroxysmal cough), PCR can be two to three times more likely than culture to detect B. pertussis in a known positive sample (101,103,112,113). As with culture, the PCR result is affected by the technique used to collect the specimen; a poorly taken nasopharyngeal swab is more likely to be negative by both culture and PCR. PCR is less affected than culture by antimicrobial therapy because the organism does not need to be viable for the test to be positive. Adults and adolescents who have specimens taken later in the course of illness, who have started antibiotic treatment, or who were vaccinated previously tend to have PCR-positive, culture-negative test results (103,114).
Although PCR testing for pertussis has been available for nearly 20 years (115), no U.S. Food and Drug Administration (FDA)-licensed PCR test kit is available. The analytical sensitivity, accuracy, and quality control of PCR-based B. pertussis tests vary widely among laboratories. PCR assays used by the majority of laboratories amplify a single gene sequence, typically within the insertion sequence IS481. Both false-positive and false-negative results have been reported with these assays; reported outbreaks of respiratory illness mistakenly attributed to pertussis have resulted in unnecessary investigation and treatment, and unnecessary chemoprophylaxis of contacts (112,(116)(117)(118)(119). Using more than one genetic target and consensus interpretation criteria for PCR diagnosis of pertussis (120,121) has been suggested as a way to provide increased assurance of specificity (122) and to allow discrimination between Bordetella species.
# Other Diagnostic Tests
Direct fluorescent antibody (DFA) tests provide rapid results (within hours), but sensitivity (10%-50%) is less than with culture (123). With use of monoclonal reagents, the specificity of DFA should be >90%. However, interpretation of the test is subjective, and, when interpreted by an inexperienced microbiologist, the specificity can be lower (110). Diagnosis of pertussis by serology requires a substantial change in titer for pertussis antigens (typically fourfold) from acute (<2 weeks after cough onset) to convalescent sera (>4 weeks after the acute sample). The results typically become available too late in the course of the illness to be useful clinically. Singlesample serologic tests for antipertussis toxin (anti-PT) IgG have been developed for research purposes; sera must be col-lected at least 2 weeks after the onset of symptoms (124). Pertussis serology assays using commercial reagents are available, but these assays are not validated clinically and do not differentiate between recent and remote infection and vaccination (125,126). No serologic assay is licensed by FDA for routine diagnostic use in the United States.
# Postexposure Prophylaxis and Treatment
A macrolide (erythromycin, azithromycin, or clarithromycin) is the preferred antimicrobial for postexposure prophylaxis and treatment of pertussis (127). Antimicrobial treatment administered in the early (catarrhal) phase of the illness can modify the severity of the symptoms (36,128,129). An antimicrobial generally does not modify the severity or the course of the illness after paroxysmal cough is established but is used to eliminate B. pertussis and halt transmission (36,(127)(128)(129). Without use of an effective antimicrobial, B. pertussis can be recovered for 6 weeks or longer from infant patients and for 21 days or longer from adult and adolescent patients. Detailed recommendations, indications, and schedules for postexposure antimicrobial prophylaxis and treatment of pertussis have been published previously (127).
Pregnant women with pertussis near term and other household contacts with pertussis are an important source of pertussis for newborn infants (6,41,42,62,64,99). Antimicrobial treatment and prophylaxis are effective in preventing transmission of pertussis to neonates. A macrolide is administered to a woman with pertussis that is acquired late in pregnancy or shortly before delivery, her household contacts, and the neonate. Early recognition of pertussis in a pregnant woman is necessary to ensure the effectiveness of this approach (42,99).
Pregnancy is not a contraindication for use of erythromycin, azithromycin, or clarithromycin. Erythromycin and azithromycin are listed as FDA Category B drugs, and clarithromycin is listed as a Category C drug (130)(131)(132). Macrolides can interact with a variety of other therapeutic agents, precluding concurrent use. Although macrolides can have gastrointestional side effects (e.g., nausea and vomiting), serious side effects (e.g., hepatic dysfunction or pseudomembranous colitis) are rare (127). Infants aged <1 month who receive erythromycin are at increased risk for infantile hypertrophic pyloric stenosis (83,(133)(134)(135)(136). For this reason, and because azithromycin is associated with fewer adverse effects than erythromycin, azithromycin is the preferred antimicrobial for prophylaxis of neonates exposed to pertussis (127). Infantile hypertrophic pyloric stenosis has been reported in two preterm infants who received azithromycin for postexposure prophylaxis (137) between infantile hypertrophic pyloric stenosis and azithromycin has not been established.
# Immunity to Pertussis
The mechanisms of protection against pertussis are incompletely understood. On the basis of studies in animals and humans, both humoral and cellular immunity are believed to play a complementary role (138)(139)(140)(141)(142)(143). The protection that results from B. pertussis infection or pertussis vaccines persists for an estimated 5-10 years or more. Protection wanes over time, leaving persons susceptible to infection or reinfection (4,75,(144)(145)(146)(147)(148)(149)(150).
# Humoral Immunity to Pertussis Vaccine Antigens
Immune responses to B. pertussis can be directed variably against a range of pertussis toxins and antigens. No level of antibody, presence of specific antibodies, or antibody profile has been accepted universally as a quantifiable serologic measure of protection (139,141,(151)(152)(153)(154)(155)(156)(157)(158). Studies of parenterally administered immune globulins for postexposure prophylaxis (159,160) or for treatment of pertussis (28,(161)(162)(163)(164)(165) report mixed results and do not clarify the role of passive antibodies in prevention or treatment of pertussis. By extrapolation, these results do not help predict the role of transplacental maternal antibodies in infant protection.
Pertussis toxin (PT), previously called lymphocytosis promoting factor (LPF), is considered one of the most important of a range of clinically relevant toxins and virulence factors of B. pertussis (including pertactin or 69-kDa protein [PRN], fimbriae types 2 and 3 [FIM], filamentous hemagglutinin [FHA]) (140,142,152,157,(166)(167)(168)(169). Detoxified PT is a component of all pertussis vaccines. The preventive efficacy of a pediatric DTaP vaccine containing detoxified PT as the only immunizing antigen was 71% (95% confidence interval [CI] = 63%-78%) against classical pertussis (170). However, the contribution to protection by anti-PT varied in analyses of the humoral immune responses to specific vaccine antigens when evaluated in two household studies. Elevated concentrations of anti-PRN and anti-FIM were associated most closely with protection in these (152,157) and other studies (171). Evidence of added protection from anti-FHA has been mixed (152,156,157,172,173).
# Cellular Immunity to Pertussis Vaccine Antigens
Cell-mediated immune mechanisms clear B. pertussis from within macrophages and other cells (52,139,(174)(175)(176)(177). In addition to humoral immune responses, B. pertussis antigens in acellular pertussis vaccines induce cell-mediated immune responses (178) after primary immunization with pediatric DTaP among infants (158,179), after booster vaccination among children (140,141,149), and after booster vaccination with reduced pertussis antigen content vaccines among adolescents (178,(180)(181)(182)(183) and adults (183,184). Protection is maintained among children whose antibody levels drop below the level of detection over time (185) suggesting that cell-mediated immunity is an important component of protection. Cell-mediated immune responses remain measurable substantially longer than antibodies to the same antigens, particularly PT, and the cell-mediated immune responses to initial doses of pertussis vaccines are believed to correlate better with long-term immunity than antibody responses (140,141,149,158,178,180,181,183,185).
# Prevalence of Pertussis-Specific Antibodies: Pregnant Women and their Infants
Although the importance of antipertussis activity in sera relative to protection remains uncertain, studies conducted since the 1930s have determined the prevalence of antipertussis activity in sera from mothers and infants using multiple assays (Tables 4-8) (37,154,(186)(187)(188)(189)(190)(191)(192)(193)(194)(195)(196)(197)(198)(199). Detectable pertussisspecific antibodies have been identified in unvaccinated women without a history of pertussis (28,187,190,192), women with a past history of pertussis (28,187,190,192), women who likely received whole-cell pertussis vaccine during childhood (195,196,(198)(199)(200), and women with a recent history of pertussis (99). With the exception of women with recent pertussis, the majority of pregnant women have low geometric mean concentrations (GMCs) of anti-PT and antibodies to other pertussis antigens (Tables 4-8) (159), consistent with generally low concentrations of antipertussis antibodies among adults surveyed in the general population (147,(201)(202)(203)(204)(205). GMCs of pertussis-specific antibodies among pregnant women typically have been low regardless of age, as demonstrated in a predominantly (80%) African-American population reported in 2005 (199). A 2006 study of pregnant Hispanics found lower GMCs among adolescents than among women aged >20 years (198).
The efficiency of maternal-fetal transfer of IgG antibodies to pertussis-specific antigens varies; the majority of investigators report similar antigen-specific concentrations in cord or neonatal infant sera and in maternal sera measured late in pregnancy or at delivery (195)(196)(197)(198)(199)(200), but higher concentrations in cord or neonatal sera than in maternal sera have been reported, which might indicate active transport in certain settings (Tables 7 and 8) (195,197,199). In a 2005 survey of mothers and their infants, anti-PT, anti-FHA, and anti-PRN were detected in maternal sera from 35%, 95%, and 80% of women, respectively, and in cord sera from 45%, 93%, and May 30, 2008 ¶ Infants were all of "premature" birth, and their specimens were obtained at age 2-9 wks. ** Infant cells were obtained at age 6-29 days (median age of immunized and nonimmunized infant groups was 10 and 11 days, respectively). The opsonic titer was calculated as the product of an arbitrary factor: 0, 1, 3, 8, and 12, respectively, for 0, 0-5, 6-20, 21-40, and >41 organisms per cell. The sum of the products defined the "opsonic titer" as "negative to weak"(0-50), "weak to moderate" (51-100), "moderate to strong" , and "strong" . 81% of infants, respectively (199). Among 17 infants studied in 1990, the half-life of transplacental maternal antibody was 36.3 days for anti-PT, 40.3 days for anti-FHA, and 55.0 days for pertussis agglutinins (195). Transplacental maternal antibody was not detectable or was negligible in the majority of infants by age 6-8 weeks (195,197) or by age 4 months (195), consistent with the results of early studies (186). By contrast, in a study of 23 unvaccinated Swedish infants whose mothers had pertussis late in pregnancy, five infants had neutralizing antibody detectable as long as 14 months and detectable anti-PT for 5 months or longer (99).
# Kinetics of Pertussis Booster Vaccination in Nonpregnant Adults and Adolescents
The majority of adults and adolescents have had exposure to B. pertussis, pertussis antigen-containing vaccines, or both, and they will have a booster response to vaccination with pertussis antigens (184,206). A rise in antibodies is measurable by 7 days after vaccination (207), and GMCs reach near-peak levels by 2 weeks after booster vaccination (207)(208)(209)(210). Antibody concentrations decline rapidly in the first few months following vaccination, after which the rate of decline slows (157,181,209,211). Anti-PT levels decline more rapidly than anti-PRN or anti-FHA levels. Among adults who received a booster dose of an acellular pertussis vaccine without tetanus or diphtheria toxoids, concentrations of IgG anti-PT and anti-PRN declined 58% and 39%, respectively, after 6 months. By 18 months after vaccination, concentrations declined 73% and 56%, respectively (209).
# Vaccinating Pregnant Women against Pertussis Tdap
No prelicensure studies were conducted with Tdap in pregnant women. In 2005, to increase understanding of the safety of Tdap in relationship to pregnancy, both Tdap manufacturers established registries to solicit voluntary reports of pregnant women who received Tdap during pregnancy or who received Tdap and were determined subsequently to be pregnant (212,213). The main utility of the registries is to signal the possibility and nature of any risk (214). All women who are vaccinated with Tdap at any time during pregnancy should be reported to the registry as early as possible during the preg-nancy. Information from pregnancy registries differs from surveillance reports, which are used to evaluate outcomes among women when an adverse outcome of pregnancy already might have occurred (e.g., an infant born with a birth defect) (214).
As of December 31, 2007, GlaxoSmithKline had received five reports of pregnancy exposure to BOOSTRIX ® within 28 days before conception or during any trimester of pregnancy, including two in the first trimester, one in the second trimester, and two during an unknown trimester. Among the two first-trimester exposures, one subject delivered a normal infant at 33 weeks' gestation, and one subject was lost to followup. Of the remaining exposures, information on the outcome of two pregnancies was not yet available, and one subject was lost to follow-up (GlaxoSmithKline, unreported data, 2008).
As of November 23, 2007, sanofi pasteur had received 107 spontaneous reports and 47 reports from postlicensing surveillance studies of exposure to ADACEL ® during pregnancy. For these 154 reports, pregnancy outcomes were 68 live infants (including 64 term deliveries [one with a congenital (215,216). Pregnancy was not an exclusion criterion for Tdap; 24 health-care personnel who received Tdap identified themselves as pregnant at the time of vaccination. Among 2,676 (59%) survey respondents, 1,792 (67%) received Tdap at an interval of >2 years after their most recent dose of Td; 17 of these respondents identified themselves as pregnant. Adverse reactions reported by the 17 pregnant women were compared with reactions reported by 472 nonpregnant female personnel aged 18-44 years. The frequencies of injection-site pain, redness, and swelling of moderate to severe intensity were not greater among the pregnant women than among the nonpregnant women. Three of the pregnant women reported feeling "feverish" after receiving Tdap. None of the 17 pregnant women reported seeking nonroutine medical attention for the adverse reaction (215,216). Among the pregnant women vaccinated with Tdap, results of the outcome of pregnancy were known for 10 women; no pregnancy resulted in premature birth or abnormality in the infant when assessed shortly after birth (Elizabeth A. Talbot, Dartmouth College, Lebanon, New Hampshire, personal communication, 2007).
# Whole-Cell Pertussis Vaccine
Five clinical trials conducted during the 1930s and 1940s evaluated vaccinating pregnant women with whole-cell per-May 30, 2008 tussis vaccine as a strategy to increase the levels of maternal pertussis-specific antibodies transferred to their infants via the placenta (Table 9) (186,189,190,192,193,217). The protective efficacy of the vaccine against pertussis in the women was not a consideration. Whole-cell pertussis vaccine was prepared from sterile extracts of killed B. pertussis. To maximize the passive transfer of maternal antibody, pregnant women were vaccinated with 2-6 doses at 1-to 2-week intervals during the third trimester.
Local reactions to vaccination in the pregnant women were common, some of which were severe. Systemic reactions were uncommon, adverse pregnancy outcomes were not reported (Table 9) (190,192,193,217).
The majority of women had substantial rise in titer to B. pertussis antigens in postvaccination sera compared with prevaccine titers (Tables 4-6) (186,189,190,192,193,217). Neither history of pertussis (190,192) nor preexisting titers of antibodies in the women correlated with maternal titers after vaccination (193). The majority of infant antibody titers were lower than (186) or similar to maternal titers (37,150,186,187,(189)(190)(191)(192)(193). Infant titers exceeded maternal titers in certain cases although higher titers might have been within the range of assay variation (37,(186)(187)(188)(189)(190)(191)193).
In subsets of infants in two studies, the duration of detectable transplacental pertussis antibodies was followed among unvaccinated infants (186,217). The mothers in both studies had received 3 doses of whole-cell pertussis vaccine during the third trimester. The mean of the agglutinin titers among infants in one study dropped from 1:160 § at birth to 1:80 at age 2 months; titers no longer were measurable at "a few months of age" (186). Of 36 infants with high agglutinin titers at birth in the other study, 16 (44%) had titers of >1:300 at age 3 months. None of 9 infants followed to age 6 months had a titer of 1:300 (217).
# Infant Protection by Transplacental Maternal Antibody
The role of transplacental maternal antibody in infant protection against pertussis remains uncertain. Prevaccine era observations concluded that infants have no "congenital immunity" and are susceptible to pertussis from the "day of birth," with the possible exception of an infant whose mother had pertussis during pregnancy (35,189,190,192,193,219). Transplacental maternal antibodies might explain the smaller proportion of infant pertussis deaths observed in the first month of life compared with the second and third months of life (Figure 1) (35,45). An alternative explanation might be that parents avoid exposing newborn infants to ill contacts (99,219).
Two retrospective surveys were conducted after early vaccine trials in pregnant women to assess infant protection (217,220). In one survey conducted during the 1940s, a subset of 100 (59%) of 170 women who received 6 doses of wholecell pertussis vaccine during the third trimester and 100 women who were not vaccinated were questioned regarding pertussis in their infants during the first year of life. During the first 6 months of life, eight exposures (three of which were "close exposures") and no cases of pertussis were reported among infants whose mothers had been vaccinated, and six exposures and three cases of infant pertussis were reported among infants whose mothers had not been vaccinated. From age 6-11 months, two cases of infant pertussis were reported in each group (220). In a second survey by the same investigators, a subset of 66 (62%) of 106 women who received 3 doses of whole-cell pertussis vaccine during the third trimester reported two exposures and no case of pertussis among their infants during the first 6 months of life (217). The results of these surveys suggested that high concentration of transplacental pertussis antibodies might provide a degree of infant protection against pertussis in the first 6 months of life (217,220).
# Inhibitory Effect of Transplacental Maternal Antibody on Infant Immunization
Transplacental maternal antibodies to pertussis antigens can interfere with the infant's response to active immunization with the pertussis components of pediatric DTP and pediatric DTaP (221). A proposed mechanism for the interference with pertussis and other vaccine antigens is maternal antibody binding to vaccine antigens, masking the vaccine antigens from the infant's B cells. Infant antigen-presenting cells also might take up maternal antibody-vaccine antigen complexes stimulating selective T-cell responses without humoral immune responses to the vaccine antigens (221)(222)(223). The concentrations and specificities of the maternal antibodies for vaccine-antigen epitopes contributes to the degree of interference (221,(223)(224)(225). The inhibitory effect of transplacental maternal antibody can be detectable for a few weeks or for more than 1 year (221,222,(224)(225)(226)(227)(228). As transplacental maternal antibody declines over time, a threshold is reached when the infant's immune system responds to vaccine antigens in subsequent doses. In theory, the threshold concentration of residual maternal antibody could be lower than the concentration of antibody needed for infant protection, but this concentration is not known for pertussis. In this setting, a theoretical window of "relative susceptibility" exists for the infant until the infant mounts a humoral immune response to a subsequent dose of vaccine (222,229).
# Interference with Pertussis Responses to Pediatric DTP
Substantially lower concentrations of infant IgG anti-PT result after 3 doses of pediatric DTP among infants with "high" (variably defined) prevaccination levels of maternal IgG anti-PT, than among infants with "low" or no measurable prevaccination level of maternal IgG anti-PT (195,(230)(231)(232)(233). The post-dose 3 concentrations of infant anti-PT in one study were 28% or 56% lower with each doubling of the concentration of transplacental maternal anti-PT, respectively, for the two DTP products studied (p <0.05) (233). The reductions in post-dose 3 concentrations also were significant for anti-FIM (18% lower) and agglutinins (15% lower) for one DTP product, and for anti-FHA (16% lower) for the other DTP product, with each doubling of the concentration of the specific transplacental maternal antibodies (p <0.05) (233).
# Interference with Pertussis Responses to Pediatric DTaP
Transplacental maternal IgG anti-PT might interfere less with infant responses after 3 doses of pediatric DTaP than § Titers of >1:320 have been reported to correlate with protection in some studies (218).
after pediatric DTP (195,196,230,233). The percentage decrease in post-dose 3 infant antibody response with each doubling of the concentration of maternal antibodies was 3% for anti-PT (not statistically significant), but was 13% for anti-PRN, 17% for anti-FIM, 10% for agglutinins, and 8% for anti-FHA (all statistically significant; p <0.05) when results from several DTaP products were combined in one study (233). The difference between interference by maternal antibody with infant responses to DTP and DTaP might result from the higher content of pertussis-specific antigens in pediatric DTaP than in pediatric DTP relative to the concentration of transplacental maternal antibody (159,222). In addition, the maternal antibodies induced by the mothers' childhood DTP vaccinations might have less specificity for the pertussis vaccine antigens in acellular pertussis vaccines (222,(234)(235)(236).
# Noninterference with Pertussis Cellular Immune Responses to Pediatric DTP or DTaP
Infants who have relatively poor humoral immune responses to active immunization with whole-cell or acellular pertussis vaccine in the presence of inhibitory concentrations of transplacental maternal antibody have evidence of T-cell priming for booster (anamestic) responses (158,237). Protection against pertussis in T-cell primed infants in the absence of specific humoral antibodies has not been established (158,(238)(239)(240)(241).
# Lactation
Existing data do not provide evidence that human colostral pertussis antibodies contribute to infant protection, although pertussis-specific antibodies present in the mother are found in colostral milk (186,190,242). Protection studies in animal models suggest human and animal colostral-derived pertussis antibodies can protect animals when the antibodies are absorbed or injected parenterally (243)(244)(245); however, the relevance of these studies for human infants is uncertain (190,246,247). Human breast milk antibodies do not enter the human neonatal circulation from the intestine in substantial amounts. In contrast, infant pigs, horses, ruminants, dogs, and cats acquire the majority of neonatal protection through intestinal uptake of colostral antibodies (245,(248)(249)(250). Maternal antibodies in human milk do not interfere with the infant immune response to pediatric vaccines (23).
# Tetanus
Tetanus is caused by Clostridium tetani spores, which are ubiquitous in the environment. Spores enter the body through disrupted skin or mucus membranes. When inoculated into oxygen-poor sites (e.g., necrotic tissue or wounds), C. tetani spores germinate to vegetative bacilli that elaborate tetanospasmin, a potent neurotoxin. More than 80% of cases of tetanus are of the generalized syndrome; the remaining cases are localized or cephalic. Persons with generalized cases typically have trismus (lockjaw), followed by rigidity and painful contractions of the skeletal muscles that can impair respiratory function. Glottic spasm, respiratory failure, and autonomic instability can result in death. The onset of tetanus typically is within 7 days of the injury (range: 0-112 days) The course of tetanus is up to 4 weeks or longer, followed by a prolonged period of convalescence (251,252).
# Obstetric and Neonatal Tetanus
Obstetric tetanus is defined as tetanus during pregnancy or with onset within 6 weeks after the termination of pregnancy (253). Obstetric tetanus occurs after contamination of wounds or abrasions during pregnancy or after unclean deliveries or abortions. In a review covering 1941-1990, an estimated 65%-80% of cases of obstetric tetanus occurred in the puerperal or postpartum period; the majority of the other cases occurred after surgical or spontaneous abortions (254).
Obstetric tetanus has the highest mortality when the incubation period is short and respiratory complications are present (255). Cases can be complicated by gram-negative sepsis (256). Case-fatality rates vary (range: 16%->50%); higher fatality rates are reported from places where access to medical intensive care is limited (255,257,258). Case-fatality rates historically have been higher for postabortal than for postpartum obstetric tetanus (254).
Neonatal tetanus (tetanus neonatorum) is associated with contamination of the umbilical stump. In nearly all cases of infant tetanus, onset occurs in the first month of life. Symptoms commonly begin at 3-14 days of life and are characterized by increasing irritability and difficulty feeding. Signs of neonatal tetanus are similar to tetanus in older age groups. Case-fatality rates vary (range: 10%-100%) (252,259). Infants who survive can have residual neurologic injury (e.g., cerebral palsy and psychomotor retardation) (252).
# Burden
Tetanus is a nationally notifiable disease in the United States (260). In 2006, a total of 41 cases were reported. No cases occurred among women aged 15-19 years or those aged 30-39 years. One case occurred among women aged 20-29 years, and three cases occurred among women aged 40-49 years. None of the women died. During 1972-2006, case reporting forms did not collect information regarding pregnancy; however, no case of obstetric tetanus was identified among more than 1,000 reports to NNDSS (CDC, unpublished data, 2006). In 1999, tetanus-specific coding became available in CDC's mortality database; no case of tetanusassociated obstetric death was reported through 2005, the most recent year for which data are available (CDC, unpublished data, 2008).
During the 1950s, approximately 100 neonatal tetanus deaths were reported annually in the United States, and neonates comprised more than one third of tetanus deaths in all age groups (261,262). During 1972During -2006, the cumulative number of reported neonatal tetanus cases decreased to 32; the most recent cases were reported in 1989, 1995, 1998, and 2001 (263). Among these 32 neonatal cases, 27 (84%) births occurred in a nonhospital setting; 30 of 31 mothers with available history reported never having received a dose of tetanus toxoid vaccine (264-266;CDC, unpublished data, 2006).
# Diagnosis and Treatment
The diagnosis of tetanus is clinical and is supported by a compatible setting, immunization history, and exclusion of other possible diseases. Anaerobic cultures of tissues or aspirates for C. tetani typically are not positive. Low or undetectable levels of serum antitoxin at the time of onset are compatible with the diagnosis of tetanus, but higher levels of antitoxin do not exclude the diagnosis (252,267). Electromyography might aid in the diagnosis of certain cases (268). Postpartum eclampsia, which typically occurs within the first few days after delivery, was the most important disease in the differential diagnosis in community-based studies (254).
Treatment of tetanus is directed at neutralizing unbound toxin with administration of human tetanus immune globulin, removing the source of infection through debridement, and use of an antimicrobial (e.g., metronidazole). The control of rigidity and spasms, attendant respiratory and autonomic dysfunction and their complications, and maintaining nutrition require careful and sustained attention that is best provided in intensive-care settings with specialty consultation (251,252,269).
# Immunity to Tetanus
The level of antitoxin that protects against obstetric and neonatal tetanus can vary with the wound characteristics, the degree of contamination, the specificity of the antitoxin, and the type of assay employed to measure the antitoxin level (270). The minimum level of antitoxin correlating with protection is 0.01 IU/mL as measured by in vivo neutralization assay. An antitoxin concentration at >0.1 IU/mL is the preferred correlate of protection based on the results of other assays (e.g., enzyme-linked immunoabsorbant assay [ELISA]), and because higher concentrations of antitoxin might be necessary to protect in certain circumstances (252,270). The serum level of tetanus antitoxin achieved in response to vaccination is determined by the number of doses of tetanus toxoid, the type of tetanus toxoid administered (adjuvanted toxoid, which is more immunogenic, has replaced fluid toxoid), the interval since the most recent dose, and individual variation in the response to vaccination (270).
# Deferring Td During Pregnancy to Substitute Tdap in the Immediate Postpartum Period
Ensuring maternal and neonatal tetanus protection as part of prenatal care is a priority for women who are due for a recommended decennial tetanus and diphtheria toxoids booster dose. For women who have not received a dose of Tdap previously, administering Td during pregnancy, followed in a few months by Tdap postpartum, theoretically could increase the risk or severity of adverse reaction, which typically is local. Moderate to severe local reactions have been associated with high levels of tetanus and diphtheria antitoxin (see Interval Between Td and Tdap). In these women, deferring the Td booster during pregnancy to substitute Tdap in the immediate postpartum period may be considered to boost protection against pertussis as well as tetanus and diphtheria. The majority of women of childbearing age who have lived in the United States since infancy or childhood have received 4-5 infant and childhood doses of tetanus toxoid with pediatric DTP or DTaP and >1 booster dose of Td (or tetanus toxoid without diphtheria toxoid [TT]) in accordance with national recommendations (1,2,271). The recommended schedule of vaccination to prevent tetanus is intended to maintain levels of antitoxin considerably higher than the minimum level required for protection against the majority of cases of tetanus, including protection among persons with intrinsically lower responses to vaccination (1,2,252,(271)(272)(273).
In 2004, women aged 15-39 years accounted for 97% of all births in the United States (3). Data from a populationbased serosurvey conducted nationwide in the United States during 1988-1994 documented tetanus antitoxin concentrations at >0.15 IU/mL among >80% of women aged 12-39 years (274,275). The proportion of women with antitoxin at >0.15 IU/mL declined with increasing age to 62% among women aged 40-49 years (274,275). Slightly lower prevalence of this titer was found among women aged 20-59 years who were not born in the United States (276). A 1999-2000 study evaluated 2,134 adult patients in an emergency department for wound management and measurement of their antitoxin titer (277). Antitoxin concentrations of >0.15 IU/mL were present among 1,051 (95%) of 1,106 adults aged 18-39 years. Among adults of all ages studied, approximately 95% of those with up-to-date vaccination histories and approximately 86% of those whose vaccinations were not up-to-date had antitoxin titers >0.15 IU/mL. The rates of a protective titer were lower for immigrants, persons with less education, and persons aged >70 years (277). Limitations of these studies are that one study did not report any connection between vaccination histories and antitoxin concentrations (274)(275)(276), and the other study included subjects who might not be representative of the U.S. population (277). However, when combined with the small number of tetanus cases among women of childbearing age in the United States, these studies suggest that when pregnant women have previously received the recommended schedule of tetanus and diphtheria toxoids vaccinations, a routine decennial Td booster during pregnancy typically can be deferred so Tdap can be substituted at delivery or before discharge from the hospital or birthing center.
# Vaccinating to Prevent Obstetric and Neonatal Tetanus
Success in preventing obstetric and neonatal tetanus relies on antitoxin being present at delivery (254). In countries where access to childhood vaccines is limited, neonatal tetanus constitutes a major cause of infant mortality; during 1978-1985, an estimated 800,000 neonatal tetanus deaths occurred annually worldwide (278). In 1974, worldwide elimination of neonatal tetanus (less than one case per 1,000 live births) through vaccine initiatives became a major focus of the Expanded Program of Immunization of the World Health Organization (WHO) (259,279). The initiative promoted clean deliveries and tetanus toxoid vaccination for pregnant women. Nonpregnant women of childbearing age also were targeted for at least 3 doses of tetanus toxoid vaccine in supplemental immunization activities.
The strategy of targeting pregnant women for vaccination to prevent neonatal tetanus was based on reports published in the 1960s concerning two vaccine trials that demonstrated that >2 doses of tetanus toxoid administered during pregnancy were >95% effective in preventing neonatal tetanus (Table 10) (280,281). Subsequent studies confirmed that 3 doses of aluminum phosphate-adjuvanted tetanus toxoid (rather than fluid toxoid) administered during pregnancy induced antitoxin levels that would protect the mother and prevent neonatal tetanus for >10 years. Adjuvanted vaccine also lowered the rates of local reactions in pregnant women (282)(283)(284).
Although the burden of obstetric tetanus has not been characterized as well as the burden of neonatal tetanus, the annual worldwide burden of obstetric tetanus deaths has been esti-mated at 15,000-30,000, accounting for approximately 5% of all maternal deaths in the 1990s (254,259). In April 2006, WHO's Strategic Advisory Group of Experts (SAGE) reported on the success of the maternal and neonatal tetanus elimination initiatives and the plan to transition from vaccination goals for women of childbearing age to universal tetanus control, to be achieved through sustained high coverage with pediatric DTP starting in infancy and childhood and booster doses to prevent tetanus throughout life (259,285,286).
# Safety of Tetanus Vaccination During Pregnancy
No evidence suggests that adverse outcomes for a mother or fetus increase after tetanus toxoid is administered to a pregnant woman (1,2,23). Tetanus toxoid administered during any trimester of pregnancy was evaluated for association with congenital abnormalities at birth during 1980-1994 in Budapest, Hungary. The rate of tetanus toxoid vaccination among 21,563 mothers of infants with congenital abnormalities was not significantly different than the rate of tetanus toxoid vaccination among 35,727 mothers of infants who were normal (0.12% and 0.09%, respectively; p = 0.39) (287). In a similar study conducted in nine countries in South America starting in 1977, approximately one half of the women had received tetanus toxoid during the first trimester of pregnancy. The rate of early tetanus toxoid vaccination among the mothers of 34,293 newborns with congenital malformations (9.2 [CI = 8.2-10.3] per 1,000 mothers) was not substantially different than the rate among the mothers of 34,477 newborns who were normal (7.6 [CI = 6.6-8.5] per 1,000 mothers) (288).
# Infant Protection by Transplacental Maternal Antibody
Tetanus toxoid is one of the most immunogenic protein antigens in any vaccine. Administration of 2 doses of tetanus toxoid to pregnant women at least 4-6 weeks before delivery stimulates antitoxin that protects the mother and readily crosses the placenta, thereby protecting the newborn against tetanus when the risk is highest (289). Pregnant women who receive a booster dose of tetanus toxoid have a measurable immune response within 5 days and a peak response in <2 weeks. The response to vaccination might be slower after a first (primary) dose or when the interval after the most recent booster dose is long (252,272). Placental transport of maternal IgG antitoxin is efficient; cord blood levels generally are similar to maternal levels (290,291). After the neonatal period, the infant is at little risk for tetanus until becoming self-mobile, typically at an age when sustained protection has been induced by 3 infant doses of pediatric DTP or DTaP (252).
# Inhibitory Effect of Transplacental Maternal Antibody on Infant Immunization
Transplacental maternal tetanus antitoxin can interfere with the infant response to active immunization after up to 3 doses of tetanus toxoid (e.g., in pediatric DTP, DTaP, or DT) (222,230,(292)(293)(294)(295)(296)(297). Certain studies (296,297), but not all (298), indicate that antitoxin inhibits the response to tetanus toxoid after vaccination with Haemophilus influenzae type b polysaccharide conjugated to tetanus toxoid. An ageaccelerated schedule results in further decrease in infant responses in the presence of maternal antitoxin (295). When levels of transplacental maternal antitoxin wane sufficiently, infants respond to subsequent doses of vaccine (229,293,294,(299)(300)(301). T-cell priming for a booster response is not substantially affected by maternal antitoxin (222,302,303). Typically, infants respond to the second dose of tetanus toxoid-containing vaccine with a protective level of antitoxin, even when the initial levels of maternal antitoxin are high; 3 doses of tetanus toxoid are required to achieve antitoxin concentrations that persist above protective levels (292,304).
# Lactation
No substantial difference in the infant immune response to tetanus toxoid (in DTP) has been identified with consumption of human milk compared with consumption of cow milk (305).
# Diphtheria
Respiratory diphtheria is an acute, severe infection caused by strains of Corynebacterium diphtheriae that produce diphtheria toxin. Rarely, toxin-producing strains of C. ulcerans cause a diphtheria-like illness (306). Respiratory diphtheria is characterized by a grayish-colored adherent membrane on the pharynx, palate, or nasal mucosa that can obstruct the airway with fatal outcome. The disease can be complicated by toxinmediated cardiac, neurologic, or renal dysfunction. Casefatality rates are >10% (307,308).
# Obstetric and Neonatal Diphtheria
Respiratory diphtheria (309)(310)(311)(312) or vulvovaginal infection (313,314) can occur during any trimester of pregnancy, at term, or in the postpartum period. The mortality rate of obstetric respiratory diphtheria is high (estimated at 50%) without infusion of diphtheria antitoxin, even with tracheostomy or intubation, and is accompanied by fetal loss or premature birth in approximately one third of survivors. Early treatment with serum diphtheria antitoxin improves survival and pregnancy outcomes, although complications of the disease might require prolonged supportive care (309)(310)(311)(312). Postpartum women with respiratory diphtheria can transmit C. diphtheriae to their neonates (310).
# Burden
Respiratory diphtheria is a nationally notifiable disease in the United States. Rare cases occur in the United States after infection with diphtheria toxin-producing strains of C. diphtheriae or other corynebacteria (315,316). During 1998-2006, seven cases of respiratory diphtheria were reported to CDC. The most recent culture-confirmed adult case of respiratory diphtheria caused by C. diphtheriae was reported in 2000, and an adult case of respiratory diphtheria caused by C. ulcerans was reported in 2005 (306). The risk for diphtheria can be increased during travel to areas in which diphtheria is endemic; a list of these areas is available at http://www.cdc. gov/travel/default.aspx. Diphtheria also can be acquired from persons with imported cases or from carriers (i.e., asymptomatic persons who are colonized with toxin-producing C. diphtheriae) (315,316).
# MMWR May 30, 2008
# Diagnosis and Treatment
The diagnosis of diphtheria is confirmed by isolation of C. diphtheriae in culture of the adherent membrane and by testing the isolate for toxin production (317). The mainstay of treatment in respiratory diphtheria is early administration of diphtheria antitoxin (equine), which is available to physicians in the United States from CDC through an FDA-Investigational New Drug protocol (24-hour telephone, 770-488-7100). Additional information is available at http://www.cdc.gov/vaccines/vpd-vac/diphtheria/dat/datmain.htm. No human-derived serum diphtheria antitoxin is available. Antibiotics are administered to limit transmission and to prevent continuing production of diphtheria toxin (318). Prompt reporting of suspect cases, investigation, culture, and antimicrobial prophylaxis of contacts and immunization of the affected community (317,318) is of critical importance. Because respiratory diphtheria does not always confer protection against future illness, patients should complete active immunization with diphtheria toxoid after recovery (286).
# Diphtheria Immunity
Protection against respiratory diphtheria is predominantly from IgG antibody to diphtheria toxin (antitoxin) induced after infection with toxin-producing C. diphtheriae or after vaccination with diphtheria toxoid. In areas with little or no endemic exposure to toxin-producing C. diphtheriae, periodic vaccination is required to maintain immunity (237,286,307,(319)(320)(321). Although the immune responses to infection and vaccination vary, antitoxin concentrations of >0.1 IU/mL typically are considered protective. Concentrations of 0.01 IU/mL-0.1 IU/mL might provide protection against severe disease; concentrations <0.01 IU/mL do not protect against diphtheria (286,307,322).
# Td Booster During Pregnancy for Diphtheria Protection
Data from a national population-based serosurvey conducted during 1988-1994 that evaluated the prevalence of immunity to diphtheria (defined as a diphtheria antitoxin concentration of >0.1 IU/mL) among women in the United States determined immunity to diphtheria to be lower than immunity to tetanus (see Tetanus: Deferring Td During Pregnancy to Substitute Tdap in the Immediate Postpartum Period). The prevalence of immunity to diphtheria decreased with increasing age (77% among women aged 12-19 years, 74% among women aged 20-29 years, 65% among women aged 30-39 years, and <45% among women aged >40 years) and with birth outside the United States or less formal education (274,276).
# Vaccinating Pregnant Women, Infant Protection by Transplacental Antibody
Diphtheria toxoid vaccine trials conducted among pregnant women in the 1940s demonstrated quantitative increases in diphtheria antitoxin after the women were vaccinated. Maternal antitoxin was transferred efficiently to the fetus (217,226,320,323,324). Several studies indicate transplacental maternal antitoxin provides newborn infants with protection against diphtheria at birth if their mother is immune (226,250,321,325).
# Safety
The safety of diphtheria toxoid (without tetanus toxoid) vaccination in pregnant women was examined during the 1970s (326). After diphtheria toxoid was administered during the first 4 months of pregnancy, 75 mother-child pairs were followed for malformations until the child reached age 7 years. Although the number of vaccinated pregnant women studied was small, the risk for malformations in their children was lower than the risk among children in a much larger group of mother-child pairs in which the women were not vaccinated with diphtheria toxoid during pregnancy (survival-and race-standardized relative risk: 0.88) (327).
# Inhibitory Effect of Transplacental Maternal Antibody on Infant Immunization
Transplacental maternal diphtheria antitoxin concentrations of <0.1 IU/mL can interfere with primary diphtheria toxoid immunization in infancy (237,292,321,(328)(329)(330)(331). The duration of interference is affected by the concentration of maternal antitoxin, the formulation and toxoid content of the infant vaccine (e.g., the limit of flocculation [Lf ] units of diphtheria toxoid, aluminum hydroxide-adsorbed, or fluid preparation), and the length of the interval between doses (229,237,292,293,295,299,321,(328)(329)(330)(331). Infants typically respond with increases in antitoxin after 2 doses of highcontent diphtheria toxoid vaccine when maternal antitoxin concentrations are 0.1 IU/mL in cord sera but not until after >3 infant doses of high-content diphtheria toxoid vaccine when maternal antitoxin concentrations are >1.0 IU/mL in cord sera (225,229,292,299,321,329,331,332). When infants receive subsequent doses of diphtheria toxoid, the responses are rapid, often within 2 weeks (330), suggesting that T-cell priming occurs in the absence of an infant antibody response to previous doses of vaccine (229,237,324,329,330).
# Lactation
Consumption of human milk does not affect the infant immune response to diphtheria toxoid-containing vaccines (292,332). Ingestion of colostrum from an immune mother does not result in an increase in the concentration of diphtheria antitoxin in infant sera (250).
# Adult and Adolescent Acellular Pertussis Combined with Tetanus and Reduced Diphtheria Toxoids (Tdap) Vaccines and Tetanus and Reduced Diphtheria Toxoids (Td) Vaccines
Both Tdap vaccines used in the United States (ADACEL ® and BOOSTRIX ® ) were licensed on the basis of clinical trials in the United States demonstrating immunogenicity not inferior to that of U.S.-licensed Td (333,334) and the pertussis components of pediatric DTaP made by the same manufacturer and an acceptable safety profile (212,213). Adsorbed Td products for adults and adolescents have been licensed in the United States since the 1950s (335). Components of these and other diphtheria and tetanus toxoids-containing vaccines have been listed (Table 1) and are available at http://www.fda. gov/cber/vaccines.htm.
In prelicensure trials, data on local and systemic adverse events were collected using standard diaries for the day of vaccination and the next 14 consecutive days (212,213,(336)(337)(338). The efficacies of the tetanus toxoid and the diphtheria toxoid components of Tdap were inferred from the immunogenicity of the antigens in Tdap compared with Td using established serologic correlates of protection in sera obtained before and approximately 1 month after vaccination. Because no wellaccepted serologic or laboratory correlate of protection is available for pertussis, the efficacy of the pertussis components of Tdap was inferred using a serologic bridge (comparison) to the immune response to vaccine antigens among infants who received 3 doses of pediatric DTaP (made by the same manufacturer) during clinical efficacy trials for pertussis during the 1990s (339). The efficacy against pertussis of an acellular pertussis vaccine without tetanus and diphtheria toxoids was 92% (CI = 32%-99%) for adults and adolescents in a randomized, controlled trial (340); these results were not considered in the evaluation of Tdap for licensure in the United States.
Selected results from the prelicensure trials are summarized below. Additional information can be found in previous ACIP statements discussing use of Tdap among adults and adolescents and in the package labels of the specific products (1,2,212,213).
# ADACEL ®
ADACEL ® contains the same tetanus toxoid, diphtheria toxoid, and five pertussis antigens as those in DAPTACEL ® (pediatric DTaP, also made by sanofi pasteur), but ADACEL ® is formulated with reduced quantities of diphtheria toxoid and detoxified PT. Prelicensure trials in the United States evaluated the immunogenicity and the safety of ADACEL ® among adults aged 18-64 years and among adolescents aged 11-17 years, randomized to receive a single dose of ADACEL ® or a single dose of Td made by the same manufacturer (Table 1) (1,2,212,333). Pregnant women were excluded.
# Immunogenicity
Tetanus and Diphtheria Toxoids. The rates of seroprotection and booster response for both antitetanus and antidiphtheria among adults and adolescents who received a single dose of ADACEL ® were noninferior to rates among those who received Td. Nearly all (>99%) subjects in the ADACEL ® and Td groups achieved seroprotective antitetanus levels (>0.1 IU/mL), and >94% of adults and >99% of adolescents achieved seroprotective antidiphtheria levels (>0.1 IU/mL) in ADACEL ® and Td groups (212,341).
Pertussis Antigens. The efficacy of the pertussis components was inferred by comparing the immune responses (GMCs) of adults and adolescents vaccinated with a single dose of ADACEL ® to those of infants vaccinated with 3 doses of DAPTACEL ® in a Swedish vaccine efficacy trial (338,342). The efficacy of 3 doses of pediatric DAPTACEL ® against WHO-defined pertussis (>21 days of paroxysmal cough with confirmation of B. pertussis infection by culture or serologic testing, or an epidemiologic link to a household member with culture-confirmed pertussis) was 85% (CI = 80%-89%) (338,342). The GMCs of anti-PT, anti-FHA, anti-PRN, and anti-FIM among adults and adolescents after a single dose of ADACEL ® were noninferior to those of infants after 3 doses of DAPTACEL. ® The prespecified criteria for booster responses also were met (1,2,212,336,341).
# Safety
The safety of ADACEL ® was evaluated in four clinical studies with data from 2,448 adults aged 18-64 years and 3,393 adolescents aged 11-17 years (212).
Immediate Events. No anaphylaxis was reported. Five adults reported an immediate event within 30 minutes of vaccination (four persons [0.2%] for ADACEL ® and one person [0.2%] for Td); three of these five events were classified as nervous system disorders (hypoesthesia/paresthesia). Eleven adolescents reported an immediate event (six persons [0.5%] for ADACEL ® and five persons [0.6%] for Td); these events included dizziness, syncope, or vasovagal reactions in addi-May 30, 2008 tion to pain and erythema at the injection site. All events resolved without sequelae (338,341,343).
Solicited Local and Systemic Adverse Events. Rates of erythema and swelling (Figures 3 and 4), or systemic (headache, generalized body aches, and tiredness [data not presented]) adverse events reported to occur during 0-14 days following vaccination with Td or Tdap were similar (1,2,212,338,341). Fever >100.4°F (>38°C) was reported with the same frequency by adults vaccinated with Td and with Tdap (Figure 3) (212); the rate of any fever reported by adolescents vaccinated with Tdap (5%) was higher than the rate for those vaccinated with Td (3%) but met the noninferiority criterion (Figure 4) (212,341). No case of whole-arm swelling was reported (341).
Serious Adverse Events. Among adults, serious adverse events (e.g., appendicitis) within 6 months after vaccination were reported for 33 (2%) of 1,752 persons in the ADACEL ® group and for 11 (2%) of 573 persons in the Td group (338,341). Two serious adverse events in ADACEL ® recipients were neuropathic and were assessed by the investigators as possibly related to vaccination. In both cases, the symptoms resolved completely over several days (1,212,338,341,343). Among adolescents, serious adverse events within 6 months after vaccination were reported for 11 (1%) of 1,184 persons in the ADACEL ® group and for eight (1%) of 792 persons in the Td group. All events were reported by investigators to be unrelated to the study vaccine (341). No physician-diagnosed Arthus reaction (see Important Local Reactions) or case of Guillain-Barré syndrome (see Neurologic and Systemic Events) was reported (1).
# Simultaneous Administration of Tdap with Other Vaccines
Trivalent Inactivated Influenza Vaccine. The safety and immunogenicity of ADACEL ® co-administered with trivalent inactivated influenza vaccine ([TIV] Fluzone, ® sanofi pasteur, Swiftwater, Pennsylvania) were evaluated in nonpregnant adults aged 19-64 years randomized to simultaneous administration in different arms (n = 359), or to TIV administered first, followed by ADACEL ® 4-6 weeks later (n = 361). Rates of fever and injection site erythema and swelling were similar following ADACEL ® administered concurrently with TIV or separately. Pain at the ADACEL ® injection site occurred more frequently after simultaneous administration than after separate administration (67% and 61%, respectively) (338). Immunogenicity criteria were met with the following exceptions: the GMC of anti-PRN was lower in the simultaneous group than in the sequential group (338,344), and the tetanus booster response rates were lower after simultaneous administration than after sequential administration (79% and 83%, respectively). However, more than 98% of subjects in both groups achieved seroprotective levels (>0.1 IU/mL) of tetanus antitoxin (338,344).
Hepatitis B Vaccine. The safety and immunogenicity of ADACEL ® administered with hepatitis B (Hep B) vaccine (Recombivax HB, ® Merck and Co., White House Station, New Jersey) were evaluated among nonpregnant adolescents Td] was 10.7% whereas the noninferiority criterion was <10%). † The rate of "any" fever was higher after Tdap than after Td (p<0.05); however, the noninferiority criterion was met for Tdap. aged 11-14 years randomized to simultaneous administration (n = 206) or to ADACEL ® administered first, followed by hepatitis B vaccine 4-6 weeks later (n = 204). Rates of solicited erythema and swelling at the ADACEL ® injection site were higher in the simultaneous group than in the sequential group, and noninferiority was not achieved (1,338). No interference was observed in the immune responses to any of the vaccine antigens when ADACEL ® and hepatitis B vaccine were administered concurrently or separately (212).
# BOOSTRIX ®
BOOSTRIX ® contains the same tetanus toxoid, diphtheria toxoid, and three pertussis antigens as those in INFANRIX ® (pediatric DTaP, also made by GlaxoSmithKline), but BOOSTRIX ® is formulated with reduced quantities of antigens. Prelicensure trials conducted in the United States evaluated the immunogenicity and safety of BOOSTRIX ® among adolescents aged 10-18 years (213,337), randomized to receive a single dose of BOOSTRIX ® or a single dose of Td (Massachusetts Public Health Biologic Laboratory, Mattapan, Massachusetts) (Table 1) (213,334,337). Pregnant adolescents were excluded.
# Immunogenicity
Tetanus and Diphtheria Toxoids. The rates of seroprotection and booster response for both antitetanus and antidiphtheria among adolescents who received a single dose of BOOSTRIX ® were noninferior to those who received Td. All adolescents had seroprotective antitetanus levels (>0.1 IU/mL); >99% of adolescents had seroprotective antidiphtheria levels (>0.1 IU/mL) (1,213,336).
Pertussis Antigens. The efficacy of the pertussis components was inferred by comparing the immune responses of adolescents vaccinated with a single dose of BOOSTRIX ® with the immune responses of infants vaccinated with 3 doses of INFANRIX ® in a German vaccine efficacy trial (213, 336,345). The efficacy of 3 doses of pediatric INFANRIX ® against WHO-defined pertussis was 89% (CI = 77%-95%) (213,345). The GMCs of anti-PT, anti-FHA, and anti-PRN after a single dose of BOOSTRIX ® were noninferior to those of infants after 3 doses of INFANRIX. ® The prespecified criteria for booster responses also were met (1,213,336,337).
# Safety
A total of 3,080 adolescents aged 10-18 years received BOOSTRIX ® in the primary safety study (213). No immediate events (i.e., those occurring within 30 minutes of vaccination) were reported (1,213,336,337).
# Solicited Local and Systemic Adverse Events.
No substantial differences were observed between the BOOSTRIX ® and Td recipients in the rates of solicited local (redness, swelling, and increase in arm circumference above baseline) (Figure 5) or systemic (headache, fatigue, gastrointestinal systemic events, fever >100.4°F [>38.0°C] [data not presented]) adverse events (1,213,336,337). No case of whole-arm swelling was reported (1).
Serious Adverse Events. Serious adverse events within 6 months after vaccination were reported among 14 (0.4%) of 3,005 adolescents vaccinated with BOOSTRIX ® and two (0.2%) of 1,003 adolescents vaccinated with Td. All events were reported by the investigators to be unrelated to the study vaccine (213,336,337,346). No physician-diagnosed Arthus reaction or case of Guillain-Barré syndrome was reported (1,213,337,346).
# Pregnant Women Vaccinated with Tdap
Pregnant women were excluded from prelicensure trials of Tdap. The outcome of pregnancy among six women who were administered ADACEL ® inadvertently during or within 1 month of conception was a healthy full-term infant (n = 3), a preterm infant (n = 1), or a miscarriage (n = 2). No infant was born with a congenital anomaly (sanofi-pasteur, unreported data, 2007). Two pregnancies occurred in BOOSTRIX ® recipients >4 months postvaccination; one subject experienced a spontaneous abortion within the first trimester, and the other subject delivered a healthy infant (337).
# Regulatory Considerations for Tdap in Pregnant Women
As with the majority of vaccines, Tdap is labeled pregnancy category C. This designation indicates that no adequate and well-controlled studies have been conducted with the vaccine in pregnant women to determine the product's safety (347,348).
# Safety Considerations for Adult and Adolescent Use of Td or Tdap
Prelicensure studies in nonpregnant adults and adolescents evaluated the safety of Tdap with respect to local and systemic adverse events (212,213). The sample sizes were insufficient to detect rare adverse events. Enrollment criteria excluded persons who were pregnant; had received vaccines containing tetanus toxoid, diphtheria toxoid, or pertussis components more recently than either the preceding 5 years for ADACEL ® (212) or the preceding 10 years for BOOSTRIX ® (213); or had certain neurologic conditions or events (336)(337)(338)341,346). Safety data are being collected by the Vaccine Adverse Event Reporting System (VAERS), and postlicensure studies continue to monitor for potential adverse reactions following widespread use of Tdap in adults and adolescents (16,17). Registries have been established by both Tdap manufacturers for reporting women vaccinated with Tdap during pregnancy.
# Interval between Td and Tdap
ACIP has made several recommendations for intervals between tetanus toxoid-and diphtheria toxoid-containing vaccines that balance the benefits of protection against the risks of moderate and severe local reactions. Moderate and severe local reactions, including Arthus reaction, are associated with frequent dosing at short intervals and larger doses of toxoid. High antitoxin levels are more likely to result when the interval between doses is short and the number of doses increases (349)(350)(351)(352)(353)(354). High preexisting antibody titers to tetanus or diphtheria toxoids also are associated with increased rates and severity of local reactions to booster doses in adults (349,(354)(355)(356).
ACIP recommends a 10-year interval for routine administration of Td (e.g., decennial Td booster), and a 5-year interval for Td when indicated for wounds management (1,2,357). Administering Td more often than every 10 years (5 years for certain nonclean, nonminor wounds) is not necessary to provide protection against tetanus or diphtheria; however, administering a single dose of Tdap at an interval shorter than 5 years after Td could provide a health benefit by adding protection against pertussis (Table 2) (1,2). When Tdap is administered to add protection against pertussis, ACIP encourages an interval of >5 years between the most recent Td and the Tdap dose for adolescents because they might receive other recommended vaccines containing tetanus or diphtheria toxoids (including quadrivalent meningococcal conjugate vaccine [MCV4] [Menactra, ® sanofi pasteur, Swiftwater, Pennsylvania]) (2). An interval as short as 2 years is recommended between the most recent Td and the single dose of Tdap for health-care personnel with direct patient contact, and a 2-year interval between the most recent Td and Tdap is suggested for adults in close contact with infants (1). ACIP allows for a shorter interval between the most recent Td and administration of Tdap in certain circumstances that might require urgent protection (1,2).
Several studies have suggested that an interval as short as 2 years between Td and a single dose of Tdap is acceptably safe. Three studies conducted among Canadian children and adolescents evaluated the safety of Tdap (ADACEL ® ) at an interval shorter than 5 years after Td or after pediatric DTP or DTaP (358)(359)(360). The largest was an open-label study of 7,001 students aged 7-19 years. Rates of local reactions were not increased among students who had received the most recent of 5 pediatric DTP or DTaP doses, or a Td dose, >2 years before Tdap, compared with >10 years before Tdap (358). The other Canadian studies demonstrated similar safety when Tdap was administered at an interval of <5 years after the previous tetanus toxoid-and diphtheria toxoid-containing vaccine (359,360).
Adverse reactions after Tdap (ADACEL ® ) administered at an interval of <2 years from the most recent Td were evaluated in a retrospective survey of 4,524 health-care personnel who received Tdap at a median age of 46 years during an outbreak of pertussis-like illness in New Hampshire in 2006 (118,215,361). For the 2,676 (59%) responses, the rates of reactions were analyzed by interval from Td to Tdap as either >2 years (n = 1,792) or <2 years (n = 370). The rates of pain, redness, or swelling of moderate or severe intensity, subjective fever, and medical visits were not higher among respondents with an interval of <2 years between administration of Td and that of Tdap. Three serious adverse events were reported among adults who received Tdap at an interval >2 years after the most recent dose of Td; causality was not assessed. The events were a case of Guillain-Barré syndrome (not requiring hospitalization) with onset 11 days after Tdap, a case of anaphylaxis-like reaction with onset 6 days after Tdap, and a case of eosinophilic nephritis with onset 6 days after Tdap in a health-care worker with a history of a renal transplant (215,216).
# Important Local Reactions Arthus Reaction
Arthus reaction (type III hypersensitivity reaction) can occur after tetanus toxoid-or diphtheria toxoid-containing vaccines (354,357,362-366;CDC, unpublished data, 2005). Arthus reaction is a local vasculitis with deposition of immune complexes and activation of complement; it occurs in the setting of high local concentration of vaccine antigens and high circulating antibody concentration (354,362,363,367). The reaction is characterized by severe pain, swelling, induration, edema, and hemorrhage, and occasionally by local necrosis. Vaccine-related arthus reaction typically resolves without sequelae. The onset of symptoms and signs is 4-12 hours after vaccination, compared with anaphylaxis (immediate type I hypersensitivity reaction), which has onset within minutes after vaccination. ACIP recommends that persons who experience an Arthus reaction after administration of a tetanus toxoid-containing vaccine not receive Td or other tetanus toxoid-containing vaccine more frequently than every 10 years, even for tetanus prophylaxis as part of wound management (1,357).
# Extensive Limb Swelling
Extensive limb swelling reactions have been reported to VAERS following administration of Td (368,369) and are described following dose 4 or dose 5 of pediatric DTaP (23,208,368,(370)(371)(372)(373). Extensive limb swelling after pediatric DTaP resolves without complication within 4-7 days (370), and is not considered a precaution or contraindication for Tdap (23).
# Neurologic and Systemic Events Pertussis Components
Concerns regarding a possible role of pertussis vaccine components in causing neurologic reactions or exacerbating underlying neurologic conditions in infants and children are long-standing (29,374). In 1991, the Institute of Medicine (IOM) concluded that evidence favored acceptance of a causal relation between pediatric DTP vaccine and acute encephalopathy (365). A subsequent retrospective analysis of >2 million children in the United States did not demonstrate that pediatric DTP was associated with an increased risk for encephalopathy after vaccination (375). Active surveillance in Canada during 1993-2002 also failed to identify any acute encephalopathy cases causally related to whole-cell or acellular pertussis vaccines among a population administered 6.5 million doses of pertussis-containing vaccines (376). Results of one recent investigation suggested that some acute encepha-lopathies attributed previously to pertussis-containing vaccines could be the result of genetically determined epileptic encephalopathies related to mutations in the sodium channel gene SCN1A (377,378). A history of encephalopathy (e.g., coma or prolonged seizures) not attributable to an identifiable cause within 7 days of administration of a vaccine with pertussis components remains a contraindication for Tdap (but not Td) in adults and adolescents.
The possibility that Tdap would complicate neurologic evaluation of chronic progressive neurologic disorders that are stable in adults (e.g., dementia) is of limited clinical concern and does not constitute a reason to delay administration of Tdap (1). Unstable or evolving neurologic conditions (e.g., cerebrovascular events or acute encephalopathic conditions) would be reason to delay administration of Tdap until the condition has stabilized (1). Among adolescents who have progressive or uncontrolled underlying neurologic disease, concerns regarding administering Tdap must be weighed against the morbidity from pertussis, which could be severe (2). ACIP does not consider a history of well-controlled seizures or a family history of seizures (febrile or afebrile) or other neurologic disorder to be a contraindication or precaution to vaccination with pertussis components (22).
# Tetanus Toxoid Component
ACIP considers Guillain-Barré syndrome within 6 weeks after receipt of a tetanus toxoid-containing vaccine to be a precaution (see Precautions and Reasons to Defer Td or Tdap) for administration of subsequent tetanus toxoid-containing vaccines (23). Although IOM concluded that evidence favored acceptance of a causal relation between tetanus toxoidcontaining vaccines and Guillain-Barré syndrome on the basis of a single well-documented case (365,379), subsequent analysis of data from both adult and pediatric populations failed to demonstrate an association (380). As of January 29, 2007, eight patients with Guillain-Barré syndrome temporally associated with receipt of Tdap or of Tdap administered on the same day with other vaccines had been reported to VAERS. The onsets were not clustered by the interval since vaccination or by a single pattern of vaccine exposure (361).
ACIP does not consider a history of brachial neuritis to be a precaution or contraindication for administration of tetanus toxoid-containing vaccines (23,381). IOM concluded that evidence from case reports and uncontrolled studies involving tetanus toxoid-containing vaccines did favor a causal relation between tetanus toxoid-containing vaccines and brachial neuritis (365); however, brachial neuritis typically is self-limited (23,381). Brachial neuritis is a compensable event through the Vaccine Injury Compensation Program (VICP) (365).
# MMWR May 30, 2008
# Economic Considerations
No study has evaluated the disease morbidity and societal costs associated with pertussis among pregnant women or modeled the cost benefit or cost effectiveness of a Tdap strategy that includes vaccination of pregnant women. The morbidity and societal cost of pertussis in adults is substantial (1,2). A retrospective assessment of medical costs of confirmed pertussis in 936 adults in Massachusetts during 1998-2000, and a prospective assessment of nonmedical costs in 203 adults during 2001-2003 (31) indicated that the mean medical and nonmedical cost per case was $326 and $447, respectively, for a societal cost of $773. If the cost of antimicrobials to treat contacts and the cost of personal time were included, the societal cost could be as high as $1,952 per adult case (31).
Cost-benefit and cost-effectiveness analyses of adult Tdap vaccination have varied in their results (382,383). When discrepancies in the models were addressed, an adult Tdap vaccination program was cost-effective when incidence of pertussis exceeded 120 cases per 100,000 population, using a benchmark of $50,000 per quality-adjusted life year saved (384)(385)(386). After adjusting for the severity of the illness at high disease incidence, little effect was observed on the overall cost effectiveness of a vaccination program. Similar results were obtained when program costs and benefits were analyzed over the lifetime of the adult cohort for decennial booster strategies (1,387).
# Implementing Tdap Preconception Assessments
Administering a dose of Tdap during routine wellness visits of adult and adolescent women of childbearing age, if indicated, is the most effective programmatic strategy to ensure that women are protected against pertussis in addition to tetanus and diphtheria and minimizes any theoretical effect of vaccination on infant immune responses should the woman become pregnant (see Immunity to Pertussis and Kinetics of Pertussis Booster Vaccination in Nonpregnant Adults and Adolescents) (1,(388)(389)(390)(391)(392). Because Tdap contains only toxoids and purified bacterial components, women who receive Tdap do not need to wait after vaccination to become pregnant (23). Assessments provide repeated opportunities for documenting the history of past doses of Td (or TT) and any serious adverse reactions to tetanus, diphtheria, and pertussis vaccines. To access and maintain immunization records, statebased immunization information systems (IIS) are increasingly becoming available to clinicians and public health officials. These confidential, computerized information systems, which consolidate vaccination data from multiple health-care providers, can generate reminder and recall notifications, assist with vaccine management and adverse events reporting, and capture lifespan vaccination histories (393). Additional guidance regarding administration of vaccines during routine assessments, record keeping, vaccine storage, and related topics has been published previously (23).
# Prenatal Visits: Deferring Td During Pregnancy to Substitute Tdap in the Immediate Postpartum Period
In 2004, a total of 96% of pregnant women started prenatal care in the first or second trimester (394). Prenatal visits provide additional opportunities for assessing the history of past vaccination with Tdap, Td, or TT and any serious adverse reactions to tetanus, diphtheria, and pertussis vaccines. Women who have not received a previous dose of Tdap can be advised that ACIP recommends Tdap postpartum before discharge from the hospital or birthing center to provide personal protection and reduce the risk for transmitting pertussis to their infants.
Health-care providers can monitor pregnant women for respiratory illness consistent with pertussis or for recent exposure to pertussis, either to themselves or to family members, and prescribe a macrolide antimicrobial for treatment of pertussis or postexposure prophylaxis, if indicated. Women and their partners should receive counseling regarding the severity of infant pertussis and ACIP's recommendation for a single dose of Tdap for adults and adolescents who anticipate contact with an infant (1,2). In a 2005 national survey of obstetricians, 72% of respondents affirmed the belief that obstetricians, pediatricians, adult primary care providers, and public health providers share responsibility to promote administration of Tdap for adults who anticipate contact with an infant, including fathers and close relatives (395). Ideally, health-care providers delivering prenatal care will encourage persons likely to have contact with an infant, including child care providers, to receive Tdap first.
When pregnant women who have not received Tdap have indications for tetanus or diphtheria booster protection (>10 years since the most recent Td), ACIP recommends receipt of Td during pregnancy (Table 2). ACIP has developed criteria for safely deferring administration of Td until delivery among women who have received past tetanus toxoidcontaining vaccinations, so the majority of these women can substitute Tdap in the immediate postpartum period for Td during pregnancy (see Deferring Td During Pregnancy to Substitute Tdap in the Immediate Postpartum Period). When the history of tetanus toxoid vaccination for the women is uncertain or lacking, health-care providers can determine the con-centration of tetanus antitoxin to ensure protective concentrations of tetanus antitoxin (>0.1 IU/mL by ELISA). Because diphtheria is rare in the United States, serologic screening for diphtheria antitoxin typically is not necessary. A woman who anticipates travel to an area in which diphtheria is endemic can improve protection against diphtheria by receiving a booster dose of Td during pregnancy or a dose of Tdap postpartum. Serologic screening to establish immunity to pertussis is not useful.
In special situations in which a pregnant woman has increased risk for tetanus, diphtheria, or pertussis, ACIP acknowledges that health-care providers may choose to administer Tdap instead of Td during pregnancy to add protection against pertussis, after discussing the theoretical benefits and risks for her, her fetus, and the pregnancy outcome with the woman before vaccination (see Considerations for Use of Tdap in Pregnant Women in Special Situations). Data to inform this decision are scarce. No theoretical risk for harm to the mother or fetus exists from Tdap, and administration of Tdap in the pregnant woman might provide a degree of early protection to the infant against pertussis. However, a theoretical risk for the infant is that the dose of Tdap in pregnancy might not result in early protection against pertussis or could increase transplacental pertussis-specific antibodies to levels that would have a negative effect on the infant's response to immunization with pediatric DTaP or with conjugate vaccines containing tetanus toxoid or diphtheria toxoid (e.g., Haemophilus influenzae type b pneumococcal conjugate vaccine) (222). Health-care providers who choose to vaccinate pregnant women with Tdap are encouraged to report such administration to the manufacturers' pregnancy registry.
# Postpartum Tdap
In 2004, a reported 99% of live births in the United States occurred in a hospital. Of out-of-hospital live births, 27% occurred at a free-standing birthing center and 65% at a residence (394). In these settings, attendants can implement protocols to ensure that postpartum women who have not received Tdap previously receive it before discharge. They also can encourage previously unvaccinated adults and adolescents who anticipate contact with an infant to receive Tdap. Tdap vaccination of the women and potential contacts before discharge rather than at a follow-up visit has the advantage of decreasing the time when new mothers and contacts of the newborns could acquire and transmit pertussis to the infants (1,2). Standing orders for postpartum Tdap vaccination before discharge have successfully raised vaccination rates to more than 80% of eligible women (396). Although obtaining a history of the most recent Td vaccination was anticipated to be a barrier to postpartum vaccination with Tdap, in practice it was not identified as a barrier (395,396).
Vaccination of parents and household contacts of premature infants has been advocated to ensure that such persons receive Tdap (397). Premature and low birth weight infants are at increased risk for severe and complicated pertussis. The case-fatality rate for pertussis is increased compared with term infants, and premature infants might respond less well than term infants to initial doses of DTaP vaccine because of comorbidities or treatments (e.g., dexamethasone) (47,53,(398)(399)(400)(401)(402)(403).
Parents should be reminded of other measures to protect infants from pertussis. To the extent feasible, parents can limit infant exposures to persons who have respiratory illness until they are determined to be noninfectious (99,219,321). When pertussis exposure occurs, antimicrobial prophylaxis of exposed contacts can be effective in preventing transmission of pertussis (42,99,404,405). Ensuring that infants begin the pediatric DTaP vaccination series at the recommended chronologic age of 6-8 weeks is critical to protection and reducing the severity of pertussis (8,45,397,406). Administration of 2 or 3 doses of pediatric DTP or DTaP can prevent hospitalization for pertussis and its complications (5,8,(407)(408)(409).
# Recommendations
Recommendations for routine use of Td and Tdap among women of childbearing age who might become pregnant have been published previously (1,2) and have been summarized (Table 2). Women are encouraged to receive a single dose of Tdap either as ADACEL ® (adults and adolescents aged 11-64 years) or as BOOSTRIX ® (adolescents aged 11-18 years) before conception (e.g., during routine wellness visits) if they have not already received Tdap. Recommendations for adults and adolescents who anticipate or have household contact with an infant aged <12 months also have been published previously (1,2) and summarized (Table 2). The dose of Tdap will provide active booster immunization against tetanus, diphtheria, and pertussis and will replace the next dose of Td according to routine recommendations. A single preconception dose of Tdap will prevent pertussis, reduce morbidity associated with pertussis, and might prevent exposing persons at increased risk for pertussis and its complications, including infants. The risk for pertussis death and severe pertussis is highest among infants in the first months of life and remains elevated until an infant has received 1-2 doses of pediatric DTaP (8,45,47).
The following sections present recommendations for use of Td and Tdap among pregnant and postpartum women, including routine vaccination, contraindications, precautions, and special situations. As with most inactivated vaccines and toxoids, pregnancy is not a contraindication for use of Tdap. Although the safety and immunogenicity of Tdap is expected to be similar in pregnant and nonpregnant women, few data on the safety of Tdap for women, fetuses, and pregnancy outcomes are available, and no information is available on the immunogenicity of Tdap in pregnant women. Vaccinating pregnant women with a single dose of Tdap might provide a degree of protection against pertussis to the infant in early life through transplacental maternal antibody, but evidence supporting this hypothesis is lacking. A concern is the unknown effect of potential interference by maternal antibody on the ability of the infant to mount an adequate immune response when the infant receives pediatric DTaP or conjugate vaccines containing tetanus toxoid or diphtheria toxoid.
In special situations, administration of Tdap during pregnancy might be warranted for pregnant women who were not vaccinated previously with Tdap. Health-care providers who choose to administer Tdap to pregnant women should discuss with the women the potential risks and benefits of immunization including the lack of data on Tdap administered during pregnancy or its unknown effects on active immunization of their infant. The following recommendations are intended to provide guidance to clinicians until additional information is available.
# Routine Tdap Vaccination
# 1-A. Recommendations for Use of Postpartum Tdap
For women who have not received Tdap previously (including women who are breastfeeding), Tdap is recommended as soon as feasible in the immediate postpartum period to protect the women from pertussis and reduce the risk for exposing their infants to pertussis. The postpartum Tdap should be administered before discharge from the hospital or birthing center. If Tdap cannot be administered at or before discharge, the dose should be administered as soon as feasible thereafter. Elevated levels of pertussis antibodies in the mother are likely within 1-2 weeks after vaccination.
Although an interval of 10 years since receipt of the most recent Td dose is recommended for the next routine Td booster, to reduce the risk for women exposing their infants to pertussis, an interval as short as 2 years between the most recent Td and administering Tdap ¶ is suggested for postpartum women.
The safety of such an interval is supported by three Canadian studies among adolescents and by a study among nonpregnant adult health-care personnel (215,(358)(359)(360), an interval shorter than 2 years may be used (see Postpartum Tdap When <2 Years Have Elapsed Since the Most Recent Td). In this setting, the benefit of Tdap to protect against pertussis typically outweighs the risk for local and systemic reactions after vaccination. Routine postpartum Tdap recommendations are supported by evidence from randomized controlled clinical trials, nonrandomized open-label trials and a retrospective survey, observational studies, and expert opinion (Box 2).
# 1-B. Dosage and Administration
The dose of Tdap or, if indicated, the dose of Td is 0.5 mL, administered intramuscularly (IM), preferably into the deltoid muscle.
# 1-C. Simultaneous Vaccination with Tdap and Other Vaccines
If two or more vaccines are indicated, they typically should be administered during the same visit (i.e., simultaneous vaccination). Each vaccine should be administered using a separate syringe at a different anatomic site. Certain experts recommend administering no more than two injections per muscle, separated by at least one inch. Administering all indicated vaccines during a single visit increases the likelihood that pregnant and postpartum women will receive recommended vaccinations (23).
# 1-D. Interchangeable Use of Tdap Vaccines
A single dose of ADACEL ® may be used for adults aged 19-64 years, and a single dose of either ADACEL ® or BOOSTRIX ® may be used for adolescents aged 11-18 years, regardless of the type or manufacturer of pediatric DTP or pediatric DTaP used for childhood vaccination.
# 1-E. Preventing Adverse Events
Attention to proper immunization technique, including use of an appropriate needle length and standard routes of administration (i.e., IM for Td and Tdap) might minimize the risk for adverse events. Guidance for administration of vaccines is available (23).
Syncope can occur after vaccination and might be more common among young adults and adolescents than among other age groups. Syncope rarely has resulted in serious injury (23,(410)(411)(412). Vaccine providers should strongly consider observing patients for 15 minutes after they are vaccinated (23,412). If syncope occurs, patients should be observed until symptoms resolve. ¶ An interval of 5 years since the most recent tetanus and diphtheria toxoidscontaining vaccine is encouraged for routine vaccination of adolescents who are not pregnant (2).
# 1-F. Inadvertent Administration of Pediatric DTaP, BOOSTRIX ® Tdap, or Purified Protein Derivative (PPD)
The potential for administration errors involving tetanus toxoid-containing vaccines (413) and other vaccines is welldocumented (414)(415)(416). Pediatric DTaP and pediatric diphtheria toxoid and tetanus toxoid vaccine (DT) formulations indicated for use in children aged 6 weeks-6 years should not be administered to adults or adolescents; these vaccines can be associated with more severe local reactions than adult formulations (350,417). Packaging of adult and adolescent Tdap vaccines, pediatric DTaP, and purified protein derivative (PPD) might appear similar. Only one formulation of Tdap, ADACEL, ® is licensed and recommended for adults aged 19-64 years. Both formulations of Tdap (BOOSTRIX ® and ADACEL ® ) are licensed and recommended for adolescents aged 11-18 years. Providers should review product labels before administering these vaccines. If pediatric DTaP is administered inadvertently to an adult or adolescent, or if BOOSTRIX ® is administered inadvertently to an adult aged >19 years, the dose should be counted as the Tdap dose, and the person should not receive an additional dose of Tdap. Adults or adolescents who receive PPD instead of Tdap should receive a dose of Tdap.
# 1-G. Record Keeping
Health-care providers who administer vaccines to adults and adolescents are required to keep permanent vaccination records of vaccines covered under the National Childhood Vaccine Injury Compensation Act. ACIP has recommended that this practice include all vaccines (23). Encouraging adults and adolescents to maintain a personal vaccination record is important to minimize administration of unnecessary vaccinations. Ideally, the personal vaccine record will document the type of the vaccine, manufacturer, anatomic site, route, and date of administration, and the name of the administering facility (23).
# Contraindications and Precautions for Use of Td and Tdap
# 2-A. Contraindications
The following conditions are contraindications for Td or Tdap:
• Td and Tdap are contraindicated for persons with a history of serious allergic reaction (i.e., anaphylaxis) to any component of the vaccine. Because of the importance of tetanus vaccination, persons with a history of anaphylaxis to components included in any Td or Tdap vaccines should be referred to an allergist to determine whether they have a specific allergy to tetanus toxoid and whether they can safely receive TT vaccination. • Tdap (but not Td) is contraindicated for adults and adolescents with a history of encephalopathy (e.g., coma or prolonged seizures) not attributable to an identifiable cause within 7 days of administration of a vaccine with pertussis components. This contraindication is for the pertussis components, and these persons should receive Td instead of Tdap.
# 2-B. Precautions and Reasons to Defer Td or Tdap
A precaution is a condition in a vaccine recipient that might increase the risk for a serious adverse reaction (23)
# 2-C. Conditions Under Which Td or Tdap May Be Administered If Otherwise Indicated
The following conditions are not contraindications or precautions for Td or Tdap:
• stable neurologic disorder, including well-controlled seizures, a history of a seizure disorder that has resolved, or cerebral palsy; • brachial neuritis after a previous dose of tetanus toxoidor diphtheria toxoid-containing vaccine; • a history of an extensive limb swelling reaction that was not an Arthus hypersensitivity reaction after pediatric DTP or DTaP or after Td; • immunosuppression, including persons with human immunodeficiency virus (HIV) (the immunogenicity of Tdap in persons with immunosuppression has not been studied and could be suboptimal); • breastfeeding; • intercurrent minor illness; and • use of antimicrobials. Latex allergies other than anaphylactic allergies (e.g., a history of contact allergy to latex gloves) are not a contraindication or precaution to Tdap (417). The tip and rubber plunger of the BOOSTRIX ® needleless syringe contain latex. The BOOSTRIX ® single dose vial and ADACEL ® preparations contain no latex. Certain Td products contain latex. The package inserts should be consulted for details (Table 1).
# Special Situations
# 3-A. Deferring Td during Pregnancy to Substitute Tdap in the Immediate Postpartum Period
Tetanus and diphtheria booster vaccination is recommended for pregnant women if >10 years have elapsed since the previous Td vaccination (1,2). To add protection against pertussis, health-care providers may defer the Td vaccination during pregnancy to substitute Tdap as soon as feasible postpartum if the woman is likely to have sufficient tetanus and diphtheria protection until delivery.
Sufficient tetanus protection is likely if:
• a pregnant woman aged <31 years has received a complete childhood series of immunization (4-5 doses of pediatric DTP, DTaP, and DT) and >1 Td booster dose during adolescence or as an adult (a primary series consisting of 3 doses of Td (or TT) administered during adolescence or as an adult substitutes for the childhood series of immunization),** • a pregnant woman aged >31 years has received a complete childhood series of immunization (4-5 doses of pediatric DTP, DTaP, and/or DT) and >2 Td booster doses, • a primary series consisting of 3 doses of Td (or TT) was administered during adolescence or as an adult substitute for the childhood series of immunization,** or • a pregnant woman has a protective level of serum tetanus antitoxin (>0.1 IU/mL by ELISA). A woman should receive Td during pregnancy if she • does not have sufficient tetanus immunity to protect against maternal and neonatal tetanus, or • requires urgent booster protection against diphtheria (e.g., for travel to an area in which diphtheria is endemic † † ). Alternatively, health-care providers may choose to administer Tdap instead of Td during pregnancy (see Considerations for Use of Tdap in Pregnant Women in Special Situations).
# 3-B. Postpartum Tdap When <2 Years Have Elapsed Since the Most Recent Td
Certain postpartum women (e.g., those who have received Td or TT within 2 years of the immediate postpartum period) might benefit from Tdap for pertussis protection. Few subjects have been evaluated to determine the risk for adverse local and systemic reactions after Tdap at intervals <2 years ** Women who have had a 3-dose series as TT instead of Td will likely have protection against tetanus but might not be protected against diphtheria.
A protective titer of diphtheria antitoxin is >0.1 IU/mL by ELISA. † † A list of areas in which diphtheria is endemic is available at www.cdc.gov/ travel/diseases/dtp.htm.
since the most recent Td (or other tetanus toxoid-or diphtheria toxoid-containing vaccine) (215). After obtaining a history to exclude women with moderate or severe adverse reactions following previous doses, health-care providers may choose to administer Tdap in postpartum women who received tetanus toxoid-or diphtheria toxoid-containing vaccine § § <2 years previously (see Precautions and Reasons to Defer Td and Tdap). Health-care providers should encourage vaccination of household and child care provider contacts of infants aged <12 months for protection against pertussis, according to current recommendations (Table 2) (1,2). Women should be advised of the symptoms of pertussis and the effectiveness of early antimicrobial prophylaxis for themselves, their infant, and members of their household, if pertussis is suspected (127).
# 3-C. History of Pertussis
Postpartum women who have a history of pertussis should receive Tdap according to the routine recommendation (see Recommendations for Use of Postpartum Tdap). This practice is preferred because the duration of protection induced by pertussis is unknown (waning might begin as early as 5-10 years after infection) (4), and a diagnosis of pertussis often is not reliably confirmed. Administering pertussis vaccine to persons with a history of pertussis presents no theoretical safety concern.
# 3-D. Considerations for Use of Tdap in Pregnant Women in Special Situations
ACIP recommends administration of Td for booster protection against tetanus and diphtheria in pregnant women. However, health-care providers may choose to administer Tdap instead of Td during pregnancy to add protection against pertussis in special situations. In these situations, the pregnant woman should be informed of the lack of data confirming the safety and immunogenicity of Tdap in pregnant women, the unknown potential for early protection of the infant against pertussis by transplacental maternal antibodies, and the possible adverse effect of maternal antibodies on the ability of the infant to mount an adequate immune response to antigens in pediatric DTaP or conjugate vaccines containing tetanus toxoid or diphtheria toxoid.
Special situations in which Tdap might be used might include instances when • a pregnant woman has insufficient tetanus or diphtheria protection until delivery, or • a pregnant woman is at increased risk for pertussis. Persons at increased risk for pertussis might include adolescents aged 11-18 years, health-care personnel, and women employed in institutions in which a pertussis outbreak is occurring or living in a community in which a pertussis outbreak is occurring.
Adverse pregnancy outcomes are most common in the first trimester (418). To minimize the perception of an association of vaccine with an adverse outcome, vaccinating with tetanus toxoid-containing vaccines during the second or third trimester is preferred.
Because information on the use of Tdap in pregnant women is lacking, both manufacturers of Tdap have established a pregnancy registry. Health-care providers are encouraged to report vaccination of pregnant women with Tdap, regardless of trimester, to the appropriate manufacturer's registry. For ADACEL, ® vaccination should be reported to sanofi pasteur, telephone 1-800-822-2463 (1-800-VACCINE), and for BOOSTRIX, ® vaccination should be reported to GlaxoSmithKline Biologicals, telephone 1-888-825-5249.
# 3-E. Tetanus Prophylaxis for Wound Management
ACIP has recommended administering tetanus toxoidcontaining vaccine and tetanus immune globulin (TIG) as part of standard wound management to prevent tetanus (Table 11) (357). A Td booster might be recommended for wound management in pregnant women if 5 years or more have elapsed since the previous Td (1,2). Health-care providers may choose to substitute Tdap for Td during pregnancy in these women (see Considerations for Use of Tdap in Pregnant Women in Special Situations). For pregnant women vaccinated previously with Tdap, Td should be used if a tetanus toxoid-containing vaccine is indicated for wound care. Pregnant women who have completed the 3-dose primary tetanus vaccination series and have received a tetanus toxoid-containing vaccine within the preceding 5 years are protected against tetanus and do not require a tetanus toxoid-containing vaccine as part of wound management.
To avoid unnecessary vaccination, health-care providers should attempt to determine whether the woman has completed the 3-dose primary tetanus vaccination series. Pregnant women with unknown or uncertain previous tetanus vaccination histories should be considered to have had no prior tetanus toxoid-containing vaccine and they should complete a 3-dose primary series of immunization to prevent maternal and neonatal tetanus (see Pregnant Women with Unknown § § Tetanus toxoid-and/or diphtheria toxoid-containing vaccines include pediatric DTP, DTaP, DT, other pediatric combination vaccines including any of these components (e.g., pediatric DTaP-inactivated poliovirus vaccine-Hep B and pediatric DTaP-Haemophilus influenzae type b), and adult and adolescent Td, Tdap, and TT). MCV4 contains diphtheria toxoid but not tetanus toxoid (2).
# MMWR May 30, 2008
or Incomplete Tetanus Vaccination). Pregnant women who have not completed the primary series might require tetanus toxoid and passive vaccination with TIG at the time of wound management (Table 11). When both TIG and a tetanus toxoid-containing vaccine are indicated, each product should be administered using a separate syringe at different anatomic sites. Pregnant women with a history of Arthus reaction after a previous dose of a tetanus toxoid-containing vaccine should not receive a tetanus toxoid-containing vaccine until 10 years or more after the most recent dose, even if they have a wound that is neither clean nor minor. If the Arthus reaction was associated with a vaccine that contained diphtheria toxoid without tetanus toxoid (e.g., MCV4), deferring Td or Tdap might leave the pregnant women inadequately protected against tetanus, and TT should be administered (see Precautions and Reasons to Defer Td or Tdap). In all circumstances, the decision to administer TIG is based on the primary vaccination history for tetanus (Table 11).
# 3-F. Pregnant Women with Unknown or Incomplete Tetanus Vaccination
Pregnant women who never have been vaccinated against tetanus (i.e., have received no dose of pediatric DTP, DTaP, or DT or of adult Td or TT) should receive a series of three vaccinations containing tetanus and diphtheria toxoids starting during pregnancy to ensure protection against maternal and neonatal tetanus. A primary series consists of a first dose administered as soon as feasible, a second dose at least 4 weeks later, and a third dose 6 calendar months after the second dose. If feasible, pregnant women who have received fewer than 3 doses of tetanus toxoid-containing vaccine should complete the 3-dose primary series during pregnancy. Td is preferred for the doses during pregnancy. Health-care providers may choose to substitute a single dose of Tdap for 1 dose of Td during pregnancy and complete the series with Td. In such cases, the women should be informed of the lack of data on safety, immunogenicity, and pregnancy outcomes for pregnant women who receive Tdap (see Considerations for Use of Tdap in Pregnant Women in Special Situations).
# Reporting Adverse Events after Vaccination
As with any newly licensed vaccine, surveillance for rare adverse events associated with administration of Tdap is important for assessing its safety in large-scale use. The National Childhood Vaccine Injury Act of 1986 requires health-care providers to report specific adverse events that follow tetanus, diphtheria, or pertussis vaccination. A table of reportable events following vaccination is available from VAERS at http://vaers.hhs.gov/reportable.htm. All clinically significant adverse events should be reported to VAERS even if causal relation to vaccination is not certain. VAERS reporting forms and information are available electronically at http://www.vaers.hhs.gov or by telephone, 1-800-822-7967. To promote better timeliness and quality of safety data, providers are encouraged to report electronically by using web-based reporting (https://secure.vaers.orgVaersDataEntryintro.htm).
# Vaccine Injury Compensation Program
VICP is a system established by the National Childhood Vaccine Injury Act of 1986 that enables compensation to be paid on behalf of a person thought to have been injured or died as a result of receiving a vaccine covered by the program. Anyone receiving a covered vaccine, regardless of age, can file * For example, wounds contaminated with dirt, feces, soil, and saliva; puncture wounds; avulsions; and wounds resulting from missiles, crushing, burns, and frostbite. † Adult tetanus and diphtheria toxoids vaccine (Td) is preferred to tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine (Tdap) for pregnant women who have never received Tdap. Tdap is preferred to Td for nonpregnant adults and adolescents who have never received Tdap. In special situations, use of Tdap during pregnancy might be warranted. Health-care providers who choose to administer Tdap during pregnancy should discuss with the women the lack of evidence of safety and effectiveness for the mother, fetus, pregnancy outcome, and the lack of evidence of the effectiveness of transplacental maternal antibodies to provide early pertussis protection to the infant. In addition, no study has examined the effectiveness of transplacental pertussis antibodies induced by Tdap on the adequacy of the infant immune response to pediatric DTaP and conjugate vaccines containing tetanus toxoid or diphtheria toxoid. Because adverse outcomes of pregnancy are most common in the first trimester, vaccinating pregnant women with Tdap during the second or third trimester is preferred to minimize the perception of an association of Tdap with an adverse outcome, unless vaccine is needed urgently. Td is preferred to tetanus toxoid vaccine (TT) for adults who received Tdap previously or who require tetanus protection when Tdap is not available. If TT and tetanus immune globulin (TIG) are both used, tetanus toxoid adsorbed rather than tetanus toxoid (fluid vaccine) should be administered.
a petition under VICP. The program is intended as an alternative to civil litigation under the traditional tort system because negligence need not be proven.
The Act establishes 1) a vaccine injury table that lists the vaccines covered by the program; 2) the injuries, disabilities, and conditions (including death) for which compensation might be paid without proof of causation; and 3) the period after vaccination during which the first symptom or substantial aggravation of the injury must appear. Persons might be compensated for an injury listed in the table or one that can be demonstrated to result from administration of a listed vaccine. All tetanus toxoid-containing vaccines and vaccines with pertussis components (e.g., Tdap, Td, and pediatric DTaP) are covered under the Act. Additional information regarding the program is available at http://www.hrsa.gov/vaccine compensation or by telephone, 1-800-338-2382.
# Areas for Future Research
Interest in vaccinating pregnant women to prevent infant pertussis declined in the late 1940s when whole-cell vaccine trials demonstrated pertussis-specific antibodies in as many as 75% of infants vaccinated starting at birth or in the first few months of life (38,186,188,218,237) and infant and childhood vaccination was adopted as the primary national strategy for protection against childhood diseases (419,420). Aside from initiatives to eliminate neonatal tetanus and more recently to prevent influenza during pregnancy, limited attention has been focused on vaccinating pregnant women as a strategy to prevent disease in the women and their infants during the first few months of life (290,(421)(422)(423)(424)(425)(426)(427)(428)(429)(430). A major barrier to conducting vaccine trials in pregnant women is the potential liability from expected adverse pregnancy outcomes that might be related temporally to vaccination (388,431,432). However, the high morbidity and mortality of certain infections that affect pregnant women and neonates warrant renewed consideration of the strategy of vaccinating pregnant women.
Ensuring the safety of vaccination for mother and fetus and for pregnancy outcomes is a public health priority. In addition, important considerations include understanding whether a degree of protection might be achieved for the mother and for her newborn by vaccinating during pregnancy, whether maternal vaccination would be required with each pregnancy to achieve these benefits (if any), and whether change in the levels of transplacental maternal antibody might affect infant responses to routine vaccination (159,222,224,228). Because few vaccines are currently recommended for pregnant women (e.g., Td and influenza), the effects of the transplacental maternal antibodies on the subsequent infant responses to rou-tine vaccination with the same antigens are not known for most vaccines. Change in the levels of transplacental antibody can affect infant susceptibility to disease at a population level. For example, a decrease over time in the level of transplacental maternal antibody from women who were immunized with measles vaccine during childhood (rather than by measles disease) resulted in susceptibility to measles among their infants at an earlier age, and to the decision to recommend infant measles vaccination at age 12 months rather than age 15-18 months in the United States (228,433,434).
Major gaps exist in the knowledge of how best to prevent pertussis in early infancy. These include 1) the safety of pertussis vaccines for pregnant women, their fetuses, and pregnancy outcomes; 2) the immunogenicity of acellular pertussis vaccines in pregnant women and transplacental maternal antibodies with respect to the timing of immunization during pregnancy; 3) the degree and duration of protection against pertussis in early infancy through transplacental maternal antibodies; and 4) the effects of transplacental maternal antibodies (induced by pertussis, DTP, DTaP, and/or Tdap) on the infant responses to active immunization with pediatric DTaP and conjugate vaccines containing tetanus toxoid or diphtheria toxoid (159,222,234,235,435). To understand the range of options for protecting women and infants from pertussis, studies are needed to determine the safety and any benefits of accelerated infant pertussis vaccination schedules or dosing (e.g., pertussis vaccination starting at birth or employing acellular vaccines that do not contain diphtheria toxoid and tetanus toxoid) (221,436,437). Alternative infant vaccination strategies examined independently or in conjunction with vaccinating pregnant women will determine the most effective and practical approaches to reduce the morbidity and mortality of pertussis.
Alternatively, health-care providers may choose to administer Tdap instead of Td during pregnancy (see Considerations for Use of Tdap in Pregnant Women in Special Situations).
# Postpartum Tdap When <2 Years Have Elapsed Since the Most Recent Dose of Td
Health-care providers should obtain a history of adverse reaction after previous doses of vaccines containing tetanus and diphtheria toxoids. Limited information is available concerning the risk for local and systemic reactions after Tdap at intervals of <2 years. Providers may choose to administer Tdap to these women postpartum for protection against pertussis after excluding a history of moderate to severe adverse reactions following previous tetanus and diphtheria-toxoidscontaining vaccines.
Health-care providers should encourage vaccination of household and child care provider contacts of infants aged <12 months. Women should be advised of the symptoms of pertussis and the effectiveness of early antimicrobial prophylaxis, if pertussis is suspected.
# Considerations for Use of Tdap in Pregnant Women in Special Situations
ACIP recommends that Td be administered when booster protection is indicated during pregnancy. Health-care providers may choose to administer Tdap instead of Td during pregnancy to add protection against pertussis in situations when Td cannot be delayed until delivery or when the risk for pertussis is increased. In such cases, the women should be informed of the lack of data on safety, immunogenicity, and pregnancy outcomes for pregnant women who receive Tdap. Whether administration of Tdap to pregnant women results in protection of the infant against pertussis through transplacental maternal antibodies is unknown. Maternal antibodies might interfere with the infant's immune response to infant doses of DTaP or conjugate vaccines containing tetanus toxoid or diphtheria toxoid.
If Tdap is administered, the second or third trimester is preferred unless protection is needed urgently. Providers are encouraged to report Tdap administrations regardless of trimester to the appropriate manufacturers' pregnancy registry: for ADACEL, ® to sanofi pasteur, telephone 1-800-822-2463 (1-800-VACCINE) and for BOOSTRIX, ® to GlaxoSmithKline Biologicals, telephone 1-888-825-5249.
# Tetanus Prophylaxis for Wound Management
ACIP recommends administration of a Td booster for wound management in pregnant women in certain situations if >5 years have elapsed since the previous Td. Health-care providers may choose to administer Tdap instead of Td during pregnancy to add protection against pertussis in these situations. In such cases, the women should be informed of the lack of data on safety, immunogenicity, and pregnancy outcomes for pregnant women who receive Tdap (see Considerations for Use of Tdap in Pregnant Women in Special Situations).
# Pregnant Women with Unknown or Incomplete Vaccination
Pregnant women who have not received 3 doses of a vaccine containing tetanus and diphtheria toxoids should complete a series of three vaccinations, including 2 doses of Td during pregnancy, to ensure protection against maternal and neonatal tetanus. The preferred schedule in pregnant women is 2 doses of Td separated by 4 weeks and 1 dose of Tdap administered 6 months after the second dose (postpartum). Health-care providers may choose to substitute a single dose of Tdap for a dose of Td during pregnancy. In such cases, the women should be informed of the lack of data on safety, immunogenicity, and pregnancy outcomes for pregnant women who receive Tdap (see Considerations for Use of Tdap in Pregnant Women in Special Situations).
# Reporting Adverse Events after Vaccination
All clinically significant adverse events should be reported to VAERS even if a causal relation to vaccination is uncertain. VAERS reporting forms and information are available at http://www.vaers.hhs.gov or by telephone, 1-800-822-7967. Providers are encouraged to report adverse events electronically at https://secure.vaers.org/VaersDataEntryintro.htm.
# Acknowledgments
This report was prepared in collaboration with ACIP's Pertussis Working Group and consultants from academic institutions, state health departments, other federal agencies, and private industry.
# Contraindications to Administration of Td and Tdap
The following conditions are contraindications to administration of Td and Tdap:
• a history of serious allergic reaction (i.e., anaphylaxis) to any component of the vaccine, or • for Tdap (but not Td), a history of encephalopathy (e.g., coma or prolonged seizures) not attributable to an identifiable cause within 7 days of administration of a vaccine with pertussis components.
# Precautions and Reasons to Defer Administration of Td or Tdap
The following conditions are reasons to defer administration of Td or Tdap:
• Guillain-Barré syndrome with onset 6 weeks or less after a previous dose of tetanus toxoid-containing vaccine; • moderate or severe acute illness; • a history of an Arthus reaction to tetanus toxoid-and/or diphtheria toxoid-containing vaccine less than 10 years previously; • for adults, unstable neurologic conditions (e.g., cerebrovascular events or acute encephalopathic conditions); or
• for adolescents, any progressive neurologic disorder, including progressive encephalopathy or uncontrolled epilepsy (until the condition has stabilized).
# Special Situations
Deferring Td During Pregnancy to Substitute Tdap in the Immediate Postpartum Period ACIP recommends administration of Td for booster vaccination during pregnancy if 10 years or more have elapsed since a previous Td booster. To add protection against pertussis, health-care providers may defer the Td vaccination during pregnancy and substitute Tdap as soon as feasible after delivery if the woman is likely to have sufficient tetanus and diphtheria protection until delivery. Sufficient tetanus protection is likely if:
• a pregnant woman aged <31 years has received a complete childhood series of immunization (4-5 doses of pediatric DTP, DTaP, and/or DT) and >1 Td booster dose during adolescence or as an adult (a primary series consisting of 3 doses of Td (or TT) administered during adolescence or as an adult substitutes for the childhood series of immunization),* • a pregnant woman aged >31 years has received a complete childhood series of immunization (4-5 doses of pediatric DTP, DTaP, and/or DT) and >2 Td booster doses, • a primary series consisting of 3 doses of Td (or TT) was administered during adolescence or as an adult substitute for the childhood series of immunization,* or • a pregnant woman has a protective level of serum tetanus antitoxin (>0.1 IU/mL by ELISA). A woman should receive Td during pregnancy if she • does not have sufficient tetanus immunity to protect against maternal and neonatal tetanus, or • requires booster protection against diphtheria (e.g., for travel to an area in which diphtheria is endemic † ).
* Women who have had a 3-dose series as TT instead of Td will likely have protection against tetanus but might not be protected against diphtheria. A protective titer of diphtheria antitoxin is >0.1 IU/mL by ELISA. † A list of areas in which diphtheria is endemic is available at www.cdc.gov/ travel/diseases/dtp.htm.
# Appendix B Abbreviations Used in This Report
| None | None |
f32aac42f320cd6ce2a67e53f74ecb2cf1d1aaa0 | cdc | None | This report will not include any discussion of the unlabeled use of a product or a product under investigational use with the exception of the discussion of off-label use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine (Tdap) by all in the following situations: A. The interval between pediatric DTP/DTaP/DT or Td and Tdap might be shorter than the 5 years indicated in the package insert; B. Progressive neurologic disorders and uncontrolled epilepsy are considered precautions and not contraindications as indicated in the package insert; C. Tdap might be used as part of the primary series for tetanus and diphtheria; and D.Inadvertent administration of Tdap and pediatric DTaP is discussed.# Introduction
Pertussis, an acute, infectious cough illness, remains endemic in the United States despite routine childhood pertussis vaccination for more than half a century and high coverage levels in children for more than a decade (1)(2)(3)(4). A primary reason for the continued circulation of Bordetella pertussis is that immunity to pertussis wanes approximately 5-10 years after completion of childhood pertussis vaccination, leaving adolescents and adults susceptible to pertussis (5)(6)(7)(8)(9)(10). Among the diseases for which universal childhood vaccination has been recommended, pertussis is the least well-controlled reportable bacterial vaccine-preventable disease in the United States (11,12).
In the United States during 1934-1943, an annual average of 200,752 pertussis cases and 4,034 pertussis-related deaths were reported (13). After the introduction of childhood pertussis vaccination during the 1940s, the number of reported pertussis cases declined dramatically, reaching an historic low of 1,010 in 1976 (Figure 1) (1). Since the 1980s, the number of reported pertussis cases has been steadily increasing, especially among adolescents and adults (4,14,15). Possible reasons for the increase in reported pertussis cases include a true increase in the burden of disease and an increase in the detection and reporting of cases; the relative contribution of each of these factors to the increase observed is unclear (4,(14)(15)(16)(17).
# Childhood Pertussis Vaccination Policy in the United States
Whole cell pertussis vaccines became available during the 1920s (18), but pediatric diphtheria and tetanus toxoids and whole cell pertussis vaccine (DTP) was not routinely recommended for children until the 1940s and 1950s (19,20). In 1991, less reactogenic pediatric acellular pertussis vaccine (diphtheria and tetanus toxoids and acellular pertussis vaccine ) was first licensed for use in children for the fourth and fifth doses of the 5-dose childhood vaccination series in the United States (21,22), and in 1996, pediatric DTaP was licensed for the first three infant doses (1). In 1997, the Advisory Committee on Immunization Practices (ACIP) recommended that pediatric DTaP be used routinely instead of pediatric DTP as a 5-dose DTaP schedule at ages 2, 4, 6, 15-18 months and 4-6 years (1,23); pediatric DTP has not been available in the United States since 2002 (CDC, unpublished data, 2005).
# Childhood and Adolescent Tetanus and Diphtheria Vaccination Policy in the United States
Vaccination against tetanus and diphtheria has markedly reduced the number of cases and deaths from tetanus and diphtheria in the United States in all age groups (24). From 1997 through spring 2005, three vaccine formulations against tetanus and diphtheria were recommended for use in the United States: pediatric DTaP routinely for children aged 7 years (1,24) (Appendix A). The formulation of choice for vaccination of persons aged >7 years has been Td rather than pediatric DT because the lower diphtheria toxoid antigen content of Td induces an adequate immune response and lower rates of adverse reactions in adults than pediatric DT (24)(25)(26)(27)(28).
To provide continued protection against tetanus and diphtheria, ACIP recommended a booster dose of Td for adolescents (24). Before 1995, the adolescent Td booster was recommended at age 14-16 years, approximately 10 years after completion of the childhood DTP series. In 1995, the first harmonized childhood vaccination schedule endorsed by ACIP, the American Academy of Pediatrics, and the American Academy of Family Physicians recommended lowering the age for Td administration to 11-12 years, but vaccination at age 14-16 years was also acceptable (29). In 1996, ACIP, in collaboration with partner organizations, recommended a routine vaccination visit at age 11-12 years to reduce adolescent morbidity associated with vaccine-preventable diseases and to improve vaccine coverage for adolescents (30). The 1996 ACIP statement emphasized that the recommended age for Td administration was 11-12 years, if at least 5 years had elapsed since administration of the last pediatric DTP/DTaP dose. Td also was recommended for older adolescents who missed the Td dose at age 11-12 years. In some states, school attendance laws continue to require that adolescents receive the Td dose 10 years after the last tetanus and diphtheria toxoids-containing vaccine, rather than at age 11-12 years (CDC, unpublished data, 2005). After the adolescent Td booster dose, ACIP has recommended Td boosters every 10 years throughout life (24,31). 1922 1930 1940 1950 1960 1970 1980 1990
# Licensure of Pertussis Vaccines for Use in Adolescents and Adults in the United States
In spring 2005, two tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine (Tdap) products were licensed in the United States for use in adolescents (and, for one product, use in adults) (32,33). The pertussis antigen composition of the adolescent and adult Tdap formulations is similar to pediatric DTaP, but some of the pertussis antigens are reduced in quantity. The tetanus and diphtheria toxoid composition of Tdap is similar to licensed adult formulations of Td (Appendix A). No preparation containing pertussis antigens alone is licensed in the United States. Acellular pertussis vaccines formulated for adolescents and adults have been available for use in other countries, including Canada, Australia, and several European countries (e.g., France, Austria and Germany) (10,(34)(35)(36)(37)(38)(39)(40).
# Background: Pertussis General Clinical Characteristics
Pertussis is an acute respiratory infection caused by Bordetella pertussis, a fastidious gram-negative coccobacillus. The organism elaborates toxins that damage respiratory epithelial tissue and have systemic effects, including promotion of lymphocytosis (41,42). Other species of Bordetella, including B. parapertussis, and less commonly B. bronchiseptica or B. holmesii, are associated with cough illness; the clinical presentation of B. parapertussis can be similar to that of classic pertussis. Illnesses caused by species of Bordetella other than B. pertussis are not preventable by pertussis vaccines (43).
Factors that affect the clinical presentation of pertussis include age, the level of immunity, and use of antimicrobials early in the course of the illness (44). The usual incubation period for pertussis is 7-10 days (range: 5-21 days) (20,44,45). Classic pertussis is characterized by three phases of illness: catarrhal, paroxysmal, and convalescent (20,44,45). During the catarrhal phase, which generally lasts 1-2 weeks, infected persons experience coryza and an intermittent cough; high fever is uncommon. The paroxysmal phase usually lasts 4-6 weeks and is characterized by spasmodic cough, posttussive vomiting, and inspiratory whoop. Absolute lymphocytosis is common in unvaccinated children (46). Symptoms slowly improve during the convalescent phase, which generally lasts 2-6 weeks, but can last months. Complications can occur during the course of pertussis, including hypoxia, pneumonia, weight loss, seizures, encephalopathy, and death (20,41,44,47).
Infants aged <12 months with pertussis are more likely than older age groups to have complications or be hospitalized during their illness (16,47,48). During 2000During -2004, an average of 2,488 cases of pertussis was reported annually among infants aged <12 months. Among these infants, 63% were hospitalized, and the median duration of hospitalization was 5 days (range: 1-152 days) (CDC, unpublished data, 2005). Two to 3 doses of pediatric DTaP (recommended at ages 2, 4, and 6 months) provide protection against severe pertussis (16,48,49). Young infants, who can present with symptoms of apnea and bradycardia without cough, are at highest risk for death from pertussis (16,47,48). During 1980During -2004, a total of 223 pertussis-related deaths in infants aged <4 months were reported to CDC (of 280 in all age groups) (48, CDC, unpublished data, 2005). Of the 100 pertussis-related deaths reported during 2000-2004, a total of 90 (90%) were among young infants aged <4 months and 76 (76%) were among infants aged <2 months (CDC, unpublished data, 2005).
B. pertussis is primarily transmitted from person to person through large respiratory droplets generated by coughing or sneezing. Persons with pertussis are most infectious during the catarrhal and early paroxysmal phases of illness (20,50). The disease is highly communicable, with attack rates as high as 80%-90% among nonimmune household contacts (20,24,44). Adolescents with pertussis can transmit the disease to infants. A study conducted using enhanced pertussis surveillance during 1999-2002 investigated the source of pertussis among infants aged <12 months. On the basis of parental interview, a source was identified among 264 (43%) of 616 infant cases. An adolescent (defined in the study as a person aged 10-19 years) was identified as the source for 43 (7%) of the 616 infants (51).
# Clinical Features and Morbidity Among Adolescents with Pertussis
The spectrum of disease caused by B. pertussis in adolescents ranges from mild cough illness to classic pertussis; infection also can be asymptomatic. When presentation is not classic, pertussis can be clinically indistinguishable from other respiratory illnesses. Adolescents reported with pertussis commonly experience a prolonged cough illness and sometimes have complications (Table 1); rates of certain clinical characteristics and complications in these types of studies probably are higher than among all adolescents with pertussis because the cases with a more classic presentation are more likely to be diagnosed and reported (52-54;CDC, unpublished data, 2005). Complications and hospitalizations related to pertussis occur in up to 2% of adolescents reported with pertussis (52,54;CDC, unpublished data, 2005). Pertussis-related deaths are rarely reported among adolescents; in the United States during 1990-2004, two pertussis-related deaths among adolescents aged 11-18 years were reported to CDC (one adolescent with malignancy and one adolescent with severe neurologic impairment) (CDC, unpublished data, 2005). A prolonged cough is a common feature of pertussis in adolescents. A study in Quebec, Canada, indicated that 97% of adolescents with pertussis coughed for >3 weeks, and 47% coughed for >9 weeks (52). Massachusetts surveillance data demonstrated that 38% of adolescents with pertussis reported during 1989-2004 had already been coughing for >1 month at the time of diagnosis (Massachusetts Department of Public Health , unpublished data, 2005).
Adolescents with pertussis often make repeated visits for medical care. Of approximately 7,000 Massachusetts adolescents with pertussis reported during 1989-2004, 41% had one, 32% had two, and 24% had three or more medical visits during their illness (MDPH, unpublished data, 2005). Adolescents with pertussis and their household contacts frequently miss school or work. Of Massachusetts adolescents with pertussis, 83% missed school (mean: 5.5 days; range: 0.4-32 days). In 43% of households with an affected adolescent, one parent or caretaker missed work (mean: 2.4 days, range: 0.1-25), and in 14% of households, a second parent or caretaker missed work (mean: 1.8 days, range: 0.1-11 days) (54).
# Pertussis Diagnosis
Many factors affect the sensitivity, specificity, and interpretation of diagnostic tests for B. pertussis, including the stage of the disease, antimicrobial administration, previous vaccination, the quality of technique used to collect the specimen, transport conditions to the testing laboratory, experience of the laboratory, contamination of the sample, and use of nonstandardized tests (55,56). In addition, tests and specimen collection materials might not be readily available to practicing clinicians.
Isolation of B. pertussis by culture is 100% specific; however, sensitivity of culture varies because fastidious growth requirements make it difficult to transport and isolate the organism. Although the sensitivity of culture can reach 80%-90% under optimal conditions, in practice, sensitivity typically ranges from 30%-60% (57). The yield of B. pertussis from culture declines in specimens taken after 2 or more weeks of cough illness, after antimicrobial treatment, or after previous pertussis vaccination (58). Within 3 weeks after onset of cough, culture is only 1%-3% sensitive (59). Although B. pertussis can be isolated in culture as early as 72 hours after plating, it takes 1-2 weeks before a culture result can definitively be called negative (60). Culture is essential to isolate B. pertussis for antimicrobial susceptibility testing and for molecular subtyping of strains.
Direct fluorescent antibody (DFA) tests provide rapid results (hours), but are generally less sensitive (sensitivity: 10%-50%) than culture. With use of monoclonal reagents, the specificity of DFA should generally be >90%; however, the interpretation of the test is subjective, and interpretation by an inexperienced microbiologist can result in lower specificity (61). Because of the limitations of DFA testing, CDC does not recommend its use. Because of increased sensitivity and shorter turn-aroundtime, DNA amplification (e.g., polymerase chain reaction ) is being used more frequently to detect B. pertussis. When symptoms of classic pertussis are present (e.g., 2 weeks of paroxysmal cough), PCR typically is 2-3 times more likely than culture to detect a positive B. pertussis sample (56,62,63). The interpretation of PCR-positive but culture-negative samples as either true positive or false positive is difficult. No U.S. Food and Drug Administration (FDA)-licensed PCR test kit and no national standardized protocols, reagents, and reporting formats are available. Approximately 100 different PCR protocols have been reported. These vary by DNA purification techniques, PCR primers, reaction conditions, and product detection methods (63). Laboratories must develop and validate their own PCR tests. As a result, the analytical sensitivity, accuracy, and quality control of PCR-based B. pertussis tests might vary widely among laboratories. The majority of laboratory validation studies have not sufficiently established the predictive value of a positive PCR test to diagnose pertussis (63). Use of PCR tests with low specificity can result in unnecessary investigation and treatment of persons with false-positive PCR test results and inappropriate chemoprophylaxis of their contacts (63). CDC Council of State and Territorial Epidemiologists (CSTE) reporting guidelines support the use of PCR to confirm the diagnosis of pertussis only when the case also meets the clinical case definition (>2 weeks of cough with paroxysms, inspiratory "whoop," or posttussive vomiting) (Appendix B) (64,65).
Diagnosis of pertussis by serology generally requires demonstration of a substantial change in titer for pertussis antigens (usually fourfold) when comparing results from acute (4 weeks after the acute sample). The results of serologic tests on paired sera generally become available late in the course of illness and can provide only retrospective diagnosis. A single sample serologic assay with age-specific antibody reference values is used as a diagnostic test for adolescents and adults in Massachusetts but is not available elsewhere (66). Other singlesample serologic assays lack standardization and do not clearly differentiate immune responses to pertussis antigens after recent clinical disease, from more remote disease, or from vaccination (43). None of these serologic assays, including the Massachusetts assay, is licensed by FDA for routine diagnostic use in the United States. For these reasons, CDC guidelines for laboratory confirmation of pertussis cases do not include serologic testing.
The only pertussis diagnostic tests that the CDC endorses are culture and PCR (when the CDC/CSTE clinical case definition is also met) (Appendix B). CDC-sponsored studies are underway to evaluate both serology and PCR testing. CDC guidance on the use of pertussis diagnostics will be updated as results of these studies become available.
# Incidence of Pertussis Among Adolescents
Pertussis is reportable in all 50 states and the District of Columbia. State health departments report confirmed and probable cases of pertussis to CDC through the passive National Notifiable Diseases Surveillance System (NNDSS); additional information for pertussis cases is collected through the Supplemental Pertussis Surveillance System (SPSS) (Appendix B) (4,16). During 2004, a total of 8,897 (34%) of the 25,827 reported U.S. cases occurred among adolescents aged 11-18 years (incidence for adolescents: 30 per 100,000 population); 17 states each reported >100 pertussis cases in adolescents (12, CDC unpublished data, 2005*). The age distribution of the other pertussis cases reported in 2004 was 3,357 (13%) among infants aged 19 years (the age was unknown for 2.5% of the cases). The incidence of pertussis in adolescents varies widely among states and from year-to-year. During 2000-2004, a total of 11 states had an annual incidence of reported pertussis in adolescents of >50 per 100,000 population during at least 1 year (Table 2) (12, CDC, unpublished data, 2005).
Data from enhanced surveillance sites and prospective studies indicate that the national passive surveillance data sub- stantially underestimate the burden of pertussis among adolescents. Reliable diagnostic tests are not widely available, and not all diagnosed cases are reported. Since the 1980s, MDPH has conducted enhanced surveillance for pertussis throughout Massachusetts. MDPH uses an in-state, standardized serologic assay for pertussis diagnosis in adolescents and adults; educates health-care providers, public health staff, and the general public about pertussis; and intensifies surveillance around cases, particularly in school settings (17,66;MDPH, unpublished data, 2005). During 1996-2004, the average annual incidence of pertussis in Massachusetts adolescents aged 11-18 years was 93 per 100,000 population, approximately 13 times greater than the incidence of 7.3 reported for adolescents in the remainder of the United States (Figure 2); reported rates among children aged <11 years were comparable between Massachusetts and the remainder of the United States (CDC, unpublished data, 2005). Massachusetts data indicated that 62% of reported pertussis cases in adolescents occurred before age 16 years, and 28% of reported cases occurred before age 14 years, suggesting that pertussis booster vaccination early in adolescence could have a substantial impact on the burden of pertussis in adolescents (Figure 3) (CDC, unpublished data, 2005).
Two prospective studies in the United States have assessed the incidence of pertussis in populations that included adolescents (67,68). In a Minnesota health maintenance organization during 1995-1996, persons aged 10-49 years were tested for pertussis if they presented with an acute paroxysmal cough or a persistent cough illness of 7-34 days duration (67). Cases were laboratory-confirmed using culture, PCR, and/or serology. On the basis of 27 identified cases, the estimated incidence of laboratory-confirmed pertussis in this study was 507 per 100,000 person-years, and the incidence in adolescents (estimated 997 per 100,000 person-years) was the highest of the age groups studied (67). During 1997-2000, a study conducted at sites in eight states estimated the incidence of pertussis among persons aged 15-64 years enrolled in the control arm of an acellular pertussis vaccine trial (68). The incidence of pertussis, defined as an acute cough illness of at least 5 days with laboratory confirmation, by culture, PCR, and/or serology, was 370 per 100,000 person-years. Applying less specific case definitions, the study suggested approximately 1,000,000 cases of pertussis occur annually among persons aged >15 years in the United States (68).
# Pertussis Outbreaks Involving Adolescents
High rates of pertussis in adolescents have been reported during community and statewide outbreaks. For example, in a 1985 outbreak that occurred in a three-county region in semirural central Wisconsin, 32% of 161 cases of pertussis occurred in adolescents aged 10-19 years for an incidence (using only culture-positive cases, the strictest case definition for confirmed cases) of 150 per 100,000 population during the 8-month outbreak period (69). Compared with the incidence of pertussis in other age groups, the incidence of pertussis in adolescents was second only to that in infants aged <1 year (496 per 100,000 population) (69). In a statewide 1996 outbreak in Vermont, younger adolescents aged 10-14 years accounted for 36% of 280 cases and had the highest incidence (235 per 100,000 population) of all age groups during the outbreak period (70).
Reported cases of pertussis in adolescents often occur in outbreaks at middle and high schools, where close interaction occurs among large numbers of students with waning vaccine- Age (yrs)
# Background: Tetanus and Diphtheria Tetanus
Tetanus is unique among diseases for which vaccination is routinely recommended in that it is noncommunicable. Clostridium tetani spores are ubiquitous in the environment and enter the body through nonintact skin. When inoculated into oxygen-poor sites, such as necrotic tissue that can result from blunt trauma or deep puncture wounds, C. tetani spores germinate to vegetative bacilli that multiply and elaborate tetanospasmin, a potent neurotoxin. Generalized tetanus typically presents with trismus (lockjaw), followed by generalized rigidity caused by painful contractions of the skeletal muscles that can impair respiratory function. Glottic spasm, respiratory failure, and autonomic instability can result in death (73). During 1998-2000, the case-fatality ratio for reported tetanus was 18% in the United States (74).
Following widespread use of tetanus toxoid-containing vaccine during the 1940s, tetanus has become uncommon in the United States, particularly in children and adolescents (73,75). During 1990-2004, a total of 624 tetanus cases were reported; 19 (3%) cases were among adolescents aged 11-18 years (76; CDC, unpublished data, 2005). A 3-dose primary series of tetanus toxoid-containing vaccine generally induces protective levels of antibody for tetanus that persist for >10 years (73). Seroprotective rates for tetanus, defined as an antitetanus concentration >0. 15 (77).
Neonatal tetanus usually occurs as the result of C. tetani infection of the umbilical stump of an infant born to a mother with a maternal antitetanus concentration insufficient to provide protection to the infant (73). Neonatal tetanus is extremely rare in the United States: three cases were reported during 1990-2004. Two of the cases occurred among children born to mothers who had no dose or 1 dose of a tetanus toxoidcontaining vaccine, and the vaccination history of the third mother was unknown (78,79;CDC, unpublished data, 2005).
# Diphtheria
Respiratory diphtheria is an acute and communicable infectious illness caused by toxigenic strains of Corynebacterium diphtheriae, and rarely by toxin-producing C. ulcerans; disease is prevented by vaccination with diphtheria toxoidcontaining vaccines. Respiratory diphtheria is characterized by a grayish-colored adherent membrane in pharynx, palate, or nasal mucosa that can obstruct the airway. In addition, toxinmediated cardiac and neurologic complications can occur (80,81).
Reports of respiratory diphtheria are rare in the United States in all age groups (80,82). During 1998-2004, seven cases of respiratory diphtheria were reported to CDC; one of the cases was imported (11,12). The last culture-confirmed case of respiratory diphtheria in a U.S. adolescent was reported in 1996 (82). Data obtained from the NHANES III serosurvey during 1988-1994 indicated that the prevalence of immunity to diphtheria, defined as an antidiphtheria concentration of >0.1 IU/mL, was approximately 80% among adolescents aged 12-19 years (77).
Exposure to diphtheria remains possible during travel to countries where diphtheria is endemic (information available at ) or from imported cases. Respiratory diphtheria also can occur following exposure to toxin-producing strains of C. ulcerans; some cases have followed contact with dairy animals or consumption of unpasteurized dairy products (80,83). Adherence to the ACIP-recommended schedule for tetanus and diphtheria toxoid-containing boosters among adolescents and adults is important to prevent sporadic cases of respiratory diphtheria. Information about the clinical management of diphtheria, including use of diphtheria antitoxin, and the public health response is available at / default.htm and reviewed elsewhere (24,80,84).
# Tetanus Toxoid, Reduced Diphtheria Toxoid and Acellular Pertussis Vaccines for Adolescents
# Criteria for Tdap Licensure
In the United States, two Tdap products were licensed for use in adolescents and, for one product, use in adults as a single dose booster immunization against tetanus, diphtheria, and pertussis on the basis of clinical trials demonstrating immunogenicity not inferior to U.S.-licensed Td or pediatric DTaP products and an overall safety profile clinically comparable to U.S.-licensed Td products (85,86). In a noninferiority trial, immunogenicity, efficacy, or safety endpoints are demonstrated when a new product is at least as good as a comparator on the basis of a predefined and narrow margin for a clinically acceptable difference between the study groups (87). The efficacy of the tetanus and diphtheria toxoid component of each Tdap was based on the immunogenicity of these antigens compared with U.S.-licensed Td using established serologic correlates of protection (73,81). The percentage of persons achieving seroprotective antitetanus and antidiphtheria concentrations (>0.1 IU/mL) and the booster response to each of these antigens 1 month postvaccination were evaluated.
In contrast to tetanus and diphtheria, no well-accepted serologic or laboratory correlate of protection for pertussis exists (88). A consensus was reached at the 1997 meeting of the Vaccines and Related Biological Products Advisory Committee that clinical endpoint efficacy studies of acellular pertussis vaccines among adolescents or adults were not required for Tdap licensure in these age groups. Rather, the efficacy of the pertussis components of Tdap administered to adolescents and adults could be inferred using a serologic bridge to infants vaccinated with pediatric DTaP during clinical endpoint efficacy trials for pertussis (89). For each Tdap product, the immune response (geometric mean antibody concentration ) of adolescents to each vaccine pertussis antigen after a single dose of Tdap was compared with the immune response of infants after three doses of pediatric DTaP that included the same pertussis components as the Tdap being assessed (32,33). The percentage of adolescents with a booster response to vaccine pertussis antigens exceeding a predefined lower limit for an acceptable booster response also was evaluated.
The safety of Tdap was evaluated by comparing rates of adverse events after vaccination in persons receiving Tdap with those receiving Td. The overall safety profile of Tdap also was assessed.
# Tdap Product Information
Data on immunogenicity and safety for the Tdap products licensed in the United States for use in adolescents (and, for one product, use in adults) are presented separately below. is formulated with reduced quantities of these antigens (Appendix A). Each antigen is adsorbed onto aluminum hydroxide. Each dose of BOOSTRIX ® (0.5 mL) is formulated to contain 5 Lf tetanus toxoid, 2.5 Lf diphtheria toxoid, 8 µg inactivated PT, 8 µg FHA and 2.5 µg PRN. Each dose of BOOSTRIX ® also contains aluminum hydroxide (<0.39 mg aluminum) as the adjuvant, 4.5 mg NaCl, <100 µg residual formaldehyde, and <100 µg polysorbate 80 (Tween 80) per 0.5-mL dose. BOOSTRIX ® contains no thimerosal or other preservative. BOOSTRIX ® is available in two presentations: a prefilled disposable syringe without a needle and a single dose vial. The tip cap and rubber plunger of the needleless prefilled syringe contain dry natural latex rubber; the single dose vial stopper preparation is latex-free (33).
# Immunogenicity and Serologic Bridge to Efficacy for Pertussis
A comparative, observer-blinded, multicenter, randomized controlled clinical trial conducted in the United States evaluated the immunogenicity of the tetanus, diphtheria, and pertussis antigens in BOOSTRIX ® among adolescents aged 10-18 years (33,85). Adolescents were randomized 3:1 to receive a single dose of BOOSTRIX ® or a single dose of Td MPHBL (manufactured by the Massachusetts Public Health Biologic Laboratories; contains diphtheria toxoid and tetanus toxoid ) (33,85). Serum samples were obtained before and approximately 1 month after vaccination (85). All assays were performed by GlaxoSmithKline Biologicals in Rixensart, Belgium, using validated methods (90).
Persons were eligible for enrollment if they were in good health and had completed routine childhood vaccination against diphtheria, tetanus, and pertussis (approximately 98% of persons had received >4 doses of pediatric DTP/DTaP). Persons were excluded if they had received the most recent pediatric DTP/DTaP during the preceding 5 years or Td during the preceding 10 years, had a history of pertussis or household exposure to pertussis during the previous 5 years, had any of the ACIP contraindications or precautions for pediatric DTP/DTaP (91), had systemic allergic or neurologic reac-tions or thrombocytopenia after a dose of tetanus or diphtheria toxoid-containing vaccine, had an acute illness, had received blood products or immunoglobulins within 3 months, had any immunodeficiency, had significant underlying disease, had certain neurologic disorders, or were pregnant (33, 85,92;GSK, unpublished data, 2005).
# Tetanus and Diphtheria
Immune responses to tetanus and diphtheria toxoids were compared between the BOOSTRIX ® (range: 2,463-2,516 persons) and Td MPHBL (range: 814-834 persons) groups. One month postvaccination, the antitetanus seroprotective (>0.1 IU/mL) and booster response rates in adolescents who had received a single dose of BOOSTRIX ® were noninferior to those who received Td MPHBL . All adolescents had seroprotective antitetanus levels >0.1 IU/mL 1 month after vaccination with either BOOSTRIX ® (95% confidence interval = 99.8%-100%) or Td MPHBL (95% CI = 99.6%-100%). The booster response rate to tetanus † in the BOOSTRIX ® group was 89.7% (95% CI = 88.4%-90.8%), compared with 92.5% (95% CI = 90.5%-94.2%) in the Td MPHBL group (33,92).
One month postvaccination, the antidiphtheria seroprotective (>0.1 IU/mL) and booster response rates among adolescents who received a single dose of BOOSTRIX ® were noninferior to those of adolescents who received Td MPHBL . Among adolescents, 99.9% had seroprotective antidiphtheria levels >0.1 IU/mL 1 month postvaccination with either BOOSTRIX ® (95% CI = 99.7%-100%) or Td MPHBL (95% CI = 99.3%-100%). The booster response rate to diphtheria † in the BOOSTRIX ® group was 90.6% (95% CI = 89.4%-91.7%), compared with 95.9% (95% CI = 94.4%-97.2%) in the Td MPHBL group (33,92).
# Pertussis
The efficacy of the pertussis components of BOOSTRIX ® was evaluated by comparing the immune responses of adolescents vaccinated with a single dose of BOOSTRIX ® with the immune responses of infants vaccinated with 3 doses of INFANRIX ® . These infants were a subset of those vaccinated with INFANRIX ® in a German vaccine efficacy trial during the 1990s (33,93). BOOSTRIX ® has the same three pertussis antigens as INFANRIX ® but in reduced quantities (Appendix A). In the infant trial, the efficacy of 3 doses of INFANRIX ® against World Health Organization (WHO)defined typical pertussis (>21 days of paroxysmal cough with confirmation of B. pertussis infection by culture and/or sero- † Booster response: In persons with prevaccination antibody concentration 0.4 IU/mL. In persons with prevaccination antibody concentration >0.1 IU/mL, an increase of at least four times the prevaccination antibody concentration.
logic testing) was 89% (95% CI = 77%-95%) (33,93). The anti-PT, anti-FHA, and anti-PRN GMCs of adolescents 1 month after a single dose of BOOSTRIX ® were noninferior to those of infants after 3 doses of INFANRIX ® (Table 4) (33,85,92). Booster response rates to the pertussis antigens § contained in BOOSTRIX ® (anti-PT, anti-FHA, and anti-PRN) among adolescents (range: 2,677-2,752 persons) 1 month after administration of BOOSTRIX ® met prespecified criteria for an acceptable response. Booster response rates to pertussis antigens were anti-PT, 84.5% (95% CI = 83.0%-85.9%); anti-FHA, 95.1% (95% CI = 94.2%-95.9%), and anti-PRN, 95.4% (95% CI = 94.5%-96.1%) (33,92).
# Safety
The primary safety study, conducted in the United States, was a randomized, observer-blinded, controlled study in which 3,080 adolescents aged 10-18 years received a single dose of BOOSTRIX ® , and 1,034 received Td MPHBL (see BOOSTRIX ® Immunogenicity and Serologic Bridge to Efficacy for Pertussis for inclusion and exclusion criteria). Data on solicited local and systemic adverse events were collected using standardized diaries for the day of vaccination and the next 14 consecutive days (i.e., within 15 days following vaccination). Unsolicited and serious adverse events were collected for 6 months following vaccination. No immediate events (within 30 minutes of vaccination) were reported in either vaccination group (33,85,92).
# Solicited Local Adverse Events
Pain at the injection site was the most frequently reported solicited local adverse event in adolescents vaccinated with BOOSTRIX ® or Td MPHBL . Within 15 days after vaccina-tion, 75.3% of persons in the BOOSTRIX ® group and 71.7% of persons in the Td MPHBL group reported pain of "any" intensity (Table 5). The rates of any pain and grade 2 or 3 pain combined (but not grade 3 alone) were significantly higher (p<0.05) in BOOSTRIX ® recipients compared with Td MPHBL recipients (Table 5). However, the rates of grade 3 pain (primary safety endpoint) were similar in each group, and the noninferiority criterion was met for BOOSTRIX ® compared with Td MPHBL . No significant differences in the rates of other solicited local adverse events (redness, swelling, and increase in arm circumference above baseline) were observed between the two study groups (33, 85,92).
Two adolescents in the study reported "large injection-site swelling" after vaccination (predefined as any local swelling with a diameter >100 mm and/or increased circumference of the injected limb >50 mm above baseline measurements and/or any diffuse swelling that interfered with or prevented normal everyday activities). Both persons had onset of symptoms within 3 days of vaccination. One person who had received BOOSTRIX ® reported grade 3 pain (Table 5) with functional impairment. This person was evaluated and treated with antimicrobials with symptom resolution within 3 days without sequelae. The second person, who had received Td MPHBL , reported grade 1 pain and did not seek medical attention. The duration of symptoms was unknown, but symptoms resolved without sequelae (85,90,92). No cases of wholearm swelling were reported in either vaccine group (GSK, unpublished data, 2005).
# Solicited Systemic Adverse Events
The most frequently reported solicited systemic adverse events within 15 days following vaccination with BOOSTRIX ® or Td MPHBL were headache and fatigue (Table 6). A statistically significantly higher rate of grade 2 or grade 3 headache combined (but not grade 3 alone) (Table 6) was reported in the BOOSTRIX ® group (15.7%), compared with the Td MPHBL group (12.7%). The proportion of adolescents reporting fever >100.4° F (38.0° C) (5.0% for BOOSTRIX ® and 4.7% for Td MPHBL ), fatigue, and gastrointestinal systemic events were comparable in both groups (33,85,92).
# Serious Adverse Events
In the primary U.S. safety study, no serious adverse events (SAEs) occurred within 1 month postvaccination with either BOOSTRIX ® or Td MPHBL . During the next 5 months of monitoring, SAEs were reported among 14 (0.4%) of the 3,005 adolescents vaccinated with BOOSTRIX ® and two (0.2%) of the 1,003 adolescents vaccinated with Td MPHBL . No SAEs that were of potential autoimmune origin, new onset and chronic in nature, or related to vaccination, as determined by the investigators, were reported (33, 85,90,92). No seizures, cases of Guillain-Barré syndrome, or physiciandiagnosed Arthus reactions were reported (33,85,90; GSK, unpublished data, 2005).
# Simultaneous Administration with other Vaccines
Safety and immunogenicity of simultaneous administration of BOOSTRIX ® with other vaccines were not evaluated during prelicensure studies (33).
# Vaccine Composition
ADACEL ™ contains the same tetanus toxoid, diphtheria toxoid, and five pertussis antigens as those in DAPTACEL ® (pediatric DTaP), but ADACEL ™ is formulated with reduced quantities of diphtheria toxoid and detoxified PT (Appendix A). Each antigen is adsorbed onto aluminum phosphate. Each dose of ADACEL ™ (0.5 mL) is formulated to contain 5 Lf tetanus toxoid, 2 Lf diphtheria toxoid, 2.5 µg detoxified PT, 5 µg FHA, 3 µg PRN, and 5 µg fimbriae types 2 and 3 (FIM). Each dose of ADACEL ™ also contains aluminum phosphate (0.33 mg aluminum) as the adjuvant, <5 µg residual formaldehyde, <50 ng residual glutaraldehyde, and 3.3 mg 2-phenoxyethanol (not as a preservative) per 0.5-mL dose. ADACEL ™ contains no thimerosal. ADACEL ™ is available in single dose vials that are latex-free (32).
# Immunogenicity and Serologic Bridge to Efficacy for Pertussis
A comparative, observer-blinded, multicenter, randomized controlled clinical trial conducted in the United States evaluated the immunogenicity of the tetanus, diphtheria, and pertussis antigens in ADACEL ™ among adolescents aged 11-17 years; adults aged 18-64 years were also studied and results are reported elsewhere (32,86). Adolescents were randomized 3:2 to receive a single dose of ADACEL ™ or a single dose of Td sp (manufactured by sanofi pasteur; contains tetanus toxoid and diphtheria toxoid ) (32,86). Sera from a subset of persons were obtained before and approximately 1 month after vaccination (32). All assays were performed at the immunology laboratories of sanofi pasteur in Toronto, Ontario, Canada or Swiftwater, Pennsylvania, using validated methods (86,94).
Persons were eligible for enrollment if they were in good health; completion of the childhood DTP/DTaP vaccination series was not required. Persons were excluded if they had received a tetanus, diphtheria, or pertussis vaccine within 5 years; had a diagnosis of pertussis within 2 years; had an allergy or sensitivity to any vaccine component; had a previous reaction to a tetanus, diphtheria or pertussis vaccine, including encephalopathy within 7 days or seizures within 3 days; had an acute respiratory illness on the day of enrollment; had daily use of oral, nonsteroidal anti-inflammatory drugs; had received blood products or immunoglobulins within 3 months; had any immunodeficiency; had significant underlying disease; had neurologic impairment; or were pregnant (32,94; sanofi pasteur, unpublished data, 2005).
# Tetanus and Diphtheria
Immune responses to tetanus and diphtheria toxoids were compared between the ADACEL ™ (N = 527) and Td sp (range: 515-516 persons) groups. One month postvaccination, the antitetanus seroprotective (>0.1 IU/mL) and booster response rates among adolescents who received ADACEL ™ were noninferior to those who received Td sp . All adolescents (95% CI = 99.3%-100% for both groups) had seroprotective antitetanus levels >0.1 IU/mL 1 month after vaccination with either ADACEL ™ or Td sp . The booster response rate to tetanus ¶ in the ADACEL ™ group was 91.7% (95% CI = 89.0%-93.9%) and 91.3% (95% CI = 88.5%-93.6%) in the Td sp group (32,86,94). One month postvaccination, the antidiphtheria seroprotective (>0.1 IU/mL) and booster response rates among adolescents who received a single dose of ADACEL ™ were noninferior to those who received Td sp . Among adolescents, 99.8% (95% CI = 98.9%-100%) had protective antidiphtheria levels >0.1 IU/mL 1 month after vaccination with either ADACEL ™ or Td sp. The booster response rate to diphtheria ¶ in the ADACEL ™ group was 95.1% (95% CI = 92.9%-96.8%) and 95.0% (95% CI = 92.7%-96.7%) in the Td sp group (32,86,94). ¶ Booster response was defined as a fourfold rise in antibody concentration, if the prevaccination antibody concentration was equal to or below the cutoff value, and a two-fold rise in antibody concentration if the prevaccination antibody concentration was above the cut-off value. The cut-off value for tetanus was 2.7 IU/mL. The cut-off value for diphtheria was 2.56 IU/mL.
# Pertussis
The efficacy of the pertussis components of ADACEL ™ was evaluated by comparing the immune responses of adolescents vaccinated with a single dose of ADACEL ™ with the immune responses of infants vaccinated with 3 doses of DAPTACEL ® in a Swedish vaccine efficacy trial during the 1990s (32,95). ADACEL ™ and DAPTACEL ® contain the same five pertussis antigens, except ADACEL ™ contains one fourth the quantity of detoxified PT in DAPTACEL ® (96) (Appendix A). In the Swedish trial, efficacy of 3 doses of DAPTACEL ® against WHO-defined pertussis (>21 days of paroxysmal cough with confirmation of B. pertussis infection by culture and/or serologic testing or an epidemiologic link to a household member with culture-confirmed pertussis) was 85% (95% CI = 80%-89%) (29,87). The anti-PT, anti-FHA, anti-PRN, and anti-FIM GMCs of adolescents 1 month after a single dose of ADACEL ™ were noninferior to those of infants following three doses of DAPTACEL ® (32,94) (Table 7).
Booster response rates to the pertussis antigens contained in ADACEL ™ (anti-PT, anti-FHA, anti-PRN, anti-FIM) among adolescents (range: 524-526 persons) 1 month fol-lowing administration of ADACEL ™ met prespecified criteria for an acceptable response. Booster response rates to pertussis antigens were anti-PT, 92.0% (95% CI = 89.3%-94.2%); anti-FHA, 85.6% (95% CI = 82.3%-88.4%); anti-PRN, 94.5% (95% CI = 92.2%-96.3%); and anti-FIM 94.9% (95% CI = 92.6%-96.6%) (32,94).
# Safety
The primary adolescent safety study, conducted in the United States, was a randomized, observer-blinded, controlled study in which 1,184 adolescents aged 11-17 years received a single dose of ADACEL ™ and 792 received Td sp (see ADACEL ™ Immunogenicity and Serologic Bridge to Efficacy for Pertussis for inclusion and exclusion criteria) (32). Adults aged 18-64 years were also studied; those results are reported elsewhere (32). Data on solicited local and systemic adverse events were collected using standardized diaries for the day of vaccination and the next 14 consecutive days (i.e., within 15 days following vaccination) (32).
# Immediate Events
Eleven adolescents experienced immediate events within 30 minutes of vaccination (ADACEL ™ , six persons and Td sp , five persons ); all events resolved without sequelae. Immediate events included dizziness, syncope, or vasovagal reactions and pain and erythema at the injection site. No anaphylaxis was reported (86,94,96).
# Solicited Local Adverse Events
Pain at the injection site was the most frequently reported solicited local adverse event among adolescents in both vaccination groups (Table 8). Within 15 days following vaccination, reports of pain of "any" intensity were more common among adolescents vaccinated with ADACEL ™ (77.8%) than among those vaccinated with Td sp (71.0%). The noninferiority criterion was not achieved for the rate of any pain following ADACEL ™ compared with the rate following Td sp . Rates of moderate/severe pain, erythema, and swelling following ADACEL ™ were comparable to the rates following Td sp (32,86,94). No cases of whole-arm swelling were reported in either vaccine group (94).
# Solicited Systemic Adverse Events
The most frequently reported solicited systemic adverse events within the 15 days following vaccination were headache, generalized body aches, and tiredness (Table 9). The proportion of adolescents reporting fever >100.4° F (>38° C) following vaccination was statistically significantly higher among adolescents vaccinated with ADACEL ™ (5.0%) than Td sp (2.7%), but noninferiority criterion for ADACEL ™ was A booster response for each antigen was defined as a fourfold rise in antibody concentration, if the prevaccination antibody concentration was equal to or below the cut-off value, and a twofold rise in antibody concentration if the prevaccination antibody concentration was above the cut-off value. The cut-off values for pertussis antigens were 85 EU/mL for pertussis toxin, 170 EU/mL for filamentous haemagglutinin, 115 EU/mL for pertactin, and 285 EU/mL for fimbriae. achieved. The rates of the other solicited systemic adverse events were comparable between the ADACEL ™ and Td sp groups (32,94).
# Serious Adverse Events
In the primary adolescent safety study, SAEs within 6 months after vaccination were reported among 11 (0.9%) of the 1,184 adolescents aged 11-17 years vaccinated with ADACEL ™ and eight (1.0%) of the 792 adolescents vaccinated with Td sp . Two adolescents (one ADACEL ™ recipient and one Td sp recipient) reported seizure events after vaccination; both persons had a history of seizure disorder. SAEs in adolescents were reported by the study investigators to be unrelated to the study vaccine (94).
The safety of ADACEL ™ among adults also was studied. In the primary adult safety study, SAEs within 6 months after vaccination were reported among 33 (1.9%) of the 1,752 adults aged 18-64 years vaccinated with ADACEL ™ and 11 (1.9%) of the 573 adults vaccinated with Td sp . Two of these SAEs were neuropathic events in ADACEL ™ recipients and were assessed by the investigators as possibly related to the study vaccine; in both cases, the symptoms resolved completely over several days (32,86,94,96). No physician-diagnosed Arthus reactions or cases of Guillain-Barré syndrome were reported in any adolescent or adult (32,86,96; sanofi pasteur, unpublished data, 2005).
# Simultaneous Administration with Other Vaccines
# Hepatitis B Vaccine
Safety and immunogenicity of ADACEL ™ co-administered with hepatitis B vaccine (Recombivax HB ® , Merck and Co., Inc., White House Station, New Jersey) was evaluated in adolescents aged 11-14 years using methods similar to the primary ADACEL ™ studies. Adolescents were randomized to one of two groups. In one group, ADACEL ™ and hepatitis B vaccine were administered simultaneously in different arms (simultaneous group; N = 206). In the other group, ADACEL ™ was administered first, followed by hepatitis B vaccine 4-6 weeks later (sequential group; N = 204) (32; sanofi pasteur, unpublished data, 2005). No interference was observed in the immune responses to any of the vaccine antigens when ADACEL ™ and hepatitis B vaccine were administered simultaneously or sequentially † † (32).
Adverse events were solicited only after ADACEL ™ vaccination (not hepatitis B vaccination) (86). Within 15 days of vaccination, the reported rates of injection site pain (at the ADACEL ™ site) and fever were comparable when ADACEL ™ and hepatitis B vaccine were administered simultaneously or sequentially (Table 10). However, rates of erythema and swelling at the ADACEL ™ injection site were higher in the simultaneous group than the sequential group, and noninferiority criteria for simultaneous vaccination were not achieved (Table 10) (86). Swollen and/or sore joints were reported in 22.5% of persons in the simultaneous group and 17.9% of persons in the sequential group. Most joint com-plaints were mild in intensity and the mean duration was 1.8 days (86).
# Trivalent Inactivated Influenza Vaccine
Safety and immunogenicity of ADACEL ™ co-administered with trivalent inactivated influenza vaccine ( Fluzone ® , sanofi pasteur, Swiftwater, Pennsylvania) was evaluated in adults aged 19-64 years using methods similar to the primary ADACEL ™ studies (32). The immunogenicity data are presented elsewhere (32). The adults were randomized to one of ¶ The rate of "Any" fever following ADACEL ™ was statistically higher than the rate following Td sp in the adolescents; however, the noninferiority criterion was achieved for ADACEL ™ (upper limit of the 95% confidence interval on the difference in the percentage of persons was <10%).
two groups. In one group, ADACEL ™ and TIV were administered simultaneously in different arms (simultaneous group; N = 359). In the other group, TIV was administered first, followed by ADACEL ™ 4-6 weeks later (sequential group; N = 361) (32; sanofi pasteur, unpublished data, 2005). Adverse events were solicited only after ADACEL ™ vaccination (not TIV) (86). Within 15 days of vaccination, rates of erythema, swelling, and fever were comparable in both vaccination groups. However, the rate of pain at the ADACEL ™ injection site was higher in the simultaneous group (66.6%) than the sequential group (60.8%), and did not meet the noninferiority criterion (upper limit of the 95% CI on the difference in percentage of persons was 13.0%, and the criterion was <10%) (86).
# Other Vaccines
Safety and immunogenicity of simultaneous administration of ADACEL ™ with other vaccines were not evaluated during prelicensure studies (32).
# Studies of Adolescent Acellular Pertussis Vaccine Impact Clinical Efficacy Trial
The efficacy against pertussis of an adolescent and adult acellular pertussis (ap) vaccine with the same pertussis antigens included in BOOSTRIX ® (without tetanus and diph-theria toxoids) was evaluated in 2,781 adolescents and adults in a prospective, randomized trial (68). Results of this study were not considered as part of Tdap licensure in the United States (see Criteria for Tdap Licensure). Persons aged 15-64 years were randomized to receive one dose of ap vaccine or hepatitis A vaccine (Havrix ® , GlaxoSmithKline Biologicals, Rixensart, Belgium). The primary outcome measure was confirmed pertussis, defined by a cough illness lasting >5 days with laboratory evidence of B. pertussis infection by culture, PCR, and/or serologic testing results (acute and convalescent). Nine persons in the hepatitis A vaccine control group and one person in the ap vaccine group had confirmed pertussis during the study period; vaccine efficacy against confirmed pertussis was 92% (95% CI = 32%-99%) (68).
# Economic Studies
The societal costs of pertussis are important, and universally vaccinating adolescents against pertussis is likely to be cost effective. In one study, the economic impact of pertussis among Massachusetts adolescents aged 10-17 years was evaluated using the state's enhanced pertussis surveillance system (54). The mean medical cost per adolescent case of pertussis was an estimated $201 and $256 for mild and severe cases of cough illness, respectively (in 2004 dollars), excluding the cost of providing antimicrobials to close contacts of the caseadolescents (53,54). The largest proportion of this cost was for medical office visits and antimicrobial therapy (54). When indirect, nonmedical costs (e.g., missed time from work for parents of adolescents) were included, total societal cost of an adolescent case of pertussis was $361 and $416 for mild and severe cough illness, respectively (in 2004 dollars) (53,54).
Two U.S. economic studies have compared adolescent vaccination with other pertussis vaccination strategies (53,97). Both studies identified a single dose of Tdap during adolescence as the most cost-effective strategy, under different assumptions about pertussis incidence, waning immunity, vaccine efficacy, vaccine coverage, and infant transmission. In the first study, a cost-benefit analysis was conducted to compare seven adolescent and/or adult pertussis vaccination strategies during a 10-year interval (2001-2010), using a single dose of a Tdap. In this analysis, the incidence of pertussis among adolescents and adults was estimated from prospective studies to be 450-507 cases per 100,000 population. Strategies included vaccinating all adolescents aged 10-19 years, vaccinating all persons aged >10 years (i.e., universal adolescent and adult vaccination), vaccinating adolescents and adults aged >15 years that were the primary care-takers of infants, and four other adult vaccination strategies. Among these strategies, vaccinating all adolescents was identified as the most costeffective strategy. Universal adolescent Tdap vaccination was cost-saving to society when the Tdap vaccine and program costs were <$37 (2002 dollars) per adolescent vaccinated (97).
In a second study, six adolescent and/or adult Tdap vaccination strategies were compared by modeling health outcomes over the course of a lifetime for hypothetical cohort of 4 million adolescents (53). Incidence rates of pertussis among adolescents and adults were estimated from Massachusetts surveillance data; baseline estimates were 155 and 11 per 100,000 population for adolescents and adults, respectively. The six strategies included no adolescent or adult vaccination, one-time adolescent vaccination at age 11 years, onetime adult vaccination, adult vaccination with decennial Tdap boosters, adolescent and adult vaccination with decennial Tdap boosters, and postpartum vaccination. The study assumed an incremental increase in Tdap price of $15 compared with Td, with a Tdap vaccination cost of $25 per person vaccinated. Universal adolescent vaccination was the most costeffective strategy. Vaccinating all adolescents once would cost $1,100 per pertussis case prevented or $20,000 per quality adjusted life year (QALY) saved, both in 2004 dollars. By contrast with the cost-benefit analysis (97), which estimated the incidence of pertussis in adolescents to be approximately 3 times higher, Tdap vaccination was not cost-saving under the second study's baseline assumptions (53). In a sensitivity analysis, results from the second study found that if the incidence of adolescent and adult pertussis was four times the base-case estimates, universal adolescent Tdap vaccination would be costsaving to society (53).
# Other Tetanus and Diphtheria Toxoids Vaccine Preparations for Adolescents
Four Td (Tetanus and Diphtheria Toxoids, Adsorbed for Adult Use) vaccines are licensed in the United States for active immunization against tetanus and diphtheria among persons aged >7 years (98)(99)(100)(101). Two tetanus toxoid vaccines (TT) also are licensed for use in this age group (102,103). Of the two TT products, one is adsorbed and is licensed for use in situations in which the combined antigen preparation (Td) is not indicated (102). The second TT preparation is a fluid vaccine (not adsorbed) and is indicated only for booster doses, not for primary immunization (103). Although TT is licensed in the United States for persons aged >7 years, Td has been preferred for routine use to provide dual protection against tetanus and diphtheria (24) (Appendix A).
# Safety Considerations for Adolescent Vaccination with Tdap or Td
Prelicensure Tdap studies support the safety of these vaccines (32,33). However, sample sizes were insufficient to detect rare adverse events, a limitation of prelicensure trials. Enrollment criteria excluded persons who had received vaccines containing tetanus toxoid, diphtheria toxoid, or pertussis components during the preceding 5 or 10 years (85,86,92,94). In addition, persons with certain neurologic conditions or events following pediatric DTP/DTaP vaccination were excluded from these studies (85,92,94). Therefore, in making recommendations on the spacing and administration sequence of vaccines containing tetanus toxoid, diphtheria toxoid, and/or pertussis components and on vaccination of adolescents with a history of certain neurologic conditions or adverse events after vaccination, ACIP considered data from a range of pre-and postlicensure studies of Tdap and other vaccines containing these components. Safety data being collected from the Vaccine Adverse Event Reporting System (VAERS) and postlicensure studies will facilitate detection of potential adverse reactions following widespread use of Tdap in adolescents (see Reporting of Adverse Events after Vaccination) (104,105).
# Spacing and Administration Sequence of Vaccines Containing Tetanus Toxoid, Diphtheria Toxoid, and Pertussis Antigens
Historically, moderate and severe local reactions following tetanus and diphtheria toxoid-containing vaccines have been associated with older, less purified vaccines, larger doses of toxoid, and frequent dosing at short intervals (106)(107)(108)(109)(110)(111). In addition, high pre-existing antibody titers to tetanus or diphtheria toxoids in children, adolescents, and adults primed with these antigens might be associated with increased rates of local reactions to booster doses of tetanus or diphtheria toxoidcontaining vaccines (26,108,111,112). Two adverse events of particular clinical interest have been associated with vaccines containing tetanus toxoid, diphtheria toxoid, and/or pertussis antigens, extensive limb swelling (ELS), and Arthus reactions.
# Extensive Limb Swelling
ELS reactions have been described following doses of pediatric DTaP and other vaccines (28,91,(113)(114)(115)(116)(117). In retrospective analyses, 2%-3% of children receiving the fourth or fifth booster doses of pediatric DTaP experienced extensive proximal limb swelling; swelling is usually greatest by 48 hours after vaccination (28,118). ELS is generally not disabling, is not often brought to medical attention, and resolves without complication within 4-7 days (118). ELS has been reported to VAERS almost as frequently following Td as following pediatric DTaP; among adolescents, the majority of reported cases of ELS have involved either Td or hepatitis B vaccine (117). The pathogenesis of ELS is not well understood; this reaction has not consistently been related to the content of tetanus toxoids, diphtheria toxoids, pertussis antigens, or aluminum adjuvants in vaccines (28,118,119). Whether children who experience ELS after receipt of pediatric DTaP are at increased risk for ELS after receipt of Tdap is unknown. Because these reactions typically resolve without sequelae, ACIP does not consider a history of ELS following pediatric DTaP or any other vaccine to be a precaution or contraindication for pediatric DTaP (91,113).
# Arthus Reactions
Arthus reactions (type III hypersensitivity reactions) are rarely reported after vaccination and can occur after tetanus toxoid-containing or diphtheria toxoid-containing vaccines (24,111,120-124;CDC, unpublished data, 2005). An Arthus reaction is a local vasculitis associated with deposition of immune complexes and activation of complement. Immune complexes form in the setting of high local concentration of vaccine antigens and high circulating antibody concentration (111,120,121,125). Arthus reactions are characterized by severe pain, swelling, induration, edema, hemorrhage, and occasionally by necrosis. These symptoms and signs usually occur 4-12 hours after vaccination; by contrast, anaphylaxis (immediate type I hypersensitivity reactions) usually occur within minutes of vaccination. As with ELS, Arthus reactions usually resolve without sequelae. ACIP has recommended that persons who experienced an Arthus reaction after a dose of tetanus toxoid-containing vaccine should not receive Td more frequently than every 10 years, even for tetanus prophylaxis as part of wound management (24).
# Interval between Td and Tdap
ACIP has recommended a 10-year interval for routine administration of Td and a 5-year minimum interval between the last pediatric DTaP and the adolescent Td dose (24,30). Administration of Td at short intervals might increase the risk for adverse events (108,109). Prelicensure clinical trials of Tdap excluded persons who had received doses of a diphtheria or tetanus toxoid-containing vaccine during the preceding 5 or 10 years (see BOOSTRIX ® and ADACEL ™ sections on Immunogenicity and Serologic Bridge to Efficacy for Pertussis for exclusion criteria) (90,94,96). Although administering Td more often than every 10 years (5 years for a tetanus-prone wound) is not necessary to provide protection against tetanus or diphtheria, administering a dose of Tdap less than 5 years after Td could provide a health benefit by protecting against pertussis.
The safety of administering a dose of Tdap at intervals less than 5 years after pediatric DTP/DTaP or Td was evaluated in Canada following the country's licensure of Tdap (ADACEL ™ ) (126). The largest Canadian study was a nonrandomized, open-label study of 7,001 students aged 7-19 years residing in Prince Edward Island. This study assessed the rates of adverse events after Tdap and compared reactogenicity of Tdap administered at year intervals of 2-9 years (eight cohorts) versus >10 years after the last tetanus and diphtheria toxoid-containing vaccine (Td, or pediatric DTP or DTaP). A year interval was defined as the integer year +0.5 years (e.g., the 2-year interval was defined as >18 months to <30 months). Vaccination history for type of pertussis vaccine(s) received (pediatric DTP and DTaP) also was assessed. The number of persons assigned to cohorts ranged from 464 in the 2-year to 925 in the 8-year cohorts. Among the persons in the 2-year cohort, 214 (46%) received the last tetanus and diphtheria toxoid-containing vaccine 18-23 months before Tdap. Adverse event diary cards were returned for 85% of study participants with a known interval; 90% of persons in the 2-year interval cohort provided safety data (126).
Four SAEs were reported in the Prince Edward Island study; none were assessed by the investigators to be related to vaccine. No Arthus reaction was reported. Rates of reported severe local adverse reactions, fever, and any pain were not increased in persons who received Tdap at intervals less than 10 years. Rates of local reactions were not increased among persons who received 5 doses of pediatric DTP, with or without Td (intervals of 2-3 years or 8-9 years). Rates of any erythema and any swelling were reported more frequently in cohorts that had received at least 1 or 2 doses of pediatric DTaP (intervals of 4-7 years), suggesting that increased rates of local reactions might occur more commonly among adolescents who received pediatric DTaP vaccines, compared with those who received a 5-dose pediatric DTP series. Limb swelling (>100 mm) was reported in 0.2% of participants and was unrelated to the interval since the last tetanus and diphtheria toxoid-containing vaccine (126).
A study was conducted in Germany to evaluate the safety of Tdap (BOOSTRIX ® ) in persons aged 9-13 years who received a 5-dose all acellular pertussis vaccine schedule (5 doses of INFANRIX ® , N = 193 or 4 doses of INFANRIX ® plus another acellular pertussis vaccine, N = 126); the interval from the fifth to sixth dose of the acellular pertussis vaccines ranged from approximately 5-6 years (GSK, unpublished data, 2005). Within 15 days after vaccination, any pain (63.6%), erythema (51.7%), and swelling (41.4%) were frequently reported symptoms, but the rate of "large injection site swelling" (see BOOSTRIX ® , solicited local adverse events for definition) was low (0.9%). Following their sixth consecutive dose of an acellular pertussis vaccine, persons reported more pain, less redness, and less swelling compared with their fifth dose of pediatric DTaP (INFANRIX ® ) (127).
Two smaller Canadian postlicensure safety studies in adolescents also showed acceptable safety when Tdap (ADACEL ™ ) was administered at intervals less than 5 years after tetanus and diphtheria toxoid-containing vaccines (128,129). Taken together, these three Canadian studies support the safety of using Tdap after Td at intervals less than 5 years. The largest study suggests intervals as short as approximately 2 years are acceptably safe (126).
# Simultaneous and Nonsimultaneous Vaccination with Tdap/Td and Diphtheria-Containing Tetravalent Meningococcal Conjugate Vaccine
Tdap, Td, and tetravalent meningococcal conjugate vaccine ( Menactra ® , sanofi pasteur, Swiftwater, Pennsylvania) contain diphtheria toxoid (32,33,130,131). Each of these vaccines is licensed for use in adolescents, but MCV4 is not indicated for active immunization against diphtheria (131). During 2005, MCV4 was recommended for routine use among adolescents (130,132). In MCV4, the diphtheria toxoid (approximately 48 µg) serves as the carrier protein that improves immune responses to meningococcal antigens. Precise comparisons cannot be made between the quantity of diphtheria toxoid in the vaccines; however, the amount in a dose of MCV4 is estimated to be comparable with the average quantity in a dose of pediatric DTaP (133).
No prelicensure studies of simultaneous or sequential vaccination with Tdap and MCV4 were done. None of the persons in the Canadian safety studies described above had received MCV4. Persons who recently received one diphtheria toxoid-containing vaccine might have increased rates of adverse reactions after a subsequent diphtheria toxoid-containing vaccine when diphtheria antibody titers remain elevated from the previous vaccination (26,108,111,112). The diphtheria GMCs were comparable or lower following Tdap compared with Td § § ; therefore, results of a co-administration trial of Td and MCV4 might be informative to infer the effect of co-administration of Tdap and MCV4. A randomized, controlled prelicensure trial assessed the safety of simultaneous versus sequential administration of Td and MCV4.
In this co-administration trial, administration of Td (approximately 8 µg of diphtheria toxoid) with MCV4 first, then placebo 28 days later (simultaneous group), or administration of Td with placebo first, then MCV4 28 days later (sequential group) was studied among 1,021 healthy adolescents aged 11-17 years (Table 11) (89,131,133). Serum samples from a subset of adolescents vaccinated with MCV4 from a different clinical trial were used for comparison. § § One month after vaccination, the antidiphtheria GMCs were ADACEL ™ Administration of MCV4 first followed by Td was not studied. Both simultaneous and sequential administration of Td and MCV4 induced immune responses to all antigens. One month postvaccination, the immune responses to diphtheria toxoid were higher when MCV4 was administered simultaneously with Td (GMT 120.9 IU/mL) than when Td was administered with placebo (GMT 8.4 IU/mL). Adolescents vaccinated with MCV4 alone also had high antidiphtheria responses 1 month following vaccination (GMT 46.5 IU/mL) (Table 11) (89,131,133). Adverse events on vaccination day and during the following 7 days were assessed among adolescents in the simultaneous and sequential groups. The overall rates of solicited local reactions were similar for the two groups: 58.0% reported local reactions at the MCV4 injection site in the simultaneous group versus 57.0% in the sequential group, and 74.7% reported local reactions at the Td injection site in the simultaneous group versus 73.3% in the sequential group. Pain was the most frequently reported reaction and pain rates were similar between groups; severe pain was uncommon (99.5° F (>37.5° C) and high fever >104° F (>40° C) were reported in <5% and <0.5% of persons, respectively (133)(134)(135). The safety of simultaneous vaccination of MCV4 with Tdap and sequential administration of Tdap first followed by MCV4 1 month later has been inferred from results of this study.
When Tdap or Td is administered after MCV4, rates of adverse reactions might be higher than when the dose is administered before MCV4 because pre-existing diphtheria antibody levels might be higher (26,108,111,112,133,135). Rates of adverse reactions were assessed in a small prelicensure study for MCV4 among 76 adolescents aged 15-17 years who received 2 doses of MCV4 spaced 3 years apart. After the second dose of MCV4, no SAEs, fever >102.2° F (>39° C), or severe local reactions were reported with the exception of one person, who reported severe pain at the injection site that lasted for 1 day (sanofi pasteur, unpublished data, 2005). No other available data exist on the safety of intervals between MCV4 and other diphtheria toxoid-containing vaccines. Postlicensure studies to provide additional information are under way (104,105).
# Neurologic and Systemic Events Associated with Vaccines with Pertussis Components or Tetanus Toxoid-Containing Vaccines
# Vaccines with Pertussis Components
Concerns about the possible role of vaccines with pertussis components in causing neurologic reactions or exacerbating underlying neurologic conditions are long-standing (20,136).
ACIP recommendations to defer pertussis vaccines in infants with suspected or evolving neurologic disease, including seizures, have been based primarily on concerns that neurologic events after vaccination (with whole cell preparations in particular) might interfere with the subsequent evaluation of the infant's neurologic status (1,136).
In 1991, the Institute of Medicine (IOM) concluded that evidence favored acceptance of a causal relation between pediatric DTP and acute encephalopathy; the IOM has not evaluated associations between pediatric DTaP and neurologic events (123). Pediatric DTaP is contraindicated for children with a history of encephalopathy not attributable to another identifiable cause occurring within 7 days after pediatric DTP/DTaP vaccination. Though active surveillance in Canada during 1993-2002 failed to ascertain any acute encephalopathy cases causally related to whole cell or acellular pertussis vaccines among a population administered 6.5 million doses of pertussis vaccines (137), research conducted in Japan during the introduction of acellular pertussis vaccines yielded rates of 1.0-1.3 attributable encephalopathy cases within 7 days of vaccination per 10 million doses (138).
ACIP has recommended that infants with evolving neurologic conditions should not be vaccinated with pediatric DTaP until a treatment regimen has been established and the condition has stabilized (1). Concerns about vaccinating adolescents with progressive or uncontrolled underlying neurologic disease must be weighed against the potential for morbidity from pertussis. Adolescents with severe neurologic conditions might be at risk for severe pertussis (48;CDC, unpublished data, 2005). ACIP does not consider a history of wellcontrolled seizures in the vaccinee or a family history of seizures (febrile or afebrile) or other neurologic disorder to be a contraindication or precaution to vaccination with pertussis components (1).
ACIP has recommended that vaccine providers and parents evaluate the risks for and benefits of administering subsequent doses of vaccines with pertussis components to young children who experienced these events after pediatric DTP/DTaP: temperature >105° F (>40.5° C) within 48 hours after pediatric DTP/DTaP, not attributable to another cause; collapse or shock-like state (hypotonic hyporesponsive episode) within 48 hours after pediatric DTP/DTaP; persistent crying lasting >3 hours, occurring within 48 hours after pediatric DTP/ DTaP; or convulsions with or without fever, occurring within 3 days after pediatric DTP/DTaP. All of these events were documented more frequently following whole cell pertussis vaccines than they have been following acellular vaccines (1,(139)(140)(141)(142). VAERS data have documented decreased reports of fever and other systemic events in infants and children fol-lowing pediatric DTaP in comparison with pediatric DTP (143). These events either do not occur in adolescents or are of less clinical concern in this age group than in infants and children (e.g., febrile seizures and hypotonic-hyporesponsive episodes). Taken together, this information supports administering Tdap to adolescents with a history of the events listed above after pediatric DTaP/DTP.
# Tetanus Toxoid-Containing Vaccines
ACIP has recommended that Guillain-Barré syndrome occurring <6 weeks after receipt of a tetanus toxoid-containing vaccine is a precaution for subsequent tetanus toxoid-containing vaccines (91). IOM concluded that evidence favored acceptance of a causal relation between tetanus toxoid-containing vaccines and Guillain-Barré syndrome (123). Evidence is based primarily on a well-documented case report (123,144). However, a subsequent analysis of active surveillance data in both adult and pediatric populations failed to demonstrate an association between receipt of a tetanus toxoid-containing vaccine and onset of Guillain-Barré syndrome within 6 weeks following vaccination (145).
IOM also has concluded that evidence from case reports and uncontrolled studies involving tetanus toxoidcontaining vaccines favored a causal relation between tetanus toxoid-containing vaccines and brachial neuritis. Brachial neuritis is considered to be a compensable event through the Vaccine Injury Compensation Program (123). However, ACIP does not consider a history of brachial neuritis to be a precaution or contraindication for administration of tetanus toxoid-containing vaccines; brachial neuritis is usually selflimited (91,143,146).
# Considerations for Vaccinating Pregnant Adolescents with Td or Tdap
ACIP has recommended Td routinely for pregnant women who received the last tetanus toxoid-containing vaccine >10 years earlier. This recommendation is primarily to prevent neonatal tetanus (24,31). In women adequately vaccinated against tetanus, passive transfer of antibodies across the placenta during pregnancy protects their newborns from neonatal tetanus (147)(148)(149). During 1999, a global maternal and neonatal tetanus elimination goal was recommended by the WHO, the United Nations Children's Fund, and the United Nations Population Fund (150).
As with tetanus, antibodies to pertussis antigens are passively transferred during pregnancy (151,152); however, serologic correlates of protection against pertussis are not known (88). Whether or not passive transfer of maternal antibodies to pertussis antigens protects neonates against pertussis is also unclear (88,153).
All licensed Td and Tdap vaccines are categorized as Pregnancy Category C agents by FDA. ¶ ¶ Pregnant women were excluded from prelicensure trials, and no animal reproduction studies have been conducted for Td or Tdap (32,33,(98)(99)(100)(101). Td has been used extensively in pregnant women worldwide, and no evidence indicates use of tetanus and diphtheria toxoids administered during pregnancy are teratogenic (24,154,155).
# Summary of the Rationale for Adolescent Tdap Recommendations
The availability of Tdap, the first pertussis vaccines formulated for use in adolescents and adults in the United States, offers a new opportunity to reduce the burden of pertussis in this country. The primary objective of vaccinating adolescents with Tdap is to protect the vaccinated adolescent against pertussis while maintaining the standard of care for protection against tetanus and diphtheria. A secondary objective of adolescent Tdap vaccination is to reduce the reservoir of pertussis within the U.S. population at large and potentially reduce the incidence of pertussis in other age groups, including infants who have the highest risk for complications from pertussis (16,48). The extent to which the secondary objective can be achieved through adolescent vaccination is unknown.
The decision to recommend routine Tdap vaccination for adolescents is based on evidence regarding the burden of pertussis among adolescents; negative effects of pertussis outbreaks involving adolescents on the community and the public health system; studies suggesting use of Tdap among adolescents will likely be safe, effective, and economical; and the established infrastructure for adolescent vaccination (30,32,33,(52)(53)(54)68).
To protect against pertussis, Tdap will be introduced into an adolescent vaccination schedule that already includes two other tetanus and/or diphtheria toxoid-containing vaccines, Td, and MCV4 (23,130). Frequent doses of tetanus and diphtheria toxoid-containing vaccines can be associated with increased local and systemic reactogenicity (108,109). ACIP has considered issues related to spacing and administration sequence of these three vaccines to develop recommendations for Tdap use in adolescents. ¶ ¶ U.S. Food and Drug Administration Pregnancy Category C: Animal studies have documented an adverse effect and no adequate and well-controlled studies in pregnant women have been conducted or no animal studies and no adequate and well-controlled studies in pregnant women have been conducted
# MMWR March 24, 2006
# Recommendations for Use of Tdap and Td Among Adolescents
The following sections present recommendations for use of Tdap and Td among adolescents aged 11-18 years and include routine Tdap vaccination, contraindications and precautions, and special situations (Appendix C). (130,132).
# Routine Tdap Vaccination
# 1-A. Recommendations for Use (
# 1-B. Dosage and Administration
The dose of Tdap is 0.5 mL, administered intramuscularly (IM), preferably into the deltoid muscle.
# 1-C. Simultaneous Vaccination with Tdap and Other Vaccines
If two or more vaccines are indicated, they should be administered during the same visit (i.e., simultaneous vaccination). Each vaccine should be administered using a separate syringe at a different anatomic site. Some experts recommend administering no more than two injections per muscle, separated by at least one inch. Administering all indicated vaccines during a single visit increases the likelihood that adolescents will receive each of the vaccines on schedule (91). Vaccine providers should administer MCV4 and Tdap (or Td) during the same visit if both vaccines are indicated and available. MCV4 contains diphtheria toxoid as a carrier protein (131) (see Safety Considerations for Adolescent Vaccination with Tdap or Td).
# 1-D. Interchangeable Use of Tdap Vaccines
A single dose of either Tdap product (BOOSTRIX ® or ADACEL ™ ) can be administered to adolescents regardless of the type or manufacturer of pediatric DTP/DTaP used for childhood vaccination.
# 1-E. Preventing Adverse Events
Syncope can occur after vaccination, might be more common among adolescents and young adults than among other age groups, and has rarely resulted in serious injury (91,156,157). Certain experts suggest a 15-20 minute observation period following vaccination (91,158). If syncope occurs, patients should be observed until symptoms resolve.
The potential for administration errors involving tetanus toxoid-containing vaccines and other products is well documented (159)(160)(161). For example, Td and TT have been inadvertently administered * Five doses of pediatric DTP/DTaP before the seventh birthday; if the fourth dose was administered on or after the fourth birthday, the fifth dose is not needed.
instead of tuberculin purified protein derivative (PPD) (159). Attention to proper vaccination technique, including use of an appropriate needle length and standard routes of administration (i.e., IM for Tdap) might minimize the risk for adverse events (91). Adverse events associated with inadvertent vaccine administration can be reported to the Vaccine Adverse Event Reporting System (VAERS) (see Reporting of Adverse Events after Vaccination).
# 1-F. Record Keeping
Health-care providers who administer vaccines are required to keep permanent vaccination records of vaccines covered under the National Childhood Vaccine Injury Act in the vaccinee's medical record; ACIP has recommended that this practice include all vaccines (91). Because documentation of tetanus toxoid-containing vaccine administration is frequently required for school or camp entry and as part of wound management, encouraging adolescents to maintain a personal vaccination record is important to minimize administration of unnecessary vaccinations. Vaccine providers can record the type of the vaccine, manufacturer, anatomic site, route, and date of administration and name of the administering facility on the personal record.
# Contraindications and Precautions for Use of Tdap and Td Among Adolescents Aged 11-18 Years
# 2-A. Contraindications
- Tdap or Td is contraindicated for persons with a history of serious allergic reaction (i.e., anaphylaxis) to any component of the vaccine. Because of the importance of tetanus vaccination, persons with a history of anaphylaxis to components included in all Tdap and Td vaccines should be referred to an allergist to determine whether they have a specific allergy to tetanus toxoid, can be desensitized to tetanus toxoid, and can safely receive TT vaccinations. - Tdap is contraindicated for adolescents with a history of encephalopathy (e.g., coma or prolonged seizures) not attributable to an identifiable cause within 7 days of administration of a vaccine with pertussis components. This contraindication is for the pertussis components and these persons should receive Td instead of Tdap.
# 2-B. Precautions and Reasons to Defer Tdap and/or Td
A precaution is a condition in a vaccine recipient that might increase the risk for a serious reaction (91)
# Special Situations for Use of Tdap and Td
# 3-A. General Principles
This section addresses special situations for Tdap and Td use. As with the routine situations, only a single dose of Tdap should be administered to an adolescent aged 11-18 years. For most, but not all, of the special situations, Tdap is preferred to Td. In some special situations or when contraindications or precautions are present, Td rather than Tdap might be indicated. The dose of Td is 0.5 mL, administered IM. Tdap (or Td) and MCV4 should be administered at the same visit during special situations if both vaccines are indicated and available, although this might not always be feasible (e.g., wound management). Simultaneous administration of Tdap (or Td) and MCV4 and an interval of at least 5 years between Td and Tdap can reduce the risk for local and systemic reactions. In certain special situations listed below, the benefit of protection against disease probably outweighs this risk.
# 3-B. Nonsimultaneous Vaccination with Tdap and
Other Vaccines, Including MCV4 ACIP has recommended that inactivated vaccines can be administered at any time before or after a different inactivated or live vaccine (i.e., nonsimultaneous vaccination), unless a contraindication exists (91). Simultaneous administration of Tdap (or Td) and MCV4 (which all contain diphtheria toxoid) during the same visit is preferred when both Tdap (or Td) and MCV4 are indicated. If simultaneous vaccination is not feasible (e.g., a vaccine is not available), MCV4 and Tdap (or Td) can be administered using any sequence. Persons who recently received one diphtheria toxoid-containing vaccine might have increased rates of adverse reactions after a subsequent diphtheria toxoidcontaining vaccine when diphtheria antibody titers remain elevated from the previous vaccination (26,108,111,112) (see Safety Considerations for Adolescent Vaccination with Tdap or Td section for a discussion of nonsimultaneous vaccination).
# 3-C. Pertussis Outbreaks and Other Settings with Increased Risk for Pertussis or its Complications
Vaccine providers can administer Tdap to adolescents aged 11-18 years at an interval less than 5 years after Td, particularly when the benefit of providing protection against pertussis is likely to be increased. The safety of an interval as short as approximately 2 years between Td and Tdap is supported by a Canadian study among children and adolescents (see Spacing and Sequence Administration of Vaccines Containing Tetanus Toxoid, Diphtheria Toxoid, and Pertussis Antigens) (126).
The benefit of using Tdap at an interval less than 5 years after Td is likely to be increased among adolescents when the adolescent is at increased risk for acquiring pertussis (e.g., during outbreaks or periods of increased pertussis activity in the community). Postexposure chemoprophylaxis and other pertussis control guidelines are described elsewhere (64,158,163). The benefit of using a shorter interval also might be increased for adolescents with severe underlying medical conditions (e.g., chronic pulmonary disease or neurologic disorders) because these adolescents might be at increased risk for pertussis-related complications.
Infants aged <12 months are at highest risk for pertussis-related complications and hospitalizations compared with older age groups; young infants have the highest risk for death from pertussis. Administering Tdap at an interval less than 5 years after Td to an adolescent who has or anticipates having close contact with an infant aged <12 months might reduce the risk for transmitting pertussis to the infant. Infants should be vaccinated on time with pediatric DTaP (1,23).
# 3-D. Lack of Availability of Tdap or MCV4
If Tdap and MCV4 are both indicated but only one vaccine is available, the available vaccine generally should be administered. When Tdap is indicated but not available, vaccine providers should administer Td or temporarily defer Tdap/Td vaccination. Td should be administered to provide protection against tetanus and diphtheria if the adolescent received the last pediatric DTP/DTaP/DT or Td >10 years earlier. Recommendations for use of Tdap among adolescents who already received Td would apply to these adolescents when Tdap becomes available (see Routine Tdap Vaccination ). Tdap/Td vaccination can be deferred temporarily if the adolescent completed the childhood DTP/DTaP vaccination series*, received the last pediatric DTP/DTaP/DT or Td <10 years earlier, and is likely to return for follow-up. If the vaccine provider defers Td in order to administer Tdap when it becomes available, a system to recall the adolescent should be maintained.
The adolescent also can be referred to another facility for Tdap administration.
# 3-E. Tetanus Prophylaxis in Wound Management
ACIP has recommended administering tetanus toxoid-containing vaccine and tetanus immune globulin (TIG) as part of standard wound management to prevent tetanus (Table 13) (24). Tdap is preferred to Td for adolescents aged 11-18 years who were vaccinated against tetanus >5 years earlier, require a tetanus toxoid-containing vaccine as part of wound management, and have not previously received Tdap.
Adolescents who have completed the 3-dose primary tetanus vaccination series and have received a tetanus toxoid-containing vaccine <5 years earlier are protected against tetanus and do not require a tetanus toxoid-containing vaccine as part of wound management. Although MCV4 and Tdap (or Td) should be administered at the same visit during routine situations if both vaccines are indicated, this might not be feasible for wound management.
A thorough attempt must be made to determine whether an adolescent has completed the 3-dose primary tetanus vaccination series. Persons with unknown or uncertain tetanus vaccination histories should be considered to have had no previous doses of a tetanus toxoid-containing vaccine (see Adolescents with History of Incomplete Pediatric DTP/ DTaP/DT or Td Vaccination ). Persons who have not completed the primary series might require a tetanus toxoid-containing vaccine and passive immunization with TIG at the time of wound management (Table 13). When both TIG and a tetanus toxoid-containing vaccine are indicated, each product should be administered using a separate syringe at different anatomic sites (24).
Adolescents with a history of an Arthus reaction after a previous dose of a tetanus toxoid-containing vaccine should not receive a tetanus toxoidcontaining vaccine until >10 years after the most recent dose, even if they have a wound that is neither clean nor minor (Table 13). If the Arthus reaction was associated with a vaccine that contained diphtheria toxoid without tetanus toxoid (e.g., MCV4), deferring Tdap or Td might leave the adolescent inadequately protected against tetanus and TT should be administered. In all circumstances, the decision to administer TIG is based on the primary vaccination history for tetanus (Table 13).
# 3-F. History of Pertussis
Adolescents aged 11-18 years who have a history of pertussis generally should receive Tdap according to the routine recommendations. This practice is preferred because duration of protection induced by pertussis is unknown (waning immunity might begin as early as 7 years after infection) and because the diagnosis of pertussis can be difficult to confirm, particularly with test results other than positive culture for B. pertussis (164). Administering pertussis vaccines to persons with a history of pertussis presents no theoretical safety concern. Adolescents who received other incomplete vaccination schedules for tetanus and diphtheria should be vaccinated with Tdap and/or Td according to guidance for catch-up vaccination (Appendix D). A single dose of Tdap can be used to substitute for any one of the Td doses in the series.
# 3-G. Adolescents with
In situations in which the adolescent probably has received vaccination against tetanus and diphtheria but cannot produce records, vaccine providers can obtain serologic testing for antibodies to tetanus and diphtheria to avoid unnecessary vaccination. If antitetanus and antidiphtheria levels are each >0.1 IU/mL, previous vaccination with tetanus and diphtheria toxoid-containing vaccines is likely and a single dose of Tdap is indicated; this Tdap dose counts as the adolescent booster dose.
# 3-I. Children Aged 7-----10 Years with Incomplete Pediatric DTP/DTaP Vaccination History
Neither Tdap vaccine is licensed for use in children aged 4 weeks after dose 1 and dose 3 is administered 6-12 months after dose 2. Children aged 7-10 years who received other incomplete vaccination schedules against tetanus, diphtheria, and pertussis should be vaccinated according to catch-up guidance (Appendix E). When these children become adolescents (aged 11-18 years), they should receive Tdap according to the routine recommendations and interval guidance used for adolescents who completed the childhood DTP/DTaP series (see Routine Tdap Vaccination ).
In situations in which the child probably has received vaccination against tetanus and diphtheria but cannot produce records, vaccine providers can obtain serologic testing for antibodies to tetanus and diphtheria to avoid unnecessary vaccination. If antitetanus and antidiphtheria levels are each >0.1 IU/mL, previous vaccination with tetanus and diphtheria toxoid-containing vaccines is likely. In this § § § Five doses of pediatric DTP/DTaP/DT before the seventh birthday; if the fourth dose was administered on or after the fourth birthday, the fifth dose is not needed. Children who began the tetanus and diphtheria vaccination series at age >7 years required 3 doses of Td to complete the primary series. ¶ ¶ ¶ A single dose of BOOSTRIX ® Tdap is licensed for persons aged 10 years and can be used instead of Td for one of the doses in children aged 10 years; if BOOSTRIX ® is administered early to a child aged 10 years, the dose counts as the adolescent Tdap dose usually administered at age 11-12 years.
situation, Td vaccination can be deferred until the child is aged 11-12 years and eligible to receive Tdap.
# 3-J. Inadvertent Administration of Tdap or Pediatric DTaP
To help prevent inadvertent administration of Tdap when pediatric DTaP is indicated or pediatric DTaP when Tdap is indicated, vaccine providers should review product labels before administering these vaccines; the packaging might appear similar. Tdap is not indicated for children aged 7 years; the increased diphtheria toxoid content is associated with higher rates of adverse reactions in older persons (24)(25)(26)(27)(28).
Guidance on the best approach to vaccination following inadvertent administration of Tdap or pediatric DTaP is based primarily on expert opinion. The family should be informed of any inadvertent vaccine administration. Adverse events associated with inadvertent vaccine administration can be reported to VAERS (see Reporting of Adverse Events after Vaccination). If Tdap is inadvertently administered instead of pediatric DTaP to a child aged <7 years as any one of the first three doses of the tetanusdiphtheria-pertussis vaccination series, the Tdap dose should not be counted as valid, and a replacement dose of pediatric DTaP should be administered. If the inadvertent administration is discovered while the child is in the office, the pediatric DTaP can be administered during the same visit. If the child has left the office, some experts suggest administering the replacement dose of pediatric DTaP within approximately 72 hours, or administering it 4 weeks later to optimize the child's immune response to the antigens in pediatric DTaP. This practice helps ensure that the child stays on the primary series schedule and has adequate protection against diphtheria and pertussis. However, the replacement dose of pediatric DTaP can be administered as soon as feasible at any interval after the inadvertent Tdap dose. The remaining doses of the pediatric DTaP series should be administered on the routine schedule, with at least a 4 week interval between the replacement dose of pediatric DTaP and the next dose of pediatric DTaP. For example, if an 8-week-old infant inadvertently received a dose of Tdap instead of the first dose of pediatric DTaP and does not receive a replacement dose of pediatric DTaP within about 72 hours, a replacement dose of pediatric DTaP can be administered 4 weeks after the inadvertent Tdap dose (age 12 weeks). The routine schedule of pediatric DTaP can then be resumed 4 weeks after the pediatric DTaP replacement dose (age 16 weeks) with the other recommended vaccines (1,23).
If Tdap is inadvertently administered as the fourth or the fifth dose in the tetanus-diphtheria-pertussis vaccination series to a child aged <7 years, the Tdap dose should be counted as valid and does not need to be repeated; the child who received Tdap as a fourth dose should complete the pediatric DTaP schedule (23). The routine adolescent Tdap vaccination recommendations would apply when this child becomes an adolescent. For example, a child who inadvertently receives Tdap at age 5 years instead of the fifth dose of pediatric DTaP should receive a second dose of Tdap at age 11-12 years.
If Tdap or pediatric DTaP is inadvertently administered to a child aged 7-9 years instead of Td as part of catch-up vaccination or for wound management, this dose can be counted as the adolescent Tdap dose, or the child can later receive an adolescent booster dose of Tdap according to the interval guidance used for Td to Tdap (see Routine Tdap Vaccination and Pertussis Outbreaks and Other Settings with Increased Risk for Pertussis or its Complications ). In either case, the child should receive a dose of vaccine containing tetanus and diphtheria toxoids no longer than 10 years after the inadvertent Tdap or pediatric DTaP dose or according to the guidance for catch-up vaccination (Appendix E).
If pediatric DTaP is inadvertently administered to an adolescent aged 11-18 years, the dose should be counted as the adolescent Tdap booster. The adolescent should receive the next dose of a vaccine containing tetanus and diphtheria toxoids 10 years after the inadvertent pediatric DTaP dose or according to the guidance for catch-up vaccination (Appendix D).
# 3-K. Vaccination during Pregnancy
As with other inactivated vaccines and toxoids (91,165), pregnancy is not considered a contraindication for Tdap vaccination. Guidance on the use of Tdap during pregnancy to protect against pertussis is under consideration by ACIP. Pregnant adolescents who received the last tetanus toxoid-containing vaccine <10 years previously should generally receive Tdap after delivery, if otherwise indicated (see Post-Partum Vaccination ).
To prevent neonatal tetanus, pregnant adolescents who received the last tetanus toxoid-containing vaccine >10 years previously should generally receive Td in preference to Tdap. ACIP has recommended that pregnant women receive Td if the last tetanus toxoid-containing vaccine was administered >10 years previously (24,31,91,165). If Td is indicated, vaccinating during the second or third trimester is preferred when feasible to minimize a perception of an association of vaccine with adverse pregnancy outcomes, which are more common during the first trimester. A pregnant adolescent who has not received the 3-dose primary tetanus vaccination series should begin this series during pregnancy, using Td. (see Adolescents with History of Incomplete Pediatric DTP/ DTaP/DT or Td Vaccination ).
Because of lack of data on the use of Tdap in pregnant women, both Tdap manufacturers have established pregnancy registries. Health-care providers are encouraged to report Tdap vaccination during pregnancy to the following registries: BOOSTRIX ® to GlaxoSmithKline Biologicals at 1-888-825-5249 and ADACEL ™ to sanofi pasteur at 1-800-822-2463 (1-800-VACCINE) (32,33).
# 3-L. Post-Partum Vaccination
Adolescents aged 11-18 years, including those who are breastfeeding, should receive a single dose of Tdap as soon as feasible in the postpartum period, according to the routine Tdap recommendations and interval guidance (see Routine Tdap Vaccination and Pertussis Outbreaks and Other Settings with Increased Risk for Pertussis or its Complications ). For adolescent mothers who have not already received Tdap, vaccinating the mother with Tdap during the postpartum period might reduce the risk for pertussis transmission to the infant. Protection of the mother against pertussis requires an estimated 1 to 2 weeks after vaccination.
# 3-M.Older Adolescents and Adults Aged >18 Years
To maintain protection against tetanus and diphtheria, ACIP has recommended decennial Td boosters for adults beginning 10 years after the adolescent dose (24,30). The safety and efficacy of Tdap (ADACEL ™ ) as a single dose booster immuniza-
# Reporting of Adverse Events After Vaccination
As with any newly licensed vaccine, surveillance for rare adverse events associated with administration of Tdap is important for assessing its safety in large-scale use. The National Childhood Vaccine Injury Act of 1986 requires health-care providers to report specific adverse events that follow tetanus, diphtheria, or pertussis vaccination (. hhs.gov/reportable.htm). All clinically significant adverse events should be reported to VAERS, even if causal relation to vaccination is not certain. VAERS reporting forms and information are available electronically at / or by telephone, (800) 822-7967. Web-based reporting is available and providers are encouraged to report electronically at to promote better timeliness and quality of safety data.
Safety surveillance for adolescent Tdap, MCV4, and other vaccines is being conducted on an ongoing basis in cooperation with FDA. Previously published safety data for Td and for tetravalent meningococcal polyscaccharide vaccine will provide some of the basis for comparison with postlicensure safety surveillance for Tdap and MCV4, respectively (130,166).
# Vaccine Injury Compensation
The National Vaccine Injury Compensation Program (VICP), established by the National Childhood Vaccine Injury Act of 1986, is a system under which compensation can be paid on behalf of a person thought to have been injured or to have died as a result of receiving a vaccine covered by the program. Anyone receiving a covered vaccine, regardless of age, can file a petition under VICP. The program is intended as an alternative to civil litigation under the traditional tort system because negligence need not be proven.
The Act establishes 1) a Vaccine Injury and conditions (including death) for which compensation might be paid without proof of causation; and 3) the period after vaccination during which the first symptom or substantial aggravation of the injury must appear. Persons might be compensated for an injury listed in the table or one that can be demonstrated to result from administration of a listed vaccine. All tetanus toxoid-containing vaccines and vaccines with pertussis components (e.g., Tdap, Td, and pediatric DTaP) are covered under the Act. Additional information about the program is available at or by calling 1-800-338-2382.
# Areas for Future Research Related to Tdap and Adolescents
With recent licensure and introduction of Tdap for adolescents, close monitoring of pertussis disease trends and vaccine safety will be high priorities for public health organizations and health-care providers. Active surveillance sites in Massachusetts and Minnesota, supported by CDC, are being established to provide additional data on the burden of pertussis in adolescents and other age groups and the impact of adolescent Tdap vaccination recommendations. Postlicensure studies and surveillance activities are planned or under way to evaluate
- changes in the incidence of pertussis;
- physicians' uptake of Tdap;
- safety and immunogenicity of simultaneous and nonsimultaneous administration of Tdap and MCV4 in adolescents (104,105); and - the prevalence of and risk factors for ELS in adolescents, including studies of adolescents who were vaccinated with 5 doses of pediatric DTaP series (during 2008, the first birth cohort for which an all-pediatric DTaP 5-dose schedule was recommended will turn 11 years of age and become eligible for adolescent vaccination with Tdap). Research is needed to evaluate and define - immunologic correlates of protection for pertussis; - improved diagnostic tests for pertussis; - methods to enhance coverage and delivery of Tdap to adolescents; and - safety and effectiveness of repeated Tdap doses. - Nonsimultaneous vaccination: : : : : If simultaneous vaccination is not feasible, inactivated vaccines can be administered at any time before or after a different inactivated or live vaccine. Tdap (or Td) and MCV4 vaccines (which all contain diphtheria toxoid) can be administered using any sequence. Persons who recently received one diphtheria toxoid-containing vaccine might have increased rates of adverse reactions after a subsequent diphtheria toxoid-containing vaccine when diphtheria antibody titers remain elevated from the previous vaccination § .
- Pertussis Outbreaks and Other Settings with Increased Risk for Pertussis or its Complications: Vaccine providers can administer Tdap to adolescents aged 11-18 years at an interval less than 5 years after Td, particularly when the benefit of providing protection against pertussis is likely to be increased (e.g., pertussis outbreaks and close contact with an infant aged 7 years required 3 doses of Td to complete the primary series. | This report will not include any discussion of the unlabeled use of a product or a product under investigational use with the exception of the discussion of off-label use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine (Tdap) by all in the following situations: A. The interval between pediatric DTP/DTaP/DT or Td and Tdap might be shorter than the 5 years indicated in the package insert; B. Progressive neurologic disorders and uncontrolled epilepsy are considered precautions and not contraindications as indicated in the package insert; C. Tdap might be used as part of the primary series for tetanus and diphtheria; and D.Inadvertent administration of Tdap and pediatric DTaP is discussed.# Introduction
Pertussis, an acute, infectious cough illness, remains endemic in the United States despite routine childhood pertussis vaccination for more than half a century and high coverage levels in children for more than a decade (1)(2)(3)(4). A primary reason for the continued circulation of Bordetella pertussis is that immunity to pertussis wanes approximately 5-10 years after completion of childhood pertussis vaccination, leaving adolescents and adults susceptible to pertussis (5)(6)(7)(8)(9)(10). Among the diseases for which universal childhood vaccination has been recommended, pertussis is the least well-controlled reportable bacterial vaccine-preventable disease in the United States (11,12).
In the United States during 1934-1943, an annual average of 200,752 pertussis cases and 4,034 pertussis-related deaths were reported (13). After the introduction of childhood pertussis vaccination during the 1940s, the number of reported pertussis cases declined dramatically, reaching an historic low of 1,010 in 1976 (Figure 1) (1). Since the 1980s, the number of reported pertussis cases has been steadily increasing, especially among adolescents and adults (4,14,15). Possible reasons for the increase in reported pertussis cases include a true increase in the burden of disease and an increase in the detection and reporting of cases; the relative contribution of each of these factors to the increase observed is unclear (4,(14)(15)(16)(17).
# Childhood Pertussis Vaccination Policy in the United States
Whole cell pertussis vaccines became available during the 1920s (18), but pediatric diphtheria and tetanus toxoids and whole cell pertussis vaccine (DTP) was not routinely recommended for children until the 1940s and 1950s (19,20). In 1991, less reactogenic pediatric acellular pertussis vaccine (diphtheria and tetanus toxoids and acellular pertussis vaccine [DTaP]) was first licensed for use in children for the fourth and fifth doses of the 5-dose childhood vaccination series in the United States (21,22), and in 1996, pediatric DTaP was licensed for the first three infant doses (1). In 1997, the Advisory Committee on Immunization Practices (ACIP) recommended that pediatric DTaP be used routinely instead of pediatric DTP as a 5-dose DTaP schedule at ages 2, 4, 6, 15-18 months and 4-6 years (1,23); pediatric DTP has not been available in the United States since 2002 (CDC, unpublished data, 2005).
# Childhood and Adolescent Tetanus and Diphtheria Vaccination Policy in the United States
Vaccination against tetanus and diphtheria has markedly reduced the number of cases and deaths from tetanus and diphtheria in the United States in all age groups (24). From 1997 through spring 2005, three vaccine formulations against tetanus and diphtheria were recommended for use in the United States: pediatric DTaP routinely for children aged <7 years, pediatric diphtheria and tetanus toxoids vaccine (DT) for children aged <7 years with contraindications or precautions for pertussis components, and adult tetanus and diphtheria toxoids vaccine (Td) routinely for persons aged >7 years (1,24) (Appendix A). The formulation of choice for vaccination of persons aged >7 years has been Td rather than pediatric DT because the lower diphtheria toxoid antigen content of Td induces an adequate immune response and lower rates of adverse reactions in adults than pediatric DT (24)(25)(26)(27)(28).
To provide continued protection against tetanus and diphtheria, ACIP recommended a booster dose of Td for adolescents (24). Before 1995, the adolescent Td booster was recommended at age 14-16 years, approximately 10 years after completion of the childhood DTP series. In 1995, the first harmonized childhood vaccination schedule endorsed by ACIP, the American Academy of Pediatrics, and the American Academy of Family Physicians recommended lowering the age for Td administration to 11-12 years, but vaccination at age 14-16 years was also acceptable (29). In 1996, ACIP, in collaboration with partner organizations, recommended a routine vaccination visit at age 11-12 years to reduce adolescent morbidity associated with vaccine-preventable diseases and to improve vaccine coverage for adolescents (30). The 1996 ACIP statement emphasized that the recommended age for Td administration was 11-12 years, if at least 5 years had elapsed since administration of the last pediatric DTP/DTaP dose. Td also was recommended for older adolescents who missed the Td dose at age 11-12 years. In some states, school attendance laws continue to require that adolescents receive the Td dose 10 years after the last tetanus and diphtheria toxoids-containing vaccine, rather than at age 11-12 years (CDC, unpublished data, 2005). After the adolescent Td booster dose, ACIP has recommended Td boosters every 10 years throughout life (24,31). 1922 1930 1940 1950 1960 1970 1980 1990
# Licensure of Pertussis Vaccines for Use in Adolescents and Adults in the United States
In spring 2005, two tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine (Tdap) products were licensed in the United States for use in adolescents (and, for one product, use in adults) (32,33). The pertussis antigen composition of the adolescent and adult Tdap formulations is similar to pediatric DTaP, but some of the pertussis antigens are reduced in quantity. The tetanus and diphtheria toxoid composition of Tdap is similar to licensed adult formulations of Td (Appendix A). No preparation containing pertussis antigens alone is licensed in the United States. Acellular pertussis vaccines formulated for adolescents and adults have been available for use in other countries, including Canada, Australia, and several European countries (e.g., France, Austria and Germany) (10,(34)(35)(36)(37)(38)(39)(40).
# Background: Pertussis General Clinical Characteristics
Pertussis is an acute respiratory infection caused by Bordetella pertussis, a fastidious gram-negative coccobacillus. The organism elaborates toxins that damage respiratory epithelial tissue and have systemic effects, including promotion of lymphocytosis (41,42). Other species of Bordetella, including B. parapertussis, and less commonly B. bronchiseptica or B. holmesii, are associated with cough illness; the clinical presentation of B. parapertussis can be similar to that of classic pertussis. Illnesses caused by species of Bordetella other than B. pertussis are not preventable by pertussis vaccines (43).
Factors that affect the clinical presentation of pertussis include age, the level of immunity, and use of antimicrobials early in the course of the illness (44). The usual incubation period for pertussis is 7-10 days (range: 5-21 days) (20,44,45). Classic pertussis is characterized by three phases of illness: catarrhal, paroxysmal, and convalescent (20,44,45). During the catarrhal phase, which generally lasts 1-2 weeks, infected persons experience coryza and an intermittent cough; high fever is uncommon. The paroxysmal phase usually lasts 4-6 weeks and is characterized by spasmodic cough, posttussive vomiting, and inspiratory whoop. Absolute lymphocytosis is common in unvaccinated children (46). Symptoms slowly improve during the convalescent phase, which generally lasts 2-6 weeks, but can last months. Complications can occur during the course of pertussis, including hypoxia, pneumonia, weight loss, seizures, encephalopathy, and death (20,41,44,47).
Infants aged <12 months with pertussis are more likely than older age groups to have complications or be hospitalized during their illness (16,47,48). During 2000During -2004, an average of 2,488 cases of pertussis was reported annually among infants aged <12 months. Among these infants, 63% were hospitalized, and the median duration of hospitalization was 5 days (range: 1-152 days) (CDC, unpublished data, 2005). Two to 3 doses of pediatric DTaP (recommended at ages 2, 4, and 6 months) provide protection against severe pertussis (16,48,49). Young infants, who can present with symptoms of apnea and bradycardia without cough, are at highest risk for death from pertussis (16,47,48). During 1980During -2004, a total of 223 pertussis-related deaths in infants aged <4 months were reported to CDC (of 280 in all age groups) (48, CDC, unpublished data, 2005). Of the 100 pertussis-related deaths reported during 2000-2004, a total of 90 (90%) were among young infants aged <4 months and 76 (76%) were among infants aged <2 months (CDC, unpublished data, 2005).
B. pertussis is primarily transmitted from person to person through large respiratory droplets generated by coughing or sneezing. Persons with pertussis are most infectious during the catarrhal and early paroxysmal phases of illness (20,50). The disease is highly communicable, with attack rates as high as 80%-90% among nonimmune household contacts (20,24,44). Adolescents with pertussis can transmit the disease to infants. A study conducted using enhanced pertussis surveillance during 1999-2002 investigated the source of pertussis among infants aged <12 months. On the basis of parental interview, a source was identified among 264 (43%) of 616 infant cases. An adolescent (defined in the study as a person aged 10-19 years) was identified as the source for 43 (7%) of the 616 infants (51).
# Clinical Features and Morbidity Among Adolescents with Pertussis
The spectrum of disease caused by B. pertussis in adolescents ranges from mild cough illness to classic pertussis; infection also can be asymptomatic. When presentation is not classic, pertussis can be clinically indistinguishable from other respiratory illnesses. Adolescents reported with pertussis commonly experience a prolonged cough illness and sometimes have complications (Table 1); rates of certain clinical characteristics and complications in these types of studies probably are higher than among all adolescents with pertussis because the cases with a more classic presentation are more likely to be diagnosed and reported (52-54;CDC, unpublished data, 2005). Complications and hospitalizations related to pertussis occur in up to 2% of adolescents reported with pertussis (52,54;CDC, unpublished data, 2005). Pertussis-related deaths are rarely reported among adolescents; in the United States during 1990-2004, two pertussis-related deaths among adolescents aged 11-18 years were reported to CDC (one adolescent with malignancy and one adolescent with severe neurologic impairment) (CDC, unpublished data, 2005). A prolonged cough is a common feature of pertussis in adolescents. A study in Quebec, Canada, indicated that 97% of adolescents with pertussis coughed for >3 weeks, and 47% coughed for >9 weeks (52). Massachusetts surveillance data demonstrated that 38% of adolescents with pertussis reported during 1989-2004 had already been coughing for >1 month at the time of diagnosis (Massachusetts Department of Public Health [MDPH], unpublished data, 2005).
Adolescents with pertussis often make repeated visits for medical care. Of approximately 7,000 Massachusetts adolescents with pertussis reported during 1989-2004, 41% had one, 32% had two, and 24% had three or more medical visits during their illness (MDPH, unpublished data, 2005). Adolescents with pertussis and their household contacts frequently miss school or work. Of Massachusetts adolescents with pertussis, 83% missed school (mean: 5.5 days; range: 0.4-32 days). In 43% of households with an affected adolescent, one parent or caretaker missed work (mean: 2.4 days, range: 0.1-25), and in 14% of households, a second parent or caretaker missed work (mean: 1.8 days, range: 0.1-11 days) (54).
# Pertussis Diagnosis
Many factors affect the sensitivity, specificity, and interpretation of diagnostic tests for B. pertussis, including the stage of the disease, antimicrobial administration, previous vaccination, the quality of technique used to collect the specimen, transport conditions to the testing laboratory, experience of the laboratory, contamination of the sample, and use of nonstandardized tests (55,56). In addition, tests and specimen collection materials might not be readily available to practicing clinicians.
Isolation of B. pertussis by culture is 100% specific; however, sensitivity of culture varies because fastidious growth requirements make it difficult to transport and isolate the organism. Although the sensitivity of culture can reach 80%-90% under optimal conditions, in practice, sensitivity typically ranges from 30%-60% (57). The yield of B. pertussis from culture declines in specimens taken after 2 or more weeks of cough illness, after antimicrobial treatment, or after previous pertussis vaccination (58). Within 3 weeks after onset of cough, culture is only 1%-3% sensitive (59). Although B. pertussis can be isolated in culture as early as 72 hours after plating, it takes 1-2 weeks before a culture result can definitively be called negative (60). Culture is essential to isolate B. pertussis for antimicrobial susceptibility testing and for molecular subtyping of strains.
Direct fluorescent antibody (DFA) tests provide rapid results (hours), but are generally less sensitive (sensitivity: 10%-50%) than culture. With use of monoclonal reagents, the specificity of DFA should generally be >90%; however, the interpretation of the test is subjective, and interpretation by an inexperienced microbiologist can result in lower specificity (61). Because of the limitations of DFA testing, CDC does not recommend its use. Because of increased sensitivity and shorter turn-aroundtime, DNA amplification (e.g., polymerase chain reaction [PCR]) is being used more frequently to detect B. pertussis. When symptoms of classic pertussis are present (e.g., 2 weeks of paroxysmal cough), PCR typically is 2-3 times more likely than culture to detect a positive B. pertussis sample (56,62,63). The interpretation of PCR-positive but culture-negative samples as either true positive or false positive is difficult. No U.S. Food and Drug Administration (FDA)-licensed PCR test kit and no national standardized protocols, reagents, and reporting formats are available. Approximately 100 different PCR protocols have been reported. These vary by DNA purification techniques, PCR primers, reaction conditions, and product detection methods (63). Laboratories must develop and validate their own PCR tests. As a result, the analytical sensitivity, accuracy, and quality control of PCR-based B. pertussis tests might vary widely among laboratories. The majority of laboratory validation studies have not sufficiently established the predictive value of a positive PCR test to diagnose pertussis (63). Use of PCR tests with low specificity can result in unnecessary investigation and treatment of persons with false-positive PCR test results and inappropriate chemoprophylaxis of their contacts (63). CDC Council of State and Territorial Epidemiologists (CSTE) reporting guidelines support the use of PCR to confirm the diagnosis of pertussis only when the case also meets the clinical case definition (>2 weeks of cough with paroxysms, inspiratory "whoop," or posttussive vomiting) (Appendix B) (64,65).
Diagnosis of pertussis by serology generally requires demonstration of a substantial change in titer for pertussis antigens (usually fourfold) when comparing results from acute (<2 weeks after cough onset) and convalescent sera (>4 weeks after the acute sample). The results of serologic tests on paired sera generally become available late in the course of illness and can provide only retrospective diagnosis. A single sample serologic assay with age-specific antibody reference values is used as a diagnostic test for adolescents and adults in Massachusetts but is not available elsewhere (66). Other singlesample serologic assays lack standardization and do not clearly differentiate immune responses to pertussis antigens after recent clinical disease, from more remote disease, or from vaccination (43). None of these serologic assays, including the Massachusetts assay, is licensed by FDA for routine diagnostic use in the United States. For these reasons, CDC guidelines for laboratory confirmation of pertussis cases do not include serologic testing.
The only pertussis diagnostic tests that the CDC endorses are culture and PCR (when the CDC/CSTE clinical case definition is also met) (Appendix B). CDC-sponsored studies are underway to evaluate both serology and PCR testing. CDC guidance on the use of pertussis diagnostics will be updated as results of these studies become available.
# Incidence of Pertussis Among Adolescents
Pertussis is reportable in all 50 states and the District of Columbia. State health departments report confirmed and probable cases of pertussis to CDC through the passive National Notifiable Diseases Surveillance System (NNDSS); additional information for pertussis cases is collected through the Supplemental Pertussis Surveillance System (SPSS) (Appendix B) (4,16). During 2004, a total of 8,897 (34%) of the 25,827 reported U.S. cases occurred among adolescents aged 11-18 years (incidence for adolescents: 30 per 100,000 population); 17 states each reported >100 pertussis cases in adolescents (12, CDC unpublished data, 2005*). The age distribution of the other pertussis cases reported in 2004 was 3,357 (13%) among infants aged <1 years, 5,441 (21%) among children aged 1-10 years, and 7,481 (29%) among adults aged >19 years (the age was unknown for 2.5% of the cases). The incidence of pertussis in adolescents varies widely among states and from year-to-year. During 2000-2004, a total of 11 states had an annual incidence of reported pertussis in adolescents of >50 per 100,000 population during at least 1 year (Table 2) (12, CDC, unpublished data, 2005).
Data from enhanced surveillance sites and prospective studies indicate that the national passive surveillance data sub- stantially underestimate the burden of pertussis among adolescents. Reliable diagnostic tests are not widely available, and not all diagnosed cases are reported. Since the 1980s, MDPH has conducted enhanced surveillance for pertussis throughout Massachusetts. MDPH uses an in-state, standardized serologic assay for pertussis diagnosis in adolescents and adults; educates health-care providers, public health staff, and the general public about pertussis; and intensifies surveillance around cases, particularly in school settings (17,66;MDPH, unpublished data, 2005). During 1996-2004, the average annual incidence of pertussis in Massachusetts adolescents aged 11-18 years was 93 per 100,000 population, approximately 13 times greater than the incidence of 7.3 reported for adolescents in the remainder of the United States (Figure 2); reported rates among children aged <11 years were comparable between Massachusetts and the remainder of the United States (CDC, unpublished data, 2005). Massachusetts data indicated that 62% of reported pertussis cases in adolescents occurred before age 16 years, and 28% of reported cases occurred before age 14 years, suggesting that pertussis booster vaccination early in adolescence could have a substantial impact on the burden of pertussis in adolescents (Figure 3) (CDC, unpublished data, 2005).
Two prospective studies in the United States have assessed the incidence of pertussis in populations that included adolescents (67,68). In a Minnesota health maintenance organization during 1995-1996, persons aged 10-49 years were tested for pertussis if they presented with an acute paroxysmal cough or a persistent cough illness of 7-34 days duration (67). Cases were laboratory-confirmed using culture, PCR, and/or serology. On the basis of 27 identified cases, the estimated incidence of laboratory-confirmed pertussis in this study was 507 per 100,000 person-years, and the incidence in adolescents (estimated 997 per 100,000 person-years) was the highest of the age groups studied (67). During 1997-2000, a study conducted at sites in eight states estimated the incidence of pertussis among persons aged 15-64 years enrolled in the control arm of an acellular pertussis vaccine trial (68). The incidence of pertussis, defined as an acute cough illness of at least 5 days with laboratory confirmation, by culture, PCR, and/or serology, was 370 per 100,000 person-years. Applying less specific case definitions, the study suggested approximately 1,000,000 cases of pertussis occur annually among persons aged >15 years in the United States (68).
# Pertussis Outbreaks Involving Adolescents
High rates of pertussis in adolescents have been reported during community and statewide outbreaks. For example, in a 1985 outbreak that occurred in a three-county region in semirural central Wisconsin, 32% of 161 cases of pertussis occurred in adolescents aged 10-19 years for an incidence (using only culture-positive cases, the strictest case definition for confirmed cases) of 150 per 100,000 population during the 8-month outbreak period (69). Compared with the incidence of pertussis in other age groups, the incidence of pertussis in adolescents was second only to that in infants aged <1 year (496 per 100,000 population) (69). In a statewide 1996 outbreak in Vermont, younger adolescents aged 10-14 years accounted for 36% of 280 cases and had the highest incidence (235 per 100,000 population) of all age groups during the outbreak period (70).
Reported cases of pertussis in adolescents often occur in outbreaks at middle and high schools, where close interaction occurs among large numbers of students with waning vaccine- Age (yrs)
# Background: Tetanus and Diphtheria Tetanus
Tetanus is unique among diseases for which vaccination is routinely recommended in that it is noncommunicable. Clostridium tetani spores are ubiquitous in the environment and enter the body through nonintact skin. When inoculated into oxygen-poor sites, such as necrotic tissue that can result from blunt trauma or deep puncture wounds, C. tetani spores germinate to vegetative bacilli that multiply and elaborate tetanospasmin, a potent neurotoxin. Generalized tetanus typically presents with trismus (lockjaw), followed by generalized rigidity caused by painful contractions of the skeletal muscles that can impair respiratory function. Glottic spasm, respiratory failure, and autonomic instability can result in death (73). During 1998-2000, the case-fatality ratio for reported tetanus was 18% in the United States (74).
Following widespread use of tetanus toxoid-containing vaccine during the 1940s, tetanus has become uncommon in the United States, particularly in children and adolescents (73,75). During 1990-2004, a total of 624 tetanus cases were reported; 19 (3%) cases were among adolescents aged 11-18 years (76; CDC, unpublished data, 2005). A 3-dose primary series of tetanus toxoid-containing vaccine generally induces protective levels of antibody for tetanus that persist for >10 years (73). Seroprotective rates for tetanus, defined as an antitetanus concentration >0. 15 (77).
Neonatal tetanus usually occurs as the result of C. tetani infection of the umbilical stump of an infant born to a mother with a maternal antitetanus concentration insufficient to provide protection to the infant (73). Neonatal tetanus is extremely rare in the United States: three cases were reported during 1990-2004. Two of the cases occurred among children born to mothers who had no dose or 1 dose of a tetanus toxoidcontaining vaccine, and the vaccination history of the third mother was unknown (78,79;CDC, unpublished data, 2005).
# Diphtheria
Respiratory diphtheria is an acute and communicable infectious illness caused by toxigenic strains of Corynebacterium diphtheriae, and rarely by toxin-producing C. ulcerans; disease is prevented by vaccination with diphtheria toxoidcontaining vaccines. Respiratory diphtheria is characterized by a grayish-colored adherent membrane in pharynx, palate, or nasal mucosa that can obstruct the airway. In addition, toxinmediated cardiac and neurologic complications can occur (80,81).
Reports of respiratory diphtheria are rare in the United States in all age groups (80,82). During 1998-2004, seven cases of respiratory diphtheria were reported to CDC; one of the cases was imported (11,12). The last culture-confirmed case of respiratory diphtheria in a U.S. adolescent was reported in 1996 (82). Data obtained from the NHANES III serosurvey during 1988-1994 indicated that the prevalence of immunity to diphtheria, defined as an antidiphtheria concentration of >0.1 IU/mL, was approximately 80% among adolescents aged 12-19 years (77).
Exposure to diphtheria remains possible during travel to countries where diphtheria is endemic (information available at http://www.cdc.gov/travel/diseases/dtp.htm) or from imported cases. Respiratory diphtheria also can occur following exposure to toxin-producing strains of C. ulcerans; some cases have followed contact with dairy animals or consumption of unpasteurized dairy products (80,83). Adherence to the ACIP-recommended schedule for tetanus and diphtheria toxoid-containing boosters among adolescents and adults is important to prevent sporadic cases of respiratory diphtheria. Information about the clinical management of diphtheria, including use of diphtheria antitoxin, and the public health response is available at http://www.cdc.gov/nip/vaccine/dat/ default.htm and reviewed elsewhere (24,80,84).
# Tetanus Toxoid, Reduced Diphtheria Toxoid and Acellular Pertussis Vaccines for Adolescents
# Criteria for Tdap Licensure
In the United States, two Tdap products were licensed for use in adolescents and, for one product, use in adults as a single dose booster immunization against tetanus, diphtheria, and pertussis on the basis of clinical trials demonstrating immunogenicity not inferior to U.S.-licensed Td or pediatric DTaP products and an overall safety profile clinically comparable to U.S.-licensed Td products (85,86). In a noninferiority trial, immunogenicity, efficacy, or safety endpoints are demonstrated when a new product is at least as good as a comparator on the basis of a predefined and narrow margin for a clinically acceptable difference between the study groups (87). The efficacy of the tetanus and diphtheria toxoid component of each Tdap was based on the immunogenicity of these antigens compared with U.S.-licensed Td using established serologic correlates of protection (73,81). The percentage of persons achieving seroprotective antitetanus and antidiphtheria concentrations (>0.1 IU/mL) and the booster response to each of these antigens 1 month postvaccination were evaluated.
In contrast to tetanus and diphtheria, no well-accepted serologic or laboratory correlate of protection for pertussis exists (88). A consensus was reached at the 1997 meeting of the Vaccines and Related Biological Products Advisory Committee that clinical endpoint efficacy studies of acellular pertussis vaccines among adolescents or adults were not required for Tdap licensure in these age groups. Rather, the efficacy of the pertussis components of Tdap administered to adolescents and adults could be inferred using a serologic bridge to infants vaccinated with pediatric DTaP during clinical endpoint efficacy trials for pertussis (89). For each Tdap product, the immune response (geometric mean antibody concentration [GMC]) of adolescents to each vaccine pertussis antigen after a single dose of Tdap was compared with the immune response of infants after three doses of pediatric DTaP that included the same pertussis components as the Tdap being assessed (32,33). The percentage of adolescents with a booster response to vaccine pertussis antigens exceeding a predefined lower limit for an acceptable booster response also was evaluated.
The safety of Tdap was evaluated by comparing rates of adverse events after vaccination in persons receiving Tdap with those receiving Td. The overall safety profile of Tdap also was assessed.
# Tdap Product Information
Data on immunogenicity and safety for the Tdap products licensed in the United States for use in adolescents (and, for one product, use in adults) are presented separately below. is formulated with reduced quantities of these antigens (Appendix A). Each antigen is adsorbed onto aluminum hydroxide. Each dose of BOOSTRIX ® (0.5 mL) is formulated to contain 5 Lf [limit of flocculation unit] tetanus toxoid, 2.5 Lf diphtheria toxoid, 8 µg inactivated PT, 8 µg FHA and 2.5 µg PRN. Each dose of BOOSTRIX ® also contains aluminum hydroxide (<0.39 mg aluminum) as the adjuvant, 4.5 mg NaCl, <100 µg residual formaldehyde, and <100 µg polysorbate 80 (Tween 80) per 0.5-mL dose. BOOSTRIX ® contains no thimerosal or other preservative. BOOSTRIX ® is available in two presentations: a prefilled disposable syringe without a needle and a single dose vial. The tip cap and rubber plunger of the needleless prefilled syringe contain dry natural latex rubber; the single dose vial stopper preparation is latex-free (33).
# Immunogenicity and Serologic Bridge to Efficacy for Pertussis
A comparative, observer-blinded, multicenter, randomized controlled clinical trial conducted in the United States evaluated the immunogenicity of the tetanus, diphtheria, and pertussis antigens in BOOSTRIX ® among adolescents aged 10-18 years (33,85). Adolescents were randomized 3:1 to receive a single dose of BOOSTRIX ® or a single dose of Td MPHBL (manufactured by the Massachusetts Public Health Biologic Laboratories; contains diphtheria toxoid [2 Lf ] and tetanus toxoid [2 Lf ]) (33,85). Serum samples were obtained before and approximately 1 month after vaccination (85). All assays were performed by GlaxoSmithKline Biologicals in Rixensart, Belgium, using validated methods (90).
Persons were eligible for enrollment if they were in good health and had completed routine childhood vaccination against diphtheria, tetanus, and pertussis (approximately 98% of persons had received >4 doses of pediatric DTP/DTaP). Persons were excluded if they had received the most recent pediatric DTP/DTaP during the preceding 5 years or Td during the preceding 10 years, had a history of pertussis or household exposure to pertussis during the previous 5 years, had any of the ACIP contraindications or precautions for pediatric DTP/DTaP (91), had systemic allergic or neurologic reac-tions or thrombocytopenia after a dose of tetanus or diphtheria toxoid-containing vaccine, had an acute illness, had received blood products or immunoglobulins within 3 months, had any immunodeficiency, had significant underlying disease, had certain neurologic disorders, or were pregnant (33, 85,92;GSK, unpublished data, 2005).
# Tetanus and Diphtheria
Immune responses to tetanus and diphtheria toxoids were compared between the BOOSTRIX ® (range: 2,463-2,516 persons) and Td MPHBL (range: 814-834 persons) groups. One month postvaccination, the antitetanus seroprotective (>0.1 IU/mL) and booster response rates in adolescents who had received a single dose of BOOSTRIX ® were noninferior to those who received Td MPHBL . All adolescents had seroprotective antitetanus levels >0.1 IU/mL 1 month after vaccination with either BOOSTRIX ® (95% confidence interval [CI] = 99.8%-100%) or Td MPHBL (95% CI = 99.6%-100%). The booster response rate to tetanus † in the BOOSTRIX ® group was 89.7% (95% CI = 88.4%-90.8%), compared with 92.5% (95% CI = 90.5%-94.2%) in the Td MPHBL group (33,92).
One month postvaccination, the antidiphtheria seroprotective (>0.1 IU/mL) and booster response rates among adolescents who received a single dose of BOOSTRIX ® were noninferior to those of adolescents who received Td MPHBL . Among adolescents, 99.9% had seroprotective antidiphtheria levels >0.1 IU/mL 1 month postvaccination with either BOOSTRIX ® (95% CI = 99.7%-100%) or Td MPHBL (95% CI = 99.3%-100%). The booster response rate to diphtheria † in the BOOSTRIX ® group was 90.6% (95% CI = 89.4%-91.7%), compared with 95.9% (95% CI = 94.4%-97.2%) in the Td MPHBL group (33,92).
# Pertussis
The efficacy of the pertussis components of BOOSTRIX ® was evaluated by comparing the immune responses of adolescents vaccinated with a single dose of BOOSTRIX ® with the immune responses of infants vaccinated with 3 doses of INFANRIX ® . These infants were a subset of those vaccinated with INFANRIX ® in a German vaccine efficacy trial during the 1990s (33,93). BOOSTRIX ® has the same three pertussis antigens as INFANRIX ® but in reduced quantities (Appendix A). In the infant trial, the efficacy of 3 doses of INFANRIX ® against World Health Organization (WHO)defined typical pertussis (>21 days of paroxysmal cough with confirmation of B. pertussis infection by culture and/or sero- † Booster response: In persons with prevaccination antibody concentration <0.1 IU/mL, postvaccination antibody concentration >0.4 IU/mL. In persons with prevaccination antibody concentration >0.1 IU/mL, an increase of at least four times the prevaccination antibody concentration.
logic testing) was 89% (95% CI = 77%-95%) (33,93). The anti-PT, anti-FHA, and anti-PRN GMCs of adolescents 1 month after a single dose of BOOSTRIX ® were noninferior to those of infants after 3 doses of INFANRIX ® (Table 4) (33,85,92). Booster response rates to the pertussis antigens § contained in BOOSTRIX ® (anti-PT, anti-FHA, and anti-PRN) among adolescents (range: 2,677-2,752 persons) 1 month after administration of BOOSTRIX ® met prespecified criteria for an acceptable response. Booster response rates to pertussis antigens were anti-PT, 84.5% (95% CI = 83.0%-85.9%); anti-FHA, 95.1% (95% CI = 94.2%-95.9%), and anti-PRN, 95.4% (95% CI = 94.5%-96.1%) (33,92).
# Safety
The primary safety study, conducted in the United States, was a randomized, observer-blinded, controlled study in which 3,080 adolescents aged 10-18 years received a single dose of BOOSTRIX ® , and 1,034 received Td MPHBL (see BOOSTRIX ® Immunogenicity and Serologic Bridge to Efficacy for Pertussis for inclusion and exclusion criteria). Data on solicited local and systemic adverse events were collected using standardized diaries for the day of vaccination and the next 14 consecutive days (i.e., within 15 days following vaccination). Unsolicited and serious adverse events were collected for 6 months following vaccination. No immediate events (within 30 minutes of vaccination) were reported in either vaccination group (33,85,92).
# Solicited Local Adverse Events
Pain at the injection site was the most frequently reported solicited local adverse event in adolescents vaccinated with BOOSTRIX ® or Td MPHBL . Within 15 days after vaccina-tion, 75.3% of persons in the BOOSTRIX ® group and 71.7% of persons in the Td MPHBL group reported pain of "any" intensity (Table 5). The rates of any pain and grade 2 or 3 pain combined (but not grade 3 alone) were significantly higher (p<0.05) in BOOSTRIX ® recipients compared with Td MPHBL recipients (Table 5). However, the rates of grade 3 pain (primary safety endpoint) were similar in each group, and the noninferiority criterion was met for BOOSTRIX ® compared with Td MPHBL . No significant differences in the rates of other solicited local adverse events (redness, swelling, and increase in arm circumference above baseline) were observed between the two study groups (33, 85,92).
Two adolescents in the study reported "large injection-site swelling" after vaccination (predefined as any local swelling with a diameter >100 mm and/or increased circumference of the injected limb >50 mm above baseline measurements and/or any diffuse swelling that interfered with or prevented normal everyday activities). Both persons had onset of symptoms within 3 days of vaccination. One person who had received BOOSTRIX ® reported grade 3 pain (Table 5) with functional impairment. This person was evaluated and treated with antimicrobials with symptom resolution within 3 days without sequelae. The second person, who had received Td MPHBL , reported grade 1 pain and did not seek medical attention. The duration of symptoms was unknown, but symptoms resolved without sequelae (85,90,92). No cases of wholearm swelling were reported in either vaccine group (GSK, unpublished data, 2005).
# Solicited Systemic Adverse Events
The most frequently reported solicited systemic adverse events within 15 days following vaccination with BOOSTRIX ® or Td MPHBL were headache and fatigue (Table 6). A statistically significantly higher rate of grade 2 or grade 3 headache combined (but not grade 3 alone) (Table 6) was reported in the BOOSTRIX ® group (15.7%), compared with the Td MPHBL group (12.7%). The proportion of adolescents reporting fever >100.4° F (38.0° C) (5.0% for BOOSTRIX ® and 4.7% for Td MPHBL ), fatigue, and gastrointestinal systemic events were comparable in both groups (33,85,92).
# Serious Adverse Events
In the primary U.S. safety study, no serious adverse events (SAEs) occurred within 1 month postvaccination with either BOOSTRIX ® or Td MPHBL . During the next 5 months of monitoring, SAEs were reported among 14 (0.4%) of the 3,005 adolescents vaccinated with BOOSTRIX ® and two (0.2%) of the 1,003 adolescents vaccinated with Td MPHBL . No SAEs that were of potential autoimmune origin, new onset and chronic in nature, or related to vaccination, as determined by the investigators, were reported (33, 85,90,92). No seizures, cases of Guillain-Barré syndrome, or physiciandiagnosed Arthus reactions were reported (33,85,90; GSK, unpublished data, 2005).
# Simultaneous Administration with other Vaccines
Safety and immunogenicity of simultaneous administration of BOOSTRIX ® with other vaccines were not evaluated during prelicensure studies (33).
# Vaccine Composition
ADACEL ™ contains the same tetanus toxoid, diphtheria toxoid, and five pertussis antigens as those in DAPTACEL ® (pediatric DTaP), but ADACEL ™ is formulated with reduced quantities of diphtheria toxoid and detoxified PT (Appendix A). Each antigen is adsorbed onto aluminum phosphate. Each dose of ADACEL ™ (0.5 mL) is formulated to contain 5 Lf tetanus toxoid, 2 Lf diphtheria toxoid, 2.5 µg detoxified PT, 5 µg FHA, 3 µg PRN, and 5 µg fimbriae types 2 and 3 (FIM). Each dose of ADACEL ™ also contains aluminum phosphate (0.33 mg aluminum) as the adjuvant, <5 µg residual formaldehyde, <50 ng residual glutaraldehyde, and 3.3 mg 2-phenoxyethanol (not as a preservative) per 0.5-mL dose. ADACEL ™ contains no thimerosal. ADACEL ™ is available in single dose vials that are latex-free (32).
# Immunogenicity and Serologic Bridge to Efficacy for Pertussis
A comparative, observer-blinded, multicenter, randomized controlled clinical trial conducted in the United States evaluated the immunogenicity of the tetanus, diphtheria, and pertussis antigens in ADACEL ™ among adolescents aged 11-17 years; adults aged 18-64 years were also studied and results are reported elsewhere (32,86). Adolescents were randomized 3:2 to receive a single dose of ADACEL ™ or a single dose of Td sp (manufactured by sanofi pasteur; contains tetanus toxoid [5 Lf ] and diphtheria toxoid [2 Lf ]) (32,86). Sera from a subset of persons were obtained before and approximately 1 month after vaccination (32). All assays were performed at the immunology laboratories of sanofi pasteur in Toronto, Ontario, Canada or Swiftwater, Pennsylvania, using validated methods (86,94).
Persons were eligible for enrollment if they were in good health; completion of the childhood DTP/DTaP vaccination series was not required. Persons were excluded if they had received a tetanus, diphtheria, or pertussis vaccine within 5 years; had a diagnosis of pertussis within 2 years; had an allergy or sensitivity to any vaccine component; had a previous reaction to a tetanus, diphtheria or pertussis vaccine, including encephalopathy within 7 days or seizures within 3 days; had an acute respiratory illness on the day of enrollment; had daily use of oral, nonsteroidal anti-inflammatory drugs; had received blood products or immunoglobulins within 3 months; had any immunodeficiency; had significant underlying disease; had neurologic impairment; or were pregnant (32,94; sanofi pasteur, unpublished data, 2005).
# Tetanus and Diphtheria
Immune responses to tetanus and diphtheria toxoids were compared between the ADACEL ™ (N = 527) and Td sp (range: 515-516 persons) groups. One month postvaccination, the antitetanus seroprotective (>0.1 IU/mL) and booster response rates among adolescents who received ADACEL ™ were noninferior to those who received Td sp . All adolescents (95% CI = 99.3%-100% for both groups) had seroprotective antitetanus levels >0.1 IU/mL 1 month after vaccination with either ADACEL ™ or Td sp . The booster response rate to tetanus ¶ in the ADACEL ™ group was 91.7% (95% CI = 89.0%-93.9%) and 91.3% (95% CI = 88.5%-93.6%) in the Td sp group (32,86,94). One month postvaccination, the antidiphtheria seroprotective (>0.1 IU/mL) and booster response rates among adolescents who received a single dose of ADACEL ™ were noninferior to those who received Td sp . Among adolescents, 99.8% (95% CI = 98.9%-100%) had protective antidiphtheria levels >0.1 IU/mL 1 month after vaccination with either ADACEL ™ or Td sp. The booster response rate to diphtheria ¶ in the ADACEL ™ group was 95.1% (95% CI = 92.9%-96.8%) and 95.0% (95% CI = 92.7%-96.7%) in the Td sp group (32,86,94). ¶ Booster response was defined as a fourfold rise in antibody concentration, if the prevaccination antibody concentration was equal to or below the cutoff value, and a two-fold rise in antibody concentration if the prevaccination antibody concentration was above the cut-off value. The cut-off value for tetanus was 2.7 IU/mL. The cut-off value for diphtheria was 2.56 IU/mL.
# Pertussis
The efficacy of the pertussis components of ADACEL ™ was evaluated by comparing the immune responses of adolescents vaccinated with a single dose of ADACEL ™ with the immune responses of infants vaccinated with 3 doses of DAPTACEL ® in a Swedish vaccine efficacy trial during the 1990s (32,95). ADACEL ™ and DAPTACEL ® contain the same five pertussis antigens, except ADACEL ™ contains one fourth the quantity of detoxified PT in DAPTACEL ® (96) (Appendix A). In the Swedish trial, efficacy of 3 doses of DAPTACEL ® against WHO-defined pertussis (>21 days of paroxysmal cough with confirmation of B. pertussis infection by culture and/or serologic testing or an epidemiologic link to a household member with culture-confirmed pertussis) was 85% (95% CI = 80%-89%) (29,87). The anti-PT, anti-FHA, anti-PRN, and anti-FIM GMCs of adolescents 1 month after a single dose of ADACEL ™ were noninferior to those of infants following three doses of DAPTACEL ® (32,94) (Table 7).
Booster response rates to the pertussis antigens** contained in ADACEL ™ (anti-PT, anti-FHA, anti-PRN, anti-FIM) among adolescents (range: 524-526 persons) 1 month fol-lowing administration of ADACEL ™ met prespecified criteria for an acceptable response. Booster response rates to pertussis antigens were anti-PT, 92.0% (95% CI = 89.3%-94.2%); anti-FHA, 85.6% (95% CI = 82.3%-88.4%); anti-PRN, 94.5% (95% CI = 92.2%-96.3%); and anti-FIM 94.9% (95% CI = 92.6%-96.6%) (32,94).
# Safety
The primary adolescent safety study, conducted in the United States, was a randomized, observer-blinded, controlled study in which 1,184 adolescents aged 11-17 years received a single dose of ADACEL ™ and 792 received Td sp (see ADACEL ™ Immunogenicity and Serologic Bridge to Efficacy for Pertussis for inclusion and exclusion criteria) (32). Adults aged 18-64 years were also studied; those results are reported elsewhere (32). Data on solicited local and systemic adverse events were collected using standardized diaries for the day of vaccination and the next 14 consecutive days (i.e., within 15 days following vaccination) (32).
# Immediate Events
Eleven adolescents experienced immediate events within 30 minutes of vaccination (ADACEL ™ , six persons [0.5%] and Td sp , five persons [0.6%]); all events resolved without sequelae. Immediate events included dizziness, syncope, or vasovagal reactions and pain and erythema at the injection site. No anaphylaxis was reported (86,94,96).
# Solicited Local Adverse Events
Pain at the injection site was the most frequently reported solicited local adverse event among adolescents in both vaccination groups (Table 8). Within 15 days following vaccination, reports of pain of "any" intensity were more common among adolescents vaccinated with ADACEL ™ (77.8%) than among those vaccinated with Td sp (71.0%). The noninferiority criterion was not achieved for the rate of any pain following ADACEL ™ compared with the rate following Td sp . Rates of moderate/severe pain, erythema, and swelling following ADACEL ™ were comparable to the rates following Td sp (32,86,94). No cases of whole-arm swelling were reported in either vaccine group (94).
# Solicited Systemic Adverse Events
The most frequently reported solicited systemic adverse events within the 15 days following vaccination were headache, generalized body aches, and tiredness (Table 9). The proportion of adolescents reporting fever >100.4° F (>38° C) following vaccination was statistically significantly higher among adolescents vaccinated with ADACEL ™ (5.0%) than Td sp (2.7%), but noninferiority criterion for ADACEL ™ was ** A booster response for each antigen was defined as a fourfold rise in antibody concentration, if the prevaccination antibody concentration was equal to or below the cut-off value, and a twofold rise in antibody concentration if the prevaccination antibody concentration was above the cut-off value. The cut-off values for pertussis antigens were 85 EU/mL for pertussis toxin, 170 EU/mL for filamentous haemagglutinin, 115 EU/mL for pertactin, and 285 EU/mL for fimbriae. achieved. The rates of the other solicited systemic adverse events were comparable between the ADACEL ™ and Td sp groups (32,94).
# Serious Adverse Events
In the primary adolescent safety study, SAEs within 6 months after vaccination were reported among 11 (0.9%) of the 1,184 adolescents aged 11-17 years vaccinated with ADACEL ™ and eight (1.0%) of the 792 adolescents vaccinated with Td sp . Two adolescents (one ADACEL ™ recipient and one Td sp recipient) reported seizure events after vaccination; both persons had a history of seizure disorder. SAEs in adolescents were reported by the study investigators to be unrelated to the study vaccine (94).
The safety of ADACEL ™ among adults also was studied. In the primary adult safety study, SAEs within 6 months after vaccination were reported among 33 (1.9%) of the 1,752 adults aged 18-64 years vaccinated with ADACEL ™ and 11 (1.9%) of the 573 adults vaccinated with Td sp . Two of these SAEs were neuropathic events in ADACEL ™ recipients and were assessed by the investigators as possibly related to the study vaccine; in both cases, the symptoms resolved completely over several days (32,86,94,96). No physician-diagnosed Arthus reactions or cases of Guillain-Barré syndrome were reported in any adolescent or adult (32,86,96; sanofi pasteur, unpublished data, 2005).
# Simultaneous Administration with Other Vaccines
# Hepatitis B Vaccine
Safety and immunogenicity of ADACEL ™ co-administered with hepatitis B vaccine (Recombivax HB ® , Merck and Co., Inc., White House Station, New Jersey) was evaluated in adolescents aged 11-14 years using methods similar to the primary ADACEL ™ studies. Adolescents were randomized to one of two groups. In one group, ADACEL ™ and hepatitis B vaccine were administered simultaneously in different arms (simultaneous group; N = 206). In the other group, ADACEL ™ was administered first, followed by hepatitis B vaccine 4-6 weeks later (sequential group; N = 204) (32; sanofi pasteur, unpublished data, 2005). No interference was observed in the immune responses to any of the vaccine antigens when ADACEL ™ and hepatitis B vaccine were administered simultaneously or sequentially † † (32).
Adverse events were solicited only after ADACEL ™ vaccination (not hepatitis B vaccination) (86). Within 15 days of vaccination, the reported rates of injection site pain (at the ADACEL ™ site) and fever were comparable when ADACEL ™ and hepatitis B vaccine were administered simultaneously or sequentially (Table 10). However, rates of erythema and swelling at the ADACEL ™ injection site were higher in the simultaneous group than the sequential group, and noninferiority criteria for simultaneous vaccination were not achieved (Table 10) (86). Swollen and/or sore joints were reported in 22.5% of persons in the simultaneous group and 17.9% of persons in the sequential group. Most joint com-plaints were mild in intensity and the mean duration was 1.8 days (86).
# Trivalent Inactivated Influenza Vaccine
Safety and immunogenicity of ADACEL ™ co-administered with trivalent inactivated influenza vaccine ([TIV] Fluzone ® , sanofi pasteur, Swiftwater, Pennsylvania) was evaluated in adults aged 19-64 years using methods similar to the primary ADACEL ™ studies (32). The immunogenicity data are presented elsewhere (32). The adults were randomized to one of ¶ The rate of "Any" fever following ADACEL ™ was statistically higher than the rate following Td sp in the adolescents; however, the noninferiority criterion was achieved for ADACEL ™ (upper limit of the 95% confidence interval on the difference in the percentage of persons [ADACEL ™ minus Td sp ] was <10%).
two groups. In one group, ADACEL ™ and TIV were administered simultaneously in different arms (simultaneous group; N = 359). In the other group, TIV was administered first, followed by ADACEL ™ 4-6 weeks later (sequential group; N = 361) (32; sanofi pasteur, unpublished data, 2005). Adverse events were solicited only after ADACEL ™ vaccination (not TIV) (86). Within 15 days of vaccination, rates of erythema, swelling, and fever were comparable in both vaccination groups. However, the rate of pain at the ADACEL ™ injection site was higher in the simultaneous group (66.6%) than the sequential group (60.8%), and did not meet the noninferiority criterion (upper limit of the 95% CI on the difference in percentage of persons [the rate following simultaneous vaccination minus the rate following sequential vaccination] was 13.0%, and the criterion was <10%) (86).
# Other Vaccines
Safety and immunogenicity of simultaneous administration of ADACEL ™ with other vaccines were not evaluated during prelicensure studies (32).
# Studies of Adolescent Acellular Pertussis Vaccine Impact Clinical Efficacy Trial
The efficacy against pertussis of an adolescent and adult acellular pertussis (ap) vaccine with the same pertussis antigens included in BOOSTRIX ® (without tetanus and diph-theria toxoids) was evaluated in 2,781 adolescents and adults in a prospective, randomized trial (68). Results of this study were not considered as part of Tdap licensure in the United States (see Criteria for Tdap Licensure). Persons aged 15-64 years were randomized to receive one dose of ap vaccine or hepatitis A vaccine (Havrix ® , GlaxoSmithKline Biologicals, Rixensart, Belgium). The primary outcome measure was confirmed pertussis, defined by a cough illness lasting >5 days with laboratory evidence of B. pertussis infection by culture, PCR, and/or serologic testing results (acute and convalescent). Nine persons in the hepatitis A vaccine control group and one person in the ap vaccine group had confirmed pertussis during the study period; vaccine efficacy against confirmed pertussis was 92% (95% CI = 32%-99%) (68).
# Economic Studies
The societal costs of pertussis are important, and universally vaccinating adolescents against pertussis is likely to be cost effective. In one study, the economic impact of pertussis among Massachusetts adolescents aged 10-17 years was evaluated using the state's enhanced pertussis surveillance system (54). The mean medical cost per adolescent case of pertussis was an estimated $201 and $256 for mild and severe cases of cough illness, respectively (in 2004 dollars), excluding the cost of providing antimicrobials to close contacts of the caseadolescents (53,54). The largest proportion of this cost was for medical office visits and antimicrobial therapy (54). When indirect, nonmedical costs (e.g., missed time from work for parents of adolescents) were included, total societal cost of an adolescent case of pertussis was $361 and $416 for mild and severe cough illness, respectively (in 2004 dollars) (53,54).
Two U.S. economic studies have compared adolescent vaccination with other pertussis vaccination strategies (53,97). Both studies identified a single dose of Tdap during adolescence as the most cost-effective strategy, under different assumptions about pertussis incidence, waning immunity, vaccine efficacy, vaccine coverage, and infant transmission. In the first study, a cost-benefit analysis was conducted to compare seven adolescent and/or adult pertussis vaccination strategies during a 10-year interval (2001-2010), using a single dose of a Tdap. In this analysis, the incidence of pertussis among adolescents and adults was estimated from prospective studies to be 450-507 cases per 100,000 population. Strategies included vaccinating all adolescents aged 10-19 years, vaccinating all persons aged >10 years (i.e., universal adolescent and adult vaccination), vaccinating adolescents and adults aged >15 years that were the primary care-takers of infants, and four other adult vaccination strategies. Among these strategies, vaccinating all adolescents was identified as the most costeffective strategy. Universal adolescent Tdap vaccination was cost-saving to society when the Tdap vaccine and program costs were <$37 (2002 dollars) per adolescent vaccinated (97).
In a second study, six adolescent and/or adult Tdap vaccination strategies were compared by modeling health outcomes over the course of a lifetime for hypothetical cohort of 4 million adolescents (53). Incidence rates of pertussis among adolescents and adults were estimated from Massachusetts surveillance data; baseline estimates were 155 and 11 per 100,000 population for adolescents and adults, respectively. The six strategies included no adolescent or adult vaccination, one-time adolescent vaccination at age 11 years, onetime adult vaccination, adult vaccination with decennial Tdap boosters, adolescent and adult vaccination with decennial Tdap boosters, and postpartum vaccination. The study assumed an incremental increase in Tdap price of $15 compared with Td, with a Tdap vaccination cost of $25 per person vaccinated. Universal adolescent vaccination was the most costeffective strategy. Vaccinating all adolescents once would cost $1,100 per pertussis case prevented or $20,000 per quality adjusted life year (QALY) saved, both in 2004 dollars. By contrast with the cost-benefit analysis (97), which estimated the incidence of pertussis in adolescents to be approximately 3 times higher, Tdap vaccination was not cost-saving under the second study's baseline assumptions (53). In a sensitivity analysis, results from the second study found that if the incidence of adolescent and adult pertussis was four times the base-case estimates, universal adolescent Tdap vaccination would be costsaving to society (53).
# Other Tetanus and Diphtheria Toxoids Vaccine Preparations for Adolescents
Four Td (Tetanus and Diphtheria Toxoids, Adsorbed for Adult Use) vaccines are licensed in the United States for active immunization against tetanus and diphtheria among persons aged >7 years (98)(99)(100)(101). Two tetanus toxoid vaccines (TT) also are licensed for use in this age group (102,103). Of the two TT products, one is adsorbed and is licensed for use in situations in which the combined antigen preparation (Td) is not indicated (102). The second TT preparation is a fluid vaccine (not adsorbed) and is indicated only for booster doses, not for primary immunization (103). Although TT is licensed in the United States for persons aged >7 years, Td has been preferred for routine use to provide dual protection against tetanus and diphtheria (24) (Appendix A).
# Safety Considerations for Adolescent Vaccination with Tdap or Td
Prelicensure Tdap studies support the safety of these vaccines (32,33). However, sample sizes were insufficient to detect rare adverse events, a limitation of prelicensure trials. Enrollment criteria excluded persons who had received vaccines containing tetanus toxoid, diphtheria toxoid, or pertussis components during the preceding 5 or 10 years (85,86,92,94). In addition, persons with certain neurologic conditions or events following pediatric DTP/DTaP vaccination were excluded from these studies (85,92,94). Therefore, in making recommendations on the spacing and administration sequence of vaccines containing tetanus toxoid, diphtheria toxoid, and/or pertussis components and on vaccination of adolescents with a history of certain neurologic conditions or adverse events after vaccination, ACIP considered data from a range of pre-and postlicensure studies of Tdap and other vaccines containing these components. Safety data being collected from the Vaccine Adverse Event Reporting System (VAERS) and postlicensure studies will facilitate detection of potential adverse reactions following widespread use of Tdap in adolescents (see Reporting of Adverse Events after Vaccination) (104,105).
# Spacing and Administration Sequence of Vaccines Containing Tetanus Toxoid, Diphtheria Toxoid, and Pertussis Antigens
Historically, moderate and severe local reactions following tetanus and diphtheria toxoid-containing vaccines have been associated with older, less purified vaccines, larger doses of toxoid, and frequent dosing at short intervals (106)(107)(108)(109)(110)(111). In addition, high pre-existing antibody titers to tetanus or diphtheria toxoids in children, adolescents, and adults primed with these antigens might be associated with increased rates of local reactions to booster doses of tetanus or diphtheria toxoidcontaining vaccines (26,108,111,112). Two adverse events of particular clinical interest have been associated with vaccines containing tetanus toxoid, diphtheria toxoid, and/or pertussis antigens, extensive limb swelling (ELS), and Arthus reactions.
# Extensive Limb Swelling
ELS reactions have been described following doses of pediatric DTaP and other vaccines (28,91,(113)(114)(115)(116)(117). In retrospective analyses, 2%-3% of children receiving the fourth or fifth booster doses of pediatric DTaP experienced extensive proximal limb swelling; swelling is usually greatest by 48 hours after vaccination (28,118). ELS is generally not disabling, is not often brought to medical attention, and resolves without complication within 4-7 days (118). ELS has been reported to VAERS almost as frequently following Td as following pediatric DTaP; among adolescents, the majority of reported cases of ELS have involved either Td or hepatitis B vaccine (117). The pathogenesis of ELS is not well understood; this reaction has not consistently been related to the content of tetanus toxoids, diphtheria toxoids, pertussis antigens, or aluminum adjuvants in vaccines (28,118,119). Whether children who experience ELS after receipt of pediatric DTaP are at increased risk for ELS after receipt of Tdap is unknown. Because these reactions typically resolve without sequelae, ACIP does not consider a history of ELS following pediatric DTaP or any other vaccine to be a precaution or contraindication for pediatric DTaP (91,113).
# Arthus Reactions
Arthus reactions (type III hypersensitivity reactions) are rarely reported after vaccination and can occur after tetanus toxoid-containing or diphtheria toxoid-containing vaccines (24,111,120-124;CDC, unpublished data, 2005). An Arthus reaction is a local vasculitis associated with deposition of immune complexes and activation of complement. Immune complexes form in the setting of high local concentration of vaccine antigens and high circulating antibody concentration (111,120,121,125). Arthus reactions are characterized by severe pain, swelling, induration, edema, hemorrhage, and occasionally by necrosis. These symptoms and signs usually occur 4-12 hours after vaccination; by contrast, anaphylaxis (immediate type I hypersensitivity reactions) usually occur within minutes of vaccination. As with ELS, Arthus reactions usually resolve without sequelae. ACIP has recommended that persons who experienced an Arthus reaction after a dose of tetanus toxoid-containing vaccine should not receive Td more frequently than every 10 years, even for tetanus prophylaxis as part of wound management (24).
# Interval between Td and Tdap
ACIP has recommended a 10-year interval for routine administration of Td and a 5-year minimum interval between the last pediatric DTaP and the adolescent Td dose (24,30). Administration of Td at short intervals might increase the risk for adverse events (108,109). Prelicensure clinical trials of Tdap excluded persons who had received doses of a diphtheria or tetanus toxoid-containing vaccine during the preceding 5 or 10 years (see BOOSTRIX ® and ADACEL ™ sections on Immunogenicity and Serologic Bridge to Efficacy for Pertussis for exclusion criteria) (90,94,96). Although administering Td more often than every 10 years (5 years for a tetanus-prone wound) is not necessary to provide protection against tetanus or diphtheria, administering a dose of Tdap less than 5 years after Td could provide a health benefit by protecting against pertussis.
The safety of administering a dose of Tdap at intervals less than 5 years after pediatric DTP/DTaP or Td was evaluated in Canada following the country's licensure of Tdap (ADACEL ™ ) (126). The largest Canadian study was a nonrandomized, open-label study of 7,001 students aged 7-19 years residing in Prince Edward Island. This study assessed the rates of adverse events after Tdap and compared reactogenicity of Tdap administered at year intervals of 2-9 years (eight cohorts) versus >10 years after the last tetanus and diphtheria toxoid-containing vaccine (Td, or pediatric DTP or DTaP). A year interval was defined as the integer year +0.5 years (e.g., the 2-year interval was defined as >18 months to <30 months). Vaccination history for type of pertussis vaccine(s) received (pediatric DTP and DTaP) also was assessed. The number of persons assigned to cohorts ranged from 464 in the 2-year to 925 in the 8-year cohorts. Among the persons in the 2-year cohort, 214 (46%) received the last tetanus and diphtheria toxoid-containing vaccine 18-23 months before Tdap. Adverse event diary cards were returned for 85% of study participants with a known interval; 90% of persons in the 2-year interval cohort provided safety data (126).
Four SAEs were reported in the Prince Edward Island study; none were assessed by the investigators to be related to vaccine. No Arthus reaction was reported. Rates of reported severe local adverse reactions, fever, and any pain were not increased in persons who received Tdap at intervals less than 10 years. Rates of local reactions were not increased among persons who received 5 doses of pediatric DTP, with or without Td (intervals of 2-3 years or 8-9 years). Rates of any erythema and any swelling were reported more frequently in cohorts that had received at least 1 or 2 doses of pediatric DTaP (intervals of 4-7 years), suggesting that increased rates of local reactions might occur more commonly among adolescents who received pediatric DTaP vaccines, compared with those who received a 5-dose pediatric DTP series. Limb swelling (>100 mm) was reported in 0.2% of participants and was unrelated to the interval since the last tetanus and diphtheria toxoid-containing vaccine (126).
A study was conducted in Germany to evaluate the safety of Tdap (BOOSTRIX ® ) in persons aged 9-13 years who received a 5-dose all acellular pertussis vaccine schedule (5 doses of INFANRIX ® , N = 193 or 4 doses of INFANRIX ® plus another acellular pertussis vaccine, N = 126); the interval from the fifth to sixth dose of the acellular pertussis vaccines ranged from approximately 5-6 years (GSK, unpublished data, 2005). Within 15 days after vaccination, any pain (63.6%), erythema (51.7%), and swelling (41.4%) were frequently reported symptoms, but the rate of "large injection site swelling" (see BOOSTRIX ® , solicited local adverse events for definition) was low (0.9%). Following their sixth consecutive dose of an acellular pertussis vaccine, persons reported more pain, less redness, and less swelling compared with their fifth dose of pediatric DTaP (INFANRIX ® ) (127).
Two smaller Canadian postlicensure safety studies in adolescents also showed acceptable safety when Tdap (ADACEL ™ ) was administered at intervals less than 5 years after tetanus and diphtheria toxoid-containing vaccines (128,129). Taken together, these three Canadian studies support the safety of using Tdap after Td at intervals less than 5 years. The largest study suggests intervals as short as approximately 2 years are acceptably safe (126).
# Simultaneous and Nonsimultaneous Vaccination with Tdap/Td and Diphtheria-Containing Tetravalent Meningococcal Conjugate Vaccine
Tdap, Td, and tetravalent meningococcal conjugate vaccine ([MCV4] Menactra ® , sanofi pasteur, Swiftwater, Pennsylvania) contain diphtheria toxoid (32,33,130,131). Each of these vaccines is licensed for use in adolescents, but MCV4 is not indicated for active immunization against diphtheria (131). During 2005, MCV4 was recommended for routine use among adolescents (130,132). In MCV4, the diphtheria toxoid (approximately 48 µg) serves as the carrier protein that improves immune responses to meningococcal antigens. Precise comparisons cannot be made between the quantity of diphtheria toxoid in the vaccines; however, the amount in a dose of MCV4 is estimated to be comparable with the average quantity in a dose of pediatric DTaP (133).
No prelicensure studies of simultaneous or sequential vaccination with Tdap and MCV4 were done. None of the persons in the Canadian safety studies described above had received MCV4. Persons who recently received one diphtheria toxoid-containing vaccine might have increased rates of adverse reactions after a subsequent diphtheria toxoid-containing vaccine when diphtheria antibody titers remain elevated from the previous vaccination (26,108,111,112). The diphtheria GMCs were comparable or lower following Tdap compared with Td § § ; therefore, results of a co-administration trial of Td and MCV4 might be informative to infer the effect of co-administration of Tdap and MCV4. A randomized, controlled prelicensure trial assessed the safety of simultaneous versus sequential administration of Td and MCV4.
In this co-administration trial, administration of Td (approximately 8 µg of diphtheria toxoid) with MCV4 first, then placebo 28 days later (simultaneous group), or administration of Td with placebo first, then MCV4 28 days later (sequential group) was studied among 1,021 healthy adolescents aged 11-17 years (Table 11) (89,131,133). Serum samples from a subset of adolescents vaccinated with MCV4 from a different clinical trial were used for comparison. § § One month after vaccination, the antidiphtheria GMCs were ADACEL ™ Administration of MCV4 first followed by Td was not studied. Both simultaneous and sequential administration of Td and MCV4 induced immune responses to all antigens. One month postvaccination, the immune responses to diphtheria toxoid were higher when MCV4 was administered simultaneously with Td (GMT 120.9 IU/mL) than when Td was administered with placebo (GMT 8.4 IU/mL). Adolescents vaccinated with MCV4 alone also had high antidiphtheria responses 1 month following vaccination (GMT 46.5 IU/mL) (Table 11) (89,131,133). Adverse events on vaccination day and during the following 7 days were assessed among adolescents in the simultaneous and sequential groups. The overall rates of solicited local reactions were similar for the two groups: 58.0% reported local reactions at the MCV4 injection site in the simultaneous group versus 57.0% in the sequential group, and 74.7% reported local reactions at the Td injection site in the simultaneous group versus 73.3% in the sequential group. Pain was the most frequently reported reaction and pain rates were similar between groups; severe pain was uncommon (<1% of persons). Fever >99.5° F (>37.5° C) and high fever >104° F (>40° C) were reported in <5% and <0.5% of persons, respectively (133)(134)(135). The safety of simultaneous vaccination of MCV4 with Tdap and sequential administration of Tdap first followed by MCV4 1 month later has been inferred from results of this study.
When Tdap or Td is administered after MCV4, rates of adverse reactions might be higher than when the dose is administered before MCV4 because pre-existing diphtheria antibody levels might be higher (26,108,111,112,133,135). Rates of adverse reactions were assessed in a small prelicensure study for MCV4 among 76 adolescents aged 15-17 years who received 2 doses of MCV4 spaced 3 years apart. After the second dose of MCV4, no SAEs, fever >102.2° F (>39° C), or severe local reactions were reported with the exception of one person, who reported severe pain at the injection site that lasted for 1 day (sanofi pasteur, unpublished data, 2005). No other available data exist on the safety of intervals between MCV4 and other diphtheria toxoid-containing vaccines. Postlicensure studies to provide additional information are under way (104,105).
# Neurologic and Systemic Events Associated with Vaccines with Pertussis Components or Tetanus Toxoid-Containing Vaccines
# Vaccines with Pertussis Components
Concerns about the possible role of vaccines with pertussis components in causing neurologic reactions or exacerbating underlying neurologic conditions are long-standing (20,136).
ACIP recommendations to defer pertussis vaccines in infants with suspected or evolving neurologic disease, including seizures, have been based primarily on concerns that neurologic events after vaccination (with whole cell preparations in particular) might interfere with the subsequent evaluation of the infant's neurologic status (1,136).
In 1991, the Institute of Medicine (IOM) concluded that evidence favored acceptance of a causal relation between pediatric DTP and acute encephalopathy; the IOM has not evaluated associations between pediatric DTaP and neurologic events (123). Pediatric DTaP is contraindicated for children with a history of encephalopathy not attributable to another identifiable cause occurring within 7 days after pediatric DTP/DTaP vaccination. Though active surveillance in Canada during 1993-2002 failed to ascertain any acute encephalopathy cases causally related to whole cell or acellular pertussis vaccines among a population administered 6.5 million doses of pertussis vaccines (137), research conducted in Japan during the introduction of acellular pertussis vaccines yielded rates of 1.0-1.3 attributable encephalopathy cases within 7 days of vaccination per 10 million doses (138).
ACIP has recommended that infants with evolving neurologic conditions should not be vaccinated with pediatric DTaP until a treatment regimen has been established and the condition has stabilized (1). Concerns about vaccinating adolescents with progressive or uncontrolled underlying neurologic disease must be weighed against the potential for morbidity from pertussis. Adolescents with severe neurologic conditions might be at risk for severe pertussis (48;CDC, unpublished data, 2005). ACIP does not consider a history of wellcontrolled seizures in the vaccinee or a family history of seizures (febrile or afebrile) or other neurologic disorder to be a contraindication or precaution to vaccination with pertussis components (1).
ACIP has recommended that vaccine providers and parents evaluate the risks for and benefits of administering subsequent doses of vaccines with pertussis components to young children who experienced these events after pediatric DTP/DTaP: temperature >105° F (>40.5° C) within 48 hours after pediatric DTP/DTaP, not attributable to another cause; collapse or shock-like state (hypotonic hyporesponsive episode) within 48 hours after pediatric DTP/DTaP; persistent crying lasting >3 hours, occurring within 48 hours after pediatric DTP/ DTaP; or convulsions with or without fever, occurring within 3 days after pediatric DTP/DTaP. All of these events were documented more frequently following whole cell pertussis vaccines than they have been following acellular vaccines (1,(139)(140)(141)(142). VAERS data have documented decreased reports of fever and other systemic events in infants and children fol-lowing pediatric DTaP in comparison with pediatric DTP (143). These events either do not occur in adolescents or are of less clinical concern in this age group than in infants and children (e.g., febrile seizures and hypotonic-hyporesponsive episodes). Taken together, this information supports administering Tdap to adolescents with a history of the events listed above after pediatric DTaP/DTP.
# Tetanus Toxoid-Containing Vaccines
ACIP has recommended that Guillain-Barré syndrome occurring <6 weeks after receipt of a tetanus toxoid-containing vaccine is a precaution for subsequent tetanus toxoid-containing vaccines (91). IOM concluded that evidence favored acceptance of a causal relation between tetanus toxoid-containing vaccines and Guillain-Barré syndrome (123). Evidence is based primarily on a well-documented case report (123,144). However, a subsequent analysis of active surveillance data in both adult and pediatric populations failed to demonstrate an association between receipt of a tetanus toxoid-containing vaccine and onset of Guillain-Barré syndrome within 6 weeks following vaccination (145).
IOM also has concluded that evidence from case reports and uncontrolled studies involving tetanus toxoidcontaining vaccines favored a causal relation between tetanus toxoid-containing vaccines and brachial neuritis. Brachial neuritis is considered to be a compensable event through the Vaccine Injury Compensation Program (123). However, ACIP does not consider a history of brachial neuritis to be a precaution or contraindication for administration of tetanus toxoid-containing vaccines; brachial neuritis is usually selflimited (91,143,146).
# Considerations for Vaccinating Pregnant Adolescents with Td or Tdap
ACIP has recommended Td routinely for pregnant women who received the last tetanus toxoid-containing vaccine >10 years earlier. This recommendation is primarily to prevent neonatal tetanus (24,31). In women adequately vaccinated against tetanus, passive transfer of antibodies across the placenta during pregnancy protects their newborns from neonatal tetanus (147)(148)(149). During 1999, a global maternal and neonatal tetanus elimination goal was recommended by the WHO, the United Nations Children's Fund, and the United Nations Population Fund (150).
As with tetanus, antibodies to pertussis antigens are passively transferred during pregnancy (151,152); however, serologic correlates of protection against pertussis are not known (88). Whether or not passive transfer of maternal antibodies to pertussis antigens protects neonates against pertussis is also unclear (88,153).
All licensed Td and Tdap vaccines are categorized as Pregnancy Category C agents by FDA. ¶ ¶ Pregnant women were excluded from prelicensure trials, and no animal reproduction studies have been conducted for Td or Tdap (32,33,(98)(99)(100)(101). Td has been used extensively in pregnant women worldwide, and no evidence indicates use of tetanus and diphtheria toxoids administered during pregnancy are teratogenic (24,154,155).
# Summary of the Rationale for Adolescent Tdap Recommendations
The availability of Tdap, the first pertussis vaccines formulated for use in adolescents and adults in the United States, offers a new opportunity to reduce the burden of pertussis in this country. The primary objective of vaccinating adolescents with Tdap is to protect the vaccinated adolescent against pertussis while maintaining the standard of care for protection against tetanus and diphtheria. A secondary objective of adolescent Tdap vaccination is to reduce the reservoir of pertussis within the U.S. population at large and potentially reduce the incidence of pertussis in other age groups, including infants who have the highest risk for complications from pertussis (16,48). The extent to which the secondary objective can be achieved through adolescent vaccination is unknown.
The decision to recommend routine Tdap vaccination for adolescents is based on evidence regarding the burden of pertussis among adolescents; negative effects of pertussis outbreaks involving adolescents on the community and the public health system; studies suggesting use of Tdap among adolescents will likely be safe, effective, and economical; and the established infrastructure for adolescent vaccination (30,32,33,(52)(53)(54)68).
To protect against pertussis, Tdap will be introduced into an adolescent vaccination schedule that already includes two other tetanus and/or diphtheria toxoid-containing vaccines, Td, and MCV4 (23,130). Frequent doses of tetanus and diphtheria toxoid-containing vaccines can be associated with increased local and systemic reactogenicity (108,109). ACIP has considered issues related to spacing and administration sequence of these three vaccines to develop recommendations for Tdap use in adolescents. ¶ ¶ U.S. Food and Drug Administration Pregnancy Category C: Animal studies have documented an adverse effect and no adequate and well-controlled studies in pregnant women have been conducted or no animal studies and no adequate and well-controlled studies in pregnant women have been conducted
# MMWR March 24, 2006
# Recommendations for Use of Tdap and Td Among Adolescents
The following sections present recommendations for use of Tdap and Td among adolescents aged 11-18 years and include routine Tdap vaccination, contraindications and precautions, and special situations (Appendix C). (130,132).
# Routine Tdap Vaccination
# 1-A. Recommendations for Use (
# 1-B. Dosage and Administration
The dose of Tdap is 0.5 mL, administered intramuscularly (IM), preferably into the deltoid muscle.
# 1-C. Simultaneous Vaccination with Tdap and Other Vaccines
If two or more vaccines are indicated, they should be administered during the same visit (i.e., simultaneous vaccination). Each vaccine should be administered using a separate syringe at a different anatomic site. Some experts recommend administering no more than two injections per muscle, separated by at least one inch. Administering all indicated vaccines during a single visit increases the likelihood that adolescents will receive each of the vaccines on schedule (91). Vaccine providers should administer MCV4 and Tdap (or Td) during the same visit if both vaccines are indicated and available. MCV4 contains diphtheria toxoid as a carrier protein (131) (see Safety Considerations for Adolescent Vaccination with Tdap or Td).
# 1-D. Interchangeable Use of Tdap Vaccines
A single dose of either Tdap product (BOOSTRIX ® or ADACEL ™ ) can be administered to adolescents regardless of the type or manufacturer of pediatric DTP/DTaP used for childhood vaccination.
# 1-E. Preventing Adverse Events
Syncope can occur after vaccination, might be more common among adolescents and young adults than among other age groups, and has rarely resulted in serious injury (91,156,157). Certain experts suggest a 15-20 minute observation period following vaccination (91,158). If syncope occurs, patients should be observed until symptoms resolve.
The potential for administration errors involving tetanus toxoid-containing vaccines and other products is well documented (159)(160)(161). For example, Td and TT have been inadvertently administered *** Five doses of pediatric DTP/DTaP before the seventh birthday; if the fourth dose was administered on or after the fourth birthday, the fifth dose is not needed.
instead of tuberculin purified protein derivative (PPD) (159). Attention to proper vaccination technique, including use of an appropriate needle length and standard routes of administration (i.e., IM for Tdap) might minimize the risk for adverse events (91). Adverse events associated with inadvertent vaccine administration can be reported to the Vaccine Adverse Event Reporting System (VAERS) (see Reporting of Adverse Events after Vaccination).
# 1-F. Record Keeping
Health-care providers who administer vaccines are required to keep permanent vaccination records of vaccines covered under the National Childhood Vaccine Injury Act in the vaccinee's medical record; ACIP has recommended that this practice include all vaccines (91). Because documentation of tetanus toxoid-containing vaccine administration is frequently required for school or camp entry and as part of wound management, encouraging adolescents to maintain a personal vaccination record is important to minimize administration of unnecessary vaccinations. Vaccine providers can record the type of the vaccine, manufacturer, anatomic site, route, and date of administration and name of the administering facility on the personal record.
# Contraindications and Precautions for Use of Tdap and Td Among Adolescents Aged 11-18 Years
# 2-A. Contraindications
• Tdap or Td is contraindicated for persons with a history of serious allergic reaction (i.e., anaphylaxis) to any component of the vaccine. Because of the importance of tetanus vaccination, persons with a history of anaphylaxis to components included in all Tdap and Td vaccines should be referred to an allergist to determine whether they have a specific allergy to tetanus toxoid, can be desensitized to tetanus toxoid, and can safely receive TT vaccinations. • Tdap is contraindicated for adolescents with a history of encephalopathy (e.g., coma or prolonged seizures) not attributable to an identifiable cause within 7 days of administration of a vaccine with pertussis components. This contraindication is for the pertussis components and these persons should receive Td instead of Tdap.
# 2-B. Precautions and Reasons to Defer Tdap and/or Td
A precaution is a condition in a vaccine recipient that might increase the risk for a serious reaction (91)
# Special Situations for Use of Tdap and Td
# 3-A. General Principles
This section addresses special situations for Tdap and Td use. As with the routine situations, only a single dose of Tdap should be administered to an adolescent aged 11-18 years. For most, but not all, of the special situations, Tdap is preferred to Td. In some special situations or when contraindications or precautions are present, Td rather than Tdap might be indicated. The dose of Td is 0.5 mL, administered IM. Tdap (or Td) and MCV4 should be administered at the same visit during special situations if both vaccines are indicated and available, although this might not always be feasible (e.g., wound management). Simultaneous administration of Tdap (or Td) and MCV4 and an interval of at least 5 years between Td and Tdap can reduce the risk for local and systemic reactions. In certain special situations listed below, the benefit of protection against disease probably outweighs this risk.
# 3-B. Nonsimultaneous Vaccination with Tdap and
Other Vaccines, Including MCV4 ACIP has recommended that inactivated vaccines can be administered at any time before or after a different inactivated or live vaccine (i.e., nonsimultaneous vaccination), unless a contraindication exists (91). Simultaneous administration of Tdap (or Td) and MCV4 (which all contain diphtheria toxoid) during the same visit is preferred when both Tdap (or Td) and MCV4 are indicated. If simultaneous vaccination is not feasible (e.g., a vaccine is not available), MCV4 and Tdap (or Td) can be administered using any sequence. Persons who recently received one diphtheria toxoid-containing vaccine might have increased rates of adverse reactions after a subsequent diphtheria toxoidcontaining vaccine when diphtheria antibody titers remain elevated from the previous vaccination (26,108,111,112) (see Safety Considerations for Adolescent Vaccination with Tdap or Td section for a discussion of nonsimultaneous vaccination).
# 3-C. Pertussis Outbreaks and Other Settings with Increased Risk for Pertussis or its Complications
Vaccine providers can administer Tdap to adolescents aged 11-18 years at an interval less than 5 years after Td, particularly when the benefit of providing protection against pertussis is likely to be increased. The safety of an interval as short as approximately 2 years between Td and Tdap is supported by a Canadian study among children and adolescents (see Spacing and Sequence Administration of Vaccines Containing Tetanus Toxoid, Diphtheria Toxoid, and Pertussis Antigens) (126).
The benefit of using Tdap at an interval less than 5 years after Td is likely to be increased among adolescents when the adolescent is at increased risk for acquiring pertussis (e.g., during outbreaks or periods of increased pertussis activity in the community). Postexposure chemoprophylaxis and other pertussis control guidelines are described elsewhere (64,158,163). The benefit of using a shorter interval also might be increased for adolescents with severe underlying medical conditions (e.g., chronic pulmonary disease or neurologic disorders) because these adolescents might be at increased risk for pertussis-related complications.
Infants aged <12 months are at highest risk for pertussis-related complications and hospitalizations compared with older age groups; young infants have the highest risk for death from pertussis. Administering Tdap at an interval less than 5 years after Td to an adolescent who has or anticipates having close contact with an infant aged <12 months might reduce the risk for transmitting pertussis to the infant. Infants should be vaccinated on time with pediatric DTaP (1,23).
# 3-D. Lack of Availability of Tdap or MCV4
If Tdap and MCV4 are both indicated but only one vaccine is available, the available vaccine generally should be administered. When Tdap is indicated but not available, vaccine providers should administer Td or temporarily defer Tdap/Td vaccination. Td should be administered to provide protection against tetanus and diphtheria if the adolescent received the last pediatric DTP/DTaP/DT or Td >10 years earlier. Recommendations for use of Tdap among adolescents who already received Td would apply to these adolescents when Tdap becomes available (see Routine Tdap Vaccination [section 1-A]). Tdap/Td vaccination can be deferred temporarily if the adolescent completed the childhood DTP/DTaP vaccination series***, received the last pediatric DTP/DTaP/DT or Td <10 years earlier, and is likely to return for follow-up. If the vaccine provider defers Td in order to administer Tdap when it becomes available, a system to recall the adolescent should be maintained.
The adolescent also can be referred to another facility for Tdap administration.
# 3-E. Tetanus Prophylaxis in Wound Management
ACIP has recommended administering tetanus toxoid-containing vaccine and tetanus immune globulin (TIG) as part of standard wound management to prevent tetanus (Table 13) (24). Tdap is preferred to Td for adolescents aged 11-18 years who were vaccinated against tetanus >5 years earlier, require a tetanus toxoid-containing vaccine as part of wound management, and have not previously received Tdap.
Adolescents who have completed the 3-dose primary tetanus vaccination series and have received a tetanus toxoid-containing vaccine <5 years earlier are protected against tetanus and do not require a tetanus toxoid-containing vaccine as part of wound management. Although MCV4 and Tdap (or Td) should be administered at the same visit during routine situations if both vaccines are indicated, this might not be feasible for wound management.
A thorough attempt must be made to determine whether an adolescent has completed the 3-dose primary tetanus vaccination series. Persons with unknown or uncertain tetanus vaccination histories should be considered to have had no previous doses of a tetanus toxoid-containing vaccine (see Adolescents with History of Incomplete Pediatric DTP/ DTaP/DT or Td Vaccination [section 3-H]). Persons who have not completed the primary series might require a tetanus toxoid-containing vaccine and passive immunization with TIG at the time of wound management (Table 13). When both TIG and a tetanus toxoid-containing vaccine are indicated, each product should be administered using a separate syringe at different anatomic sites (24).
Adolescents with a history of an Arthus reaction after a previous dose of a tetanus toxoid-containing vaccine should not receive a tetanus toxoidcontaining vaccine until >10 years after the most recent dose, even if they have a wound that is neither clean nor minor (Table 13). If the Arthus reaction was associated with a vaccine that contained diphtheria toxoid without tetanus toxoid (e.g., MCV4), deferring Tdap or Td might leave the adolescent inadequately protected against tetanus and TT should be administered. In all circumstances, the decision to administer TIG is based on the primary vaccination history for tetanus (Table 13).
# 3-F. History of Pertussis
Adolescents aged 11-18 years who have a history of pertussis generally should receive Tdap according to the routine recommendations. This practice is preferred because duration of protection induced by pertussis is unknown (waning immunity might begin as early as 7 years after infection) and because the diagnosis of pertussis can be difficult to confirm, particularly with test results other than positive culture for B. pertussis (164). Administering pertussis vaccines to persons with a history of pertussis presents no theoretical safety concern. Adolescents who received other incomplete vaccination schedules for tetanus and diphtheria should be vaccinated with Tdap and/or Td according to guidance for catch-up vaccination (Appendix D). A single dose of Tdap can be used to substitute for any one of the Td doses in the series.
# 3-G. Adolescents with
In situations in which the adolescent probably has received vaccination against tetanus and diphtheria but cannot produce records, vaccine providers can obtain serologic testing for antibodies to tetanus and diphtheria to avoid unnecessary vaccination. If antitetanus and antidiphtheria levels are each >0.1 IU/mL, previous vaccination with tetanus and diphtheria toxoid-containing vaccines is likely and a single dose of Tdap is indicated; this Tdap dose counts as the adolescent booster dose.
# 3-I. Children Aged 7-----10 Years with Incomplete Pediatric DTP/DTaP Vaccination History
Neither Tdap vaccine is licensed for use in children aged <10 years (32,33). Children aged 7-10 years who never received a pediatric DTP/DTaP/DT dose or a Td dose generally should receive 3 doses of Td ¶ ¶ ¶ : dose 2 is administered >4 weeks after dose 1 and dose 3 is administered 6-12 months after dose 2. Children aged 7-10 years who received other incomplete vaccination schedules against tetanus, diphtheria, and pertussis should be vaccinated according to catch-up guidance (Appendix E). When these children become adolescents (aged 11-18 years), they should receive Tdap according to the routine recommendations and interval guidance used for adolescents who completed the childhood DTP/DTaP series (see Routine Tdap Vaccination [section 1-A]).
In situations in which the child probably has received vaccination against tetanus and diphtheria but cannot produce records, vaccine providers can obtain serologic testing for antibodies to tetanus and diphtheria to avoid unnecessary vaccination. If antitetanus and antidiphtheria levels are each >0.1 IU/mL, previous vaccination with tetanus and diphtheria toxoid-containing vaccines is likely. In this § § § Five doses of pediatric DTP/DTaP/DT before the seventh birthday; if the fourth dose was administered on or after the fourth birthday, the fifth dose is not needed. Children who began the tetanus and diphtheria vaccination series at age >7 years required 3 doses of Td to complete the primary series. ¶ ¶ ¶ A single dose of BOOSTRIX ® Tdap is licensed for persons aged 10 years and can be used instead of Td for one of the doses in children aged 10 years; if BOOSTRIX ® is administered early to a child aged 10 years, the dose counts as the adolescent Tdap dose usually administered at age 11-12 years.
situation, Td vaccination can be deferred until the child is aged 11-12 years and eligible to receive Tdap.
# 3-J. Inadvertent Administration of Tdap or Pediatric DTaP
To help prevent inadvertent administration of Tdap when pediatric DTaP is indicated or pediatric DTaP when Tdap is indicated, vaccine providers should review product labels before administering these vaccines; the packaging might appear similar. Tdap is not indicated for children aged <10 years. Tdap contains lower amounts of diphtheria toxoid and lower amounts of some pertussis antigens compared with pediatric DTaP. Studies of the immune responses to Tdap among infants have not been conducted. Pediatric DTaP is not indicated for persons aged >7 years; the increased diphtheria toxoid content is associated with higher rates of adverse reactions in older persons (24)(25)(26)(27)(28).
Guidance on the best approach to vaccination following inadvertent administration of Tdap or pediatric DTaP is based primarily on expert opinion. The family should be informed of any inadvertent vaccine administration. Adverse events associated with inadvertent vaccine administration can be reported to VAERS (see Reporting of Adverse Events after Vaccination). If Tdap is inadvertently administered instead of pediatric DTaP to a child aged <7 years as any one of the first three doses of the tetanusdiphtheria-pertussis vaccination series, the Tdap dose should not be counted as valid, and a replacement dose of pediatric DTaP should be administered. If the inadvertent administration is discovered while the child is in the office, the pediatric DTaP can be administered during the same visit. If the child has left the office, some experts suggest administering the replacement dose of pediatric DTaP within approximately 72 hours, or administering it 4 weeks later to optimize the child's immune response to the antigens in pediatric DTaP. This practice helps ensure that the child stays on the primary series schedule and has adequate protection against diphtheria and pertussis. However, the replacement dose of pediatric DTaP can be administered as soon as feasible at any interval after the inadvertent Tdap dose. The remaining doses of the pediatric DTaP series should be administered on the routine schedule, with at least a 4 week interval between the replacement dose of pediatric DTaP and the next dose of pediatric DTaP. For example, if an 8-week-old infant inadvertently received a dose of Tdap instead of the first dose of pediatric DTaP and does not receive a replacement dose of pediatric DTaP within about 72 hours, a replacement dose of pediatric DTaP can be administered 4 weeks after the inadvertent Tdap dose (age 12 weeks). The routine schedule of pediatric DTaP can then be resumed 4 weeks after the pediatric DTaP replacement dose (age 16 weeks) with the other recommended vaccines (1,23).
If Tdap is inadvertently administered as the fourth or the fifth dose in the tetanus-diphtheria-pertussis vaccination series to a child aged <7 years, the Tdap dose should be counted as valid and does not need to be repeated; the child who received Tdap as a fourth dose should complete the pediatric DTaP schedule (23). The routine adolescent Tdap vaccination recommendations would apply when this child becomes an adolescent. For example, a child who inadvertently receives Tdap at age 5 years instead of the fifth dose of pediatric DTaP should receive a second dose of Tdap at age 11-12 years.
If Tdap or pediatric DTaP is inadvertently administered to a child aged 7-9 years instead of Td as part of catch-up vaccination or for wound management, this dose can be counted as the adolescent Tdap dose, or the child can later receive an adolescent booster dose of Tdap according to the interval guidance used for Td to Tdap (see Routine Tdap Vaccination [section 1-A] and Pertussis Outbreaks and Other Settings with Increased Risk for Pertussis or its Complications [section 3-C]). In either case, the child should receive a dose of vaccine containing tetanus and diphtheria toxoids no longer than 10 years after the inadvertent Tdap or pediatric DTaP dose or according to the guidance for catch-up vaccination (Appendix E).
If pediatric DTaP is inadvertently administered to an adolescent aged 11-18 years, the dose should be counted as the adolescent Tdap booster. The adolescent should receive the next dose of a vaccine containing tetanus and diphtheria toxoids 10 years after the inadvertent pediatric DTaP dose or according to the guidance for catch-up vaccination (Appendix D).
# 3-K. Vaccination during Pregnancy
As with other inactivated vaccines and toxoids (91,165), pregnancy is not considered a contraindication for Tdap vaccination. Guidance on the use of Tdap during pregnancy to protect against pertussis is under consideration by ACIP. Pregnant adolescents who received the last tetanus toxoid-containing vaccine <10 years previously should generally receive Tdap after delivery, if otherwise indicated (see Post-Partum Vaccination [section 3-L]).
To prevent neonatal tetanus, pregnant adolescents who received the last tetanus toxoid-containing vaccine >10 years previously should generally receive Td in preference to Tdap. ACIP has recommended that pregnant women receive Td if the last tetanus toxoid-containing vaccine was administered >10 years previously (24,31,91,165). If Td is indicated, vaccinating during the second or third trimester is preferred when feasible to minimize a perception of an association of vaccine with adverse pregnancy outcomes, which are more common during the first trimester. A pregnant adolescent who has not received the 3-dose primary tetanus vaccination series should begin this series during pregnancy, using Td. (see Adolescents with History of Incomplete Pediatric DTP/ DTaP/DT or Td Vaccination [section 3-H]).
Because of lack of data on the use of Tdap in pregnant women, both Tdap manufacturers have established pregnancy registries. Health-care providers are encouraged to report Tdap vaccination during pregnancy to the following registries: BOOSTRIX ® to GlaxoSmithKline Biologicals at 1-888-825-5249 and ADACEL ™ to sanofi pasteur at 1-800-822-2463 (1-800-VACCINE) (32,33).
# 3-L. Post-Partum Vaccination
Adolescents aged 11-18 years, including those who are breastfeeding, should receive a single dose of Tdap as soon as feasible in the postpartum period, according to the routine Tdap recommendations and interval guidance (see Routine Tdap Vaccination [section 1-A] and Pertussis Outbreaks and Other Settings with Increased Risk for Pertussis or its Complications [section 3-C]). For adolescent mothers who have not already received Tdap, vaccinating the mother with Tdap during the postpartum period might reduce the risk for pertussis transmission to the infant. Protection of the mother against pertussis requires an estimated 1 to 2 weeks after vaccination.
# 3-M.Older Adolescents and Adults Aged >18 Years
To maintain protection against tetanus and diphtheria, ACIP has recommended decennial Td boosters for adults beginning 10 years after the adolescent dose (24,30). The safety and efficacy of Tdap (ADACEL ™ ) as a single dose booster immuniza-
# Reporting of Adverse Events After Vaccination
As with any newly licensed vaccine, surveillance for rare adverse events associated with administration of Tdap is important for assessing its safety in large-scale use. The National Childhood Vaccine Injury Act of 1986 requires health-care providers to report specific adverse events that follow tetanus, diphtheria, or pertussis vaccination (http://vaers. hhs.gov/reportable.htm). All clinically significant adverse events should be reported to VAERS, even if causal relation to vaccination is not certain. VAERS reporting forms and information are available electronically at http://www.vaers.hhs.gov/ or by telephone, (800) 822-7967. Web-based reporting is available and providers are encouraged to report electronically at https://secure.vaers.org/VaersDataEntryintro.htm to promote better timeliness and quality of safety data.
Safety surveillance for adolescent Tdap, MCV4, and other vaccines is being conducted on an ongoing basis in cooperation with FDA. Previously published safety data for Td and for tetravalent meningococcal polyscaccharide vaccine will provide some of the basis for comparison with postlicensure safety surveillance for Tdap and MCV4, respectively (130,166).
# Vaccine Injury Compensation
The National Vaccine Injury Compensation Program (VICP), established by the National Childhood Vaccine Injury Act of 1986, is a system under which compensation can be paid on behalf of a person thought to have been injured or to have died as a result of receiving a vaccine covered by the program. Anyone receiving a covered vaccine, regardless of age, can file a petition under VICP. The program is intended as an alternative to civil litigation under the traditional tort system because negligence need not be proven.
The Act establishes 1) a Vaccine Injury and conditions (including death) for which compensation might be paid without proof of causation; and 3) the period after vaccination during which the first symptom or substantial aggravation of the injury must appear. Persons might be compensated for an injury listed in the table or one that can be demonstrated to result from administration of a listed vaccine. All tetanus toxoid-containing vaccines and vaccines with pertussis components (e.g., Tdap, Td, and pediatric DTaP) are covered under the Act. Additional information about the program is available at http://www.hrsa.gov/osp/vicp or by calling 1-800-338-2382.
# Areas for Future Research Related to Tdap and Adolescents
With recent licensure and introduction of Tdap for adolescents, close monitoring of pertussis disease trends and vaccine safety will be high priorities for public health organizations and health-care providers. Active surveillance sites in Massachusetts and Minnesota, supported by CDC, are being established to provide additional data on the burden of pertussis in adolescents and other age groups and the impact of adolescent Tdap vaccination recommendations. Postlicensure studies and surveillance activities are planned or under way to evaluate
• changes in the incidence of pertussis;
• physicians' uptake of Tdap;
• safety and immunogenicity of simultaneous and nonsimultaneous administration of Tdap and MCV4 in adolescents (104,105); and • the prevalence of and risk factors for ELS in adolescents, including studies of adolescents who were vaccinated with 5 doses of pediatric DTaP series (during 2008, the first birth cohort for which an all-pediatric DTaP 5-dose schedule was recommended will turn 11 years of age and become eligible for adolescent vaccination with Tdap). Research is needed to evaluate and define • immunologic correlates of protection for pertussis; • improved diagnostic tests for pertussis; • methods to enhance coverage and delivery of Tdap to adolescents; and • safety and effectiveness of repeated Tdap doses. • Nonsimultaneous vaccination: : : : : If simultaneous vaccination is not feasible, inactivated vaccines can be administered at any time before or after a different inactivated or live vaccine. Tdap (or Td) and MCV4 vaccines (which all contain diphtheria toxoid) can be administered using any sequence. Persons who recently received one diphtheria toxoid-containing vaccine might have increased rates of adverse reactions after a subsequent diphtheria toxoid-containing vaccine when diphtheria antibody titers remain elevated from the previous vaccination § [3-B].
• Pertussis Outbreaks and Other Settings with Increased Risk for Pertussis or its Complications: Vaccine providers can administer Tdap to adolescents aged 11-18 years at an interval less than 5 years after Td, particularly when the benefit of providing protection against pertussis is likely to be increased (e.g., pertussis outbreaks and close contact with an infant aged <12 months) . ¶ Five doses of pediatric DT before the seventh birthday; if the fourth dose was administered on or after the fourth birthday, the fifth dose is not needed. Children who began the tetanus and diphtheria vaccination series at age >7 years required 3 doses of Td to complete the primary series.
.
# Acknowledgements
This report was prepared in collaboration with the Advisory Committee on Immunization Practices Pertussis Working Group. We acknowledge our U.S. Food
#
• a cough illness lasting at least 2 weeks with one of the following: paroxysms of coughing, inspiratory "whoop," or posttussive vomiting, and without other apparent cause (as reported by a health-care professional)
# Laboratory Criteria for Diagnosis
• isolation of Bordetella pertussis from a clinical specimen, or • positive polymerase chain reaction (PCR) assay for B. pertussis
# Case Classification
# Confirmed
• an acute cough illness of any duration associated with B. pertussis isolation, or • a case that meets the clinical case definition and is confirmed by PCR, or • a case that meets the clinical definition and is epidemiologically linked directly to a case confirmed by either culture or PCR
# Probable
• a case that meets the clinical case definition, is not laboratory confirmed by culture or PCR, and is not epidemiologically linked directly to a laboratory-confirmed case.
SOURCES: Guidelines for the control of pertussis outbreaks. Atlanta, GA: CDC. Available at http://www.cdc.gov/nip/publications/pertussis/ guide.htm. Council of State and Territorial Epidemiologists. CSTE position statement, 1997-ID-9: Public health surveillance control and prevention of pertussis, available at http://www.cste.org/ps/1997/1997-id-09.htm. * Both probable and confirmed cases should be reported to the National Notifiable Diseases Surveillance System (http://www.cdc.gov/epo/ dphsi/nndsshis.htm).
# Appendix C
Summary of recommendations for tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine (Tdap) and tetanus and diphtheria toxoids (Td) use among adolescents aged 11-18 years* * Consult recommendations in text for details.
† Five doses of pediatric DTP/DTaP before the seventh birthday; if the fourth dose was administered on or after the fourth birthday, the fifth dose is not needed. § A prelicensure study demonstrated that simultaneous vaccination with Td and MCV4 was acceptably safe; the safety of simultaneous vaccination with Tdap and MCV4 has been inferred from this study. Td followed 1 month later by MCV4 was studied, and rates of local reactions were comparable to simultaneous vaccination. Other schedules of MCV4 and Td and MCV4 and Tdap have not been studied (http://www.fda.gov/cber/label/mpdtave011405LB.pdf ).
# Routine Tdap vaccination
# Appendix E
Guide to catch-up vaccination with Td for children aged 7-10 years*
# INSTRUCTIONS ACCREDITATION Continuing Medical Education (CME).
CDC is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians. CDC designates this educational activity for a maximum of 2.75 hours in category 1 credit toward the AMA Physician's Recognition Award. Each physician should claim only those hours of credit that he/she actually spent in the educational activity.
# Goal and Objectives
This report provides information about the safety and use of two new tetanus toxoid, reduced diphtheria toxoid and acellular pertussis (Tdap) vaccine products. The goal of the report is to improve immunization practices in the United States. Upon completion of this educational activity, the reader should be able to 1) describe the impact of pertussis among adolescents, 2) describe the characteristics of Tdap vaccine, 3) list Advisory Committee on Immunization Practices (ACIP) recommendations for the use of Tdap vaccine among adolescents, and 4) identify contraindications to the use of Tdap vaccine among adolescents.
To receive continuing education credit, please answer all of the following questions.
# What proportion of reported cases of pertussis in the United
# What is the recommendation for use of Tdap among adolescents who did not receive pertussis vaccine as a child?
A. Three doses of Tdap. B. Two doses of Tdap followed by one dose of tetanus-diphtheria toxoid (Td). C. Two doses of Tdap followed by two doses of Td. D. One dose of Tdap followed by two doses of Td. E. Tdap vaccine should not be administered to adolescents who did not receive pertussis vaccine as a child. | None | None |
359372cac27db7a1bb1c4741811a6bc9fb1f23ad | cdc | None | # II. Recommendations for prevention of infections in health care
. Summary of suggested work restrictions for health care personnel exposed to or infected with infectious diseases of importance in health care settings, in the absence of state and local regulations 299 Table 4. Recommendation for postexposure prophylaxis for percutaneous or permucosal exposure to hepatitis B virus, United States 303 Table 5. Selected reported etiologic agents causing community or nosocomially acquired gastrointestinal 307 infections in developed countries Table 6. Pregnant health care personnel: Pertinent facts to guide management of occupational exposures to 322 infectious agents Appendix A. Recommended readings for infection control in health care personnel 354
Part I. Infection control issues for health care personnel: An overview
# A. EXECUTIVE SUMMARY
This guideline updates and replaces the previ ous edition of the Centers for Disease Control and Prevention (CDC) "Guideline for Infection Control in Hospital Personnel," published in 1983. The revised guideline, designed to provide methods for reducing the transmission of infections from patients to health care personnel and from per sonnel to patients, also provides an overview of the evidence for recommendations considered prudent by consensus of the Hospital Infection Control Practices Advisory Committee members. A working draft of this guideline was also reviewed by experts in infection control, occupa tional health, and infectious diseases; however, all recommendations contained in the guideline may not reflect the opinion of all reviewers.
This document focuses on the epidemiology of and preventive strategies for infections known to be transmitted in health care settings and those for which there are adequate scientific data on which to base recommendations for prevention.
The prevention strategies addressed in this docu ment include immunizations for vaccine-pre ventable diseases, isolation precautions to pre vent exposures to infectious agents, management of health care personnel exposure to infected per sons, including postexposure prophylaxis, and work restrictions for exposed or infected health care personnel. In addition, because latex barri ers are frequently used to protect personnel against transmission of infectious agents, this guideline addresses issues related to latex hyper sensitivity and provides recommendations to pre vent sensitization and reactions among health care personnel.
# B. INTRODUCTION
In the United States, there are an estimated 8.8 million persons who work in health care profes sions and about 6 million persons work in more than 6000 hospitals. However, health care is increasingly being provided outside hospitals in facilities such as nursing homes, freestanding sur gical and outpatient centers, emergency care clin ics, and in patients' homes or during prehospital emergency care. Hospital-based personnel and personnel who provide health care outside hospi tals may acquire infections from or transmit infections to patients, other personnel, household members, or other community contacts. 1,2 In this document, the term health care person nel refers to all paid and unpaid persons work ing in health care settings who have the poten tial for exposure to infectious materials, includ ing body substances, contaminated medical supplies and equipment, contaminated environ mental surfaces, or contaminated air. These personnel may include but are not limited to emergency medical service personnel, dental personnel, laboratory personnel, autopsy per sonnel, nurses, nursing assistants, physicians, technicians, therapists, pharmacists, students and trainees, contractual staff not employed by the health care facility, and persons not directly involved in patient care but potentially exposed to infectious agents (e.g., clerical, dietary, housekeeping, maintenance, and volunteer per sonnel). In general, health care personnel in or outside hospitals who have contact with patients, body fluids, or specimens have a high er risk of acquiring or transmitting infections than do other health care personnel who have only brief casual contact with patients and their environment (e.g., beds, furniture, bathrooms, food trays, medical equipment).
# AJIC June 1998
Throughout this document, terms are used to describe routes of transmission of infections. These terms have been fully described in the "Guideline for Isolation Precautions in Hospitals." 3 They are summarized as follows: direct contact refers to body surface-to-body sur face contact and physical transfer of microorgan isms between a susceptible host and an infected or colonized person (e.g., while performing oral care or procedures); indirect contact refers to con tact of a susceptible host with a contaminated object (e.g., instruments, hands); droplet contact refers to conjunctival, nasal, or oral mucosa con tact with droplets containing microorganisms generated from an infected person (by coughing, sneezing, and talking, or during certain proce dures such as suctioning and bronchoscopy) that are propelled a short distance; airborne transmis sion refers to contact with droplet nuclei contain ing microorganisms that can remain suspended in the air for long periods or to contact with dust particles containing an infectious agent that can be widely disseminated by air currents; and, final ly, common vehicle transmission refers to contact with contaminated items such as food, water, medications, devices, and equipment.
In 1983 the CDC published the "Guideline for Infection Control in Hospital Personnel." 4 The document focused on the prevention of infec tions known to be transmitted to and from health care personnel. This revision of the guide line has been expanded to include (a) recom mendations for non-patient care personnel, both in and outside hospitals, (b) management of exposures, (c) prevention of transmission of infections in microbiologic and biomedical labo ratories, and, because of the common use of latex barriers to prevent infections, (d) preven tion of latex hypersensitivity reactions. As in the 1983 guideline, readers are frequently referred to the "Guideline for Isolation Precautions in Hospitals" 3 and other published guidelines and recommendations for precautions that health care personnel may use when caring for patients or handling patient equipment or specimens. 5,6
# C. INFECTION CONTROL OBJECTIVES FOR A PERSONNEL HEALTH SERVICE
The infection control objectives of the person nel health service should be an integral part of a health care organization's general program for infection control. The objectives usually include the following: (a) educating personnel about the principles of infection control and stressing indi vidual responsibility for infection control, (b) col laborating with the infection control department in monitoring and investigating potentially harm ful infectious exposures and outbreaks among personnel, (c) providing care to personnel for work-related illnesses or exposures, (d) identify ing work-related infection risks and instituting appropriate preventive measures, and (e) contain ing costs by preventing infectious diseases that result in absenteeism and disability. These objec tives cannot be met without the support of the health care organization's administration, med ical staff, and other health care personnel. Documents that provide more detailed informa tion regarding infection control issues for person nel health are listed in Appendix A.
# D. ELEMENTS OF A PERSONNEL HEALTH SERVICE FOR INFECTION CONTROL
Certain elements are necessary to attain the infection control goals of a personnel health ser vice: (a) coordination with other departments, (b) medical evaluations, (c) health and safety educa tion, (d) immunization programs, (e) manage ment of job-related illnesses and exposures to infectious diseases, including policies for work restrictions for infected or exposed personnel, (f) counseling services for personnel on infection risks related to employment or special conditions, and (g) maintenance and confidentiality of per sonnel health records.
The organization of a personnel health service may be influenced by the size of the institution, the number of personnel, and the services offered. To ensure that contractual personnel who are not paid by the health care facility receive appropriate personnel health services, contractual agreements with their employers should contain provisions consistent with the policies of the facility that uses those employees. Personnel with specialized training and qualifications in occupational health can facilitate the provision of effective services.
# Coordination with other departments
For infection control objectives to be achieved, the activities of the personnel health service must be coordinated with infection control and other appropriate departmental personnel. This coordi nation will help ensure adequate surveillance of infections in personnel and provision of preven tive services. Coordinating activities will also help to ensure that investigations of exposures and out breaks are conducted efficiently and preventive measures implemented promptly.
CDC Personnel Health Guideline 293
# Medical evaluations
Medical evaluations before placement can ensure that personnel are not placed in jobs that would pose undue risk of infection to them, other personnel, patients, or visitors. An important com ponent of the placement evaluation is a health inventory. This usually includes determining immunization status and obtaining histories of any conditions that might predispose personnel to acquiring or transmitting communicable diseases. This information will assist in decisions about immunizations or postexposure management.
A physical examination, another component of the medical evaluation, can be used to screen personnel for conditions that might increase the risk of transmitting or acquiring work-relat ed diseases and can serve as a baseline for determining whether future diseases are work related. However, the cost-effectiveness of rou tine physical examinations, including laborato ry testing (such as complete blood cell counts, serologic tests for syphilis, urinalysis, and chest radiographs) and screening for enteric or other pathogens for infection control purposes, has not been demonstrated. Conversely, screening for some vaccine-preventable diseases, such as hepatitis B, measles, mumps, rubella, or vari cella, may be cost-effective. In general, the health inventory can be used to guide decisions regarding physical examinations or laboratory tests. However, some local public health ordi nances may mandate that certain screening procedures be used.
Periodic evaluations may be done as indicat ed for job reassignment, for ongoing programs (e.g., TB screening), or for evaluation of workrelated problems.
# Personnel health and safety education
Personnel are more likely to comply with an infection control program if they understand its rationale. Thus, personnel education is a cardinal element of an effective infection control program. Clearly written policies, guidelines, and proce dures ensure uniformity, efficiency, and effective coordination of activities. However, because the risk of infection varies by job category, infection control education should be modified accordingly. In addition, some personnel may need specialized education on infection risks related to their employment and on preventive measures that will reduce those risks. Furthermore, educational materials need to be appropriate in content and vocabulary to the educational level, literacy, and are also likely to be susceptible to rubella least 1 mo mentation of (a) receipt of (including HIV-infect and/or mumps; persons vaccinated later two doses of live vaccine on ed persons with between 1963 and 1967 with (a) a killed or after their 1st birthday, (b) severe immunosup measles vaccine alone, (b) killed vaccine physician-diagnosed pression) history of followed by live vaccine, or (c) a vaccine measles, or (c) laboratory anaphylactic reac of unknown type should be revaccinated evidence of immunity; vac tions after gelatin with two doses of live measles vaccine cine should be considered ingestion or receipt for all personnel, including of neomycin; or those born before 1957, who recent receipt of have no proof of immunity immune globulin Mumps live-One dose SC; Health care personnel Pregnancy; immuno-MMR is the vaccine of choice if recipients virus vaccine no booster believed to be susceptible compromised- state; are also likely to be susceptible to can be vaccinated; adults history of anaphylac measles and rubella born before 1957 can be tic reaction after considered immune gelatin ingestion or receipt of neomycin Rubella live-One dose SC; Health care personnel, both Pregnancy; immuno-Women pregnant when vaccinated or who virus vaccine no booster male and female, who lack compromised- state; become pregnant within 3 mo of vaccina documentation of receipt of history of anaphylac tion should be counseled on the theoretic live vaccine on or after their tic reaction after risks to the fetus, the risk of rubella vac 1st birthday, or of laboratory receipt of neomycin cine-associated malformations in these evidence of immunity; adults women is negligible; MMR is the vaccine born before 1957 can be of choice if recipients are also likely to be considered immune, except susceptible to measles or mumps women of childbearing age
# Immunization programs
Ensuring that personnel are immune to vac cine-preventable diseases is an essential part of successful personnel health programs. Optimal use of vaccines can prevent transmission of vac cine-preventable diseases and eliminate unneces sary work restriction. Prevention of illness through comprehensive personnel immunization programs is far more cost-effective than case management and outbreak control. Mandatory immunization programs, which include both newly hired and currently employed persons, are more effective than voluntary programs in ensur ing that susceptible persons are vaccinated. 7 National guidelines for immunization of and postexposure prophylaxis for health care person nel are provided by the U.S. Public Health Service's Advisory Committee on Immunization Practices (ACIP; Table 1). 8,9 ACIP guidelines also contain (a) detailed information on the epidemi ology of vaccine-preventable diseases, (b) data on the safety and efficacy of vaccines and immune globulin preparations, and (c) recommenda tions for immunization of immunocompromised persons- (Table 2). 16,23 The recommendations in this guideline have been adapted from the ACIP recommendations. 9 In addition, individual states and professional organizations have regulations or recommendations on the vaccination of health care personnel. 24 Decisions about which vaccines to include in immunization programs have been made by con sidering (a) the likelihood of personnel exposure to vaccine-preventable diseases and the potential con sequences of not vaccinating personnel, (b) the nature of employment (type of contact with patients and their environment), and (c) the characteristics of the patient population within the health care organization. Immunization of personnel before they enter high-risk situations is the most efficient and effective use of vaccines in health care settings.
Screening tests are available to determine sus ceptibility to certain vaccine-preventable diseases *The term immunocompromised includes persons who are immunocompromised from immune deficiency diseases, HIV infection, leukemia, lymphoma, or generalized malig nancy, or immunosuppressed as a result of therapy with cor ticosteroids, alkylating drugs, antimetabolites, or radiation. (e.g., hepatitis B, measles, mumps, rubella, and varicella). Such screening programs need to be combined with tracking systems to ensure accu rate maintenance of personnel immunization records. Accurate immunization records ensure that susceptible personnel are promptly identified and appropriately vaccinated.
# CDC Personnel Health Guideline 297
# Management of job-related illnesses and exposures
Primary functions of the personnel health ser vice are to arrange for prompt diagnosis and man agement of job-related illnesses and to provide appropriate postexposure prophylaxis after jobrelated exposures.
It is the responsibility of the health care orga nization to implement measures to prevent fur ther transmission of infection, which some times warrants exclusion of personnel from work or patient contact. 25 Decisions on work restrictions are based on the mode of transmis sion and the epidemiology of the disease (Table 3). The term exclude from duty in this document should be interpreted as exclusion from the health care facility and from health care activi ties outside the facility. Personnel who are excluded should avoid contact with susceptible persons both in the facility and in the commu nity. Exclusion policies should include a state ment of authority defining who may exclude personnel. The policies also need to be designed to encourage personnel to report their illnesses or exposures and not to penalize them with loss of wages, benefits, or job status. Workers' com pensation laws do not cover exclusion from duty for exposures to infectious diseases; poli cies therefore should include a method for pro viding wages during the period that personnel are not able to work. In addition, exclusion policies must be enforceable and all personnel, especially department heads, supervisors, and nurse managers, should know which infections may warrant exclusion and where to report the illnesses 24 hours a day. Health care personnel who have contact with infectious patients out side of hospitals also need to be included in the postexposure program and encouraged to report any suspected or known exposures promptly. Notification of emergency-response personnel possibly exposed to selected infec tious disease is mandatory (1990 Ryan White Act, Subtitle B, 42 USC 300ff-80).
CDC Personnel Health Guideline 299
# Health counseling
Access to adequate health counseling for per sonnel is another crucial element of an effective personnel health service. Health counseling allows personnel to receive individually targeted information regarding (a) the risk and prevention of occupationally acquired infections, (b) the risk of illness or other adverse outcome after expo sures, (c) management of exposures, including the risks and benefits of postexposure prophylaxis regimens, and (d) the potential consequences of exposures or communicable diseases for family members, patients, or other personnel, both inside and outside the health care facility.
# Maintenance of records, data management, and confidentiality
Maintenance of records on medical evaluations, immunizations, exposures, postexposure prophy laxis, and screening tests in a retrievable, prefer ably computerized, database allows efficient mon itoring of the health status of personnel. Such record keeping also helps to ensure that the orga nization will provide consistent and appropriate services to health care personnel.
Individual records for all personnel should be maintained in accordance with the Occu pational Safety and Health Administration (OSHA) medical records standard, which requires the employer to retain records, main tain employee confidentiality, and provide records to employees when they ask to review them. 26 In addition, the 1991 OSHA "Occu pational Exposure to Bloodborne Pathogens; Final Rule" 27 requires employers, including health care facilities, to establish and maintain an accurate record for each employee with occu pational exposure to bloodborne pathogens. The standard also requires that each employer ensure that the employee medical records are (a) kept confidential, (b) not disclosed or report ed without the employee's express written con sent to any person within or outside the work place, except as required by law, and (c) main tained by the employer for at least the duration of the worker's employment plus 30 years.
OSHA's record keeping regulation also requires employers to record work-related injuries and ill nesses on the OSHA 200 log and the OSHA 101 form. The records include all occupational fatali ties, all occupational illnesses, and occupational injuries that result in loss of consciousness, restriction of work or motion, transfer to another job, or medical treatment beyond first aid. Infectious diseases are recordable if they are work related and result in illness. 28 More recently, OSHA developed policies that require the recording of positive tuberculin skintest results. 29 It would be beneficial to health care organizations and personnel if the principles of record keeping and confidentiality mandated by OSHA were to be expanded to other work-related exposures and incidents, immunizations, TB screening, and investigation and management of nosocomial outbreaks.
# E. EPIDEMIOLOGY AND CONTROL OF SELECTED INFECTIONS TRANSMITTED AMONG HEALTH CARE PERSONNEL AND PATIENTS
Almost any transmissible infection may occur in the community at large or within health care organizations and can affect both personnel and patients. Only those infectious diseases that occur frequently in the health care setting or are most important to personnel are discussed here.
# Bloodborne pathogens a. Overview
Assessment of the risk and prevention of trans mission of bloodborne pathogens, such as hepati tis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV), in health care settings are based on information from a variety of sources, including surveillance and investigation of suspected cases of transmission to health care personnel and patients, seropreva lence surveys of health care personnel and patients, and studies of the risk of seroconversion after exposure to blood or other body fluids from infected persons. In this document, the emphasis of the discussion of bloodborne pathogens will be on patient-to-personnel transmission.
The CDC has periodically issued and updated recommendations for prevention of transmission of bloodborne pathogens in health care settings; these provide detailed information and guid ance. Also, in 1991 OSHA published a bloodborne pathogen standard that was based on the concept of universal precautions to prevent occu pational exposure to bloodborne pathogens. 27 The use of standard precautions (which incorporates universal precautions), including appropriate handwashing and barrier precautions, will reduce contact with blood and body fluids. 3,30,31,41 The use of engineering controls (e.g., safety devices) and changes in work practices (e.g., techniques to reduce handling of sharp instruments) can reduce the frequency of percutaneous injuries. 41,42 In set tings such as the operating room, changes in AJIC June 1998 instrument design and techniques for performing surgical procedures and modified personal barri ers have been shown to reduce blood contacts. 43,44 Despite adherence to standard precautions and implementation of some new techniques and devices, percutaneous injuries continue to occur. This is of concern because percutaneous injuries represent the greatest risk of transmission of bloodborne pathogens to health care personnel. 45 Only a few studies evaluating a limited number of safety devices have demonstrated a reduction in percutaneous injuries among health care work ers. 46,47 This document will not address the use of safety devices, because the Public Health Service is assessing the need for further guidance on selection, implementation, and evaluation of such devices in health care settings.
The risk posed to patients by health care per sonnel infected with bloodborne pathogens such as HBV and HIV has been the subject of much concern and debate. There are no data to indi cate that infected workers who do not perform invasive procedures pose a risk to patients. Consequently, work restrictions for these work ers are not appropriate. However, the extent to which infected workers who perform certain types of invasive procedures pose a risk to patients and the restrictions that should be imposed on these workers have been much more controversial. In 1991, CDC recommendations on this issue were published. 48 Subsequently, Congress mandated that each state implement the CDC guidelines or equivalent as a condition for continued federal public health funding to that state. Although all states have complied with this mandate, there is a fair degree of state-to state variation regarding specific provisions. Local or state public health officials should be contacted to determine the regulations or rec ommendations applicable in a given area. CDC is currently in the process of reviewing relevant data regarding health care personnel-to-patient transmission of bloodborne pathogens.
# b. Hepatitis B
Nosocomial transmission of HBV is a serious risk for health care personnel. Approximately 1000 health care personnel were estimated to have become infected with HBV in 1994. This 90% decline since 1985 is attributable to the use of vaccine and adherence to other preventive mea sures (e.g., standard precautions). 54 During the past decade, an estimated 100 to 200 health care personnel annually have died of occupationally acquired HBV infection. 54 The risk of acquiring CDC Personnel Health Guideline 303 HBV infection from occupational exposure is dependent on the nature and frequency of expo sure to blood or to body fluids containing blood. 49,53 The risk of infection is at least 30% after a percutaneous exposure to blood from a hepatitis B e antigen-seropositive source. 54 HBV is transmitted by percutaneous or mucosal exposure to blood and serum-derived body fluids from persons who have either acute or chronic HBV infection. The incubation peri od is 45 to 180 days (average 60 to 90 days). Any person seropositive for hepatitis B surface anti gen (HBsAg) is potentially infectious.
Hepatitis B vaccination of health care personnel who have contact with blood and body fluids can prevent transmission of HBV and is strongly rec ommended. 9,10,40 The OSHA bloodborne pathogen standard mandates that hepatitis B vaccine be made available, at the employer's expense, to all health care personnel with occupational exposure to blood or other potentially infectious materials. 27 Provision of vaccine during training of health care professionals before such blood exposure occurs may both increase the vaccination rates among personnel and prevent infection among trainees, who are at increased risk for unintentional injuries while they are learning techniques.
Prevaccination serologic screening for suscepti bility to HBV infection is not indicated for per sons being vaccinated, unless the health care organization considers such screening to be costeffective. Postvaccination screening for antibody to HBsAg (anti-HBs) is advised for personnel at ongoing risk for blood exposure to determine whether response to vaccinations has occurred and to aid in determining the appropriate postex posure prophylaxis or the need for revaccination. Personnel who do not respond to or do not com plete the primary vaccination series should be revaccinated with a second three-dose vaccine series or evaluated to determine whether they are HBsAg seropositive. Revaccinated persons should be tested for anti-HBs at the completion of the second vaccine series. 9 If they do not respond, no further vaccination series should be given and they should be evaluated for the presence of HBsAg (possible chronic HBV infection). No spe cific work restrictions are recommended for nonresponders; in the event of percutaneous exposure to blood or body fluids, however, they should see their health care providers as soon as possible to evaluate the need for postexposure prophylaxis. Personnel in chronic dialysis centers who do not respond to vaccine need to be screened for HBsAg and anti-HBs every 6 months. 55 Vaccine-induced antibodies decline gradually with time, and as many as 60% of those who ini tially respond to vaccination will lose detectable anti-HBs by 8 years. 56 Booster doses of vaccine are not routinely recommended, because per sons who respond to the initial vaccine series remain protected against clinical hepatitis and chronic infection even when their anti-HBs lev els become low or undetectable. 57 The need for postexposure prophylaxis, vacci nation, or both depends on the HBsAg status of the source of the exposure as well as the immu nization status of the person exposed (Table 4). 40 Vaccine should be offered after any exposure in an unvaccinated person; if the source is known to be HBsAg seropositive, hepatitis B immune glob ulin (HBIG) should be given, preferably within 24 hours. The effectiveness of HBIG given later than 7 days after HBV exposure is unknown. 8,10,40 If the source is HBsAg seropositive and the exposed person is known not to have responded to a threedose vaccine series, a single dose of HBIG and a dose of hepatitis B vaccine need to be given as soon as possible after the exposure with subse quent vaccine doses given at 1 month and 6 months after the initial dose. If the exposed per son is known not to have responded to a threedose vaccine series and to revaccination, two doses of HBIG need to be given, one dose as soon as possible after exposure and the second dose 1 month later.
# c. Hepatitis C
HCV is the etiologic agent in most cases of par enterally transmitted non-A, non-B hepatitis in the United States. 58,59 During the past decade, the annual number of newly acquired HCV infections has ranged from an estimated 180,000 in 1984 to an estimated 28,000 in 1995. Of these, an estimat ed 2% to 4% occurred among health care person nel who were occupationally exposed to blood. 59 A case-control study of patients with acute non-A, non-B hepatitis, conducted before the identification of HCV, showed a significant asso ciation between acquisition of disease and health care employment, specifically patient care or laboratory work. 60 Seroprevalence stud ies among hospital-based health care personnel have shown seroprevalence rates of antibody to HCV (anti-HCV) ranging from 1% to 2%. In a study that assessed risk factors for infection in health care personnel, a history of accidental needlesticks was independently associated with anti-HCV seropositivity. 61 Several case reports have documented transmis sion of HCV infection from anti-HCV-seropositive patients to health care personnel as a result of accidental needlesticks or cuts with sharp instru ments. 65,66 In follow-up studies of health care per sonnel who sustained percutaneous exposures to blood from anti-HCV-seropositive patients, the rate of anti-HCV seroconversion averaged 1.8% (range 0% to 7%). In a study in which HCV RNA polymerase chain reaction methods were used to measure HCV infection, the rate of HCV transmission was 10%. 70 The incubation period for hepatitis C is 6 to 7 weeks, and nearly all persons with acute infec-AJIC June 1998 tion will have chronic HCV infection occur with persistent viremia and the potential for trans mission of HCV to others.
Serologic assays to detect anti-HCV are com mercially available. The interpretation of anti-HCV test results is limited by several factors: (a) these assays will not detect anti-HCV in approxi mately 5% of persons infected with HCV; (b) these assays do not distinguish between acute, chronic, and past infection; (c) there may be a prolonged interval between the onset of acute illness with HCV and seroconversion; and (d) when the assays are used in populations with a low prevalence of HCV infection, commercial screening assays for anti-HCV yield a high proportion (as great as 50%) of false-positive results. 34,59 Although no true confirmatory test has been developed, supplemen tal tests for specificity are available and should be used to judge the validity of repeatedly reactive results by screening assays.
Although the value of immune globulin for postexposure prophylaxis after occupational exposure to HCV has been difficult to assess, postexposure prophylaxis with immune globulin does not appear to be effective in preventing HCV infection. Current immune globulin preparations are manufactured from plasma that has been screened for HCV antibody; positive lots are excluded from use. An experimental study in chimpanzees found that administration 1 hour after exposure to HCV of immune globulin manu factured from anti-HCV-screened plasma did not prevent infection or disease. 74 Thus, available data do not support the use of immune globulin for postexposure prophylaxis against hepatitis C, and its use is not recommended. There is no informa tion regarding the use of antiviral agents, such as interferon alfa, in the postexposure setting, and such prophylaxis is not recommended. 37 Health care institutions should consider imple menting recommended policies and procedures for follow-up for HCV infection after percuta neous or mucosal exposures to blood. At a mini mum, such policies can include (1) baseline test ing of the source for anti-HCV, (2) baseline and follow-up testing (e.g., 6 months) for anti-HCV and alanine aminotransferase activity of the per son exposed to an anti-HCV seropositive source, (3) confirmation by supplemental anti-HCV test ing of all anti-HCV results reported as repeatedly active by enzyme immunoassay, (4) recommen dation against postexposure prophylaxis with immune globulin or antiviral agents (e.g., inter feron), and (5) education of health care personnel about the risk for and prevention of bloodborne infections, including HCV, in occupational set tings, with the information routinely updated to ensure accuracy. 37 Among health care personnel in the postexposure period, onset of HCV infec tion may be detected earlier by measuring HCV RNA with polymerase chain reaction rather than by measuring anti-HCV with enzyme immunoas say. However, polymerase chain reaction is not a licensed assay, and the accuracy of the results are highly variable. 37
# d. Human immunodeficiency virus
Nosocomial transmission of human immuno deficiency virus (HIV) infection from patients to health care personnel may occur after percuta neous or, infrequently, mucocutaneous exposure to blood or body fluids containing blood. According to prospective studies of health care personnel percutaneously exposed to HIV-infect ed blood, the average risk for HIV infection has been estimated to be 0.3%. 45, A retrospective case-control study to identify risk factors for HIV seroconversion among health care personnel after a percutaneous exposure to HIV-infected blood found that they were more likely to become infected if they were exposed to a larger quantity of blood, represented in the study as (1) presence of visible blood on the device before injury, (2) a procedure that involved a needle placed directly in the patient's vein or artery, or (3) deep injury. 45 Transmission of HIV infection also was associat ed with injuries in which the source patient was terminally ill with AIDS; this may be attributable to the increased titer of HIV in blood that is known to accompany late stages of illness or pos sibly to other factors, such as the presence of syn cytia-inducing strains of HIV in these patients. In addition, the findings of this study suggested that the postexposure use of zidovudine may be pro tective for health care personnel. 45 Factors that determine health care personnel's risk of infection with HIV include the prevalence of infection among patients, the risk of infection transmission after an exposure, and the fre quency and nature of exposures. 79 Most person nel who acquire infection after percutaneous exposure have HIV antibody develop within 6 months of exposure. HIV-infected persons are likely to transmit virus from the time of early infection throughout life.
In 1990, CDC published guidelines for postex posure management of occupational exposure to HIV, 33 and provisional recommendations for postexposure chemoprophylaxis were published CDC Personnel Health Guideline 305 in 1996. 80 In 1998, both of these documents were updated and consolidated to reflect current sci entific knowledge on the efficacy of postexpo sure prophylaxis and the use of antiretroviral therapies. 81 The U.S. Public Health Service will periodically review scientific information on antiretroviral therapies and publish updated recommendations for their use as postexposure prophylaxis as necessary.
# Conjunctivitis
Although conjunctivitis can be caused by a vari ety of bacteria and viruses, adenovirus has been the primary cause of nosocomial outbreaks of conjunctivitis. Nosocomial outbreaks of conjunc tivitis caused by other pathogens are rare.
Adenoviruses, which can cause respiratory, ocular, genitourinary, and gastrointestinal infections, are a major cause of epidemic kera toconjunctivitis in the community and health care settings. Nosocomial outbreaks have pri marily occurred in eye clinics or offices but have also been reported in neonatal intensive care units and long-term care facilities. Patients and health care personnel have acquired and transmitted epidemic keratocon junctivitis during these outbreaks. The incuba tion period ranges from 5 to 12 days, and shed ding of virus occurs from late in the incubation period to as long as 14 days after onset of dis ease. 83 Adenovirus survives for long periods on environmental surfaces; ophthalmologic instru ments and equipment can become contaminat ed and transmit infection. Contaminated hands are also a major source of person-to-person transmission of adenovirus, both from patients to health care personnel and from health care personnel to patients. Handwashing, glove use, and disinfection of instruments can prevent the transmission of adenovirus. 82,83 Infected personnel should not provide patient care for the duration of symptoms after onset of epidemic keratoconjunctivitis 82,83 or purulent con junctivitis caused by other pathogens.
# Cytomegalovirus
There are two principal reservoirs of cytomegalovirus (CMV) in health care institu tions: (a) infants and young children infected with CMV and (b) immunocompromised patients, such as those undergoing solid-organ or bone-marrow transplantation or those with AIDS. However, personnel who provide care to such high-risk patients have a rate of primary CMV infection that is no higher than that among personnel without such patient contact (3% vs 2%). In areas where there are patient populations with a high prevalence of CMV, seroprevalence studies and epidemiologic investigations have also demon strated that personnel who care for patients have no greater risk of acquiring CMV than do person nel who have no patient contact. 92,100, In addition, epidemiologic studies that included DNA testing of viral strains have demonstrated that personnel who acquired CMV infections while providing care to CMV-infected infants had not acquired their infections from the CMV-infect ed patients. 88,92,96, CMV transmission appears to occur directly either through close, intimate contact with an excreter of CMV or through contact with contaminated secre tions or excretions, especially saliva or urine. 101, Transmission by the hands of personnel or infected persons has also been suggested. 92,115 The incubation period for person-to-person transmission is not known. Although CMV can survive on environmen tal surfaces and other objects for short periods, 116 there is no evidence that the environment plays a role in the transmission of infection. 92 Because infection with CMV during pregnancy may have adverse effects on the fetus, women of childbearing age need to be counseled regarding the risks and prevention of transmission of CMV in both nonoccupational and occupational set tings. 117 Although most fetal infections follow pri mary maternal infection, fetal infection may fol low maternal reinfection or reactivation. 118,119 There are no studies that clearly indicate that seronegative personnel may be protected from infection by transfer to areas with less contact with patients likely to be reservoirs for CMV infec tion. 88,92,102,105,106,119,120 Serologic or virologic screening programs to identify CMV-infected patients or seronegative female personnel of childbearing age are imprac tical and costly for the following reasons: (a) the virus can be intermittently shed, 121 and repeated screening tests may be needed to identify shed ders; (b) seropositivity for CMV does not offer complete protection against maternal reinfection or reactivation and subsequent fetal infec tion 118,119 ; and (c) no currently available vac cines or prophylactic therapy 90, can pro vide protection against primary infection.
Work restrictions for personnel who contract CMV illnesses are not necessary. The risk of transmission of CMV can be reduced by careful adherence to handwashing and standard precautions. 3,119,130 AJIC June 1998
# Diphtheria
Nosocomial transmission of diphtheria among patients and personnel has been reported. Diphtheria is currently a rare disease in the United States. During 1980 through 1994, only 41 diphthe ria cases were reported 134 ; however, community out breaks of diphtheria have occurred in the past, 135 and clusters of infection may occur in communities where diphtheria was previously endemic. 136 In addition, diphtheria epidemics have been occurring since 1990 in the new independent states of the for mer Soviet Union and in Thailand. 140 At least 20 imported cases of diphtheria have been reported in countries in Europe, 139,141 and two cases occurred in U.S. citizens visiting or working in the Russian Federation and Ukraine. 142 Health care personnel are not at substantially higher risk than the general adult population for acquiring diphtheria; however, there is a potential for sporadic or imported cases to require medical care in the United States.
Diphtheria, caused by Corynebacterium diphthe riae, is transmitted by contact with respiratory droplets or contact with skin lesions of infected patients. The incubation period is usually 2 to 5 days. Patients with diphtheria are usually infec tious for 2 weeks or less, but communicability can persist for several months. 143 Droplet precautions are recommended for patients with pharyngeal symptoms, and contact precautions are recom mended for patients with cutaneous lesions. Precautions need to be maintained until antibiotic therapy is completed and results of two cultures taken at least 24 hours apart are negative. 3 Limited serosurveys conducted since 1977 in the United States indicate that 22% to 62% of adults 18 to 39 years old may lack protective diphtheria antibody levels. Prevention of diphtheria is best accomplished by maintaining high levels of diphtheria immunity among children and adults. 19,137,138 Immunization with tetanus and diphtheria toxoid (Td) is recommended every 10 years for all adults who have completed the pri mary immunization series (Table 1). 9,19 Health care personnel need to consider obtaining Td immu nization from their health care providers. 9 To determine whether health care personnel directly exposed to oral secretions of patients infected with toxigenic strains of C. diphtheriae are carriers, cultures of the nasopharynx may be obtained. Exposed personnel need to be evaluated for evidence of disease daily for 1 week. 149 Although the efficacy of antimicrobial prophylaxis in pre venting secondary disease has not been proved, prophylaxis with either a single intramuscular CDC Personnel Health Guideline 307 injection of benzathine penicillin (1.2 mouse units) or oral erythromycin (1 gm/day) for 7 days has been recommended. 19 Follow-up nasopharyngeal cultures for C. diphtheriae need to be obtained at least 2 weeks after antimicrobial therapy is com pleted. If the organism has not been eradicated, a 10-day course of erythromycin needs to be given. 149 In addition, previously immunized exposed per sonnel need to receive a dose of Td if they have not been vaccinated within the previous 5 years. 19 Exclusion from duty is indicated for personnel with C. diphtheriae infection or those determined to be asymptomatic carriers until antimicrobial ther apy is completed and nasopharyngeal culture results are negative.
# Gastrointestinal infections, acute
Gastrointestinal infections may be caused by a variety of agents, including bacteria, viruses, and protozoa. However, only a few agents have been documented in nosocomial transmission (Table 5). Nosocomial transmission of agents that cause gastrointestinal infections usually results from contact with infected individuals, 150,161,163,169 from consumption of contaminated food, water, or other beverages, 150,166,169,170 or from exposure to contaminated objects or environmental sur faces. 152,153,171 Airborne transmission of small round-structured viruses (Norwalk-like viruses) has been postulated but not proved. 164,165, Inadequate handwashing by health care person nel 176 and inadequate sterilization or disinfection of patient-care equipment and environmental sur faces increase the likelihood of transmission of agents that cause gastrointestinal infections. Generally, adherence to good personal hygiene by personnel before and after all contacts with patients or food and to either standard or contact precautions 3 will minimize the risk of transmit ting enteric pathogens. 167,177 Laboratory personnel who handle infectious materials also may be at risk for occupational acquisition of gastrointestinal infections, most commonly with Salmonella typhi. Although the incidence of laboratory-acquired S. typhi infec tion has decreased substantially since 1955, infections continue to occur among laboratory workers, particularly those performing profi ciency exercises or research tests. 151,162 Several typhoid vaccines are available for use in labo ratory workers who regularly work with cul tures or clinical materials containing S. typhi. 178 The oral live-attenuated Ty21a vaccine, the intramuscular Vi capsular polysaccharide vaccine, or the subcutaneous inactivated vac cine may be given (Table 1). 178 Booster doses of vaccine are required at 2-to 5-year intervals, depending on the preparation used. The liveattenuated Ty21a vaccine should not be used for immunocompromised persons, including those known to be infected with HIV. 178 Personnel who acquire an acute gastroin testinal illness (defined as vomiting, diarrhea, or both, with or without associated symptoms such as fever, nausea, and abdominal pain) are likely to have high concentrations of the infect ing agent in their feces (bacteria, viruses, and parasites) or vomitus (viruses and para sites). 165,179,180 It is important to determine the etiology of gastrointestinal illness in health care personnel who care for patients at high risk for severe disease (e.g., neonates, elderly persons, and immunocompromised patients). The initial evaluation of personnel with gas troenteritis needs to include a thorough history and determination of the need for specific lab oratory tests, such as stool or blood cultures, staining procedures, and serologic or antigenantibody tests. 162,171,181,182 After resolution of some acute bacterial gas trointestinal illnesses, some personnel may have persistent carriage of the infectious agent. Once the person has clinically recovered and is having formed stools, however, the risk of trans mission of enteric pathogens is minimized by adherence to standard precautions. 3,167 In addi tion, appropriate antimicrobial therapy may eradicate fecal carriage of Shigella 183 or Campylobacter. 184 In contrast, antimicrobial or antiparasitic therapy may not eliminate car riage of Salmonella 185 or Cryptosporidium. Moreover, antimicrobials may prolong excre tion of Salmonella 186 and lead to emergence of resistant strains. 187 However, transmission of Salmonella to patients from personnel who are asymptomatic carriers of Salmonella has not been well documented. 167 In general, antimicro bial therapy is not recommended, unless the person is at high risk for severe disease. 188 When antibiotics are given, stool cultures AJIC June 1998 should be obtained at least 48 hours after com pletion of antibiotic therapy.
Restriction from patient care and the patient's environment or from food handling is indicated for personnel with diarrhea or acute gastrointestinal symptoms, regardless of the causative agent. 3,171 Some local and state agen cies have regulations that require work exclu sion for health care personnel, food handlers, or both who have gastrointestinal infections caused by Salmonella or Shigella. These regula tions may require such personnel to be restrict ed from duty until results of at least two con secutive stool cultures obtained at least 24 hours apart are negative.
# Hepatitis A
Nosocomial hepatitis A occurs infrequently, and transmission to personnel usually occurs when the source patient has unrecognized hepatitis and is fecally incontinent or has diarrhea. Other risk factors for hepatitis A virus (HAV) transmission to personnel include activities that increase the risk of fecal-oral contamination such as (a) eating or drinking in patient care areas, 189,191,193,199 (b) not washing hands after handling an infected infant, 191,199,200 and (c) sharing food, beverages, or cigarettes with patients, their families, or other staff members. 189,191 HAV is transmitted primarily by the fecal-oral route. It has not been reported to occur after inadvertent needlesticks or other contact with blood, but it has rarely been reported to be transmitted by transfusion of blood prod ucts. 193,201,202 The incubation period for HAV is 15 to 50 days. Fecal excretion of HAV is greatest during the incubation period of disease before the onset of jaundice. 203 Once disease is clini cally obvious, the risk of transmitting infection is decreased. However, some patients admitted to the hospital with HAV, particularly immuno compromised patients, may still be shedding virus because of prolonged or relapsing disease, and such patients are potentially infective. 190,203 Fecal shedding of HAV, formerly believed to continue only as long as 2 weeks after onset of dark urine, 203 has been shown to occur as late as 6 months after diagnosis of infection in prema ture infants. 189 Anicteric infection is typical in young children and infants. 204 Personnel can protect themselves and others from infection with HAV by adhering to stan dard precautions. 3 Food-borne transmission of hepatitis A is not discussed in this guideline, but it has occurred in health care settings. 205,206 Two inactivated hepatitis A vaccines are now available and provide long-term preexposure protection against clinical infection with greater than 94% efficacy. 204 Serologic surveys among health care personnel have not shown greater prevalence of HAV infection than in control populations 52,192,207,208 ; therefore, routine administration of vaccine in health care person nel is not recommended. Vaccine may be useful for personnel working or living in areas where HAV is highly endemic and is indicated for per sonnel who handle HAV-infected primates or are exposed to HAV in a research laboratory. The role of hepatitis A vaccine in controlling outbreaks has not been adequately investigat ed. 9 Immune globulin given within 2 weeks after an HAV exposure is more than 85% effec tive in preventing HAV infection 204 and may be advisable in some outbreak situations. 9,204 Restriction from patient care areas or food handling is indicated for personnel with HAV infection. They may return to regular duties 1 week after onset of illness. 9
# Herpes simplex
Nosocomial transmission of herpes simplex virus (HSV) is rare. Nosocomial transmission has been reported in nurseries and intensive care units 212,213 where high-risk patients (e.g., neonates, patients with severe malnutrition, patients with severe burns or eczema, and immunocompromised patients) are located. Nosocomial transmission of HSV occurs primarily through contact either with primary or recurrent lesions or with virus-contain ing secretions, such as saliva, vaginal secretions, or amniotic fluid. 210,212,214 Exposed areas of skin are the most likely sites of nosocomial infection, par ticularly when minor cuts, abrasions, or other skin lesions are present. 213 The incubation period of HSV is 2 to 14 days. 215 The duration of viral shed ding has not been well defined. 216 Personnel may acquire a herpetic infection of the fingers (herpetic whitlow or paronychia) from exposure to contaminated oral secretions. 213,214 Such exposures are a distinct hazard for nurses, anesthesiologists, dentists, respiratory care per sonnel, and other personnel who have direct (usu ally hand) contact with either oral lesions or res piratory secretions from patients. 213 Less fre quently, personnel may acquire mucocutaneous infection on other body sites from contact with infectious body secretions. 217
# CDC Personnel Health Guideline 309
Personnel with active infection of the hands (her petic whitlow) can potentially transmit HSV infec tion to patients with whom they have contact. 214 Transmission of HSV from personnel with orofa cial HSV infection to patients has also been infre quently documented 209 ; however, the magnitude of this risk is unknown. 211,218 Although asymptomatic infected persons can shed the virus, they are less infectious than persons with active lesions. 216,219 Personnel can protect themselves from acquiring HSV by adhering to standard precau tions. 3 The risk of transmission of HSV from personnel with orofacial infections to patients can be reduced by handwashing before all patient care and by the use of appropriate bar riers, such as a mask or gauze dressing, to pre vent hand contact with the lesion.
Because personnel with orofacial lesions may touch their lesions and potentially transmit infec tions, they should be evaluated to determine their potential for transmitting herpes simplex to patients at high risk for serious disease (e.g., neonates, patients with severe malnutrition, patients with severe burns or eczema, and immunocompromised patients) and excluded from the care of such patients as indicated. The evaluation should consider the extent of the lesion and the severity of illness in the patient population that personnel will contact. Personnel with HSV infections of the fingers or hands can more easily transmit infection and therefore need to be excluded from patient care until their lesions have crusted. In addition, herpetic lesions may be secondarily infected by Staphylococcus and Streptococcus, and personnel with such infections should be evaluated to determine whether they need to be excluded from patient contact until the secondary infection has resolved. There have been no reports that person nel with genital HSV infections have transmitted HSV to patients; therefore, work restrictions for personnel with genital herpes are not indicated.
# Measles
Nosocomial transmission of measles virus (sporadic and epidemic) has been well described. From 1985 through 1991, approx imately 3000 (4%) of all reported episodes of measles in the United States were probably acquired in a medical facility; of these, more than 700 (25%) occurred in health care personnel, many of whom were not vaccinated. 9 Data have suggested that health care personnel have a risk of measles 13-fold that of the general population. 9 Of the 2765 episodes of measles reported during 1992 through 1995, 385 (13.9%) occurred in health care settings. 221,230 Measles is transmitted both by large droplets during close contact between infected and sus ceptible persons and by the airborne route. 229,231 Measles is highly transmissible and frequently misdiagnosed during the prodromal stage. The incubation period for measles is 5 to 21 days. Immunocompetent persons with measles shed the virus from the nasopharynx, beginning with the prodrome until 3 to 4 days after rash onset; immunocompromised persons with measles may shed virus for extended periods. 232 Strategies to prevent nosocomial transmis sion of measles include (a) documentation of measles immunity in health care personnel, (b) prompt identification and isolation of persons with fever and rash, and (c) adherence to air borne precautions for suspected and proven cases of measles. 3 It is essential that all personnel have docu mentation of measles immunity, regardless of their length of employment or whether they are involved in patient care. Further, some states have regulations requiring measles immunity for health care personnel. Although persons born before 1957 are generally considered to be immune to measles, serologic studies indicate that 5% to 9% of health care personnel born immune. 9,233,234 before 1957 may not be Furthermore, during 1985 through 1989, 29% of all measles cases in U.S. health care person nel occurred in those born before 1957. 221 Consideration should be given to recommend ing a dose of measles-mumps-rubella trivalent vaccine (MMR) to personnel born before 1957 who are unvaccinated and who lack (a) a histo ry of previous measles disease, (b) documenta tion of receipt of one dose of live-measles vac cine, and (c) serologic evidence of measles immunity. 9 Health care personnel born during or after 1957 should be considered immune to measles when they have (a) documentation of physician-diagnosed measles, (b) documenta tion of two doses of live measles vaccine on or after their first birthday, or (c) serologic evi dence of measles immunity (persons with an "indeterminate" level of immunity on testing should be considered susceptible). Persons born between 1957 and 1984 who received childhood measles immunization were given only one dose of vaccine during infancy and may require a second dose of vaccine. 8
# AJIC
# June 1998
Serologic screening for measles immunity is not necessary before administration of measles vaccine, unless the medical facility considers it cost-effective or the person to be vaccinated requests it. When serologic screening before vaccination is done, tracking systems are needed to ensure that those identified as susceptible are subsequently vaccinated in a timely manner. 237 During measles outbreaks, serologic screening before vaccination is not necessary. In outbreak situations, prompt administration of vaccine is necessary to halt disease transmission.
Work restrictions are necessary for personnel who acquire measles; they need to be excluded from duty for 7 days after the rash appears. Likewise, personnel not immune to measles need to be excluded from duty from 5 days after the first exposure to 21 days after the last exposure to measles.
# Meningococcal disease
Community-acquired meningococcal disease is typically caused by a variety of serogroups of Neisseria meningitidis; serogroups B and C cause 46% and 45% of the endemic cases, respectively. Serogroups A, Y, and W-135 account for nearly all the remaining endemic cases. 15 In contrast, epidem ic meningococcal disease has, since the early 1990s, been caused increasingly by serogroup C. 15,239,240 Nosocomial transmission of N. meningitidis is uncommon. In rare instances, when proper pre cautions were not used, N. meningitidis has been transmitted from patient to personnel, through contact with the respiratory secretions of patients with meningococcemia or meningo coccal meningitis, or through handling laboratory specimens. 241 Lower respiratory tract infections caused by N. meningitidis may present a greater risk of transmission than either meningococcemia or meningitis, 243,244 especially if the patient has an active, produc tive cough. 244 The risk of personnel acquisition of meningococcal disease from casual contact (e.g., cleaning rooms or delivering food trays) appears to be negligible. 244 N. meningitidis infection is probably transmit ted by large droplets; the incubation period is from 2 to 10 days, and patients infected with N. meningitidis are rendered noninfectious by 24 hours of effective therapy. Personnel who care for patients with suspected N. meningitidis infection can decrease their risk of infection by adhering to droplet precautions. 3 Postexposure prophylaxis is advised for persons who have had intensive, unprotected contact (i.e., without wearing a mask) with infected patients (e.g., mouth-to-mouth resuscitation, endotracheal intubation, endotracheal tube management, or close examination of the oropharynx of patients). 15 Antimicrobial prophylaxis can eradi cate carriage of N. meningitidis and prevent infec tions in personnel who have unprotected exposure to patients with meningococcal infections. 245,246 Because secondary cases of N. meningitidis occur rapidly (within the first week) after expo sure to persons with meningococcal disease, 247 it is important to begin prophylactic therapy immediately after an intensive, unprotected exposure, often before results of antimicrobial testing are available. Prophylaxis administered later than 14 days after exposure is probably of limited or no value. 15 Rifampin (600 mg orally every 12 hours for 2 days) is effective in eradi cating nasopharyngeal carriage of N. meningi tidis. 245 Ciprofloxacin (500 mg orally) and ceftri axone (250 mg intramuscularly) in single-dose regimens are also effective in reducing nasopha ryngeal carriage of N. meningitidis and are rea sonable alternatives to the multidose rifampin regimen. 15,246 These antimicrobials may be useful when infections are caused by rifampin-resistant meningococci or rifampin is contraindicated. Rifampin and ciprofloxacin are not recommend ed for pregnant women. 15,106,248,249 The quadrivalent A,C,Y,W-135 polysaccharide vaccine has been used successfully to control community outbreaks caused by serogroup C, 15,239,240,248 but its use is not recommended for postexposure prophylaxis in health care settings. 15 However, preexposure vaccination may be consid ered for laboratory personnel who routinely han 15,241 dle soluble preparations of N. meningitidis.
Healthy persons may have nasopharyngeal car riage of N. meningitidis. 245, Nosocomial trans mission from carriers to personnel has not been reported. In the absence of exposures to patients with N. meningitidis infection, personnel who are asymptomatic carriers need not be identified, treated, or removed from patient care activities. However, personnel with meningococcal infection need to be excluded from duty until 24 hours after the start of effective therapy.
# Mumps
Mumps transmission has occurred in hospi tals and long-term care facilities housing adoles cents and young adults. 253,254 Most cases of CDC Personnel Health Guideline 311 mumps in health care personnel have been com munity acquired.
Mumps is transmitted by contact with viruscontaining respiratory secretions, including sali va; the portals of entry are the nose and mouth. The incubation period varies from 12 to 25 days and is usually 16 to 18 days. The virus may be pre sent in saliva for 6 to 7 days before parotitis and may persist for as long as 9 days after onset of dis ease. Exposed personnel may be infectious for 12 to 25 days after their exposure, and many infected persons remain asymptomatic. 255 Droplet precau tions are recommended for patients with mumps; such precautions should be continued for 9 days after the onset of parotitis. 3 An effective vaccination program is the best approach to prevention of nosocomial mumps transmission. 12 Vaccination with mumps virus vac cine is recommended, unless otherwise con traindicated, for all those who are susceptible to mumps; 12,256 combined MMR is the vaccine of choice, 257 especially when the recipient also is like ly to be susceptible to measles, rubella, or both.
Personnel should be considered immune to mumps if they have (a) documentation of physi cian-diagnosed mumps, (b) documentation of receipt of one dose of live mumps vaccine on or after their first birthday, or (c) serologic evidence of immunity (individuals who have an "indeter minate" antibody level should be considered sus ceptible). 12 Most persons born before 1957 are likely to have been infected naturally and may be considered to be immune, even though they may not have had clinically recognized mumps. Outbreaks among highly vaccinated populations have occurred and have been attributed to pri mary vaccine failure. 258 Work restrictions are necessary for personnel who acquire mumps; such restrictions should be imposed for 9 days after the onset of parotitis. Likewise, susceptible personnel who are exposed to mumps need to be excluded from duty from the 12th day after the first exposure until the 26th day after the last exposure. 9,255
# Parvovirus
Human parvovirus B19 (B19) is the cause of erythema infectiosum (fifth disease), a common rash illness that is usually acquired in childhood. Immunocompetent persons infected with B19 may have an acute, self-limited arthropathy, with or without a rash or anemia of short duration. However, patients with preexisting anemia (e.g., patients with sickle-cell anemia or thalassemia) may have aplastic crisis occur. Immunodeficient patients (e.g., patients with leukemia or AIDS) may become chronically infected with B19 and have chronic anemia. 259,260 Transmission of B19 to health care personnel from infected patients appears to be rare but has been reported. In two investigations of health care personnel exposures to B19, the rate of infec tion among exposed nurses was not higher than the rate among unexposed control subjects. 266,267 In another investigation of health care personnel exposed to a patient with undetected chronic B19 infection, none of the susceptible employees became infected. 268 Personnel have acquired infection while working in laboratories or during the care of patients with B19-associated sickle-cell aplastic crises. B19 may be transmitted through contact with infected persons, fomites, or large droplets. 266,272,273 The incubation period is variable, depending on the clinical manifestation of disease, and ranges from 6 to 10 days. 260 The period of infectivity also varies, depending on the clinical presentation or stage of disease. Persons with erythema infectio sum are infectious before the appearance of the rash, those with infection and aplastic crises for as long as 7 days after onset of illness, and persons with chronic infection for years.
Pregnant personnel are at no greater risk of acquiring B19 infection than are nonpregnant per sonnel; however, if a pregnant woman does acquire B19 infection during the first half of pregnancy, the risk of fetal death (fetal hydrops, spontaneous abor tion, and stillbirth) is increased. 274,275 Because of the serious nature of the consequences for the fetus, female personnel of childbearing age need to be counseled regarding the risk of transmission of B19 and appropriate infection control precautions. 3 Isolation precautions are not indicated for most patients with erythema infectiosum because they are past their period of infectiousness at the time of clinical illness. 271,274 However, patients in aplas tic crisis from B19 or patients with chronic B19 infection may transmit the virus to susceptible health care personnel or other patients; therefore, patients with preexisting anemia who are admit ted to the hospital with febrile illness and tran sient aplastic crises should remain on droplet pre cautions for 7 days and patients with known or suspected chronic infection with B19 should be placed on droplet precautions on admission and for the duration of hospitalization. 3,263 Work restrictions are not necessary for personnel exposed to B19.
AJIC June 1998
# Pertussis
Nosocomial transmission of Bordetella pertus sis has involved both patients and personnel; nonimmunized children are at greatest risk. Serologic studies of health care personnel indi cate that personnel may be exposed to and infected with pertussis much more frequently than indicated by the occurrence of recognized clinical illness. 277,279,281,282 In one such study, the level of pertussis agglutination antibodies was found to correlate with the degree of patient con tact; the prevalence of such antibody was highest in pediatric house staff (82%) and ward nurses (71%) and lowest in nurses with administrative responsibilities (35%). 277 Pertussis is highly contagious; secondary attack rates exceed 80% in susceptible household con tacts. B. pertussis transmission occurs by con tact with respiratory secretions or large aerosol droplets from the respiratory tracts of infected per sons. The incubation period is usually 7 to 10 days. The period of communicability starts at the onset of the catarrhal stage and extends into the paroxysmal stage up to 3 weeks after onset of symptoms. Prevention of secondary transmission of pertussis is especially difficult during the early stages of the dis ease because pertussis is highly communicable in the catarrhal stage, when the symptoms are non specific and the diagnosis is uncertain.
During nosocomial pertussis outbreaks, the risk of acquiring infection among patients or personnel is often difficult to quantify because exposure is not easily determined. Furthermore, clinical symptoms in adults are less severe than in children and may not be recognized as pertussis. Pertussis should be considered for any person seeking treatment with an acute cough lasting at least 7 days, particularly if accompanied by paroxysms of coughing, inspira tory whoop, or posttussive vomiting. 280,281 Prevention of transmission of B. pertussis in health care settings involves (a) early diagnosis and treatment of patients with clinical infection, (b) implementation of droplet precautions for infectious patients, 3 (c) exclusion of infectious personnel from work, and (d) administration of postexposure prophylaxis to persons exposed to infectious patients. 279 Patients with suspected or confirmed pertussis who are admitted to the hos pital need to be placed on droplet precautions until they have clinical improvement and have received antimicrobial therapy for at least 5 days.
Vaccination of adolescents and adults with whole-cell B. pertussis vaccine is not recommend ed 19 because local and systemic reactions have been observed more frequently in these groups than in children. Acellular pertussis vaccine is immunogenic in adults and carries a lower risk of adverse events than does whole-cell vaccine. 280,286 However, the acellular vaccine has not been licensed for use in persons 7 years old or older. Because immunity among vaccine recipients wanes 5 to 10 years after the last vaccine dose (usually given at 4 to 6 years of age), personnel may play an important role in transmitting pertus sis to susceptible infants. However, additional studies are needed to assess whether booster doses of acellular vaccines are indicated for adults.
Postexposure prophylaxis is indicated for person nel exposed to pertussis; a 14-day course of either erythromycin (500 mg orally four times daily) or trimethoprim-sulfamethoxazole (one tablet twice daily) has been used for this purpose. The efficacy of such prophylaxis has not been well documented, but studies suggest that it may minimize transmis sion. 19,279,287,288 There are no data on the efficacy of newer macrolides (clarithromycin or azithromycin) for prophylaxis in persons exposed to pertussis.
Restriction from duty is indicated for personnel with pertussis from the beginning of the catarrhal stage through the third week after onset of parox ysms, or until 5 days after the start of effective antimicrobial therapy. Exposed personnel do not need to be excluded from duty.
# Poliomyelitis
The last cases of indigenously acquired wildvirus poliomyelitis occurred in the United States in 1979. 289 Since then, all cases of endemic poliomyelitis reported in the United States (5 to 10 endemic cases/year) have been related to the administration of oral polio vaccine (OPV). 21 Although the risk of transmission of poliovirus in the United States is very low, wild poliovirus may potentially be introduced into susceptible popula tions with low immunization levels.
Poliovirus is transmitted through contact with feces or urine of infected persons but can be spread by contact with respiratory secretions and, in rare instances, through items contami nated with feces. The incubation period for nonparalytic poliomyelitis is 3 to 6 days, but is usu ally 7 to 21 days for paralytic polio. 290 Com municability is greatest immediately before and after the onset of symptoms, when the virus is in the throat and excreted in high concentration in feces. The virus can be recovered from the throat for 1 week and from feces for several weeks to months after onset of symptoms.
# CDC Personnel Health Guideline 313
Vaccine-associated poliomyelitis may occur in the recipient (7 to 21 days after vaccine administration) or susceptible contacts of the vaccine recipient (20 to 29 days after vaccine administration). 289 Adults have a slightly increased risk of vaccine-associated para lytic poliomyelitis after receipt of OPV; therefore, inactivated poliovirus vaccine (IPV) should be used when adult immunization is warranted. 8,16,21 Also, because immunocompromised persons may be at greater risk for development of poliomyelitis after exposure to vaccine virus, IPV rather than OPV is rec ommended when vaccinating pregnant or immuno compromised personnel, or personnel who may have contact with immunocompromised patients. 8,16,21,290 Health care personnel who may have contact with patients excreting wild virus (e.g., imported poliomyelitis case) and laboratory personnel han dling specimens containing poliovirus or per forming cultures to amplify virus should receive a complete series of polio vaccine; if previously vac cinated, they may require a booster dose of either IPV or OPV. 8,21 For situations where immediate protection is necessary (e.g., an imported case of wild-virus poliomyelitis requiring care), addition al doses of OPV should be given to adults who have previously completed a polio vaccine series. 21
# Rabies
Human rabies cases occur primarily from exposure to rabid animals. Cases of human rabies have increased in the United States during the 1990s. 291 Laboratory and animal care personnel who are exposed to infected animals, their tis sues, and their excretions are at risk for the dis ease. Also, rabies transmission to laboratory per sonnel has been reported in vaccine production and research facilities after exposure to high titered infectious aerosols. 292,293 Theoretically, rabies may be transmitted to health care person nel from exposures (bite and nonbite) to saliva from infected patients, but no cases have been documented after these types of exposures. 294 It is also possible for rabies to be transmitted when other potentially infectious material (such as brain tissue) comes into contact with nonintact skin or mucous membranes. 22,294 Bites that pene trate the skin, especially bites to the face and hands, pose the greatest risk of transmission of rabies virus from animals to human beings. 22 The incubation period for rabies is usually 1 to 3 months, but longer periods have been reported. 295 Exposures to rabies can be minimized by adher ing to standard precautions when caring for per sons with suspected or confirmed rabies 3 and by using proper biosafety precautions in laborato ries. 5 Preexposure vaccination has been recom mended for all personnel who (a) work with rabies virus or infected animals or (b) engage in diagnostic, production, or research activities with rabies virus. 5,22 Consideration also may be given to providing preexposure vaccination to animal han dlers when research animals are obtained from the wild, rather than from a known supplier that breeds the animals.
Postexposure prophylaxis has been adminis tered to health care personnel after exposures to patients with rabies (Table 1), but decisions regarding postexposure prophylaxis should be made on a case-by-case basis after discussion with public health authorities. 22
# Rubella
Nosocomial transmission of rubella has occurred from both male and female personnel to other susceptible personnel and patients, as well as from patients to susceptible personnel and other patients. Rubella is transmitted by contact with nasopha ryngeal droplets from infected persons. The incu bation period is variable but may range from 12 to 23 days; most persons have the rash 14 to 16 days after exposure. The disease is most contagious when the rash is erupting, but virus may be shed from 1 week before to 5 to 7 days after the onset of the rash. 306 Rubella in adults is usually a mild disease, lasting only a few days; 30% to 50% of cases may be subclinical or inapparent.
Droplet precautions are used to prevent trans mission of rubella. Infants with congenital rubella may excrete virus for months to years; when caring for such patients, it is therefore advisable to use contact precautions for the first year of life, unless nasopharyngeal and urine culture results are nega tive for rubella virus after 3 months of age. 3 Ensuring immunity among all health care per sonnel (male and female) is the most effective way to eliminate nosocomial transmission of rubella. 8,9,14,256,307 Persons should be considered susceptible to rubella if they lack (a) documenta tion of one dose of live rubella vaccine on or after their first birthday and (b) laboratory evi dence of immunity (persons with indeterminate levels are considered susceptible). A history of previous rubella infection is unreliable and should not be considered indicative of immunity to rubella. Although birth before 1957 is general ly considered acceptable evidence of rubella immunity, a dose of MMR has been recommend-June 1998 ed for those health care personnel that do not have laboratory evidence of immunity. 9 In addi tion, birth before 1957 is not considered accept able evidence of rubella immunity for women of childbearing age; history of vaccination or labo ratory evidence of rubella immunity is particu larly important for women who may become pregnant. 9 Voluntary immunization programs are usually inadequate to ensure personnel pro tection. 7,308 Because many health departments mandate rubella immunity for health care per sonnel, personnel health programs should con sult with their local or state health departments before establishing policies for their facilities.
Serologic screening of personnel for immunity to rubella need not be done before vaccinating against rubella, unless the medical facility consid ers it cost-effective or the person getting vaccinat ed requests it. 7, When serologic screening before vaccination is done, tracking systems are needed to ensure that those identified as suscepti ble are subsequently vaccinated in a timely man ner. 237 Likewise, during rubella outbreaks, sero logic screening is not necessary. Pregnant women who are already immune to rubella are not at increased risk for adverse advents. 309 However, for theoretic reasons, a risk to the fetus from admin istration of live-virus vaccines cannot be excluded. Women should be counseled to avoid pregnancy for 30 days after administration of MMR or other rubella-containing vaccines. Routine precautions for vaccinating postpubertal women include (a) asking whether they are or may be pregnant, (b) not vaccinating those who say they are or may be pregnant, and (c) vaccinating those who state they are not pregnant after the potential risk to the fetus has been explained. If a pregnant woman is vaccinated or a woman becomes pregnant within 3 months after vaccination, she should be coun seled about the theoretic basis of concern for the fetus, but MMR vaccination during pregnancy should not ordinarily be a reason to consider ter mination of pregnancy. Rubella-susceptible women who are not vaccinated because of preg nancy should be counseled about the importance of being vaccinated as soon as they are no longer pregnant. 9 MMR is the vaccine of choice for rubel la, especially when the recipient also is likely to be susceptible to measles, mumps, or both (Table 2).
Work restrictions are necessary for personnel who acquire rubella; ill personnel need to be excluded from duty for 5 days after the rash appears. Likewise, personnel susceptible to rubel la require exclusion from duty from the seventh day after the first exposure through the 21st day after the last exposure (Table 3).
# Scabies and pediculosis a. Scabies
Scabies is caused by infestation with the mite Sarcoptes scabiei. The conventional (typical) clini cal presentation of scabies includes intense pruri tus and cutaneous tracks, where mites have bur rowed into the skin. Crusted or "Norwegian" sca bies may develop among immunocompromised and elderly individuals in which their skin may become hyperkeratotic; pruritus may not be pre sent, which also makes diagnosis difficult. In con ventional scabies, 10 to 15 mites are present, whereas in crusted scabies, thousands of mites are harbored in the skin, increasing the potential for transmission. 310,311 Nosocomial outbreaks of scabies have occurred in a variety of health care settings, including intensive care units, 312 rehabilitation centers, 313 long-term care facilities, 314,315 hospital wards, 316 a dialysis unit, 317 and a health care laundry. 318 In recent years there has been an increase in the occurrence of crusted scabies among immunocompromised patients, particu larly persons with HIV, which has led to the transmission of scabies among personnel, patients, and their families. 310, Nosocomial transmission of scabies occurs primarily through prolonged skin-to-skin con tact with an infested person who has conven tional scabies. 310,322 Shorter periods of skin-to skin contact with persons who have crusted sca bies may result in transmission of scabies. 323 Personnel have acquired scabies while perform ing patient care duties such as sponge bathing, lifting, or applying body lotions. 310,311,319,324 Transmission by casual contact, such as by hold ing hands, or through inanimate objects, such as infested bedding, clothes, or other fomites, has been reported infrequently. 317,318 The use of contact precautions when taking care of infested patients before application of scabicides can decrease the risk of transmission to personnel. 3,311 Routine cleaning of the environ ment of patients with typical scabies, especially bed linens and upholstered furniture, will aid in eliminating the mites. Additional environmental cleaning procedures may be warranted for crust ed scabies. 310,311, Recommendations for treatment and control of scabies in health care institutions have been published previously. 310,311, The recommend-
CDC Personnel Health Guideline 315
ed topical scabicides include permethrin cream (5%), crotamiton (10%), and lindane (1%) lotion; resistance to and adverse effects from lindane have been reported. 329 Single-dose oral iver mectin has recently been shown to be an effec tive therapy for scabies 323,330,332 but has not received Food and Drug Administration (FDA) approval for this purpose.
Most infested health care workers have typical scabies with low mite loads 333 ; a single correct application of a scabicide is adequate and imme diately decreases the risk of transmis sion. 25,319,322,324,334 There are no controlled evaluations of the efficacy of prophylactic scabi cide therapy among health care personnel, and some experts recommend two applications of scabicide for all infested personnel. 311,315,321 If personnel continue to have symptoms after ini tial treatment, another application of scabicide may be needed. Persistent symptoms likely rep resent newly hatched mites rather than new infestation; however, pruritus after scabies infes tation and treatment may persist for as long as 2 weeks, even without infestation. 25 Patients with crusted scabies may require repeated treatments and should be observed for recurrence of the mite infestation. 310,311,314,326 Personnel who are exposed to scabies but lack signs of infestation do not usually require prophylactic treatment with scabicides. In outbreak situations where transmission continues to occur, prophylaxis may be warranted for both patients and exposed health care personnel. 311,313 Restrictions from patient care are indicated for personnel infested with scabies until after they receive initial treatment and have been medically evaluated and determined to be free of infestation. They should be advised to report for further eval uation if symptoms do not subside.
# b. Pediculosis
Pediculosis is caused by infestation with any of three species of lice: Pediculus humanus capitus (human head louse), Pediculus humanus corporis (human body louse), and Phthirus pubis (pubic or crab louse).
Head lice are transmitted by head-to-head con tact or by contact with infested fomites such as hats, combs, or brushes. Nosocomial transmis sion, although not common, has occurred. 310 Body lice are usually associated with poor hygiene and overcrowded conditions. Trans mission occurs by contact with the skin or cloth ing of an infested person. Nosocomial transmis sion is unlikely.
Pubic lice are primarily found in the pubic hair but can be found in the axilla, eyelashes, or eyebrows. Transmission occurs primarily through intimate physical or sexual contact. Transmission by fomites, such as toilet seats or bedding, is uncommon. Nosocomial transmis sion is very unlikely.
Recommendations for control of pediculosis have been published previously. 310,327,335 The drugs recommended for treatment include permethrin cream 1%, pyrethrins with piperonyl butoxide, 1%. 328-330,335 malathion 0.5%, and lindane Resistance to various drugs has been reported. Local health departments may have information about drugs that are effective in their areas. Health care personnel exposed to patients with pediculosis do not require treatment, unless they show evidence of infestation.
Restriction from patient care is indicated for personnel with pediculosis until after they receive initial treatment and are found to be free of adult and immature lice. If symptoms do not subside after initial treatment, they should be advised to report for further evaluation.
# Staphylococcus aureus infection and carriage
Staphylococcal infection and carriage occur fre quently in human beings. In hospitals, the most important sources of S. aureus are infected and colonized patients. Previously, methicillin-suscep tible (but penicillin-resistant) S. aureus accounted for most staphylococcal infections. In recent years, however, methicillin-resistant S. aureus has accounted for approximately 80% of all S. aureus isolates reported to the National Nosocomial Infections Surveillance System. 336,337 The epidemi ology of methicillin-resistant S. aureus does not appear to differ from that of methicillin-suscepti ble, penicillin-resistant S. aureus, except that out breaks of methicillin-resistant S. aureus tend to occur more frequently among elderly or immuno compromised patients or among patients with severe underlying conditions. 338,339 Nosocomial transmission of S. aureus occurs primarily by the hands of personnel, which can become contaminated by contact with the colo nized or infected body sites of patients. 339,340 Hospital personnel who are infected or colonized with S. aureus also can serve as reservoirs and dis seminators of S. aureus, and infected dietary personnel have been implicated in staphylococcal food poisoning. 345 The role of contaminated envi ronmental surfaces in transmission of S. aureus AJIC June 1998 has rarely been well documented 346 and remains controversial, although heavy contamination of fomites may facilitate transmission to patients by hands of personnel. 339 The incubation period for S. aureus infections varies by type of disease. For food-borne illness it is 30 minutes to 6 hours, for bullous impetigo it is 1 to 10 days, for toxic shock syndrome it is usually 2 days, and for other types of infection it is variable. 347 Carriage of S. aureus is most common in the anterior nares, but other sites, such as the hands, axilla, perineum, nasopharynx, and oropharynx, may also be involved. 339 The frequency of nasal carriage of S. aureus among health care personnel ranges between 20% and 90%, but fewer than 10% of healthy nasal carriers disperse the organisms into the air. 342 Nasal carriers with upper respirato ry symptoms can disseminate the organism more effectively. 342 Carriage of S. aureus in the nares has been shown to correspond to hand carriage, 336 and persons with skin lesions caused by S. aureus are more likely than asymptomatic nasal carriers to disseminate the organism.
Culture surveys of personnel can detect carriers of S. aureus but do not indicate which carriers are likely to disseminate organisms. Thus, such sur veys are not cost-effective and may subject per sonnel with positive culture results to unneces sary treatment and removal from duty. A more reasonable approach is to conduct active surveil lance for nosocomial S. aureus infections. Culture surveys may be indicated if, after a thorough epi demiologic investigation, personnel are linked to infections. Such implicated personnel can then be removed from clinical duties until carriage has been eradicated. 339,341, Several antimicrobial regimens have been used successfully to eradicate staphylococcal carriage in health care personnel. These regimens include orally administered antimicrobial agents (e.g., rifampin, clindamycin, or ciprofloxacin) alone or in combination with another oral (e.g., trimetho prim-sulfamethoxazole) or topical (mupirocin) antimicrobial. 349, Resistant S. aureus strains have emerged after the use of these oral or topical antimicrobial agents for eradication of S. aureus colonization. 18,210,349,353, Thus, antimicrobial treatment to eradicate carriage may be best if lim ited to personnel who are carriers epidemiological ly linked to disease transmission. Nosocomial transmission of S. aureus can be prevented by adherence to standard precautions and other forms of transmission-based precautions as needed. 3 Restriction from patient-care activities or food handling is indicated for personnel who have draining skin lesions that are infected with S. aureus until they have received appropriate thera py and the infection has resolved. No work restric tions are necessary for personnel who are colo nized with S. aureus, unless they have been epi demiologically implicated in S. aureus transmis sion within the facility.
# Streptococcus, group A infection
Group A Streptococcus (GAS) has been trans mitted from infected patients to health care per sonnel after contact with infected secretions, and the infected personnel have subsequently acquired a variety of GAS-related illnesses (e.g., toxic shock-like syndrome, cellulitis, lymphangi tis, and pharyngitis). Health care personnel who were GAS carriers have infrequently been linked to sporadic outbreaks of surgical site, postpartum, or burn wound infections and to food-borne transmission of GAS causing pharyngitis. 377 In these outbreaks, GAS carriage was documented in the pharynx, 369,372,378 the skin, 369,370 the rec tum, 369,375 and the female genital tract of the infected personnel. 369,374,379 The incubation period for GAS pharyngitis is 2 to 5 days, but for impetigo is 7 to 10 days. The incu bation period is variable for other GAS infections. 380 Culture surveys to detect GAS carriage among personnel are not warranted, unless personnel are epidemiologically linked to cases of nosocomial infection. 378 In instances where thorough epi demiologic investigation has implicated person nel in nosocomial transmission, cultures may be obtained from skin lesions, pharynx, rectum, and vagina; GAS isolates obtained from personnel and patients can be serotyped to determine strain relatedness. 373 Treatment of personnel carriers needs to be individually determined because (a) experience is limited regarding the treatment of personnel carriers implicated in GAS outbreaks and (b) carriage of the organism by personnel may be recurrent through long periods. 374 Contact is the major mode of transmission of GAS in these health care settings. Airborne transmis sion during outbreaks has been suggested by sev eral investigators, and some have demonstrated that exercising and changing of clothing can lead to airborne dissemination of GAS from rectal and vaginal carriage. 369,374,375,379 Nosocomial transmis sion of GAS to personnel can be prevented by adherence to standard precautions or other transmission-based precautions as needed. 3
# CDC Personnel Health Guideline 317
Restriction from patient care activities and food handling is indicated for personnel with GAS infec tions until 24 hours after they have received appro priate therapy. However, no work restrictions are necessary for personnel who are colonized with GAS, unless they have been epidemiologically linked to transmission of infection within the facility.
# Tuberculosis
Nosocomial transmission of tuberculosis (TB) is well documented, but such transmission in the United States is generally low. However, the risk may be increased in health care facilities located in communities with (a) high rates of HIV, (b) high numbers of persons from TB-endemic coun tries, and (c) communities with a high prevalence of TB infection. 381,382 In some areas in the United States, the incidence and prevalence of mul tidrug-resistant Mycobacterium tuberculosis (MDR-TB) have also increased, and nosocomial MDR-TB outbreaks have occurred. The increased risk of occupational acquisition of TB by health care personnel has been reported for decades, and it dramatically decreased after the introduction of effective antituberculous drugs. 392,393 Skin-test conversion rates among health care personnel after routine skin testing have ranged from 0.11% to 10%. 394 Among health care personnel with known exposure to an infec tious patient with TB or involved in prolonged nosocomial outbreaks of TB, the skin-test conver sion rates have ranged from 18% to 55%. 383 385,388,389,393,395-401 Health care personnel with severely compromised immune systems, especial ly those infected with HIV 381,402 and including those with malignancies or receiving immuno suppressive therapy, are at high risk for develop ment of active disease after acquisition of tuber culous infection. It has been estimated that per sons infected with M. tuberculosis and coinfected with HIV have an 8% to 10% risk per year for development of active TB, whereas immunocom petent persons infected with TB have a 10% life time risk for active disease. 403 The transmission of TB in health care facilities has been primarily caused by incomplete imple mentation of recommended TB infection control measures. 396 In 1994, the CDC published detailed recommendations for the prevention of trans mission of TB in health care settings, "Guidelines for Preventing the Transmission of M. tuberculosis in Health Care Facilities, 1994." 382 A summary of the recommendations pertaining to personnel health follows.
# a. Strategies for prevention of transmission of TB
The risk of transmission of TB to or from per sonnel in a health care facility varies according to the type and size of the facility, the preva lence of TB in the community, the patient pop ulation served by the facility, the occupational group the person represents, the area of the facility where the person works, and the effec tiveness of the facility's TB control program. A detailed risk assessment is essential in identify ing the nature of TB control measures that are appropriate for a particular facility, as well as for specific areas and occupational groups within a facility. 382,404 A risk assessment should include the following: (a) review of the commu nity TB profile, (b) review of the number of patients with TB who were treated in each area of the facility, (c) review of the drug-suscepti bility patterns of TB isolates from patients treated in the facility, (d) an analysis of purified protein derivative (PPD) skin-test results of health care personnel by work area or occupa tional group, (e) an evaluation of infection con trol parameters, including isolation policies, laboratory diagnostic capabilities, and antitu berculous therapy regimens, (f) an observation al review of TB infection control practices, and (g) evaluation of the function and maintenance of environmental controls. 382 Transmission of TB can be minimized by developing and implementing an effective TB control program that is based on a hierarchy of controls: (a) administrative controls, (b) engi neering controls, and (c) personal respiratory protection. 382,384,386,393,396,404,405
# b. TB screening program
A TB screening program for personnel is an inte gral part of a health care facility's comprehensive TB control program. The screening program should be based on the facility-specific risk assess ment. It may be advisable to screen immunocom promised personnel every 6 months. 382 Baseline PPD testing of all personnel (including personnel with a history of bacille Calmette-Guérin vaccination) during their preem ployment physical examination or their applica tion for hospital privileges will identify personnel who have been previously infected. For the base line testing, a two-step procedure for personnel without a PPD test in the past 12 months can be used to minimize the likelihood of confusing reac tivity from an old infection (boosting) with reac tivity from a recent infection (conversion). Decisions concerning the use of the two-step pro-AJIC June 1998 cedure for baseline testing in a particular facility should be based on the frequency of boosting in that facility. Criteria used for interpretation of a PPD-test reaction may vary depending on (a) the purpose (diagnostic or epidemiologic) of the test, (b) the prevalence of TB infection in the popula tion being tested, (c) the immune status of the host, and (d) any previous receipt of BCG immu nization. Detailed recommendations for perform ing and interpreting skin tests have been pub lished. 382,
# c. Follow-up evaluation
The risk assessment will show which health care personnel have the potential for exposure to M. tuberculosis and determine how frequently they should receive PPD testing. At a minimum, annual PPD testing is indicated for personnel with the potential for exposure to TB.
It is also important to obtain an initial chest radiograph for personnel with positive PPD-test reactions, documented PPD-test conversions, or pulmonary symptoms suggestive of TB. There are no data to support the use of routine chest radiographic examinations for asymptomatic PPD-negative personnel. In addition, personnel who have positive PPD-test reactions but also received adequate preventive treatment do not need repeat chest films, unless they have pul monary symptoms suggestive of TB. Repeat chest radiographic examinations of such persons have not been shown to be beneficial or costeffective in monitoring persons for development of disease. However, more frequent monitoring for symptoms of TB may be considered for per sonnel who had recent conversion of their PPD test and those persons who, if infected, are at increased risk for development of active TB (e.g., HIV-infected or otherwise severely immunocom promised persons). 382 Routine anergy testing of HIV-seropositive individuals is limited in its use fulness; however, anergy testing may be useful in guiding individual decisions regarding preven tive therapy in selected situations. 408
# d. Management of personnel after exposure to TB
It is important to administer PPD tests to per sonnel as soon as possible after TB exposures are recognized. Such immediate PPD testing estab lishes a baseline with which subsequent PPD tests can be compared. A PPD test performed 12 weeks after the last exposure will indicate whether infection has occurred. Persons already known to have reactive PPD tests need not be retested. Personnel with evidence of new infec tion (i.e., PPD-test conversions) need to be evalu ated for active TB. If active TB is not diagnosed, preventive therapy should be considered. 382
# e. Preventive therapy
For workers with positive PPD-test results who were probably exposed to drug-susceptible TB, preventive therapy with isoniazid is indicated, unless there are contraindications to such thera py. 382,407 Alternative preventive regimens have been proposed for persons who have positive PPD-test results after exposure to drug-resistant TB. 409
# f. Work restrictions
Personnel with active pulmonary or laryngeal TB may be highly infectious; exclusion from duty is indicated until they are noninfectious. If personnel are excluded from duty because of active TB, the facility should have documentation from their health care providers that personnel are noninfec tious before they are allowed to return to duty. The documentation needs to include evidence that (a) adequate therapy is being received, (b) the cough has resolved, and (c) results of three consecutive sputum acid-fast bacilli (AFB) smears collected on different days are negative. After personnel resume duty and while they remain on anti-TB therapy, periodic documentation from their health care providers is needed to show that effective drug therapy is being maintained for the recommended period and that their sputum AFB smear results continue to be negative. If personnel discontinue their treatment, they need to be evaluated for active TB; directly observed therapy may be considered.
Work restrictions are not necessary for person nel receiving preventive treatment for latent TB (positive PPD-test result without active disease) or for personnel with latent TB who do not accept preventive therapy. However, these personnel should be instructed to seek evaluation promptly if symptoms suggestive of TB develop.
# g. Considerations for BCG vaccine
# BCG has not been routinely used in the United
States to protect health care personnel. Never theless, because of the resurgence of TB in the United States and new information about the pro tective effect of BCG, 410,411 the role of BCG vaccina tion in the prevention and control of TB in the coun try has been reevaluated. 412 The following is a sum mary of the joint statement by the Advisory Council for the Elimination of Tuberculosis and ACIP regarding the use of BCG in health care personnel.
Two recent metaanalyses of 18 410 and 26 411 BCG studies, respectively, indicate that the efficacy of BCG vaccine in preventing serious TB is high (>80%) in children and suggest 50% efficacy in adults. However, the protective efficacy of the vac-CDC Personnel Health Guideline 319 cine in adolescents and adults, including health care personnel and HIV-infected children and adults, has not been determined. 412 BCG vaccination should not be used as a pri mary TB control strategy because (a) the protec tive efficacy of the vaccine in health care person nel is uncertain and (b) even if vaccination is effective in an individual, other persons in the health care facility are not protected against pos sible exposure to and infection with drug-resistant strains of M. tuberculosis. However, BCG vaccina tion may be indicated for health care personnel in a few geographic areas where the prevalence of MDR-TB is high, transmission of TB is likely, and TB infection control measures have been imple mented but have not been successful in control ling nosocomial transmission. 412 Consultation with local and state health departments is advis able when determining whether to provide BCG vaccination to health care personnel.
BCG vaccination often results in local adverse effects (such as muscular soreness, erythema, purulent drainage, and axillary or cervical lym phadenopathy) for as long as 3 months after vacci nation; serious long-term complications (such as musculoskeletal lesions, multiple lymphadenitis, and disseminated BCG disease) are infrequent. The safety of BCG vaccination in immunocompro mised populations (i.e., immunocompromised from immune deficiency diseases, HIV infection, leukemia, lymphoma, or generalized malignancy, or immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabolites, or radiation) has not been determined by adequate epidemiologic studies. However, because of the possibility of disseminated BCG infection in such persons, BCG vaccination is not recommend ed for immunocompromised personnel. 412 The safety of BCG vaccination in pregnant women has also not been evaluated; therefore, it is not recom mended for pregnant personnel. 412 PPD testing is not contraindicated for persons who have received BCG vaccine and can be used to support or exclude the diagnosis of infection with M. tuberculosis. 412 PPD-test reactivity caused by BCG vaccination wanes with time and is unlikely to persist longer than 10 years after vac cination in the absence of infection with M. tuber culosis. 420,421 After a person has been vaccinated with BCG, the presence or size of a PPD-test reac tion cannot be used to predict whether BCG will provide any protection against TB disease 423,424 or to determine whether the reaction is caused by M. tuberculosis infection or the previous BCG vaccination. 425 However, a BCG-vaccinated per son who has a PPD-test reaction of ≥ 10 mm induration should be considered infected with TB, especially if the vaccinee (a) is a contact of a person with infectious TB, particularly if the infectious person has transmitted M. tuberculosis to others, (b) is from a country with high preva lence of TB, or (c) is continually exposed to pop ulations in which the prevalence of TB is high. 412
# Vaccinia (smallpox)
Through aggressive surveillance for smallpox combined with the effective use of smallpox vac cine (vaccinia virus vaccine), the World Health Organization was able to declare the world free of smallpox in 1980. The smallpox vaccine licensed for use in the United States is derived from infec tious vaccinia virus. After vaccination, the virus can be cultured from the vaccination site until the scab has separated from the skin (2 to 21 days after vaccination); thus, susceptible persons may acquire vaccinia from a recently vaccinated per son. Covering the vaccination site and wash ing hands after contact with the vaccination site (including bandages) will prevent transmission. Recently, recombinant vaccinia viruses have been engineered to express immunizing agents of sev eral viruses (e.g., herpesvirus, HBV, influenza). There is a theoretic risk that transmission could occur from contact with contaminated dressings or by contact with recombinant vaccine, but no such transmission has been reported among per sonnel who provide care to recipients of the recombinant vaccine. Infections also have been reported among laboratory personnel who handle viral cultures or materials contaminated with vac cinia or recombinant viruses. 18,162 Smallpox vaccination (every 10 years) is indicat ed for personnel who work directly with orthopox viruses (e.g., monkeypox, vaccinia, variola) or in animal care areas where orthopox viruses are stud ied. In selected instances, vaccination may be con sidered for personnel who provide care to recipients of recombinant vaccinia vaccine. 9,18 Personnel who receive the vaccine may continue to have contact with patients if the vaccination site is covered and handwashing is strictly observed. 18 Vaccine is not recommended for personnel with immunosuppres sion or eczema or for personnel who are pregnant.
# Varicella
Nosocomial transmission of varicella-zoster virus (VZV) is well recognized. Sources for nosoco mial exposures have included patients, health care AJIC June 1998 personnel, and visitors (including the children of personnel) with either varicella or herpes zoster.
All susceptible adults in health care settings are at risk for varicella and its complications. During 1990 through 1994, fewer than 5% of varicella cases occurred among adults older than 20 years, but they accounted for 55% of varicella-related deaths. Certain persons are at higher risk for severe disease and secondary complications: preg nant women, premature infants born to varicellasusceptible mothers, infants born at less than 28 weeks' gestation or weighing ≤ 1000 gm (regard less of maternal immune status), and immuno compromised patients. 13 The incubation period for varicella is usually 14 to 16 days but may be from 10 to 21 days after exposure, although the incubation period may be shorter in immunocompromised persons. 442 In persons who receive postexposure VZV immune globulin, the incubation period may be as long as 28 days after exposure. Transmission of infection may occur from 2 days before onset of rash and usually as long as 5 days after rash onset. 442 VZV is transmitted by the contact with infect ed lesions and, in hospitals, airborne transmis sion has occurred from patients with varicella or zoster to susceptible persons who had no direct contact with the infected patient. Adher ence to airborne and contact precautions when caring for patients with known or suspected VZV infection can reduce the risk of transmis sion to personnel. 3 It is generally advisable to allow only personnel who are immune to varicella to take care of patients with VZV. Because of the possibility of transmission to and development of severe illness in high-risk patients, personnel with localized zoster should not take care of such patients until all lesions are dry and crusted. 13,447 Personnel with localized zoster are not likely to transmit infection to immunocompetent patients if their lesions can be covered. However, some institutions may exclude personnel with zoster from work until their lesions dry and crust. 439
# a. Varicella screening and vaccination
Serologic tests have been used to assess the accuracy of reported histories of chicken pox. 440, In adults, a history of varicella is highly predictive of serologic immunity (97% to 99% seropositive). Most adults who have negative or uncertain histories of varicella are also seropositive (71% to 93%). In health care institutions, serologic screening of personnel who have negative or uncertain histories is likely to be cost-effective, depending on the rel ative costs of the test and vaccine. 9,13 A variety of methods have been used for detect ing varicella antibody, but a commercially avail able latex agglutination test provides prompt, sen sitive, and specific serologic results at a reason able cost. The latex agglutination test may not detect low levels of protective antibody that can occur after vaccination; however, a test with increased sensitivity and specificity is currently under development. Routine testing for varicella immunity after vaccination is not necessary, because 99% of persons are seropositive after the second dose. Moreover, seroconversion does not always result in full protection against disease. However, testing vaccinees after exposures may be warranted. In addition, vaccinated persons who are exposed to varicella but lack antibody may be retested in 5 to 6 days to determine whether they are antibody seropositive after the second test and therefore unlikely to acquire varicella. 13 In March 1995, a live-attenuated varicella vac cine was licensed for use in the United States. Administration of varicella vaccine is recom mended for all susceptible health care person nel, especially those who will have close contact with persons at high risk for serious complica tions. 9,13,451,452 Effective varicella vaccination pro grams require two doses of vaccine to achieve high seroconversion rates in adults; 451 the need for and response to booster doses of vaccine are unknown. Vaccination provides approximately 70% protection against infection and 95% pro tection against severe disease in follow-up from 7 to 10 years after vaccination. 13 Cases of vari cella have occurred among vaccinees after expo sure to wild-type virus ("breakthrough infec tion"). Data from vaccine trials in which vacci nees of all ages were followed up for as long as 9 years indicate that 1% to 4% of vaccine recip ients per year acquire varicella, depending on the vaccine lot and interval after vaccination. 9,13 However, vaccinated persons have milder dis ease (e.g., afebrile, a mean of 50 skin lesions that are often not vesicular, and shorter duration of illness) than do unvaccinated individuals (e.g., febrile with several hundred vesicular lesions) 453,454 and are less likely to transmit dis ease than unvaccinated persons.
The rate of transmission of disease from vac cinees who contract varicella is low for vacci nated children but has not been studied in adults. Active surveillance for 1 to 8 years after vaccination of 2141 children between 1981 and CDC Personnel Health Guideline 321 1989 in 10 different trials 9 resulted in reports of breakthrough infections in 78 children, which further resulted in secondary cases in 12.2% (11/90) of vaccinated siblings. Illness was mild in both index and secondary cases. There also has been a report of transmission from a vacci nated child in whom breakthrough disease occurred to a susceptible mother. 9 All information currently available on vaccine efficacy and the persistence of antibody in vac cinees is based on research conducted in set tings where infection is highly prevalent and not affected by the wide use of vaccine. Thus, the extent to which the protection provided by vac cination has been increased by boosting from exposure to natural virus and whether longer term immunity may wane as the prevalence of natural VZV decreases are unknown.
# b. Transmission of vaccine virus
In clinical trials, 3.8% of children and 5.5% of adolescents and adults acquired a nonlocalized rash (median five lesions) after the first injection, and 0.9% of adolescents and adults acquired a nonlocalized rash after the second injection. Available data suggest that healthy children have limited potential to transmit vaccine virus to sus ceptible contacts (estimated to be <1%) but that the risk of transmission from immunocompro mised vaccinees is higher. 13,455,456 Tertiary trans mission of vaccine virus to a second healthy sib ling of a vaccinated leukemic child has also occurred. 456 These data suggest that healthy, vac cinated individuals have a very small risk of trans mitting vaccine virus to their contacts; this risk may be higher in those who acquire a varicellalike rash after vaccination.
Although the risk of transmission of vaccine virus from vaccinees is not known, the risk if any appears to be very low, and the benefits of vacci nating susceptible health care personnel clearly outweigh this potential risk. As a safeguard, insti tutions may wish to consider precautions for vac cinated personnel who acquire a rash or who will have contact with susceptible persons at high risk for serious complications.
# c. Management of health care personnel exposed to varicella
When unvaccinated susceptible personnel are exposed to varicella, they are potentially infec tious 10 to 21 days after exposure, and exclusion from duty is indicated from the tenth day after the first exposure through the 21st day after the last exposure, or until all lesions are dry and crusted if varicella occurs (Table 3). 256 June 1998 If vaccinated health care personnel are exposed to varicella, they may be serotested immediately after exposure to assess the presence of anti body. 452 If they are seronegative, they may be excluded from duty or monitored daily for devel opment of symptoms. Exclusion from duty is indi cated if symptoms (fever, upper respiratory tract symptoms, or rash) develop.
Vaccination should be considered for exposed unvaccinated health care personnel without docu mented immunity. 441,452 Because the efficacy of postexposure vaccination is unknown, however, persons vaccinated after an exposure should be managed as previously recommended for unvaccinated persons.
The routine postexposure use of VZV immune globulin (VZIG) is not recommended among immunocompetent health care personnel. 13 VZIG can be costly, does not necessarily prevent varicel la, and may prolong the incubation period by a week or more, thus extending the time that per sonnel will be restricted from duty. The use of VZIG may be considered for immunocompro mised (e.g., HIV infected) or pregnant health care personnel. 13,457 Postexposure use of acyclovir may be effective and less costly than the use of VZIG in some susceptible persons. 457 However, additional data concerning the efficacy of acyclovir for postexposure prophylaxis are needed before such use can be recommended. 9,13,441,458
# Viral respiratory infections
Viral respiratory infections are common prob lems in health care settings. Nosocomial respira tory infections can be caused by a number of viruses, including adenoviruses, influenza virus, parainfluenza viruses, respiratory syncytial virus (RSV), and rhinoviruses. Because influenza and RSV substantially contribute to the morbidity and mortality associated with viral pneumonia and both have been well studied epidemiologically, this section focuses on prevention of these two viral infections among personnel. Additional information on influenza and RSV can be found in the "Guideline for Prevention of Nosocomial Pneumonia." 459 a. Influenza Nosocomial transmission of influenza has been reported in acute and long-term care facil ities. Transmission has occurred from patients to health care personnel, 462,464 from health care personnel to patients, 466 and among health care personnel. 465, Influenza is believed to be transmitted from person to person by direct deposition of virus-CDC Personnel Health Guideline 323 laden large droplets onto the mucosal surfaces of the upper respiratory tract of an individual during close contact with an infected person, as well as by droplet nuclei or small-particle aerosols. 21,290,473 Although the extent of transmission by virus-con taminated hands or fomites is not known, it is not the primary mode of transmission. 473 The incubation period of influenza is usually 1 to 5 days, and the period of greatest communica bility is during the first 3 days of illness. However, virus can be shed before the onset of symptoms and as long as 7 days after illness onset. Persons at greatest risk for influenzarelated complications include (a) persons older than 65 years, (b) residents of nursing homes and other chronic care facilities, (c) persons with chronic pulmonary or cardiovascular conditions, and (d) persons with diabetes mellitus. 17 Adherence to droplet precautions may prevent nosocomial transmission. 3 Administration of influenza vaccine to health care personnel, including pregnant women, 9 before the beginning of each influenza season can help to (a) reduce the risk to health care personnel of influenza infection, (b) prevent transmission of influenza from personnel to persons at high risk for complications, and (c) reduce personnel absenteeism during community outbreaks. Innovative methods may be needed to increase influenza immunization rates among health care personnel. 477 Immunization rates may also be increased by providing data to health care person nel on the low rates of systemic reactions to influenza vaccine among healthy adults. 478 During institutional outbreaks of influenza, prophylactic antiviral agents (e.g., amantadine and rimantadine) may be used in conjunction with influenza vaccine to reduce the severity and duration of illness among unvaccinated health care personnel. Amantadine and rimanta dine may be administered for 2 weeks after per sonnel vaccination or, in unvaccinated person nel, for the duration of influenza activity in the community. 17,459,465,479
# b. Respiratory syncytial virus
Nosocomial transmission of respiratory syncy tial virus (RSV) is greatest during the early winter when community RSV outbreaks occur; patients, visitors, and health care personnel may transmit the virus in the health care setting. RSV infection is most common among infants and children, who are likely to acquire more severe disease. Because RSV infection can also occur simultaneously with other respiratory viruses, it may go unrecog nized. 480,481 Nosocomial transmission has been reported most frequently among newborn and pediatric patients, 482,483 but outbreaks associated with substantial morbidity and mortality have been reported among adults in bone-marrow transplant centers, 484 intensive care units, 485 and long-term care facilities. 486,487 RSV is present in large numbers in the respira tory secretions of persons symptomatically infect ed with the virus and can be transmitted directly through large droplets during close contact with such persons or indirectly by hands or fomites that are contaminated with RSV. Hands can become contaminated through handling of infect ed persons' respiratory secretions or contaminat ed fomites and can transmit RSV by touching the eyes or nose. 459 The incubation period ranges from 2 to 8 days; 4 to 6 days is most common. In general, infected persons shed the virus for 3 to 8 days, but young infants may shed virus for as long as 3 to 4 weeks. Adherence to contact precautions effectively prevents nosocomial transmission.
# c. Work restrictions
Because large numbers of personnel may have viral respiratory illnesses during the winter, it may not be possible to restrict infected personnel from all patient care duties. Nevertheless, it may be prudent to restrict personnel with acute viral respiratory infections from the care of high-risk patients during community outbreaks of RSV and influenza. 488
# F. PREGNANT PERSONNEL
Immunologic changes occur during pregnancy, primarily depression of certain aspects of cell-medi ated immunity such as decreased levels of helper T cells. These changes permit fetal development with out rejection but generally do not increase maternal susceptibility to infectious diseases. Occupational acquisition of infections is of special concern to female health care personnel of childbearing age for several reasons. Some infections, such as varicella, may be more severe during pregnancy. Transplacental infections with viruses such as par vovirus, varicella, and rubella have been associated with abortion, congenital anomaly, and mental retardation. Other diseases in which the infectious agent may be transmitted to the fetus include CMV, hepatitis B, herpes simplex, influenza, and measles. In addition, certain drugs used to treat or prevent some infections, for example tuberculosis, may be contraindicated during pregnancy.
In general, pregnant health care personnel do not have an increased risk for acquiring infections AJIC June 1998 in the workplace. The risks to pregnant personnel and methods for prevention are discussed in the various sections of this document and are sum marized in Table 6. Female personnel of child bearing age should be strongly encouraged to receive immunizations for vaccine-preventable diseases before pregnancy. Such personnel may also decrease their risk of acquiring infection by adhering to appropriate infection control prac tices, including standard precautions when caring for all patients. Additional information on occu pational risks for pregnant health care personnel has been published elsewhere.
# G. LABORATORY PERSONNEL
Despite the availability of improved engineering controls, work practices, and personal protective equipment, laboratory personnel remain at risk for occupational acquisition of infectious agents. 5,18,53,151,162,241,492,493 Furthermore, newer technologies that require the use of large or con centrated specimens may further increase the risk of occupationally acquired infections among lab oratory personnel. 494 In a review of laboratory-acquired infections from 1950 through 1974, more than 4000 labora tory-associated infections were documented in the United States 492 ; the 10 most commonly reported infections were brucellosis, Q fever, hepatitis (especially hepatitis B), typhoid fever, tularemia, tuberculosis, dermatomycosis, vene zuelan equine encephalitis, psittacosis, and coc cidioidomycosis. However, laboratory-associated infections also have been caused by a wide vari ety of other pathogens. 162,492,493 More recently, viral agents have accounted for a larger propor tion of laboratory-associated infections than have bacterial agents. Laboratory personnel may acquire infection by aerosolization of specimens, mouth pipetting, or percutaneous injury. Information on the risks of laboratory-associated infections and appropriate biosafety procedures and precautions for labora tories have been published. 5,6,494,499,500 In addition to biosafety precautions, preventive measures (e.g., immunizations and postexposure prophylaxis) may also be indicated for laboratory personnel who handle infectious agents. In this document, disease-specific information and guid ance are provided for prevention of laboratoryassociated infections and for management of labo ratory personnel exposed to infectious agents. Health care institutions need to ensure that labo ratory personnel who may be exposed to infectious agents are well informed about the risks of acquir ing infections and about biosafety procedures to prevent transmission of infectious agents.
# H. EMERGENCY-RESPONSE PERSONNEL
Emergency medical technicians, firefighters, policemen, and others who attend to and trans port patients to the hospital may be exposed to recognized or undiagnosed transmissible infec tious diseases in the patients with whom they come in contact. Subtitle B (42 USC 300ff-80) of the 1990 Ryan White Comprehensive AIDS Resources Emergency Act requires the establish ment of notification systems in each state to ensure that emergency-response employees (including emergency medical technicians, fire fighters, and the like) are informed when they have been exposed to an emergency medical patient with an infectious, potentially fatal disease such as HIV or meningococcemia. CDC published a list of diseases for which emergency-response employees must be informed of an exposure. 501
# I. LATEX HYPERSENSITIVITY
Since the introduction of universal precautions, the use of latex gloves has become commonplace in health care settings. 31,502 The increased use of latex gloves has been accompanied by increasing reports of allergic reactions to natural rubber latex among health care personnel. Natural rubber latex is a combination of heatand water-soluble proteins derived from the tree Hevea braziliensis. Reactions to latex gloves may be localized or systemic and include dermatitis, conjunctivitis, rhinitis, urticaria, angioedema, asthma, and anaphylaxis. Most local reac tions associated with latex glove use are not immunologically mediated and result from chem icals (e.g., thiurams, carbamates, mercaptoben zothiazole, phenylenediamine), accelerants or antioxidants added to gloves during manufactur ing. 502,507, It may be clinically difficult to dif ferentiate irritant reactions from allergic contact dermatitis reactions; both may be manifested by itching, dryness, erythema, bleeding, or scaling of the hands. Nevertheless, neither of the types of local reactions to latex gloves are good predictors of latex allergy 503,516 ; only a subset of health care personnel reporting glove-associated skin irrita tion will have immunoglobulin E (IgE) antibod ies specific for latex. 513, In contrast, systemic reactions to natural rub ber latex, including urticaria, are mediated by antilatex IgE antibodies 509,520,521 and may result CDC Personnel Health Guideline 325 from direct skin contact or from exposure to air borne latex allergen adsorbed to glove powder. Occupational asthma from latex is becoming increasingly recognized. 520, Asthmatic responses to latex may occur early (8 hours) after exposure. Local reactions (i.e., irritant or allergic contact dermatitis) to latex gloves account for most reported reactions among health care person nel. 503,506 The risk of progression from localized to systemic reactions is unknown.
Latex gloves may vary considerably in total protein content from brand to brand and from lot to lot within brands. 528,529 However, the total protein concentrations and allergenicity of latex gloves are not always directly correlated, 528 sug gesting that total protein concentrations are not necessarily a measure of the allergenic proper ties of latex gloves. Currently, the amount of latex allergen exposure required to produce sen sitization or to elicit reactions in previously sen sitized persons is unknown. The FDA has man dated labeling of all medical devices that contain natural rubber latex. 530 Another recognized contributor to latex sensiti zation and reactions is the powder or cornstarch used as a lubricant for gloves. Levels of extractable protein and allergen in a given glove have been shown to be correlated with the pres ence of powder. Also, investigators have demon strated that latex proteins adhere to the powder on gloves and that aerosolized latex protein-pow der particles can provoke allergic respiratory symptoms if inhaled by a latex-sensitive individ ual 531 ; similar adherence has not been detected with powdered vinyl gloves. In one study, person nel wearing powdered latex gloves had a signifi cantly higher rate of reaction than did workers who wore washed latex gloves, from which the powder had been removed (60% vs 28%); none of these workers had positive skin-test reactions to industrial or commercial cornstarch or powder. 504 Although many health care personnel or clini cians may implicate the powder or cornstarch on gloves as the cause of their reactions, documented reactions to cornstarch powder are rare.
# a. Prevalence and risk factors
In studies of health care personnel, the reported prevalence of IgE-mediated allergy to latex varies considerably, ranging from 2.9% to 17%. The broad range of prevalence rates reported likely represent differences in the personnel groups studied and the methods used for estimating sen sitization or allergy. 518,519,522,532,533 The prevalence detected in some studies also has been biased by enrollment or testing of only personnel with symptoms. 504,508 However, it is estimated that a minority of health care personnel seek medical evaluation or treatment for latex-allergic condi tions, even if they have symptoms. Thus, the true prevalence of these reactions among health care personnel is unknown.
The prevalence of sensitization to latex among health care personnel has been shown to vary by job category and by location within a facility. 506,533 In one study of 224 health care personnel, the overall prevalence of skin-prick reactivity to latex was 17% but ranged from 0% (0/17) among house keepers and clerical workers to 38% (5/13) among dental residents and assistants. 506 In another sur vey of 512 health care personnel, the prevalence among physicians (6.5%, 7/108) was greater than that among nurses (2.2%, 7/325) or other hospital personnel (1.3%, 1/79). Also, operating room per sonnel (6.2%, 9/145) were significantly more like ly to be sensitized than were personnel assigned to general wards or laboratories (1.6%, 6/367); oper ating room nurses had fourfold the prevalence of general ward nurses (5.6% vs 1.2%). 533 Measurable levels of latex aeroallergen have been detected in the breathing zones of operating room personnel and may vary as much as 100-fold, depending on the invasiveness of the procedure and frequency of glove changes. 534 Several factors have been linked with latex sen sitization among health care personnel, including the presence of other allergic conditions (e.g., asthma, eczema, hay fever), 503,516,518,519,522,532,533 nonwhite ethnicity, 519,532 elevated total IgE lev els, 519 allergy to cosmetic powders or foods, 535 years or status (full-time vs part-time) of employ ment, and frequency or duration of glove use. 503,516,522,533 Coexistent allergy to certain fruits (e.g., bananas, 536,537 avocados, 538,539 and chest nuts 540 ) also has been described in latex-allergic health care personnel.
Skin irritation and eczematous dermatitis 516,533 (conditions that may allow passage of latex pro teins through the skin) and use of other latex products (e.g., condoms, diaphragms) have not been consistently linked to latex sensitization in health care personnel.
# b. Diagnosis and identification
Diagnosis of latex allergy in personnel relies largely on a clinical history of symptoms elicited by exposure to latex products (e.g., balloons, gloves). Clinical symptoms, such as urticaria, may be good predictors of IgE-medicated allergy. 516,519 AJIC June 1998 A variety of methods have been used to aid in the identification of latex-allergic persons; most are experimental and have not been approved for clinical use. Skin-prick testing may be the most sensitive method for diagnosis of IgE-mediated allergy, but no standardized FDA-approved anti gen is currently available in the United States for detection of latex-specific IgE antibodies. Moreover, the use of some skin-test reagents in highly sensitized persons has been associated with adverse outcomes, 541 suggesting that these nonstandardized reagents may not be safe for rou tine use. In Europe, where a standardized testing antigen has been developed, skin-prick testing has been used successfully.
FDA-approved immunoassays are available for detection of latex-specific IgE antibodies in blood. The FDA has recommended that these assays be used as confirmatory tests, rather than screening tests, for persons in whom latex allergy is sus pected on the basis of clinical history and find ings. Levels of detectable antibody appear to be associated with symptoms, 504,519 but, as with other allergens, the correlation between serum concen trations of latex-specific IgE antibodies and symp tom severity may not be predictable. 312,504,516
# c. Prevention strategies
Avoiding latex products remains the cornerstone of preventing sensitization (primary prevention) and reactions (secondary prevention) to natural rubber latex products. Proposed strategies to reduce the risk of reactions to natural rubber latex have included the use of the following: (a) nonla tex (e.g., vinyl) products alone or in combination with latex gloves, (b) powder-free latex gloves, (c) powdered latex gloves washed to remove powder, and (d) "low-protein" latex gloves. However, none of these interventions has been prospectively stud ied in controlled trials to assess cost-effectiveness or efficacy in preventing sensitization or reactions.
Because latex proteins can be aerosolized when powdered gloves are donned or removed, systemic symptoms caused by latex aeroallergens may not be alleviated by simply avoiding latex products, particularly if coworkers of the affected worker continue to use powdered latex gloves. Although the risk of a worker's exposure is greatest when gloves are donned or removed, allergenic proteins also may settle on environmental surfaces, surgi cal gowns, or other clothing and become resus pended. The use of powder-free or low-protein gloves appears more effective and less costly than either laminar-flow or high-efficiency particulate air-filtered glove-changing stations in reducing latex aeroallergens. 534 For personnel with sys temic manifestations of latex allergy, workplace restriction or reassignment may be necessary.
# J. THE AMERICANS WITH DISABILITIES ACT
The Americans With Disabilities Act provides guidelines for hiring and placing employees with disabilities, as defined in the Act. In general, employers must assess applicants for their qualifications to perform the tasks inher ent to the job for which the employee is being considered. Applicants may be asked about their ability to perform specific job functions but may not be asked about the existence, nature, or severity of a disability. Employers must make a "reasonable accommodation" to allow an indi vidual to perform the essential functions of a job, unless the employer can prove that this would create undue hardship because of signifi cant difficulty or expense.
The provisions of the Americans With Disabilities Act need to be incorporated into infec-CDC Personnel Health Guideline 327 tion control policies for health care personnel. For example, applicants with a communicable disease spread by aerosol could justifiably be denied employment (until they are no longer infectious) because they could pose a direct threat to others. On the other hand, applicants who are immuno compromised may not necessarily be excluded because of an increased risk for acquiring an infection in the hospital if the employer can make reasonable accommodations that prevent expo sure. Health care personnel who are known to be immunocompromised need to be referred to per sonnel health professionals who can individually counsel the employees on their risk for infection. At the request of the immunocompromised health care personnel, employers should offer but not compel a work setting in which health care per sonnel would have the lowest possible risk for occupational exposure to infectious agents. Evaluation of individual situations also needs to include consideration of the provisions of other applicable federal, state, and local laws.
# A. INTRODUCTION
In this document, the term health care personnel refers to all paid and unpaid persons working in health care settings who have the potential for exposure to infectious materials including body substances, contaminated medical supplies and equipment, contaminated environmental sur faces, or contaminated air. These personnel may include but are not limited to physicians, nurses, technicians, therapists, pharmacists, nursing assistants, laboratory personnel, autopsy person nel, emergency medical service personnel, dental personnel, students and trainees, contractual staff not employed by the health care facility, and per sons not directly involved in patient care but potentially exposed to infectious agents (e.g., vol unteer, dietary, housekeeping, maintenance, and clerical personnel).
As in previous CDC guidelines, each recommen dation is categorized on the basis of existing sci entific data, theoretic rationale, applicability, and potential economic impact. The system for cate gorizing recommendations is as follows:
Category IA Strongly recommended for all hospitals and strongly supported by well-designed experimental or epidemiologic studies.
# Category IB
Strongly recommended for all hospitals and reviewed as effective by experts in the field and a consensus of Hospital Infection Control Practices Advisory Committee members on the basis of strong rationale and suggestive evi dence, even though definitive scientific studies have not been done.
# Category II
Suggested for implementation in many hospi tals. Recommendations may be supported by sug gestive clinical or epidemiologic studies, a strong theoretic rationale, or definitive studies applica ble to some but not all hospitals.
# No recommendation; unresolved issue
Practices for which insufficient evidence or consensus regarding efficacy exists. 8,9 (b) well informed about indications, storage, dosage, preparation, side effects, and contraindications for each of the vaccines, toxoids, and immune globu lins used, 8,9,24 and (c) kept updated on nation al and local recommendations regarding vac cination of health care personnel (Tables 1 and 2). Category IB 3. Ensure that immunization product informa tion is available at all times and that a perti nent health history, especially a history of allergy and potential vaccine contraindica tions, is obtained from each person before an agent is given (Table 2). Category IB 4. Develop a list of needed immunizations for each employee during screening and an indi vidual plan to provide the necessary vac cines. Category IB 5. In the absence of a known occupational exposure, provide personnel with on-site immunizations or refer personnel to their own health care providers for routine non-occupation-related immunizations against diphtheria, pneumococcal disease, hepatitis A, or tetanus (Table 1). Category IB 6. Provide vaccine to personnel who may have occupational exposure to uncommon dis-
# Bloodborne pathogens, general recommen dation
Ensure that health care personnel are famil iar with precautions to prevent occupational transmission of bloodborne pathogens. 3,6,30,31,39 Category IA Follow state and federal guidelines and strategies for determining the need for work restrictions for health care personnel infected with bloodborne pathogens. 48 1). 9 Category IA e. Administer rubella vaccine- in the postpar tum period to female personnel not known to be immune. Category IA f. Exclude susceptible personnel who are exposed to rubella from duty from the sev enth day after the first exposure through the 21st day after the last exposure (Table 3). 9 Category IB g. Exclude personnel who acquire rubella from duty until 7 days after the beginning of the rash (Table 3 3). 369 371,374 Category IB b. Do not routinely exclude personnel with sus pected or confirmed carriage of group A Streptococcus from patient care or food han dling unless it is shown epidemiologically that they are responsible for disseminating the organism in the health care setting (Table 3). 369,373,378 1) Exclude personnel with infectious pul monary or laryngeal TB from the workplace until the facility has documentation from their health care provider that they are receiving adequate therapy, their coughs have resolved, and that they have had three consecutive sputum smears collected on dif ferent days with negative results for AFB. After personnel return to work, obtain peri odic documentation from their health care provider that effective drug therapy has been maintained for the recommended peri od and that sputum smear results remain negative for AFB ( 1). 9,18 Category IB b. Consider administering vaccinia vaccine to personnel who provide clinical care to recip ients of recombinant vaccinia virus vaccines (Table 1). 9,18 Category II c. Do not administer vaccinia vaccine to pregnant personnel or personnel with immunosuppres sion or eczema (Tables 1 and 2). Category IB d. Do not exclude from duty personnel who receive the vaccine, if they keep the vaccina tion site covered and adhere to handwashing practices. 18 Category IB
# Varicella
a. Administer varicella vaccine to susceptible personnel, especially those that will have contact with patients at high risk for serious complications (Table 1). 9,13 Category IA b. Do not perform serologic screening of per sons with negative or uncertain history of varicella before administering varicella vac cine to personnel, unless the institution con siders it cost-effective. 9,13 Category IB c. Do not routinely perform postvaccination testing of personnel for antibodies to vari cella. 9 Category IB d. NO RECOMMENDATION for administering postexposure varicella vaccination for the protection of exposed, susceptible person nel. 9 UNRESOLVED ISSUE e. Develop guidelines for managing health care personnel who receive varicella vaccine; for example, consider precautions for personnel who acquire a rash after receipt of varicella vac cine and for other health care personnel who June 1998 receive varicella vaccine and will have contact with susceptible persons at high risk for serious complications from varicella. 9 Category IB f. Develop written guidelines for postexposure management of vaccinated or susceptible personnel who are exposed to wild-type vari cella. 9 Category IB g. Exclude personnel from work who have onset of varicella until all lesions have dried and crusted (Table 3). 3 Category IB h. Exclude from duty after exposure to varicella personnel who are not known to be immune to varicella (by history or serology), begin ning on the tenth day after the first exposure until the 21st day after the last exposure (28th day if VZIG was given; Table 3). 9 Category IB i. Restrict immunocompetent personnel with localized zoster from the care of high-risk patients until lesions are crusted; allow them to care for other patients with lesions cov ered. 9 Category IB j. Restrict immunocompromised personnel with zoster from contact with patients until their lesions are crusted (Table 3). 9 Category IB k. Restrict susceptible personnel exposed to zoster from patient contact from the tenth day after the first exposure through the 21st day after the last exposure (28th day if VZIG was given; Table 3). 9 Category IB l. Perform serologic screening for immunity to varicella on exposed personnel who have not had varicella or are unvaccinated against varicella. 9,13 Category IB m. Consider performing serologic screening for immunity to varicella on exposed, vacci nated personnel whose antibody status is not known. If the initial test result is negative, retest 5 to 6 days after exposure to determine whether an immune response occurred. Category IB n. Consider excluding vaccinated personnel from work beginning on the 10th day after the first exposure through the 21st day after the last exposure if they do not have detectable antibodies to varicella, or screen daily for symptoms of varicella (Table 3). 9 Category IB o. Do not routinely give VZIG to exposed sus ceptible personnel, unless immunosup pressed, HIV infected, or pregnant. If VZIG is given, exclude personnel from duty from the 10th day after the first exposure through the 28th day after the last exposure (Tables 1 and 3). 9,13 Category IB
# Viral respiratory infections
a. Administer influenza vaccine annually to all personnel, including pregnant women, before the influenza season, unless otherwise contraindicated (Table 1). 9,17 Category IB b. Consider the use of antiviral postexposure prophylaxis for unvaccinated health care per sonnel during institutional or community outbreaks of influenza for the duration of influenza activity, or consider giving vaccine to unvaccinated personnel and providing them with antiviral postexposure prophylaxis for 2 weeks after vaccination (Table 1). 3,17,459 Category IB c. Consider excluding personnel with acute febrile respiratory infections or with lab oratory evidence of epidemiologically significant viruses from the care of highrisk patients (e.g., neonates, young infants, patients with chronic obstructive lung disease, and immunocompromised patients) during community outbreaks of influenza or RSV infections (Table 3). 3
# Category IB
# H. SPECIAL ISSUES
1. Pregnancy a. Counsel pregnant women and women of childbearing age regarding the risk of transmission of particular infectious dis eases (e.g., CMV, hepatitis, herpes simplex, HIV, parvovirus, rubella) that, if acquired during pregnancy, may have adverse effects on the fetus, whether the infection is acquired in nonoccupational or occupa tional environments. Provide such women with information on standard and transmission-based precautions appropriate for each infection (Table 6). 3, Category IB b. Do not routinely exclude women only on the basis of their pregnancy or intent to be pregnant from the care of patients with particular infections that have potential to harm the fetus (e.g., CMV, HIV, hepatitis, herpes simplex, parvovirus, rubella, and varicella; Table 6). Category IB a. Develop an institutional protocol for (1) evaluating and managing personnel with suspected or known latex allergy, (2) establishing surveillance for latex reac tions within the facility, (3) purchasing gloves, and (4) measuring the impact of preventive measures. Educational materi als and activities should be provided to inform personnel about appropriate glove use and the manifestations and potential risk of latex allergy. 31,546 Category IB b. Glove purchasers should review information on the barrier effectiveness of gloves and consider worker acceptance (e.g., comfort and fit) when selecting gloves for use in the health care organization. 31, Category IB c. To facilitate the appropriate selection of gloves, the occupational health service should maintain a list of all gloves used the institution according to whether they do or do not contain latex. Category II d. Evaluate personnel with symptoms sugges tive of latex allergy (e.g., localized dermati tis and workplace-related asthma). 522 Use serologic tests only for those who, on the basis of this evaluation, have suspected latex allergy. 504,516 Category IB e. Avoid the use of all latex products by per sonnel with a history of systemic reactions to latex. 520, Category IB f. Use nonlatex gloves for personnel with localized reactions to latex. 502,507, Category IB The opinions of all the reviewers might not be reflected in all the rec ommendations contained in this document. | # II. Recommendations for prevention of infections in health care
3
. Summary of suggested work restrictions for health care personnel exposed to or infected with infectious diseases of importance in health care settings, in the absence of state and local regulations 299 Table 4. Recommendation for postexposure prophylaxis for percutaneous or permucosal exposure to hepatitis B virus, United States 303 Table 5. Selected reported etiologic agents causing community or nosocomially acquired gastrointestinal 307 infections in developed countries Table 6. Pregnant health care personnel: Pertinent facts to guide management of occupational exposures to 322 infectious agents Appendix A. Recommended readings for infection control in health care personnel 354
Part I. Infection control issues for health care personnel: An overview
# A. EXECUTIVE SUMMARY
This guideline updates and replaces the previ ous edition of the Centers for Disease Control and Prevention (CDC) "Guideline for Infection Control in Hospital Personnel," published in 1983. The revised guideline, designed to provide methods for reducing the transmission of infections from patients to health care personnel and from per sonnel to patients, also provides an overview of the evidence for recommendations considered prudent by consensus of the Hospital Infection Control Practices Advisory Committee members. A working draft of this guideline was also reviewed by experts in infection control, occupa tional health, and infectious diseases; however, all recommendations contained in the guideline may not reflect the opinion of all reviewers.
This document focuses on the epidemiology of and preventive strategies for infections known to be transmitted in health care settings and those for which there are adequate scientific data on which to base recommendations for prevention.
The prevention strategies addressed in this docu ment include immunizations for vaccine-pre ventable diseases, isolation precautions to pre vent exposures to infectious agents, management of health care personnel exposure to infected per sons, including postexposure prophylaxis, and work restrictions for exposed or infected health care personnel. In addition, because latex barri ers are frequently used to protect personnel against transmission of infectious agents, this guideline addresses issues related to latex hyper sensitivity and provides recommendations to pre vent sensitization and reactions among health care personnel.
# B. INTRODUCTION
In the United States, there are an estimated 8.8 million persons who work in health care profes sions and about 6 million persons work in more than 6000 hospitals. However, health care is increasingly being provided outside hospitals in facilities such as nursing homes, freestanding sur gical and outpatient centers, emergency care clin ics, and in patients' homes or during prehospital emergency care. Hospital-based personnel and personnel who provide health care outside hospi tals may acquire infections from or transmit infections to patients, other personnel, household members, or other community contacts. 1,2 In this document, the term health care person nel refers to all paid and unpaid persons work ing in health care settings who have the poten tial for exposure to infectious materials, includ ing body substances, contaminated medical supplies and equipment, contaminated environ mental surfaces, or contaminated air. These personnel may include but are not limited to emergency medical service personnel, dental personnel, laboratory personnel, autopsy per sonnel, nurses, nursing assistants, physicians, technicians, therapists, pharmacists, students and trainees, contractual staff not employed by the health care facility, and persons not directly involved in patient care but potentially exposed to infectious agents (e.g., clerical, dietary, housekeeping, maintenance, and volunteer per sonnel). In general, health care personnel in or outside hospitals who have contact with patients, body fluids, or specimens have a high er risk of acquiring or transmitting infections than do other health care personnel who have only brief casual contact with patients and their environment (e.g., beds, furniture, bathrooms, food trays, medical equipment).
# AJIC June 1998
Throughout this document, terms are used to describe routes of transmission of infections. These terms have been fully described in the "Guideline for Isolation Precautions in Hospitals." 3 They are summarized as follows: direct contact refers to body surface-to-body sur face contact and physical transfer of microorgan isms between a susceptible host and an infected or colonized person (e.g., while performing oral care or procedures); indirect contact refers to con tact of a susceptible host with a contaminated object (e.g., instruments, hands); droplet contact refers to conjunctival, nasal, or oral mucosa con tact with droplets containing microorganisms generated from an infected person (by coughing, sneezing, and talking, or during certain proce dures such as suctioning and bronchoscopy) that are propelled a short distance; airborne transmis sion refers to contact with droplet nuclei contain ing microorganisms that can remain suspended in the air for long periods or to contact with dust particles containing an infectious agent that can be widely disseminated by air currents; and, final ly, common vehicle transmission refers to contact with contaminated items such as food, water, medications, devices, and equipment.
In 1983 the CDC published the "Guideline for Infection Control in Hospital Personnel." 4 The document focused on the prevention of infec tions known to be transmitted to and from health care personnel. This revision of the guide line has been expanded to include (a) recom mendations for non-patient care personnel, both in and outside hospitals, (b) management of exposures, (c) prevention of transmission of infections in microbiologic and biomedical labo ratories, and, because of the common use of latex barriers to prevent infections, (d) preven tion of latex hypersensitivity reactions. As in the 1983 guideline, readers are frequently referred to the "Guideline for Isolation Precautions in Hospitals" 3 and other published guidelines and recommendations for precautions that health care personnel may use when caring for patients or handling patient equipment or specimens. 5,6
# C. INFECTION CONTROL OBJECTIVES FOR A PERSONNEL HEALTH SERVICE
The infection control objectives of the person nel health service should be an integral part of a health care organization's general program for infection control. The objectives usually include the following: (a) educating personnel about the principles of infection control and stressing indi vidual responsibility for infection control, (b) col laborating with the infection control department in monitoring and investigating potentially harm ful infectious exposures and outbreaks among personnel, (c) providing care to personnel for work-related illnesses or exposures, (d) identify ing work-related infection risks and instituting appropriate preventive measures, and (e) contain ing costs by preventing infectious diseases that result in absenteeism and disability. These objec tives cannot be met without the support of the health care organization's administration, med ical staff, and other health care personnel. Documents that provide more detailed informa tion regarding infection control issues for person nel health are listed in Appendix A.
# D. ELEMENTS OF A PERSONNEL HEALTH SERVICE FOR INFECTION CONTROL
Certain elements are necessary to attain the infection control goals of a personnel health ser vice: (a) coordination with other departments, (b) medical evaluations, (c) health and safety educa tion, (d) immunization programs, (e) manage ment of job-related illnesses and exposures to infectious diseases, including policies for work restrictions for infected or exposed personnel, (f) counseling services for personnel on infection risks related to employment or special conditions, and (g) maintenance and confidentiality of per sonnel health records.
The organization of a personnel health service may be influenced by the size of the institution, the number of personnel, and the services offered. To ensure that contractual personnel who are not paid by the health care facility receive appropriate personnel health services, contractual agreements with their employers should contain provisions consistent with the policies of the facility that uses those employees. Personnel with specialized training and qualifications in occupational health can facilitate the provision of effective services.
# Coordination with other departments
For infection control objectives to be achieved, the activities of the personnel health service must be coordinated with infection control and other appropriate departmental personnel. This coordi nation will help ensure adequate surveillance of infections in personnel and provision of preven tive services. Coordinating activities will also help to ensure that investigations of exposures and out breaks are conducted efficiently and preventive measures implemented promptly.
CDC Personnel Health Guideline 293
# Medical evaluations
Medical evaluations before placement can ensure that personnel are not placed in jobs that would pose undue risk of infection to them, other personnel, patients, or visitors. An important com ponent of the placement evaluation is a health inventory. This usually includes determining immunization status and obtaining histories of any conditions that might predispose personnel to acquiring or transmitting communicable diseases. This information will assist in decisions about immunizations or postexposure management.
A physical examination, another component of the medical evaluation, can be used to screen personnel for conditions that might increase the risk of transmitting or acquiring work-relat ed diseases and can serve as a baseline for determining whether future diseases are work related. However, the cost-effectiveness of rou tine physical examinations, including laborato ry testing (such as complete blood cell counts, serologic tests for syphilis, urinalysis, and chest radiographs) and screening for enteric or other pathogens for infection control purposes, has not been demonstrated. Conversely, screening for some vaccine-preventable diseases, such as hepatitis B, measles, mumps, rubella, or vari cella, may be cost-effective. In general, the health inventory can be used to guide decisions regarding physical examinations or laboratory tests. However, some local public health ordi nances may mandate that certain screening procedures be used.
Periodic evaluations may be done as indicat ed for job reassignment, for ongoing programs (e.g., TB screening), or for evaluation of workrelated problems.
# Personnel health and safety education
Personnel are more likely to comply with an infection control program if they understand its rationale. Thus, personnel education is a cardinal element of an effective infection control program. Clearly written policies, guidelines, and proce dures ensure uniformity, efficiency, and effective coordination of activities. However, because the risk of infection varies by job category, infection control education should be modified accordingly. In addition, some personnel may need specialized education on infection risks related to their employment and on preventive measures that will reduce those risks. Furthermore, educational materials need to be appropriate in content and vocabulary to the educational level, literacy, and are also likely to be susceptible to rubella least 1 mo mentation of (a) receipt of (including HIV-infect and/or mumps; persons vaccinated later two doses of live vaccine on ed persons with between 1963 and 1967 with (a) a killed or after their 1st birthday, (b) severe immunosup measles vaccine alone, (b) killed vaccine physician-diagnosed pression) history of followed by live vaccine, or (c) a vaccine measles, or (c) laboratory anaphylactic reac of unknown type should be revaccinated evidence of immunity; vac tions after gelatin with two doses of live measles vaccine cine should be considered ingestion or receipt for all personnel, including of neomycin; or those born before 1957, who recent receipt of have no proof of immunity immune globulin Mumps live-One dose SC; Health care personnel Pregnancy; immuno-MMR is the vaccine of choice if recipients virus vaccine no booster believed to be susceptible compromised* state; are also likely to be susceptible to can be vaccinated; adults history of anaphylac measles and rubella born before 1957 can be tic reaction after considered immune gelatin ingestion or receipt of neomycin Rubella live-One dose SC; Health care personnel, both Pregnancy; immuno-Women pregnant when vaccinated or who virus vaccine no booster male and female, who lack compromised* state; become pregnant within 3 mo of vaccina documentation of receipt of history of anaphylac tion should be counseled on the theoretic live vaccine on or after their tic reaction after risks to the fetus, the risk of rubella vac 1st birthday, or of laboratory receipt of neomycin cine-associated malformations in these evidence of immunity; adults women is negligible; MMR is the vaccine born before 1957 can be of choice if recipients are also likely to be considered immune, except susceptible to measles or mumps women of childbearing age
# Immunization programs
Ensuring that personnel are immune to vac cine-preventable diseases is an essential part of successful personnel health programs. Optimal use of vaccines can prevent transmission of vac cine-preventable diseases and eliminate unneces sary work restriction. Prevention of illness through comprehensive personnel immunization programs is far more cost-effective than case management and outbreak control. Mandatory immunization programs, which include both newly hired and currently employed persons, are more effective than voluntary programs in ensur ing that susceptible persons are vaccinated. 7 National guidelines for immunization of and postexposure prophylaxis for health care person nel are provided by the U.S. Public Health Service's Advisory Committee on Immunization Practices (ACIP; Table 1). 8,9 ACIP guidelines also contain (a) detailed information on the epidemi ology of vaccine-preventable diseases, (b) data on the safety and efficacy of vaccines and immune globulin preparations, [8][9][10][11][12][13][14][15][16][17][18][19][20][21][22] and (c) recommenda tions for immunization of immunocompromised persons* (Table 2). 16,23 The recommendations in this guideline have been adapted from the ACIP recommendations. 9 In addition, individual states and professional organizations have regulations or recommendations on the vaccination of health care personnel. 24 Decisions about which vaccines to include in immunization programs have been made by con sidering (a) the likelihood of personnel exposure to vaccine-preventable diseases and the potential con sequences of not vaccinating personnel, (b) the nature of employment (type of contact with patients and their environment), and (c) the characteristics of the patient population within the health care organization. Immunization of personnel before they enter high-risk situations is the most efficient and effective use of vaccines in health care settings.
Screening tests are available to determine sus ceptibility to certain vaccine-preventable diseases *The term immunocompromised includes persons who are immunocompromised from immune deficiency diseases, HIV infection, leukemia, lymphoma, or generalized malig nancy, or immunosuppressed as a result of therapy with cor ticosteroids, alkylating drugs, antimetabolites, or radiation. (e.g., hepatitis B, measles, mumps, rubella, and varicella). Such screening programs need to be combined with tracking systems to ensure accu rate maintenance of personnel immunization records. Accurate immunization records ensure that susceptible personnel are promptly identified and appropriately vaccinated.
# CDC Personnel Health Guideline 297
# Management of job-related illnesses and exposures
Primary functions of the personnel health ser vice are to arrange for prompt diagnosis and man agement of job-related illnesses and to provide appropriate postexposure prophylaxis after jobrelated exposures.
It is the responsibility of the health care orga nization to implement measures to prevent fur ther transmission of infection, which some times warrants exclusion of personnel from work or patient contact. 25 Decisions on work restrictions are based on the mode of transmis sion and the epidemiology of the disease (Table 3). The term exclude from duty in this document should be interpreted as exclusion from the health care facility and from health care activi ties outside the facility. Personnel who are excluded should avoid contact with susceptible persons both in the facility and in the commu nity. Exclusion policies should include a state ment of authority defining who may exclude personnel. The policies also need to be designed to encourage personnel to report their illnesses or exposures and not to penalize them with loss of wages, benefits, or job status. Workers' com pensation laws do not cover exclusion from duty for exposures to infectious diseases; poli cies therefore should include a method for pro viding wages during the period that personnel are not able to work. In addition, exclusion policies must be enforceable and all personnel, especially department heads, supervisors, and nurse managers, should know which infections may warrant exclusion and where to report the illnesses 24 hours a day. Health care personnel who have contact with infectious patients out side of hospitals also need to be included in the postexposure program and encouraged to report any suspected or known exposures promptly. Notification of emergency-response personnel possibly exposed to selected infec tious disease is mandatory (1990 Ryan White Act, Subtitle B, 42 USC 300ff-80).
CDC Personnel Health Guideline 299
# Health counseling
Access to adequate health counseling for per sonnel is another crucial element of an effective personnel health service. Health counseling allows personnel to receive individually targeted information regarding (a) the risk and prevention of occupationally acquired infections, (b) the risk of illness or other adverse outcome after expo sures, (c) management of exposures, including the risks and benefits of postexposure prophylaxis regimens, and (d) the potential consequences of exposures or communicable diseases for family members, patients, or other personnel, both inside and outside the health care facility.
# Maintenance of records, data management, and confidentiality
Maintenance of records on medical evaluations, immunizations, exposures, postexposure prophy laxis, and screening tests in a retrievable, prefer ably computerized, database allows efficient mon itoring of the health status of personnel. Such record keeping also helps to ensure that the orga nization will provide consistent and appropriate services to health care personnel.
Individual records for all personnel should be maintained in accordance with the Occu pational Safety and Health Administration (OSHA) medical records standard, which requires the employer to retain records, main tain employee confidentiality, and provide records to employees when they ask to review them. 26 In addition, the 1991 OSHA "Occu pational Exposure to Bloodborne Pathogens; Final Rule" 27 requires employers, including health care facilities, to establish and maintain an accurate record for each employee with occu pational exposure to bloodborne pathogens. The standard also requires that each employer ensure that the employee medical records are (a) kept confidential, (b) not disclosed or report ed without the employee's express written con sent to any person within or outside the work place, except as required by law, and (c) main tained by the employer for at least the duration of the worker's employment plus 30 years.
OSHA's record keeping regulation also requires employers to record work-related injuries and ill nesses on the OSHA 200 log and the OSHA 101 form. The records include all occupational fatali ties, all occupational illnesses, and occupational injuries that result in loss of consciousness, restriction of work or motion, transfer to another job, or medical treatment beyond first aid. Infectious diseases are recordable if they are work related and result in illness. 28 More recently, OSHA developed policies that require the recording of positive tuberculin skintest results. 29 It would be beneficial to health care organizations and personnel if the principles of record keeping and confidentiality mandated by OSHA were to be expanded to other work-related exposures and incidents, immunizations, TB screening, and investigation and management of nosocomial outbreaks.
# E. EPIDEMIOLOGY AND CONTROL OF SELECTED INFECTIONS TRANSMITTED AMONG HEALTH CARE PERSONNEL AND PATIENTS
Almost any transmissible infection may occur in the community at large or within health care organizations and can affect both personnel and patients. Only those infectious diseases that occur frequently in the health care setting or are most important to personnel are discussed here.
# Bloodborne pathogens a. Overview
Assessment of the risk and prevention of trans mission of bloodborne pathogens, such as hepati tis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV), in health care settings are based on information from a variety of sources, including surveillance and investigation of suspected cases of transmission to health care personnel and patients, seropreva lence surveys of health care personnel and patients, and studies of the risk of seroconversion after exposure to blood or other body fluids from infected persons. In this document, the emphasis of the discussion of bloodborne pathogens will be on patient-to-personnel transmission.
The CDC has periodically issued and updated recommendations for prevention of transmission of bloodborne pathogens in health care settings; these provide detailed information and guid ance. [30][31][32][33][34][35][36][37][38][39][40] Also, in 1991 OSHA published a bloodborne pathogen standard that was based on the concept of universal precautions to prevent occu pational exposure to bloodborne pathogens. 27 The use of standard precautions (which incorporates universal precautions), including appropriate handwashing and barrier precautions, will reduce contact with blood and body fluids. 3,30,31,41 The use of engineering controls (e.g., safety devices) and changes in work practices (e.g., techniques to reduce handling of sharp instruments) can reduce the frequency of percutaneous injuries. 41,42 In set tings such as the operating room, changes in AJIC June 1998 instrument design and techniques for performing surgical procedures and modified personal barri ers have been shown to reduce blood contacts. 43,44 Despite adherence to standard precautions and implementation of some new techniques and devices, percutaneous injuries continue to occur. This is of concern because percutaneous injuries represent the greatest risk of transmission of bloodborne pathogens to health care personnel. 45 Only a few studies evaluating a limited number of safety devices have demonstrated a reduction in percutaneous injuries among health care work ers. 46,47 This document will not address the use of safety devices, because the Public Health Service is assessing the need for further guidance on selection, implementation, and evaluation of such devices in health care settings.
The risk posed to patients by health care per sonnel infected with bloodborne pathogens such as HBV and HIV has been the subject of much concern and debate. There are no data to indi cate that infected workers who do not perform invasive procedures pose a risk to patients. Consequently, work restrictions for these work ers are not appropriate. However, the extent to which infected workers who perform certain types of invasive procedures pose a risk to patients and the restrictions that should be imposed on these workers have been much more controversial. In 1991, CDC recommendations on this issue were published. 48 Subsequently, Congress mandated that each state implement the CDC guidelines or equivalent as a condition for continued federal public health funding to that state. Although all states have complied with this mandate, there is a fair degree of state-to state variation regarding specific provisions. Local or state public health officials should be contacted to determine the regulations or rec ommendations applicable in a given area. CDC is currently in the process of reviewing relevant data regarding health care personnel-to-patient transmission of bloodborne pathogens.
# b. Hepatitis B
Nosocomial transmission of HBV is a serious risk for health care personnel. [49][50][51][52][53] Approximately 1000 health care personnel were estimated to have become infected with HBV in 1994. This 90% decline since 1985 is attributable to the use of vaccine and adherence to other preventive mea sures (e.g., standard precautions). 54 During the past decade, an estimated 100 to 200 health care personnel annually have died of occupationally acquired HBV infection. 54 The risk of acquiring CDC Personnel Health Guideline 303 HBV infection from occupational exposure is dependent on the nature and frequency of expo sure to blood or to body fluids containing blood. 49,53 The risk of infection is at least 30% after a percutaneous exposure to blood from a hepatitis B e antigen-seropositive source. 54 HBV is transmitted by percutaneous or mucosal exposure to blood and serum-derived body fluids from persons who have either acute or chronic HBV infection. The incubation peri od is 45 to 180 days (average 60 to 90 days). Any person seropositive for hepatitis B surface anti gen (HBsAg) is potentially infectious.
Hepatitis B vaccination of health care personnel who have contact with blood and body fluids can prevent transmission of HBV and is strongly rec ommended. 9,10,40 The OSHA bloodborne pathogen standard mandates that hepatitis B vaccine be made available, at the employer's expense, to all health care personnel with occupational exposure to blood or other potentially infectious materials. 27 Provision of vaccine during training of health care professionals before such blood exposure occurs may both increase the vaccination rates among personnel and prevent infection among trainees, who are at increased risk for unintentional injuries while they are learning techniques.
Prevaccination serologic screening for suscepti bility to HBV infection is not indicated for per sons being vaccinated, unless the health care organization considers such screening to be costeffective. Postvaccination screening for antibody to HBsAg (anti-HBs) is advised for personnel at ongoing risk for blood exposure to determine whether response to vaccinations has occurred and to aid in determining the appropriate postex posure prophylaxis or the need for revaccination. Personnel who do not respond to or do not com plete the primary vaccination series should be revaccinated with a second three-dose vaccine series or evaluated to determine whether they are HBsAg seropositive. Revaccinated persons should be tested for anti-HBs at the completion of the second vaccine series. 9 If they do not respond, no further vaccination series should be given and they should be evaluated for the presence of HBsAg (possible chronic HBV infection). No spe cific work restrictions are recommended for nonresponders; in the event of percutaneous exposure to blood or body fluids, however, they should see their health care providers as soon as possible to evaluate the need for postexposure prophylaxis. Personnel in chronic dialysis centers who do not respond to vaccine need to be screened for HBsAg and anti-HBs every 6 months. 55 Vaccine-induced antibodies decline gradually with time, and as many as 60% of those who ini tially respond to vaccination will lose detectable anti-HBs by 8 years. 56 Booster doses of vaccine are not routinely recommended, because per sons who respond to the initial vaccine series remain protected against clinical hepatitis and chronic infection even when their anti-HBs lev els become low or undetectable. 57 The need for postexposure prophylaxis, vacci nation, or both depends on the HBsAg status of the source of the exposure as well as the immu nization status of the person exposed (Table 4). 40 Vaccine should be offered after any exposure in an unvaccinated person; if the source is known to be HBsAg seropositive, hepatitis B immune glob ulin (HBIG) should be given, preferably within 24 hours. The effectiveness of HBIG given later than 7 days after HBV exposure is unknown. 8,10,40 If the source is HBsAg seropositive and the exposed person is known not to have responded to a threedose vaccine series, a single dose of HBIG and a dose of hepatitis B vaccine need to be given as soon as possible after the exposure with subse quent vaccine doses given at 1 month and 6 months after the initial dose. If the exposed per son is known not to have responded to a threedose vaccine series and to revaccination, two doses of HBIG need to be given, one dose as soon as possible after exposure and the second dose 1 month later.
# c. Hepatitis C
HCV is the etiologic agent in most cases of par enterally transmitted non-A, non-B hepatitis in the United States. 58,59 During the past decade, the annual number of newly acquired HCV infections has ranged from an estimated 180,000 in 1984 to an estimated 28,000 in 1995. Of these, an estimat ed 2% to 4% occurred among health care person nel who were occupationally exposed to blood. 59 A case-control study of patients with acute non-A, non-B hepatitis, conducted before the identification of HCV, showed a significant asso ciation between acquisition of disease and health care employment, specifically patient care or laboratory work. 60 Seroprevalence stud ies among hospital-based health care personnel have shown seroprevalence rates of antibody to HCV (anti-HCV) ranging from 1% to 2%. [61][62][63][64] In a study that assessed risk factors for infection in health care personnel, a history of accidental needlesticks was independently associated with anti-HCV seropositivity. 61 Several case reports have documented transmis sion of HCV infection from anti-HCV-seropositive patients to health care personnel as a result of accidental needlesticks or cuts with sharp instru ments. 65,66 In follow-up studies of health care per sonnel who sustained percutaneous exposures to blood from anti-HCV-seropositive patients, the rate of anti-HCV seroconversion averaged 1.8% (range 0% to 7%). [67][68][69][70] In a study in which HCV RNA polymerase chain reaction methods were used to measure HCV infection, the rate of HCV transmission was 10%. 70 The incubation period for hepatitis C is 6 to 7 weeks, and nearly all persons with acute infec-AJIC June 1998 tion will have chronic HCV infection occur with persistent viremia and the potential for trans mission of HCV to others.
Serologic assays to detect anti-HCV are com mercially available. The interpretation of anti-HCV test results is limited by several factors: (a) these assays will not detect anti-HCV in approxi mately 5% of persons infected with HCV; (b) these assays do not distinguish between acute, chronic, and past infection; (c) there may be a prolonged interval between the onset of acute illness with HCV and seroconversion; and (d) when the assays are used in populations with a low prevalence of HCV infection, commercial screening assays for anti-HCV yield a high proportion (as great as 50%) of false-positive results. 34,59 Although no true confirmatory test has been developed, supplemen tal tests for specificity are available and should be used to judge the validity of repeatedly reactive results by screening assays.
Although the value of immune globulin for postexposure prophylaxis after occupational exposure to HCV has been difficult to assess, [71][72][73] postexposure prophylaxis with immune globulin does not appear to be effective in preventing HCV infection. Current immune globulin preparations are manufactured from plasma that has been screened for HCV antibody; positive lots are excluded from use. An experimental study in chimpanzees found that administration 1 hour after exposure to HCV of immune globulin manu factured from anti-HCV-screened plasma did not prevent infection or disease. 74 Thus, available data do not support the use of immune globulin for postexposure prophylaxis against hepatitis C, and its use is not recommended. There is no informa tion regarding the use of antiviral agents, such as interferon alfa, in the postexposure setting, and such prophylaxis is not recommended. 37 Health care institutions should consider imple menting recommended policies and procedures for follow-up for HCV infection after percuta neous or mucosal exposures to blood. At a mini mum, such policies can include (1) baseline test ing of the source for anti-HCV, (2) baseline and follow-up testing (e.g., 6 months) for anti-HCV and alanine aminotransferase activity of the per son exposed to an anti-HCV seropositive source, (3) confirmation by supplemental anti-HCV test ing of all anti-HCV results reported as repeatedly active by enzyme immunoassay, (4) recommen dation against postexposure prophylaxis with immune globulin or antiviral agents (e.g., inter feron), and (5) education of health care personnel about the risk for and prevention of bloodborne infections, including HCV, in occupational set tings, with the information routinely updated to ensure accuracy. 37 Among health care personnel in the postexposure period, onset of HCV infec tion may be detected earlier by measuring HCV RNA with polymerase chain reaction rather than by measuring anti-HCV with enzyme immunoas say. However, polymerase chain reaction is not a licensed assay, and the accuracy of the results are highly variable. 37
# d. Human immunodeficiency virus
Nosocomial transmission of human immuno deficiency virus (HIV) infection from patients to health care personnel may occur after percuta neous or, infrequently, mucocutaneous exposure to blood or body fluids containing blood. According to prospective studies of health care personnel percutaneously exposed to HIV-infect ed blood, the average risk for HIV infection has been estimated to be 0.3%. 45,[75][76][77][78] A retrospective case-control study to identify risk factors for HIV seroconversion among health care personnel after a percutaneous exposure to HIV-infected blood found that they were more likely to become infected if they were exposed to a larger quantity of blood, represented in the study as (1) presence of visible blood on the device before injury, (2) a procedure that involved a needle placed directly in the patient's vein or artery, or (3) deep injury. 45 Transmission of HIV infection also was associat ed with injuries in which the source patient was terminally ill with AIDS; this may be attributable to the increased titer of HIV in blood that is known to accompany late stages of illness or pos sibly to other factors, such as the presence of syn cytia-inducing strains of HIV in these patients. In addition, the findings of this study suggested that the postexposure use of zidovudine may be pro tective for health care personnel. 45 Factors that determine health care personnel's risk of infection with HIV include the prevalence of infection among patients, the risk of infection transmission after an exposure, and the fre quency and nature of exposures. 79 Most person nel who acquire infection after percutaneous exposure have HIV antibody develop within 6 months of exposure. HIV-infected persons are likely to transmit virus from the time of early infection throughout life.
In 1990, CDC published guidelines for postex posure management of occupational exposure to HIV, 33 and provisional recommendations for postexposure chemoprophylaxis were published CDC Personnel Health Guideline 305 in 1996. 80 In 1998, both of these documents were updated and consolidated to reflect current sci entific knowledge on the efficacy of postexpo sure prophylaxis and the use of antiretroviral therapies. 81 The U.S. Public Health Service will periodically review scientific information on antiretroviral therapies and publish updated recommendations for their use as postexposure prophylaxis as necessary.
# Conjunctivitis
Although conjunctivitis can be caused by a vari ety of bacteria and viruses, adenovirus has been the primary cause of nosocomial outbreaks of conjunctivitis. Nosocomial outbreaks of conjunc tivitis caused by other pathogens are rare.
Adenoviruses, which can cause respiratory, ocular, genitourinary, and gastrointestinal infections, are a major cause of epidemic kera toconjunctivitis in the community and health care settings. Nosocomial outbreaks have pri marily occurred in eye clinics or offices but have also been reported in neonatal intensive care units and long-term care facilities. [82][83][84][85][86] Patients and health care personnel have acquired and transmitted epidemic keratocon junctivitis during these outbreaks. The incuba tion period ranges from 5 to 12 days, and shed ding of virus occurs from late in the incubation period to as long as 14 days after onset of dis ease. 83 Adenovirus survives for long periods on environmental surfaces; ophthalmologic instru ments and equipment can become contaminat ed and transmit infection. Contaminated hands are also a major source of person-to-person transmission of adenovirus, both from patients to health care personnel and from health care personnel to patients. Handwashing, glove use, and disinfection of instruments can prevent the transmission of adenovirus. 82,83 Infected personnel should not provide patient care for the duration of symptoms after onset of epidemic keratoconjunctivitis 82,83 or purulent con junctivitis caused by other pathogens.
# Cytomegalovirus
There are two principal reservoirs of cytomegalovirus (CMV) in health care institu tions: (a) infants and young children infected with CMV and (b) immunocompromised patients, such as those undergoing solid-organ or bone-marrow transplantation or those with AIDS. [87][88][89][90][91][92][93][94] However, personnel who provide care to such high-risk patients have a rate of primary CMV infection that is no higher than that among personnel without such patient contact (3% vs 2%). [95][96][97][98][99][100][101] In areas where there are patient populations with a high prevalence of CMV, seroprevalence studies and epidemiologic investigations have also demon strated that personnel who care for patients have no greater risk of acquiring CMV than do person nel who have no patient contact. 92,[95][96][97][98]100,[102][103][104][105][106][107] In addition, epidemiologic studies that included DNA testing of viral strains have demonstrated that personnel who acquired CMV infections while providing care to CMV-infected infants had not acquired their infections from the CMV-infect ed patients. 88,92,96,[108][109][110] CMV transmission appears to occur directly either through close, intimate contact with an excreter of CMV or through contact with contaminated secre tions or excretions, especially saliva or urine. 101,[111][112][113][114] Transmission by the hands of personnel or infected persons has also been suggested. 92,115 The incubation period for person-to-person transmission is not known. Although CMV can survive on environmen tal surfaces and other objects for short periods, 116 there is no evidence that the environment plays a role in the transmission of infection. 92 Because infection with CMV during pregnancy may have adverse effects on the fetus, women of childbearing age need to be counseled regarding the risks and prevention of transmission of CMV in both nonoccupational and occupational set tings. 117 Although most fetal infections follow pri mary maternal infection, fetal infection may fol low maternal reinfection or reactivation. 118,119 There are no studies that clearly indicate that seronegative personnel may be protected from infection by transfer to areas with less contact with patients likely to be reservoirs for CMV infec tion. 88,92,[95][96][97]102,105,106,119,120 Serologic or virologic screening programs to identify CMV-infected patients or seronegative female personnel of childbearing age are imprac tical and costly for the following reasons: (a) the virus can be intermittently shed, 121 and repeated screening tests may be needed to identify shed ders; (b) seropositivity for CMV does not offer complete protection against maternal reinfection or reactivation and subsequent fetal infec tion 118,119 ; and (c) no currently available vac cines [122][123][124][125] or prophylactic therapy 90,[126][127][128][129] can pro vide protection against primary infection.
Work restrictions for personnel who contract CMV illnesses are not necessary. The risk of transmission of CMV can be reduced by careful adherence to handwashing and standard precautions. 3,119,130 AJIC June 1998
# Diphtheria
Nosocomial transmission of diphtheria among patients and personnel has been reported. [131][132][133] Diphtheria is currently a rare disease in the United States. During 1980 through 1994, only 41 diphthe ria cases were reported 134 ; however, community out breaks of diphtheria have occurred in the past, 135 and clusters of infection may occur in communities where diphtheria was previously endemic. 136 In addition, diphtheria epidemics have been occurring since 1990 in the new independent states of the for mer Soviet Union [137][138][139] and in Thailand. 140 At least 20 imported cases of diphtheria have been reported in countries in Europe, 139,141 and two cases occurred in U.S. citizens visiting or working in the Russian Federation and Ukraine. 142 Health care personnel are not at substantially higher risk than the general adult population for acquiring diphtheria; however, there is a potential for sporadic or imported cases to require medical care in the United States.
Diphtheria, caused by Corynebacterium diphthe riae, is transmitted by contact with respiratory droplets or contact with skin lesions of infected patients. The incubation period is usually 2 to 5 days. Patients with diphtheria are usually infec tious for 2 weeks or less, but communicability can persist for several months. 143 Droplet precautions are recommended for patients with pharyngeal symptoms, and contact precautions are recom mended for patients with cutaneous lesions. Precautions need to be maintained until antibiotic therapy is completed and results of two cultures taken at least 24 hours apart are negative. 3 Limited serosurveys conducted since 1977 in the United States indicate that 22% to 62% of adults 18 to 39 years old may lack protective diphtheria antibody levels. [144][145][146][147][148] Prevention of diphtheria is best accomplished by maintaining high levels of diphtheria immunity among children and adults. 19,137,138 Immunization with tetanus and diphtheria toxoid (Td) is recommended every 10 years for all adults who have completed the pri mary immunization series (Table 1). 9,19 Health care personnel need to consider obtaining Td immu nization from their health care providers. 9 To determine whether health care personnel directly exposed to oral secretions of patients infected with toxigenic strains of C. diphtheriae are carriers, cultures of the nasopharynx may be obtained. Exposed personnel need to be evaluated for evidence of disease daily for 1 week. 149 Although the efficacy of antimicrobial prophylaxis in pre venting secondary disease has not been proved, prophylaxis with either a single intramuscular CDC Personnel Health Guideline 307 injection of benzathine penicillin (1.2 mouse units) or oral erythromycin (1 gm/day) for 7 days has been recommended. 19 Follow-up nasopharyngeal cultures for C. diphtheriae need to be obtained at least 2 weeks after antimicrobial therapy is com pleted. If the organism has not been eradicated, a 10-day course of erythromycin needs to be given. 149 In addition, previously immunized exposed per sonnel need to receive a dose of Td if they have not been vaccinated within the previous 5 years. 19 Exclusion from duty is indicated for personnel with C. diphtheriae infection or those determined to be asymptomatic carriers until antimicrobial ther apy is completed and nasopharyngeal culture results are negative.
# Gastrointestinal infections, acute
Gastrointestinal infections may be caused by a variety of agents, including bacteria, viruses, and protozoa. However, only a few agents have been documented in nosocomial transmission (Table 5). [150][151][152][153][154][155][156][157][158][159][160][161][162][163][164][165][166][167][168] Nosocomial transmission of agents that cause gastrointestinal infections usually results from contact with infected individuals, 150,161,163,169 from consumption of contaminated food, water, or other beverages, 150,166,169,170 or from exposure to contaminated objects or environmental sur faces. 152,153,171 Airborne transmission of small round-structured viruses (Norwalk-like viruses) has been postulated but not proved. 164,165,[172][173][174][175] Inadequate handwashing by health care person nel 176 and inadequate sterilization or disinfection of patient-care equipment and environmental sur faces increase the likelihood of transmission of agents that cause gastrointestinal infections. Generally, adherence to good personal hygiene by personnel before and after all contacts with patients or food and to either standard or contact precautions 3 will minimize the risk of transmit ting enteric pathogens. 167,177 Laboratory personnel who handle infectious materials also may be at risk for occupational acquisition of gastrointestinal infections, most commonly with Salmonella typhi. Although the incidence of laboratory-acquired S. typhi infec tion has decreased substantially since 1955, infections continue to occur among laboratory workers, particularly those performing profi ciency exercises or research tests. 151,162 Several typhoid vaccines are available for use in labo ratory workers who regularly work with cul tures or clinical materials containing S. typhi. 178 The oral live-attenuated Ty21a vaccine, the intramuscular Vi capsular polysaccharide vaccine, or the subcutaneous inactivated vac cine may be given (Table 1). 178 Booster doses of vaccine are required at 2-to 5-year intervals, depending on the preparation used. The liveattenuated Ty21a vaccine should not be used for immunocompromised persons, including those known to be infected with HIV. 178 Personnel who acquire an acute gastroin testinal illness (defined as vomiting, diarrhea, or both, with or without associated symptoms such as fever, nausea, and abdominal pain) are likely to have high concentrations of the infect ing agent in their feces (bacteria, viruses, and parasites) or vomitus (viruses and para sites). 165,179,180 It is important to determine the etiology of gastrointestinal illness in health care personnel who care for patients at high risk for severe disease (e.g., neonates, elderly persons, and immunocompromised patients). The initial evaluation of personnel with gas troenteritis needs to include a thorough history and determination of the need for specific lab oratory tests, such as stool or blood cultures, staining procedures, and serologic or antigenantibody tests. 162,171,181,182 After resolution of some acute bacterial gas trointestinal illnesses, some personnel may have persistent carriage of the infectious agent. Once the person has clinically recovered and is having formed stools, however, the risk of trans mission of enteric pathogens is minimized by adherence to standard precautions. 3,167 In addi tion, appropriate antimicrobial therapy may eradicate fecal carriage of Shigella 183 or Campylobacter. 184 In contrast, antimicrobial or antiparasitic therapy may not eliminate car riage of Salmonella 185 or Cryptosporidium. Moreover, antimicrobials may prolong excre tion of Salmonella 186 and lead to emergence of resistant strains. 187 However, transmission of Salmonella to patients from personnel who are asymptomatic carriers of Salmonella has not been well documented. 167 In general, antimicro bial therapy is not recommended, unless the person is at high risk for severe disease. 188 When antibiotics are given, stool cultures AJIC June 1998 should be obtained at least 48 hours after com pletion of antibiotic therapy.
Restriction from patient care and the patient's environment or from food handling is indicated for personnel with diarrhea or acute gastrointestinal symptoms, regardless of the causative agent. 3,171 Some local and state agen cies have regulations that require work exclu sion for health care personnel, food handlers, or both who have gastrointestinal infections caused by Salmonella or Shigella. These regula tions may require such personnel to be restrict ed from duty until results of at least two con secutive stool cultures obtained at least 24 hours apart are negative.
# Hepatitis A
Nosocomial hepatitis A occurs infrequently, and transmission to personnel usually occurs when the source patient has unrecognized hepatitis and is fecally incontinent or has diarrhea. [189][190][191][192][193][194][195][196][197][198] Other risk factors for hepatitis A virus (HAV) transmission to personnel include activities that increase the risk of fecal-oral contamination such as (a) eating or drinking in patient care areas, 189,191,193,199 (b) not washing hands after handling an infected infant, 191,199,200 and (c) sharing food, beverages, or cigarettes with patients, their families, or other staff members. 189,191 HAV is transmitted primarily by the fecal-oral route. It has not been reported to occur after inadvertent needlesticks or other contact with blood, but it has rarely been reported to be transmitted by transfusion of blood prod ucts. 193,201,202 The incubation period for HAV is 15 to 50 days. Fecal excretion of HAV is greatest during the incubation period of disease before the onset of jaundice. 203 Once disease is clini cally obvious, the risk of transmitting infection is decreased. However, some patients admitted to the hospital with HAV, particularly immuno compromised patients, may still be shedding virus because of prolonged or relapsing disease, and such patients are potentially infective. 190,203 Fecal shedding of HAV, formerly believed to continue only as long as 2 weeks after onset of dark urine, 203 has been shown to occur as late as 6 months after diagnosis of infection in prema ture infants. 189 Anicteric infection is typical in young children and infants. 204 Personnel can protect themselves and others from infection with HAV by adhering to stan dard precautions. 3 Food-borne transmission of hepatitis A is not discussed in this guideline, but it has occurred in health care settings. 205,206 Two inactivated hepatitis A vaccines are now available and provide long-term preexposure protection against clinical infection with greater than 94% efficacy. 204 Serologic surveys among health care personnel have not shown greater prevalence of HAV infection than in control populations 52,192,207,208 ; therefore, routine administration of vaccine in health care person nel is not recommended. Vaccine may be useful for personnel working or living in areas where HAV is highly endemic and is indicated for per sonnel who handle HAV-infected primates or are exposed to HAV in a research laboratory. The role of hepatitis A vaccine in controlling outbreaks has not been adequately investigat ed. 9 Immune globulin given within 2 weeks after an HAV exposure is more than 85% effec tive in preventing HAV infection 204 and may be advisable in some outbreak situations. 9,204 Restriction from patient care areas or food handling is indicated for personnel with HAV infection. They may return to regular duties 1 week after onset of illness. 9
# Herpes simplex
Nosocomial transmission of herpes simplex virus (HSV) is rare. Nosocomial transmission has been reported in nurseries [209][210][211] and intensive care units 212,213 where high-risk patients (e.g., neonates, patients with severe malnutrition, patients with severe burns or eczema, and immunocompromised patients) are located. Nosocomial transmission of HSV occurs primarily through contact either with primary or recurrent lesions or with virus-contain ing secretions, such as saliva, vaginal secretions, or amniotic fluid. 210,212,214 Exposed areas of skin are the most likely sites of nosocomial infection, par ticularly when minor cuts, abrasions, or other skin lesions are present. 213 The incubation period of HSV is 2 to 14 days. 215 The duration of viral shed ding has not been well defined. 216 Personnel may acquire a herpetic infection of the fingers (herpetic whitlow or paronychia) from exposure to contaminated oral secretions. 213,214 Such exposures are a distinct hazard for nurses, anesthesiologists, dentists, respiratory care per sonnel, and other personnel who have direct (usu ally hand) contact with either oral lesions or res piratory secretions from patients. 213 Less fre quently, personnel may acquire mucocutaneous infection on other body sites from contact with infectious body secretions. 217
# CDC Personnel Health Guideline 309
Personnel with active infection of the hands (her petic whitlow) can potentially transmit HSV infec tion to patients with whom they have contact. 214 Transmission of HSV from personnel with orofa cial HSV infection to patients has also been infre quently documented 209 ; however, the magnitude of this risk is unknown. 211,218 Although asymptomatic infected persons can shed the virus, they are less infectious than persons with active lesions. 216,219 Personnel can protect themselves from acquiring HSV by adhering to standard precau tions. 3 The risk of transmission of HSV from personnel with orofacial infections to patients can be reduced by handwashing before all patient care and by the use of appropriate bar riers, such as a mask or gauze dressing, to pre vent hand contact with the lesion.
Because personnel with orofacial lesions may touch their lesions and potentially transmit infec tions, they should be evaluated to determine their potential for transmitting herpes simplex to patients at high risk for serious disease (e.g., neonates, patients with severe malnutrition, patients with severe burns or eczema, and immunocompromised patients) and excluded from the care of such patients as indicated. The evaluation should consider the extent of the lesion and the severity of illness in the patient population that personnel will contact. Personnel with HSV infections of the fingers or hands can more easily transmit infection and therefore need to be excluded from patient care until their lesions have crusted. In addition, herpetic lesions may be secondarily infected by Staphylococcus and Streptococcus, and personnel with such infections should be evaluated to determine whether they need to be excluded from patient contact until the secondary infection has resolved. There have been no reports that person nel with genital HSV infections have transmitted HSV to patients; therefore, work restrictions for personnel with genital herpes are not indicated.
# Measles
Nosocomial transmission of measles virus (sporadic and epidemic) has been well described. [220][221][222][223][224][225][226][227][228][229] From 1985 through 1991, approx imately 3000 (4%) of all reported episodes of measles in the United States were probably acquired in a medical facility; of these, more than 700 (25%) occurred in health care personnel, many of whom were not vaccinated. 9 Data have suggested that health care personnel have a risk of measles 13-fold that of the general population. 9 Of the 2765 episodes of measles reported during 1992 through 1995, 385 (13.9%) occurred in health care settings. 221,230 Measles is transmitted both by large droplets during close contact between infected and sus ceptible persons and by the airborne route. 229,231 Measles is highly transmissible and frequently misdiagnosed during the prodromal stage. The incubation period for measles is 5 to 21 days. Immunocompetent persons with measles shed the virus from the nasopharynx, beginning with the prodrome until 3 to 4 days after rash onset; immunocompromised persons with measles may shed virus for extended periods. 232 Strategies to prevent nosocomial transmis sion of measles include (a) documentation of measles immunity in health care personnel, (b) prompt identification and isolation of persons with fever and rash, and (c) adherence to air borne precautions for suspected and proven cases of measles. 3 It is essential that all personnel have docu mentation of measles immunity, regardless of their length of employment or whether they are involved in patient care. Further, some states have regulations requiring measles immunity for health care personnel. Although persons born before 1957 are generally considered to be immune to measles, serologic studies indicate that 5% to 9% of health care personnel born immune. 9,233,234 before 1957 may not be Furthermore, during 1985 through 1989, 29% of all measles cases in U.S. health care person nel occurred in those born before 1957. 221 Consideration should be given to recommend ing a dose of measles-mumps-rubella trivalent vaccine (MMR) to personnel born before 1957 who are unvaccinated and who lack (a) a histo ry of previous measles disease, (b) documenta tion of receipt of one dose of live-measles vac cine, and (c) serologic evidence of measles immunity. 9 Health care personnel born during or after 1957 should be considered immune to measles when they have (a) documentation of physician-diagnosed measles, (b) documenta tion of two doses of live measles vaccine on or after their first birthday, or (c) serologic evi dence of measles immunity (persons with an "indeterminate" level of immunity on testing should be considered susceptible). Persons born between 1957 and 1984 who received childhood measles immunization were given only one dose of vaccine during infancy and may require a second dose of vaccine. 8
# AJIC
# June 1998
Serologic screening for measles immunity is not necessary before administration of measles vaccine, unless the medical facility considers it cost-effective or the person to be vaccinated requests it. [235][236][237][238] When serologic screening before vaccination is done, tracking systems are needed to ensure that those identified as susceptible are subsequently vaccinated in a timely manner. 237 During measles outbreaks, serologic screening before vaccination is not necessary. In outbreak situations, prompt administration of vaccine is necessary to halt disease transmission.
Work restrictions are necessary for personnel who acquire measles; they need to be excluded from duty for 7 days after the rash appears. Likewise, personnel not immune to measles need to be excluded from duty from 5 days after the first exposure to 21 days after the last exposure to measles.
# Meningococcal disease
Community-acquired meningococcal disease is typically caused by a variety of serogroups of Neisseria meningitidis; serogroups B and C cause 46% and 45% of the endemic cases, respectively. Serogroups A, Y, and W-135 account for nearly all the remaining endemic cases. 15 In contrast, epidem ic meningococcal disease has, since the early 1990s, been caused increasingly by serogroup C. 15,239,240 Nosocomial transmission of N. meningitidis is uncommon. In rare instances, when proper pre cautions were not used, N. meningitidis has been transmitted from patient to personnel, through contact with the respiratory secretions of patients with meningococcemia or meningo coccal meningitis, [241][242][243] or through handling laboratory specimens. 241 Lower respiratory tract infections caused by N. meningitidis may present a greater risk of transmission than either meningococcemia or meningitis, 243,244 especially if the patient has an active, produc tive cough. 244 The risk of personnel acquisition of meningococcal disease from casual contact (e.g., cleaning rooms or delivering food trays) appears to be negligible. 244 N. meningitidis infection is probably transmit ted by large droplets; the incubation period is from 2 to 10 days, and patients infected with N. meningitidis are rendered noninfectious by 24 hours of effective therapy. Personnel who care for patients with suspected N. meningitidis infection can decrease their risk of infection by adhering to droplet precautions. 3 Postexposure prophylaxis is advised for persons who have had intensive, unprotected contact (i.e., without wearing a mask) with infected patients (e.g., mouth-to-mouth resuscitation, endotracheal intubation, endotracheal tube management, or close examination of the oropharynx of patients). 15 Antimicrobial prophylaxis can eradi cate carriage of N. meningitidis and prevent infec tions in personnel who have unprotected exposure to patients with meningococcal infections. 245,246 Because secondary cases of N. meningitidis occur rapidly (within the first week) after expo sure to persons with meningococcal disease, 247 it is important to begin prophylactic therapy immediately after an intensive, unprotected exposure, often before results of antimicrobial testing are available. Prophylaxis administered later than 14 days after exposure is probably of limited or no value. 15 Rifampin (600 mg orally every 12 hours for 2 days) is effective in eradi cating nasopharyngeal carriage of N. meningi tidis. 245 Ciprofloxacin (500 mg orally) and ceftri axone (250 mg intramuscularly) in single-dose regimens are also effective in reducing nasopha ryngeal carriage of N. meningitidis and are rea sonable alternatives to the multidose rifampin regimen. 15,246 These antimicrobials may be useful when infections are caused by rifampin-resistant meningococci or rifampin is contraindicated. Rifampin and ciprofloxacin are not recommend ed for pregnant women. 15,106,248,249 The quadrivalent A,C,Y,W-135 polysaccharide vaccine has been used successfully to control community outbreaks caused by serogroup C, 15,239,240,248 but its use is not recommended for postexposure prophylaxis in health care settings. 15 However, preexposure vaccination may be consid ered for laboratory personnel who routinely han 15,241 dle soluble preparations of N. meningitidis.
Healthy persons may have nasopharyngeal car riage of N. meningitidis. 245,[250][251][252] Nosocomial trans mission from carriers to personnel has not been reported. In the absence of exposures to patients with N. meningitidis infection, personnel who are asymptomatic carriers need not be identified, treated, or removed from patient care activities. However, personnel with meningococcal infection need to be excluded from duty until 24 hours after the start of effective therapy.
# Mumps
Mumps transmission has occurred in hospi tals and long-term care facilities housing adoles cents and young adults. 253,254 Most cases of CDC Personnel Health Guideline 311 mumps in health care personnel have been com munity acquired.
Mumps is transmitted by contact with viruscontaining respiratory secretions, including sali va; the portals of entry are the nose and mouth. The incubation period varies from 12 to 25 days and is usually 16 to 18 days. The virus may be pre sent in saliva for 6 to 7 days before parotitis and may persist for as long as 9 days after onset of dis ease. Exposed personnel may be infectious for 12 to 25 days after their exposure, and many infected persons remain asymptomatic. 255 Droplet precau tions are recommended for patients with mumps; such precautions should be continued for 9 days after the onset of parotitis. 3 An effective vaccination program is the best approach to prevention of nosocomial mumps transmission. 12 Vaccination with mumps virus vac cine is recommended, unless otherwise con traindicated, for all those who are susceptible to mumps; 12,256 combined MMR is the vaccine of choice, 257 especially when the recipient also is like ly to be susceptible to measles, rubella, or both.
Personnel should be considered immune to mumps if they have (a) documentation of physi cian-diagnosed mumps, (b) documentation of receipt of one dose of live mumps vaccine on or after their first birthday, or (c) serologic evidence of immunity (individuals who have an "indeter minate" antibody level should be considered sus ceptible). 12 Most persons born before 1957 are likely to have been infected naturally and may be considered to be immune, even though they may not have had clinically recognized mumps. Outbreaks among highly vaccinated populations have occurred and have been attributed to pri mary vaccine failure. 258 Work restrictions are necessary for personnel who acquire mumps; such restrictions should be imposed for 9 days after the onset of parotitis. Likewise, susceptible personnel who are exposed to mumps need to be excluded from duty from the 12th day after the first exposure until the 26th day after the last exposure. 9,255
# Parvovirus
Human parvovirus B19 (B19) is the cause of erythema infectiosum (fifth disease), a common rash illness that is usually acquired in childhood. Immunocompetent persons infected with B19 may have an acute, self-limited arthropathy, with or without a rash or anemia of short duration. However, patients with preexisting anemia (e.g., patients with sickle-cell anemia or thalassemia) may have aplastic crisis occur. Immunodeficient patients (e.g., patients with leukemia or AIDS) may become chronically infected with B19 and have chronic anemia. 259,260 Transmission of B19 to health care personnel from infected patients appears to be rare but has been reported. [261][262][263][264][265] In two investigations of health care personnel exposures to B19, the rate of infec tion among exposed nurses was not higher than the rate among unexposed control subjects. 266,267 In another investigation of health care personnel exposed to a patient with undetected chronic B19 infection, none of the susceptible employees became infected. 268 Personnel have acquired infection while working in laboratories or during the care of patients with B19-associated sickle-cell aplastic crises. [263][264][265][269][270][271] B19 may be transmitted through contact with infected persons, fomites, or large droplets. 266,272,273 The incubation period is variable, depending on the clinical manifestation of disease, and ranges from 6 to 10 days. 260 The period of infectivity also varies, depending on the clinical presentation or stage of disease. Persons with erythema infectio sum are infectious before the appearance of the rash, those with infection and aplastic crises for as long as 7 days after onset of illness, and persons with chronic infection for years.
Pregnant personnel are at no greater risk of acquiring B19 infection than are nonpregnant per sonnel; however, if a pregnant woman does acquire B19 infection during the first half of pregnancy, the risk of fetal death (fetal hydrops, spontaneous abor tion, and stillbirth) is increased. 274,275 Because of the serious nature of the consequences for the fetus, female personnel of childbearing age need to be counseled regarding the risk of transmission of B19 and appropriate infection control precautions. 3 Isolation precautions are not indicated for most patients with erythema infectiosum because they are past their period of infectiousness at the time of clinical illness. 271,274 However, patients in aplas tic crisis from B19 or patients with chronic B19 infection may transmit the virus to susceptible health care personnel or other patients; therefore, patients with preexisting anemia who are admit ted to the hospital with febrile illness and tran sient aplastic crises should remain on droplet pre cautions for 7 days and patients with known or suspected chronic infection with B19 should be placed on droplet precautions on admission and for the duration of hospitalization. 3,263 Work restrictions are not necessary for personnel exposed to B19.
AJIC June 1998
# Pertussis
Nosocomial transmission of Bordetella pertus sis has involved both patients and personnel; nonimmunized children are at greatest risk. [276][277][278][279][280] Serologic studies of health care personnel indi cate that personnel may be exposed to and infected with pertussis much more frequently than indicated by the occurrence of recognized clinical illness. 277,279,281,282 In one such study, the level of pertussis agglutination antibodies was found to correlate with the degree of patient con tact; the prevalence of such antibody was highest in pediatric house staff (82%) and ward nurses (71%) and lowest in nurses with administrative responsibilities (35%). 277 Pertussis is highly contagious; secondary attack rates exceed 80% in susceptible household con tacts. [283][284][285] B. pertussis transmission occurs by con tact with respiratory secretions or large aerosol droplets from the respiratory tracts of infected per sons. The incubation period is usually 7 to 10 days. The period of communicability starts at the onset of the catarrhal stage and extends into the paroxysmal stage up to 3 weeks after onset of symptoms. Prevention of secondary transmission of pertussis is especially difficult during the early stages of the dis ease because pertussis is highly communicable in the catarrhal stage, when the symptoms are non specific and the diagnosis is uncertain.
During nosocomial pertussis outbreaks, the risk of acquiring infection among patients or personnel is often difficult to quantify because exposure is not easily determined. Furthermore, clinical symptoms in adults are less severe than in children and may not be recognized as pertussis. Pertussis should be considered for any person seeking treatment with an acute cough lasting at least 7 days, particularly if accompanied by paroxysms of coughing, inspira tory whoop, or posttussive vomiting. 280,281 Prevention of transmission of B. pertussis in health care settings involves (a) early diagnosis and treatment of patients with clinical infection, (b) implementation of droplet precautions for infectious patients, 3 (c) exclusion of infectious personnel from work, and (d) administration of postexposure prophylaxis to persons exposed to infectious patients. 279 Patients with suspected or confirmed pertussis who are admitted to the hos pital need to be placed on droplet precautions until they have clinical improvement and have received antimicrobial therapy for at least 5 days.
Vaccination of adolescents and adults with whole-cell B. pertussis vaccine is not recommend ed 19 because local and systemic reactions have been observed more frequently in these groups than in children. Acellular pertussis vaccine is immunogenic in adults and carries a lower risk of adverse events than does whole-cell vaccine. 280,286 However, the acellular vaccine has not been licensed for use in persons 7 years old or older. Because immunity among vaccine recipients wanes 5 to 10 years after the last vaccine dose (usually given at 4 to 6 years of age), personnel may play an important role in transmitting pertus sis to susceptible infants. However, additional studies are needed to assess whether booster doses of acellular vaccines are indicated for adults.
Postexposure prophylaxis is indicated for person nel exposed to pertussis; a 14-day course of either erythromycin (500 mg orally four times daily) or trimethoprim-sulfamethoxazole (one tablet twice daily) has been used for this purpose. The efficacy of such prophylaxis has not been well documented, but studies suggest that it may minimize transmis sion. 19,279,287,288 There are no data on the efficacy of newer macrolides (clarithromycin or azithromycin) for prophylaxis in persons exposed to pertussis.
Restriction from duty is indicated for personnel with pertussis from the beginning of the catarrhal stage through the third week after onset of parox ysms, or until 5 days after the start of effective antimicrobial therapy. Exposed personnel do not need to be excluded from duty.
# Poliomyelitis
The last cases of indigenously acquired wildvirus poliomyelitis occurred in the United States in 1979. 289 Since then, all cases of endemic poliomyelitis reported in the United States (5 to 10 endemic cases/year) have been related to the administration of oral polio vaccine (OPV). 21 Although the risk of transmission of poliovirus in the United States is very low, wild poliovirus may potentially be introduced into susceptible popula tions with low immunization levels.
Poliovirus is transmitted through contact with feces or urine of infected persons but can be spread by contact with respiratory secretions and, in rare instances, through items contami nated with feces. The incubation period for nonparalytic poliomyelitis is 3 to 6 days, but is usu ally 7 to 21 days for paralytic polio. 290 Com municability is greatest immediately before and after the onset of symptoms, when the virus is in the throat and excreted in high concentration in feces. The virus can be recovered from the throat for 1 week and from feces for several weeks to months after onset of symptoms.
# CDC Personnel Health Guideline 313
Vaccine-associated poliomyelitis may occur in the recipient (7 to 21 days after vaccine administration) or susceptible contacts of the vaccine recipient (20 to 29 days after vaccine administration). 289 Adults have a slightly increased risk of vaccine-associated para lytic poliomyelitis after receipt of OPV; therefore, inactivated poliovirus vaccine (IPV) should be used when adult immunization is warranted. 8,16,21 Also, because immunocompromised persons may be at greater risk for development of poliomyelitis after exposure to vaccine virus, IPV rather than OPV is rec ommended when vaccinating pregnant or immuno compromised personnel, or personnel who may have contact with immunocompromised patients. 8,16,21,290 Health care personnel who may have contact with patients excreting wild virus (e.g., imported poliomyelitis case) and laboratory personnel han dling specimens containing poliovirus or per forming cultures to amplify virus should receive a complete series of polio vaccine; if previously vac cinated, they may require a booster dose of either IPV or OPV. 8,21 For situations where immediate protection is necessary (e.g., an imported case of wild-virus poliomyelitis requiring care), addition al doses of OPV should be given to adults who have previously completed a polio vaccine series. 21
# Rabies
Human rabies cases occur primarily from exposure to rabid animals. Cases of human rabies have increased in the United States during the 1990s. 291 Laboratory and animal care personnel who are exposed to infected animals, their tis sues, and their excretions are at risk for the dis ease. Also, rabies transmission to laboratory per sonnel has been reported in vaccine production and research facilities after exposure to high titered infectious aerosols. 292,293 Theoretically, rabies may be transmitted to health care person nel from exposures (bite and nonbite) to saliva from infected patients, but no cases have been documented after these types of exposures. 294 It is also possible for rabies to be transmitted when other potentially infectious material (such as brain tissue) comes into contact with nonintact skin or mucous membranes. 22,294 Bites that pene trate the skin, especially bites to the face and hands, pose the greatest risk of transmission of rabies virus from animals to human beings. 22 The incubation period for rabies is usually 1 to 3 months, but longer periods have been reported. 295 Exposures to rabies can be minimized by adher ing to standard precautions when caring for per sons with suspected or confirmed rabies 3 and by using proper biosafety precautions in laborato ries. 5 Preexposure vaccination has been recom mended for all personnel who (a) work with rabies virus or infected animals or (b) engage in diagnostic, production, or research activities with rabies virus. 5,22 Consideration also may be given to providing preexposure vaccination to animal han dlers when research animals are obtained from the wild, rather than from a known supplier that breeds the animals.
Postexposure prophylaxis has been adminis tered to health care personnel after exposures to patients with rabies (Table 1), [295][296][297] but decisions regarding postexposure prophylaxis should be made on a case-by-case basis after discussion with public health authorities. 22
# Rubella
Nosocomial transmission of rubella has occurred from both male and female personnel to other susceptible personnel and patients, as well as from patients to susceptible personnel and other patients. [298][299][300][301][302][303][304][305] Rubella is transmitted by contact with nasopha ryngeal droplets from infected persons. The incu bation period is variable but may range from 12 to 23 days; most persons have the rash 14 to 16 days after exposure. The disease is most contagious when the rash is erupting, but virus may be shed from 1 week before to 5 to 7 days after the onset of the rash. 306 Rubella in adults is usually a mild disease, lasting only a few days; 30% to 50% of cases may be subclinical or inapparent.
Droplet precautions are used to prevent trans mission of rubella. Infants with congenital rubella may excrete virus for months to years; when caring for such patients, it is therefore advisable to use contact precautions for the first year of life, unless nasopharyngeal and urine culture results are nega tive for rubella virus after 3 months of age. 3 Ensuring immunity among all health care per sonnel (male and female) is the most effective way to eliminate nosocomial transmission of rubella. 8,9,14,256,307 Persons should be considered susceptible to rubella if they lack (a) documenta tion of one dose of live rubella vaccine on or after their first birthday and (b) laboratory evi dence of immunity (persons with indeterminate levels are considered susceptible). A history of previous rubella infection is unreliable and should not be considered indicative of immunity to rubella. Although birth before 1957 is general ly considered acceptable evidence of rubella immunity, a dose of MMR has been recommend-June 1998 ed for those health care personnel that do not have laboratory evidence of immunity. 9 In addi tion, birth before 1957 is not considered accept able evidence of rubella immunity for women of childbearing age; history of vaccination or labo ratory evidence of rubella immunity is particu larly important for women who may become pregnant. 9 Voluntary immunization programs are usually inadequate to ensure personnel pro tection. 7,308 Because many health departments mandate rubella immunity for health care per sonnel, personnel health programs should con sult with their local or state health departments before establishing policies for their facilities.
Serologic screening of personnel for immunity to rubella need not be done before vaccinating against rubella, unless the medical facility consid ers it cost-effective or the person getting vaccinat ed requests it. 7,[235][236][237] When serologic screening before vaccination is done, tracking systems are needed to ensure that those identified as suscepti ble are subsequently vaccinated in a timely man ner. 237 Likewise, during rubella outbreaks, sero logic screening is not necessary. Pregnant women who are already immune to rubella are not at increased risk for adverse advents. 309 However, for theoretic reasons, a risk to the fetus from admin istration of live-virus vaccines cannot be excluded. Women should be counseled to avoid pregnancy for 30 days after administration of MMR or other rubella-containing vaccines. Routine precautions for vaccinating postpubertal women include (a) asking whether they are or may be pregnant, (b) not vaccinating those who say they are or may be pregnant, and (c) vaccinating those who state they are not pregnant after the potential risk to the fetus has been explained. If a pregnant woman is vaccinated or a woman becomes pregnant within 3 months after vaccination, she should be coun seled about the theoretic basis of concern for the fetus, but MMR vaccination during pregnancy should not ordinarily be a reason to consider ter mination of pregnancy. Rubella-susceptible women who are not vaccinated because of preg nancy should be counseled about the importance of being vaccinated as soon as they are no longer pregnant. 9 MMR is the vaccine of choice for rubel la, especially when the recipient also is likely to be susceptible to measles, mumps, or both (Table 2).
Work restrictions are necessary for personnel who acquire rubella; ill personnel need to be excluded from duty for 5 days after the rash appears. Likewise, personnel susceptible to rubel la require exclusion from duty from the seventh day after the first exposure through the 21st day after the last exposure (Table 3).
# Scabies and pediculosis a. Scabies
Scabies is caused by infestation with the mite Sarcoptes scabiei. The conventional (typical) clini cal presentation of scabies includes intense pruri tus and cutaneous tracks, where mites have bur rowed into the skin. Crusted or "Norwegian" sca bies may develop among immunocompromised and elderly individuals in which their skin may become hyperkeratotic; pruritus may not be pre sent, which also makes diagnosis difficult. In con ventional scabies, 10 to 15 mites are present, whereas in crusted scabies, thousands of mites are harbored in the skin, increasing the potential for transmission. 310,311 Nosocomial outbreaks of scabies have occurred in a variety of health care settings, including intensive care units, 312 rehabilitation centers, 313 long-term care facilities, 314,315 hospital wards, 316 a dialysis unit, 317 and a health care laundry. 318 In recent years there has been an increase in the occurrence of crusted scabies among immunocompromised patients, particu larly persons with HIV, which has led to the transmission of scabies among personnel, patients, and their families. 310,[312][313][314][315][316][319][320][321] Nosocomial transmission of scabies occurs primarily through prolonged skin-to-skin con tact with an infested person who has conven tional scabies. 310,322 Shorter periods of skin-to skin contact with persons who have crusted sca bies may result in transmission of scabies. 323 Personnel have acquired scabies while perform ing patient care duties such as sponge bathing, lifting, or applying body lotions. 310,311,319,324 Transmission by casual contact, such as by hold ing hands, or through inanimate objects, such as infested bedding, clothes, or other fomites, has been reported infrequently. 317,318 The use of contact precautions when taking care of infested patients before application of scabicides can decrease the risk of transmission to personnel. 3,311 Routine cleaning of the environ ment of patients with typical scabies, especially bed linens and upholstered furniture, will aid in eliminating the mites. Additional environmental cleaning procedures may be warranted for crust ed scabies. 310,311,[325][326][327] Recommendations for treatment and control of scabies in health care institutions have been published previously. 310,311,[327][328][329][330][331] The recommend-
CDC Personnel Health Guideline 315
ed topical scabicides include permethrin cream (5%), crotamiton (10%), and lindane (1%) lotion; resistance to and adverse effects from lindane have been reported. 329 Single-dose oral iver mectin has recently been shown to be an effec tive therapy for scabies 323,330,332 but has not received Food and Drug Administration (FDA) approval for this purpose.
Most infested health care workers have typical scabies with low mite loads 333 ; a single correct application of a scabicide is adequate and imme diately decreases the risk of transmis sion. 25,[315][316][317]319,322,324,334 There are no controlled evaluations of the efficacy of prophylactic scabi cide therapy among health care personnel, and some experts recommend two applications of scabicide for all infested personnel. 311,315,321 If personnel continue to have symptoms after ini tial treatment, another application of scabicide may be needed. Persistent symptoms likely rep resent newly hatched mites rather than new infestation; however, pruritus after scabies infes tation and treatment may persist for as long as 2 weeks, even without infestation. 25 Patients with crusted scabies may require repeated treatments and should be observed for recurrence of the mite infestation. 310,311,314,326 Personnel who are exposed to scabies but lack signs of infestation do not usually require prophylactic treatment with scabicides. In outbreak situations where transmission continues to occur, prophylaxis may be warranted for both patients and exposed health care personnel. 311,313 Restrictions from patient care are indicated for personnel infested with scabies until after they receive initial treatment and have been medically evaluated and determined to be free of infestation. They should be advised to report for further eval uation if symptoms do not subside.
# b. Pediculosis
Pediculosis is caused by infestation with any of three species of lice: Pediculus humanus capitus (human head louse), Pediculus humanus corporis (human body louse), and Phthirus pubis (pubic or crab louse).
Head lice are transmitted by head-to-head con tact or by contact with infested fomites such as hats, combs, or brushes. Nosocomial transmis sion, although not common, has occurred. 310 Body lice are usually associated with poor hygiene and overcrowded conditions. Trans mission occurs by contact with the skin or cloth ing of an infested person. Nosocomial transmis sion is unlikely.
Pubic lice are primarily found in the pubic hair but can be found in the axilla, eyelashes, or eyebrows. Transmission occurs primarily through intimate physical or sexual contact. Transmission by fomites, such as toilet seats or bedding, is uncommon. Nosocomial transmis sion is very unlikely.
Recommendations for control of pediculosis have been published previously. 310,327,335 The drugs recommended for treatment include permethrin cream 1%, pyrethrins with piperonyl butoxide, 1%. 328-330,335 malathion 0.5%, and lindane Resistance to various drugs has been reported. Local health departments may have information about drugs that are effective in their areas. Health care personnel exposed to patients with pediculosis do not require treatment, unless they show evidence of infestation.
Restriction from patient care is indicated for personnel with pediculosis until after they receive initial treatment and are found to be free of adult and immature lice. If symptoms do not subside after initial treatment, they should be advised to report for further evaluation.
# Staphylococcus aureus infection and carriage
Staphylococcal infection and carriage occur fre quently in human beings. In hospitals, the most important sources of S. aureus are infected and colonized patients. Previously, methicillin-suscep tible (but penicillin-resistant) S. aureus accounted for most staphylococcal infections. In recent years, however, methicillin-resistant S. aureus has accounted for approximately 80% of all S. aureus isolates reported to the National Nosocomial Infections Surveillance System. 336,337 The epidemi ology of methicillin-resistant S. aureus does not appear to differ from that of methicillin-suscepti ble, penicillin-resistant S. aureus, except that out breaks of methicillin-resistant S. aureus tend to occur more frequently among elderly or immuno compromised patients or among patients with severe underlying conditions. 338,339 Nosocomial transmission of S. aureus occurs primarily by the hands of personnel, which can become contaminated by contact with the colo nized or infected body sites of patients. 339,340 Hospital personnel who are infected or colonized with S. aureus also can serve as reservoirs and dis seminators of S. aureus, [341][342][343][344] and infected dietary personnel have been implicated in staphylococcal food poisoning. 345 The role of contaminated envi ronmental surfaces in transmission of S. aureus AJIC June 1998 has rarely been well documented 346 and remains controversial, although heavy contamination of fomites may facilitate transmission to patients by hands of personnel. 339 The incubation period for S. aureus infections varies by type of disease. For food-borne illness it is 30 minutes to 6 hours, for bullous impetigo it is 1 to 10 days, for toxic shock syndrome it is usually 2 days, and for other types of infection it is variable. 347 Carriage of S. aureus is most common in the anterior nares, but other sites, such as the hands, axilla, perineum, nasopharynx, and oropharynx, may also be involved. 339 The frequency of nasal carriage of S. aureus among health care personnel ranges between 20% and 90%, but fewer than 10% of healthy nasal carriers disperse the organisms into the air. 342 Nasal carriers with upper respirato ry symptoms can disseminate the organism more effectively. 342 Carriage of S. aureus in the nares has been shown to correspond to hand carriage, 336 and persons with skin lesions caused by S. aureus are more likely than asymptomatic nasal carriers to disseminate the organism.
Culture surveys of personnel can detect carriers of S. aureus but do not indicate which carriers are likely to disseminate organisms. Thus, such sur veys are not cost-effective and may subject per sonnel with positive culture results to unneces sary treatment and removal from duty. A more reasonable approach is to conduct active surveil lance for nosocomial S. aureus infections. Culture surveys may be indicated if, after a thorough epi demiologic investigation, personnel are linked to infections. Such implicated personnel can then be removed from clinical duties until carriage has been eradicated. 339,341,[348][349][350] Several antimicrobial regimens have been used successfully to eradicate staphylococcal carriage in health care personnel. These regimens include orally administered antimicrobial agents (e.g., rifampin, clindamycin, or ciprofloxacin) alone or in combination with another oral (e.g., trimetho prim-sulfamethoxazole) or topical (mupirocin) antimicrobial. 349,[351][352][353][354][355][356][357][358][359][360][361][362][363] Resistant S. aureus strains have emerged after the use of these oral or topical antimicrobial agents for eradication of S. aureus colonization. 18,210,349,353,[364][365][366] Thus, antimicrobial treatment to eradicate carriage may be best if lim ited to personnel who are carriers epidemiological ly linked to disease transmission. Nosocomial transmission of S. aureus can be prevented by adherence to standard precautions and other forms of transmission-based precautions as needed. 3 Restriction from patient-care activities or food handling is indicated for personnel who have draining skin lesions that are infected with S. aureus until they have received appropriate thera py and the infection has resolved. No work restric tions are necessary for personnel who are colo nized with S. aureus, unless they have been epi demiologically implicated in S. aureus transmis sion within the facility.
# Streptococcus, group A infection
Group A Streptococcus (GAS) has been trans mitted from infected patients to health care per sonnel after contact with infected secretions, [367][368][369] and the infected personnel have subsequently acquired a variety of GAS-related illnesses (e.g., toxic shock-like syndrome, cellulitis, lymphangi tis, and pharyngitis). Health care personnel who were GAS carriers have infrequently been linked to sporadic outbreaks of surgical site, postpartum, or burn wound infections [370][371][372][373][374][375][376] and to food-borne transmission of GAS causing pharyngitis. 377 In these outbreaks, GAS carriage was documented in the pharynx, 369,372,378 the skin, 369,370 the rec tum, 369,375 and the female genital tract of the infected personnel. 369,374,379 The incubation period for GAS pharyngitis is 2 to 5 days, but for impetigo is 7 to 10 days. The incu bation period is variable for other GAS infections. 380 Culture surveys to detect GAS carriage among personnel are not warranted, unless personnel are epidemiologically linked to cases of nosocomial infection. 378 In instances where thorough epi demiologic investigation has implicated person nel in nosocomial transmission, cultures may be obtained from skin lesions, pharynx, rectum, and vagina; GAS isolates obtained from personnel and patients can be serotyped to determine strain relatedness. 373 Treatment of personnel carriers needs to be individually determined because (a) experience is limited regarding the treatment of personnel carriers implicated in GAS outbreaks and (b) carriage of the organism by personnel may be recurrent through long periods. [369][370][371]374 Contact is the major mode of transmission of GAS in these health care settings. Airborne transmis sion during outbreaks has been suggested by sev eral investigators, and some have demonstrated that exercising and changing of clothing can lead to airborne dissemination of GAS from rectal and vaginal carriage. 369,374,375,379 Nosocomial transmis sion of GAS to personnel can be prevented by adherence to standard precautions or other transmission-based precautions as needed. 3
# CDC Personnel Health Guideline 317
Restriction from patient care activities and food handling is indicated for personnel with GAS infec tions until 24 hours after they have received appro priate therapy. However, no work restrictions are necessary for personnel who are colonized with GAS, unless they have been epidemiologically linked to transmission of infection within the facility.
# Tuberculosis
Nosocomial transmission of tuberculosis (TB) is well documented, but such transmission in the United States is generally low. However, the risk may be increased in health care facilities located in communities with (a) high rates of HIV, (b) high numbers of persons from TB-endemic coun tries, and (c) communities with a high prevalence of TB infection. 381,382 In some areas in the United States, the incidence and prevalence of mul tidrug-resistant Mycobacterium tuberculosis (MDR-TB) have also increased, and nosocomial MDR-TB outbreaks have occurred. [383][384][385][386][387][388][389][390][391] The increased risk of occupational acquisition of TB by health care personnel has been reported for decades, and it dramatically decreased after the introduction of effective antituberculous drugs. 392,393 Skin-test conversion rates among health care personnel after routine skin testing have ranged from 0.11% to 10%. 394 Among health care personnel with known exposure to an infec tious patient with TB or involved in prolonged nosocomial outbreaks of TB, the skin-test conver sion rates have ranged from 18% to 55%. 383 385,388,389,393,395-401 Health care personnel with severely compromised immune systems, especial ly those infected with HIV 381,402 and including those with malignancies or receiving immuno suppressive therapy, are at high risk for develop ment of active disease after acquisition of tuber culous infection. It has been estimated that per sons infected with M. tuberculosis and coinfected with HIV have an 8% to 10% risk per year for development of active TB, whereas immunocom petent persons infected with TB have a 10% life time risk for active disease. 403 The transmission of TB in health care facilities has been primarily caused by incomplete imple mentation of recommended TB infection control measures. 396 In 1994, the CDC published detailed recommendations for the prevention of trans mission of TB in health care settings, "Guidelines for Preventing the Transmission of M. tuberculosis in Health Care Facilities, 1994." 382 A summary of the recommendations pertaining to personnel health follows.
# a. Strategies for prevention of transmission of TB
The risk of transmission of TB to or from per sonnel in a health care facility varies according to the type and size of the facility, the preva lence of TB in the community, the patient pop ulation served by the facility, the occupational group the person represents, the area of the facility where the person works, and the effec tiveness of the facility's TB control program. A detailed risk assessment is essential in identify ing the nature of TB control measures that are appropriate for a particular facility, as well as for specific areas and occupational groups within a facility. 382,404 A risk assessment should include the following: (a) review of the commu nity TB profile, (b) review of the number of patients with TB who were treated in each area of the facility, (c) review of the drug-suscepti bility patterns of TB isolates from patients treated in the facility, (d) an analysis of purified protein derivative (PPD) skin-test results of health care personnel by work area or occupa tional group, (e) an evaluation of infection con trol parameters, including isolation policies, laboratory diagnostic capabilities, and antitu berculous therapy regimens, (f) an observation al review of TB infection control practices, and (g) evaluation of the function and maintenance of environmental controls. 382 Transmission of TB can be minimized by developing and implementing an effective TB control program that is based on a hierarchy of controls: (a) administrative controls, (b) engi neering controls, and (c) personal respiratory protection. 382,384,386,393,396,404,405
# b. TB screening program
A TB screening program for personnel is an inte gral part of a health care facility's comprehensive TB control program. The screening program should be based on the facility-specific risk assess ment. It may be advisable to screen immunocom promised personnel every 6 months. 382 Baseline PPD testing of all personnel (including personnel with a history of bacille Calmette-Guérin [BCG] vaccination) during their preem ployment physical examination or their applica tion for hospital privileges will identify personnel who have been previously infected. For the base line testing, a two-step procedure for personnel without a PPD test in the past 12 months can be used to minimize the likelihood of confusing reac tivity from an old infection (boosting) with reac tivity from a recent infection (conversion). Decisions concerning the use of the two-step pro-AJIC June 1998 cedure for baseline testing in a particular facility should be based on the frequency of boosting in that facility. Criteria used for interpretation of a PPD-test reaction may vary depending on (a) the purpose (diagnostic or epidemiologic) of the test, (b) the prevalence of TB infection in the popula tion being tested, (c) the immune status of the host, and (d) any previous receipt of BCG immu nization. Detailed recommendations for perform ing and interpreting skin tests have been pub lished. 382,[406][407][408]
# c. Follow-up evaluation
The risk assessment will show which health care personnel have the potential for exposure to M. tuberculosis and determine how frequently they should receive PPD testing. At a minimum, annual PPD testing is indicated for personnel with the potential for exposure to TB.
It is also important to obtain an initial chest radiograph for personnel with positive PPD-test reactions, documented PPD-test conversions, or pulmonary symptoms suggestive of TB. There are no data to support the use of routine chest radiographic examinations for asymptomatic PPD-negative personnel. In addition, personnel who have positive PPD-test reactions but also received adequate preventive treatment do not need repeat chest films, unless they have pul monary symptoms suggestive of TB. Repeat chest radiographic examinations of such persons have not been shown to be beneficial or costeffective in monitoring persons for development of disease. However, more frequent monitoring for symptoms of TB may be considered for per sonnel who had recent conversion of their PPD test and those persons who, if infected, are at increased risk for development of active TB (e.g., HIV-infected or otherwise severely immunocom promised persons). 382 Routine anergy testing of HIV-seropositive individuals is limited in its use fulness; however, anergy testing may be useful in guiding individual decisions regarding preven tive therapy in selected situations. 408
# d. Management of personnel after exposure to TB
It is important to administer PPD tests to per sonnel as soon as possible after TB exposures are recognized. Such immediate PPD testing estab lishes a baseline with which subsequent PPD tests can be compared. A PPD test performed 12 weeks after the last exposure will indicate whether infection has occurred. Persons already known to have reactive PPD tests need not be retested. Personnel with evidence of new infec tion (i.e., PPD-test conversions) need to be evalu ated for active TB. If active TB is not diagnosed, preventive therapy should be considered. 382
# e. Preventive therapy
For workers with positive PPD-test results who were probably exposed to drug-susceptible TB, preventive therapy with isoniazid is indicated, unless there are contraindications to such thera py. 382,407 Alternative preventive regimens have been proposed for persons who have positive PPD-test results after exposure to drug-resistant TB. 409
# f. Work restrictions
Personnel with active pulmonary or laryngeal TB may be highly infectious; exclusion from duty is indicated until they are noninfectious. If personnel are excluded from duty because of active TB, the facility should have documentation from their health care providers that personnel are noninfec tious before they are allowed to return to duty. The documentation needs to include evidence that (a) adequate therapy is being received, (b) the cough has resolved, and (c) results of three consecutive sputum acid-fast bacilli (AFB) smears collected on different days are negative. After personnel resume duty and while they remain on anti-TB therapy, periodic documentation from their health care providers is needed to show that effective drug therapy is being maintained for the recommended period and that their sputum AFB smear results continue to be negative. If personnel discontinue their treatment, they need to be evaluated for active TB; directly observed therapy may be considered.
Work restrictions are not necessary for person nel receiving preventive treatment for latent TB (positive PPD-test result without active disease) or for personnel with latent TB who do not accept preventive therapy. However, these personnel should be instructed to seek evaluation promptly if symptoms suggestive of TB develop.
# g. Considerations for BCG vaccine
# BCG has not been routinely used in the United
States to protect health care personnel. Never theless, because of the resurgence of TB in the United States and new information about the pro tective effect of BCG, 410,411 the role of BCG vaccina tion in the prevention and control of TB in the coun try has been reevaluated. 412 The following is a sum mary of the joint statement by the Advisory Council for the Elimination of Tuberculosis and ACIP regarding the use of BCG in health care personnel.
Two recent metaanalyses of 18 410 and 26 411 BCG studies, respectively, indicate that the efficacy of BCG vaccine in preventing serious TB is high (>80%) in children and suggest 50% efficacy in adults. However, the protective efficacy of the vac-CDC Personnel Health Guideline 319 cine in adolescents and adults, including health care personnel and HIV-infected children and adults, has not been determined. 412 BCG vaccination should not be used as a pri mary TB control strategy because (a) the protec tive efficacy of the vaccine in health care person nel is uncertain and (b) even if vaccination is effective in an individual, other persons in the health care facility are not protected against pos sible exposure to and infection with drug-resistant strains of M. tuberculosis. However, BCG vaccina tion may be indicated for health care personnel in a few geographic areas where the prevalence of MDR-TB is high, transmission of TB is likely, and TB infection control measures have been imple mented but have not been successful in control ling nosocomial transmission. 412 Consultation with local and state health departments is advis able when determining whether to provide BCG vaccination to health care personnel.
BCG vaccination often results in local adverse effects (such as muscular soreness, erythema, purulent drainage, and axillary or cervical lym phadenopathy) for as long as 3 months after vacci nation; serious long-term complications (such as musculoskeletal lesions, multiple lymphadenitis, and disseminated BCG disease) are infrequent. [413][414][415] The safety of BCG vaccination in immunocompro mised populations (i.e., immunocompromised from immune deficiency diseases, HIV infection, leukemia, lymphoma, or generalized malignancy, or immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabolites, or radiation) has not been determined by adequate epidemiologic studies. However, because of the possibility of disseminated BCG infection in such persons, [416][417][418][419] BCG vaccination is not recommend ed for immunocompromised personnel. 412 The safety of BCG vaccination in pregnant women has also not been evaluated; therefore, it is not recom mended for pregnant personnel. 412 PPD testing is not contraindicated for persons who have received BCG vaccine and can be used to support or exclude the diagnosis of infection with M. tuberculosis. 412 PPD-test reactivity caused by BCG vaccination wanes with time [420][421][422] and is unlikely to persist longer than 10 years after vac cination in the absence of infection with M. tuber culosis. 420,421 After a person has been vaccinated with BCG, the presence or size of a PPD-test reac tion cannot be used to predict whether BCG will provide any protection against TB disease 423,424 or to determine whether the reaction is caused by M. tuberculosis infection or the previous BCG vaccination. 425 However, a BCG-vaccinated per son who has a PPD-test reaction of ≥ 10 mm induration should be considered infected with TB, especially if the vaccinee (a) is a contact of a person with infectious TB, particularly if the infectious person has transmitted M. tuberculosis to others, (b) is from a country with high preva lence of TB, or (c) is continually exposed to pop ulations in which the prevalence of TB is high. 412
# Vaccinia (smallpox)
Through aggressive surveillance for smallpox combined with the effective use of smallpox vac cine (vaccinia virus vaccine), the World Health Organization was able to declare the world free of smallpox in 1980. The smallpox vaccine licensed for use in the United States is derived from infec tious vaccinia virus. After vaccination, the virus can be cultured from the vaccination site until the scab has separated from the skin (2 to 21 days after vaccination); thus, susceptible persons may acquire vaccinia from a recently vaccinated per son. [426][427][428][429] Covering the vaccination site and wash ing hands after contact with the vaccination site (including bandages) will prevent transmission. Recently, recombinant vaccinia viruses have been engineered to express immunizing agents of sev eral viruses (e.g., herpesvirus, HBV, influenza). There is a theoretic risk that transmission could occur from contact with contaminated dressings or by contact with recombinant vaccine, but no such transmission has been reported among per sonnel who provide care to recipients of the recombinant vaccine. Infections also have been reported among laboratory personnel who handle viral cultures or materials contaminated with vac cinia or recombinant viruses. 18,162 Smallpox vaccination (every 10 years) is indicat ed for personnel who work directly with orthopox viruses (e.g., monkeypox, vaccinia, variola) or in animal care areas where orthopox viruses are stud ied. In selected instances, vaccination may be con sidered for personnel who provide care to recipients of recombinant vaccinia vaccine. 9,18 Personnel who receive the vaccine may continue to have contact with patients if the vaccination site is covered and handwashing is strictly observed. 18 Vaccine is not recommended for personnel with immunosuppres sion or eczema or for personnel who are pregnant.
# Varicella
Nosocomial transmission of varicella-zoster virus (VZV) is well recognized. [430][431][432][433][434][435][436][437][438][439][440][441] Sources for nosoco mial exposures have included patients, health care AJIC June 1998 personnel, and visitors (including the children of personnel) with either varicella or herpes zoster.
All susceptible adults in health care settings are at risk for varicella and its complications. During 1990 through 1994, fewer than 5% of varicella cases occurred among adults older than 20 years, but they accounted for 55% of varicella-related deaths. Certain persons are at higher risk for severe disease and secondary complications: preg nant women, premature infants born to varicellasusceptible mothers, infants born at less than 28 weeks' gestation or weighing ≤ 1000 gm (regard less of maternal immune status), and immuno compromised patients. 13 The incubation period for varicella is usually 14 to 16 days but may be from 10 to 21 days after exposure, although the incubation period may be shorter in immunocompromised persons. 442 In persons who receive postexposure VZV immune globulin, the incubation period may be as long as 28 days after exposure. Transmission of infection may occur from 2 days before onset of rash and usually as long as 5 days after rash onset. 442 VZV is transmitted by the contact with infect ed lesions and, in hospitals, airborne transmis sion has occurred from patients with varicella or zoster to susceptible persons who had no direct contact with the infected patient. [443][444][445][446][447] Adher ence to airborne and contact precautions when caring for patients with known or suspected VZV infection can reduce the risk of transmis sion to personnel. 3 It is generally advisable to allow only personnel who are immune to varicella to take care of patients with VZV. Because of the possibility of transmission to and development of severe illness in high-risk patients, personnel with localized zoster should not take care of such patients until all lesions are dry and crusted. 13,447 Personnel with localized zoster are not likely to transmit infection to immunocompetent patients if their lesions can be covered. However, some institutions may exclude personnel with zoster from work until their lesions dry and crust. 439
# a. Varicella screening and vaccination
Serologic tests have been used to assess the accuracy of reported histories of chicken pox. 440,[448][449][450] In adults, a history of varicella is highly predictive of serologic immunity (97% to 99% seropositive). Most adults who have negative or uncertain histories of varicella are also seropositive (71% to 93%). In health care institutions, serologic screening of personnel who have negative or uncertain histories is likely to be cost-effective, depending on the rel ative costs of the test and vaccine. 9,13 A variety of methods have been used for detect ing varicella antibody, but a commercially avail able latex agglutination test provides prompt, sen sitive, and specific serologic results at a reason able cost. The latex agglutination test may not detect low levels of protective antibody that can occur after vaccination; however, a test with increased sensitivity and specificity is currently under development. Routine testing for varicella immunity after vaccination is not necessary, because 99% of persons are seropositive after the second dose. Moreover, seroconversion does not always result in full protection against disease. However, testing vaccinees after exposures may be warranted. In addition, vaccinated persons who are exposed to varicella but lack antibody may be retested in 5 to 6 days to determine whether they are antibody seropositive after the second test and therefore unlikely to acquire varicella. 13 In March 1995, a live-attenuated varicella vac cine was licensed for use in the United States. Administration of varicella vaccine is recom mended for all susceptible health care person nel, especially those who will have close contact with persons at high risk for serious complica tions. 9,13,451,452 Effective varicella vaccination pro grams require two doses of vaccine to achieve high seroconversion rates in adults; 451 the need for and response to booster doses of vaccine are unknown. Vaccination provides approximately 70% protection against infection and 95% pro tection against severe disease in follow-up from 7 to 10 years after vaccination. 13 Cases of vari cella have occurred among vaccinees after expo sure to wild-type virus ("breakthrough infec tion"). Data from vaccine trials in which vacci nees of all ages were followed up for as long as 9 years indicate that 1% to 4% of vaccine recip ients per year acquire varicella, depending on the vaccine lot and interval after vaccination. 9,13 However, vaccinated persons have milder dis ease (e.g., afebrile, a mean of 50 skin lesions that are often not vesicular, and shorter duration of illness) than do unvaccinated individuals (e.g., febrile with several hundred vesicular lesions) 453,454 and are less likely to transmit dis ease than unvaccinated persons.
The rate of transmission of disease from vac cinees who contract varicella is low for vacci nated children but has not been studied in adults. Active surveillance for 1 to 8 years after vaccination of 2141 children between 1981 and CDC Personnel Health Guideline 321 1989 in 10 different trials 9 resulted in reports of breakthrough infections in 78 children, which further resulted in secondary cases in 12.2% (11/90) of vaccinated siblings. Illness was mild in both index and secondary cases. There also has been a report of transmission from a vacci nated child in whom breakthrough disease occurred to a susceptible mother. 9 All information currently available on vaccine efficacy and the persistence of antibody in vac cinees is based on research conducted in set tings where infection is highly prevalent and not affected by the wide use of vaccine. Thus, the extent to which the protection provided by vac cination has been increased by boosting from exposure to natural virus and whether longer term immunity may wane as the prevalence of natural VZV decreases are unknown.
# b. Transmission of vaccine virus
In clinical trials, 3.8% of children and 5.5% of adolescents and adults acquired a nonlocalized rash (median five lesions) after the first injection, and 0.9% of adolescents and adults acquired a nonlocalized rash after the second injection. Available data suggest that healthy children have limited potential to transmit vaccine virus to sus ceptible contacts (estimated to be <1%) but that the risk of transmission from immunocompro mised vaccinees is higher. 13,455,456 Tertiary trans mission of vaccine virus to a second healthy sib ling of a vaccinated leukemic child has also occurred. 456 These data suggest that healthy, vac cinated individuals have a very small risk of trans mitting vaccine virus to their contacts; this risk may be higher in those who acquire a varicellalike rash after vaccination.
Although the risk of transmission of vaccine virus from vaccinees is not known, the risk if any appears to be very low, and the benefits of vacci nating susceptible health care personnel clearly outweigh this potential risk. As a safeguard, insti tutions may wish to consider precautions for vac cinated personnel who acquire a rash or who will have contact with susceptible persons at high risk for serious complications.
# c. Management of health care personnel exposed to varicella
When unvaccinated susceptible personnel are exposed to varicella, they are potentially infec tious 10 to 21 days after exposure, and exclusion from duty is indicated from the tenth day after the first exposure through the 21st day after the last exposure, or until all lesions are dry and crusted if varicella occurs (Table 3). 256 June 1998 If vaccinated health care personnel are exposed to varicella, they may be serotested immediately after exposure to assess the presence of anti body. 452 If they are seronegative, they may be excluded from duty or monitored daily for devel opment of symptoms. Exclusion from duty is indi cated if symptoms (fever, upper respiratory tract symptoms, or rash) develop.
Vaccination should be considered for exposed unvaccinated health care personnel without docu mented immunity. 441,452 Because the efficacy of postexposure vaccination is unknown, however, persons vaccinated after an exposure should be managed as previously recommended for unvaccinated persons.
The routine postexposure use of VZV immune globulin (VZIG) is not recommended among immunocompetent health care personnel. 13 VZIG can be costly, does not necessarily prevent varicel la, and may prolong the incubation period by a week or more, thus extending the time that per sonnel will be restricted from duty. The use of VZIG may be considered for immunocompro mised (e.g., HIV infected) or pregnant health care personnel. 13,457 Postexposure use of acyclovir may be effective and less costly than the use of VZIG in some susceptible persons. 457 However, additional data concerning the efficacy of acyclovir for postexposure prophylaxis are needed before such use can be recommended. 9,13,441,458
# Viral respiratory infections
Viral respiratory infections are common prob lems in health care settings. Nosocomial respira tory infections can be caused by a number of viruses, including adenoviruses, influenza virus, parainfluenza viruses, respiratory syncytial virus (RSV), and rhinoviruses. Because influenza and RSV substantially contribute to the morbidity and mortality associated with viral pneumonia and both have been well studied epidemiologically, this section focuses on prevention of these two viral infections among personnel. Additional information on influenza and RSV can be found in the "Guideline for Prevention of Nosocomial Pneumonia." 459 a. Influenza Nosocomial transmission of influenza has been reported in acute and long-term care facil ities. [460][461][462][463][464][465] Transmission has occurred from patients to health care personnel, 462,464 from health care personnel to patients, 466 and among health care personnel. 465,[467][468][469][470][471][472] Influenza is believed to be transmitted from person to person by direct deposition of virus-CDC Personnel Health Guideline 323 laden large droplets onto the mucosal surfaces of the upper respiratory tract of an individual during close contact with an infected person, as well as by droplet nuclei or small-particle aerosols. 21,290,473 Although the extent of transmission by virus-con taminated hands or fomites is not known, it is not the primary mode of transmission. 473 The incubation period of influenza is usually 1 to 5 days, and the period of greatest communica bility is during the first 3 days of illness. However, virus can be shed before the onset of symptoms and as long as 7 days after illness onset. [474][475][476] Persons at greatest risk for influenzarelated complications include (a) persons older than 65 years, (b) residents of nursing homes and other chronic care facilities, (c) persons with chronic pulmonary or cardiovascular conditions, and (d) persons with diabetes mellitus. 17 Adherence to droplet precautions may prevent nosocomial transmission. 3 Administration of influenza vaccine to health care personnel, including pregnant women, 9 before the beginning of each influenza season can help to (a) reduce the risk to health care personnel of influenza infection, (b) prevent transmission of influenza from personnel to persons at high risk for complications, and (c) reduce personnel absenteeism during community outbreaks. Innovative methods may be needed to increase influenza immunization rates among health care personnel. 477 Immunization rates may also be increased by providing data to health care person nel on the low rates of systemic reactions to influenza vaccine among healthy adults. 478 During institutional outbreaks of influenza, prophylactic antiviral agents (e.g., amantadine and rimantadine) may be used in conjunction with influenza vaccine to reduce the severity and duration of illness among unvaccinated health care personnel. Amantadine and rimanta dine may be administered for 2 weeks after per sonnel vaccination or, in unvaccinated person nel, for the duration of influenza activity in the community. 17,459,465,479
# b. Respiratory syncytial virus
Nosocomial transmission of respiratory syncy tial virus (RSV) is greatest during the early winter when community RSV outbreaks occur; patients, visitors, and health care personnel may transmit the virus in the health care setting. RSV infection is most common among infants and children, who are likely to acquire more severe disease. Because RSV infection can also occur simultaneously with other respiratory viruses, it may go unrecog nized. 480,481 Nosocomial transmission has been reported most frequently among newborn and pediatric patients, 482,483 but outbreaks associated with substantial morbidity and mortality have been reported among adults in bone-marrow transplant centers, 484 intensive care units, 485 and long-term care facilities. 486,487 RSV is present in large numbers in the respira tory secretions of persons symptomatically infect ed with the virus and can be transmitted directly through large droplets during close contact with such persons or indirectly by hands or fomites that are contaminated with RSV. Hands can become contaminated through handling of infect ed persons' respiratory secretions or contaminat ed fomites and can transmit RSV by touching the eyes or nose. 459 The incubation period ranges from 2 to 8 days; 4 to 6 days is most common. In general, infected persons shed the virus for 3 to 8 days, but young infants may shed virus for as long as 3 to 4 weeks. Adherence to contact precautions effectively prevents nosocomial transmission.
# c. Work restrictions
Because large numbers of personnel may have viral respiratory illnesses during the winter, it may not be possible to restrict infected personnel from all patient care duties. Nevertheless, it may be prudent to restrict personnel with acute viral respiratory infections from the care of high-risk patients during community outbreaks of RSV and influenza. 488
# F. PREGNANT PERSONNEL
Immunologic changes occur during pregnancy, primarily depression of certain aspects of cell-medi ated immunity such as decreased levels of helper T cells. These changes permit fetal development with out rejection but generally do not increase maternal susceptibility to infectious diseases. Occupational acquisition of infections is of special concern to female health care personnel of childbearing age for several reasons. Some infections, such as varicella, may be more severe during pregnancy. Transplacental infections with viruses such as par vovirus, varicella, and rubella have been associated with abortion, congenital anomaly, and mental retardation. Other diseases in which the infectious agent may be transmitted to the fetus include CMV, hepatitis B, herpes simplex, influenza, and measles. In addition, certain drugs used to treat or prevent some infections, for example tuberculosis, may be contraindicated during pregnancy.
In general, pregnant health care personnel do not have an increased risk for acquiring infections AJIC June 1998 in the workplace. The risks to pregnant personnel and methods for prevention are discussed in the various sections of this document and are sum marized in Table 6. Female personnel of child bearing age should be strongly encouraged to receive immunizations for vaccine-preventable diseases before pregnancy. Such personnel may also decrease their risk of acquiring infection by adhering to appropriate infection control prac tices, including standard precautions when caring for all patients. Additional information on occu pational risks for pregnant health care personnel has been published elsewhere. [489][490][491]
# G. LABORATORY PERSONNEL
Despite the availability of improved engineering controls, work practices, and personal protective equipment, laboratory personnel remain at risk for occupational acquisition of infectious agents. 5,18,53,151,162,241,492,493 Furthermore, newer technologies that require the use of large or con centrated specimens may further increase the risk of occupationally acquired infections among lab oratory personnel. 494 In a review of laboratory-acquired infections from 1950 through 1974, more than 4000 labora tory-associated infections were documented in the United States 492 ; the 10 most commonly reported infections were brucellosis, Q fever, hepatitis (especially hepatitis B), typhoid fever, tularemia, tuberculosis, dermatomycosis, vene zuelan equine encephalitis, psittacosis, and coc cidioidomycosis. However, laboratory-associated infections also have been caused by a wide vari ety of other pathogens. 162,492,493 More recently, viral agents have accounted for a larger propor tion of laboratory-associated infections than have bacterial agents. [493][494][495][496][497][498] Laboratory personnel may acquire infection by aerosolization of specimens, mouth pipetting, or percutaneous injury. Information on the risks of laboratory-associated infections and appropriate biosafety procedures and precautions for labora tories have been published. 5,6,494,499,500 In addition to biosafety precautions, preventive measures (e.g., immunizations and postexposure prophylaxis) may also be indicated for laboratory personnel who handle infectious agents. In this document, disease-specific information and guid ance are provided for prevention of laboratoryassociated infections and for management of labo ratory personnel exposed to infectious agents. Health care institutions need to ensure that labo ratory personnel who may be exposed to infectious agents are well informed about the risks of acquir ing infections and about biosafety procedures to prevent transmission of infectious agents.
# H. EMERGENCY-RESPONSE PERSONNEL
Emergency medical technicians, firefighters, policemen, and others who attend to and trans port patients to the hospital may be exposed to recognized or undiagnosed transmissible infec tious diseases in the patients with whom they come in contact. Subtitle B (42 USC 300ff-80) of the 1990 Ryan White Comprehensive AIDS Resources Emergency Act requires the establish ment of notification systems in each state to ensure that emergency-response employees (including emergency medical technicians, fire fighters, and the like) are informed when they have been exposed to an emergency medical patient with an infectious, potentially fatal disease such as HIV or meningococcemia. CDC published a list of diseases for which emergency-response employees must be informed of an exposure. 501
# I. LATEX HYPERSENSITIVITY
Since the introduction of universal precautions, the use of latex gloves has become commonplace in health care settings. 31,502 The increased use of latex gloves has been accompanied by increasing reports of allergic reactions to natural rubber latex among health care personnel. [503][504][505][506][507][508] Natural rubber latex is a combination of heatand water-soluble proteins derived from the tree Hevea braziliensis. Reactions to latex gloves may be localized or systemic and include dermatitis, conjunctivitis, rhinitis, urticaria, angioedema, asthma, and anaphylaxis. [509][510][511][512] Most local reac tions associated with latex glove use are not immunologically mediated and result from chem icals (e.g., thiurams, carbamates, mercaptoben zothiazole, phenylenediamine), accelerants or antioxidants added to gloves during manufactur ing. 502,507,[513][514][515] It may be clinically difficult to dif ferentiate irritant reactions from allergic contact dermatitis reactions; both may be manifested by itching, dryness, erythema, bleeding, or scaling of the hands. Nevertheless, neither of the types of local reactions to latex gloves are good predictors of latex allergy 503,516 ; only a subset of health care personnel reporting glove-associated skin irrita tion will have immunoglobulin E (IgE) antibod ies specific for latex. 513,[517][518][519] In contrast, systemic reactions to natural rub ber latex, including urticaria, are mediated by antilatex IgE antibodies 509,520,521 and may result CDC Personnel Health Guideline 325 from direct skin contact or from exposure to air borne latex allergen adsorbed to glove powder. Occupational asthma from latex is becoming increasingly recognized. 520,[522][523][524] Asthmatic responses to latex may occur early (<8 hours) or late (>8 hours) after exposure. [525][526][527] Local reactions (i.e., irritant or allergic contact dermatitis) to latex gloves account for most reported reactions among health care person nel. 503,506 The risk of progression from localized to systemic reactions is unknown.
Latex gloves may vary considerably in total protein content from brand to brand and from lot to lot within brands. 528,529 However, the total protein concentrations and allergenicity of latex gloves are not always directly correlated, 528 sug gesting that total protein concentrations are not necessarily a measure of the allergenic proper ties of latex gloves. Currently, the amount of latex allergen exposure required to produce sen sitization or to elicit reactions in previously sen sitized persons is unknown. The FDA has man dated labeling of all medical devices that contain natural rubber latex. 530 Another recognized contributor to latex sensiti zation and reactions is the powder or cornstarch used as a lubricant for gloves. Levels of extractable protein and allergen in a given glove have been shown to be correlated with the pres ence of powder. Also, investigators have demon strated that latex proteins adhere to the powder on gloves and that aerosolized latex protein-pow der particles can provoke allergic respiratory symptoms if inhaled by a latex-sensitive individ ual 531 ; similar adherence has not been detected with powdered vinyl gloves. In one study, person nel wearing powdered latex gloves had a signifi cantly higher rate of reaction than did workers who wore washed latex gloves, from which the powder had been removed (60% vs 28%); none of these workers had positive skin-test reactions to industrial or commercial cornstarch or powder. 504 Although many health care personnel or clini cians may implicate the powder or cornstarch on gloves as the cause of their reactions, documented reactions to cornstarch powder are rare.
# a. Prevalence and risk factors
In studies of health care personnel, the reported prevalence of IgE-mediated allergy to latex varies considerably, ranging from 2.9% to 17%. The broad range of prevalence rates reported likely represent differences in the personnel groups studied and the methods used for estimating sen sitization or allergy. 518,519,522,532,533 The prevalence detected in some studies also has been biased by enrollment or testing of only personnel with symptoms. 504,508 However, it is estimated that a minority of health care personnel seek medical evaluation or treatment for latex-allergic condi tions, even if they have symptoms. Thus, the true prevalence of these reactions among health care personnel is unknown.
The prevalence of sensitization to latex among health care personnel has been shown to vary by job category and by location within a facility. 506,533 In one study of 224 health care personnel, the overall prevalence of skin-prick reactivity to latex was 17% but ranged from 0% (0/17) among house keepers and clerical workers to 38% (5/13) among dental residents and assistants. 506 In another sur vey of 512 health care personnel, the prevalence among physicians (6.5%, 7/108) was greater than that among nurses (2.2%, 7/325) or other hospital personnel (1.3%, 1/79). Also, operating room per sonnel (6.2%, 9/145) were significantly more like ly to be sensitized than were personnel assigned to general wards or laboratories (1.6%, 6/367); oper ating room nurses had fourfold the prevalence of general ward nurses (5.6% vs 1.2%). 533 Measurable levels of latex aeroallergen have been detected in the breathing zones of operating room personnel and may vary as much as 100-fold, depending on the invasiveness of the procedure and frequency of glove changes. 534 Several factors have been linked with latex sen sitization among health care personnel, including the presence of other allergic conditions (e.g., asthma, eczema, hay fever), 503,516,518,519,522,532,533 nonwhite ethnicity, 519,532 elevated total IgE lev els, 519 allergy to cosmetic powders or foods, 535 years or status (full-time vs part-time) of employ ment, and frequency or duration of glove use. 503,516,522,533 Coexistent allergy to certain fruits (e.g., bananas, 536,537 avocados, 538,539 and chest nuts 540 ) also has been described in latex-allergic health care personnel.
Skin irritation and eczematous dermatitis 516,533 (conditions that may allow passage of latex pro teins through the skin) and use of other latex products (e.g., condoms, diaphragms) have not been consistently linked to latex sensitization in health care personnel.
# b. Diagnosis and identification
Diagnosis of latex allergy in personnel relies largely on a clinical history of symptoms elicited by exposure to latex products (e.g., balloons, gloves). Clinical symptoms, such as urticaria, may be good predictors of IgE-medicated allergy. 516,519 AJIC June 1998 A variety of methods have been used to aid in the identification of latex-allergic persons; most are experimental and have not been approved for clinical use. Skin-prick testing may be the most sensitive method for diagnosis of IgE-mediated allergy, but no standardized FDA-approved anti gen is currently available in the United States for detection of latex-specific IgE antibodies. Moreover, the use of some skin-test reagents in highly sensitized persons has been associated with adverse outcomes, 541 suggesting that these nonstandardized reagents may not be safe for rou tine use. In Europe, where a standardized testing antigen has been developed, skin-prick testing has been used successfully.
FDA-approved immunoassays are available for detection of latex-specific IgE antibodies in blood. The FDA has recommended that these assays be used as confirmatory tests, rather than screening tests, for persons in whom latex allergy is sus pected on the basis of clinical history and find ings. Levels of detectable antibody appear to be associated with symptoms, 504,519 but, as with other allergens, the correlation between serum concen trations of latex-specific IgE antibodies and symp tom severity may not be predictable. 312,504,516
# c. Prevention strategies
Avoiding latex products remains the cornerstone of preventing sensitization (primary prevention) and reactions (secondary prevention) to natural rubber latex products. Proposed strategies to reduce the risk of reactions to natural rubber latex have included the use of the following: (a) nonla tex (e.g., vinyl) products alone or in combination with latex gloves, (b) powder-free latex gloves, (c) powdered latex gloves washed to remove powder, and (d) "low-protein" latex gloves. However, none of these interventions has been prospectively stud ied in controlled trials to assess cost-effectiveness or efficacy in preventing sensitization or reactions.
Because latex proteins can be aerosolized when powdered gloves are donned or removed, systemic symptoms caused by latex aeroallergens may not be alleviated by simply avoiding latex products, particularly if coworkers of the affected worker continue to use powdered latex gloves. Although the risk of a worker's exposure is greatest when gloves are donned or removed, allergenic proteins also may settle on environmental surfaces, surgi cal gowns, or other clothing and become resus pended. The use of powder-free or low-protein gloves appears more effective and less costly than either laminar-flow or high-efficiency particulate air-filtered glove-changing stations in reducing latex aeroallergens. 534 For personnel with sys temic manifestations of latex allergy, workplace restriction or reassignment may be necessary.
# J. THE AMERICANS WITH DISABILITIES ACT
The Americans With Disabilities Act provides guidelines for hiring and placing employees with disabilities, as defined in the Act. [542][543][544][545] In general, employers must assess applicants for their qualifications to perform the tasks inher ent to the job for which the employee is being considered. Applicants may be asked about their ability to perform specific job functions but may not be asked about the existence, nature, or severity of a disability. Employers must make a "reasonable accommodation" to allow an indi vidual to perform the essential functions of a job, unless the employer can prove that this would create undue hardship because of signifi cant difficulty or expense.
The provisions of the Americans With Disabilities Act need to be incorporated into infec-CDC Personnel Health Guideline 327 tion control policies for health care personnel. For example, applicants with a communicable disease spread by aerosol could justifiably be denied employment (until they are no longer infectious) because they could pose a direct threat to others. On the other hand, applicants who are immuno compromised may not necessarily be excluded because of an increased risk for acquiring an infection in the hospital if the employer can make reasonable accommodations that prevent expo sure. Health care personnel who are known to be immunocompromised need to be referred to per sonnel health professionals who can individually counsel the employees on their risk for infection. At the request of the immunocompromised health care personnel, employers should offer but not compel a work setting in which health care per sonnel would have the lowest possible risk for occupational exposure to infectious agents. Evaluation of individual situations also needs to include consideration of the provisions of other applicable federal, state, and local laws.
# A. INTRODUCTION
In this document, the term health care personnel refers to all paid and unpaid persons working in health care settings who have the potential for exposure to infectious materials including body substances, contaminated medical supplies and equipment, contaminated environmental sur faces, or contaminated air. These personnel may include but are not limited to physicians, nurses, technicians, therapists, pharmacists, nursing assistants, laboratory personnel, autopsy person nel, emergency medical service personnel, dental personnel, students and trainees, contractual staff not employed by the health care facility, and per sons not directly involved in patient care but potentially exposed to infectious agents (e.g., vol unteer, dietary, housekeeping, maintenance, and clerical personnel).
As in previous CDC guidelines, each recommen dation is categorized on the basis of existing sci entific data, theoretic rationale, applicability, and potential economic impact. The system for cate gorizing recommendations is as follows:
Category IA Strongly recommended for all hospitals and strongly supported by well-designed experimental or epidemiologic studies.
# Category IB
Strongly recommended for all hospitals and reviewed as effective by experts in the field and a consensus of Hospital Infection Control Practices Advisory Committee members on the basis of strong rationale and suggestive evi dence, even though definitive scientific studies have not been done.
# Category II
Suggested for implementation in many hospi tals. Recommendations may be supported by sug gestive clinical or epidemiologic studies, a strong theoretic rationale, or definitive studies applica ble to some but not all hospitals.
# No recommendation; unresolved issue
Practices for which insufficient evidence or consensus regarding efficacy exists. 8,9 (b) well informed about indications, storage, dosage, preparation, side effects, and contraindications for each of the vaccines, toxoids, and immune globu lins used, 8,9,24 and (c) kept updated on nation al and local recommendations regarding vac cination of health care personnel (Tables 1 and 2). Category IB 3. Ensure that immunization product informa tion is available at all times and that a perti nent health history, especially a history of allergy and potential vaccine contraindica tions, is obtained from each person before an agent is given (Table 2). Category IB 4. Develop a list of needed immunizations for each employee during screening and an indi vidual plan to provide the necessary vac cines. Category IB 5. In the absence of a known occupational exposure, provide personnel with on-site immunizations or refer personnel to their own health care providers for routine non-occupation-related immunizations against diphtheria, pneumococcal disease, hepatitis A, or tetanus (Table 1). Category IB 6. Provide vaccine to personnel who may have occupational exposure to uncommon dis-
# Bloodborne pathogens, general recommen dation
Ensure that health care personnel are famil iar with precautions to prevent occupational transmission of bloodborne pathogens. 3,6,30,31,39 Category IA Follow state and federal guidelines and strategies for determining the need for work restrictions for health care personnel infected with bloodborne pathogens. 48 1). 9 Category IA e. Administer rubella vaccine* in the postpar tum period to female personnel not known to be immune. Category IA f. Exclude susceptible personnel who are exposed to rubella from duty from the sev enth day after the first exposure through the 21st day after the last exposure (Table 3). 9 Category IB g. Exclude personnel who acquire rubella from duty until 7 days after the beginning of the rash (Table 3 3). 369 371,374 Category IB b. Do not routinely exclude personnel with sus pected or confirmed carriage of group A Streptococcus from patient care or food han dling unless it is shown epidemiologically that they are responsible for disseminating the organism in the health care setting (Table 3). 369,373,378 1) Exclude personnel with infectious pul monary or laryngeal TB from the workplace until the facility has documentation from their health care provider that they are receiving adequate therapy, their coughs have resolved, and that they have had three consecutive sputum smears collected on dif ferent days with negative results for AFB. After personnel return to work, obtain peri odic documentation from their health care provider that effective drug therapy has been maintained for the recommended peri od and that sputum smear results remain negative for AFB ( 1). 9,18 Category IB b. Consider administering vaccinia vaccine to personnel who provide clinical care to recip ients of recombinant vaccinia virus vaccines (Table 1). 9,18 Category II c. Do not administer vaccinia vaccine to pregnant personnel or personnel with immunosuppres sion or eczema (Tables 1 and 2). Category IB d. Do not exclude from duty personnel who receive the vaccine, if they keep the vaccina tion site covered and adhere to handwashing practices. 18 Category IB
# Varicella
a. Administer varicella vaccine to susceptible personnel, especially those that will have contact with patients at high risk for serious complications (Table 1). 9,13 Category IA b. Do not perform serologic screening of per sons with negative or uncertain history of varicella before administering varicella vac cine to personnel, unless the institution con siders it cost-effective. 9,13 Category IB c. Do not routinely perform postvaccination testing of personnel for antibodies to vari cella. 9 Category IB d. NO RECOMMENDATION for administering postexposure varicella vaccination for the protection of exposed, susceptible person nel. 9 UNRESOLVED ISSUE e. Develop guidelines for managing health care personnel who receive varicella vaccine; for example, consider precautions for personnel who acquire a rash after receipt of varicella vac cine and for other health care personnel who June 1998 receive varicella vaccine and will have contact with susceptible persons at high risk for serious complications from varicella. 9 Category IB f. Develop written guidelines for postexposure management of vaccinated or susceptible personnel who are exposed to wild-type vari cella. 9 Category IB g. Exclude personnel from work who have onset of varicella until all lesions have dried and crusted (Table 3). 3 Category IB h. Exclude from duty after exposure to varicella personnel who are not known to be immune to varicella (by history or serology), begin ning on the tenth day after the first exposure until the 21st day after the last exposure (28th day if VZIG was given; Table 3). 9 Category IB i. Restrict immunocompetent personnel with localized zoster from the care of high-risk patients until lesions are crusted; allow them to care for other patients with lesions cov ered. 9 Category IB j. Restrict immunocompromised personnel with zoster from contact with patients until their lesions are crusted (Table 3). 9 Category IB k. Restrict susceptible personnel exposed to zoster from patient contact from the tenth day after the first exposure through the 21st day after the last exposure (28th day if VZIG was given; Table 3). 9 Category IB l. Perform serologic screening for immunity to varicella on exposed personnel who have not had varicella or are unvaccinated against varicella. 9,13 Category IB m. Consider performing serologic screening for immunity to varicella on exposed, vacci nated personnel whose antibody status is not known. If the initial test result is negative, retest 5 to 6 days after exposure to determine whether an immune response occurred. Category IB n. Consider excluding vaccinated personnel from work beginning on the 10th day after the first exposure through the 21st day after the last exposure if they do not have detectable antibodies to varicella, or screen daily for symptoms of varicella (Table 3). 9 Category IB o. Do not routinely give VZIG to exposed sus ceptible personnel, unless immunosup pressed, HIV infected, or pregnant. If VZIG is given, exclude personnel from duty from the 10th day after the first exposure through the 28th day after the last exposure (Tables 1 and 3). 9,13 Category IB
# Viral respiratory infections
a. Administer influenza vaccine annually to all personnel, including pregnant women, before the influenza season, unless otherwise contraindicated (Table 1). 9,17 Category IB b. Consider the use of antiviral postexposure prophylaxis for unvaccinated health care per sonnel during institutional or community outbreaks of influenza for the duration of influenza activity, or consider giving vaccine to unvaccinated personnel and providing them with antiviral postexposure prophylaxis for 2 weeks after vaccination (Table 1). 3,17,459 Category IB c. Consider excluding personnel with acute febrile respiratory infections or with lab oratory evidence of epidemiologically significant viruses from the care of highrisk patients (e.g., neonates, young infants, patients with chronic obstructive lung disease, and immunocompromised patients) during community outbreaks of influenza or RSV infections (Table 3). 3
# Category IB
# H. SPECIAL ISSUES
1. Pregnancy a. Counsel pregnant women and women of childbearing age regarding the risk of transmission of particular infectious dis eases (e.g., CMV, hepatitis, herpes simplex, HIV, parvovirus, rubella) that, if acquired during pregnancy, may have adverse effects on the fetus, whether the infection is acquired in nonoccupational or occupa tional environments. Provide such women with information on standard and transmission-based precautions appropriate for each infection (Table 6). 3,[489][490][491] Category IB b. Do not routinely exclude women only on the basis of their pregnancy or intent to be pregnant from the care of patients with particular infections that have potential to harm the fetus (e.g., CMV, HIV, hepatitis, herpes simplex, parvovirus, rubella, and varicella; Table 6). [489][490][491] Category IB a. Develop an institutional protocol for (1) evaluating and managing personnel with suspected or known latex allergy, (2) establishing surveillance for latex reac tions within the facility, (3) purchasing gloves, and (4) measuring the impact of preventive measures. Educational materi als and activities should be provided to inform personnel about appropriate glove use and the manifestations and potential risk of latex allergy. 31,546 Category IB b. Glove purchasers should review information on the barrier effectiveness of gloves and consider worker acceptance (e.g., comfort and fit) when selecting gloves for use in the health care organization. 31,[547][548][549] Category IB c. To facilitate the appropriate selection of gloves, the occupational health service should maintain a list of all gloves used the institution according to whether they do or do not contain latex. Category II d. Evaluate personnel with symptoms sugges tive of latex allergy (e.g., localized dermati tis and workplace-related asthma). 522 Use serologic tests only for those who, on the basis of this evaluation, have suspected latex allergy. 504,516 Category IB e. Avoid the use of all latex products by per sonnel with a history of systemic reactions to latex. [509][510][511][512]520,[522][523][524] Category IB f. Use nonlatex gloves for personnel with localized reactions to latex. 502,507,[513][514][515] Category IB The opinions of all the reviewers might not be reflected in all the rec ommendations contained in this document. | None | None |
eddd215c59d50e487c326c4dd6adce6a29c42370 | cdc | None | While NIOSH estimates that no more than 500 US workers are subject to nickel carbonyl exposure from activities directly relating to these industrial operations, this number may increase by an order of magnitude when considering the possible inadvertent formation of nickel carbonyl. Such can occur with the use of nickel catalysts in hydrogenation, in coal gasification, and in petroleum refining.
Nickel carbonyl is an extremely volatile and flammable liquid (igniting spontaneously in air at room temperature) whose toxicity in the vapor form is well documented.
Toxic effects in animals have resulted from inhalation exposures of 17-70 mg nickel carbonyl/cu m (2400-10,000 ppb) for 5-30 minutes and included edema of the lungs and brain and high mortality . Human effects resulting from accidental exposure to nickel carbonyl have included pulmonary edema, interstitial pneumonitis, reduced lung capacity, cardiac irregularities, liver enlargement, and in severe exposure cases, death .
In animal carcinogenicity studies-, rats developed lung tumors from both long-term (inhalation of 30 mg/cu m air (4300 ppb), for 30 minutes, 3 times weekly, for 1 year) and acute (single dose of 600 mg/cu m (8 6 , 0 0 0 ppb) for 30 minutes) exposure to nickel carbonyl vapor . Induction of malignant tumors of several organs has also been reported following intravenous injections of nickel carbonyl.
From an occupational health viewpoint, those occurring following inhalation of nickel carbonyl vapor are considered of greater relevance. The nature of its biochemical interactions may support a carcinogenic potential for nickel carbonyl . For many years the increased incidence of lung and nasal cancers occurring in nickel refinery workers was attributed to nickel carbonyl. A later analysis of these workers refuted this association. At the present time human epidemiologic data are insufficient to either confirm or deny a causal relationship.
In view of its extreme toxicity from either acute or chronic exposure, nickel carbonyl should be designated as a highly hazardous material and regulated as a carcinogen. After a review of the existing data NIOSH supports the current US standard for nickel carbonyl of 1 ppb which approximates the least detectable level for this substance and does not recommend a change in the environmental level. The 1 ppb standard should protect workers from any carcinogenic potential which nickel carbonyl may have, as well as any of the other adverse health effects associated with nickel carbonyl exposure. In 1951, Barnes and Denz exposed rats to nickel carbonyl at concentrations ranging from 17-70 milligrams per cubic meter of air (mg/cu m) (2400-10,000 ppb) for 5-30 minutes and rabbits at concentrations ranging from 10-32 mg/cu m (1400-4600 ppb) for 10-30 minutes. The animals were killed at intervals up to several months after exposure. Mortality and the effects seen upon gross and microscopic examination were very similar to those described by Armit . In addition, they described the presence of an early compensatory fibrogenic lung reaction in those animals which were killed between one and four months after exposure and a complete resolution of that reaction in animals which were killed a year or more after exposure. Also, they found that only 5 to 10% of the calculated amount of nickel inhaled by the animals was retained in the lungs, suggesting rapid relocation and excretion of that which was absorbed.
Sunderman and Selin investigated the metabolism of nickel carbonyl. Radioactive nickel carbonyl was administered to 78 adult male rats by either intravenous (IV) injection or inhalation. The LD50 value of 5juL/100g body weight, as determined by Hackett and Sunderman , was used.
Determination of radioactive nickel in urine, feces, and expired air revealed that 38.4% of the injected dose was exhaled as nickel carbonyl, 31.2% was excreted in the urine, and 2.4% was excreted in the feces. A total of 66.2% of the injected dose was excreted within 24 hours following exposure.
Further excretion of nickel carbonyl was extremely slow and reached a maximum of 72.0% of the injected dose at the end of the fourth day. Tissue analyses of rats killed 24 hours after injection revealed 7.3% of the dose in muscle and fat, 5.5% in bone and connective tissue, 4.7% in viscera and blood, and 0.2% in the brain and spinal cord. According to the authors, excretion values obtained after inhalation were not practicable in that there was significant fecal and exhalant contamination as a result of nickel carbonyl adsorbed onto the animals' fur during exposure.
# B. Carcinogenicity in Animals
Three animal studies have been conducted to assess the carcinogenic potential of nickel carbonyl. Two studies were conducted by inhalation and one by intravenous injection using either multiple or single exposures. Details of the experimental design and pertinent results are presented in Table I.
In the first two studies Sunderman and his coworkers observed a single pulmonary carcinoma in each of six groups of exposed rats. A total of six lung cancers occurred in 157 nickel carbonyl-exposed rats that survived at least 12 months. No lung cancers were observed in 82 controls.
This difference is of only marginal statistical significance (P=.073).
Spontaneously occurring lung cancer is extremely rare in rats and according to Sunderman and Donnelly none had been observed in their 12-year series of experiments.
Comparing the incidence of lung cancer in nickel carbonyl-exposed rats to this much larger, historical control population would increase the level of significance.
These six lung cancers consisted of 2 squamous cell carcinomas, 2 adenocarcinomas, and 2 anaplastic carcinomas, all found between 24-27 months after initial exposure.
In addition, lung cancers occurred equally in rats subjected to either a large single exposure or repeated exposures at much lower levels for a long period of time. The major sites of metastases were the kidneys, liver, and heart ,
A wide variety of tumors other than pulmonary cancers was observed in both nickel carbonyl-exposed and control groups in the second Sunderman study .
While the total incidence of tumors in the nickel carbonylexposed rats was greater than that in the controls, 50% vs 33%, a causal relationship was considered doubtful . There were no tumors other than the lung cancers reported in the Sunderman et al. study. However, the number of animals that survived to 24 months was very small and the thoroughness of the pathology examination could not be ascertained from the report.
In the studies of Lau et al. , nickel carbonyl was injected intravenously into the tail vein of Sprague-Dawley rats, either as a single injection or in six injections administered 2-4 weeks apart. The total dose administered to the multiple -dose group was approximately 2 1 / 2 times that of the single-injection group.
For the single-injected group, there was little overall difference in the survival or in the incidences of benign tumors of treated and control animals. The incidence of malignant tumors was slightly increased over the controls, 8.3% vs 4.3%. Rats administered multiple injections had a greater increase, 15% vs 4.3%, in the overall incidence of malignant tumors which was of statistical significance (P<0.05). Other than two pulmonary lymphomas, no malignant tumors were observed in the controls. Considering only non-lymphomatous malignant tumors, the difference between the exposed and control groups is of greater statistical significance (P<0.02). The tumors originated in many organs and most were observed to have metastasized.
In an additional study, not tabulated in Table I, Sanina reported the induction of malignant tumors in various organs including the uterus, ovaries and mammary glands in rats exposed by inhalation for two hours, once every two weeks, at a concentration of 0.0005 -0.0017 mg/L (70-240 ppb) . Tumors were found during examination after having killed the animals at various time intervals up to six months. While the report indicated no tumors in the controls, the total number of exposed animals was small (2 0 ) and no data were given on the incidence of each type of tumor or on the time of killing. Due to its lack of details, very little information can be derived from this report.
Thus, the carcinogenicity of nickel carbonyl has been demonstrated in at least three different experiments, by two routes of exposure (inhalation and intravenous injection) and in different organ systems. Perhaps, the most pertinent finding is that of lung cancers in the inhalation studies, closely simulating the most probable route of occupational exposure to this compound.
The extent of carcinogen testing has been limited to only one species, the rat. While it is difficult to determine whether other species, and indeed man, would show a similar response to that of the rat, Laskin and Sellakumar concluded that the common laboratory rat most clearly meets the requirements of the ideal animal model for respiratory carcinogenesis.
Their conclusion was based upon the induction of tumors in rats which are similar in morphology and origin to those of man, and the extreme rarity with which these tumors spontaneously occur.
In addition, the inhalation and retention kinetics of inhaled particulates and vapors of the rat resembles that of man moreso than do those of the smaller laboratory rodents.
# C. Toxic Effects in Humans
In view of its volatility and its general use in the vapor state, the major occupational exposure to nickel carbonyl is by inhalation. Skin absorption and ingestion also may be routes of entry into the body.
The initial signs and symptoms resulting from exposure to toxic amounts of nickel carbonyl have been most often described as dyspnea, fatigue, nausea, and headache . These signs and symptoms, except in the most severe exposures, usually ceased in the first 24 .
In the two fatal-exposure cases, the investigators, Brandes in 1934 and Jones in 1973 reported finding edema of the brain in addition to damage of the lungs in the decedents.
A report was published in Lancet in 1903 concerning two other deaths associated with exposure to nickel carbonyl but the description of pathologic changes found in the bodies of the victims is of questionable accuracy.
Cardiac irregularities , liver enlargement , and spleen enlargement are some of the other significant human health effects of nickel carbonyl exposure reported in the literature. A case of an allergic reaction known as Loffler's Syndrome was attributed to nickel carbonyl exposure by Sunderman and Sunderman .
# D. Epidemiology Studies of Cancer in Humans
In 1939, Hill observed an apparent increase in lung and nasal cavity cancers occurring in Mond nickel refinery workers in South Wales.
Morgan and Doll et al. conducted followup studies on these same workers and confirmed Hill's earlier findings.
Of 482 workers, 113 died of lung cancer and 39 of nasal cancer. Of these, all nasal cancers and all but 8 lung cancers occurred in workers employed prior to 1925. The risk of developing lung cancer for those employed prior to 1925 was 5-10 times that expected and that for nasal cancer, 100-900 times that expected . For those employed after 1925, the observed incidences approximated the national averages, perhaps indicating the reduction or elimination of a causal factor.
Based upon the observations of Hill the British government attributed nickel carbonyl as the causative agent for development of these cancers .
Morgan and Doll et al. refuted an association with exposure to nickel carbonyl and believed that metal dust, copper sulfate, and/or arsenic were the more likely causative agents. This conclusion was based upon the following considerations; (1 ) although no changes had been made in the nickel carbonyl process for 50 years prior to 1958, the occurrence of lung and nasal cancers was confined exclusively to those workers employed prior to 1925, (2) very few cases of acute toxicity attributable to nickel carbonyl inhalation were recorded, indicating that substantial exposure to the vapor of nickel carbonyl was unlikely, (3) between 1920 and 1925, major changes were made in the refinery that resulted in less dust, use of masks to reduce dust inhalation, and use of arsenic-free sulfuric acid, and (4) studies of the personnel in nickel refineries not using the nickel carbonyl process also indicated an increased risk to develop cancers of the lungs and nasal sinuses .
Additionally, Doll et al. have speculated that differences in cigarette smoking might help to account for the difference between the incidences of cancer of the lungs in the Welsh workers hired before and after 1925.
From a review of the epidemiologic data it is not possible to confirm or deny an association of lung cancer with nickel carbonyl exposure .
# D. Engineering and Other Control Technology
Areas where nickel carbonyl is manufactured, used, or stored, should be isolated from all other process areas.
In any event, regulated areas, except for outdoor systems, should be maintained under pressure, negative with respect to non-regulated areas.
In order to accomplish this, each nickel carbonyl operation should be provided with continuous local exhaust ventilation so that air movement is always from nonregulated to regulated areas. Where a fan is used to affect such air movement, the fan blades and 1 8
throat should be made of a nonsparking material.
Exhaust air should not be discharged to regulated areas, nonregulated areas or the external environment unless decontaminated. This may be accomplished by discharging exhaust air directly to the fire box of a decontamination furnace, with subsequent discharge of this air to the environment. A portable suctionvent system is recommended so that in the event of a localized leakage of process gas into the regulated area, a hood and suction hose could be placed near the leak for direct removal of the process gas.
Laboratory work involving the use of nickel carbonyl should adhere to the same ventilation and decontamination strategies as stated above.
All work should be done under laboratory hoods and only the amount of nickel carbonyl needed for that day's work should be at hand. There should be no connection between the regulated laboratory areas and nonregulated areas through the ventilation system.
# E. Confined Spaces
Entry into such confined spaces as tanks, pits, process vessels, and trenches should be restricted to authorized personnel only and the following precautionary measures should be instituted: Non-sophisticated instruments and methods have been developed for detecting nickel carbonyl leaks. The color change of a butane flame in the presence of nickel carbonyl has been used for leak testing with a reported sensitivity of 1-2 ppm (1000-2000 ppb) . A Draeger tube with a sensitivity of 50 ppb and a "Sniffer" , with a detection range of 4-70 ppm (4000-70,000 ppb), have also been used. The second generally accepted instrumental method for continuous monitoring of nickel carbonyl is plasma chromatography. The plasma chromatograph has a detection range of 0.2-2.0 ppb . Both the FTIR and the plasma chromatograph are commercially available.
A third instrumental method which is not commercially available has been developed by Stedman and Tammara [2 \ They have demonstrated the chemilumunescent detection of nickel carbonyl in air using a reaction with oxygen/ozone and purified CO. Th detection limit of their prototype detector is 0.01 ppb. Since their original system was conceived, a portable detector has been built which has a response time of 3-5
seconds, with about a 1 . 0 ppb detection limit (written communication, David A. Tammaro, 1976).
In analyses performed in the field, plasma chromatography and FTIR have been superior to chemical methods for area monitoring of nickel carbonyl at the 1 ppb level . While the major users of nickel carbonyl have been innovative in the development of these superior instrumental methods of analysis, their cost may be prohibitive to the short-term or intermittent user of nickel carbonyl.
Only for this reason should the following chemical method be used as an alternative.
The chemical method .
In general, an air sample containing nickel carbonyl is bubbled through an alcoholic-iodine solution. The entire bubbler solution is dried and dissolved in dilute acid, this solution is neutralized and alpha-furildioxime is added to form a chloroform-extractable complex with nickel. The absorbance at 425 nanometers (nm) is determined and compared to the absorbance of standards.
The detection limit of nickel carbonyl is in the sub-ppb to ppm range.
The specific materials and methods used to carry-out this analysis are as follows:
# Collection of samples
The air sample is bubbled through 80-100 ml of alcoholic-iodine solution. A 0.8 micron millipore filter is placed in front of the scrubber to exclude nickel particulates. For long collection times, the scrubbing liquid volume may be replenished with isopropyl alcohol. The sampling rate is measured at the start and end of the sample period, and the average of the two rates is used to calculate the volume of air sampled. Sampling times usually range from 6-24 hours. Nickel carbonyl has found some application in the nickel plating industry . By using nickel carbonyl, nickel can be deposited on metal or other surfaces without the use of electric current. The process simply involves decomposition of nickel carbonyl vapor by heat in the presence of the target surface.
irregularity, liver enlargement, elevated blood and urinary glucose levels, and in severe cases, death.
# Chronic Long-term Effects
If treatment is prompt and effective or if exposure is only slight the adverse health effects should disappear in 2-3 weeks. However, in one reported case, four patients who had appeared to have recovered were found to have radiographic evidence of fibrosis, a year after exposure.
# C. Reporting Signs and Symptoms
Signs and symptoms of acute exposure to nickel carbonyl can include, shortness of breath, fatigue, nausea, and headache. These initial signs and symptoms may pass away except in the case of massive exposures. In most exposure cases, the effects are not immediately disabling and the exposed persons are able to report to the appropriate health personnel under their own power. In extreme cases where the degree of asphyxia is severe, the immediate treatment should be that for carbon monoxide 32 poisoning.
A mixture of 95% oxygen and 5% carbon dioxide should be administered.
It is of great importance to keep the patient warm but if no oxygen supply equipment is available, he should be removed into fresh air regardless of the surrounding temperature.
In addition it may be necessary to apply artificial respiration.
If so, the arm-lift-back pressure (Nielsen) method should be employed and not mouth-to-mouth resuscitation.
# B. Precautions for Safe Use
Precautions taken in any area where nickel carbonyl is manufactured and/or used should include proper ventilation. Continuous local exhaust ventilation should provide air movement which is always from non-nickel carbonyl areas to areas containing nickel carbonyl. Where a fan is used to affect such air movement, the fan blades and throat should be made of a nonsparking material. Further, the exhaust from such exposure-risk areas should pass through a decontamination furnace before emission into the environment. These practices should be followed in the laboratory as well as in the commercial processing plant.
# C. Handling and Storage Precautions
Because nickel carbonyl is extremely volatile and flammable, it should be handled only when it is contained in steel bottles. Carbon dioxide fire extinguishers should be readily accessible in all nickel carbonyl storage and handling areas.
# IV. RESPIRATORS AND PROTECTIVE CLOTHING
# A. Respirators
In all areas where nickel carbonyl is manufactured, stored, or used, workers should wear full facepiece supplied-air respirators. The extreme toxicity and volatility of nickel carbonyl coupled with its nearly undetectable odor emphasize the need for careful observance of this recommendation.
# B. Protective Clothing
Absorption of nickel carbonyl through the skin has not been demonstrated but has been suggested. Therefore, the necessity for the use of protective gloves and impervious (e.g., rubber) clothing is uncertain.
However, in view of nickel carbonyl's volatility and the major threat of exposure to its vapor, the use of protective clothing is not suggested. | #
While NIOSH estimates that no more than 500 US workers are subject to nickel carbonyl exposure from activities directly relating to these industrial operations, this number may increase by an order of magnitude when considering the possible inadvertent formation of nickel carbonyl. Such can occur with the use of nickel catalysts in hydrogenation, in coal gasification, and in petroleum refining.
Nickel carbonyl is an extremely volatile and flammable liquid (igniting spontaneously in air at room temperature) whose toxicity in the vapor form is well documented.
Toxic effects in animals have resulted from inhalation exposures of 17-70 mg nickel carbonyl/cu m (2400-10,000 ppb) for 5-30 minutes and included edema of the lungs and brain and high mortality [5]. Human effects resulting from accidental exposure to nickel carbonyl have included pulmonary edema, interstitial pneumonitis, reduced lung capacity, cardiac irregularities, liver enlargement, and in severe exposure cases, death [26][27][28][29][30] .
In animal carcinogenicity studies-, rats developed lung tumors from both long-term (inhalation of 30 mg/cu m air (4300 ppb), for 30 minutes, 3 times weekly, for 1 year) and acute (single dose of 600 mg/cu m (8 6 , 0 0 0 ppb) for 30 minutes) exposure to nickel carbonyl vapor [9,10]. Induction of malignant tumors of several organs has also been reported following intravenous injections of nickel carbonyl.
From an occupational health viewpoint, those occurring following inhalation of nickel carbonyl vapor are considered of greater relevance. The nature of its biochemical interactions may support a carcinogenic potential for nickel carbonyl [14][15][16]. For many years the increased incidence of lung and nasal cancers occurring in nickel refinery workers was attributed to nickel carbonyl. A later analysis of these workers refuted this association. At the present time human epidemiologic data [32][33][34][35][36][37][38] are insufficient to either confirm or deny a causal relationship.
In view of its extreme toxicity from either acute or chronic exposure, nickel carbonyl should be designated as a highly hazardous material and regulated as a carcinogen. After a review of the existing data NIOSH supports the current US standard for nickel carbonyl of 1 ppb which approximates the least detectable level for this substance and does not recommend a change in the environmental level. The 1 ppb standard should protect workers from any carcinogenic potential which nickel carbonyl may have, as well as any of the other adverse health effects associated with nickel carbonyl exposure. In 1951, Barnes and Denz [6 ] exposed rats to nickel carbonyl at concentrations ranging from 17-70 milligrams per cubic meter of air (mg/cu m) (2400-10,000 ppb) for 5-30 minutes and rabbits at concentrations ranging from 10-32 mg/cu m (1400-4600 ppb) for 10-30 minutes. The animals were killed at intervals up to several months after exposure. Mortality and the effects seen upon gross and microscopic examination were very similar to those described by Armit [5]. In addition, they described the presence of an early compensatory fibrogenic lung reaction in those animals which were killed between one and four months after exposure and a complete resolution of that reaction in animals which were killed a year or more after exposure. Also, they found that only 5 to 10% of the calculated amount of nickel inhaled by the animals was retained in the lungs, suggesting rapid relocation and excretion of that which was absorbed.
Sunderman and Selin [7] investigated the metabolism of nickel carbonyl. Radioactive nickel carbonyl was administered to 78 adult male rats by either intravenous (IV) injection or inhalation. The LD50 value of 5juL/100g body weight, as determined by Hackett and Sunderman [8 ], was used.
Determination of radioactive nickel in urine, feces, and expired air revealed that 38.4% of the injected dose was exhaled as nickel carbonyl, 31.2% was excreted in the urine, and 2.4% was excreted in the feces. A total of 66.2% of the injected dose was excreted within 24 hours following exposure.
Further excretion of nickel carbonyl was extremely slow and reached a maximum of 72.0% of the injected dose at the end of the fourth day. Tissue analyses of rats killed 24 hours after injection revealed 7.3% of the dose in muscle and fat, 5.5% in bone and connective tissue, 4.7% in viscera and blood, and 0.2% in the brain and spinal cord. According to the authors, excretion values obtained after inhalation were not practicable in that there was significant fecal and exhalant contamination as a result of nickel carbonyl adsorbed onto the animals' fur during exposure.
# B. Carcinogenicity in Animals
Three animal studies [9][10][11] have been conducted to assess the carcinogenic potential of nickel carbonyl. Two studies were conducted by inhalation and one by intravenous injection using either multiple or single exposures. Details of the experimental design and pertinent results are presented in Table I.
In the first two studies [9,10] Sunderman and his coworkers observed a single pulmonary carcinoma in each of six groups of exposed rats. A total of six lung cancers occurred in 157 nickel carbonyl-exposed rats that survived at least 12 months. No lung cancers were observed in 82 controls.
This difference is of only marginal statistical significance (P=.073).
Spontaneously occurring lung cancer is extremely rare in rats and according to Sunderman and Donnelly [10] none had been observed in their 12-year series of experiments.
Comparing the incidence of lung cancer in nickel carbonyl-exposed rats to this much larger, historical control population would increase the level of significance.
These six lung cancers consisted of 2 squamous cell carcinomas, 2 adenocarcinomas, and 2 anaplastic carcinomas, all found between 24-27 months after initial exposure.
In addition, lung cancers occurred equally in rats subjected to either a large single exposure or repeated exposures at much lower levels for a long period of time. The major sites of metastases were the kidneys, liver, and heart [1 0 ],
A wide variety of tumors other than pulmonary cancers was observed in both nickel carbonyl-exposed and control groups in the second Sunderman study [10].
While the total incidence of tumors in the nickel carbonylexposed rats was greater than that in the controls, 50% vs 33%, a causal relationship was considered doubtful [10]. There were no tumors other than the lung cancers reported in the Sunderman et al. [9] study. However, the number of animals that survived to 24 months was very small and the thoroughness of the pathology examination could not be ascertained from the report.
In the studies of Lau et al. [11], nickel carbonyl was injected intravenously into the tail vein of Sprague-Dawley rats, either as a single injection or in six injections administered 2-4 weeks apart. The total dose administered to the multiple -dose group was approximately 2 1 / 2 times that of the single-injection group.
For the single-injected group, there was little overall difference in the survival or in the incidences of benign tumors of treated and control animals. The incidence of malignant tumors was slightly increased over the controls, 8.3% vs 4.3%. Rats administered multiple injections had a greater increase, 15% vs 4.3%, in the overall incidence of malignant tumors which was of statistical significance (P<0.05). Other than two pulmonary lymphomas, no malignant tumors were observed in the controls. Considering only non-lymphomatous malignant tumors, the difference between the exposed and control groups is of greater statistical significance (P<0.02). The tumors originated in many organs and most were observed to have metastasized.
In an additional study, not tabulated in Table I, Sanina [12] reported the induction of malignant tumors in various organs including the uterus, ovaries and mammary glands in rats exposed by inhalation for two hours, once every two weeks, at a concentration of 0.0005 -0.0017 mg/L (70-240 ppb) . Tumors were found during examination after having killed the animals at various time intervals up to six months. While the report indicated no tumors in the controls, the total number of exposed animals was small (2 0 ) and no data were given on the incidence of each type of tumor or on the time of killing. Due to its lack of details, very little information can be derived from this report.
Thus, the carcinogenicity of nickel carbonyl has been demonstrated in at least three different experiments, by two routes of exposure (inhalation and intravenous injection) and in different organ systems. Perhaps, the most pertinent finding is that of lung cancers in the inhalation studies, closely simulating the most probable route of occupational exposure to this compound.
The extent of carcinogen testing has been limited to only one species, the rat. While it is difficult to determine whether other species, and indeed man, would show a similar response to that of the rat, Laskin and Sellakumar [13] concluded that the common laboratory rat most clearly meets the requirements of the ideal animal model for respiratory carcinogenesis.
Their conclusion was based upon the induction of tumors in rats which are similar in morphology and origin to those of man, and the extreme rarity with which these tumors spontaneously occur.
In addition, the inhalation and retention kinetics of inhaled particulates and vapors of the rat resembles that of man moreso than do those of the smaller laboratory rodents.
# C. Toxic Effects in Humans
In view of its volatility and its general use in the vapor state, the major occupational exposure to nickel carbonyl is by inhalation. Skin absorption [17] and ingestion [18] also may be routes of entry into the body.
The initial signs and symptoms resulting from exposure to toxic amounts of nickel carbonyl have been most often described as dyspnea, fatigue, nausea, and headache [19][20][21]. These signs and symptoms, except in the most severe exposures, usually ceased in the first 24 [19,20,22,[26][27][28][29][30].
In the two fatal-exposure cases, the investigators, Brandes [27] in 1934 and Jones [30] in 1973 reported finding edema of the brain in addition to damage of the lungs in the decedents.
A report was published in Lancet [23] in 1903 concerning two other deaths associated with exposure to nickel carbonyl but the description of pathologic changes found in the bodies of the victims is of questionable accuracy.
Cardiac irregularities [28], liver enlargement [28], and spleen enlargement [31] are some of the other significant human health effects of nickel carbonyl exposure reported in the literature. A case of an allergic reaction known as Loffler's Syndrome was attributed to nickel carbonyl exposure by Sunderman and Sunderman [26].
# D. Epidemiology Studies of Cancer in Humans
In 1939, Hill [32] observed an apparent increase in lung and nasal cavity cancers occurring in Mond nickel refinery workers in South Wales.
Morgan [33] and Doll et al. [34] conducted followup studies on these same workers and confirmed Hill's earlier findings.
Of 482 workers, 113 died of lung cancer and 39 of nasal cancer. Of these, all nasal cancers and all but 8 lung cancers occurred in workers employed prior to 1925. The risk of developing lung cancer for those employed prior to 1925 was 5-10 times that expected and that for nasal cancer, 100-900 times that expected [32][33][34]. For those employed after 1925, the observed incidences approximated the national averages, perhaps indicating the reduction or elimination of a causal factor.
Based upon the observations of Hill [32] the British government attributed nickel carbonyl as the causative agent for development of these cancers [34].
Morgan [33] and Doll et al. [34] refuted an association with exposure to nickel carbonyl and believed that metal dust, copper sulfate, and/or arsenic were the more likely causative agents. This conclusion was based upon the following considerations; (1 ) although no changes had been made in the nickel carbonyl process for 50 years prior to 1958, the occurrence of lung and nasal cancers was confined exclusively to those workers employed prior to 1925, (2) very few cases of acute toxicity attributable to nickel carbonyl inhalation were recorded, indicating that substantial exposure to the vapor of nickel carbonyl was unlikely, (3) between 1920 and 1925, major changes were made in the refinery that resulted in less dust, use of masks to reduce dust inhalation, and use of arsenic-free sulfuric acid, and (4) studies of the personnel in nickel refineries not using the nickel carbonyl process also indicated an increased risk to develop cancers of the lungs and nasal sinuses [35][36][37][38].
Additionally, Doll et al. [34] have speculated that differences in cigarette smoking might help to account for the difference between the incidences of cancer of the lungs in the Welsh workers hired before and after 1925.
From a review of the epidemiologic data it is not possible to confirm or deny an association of lung cancer with nickel carbonyl exposure .
# D. Engineering and Other Control Technology
Areas where nickel carbonyl is manufactured, used, or stored, should be isolated from all other process areas.
In any event, regulated areas, except for outdoor systems, should be maintained under pressure, negative with respect to non-regulated areas.
In order to accomplish this, each nickel carbonyl operation should be provided with continuous local exhaust ventilation so that air movement is always from nonregulated to regulated areas. Where a fan is used to affect such air movement, the fan blades and 1 8
throat should be made of a nonsparking material.
Exhaust air should not be discharged to regulated areas, nonregulated areas or the external environment unless decontaminated. This may be accomplished by discharging exhaust air directly to the fire box of a decontamination furnace, with subsequent discharge of this air to the environment. A portable suctionvent system is recommended so that in the event of a localized leakage of process gas into the regulated area, a hood and suction hose could be placed near the leak for direct removal of the process gas.
Laboratory work involving the use of nickel carbonyl should adhere to the same ventilation and decontamination strategies as stated above.
All work should be done under laboratory hoods and only the amount of nickel carbonyl needed for that day's work should be at hand. There should be no connection between the regulated laboratory areas and nonregulated areas through the ventilation system.
# E. Confined Spaces
Entry into such confined spaces as tanks, pits, process vessels, and trenches should be restricted to authorized personnel only and the following precautionary measures should be instituted: Non-sophisticated instruments and methods have been developed for detecting nickel carbonyl leaks. The color change of a butane flame in the presence of nickel carbonyl has been used for leak testing with a reported sensitivity of 1-2 ppm (1000-2000 ppb) [42] . A Draeger tube [43] with a sensitivity of 50 ppb and a "Sniffer" [42], with a detection range of 4-70 ppm (4000-70,000 ppb), have also been used. The second generally accepted instrumental method for continuous monitoring of nickel carbonyl is plasma chromatography. The plasma chromatograph has a detection range of 0.2-2.0 ppb [42]. Both the FTIR and the plasma chromatograph are commercially available.
A third instrumental method which is not commercially available has been developed by Stedman and Tammara [2 \ They have demonstrated the chemilumunescent detection of nickel carbonyl in air using a reaction with oxygen/ozone and purified CO. Th detection limit of their prototype detector is 0.01 ppb. Since their original system was conceived, a portable detector has been built which has a response time of 3-5
seconds, with about a 1 . 0 ppb detection limit (written communication, David A. Tammaro, 1976).
In analyses performed in the field, plasma chromatography and FTIR have been superior to chemical methods for area monitoring of nickel carbonyl at the 1 ppb level [4 2 ] . While the major users of nickel carbonyl have been innovative in the development of these superior instrumental methods of analysis, their cost may be prohibitive to the short-term or intermittent user of nickel carbonyl.
Only for this reason should the following chemical method be used as an alternative.
The chemical method [42} suggested is a modification of the colorimetric one developed by Brief et al. [44].
In general, an air sample containing nickel carbonyl is bubbled through an alcoholic-iodine solution. The entire bubbler solution is dried and dissolved in dilute acid, this solution is neutralized and alpha-furildioxime is added to form a chloroform-extractable complex with nickel. The absorbance at 425 nanometers (nm) is determined and compared to the absorbance of standards.
The detection limit of nickel carbonyl is in the sub-ppb to ppm range.
The specific materials and methods used to carry-out this analysis are as follows:
# Collection of samples
The air sample is bubbled through 80-100 ml of alcoholic-iodine solution. A 0.8 micron millipore filter is placed in front of the scrubber to exclude nickel particulates. For long collection times, the scrubbing liquid volume may be replenished with isopropyl alcohol. The sampling rate is measured at the start and end of the sample period, and the average of the two rates is used to calculate the volume of air sampled. Sampling times usually range from 6-24 hours. Nickel carbonyl has found some application in the nickel plating industry [1]. By using nickel carbonyl, nickel can be deposited on metal or other surfaces without the use of electric current. The process simply involves decomposition of nickel carbonyl vapor by heat in the presence of the target surface.
irregularity, liver enlargement, elevated blood and urinary glucose levels, and in severe cases, death.
# Chronic Long-term Effects
If treatment is prompt and effective or if exposure is only slight the adverse health effects should disappear in 2-3 weeks. However, in one reported case, four patients who had appeared to have recovered were found to have radiographic evidence of fibrosis, a year after exposure.
# C. Reporting Signs and Symptoms
Signs and symptoms of acute exposure to nickel carbonyl can include, shortness of breath, fatigue, nausea, and headache. These initial signs and symptoms may pass away except in the case of massive exposures. In most exposure cases, the effects are not immediately disabling and the exposed persons are able to report to the appropriate health personnel under their own power. In extreme cases where the degree of asphyxia is severe, the immediate treatment should be that for carbon monoxide 32 poisoning.
A mixture of 95% oxygen and 5% carbon dioxide should be administered.
It is of great importance to keep the patient warm but if no oxygen supply equipment is available, he should be removed into fresh air regardless of the surrounding temperature.
In addition it may be necessary to apply artificial respiration.
If so, the arm-lift-back pressure (Nielsen) method should be employed and not mouth-to-mouth resuscitation.
# B. Precautions for Safe Use
Precautions taken in any area where nickel carbonyl is manufactured and/or used should include proper ventilation. Continuous local exhaust ventilation should provide air movement which is always from non-nickel carbonyl areas to areas containing nickel carbonyl. Where a fan is used to affect such air movement, the fan blades and throat should be made of a nonsparking material. Further, the exhaust from such exposure-risk areas should pass through a decontamination furnace before emission into the environment. These practices should be followed in the laboratory as well as in the commercial processing plant.
# C. Handling and Storage Precautions
Because nickel carbonyl is extremely volatile and flammable, it should be handled only when it is contained in steel bottles. Carbon dioxide fire extinguishers should be readily accessible in all nickel carbonyl storage and handling areas.
# IV. RESPIRATORS AND PROTECTIVE CLOTHING
# A. Respirators
In all areas where nickel carbonyl is manufactured, stored, or used, workers should wear full facepiece supplied-air respirators. The extreme toxicity and volatility of nickel carbonyl coupled with its nearly undetectable odor emphasize the need for careful observance of this recommendation.
# B. Protective Clothing
Absorption of nickel carbonyl through the skin has not been demonstrated but has been suggested. Therefore, the necessity for the use of protective gloves and impervious (e.g., rubber) clothing is uncertain.
However, in view of nickel carbonyl's volatility and the major threat of exposure to its vapor, the use of protective clothing is not suggested.
34
# ACKNOWLEDGEMENTS
# APPENDIX A PROCESS DESCRIPTIONS FOR MAJOR USES OF NICKEL CARBONYL
Nickel carbonyl is used world-wide as an intermediate in the Mond process for extracting pure nickel from its ores [3].
In this process, crude nickel is exposed to carbon monoxide gas at controlled temperature and pressure [4]. This results in the formation of nickel carbonyl vapor which is diverted to a decomposition chamber.
In this chamber, the combination of higher temperature and the existence of a "seeded" nickel compound promotes the formation of tiny nickel particles and the release of carbon monoxide.
The nickel particles are allowed to "grow" until they reach the size of small pellets, termed "nickel shot" at which time they are removed from the process.
Similarly, nickel is recovered from nickel sulfide by the carbonyl process [4]. The nickel sulfide, NiS and/or Ni3S2, is "roasted" (oxidized)
to produce the oxide, NiO, which is then reduced with "water gas" to form crude "sponge nickel". The "sponge nickel" is then treated with carbon monoxide to form nickel carbonyl which is decomposed with heat (as described earlier) to make nickel pellets or nickel powder.
In a process to produce methyl and ethyl acrylate monomers, nickel carbonyl, acetylene, carbon monoxide, an alcohol, and hydrogen chloride react continuously in carefully controlled ratios [42], Although carbon monoxide gas will not enter into this reaction initially, once the reaction has started CO will react with acetylene and alcohol to produce acrylate. | None | None |
a3733dd582c204fe5650cde481ec85fa13701a3a | cdc | None | The National Institute fo r Occupational Safety and Health (NIOSH) recommends that worker exposure to carbon tetrachloride in the workplace be controlled by adherence to the follow ing sections. The standard is designed to protect the health and provide fo r the safety of workers for up to a 10-hour workday, 40-hour workweek over a working lifetim e. Compliance w ith all sections of the standard should prevent the adverse effects currently reported from exposure to carbon tetrachloride in the workplace and m aterially reduce the risk of cancer from occupational exposure to carbon tetrachloride. The standard is meas urable by techniques tha t are valid, reproduc ible, and available. Sufficient technology exists to perm it com pliance w ith the recommended standard. The standard w ill be subject to fu r the r review and revision as necessary. " Occu pational exposure to carbon te trach lorid e" is defined as exposure to carbon tetrachloride in any establishm ent where carbon tetrachloride is used, m anufactured, or stored. Exposure to carbon tetrachloride under any of the above conditions w ill require adherence to all of the follow ing sections.
# Section 1 -Environmental (Workplace Air)
Carbon tetrachloride shall be controlled in the workplace so that the concentration of carbon tetrachloride is not greater than 2 ppm (12.6mg m3) of breathing zone air in a 45 liter a ir sample taken over a period not to exceed 1 hour in duration.
Procedures for sam pling and analysis of carbon tetrachloride in air shall be as provided in Appendices I and II, or by any method shown to be equivalent in precision, accuracy, and sensitivity to the methods specified.
Section 2 -Medical (a) Comprehensive preplacement and an nual medical examinations shall be made avail able to all workers exposed to carbon te tra chloride unless a different frequency is in d i cated by professional medical judgm ent based on such factors as emergencies, variations in work periods, and preexisting health status of individual workers.
(b) These examinations shall include, but shall not be lim ited to:
(1) A comprehensive and interim med ical and work history to include occurrence of nausea, vom iting, visual disturbances, and use of alcohol and barbiturates.
(2) A comprehensive medical examina tion, giving particular attention to kidneys, eyes (black and white and color visual fields), and appropriate tests of liver function.
(3) An evaluation of the w orker's phys ical a b ility to safely wear a respirator.
(c) Employees shall be counseled regard ing the increased hazards of working w ith car bon tetrachloride resulting from use of alcohol and barbiturates.
(d) Medical records shall be maintained for all persons employed in work involving occupational exposure to carbon tetrachloride fo r at least 30 years after the individu al's em ploym ent is term inated. The medical rep resentatives of the Secretary of Health, Educa tion, and Welfare, of the Secretary of Labor, of the employer, and of the employee or form er employee shall have access to these records.
(e) Initial exam inations for presently em ployed workers shall be offered w ithin 6 months of the prom ulgation of a standard in corporating these recommendations. (b) In areas where there is occupational exposure to carbon tetrachloride, the follow ing w arning sign shall be posted in readily visible locations, particularly at the entrances to the area.
# DANGER! EXTREME HEALTH HAZARD CANCER-SUSPECT AGENT USED IN THIS AREA UNAUTHORIZED PERSONS KEEP OUT
The sign shall be printed both in English and in the predom inant language of non-Englishspeaking workers, if any, unless employers use other equally effective means to ensure that these workers know the hazards associated w ith carbon tetrachloride and the locations of areas in which there is occupational exposure to carbon tetrachloride. Employers shall en sure that illiterate workers also know these hazards and the locations of these areas.
# Section 4 -Personal Protective Equipment
and Protective Clothing (a) Protective Clothing (1) Coveralls or other full-body protec tive clothing shall be worn in areas where there is occupational exposure to carbon tetrachlo ride. Protective clothing shall be changed at least daily at the end of the sh ift and more frequently if it should become grossly con tam inated.
(2) Impervious gloves, aprons, and footwear shall be worn at operations where carbon tetrachloride may contact the skin.
(3) Eye protective devices shall be provided by the employer and used by the employees where contact of carbon te tra chloride w ith eyes is likely. Selection, use, and maintenance of eye protective equipm ent shall follow the Standard Practice fo r Occupa tional and Educational Eye and Face Protec tion, ANSI Z87.1-1968. Unless eye protection is afforded by a respirator hood or facepiece, protective goggles or a face shield shall be worn at operations where there is danger of contact of the eyes w ith wet m aterials contain ing carbon, tetrachloride because of spills, splashes, or excessive vapors in the air.
(4) The em ployer shall ensure that all personal protective devices are inspected reg ularly and maintained in clean and satisfactory working condition.
(5) Work clothing may not be taken home by employees. The em ployer shall pro vide for maintenance and laundering of pro tective clothing.
(6)The employer shall ensure that pre cautions necessary to protect laundry person nel are taken while soiled protective clothing is being laundered.
(7) The employer shall ensure that carbon tetrachloride is not discharged into m unicipal waste treatm ent systems or the com m unity air.
(b) Respiratory Protection from Carbon Tetrachloride.
Engineering controls shall be used w her ever feasible to m aintain carbon tetrachloride concentrations at or below that recommended in Section 1 above. Compliance with the en vironm ental exposure lim it by the use of respi rators is allowed only when carbon tetrachlo ride concentrations are in excess of the work place environmental lim it because required engineering controls are being installed or tested, when nonroutine maintenance or re pair is being accomplished, or during emer gencies. When a respirator is thus perm itted, it shall be selected and used in accordance w ith the follow ing requirem ents:
(1) For the purpose of determ ining if it is necessary fo r workers to wear respirators, the employer shall measure the concentration of carbon tetrachloride in the workplace in i tia lly and thereafter whenever process, work site, clim ate, or control changes occur which are likely to increase the concentration of car bon tetrachloride.
(2) The em ployer shall ensure that no worker is exposed to carbon tetrachloride above the workplace environm ental lim it be cause of im proper respirator selection, fit, use, or maintenance.
(3) A respiratory protection program meeting the requirem ents of 29 CFR 1910.134 and 30 CFR 11 which incorporates the Am eri can National Standard Practices for Respira tory Protection Z88.2-1969 shall be established and enforced by the employer.
(4) The employer shall provide res pirators in accordance with Table 1-1 and shall ensure that the employee uses the respirator provided anytime the concentration of carbon tetrachloride exceeds the level described in Section 1.
(5) Respirators described in Table 1-1 shall be those approved under the provisions of 29 CFR 1910.134 and 30 CFR 11. (6) The employer shall ensure that res pirators are adequately cleaned, and that em ployees are instructed on the use of respirators assigned to them, th e ir location in the work place, and on how to test for leakage.
(7) Where an emergency may develop which could result in employee injury from carbon tetrachloride, the em ployer shall pro vide an escape device as listed in At the beginning of em ploym ent or assign ment fo r work in a carbon tetrachloride area, employees w ith occupational exposure to car bon tetrachloride shall be inform ed of the hazards, relevant signs and symptoms of over exposure, appropriate emergency procedures, and proper conditions and precautions for the safe use of carbon tetrachloride.
Instruction shall include, as a m inim um , all inform ation in Appendix III which is a ppli cable to the specific carbon tetrachloride product or material to which there is exposure, as well as inform ation which indicates that carbon tetrachloride causes cancer in experi mental animals. The inform ation shall be posted in the work area and kept on file, read ily accessible to the worker at all places of em ploym ent where carbon tetrachloride is in volved in unit processes and operations.
A continuing educational program shall be instituted to ensure that all workers have cur rent knowledge of job hazards, proper m ain tenance procedures, and cleanup methods, and that they know how to use respiratory protective equipm ent and protective clothing correctly.
Inform ation as specified in Appendix III shall be recorded on the Material Safety Data Sheet or a sim ilar form approved by the Occu pational Safety and Health A dm inistration, US Department of Labor.
# Section 6 -Work Practices (a) Control of Airborne Contamination
Emission of vapors of carbon tetrachloride shall be controlled at the sources of dispersion by means of effective and properly m aintained methods such as fu lly enclosed operations and local exhaust ventilation, under negative pres sure, if possible. No recirculation of control ventilation or process air shall bë" perm itted. Other methods may be used if they are shown to effectively control airborne concentrations of carbon tetrachloride w ithin the lim it of the recommended standard.
# (b) Control of Contact w ith Skin and Eyes
(1) Employees working in areas where contact of skin or eyes w ith carbon te tra chloride is possible shall wear full-body pro tective clothing, including neck and head coverings, and gloves, in accord w ith Section 4(a).
(2) Clean protective clothing shall be put on before each work shift.
(3) If, during the shift, the clothing becomes wetted w ith carbon tetrachloride, it shall be removed prom ptly and placed in a special container for garments for decontam i nation or disposal. The employee shall wash the contam inated skin area thoroughly with soap and a copious am ount of water. A com plete shower is preferred after anything but lim ited, m inor contact. Then, clean protective clothing shall be put on before resuming work.
(4) Small areas of skin (principally the hands) contam inated by contact w ith carbon tetrachloride shall be washed im m ediately and thoroughly with an abundance of water. Water shall be easily accessible in the work areas as low-pressure, free-running hose lines or showers.
(5) If carbon tetrachloride comes into contact with the eyes, the eyes should be flushed with a large volume of low-pressure flowing water for at least 15 minutes. Medical attention shall be obtained w ithout delay, but not at the expense of im m ediate and thorough flushing of the eyes.
(c) Procedures for emergencies, including firefighting, shall be established to meet fore seeable events. Necessary emergency equip ment, including appropriate respiratory pro tective devices, shall be kept in readily ac cessible locations. Only self-contained breath ing apparatus w ith positive pressure in the facepiece shall be used in firefighting. Appro priate respirators shall be available for use during evacuation.
(d) Special supervision and care shall be exercised to ensure tha t the exposures of re pair and maintenance personnel to carbon tetrachloride are w ithin the lim it prescribed by this standard.
(e) Prompt cleaning of spills of carbon tetrachloride:
Spills shall be channeled for appro priate treatm ent or collection for disposal. They may not be channeled directly into the m unicipal sanitary sewer system.
(f) General requirements:
(1) Good housekeeping practices shall be observed to prevent or m inim ize contam ina tion of areas and equipm ent and to prevent build-up of such contam ination.
(2) Good personal hygiene practices shall be encouraged.
(3) Equipm ent shall be kept in good repair and free of leaks.
(4) Containers of carbon tetrachloride shall be kept covered insofar as is practical.
(g) A regulated area shall be established and maintained where:
(1) Carbon tetrachloride is m anufac tured, reacted, mixed w ith other substances, repackaged, stored, handled, or used.
(2) Concentrations of carbon tetrachlo ride are in excess of the workplace environ mental lim it in Section 1.
(h) Access to the regulated areas desig nated by Section 6(g) shall be lim ited to authorized persons. A daily roster shall be made of persons authorized to enter; these rosters shall be m aintained fo r 30 years.
(i) Employers shall ensure that before employees leave a regulated area they remove and leave protective clothing at that point.
# Section 7 -Sanitation
(a) Washing Facilities Emergency showers and eye-flushing foun tains with cool water under adequate pressure shall be provided and readily accessible in areas where contact of skin or eyes w ith car bon tetrachloride may occur. This equipm ent shall be frequently inspected and maintained in good working condition.
Showers and washbasins shall be provided in the employees' locker areas. Employers shall ensure that employees exposed to car bon tetrachloride during th e ir work s h ift shall wash before eating or smoking periods taken during the work shift.
(b) Food Facilities Food storage and preparation as well as eating shall be prohibited in areas where car bon tetrachloride is handled, processed, or stored. Eating facilities provided for employees shall be located in areas ventilated in such a manner to ensure that contam ination from carbon tetrachloride is prevented. Surfaces in these areas shall be kept free of carbon tetrachloride. Employers shall ensure that be fore employees enter premises reserved for eating, food storage, or food preparation, they remove protective clothing. Washing facilities should be accessible nearby.
(c) Employees may not smoke in areas where carbon tetrachloride is handled, proc essed, or stored.
(d) Clothing and Locker Room Facilities Locker room fa c ilitie s for employees re quired to change clothing before and after work shall be provided in an area separate and ventilated in such a manner to ensure that contam ination from carbon tetrachloride is non-existent. The fa cilitie s shall provide for the storing of street clothing and clean work clothing separately from soiled work clothing. Showers and washbasins should be located in the locker area to encourage good personal hygiene.
Covered containers should be provided for work clothing discarded at the end of the sh ift or after a contam ination incident. The clothing shall be held in these containers until removed for decontam ination or disposal.
# Section 8 -M onitoring and Recordkeeping Requirements
In any workplace where carbon tetrachlo ride is handled or processed, surveys shall be repeated semi-annually. Requirements set forth below apply to areas in which there is occupational exposure to carbon tetrachloride.
Employers shall m aintain records of work place environm ental exposures to carbon te t rachloride based on the follow ing sampling, analytical, and recording schedules:
(a) In all monitoring, samples representa tive of the exposure in the breathing zone of employees shall be collected by personal samplers.
(b) An adequate num ber of samples shall be taken in order to determ ine the occupa tional exposure of each employee.
(c) The firs t determ ination of employee exposure to carbon tetrachloride shall be completed w ithin 6 months after the prom ul gation of a standard incorporating these recom mendations.
(d) A réévaluation of the exposure of em ployees to carbon tetrachloride shall be made w ithin 30 days after installation of a new process or process changes.
(e) A réévaluation of employee exposure to carbon tetrachloride shall be repeated at 1-week intervals when the airborne concen tration has been found to exceed the recom mended workplace environm ental lim it. In such cases, suitable controls shall be instituted and m onitoring shall continue at 1-week in te r vals until 3 consecutive surveys indicate the adequacy of controls.
(f) Records of all sam pling and analysis of carbon tetrachloride and of m edical exam ina tions shall be maintained for at least 30 years after the individual's em ploym ent is te rm i nated. Records shall indicate the details of (1) type of personal protective devices, if any, in use at the tim e of sampling, and (2) methods of sam pling and analysis used. Each employee shall be able to obtain inform ation on his own exposure. If the employer who has or has had employees w ith occupational exposure to car bon tetrachloride ceases business w ithout a successor, he shall forward th e ir records by registered mail to the Director, National Insti tute for Occupational Safety and Health.
# D E P A R T M E N T O F H E A L T H , E D U C A T I O N , A N D W E L F A R E PUBLIC HEALTH SERVICE C E N T E R F O R D I S E A S E C O N T R O L N A T I O N A L I N S T I T U T E F O R O C C U P A T I O N A L S A F E T Y A N D H E A L T H R O B E R T A . T A F T L A B O R | #
The National Institute fo r Occupational Safety and Health (NIOSH) recommends that worker exposure to carbon tetrachloride in the workplace be controlled by adherence to the follow ing sections. The standard is designed to protect the health and provide fo r the safety of workers for up to a 10-hour workday, 40-hour workweek over a working lifetim e. Compliance w ith all sections of the standard should prevent the adverse effects currently reported from exposure to carbon tetrachloride in the workplace and m aterially reduce the risk of cancer from occupational exposure to carbon tetrachloride. The standard is meas urable by techniques tha t are valid, reproduc ible, and available. Sufficient technology exists to perm it com pliance w ith the recommended standard. The standard w ill be subject to fu r the r review and revision as necessary. " Occu pational exposure to carbon te trach lorid e" is defined as exposure to carbon tetrachloride in any establishm ent where carbon tetrachloride is used, m anufactured, or stored. Exposure to carbon tetrachloride under any of the above conditions w ill require adherence to all of the follow ing sections.
# Section 1 -Environmental (Workplace Air)
Carbon tetrachloride shall be controlled in the workplace so that the concentration of carbon tetrachloride is not greater than 2 ppm (12.6mg m3) of breathing zone air in a 45 liter a ir sample taken over a period not to exceed 1 hour in duration.
Procedures for sam pling and analysis of carbon tetrachloride in air shall be as provided in Appendices I and II, or by any method shown to be equivalent in precision, accuracy, and sensitivity to the methods specified.
Section 2 -Medical (a) Comprehensive preplacement and an nual medical examinations shall be made avail able to all workers exposed to carbon te tra chloride unless a different frequency is in d i cated by professional medical judgm ent based on such factors as emergencies, variations in work periods, and preexisting health status of individual workers.
(b) These examinations shall include, but shall not be lim ited to:
(1) A comprehensive and interim med ical and work history to include occurrence of nausea, vom iting, visual disturbances, and use of alcohol and barbiturates.
(2) A comprehensive medical examina tion, giving particular attention to kidneys, eyes (black and white and color visual fields), and appropriate tests of liver function.
(3) An evaluation of the w orker's phys ical a b ility to safely wear a respirator.
(c) Employees shall be counseled regard ing the increased hazards of working w ith car bon tetrachloride resulting from use of alcohol and barbiturates.
(d) Medical records shall be maintained for all persons employed in work involving occupational exposure to carbon tetrachloride fo r at least 30 years after the individu al's em ploym ent is term inated. The medical rep resentatives of the Secretary of Health, Educa tion, and Welfare, of the Secretary of Labor, of the employer, and of the employee or form er employee shall have access to these records.
(e) Initial exam inations for presently em ployed workers shall be offered w ithin 6 months of the prom ulgation of a standard in corporating these recommendations. (b) In areas where there is occupational exposure to carbon tetrachloride, the follow ing w arning sign shall be posted in readily visible locations, particularly at the entrances to the area.
# DANGER! EXTREME HEALTH HAZARD CANCER-SUSPECT AGENT USED IN THIS AREA UNAUTHORIZED PERSONS KEEP OUT
The sign shall be printed both in English and in the predom inant language of non-Englishspeaking workers, if any, unless employers use other equally effective means to ensure that these workers know the hazards associated w ith carbon tetrachloride and the locations of areas in which there is occupational exposure to carbon tetrachloride. Employers shall en sure that illiterate workers also know these hazards and the locations of these areas.
# Section 4 -Personal Protective Equipment
and Protective Clothing (a) Protective Clothing (1) Coveralls or other full-body protec tive clothing shall be worn in areas where there is occupational exposure to carbon tetrachlo ride. Protective clothing shall be changed at least daily at the end of the sh ift and more frequently if it should become grossly con tam inated.
(2) Impervious gloves, aprons, and footwear shall be worn at operations where carbon tetrachloride may contact the skin.
(3) Eye protective devices shall be provided by the employer and used by the employees where contact of carbon te tra chloride w ith eyes is likely. Selection, use, and maintenance of eye protective equipm ent shall follow the Standard Practice fo r Occupa tional and Educational Eye and Face Protec tion, ANSI Z87.1-1968. Unless eye protection is afforded by a respirator hood or facepiece, protective goggles or a face shield shall be worn at operations where there is danger of contact of the eyes w ith wet m aterials contain ing carbon, tetrachloride because of spills, splashes, or excessive vapors in the air.
(4) The em ployer shall ensure that all personal protective devices are inspected reg ularly and maintained in clean and satisfactory working condition.
(5) Work clothing may not be taken home by employees. The em ployer shall pro vide for maintenance and laundering of pro tective clothing.
(6)The employer shall ensure that pre cautions necessary to protect laundry person nel are taken while soiled protective clothing is being laundered.
(7) The employer shall ensure that carbon tetrachloride is not discharged into m unicipal waste treatm ent systems or the com m unity air.
(b) Respiratory Protection from Carbon Tetrachloride.
Engineering controls shall be used w her ever feasible to m aintain carbon tetrachloride concentrations at or below that recommended in Section 1 above. Compliance with the en vironm ental exposure lim it by the use of respi rators is allowed only when carbon tetrachlo ride concentrations are in excess of the work place environmental lim it because required engineering controls are being installed or tested, when nonroutine maintenance or re pair is being accomplished, or during emer gencies. When a respirator is thus perm itted, it shall be selected and used in accordance w ith the follow ing requirem ents:
(1) For the purpose of determ ining if it is necessary fo r workers to wear respirators, the employer shall measure the concentration of carbon tetrachloride in the workplace in i tia lly and thereafter whenever process, work site, clim ate, or control changes occur which are likely to increase the concentration of car bon tetrachloride.
(2) The em ployer shall ensure that no worker is exposed to carbon tetrachloride above the workplace environm ental lim it be cause of im proper respirator selection, fit, use, or maintenance.
(3) A respiratory protection program meeting the requirem ents of 29 CFR 1910.134 and 30 CFR 11 which incorporates the Am eri can National Standard Practices for Respira tory Protection Z88.2-1969 shall be established and enforced by the employer.
(4) The employer shall provide res pirators in accordance with Table 1-1 and shall ensure that the employee uses the respirator provided anytime the concentration of carbon tetrachloride exceeds the level described in Section 1.
(5) Respirators described in Table 1-1 shall be those approved under the provisions of 29 CFR 1910.134 and 30 CFR 11. (6) The employer shall ensure that res pirators are adequately cleaned, and that em ployees are instructed on the use of respirators assigned to them, th e ir location in the work place, and on how to test for leakage.
(7) Where an emergency may develop which could result in employee injury from carbon tetrachloride, the em ployer shall pro vide an escape device as listed in At the beginning of em ploym ent or assign ment fo r work in a carbon tetrachloride area, employees w ith occupational exposure to car bon tetrachloride shall be inform ed of the hazards, relevant signs and symptoms of over exposure, appropriate emergency procedures, and proper conditions and precautions for the safe use of carbon tetrachloride.
Instruction shall include, as a m inim um , all inform ation in Appendix III which is a ppli cable to the specific carbon tetrachloride product or material to which there is exposure, as well as inform ation which indicates that carbon tetrachloride causes cancer in experi mental animals. The inform ation shall be posted in the work area and kept on file, read ily accessible to the worker at all places of em ploym ent where carbon tetrachloride is in volved in unit processes and operations.
A continuing educational program shall be instituted to ensure that all workers have cur rent knowledge of job hazards, proper m ain tenance procedures, and cleanup methods, and that they know how to use respiratory protective equipm ent and protective clothing correctly.
Inform ation as specified in Appendix III shall be recorded on the Material Safety Data Sheet or a sim ilar form approved by the Occu pational Safety and Health A dm inistration, US Department of Labor.
# Section 6 -Work Practices (a) Control of Airborne Contamination
Emission of vapors of carbon tetrachloride shall be controlled at the sources of dispersion by means of effective and properly m aintained methods such as fu lly enclosed operations and local exhaust ventilation, under negative pres sure, if possible. No recirculation of control ventilation or process air shall bë" perm itted. Other methods may be used if they are shown to effectively control airborne concentrations of carbon tetrachloride w ithin the lim it of the recommended standard.
# (b) Control of Contact w ith Skin and Eyes
(1) Employees working in areas where contact of skin or eyes w ith carbon te tra chloride is possible shall wear full-body pro tective clothing, including neck and head coverings, and gloves, in accord w ith Section 4(a).
(2) Clean protective clothing shall be put on before each work shift.
(3) If, during the shift, the clothing becomes wetted w ith carbon tetrachloride, it shall be removed prom ptly and placed in a special container for garments for decontam i nation or disposal. The employee shall wash the contam inated skin area thoroughly with soap and a copious am ount of water. A com plete shower is preferred after anything but lim ited, m inor contact. Then, clean protective clothing shall be put on before resuming work.
(4) Small areas of skin (principally the hands) contam inated by contact w ith carbon tetrachloride shall be washed im m ediately and thoroughly with an abundance of water. Water shall be easily accessible in the work areas as low-pressure, free-running hose lines or showers.
(5) If carbon tetrachloride comes into contact with the eyes, the eyes should be flushed with a large volume of low-pressure flowing water for at least 15 minutes. Medical attention shall be obtained w ithout delay, but not at the expense of im m ediate and thorough flushing of the eyes.
(c) Procedures for emergencies, including firefighting, shall be established to meet fore seeable events. Necessary emergency equip ment, including appropriate respiratory pro tective devices, shall be kept in readily ac cessible locations. Only self-contained breath ing apparatus w ith positive pressure in the facepiece shall be used in firefighting. Appro priate respirators shall be available for use during evacuation.
(d) Special supervision and care shall be exercised to ensure tha t the exposures of re pair and maintenance personnel to carbon tetrachloride are w ithin the lim it prescribed by this standard.
(e) Prompt cleaning of spills of carbon tetrachloride:
Spills shall be channeled for appro priate treatm ent or collection for disposal. They may not be channeled directly into the m unicipal sanitary sewer system.
(f) General requirements:
(1) Good housekeeping practices shall be observed to prevent or m inim ize contam ina tion of areas and equipm ent and to prevent build-up of such contam ination.
(2) Good personal hygiene practices shall be encouraged.
(3) Equipm ent shall be kept in good repair and free of leaks.
(4) Containers of carbon tetrachloride shall be kept covered insofar as is practical.
(g) A regulated area shall be established and maintained where:
(1) Carbon tetrachloride is m anufac tured, reacted, mixed w ith other substances, repackaged, stored, handled, or used.
(2) Concentrations of carbon tetrachlo ride are in excess of the workplace environ mental lim it in Section 1.
(h) Access to the regulated areas desig nated by Section 6(g) shall be lim ited to authorized persons. A daily roster shall be made of persons authorized to enter; these rosters shall be m aintained fo r 30 years.
(i) Employers shall ensure that before employees leave a regulated area they remove and leave protective clothing at that point.
# Section 7 -Sanitation
(a) Washing Facilities Emergency showers and eye-flushing foun tains with cool water under adequate pressure shall be provided and readily accessible in areas where contact of skin or eyes w ith car bon tetrachloride may occur. This equipm ent shall be frequently inspected and maintained in good working condition.
Showers and washbasins shall be provided in the employees' locker areas. Employers shall ensure that employees exposed to car bon tetrachloride during th e ir work s h ift shall wash before eating or smoking periods taken during the work shift.
(b) Food Facilities Food storage and preparation as well as eating shall be prohibited in areas where car bon tetrachloride is handled, processed, or stored. Eating facilities provided for employees shall be located in areas ventilated in such a manner to ensure that contam ination from carbon tetrachloride is prevented. Surfaces in these areas shall be kept free of carbon tetrachloride. Employers shall ensure that be fore employees enter premises reserved for eating, food storage, or food preparation, they remove protective clothing. Washing facilities should be accessible nearby.
(c) Employees may not smoke in areas where carbon tetrachloride is handled, proc essed, or stored.
(d) Clothing and Locker Room Facilities Locker room fa c ilitie s for employees re quired to change clothing before and after work shall be provided in an area separate and ventilated in such a manner to ensure that contam ination from carbon tetrachloride is non-existent. The fa cilitie s shall provide for the storing of street clothing and clean work clothing separately from soiled work clothing. Showers and washbasins should be located in the locker area to encourage good personal hygiene.
Covered containers should be provided for work clothing discarded at the end of the sh ift or after a contam ination incident. The clothing shall be held in these containers until removed for decontam ination or disposal.
# Section 8 -M onitoring and Recordkeeping Requirements
In any workplace where carbon tetrachlo ride is handled or processed, surveys shall be repeated semi-annually. Requirements set forth below apply to areas in which there is occupational exposure to carbon tetrachloride.
Employers shall m aintain records of work place environm ental exposures to carbon te t rachloride based on the follow ing sampling, analytical, and recording schedules:
(a) In all monitoring, samples representa tive of the exposure in the breathing zone of employees shall be collected by personal samplers.
(b) An adequate num ber of samples shall be taken in order to determ ine the occupa tional exposure of each employee.
(c) The firs t determ ination of employee exposure to carbon tetrachloride shall be completed w ithin 6 months after the prom ul gation of a standard incorporating these recom mendations.
(d) A réévaluation of the exposure of em ployees to carbon tetrachloride shall be made w ithin 30 days after installation of a new process or process changes.
(e) A réévaluation of employee exposure to carbon tetrachloride shall be repeated at 1-week intervals when the airborne concen tration has been found to exceed the recom mended workplace environm ental lim it. In such cases, suitable controls shall be instituted and m onitoring shall continue at 1-week in te r vals until 3 consecutive surveys indicate the adequacy of controls.
(f) Records of all sam pling and analysis of carbon tetrachloride and of m edical exam ina tions shall be maintained for at least 30 years after the individual's em ploym ent is te rm i nated. Records shall indicate the details of (1) type of personal protective devices, if any, in use at the tim e of sampling, and (2) methods of sam pling and analysis used. Each employee shall be able to obtain inform ation on his own exposure. If the employer who has or has had employees w ith occupational exposure to car bon tetrachloride ceases business w ithout a successor, he shall forward th e ir records by registered mail to the Director, National Insti tute for Occupational Safety and Health.
# D E P A R T M E N T O F H E A L T H , E D U C A T I O N , A N D W E L F A R E PUBLIC HEALTH SERVICE C E N T E R F O R D I S E A S E C O N T R O L N A T I O N A L I N S T I T U T E F O R O C C U P A T I O N A L S A F E T Y A N D H E A L T H R O B E R T A . T A F T L A B O R
| None | None |
de525cf852a4ba8e51c97cf9128cdb7420bf260c | cdc | None | depar depar depar depar department of health and human ser tment of health and human ser tment of health and human ser tment of health and human ser tment of health and human services vices vices vices vices# Introduction
Influenza transmission and outbreaks in hospitals (1)(2)(3)(4)(5)(6)(7)(8) and nursing homes (9-13) are well documented. HCP can acquire influenza from patients or transmit influenza to patients and other staff. Despite the documented benefits of HCP influenza vaccination on patient outcomes (14,15) and HCP absenteeism (16) and on reducing influenza infection among staff (16,17), vaccination coverage among HCP remain low (i.e., 65 years) and those who have underlying chronic medical conditions or who might be pregnant are at increased risk for influenza-related complications. Achieving and sustaining high vaccination coverage among HCP will protect staff and their patients, and reduce disease burden and health-care costs.
This report summarizes recommendations of the Healthcare Infection Control Practices Advisory Committee (HICPAC) and the Advisory Committee on Immunization Practices (ACIP) concerning influenza vaccination of health-care personnel (HCP)- in the United States. These recommendations are targeted at health-care facility administrators, infection control professionals, and occupational health professionals responsible for influenza vaccination programs and influenza infection control programs in their institutions. HICPAC and ACIP recommend that all HCP be vaccinated annually against influenza. Facilities that employ HCP are strongly encouraged to provide vaccine to their staff by using - In this report, the term HCP refers to all paid and unpaid persons working in health-care settings who have the potential for exposure to infectious materials, including body substances, contaminated medical supplies and equipment, contaminated environmental surfaces, or contaminated air. HCP might include (but are not limited to) physicians, nurses, nursing assistants, therapists, technicians, emergency medical service personnel, dental personnel, pharmacists, laboratory personnel, autopsy personnel, students and trainees, contractual staff not employed by the health-care facility, and persons (e.g., clerical, dietary, housekeeping, maintenance, and volunteers) not directly involved in patient care but potentially exposed to infectious agents that can be transmitted to and from HCP. The recommendations in this report apply to HCP in acute care hospitals, nursing homes, skilled nursing facilities, physician's offices, urgent care centers, and outpatient clinics, and to persons who provide home health care and emergency medical services.
# Summary Recommendations
The summary recommendations contained in this report are categorized by using the HICPAC evidence ranking system (Table 1). The recommendations were drafted after review of peer-reviewed scientific articles, and whenever possible are based on well-designed studies; certain recommendations are based on strong theoretic rationale and expert opinion. All recommendations have been approved by HICPAC and ACIP. The committees involved in drafting and reviewing these recommendations included persons with expertise in infectious diseases, infection control, pediatrics, vaccinology, internal medicine, and public health. The recommendations are as follows:
- Educate HCP regarding the benefits of influenza vaccination and the potential health consequences of influenza illness for themselves and their patients, the epidemiology and modes of transmission, diagnosis, treatment, and nonvaccine infection control strategies, in accordance with their level of responsibility in preventing health-care-associated influenza (category IB).
# Background Influenza Among HCP
A limited number of prospective and cross-sectional studies provide estimates of incidence of influenza and influenza-like illness (ILI) among HCP (17,19,20). In one serosurvey of HCP, 23% of HCP had documented serologic evidence of influenza infection after a mild influenza season; however, of these, 59% could not recall having influenza, and 28% could not recall any respiratory infection, suggesting a high proportion of asymptomatic illness (17). In a randomized trial of influenza vaccine among HCP, 13% of placebo recipients subsequently had influenza infection (18). In a cross-sectional survey of house staff, 37% reported ILI during an 8-month period (September-April); 9% reported more than one illness. Length of illness varied (range: 1-10 days; mean: 7 days), as did the number of days of work missed (range: 0-10 days; mean: 0.7 days) (20).
# Efficacy and Effectiveness of Influenza Vaccines Among Adults
Trivalent inactivated influenza vaccine prevents influenza illness among approximately 70%-90% of healthy adults aged 65 years and persons with certain chronic conditions (e.g., diabetes, human immunodeficiency virus (HIV), or chronic obstructive pulmonary disease) (24)(25)(26)(27)(28). Vaccination of healthy adults also decreases work absenteeism and use of health-care resources, including antibiotics, when the vaccine and circulating viruses are well matched (17,21,23,(29)(30)(31). In addition, influenza vaccine prevents secondary complications and reduces the risk for influenza-related hospitalization and death among adults aged >65 years with and without high-risk medical conditions (e.g., heart disease and diabetes) (32)(33)(34)(35)(36).
LAIV has demonstrated similar benefits in randomized controlled trials among healthy working adults aged 18-64 years. In one study, vaccination with LAIV reduced severe febrile illnesses 19% and upper respiratory tract illnesses 24%; LAIV use also was associated with fewer days of illness and of work lost, fewer health-care provider visits, and reduced use of prescription antibiotics and over-the-counter medications (37). These results were recorded during a season in which the vaccine and circulating influenza A (H3N2) strains were not well matched. In the same study, LAIV vaccination yielded similar benefits among a subset of healthy adults aged 18-49 years, and antibiotic use in this age group decreased 41%-51% (37). In one study, overall efficacy of LAIV and inactivated influenza vaccine in preventing laboratory-documented influenza was 85% and 71%, respectively (38).
# Impact of HCP Vaccination on Influenza in Health-Care Settings
Vaccination of HCP is an important component of influenza prevention programs in the United States (18). Vaccination of HCP reduces transmission of influenza in health-care settings, staff illness and absenteeism, and influenza-related morbidity and mortality among persons at increased risk for severe influenza illness (14-17). Use of antiviral drugs used for chemoprophylaxis or treatment of influenza is an adjunct to (but not a substitute for) vaccination (18).
# Transmission of Influenza in Health-Care Settings
Influenza outbreaks in hospitals (4,39) and long-term-care facilities (40) have been associated with low vaccination rates among HCP. In addition, higher vaccination levels among staff have been associated with a lower incidence of nosocomial influenza cases (14,15,39).
In one tertiary care facility in which routine surveillance for influenza was conducted, the relation between staff vaccination coverage and annual incidence of nosocomial influenza was assessed for 12 influenza seasons during 1987-2000. During this period, staff vaccination coverage increased from 4% during 1987-1988 to 67% during 1999-2000 (p<0.0001), and the proportion of laboratory-confirmed cases of influenza that occurred among HCP decreased from 42% during 1990-1993 to 9% during 1997-2000 (p<0.0001). The proportion of nosocomial cases among hospitalized patients decreased 32% to 0 (p<0.0001). After controlling for potential confounders by using logistic regression, a significant and inverse relationship was demonstrated between vaccination rates among HCP and the rate of nosocomial influenza among patients, suggesting that staff vaccination contributed to the observed decline in the number of nosocomial influenza cases (39).
# Staff Illness and Absenteeism
During an influenza season, HCP might acquire influenza from infected patients with resulting morbidity and absenteeism. The impact of influenza vaccination on staff illness and absenteeism has been evaluated in two randomized, placebocontrolled, double-blind trials. In one trial, HCP who received vaccine had 28% fewer documented lost work days attributable to respiratory infections (1.0 and 1.4, respectively; p = 0.02) and 28% fewer days on which they felt unable to work, whether they were on or off duty (2.5 and 3.5, respectively; p = 0.02). Vaccination did not reduce either the number of episodes (1.8 and 2.0, respectively) or the total number of days (13.5 and 14.6, respectively) of respiratory infection (16). In a second trial conducted in two large teaching hospitals for 3 consecutive years that measured serologically confirmed influenza, days of febrile respiratory illness, and days absent from work, HCP who received influenza vaccine had a substantially lower incidence of influenza than controls (1.7% and 13.4%, respectively) with an estimated vaccine efficacy against serologically defined influenza A and influenza B infection of 88% and 89%, respectively. HCP who received influenza vaccine also tended to have fewer total respiratory illnesses (28.7 and 40.6 per 100 persons, respectively; p = 0.57) and days of lost work (9.9 and 21.1 per 100 persons, respectively; p = 0.41) than did controls (17).
In a cross-sectional survey, similar reductions in staff illness episodes and days of illness were reported (20). Overall, compared with unvaccinated coworkers, vaccinated house staff reported 23% fewer ILIs (42 and 54 per 100 persons, respectively; p = 0.03), 27% fewer days of illness (80 and 115 per 100 persons, respectively; p = 0.02), and a 59% reduction in illness during vacation time (1.7% and 4.0% of persons, respectively; p = 0.08). The two groups had a similar number of lost work days attributable to ILI (18 and 21 per 100 subjects, respectively; p = 0.69). During influenza season, vaccination was associated with reductions of 30% in ILI (p = 0.05), 43% in the proportion of house staff reporting illnesses associated with fever and cough (p = 0.05), and 63% in illnesses associated with fever and cough (p = 0.03). The inability to consistently demonstrate statistically significant decreases in absenteeism among staff who received vaccination is likely attributable to the finding that HCP tend to work despite illness (17,41).
# Patient Outcomes
HCP who are clinically or subclinically infected can transmit influenza virus to other persons. Decreasing transmission of influenza from caregivers to persons at high risk might reduce influenza-related deaths among persons at high risk for complications from influenza.
Residents of long-term-care facilities are particularly vulnerable to influenza and influenza-related complications. In1999, an estimated 1.6 million persons resided in nursing homes in the United States (42). During influenza outbreaks in long-term-care facilities, attack rates among residents have ranged as high as 25%-60%, with case-fatality rates of 10%-20% (13,(43)(44)(45). When vaccine and epidemic strains are well matched, achieving increased vaccination rates among persons living in closed settings (e.g., nursing homes and other chronic-care facilities) and among staff can reduce the risk for outbreaks by inducing herd immunity (32).
Two randomized controlled trials have evaluated the impact of influenza vaccination of HCP on the outcomes of residents in nursing homes. In one study, staff vaccination was associated with a 43% decrease in incidence of ILI (odds ratio = 0.6; 95% confidence interval = 0.3-0.9) and a 44% decrease in overall mortality among facility residents, from 17% to 10% (OR = 0.6; 95% CI = 0.4-0.8) (15). No virologic data were provided in this study. In a second study, 20 long-term-care facilities were randomized to have vaccine routinely offered (intervention facilities) or not offered (control facilities) to their staff (14). Facilities were paired by number of beds and patient vaccination policies. Staff vaccination coverage was higher in intervention facilities than in control facilities (50.9% and 4.9%, respectively). Crude mortality rates were 42% lower among residents in facilities with higher staff vaccination coverage than those in control facilities (13.6% and 22.4%, respectively; OR = 0.6; 95% CI = 0.4-0.8; p = 0.014). Incidence of laboratory-confirmed influenza did not differ between the two groups (5.4% and 6.7%, respectively), but postmortem samples from pa-tients in control facilities were more likely to be positive for influenza by a polymerase chain reaction test than samples from patients in intervention facilities (six of 30 and none of 17, respectively; p = 0.055), suggesting that in this study population, HCP vaccination reduced influenza-related mortality in patients despite not reducing the incidence of non-fatal influenza infection. In neither study was a significant association demonstrated between patient vaccination and mortality. Randomized trials assessing the impact of staff vaccination on patient outcomes in acute care facilities have not been conducted, but low staff vaccination coverage has been correlated with influenza outbreaks in hospitals (4,39).
# Cost-Effectiveness of Influenza Vaccine
Cost-effectiveness studies of adults aged 70% of the costs prevented were associated with reductions in lost work productivity.
# Vaccination Coverage Levels Among HCP
During 1989-2003, HCP vaccination coverage levels in the United States increased substantially, from 10% to 40%; however, coverage levels have remained relatively constant since 1997 (18). One of the national health objectives for 2010 is to achieve HCP vaccination coverage levels of 60% (objective no. 14-29g) (51). Substantially lower vaccination rates have been reported among HCP who have contact with certain populations at high risk (12,(52)(53)(54). In addition, HCP vaccination coverage varies by level and years of training, age, occupational group, and facility type (20,55,56).
# Barriers to HCP Vaccination
Reported barriers to HCP receipt or acceptance of influenza vaccination include fear of vaccine side effects (particularly ILI symptoms) (20,55,(57)(58)(59)(60)(61), insufficient time or inconvenience (20), perceived ineffectiveness of the vaccine (20,55,58,59), medical contraindication (55), perceived low likelihood of contracting influenza (55,60,62), reliance on treatment with homeopathic medications (55,62), avoidance of medications (57), and fear of needles (57,59). Factors facilitating vaccine acceptance include a desire for selfprotection (20,58,61), previous receipt of influenza vaccine (57,58,(63)(64)(65), a desire to protect patients (61), and perceived effectiveness of vaccine (20).
# Strategies for Improving HCP Vaccination Rates
Facilities that employ HCP are strongly encouraged to provide vaccine to staff by using evidence-based approaches that maximize vaccination rates. Successful HCP vaccination programs are multifaceted and combine publicity and education to combat fears and misconceptions about influenza and influenza vaccines, use of reminder recall systems, efforts to remove administrative and financial barriers, role modeling, and monitoring and feedback on vaccination coverage (66). In contrast, single-component interventions will likely have minimal effectiveness in achieving desired vaccination coverage levels (66,67).
# Education and Campaigns
HCP knowledge, perceptions, and attitudes regarding influenza and influenza vaccination vary (20). Basic knowledge about influenza and influenza vaccination has been associated with vaccine receipt (57,68,69), and participation in structured in-service education or conferences has been associated with improved vaccination rates (62,65). Educational programs should emphasize the benefits of HCP vaccination for staff and patients (70). Organized campaigns that promote and make vaccine accessible can improve vaccination rates among HCP (52,71).
# Role Models
Vaccination of senior medical staff or opinion leaders has been associated with higher vaccination acceptance among staff members under their leadership (55,69,72,73). For example, medical students who have contact with infectious disease specialists are more likely to be vaccinated (69).
# Improved Access
Removing administrative barriers (e.g., costs) (71) and providing vaccine in locations and at times easily accessible by HCP can substantially improve vaccine acceptance (40,52,55,72,74,75). In one survey, 33% of HCP reported that they would reject vaccination if they were required to pay for the vaccine (76).
Making vaccine readily accessible at congregate areas (e.g., clinics), during conferences, or by use of mobile carts (40,52,55,72) has been demonstrated to improve vaccination coverage rates. Use of mobile carts has been associated with increased vaccine acceptance during outbreaks and nonoutbreak situations (75,76) . In a 3-year prospective study in a 630-bed acute care hospital, a sustained four-to fivefold increase in vaccination rates was associated with using mobile carts to deliver vaccine to staff rather than requiring HCP to visit an employee health center to receive vaccine. Provision of modest incentives also has been associated with improved vaccine acceptance among HCP (77). However, the benefits of vaccine deputies or peer-vaccinators have not been consistently associated with improved HCP vaccination (52).
# Measurement and Feedback
HCP influenza vaccination coverage should be regularly measured and reported. Posting of vaccination coverage levels in different areas of the hospital is a component of successful vaccination programs (6). Monitoring vaccination coverage by facility area (e.g., ward or unit) or occupational group allows facilities to identify where vaccination levels are low and interventions should be targeted. In addition, HICPAC has recommended that HCP influenza vaccination coverage be used as a health-care quality measure in those states that mandate public reporting of health-care-associated infections (78).
The independent contribution of signed declination statements to improving HCP vaccination has not been studied. However, obtaining declination statements from HCP who refuse vaccination for reasons other than medical contraindications can assist facilities in identifying personnel who might require targeted education or other interventions to overcome barriers to vaccine acceptance. In addition, collection of such information will allow health-care facilities to determine what proportion of their staff are reached and offered vaccine.
# Legislation and Regulation
Legislative and regulatory efforts have favorably affected hepatitis B vaccination rates among HCP (79,80). As of January 2005, a total of 13 states (Alabama, Arkansas, Kentucky, Maine, Maryland, New Hampshire, New York, Oklahoma, Oregon, Pennsylvania, Rhode Island, Texas, and Utah) and the District of Columbia were reported to have enacted regulations regarding influenza vaccination of staff in long-termcare facilities (67,81). However, because only one state (Pennsylvania) has monitored the impact of its laws on nursing home staff vaccination rates, data are insufficient to assess the overall impact of these legislative efforts on HCP influenza vaccination coverage (CDC, unpublished data, 2005).
# Recommendations for Using Inactivated Influenza Vaccine and LAIV Among HCP
All HCP should be vaccinated annually against influenza. Either inactivated influenza vaccine or LAIV can be used to reduce the risk for influenza among HCP ( 3).
# Inactivated Influenza Vaccine Recommendations Dosage and Route
Because immunity declines during the year after vaccination, HCP eligible to receive inactivated influenza vaccine should be administered 1 dose of the current year's vaccine each year (82,83). The intramuscular route is recommended for inactivated influenza vaccine. Adults should be vaccinated in the deltoid muscle, ideally by using a needle of length >1 inch because needles of length <1 inch might not penetrate muscle tissue in certain adults (84).
# Persons Who Should Not Be Vaccinated with Inactivated Influenza Vaccine
Inactivated influenza vaccine should not be administered to persons known to have anaphylactic hypersensitivity to eggs or to other components of the influenza vaccine without first consulting a physician (see Side Effects and Adverse Reactions Associated with Vaccination). Prophylactic use of antiviral agents is an option for preventing influenza among such persons. However, persons who have a history of anaphylactic hypersensitivity to vaccine components but who are also at high risk for complications from influenza can benefit from vaccine after appropriate allergy evaluation and desensitization (18). Information regarding vaccine components is located in package inserts from each manufacturer. Persons with acute febrile illness typically should not be vaccinated until their symptoms have abated. However, minor illnesses with or without fever do not contraindicate use of influenza vaccine.
# LAIV Recommendations
LAIV licensed for use in the United States (FluMist ™ manufactured by MedImmune, Inc., Gaithersburg, Maryland ) is a live, trivalent, intranasally administered vaccine that is - attenuated, producing mild or no signs or symptoms related to influenza virus infection; - temperature-sensitive, a property that limits the replication of the vaccine viruses at 100.4°-102.2° F (38° C-39° C) and thus restricts LAIV viruses from replicating efficiently in human lower airways; and - cold-adapted, replicating efficiently at 77° F (25° C), a temperature that is permissive for replication of LAIV viruses but restrictive for replication of different wild-type viruses. The immunogenicity of the approved LAIV has been assessed in multiple studies (85)(86)(87)(88)(89)(90)(91). LAIV virus strains replicate primarily in nasopharyngeal epithelial cells. The protective mechanisms induced by vaccination with LAIV are not completely understood but appear to involve both serum and nasal secretory antibodies. No single laboratory measurement closely correlates with protective immunity induced by LAIV.
# Shedding and Transmission of Vaccine Viruses
One concern regarding use of LAIV among HCP has been the potential for transmitting vaccine virus from persons receiving vaccine to nonimmune patients at high risk. Available data indicate that children and adults vaccinated with LAIV can shed vaccine viruses for >2 days after vaccination, although in lower titers than typically occur with shedding of wild-type influenza viruses. Shedding should not be equated with person-to-person transmission of vaccine viruses, although transmission of shed vaccine viruses from vaccinated persons to nonvaccinated persons has been documented in rare instances among children in a day care center (92).
In one study of 20 healthy vaccinated adults aged 18-49 years, the majority of vaccine virus shedding occurred within the first 3 days after vaccination, although in one vaccinated person, viral shedding was detected on day 7 after vaccination (93). No vaccine viruses were shed >10 days after vaccination, and duration or type of symptoms associated with receipt of LAIV did not correlate with duration of shedding of vaccine viruses (93). In another study of 14 healthy adults aged 18-49 years, 50% of vaccinated persons had viral antigen detected by direct immunofluorescence or rapid antigen tests within 7 days of vaccination; the majority of viral shedding was detected on day 2 or 3 (94). Person-to-person transmission of vaccine viruses was not assessed in either of these studies.
One study conducted in a child care center assessed transmissibility of vaccine viruses from 98 vaccinated persons to 99 unvaccinated controls aged 8-36 months; 80% of vaccine recipients shed one or more virus strains (mean duration: 7.6 days). One influenza type B isolate was recovered from a placebo recipient and confirmed to be vaccine-type virus; the isolate retained the cold-adapted, temperature-sensitive, attenuated phenotype and possessed the same genetic sequence as a virus shed from a vaccine recipient in the same children's play group. The placebo recipient from whom the influenza type B vaccine virus was isolated exhibited symptoms that were similar to those experienced by vaccine recipients. The estimated probability of acquiring vaccine virus after close contact with a single LAIV recipient in this child care population was 0.6%-2.4% (92).
# Using LAIV for HCP
LAIV may be used for vaccination of healthy, nonpregnant persons aged 5-49 years, including HCP. When feasible, use of LAIV for vaccination of eligible HCP is especially encouraged during periods of limited supply of inactivated influenza vaccine because use of LAIV for HCP might increase availability of inactivated influenza vaccine for persons at high risk. Use of LAIV also provides an alternative vaccine strategy for HCP who avoid influenza vaccination because of an aversion to intramuscular injections.
# Persons Who Should Not Receive LAIV
The following populations should not receive LAIV:
# LAIV Dosage and Administration
Eligible HCP should receive 1 dose of LAIV. LAIV is intended only for intranasal administration and should not be administered by the intramuscular, intradermal, or intra-venous route. Administration can be accomplished by holding an individual sprayer in the palm of the hand until thawed, with subsequent immediate administration. Alternatively, the vaccine can be thawed in a refrigerator and stored at 35.6° F-46.4° F (2° C-8° C) for <60 hours before use. Vaccine should not be refrozen after thawing. LAIV is supplied in a prefilled single-use sprayer containing 0.5 mL of vaccine. Approximately 0.25 mL is sprayed into the first nostril while the recipient is in the upright position. An attached dosedivider clip is removed from the sprayer to administer the second half of the dose into the other nostril. If the vaccine recipient sneezes after administration, the dose should not be repeated.
LAIV may be administered to persons with minor acute illnesses (e.g., diarrhea or mild upper respiratory tract infection, with or without fever). However, if clinical judgment indicates the presence of nasal congestion that might impede delivery of vaccine to the nasopharyngeal mucosa, deferral of administration should be considered until resolution of the illness.
Whether concurrent administration of LAIV with other vaccines affects the safety or efficacy of either LAIV or the simultaneously administered vaccine is unknown. In the absence of specific data indicating interference, adherence to ACIP's general recommendations for vaccination is prudent (95). Inactivated vaccines do not interfere with the immune response to other inactivated vaccines or to live vaccines. An inactivated vaccine can be administered either simultaneously or at any time before or after LAIV. Whenever possible, two live vaccines not administered on the same day should be administered >4 weeks apart.
# Recommended Vaccines for HCP Who Have Close Contact with Severely Immunosuppressed Persons
Inactivated influenza vaccine is the preferred vaccine for use among HCP who have close contact with severely immunosuppressed persons (e.g., patients with hematopoietic stem cell transplants) during those periods in which the immunosuppressed person requires care in a protective environment. The rationale for not using LAIV among HCP caring for such patients is the theoretic risk that a live, attenuated vaccine virus could be transmitted to the severely immunosuppressed person. HCP who receive LAIV should refrain from contact with severely immunosuppressed patients for 7 days after vaccine receipt. In addition, visitors who have received LAIV should refrain from contact with severely immunosuppressed persons for 7 days after vaccination; however, such persons need not be excluded from visitation of patients who are not severely immunosuppressed. Either inactivated influenza vaccine or LAIV can be used to vaccinate HCP who have close contact with persons with lesser degrees of immunosuppression (e.g., persons with diabetes, persons with asthma taking corticosteroids, or persons infected with human immunodeficiency virus) or who are in close contact with all other persons at high risk.
# Personnel Who May Administer LAIV
The risk of acquiring vaccine viruses from the environment is unknown but likely small. Nevertheless, severely immunosuppressed persons should not administer LAIV because introduction of low levels of vaccine virus into the environment probably cannot be avoided when administering LAIV. However, other persons with conditions placing them at high risk for influenza complications (e.g., pregnant women, persons with asthma, and persons aged >50 years) may administer LAIV.
# LAIV and Use of Influenza Antiviral Medications
How LAIV coadministration with influenza antiviral medications affects safety and efficacy has not been studied. However, because influenza antivirals reduce replication of influenza viruses, LAIV should not be administered until 48 hours after cessation of influenza antiviral therapy, and influenza antiviral medications should not be administered for 2 weeks after receipt of LAIV.
# LAIV Storage
LAIV must be stored at -59° F (-15° C) or colder. LAIV may be stored in frost-free freezers without using a freezer-box. LAIV can be thawed in a refrigerator and stored at 35.6° F-46.4° F (2 º C-8 º C) for <60 hours before use. It should not be refrozen after thawing. Additional information regarding LAIV storage is available at .
# Vaccination of Specific HCP Populations Pregnant Women
Pregnant women are at increased risk for influenza-related complications (96)(97)(98)(99)(100)(101)(102)(103) and hospitalizations (104). Therefore, all HCP who are pregnant during the influenza season should be vaccinated against influenza. However, pregnant women should receive only inactivated influenza vaccine; LAIV is not recommended for use during pregnancy. Inactivated influenza vaccine may be administered in any trimester. One study of influenza vaccination of approximately 2,000 pregnant women demonstrated no adverse fetal effects associated with receipt of inactivated influenza vaccine (105).
# Breastfeeding Mothers
Influenza vaccine does not affect the safety of mothers who are breastfeeding or their infants. Breastfeeding does not adversely affect the immune response and is not a contraindication for vaccination.
# Persons Infected with HIV
Detailed information on the use of influenza vaccine among persons infected with HIV has been published previously (18). Because influenza can result in serious illness and influenza vaccination can result in the production of protective antibody titers, vaccination with inactivated vaccine will benefit HIV-infected persons, including those that are pregnant.
# Timing of Annual Influenza Vaccination of HCP
# Timing of Organized Vaccination Campaigns
Planning for influenza campaigns should begin as early as February or March (106). The optimal time to vaccinate HCP is during October-November. Beginning in October each year, health-care facilities should offer influenza vaccinations to all full-and part-time staff. Particular emphasis should be placed on vaccinating HCP who care for persons at high risk. Vaccination programs should educate HCP regarding the benefits of vaccination and the potential health consequences of influenza illness for themselves and their patients. As part of employee health programs, all HCP should be provided convenient access to free influenza vaccine at the work site (107).
# Vaccination in December and Later
To improve vaccine coverage among HCP, influenza vaccine should continue to be offered in December and throughout the influenza season as long as vaccine supplies are available, even after influenza activity has been documented in the community. In the United States, seasonal influenza activity can increase as early as October or November, but influenza activity has not reached peak levels in the majority of recent seasons until late December-early March. Therefore, although the timing of influenza activity can vary by region, vaccine administered after November is likely to be beneficial in the majority of influenza seasons. Adults achieve peak antibody protection against influenza infection 2 weeks after vaccination (108,109).
# MMWR February 24,
# Recommendations for Prioritization of Influenza Vaccination During the 2005-06 Influenza Season
As a result of influenza vaccine distribution delays or supply shortages in the United States during recent influenza seasons (110,111), in September 2005, CDC issued recommendations for prioritizing the use of inactivated vaccine during the 2005-06 influenza season to ensure that early vaccine is available for those at the highest risk for complications from influenza (112). On the basis of uncertainties in doses and distribution, CDC recommended that the following groups receive priority for inactivated influenza vaccine until October 24, 2005:
- persons aged >65 years with and without comorbid conditions, - residents of long-term-care facilities, - persons aged 2-64 years with comorbid conditions, - children aged 6-23 months, - pregnant women, - HCP who provide direct patient care, and - household contacts and out-of-home caregivers of children aged <6 months (112). These groups correspond to tiers 1A-1C in the table of inactivated influenza vaccine priority groups in the event of vaccination supply disruption that was published previously (113). After October 24, 2005, all persons were eligible for vaccination.
Tiered use of prioritization was not recommended for LAIV administration. LAIV may be administered at any time for vaccination of nonpregnant healthy persons aged 5-49 years, including the majority of HCP, other persons in close contact with persons at high risk for influenza-related complications, and others desiring protection against influenza (18).
# Side Effects and Adverse Reactions Associated with Vaccination Inactivated Influenza Vaccine
When educating HCP regarding potential side effects, providers should emphasize that 1) inactivated influenza vaccine contains noninfectious killed viruses and cannot cause influenza; and 2) coincidental respiratory disease unrelated to influenza vaccination can occur after vaccination. The occurrence of vaccine-related side effects has had limited to no impact on rates of absenteeism among HCP (16,17).
# Local Reactions
The most frequent side effect of vaccination (affecting 10%-64% of patients) is soreness at the vaccination site, typically lasting <2 days (21,(114)(115)(116). Local reactions typically are mild and rarely interfere with a person's ability to conduct everyday activities. In a controlled trial, only body aches (25.1%) were reported more frequently after inactivated influenza vaccine than placebo-injection (20.8%) (117).
# Systemic Reactions
Fever, malaise, myalgia, and other systemic symptoms can occur after vaccination with inactivated vaccine and most often affect persons (e.g., infants) with no previous exposure to the influenza virus antigens in the vaccine (118,119). Such reactions typically begin 6-12 hours after vaccination and can persist for 1-2 days. Recent placebo-controlled trials demonstrate that among older persons and healthy young adults, administration of split-virus (i.e., detergent-disrupted virion) influenza vaccine is not associated with higher rates of systemic symptoms (e.g., fever, malaise, myalgia, and headache) compared with placebo injections (21,(114)(115)(116). No increase in asthma exacerbations has been documented in association with receipt of influenza vaccine (117).
# Severe Adverse Events
Immediate and presumably allergic reactions (e.g., hives, angioedema, allergic asthma, and systemic anaphylaxis) rarely occur after influenza vaccination (120). These reactions probably result from hypersensitivity to certain vaccine components; the majority of reactions probably are caused by residual egg protein. Although current influenza vaccines contain only a limited quantity of egg protein, this protein can induce immediate hypersensitivity reactions among persons who have severe egg allergy. Persons who have had hives or swelling of the lips or tongue, or who have experienced acute respiratory distress or collapse after eating eggs should consult a physician for appropriate evaluation to help determine if vaccine should be administered. Persons who have documented immunoglobulin E (IgE)-mediated hypersensitivity to eggs, including those who have had occupational asthma or other allergic responses to egg protein, might also be at increased risk for allergic reactions to influenza vaccine, and consultation with a physician should be considered. Protocols have been published for administering influenza vaccine safely to persons with egg allergies (121)(122)(123).
Hypersensitivity reactions to any vaccine component can occur. Although exposure to vaccines containing thimerosal can lead to induction of hypersensitivity, the majority of patients do not have reactions to thimerosal when it is administered as a component of vaccines, even when patch or intradermal tests for thimerosal allergy indicate hypersensitivity (124,125). When reported, hypersensitivity to thimerosal typically has consisted of local, delayed hypersensitivity reactions (124).
# GBS
Investigations to date indicate no substantial increase in GBS associated with influenza vaccines (other than the 1976 swine influenza vaccine) (126)(127)(128)(129)(130). If current influenza vaccines pose a risk for GBS, the estimated risk is approximately one additional case per million persons vaccinated, with the total combined number of GBS cases peaking 2 weeks after vaccination (131). This estimated risk for GBS is substantially less than the risk for severe influenza, which can be prevented by vaccination among all age groups, especially persons aged >65 years and those who have medical indications for influenza vaccination. The potential benefits of influenza vaccination in preventing serious illness, hospitalization, and death substantially outweigh the possible risks for experiencing vaccineassociated GBS. The average case-fatality ratio for GBS is 6% and increases with age (132,133). No evidence indicates that the case-fatality ratio for GBS differs among vaccinated persons and those not vaccinated.
Incidence of GBS among the general population is low, but persons with a history of GBS have a substantially greater likelihood of subsequently experiencing GBS than persons without such a history (128,134). Whether influenza vaccination might increase the risk for recurrence of GBS is unknown; for this reason, persons who are not at high risk for severe influenza complications and who are known to have experienced GBS within 6 weeks after a previous influenza vaccination should not receive vaccine. Chemoprophylaxis using influenza antivirals might be an alternative for such persons. Although data are limited, for the majority of persons who have a history of GBS and who are at high risk for severe complications from influenza, the established benefits of influenza vaccination justify yearly vaccination. Health-care professionals should promptly report all clinically significant adverse events after influenza vaccination to the Vaccine Adverse Event Reporting System (VAERS), even if evidence is lacking that the vaccine caused the event.
# LAIV
Until additional data are available, persons at high risk for experiencing complications from influenza infection (e.g., immunocompromised patients; patients with asthma, cystic fibrosis, or chronic obstructive pulmonary disease; or persons aged >65 years) should not be vaccinated with LAIV. Protection from influenza among these groups should be accomplished by using inactivated influenza vaccine.
Among adults, runny nose or nasal congestion (28%-78%), headache (16%-44%), and sore throat (15%-27%) have been reported more often among vaccine recipients than placebo recipients (37,135,136). In one clinical trial among a subset of healthy adults aged 18-49 years, signs and symptoms reported more frequently among LAIV recipients (n = 2,548) than placebo recipients (n = 1,290) within 7 days after each dose included cough (13.9% and 10.8%, respectively); runny nose (44.5% and 27.1%, respectively); sore throat (27.8% and 17.1%, respectively); chills (8.6% and 6.0%, respectively); and tiredness or weakness (25.7% and 21.6%, respectively) (37). Pneumonia, bronchitis, bronchiolitis, or central nervous system events have not been observed more frequently among LAIV than among placebo recipients.
# Severe Adverse Events
Serious adverse events associated with receipt of LAIV among healthy adults aged 18-49 years occur at a rate of <1% (137). However, surveillance should continue for adverse events that might not have been detected in previous studies. Health-care professionals should promptly report to VAERS all clinically significant adverse events after LAIV administration, even if evidence is lacking that the vaccine caused the event.
# Additional Information Regarding Influenza Infection Control in Health-Care Settings
Additional information on controlling and preventing influenza in health-care settings is available in the following publications:
- CDC. Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP | depar depar depar depar department of health and human ser tment of health and human ser tment of health and human ser tment of health and human ser tment of health and human services vices vices vices vices# Introduction
Influenza transmission and outbreaks in hospitals (1)(2)(3)(4)(5)(6)(7)(8) and nursing homes (9-13) are well documented. HCP can acquire influenza from patients or transmit influenza to patients and other staff. Despite the documented benefits of HCP influenza vaccination on patient outcomes (14,15) and HCP absenteeism (16) and on reducing influenza infection among staff (16,17), vaccination coverage among HCP remain low (i.e., <50%) (18). Because HCP provide care to patients at high risk for complications of influenza, HCP should be considered a high priority for expanding influenza vaccine use. In addition, older HCP (i.e., aged >65 years) and those who have underlying chronic medical conditions or who might be pregnant are at increased risk for influenza-related complications. Achieving and sustaining high vaccination coverage among HCP will protect staff and their patients, and reduce disease burden and health-care costs.
This report summarizes recommendations of the Healthcare Infection Control Practices Advisory Committee (HICPAC) and the Advisory Committee on Immunization Practices (ACIP) concerning influenza vaccination of health-care personnel (HCP)* in the United States. These recommendations are targeted at health-care facility administrators, infection control professionals, and occupational health professionals responsible for influenza vaccination programs and influenza infection control programs in their institutions. HICPAC and ACIP recommend that all HCP be vaccinated annually against influenza. Facilities that employ HCP are strongly encouraged to provide vaccine to their staff by using * In this report, the term HCP refers to all paid and unpaid persons working in health-care settings who have the potential for exposure to infectious materials, including body substances, contaminated medical supplies and equipment, contaminated environmental surfaces, or contaminated air. HCP might include (but are not limited to) physicians, nurses, nursing assistants, therapists, technicians, emergency medical service personnel, dental personnel, pharmacists, laboratory personnel, autopsy personnel, students and trainees, contractual staff not employed by the health-care facility, and persons (e.g., clerical, dietary, housekeeping, maintenance, and volunteers) not directly involved in patient care but potentially exposed to infectious agents that can be transmitted to and from HCP. The recommendations in this report apply to HCP in acute care hospitals, nursing homes, skilled nursing facilities, physician's offices, urgent care centers, and outpatient clinics, and to persons who provide home health care and emergency medical services.
# Summary Recommendations
The summary recommendations contained in this report are categorized by using the HICPAC evidence ranking system (Table 1). The recommendations were drafted after review of peer-reviewed scientific articles, and whenever possible are based on well-designed studies; certain recommendations are based on strong theoretic rationale and expert opinion. All recommendations have been approved by HICPAC and ACIP. The committees involved in drafting and reviewing these recommendations included persons with expertise in infectious diseases, infection control, pediatrics, vaccinology, internal medicine, and public health. The recommendations are as follows:
• Educate HCP regarding the benefits of influenza vaccination and the potential health consequences of influenza illness for themselves and their patients, the epidemiology and modes of transmission, diagnosis, treatment, and nonvaccine infection control strategies, in accordance with their level of responsibility in preventing health-care-associated influenza (category IB).
# Background Influenza Among HCP
A limited number of prospective and cross-sectional studies provide estimates of incidence of influenza and influenza-like illness (ILI) among HCP (17,19,20). In one serosurvey of HCP, 23% of HCP had documented serologic evidence of influenza infection after a mild influenza season; however, of these, 59% could not recall having influenza, and 28% could not recall any respiratory infection, suggesting a high proportion of asymptomatic illness (17). In a randomized trial of influenza vaccine among HCP, 13% of placebo recipients subsequently had influenza infection (18). In a cross-sectional survey of house staff, 37% reported ILI during an 8-month period (September-April); 9% reported more than one illness. Length of illness varied (range: 1-10 days; mean: 7 days), as did the number of days of work missed (range: 0-10 days; mean: 0.7 days) (20).
# Efficacy and Effectiveness of Influenza Vaccines Among Adults
Trivalent inactivated influenza vaccine prevents influenza illness among approximately 70%-90% of healthy adults aged <65 years when the vaccine and circulating viruses are anti- genically similar (17,(21)(22)(23). The effectiveness of inactivated influenza vaccine in preventing influenza illness might be lower when vaccine and circulating viruses are not well matched or among adults aged >65 years and persons with certain chronic conditions (e.g., diabetes, human immunodeficiency virus (HIV), or chronic obstructive pulmonary disease) (24)(25)(26)(27)(28). Vaccination of healthy adults also decreases work absenteeism and use of health-care resources, including antibiotics, when the vaccine and circulating viruses are well matched (17,21,23,(29)(30)(31). In addition, influenza vaccine prevents secondary complications and reduces the risk for influenza-related hospitalization and death among adults aged >65 years with and without high-risk medical conditions (e.g., heart disease and diabetes) (32)(33)(34)(35)(36).
LAIV has demonstrated similar benefits in randomized controlled trials among healthy working adults aged 18-64 years. In one study, vaccination with LAIV reduced severe febrile illnesses 19% and upper respiratory tract illnesses 24%; LAIV use also was associated with fewer days of illness and of work lost, fewer health-care provider visits, and reduced use of prescription antibiotics and over-the-counter medications (37). These results were recorded during a season in which the vaccine and circulating influenza A (H3N2) strains were not well matched. In the same study, LAIV vaccination yielded similar benefits among a subset of healthy adults aged 18-49 years, and antibiotic use in this age group decreased 41%-51% (37). In one study, overall efficacy of LAIV and inactivated influenza vaccine in preventing laboratory-documented influenza was 85% and 71%, respectively (38).
# Impact of HCP Vaccination on Influenza in Health-Care Settings
Vaccination of HCP is an important component of influenza prevention programs in the United States (18). Vaccination of HCP reduces transmission of influenza in health-care settings, staff illness and absenteeism, and influenza-related morbidity and mortality among persons at increased risk for severe influenza illness (14-17). Use of antiviral drugs used for chemoprophylaxis or treatment of influenza is an adjunct to (but not a substitute for) vaccination (18).
# Transmission of Influenza in Health-Care Settings
Influenza outbreaks in hospitals (4,39) and long-term-care facilities (40) have been associated with low vaccination rates among HCP. In addition, higher vaccination levels among staff have been associated with a lower incidence of nosocomial influenza cases (14,15,39).
In one tertiary care facility in which routine surveillance for influenza was conducted, the relation between staff vaccination coverage and annual incidence of nosocomial influenza was assessed for 12 influenza seasons during 1987-2000. During this period, staff vaccination coverage increased from 4% during 1987-1988 to 67% during 1999-2000 (p<0.0001), and the proportion of laboratory-confirmed cases of influenza that occurred among HCP decreased from 42% during 1990-1993 to 9% during 1997-2000 (p<0.0001). The proportion of nosocomial cases among hospitalized patients decreased 32% to 0 (p<0.0001). After controlling for potential confounders by using logistic regression, a significant and inverse relationship was demonstrated between vaccination rates among HCP and the rate of nosocomial influenza among patients, suggesting that staff vaccination contributed to the observed decline in the number of nosocomial influenza cases (39).
# Staff Illness and Absenteeism
During an influenza season, HCP might acquire influenza from infected patients with resulting morbidity and absenteeism. The impact of influenza vaccination on staff illness and absenteeism has been evaluated in two randomized, placebocontrolled, double-blind trials. In one trial, HCP who received vaccine had 28% fewer documented lost work days attributable to respiratory infections (1.0 and 1.4, respectively; p = 0.02) and 28% fewer days on which they felt unable to work, whether they were on or off duty (2.5 and 3.5, respectively; p = 0.02). Vaccination did not reduce either the number of episodes (1.8 and 2.0, respectively) or the total number of days (13.5 and 14.6, respectively) of respiratory infection (16). In a second trial conducted in two large teaching hospitals for 3 consecutive years that measured serologically confirmed influenza, days of febrile respiratory illness, and days absent from work, HCP who received influenza vaccine had a substantially lower incidence of influenza than controls (1.7% and 13.4%, respectively) with an estimated vaccine efficacy against serologically defined influenza A and influenza B infection of 88% and 89%, respectively. HCP who received influenza vaccine also tended to have fewer total respiratory illnesses (28.7 and 40.6 per 100 persons, respectively; p = 0.57) and days of lost work (9.9 and 21.1 per 100 persons, respectively; p = 0.41) than did controls (17).
In a cross-sectional survey, similar reductions in staff illness episodes and days of illness were reported (20). Overall, compared with unvaccinated coworkers, vaccinated house staff reported 23% fewer ILIs (42 and 54 per 100 persons, respectively; p = 0.03), 27% fewer days of illness (80 and 115 per 100 persons, respectively; p = 0.02), and a 59% reduction in illness during vacation time (1.7% and 4.0% of persons, respectively; p = 0.08). The two groups had a similar number of lost work days attributable to ILI (18 and 21 per 100 subjects, respectively; p = 0.69). During influenza season, vaccination was associated with reductions of 30% in ILI (p = 0.05), 43% in the proportion of house staff reporting illnesses associated with fever and cough (p = 0.05), and 63% in illnesses associated with fever and cough (p = 0.03). The inability to consistently demonstrate statistically significant decreases in absenteeism among staff who received vaccination is likely attributable to the finding that HCP tend to work despite illness (17,41).
# Patient Outcomes
HCP who are clinically or subclinically infected can transmit influenza virus to other persons. Decreasing transmission of influenza from caregivers to persons at high risk might reduce influenza-related deaths among persons at high risk for complications from influenza.
Residents of long-term-care facilities are particularly vulnerable to influenza and influenza-related complications. In1999, an estimated 1.6 million persons resided in nursing homes in the United States (42). During influenza outbreaks in long-term-care facilities, attack rates among residents have ranged as high as 25%-60%, with case-fatality rates of 10%-20% (13,(43)(44)(45). When vaccine and epidemic strains are well matched, achieving increased vaccination rates among persons living in closed settings (e.g., nursing homes and other chronic-care facilities) and among staff can reduce the risk for outbreaks by inducing herd immunity (32).
Two randomized controlled trials have evaluated the impact of influenza vaccination of HCP on the outcomes of residents in nursing homes. In one study, staff vaccination was associated with a 43% decrease in incidence of ILI (odds ratio [OR] = 0.6; 95% confidence interval [CI] = 0.3-0.9) and a 44% decrease in overall mortality among facility residents, from 17% to 10% (OR = 0.6; 95% CI = 0.4-0.8) (15). No virologic data were provided in this study. In a second study, 20 long-term-care facilities were randomized to have vaccine routinely offered (intervention facilities) or not offered (control facilities) to their staff (14). Facilities were paired by number of beds and patient vaccination policies. Staff vaccination coverage was higher in intervention facilities than in control facilities (50.9% and 4.9%, respectively). Crude mortality rates were 42% lower among residents in facilities with higher staff vaccination coverage than those in control facilities (13.6% and 22.4%, respectively; OR = 0.6; 95% CI = 0.4-0.8; p = 0.014). Incidence of laboratory-confirmed influenza did not differ between the two groups (5.4% and 6.7%, respectively), but postmortem samples from pa-tients in control facilities were more likely to be positive for influenza by a polymerase chain reaction test than samples from patients in intervention facilities (six [20%] of 30 and none of 17, respectively; p = 0.055), suggesting that in this study population, HCP vaccination reduced influenza-related mortality in patients despite not reducing the incidence of non-fatal influenza infection. In neither study was a significant association demonstrated between patient vaccination and mortality. Randomized trials assessing the impact of staff vaccination on patient outcomes in acute care facilities have not been conducted, but low staff vaccination coverage has been correlated with influenza outbreaks in hospitals (4,39).
# Cost-Effectiveness of Influenza Vaccine
Cost-effectiveness studies of adults aged <65 years indicate that vaccination can reduce both direct medical costs and indirect costs from work absenteeism (21,23,29,30,46,47), resulting in 13%-44% fewer health-care provider visits, 18%-45% fewer lost workdays, 18%-28% fewer days working with reduced effectiveness, and a 25% decrease in antibiotic use for ILI (21,29,48,49). Among healthy persons aged 18-64 years, vaccination can save an estimated $60-$4,000 per illness, depending on the cost of vaccination, the influenza attack rate, and vaccine effectiveness against ILI (23). In another economic analysis, vaccination resulted in an average annual cost savings of $13.66 per person vaccinated (50); however, other analyses have not demonstrated cost savings (21). Among studies of healthy young adults, >70% of the costs prevented were associated with reductions in lost work productivity.
# Vaccination Coverage Levels Among HCP
During 1989-2003, HCP vaccination coverage levels in the United States increased substantially, from 10% to 40%; however, coverage levels have remained relatively constant since 1997 (18). One of the national health objectives for 2010 is to achieve HCP vaccination coverage levels of 60% (objective no. 14-29g) (51). Substantially lower vaccination rates have been reported among HCP who have contact with certain populations at high risk (12,(52)(53)(54). In addition, HCP vaccination coverage varies by level and years of training, age, occupational group, and facility type (20,55,56).
# Barriers to HCP Vaccination
Reported barriers to HCP receipt or acceptance of influenza vaccination include fear of vaccine side effects (particularly ILI symptoms) (20,55,(57)(58)(59)(60)(61), insufficient time or inconvenience (20), perceived ineffectiveness of the vaccine (20,55,58,59), medical contraindication (55), perceived low likelihood of contracting influenza (55,60,62), reliance on treatment with homeopathic medications (55,62), avoidance of medications (57), and fear of needles (57,59). Factors facilitating vaccine acceptance include a desire for selfprotection (20,58,61), previous receipt of influenza vaccine (57,58,(63)(64)(65), a desire to protect patients (61), and perceived effectiveness of vaccine (20).
# Strategies for Improving HCP Vaccination Rates
Facilities that employ HCP are strongly encouraged to provide vaccine to staff by using evidence-based approaches that maximize vaccination rates. Successful HCP vaccination programs are multifaceted and combine publicity and education to combat fears and misconceptions about influenza and influenza vaccines, use of reminder recall systems, efforts to remove administrative and financial barriers, role modeling, and monitoring and feedback on vaccination coverage (66). In contrast, single-component interventions will likely have minimal effectiveness in achieving desired vaccination coverage levels (66,67).
# Education and Campaigns
HCP knowledge, perceptions, and attitudes regarding influenza and influenza vaccination vary (20). Basic knowledge about influenza and influenza vaccination has been associated with vaccine receipt (57,68,69), and participation in structured in-service education or conferences has been associated with improved vaccination rates (62,65). Educational programs should emphasize the benefits of HCP vaccination for staff and patients (70). Organized campaigns that promote and make vaccine accessible can improve vaccination rates among HCP (52,71).
# Role Models
Vaccination of senior medical staff or opinion leaders has been associated with higher vaccination acceptance among staff members under their leadership (55,69,72,73). For example, medical students who have contact with infectious disease specialists are more likely to be vaccinated (69).
# Improved Access
Removing administrative barriers (e.g., costs) (71) and providing vaccine in locations and at times easily accessible by HCP can substantially improve vaccine acceptance (40,52,55,72,74,75). In one survey, 33% of HCP reported that they would reject vaccination if they were required to pay for the vaccine (76).
Making vaccine readily accessible at congregate areas (e.g., clinics), during conferences, or by use of mobile carts (40,52,55,72) has been demonstrated to improve vaccination coverage rates. Use of mobile carts has been associated with increased vaccine acceptance during outbreaks and nonoutbreak situations (75,76) . In a 3-year prospective study in a 630-bed acute care hospital, a sustained four-to fivefold increase in vaccination rates was associated with using mobile carts to deliver vaccine to staff rather than requiring HCP to visit an employee health center to receive vaccine. Provision of modest incentives also has been associated with improved vaccine acceptance among HCP (77). However, the benefits of vaccine deputies or peer-vaccinators have not been consistently associated with improved HCP vaccination (52).
# Measurement and Feedback
HCP influenza vaccination coverage should be regularly measured and reported. Posting of vaccination coverage levels in different areas of the hospital is a component of successful vaccination programs (6). Monitoring vaccination coverage by facility area (e.g., ward or unit) or occupational group allows facilities to identify where vaccination levels are low and interventions should be targeted. In addition, HICPAC has recommended that HCP influenza vaccination coverage be used as a health-care quality measure in those states that mandate public reporting of health-care-associated infections (78).
The independent contribution of signed declination statements to improving HCP vaccination has not been studied. However, obtaining declination statements from HCP who refuse vaccination for reasons other than medical contraindications can assist facilities in identifying personnel who might require targeted education or other interventions to overcome barriers to vaccine acceptance. In addition, collection of such information will allow health-care facilities to determine what proportion of their staff are reached and offered vaccine.
# Legislation and Regulation
Legislative and regulatory efforts have favorably affected hepatitis B vaccination rates among HCP (79,80). As of January 2005, a total of 13 states (Alabama, Arkansas, Kentucky, Maine, Maryland, New Hampshire, New York, Oklahoma, Oregon, Pennsylvania, Rhode Island, Texas, and Utah) and the District of Columbia were reported to have enacted regulations regarding influenza vaccination of staff in long-termcare facilities (67,81). However, because only one state (Pennsylvania) has monitored the impact of its laws on nursing home staff vaccination rates, data are insufficient to assess the overall impact of these legislative efforts on HCP influenza vaccination coverage (CDC, unpublished data, 2005).
# Recommendations for Using Inactivated Influenza Vaccine and LAIV Among HCP
All HCP should be vaccinated annually against influenza. Either inactivated influenza vaccine or LAIV can be used to reduce the risk for influenza among HCP ( 3).
# Inactivated Influenza Vaccine Recommendations Dosage and Route
Because immunity declines during the year after vaccination, HCP eligible to receive inactivated influenza vaccine should be administered 1 dose of the current year's vaccine each year (82,83). The intramuscular route is recommended for inactivated influenza vaccine. Adults should be vaccinated in the deltoid muscle, ideally by using a needle of length >1 inch because needles of length <1 inch might not penetrate muscle tissue in certain adults (84).
# Persons Who Should Not Be Vaccinated with Inactivated Influenza Vaccine
Inactivated influenza vaccine should not be administered to persons known to have anaphylactic hypersensitivity to eggs or to other components of the influenza vaccine without first consulting a physician (see Side Effects and Adverse Reactions Associated with Vaccination). Prophylactic use of antiviral agents is an option for preventing influenza among such persons. However, persons who have a history of anaphylactic hypersensitivity to vaccine components but who are also at high risk for complications from influenza can benefit from vaccine after appropriate allergy evaluation and desensitization (18). Information regarding vaccine components is located in package inserts from each manufacturer. Persons with acute febrile illness typically should not be vaccinated until their symptoms have abated. However, minor illnesses with or without fever do not contraindicate use of influenza vaccine.
# LAIV Recommendations
LAIV licensed for use in the United States (FluMist ™ manufactured by MedImmune, Inc., Gaithersburg, Maryland [http//www.medimmune.com]) is a live, trivalent, intranasally administered vaccine that is • attenuated, producing mild or no signs or symptoms related to influenza virus infection; • temperature-sensitive, a property that limits the replication of the vaccine viruses at 100.4°-102.2° F (38° C-39° C) and thus restricts LAIV viruses from replicating efficiently in human lower airways; and • cold-adapted, replicating efficiently at 77° F (25° C), a temperature that is permissive for replication of LAIV viruses but restrictive for replication of different wild-type viruses. The immunogenicity of the approved LAIV has been assessed in multiple studies (85)(86)(87)(88)(89)(90)(91). LAIV virus strains replicate primarily in nasopharyngeal epithelial cells. The protective mechanisms induced by vaccination with LAIV are not completely understood but appear to involve both serum and nasal secretory antibodies. No single laboratory measurement closely correlates with protective immunity induced by LAIV.
# Shedding and Transmission of Vaccine Viruses
One concern regarding use of LAIV among HCP has been the potential for transmitting vaccine virus from persons receiving vaccine to nonimmune patients at high risk. Available data indicate that children and adults vaccinated with LAIV can shed vaccine viruses for >2 days after vaccination, although in lower titers than typically occur with shedding of wild-type influenza viruses. Shedding should not be equated with person-to-person transmission of vaccine viruses, although transmission of shed vaccine viruses from vaccinated persons to nonvaccinated persons has been documented in rare instances among children in a day care center (92).
In one study of 20 healthy vaccinated adults aged 18-49 years, the majority of vaccine virus shedding occurred within the first 3 days after vaccination, although in one vaccinated person, viral shedding was detected on day 7 after vaccination (93). No vaccine viruses were shed >10 days after vaccination, and duration or type of symptoms associated with receipt of LAIV did not correlate with duration of shedding of vaccine viruses (93). In another study of 14 healthy adults aged 18-49 years, 50% of vaccinated persons had viral antigen detected by direct immunofluorescence or rapid antigen tests within 7 days of vaccination; the majority of viral shedding was detected on day 2 or 3 (94). Person-to-person transmission of vaccine viruses was not assessed in either of these studies.
One study conducted in a child care center assessed transmissibility of vaccine viruses from 98 vaccinated persons to 99 unvaccinated controls aged 8-36 months; 80% of vaccine recipients shed one or more virus strains (mean duration: 7.6 days). One influenza type B isolate was recovered from a placebo recipient and confirmed to be vaccine-type virus; the isolate retained the cold-adapted, temperature-sensitive, attenuated phenotype and possessed the same genetic sequence as a virus shed from a vaccine recipient in the same children's play group. The placebo recipient from whom the influenza type B vaccine virus was isolated exhibited symptoms that were similar to those experienced by vaccine recipients. The estimated probability of acquiring vaccine virus after close contact with a single LAIV recipient in this child care population was 0.6%-2.4% (92).
# Using LAIV for HCP
LAIV may be used for vaccination of healthy, nonpregnant persons aged 5-49 years, including HCP. When feasible, use of LAIV for vaccination of eligible HCP is especially encouraged during periods of limited supply of inactivated influenza vaccine because use of LAIV for HCP might increase availability of inactivated influenza vaccine for persons at high risk. Use of LAIV also provides an alternative vaccine strategy for HCP who avoid influenza vaccination because of an aversion to intramuscular injections.
# Persons Who Should Not Receive LAIV
The following populations should not receive LAIV:
•
# LAIV Dosage and Administration
Eligible HCP should receive 1 dose of LAIV. LAIV is intended only for intranasal administration and should not be administered by the intramuscular, intradermal, or intra-venous route. Administration can be accomplished by holding an individual sprayer in the palm of the hand until thawed, with subsequent immediate administration. Alternatively, the vaccine can be thawed in a refrigerator and stored at 35.6° F-46.4° F (2° C-8° C) for <60 hours before use. Vaccine should not be refrozen after thawing. LAIV is supplied in a prefilled single-use sprayer containing 0.5 mL of vaccine. Approximately 0.25 mL is sprayed into the first nostril while the recipient is in the upright position. An attached dosedivider clip is removed from the sprayer to administer the second half of the dose into the other nostril. If the vaccine recipient sneezes after administration, the dose should not be repeated.
LAIV may be administered to persons with minor acute illnesses (e.g., diarrhea or mild upper respiratory tract infection, with or without fever). However, if clinical judgment indicates the presence of nasal congestion that might impede delivery of vaccine to the nasopharyngeal mucosa, deferral of administration should be considered until resolution of the illness.
Whether concurrent administration of LAIV with other vaccines affects the safety or efficacy of either LAIV or the simultaneously administered vaccine is unknown. In the absence of specific data indicating interference, adherence to ACIP's general recommendations for vaccination is prudent (95). Inactivated vaccines do not interfere with the immune response to other inactivated vaccines or to live vaccines. An inactivated vaccine can be administered either simultaneously or at any time before or after LAIV. Whenever possible, two live vaccines not administered on the same day should be administered >4 weeks apart.
# Recommended Vaccines for HCP Who Have Close Contact with Severely Immunosuppressed Persons
Inactivated influenza vaccine is the preferred vaccine for use among HCP who have close contact with severely immunosuppressed persons (e.g., patients with hematopoietic stem cell transplants) during those periods in which the immunosuppressed person requires care in a protective environment. The rationale for not using LAIV among HCP caring for such patients is the theoretic risk that a live, attenuated vaccine virus could be transmitted to the severely immunosuppressed person. HCP who receive LAIV should refrain from contact with severely immunosuppressed patients for 7 days after vaccine receipt. In addition, visitors who have received LAIV should refrain from contact with severely immunosuppressed persons for 7 days after vaccination; however, such persons need not be excluded from visitation of patients who are not severely immunosuppressed. Either inactivated influenza vaccine or LAIV can be used to vaccinate HCP who have close contact with persons with lesser degrees of immunosuppression (e.g., persons with diabetes, persons with asthma taking corticosteroids, or persons infected with human immunodeficiency virus) or who are in close contact with all other persons at high risk.
# Personnel Who May Administer LAIV
The risk of acquiring vaccine viruses from the environment is unknown but likely small. Nevertheless, severely immunosuppressed persons should not administer LAIV because introduction of low levels of vaccine virus into the environment probably cannot be avoided when administering LAIV. However, other persons with conditions placing them at high risk for influenza complications (e.g., pregnant women, persons with asthma, and persons aged >50 years) may administer LAIV.
# LAIV and Use of Influenza Antiviral Medications
How LAIV coadministration with influenza antiviral medications affects safety and efficacy has not been studied. However, because influenza antivirals reduce replication of influenza viruses, LAIV should not be administered until 48 hours after cessation of influenza antiviral therapy, and influenza antiviral medications should not be administered for 2 weeks after receipt of LAIV.
# LAIV Storage
LAIV must be stored at -59° F (-15° C) or colder. LAIV may be stored in frost-free freezers without using a freezer-box. LAIV can be thawed in a refrigerator and stored at 35.6° F-46.4° F (2 º C-8 º C) for <60 hours before use. It should not be refrozen after thawing. Additional information regarding LAIV storage is available at http://www.FluMist.com.
# Vaccination of Specific HCP Populations Pregnant Women
Pregnant women are at increased risk for influenza-related complications (96)(97)(98)(99)(100)(101)(102)(103) and hospitalizations (104). Therefore, all HCP who are pregnant during the influenza season should be vaccinated against influenza. However, pregnant women should receive only inactivated influenza vaccine; LAIV is not recommended for use during pregnancy. Inactivated influenza vaccine may be administered in any trimester. One study of influenza vaccination of approximately 2,000 pregnant women demonstrated no adverse fetal effects associated with receipt of inactivated influenza vaccine (105).
# Breastfeeding Mothers
Influenza vaccine does not affect the safety of mothers who are breastfeeding or their infants. Breastfeeding does not adversely affect the immune response and is not a contraindication for vaccination.
# Persons Infected with HIV
Detailed information on the use of influenza vaccine among persons infected with HIV has been published previously (18). Because influenza can result in serious illness and influenza vaccination can result in the production of protective antibody titers, vaccination with inactivated vaccine will benefit HIV-infected persons, including those that are pregnant.
# Timing of Annual Influenza Vaccination of HCP
# Timing of Organized Vaccination Campaigns
Planning for influenza campaigns should begin as early as February or March (106). The optimal time to vaccinate HCP is during October-November. Beginning in October each year, health-care facilities should offer influenza vaccinations to all full-and part-time staff. Particular emphasis should be placed on vaccinating HCP who care for persons at high risk. Vaccination programs should educate HCP regarding the benefits of vaccination and the potential health consequences of influenza illness for themselves and their patients. As part of employee health programs, all HCP should be provided convenient access to free influenza vaccine at the work site (107).
# Vaccination in December and Later
To improve vaccine coverage among HCP, influenza vaccine should continue to be offered in December and throughout the influenza season as long as vaccine supplies are available, even after influenza activity has been documented in the community. In the United States, seasonal influenza activity can increase as early as October or November, but influenza activity has not reached peak levels in the majority of recent seasons until late December-early March. Therefore, although the timing of influenza activity can vary by region, vaccine administered after November is likely to be beneficial in the majority of influenza seasons. Adults achieve peak antibody protection against influenza infection 2 weeks after vaccination (108,109).
# MMWR February 24,
# Recommendations for Prioritization of Influenza Vaccination During the 2005-06 Influenza Season
As a result of influenza vaccine distribution delays or supply shortages in the United States during recent influenza seasons (110,111), in September 2005, CDC issued recommendations for prioritizing the use of inactivated vaccine during the 2005-06 influenza season to ensure that early vaccine is available for those at the highest risk for complications from influenza (112). On the basis of uncertainties in doses and distribution, CDC recommended that the following groups receive priority for inactivated influenza vaccine until October 24, 2005:
• persons aged >65 years with and without comorbid conditions, • residents of long-term-care facilities, • persons aged 2-64 years with comorbid conditions, • children aged 6-23 months, • pregnant women, • HCP who provide direct patient care, and • household contacts and out-of-home caregivers of children aged <6 months (112). These groups correspond to tiers 1A-1C in the table of inactivated influenza vaccine priority groups in the event of vaccination supply disruption that was published previously (113). After October 24, 2005, all persons were eligible for vaccination.
Tiered use of prioritization was not recommended for LAIV administration. LAIV may be administered at any time for vaccination of nonpregnant healthy persons aged 5-49 years, including the majority of HCP, other persons in close contact with persons at high risk for influenza-related complications, and others desiring protection against influenza (18).
# Side Effects and Adverse Reactions Associated with Vaccination Inactivated Influenza Vaccine
When educating HCP regarding potential side effects, providers should emphasize that 1) inactivated influenza vaccine contains noninfectious killed viruses and cannot cause influenza; and 2) coincidental respiratory disease unrelated to influenza vaccination can occur after vaccination. The occurrence of vaccine-related side effects has had limited to no impact on rates of absenteeism among HCP (16,17).
# Local Reactions
The most frequent side effect of vaccination (affecting 10%-64% of patients) is soreness at the vaccination site, typically lasting <2 days (21,(114)(115)(116). Local reactions typically are mild and rarely interfere with a person's ability to conduct everyday activities. In a controlled trial, only body aches (25.1%) were reported more frequently after inactivated influenza vaccine than placebo-injection (20.8%) (117).
# Systemic Reactions
Fever, malaise, myalgia, and other systemic symptoms can occur after vaccination with inactivated vaccine and most often affect persons (e.g., infants) with no previous exposure to the influenza virus antigens in the vaccine (118,119). Such reactions typically begin 6-12 hours after vaccination and can persist for 1-2 days. Recent placebo-controlled trials demonstrate that among older persons and healthy young adults, administration of split-virus (i.e., detergent-disrupted virion) influenza vaccine is not associated with higher rates of systemic symptoms (e.g., fever, malaise, myalgia, and headache) compared with placebo injections (21,(114)(115)(116). No increase in asthma exacerbations has been documented in association with receipt of influenza vaccine (117).
# Severe Adverse Events
Immediate and presumably allergic reactions (e.g., hives, angioedema, allergic asthma, and systemic anaphylaxis) rarely occur after influenza vaccination (120). These reactions probably result from hypersensitivity to certain vaccine components; the majority of reactions probably are caused by residual egg protein. Although current influenza vaccines contain only a limited quantity of egg protein, this protein can induce immediate hypersensitivity reactions among persons who have severe egg allergy. Persons who have had hives or swelling of the lips or tongue, or who have experienced acute respiratory distress or collapse after eating eggs should consult a physician for appropriate evaluation to help determine if vaccine should be administered. Persons who have documented immunoglobulin E (IgE)-mediated hypersensitivity to eggs, including those who have had occupational asthma or other allergic responses to egg protein, might also be at increased risk for allergic reactions to influenza vaccine, and consultation with a physician should be considered. Protocols have been published for administering influenza vaccine safely to persons with egg allergies (121)(122)(123).
Hypersensitivity reactions to any vaccine component can occur. Although exposure to vaccines containing thimerosal can lead to induction of hypersensitivity, the majority of patients do not have reactions to thimerosal when it is administered as a component of vaccines, even when patch or intradermal tests for thimerosal allergy indicate hypersensitivity (124,125). When reported, hypersensitivity to thimerosal typically has consisted of local, delayed hypersensitivity reactions (124).
# GBS
Investigations to date indicate no substantial increase in GBS associated with influenza vaccines (other than the 1976 swine influenza vaccine) (126)(127)(128)(129)(130). If current influenza vaccines pose a risk for GBS, the estimated risk is approximately one additional case per million persons vaccinated, with the total combined number of GBS cases peaking 2 weeks after vaccination (131). This estimated risk for GBS is substantially less than the risk for severe influenza, which can be prevented by vaccination among all age groups, especially persons aged >65 years and those who have medical indications for influenza vaccination. The potential benefits of influenza vaccination in preventing serious illness, hospitalization, and death substantially outweigh the possible risks for experiencing vaccineassociated GBS. The average case-fatality ratio for GBS is 6% and increases with age (132,133). No evidence indicates that the case-fatality ratio for GBS differs among vaccinated persons and those not vaccinated.
Incidence of GBS among the general population is low, but persons with a history of GBS have a substantially greater likelihood of subsequently experiencing GBS than persons without such a history (128,134). Whether influenza vaccination might increase the risk for recurrence of GBS is unknown; for this reason, persons who are not at high risk for severe influenza complications and who are known to have experienced GBS within 6 weeks after a previous influenza vaccination should not receive vaccine. Chemoprophylaxis using influenza antivirals might be an alternative for such persons. Although data are limited, for the majority of persons who have a history of GBS and who are at high risk for severe complications from influenza, the established benefits of influenza vaccination justify yearly vaccination. Health-care professionals should promptly report all clinically significant adverse events after influenza vaccination to the Vaccine Adverse Event Reporting System (VAERS), even if evidence is lacking that the vaccine caused the event.
# LAIV
Until additional data are available, persons at high risk for experiencing complications from influenza infection (e.g., immunocompromised patients; patients with asthma, cystic fibrosis, or chronic obstructive pulmonary disease; or persons aged >65 years) should not be vaccinated with LAIV. Protection from influenza among these groups should be accomplished by using inactivated influenza vaccine.
Among adults, runny nose or nasal congestion (28%-78%), headache (16%-44%), and sore throat (15%-27%) have been reported more often among vaccine recipients than placebo recipients (37,135,136). In one clinical trial among a subset of healthy adults aged 18-49 years, signs and symptoms reported more frequently among LAIV recipients (n = 2,548) than placebo recipients (n = 1,290) within 7 days after each dose included cough (13.9% and 10.8%, respectively); runny nose (44.5% and 27.1%, respectively); sore throat (27.8% and 17.1%, respectively); chills (8.6% and 6.0%, respectively); and tiredness or weakness (25.7% and 21.6%, respectively) (37). Pneumonia, bronchitis, bronchiolitis, or central nervous system events have not been observed more frequently among LAIV than among placebo recipients.
# Severe Adverse Events
Serious adverse events associated with receipt of LAIV among healthy adults aged 18-49 years occur at a rate of <1% (137). However, surveillance should continue for adverse events that might not have been detected in previous studies. Health-care professionals should promptly report to VAERS all clinically significant adverse events after LAIV administration, even if evidence is lacking that the vaccine caused the event.
# Additional Information Regarding Influenza Infection Control in Health-Care Settings
Additional information on controlling and preventing influenza in health-care settings is available in the following publications:
• CDC. Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP | None | None |
da06ffd685c40151bd4abd3a54b2b40cd452ff02 | cdc | None | Concerned by reports that the precast concrete products industry (SIC 3272) has an injury incidence rate which is consistently at least twice that of the national average, the National Institute for Occupational Safety and Health (NIOSH) began developing this document with the intent of providing recommendations aimed at reducing worker exposure to hazards.# PREFACE
The Occupational Safety and Health Act of 1970 (Public Law 91-596), states that the purpose of Congress expressed in the Act is "to assure so far as possible every working man and woman in the Nation safe and healthful working conditions and to preserve our human resources...by," among other things, "providing for research in the field of occupational safety and health...and by developing innovative methods, techniques, and approaches for dealing with occupational safety and health problems."
Later in the Act, the National Institute for Occupational Safety and Health (NIOSH) is charged with carrying out this policy.
One method by which NIOSH responds to this charge is to publish Technical Guidelines.
Technical Guidelines present the results of comprehensive systematic analyses of occupational hazards, and suggestions for preventing injury and disease among workers.
They are intended to supplement existing Federal safety and health standards and may provide background useful in formulating new standards for development.
In the interest of wide dissemination of this information, NIOSH distributes Technical Guidelines to other appropriate governmental agencies, organized labor, industry, and public interest groups. We welcome suggestions concerning the content, style, and distribution.
This document provides guidance for protecting workers in the precast concrete products industry. It was prepared by the staff of the Division of Safety Research in conjunction with the Division of Standards Development and Technology Transfer, NIOSH.
I am pleased to acknowledge the many contributions made by reviewers selected by the Prestressed Concrete Institute (PCI), the American Concrete Pipe Association (ACPA), and the National Precast Concrete Association (NPCA); other reviewers and consultants; representatives of other Federal agencies; and the staff of the Institute. However, responsibility for the conclusions and recommendations belongs solely to the Institute. All comments by reviewers, whether or not incorporated into the final version, are being sent with this document to the Occupational Safety and Health ^Administration (OSHA^ for consideration in standard setting.
The document characterizes the industry and describes the operations, tasks and processes required to manufacture precast concrete products.
The magnitude of the occupational safety problem in the precast concrete products industry is defined through presentation of injury and illness incidence rates.
In support of the document's systematic approach to the identification of industry hazards, a detailed analysis of 1,319 accident case histories was performed.
This analysis identifies the tasks, tools, and equipment that are the most hazardous to the worker.
For example, materials handling tasks, both manual and mechanical, accounted for 28.0% of the total injuries studied.
Tasks associated with welding, burning and cutting accounted for 4.6% of the total injuries. Some of the specific tools found to be particularly hazardous to precast concrete workers include: hoists and cranes, which accounted for 4.4% of the total injuries and 40% of the fatalities; unpowered handtools, which accounted for 5.7% of the total injuries; and powered handtools, which accounted for 5.8% of total injuries. The determination of how workers are injured during precasting operations led to the formulation of comprehensive safety recommendations.
The recom mended engineering controls and/or operational safe work practices offered are applicable to product manufacture and delivery to a construction site only, and do not address erection or installation procedures.
To further enhance the document's usability for small to middle-sized pre casting plants, a chapter addressing safety management principles is presented. The Romans used the product in ashlar work (stone and brick) and as concrete in building harbors, piers, canals, and water supply and sewerage systems.
The remains of ancient structures reveal that building materials progressed from relatively simple applications of natural materials to cast concrete, one of the earliest substitutes for natural stone. Despite the ravages of time, weather, and warfare, many ancient concrete structures remain to give testimony to their durability.
Following the Roman period, the use of cement and concrete had a long period of dormancy until the emergence of studies by the early British civil engineers in the late 18th century.
During the 19th century, after the successful development of the Erie Canal under Governor DeWitt Clinton of New York, engineering projects increased the need for cement and concrete. New sources and techniques were developed, transportation improved, industrial growth expanded, and concern for public health emerged. Transportation requirements created a demand for railways, highways, storm drainage, and bridges; buildings required structural and architectural elements; and improvements in public health called for sewerage, water storage, and water distribution systems.
Technological advances, beginning with reinforced concrete and culminating in contemporary prestressing methods, have made longer, stronger concrete members possible.
Thus, concrete has grown out of a mere supplemental relationship with steel into direct competition with it in construction of varying projects.
The widespread use of standardized precast/prestressed concrete products, such as architectural panels, pipe, etc., has brought about the prevalence of fixed, permanent plants for manufacturing concrete products.
The improvement of transportational methods and systems has contributed to the evolution of the precast concrete plant, in that it has become cost efficient to mass produce concrete products and transport them to the various construction sites rather than cast members on-site.
Such plants capably produce job-specific, one-of-a-kind product as well, offering an alternative to poured-in-place operations, or casting operations adjacent to actual construction sites.
# B . Scope
This document concerns occupational exposure in the manufacturing of precast concrete products (SIC 3272). Examples of products manufactured within SIC 3272 are contained in Appendix A.
Contractors engaged in concrete construction work including on-site precasting of concrete products are classified in the construction industries and are not considered in this document. Other industries concerned with manufacture of concrete products which are excluded from the scope of this document are:
# CHAPTER II DESCRIPTION OF THE PRECAST CONCRETE PRODUCTS INDUSTRY
In this chapter the precast concrete products industry is described, its structure is examined, the number of plants and the size of the work force are defined, and the labor and trade organizations associated with the industry are identified. An operations approach that follows the production flow is used to give a description of specific manufacturing techniques or processes, the tasks performed by workers within each operation, and the tools and equipment associated with such operations.
Concrete is a building material made by thoroughly mixing cement; sand; aggregate, such as gravel or crushed stone; and water in desired proportions.
The cementitious material usually is a hydraulic cement that sets and hardens in water.
Initially, the concrete mix is a plastic material that assumes the shape of the mold into which it is cast.
The mixture is poured into a cavity, an excavation in the ground, or a form designed for a specific purpose.
After hardening, concrete has the appearance and structure of stone.
In fact, it may be thought of as "moldable stone." When the mixture is deposited in its final position, it is known as cast-in-place concrete.
When a concrete product or element is cast elsewhere (whether in a plant or on a field site) and then brought to its final position, it is termed precast concrete.
Precasting is a manufacturing procedure, whereas casting-in-place is a construction procedure.
Being a manufacturing operation, precasting can have certain advantages: o Work can be performed at a fixed site with accelerated curing facilities. o A single location for batching and mixing concrete can be provided, o A convenient source of water and other raw materials can be used, o A location convenient to transportation facilities can be selected, o Mass production techniques can be employed. o Opportunities for storing product and working under shelter reduce the impacts of cyclical demand and weather conditions.
# A. Plant Census and Worker Population
The precast concrete products industry is entrepreneurial, highly diversi fied, and geographically dispersed, with nearly 4,000 disparate plants manu facturing more than 600 different products.
The NIOSH Industrial Profile data for 1980 (Table II-1) show that 3,930 precast concrete manufacturing plants employ about 82,049 workers .
These figures compare well with information derived from the 1979 Pennsylvania Industrial Directory . , 1979 Pennsylvania Industrial Directory , and 1977 Census of Manufacturers , Information supplied by trade associations also verifies the plant census figures in the NIOSH profile. The American Concrete Pipe Association (ACPA) , the Prestressed Concrete Institute (PCI) and the National Precast Concrete Association (NPCA) estimations of worker population corroborate the NIOSH profile figures. Further, the trade associations estimate that the precast concrete industry is comprised of approximately 62,500 production workers. This equates well with the aforementioned NIOSH profile total population of 82,049 workers, and the Department of Commerce Census estimation that approximately 77% (or 63,178) of the total worker population in the industry are production workers.
Table II-3 presents these trade association estimates.
For the purposes of this study, the NIOSH Industrial Profile data was used since it was the latest compilation of data on the industry. *From Duffy J. J. American Concrete Pipe Association . From Freedman S. Prestressed Concrete Institute . *From Tilford J. E. National Precast Concrete Asso ciation .
# B. Process and Task Descriptions
This section describes the operations, tasks, and equipment required to manufacture precast concrete products. These descriptions are presented in organizational groupings that follow the primary production steps necessary in the precasting process. In many instances, the operations, tasks, and equipment described under a particular process heading are not unique only to that specific process; however, it is convenient to present the task descriptions in the sequence of the production flow. An additional section on materials handling is presented following the production task descriptions.
# Forming
Forms or molds used for the casting of precast concrete products us ually are made of steel or wood.
However, they may be constructed of any material that remains stable during casting and is able to withstand the abuse of preparation, installation of steel reinforcement, oiling, curing, stripping, and reuse. Wood is commonly used for the construction of forms expected to have a limited use; that is, forms built for the casting of fairly unique concrete products. Concrete is sometimes used as a form because it can be cast into intricate shapes. With a dense, smooth surface finish and the application of form release agents, concrete is an excellent form material for products requiring smooth or curvilinear surfaces. Styrofoam, fiber glass, rubber matting, and various paperboards are also occasionally used to make forms or form liners for special surface effects.
Because many of the products manufactured in the industry are produced repetitively, steel forms are common.
Such forms are usually made to design specification by other departments or are purchased as standard equipment from other form manufacturers.
Occasionally, it is necessary to modify or customize steel forms; that is, holes, notches, and sections may be burned out or fillets, boxouts, and seats may be welded in place as needed.
Large forms may be equipped with access ladders, stairways, work platforms, conveyor connections for receiving concrete, and external vibrators for consolidation.
Steel forms are hammered, vibrated, modified, and moved, creating dents, holes, and misalignments that require periodic repair and mainten ance.
In addition to welding shops, many plants have portable welding equipment for repair and modification of forms too large and unwieldy to move. Welds and patches are occasionally required to fill in depressed spots; chipping and grinding operations are used to smooth rough areas.
The form surface against which the concrete will be cast must be clean and smooth (unless specifically designed otherwise).
Forms are cleaned for reuse by chipping, wire brushing, scraping, scrubbing with water, sanding, and/or air blowing.
Form assembly follows repair and cleaning. Large forms are moved to the casting station by overhead hoists or cranes, or by lift truck.
Many products have interior and exterior forms.
Often, the interior form is placed and fixed to a cleaned steel plate, or pallet ring that forms the bottom of the product.
Exterior forms are then locked into place with various fittings (makeup bolts, tack welding) that both fix its position and maintain the required dimension between the interior and exterior form.
Forms for long or flat products require minimum assembly, except to position the edges, bulkheads, and boxouts at the desired locations. Edges and bulkheads usually require appropriate spacers, spreaders, braces, and stiffeners.
These pieces are usually cut from wood to the proper length, hammered into place, and held by nails. Hammers are used for driving nails and tacking chamfer strips in wood forms. Sledge hammers, crowbars, and prybars are used in the alignment of forms as well as during the placement and removal of bulkheads.
The tasks and equipment used during the construction of the forms are typical to wood, Styrofoam, or fiber glass assembly/manufacturing pro cesses.
Most companies have carpenters' shops or areas equipped with hand and power tools for form construction.
Larger companies usually have full-time personnel to use this equipment while smaller companies usually assign workers the task of making the form as part of their other routine responsibilities (casting, oiling, mixing, etc.).
# Oiling
The form surface is coated with a release agent to keep the fresh concrete from bonding to the form. Form release agents usually have a kerosene or paraffin base and are applied to the form by swabbing or spraying before the reinforcing steel is placed.
Swabbing is the hand application and spreading of the agent on the interior surface of the form with the use of brooms, mops, rags, or brushes. Swabbing operations require a worker to fill a container (buc ket) with form oil from a drum, transfer it t:o the form, and physically apply it to the form walls. Usually the worker will swab while standing and walking in the form. Some forms (vertical walls) may require the worker to stand on the form structure and mop the walls.
Most spray application of form oil is by hand-pumped, hand-carried sprayers similar to garden insecticide sprayers.
The pump is filled from a central drum and carried by the worker to the form.
Typically, the worker will walk along the edge of the form and spray the required surfaces.
Some precast plants use a central pressurized air venturi system instead of hand pumps to spread the form oil.
# Reinforcing
The reinforcing operation includes the fabrication and placement of steel reinforcement into the product forms. The tasks associated with this operation are cutting, bending, tying and welding of rebar, wire and wire mesh; and stringing and stressing of steel strand. The reinforcement, once sized and shaped, may be assembled in the form or fabricated outside of the form in a separate area or shop. The movement or placement of the steel may be done mechanically or by manual means.
# a. Plant Fabricated Steel
Manual fabrication of reinforcing assemblies is common. Some times reinforcing bars or welded wire fabric are placed and tied in the form. For more complex assemblies, a jig is built to position bars. Transverse and shear steel is manually tied to the longitud inal steel with wire and pliers or with looped-end wire ties and a special "pigtail" tool that twists the two ends of the wire tie together when pulled. To produce reinforcing bars with the bends, loops, angles, and hooks specified by the design, a rebar bender is used. A cage or mat can be made to any desired size or shape. The completed plant fabricated reinforcing steel assembly is then lifted and placed in the form by manual or mechanical means. With prestressed concrete products, individual stirrups or welded wire fabric used for shear reinforcement are hand placed and may be tied to the prestressing steel.
Circular or elliptical reinforcing cages for concrete pipe are usually made of welded wire fabric (2-to 4-inch mesh made from 1/8-to 3/o-inch wire) or cold-drawn steel wire.
A wire roller forms rolls or flat mats of welded wire fabric into the desired circular shape, which is then cut and spot welded to make the cage.
Both cage machines or mandrels can be used to form steel wire into cages.
In a cage machine, the operation is continuous and the endless cage produced is cut to the required length; in a mandrel operation, each cage is made individually to the desired diameter and length. Both techniques require that the wire mesh be shaped into a cylinder (by rolling or bending), the ends joined (by welding or using tie wires), and the finished reinforcing cage placed into the annular space of the pipe form.
# b. Prefabricated Steel
Many small precast concrete products are reinforced by prefab ricated steel manufactured to specification by others. This prefabricated steel is placed, tied, or secured into the form or pressed into the freshly cast concrete at the desired locations.
# c. Steel Plates and Rolled Sections
For connecting some structural and architectural precast concrete products, small, rolled, sectioned steel plates with reinforcing bars or studs welded to them are tied to the cages inserted in the freshly placed concrete.
Wire loops of prestressing strand or reinforcing bars are tied in place or inserted manually for lifting and handling the finished product.
Connection and handling steel is called "hardware," and should be designed by the plant engineering staff or the project engineer.
The tasks necessary when using steel plates are similar to those described in the preceding sections.
# d. Prestressing Steel Strand
Prestressing steel is usually seven-wire strand that is manually or mechanically strung in the form before concrete is cast.
Manual strand stringing is performed by a worker physically pulling the length of strand down the bed from a reel stationed at one end of the bed.
The strand is then cut by torch or strand saw, and the process is repeated. Mechanical stringers pull multiple lengths of strand from separate reels at the same time.
Single or multiple strands may be threaded through cages of reinforcing steel and through bulkheads used to separate adjacent members.
The steel wire strands are laid in the stressing bed (a long form up to several hundred feet in length with the cross section of the desired shape) and fixed at the ends (abutments).
The stressing bed is the mold for several precast units along its length.
For example, if 50-foot-long "double tees" are desired and a 610-foot-long stressing bed is used, 12 such units can be produced in one bed, each separated by a bulkhead. Some beds are designed as selfstressing forms, eliminating the need for end abutments.
Once the strands are in place they are then stressed. This operation is the tensioning (stretching) of wire strands previously positioned in the form.
Stressing includes strand vise placement, jacking, tensioning, harping, and detensioning.
The stressing operation can be done by single strand jacking or multiple strand jacking where all the strands are tensioned at the same time.
The strands to be stressed (usually 1/2-inch, seven-wire strand , tensioned to approximately 200,000 pounds per square inch (psi) or a 30,000 pound load) are anchored at one end of the bed with a strand vise.
The strand vise barrel has a truncated conical hole along its longitudinal axis that holds the three jaws of a chuck.
The chuck is serrated on the inside surface and conical in shape outside. The jaws permit free movement of the strand in one direction.
In the other direction, they grip the strand and wedge themselves into the conical hole in the barrel of the strand vise.
A strand vise is placed over each length of strand at the anchor end abutment, which fixes it in place. At the jacking abutment, two strand vises are placed on the strand in opposing directions.
One is seated against the end abutment and allows the strand to be pulled through as the jack tensions the strand.
This strand vise also holds and anchors the tensioned steel to the abutment. The other strand vise provides a grip for the jack.
Figure II-l shows a rectangular prestressed beam form with strands stressed and reinforcement in place.
The steel strand may run straight through the bed and may be stressed in this position.
Alternatively, the strands may be depressed within the form for each member along the bed to create an upward force that improves structural efficiency . This technique is called draping or harping.
The term "draping" describes the profile of the steel strand, which is "draped" from its high point near the ends of each precast member to the low point at the midspan of each member.
Strands can either be depressed or pulled up.
Tine strands are passed through and over pin and roller fixtures that minimize friction at the points of change in the steel strand profile.
Figure II-2 shows the strands depressed at the midpoint of a member, thus creating the appearance of strings on a harp. Some designs may require other holddown locations for each member.
After the concrete is cast and has gained the specified strength (us ually 3,500 psi or more ), the strand tension is released, or detensioned.
In some cases, strands are individually cut by torch; however, with hydraulic jacks, the tension is gradually released from the header.
# FIGURE II-2. A "SINGLE TEE" SLAB WITH THE STRANDS HELD DOWN AT THE MIDPOINT
TO "HARP" THE PRETENSIONED STEEL Adapted from Bennett W. B. Jr. .
Detensioning transfers the stress from the steel to the concrete to which it has bonded, precompressing the concrete.
# Concrete Mixing
Concrete may be batched and mixed at the products plant or purchased from a ready-mix concrete producer. The correctly weighed proportions of cement, aggregates, and water are charged into a drum mixer, pan mixer, or a transit mix truck.
Small mixers that are used in many miscellaneous products plants are gas, diesel, or electrically powered.
Cement may be delivered to the plant in bulk cement trucks or railroad cars and unloaded by a totally enclosed, screw auger pneumatic system that carries the cement to an elevated hopper or silo.
Aggregates for larger plants are unloaded in much the same way as cement, except that open conveyors may be used.
The material stored at a higher elevation is weighed and chuted by gravity (charged) into the mixer.
The proper weight of water is added, and the mixer blends the components into a homogeneous mixture by rotating paddles inside an enclosed vessel at speeds of 2-15 revolutions per minute (rprn), or approximately 2 linear feet per second.
The two most common types of mixers used in the industry are drum mixers and pan mixers.
A drum mixer is a rotating cylinder in which sta tionary paddles, mounted along the cylinder, mix the concrete (truck mixers are of the drum type, inclined from the horizontal).
The pan mixer consists of a shorter cylinder than the drum mixer and is vertically oriented; paddles are mounted vertically and rotate to mix the concrete in the stationary cylinder.
The mixer is usually positioned 10-15 feet above the adjacent working surface to allow gravity discharge of the mixed concrete into buckets, trucks, or other means of conveyance to the casting area.
Access for cleaning, maintenance, or concrete quality control is provided by ladder or steps to a working platform that will partially or totally encircle the mixer.
Figure II-3 depicts a concrete batching, mixing, discharge, and transport system.
At the end of each shift or after mixing is completed for the day, the mixers are cleaned.
In addition to daily cleaning and flushing of concrete mixers, it may be necessary to hammer or chip away built-up en crustations of concrete on a periodic basis.
Mixers also require maintenance, paddle replacement, and repair.
All of these tasks may require workers to enter the mixers.
# Concrete Delivery and Casting
Casting of small products can be a manual operation; a quantity of mix is made available to the operator, who trowels or shovels it into a prepared mold around the reinforcement. The material may be hand tamped or vibrated to consolidate the mix.
Many small products are made with high production, automated equipment.
For casting larger pieces, the concrete is delivered from a truck, a concrete bucket, or a concrete buggy moved to the location where the concrete is to be used.
For very large pieces or for long-line prestressing beds, the concrete may be delivered by a monorail bucket system, overhead bridge crane, or other mechanical means and deposited directly in the form, where it is vibrated and consolidated by machinery or by manually inserted spud vibrators.
Usually two to five employees will be directly involved in these tasks.
In addition, concrete may be extruded through a die to form products such as hollow-core slabs.
Systems used to deliver the mixed concrete to the placement location vary from simple manual handling to totally automated, enclosed convey ances.
Concrete mixed in small power mixers is delivered by direct deposit (when the mixer or form is portable), by front-end loader (which carries concrete from mixer to form), or by wheelbarrow.
Ready-mix trucks frequently are used to deliver concrete because they can carry, and continuously mix, large volumes (up to 12 cubic yards) directly to or near the forms for placement. A chute, attached to a lip below the discharge opening of the truck's drum mixer, is directed by a worker to deposit the concrete.
The chute is moved around during the casting process to spread the concrete and reduce shoveling or raking.
As parts of the form are filled with concrete, the truck moves along the form, placing concrete to the desired level.
The process continues, FIGURE II-3. CONCRETE BATCHING, MIXING, DISCHARGE, AND TRANSPORT SYSTEM using additional ready-mix trucks with loads of concrete, to completely cast the products being made. During casting, workers will be engaged in a series of continuous tasks directed at filling the form with concrete.
When a ready-mix truck is used, workers will be working adjacent to and along with the movement of the delivery truck. Access (steps or ramps) to low forms (1-3 feet high) is usually limited or nonexistent. Employees will frequently be working and moving among multiple form tiedowns, spacers, and spreaders as well as walking on the reinforcing mats while filling and vibrating the forms. When it is not possible for a truck to deposit concrete directly into the form, wheelbarrows, hoisted concrete buckets, or concrete delivery vehicles are used.
Workers may push wheelbarrows along walkways, planks, or ramps to fill the form with concrete.
Another method of delivering concrete is by transporter, which takes mixed concrete from a central mixer and carries it directly to the forms.
Enclosed transporters have a smaller capacity (up to 6 cubic yards) and are usually lighter, smaller, and more maneuverable than ready-mix trucks. This method of depositing concrete is similar to that for ready-mix trucks except that the chute is tubular in shape, with an enclosed auger or conveyor belt, allowing concrete to be pushed to higher elevations instead of depending on gravity. Some transporters consist of wheeled or tracked carriers that take large buckets or hoppers of mixed concrete (up to 4 cubic yards) to placing or casting machines.
Transporters may travel on aisleways, rails, or roadways at speeds of up to 500 feet per minute.
Transfer, turnaround, or backing areas may be provided at the end of the travelway s for moving the transporters laterally relative to the casting areas or for access to the concrete mixers.
Visibility may be limited because of walls, corners, other equipment, storage, or layout. Once the concrete buckets have been delivered to the casting area, an overhead hoist, which may be an integral part of a casting machine, will be used to hoist and position the bucket over the form or casting hopper.
Conveyors are frequently used to deliver concrete to the point of placement, especially in the miscellaneous and pipe sectors of the industry.
The forms can be set up under the discharge end of the conveyor, or a portable conveyor can be set up with its discharge over the forms (depending on form mobility).
Concrete is deposited onto the conveyor and moved along the conveyor system (which can be arranged to move the concrete around corners, to different elevations, or to remote plant locations) to the point of discharge.
Access to elevated forms during casting is usually provided by plat forms, stairs, movable scaffolds, or ramps.
Large pipe forms and mis cellaneous products forms will sometimes have walkway platforms built around the forms or attached for the casting operations.
Ramps are a convenient means of access to forms at elevations different from the surrounding working surface; otherwise, stairs are used.
Access to lower beds up to 3 feet above the plant or yard surface usually is by stepping up and jumping down; it is uncommon for steps or ramps to be provided- In mechanized plants, placement of concrete into lorigbed forms is accomplished by placing or casting machines, similar to pavers or extru ders.
The concrete is spread, vibrated, compacted, screeded, and finished as the machine passes over the form, or is extruded as it moves along the bed. Drive controls are located in a cab on the machine or on a panel reached by workers from the side of the machine.
One method of casting utilized in the manufacture of pipe and many miscellaneous circular products requires a concrete mix that is wet com pared to the mixes used in dry mix processes.
Using both inner and outer forms, a cone is placed on the inner form to direct concrete down into the annular space between the forms. The concrete is then consolidated by stick vibrators or external vibrators, and the exposed top surface shaped and finished as required by hand, using edgers, trowels, and brushes.
# Figure II-4 depicts an automated vertical pipe casting operation.
Employees work from scaffolds that are rolled into place around the perim eter of the external pipe form.
As the concrete discharge chute rotates around the form, workers using shovels, boards, tampers, and/or vibrators ensure the proper placement and consolidation of the concrete.
Most concrete pipe is cast with a relatively dry, low-slump mix that is mechanically placed and consolidated in the form.
Two of the four mechanical methods use both inner and outer forms, which vibrate with either tampers or vibrators while the dry-mixed concrete is cast into the annular space between them.
In the tamping method, compaction is performed directly by vertically operated tampers.
In the dry cast method, consolidation is done by external vibration of the inner or outer form.
The other two mechanical methods use only the outer form and either spin the pipe horizontally while centrifugal forces distribute the concrete delivered by conveyor, or spin a mandrel-like packerhead that is drawn up inside the pipe as concrete is cast from above, compacting as it goes.
These four mechanical, dry-type mix methods of casting pipe are shown in Figure II--5. Metal pipe forms are placed by forklift or man ual or automated cranes onto openings in a circular casting floor.
The floor rotates (at slow speeds) to position the form in the operational packerhead area.
An employee on an elevated platform controls the packerhead spinning speeds, the up-and-down motion of the packerhead, and the flow of concrete into the form. When the casting is complete, the floor rotates an empty form into place and the forklift removes the cast pipe and mold to a curing area. per second (rps) while vibrating and depositing concrete, and at speeds up to 10-12 rps while "throwing" the concrete and compressing it against the rotating form. In the centrifugal process, excess water is removed, further lowering the water/cement ratio of the concrete.
Figure II-7 depicts one method of pipe spin-casting.
In this method, the pipe form is assembled by bolting or clamping the halves together. The form is placed by hoist onto a rotating pipe machine.
Horizontal pipe machines are usually constructed from groupings of auto/truck tires that serve to cradle and spin the form.
In this figure, the rotating force is applied by overhead tires that spin the pipe form at the required speeds. Concrete is added by a movable extruder, operated by a worker who is positioned to visually inspect the centrifugal consolidation during the placement process.
Internal finish work is usually performed by a hand-held, dowel-mounted trowel.
A worker runs it in and out of the pipe orifice while the form is spinning.
# FIGURE II-7. HORIZONTAL PIPE SPIN CASTING
Casting large miscellaneous products is similar to the tamping, dry cast, or wet cast methods used for pipe manufacture; however, the form may be square or rectangular as for burial vaults or septic tanks.
# Finishing
Wet finishing includes tasks such as screeding, floating, troweling, patching, rubbing, and cleaning surfaces not in contact with the form. Screeding is the back-and-forth motion of a strike off (a wood 2 by 4 or steel channel) resting on a screed guide to form the surface of the con crete to be finished. Workers may have to reach, bend over, and pull to perform this task.
Floating, the smoothing of the surface with a wood, aluminum, or magnesium float, is manual work requiring bending, kneeling, and reaching.
Troweling smooths and compacts the floated surface when the surface is hard enough to walk on without leaving indentations.
Additional treatment of the formed surface may take place after the form has been removed and the product has cured. This is particularly true for architectural panels, when the surface texture is important. Techniques such as grinding, bush hammering, sand blasting, water washing of retarded surfaces, or acid etching are used to produce a variety of desired architectural effects.
Bush hammering is the roughening of the hardened concrete surface with a vibrating hammer, the head of which is serrated with a series of pointed teeth. Sand blasting is the high-pressure spraying of sand onto the exterior concrete surface to clean or smooth it. Water washing (up to 300 psi) is the flushing of cement paste that purposely has been retarded in setting to expose the surface of the aggregate.
Acid etching serves a similar purpose, but does not expose as much of the aggregate.
This procedure involves the mixing, dilution, and application of muriatic acid, an industrial grade of hydrochloric acid.
In some instances, precast concrete products are cut to length or have portions removed by sawing them with a concrete saw.
This type of saw is similar to that of a carpenter's circular skill saw except that the blade size ranges from 1-3 feet (or more) in diameter.
During repetitive operations, or when using larger blades, saws may be semiautomated and suspended overhead. The power source for the concrete saws may be electricity or pressurized air, although some of the smaller, portable models may be powered by gasoline engines. Most saws are not provided with a lower (exposed) blade guard.
# Curing
Three fundamental factors in all methods of curing concrete are time, temperature, and moisture.
Within limits, an increase in temperature shortens the curing period by accelerating strength gain.
The time/temperature relationship is not the same for all mixtures, materials, and conditions and is determined empirically.
# I
The curing of many larger precast products is accelerated by radiant heat, steam, hot water, or hot oil. In some instances, the cast product is exposed to live, low-pressure steam within an insulated kiln or steam shed. Pipe or other products to be steam or heat cured will usually be transferred from the casting area to the heated shed by conveyor, forklift, hoist, or, in some instances, by rolling.
The products remain in the steam shed for 2-8 hours (frequently overnight) before being removed and the form stripped.
In some instances, the form is stripped before the product is steam cured.
Large pipe is frequently enclosed (in the place where it was cast) by canvas, plastic, or other material into which steam or warm, moist air is introduced.
Steam and hot water for accelerated curing procedures are usually generated at the plant by a low-pressure boiler and piped to designated locations prior to release into the curing shed.
Occasionally, a chemical curing compound is sprayed on the finished surface of the concrete.
# Form Stripping
Once a concrete product has cured sufficiently to be handled, it is necessary to remove it from the forms it was cast in or, conversely, to remove the forms from the product. The tasks and equipment used in form stripping operations vary considerably with the nature of the product. Reusable metal forms, such as those used during the manufacture of pipe, are usually handled by overhead hoist. The inner form is rigged to the crane and removed-a task made more difficult because the product fre quently adheres to the form surface.
In some instances, striking the form with a hard rubber mallet is sufficient to jar the concrete loose. In others, a hoist is used to shake the form and/or to pull the form free. Large pipe forms are frequently equipped with a means to collapse the internal form within the pipe bore.
Workers enter the pipe bore to release retaining clamps.
Rigging of the hoist to large form members requires that employees gain access to elevated areas. This may be done by ladder, rolling scaffolding, or climbing the form structure itself if it provides safe access. With low-slump, consolidated pipe, the mold is removed at the kiln prior to accelerated curing.
Flat products are removed from the mold by means of a vacuum lifter, or by lifting the product from the mold utilizing "lifting eyes" previous ly inserted in the product.
Girders, beams, or other large, vertical products may have side forms to be removed before the product is freed from the forms.
Bolts and other connectors are removed, and the side form panels pulled away or dropped to the ground. Some concrete products may require dismantling of the forms for re moval either because the form material will not be used again or because this is the only practical means of removing the completed product. Depending on the size and shape of the form, workers may perform the dismantling from the plant floor, from the elevated casting beds, from rolling ladder/scaffolds, or from the form itself. Workers will usually be performing their tasks on and among the equipment and material used during the form stripping process.
Prybars, crowbars, sledge hammers, and wrenches will be used to pull nails and remove the spreaders, stiffeners, and bulkhead-retaining tie rods.
Sledges and prybars will be used to force the separation of bulkheads from the product and/or other form structures.
This frequently involves workers pushing or pulling on the bar until the adherence forces release, sometimes suddenly.
# Material/Product Storage
Material storage in the precast concrete products industry follows a usage pattern typical to most manufacturing processes.
Raw materials necessary to produce the product will be shipped and temporarily stored in a yard. Usually raw materials will consist of the basic ingredients of the concrete (cement, sand, aggregate), the reinforcing materials (reinforcing steel, strand, wire mesh, hardware), and a variety of ancillary materials (blasting sand, equipment maintenance materials, etching acids, etc.) necessary for the production of a finished concrete product.
The bulk ingredients for the production of concrete may be hauled in by truck and dumped in covered bays or, in smaller plants, a convenient place on the prenises. Larger, more automated plants may yard consider able volumes of various sized aggregates and cement prior to transfer to mixers.
Cement may be bagged, palletized, and stored in weatherproof areas or it may be delivered by bulk tankers and stored in silos. These 94-pound bags of cement may be stacked higher than a worker's head, requiring access to the upper levels.
Reinforcing steel bars are usually received in banded lots of various lengths, ranging up to 40 feet or more.
Prior to cutting to required lengths, the rebars will usually be stored on the ground on cribbing material. Spooled or reeled material (e.g., wire mesh) is frequently stored in stacked rows.
The end spools are chocked to prevent rolling or shifting; second level spools are nestled in the spool interface.
Since forklifts or mobile cranes will be used to move these heavy rolls, adequate access space between rows of stored materials should be considered.
Product storage methods vary considerably with the size and shape of the product.
Small miscellaneous products are frequently produced in a variety of shapes at the same plant.
Yard areas are usually limited, necessitating multilayered stacking of the pieces.
Layers may be separated by cribbing and/or pallets to both protect the finished surface and to increase the load-bearing surface stability.
Larger and heavier shapes, such as vaults and manholes, are frequently stacked with cribbing layers between them to provide access for forklifts or rigging material.
Pipes and cylindrical products are stored in the manner described for rolls and reels. Pipes of the same size are stored in the same stack.
Again, care must be taken to allow adequate access for materials handling equipment and to prevent stack shifting. Large pipes are usually stored vertically.
Discarded products, broken pieces, metal scrap from forms, reinforcement, tie-wire, wood scrap, nails, chamfer strip, rejected hardware, concrete, forms, and the remainder of unused raw materials can be found in plants in this industry.
Many plants have a "bone yard" in which such discarded material is kept, pending burial or removal.
# Materials Handling
Materials handling operations are performed throughout all phases of the production of precast concrete products.
At the simplest (and fre quently overlooked) level, employees lift, carry, push, or pull everything from concrete debris to wood form material to smaller, finished products.
In fact, throughout the industry, manual handling is necessary to perform many of the tasks required in the production process, including: Individual, small miscellaneous products may be loaded or unloaded by hand. When several small items of the same variety are to be handled, they usually are strapped and palletized.
Larger products and concrete pipe require the use of lifting and unloading equipment.
Architectural and structural products usually are large, bulky, and heavy, requiring the use of cranes and special loading and handling techniques such as "A" frame holders and wood and metal chocking for security, for bolting to the trailer bed, and for single-product loads.
Since precast concrete products and their components are heavy by their nature, the industry makes use of a variety of mechanical devices to assist in handling and movement operations.
# a. Hoists and Cranes
For the most part, the types and varieties of hoists and cranes that are used in precasting operations do not differ significantly from those used in other industries.
However, because of the weight of the material and products being moved, crane and hoist usage may be more prevalent.
Smaller plants may use rubber-tired cranes with hydraulic booms to move material and products around the yard, onto trucks for trans port, and from the casting bed to the storage yard.
These mobile cranes are prevalent throughout the industry for movement of yarded material and products.
In most instances, the crane operator will work in tandem with other employees charged with the material rigging responsibilities.
Products may be manufactured with integral picking eyes that facilitate proper rigging and load balance.
In other instances, the rigging and hoisting will be performed on material necessitating new or single instance handling procedures.
Load weights and balance points must be identified by the workers as part of the rigging operation.
Larger, more automated plants are likely to have semipermanent work stations and fairly repetitive product design.
These plants are likely to use a number of overhead hoists. Overhead hoists may run on tracks and be located to service multiple operations in the manufacturing process. Larger overhead cranes are controlled by an operator located in the crane cab. Work stations may be serviced by smaller, 2-to 10-ton jib cranes.
Although a jib crane may be mounted on an independent vertical column, the horizontal "jib" is most frequently affixed to a vertical column integral to the plant's structure.
Employees at the work station operate the jib crane by using a wire-attached pendant control, which allows the worker to control the up/down and back/forth movements, or other functions of the crane, from the floor of the plant.
In these instances, the hoist operator is usually the same worker that performs the rigging.
He is also likely to accompany, with hands on, the load being transported to its destination.
Straddle carriers are large, four-wheeled, wide-spaced, high legged movers that straddle large products (such as girders, planks, or other structural elements) pick them out of forms and move
them. This open-framed machine, basically square in configuration, hoists and carries the load within a large open bay between the four wheels on which it travels. The operator's cab is located on the extreme left-hand side between the front and rear wheels. Loads suspended in the bay often obscure the driver's view of the right side wheels.
The machine ordinarily moves at about 2 miles per hour (mph) and has a maximum speed of about 10 mph.
# b. Forklifts
Many of the palletized raw materials and finished products used in precast plants are moved by forklifts.
Fork extenders may be used to increase the bearing surface of the forklift.
In some instances, a jib may be added to the forklift to convert it to a small, movable crane.
Pipe and other circular products are moved by forklifts with specially designed long forks or fitted forks with curved surfaces to cradle the product. Some forklifts are equipped with clamping forks used for attaching to and moving forms or other compatible shapes.
The power source on forklifts is most frequently propane or diesel fuel.
# CHAPTER III IDENTIFICATION OF THE SAFETY HAZARDS AND DEFINITION OF THE PROBLEMS
This chapter is divided into two major areas of emphasis: the development and presentation of data pertaining to injury incidence rates for the precast concrete products industry (SIC 3272), and the identification of those tasks performed that are hazardous to the worker.
Additionally, an estimation of the cost of injuries sustained by workers in the precast concrete products industry is presented.
# A. Injury and Illness Incidence Rates
The yearly compilations of occupational injury and illness data, prepared by the BLS, show that between 1976 and 1980, the precast concrete products industry had an average incidence rate of about 23 cases per 100 employees (Table III-l) .
In comparison, the incidence rate for all private sector industries averaged about 9.2 during the same interval. Workers in the precast concrete products industry have been consistently injured at a rate nearly 2.5 times the national average. Also, between 1976 and 1980 the average incidence rate for all durable goods manufacturing industries (which include SIC 3272) was about 14, which is substantially less than the rate for manufacturers of precast concrete products (Tables III-l and III-2). The incidence rates for precast concrete products are among the highest rates within the manufacturing sector (top 3%). A representative selection of the manufacturing industries is shown in Table III
Table III-3 demonstrates that the occupational incidence rate per 100 employees in the precast concrete products industry was higher than those for concrete block and brick manufacturers and ready-mixed concrete, which exhibited incidence rates of 15.8 and 13.7, respectively.
The incidence rate for concrete products was also substantially higher than for blast furnaces and steel mills (9.5), which is a heavy industry involving additional injury potentials attendant to the handling of molten metal.
The severity of injuries sustained by employees of the precast concrete products industry was also shown to be high.
The lost workday cases and lost workdays incidence rates, represent a general measurement of the seriousness of occupational injuries and illnesses.
The lost workday cases incidence rate for the precast concrete products industry (SIC 3272) in 1980 was reported by the BLS as 10.4 (Table III
-l).
This figure ranged from a reported high of 12.1 in 1979 to a low of 9.1 in 1976, with an average of about 10.7 for the years between 1976 and 1980 (Table III
-l).
The lost workday cases incidence rate for all private sector industries in 1980 was reported by the BLS as 4.0 and for the durable goods manufacturing industries as 5.6 (Table III
Furthermore, for every 100 employees in the precast concrete products industry in 1980, a total of about 158 days were lost due to disabling injuries and illnesses (Table III
-l).
The Although the estimates of direct costs of worker injuries are not precise, they do reflect the magnitude of the problem.
Estimates derived from National Safety Council data indicate that full costs of work-related accidents are more than 3.4 times the direct wage loss and medical expense costs.
Since the indemnity payments are normally less than wage loss, the real accident costs for the precast concrete products industry are estimated to exceed $105 million per year (3.4 x $30.9 million).
In addition to medical and indemnity expenses, estimates of the real cost of accidents include:
# C. Identification of the Hazards
The preceding section of this chapter defined the magnitude of the safety problem in the precast concrete products industry.
The next step in a systematic approach to effectively lowering worker accident/injury exposure is the identification of how workers are injured while performing the tasks required to produce precast concrete products.
# The Supplementary Data System (SDS)
Currently, occupational accident and injury information from participat ing states, which is taken from employers' first report of injury forms, ' Production workers comprise about 77% of the total work force for this industry . Seventy-seven percent of the reported 1977 employment figure of 67,300 (Table III-l) is 51,821 production workers.
Compensation losses of $30,855,454 divided by 51,821 production workers yields about $595 per production worker. is compiled and reported by the BLS Supplementary Data System (SDS) . The SDS is intended to alert users to patterns and relationships of injury causal factors.
The information is entered into each of four major groupings: The frequency and percentage distribution of the injuries reported to SDS by the precast concrete products industry for the years 1976 -1979 are presented in Table III-4 for each of the groupings mentioned above. The percentages do not indicate that one category represents a greater hazard than another, since data clarifying worker exposure are not available.
# Accident/Injury Analysis
The SDS data are limited when used in the analysis of a specific industry because the "source of injury" category contains subcategories which do not apply to the industry under study, and does not contain subcategories which are related to industry-specific tools and equipment.
Further, the "source of injury" reported is the object most responsible for causing the injury.
Thus, if a worker falls from a ladder and fractures his leg on the plant floor, the "source of injury" is the floor, which probably contributed little to the actual cause of the accident.
Despite the constraints, the SDS data reported by the precast concrete industry for 1976 -1979, which included 15,208 injuries, were analyzed to identify specific industry hazards.
The analysis included 37 categories that identified injury sources within precasting operations.
The results of the cross-analysis of the SDS data are summarized in Table III
The total number of accidents/injuries appears in the "Source of Injury" column.
The numbers associated with "Type of Acci dent," "Nature of Injury" and "Body Part" do not agree with the "Source of Injury" totals since the figures given are merely the most frequent subcategories.
# Analysis of Accident Case Histories
For a more complete understanding of accident/injury causal factors, full text copies of employers' first report of injury forms filed by SIC 3272 industries were requested from all 50 States.
In most instances, the state agencies were not able to provide information.
However, 10 States 1 did provide copies of 2,250 first report of injury forms from California, Hawaii, Iowa, Kentucky, Michigan, Montana, Maryland, Washington, Wyoming, and Vermont. Of the 2,250 accident/injury reports, 1,319 (about 59%) were included in the analysis.
Of these 1,319 injuries, 34 resulted in a fatality.
Those reports not included in the analysis primarily contained injury information, and were found to contain insufficient data to determine accident causal factors.
A preliminary analysis of these accident case histories was performed to determine whether the accident data base was indicative of accidents occurring to workers in precasting operations nationwide.
Each report was categorized by type of accident ("struck by," "caught between," "fall").
Numerical and percentage values of the "type of accident" categories were compared to the national SDS figures (Table III-4). The comparison (Table III-6) shows markedly similar ratios; e.g., the percentage of "struck by" and/or "caught between" accident types are reasonably consistent in both data bases.
Because of the similarities between data from the sources considered, it was concluded that the accident/injury case histories used in this report are representative of accidents that occur to workers in the precast concrete products industry.
The first step in the analysis was the identification of the specific task, tool, type of material, piece of equipment, or plant area most closely associated with the accident in each case.
This procedure made possible more precise and industry-specific classification than the SDS "Source of Injury" category could provide. Then, a causal factor was identified in each case (e.g. improper tool use, lack of personal protective equipment, lack of adequate guarding, improper materials handling procedures).
The task/tool/equipment factors and accident causal factors were then cross-indexed to allow the identification of problem areas.
The following narrative descriptions of how workers are injured in the precast concrete products industry are based on analysis of SDS data (Table III -5) and the accident case histories. The percentage that follows each category or factor is the percentage of the total number of accidents (1,319) from the case history analysis.
Section a covers general accident factors; i.e., tasks, tools and items of equipment that are not specific to the precast industry.
Section b presents factors that are specific to precasting processes.
Section c describes accident causal factor patterns, groups of factors which may encompass several task/tool/equipment categories. Essentially, the organization of sections a, b, and £ is followed in the presentation of the recommendations in Chapter IV.
# a. General Accident Factors
The following narrative paragraphs describe the ways workers are injured due to task/tool/equipment factors which are not necessarily specific to the precast concrete products industry. Although these general factors are arranged in order from highest to lowest percentage of occurrence, this grouping does not suggest that one factor represents a more significant hazard than another, since no data clarifying worker exposure are available.
(1) Materials Handling (28.0%) (a) Manual (19.9%)
(i) Lifting (9.6%)
The act of lifting items resulted in nearly 10% of the injuries in the industry. Approximately 81% of these incidents involved overexertion to the back while manually handling materials.
Loss of grip accounted for 9% of the lifting accidents. These usually resulted in injuries either to the lower extremities when the load was dropped or to the fingers when the load was set down with inadequate clearance.
(ii) Mechanical Materials Transport (7.1%) This category presents a variety of tasks associated with materials handling as well as a variety of other accident causal factors.
Included in this activity are interface of manual and mechanical load handling procedures performed on flatbed trucks and the manual transfer of materials to forklifts. Manual materials handling and gripping of materials accounted for 27% of the injuries in approximately the same causal/injury breakdown as cited in the discussion of the lifting category. Improper stacking and binding of materials was reported to be the cause of about 27% of these accidents, usually from the material falling onto the worker.
An additional 12% of the accidents occurred to workers attempting to climb onto the transport vehicle or the material itself when access was not provided.
(iii) Carrying and Holding (1.8%) This category of activity includes the manual tasks, by one or more workers, of carrying or handling materials.
Many of the injuries were sprains and strains that usually occurred from overexertion during the procedure.
About Hand operation of the hoists necessitated close proximity to the hoisted loads and contributed to employee exposure to hoist or rig failure.
(iv) Conveyors (0.6%) Although only 0.6% of the accidents involved con veyors, they accounted for nearly 9% of the fatal injuries.
These accidents occurred when the conveyor jammed and the operator/worker attempted to free the jam without deenergizing and locking out the system.
Workers were caught by or in exposed moving portions of the conveyors.
Lack of guarding of exposed moving parts and/ or nonlimiting access to the area were cited as contributing factors to the accidents.
Similarly, the nonfatal incidents usually involved the upper extremities being caught in or between the conveyor mechanisms as shown in Table III In the latter accidents, the injured workers were in the path of travel of the loaders and were either caught between it and another object or they were run over by the moving equipment.
Inaudible or nonfunctioning backup alarms as well as operator inability to see coworkers were cited as contributing factors.
(2) Handtools (11.5%) (a) Handtools, Powered (5.8%) Nearly all of the injuries attributable to the use of powered handtools resulted from deficiencies in three areas: guarding, tool usage, and lack of eye protection.
The injury analysis revealed that most eye injuries occur during use of grinders. The remaining grinder-related accidents were the result of inadequate or non-existent guards that failed to prevent finger contact or protect against stone disintegration.
In some instances, while using the grinder, part of an employee's body, usually the thigh, came into contact with the abrasive stone.
In the SDS accident/injury analysis (Table III-5), eye injuries occurring during grinding activities were not listed with grinders; rather, they were tabulated in the "Particles" category.
Although lack of eye protection contributed to 20% of the powersaw injuries, the single, consistent accident causal factor was inadequate or nonexistent saw blade guards (58%).
Included in this category were instances when anti-kickback devices were not used during ripping operations. The majority of injuries resulting from lack of saw guards were lacerations and amputations of fingers.
Two eye injury accidents also occurred while using concrete saws.
The accident analysis shows that most accidents during drilling tasks occurred when large-diameter (1-inch or larger) holes were drilled through forms.
The drill bit would bind and the drill motor would continue to turn, catching the workers' hands between the motor and adjacent items, usually the form. This may be interpreted as improper tool use or as improper worker position relative to the task. Lack of eye protection accounted for one-third of the reported injuries that occurred while using airhammers. In some instances, airhammers were used in awkward positions, resulting in strains and sprains of the back and/or arms.
In three instances, the airhammer was positioned for use too close to the edge of either a form or product, and the worker's hands or fingers were caught. Table III-5 indicates that powered hammers as a source of injury resulted in injuries to the back because of worker overexertion and to fingers that were struck by the hammer. The injury reports indicated that many injuries were associated with over loading the shovel, twisting the body, and handling the load from too great a distance (see Table III-5, "Shovel" and "Concrete aggregate"). The activity of "prying" is frequently performed by workers dismantling forms and separating the product from the form.
Referring back to Table III-5, 47% of the accidents involving crowbars, a tool routinely used for prying, were classified by the SDS as "struck by" accident types resulting in contusions and sprains and strains.
The most frequent areas of the body injured were the back and finger.
The analysis of the accident cases showed that 65% of the prying accidents were reported to be caused by improper worker position relative to the task. When the prying implement slipped, the tool usually either struck the worker or the worker slipped and fell.
Most of the remaining accidents involving prying activities resulted from improper tool use. Shovels were commonly misused by workers attempting to pry forms loose from cured concrete.
The most common type of accident that occurs during the use of handtools is the "struck by" variety (Table III-5), most frequently caused by improper position of the worker relative to the task.
The analysis indicated that glancing blows are commonly cited as the cause of the accident.
Fingers and hands were struck by hammers and sledge hammers when part of a worker's body was in the path of the deflected hammer movement.
Use of improper tools contributed to 25% of the hammering accidents. Typical cases involved shovels, wrenches, and boards used to hammer forms, nails, or other materials.
The analysis indicated that fingers were the most frequent part of the body injured while using a wrench; usually, the wrench slipped off a nut or bolt.
The injury reports indicated that many accidents associated with tool slippage were caused by improper tool usage (size and/or adjustment).
The accident probability was compounded by improper worker position relative to the task.
The information in Table III-5 indicates that workers suffered sprains and strains from excessive physical effort while using wrenches. This could possibly be a result of using wrenches of improper size for the job.
(3) Worker Proximity to Operations (7.4%) (a) Walking Through Work Areas (6.3%)
In a number of instances a specific task or activity description was not included in the accident report. The worker was "walking" in an unspecified section of the plant. Almost 29% of these injuries were nail punctures of the foot. More than 45% were falls to the working/walking surface caused by slipping on wet, slippery surfaces or tripping on material, usually pieces of concrete debris, rebar, welding stubs, or leads.
(b) Working Near Operations (1.1%) This category includes workers injured by tasks or operations that were independent from their assigned tasks.
The most prevalent accident/injury in this grouping was flash burns from nearby welding operations. In fact, 45% of the reported flash burns occurred to workers who were not involved in the actual welding process. Two workers were also injured by particles from nearby metal grinding operations.
(4) Welding, Cutting, Burning (4.6%)
The data indicated most of the injuries (54%) that occurred in welding, cutting, and burning activities were typified by foreign bodies in the eye that were caused by slag or weld "pop."
In these instances, the workers were not wearing eye protection.
An additional 20% of the injuries were flash burns to the workers performing the welding operations.
In these cases, the worker was usually inadequately protected because cutting goggles were being used instead of approved welding hoods during short welding operations.
The SDS data (Table III -5) indicate that welders flash burns account for 1% of the industry's injuries.
(5) Chemical Handling (4.6%) More than 44% of the incidents in this category involved chemical dermatitis caused by direct skin contact with moist concrete.
Concrete burns, most commonly to hands and forearms, were usually sustained during casting or cleanup operations.
In a few instances, concrete dermatitis developed during the dry mixing of the concrete.
Lack of respiratory protection accounted for four of the incidents involving cement dust.
Lack of personal protective equipment, mostly eye protection, was a contributing factor in 30% of the chemical handling injuries.
Workers received eye injuries during mixing, casting, and cleanup operations.
Lack of eye protection was also a causal factor in four eye injuries that occurred during spray application of form release agents.
Sprayers were overpressurized by misapplication of unregulated systems, resulting in explosions of the canisters in two instances. Analysis of the accident data indicates that 46% of the materials storage accidents were the direct result of improper stacking and/or binding procedures.
Product storage (multi level) stacks were not stable enough to support their height and weight. Most of the injuries occurred while workers were in the process of adding additional material to the stack. The second most frequent cause of injury in materials storage activities was related to manual materials handling and improper gripping of the load. Fingers and toes were most at risk during these activities.
(7) Ladders and Scaffolds (3.9%) One-fourth (25%) of the ladder/scaffold accidents were directly attributable to working from makeshift platforms (improper tools).
The accidents that occurred on makeshift scaffolds were usually falls to the level below. Two scaffold accidents (one fatal) involved scaffolds with inadequate or nonexistent guardrails.
Slippery (wet, icy) conditions on the ladders/scaffolds were cited in more than 22% of the accidents, mostly resulting in falls to the working surface of the scaffold.
Inadequate securing of ladders against slipping (chocking, blocking, or tying) caused six of the accidents that were falls to levels below.
In two instances, ladders were placed in the paths of moving vehicles (forklift, crane), resulting in collisions and serious injuries. The majority of injuries that occurred to workers cleaning forms, products, or mixers probably would have been prevented by eye protection.
The second largest accident causal factor in chipping/cleaning tasks was inadequate or nonexistent access to the area; makeshift worker platforms were common.
# b. Process-specific Accident Factors
The following narrative paragraphs describe the ways workers are injured due to task/tool/equipment factors specific to the precasting processes.
In the absence of data clarifying worker exposure, the percentage ranking is not intended to imply that any one factor represents a more significant hazard than another.
(1) Form Work (7.2%) (a) Form Assembly/Disassembly (4.9%) Form assembly and dismantling are frequently manual procedures that involve physical manipulation of form components.
Consequently, the accident/causal factors associated with form assembly primarily fall into the categories that typify physical procedures; e.g., the worker's position relative to the task, and gripping and handling form components.
Many of the injuries that occurred in form assembly tasks were sprains and strains of the back, and injuries to the fingers.
In two instances, workers were struck by form sections being turned by overhead hoists.
Inadequate chocking and bracing of form sections during assembly or stripping contributed to many of the more serious injuries.
In the instances when the form component adhered to the cured concrete, workers were struck by or caught beneath a portion of the form that was suddenly released and fell. Additional information concerning injuries resulting from form work can be found in Table III Binding and unexpected release of the inner cores or outer forms of pipe molds typified most of the accidents in this group.
"Caught between" accidents resulting in injuries to the fingers were the most common.
(r.) Form Stripping (1.2%)
The most common cause of accidents in form stripping activities involved improper tool usage. Most frequently, these accidents resulted from using shovels as levers to pry form walls loose from the cured concrete.
The most serious accidents, one of which was fatal, involved inadequate or nonexistent cribbing or blocking of form walls.
The fatality resulted when a worker crawled under a portion of form wall no longer integral to the remainder of the form or the product to determine where the form was still "hung up." The form wall fell while the worker was under it. Additional injury information is contained in Table III
-5, "Reinforcement". (b) Stressing (1.5%)
The accidents that most frequently occurred during stressing operations were similar to accidents which occurred during other forming and casting operations. Lack of eye protection accounted for more than 32% of the incidents-most of these caused by metal particles (scale) flicking off during the handling of the strand. The more serious accidents occurred during the actual stressing procedure and involved inadequate or nonexistent means for controlling employee access to the stressing area.
The high tension stretching of the steel strand poses a somewhat unique hazard to the industry.
Since stressing is used in only about 10% of the precasting plants, the relatively small number of accident cases (19) may not reflect the frequency of accidents occurring in the actual stressing operation.
The static forces contained in stressed strand are potentially hazardous. When these forces are accidentally released, workers within range of strand whiplash are exposed to potentially serious injury.
(c) Metalworking Machinery (1.3%) Metalworking machinery (cage rollers, rebar benders and cutters, press brakes) are used in the precast concrete products industry to manufacture the shapes necessary for reinforcing concrete. More than 1% of the accidents that occurred to precast concrete workers happened during metalworking tasks related to the production of the reinforcing steel shapes.
Inadequate and nonexistent guarding was the major accident causal factor associated with metalworking tools and operations.
Cage rollers (0.6%) accounted for nearly one-half of these accidents. Failure to guard in-rolling nip points on the cage rollers resulted in two of the more serious injuries. Other accidents occurred while handling the metal items during bending, cutting, or rolling operations. Frequently, these were either lacerations of the hands caused by sharp edges or crushing injuries due to hands-on manipulation of the metal while the machine was in operation.
Additional information concerning injuries from machinery can be found in Table III-5.
(3) Oiling Analysis of the accident reports failed to identify accidents which were specifically ascribed to the oiling process. Factors which may influence the occurrence of accidents during oiling procedures include contact with form release agents, access to forms or product, and working/walking surfaces. These factors are discussed in the paragraphs on Chemical Handling in section a, and in the paragraphs on Personal Protective Equipment, Access, and Working/Walking Surfaces in section £. Failure to lockout or tagout an energy source before entering or reaching into concrete mixing equipment accounted for 25% of the accidents involving concrete mixing and 3 of the 6 lockout/tagout related fatalities. Twelve percent of these accidents occurred when workers were attempting to access mixers.
Fifteen percent of these accidents involved workers who were caught in or struck by chutes or hatches when they were not secured in place.
(b) Concrete Transport (0.8%) Ready-mix concrete delivery trucks accounted for most of the accidents in this category.
Usually the worker was struck by or caught between the delivery chute and the form.
The more serious injuries happened during cleaning/maintenance operations on the trucks and were caused by lack of adequate energy control procedures. The accidents that occurred during casting operations were most commonly caused by lack of access to the casting beds or between forms. Workers must continually get up onto and down from forms, or move back and forth between forms.
In these instances, access was either not provided or was located in an area away from the work activity.
Slipping or tripping on working surfaces caused almost 24% of the casting accidents. Most of the accidents were falls from or onto the casting bed, or involuntary recovery from slips or falls resulting in sprains, fractures, and contusions. Accidents that were more task or tool specific (concrete delivery, pipe machine, scaffolds), yet still operationally part of the overall casting procedure, were included in the more specific category.
(b) Concrete Buckets (0.5%)
The injuries occurring to workers using concrete buckets were caused by the opening and closing mechanisms on the bucket's pour hatch. The latch bar frequently caught fingers and hands between the handle and the bucket.
(c) Pipe Manufacturing Equipment (0.4%)
The serious injuries to workers during mechanical pipe operations (packerhead and horizontal pipe spinning) were the result of inadequate machine guarding or isolation of the operation and the moving mechanical parts. A packerhead table with a gap between the table and the adjacent working surface caused a serious leg injury. Inadvertent entanglement with a horizontal pipe spinner injured another worker. Workers' eyes are also at risk in these operations.
The rotating speeds used in these casting operations tend to "throw" cement and aggregate out into the adjacent work area. This classification of equipment is comprised of various types of trucks (flatbeds, pickups) that are used to transport products on or off of the plant premises. More than 82% of these accidents occurred while workers were attempting to get onto or off of the vehicle bed (access).
The beds of these vehicles are typically 3 The most serious accident occurred when a crane was used to lift a product from a form to which the product remained adherent. When the crane attempted to hoist the product, the weight of the adhered form, an unknown force, resulted in crane overload and failure.
One worker was killed.
Inadequate cribbing or blocking of the product during product removal tasks also resulted in serious injuries to workers (one was fatal). Workers under the product attempting to position rigging material or guide the load were injured when the product shifted, catching them under the load.
(c) Rolling Stock (Pipe) (0.8%) Handling and storage of rolling stock (concrete pipe) resulted in 0.8% of the injuries in the industry.
More than 55% of these accidents were the result of improper or nonexistent binding or chocking of the pipe. Although the back, hands and fingers were the most frequent parts of the body injured, the lower extremities were more seriously injured.
Most of the remaining accident case histories cited rigging failure during stacking as the cause of the accident.
# c. Accident Causal Factor Patterns
The method used to analyze the accident case histories allowed the identification of significant accident patterns by the grouping of related accident causal factors.
For example, injuries attributed to wet, icy, or slippery surfaces; tripping; or puncture; are discussed below under the general heading "Working/Walking Surfaces."
These accident patterns indicate hazardous activities or conditions that encompass various tasks, industrial processes, tools, and items of equipment utilized in the precast concrete products industry. The arrangement of these patterns by percentage, in order from highest to lowest, is not intended to suggest that one accident pattern represents greater hazard to workers than another pattern, since data clarifying worker exposure are not available.
(1) Manual Materials Handling (17.6%) There are two major accident types that occur as the result of improper manual materials handling procedures: overexertion accidents that cause sprains and strains of the back and shoulders, and materials movement accidents (dropped load, load placed on fingers) that usually result in lacerations, contusions, and fractures of fingers or toes.
There is very little task specificity in manual materials handling accidents. Workers are required to lift and handle materials and tools throughout all precasting operations.
They appear to be injured in proportion to the expected amount of manual materials handling likely to be used in any given task.
(2) Working/Walking Surfaces (12.4%)
The production processes of forming, pouring, stripping, and cleaning forms produce water, excess concrete, forming material, and a variety of tools and equipment that clutter walking and working surfaces.
These hazards result in worker falls to the working surface and/or involuntary recovery injuries (sprains and strains that happen when a worker attempts to recover his balance).
The SDS data (Table III-5) indicate that bodily motion (not including lifting, pushing or pulling) was the source of injury in 5% of the industry's accidents. Additionally, working surfaces were the source of injury in 12% of the accidents when workers fell while performing their duties.
Workers in form stripping operations (most likely responsible for exposed nails) are not the individuals usually injured by nails.
The pattern of accidents related to nail puncture indicates that frequently (56%) it is a person walking through the area who steps on an exposed nail.
Table III-5 indicates that nails were involved in 1% of all injuries, resulting most frequently in punctures to the foot.
(3) Personal Protective Equipment (10.7%)
The lack of personal protective equipment is not, in itself, a cause of accidents.
However, during activities associated with some tasks or tools, workers are exposed to hazards likely to result in injuries. For example, cutting torch tasks cause metal particles to fly through the air, increasing the probability of eye injuries; or, mixing and placement of concrete may result in material splashes that cause eye injuries; or, loads may fall or be dropped onto workers feet resulting in toe injuries.
In precasting operations, 10.7% of the injuries were likely to have been prevented by the employee wearing proper personal protective equipment.
In most instances resulting in injury, the type of protective device found lacking was eye protective equipment.
Concrete splashes, slag from cutting operations, metal particles from grinding, sawdust, particles falling from or blowing off forms, curing compounds, and general airborne dirt all resulted in eye injuries.
Although safety glasses (eye protection) may not have prevented all of the reported injuries, their use certainly would have lowered the incidence of occupational eye injury.
Two fatal accidents in this category involved employees working from elevated areas and were directly attributable to the lack of fall protective devices.
In both cases, the workers were performing tasks, on or from forms, without the protection of a safety belt and lanyard.
The use of an adequate scaffold, including guardrails, would also have provided worker protection.
Crushing injuries to toes and feet resulting from the impact of heavy products and materials are not likely to be entirely eliminated by the wearing of safety-toed boots. However, such protective footwear would likely have prevented some of the injuries and reduced the severity of others in many of the cited instances.
(4) Access (9.8%) Inadequate or nonexistent access to work areas was the primary causal factor in 9.8% of the accidents. As an accident causal factor, lack of adequate access resulted in workers being injured while performing most tasks and activities directly involved in the manufacture of precast concrete products. Workers attempting to move or work on casting beds and/or forms accounted for 38% of the "access" accidents.
Most of these accidents were falls to lower levels; that is, off of the form or casting bed and onto the adjacent working surface (see Table III-5, "Working/walking surfaces"). Injuries ranged from simple bruises and lacerations to fractures. Many of the remaining "access" accidents were related to equipment; more than half of the vehicle access accidents involved workers climbing onto or down from truck beds. Again, the injuries usually were caused by falls to below.
(5) Mechanical Materials Handling (7.6%)
Mechanical materials handling accidents comprised 38% (13) of the fatalities analyzed; half of these occurred to coworkers that were struck by a moving vehicle (crane, forklift). Twenty-three percent of the fatalities in mechanical materials handling were caused by rigging overloads. There were two incidents of crane "two-blocking" that resulted in fatal injury to workers.
The use of hoists, cranes, and forklifts is common throughout the industry.
In many instances, the product is simply too heavy to move by other means.
In some instances, the material is also too heavy to be moved by the selected mechanical method.
Employees frequently work in close proximity to moving equipment.
This interface, man and moving equipment, when compounded by the distractions of ongoing work and background noise, contributes to fatal accidents in precasting operations.
(6) Guarding (2.7%) Inadequate or nonexistent guards were cited in 2.7% of the accidents.
All but 2 of these 36 accidents occurred in con junction with exposed moving parts of machinery and/or tools. Unguarded saws injured workers most frequently (31%), and un guarded grinders (abrasive stone) accounted for 17% of the injuries related to guarding. Conveyors may jam during operation.
Workers were injured while attempting to remove the jammed objects without first controlling the systems' energy sources.
# D. New Employee Injury Rates
Analysis of the 1,319 accident case histories shows that 513 (54%) of the 950 reports that included length of employment information involved workers employed less than 1 year.
In fact, 408 (43%) of the injuries were actually sustained by workers employed for less than 6 months.
Several factors may influence the apparent prevalence of injuries to new employees. Although some plants experience a relatively high turnover rate, many smaller plants seem to have a stable work force.
These plants will layoff and rehire the same workers in accordance with seasonal or economic demands. Therefore, an injured employee reported as "new" on an injury report form, may actually be an experienced worker.
Further, new employees may perform the more hazardous tasks.
Or, new employees may typically comprise about 50% of the work force.
No information which identifies either the distribution of tasks among workers of varying experience or the number of relatively new employees that make up the worker population at any given time is available.
However, there is evidence to suggest that new employees or employees performing new tasks suffer significantly higher rates of injury than the employed population in general .
# E. Summary of the Problem
Accident and injury statistics for 1980 indicate that the injury and illness incidence rate for the precast concrete products industry (SIC 3272) was 2.5 times the rate for all private sector industries. Not only does the precast concrete products industry have the problem of high injury incidence rates relative to all private sector industries, but within the manufacturing sector where there are similar tasks and operations, only 8, or 3.4%, of the 235 four-digit SIC code industries had higher incidence rates than this industry in 1980.
Analysis of 1,319 accident case histories has demonstrated how employees in the precast concrete products industry are injured while performing those tasks necessary to manufacture concrete products.
Furthermore, patterns of accident causal factors common throughout the industry have been identified.
It is concluded that the primary safety needs of the precast concrete products industry are:
1) implementation of the recommendations for safe work practices presented in Chapter IV; and 2) implementation of a safety management program, such as the one presented in Chapter V.
# CHAPTER IV RECOMMENDATIONS FOR SAFE WORK PRACTICES FOR THE PRECAST CONCRETE PRODUCTS INDUSTRY
The safe work practices recommended in this chapter are presented as ways to reduce and control injuries resulting from precasting operations. The hazardous tasks identified, as well as the patterns of accident causal factors developed in Chapter III, indicate potential problem areas that have been given insufficient emphasis by the precasting industry.
The solutions offered in the following safety recommendations may not be entirely suitable for a specific plant.
In some instances, management may even view the recommendations as counterproductive to their operations. In these instances, the responsible persons (plant managers, safety managers, and/or plant owners) should interpret and modify the recommendations to make them applicable to their specific needs.
It is essential that, in any modification of the recommended safe work practices, a similar quality of worker protection be provided.
Considerable emphasis has been placed on the safety recommendations directed at hoist and crane activities.
In the cases analyzed, 41% of the fatal accidents occurred due to misuse of hoists and cranes.
Expertise specific to hoisting equipment may be less developed than supervisory expertise particular to production; therefore, hoist and crane safety has been presented in detail.
The goal of this study has been to identify hazards in precasting opera tions and to recommend applicable and manageable means to alleviate them. The safety recommendations presented are not meant to be all-inclusive or to supersede the OSHA General Industry Standards, which offer adequate regulatory guidelines for many of the tasks, tools, and equipment used in the precast concrete products industry.
Emphasis has been placed on recommendations for safe work practices which address tasks, activities, and tools commonly associated with injuries. This preliminary section presents safe work practices for the tasks, acti vities, and tools that are commonly used throughout precasting operations. Included in this section are the recommendations for manual and mechanical materials handling, handtools, worker proximity to operations, welding and cutting, chemical handling, ladders and scaffolding, and chipping/cleaning.
# Manual Materials Handling
A wide range of manual materials handling activities are inherent to the precast concrete products industry.
Workers may be required to lift, carry, push and pull raw materials and/or finished products during loading/unloading, processing, storage and cleanup operations.
The handling and manipulation of loads can markedly increase the stresses imposed on workers' musculoskeletal systems and increase the likelihood of injuries to certain body areas (e.g. back, extremities) .
The application of proper handling techniques can minimize these stresses and help reduce the incidence of musculoskeletal injuries.
A number of factors can directly influence the likelihood of an individual suffering a musculoskeletal injury during the performance of manual materials handling activities.
These are discussed in NIOSH's "Work Practices Guide for Manual Lifting" The proper use of safe handling techniques by workers performing manual materials handling activities is one of the most important factors in avoiding injury, since the techniques reduce body stresses and their application are at the discretion of the worker.
NIOSH's publication "How to Lift Safely" illustrates several of the important points in materials handling.
# Key points include:
- Workers should assess the size, shape and weight of objects to be lifted or carried. Objects deemed to be beyond the physical capacity of one worker should be handled by two or more workers. o Workers should spread their feet apart to provide a wide base of support during manual materials handling, o When lifting objects, workers should bend their knees to a degree which is comfortable to them and then get a good firm grip on the item to be lifted. Lifting should be accom plished through the use of leg muscles in straightening the knees rather than using the back muscles, o Workers should handle objects as close to the body's center of gravity as possible, o Workers should avoid twisting the trunk when handling ob jects.
# b. Assistive Devices
A number of assistive devices can reduce or eliminate the need for stressful manual materials handling. For example, rebar can be stored on surfaces which correspond to the height of the bending and cutting machines so that the worker does not need to lift the rebar from the floor level to the cutting or bending surface.
It is even better to have the rebar storage surface gently slope toward the cutting and bending machine.
This reduces the stress required to pull the rebar to the cutting or bending position. .
These methods also represent a wide range of costs to employers under various financial restraints. Training programs are means of conveying information to workers. A goal of training programs is that workers will alter their work habits by substituting safer work practices for various unsafe techniques. This form of behavioral modification usually requires feedback to the workers.
Supervisors and employers must take the time to positively reinforce safe practices and constructively criticize unsafe practices. Effective training is approached as an ongoing interaction among all plant employees and not a one time exposure to the training material . o Approved boom stops installed to preclude travel beyond the angle of 85 degrees above the hori zontal plane o Boom angle indicators for booms capable of moving in the vertical plane o Automatic devices to stop boom drum motion when the maximum permissible boom angle is reached o Boom length indicators for telescopic booms o Automatic "anti-two-blocking" devices for hydraulic extending booms o An effective audible warning signal (horn) mounted outside the cab with controls easily within reach of the operator o A spirit level at the outrigger controls for level ing o Adequate lighting for night operation, including backup lights for mobile units o Wheel chocks on mobile units to block movement on slopes when the equipment is left unattended or is undergoing maintenance o A fire extinguisher and a first-aid kit o Rearview mirrors on both sides of mobile equip ment o Self-closing filler caps and flame arresters on fuel tanks o Slip-resistant material on crane surfaces subject to foot traffic .
# Mechanical Materials
(c) Equipment should be safety inspected frequently (daily to weekly). Inspectors should :
- Check brakes, clutches, and safety devices for prop er adjustment and operation (if possible, check load brakes by lifting a capacity or near capacity load a few inches off the ground) o Daily, visually inspect each component of the equip ment used in lifting, swinging, or lowering the load and components used to lift and lower the boom, for any defects that might result in unsafe operation o Check for freedom of rotation of all swivels o Check all functional, operating mechanisms such as sheaves, drums, brakes, locking mechanisms, hooks, boom, jib, hook roller brackets, outrigger compo nents, limit switches, safety devices, hydraulic cylinders, instruments, and lights o On cranes, daily, visually inspect the boom and jib for straightness and for any evidence of physical damage such as cracking, bending, or other deforma tion of the steel elements or welds (this precau tion is especially important on lattice and tubular booms, where every component should be straight and free from dents) o Inspect wire ropes (including standing ropes), rig ging hardware, and attachments o On cranes, check that the counterweight is secure and that the weight and capacity are permanently and legibly stamped on jibs, blocks, equalizer beams, and all other accessories o Daily, visually inspect the equipment for fluid or air leaks o Ensure that all walking surfaces of the equipment are clean and free from tackle, grease, and oil.
(d) All capacities listed on the load chart for machine "on outriggers" and "on tires" are based on the crane being level and on solid support. The importance of leveling cannot be overemphasized. The manufacturers' capacity tables should be referred to for both outriggers and tires, since lifting capacity is reduced markedly when the crane is not level .
(e) If a crane has to make its lifts on rubber, always use wheel chocks to block the wheels and apply the airbrakes to hold the crane in position.
If the machine is of two-engine design, keep the carrier engine running to maintain air pressure.
Ensure that the tires are properly inflated; if they are not, then the capacity and crane stability will be reduced .
(f) Dunnage under outriggers must be strong enough to support the imposed load.
If more than one layer is needed, then proper "cross-hatched" stacking must be used to prevent tipping.
Reset outriggers before a lift if necessary.
If floats are allowed to settle into the ground, they lose their effectiveness, making continued operation unsafe .
(2) Competent operation of equipment (a) Only thoroughly trained and tested workers are permitted to operate a crane.
When an operator is assigned to a new crane, competence with that crane must be demonstrated.
Training and testing must be sufficient to demonstrate that the operator fully understands and is capable of safely performing all tasks.
The testing should include a performance evaluation of: o Never allow his attention to be diverted from the operation of the crane (coworkers should not be per mitted to talk to the operator while he is working) o Allow no passengers (excepting an oiler) on a crane in motion or operating, especially during mobile yarding operations o Not back up the machine without first making certain that no one will be endangered (when vision of the area behind the crane is blocked, use a signalman) o Sound an audible alarm (horn) before moving a crane and whenever the crane is approaching other workers o Sound an audible alarm whenever a suspended load is approaching employees to give them time to move o Never operate the crane within 10 feet of energized high-voltage powerlines.
(c) During operations, management should:
- Prohibit employees from performing any maintenance work on equipment while it is in service o Barricade the swing radius of the crane structure to prevent employees from being trapped and crushed be tween rotating portions of the crane and adjacent structures o Prohibit oilers, helpers, or other workers from areas within the swing radius of the crane carriage while the crane is rotating or under load o See that oilers, helpers, or other workers are not under any portion of the crane body while a load is suspended.
(3) Rigging the Load
The proper selection and integrity of rigging material and the methods used to attach the load to the hoist are vital to safe hoisting operations .
(a) The load should be rigged so that the load is stable in the saddle of the hook.
(b) The worker should know the safe load limits of rigging equipment, which must not be exceeded. The employer can accomplish this by permanently attaching tags to, or painting a section on, each sling, rope, and chain that identifies its capacity.
(c) The employer should train all riggers in the safe operating procedures of rigging, including:
- Keeping hands away from pinch points as the slack is being taken up o Examining all hardware, equipment, tackle, and slings before use and destroying defective compo nents o Making sure that all slings are of the same capaci ty and length when two or more slings are used on a load o Making sure that the hoist rope or chain is never wrapped around the load or completely wrapped around a hook o Attaching the load to the hook by slings or other rigging devices that are adequate for the load being lifted o Securing the unused legs of a multileg sling before lifting loads with one leg o Remembering when a bundled load is picked up that the material will tend to "nest" and create pinch points, and when a load is landed, it will tend to roll or spread out o Making sure wood blocks or short lengths of steel are not carried loosely on tops of loads o Making sure wire rope or chain is never allowed to lie on the ground for any length of time or on damp or wet surfaces, rusty steel, or near corrosive substances o Avoiding draping rope slings from beneath loads o Keeping all rope or chain clear of flame cutting and electric welding operations o Making sure shackles are not rigged with the run ning rope against the pin, causing it to "spin out" and drop the load o Ensuring proper load/shackle alignment by using spacers such as washers o Keeping the load under control with guide ropes or tag lines. (e) Slings, ropes, or chains should not be left on the floor or ground where they can be subjected to abrasion or create a tripping hazard. They should be hung from a rack and looped so that they do not touch the floor.
(f) All hooks should have safety latches.
(g) Sharp bends, pinching, and crushing of ropes and slings must be avoided. Sharp edges or corners of heavy loads should be padded as protection for slings by the use of large-diameter split pipe sections, corner saddles, or other, softer material. The load should not be "picked" until the signal is received from the signalman. All signals must be clearly understood by the operator.
If there is any doubt, the operator should stop operations until the signal has been clarified. The crane operator should receive signals from only one person; this does not exclude relay signaling or emergency stop signals.
Signalmen may be supplied with orange gloves for maximum signal visibility.
(b) Crane/hoist operators should remain at the controls whenever a load is suspended.
(c) When preparing for new and near-capacity picks, the operator should make a practice run, going through all the motions without the load, anticipating the actions that should be taken to make a safe lift and a smooth operation.
(d) The crane should never be loaded beyond its rated capacity.
(e) Handling loads during high winds should be avoided.
# b. Straddle Carriers
(1) Straddle carrier operators must be thoroughly trained.
(2) Straddle carriers must be thoroughly inspected before beginning operation each day. Particular attention should be given to brakes and hydraulic systems. Visual inspections of the bridge, rigging, and lifting hardware should be made to ensure their integrity. All wire ropes should be inspected and special safety devices should be in working order.
The inspection should be performed and documented by qualified maintenance personnel.
(3) The rated load of the straddle crane should be posted in a conspicuous location on the equipment and in the operator's cab.
(4) When operator visibility is restricted, a signalman must be provided.
(5) Visible and audible alarms should be in operation during any moving task.
(6) No one should ride on the carrier unless such a procedure is approved by the plant manager.
Where approval is granted, a seat or cage, located so that it will not interfere with operator vision or in itself be a hazard, should be provided.
The rider should be in the seat or cage before the carrier is moved and should not move around on the carrier until it is stopped.
# c. Forklifts
(1) Only workers authorized by the employer and trained in the safe operation of industrial trucks, forklifts, or industrial tow tractors should be permitted to operate these types of vehicles.
(2) Forklifts and industrial vehicles should be equipped with audible backup alarms. (4) Employees should not be permitted to place any part of their bodies outside the cab or protected area of an industrial truck or between mast uprights or other parts of a truck where shearing or crushing hazards exist.
(5) Passengers are not permitted on industrial vehicles.
(6) Employees should not be allowed to stand, pass, or work under the elevated portion of any industrial vehicle, loaded or empty, unless it is effectively blocked to prevent it from falling.
(7) When loading or unloading trucks or trailers, the brakes must be set and the rear wheels chocked.
(8) Forklift forks should be carried as low as possible.
(9) Industrial vehicles should not run onto floors, platforms, or other surfaces that will not safely support the loaded vehicle.
(10) Vehicle loads must not exceed rated capacities.
A loaded industrial vehicle should not be moved until the load is secure.
(11) When leaving the vehicle, the worker should shut off the engine, set the brakes, and lower the lifting forks to the ground.
(12) All traffic regulations should be observed including plant speed limits. The operator of an industrial vehicle is required to slow down and sound the horn at cross aisles and other locations where vision is obstructed.
(13) No person should operate or be in physical control of a motorized vehicle or piece of equipment if he is under the influence of or is using alcohol or drugs.
# d. Chain Hoists
(1) Chain hoists or "come-a-longs" should be inspected and maintained as part of a preventative maintenance program. Inspection should include:
- Checking the integrity of the chain or wire rope for worn links, deformations, kinks, rust, or excessive stretch o Examining the hook for deformity, cracks, or bending o Ensuring that the clutch and brakes are within the manu facturers' tolerances.
(2) Employees lifting material with mechanical hoists should:
- Use proper and accepted rigging methods o Use safety latch hooks o Chock or block loads before working under them o Not use "cheaters" on the hoist handles. The handle length is matched to the safe lifting capacity of the hoist, and while the cheater extension may temporarily enable a greater load to be lifted, it may tax the hoist and lead to failure.
# e. Conveyors
(1) Conveyors should be adequately guarded to prevent workers from being caught on moving parts or being injured by falling materials.
(2) Conveyors should have delay startup warning devices with controls for emergency stops. All chain drives, gears, nip or shear points, and revolving shafts should be guarded.
(3) Personnel working near conveyors should wear close-fitting clothing that cannot be caught in moving parts.
(4) Employees should be instructed in safe practices for freeing "jammed" conveyors, including use of special tools. A lockout system should be mandatory.
(5) Chutes or other devices that depend on gravity for moving materials should be guarded. (2) Front-end loaders should be equipped with a backup warning device.
The device should be audible and sufficiently distinct to be heard under the prevailing conditions. The device should operate automatically upon commencement of backward motion and should operate during the entire backing operation .
(3) Loader operators should be sure other workers are in the clear before starting or moving the machine .
(A) Operators should not move loads over the heads of other workmen or over truck cabs .
(5) The loader bucket should be carried as low as possible and tilted back. This provides better operator visibility and minimizes machine bounce .
# Handtools a. Powered
Handtools (powered) should be used according to the following safety recommendations:
(1) Hand-held powered circular saws, chain saws, and percussion tools without a positive accessory holding means must be equipped with a constant pressure switch .
(2) Portable, power-driven circular saws must have guards above and below the base plate or shoe. The upper guard should cover the saw to the depth of the teeth, except for the minimum arc required to permit the base to be tilted for bevel cuts.
The lower guard should cover the saw to the depth of the teeth, except for the minimum arc required to allow proper retraction and contact with the work. When the tool is withdrawn from the work, the lower guard must automatically and instantly return to the covering position .
(3) Abrasive wheels and stones must have a safety guard cover ing the spindle end, nut, and flange projections. The safety guard should be mounted to maintain proper alignment with the wheel; the strength of the fastenings should exceed the strength of the guard .
(a) Prior to use, abrasive stone wheels should be inspected to ensure that: o They have not been damaged in transit or handling, which is checked by means of sounding with a ring test o Wheels fit freely on the spindle and remain free through an entire turn of the wheel, and that the free clearance between wheel and guard does not ex ceed one-fourth inch o A controlled clearance between the wheel hole and the machine spindle (or wheel sleeves or adaptors) is sufficient to prevent excessive pressure from mount ing and spindle expansion o All contact surfaces of wheels, blotters, and flang es are flat and free of foreign matter' o When a bushing is used in the wheel hole, it does not exceed the width of the wheel and does not contact the flanges.
(b) The safe operating speeds of abrasive grinding stones should not be exceeded .
(4) Hand-held powered drills; tappers; fastener drivers; hori zontal, vertical, and angle grinders; disk and belt sanders; reciprocating, saber, scroll, and jig saws; and similar tools must be equipped with constant pressure switches.
Other handheld powered tools, such as platen sanders; grinders; disk sanders; routers; planers; and saber, scroll, and jig saws, should be equipped with either a positive on-off control or a constant pressure switch .
# b. Unpowered
The following safe practices should be observed when unpowered handtools are being used :
(1) Train employees to select the correct tool for the job, and ensure that the tools are available.
(2) Keep all hand tools in a safe condition. Handles of tools shall be kept tight in the tool. Wooden handles shall be free of splinters or cracks.
Wedges, chisels, and other struck tools should be dressed as soon as the struck surfaces begin to mushroom.
Discard wrenches which are sprung to the extent that slippage occurs. The crowbar should have a point or toe that will grip the object to be moved, and a heel to act as a pivot point. Sometimes it is necessary to use a block of wood under the heel to prevent the crowbar from slipping and injuring the hand. Workers should position themselves so that their bodies will not be in the path of travel if the prybar slips.
Additionally, they should brace/position themselves so that they will not fall if the prying forces are released suddenly. Guardrails may be necessary to prevent workers from falling to lower levels.
(d) Employees should be aware that when using torsion tools such as wrenches, there is always a possibility that the tool may slip. Therefore, the employee should be in a braced position to maintain bodily balance should the tool slip.
Wrenches should be inspected for flaws. Wrenches should never be ground to change their dimensions to make them fit in close quarters. A wrench of proper size for the job must be selected.
# Worker Proximity to Operations a. Walking Through Work Areas
Work areas should be kept free of litter, trash, gravel, excess concrete spills, welding rod stubs and other junk.
All scrap, salvageable material, unused forming or reinforcing materials and equipment should be removed.
Protruding nails in wood forming material should either be removed or benl: over. Aisles around work areas should be kept clear of such items as reinforcement, welding hoses or leads, lumber, power cords, and concrete working tools.
# b. Working Near Operations
Of particular interest in this category is the need to protect workers in the vicinity of welding operations from flash burns. Whenever possible, resistance welding operations should be isolated to protect workers in the vicinity of the welding operations from exposure to the direct or reflected light rays.
This can be accomplished either by use of booths for regular welding production operations or by portable welding screens for welding being performed intermittently throughout the plant .
# Welding, Cutting, Burning
Welding, cutting, and burning necessary for making precast concrete products should be done in accordance with the following safe work practices: a. Workers performing welding and cutting tasks should be trained. c. Welding and cutting should be done in an area having a nonflam mable floor, such as concrete, but not on the concrete floor, because of the possibility of explosive spalling of the concrete.
The material to be cut should be raised above the concrete or the concrete shielded from the flame.
If welding must be done over wooden floors, a noncombustible covering material should be placed over the floor to provide fire protection and to prevent spatter from dripping through openings in the floor. The use of wet sand or metal coverings, however, may create electric shock hazards that otherwise would not exist. o Persons involved in grinding, chipping, wire brushing, and/or scraping should wear goggles or safety glasses with side shields under a face shield, o Since the chipping/cleaning tasks which utilize power tools can cause particles to be airborne for considerable distance (10 -30 feet), the operations should be isolated from other workers. If this is not practical, then workers in the vicinity of these op erations should also wear adequate eye and face protection.
# B. Safe Work Practices for Precasting Processes
Safe work practices for procedures used in the manufacture of precast concrete products are presented in this section.
Included are safety recom mendations that address the hazards of processes used in the precasting industry as well as the application of tools or equipment used in a specific process.
# Form Work a. Forms and Forming
(1) Forms and beds for casting should be: o Arranged or laid out to provide a working space, aisle way, or working platform clear of obstructions and suffi ciently wide to provide ample room for the safe movement of materials and vehicles o Provided with access steps or ramps at convenient inter vals along the bed or form o Equipped with standard guardrails, if over 4 feet high.
(2) Forms should be structurally sound so that they do not present a hazard to employees as they are built, repaired, cleaned, modified, or moved.
(3) During form assembly, components should be chocked and/or braced to prevent displacement.
(4) Safe access during vertical pipe form assembly should be provided for workers during assembly, aligning of hoisted parts, and attaching of hoist hooks.
(5) The floor, yard, platform, or other surface on which a form is placed, built, or erected should be free of litter, debris, and other loose materials that can cause tripping hazards. Also, these surfaces should be well drained and free of potholes, cracks, unevenness, or standing water that may contribute to slips and falls.. (6) Tilt tables should be capable of supporting the temporary loads of employees during forming operations in addition to the imposed load of product. They should also be chocked when in the upright position for cleaning, product removal, or maintenance to avoid collapse.
# b. Form Stripping
(1) Employees should be instructed that form bulkheads, etc., may temporarily adhere to the concrete product. The bulkheads may release suddenly.
Workers (and their body parts) should not be positioned where they may be caught between either the bulkhead, the product, and/or the form.
(2) During form stripping and product removal tasks, it is important that form bulkheads and components be cribbed, braced, or suspended by hoist to prevent their falling unexpectedly.
(3) Prying tasks should only be performed with the proper tool (crowbar or prybar). Shovels should not be used as substi tute s.
(4) Cranes or hoists should not be used to remove products lodged or stuck to the forms. The crane's safe lifting capacity should not be exceeded.
Use of properly adjusted crane load indicating devices will help avoid exceeding crane capacities.
(5) As forms are stripped, all excess material, wood, nails, and bits of wire should be removed so that the area is clean and safe. After forms are stripped, all nails should be bent or pulled immediately.
# Reinforcing a. Reinforcing Materials/Assemblies
(1) Reinforcing assemblies should be fabricated with a working level jig to avoid constant bending over to tie or weld.
(2) In the handling of reinforcing steel and fabricated assemblies, the following precautions should be taken: o Employees must be instructed and required to use correct lifting techniques, o Finished cages for pipes, columns, and beams should be moved to their final locations in the forms with consider ation of their weight and the physical capabilities of the employees assigned, o Mechanical lift assistance should be provided to safely lift pieces too bulky or heavy to be handled manually, o Bundles of reinforcing steel moved by crane or other means should be securely tied and wedged together to prevent slipping. o Rebar bundles lifted by hoist should be rigged by 2-point suspension chokers and moved in a balanced horizontal posi tion. They should not be moved in the vertical plane, o When bars carried by hand are long, bulky, or heavy, more than one worker should be utilized, o Rebar materials used in cutting and bending operations should be located such as to minimize or eliminate the need for the worker to lift the bar from ground level to the cutting or bending height, o Gloves should be worn during strand stringing, vise plac ing, rebar tying or handling, mesh placement, and cage handling tasks .
# b. Metalworking Equipment
Metalworking equipment should meet the following requirements:
- Cage rollers should be equipped with deadman switches and positive braking mechanisms that immediately stop the move ment of the rollers, o Cage or wire rollers should be equipped with trip wire mechanisms at the in-rolling nip points, that automati cally shut down the rollers when inadvertent contact is made. o Shearing machines should be equipped with physical guards and/or proximity detectors. (b) Welding or cutting should not be allowed in any stressing bed where strand has been strung or tensioned, or in any other location where strand is stored. If an electric arc jumps to or from the strand, the molecular structure of the strand is altered and a loss of strength occurs.
# c. Stressing
Heat from molten metal or torch cutting will also change the mechanical properties of steel wire strand.
(c) Strand vises used to secure strand at the anchor abut ments should be placed away from a burned end to avoid the area of altered strand strength. This distance should be at least 12 diameters of the strand or 6 inches, whichever is greater.
(d) Strand previously gripped by vises, and therefore nicked, must not be reused.
Strand vises should be cleaned and inspected between each use and lubricated as necessary. Grips that become visibly worn or distorted, or allow excessive slippage should be discarded.
(e) Check that the strands in the form are not crossed or tangled before tensioning.
(f) Audible and visible alarm signals should be turned on and remain on during tensioning. Any personnel not directly involved in stressing operations should be cleared from the "designated area" and remain clear until audible and visual signals are turned off.
(g) The "designated area" should be the entire length of the bed being stressed, including both ends and the sides out to the center line of any adjacent bed, or one-half the length of the longest member, but not less than 20 feet.
(h) Only stressing crew personnel directly involved in tensioning are to be permitted in the vicinity of the bed.
(i) Personnel in the stressing crew must not stand behind the jack or in line with the tensioned steel, since ruptured strand tends to retract along the line of tension.
(j) No employees should be in the jacking area (the area within the possible swing radius of the stressing jacks) during stressing.
(k) Elongation should be measured by means of a template, jig, or scale attached to the stressing jack that can be viewed from a safe distance.
(1) Workers involved in tensioning should be protected by bed end protection, a pumphouse, or a portable booth to shield them from flying strands or bulkheads resulting from strand breakage.
(m) An employee should be posted in a location with an unobstructed view of the designated area in order to warn personnel who inadvertently approach the re stricted area. Shields must be designed to withstand the forces applied against them by recoiling strand, flying bulkheads, and other material that may be launched as a result of strand failures during stressing.
Shields can be fabricated of sheet steel; heavy duty, small aperture expanded metal; or concrete with a supporting frame of angle iron, channel, or pipe. The purpose of bed end protection is to shield those workers who are involved in the tensioning or detensioning operation from flying chucks, strand, or bulkheads resulting from chuck or strand breakage.
The following recommendations describe possible methods of bed end protection.
Staff engineers should develop measures which are specific to the protection needs in each plant . The secondary barrier should be constructed of concrete, steel, or other material able to withstand the force of a chuck and strand retracting through the pulling head.
Alternatively., an angled trough that is of sufficient strength and dimension to collect a retracting strand and direct it toward the ground should be permanently installed at the pulling head. on the harping dowel large enough to be visible from a safe location during the harping sequence.
During harping the following safety recommendations should be followed: o All unnecessary employees should be cleared from the immediate area, o Audible and visible alarms should alert personnel that harping operations are taking place, o An employee should be stationed in a safe area to en sure that personnel do not enter the "designated area" while harping operations are in progress, o A mirror can be set up on the form so that an employee can observe the depressing clip from a safe location, o Entangled or misaligned strand should be restored to its original position and then correctly harped. Work ers must not attempt to shift strand while it is de pressed .
There are different types of harping operations, and each type requires special precautions. More detailed procedures and safe work practices are contained in the Prestressed Adapted from PCI Safety and Loss Prevention Manual .
# Concrete
Institute publication, "PCI Safety and Loss Prevention Manual" .
(4) Dejacking Dejacking, used to release a strand that is misplaced or fouled, requires extreme care.
The following precautions should be taken: o Hands and fingers must not be placed between the chuck face and the jackhead. o Jaws should be removed with a hook tool or other device recommended by the manufacturer, o Tension on strand should be released slowly. o Prior to stressing, place a solid steel cylinder, called a spacer (approximately 2 inches long and slotted to fit the strand), between the chuck and the jackhead and tape it to the chuck, o After casting and curing, remove the tape; place a "detensioning stand" over the strand; and stress the strand slowly until the spacer falls out. o Use long-handled pliers or tongs to insert a removal tool in its place; remove the chuck cap, and slowly release tension until the removal tool has forced the jaws from the barrel. When the jaws are access ible, pull them free of the retaining ring, remove them from the strand, and release tension slowly, o Keep hands out of the "detensioning stand" by using long-handled tools, o Allow no employees other than the detensioning crew in the "designated area." o Do not regrip the strand on or near the previous jaw marks. o Use warning lights and horns and enforce "designated area" precautions as when tensioning.
# Oiling
a. Supplied air pressure vessels, used for spraying form release agents, should have both a visible pressure gauge and a pressure relief valve in proper operating order. Supplied air sprayers should be labeled for their maximum safe operating pressure and this pressure should not be exceeded.
b. Form release agents should be stored neatly in cabinets or areas specially set aside for that purpose. Aisles should be maintained to allow unobstructed movement of personnel and equipment, and to avoid tripping and slipping hazards. c. Material Safety Data Sheets for all form release agents should be requested, and all applicable safety and health precautions should be followed.
d. Eye and face protection, such as a face shield, should be manda tory during spray application of form release agents.
e. A minimum of safety glasses should be used during hand applica tions (swabbing, rolling) and during all transfers of form release agents. (2) Employees should be adequately instructed in preventive measures to avoid skin burns that can occur from prolonged, direct contact between skin surfaces and fresh (moist) concrete or clothing saturated by it.
(3) Where cement, sand or gravel are stored in silos, bins or hoppers, the following procedures should be followed:
(a) Workers should be made aware that fine materials such as cement, sand and gravel can freeze or bond and crust over in cold or wet conditions. This crust can collapse under the weight of an employee standing or walking on it to free it up.
The individual could sink into the quicksand-like material and suffocate. Further information on working safely in confined spaces is contained in the NIOSH criteria document "Working in Confined Spaces" .
(4) NIOSH/MSHA-approved respirators should be worn in areas where dust levels are excessive. The threshold limit value (TLV) for specific dusts and exposure levels are cited in the 1981 TLV booklet of the American Conference of Governmental Industrial Hygienists (ACGIH) .
(5) In high-noise areas, the following; recommendations should be adhered to :
- A continuously effective hearing conservation program, in cluding annual audiometric testing of exposed employees, must be established when noise levels are found to exceed 85 dB(A) for an 8-hour time-weighted average (TWA), o Administrative or engineering controls, including rotation of exposed employees and acoustical booth isolation where feasible, should be applied to reduce exposure time, o All employees must be provided with hearing protection de vices if feasible engineering controls are inadequate in reducing noise to levels below 85 dB(A) for an 8-hour TWA.
# b. Concrete Transport
(1) A signalman should be available at times of entry, movement, and exit to ensure safe passage of concrete delivery trucks to casting areas.
(2) Backing lanes should be free of equipment, material, and workers .
(3) Movement of personnel and job equipment should be routed to avoid crossing truck lanes, tracks, aisleways, or transfer areas.
(4) Concrete delivery transporters should be equipped with audible and visible alarms, including backup alarms to warn of their approach, and mirrors to eliminate blindspots.
# Casting Concrete a. General
During the casting of concrete product, the following safety recommendations should be followed:
(1) Concrete buckets should not be transported over workers . Workers should not step under overhead buckets.
(2) Buckets should have a positive locking gate .
(3) Concrete buckets should be equipped with a release latch (bar, handle) designed and located to prevent fingers from being caught between the latch bar and the bucket.
(4) Electric cords must meet OSHA standards and be free of breaks and in safe condition. The cords should be placed or protected so that they will not be run over and damaged or be allowed to rest in water.
(5) Safe access to the points of concrete placement and consol idation should be provided by stairs, ramps, or ladders. Also, a properly guarded walking and working surface must be available. ( 6) Safe work platforms should be provided for elevated casting operations such as vertical wet casting of pipe. (7) Rolling stair scaffolds must be equipped with adequate guardrails on all exposed sides, particularly the ends of the scaffold and the interface between the form and the scaffold if a floor or wall opening exists. ( 8 o Ensuring that broken or missing handholds and footholds are repaired or replaced o Removing and refitting unsuitable handholds and footholds o Adding new handholds and footholds where they are needed for worker access o Providing non-skid surfaces on all access systems which might become slippery o Providing a handhold, long enough to be accessible by the majority of drivers, on the right of the tractor driver's door o Providing portable access stairs for pickup and trailer beds. f. Concrete products should be unloaded in accordance with the following safety recommendations:
- The safe lifting capacity of the equipment should not be exceeded. o Loads that are long, oddly shaped, or difficult to rig should be raised only a short distance until it is apparent they will not spring, slip, or tip. o Pipe or circular products should be off-loaded with skids, ropes, or automatic unloaders, o The job site unloading area should be examined for access, stability, and temporary storage capability, o Before unattended vehicles are unloaded, all wheels should be chocked and the parking brakes set. o Trailers should be loaded and unloaded evenly so as not to tip the load or the trailer.
# Personal Protective Equipment
To protect workers, the use of various personal protective equipment should become an integral part of the safety program.
The most common personal protective equipment that should be used are contained in Table IV
Requirements for personal protective equipment are covered in the OSHA standards .
# Mechanical Materials Handling
Recommendations for control of hazards encountered in mechanical materials handling activities are contained in paragraph A.2. of this chapter.
# Guarding
Guarding of machinery should conform to the following:
(a) Drives for machinery must be properly guarded at chains, belts, and pulleys in full accordance with the following requirements:
- Pulleys, belts, or chain drives 7 feet (within reach) or less from the floor should be guarded, o Gears should be guarded by a complete enclosure, o Sprocket wheels and chains should be enclosed if less than 7 feet above the floor or platform . (d) Circular, hand-fed ripsaws and crosscut table saws must be guarded by a hood that encloses the portion of the saw above the table prior to cutting and above the material being cut (the hood should automatically adjust itself to the thickness of, and remain in contact with, the material being cut) .
(e) All p< tions of the saw blade on bandsaws must be :
- Enclosed or guarded, except for the working portion of the blade between the bottom of the guide rolls and the table (bandsaw wheels should be fully encased)
- Guarded to prevent hands from contact with the in-running rolls.
(f) Radial saws should be provided with:
- A hood to protect the operator from flying splinters, broken sawteeth, and sawdust o A guard on the upper hood completely enclosing the upper por tion of the blade down to the end of the saw arbor o A lower blade guard that automatically adjusts to the thick ness of the stock and that remains in contact with the stock being cut o Nonkickback fingers or dogs located on both sides of the saw to oppose the tendency of the saw to pick up the material or throw it back toward the operator.. Further information regarding hazardous energy control is contained in the NIOSH document "Guidelines for Controlling Hazardous Energy During Maintenance and Servicing" .
# Chapter V SAFETY MANAGEMENT
There should be little disagreement that safety is ultimately the re sponsibility of management.
In addition to the fact that the Occupational Safety and Health Act of 1970 (OSHA) requires each employer to furnish each employee a place of employment that is free from recognized hazards likely to cause death or serious physical harm, worker accidents and injuries are counter-productive and costly.
As shown in Chapter III of this document (specifically Table III-3), the occupational injury and illness incidence rate for the precast concrete products industry in 1980 was in the top 3% of the durable goods manufacturing industries.
Since 1977, the estimated cost of actual paid-out medical and indemnity expenses of occupational injuries in this industry has averaged more than $30.9 million per year.
The National Safety Council estimates that the full costs of work-related accidents have been 3.4 times greater than the cost of actual paid-out claims, or over $105 million per year (see Chapter III).
These needless losses can be controlled by managing successful safety programs.
However, safety programs can only be successful when plant management provides an environment responsive to worker safety and is committed to providing a safe workplace.
Safety recommendations such as those presented in Chapter IV or safety standards such as those promulgated by OSHA will not, by themselves, reduce occupational injuries.
Management must accept the responsibility of implementing a safety program which is designed for successful accident prevention.
Such success requires an organized approach.
No individual level of management can do the job by itself.
It takes a combined effort of all -from the plant manager down through the first-line supervisor to the employees. This chapter presents the basic elements of safety program management.
It outlines criteria for evaluation of present safety programs and suggests implementation of critical elements which are indicative of safety being a management function.
It is recognized that each company will need to tailor its safety program to fit the various characteristics of its particular operation.
# A. Pre-Assessment of Present Program
Before revising an on-going safety program or attempting to design a new program, it is advisable that management assess its existing safety status within the plant. An evaluation of the present safety status will help out line where changes and additions are essential.
It will yield answers to the seriousness of the plant's accident problem, it will identify the major organizational deficiencies which have an adverse effect on the safety program, and it will identify the major accident prevention deficiencies within the program itself. Assessment of the following basic elements of the safety program should be made:
1. Management leadership 2. Assignment of responsibility 3. Identification and control of hazards 4. Employee and supervisory training 5. Accident reporting and investigation 6. Emergency plans 7. Employee awareness. Utilization of pre-assessment tools such as the American Society of Safety Engineers (ASSE) Safety Audit contained in Appendix C, or the example assessment forms contained in Appendix D can provide insight into safety program weaknesses which need management's attention. B. Basic Elements of a Safety Program It is difficult to outline a safety program that will be applicable to all precast concrete plants, since a program must vary with the specific needs of each company. It is important that a safety program be tailored for the processes and operations of an individual company. It becomes the responsibility of management to design and define a program within the constraints of a specific plant's operation. A safety program should, however, include aspects of the following basic elements:
1. Management Leadership Management's interest in safety must be sincere and visible to employees. Therefore, senior management must establish achievable safety program objectives and communicate these to all employees. The safety program objectives should receive the same management scrutiny as that given for the control of quality, cost, and production. Once the objectives are established, then management must plan, organize and control the overall program to meet the objectives. Management's leadership and support should contain the following key elements: a. Written Policy A written safety policy is management's method of communicating a direction to be followed. It is the first step in organizing to meet the stated objectives. It is important that the policy be in writing to reduce confusion concerning direction and assignment of responsibility.
The written policy should be concise, to the point, and should address the following areas: safety and health conditions . Employee participation can be encouraged by conducting safety meetings and by forming a plant safety committee. Holding safety meetings is a useful technique for communicating safety to employees. These meetings are more commonly referred to as safety huddles, tailgate sessions, or toolbox sessions. These are short
# SAFETY AND HEALTH POLICY
It is the policy of this company to provide every employee with a safe and healthful workplace. When a person enters the employ of our company, they have the right to ex pect to be provided with a proper place in which to work, as well as proper and safe machines and tools with which to do the job, and that the employee will be able to devote his or her energies to the work without undue danger. Only under these circumstances can the association between employee and em ployer be mutually profitable and harmonious. It is our desire, intention, and responsibility to provide a safe workplace, safe equipment, and proper materials and to establish and insist on safe methods and practices at all t ime s. People are our most important asset-their safety is our greatest responsibility. It is a basic responsibility for all employees of this company to make the SAFETY of fellow human beings a part of their daily, hourly concern. This responsibility must be accepted by each person who conducts the affairs of the company, regardless of the capacity in which they function. Employees are expected to know the SAFETY rules applicable to their job and must use the SAFETY equipment provided. Rules of conduct and rules of SAFETY shall be observed by all employees. SAFETY equipment must not be destroyed or abused. The joint cooperation of employees and management in the observance of this policy will provide safe working conditions and accident-free performance to our mutual advantage. We consider the SAFETY of our personnel to be of first importance, and we ask your full cooperation in making this policy effective.
# Company President FIGURE V-l. EXAMPLE OF A PLANT SAFETY AND HEALTH POLICY
Adapted from American Society for Personnel Administration, 19 Church Street, Berea, OH 44017.
As we are known and recognized for our products and service, so should we te known for our safety performance. No job must ever become so routine or so urgent that every safety precaution is not observed. Prevention of personal injury and damage to the property and equipment of both the company and its customers must always re main uppermost in the mind of every employee.
It is the policy of ABC PRECAST CONCRETE CORPORATION to develop and maintain safe and efficient operations. Our safety program has been designed, in accordance with the Williams-Steiger Occupational Safety and Health Act of 1970, to develop safe working conditions. The success of our program requires the full support of each and every employee.
# President FIGURE V-2. EXAMPLE OF A PLANT SAFETY POLICY STATEMENT
Adapted from Summary Plant Observation Report and Evaluation . meetings usually conducted by the supervisor with all his employees. The primary functions of such meetings are to foster communication between management (supervisor) and employees relating to safety consciousness,and to disseminate safety concepts. The subject should be specific to work being performed or planned for the upcoming week. The session should take place at the work site and last 10-15 minutes. Employees knowledgeable in specific safety subject areas should be requested to lead the safety discussions, thereby encouraging peer participation. Establishment of a safety committee is another technique which demonstrates management's desire that employees participate in the plant safety program. Committees may vary considerably in different organizations, but should have the basic functions of developing, promoting, and maintaining safety practices in the plant. Such committees should also serve as a means for communicating safety policies to both management and labor.
# Assignment of Responsibility
Management has the responsibility for controlling unsafe acts of employees and unsafe working conditions. Ultimately, the plant manager has the overall responsibility for meeting the plant's safety program objectives.
Since plant size and organizational structure vary widely throughout the precast concrete products industry, assignment of safety responsibilities must be appropriate for the management structure within the plant. In very small plants, the owner/operator may have sole responsibility; in larger plants, responsibility is assigned to the plant manager, middle managers and first-lin e supervisors. Additionally, the employees must also be assigned responsibilities in order to meet the stated safety program objectives.
# I d e n t if ic a ti o n and C o n tro l of H azards
Whenever management decides to either implement an accident prevention program or to overhaul an existing program, employees are inclined to be skeptical of projected results and tend to take a "wait and see" attitude. A vigorous management effort to eliminate longstanding hazards and to provide a safer workplace can convince employees that management is truly concerned about their on-the-job well being.
However, prior to eliminating these hazards, management must first identify them. Identification of hazards requires a fairly complete inspection of all precast operating areas. The inspection should be made by a small group composed of someone from production, someone from maintenance, and the safety program coordinator.
The hazard identification process should be done in phases to reduce interference with normal work routines.
Safety inspection checklists may be helpful in directing the group's inspection to the operating areas with the more hazardous work exposures. Management can either obtain checklists from insurance companies, or develop one specifically for their plant after analysis of the injury data presented in Chapter III, Table III-5. As an example, analyze nails as a source of injury. The table shows that nails mostly resulted in puncture injuries to employee's feet. Therefore, it is assumed that when wooden forms are removed from cured product, the nails are not bent over or removed, thereby creating a hazard to workers. Analysis of the "machinery" source indicates that lack of adequate guards are creating a hazard. If these sources of injury are present within the plant, the checklist should address these items. After the in itial inspection has been performed, a program for correcting the noted deficiencies and performing periodic inspections should be established. Identifying hazards by means of inspection and promptly eliminating or controlling them is one of the best methods management can use to demonstrate its interest and concern for accident prevention to employees. both new employees and employees new to a particular task. Newly hired employees should always receive instruction and orientation about the company, the plant, the product, organizational arrangements, lines of authority, and safety policies and rules. Specific training, including supervised on-the-job training, must be provided to each employee.
During orientation to the plant, a new employee should be given copies of the company's safety policy, and safety rules and regulations. If an employee starts a new task, changes tasks, or uses new or modified equipment, it is essential that quality training for this job be provided. Training may be necessary to develop a particular skill that cannot be performed safely without specific knowledge; e.g., working at a rebar bender, casting concrete, or operating a forklift. Safety training is based on the general assumption that the development of a positive mental attitude predisposes an individual to safe habits of work and conduct. A job should be explained in detail by breaking it down into manageable parts. If personal protective equipment is required, employees must understand why it must be used and what may happen if it is not used properly. Hazards should be identified, and precautions or safe work practices demonstrated. Training should take a new employee through each step, and each step should be fully demonstrated. In addition, the supervisor should verify, at regular intervals, that the original lessons are being followed and that the employee is not developing bad habits or taking dangerous shortcuts. The type of training required, by employee group, is presented in Table
V-l.
Other training, such as first-aid courses, cardiopulmonary resuscita tion (CPR), fire extinguisher use, and other emergency procedures may be required.
Training is a continuous process, and attention must be paid to all employees. An employee who continues to repeat an unsafe procedure is not working safely, even if an accident has not occurred. The following indicators might show a need for training or retraining: o High incidence of injury o An increase in the number of "near misses" that could have re sulted in accidents o A change in a process or introduction of a new process o A recent upswing in actual accident experience o Excessive waste or scrap due to poor housekeeping.
# Accident Investigation
The investigation of accidents is an important part of the safety/accident prevention program. It identifies accident causes so that similar situations can be prevented by management actions such as mechanical im provements, better supervision, or employee training. It determines the "changes" or deviation that produced an "error" resulting in an accident; it publicizes the particular hazard among employees and their supervisors; and it directs attention to accident prevention in general. Since nothing is learned from unreported accidents, even minor injuries and near misses should be investigated. The investigation of accidents is the responsibility of all levels of management. However, the firstline supervisor is perhaps the best quali fied, since he is close to the jobs, working conditions, and workers. The supervisor must be trained and have the ability to recognize the cause of accidents. This evaluation may require the assistance of management, equipment suppliers, and insurance representatives. Figure V-3 shows an example of an accident investigation form.
The basic problem confronting any supervisor interviewing a person involved in an accident is obtaining complete facts. Often a worker is reluctant to cooperate for fear of ridicule, sarcasm, or reprimand. It is important to stress the need for facts so that recurrence can be prevented in the future. It is also helpful to ask individuals involved in accidents for their ideas on making the job safer.
Witnesses are important sources of accident information. When a fatal injury occurs, a witness may be the only direct source of information available. When a serious injury occurs, a witness may be the only means of verifying incoherent pieces of the injured's account. For minor injuries, a witness may be able to clarify some of the circumstances surrounding the accident better than the injured person himself. This is also true of near accidents that have a potential for serious injury.
In all cases, all levels of management can learn how to prevent accidents through investigations. By investigating accidents, similar unsafe practices and conditions can be monitored in the future. The information compiled can also help to design better training programs, emphasize areas needing management's attention, and generally prevent future potential problems.
Management's participation is highly important to a functioning safety program in the precast concrete products industry. Efforts should be made to reduce the unnecessary costs of worker injury and illness, loss in production time, as well as repair and replacement of damaged machinery and products.
# Emergency Plans
Management should have a written plan of action outlining procedures to be taken in emergency situations such as employee injury and fire. The purpose of the plan is to eliminate as much confusion as possible in order that immediate positive response will be taken to minimize the dangers of the emergency. firefighting equipment appropriate to the work space, materials, and expected hazards. Canada also requires that facilities for producing prestressed con crete elements include measuring equipment for setting up and checking alignments and levels. Canada requires that there be adequate dustcollecting and ventilating capabilities when personnel are in woodworking shops where wood or plastic forms are made.
# Reinforcing
Canada requires that work benches or gigs where welding is performed be arranged so that employees are protected from welding flashes and that the areas be ventilated to avoid exposure to excessive welding fumes.
PCI refers to the OSHA General Industry Standards in 29 CFR 1910.217 and requires welding areas to be ventilated and protected to prevent welding flash.
# Stressing
Both Canada and the PCI have safety requirements for stressing opera tions. The PCI requires that a shield or guard be provided for bed end protection of the jacking area. There are suggestions for the materials for a barrier, but no specific requirements.
# Oiling
There are no unique safety standards in any international or consensus standards that address the tasks of this operation, except those discussing walking and working surfaces in the PCI "Safety and Loss Pre vention Manual" .
# Mixing
The PCI has no specific safety standards regarding batching and mixing that relate to safety. The Canadian standards require that the batch plant be kept clean at all times.
# Casting
The PCI recommends that gloves, long-sleeved shirts, and long trousers be worn when employees are performing any of the various tasks related to concrete operations, such as shoveling, raking, vibrating, and screeding. The PCI requires that personnel performing the shoveling tasks be trained in proper procedures to reduce the potential for back strains. They also require that extruder hoppers have guards and that all electrical connections be insulated or guarded.
The PCI refers to requirements regarding noise in 29 CFR 1926.52 and CFR 1910.95.
# S trip p in g
There are no specific requirements in the PCI, ACPA, or Canadian standards that apply to tasks in the stripping operation.
# Curing
The PCI has both recommendations and specific requirements concerning steam, hot oil, electric, and moisture curing. They include requirements for the insulation of steam, hot: oil, and hot water lines and for thermostats, timers, and circuit breakers for electric curing.
# Finishing
The PCI "Safety and Loss Prevention Manual" recommends the use of rubbersoled shoes where there are slippery surfaces and requires the use of hard hats, eye protection, knee pads, and gloves in the performance of certain operations; e.g., gloves are required for all finishers working with concrete; eye protection is required while concrete is poured; and eye protection is required whenever finishers are chipping, burning, drillling, or grinding. During special finishing processes such as sand blasting, the PCI re quires adequate exhaust ventilation and respiratory protective equipment. When acid etching is used as a finishing technique, the PCI requires that warning signs be posted and visible, that all caustic and acid products be labeled, and that employees know the location of the nearest portable water supply. It also recommends the use of protective face, hand, foot, and body clothing for employees performing these tasks.
# Materials
Handling PCI refers to 29 CFR 1926.600 for certain general requirements, but also specifies in its "Safety and Loss Prevention Manual" that operators be trained and qualified, be able to pass at least a verbal examination, be specifically designated to a particular task, and make a daily minimum check of their equipment. PCI also requires that the grounds be properly maintained for safe operations and prohibits the carrying or holding of loads over work areas where other employees are present. The ACPA requires that product handling conform with the standard recommendations in its handbook.
Canada requires that all physical production facilities be laid out, designed, and constructed so that there will be adequate space for mate rials, storage, equipment, and production facilities, with sufficient capacity so that production can be adequately maintained without adversely affecting the safety of plant, personnel, or products.
The PCI has both general and specific recommendations for yard storage, including storage area, dunnage, stacking, personnel safety, strand, and rebar storage. They also have recommendations regarding product trans portation, including operating rules for driving in hazardous weather. The PCI prohibits the use of drugs and alcohol; it also requires that drivers wear hardhats and safety shoes.
The OSHA General Industry Standards in 29 CFR 1910 regulate safety and health in the precast concrete products industry (SIC 3272); however, the standards do not apply to all operations, tasks, and conditions specific to the industry. Those items in the existing standards that are related to the manufacture and delivery of precast concrete products are presented in Table B E. Summary OSHA General Industry Standards apply to many of the operations, tasks, and conditions typical of precast concrete manufacturing operations. These OSHA regulations address subjects such as walking and working surfaces, handtools, ventilation, noise, fire prevention, respiratory protection, machine guarding, ladders, scaffolding, and welding or cutting. OSHA standards do not, however, regulate some of the tasks, equipment, and opera tions that are specific to the precast concrete products industry, such as forming, stressing, detensioning, oiling, concrete transport and casting. Existing international standards and trade association guidelines address many of the hazards that are unique to tasks in the precast concrete indus try. PCI provides guidelines for worker protection in such areas as ten sioning, architectural and structural product storage, yard layout and cleanliness, product shipping, and steel placement. ACPA guidelines address the areas of pipe handling and unloading. In addition to ef fective accident analysis, results are used to pinpoint accident causes so accident prevention objectives can be established. Written requirement that all property damage accidents of $50 & more will be investigated. higher range (generally between 30° C and 70° C), the term "accelerated curing" is used.
# Investigation of property damage.
The process of creating draped strand.
The release of tension from the tendon, usually occurring at the time the prestressing force is transferred from the bed anchorage to the individual pieces cast in the bed.
The minimum concrete strength specified for individual concrete elements before the prestressing force may be transferred to them. A strand that is held up at specific points, and held down at others, to form a special desired profile.
Concrete designed with very low water/cement ratios and slumps to be used with special consolidation methods, tamping, or extrusion production equipment. Materials (usually wood) used for keeping concrete products from touching each other or other materials during storage and transportation.
A structure or mold for the support of concrete while it is setting and gaining sufficient strength to be selfsupporting .
A substance applied to the forms for the purpose of pre venting a bond between the form and the concrete cast in it.
The system of support for freshly placed concrete, including the mold or sheathing that contacts the concrete as well as all supporting members. The parts of a strand vise that actually contact or grip the wires or strands.
A collective term used to cover all items embedded in the concrete (other than reinforcement) or otherwise used in connecting precast elements or attaching or accommodating adjacent materials or equipment:.
A device to align parts of an assembly, usually for pre assembling reinforcing steel and hardware cages, with a minimum of measurement and consistent accuracy, from one cage to the next. A device designed to provide two or more lifting points of a precast concrete element with predictable load dis tribution and prearranged direction of pulling force during lifting. Products cast by one or more machines specifically design ed for the purpose. Slipform and extrusion machines are types of casting equipment used to make solid or hollow-core slabs. Finishes applied by special tools while the concrete is s till in the forms and plastic.
Concrete with a near-zero slump to be used with special consolidation methods, tamping, or extrusion production equipment.
A concrete element cast in a location other than its final position in service. Precast concrete may be produced at the job site, in temporary plants, or in permanent factories.
A general term for any precast product regardless of classification or application. The term includes any nonconcrete items incorporated in the element at the time of manufacture.
The platform and abutments needed to support the forms and maintain the tendons in a stressed condition during placing and curing of the concrete.
An admixture that delays the setting of concrete paste.
The smoothing or leveling off of freshly cast concrete by manual or mechanical means. A screed usually has a wooden or metal edge that is moved horizontally across the concrete, pushing excess material in front of it and filling in low places.
Equipment that, in addition to serving as forms for con crete, accommodates the pretensioned strands (or wires) and sustains the total prestressing force by suitable end bulkheads and sufficient cross-sectional strength.
The drop from the top of a slump cone to the top of the unsupported concrete after the sudden removal of the supporting slump cone. The difference in height, measured in inches or centimeters, is the slump of the concrete. A wet or soft mix slumps more than a dry or stiff mix. strand chuck A device for holding a strand under tension, or vise stripping
The process of removing a precast concrete element from the form in which it was cast.
# two-blocking
The action of the crane hook block being pulled into the crane boom head. water/cement
The weight of water relative to the weight of cement in a ratio concrete mix. Enough water must be added to the mix to provide hydration. Excess water improves workability but reduces strength.
Occupational safety and health standards that address operations in the precast concrete products industry were requested from Germany, the United Kingdom, France, the Netherlands, Belgium, Australia, Canada, and Mexico. The Canadian standards that regulate architectural and structural operations are included for evaluation. Australia, France, and Belgium have standards for the concrete construction industry, but do not regulate manufacturing operations.
The remaining countries do not have safety standards that specifically address precast concrete operations.
# B. Trade Association Guidelines
The ACPA has published a "Concrete Pipe Handbook" that contains some suggestions on handling, unloading, and site storage. The PCI has developed a "Safety and Loss Prevention Manual" that includes sections on subjects such as training motivation, yard storage, tensioning equipment, stressing operations, steel placement, travelifts, chucks, and harping. These subjects are specifically related to tasks or operations in the architectural and structural sectors of the industry.
# C. Foreign Standards vs. Trade Association Guidelines
International standards and guidelines are incorporated, where appro priate, in the comprehensive safety recommendations presented in Chapter IV. A comparison of these standards and guidelines are presented topically, by operation, in the following section.
# Forming
Canada requires that, in facilities for making forms and accessories, the construction of the forms be within the tolerances required for the product. They also require that all form-making shops have exits and A tool used to spread out and smooth the concrete.
An air-powered reciprocating tool used to give a textured appearance to architectural concrete products by roughening the surface.
(a) The upward deflection that occurs in prestressed concrete elements due to the net bending resulting from stressing forces and self-weight. It specifically does not include dimensional inaccuracies. (b) A built-in upward curvature in some molds for precast concrete other than prestressed to avoid deflection under load to below a defined line of finished product. Any of various construction adhesives, consisting essen tially of powdered, calcined rock and clay materials, that form a paste with water and can be molded or poured to set as a solid mass.
A mixture of cement, sand, and aggregate with water that hardens by chemical curing into a final product similar to stone in texture, weight, and durability.
A device for attachment of precast concrete elements to each other or to a building structure.
The maintenance of humidity and temperature of freshly placed concrete during some definite period following placing, casting, or finishing to ensure satisfactory hydration of the cementitious materials and proper hardening of the concrete. When the curing temperature remains in the normal environmental range (generally between 10° C and 30° C) , the term "normal curing" is used. When the curing temperature is increased to a | Concerned by reports that the precast concrete products industry (SIC 3272) has an injury incidence rate which is consistently at least twice that of the national average, the National Institute for Occupational Safety and Health (NIOSH) began developing this document with the intent of providing recommendations aimed at reducing worker exposure to hazards.# PREFACE
The Occupational Safety and Health Act of 1970 (Public Law 91-596), states that the purpose of Congress expressed in the Act is "to assure so far as possible every working man and woman in the Nation safe and healthful working conditions and to preserve our human resources...by," among other things, "providing for research in the field of occupational safety and health...and by developing innovative methods, techniques, and approaches for dealing with occupational safety and health problems."
Later in the Act, the National Institute for Occupational Safety and Health (NIOSH) is charged with carrying out this policy.
One method by which NIOSH responds to this charge is to publish Technical Guidelines.
Technical Guidelines present the results of comprehensive systematic analyses of occupational hazards, and suggestions for preventing injury and disease among workers.
They are intended to supplement existing Federal safety and health standards and may provide background useful in formulating new standards for development.
In the interest of wide dissemination of this information, NIOSH distributes Technical Guidelines to other appropriate governmental agencies, organized labor, industry, and public interest groups. We welcome suggestions concerning the content, style, and distribution.
This document provides guidance for protecting workers in the precast concrete products industry. It was prepared by the staff of the Division of Safety Research in conjunction with the Division of Standards Development and Technology Transfer, NIOSH.
I am pleased to acknowledge the many contributions made by reviewers selected by the Prestressed Concrete Institute (PCI), the American Concrete Pipe Association (ACPA), and the National Precast Concrete Association (NPCA); other reviewers and consultants; representatives of other Federal agencies; and the staff of the Institute. However, responsibility for the conclusions and recommendations belongs solely to the Institute. All comments by reviewers, whether or not incorporated into the final version, are being sent with this document to the Occupational Safety and Health ^Administration (OSHA^ for consideration in standard setting.
The document characterizes the industry and describes the operations, tasks and processes required to manufacture precast concrete products.
The magnitude of the occupational safety problem in the precast concrete products industry is defined through presentation of injury and illness incidence rates.
In support of the document's systematic approach to the identification of industry hazards, a detailed analysis of 1,319 accident case histories was performed.
This analysis identifies the tasks, tools, and equipment that are the most hazardous to the worker.
For example, materials handling tasks, both manual and mechanical, accounted for 28.0% of the total injuries studied.
Tasks associated with welding, burning and cutting accounted for 4.6% of the total injuries. Some of the specific tools found to be particularly hazardous to precast concrete workers include: hoists and cranes, which accounted for 4.4% of the total injuries and 40% of the fatalities; unpowered handtools, which accounted for 5.7% of the total injuries; and powered handtools, which accounted for 5.8% of total injuries. The determination of how workers are injured during precasting operations led to the formulation of comprehensive safety recommendations.
The recom mended engineering controls and/or operational safe work practices offered are applicable to product manufacture and delivery to a construction site only, and do not address erection or installation procedures.
To further enhance the document's usability for small to middle-sized pre casting plants, a chapter addressing safety management principles is presented. The Romans used the product in ashlar work (stone and brick) and as concrete in building harbors, piers, canals, and water supply and sewerage systems.
The remains of ancient structures reveal that building materials progressed from relatively simple applications of natural materials to cast concrete, one of the earliest substitutes for natural stone. Despite the ravages of time, weather, and warfare, many ancient concrete structures remain to give testimony to their durability.
Following the Roman period, the use of cement and concrete had a long period of dormancy until the emergence of studies by the early British civil engineers in the late 18th century.
During the 19th century, after the successful development of the Erie Canal under Governor DeWitt Clinton of New York, engineering projects increased the need for cement and concrete. New sources and techniques were developed, transportation improved, industrial growth expanded, and concern for public health emerged. Transportation requirements created a demand for railways, highways, storm drainage, and bridges; buildings required structural and architectural elements; and improvements in public health called for sewerage, water storage, and water distribution systems.
Technological advances, beginning with reinforced concrete and culminating in contemporary prestressing methods, have made longer, stronger concrete members possible.
Thus, concrete has grown out of a mere supplemental relationship with steel into direct competition with it in construction of varying projects.
The widespread use of standardized precast/prestressed concrete products, such as architectural panels, pipe, etc., has brought about the prevalence of fixed, permanent plants for manufacturing concrete products.
The improvement of transportational methods and systems has contributed to the evolution of the precast concrete plant, in that it has become cost efficient to mass produce concrete products and transport them to the various construction sites rather than cast members on-site.
Such plants capably produce job-specific, one-of-a-kind product as well, offering an alternative to poured-in-place operations, or casting operations adjacent to actual construction sites.
# B . Scope
This document concerns occupational exposure in the manufacturing of precast concrete products (SIC 3272). Examples of products manufactured within SIC 3272 are contained in Appendix A.
Contractors engaged in concrete construction work including on-site precasting of concrete products are classified in the construction industries and are not considered in this document. Other industries concerned with manufacture of concrete products which are excluded from the scope of this document are:
o
# CHAPTER II DESCRIPTION OF THE PRECAST CONCRETE PRODUCTS INDUSTRY
In this chapter the precast concrete products industry is described, its structure is examined, the number of plants and the size of the work force are defined, and the labor and trade organizations associated with the industry are identified. An operations approach that follows the production flow is used to give a description of specific manufacturing techniques or processes, the tasks performed by workers within each operation, and the tools and equipment associated with such operations.
Concrete is a building material made by thoroughly mixing cement; sand; aggregate, such as gravel or crushed stone; and water in desired proportions.
The cementitious material usually is a hydraulic cement that sets and hardens in water.
Initially, the concrete mix is a plastic material that assumes the shape of the mold into which it is cast.
The mixture is poured into a cavity, an excavation in the ground, or a form designed for a specific purpose.
After hardening, concrete has the appearance and structure of stone.
In fact, it may be thought of as "moldable stone." When the mixture is deposited in its final position, it is known as cast-in-place concrete.
When a concrete product or element is cast elsewhere (whether in a plant or on a field site) and then brought to its final position, it is termed precast concrete.
Precasting is a manufacturing procedure, whereas casting-in-place is a construction procedure.
Being a manufacturing operation, precasting can have certain advantages: o Work can be performed at a fixed site with accelerated curing facilities. o A single location for batching and mixing concrete can be provided, o A convenient source of water and other raw materials can be used, o A location convenient to transportation facilities can be selected, o Mass production techniques can be employed. o Opportunities for storing product and working under shelter reduce the impacts of cyclical demand and weather conditions.
# A. Plant Census and Worker Population
The precast concrete products industry is entrepreneurial, highly diversi fied, and geographically dispersed, with nearly 4,000 disparate plants manu facturing more than 600 different products.
The NIOSH Industrial Profile data for 1980 (Table II-1) show that 3,930 precast concrete manufacturing plants employ about 82,049 workers [1].
These figures compare well with information derived from the 1979 Pennsylvania Industrial Directory [2], and the U.S. Department of Commerce 1977 Census of Manufacturers [3](Table II-2). [1], 1979 Pennsylvania Industrial Directory [2], and 1977 Census of Manufacturers [3], Information supplied by trade associations also verifies the plant census figures in the NIOSH profile. The American Concrete Pipe Association (ACPA) [4], the Prestressed Concrete Institute (PCI) [5] and the National Precast Concrete Association (NPCA) [6] estimations of worker population corroborate the NIOSH profile figures. Further, the trade associations estimate that the precast concrete industry is comprised of approximately 62,500 production workers. This equates well with the aforementioned NIOSH profile total population of 82,049 workers, and the Department of Commerce Census estimation that approximately 77% (or 63,178) of the total worker population in the industry are production workers.
Table II-3 presents these trade association estimates.
For the purposes of this study, the NIOSH Industrial Profile data was used since it was the latest compilation of data on the industry. *From Duffy J. J. American Concrete Pipe Association [4]. **From Freedman S. Prestressed Concrete Institute [5]. ***From Tilford J. E. National Precast Concrete Asso ciation [6] .
# B. Process and Task Descriptions
This section describes the operations, tasks, and equipment required to manufacture precast concrete products. These descriptions are presented in organizational groupings that follow the primary production steps necessary in the precasting process. In many instances, the operations, tasks, and equipment described under a particular process heading are not unique only to that specific process; however, it is convenient to present the task descriptions in the sequence of the production flow. An additional section on materials handling is presented following the production task descriptions.
# Forming
Forms or molds used for the casting of precast concrete products us ually are made of steel or wood.
However, they may be constructed of any material that remains stable during casting and is able to withstand the abuse of preparation, installation of steel reinforcement, oiling, curing, stripping, and reuse. Wood is commonly used for the construction of forms expected to have a limited use; that is, forms built for the casting of fairly unique concrete products. Concrete is sometimes used as a form because it can be cast into intricate shapes. With a dense, smooth surface finish and the application of form release agents, concrete is an excellent form material for products requiring smooth or curvilinear surfaces. Styrofoam, fiber glass, rubber matting, and various paperboards are also occasionally used to make forms or form liners for special surface effects.
Because many of the products manufactured in the industry are produced repetitively, steel forms are common.
Such forms are usually made to design specification by other departments or are purchased as standard equipment from other form manufacturers.
Occasionally, it is necessary to modify or customize steel forms; that is, holes, notches, and sections may be burned out or fillets, boxouts, and seats may be welded in place as needed.
Large forms may be equipped with access ladders, stairways, work platforms, conveyor connections for receiving concrete, and external vibrators for consolidation.
Steel forms are hammered, vibrated, modified, and moved, creating dents, holes, and misalignments that require periodic repair and mainten ance.
In addition to welding shops, many plants have portable welding equipment for repair and modification of forms too large and unwieldy to move. Welds and patches are occasionally required to fill in depressed spots; chipping and grinding operations are used to smooth rough areas.
The form surface against which the concrete will be cast must be clean and smooth (unless specifically designed otherwise).
Forms are cleaned for reuse by chipping, wire brushing, scraping, scrubbing with water, sanding, and/or air blowing.
Form assembly follows repair and cleaning. Large forms are moved to the casting station by overhead hoists or cranes, or by lift truck.
Many products have interior and exterior forms.
Often, the interior form is placed and fixed to a cleaned steel plate, or pallet ring that forms the bottom of the product.
Exterior forms are then locked into place with various fittings (makeup bolts, tack welding) that both fix its position and maintain the required dimension between the interior and exterior form.
Forms for long or flat products require minimum assembly, except to position the edges, bulkheads, and boxouts at the desired locations. Edges and bulkheads usually require appropriate spacers, spreaders, braces, and stiffeners.
These pieces are usually cut from wood to the proper length, hammered into place, and held by nails. Hammers are used for driving nails and tacking chamfer strips in wood forms. Sledge hammers, crowbars, and prybars are used in the alignment of forms as well as during the placement and removal of bulkheads.
The tasks and equipment used during the construction of the forms are typical to wood, Styrofoam, or fiber glass assembly/manufacturing pro cesses.
Most companies have carpenters' shops or areas equipped with hand and power tools for form construction.
Larger companies usually have full-time personnel to use this equipment while smaller companies usually assign workers the task of making the form as part of their other routine responsibilities (casting, oiling, mixing, etc.).
# Oiling
The form surface is coated with a release agent to keep the fresh concrete from bonding to the form. Form release agents usually have a kerosene or paraffin base and are applied to the form by swabbing or spraying before the reinforcing steel is placed.
Swabbing is the hand application and spreading of the agent on the interior surface of the form with the use of brooms, mops, rags, or brushes. Swabbing operations require a worker to fill a container (buc ket) with form oil from a drum, transfer it t:o the form, and physically apply it to the form walls. Usually the worker will swab while standing and walking in the form. Some forms (vertical walls) may require the worker to stand on the form structure and mop the walls.
Most spray application of form oil is by hand-pumped, hand-carried sprayers similar to garden insecticide sprayers.
The pump is filled from a central drum and carried by the worker to the form.
Typically, the worker will walk along the edge of the form and spray the required surfaces.
Some precast plants use a central pressurized air venturi system instead of hand pumps to spread the form oil.
# Reinforcing
The reinforcing operation includes the fabrication and placement of steel reinforcement into the product forms. The tasks associated with this operation are cutting, bending, tying and welding of rebar, wire and wire mesh; and stringing and stressing of steel strand. The reinforcement, once sized and shaped, may be assembled in the form or fabricated outside of the form in a separate area or shop. The movement or placement of the steel may be done mechanically or by manual means.
# a. Plant Fabricated Steel
Manual fabrication of reinforcing assemblies is common. Some times reinforcing bars or welded wire fabric are placed and tied in the form. For more complex assemblies, a jig is built to position bars. Transverse and shear steel is manually tied to the longitud inal steel with wire and pliers or with looped-end wire ties and a special "pigtail" tool that twists the two ends of the wire tie together when pulled. To produce reinforcing bars with the bends, loops, angles, and hooks specified by the design, a rebar bender is used. A cage or mat can be made to any desired size or shape. The completed plant fabricated reinforcing steel assembly is then lifted and placed in the form by manual or mechanical means. With prestressed concrete products, individual stirrups or welded wire fabric used for shear reinforcement are hand placed and may be tied to the prestressing steel.
Circular or elliptical reinforcing cages for concrete pipe are usually made of welded wire fabric (2-to 4-inch mesh made from 1/8-to 3/o-inch wire) or cold-drawn steel wire.
A wire roller forms rolls or flat mats of welded wire fabric into the desired circular shape, which is then cut and spot welded to make the cage.
Both cage machines or mandrels can be used to form steel wire into cages.
In a cage machine, the operation is continuous and the endless cage produced is cut to the required length; in a mandrel operation, each cage is made individually to the desired diameter and length. Both techniques require that the wire mesh be shaped into a cylinder (by rolling or bending), the ends joined (by welding or using tie wires), and the finished reinforcing cage placed into the annular space of the pipe form.
# b. Prefabricated Steel
Many small precast concrete products are reinforced by prefab ricated steel manufactured to specification by others. This prefabricated steel is placed, tied, or secured into the form or pressed into the freshly cast concrete at the desired locations.
# c. Steel Plates and Rolled Sections
For connecting some structural and architectural precast concrete products, small, rolled, sectioned steel plates with reinforcing bars or studs welded to them are tied to the cages inserted in the freshly placed concrete.
Wire loops of prestressing strand or reinforcing bars are tied in place or inserted manually for lifting and handling the finished product.
Connection and handling steel is called "hardware," and should be designed by the plant engineering staff or the project engineer.
The tasks necessary when using steel plates are similar to those described in the preceding sections.
# d. Prestressing Steel Strand
Prestressing steel is usually seven-wire strand that is manually or mechanically strung in the form before concrete is cast.
Manual strand stringing is performed by a worker physically pulling the length of strand down the bed from a reel stationed at one end of the bed.
The strand is then cut by torch or strand saw, and the process is repeated. Mechanical stringers pull multiple lengths of strand from separate reels at the same time.
Single or multiple strands may be threaded through cages of reinforcing steel and through bulkheads used to separate adjacent members.
The steel wire strands are laid in the stressing bed (a long form up to several hundred feet in length with the cross section of the desired shape) and fixed at the ends (abutments).
The stressing bed is the mold for several precast units along its length.
For example, if 50-foot-long "double tees" are desired and a 610-foot-long stressing bed is used, 12 such units can be produced in one bed, each separated by a bulkhead. Some beds are designed as selfstressing forms, eliminating the need for end abutments.
Once the strands are in place they are then stressed. This operation is the tensioning (stretching) of wire strands previously positioned in the form.
Stressing includes strand vise placement, jacking, tensioning, harping, and detensioning.
The stressing operation can be done by single strand jacking or multiple strand jacking where all the strands are tensioned at the same time.
The strands to be stressed (usually 1/2-inch, seven-wire strand [7], tensioned to approximately 200,000 pounds per square inch (psi) or a 30,000 pound load) are anchored at one end of the bed with a strand vise.
The strand vise barrel has a truncated conical hole along its longitudinal axis that holds the three jaws of a chuck.
The chuck is serrated on the inside surface and conical in shape outside. The jaws permit free movement of the strand in one direction.
In the other direction, they grip the strand and wedge themselves into the conical hole in the barrel of the strand vise.
A strand vise is placed over each length of strand at the anchor end abutment, which fixes it in place. At the jacking abutment, two strand vises are placed on the strand in opposing directions.
One is seated against the end abutment and allows the strand to be pulled through as the jack tensions the strand.
This strand vise also holds and anchors the tensioned steel to the abutment. The other strand vise provides a grip for the jack.
Figure II-l shows a rectangular prestressed beam form with strands stressed and reinforcement in place.
The steel strand may run straight through the bed and may be stressed in this position.
Alternatively, the strands may be depressed within the form for each member along the bed to create an upward force that improves structural efficiency [7]. This technique is called draping or harping.
The term "draping" describes the profile of the steel strand, which is "draped" from its high point near the ends of each precast member to the low point at the midspan of each member.
Strands can either be depressed or pulled up.
Tine strands are passed through and over pin and roller fixtures that minimize friction at the points of change in the steel strand profile.
Figure II-2 shows the strands depressed at the midpoint of a member, thus creating the appearance of strings on a harp. Some designs may require other holddown locations for each member.
After the concrete is cast and has gained the specified strength (us ually 3,500 psi or more [7]), the strand tension is released, or detensioned.
In some cases, strands are individually cut by torch; however, with hydraulic jacks, the tension is gradually released from the header.
# FIGURE II-2. A "SINGLE TEE" SLAB WITH THE STRANDS HELD DOWN AT THE MIDPOINT
TO "HARP" THE PRETENSIONED STEEL Adapted from Bennett W. B. Jr. [7].
Detensioning transfers the stress from the steel to the concrete to which it has bonded, precompressing the concrete.
# Concrete Mixing
Concrete may be batched and mixed at the products plant or purchased from a ready-mix concrete producer. The correctly weighed proportions of cement, aggregates, and water are charged into a drum mixer, pan mixer, or a transit mix truck.
Small mixers that are used in many miscellaneous products plants are gas, diesel, or electrically powered.
Cement may be delivered to the plant in bulk cement trucks or railroad cars and unloaded by a totally enclosed, screw auger pneumatic system that carries the cement to an elevated hopper or silo.
Aggregates for larger plants are unloaded in much the same way as cement, except that open conveyors may be used.
The material stored at a higher elevation is weighed and chuted by gravity (charged) into the mixer.
The proper weight of water is added, and the mixer blends the components into a homogeneous mixture by rotating paddles inside an enclosed vessel at speeds of 2-15 revolutions per minute (rprn), or approximately 2 linear feet per second.
The two most common types of mixers used in the industry are drum mixers and pan mixers.
A drum mixer is a rotating cylinder in which sta tionary paddles, mounted along the cylinder, mix the concrete (truck mixers are of the drum type, inclined from the horizontal).
The pan mixer consists of a shorter cylinder than the drum mixer and is vertically oriented; paddles are mounted vertically and rotate to mix the concrete in the stationary cylinder.
The mixer is usually positioned 10-15 feet above the adjacent working surface to allow gravity discharge of the mixed concrete into buckets, trucks, or other means of conveyance to the casting area.
Access for cleaning, maintenance, or concrete quality control is provided by ladder or steps to a working platform that will partially or totally encircle the mixer.
Figure II-3 depicts a concrete batching, mixing, discharge, and transport system.
At the end of each shift or after mixing is completed for the day, the mixers are cleaned.
In addition to daily cleaning and flushing of concrete mixers, it may be necessary to hammer or chip away built-up en crustations of concrete on a periodic basis.
Mixers also require maintenance, paddle replacement, and repair.
All of these tasks may require workers to enter the mixers.
# Concrete Delivery and Casting
Casting of small products can be a manual operation; a quantity of mix is made available to the operator, who trowels or shovels it into a prepared mold around the reinforcement. The material may be hand tamped or vibrated to consolidate the mix.
Many small products are made with high production, automated equipment.
For casting larger pieces, the concrete is delivered from a truck, a concrete bucket, or a concrete buggy moved to the location where the concrete is to be used.
For very large pieces or for long-line prestressing beds, the concrete may be delivered by a monorail bucket system, overhead bridge crane, or other mechanical means and deposited directly in the form, where it is vibrated and consolidated by machinery or by manually inserted spud vibrators.
Usually two to five employees will be directly involved in these tasks.
In addition, concrete may be extruded through a die to form products such as hollow-core slabs.
Systems used to deliver the mixed concrete to the placement location vary from simple manual handling to totally automated, enclosed convey ances.
Concrete mixed in small power mixers is delivered by direct deposit (when the mixer or form is portable), by front-end loader (which carries concrete from mixer to form), or by wheelbarrow.
Ready-mix trucks frequently are used to deliver concrete because they can carry, and continuously mix, large volumes (up to 12 cubic yards) directly to or near the forms for placement. A chute, attached to a lip below the discharge opening of the truck's drum mixer, is directed by a worker to deposit the concrete.
The chute is moved around during the casting process to spread the concrete and reduce shoveling or raking.
As parts of the form are filled with concrete, the truck moves along the form, placing concrete to the desired level.
The process continues, FIGURE II-3. CONCRETE BATCHING, MIXING, DISCHARGE, AND TRANSPORT SYSTEM using additional ready-mix trucks with loads of concrete, to completely cast the products being made. During casting, workers will be engaged in a series of continuous tasks directed at filling the form with concrete.
When a ready-mix truck is used, workers will be working adjacent to and along with the movement of the delivery truck. Access (steps or ramps) to low forms (1-3 feet high) is usually limited or nonexistent. Employees will frequently be working and moving among multiple form tiedowns, spacers, and spreaders as well as walking on the reinforcing mats while filling and vibrating the forms. When it is not possible for a truck to deposit concrete directly into the form, wheelbarrows, hoisted concrete buckets, or concrete delivery vehicles are used.
Workers may push wheelbarrows along walkways, planks, or ramps to fill the form with concrete.
Another method of delivering concrete is by transporter, which takes mixed concrete from a central mixer and carries it directly to the forms.
Enclosed transporters have a smaller capacity (up to 6 cubic yards) and are usually lighter, smaller, and more maneuverable than ready-mix trucks. This method of depositing concrete is similar to that for ready-mix trucks except that the chute is tubular in shape, with an enclosed auger or conveyor belt, allowing concrete to be pushed to higher elevations instead of depending on gravity. Some transporters consist of wheeled or tracked carriers that take large buckets or hoppers of mixed concrete (up to 4 cubic yards) to placing or casting machines.
Transporters may travel on aisleways, rails, or roadways at speeds of up to 500 feet per minute.
Transfer, turnaround, or backing areas may be provided at the end of the travelway s for moving the transporters laterally relative to the casting areas or for access to the concrete mixers.
Visibility may be limited because of walls, corners, other equipment, storage, or layout. Once the concrete buckets have been delivered to the casting area, an overhead hoist, which may be an integral part of a casting machine, will be used to hoist and position the bucket over the form or casting hopper.
Conveyors are frequently used to deliver concrete to the point of placement, especially in the miscellaneous and pipe sectors of the industry.
The forms can be set up under the discharge end of the conveyor, or a portable conveyor can be set up with its discharge over the forms (depending on form mobility).
Concrete is deposited onto the conveyor and moved along the conveyor system (which can be arranged to move the concrete around corners, to different elevations, or to remote plant locations) to the point of discharge.
Access to elevated forms during casting is usually provided by plat forms, stairs, movable scaffolds, or ramps.
Large pipe forms and mis cellaneous products forms will sometimes have walkway platforms built around the forms or attached for the casting operations.
Ramps are a convenient means of access to forms at elevations different from the surrounding working surface; otherwise, stairs are used.
Access to lower beds up to 3 feet above the plant or yard surface usually is by stepping up and jumping down; it is uncommon for steps or ramps to be provided• In mechanized plants, placement of concrete into lorigbed forms is accomplished by placing or casting machines, similar to pavers or extru ders.
The concrete is spread, vibrated, compacted, screeded, and finished as the machine passes over the form, or is extruded as it moves along the bed. Drive controls are located in a cab on the machine or on a panel reached by workers from the side of the machine.
One method of casting utilized in the manufacture of pipe and many miscellaneous circular products requires a concrete mix that is wet com pared to the mixes used in dry mix processes.
Using both inner and outer forms, a cone is placed on the inner form to direct concrete down into the annular space between the forms. The concrete is then consolidated by stick vibrators or external vibrators, and the exposed top surface shaped and finished as required by hand, using edgers, trowels, and brushes.
# Figure II-4 depicts an automated vertical pipe casting operation.
Employees work from scaffolds that are rolled into place around the perim eter of the external pipe form.
As the concrete discharge chute rotates around the form, workers using shovels, boards, tampers, and/or vibrators ensure the proper placement and consolidation of the concrete.
Most concrete pipe is cast with a relatively dry, low-slump mix that is mechanically placed and consolidated in the form.
Two of the four mechanical methods use both inner and outer forms, which vibrate with either tampers or vibrators while the dry-mixed concrete is cast into the annular space between them.
In the tamping method, compaction is performed directly by vertically operated tampers.
In the dry cast method, consolidation is done by external vibration of the inner or outer form.
The other two mechanical methods use only the outer form and either spin the pipe horizontally while centrifugal forces distribute the concrete delivered by conveyor, or spin a mandrel-like packerhead that is drawn up inside the pipe as concrete is cast from above, compacting as it goes.
These four mechanical, dry-type mix methods of casting pipe are shown in Figure II--5. Metal pipe forms are placed by forklift or man ual or automated cranes onto openings in a circular casting floor.
The floor rotates (at slow speeds) to position the form in the operational packerhead area.
An employee on an elevated platform controls the packerhead spinning speeds, the up-and-down motion of the packerhead, and the flow of concrete into the form. When the casting is complete, the floor rotates an empty form into place and the forklift removes the cast pipe and mold to a curing area. per second (rps) while vibrating and depositing concrete, and at speeds up to 10-12 rps while "throwing" the concrete and compressing it against the rotating form. In the centrifugal process, excess water is removed, further lowering the water/cement ratio of the concrete.
Figure II-7 depicts one method of pipe spin-casting.
In this method, the pipe form is assembled by bolting or clamping the halves together. The form is placed by hoist onto a rotating pipe machine.
Horizontal pipe machines are usually constructed from groupings of auto/truck tires that serve to cradle and spin the form.
In this figure, the rotating force is applied by overhead tires that spin the pipe form at the required speeds. Concrete is added by a movable extruder, operated by a worker who is positioned to visually inspect the centrifugal consolidation during the placement process.
Internal finish work is usually performed by a hand-held, dowel-mounted trowel.
A worker runs it in and out of the pipe orifice while the form is spinning.
# FIGURE II-7. HORIZONTAL PIPE SPIN CASTING
Casting large miscellaneous products is similar to the tamping, dry cast, or wet cast methods used for pipe manufacture; however, the form may be square or rectangular as for burial vaults or septic tanks.
# Finishing
Wet finishing includes tasks such as screeding, floating, troweling, patching, rubbing, and cleaning surfaces not in contact with the form. Screeding is the back-and-forth motion of a strike off (a wood 2 by 4 or steel channel) resting on a screed guide to form the surface of the con crete to be finished. Workers may have to reach, bend over, and pull to perform this task.
Floating, the smoothing of the surface with a wood, aluminum, or magnesium float, is manual work requiring bending, kneeling, and reaching.
Troweling smooths and compacts the floated surface when the surface is hard enough to walk on without leaving indentations.
Additional treatment of the formed surface may take place after the form has been removed and the product has cured. This is particularly true for architectural panels, when the surface texture is important. Techniques such as grinding, bush hammering, sand blasting, water washing of retarded surfaces, or acid etching are used to produce a variety of desired architectural effects.
Bush hammering is the roughening of the hardened concrete surface with a vibrating hammer, the head of which is serrated with a series of pointed teeth. Sand blasting is the high-pressure spraying of sand onto the exterior concrete surface to clean or smooth it. Water washing (up to 300 psi) is the flushing of cement paste that purposely has been retarded in setting to expose the surface of the aggregate.
Acid etching serves a similar purpose, but does not expose as much of the aggregate.
This procedure involves the mixing, dilution, and application of muriatic acid, an industrial grade of hydrochloric acid.
In some instances, precast concrete products are cut to length or have portions removed by sawing them with a concrete saw.
This type of saw is similar to that of a carpenter's circular skill saw except that the blade size ranges from 1-3 feet (or more) in diameter.
During repetitive operations, or when using larger blades, saws may be semiautomated and suspended overhead. The power source for the concrete saws may be electricity or pressurized air, although some of the smaller, portable models may be powered by gasoline engines. Most saws are not provided with a lower (exposed) blade guard.
# Curing
Three fundamental factors in all methods of curing concrete are time, temperature, and moisture.
Within limits, an increase in temperature shortens the curing period by accelerating strength gain.
The time/temperature relationship is not the same for all mixtures, materials, and conditions and is determined empirically.
# I
The curing of many larger precast products is accelerated by radiant heat, steam, hot water, or hot oil. In some instances, the cast product is exposed to live, low-pressure steam within an insulated kiln or steam shed. Pipe or other products to be steam or heat cured will usually be transferred from the casting area to the heated shed by conveyor, forklift, hoist, or, in some instances, by rolling.
The products remain in the steam shed for 2-8 hours (frequently overnight) before being removed and the form stripped.
In some instances, the form is stripped before the product is steam cured.
Large pipe is frequently enclosed (in the place where it was cast) by canvas, plastic, or other material into which steam or warm, moist air is introduced.
Steam and hot water for accelerated curing procedures are usually generated at the plant by a low-pressure boiler and piped to designated locations prior to release into the curing shed.
Occasionally, a chemical curing compound is sprayed on the finished surface of the concrete.
# Form Stripping
Once a concrete product has cured sufficiently to be handled, it is necessary to remove it from the forms it was cast in or, conversely, to remove the forms from the product. The tasks and equipment used in form stripping operations vary considerably with the nature of the product. Reusable metal forms, such as those used during the manufacture of pipe, are usually handled by overhead hoist. The inner form is rigged to the crane and removed-a task made more difficult because the product fre quently adheres to the form surface.
In some instances, striking the form with a hard rubber mallet is sufficient to jar the concrete loose. In others, a hoist is used to shake the form and/or to pull the form free. Large pipe forms are frequently equipped with a means to collapse the internal form within the pipe bore.
Workers enter the pipe bore to release retaining clamps.
Rigging of the hoist to large form members requires that employees gain access to elevated areas. This may be done by ladder, rolling scaffolding, or climbing the form structure itself if it provides safe access. With low-slump, consolidated pipe, the mold is removed at the kiln prior to accelerated curing.
Flat products are removed from the mold by means of a vacuum lifter, or by lifting the product from the mold utilizing "lifting eyes" previous ly inserted in the product.
Girders, beams, or other large, vertical products may have side forms to be removed before the product is freed from the forms.
Bolts and other connectors are removed, and the side form panels pulled away or dropped to the ground. Some concrete products may require dismantling of the forms for re moval either because the form material will not be used again or because this is the only practical means of removing the completed product. Depending on the size and shape of the form, workers may perform the dismantling from the plant floor, from the elevated casting beds, from rolling ladder/scaffolds, or from the form itself. Workers will usually be performing their tasks on and among the equipment and material used during the form stripping process.
Prybars, crowbars, sledge hammers, and wrenches will be used to pull nails and remove the spreaders, stiffeners, and bulkhead-retaining tie rods.
Sledges and prybars will be used to force the separation of bulkheads from the product and/or other form structures.
This frequently involves workers pushing or pulling on the bar until the adherence forces release, sometimes suddenly.
# Material/Product Storage
Material storage in the precast concrete products industry follows a usage pattern typical to most manufacturing processes.
Raw materials necessary to produce the product will be shipped and temporarily stored in a yard. Usually raw materials will consist of the basic ingredients of the concrete (cement, sand, aggregate), the reinforcing materials (reinforcing steel, strand, wire mesh, hardware), and a variety of ancillary materials (blasting sand, equipment maintenance materials, etching acids, etc.) necessary for the production of a finished concrete product.
The bulk ingredients for the production of concrete may be hauled in by truck and dumped in covered bays or, in smaller plants, a convenient place on the prenises. Larger, more automated plants may yard consider able volumes of various sized aggregates and cement prior to transfer to mixers.
Cement may be bagged, palletized, and stored in weatherproof areas or it may be delivered by bulk tankers and stored in silos. These 94-pound bags of cement may be stacked higher than a worker's head, requiring access to the upper levels.
Reinforcing steel bars are usually received in banded lots of various lengths, ranging up to 40 feet or more.
Prior to cutting to required lengths, the rebars will usually be stored on the ground on cribbing material. Spooled or reeled material (e.g., wire mesh) is frequently stored in stacked rows.
The end spools are chocked to prevent rolling or shifting; second level spools are nestled in the spool interface.
Since forklifts or mobile cranes will be used to move these heavy rolls, adequate access space between rows of stored materials should be considered.
Product storage methods vary considerably with the size and shape of the product.
Small miscellaneous products are frequently produced in a variety of shapes at the same plant.
Yard areas are usually limited, necessitating multilayered stacking of the pieces.
Layers may be separated by cribbing and/or pallets to both protect the finished surface and to increase the load-bearing surface stability.
Larger and heavier shapes, such as vaults and manholes, are frequently stacked with cribbing layers between them to provide access for forklifts or rigging material.
Pipes and cylindrical products are stored in the manner described for rolls and reels. Pipes of the same size are stored in the same stack.
Again, care must be taken to allow adequate access for materials handling equipment and to prevent stack shifting. Large pipes are usually stored vertically.
Discarded products, broken pieces, metal scrap from forms, reinforcement, tie-wire, wood scrap, nails, chamfer strip, rejected hardware, concrete, forms, and the remainder of unused raw materials can be found in plants in this industry.
Many plants have a "bone yard" in which such discarded material is kept, pending burial or removal.
# Materials Handling
Materials handling operations are performed throughout all phases of the production of precast concrete products.
At the simplest (and fre quently overlooked) level, employees lift, carry, push, or pull everything from concrete debris to wood form material to smaller, finished products.
In fact, throughout the industry, manual handling is necessary to perform many of the tasks required in the production process, including: Individual, small miscellaneous products may be loaded or unloaded by hand. When several small items of the same variety are to be handled, they usually are strapped and palletized.
Larger products and concrete pipe require the use of lifting and unloading equipment.
Architectural and structural products usually are large, bulky, and heavy, requiring the use of cranes and special loading and handling techniques such as "A" frame holders and wood and metal chocking for security, for bolting to the trailer bed, and for single-product loads.
Since precast concrete products and their components are heavy by their nature, the industry makes use of a variety of mechanical devices to assist in handling and movement operations.
# a. Hoists and Cranes
For the most part, the types and varieties of hoists and cranes that are used in precasting operations do not differ significantly from those used in other industries.
However, because of the weight of the material and products being moved, crane and hoist usage may be more prevalent.
Smaller plants may use rubber-tired cranes with hydraulic booms to move material and products around the yard, onto trucks for trans port, and from the casting bed to the storage yard.
These mobile cranes are prevalent throughout the industry for movement of yarded material and products.
In most instances, the crane operator will work in tandem with other employees charged with the material rigging responsibilities.
Products may be manufactured with integral picking eyes that facilitate proper rigging and load balance.
In other instances, the rigging and hoisting will be performed on material necessitating new or single instance handling procedures.
Load weights and balance points must be identified by the workers as part of the rigging operation.
Larger, more automated plants are likely to have semipermanent work stations and fairly repetitive product design.
These plants are likely to use a number of overhead hoists. Overhead hoists may run on tracks and be located to service multiple operations in the manufacturing process. Larger overhead cranes are controlled by an operator located in the crane cab. Work stations may be serviced by smaller, 2-to 10-ton jib cranes.
Although a jib crane may be mounted on an independent vertical column, the horizontal "jib" is most frequently affixed to a vertical column integral to the plant's structure.
Employees at the work station operate the jib crane by using a wire-attached pendant control, which allows the worker to control the up/down and back/forth movements, or other functions of the crane, from the floor of the plant.
In these instances, the hoist operator is usually the same worker that performs the rigging.
He is also likely to accompany, with hands on, the load being transported to its destination.
Straddle carriers are large, four-wheeled, wide-spaced, high legged movers that straddle large products (such as girders, planks, or other structural elements) pick them out of forms and move
them. This open-framed machine, basically square in configuration, hoists and carries the load within a large open bay between the four wheels on which it travels. The operator's cab is located on the extreme left-hand side between the front and rear wheels. Loads suspended in the bay often obscure the driver's view of the right side wheels.
The machine ordinarily moves at about 2 miles per hour (mph) and has a maximum speed of about 10 mph.
# b. Forklifts
Many of the palletized raw materials and finished products used in precast plants are moved by forklifts.
Fork extenders may be used to increase the bearing surface of the forklift.
In some instances, a jib may be added to the forklift to convert it to a small, movable crane.
Pipe and other circular products are moved by forklifts with specially designed long forks or fitted forks with curved surfaces to cradle the product. Some forklifts are equipped with clamping forks used for attaching to and moving forms or other compatible shapes.
The power source on forklifts is most frequently propane or diesel fuel.
# CHAPTER III IDENTIFICATION OF THE SAFETY HAZARDS AND DEFINITION OF THE PROBLEMS
This chapter is divided into two major areas of emphasis: the development and presentation of data pertaining to injury incidence rates for the precast concrete products industry (SIC 3272), and the identification of those tasks performed that are hazardous to the worker.
Additionally, an estimation of the cost of injuries sustained by workers in the precast concrete products industry is presented.
# A. Injury and Illness Incidence Rates
The yearly compilations of occupational injury and illness data, prepared by the BLS, show that between 1976 and 1980, the precast concrete products industry had an average incidence rate of about 23 cases per 100 employees (Table III-l) [9][10][11][12].
In comparison, the incidence rate for all private sector industries averaged about 9.2 during the same interval. Workers in the precast concrete products industry have been consistently injured at a rate nearly 2.5 times the national average. Also, between 1976 and 1980 the average incidence rate for all durable goods manufacturing industries (which include SIC 3272) was about 14, which is substantially less than the rate for manufacturers of precast concrete products (Tables III-l and III-2). The incidence rates for precast concrete products are among the highest rates within the manufacturing sector (top 3%). A representative selection of the manufacturing industries is shown in Table III
-3.
Table III-3 demonstrates that the occupational incidence rate per 100 employees in the precast concrete products industry was higher than those for concrete block and brick manufacturers and ready-mixed concrete, which exhibited incidence rates of 15.8 and 13.7, respectively.
The incidence rate for concrete products was also substantially higher than for blast furnaces and steel mills (9.5), which is a heavy industry involving additional injury potentials attendant to the handling of molten metal.
The severity of injuries sustained by employees of the precast concrete products industry was also shown to be high.
The lost workday cases and lost workdays incidence rates, represent a general measurement of the seriousness of occupational injuries and illnesses.
The lost workday cases incidence rate for the precast concrete products industry (SIC 3272) in 1980 was reported by the BLS as 10.4 (Table III
-l).
This figure ranged from a reported high of 12.1 in 1979 to a low of 9.1 in 1976, with an average of about 10.7 for the years between 1976 and 1980 (Table III
-l).
The lost workday cases incidence rate for all private sector industries in 1980 was reported by the BLS as 4.0 [12] and for the durable goods manufacturing industries as 5.6 (Table III
-2).
Furthermore, for every 100 employees in the precast concrete products industry in 1980, a total of about 158 days were lost due to disabling injuries and illnesses (Table III
-l).
The Although the estimates of direct costs of worker injuries are not precise, they do reflect the magnitude of the problem.
Estimates derived from National Safety Council [22] data indicate that full costs of work-related accidents are more than 3.4 times the direct wage loss and medical expense costs.
Since the indemnity payments are normally less than wage loss, the real accident costs for the precast concrete products industry are estimated to exceed $105 million per year (3.4 x $30.9 million).
In addition to medical and indemnity expenses, estimates of the real cost of accidents include:
# C. Identification of the Hazards
The preceding section of this chapter defined the magnitude of the safety problem in the precast concrete products industry.
The next step in a systematic approach to effectively lowering worker accident/injury exposure is the identification of how workers are injured while performing the tasks required to produce precast concrete products.
# The Supplementary Data System (SDS)
Currently, occupational accident and injury information from participat ing states, which is taken from employers' first report of injury forms, ■ ' ■Production workers comprise about 77% of the total work force for this industry [3]. Seventy-seven percent of the reported 1977 employment figure of 67,300 (Table III-l) is 51,821 production workers.
Compensation losses of $30,855,454 divided by 51,821 production workers yields about $595 per production worker. is compiled and reported by the BLS Supplementary Data System (SDS) [23,24]. The SDS is intended to alert users to patterns and relationships of injury causal factors.
The information is entered into each of four major groupings: The frequency and percentage distribution of the injuries reported to SDS by the precast concrete products industry for the years 1976 -1979 are presented in Table III-4 for each of the groupings mentioned above. The percentages do not indicate that one category represents a greater hazard than another, since data clarifying worker exposure are not available.
o
# Accident/Injury Analysis
The SDS data are limited when used in the analysis of a specific industry because the "source of injury" category contains subcategories which do not apply to the industry under study, and does not contain subcategories which are related to industry-specific tools and equipment.
Further, the "source of injury" reported is the object most responsible for causing the injury.
Thus, if a worker falls from a ladder and fractures his leg on the plant floor, the "source of injury" is the floor, which probably contributed little to the actual cause of the accident.
Despite the constraints, the SDS data reported by the precast concrete industry for 1976 -1979, which included 15,208 injuries, were analyzed to identify specific industry hazards.
The analysis included 37 categories that identified injury sources within precasting operations.
The results of the cross-analysis of the SDS data are summarized in Table III
-5.
The total number of accidents/injuries appears in the "Source of Injury" column.
The numbers associated with "Type of Acci dent," "Nature of Injury" and "Body Part" do not agree with the "Source of Injury" totals since the figures given are merely the most frequent subcategories.
# Analysis of Accident Case Histories
For a more complete understanding of accident/injury causal factors, full text copies of employers' first report of injury forms filed by SIC 3272 industries were requested from all 50 States.
In most instances, the state agencies were not able to provide information.
However, 10 States 1 did provide copies of 2,250 first report of injury forms from ■California, Hawaii, Iowa, Kentucky, Michigan, Montana, Maryland, Washington, Wyoming, and Vermont. Of the 2,250 accident/injury reports, 1,319 (about 59%) were included in the analysis.
Of these 1,319 injuries, 34 resulted in a fatality.
Those reports not included in the analysis primarily contained injury information, and were found to contain insufficient data to determine accident causal factors.
A preliminary analysis of these accident case histories was performed to determine whether the accident data base was indicative of accidents occurring to workers in precasting operations nationwide.
Each report was categorized by type of accident ("struck by," "caught between," "fall").
Numerical and percentage values of the "type of accident" categories were compared to the national SDS figures (Table III-4). The comparison (Table III-6) shows markedly similar ratios; e.g., the percentage of "struck by" and/or "caught between" accident types are reasonably consistent in both data bases.
Because of the similarities between data from the sources considered, it was concluded that the accident/injury case histories used in this report are representative of accidents that occur to workers in the precast concrete products industry.
The first step in the analysis was the identification of the specific task, tool, type of material, piece of equipment, or plant area most closely associated with the accident in each case.
This procedure made possible more precise and industry-specific classification than the SDS "Source of Injury" category could provide. Then, a causal factor was identified in each case (e.g. improper tool use, lack of personal protective equipment, lack of adequate guarding, improper materials handling procedures).
The task/tool/equipment factors and accident causal factors were then cross-indexed to allow the identification of problem areas.
The following narrative descriptions of how workers are injured in the precast concrete products industry are based on analysis of SDS data (Table III -5) and the accident case histories. The percentage that follows each category or factor is the percentage of the total number of accidents (1,319) from the case history analysis.
Section a covers general accident factors; i.e., tasks, tools and items of equipment that are not specific to the precast industry.
Section b presents factors that are specific to precasting processes.
Section c describes accident causal factor patterns, groups of factors which may encompass several task/tool/equipment categories. Essentially, the organization of sections a, b, and £ is followed in the presentation of the recommendations in Chapter IV.
# a. General Accident Factors
The following narrative paragraphs describe the ways workers are injured due to task/tool/equipment factors which are not necessarily specific to the precast concrete products industry. Although these general factors are arranged in order from highest to lowest percentage of occurrence, this grouping does not suggest that one factor represents a more significant hazard than another, since no data clarifying worker exposure are available.
(1) Materials Handling (28.0%) (a) Manual (19.9%)
(i) Lifting (9.6%)
The act of lifting items resulted in nearly 10% of the injuries in the industry. Approximately 81% of these incidents involved overexertion to the back while manually handling materials.
Loss of grip accounted for 9% of the lifting accidents. These usually resulted in injuries either to the lower extremities when the load was dropped or to the fingers when the load was set down with inadequate clearance.
(ii) Mechanical Materials Transport (7.1%) This category presents a variety of tasks associated with materials handling as well as a variety of other accident causal factors.
Included in this activity are interface of manual and mechanical load handling procedures performed on flatbed trucks and the manual transfer of materials to forklifts. Manual materials handling and gripping of materials accounted for 27% of the injuries in approximately the same causal/injury breakdown as cited in the discussion of the lifting category. Improper stacking and binding of materials was reported to be the cause of about 27% of these accidents, usually from the material falling onto the worker.
An additional 12% of the accidents occurred to workers attempting to climb onto the transport vehicle or the material itself when access was not provided.
(iii) Carrying and Holding (1.8%) This category of activity includes the manual tasks, by one or more workers, of carrying or handling materials.
Many of the injuries were sprains and strains that usually occurred from overexertion during the procedure.
About Hand operation of the hoists necessitated close proximity to the hoisted loads and contributed to employee exposure to hoist or rig failure.
(iv) Conveyors (0.6%) Although only 0.6% of the accidents involved con veyors, they accounted for nearly 9% of the fatal injuries.
These accidents occurred when the conveyor jammed and the operator/worker attempted to free the jam without deenergizing and locking out the system.
Workers were caught by or in exposed moving portions of the conveyors.
Lack of guarding of exposed moving parts and/ or nonlimiting access to the area were cited as contributing factors to the accidents.
Similarly, the nonfatal incidents usually involved the upper extremities being caught in or between the conveyor mechanisms as shown in Table III In the latter accidents, the injured workers were in the path of travel of the loaders and were either caught between it and another object or they were run over by the moving equipment.
Inaudible or nonfunctioning backup alarms as well as operator inability to see coworkers were cited as contributing factors.
(2) Handtools (11.5%) (a) Handtools, Powered (5.8%) Nearly all of the injuries attributable to the use of powered handtools resulted from deficiencies in three areas: guarding, tool usage, and lack of eye protection.
The injury analysis revealed that most eye injuries occur during use of grinders. The remaining grinder-related accidents were the result of inadequate or non-existent guards that failed to prevent finger contact or protect against stone disintegration.
In some instances, while using the grinder, part of an employee's body, usually the thigh, came into contact with the abrasive stone.
In the SDS accident/injury analysis (Table III-5), eye injuries occurring during grinding activities were not listed with grinders; rather, they were tabulated in the "Particles" category.
Although lack of eye protection contributed to 20% of the powersaw injuries, the single, consistent accident causal factor was inadequate or nonexistent saw blade guards (58%).
Included in this category were instances when anti-kickback devices were not used during ripping operations. The majority of injuries resulting from lack of saw guards were lacerations and amputations of fingers.
Two eye injury accidents also occurred while using concrete saws.
The accident analysis shows that most accidents during drilling tasks occurred when large-diameter (1-inch or larger) holes were drilled through forms.
The drill bit would bind and the drill motor would continue to turn, catching the workers' hands between the motor and adjacent items, usually the form. This may be interpreted as improper tool use or as improper worker position relative to the task. Lack of eye protection accounted for one-third of the reported injuries that occurred while using airhammers. In some instances, airhammers were used in awkward positions, resulting in strains and sprains of the back and/or arms.
In three instances, the airhammer was positioned for use too close to the edge of either a form or product, and the worker's hands or fingers were caught. Table III-5 indicates that powered hammers as a source of injury resulted in injuries to the back because of worker overexertion and to fingers that were struck by the hammer. The injury reports indicated that many injuries were associated with over loading the shovel, twisting the body, and handling the load from too great a distance (see Table III-5, "Shovel" and "Concrete aggregate"). The activity of "prying" is frequently performed by workers dismantling forms and separating the product from the form.
Referring back to Table III-5, 47% of the accidents involving crowbars, a tool routinely used for prying, were classified by the SDS as "struck by" accident types resulting in contusions and sprains and strains.
The most frequent areas of the body injured were the back and finger.
The analysis of the accident cases showed that 65% of the prying accidents were reported to be caused by improper worker position relative to the task. When the prying implement slipped, the tool usually either struck the worker or the worker slipped and fell.
Most of the remaining accidents involving prying activities resulted from improper tool use. Shovels were commonly misused by workers attempting to pry forms loose from cured concrete.
The most common type of accident that occurs during the use of handtools is the "struck by" variety (Table III-5), most frequently caused by improper position of the worker relative to the task.
The analysis indicated that glancing blows are commonly cited as the cause of the accident.
Fingers and hands were struck by hammers and sledge hammers when part of a worker's body was in the path of the deflected hammer movement.
Use of improper tools contributed to 25% of the hammering accidents. Typical cases involved shovels, wrenches, and boards used to hammer forms, nails, or other materials.
The analysis indicated that fingers were the most frequent part of the body injured while using a wrench; usually, the wrench slipped off a nut or bolt.
The injury reports indicated that many accidents associated with tool slippage were caused by improper tool usage (size and/or adjustment).
The accident probability was compounded by improper worker position relative to the task.
The information in Table III-5 indicates that workers suffered sprains and strains from excessive physical effort while using wrenches. This could possibly be a result of using wrenches of improper size for the job.
(3) Worker Proximity to Operations (7.4%) (a) Walking Through Work Areas (6.3%)
In a number of instances a specific task or activity description was not included in the accident report. The worker was "walking" in an unspecified section of the plant. Almost 29% of these injuries were nail punctures of the foot. More than 45% were falls to the working/walking surface caused by slipping on wet, slippery surfaces or tripping on material, usually pieces of concrete debris, rebar, welding stubs, or leads.
(b) Working Near Operations (1.1%) This category includes workers injured by tasks or operations that were independent from their assigned tasks.
The most prevalent accident/injury in this grouping was flash burns from nearby welding operations. In fact, 45% of the reported flash burns occurred to workers who were not involved in the actual welding process. Two workers were also injured by particles from nearby metal grinding operations.
(4) Welding, Cutting, Burning (4.6%)
The data indicated most of the injuries (54%) that occurred in welding, cutting, and burning activities were typified by foreign bodies in the eye that were caused by slag or weld "pop."
In these instances, the workers were not wearing eye protection.
An additional 20% of the injuries were flash burns to the workers performing the welding operations.
In these cases, the worker was usually inadequately protected because cutting goggles were being used instead of approved welding hoods during short welding operations.
The SDS data (Table III -5) indicate that welders flash burns account for 1% of the industry's injuries.
(5) Chemical Handling (4.6%) More than 44% of the incidents in this category involved chemical dermatitis caused by direct skin contact with moist concrete.
Concrete burns, most commonly to hands and forearms, were usually sustained during casting or cleanup operations.
In a few instances, concrete dermatitis developed during the dry mixing of the concrete.
Lack of respiratory protection accounted for four of the incidents involving cement dust.
Lack of personal protective equipment, mostly eye protection, was a contributing factor in 30% of the chemical handling injuries.
Workers received eye injuries during mixing, casting, and cleanup operations.
Lack of eye protection was also a causal factor in four eye injuries that occurred during spray application of form release agents.
Sprayers were overpressurized by misapplication of unregulated systems, resulting in explosions of the canisters in two instances. Analysis of the accident data indicates that 46% of the materials storage accidents were the direct result of improper stacking and/or binding procedures.
Product storage (multi level) stacks were not stable enough to support their height and weight. Most of the injuries occurred while workers were in the process of adding additional material to the stack. The second most frequent cause of injury in materials storage activities was related to manual materials handling and improper gripping of the load. Fingers and toes were most at risk during these activities.
(7) Ladders and Scaffolds (3.9%) One-fourth (25%) of the ladder/scaffold accidents were directly attributable to working from makeshift platforms (improper tools).
The accidents that occurred on makeshift scaffolds were usually falls to the level below. Two scaffold accidents (one fatal) involved scaffolds with inadequate or nonexistent guardrails.
Slippery (wet, icy) conditions on the ladders/scaffolds were cited in more than 22% of the accidents, mostly resulting in falls to the working surface of the scaffold.
Inadequate securing of ladders against slipping (chocking, blocking, or tying) caused six of the accidents that were falls to levels below.
In two instances, ladders were placed in the paths of moving vehicles (forklift, crane), resulting in collisions and serious injuries. The majority of injuries that occurred to workers cleaning forms, products, or mixers probably would have been prevented by eye protection.
The second largest accident causal factor in chipping/cleaning tasks was inadequate or nonexistent access to the area; makeshift worker platforms were common.
# b. Process-specific Accident Factors
The following narrative paragraphs describe the ways workers are injured due to task/tool/equipment factors specific to the precasting processes.
In the absence of data clarifying worker exposure, the percentage ranking is not intended to imply that any one factor represents a more significant hazard than another.
(1) Form Work (7.2%) (a) Form Assembly/Disassembly (4.9%) Form assembly and dismantling are frequently manual procedures that involve physical manipulation of form components.
Consequently, the accident/causal factors associated with form assembly primarily fall into the categories that typify physical procedures; e.g., the worker's position relative to the task, and gripping and handling form components.
Many of the injuries that occurred in form assembly tasks were sprains and strains of the back, and injuries to the fingers.
In two instances, workers were struck by form sections being turned by overhead hoists.
Inadequate chocking and bracing of form sections during assembly or stripping contributed to many of the more serious injuries.
In the instances when the form component adhered to the cured concrete, workers were struck by or caught beneath a portion of the form that was suddenly released and fell. Additional information concerning injuries resulting from form work can be found in Table III Binding and unexpected release of the inner cores or outer forms of pipe molds typified most of the accidents in this group.
"Caught between" accidents resulting in injuries to the fingers were the most common.
(r.) Form Stripping (1.2%)
The most common cause of accidents in form stripping activities involved improper tool usage. Most frequently, these accidents resulted from using shovels as levers to pry form walls loose from the cured concrete.
The most serious accidents, one of which was fatal, involved inadequate or nonexistent cribbing or blocking of form walls.
The fatality resulted when a worker crawled under a portion of form wall no longer integral to the remainder of the form or the product to determine where the form was still "hung up." The form wall fell while the worker was under it. Additional injury information is contained in Table III
-5, "Reinforcement". (b) Stressing (1.5%)
The accidents that most frequently occurred during stressing operations were similar to accidents which occurred during other forming and casting operations. Lack of eye protection accounted for more than 32% of the incidents-most of these caused by metal particles (scale) flicking off during the handling of the strand. The more serious accidents occurred during the actual stressing procedure and involved inadequate or nonexistent means for controlling employee access to the stressing area.
The high tension stretching of the steel strand poses a somewhat unique hazard to the industry.
Since stressing is used in only about 10% of the precasting plants, the relatively small number of accident cases (19) may not reflect the frequency of accidents occurring in the actual stressing operation.
The static forces contained in stressed strand are potentially hazardous. When these forces are accidentally released, workers within range of strand whiplash are exposed to potentially serious injury.
(c) Metalworking Machinery (1.3%) Metalworking machinery (cage rollers, rebar benders and cutters, press brakes) are used in the precast concrete products industry to manufacture the shapes necessary for reinforcing concrete. More than 1% of the accidents that occurred to precast concrete workers happened during metalworking tasks related to the production of the reinforcing steel shapes.
Inadequate and nonexistent guarding was the major accident causal factor associated with metalworking tools and operations.
Cage rollers (0.6%) accounted for nearly one-half of these accidents. Failure to guard in-rolling nip points on the cage rollers resulted in two of the more serious injuries. Other accidents occurred while handling the metal items during bending, cutting, or rolling operations. Frequently, these were either lacerations of the hands caused by sharp edges or crushing injuries due to hands-on manipulation of the metal while the machine was in operation.
Additional information concerning injuries from machinery can be found in Table III-5.
(3) Oiling Analysis of the accident reports failed to identify accidents which were specifically ascribed to the oiling process. Factors which may influence the occurrence of accidents during oiling procedures include contact with form release agents, access to forms or product, and working/walking surfaces. These factors are discussed in the paragraphs on Chemical Handling in section a, and in the paragraphs on Personal Protective Equipment, Access, and Working/Walking Surfaces in section £. Failure to lockout or tagout an energy source before entering or reaching into concrete mixing equipment accounted for 25% of the accidents involving concrete mixing and 3 of the 6 lockout/tagout related fatalities. Twelve percent of these accidents occurred when workers were attempting to access mixers.
Fifteen percent of these accidents involved workers who were caught in or struck by chutes or hatches when they were not secured in place.
(b) Concrete Transport (0.8%) Ready-mix concrete delivery trucks accounted for most of the accidents in this category.
Usually the worker was struck by or caught between the delivery chute and the form.
The more serious injuries happened during cleaning/maintenance operations on the trucks and were caused by lack of adequate energy control procedures. The accidents that occurred during casting operations were most commonly caused by lack of access to the casting beds or between forms. Workers must continually get up onto and down from forms, or move back and forth between forms.
In these instances, access was either not provided or was located in an area away from the work activity.
Slipping or tripping on working surfaces caused almost 24% of the casting accidents. Most of the accidents were falls from or onto the casting bed, or involuntary recovery from slips or falls resulting in sprains, fractures, and contusions. Accidents that were more task or tool specific (concrete delivery, pipe machine, scaffolds), yet still operationally part of the overall casting procedure, were included in the more specific category.
(b) Concrete Buckets (0.5%)
The injuries occurring to workers using concrete buckets were caused by the opening and closing mechanisms on the bucket's pour hatch. The latch bar frequently caught fingers and hands between the handle and the bucket.
(c) Pipe Manufacturing Equipment (0.4%)
The serious injuries to workers during mechanical pipe operations (packerhead and horizontal pipe spinning) were the result of inadequate machine guarding or isolation of the operation and the moving mechanical parts. A packerhead table with a gap between the table and the adjacent working surface caused a serious leg injury. Inadvertent entanglement with a horizontal pipe spinner injured another worker. Workers' eyes are also at risk in these operations.
The rotating speeds used in these casting operations tend to "throw" cement and aggregate out into the adjacent work area. This classification of equipment is comprised of various types of trucks (flatbeds, pickups) that are used to transport products on or off of the plant premises. More than 82% of these accidents occurred while workers were attempting to get onto or off of the vehicle bed (access).
The beds of these vehicles are typically 3 The most serious accident occurred when a crane was used to lift a product from a form to which the product remained adherent. When the crane attempted to hoist the product, the weight of the adhered form, an unknown force, resulted in crane overload and failure.
One worker was killed.
Inadequate cribbing or blocking of the product during product removal tasks also resulted in serious injuries to workers (one was fatal). Workers under the product attempting to position rigging material or guide the load were injured when the product shifted, catching them under the load.
(c) Rolling Stock (Pipe) (0.8%) Handling and storage of rolling stock (concrete pipe) resulted in 0.8% of the injuries in the industry.
More than 55% of these accidents were the result of improper or nonexistent binding or chocking of the pipe. Although the back, hands and fingers were the most frequent parts of the body injured, the lower extremities were more seriously injured.
Most of the remaining accident case histories cited rigging failure during stacking as the cause of the accident.
# c. Accident Causal Factor Patterns
The method used to analyze the accident case histories allowed the identification of significant accident patterns by the grouping of related accident causal factors.
For example, injuries attributed to wet, icy, or slippery surfaces; tripping; or puncture; are discussed below under the general heading "Working/Walking Surfaces."
These accident patterns indicate hazardous activities or conditions that encompass various tasks, industrial processes, tools, and items of equipment utilized in the precast concrete products industry. The arrangement of these patterns by percentage, in order from highest to lowest, is not intended to suggest that one accident pattern represents greater hazard to workers than another pattern, since data clarifying worker exposure are not available.
(1) Manual Materials Handling (17.6%) There are two major accident types that occur as the result of improper manual materials handling procedures: overexertion accidents that cause sprains and strains of the back and shoulders, and materials movement accidents (dropped load, load placed on fingers) that usually result in lacerations, contusions, and fractures of fingers or toes.
There is very little task specificity in manual materials handling accidents. Workers are required to lift and handle materials and tools throughout all precasting operations.
They appear to be injured in proportion to the expected amount of manual materials handling likely to be used in any given task.
(2) Working/Walking Surfaces (12.4%)
The production processes of forming, pouring, stripping, and cleaning forms produce water, excess concrete, forming material, and a variety of tools and equipment that clutter walking and working surfaces.
These hazards result in worker falls to the working surface and/or involuntary recovery injuries (sprains and strains that happen when a worker attempts to recover his balance).
The SDS data (Table III-5) indicate that bodily motion (not including lifting, pushing or pulling) was the source of injury in 5% of the industry's accidents. Additionally, working surfaces were the source of injury in 12% of the accidents when workers fell while performing their duties.
Workers in form stripping operations (most likely responsible for exposed nails) are not the individuals usually injured by nails.
The pattern of accidents related to nail puncture indicates that frequently (56%) it is a person walking through the area who steps on an exposed nail.
Table III-5 indicates that nails were involved in 1% of all injuries, resulting most frequently in punctures to the foot.
(3) Personal Protective Equipment (10.7%)
The lack of personal protective equipment is not, in itself, a cause of accidents.
However, during activities associated with some tasks or tools, workers are exposed to hazards likely to result in injuries. For example, cutting torch tasks cause metal particles to fly through the air, increasing the probability of eye injuries; or, mixing and placement of concrete may result in material splashes that cause eye injuries; or, loads may fall or be dropped onto workers feet resulting in toe injuries.
In precasting operations, 10.7% of the injuries were likely to have been prevented by the employee wearing proper personal protective equipment.
In most instances resulting in injury, the type of protective device found lacking was eye protective equipment.
Concrete splashes, slag from cutting operations, metal particles from grinding, sawdust, particles falling from or blowing off forms, curing compounds, and general airborne dirt all resulted in eye injuries.
Although safety glasses (eye protection) may not have prevented all of the reported injuries, their use certainly would have lowered the incidence of occupational eye injury.
Two fatal accidents in this category involved employees working from elevated areas and were directly attributable to the lack of fall protective devices.
In both cases, the workers were performing tasks, on or from forms, without the protection of a safety belt and lanyard.
The use of an adequate scaffold, including guardrails, would also have provided worker protection.
Crushing injuries to toes and feet resulting from the impact of heavy products and materials are not likely to be entirely eliminated by the wearing of safety-toed boots. However, such protective footwear would likely have prevented some of the injuries and reduced the severity of others in many of the cited instances.
(4) Access (9.8%) Inadequate or nonexistent access to work areas was the primary causal factor in 9.8% of the accidents. As an accident causal factor, lack of adequate access resulted in workers being injured while performing most tasks and activities directly involved in the manufacture of precast concrete products. Workers attempting to move or work on casting beds and/or forms accounted for 38% of the "access" accidents.
Most of these accidents were falls to lower levels; that is, off of the form or casting bed and onto the adjacent working surface (see Table III-5, "Working/walking surfaces"). Injuries ranged from simple bruises and lacerations to fractures. Many of the remaining "access" accidents were related to equipment; more than half of the vehicle access accidents involved workers climbing onto or down from truck beds. Again, the injuries usually were caused by falls to below.
(5) Mechanical Materials Handling (7.6%)
Mechanical materials handling accidents comprised 38% (13) of the fatalities analyzed; half of these occurred to coworkers that were struck by a moving vehicle (crane, forklift). Twenty-three percent of the fatalities in mechanical materials handling were caused by rigging overloads. There were two incidents of crane "two-blocking" that resulted in fatal injury to workers.
The use of hoists, cranes, and forklifts is common throughout the industry.
In many instances, the product is simply too heavy to move by other means.
In some instances, the material is also too heavy to be moved by the selected mechanical method.
Employees frequently work in close proximity to moving equipment.
This interface, man and moving equipment, when compounded by the distractions of ongoing work and background noise, contributes to fatal accidents in precasting operations.
(6) Guarding (2.7%) Inadequate or nonexistent guards were cited in 2.7% of the accidents.
All but 2 of these 36 accidents occurred in con junction with exposed moving parts of machinery and/or tools. Unguarded saws injured workers most frequently (31%), and un guarded grinders (abrasive stone) accounted for 17% of the injuries related to guarding. Conveyors may jam during operation.
Workers were injured while attempting to remove the jammed objects without first controlling the systems' energy sources.
# D. New Employee Injury Rates
Analysis of the 1,319 accident case histories shows that 513 (54%) of the 950 reports that included length of employment information involved workers employed less than 1 year.
In fact, 408 (43%) of the injuries were actually sustained by workers employed for less than 6 months.
Several factors may influence the apparent prevalence of injuries to new employees. Although some plants experience a relatively high turnover rate, many smaller plants seem to have a stable work force.
These plants will layoff and rehire the same workers in accordance with seasonal or economic demands. Therefore, an injured employee reported as "new" on an injury report form, may actually be an experienced worker.
Further, new employees may perform the more hazardous tasks.
Or, new employees may typically comprise about 50% of the work force.
No information which identifies either the distribution of tasks among workers of varying experience or the number of relatively new employees that make up the worker population at any given time is available.
However, there is evidence to suggest that new employees or employees performing new tasks suffer significantly higher rates of injury than the employed population in general [25,26].
# E. Summary of the Problem
Accident and injury statistics for 1980 indicate that the injury and illness incidence rate for the precast concrete products industry (SIC 3272) was 2.5 times the rate for all private sector industries. Not only does the precast concrete products industry have the problem of high injury incidence rates relative to all private sector industries, but within the manufacturing sector where there are similar tasks and operations, only 8, or 3.4%, of the 235 four-digit SIC code industries had higher incidence rates than this industry in 1980.
Analysis of 1,319 accident case histories has demonstrated how employees in the precast concrete products industry are injured while performing those tasks necessary to manufacture concrete products.
Furthermore, patterns of accident causal factors common throughout the industry have been identified.
It is concluded that the primary safety needs of the precast concrete products industry are:
1) implementation of the recommendations for safe work practices presented in Chapter IV; and 2) implementation of a safety management program, such as the one presented in Chapter V.
# CHAPTER IV RECOMMENDATIONS FOR SAFE WORK PRACTICES FOR THE PRECAST CONCRETE PRODUCTS INDUSTRY
The safe work practices recommended in this chapter are presented as ways to reduce and control injuries resulting from precasting operations. The hazardous tasks identified, as well as the patterns of accident causal factors developed in Chapter III, indicate potential problem areas that have been given insufficient emphasis by the precasting industry.
The solutions offered in the following safety recommendations may not be entirely suitable for a specific plant.
In some instances, management may even view the recommendations as counterproductive to their operations. In these instances, the responsible persons (plant managers, safety managers, and/or plant owners) should interpret and modify the recommendations to make them applicable to their specific needs.
It is essential that, in any modification of the recommended safe work practices, a similar quality of worker protection be provided.
Considerable emphasis has been placed on the safety recommendations directed at hoist and crane activities.
In the cases analyzed, 41% of the fatal accidents occurred due to misuse of hoists and cranes.
Expertise specific to hoisting equipment may be less developed than supervisory expertise particular to production; therefore, hoist and crane safety has been presented in detail.
The goal of this study has been to identify hazards in precasting opera tions and to recommend applicable and manageable means to alleviate them. The safety recommendations presented are not meant to be all-inclusive or to supersede the OSHA General Industry Standards, which offer adequate regulatory guidelines for many of the tasks, tools, and equipment used in the precast concrete products industry.
Emphasis has been placed on recommendations for safe work practices which address tasks, activities, and tools commonly associated with injuries. This preliminary section presents safe work practices for the tasks, acti vities, and tools that are commonly used throughout precasting operations. Included in this section are the recommendations for manual and mechanical materials handling, handtools, worker proximity to operations, welding and cutting, chemical handling, ladders and scaffolding, and chipping/cleaning.
# Manual Materials Handling
A wide range of manual materials handling activities are inherent to the precast concrete products industry.
Workers may be required to lift, carry, push and pull raw materials and/or finished products during loading/unloading, processing, storage and cleanup operations.
The handling and manipulation of loads can markedly increase the stresses imposed on workers' musculoskeletal systems and increase the likelihood of injuries to certain body areas (e.g. back, extremities) [27].
The application of proper handling techniques can minimize these stresses and help reduce the incidence of musculoskeletal injuries.
A number of factors can directly influence the likelihood of an individual suffering a musculoskeletal injury during the performance of manual materials handling activities.
These are discussed in NIOSH's "Work Practices Guide for Manual Lifting" [28] The proper use of safe handling techniques by workers performing manual materials handling activities is one of the most important factors in avoiding injury, since the techniques reduce body stresses and their application are at the discretion of the worker.
NIOSH's publication "How to Lift Safely" [29] illustrates several of the important points in materials handling.
# Key points include:
o Workers should assess the size, shape and weight of objects to be lifted or carried. Objects deemed to be beyond the physical capacity of one worker should be handled by two or more workers. o Workers should spread their feet apart to provide a wide base of support during manual materials handling, o When lifting objects, workers should bend their knees to a degree which is comfortable to them and then get a good firm grip on the item to be lifted. Lifting should be accom plished through the use of leg muscles in straightening the knees rather than using the back muscles, o Workers should handle objects as close to the body's center of gravity as possible, o Workers should avoid twisting the trunk when handling ob jects.
# b. Assistive Devices
A number of assistive devices can reduce or eliminate the need for stressful manual materials handling. For example, rebar can be stored on surfaces which correspond to the height of the bending and cutting machines so that the worker does not need to lift the rebar from the floor level to the cutting or bending surface.
It is even better to have the rebar storage surface gently slope toward the cutting and bending machine.
This reduces the stress required to pull the rebar to the cutting or bending position. [30].
These methods also represent a wide range of costs to employers under various financial restraints. Training programs are means of conveying information to workers. A goal of training programs is that workers will alter their work habits by substituting safer work practices for various unsafe techniques. This form of behavioral modification usually requires feedback to the workers.
Supervisors and employers must take the time to positively reinforce safe practices and constructively criticize unsafe practices. Effective training is approached as an ongoing interaction among all plant employees and not a one time exposure to the training material [31]. o Approved boom stops installed to preclude travel beyond the angle of 85 degrees above the hori zontal plane [32] o Boom angle indicators for booms capable of moving in the vertical plane [33] o Automatic devices to stop boom drum motion when the maximum permissible boom angle is reached [33] o Boom length indicators for telescopic booms [33] o Automatic "anti-two-blocking" devices for hydraulic extending booms [33] o An effective audible warning signal (horn) mounted outside the cab with controls easily within reach of the operator [33] o A spirit level at the outrigger controls for level ing [33] o Adequate lighting for night operation, including backup lights for mobile units [33] o Wheel chocks on mobile units to block movement on slopes when the equipment is left unattended or is undergoing maintenance [33] o A fire extinguisher and a first-aid kit [32] o Rearview mirrors on both sides of mobile equip ment [33] o Self-closing filler caps and flame arresters on fuel tanks [33] o Slip-resistant material on crane surfaces subject to foot traffic [33].
# Mechanical Materials
(c) Equipment should be safety inspected frequently (daily to weekly). Inspectors should [33]:
o Check brakes, clutches, and safety devices for prop er adjustment and operation (if possible, check load brakes by lifting a capacity or near capacity load a few inches off the ground) o Daily, visually inspect each component of the equip ment used in lifting, swinging, or lowering the load and components used to lift and lower the boom, for any defects that might result in unsafe operation o Check for freedom of rotation of all swivels o Check all functional, operating mechanisms such as sheaves, drums, brakes, locking mechanisms, hooks, boom, jib, hook roller brackets, outrigger compo nents, limit switches, safety devices, hydraulic cylinders, instruments, and lights o On cranes, daily, visually inspect the boom and jib for straightness and for any evidence of physical damage such as cracking, bending, or other deforma tion of the steel elements or welds (this precau tion is especially important on lattice and tubular booms, where every component should be straight and free from dents) o Inspect wire ropes (including standing ropes), rig ging hardware, and attachments o On cranes, check that the counterweight is secure and that the weight and capacity are permanently and legibly stamped on jibs, blocks, equalizer beams, and all other accessories o Daily, visually inspect the equipment for fluid or air leaks o Ensure that all walking surfaces of the equipment are clean and free from tackle, grease, and oil.
(d) All capacities listed on the load chart for machine "on outriggers" and "on tires" are based on the crane being level and on solid support. The importance of leveling cannot be overemphasized. The manufacturers' capacity tables should be referred to for both outriggers and tires, since lifting capacity is reduced markedly when the crane is not level [33].
(e) If a crane has to make its lifts on rubber, always use wheel chocks to block the wheels and apply the airbrakes to hold the crane in position.
If the machine is of two-engine design, keep the carrier engine running to maintain air pressure.
Ensure that the tires are properly inflated; if they are not, then the capacity and crane stability will be reduced [34].
(f) Dunnage under outriggers must be strong enough to support the imposed load.
If more than one layer is needed, then proper "cross-hatched" stacking must be used to prevent tipping.
Reset outriggers before a lift if necessary.
If floats are allowed to settle into the ground, they lose their effectiveness, making continued operation unsafe [34].
(2) Competent operation of equipment (a) Only thoroughly trained and tested workers are permitted to operate a crane.
When an operator is assigned to a new crane, competence with that crane must be demonstrated.
Training and testing must be sufficient to demonstrate that the operator fully understands and is capable of safely performing all tasks.
The testing should include a performance evaluation of: o Never allow his attention to be diverted from the operation of the crane (coworkers should not be per mitted to talk to the operator while he is working) o Allow no passengers (excepting an oiler) on a crane in motion or operating, especially during mobile yarding operations o Not back up the machine without first making certain that no one will be endangered (when vision of the area behind the crane is blocked, use a signalman) o Sound an audible alarm (horn) before moving a crane and whenever the crane is approaching other workers o Sound an audible alarm whenever a suspended load is approaching employees to give them time to move o Never operate the crane within 10 feet of energized high-voltage powerlines.
(c) During operations, management should:
o Prohibit employees from performing any maintenance work on equipment while it is in service o Barricade the swing radius of the crane structure to prevent employees from being trapped and crushed be tween rotating portions of the crane and adjacent structures o Prohibit oilers, helpers, or other workers from areas within the swing radius of the crane carriage while the crane is rotating or under load o See that oilers, helpers, or other workers are not under any portion of the crane body while a load is suspended.
(3) Rigging the Load
The proper selection and integrity of rigging material and the methods used to attach the load to the hoist are vital to safe hoisting operations [33,34].
(a) The load should be rigged so that the load is stable in the saddle of the hook.
(b) The worker should know the safe load limits of rigging equipment, which must not be exceeded. The employer can accomplish this by permanently attaching tags to, or painting a section on, each sling, rope, and chain that identifies its capacity.
(c) The employer should train all riggers in the safe operating procedures of rigging, including:
o Keeping hands away from pinch points as the slack is being taken up o Examining all hardware, equipment, tackle, and slings before use and destroying defective compo nents o Making sure that all slings are of the same capaci ty and length when two or more slings are used on a load o Making sure that the hoist rope or chain is never wrapped around the load or completely wrapped around a hook o Attaching the load to the hook by slings or other rigging devices that are adequate for the load being lifted o Securing the unused legs of a multileg sling before lifting loads with one leg o Remembering when a bundled load is picked up that the material will tend to "nest" and create pinch points, and when a load is landed, it will tend to roll or spread out o Making sure wood blocks or short lengths of steel are not carried loosely on tops of loads o Making sure wire rope or chain is never allowed to lie on the ground for any length of time or on damp or wet surfaces, rusty steel, or near corrosive substances o Avoiding draping rope slings from beneath loads o Keeping all rope or chain clear of flame cutting and electric welding operations o Making sure shackles are not rigged with the run ning rope against the pin, causing it to "spin out" and drop the load o Ensuring proper load/shackle alignment by using spacers such as washers o Keeping the load under control with guide ropes or tag lines. (e) Slings, ropes, or chains should not be left on the floor or ground where they can be subjected to abrasion or create a tripping hazard. They should be hung from a rack and looped so that they do not touch the floor.
(f) All hooks should have safety latches.
(g) Sharp bends, pinching, and crushing of ropes and slings must be avoided. Sharp edges or corners of heavy loads should be padded as protection for slings by the use of large-diameter split pipe sections, corner saddles, or other, softer material. The load should not be "picked" until the signal is received from the signalman. All signals must be clearly understood by the operator.
If there is any doubt, the operator should stop operations until the signal has been clarified. The crane operator should receive signals from only one person; this does not exclude relay signaling or emergency stop signals.
Signalmen may be supplied with orange gloves for maximum signal visibility.
(b) Crane/hoist operators should remain at the controls whenever a load is suspended.
(c) When preparing for new and near-capacity picks, the operator should make a practice run, going through all the motions without the load, anticipating the actions that should be taken to make a safe lift and a smooth operation.
(d) The crane should never be loaded beyond its rated capacity.
(e) Handling loads during high winds should be avoided.
# b. Straddle Carriers
(1) Straddle carrier operators must be thoroughly trained.
(2) Straddle carriers must be thoroughly inspected before beginning operation each day. Particular attention should be given to brakes and hydraulic systems. Visual inspections of the bridge, rigging, and lifting hardware should be made to ensure their integrity. All wire ropes should be inspected and special safety devices should be in working order.
The inspection should be performed and documented by qualified maintenance personnel.
(3) The rated load of the straddle crane should be posted in a conspicuous location on the equipment and in the operator's cab.
(4) When operator visibility is restricted, a signalman must be provided.
(5) Visible and audible alarms should be in operation during any moving task.
(6) No one should ride on the carrier unless such a procedure is approved by the plant manager.
Where approval is granted, a seat or cage, located so that it will not interfere with operator vision or in itself be a hazard, should be provided.
The rider should be in the seat or cage before the carrier is moved and should not move around on the carrier until it is stopped.
# c. Forklifts
(1) Only workers authorized by the employer and trained in the safe operation of industrial trucks, forklifts, or industrial tow tractors should be permitted to operate these types of vehicles.
(2) Forklifts and industrial vehicles should be equipped with audible backup alarms. (4) Employees should not be permitted to place any part of their bodies outside the cab or protected area of an industrial truck or between mast uprights or other parts of a truck where shearing or crushing hazards exist.
(5) Passengers are not permitted on industrial vehicles.
(6) Employees should not be allowed to stand, pass, or work under the elevated portion of any industrial vehicle, loaded or empty, unless it is effectively blocked to prevent it from falling.
(7) When loading or unloading trucks or trailers, the brakes must be set and the rear wheels chocked.
(8) Forklift forks should be carried as low as possible.
(9) Industrial vehicles should not run onto floors, platforms, or other surfaces that will not safely support the loaded vehicle.
(10) Vehicle loads must not exceed rated capacities.
A loaded industrial vehicle should not be moved until the load is secure.
(11) When leaving the vehicle, the worker should shut off the engine, set the brakes, and lower the lifting forks to the ground.
(12) All traffic regulations should be observed including plant speed limits. The operator of an industrial vehicle is required to slow down and sound the horn at cross aisles and other locations where vision is obstructed.
(13) No person should operate or be in physical control of a motorized vehicle or piece of equipment if he is under the influence of or is using alcohol or drugs.
# d. Chain Hoists
(1) Chain hoists or "come-a-longs" should be inspected and maintained as part of a preventative maintenance program. Inspection should include:
o Checking the integrity of the chain or wire rope for worn links, deformations, kinks, rust, or excessive stretch o Examining the hook for deformity, cracks, or bending o Ensuring that the clutch and brakes are within the manu facturers' tolerances.
(2) Employees lifting material with mechanical hoists should:
o Use proper and accepted rigging methods o Use safety latch hooks o Chock or block loads before working under them o Not use "cheaters" on the hoist handles. The handle length is matched to the safe lifting capacity of the hoist, and while the cheater extension may temporarily enable a greater load to be lifted, it may tax the hoist and lead to failure.
# e. Conveyors
(1) Conveyors should be adequately guarded to prevent workers from being caught on moving parts or being injured by falling materials.
(2) Conveyors should have delay startup warning devices with controls for emergency stops. All chain drives, gears, nip or shear points, and revolving shafts should be guarded.
(3) Personnel working near conveyors should wear close-fitting clothing that cannot be caught in moving parts.
(4) Employees should be instructed in safe practices for freeing "jammed" conveyors, including use of special tools. A lockout system should be mandatory.
(5) Chutes or other devices that depend on gravity for moving materials should be guarded. (2) Front-end loaders should be equipped with a backup warning device.
The device should be audible and sufficiently distinct to be heard under the prevailing conditions. The device should operate automatically upon commencement of backward motion and should operate during the entire backing operation [36].
(3) Loader operators should be sure other workers are in the clear before starting or moving the machine [36].
(A) Operators should not move loads over the heads of other workmen or over truck cabs [36].
(5) The loader bucket should be carried as low as possible and tilted back. This provides better operator visibility and minimizes machine bounce [36].
# Handtools a. Powered
Handtools (powered) should be used according to the following safety recommendations:
(1) Hand-held powered circular saws, chain saws, and percussion tools without a positive accessory holding means must be equipped with a constant pressure switch [32].
(2) Portable, power-driven circular saws must have guards above and below the base plate or shoe. The upper guard should cover the saw to the depth of the teeth, except for the minimum arc required to permit the base to be tilted for bevel cuts.
The lower guard should cover the saw to the depth of the teeth, except for the minimum arc required to allow proper retraction and contact with the work. When the tool is withdrawn from the work, the lower guard must automatically and instantly return to the covering position [32].
(3) Abrasive wheels and stones must have a safety guard cover ing the spindle end, nut, and flange projections. The safety guard should be mounted to maintain proper alignment with the wheel; the strength of the fastenings should exceed the strength of the guard [32].
(a) Prior to use, abrasive stone wheels should be inspected to ensure that: o They have not been damaged in transit or handling, which is checked by means of sounding with a ring test o Wheels fit freely on the spindle and remain free through an entire turn of the wheel, and that the free clearance between wheel and guard does not ex ceed one-fourth inch o A controlled clearance between the wheel hole and the machine spindle (or wheel sleeves or adaptors) is sufficient to prevent excessive pressure from mount ing and spindle expansion o All contact surfaces of wheels, blotters, and flang es are flat and free of foreign matter' o When a bushing is used in the wheel hole, it does not exceed the width of the wheel and does not contact the flanges.
(b) The safe operating speeds of abrasive grinding stones should not be exceeded [32].
(4) Hand-held powered drills; tappers; fastener drivers; hori zontal, vertical, and angle grinders; disk and belt sanders; reciprocating, saber, scroll, and jig saws; and similar tools must be equipped with constant pressure switches.
Other handheld powered tools, such as platen sanders; grinders; disk sanders; routers; planers; and saber, scroll, and jig saws, should be equipped with either a positive on-off control or a constant pressure switch [32].
# b. Unpowered
The following safe practices should be observed when unpowered handtools are being used [37]:
(1) Train employees to select the correct tool for the job, and ensure that the tools are available.
(2) Keep all hand tools in a safe condition. Handles of tools shall be kept tight in the tool. Wooden handles shall be free of splinters or cracks.
Wedges, chisels, and other struck tools should be dressed as soon as the struck surfaces begin to mushroom.
Discard wrenches which are sprung to the extent that slippage occurs. The crowbar should have a point or toe that will grip the object to be moved, and a heel to act as a pivot point. Sometimes it is necessary to use a block of wood under the heel to prevent the crowbar from slipping and injuring the hand. Workers should position themselves so that their bodies will not be in the path of travel if the prybar slips.
Additionally, they should brace/position themselves so that they will not fall if the prying forces are released suddenly. Guardrails may be necessary to prevent workers from falling to lower levels.
(d) Employees should be aware that when using torsion tools such as wrenches, there is always a possibility that the tool may slip. Therefore, the employee should be in a braced position to maintain bodily balance should the tool slip.
Wrenches should be inspected for flaws. Wrenches should never be ground to change their dimensions to make them fit in close quarters. A wrench of proper size for the job must be selected.
# Worker Proximity to Operations a. Walking Through Work Areas
Work areas should be kept free of litter, trash, gravel, excess concrete spills, welding rod stubs and other junk.
All scrap, salvageable material, unused forming or reinforcing materials and equipment should be removed.
Protruding nails in wood forming material should either be removed or benl: over. Aisles around work areas should be kept clear of such items as reinforcement, welding hoses or leads, lumber, power cords, and concrete working tools.
# b. Working Near Operations
Of particular interest in this category is the need to protect workers in the vicinity of welding operations from flash burns. Whenever possible, resistance welding operations should be isolated to protect workers in the vicinity of the welding operations from exposure to the direct or reflected light rays.
This can be accomplished either by use of booths for regular welding production operations or by portable welding screens for welding being performed intermittently throughout the plant [38].
# Welding, Cutting, Burning
Welding, cutting, and burning necessary for making precast concrete products should be done in accordance with the following safe work practices: a. Workers performing welding and cutting tasks should be trained. c. Welding and cutting should be done in an area having a nonflam mable floor, such as concrete, but not on the concrete floor, because of the possibility of explosive spalling of the concrete.
The material to be cut should be raised above the concrete or the concrete shielded from the flame.
If welding must be done over wooden floors, a noncombustible covering material should be placed over the floor to provide fire protection and to prevent spatter from dripping through openings in the floor. The use of wet sand or metal coverings, however, may create electric shock hazards that otherwise would not exist. o Persons involved in grinding, chipping, wire brushing, and/or scraping should wear goggles or safety glasses with side shields under a face shield, o Since the chipping/cleaning tasks which utilize power tools can cause particles to be airborne for considerable distance (10 -30 feet), the operations should be isolated from other workers. If this is not practical, then workers in the vicinity of these op erations should also wear adequate eye and face protection.
# B. Safe Work Practices for Precasting Processes
Safe work practices for procedures used in the manufacture of precast concrete products are presented in this section.
Included are safety recom mendations that address the hazards of processes used in the precasting industry as well as the application of tools or equipment used in a specific process.
# Form Work a. Forms and Forming
(1) Forms and beds for casting should be: o Arranged or laid out to provide a working space, aisle way, or working platform clear of obstructions and suffi ciently wide to provide ample room for the safe movement of materials and vehicles o Provided with access steps or ramps at convenient inter vals along the bed or form o Equipped with standard guardrails, if over 4 feet high.
(2) Forms should be structurally sound so that they do not present a hazard to employees as they are built, repaired, cleaned, modified, or moved.
(3) During form assembly, components should be chocked and/or braced to prevent displacement.
(4) Safe access during vertical pipe form assembly should be provided for workers during assembly, aligning of hoisted parts, and attaching of hoist hooks.
(5) The floor, yard, platform, or other surface on which a form is placed, built, or erected should be free of litter, debris, and other loose materials that can cause tripping hazards. Also, these surfaces should be well drained and free of potholes, cracks, unevenness, or standing water that may contribute to slips and falls.. (6) Tilt tables should be capable of supporting the temporary loads of employees during forming operations in addition to the imposed load of product. They should also be chocked when in the upright position for cleaning, product removal, or maintenance to avoid collapse.
# b. Form Stripping
(1) Employees should be instructed that form bulkheads, etc., may temporarily adhere to the concrete product. The bulkheads may release suddenly.
Workers (and their body parts) should not be positioned where they may be caught between either the bulkhead, the product, and/or the form.
(2) During form stripping and product removal tasks, it is important that form bulkheads and components be cribbed, braced, or suspended by hoist to prevent their falling unexpectedly.
(3) Prying tasks should only be performed with the proper tool (crowbar or prybar). Shovels should not be used as substi tute s.
(4) Cranes or hoists should not be used to remove products lodged or stuck to the forms. The crane's safe lifting capacity should not be exceeded.
Use of properly adjusted crane load indicating devices will help avoid exceeding crane capacities.
(5) As forms are stripped, all excess material, wood, nails, and bits of wire should be removed so that the area is clean and safe. After forms are stripped, all nails should be bent or pulled immediately.
# Reinforcing a. Reinforcing Materials/Assemblies
(1) Reinforcing assemblies should be fabricated with a working level jig to avoid constant bending over to tie or weld.
(2) In the handling of reinforcing steel and fabricated assemblies, the following precautions should be taken: o Employees must be instructed and required to use correct lifting techniques, o Finished cages for pipes, columns, and beams should be moved to their final locations in the forms with consider ation of their weight and the physical capabilities of the employees assigned, o Mechanical lift assistance should be provided to safely lift pieces too bulky or heavy to be handled manually, o Bundles of reinforcing steel moved by crane or other means should be securely tied and wedged together to prevent slipping. o Rebar bundles lifted by hoist should be rigged by 2-point suspension chokers and moved in a balanced horizontal posi tion. They should not be moved in the vertical plane, o When bars carried by hand are long, bulky, or heavy, more than one worker should be utilized, o Rebar materials used in cutting and bending operations should be located such as to minimize or eliminate the need for the worker to lift the bar from ground level to the cutting or bending height, o Gloves should be worn during strand stringing, vise plac ing, rebar tying or handling, mesh placement, and cage handling tasks [39].
# b. Metalworking Equipment
Metalworking equipment should meet the following requirements:
o Cage rollers should be equipped with deadman switches and positive braking mechanisms that immediately stop the move ment of the rollers, o Cage or wire rollers should be equipped with trip wire mechanisms at the in-rolling nip points, that automati cally shut down the rollers when inadvertent contact is made. o Shearing machines should be equipped with physical guards and/or proximity detectors. (b) Welding or cutting should not be allowed in any stressing bed where strand has been strung or tensioned, or in any other location where strand is stored. If an electric arc jumps to or from the strand, the molecular structure of the strand is altered and a loss of strength occurs.
# c. Stressing
Heat from molten metal or torch cutting will also change the mechanical properties of steel wire strand.
(c) Strand vises used to secure strand at the anchor abut ments should be placed away from a burned end to avoid the area of altered strand strength. This distance should be at least 12 diameters of the strand or 6 inches, whichever is greater.
(d) Strand previously gripped by vises, and therefore nicked, must not be reused.
Strand vises should be cleaned and inspected between each use and lubricated as necessary. Grips that become visibly worn or distorted, or allow excessive slippage should be discarded.
(e) Check that the strands in the form are not crossed or tangled before tensioning.
(f) Audible and visible alarm signals should be turned on and remain on during tensioning. Any personnel not directly involved in stressing operations should be cleared from the "designated area" and remain clear until audible and visual signals are turned off.
(g) The "designated area" should be the entire length of the bed being stressed, including both ends and the sides out to the center line of any adjacent bed, or one-half the length of the longest member, but not less than 20 feet.
(h) Only stressing crew personnel directly involved in tensioning are to be permitted in the vicinity of the bed.
(i) Personnel in the stressing crew must not stand behind the jack or in line with the tensioned steel, since ruptured strand tends to retract along the line of tension.
(j) No employees should be in the jacking area (the area within the possible swing radius of the stressing jacks) during stressing.
(k) Elongation should be measured by means of a template, jig, or scale attached to the stressing jack that can be viewed from a safe distance.
(1) Workers involved in tensioning should be protected by bed end protection, a pumphouse, or a portable booth to shield them from flying strands or bulkheads resulting from strand breakage.
(m) An employee should be posted in a location with an unobstructed view of the designated area in order to warn personnel who inadvertently approach the re stricted area. Shields must be designed to withstand the forces applied against them by recoiling strand, flying bulkheads, and other material that may be launched as a result of strand failures during stressing.
Shields can be fabricated of sheet steel; heavy duty, small aperture expanded metal; or concrete with a supporting frame of angle iron, channel, or pipe. The purpose of bed end protection is to shield those workers who are involved in the tensioning or detensioning operation from flying chucks, strand, or bulkheads resulting from chuck or strand breakage.
The following recommendations describe possible methods of bed end protection.
Staff engineers should develop measures which are specific to the protection needs in each plant [39]. The secondary barrier should be constructed of concrete, steel, or other material able to withstand the force of a chuck and strand retracting through the pulling head.
Alternatively., an angled trough that is of sufficient strength and dimension to collect a retracting strand and direct it toward the ground should be permanently installed at the pulling head. on the harping dowel large enough to be visible from a safe location during the harping sequence.
During harping the following safety recommendations should be followed: o All unnecessary employees should be cleared from the immediate area, o Audible and visible alarms should alert personnel that harping operations are taking place, o An employee should be stationed in a safe area to en sure that personnel do not enter the "designated area" while harping operations are in progress, o A mirror can be set up on the form so that an employee can observe the depressing clip from a safe location, o Entangled or misaligned strand should be restored to its original position and then correctly harped. Work ers must not attempt to shift strand while it is de pressed .
There are different types of harping operations, and each type requires special precautions. More detailed procedures and safe work practices are contained in the Prestressed Adapted from PCI Safety and Loss Prevention Manual [39].
# Concrete
Institute publication, "PCI Safety and Loss Prevention Manual" [39].
(4) Dejacking Dejacking, used to release a strand that is misplaced or fouled, requires extreme care.
The following precautions should be taken: o Hands and fingers must not be placed between the chuck face and the jackhead. o Jaws should be removed with a hook tool or other device recommended by the manufacturer, o Tension on strand should be released slowly. o Prior to stressing, place a solid steel cylinder, called a spacer (approximately 2 inches long and slotted to fit the strand), between the chuck and the jackhead and tape it to the chuck, o After casting and curing, remove the tape; place a "detensioning stand" over the strand; and stress the strand slowly until the spacer falls out. o Use long-handled pliers or tongs to insert a removal tool in its place; remove the chuck cap, and slowly release tension until the removal tool has forced the jaws from the barrel. When the jaws are access ible, pull them free of the retaining ring, remove them from the strand, and release tension slowly, o Keep hands out of the "detensioning stand" by using long-handled tools, o Allow no employees other than the detensioning crew in the "designated area." o Do not regrip the strand on or near the previous jaw marks. o Use warning lights and horns and enforce "designated area" precautions as when tensioning.
# Oiling
a. Supplied air pressure vessels, used for spraying form release agents, should have both a visible pressure gauge and a pressure relief valve in proper operating order. Supplied air sprayers should be labeled for their maximum safe operating pressure and this pressure should not be exceeded.
b. Form release agents should be stored neatly in cabinets or areas specially set aside for that purpose. Aisles should be maintained to allow unobstructed movement of personnel and equipment, and to avoid tripping and slipping hazards. c. Material Safety Data Sheets for all form release agents should be requested, and all applicable safety and health precautions should be followed.
d. Eye and face protection, such as a face shield, should be manda tory during spray application of form release agents.
e. A minimum of safety glasses should be used during hand applica tions (swabbing, rolling) and during all transfers of form release agents. (2) Employees should be adequately instructed in preventive measures to avoid skin burns that can occur from prolonged, direct contact between skin surfaces and fresh (moist) concrete or clothing saturated by it.
(3) Where cement, sand or gravel are stored in silos, bins or hoppers, the following procedures should be followed:
(a) Workers should be made aware that fine materials such as cement, sand and gravel can freeze or bond and crust over in cold or wet conditions. This crust can collapse under the weight of an employee standing or walking on it to free it up.
The individual could sink into the quicksand-like material and suffocate. Further information on working safely in confined spaces is contained in the NIOSH criteria document "Working in Confined Spaces" [40].
(4) NIOSH/MSHA-approved respirators should be worn in areas where dust levels are excessive. The threshold limit value (TLV) for specific dusts and exposure levels are cited in the 1981 TLV booklet of the American Conference of Governmental Industrial Hygienists (ACGIH) [41].
(5) In high-noise areas, the following; recommendations should be adhered to [32]:
o A continuously effective hearing conservation program, in cluding annual audiometric testing of exposed employees, must be established when noise levels are found to exceed 85 dB(A) for an 8-hour time-weighted average (TWA), o Administrative or engineering controls, including rotation of exposed employees and acoustical booth isolation where feasible, should be applied to reduce exposure time, o All employees must be provided with hearing protection de vices if feasible engineering controls are inadequate in reducing noise to levels below 85 dB(A) for an 8-hour TWA.
# b. Concrete Transport
(1) A signalman should be available at times of entry, movement, and exit to ensure safe passage of concrete delivery trucks to casting areas.
(2) Backing lanes should be free of equipment, material, and workers [39].
(3) Movement of personnel and job equipment should be routed to avoid crossing truck lanes, tracks, aisleways, or transfer areas.
(4) Concrete delivery transporters should be equipped with audible and visible alarms, including backup alarms to warn of their approach, and mirrors to eliminate blindspots.
# Casting Concrete a. General
During the casting of concrete product, the following safety recommendations should be followed:
(1) Concrete buckets should not be transported over workers [42]. Workers should not step under overhead buckets.
(2) Buckets should have a positive locking gate [39].
(3) Concrete buckets should be equipped with a release latch (bar, handle) designed and located to prevent fingers from being caught between the latch bar and the bucket.
(4) Electric cords must meet OSHA standards and be free of breaks and in safe condition. The cords should be placed or protected so that they will not be run over and damaged or be allowed to rest in water.
(5) Safe access to the points of concrete placement and consol idation should be provided by stairs, ramps, or ladders. Also, a properly guarded walking and working surface must be available. ( 6) Safe work platforms should be provided for elevated casting operations such as vertical wet casting of pipe. (7) Rolling stair scaffolds must be equipped with adequate guardrails on all exposed sides, particularly the ends of the scaffold and the interface between the form and the scaffold if a floor or wall opening exists. ( 8 o Ensuring that broken or missing handholds and footholds are repaired or replaced [42] o Removing and refitting unsuitable handholds and footholds [42] o Adding new handholds and footholds where they are needed for worker access [42] o Providing non-skid surfaces on all access systems which might become slippery [42] o Providing a handhold, long enough to be accessible by the majority of drivers, on the right of the tractor driver's door o Providing portable access stairs for pickup and trailer beds. f. Concrete products should be unloaded in accordance with the following safety recommendations:
o The safe lifting capacity of the equipment should not be exceeded. o Loads that are long, oddly shaped, or difficult to rig should be raised only a short distance until it is apparent they will not spring, slip, or tip. o Pipe or circular products should be off-loaded with skids, ropes, or automatic unloaders, o The job site unloading area should be examined for access, stability, and temporary storage capability, o Before unattended vehicles are unloaded, all wheels should be chocked and the parking brakes set. o Trailers should be loaded and unloaded evenly so as not to tip the load or the trailer.
# Personal Protective Equipment
To protect workers, the use of various personal protective equipment should become an integral part of the safety program.
The most common personal protective equipment that should be used are contained in Table IV
-1.
Requirements for personal protective equipment are covered in the OSHA standards [32].
# Mechanical Materials Handling
Recommendations for control of hazards encountered in mechanical materials handling activities are contained in paragraph A.2. of this chapter.
# Guarding
Guarding of machinery should conform to the following:
(a) Drives for machinery must be properly guarded at chains, belts, and pulleys in full accordance with the following requirements:
o Pulleys, belts, or chain drives 7 feet (within reach) or less from the floor should be guarded, o Gears should be guarded by a complete enclosure, o Sprocket wheels and chains should be enclosed if less than 7 feet above the floor or platform [32]. (d) Circular, hand-fed ripsaws and crosscut table saws must be guarded by a hood that encloses the portion of the saw above the table prior to cutting and above the material being cut (the hood should automatically adjust itself to the thickness of, and remain in contact with, the material being cut) [32].
(e) All p< tions of the saw blade on bandsaws must be [32]:
o Enclosed or guarded, except for the working portion of the blade between the bottom of the guide rolls and the table (bandsaw wheels should be fully encased)
o Guarded to prevent hands from contact with the in-running rolls.
(f) Radial saws should be provided with:
o A hood to protect the operator from flying splinters, broken sawteeth, and sawdust o A guard on the upper hood completely enclosing the upper por tion of the blade down to the end of the saw arbor o A lower blade guard that automatically adjusts to the thick ness of the stock and that remains in contact with the stock being cut o Nonkickback fingers or dogs located on both sides of the saw to oppose the tendency of the saw to pick up the material or throw it back toward the operator.. Further information regarding hazardous energy control is contained in the NIOSH document "Guidelines for Controlling Hazardous Energy During Maintenance and Servicing" [43].
# Chapter V SAFETY MANAGEMENT
There should be little disagreement that safety is ultimately the re sponsibility of management.
In addition to the fact that the Occupational Safety and Health Act of 1970 (OSHA) requires each employer to furnish each employee a place of employment that is free from recognized hazards likely to cause death or serious physical harm, worker accidents and injuries are counter-productive and costly.
As shown in Chapter III of this document (specifically Table III-3), the occupational injury and illness incidence rate for the precast concrete products industry in 1980 was in the top 3% of the durable goods manufacturing industries.
Since 1977, the estimated cost of actual paid-out medical and indemnity expenses of occupational injuries in this industry has averaged more than $30.9 million per year.
The National Safety Council estimates that the full costs of work-related accidents have been 3.4 times greater than the cost of actual paid-out claims, or over $105 million per year (see Chapter III).
These needless losses can be controlled by managing successful safety programs.
However, safety programs can only be successful when plant management provides an environment responsive to worker safety and is committed to providing a safe workplace.
Safety recommendations such as those presented in Chapter IV or safety standards such as those promulgated by OSHA will not, by themselves, reduce occupational injuries.
Management must accept the responsibility of implementing a safety program which is designed for successful accident prevention.
Such success requires an organized approach.
No individual level of management can do the job by itself.
It takes a combined effort of all -from the plant manager down through the first-line supervisor to the employees. This chapter presents the basic elements of safety program management.
It outlines criteria for evaluation of present safety programs and suggests implementation of critical elements which are indicative of safety being a management function.
It is recognized that each company will need to tailor its safety program to fit the various characteristics of its particular operation.
# A. Pre-Assessment of Present Program
Before revising an on-going safety program or attempting to design a new program, it is advisable that management assess its existing safety status within the plant. An evaluation of the present safety status will help out line where changes and additions are essential.
It will yield answers to the seriousness of the plant's accident problem, it will identify the major organizational deficiencies which have an adverse effect on the safety program, and it will identify the major accident prevention deficiencies within the program itself. Assessment of the following basic elements of the safety program should be made:
1. Management leadership 2. Assignment of responsibility 3. Identification and control of hazards 4. Employee and supervisory training 5. Accident reporting and investigation 6. Emergency plans 7. Employee awareness. Utilization of pre-assessment tools such as the American Society of Safety Engineers (ASSE) Safety Audit contained in Appendix C, or the example assessment forms contained in Appendix D can provide insight into safety program weaknesses which need management's attention. B. Basic Elements of a Safety Program It is difficult to outline a safety program that will be applicable to all precast concrete plants, since a program must vary with the specific needs of each company. It is important that a safety program be tailored for the processes and operations of an individual company. It becomes the responsibility of management to design and define a program within the constraints of a specific plant's operation. A safety program should, however, include aspects of the following basic elements:
1. Management Leadership Management's interest in safety must be sincere and visible to employees. Therefore, senior management must establish achievable safety program objectives and communicate these to all employees. The safety program objectives should receive the same management scrutiny as that given for the control of quality, cost, and production. Once the objectives are established, then management must plan, organize and control the overall program to meet the objectives. Management's leadership and support should contain the following key elements: a. Written Policy A written safety policy is management's method of communicating a direction to be followed. It is the first step in organizing to meet the stated objectives. It is important that the policy be in writing to reduce confusion concerning direction and assignment of responsibility.
The written policy should be concise, to the point, and should address the following areas: safety and health conditions [45]. Employee participation can be encouraged by conducting safety meetings and by forming a plant safety committee. Holding safety meetings is a useful technique for communicating safety to employees. These meetings are more commonly referred to as safety huddles, tailgate sessions, or toolbox sessions. These are short
# SAFETY AND HEALTH POLICY
It is the policy of this company to provide every employee with a safe and healthful workplace. When a person enters the employ of our company, they have the right to ex pect to be provided with a proper place in which to work, as well as proper and safe machines and tools with which to do the job, and that the employee will be able to devote his or her energies to the work without undue danger. Only under these circumstances can the association between employee and em ployer be mutually profitable and harmonious. It is our desire, intention, and responsibility to provide a safe workplace, safe equipment, and proper materials and to establish and insist on safe methods and practices at all t ime s. People are our most important asset-their safety is our greatest responsibility. It is a basic responsibility for all employees of this company to make the SAFETY of fellow human beings a part of their daily, hourly concern. This responsibility must be accepted by each person who conducts the affairs of the company, regardless of the capacity in which they function. Employees are expected to know the SAFETY rules applicable to their job and must use the SAFETY equipment provided. Rules of conduct and rules of SAFETY shall be observed by all employees. SAFETY equipment must not be destroyed or abused. The joint cooperation of employees and management in the observance of this policy will provide safe working conditions and accident-free performance to our mutual advantage. We consider the SAFETY of our personnel to be of first importance, and we ask your full cooperation in making this policy effective.
# Company President FIGURE V-l. EXAMPLE OF A PLANT SAFETY AND HEALTH POLICY
Adapted from American Society for Personnel Administration, 19 Church Street, Berea, OH 44017.
As we are known and recognized for our products and service, so should we te known for our safety performance. No job must ever become so routine or so urgent that every safety precaution is not observed. Prevention of personal injury and damage to the property and equipment of both the company and its customers must always re main uppermost in the mind of every employee.
It is the policy of ABC PRECAST CONCRETE CORPORATION to develop and maintain safe and efficient operations. Our safety program has been designed, in accordance with the Williams-Steiger Occupational Safety and Health Act of 1970, to develop safe working conditions. The success of our program requires the full support of each and every employee.
# President FIGURE V-2. EXAMPLE OF A PLANT SAFETY POLICY STATEMENT
Adapted from Summary Plant Observation Report and Evaluation [46]. meetings usually conducted by the supervisor with all his employees. The primary functions of such meetings are to foster communication between management (supervisor) and employees relating to safety consciousness,and to disseminate safety concepts. The subject should be specific to work being performed or planned for the upcoming week. The session should take place at the work site and last 10-15 minutes. Employees knowledgeable in specific safety subject areas should be requested to lead the safety discussions, thereby encouraging peer participation. Establishment of a safety committee is another technique which demonstrates management's desire that employees participate in the plant safety program. Committees may vary considerably in different organizations, but should have the basic functions of developing, promoting, and maintaining safety practices in the plant. Such committees should also serve as a means for communicating safety policies to both management and labor.
# Assignment of Responsibility
Management has the responsibility for controlling unsafe acts of employees and unsafe working conditions. Ultimately, the plant manager has the overall responsibility for meeting the plant's safety program objectives.
Since plant size and organizational structure vary widely throughout the precast concrete products industry, assignment of safety responsibilities must be appropriate for the management structure within the plant. In very small plants, the owner/operator may have sole responsibility; in larger plants, responsibility is assigned to the plant manager, middle managers and first-lin e supervisors. Additionally, the employees must also be assigned responsibilities in order to meet the stated safety program objectives.
# I d e n t if ic a ti o n and C o n tro l of H azards
Whenever management decides to either implement an accident prevention program or to overhaul an existing program, employees are inclined to be skeptical of projected results and tend to take a "wait and see" attitude. A vigorous management effort to eliminate longstanding hazards and to provide a safer workplace can convince employees that management is truly concerned about their on-the-job well being.
However, prior to eliminating these hazards, management must first identify them. Identification of hazards requires a fairly complete inspection of all precast operating areas. The inspection should be made by a small group composed of someone from production, someone from maintenance, and the safety program coordinator.
The hazard identification process should be done in phases to reduce interference with normal work routines.
Safety inspection checklists may be helpful in directing the group's inspection to the operating areas with the more hazardous work exposures. Management can either obtain checklists from insurance companies, or develop one specifically for their plant after analysis of the injury data presented in Chapter III, Table III-5. As an example, analyze nails as a source of injury. The table shows that nails mostly resulted in puncture injuries to employee's feet. Therefore, it is assumed that when wooden forms are removed from cured product, the nails are not bent over or removed, thereby creating a hazard to workers. Analysis of the "machinery" source indicates that lack of adequate guards are creating a hazard. If these sources of injury are present within the plant, the checklist should address these items. After the in itial inspection has been performed, a program for correcting the noted deficiencies and performing periodic inspections should be established. Identifying hazards by means of inspection and promptly eliminating or controlling them is one of the best methods management can use to demonstrate its interest and concern for accident prevention to employees. both new employees and employees new to a particular task. Newly hired employees should always receive instruction and orientation about the company, the plant, the product, organizational arrangements, lines of authority, and safety policies and rules. Specific training, including supervised on-the-job training, must be provided to each employee.
During orientation to the plant, a new employee should be given copies of the company's safety policy, and safety rules and regulations. If an employee starts a new task, changes tasks, or uses new or modified equipment, it is essential that quality training for this job be provided. Training may be necessary to develop a particular skill that cannot be performed safely without specific knowledge; e.g., working at a rebar bender, casting concrete, or operating a forklift. Safety training is based on the general assumption that the development of a positive mental attitude predisposes an individual to safe habits of work and conduct. A job should be explained in detail by breaking it down into manageable parts. If personal protective equipment is required, employees must understand why it must be used and what may happen if it is not used properly. Hazards should be identified, and precautions or safe work practices demonstrated. Training should take a new employee through each step, and each step should be fully demonstrated. In addition, the supervisor should verify, at regular intervals, that the original lessons are being followed and that the employee is not developing bad habits or taking dangerous shortcuts. The type of training required, by employee group, is presented in Table
V-l.
Other training, such as first-aid courses, cardiopulmonary resuscita tion (CPR), fire extinguisher use, and other emergency procedures may be required.
Training is a continuous process, and attention must be paid to all employees. An employee who continues to repeat an unsafe procedure is not working safely, even if an accident has not occurred. The following indicators might show a need for training or retraining: o High incidence of injury o An increase in the number of "near misses" that could have re sulted in accidents o A change in a process or introduction of a new process o A recent upswing in actual accident experience o Excessive waste or scrap due to poor housekeeping.
# Accident Investigation
The investigation of accidents is an important part of the safety/accident prevention program. It identifies accident causes so that similar situations can be prevented by management actions such as mechanical im provements, better supervision, or employee training. It determines the "changes" or deviation that produced an "error" resulting in an accident; it publicizes the particular hazard among employees and their supervisors; and it directs attention to accident prevention in general. Since nothing is learned from unreported accidents, even minor injuries and near misses should be investigated. The investigation of accidents is the responsibility of all levels of management. However, the firstline supervisor is perhaps the best quali fied, since he is close to the jobs, working conditions, and workers. The supervisor must be trained and have the ability to recognize the cause of accidents. This evaluation may require the assistance of management, equipment suppliers, and insurance representatives. Figure V-3 shows an example of an accident investigation form.
The basic problem confronting any supervisor interviewing a person involved in an accident is obtaining complete facts. Often a worker is reluctant to cooperate for fear of ridicule, sarcasm, or reprimand. It is important to stress the need for facts so that recurrence can be prevented in the future. It is also helpful to ask individuals involved in accidents for their ideas on making the job safer.
Witnesses are important sources of accident information. When a fatal injury occurs, a witness may be the only direct source of information available. When a serious injury occurs, a witness may be the only means of verifying incoherent pieces of the injured's account. For minor injuries, a witness may be able to clarify some of the circumstances surrounding the accident better than the injured person himself. This is also true of near accidents that have a potential for serious injury.
In all cases, all levels of management can learn how to prevent accidents through investigations. By investigating accidents, similar unsafe practices and conditions can be monitored in the future. The information compiled can also help to design better training programs, emphasize areas needing management's attention, and generally prevent future potential problems.
Management's participation is highly important to a functioning safety program in the precast concrete products industry. Efforts should be made to reduce the unnecessary costs of worker injury and illness, loss in production time, as well as repair and replacement of damaged machinery and products.
# Emergency Plans
Management should have a written plan of action outlining procedures to be taken in emergency situations such as employee injury and fire. The purpose of the plan is to eliminate as much confusion as possible in order that immediate positive response will be taken to minimize the dangers of the emergency. firefighting equipment appropriate to the work space, materials, and expected hazards. Canada also requires that facilities for producing prestressed con crete elements include measuring equipment for setting up and checking alignments and levels. Canada requires that there be adequate dustcollecting and ventilating capabilities when personnel are in woodworking shops where wood or plastic forms are made.
# Reinforcing
Canada requires that work benches or gigs where welding is performed be arranged so that employees are protected from welding flashes and that the areas be ventilated to avoid exposure to excessive welding fumes.
PCI refers to the OSHA General Industry Standards in 29 CFR 1910.217 and requires welding areas to be ventilated and protected to prevent welding flash.
# Stressing
Both Canada and the PCI have safety requirements for stressing opera tions. The PCI requires that a shield or guard be provided for bed end protection of the jacking area. There are suggestions for the materials for a barrier, but no specific requirements.
# Oiling
There are no unique safety standards in any international or consensus standards that address the tasks of this operation, except those discussing walking and working surfaces in the PCI "Safety and Loss Pre vention Manual" [39].
# Mixing
The PCI has no specific safety standards regarding batching and mixing that relate to safety. The Canadian standards require that the batch plant be kept clean at all times.
# Casting
The PCI recommends that gloves, long-sleeved shirts, and long trousers be worn when employees are performing any of the various tasks related to concrete operations, such as shoveling, raking, vibrating, and screeding. The PCI requires that personnel performing the shoveling tasks be trained in proper procedures to reduce the potential for back strains. They also require that extruder hoppers have guards and that all electrical connections be insulated or guarded.
The PCI refers to requirements regarding noise in 29 CFR 1926.52 and CFR 1910.95.
# S trip p in g
There are no specific requirements in the PCI, ACPA, or Canadian standards that apply to tasks in the stripping operation.
# Curing
The PCI has both recommendations and specific requirements concerning steam, hot oil, electric, and moisture curing. They include requirements for the insulation of steam, hot: oil, and hot water lines and for thermostats, timers, and circuit breakers for electric curing.
# Finishing
The PCI "Safety and Loss Prevention Manual" [39] recommends the use of rubbersoled shoes where there are slippery surfaces and requires the use of hard hats, eye protection, knee pads, and gloves in the performance of certain operations; e.g., gloves are required for all finishers working with concrete; eye protection is required while concrete is poured; and eye protection is required whenever finishers are chipping, burning, drillling, or grinding. During special finishing processes such as sand blasting, the PCI re quires adequate exhaust ventilation and respiratory protective equipment. When acid etching is used as a finishing technique, the PCI requires that warning signs be posted and visible, that all caustic and acid products be labeled, and that employees know the location of the nearest portable water supply. It also recommends the use of protective face, hand, foot, and body clothing for employees performing these tasks.
# Materials
Handling PCI refers to 29 CFR 1926.600 for certain general requirements, but also specifies in its "Safety and Loss Prevention Manual" [39] that operators be trained and qualified, be able to pass at least a verbal examination, be specifically designated to a particular task, and make a daily minimum check of their equipment. PCI also requires that the grounds be properly maintained for safe operations and prohibits the carrying or holding of loads over work areas where other employees are present. The ACPA requires that product handling conform with the standard recommendations in its handbook.
Canada requires that all physical production facilities be laid out, designed, and constructed so that there will be adequate space for mate rials, storage, equipment, and production facilities, with sufficient capacity so that production can be adequately maintained without adversely affecting the safety of plant, personnel, or products.
The PCI has both general and specific recommendations for yard storage, including storage area, dunnage, stacking, personnel safety, strand, and rebar storage. They also have recommendations regarding product trans portation, including operating rules for driving in hazardous weather. The PCI prohibits the use of drugs and alcohol; it also requires that drivers wear hardhats and safety shoes.
The OSHA General Industry Standards in 29 CFR 1910 [32] regulate safety and health in the precast concrete products industry (SIC 3272); however, the standards do not apply to all operations, tasks, and conditions specific to the industry. Those items in the existing standards that are related to the manufacture and delivery of precast concrete products are presented in Table B E. Summary OSHA General Industry Standards apply to many of the operations, tasks, and conditions typical of precast concrete manufacturing operations. These OSHA regulations address subjects such as walking and working surfaces, handtools, ventilation, noise, fire prevention, respiratory protection, machine guarding, ladders, scaffolding, and welding or cutting. OSHA standards do not, however, regulate some of the tasks, equipment, and opera tions that are specific to the precast concrete products industry, such as forming, stressing, detensioning, oiling, concrete transport and casting. Existing international standards and trade association guidelines address many of the hazards that are unique to tasks in the precast concrete indus try. PCI provides guidelines for worker protection in such areas as ten sioning, architectural and structural product storage, yard layout and cleanliness, product shipping, and steel placement. ACPA guidelines address the areas of pipe handling and unloading. In addition to ef fective accident analysis, results are used to pinpoint accident causes so accident prevention objectives can be established. Written requirement that all property damage accidents of $50 & more will be investigated. higher range (generally between 30° C and 70° C), the term "accelerated curing" is used.
# Investigation of property damage.
The process of creating draped strand.
The release of tension from the tendon, usually occurring at the time the prestressing force is transferred from the bed anchorage to the individual pieces cast in the bed.
The minimum concrete strength specified for individual concrete elements before the prestressing force may be transferred to them. A strand that is held up at specific points, and held down at others, to form a special desired profile.
Concrete designed with very low water/cement ratios and slumps to be used with special consolidation methods, tamping, or extrusion production equipment. Materials (usually wood) used for keeping concrete products from touching each other or other materials during storage and transportation.
A structure or mold for the support of concrete while it is setting and gaining sufficient strength to be selfsupporting .
A substance applied to the forms for the purpose of pre venting a bond between the form and the concrete cast in it.
The system of support for freshly placed concrete, including the mold or sheathing that contacts the concrete as well as all supporting members. The parts of a strand vise that actually contact or grip the wires or strands.
A collective term used to cover all items embedded in the concrete (other than reinforcement) or otherwise used in connecting precast elements or attaching or accommodating adjacent materials or equipment:.
A device to align parts of an assembly, usually for pre assembling reinforcing steel and hardware cages, with a minimum of measurement and consistent accuracy, from one cage to the next. A device designed to provide two or more lifting points of a precast concrete element with predictable load dis tribution and prearranged direction of pulling force during lifting. Products cast by one or more machines specifically design ed for the purpose. Slipform and extrusion machines are types of casting equipment used to make solid or hollow-core slabs. Finishes applied by special tools while the concrete is s till in the forms and plastic.
Concrete with a near-zero slump to be used with special consolidation methods, tamping, or extrusion production equipment.
A concrete element cast in a location other than its final position in service. Precast concrete may be produced at the job site, in temporary plants, or in permanent factories.
A general term for any precast product regardless of classification or application. The term includes any nonconcrete items incorporated in the element at the time of manufacture.
The platform and abutments needed to support the forms and maintain the tendons in a stressed condition during placing and curing of the concrete.
An admixture that delays the setting of concrete paste.
The smoothing or leveling off of freshly cast concrete by manual or mechanical means. A screed usually has a wooden or metal edge that is moved horizontally across the concrete, pushing excess material in front of it and filling in low places.
Equipment that, in addition to serving as forms for con crete, accommodates the pretensioned strands (or wires) and sustains the total prestressing force by suitable end bulkheads and sufficient cross-sectional strength.
The drop from the top of a slump cone to the top of the unsupported concrete after the sudden removal of the supporting slump cone. The difference in height, measured in inches or centimeters, is the slump of the concrete. A wet or soft mix slumps more than a dry or stiff mix. strand chuck A device for holding a strand under tension, or vise stripping
The process of removing a precast concrete element from the form in which it was cast.
# two-blocking
The action of the crane hook block being pulled into the crane boom head. water/cement
The weight of water relative to the weight of cement in a ratio concrete mix. Enough water must be added to the mix to provide hydration. Excess water improves workability but reduces strength.
#
[32]
.
Occupational safety and health standards that address operations in the precast concrete products industry were requested from Germany, the United Kingdom, France, the Netherlands, Belgium, Australia, Canada, and Mexico. The Canadian standards [49,50] that regulate architectural and structural operations are included for evaluation. Australia, France, and Belgium have standards for the concrete construction industry, but do not regulate manufacturing operations.
The remaining countries do not have safety standards that specifically address precast concrete operations.
# B. Trade Association Guidelines
The ACPA has published a "Concrete Pipe Handbook" [8] that contains some suggestions on handling, unloading, and site storage. The PCI has developed a "Safety and Loss Prevention Manual" [39] that includes sections on subjects such as training motivation, yard storage, tensioning equipment, stressing operations, steel placement, travelifts, chucks, and harping. These subjects are specifically related to tasks or operations in the architectural and structural sectors of the industry.
# C. Foreign Standards vs. Trade Association Guidelines
International standards and guidelines are incorporated, where appro priate, in the comprehensive safety recommendations presented in Chapter IV. A comparison of these standards and guidelines are presented topically, by operation, in the following section.
# Forming
Canada requires that, in facilities for making forms and accessories, the construction of the forms be within the tolerances required for the product. They also require that all form-making shops have exits and A tool used to spread out and smooth the concrete.
An air-powered reciprocating tool used to give a textured appearance to architectural concrete products by roughening the surface.
(a) The upward deflection that occurs in prestressed concrete elements due to the net bending resulting from stressing forces and self-weight. It specifically does not include dimensional inaccuracies. (b) A built-in upward curvature in some molds for precast concrete other than prestressed to avoid deflection under load to below a defined line of finished product. Any of various construction adhesives, consisting essen tially of powdered, calcined rock and clay materials, that form a paste with water and can be molded or poured to set as a solid mass.
A mixture of cement, sand, and aggregate with water that hardens by chemical curing into a final product similar to stone in texture, weight, and durability.
A device for attachment of precast concrete elements to each other or to a building structure.
The maintenance of humidity and temperature of freshly placed concrete during some definite period following placing, casting, or finishing to ensure satisfactory hydration of the cementitious materials and proper hardening of the concrete. When the curing temperature remains in the normal environmental range (generally between 10° C and 30° C) , the term "normal curing" is used. When the curing temperature is increased to a | None | None |
58bb5bbd76e515f34f12b30df2682ca8619877ef | cdc | None | # Table of Contents
# Background and Purpose
The Centers for Disease Control and Prevention (CDC) established the Vessel Sanitation Program (VSP) in 1975 as a cooperative endeavor with the cruise vessel industry. VSP's goal is to assist the industry to develop and implement comprehensive sanitation programs to protect the health of passengers and crew aboard cruise vessels.
Every cruise vessel that has a foreign itinerary, carries 13 or more passengers, and calls on a U.S. port is subject to biannual operational inspections and when necessary, re-inspection by VSP. The vessel owner pays a fee, based on gross registered tonnage (GRT) of the vessel, for all operational inspections. The Vessel Sanitation Program Operations Manual (VSP Operations Manual), which is available on the VSP Web site (www.cdc.gov/nceh/vsp), covers details of these inspections.
Additionally, cruise vessel owners or shipyards that build or renovate cruise vessels may voluntarily request plan reviews, on-site shipyard construction inspections and/or final construction inspections of new or remodeled vessels before their first or next operational inspection. The vessel owner or shipyard pays a fee, based on GRT of the vessel, for on-site and final construction inspections. VSP does not charge a fee for plan reviews or consultations. Section 3.0, Procedures for Making Requests for Plan Reviews and Construction-Related Inspections covers details pertaining to plan reviews, consultations, or construction inspections.
The Recommended Shipbuilding Construction Guidelines for Cruise Vessels Destined to Call on U.S. Ports, has been renamed as the Vessel Sanitation Program Construction Manual (referred to in this documents as "these guidelines"). The main purpose of these guidelines is to provide a framework of consistent construction and design guidelines that protect passenger and crew health. CDC is committed to promoting high construction standards to protect the public's health. Compliance with these guidelines will help to ensure a healthy environment on cruise vessels.
CDC reviewed many references from a variety of sources to develop this document. These references are indicated in Section 32.2, Standards, Codes and Other References Reviewed for Guidance.
These guidelines cover various components of the vessel's facilities related to public health, including food storage, preparation, and service; water bunkering, storage, disinfection, and distribution. Vessel owners and operators may select the design and equipment that best meets their needs. However, the design and equipment must also meet the sanitary design criteria of the American National Standards Institute (ANSI) or equivalent organization, and VSP's routine operational inspection requirements.
These guidelines are not meant to limit the introduction of new designs, materials or technology for shipbuilding. A shipbuilder, owner, manufacturer, or other interested party may request VSP to periodically review or revise these guidelines in relation to new information or technology. VSP reviews such requests in accordance with the criteria described in Section 2.0, "Revisions and Recommended Changes."
New cruise vessels must comply with all international code requirements (e.g., International Maritime Organization Conventions). Those include requirements of the Safety of Life-at-Sea Convention (SOLAS), International Convention for the Prevention of Pollution from Ships (MARPOL), Tonnage and Load Line Convention, International Electrical Code (IEC), International Plumbing Code (IPC), and International Standards Organization (ISO). This document does not cross-reference related and sometimes overlapping standards that new cruise vessels must meet.
These guidelines went into effect on June 1, 2005. They apply to vessels that lay keel or perform any major renovation (e.g., any changes to the structural elements of the vessel covered by these guidelines) after this date. The guidelines do not apply to minor renovations such as the installation or removal of single pieces of equipment, (refrigerator units, bains-marie units, etc.) or single pipe runs. These guidelines will apply to all areas of the vessel affected by a renovation. VSP will inspect the entire vessel in accordance with the VSP Operations Manual during routine vessel sanitation inspections and reinspections.
# Revisions and Changes
VSP periodically reviews and revises these recommendations in coordination with industry representatives and other interested parties to stay abreast with industry innovations. A shipbuilder, owner, manufacturer, or other interested parties may ask VSP to review a construction guideline on the basics of new technologies, concepts, or methods. Recommendations for changes or additions to these guidelines must be submitted in writing, to the Chief, VSP (see Section 33.2 for contact information). The recommendation should:
- identify the section to be revised,
- describe the proposed change or addition,
- state the reason for recommending the change or addition, and - include research or test results and any other pertinent information that support change or addition.
# Procedures for requesting Plan Reviews, Consultations, and Construction-Related Inspections
VSP will coordinate a professional evaluation and consult with industry to determine whether to include the recommendation in the next revision.
VSP gives special consideration to shipyards and owners of vessels that have had plan reviews conducted before an effective date of a revision of these guidelines. This helps limit any burden placed on the shipyards and owners to make excessive changes to previously agreed upon plans.
VSP will ask industry representatives and other knowledgeable parties to meet with VSP representatives periodically to review the guidelines and determine whether changes are necessary to keep up with the innovations in the industry.
To coordinate or schedule a plan review or construction-related inspection submit an official written request to the VSP Chief as early as possible in the planning, construction, or renovation process. Requests that require foreign travel must be received in writing at least 60 days before the intended visit. The request will be honored, depending on VSP staff availability. A complete listing of contact addresses and telephone numbers can be found in Section 33.2.
After the initial contact, VSP assigns primary and secondary officers to coordinate with the vessel owner and shipyard. Normally two officers will be assigned. These officers are the points of contact for the vessel from the time the plan review and subsequent consultations take place through the final construction inspection.
The vessel representatives should provide points of contact to represent the owners, the shipyard, and key subcontractors. All parties will use these points of contact during consultations between any of the parties and VSP to ensure awareness of all consultative activities after conducting the plan review.
# Plan Reviews and Consultations
VSP normally conducts plan reviews for new construction a minimum of 18-24 months before the vessel is scheduled for delivery. The time required for major renovations varies. To allow time for any necessary changes, VSP coordinates the plan reviews for such projects well before the work begins. Plan reviews normally take two working days. They are conducted in Atlanta, Georgia; Fort Lauderdale, Florida; or other agreed upon sites. Normally, two VSP officers will be assigned to the project. Representatives from the shipyard, the vessel owner, and the subcontractor(s) who will be doing most of the work should attend the review. They should bring all pertinent plans or drawings and equipment specifications for the areas covered in these guidelines. That includes but is not limited to the following:
- general arrangement plans;
- all food-related storage, preparation, and service area plans;
- potable and non-potable water system plans with details on water inlets, (e.g., sea chests, overboard discharge points, and backflow protection devices); - ventilation system plans; and, if applicable;
- swimming pool and whirlpool spa plans.
VSP will prepare a Plan Review Report summarizing the recommendations made during the plan review and will submit the report to the shipyard and owner representatives.
Following the plan review, the shipyard will provide: 1) a complete set of plans or drawings and specifications for the vessel; 2) any redrawn plans and; 3) a statement of corrective action outlining how each of the items identified in the Plan Review Report will be corrected, and 4) copies of any major change orders in the areas covered by these guidelines that are made after the plan review.
While the vessel is being built, shipyard representatives, the owner or other vessel representatives may direct questions or requests for consultative services to the VSP project officers. Direct these questions or requests in writing to the officer(s) assigned to the project. Include fax number(s) and an e-mail address(es) for appropriate contacts. VSP officer(s) will coordinate the request with the owner and shipyard points of contact designated during the plan review.
# On-Site Construction Inspections
VSP conducts most on-site or shipyard construction inspections in shipyards outside the United States. A formal written request must be submitted to the VSP Chief 60 days before the inspection date so that VSP can process the required foreign travel orders for VSP officers (see Section 3.0). A sample of a request is shown in Section 33.1. VSP encourages shipyards to contact the Chief, VSP to and coordinate on-site construction inspections well before the 60 day minimum to better plan the actual inspection dates. If a shipyard requests an on-site construction inspection, VSP will advise the vessel owner of the inspection dates so that the owner's representatives are present. An on-site construction inspection normally requires the expertise of one to three officers, depending on the size of the vessel and whether it is the first of a hull design class or a subsequent hull in a series of the same class of vessels. The inspection, including travel, generally takes 5 working days. The on-site inspection should be conducted approximately 4 to 5 weeks before delivery of the vessel when 90% of the areas of the vessel to be inspected are completed. VSP will provide a written report to the party that requested the inspection. After the inspection, and before the ship's arrival in the United States, the shipyard will submit to VSP a statement of corrective action outlining how it will address and correct each item identified in the inspection report.
# Final Construction Inspections
At the request of a vessel owner or shipyard, VSP may conduct a final construction inspection. To schedule the inspection, the vessel owner or shipyard will submit a formal, written request the Chief, VSP as soon as possible after the vessel is completed, or a minimum of 10 days before its arrival in the United States. At the request of a vessel owner or shipyard and provided the vessel is not entering the United States market immediately, VSP may conduct final construction inspections outside the United States (see requirements for foreign travel in section 3.2 On-Site Construction Inspections). If a final construction inspection is not requested, VSP generally will conduct an unannounced operational inspection within 4 weeks following the vessel's arrival in the United States. VSP conducts operational inspections in accordance with the VSP Operations Manual.
As soon as possible after the final construction inspection, the vessel owner or shipyard will submit a statement of corrective action to VSP. The statement will outline how they will address each item cited in the inspection report, including the projected date of completion. VSP generally schedules vessels that undergo final construction inspection in the United States for an unannounced operational inspection within 6 weeks of the vessel's final construction inspection. VSP conducts operational inspections in accordance with the VSP Operations Manual.
# Equipment Standards, Testing, and Certification
Although these guidelines establish certain standards for equipment and materials installed on cruise vessels, VSP does not test, certify, or otherwise endorse any equipment or materials used by the cruise industry. Instead, VSP recognizes certification from independent testing laboratories such as NSF International, Underwriter's Laboratories (UL), the American National Standards Institute (ANSI), or other accredited institutions.
In most cases, independent testing laboratories test equipment and materials to certain minimum standards which generally, but not always meet the recommended standards established by these guidelines. Equipment built to questionable standards will be reviewed by a committee of VSP, the cruise ship industry and independent testing organization participants. The committee will determine if the equipment meets the recommended standards established in these guidelines. Copies of test or certification standards are available from the independent testing laboratories. Equipment manufacturers and suppliers will not refer to VSP to approve their products.
# General Definitions
Accessible -Can be exposed for cleaning and inspection with the use of simple tools such as a screwdriver, pliers, or an open-end wrench.
Air-break -A piping arrangement in which a drain from a fixture, appliance, or device discharges indirectly into another fixture, receptacle, or interceptor at a point below the flood-level rim. (Figure 1)
Air-gap -The unobstructed vertical distance through the free atmosphere between the lowest opening from any pipe or faucet supplying water to a tank, plumbing fixture, or other device and the flood-level rim of the receptacle or receiving fixture. The air-gap must be at least twice the diameter of the supply pipe or faucet or at least 25 mm (1 inch). (Figure 2) Backflow -The flow of water or other liquids, mixtures, or substances into the distribution pipes of a potable supply of water from any source or sources other than the potable water supply. Back-siphonage and back-pressure are forms of backflow.
Backflow, check, or non-return valve -A mechanical device installed in a waste line to prevent the reversal of flow under conditions of back-pressure. In check-valves, the flap should swing into a recess when the line is flowing full so that it does not obstruct the flow.
Backflow preventer-An approved backflow prevention plumbing device that must be used on potable water distribution lines where there is a direct connection or a potential connection between the potable water distribution system and other liquids, mixtures, or substances from any source other than the potable water supply. Some devices are designed for use under continuous water pressure, whereas others are non-continuous pressure types. Perform a thorough review of the water system to ensure proper protection of the water supply, to confirm that the appropriate device is selected for each specific application. The following are general types of backflow preventers and their uses:
- Atmospheric vacuum breaker -An approved backflow prevention plumbing device used on potable water lines where shut-off valves do not exist downstream from the device. The device is not approved for use under continuous water pressure. An atmospheric vacuum breaker must be installed at least 152 mm (6 inches) above the flood level rim of the fixture or container to which it is supplying water.
- Continuous pressure backflow preventer -An approved backflow prevention plumbing device with two check valves and an intermediate atmospheric vent. It is designed and approved for use under continuous water pressure (e.g., when shut-off valves are located downstream from the device).
- Hose bib connection vacuum breaker -An approved backflow prevention plumbing device that attaches directly to a hose bib by way of a threaded head. This device uses a single check valve and vacuum breaker vent. It is not approved for use under continuous pressure (e.g., when a shut-off valve is located downstream from the device).
- Reduced Pressure Principle Backflow Prevention Assembly (RP assembly) -An assembly containing two independently acting approved check valves together with a hydraulically operating, mechanically independent pressure differential relief valve located between the check valves and at the same time below the first check valve. The unit must include properly located resilient seated test cocks and tightly closing resilient seated shutoff valves at each end of the assembly.
Back-siphonage -The backward flow of used, contaminated, or polluted water from a plumbing fixture or vessel or other source into a water-supply pipe as a result of negative pressure in the pipe.
Black water -Waste from toilets, urinals, medical sinks, and similar facilities.
Blast chiller -A unit specifically designed for rapid intermediate chilling of food products to 21°C (70°F) within 2 hours and 5°C (41°F) within an additional 4 hours.
Child activity facility -A designated area for use by children who do not require assistance using toilet rooms and who may be old enough to come and go on their own.
Child care facility -A designated area for use by children who are not yet out of diapers or require supervision when using the toilet rooms, and who are cared for by vessel staff.
Child-size toilet -Toilets whose toilet seat height is between 280-380 mm (11-15 inches) and the water closet center line is between 305-380 mm (12-15 inches). This can be achieved by installing a smaller water closet or by providing a deck platform at the front of the water closet and variably sized, fold-down toilet seats.
Cleaning room -A room specifically designed for storage of cleaning equipment such as mops, brooms, floor scrubbing machines, and cleaning chemicals. The room may or may not include a sink for filling buckets and washing mops.
Corrosion-resistant -Material that maintains its original surface characteristics through prolonged influence by the use environment, food contact, and normal use of cleaning compounds and sanitizing solutions.
Coved -A curved or concave surface, molding, or other design that eliminates the usual joint angles of 90° or less. (Figures 3 and 4)
Crew toilet room -Those toilets located near food preparation areas and intended for use by food service personnel.
Cross-connection -Any unprotected, actual or potential connection or structural arrangement between a public or a consumer's potable water system and any other source or system through which it is possible to introduce into any part of the potable system any used water, industrial fluid, gas, or substance other than the intended potable water with which the system is supplied. Bypass arrangements, jumper connection, removable section, swivel or change-over devices and other temporary or permanent devices which or because of which backflow can occur are considered to be cross-connections.
Deck drain -The physical connection between decks, scuppers, or deck sinks to the gray or black water systems.
Deck sink -A sink recessed into the deck, sized to contain waste liquids from tilting kettles and tilting pans.
Drip tray -Readily removable tray to collect dripping food from a food dispensing mechanism.
Easily cleanable -Fabricated with a material, finish, and design that allows for cleaning by normal methods.
Food contact surfaces -Surfaces (food zone, splash zone) of equipment and utensils with which food normally comes in contact and surfaces from which food may drain, drip, or splash back onto surfaces normally in contact with food. This includes those areas of ice-making machines where the ice is produced and above the connecting chute between the maker and the storage bin. It does not include the technical compartment where the compressor is located. (figure 5)
Food display areas -Any area where food is displayed for consumption by passengers and/or crew.
Food handling areas -Any area where food is stored, processed, prepared, or served.
Food preparation areas -Any area where food is processed, cooked, or prepared for service.
Food service areas -Any area where food is presented to passengers or crew members (excluding individual cabin service).
Food storage areas -Any area where food or food products are stored.
Food transport areas -Any area through which unprepared or prepared food is transported during food storage, preparation, and service operations (excluding public areas and individual cabin service).
Food waste system -Food waste transport system (e.g., pulper, vacuum system).
Gray water -All wastewater including drainage from galleys, dishwashers, showers, laundries, bath, washbasin, deck drains, and swimming pool and whirlpool spas. It does not include black water or bilge water from the machinery spaces.
# Gutterway -See scupper
Keel laying -The date at which construction identifiable with a specific ship begins and when assembly of that ship comprises at least 50 tons or 1% of the estimated mass of all structural material, whichever is less.
Non-food contact surfaces (non-food zone) -All exposed surfaces, other than food contact or splash contact surfaces, of equipment located in food storage, preparation and service areas. (figure 5) nonabsorbent nontoxic Non-potable water (Technical Water) -Fresh water that may not be halogenated and is intended for use in technical and other areas where potable water is not required (e.g., laundries, engine room, toilets, waste-treatment areas, and for washing decks in areas other than the vessel's hospital, food service, preparation, or storage areas).
Potable water -Fresh water that is intended for drinking, washing, bathing, or showering; for use in fresh water swimming pools and whirlpool spas; for use in the vessel's hospital; for handling, preparing, or cooking food; and for cleaning food storage and preparation areas, utensils, and equipment.
Potable water tanks -All tanks in which potable water is stored from bunkering and production for distribution and use as potable water.
Portable -A description of equipment that is readily removable or mounted on casters, gliders, or rollers; provided with a mechanical means so that it can be tilted safely for cleaning; or readily movable by one person.
Readily accessible -Exposed or capable of being exposed for cleaning or inspection without the use of tools.
Readily removable -Capable of being detached from the main unit without the use of tools.
Removable -Capable of being detached from the main unit with the use of simple tools such as a screwdriver, pliers, or an open end wrench.
Safe material -An article or material that would not be expected to become a component of any food or otherwise affect the characteristics of any food. Also, an additive or other materials used as specified in Section 409 or 706 of the Federal Food, Drug, and Cosmetic Act or in conformity with applicable regulations of the U.S. Food and Drug Administration (FDA).
Scupper -A conduit or collection basin that channels liquid runoff to a deck drain.
Sealant -Material used to fill seams to prevent the entry or leakage of liquid or moisture.
Sealed -Having no openings present that will permit the entry of soiled material or seepage of liquids.
Sealed seam -A seam that has no openings that would permit the entry of soil or liquid seepage.
Seam -An open juncture between two similar or dissimilar materials. Continuously welded junctures, ground and polished smooth, are not considered seams.
Sewage (black water) -Any liquid waste that contains animal or vegetable matter in suspension or solution, including liquids that contain chemicals in solution.
Smooth -means: a) A food contact surface that is free of pits and inclusions with a cleanability equal to or exceeding that of a No. 3 finish (100 grit) on stainless steel; b) A non-food contact surface of equipment that is equal to commercial grade hot-rolled steel and is free of visible scale; and c) A deck, bulkhead, or deckhead that has an even or level surface with no roughness or projections that renders it difficult to clean.
Spa pool -A fresh or saltwater supplied pool with temperatures and turbulence comparable to a whirlpool spa, but with a water depth and volume more comparable to a swimming pool. General characteristics are - water temperature of 30°C-40°C or 86°F-104°F,
- bubbling or jetted water effects that physically break at the water surface,
- depth of more than 1 m (3 feet),
- shape is normally non-circular, and - volume exceeds 6 tons of water.
# Splash contact surfaces (non-food zone)
-Surfaces that are subject to routine splash, spillage or other soiling during normal use.
Direct splash surfaces -Areas adjacent to food contact surfaces that are subject to splash, drainage, or drippage onto food contact surfaces. Considered food contact surfaces.
Indirect splash surfaces -Areas adjacent to food contact surfaces that are subject to splash, drainage, drippage, condensation, or spillage from food preparation and storage. Considered non-food contact surfaces.
Technical water -Fresh water NOT intended for: 1) drinking, washing, bathing, or showering; 2) use in the vessel's hospital; 3) handling, preparing, or cooking food; or 4) cleaning food storage and preparation areas, utensils, and equipment.
Temperature measuring devices (TMDs) -Thermometers or other instruments that measure relative heat and cold according to an established scale. TMDs that are scaled in Celsius, Fahrenheit, or both must be designed to be easily readable and accurate to ± 1.5°C or 3°F.
Transportation corridors -Areas primarily intended to move unprepared or prepared food during food preparation, storage, and service operations (e.g., service lift (elevator) vestibules to food preparation service and storage areas, and corridors connecting preparation areas and service areas). Marshalling, provisions areas, passenger/corridors, public areas, and dinning rooms connected to galleys are excluded.
TMD -See temperature measuring device.
Utility sink -Any sink located in a food service area not intended for handwashing and/or warewashing.
Whirlpool spa -A freshwater pool designed to operate at a minimum temperature of 30°C (86°F) and equipped with either water or air jets.
# General Facilities Requirements
# Size and Flow
Many factors determine and influence the size of rooms and work areas and the flow of food through a vessel. Those can include the size of the vessel, number of passengers and crew, types of foods or menus, number of meals or mealtimes, service or presentation of meals, itinerary, and the vessel owner's experience. In general, food storage, preparation, and service areas; warewashing areas; and waste management areas must be sized to accommodate the vessel's full capacity of passengers and crew. Bulk food storage areas or provision rooms (e.g., frozen stores, refrigerated stores, and dry stores) must be sized to prevent bulk foods from being stored in provisions passageways unless specifically designed to meet provision room standards (Section 15.0). Refrigeration and hot-food holding facilities, including temporary storage facilities, must be available for all food preparation and service areas and for foods being transported to remote areas.
Arrange the flow of food through a vessel in a logical sequence that eliminates or minimizes cross-traffic or backtracking and that allows clear separation of clean and soiled operations. Provide an orderly, functional flow of food from the purveyor at dockside through the storage, preparation, and finishing areas to the service areas and finally, to the waste management area. The goal is to prepare and serve food smoothly and rapidly in accordance with strict time and temperature-control requirements and to minimize time and handling.
VSP evaluates the size of a particular room or area and the flow of food through the vessel to those rooms or areas initially and primarily during the plan review process.
# Equipment Requirements
The following is a list of equipment required in galleys, depending on the level, and type of service, with recommendation for other areas:
6.2.1.1 Blast chillers incorporated into the design of passenger and crew galleys. More than one unit may be necessary depending on the size of the vessel, the unit's intended application, and the distances between the chillers and the storage and service areas.
Food preparation sinks in as many areas as necessary (e.g., in all meat, fish, and vegetable preparation rooms; cold pantries or garde mangers; and in any other areas where personnel wash or soak food). An automatic vegetable washing machine may be used in addition to food preparation sinks in vegetable preparation rooms;
Equip the main pot washing area that serves the full galley operation with a minimum of a three-compartment sink with a prewash station or a four compartment sink with an insert pan and an overhead spray. Install a sink that is large enough to accommodate the largest piece of equipment (pots, tableware, etc.) used in its designated serving area. If desired, use an automatic warewashing machine with separate prewash stations in addition to the threecompartment sinks, if the machines are sized to accommodate the equipment being washed. A front-loading, pass-through, or conveyor type warewashing machine is preferable to an under counter model.
Provide additional three-compartment sinks with prewash stations or fourcompartment sinks with insert pans and overhead spray in heavy-use areas.
Those may include bakeries, butcher shops, and other preparation areas where the size of the facility or distance makes use of a central pot washing area impractical.
Equip all food preparation areas with easy access to a three-compartment sink, or a warewashing machine with an adjacent dump sink and pre-wash hose.
Furnish beverage dispensing equipment with readily removable drip trays or built-in drains in the tabletop. Furnish bulk milk dispensers with readily removable drip trays.
Provide readily removable drip trays for condiment dispensing equipment.
Design storage areas to accommodate all equipment and utensils used in food preparation areas such as ladles and cutting blades.
Ensure that the design of installed equipment directs food and wash water drainage into a deck drain, scupper, or deck sink, and not directly or indirectly onto a deck.
Provide a utility sink in areas such as beverage stations where it is necessary to refill pitchers or dispensers or discard liquids such as coffee.
Provide ice cream, sherbet, or a similar product dipper wells with running water and proper drainage.
Provide tight-fitting doors or protective closures to ice bins, food display cases, and other food and ice holding units to prevent contamination of stored products.
Protect countertop openings and rims of food cold tops, bains-marie, ice wells, and other drop-in type food and ice holding units with a raised integral edge or rim of at least 5 mm (3/16 inch) above the counter level around the opening.
# Equipment Surfaces
Ensure that material used for food contact, splash contact and exposed non-food contact surfaces are smooth, durable, and non-corroding. They should be easily cleanable and designed without unnecessary edges, projections, or crevices.
Use only materials approved for contact with food on food contact surfaces. Make all food contact surfaces smooth, durable, non-corroding, easily cleanable, readily accessible, and maintainable. Provide coved preferable seamless corners in accordance with current sanitary standards for food service equipment. Form external corners and angles with a sufficient radius to permit proper drainage and without sharp edges. Use only sealants approved for food contact surfaces (certified to ANSI/NSF Standard 51, or equivalent criteria) on food contact and food splash surfaces. Use approved sealants in limited application when practical function or design requires, such as the joining surfaces between ice makers and bins. Avoid excessive use of sealant.
Use materials approved for food contact surfaces for splash contact surfaces. Design surfaces so they are smooth with no sharp edges, durable, non corroding, readily accessible, and easily cleanable.
Use durable and non-corroding material for non-food contact surfaces. Design surfaces so that they are smooth, easily cleanable, and accessible material.
# Bulkheads, Deckheads and Decks
6.4.1 Do not use exposed fasteners in bulkhead and deckhead construction. Seal all seams between adjoining bulkhead panels, deckhead panels, and between bulkhead and deckhead panels. Seal seams greater than 0.8 mm (1/32 inch), but less than 3 mm (⅛ inch), with an appropriate sealant or appropriate profile strips. Cover all seams greater than 3 mm (⅛ inch) with appropriate profile strips. Seal all bulkhead, deckhead, and deck penetrations through which pipes or other conduits pass, including those located inside technical compartments. Use durable and corrosion-resistant collars where gaps are greater than 3 mm (⅛ inch).
Reinforce all bulkheads sufficiently to prevent panels from buckling or becoming detached under normal operating conditions.
Weld door penetration indentations completely so that there are no open voids. Ensure that locking and latch pins insert into inverted nipple recesses. This also applies to the penetrations around fire doors, in thresholds, and bulkhead openings.
Install durable coving of at least a 9.5 mm (3/8 inch) radius or open design (> 90 degrees ) as an integral part of the deck and bulkhead interface and at the juncture between decks and equipment foundations. Provide coving that is durable, of sufficient thickness, and securely fastened.
Use material for decks that is hard, durable, easily cleanable, non-skid, and non-absorbent.
Install durable vinyl or linoleum deck coverings in staff, crew or officer dining areas only.
Seal all pipe and conduit deck penetrations.
Use compatible metals to minimize corrosion due to galvanic action or provide effective insulation techniques between dissimilar metals to protect them from corrosion.
# Deck Drains, Deck Sinks and Scuppers
6.5.1 Construct deck drains, scuppers, and deck sinks from stainless steel with smooth finished surfaces that are accessible for cleaning, designed to drain completely, and large enough to prevent overflow to adjacent deck surfaces.
Construct scupper, and deck sink cover grates from stainless steel or other materials that: 1) meet the requirements for a smooth, easily cleanable surface; 2) are strong enough to maintain the original shape; and 3) exhibit no sharp edges. Install scupper and deck sink cover grates that are tight-fitting, readily removable for cleaning, and uniform in length where practical (e.g., 1,000 mm or 40 inches), so that they are interchangeable.
Place deck drains, and deck sinks in low-traffic areas such as in front of soup kettles, boilers, tilting pans, or braising pans. Size the deck drains, scuppers, and sinks in order to eliminate spillage and overflow to adjacent deck surfaces.
Provide sufficient deck drainage in all food service areas to prevent liquids from pooling on the decks. 6.5.5 Design deck and scupper drain lines to drain at a sufficient rate, relative to nearby water supplies, to avoid pooling. Provide cross-drain connections to prevent ponding and spillage from the scupper when the vessel is listing. 6.5.6 Do not use deck sinks as substitutes for deck drains. Independent deck drains are required.
6.6 Ramps 6.6.1 Ensure that ramps over thresholds are easily removable or sealed in place, sloped for easy roll-in and roll-out of trolleys, and are strong enough to maintain their shape. If ramps over scupper covers are built as an integral part of the scupper system, construct them of cleanable and durable material. 6.7 Gray and black water drain lines 6.7.1 Limit the installation of drain lines that carry sewage or other liquid waste directly overhead or horizontally through spaces used for food preparation or storage. That includes areas for washing or storage of utensils and equipment, such as bars, deck pantries, and over buffet counters. Sleeve-weld, or butt weld steel pipe; and heat fuse, or chemically weld plastic pipe. Do not use push-fit or press-fit piping over these areas.
# General Hygiene Facilities Requirements
# Handwashing Stations
7.1.1 Provide hot and cold potable water to all handwashing sinks. 7.1.1.a Equip handwashing sinks to provide water at a temperature between 43°C (110°F) and 52°C (125°F) through a mixing valve or combination faucet.
Construct handwashing sinks of stainless steel in food handling, preparation and storage areas. Construct handwashing sinks in food service areas of stainless steel or similar, durable materials.
Provide handwashing stations that include a suitable soap dispenser, paper towel dispenser, corrosion-resistant waste receptacle, and where necessary, splash panels to protect adjoining equipment. If attached to the bulkhead, permanently seal or make readily removable for cleaning paper towel dispensers and waste towel receptacles.
Provide at least one bucket filling station in each area of the galleys (e.g., cold galley, hot galley, bakery, etc.), food storage, and food preparation areas, below the handwashing sinks. Supply hot and cold potable water through a mixing valve to a faucet with the appropriate backflow protection at each bucket filling station. Provide appropriate deck drainage (e.g., scupper or sloping deck to deck drain) under all bucket filling stations to eliminate any pooling of water on the decks below the bucket filling station. 7.1.5 Locate handwashing stations throughout food handling, preparation, and warewash areas, so that no employee must walk more than 8000 mm (25 feet) to reach a station or pass through a normally closed door. 7.1.5.a Install handwash sinks approximately 750 mm (30 inches) above the deck.
# 7.1.5.b
Position the handwash sink so employees do not have to squat or reach excessively to wash their hands. 7.1.5.c Provide a handwashing station at food dispensing waiter stations (e.g., soups, ice, etc.), where the staff does not routinely return to an area with a handwashing station. 7.1.5.d Provide a handwashing station in provision areas where bulk raw foods are handled by provisioning staff. 7.1.5.e Provide at least one handwashing station for every 100 seats, (e.g., 1-100 seats = one handwashing station, 101-200 seats = two handwashing stations, etc.) at the entrance of all officer/staff/crew mess areas where food service lines are "self-service."
Install a sufficient number of handwashing sinks at the soiled dish drop-off area(s) in the main galley to allow quick turn-around time for employees bringing soiled dishware from the dining rooms or other food service areas and to prevent long waiting lines at handwashing stations.
Provide at least one handwashing station at soiled linen handling areas of the main laundry.
Install easy-to-operate, sanitary faucet handles, (e.g., elephant ear handles, foot pedals, knee pedals, or electronic sensors) on handwashing sinks in food service areas. If a faucet is self-closing, slow-closing, or metering, provide a water flow of at least 15 seconds without the need to reactivate the faucet.
Install permanent signs in English, and in other languages where appropriate, stating at a minimum, "WASH HANDS OFTEN."
# Crew Toilet Rooms
Install employee toilet rooms in proximity to the work area of all food preparation areas.
Supply toilet rooms with exhaust ventilation and equip them with handwashing facilities. Install permanent signs in English, and other languages where appropriate, stating at a minimum "WASH HANDS AFTER USING TOILET."
Install tight-fitting, self-closing doors to control insects/vermin and odors in toilet rooms or water closets inside toilet rooms.
Construct decks of hard, durable materials and cove the bulkhead-deck juncture.
Install easily cleanable deckheads and bulkheads.
# Equipment Placement and Mounting
Provide at least 150 mm (6 inches) of clear, unobstructed space between adjacent equipment and between the equipment and bulkheads, when the distance to be cleaned is less than 600 mm (24 inches).
Provide at least 200 mm (8 inches) of clear, unobstructed space between adjacent equipment and between the equipment and bulkheads when the distance to be cleaned is greater than 600 mm (24 inches) but less than 1200 mm (48 inches) long.
Provide at least 300 mm (12 inches) of clear, unobstructed space between adjacent equipment and between the equipment and bulkheads when the distance to be cleaned is greater than 1200 mm (48 inches) but less than 1800 mm (72 inches) long.
Provide at least 460 mm (18 inches) of clear, unobstructed space between adjacent equipment and between the equipment and bulkheads when the distance to be cleaned is greater than 1800 mm (72 inches).
Continuous weld all equipment that is not classified as portable to stainless steel pads or plates on the deck. Make sure the welds have smooth edges, rounded corners, and no gaps. Attach equipment as an integral part of the deck surface with glue, epoxy, or other durable adhesive product. Ensure that the arrangement is smooth and easily cleanable.
Seal deck-mounted equipment that is not easily movable to the deck or elevate it on legs that provide at least a 150 mm (6 inch) clearance between the deck and the equipment. If no part of the deck under the deck-mounted equipment is more than 150 mm (6 inches) from the point of cleaning access, the clearance space may be only 100 mm (4 inches). Exceptions also may be granted if there are no barriers to cleanability, (e.g., equipment, such as waste handling systems and warewashing machines with pipelines, motors, and cables below whiche 150 mm clearance from the deck may not be practical).
Provide a minimum of at least 150 mm (6 inches) between equipment and the deckheads. If proper clearance cannot be achieved, extend the equipment through the deckhead panels and seal appropriately.
Mount equipment that is on a foundation or coaming at least 100 mm (4 inches) above the finished deck. Use cement or a continuous weld to seal equipment to the foundation or coaming. Provide a sealed-type foundation or coaming for equipment not mounted on legs. Do not allow equipment to overhang the foundation or coaming by more than 100 mm (4 inches). Completely seal any overhang(ing) equipment along the bottom (Figure 6).
Seal table-mounted equipment, unless portable, to the tabletop or mount on legs.
The length of the legs is dependent upon the horizontal distance of the table top under the equipment from either end to the farthest point requiring cleaning.
8.6.1.a Mount the equipment on legs at least 100 mm (4 inches) above the tabletop if the horizontal distance of the table top under the equipment is 500 mm (20 inches) or greater from the point of access for cleaning.
# 8.6.1.b
Mount the equipment on legs at least 75 mm (3 inches) above the tabletop if the horizontal distance of the table top under the equipment is less than 500 mm (20 inches) or greater than 75 mm (3 inches) from the point of access for cleaning.
# 8.6.1.c
Mount the equipment on legs at least 50 mm (2 inches) above the tabletop if the horizontal distance of the table top under the equipment less than 75 mm (3 inches) from the point of access for cleaning. 8.6.2 Provide access behind tabletop mounted equipment, including beverage line equipment, for cleaning.
# Fasteners and Requirements for Securing and Sealing Equipment
9.1 Food Contact Surfaces 9.1.1 Attach all food contact surfaces or connections from food contact surfaces to adjacent splash zones to ensure a seamless, coved corner. Reinforce all bulkheads, deckheads, or decks receiving such attachments. 9.1.2 Use low profile, non-slotted, non-corroding, and easy to clean fasteners on food contact surfaces and in food splash zones. The use of exposed slotted screws, Phillips head screws or pot rivets in these areas is prohibited.
# Non-Food Contact Surfaces
9.2.1 Seal non-food contact surfaces of equipment, gaps, and seams less than 3 mm (⅛ inch) with an appropriate sealant. Use only stainless steel profile strips on surfaces exposed to extreme temperatures (e.g., freezers, and above cook tops, grills, and fryers) or for gaps greater than 3 mm (⅛ inch). Avoid excessive use of sealant.
Construct slotted or Phillips head screws, pop rivets, and other fasteners used in non-food contact areas of corrosion-resistant materials.
# Use of Sealants
Use approved food grade sealants in food contact and food splash zones.
# Latches, Hinges, and Handles
10.1 Use durable, non-corroding, and easily cleanable built-in equipment latches, hinges, and handles. Do not use piano hinges in food contact or splash zones.
# Gaskets
11.1 Use smooth, non-absorbent, non-porous materials for equipment gaskets in reach-in refrigerators, steamers, ice bins, ice cream freezers, and similar equipment.
Close and seal exposed surfaces of gaskets at their ends and corners.
Use refrigerator door gaskets that are designed to be removable.
Follow the requirements in Section 9.0 when using fasteners to install gaskets.
# Equipment Drain Lines:
12.1 Connect drain lines from the following to appropriate waste systems by means of an or air-break all fixtures, sinks, appliances, compartments, refrigeration units, or devices that are used, designed for, or intended to be used in the preparation, processing, storage, or handling of food, ice, or drinks.
12.1.1 Use stainless steel or other easily cleanable rigid or flexible material in the construction of drain lines. Size drain lines appropriately, with a minimum interior diameter of 25 mm (1 inch) for custom-built equipment.
12.1.2 Slope walk-in refrigerators and freezer evaporator drain lines, and extend them through the bulkheads or decks. Direct drain lines through an accessible air-break to a deck scupper or drain below the deck level or to a scupper outside.
12.1.3 Install drain lines to minimize the horizontal distance from the source of the drainage to the discharge.
12.1.4 Install horizontal drain lines at least 100 mm (4 inches) above the deck and slope to drain.
12.2 All drain lines (except condensate drain lines) from hood washing systems, cold top tables, bains-marie, dipper wells, food preparation sinks and warewashing sinks or machines must: 12.2.1 be less than 1000 mm (40 inches) and free of sharp angles or corners, if designed to be cleaned in place by a brush.
12.2.2 be readily removable for cleaning, if greater than 1000 mm (40 inches).
# drain through an air-break to a drain or scupper.
12.3 Extend all installed equipment drain lines in a vertical line to a scupper, or deck drain, when possible. If not possible, keep the horizontal distance of the line to a minimum.
Handwashing sinks, mop sinks and drinking fountains are not required to drain through an air-break.
# Electrical Connections, Pipelines, and other Attached Equipment
13.1 Encase electrical wiring from permanently installed equipment in durable and easily cleanable material. Do not use braided or woven stainless steel electrical conduit outside of technical spaces or where it is subject to splash or soiling, unless encased in easily cleanable plastic or similar easily cleanable material. For equipment that is not permanently mounted, adjust the length of electrical cords or fasten them in a manner that prevents the cords from lying on countertops.
13.2 Tightly seal bulkhead or deckhead-mounted equipment (phones, speakers, electrical control panels, outlet boxes, etc.) with the bulkhead or deckhead panels. Do not locate such equipment in areas exposed to food splash.
Tightly seal any areas where electrical lines, steam or water pipelines, etc., penetrate the panels or tiles of the deck, bulkhead, or deckhead, including inside technical spaces located above or below equipment or work surfaces. Seal any openings or voids around the electrical lines or the steam or water pipelines and the surrounding conduit or pipelines.
Enclose steam and water pipelines to kettles and boilers in stainless steel cabinets or position the pipelines behind bulkhead panels. Minimize the number of exposed pipelines. Cover any exposed, insulated pipelines with stainless steel or other durable, easily cleanable material.
# Hood Systems
14.1 Install hood systems or direct duct exhaust over warewashing equipment (except undercounter warewashing machines) and over three-compartment sinks in pot wash areas where hot water is used for sanitizing.
Directly connect warewashing machines that have a direct duct exhaust, to the hood exhaust trunk.
Design exhaust hoods over warewashing equipment or threecompartment sinks to have a minimum 150 mm (6 inches) overhang from the edge of equipment to capture excess steam and heat.
Install a clean-out port in the direct exhaust ducts of the ventilation systems between the top of the warewashing machine and the hood system or deckhead.
Provide accessible and removable flat condensate drip trays in the ducts from the warewashing machines.
Install hood or canopy systems above cooking equipment in accordance with SOLAS requirements to ensure that they adequately remove excess steam and grease-laden vapors.
Install hood systems or dedicated local exhaust ventilation to control excess heat and steam from bains-marie or steam tables.
Select proper sized exhaust and supply vents. Position and balance them appropriately for expected operating conditions to ensure proper air conditioning, and capture and exhaust of heat and steam.
Where used, provide readily removable, and cleanable filters.
Provide access for cleaning vents and ductwork (Automatic clean-in-place systems are recommended for removal of grease generated from cooking equipment).
Locate the automatic clean-in-place hood wash control panels that have detergent reservoirs so they are not over food preparation equipment or counters.
Construct hoods systems of stainless steel with coved corners of at least 9.5 mm (3/8 inch) radius. Use continuous welds or profile strips on adjoining pieces of stainless steel.
A drainage system is not required for normal grease and condensate hoods, or if cleaning solutions are applied manually to hood assemblies.
Install drainage for automatic clean-in-place hood washing systems.
Install ventilation systems in accordance with the manufacturer's recommendations. Test the system by utilizing a method that determines if the system is properly balanced for normal operating conditions.
# Provision Rooms, Walk-in Refrigerators and Freezers, and Transportation Corridors
# Bulkheads and and Deckheads
15.1.1 Provide tight-fitting, stainless steel bulkheads in walk-in refrigerators and freezers. Line doors with stainless steel.
# 15.1.2.a
Light colored painted steel is acceptable for provision passageways and transportation corridors.
# 15.1.2.b
Stainless steel panels are preferable but not required in dry storage areas.
Provide protection to prevent damage to bulkheads from pallet handling equipment (e.g., forklifts, pallet jacks, etc.) in areas through which food is stored or transferred.
Close deckhead-mounted cable trays, piping or other difficult to clean deckhead-mounted equipment, or close the deckhead to prevent food contamination from dust and debris falling from deckheads and deckhead mounted equipment and utilities (painted sheet metal ceilings are acceptable in these areas).
# Decks
15.2.1 Use hard, durable, non-absorbent decking, (e.g., tiles, or diamond plate corrugated stainless steel deck panels) in refrigerated provision rooms. Install durable covings, and provision rooms s, and provision rooms as an integral part of the deck and bulkhead interface and at the juncture between decks and equipment foundations. If installed, use a sufficient thickness on stainless steel or other coving to make durable and secure. Sufficiently reinforce stainless steel decking to prevent buckling if pallet handling equipment will be used in these areas.
Steel decking is acceptable in provisions passageways, transportation corridors, and dry-stores areas.
# Cold Room Evaporators, Drip Pan, and Drain Lines
15.3.1 Enclose piping, wiring, coils, and other difficult-to-clean components of evaporators in walk-in refrigerators, freezers, and dry storerooms with stainless steel panels.
Use stainless steel evaporator drip pan that have coved corners, are sloped to drain and strong enough to maintain slope, and are readily accessible for cleaning.
Place non-corroding spacers between the drip pan brackets and the interior edges of the pans.
Follow all fastener guidelines in Section 9.0.
Provide a heater coil for freezer drip pan. Attach the coil to a stainless steel insert panel or to the underside of the drip pan. Use easily removable coils so that the drip pan can be cleaned. Make sure that heating coils provided for drain lines are installed inside of the lines.
Position and size the evaporator drip pan to collect all condensate dripping from the evaporator unit.
Encase thermometer probes in a stainless steel conduit. Position probes in the warmest part of the room where food is normally stored.
# Galleys, Food Preparation Rooms, and Pantries
# Bulkheads and Deckheads
16.1.1 Construct bulkheads and deckheads (including doors, door frames, and columns) with a high quality, corrosion-resistant stainless steel. Use a thick enough gauge so that the panels do not warp, flex, or separate under normal conditions. Use an appropriate sealant for seams greater than 1 mm (1/32 inch), but less than 3 mm (⅛ inch). Use only stainless steel profile strips for bulkhead and deckhead seams greater than 3 mm (⅛ inch).
# 16.1.1.a
Minimize gaps around fire shutters, sliding doors, and pass-through windows.
# 16.1.1.b
Provide cleaning access to void spaces of sliding doors and sliding pass-through windows.
Construct bulkheads of sufficient thickness or reinforce the areas where equipment is installed to allow the use of fasteners or welding without compromising the quality and construction of the panels.
Install utility line connections through a stainless steel or other easily cleanable, food service approved conduit that is mounted away from bulkheads for ease in cleaning.
Attach backsplashes to the bulkhead with low profile, non-slotted fasteners or continuous-or tack-welds, polished smooth. Use an appropriate sealant to make the backsplash attachment watertight.
Seal all openings where piping and other items penetrate the bulkheads and deckheads, including inside technical compartments.
# Decks
16.2.1 Construct decks from hard, durable, non-absorbent, non-skid material. Install durable coving as an integral part of the deck and bulkhead interface and at the juncture between decks and equipment foundations.
# Decks
Install hard, durable, non-absorbent decks at all buffet lines that are at least 1000 mm (40 inches) in width measured from the edge of the service counter or from the outside edge of the tray rail (if such a rail is present).
Install hard, durable, non-absorbent decks (e.g., tile, sealed granite, or marble) that extends at least 600 mm (24 inches) from the edge of the working side of the dining room service stations.
Construct and cove decks behind service counters, under equipment, and in technical spaces of hard, durable, non-absorbent materials (e.g., tiles, epoxy resin, or stainless steel). Do not use painted steel or concrete decking.
Durable linoleum, vinyl tile, or deck covering may be used only in staff, crew, or officers dining areas.
Cove and tightly seal all bulkhead and deck junctures (including deck/buffet, deck/bar, deck/waiter station).
# Food Display Protection
Provide effective means to protect food (e.g., sneeze shields or display cases) in all areas where food is on display for self-service.
Following these criteria for sneeze guards: 17.3.2.1 Sneeze guards may be temporary (portable), built-in and integral parts of display tables, bains-marie, or cold-top tables.
Sneeze guard panels must be durable plastic or glass that is smooth and easily cleanable. Use sections of manageable lengths that are removable for cleaning.
Position sneeze guards so that the panels intercept the line between the consumer's mouth and the displayed foods, in accordance with ANSI/NSF Standard 2 for food equipment. Take into account factors such as the height of the food display counter, the presence or absence of a tray rail, and the distance between the edge of the display counter and the actual placement of the food (Figure 7).
# 17.3.2.3.a
Install side protection for sneeze guards if the distance between exposed food and where people are expected to stand is less than 1000 mm (40 inches).
Use tray rail surfaces that are sealed, coved, or have an open design and easily cleanable in accordance with guidelines for food splash zones.
# Beverage Delivery System
17.4.1 Install a stainless steel, vented, double-check valve backflow prevention device on carbonation systems with brass or copper fittings (e.g., multi-flow beverage dispensing systems). Install the device before the carbonator and downstream from any copper or copper-alloy (e.g., brass) in the potable watersupply line.
Encase supply lines to the dispensing guns in a single tube. If the tube penetrates through any bulkhead or countertop, seal the penetration with a grommet.
Incorporate, into the design of bulk dispensers of beverage delivery systems, a clean-in-place system that provides a means of flushing, and sanitizing the entire interior of the dispensing lines in accordance with manufacturers' instructions.
# Warewashing
18.1 Provide rinse hoses for prewashing (not required but recommended in bar and deck pantries). If a sink is to be used for prerinsing, provide a removable strainer.
Provide space for trash cans, garbage grinder, or food waste handling systems. Grinders are optional in pantries and bars.
Provide a food waste trough that extends the full length of soiled landing tables with food waste handling systems.
Seal the back edge of the soiled landing table to the bulkhead or provide a minimum of 460 mm (18.4 inches) clearance between the table and the bulkhead.
Design soiled landing tables to drain waste liquids and to prevent contamination of adjacent clean surfaces.
Provide across-the-counter gutters with drains, and slope the clean landing tables to the gutters at the exit from the warewashing machines to prevent water from pooling. If the first gutter does not effectively remove the pooled water, install additional gutter(s) and drain line(s). Minimize the length of drain lines and when possible direct them in a straight line to the deck scupper.
Provide sufficient space for cleaning around and behind equipment (e.g., food waste systems and warewashing machines). Refer to section 8.0 for spacing requirements.
18.8 Encase food waste system wiring in a durable and easy to clean stainless steel or non-metallic watertight conduit and raise it at least 150 mm (6 inches) above the deck. Elevate all warewashing machine components at least 150 mm (6 inches) above the deck, except as noted in Section 8.3.
Construct removable splash panels of stainless steel to protect the food waste system and technical areas.
Construct grinder cones, food waste system tables, and dish-landing tables from stainless steel with continuous welding. Construct platforms for supporting warewashing equipment from stainless steel.
Design and size warewashing machines for their intended use and install them according to the manufacturer's recommendations.
Equip warewashing machines with a device that audibly or visually indicates that the sanitizing temperature or the chemical sanitizer level has dropped below the levels stated on the machine data plate.
Display the data plate affixed to warewashing machines by the manufacturer so that the information is easily accessible and readable. The data plate provides the following information: 18.12 a) temperatures required for washing, rinsing, and sanitizing; 18.12 b) pressure required for the fresh water sanitizing rinse unless the machine is designed to use only a pumped sanitizing rinse; 18.12 c) conveyor speed for conveyor machines or cycle time for stationary rack machines; and 18.12 d) chemical concentration (if chemical sanitizers are used).
Correctly size three-compartment warewashing, and potwashing sinks for their intended use. Use sinks that are large enough to submerge the largest piece of equipment used in the area that is served. Use sinks that have coved, continuously welded internal corners that are integral to the interior surfaces.
18.14 Install one of the following arrangements to prevent excessive contamination of rinse water with wash water splash: 18.14 a) an across-the-counter gutter with a drain that divides the wash compartment from the rinse compartment 18.14 b) a splash shield at least 100 mm (4 inches) above the flood level rim of the sink between the wash and rinse compartments 18.14 c) an overflow drain in the wash compartment 100 mm (4 inches) below the flood level.
Equip hot water sanitizing sinks with accessible and easily readable thermometers, a utensil retrieval system (e.g., long-handled stainless steel wire basket, or other retrieval system), a jacketed or coiled steam supply with a temperature control valve to control water temperature, or electric heating system. (Three-compartment sinks that utilize chemical sanitizers for the sanitization step do not require those items).
Provide adequate ventilation to prevent condensation on the deckhead or adjacent bulkheads. Ensure that any filters installed over warewashing equipment are easily removable, and fans are accessible for cleaning.
# Lighting
19.1 Provide a minimum of 220 lux (20 foot candles) of light at the work surface level in all food preparation, food service, and warewashing areas when all equipment is installed. Provide 220 lux (20 foot candles) of lighting for equipment storage, garbage and food lifts, garbage rooms, and toilet rooms, measured at 760 mm (30 inches) above the deck.
Provide a minimum light level of 110 lux (10 foot-candles) behind and around equipment measured at a distance of 760 mm (30 inches) above the deck (e.g., ice machines, combi-ovens, etc.).
Provide a minimum light level of 220 lux (20 foot-candles) at counter tops (e.g., beverage lines, etc.).
For effective illumination, place the deckhead mounted light fixtures above the work surfaces and positioned them in an "L" pattern rather than a straight line pattern.
# Install light fixtures tightly against the bulkhead and deckhead panels.
Completely seal electrical penetrations to permit easy cleaning around the fixtures.
Use shatter-resistant and removable light shields for light fixtures. Completely enclose the entire light bulb or fluorescent light tube(s).
Provide lighting levels of at least of 220 lux (20 foot candles) in provision rooms, measured at 760 mm (30 inches) above the deck while the rooms are empty. During normal operations when foods are stored in the rooms, provide lighting levels of at least 110 lux (10 foot candles), measured at a distance of 760 mm (30 inches) above the deck.
In bars and over dining room waiters' stations designed for lowered lighting during normal operations, provide lighting that can be raised to 220 lux (20 foot candles) during cleaning operations, as measured at 760 mm (30 inches) above the deck.
Use shielded, coated, or otherwise shatter-resistant light bulbs in areas where there is exposed food; clean equipment, utensils, and linens; or unwrapped single-service, and single-use articles.
Use shields that surround and extend beyond bulbs on infrared or other heat lamps to protect against breakage. Allow only the face of the bulb to be exposed.
Decorative track or recessed deckhead-mounted lights above bar countertops, buffets, and other similar areas may be mounted on, or recessed within the deckhead panels without being shielded. However, install speciallycoated, shatter-resistant bulbs in the light fixtures in this area.
Install a drain at the bottom of all lift shafts including provision platform lifts, and dumbwaiters.
Construct the interiors of dumbwaiters of stainless steel with coved bulkhead and deck junctures and meets the standards of Section 16.0.
Provide light fixtures that are recessed or fitted with stainless steel guards to prevent breakage.
If installed, construct garbage chutes of stainless steel, with an automatic washing system, and in accordance with SOLAS and classification society requirements.
# Trolley, Waste Container, and Cleaning Equipment Wash Rooms
# Construct bulkheads, deckheads, and decks to the same standards as
Section 16.0.
Provide a bulkhead-mounted pressure washing system with a deck sink and drain (An enclosed automatic equipment washing machine or room may be used in place of the pressure washing system and deck sink).
Provide an easily accessible handwashing station with potable hot and cold water, a hose connection, and a deck drain.
Provide ventilation for the extraction of steam and heat.
# Garbage Holding Facilities
Construct garbage and refuse storage or holding rooms sized to hold unprocessed waste for the longest expected period when off-loading of waste is not possible. Separate the refuse-storage room from all food preparation and storage areas.
Provide supply and exhaust ventilation to control odors, temperature, and humidity.
Provide a sealed, refrigerated space for storing wet garbage that meets the standards of 15.0.
Provide an easily accessible handwashing station with potable hot and cold water, a hose connection, and a deck drain.
Provide sufficient deck drainage to prevent pooling of any water.
Ensure that all bulkheads and decks are durable and easily cleanable.
# Garbage Processing Areas
Appropriately size the garbage processing area for the operation and supply a sufficient number of sorting tables.
Provide stainless steel sorting tables with coved corners. If provided, use deck coaming that is at least 80 mm (3 inches) and coved. If the tables have drains, direct the table drains to a deck drain and install a strainer in the deck drain.
Provide an easily accessible handwashing station with potable hot and cold water, a hose connection, and a deck drain.
Provide a storage locker for cleaning materials. Follow storage locker guidelines in Section 26.1.
Ensure that bulkheads and decks are durable and easily cleanable. Provide deck drains to prevent liquids from pooling on the decks. Provide berm/coaming around all waste-processing equipment and ensure there is proper deck drainage inside the berms.
Provide light levels of at least 220 lux (20 foot candles) at work surface levels.
Equip a sink with a pressure washer or an automatic washing machine for washing equipment, storage containers, and garbage barrels.
# Sewage Systems
Limit the installation of drain lines that carry sewage or other liquid waste directly overhead or horizontally through spaces used for food preparation or storage. That includes areas for washing or storage of utensils and equipment, such as bars, deck pantries, and over buffet counters. Sleeve-weld, or butt weld steel pipe; and heat fuse, or chemically weld plastic pipe. Do not use push-fit or press-fit piping over these areas.
Design black and gray water drain systems from cabins, food areas, and public spaces to prevent the back-up of waste and the emission of odors or gases into these areas.
Vent sewage-holding tanks to the outside of the vessel so that they are independent of all other tanks and are away from any air intakes.
# Potable Water System
# Bunker Stations
Position the filling lines at least 450 mm (18 inches) above the deck; paint or stripe them auxiliary blue or in accordance with ISO 14726.
Equip filling lines with tight-fitting caps that are fastened by a non corroding chain so that the cap does not touch the deck when hanging.
Use unique screw connections for the hose attachments that only fit potable water hoses.
Label the filling lines "POTABLE WATER FILLING" with at least 13 mm (½ inch) high lettering stamped, stenciled, or painted on the bulkhead in the area of the bunker line.
If used, locate filters in the bunkering line before the halogenation injection point, accessible for inspection and removable for cleaning.
# Filling Hoses
Provide hoses designed for potable water use that are durable with smooth, impervious linings, caps on each end, and fittings unique to the potable water connections.
Provide at least two 15 m (50 feet) hoses per bunker station.
Label potable water hoses "POTABLE WATER ONLY."
# Filling Hose Storage
Construct potable water hose lockers from smooth, non-toxic, corrosionresistant, and easily cleanable material.
Mount potable water hose lockers at least 450 mm (18 inches) above the deck. Design hose lockers to be self-draining.
# Label potable water hose lockers "POTABLE WATER HOSE AND FITTING STORAGE
" in letters at least 13 mm (½ inch) high.
Provide storage space for at least four 15 m (50 feet) potable water bunker hoses per bunker station.
# International Fire Shore Connections and Fire Sprinkler Shore Connections
Install an RP assembly on all connections where hoses from potable water supplies on shore will be connected to non-potable systems onboard the vessel.
# Storage and Production Capacity for Potable Water
21.5.1.a Provide a minimum of 2 days storage capacity that assumes 120 liters (30 gallons) of water per day per person, and provide potable water production capacity of 120 liters (30 gallons) per day per person for the maximum capacity of crew and passengers on the vessel.
# Potable Water Storage Tanks
21.6.1 General Requirements 21.6.1.1 Ensure that the tanks are independent of the shell of the vessel and do not share a common wall with tanks containing non-potable water or other liquids. Provide a 450 mm (18 inch) cofferdam above and between tanks that are not for storage of potable water and also between the tanks and the hull. Skin or double-bottom tanks are not allowed for potable water storage.
Use an approved potable water tank coating. Follow all of the manufacturers' recommendations for applying and drying or curing the coating. Provide written documentation for these.
Coat all items that penetrate the tank (e.g., bolts, pipes, pipe flanges) with the same product used for the tank's interior.
Design tanks to be super-chlorinated one tank at a time.
Ensure that lines for non-potable liquids do not pass through potable water tanks. Minimize the use of non-potable lines above potable water tanks. Do not use mechanical couplings on lines above tanks. If coaming is present along the edges of the tank, provide slots along the top of the tank to allow leaking liquid to run off and be detected.
Treat welded pipes over the tanks in order to make them corrosionresistant.
Treat all potable water lines inside potable water tanks so as to make them jointless and corrosion-resistant.
Label each potable water tank on its side and where clearly visible, with a number and the words "POTABLE WATER" in letters a minimum of 13 mm (½ inch) high.
Install at least one sample cock located above the deck plating on each tank. 21.6.1.9.a Point sample cocks down; identify and number them for each tank.
# Storage Tank Access Holes
Install access holes on the sides of potable water tanks.
# Storage Tank
# 21.6.5.3.b
Locate the drain in the pump discharge line ahead of any branch take offs to the distribution system. Provide a valve on the distribution main immediately beyond the drain line take-off. (Figure 8).
# Suction Lines
Place suction lines at least 150 mm (6 inches) from the tank bottom or sump bottom.
# Potable Water Distribution System
Locate distribution lines at least 450 mm (18 inches) above the deck plating or the normal bilge water level.
Do not cross connect potable water distribution lines with the piping of any non-potable water system lines.
Do not use lead or cadmium pipes, fittings, or solder.
Install only potable water taps in food areas, the hospital, and the cabin showers and sinks.
Paint or stripe potable water piping and fittings in auxiliary blue, or in accordance with ISO 14726 at 5000 mm (15 feet) intervals and on each side of partitions, decks, and bulkheads except where decor would be marred by such markings.
Use only potable water for steam that is applied directly to food and food contact surfaces. Generate the steam locally from food service equipment designed for this purpose (e.g., vegetable steamers, combi-ovens, etc.). Only apply non-potable water steam indirectly to food or food equipment. Route that steam through coils, tubes, or separate chambers.
Ensure that an air-gap or approved backflow prevention device is present if potable water is supplied to a bilge, waste, ballast, or laundry tank.
Clean, disinfect, and flush potable water tanks and any parts of the potable water distribution system with potable water before the system is placed in service.
# Potable Water Pressure Tanks
21.9.1 Do not cross-connect potable water hydrophore tanks to non-potable water tanks through the main air compressor.
Provide a filtered air supply from a non-permanent, quick disconnect, or independent compressor. The compressor shall not emit oil into the final air product.
# Potable Water Pumps
Size the potable water pumps to meet the service demands; do not use them for any other purpose.
Use pumps that prime automatically and not manually. Use a direct connection, not an air-gap, when supplying water to a potable water pump.
Properly size potable water pumps and distribution lines so that pressure is maintained at all times and at levels adequate levels to operate all equipment.
# Evaporators and Reverse Osmosis Plants
Locate the seawater inlets (sea chests) forward of all overboard waste water, swimming pool and whirlpool spa, and ballast tank discharge outlets.
Use only direct connections to the potable water system. Do not use swing lines.
Provide an air-gap or RP assembly between the potable water system and the non-potable water system. (Fresh water produced by an evaporator, or reverse osmosis plant is not considered potable until after it has been pH adjusted to the proper level.) 21.11.4 Post operating instructions for the evaporators, or reverse osmosis plants near the units.
Ensure that high and low-pressure units connected directly to the potable water lines have the ability to discharge to the waste system if the distillate is not fit for use.
Install units that have a low-range salinity indicator, an operation temperature indicator, an automatic discharge to waste, and an alarm with trip setting.
Route the high-saline discharge to the bilge or overboard through an airgap or RP assembly.
# Halogenation
21.12.1 Bunkering and Production 21.12.1.1 Provide labeled potable water taps with appropriate backflow preventers at the halogen supply tanks. 21.12.1.2 Provide a labeled sample cock at least 3000 mm (120 inches) downstream of the halogen injection point.
# Control halogen injection by a flow meter or analyzer.
21.12.1.4 Provide pH adjustment equipment for water bunkering and production. Install analyzer, controller, and dosing pumps that are designed to accommodate changes in flow rates.
# Distribution
21.12.2.1 Provide a completely automatic halogenation system that is analyzer controlled.
Use halogenation probes that measure free halogen; link them to an analyzer/controller and dosing pump.
Provide a back-up halogenation system with an automatic switchover that begins pumping halogen when the primary (in-use) pump fails or cannot meet the preset halogenation level.
Locate analyzer probes at a distant point in the system where significant water flow exists. 21.12.2.5 Provide an audible alarm in a continually occupied watch station, (e.g., the engine-control room), to indicate low free-halogen readings at the distantpoint analyzer.
Provide labeled potable water taps with appropriate backflow preventers at halogen supply tanks.
Locate a labeled sample cock at least 3000 mm (120 inches) downstream of the halogen injection point.
Provide free-halogen analyzer-chart recorders with ranges of 0.0 to 5.0 ppm and continuous recording periods indicating the level of free-halogen for 24 hour time periods, (e.g., circular 24 hour charts). 21.12.8.a Electronic data loggers with certified data security features may be installed in lieu of chart recorders. Acceptable data loggers produce records that conform to the principles of operation and data display required of the analog charts, including printing the records. Use electronic data loggers that log times in increments of <15 minutes.
# Disinfection of the Potable Water System
21.13.1 Disinfect the entire distribution system with a free halogen concentration of at least 50 mg/L (ppm) for at least 4 hours. Prior VSP agreement is required if alternative approved disinfection practices are used.
Provide written documentation of the distribution system disinfection.
# Backflow Prevention
22.1 Use appropriate backflow prevention (e.g., air-gaps, RP assemblies, pressure vacuum breakers, atmospheric vacuum beakers, pressure-type backflow preventers, or double-check valves with intermediate atmospheric vent) for all non-potable connections in the potable water system.
Use air-gaps that are at least twice the diameter of the supply pipe measured vertically above the flood level rim of the receiving vessel. The air-gap must at least 25 mm (1 inch).
Install RP assemblies in high-hazard situations where air-gaps are not practical.
If RP backflow prevention assemblies are used, provide a test kit for testing the devices.
# 22.4.a Test all RP's after installation.
22.5 Use mechanical backflow prevention devices when water must be supplied under pressure.
Install atmospheric vacuum breakers 150 mm (6 inches) above the fixture flood level rim with no valves downstream from the device.
Connect potable water through an air-gap when it is directed to a black water tank for rinse down or other such uses. RP assemblies are inadequate in this high hazard condition.
Protect the following connections to the potable water system against backflow or back-siphonage by air-gaps or mechanical backflow prevention devices:
Potable water supply lines to swimming pools, whirlpool spas, hot tubs, bathtubs, showers, and similar facilities. 22.8.12 Potable water, bilge, and sanitary pumps that require priming.
Freshwater or saltwater ballast systems.
International fire and fire sprinkler water connections.
The potable water supply to automatic window washing systems which utilize chemicals or chemical mix tanks.
Water softeners for non-potable fresh water if located before an airgap.
Water softener and mineralizer drain lines must be protected by an air-gap or RP assembly.
Any other connection between potable and non-potable water systems.
22.9 Heat Exchangers used for cooling potable water 22.9.1 Fabricate heat exchangers, using, or for cooling potable water so a single failure of any barrier will not cause a cross-connection or permit back-siphonage of contaminants into the potable water system. 22.9.2 Design heat exchangers where both potable water and any non-potable liquid are used to protect the potable water from contamination by one of the following designs; 22.9.2.a Double-wall construction between the potable and non-potable liquids, with a void space to allow any leaking liquid to drain away; and 22.9.2.a.1 An alarm system to indicate a leak in the double wall.
# 22.9.2.b
Single-wall construction with the following safety features: 22.9.2.b.1 Higher pressure of at least 1 bar on the potable water side of the heat exchanger; 22.9.2.b.2 An automatic diverter valve that directs potable water from the heat exchanger when the pressure difference is less than 1 bar; and 22.9.2.b.3 An alarm system that sounds when the diverter valve directs potable water from the heat exchanger.
# Swimming Pools
23.1 Use seawater, or a potable water supply passing through an air-gap or backflow preventer to fill swimming pools.
Provide an independent pool drainage system. If swimming pool drains are connected to another drainage system, provide a double-check valve between the two.
# 23.2.a
Install a drain at the lowest point in the pool.
Slope the bottom of the pool towards the drains to achieve complete drainage.
Provide anti-entrapment type drain covers that are constructed of durable easily visible, easily cleanable material and that meet ASME/ANSI A112.19.8M voluntary standard for suction fittings (figure 9a-9c), or other drains that prevent entrapment hazards as specified in U.S. Consumer Product Safety Publication 363-009801 (figure 9-10b). Dual drains meet the anti-entrapment requirements.
Ensure that the fill level of the pool is at the skim gutter level.
Ensure that pool overflows are either directed by gravity to the make-up tank for recirculation through the filter system or disposed of as waste.
Install recirculation, filtration, and disinfection equipment.
Use pool equipment (e.g., pumps and filters) that has the capacity to turnover the pool water at least four times every 24 hours (i.e., once every 6 hours or less).
Use self-priming, centrifugal pumps to re-circulate pool water.
Install pumps large enough to re-circulate the entire volume of the pool in 6 hours.
Install surface skimmers or gutters that are capable of handling approximately 80% of the filter flow of the recirculation system.
If skimmers are used instead of gutters, install is at least one skimmer for each 47 m² (500 square feet) of pool surface area.
Provide a hair strainer between the pool outlet and the suction side of the pumps to remove foreign debris such as hair, lint, pins, etc.
Ensure that the removable portion of the strainer is corrosion-resistant and has holes no greater than 6 mm (¼ inch) in diameter.
Use filters that are designed to remove all particles greater than 20 micrometers from the entire volume of the pool in 6 hours or less.
Use cartridge or media-type filters (e.g., rapid-pressure sand filters, high rate sand filters, diatomaceous earth filters, or gravity sand filters). Make filter sizing consistent with ANSI standards for public pools.
Use media-type filters that are capable of being back-washed.
Provide filter accessories, such as pressure gauges, air-relief valves, and rate-of-flow indicators.
Provide automatic dosing of chemicals for disinfection and pH adjustment.
If desired, use a make-up tank to replace water lost by splashing and evaporation. If the tank is supplied with potable water, ensure that the supply enters through an air-gap or backflow preventer. An overflow line at least twice the diameter of the supply line and located below the tank supply line as backflow prevention is acceptable provided it drains through a visible air-break.
Provide easy access to the media filters so that they can be inspected at least on a weekly basis and the media can be changed periodically.
Provide water sample points on the system for halogen level testing and routinely calibrating the analyzer.
Provide analyzer controlled halogen-based disinfection equipment.
Ensure that pH adjustment is accomplished by using appropriate acids and bases and that a buffering agent is used to stabilize the pH. Control the injection of acids and bases by an analyzer.
Make pool mechanical rooms accessible, well-ventilated, and provide a potable water tap with appropriate backflow protection.
Mark all piping with directional-flow arrows and maintain a flow diagram and operational instructions in a readily available location.
Design the pool mechanical room and recirculation system for easy and safe chemical storage and re-filling of chemical feed tanks.
Install drains in the pool mechanical room that allow rapid draining of the entire pump and filter system; install a minimum 80 mm (3 inch) drain on the lowest point of the system.
Provide a drain in the make-up tanks to allow complete draining.
Prominently display the depth of the pool so that it can be seen from the deck and in the pool. Label depth markers either in feet or meters, or both. Install additional depth markers for every 1 m (3 feet) change of depth and prominently display them so that they can be seen from the deck and in the pool.
# Children's Pools
24.1 Follow all requirements in Section 23.0.
Provide an independent recirculation, filtration and halogenation system in children's pools.
Use a water turn-over rate of is at least once every 30 minutes.
# Whirlpool Spas
25.1 Supply potable water whirlpool systems through an air-gap or approved backflow preventer.
Use water filtration equipment (e.g., pumps, filters, etc.) that ensures a turn over rate of at least once every 30 minutes and halogenation equipment that is capable of maintaining the appropriate levels of free-halogen throughout the use period.
Provide a temperature control mechanism to prevent the temperature from exceeding 40ºC (104ºF).
Design the overflow system so that water level is maintained.
If skimmers are used instead of gutters, use one skimmer for every 14 m² (150 square feet) or fraction thereof of water surface area.
Provide an independent whirlpool drainage system. If the whirlpool drainage system is connected to another drainage system, provide a double-check valve between the two.
Provide drains and ensure the bottom of the whirlpool slopes toward the drains to affect complete drainage.
# 25.7.a
Use whirlpools seating areas that drain completely.
Provide anti-entrapment type drain covers constructed of durable easily visible, easily cleanable material and that meet ASME/ANSI A112.19.8M voluntary standard for suction fittings (figure 9a-9c), or other drains that prevent entrapment hazards as specified in U.S. Consumer Product Safety Publication 363-009801 (figures 9a-10b) dual drains meet the anti-entrapment requirements.
Design the system to permit daily shock treatment or super-halogenation in accordance with the VSP Operations Manual.
Install systems in a manner that permits routine visual inspection of the granular media filters in accordance with the VSP Operations Manual.
Ensure that the fill level of the whirlpool is at the skim gutter level.
Ensure that whirlpool overflows are either directed by gravity to the make up tank for recirculation through the filter system or disposed of as waste.
Use self-priming, centrifugal pumps to re-circulate whirlpool water.
25.14 Provide a hair strainer between the whirlpool outlet and the suction side of the pumps to remove foreign debris such as hair, lint, pins, etc.
Ensure that the removable portion of the strainer is corrosion-resistant and has no holes greater than 6 mm (¼ inch) in diameter.
Use filters that are designed to remove all particles greater than 20 micrometers from the entire volume of the whirlpool in 30 minutes or less.
Use filters that are cartridge, or media type (e.g., rapid-pressure sand filters, high-rate sand filters, diatomaceous earth filters, or gravity sand filters). Make filter sizing consistent with ANSI standards for public pools.
Provide a clear sight glass on the backwash side of the filters.
Design and install filters in a manner that allows for easy access for inspection and maintenance.
Make all media-type filters capable of being back-washed.
Provide filter accessories, such as pressure gauges, air-relief valves, and rate-of-flow indicators.
A make-up tank may be used to replace water lost by splashing and evaporation. If the tank is supplied with potable water, ensure that the supply enters through an air-gap or backflow preventer. An overflow line at least twice the diameter of the supply line and located below the tank supply line may be used as backflow prevention.
Provide analyzer controlled chemical dosing for both pH and disinfection.
Accomplish disinfection by chlorination or bromination.
Provide water sample points on the system for the testing of halogen levels and routine calibration of the analyzer.
Accomplish pH adjustment by using appropriate acids and bases and that a buffering agent is used to stabilize the pH. Control acid and bases injections by an analyzer.
Make the whirlpool mechanical room accessible and well-ventilated and provide a potable water tap.
Mark all piping with directional-flow arrows and maintain a flow diagram and operational instructions in a readily available location.
Design the pool mechanical room and recirculation system for easy and safe chemical storage and re-filling of chemical feed tanks.
Install drains in the whirlpool mechanical room to allow for rapid draining of the entire pump and filter system; install them so that a minimum 80 mm (3 inch) drain is on the lowest point of the system.
Provide a drain in the make-up tanks to allow complete draining.
Make sure that all decorative features of whirlpool spas are completely draining, non-porous and easy to clean.
# Miscellaneous
# Facilities and Lockers for Cleaning Materials
26.1.1 Provide bulkhead-mounted racks on which hang wet brooms and mops, or provide sufficient space and hanging brackets within a cleaning locker. Locate bulkhead-mounted racks outside of food storage, preparation, or service areas.
Provide stainless steel vented lockers, with coved deck and wall junctures, for storing buckets, detergents, sanitizers, cloths, etc.
The number of lockers and the location and size of lockers is determined by the needs of the vessel. Make access to lockers containing cleaning materials convenient.
# 26.1.3.a
# Drinking Fountains
Ensure that the water jet orifices from drinking fountains are slanted and that the orifice is protected by a cover to prevent contamination. Do not allow lead in the water storage tanks and plumbing serving water fountains.
Provide drinking fountains with stainless steel cabinets and without filling spouts in food preparation areas.
Provide drinking fountains that will allow the user to control the water stream.
Install drinking fountains that are accessible to galley personnel.
# Facility for Cleaning of Maintenance Equipment
26.4.1 Provide facilities (e.g., deep utility sinks) with hot and cold water or a pressure-washing system with a deck sink and drain for cleaning of maintenance equipment such as brooms and mops. Provide bulkhead-mounted racks or hooks for hanging the equipment for drying. Separate room(s) designated for this purpose from food preparation and warewashing areas.
# Ventilation Systems
# Air Supply Systems
27.1.1 Design fan rooms so that they are accessible for periodic inspections and air intake filter changing.
# Design air condition condensation collection pans to drain completely.
# 27.1.2.a
Use air conditioner condensation collection pans that are designed to drain through closed piping to prevent condensate from pooling on the decks.
Locate air intakes for fan rooms so that any ventilation or processed exhaust air is not drawn back into the vessel.
Provide a sufficient air supply in all food preparation, warewashing, cleaning rooms, and toilet rooms.
# Design all cabin air vent diffusers for easy removal and cleaning.
27.1.6 Make air handling unit condensate drain pans easily accessible for inspection and cleaning, and accessible for maintenance. Make sure that all major air supply trunks have access panels to allow for periodic inspection and cleaning.
Provide a separate, independent air supply system for the engine room and other mechanical compartments, (e.g., fuel separation, purifying, and black water treatment rooms) which are located in and around the engine room.
# Air Exhaust Systems
Air handling devices in the following areas must exhaust air through independent systems that are completely separated from systems using re circulated air:
# Engine rooms and other mechanical spaces;
27.2.1.2 Hospitals, infirmaries, and any rooms used for patient care or isolation;
Indoor swimming pools swimming pool: , dome type swimming pools when closed; whirlpool spa facilities, and supporting mechanical rooms.
# An adjacent handwashing station; and
28.2.4 A sign advising child care facility staff to wash their hands after each diaper change.
Provide separate toilet and handwashing facilities for child care providers.
# Housekeeping
29.1 Provide handwashing stations for housekeeping staff. VSP will evaluate the number and location for these handwashing stations during the plan review process.
# Public Toilet Rooms
# Decorative Fountains
31.1 Provide potable water to all decorative fountains.
Ensure that fountains are designed to be maintained free of algae and mold. | # Table of Contents
# Background and Purpose
The Centers for Disease Control and Prevention (CDC) established the Vessel Sanitation Program (VSP) in 1975 as a cooperative endeavor with the cruise vessel industry. VSP's goal is to assist the industry to develop and implement comprehensive sanitation programs to protect the health of passengers and crew aboard cruise vessels.
Every cruise vessel that has a foreign itinerary, carries 13 or more passengers, and calls on a U.S. port is subject to biannual operational inspections and when necessary, re-inspection by VSP. The vessel owner pays a fee, based on gross registered tonnage (GRT) of the vessel, for all operational inspections. The Vessel Sanitation Program Operations Manual (VSP Operations Manual), which is available on the VSP Web site (www.cdc.gov/nceh/vsp), covers details of these inspections.
Additionally, cruise vessel owners or shipyards that build or renovate cruise vessels may voluntarily request plan reviews, on-site shipyard construction inspections and/or final construction inspections of new or remodeled vessels before their first or next operational inspection. The vessel owner or shipyard pays a fee, based on GRT of the vessel, for on-site and final construction inspections. VSP does not charge a fee for plan reviews or consultations. Section 3.0, Procedures for Making Requests for Plan Reviews and Construction-Related Inspections covers details pertaining to plan reviews, consultations, or construction inspections.
The Recommended Shipbuilding Construction Guidelines for Cruise Vessels Destined to Call on U.S. Ports, has been renamed as the Vessel Sanitation Program Construction Manual (referred to in this documents as "these guidelines"). The main purpose of these guidelines is to provide a framework of consistent construction and design guidelines that protect passenger and crew health. CDC is committed to promoting high construction standards to protect the public's health. Compliance with these guidelines will help to ensure a healthy environment on cruise vessels.
CDC reviewed many references from a variety of sources to develop this document. These references are indicated in Section 32.2, Standards, Codes and Other References Reviewed for Guidance.
These guidelines cover various components of the vessel's facilities related to public health, including food storage, preparation, and service; water bunkering, storage, disinfection, and distribution. Vessel owners and operators may select the design and equipment that best meets their needs. However, the design and equipment must also meet the sanitary design criteria of the American National Standards Institute (ANSI) or equivalent organization, and VSP's routine operational inspection requirements.
These guidelines are not meant to limit the introduction of new designs, materials or technology for shipbuilding. A shipbuilder, owner, manufacturer, or other interested party may request VSP to periodically review or revise these guidelines in relation to new information or technology. VSP reviews such requests in accordance with the criteria described in Section 2.0, "Revisions and Recommended Changes."
New cruise vessels must comply with all international code requirements (e.g., International Maritime Organization [IMO] Conventions). Those include requirements of the Safety of Life-at-Sea Convention (SOLAS), International Convention for the Prevention of Pollution from Ships (MARPOL), Tonnage and Load Line Convention, International Electrical Code (IEC), International Plumbing Code (IPC), and International Standards Organization (ISO). This document does not cross-reference related and sometimes overlapping standards that new cruise vessels must meet.
These guidelines went into effect on June 1, 2005. They apply to vessels that lay keel or perform any major renovation (e.g., any changes to the structural elements of the vessel covered by these guidelines) after this date. The guidelines do not apply to minor renovations such as the installation or removal of single pieces of equipment, (refrigerator units, bains-marie units, etc.) or single pipe runs. These guidelines will apply to all areas of the vessel affected by a renovation. VSP will inspect the entire vessel in accordance with the VSP Operations Manual during routine vessel sanitation inspections and reinspections.
# Revisions and Changes
VSP periodically reviews and revises these recommendations in coordination with industry representatives and other interested parties to stay abreast with industry innovations. A shipbuilder, owner, manufacturer, or other interested parties may ask VSP to review a construction guideline on the basics of new technologies, concepts, or methods. Recommendations for changes or additions to these guidelines must be submitted in writing, to the Chief, VSP (see Section 33.2 for contact information). The recommendation should:
• identify the section to be revised,
• describe the proposed change or addition,
• state the reason for recommending the change or addition, and • include research or test results and any other pertinent information that support change or addition.
# Procedures for requesting Plan Reviews, Consultations, and Construction-Related Inspections
VSP will coordinate a professional evaluation and consult with industry to determine whether to include the recommendation in the next revision.
VSP gives special consideration to shipyards and owners of vessels that have had plan reviews conducted before an effective date of a revision of these guidelines. This helps limit any burden placed on the shipyards and owners to make excessive changes to previously agreed upon plans.
VSP will ask industry representatives and other knowledgeable parties to meet with VSP representatives periodically to review the guidelines and determine whether changes are necessary to keep up with the innovations in the industry.
To coordinate or schedule a plan review or construction-related inspection submit an official written request to the VSP Chief as early as possible in the planning, construction, or renovation process. Requests that require foreign travel must be received in writing at least 60 days before the intended visit. The request will be honored, depending on VSP staff availability. A complete listing of contact addresses and telephone numbers can be found in Section 33.2.
After the initial contact, VSP assigns primary and secondary officers to coordinate with the vessel owner and shipyard. Normally two officers will be assigned. These officers are the points of contact for the vessel from the time the plan review and subsequent consultations take place through the final construction inspection.
The vessel representatives should provide points of contact to represent the owners, the shipyard, and key subcontractors. All parties will use these points of contact during consultations between any of the parties and VSP to ensure awareness of all consultative activities after conducting the plan review.
# Plan Reviews and Consultations
VSP normally conducts plan reviews for new construction a minimum of 18-24 months before the vessel is scheduled for delivery. The time required for major renovations varies. To allow time for any necessary changes, VSP coordinates the plan reviews for such projects well before the work begins. Plan reviews normally take two working days. They are conducted in Atlanta, Georgia; Fort Lauderdale, Florida; or other agreed upon sites. Normally, two VSP officers will be assigned to the project. Representatives from the shipyard, the vessel owner, and the subcontractor(s) who will be doing most of the work should attend the review. They should bring all pertinent plans or drawings and equipment specifications for the areas covered in these guidelines. That includes but is not limited to the following:
• general arrangement plans;
• all food-related storage, preparation, and service area plans;
• potable and non-potable water system plans with details on water inlets, (e.g., sea chests, overboard discharge points, and backflow protection devices); • ventilation system plans; and, if applicable;
• swimming pool and whirlpool spa plans.
VSP will prepare a Plan Review Report summarizing the recommendations made during the plan review and will submit the report to the shipyard and owner representatives.
Following the plan review, the shipyard will provide: 1) a complete set of plans or drawings and specifications for the vessel; 2) any redrawn plans and; 3) a statement of corrective action outlining how each of the items identified in the Plan Review Report will be corrected, and 4) copies of any major change orders in the areas covered by these guidelines that are made after the plan review.
While the vessel is being built, shipyard representatives, the owner or other vessel representatives may direct questions or requests for consultative services to the VSP project officers. Direct these questions or requests in writing to the officer(s) assigned to the project. Include fax number(s) and an e-mail address(es) for appropriate contacts. VSP officer(s) will coordinate the request with the owner and shipyard points of contact designated during the plan review.
# On-Site Construction Inspections
VSP conducts most on-site or shipyard construction inspections in shipyards outside the United States. A formal written request must be submitted to the VSP Chief 60 days before the inspection date so that VSP can process the required foreign travel orders for VSP officers (see Section 3.0). A sample of a request is shown in Section 33.1. VSP encourages shipyards to contact the Chief, VSP to and coordinate on-site construction inspections well before the 60 day minimum to better plan the actual inspection dates. If a shipyard requests an on-site construction inspection, VSP will advise the vessel owner of the inspection dates so that the owner's representatives are present. An on-site construction inspection normally requires the expertise of one to three officers, depending on the size of the vessel and whether it is the first of a hull design class or a subsequent hull in a series of the same class of vessels. The inspection, including travel, generally takes 5 working days. The on-site inspection should be conducted approximately 4 to 5 weeks before delivery of the vessel when 90% of the areas of the vessel to be inspected are completed. VSP will provide a written report to the party that requested the inspection. After the inspection, and before the ship's arrival in the United States, the shipyard will submit to VSP a statement of corrective action outlining how it will address and correct each item identified in the inspection report.
# Final Construction Inspections
At the request of a vessel owner or shipyard, VSP may conduct a final construction inspection. To schedule the inspection, the vessel owner or shipyard will submit a formal, written request the Chief, VSP as soon as possible after the vessel is completed, or a minimum of 10 days before its arrival in the United States. At the request of a vessel owner or shipyard and provided the vessel is not entering the United States market immediately, VSP may conduct final construction inspections outside the United States (see requirements for foreign travel in section 3.2 On-Site Construction Inspections). If a final construction inspection is not requested, VSP generally will conduct an unannounced operational inspection within 4 weeks following the vessel's arrival in the United States. VSP conducts operational inspections in accordance with the VSP Operations Manual.
As soon as possible after the final construction inspection, the vessel owner or shipyard will submit a statement of corrective action to VSP. The statement will outline how they will address each item cited in the inspection report, including the projected date of completion. VSP generally schedules vessels that undergo final construction inspection in the United States for an unannounced operational inspection within 6 weeks of the vessel's final construction inspection. VSP conducts operational inspections in accordance with the VSP Operations Manual.
# Equipment Standards, Testing, and Certification
Although these guidelines establish certain standards for equipment and materials installed on cruise vessels, VSP does not test, certify, or otherwise endorse any equipment or materials used by the cruise industry. Instead, VSP recognizes certification from independent testing laboratories such as NSF International, Underwriter's Laboratories (UL), the American National Standards Institute (ANSI), or other accredited institutions.
In most cases, independent testing laboratories test equipment and materials to certain minimum standards which generally, but not always meet the recommended standards established by these guidelines. Equipment built to questionable standards will be reviewed by a committee of VSP, the cruise ship industry and independent testing organization participants. The committee will determine if the equipment meets the recommended standards established in these guidelines. Copies of test or certification standards are available from the independent testing laboratories. Equipment manufacturers and suppliers will not refer to VSP to approve their products.
# General Definitions
Accessible -Can be exposed for cleaning and inspection with the use of simple tools such as a screwdriver, pliers, or an open-end wrench.
Air-break -A piping arrangement in which a drain from a fixture, appliance, or device discharges indirectly into another fixture, receptacle, or interceptor at a point below the flood-level rim. (Figure 1)
Air-gap -The unobstructed vertical distance through the free atmosphere between the lowest opening from any pipe or faucet supplying water to a tank, plumbing fixture, or other device and the flood-level rim of the receptacle or receiving fixture. The air-gap must be at least twice the diameter of the supply pipe or faucet or at least 25 mm (1 inch). (Figure 2) Backflow -The flow of water or other liquids, mixtures, or substances into the distribution pipes of a potable supply of water from any source or sources other than the potable water supply. Back-siphonage and back-pressure are forms of backflow.
Backflow, check, or non-return valve -A mechanical device installed in a waste line to prevent the reversal of flow under conditions of back-pressure. In check-valves, the flap should swing into a recess when the line is flowing full so that it does not obstruct the flow.
Backflow preventer-An approved backflow prevention plumbing device that must be used on potable water distribution lines where there is a direct connection or a potential connection between the potable water distribution system and other liquids, mixtures, or substances from any source other than the potable water supply. Some devices are designed for use under continuous water pressure, whereas others are non-continuous pressure types. Perform a thorough review of the water system to ensure proper protection of the water supply, to confirm that the appropriate device is selected for each specific application. The following are general types of backflow preventers and their uses:
• Atmospheric vacuum breaker -An approved backflow prevention plumbing device used on potable water lines where shut-off valves do not exist downstream from the device. The device is not approved for use under continuous water pressure. An atmospheric vacuum breaker must be installed at least 152 mm (6 inches) above the flood level rim of the fixture or container to which it is supplying water.
• Continuous pressure backflow preventer -An approved backflow prevention plumbing device with two check valves and an intermediate atmospheric vent. It is designed and approved for use under continuous water pressure (e.g., when shut-off valves are located downstream from the device).
• Hose bib connection vacuum breaker -An approved backflow prevention plumbing device that attaches directly to a hose bib by way of a threaded head. This device uses a single check valve and vacuum breaker vent. It is not approved for use under continuous pressure (e.g., when a shut-off valve is located downstream from the device).
• Reduced Pressure Principle Backflow Prevention Assembly (RP assembly) -An assembly containing two independently acting approved check valves together with a hydraulically operating, mechanically independent pressure differential relief valve located between the check valves and at the same time below the first check valve. The unit must include properly located resilient seated test cocks and tightly closing resilient seated shutoff valves at each end of the assembly.
Back-siphonage -The backward flow of used, contaminated, or polluted water from a plumbing fixture or vessel or other source into a water-supply pipe as a result of negative pressure in the pipe.
Black water -Waste from toilets, urinals, medical sinks, and similar facilities.
Blast chiller -A unit specifically designed for rapid intermediate chilling of food products to 21°C (70°F) within 2 hours and 5°C (41°F) within an additional 4 hours.
Child activity facility -A designated area for use by children who do not require assistance using toilet rooms and who may be old enough to come and go on their own.
Child care facility -A designated area for use by children who are not yet out of diapers or require supervision when using the toilet rooms, and who are cared for by vessel staff.
Child-size toilet -Toilets whose toilet seat height is between 280-380 mm (11-15 inches) and the water closet center line is between 305-380 mm (12-15 inches). This can be achieved by installing a smaller water closet or by providing a deck platform at the front of the water closet and variably sized, fold-down toilet seats.
Cleaning room -A room specifically designed for storage of cleaning equipment such as mops, brooms, floor scrubbing machines, and cleaning chemicals. The room may or may not include a sink for filling buckets and washing mops.
Corrosion-resistant -Material that maintains its original surface characteristics through prolonged influence by the use environment, food contact, and normal use of cleaning compounds and sanitizing solutions.
Coved -A curved or concave surface, molding, or other design that eliminates the usual joint angles of 90° or less. (Figures 3 and 4)
Crew toilet room -Those toilets located near food preparation areas and intended for use by food service personnel.
Cross-connection -Any unprotected, actual or potential connection or structural arrangement between a public or a consumer's potable water system and any other source or system through which it is possible to introduce into any part of the potable system any used water, industrial fluid, gas, or substance other than the intended potable water with which the system is supplied. Bypass arrangements, jumper connection, removable section, swivel or change-over devices and other temporary or permanent devices which or because of which backflow can occur are considered to be cross-connections.
Deck drain -The physical connection between decks, scuppers, or deck sinks to the gray or black water systems.
Deck sink -A sink recessed into the deck, sized to contain waste liquids from tilting kettles and tilting pans.
Drip tray -Readily removable tray to collect dripping food from a food dispensing mechanism.
Easily cleanable -Fabricated with a material, finish, and design that allows for cleaning by normal methods.
Food contact surfaces -Surfaces (food zone, splash zone) of equipment and utensils with which food normally comes in contact and surfaces from which food may drain, drip, or splash back onto surfaces normally in contact with food. This includes those areas of ice-making machines where the ice is produced and above the connecting chute between the maker and the storage bin. It does not include the technical compartment where the compressor is located. (figure 5)
Food display areas -Any area where food is displayed for consumption by passengers and/or crew.
Food handling areas -Any area where food is stored, processed, prepared, or served.
Food preparation areas -Any area where food is processed, cooked, or prepared for service.
Food service areas -Any area where food is presented to passengers or crew members (excluding individual cabin service).
Food storage areas -Any area where food or food products are stored.
Food transport areas -Any area through which unprepared or prepared food is transported during food storage, preparation, and service operations (excluding public areas and individual cabin service).
Food waste system -Food waste transport system (e.g., pulper, vacuum system).
Gray water -All wastewater including drainage from galleys, dishwashers, showers, laundries, bath, washbasin, deck drains, and swimming pool and whirlpool spas. It does not include black water or bilge water from the machinery spaces.
# Gutterway -See scupper
Keel laying -The date at which construction identifiable with a specific ship begins and when assembly of that ship comprises at least 50 tons or 1% of the estimated mass of all structural material, whichever is less.
Non-food contact surfaces (non-food zone) -All exposed surfaces, other than food contact or splash contact surfaces, of equipment located in food storage, preparation and service areas. (figure 5) nonabsorbent nontoxic Non-potable water (Technical Water) -Fresh water that may not be halogenated and is intended for use in technical and other areas where potable water is not required (e.g., laundries, engine room, toilets, waste-treatment areas, and for washing decks in areas other than the vessel's hospital, food service, preparation, or storage areas).
Potable water -Fresh water that is intended for drinking, washing, bathing, or showering; for use in fresh water swimming pools and whirlpool spas; for use in the vessel's hospital; for handling, preparing, or cooking food; and for cleaning food storage and preparation areas, utensils, and equipment.
Potable water tanks -All tanks in which potable water is stored from bunkering and production for distribution and use as potable water.
Portable -A description of equipment that is readily removable or mounted on casters, gliders, or rollers; provided with a mechanical means so that it can be tilted safely for cleaning; or readily movable by one person.
Readily accessible -Exposed or capable of being exposed for cleaning or inspection without the use of tools.
Readily removable -Capable of being detached from the main unit without the use of tools.
Removable -Capable of being detached from the main unit with the use of simple tools such as a screwdriver, pliers, or an open end wrench.
Safe material -An article or material that would not be expected to become a component of any food or otherwise affect the characteristics of any food. Also, an additive or other materials used as specified in Section 409 or 706 of the Federal Food, Drug, and Cosmetic Act or in conformity with applicable regulations of the U.S. Food and Drug Administration (FDA).
Scupper -A conduit or collection basin that channels liquid runoff to a deck drain.
Sealant -Material used to fill seams to prevent the entry or leakage of liquid or moisture.
Sealed -Having no openings present that will permit the entry of soiled material or seepage of liquids.
Sealed seam -A seam that has no openings that would permit the entry of soil or liquid seepage.
Seam -An open juncture between two similar or dissimilar materials. Continuously welded junctures, ground and polished smooth, are not considered seams.
Sewage (black water) -Any liquid waste that contains animal or vegetable matter in suspension or solution, including liquids that contain chemicals in solution.
Smooth -means: a) A food contact surface that is free of pits and inclusions with a cleanability equal to or exceeding that of a No. 3 finish (100 grit) on stainless steel; b) A non-food contact surface of equipment that is equal to commercial grade hot-rolled steel and is free of visible scale; and c) A deck, bulkhead, or deckhead that has an even or level surface with no roughness or projections that renders it difficult to clean.
Spa pool -A fresh or saltwater supplied pool with temperatures and turbulence comparable to a whirlpool spa, but with a water depth and volume more comparable to a swimming pool. General characteristics are • water temperature of 30°C-40°C or 86°F-104°F,
• bubbling or jetted water effects that physically break at the water surface,
• depth of more than 1 m (3 feet),
• shape is normally non-circular, and • volume exceeds 6 tons of water.
# Splash contact surfaces (non-food zone)
-Surfaces that are subject to routine splash, spillage or other soiling during normal use.
Direct splash surfaces -Areas adjacent to food contact surfaces that are subject to splash, drainage, or drippage onto food contact surfaces. Considered food contact surfaces.
Indirect splash surfaces -Areas adjacent to food contact surfaces that are subject to splash, drainage, drippage, condensation, or spillage from food preparation and storage. Considered non-food contact surfaces.
Technical water -Fresh water NOT intended for: 1) drinking, washing, bathing, or showering; 2) use in the vessel's hospital; 3) handling, preparing, or cooking food; or 4) cleaning food storage and preparation areas, utensils, and equipment.
Temperature measuring devices (TMDs) -Thermometers or other instruments that measure relative heat and cold according to an established scale. TMDs that are scaled in Celsius, Fahrenheit, or both must be designed to be easily readable and accurate to ± 1.5°C or 3°F.
Transportation corridors -Areas primarily intended to move unprepared or prepared food during food preparation, storage, and service operations (e.g., service lift (elevator) vestibules to food preparation service and storage areas, and corridors connecting preparation areas and service areas). Marshalling, provisions areas, passenger/corridors, public areas, and dinning rooms connected to galleys are excluded.
TMD -See temperature measuring device.
Utility sink -Any sink located in a food service area not intended for handwashing and/or warewashing.
Whirlpool spa -A freshwater pool designed to operate at a minimum temperature of 30°C (86°F) and equipped with either water or air jets.
# General Facilities Requirements
# Size and Flow
Many factors determine and influence the size of rooms and work areas and the flow of food through a vessel. Those can include the size of the vessel, number of passengers and crew, types of foods or menus, number of meals or mealtimes, service or presentation of meals, itinerary, and the vessel owner's experience. In general, food storage, preparation, and service areas; warewashing areas; and waste management areas must be sized to accommodate the vessel's full capacity of passengers and crew. Bulk food storage areas or provision rooms (e.g., frozen stores, refrigerated stores, and dry stores) must be sized to prevent bulk foods from being stored in provisions passageways unless specifically designed to meet provision room standards (Section 15.0). Refrigeration and hot-food holding facilities, including temporary storage facilities, must be available for all food preparation and service areas and for foods being transported to remote areas.
Arrange the flow of food through a vessel in a logical sequence that eliminates or minimizes cross-traffic or backtracking and that allows clear separation of clean and soiled operations. Provide an orderly, functional flow of food from the purveyor at dockside through the storage, preparation, and finishing areas to the service areas and finally, to the waste management area. The goal is to prepare and serve food smoothly and rapidly in accordance with strict time and temperature-control requirements and to minimize time and handling.
VSP evaluates the size of a particular room or area and the flow of food through the vessel to those rooms or areas initially and primarily during the plan review process.
# Equipment Requirements
# 6.2.1
The following is a list of equipment required in galleys, depending on the level, and type of service, with recommendation for other areas:
6.2.1.1 Blast chillers incorporated into the design of passenger and crew galleys. More than one unit may be necessary depending on the size of the vessel, the unit's intended application, and the distances between the chillers and the storage and service areas.
# 6.2.1.2
Food preparation sinks in as many areas as necessary (e.g., in all meat, fish, and vegetable preparation rooms; cold pantries or garde mangers; and in any other areas where personnel wash or soak food). An automatic vegetable washing machine may be used in addition to food preparation sinks in vegetable preparation rooms;
# 6.2.2
Equip the main pot washing area that serves the full galley operation with a minimum of a three-compartment sink with a prewash station or a four compartment sink with an insert pan and an overhead spray. Install a sink that is large enough to accommodate the largest piece of equipment (pots, tableware, etc.) used in its designated serving area. If desired, use an automatic warewashing machine with separate prewash stations in addition to the threecompartment sinks, if the machines are sized to accommodate the equipment being washed. A front-loading, pass-through, or conveyor type warewashing machine is preferable to an under counter model.
# 6.2.3
Provide additional three-compartment sinks with prewash stations or fourcompartment sinks with insert pans and overhead spray in heavy-use areas.
Those may include bakeries, butcher shops, and other preparation areas where the size of the facility or distance makes use of a central pot washing area impractical.
# 6.2.4
Equip all food preparation areas with easy access to a three-compartment sink, or a warewashing machine with an adjacent dump sink and pre-wash hose.
# 6.2.5
Furnish beverage dispensing equipment with readily removable drip trays or built-in drains in the tabletop. Furnish bulk milk dispensers with readily removable drip trays.
# 6.2.6
Provide readily removable drip trays for condiment dispensing equipment.
# 6.2.7
Design storage areas to accommodate all equipment and utensils used in food preparation areas such as ladles and cutting blades.
# 6.2.8
Ensure that the design of installed equipment directs food and wash water drainage into a deck drain, scupper, or deck sink, and not directly or indirectly onto a deck.
# 6.2.9
Provide a utility sink in areas such as beverage stations where it is necessary to refill pitchers or dispensers or discard liquids such as coffee.
# 6.2.10
Provide ice cream, sherbet, or a similar product dipper wells with running water and proper drainage.
# 6.2.11
Provide tight-fitting doors or protective closures to ice bins, food display cases, and other food and ice holding units to prevent contamination of stored products.
# 6.2.12
Protect countertop openings and rims of food cold tops, bains-marie, ice wells, and other drop-in type food and ice holding units with a raised integral edge or rim of at least 5 mm (3/16 inch) above the counter level around the opening.
# Equipment Surfaces
# 6.3.1
Ensure that material used for food contact, splash contact and exposed non-food contact surfaces are smooth, durable, and non-corroding. They should be easily cleanable and designed without unnecessary edges, projections, or crevices.
# 6.3.2
Use only materials approved for contact with food on food contact surfaces. Make all food contact surfaces smooth, durable, non-corroding, easily cleanable, readily accessible, and maintainable. Provide coved preferable seamless corners in accordance with current sanitary standards for food service equipment. Form external corners and angles with a sufficient radius to permit proper drainage and without sharp edges. Use only sealants approved for food contact surfaces (certified to ANSI/NSF Standard 51, or equivalent criteria) on food contact and food splash surfaces. Use approved sealants in limited application when practical function or design requires, such as the joining surfaces between ice makers and bins. Avoid excessive use of sealant.
# 6.3.3
Use materials approved for food contact surfaces for splash contact surfaces. Design surfaces so they are smooth with no sharp edges, durable, non corroding, readily accessible, and easily cleanable.
# 6.3.4
Use durable and non-corroding material for non-food contact surfaces. Design surfaces so that they are smooth, easily cleanable, and accessible material.
# Bulkheads, Deckheads and Decks
6.4.1 Do not use exposed fasteners in bulkhead and deckhead construction. Seal all seams between adjoining bulkhead panels, deckhead panels, and between bulkhead and deckhead panels. Seal seams greater than 0.8 mm (1/32 inch), but less than 3 mm (⅛ inch), with an appropriate sealant or appropriate profile strips. Cover all seams greater than 3 mm (⅛ inch) with appropriate profile strips. Seal all bulkhead, deckhead, and deck penetrations through which pipes or other conduits pass, including those located inside technical compartments. Use durable and corrosion-resistant collars where gaps are greater than 3 mm (⅛ inch).
# 6.4.2
Reinforce all bulkheads sufficiently to prevent panels from buckling or becoming detached under normal operating conditions.
# 6.4.3
Weld door penetration indentations completely so that there are no open voids. Ensure that locking and latch pins insert into inverted nipple recesses. This also applies to the penetrations around fire doors, in thresholds, and bulkhead openings.
# 6.4.4
Install durable coving of at least a 9.5 mm (3/8 inch) radius or open design (> 90 degrees [see definition]) as an integral part of the deck and bulkhead interface and at the juncture between decks and equipment foundations. Provide coving that is durable, of sufficient thickness, and securely fastened.
# 6.4.5
Use material for decks that is hard, durable, easily cleanable, non-skid, and non-absorbent.
# 6.4.5.1
Install durable vinyl or linoleum deck coverings in staff, crew or officer dining areas only.
# 6.4.5.2
Seal all pipe and conduit deck penetrations.
# 6.4.6
Use compatible metals to minimize corrosion due to galvanic action or provide effective insulation techniques between dissimilar metals to protect them from corrosion.
# Deck Drains, Deck Sinks and Scuppers
6.5.1 Construct deck drains, scuppers, and deck sinks from stainless steel with smooth finished surfaces that are accessible for cleaning, designed to drain completely, and large enough to prevent overflow to adjacent deck surfaces.
# 6.5.2
Construct scupper, and deck sink cover grates from stainless steel or other materials that: 1) meet the requirements for a smooth, easily cleanable surface; 2) are strong enough to maintain the original shape; and 3) exhibit no sharp edges. Install scupper and deck sink cover grates that are tight-fitting, readily removable for cleaning, and uniform in length where practical (e.g., 1,000 mm or 40 inches), so that they are interchangeable.
# 6.5.3
Place deck drains, and deck sinks in low-traffic areas such as in front of soup kettles, boilers, tilting pans, or braising pans. Size the deck drains, scuppers, and sinks in order to eliminate spillage and overflow to adjacent deck surfaces.
# 6.5.4
Provide sufficient deck drainage in all food service areas to prevent liquids from pooling on the decks. 6.5.5 Design deck and scupper drain lines to drain at a sufficient rate, relative to nearby water supplies, to avoid pooling. Provide cross-drain connections to prevent ponding and spillage from the scupper when the vessel is listing. 6.5.6 Do not use deck sinks as substitutes for deck drains. Independent deck drains are required.
6.6 Ramps 6.6.1 Ensure that ramps over thresholds are easily removable or sealed in place, sloped for easy roll-in and roll-out of trolleys, and are strong enough to maintain their shape. If ramps over scupper covers are built as an integral part of the scupper system, construct them of cleanable and durable material. 6.7 Gray and black water drain lines 6.7.1 Limit the installation of drain lines that carry sewage or other liquid waste directly overhead or horizontally through spaces used for food preparation or storage. That includes areas for washing or storage of utensils and equipment, such as bars, deck pantries, and over buffet counters. Sleeve-weld, or butt weld steel pipe; and heat fuse, or chemically weld plastic pipe. Do not use push-fit or press-fit piping over these areas.
# General Hygiene Facilities Requirements
# Handwashing Stations
7.1.1 Provide hot and cold potable water to all handwashing sinks. 7.1.1.a Equip handwashing sinks to provide water at a temperature between 43°C (110°F) and 52°C (125°F) through a mixing valve or combination faucet.
# 7.1.2
Construct handwashing sinks of stainless steel in food handling, preparation and storage areas. Construct handwashing sinks in food service areas of stainless steel or similar, durable materials.
# 7.1.3
Provide handwashing stations that include a suitable soap dispenser, paper towel dispenser, corrosion-resistant waste receptacle, and where necessary, splash panels to protect adjoining equipment. If attached to the bulkhead, permanently seal or make readily removable for cleaning paper towel dispensers and waste towel receptacles.
# 7.1.4
Provide at least one bucket filling station in each area of the galleys (e.g., cold galley, hot galley, bakery, etc.), food storage, and food preparation areas, below the handwashing sinks. Supply hot and cold potable water through a mixing valve to a faucet with the appropriate backflow protection at each bucket filling station. Provide appropriate deck drainage (e.g., scupper or sloping deck to deck drain) under all bucket filling stations to eliminate any pooling of water on the decks below the bucket filling station. 7.1.5 Locate handwashing stations throughout food handling, preparation, and warewash areas, so that no employee must walk more than 8000 mm (25 feet) to reach a station or pass through a normally closed door. 7.1.5.a Install handwash sinks approximately 750 mm (30 inches) above the deck.
# 7.1.5.b
Position the handwash sink so employees do not have to squat or reach excessively to wash their hands. 7.1.5.c Provide a handwashing station at food dispensing waiter stations (e.g., soups, ice, etc.), where the staff does not routinely return to an area with a handwashing station. 7.1.5.d Provide a handwashing station in provision areas where bulk raw foods are handled by provisioning staff. 7.1.5.e Provide at least one handwashing station for every 100 seats, (e.g., 1-100 seats = one handwashing station, 101-200 seats = two handwashing stations, etc.) at the entrance of all officer/staff/crew mess areas where food service lines are "self-service."
# 7.1.6
Install a sufficient number of handwashing sinks at the soiled dish drop-off area(s) in the main galley to allow quick turn-around time for employees bringing soiled dishware from the dining rooms or other food service areas and to prevent long waiting lines at handwashing stations.
# 7.1.7
Provide at least one handwashing station at soiled linen handling areas of the main laundry.
# 7.1.8
Install easy-to-operate, sanitary faucet handles, (e.g., elephant ear handles, foot pedals, knee pedals, or electronic sensors) on handwashing sinks in food service areas. If a faucet is self-closing, slow-closing, or metering, provide a water flow of at least 15 seconds without the need to reactivate the faucet.
# 7.1.9
Install permanent signs in English, and in other languages where appropriate, stating at a minimum, "WASH HANDS OFTEN."
# Crew Toilet Rooms
# 7.2.1
Install employee toilet rooms in proximity to the work area of all food preparation areas.
# 7.2.2
Supply toilet rooms with exhaust ventilation and equip them with handwashing facilities. Install permanent signs in English, and other languages where appropriate, stating at a minimum "WASH HANDS AFTER USING TOILET."
# 7.2.3
Install tight-fitting, self-closing doors to control insects/vermin and odors in toilet rooms or water closets inside toilet rooms.
# 7.2.4
Construct decks of hard, durable materials and cove the bulkhead-deck juncture.
# 7.2.5
Install easily cleanable deckheads and bulkheads.
# Equipment Placement and Mounting
# 8.1.1
Provide at least 150 mm (6 inches) of clear, unobstructed space between adjacent equipment and between the equipment and bulkheads, when the distance to be cleaned is less than 600 mm (24 inches).
# 8.1.2
Provide at least 200 mm (8 inches) of clear, unobstructed space between adjacent equipment and between the equipment and bulkheads when the distance to be cleaned is greater than 600 mm (24 inches) but less than 1200 mm (48 inches) long.
# 8.1.3
Provide at least 300 mm (12 inches) of clear, unobstructed space between adjacent equipment and between the equipment and bulkheads when the distance to be cleaned is greater than 1200 mm (48 inches) but less than 1800 mm (72 inches) long.
# 8.1.4
Provide at least 460 mm (18 inches) of clear, unobstructed space between adjacent equipment and between the equipment and bulkheads when the distance to be cleaned is greater than 1800 mm (72 inches).
# 8.2
Continuous weld all equipment that is not classified as portable to stainless steel pads or plates on the deck. Make sure the welds have smooth edges, rounded corners, and no gaps. Attach equipment as an integral part of the deck surface with glue, epoxy, or other durable adhesive product. Ensure that the arrangement is smooth and easily cleanable.
# 8.3
Seal deck-mounted equipment that is not easily movable to the deck or elevate it on legs that provide at least a 150 mm (6 inch) clearance between the deck and the equipment. If no part of the deck under the deck-mounted equipment is more than 150 mm (6 inches) from the point of cleaning access, the clearance space may be only 100 mm (4 inches). Exceptions also may be granted if there are no barriers to cleanability, (e.g., equipment, such as waste handling systems and warewashing machines with pipelines, motors, and cables below whiche 150 mm [6 inches] clearance from the deck may not be practical).
# 8.4
Provide a minimum of at least 150 mm (6 inches) between equipment and the deckheads. If proper clearance cannot be achieved, extend the equipment through the deckhead panels and seal appropriately.
# 8.5
Mount equipment that is on a foundation or coaming at least 100 mm (4 inches) above the finished deck. Use cement or a continuous weld to seal equipment to the foundation or coaming. Provide a sealed-type foundation or coaming for equipment not mounted on legs. Do not allow equipment to overhang the foundation or coaming by more than 100 mm (4 inches). Completely seal any overhang(ing) equipment along the bottom (Figure 6).
# 8.6
Seal table-mounted equipment, unless portable, to the tabletop or mount on legs.
# 8.6.1
The length of the legs is dependent upon the horizontal distance of the table top under the equipment from either end to the farthest point requiring cleaning.
8.6.1.a Mount the equipment on legs at least 100 mm (4 inches) above the tabletop if the horizontal distance of the table top under the equipment is 500 mm (20 inches) or greater from the point of access for cleaning.
# 8.6.1.b
Mount the equipment on legs at least 75 mm (3 inches) above the tabletop if the horizontal distance of the table top under the equipment is less than 500 mm (20 inches) or greater than 75 mm (3 inches) from the point of access for cleaning.
# 8.6.1.c
Mount the equipment on legs at least 50 mm (2 inches) above the tabletop if the horizontal distance of the table top under the equipment less than 75 mm (3 inches) from the point of access for cleaning. 8.6.2 Provide access behind tabletop mounted equipment, including beverage line equipment, for cleaning.
# Fasteners and Requirements for Securing and Sealing Equipment
9.1 Food Contact Surfaces 9.1.1 Attach all food contact surfaces or connections from food contact surfaces to adjacent splash zones to ensure a seamless, coved corner. Reinforce all bulkheads, deckheads, or decks receiving such attachments. 9.1.2 Use low profile, non-slotted, non-corroding, and easy to clean fasteners on food contact surfaces and in food splash zones. The use of exposed slotted screws, Phillips head screws or pot rivets in these areas is prohibited.
# Non-Food Contact Surfaces
9.2.1 Seal non-food contact surfaces of equipment, gaps, and seams less than 3 mm (⅛ inch) with an appropriate sealant. Use only stainless steel profile strips on surfaces exposed to extreme temperatures (e.g., freezers, and above cook tops, grills, and fryers) or for gaps greater than 3 mm (⅛ inch). Avoid excessive use of sealant.
# 9.2.2
Construct slotted or Phillips head screws, pop rivets, and other fasteners used in non-food contact areas of corrosion-resistant materials.
# Use of Sealants
# 9.3.1
Use approved food grade sealants in food contact and food splash zones.
# Latches, Hinges, and Handles
10.1 Use durable, non-corroding, and easily cleanable built-in equipment latches, hinges, and handles. Do not use piano hinges in food contact or splash zones.
# Gaskets
11.1 Use smooth, non-absorbent, non-porous materials for equipment gaskets in reach-in refrigerators, steamers, ice bins, ice cream freezers, and similar equipment.
# 11.2
Close and seal exposed surfaces of gaskets at their ends and corners.
# 11.3
Use refrigerator door gaskets that are designed to be removable.
# 11.4
Follow the requirements in Section 9.0 when using fasteners to install gaskets.
# Equipment Drain Lines:
12.1 Connect drain lines from the following to appropriate waste systems by means of an or air-break all fixtures, sinks, appliances, compartments, refrigeration units, or devices that are used, designed for, or intended to be used in the preparation, processing, storage, or handling of food, ice, or drinks.
12.1.1 Use stainless steel or other easily cleanable rigid or flexible material in the construction of drain lines. Size drain lines appropriately, with a minimum interior diameter of 25 mm (1 inch) for custom-built equipment.
12.1.2 Slope walk-in refrigerators and freezer evaporator drain lines, and extend them through the bulkheads or decks. Direct drain lines through an accessible air-break to a deck scupper or drain below the deck level or to a scupper outside.
12.1.3 Install drain lines to minimize the horizontal distance from the source of the drainage to the discharge.
12.1.4 Install horizontal drain lines at least 100 mm (4 inches) above the deck and slope to drain.
12.2 All drain lines (except condensate drain lines) from hood washing systems, cold top tables, bains-marie, dipper wells, food preparation sinks and warewashing sinks or machines must: 12.2.1 be less than 1000 mm (40 inches) and free of sharp angles or corners, if designed to be cleaned in place by a brush.
12.2.2 be readily removable for cleaning, if greater than 1000 mm (40 inches).
# drain through an air-break to a drain or scupper.
12.3 Extend all installed equipment drain lines in a vertical line to a scupper, or deck drain, when possible. If not possible, keep the horizontal distance of the line to a minimum.
# 12.4
Handwashing sinks, mop sinks and drinking fountains are not required to drain through an air-break.
# Electrical Connections, Pipelines, and other Attached Equipment
13.1 Encase electrical wiring from permanently installed equipment in durable and easily cleanable material. Do not use braided or woven stainless steel electrical conduit outside of technical spaces or where it is subject to splash or soiling, unless encased in easily cleanable plastic or similar easily cleanable material. For equipment that is not permanently mounted, adjust the length of electrical cords or fasten them in a manner that prevents the cords from lying on countertops.
13.2 Tightly seal bulkhead or deckhead-mounted equipment (phones, speakers, electrical control panels, outlet boxes, etc.) with the bulkhead or deckhead panels. Do not locate such equipment in areas exposed to food splash.
# 13.3
Tightly seal any areas where electrical lines, steam or water pipelines, etc., penetrate the panels or tiles of the deck, bulkhead, or deckhead, including inside technical spaces located above or below equipment or work surfaces. Seal any openings or voids around the electrical lines or the steam or water pipelines and the surrounding conduit or pipelines.
# 13.4
Enclose steam and water pipelines to kettles and boilers in stainless steel cabinets or position the pipelines behind bulkhead panels. Minimize the number of exposed pipelines. Cover any exposed, insulated pipelines with stainless steel or other durable, easily cleanable material.
# Hood Systems
14.1 Install hood systems or direct duct exhaust over warewashing equipment (except undercounter warewashing machines) and over three-compartment sinks in pot wash areas where hot water is used for sanitizing.
# 14.1.1
Directly connect warewashing machines that have a direct duct exhaust, to the hood exhaust trunk.
# 14.1.2
Design exhaust hoods over warewashing equipment or threecompartment sinks to have a minimum 150 mm (6 inches) overhang from the edge of equipment to capture excess steam and heat.
# 14.1.3
Install a clean-out port in the direct exhaust ducts of the ventilation systems between the top of the warewashing machine and the hood system or deckhead.
# 14.1.4
Provide accessible and removable flat condensate drip trays in the ducts from the warewashing machines.
# 14.2
Install hood or canopy systems above cooking equipment in accordance with SOLAS requirements to ensure that they adequately remove excess steam and grease-laden vapors.
# 14.2.1
Install hood systems or dedicated local exhaust ventilation to control excess heat and steam from bains-marie or steam tables.
# 14.3
Select proper sized exhaust and supply vents. Position and balance them appropriately for expected operating conditions to ensure proper air conditioning, and capture and exhaust of heat and steam.
# 14.4
Where used, provide readily removable, and cleanable filters.
# 14.5
Provide access for cleaning vents and ductwork (Automatic clean-in-place systems are recommended for removal of grease generated from cooking equipment).
# 14.6
Locate the automatic clean-in-place hood wash control panels that have detergent reservoirs so they are not over food preparation equipment or counters.
# 14.7
Construct hoods systems of stainless steel with coved corners of at least 9.5 mm (3/8 inch) radius. Use continuous welds or profile strips on adjoining pieces of stainless steel.
# 14.7.1
A drainage system is not required for normal grease and condensate hoods, or if cleaning solutions are applied manually to hood assemblies.
# 14.7.2
Install drainage for automatic clean-in-place hood washing systems.
# 14.8
Install ventilation systems in accordance with the manufacturer's recommendations. Test the system by utilizing a method that determines if the system is properly balanced for normal operating conditions.
# Provision Rooms, Walk-in Refrigerators and Freezers, and Transportation Corridors
# Bulkheads and and Deckheads
15.1.1 Provide tight-fitting, stainless steel bulkheads in walk-in refrigerators and freezers. Line doors with stainless steel.
# 15.1.2.a
Light colored painted steel is acceptable for provision passageways and transportation corridors.
# 15.1.2.b
Stainless steel panels are preferable but not required in dry storage areas.
# 15.1.3
Provide protection to prevent damage to bulkheads from pallet handling equipment (e.g., forklifts, pallet jacks, etc.) in areas through which food is stored or transferred.
# 15.1.4
Close deckhead-mounted cable trays, piping or other difficult to clean deckhead-mounted equipment, or close the deckhead to prevent food contamination from dust and debris falling from deckheads and deckhead mounted equipment and utilities (painted sheet metal ceilings are acceptable in these areas).
# Decks
15.2.1 Use hard, durable, non-absorbent decking, (e.g., tiles, or diamond plate corrugated stainless steel deck panels) in refrigerated provision rooms. Install durable covings, and provision rooms s, and provision rooms as an integral part of the deck and bulkhead interface and at the juncture between decks and equipment foundations. If installed, use a sufficient thickness on stainless steel or other coving to make durable and secure. Sufficiently reinforce stainless steel decking to prevent buckling if pallet handling equipment will be used in these areas.
# 15.2.2
Steel decking is acceptable in provisions passageways, transportation corridors, and dry-stores areas.
# Cold Room Evaporators, Drip Pan, and Drain Lines
15.3.1 Enclose piping, wiring, coils, and other difficult-to-clean components of evaporators in walk-in refrigerators, freezers, and dry storerooms with stainless steel panels.
# 15.3.2
Use stainless steel evaporator drip pan that have coved corners, are sloped to drain and strong enough to maintain slope, and are readily accessible for cleaning.
# 15.3.3
Place non-corroding spacers between the drip pan brackets and the interior edges of the pans.
# 15.3.4
Follow all fastener guidelines in Section 9.0.
# 15.3.5
Provide a heater coil for freezer drip pan. Attach the coil to a stainless steel insert panel or to the underside of the drip pan. Use easily removable coils so that the drip pan can be cleaned. Make sure that heating coils provided for drain lines are installed inside of the lines.
# 15.3.6
Position and size the evaporator drip pan to collect all condensate dripping from the evaporator unit.
# 15.3.7
Encase thermometer probes in a stainless steel conduit. Position probes in the warmest part of the room where food is normally stored.
# Galleys, Food Preparation Rooms, and Pantries
# Bulkheads and Deckheads
16.1.1 Construct bulkheads and deckheads (including doors, door frames, and columns) with a high quality, corrosion-resistant stainless steel. Use a thick enough gauge so that the panels do not warp, flex, or separate under normal conditions. Use an appropriate sealant for seams greater than 1 mm (1/32 inch), but less than 3 mm (⅛ inch). Use only stainless steel profile strips for bulkhead and deckhead seams greater than 3 mm (⅛ inch).
# 16.1.1.a
Minimize gaps around fire shutters, sliding doors, and pass-through windows.
# 16.1.1.b
Provide cleaning access to void spaces of sliding doors and sliding pass-through windows.
# 16.1.2
Construct bulkheads of sufficient thickness or reinforce the areas where equipment is installed to allow the use of fasteners or welding without compromising the quality and construction of the panels.
# 16.1.3
Install utility line connections through a stainless steel or other easily cleanable, food service approved conduit that is mounted away from bulkheads for ease in cleaning.
# 16.1.4
Attach backsplashes to the bulkhead with low profile, non-slotted fasteners or continuous-or tack-welds, polished smooth. Use an appropriate sealant to make the backsplash attachment watertight.
# 16.1.5
Seal all openings where piping and other items penetrate the bulkheads and deckheads, including inside technical compartments.
# Decks
16.2.1 Construct decks from hard, durable, non-absorbent, non-skid material. Install durable coving as an integral part of the deck and bulkhead interface and at the juncture between decks and equipment foundations.
# 16.2.2
# Decks
# 17.2.1
Install hard, durable, non-absorbent decks at all buffet lines that are at least 1000 mm (40 inches) in width measured from the edge of the service counter or from the outside edge of the tray rail (if such a rail is present).
# 17.2.2
Install hard, durable, non-absorbent decks (e.g., tile, sealed granite, or marble) that extends at least 600 mm (24 inches) from the edge of the working side of the dining room service stations.
# 17.2.3
Construct and cove decks behind service counters, under equipment, and in technical spaces of hard, durable, non-absorbent materials (e.g., tiles, epoxy resin, or stainless steel). Do not use painted steel or concrete decking.
# 17.2.4
Durable linoleum, vinyl tile, or deck covering may be used only in staff, crew, or officers dining areas.
# 17.2.5
Cove and tightly seal all bulkhead and deck junctures (including deck/buffet, deck/bar, deck/waiter station).
# Food Display Protection
# 17.3.1
Provide effective means to protect food (e.g., sneeze shields or display cases) in all areas where food is on display for self-service.
# 17.3.2
Following these criteria for sneeze guards: 17.3.2.1 Sneeze guards may be temporary (portable), built-in and integral parts of display tables, bains-marie, or cold-top tables.
# 17.3.2.2
Sneeze guard panels must be durable plastic or glass that is smooth and easily cleanable. Use sections of manageable lengths that are removable for cleaning.
# 17.3.2.3
Position sneeze guards so that the panels intercept the line between the consumer's mouth and the displayed foods, in accordance with ANSI/NSF Standard 2 for food equipment. Take into account factors such as the height of the food display counter, the presence or absence of a tray rail, and the distance between the edge of the display counter and the actual placement of the food (Figure 7).
# 17.3.2.3.a
Install side protection for sneeze guards if the distance between exposed food and where people are expected to stand is less than 1000 mm (40 inches).
# 17.3.3
Use tray rail surfaces that are sealed, coved, or have an open design and easily cleanable in accordance with guidelines for food splash zones.
# Beverage Delivery System
17.4.1 Install a stainless steel, vented, double-check valve backflow prevention device on carbonation systems with brass or copper fittings (e.g., multi-flow beverage dispensing systems). Install the device before the carbonator and downstream from any copper or copper-alloy (e.g., brass) in the potable watersupply line.
# 17.4.2
Encase supply lines to the dispensing guns in a single tube. If the tube penetrates through any bulkhead or countertop, seal the penetration with a grommet.
# 17.4.3
Incorporate, into the design of bulk dispensers of beverage delivery systems, a clean-in-place system that provides a means of flushing, and sanitizing the entire interior of the dispensing lines in accordance with manufacturers' instructions.
# Warewashing
18.1 Provide rinse hoses for prewashing (not required but recommended in bar and deck pantries). If a sink is to be used for prerinsing, provide a removable strainer.
# 18.2
Provide space for trash cans, garbage grinder, or food waste handling systems. Grinders are optional in pantries and bars.
# 18.3
Provide a food waste trough that extends the full length of soiled landing tables with food waste handling systems.
# 18.4
Seal the back edge of the soiled landing table to the bulkhead or provide a minimum of 460 mm (18.4 inches) clearance between the table and the bulkhead.
# 18.5
Design soiled landing tables to drain waste liquids and to prevent contamination of adjacent clean surfaces.
# 18.6
Provide across-the-counter gutters with drains, and slope the clean landing tables to the gutters at the exit from the warewashing machines to prevent water from pooling. If the first gutter does not effectively remove the pooled water, install additional gutter(s) and drain line(s). Minimize the length of drain lines and when possible direct them in a straight line to the deck scupper.
# 18.7
Provide sufficient space for cleaning around and behind equipment (e.g., food waste systems and warewashing machines). Refer to section 8.0 for spacing requirements.
18.8 Encase food waste system wiring in a durable and easy to clean stainless steel or non-metallic watertight conduit and raise it at least 150 mm (6 inches) above the deck. Elevate all warewashing machine components at least 150 mm (6 inches) above the deck, except as noted in Section 8.3.
# 18.9
Construct removable splash panels of stainless steel to protect the food waste system and technical areas.
# 18.10
Construct grinder cones, food waste system tables, and dish-landing tables from stainless steel with continuous welding. Construct platforms for supporting warewashing equipment from stainless steel.
# 18.11
Design and size warewashing machines for their intended use and install them according to the manufacturer's recommendations.
# 18.11.1
Equip warewashing machines with a device that audibly or visually indicates that the sanitizing temperature or the chemical sanitizer level has dropped below the levels stated on the machine data plate.
# 18.12
Display the data plate affixed to warewashing machines by the manufacturer so that the information is easily accessible and readable. The data plate provides the following information: 18.12 a) temperatures required for washing, rinsing, and sanitizing; 18.12 b) pressure required for the fresh water sanitizing rinse unless the machine is designed to use only a pumped sanitizing rinse; 18.12 c) conveyor speed for conveyor machines or cycle time for stationary rack machines; and 18.12 d) chemical concentration (if chemical sanitizers are used).
# 18.13
Correctly size three-compartment warewashing, and potwashing sinks for their intended use. Use sinks that are large enough to submerge the largest piece of equipment used in the area that is served. Use sinks that have coved, continuously welded internal corners that are integral to the interior surfaces.
18.14 Install one of the following arrangements to prevent excessive contamination of rinse water with wash water splash: 18.14 a) an across-the-counter gutter with a drain that divides the wash compartment from the rinse compartment 18.14 b) a splash shield at least 100 mm (4 inches) above the flood level rim of the sink between the wash and rinse compartments 18.14 c) an overflow drain in the wash compartment 100 mm (4 inches) below the flood level.
# 18.15
Equip hot water sanitizing sinks with accessible and easily readable thermometers, a utensil retrieval system (e.g., long-handled stainless steel wire basket, or other retrieval system), a jacketed or coiled steam supply with a temperature control valve to control water temperature, or electric heating system. (Three-compartment sinks that utilize chemical sanitizers for the sanitization step do not require those items).
# 18.17
Provide adequate ventilation to prevent condensation on the deckhead or adjacent bulkheads. Ensure that any filters installed over warewashing equipment are easily removable, and fans are accessible for cleaning.
# Lighting
19.1 Provide a minimum of 220 lux (20 foot candles) of light at the work surface level in all food preparation, food service, and warewashing areas when all equipment is installed. Provide 220 lux (20 foot candles) of lighting for equipment storage, garbage and food lifts, garbage rooms, and toilet rooms, measured at 760 mm (30 inches) above the deck.
# 19.1.1
Provide a minimum light level of 110 lux (10 foot-candles) behind and around equipment measured at a distance of 760 mm (30 inches) above the deck (e.g., ice machines, combi-ovens, etc.).
# 19.1.2
Provide a minimum light level of 220 lux (20 foot-candles) at counter tops (e.g., beverage lines, etc.).
# 19.2
For effective illumination, place the deckhead mounted light fixtures above the work surfaces and positioned them in an "L" pattern rather than a straight line pattern.
# Install light fixtures tightly against the bulkhead and deckhead panels.
Completely seal electrical penetrations to permit easy cleaning around the fixtures.
# 19.4
Use shatter-resistant and removable light shields for light fixtures. Completely enclose the entire light bulb or fluorescent light tube(s).
# 19.5
Provide lighting levels of at least of 220 lux (20 foot candles) in provision rooms, measured at 760 mm (30 inches) above the deck while the rooms are empty. During normal operations when foods are stored in the rooms, provide lighting levels of at least 110 lux (10 foot candles), measured at a distance of 760 mm (30 inches) above the deck.
# 19.6
In bars and over dining room waiters' stations designed for lowered lighting during normal operations, provide lighting that can be raised to 220 lux (20 foot candles) during cleaning operations, as measured at 760 mm (30 inches) above the deck.
# 19.7
Use shielded, coated, or otherwise shatter-resistant light bulbs in areas where there is exposed food; clean equipment, utensils, and linens; or unwrapped single-service, and single-use articles.
# 19.8
Use shields that surround and extend beyond bulbs on infrared or other heat lamps to protect against breakage. Allow only the face of the bulb to be exposed.
# 19.9
Decorative track or recessed deckhead-mounted lights above bar countertops, buffets, and other similar areas may be mounted on, or recessed within the deckhead panels without being shielded. However, install speciallycoated, shatter-resistant bulbs in the light fixtures in this area.
# 20.1.4
Install a drain at the bottom of all lift shafts including provision platform lifts, and dumbwaiters.
# 20.1.5
Construct the interiors of dumbwaiters of stainless steel with coved bulkhead and deck junctures and meets the standards of Section 16.0.
# 20.1.6
Provide light fixtures that are recessed or fitted with stainless steel guards to prevent breakage.
# 20.1.7
If installed, construct garbage chutes of stainless steel, with an automatic washing system, and in accordance with SOLAS and classification society requirements.
# Trolley, Waste Container, and Cleaning Equipment Wash Rooms
# Construct bulkheads, deckheads, and decks to the same standards as
Section 16.0.
# 20.2.2
Provide a bulkhead-mounted pressure washing system with a deck sink and drain (An enclosed automatic equipment washing machine or room may be used in place of the pressure washing system and deck sink).
# 20.2.3
Provide an easily accessible handwashing station with potable hot and cold water, a hose connection, and a deck drain.
# 20.2.4
Provide ventilation for the extraction of steam and heat.
# Garbage Holding Facilities
# 20.3.1
Construct garbage and refuse storage or holding rooms sized to hold unprocessed waste for the longest expected period when off-loading of waste is not possible. Separate the refuse-storage room from all food preparation and storage areas.
# 20.3.2
Provide supply and exhaust ventilation to control odors, temperature, and humidity.
# 20.3.3
Provide a sealed, refrigerated space for storing wet garbage that meets the standards of 15.0.
# 20.3.4
Provide an easily accessible handwashing station with potable hot and cold water, a hose connection, and a deck drain.
# 20.3.5
Provide sufficient deck drainage to prevent pooling of any water.
# 20.3.6
Ensure that all bulkheads and decks are durable and easily cleanable.
# Garbage Processing Areas
# 20.4.1
Appropriately size the garbage processing area for the operation and supply a sufficient number of sorting tables.
# 20.4.2
Provide stainless steel sorting tables with coved corners. If provided, use deck coaming that is at least 80 mm (3 inches) and coved. If the tables have drains, direct the table drains to a deck drain and install a strainer in the deck drain.
# 20.4.3
Provide an easily accessible handwashing station with potable hot and cold water, a hose connection, and a deck drain.
# 20.4.4
Provide a storage locker for cleaning materials. Follow storage locker guidelines in Section 26.1.
# 20.4.5
Ensure that bulkheads and decks are durable and easily cleanable. Provide deck drains to prevent liquids from pooling on the decks. Provide berm/coaming around all waste-processing equipment and ensure there is proper deck drainage inside the berms.
# 20.4.6
Provide light levels of at least 220 lux (20 foot candles) at work surface levels.
# 20.4.7
Equip a sink with a pressure washer or an automatic washing machine for washing equipment, storage containers, and garbage barrels.
# Sewage Systems
# 20.5.1
Limit the installation of drain lines that carry sewage or other liquid waste directly overhead or horizontally through spaces used for food preparation or storage. That includes areas for washing or storage of utensils and equipment, such as bars, deck pantries, and over buffet counters. Sleeve-weld, or butt weld steel pipe; and heat fuse, or chemically weld plastic pipe. Do not use push-fit or press-fit piping over these areas.
# 20.5.2
Design black and gray water drain systems from cabins, food areas, and public spaces to prevent the back-up of waste and the emission of odors or gases into these areas.
# 20.5.3
Vent sewage-holding tanks to the outside of the vessel so that they are independent of all other tanks and are away from any air intakes.
# Potable Water System
# Bunker Stations
# 21.1.1
Position the filling lines at least 450 mm (18 inches) above the deck; paint or stripe them auxiliary blue or in accordance with ISO 14726.
# 21.1.2
Equip filling lines with tight-fitting caps that are fastened by a non corroding chain so that the cap does not touch the deck when hanging.
# 21.1.3
Use unique screw connections for the hose attachments that only fit potable water hoses.
# 21.1.4
Label the filling lines "POTABLE WATER FILLING" with at least 13 mm (½ inch) high lettering stamped, stenciled, or painted on the bulkhead in the area of the bunker line.
# 21.1.5
If used, locate filters in the bunkering line before the halogenation injection point, accessible for inspection and removable for cleaning.
# Filling Hoses
# 21.2.1
Provide hoses designed for potable water use that are durable with smooth, impervious linings, caps on each end, and fittings unique to the potable water connections.
# 21.2.2
Provide at least two 15 m (50 feet) hoses per bunker station.
# 21.2.3
Label potable water hoses "POTABLE WATER ONLY."
# Filling Hose Storage
# 21.3.1
Construct potable water hose lockers from smooth, non-toxic, corrosionresistant, and easily cleanable material.
# 21.3.2
Mount potable water hose lockers at least 450 mm (18 inches) above the deck. Design hose lockers to be self-draining.
# Label potable water hose lockers "POTABLE WATER HOSE AND FITTING STORAGE
" in letters at least 13 mm (½ inch) high.
# 21.3.4
Provide storage space for at least four 15 m (50 feet) potable water bunker hoses per bunker station.
# International Fire Shore Connections and Fire Sprinkler Shore Connections
# 21.4.1
Install an RP assembly on all connections where hoses from potable water supplies on shore will be connected to non-potable systems onboard the vessel.
# Storage and Production Capacity for Potable Water
21.5.1.a Provide a minimum of 2 days storage capacity that assumes 120 liters (30 gallons) of water per day per person, and provide potable water production capacity of 120 liters (30 gallons) per day per person for the maximum capacity of crew and passengers on the vessel.
# Potable Water Storage Tanks
21.6.1 General Requirements 21.6.1.1 Ensure that the tanks are independent of the shell of the vessel and do not share a common wall with tanks containing non-potable water or other liquids. Provide a 450 mm (18 inch) cofferdam above and between tanks that are not for storage of potable water and also between the tanks and the hull. Skin or double-bottom tanks are not allowed for potable water storage.
# 21.6.1.2
Use an approved potable water tank coating. Follow all of the manufacturers' recommendations for applying and drying or curing the coating. Provide written documentation for these.
# 21.6.1.3
Coat all items that penetrate the tank (e.g., bolts, pipes, pipe flanges) with the same product used for the tank's interior.
# 21.6.1.4
Design tanks to be super-chlorinated one tank at a time.
# 21.6.1.5
Ensure that lines for non-potable liquids do not pass through potable water tanks. Minimize the use of non-potable lines above potable water tanks. Do not use mechanical couplings on lines above tanks. If coaming is present along the edges of the tank, provide slots along the top of the tank to allow leaking liquid to run off and be detected.
# 21.6.1.6
Treat welded pipes over the tanks in order to make them corrosionresistant.
# 21.6.1.7
Treat all potable water lines inside potable water tanks so as to make them jointless and corrosion-resistant.
# 21.6.1.8
Label each potable water tank on its side and where clearly visible, with a number and the words "POTABLE WATER" in letters a minimum of 13 mm (½ inch) high.
# 21.6.1.9
Install at least one sample cock located above the deck plating on each tank. 21.6.1.9.a Point sample cocks down; identify and number them for each tank.
# Storage Tank Access Holes
# 21.6.2.1
Install access holes on the sides of potable water tanks.
# Storage Tank
# 21.6.5.3.b
Locate the drain in the pump discharge line ahead of any branch take offs to the distribution system. Provide a valve on the distribution main immediately beyond the drain line take-off. (Figure 8).
# Suction Lines
# 21.7.1
Place suction lines at least 150 mm (6 inches) from the tank bottom or sump bottom.
# Potable Water Distribution System
# 21.8.1
Locate distribution lines at least 450 mm (18 inches) above the deck plating or the normal bilge water level.
# 21.8.2
Do not cross connect potable water distribution lines with the piping of any non-potable water system lines.
# 21.8.3
Do not use lead or cadmium pipes, fittings, or solder.
# 21.8.4
Install only potable water taps in food areas, the hospital, and the cabin showers and sinks.
# 21.8.5
Paint or stripe potable water piping and fittings in auxiliary blue, or in accordance with ISO 14726 at 5000 mm (15 feet) intervals and on each side of partitions, decks, and bulkheads except where decor would be marred by such markings.
# 21.8.6
Use only potable water for steam that is applied directly to food and food contact surfaces. Generate the steam locally from food service equipment designed for this purpose (e.g., vegetable steamers, combi-ovens, etc.). Only apply non-potable water steam indirectly to food or food equipment. Route that steam through coils, tubes, or separate chambers.
# 21.8.7
Ensure that an air-gap or approved backflow prevention device is present if potable water is supplied to a bilge, waste, ballast, or laundry tank.
# 21.8.8
Clean, disinfect, and flush potable water tanks and any parts of the potable water distribution system with potable water before the system is placed in service.
# Potable Water Pressure Tanks
21.9.1 Do not cross-connect potable water hydrophore tanks to non-potable water tanks through the main air compressor.
# 21.9.2
Provide a filtered air supply from a non-permanent, quick disconnect, or independent compressor. The compressor shall not emit oil into the final air product.
# Potable Water Pumps
# 21.10.1
Size the potable water pumps to meet the service demands; do not use them for any other purpose.
# 21.10.2
Use pumps that prime automatically and not manually. Use a direct connection, not an air-gap, when supplying water to a potable water pump.
# 21.10.3
Properly size potable water pumps and distribution lines so that pressure is maintained at all times and at levels adequate levels to operate all equipment.
# Evaporators and Reverse Osmosis Plants
# 21.11.1
Locate the seawater inlets (sea chests) forward of all overboard waste water, swimming pool and whirlpool spa, and ballast tank discharge outlets.
# 21.11.2
Use only direct connections to the potable water system. Do not use swing lines.
# 21.11.3
Provide an air-gap or RP assembly between the potable water system and the non-potable water system. (Fresh water produced by an evaporator, or reverse osmosis plant is not considered potable until after it has been pH adjusted to the proper level.) 21.11.4 Post operating instructions for the evaporators, or reverse osmosis plants near the units.
# 21.11.5
Ensure that high and low-pressure units connected directly to the potable water lines have the ability to discharge to the waste system if the distillate is not fit for use.
# 21.11.6
Install units that have a low-range salinity indicator, an operation temperature indicator, an automatic discharge to waste, and an alarm with trip setting.
# 21.11.7
Route the high-saline discharge to the bilge or overboard through an airgap or RP assembly.
# Halogenation
21.12.1 Bunkering and Production 21.12.1.1 Provide labeled potable water taps with appropriate backflow preventers at the halogen supply tanks. 21.12.1.2 Provide a labeled sample cock at least 3000 mm (120 inches) downstream of the halogen injection point.
# Control halogen injection by a flow meter or analyzer.
21.12.1.4 Provide pH adjustment equipment for water bunkering and production. Install analyzer, controller, and dosing pumps that are designed to accommodate changes in flow rates.
# Distribution
21.12.2.1 Provide a completely automatic halogenation system that is analyzer controlled.
# 21.12.2.2
Use halogenation probes that measure free halogen; link them to an analyzer/controller and dosing pump.
# 21.12.2.3
Provide a back-up halogenation system with an automatic switchover that begins pumping halogen when the primary (in-use) pump fails or cannot meet the preset halogenation level.
# 21.12.2.4
Locate analyzer probes at a distant point in the system where significant water flow exists. 21.12.2.5 Provide an audible alarm in a continually occupied watch station, (e.g., the engine-control room), to indicate low free-halogen readings at the distantpoint analyzer.
# 21.12.2.6
Provide labeled potable water taps with appropriate backflow preventers at halogen supply tanks.
# 21.12.2.7
Locate a labeled sample cock at least 3000 mm (120 inches) downstream of the halogen injection point.
# 21.12.2.8
Provide free-halogen analyzer-chart recorders with ranges of 0.0 to 5.0 ppm and continuous recording periods indicating the level of free-halogen for 24 hour time periods, (e.g., circular 24 hour charts). 21.12.8.a Electronic data loggers with certified data security features may be installed in lieu of chart recorders. Acceptable data loggers produce records that conform to the principles of operation and data display required of the analog charts, including printing the records. Use electronic data loggers that log times in increments of <15 minutes.
# Disinfection of the Potable Water System
21.13.1 Disinfect the entire distribution system with a free halogen concentration of at least 50 mg/L (ppm) for at least 4 hours. Prior VSP agreement is required if alternative approved disinfection practices are used.
# 21.13.2
Provide written documentation of the distribution system disinfection.
# Backflow Prevention
22.1 Use appropriate backflow prevention (e.g., air-gaps, RP assemblies, pressure vacuum breakers, atmospheric vacuum beakers, pressure-type backflow preventers, or double-check valves with intermediate atmospheric vent) for all non-potable connections in the potable water system.
# 22.2
Use air-gaps that are at least twice the diameter of the supply pipe measured vertically above the flood level rim of the receiving vessel. The air-gap must at least 25 mm (1 inch).
# 22.3
Install RP assemblies in high-hazard situations where air-gaps are not practical.
# 22.4
If RP backflow prevention assemblies are used, provide a test kit for testing the devices.
# 22.4.a Test all RP's after installation.
22.5 Use mechanical backflow prevention devices when water must be supplied under pressure.
# 22.6
Install atmospheric vacuum breakers 150 mm (6 inches) above the fixture flood level rim with no valves downstream from the device.
# 22.7
Connect potable water through an air-gap when it is directed to a black water tank for rinse down or other such uses. RP assemblies are inadequate in this high hazard condition.
# 22.8
Protect the following connections to the potable water system against backflow or back-siphonage by air-gaps or mechanical backflow prevention devices:
# 22.8.1
Potable water supply lines to swimming pools, whirlpool spas, hot tubs, bathtubs, showers, and similar facilities. 22.8.12 Potable water, bilge, and sanitary pumps that require priming.
# 22.8.13
Freshwater or saltwater ballast systems.
# 22.8.14
International fire and fire sprinkler water connections.
# 22.8.15
The potable water supply to automatic window washing systems which utilize chemicals or chemical mix tanks.
# 22.8.16
Water softeners for non-potable fresh water if located before an airgap.
# 22.8.17
Water softener and mineralizer drain lines must be protected by an air-gap or RP assembly.
# 22.8.18
Any other connection between potable and non-potable water systems.
22.9 Heat Exchangers used for cooling potable water 22.9.1 Fabricate heat exchangers, using, or for cooling potable water so a single failure of any barrier will not cause a cross-connection or permit back-siphonage of contaminants into the potable water system. 22.9.2 Design heat exchangers where both potable water and any non-potable liquid are used to protect the potable water from contamination by one of the following designs; 22.9.2.a Double-wall construction between the potable and non-potable liquids, with a void space to allow any leaking liquid to drain away; and 22.9.2.a.1 An alarm system to indicate a leak in the double wall.
# 22.9.2.b
Single-wall construction with the following safety features: 22.9.2.b.1 Higher pressure of at least 1 bar on the potable water side of the heat exchanger; 22.9.2.b.2 An automatic diverter valve that directs potable water from the heat exchanger when the pressure difference is less than 1 bar; and 22.9.2.b.3 An alarm system that sounds when the diverter valve directs potable water from the heat exchanger.
# Swimming Pools
23.1 Use seawater, or a potable water supply passing through an air-gap or backflow preventer to fill swimming pools.
# 23.2
Provide an independent pool drainage system. If swimming pool drains are connected to another drainage system, provide a double-check valve between the two.
# 23.2.a
Install a drain at the lowest point in the pool.
# 23.3
Slope the bottom of the pool towards the drains to achieve complete drainage.
# 23.4
Provide anti-entrapment type drain covers that are constructed of durable easily visible, easily cleanable material and that meet ASME/ANSI A112.19.8M voluntary standard for suction fittings (figure 9a-9c), or other drains that prevent entrapment hazards as specified in U.S. Consumer Product Safety Publication 363-009801 (figure 9-10b). Dual drains meet the anti-entrapment requirements.
# 23.5
Ensure that the fill level of the pool is at the skim gutter level.
# 23.6
Ensure that pool overflows are either directed by gravity to the make-up tank for recirculation through the filter system or disposed of as waste.
# 23.7
Install recirculation, filtration, and disinfection equipment.
# 23.8
Use pool equipment (e.g., pumps and filters) that has the capacity to turnover the pool water at least four times every 24 hours (i.e., once every 6 hours or less).
# 23.9
Use self-priming, centrifugal pumps to re-circulate pool water.
# 23.10
Install pumps large enough to re-circulate the entire volume of the pool in 6 hours.
# 23.11
Install surface skimmers or gutters that are capable of handling approximately 80% of the filter flow of the recirculation system.
# 23.12
If skimmers are used instead of gutters, install is at least one skimmer for each 47 m² (500 square feet) of pool surface area.
# 23.13
Provide a hair strainer between the pool outlet and the suction side of the pumps to remove foreign debris such as hair, lint, pins, etc.
# 23.14
Ensure that the removable portion of the strainer is corrosion-resistant and has holes no greater than 6 mm (¼ inch) in diameter.
# 23.15
Use filters that are designed to remove all particles greater than 20 micrometers from the entire volume of the pool in 6 hours or less.
# 23.16
Use cartridge or media-type filters (e.g., rapid-pressure sand filters, high rate sand filters, diatomaceous earth filters, or gravity sand filters). Make filter sizing consistent with ANSI standards for public pools.
# 23.17
Use media-type filters that are capable of being back-washed.
# 23.18
Provide filter accessories, such as pressure gauges, air-relief valves, and rate-of-flow indicators.
# 23.19
Provide automatic dosing of chemicals for disinfection and pH adjustment.
# 23.20
If desired, use a make-up tank to replace water lost by splashing and evaporation. If the tank is supplied with potable water, ensure that the supply enters through an air-gap or backflow preventer. An overflow line at least twice the diameter of the supply line and located below the tank supply line as backflow prevention is acceptable provided it drains through a visible air-break.
# 23.21
Provide easy access to the media filters so that they can be inspected at least on a weekly basis and the media can be changed periodically.
# 23.22
Provide water sample points on the system for halogen level testing and routinely calibrating the analyzer.
# 23.23
Provide analyzer controlled halogen-based disinfection equipment.
# 23.24
Ensure that pH adjustment is accomplished by using appropriate acids and bases and that a buffering agent is used to stabilize the pH. Control the injection of acids and bases by an analyzer.
# 23.25
Make pool mechanical rooms accessible, well-ventilated, and provide a potable water tap with appropriate backflow protection.
# 23.26
Mark all piping with directional-flow arrows and maintain a flow diagram and operational instructions in a readily available location.
# 23.27
Design the pool mechanical room and recirculation system for easy and safe chemical storage and re-filling of chemical feed tanks.
# 23.28
Install drains in the pool mechanical room that allow rapid draining of the entire pump and filter system; install a minimum 80 mm (3 inch) drain on the lowest point of the system.
# 23.29
Provide a drain in the make-up tanks to allow complete draining.
# 23.30
Prominently display the depth of the pool so that it can be seen from the deck and in the pool. Label depth markers either in feet or meters, or both. Install additional depth markers for every 1 m (3 feet) change of depth and prominently display them so that they can be seen from the deck and in the pool.
# Children's Pools
24.1 Follow all requirements in Section 23.0.
# 24.2
Provide an independent recirculation, filtration and halogenation system in children's pools.
# 24.3
Use a water turn-over rate of is at least once every 30 minutes.
# Whirlpool Spas
25.1 Supply potable water whirlpool systems through an air-gap or approved backflow preventer.
# 25.2
Use water filtration equipment (e.g., pumps, filters, etc.) that ensures a turn over rate of at least once every 30 minutes and halogenation equipment that is capable of maintaining the appropriate levels of free-halogen throughout the use period.
# 25.3
Provide a temperature control mechanism to prevent the temperature from exceeding 40ºC (104ºF).
# 25.4
Design the overflow system so that water level is maintained.
# 25.5
If skimmers are used instead of gutters, use one skimmer for every 14 m² (150 square feet) or fraction thereof of water surface area.
# 25.6
Provide an independent whirlpool drainage system. If the whirlpool drainage system is connected to another drainage system, provide a double-check valve between the two.
# 25.7
Provide drains and ensure the bottom of the whirlpool slopes toward the drains to affect complete drainage.
# 25.7.a
Use whirlpools seating areas that drain completely.
# 25.8
Provide anti-entrapment type drain covers constructed of durable easily visible, easily cleanable material and that meet ASME/ANSI A112.19.8M voluntary standard for suction fittings (figure 9a-9c), or other drains that prevent entrapment hazards as specified in U.S. Consumer Product Safety Publication 363-009801 (figures 9a-10b) dual drains meet the anti-entrapment requirements.
# 25.9
Design the system to permit daily shock treatment or super-halogenation in accordance with the VSP Operations Manual.
# 25.10
Install systems in a manner that permits routine visual inspection of the granular media filters in accordance with the VSP Operations Manual.
# 25.11
Ensure that the fill level of the whirlpool is at the skim gutter level.
# 25.12
Ensure that whirlpool overflows are either directed by gravity to the make up tank for recirculation through the filter system or disposed of as waste.
# 25.13
Use self-priming, centrifugal pumps to re-circulate whirlpool water.
25.14 Provide a hair strainer between the whirlpool outlet and the suction side of the pumps to remove foreign debris such as hair, lint, pins, etc.
# 25.15
Ensure that the removable portion of the strainer is corrosion-resistant and has no holes greater than 6 mm (¼ inch) in diameter.
# 25.16
Use filters that are designed to remove all particles greater than 20 micrometers from the entire volume of the whirlpool in 30 minutes or less.
# 25.17
Use filters that are cartridge, or media type (e.g., rapid-pressure sand filters, high-rate sand filters, diatomaceous earth filters, or gravity sand filters). Make filter sizing consistent with ANSI standards for public pools.
# 25.17.1
Provide a clear sight glass on the backwash side of the filters.
# 25.18
Design and install filters in a manner that allows for easy access for inspection and maintenance.
# 25.19
Make all media-type filters capable of being back-washed.
# 25.20
Provide filter accessories, such as pressure gauges, air-relief valves, and rate-of-flow indicators.
# 25.21
A make-up tank may be used to replace water lost by splashing and evaporation. If the tank is supplied with potable water, ensure that the supply enters through an air-gap or backflow preventer. An overflow line at least twice the diameter of the supply line and located below the tank supply line may be used as backflow prevention.
# 25.22
Provide analyzer controlled chemical dosing for both pH and disinfection.
# 25.23
Accomplish disinfection by chlorination or bromination.
# 25.24
Provide water sample points on the system for the testing of halogen levels and routine calibration of the analyzer.
# 25.25
Accomplish pH adjustment by using appropriate acids and bases and that a buffering agent is used to stabilize the pH. Control acid and bases injections by an analyzer.
# 25.26
Make the whirlpool mechanical room accessible and well-ventilated and provide a potable water tap.
# 25.27
Mark all piping with directional-flow arrows and maintain a flow diagram and operational instructions in a readily available location.
# 25.28
Design the pool mechanical room and recirculation system for easy and safe chemical storage and re-filling of chemical feed tanks.
# 25.29
Install drains in the whirlpool mechanical room to allow for rapid draining of the entire pump and filter system; install them so that a minimum 80 mm (3 inch) drain is on the lowest point of the system.
# 25.30
Provide a drain in the make-up tanks to allow complete draining.
# 25.31
Make sure that all decorative features of whirlpool spas are completely draining, non-porous and easy to clean.
# Miscellaneous
# Facilities and Lockers for Cleaning Materials
26.1.1 Provide bulkhead-mounted racks on which hang wet brooms and mops, or provide sufficient space and hanging brackets within a cleaning locker. Locate bulkhead-mounted racks outside of food storage, preparation, or service areas.
# 26.1.2
Provide stainless steel vented lockers, with coved deck and wall junctures, for storing buckets, detergents, sanitizers, cloths, etc.
# 26.1.3
The number of lockers and the location and size of lockers is determined by the needs of the vessel. Make access to lockers containing cleaning materials convenient.
# 26.1.3.a
# Drinking Fountains
# 26.3.1
Ensure that the water jet orifices from drinking fountains are slanted and that the orifice is protected by a cover to prevent contamination. Do not allow lead in the water storage tanks and plumbing serving water fountains.
# 26.3.2
Provide drinking fountains with stainless steel cabinets and without filling spouts in food preparation areas.
# 26.3.3
Provide drinking fountains that will allow the user to control the water stream.
# 26.3.4
Install drinking fountains that are accessible to galley personnel.
# Facility for Cleaning of Maintenance Equipment
26.4.1 Provide facilities (e.g., deep utility sinks) with hot and cold water or a pressure-washing system with a deck sink and drain for cleaning of maintenance equipment such as brooms and mops. Provide bulkhead-mounted racks or hooks for hanging the equipment for drying. Separate room(s) designated for this purpose from food preparation and warewashing areas.
# Ventilation Systems
# Air Supply Systems
27.1.1 Design fan rooms so that they are accessible for periodic inspections and air intake filter changing.
# Design air condition condensation collection pans to drain completely.
# 27.1.2.a
Use air conditioner condensation collection pans that are designed to drain through closed piping to prevent condensate from pooling on the decks.
# 27.1.3
Locate air intakes for fan rooms so that any ventilation or processed exhaust air is not drawn back into the vessel.
# 27.1.4
Provide a sufficient air supply in all food preparation, warewashing, cleaning rooms, and toilet rooms.
# Design all cabin air vent diffusers for easy removal and cleaning.
27.1.6 Make air handling unit condensate drain pans easily accessible for inspection and cleaning, and accessible for maintenance. Make sure that all major air supply trunks have access panels to allow for periodic inspection and cleaning.
# 27.1.7
Provide a separate, independent air supply system for the engine room and other mechanical compartments, (e.g., fuel separation, purifying, and black water treatment rooms) which are located in and around the engine room.
# Air Exhaust Systems
# 27.2.1
Air handling devices in the following areas must exhaust air through independent systems that are completely separated from systems using re circulated air:
# Engine rooms and other mechanical spaces;
27.2.1.2 Hospitals, infirmaries, and any rooms used for patient care or isolation;
# 27.2.1.3
Indoor swimming pools swimming pool: , dome type swimming pools when closed; whirlpool spa facilities, and supporting mechanical rooms.
# An adjacent handwashing station; and
28.2.4 A sign advising child care facility staff to wash their hands after each diaper change.
# 28.3
Provide separate toilet and handwashing facilities for child care providers.
# Housekeeping
29.1 Provide handwashing stations for housekeeping staff. VSP will evaluate the number and location for these handwashing stations during the plan review process.
# Public Toilet Rooms
# Decorative Fountains
31.1 Provide potable water to all decorative fountains.
# 31.2
Ensure that fountains are designed to be maintained free of algae and mold.
# Acknowledgements
# Individuals
This document is a result of the cooperative effort of many individuals from both the government and private industry, and the public. VSP staff thanks all of those who submitted comments and participated throughout this lengthy process. We request the presence of USPHS representatives to conduct a construction inspection on the cruise vessel (NAME). We tentatively expect to deliver the vessel on (DATE). We would like to schedule the inspection for (DATE). We expect the inspection to take approximately (NUMBER OF DAYS). We will pay CDC in accordance with the inspection fees published in the Federal Register. For inspections occurring outside of the United States, we will reimburse the Vessel Sanitation Program for all expenses in connection with the on-site Vessel Sanitation inspection and will make all necessary arrangements for lodging and transportation, which includes airfare and ground transportation in (CITY, STATE, COUNTRY). We will provide in-kind lodging, airfare, and local transportation expenses. We will reimburse the CDC for en-route per diem, meals and miscellaneous expenses, and ground transportation to and from the airport nearest the representative's work site or residence. No honorarium will be given. No U.S. federal funds will be used. Send an invoice to:
# Standards, Codes, and Other References Reviewed For Guidance
# Sample Letter of Request for Construction Inspection
# 32.2.11
# Appendices
| None | None |
1045fe6f97056e3790a1ad60aae3bfe48b8a1258 | cdc | None | # ¡¡S MMWR
Septem ber 28, 1 984 This statem ent, a com pendium o f ACIP recom m endations, w ill n o t be updated regularly. The ACIP p e rio dica lly review s in d ivid u a l im m u n iza tio n statem ents, and revised statem e nts are pu b lish e d in the MMWR. The reader m u s t use the detailed, u p -to -d a te in d ivid u a l s ta te m en ts in conjunction w ith th is com pendium in order to keep abreast o f current inform ation.
# V A C C IN E-P R EV E N T A B LE D IS E A S E S AN D T H E IR
# IN TRO D U CTIO N
In general, immunization policies have been directed towards vaccinating infants, children, and adolescents. While immunization is a routine measure in pediatric practice, it is not usually routine in the practice of physicians who treat adults.
The widespread and successful implementation of childhood immunization programs has greatly reduced the occurrence of many vaccine-preventable diseases. However, successful childhood immunization alone will not necessarily eliminate specific disease problems. A sub stantial proportion of the remaining morbidity and mortality from vaccine-preventable dis eases now occurs in older adolescents and adults. Persons who escaped natural infection or were not immunized with vaccines and toxoids against diphtheria, tetanus, measles, mumps, rubella, and poliomyelitis may be at risk of these diseases and their complications.
To reduce further the unnecessary occurrence of these vaccine-preventable diseases, all those who provide health care to older adolescents and adults should provide immunizations as a routine part of their practice. In addition, the epidemiology of other vaccine-preventable diseases (e.g., hepatitis B, rabies, influenza, and pneumococcal disease) indicates that indi viduals in certain age, occupational, environmental, and lifestyle groups and individuals who have special health problems are at increased risk of these illnesses and should be immunized. Travelers to some countries may be at increased risk of exposure to vaccine-preventable ill nesses. Finally, foreign students, immigrants, and refugees may be susceptible to these diseases.
A system atic approach to immunization is necessary to ensure that every adult is appropri ately protected against vaccine-preventable diseases. Every visit by an adult to a health-care provider should be an opportunity to provide this protection. Several factors need to be con sidered before any patient is vaccinated. These include the susceptibility of the patient, the risk of exposure to the disease, the risk from the disease, and the benefits and risks from the immunizing agent. Physicians should maintain detailed information about previous vaccina tions received by each individual, including type of vaccination, date of receipt, and adverse events, if any, following vaccination. Information should also include the person's history of vaccine-preventable illnesses, occupation, and lifestyle. Vaccine histories ideally should be based on written documentation to ascertain whether vaccines and toxoids were administered at appropriate ages and at proper intervals. Close attention to factors such as military service and age may be helpful in determining whether any vaccines or toxoids are advisable for an in dividual. After the administration of any immunobiologic, the patient should be given written documentation of its receipt and information on which vaccines or toxoids will be needed in
# 2S
# MMWR
Septem ber 28, 1984 the future. For this purpose an immunization record form such as the suggested form found in Appendix 1 should be used routinely.
The patient or responsible person should be given information on the risks of immunobio logies as well as their major benefits in preventing disease both in individuals and in the com munity. No formal, legally acceptable statement has been universally adopted for the private medical sector. Thus, the ACIP recommends that there be ample opportunity for questions before each immunization. C D C has developed "Important Information Statem ents" for use with federally purchased vaccines given in public health clinics. Practitioners may wish to con sider these or similar materials for patients. Examples of "Important Information Statements" can be obtained from state and many local health departments.
Modern immunobiologies are extremely safe and effective, but not completely so. All im munobiologies have had adverse events reported after administration. These range from fre quent, minor, local reactions to extremely rare, severe system ic illness, such as paralysis asso ciated with oral poliovirus vaccine (OPV). It is frequently impossible to establish causeand-effect relationships when untoward events occur after vaccination since temporal asso ci ation alone does not necessarily indicate causation. To improve knowledge about adverse reactions, all temporally associated events severe enough to require the recipient to seek medical attention should be evaluated and reported in detail to local or state health officials and to the manufacturer of the immunobiologic.
General immunization considerations and recommendations are found in the ACIP state ment "General Recommendations on Immunization" ( 1).
The following recommendations apply generally to individuals in the indicated groups. For more detailed information on immunobiologies, including indications, side effects, adverse reactions, precautions, contraindications, dosage, and route of administration, providers are urged to refer to the following section on individual immunobiologies, the ACIP statements on specific immunobiologies (Appendix 2), and the tables and appendices at the back of this sup plement. Appendix 3 provides a list of vaccines, toxoids, and immune globulins available in the United States as of June 1 984.
# Age Groups
The following text and Table 1 summarize the vaccines and toxoids recommended for most adults in the specific age groups. The reader is referred to the section on specific immu nobiologies for essential information.
# A d u lts 1 8 -2 4 Years O ld
All young adults should complete a primary series of diphtheria and tetanus toxoids. A pri mary series for adults is three doses of preparations containing tetanus and diphtheria toxoids, with the first two doses given at least 4 weeks apart and the third dose given 6-1 2 months after the second. Those who have completed a primary series should receive a boos ter dose every 10 years. There is no need to repeat doses when the series schedule is delayed. The combined tetanus-diphtheria toxoids for adult use, Td, should be used to en hance protection against both diseases. Persons with unknown or uncertain histories of re ceiving tetanus or diphtheria toxoids should be considered unimmunized and should receive a full three-dose primary series of Td.
Young adults should also be immune to measles, rubella, and mumps. Persons are consid ered immune to measles and mumps if they have a dated record of vaccination with live vac cines on or after their first birthday, documentation of physician-diagnosed disease, or labora tory evidence of immunity. Persons vaccinated in the period 1 9 6 3 -1 9 6 7 with inactivated-measles-virus vaccine or with a measles vaccine of unknown type should be revaccinated with live-m easles-virus vaccine to prevent measles disease or atypical measles syndrome if exposed to wild measles virus. Persons are considered immune to rubella only if they have a record of vaccination with rubella vaccine on or after their first birthday or laboratory evidence of immunity. The combined measles, mumps, rubella (MMR) vaccine is the vaccine of choice if recipients are likely to be susceptible to more than one of the three diseases. Persons lacking adequate documentation as noted above should be vaccinated.
# A d u lts 2 5 -6 4 Years O ld
All adults 2 5 -6 4 years of age should complete a primary series of tetanus and diphtheria toxoids. A primary series for adults is three doses of preparations containing tetanus and diphtheria toxoids, with the first two doses given at least 4 weeks apart and the third dose given 6-1 2 months after the second. Those who have completed a primary series should re ceive a booster dose every 10 years. The combined toxoids for adult use, Td, should be used to enhance protection against both diseases. Persons with unknown or uncertain histories of receiving tetanus or diphtheria toxoids should be considered unimmunized and should receive a full three-dose primary series of Td.
Adults born in 1957 or later should receive measles vaccine unless they have a dated record of vaccination with live-measles vaccine on or after their first birthday, documentation of physician-diagnosed disease, or laboratory evidence of immunity. Adults born before 1 957 can be considered immune to measles, since measles was a universal infection before measles vaccine became available. While most adults are likely to have been infected naturally with mumps, mumps vaccine may be given to adults, especially males, who are considered susceptible. Unless proof of vaccination with rubella vaccine or laboratory evidence of im munity is available, rubella vaccine is recommended for women of childbearing age and for other adults who may find themselves in places where rubella transmission is likely to occur, such as hospitals, all types of schools, and other places where young people are likely to con gregate. The combined MMR vaccine is the vaccine of choice if recipients are likely to be su s ceptible to more than one of these three diseases.
# A d u lts 6 5 Years O ld o r O lder
All older adults should complete a primary series of tetanus and diphtheria toxoids. A pri mary series for adults is three doses of preparations containing tetanus and diphtheria toxoids, with the first two doses given at least 4 weeks apart and the third dose given 6-1 2 months after the second. Those who have completed a primary series should receive a boos ter dose every 10 years. The combined toxoids for adult use, Td, should be used to enhance protection against both diseases. Persons with unknown or uncertain histories of receiving tetanus or diphtheria toxoids should be considered unimmunized and should receive a full three-dose primary series of Td All older adults should receive influenza vaccine annually. They should also receive a single dose of pneumococcal polysaccharide vaccine.
# Special O ccupations
Persons in specific occupations may be at increased risk of exposure to certain vaccinepreventable illnesses. Such persons may need selected vaccines and toxoids in addition to those routinely recommended for their age group. Table 2 provides a summary of immunobio logies recommended for various special occupational groups. The reader is referred to the section on specific immunobiologies for essential information.
# MMWR
Septem ber 28, 1984
# H e a lth -R e la te d O ccu p a tio n s
Medical, dental, laboratory, and other support personnel who may have contact with blood or blood products should be immune to hepatitis B virus (HBV) infection. The groups at high est risk for acquiring HBV infection and for whom HB vaccine is recommended include medical technicians, operating room staff, phlebotomists, physicians (particularly surgeons and pa thologists), nurses (particularly intravenous-therapy nurses and nurses on oncology and dialy sis units), dentists and oral surgeons, laboratory and blood-bank technicians, and emergencyroom staff. Morticians and their assistants who have routine contact with blood and secre tions are also at high risk of HBV infection. Selected staff of institutions for the mentally retarded may be at increased risk of HBV infection because of exposure to bites and contact with skin lesions, saliva, and other potentially infected secretions in addition to blood.
Am ong health-care personnel with frequent exposure to blood, the prevalence of serologic evidence of HBV infection is estimated to range between 10% and 30%. Since the cost effec tiveness of serologic screening to detect susceptible individuals among health-care personnel depends on the prevalence of infection, each institution must decide whether serologic screening is cost effective. Vaccination of individuals who already have antibodies to HBV has not been shown to cause adverse effects.
The duration of protection from a three-dose series of HB vaccine or the need for booster doses has not yet been determined.
Transmission of rubella in health facilities (hospitals, physician or dentist offices, clinics, etc.) can disrupt hospital or office routines and cause considerable expense. Although no cases of congenital rubella syndrome (CRS) have been reported in association with rubella transmission in health facilities, therapeutic abortions have been sought by pregnant staff members following rubella infection (2). To prevent such situations, all medical, dental, laboratory, and other support health personnel, both male and female, who might be at risk of exposure to patients infected with rubella, or who might have contact with pregnant patients, should be immune. Rubella vaccine is recommended for all such personnel unless they have either proof of vaccination with rubella vaccine on or after their first birthday or laboratory evi dence of immunity. Combined MMR vaccine is the vaccine of choice if recipients are likely to be susceptible to measles and/or mumps as well as to rubella.
Measles transmission in health facilities can also be disruptive and costly. To prevent such situations, all health personnel born in 1957 or later who may have contact with patients in fected with measles should be immune. Such persons can be considered immune only if they have documentation of having received live-m easles vaccine on or after their first birthday, a record of physician-diagnosed measles, or laboratory evidence of immunity. Measles vaccine is recommended for all persons lacking such documentation. Combined MMR vaccine is the vaccine of choice if recipients are likely to be susceptible to rubella and/or mumps as well as to measles. Adults born before 1957 can be considered immune to measles since measles w as a universal infection before the availability of measles vaccine.
Poliovirus vaccine is not routinely recommended for persons older than high school age (18-19 years old). However, hospital personnel having close contact with patients who may be excreting wild polioviruses, and laboratory personnel handling specim ens that may contain wild polioviruses, should have completed a primary series of poliovirus vaccine. For personnel who do not have proof of having completed a primary series, completion is recommended with inactivated poliovirus vaccine (IPV). IPV is preferred because there is a slightly increased risk in adults of vaccine-associated paralysis following receipt of OPV. In addition, since v ac cine poliovirus may be excreted by O PV recipients for 30 or more days, the use of O PV in creases the risk of acquiring vaccine-associated paralytic poliomyelitis among susceptible im munocompromised contacts and susceptible close contacts of O PV recipients.
# MMWR 5 S
Sm allpox vaccination is indicated only for laboratory workers involved with orthopox viruses or in producing and testing smallpox vaccine. When indicated, smallpox vaccination should be given at least every years.
Plague vaccine is indicated for laboratory personnel working with Yersinia p e stis possibly resistant to antimicrobial agents and for persons performing Y. p e stis aerosol experiments.
Preexposure rabies vaccination is indicated for laboratory workers directly involved with testing or isolating rabies virus.
# Veterinarians an d A n im a l H a n d lers
Veterinarians and animal handlers are at risk of rabies exposure because of occupational contact with both domestic and wild animals. They should receive preexposure rabies-vaccine prophylaxis with human diploid cell rabies vaccine (HDCV). Preexposure vaccination against rabies does n o t eliminate the need for additional therapy after exposure to rabies; it does, however, simplify postexposure therapy by eliminating the need for human rabies immune globulin (HRIG) and by decreasing the number of postexposure doses of vaccine needed. Per sons at continued risk of frequent exposure should receive a booster dose of H D CV every 2 years or have their serum tested for rabies antibody every 2 years and, if the titer is inadequate ( < 5 by the rapid fluorescent-focus inhibition test), receive a booster dose.
# S e le c te d F ie ld P e rso n n e l
Plague vaccine is indicated for field personnel who cannot avoid regular exposure to poten tially plague-infected wild rodents and rabbits and their fleas.
Preexposure rabies vaccine prophylaxis should be considered for field personnel who are likely to have contact with potentially rabid dogs, cats, skunks, raccoons, bats, or other w ild life species.
# S e w a g e W orkers
Sew age workers, as all other adults, should be adequately vaccinated against diphtheria and tetanus.
Poliovirus and typhoid vaccines and immune globulin are not routinely recommended for sew age workers.
# Lifestyles
Various lifestyles may increase the risk of exposure to certain vaccine-preventable ill nesses. Persons with these lifestyles may require vaccines in addition to those routinely recommended for their age group. Table 2 provides a summary of the vaccines recommended.
# H o m o s e x u a lly A c t iv e M a le s
Homosexually active males are at high risk of HBV infection. Between 35% and 80°o have serologic evidence of HBV infection. Susceptible homosexual males should be vaccinated with HB vaccine as early as possible after they begin homosexual activity because they can be expected to acquire HBV infection at a rate of 10% -20% per year. The duration of protection from a three-dose series of HB vaccine and the need for booster doses have not yet been determined. Because of the high prevalence of infection, prevaccination serologic screening of homosexual males may be cost effective regardless of their age or of how long they have been homosexually active.
# MMWR
Sep tem b er 28, 1 984
# U se rs o f Illic it In je cta b le D ru gs
Users of illicit injectable drugs are at high risk of HBV infection. Serologic evidence of HBV infection has been found in 60% -80% of these individuals. Efforts should be made to vaccinate susceptible users with HB vaccine as early as possible after their drug use begins because they can be expected to acquire HBV infection at a rate of 10% -20% per year. The duration of protection from a three-dose series of HB vaccine and the need for booster doses have not yet been determined Because of the high prevalence of infection, prevaccination serologic screening of users of illicit injectable drugs to avoid unnecessary immunization is cost effective.
These drug users are also at increased risk of tetanus, and their tetanus immunization status should be kept up to date with Td.
# Environmental Situations
Certain environments may place an individual at increased risk of certain vaccinepreventable diseases. Table 2 sum marizes additional vaccines recommended for persons in selected environments. The reader is referred to the section on specific immunobiologies for essential information.
# In m a te s o f Lo n g -Term C o rre ctio n a l F a c ilit ie s
Serologic evidence of HBV infection has been found in 10% -80% of male prisoners. A l though the frequency of transmission during imprisonment has not been documented, the en vironment of long-term correctional facilities may be associated with a high risk of transm is sion of HBV infection because of the frequency of use of illicit injectable drugs and of homo sexual behavior. In selected long-term institutional settings, prison officials may elect to un dertake serologic HBV screening and vaccination programs. The duration of protection from a three-dose series of HB vaccine and the need for booster doses have not yet been determined.
# R e s id e n ts o f In stitu tio n s fo r the M e n ta lly R e ta rd e d
Institutions for the mentally retarded provide a setting conducive to the transmission of HBV infection through bites and contact with blood, skin lesions, saliva, and other potentially infectious secretions. Serologic evidence of HBV infection has been found in 35% -80% of resi dents of such institutions. New adm issions to these institutions should be vaccinated as soon as possible. For current residents, screening and vaccination of susceptible residents is recom mended. Because of the high prevalence of infection, preimmunization serologic screening of those already institutionalized may be cost effective; however, screening of new admissions very likely will not be. Residents of group homes, foster homes, and similar settings who have household contact with a carrier of HBV should also be vaccinated. The duration of protection from a three-dose series of HB vaccine and the need for booster doses have not yet been determined.
# Travel
The risk of acquiring illness during international travel depends on the areas of the world to be visited and the extent to which the traveler is likely to be exposed to vaccine-preventable diseases. When considering travel, people often seek advice from health-care personnel on immunization. This provides a good opportunity to review the person's immunization status and administer primary series or booster doses, if needed.
# MMWR 7S
In most countries, measles, mumps, and rubella remain uncontrolled. Therefore, the risk of acquiring these diseases while traveling outside the United States is greater than the risk in curred within the United States. Approximately 50S, of imported measles cases reported for 1 980-1 9 8 3 occurred in citizens returning to the United States (3). To minimize importations by U.S. citizens, all travelers born in 1 957 or later should be immune to measles. Women trav elers of childbearing ages should be immune to rubella before leaving the United States.
In developed countries such as Japan, Canada, Australia, New Zealand, and the European countries, the risk of acquiring other vaccine-preventable diseases such as poliomyelitis, diphtheria, and tetanus is usually no greater than the risk incurred while traveling in the United States. In contrast, travelers to developing countries are, in general, at increased risk of expo sure to many infections, including wild polioviruses and diphtheria. Accordingly, such travelers should be immune to poliomyelitis and diphtheria, in particular.
For protection against poliomyelitis, unimmunized adults should receive at least two doses of IPV 1 month apart, and preferably a complete primary series, before traveling to a develop ing country. If an individual's travel plans do not permit this interval, then a single dose of OPV is recommended. For adults previously incompletely immunized with O PV or IPV, the remain ing doses of either vaccine required for completion of the primary series should be given, regardless of the interval since the last dose or the type of vaccine previously received. A single additional dose of either O PV or IPV should be given to travelers who have previously completed a primary series of O PV or IPV Selective immunization of travelers with vaccines against yellow fever, cholera, typhoid, plague, m eningococcal disease, rabies, or HBV infection or administration of immune globulin (IG) to prevent hepatitis A is recommended on the basis of known, or perceived, diseasespecific risks in the country(ies) to be visited and the type and duration of travel within a coun try. In the instances of cholera and yellow fever, vaccination requirements may have been es tablished by the country to be visited. Countries currently reporting yellow fever, cholera, and plague are identified biweekly in the S um m a ry o f H ealth Inform a tion fo r In tern ation al Travel. and information on known or probably infected areas is published annually in H ealth In fo rm a tion fo r In tern ation al Travel, which also lists specific requirements for cholera and yellow fever vaccinations for each country. All state health departments and many county and city health departments receive both publications. For entry into countries requiring yellow fever or cholera vaccination, travelers must have an International Certificate of Vaccination validat ed by an appropriate authority. State or local health departments can provide the addresses of persons or centers able to validate certificates.
More information on specific vaccine-preventable illnesses that a traveler might encounter is provided in the sections describing specific vaccines.
# Foreign Students, Im m igrants, and Refugees
In many countries children and adolescents are not routinely immunized against diphtheria, tetanus, measles, mumps, rubella, and poliomyelitis. A s a result, persons entering the United States to pursue college and postgraduate studies or as immigrants or refugees may be su s ceptible to one or more of these diseases.
Unless foreign students, immigrants, and refugees can provide a vaccination record docu menting the receipt of recommended vaccines or toxoids at appropriate ages and intervals or laboratory evidence of immunity, they should receive the appropriate vaccines for their age as noted in age-specific recommendations (see page 2S) and in
# Special Health Status
Som e vaccines may be contraindicated for persons with certain health problems; other vaccines may be indicated because of an underlying health condition. Table 3 provides a sum mary of immunobiologies indicated or contraindicated for persons with selected health problems.
# P re g n a n c y
When any vaccine or toxoid is to be given during pregnancy, waiting until the second or third trimester, when possible, is a reasonable precaution to minimize concern about possible teratogenicity.
Pregnant women not vaccinated previously against tetanus and diphtheria should receive two doses of Td properly spaced. Those who have previously received one or two doses of tetanus or diphtheria toxoid should complete their primary series during pregnancy. A primary series is three doses of preparations containing tetanus and diphtheria toxoids, with the first two doses given at least 4 weeks apart and the third dose given 6 -1 2 months after the second. Pregnant women who have completed a primary series should receive a booster dose of Td if 10 or more years have elapsed since their last dose.
Because of a theoretical risk to the developing fetus, live-virus vaccines should not usually be given to pregnant women or to those likely to become pregnant within 3 months. If, how ever, immediate protection against poliomyelitis or yellow fever is needed because of immi nent exposure, O PV or yellow fever vaccine may be given. If the only reason to vaccinate a pregnant woman with yellow fever vaccine is an international travel requirement, efforts should be made to obtain a waiver letter (see page 1 9S).
It is strongly recommended that rubella vaccine be administered in the postpartum period to women not known to be immune, preferably before discharge from the hospital.
Information about immunobiologies and vaccine-preventable diseases during pregnancy is summarized in Appendix 4.
# C o n d itio n s That C o m p ro m ise the Im m u n e S y s te m
Persons with conditions that compromise their immune responses (e.g., leukemia, lym pho ma, and generalized malignancy or immunosuppressive therapies) should receive annual in fluenza vaccination with the currently formulated vaccine. Persons with conditions associated with increased risk of pneumococcal disease or its complications should receive a single dose of pneumococcal polysaccharide vaccine. The effectiveness of these vaccines in such per sons may be limited, but the risk of disease is substantial and adverse reactions are minimal.
In general, live-virus vaccines should not be given to persons who are immunocompro mised as a result of immune deficiency diseases, leukemia, lymphoma, or generalized m alignancy or are immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabolites, or radiation. However, susceptible patients with leukemia in remission who have not had chemotherapy for at least 3 months may receive live-virus vaccines. The exact interval between discontinuing im m unosuppressives and regaining the ability to respond to individual vaccines is not known. Estimates of experts vary from 3 months to 1 year.
Short-term (less than 2 weeks) corticosteroid therapy, topical steroid therapy (e.g., nasal or skin), and intraarticular, bursal, or tendon injections with corticosteroids should not be im munosuppressive and do not necessarily contraindicate vaccination with live-virus vaccines. Vaccination should be avoided if system ic immunosuppressive levels are achieved by topical application.
# MMWR 9S
# H e m o d ia ly sis
Persons receiving hemodialysis have been at high risk of infection with HBV, although envi ronmental control measures have reduced this risk during the past few years. Nationwide, an estimated 1 5% of hemodialysis patients have serologic evidence of HBV infection, and routine serologic screening of hemodialysis patients is currently recommended. Susceptible patients who will soon require or are currently receiving long-term hemodialysis should receive three double doses of HB vaccine as soon as possible. Double the normal dose is recommended for these patients because of lower vaccine immunogenicity in this group. Postvaccination screening to demonstrate antibody to hepatitis B surface antigen (HBsAg) is recommended in this group. Approximately 60% of hemodialysis patients who receive double doses of HB vac cine demonstrate antibodies against HBV. The duration of protection from a three-dose series of HB vaccine and the need for booster doses have not yet been determined.
Because persons with chronic renal disease are at increased risk of adverse consequences from infections of the lower respiratory tract, hemodialysis patients should receive annual in fluenza vaccination with the current formulated vaccine. These patients are also at increased risk of developing pneumococcal infection, as well as of experiencing more severe pneumo coccal disease, and should receive pneumococcal polysaccharide vaccine.
# S p le n ic D y sfu n c tio n or A n a to m ic A sp le n ia
Persons with splenic dysfunction or anatomic asplenia are known to be at increased risk of contracting fatal pneumococcal bacteremia and should receive pneumococcal polysaccharide vaccine. Persons scheduled for elective splenectomy should receive pneumococcal polysac charide vaccine at least 2 weeks before the operation.
# F a c to r V III a n d I X D e fic ie n c ie s
Patients with clotting disorders who receive factor VIII or IX concentrates have an in creased risk of HBV infection. Vaccination with HB vaccine is recommended for susceptible patients. The degree and duration of protection from a three-dose series of HB vaccine and the need for booster doses have not yet been determined.
Prevaccination serologic screening for HBV markers is recommended for patients who have already received multiple infusions of these products.
# C h ro n ic A lco h o lism
Persons with chronic alcoholism may be at increased risk of contracting a pneumococcal infection or having a more severe pneumococcal illness. Such persons, especially those with cirrhosis, should receive pneumococcal polysaccharide vaccine.
# H ig h -R is k D is e a s e s
Persons with disease conditions that increase the risk of adverse consequences from lower-respiratory-tract infections should receive annual influenza vaccination with the current formulated vaccine. These conditions include:
(a) Acquired or congenital heart disease with actual or potentially altered circulatory dynamics. (b) Any chronic disorder or condition that compromises pulmonary function. (c) Diabetes mellitus or other metabolic diseases that increase the likelihood that infections will be more severe than for persons without such conditions. (d) Chronic renal disease with azotemia or nephrotic syndrome. (e) Chronic, severe anemia, such as sickle cell disease. Som e chronic illnesses (e.g., chronic pulmonary disease, congestive heart failure, diabetes mellitis) predispose individuals to an increased risk of pneumococcal illness or its com plica tions. While data on the effectiveness of pneumococcal polysaccharide vaccine for chronical ly ill persons are not conclusive, such persons should receive the vaccine.
# V A C C IN E -P R E V E N T A B LE D IS E A S E S AN D TH EIR IM MU NO BIO LO G IC S
Vaccines, toxoids, and immune globulins are available for use in the prevention of a number of diseases. These diseases and their specific immunobiologies are presented in this section. For each immunobiologic, dosage, route of delivery, indications for use, side effects, adverse reactions, precautions, and contraindications to be considered before administration are described here and are summarized in Table 4.
# Toxoids
# D iphth eria
The occurrence of diphtheria has decreased dramatically in the United States, largely be cause of the widespread use of diphtheria toxoid. Only 11 cases of diphtheria were reported in the period 1 9 8 0 -1 9 8 2 . From 1977 through 1982 , 56% of the 34 reported cases of re spiratory diphtheria occurred in adults 20 years of age or older, and 24% of the cases o c curred in adults 50 years of age or older. The age distribution for persons who died from diphtheria w as similar. Diphtheria occurs primarily among unimmunized or inadequately immunized individuals. Limited serosurveys done since 1977 indicated that 62% of adults 1 8 -3 9 years of age and 41% -84% of those 60 years of age or older lacked protective levels of circulating antitoxin against diphtheria (4 -6 ).
# Diphtheria toxoid
Complete and appropriately timed immunization is at least 95% effective in preventing diphtheria. The combined preparation Td is recommended for use in adults since a large pro portion of adults lack protective levels of circulating antibody against tetanus (4)(5)(6). Further more, Td contains much less diphtheria toxoid than other diphtheria toxoid-containing pro ducts, and as a result, reactions to the diphtheria component are less likely. Immunization with toxoid does not, however, prevent or eliminate carriage of Corynebacterium diphtheriae.
# Toxoid indications
All adults lacking a completed primary series of tetanus and diphtheria toxoids should complete the series with Td. A primary series for adults is three doses of preparations con taining tetanus and diphtheria toxoids, with the first two doses given at least 4 weeks apart and the third dose given 6-1 2 months after the second. All adults for whom 10 years or more have elapsed since completion of their primary series or since their last booster dose should receive a dose of Td. Thereafter, a booster dose of Td should be administered every 1 0 years. There is no need to repeat doses if the schedule for the primary series or booster doses is delayed. (For toxoid side effects and adverse reactions, and precautions and contraindications, see page 1 2S).
# Tetanus
The occurrence of tetanus has decreased dramatically, largely because of the widespread use of tetanus toxoid. Nevertheless, the number of cases remained relatively constant from M M W R I I S 1 973 through 1 982, averaging 88 reported cases per year. Tetanus occurs almost exclusive ly in unimmunized or inadequately immunized individuals. Immune pregnant women confer temporary protection against tetanus to their infants through transplacental maternal anti body. In the period 1 977-1 982, persons 20 years of age or older accounted for 89% of the 50 4 reported tetanus cases for which patient ages were known; persons 60 years of age or older accounted for 55%. The age distribution of persons who died from tetanus w as similar. Serosurveys done since 1977 indicated that 110/-of adults 1 8 -3 9 years of age and 49° j-66% of those 60 years of age or older lacked protective levels of circulating antitoxin against tetanus (4-6).
# Tetanus toxoid
Complete and appropriately timed immunization is nearly 100% effective in preventing tetanus. The combined preparation, Td, is the preferred preparation for active tetanus immuni zation of adults since a large proportion of adults lack protective levels of circulating antitoxin against diphtheria (4-6).
# Toxoid indications
All adults lacking a complete primary series of tetanus and diphtheria toxoids should com plete the series with Td. A primary series for adults is three doses of preparations containing tetanus and diphtheria toxoids, with the first two doses given at least 4 weeks apart and the third dose given 6 -1 2 months after the second. All adults for whom 10 years or more have elapsed since completion of their primary series or since their last booster dose should receive a booster dose of Td. Thereafter, a booster dose of Td should be administered every 10 years. There is no need to repeat doses if the primary schedule for the series or booster doses is delayed.
The recommended pediatric schedule for DTP vaccine includes a booster dose at age 4 -6 years. The first Td booster is recommended at age 14-1 6 years (10 years after the dose at age 4 -6 years). One means of ensuring that persons continue to receive boosters every 10 years is to vaccinate persons routinely at mid-decade ages, e.g., 25 years, 35 years, etc.
For wound management the need for active immunization, with or without passive immuni zation, depends on the condition of the wound and the patient's immunization history. A sum mary of the indications for active and passive immunization is provided in Table 5. Only rarely have cases of tetanus occurred in persons with a documented primary series of toxoid injections.
Evidence indicates that complete primary immunization with tetanus toxoid provides longlasting protection-10 years or more in most recipients. Consequently, after complete primary tetanus immunization, boosters are recommended at 10-year intervals. For clean and minor wounds occurring during the 10-year interval no additional booster is recommended. For other wounds, a booster is appropriate if the patient has not received tetanus toxoid within the preceding 5 years. Antitoxin antibodies develop rapidly in persons who have previously re ceived at least two doses of tetanus toxoid.
Persons who have not completed a full primary series of injections or whose immunization status is unknown or uncertain may require tetanus toxoid and passive immunization at the time of wound cleaning and debridement. It is not sufficient to ascertain the interval since the most recent toxoid dose. A careful attempt should be made to determine whether a patient has previously completed primary immunization and, if not, how many doses have been given. Persons with unknown or uncertain previous immunization histories should be consid ered to have had no previous tetanus toxoid doses.
Td is the preferred preparation for active tetanus immunization in managing the wounds of adults. Td is used to enhance protection against diphtheria concurrently, since a large propor
# MMWR
Sep tem b er 28, 1 9 8 4 tion of adults are susceptible. Thus, if advantage is taken of visits for care of acute health problems, such as for wound management, some patients who otherwise would remain su s ceptible can be protected against both diseases. Primary immunization should ultimately be completed for persons documented to have received fewer than the recommended number of doses, including doses given as part of wound management. If passive immunization is needed, human tetanus immune globulin (TIG) is the product of choice. The currently recommended prophylactic dose of TIG for wounds of average severity is 2 5 0 units, intramuscularly (IM). When tetanus toxoid and TIG are given concurrently, separ ate syringes and separate sites should be used. Most experts consider the use of adsorbed toxoid mandatory in this situation.
# To xo id (Td) S id e E f f e c t s a n d A d v e rs e R e a ctio n s
Local reactions, generally erythema and induration with or without tenderness, can occur after the administration of Td. Fever and other system ic sym ptom s are less common.
Arthus-type hypersensitivity reactions characterized by severe local reactions generally starting 2 -8 hours after an injection and often associated with fever and malaise may occur, particularly in persons who have received multiple boosters of tetanus toxoid.
Rarely, severe system ic reactions such as generalized urticaria, anaphylaxis, or neurologic com plications have been reported after administration of tetanus and diphtheria toxoids. Peripheral neuropathy has been reported rarely after administration of tetanus toxoid, al though a causal relationship has not been established.
# To x o id (Td ) P re ca u tio n s an d C o n tra in d ica tio n s
Although there is no evidence that tetanus and diphtheria toxoids are teratogenic, waiting until the second trimester of pregnancy to administer Td is a reasonable precaution to mini mize any concern over teratogenicity.
A history of a neurologic reaction or a severe hypersensitivity reaction (e.g., generalized ur ticaria or anaphylaxis) following a previous dose is a contraindication to tetanus and diphtheria toxoids. Local side effects alone do not preclude continued use. If a prior system ic reaction is suspected of representing allergic hypersensitivity, appropriate skin testing to document im mediate hypersensitivity may be useful before tetanus toxoid immunization is discontinued (7). Mild, nonspecific skin-test reactivity to tetanus toxoid is common. Most vaccinees develop cutaneous delayed hypersensitivity to the toxoid.
Persons experiencing severe Arthus-type hypersensitivity reactions to a prior dose of tetanus toxoid usually have very high serum tetanus antitoxin levels and should not be given even emergency booster doses of Td more frequently than every 10 years.
Although a minor illness, such as a mild upper-respiratory infection, should not be cause for postponing vaccination, a severe febrile illness is reason to defer routine vaccination.
# Live-V irus Vaccines
# M e a sle s
In 1983, only 5.6% of the 3 ,1 3 9 counties in the United States reported cases of measles. Indigenous transmission of measles has been eliminated from most of the United States be cause of widespread vaccination. However, importations of disease are frequent (more than 1 0 0 each year), and there is a continued risk of exposure, particularly for young adults attend ing college or universities or traveling abroad.
In 1982, 1 1.7% of measles patients whose ages were reported were 20 years of age or older. Outbreaks continue to occur in universities and colleges and other places where young MMWR 13S
adults congregate. In the first half of 1983, 51% of reported cases were among college stu dents or were epidemiologically linked to cam pus outbreaks. It is estimated that as many as 20% of young adults lack detectable antibody and may be susceptible to measles. Encephalitis or death follows measles disease in approximately one case per 1,000. The risk of encephalitis is greatest in adult patients. Aside from infants, the highest measles casefatality ratio occurs in adults.
Measles illness during pregnancy increases rates of spontaneous abortion, premature labor, and low birth weight for infants. Although cases of congenital malformation following m easles infection during pregnancy have been reported, no consistent patterns have been demonstrated.
# M easles vaccine
Measles vaccine produces a mild or inapparent noncommunicable infection. A single sub cutaneously (SC) administered dose of live-m easles vaccine provides durable protection against measles illness in approximately 95% of vaccinees, extending probably for their life time. Combined MMR vaccine is the vaccine of choice if recipients are likely to be susceptible to rubella and/or mumps as well as to measles. Although reactions following measles, mumps, and rubella vaccines in persons previously immune have been reported, evidence and experience overwhelmingly suggest that vaccination with MMR of persons who were pre viously immune to one or more of its components is not associated with significant adverse effects.
# Vaccine indications
Measles vaccine is indicated for all persons born in 1 957 or later who lack documentation of receipt of live-m easles vaccine on or after their first birthday, physician-diagnosed measles, or laboratory evidence of immunity. Persons born before 1957 can generally be considered immune since measles w as a universal infection before measles vaccine became available. In dividuals who received vaccine before their first birthday, killed-measles vaccine, killedmeasles vaccine followed within 3 months by live-m easles vaccine, or a measles vaccine of unknown type in the period 1 9 6 3 -1 9 6 7 should be revaccinated. An estimated 6 0 0 ,0 0 0 -9 0 0 ,0 0 0 persons in the United States received killed-measles vaccine in the years 1 9 6 3 -1 9 6 7 .
Because the risk of acquiring measles outside the United States is greater than the risk in curred in the United States, travelers should be immune to measles before leaving the United States.
Generally, young adults who are exposed to measles and who have no or uncertain docu mentation of live-m easles vaccination on or after their first birthday, no record of physiciandiagnosed measles, and no laboratory evidence of immunity should be vaccinated within 72 hours after exposure, when vaccination is most likely to be protective. If the exposure did not result in infection, the vaccine should induce protection against subsequent measles infection. An acceptable alternative is to use IG, which can prevent or modify infection if administered within 6 days after exposure. IG is principally indicated when measles vaccine is contraindicat ed. IG should not be used in an attempt to control measles outbreaks. The recommended dose of IG is 0.25 ml/kg IM, not to exceed 1 5 ml. Live-m easles vaccine should be given 3 months after IG is administered, by which time the passive measles entibodies should have disappeared.
# Vaccine side effects and adverse reactions
Reactions to measles vaccine do not appear to be age related. About 5%-1 5% of vaccinees may develop a temperature of 103°F (39.4°C) or higher, generally beginning between days 5 and 12 after vaccination; fever usually lasts 1-2 days and, rarely, up to 5 days. Transient
# 14S MMWR
Sep tem b er 28, 1 984 rashes have been reported in approximately 5% of vaccinees. The incidence rate of encephali tis or encephalopathy following measles vaccination is lower than the observed background incidence rate of encephalitis of unknown etiology and much lower than that following natural measles.
Reactions after live-measles vaccination occur in 4% -55% of prior recipients of killedmeasles vaccine. The reactions are generally mild, consisting of a local reaction with or with out a low-grade fever of 1-2 days' duration. Such reactions are considerably milder than atypical measles syndrome, an illness which may affect prior recipients of killed-measles vac cine who are exposed to natural measles.
# Vaccine precautions and contraindications
Vaccination should not be postponed because of a minor illness, such as a mild upperrespiratory infection. However, vaccination of persons with severe febrile illnesses should be postponed until recovery. Vaccine should be given 14 days before or deferred for at least 6 weeks, and preferably 3 months, after a person has received IG, whole blood, or other blood products containing antibody.
Because of a theoretical risk to the developing fetus, measles vaccine should not be given to pregnant women.
Measles vaccine should not be given to persons who are immunocompromised as a result of immune deficiency diseases, leukemia, lymphoma, or generalized malignancy or are immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabolites, or radiation. (See "Conditions That Com prom ise the Immune System ," page 8S.)
There is no evidence that live-measles vaccine exacerbates tuberculosis. If tuberculin skin testing is needed, it should be done on the day of vaccination and read 4 8 -7 2 hours later. For a recent vaccinee, it is prudent to wait 4 -6 weeks after receipt of measles vaccine before ad ministering a tuberculin skin test since measles vaccination may temporarily suppress tubercu lin reactivity.
Persons with a history of any sign or symptom of an anaphylactic reaction (i.e., hives, swelling of the mouth and throat, difficulty in breathing, hypotension, or shock) following in gestion of eggs or receipt of neomycin should be given measles vaccine only with extreme caution. Protocols have been developed for vaccinating such persons (S). Persons with reac tions that are not anaphylactic are not at increased risk and can be vaccinated.
# M u m p s
The occurrence of reported mumps cases in the United States has decreased steadily since the introduction of live-m um ps-virus vaccine. In 1983, a record low of 3,2 9 7 cases were reported provisionally; this number represented a 98% decline from the 1 85,691 cases reported in 1967, the year live-m umps vaccine w as licensed. In 1982, 5 ,2 7 0 cases were reported, of which 9% occurred in persons 20 years of age or older.
Although mumps disease is generally self-limiting, meningeal signs may appear in up to 1 5% of cases, and orchitis in up to 20% of clinical cases among postpubertal males. Sterility is a rare sequela of mumps orchitis among males. Deafness occurs at a rate of one case per 1 5 ,0 0 0 cases of mumps.
Serologic surveys indicate that most individuals have been infected with mumps by 20 years of age.
# M umps vaccine
Live-m um ps vaccine has been available since 1967. A single dose of live-m umps vaccine administered S C provides protective and long-lasting levels of antibody in over 90% of reci pients. Reported clinical vaccine efficacy ranges between 75% and 90%. MMR is the vaccine
# MMWR 15S
-f choice if recipients are likely to be susceptible to measles and/or rubella as well as to mumps. Although reactions following measles, mumps, and rubella vaccines in persons pre viously immune have been reported, evidence and experience overwhelmingly suggest that the vaccination with MMR of persons who were previously immune to one or more of its components is not associated with significant adverse effects.
# Vaccine indications
Mumps vaccine is indicated for all adults, particularly males, believed to be susceptible. Most adults are likely to have been infected naturally and generally can be considered immune, even if they did not have clinically recognizable mumps disease. Killed-m um ps vac cine w as available from 1 9 5 0 until 1 978. Persons who received killed-mumps vaccine might benefit from vaccination with live-mumps vaccine.
# Vaccine side e ffe cts and adverse reactions
Parotitis after vaccination has been reported rarely. Allergic reactions including rash, pru ritus, and purpura have been associated temporally with mumps vaccination but are uncom mon, usually mild, and of brief duration. The frequency of reported central nervous system (CNS) dysfunction following mumps vaccination is lower than the observed background inci dence rate in the general population.
# Vaccine precautions and contraindications
Vaccine should be given at least 14 days before or deferred for at least 6 weeks, and preferably 3 months, after a person has received IG, whole blood, or other blood products containing antibody.
Because of the theoretical risk of fetal damage following administration of a live-virus vac cine to a pregnant woman, it is prudent to avoid giving mumps vaccine to pregnant women.
Mumps vaccine should not be given to persons who are immunocompromised as a result of immune deficiency diseases, leukemia, lymphoma, or generalized m alignancy or are immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabolites, or radiation. (See "Conditions That Com prom ise the Immune System ," page 8S.)
Persons with a history of any sign or symptom of an anaphylactic reaction (i.e., hives, swelling of the mouth and throat, difficulty in breathing, hypotension, or shock) following in gestion of eggs or receipt of neomycin should be vaccinated only with extreme caution. Proto cols have been developed for vaccinating persons with severe egg allergy (8). Persons with reactions that are not anaphylactic are not at increased risk and can be vaccinated.
# R u b e lla
Preventing fetal infection and consequent C R S are the objectives of rubella immunization. Fetal infection occurring during the first trimester of pregnancy can lead to C R S in up to 80% of fetuses. In addition, fetal wastage due to miscarriage or therapeutic abortion following m a ternal rubella disease or exposure during the first trimester remains a frequent occurrence.
The number of reported rubella cases has decreased steadily from over 5 6 ,0 0 0 cases in 1 9 69, the year rubella vaccine w as licensed, to 2 ,325 cases in 1 982. In 1 982, only 11.7% of the 3,1 37 counties in the United States reported cases of rubella. The 1 9 8 3 provisional total of 9 5 4 cases is an all-time low. Because, until recently, many adolescents and young adults had not been vaccinated, decreases in incidence rates of reported rubella were observed pri marily for children. Recent efforts to increase delivery of vaccine to cellege-age and older per sons have led to the current decline in the incidence rates for these age groups. However, an estimated 1 0%-1 5% of young adults remain susceptible to rubella, and limited outbreaks con tinue to be reported in universities, colleges, and places of employment-notably hospitals. Vaccination of young children has prevented widespread epidemics of rubella and of C R S and eventually will lead to the elimination of C R S as vaccinated cohorts enter the childbearing age. However, increased efforts to ensure that all women of childbearing age, in particular, are vaccinated will hasten the elimination of rubella and C R S in the United States. Additional aids to elimination of rubella and C R S include 1) achieving and maintaining high immunization levels, 2) maintaining vigorous surveillance, and 3) practicing aggressive outbreak control.
# Rubella vaccine
A single S C administered dose of live, attenuated rubella vaccine provides long-term, probably lifetime, immunity in approximately 95% of vaccinees. Moreover, there is no risk to susceptible contacts of vaccinees. MMR is the vaccine of choice if recipients are likely to be susceptible to measles and/or mumps as well as to rubella. Although reactions following ad ministration of measles, mumps, and rubella vaccines to persons previously immune have been reported, evidence and experience overwhelmingly suggest that the vaccination with MMR of persons who are already immune to one or more of its components is not associated with significant adverse effects.
# Vaccine indications
Rubella vaccine is recommended for adults, particularly females, unless proof of immunity is available (i.e., documented rubella vaccination on or after the first birthday or a positive serologic test) or unless the vaccine is specifically contraindicated. In particular, nonpregnant susceptible women of childbearing age should be provided rubella vaccination 1) during rou tine internal medicine and gynecologic outpatient care, 2) during routine care in a family plan ning clinic, 3) following premarital screening, 4) before discharge from a hospital for any reason, and 5) after childbirth or abortion. Ideally, any contact with the health-care system should be used as an opportunity to vaccinate susceptible women. In addition, evidence of rubella immunity should be required for all individuals in colleges and universities. Health-care programs in work places and in other places where women of childbearing age congregate should ensure that the rubella immune status of every employee is ascertained and that rubella immunization is made available. All hospital personnel (male and female) who might be at risk of exposure to patients infected with rubella or who might have contact with pregnant pa tients or personnel should be immune to rubella. Consideration should be given to making rubella immunity a condition for employment. Finally, since the risk of acquiring rubella while traveling outside the United States is greater than the risk incurred within the United States, all women travelers, particularly those of childbearing age, should be immune before leaving the United States.
# Vaccine side effects and adverse reactions
Up to 40% of susceptible adult vaccinees in large-scale field trials have had joint pain, usu ally of the small peripheral joints, after vaccination; frank arthritis is reported infrequently. A r thralgia and transient arthritis occur more frequently and tend to be more severe in susceptible women than in children. When joint sym ptom s or other types of pain and paresthesias do occur, they generally begin 3 -2 5 days after vaccination, persist for 1-11 days, and rarely recur. Adults with joint problems usually have not had to disrupt work activities. Complaints of transient peripheral neuritis such as paresthesias and pain in the arms and legs have o c curred very rarely and only in susceptible vaccinees.
# Vaccine precautions and contraindications
Rubella vaccine should be given at least 14 days before administration of IG or deferred for at least 6 weeks, and preferably 3 months, after administration. On the other hand, previ ous administration of whole blood or other blood products containing antibody (e.g., human anti-Rho immune globulin) does not generally interfere with an immune response and is not a contraindication to postpartum vaccination. However, in this situation, serologic testing should be done 6 -8 weeks after vaccination to assure that seroconversion has occurred.
# MMWR 17S
Rubella vaccine should not be given to pregnant women or to those likely to become preg nant within 3 months after receiving the vaccine. Through 1 983, C D C monitored prospective ly 2 1 4 susceptible pregnant women who had received rubella vaccine within 3 months before or after conception and carried their pregnancies to term (94 received Cendehill or H PV-77, 11 9 received RA 27/3, and one received an unknown strain of vaccine). None of the infants had malformations compatible with C R S. The ACIP believes that the risk of vaccineassociated malformation is so small as to be negligible. Although a final decision must rest with the individual patient and her physician, the ACIP believes that rubella vaccination during pregnancy should not ordinarily be a reason to recommend interruption of pregnancy.
Because of the theoretical risk to the fetus, reasonable precautions should be taken before women of childbearing age are vaccinated. These precautions include 1) asking women if they are pregnant, 2) excluding those who say they are, and 3) explaining the theoretical risks of the vaccine to the others and counseling them not to become pregnant for 3 months after vaccination. If a pregnant woman is vaccinated or if a woman becomes pregnant within 3 months after vaccination, she should be counseled on the theoretical risks to the fetus. In stances of vaccination of k n o w n susceptible women who are pregnant or become pregnant within 3 months should be reported through state health departments to the Division of Im munization, CDC.
In general, rubella vaccine should not be given to persons who are immunocompromised as a result of immune deficiency diseases, leukemia, lymphoma, or generalized m alignancy or are immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antime tabolites, or radiation. (See "Conditions That Com prom ise the Immune System ," page 8S.)
Rubella vaccine is prepared in human diploid cell cultures and has not been reported to be associated with allergic reactions. The vaccine does contain trace amounts of neomycin to which patients may be allergic. Persons with a history of any sign or symptom of an anaphylactic reaction (i.e., hives, swelling of the mouth and throat, difficulty in breathing, hy potension, or shock) following receipt of neomycin should not receive rubella vaccine. Persons with reactions to neomycin that are not anaphylactic are not at increased risk and can be v ac cinated. Rubella vaccine does not contain penicillin.
# S m a llp o x
In May 1 9 80, the World Health Organization (WHO) declared the world free of smallpox. A smallpox vaccination certificate is not required by any country as a condition of entry for inter national travelers. In May 1983, the distribution of smallpox vaccine for civilian use in the United States w as discontinued.
# Vaccine indications
There is no evidence that smallpox vaccination has therapeutic value in the treatment of recurrent herpes simplex infection, warts, or any other disease. Sm allpox vaccine should never be used therapeutically for these or any other conditions.
Except for persons working with orthopox viruses or involved in producing and testing smallpox vaccine, there are no indications for the use of smallpox vaccine in civilian popula tions. When indicated, smallpox vaccination should be given at least every 3 years. For advice on vaccine administration and contraindications, contact the International Health Program Office, C D C , Atlanta, Georgia 30 3 3 3 .
# Y ello w F e v e r
C ases of yellow fever are reported only from Africa and South America. Two form s of yellow fever-urban and jungle -are distinguishable epidemiologically. Clinically and ecologi cally they are identical.
# 18S
# MMWR
# Septem ber 28, 1984
Urban yellow fever is an epidemic viral disease transmitted from infected to susceptible persons by the Aedes a e g yp ti mosquito. In areas where the A. a e g yp ti mosquito has been eliminated or suppressed, urban yellow fever has disappeared. In W est Africa, A. aegyptitransmitted epidemics involving town and village populations continue to occur at frequent intervals.
Jungle yellow fever is an enzootic viral disease transmitted among nonhuman hosts by a variety of mosquito vectors. It is currently observed only in forested areas of South America and forest-savannah zones of tropical Africa, but occasionally extends into Central America and the Caribbean. In tropical America 2 0 0 -4 0 0 cases are recognized annually, mainly among persons with occupational exposure to the vector in forested areas; the disease is, however, believed to be greatly underreported. In Africa, epidemics that are spread by forest mosquito vectors affect tens of thousands of persons every few years, but few cases are officially reported. The jungle yellow fever cycle may be active but unrecognized in forested areas of countries within the zone with endemic yellow fever (Figure 1).
# Yellow fever vaccine
The yellow fever vaccine available in the United States is an attenuated, live-virus vaccine prepared from the 1 7D strain of virus grown in chick embryo. Immunity is induced by a single S C injection of 0.5 ml of reconstituted vaccine and persists for more than 10 years.
Yellow fever vaccines must be approved by W HO and administered at an approved Yellow Fever Vaccination Center. Centers can be identified by contacting state and local health departments. Vaccinees should have an International Certificate of Vaccination filled out, dated, signed, and validated with the stamp of the center where the vaccine is given. Vaccine must be received 6 days to 10 years before travel in order for the certificate to be valid.
# Vaccine indications
Vaccination is recommended for persons traveling or living in areas where yellow fever in fection o ccu rs-currently parts of Africa and South America. tries currently reporting yellow fever are noted biweekly in S um m ary o f H ealth In fo rm a tio n fo r In te rn a tio n a l Travel. All state health departments and many county and city health depart ments receive these publications. It should be emphasized that the actual areas of yellow fever activity far exceed the zones officially reported to be infected. Vaccination is also recommended for laboratory personnel who might be exposed to virulent yellow fever virus. Booster doses are needed at 1 O-year intervals. Som e countries, especially in Africa, require evidence of vaccination from all entering trav elers. Other countries may waive the requirements for travelers coming from noninfected areas and staying less than 2 weeks. Som e countries require a traveler, even if only in transit, to have a valid certificate if the traveler has visited any country thought to harbor yellow fever virus. Requirements of individual countries may change, and the most current information is published biweekly in S um m ary o f H ealth In fo rm a tio n fo r In tern ation al Travel and summarized annually in H ealth Inform a tion fo r Intern ation al Travel.
# Vaccine side effects and adverse reactions
Reactions to 17D yellow fever vaccine are generally mild. From 2% to 5% of vaccinees have mild headache, myalgia, low-grade fever, or other minor sym ptom s 5 -1 0 days after vac cination. Fewer than 0.2% curtail regular activities. Immediate hypersensitivity reactions, char acterized by rash, urticaria, and/or asthma, are extremely uncommon and occur principally in persons with a history of egg allergy. Although more than 34 million doses of vaccines have been distributed, only two cases of encephalitis temporally associated with vaccinations have been reported in the United States; in one fatal case, 1 7D virus w as isolated from the brain.
# Vaccine precautions and contraindications
Yellow fever vaccine should not be given to persons who are immunocompromised as a result of immune deficiency diseases, leukemia, lymphoma, or generalized m alignancy or are immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabo lites, or radiation. (See "Conditions That Com prom ise the Immune System ," page 8S.)
Although specific information is not available on adverse effects of yellow fever vaccine on the developing fetus, it is prudent on theoretical grounds to avoid vaccinating pregnant women and to advise that they postpone travel to areas where yellow fever occurs until after delivery. Pregnant women who must travel to areas where the risk of yellow fever is high should be vaccinated. It is believed that under these circum stances, the risk of yellow fever in fection far outweighs the small theoretical risk to mother and fetus from vaccination. Howev er, if international travel regulations constitute the only reason to vaccinate a pregnant woman or a patient hypersensitive to eggs, efforts should be made to obtain a letter of waiver from a physician clearly stating the contraindication to vaccination. Ideally, this letter should be writ ten on letterhead stationery and bear the stamp used by health departments and official im munization centers to validate the International Certificates of Vaccination. Such a letter of waiver has been acceptable to some governments. Under these conditions, it is also useful for the traveler to obtain specific, authoritative advice from the country or countries he or she plans to visit. Their em bassies or consulates may be contacted, and a letter substantiating the waiver of requirements obtained.
Since live yellow fever vaccine is produced in chick embryos, persons with a history of any signs or sym ptom s of an anaphylactic reaction (i.e., hives, swelling of the mouth and throat, difficulty in breathing, hypotension, or shock) after eating eggs should not receive yellow fever vaccine. If vaccination of an individual with a questionable history of egg hypersensitivity is considered essential because of a high risk of exposure, an intradermal (ID) test dose may be administered under close medical supervision. Specific directions for skin testing are found in the package insert. Som e data have indicated that persons given yellow fever and cholera vaccines simultane ously or 1-3 weeks apart had lower-than-normal antibody responses to both vaccines. Unless there are time constraints, cholera and yellow fever vaccines should be administered at a minimal interval of 3 weeks. If the vaccines cannot be administered at least 3 weeks apart, then they should preferably be given simultaneously.
Yellow fever vaccine and commercially available IG may be given simultaneously.
# Both Live-V irus and Inactivated-Virus Vaccines
# P o lio m y e litis
The risk of poliomyelitis is very small in the United States; however, epidemics could occur if the high immunity level of the general population is not maintained by immunizing children routinely or if wild poliovirus is introduced into susceptible populations in communi ties with low immunization levels. In the United States inapparent infection with wild poliovirus strains no longer contributes significantly to establishing or maintaining immunity. Most adults are already immune.
# Poliovirus vaccines
Two types of poliovirus vaccines are currently licensed in the United States: O PV and IPV. A primary vaccination series with either vaccine produces immunity to all three types of polio virus in more than 95% of recipients. The primary series of O PV consists of three doses: two doses given 6 -8 weeks apart and a third dose given at least 6 weeks and customarily 6 -1 2 months after the second. The primary series for IPV consists of four doses: three doses each given 4 -8 weeks apart and a fourth dose given 6 -1 2 months after the third. In general, it is not necessary to give a primary vaccine series to adults living in the United States who have not had a primary series as children. However, for adults who have not had a primary series and who are at greater risk than the general population of exposure to wild polioviruses be cause of foreign travel or health occupation, IPV is preferred since the risk of O PV-associated paralysis is slightly higher in adults than in children.
Poliovirus vaccine is not routinely recommended for persons older than high school age (1 8 -1 9 years old).
# Vaccine indications
Travelers to areas where wild poliovirus is epidemic or endemic should have completed a primary series of poliovirus vaccine. For previously unimmunized persons, IPV is indicated. However, if less than 4 weeks are available before protection is needed, a single dose of OPV is recommended. Travelers who have previously received less than a full primary course of O PV or IPV should be given the remaining required doses of either vaccine, regardless of the interval since the last dose and the type of vaccine previously received. Travelers to develop ing countries who have previously completed a primary series of O PV should receive a single dose of OPV. Additional booster doses of O PV are probably not necessary. Those who have previously received a primary series of IPV should receive a dose of either O PV or IPV. If IPV is used exclusively, an additional dose may be given every 5 years if exposure continues or recurs, although the need for these boosters has not been established.
Health-care personnel in close contact with patients who may be excreting wild poliovi ruses, and laboratory personnel handling specim ens that may contain wild polioviruses, should have completed a primary series of poliovirus vaccine. IPV is indicated because of the slightly increased risk to adults of vaccine-associated paralysis after O PV administration; also, virus may be shed after receipt of O PV vaccine and inadvertently expose susceptible im munocompromised contacts to live vaccine virus.
# MMWR
# 21S
# Vaccine adverse reactions
In a ctiva te d po lio viru s vaccine. No serious side effects of currently available IPV have been documented. Since IPV contains trace amounts of streptomycin and neomycin, hypersensitivi ty reactions are possible in individuals sensitive to these antibiotics. Persons with signs and sym ptom s of an anaphylactic reaction (i.e., hives, swelling of mouth and throat, difficulty in breathing, hypotension, or shock) following receipt of streptomycin or neomycin should not receive IPV. Persons with reactions that are not anaphylactic are not at increased risk and can be vaccinated.
O ral p o lio viru s vaccine. In rare instances, administration of O PV has been associated with paralysis in healthy recipients and their contacts. Although the risk of vaccine-associated paralytic poliomyelitis is extremely small for immunologically normal vaccinees (approximate ly one case per 9 million doses distributed) and their susceptible, immunologically normal household contacts (approximately one case per 7 million doses distributed), vaccinees should be informed of this risk.
# Vaccine precautions and contraindications
In a ctiva te d p o lio viru s vaccine. There is no convincing evidence of adverse effects of IPV for the pregnant woman or developing fetus; regardless, it is prudent on theoretical grounds to avoid vaccinating pregnant women. However, if immediate protection against poliomyelitis is needed. OPV, not IPV, is recommended.
O ral po lio viru s vaccine. Unlike other live-virus vaccines, which are administered parenteral ly, O PV is administered orally. IG and other antibody-containing blood products do not appear to interfere with the immune response to OPV.
OPV should not be given to persons who are or may be immunocompromised as a result of immune deficiency diseases, leukemia, lymphoma, or generalized malignancy or immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabolites, or ra diation. (See "Conditions That Com prom ise the Immune System ," page 8S.) If immunization against poliomyelitis is indicated in such persons, IPV should be used, and some protection may result.
OPV should not be used for immunizing household contacts of patients immunocompro mised as a result of immune deficiency disease, leukemia, lymphoma, or generalized malignancy or immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabolites, or radiation. If protection is indicated, IPV should be used for immuniz ing household contacts of such patients. O PV should not be given to anyone in a family with a known family history of immunodeficiency until the immune status of all family members is documented.
When children in the household are given O PV, adults who are not adequately immunized against poliomyelitis are at a very small risk of contracting O PV-associated paralytic polio myelitis. Because of the overriding importance of ensuring prompt and complete immunization of the child and the extreme rarity of O PV-associated disease in contacts of vaccinees, the ACIP recommends the administration of O PV to a child regardless of the poliovirus-vaccine status of adult household contacts. This is the usual practice in the United States. The re sponsible adult should be informed of the small risk involved and of precautions to be taken, such as hand washing after changing a diaper. An acceptable alternative, if there is strong assurance that ultimate, full immunization of the child will not be jeopardized or unduly delayed, is to immunize adults with IPV or OPV, as appropriate to their immunity status, before giving O PV to the child.
# Inactivated-Virus Vaccines
# H e p a titis B Virus In fe ctio n
The estimated lifetime risk of acquiring HBV infection in the United States is approximately 5% for the population as a whole but may approach 100% for the highest risk groups. Annual ly, an estimated 1 0 0 ,0 0 0 sym ptom atic cases of hepatitis B disease occur in the United States, leading to approximately 10,000 hospitalizations and 190 fulminant cases. Threefourths of persons with fulminant disease die.
In 1982, 88% of hepatitis B cases for which patient age w as known occurred in persons 20 years of age or older. Between 6% and 10% of adults with HBV infection become carriers. The United States currently has 4 0 0 ,0 0 0 -8 0 0 ,0 0 0 carriers. Chronic active hepatitis occurs in 25% of carriers. Each year in the United States, approximately 4 ,0 0 0 persons die of HBVrelated cirrhosis, and 8 00, of HBV-related liver cancer.
# Hepatitis B vaccine
A series of three 1 -ml IM doses of HB vaccine, each containing 20 /ug/ml of HBsAg protein, provides protective antibody in over 90% of healthy adult recipients and is 80% -95% effective in preventing infection for at least 2 years. The first two doses should be given 1 month apart, and the third dose, 5 months after the second. The duration of vaccine-induced protection and the need for booster doses are not yet known. For susceptible hem odialysis patients, three 2-m l doses given at the above intervals are recommended. Because the prevalence of HBV varies widely among various population groups, serologic screening to detect susceptible individuals before vaccination may or may not be cost effective. Cost effectiveness depends on the known or perceived risk of infection, the cost of screening, and the cost of HB vaccine.
# Vaccine indications
Immunization is recommended for adults at increased risk of occupational, social, family, environmental, or illness-related exposure to HBV. These include homosexual males, users of illicit injectable drugs, household and sexual contacts of HBV carriers, workers in healthrelated occupations requiring frequent exposure to blood, residents and staff of institutions for the mentally retarded, hemodialysis patients, recipients of factor VIII or IX concentrates, and morticians and their assistants. Inmates in some long-term correctional facilities may also be candidates for vaccination.
Vaccination should also be considered for persons who plan to reside for more than 6 months in areas with high levels of endemic HBV and who will have close contact with the local population and for travelers intending a short stay who are likely to have contact with blood from or sexual contact with residents of areas with high levels of endemic disease (par ticularly areas of eastern Asia and Sub-Saharan Africa). Such persons should allow 6 months before travel in order to complete the HB vaccine primary series.
HB vaccine is intended primarily for preexposure prophylaxis. However, it has recently been recommended for postexposure use in certain situations, particularly for persons who belong to a high-risk group for whom preexposure administration of vaccine is recommended ( 3 ). HB vaccine in combination with HBIG provides sustained protective levels of antibody and obviates the need for a second dose of HBIG in such exposures. Therefore, a normal series of HB vaccine, combined with a single dose (0.06 ml/kg or 5 ml for adults) of HBIG given at a dif ferent site, is recommended for postexposure prophylaxis of health workers following acci dental percutaneous or mucous-membrane exposure to blood containing HBsAg, and of su s ceptible homosexual men following sexual exposure to an H BsAg-positive man. HBIG alone (in the same dose) is recommended for postexposure prophylaxis of persons with heterosexu al exposures. - Vaccine side effects and adverse reactions
In vaccine trials, soreness at the site of injection w as the only side effect that occurred more frequently for vaccinees than for controls. Since its licensure in 1981 through August 1 983, HB vaccine is estimated to have been administered to over 3 5 0 ,0 0 0 individuals in the United States. A s of May 1 984, adverse events following immunization had been reported for 8 9 0 vaccinees. The reported adverse events represent temporal associations with vaccination and are not necessarily caused by the vaccine. Forty-eight persons had serious events such as transverse myelitis, grand mal seizures, aseptic meningitis, erythema multiforme, or Guillain-Barre syndrome (GBS).
# Vaccine precautions and contraindications
Pregnancy should not be considered a contraindication to vaccinating women who are oth erwise candidates for receiving HB vaccine. While data are not available on the safety of the vaccine for the developing fetus, HB vaccine contains only noninfectious HBsAg particles and should pose no risk to the fetus. In contrast, HBV infection in a pregnant woman may result in a severe disease for the mother and chronic infection for the newborn.
Since HB vaccine is made from human plasma, the possibility that it may contain an etiologic agent of acquired immunodeficiency syndrome (AIDS) has been raised. The purification and inactivation process used in preparing HB vaccine inactivates representatives of all known groups of viruses. There are no microbiologic, epidemiologic, or empiric data to suggest that the HB vaccine carries any etiologic risk for AIDS.
# In flu e n za
Influenza viruses have continually demonstrated the ability to cause major epidem ics of re spiratory disease. High attack rates of acute illness and the frequent occurrence of lowerrespiratory-tract complications usually result in dramatic rises in visits to physicians' offices and hospital emergency rooms. Furthermore, influenza frequently infects individuals who, be cause of their age or underlying health status, are poorly able to cope with the disease and often require medical attention, including hospitalization. Such persons are considered to be medically at "high risk" in epidemics. In one recent study, for example, rates of hospitalization for adults with "high-risk" medical conditions increased during major epidemics by about two-to fivefold in different age groups, reaching a maximum rate of about 8 0 0 per 1 0 0 ,0 0 0 population.
Influenza epidemics cause excess mortality, which is attributable not only to influenza pneumonia, but also to cardiopulmonary disease. Fifteen times in the years 1 9 5 7 -1 9 8 2 , epidemics have been associated with 10 ,0 0 0 or more excess deaths; in 1983, excess mor tality again exceeded the epidemic threshold.
The greatest impact of influenza is normally seen when new strains appear against which most of the population lacks immunity. In these circum stances (e.g., 1957 and 1968), pandemics occur. During pandemics, a quarter or more of the United States population have been affected over a period of 2 -3 months.
Because the proportion of elderly persons in the United States is increasing, and because age and its associated chronic diseases are risk factors for severe influenza illness, the toll of influenza may also increase unless control measures are used more vigorously than in the past.
# Influenza vaccine
Influenza A viruses are classified into subtypes on the basis of two antigens: hemagglutinin (H) and neuraminidase (N). Three subtypes of hemagglutinin (H1, H2, H3) and two subtypes of neuraminidases (N1, N2) are recognized among influenza A viruses that have caused w ide spread human disease. Immunity to these antigens, especially hemagglutinin, reduces the likelihood of infection and the severity of disease if a person does become infected. However, there may be sufficient antigenic variation (antigenic drift) within the same subtype overtime, so that infection or vaccination with one strain may not induce immunity to distantly related strains of the same subtype. Although influenza B viruses have shown much more antigenic stability than influenza A viruses, antigenic variation does occur. A s a consequence, the an tigenic characteristics of current strains provide the basis for selecting virus strains to be included in the vaccine for a given year. Potency of present vaccines is such that nearly all vaccinated young adults develop hemagglutination-inhibition antibody titers that are likely to protect them against infection by strains like those in the vaccine, and often by related variants that emerge. The elderly, the very young, and patients with certain chronic diseases may develop lower postvaccination an tibody titers than do young adults. Under these circum stances, influenza vaccine may be more effective in preventing lower-respiratory-tract involvement, or other complications of in fluenza, than in preventing upper-respiratory-tract involvement. Influenza vaccine will not pre vent primary illnesses caused by other respiratory pathogens.
# Vaccine indications
Use of inactivated influenza vaccine is the single most important measure in the prevention and/or attenuation of influenza infection. Since 1 963, annual vaccination against influenza has been recommended for individuals at high risk of lower-respiratory-tract complications and death following influenza infection (i.e., the elderly and persons with chronic disorders of the cardiovascular, pulmonary, and/or renal system s; metabolic diseases; severe anemia; and/or compromised immune function). These groups have been identified primarily by review of death certificate data, supported by hospital-based or population-based studies. W ithin each broadly defined "high-risk" category, however, some persons are more likely than others to suffer severe complications from influenza infection.
Am ong nursing-home residents, chronic diseases and other debilitating conditions are common, and spread of influenza can often be explosive, with attack rates as high as 60% and case-fatality ratios up to 30% or higher. In addition, recent retrospective studies of nonin stitutionalized patients suggest that chronic underlying diseases, particularly those that affect the cardiovascular and pulmonary system s, may contribute more to the severity of illness than does age alone.
Medical personnel may transmit influenza infections to their high-risk patients while they are themselves incubating an infection, undergoing a subclinical infection, or working while they have mild sym ptom s. Nosocom ial outbreaks of influenza are reported. The potential for introducing influenza to a high-risk group such as patients with severely compromised cardio pulmonary or immune system s or infants in neonatal intensive care units should be reduced by targeted vaccination programs of medical personnel.
Based on these observations, the previous, broadly defined "high-risk" adult groups have been further assigned priority for receiving vaccine in order that special efforts can be directed at providing vaccine to those who may derive the greatest benefit.
1. Adults at high risk of severe influenza illness who most warrant active, targeted v acci nation efforts: (a) Adults with chronic disorders of the cardiovascular or pulmonary system s that are severe enough to require regular medical follow-up or to have caused hospitalization during the preceding year.
(b) Residents of nursing homes and other chronic-care facilities (e.g., institutions hous ing patients of any age with chronic medical conditions). Achievement of high vacci nation rates (e.g., 80%) may induce herd immunity in such populations and thereby MMVIIR 2 5 S lower the frequency of outbreaks, as well as reducing the frequency of severe illness when outbreaks do occur. 2. Physicians, nurses, and other personnel who have extensive contact with high-risk pa tients (e.g., primary-care and certain specialty clinicians and staff of intensive-care units). These persons should receive influenza vaccination annually to reduce the po ssi bility for nosocomial spread of influenza to high-risk patients. 3. Other adults who are at moderately increased risk of serious illness compared with the general population. Special programs to make vaccine readily available to these groups should also be given high priority:
(a) Healthy individuals over 65 years of age.
(b) Adults with a chronic metabolic disease (including diabetes mellitus), renal dysfunc tion (including those in chronic dialysis), anemia, immunosuppression, or asthma that is severe enough to require regular medical follow-up or to have caused hospi talization during the preceding year. In addition, influenza vaccine may be offered to persons who provide essential community service or to any adult who w ishes to reduce the likelihood of an influenza infection.
Effective programs for giving influenza vaccine are needed in nursing homes and other chronic-care facilities, in physicians' offices, and in hospital settings. Residents of nursing homes and chronic-care facilities should receive routine annual vaccination. Other adult highpriority groups should receive influenza vaccine at the time of regular medical follow -ups in the fall, or should be notified to come in specifically to receive the vaccine. Patients with high risk conditions who are hospitalized during the fall should be considered for influenza vaccine before discharge from the hospital.
There is considerable overlap in the target groups for influenza vaccination and those for pneumococcal polysaccharide vaccine. Pneum ococcal polysacchraride vaccine and influenza vaccine can be given at the same time at different sites without an increase in side effects; however, it should be emphasized that whereas influenza vaccine is given annually, pneumo coccal polysaccharide vaccine should be given only once to adults. Detailed immunization records should be provided to each patient to help ensure that additional doses of pneumo coccal polysaccharide vaccine are not given.
Amantadine hydrochloride, an antiviral drug, can prevent influenza A or be used therapeuti cally to reduce sym ptom s of influenza A infections. It is n o t a substitute for vaccine. Specific circum stances in which amantadine prophylaxis is recommended are described in the ACIP recommendations on prevention and control of influenza.
# Vaccine side effects and adverse reactions
Vaccines used in recent years have generally been associated with only a few reactions. Fewer than one-third of vaccinees have been reported to develop local redness or induration for 1 or 2 days at the site of injection.
System ic reactions have been of two types. First, malaise, myalgia, and other system ic sym ptom s of toxicity, although infrequent, most often affect those who have had no experi ence with the influenza virus antigens contained in the vaccine. These reactions, which begin 6 -1 2 hours after vaccination and persist for 1-2 days, are usually attributed to the influenza antigens (even though the virus is inactivated) and constitute most of the system ic side ef fects of influenza vaccination.
Second, immediate, presumably allergic, responses such as flare and wheal or various respiratory-tract sym ptom s of hypersensitivity occur extremely rarely after influenza vaccina tion. These sym ptom s probably result from sensitivity to some vaccine component -most likely residual egg protein. Although current influenza vaccines contain only a small quantity of egg protein, on rare occasions vaccine can induce hypersensitivity reactions. Unlike the MMWR Septem ber 28, 1984
1 976 swine influenza vaccine, vaccines used subsequently have not been associated with an increased frequency of GBS.
# Vaccine precautions and contraindications
Pregnancy has not been demonstrated to be a risk factor for severe influenza infection except in the largest pandemics of 1 9 1 8 -1 9 1 9 and 1 957-1 958. Influenza vaccine is consid ered to be generally safe for pregnant women. Nonetheless, when vaccine is to be given during pregnancy, waiting until the second or third trimester is a reasonable precaution to minimize any concern over theoretical teratogenicity.
Persons with a history of any signs or sym ptom s of an anaphylactic reaction (i.e., hives, swelling of the mouth and throat, difficulty in breathing, hypotension, or shock) after eating eggs should not be given inactivated influenza vaccine.
Persons with acute febrile illnesses normally should not be vaccinated until their temporary sym ptom s have abated.
# R a b ie s
Although rabies rarely affects humans in the United States, thousands of persons receive rabies vaccine every year, principally for postexposure prophylaxis. The likelihood of human exposure to rabies from domestic animals has decreased greatly in recent years. In every year since 1 976, more than 85% of all reported cases of animal rabies have been among wild ani mals, the most important source of possible infection for humans in the United States. How ever, for persons traveling overseas to developing countries with endemic rabies, the dog re mains the animal most likely to transmit rabies.
# Rabies vaccine
Both whole-virion and subvirion human diploid cell rabies vaccines (HDCV) are available. For preexposure rabies prophylaxis a three-dose series of H D CV of either type given as 1 -ml doses IM on days 0, 7, and 28 provides adequate antibody levels in virtually all recipients (10). The C D C currently accepts a titer of 5 by the rapid fluorescent-focus inhibition test as adequate.
The whole-virion H D CV produced by the Merieux Institute has been used for preexposure immunization in a regimen of three 0 .1 -ml doses given intradermally (ID) in the lateral aspect of the upper arm in the deltoid area, one dose on each of days 0, 7, and 28. Experience gained with over 2 ,0 0 0 persons vaccinated in the United States by the ID route has shown that anti body is produced in all recipients, although the mean response is somewhat lower and may be of shorter duration than with comparable IM immunization. Except for persons suspected of being immunosuppressed, postvaccination serology is not necessary following IM or ID im munization in the United States. Antibody response in some groups vaccinated ID outside the United States has been found to be inadequate for reasons not yet determined (11). Prelimi nary data suggest that concurrent administration of malaria chem oprophylaxis may be a factor in the lowered immunologic response of persons vaccinated overseas. It should be noted that Merieux Institute, the manufacturer, has not yet met the packaging and labeling re quirements necessary to obtain approval by the FDA for the ID route of administration. The 1 -ml vial presently available is intended for IM use and contains no preservatives. To minimize the risk of contamination and loss of vaccine potency, the reconstituted vaccine must be used immediately. Data on ID immunization are not available for W yeth Laboratories vaccine.
Proper postexposure rabies prophylaxis is determined by whether or not the person has had previous preexposure or postexposure prophylaxis. 1) Persons who (a) have previously received postexposure prophylaxis with HDCV, (b) have received a three-dose IM preexposure regimen of HDCV, (c) have received a three-dose ID preexposure regimen of H D CV in the United States, or (d) have a previously documented adequate rabies titer should receive two 1-ml IM doses of H D C V -one dose on each of days 0 and 3. HRIG is not recommended in these circum stances. 2) Persons not meeting the above criteria should be treated with a single, 20-international units (IU)/kg dose of HRIG and five 1-ml doses IM of H D CV -one on each of days 0, 3, 7, 14, and 28. HRIG should be administered at the beginning of H D CV post exposure prophylaxis but can be given up to the eighth day after the first dose of H D CV was given. The HRIG dose should be divided; up to half should be infiltrated into the area of the wound, if possible, and the rest administered IM, but not in the same site as HDCV. O nly IM ad ministration of HD CV is indicated for postexposure prophylaxis.
# Vaccine indications
Preexposure immunization should be considered for high-risk groups: animal handlers, cer tain laboratory workers and field personnel, and persons planning to be in countries or areas of countries for more than 1 month where rabies is a constant threat. Persons whose voca tions or avocations bring them into contact with potentially rabid animals should also be con sidered for preexposure immunization. Persons with continuing risk of exposure should re ceive a booster dose every 2 years or have their serum tested for rabies antibody every 2 years and, if the titer is inadequate, be given a booster dose. If there is substantial risk of expo sure to rabies, preexposure rabies prophylaxis may be indicated during pregnancy.
The decision to provide specific postexposure antirabies treatment should include the fol lowing considerations:
1 Type of exposure-rabies is transmitted primarily by the bite of infected animals. It may also be transmitted by introducing the virus into open cuts or wounds in skin or via m ucous membranes by saliva or other potentially infectious material from a rabid animal and, rarely, by aerosol exposure. 2. Species of biting animal -carnivorous wild animals (especially skunks, raccoons, and foxes) and bats are most commonly infected with rabies in the United States. Elsewhere in the world, dogs, cats, carnivorous wildlife, and bats are the major vectors. The likeli hood that domestic cats or dogs in the United States will be infected varies from region to region. Rodents are rarely infected. Consultations with the state or local health department may be helpful. 3. Circum stances of biting incident -an unprovoked attack is more indicative of a rabid animal than a provoked attack.
- Vaccine side effects and adverse reactions Following postexposure prophylaxis, local reactions, such as pain, erythema, and swelling or itching at the injection site, are very common, and mild system ic reactions, such as head ache, nausea, abdominal pain, muscle aches, and dizziness, are reported by about 20% of reci pients. System ic allergic reactions ranging from hives to anaphylaxis occur in an estimated 11 per 10,000 vaccinees. Mild immune-complex-like hypersensitivity reactions consisting of hives, itching, and angio-edema have occurred 2-21 days after booster doses of H D CV and are the most frequently reported allergic reactions ( 12 ). Four cases of transient neuroparalytic illness have been temporally associated with H D CV administration: two following administra tion of whole-virion vaccine and two following administration of subvirion vaccine (13). No permanent sequelae or deaths have been associated with administration of HDCV.
# Vaccine precautions and contraindications
Corticosteroids and other immunosuppressive agents can interfere with the development of active immunity and should not be administered during preexposure therapy. When rabies postexposure prophylaxis is administered to persons known or suspected of being immunosuppressed, or to those who are receiving steroids or immunosuppressive therapy, it is espe cially important that serum be tested to ensure an adequate rabies antibody response. If a person experiences an anaphylactic reaction (i.e., hives, swelling of the mouth and throat, difficulty in breathing, hypotension, or shock) after receiving HDCV, no further preex posure doses of H D CV should be given. By contrast, if a person needing postexposure therapy has had a previous anaphylactic reaction to H D CV or has such a reaction during the postexpo sure course, H D CV therapy should continue; however, the person should receive the required doses in an appropriate medical setting.
# Inactivated-Bacteria Vaccines
# Ch o le ra
Cholera continues to be a health risk in Africa and Asia. Countries currently reporting chol era are listed in the biweekly publication S um m a ry o f H ealth Inform a tion fo r In tern ation al Travel. All state health departments and many county and city health departments receive this publication. Persons who follow the usual tourist itinerary and who use tourist accom m o dations in countries affected by cholera are at virtually no risk of infection. The traveler's best protection against cholera is avoiding food and water that might be contaminated.
# Cholera vaccine
The vaccine may be administered as a 0.5-m l dose S C or IM or as a 0.2-m l dose ID. A l though a single dose of vaccine is sufficient for entry into most countries, some countries may require evidence of a complete primary series of two doses given 1 week to 1 month or more apart, or a booster dose within 6 months before arrival.
The currently available cholera vaccine has been shown in field trials to be only about 50% effective in preventing clinical illness for a period of 3 -6 months. The vaccine does not prevent transmission of infection. The risk of cholera to most U.S. travelers is so low that it is doubtful that vaccination is of benefit. W HO no longer recommends cholera vaccination for travel to or from cholera-infected areas. However, some countries affected or threatened by cholera re quire evidence of cholera vaccination as a condition of entry. Current information on choleravaccination requirements of individual countries is published annually in H ealth Inform a tion fo r International. Travel. All state health departments and many county and city health depart ments receive this publication. Travelers to countries with cholera-vaccination requirements should have an International Certificate of Vaccination filled in, dated, signed, and validated showing receipt of the vaccine 6 days to 6 months before entry into the country. Most city, county, and state health departments can validate certificates. Failure to secure validation may cause travelers to be revaccinated or quarantined
# Vaccine indications
Cholera vaccine is indicated only for travelers to countries requiring evidence of cholera vaccination for entry. Boosters may be given every 6 months if required by a country.
# Vaccine side effects and adverse reactions
Vaccination often results in 1 -2 days of pain, erythema, and induration at the site of injec tion. The local reaction may be accompanied by fever, malaise, and headache. Serious reac tions, including neurologic reactions, following cholera vaccination are extremely rare.
# Vaccine precautions and contraindications
No specific information is available on the safety of cholera vaccine during pregnancy. Be cause cholera disease during pregnancy is a serious illness, whether to use cholera vaccine should be determined in individual circum stances based on the actual risk of disease and the probable benefits of the vaccine.
The only contraindication to cholera vaccine is a history of a severe reaction following a previous dose. Most governments will permit an unvaccinated traveler to enter the country if
MMWR 2 9 S
he or she carries a physician's statement of medical contraindication. However, some coun tries may quarantine such unvaccinated persons or place them under surveillance if they come from areas with cholera. Som e data have indicated that persons given yellow fever and cholera vaccines simultane ously or 1-3 weeks apart had lower-than-normal antibody responses to both vaccines. Unless there are time constraints, cholera and yellow fever vaccines should be administered at a minimal interval of 3 weeks. If the vaccines cannot be administered at least 3 weeks apart, then they should preferably be given simultaneously.
# M e n in g o co cca l D is e a s e
Meningococcal disease is endemic throughout the world but may also occur in epidemics. Am ong U.S. civilians, m eningococcal disease occurs primarily as single, isolated cases or, in frequently, in small, localized clusters. A third of all cases of m eningococcal disease occur in patients 20 years old or older. Serogroup B strains cause the majority of U.S. cases, with serogroups C and W1 35 strains accounting for most of the remainder.
# M eningococcal polysaccharide vaccine
Two m eningococcal polysaccharide vaccines, bivalent A -C and quadrivalent A, C, Y, and W1 35 vaccines, are available for use in the United States. Each is given as a single dose, and each induces specific serogroup immunity. The duration of immunity conferred by the v ac cines is not known.
# Vaccine indications
Vaccine may be of benefit as an adjunct to antibiotic chem oprophylaxis for household and other close contacts of persons with m eningococcal disease caused by serogroups A, C, Y, and W 1 3 5 and for travelers to areas with epidemic m eningococcal disease. The need for booster doses has not been established.
Routine vaccination of U.S. civilians with m eningococcal polysaccharide vaccine is not recommended because of the lack of availability of a group B vaccine and the low risk of in fection in the United States.
# Vaccine side effects and adverse reactions
Adverse reactions to meningococcal polysaccharide vaccines are infrequent and mild, con sisting principally of localized erythema lasting 1 -2 days.
# Vaccine precautions and contraindications
The safety of meningococcal polysaccharide vaccines for pregnant women has not been established. On theoretical grounds, it is prudent not to use them unless there is a substantial risk of infection.
# P lagu e
Plague is a natural infection of rodents and their fleas. In the United States a few human cases occur yearly in humans exposed in the Western states to infected animals, primarily ro dents, and their fleas. Other countries currently reporting plague infections are noted in the biweekly publication S um m a ry o f H ealth In fo rm a tio n fo r In tern ation al Travel. All state health departments and many county and city health departments receive this publication. A number of countries in Africa, Asia, and South America continue to report sporadic, epidemic, and epi zootic infection. In most of these countries, the risk of exposure exists primarily in rural or semirural areas.
- Plague vaccine A primary series of plague vaccine consists of three IM doses. The first dose, 1 ml, is fol lowed in 4 weeks by a second dose of 0.2 ml. The third dose, also 0.2 ml, is administered 5 months after the second. The effectiveness of a primary series of plague vaccine has never been measured precisely. Field experience indicates that vaccination with plague vaccine reduces the incidence and severity of disease resulting from the bite of infected fleas. The degree of protection offered against primary pneumonic infection is unknown. Since plague vaccination may only ameliorate illness, prophylactic antibiotics may be indicated whenever a person, vaccinated or not, has a definite exposure.
# Vaccine indications
Vaccination is indicated for certain vocational groups. These include all laboratory and field personnel working with Yersinia pe stis organisms that may be resistant to antimicro bials, persons engaged in aerosol experiments with Y. pestis, and field personnel engaged in operations in areas with enzootic or epidemic plague where preventing exposure to rodents and fleas is impossible. Plague vaccination should be considered for laboratory personnel regularly working with Y. p e stis or plague-infected rodents and for persons whose vocation regularly exposes them to wild rodents or rabbits in areas with enzootic plague.
Vaccine may also be considered for travelers to areas known to have endemic plague in countries reporting plague, particularly if travel will not be limited to urban areas with tourist hotel accommodations.
For persons with continuing exposure, three booster doses, each 0.1-0.2 ml, should be given at approximately 6-m onth intervals. Thereafter, booster doses at 1-to 2-year intervals should provide good protection.
# Vaccine side e ffe cts and adverse reactions
For about 10% of recipients, primary vaccination may result in general malaise, headache, fever, mild lymphadenopathy, and/or erythema and induration at the injection site. These reactions occur more commonly with repeated injections. Sterile abscesses occur rarely. Se n sitivity reactions manifested by urticarial and asthmatic phenomena have occasionally been reported.
# Vaccine precautions and contraindications
Neither the safety nor efficacy of vaccination with plague vaccine during pregnancy has been determined; therefore, it should not be used unless there is a substantial risk of infection.
Plague vaccine should not be administered to anyone with a known hypersensitivity to any of its constituents (beef protein, soy, casein, and phenol). Patients who have had severe local or system ic reactions to plague vaccine should not be revaccinated.
# P n e u m o c o c c a l D is e a s e
Precise data on the occurrence of serious pneumococcal disease in the United States are not available: however, the annual incidence rate of pneumococcal pneumonia is estimated to be 68 cases to 2 6 0 cases per 1 0 0 ,0 0 0 population, and of bacteremia, 7 -2 5 /1 0 0 ,0 0 0 . The incidence of pneumococcal pneumonia, which causes a substantial number of deaths annual ly, increases in those over 4 0 years old, and show s a twofold increase in those over 60 years of age. Mortality from pneumococcal disease is highest among patients who have bacteremia or meningitis, patients with underlying medical conditions, and older persons.
Patients with certain underlying conditions are clearly at increased risk both of contracting pneumococcal infection and of experiencing more severe pneumococcal illness. These condi tions include sickle cell anemia, multiple myeloma, cirrhosis, alcoholism, nephrotic syndrome, renal failure, splenic dysfunction, anatomic asplenia, and organ transplant. Persons suffering from diabetes mellitus, chronic pulmonary disease, cardiovascular disease, or conditions asso ciated with immunosuppression may be at increased risk of contracting pneumococcal infec tion or of having more severe illness.
# MMWR 3 1 S - Pneum ococcal polysaccharide vaccine
The pneumococcal polysaccharide vaccine currently available contains purified capsular materials of the 23 types of S treptococcus pneum oniae responsible for 87% of recent bacteremic pneumococcal disease in the United States. Most healthy adults show a twofold rise in type-specific antibody 2-3 weeks after administration of a single dose of vaccine. The titer of antibody that is protective against each serotype has not been determined.
The duration of vaccine-induced immunity is unknown. Studies of persistence of vaccineinduced antibody show elevated titers 3 -5 years after immunization. Booster doses are not recommended because of increased adverse reactions to subsequent doses.
Patients who have received the earlier pneumococcal polysaccharide vaccine containing capsular material from only 14 types of S. pneum oniae should not receive a dose of the 2 3valent pneumococcal polysaccharide vaccine since the modest increase in coverage does not warrant the increased risk of adverse reactions.
# Vaccine indications
Newly available data regarding vaccine efficacy support the broader use of pneumococcal polysaccharide vaccine in the United States. Vaccination is particularly recommended for the following:
1) Adults with chronic illnesses, especially those with cardiovascular disease and chronic pulmonary disease, who sustain increased morbidity with respiratory infections. 2) Adults with chronic illnesses specifically associated with an increased risk of pneumo coccal disease or its complications. These include splenic dysfunction or anatomic asplenia, Hodgkins' disease, multiple myeloma, cirrhosis, alcoholism, renal failure (including those on chronic dialysis), cerebrospinal-fluid leaks, and conditions associat ed with immunosuppression. 3) Older adults, especially those age 65 and over, who are healthy. Program s for vaccine delivery in the recommended high-risk groups need to be developed further. Specifically, more effective programs are needed for giving vaccine in physicians' of fices, in hospitals, and in nursing homes and other chronic-care facilities.
Since two-thirds of persons with serious pneumococcal disease have been hospitalized within 5 years before the pneumococcal illness ( 14), vaccine should be given to hospitalized patients in the high-risk groups before discharge, in order to prevent future adm issions for pneumococcal disease. In addition, persons with chronic conditions who visit physicians fre quently are probably at higher risk of pneumococcal infection than those who require infre quent visits. Office-based programs to identify and immunize patients requiring frequent medical care should help prevent pneumococcal illness. Furthermore, pneumococcal polysac charide vaccine and influenza vaccine can be given at different sites at the same time without an increase in side effects (7 5 ).
Medicare has partially reimbursed the cost of pneumococcal polysaccharide vaccination since 1981. It has been determined that hospitals may be reimbursed for pneumococcal im munization of Medicare recipients independent of reimbursement based on system s of pros pective payments.
# Vaccine side e ffe cts and adverse reactions
About half of the persons given pneumococcal polysaccharide vaccine experience mild side effects such as erythema and pain at the site of injection. Fever and m yalgias have been reported by fewer than 1% of those given pneumococcal polysaccharide vaccine (7 6).
Severe adverse effects such as anaphylactic reactions have rarely been reported -about five cases per million doses administered.
Arthus reactions and system ic reactions have been common among adults given second doses (1 7). They are thought to result from localized antigen-antibody reactions involving an tibody induced by previous vaccination. Therefore, second, or "booster," doses are not recommended.
# Vaccine precautions and contraindications
The safety of pneumococcal polysaccharide vaccine in pregnant women has not been evaluated. It should not be given to healthy pregnant women. Women at high risk of pneumo coccal disease ideally should be vaccinated before pregnancy.
Because of a marked increase in adverse reactions with second injections of pneumococcal polysaccharide vaccine, second, or "booster," doses should not be given. However, when there is doubt or no information on whether a person in one of the high-risk groups has ever received pneumococcal polysaccharide vaccine, vaccine should be given. Complete records of vaccination can help to avoid repeat doses.
# Typhoid
The occurrence of typhoid fever remained constant in the period 1 9 7 2 -1 9 8 2 , with an average of 4 8 6 cases reported annually. During the years 1 9 7 8 -1 9 8 2 , 57% of cases for which the patient's age w as known occurred in patients 20 years of age or older. Approxi mately 62% of typhoid cases reported in the United States during 1 977-1 979 were acquired by travelers to other countries, and an additional 27% occurred in contacts of typhoid carriers.
# Typhoid vaccine
A primary series of two 0.5-m l doses of typhoid vaccine given S C 4 weeks apart has been shown to protect 70% -90% of recipients.
# Vaccine indications
Immunization is indicated for travelers to areas where a recognized risk of exposure to ty phoid exists. It should be emphasized that even after typhoid vaccination, food and water should be selected carefully in these areas. Typhoid vaccination is not recommended in the United States or in areas of natural disaster. Booster doses should be given at least every 3 years to persons with continued or repeated exposure; these may be given S C (0.5 ml) or ID (0.1 ml). The acetone-killed and -dried vaccine should not be given ID. This preparation is available only to the U.S. Armed Forces.
# Vaccine side effects and adverse reactions
Typhoid vaccination often results in 1-2 days of discom fort at the site of injection. The local reaction may be accompanied by fever, malaise, and headache.
# Vaccine precautions and contraindications
The only contraindication to typhoid vaccine is a history of a severe local or system ic reac tion following a previous dose.
# Live-Bacteria V accines T u b e rcu lo sis
The number of tuberculosis cases in the United States has declined steadily since reporting began in the 1 9th century. Between 1 972 and 1 9 82, the annual incidence of tuberculosis de clined from 15.8 cases per 1 0 0 ,0 0 0 population to 1 1 .0/100 ,000, a decrease of 30%. In 1 982, approximately 92% of 2 5 ,0 5 9 reported cases with patient ages known occurred in per sons 20 years of age or older. Reported cases usually are typical postprimary pulmonary dis ease. The risk of infection is greatest for those who have repeated exposure to persons with unrecognized or untreated sputum -positive pulmonary tuberculosis. In the United States, ef forts to control tuberculosis are directed toward early identification and treatment of cases.
# MMWR 33 S
preventive therapy with isoniazid for infected persons at high risk of developing disease, and prevention of transmission to others.
# BCG vaccine
Although BCG vaccine is widely used in many areas of the world, results of a recent largescale field trial in India have raised questions about its efficacy (18). BCG vaccines currently available in the United States differ from the products used in the published field trials, and their efficacy has not been demonstrated directly. In the United States, vaccines for ID and for percutaneous administration are licensed. (For percutaneous administration, one drop of vac cine is placed on the skin and introduced through the skin by multiple punctures with a bifurcated or other needle.) Vaccination should be only by the route indicated on the package labeling.
# Vaccine indications
In the United States the only situations in which BCG might be considered are 1) for indi viduals in prolonged close contact with patients with active tuberculosis that is untreated, ineffectually treated, or resistant to treatment; 2) for health-worker groups, such as hospital staffs, with an annual new-infection rate of 1% or higher in spite of other tuberculosis control measures; and 3) for other groups in which an excessive rate of new infection can be demonstrated and the usual surveillance and treatment programs have failed or are not feasible. - Vaccine side effects and adverse reactions BCG has been associated with severe or prolonged ulceration at the vaccination site, re gional adenitis, disseminated BCG infection, and osteitis. Severe ulceration and adenitis occur in approximately 1 % -10% of vaccinees, and disseminated infections and osteitis are quite rare (1-10 per million doses).
# Vaccine precautions and contraindications
Although no harmful effects of BCG on the fetus have been observed, it is prudent to avoid vaccination during pregnancy unless there is immediate excessive risk of exposure to in fective tuberculosis.
Since BCG is a live-bacteria vaccine, it should not be given to persons immunocompro mised as a result of immune deficiency diseases, leukemia, lymphoma, or generalized m alignancy or to persons immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabolites, or radiation. (See "Conditions That Com prom ise the Immune System ," page 8S.)
# Other Licensed Vaccines
# A d e n o v iru s a n d A d e n o v iru s V a ccin e
Adenovirus types 4 and 7 have frequently been the cause of outbreaks of acute, febrile, respiratory-tract disease in young adults during military training. Live, oral adenovirus vaccines for types 4 and 7 are available for immunization of military populations. Use of the vaccines in other populations is not recommended.
# A n th ra x an d A n th ra x V a ccin e
Anthrax is infrequently encountered. Anthrax vaccine is recommended only for individuals who come in contact with imported animal hides, furs, bonemeal, wool, animal hair (especially goat hair), and bristles in the workplace and for individuals undertaking investigational studies involving Bacillus anthracis.
Primary immunization consists of six S C 0.5-m l injections, the first three at 2-w eek inter vals and the other three at 6-m onth intervals. Booster doses of 0.5-m l S C are recommended at 1-year intervals. The vaccine is only available from the Biologic Products Program, Michi
# P e rtu ss is a n d P e rtu s s is V a ccin e
Pertussis disease in adults is generally milder than in children and is not known to result in death. Pertussis can be transmitted from adult patients to close contacts, especially unimmu nized children. Such transmission may occur in the household and in hospitals, where chains of transmission have involved patients and staff.
In general, pertussis vaccine is not recommended for adults because both local and sy s temic reactions are thought to be more frequent and severe than in children under 7 years of age and because the disease itself is less severe in adults. In specific situations, such as docu mented transmission to and from personnel in a hospital, single-antigen pertussis vaccine in a 0.2-m l IM dose has been given as a part of control efforts. Single-antigen pertussis vaccine, adsorbed, is available only from the Biologic Products Program, Michigan Department of Public Health.
# Immune Globulins
IG and specific immune globulins, i.e., HBIG, TIG, HRIG, and varicella zoster immune globulin (VZIG), are indicated for use in order to prevent or modify certain diseases in specific circumstances.
# Im m u n e G lobulin fo r In tra m u scu la r U se
IG is given IM for preexposure prophylaxis against hepatitis A to travelers in areas where contact with potentially contaminated food and water is unavoidable. For travelers at risk for 2-3 months, a single IM dose of 0.02 ml/kg is recommended. For more prolonged travel 0.06 ml/kg should be given every 5 months. IG is also indicated for postexposure prophylaxis for close household and sexual contacts of persons with hepatitis A, staff and attendees of day care centers and household contacts of diapered children in day-care centers in which hepati tis A transmission is occurring, selected staff and clients of custodial institutions in which an outbreak is occurring, and co-workers of food handlers with hepatitis A. For such contacts a single dose of 0.02 ml/kg of IG is recommended as soon as possible after exposure. IG should be given within 2 weeks after exposure.
IG can be used to prevent or modify measles disease in susceptible contacts of persons with measles, especially those for whom measles vaccine is contraindicated, if given within 6 days after exposure. The recommended dose is 0.25 ml/kg (maximum dose = 15 ml). IG should not be used to control measles outbreaks.
# Im m u n e G lobulin fo r In tra ve n o u s U se
IG modified for IV administration may be given to prevent acute infections in patients with defective antibody synthesis or as prophylaxis against hepatitis A for patients for whom the IM preparation is contraindicated because of thrombocytopenia or disorders that can cause IM hemorrhage. ONLY IG MODIFIED FOR IN TRAVENO US U SE CAN BE GIVEN INTRAVE NOUSLY. The IV dose is 100 mg/kg, given slowly. The IV preparation is supplied in 50-m l vials containing 2.5 g of IG.
# H e p a titis B Im m u n e G lobulin
HBIG, alone or in combination with HB vaccine, is used for postexposure prophylaxis of HBV infection. For percutaneous or mucous membrane exposure to blood known to be HBsAg positive or from a bite by an HBV carrier, a single dose of HBIG (0.06 ml/kg or 5 ml for adults) should be given as soon as possible, and a series of three doses of HB vaccine begun within 1 week after exposure. Vaccine and HBIG may be given simultaneously, but in different sites.
For those who choose not to take HB vaccine, a second identical dose of HBIG should be given 1 month later. Following percutaneous exposure to blood from individuals at high risk of being HBsAg positive (such as persons with acute, unconfirmed viral hepatitis) or from patients at high risk of being infected with hepatitis B (such as male homosexuals, users of illicit IV drugs, and hemodialysis patients), IG should be given immediately to the exposed person as an IM dose of 0.06 ml/kg. Then serologic confirmation of the HBsAg status of the suspected high-risk patient should be obtained as soon as possible, and certainly within 7 days. If the suspected high-risk patient is HBsAg positive, the exposed person should immediately receive HBIG and hepatitis B vaccine according to the schedule above. The value of HBIG given beyond 7 days after exposure is unclear.
For homosexual exposure to HBsAg-positive males (known carriers or persons with acute cases), a single dose of HBIG should be given to susceptible contacts within 1 4 days after the last sexual exposure. Since HB vaccine is routinely recommended for male homosexuals, an HB vaccine series should be started within 7 days after HBIG administration.
For heterosexual exposures to persons with acute cases of hepatitis B, a single dose of HBIG (0.06 ml/kg or 5 ml for adults) should be given within 14 days of the last sexual contact. If the index case remains HBsAg positive at 3 months and exposure continues, the contact should be given a second dose of HBIG. If the index case becomes an HBV carrier (HGsAg positive for 6 months), the HB vaccine series should be given to the contact.
# Tetanus Im m u n e G lobulin
TIG is indicated in tetanus prophylaxis as part of the management of wounds other than clean, minor wounds in persons 1) whose previous tetanus toxoid immunization status is un known or uncertain, 2) who have received fewer than two previous tetanus toxoid doses, or 3) who have received only two previous tetanus toxoid doses and whose wound is more than 24 hours old. The currently recommended prophylactic dose for wounds of average severity is 2 5 0 units IM Td should be given at the same time but at a separate site.
A summary of the indications for active and passive immunization in the management of wounds is provided in Table 5.
# H um an R a b ie s Im m u n e G lobulin
Postexposure prophylaxis for rabies should always include HRIG with one exception: per sons who have been previously immunized with the recommended preexposure or postexpo sure regimens of HD CV or have been immunized with other types of rabies vaccines and have a history of documented adequate rabies antibody titer should not receive HRIG (Table 4). The recommended dose of HRIG is 20 Ill/kg body weight. If anatomically feasible, up to onehalf the dose of HRIG should be thoroughly infiltrated in the area around the wound, the rest should be administered IM.
# V a rice lla -Z o s te r Im m u n e G lobulin
Most adults (85%-95%) with negative or unknown histories of varicella disease (chickenpox) are likely to be immune. (Susceptibility rates for adults raised in some tropical areas, par ticularly remote areas, may be somewhat higher.) Rates of complications and death for immu nocompromised adults who contract varicella are likely to be substantially greater than for normal adults. After careful, individual evaluation, an immunocompromised patient who is be lieved to be susceptible and who has had significant exposure to varicella should receive VZIG to prevent complications. Significant exposure to a person with varicella includes household contact, close contact indoors of longer than 1 hour, sharing the same two-to four-bed hospital room, or prolonged, direct, face-to-face contact such as occurs with nurses or doctors who take care of the patient.
Chickenpox can be more severe in adults than in normal children. The decision to adminis ter VZIG to a normal adult should be made on an individual basis. The objective of VZIG use for normal adults is to modify rather than prevent illness in hopes of inducing lifelong immuni ty. When deciding whether to administer VZIG , the clinician should consider the patient's health status, the type of exposure, and the likelihood of previous infection. It is likely that adults who were older siblings in large families or whose children have had varicella are immune. If, after careful evaluation, a normal adult with significant exposure to varicella is be lieved to be susceptible, VZIG may be administered. Pregnant women and potentially su s ceptible hospital personnel should be evaluated in the same way as other adults. Supplies of V ZIG are limited, and indiscriminate administration of VZIG to normal adults would quickly ex haust supplies and prevent prophylaxis for known high-risk individuals. The cost of a five-vial adult dose is approximately $ 3 7 5 .
VZIG, available through some American Red C ro ss distribution centers (Appendix 5), is supplied in vials containing 1 25 units. W hereas 1 25 units/1 0 kg of body weight up to a m axi mum of 625 units generally is considered likely to prevent or modify varicella in normal adults, higher doses may be necessary for the immunocompromised adult. However, the ap propriate dose for immunocompromised adults has not been determined. VZIG should be ad ministered IM as directed by the manufacturer. While the duration of protection is unknown, it seems reasonable that protection should last for at least one half-life of the immune globulin, that is, approximately 3 weeks.
# Im m u n e G lo bu lin S id e E f f e c t s a n d A d v e rs e R e a c tio n s
Serious adverse effects have been rare from immune globulins administered as recommended.
# Im m u n e G lo bu lin P re ca u tio n s a n d C o n tra in d ica tio n s
Immune globulins, if needed, are not contraindicated for pregnant women. Except for the IV preparation of IG, immune globulins are prepared for IM use and should no t be given IV. The various preparations intended for IM use should not be given to patients with severe thrombocytopenia or other coagulation disorders that would ordinarily contraindicate IM in jections unless the expected benefits outweigh the risks.
Parenterally administered live-virus vaccines (e.g., MMR or other combinations) should be given at least 1 4 days before or at least 6 weeks, and preferably 3 months, after the adminis tration of immune globulins. If an immune globulin must be administered within 14 days after the administration of most live-virus vaccines, the vaccine should be administered again 3 months after the immune globulin is given. If the interval between vaccine receipt and immune globulin receipt is longer, the vaccine need not be readministered.
Preliminary data indicate that immune globulins do not interfere with the immune response to either O PV or yellow fever vaccine.
In Ju ly 1983 , a W HO Consultative Group reviewed data on both normal and specific immune globulins prepared from plasma collected mainly in the United States, including dona "Several other vaccines, toxoids, and immune globulins are licensed and available. These are noted in Appendix 3. In addition, the following antitoxins are licensed and available: (1) botulism antitoxin, trivalent (ABE) equine (distributed by C D C only), (2) tetanus antitoxin (equine), (3) diphtheria antitoxin (equine), and (4) rabies antitoxin (equine). Several vaccines and toxoids are in "Investigation of New Drug" (IND) status and available only through the Division of Host Factors, Center for Infectious Disease, CD C. These are: (1) pentavalent (ABCDE) botulinum toxoid, (2) eastern equine encephalitis (EEE) vaccine, (3) Venezualan equine encephalitis (VEE) vaccine, and (4) tularemia vaccine §When any vaccine or toxoid is indicated during pregnancy, waiting until the second or the third trimester, when possible, is a reasonable precaution that minimizes concern about teratogenicity.
Persons immunocompromised because of immune deficiency diseases, leukemia, lymphoma or generalized m alignancy or immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabolites or radiation. Although a protective immune response to IPV in the immunocompromised individual cannot be assured, the vaccine is safe and some protection may result from its administration. 'Several other vaccines, toxoids, and immune globulins are licensed and available. These are noted in Appendix 3. In addition, the following antitoxins are licensed and available: (1) botulism antitoxin, trivalent (ABE) equine (distributed by CD C only), (2) tetanus antitoxin (equine), (3) diphtheria antitoxin (equine), and (4) rabies antitoxin (equine). Several vaccines and toxoids are in "Investigation of New Drug" (IND) status and available only through the Division of Host Factors, Center for Infectious Disease, CD C. These are: (1) pentavalent (ABCDE) botulinum toxoid, (2) eastern equine encephalitis (EEE) vaccine, (3) Venezualan equine encephalitis (VEE) vaccine, and (4) tularemia vaccine §When any vaccine or toxoid is indicated during pregnancy, waiting until the second or the third trimester, when possible, is a reasonable precaution that minimizes concern about teratogenicity.
# L IV E -V IR U S A N D IN A C TIV A TED -V IR U S V A C C IN ES
# IN A C T IV A T ED -V IR U S V A C C IN ES
Persons immunocompromised because of immune deficiency diseases, leukemia, lymphoma or generalized m alignancy or immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabolites or radiation. "Several other vaccines, toxoids, and immune globulins are licensed and available. These are noted in Appendix 3. In addition, the following antitoxins are licensed and available: (1) botulism antitoxin, trivalent (ABE) equine (distributed by CD C only), (2) tetanus antitoxin (equine), (3) diphtheria antitoxin (equine), and (4) rabies antitoxin (equine). Several vaccines and toxoids are in "Investigation of New Drug" (IND) status and available only through the Division of Host Factors, Center for Infectious Disease, CD C. These are: (1) pentavalent (ABCDE) botulinum toxoid, (2) eastern equine encephalitis (EEE) vaccine, (3) Venezuelan equine encephalitis (VEE) vaccine, and (4) tularemia vaccine §When any vaccine or toxoid is indicated during pregnancy, waiting until the second or the third trimester, when possible, is a reasonable precaution that minimizes concern about teratogenicity. 'Several other vaccines, toxoids, and immune globulins are licensed and available. These are noted in Appendix 3. In addition, the following antitoxins are licensed and available: (1) botulism antitoxin, trivalent (ABE) equine (distributed by C D C only), (2) tetanus antitoxin (equine), (3) diphtheria antitoxin (equine), and (4) rabies antitoxin (equine). Several vaccines and toxoids are in "Investigation of New D rug" (IND) status and available only through the Division of Host Factors, Center for Infectious Disease, CD C. These are: (1) pentavalent (ABCDE) botulinum toxoid, (2) eastern equine encephalitis (EEE) vaccine, (3) Venezualan equine encephalitis (VEE) vaccine, and (4) tularemia vaccine §When any vaccine or toxoid is indicated during pregnancy, waiting until the second or the third trimester, when possible, is a reasonable precaution that minimizes concern about teratogenicity.
Persons immunocompromised because of immune deficiency diseases, leukemia, lymphoma or generalized m alignancy or immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabolites or radiation Although preferable to be given with the 1 st dose of vaccine, can be given up to the 8th day after the 1 st dose of vaccine.
Varicella-zoster immune globulin (VZIG) '
Persons ^ 50 kg: 125 units/10kg IM; persons > 50 kg: 6 25 u n its"
Immunocompromised patients known or likely to be su s ceptible with close and pro longed exposure to a house hold contact case or to an infectious hospital staff member or hospital roommate.N O TE: Refer to text on specific vaccines or toxoids for further details on indications, contraindications, precautions, dosages, side effects, and adverse reactions, and special considerations and individual ACIP statements (see list of published ACIP statements in Appendix 2). ' Several other vaccines, toxoids, and immune globulins are licensed and available. These are noted in Appendix 3. In addition, the following antitoxins are licensed and available: (1) botulism antitoxin, trivalent (ABE) equine (distributed by CD C only), (2) tetanus antitoxin (equine), (3) diphtheria antitoxin (equine), and (4) rabies antitoxin (equine).
Several vaccines and toxoids are in "Investigation of New Drug" (IND) status and available only through the Division of Host Factors, Center for Infectious Disease, CDC. These are: (1) pentavalent (ABCDE) botulinum toxoid, (2) eastern equine encephalitis (EEE) vaccine, (3) Venezualan equine encephalitis (VEE) vaccine, and (4) tularemia vaccine §When any vaccine or toxoid is indicated during pregnancy, waiting until the second or the third trimester, when possible, is a reasonable precaution that minimizes concern about teratogenicity.
Persons immunocompromised because of immune deficiency diseases, leukemia, lymphoma or generalized m alignancy or immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabolites or radiation.
# MMWR 37 S
tions from homosexuals. The data indicated that although about 19.5 million 2-m l to 10-m l doses of immune globulin had been prepared during the preceding 4 years, no transmission of hepatitis B or any other infectious agents and no cases of A ID S had been reported in persons observed for 1-4 years after receiving immune globulin. Therefore, the Consultative Group confirmed that, at present, there is no evidence of risk attached to the use of normal or specif ic immune globulins prepared by the universally accepted methods ( 19).
R eferences 1. Immunization Practices Advisory Committee, General recommendations on immunizations. MMWR 1 9 8 3 ;3 2 :1 -8 , 13-7. 2. CD C. Rubella in hospitals -California. MMWR 1 9 8 3 ;3 2 :3 7 -9 . 3. Amler RW, Bloch AB, Orenstein WA, Bart K J, Turner PM Jr, Hinman AR. Imported m easles in the United States. JA M A 1 9 8 2 ;2 4 8 :2 1 2 9 -3 3 . 4. W eiss BP, Strassburg MA, Feeley J C . Tetanus and diphtheria immunity in an elderly population in Los Angeles County, Am J Pub Health 1 9 8 3 ;7 3 :8 0 2 -4 . 5. Crossley K, Irvine P, Warren JB , Lee BK, Mead K. Tetanus and diphtheria immunity in urban Min nesota adults. JA M A 1 9 7 9 :2 4 2 :2 2 9 8 -3 0 0 0 . 6. Ruben FL, Nagel J , Fireman P Antitoxin responses in the elderly to tetanus-diphtheria (Td) immuni zation. Am J Epidemiol 1978; 1 0 8 :1 4 5 -9 . 7. Ja c o b s RL, Lowe RS, Lanier BQ. Adverse reactions to tetanus toxoid. JA M A 1 9 8 2 :2 4 7 :40-2. 8. Herman J J , Radin R, Schneiderm an R. Allergic reactions to m easles (rubeola) vaccine in patients hy persensitive to egg protein. J Pediatr 1 983; 1 0 2 :1 9 6 -9 . 9. CD C. Postexposure prophylaxis of hepatitis B. MMWR 1 9 8 4 ;3 3 :2 8 5 -9 0 . 10. Turner G S, Nicholson KG, Tyrrell D A J, Akoi FY. Evaluation of a human diploid cell strain rabies va c cine: final report of a three year study of pre-exposure immunization. J Hyg 1 9 8 2 ;8 9 :1 0 1 -1 0 . 1 1. CD C. Field evaluations of pre-exposure use of human diploid cell rabies vaccine. MMWR 1 9 8 3 :3 2 :6 0 1 -3 . 12. C D C System ic allergic reactions following immunization with human diploid cell rabies vaccine.
MMWR 1 9 8 4 ;3 3 :1 8 5 -7 . 13. Bernard KW , Sm ith PW, Kader F J, Moran MJ. Neuroparalytic illness and human diploid cell rabies vaccine. JA M A 1 9 8 2 :2 4 8 :3 1 36 -8 14. Fedson DS, Chiarello LA. Previous hospital care and pneum ococcal bacteremia: importance for pneum ococcal immunization. Arch Intern Med 1 9 83; 1 4 3 :8 8 5 -9 . 1 5. DeStefano F, Goodman RA, Noble GR, et al. Sim ultaneous administration of influenza and pneumo coccal vaccines. JA M A 1 9 8 2 ;2 4 7 :2 5 5 1 -4. 16. Sem el JD , Seskind C. Severe febrile reaction to pneum ococcal vaccine. JA M A 1 9 7 9 :2 4 1 :1 792. General recommendations on immunizations 1 9 8 3 :3 2 :1 -8 ,1 3 -7 Diphtheria, tetanus, and pertussis. 1 9 8 1 :3 0 :3 9 2 -9 6 ,4 0 1 -7 guidelines for vaccine prophylaxis and Erratum. 1 981 ;3 0 :4 2 0 other preventive measures M easles prevention 1 9 8 2 ;3 1 :2 1 7 -2 4 ,2 2 9 -3 1
Mumps vaccine 1 9 8 2 :3 1 :6 1 7 -2 0 ,6 2 5
Rubella prevention 1 9 8 4 :3 3 :3 0 1 -1 0 ,3 1 5 -8
Yellow fever vaccine 1 9 8 4 :3 2 :6 7 9 -8 2 ,6 8 7 -8
Poliomyelitis prevention 1 9 82;31 22-6,31 -4
Prevention and control of influenza- 1 9 8 4 :3 3 :2 5 3 -6 0 ,2 6 5 -6
Inactivated hepatitis B virus vaccine 1 9 8 2 :3 1 :3 1 7 -2 2 ,3 2 7 -8
Postexposure prophylaxis of hepatitis B 1 9 8 4 :3 3 :2 8 5 -9 0
Rabies prevention Supplem entary statement on rabies vaccine and serologic testing 1 9 8 1 ;3 0 :5 3 5 -6 Rabies 1 9 8 4 ;3 3 :3 9 3 -4 0 2 ,4 0 7 -8
Supplem entary statement on 1 9 8 2 :3 1 :2 7 9 -8 0 ,2 8 5 pre-exposure rabies prophylaxis by the intradermal route Cholera vaccine 1 9 7 8 :2 7 :1 7 3 -4 M eningococcal polysaccharide vaccine 1 9 7 8 :2 7 :3 2 7 -9
Plague vaccine 1 9 8 2 ;3 1 :3 0 1 -4
Update: Pneum ococcal polysaccharide vaccine 1 9 8 4 :3 3 :2 7 3 -6 ,8 1 usage -United States Typhoid vaccine 1 9 7 8 ;2 7 :2 3 1 -3 BCG vaccines 1 9 7 9 ;2 8 :2 4 1 -4
Immune globulins for protection against viral hepatitis 1 9 8 1 :3 0 :4 2 3 -8 ,4 3 3 -5
Varicella-zoster immune globulin for the prevention of chickenpox 1 9 8 4 :3 3 :8 4 -9 0 ,9 5 -1 0 0 'T h e Immunization Practices A dvisory Committee (ACIP) periodically reviews recommendations on v a c cination and prophylaxis. W hen recommendations are revised, they are published individually in the MMWR.
Each year influenza vaccine recommendations are reviewed and amended to reflect updated informa tion on influenza activity in the United States for the preceding influenza season and to provide inform a tion on the vaccine available for the upcoming influenza season. These recommendations are published in the MMWR annually, usually during June or July. The Greater New York Blood Program 1 50 Am sterdam Ave. New York, NY 10023 (212) 5 7 0 -3 0 6 7 (212) 5 7 0 -3 0 6 8 (night) Am erican Red Cross Blood Services Northeastern New York Region Hackett Blvd. at Clara Barton Dr. Albany, N Y 12208 (518) 4 4 9 -5 0 2 0 (518) 4 6 2 -7 4 6 1 (518) 4 6 2 -6 9 6 4 (night) Am erican Red Cross Blood Services Greater Buffalo Chapter 786 Delaware Ave. Buffalo, NY 1 4209 (716) 8 8 6 -7 5 0 6 3 1 0 8 (314) 6 5 8 -2 0 0 0 (314) 6 5 8 -2 1 3 6 (
# IN A C T IV A TE D -V IR U S V A C C IN ES
# IN A C T IV A T E D -B A C T E R IA V A C C IN ES | # ¡¡S MMWR
Septem ber 28, 1 984 This statem ent, a com pendium o f ACIP recom m endations, w ill n o t be updated regularly. The ACIP p e rio dica lly review s in d ivid u a l im m u n iza tio n statem ents, and revised statem e nts are pu b lish e d in the MMWR. The reader m u s t use the detailed, u p -to -d a te in d ivid u a l s ta te m en ts in conjunction w ith th is com pendium in order to keep abreast o f current inform ation.
# V A C C IN E-P R EV E N T A B LE D IS E A S E S AN D T H E IR
# IN TRO D U CTIO N
In general, immunization policies have been directed towards vaccinating infants, children, and adolescents. While immunization is a routine measure in pediatric practice, it is not usually routine in the practice of physicians who treat adults.
The widespread and successful implementation of childhood immunization programs has greatly reduced the occurrence of many vaccine-preventable diseases. However, successful childhood immunization alone will not necessarily eliminate specific disease problems. A sub stantial proportion of the remaining morbidity and mortality from vaccine-preventable dis eases now occurs in older adolescents and adults. Persons who escaped natural infection or were not immunized with vaccines and toxoids against diphtheria, tetanus, measles, mumps, rubella, and poliomyelitis may be at risk of these diseases and their complications.
To reduce further the unnecessary occurrence of these vaccine-preventable diseases, all those who provide health care to older adolescents and adults should provide immunizations as a routine part of their practice. In addition, the epidemiology of other vaccine-preventable diseases (e.g., hepatitis B, rabies, influenza, and pneumococcal disease) indicates that indi viduals in certain age, occupational, environmental, and lifestyle groups and individuals who have special health problems are at increased risk of these illnesses and should be immunized. Travelers to some countries may be at increased risk of exposure to vaccine-preventable ill nesses. Finally, foreign students, immigrants, and refugees may be susceptible to these diseases.
A system atic approach to immunization is necessary to ensure that every adult is appropri ately protected against vaccine-preventable diseases. Every visit by an adult to a health-care provider should be an opportunity to provide this protection. Several factors need to be con sidered before any patient is vaccinated. These include the susceptibility of the patient, the risk of exposure to the disease, the risk from the disease, and the benefits and risks from the immunizing agent. Physicians should maintain detailed information about previous vaccina tions received by each individual, including type of vaccination, date of receipt, and adverse events, if any, following vaccination. Information should also include the person's history of vaccine-preventable illnesses, occupation, and lifestyle. Vaccine histories ideally should be based on written documentation to ascertain whether vaccines and toxoids were administered at appropriate ages and at proper intervals. Close attention to factors such as military service and age may be helpful in determining whether any vaccines or toxoids are advisable for an in dividual. After the administration of any immunobiologic, the patient should be given written documentation of its receipt and information on which vaccines or toxoids will be needed in
# 2S
# MMWR
Septem ber 28, 1984 the future. For this purpose an immunization record form such as the suggested form found in Appendix 1 should be used routinely.
The patient or responsible person should be given information on the risks of immunobio logies as well as their major benefits in preventing disease both in individuals and in the com munity. No formal, legally acceptable statement has been universally adopted for the private medical sector. Thus, the ACIP recommends that there be ample opportunity for questions before each immunization. C D C has developed "Important Information Statem ents" for use with federally purchased vaccines given in public health clinics. Practitioners may wish to con sider these or similar materials for patients. Examples of "Important Information Statements" can be obtained from state and many local health departments.
Modern immunobiologies are extremely safe and effective, but not completely so. All im munobiologies have had adverse events reported after administration. These range from fre quent, minor, local reactions to extremely rare, severe system ic illness, such as paralysis asso ciated with oral poliovirus vaccine (OPV). It is frequently impossible to establish causeand-effect relationships when untoward events occur after vaccination since temporal asso ci ation alone does not necessarily indicate causation. To improve knowledge about adverse reactions, all temporally associated events severe enough to require the recipient to seek medical attention should be evaluated and reported in detail to local or state health officials and to the manufacturer of the immunobiologic.
General immunization considerations and recommendations are found in the ACIP state ment "General Recommendations on Immunization" ( 1).
The following recommendations apply generally to individuals in the indicated groups. For more detailed information on immunobiologies, including indications, side effects, adverse reactions, precautions, contraindications, dosage, and route of administration, providers are urged to refer to the following section on individual immunobiologies, the ACIP statements on specific immunobiologies (Appendix 2), and the tables and appendices at the back of this sup plement. Appendix 3 provides a list of vaccines, toxoids, and immune globulins available in the United States as of June 1 984.
# Age Groups
The following text and Table 1 summarize the vaccines and toxoids recommended for most adults in the specific age groups. The reader is referred to the section on specific immu nobiologies for essential information.
# A d u lts 1 8 -2 4 Years O ld
All young adults should complete a primary series of diphtheria and tetanus toxoids. A pri mary series for adults is three doses of preparations containing tetanus and diphtheria toxoids, with the first two doses given at least 4 weeks apart and the third dose given 6-1 2 months after the second. Those who have completed a primary series should receive a boos ter dose every 10 years. There is no need to repeat doses when the series schedule is delayed. The combined tetanus-diphtheria toxoids for adult use, Td, should be used to en hance protection against both diseases. Persons with unknown or uncertain histories of re ceiving tetanus or diphtheria toxoids should be considered unimmunized and should receive a full three-dose primary series of Td.
Young adults should also be immune to measles, rubella, and mumps. Persons are consid ered immune to measles and mumps if they have a dated record of vaccination with live vac cines on or after their first birthday, documentation of physician-diagnosed disease, or labora tory evidence of immunity. Persons vaccinated in the period 1 9 6 3 -1 9 6 7 with inactivated-measles-virus vaccine or with a measles vaccine of unknown type should be revaccinated with live-m easles-virus vaccine to prevent measles disease or atypical measles syndrome if exposed to wild measles virus. Persons are considered immune to rubella only if they have a record of vaccination with rubella vaccine on or after their first birthday or laboratory evidence of immunity. The combined measles, mumps, rubella (MMR) vaccine is the vaccine of choice if recipients are likely to be susceptible to more than one of the three diseases. Persons lacking adequate documentation as noted above should be vaccinated.
# A d u lts 2 5 -6 4 Years O ld
All adults 2 5 -6 4 years of age should complete a primary series of tetanus and diphtheria toxoids. A primary series for adults is three doses of preparations containing tetanus and diphtheria toxoids, with the first two doses given at least 4 weeks apart and the third dose given 6-1 2 months after the second. Those who have completed a primary series should re ceive a booster dose every 10 years. The combined toxoids for adult use, Td, should be used to enhance protection against both diseases. Persons with unknown or uncertain histories of receiving tetanus or diphtheria toxoids should be considered unimmunized and should receive a full three-dose primary series of Td.
Adults born in 1957 or later should receive measles vaccine unless they have a dated record of vaccination with live-measles vaccine on or after their first birthday, documentation of physician-diagnosed disease, or laboratory evidence of immunity. Adults born before 1 957 can be considered immune to measles, since measles was a universal infection before measles vaccine became available. While most adults are likely to have been infected naturally with mumps, mumps vaccine may be given to adults, especially males, who are considered susceptible. Unless proof of vaccination with rubella vaccine or laboratory evidence of im munity is available, rubella vaccine is recommended for women of childbearing age and for other adults who may find themselves in places where rubella transmission is likely to occur, such as hospitals, all types of schools, and other places where young people are likely to con gregate. The combined MMR vaccine is the vaccine of choice if recipients are likely to be su s ceptible to more than one of these three diseases.
# A d u lts 6 5 Years O ld o r O lder
All older adults should complete a primary series of tetanus and diphtheria toxoids. A pri mary series for adults is three doses of preparations containing tetanus and diphtheria toxoids, with the first two doses given at least 4 weeks apart and the third dose given 6-1 2 months after the second. Those who have completed a primary series should receive a boos ter dose every 10 years. The combined toxoids for adult use, Td, should be used to enhance protection against both diseases. Persons with unknown or uncertain histories of receiving tetanus or diphtheria toxoids should be considered unimmunized and should receive a full three-dose primary series of Td All older adults should receive influenza vaccine annually. They should also receive a single dose of pneumococcal polysaccharide vaccine.
# Special O ccupations
Persons in specific occupations may be at increased risk of exposure to certain vaccinepreventable illnesses. Such persons may need selected vaccines and toxoids in addition to those routinely recommended for their age group. Table 2 provides a summary of immunobio logies recommended for various special occupational groups. The reader is referred to the section on specific immunobiologies for essential information.
# MMWR
Septem ber 28, 1984
# H e a lth -R e la te d O ccu p a tio n s
Medical, dental, laboratory, and other support personnel who may have contact with blood or blood products should be immune to hepatitis B virus (HBV) infection. The groups at high est risk for acquiring HBV infection and for whom HB vaccine is recommended include medical technicians, operating room staff, phlebotomists, physicians (particularly surgeons and pa thologists), nurses (particularly intravenous-therapy nurses and nurses on oncology and dialy sis units), dentists and oral surgeons, laboratory and blood-bank technicians, and emergencyroom staff. Morticians and their assistants who have routine contact with blood and secre tions are also at high risk of HBV infection. Selected staff of institutions for the mentally retarded may be at increased risk of HBV infection because of exposure to bites and contact with skin lesions, saliva, and other potentially infected secretions in addition to blood.
Am ong health-care personnel with frequent exposure to blood, the prevalence of serologic evidence of HBV infection is estimated to range between 10% and 30%. Since the cost effec tiveness of serologic screening to detect susceptible individuals among health-care personnel depends on the prevalence of infection, each institution must decide whether serologic screening is cost effective. Vaccination of individuals who already have antibodies to HBV has not been shown to cause adverse effects.
The duration of protection from a three-dose series of HB vaccine or the need for booster doses has not yet been determined.
Transmission of rubella in health facilities (hospitals, physician or dentist offices, clinics, etc.) can disrupt hospital or office routines and cause considerable expense. Although no cases of congenital rubella syndrome (CRS) have been reported in association with rubella transmission in health facilities, therapeutic abortions have been sought by pregnant staff members following rubella infection (2). To prevent such situations, all medical, dental, laboratory, and other support health personnel, both male and female, who might be at risk of exposure to patients infected with rubella, or who might have contact with pregnant patients, should be immune. Rubella vaccine is recommended for all such personnel unless they have either proof of vaccination with rubella vaccine on or after their first birthday or laboratory evi dence of immunity. Combined MMR vaccine is the vaccine of choice if recipients are likely to be susceptible to measles and/or mumps as well as to rubella.
Measles transmission in health facilities can also be disruptive and costly. To prevent such situations, all health personnel born in 1957 or later who may have contact with patients in fected with measles should be immune. Such persons can be considered immune only if they have documentation of having received live-m easles vaccine on or after their first birthday, a record of physician-diagnosed measles, or laboratory evidence of immunity. Measles vaccine is recommended for all persons lacking such documentation. Combined MMR vaccine is the vaccine of choice if recipients are likely to be susceptible to rubella and/or mumps as well as to measles. Adults born before 1957 can be considered immune to measles since measles w as a universal infection before the availability of measles vaccine.
Poliovirus vaccine is not routinely recommended for persons older than high school age (18-19 years old). However, hospital personnel having close contact with patients who may be excreting wild polioviruses, and laboratory personnel handling specim ens that may contain wild polioviruses, should have completed a primary series of poliovirus vaccine. For personnel who do not have proof of having completed a primary series, completion is recommended with inactivated poliovirus vaccine (IPV). IPV is preferred because there is a slightly increased risk in adults of vaccine-associated paralysis following receipt of OPV. In addition, since v ac cine poliovirus may be excreted by O PV recipients for 30 or more days, the use of O PV in creases the risk of acquiring vaccine-associated paralytic poliomyelitis among susceptible im munocompromised contacts and susceptible close contacts of O PV recipients.
# MMWR 5 S
Sm allpox vaccination is indicated only for laboratory workers involved with orthopox viruses or in producing and testing smallpox vaccine. When indicated, smallpox vaccination should be given at least every years.
Plague vaccine is indicated for laboratory personnel working with Yersinia p e stis possibly resistant to antimicrobial agents and for persons performing Y. p e stis aerosol experiments.
Preexposure rabies vaccination is indicated for laboratory workers directly involved with testing or isolating rabies virus.
# Veterinarians an d A n im a l H a n d lers
Veterinarians and animal handlers are at risk of rabies exposure because of occupational contact with both domestic and wild animals. They should receive preexposure rabies-vaccine prophylaxis with human diploid cell rabies vaccine (HDCV). Preexposure vaccination against rabies does n o t eliminate the need for additional therapy after exposure to rabies; it does, however, simplify postexposure therapy by eliminating the need for human rabies immune globulin (HRIG) and by decreasing the number of postexposure doses of vaccine needed. Per sons at continued risk of frequent exposure should receive a booster dose of H D CV every 2 years or have their serum tested for rabies antibody every 2 years and, if the titer is inadequate ( < 5 by the rapid fluorescent-focus inhibition test), receive a booster dose.
# S e le c te d F ie ld P e rso n n e l
Plague vaccine is indicated for field personnel who cannot avoid regular exposure to poten tially plague-infected wild rodents and rabbits and their fleas.
Preexposure rabies vaccine prophylaxis should be considered for field personnel who are likely to have contact with potentially rabid dogs, cats, skunks, raccoons, bats, or other w ild life species.
# S e w a g e W orkers
Sew age workers, as all other adults, should be adequately vaccinated against diphtheria and tetanus.
Poliovirus and typhoid vaccines and immune globulin are not routinely recommended for sew age workers.
# Lifestyles
Various lifestyles may increase the risk of exposure to certain vaccine-preventable ill nesses. Persons with these lifestyles may require vaccines in addition to those routinely recommended for their age group. Table 2 provides a summary of the vaccines recommended.
# H o m o s e x u a lly A c t iv e M a le s
Homosexually active males are at high risk of HBV infection. Between 35% and 80°o have serologic evidence of HBV infection. Susceptible homosexual males should be vaccinated with HB vaccine as early as possible after they begin homosexual activity because they can be expected to acquire HBV infection at a rate of 10% -20% per year. The duration of protection from a three-dose series of HB vaccine and the need for booster doses have not yet been determined. Because of the high prevalence of infection, prevaccination serologic screening of homosexual males may be cost effective regardless of their age or of how long they have been homosexually active.
# MMWR
Sep tem b er 28, 1 984
# U se rs o f Illic it In je cta b le D ru gs
Users of illicit injectable drugs are at high risk of HBV infection. Serologic evidence of HBV infection has been found in 60% -80% of these individuals. Efforts should be made to vaccinate susceptible users with HB vaccine as early as possible after their drug use begins because they can be expected to acquire HBV infection at a rate of 10% -20% per year. The duration of protection from a three-dose series of HB vaccine and the need for booster doses have not yet been determined Because of the high prevalence of infection, prevaccination serologic screening of users of illicit injectable drugs to avoid unnecessary immunization is cost effective.
These drug users are also at increased risk of tetanus, and their tetanus immunization status should be kept up to date with Td.
# Environmental Situations
Certain environments may place an individual at increased risk of certain vaccinepreventable diseases. Table 2 sum marizes additional vaccines recommended for persons in selected environments. The reader is referred to the section on specific immunobiologies for essential information.
# In m a te s o f Lo n g -Term C o rre ctio n a l F a c ilit ie s
Serologic evidence of HBV infection has been found in 10% -80% of male prisoners. A l though the frequency of transmission during imprisonment has not been documented, the en vironment of long-term correctional facilities may be associated with a high risk of transm is sion of HBV infection because of the frequency of use of illicit injectable drugs and of homo sexual behavior. In selected long-term institutional settings, prison officials may elect to un dertake serologic HBV screening and vaccination programs. The duration of protection from a three-dose series of HB vaccine and the need for booster doses have not yet been determined.
# R e s id e n ts o f In stitu tio n s fo r the M e n ta lly R e ta rd e d
Institutions for the mentally retarded provide a setting conducive to the transmission of HBV infection through bites and contact with blood, skin lesions, saliva, and other potentially infectious secretions. Serologic evidence of HBV infection has been found in 35% -80% of resi dents of such institutions. New adm issions to these institutions should be vaccinated as soon as possible. For current residents, screening and vaccination of susceptible residents is recom mended. Because of the high prevalence of infection, preimmunization serologic screening of those already institutionalized may be cost effective; however, screening of new admissions very likely will not be. Residents of group homes, foster homes, and similar settings who have household contact with a carrier of HBV should also be vaccinated. The duration of protection from a three-dose series of HB vaccine and the need for booster doses have not yet been determined.
# Travel
The risk of acquiring illness during international travel depends on the areas of the world to be visited and the extent to which the traveler is likely to be exposed to vaccine-preventable diseases. When considering travel, people often seek advice from health-care personnel on immunization. This provides a good opportunity to review the person's immunization status and administer primary series or booster doses, if needed.
# MMWR 7S
In most countries, measles, mumps, and rubella remain uncontrolled. Therefore, the risk of acquiring these diseases while traveling outside the United States is greater than the risk in curred within the United States. Approximately 50S, of imported measles cases reported for 1 980-1 9 8 3 occurred in citizens returning to the United States (3). To minimize importations by U.S. citizens, all travelers born in 1 957 or later should be immune to measles. Women trav elers of childbearing ages should be immune to rubella before leaving the United States.
In developed countries such as Japan, Canada, Australia, New Zealand, and the European countries, the risk of acquiring other vaccine-preventable diseases such as poliomyelitis, diphtheria, and tetanus is usually no greater than the risk incurred while traveling in the United States. In contrast, travelers to developing countries are, in general, at increased risk of expo sure to many infections, including wild polioviruses and diphtheria. Accordingly, such travelers should be immune to poliomyelitis and diphtheria, in particular.
For protection against poliomyelitis, unimmunized adults should receive at least two doses of IPV 1 month apart, and preferably a complete primary series, before traveling to a develop ing country. If an individual's travel plans do not permit this interval, then a single dose of OPV is recommended. For adults previously incompletely immunized with O PV or IPV, the remain ing doses of either vaccine required for completion of the primary series should be given, regardless of the interval since the last dose or the type of vaccine previously received. A single additional dose of either O PV or IPV should be given to travelers who have previously completed a primary series of O PV or IPV Selective immunization of travelers with vaccines against yellow fever, cholera, typhoid, plague, m eningococcal disease, rabies, or HBV infection or administration of immune globulin (IG) to prevent hepatitis A is recommended on the basis of known, or perceived, diseasespecific risks in the country(ies) to be visited and the type and duration of travel within a coun try. In the instances of cholera and yellow fever, vaccination requirements may have been es tablished by the country to be visited. Countries currently reporting yellow fever, cholera, and plague are identified biweekly in the S um m a ry o f H ealth Inform a tion fo r In tern ation al Travel. and information on known or probably infected areas is published annually in H ealth In fo rm a tion fo r In tern ation al Travel, which also lists specific requirements for cholera and yellow fever vaccinations for each country. All state health departments and many county and city health departments receive both publications. For entry into countries requiring yellow fever or cholera vaccination, travelers must have an International Certificate of Vaccination validat ed by an appropriate authority. State or local health departments can provide the addresses of persons or centers able to validate certificates.
More information on specific vaccine-preventable illnesses that a traveler might encounter is provided in the sections describing specific vaccines.
# Foreign Students, Im m igrants, and Refugees
In many countries children and adolescents are not routinely immunized against diphtheria, tetanus, measles, mumps, rubella, and poliomyelitis. A s a result, persons entering the United States to pursue college and postgraduate studies or as immigrants or refugees may be su s ceptible to one or more of these diseases.
Unless foreign students, immigrants, and refugees can provide a vaccination record docu menting the receipt of recommended vaccines or toxoids at appropriate ages and intervals or laboratory evidence of immunity, they should receive the appropriate vaccines for their age as noted in age-specific recommendations (see page 2S) and in
# Special Health Status
Som e vaccines may be contraindicated for persons with certain health problems; other vaccines may be indicated because of an underlying health condition. Table 3 provides a sum mary of immunobiologies indicated or contraindicated for persons with selected health problems.
# P re g n a n c y
When any vaccine or toxoid is to be given during pregnancy, waiting until the second or third trimester, when possible, is a reasonable precaution to minimize concern about possible teratogenicity.
Pregnant women not vaccinated previously against tetanus and diphtheria should receive two doses of Td properly spaced. Those who have previously received one or two doses of tetanus or diphtheria toxoid should complete their primary series during pregnancy. A primary series is three doses of preparations containing tetanus and diphtheria toxoids, with the first two doses given at least 4 weeks apart and the third dose given 6 -1 2 months after the second. Pregnant women who have completed a primary series should receive a booster dose of Td if 10 or more years have elapsed since their last dose.
Because of a theoretical risk to the developing fetus, live-virus vaccines should not usually be given to pregnant women or to those likely to become pregnant within 3 months. If, how ever, immediate protection against poliomyelitis or yellow fever is needed because of immi nent exposure, O PV or yellow fever vaccine may be given. If the only reason to vaccinate a pregnant woman with yellow fever vaccine is an international travel requirement, efforts should be made to obtain a waiver letter (see page 1 9S).
It is strongly recommended that rubella vaccine be administered in the postpartum period to women not known to be immune, preferably before discharge from the hospital.
Information about immunobiologies and vaccine-preventable diseases during pregnancy is summarized in Appendix 4.
# C o n d itio n s That C o m p ro m ise the Im m u n e S y s te m
Persons with conditions that compromise their immune responses (e.g., leukemia, lym pho ma, and generalized malignancy or immunosuppressive therapies) should receive annual in fluenza vaccination with the currently formulated vaccine. Persons with conditions associated with increased risk of pneumococcal disease or its complications should receive a single dose of pneumococcal polysaccharide vaccine. The effectiveness of these vaccines in such per sons may be limited, but the risk of disease is substantial and adverse reactions are minimal.
In general, live-virus vaccines should not be given to persons who are immunocompro mised as a result of immune deficiency diseases, leukemia, lymphoma, or generalized m alignancy or are immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabolites, or radiation. However, susceptible patients with leukemia in remission who have not had chemotherapy for at least 3 months may receive live-virus vaccines. The exact interval between discontinuing im m unosuppressives and regaining the ability to respond to individual vaccines is not known. Estimates of experts vary from 3 months to 1 year.
Short-term (less than 2 weeks) corticosteroid therapy, topical steroid therapy (e.g., nasal or skin), and intraarticular, bursal, or tendon injections with corticosteroids should not be im munosuppressive and do not necessarily contraindicate vaccination with live-virus vaccines. Vaccination should be avoided if system ic immunosuppressive levels are achieved by topical application.
# MMWR 9S
# H e m o d ia ly sis
Persons receiving hemodialysis have been at high risk of infection with HBV, although envi ronmental control measures have reduced this risk during the past few years. Nationwide, an estimated 1 5% of hemodialysis patients have serologic evidence of HBV infection, and routine serologic screening of hemodialysis patients is currently recommended. Susceptible patients who will soon require or are currently receiving long-term hemodialysis should receive three double doses of HB vaccine as soon as possible. Double the normal dose is recommended for these patients because of lower vaccine immunogenicity in this group. Postvaccination screening to demonstrate antibody to hepatitis B surface antigen (HBsAg) is recommended in this group. Approximately 60% of hemodialysis patients who receive double doses of HB vac cine demonstrate antibodies against HBV. The duration of protection from a three-dose series of HB vaccine and the need for booster doses have not yet been determined.
Because persons with chronic renal disease are at increased risk of adverse consequences from infections of the lower respiratory tract, hemodialysis patients should receive annual in fluenza vaccination with the current formulated vaccine. These patients are also at increased risk of developing pneumococcal infection, as well as of experiencing more severe pneumo coccal disease, and should receive pneumococcal polysaccharide vaccine.
# S p le n ic D y sfu n c tio n or A n a to m ic A sp le n ia
Persons with splenic dysfunction or anatomic asplenia are known to be at increased risk of contracting fatal pneumococcal bacteremia and should receive pneumococcal polysaccharide vaccine. Persons scheduled for elective splenectomy should receive pneumococcal polysac charide vaccine at least 2 weeks before the operation.
# F a c to r V III a n d I X D e fic ie n c ie s
Patients with clotting disorders who receive factor VIII or IX concentrates have an in creased risk of HBV infection. Vaccination with HB vaccine is recommended for susceptible patients. The degree and duration of protection from a three-dose series of HB vaccine and the need for booster doses have not yet been determined.
Prevaccination serologic screening for HBV markers is recommended for patients who have already received multiple infusions of these products.
# C h ro n ic A lco h o lism
Persons with chronic alcoholism may be at increased risk of contracting a pneumococcal infection or having a more severe pneumococcal illness. Such persons, especially those with cirrhosis, should receive pneumococcal polysaccharide vaccine.
# H ig h -R is k D is e a s e s
Persons with disease conditions that increase the risk of adverse consequences from lower-respiratory-tract infections should receive annual influenza vaccination with the current formulated vaccine. These conditions include:
(a) Acquired or congenital heart disease with actual or potentially altered circulatory dynamics. (b) Any chronic disorder or condition that compromises pulmonary function. (c) Diabetes mellitus or other metabolic diseases that increase the likelihood that infections will be more severe than for persons without such conditions. (d) Chronic renal disease with azotemia or nephrotic syndrome. (e) Chronic, severe anemia, such as sickle cell disease. Som e chronic illnesses (e.g., chronic pulmonary disease, congestive heart failure, diabetes mellitis) predispose individuals to an increased risk of pneumococcal illness or its com plica tions. While data on the effectiveness of pneumococcal polysaccharide vaccine for chronical ly ill persons are not conclusive, such persons should receive the vaccine.
# V A C C IN E -P R E V E N T A B LE D IS E A S E S AN D TH EIR IM MU NO BIO LO G IC S
Vaccines, toxoids, and immune globulins are available for use in the prevention of a number of diseases. These diseases and their specific immunobiologies are presented in this section. For each immunobiologic, dosage, route of delivery, indications for use, side effects, adverse reactions, precautions, and contraindications to be considered before administration are described here and are summarized in Table 4.
# Toxoids
# D iphth eria
The occurrence of diphtheria has decreased dramatically in the United States, largely be cause of the widespread use of diphtheria toxoid. Only 11 cases of diphtheria were reported in the period 1 9 8 0 -1 9 8 2 . From 1977 through 1982 , 56% of the 34 reported cases of re spiratory diphtheria occurred in adults 20 years of age or older, and 24% of the cases o c curred in adults 50 years of age or older. The age distribution for persons who died from diphtheria w as similar. Diphtheria occurs primarily among unimmunized or inadequately immunized individuals. Limited serosurveys done since 1977 indicated that 62% of adults 1 8 -3 9 years of age and 41% -84% of those 60 years of age or older lacked protective levels of circulating antitoxin against diphtheria (4 -6 ).
# • Diphtheria toxoid
Complete and appropriately timed immunization is at least 95% effective in preventing diphtheria. The combined preparation Td is recommended for use in adults since a large pro portion of adults lack protective levels of circulating antibody against tetanus (4)(5)(6). Further more, Td contains much less diphtheria toxoid than other diphtheria toxoid-containing pro ducts, and as a result, reactions to the diphtheria component are less likely. Immunization with toxoid does not, however, prevent or eliminate carriage of Corynebacterium diphtheriae.
# • Toxoid indications
All adults lacking a completed primary series of tetanus and diphtheria toxoids should complete the series with Td. A primary series for adults is three doses of preparations con taining tetanus and diphtheria toxoids, with the first two doses given at least 4 weeks apart and the third dose given 6-1 2 months after the second. All adults for whom 10 years or more have elapsed since completion of their primary series or since their last booster dose should receive a dose of Td. Thereafter, a booster dose of Td should be administered every 1 0 years. There is no need to repeat doses if the schedule for the primary series or booster doses is delayed. (For toxoid side effects and adverse reactions, and precautions and contraindications, see page 1 2S).
# Tetanus
The occurrence of tetanus has decreased dramatically, largely because of the widespread use of tetanus toxoid. Nevertheless, the number of cases remained relatively constant from M M W R I I S 1 973 through 1 982, averaging 88 reported cases per year. Tetanus occurs almost exclusive ly in unimmunized or inadequately immunized individuals. Immune pregnant women confer temporary protection against tetanus to their infants through transplacental maternal anti body. In the period 1 977-1 982, persons 20 years of age or older accounted for 89% of the 50 4 reported tetanus cases for which patient ages were known; persons 60 years of age or older accounted for 55%. The age distribution of persons who died from tetanus w as similar. Serosurveys done since 1977 indicated that 110/-of adults 1 8 -3 9 years of age and 49° j-66% of those 60 years of age or older lacked protective levels of circulating antitoxin against tetanus (4-6).
# • Tetanus toxoid
Complete and appropriately timed immunization is nearly 100% effective in preventing tetanus. The combined preparation, Td, is the preferred preparation for active tetanus immuni zation of adults since a large proportion of adults lack protective levels of circulating antitoxin against diphtheria (4-6).
# • Toxoid indications
All adults lacking a complete primary series of tetanus and diphtheria toxoids should com plete the series with Td. A primary series for adults is three doses of preparations containing tetanus and diphtheria toxoids, with the first two doses given at least 4 weeks apart and the third dose given 6 -1 2 months after the second. All adults for whom 10 years or more have elapsed since completion of their primary series or since their last booster dose should receive a booster dose of Td. Thereafter, a booster dose of Td should be administered every 10 years. There is no need to repeat doses if the primary schedule for the series or booster doses is delayed.
The recommended pediatric schedule for DTP vaccine includes a booster dose at age 4 -6 years. The first Td booster is recommended at age 14-1 6 years (10 years after the dose at age 4 -6 years). One means of ensuring that persons continue to receive boosters every 10 years is to vaccinate persons routinely at mid-decade ages, e.g., 25 years, 35 years, etc.
For wound management the need for active immunization, with or without passive immuni zation, depends on the condition of the wound and the patient's immunization history. A sum mary of the indications for active and passive immunization is provided in Table 5. Only rarely have cases of tetanus occurred in persons with a documented primary series of toxoid injections.
Evidence indicates that complete primary immunization with tetanus toxoid provides longlasting protection-10 years or more in most recipients. Consequently, after complete primary tetanus immunization, boosters are recommended at 10-year intervals. For clean and minor wounds occurring during the 10-year interval no additional booster is recommended. For other wounds, a booster is appropriate if the patient has not received tetanus toxoid within the preceding 5 years. Antitoxin antibodies develop rapidly in persons who have previously re ceived at least two doses of tetanus toxoid.
Persons who have not completed a full primary series of injections or whose immunization status is unknown or uncertain may require tetanus toxoid and passive immunization at the time of wound cleaning and debridement. It is not sufficient to ascertain the interval since the most recent toxoid dose. A careful attempt should be made to determine whether a patient has previously completed primary immunization and, if not, how many doses have been given. Persons with unknown or uncertain previous immunization histories should be consid ered to have had no previous tetanus toxoid doses.
Td is the preferred preparation for active tetanus immunization in managing the wounds of adults. Td is used to enhance protection against diphtheria concurrently, since a large propor
# MMWR
Sep tem b er 28, 1 9 8 4 tion of adults are susceptible. Thus, if advantage is taken of visits for care of acute health problems, such as for wound management, some patients who otherwise would remain su s ceptible can be protected against both diseases. Primary immunization should ultimately be completed for persons documented to have received fewer than the recommended number of doses, including doses given as part of wound management. If passive immunization is needed, human tetanus immune globulin (TIG) is the product of choice. The currently recommended prophylactic dose of TIG for wounds of average severity is 2 5 0 units, intramuscularly (IM). When tetanus toxoid and TIG are given concurrently, separ ate syringes and separate sites should be used. Most experts consider the use of adsorbed toxoid mandatory in this situation.
# To xo id (Td) S id e E f f e c t s a n d A d v e rs e R e a ctio n s
Local reactions, generally erythema and induration with or without tenderness, can occur after the administration of Td. Fever and other system ic sym ptom s are less common.
Arthus-type hypersensitivity reactions characterized by severe local reactions generally starting 2 -8 hours after an injection and often associated with fever and malaise may occur, particularly in persons who have received multiple boosters of tetanus toxoid.
Rarely, severe system ic reactions such as generalized urticaria, anaphylaxis, or neurologic com plications have been reported after administration of tetanus and diphtheria toxoids. Peripheral neuropathy has been reported rarely after administration of tetanus toxoid, al though a causal relationship has not been established.
# To x o id (Td ) P re ca u tio n s an d C o n tra in d ica tio n s
Although there is no evidence that tetanus and diphtheria toxoids are teratogenic, waiting until the second trimester of pregnancy to administer Td is a reasonable precaution to mini mize any concern over teratogenicity.
A history of a neurologic reaction or a severe hypersensitivity reaction (e.g., generalized ur ticaria or anaphylaxis) following a previous dose is a contraindication to tetanus and diphtheria toxoids. Local side effects alone do not preclude continued use. If a prior system ic reaction is suspected of representing allergic hypersensitivity, appropriate skin testing to document im mediate hypersensitivity may be useful before tetanus toxoid immunization is discontinued (7). Mild, nonspecific skin-test reactivity to tetanus toxoid is common. Most vaccinees develop cutaneous delayed hypersensitivity to the toxoid.
Persons experiencing severe Arthus-type hypersensitivity reactions to a prior dose of tetanus toxoid usually have very high serum tetanus antitoxin levels and should not be given even emergency booster doses of Td more frequently than every 10 years.
Although a minor illness, such as a mild upper-respiratory infection, should not be cause for postponing vaccination, a severe febrile illness is reason to defer routine vaccination.
# Live-V irus Vaccines
# M e a sle s
In 1983, only 5.6% of the 3 ,1 3 9 counties in the United States reported cases of measles. Indigenous transmission of measles has been eliminated from most of the United States be cause of widespread vaccination. However, importations of disease are frequent (more than 1 0 0 each year), and there is a continued risk of exposure, particularly for young adults attend ing college or universities or traveling abroad.
In 1982, 1 1.7% of measles patients whose ages were reported were 20 years of age or older. Outbreaks continue to occur in universities and colleges and other places where young MMWR 13S
adults congregate. In the first half of 1983, 51% of reported cases were among college stu dents or were epidemiologically linked to cam pus outbreaks. It is estimated that as many as 20% of young adults lack detectable antibody and may be susceptible to measles. Encephalitis or death follows measles disease in approximately one case per 1,000. The risk of encephalitis is greatest in adult patients. Aside from infants, the highest measles casefatality ratio occurs in adults.
Measles illness during pregnancy increases rates of spontaneous abortion, premature labor, and low birth weight for infants. Although cases of congenital malformation following m easles infection during pregnancy have been reported, no consistent patterns have been demonstrated.
# * M easles vaccine
Measles vaccine produces a mild or inapparent noncommunicable infection. A single sub cutaneously (SC) administered dose of live-m easles vaccine provides durable protection against measles illness in approximately 95% of vaccinees, extending probably for their life time. Combined MMR vaccine is the vaccine of choice if recipients are likely to be susceptible to rubella and/or mumps as well as to measles. Although reactions following measles, mumps, and rubella vaccines in persons previously immune have been reported, evidence and experience overwhelmingly suggest that vaccination with MMR of persons who were pre viously immune to one or more of its components is not associated with significant adverse effects.
# * Vaccine indications
Measles vaccine is indicated for all persons born in 1 957 or later who lack documentation of receipt of live-m easles vaccine on or after their first birthday, physician-diagnosed measles, or laboratory evidence of immunity. Persons born before 1957 can generally be considered immune since measles w as a universal infection before measles vaccine became available. In dividuals who received vaccine before their first birthday, killed-measles vaccine, killedmeasles vaccine followed within 3 months by live-m easles vaccine, or a measles vaccine of unknown type in the period 1 9 6 3 -1 9 6 7 should be revaccinated. An estimated 6 0 0 ,0 0 0 -9 0 0 ,0 0 0 persons in the United States received killed-measles vaccine in the years 1 9 6 3 -1 9 6 7 .
Because the risk of acquiring measles outside the United States is greater than the risk in curred in the United States, travelers should be immune to measles before leaving the United States.
Generally, young adults who are exposed to measles and who have no or uncertain docu mentation of live-m easles vaccination on or after their first birthday, no record of physiciandiagnosed measles, and no laboratory evidence of immunity should be vaccinated within 72 hours after exposure, when vaccination is most likely to be protective. If the exposure did not result in infection, the vaccine should induce protection against subsequent measles infection. An acceptable alternative is to use IG, which can prevent or modify infection if administered within 6 days after exposure. IG is principally indicated when measles vaccine is contraindicat ed. IG should not be used in an attempt to control measles outbreaks. The recommended dose of IG is 0.25 ml/kg IM, not to exceed 1 5 ml. Live-m easles vaccine should be given 3 months after IG is administered, by which time the passive measles entibodies should have disappeared.
# * Vaccine side effects and adverse reactions
Reactions to measles vaccine do not appear to be age related. About 5%-1 5% of vaccinees may develop a temperature of 103°F (39.4°C) or higher, generally beginning between days 5 and 12 after vaccination; fever usually lasts 1-2 days and, rarely, up to 5 days. Transient
# 14S MMWR
Sep tem b er 28, 1 984 rashes have been reported in approximately 5% of vaccinees. The incidence rate of encephali tis or encephalopathy following measles vaccination is lower than the observed background incidence rate of encephalitis of unknown etiology and much lower than that following natural measles.
Reactions after live-measles vaccination occur in 4% -55% of prior recipients of killedmeasles vaccine. The reactions are generally mild, consisting of a local reaction with or with out a low-grade fever of 1-2 days' duration. Such reactions are considerably milder than atypical measles syndrome, an illness which may affect prior recipients of killed-measles vac cine who are exposed to natural measles.
# • Vaccine precautions and contraindications
Vaccination should not be postponed because of a minor illness, such as a mild upperrespiratory infection. However, vaccination of persons with severe febrile illnesses should be postponed until recovery. Vaccine should be given 14 days before or deferred for at least 6 weeks, and preferably 3 months, after a person has received IG, whole blood, or other blood products containing antibody.
Because of a theoretical risk to the developing fetus, measles vaccine should not be given to pregnant women.
Measles vaccine should not be given to persons who are immunocompromised as a result of immune deficiency diseases, leukemia, lymphoma, or generalized malignancy or are immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabolites, or radiation. (See "Conditions That Com prom ise the Immune System ," page 8S.)
There is no evidence that live-measles vaccine exacerbates tuberculosis. If tuberculin skin testing is needed, it should be done on the day of vaccination and read 4 8 -7 2 hours later. For a recent vaccinee, it is prudent to wait 4 -6 weeks after receipt of measles vaccine before ad ministering a tuberculin skin test since measles vaccination may temporarily suppress tubercu lin reactivity.
Persons with a history of any sign or symptom of an anaphylactic reaction (i.e., hives, swelling of the mouth and throat, difficulty in breathing, hypotension, or shock) following in gestion of eggs or receipt of neomycin should be given measles vaccine only with extreme caution. Protocols have been developed for vaccinating such persons (S). Persons with reac tions that are not anaphylactic are not at increased risk and can be vaccinated.
# M u m p s
The occurrence of reported mumps cases in the United States has decreased steadily since the introduction of live-m um ps-virus vaccine. In 1983, a record low of 3,2 9 7 cases were reported provisionally; this number represented a 98% decline from the 1 85,691 cases reported in 1967, the year live-m umps vaccine w as licensed. In 1982, 5 ,2 7 0 cases were reported, of which 9% occurred in persons 20 years of age or older.
Although mumps disease is generally self-limiting, meningeal signs may appear in up to 1 5% of cases, and orchitis in up to 20% of clinical cases among postpubertal males. Sterility is a rare sequela of mumps orchitis among males. Deafness occurs at a rate of one case per 1 5 ,0 0 0 cases of mumps.
Serologic surveys indicate that most individuals have been infected with mumps by 20 years of age.
# • M umps vaccine
Live-m um ps vaccine has been available since 1967. A single dose of live-m umps vaccine administered S C provides protective and long-lasting levels of antibody in over 90% of reci pients. Reported clinical vaccine efficacy ranges between 75% and 90%. MMR is the vaccine
# MMWR 15S
of choice if recipients are likely to be susceptible to measles and/or rubella as well as to mumps. Although reactions following measles, mumps, and rubella vaccines in persons pre viously immune have been reported, evidence and experience overwhelmingly suggest that the vaccination with MMR of persons who were previously immune to one or more of its components is not associated with significant adverse effects.
# • Vaccine indications
Mumps vaccine is indicated for all adults, particularly males, believed to be susceptible. Most adults are likely to have been infected naturally and generally can be considered immune, even if they did not have clinically recognizable mumps disease. Killed-m um ps vac cine w as available from 1 9 5 0 until 1 978. Persons who received killed-mumps vaccine might benefit from vaccination with live-mumps vaccine.
# • Vaccine side e ffe cts and adverse reactions
Parotitis after vaccination has been reported rarely. Allergic reactions including rash, pru ritus, and purpura have been associated temporally with mumps vaccination but are uncom mon, usually mild, and of brief duration. The frequency of reported central nervous system (CNS) dysfunction following mumps vaccination is lower than the observed background inci dence rate in the general population.
# • Vaccine precautions and contraindications
Vaccine should be given at least 14 days before or deferred for at least 6 weeks, and preferably 3 months, after a person has received IG, whole blood, or other blood products containing antibody.
Because of the theoretical risk of fetal damage following administration of a live-virus vac cine to a pregnant woman, it is prudent to avoid giving mumps vaccine to pregnant women.
Mumps vaccine should not be given to persons who are immunocompromised as a result of immune deficiency diseases, leukemia, lymphoma, or generalized m alignancy or are immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabolites, or radiation. (See "Conditions That Com prom ise the Immune System ," page 8S.)
Persons with a history of any sign or symptom of an anaphylactic reaction (i.e., hives, swelling of the mouth and throat, difficulty in breathing, hypotension, or shock) following in gestion of eggs or receipt of neomycin should be vaccinated only with extreme caution. Proto cols have been developed for vaccinating persons with severe egg allergy (8). Persons with reactions that are not anaphylactic are not at increased risk and can be vaccinated.
# R u b e lla
Preventing fetal infection and consequent C R S are the objectives of rubella immunization. Fetal infection occurring during the first trimester of pregnancy can lead to C R S in up to 80% of fetuses. In addition, fetal wastage due to miscarriage or therapeutic abortion following m a ternal rubella disease or exposure during the first trimester remains a frequent occurrence.
The number of reported rubella cases has decreased steadily from over 5 6 ,0 0 0 cases in 1 9 69, the year rubella vaccine w as licensed, to 2 ,325 cases in 1 982. In 1 982, only 11.7% of the 3,1 37 counties in the United States reported cases of rubella. The 1 9 8 3 provisional total of 9 5 4 cases is an all-time low. Because, until recently, many adolescents and young adults had not been vaccinated, decreases in incidence rates of reported rubella were observed pri marily for children. Recent efforts to increase delivery of vaccine to cellege-age and older per sons have led to the current decline in the incidence rates for these age groups. However, an estimated 1 0%-1 5% of young adults remain susceptible to rubella, and limited outbreaks con tinue to be reported in universities, colleges, and places of employment-notably hospitals. Vaccination of young children has prevented widespread epidemics of rubella and of C R S and eventually will lead to the elimination of C R S as vaccinated cohorts enter the childbearing age. However, increased efforts to ensure that all women of childbearing age, in particular, are vaccinated will hasten the elimination of rubella and C R S in the United States. Additional aids to elimination of rubella and C R S include 1) achieving and maintaining high immunization levels, 2) maintaining vigorous surveillance, and 3) practicing aggressive outbreak control.
# • Rubella vaccine
A single S C administered dose of live, attenuated rubella vaccine provides long-term, probably lifetime, immunity in approximately 95% of vaccinees. Moreover, there is no risk to susceptible contacts of vaccinees. MMR is the vaccine of choice if recipients are likely to be susceptible to measles and/or mumps as well as to rubella. Although reactions following ad ministration of measles, mumps, and rubella vaccines to persons previously immune have been reported, evidence and experience overwhelmingly suggest that the vaccination with MMR of persons who are already immune to one or more of its components is not associated with significant adverse effects.
# • Vaccine indications
Rubella vaccine is recommended for adults, particularly females, unless proof of immunity is available (i.e., documented rubella vaccination on or after the first birthday or a positive serologic test) or unless the vaccine is specifically contraindicated. In particular, nonpregnant susceptible women of childbearing age should be provided rubella vaccination 1) during rou tine internal medicine and gynecologic outpatient care, 2) during routine care in a family plan ning clinic, 3) following premarital screening, 4) before discharge from a hospital for any reason, and 5) after childbirth or abortion. Ideally, any contact with the health-care system should be used as an opportunity to vaccinate susceptible women. In addition, evidence of rubella immunity should be required for all individuals in colleges and universities. Health-care programs in work places and in other places where women of childbearing age congregate should ensure that the rubella immune status of every employee is ascertained and that rubella immunization is made available. All hospital personnel (male and female) who might be at risk of exposure to patients infected with rubella or who might have contact with pregnant pa tients or personnel should be immune to rubella. Consideration should be given to making rubella immunity a condition for employment. Finally, since the risk of acquiring rubella while traveling outside the United States is greater than the risk incurred within the United States, all women travelers, particularly those of childbearing age, should be immune before leaving the United States.
# • Vaccine side effects and adverse reactions
Up to 40% of susceptible adult vaccinees in large-scale field trials have had joint pain, usu ally of the small peripheral joints, after vaccination; frank arthritis is reported infrequently. A r thralgia and transient arthritis occur more frequently and tend to be more severe in susceptible women than in children. When joint sym ptom s or other types of pain and paresthesias do occur, they generally begin 3 -2 5 days after vaccination, persist for 1-11 days, and rarely recur. Adults with joint problems usually have not had to disrupt work activities. Complaints of transient peripheral neuritis such as paresthesias and pain in the arms and legs have o c curred very rarely and only in susceptible vaccinees.
# • Vaccine precautions and contraindications
Rubella vaccine should be given at least 14 days before administration of IG or deferred for at least 6 weeks, and preferably 3 months, after administration. On the other hand, previ ous administration of whole blood or other blood products containing antibody (e.g., human anti-Rho [D] immune globulin) does not generally interfere with an immune response and is not a contraindication to postpartum vaccination. However, in this situation, serologic testing should be done 6 -8 weeks after vaccination to assure that seroconversion has occurred.
# MMWR 17S
Rubella vaccine should not be given to pregnant women or to those likely to become preg nant within 3 months after receiving the vaccine. Through 1 983, C D C monitored prospective ly 2 1 4 susceptible pregnant women who had received rubella vaccine within 3 months before or after conception and carried their pregnancies to term (94 received Cendehill or H PV-77, 11 9 received RA 27/3, and one received an unknown strain of vaccine). None of the infants had malformations compatible with C R S. The ACIP believes that the risk of vaccineassociated malformation is so small as to be negligible. Although a final decision must rest with the individual patient and her physician, the ACIP believes that rubella vaccination during pregnancy should not ordinarily be a reason to recommend interruption of pregnancy.
Because of the theoretical risk to the fetus, reasonable precautions should be taken before women of childbearing age are vaccinated. These precautions include 1) asking women if they are pregnant, 2) excluding those who say they are, and 3) explaining the theoretical risks of the vaccine to the others and counseling them not to become pregnant for 3 months after vaccination. If a pregnant woman is vaccinated or if a woman becomes pregnant within 3 months after vaccination, she should be counseled on the theoretical risks to the fetus. In stances of vaccination of k n o w n susceptible women who are pregnant or become pregnant within 3 months should be reported through state health departments to the Division of Im munization, CDC.
In general, rubella vaccine should not be given to persons who are immunocompromised as a result of immune deficiency diseases, leukemia, lymphoma, or generalized m alignancy or are immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antime tabolites, or radiation. (See "Conditions That Com prom ise the Immune System ," page 8S.)
Rubella vaccine is prepared in human diploid cell cultures and has not been reported to be associated with allergic reactions. The vaccine does contain trace amounts of neomycin to which patients may be allergic. Persons with a history of any sign or symptom of an anaphylactic reaction (i.e., hives, swelling of the mouth and throat, difficulty in breathing, hy potension, or shock) following receipt of neomycin should not receive rubella vaccine. Persons with reactions to neomycin that are not anaphylactic are not at increased risk and can be v ac cinated. Rubella vaccine does not contain penicillin.
# S m a llp o x
In May 1 9 80, the World Health Organization (WHO) declared the world free of smallpox. A smallpox vaccination certificate is not required by any country as a condition of entry for inter national travelers. In May 1983, the distribution of smallpox vaccine for civilian use in the United States w as discontinued.
# * Vaccine indications
There is no evidence that smallpox vaccination has therapeutic value in the treatment of recurrent herpes simplex infection, warts, or any other disease. Sm allpox vaccine should never be used therapeutically for these or any other conditions.
Except for persons working with orthopox viruses or involved in producing and testing smallpox vaccine, there are no indications for the use of smallpox vaccine in civilian popula tions. When indicated, smallpox vaccination should be given at least every 3 years. For advice on vaccine administration and contraindications, contact the International Health Program Office, C D C , Atlanta, Georgia 30 3 3 3 .
# Y ello w F e v e r
C ases of yellow fever are reported only from Africa and South America. Two form s of yellow fever-urban and jungle -are distinguishable epidemiologically. Clinically and ecologi cally they are identical.
# 18S
# MMWR
# Septem ber 28, 1984
Urban yellow fever is an epidemic viral disease transmitted from infected to susceptible persons by the Aedes a e g yp ti mosquito. In areas where the A. a e g yp ti mosquito has been eliminated or suppressed, urban yellow fever has disappeared. In W est Africa, A. aegyptitransmitted epidemics involving town and village populations continue to occur at frequent intervals.
Jungle yellow fever is an enzootic viral disease transmitted among nonhuman hosts by a variety of mosquito vectors. It is currently observed only in forested areas of South America and forest-savannah zones of tropical Africa, but occasionally extends into Central America and the Caribbean. In tropical America 2 0 0 -4 0 0 cases are recognized annually, mainly among persons with occupational exposure to the vector in forested areas; the disease is, however, believed to be greatly underreported. In Africa, epidemics that are spread by forest mosquito vectors affect tens of thousands of persons every few years, but few cases are officially reported. The jungle yellow fever cycle may be active but unrecognized in forested areas of countries within the zone with endemic yellow fever (Figure 1).
# • Yellow fever vaccine
The yellow fever vaccine available in the United States is an attenuated, live-virus vaccine prepared from the 1 7D strain of virus grown in chick embryo. Immunity is induced by a single S C injection of 0.5 ml of reconstituted vaccine and persists for more than 10 years.
Yellow fever vaccines must be approved by W HO and administered at an approved Yellow Fever Vaccination Center. Centers can be identified by contacting state and local health departments. Vaccinees should have an International Certificate of Vaccination filled out, dated, signed, and validated with the stamp of the center where the vaccine is given. Vaccine must be received 6 days to 10 years before travel in order for the certificate to be valid.
# • Vaccine indications
Vaccination is recommended for persons traveling or living in areas where yellow fever in fection o ccu rs-currently parts of Africa and South America. tries currently reporting yellow fever are noted biweekly in S um m ary o f H ealth In fo rm a tio n fo r In te rn a tio n a l Travel. All state health departments and many county and city health depart ments receive these publications. It should be emphasized that the actual areas of yellow fever activity far exceed the zones officially reported to be infected. Vaccination is also recommended for laboratory personnel who might be exposed to virulent yellow fever virus. Booster doses are needed at 1 O-year intervals. Som e countries, especially in Africa, require evidence of vaccination from all entering trav elers. Other countries may waive the requirements for travelers coming from noninfected areas and staying less than 2 weeks. Som e countries require a traveler, even if only in transit, to have a valid certificate if the traveler has visited any country thought to harbor yellow fever virus. Requirements of individual countries may change, and the most current information is published biweekly in S um m ary o f H ealth In fo rm a tio n fo r In tern ation al Travel and summarized annually in H ealth Inform a tion fo r Intern ation al Travel.
# • Vaccine side effects and adverse reactions
Reactions to 17D yellow fever vaccine are generally mild. From 2% to 5% of vaccinees have mild headache, myalgia, low-grade fever, or other minor sym ptom s 5 -1 0 days after vac cination. Fewer than 0.2% curtail regular activities. Immediate hypersensitivity reactions, char acterized by rash, urticaria, and/or asthma, are extremely uncommon and occur principally in persons with a history of egg allergy. Although more than 34 million doses of vaccines have been distributed, only two cases of encephalitis temporally associated with vaccinations have been reported in the United States; in one fatal case, 1 7D virus w as isolated from the brain.
# • Vaccine precautions and contraindications
Yellow fever vaccine should not be given to persons who are immunocompromised as a result of immune deficiency diseases, leukemia, lymphoma, or generalized m alignancy or are immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabo lites, or radiation. (See "Conditions That Com prom ise the Immune System ," page 8S.)
Although specific information is not available on adverse effects of yellow fever vaccine on the developing fetus, it is prudent on theoretical grounds to avoid vaccinating pregnant women and to advise that they postpone travel to areas where yellow fever occurs until after delivery. Pregnant women who must travel to areas where the risk of yellow fever is high should be vaccinated. It is believed that under these circum stances, the risk of yellow fever in fection far outweighs the small theoretical risk to mother and fetus from vaccination. Howev er, if international travel regulations constitute the only reason to vaccinate a pregnant woman or a patient hypersensitive to eggs, efforts should be made to obtain a letter of waiver from a physician clearly stating the contraindication to vaccination. Ideally, this letter should be writ ten on letterhead stationery and bear the stamp used by health departments and official im munization centers to validate the International Certificates of Vaccination. Such a letter of waiver has been acceptable to some governments. Under these conditions, it is also useful for the traveler to obtain specific, authoritative advice from the country or countries he or she plans to visit. Their em bassies or consulates may be contacted, and a letter substantiating the waiver of requirements obtained.
Since live yellow fever vaccine is produced in chick embryos, persons with a history of any signs or sym ptom s of an anaphylactic reaction (i.e., hives, swelling of the mouth and throat, difficulty in breathing, hypotension, or shock) after eating eggs should not receive yellow fever vaccine. If vaccination of an individual with a questionable history of egg hypersensitivity is considered essential because of a high risk of exposure, an intradermal (ID) test dose may be administered under close medical supervision. Specific directions for skin testing are found in the package insert. Som e data have indicated that persons given yellow fever and cholera vaccines simultane ously or 1-3 weeks apart had lower-than-normal antibody responses to both vaccines. Unless there are time constraints, cholera and yellow fever vaccines should be administered at a minimal interval of 3 weeks. If the vaccines cannot be administered at least 3 weeks apart, then they should preferably be given simultaneously.
Yellow fever vaccine and commercially available IG may be given simultaneously.
# Both Live-V irus and Inactivated-Virus Vaccines
# P o lio m y e litis
The risk of poliomyelitis is very small in the United States; however, epidemics could occur if the high immunity level of the general population is not maintained by immunizing children routinely or if wild poliovirus is introduced into susceptible populations in communi ties with low immunization levels. In the United States inapparent infection with wild poliovirus strains no longer contributes significantly to establishing or maintaining immunity. Most adults are already immune.
# • Poliovirus vaccines
Two types of poliovirus vaccines are currently licensed in the United States: O PV and IPV. A primary vaccination series with either vaccine produces immunity to all three types of polio virus in more than 95% of recipients. The primary series of O PV consists of three doses: two doses given 6 -8 weeks apart and a third dose given at least 6 weeks and customarily 6 -1 2 months after the second. The primary series for IPV consists of four doses: three doses each given 4 -8 weeks apart and a fourth dose given 6 -1 2 months after the third. In general, it is not necessary to give a primary vaccine series to adults living in the United States who have not had a primary series as children. However, for adults who have not had a primary series and who are at greater risk than the general population of exposure to wild polioviruses be cause of foreign travel or health occupation, IPV is preferred since the risk of O PV-associated paralysis is slightly higher in adults than in children.
Poliovirus vaccine is not routinely recommended for persons older than high school age (1 8 -1 9 years old).
# • Vaccine indications
Travelers to areas where wild poliovirus is epidemic or endemic should have completed a primary series of poliovirus vaccine. For previously unimmunized persons, IPV is indicated. However, if less than 4 weeks are available before protection is needed, a single dose of OPV is recommended. Travelers who have previously received less than a full primary course of O PV or IPV should be given the remaining required doses of either vaccine, regardless of the interval since the last dose and the type of vaccine previously received. Travelers to develop ing countries who have previously completed a primary series of O PV should receive a single dose of OPV. Additional booster doses of O PV are probably not necessary. Those who have previously received a primary series of IPV should receive a dose of either O PV or IPV. If IPV is used exclusively, an additional dose may be given every 5 years if exposure continues or recurs, although the need for these boosters has not been established.
Health-care personnel in close contact with patients who may be excreting wild poliovi ruses, and laboratory personnel handling specim ens that may contain wild polioviruses, should have completed a primary series of poliovirus vaccine. IPV is indicated because of the slightly increased risk to adults of vaccine-associated paralysis after O PV administration; also, virus may be shed after receipt of O PV vaccine and inadvertently expose susceptible im munocompromised contacts to live vaccine virus.
# MMWR
# 21S
# • Vaccine adverse reactions
In a ctiva te d po lio viru s vaccine. No serious side effects of currently available IPV have been documented. Since IPV contains trace amounts of streptomycin and neomycin, hypersensitivi ty reactions are possible in individuals sensitive to these antibiotics. Persons with signs and sym ptom s of an anaphylactic reaction (i.e., hives, swelling of mouth and throat, difficulty in breathing, hypotension, or shock) following receipt of streptomycin or neomycin should not receive IPV. Persons with reactions that are not anaphylactic are not at increased risk and can be vaccinated.
O ral p o lio viru s vaccine. In rare instances, administration of O PV has been associated with paralysis in healthy recipients and their contacts. Although the risk of vaccine-associated paralytic poliomyelitis is extremely small for immunologically normal vaccinees (approximate ly one case per 9 million doses distributed) and their susceptible, immunologically normal household contacts (approximately one case per 7 million doses distributed), vaccinees should be informed of this risk.
# • Vaccine precautions and contraindications
In a ctiva te d p o lio viru s vaccine. There is no convincing evidence of adverse effects of IPV for the pregnant woman or developing fetus; regardless, it is prudent on theoretical grounds to avoid vaccinating pregnant women. However, if immediate protection against poliomyelitis is needed. OPV, not IPV, is recommended.
O ral po lio viru s vaccine. Unlike other live-virus vaccines, which are administered parenteral ly, O PV is administered orally. IG and other antibody-containing blood products do not appear to interfere with the immune response to OPV.
OPV should not be given to persons who are or may be immunocompromised as a result of immune deficiency diseases, leukemia, lymphoma, or generalized malignancy or immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabolites, or ra diation. (See "Conditions That Com prom ise the Immune System ," page 8S.) If immunization against poliomyelitis is indicated in such persons, IPV should be used, and some protection may result.
OPV should not be used for immunizing household contacts of patients immunocompro mised as a result of immune deficiency disease, leukemia, lymphoma, or generalized malignancy or immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabolites, or radiation. If protection is indicated, IPV should be used for immuniz ing household contacts of such patients. O PV should not be given to anyone in a family with a known family history of immunodeficiency until the immune status of all family members is documented.
When children in the household are given O PV, adults who are not adequately immunized against poliomyelitis are at a very small risk of contracting O PV-associated paralytic polio myelitis. Because of the overriding importance of ensuring prompt and complete immunization of the child and the extreme rarity of O PV-associated disease in contacts of vaccinees, the ACIP recommends the administration of O PV to a child regardless of the poliovirus-vaccine status of adult household contacts. This is the usual practice in the United States. The re sponsible adult should be informed of the small risk involved and of precautions to be taken, such as hand washing after changing a diaper. An acceptable alternative, if there is strong assurance that ultimate, full immunization of the child will not be jeopardized or unduly delayed, is to immunize adults with IPV or OPV, as appropriate to their immunity status, before giving O PV to the child.
# Inactivated-Virus Vaccines
# H e p a titis B Virus In fe ctio n
The estimated lifetime risk of acquiring HBV infection in the United States is approximately 5% for the population as a whole but may approach 100% for the highest risk groups. Annual ly, an estimated 1 0 0 ,0 0 0 sym ptom atic cases of hepatitis B disease occur in the United States, leading to approximately 10,000 hospitalizations and 190 fulminant cases. Threefourths of persons with fulminant disease die.
In 1982, 88% of hepatitis B cases for which patient age w as known occurred in persons 20 years of age or older. Between 6% and 10% of adults with HBV infection become carriers. The United States currently has 4 0 0 ,0 0 0 -8 0 0 ,0 0 0 carriers. Chronic active hepatitis occurs in 25% of carriers. Each year in the United States, approximately 4 ,0 0 0 persons die of HBVrelated cirrhosis, and 8 00, of HBV-related liver cancer.
# • Hepatitis B vaccine
A series of three 1 -ml IM doses of HB vaccine, each containing 20 /ug/ml of HBsAg protein, provides protective antibody in over 90% of healthy adult recipients and is 80% -95% effective in preventing infection for at least 2 years. The first two doses should be given 1 month apart, and the third dose, 5 months after the second. The duration of vaccine-induced protection and the need for booster doses are not yet known. For susceptible hem odialysis patients, three 2-m l doses given at the above intervals are recommended. Because the prevalence of HBV varies widely among various population groups, serologic screening to detect susceptible individuals before vaccination may or may not be cost effective. Cost effectiveness depends on the known or perceived risk of infection, the cost of screening, and the cost of HB vaccine.
# • Vaccine indications
Immunization is recommended for adults at increased risk of occupational, social, family, environmental, or illness-related exposure to HBV. These include homosexual males, users of illicit injectable drugs, household and sexual contacts of HBV carriers, workers in healthrelated occupations requiring frequent exposure to blood, residents and staff of institutions for the mentally retarded, hemodialysis patients, recipients of factor VIII or IX concentrates, and morticians and their assistants. Inmates in some long-term correctional facilities may also be candidates for vaccination.
Vaccination should also be considered for persons who plan to reside for more than 6 months in areas with high levels of endemic HBV and who will have close contact with the local population and for travelers intending a short stay who are likely to have contact with blood from or sexual contact with residents of areas with high levels of endemic disease (par ticularly areas of eastern Asia and Sub-Saharan Africa). Such persons should allow 6 months before travel in order to complete the HB vaccine primary series.
HB vaccine is intended primarily for preexposure prophylaxis. However, it has recently been recommended for postexposure use in certain situations, particularly for persons who belong to a high-risk group for whom preexposure administration of vaccine is recommended ( 3 ). HB vaccine in combination with HBIG provides sustained protective levels of antibody and obviates the need for a second dose of HBIG in such exposures. Therefore, a normal series of HB vaccine, combined with a single dose (0.06 ml/kg or 5 ml for adults) of HBIG given at a dif ferent site, is recommended for postexposure prophylaxis of health workers following acci dental percutaneous or mucous-membrane exposure to blood containing HBsAg, and of su s ceptible homosexual men following sexual exposure to an H BsAg-positive man. HBIG alone (in the same dose) is recommended for postexposure prophylaxis of persons with heterosexu al exposures. • Vaccine side effects and adverse reactions
In vaccine trials, soreness at the site of injection w as the only side effect that occurred more frequently for vaccinees than for controls. Since its licensure in 1981 through August 1 983, HB vaccine is estimated to have been administered to over 3 5 0 ,0 0 0 individuals in the United States. A s of May 1 984, adverse events following immunization had been reported for 8 9 0 vaccinees. The reported adverse events represent temporal associations with vaccination and are not necessarily caused by the vaccine. Forty-eight persons had serious events such as transverse myelitis, grand mal seizures, aseptic meningitis, erythema multiforme, or Guillain-Barre syndrome (GBS).
# • Vaccine precautions and contraindications
Pregnancy should not be considered a contraindication to vaccinating women who are oth erwise candidates for receiving HB vaccine. While data are not available on the safety of the vaccine for the developing fetus, HB vaccine contains only noninfectious HBsAg particles and should pose no risk to the fetus. In contrast, HBV infection in a pregnant woman may result in a severe disease for the mother and chronic infection for the newborn.
Since HB vaccine is made from human plasma, the possibility that it may contain an etiologic agent of acquired immunodeficiency syndrome (AIDS) has been raised. The purification and inactivation process used in preparing HB vaccine inactivates representatives of all known groups of viruses. There are no microbiologic, epidemiologic, or empiric data to suggest that the HB vaccine carries any etiologic risk for AIDS.
# In flu e n za
Influenza viruses have continually demonstrated the ability to cause major epidem ics of re spiratory disease. High attack rates of acute illness and the frequent occurrence of lowerrespiratory-tract complications usually result in dramatic rises in visits to physicians' offices and hospital emergency rooms. Furthermore, influenza frequently infects individuals who, be cause of their age or underlying health status, are poorly able to cope with the disease and often require medical attention, including hospitalization. Such persons are considered to be medically at "high risk" in epidemics. In one recent study, for example, rates of hospitalization for adults with "high-risk" medical conditions increased during major epidemics by about two-to fivefold in different age groups, reaching a maximum rate of about 8 0 0 per 1 0 0 ,0 0 0 population.
Influenza epidemics cause excess mortality, which is attributable not only to influenza pneumonia, but also to cardiopulmonary disease. Fifteen times in the years 1 9 5 7 -1 9 8 2 , epidemics have been associated with 10 ,0 0 0 or more excess deaths; in 1983, excess mor tality again exceeded the epidemic threshold.
The greatest impact of influenza is normally seen when new strains appear against which most of the population lacks immunity. In these circum stances (e.g., 1957 and 1968), pandemics occur. During pandemics, a quarter or more of the United States population have been affected over a period of 2 -3 months.
Because the proportion of elderly persons in the United States is increasing, and because age and its associated chronic diseases are risk factors for severe influenza illness, the toll of influenza may also increase unless control measures are used more vigorously than in the past.
# • Influenza vaccine
Influenza A viruses are classified into subtypes on the basis of two antigens: hemagglutinin (H) and neuraminidase (N). Three subtypes of hemagglutinin (H1, H2, H3) and two subtypes of neuraminidases (N1, N2) are recognized among influenza A viruses that have caused w ide spread human disease. Immunity to these antigens, especially hemagglutinin, reduces the likelihood of infection and the severity of disease if a person does become infected. However, there may be sufficient antigenic variation (antigenic drift) within the same subtype overtime, so that infection or vaccination with one strain may not induce immunity to distantly related strains of the same subtype. Although influenza B viruses have shown much more antigenic stability than influenza A viruses, antigenic variation does occur. A s a consequence, the an tigenic characteristics of current strains provide the basis for selecting virus strains to be included in the vaccine for a given year. Potency of present vaccines is such that nearly all vaccinated young adults develop hemagglutination-inhibition antibody titers that are likely to protect them against infection by strains like those in the vaccine, and often by related variants that emerge. The elderly, the very young, and patients with certain chronic diseases may develop lower postvaccination an tibody titers than do young adults. Under these circum stances, influenza vaccine may be more effective in preventing lower-respiratory-tract involvement, or other complications of in fluenza, than in preventing upper-respiratory-tract involvement. Influenza vaccine will not pre vent primary illnesses caused by other respiratory pathogens.
# • Vaccine indications
Use of inactivated influenza vaccine is the single most important measure in the prevention and/or attenuation of influenza infection. Since 1 963, annual vaccination against influenza has been recommended for individuals at high risk of lower-respiratory-tract complications and death following influenza infection (i.e., the elderly and persons with chronic disorders of the cardiovascular, pulmonary, and/or renal system s; metabolic diseases; severe anemia; and/or compromised immune function). These groups have been identified primarily by review of death certificate data, supported by hospital-based or population-based studies. W ithin each broadly defined "high-risk" category, however, some persons are more likely than others to suffer severe complications from influenza infection.
Am ong nursing-home residents, chronic diseases and other debilitating conditions are common, and spread of influenza can often be explosive, with attack rates as high as 60% and case-fatality ratios up to 30% or higher. In addition, recent retrospective studies of nonin stitutionalized patients suggest that chronic underlying diseases, particularly those that affect the cardiovascular and pulmonary system s, may contribute more to the severity of illness than does age alone.
Medical personnel may transmit influenza infections to their high-risk patients while they are themselves incubating an infection, undergoing a subclinical infection, or working while they have mild sym ptom s. Nosocom ial outbreaks of influenza are reported. The potential for introducing influenza to a high-risk group such as patients with severely compromised cardio pulmonary or immune system s or infants in neonatal intensive care units should be reduced by targeted vaccination programs of medical personnel.
Based on these observations, the previous, broadly defined "high-risk" adult groups have been further assigned priority for receiving vaccine in order that special efforts can be directed at providing vaccine to those who may derive the greatest benefit.
1. Adults at high risk of severe influenza illness who most warrant active, targeted v acci nation efforts: (a) Adults with chronic disorders of the cardiovascular or pulmonary system s that are severe enough to require regular medical follow-up or to have caused hospitalization during the preceding year.
(b) Residents of nursing homes and other chronic-care facilities (e.g., institutions hous ing patients of any age with chronic medical conditions). Achievement of high vacci nation rates (e.g., 80%) may induce herd immunity in such populations and thereby MMVIIR 2 5 S lower the frequency of outbreaks, as well as reducing the frequency of severe illness when outbreaks do occur. 2. Physicians, nurses, and other personnel who have extensive contact with high-risk pa tients (e.g., primary-care and certain specialty clinicians and staff of intensive-care units). These persons should receive influenza vaccination annually to reduce the po ssi bility for nosocomial spread of influenza to high-risk patients. 3. Other adults who are at moderately increased risk of serious illness compared with the general population. Special programs to make vaccine readily available to these groups should also be given high priority:
(a) Healthy individuals over 65 years of age.
(b) Adults with a chronic metabolic disease (including diabetes mellitus), renal dysfunc tion (including those in chronic dialysis), anemia, immunosuppression, or asthma that is severe enough to require regular medical follow-up or to have caused hospi talization during the preceding year. In addition, influenza vaccine may be offered to persons who provide essential community service or to any adult who w ishes to reduce the likelihood of an influenza infection.
Effective programs for giving influenza vaccine are needed in nursing homes and other chronic-care facilities, in physicians' offices, and in hospital settings. Residents of nursing homes and chronic-care facilities should receive routine annual vaccination. Other adult highpriority groups should receive influenza vaccine at the time of regular medical follow -ups in the fall, or should be notified to come in specifically to receive the vaccine. Patients with high risk conditions who are hospitalized during the fall should be considered for influenza vaccine before discharge from the hospital.
There is considerable overlap in the target groups for influenza vaccination and those for pneumococcal polysaccharide vaccine. Pneum ococcal polysacchraride vaccine and influenza vaccine can be given at the same time at different sites without an increase in side effects; however, it should be emphasized that whereas influenza vaccine is given annually, pneumo coccal polysaccharide vaccine should be given only once to adults. Detailed immunization records should be provided to each patient to help ensure that additional doses of pneumo coccal polysaccharide vaccine are not given.
Amantadine hydrochloride, an antiviral drug, can prevent influenza A or be used therapeuti cally to reduce sym ptom s of influenza A infections. It is n o t a substitute for vaccine. Specific circum stances in which amantadine prophylaxis is recommended are described in the ACIP recommendations on prevention and control of influenza.
# * Vaccine side effects and adverse reactions
Vaccines used in recent years have generally been associated with only a few reactions. Fewer than one-third of vaccinees have been reported to develop local redness or induration for 1 or 2 days at the site of injection.
System ic reactions have been of two types. First, malaise, myalgia, and other system ic sym ptom s of toxicity, although infrequent, most often affect those who have had no experi ence with the influenza virus antigens contained in the vaccine. These reactions, which begin 6 -1 2 hours after vaccination and persist for 1-2 days, are usually attributed to the influenza antigens (even though the virus is inactivated) and constitute most of the system ic side ef fects of influenza vaccination.
Second, immediate, presumably allergic, responses such as flare and wheal or various respiratory-tract sym ptom s of hypersensitivity occur extremely rarely after influenza vaccina tion. These sym ptom s probably result from sensitivity to some vaccine component -most likely residual egg protein. Although current influenza vaccines contain only a small quantity of egg protein, on rare occasions vaccine can induce hypersensitivity reactions. Unlike the MMWR Septem ber 28, 1984
1 976 swine influenza vaccine, vaccines used subsequently have not been associated with an increased frequency of GBS.
# • Vaccine precautions and contraindications
Pregnancy has not been demonstrated to be a risk factor for severe influenza infection except in the largest pandemics of 1 9 1 8 -1 9 1 9 and 1 957-1 958. Influenza vaccine is consid ered to be generally safe for pregnant women. Nonetheless, when vaccine is to be given during pregnancy, waiting until the second or third trimester is a reasonable precaution to minimize any concern over theoretical teratogenicity.
Persons with a history of any signs or sym ptom s of an anaphylactic reaction (i.e., hives, swelling of the mouth and throat, difficulty in breathing, hypotension, or shock) after eating eggs should not be given inactivated influenza vaccine.
Persons with acute febrile illnesses normally should not be vaccinated until their temporary sym ptom s have abated.
# R a b ie s
Although rabies rarely affects humans in the United States, thousands of persons receive rabies vaccine every year, principally for postexposure prophylaxis. The likelihood of human exposure to rabies from domestic animals has decreased greatly in recent years. In every year since 1 976, more than 85% of all reported cases of animal rabies have been among wild ani mals, the most important source of possible infection for humans in the United States. How ever, for persons traveling overseas to developing countries with endemic rabies, the dog re mains the animal most likely to transmit rabies.
# • Rabies vaccine
Both whole-virion and subvirion human diploid cell rabies vaccines (HDCV) are available. For preexposure rabies prophylaxis a three-dose series of H D CV of either type given as 1 -ml doses IM on days 0, 7, and 28 provides adequate antibody levels in virtually all recipients (10). The C D C currently accepts a titer of 5 by the rapid fluorescent-focus inhibition test as adequate.
The whole-virion H D CV produced by the Merieux Institute has been used for preexposure immunization in a regimen of three 0 .1 -ml doses given intradermally (ID) in the lateral aspect of the upper arm in the deltoid area, one dose on each of days 0, 7, and 28. Experience gained with over 2 ,0 0 0 persons vaccinated in the United States by the ID route has shown that anti body is produced in all recipients, although the mean response is somewhat lower and may be of shorter duration than with comparable IM immunization. Except for persons suspected of being immunosuppressed, postvaccination serology is not necessary following IM or ID im munization in the United States. Antibody response in some groups vaccinated ID outside the United States has been found to be inadequate for reasons not yet determined (11). Prelimi nary data suggest that concurrent administration of malaria chem oprophylaxis may be a factor in the lowered immunologic response of persons vaccinated overseas. It should be noted that Merieux Institute, the manufacturer, has not yet met the packaging and labeling re quirements necessary to obtain approval by the FDA for the ID route of administration. The 1 -ml vial presently available is intended for IM use and contains no preservatives. To minimize the risk of contamination and loss of vaccine potency, the reconstituted vaccine must be used immediately. Data on ID immunization are not available for W yeth Laboratories vaccine.
Proper postexposure rabies prophylaxis is determined by whether or not the person has had previous preexposure or postexposure prophylaxis. 1) Persons who (a) have previously received postexposure prophylaxis with HDCV, (b) have received a three-dose IM preexposure regimen of HDCV, (c) have received a three-dose ID preexposure regimen of H D CV in the United States, or (d) have a previously documented adequate rabies titer should receive two 1-ml IM doses of H D C V -one dose on each of days 0 and 3. HRIG is not recommended in these circum stances. 2) Persons not meeting the above criteria should be treated with a single, 20-international units (IU)/kg dose of HRIG and five 1-ml doses IM of H D CV -one on each of days 0, 3, 7, 14, and 28. HRIG should be administered at the beginning of H D CV post exposure prophylaxis but can be given up to the eighth day after the first dose of H D CV was given. The HRIG dose should be divided; up to half should be infiltrated into the area of the wound, if possible, and the rest administered IM, but not in the same site as HDCV. O nly IM ad ministration of HD CV is indicated for postexposure prophylaxis.
# • Vaccine indications
Preexposure immunization should be considered for high-risk groups: animal handlers, cer tain laboratory workers and field personnel, and persons planning to be in countries or areas of countries for more than 1 month where rabies is a constant threat. Persons whose voca tions or avocations bring them into contact with potentially rabid animals should also be con sidered for preexposure immunization. Persons with continuing risk of exposure should re ceive a booster dose every 2 years or have their serum tested for rabies antibody every 2 years and, if the titer is inadequate, be given a booster dose. If there is substantial risk of expo sure to rabies, preexposure rabies prophylaxis may be indicated during pregnancy.
The decision to provide specific postexposure antirabies treatment should include the fol lowing considerations:
1 Type of exposure-rabies is transmitted primarily by the bite of infected animals. It may also be transmitted by introducing the virus into open cuts or wounds in skin or via m ucous membranes by saliva or other potentially infectious material from a rabid animal and, rarely, by aerosol exposure. 2. Species of biting animal -carnivorous wild animals (especially skunks, raccoons, and foxes) and bats are most commonly infected with rabies in the United States. Elsewhere in the world, dogs, cats, carnivorous wildlife, and bats are the major vectors. The likeli hood that domestic cats or dogs in the United States will be infected varies from region to region. Rodents are rarely infected. Consultations with the state or local health department may be helpful. 3. Circum stances of biting incident -an unprovoked attack is more indicative of a rabid animal than a provoked attack.
• Vaccine side effects and adverse reactions Following postexposure prophylaxis, local reactions, such as pain, erythema, and swelling or itching at the injection site, are very common, and mild system ic reactions, such as head ache, nausea, abdominal pain, muscle aches, and dizziness, are reported by about 20% of reci pients. System ic allergic reactions ranging from hives to anaphylaxis occur in an estimated 11 per 10,000 vaccinees. Mild immune-complex-like hypersensitivity reactions consisting of hives, itching, and angio-edema have occurred 2-21 days after booster doses of H D CV and are the most frequently reported allergic reactions ( 12 ). Four cases of transient neuroparalytic illness have been temporally associated with H D CV administration: two following administra tion of whole-virion vaccine and two following administration of subvirion vaccine (13). No permanent sequelae or deaths have been associated with administration of HDCV.
# • Vaccine precautions and contraindications
Corticosteroids and other immunosuppressive agents can interfere with the development of active immunity and should not be administered during preexposure therapy. When rabies postexposure prophylaxis is administered to persons known or suspected of being immunosuppressed, or to those who are receiving steroids or immunosuppressive therapy, it is espe cially important that serum be tested to ensure an adequate rabies antibody response. If a person experiences an anaphylactic reaction (i.e., hives, swelling of the mouth and throat, difficulty in breathing, hypotension, or shock) after receiving HDCV, no further preex posure doses of H D CV should be given. By contrast, if a person needing postexposure therapy has had a previous anaphylactic reaction to H D CV or has such a reaction during the postexpo sure course, H D CV therapy should continue; however, the person should receive the required doses in an appropriate medical setting.
# Inactivated-Bacteria Vaccines
# Ch o le ra
Cholera continues to be a health risk in Africa and Asia. Countries currently reporting chol era are listed in the biweekly publication S um m a ry o f H ealth Inform a tion fo r In tern ation al Travel. All state health departments and many county and city health departments receive this publication. Persons who follow the usual tourist itinerary and who use tourist accom m o dations in countries affected by cholera are at virtually no risk of infection. The traveler's best protection against cholera is avoiding food and water that might be contaminated.
# • Cholera vaccine
The vaccine may be administered as a 0.5-m l dose S C or IM or as a 0.2-m l dose ID. A l though a single dose of vaccine is sufficient for entry into most countries, some countries may require evidence of a complete primary series of two doses given 1 week to 1 month or more apart, or a booster dose within 6 months before arrival.
The currently available cholera vaccine has been shown in field trials to be only about 50% effective in preventing clinical illness for a period of 3 -6 months. The vaccine does not prevent transmission of infection. The risk of cholera to most U.S. travelers is so low that it is doubtful that vaccination is of benefit. W HO no longer recommends cholera vaccination for travel to or from cholera-infected areas. However, some countries affected or threatened by cholera re quire evidence of cholera vaccination as a condition of entry. Current information on choleravaccination requirements of individual countries is published annually in H ealth Inform a tion fo r International. Travel. All state health departments and many county and city health depart ments receive this publication. Travelers to countries with cholera-vaccination requirements should have an International Certificate of Vaccination filled in, dated, signed, and validated showing receipt of the vaccine 6 days to 6 months before entry into the country. Most city, county, and state health departments can validate certificates. Failure to secure validation may cause travelers to be revaccinated or quarantined
# • Vaccine indications
Cholera vaccine is indicated only for travelers to countries requiring evidence of cholera vaccination for entry. Boosters may be given every 6 months if required by a country.
# • Vaccine side effects and adverse reactions
Vaccination often results in 1 -2 days of pain, erythema, and induration at the site of injec tion. The local reaction may be accompanied by fever, malaise, and headache. Serious reac tions, including neurologic reactions, following cholera vaccination are extremely rare.
# • Vaccine precautions and contraindications
No specific information is available on the safety of cholera vaccine during pregnancy. Be cause cholera disease during pregnancy is a serious illness, whether to use cholera vaccine should be determined in individual circum stances based on the actual risk of disease and the probable benefits of the vaccine.
The only contraindication to cholera vaccine is a history of a severe reaction following a previous dose. Most governments will permit an unvaccinated traveler to enter the country if
MMWR 2 9 S
he or she carries a physician's statement of medical contraindication. However, some coun tries may quarantine such unvaccinated persons or place them under surveillance if they come from areas with cholera. Som e data have indicated that persons given yellow fever and cholera vaccines simultane ously or 1-3 weeks apart had lower-than-normal antibody responses to both vaccines. Unless there are time constraints, cholera and yellow fever vaccines should be administered at a minimal interval of 3 weeks. If the vaccines cannot be administered at least 3 weeks apart, then they should preferably be given simultaneously.
# M e n in g o co cca l D is e a s e
Meningococcal disease is endemic throughout the world but may also occur in epidemics. Am ong U.S. civilians, m eningococcal disease occurs primarily as single, isolated cases or, in frequently, in small, localized clusters. A third of all cases of m eningococcal disease occur in patients 20 years old or older. Serogroup B strains cause the majority of U.S. cases, with serogroups C and W1 35 strains accounting for most of the remainder.
# • M eningococcal polysaccharide vaccine
Two m eningococcal polysaccharide vaccines, bivalent A -C and quadrivalent A, C, Y, and W1 35 vaccines, are available for use in the United States. Each is given as a single dose, and each induces specific serogroup immunity. The duration of immunity conferred by the v ac cines is not known.
# • Vaccine indications
Vaccine may be of benefit as an adjunct to antibiotic chem oprophylaxis for household and other close contacts of persons with m eningococcal disease caused by serogroups A, C, Y, and W 1 3 5 and for travelers to areas with epidemic m eningococcal disease. The need for booster doses has not been established.
Routine vaccination of U.S. civilians with m eningococcal polysaccharide vaccine is not recommended because of the lack of availability of a group B vaccine and the low risk of in fection in the United States.
# • Vaccine side effects and adverse reactions
Adverse reactions to meningococcal polysaccharide vaccines are infrequent and mild, con sisting principally of localized erythema lasting 1 -2 days.
# • Vaccine precautions and contraindications
The safety of meningococcal polysaccharide vaccines for pregnant women has not been established. On theoretical grounds, it is prudent not to use them unless there is a substantial risk of infection.
# P lagu e
Plague is a natural infection of rodents and their fleas. In the United States a few human cases occur yearly in humans exposed in the Western states to infected animals, primarily ro dents, and their fleas. Other countries currently reporting plague infections are noted in the biweekly publication S um m a ry o f H ealth In fo rm a tio n fo r In tern ation al Travel. All state health departments and many county and city health departments receive this publication. A number of countries in Africa, Asia, and South America continue to report sporadic, epidemic, and epi zootic infection. In most of these countries, the risk of exposure exists primarily in rural or semirural areas.
• Plague vaccine A primary series of plague vaccine consists of three IM doses. The first dose, 1 ml, is fol lowed in 4 weeks by a second dose of 0.2 ml. The third dose, also 0.2 ml, is administered 5 months after the second. The effectiveness of a primary series of plague vaccine has never been measured precisely. Field experience indicates that vaccination with plague vaccine reduces the incidence and severity of disease resulting from the bite of infected fleas. The degree of protection offered against primary pneumonic infection is unknown. Since plague vaccination may only ameliorate illness, prophylactic antibiotics may be indicated whenever a person, vaccinated or not, has a definite exposure.
# • Vaccine indications
Vaccination is indicated for certain vocational groups. These include all laboratory and field personnel working with Yersinia pe stis organisms that may be resistant to antimicro bials, persons engaged in aerosol experiments with Y. pestis, and field personnel engaged in operations in areas with enzootic or epidemic plague where preventing exposure to rodents and fleas is impossible. Plague vaccination should be considered for laboratory personnel regularly working with Y. p e stis or plague-infected rodents and for persons whose vocation regularly exposes them to wild rodents or rabbits in areas with enzootic plague.
Vaccine may also be considered for travelers to areas known to have endemic plague in countries reporting plague, particularly if travel will not be limited to urban areas with tourist hotel accommodations.
For persons with continuing exposure, three booster doses, each 0.1-0.2 ml, should be given at approximately 6-m onth intervals. Thereafter, booster doses at 1-to 2-year intervals should provide good protection.
# • Vaccine side e ffe cts and adverse reactions
For about 10% of recipients, primary vaccination may result in general malaise, headache, fever, mild lymphadenopathy, and/or erythema and induration at the injection site. These reactions occur more commonly with repeated injections. Sterile abscesses occur rarely. Se n sitivity reactions manifested by urticarial and asthmatic phenomena have occasionally been reported.
# • Vaccine precautions and contraindications
Neither the safety nor efficacy of vaccination with plague vaccine during pregnancy has been determined; therefore, it should not be used unless there is a substantial risk of infection.
Plague vaccine should not be administered to anyone with a known hypersensitivity to any of its constituents (beef protein, soy, casein, and phenol). Patients who have had severe local or system ic reactions to plague vaccine should not be revaccinated.
# P n e u m o c o c c a l D is e a s e
Precise data on the occurrence of serious pneumococcal disease in the United States are not available: however, the annual incidence rate of pneumococcal pneumonia is estimated to be 68 cases to 2 6 0 cases per 1 0 0 ,0 0 0 population, and of bacteremia, 7 -2 5 /1 0 0 ,0 0 0 . The incidence of pneumococcal pneumonia, which causes a substantial number of deaths annual ly, increases in those over 4 0 years old, and show s a twofold increase in those over 60 years of age. Mortality from pneumococcal disease is highest among patients who have bacteremia or meningitis, patients with underlying medical conditions, and older persons.
Patients with certain underlying conditions are clearly at increased risk both of contracting pneumococcal infection and of experiencing more severe pneumococcal illness. These condi tions include sickle cell anemia, multiple myeloma, cirrhosis, alcoholism, nephrotic syndrome, renal failure, splenic dysfunction, anatomic asplenia, and organ transplant. Persons suffering from diabetes mellitus, chronic pulmonary disease, cardiovascular disease, or conditions asso ciated with immunosuppression may be at increased risk of contracting pneumococcal infec tion or of having more severe illness.
# MMWR 3 1 S * Pneum ococcal polysaccharide vaccine
The pneumococcal polysaccharide vaccine currently available contains purified capsular materials of the 23 types of S treptococcus pneum oniae responsible for 87% of recent bacteremic pneumococcal disease in the United States. Most healthy adults show a twofold rise in type-specific antibody 2-3 weeks after administration of a single dose of vaccine. The titer of antibody that is protective against each serotype has not been determined.
The duration of vaccine-induced immunity is unknown. Studies of persistence of vaccineinduced antibody show elevated titers 3 -5 years after immunization. Booster doses are not recommended because of increased adverse reactions to subsequent doses.
Patients who have received the earlier pneumococcal polysaccharide vaccine containing capsular material from only 14 types of S. pneum oniae should not receive a dose of the 2 3valent pneumococcal polysaccharide vaccine since the modest increase in coverage does not warrant the increased risk of adverse reactions.
# * Vaccine indications
Newly available data regarding vaccine efficacy support the broader use of pneumococcal polysaccharide vaccine in the United States. Vaccination is particularly recommended for the following:
1) Adults with chronic illnesses, especially those with cardiovascular disease and chronic pulmonary disease, who sustain increased morbidity with respiratory infections. 2) Adults with chronic illnesses specifically associated with an increased risk of pneumo coccal disease or its complications. These include splenic dysfunction or anatomic asplenia, Hodgkins' disease, multiple myeloma, cirrhosis, alcoholism, renal failure (including those on chronic dialysis), cerebrospinal-fluid leaks, and conditions associat ed with immunosuppression. 3) Older adults, especially those age 65 and over, who are healthy. Program s for vaccine delivery in the recommended high-risk groups need to be developed further. Specifically, more effective programs are needed for giving vaccine in physicians' of fices, in hospitals, and in nursing homes and other chronic-care facilities.
Since two-thirds of persons with serious pneumococcal disease have been hospitalized within 5 years before the pneumococcal illness ( 14), vaccine should be given to hospitalized patients in the high-risk groups before discharge, in order to prevent future adm issions for pneumococcal disease. In addition, persons with chronic conditions who visit physicians fre quently are probably at higher risk of pneumococcal infection than those who require infre quent visits. Office-based programs to identify and immunize patients requiring frequent medical care should help prevent pneumococcal illness. Furthermore, pneumococcal polysac charide vaccine and influenza vaccine can be given at different sites at the same time without an increase in side effects (7 5 ).
Medicare has partially reimbursed the cost of pneumococcal polysaccharide vaccination since 1981. It has been determined that hospitals may be reimbursed for pneumococcal im munization of Medicare recipients independent of reimbursement based on system s of pros pective payments.
# * Vaccine side e ffe cts and adverse reactions
About half of the persons given pneumococcal polysaccharide vaccine experience mild side effects such as erythema and pain at the site of injection. Fever and m yalgias have been reported by fewer than 1% of those given pneumococcal polysaccharide vaccine (7 6).
Severe adverse effects such as anaphylactic reactions have rarely been reported -about five cases per million doses administered.
Arthus reactions and system ic reactions have been common among adults given second doses (1 7). They are thought to result from localized antigen-antibody reactions involving an tibody induced by previous vaccination. Therefore, second, or "booster," doses are not recommended.
# • Vaccine precautions and contraindications
The safety of pneumococcal polysaccharide vaccine in pregnant women has not been evaluated. It should not be given to healthy pregnant women. Women at high risk of pneumo coccal disease ideally should be vaccinated before pregnancy.
Because of a marked increase in adverse reactions with second injections of pneumococcal polysaccharide vaccine, second, or "booster," doses should not be given. However, when there is doubt or no information on whether a person in one of the high-risk groups has ever received pneumococcal polysaccharide vaccine, vaccine should be given. Complete records of vaccination can help to avoid repeat doses.
# Typhoid
The occurrence of typhoid fever remained constant in the period 1 9 7 2 -1 9 8 2 , with an average of 4 8 6 cases reported annually. During the years 1 9 7 8 -1 9 8 2 , 57% of cases for which the patient's age w as known occurred in patients 20 years of age or older. Approxi mately 62% of typhoid cases reported in the United States during 1 977-1 979 were acquired by travelers to other countries, and an additional 27% occurred in contacts of typhoid carriers.
# • Typhoid vaccine
A primary series of two 0.5-m l doses of typhoid vaccine given S C 4 weeks apart has been shown to protect 70% -90% of recipients.
# • Vaccine indications
Immunization is indicated for travelers to areas where a recognized risk of exposure to ty phoid exists. It should be emphasized that even after typhoid vaccination, food and water should be selected carefully in these areas. Typhoid vaccination is not recommended in the United States or in areas of natural disaster. Booster doses should be given at least every 3 years to persons with continued or repeated exposure; these may be given S C (0.5 ml) or ID (0.1 ml). The acetone-killed and -dried vaccine should not be given ID. This preparation is available only to the U.S. Armed Forces.
# • Vaccine side effects and adverse reactions
Typhoid vaccination often results in 1-2 days of discom fort at the site of injection. The local reaction may be accompanied by fever, malaise, and headache.
# • Vaccine precautions and contraindications
The only contraindication to typhoid vaccine is a history of a severe local or system ic reac tion following a previous dose.
# Live-Bacteria V accines T u b e rcu lo sis
The number of tuberculosis cases in the United States has declined steadily since reporting began in the 1 9th century. Between 1 972 and 1 9 82, the annual incidence of tuberculosis de clined from 15.8 cases per 1 0 0 ,0 0 0 population to 1 1 .0/100 ,000, a decrease of 30%. In 1 982, approximately 92% of 2 5 ,0 5 9 reported cases with patient ages known occurred in per sons 20 years of age or older. Reported cases usually are typical postprimary pulmonary dis ease. The risk of infection is greatest for those who have repeated exposure to persons with unrecognized or untreated sputum -positive pulmonary tuberculosis. In the United States, ef forts to control tuberculosis are directed toward early identification and treatment of cases.
# MMWR 33 S
preventive therapy with isoniazid for infected persons at high risk of developing disease, and prevention of transmission to others.
# • BCG vaccine
Although BCG vaccine is widely used in many areas of the world, results of a recent largescale field trial in India have raised questions about its efficacy (18). BCG vaccines currently available in the United States differ from the products used in the published field trials, and their efficacy has not been demonstrated directly. In the United States, vaccines for ID and for percutaneous administration are licensed. (For percutaneous administration, one drop of vac cine is placed on the skin and introduced through the skin by multiple punctures with a bifurcated or other needle.) Vaccination should be only by the route indicated on the package labeling.
# • Vaccine indications
In the United States the only situations in which BCG might be considered are 1) for indi viduals in prolonged close contact with patients with active tuberculosis that is untreated, ineffectually treated, or resistant to treatment; 2) for health-worker groups, such as hospital staffs, with an annual new-infection rate of 1% or higher in spite of other tuberculosis control measures; and 3) for other groups in which an excessive rate of new infection can be demonstrated and the usual surveillance and treatment programs have failed or are not feasible. * Vaccine side effects and adverse reactions BCG has been associated with severe or prolonged ulceration at the vaccination site, re gional adenitis, disseminated BCG infection, and osteitis. Severe ulceration and adenitis occur in approximately 1 % -10% of vaccinees, and disseminated infections and osteitis are quite rare (1-10 per million doses).
# * Vaccine precautions and contraindications
Although no harmful effects of BCG on the fetus have been observed, it is prudent to avoid vaccination during pregnancy unless there is immediate excessive risk of exposure to in fective tuberculosis.
Since BCG is a live-bacteria vaccine, it should not be given to persons immunocompro mised as a result of immune deficiency diseases, leukemia, lymphoma, or generalized m alignancy or to persons immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabolites, or radiation. (See "Conditions That Com prom ise the Immune System ," page 8S.)
# Other Licensed Vaccines
# A d e n o v iru s a n d A d e n o v iru s V a ccin e
Adenovirus types 4 and 7 have frequently been the cause of outbreaks of acute, febrile, respiratory-tract disease in young adults during military training. Live, oral adenovirus vaccines for types 4 and 7 are available for immunization of military populations. Use of the vaccines in other populations is not recommended.
# A n th ra x an d A n th ra x V a ccin e
Anthrax is infrequently encountered. Anthrax vaccine is recommended only for individuals who come in contact with imported animal hides, furs, bonemeal, wool, animal hair (especially goat hair), and bristles in the workplace and for individuals undertaking investigational studies involving Bacillus anthracis.
Primary immunization consists of six S C 0.5-m l injections, the first three at 2-w eek inter vals and the other three at 6-m onth intervals. Booster doses of 0.5-m l S C are recommended at 1-year intervals. The vaccine is only available from the Biologic Products Program, Michi
# P e rtu ss is a n d P e rtu s s is V a ccin e
Pertussis disease in adults is generally milder than in children and is not known to result in death. Pertussis can be transmitted from adult patients to close contacts, especially unimmu nized children. Such transmission may occur in the household and in hospitals, where chains of transmission have involved patients and staff.
In general, pertussis vaccine is not recommended for adults because both local and sy s temic reactions are thought to be more frequent and severe than in children under 7 years of age and because the disease itself is less severe in adults. In specific situations, such as docu mented transmission to and from personnel in a hospital, single-antigen pertussis vaccine in a 0.2-m l IM dose has been given as a part of control efforts. Single-antigen pertussis vaccine, adsorbed, is available only from the Biologic Products Program, Michigan Department of Public Health.
# Immune Globulins
IG and specific immune globulins, i.e., HBIG, TIG, HRIG, and varicella zoster immune globulin (VZIG), are indicated for use in order to prevent or modify certain diseases in specific circumstances.
# Im m u n e G lobulin fo r In tra m u scu la r U se
IG is given IM for preexposure prophylaxis against hepatitis A to travelers in areas where contact with potentially contaminated food and water is unavoidable. For travelers at risk for 2-3 months, a single IM dose of 0.02 ml/kg is recommended. For more prolonged travel 0.06 ml/kg should be given every 5 months. IG is also indicated for postexposure prophylaxis for close household and sexual contacts of persons with hepatitis A, staff and attendees of day care centers and household contacts of diapered children in day-care centers in which hepati tis A transmission is occurring, selected staff and clients of custodial institutions in which an outbreak is occurring, and co-workers of food handlers with hepatitis A. For such contacts a single dose of 0.02 ml/kg of IG is recommended as soon as possible after exposure. IG should be given within 2 weeks after exposure.
IG can be used to prevent or modify measles disease in susceptible contacts of persons with measles, especially those for whom measles vaccine is contraindicated, if given within 6 days after exposure. The recommended dose is 0.25 ml/kg (maximum dose = 15 ml). IG should not be used to control measles outbreaks.
# Im m u n e G lobulin fo r In tra ve n o u s U se
IG modified for IV administration may be given to prevent acute infections in patients with defective antibody synthesis or as prophylaxis against hepatitis A for patients for whom the IM preparation is contraindicated because of thrombocytopenia or disorders that can cause IM hemorrhage. ONLY IG MODIFIED FOR IN TRAVENO US U SE CAN BE GIVEN INTRAVE NOUSLY. The IV dose is 100 mg/kg, given slowly. The IV preparation is supplied in 50-m l vials containing 2.5 g of IG.
# H e p a titis B Im m u n e G lobulin
HBIG, alone or in combination with HB vaccine, is used for postexposure prophylaxis of HBV infection. For percutaneous or mucous membrane exposure to blood known to be HBsAg positive or from a bite by an HBV carrier, a single dose of HBIG (0.06 ml/kg or 5 ml for adults) should be given as soon as possible, and a series of three doses of HB vaccine begun within 1 week after exposure. Vaccine and HBIG may be given simultaneously, but in different sites.
For those who choose not to take HB vaccine, a second identical dose of HBIG should be given 1 month later. Following percutaneous exposure to blood from individuals at high risk of being HBsAg positive (such as persons with acute, unconfirmed viral hepatitis) or from patients at high risk of being infected with hepatitis B (such as male homosexuals, users of illicit IV drugs, and hemodialysis patients), IG should be given immediately to the exposed person as an IM dose of 0.06 ml/kg. Then serologic confirmation of the HBsAg status of the suspected high-risk patient should be obtained as soon as possible, and certainly within 7 days. If the suspected high-risk patient is HBsAg positive, the exposed person should immediately receive HBIG and hepatitis B vaccine according to the schedule above. The value of HBIG given beyond 7 days after exposure is unclear.
For homosexual exposure to HBsAg-positive males (known carriers or persons with acute cases), a single dose of HBIG should be given to susceptible contacts within 1 4 days after the last sexual exposure. Since HB vaccine is routinely recommended for male homosexuals, an HB vaccine series should be started within 7 days after HBIG administration.
For heterosexual exposures to persons with acute cases of hepatitis B, a single dose of HBIG (0.06 ml/kg or 5 ml for adults) should be given within 14 days of the last sexual contact. If the index case remains HBsAg positive at 3 months and exposure continues, the contact should be given a second dose of HBIG. If the index case becomes an HBV carrier (HGsAg positive for 6 months), the HB vaccine series should be given to the contact.
# Tetanus Im m u n e G lobulin
TIG is indicated in tetanus prophylaxis as part of the management of wounds other than clean, minor wounds in persons 1) whose previous tetanus toxoid immunization status is un known or uncertain, 2) who have received fewer than two previous tetanus toxoid doses, or 3) who have received only two previous tetanus toxoid doses and whose wound is more than 24 hours old. The currently recommended prophylactic dose for wounds of average severity is 2 5 0 units IM Td should be given at the same time but at a separate site.
A summary of the indications for active and passive immunization in the management of wounds is provided in Table 5.
# H um an R a b ie s Im m u n e G lobulin
Postexposure prophylaxis for rabies should always include HRIG with one exception: per sons who have been previously immunized with the recommended preexposure or postexpo sure regimens of HD CV or have been immunized with other types of rabies vaccines and have a history of documented adequate rabies antibody titer should not receive HRIG (Table 4). The recommended dose of HRIG is 20 Ill/kg body weight. If anatomically feasible, up to onehalf the dose of HRIG should be thoroughly infiltrated in the area around the wound, the rest should be administered IM.
# V a rice lla -Z o s te r Im m u n e G lobulin
Most adults (85%-95%) with negative or unknown histories of varicella disease (chickenpox) are likely to be immune. (Susceptibility rates for adults raised in some tropical areas, par ticularly remote areas, may be somewhat higher.) Rates of complications and death for immu nocompromised adults who contract varicella are likely to be substantially greater than for normal adults. After careful, individual evaluation, an immunocompromised patient who is be lieved to be susceptible and who has had significant exposure to varicella should receive VZIG to prevent complications. Significant exposure to a person with varicella includes household contact, close contact indoors of longer than 1 hour, sharing the same two-to four-bed hospital room, or prolonged, direct, face-to-face contact such as occurs with nurses or doctors who take care of the patient.
Chickenpox can be more severe in adults than in normal children. The decision to adminis ter VZIG to a normal adult should be made on an individual basis. The objective of VZIG use for normal adults is to modify rather than prevent illness in hopes of inducing lifelong immuni ty. When deciding whether to administer VZIG , the clinician should consider the patient's health status, the type of exposure, and the likelihood of previous infection. It is likely that adults who were older siblings in large families or whose children have had varicella are immune. If, after careful evaluation, a normal adult with significant exposure to varicella is be lieved to be susceptible, VZIG may be administered. Pregnant women and potentially su s ceptible hospital personnel should be evaluated in the same way as other adults. Supplies of V ZIG are limited, and indiscriminate administration of VZIG to normal adults would quickly ex haust supplies and prevent prophylaxis for known high-risk individuals. The cost of a five-vial adult dose is approximately $ 3 7 5 .
VZIG, available through some American Red C ro ss distribution centers (Appendix 5), is supplied in vials containing 1 25 units. W hereas 1 25 units/1 0 kg of body weight up to a m axi mum of 625 units generally is considered likely to prevent or modify varicella in normal adults, higher doses may be necessary for the immunocompromised adult. However, the ap propriate dose for immunocompromised adults has not been determined. VZIG should be ad ministered IM as directed by the manufacturer. While the duration of protection is unknown, it seems reasonable that protection should last for at least one half-life of the immune globulin, that is, approximately 3 weeks.
# Im m u n e G lo bu lin S id e E f f e c t s a n d A d v e rs e R e a c tio n s
Serious adverse effects have been rare from immune globulins administered as recommended.
# Im m u n e G lo bu lin P re ca u tio n s a n d C o n tra in d ica tio n s
Immune globulins, if needed, are not contraindicated for pregnant women. Except for the IV preparation of IG, immune globulins are prepared for IM use and should no t be given IV. The various preparations intended for IM use should not be given to patients with severe thrombocytopenia or other coagulation disorders that would ordinarily contraindicate IM in jections unless the expected benefits outweigh the risks.
Parenterally administered live-virus vaccines (e.g., MMR or other combinations) should be given at least 1 4 days before or at least 6 weeks, and preferably 3 months, after the adminis tration of immune globulins. If an immune globulin must be administered within 14 days after the administration of most live-virus vaccines, the vaccine should be administered again 3 months after the immune globulin is given. If the interval between vaccine receipt and immune globulin receipt is longer, the vaccine need not be readministered.
Preliminary data indicate that immune globulins do not interfere with the immune response to either O PV or yellow fever vaccine.
In Ju ly 1983 , a W HO Consultative Group reviewed data on both normal and specific immune globulins prepared from plasma collected mainly in the United States, including dona "Several other vaccines, toxoids, and immune globulins are licensed and available. These are noted in Appendix 3. In addition, the following antitoxins are licensed and available: (1) botulism antitoxin, trivalent (ABE) equine (distributed by C D C only), (2) tetanus antitoxin (equine), (3) diphtheria antitoxin (equine), and (4) rabies antitoxin (equine). Several vaccines and toxoids are in "Investigation of New Drug" (IND) status and available only through the Division of Host Factors, Center for Infectious Disease, CD C. These are: (1) pentavalent (ABCDE) botulinum toxoid, (2) eastern equine encephalitis (EEE) vaccine, (3) Venezualan equine encephalitis (VEE) vaccine, and (4) tularemia vaccine §When any vaccine or toxoid is indicated during pregnancy, waiting until the second or the third trimester, when possible, is a reasonable precaution that minimizes concern about teratogenicity.
Persons immunocompromised because of immune deficiency diseases, leukemia, lymphoma or generalized m alignancy or immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabolites or radiation. Although a protective immune response to IPV in the immunocompromised individual cannot be assured, the vaccine is safe and some protection may result from its administration. 'Several other vaccines, toxoids, and immune globulins are licensed and available. These are noted in Appendix 3. In addition, the following antitoxins are licensed and available: (1) botulism antitoxin, trivalent (ABE) equine (distributed by CD C only), (2) tetanus antitoxin (equine), (3) diphtheria antitoxin (equine), and (4) rabies antitoxin (equine). Several vaccines and toxoids are in "Investigation of New Drug" (IND) status and available only through the Division of Host Factors, Center for Infectious Disease, CD C. These are: (1) pentavalent (ABCDE) botulinum toxoid, (2) eastern equine encephalitis (EEE) vaccine, (3) Venezualan equine encephalitis (VEE) vaccine, and (4) tularemia vaccine §When any vaccine or toxoid is indicated during pregnancy, waiting until the second or the third trimester, when possible, is a reasonable precaution that minimizes concern about teratogenicity.
# L IV E -V IR U S A N D IN A C TIV A TED -V IR U S V A C C IN ES
# IN A C T IV A T ED -V IR U S V A C C IN ES
Persons immunocompromised because of immune deficiency diseases, leukemia, lymphoma or generalized m alignancy or immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabolites or radiation. "Several other vaccines, toxoids, and immune globulins are licensed and available. These are noted in Appendix 3. In addition, the following antitoxins are licensed and available: (1) botulism antitoxin, trivalent (ABE) equine (distributed by CD C only), (2) tetanus antitoxin (equine), (3) diphtheria antitoxin (equine), and (4) rabies antitoxin (equine). Several vaccines and toxoids are in "Investigation of New Drug" (IND) status and available only through the Division of Host Factors, Center for Infectious Disease, CD C. These are: (1) pentavalent (ABCDE) botulinum toxoid, (2) eastern equine encephalitis (EEE) vaccine, (3) Venezuelan equine encephalitis (VEE) vaccine, and (4) tularemia vaccine §When any vaccine or toxoid is indicated during pregnancy, waiting until the second or the third trimester, when possible, is a reasonable precaution that minimizes concern about teratogenicity. 'Several other vaccines, toxoids, and immune globulins are licensed and available. These are noted in Appendix 3. In addition, the following antitoxins are licensed and available: (1) botulism antitoxin, trivalent (ABE) equine (distributed by C D C only), (2) tetanus antitoxin (equine), (3) diphtheria antitoxin (equine), and (4) rabies antitoxin (equine). Several vaccines and toxoids are in "Investigation of New D rug" (IND) status and available only through the Division of Host Factors, Center for Infectious Disease, CD C. These are: (1) pentavalent (ABCDE) botulinum toxoid, (2) eastern equine encephalitis (EEE) vaccine, (3) Venezualan equine encephalitis (VEE) vaccine, and (4) tularemia vaccine §When any vaccine or toxoid is indicated during pregnancy, waiting until the second or the third trimester, when possible, is a reasonable precaution that minimizes concern about teratogenicity.
Persons immunocompromised because of immune deficiency diseases, leukemia, lymphoma or generalized m alignancy or immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabolites or radiation Although preferable to be given with the 1 st dose of vaccine, can be given up to the 8th day after the 1 st dose of vaccine.
Varicella-zoster immune globulin (VZIG) '
Persons ^ 50 kg: 125 units/10kg IM; persons > 50 kg: 6 25 u n its"
Immunocompromised patients known or likely to be su s ceptible with close and pro longed exposure to a house hold contact case or to an infectious hospital staff member or hospital roommate.N O TE: Refer to text on specific vaccines or toxoids for further details on indications, contraindications, precautions, dosages, side effects, and adverse reactions, and special considerations and individual ACIP statements (see list of published ACIP statements in Appendix 2). ' Several other vaccines, toxoids, and immune globulins are licensed and available. These are noted in Appendix 3. In addition, the following antitoxins are licensed and available: (1) botulism antitoxin, trivalent (ABE) equine (distributed by CD C only), (2) tetanus antitoxin (equine), (3) diphtheria antitoxin (equine), and (4) rabies antitoxin (equine).
Several vaccines and toxoids are in "Investigation of New Drug" (IND) status and available only through the Division of Host Factors, Center for Infectious Disease, CDC. These are: (1) pentavalent (ABCDE) botulinum toxoid, (2) eastern equine encephalitis (EEE) vaccine, (3) Venezualan equine encephalitis (VEE) vaccine, and (4) tularemia vaccine §When any vaccine or toxoid is indicated during pregnancy, waiting until the second or the third trimester, when possible, is a reasonable precaution that minimizes concern about teratogenicity.
Persons immunocompromised because of immune deficiency diseases, leukemia, lymphoma or generalized m alignancy or immunosuppressed as a result of therapy with corticosteroids, alkylating drugs, antimetabolites or radiation.
# MMWR 37 S
tions from homosexuals. The data indicated that although about 19.5 million 2-m l to 10-m l doses of immune globulin had been prepared during the preceding 4 years, no transmission of hepatitis B or any other infectious agents and no cases of A ID S had been reported in persons observed for 1-4 years after receiving immune globulin. Therefore, the Consultative Group confirmed that, at present, there is no evidence of risk attached to the use of normal or specif ic immune globulins prepared by the universally accepted methods ( 19).
R eferences 1. Immunization Practices Advisory Committee, General recommendations on immunizations. MMWR 1 9 8 3 ;3 2 :1 -8 , 13-7. 2. CD C. Rubella in hospitals -California. MMWR 1 9 8 3 ;3 2 :3 7 -9 . 3. Amler RW, Bloch AB, Orenstein WA, Bart K J, Turner PM Jr, Hinman AR. Imported m easles in the United States. JA M A 1 9 8 2 ;2 4 8 :2 1 2 9 -3 3 . 4. W eiss BP, Strassburg MA, Feeley J C . Tetanus and diphtheria immunity in an elderly population in Los Angeles County, Am J Pub Health 1 9 8 3 ;7 3 :8 0 2 -4 . 5. Crossley K, Irvine P, Warren JB , Lee BK, Mead K. Tetanus and diphtheria immunity in urban Min nesota adults. JA M A 1 9 7 9 :2 4 2 :2 2 9 8 -3 0 0 0 . 6. Ruben FL, Nagel J , Fireman P Antitoxin responses in the elderly to tetanus-diphtheria (Td) immuni zation. Am J Epidemiol 1978; 1 0 8 :1 4 5 -9 . 7. Ja c o b s RL, Lowe RS, Lanier BQ. Adverse reactions to tetanus toxoid. JA M A 1 9 8 2 :2 4 7 :40-2. 8. Herman J J , Radin R, Schneiderm an R. Allergic reactions to m easles (rubeola) vaccine in patients hy persensitive to egg protein. J Pediatr 1 983; 1 0 2 :1 9 6 -9 . 9. CD C. Postexposure prophylaxis of hepatitis B. MMWR 1 9 8 4 ;3 3 :2 8 5 -9 0 . 10. Turner G S, Nicholson KG, Tyrrell D A J, Akoi FY. Evaluation of a human diploid cell strain rabies va c cine: final report of a three year study of pre-exposure immunization. J Hyg 1 9 8 2 ;8 9 :1 0 1 -1 0 . 1 1. CD C. Field evaluations of pre-exposure use of human diploid cell rabies vaccine. MMWR 1 9 8 3 :3 2 :6 0 1 -3 . 12. C D C System ic allergic reactions following immunization with human diploid cell rabies vaccine.
MMWR 1 9 8 4 ;3 3 :1 8 5 -7 . 13. Bernard KW , Sm ith PW, Kader F J, Moran MJ. Neuroparalytic illness and human diploid cell rabies vaccine. JA M A 1 9 8 2 :2 4 8 :3 1 36 -8 14. Fedson DS, Chiarello LA. Previous hospital care and pneum ococcal bacteremia: importance for pneum ococcal immunization. Arch Intern Med 1 9 83; 1 4 3 :8 8 5 -9 . 1 5. DeStefano F, Goodman RA, Noble GR, et al. Sim ultaneous administration of influenza and pneumo coccal vaccines. JA M A 1 9 8 2 ;2 4 7 :2 5 5 1 -4. 16. Sem el JD , Seskind C. Severe febrile reaction to pneum ococcal vaccine. JA M A 1 9 7 9 :2 4 1 :1 792. General recommendations on immunizations 1 9 8 3 :3 2 :1 -8 ,1 3 -7 Diphtheria, tetanus, and pertussis. 1 9 8 1 :3 0 :3 9 2 -9 6 ,4 0 1 -7 guidelines for vaccine prophylaxis and Erratum. 1 981 ;3 0 :4 2 0 other preventive measures M easles prevention 1 9 8 2 ;3 1 :2 1 7 -2 4 ,2 2 9 -3 1
Mumps vaccine 1 9 8 2 :3 1 :6 1 7 -2 0 ,6 2 5
Rubella prevention 1 9 8 4 :3 3 :3 0 1 -1 0 ,3 1 5 -8
Yellow fever vaccine 1 9 8 4 :3 2 :6 7 9 -8 2 ,6 8 7 -8
Poliomyelitis prevention 1 9 82;31 22-6,31 -4
Prevention and control of influenza* 1 9 8 4 :3 3 :2 5 3 -6 0 ,2 6 5 -6
Inactivated hepatitis B virus vaccine 1 9 8 2 :3 1 :3 1 7 -2 2 ,3 2 7 -8
Postexposure prophylaxis of hepatitis B 1 9 8 4 :3 3 :2 8 5 -9 0
Rabies prevention Supplem entary statement on rabies vaccine and serologic testing 1 9 8 1 ;3 0 :5 3 5 -6 Rabies 1 9 8 4 ;3 3 :3 9 3 -4 0 2 ,4 0 7 -8
Supplem entary statement on 1 9 8 2 :3 1 :2 7 9 -8 0 ,2 8 5 pre-exposure rabies prophylaxis by the intradermal route Cholera vaccine 1 9 7 8 :2 7 :1 7 3 -4 M eningococcal polysaccharide vaccine 1 9 7 8 :2 7 :3 2 7 -9
Plague vaccine 1 9 8 2 ;3 1 :3 0 1 -4
Update: Pneum ococcal polysaccharide vaccine 1 9 8 4 :3 3 :2 7 3 -6 ,8 1 usage -United States Typhoid vaccine 1 9 7 8 ;2 7 :2 3 1 -3 BCG vaccines 1 9 7 9 ;2 8 :2 4 1 -4
Immune globulins for protection against viral hepatitis 1 9 8 1 :3 0 :4 2 3 -8 ,4 3 3 -5
Varicella-zoster immune globulin for the prevention of chickenpox 1 9 8 4 :3 3 :8 4 -9 0 ,9 5 -1 0 0 'T h e Immunization Practices A dvisory Committee (ACIP) periodically reviews recommendations on v a c cination and prophylaxis. W hen recommendations are revised, they are published individually in the MMWR.
Each year influenza vaccine recommendations are reviewed and amended to reflect updated informa tion on influenza activity in the United States for the preceding influenza season and to provide inform a tion on the vaccine available for the upcoming influenza season. These recommendations are published in the MMWR annually, usually during June or July. The Greater New York Blood Program 1 50 Am sterdam Ave. New York, NY 10023 (212) 5 7 0 -3 0 6 7 (212) 5 7 0 -3 0 6 8 (night) Am erican Red Cross Blood Services Northeastern New York Region Hackett Blvd. at Clara Barton Dr. Albany, N Y 12208 (518) 4 4 9 -5 0 2 0 (518) 4 6 2 -7 4 6 1 (518) 4 6 2 -6 9 6 4 (night) Am erican Red Cross Blood Services Greater Buffalo Chapter 786 Delaware Ave. Buffalo, NY 1 4209 (716) 8 8 6 -7 5 0 6 3 1 0 8 (314) 6 5 8 -2 0 0 0 (314) 6 5 8 -2 1 3 6 (
# IN A C T IV A TE D -V IR U S V A C C IN ES
# IN A C T IV A T E D -B A C T E R IA V A C C IN ES
| None | None |
b6d2ee25c9d9d682541ca70ff44517f258f1e804 | cdc | None | Monitoring human immunodeficiency virus type 1 (HIV-1) ribonucleic acid levels (also known as HIV viral load ) has become the standard of care for monitoring response to therapy in HIV-infected patients. In 1999, CDC published updated surveillance case definitions for HIV infection and acquired immunodeficiency syndrome (AIDS) reporting, including positive results of HIV-1 viral detection tests (CDC. Guidelines for national human immunodeficiency virus case surveillance, including monitoring for human immunodeficiency virus infection and acquired immunodeficiency syndrome. MMWR 1999;48:1-28). Since 1996, an increased number of public and private laboratories have begun performing viral load tests. Results obtained with available test methods are variable, and laboratories present these results in different ways, indicating that guidelines to promote standard practice in reporting of test results are warranted. This report provides guidelines for standardized reporting of viral load test results by licensed laboratories to health-care providers and facilities for public health case reporting of HIV infection and AIDS. Recommended standards were developed through data review, input involving a working group of physicians and laboratorians experienced in viral load testing, and an assessment of laboratory practices. These guidelines were discussed, refined, and endorsed at the annual Human Retrovirus and Hepatitis C Laboratory Testing Conference, held March 6-9, 2000, in Charlotte, North Carolina, with participation of representatives from public health, hospital, independent, and blood-collectionfacility laboratories. Adoption of these guidelines by all public and private laboratories that perform HIV viral load testing will improve the quality and usefulness of viral load test results for the physician ordering the test and for reporting to public health departments.# INTRODUCTION
Using highly active antiretroviral therapy (HAART) and monitoring therapy response by using viral load testing have contributed to clinical management of persons infected with human immunodeficiency virus (HIV) . Measurements of viral load and CD4 + lymphocytes are used to determine when antiretroviral therapy should be initiated and to monitor treatment efficacy (27)(28)(29)(30)(31)(32)(33)(34)(35). Since 1996, an increasing number of laboratories have been performing viral load tests. In 1999, CDC's Model Performance Evaluation Program (MPEP) conducted a laboratory questionnaire survey, which determined that 51% of the laboratories performing viral load tests had begun doing so in the previous 2 years and 37% had begun in the previous 3-4 years. No test reporting standardization exists; specifically, standard units of measurement of test method have not been established. Laboratory viral load test reports should be accurate and adequate for patient treatment and public health monitoring of the HIV and acquired immunodeficiency syndrome (AIDS) epidemic. To assure test reporting comparability among laboratories, standard methods are needed; moreover, standardized results are needed for early detection of infection, early access to patient care, and early detection of treatment failure.
On January 1, 2000, the CDC HIV-infection surveillance case definition was expanded to include viral load test results (34 ). HIV ribonucleic acid (RNA) viral load reporting is critical in monitoring patients' progression toward AIDS and response to HAART. For public health purposes, viral load reporting is key to expanding surveillance of HIVinfection reporting and improving monitoring of the epidemic. Surveillance programs for HIV/AIDS in the United States, specifically states initiating HIV-infection reporting, will rely on laboratory viral load test reporting to identify prevalent HIV infections among persons who are in care and receiving routine viral load monitoring. Test-reporting standardization will facilitate progress toward electronic laboratory reporting, which is key to increasing efficiency among disease surveillance programs.
On November 30, 1999, CDC convened a working group of physicians and laboratorians experienced in HIV testing and representing the Food and Drug Administration (FDA), the Association of Public Health Laboratories (APHL), and the College of American Pathologists to address standardization of laboratory reporting of HIV type 1 (HIV-1) viral load testing results. The working group reviewed information regarding variations in test reporting and interkit variation of test results. At the conclusion of this meeting, the working group developed recommendations, which were discussed, refined, and endorsed at the annual Human Retrovirus and Hepatitis C Laboratory Testing Conference, held March 6-9, 2000, in Charlotte, North Carolina, and sponsored by APHL, with participation of representatives from public health, hospital, independent, and bloodcollection-facility laboratories.- This report provides recommendations for standardizing viral load test reports from licensed laboratories to health-care providers and facilities and reporting HIV infection and AIDS cases for public health surveillance. These guidelines do not include a) recommendations for using viral load tests for clinical management, which are reported elsewhere (35,36 ); b) laboratory safety standards; c) specimen collection, transport, integrity, storage, processing, and analysis; d) data analysis, storage, and transmission; or quality assurance, which is also reported elsewhere (37 ).
# BACKGROUND Available Viral Load Tests
Three commercially available test kits are routinely used for detecting and quantitating HIV RNA in plasma, including a) the Roche ® Amplicor HIV-1 Monitor™ (Roche Diag- The methods these kits employ and their range of detection sensitivities are provided in this report (Table 1).
The Roche assay is based on a target amplification system and uses reverse transcriptase-polymerase chain reaction (RT-PCR) technology. This assay is available in two versions, 1.0 and 1.5. Version 1.0 is the standard assay and the only FDA-approved assay. The manufacturer has developed a method to increase the sensitivity of the standard assay, and this ultrasensitive method can be used only with version 1.0. Version 1.0 was developed for quantitation of HIV-1 subtype B, the predominant subtype in North America, whereas version 1.5 has been designed to improve equivalent quantitation of non-B subtypes. The Bayer assay, versions 2.0 and 3.0, are based on signal amplification that uses bDNA technology. The Organon Teknika assay is a transcription-based isothermal target amplification method employing nucleic acid sequence-based amplification (NASBA) technology. The NucliSens HIV-1 QT is the present version of the Organon Teknika assay.- Sensitivities of HIV viral load detection vary by test kit type. The Roche standard assay kit has a reportable range of 400-750,000 copies/mL of plasma, whereas the ultrasensitive method has a range of 50-75,000 copies/mL (38 ). Bayer assay versions 2.0 and 3.0 have a detection range of 500-1,600,000 and 50-500,000 copies/mL, respectively (39 ). The Organon Teknika's initial NASBA HIV-1 RNA QT detection range was 400-15,000,000 copies/mL, but the NucliSens HIV-1 QT has a detection range of 40-10,000,000 copies/mL (40 ).
# Laboratory Practices for HIV Viral Load Testing
In 1997, CDC's MPEP implemented an ongoing performance evaluation of laboratories that perform viral load testing. Coded plasma samples of varying RNA levels, which have been obtained from individual- HIV-1 infected and uninfected donors, are frozen and mailed to approximately 200 MPEP participating laboratories. The laboratories are asked to test the samples in the same manner they test routine or clinical specimens and to provide MPEP with test results, test kit manufacturer information, test control/ calibrators/standards results, and quality-control practices. To assess intrashipment reproducibility, selected samples in a panel are duplicated. To assess intershipment reproducibility, all samples in each of two subsequent (i.e., replicate) shipments are identical, except that the vial labeling and sequence are changed so that laboratories will not receive samples containing the same coding or coding within an identical sequence as the original survey. Before each survey, donor samples are characterized by reference laboratories that use kits manufactured by Roche, Bayer, and Organon Teknika.
The distribution of laboratory types voluntarily participating in MPEP remained approximately the same during June 1997-February 2000 and included hospitals (52%), independent laboratories (20.5%), health departments (17%), others (10%), and blood banks (0.5%). Approximately 70% of the participating laboratories used the Roche kit in all six survey periods; 22% used a Bayer kit; 6% used an Organon Teknika kit; and 2% used an in-house-developed kit. Of the laboratories using the Roche Amplicor HIV-1 Monitor kit, approximately 25% indicated they had begun using the ultrasensitive procedure. By the last two surveys, all laboratories using the Bayer kit were using the Bayer HIV-1 RNA 3.0 Assay (bDNA); among the nine laboratories using an Organon Teknika kit, all but one were using the NucliSens HIV-1 QT kit.
To provide information regarding the variability among laboratory test reporting, results from within test kit manufacturers and within each survey during the six survey periods were examined (Table 2). The median values determined from duplicate sample testing results were reproducible, although variability occurred among the results reported by laboratories using the same test kit and testing the same donor samples (i.e., the duplicate) within a survey or the same donor sample (i.e., the replicate) used in a later survey. When the minimum and maximum values of the reported results were examined for laboratories using the Roche Amplicor HIV-1 Monitor kit, the log difference ranged from 0.8 to 2.2. Similarly, examination of the minimum and maximum reported values for laboratories using the Organon Teknika NucliSens HIV-1 QT kit demonstrated a log difference range of 0.3-0.6. In comparison, a 0.5-log difference occurred within the minimum and maximum reported results from laboratories using the Bayer HIV-1 RNA 3.0 Assay (bDNA), which was the observed difference with all results reported for the same donor sample within and among survey periods (Table 2). Among test kit manufacturers, the *Samples are obtained from individual donors; samples from different donors are not pooled, and individual samples are not diluted. median values determined from results reported by laboratories using the Roche Amplicor HIV-1 Monitor and Organon Teknika NucliSens HIV-1 QT were consistently higher than the median values determined from testing results reported by laboratories using the Bayer HIV-1 RNA 3.0 Quantitative Assay (bDNA). This observation was true only for the original sample in a survey and its duplicate. For the same sample used in a later survey (i.e., the replicate), this observation was not true. Instead, good reproducibility- existed among the values reported for the replicate sample by laboratories using all three manufacturers' test kits. For these surveys, more laboratories use the Roche Amplicor HIV-1 Monitor test kit than the other two kits. If the number of laboratories using the other test kits matched the number of laboratories using the Roche Amplicor HIV-1 Monitor, the range in log difference for results reported by laboratories using the other two test kits would probably increase.
# Variation Among Laboratory Viral Load Test Reports
To understand laboratory practices regarding HIV viral load test reporting, a telephone survey was conducted by San Diego State University (SDSU), under a cooperative agreement with CDC, of randomly selected laboratories from three source groups: medical schools, national commercial laboratories, and laboratories participating in CDC MPEP. Laboratorians who are knowledgeable regarding HIV testing were interviewed, and respondents were asked to fax or mail a copy of a negative and positive HIV RNA report without patient identifiers.
A total of 212/279 (76%) telephone surveys were completed; of these, 112 (52.8%) respondents performed HIV RNA testing. Of the respondents performing HIV RNA testing, 3 (2.7%) were blood banks; 69 (61.6%) were hospitals; 11 (9.8%) were health departments; 24 (21.4%) were independent laboratories; and 5 (4.5%) were other laboratory types. Among the 112 respondents, (76.8%) used the Roche Amplicor HIV-1 Monitor; 27 (24.1%) used the Bayer HIV-1 RNA 3.0 Quantitative Assay (bDNA); 11 (9.8%) used the Organon Teknika NucliSens HIV-1 QT kit; and 6 (5.4%) used other methods (e.g., Digene™ and in-house-developed reagents). Multiple test kits were used by 15/112 (13.4%) responding laboratories. A total of 37 different laboratories, 9 (24.3%) independent, 7 (18.9%) health department, 19 (51.4%) hospital, and 2 (5.4%) other laboratories furnished HIV RNA test reports. Of these 37 laboratories, all results were reported in copies/ mL; 5 (13.5%) reported in both copies/mL and log 10 transformation.
Laboratories used different terminology to specify test limits, including the terms linear range, reportable range, sensitivity level, detection levels or limits, and assay limits. Using >1 terms, 26/37 (70.3%) laboratories specified the test kit's lower limits; 12 (32.4%) reported upper limits; and 11 did not provide test limits. One laboratory that specified both a lower limit and an upper limit when results were outside test kit limits did not report the test limits when the results were within the test limit range. When the result was outside the test limits, the report stated that the linear response range for the Roche Amplicor HIV-1 Monitor Test was determined to be within 400-750,000 HIV-1 RNA copies/mL, which is the linear range stated in the manufacturer's insert (38 ). However, when results were within test limits, the laboratory did not provide the statement indicating the manufacturer's linear range, which indicated information inconsistency among test reports.
In certain cases, laboratory slips indicated that HIV had been detected at a value below the test's lower limit (e.g., HIV detected was <400 copies/mL), or the laboratory slip provided an actual number of copies outside of the stated reportable range. The test kit used was reported on the test report form by 9/37 (24.3%) laboratories. Examples of items appearing on the test reports that could introduce difficulty in interpreting test results are provided in this report (Box).
- Assay detection limits not provided.
# BOX. Items appearing on the human immunodeficiency virus type 1 viral load test reports- that could cause difficulty in interpreting results
# RECOMMENDATIONS
The following recommendations were endorsed at the Human Retrovirus and Hepatitis C Laboratory Testing Conference (sponsored by APHL), held March 6-9, 2000, in Charlotte, North Carolina. Good laboratory practice- requires that a discrete patient identifier be provided to the laboratory with each specimen submitted for retrovirus testing. Because laboratory reporting is critical to public health practice, information regarding date of birth, sex, and racial/ethnic group should be included on the test report form when available. Moreover, the laboratory report should be concise.
# Required Items To Report
The following items must be included on the report form:
- Correct nomenclature for retroviruses.
- Name and address of the laboratory that performed the test.
- Date of specimen collection and receipt and report date.
- Identification of specimens having doubtful quality.
- Test kit name, manufacturer, and version.
- If required, correct wording regarding analyte specific reagents (ASR).
- Results obtained (laboratories must report test results according to the reportable range specified in the manufacturer's package insert and should not report values outside that range).
-Results must be reported as a value in copies/mL and log 10 transformation (e.g., 500,000 copies/mL and log 10 = 5.7).
-When the result is below the test's lower detection limit, the result must be reported as less than the lower limit of quantification for the test kit being used (e.g., <400 copies/mL or <50 copies/mL).
-When the result is above the upper detection limit, the result must be reported as greater than the upper limit of quantification for the test kit being used (e.g., >750,000 copies/mL or >500,000 copies/mL).
# Optional Items To Report
The following items are optional for test report forms:
- Disclaimer stating that the test should not be used for unintended purposes.
- Changes from patient's baseline and previous viral load values.
- Narrative explanations or results interpretation.
*Good laboratory practice is defined as an acceptable way to perform a basic activity that is known to influence the quality of its output (Source: Taylor JK. Good laboratory and good measurement practices. In: Quality assurance of chemical measurements. Chelsea, MI: Lewis Publishers, Inc., 1987;112-3.)
# MMWR November 16, 2001
- Reportable ranges, as specified in the manufacturer's package insert.
- Statements regarding clinical consequences of recognizing variability among assays.
# Items Not To Be Included on Reports
The following items should not be included on the report form:
- Nonstandard abbreviations, clichés, and jargon.
- Statements regarding the sensitivity or specificity of results.
- Statements regarding confidentiality.
- Statements regarding AIDS.
- Statements regarding counseling.
- Information regarding primer, optical density, dilution factor, or preparation method or assay number used.
- Prefinal results that require manipulations to obtain final results.
# DISCUSSION
Although results from laboratories that use the three commercially produced assays are strongly correlated, the absolute values of HIV viral load measured in the same plasma sample by using two different assays can differ by >2-fold. Data from the MPEP performance surveys demonstrate these differences and illustrate the need for continued surveillance of manufactured tests and laboratory performance. Until a common standard is available to use for normalizing values obtained with different assay methods, choosing one assay method is advisable when HIV RNA levels are monitored to guide therapeutic decision-making. The goal to develop a common standard for normalizing values obtained with different test kits has recently been reported (41 ). In that study, 26 laboratories, representing 10 different countries, collaborated in establishing the first international standard for HIV-1 RNA that can be used for nucleic acid-based techniques. According to the SDSU survey of laboratory practices, <50% of the laboratories indicated on the results slip what test had been used. Because this information is used to interpret results, whether for clinical care or public health purposes, assay methods and test kit manufacturers should be noted on all viral load test reports.
SDSU's survey indicated that all laboratories reported results in copies/mL, and certain laboratories also provided log 10 transformation. Although changes can be monitored by using either absolute or log 10 values, absolute values are used to determine therapy initiation. In addition, results expressed in both copies/mL and log 10 might be useful to health-care providers; therefore, reporting both is strongly recommended.
Available tests are not licensed for diagnosing HIV infection, but the viral load test results are used for reporting HIV infection to local and state health departments (34 ). Although future versions of these tests might be licensed for diagnostic purposes, healthcare providers should be aware that available viral load tests are only useful for monitoring clinical status after an HIV diagnosis (35 ).
Available test kits perform differently in detecting non-B subtypes (42)(43)(44)(45)(46)(47)(48). In the United States, the Roche Amplicor HIV-1 Monitor version 1.0 is the most popular test for determining viral load. However, it underdetects and underestimates non-B subtypes (e.g., A, E, F, and G) when quantifying viral load (42)(43)(44)(45)(46)(47). The Bayer HIV-1 RNA 3.0 Quantitative Assay (bDNA) probably quantifies RNA of different HIV-1 subtypes accurately as a result of redundancy of multiple probes (43)(44)(45). The Organon Teknika NucliSens HIV-1 QT assay also underdetects and underestimates divergent subtypes (e.g., A and E) (43)(44)(45). All assays have problems amplifying HIV-1 group O and do not amplify HIV-2. The Roche Monitor version 1.5 kit uses a new set of probes and primers that reportedly detect and quantitate non-B subtypes with greater efficiency than the previous version (42)(43)(44)(45)(46).
Plasma HIV RNA level provides a valid measure of antiretroviral therapy efficacy for HIV-infected persons. Antiretroviral therapy suppression of HIV RNA level followed by rebound levels might signal the emergence of drug-resistant HIV variants, suboptimal adherence to the antiretroviral therapy regimen, decreased absorption of antiretroviral drugs, altered drug metabolism because of physiologic changes, drug interactions, vaccinations, or concurrent infections. An HIV RNA level might be transiently elevated among patients on therapy; the consequences of such elevations is unknown. HIV RNA levels can vary by approximately threefold (0.5 log 10 ) in either direction upon repeated measurements among clinically stable, HIV-infected persons. Changes >0.5 log 10 usually cannot be explained by inherent biological or assay variability and likely reflect a biologically and clinically relevant change in the level of plasma HIV RNA. However, plasma HIV RNA assays vary greater toward the lower limits of sensitivity. Thus, differences between repeated measures of >0.5 log 10 might occur at low plasma HIV RNA values and might not reflect a substantive biological or clinical change.
Viral load reporting has implications for clinical care and HIV/AIDS surveillance. State public health programs are implementing recommendations by the Council of State and Territorial Epidemiologists and CDC for nationwide HIV surveillance, including reporting detectable RNA viral loads (34 ). As part of this reporting, laboratories and health-care providers would be required to report HIV-infection cases to state and territorial health departments. Standard methods are needed for viral load test reporting to providers and health departments so that clinicians and public health professionals will have a common language to use in conducting patient care and monitoring the epidemic.
To facilitate developing that common language, CDC and the Council of State and Territorial Epidemiologists recommend that all states adopt rules or regulations to require reporting of detectable viral loads to public health departments. One state requires reporting of undetectable viral load results based on the lower limit sensitivities of the manufactured kits, but then follows up with health-care providers to document whether the patient has other test results or clinical evidence indicative of infection with HIV. Reporting of viral load test results by using standard nomenclature, test results presentation, and electronic data transfer will permit reporting of HIV cases in a way that is compatible with electronic laboratory efforts being developed for national notifiable disease reporting (49 ).
All MMWR references are available on the Internet at . Use the search function to find specific articles.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services.
# MMWR The Morbidity and Mortality Weekly Report (MMWR) Series is prepared by the Centers for Disease Control and Prevention (CDC) and is available free of charge in electronic format and on a paid subscription basis for paper copy. To receive an electronic copy on | Monitoring human immunodeficiency virus type 1 (HIV-1) ribonucleic acid levels (also known as HIV viral load ) has become the standard of care for monitoring response to therapy in HIV-infected patients. In 1999, CDC published updated surveillance case definitions for HIV infection and acquired immunodeficiency syndrome (AIDS) reporting, including positive results of HIV-1 viral detection tests (CDC. Guidelines for national human immunodeficiency virus case surveillance, including monitoring for human immunodeficiency virus infection and acquired immunodeficiency syndrome. MMWR 1999;48[No. RR-13]:1-28). Since 1996, an increased number of public and private laboratories have begun performing viral load tests. Results obtained with available test methods are variable, and laboratories present these results in different ways, indicating that guidelines to promote standard practice in reporting of test results are warranted. This report provides guidelines for standardized reporting of viral load test results by licensed laboratories to health-care providers and facilities for public health case reporting of HIV infection and AIDS. Recommended standards were developed through data review, input involving a working group of physicians and laboratorians experienced in viral load testing, and an assessment of laboratory practices. These guidelines were discussed, refined, and endorsed at the annual Human Retrovirus and Hepatitis C Laboratory Testing Conference, held March 6-9, 2000, in Charlotte, North Carolina, with participation of representatives from public health, hospital, independent, and blood-collectionfacility laboratories. Adoption of these guidelines by all public and private laboratories that perform HIV viral load testing will improve the quality and usefulness of viral load test results for the physician ordering the test and for reporting to public health departments.# INTRODUCTION
Using highly active antiretroviral therapy (HAART) and monitoring therapy response by using viral load testing have contributed to clinical management of persons infected with human immunodeficiency virus (HIV) . Measurements of viral load and CD4 + lymphocytes are used to determine when antiretroviral therapy should be initiated and to monitor treatment efficacy (27)(28)(29)(30)(31)(32)(33)(34)(35). Since 1996, an increasing number of laboratories have been performing viral load tests. In 1999, CDC's Model Performance Evaluation Program (MPEP) conducted a laboratory questionnaire survey, which determined that 51% of the laboratories performing viral load tests had begun doing so in the previous 2 years and 37% had begun in the previous 3-4 years. No test reporting standardization exists; specifically, standard units of measurement of test method have not been established. Laboratory viral load test reports should be accurate and adequate for patient treatment and public health monitoring of the HIV and acquired immunodeficiency syndrome (AIDS) epidemic. To assure test reporting comparability among laboratories, standard methods are needed; moreover, standardized results are needed for early detection of infection, early access to patient care, and early detection of treatment failure.
On January 1, 2000, the CDC HIV-infection surveillance case definition was expanded to include viral load test results (34 ). HIV ribonucleic acid (RNA) viral load reporting is critical in monitoring patients' progression toward AIDS and response to HAART. For public health purposes, viral load reporting is key to expanding surveillance of HIVinfection reporting and improving monitoring of the epidemic. Surveillance programs for HIV/AIDS in the United States, specifically states initiating HIV-infection reporting, will rely on laboratory viral load test reporting to identify prevalent HIV infections among persons who are in care and receiving routine viral load monitoring. Test-reporting standardization will facilitate progress toward electronic laboratory reporting, which is key to increasing efficiency among disease surveillance programs.
On November 30, 1999, CDC convened a working group of physicians and laboratorians experienced in HIV testing and representing the Food and Drug Administration (FDA), the Association of Public Health Laboratories (APHL), and the College of American Pathologists to address standardization of laboratory reporting of HIV type 1 (HIV-1) viral load testing results. The working group reviewed information regarding variations in test reporting and interkit variation of test results. At the conclusion of this meeting, the working group developed recommendations, which were discussed, refined, and endorsed at the annual Human Retrovirus and Hepatitis C Laboratory Testing Conference, held March 6-9, 2000, in Charlotte, North Carolina, and sponsored by APHL, with participation of representatives from public health, hospital, independent, and bloodcollection-facility laboratories.* This report provides recommendations for standardizing viral load test reports from licensed laboratories to health-care providers and facilities and reporting HIV infection and AIDS cases for public health surveillance. These guidelines do not include a) recommendations for using viral load tests for clinical management, which are reported elsewhere (35,36 ); b) laboratory safety standards; c) specimen collection, transport, integrity, storage, processing, and analysis; d) data analysis, storage, and transmission; or quality assurance, which is also reported elsewhere (37 ).
# BACKGROUND Available Viral Load Tests
Three commercially available test kits are routinely used for detecting and quantitating HIV RNA in plasma, including a) the Roche ® Amplicor HIV-1 Monitor™ (Roche Diag- The methods these kits employ and their range of detection sensitivities are provided in this report (Table 1).
The Roche assay is based on a target amplification system and uses reverse transcriptase-polymerase chain reaction (RT-PCR) technology. This assay is available in two versions, 1.0 and 1.5. Version 1.0 is the standard assay and the only FDA-approved assay. The manufacturer has developed a method to increase the sensitivity of the standard assay, and this ultrasensitive method can be used only with version 1.0. Version 1.0 was developed for quantitation of HIV-1 subtype B, the predominant subtype in North America, whereas version 1.5 has been designed to improve equivalent quantitation of non-B subtypes. The Bayer assay, versions 2.0 and 3.0, are based on signal amplification that uses bDNA technology. The Organon Teknika assay is a transcription-based isothermal target amplification method employing nucleic acid sequence-based amplification (NASBA) technology. The NucliSens HIV-1 QT is the present version of the Organon Teknika assay.* Sensitivities of HIV viral load detection vary by test kit type. The Roche standard assay kit has a reportable range of 400-750,000 copies/mL of plasma, whereas the ultrasensitive method has a range of 50-75,000 copies/mL (38 ). Bayer assay versions 2.0 and 3.0 have a detection range of 500-1,600,000 and 50-500,000 copies/mL, respectively (39 ). The Organon Teknika's initial NASBA HIV-1 RNA QT detection range was 400-15,000,000 copies/mL, but the NucliSens HIV-1 QT has a detection range of 40-10,000,000 copies/mL (40 ).
# Laboratory Practices for HIV Viral Load Testing
In 1997, CDC's MPEP implemented an ongoing performance evaluation of laboratories that perform viral load testing. Coded plasma samples of varying RNA levels, which have been obtained from individual* HIV-1 infected and uninfected donors, are frozen and mailed to approximately 200 MPEP participating laboratories. The laboratories are asked to test the samples in the same manner they test routine or clinical specimens and to provide MPEP with test results, test kit manufacturer information, test control/ calibrators/standards results, and quality-control practices. To assess intrashipment reproducibility, selected samples in a panel are duplicated. To assess intershipment reproducibility, all samples in each of two subsequent (i.e., replicate) shipments are identical, except that the vial labeling and sequence are changed so that laboratories will not receive samples containing the same coding or coding within an identical sequence as the original survey. Before each survey, donor samples are characterized by reference laboratories that use kits manufactured by Roche, Bayer, and Organon Teknika.
The distribution of laboratory types voluntarily participating in MPEP remained approximately the same during June 1997-February 2000 and included hospitals (52%), independent laboratories (20.5%), health departments (17%), others (10%), and blood banks (0.5%). Approximately 70% of the participating laboratories used the Roche kit in all six survey periods; 22% used a Bayer kit; 6% used an Organon Teknika kit; and 2% used an in-house-developed kit. Of the laboratories using the Roche Amplicor HIV-1 Monitor kit, approximately 25% indicated they had begun using the ultrasensitive procedure. By the last two surveys, all laboratories using the Bayer kit were using the Bayer HIV-1 RNA 3.0 Assay (bDNA); among the nine laboratories using an Organon Teknika kit, all but one were using the NucliSens HIV-1 QT kit.
To provide information regarding the variability among laboratory test reporting, results from within test kit manufacturers and within each survey during the six survey periods were examined (Table 2). The median values determined from duplicate sample testing results were reproducible, although variability occurred among the results reported by laboratories using the same test kit and testing the same donor samples (i.e., the duplicate) within a survey or the same donor sample (i.e., the replicate) used in a later survey. When the minimum and maximum values of the reported results were examined for laboratories using the Roche Amplicor HIV-1 Monitor kit, the log difference ranged from 0.8 to 2.2. Similarly, examination of the minimum and maximum reported values for laboratories using the Organon Teknika NucliSens HIV-1 QT kit demonstrated a log difference range of 0.3-0.6. In comparison, a 0.5-log difference occurred within the minimum and maximum reported results from laboratories using the Bayer HIV-1 RNA 3.0 Assay (bDNA), which was the observed difference with all results reported for the same donor sample within and among survey periods (Table 2). Among test kit manufacturers, the *Samples are obtained from individual donors; samples from different donors are not pooled, and individual samples are not diluted. median values determined from results reported by laboratories using the Roche Amplicor HIV-1 Monitor and Organon Teknika NucliSens HIV-1 QT were consistently higher than the median values determined from testing results reported by laboratories using the Bayer HIV-1 RNA 3.0 Quantitative Assay (bDNA). This observation was true only for the original sample in a survey and its duplicate. For the same sample used in a later survey (i.e., the replicate), this observation was not true. Instead, good reproducibility* existed among the values reported for the replicate sample by laboratories using all three manufacturers' test kits. For these surveys, more laboratories use the Roche Amplicor HIV-1 Monitor test kit than the other two kits. If the number of laboratories using the other test kits matched the number of laboratories using the Roche Amplicor HIV-1 Monitor, the range in log difference for results reported by laboratories using the other two test kits would probably increase.
# Variation Among Laboratory Viral Load Test Reports
To understand laboratory practices regarding HIV viral load test reporting, a telephone survey was conducted by San Diego State University (SDSU), under a cooperative agreement with CDC, of randomly selected laboratories from three source groups: medical schools, national commercial laboratories, and laboratories participating in CDC MPEP. Laboratorians who are knowledgeable regarding HIV testing were interviewed, and respondents were asked to fax or mail a copy of a negative and positive HIV RNA report without patient identifiers.
A total of 212/279 (76%) telephone surveys were completed; of these, 112 (52.8%) respondents performed HIV RNA testing. Of the respondents performing HIV RNA testing, 3 (2.7%) were blood banks; 69 (61.6%) were hospitals; 11 (9.8%) were health departments; 24 (21.4%) were independent laboratories; and 5 (4.5%) were other laboratory types. Among the 112 respondents, (76.8%) used the Roche Amplicor HIV-1 Monitor; 27 (24.1%) used the Bayer HIV-1 RNA 3.0 Quantitative Assay (bDNA); 11 (9.8%) used the Organon Teknika NucliSens HIV-1 QT kit; and 6 (5.4%) used other methods (e.g., Digene™ and in-house-developed reagents). Multiple test kits were used by 15/112 (13.4%) responding laboratories. A total of 37 different laboratories, 9 (24.3%) independent, 7 (18.9%) health department, 19 (51.4%) hospital, and 2 (5.4%) other laboratories furnished HIV RNA test reports. Of these 37 laboratories, all results were reported in copies/ mL; 5 (13.5%) reported in both copies/mL and log 10 transformation.
Laboratories used different terminology to specify test limits, including the terms linear range, reportable range, sensitivity level, detection levels or limits, and assay limits. Using >1 terms, 26/37 (70.3%) laboratories specified the test kit's lower limits; 12 (32.4%) reported upper limits; and 11 did not provide test limits. One laboratory that specified both a lower limit and an upper limit when results were outside test kit limits did not report the test limits when the results were within the test limit range. When the result was outside the test limits, the report stated that the linear response range for the Roche Amplicor HIV-1 Monitor Test was determined to be within 400-750,000 HIV-1 RNA copies/mL, which is the linear range stated in the manufacturer's insert (38 ). However, when results were within test limits, the laboratory did not provide the statement indicating the manufacturer's linear range, which indicated information inconsistency among test reports.
In certain cases, laboratory slips indicated that HIV had been detected at a value below the test's lower limit (e.g., HIV detected was <400 copies/mL), or the laboratory slip provided an actual number of copies outside of the stated reportable range. The test kit used was reported on the test report form by 9/37 (24.3%) laboratories. Examples of items appearing on the test reports that could introduce difficulty in interpreting test results are provided in this report (Box).
• Assay detection limits not provided.
# BOX. Items appearing on the human immunodeficiency virus type 1 viral load test reports* that could cause difficulty in interpreting results
# RECOMMENDATIONS
The following recommendations were endorsed at the Human Retrovirus and Hepatitis C Laboratory Testing Conference (sponsored by APHL), held March 6-9, 2000, in Charlotte, North Carolina. Good laboratory practice* requires that a discrete patient identifier be provided to the laboratory with each specimen submitted for retrovirus testing. Because laboratory reporting is critical to public health practice, information regarding date of birth, sex, and racial/ethnic group should be included on the test report form when available. Moreover, the laboratory report should be concise.
# Required Items To Report
The following items must be included on the report form:
• Correct nomenclature for retroviruses.
• Name and address of the laboratory that performed the test.
• Date of specimen collection and receipt and report date.
• Identification of specimens having doubtful quality.
• Test kit name, manufacturer, and version.
• If required, correct wording regarding analyte specific reagents (ASR).
• Results obtained (laboratories must report test results according to the reportable range specified in the manufacturer's package insert and should not report values outside that range).
-Results must be reported as a value in copies/mL and log 10 transformation (e.g., 500,000 copies/mL and log 10 = 5.7).
-When the result is below the test's lower detection limit, the result must be reported as less than the lower limit of quantification for the test kit being used (e.g., <400 copies/mL or <50 copies/mL).
-When the result is above the upper detection limit, the result must be reported as greater than the upper limit of quantification for the test kit being used (e.g., >750,000 copies/mL or >500,000 copies/mL).
# Optional Items To Report
The following items are optional for test report forms:
• Disclaimer stating that the test should not be used for unintended purposes.
• Changes from patient's baseline and previous viral load values.
• Narrative explanations or results interpretation.
*Good laboratory practice is defined as an acceptable way to perform a basic activity that is known to influence the quality of its output (Source: Taylor JK. Good laboratory and good measurement practices. In: Quality assurance of chemical measurements. Chelsea, MI: Lewis Publishers, Inc., 1987;112-3.)
# MMWR November 16, 2001
• Reportable ranges, as specified in the manufacturer's package insert.
• Statements regarding clinical consequences of recognizing variability among assays.
# Items Not To Be Included on Reports
The following items should not be included on the report form:
• Nonstandard abbreviations, clichés, and jargon.
• Statements regarding the sensitivity or specificity of results.
• Statements regarding confidentiality.
• Statements regarding AIDS.
• Statements regarding counseling.
• Information regarding primer, optical density, dilution factor, or preparation method or assay number used.
• Prefinal results that require manipulations to obtain final results.
# DISCUSSION
Although results from laboratories that use the three commercially produced assays are strongly correlated, the absolute values of HIV viral load measured in the same plasma sample by using two different assays can differ by >2-fold. Data from the MPEP performance surveys demonstrate these differences and illustrate the need for continued surveillance of manufactured tests and laboratory performance. Until a common standard is available to use for normalizing values obtained with different assay methods, choosing one assay method is advisable when HIV RNA levels are monitored to guide therapeutic decision-making. The goal to develop a common standard for normalizing values obtained with different test kits has recently been reported (41 ). In that study, 26 laboratories, representing 10 different countries, collaborated in establishing the first international standard for HIV-1 RNA that can be used for nucleic acid-based techniques. According to the SDSU survey of laboratory practices, <50% of the laboratories indicated on the results slip what test had been used. Because this information is used to interpret results, whether for clinical care or public health purposes, assay methods and test kit manufacturers should be noted on all viral load test reports.
SDSU's survey indicated that all laboratories reported results in copies/mL, and certain laboratories also provided log 10 transformation. Although changes can be monitored by using either absolute or log 10 values, absolute values are used to determine therapy initiation. In addition, results expressed in both copies/mL and log 10 might be useful to health-care providers; therefore, reporting both is strongly recommended.
Available tests are not licensed for diagnosing HIV infection, but the viral load test results are used for reporting HIV infection to local and state health departments (34 ). Although future versions of these tests might be licensed for diagnostic purposes, healthcare providers should be aware that available viral load tests are only useful for monitoring clinical status after an HIV diagnosis (35 ).
Available test kits perform differently in detecting non-B subtypes (42)(43)(44)(45)(46)(47)(48). In the United States, the Roche Amplicor HIV-1 Monitor version 1.0 is the most popular test for determining viral load. However, it underdetects and underestimates non-B subtypes (e.g., A, E, F, and G) when quantifying viral load (42)(43)(44)(45)(46)(47). The Bayer HIV-1 RNA 3.0 Quantitative Assay (bDNA) probably quantifies RNA of different HIV-1 subtypes accurately as a result of redundancy of multiple probes (43)(44)(45). The Organon Teknika NucliSens HIV-1 QT assay also underdetects and underestimates divergent subtypes (e.g., A and E) (43)(44)(45). All assays have problems amplifying HIV-1 group O and do not amplify HIV-2. The Roche Monitor version 1.5 kit uses a new set of probes and primers that reportedly detect and quantitate non-B subtypes with greater efficiency than the previous version (42)(43)(44)(45)(46).
Plasma HIV RNA level provides a valid measure of antiretroviral therapy efficacy for HIV-infected persons. Antiretroviral therapy suppression of HIV RNA level followed by rebound levels might signal the emergence of drug-resistant HIV variants, suboptimal adherence to the antiretroviral therapy regimen, decreased absorption of antiretroviral drugs, altered drug metabolism because of physiologic changes, drug interactions, vaccinations, or concurrent infections. An HIV RNA level might be transiently elevated among patients on therapy; the consequences of such elevations is unknown. HIV RNA levels can vary by approximately threefold (0.5 log 10 ) in either direction upon repeated measurements among clinically stable, HIV-infected persons. Changes >0.5 log 10 usually cannot be explained by inherent biological or assay variability and likely reflect a biologically and clinically relevant change in the level of plasma HIV RNA. However, plasma HIV RNA assays vary greater toward the lower limits of sensitivity. Thus, differences between repeated measures of >0.5 log 10 might occur at low plasma HIV RNA values and might not reflect a substantive biological or clinical change.
Viral load reporting has implications for clinical care and HIV/AIDS surveillance. State public health programs are implementing recommendations by the Council of State and Territorial Epidemiologists and CDC for nationwide HIV surveillance, including reporting detectable RNA viral loads (34 ). As part of this reporting, laboratories and health-care providers would be required to report HIV-infection cases to state and territorial health departments. Standard methods are needed for viral load test reporting to providers and health departments so that clinicians and public health professionals will have a common language to use in conducting patient care and monitoring the epidemic.
To facilitate developing that common language, CDC and the Council of State and Territorial Epidemiologists recommend that all states adopt rules or regulations to require reporting of detectable viral loads to public health departments. One state requires reporting of undetectable viral load results based on the lower limit sensitivities of the manufactured kits, but then follows up with health-care providers to document whether the patient has other test results or clinical evidence indicative of infection with HIV. Reporting of viral load test results by using standard nomenclature, test results presentation, and electronic data transfer will permit reporting of HIV cases in a way that is compatible with electronic laboratory efforts being developed for national notifiable disease reporting (49 ).
#
All MMWR references are available on the Internet at <http://www.cdc.gov/mmwr/>. Use the search function to find specific articles.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services.
# MMWR The Morbidity and Mortality Weekly Report (MMWR) Series is prepared by the Centers for Disease Control and Prevention (CDC) and is available free of charge in electronic format and on a paid subscription basis for paper copy. To receive an electronic copy on
| None | None |
af16f2bf999592e6cda5a574da89e1601fcb8391 | cdc | None | World No-Tobacco Day is May 31, 2001. The theme, "Second-Hand Smoke Kills-Let's Clear the Air," was designated by the World Health Organization (WHO) to raise awareness of the hazards of exposure to second-hand smoke. Tobacco use worldwide will cause an estimated 10 million deaths annually by 2030 (1 ). An effective strategy to promote and encourage tobacco-free policies is to link them with sporting events. Such policies also reduce nonsmokers' exposure to second-hand smoke (2 ). The 1988 Olympic Winter Games in Calgary, Alberta, Canada, was the first tobacco-free Olympics. Since then, all of the Olympic Games have had tobacco-free policies (3 ). For the 2002 games, the Olympic organizing committee for Salt Lake City, Utah, will implement a public information campaign using Olympic athletes to promote healthy lifestyles and sports as an alternative to tobacco use. Plans also include information to increase awareness of the tobacco-free policy among visitors, media, athletes, and officials from participating countries. Another media campaign is "Tobacco Kills-Don't Be Duped," which aims to ban tobacco advertising and promotion at sporting events globally. Additional information about World No-Tobacco Day 2001 is available at *, and http:// www.cdc.gov/tobacco; telephone (800) 232-1311. References 1. World Health Organization. Combating the tobacco epidemic. World Health Organization's world health report 1999. Geneva, Switzerland: World Health Organization, 1999:6579. 2. CDC. National report on human exposure to environmental chemicals. Atlanta, Georgia:#
- Persons aged >18 years who reported having smoked >100 cigarettes in their entire life and who reported smoking every day or some days. † Confidence interval. § Significant value: two-tailed p<0.05.
# MMWR May 25, 2001
Tobacco Use Among Adults -Continued Asked about smoking and advised to stop smoking by a dentist? 9.9 (±4.5) 24.9 (±4.7) ¶ - Persons aged >18 years who reported having smoked >100 cigarettes in their entire life and who reported smoking every day or some days. † Confidence interval. § Includes physicians, nurse practitioners, or physician assistants. ¶ Significant value: two-tailed p<0.05. Asked of respondents who visited a dentist during the year preceding the survey. Editorial Note: The results of the 1996 and 1999 Arizona ATS indicate that the prevalence of cigarette use among Arizona adults decreased substantially following the implementation of the statewide Arizona TEPP. The decrease in smoking prevalence among low income and low education groups also indicates a narrowing in disparities in cigarette use.
TEPP directed many of its activities toward Hispanics, which may, in part, explain the substantial decrease in cigarette smoking in that population. TEPP serves the Hispanic population through its Spanish language statewide media campaign and telephone helpline and through local cessation and prevention services. TEPP uses methods appropriate for this population, including Promotoras de Salud (lay health workers) and culturally appropriate materials and curricula.
The Arizona ATS results also showed a substantial increase in the proportion of smokers who reported that either a health-care provider or a dentist both asked about tobacco use and advised them to quit. Health-care providers can play a key role in assisting MMWR 405
Tobacco Use Among Adults -Continued patients to quit smoking (2 ), and brief physician advice substantially increases successful quitting (2 ). TEPP, through statewide and local projects, provides training for healthcare providers to increase the number of patients with whom they briefly discuss stopping smoking. The findings in this report are subject to at least five limitations. First, it is difficult to separate the effects of TEPP from price increases. The cigarette tax in Arizona increased from $0.18 to $0.58 per pack in November 1994, which may have contributed to the decline in adult smoking prevalence. Although the tax increase occurred more than a year before the first survey, the average retail price of cigarettes in Arizona continued to increase from $2.08 in 1996 to $2.50 in 1999 (3 ). Second, some segments of the population in Arizona, including some low income residents, are more likely than others to lack telephone service and therefore not be included in the study sample. Third, the response rate in 1999 was almost nine percentage points lower than the response rate in 1996, which may have influenced the results. Fourth, health-care provider communication data about smoking was based on self-reported recall for an entire year; the validity of these self-reports was not determined. Finally, although declines in smoking rates in Arizona may be a result of TEPP, a cause-and-effect relation cannot be established by comparing data from the cross-sectional ATS surveys alone. Comparing Arizona smoking prevalence trends and trends in other states with varying levels of interventions during 1996-1999 could help to determine how much of the decline may be related to the Arizona TEPP rather than to regional or national influences.
Arizona is one of seven states that meet CDC's funding recommendations for FY 2001 (4,5 ). The Arizona TEPP incorporates all nine components of a comprehensive tobaccocontrol program as recommended by CDC (4 ). The program added a certification program for smoking cessation counselors. The Arizona TEPP has been implementing strategies recommended in the Surgeon General's report Reducing Tobacco Use (6 ), CDC's Best Practices for Comprehensive Tobacco Control Programs (4 ), the Clinical Practice Guidelines for Treating Tobacco Use and Dependence (2 ), and the Task Force on Community Preventive Services (7 ). The findings of the 1996 and 1999 Arizona ATS suggest that an adequately funded and comprehensive program can substantially reduce tobacco use overall and across diverse demographic groups. Recent reports from California indicate that sustaining such a program for at least 9 years also could result in reductions in lung and bronchial cancer and coronary heart disease rates (8,9 ). Attainment of the 2010 national health objective (10 ) to reduce adult smoking rates to <12% will require similar programs to be implemented across the United States.
# MMWR May 25, 2001
Tobacco Use Among Adults -Continued
# Protracted Outbreaks of Cryptosporidiosis Associated With Swimming Pool Use -Ohio and Nebraska, 2000
Swimming is the second most popular exercise in the United States with approximately 400 million pool visits annually (1 ). During the summer of 2000, five outbreaks of cryptosporidiosis linked to swimming pools were reported to CDC. This report summarizes the investigations of two of these outbreaks involving approximately 1000 cases and provides recommendations to reduce the transmission of pool-related disease.
# Ohio
In July 2000, the Delaware City/County Health Department (DCCHD) learned of several laboratory-confirmed cases of cryptosporidiosis potentially linked to a private swim club. To determine associated exposures, DCCHD, in collaboration with the Ohio State Health Department and CDC, conducted an investigation.
A descriptive study and two telephone-based case-control studies were conducted: a community-based study to examine potential sources of the outbreak and a swim clubbased study to identify club-related risk factors. Persons were asked about source of drinking water, recent travel, visits to pools and lakes, swimming behaviors, contact with ill persons or young animals, and day care attendance.
A clinical case was defined as diarrhea (three loose stools during a 24-hour period) in a person for at least 1 day. A laboratory-confirmed case was defined as diarrhea, vomiting, or abdominal cramps in a person and a stool specimen that tested positive for Cryptosporidium parvum. All case-patients were in central Ohio during June 17-August 18. Case-patients and controls were frequency matched by age. DCCHD identified 700 clinical cases among residents of Delaware County and three neighboring counties. The outbreak began in late June and continued through September (Figure 1). The club closed during July 28-August 4. Of 268 stool samples submitted to DCCHD, 186 (70%) tested positive for Cryptosporidium; 47 laboratory-confirmed casepatients were enrolled in the two case-control studies. The median age of these casepatients was 6 years (range: 1-46 years) and 28 (61%) were female. The median duration of illness was 7 days (range: 1-36 days). Symptoms included diarrhea (91%), loss of appetite (87%), abdominal cramps (83%), and vomiting (35%). Nearly half (45%) reported intermittent diarrhea. Swimming at the private club was strongly associated with illness in the community case-control study. Of the 47 case-patients, 40 (93.6%) went swimming in the pool, compared with 24 (55%) of 44 controls (odds ratio =42.3; 95% confidence interval =12. 3-144.9). In the club-based case-control study, activities that increased the risk for pool water getting in the mouth (e.g., standing under a pool sprinkler) increased the risk for illness (OR=8.4; 95% CI=1.8-54.8). At least five fecal accidents, one of which was diarrheal, were observed.
# Nebraska
In August 2000, the Douglas County Health Department, Nebraska, detected an increase in laboratory-reported cases of cryptosporidiosis. Initial cases were linked to a private club with swimming facilities (club A). Additional case-patients reported swimming at club A, at another nearby private club (club B), or at other local pools. The pools at clubs A and B subsequently closed for 2 weeks in mid-August.
A case-control study was conducted at club A to identify community and club-specific risk factors. A clinical case was defined as diarrhea (three loose stools during a 24-hour period) in a person who was a member of club A. A laboratory-confirmed case was defined as diarrhea, vomiting, or cramps in a person who had a stool specimen that tested positive for Cryptosporidium. All case-patients were in the Douglas County area during June 3-September 28. Members of club A with laboratory-confirmed or clinical cases of cryptosporidiosis were enrolled in the study. Controls were randomly selected from the club A membership list and frequency matched by age.
The outbreak began in mid-June, peaked in mid-August, and tapered off in September, coinciding with the end of the outdoor swimming season in Nebraska (Figure 2 Symptoms included diarrhea (94%), abdominal cramps (83%), loss of appetite (74%), nausea (60%), and vomiting (43%). The median duration of diarrhea was 7 days (range: 1-44 days), and nearly half (46%) of patients reported intermittent diarrhea. Thirty-seven case-patients and 36 controls were included in the case-control study at club A. Illness was associated with swimming at club A (OR=5.0; 95% CI=1.48-17.7) and having been splashed with pool water (OR=5.3; 95% CI=1.6-18.9).
Swimmers often swam at multiple pool facilities and swim/dive team meets were held at both clubs A and B. Approximately 18% of the case-patients reported swimming while symptomatic, and nearly one third (32%) swam either during illness or during the 2-week period after symptoms subsided. Fecal accidents were observed at both clubs. Editorial Note: Outbreaks of gastrointestinal illness associated with treated recreational water (e.g., swimming pools) appear to have increased in recent years with most being caused by Cryptosporidium (2,3 ). Although a fecal accident by a swimmer can expose other swimmers to various disease-causing organisms, the probability of transmission of cryptosporidiosis is higher in this setting for two reasons. First, Cryptosporidium oocysts are extremely resistant to chlorine and may remain infective for several days in swimming pool water containing recommended chlorine concentrations (4 ) and, because of their small size, may not be removed efficiently by conventional pool filters. Second, the high titer of Cryptosporidium in diarrhea from infected persons (5 ) and the low 6) make it possible for a single fecal accident to sufficiently contaminate an entire pool such that accidental ingestion of a few mouthfuls of water can result in infection.
The protracted nature of these two outbreaks highlights the challenges faced by health departments and pool managers in detecting and controlling pool-associated cryptosporidiosis outbreaks. The outbreaks went unreported for several weeks, possibly because ill persons often do not seek health care for diarrheal illness (U.S. Department of Agriculture, unpublished data, 1997). During this time, ill persons continued to swim, increasing the likelihood that contamination of the pools continued to occur. It is unclear whether extended pool closure reduced the potential for exposure or contributed to transmission at other pools. A multicomponent approach to outbreak prevention is needed that combines education of swimmers and pool staff, pool design modifications, and improved operations and maintenance procedures.
The high incidence of diarrhea in the United States (7 ) and the continued use of the pools during illness suggest that education of the public is an important component of any prevention strategy. To reduce pool contamination and the spread of cryptosporidiosis and other diarrheal illnesses, public health officials and pool managers should educate staff and patrons about key messages that may reduce recreational water illness transmission. To prevent transmission, persons with diarrhea should not swim, swimmers should avoid swallowing pool water, and persons should practice good hygiene before swimming, after using the restroom, and after changing a diaper.
Improved design and management of pools also may reduce the risk for disease transmission. Public health officials and pool operators should consider 1) using separate filtration systems for "kiddie" pools and other pools to decrease the potential for cross-contamination; 2) optimizing filtration rates of kiddie pools without facilitating suction injuries to decrease the length of time that swimmers would be exposed to pathogens; and 3) ensuring that restrooms and diaper changing areas are close to the pool and are clean and adequate in number. Management practices should 1) reinforce that pool operators regularly maintain and monitor pH and free residual chlorine levels to help prevent transmission of most waterborne pathogens; 2) develop policies for pool disinfection following a fecal accident (8,9 ); 3) train staff about prevention of recreational water illness transmission; and 4) institute frequent restroom breaks for young swimmers to reduce the potential for fecal accidents.
During a pool-associated or other local outbreak of cryptosporidiosis, extra vigilance is necessary to prevent swimming-related disease transmission. Those at risk for serious illness (e.g., immunocompromised persons) should consider not swimming during an outbreak. In addition, because persons ill with cryptosporidiosis often have intermittent diarrhea and Cryptosporidium can be excreted for several weeks after diarrhea subsides (10 ), ill swimmers should refrain from swimming while ill with diarrhea and should also not swim for a 2-week period after cessation of diarrhea. Operators of implicated pools should intensify education efforts and consider prohibiting diaper-and toddleraged children from swimming during the outbreak. In addition, health officials should alert pool operators in the geographic area so they can undertake intensive education efforts to prevent infected persons from swimming in and potentially contaminating their pools. Further evaluation is needed to determine the efficacy of extended pool closures on preventing Cryptosporidium transmission. Additional information about prevention of recreational water illness is available at .
# Prevalence of Parasites in Fecal Material from Chlorinated Swimming Pools -United States, 1999
As a result of the 1998 outbreak of infection with the chlorine-sensitive pathogen Escherichia coli O157:H7 at a waterpark in Georgia (1 ), many public health departments updated their guidelines for disinfecting pools following a fecal accident. Many of these guidelines recommended treating all fecal accidents as if they contained the highly chlorine-resistant parasite Cryptosporidium parvum (2 ), generally resulting in hyperchlorination and pool closures of up to a day. To determine whether fecal accidents commonly contained Cryptosporidium, the prevalence of this parasite and the moderately chlorine sensitive parasite Giardia intestinalis (3 ) was assessed by asking swimming pool operators throughout the United States to collect formed stools from fecal accidents in their pools. This report summarizes the results of this study and provides recommendations for disinfecting pools following fecal accidents.
During 1999, 47 swimming pools, waterparks, or aquatics centers were enrolled in the survey by telephone. Sample collection began Memorial Day weekend (May 29) and ended after Labor Day weekend (September 6). Samples of each fecal accident were collected into vials containing 10% formalin. Labels included no pool-specific identifiers. Samples were tested for Cryptosporidiumand Giardia-specific stool antigen without prior concentration. All positive specimens were verified using an immunofluorescent antibody mixture specific to Cryptosporidium and Giardia followed by microscopic identification.
# Parasites in Chlorinated Swimming Pools -Continued
None of 293 formed stools from fecal accidents collected by pool operators contained Cryptosporidium. Giardia was found in 13 (4.4%) of the samples. Because this study addressed parasite prevalence in only formed stool, no information relating to disinfection procedures for diarrheal fecal accidents was obtained. Editorial Note: During the 1990s, reports of outbreaks of gastrointestinal disease associated with the use of disinfected recreational water (i.e., swimming and wading pools, waterparks, fountains, hot tubs, and spas) have gradually increased (4 ). During 1989-1998, approximately 10,000 cases of diarrheal illness were associated with 32 recreational waterborne disease outbreaks in disinfected water venues in the United States. Ten outbreaks occurred during 1997-1998, the highest number of recreational water outbreaks ever reported (4 ). Because diarrheal illness is underreported to public health authorities, the number of outbreaks associated with recreational water use is probably higher (5 ). The number of swimming exposures in the United States (approximately 400 million annual visits) (6 ) and increasing attendance at high capacity recreational water venues provide strong incentives to review and improve recommendations to reduce the transmission of gastrointestinal illness resulting from recreational water use.
Because swimming typically involves sharing water with many other persons in a pool, the water contains various bodily fluids, fecal matter, dirt, and debris that wash off bodies during swimming activities. Fecal matter is regularly introduced into the water when someone has a fecal accident through release of formed stool or diarrhea into the water, or residual fecal material on swimmers' bodies is washed into the pool. Fecal contamination may be more likely to occur when there is a high density of bathers, particularly diaper-and toddler-aged children. Swallowing this fecally contaminated water is the primary mode for transmission of enteric pathogens in recreational water outbreaks.
Although chlorine is an effective disinfectant, it does not instantly kill all pathogens (7 ). In addition, some pathogens, such as the parasite Cryptosporidium, are highly resistant to chlorine concentrations routinely used in pools (2 ). Because of frequent fecal contamination, the inability of chlorine disinfection to rapidly inactivate several pathogens and the common occurrence of accidental ingestion of pool water, transmission of pathogens can occur even in well-maintained pools.
The low prevalence of Cryptosporidium in formed fecal accidents in this study indicates that regulators can adopt less stringent disinfection guidelines by disinfecting pool water as if it contained the moderately chlorine-resistant parasite Giardia. Although there is a large differential between inactivation times for Cryptosporidium, Giardia, and E. coli (approximately 7 days, <1 hour, and <1 minute, respectively, at 1 mg/L free available chlorine ), responding to formed fecal accidents with water treatment sufficient to inactivate Giardia also should be sufficient to inactivate other known viral and bacterial waterborne pathogens, including E. coli O157:H7 (8 ).
On the basis of these findings, CDC has prepared recommendations for responding to fecal accidents in disinfected recreational water venues (see Notice to Readers, page ). These recommendations assume the presence of Giardia in formed stool accidents and the presence of Cryptosporidium in diarrheal accidents. The prevalence of Cryptosporidium in diarrhetic and nondiarrhetic stools requires further investigation.
The Giardia inactivation guidelines are based on data developed by the Environmental Protection Agency for disinfection of Giardia in drinking water (9 ). Pool operators should consult with their local or state health authorities for specific fecal accident disinfection procedures. These recommendations are intended to minimize infectious disease transmission by observed fecal accidents (primarily formed stool); however, the unique circulation patterns found in pools often result in areas of poor pool circulation (i.e., "dead spots") making it unlikely that disease transmission can be fully prevented. In addition, the higher risk associated with diarrheal accidents, which may rarely be observed and/or responded to, makes it important that public health professionals and the aquatics industry address other critical recreational water illness prevention components. These may include improving aquatics industry policies, planning, and practices and educating aquatics staff and patrons about the potential for recreational water illness transmission. Swimmers should be informed by public health professionals and the aquatics industry that healthy swimming practices necessitate that patrons refrain from swimming while ill with diarrhea and avoid swallowing pool water. Improved hygiene before and during swimming (e.g., showering, handwashing, frequent restroom breaks for young children, and appropriate diaper changing) also should be promoted. Additional information about prevention of recreational water illness is available at / healthyswimming.
# Drowning -Louisiana, 1998
Drowning is the third leading cause of death from unintentional injuries in Louisiana. In 1998, the fatality rate from drowning for Louisiana residents was 3.1 per 100,000 population, higher than the U.S. rate of 1.9 per 100,000, and more than twice the 2000 national target of 1.3 per 100,000 population. This report describes the demographics and risk factors associated with drownings in Louisiana in 1998. Findings indicate that alcohol or illicit drug use was found in approximately 60% of tested victims aged >13 years and that none of the victims of boating-related drowning were correctly wearing a personal flotation device (PFD). Prevention efforts should focus on decreasing alcohol and illicit drug use and increasing the proper use of PFDs among boaters and others involved in water recreation.
The Louisiana Office of Public Health examined three sources of data on persons who died by drowning: 1998 death certificates, coroners' records, and records of investigations performed by the Louisiana Department of Wildlife and Fisheries (LDWF). A case was defined as death in a resident of Louisiana coded on the death certificate as having drowned in the state during 1998. Using death certificates, 137 cases were identified. Of these, 114 investigative reports were reviewed: 96 with coroners' records, six with LDWF reports, and 12 with both; investigative reports for 23 (17%) cases could not be obtained. In addition, modifiable risk factors were analyzed. Alcohol and illicit drug use were examined in the deaths of persons aged >13 years. Use was determined by the presence of ethanol or metabolites of illicit drugs in samples collected at autopsy. Among deaths that occurred in a swimming pool, pool fencing was described as present or absent, and PFD use was recorded for investigative reports of boating-related drowning.
Of the 137 drowning cases, 115 (84%) occurred among males. Blacks and whites died in almost equal numbers, 68 (50%) and 67 (49%), respectively; however, the rate of drowning among blacks was more than twice the rate of whites, 4.8 per 100,000 and 2.3 per 100,000, respectively. The median age of drowned persons was 32 years (range: 10 months-94 years). The highest drowning rate was among persons aged 25-35 years (3.8 per 100,000). Children aged <4 years accounted for 10% of the total deaths and had the second highest rate (3.5 per 100,000). Among those cases in which the manner of death could be determined, 122 (95%) were classified as "accident" (unintentional); seven (5%) were classified as suicide. Twelve (9%) drowning deaths were work-related.
Of 114 deaths with coroner or LDWF records, 83 (73%) occurred in natural bodies of water (e.g., lakes, bayous, rivers, and the Gulf of Mexico), 19 (17%) in swimming pools, and seven (6%) in bathtubs or hot tubs. Four deaths were classified to have occurred in an "other setting" and in one death the setting was unknown. Alcohol testing was recorded in 72 (76%) of the 94 decedents aged >13 years; 43 (60%) had evidence for the presence of alcohol and/or illicit drugs. Thirteen (30%) decedents were positive for alcohol and illicit drugs, 28 (67%) were positive for alcohol, and one (2%) was positive for illicit drugs.
Among the 19 deaths that occurred in a swimming pool, 11 (58%) were in children aged <14 years. Children aged <4 years died in swimming pools at the highest rate (1.3 per 100,000). The presence or absence of fences was noted in eight (42%) deaths. Six pools had and two did not have fencing. May 25, 2001
# Drowning -Continued
Coroner and LDWF reports indicated that 35 (31%) of 114 deaths occurred during boating-related activities: 11 (31%) involved a fall from the boat, seven (20%) occurred when the boat capsized, and six (17%) involved a collision. Five (14%) persons who drowned had entered the water voluntarily, and six (17%) had entered the water for unknown reasons. PFD use was recorded for 22 (63%) boating-related drownings; only one decedent had been wearing a PFD and it was unfastened. Among persons aged >13 years, 34 drownings occurred; 13 (48%) tested positive for alcohol or illicit drugs. Editorial Note: The circumstances of drowning identified in this report highlight ways to prevent drowning deaths. Drowning in Louisiana occurred most often in natural bodies of water. Approximately 30% of the deaths during 1998 were associated with boating, which is proportionately more than in the entire United States, where boating accounts for 20% of drowning (1 ). In this investigation, the findings indicated that alcohol or illicit drug use was present in nearly half of the tested boating-related deaths among persons aged >13 years, that none of the boating-related decedents had been wearing a PFD correctly, and that during 1998, drowning in swimming pools accounted for 17% of deaths, with children aged <4 years at highest risk. Louisiana state regulations pertaining to alcohol use focus only on boat operators, and state regulations on wearing PFD pertain only to children aged <13 years.
The findings in this report are subject to at least two limitations. First, some investigative reports were not available. Second, risk factor information was missing in many of the reports that were examined. Both of these limitations could effect the reported prevalence of risk behaviors.
By analyzing the state-level data described in this report, the Louisiana Office of Public Health determined that drowning prevention efforts should include: 1) decreasing alcohol and illicit drug use among both boating passengers and operators; 2) focusing on the proper use of PFDs not only among children but among persons of all ages; and 3) instructing caretakers to supervise children and maintain adequate fencing around swimming pools (2 ). For a pool fence to protect against drowning, the fence must completely enclose the pool and must be at least 4 feet high with vertical openings <4 inches wide and with a functional self-latching gate (3 ). All of these prevention efforts need to be delivered in a manner culturally appropriate for the highest risk populations.
# Notice to Readers
# National Safe Boating Week -May 19-25, 2001
National Safe Boating Week is May 19-25, 2001. Boating safety improved in the United States throughout the 1990s. Despite a 15% increase in boats registered, the boating fatality rate declined 32% from 1990 to 1999. However, boating-related deaths continue to occur. In 1999, 734 persons died in boating incidents. Boaters routinely should adopt safety practices.
All boaters should wear personal flotation devices (PFDs). Capsizing and falling overboard account for more than half of all recreational boating deaths each year (1 ). Although all states and territories (except Guam, Hawaii, and Idaho) have regulations on wearing life jackets, most affect only children aged <12 years.
Boaters should avoid alcoholic beverages while boating. Alcohol use affects judgment, vision, balance, and coordination. Approximately one third of all deaths caused by a collision involved alcohol use.
Boaters should be aware of the risk for carbon monoxide (CO) poisoning. Potential sources of CO poisoning include using air conditioning powered by an onboard motor generator, operating a gasoline powered engine while docked and/or rafted with other boats operating engines, or being underway with improper cabin ventilation. To avoid CO poisoning, boaters should have sufficient ventilation, properly install and maintain equipment, and use CO detectors.
Boaters should be aware of potential hazards and the regulations of operating a boat. Boating education courses teach the regulatory and statutory rules for safely operating and navigating recreational boats. The U.S. Coast Guard Auxiliary and U.S. Power Squadron offer the Vessel Safety Check (VSC) program to promote boating safety. Volunteers check safety equipment and provide information about equipment purpose, safety procedures, and applicable regulations.
Additional
# MMWR May 25, 2001
Notice to Readers -Continued
# Notice to Readers
# Responding to Fecal Accidents in Disinfected Swimming Venues
These recommendations are solely for management of fecal accidents in disinfected recreational water venues. The recommendations do not address use of other nonchlorine disinfectants because there is limited pathogen inactivation data for many of these compounds. Because improper handling of chlorinated disinfectants could cause injury, appropriate occupational safety and health requirements should be followed.
A. Formed stool (solid, nonliquid)
1. Direct everyone to leave all pools into which water containing the feces is circulated. Do not allow anyone to enter the contaminated pool(s) until all decontamination procedures are completed.
2. Remove as much of the fecal material as possible using a net or scoop and dispose of it in a sanitary manner. Clean and disinfect the net or scoop (e.g., after cleaning, leave the net or scoop immersed in the pool during disinfection). Vacuuming stool from the pool is not recommended*.
3. Raise the free available chlorine concentration to 2 mg/L, pH 7.2-7.5, if it is <2.0 mg/L. Ensure this concentration is found throughout all co-circulating pools by sampling at least three widely spaced locations away from return water outlets. This free available chlorine concentration was selected to keep the pool closure time to approximately 30 minutes. Other concentrations or closure times can be used as long as the CT inactivation value † is kept constant (Table 1).
4. Maintain the free available chlorine concentration at 2.0 mg/L, pH 7.2-7.5, for at least 25 minutes before reopening the pool. State or local regulators may require higher free available chlorine levels in the presence of chlorine stabilizers such as chlorinated isocyanurates § . Ensure that the filtration system is operating while the pool reaches and maintains the proper free available chlorine concentration during the disinfection process.
5. Establish a fecal accident log. Document each fecal accident by recording date and time of the event, formed stool or diarrhea, free available chlorine concentration at the time or observation of the event and before opening the pool, the pH, the procedures followed to respond to the fecal accident (including the process used to increase free chlorine residual if necessary), and the contact time.
# B. Diarrhea (liquid stool)
1. See A1.
2. See A2.
3. Raise the free available chlorine concentration to 20 mg/L ¶ and maintain the pH between 7.2 and 7.5. Ensure this concentration is found throughout all co-circulating pools by sampling at least three widely spaced locations away from return water outlets. This chlorine and pH level should be sufficient to inactivate Cryptosporidium and should be maintained for at least 8 hours, equivalent to a CT inactivation value of 9600. A higher or lower free available chlorine level/inactivation time can be used as long as a CT inactivation value equaling 9600 is maintained for Cryptosporidium inactivation. State or local regulators may require higher free available chlorine levels in the presence of chlorine stabilizers such as chlorinated isocyanurates. If necessary, consult an aquatics professional to determine and identify the feasibility, practical methods, and safety considerations before attempting the hyperchlorination of any pool.
4. Ensure that the filtration system is operating while the pool reaches and maintains the proper free available chlorine concentration during disinfection.
5. Backwash the filter thoroughly after reaching the CT value. Be sure the effluent is discharged directly to waste and in accordance with state or local regulations. Do not return the backwash through the filter. Where appropriate, replace the filter media.
6. Swimmers may be allowed into the pool after the required CT value has been achieved and the free available chlorine level has been returned to the normal operating range allowed - No uniform recommendations for disinfection of vacuum systems are available. However, if a vacuum system is accidentally used, the waste should be discharged directly to a sewer or other approved waste disposal system and not through the filtration system. The dilution effect of the pool water going through the hose may reduce the risk for high-level contamination of the vacuum system. † CT refers to concentration (C) of free available chlorine in mg/L or ppm multiplied by time (T) in minutes. If pool operators want to use a different chlorine concentration or inactivation time, they need to ensure that CT values always remain the same. For example, if an operator finds a formed fecal accident in the pool and his pool has a free available chlorine reading of 3 mg/L and a pH of 7.5, to determine how long the pool should be closed to swimmers, locate 3 mg/L in the left column of the table and then move right and read the pool closure time. The pool should be closed for 19 minutes. Example 2: The CT inactivation value for Cryptosporidium is 9600, which equals (20 mg/L)(480 minutes) (i.e., 8 hours). After a diarrheal accident in the pool, an operator determines she can only maintain 15 mg/L. How long would hyperchlorination take? Answer: 9600=CT=;T=9600/15=640 minutes=10.7 hours. § The impact of chlorine stabilizers (e.g., chlorinated isocyanurates) on pathogen inactivation and disinfectant measurement is unclear and requires further investigation. State or local regulations on chlorinated isocyanurates use should be consulted. ¶ Many conventional test kits cannot measure free available chlorine levels this high. Use chlorine test strips that can measure free available chlorine in a range that includes 20mg/L (such as those used in the food industry) or make dilutions for use in a standard DPD (N, N-diethyl-p-phenylenediamine) test kit using chlorine-free water. May 25, 2001
Notice to Readers -Continued
# Notice to Readers
# Deferral of Routine Booster Doses of Tetanus and Diphtheria Toxoids for Adolescents and Adults
A shortage of tetanus and diphtheria toxoids (Td) and tetanus toxoid (TT) in the United States has resulted because one of two manufacturers discontinued production of tetanus toxoid-containing products (1 ). Aventis Pasteur (Swiftwater, Pennsylvania) is the only major manufacturer of tetanus and Td in the United States. In response to the shortage, Aventis Pasteur has increased production of Td to meet national needs; however, because 11 months are required for vaccine production, the shortage is expected to last for the remainder of 2001.
To assure vaccine availability for priority indications (2 ), all routine Td boosters in adolescents and adults should be delayed until 2002. Td use should follow existing recommendations for all other indications, which include 1) persons traveling to a country where the risk for diphtheria is high*; 2) persons requiring tetanus vaccination for prophylaxis in wound management; 3) persons who have received <3 doses of any vaccine containing Td; and 4) pregnant women who have not been vaccinated with Td during the preceding 10 years.
CDC recommends that health-care providers, including clinic personnel, record the names of patients whose booster dose is delayed during the shortage. When Td supplies are restored, these patients should be notified to return to their health-care provider for vaccination. According to Aventis Pasteur, sufficient vaccine will be available in early 2002 to supply the national demand.
Health-care providers using Td for wound management should follow recommendations from the Advisory Committee on Immunization Practices for wound management (3 ). All wound patients should receive Td if they have received 3 doses of TT-containing vaccine and severe or contaminated wounds, Td should be given only if >5 years have passed since the last dose of tetanuscontaining vaccine. For clean and minor wounds, Td should be given only if the patient has not received a tetanus-containing vaccine during the preceding 10 years. Healthcare providers should inquire from patients presenting for wound management about the timing of their last tetanus-containing vaccine to avoid unnecessary vaccination.
Pediatric formulations of diphtheria and tetanus toxoids (DT) and diphtheria and tetanus toxoids and acellular pertussis vaccine (DTaP) should not be used for persons aged >7 years. Although TT might be considered a substitute for Td in wound management Because of changes in reporting methods in this Pennsylvania city, these numbers are partial counts for the current week. Complete counts will be available in 4 to 6 weeks. ¶ Total includes unknown ages.
# Contributors to the Production of the MMWR (Weekly)
Weekly
when Td is not available, TT is not available for national distribution. Existing stocks of TT are extremely limited and are mainly reserved for production of tetanus immune globulin and other special circumstances. Health-care providers and institutions requiring Td for priority indications should contact Aventis Pasteur, telephone (800) 822-2463 or (800) VACCINE. Institutions should place orders for their anticipated needs for priority indications only. Limiting quantities of vaccine in each order is necessary to assure the widest possible distribution of available vaccine. For emergency situations (e.g., natural disasters) requiring increased use of Td, Aventis Pasteur can provide vaccine within 24 hours.
# The Morbidity and Mortality Weekly Report (MMWR) Series is prepared by the Centers for Disease Control and Prevention (CDC) and is available free of charge in electronic format and on a paid subscription basis for paper copy.
To receive an electronic copy on Friday of each week, send an e-mail message to [email protected]. The body content should read SUBscribe mmwr-toc. Electronic copy also is available from CDC's World-Wide Web server at or from CDC's file transfer protocol server at ftp/ Publications/mmwr. To subscribe for paper copy, contact Superintendent of Documents, U.S. Government Printing Office, Washington, DC 20402; telephone (202) 512-1800.
Data in the weekly MMWR are provisional, based on weekly reports to CDC by state health departments. The reporting week concludes at close of business on Friday; compiled data on a national basis are officially released to the public on the following Friday. Address inquiries about the MMWR Series, including material to be considered for publication, to: Editor, MMWR Series, Mailstop C-08, CDC, 1600 Clifton Rd., N.E., Atlanta, GA 30333; telephone (888) 232-3228.
All material in the MMWR Series is in the public domain and may be used and reprinted without permission; citation as to source, however, is appreciated.
# IU.S. Government Printing | World No-Tobacco Day is May 31, 2001. The theme, "Second-Hand Smoke Kills-Let's Clear the Air," was designated by the World Health Organization (WHO) to raise awareness of the hazards of exposure to second-hand smoke. Tobacco use worldwide will cause an estimated 10 million deaths annually by 2030 (1 ). An effective strategy to promote and encourage tobacco-free policies is to link them with sporting events. Such policies also reduce nonsmokers' exposure to second-hand smoke (2 ). The 1988 Olympic Winter Games in Calgary, Alberta, Canada, was the first tobacco-free Olympics. Since then, all of the Olympic Games have had tobacco-free policies (3 ). For the 2002 games, the Olympic organizing committee for Salt Lake City, Utah, will implement a public information campaign using Olympic athletes to promote healthy lifestyles and sports as an alternative to tobacco use. Plans also include information to increase awareness of the tobacco-free policy among visitors, media, athletes, and officials from participating countries. Another media campaign is "Tobacco Kills-Don't Be Duped," which aims to ban tobacco advertising and promotion at sporting events globally. Additional information about World No-Tobacco Day 2001 is available at http://tobacco.who.int*, and http:// www.cdc.gov/tobacco; telephone (800) 232-1311. References 1. World Health Organization. Combating the tobacco epidemic. World Health Organization's world health report 1999. Geneva, Switzerland: World Health Organization, 1999:6579. 2. CDC. National report on human exposure to environmental chemicals. Atlanta, Georgia:#
* Persons aged >18 years who reported having smoked >100 cigarettes in their entire life and who reported smoking every day or some days. † Confidence interval. § Significant value: two-tailed p<0.05.
# MMWR May 25, 2001
Tobacco Use Among Adults -Continued Asked about smoking and advised to stop smoking by a dentist? 9.9 (±4.5) 24.9 (±4.7) ¶ * Persons aged >18 years who reported having smoked >100 cigarettes in their entire life and who reported smoking every day or some days. † Confidence interval. § Includes physicians, nurse practitioners, or physician assistants. ¶ Significant value: two-tailed p<0.05. **Asked of respondents who visited a dentist during the year preceding the survey. Editorial Note: The results of the 1996 and 1999 Arizona ATS indicate that the prevalence of cigarette use among Arizona adults decreased substantially following the implementation of the statewide Arizona TEPP. The decrease in smoking prevalence among low income and low education groups also indicates a narrowing in disparities in cigarette use.
TEPP directed many of its activities toward Hispanics, which may, in part, explain the substantial decrease in cigarette smoking in that population. TEPP serves the Hispanic population through its Spanish language statewide media campaign and telephone helpline and through local cessation and prevention services. TEPP uses methods appropriate for this population, including Promotoras de Salud (lay health workers) and culturally appropriate materials and curricula.
The Arizona ATS results also showed a substantial increase in the proportion of smokers who reported that either a health-care provider or a dentist both asked about tobacco use and advised them to quit. Health-care providers can play a key role in assisting MMWR 405
Tobacco Use Among Adults -Continued patients to quit smoking (2 ), and brief physician advice substantially increases successful quitting (2 ). TEPP, through statewide and local projects, provides training for healthcare providers to increase the number of patients with whom they briefly discuss stopping smoking. The findings in this report are subject to at least five limitations. First, it is difficult to separate the effects of TEPP from price increases. The cigarette tax in Arizona increased from $0.18 to $0.58 per pack in November 1994, which may have contributed to the decline in adult smoking prevalence. Although the tax increase occurred more than a year before the first survey, the average retail price of cigarettes in Arizona continued to increase from $2.08 in 1996 to $2.50 in 1999 (3 ). Second, some segments of the population in Arizona, including some low income residents, are more likely than others to lack telephone service and therefore not be included in the study sample. Third, the response rate in 1999 was almost nine percentage points lower than the response rate in 1996, which may have influenced the results. Fourth, health-care provider communication data about smoking was based on self-reported recall for an entire year; the validity of these self-reports was not determined. Finally, although declines in smoking rates in Arizona may be a result of TEPP, a cause-and-effect relation cannot be established by comparing data from the cross-sectional ATS surveys alone. Comparing Arizona smoking prevalence trends and trends in other states with varying levels of interventions during 1996-1999 could help to determine how much of the decline may be related to the Arizona TEPP rather than to regional or national influences.
Arizona is one of seven states that meet CDC's funding recommendations for FY 2001 (4,5 ). The Arizona TEPP incorporates all nine components of a comprehensive tobaccocontrol program as recommended by CDC (4 ). The program added a certification program for smoking cessation counselors. The Arizona TEPP has been implementing strategies recommended in the Surgeon General's report Reducing Tobacco Use (6 ), CDC's Best Practices for Comprehensive Tobacco Control Programs (4 ), the Clinical Practice Guidelines for Treating Tobacco Use and Dependence (2 ), and the Task Force on Community Preventive Services (7 ). The findings of the 1996 and 1999 Arizona ATS suggest that an adequately funded and comprehensive program can substantially reduce tobacco use overall and across diverse demographic groups. Recent reports from California indicate that sustaining such a program for at least 9 years also could result in reductions in lung and bronchial cancer and coronary heart disease rates (8,9 ). Attainment of the 2010 national health objective (10 ) to reduce adult smoking rates to <12% will require similar programs to be implemented across the United States.
# MMWR May 25, 2001
Tobacco Use Among Adults -Continued
# Protracted Outbreaks of Cryptosporidiosis Associated With Swimming Pool Use -Ohio and Nebraska, 2000
Swimming is the second most popular exercise in the United States with approximately 400 million pool visits annually (1 ). During the summer of 2000, five outbreaks of cryptosporidiosis linked to swimming pools were reported to CDC. This report summarizes the investigations of two of these outbreaks involving approximately 1000 cases and provides recommendations to reduce the transmission of pool-related disease.
# Ohio
In July 2000, the Delaware City/County Health Department (DCCHD) learned of several laboratory-confirmed cases of cryptosporidiosis potentially linked to a private swim club. To determine associated exposures, DCCHD, in collaboration with the Ohio State Health Department and CDC, conducted an investigation.
A descriptive study and two telephone-based case-control studies were conducted: a community-based study to examine potential sources of the outbreak and a swim clubbased study to identify club-related risk factors. Persons were asked about source of drinking water, recent travel, visits to pools and lakes, swimming behaviors, contact with ill persons or young animals, and day care attendance.
A clinical case was defined as diarrhea (three loose stools during a 24-hour period) in a person for at least 1 day. A laboratory-confirmed case was defined as diarrhea, vomiting, or abdominal cramps in a person and a stool specimen that tested positive for Cryptosporidium parvum. All case-patients were in central Ohio during June 17-August 18. Case-patients and controls were frequency matched by age. DCCHD identified 700 clinical cases among residents of Delaware County and three neighboring counties. The outbreak began in late June and continued through September (Figure 1). The club closed during July 28-August 4. Of 268 stool samples submitted to DCCHD, 186 (70%) tested positive for Cryptosporidium; 47 laboratory-confirmed casepatients were enrolled in the two case-control studies. The median age of these casepatients was 6 years (range: 1-46 years) and 28 (61%) were female. The median duration of illness was 7 days (range: 1-36 days). Symptoms included diarrhea (91%), loss of appetite (87%), abdominal cramps (83%), and vomiting (35%). Nearly half (45%) reported intermittent diarrhea. Swimming at the private club was strongly associated with illness in the community case-control study. Of the 47 case-patients, 40 (93.6%) went swimming in the pool, compared with 24 (55%) of 44 controls (odds ratio [OR]=42.3; 95% confidence interval [CI]=12. 3-144.9). In the club-based case-control study, activities that increased the risk for pool water getting in the mouth (e.g., standing under a pool sprinkler) increased the risk for illness (OR=8.4; 95% CI=1.8-54.8). At least five fecal accidents, one of which was diarrheal, were observed.
# Nebraska
In August 2000, the Douglas County Health Department, Nebraska, detected an increase in laboratory-reported cases of cryptosporidiosis. Initial cases were linked to a private club with swimming facilities (club A). Additional case-patients reported swimming at club A, at another nearby private club (club B), or at other local pools. The pools at clubs A and B subsequently closed for 2 weeks in mid-August.
A case-control study was conducted at club A to identify community and club-specific risk factors. A clinical case was defined as diarrhea (three loose stools during a 24-hour period) in a person who was a member of club A. A laboratory-confirmed case was defined as diarrhea, vomiting, or cramps in a person who had a stool specimen that tested positive for Cryptosporidium. All case-patients were in the Douglas County area during June 3-September 28. Members of club A with laboratory-confirmed or clinical cases of cryptosporidiosis were enrolled in the study. Controls were randomly selected from the club A membership list and frequency matched by age.
The outbreak began in mid-June, peaked in mid-August, and tapered off in September, coinciding with the end of the outdoor swimming season in Nebraska (Figure 2 Symptoms included diarrhea (94%), abdominal cramps (83%), loss of appetite (74%), nausea (60%), and vomiting (43%). The median duration of diarrhea was 7 days (range: 1-44 days), and nearly half (46%) of patients reported intermittent diarrhea. Thirty-seven case-patients and 36 controls were included in the case-control study at club A. Illness was associated with swimming at club A (OR=5.0; 95% CI=1.48-17.7) and having been splashed with pool water (OR=5.3; 95% CI=1.6-18.9).
Swimmers often swam at multiple pool facilities and swim/dive team meets were held at both clubs A and B. Approximately 18% of the case-patients reported swimming while symptomatic, and nearly one third (32%) swam either during illness or during the 2-week period after symptoms subsided. Fecal accidents were observed at both clubs. Editorial Note: Outbreaks of gastrointestinal illness associated with treated recreational water (e.g., swimming pools) appear to have increased in recent years with most being caused by Cryptosporidium (2,3 ). Although a fecal accident by a swimmer can expose other swimmers to various disease-causing organisms, the probability of transmission of cryptosporidiosis is higher in this setting for two reasons. First, Cryptosporidium oocysts are extremely resistant to chlorine and may remain infective for several days in swimming pool water containing recommended chlorine concentrations (4 ) and, because of their small size, may not be removed efficiently by conventional pool filters. Second, the high titer of Cryptosporidium in diarrhea from infected persons (5 ) and the low 6) make it possible for a single fecal accident to sufficiently contaminate an entire pool such that accidental ingestion of a few mouthfuls of water can result in infection.
The protracted nature of these two outbreaks highlights the challenges faced by health departments and pool managers in detecting and controlling pool-associated cryptosporidiosis outbreaks. The outbreaks went unreported for several weeks, possibly because ill persons often do not seek health care for diarrheal illness (U.S. Department of Agriculture, unpublished data, 1997). During this time, ill persons continued to swim, increasing the likelihood that contamination of the pools continued to occur. It is unclear whether extended pool closure reduced the potential for exposure or contributed to transmission at other pools. A multicomponent approach to outbreak prevention is needed that combines education of swimmers and pool staff, pool design modifications, and improved operations and maintenance procedures.
The high incidence of diarrhea in the United States (7 ) and the continued use of the pools during illness suggest that education of the public is an important component of any prevention strategy. To reduce pool contamination and the spread of cryptosporidiosis and other diarrheal illnesses, public health officials and pool managers should educate staff and patrons about key messages that may reduce recreational water illness transmission. To prevent transmission, persons with diarrhea should not swim, swimmers should avoid swallowing pool water, and persons should practice good hygiene before swimming, after using the restroom, and after changing a diaper.
Improved design and management of pools also may reduce the risk for disease transmission. Public health officials and pool operators should consider 1) using separate filtration systems for "kiddie" pools and other pools to decrease the potential for cross-contamination; 2) optimizing filtration rates of kiddie pools without facilitating suction injuries to decrease the length of time that swimmers would be exposed to pathogens; and 3) ensuring that restrooms and diaper changing areas are close to the pool and are clean and adequate in number. Management practices should 1) reinforce that pool operators regularly maintain and monitor pH and free residual chlorine levels to help prevent transmission of most waterborne pathogens; 2) develop policies for pool disinfection following a fecal accident (8,9 ); 3) train staff about prevention of recreational water illness transmission; and 4) institute frequent restroom breaks for young swimmers to reduce the potential for fecal accidents.
During a pool-associated or other local outbreak of cryptosporidiosis, extra vigilance is necessary to prevent swimming-related disease transmission. Those at risk for serious illness (e.g., immunocompromised persons) should consider not swimming during an outbreak. In addition, because persons ill with cryptosporidiosis often have intermittent diarrhea and Cryptosporidium can be excreted for several weeks after diarrhea subsides (10 ), ill swimmers should refrain from swimming while ill with diarrhea and should also not swim for a 2-week period after cessation of diarrhea. Operators of implicated pools should intensify education efforts and consider prohibiting diaper-and toddleraged children from swimming during the outbreak. In addition, health officials should alert pool operators in the geographic area so they can undertake intensive education efforts to prevent infected persons from swimming in and potentially contaminating their pools. Further evaluation is needed to determine the efficacy of extended pool closures on preventing Cryptosporidium transmission. Additional information about prevention of recreational water illness is available at http://www.cdc.gov/healthyswimming.
# Prevalence of Parasites in Fecal Material from Chlorinated Swimming Pools -United States, 1999
As a result of the 1998 outbreak of infection with the chlorine-sensitive pathogen Escherichia coli O157:H7 at a waterpark in Georgia (1 ), many public health departments updated their guidelines for disinfecting pools following a fecal accident. Many of these guidelines recommended treating all fecal accidents as if they contained the highly chlorine-resistant parasite Cryptosporidium parvum (2 ), generally resulting in hyperchlorination and pool closures of up to a day. To determine whether fecal accidents commonly contained Cryptosporidium, the prevalence of this parasite and the moderately chlorine sensitive parasite Giardia intestinalis (3 ) was assessed by asking swimming pool operators throughout the United States to collect formed stools from fecal accidents in their pools. This report summarizes the results of this study and provides recommendations for disinfecting pools following fecal accidents.
During 1999, 47 swimming pools, waterparks, or aquatics centers were enrolled in the survey by telephone. Sample collection began Memorial Day weekend (May 29) and ended after Labor Day weekend (September 6). Samples of each fecal accident were collected into vials containing 10% formalin. Labels included no pool-specific identifiers. Samples were tested for Cryptosporidiumand Giardia-specific stool antigen without prior concentration. All positive specimens were verified using an immunofluorescent antibody mixture specific to Cryptosporidium and Giardia followed by microscopic identification.
# Parasites in Chlorinated Swimming Pools -Continued
None of 293 formed stools from fecal accidents collected by pool operators contained Cryptosporidium. Giardia was found in 13 (4.4%) of the samples. Because this study addressed parasite prevalence in only formed stool, no information relating to disinfection procedures for diarrheal fecal accidents was obtained. Editorial Note: During the 1990s, reports of outbreaks of gastrointestinal disease associated with the use of disinfected recreational water (i.e., swimming and wading pools, waterparks, fountains, hot tubs, and spas) have gradually increased (4 ). During 1989-1998, approximately 10,000 cases of diarrheal illness were associated with 32 recreational waterborne disease outbreaks in disinfected water venues in the United States. Ten outbreaks occurred during 1997-1998, the highest number of recreational water outbreaks ever reported (4 ). Because diarrheal illness is underreported to public health authorities, the number of outbreaks associated with recreational water use is probably higher (5 ). The number of swimming exposures in the United States (approximately 400 million annual visits) (6 ) and increasing attendance at high capacity recreational water venues provide strong incentives to review and improve recommendations to reduce the transmission of gastrointestinal illness resulting from recreational water use.
Because swimming typically involves sharing water with many other persons in a pool, the water contains various bodily fluids, fecal matter, dirt, and debris that wash off bodies during swimming activities. Fecal matter is regularly introduced into the water when someone has a fecal accident through release of formed stool or diarrhea into the water, or residual fecal material on swimmers' bodies is washed into the pool. Fecal contamination may be more likely to occur when there is a high density of bathers, particularly diaper-and toddler-aged children. Swallowing this fecally contaminated water is the primary mode for transmission of enteric pathogens in recreational water outbreaks.
Although chlorine is an effective disinfectant, it does not instantly kill all pathogens (7 ). In addition, some pathogens, such as the parasite Cryptosporidium, are highly resistant to chlorine concentrations routinely used in pools (2 ). Because of frequent fecal contamination, the inability of chlorine disinfection to rapidly inactivate several pathogens and the common occurrence of accidental ingestion of pool water, transmission of pathogens can occur even in well-maintained pools.
The low prevalence of Cryptosporidium in formed fecal accidents in this study indicates that regulators can adopt less stringent disinfection guidelines by disinfecting pool water as if it contained the moderately chlorine-resistant parasite Giardia. Although there is a large differential between inactivation times for Cryptosporidium, Giardia, and E. coli (approximately 7 days, <1 hour, and <1 minute, respectively, at 1 mg/L free available chlorine [2,3,8 ]), responding to formed fecal accidents with water treatment sufficient to inactivate Giardia also should be sufficient to inactivate other known viral and bacterial waterborne pathogens, including E. coli O157:H7 (8 ).
On the basis of these findings, CDC has prepared recommendations for responding to fecal accidents in disinfected recreational water venues (see Notice to Readers, page ). These recommendations assume the presence of Giardia in formed stool accidents and the presence of Cryptosporidium in diarrheal accidents. The prevalence of Cryptosporidium in diarrhetic and nondiarrhetic stools requires further investigation.
The Giardia inactivation guidelines are based on data developed by the Environmental Protection Agency for disinfection of Giardia in drinking water (9 ). Pool operators should consult with their local or state health authorities for specific fecal accident disinfection procedures. These recommendations are intended to minimize infectious disease transmission by observed fecal accidents (primarily formed stool); however, the unique circulation patterns found in pools often result in areas of poor pool circulation (i.e., "dead spots") making it unlikely that disease transmission can be fully prevented. In addition, the higher risk associated with diarrheal accidents, which may rarely be observed and/or responded to, makes it important that public health professionals and the aquatics industry address other critical recreational water illness prevention components. These may include improving aquatics industry policies, planning, and practices and educating aquatics staff and patrons about the potential for recreational water illness transmission. Swimmers should be informed by public health professionals and the aquatics industry that healthy swimming practices necessitate that patrons refrain from swimming while ill with diarrhea and avoid swallowing pool water. Improved hygiene before and during swimming (e.g., showering, handwashing, frequent restroom breaks for young children, and appropriate diaper changing) also should be promoted. Additional information about prevention of recreational water illness is available at http://www.cdc.gov/ healthyswimming.
# Drowning -Louisiana, 1998
Drowning is the third leading cause of death from unintentional injuries in Louisiana. In 1998, the fatality rate from drowning for Louisiana residents was 3.1 per 100,000 population, higher than the U.S. rate of 1.9 per 100,000, and more than twice the 2000 national target of 1.3 per 100,000 population. This report describes the demographics and risk factors associated with drownings in Louisiana in 1998. Findings indicate that alcohol or illicit drug use was found in approximately 60% of tested victims aged >13 years and that none of the victims of boating-related drowning were correctly wearing a personal flotation device (PFD). Prevention efforts should focus on decreasing alcohol and illicit drug use and increasing the proper use of PFDs among boaters and others involved in water recreation.
The Louisiana Office of Public Health examined three sources of data on persons who died by drowning: 1998 death certificates, coroners' records, and records of investigations performed by the Louisiana Department of Wildlife and Fisheries (LDWF). A case was defined as death in a resident of Louisiana coded on the death certificate as having drowned in the state during 1998. Using death certificates, 137 cases were identified. Of these, 114 investigative reports were reviewed: 96 with coroners' records, six with LDWF reports, and 12 with both; investigative reports for 23 (17%) cases could not be obtained. In addition, modifiable risk factors were analyzed. Alcohol and illicit drug use were examined in the deaths of persons aged >13 years. Use was determined by the presence of ethanol or metabolites of illicit drugs in samples collected at autopsy. Among deaths that occurred in a swimming pool, pool fencing was described as present or absent, and PFD use was recorded for investigative reports of boating-related drowning.
Of the 137 drowning cases, 115 (84%) occurred among males. Blacks and whites died in almost equal numbers, 68 (50%) and 67 (49%), respectively; however, the rate of drowning among blacks was more than twice the rate of whites, 4.8 per 100,000 and 2.3 per 100,000, respectively. The median age of drowned persons was 32 years (range: 10 months-94 years). The highest drowning rate was among persons aged 25-35 years (3.8 per 100,000). Children aged <4 years accounted for 10% of the total deaths and had the second highest rate (3.5 per 100,000). Among those cases in which the manner of death could be determined, 122 (95%) were classified as "accident" (unintentional); seven (5%) were classified as suicide. Twelve (9%) drowning deaths were work-related.
Of 114 deaths with coroner or LDWF records, 83 (73%) occurred in natural bodies of water (e.g., lakes, bayous, rivers, and the Gulf of Mexico), 19 (17%) in swimming pools, and seven (6%) in bathtubs or hot tubs. Four deaths were classified to have occurred in an "other setting" and in one death the setting was unknown. Alcohol testing was recorded in 72 (76%) of the 94 decedents aged >13 years; 43 (60%) had evidence for the presence of alcohol and/or illicit drugs. Thirteen (30%) decedents were positive for alcohol and illicit drugs, 28 (67%) were positive for alcohol, and one (2%) was positive for illicit drugs.
Among the 19 deaths that occurred in a swimming pool, 11 (58%) were in children aged <14 years. Children aged <4 years died in swimming pools at the highest rate (1.3 per 100,000). The presence or absence of fences was noted in eight (42%) deaths. Six pools had and two did not have fencing. May 25, 2001
# Drowning -Continued
Coroner and LDWF reports indicated that 35 (31%) of 114 deaths occurred during boating-related activities: 11 (31%) involved a fall from the boat, seven (20%) occurred when the boat capsized, and six (17%) involved a collision. Five (14%) persons who drowned had entered the water voluntarily, and six (17%) had entered the water for unknown reasons. PFD use was recorded for 22 (63%) boating-related drownings; only one decedent had been wearing a PFD and it was unfastened. Among persons aged >13 years, 34 drownings occurred; 13 (48%) tested positive for alcohol or illicit drugs. Editorial Note: The circumstances of drowning identified in this report highlight ways to prevent drowning deaths. Drowning in Louisiana occurred most often in natural bodies of water. Approximately 30% of the deaths during 1998 were associated with boating, which is proportionately more than in the entire United States, where boating accounts for 20% of drowning (1 ). In this investigation, the findings indicated that alcohol or illicit drug use was present in nearly half of the tested boating-related deaths among persons aged >13 years, that none of the boating-related decedents had been wearing a PFD correctly, and that during 1998, drowning in swimming pools accounted for 17% of deaths, with children aged <4 years at highest risk. Louisiana state regulations pertaining to alcohol use focus only on boat operators, and state regulations on wearing PFD pertain only to children aged <13 years.
The findings in this report are subject to at least two limitations. First, some investigative reports were not available. Second, risk factor information was missing in many of the reports that were examined. Both of these limitations could effect the reported prevalence of risk behaviors.
By analyzing the state-level data described in this report, the Louisiana Office of Public Health determined that drowning prevention efforts should include: 1) decreasing alcohol and illicit drug use among both boating passengers and operators; 2) focusing on the proper use of PFDs not only among children but among persons of all ages; and 3) instructing caretakers to supervise children and maintain adequate fencing around swimming pools (2 ). For a pool fence to protect against drowning, the fence must completely enclose the pool and must be at least 4 feet high with vertical openings <4 inches wide and with a functional self-latching gate (3 ). All of these prevention efforts need to be delivered in a manner culturally appropriate for the highest risk populations.
# Notice to Readers
# National Safe Boating Week -May 19-25, 2001
National Safe Boating Week is May 19-25, 2001. Boating safety improved in the United States throughout the 1990s. Despite a 15% increase in boats registered, the boating fatality rate declined 32% from 1990 to 1999. However, boating-related deaths continue to occur. In 1999, 734 persons died in boating incidents. Boaters routinely should adopt safety practices.
All boaters should wear personal flotation devices (PFDs). Capsizing and falling overboard account for more than half of all recreational boating deaths each year (1 ). Although all states and territories (except Guam, Hawaii, and Idaho) have regulations on wearing life jackets, most affect only children aged <12 years.
Boaters should avoid alcoholic beverages while boating. Alcohol use affects judgment, vision, balance, and coordination. Approximately one third of all deaths caused by a collision involved alcohol use.
Boaters should be aware of the risk for carbon monoxide (CO) poisoning. Potential sources of CO poisoning include using air conditioning powered by an onboard motor generator, operating a gasoline powered engine while docked and/or rafted with other boats operating engines, or being underway with improper cabin ventilation. To avoid CO poisoning, boaters should have sufficient ventilation, properly install and maintain equipment, and use CO detectors.
Boaters should be aware of potential hazards and the regulations of operating a boat. Boating education courses teach the regulatory and statutory rules for safely operating and navigating recreational boats. The U.S. Coast Guard Auxiliary and U.S. Power Squadron offer the Vessel Safety Check (VSC) program to promote boating safety. Volunteers check safety equipment and provide information about equipment purpose, safety procedures, and applicable regulations.
Additional
# MMWR May 25, 2001
Notice to Readers -Continued
# Notice to Readers
# Responding to Fecal Accidents in Disinfected Swimming Venues
These recommendations are solely for management of fecal accidents in disinfected recreational water venues. The recommendations do not address use of other nonchlorine disinfectants because there is limited pathogen inactivation data for many of these compounds. Because improper handling of chlorinated disinfectants could cause injury, appropriate occupational safety and health requirements should be followed.
A. Formed stool (solid, nonliquid)
1. Direct everyone to leave all pools into which water containing the feces is circulated. Do not allow anyone to enter the contaminated pool(s) until all decontamination procedures are completed.
2. Remove as much of the fecal material as possible using a net or scoop and dispose of it in a sanitary manner. Clean and disinfect the net or scoop (e.g., after cleaning, leave the net or scoop immersed in the pool during disinfection). Vacuuming stool from the pool is not recommended*.
3. Raise the free available chlorine concentration to 2 mg/L, pH 7.2-7.5, if it is <2.0 mg/L. Ensure this concentration is found throughout all co-circulating pools by sampling at least three widely spaced locations away from return water outlets. This free available chlorine concentration was selected to keep the pool closure time to approximately 30 minutes. Other concentrations or closure times can be used as long as the CT inactivation value † is kept constant (Table 1).
4. Maintain the free available chlorine concentration at 2.0 mg/L, pH 7.2-7.5, for at least 25 minutes before reopening the pool. State or local regulators may require higher free available chlorine levels in the presence of chlorine stabilizers such as chlorinated isocyanurates § . Ensure that the filtration system is operating while the pool reaches and maintains the proper free available chlorine concentration during the disinfection process.
5. Establish a fecal accident log. Document each fecal accident by recording date and time of the event, formed stool or diarrhea, free available chlorine concentration at the time or observation of the event and before opening the pool, the pH, the procedures followed to respond to the fecal accident (including the process used to increase free chlorine residual if necessary), and the contact time.
# B. Diarrhea (liquid stool)
1. See A1.
2. See A2.
3. Raise the free available chlorine concentration to 20 mg/L ¶ and maintain the pH between 7.2 and 7.5. Ensure this concentration is found throughout all co-circulating pools by sampling at least three widely spaced locations away from return water outlets. This chlorine and pH level should be sufficient to inactivate Cryptosporidium and should be maintained for at least 8 hours, equivalent to a CT inactivation value of 9600. A higher or lower free available chlorine level/inactivation time can be used as long as a CT inactivation value equaling 9600 is maintained for Cryptosporidium inactivation. State or local regulators may require higher free available chlorine levels in the presence of chlorine stabilizers such as chlorinated isocyanurates. If necessary, consult an aquatics professional to determine and identify the feasibility, practical methods, and safety considerations before attempting the hyperchlorination of any pool.
4. Ensure that the filtration system is operating while the pool reaches and maintains the proper free available chlorine concentration during disinfection.
5. Backwash the filter thoroughly after reaching the CT value. Be sure the effluent is discharged directly to waste and in accordance with state or local regulations. Do not return the backwash through the filter. Where appropriate, replace the filter media.
6. Swimmers may be allowed into the pool after the required CT value has been achieved and the free available chlorine level has been returned to the normal operating range allowed * No uniform recommendations for disinfection of vacuum systems are available. However, if a vacuum system is accidentally used, the waste should be discharged directly to a sewer or other approved waste disposal system and not through the filtration system. The dilution effect of the pool water going through the hose may reduce the risk for high-level contamination of the vacuum system. † CT refers to concentration (C) of free available chlorine in mg/L or ppm multiplied by time (T) in minutes. If pool operators want to use a different chlorine concentration or inactivation time, they need to ensure that CT values always remain the same. For example, if an operator finds a formed fecal accident in the pool and his pool has a free available chlorine reading of 3 mg/L and a pH of 7.5, to determine how long the pool should be closed to swimmers, locate 3 mg/L in the left column of the table and then move right and read the pool closure time. The pool should be closed for 19 minutes. Example 2: The CT inactivation value for Cryptosporidium is 9600, which equals (20 mg/L)(480 minutes) (i.e., 8 hours). After a diarrheal accident in the pool, an operator determines she can only maintain 15 mg/L. How long would hyperchlorination take? Answer: 9600=CT=[(15)(T)];T=9600/15=640 minutes=10.7 hours. § The impact of chlorine stabilizers (e.g., chlorinated isocyanurates) on pathogen inactivation and disinfectant measurement is unclear and requires further investigation. State or local regulations on chlorinated isocyanurates use should be consulted. ¶ Many conventional test kits cannot measure free available chlorine levels this high. Use chlorine test strips that can measure free available chlorine in a range that includes 20mg/L (such as those used in the food industry) or make dilutions for use in a standard DPD (N, N-diethyl-p-phenylenediamine) test kit using chlorine-free water. May 25, 2001
Notice to Readers -Continued
# Notice to Readers
# Deferral of Routine Booster Doses of Tetanus and Diphtheria Toxoids for Adolescents and Adults
A shortage of tetanus and diphtheria toxoids (Td) and tetanus toxoid (TT) in the United States has resulted because one of two manufacturers discontinued production of tetanus toxoid-containing products (1 ). Aventis Pasteur (Swiftwater, Pennsylvania) is the only major manufacturer of tetanus and Td in the United States. In response to the shortage, Aventis Pasteur has increased production of Td to meet national needs; however, because 11 months are required for vaccine production, the shortage is expected to last for the remainder of 2001.
To assure vaccine availability for priority indications (2 ), all routine Td boosters in adolescents and adults should be delayed until 2002. Td use should follow existing recommendations for all other indications, which include 1) persons traveling to a country where the risk for diphtheria is high*; 2) persons requiring tetanus vaccination for prophylaxis in wound management; 3) persons who have received <3 doses of any vaccine containing Td; and 4) pregnant women who have not been vaccinated with Td during the preceding 10 years.
CDC recommends that health-care providers, including clinic personnel, record the names of patients whose booster dose is delayed during the shortage. When Td supplies are restored, these patients should be notified to return to their health-care provider for vaccination. According to Aventis Pasteur, sufficient vaccine will be available in early 2002 to supply the national demand.
Health-care providers using Td for wound management should follow recommendations from the Advisory Committee on Immunization Practices for wound management (3 ). All wound patients should receive Td if they have received <3 tetanus-containing vaccines or if vaccination history is uncertain. These patients also should receive tetanus immune globulin for wounds that are contaminated with dirt, feces, soil or saliva, puncture wounds, and avulsions and wounds resulting from missiles, crushing, burns or frostbite (3 ). For persons with >3 doses of TT-containing vaccine and severe or contaminated wounds, Td should be given only if >5 years have passed since the last dose of tetanuscontaining vaccine. For clean and minor wounds, Td should be given only if the patient has not received a tetanus-containing vaccine during the preceding 10 years. Healthcare providers should inquire from patients presenting for wound management about the timing of their last tetanus-containing vaccine to avoid unnecessary vaccination.
Pediatric formulations of diphtheria and tetanus toxoids (DT) and diphtheria and tetanus toxoids and acellular pertussis vaccine (DTaP) should not be used for persons aged >7 years. Although TT might be considered a substitute for Td in wound management Because of changes in reporting methods in this Pennsylvania city, these numbers are partial counts for the current week. Complete counts will be available in 4 to 6 weeks. ¶ Total includes unknown ages.
# Contributors to the Production of the MMWR (Weekly)
Weekly
when Td is not available, TT is not available for national distribution. Existing stocks of TT are extremely limited and are mainly reserved for production of tetanus immune globulin and other special circumstances. Health-care providers and institutions requiring Td for priority indications should contact Aventis Pasteur, telephone (800) 822-2463 or (800) VACCINE. Institutions should place orders for their anticipated needs for priority indications only. Limiting quantities of vaccine in each order is necessary to assure the widest possible distribution of available vaccine. For emergency situations (e.g., natural disasters) requiring increased use of Td, Aventis Pasteur can provide vaccine within 24 hours.
# The Morbidity and Mortality Weekly Report (MMWR) Series is prepared by the Centers for Disease Control and Prevention (CDC) and is available free of charge in electronic format and on a paid subscription basis for paper copy.
To receive an electronic copy on Friday of each week, send an e-mail message to [email protected]. The body content should read SUBscribe mmwr-toc. Electronic copy also is available from CDC's World-Wide Web server at http://www.cdc.gov/mmwr or from CDC's file transfer protocol server at ftp://ftp.cdc.gov/pub/ Publications/mmwr. To subscribe for paper copy, contact Superintendent of Documents, U.S. Government Printing Office, Washington, DC 20402; telephone (202) 512-1800.
Data in the weekly MMWR are provisional, based on weekly reports to CDC by state health departments. The reporting week concludes at close of business on Friday; compiled data on a national basis are officially released to the public on the following Friday. Address inquiries about the MMWR Series, including material to be considered for publication, to: Editor, MMWR Series, Mailstop C-08, CDC, 1600 Clifton Rd., N.E., Atlanta, GA 30333; telephone (888) 232-3228.
All material in the MMWR Series is in the public domain and may be used and reprinted without permission; citation as to source, however, is appreciated.
# IU.S. Government Printing
| None | None |
eb4980ab283a68e2e91ea255ba3fc9ba595b8a97 | cdc | None | depar depar depar depar department of health and human ser tment of health and human ser tment of health and human ser tment of health and human ser tment of health and human services vices vices vices vices#
This report summarizes the results of that analysis, which indicated that the homicide rate in Brazil more than doubled during this period (Figure 1). Since 2001, Brazilian authorities have implemented several initiatives to reduce the number of homicides, including a law that controls gun ownership and prohibits anyone other than police and members of the armed forces from carrying guns. However, homicides among adolescents and young adults remain a substantial public health problem in Brazil, and additional prevention strategies that target young persons are needed.
Data were obtained from the Mortality Information System operated by Brazil's Ministry of Health. This database includes information from death certificates for all states in Brazil. Additional data for São Paulo city were obtained from the Program for Quality Improvement of Mortality Information. Homicide was defined as a death resulting from an injury that was inflicted purposefully by another (including legal intervention) for which the underlying cause listed on the death certificate corresponds to codes E960-E978 and E970-E978 of the International Classification of Diseases, Ninth Revision for 1980-1996, and codes X85-Y09 and Y35 of the Tenth Revision for 1997-2002. Population data for Brazil and São Paulo city were obtained from BGSI. Crude, age-, and sex-specific rates were calculated per 100,000 population. To examine the association between socioeconomic status and homicide rates in São Paulo city, SHDSP obtained data on the monthly average income of heads of households in all 96 city districts from the 2000 Brazil Population Census. Pearson correlation analysis was used to test this association. Other countries in the Americas have experienced similar increases in homicide rates during this period (3). In 2002, Brazil had one of the world's highest homicide rates, nearly four times higher than that for the United States (4). In 2000, Brazil accounted for an estimated 28% of all the homicides that occurred in the Americas, a region that has the highest homicide rate (4).
Factors that might have contributed to increased violence include increasing urbanization, expansion of illegal drug and firearms trafficking, a lengthy economic crisis, increased unemployment, and widening income inequality (5)(6)(7). The strong negative correlation between monthly average income and homicide rates in São Paulo city described in this report is consistent with homicide research in other urban areas worldwide (8). Further research is needed to better understand the association between violence and poverty so appropriate interventions can be developed. This association might be attributed to income inequality and disparities in job and education prospects.
Brazil has adopted measures to reduce the number of homicides. In 2001, the Brazil Ministry of Health issued a national policy to reduce injury-related morbidity and mortality and, in 2002, Brazil issued guidelines for the reporting of child maltreatment by health professionals. In December 2003, the Brazilian Congress passed a law that controls gun ownership and prohibits anyone other than police and members of the armed forces from carrying guns. The law also established tougher penalties for international firearms trafficking. The country also plans to implement an emergency departmentbased registry for injuries. In 2002, the government of São Paulo state passed legislation to establish an injury surveillance system. Improved surveillance data can help guide program and policy design and monitor progress toward reducing levels of violence (4).
Several violence-prevention initiatives have been developed in Brazil. In Rio de Janeiro, Viva Rio, a nongovernment organization, directs projects for 1) promoting awareness about the risks of using or carrying firearms, 2) reducing firearm injuries, 3) promoting peace, and 4) providing vocational training for youths who live in impoverished communities. In São Paulo state, a coalition of private sector investor groups, state banking organizations, advertising and media companies, and research centers established the São Paulo Institute Against Violence to support projects for violence prevention. In addition, the local government of São Paulo city implemented the Renda Minima Program, which provides financial support to low-income families, and the Bolsa Trabalho Program, which promotes youth employment; both programs might help reduce the homicide rate. The impact of these efforts should be evaluated to guide development of interventions in other communities.
The findings in this report are subject to at least two limitations. First, data from death certificates might underestimate the proportion of firearm-related homicides. Studies based on medical examiners' records have documented that, in large Brazilian cities like Recife, >90% of homicides involve firearms, whereas death certificates indicate that <70% of deaths were firearm related (9). Second, information is lacking about perpetrator characteristics or circumstances of these deaths (e.g., place of occurrence, relationship between victim and offender, and the use of alcohol and other substances). A homicide surveillance system is being planned for São Paulo city that will link information from death certificates with medical examiner and police records to guide public policies.
Homicides among adolescents and young adults constitute a substantial public health problem in Brazil, and additional prevention strategies that target young persons are needed. These strategies should include partnerships among the government, universities, the private sector, nongovernment organizations, and communities.
# Hypothermia-Related Deaths -United States, 2003
Hypothermia, a preventable lowering of the core body temperature to <95° F (<35° C) (1), causes approximately 600 deaths each year in the United States (2). Exposure to excessive cold (or excessive exposure to cold) slows enzymatic activity throughout the body, leading to potentially fatal rhabdomyolysis, coagulopathy, renal failure, and dysrhythmias (3). Alcohol intake, activity level, and type of clothing are among the modifiable factors associated with hypothermia (4). Understanding the epidemiology and pathophysiology of hypothermia is important to preventing hypothermiarelated mortality. This report describes three cases of fatal hypothermia that occurred during 2003, reviews national statistics on mortality from cold exposure in 2001, and provides recommendations for the diagnosis, treatment, and prevention of hypothermia. Public health strategies tailored to U.S. populations at increased risk for exposure to excessive cold can help reduce mortality and morbidity from hypothermia.
# Case Reports
Case 1. In the fall of 2003, a man aged 44 years was found dead outdoors in Vermont. He wore a T-shirt, long-sleeved shirt, two sweatshirts, underpants, pants, socks, and boots. His clothes were wet, and an empty vodka bottle was nearby. Local investigators reported that he looked as though he "lay down and went to sleep." Overnight, the temperature had dropped to <32° F (<0° C). Autopsy findings were unremarkable except for a fatty liver. A toxicology screen was negative except for an elevated blood alcohol concentration (BAC) of 0.30 g/dL, nearly four times the legal intoxication limit of 0.08 g/dL in Vermont. Cause of death was certified as hypothermia, with alcohol intoxication as a contributing factor. Case 2. In the spring of 2003, a man aged 76 years with Alzheimer's disease was reported missing from his home in Vermont. The next day, a farmer found the man lying in a swampy area where his car had become stuck in the mud. Overnight, the temperature had dropped to <32° F (<0° C). The man was pronounced dead at the scene; cause of death was hypothermia precipitated by a cold, wet environment. Case 3. In the fall of 2003, Alaska state troopers reported that a hiker aged 35 years was found dead alongside a highway. The hiker was not clothed from the waist up and was missing a shoe. The overnight temperature was 44° F (6.7° C), but conditions were wet and windy. The hiker's BAC was 0.28 g/dL, nearly four times the legal intoxication limit of 0.08 g/dL in Alaska; his toxicology screen was positive for cocaine and marijuana. Cause of death was hypothermia, with drug and alcohol intoxication as contributing factors.
# United States
In the United States, certain populations (e.g., alcoholics; drug users; elderly, homeless, and chronically ill persons; and those with preexisting heart disease) are at increased risk for dying from hypothermia. During 2001, a total of 599 persons in the United States (2) died from "exposure to excessive natural cold" (code X31), as categorized in the International Classification of Diseases, Tenth Revision. Of these victims, 67% were male, and 51% were aged >65 years. As persons age, their risk for dying from hypothermia increases (Figure Editorial Note: Hypothermia causes multiple dysfunctions, including cardiac arrhythmias, renal insufficiency, and hemoconcentration. In late stages of hypothermia, brain function deteriorates, predisposing persons to poor judgment and increasing their risk for further exposure to excessive cold.
Improper clothing and comorbidities can interfere with the balance between the body's heat production and cooling. Wet clothing cannot retain body heat; warm clothing keeps the body dry and helps to decrease heat loss, which can save a person's life during excessively cold weather. Advanced age, immobility, and existing medical conditions can increase the risk for hypothermia and death during cold weather. Certain medical conditions (e.g., hypothyroidism, congestive heart failure, and diabetes) can affect a person's ability to recognize warning symptoms of hypothermia, compensate for the cold, or to seek shelter from the cold.
Use of alcohol or other mood-altering drugs often is associated with cases of hypothermia. The vasodilatation caused by alcohol provides a sensation of warmth but also increases heat loss through radiation. In addition, alcohol and other drugs impair hand coordination, mobility, and decision-making abilities.
Treatment of hypothermia focuses on returning the core body temperature to normal while providing supportive care. The method chosen to rewarm a patient depends on the severity of the hypothermia (Box). With rewarming and supportive care, even persons who appear to be dead might survive hypothermia (5).
Prevention of hypothermia requires public health strategies that target persons at greatest risk. Such strategies can include creating community programs for checking on the well-being of elderly persons, opening temporary shelters for the homeless, and urging persons with cardiovascular disease to avoid outdoor exercise during cold weather (6).
# Epidemiology
# Alcohol Use Among Adolescents and Adults -New Hampshire, 1991-2003
Alcohol abuse is the third leading preventable cause of death in the United States (1). Because binge and heavy drinking increase the risk for cirrhosis, cancer, heart disease, stroke, injury, and depression (2,3), public health efforts have focused on reducing these patterns of alcohol use. The Council of State and Territorial Epidemiologists, the Association of State and Territorial Chronic Disease Program Directors, and CDC developed Indicators for Chronic Disease Surveillance (4), which provides a standard set of measures for alcohol surveillance. The New Hampshire Department of Health and Human Services used these measures to facilitate statewide trend analysis of alcohol use among adolescents and adults. This report summarizes the results of that analysis, which indicated that, in 2003, a total of 30.6% of adolescents reported binge drinking. In 2001, a total of 15.8% of adults reported binge drinking, and 6.3% reported heavy drinking. Interventions are needed to prevent adolescent drinking and to reduce excessive alcohol use among adults.
Three data sources were used to examine trends in alcohol use: New Hampshire (NH) Youth Risk Behavior Survey (NHYRBS), NH Behavioral Risk Factor Surveillance System (NHBRFSS), and NH Vital Records (NHVR). NHYRBS is a biennial, self-administered, school-based survey of students in grades 9-12; NHYRBS was conducted in odd-numbered years during 1995-2003. Because the statewide response rate was 18 years. Alcohol-related questions were asked annually during 1991-1993 and in odd-numbered years during 1995-2001 (response rate: 42.5%-70.9%). NHVR maintains and analyzes death-related data that are reported according to state law. The cause of death reported is the underlying cause of death or the specific disease, condition, or injury that leads to death.
For this analysis, seven public health indicators of alcoholrelated impact were assessed: binge drinking among adults, women of child-bearing age (i.e., aged 18-44 years), and adolescents (indicators 1-3); heavy drinking among adult men and women (indicators 4-5); alcohol use among adolescents (indicator 6); and mortality from chronic liver disease (indicator 7). Binge drinking was defined as having five or more drinks on one or more occasions during the 30 days preceding the survey. Heavy drinking was defined as an average daily consumption of greater than two drinks for men and one drink for women. Alcohol use among adolescents was defined as having one or more drinks during the 30 days preceding the survey. Mortality from chronic liver disease was determined by using the underlying primary cause of death from International Classification of Diseases, Tenth Revision codes K70 or K73-K74 or, for years before 1999, Ninth Revision code 571. Age-standardized prevalence estimates were calculated by using the 2000 U.S. standard population for all indicators except those that were age specific.
In the 2003 NHYRBS, 47.1% of high school students reported alcohol use, and 30.6% reported binge drinking; in comparison with 1995 results, changes were not statistically significant (Table 1). Both alcohol use and binge drinking among students increased significantly in grades 9 and 12 in 1995 and 2003.
In the 2001 NHBRFSS, 15.8% of adults reported binge drinking. During 1991-2001, men were two to three times more likely than women to report binge drinking (Table 2). In 2001, women of child-bearing age were six times more likely to report binge drinking than women aged >45 years (14.2% versus 2.3% ). In 2001, a total of 6.3% of adults reported heavy drinking (Table 3). No statistically significant differences were observed in heavy drinking between men and women during 1991-2001.
According to the 2001 NHVR, 9.7 deaths per 100,000 New Hampshire residents were attributable to chronic liver disease. (6). The findings in this report are subject to at least four limitations. First, because approximately half of all adults and high school students reported no alcohol use, the prevalence of binge drinking among current drinkers was underestimated. Second, a trend analysis of alcohol use among high school students could not be performed because weighted data from NHYRBS during 1997-2001 were unavailable. Third, analysis of annual data at the substate level was not possible because of sample size limitations. Finally, the full burden of alcohol-related disease and death, including injuries, violence, and other health impacts, could not be determined because analysis of alcohol-related health effects was limited to deaths caused by chronic liver disease.
New Hampshire was one of 12 states that included a module on binge drinking in its 2003 BRFSS survey, which will provide more recent and comprehensive information on adult binge drinking, including the type and quantity of alcohol consumed, the location of consumption, and alcohol-impaired driving that might have resulted from binge drinking. Alcohol surveillance information in New Hampshire was published for the first time in 2003 (6); the report will be updated annually to help policymakers and public health authorities implement programs to prevent adolescent drinking and excessive alcohol use among adults. | depar depar depar depar department of health and human ser tment of health and human ser tment of health and human ser tment of health and human ser tment of health and human services vices vices vices vices#
This report summarizes the results of that analysis, which indicated that the homicide rate in Brazil more than doubled during this period (Figure 1). Since 2001, Brazilian authorities have implemented several initiatives to reduce the number of homicides, including a law that controls gun ownership and prohibits anyone other than police and members of the armed forces from carrying guns. However, homicides among adolescents and young adults remain a substantial public health problem in Brazil, and additional prevention strategies that target young persons are needed.
Data were obtained from the Mortality Information System operated by Brazil's Ministry of Health. This database includes information from death certificates for all states in Brazil. Additional data for São Paulo city were obtained from the Program for Quality Improvement of Mortality Information. Homicide was defined as a death resulting from an injury that was inflicted purposefully by another (including legal intervention) for which the underlying cause listed on the death certificate corresponds to codes E960-E978 and E970-E978 of the International Classification of Diseases, Ninth Revision for 1980-1996, and codes X85-Y09 and Y35 of the Tenth Revision for 1997-2002. Population data for Brazil and São Paulo city were obtained from BGSI. Crude, age-, and sex-specific rates were calculated per 100,000 population. To examine the association between socioeconomic status and homicide rates in São Paulo city, SHDSP obtained data on the monthly average income of heads of households in all 96 city districts from the 2000 Brazil Population Census. Pearson correlation analysis was used to test this association. Other countries in the Americas have experienced similar increases in homicide rates during this period (3). In 2002, Brazil had one of the world's highest homicide rates, nearly four times higher than that for the United States (4). In 2000, Brazil accounted for an estimated 28% of all the homicides that occurred in the Americas, a region that has the highest homicide rate (4).
Factors that might have contributed to increased violence include increasing urbanization, expansion of illegal drug and firearms trafficking, a lengthy economic crisis, increased unemployment, and widening income inequality (5)(6)(7). The strong negative correlation between monthly average income and homicide rates in São Paulo city described in this report is consistent with homicide research in other urban areas worldwide (8). Further research is needed to better understand the association between violence and poverty so appropriate interventions can be developed. This association might be attributed to income inequality and disparities in job and education prospects.
Brazil has adopted measures to reduce the number of homicides. In 2001, the Brazil Ministry of Health issued a national policy to reduce injury-related morbidity and mortality and, in 2002, Brazil issued guidelines for the reporting of child maltreatment by health professionals. In December 2003, the Brazilian Congress passed a law that controls gun ownership and prohibits anyone other than police and members of the armed forces from carrying guns. The law also established tougher penalties for international firearms trafficking. The country also plans to implement an emergency departmentbased registry for injuries. In 2002, the government of São Paulo state passed legislation to establish an injury surveillance system. Improved surveillance data can help guide program and policy design and monitor progress toward reducing levels of violence (4).
Several violence-prevention initiatives have been developed in Brazil. In Rio de Janeiro, Viva Rio, a nongovernment organization, directs projects for 1) promoting awareness about the risks of using or carrying firearms, 2) reducing firearm injuries, 3) promoting peace, and 4) providing vocational training for youths who live in impoverished communities. In São Paulo state, a coalition of private sector investor groups, state banking organizations, advertising and media companies, and research centers established the São Paulo Institute Against Violence to support projects for violence prevention. In addition, the local government of São Paulo city implemented the Renda Minima Program, which provides financial support to low-income families, and the Bolsa Trabalho Program, which promotes youth employment; both programs might help reduce the homicide rate. The impact of these efforts should be evaluated to guide development of interventions in other communities.
The findings in this report are subject to at least two limitations. First, data from death certificates might underestimate the proportion of firearm-related homicides. Studies based on medical examiners' records have documented that, in large Brazilian cities like Recife, >90% of homicides involve firearms, whereas death certificates indicate that <70% of deaths were firearm related (9). Second, information is lacking about perpetrator characteristics or circumstances of these deaths (e.g., place of occurrence, relationship between victim and offender, and the use of alcohol and other substances). A homicide surveillance system is being planned for São Paulo city that will link information from death certificates with medical examiner and police records to guide public policies.
Homicides among adolescents and young adults constitute a substantial public health problem in Brazil, and additional prevention strategies that target young persons are needed. These strategies should include partnerships among the government, universities, the private sector, nongovernment organizations, and communities.
# Hypothermia-Related Deaths -United States, 2003
Hypothermia, a preventable lowering of the core body temperature to <95° F (<35° C) (1), causes approximately 600 deaths each year in the United States (2). Exposure to excessive cold (or excessive exposure to cold) slows enzymatic activity throughout the body, leading to potentially fatal rhabdomyolysis, coagulopathy, renal failure, and dysrhythmias (3). Alcohol intake, activity level, and type of clothing are among the modifiable factors associated with hypothermia (4). Understanding the epidemiology and pathophysiology of hypothermia is important to preventing hypothermiarelated mortality. This report describes three cases of fatal hypothermia that occurred during 2003, reviews national statistics on mortality from cold exposure in 2001, and provides recommendations for the diagnosis, treatment, and prevention of hypothermia. Public health strategies tailored to U.S. populations at increased risk for exposure to excessive cold can help reduce mortality and morbidity from hypothermia.
# Case Reports
Case 1. In the fall of 2003, a man aged 44 years was found dead outdoors in Vermont. He wore a T-shirt, long-sleeved shirt, two sweatshirts, underpants, pants, socks, and boots. His clothes were wet, and an empty vodka bottle was nearby. Local investigators reported that he looked as though he "lay down and went to sleep." Overnight, the temperature had dropped to <32° F (<0° C). Autopsy findings were unremarkable except for a fatty liver. A toxicology screen was negative except for an elevated blood alcohol concentration (BAC) of 0.30 g/dL, nearly four times the legal intoxication limit of 0.08 g/dL in Vermont. Cause of death was certified as hypothermia, with alcohol intoxication as a contributing factor. Case 2. In the spring of 2003, a man aged 76 years with Alzheimer's disease was reported missing from his home in Vermont. The next day, a farmer found the man lying in a swampy area where his car had become stuck in the mud. Overnight, the temperature had dropped to <32° F (<0° C). The man was pronounced dead at the scene; cause of death was hypothermia precipitated by a cold, wet environment. Case 3. In the fall of 2003, Alaska state troopers reported that a hiker aged 35 years was found dead alongside a highway. The hiker was not clothed from the waist up and was missing a shoe. The overnight temperature was 44° F (6.7° C), but conditions were wet and windy. The hiker's BAC was 0.28 g/dL, nearly four times the legal intoxication limit of 0.08 g/dL in Alaska; his toxicology screen was positive for cocaine and marijuana. Cause of death was hypothermia, with drug and alcohol intoxication as contributing factors.
# United States
In the United States, certain populations (e.g., alcoholics; drug users; elderly, homeless, and chronically ill persons; and those with preexisting heart disease) are at increased risk for dying from hypothermia. During 2001, a total of 599 persons in the United States (2) died from "exposure to excessive natural cold" (code X31), as categorized in the International Classification of Diseases, Tenth Revision. Of these victims, 67% were male, and 51% were aged >65 years. As persons age, their risk for dying from hypothermia increases (Figure Editorial Note: Hypothermia causes multiple dysfunctions, including cardiac arrhythmias, renal insufficiency, and hemoconcentration. In late stages of hypothermia, brain function deteriorates, predisposing persons to poor judgment and increasing their risk for further exposure to excessive cold.
Improper clothing and comorbidities can interfere with the balance between the body's heat production and cooling. Wet clothing cannot retain body heat; warm clothing keeps the body dry and helps to decrease heat loss, which can save a person's life during excessively cold weather. Advanced age, immobility, and existing medical conditions can increase the risk for hypothermia and death during cold weather. Certain medical conditions (e.g., hypothyroidism, congestive heart failure, and diabetes) can affect a person's ability to recognize warning symptoms of hypothermia, compensate for the cold, or to seek shelter from the cold.
Use of alcohol or other mood-altering drugs often is associated with cases of hypothermia. The vasodilatation caused by alcohol provides a sensation of warmth but also increases heat loss through radiation. In addition, alcohol and other drugs impair hand coordination, mobility, and decision-making abilities.
Treatment of hypothermia focuses on returning the core body temperature to normal while providing supportive care. The method chosen to rewarm a patient depends on the severity of the hypothermia (Box). With rewarming and supportive care, even persons who appear to be dead might survive hypothermia (5).
Prevention of hypothermia requires public health strategies that target persons at greatest risk. Such strategies can include creating community programs for checking on the well-being of elderly persons, opening temporary shelters for the homeless, and urging persons with cardiovascular disease to avoid outdoor exercise during cold weather (6).
# Epidemiology
# Alcohol Use Among Adolescents and Adults -New Hampshire, 1991-2003
Alcohol abuse is the third leading preventable cause of death in the United States (1). Because binge and heavy drinking increase the risk for cirrhosis, cancer, heart disease, stroke, injury, and depression (2,3), public health efforts have focused on reducing these patterns of alcohol use. The Council of State and Territorial Epidemiologists, the Association of State and Territorial Chronic Disease Program Directors, and CDC developed Indicators for Chronic Disease Surveillance (4), which provides a standard set of measures for alcohol surveillance. The New Hampshire Department of Health and Human Services used these measures to facilitate statewide trend analysis of alcohol use among adolescents and adults. This report summarizes the results of that analysis, which indicated that, in 2003, a total of 30.6% of adolescents reported binge drinking. In 2001, a total of 15.8% of adults reported binge drinking, and 6.3% reported heavy drinking. Interventions are needed to prevent adolescent drinking and to reduce excessive alcohol use among adults.
Three data sources were used to examine trends in alcohol use: New Hampshire (NH) Youth Risk Behavior Survey (NHYRBS), NH Behavioral Risk Factor Surveillance System (NHBRFSS), and NH Vital Records (NHVR). NHYRBS is a biennial, self-administered, school-based survey of students in grades 9-12; NHYRBS was conducted in odd-numbered years during 1995-2003. Because the statewide response rate was <60% during 1997-2001, analysis of NHYRBS data was restricted to 1995 and 2003 (response rate: 65% and 62%, respectively). NHBRFSS is an annual population-based, random-digit-dialed telephone survey of the noninstitutionalized, civilian population aged >18 years. Alcohol-related questions were asked annually during 1991-1993 and in odd-numbered years during 1995-2001 (response rate: 42.5%-70.9%). NHVR maintains and analyzes death-related data that are reported according to state law. The cause of death reported is the underlying cause of death or the specific disease, condition, or injury that leads to death.
For this analysis, seven public health indicators of alcoholrelated impact were assessed: binge drinking among adults, women of child-bearing age (i.e., aged 18-44 years), and adolescents (indicators 1-3); heavy drinking among adult men and women (indicators 4-5); alcohol use among adolescents (indicator 6); and mortality from chronic liver disease (indicator 7). Binge drinking was defined as having five or more drinks on one or more occasions during the 30 days preceding the survey. Heavy drinking was defined as an average daily consumption of greater than two drinks for men and one drink for women. Alcohol use among adolescents was defined as having one or more drinks during the 30 days preceding the survey. Mortality from chronic liver disease was determined by using the underlying primary cause of death from International Classification of Diseases, Tenth Revision codes K70 or K73-K74 or, for years before 1999, Ninth Revision code 571. Age-standardized prevalence estimates were calculated by using the 2000 U.S. standard population for all indicators except those that were age specific.
In the 2003 NHYRBS, 47.1% of high school students reported alcohol use, and 30.6% reported binge drinking; in comparison with 1995 results, changes were not statistically significant (Table 1). Both alcohol use and binge drinking among students increased significantly in grades 9 and 12 in 1995 and 2003.
In the 2001 NHBRFSS, 15.8% of adults reported binge drinking. During 1991-2001, men were two to three times more likely than women to report binge drinking (Table 2). In 2001, women of child-bearing age were six times more likely to report binge drinking than women aged >45 years (14.2% [95% confidence interval (CI) = 11.8%-16.6%] versus 2.3% [95% CI = 1.4%-3.2%]). In 2001, a total of 6.3% of adults reported heavy drinking (Table 3). No statistically significant differences were observed in heavy drinking between men and women during 1991-2001.
According to the 2001 NHVR, 9.7 deaths per 100,000 New Hampshire residents were attributable to chronic liver disease. (6). The findings in this report are subject to at least four limitations. First, because approximately half of all adults and high school students reported no alcohol use, the prevalence of binge drinking among current drinkers was underestimated. Second, a trend analysis of alcohol use among high school students could not be performed because weighted data from NHYRBS during 1997-2001 were unavailable. Third, analysis of annual data at the substate level was not possible because of sample size limitations. Finally, the full burden of alcohol-related disease and death, including injuries, violence, and other health impacts, could not be determined because analysis of alcohol-related health effects was limited to deaths caused by chronic liver disease.
New Hampshire was one of 12 states that included a module on binge drinking in its 2003 BRFSS survey, which will provide more recent and comprehensive information on adult binge drinking, including the type and quantity of alcohol consumed, the location of consumption, and alcohol-impaired driving that might have resulted from binge drinking. Alcohol surveillance information in New Hampshire was published for the first time in 2003 (6); the report will be updated annually to help policymakers and public health authorities implement programs to prevent adolescent drinking and excessive alcohol use among adults.
# Acknowledgment
The findings in this report are based on data contributed by K Vandole, New Hampshire Dept of Health and Human Svcs.
# MMWR March 5, 2004
Brief Report
# Exposure to Tear Gas from a Theft-Deterrent Device on a Safe -Wisconsin, December 2003
On December 4, 2003, a hazardous materials (HazMat) release occurred at a jewelry store in Beloit, Wisconsin, when the store owner tightened a screw on the door of an old safe outfitted with a chemical theft-deterrent device. The device included a metal housing containing a glass vial of liquid, which cracked as the screw tightened, releasing approximately 4 ounces of tear gas. The store owner sustained eye and skin irritation and was treated at a hospital and released. Twelve persons in the building and persons in adjacent businesses were evacuated for 3 hours while a certified Level A HazMat team*, city firefighters, and emergency medical technicians responded to the release. This report summarizes the response to this event and underscores the need for persons who use old safes and vaults to know how to identify these devices and avoid tampering with them.
Beginning in the 1920s, certain safes and vaults included (or were fitted with) theft-deterrent devices containing chemical vials (Figure). Chloropicrin † was used commonly in these devices. Other tear gas agents reportedly were used in similar theft-deterrent devices. The metal casing of these devices usually is approximately 3 inches wide and 6-8 inches tall; the device is fastened to the back of a safe door with screws. A major manufacturer of these devices was located in Wisconsin during the 1920s-1950s, and other companies sold similar devices. One such device was found in an Iowa bank in 1999 after a vial shattered, releasing chloropicrin and causing a pregnant bank employee to suffer eye, skin, and throat irritation (2). The number of these devices sold or still in circulation is unknown.
Chloropicrin was used as a chemical weapon during World War I (2). Documented symptoms of chloropicrin exposure include 1) irritation of the eyes, skin, and respiratory system; 2) lacrimation (i.e., tearing); 3) cough; 4) pulmonary edema; and 5) nausea and vomiting (1).
The 2003 chloropicrin release was reported to the Hazardous Substances Emergency Events Surveillance (HSEES) system operated by the Wisconsin Department of Health and Family Services. Created and funded by the Agency for Toxic Substances and Disease Registry (3), HSEES is a multistate § health department surveillance system that tracks morbidity and mortality resulting from events ¶ involving the release or potential release of a hazardous substance**. However, because reporting HazMat events to HSEES is not mandatory, participating state health departments might not be informed about every event. In addition, how many chemical releases from theft-deterrent devices occur in nonparticipating states is unknown.
Persons who use or are around older safes and vaults (e.g., bankers, jewelers, locksmiths, and vault technicians) should know how to identify these devices and should avoid tampering with them. If a device is identified, only trained persons (e.g., experienced locksmiths or HazMat personnel) should attempt to remove or neutralize these devices. In addition, appropriate personal protective equipment should be used when attempting to dismantle these devices (4). If the contents of a device are released, the area should be evacuated immediately. Persons who have adverse health effects (e.g., eye, skin, or respiratory irritation) should seek medical attention immediately.
# FIGURE. Chemical theft-deterrent device used on a safe
# Front view
Rear view Photo/Charles Eastwood § Alabama, Colorado, Iowa, Louisiana, Minnesota, Mississippi, Missouri, New Jersey, New York, North Carolina, Oregon, Texas, Utah, Washington, and Wisconsin. ¶ An event is the release or threatened release of a hazardous substance(s) in an amount requiring removal, cleaning up, or neutralizing according to federal, state, or local law (3). ** A substance that can reasonably be expected to cause an adverse health effect.
# Notice to Readers
# Updated Recommendations on the Use of Pneumococcal Conjugate Vaccine: Suspension of Recommendation for Third and Fourth Dose
On March 2, this notice was posted on the MMWR website (http://www.cdc.gov/mmwr).
On February 13, 2004, CDC recommended that healthcare providers temporarily suspend routine use of the fourth dose of 7-valent pneumococcal conjugate vaccine (PCV7) when vaccinating healthy children (1). This action was taken to conserve vaccine and minimize the likelihood of shortages until Wyeth Vaccines, the only U.S. supplier of PCV7 (marketed as Prevnar ® ), restores sufficient production capacity to meet the national need. Since that recommendation, PCV7 production has been much less than expected because of continuing problems with the PCV7 vial-filling production line. Shipments have been delayed, resulting in spot shortages that might continue beyond summer 2004 and become widespread. Effective immediately, to further conserve vaccine, CDC recommends that all health-care providers temporarily suspend routine administration of both the third and fourth doses to healthy children.
Approximately 1.3 million doses of PCV7 are needed each month to provide every infant in the United States with the full, 4-dose vaccination series. For January-April 2004, total shipments are estimated to be <55% of the amount needed. Limiting healthy children to 2 doses of PCV7 will conserve vaccine and permit more children to receive at least 2 doses. More vaccine is expected to become available for distribution in May and June, but availability cannot be guaranteed. CDC will continue to update health-care providers on the status of vaccine supplies while the shortage persists.
PCV7 is highly effective. The routinely recommended 4-dose series has been 97% (95% confidence interval [CI] = 76%-100%) effective against invasive disease caused by serotypes represented in the vaccine; effectiveness in children who received 3 doses before age 1 year has been 87% (95% CI = 71%-94%), and effectiveness in children who received 2 doses has been 94% (95% CI = 84%-98%) (CDC, unpublished data, 2004). Efficacy data from a randomized, controlled trial suggest that 1-2 doses of pneumococcal conjugate vaccine are protective during the 2-month interval before the next dose, with 86% effectiveness (but a 95% CI that includes zero) (2). Although limited data support a 2-dose schedule among infants, this regimen is preferable to vaccinating certain children with 3 doses and not vaccinating others. Because PCV7 is a new vaccine, no long-term data on vaccine effectiveness are available. However, the incidence of invasive pneumococcal disease declines rapidly after age 2 years, even in unvaccinated children. In 1998, before PCV7 was licensed, the incidence of invasive disease was 203 per 100,000 infants aged 1 year and 63 per 100,000 children aged 2 years (3).
To ensure that every child is protected against pneumococcal disease despite the PCV7 shortage, CDC, in consultation with the American Academy of Family Physicians, the American Academy of Pediatrics, and the Advisory Committee on Immunization Practices, recommends that all health-care providers temporarily discontinue administering the third and fourth dose of PCV7 to healthy children. Health-care providers should continue to administer the routine 4-dose series to children at increased risk for severe disease*. Unvaccinated, healthy children aged 12-23 months should receive a single dose of PCV7. For children aged >2 years, PCV7 is not recommended routinely.
This recommendation reflects CDC's assessment of the existing national PCV7 supply and will be changed if the supply changes. Updated information about the national PCV7 supply is available from CDC at http://www.cdc.gov/nip/ news/shortages/default.htm. * Including children with sickle cell disease and other hemoglobinopathies, anatomic asplenia, chronic diseases (e.g., chronic cardiac and pulmonary disease and diabetes), cerebrospinal fluid leak, human immunodeficiency virus infection and other immunocompromising conditions, immunosuppressive chemotherapy or long-term systemic corticosteroid use; children who have undergone solid organ transplantation, and children who either have received or will receive cochlear implants (4). All these children have been identified as being at either "high risk" or "presumed high risk" for severe invasive pneumoccocal disease (5).
Health-care providers should maintain lists of children for whom conjugate vaccine has been deferred so it can be administered when the supply allows. The highest priority for vaccination among children who have been deferred is children vaccinated with <2 doses who are aged <1 year.
Because data on the long-term efficacy of 3-dose or 2-dose vaccine regimens are limited, health-care providers should consider the diagnosis of invasive pneumococcal disease in incompletely vaccinated children and are encouraged to report invasive pneumococcal disease after any regimen of pneumococcal conjugate vaccine to CDC through state health departments. If a pneumococcal isolate is available from a vaccinated child, CDC will perform serotyping to determine whether the type is included in the vaccine.
- D.C. -582 542 - - - - - - Kans. - 7 1,195 1,042 N N 9 - - - S. ATLANTIC - 1,118 16,556 22,125 - - 64 156 1 57 Del. - 30 447 466 N N - 1 - - Md. - 103 2,844 2,358 - - 6 6 - | None | None |
36970ec88a51df8471cac3f2e40f6d183385db2f | cdc | None | postage-paid form, which is available by calling 800-822-7967 (toll-free). ACIP will review these recommendations periodically as new information becomes available related to smallpox disease, smallpox vaccines, the risk of smallpox attack, smallpox vaccine adverse events, and the experience gained as recent recommendations are implemented. Revised recommendations will be developed as needed.# Summary
. This supplemental report provides recommendations for using smallpox vaccine in the pre-event vaccination program in the United States.
To facilitate preparedness and response, smallpox vaccination is recommended for persons designated by public health authorities to conduct investigation and follow-up of initial smallpox cases that might necessitate direct patient contact. ACIP recommends that each state and territory establish and maintain >1 smallpox response team. ACIP and the Healthcare Infection Control Practices Advisory Committee (HICPAC) recommend that each acute-care hospital identify health-care workers who can be vaccinated and trained to provide direct medical care for the first smallpox patients requiring hospital admission and to evaluate and manage patients who are suspected as having smallpox. When feasible, the first-stage vaccination program should include previously vaccinated health-care personnel to decrease the potential for adverse events. Additionally, persons administering smallpox vaccine in this pre-event vaccination program should be vaccinated.
Smallpox vaccine is administered by using the multiple-puncture technique with a bifurcated needle, packaged with the vaccine and diluent. According to the product labeling, 2-3 punctures are recommended for primary vaccination and 15 punctures for revaccination. A trace of blood should appear at the vaccination site after 15-20 seconds; if no trace of blood is visible, an additional 3 insertions should be made by using the same bifurcated needle without reinserting the needle into the vaccine vial. If no evidence of vaccine take is apparent after 7 days, the person can be vaccinated again.
Optimal infection-control practices and appropriate site care should prevent transmission of vaccinia virus from vaccinated health-care workers to patients. Health-care personnel providing direct patient care should keep their vaccination sites covered with gauze in combination with a semipermeable membrane dressing to absorb exudates and to provide a barrier for containment of vaccinia virus to minimize the risk of transmission; the dressing should also be covered by a layer of clothing. Dressings used to cover the site should be changed frequently to prevent accumulation of exudates and consequent maceration. The most critical measure in preventing contact transmission is consistent hand hygiene. Hospitals should designate staff to assess dressings for all vaccinated health-care workers. When feasible, staff responsible for dressing changes for smallpox health-care teams should be vaccinated; all persons handling dressings should observe contact precautions. Administrative leave is not required routinely for newly vaccinated health-care personnel, unless they are physically unable to work as a result of systemic signs and symptoms of illness; have extensive skin lesions that cannot be adequately covered; or if they are unable to adhere to the recommended infectioncontrol precautions. Persons outside the patient-care setting can keep their vaccination sites covered with a porous dressing; hand hygiene remains key to preventing inadvertent inoculation. FDA has recommended that recipients of smallpox vaccine be deferred from donating blood for 21 days or until the scab has separated. Contacts of vaccinees, who have inadvertently contracted vaccinia, also should be deferred from donating blood for 14 days after complete resolution of their complication.
In the pre-event vaccination program, smallpox vaccination is contraindicated for persons with a history or presence of eczema or atopic dermatitis; who have other acute, chronic, or exfoliative skin conditions; who have conditions associated with immunosuppression; are aged <1 year; who have a serious allergy to any component of the vaccine; or who are pregnant or breastfeeding. ACIP does not recommend smallpox vaccination for children and adolescents aged <18 years during the pre-event vaccination program. Pre-event vaccination also is contraindicated among persons with household contacts who have a history or presence of eczema or atopic dermatitis; who have other acute, chronic, or exfoliative skin conditions; who have conditions associated with immunosuppression; or who are pregnant. For purposes of screening for contraindications for pre-event vaccination, household contacts include persons with prolonged intimate contact (e.g., sexual contacts) with the potential vaccinee and others who might have direct contact with the vaccination site. Persons with inflammatory eye disease might be at increased risk for inadvertent inoculation as a result of touching or rubbing the eye. Therefore, deferring vaccination is prudent for persons with inflammatory eye diseases requiring steroid treatment until the condition resolves and the course of therapy is complete.
Eczema vaccinatum, a serious form of disseminated vaccinia infection, can occur among persons with atopic dermatitis and other dermatologic conditions. Potential vaccinees should be queried regarding the diagnosis of atopic dermatitis or eczema in themselves or any member of their household, or regarding the presence of chronic or recurrent rashes consistent with these diagnoses. Persons reporting such a rash in themselves or household members should not be vaccinated, unless a health-care provider determines that the rash is not eczema or atopic dermatitis.
Before vaccination, women of childbearing age should be asked if they are pregnant or intend to become pregnant during the next 4 weeks; women who respond positively should not be vaccinated. Any woman who thinks she might be pregnant or who wants additional assurance that she is not pregnant should perform a urine pregnancy test on the day scheduled for vaccination. If a pregnant woman is inadvertently vaccinated or if she becomes pregnant within 4
# Introduction
In June 2001, the Advisory Committee on Immunization Practices (ACIP) made recommendations for using smallpox (vaccinia) vaccine to protect persons working with orthopoxviruses and to prepare for and respond to a possible terrorist attack involving smallpox (1). Because of the terrorist attacks in 2001, CDC asked ACIP to review its previous recommendations for smallpox vaccination. These supplemental recommendations update the 2001 recommendations for vaccination of persons designated to respond to or care for a suspected or confirmed case of smallpox. In addition, they clarify and expand the primary strategy for control and containment of smallpox in the event of an outbreak (see Box for clinical summary). Recommendations remain unchanged for vaccination of laboratory workers who directly handle recombinant vaccinia viruses derived from nonhighly attenuated vaccinia strains or other orthopoxviruses that infect humans (e.g., monkeypox, cowpox, vaccinia, and variola) (1). The following recommendations were developed after formation of a joint working group of ACIP and the National Vaccine Advisory Committee (NVAC) in April 2002. That working group was joined in September 2002 by the Healthcare Infection Control Practices Advisory Committee (HICPAC). A series of public meetings and forums also were held to review available data related to smallpox, smallpox vaccine, smallpox-control strategies, and other concerns related to smallpox vaccination.
# Smallpox Transmission and Control
Smallpox is transmitted from an infected person to another person. Patients are most infectious during the first 7-10 days after rash onset; transmission can occur during the prodromal period, immediately before rash onset, when lesions in the mouth ulcerate, releasing virus into oral secretions. Infection is transmitted by large-droplet nuclei and occasionally by direct contact or contact with fomites (e.g., clothes or bedding). Airborne transmission has occurred rarely (2). Epidemiologic studies have demonstrated that smallpox has a lower rate of transmission than certain other diseases (e.g., measles, pertussis, and influenza) (2,3). The greatest risk for infection occurs among household members and close contacts of persons with smallpox, especially those with prolonged face-to-face exposure. Isolation of infected patients and vaccination and close monitoring of contacts of patients at greatest risk for infection have been demonstrated to interrupt transmission of smallpox (4,5). During the smallpox era, inadequate infection-control practices sometimes resulted in transmission in hospitals (6,7); a review of importations into Europe during 1950-1971 determined that >50% of the spread cases were associated with hospitals, with approximately 20% of all spread cases related to infections among health-care workers (6). In a review of European smallpox outbreaks, the communicability of smallpox decreased by approximately one half when hospital-based transmission was excluded (8).
The primary strategy to control a smallpox outbreak and interrupt disease transmission is surveillance and containment, which includes isolation of smallpox cases and vaccination of persons at risk for contracting smallpox. This strategy involves identification of infected persons through intensive surveillance, isolation of smallpox patients to prevent further transmission, vaccination of household contacts and other close contacts of infected persons (i.e., primary contacts), and vaccination of close contacts of the primary contact (i.e., a secondary contact who would be exposed if disease developed in the primary contact). This strategy was instrumental in the eradication of smallpox as a naturally occurring disease, including in areas that had low vaccination coverage (4).
During the smallpox eradication era, depending on the size of the smallpox outbreak and the resources that were available for rapid and thorough contact tracing, surveillance and containment activities in areas with identified smallpox cases were sometimes supplemented with vaccination of other persons in the area where the outbreak occurred. This was done to expand the ring of immune persons within an outbreak area and to further reduce the chance of secondary transmission from smallpox patients before they could be identified and isolated. Regardless of the geographic distribution, number of cases, or number of concurrent outbreaks, surveillance and containment activities remained the primary disease-control strategy (4).
# Critical Considerations
Multiple factors and assumptions were used in developing these supplemental recommendations, as follows:
- Level of Disease Risk and Threat. Information provided to ACIP indicated that a risk for smallpox occurring as a result of a deliberate release by terrorists exists; however, this risk is low, and the population at risk for such an exposure cannot be determined. ACIP also assumed that, regardless of the mode, magnitude, or duration of a terrorism release, the epidemiology of subsequent personto-person transmission would be consistent with prior experience. These recommendations also are based on the assumption that, in addition to vaccination, health-care workers and others would be afforded a certain level of protection from infection through appropriate infectioncontrol measures, including use of appropriate personal protective equipment. - Expected Severe Adverse Reactions to Vaccination.
ACIP assumes that appropriate screening for contraindications to vaccination will be implemented and will include both vaccinated persons as well as their household contacts. ACIP further assumes that recommended precautions will be taken to minimize both the risk for MMWR April 4,
# BOX. Clinical summary of recommendations for using smallpox vaccine in a pre-event vaccination program
To facilitate preparedness and response, smallpox vaccination is recommended for persons designated by public health authorities to conduct investigation and follow-up of initial smallpox cases that might necessitate direct patient contact. ACIP recommends that each state and territory establish and maintain >1 smallpox response team.
# Background
- During the smallpox era, the greatest risk for smallpox occurred among household members and close contacts of persons with smallpox, especially those with prolonged face-to-face exposure. Therefore, the primary strategy for controlling a smallpox outbreak and interrupting disease transmission is surveillance and containment, which includes isolation of smallpox patients and vaccination of persons at risk for contracting smallpox. In the event of a terrorist attack using smallpox, this strategy might be supplemented by expanded vaccination; state and local health departments should be able to vaccinate entire populations in a timely manner. adverse events among vaccinees as well as the risk for transmission of vaccinia to their contacts (e.g., patients or household members) and resulting adverse events among those contacts.
# Smallpox Vaccine and Vaccinia Immune Globulin
Supply. ACIP assumes that both smallpox vaccine and vaccinia immune globulin (VIG) will be available for use, in sufficient supply, handled and administered according to standard protocols, and that any pre-event use of smallpox vaccine will be voluntary.
# State and Local Vaccination Capacity and Capability.
State and local health departments should be able to conduct surveillance and containment, including ring vaccination, as the primary strategy for controlling and containing smallpox. In addition, state and local health departments should be able, if necessary, to expand vaccination to additional groups, including entire populations, in a timely manner. CDC has recently issued large-scale vaccination clinic guidelines to assist state and local health departments in developing this capacity (9).
# Smallpox Vaccines and VIG Availability
The only smallpox vaccine licensed in the United States is Dryvax ® (manufactured by Wyeth Laboratories, Inc., Marietta, Pennsylvania), which is a dried calf-lymph-type vaccine. Dryvax is a lyophilized preparation of live vaccinia virus grown on the skin of calves (Wyeth Laboratories. Dryvax . Marietta, PA: Wyeth Laboratories, 1994). On October 25, 2002, the Food and Drug Administration (FDA) approved a labeling supplement and a manufacturing supplement to Wyeth's biologics license application for Dryvax. The manufacturing supplement provides for a new kit that includes lyophilized vaccine in a 100-dose vial, a new supply of diluent (one prefilled diluent syringe), one transfer needle, and 100 individually wrapped bifurcated needles. With approval of this supplement, Dryvax can again be distributed and used as a licensed product. Licensed lots must meet lot-release specifications, which include recent testing to demonstrate that the vaccine retains its potency.- As of December 16, 2002, two lots that included a total of 2.7 million doses of Dryvax had full approval for use as a licensed product. Additional lots of Dryvax are expected to be released by FDA under the license.
Licensed Dryvax vaccine for civilian use will only be available through CDC. Licensed vaccine will be used for vaccinating laboratory or health-care workers who directly handle cultures, animals, or contaminated materials containing nonhighly attenuated vaccinia or recombinant vaccinia viruses, or other orthopoxviruses that infect humans (1)
# Surveillance
Cases of febrile rash illnesses for which smallpox is considered in the differential diagnosis should be immediately reported to local or state health departments. After evaluation by the health departments, if smallpox laboratory diagnostics are considered necessary, CDC's Rash Illness Evaluation Team should be consulted at 770-488-7100. Because smallpox was officially certified as eradicated in 1980 and no longer occurs naturally, an initial case of smallpox must be laboratoryconfirmed, which is available only at CDC. Clinical consultation and a preliminary laboratory diagnosis can be completed within 8-24 hours.
To assist medical and public health personnel in evaluating the likelihood of smallpox among patients with febrile rash illnesses, CDC has developed a rash illness assessment algorithm. † To enhance public health preparedness and response for smallpox control, specific teams at the federal, state, and local levels should be established to facilitate diagnostic evaluation of initial suspected cases of smallpox and to initiate control measures. These smallpox response teams might include persons designated as medical team leaders, public health advisors, medical epidemiologists, disease investigators, diagnostic laboratory scientists, nurses, personnel who could administer smallpox vaccines, security or law enforcement personnel, and other medical personnel to assist in evaluating suspected smallpox cases. ACIP recommends that each state and territory establish and maintain >1 smallpox response team. Considerations for additional teams should include population and geographic concerns and should be developed in accordance with federal, state, and local terrorism-response plans.
# Smallpox Health-Care Teams
ACIP and HICPAC recommend that in the first stage of the pre-event smallpox vaccination program, each acute-care hospital identify groups of health-care workers to be vaccinated and trained to provide direct medical care for the first smallpox patients requiring hospital admission and to evaluate and manage patients who are examined at emergency departments with suspected smallpox. This team should provide care 24 hours/day for the first >2 days after patients with smallpox have been identified, until additional health-care personnel are vaccinated. Nonvaccinated workers should be restricted from entering the rooms of smallpox patients or, under emergency conditions, should wear personal protective equipment.
ACIP and HICPAC recommend that smallpox health-care teams include
- emergency department staff, including physicians and nurses caring for children and adults; - intensive-care-unit staff, including physicians, nurses, and in hospitals that care for infants and children, pediatricians and pediatric intensive care specialists; - general medical unit staff, including nurses, internists, pediatricians, hospitalists (i.e., physicians whose practice emphasizes providing care for hospitalized patients), and family physicians in institutions where these persons are the essential providers of in-patient medical care; - primary-care house staff (i.e., medical, pediatric, and family physicians); - medical subspecialists, including infectious disease specialists; ¶ - infection-control professionals; - respiratory therapists; - radiology technicians; - security personnel; and - housekeeping staff (e.g., those staff involved in maintaining the health-care environment and decreasing the risk for fomite transmission). ACIP and HICPAC anticipate that the size and composition of smallpox health-care teams will vary according to the institutions and their patient populations, but each hospital should ideally have enough vaccinated personnel from each occupational category to ensure continuity of care. When feasible, the first-stage vaccination program should include previously vaccinated health-care personnel to further decrease the potential for adverse events, because adverse events occur less commonly among previously vaccinated persons.
Clinical laboratory workers are not recommended for inclusion in the initial phase of pre-event smallpox vaccination because the quantity of smallpox virus likely to be in clinical specimens of blood and body fluids is low. Consistent adherence to the Standard Precautions and biosafety protocols for protection of laboratory workers will prevent exposure to smallpox virus in clinical specimens (11)(12)(13)(14). § Additional information regarding surveillance activities after laboratory confirmation of a smallpox outbreak is located in CDC's Smallpox Response Plan and Guidelines (/ index.asp). ¶ This might involve creating regional teams of subspecialists (e.g., local medical consultants with smallpox experience, dermatologists, ophthalmologists, pathologists, surgeons, anesthesiologists in facilities where intensivists are not trained in anesthesia) to deliver consultative services.
# Vaccination Method
The skin over the insertion of the deltoid muscle or the posterior aspect of the arm over the triceps muscle is the preferred site for smallpox vaccination. Skin preparation for vaccination is not required unless the area is grossly contaminated, in which case soap and water should be used to clean the site. If alcohol or another chemical antiseptic is used, the skin must be allowed to dry thoroughly to prevent inactivation of the vaccine virus by the antiseptic. The multiple-puncture technique uses a presterilized bifurcated needle that is inserted vertically into the vaccine vial, causing a small droplet of vaccine (approximately 0.0025 mL) to adhere between the prongs of the needle. The droplet contains the recommended dosage of vaccine, and its presence within the prongs of the bifurcated needle should be confirmed visually. Holding the bifurcated needle perpendicular to the skin, punctures are made rapidly, with strokes vigorous enough to allow a trace of blood to appear after 15-20 seconds (4). According to the product labeling, 2-3 punctures are recommended for primary vaccination and 15 punctures for revaccination. If no trace of blood is visible after vaccination, an additional three insertions should be made by using the same bifurcated needle without reinserting the needle into the vaccine vial. If no evidence of vaccine take is apparent after 7 days, the person can be vaccinated again. Any remaining vaccine should be wiped off the skin with dry sterile gauze and the gauze disposed of in a biohazard waste container.
# Vaccinating Persons Administering Smallpox Vaccine in the Pre-Event Vaccination Program
Historically, vaccinators were administering smallpox vaccine as part of a disease control or eradication program and were revaccinated frequently. No data exist regarding the risks for inadvertent inoculation of vaccinia among susceptible vaccinators, but they are assumed to have a certain level of risk. The risk might be analogous to that observed among laboratory workers handling nonhighly attenuated vaccinia strains; ACIP recommends that these workers be vaccinated (1). Prior vaccination probably confers substantial protection, but local reactions can occur among revaccinees; thus, protection from clinically significant inadvertent inoculation cannot be considered absolute (15).
ACIP and HICPAC recommend that persons administering smallpox vaccine in the pre-event vaccination program be vaccinated to minimize clinical effects of inadvertent inoculation, if inadvertent inoculation occurs. Ideally, vaccinators should have a confirmed vaccine take before vaccinating others, but administering vaccine to vaccinators immediately before beginning work in vaccination clinics is acceptable. Vaccination of this group will also contribute to preparedness for smallpox response. If a smallpox release occurs, experienced vaccinators could immediately be deployed for terrorism response.
# Preventing Contact Transmission of Vaccinia Virus
After primary smallpox vaccination, vaccinia virus can be isolated from the vaccination site, beginning with development of a papule (i.e., 2-5 days after vaccination) until the scab separates from the skin lesion (i.e., 14-21 days after vaccination), with maximal shedding at 4-14 days after vaccination. Viral shedding might be of shorter duration among revaccinees (16,17). During the interval in which vaccinia virus is shed, inadvertent inoculation can occur from the vaccination site to another area of the body, most commonly the face, eyelid, nose, lips, genitalia, or anus. In addition, transmission could occur to another nonimmune person, leading to self-limited infections or to more serious complications, particularly among persons with medical contraindications to vaccination. The risk for mortality from eczema vaccinatum might be higher among infected contacts than among vaccinees (10,18,19).
Data from the smallpox eradication era indicate that primary vaccinees were the major source of vaccinia infection among contacts, presumably because they had a larger or longer duration of viral shedding than did revaccinees (16,18). Transmission usually required close interaction, occurred most often in the home, and often involved children (18). Nosocomial transmission of vaccinia from either patients or healthcare workers to patients has rarely been described; in the majority of instances, the source of vaccinia was a patient suffering from an adverse event after vaccination. The majority of these cases involved direct person-to-person transmission, though for certain persons, the mode of spread was not determined (18,(20)(21)(22). These data indicate that secondary transmission of vaccinia virus occurs infrequently, especially from adults, and requires close contact. However, today, both the risk for transmission and the risk that a serious adverse event might result if transmission occurs might be greater than during the smallpox era. At the time of the earlier studies, the majority of health-care workers would have been vaccinated previously and therefore were less likely to transmit vaccinia; moreover, the majority of patients were vaccinated also and were less likely to be susceptible to vaccinia. The number of health-care workers who had been vaccinated during these earlier study periods is unknown, but vaccination of healthcare workers was routinely recommended. The number of hospitalized patients at risk for serious complications of vaccinia infection is higher now and includes those persons with compromised immune systems from human immunodeficiency virus (HIV) infection or acquired immunodeficiency syndrome (AIDS), chemotherapy, or other immunosuppressive medications, organ transplantation, or similar conditions. More patients with indwelling invasive devices requiring frequent manipulation (e.g., intravenous lines, arterial lines, dialysis, ostomies, or central venous lines) are being cared for on hospital wards. Infection-control practices have improved also, and health-care workers are more cognizant of infectioncontrol practices than in earlier years. Additionally, new approaches to vaccination site care (i.e., semipermeable dressings) provide an effective barrier for containment of vaccinia virus (16,23).
After considering the data and the caveats noted previously, ACIP and HICPAC concluded that optimal infectioncontrol practices should essentially eliminate the risk of vaccinated health-care workers transmitting vaccinia to patients, and that placing health-care workers on administrative leave could create staffing shortages that might pose a risk to patients (24,25).
Consequently, ACIP and HICPAC recommend that, after smallpox vaccination, health-care personnel providing direct patient care should keep their vaccination sites covered with gauze or a similar absorbent material in combination with a semipermeable dressing to absorb exudates that develop and to provide a barrier for containment of vaccinia virus to minimize the risk of transmission (16,23). Alternatively, products combining an absorbent base with an overlying semipermeable layer can be used to cover the site. Semipermeable dressings provide an effective barrier to vaccinia virus, but use of a semipermeable dressing alone is associated with maceration of the vaccination site and increased irritation and itching at the site (23), thereby causing touching, scratching, and possible contamination of the hands. The vaccination site should be covered with gauze, a semipermeable dressing, and a layer of clothing during direct patient care until the scab separates. Dressings used to cover the site should be changed frequently (e.g., every 3-5 days or more frequently if exudates accumulate) to prevent buildup of exudates and consequent maceration.
The most critical measure in preventing contact transmission is consistent hand hygiene with antimicrobial soap and water or an approved alcohol-based hand-rub (i.e., one that contains >60% alcohol) after any contact with the vaccination site or with materials that have come into contact with the site and before patient contact (26). In addition, care should be taken to prevent contact with the site or contaminated materials from the site.
Hospitals should include a vaccination site-care component in their smallpox vaccination programs in which designated staff assess dressings for all vaccinated health-care workers daily (whether the workers are involved in direct patient care or in other duties), determine if dressings need changing (e.g., when accumulation of purulent material is visible or the integrity of the dressing has been disrupted), and change the dressing, if indicated. These designated staff should assess the vaccination site for local reactions and for vaccine take; reinforce education of vaccinees regarding the need for meticulous hand hygiene; and record and report serious adverse events after vaccination (see Reporting and Managing Adverse Events). When feasible, staff responsible for dressing changes for teams should be vaccinated, but having nonvaccinated staff change dressings is acceptable. All persons handling bandages should observe contact precautions.
Persons outside the patient-care setting (e.g., members of public health response teams not involved in patient care, or health-care workers who are not at work) can keep their vaccination sites covered with a porous dressing (e.g., gauze); hand hygiene remains critical in preventing inadvertent inoculation. In nonpatient-care settings in which transmission of vaccinia is a concern because of close personal contact with children or other persons, the vaccination site should be covered with gauze or a similar absorbent material and covered with clothing. Hypoallergenic tape should be used for persons who experience tape hypersensitivity.
The vaccination site should be kept dry, although normal showering or bathing can continue. A waterproof dressing might decrease the risk for autoinoculation while washing; if the site is uncovered, care should be taken to avoid touching it. After showering, if the vaccination site is wet, it should be blotted dry with gauze, which is then discarded. If a towel is used to dry the site, the towel should not be used to dry the rest of the body. Alternatively, the site can be allowed to air dry before replacing the bandage. No salves, creams, or ointments should be placed on the site. Contaminated bandages and, if possible, the vaccination site scab, after it has fallen off, should be placed in sealed plastic bags before disposal in the trash to further decrease the potential for inadvertent transmission of the live virus contained in the materials. Clothing, towels, and other cloth materials that have had contact with the site can be decontaminated with routine laundering in hot water (27,28). FDA guidance is available at / smpoxdefquar.htm.
# Administrative Leave for Vaccinated Health-Care Workers
Administrative leave is not required routinely for newly vaccinated health-care personnel unless they 1) are physically unable to work because of systemic signs and symptoms of illness; 2) have extensive skin lesions that cannot be covered adequately; or 3) are unable to adhere to the recommended infection-control precautions. The close contact required for transmission of vaccinia to household contacts is unlikely to occur in the health-care setting.
# Vaccination and Blood Donation
FDA has recommended that vaccinees be deferred from donating blood for 21 days or until the scab has separated. Contacts of vaccinees who have inadvertently contracted vaccinia also should be deferred from donating blood for 14 days after complete resolution of their complication. If a substantial number of persons are vaccinated within a brief period, the resulting donor deferrals could impact blood availability. Blood supply shortages can be serious. Blood and platelet donors can help sustain blood supplies by donating immediately before being vaccinated and donating again after they are eligible. Because the donor deferral period needs to be documented carefully, all vaccinees should save the written record of their vaccination. Saving this record also will help to determine vaccination status and donor eligibility in the event of a smallpox outbreak.
# Contraindications for Use of Smallpox Vaccine in the Pre-Event Vaccination Program
The conditions discussed in this section are contraindications in the pre-event vaccination program. No absolute contraindications exist to defer vaccination for persons with high-risk exposure to smallpox; persons at greatest risk for experiencing serious vaccination complications are also at greatest risk for death if they become infected with the smallpox virus. If a relative contraindication to vaccination exists in the setting of a terrorism threat or exposure, the risk of experiencing serious vaccination complications must be weighed against the risk of experiencing a potentially fatal smallpox infection (1).
In the pre-event vaccination program, smallpox vaccination is contraindicated (Table ) for persons Atopic dermatitis, irrespective of disease severity or activity, is a risk factor for developing eczema vaccinatum after smallpox vaccination among either vaccinees or their close contacts (10,(29)(30)(31)(32)(33), but no data exist to predict the absolute risk for this population. Because the majority of primary-care providers do not distinguish between eczema and atopic dermatitis, including when describing chronic exfoliative skin conditions among infants (34,35), ACIP recommends that smallpox vaccine not be administered to persons with a history of eczema or atopic dermatitis, irrespective of disease severity or activity.
Persons with other active acute, chronic, or exfoliative conditions (e.g., burns, impetigo, varicella zoster, herpes, severe acne, severe diaper dermatitis with extensive areas of denuded skin, or psoriasis) are at higher risk for clinically severe inadvertent inoculation and should not be vaccinated until the condition resolves. Additionally, persons with Darier disease (keratosis follicularis) can develop eczema vaccinatum and therefore should not be vaccinated (32,36).
Replication of vaccinia virus can be enhanced among persons with cellular or humoral immunodeficiencies and among those with immunosuppression (e.g., HIV/AIDS, leukemia, lymphoma, generalized malignancy, solid organ transplantation, or therapy with alkylating agents, antimetabolites, radiation, or high-dose corticosteroids ). Persons who are taking or have taken high-dose corticosteroids should not be vaccinated within 1 month of completing corticosteroid therapy, and persons treated with other immunosuppressive drugs within the previous 3 months should not be vaccinated (37). Persons with immunosuppression also include hematopoietic stem cell transplant recipients who are 24 months posttransplant, but have graftversus-host disease or disease relapse. Patients with severe clinical manifestations of certain autoimmune diseases (e.g., systemic lupus erythematosis) might have a degree of immunocompromise as a component of the disease (38). Although no data exist to indicate that a person is at risk from live-virus vaccines because of severe autoimmune disease in the absence of immunosuppressive therapy, persons with immunodeficiency as a clinical component of their autoimmune disease should not receive smallpox vaccine during the pre-event vaccination program.
According to product labeling, smallpox vaccine is not recommended for use among breastfeeding women (Wyeth Laboratories. Dryvax . Marietta, PA: Wyeth Laboratories, 1994); whether vaccine virus or antibodies are excreted in human milk is unknown. ACIP does not recommend smallpox vaccination of children and adolescents aged <18 years in the pre-event vaccination program, and smallpox vaccine is contraindicated for infants aged <1 year.
Pre-event vaccination is also contraindicated among persons with household contacts who have a history or presence of eczema or atopic dermatitis, irrespective of disease severity or activity; who have other acute, chronic, or exfoliative skin conditions; who have conditions associated with immunosuppression (see previous discussion); or who are pregnant. For purposes of screening for contraindications for pre-event vaccination, household contacts include persons with prolonged intimate contact with the potential vaccinee (e.g., sexual contacts) and others who might have direct contact with the vaccination site.
The presence of an adolescent or child (including an infant) in the household is not a contraindication to vaccination of adult members of the household; the risk for serious complications from transmission from an adult to a child is limited. Nonetheless, ACIP recognizes that programs might defer vaccination of household contacts of infants aged <1 year because of data indicating a higher risk for adverse events among primary vaccinees in this age group, compared with that among older children (31). The presence of a breastfeeding woman or a person with a vaccine component allergy in the household is also not a contraindication to vaccination of other household members (Table ).
# Precautions for Smallpox Vaccination
Persons with inflammatory eye diseases can be at increased risk for inadvertent inoculation as a result of touching or rubbing the eye. Therefore, deferring vaccination of persons with inflammatory eye diseases requiring steroid treatment is prudent until the condition resolves and the course of therapy is complete.
# Screening for Atopic Dermatitis as a Contraindication for Vaccination
To assist providers in identifying persons who should defer smallpox vaccination, ACIP recommends using two screening questions (Figure). Although sensitive, this approach to screening might preclude vaccination of persons who could otherwise be safely vaccinated. Certain organizations (e.g., the military or CDC) might elect to develop more precise screening tools for persons among whom the dermatologic risk factor or diagnosis is uncertain. These secondary screening tools should weigh the person's risk of developing an adverse event with the requirement of occupational readiness through safe smallpox vaccination.
# Screening for Pregnancy as a Contraindication for Vaccination
Fetal vaccinia is a rare, but serious, complication of smallpox vaccination during pregnancy or immediately before conception. Infection, which can spread to the fetus if viremia
# TABLE. Contraindications to using smallpox vaccine among vaccinees and their household contacts in the pre-event vaccination program
# Household Contraindication
Vaccinees contacts- History or presence of eczema or atopic dermatitis X X Other acute, chronic, or exfoliative skin conditions † X X Immunosuppression § X X Pregnancy X X Breastfeeding X Aged <1 year ¶ X Vaccine component allergy X - For purposes of screening for contraindications for pre-event vaccination, household contacts include persons with prolonged intimate contact with the potential vaccinee (e.g., sexual contacts) and others who might have direct contact with the vaccination site. † Conditions include burns, impetigo, varicella zoster, herpes, severe acne, or psoriasis. Persons with these conditions should not be vaccinated until the dermatologic condition resolves. § Conditions include human immunodeficiency virus, acquired immunodeficiency syndrome, leukemia, lymphoma, generalized malignancy, solid organ transplantation, cellular or humoral immunodeficiencies, or therapy with alkylating agents, antimetabolites, radiation, or high-dose corticosteroids. ¶ Vaccination of infants aged <1 year is contraindicated. Additionally, the Advisory Committee on Immunization Practices does not recommend vaccinating children and adolescents aged <18 years in the pre-event smallpox vaccination program.
-ccurs after vaccination, is manifested by typical skin lesions, organ involvement, and fetal or early neonatal death (39). During 1932During -1972, of 20 affected pregnancies, 18 occurred when the pregnant woman was vaccinated, and two occurred among pregnant contacts; 13 occurred among primary vaccinees, and three among those being revaccinated. Seven occurred during the first trimester, and 13 in the second trimester. Only one of 20 pregnancies was maintained until term, and of 21 affected births (one birth was of twins), three infants survived (39). A cohort study of pregnant women vaccinated during a mass campaign in Sweden in 1963 demonstrated a higher than expected rate of fetal loss (40); however, pathology was not performed to evaluate causation, and vaccinees might have been at higher risk for adverse outcomes of pregnancy. Smallpox vaccination of pregnant women has not been associated with an increased risk for congenital malformations (41).
Because of the limited risk but severe consequences of fetal infection, smallpox vaccine should not be administered in a pre-event setting to pregnant women or to women who are trying to become pregnant. Before vaccination, women of childbearing age should be asked if they are pregnant or intend to become pregnant in the next 4 weeks; women who respond positively should not be vaccinated. To further reduce the risk for inadvertently vaccinating a woman who is pregnant, at the time of prescreening women of childbearing age should be educated regarding what is known about fetal vaccinia. Women should be counseled to avoid becoming pregnant until >4 weeks after vaccination, and abstinence or highly effective contraceptive measures should be recommended to reduce the risk of pregnancy before or within 4 weeks after vaccination. Any woman who believes she might be pregnant or who wants additional assurance that she is not pregnant should perform a urine pregnancy test by using her firstmorning-void urine on the day scheduled for vaccination. Such tests could be made available at the prescreening and vaccination sites to avoid cost or other barriers to testing. However, women should be informed that a negative urine pregnancy test cannot exclude a very early pregnancy, and therefore, they and their health-care providers should not base a decision regarding their pregnancy status solely on a urine pregnancy test result (42).
If a pregnant woman is inadvertently vaccinated or if she becomes pregnant within 4 weeks after smallpox vaccination, she should be counseled regarding concern for the fetus. Smallpox vaccination during pregnancy should not ordinarily be a reason to terminate pregnancy. To expand understanding of the risk for fetal vaccinia and to document whether other adverse pregnancy outcomes might be associated with vaccination, CDC has established a pregnancy registry to prospectively follow the outcome of such pregnancies and facilitate the investigation of any adverse pregnancy outcome among pregnant women who were inadvertently vaccinated. For enrollment in the registry, contact CDC at 404-639-8253.
# Screening for HIV Infection as a Contraindication for Vaccination
Persons with HIV infection or AIDS might have an increased risk for severe adverse reactions resulting from live-virus vaccines. Because the HIV epidemic began after the cessation of routine smallpox vaccination, data are limited regarding the risks from vaccination among HIV-infected persons. A single case report has been published of a U.S. military recruit who developed disseminated vaccinia after smallpox vaccination and who was successfully treated with VIG, but later died from complications of AIDS (43). Although the exact number of HIV-infected persons who were vaccinated in the military program is unclear, 732 recruits who were in the service during 1981-1985, when vaccinations were administered, tested HIV-positive during 1985-1988, for an estimated fre-FIGURE. Questions used to screen for eczema and atopic dermatitis among potential recipients of smallpox vaccine.
# Question 1:
Have you or a member of your household ever been diagnosed with eczema or atopic dermatitis? Do not vaccinate. Question 2: Eczema or atopic dermatitis is an itchy, red, scaly rash that comes and goes but usually lasts >2 weeks. Have you or a member of your household ever had a rash like that? Continue screening process for other contraindications.
Do not vaccinate unless the vaccinee and his or her health-care provider are certain that the rash is not eczema or atopic dermatitis.
# No
No Yes Yes quency of serious adverse events among HIV-positive persons of 1/732, or 0.137% (95% confidence interval = 0.084%-0.22%); if only half were HIV-positive at the time of vaccination, the frequency increases to 1/366, or 0.273% (95% CI = 0.17%-0.44%) (Col. Deborah L. Birx, M.D., Walter Reed Army Institute of Medicine, personal communication, September 2002). Because the immunologic status of an HIVinfected person is probably the key to the risk from vaccination and the immunologic status of the recruits at the time of vaccination was unknown, these estimated rates might not apply to other groups of HIV-infected persons.
An estimated 850,000-950,000 HIV-infected persons are living in the United States (prevalence: 0.3%), and of these, an estimated 180,000-280,000 are unaware that they are infected (44). Estimates of the number of HIV-infected healthcare workers range from approximately 21,000 to 48,000 (CDC, Division of Health Care Quality Promotion, unpublished data, 2002), and the proportion of these infected healthcare workers who remain undiagnosed is unknown. Risk assessment followed by counseling and testing is useful in identifying persons with HIV infection. However, substantial numbers of HIV-infected persons might not recognize or acknowledge their risk during risk-assessment screening (45).
Smallpox vaccine should not be administered to persons with HIV infection or AIDS as part of a pre-event program because of their increased risk for progressive vaccinia (vaccinia necrosum). Before vaccination, potential vaccinees should be educated regarding the risk for severe vaccinial complications among persons with HIV infection or other immunosuppressive conditions; persons who think they might have one of these conditions should not be vaccinated.
ACIP does not recommend mandatory HIV testing before smallpox vaccination, but recommends that HIV testing should be readily available to all persons considering smallpox vaccination. HIV testing is recommended for persons who have any history of a risk factor for HIV infection and who are unsure of their HIV infection status. Because known risk factors cannot be identified for certain persons with HIV infection, anyone who is concerned that they could have HIV infection also should be tested. HIV testing should be available in a confidential or anonymous setting, as allowed by local laws and regulations, with results communicated to the potential vaccinee before the planned date of vaccination. Persons with a positive test result should be advised not to be vaccinated. Information regarding local testing options should be provided to all potential vaccinees, including sites where testing is performed at no cost. The recently licensed rapid HIV test might facilitate availability of HIV testing to potential vaccinees (46).
# Simultaneous Administration of Smallpox Vaccine with Other Vaccines
Simultaneously administering the most widely used live and inactivated vaccines has produced seroconversion rates and rates of adverse reactions similar to those observed when the vaccines are administered separately (47)(48)(49)(50). Inactivated vaccines do not interfere with the immune response to other inactivated vaccines or to live vaccines. An inactivated vaccine can be administered either simultaneously or at any time before or after a different inactivated vaccine or live vaccine. The immune response to one live-virus vaccine might be impaired if administered within 30 days of another live-virus vaccine, if not administered simultaneously (51,52). To minimize the potential risk for interference, parenterally administered live vaccines not administered on the same day should be administered >4 weeks apart, whenever possible. If parenterally administered live vaccines are separated by 4 weeks after the last, invalid dose (37).
Smallpox vaccine can be administered at the same time as certain other vaccines, with levels of safety and efficacy comparable to those observed when the vaccines are administered separately (53). Vaccines that have been documented to be effective when administered simultaneously with smallpox vaccine include oral polio vaccine, bacille of Calmette-Guérin (BCG) vaccine, yellow fever vaccine, measles vaccine, and diphtheria and tetanus toxoids and whole-cell pertussis vaccine (53). However, no data exist regarding simultaneous administration of smallpox vaccine with other vaccines now routinely administered to children and adults in the United States.
Varicella vaccine virus lesions might be confused with vaccinia lesions if the vaccines were administered simultaneously. In uncontrolled trials of persons aged >13 years, approximately 1,600 vaccinees who received 1 dose and 955 who received 2 doses of varicella vaccine were monitored for 42 days for adverse events (Merck and Co., Inc. Varivax . West Point, PA: Merck and Co., 1995). After the first and second doses, a nonlocalized rash consisting of a median number of five lesions developed in 5.5% and 0.9% of vaccinees, respectively, and occurred at a peak of 7-21 days and 0-23 days postvaccination, respectively (54).
Smallpox vaccine can be administered simultaneously with any inactivated vaccine (e.g., influenza vaccine) to encourage appropriate receipt of all indicated vaccines (e.g., among such populations as health-care workers). With the exception of varicella vaccine, smallpox vaccine can be administered simultaneously with other live-virus vaccines. To avoid confusion in ascertaining which vaccine might have caused postvaccination skin lesions or other adverse events, and facilitate managing such events, varicella vaccine and smallpox vaccine should only be administered >4 weeks apart.
# Timing of Tuberculosis Screening and Smallpox Vaccination
Suppression of tuberculin skin test (purified protein derivative ) reactivity has been demonstrated after administration of smallpox vaccine (55), as has been observed after administration of other parenteral live-virus vaccines (37). Health-care workers scheduled to receive an annual PPD skin test should not receive the skin test for 1 month after smallpox vaccination to prevent possible false-negative reactions.
# Reporting and Managing Adverse Events
Persons with progressive vaccinia, eczema vaccinatum, and severe generalized vaccinia or inadvertent inoculation might benefit from therapy with VIG or cidofovir, although the latter has not been approved by FDA for this indication. Suspected cases of these illnesses or other serious adverse events after smallpox vaccination should be reported immediately to state health departments. VIG and cidofovir are available from CDC for treatment of adverse events among smallpox vaccine recipients and their contacts under IND protocols. Recommendations regarding treatment of adverse events have been published recently (56).
Additionally, serious adverse events after smallpox vaccination should be reported to the Vaccine Adverse Event Reporting System (VAERS). Reports can be submitted through a secure Internet-based system at / VaersDataEntryintro.htm. Printable VAERS forms are located online at , or postagepaid forms can be obtained by calling 800-822-7967 (tollfree). Submission of VAERS reports by Internet is encouraged to expedite processing and data entry. Completed forms can be faxed to 877-721-0366 (toll-free) or mailed to P.O. Box 1100, Rockville, MD 20894-1100. Additional information related to VAERS reporting can be obtained by calling 800-822-7967 or by e-mail at [email protected].
# Future Directions
ACIP will review these recommendations periodically or more urgently, if necessary. These reviews will include new information or developments related to smallpox disease, smallpox vaccines (including licensure of additional smallpox vaccines), risk of smallpox attack, smallpox vaccine adverse events, and the experience gained in the implementation of these recommendations. Revised recommendations will be developed as needed. | postage-paid form, which is available by calling 800-822-7967 (toll-free). ACIP will review these recommendations periodically as new information becomes available related to smallpox disease, smallpox vaccines, the risk of smallpox attack, smallpox vaccine adverse events, and the experience gained as recent recommendations are implemented. Revised recommendations will be developed as needed.# Summary
. This supplemental report provides recommendations for using smallpox vaccine in the pre-event vaccination program in the United States.
To facilitate preparedness and response, smallpox vaccination is recommended for persons designated by public health authorities to conduct investigation and follow-up of initial smallpox cases that might necessitate direct patient contact. ACIP recommends that each state and territory establish and maintain >1 smallpox response team. ACIP and the Healthcare Infection Control Practices Advisory Committee (HICPAC) recommend that each acute-care hospital identify health-care workers who can be vaccinated and trained to provide direct medical care for the first smallpox patients requiring hospital admission and to evaluate and manage patients who are suspected as having smallpox. When feasible, the first-stage vaccination program should include previously vaccinated health-care personnel to decrease the potential for adverse events. Additionally, persons administering smallpox vaccine in this pre-event vaccination program should be vaccinated.
Smallpox vaccine is administered by using the multiple-puncture technique with a bifurcated needle, packaged with the vaccine and diluent. According to the product labeling, 2-3 punctures are recommended for primary vaccination and 15 punctures for revaccination. A trace of blood should appear at the vaccination site after 15-20 seconds; if no trace of blood is visible, an additional 3 insertions should be made by using the same bifurcated needle without reinserting the needle into the vaccine vial. If no evidence of vaccine take is apparent after 7 days, the person can be vaccinated again.
Optimal infection-control practices and appropriate site care should prevent transmission of vaccinia virus from vaccinated health-care workers to patients. Health-care personnel providing direct patient care should keep their vaccination sites covered with gauze in combination with a semipermeable membrane dressing to absorb exudates and to provide a barrier for containment of vaccinia virus to minimize the risk of transmission; the dressing should also be covered by a layer of clothing. Dressings used to cover the site should be changed frequently to prevent accumulation of exudates and consequent maceration. The most critical measure in preventing contact transmission is consistent hand hygiene. Hospitals should designate staff to assess dressings for all vaccinated health-care workers. When feasible, staff responsible for dressing changes for smallpox health-care teams should be vaccinated; all persons handling dressings should observe contact precautions. Administrative leave is not required routinely for newly vaccinated health-care personnel, unless they are physically unable to work as a result of systemic signs and symptoms of illness; have extensive skin lesions that cannot be adequately covered; or if they are unable to adhere to the recommended infectioncontrol precautions. Persons outside the patient-care setting can keep their vaccination sites covered with a porous dressing; hand hygiene remains key to preventing inadvertent inoculation. FDA has recommended that recipients of smallpox vaccine be deferred from donating blood for 21 days or until the scab has separated. Contacts of vaccinees, who have inadvertently contracted vaccinia, also should be deferred from donating blood for 14 days after complete resolution of their complication.
In the pre-event vaccination program, smallpox vaccination is contraindicated for persons with a history or presence of eczema or atopic dermatitis; who have other acute, chronic, or exfoliative skin conditions; who have conditions associated with immunosuppression; are aged <1 year; who have a serious allergy to any component of the vaccine; or who are pregnant or breastfeeding. ACIP does not recommend smallpox vaccination for children and adolescents aged <18 years during the pre-event vaccination program. Pre-event vaccination also is contraindicated among persons with household contacts who have a history or presence of eczema or atopic dermatitis; who have other acute, chronic, or exfoliative skin conditions; who have conditions associated with immunosuppression; or who are pregnant. For purposes of screening for contraindications for pre-event vaccination, household contacts include persons with prolonged intimate contact (e.g., sexual contacts) with the potential vaccinee and others who might have direct contact with the vaccination site. Persons with inflammatory eye disease might be at increased risk for inadvertent inoculation as a result of touching or rubbing the eye. Therefore, deferring vaccination is prudent for persons with inflammatory eye diseases requiring steroid treatment until the condition resolves and the course of therapy is complete.
Eczema vaccinatum, a serious form of disseminated vaccinia infection, can occur among persons with atopic dermatitis and other dermatologic conditions. Potential vaccinees should be queried regarding the diagnosis of atopic dermatitis or eczema in themselves or any member of their household, or regarding the presence of chronic or recurrent rashes consistent with these diagnoses. Persons reporting such a rash in themselves or household members should not be vaccinated, unless a health-care provider determines that the rash is not eczema or atopic dermatitis.
Before vaccination, women of childbearing age should be asked if they are pregnant or intend to become pregnant during the next 4 weeks; women who respond positively should not be vaccinated. Any woman who thinks she might be pregnant or who wants additional assurance that she is not pregnant should perform a urine pregnancy test on the day scheduled for vaccination. If a pregnant woman is inadvertently vaccinated or if she becomes pregnant within 4
# Introduction
In June 2001, the Advisory Committee on Immunization Practices (ACIP) made recommendations for using smallpox (vaccinia) vaccine to protect persons working with orthopoxviruses and to prepare for and respond to a possible terrorist attack involving smallpox (1). Because of the terrorist attacks in 2001, CDC asked ACIP to review its previous recommendations for smallpox vaccination. These supplemental recommendations update the 2001 recommendations for vaccination of persons designated to respond to or care for a suspected or confirmed case of smallpox. In addition, they clarify and expand the primary strategy for control and containment of smallpox in the event of an outbreak (see Box for clinical summary). Recommendations remain unchanged for vaccination of laboratory workers who directly handle recombinant vaccinia viruses derived from nonhighly attenuated vaccinia strains or other orthopoxviruses that infect humans (e.g., monkeypox, cowpox, vaccinia, and variola) (1). The following recommendations were developed after formation of a joint working group of ACIP and the National Vaccine Advisory Committee (NVAC) in April 2002. That working group was joined in September 2002 by the Healthcare Infection Control Practices Advisory Committee (HICPAC). A series of public meetings and forums also were held to review available data related to smallpox, smallpox vaccine, smallpox-control strategies, and other concerns related to smallpox vaccination.
# Smallpox Transmission and Control
Smallpox is transmitted from an infected person to another person. Patients are most infectious during the first 7-10 days after rash onset; transmission can occur during the prodromal period, immediately before rash onset, when lesions in the mouth ulcerate, releasing virus into oral secretions. Infection is transmitted by large-droplet nuclei and occasionally by direct contact or contact with fomites (e.g., clothes or bedding). Airborne transmission has occurred rarely (2). Epidemiologic studies have demonstrated that smallpox has a lower rate of transmission than certain other diseases (e.g., measles, pertussis, and influenza) (2,3). The greatest risk for infection occurs among household members and close contacts of persons with smallpox, especially those with prolonged face-to-face exposure. Isolation of infected patients and vaccination and close monitoring of contacts of patients at greatest risk for infection have been demonstrated to interrupt transmission of smallpox (4,5). During the smallpox era, inadequate infection-control practices sometimes resulted in transmission in hospitals (6,7); a review of importations into Europe during 1950-1971 determined that >50% of the spread cases were associated with hospitals, with approximately 20% of all spread cases related to infections among health-care workers (6). In a review of European smallpox outbreaks, the communicability of smallpox decreased by approximately one half when hospital-based transmission was excluded (8).
The primary strategy to control a smallpox outbreak and interrupt disease transmission is surveillance and containment, which includes isolation of smallpox cases and vaccination of persons at risk for contracting smallpox. This strategy involves identification of infected persons through intensive surveillance, isolation of smallpox patients to prevent further transmission, vaccination of household contacts and other close contacts of infected persons (i.e., primary contacts), and vaccination of close contacts of the primary contact (i.e., a secondary contact who would be exposed if disease developed in the primary contact). This strategy was instrumental in the eradication of smallpox as a naturally occurring disease, including in areas that had low vaccination coverage (4).
During the smallpox eradication era, depending on the size of the smallpox outbreak and the resources that were available for rapid and thorough contact tracing, surveillance and containment activities in areas with identified smallpox cases were sometimes supplemented with vaccination of other persons in the area where the outbreak occurred. This was done to expand the ring of immune persons within an outbreak area and to further reduce the chance of secondary transmission from smallpox patients before they could be identified and isolated. Regardless of the geographic distribution, number of cases, or number of concurrent outbreaks, surveillance and containment activities remained the primary disease-control strategy (4).
# Critical Considerations
Multiple factors and assumptions were used in developing these supplemental recommendations, as follows:
• Level of Disease Risk and Threat. Information provided to ACIP indicated that a risk for smallpox occurring as a result of a deliberate release by terrorists exists; however, this risk is low, and the population at risk for such an exposure cannot be determined. ACIP also assumed that, regardless of the mode, magnitude, or duration of a terrorism release, the epidemiology of subsequent personto-person transmission would be consistent with prior experience. These recommendations also are based on the assumption that, in addition to vaccination, health-care workers and others would be afforded a certain level of protection from infection through appropriate infectioncontrol measures, including use of appropriate personal protective equipment. • Expected Severe Adverse Reactions to Vaccination.
ACIP assumes that appropriate screening for contraindications to vaccination will be implemented and will include both vaccinated persons as well as their household contacts. ACIP further assumes that recommended precautions will be taken to minimize both the risk for MMWR April 4,
# BOX. Clinical summary of recommendations for using smallpox vaccine in a pre-event vaccination program
To facilitate preparedness and response, smallpox vaccination is recommended for persons designated by public health authorities to conduct investigation and follow-up of initial smallpox cases that might necessitate direct patient contact. ACIP recommends that each state and territory establish and maintain >1 smallpox response team.
# Background
• During the smallpox era, the greatest risk for smallpox occurred among household members and close contacts of persons with smallpox, especially those with prolonged face-to-face exposure. Therefore, the primary strategy for controlling a smallpox outbreak and interrupting disease transmission is surveillance and containment, which includes isolation of smallpox patients and vaccination of persons at risk for contracting smallpox. In the event of a terrorist attack using smallpox, this strategy might be supplemented by expanded vaccination; state and local health departments should be able to vaccinate entire populations in a timely manner. adverse events among vaccinees as well as the risk for transmission of vaccinia to their contacts (e.g., patients or household members) and resulting adverse events among those contacts.
# • Smallpox Vaccine and Vaccinia Immune Globulin
Supply. ACIP assumes that both smallpox vaccine and vaccinia immune globulin (VIG) will be available for use, in sufficient supply, handled and administered according to standard protocols, and that any pre-event use of smallpox vaccine will be voluntary.
# • State and Local Vaccination Capacity and Capability.
State and local health departments should be able to conduct surveillance and containment, including ring vaccination, as the primary strategy for controlling and containing smallpox. In addition, state and local health departments should be able, if necessary, to expand vaccination to additional groups, including entire populations, in a timely manner. CDC has recently issued large-scale vaccination clinic guidelines to assist state and local health departments in developing this capacity (9).
# Smallpox Vaccines and VIG Availability
The only smallpox vaccine licensed in the United States is Dryvax ® (manufactured by Wyeth Laboratories, Inc., Marietta, Pennsylvania), which is a dried calf-lymph-type vaccine. Dryvax is a lyophilized preparation of live vaccinia virus grown on the skin of calves (Wyeth Laboratories. Dryvax [Package insert]. Marietta, PA: Wyeth Laboratories, 1994). On October 25, 2002, the Food and Drug Administration (FDA) approved a labeling supplement and a manufacturing supplement to Wyeth's biologics license application for Dryvax. The manufacturing supplement provides for a new kit that includes lyophilized vaccine in a 100-dose vial, a new supply of diluent (one prefilled diluent syringe), one transfer needle, and 100 individually wrapped bifurcated needles. With approval of this supplement, Dryvax can again be distributed and used as a licensed product. Licensed lots must meet lot-release specifications, which include recent testing to demonstrate that the vaccine retains its potency.* As of December 16, 2002, two lots that included a total of 2.7 million doses of Dryvax had full approval for use as a licensed product. Additional lots of Dryvax are expected to be released by FDA under the license.
Licensed Dryvax vaccine for civilian use will only be available through CDC. Licensed vaccine will be used for vaccinating laboratory or health-care workers who directly handle cultures, animals, or contaminated materials containing nonhighly attenuated vaccinia or recombinant vaccinia viruses, or other orthopoxviruses that infect humans (1)
# Surveillance
Cases of febrile rash illnesses for which smallpox is considered in the differential diagnosis should be immediately reported to local or state health departments. After evaluation by the health departments, if smallpox laboratory diagnostics are considered necessary, CDC's Rash Illness Evaluation Team should be consulted at 770-488-7100. Because smallpox was officially certified as eradicated in 1980 and no longer occurs naturally, an initial case of smallpox must be laboratoryconfirmed, which is available only at CDC. Clinical consultation and a preliminary laboratory diagnosis can be completed within 8-24 hours.
To assist medical and public health personnel in evaluating the likelihood of smallpox among patients with febrile rash illnesses, CDC has developed a rash illness assessment algorithm. † To enhance public health preparedness and response for smallpox control, specific teams at the federal, state, and local levels should be established to facilitate diagnostic evaluation of initial suspected cases of smallpox and to initiate control measures. These smallpox response teams might include persons designated as medical team leaders, public health advisors, medical epidemiologists, disease investigators, diagnostic laboratory scientists, nurses, personnel who could administer smallpox vaccines, security or law enforcement personnel, and other medical personnel to assist in evaluating suspected smallpox cases. ACIP recommends that each state and territory establish and maintain >1 smallpox response team. Considerations for additional teams should include population and geographic concerns and should be developed in accordance with federal, state, and local terrorism-response plans.
# Smallpox Health-Care Teams
ACIP and HICPAC recommend that in the first stage of the pre-event smallpox vaccination program, each acute-care hospital identify groups of health-care workers to be vaccinated and trained to provide direct medical care for the first smallpox patients requiring hospital admission and to evaluate and manage patients who are examined at emergency departments with suspected smallpox. This team should provide care 24 hours/day for the first >2 days after patients with smallpox have been identified, until additional health-care personnel are vaccinated. Nonvaccinated workers should be restricted from entering the rooms of smallpox patients or, under emergency conditions, should wear personal protective equipment.
ACIP and HICPAC recommend that smallpox health-care teams include
• emergency department staff, including physicians and nurses caring for children and adults; • intensive-care-unit staff, including physicians, nurses, and in hospitals that care for infants and children, pediatricians and pediatric intensive care specialists; • general medical unit staff, including nurses, internists, pediatricians, hospitalists (i.e., physicians whose practice emphasizes providing care for hospitalized patients), and family physicians in institutions where these persons are the essential providers of in-patient medical care; • primary-care house staff (i.e., medical, pediatric, and family physicians); • medical subspecialists, including infectious disease specialists; ¶ • infection-control professionals; • respiratory therapists; • radiology technicians; • security personnel; and • housekeeping staff (e.g., those staff involved in maintaining the health-care environment and decreasing the risk for fomite transmission). ACIP and HICPAC anticipate that the size and composition of smallpox health-care teams will vary according to the institutions and their patient populations, but each hospital should ideally have enough vaccinated personnel from each occupational category to ensure continuity of care. When feasible, the first-stage vaccination program should include previously vaccinated health-care personnel to further decrease the potential for adverse events, because adverse events occur less commonly among previously vaccinated persons.
Clinical laboratory workers are not recommended for inclusion in the initial phase of pre-event smallpox vaccination because the quantity of smallpox virus likely to be in clinical specimens of blood and body fluids is low. Consistent adherence to the Standard Precautions and biosafety protocols for protection of laboratory workers will prevent exposure to smallpox virus in clinical specimens (11)(12)(13)(14). § Additional information regarding surveillance activities after laboratory confirmation of a smallpox outbreak is located in CDC's Smallpox Response Plan and Guidelines (http://www.bt.cdc.gov/agent/smallpox/response-plan/ index.asp). ¶ This might involve creating regional teams of subspecialists (e.g., local medical consultants with smallpox experience, dermatologists, ophthalmologists, pathologists, surgeons, anesthesiologists in facilities where intensivists [i.e., physicians who are board-certified in a medical specialty and who receive special training in critical care] are not trained in anesthesia) to deliver consultative services.
# Vaccination Method
The skin over the insertion of the deltoid muscle or the posterior aspect of the arm over the triceps muscle is the preferred site for smallpox vaccination. Skin preparation for vaccination is not required unless the area is grossly contaminated, in which case soap and water should be used to clean the site. If alcohol or another chemical antiseptic is used, the skin must be allowed to dry thoroughly to prevent inactivation of the vaccine virus by the antiseptic. The multiple-puncture technique uses a presterilized bifurcated needle that is inserted vertically into the vaccine vial, causing a small droplet of vaccine (approximately 0.0025 mL) to adhere between the prongs of the needle. The droplet contains the recommended dosage of vaccine, and its presence within the prongs of the bifurcated needle should be confirmed visually. Holding the bifurcated needle perpendicular to the skin, punctures are made rapidly, with strokes vigorous enough to allow a trace of blood to appear after 15-20 seconds (4). According to the product labeling, 2-3 punctures are recommended for primary vaccination and 15 punctures for revaccination. If no trace of blood is visible after vaccination, an additional three insertions should be made by using the same bifurcated needle without reinserting the needle into the vaccine vial. If no evidence of vaccine take is apparent after 7 days, the person can be vaccinated again. Any remaining vaccine should be wiped off the skin with dry sterile gauze and the gauze disposed of in a biohazard waste container.
# Vaccinating Persons Administering Smallpox Vaccine in the Pre-Event Vaccination Program
Historically, vaccinators were administering smallpox vaccine as part of a disease control or eradication program and were revaccinated frequently. No data exist regarding the risks for inadvertent inoculation of vaccinia among susceptible vaccinators, but they are assumed to have a certain level of risk. The risk might be analogous to that observed among laboratory workers handling nonhighly attenuated vaccinia strains; ACIP recommends that these workers be vaccinated (1). Prior vaccination probably confers substantial protection, but local reactions can occur among revaccinees; thus, protection from clinically significant inadvertent inoculation cannot be considered absolute (15).
ACIP and HICPAC recommend that persons administering smallpox vaccine in the pre-event vaccination program be vaccinated to minimize clinical effects of inadvertent inoculation, if inadvertent inoculation occurs. Ideally, vaccinators should have a confirmed vaccine take before vaccinating others, but administering vaccine to vaccinators immediately before beginning work in vaccination clinics is acceptable. Vaccination of this group will also contribute to preparedness for smallpox response. If a smallpox release occurs, experienced vaccinators could immediately be deployed for terrorism response.
# Preventing Contact Transmission of Vaccinia Virus
After primary smallpox vaccination, vaccinia virus can be isolated from the vaccination site, beginning with development of a papule (i.e., 2-5 days after vaccination) until the scab separates from the skin lesion (i.e., 14-21 days after vaccination), with maximal shedding at 4-14 days after vaccination. Viral shedding might be of shorter duration among revaccinees (16,17). During the interval in which vaccinia virus is shed, inadvertent inoculation can occur from the vaccination site to another area of the body, most commonly the face, eyelid, nose, lips, genitalia, or anus. In addition, transmission could occur to another nonimmune person, leading to self-limited infections or to more serious complications, particularly among persons with medical contraindications to vaccination. The risk for mortality from eczema vaccinatum might be higher among infected contacts than among vaccinees (10,18,19).
Data from the smallpox eradication era indicate that primary vaccinees were the major source of vaccinia infection among contacts, presumably because they had a larger or longer duration of viral shedding than did revaccinees (16,18). Transmission usually required close interaction, occurred most often in the home, and often involved children (18). Nosocomial transmission of vaccinia from either patients or healthcare workers to patients has rarely been described; in the majority of instances, the source of vaccinia was a patient suffering from an adverse event after vaccination. The majority of these cases involved direct person-to-person transmission, though for certain persons, the mode of spread was not determined (18,(20)(21)(22). These data indicate that secondary transmission of vaccinia virus occurs infrequently, especially from adults, and requires close contact. However, today, both the risk for transmission and the risk that a serious adverse event might result if transmission occurs might be greater than during the smallpox era. At the time of the earlier studies, the majority of health-care workers would have been vaccinated previously and therefore were less likely to transmit vaccinia; moreover, the majority of patients were vaccinated also and were less likely to be susceptible to vaccinia. The number of health-care workers who had been vaccinated during these earlier study periods is unknown, but vaccination of healthcare workers was routinely recommended. The number of hospitalized patients at risk for serious complications of vaccinia infection is higher now and includes those persons with compromised immune systems from human immunodeficiency virus (HIV) infection or acquired immunodeficiency syndrome (AIDS), chemotherapy, or other immunosuppressive medications, organ transplantation, or similar conditions. More patients with indwelling invasive devices requiring frequent manipulation (e.g., intravenous lines, arterial lines, dialysis, ostomies, or central venous lines) are being cared for on hospital wards. Infection-control practices have improved also, and health-care workers are more cognizant of infectioncontrol practices than in earlier years. Additionally, new approaches to vaccination site care (i.e., semipermeable dressings) provide an effective barrier for containment of vaccinia virus (16,23).
After considering the data and the caveats noted previously, ACIP and HICPAC concluded that optimal infectioncontrol practices should essentially eliminate the risk of vaccinated health-care workers transmitting vaccinia to patients, and that placing health-care workers on administrative leave could create staffing shortages that might pose a risk to patients (24,25).
Consequently, ACIP and HICPAC recommend that, after smallpox vaccination, health-care personnel providing direct patient care should keep their vaccination sites covered with gauze or a similar absorbent material in combination with a semipermeable dressing to absorb exudates that develop and to provide a barrier for containment of vaccinia virus to minimize the risk of transmission (16,23). Alternatively, products combining an absorbent base with an overlying semipermeable layer can be used to cover the site. Semipermeable dressings provide an effective barrier to vaccinia virus, but use of a semipermeable dressing alone is associated with maceration of the vaccination site and increased irritation and itching at the site (23), thereby causing touching, scratching, and possible contamination of the hands. The vaccination site should be covered with gauze, a semipermeable dressing, and a layer of clothing during direct patient care until the scab separates. Dressings used to cover the site should be changed frequently (e.g., every 3-5 days or more frequently if exudates accumulate) to prevent buildup of exudates and consequent maceration.
The most critical measure in preventing contact transmission is consistent hand hygiene with antimicrobial soap and water or an approved alcohol-based hand-rub (i.e., one that contains >60% alcohol) after any contact with the vaccination site or with materials that have come into contact with the site and before patient contact (26). In addition, care should be taken to prevent contact with the site or contaminated materials from the site.
Hospitals should include a vaccination site-care component in their smallpox vaccination programs in which designated staff assess dressings for all vaccinated health-care workers daily (whether the workers are involved in direct patient care or in other duties), determine if dressings need changing (e.g., when accumulation of purulent material is visible or the integrity of the dressing has been disrupted), and change the dressing, if indicated. These designated staff should assess the vaccination site for local reactions and for vaccine take; reinforce education of vaccinees regarding the need for meticulous hand hygiene; and record and report serious adverse events after vaccination (see Reporting and Managing Adverse Events). When feasible, staff responsible for dressing changes for teams should be vaccinated, but having nonvaccinated staff change dressings is acceptable. All persons handling bandages should observe contact precautions.
Persons outside the patient-care setting (e.g., members of public health response teams not involved in patient care, or health-care workers who are not at work) can keep their vaccination sites covered with a porous dressing (e.g., gauze); hand hygiene remains critical in preventing inadvertent inoculation. In nonpatient-care settings in which transmission of vaccinia is a concern because of close personal contact with children or other persons, the vaccination site should be covered with gauze or a similar absorbent material and covered with clothing. Hypoallergenic tape should be used for persons who experience tape hypersensitivity.
The vaccination site should be kept dry, although normal showering or bathing can continue. A waterproof dressing might decrease the risk for autoinoculation while washing; if the site is uncovered, care should be taken to avoid touching it. After showering, if the vaccination site is wet, it should be blotted dry with gauze, which is then discarded. If a towel is used to dry the site, the towel should not be used to dry the rest of the body. Alternatively, the site can be allowed to air dry before replacing the bandage. No salves, creams, or ointments should be placed on the site. Contaminated bandages and, if possible, the vaccination site scab, after it has fallen off, should be placed in sealed plastic bags before disposal in the trash to further decrease the potential for inadvertent transmission of the live virus contained in the materials. Clothing, towels, and other cloth materials that have had contact with the site can be decontaminated with routine laundering in hot water (27,28). ** FDA guidance is available at http://www.fda.gov/cber/gdlns/ smpoxdefquar.htm.
# Administrative Leave for Vaccinated Health-Care Workers
Administrative leave is not required routinely for newly vaccinated health-care personnel unless they 1) are physically unable to work because of systemic signs and symptoms of illness; 2) have extensive skin lesions that cannot be covered adequately; or 3) are unable to adhere to the recommended infection-control precautions. The close contact required for transmission of vaccinia to household contacts is unlikely to occur in the health-care setting.
# Vaccination and Blood Donation
FDA has recommended that vaccinees be deferred from donating blood for 21 days or until the scab has separated. Contacts of vaccinees who have inadvertently contracted vaccinia also should be deferred from donating blood for 14 days after complete resolution of their complication.** If a substantial number of persons are vaccinated within a brief period, the resulting donor deferrals could impact blood availability. Blood supply shortages can be serious. Blood and platelet donors can help sustain blood supplies by donating immediately before being vaccinated and donating again after they are eligible. Because the donor deferral period needs to be documented carefully, all vaccinees should save the written record of their vaccination. Saving this record also will help to determine vaccination status and donor eligibility in the event of a smallpox outbreak.
# Contraindications for Use of Smallpox Vaccine in the Pre-Event Vaccination Program
The conditions discussed in this section are contraindications in the pre-event vaccination program. No absolute contraindications exist to defer vaccination for persons with high-risk exposure to smallpox; persons at greatest risk for experiencing serious vaccination complications are also at greatest risk for death if they become infected with the smallpox virus. If a relative contraindication to vaccination exists in the setting of a terrorism threat or exposure, the risk of experiencing serious vaccination complications must be weighed against the risk of experiencing a potentially fatal smallpox infection (1).
In the pre-event vaccination program, smallpox vaccination is contraindicated (Table ) for persons Atopic dermatitis, irrespective of disease severity or activity, is a risk factor for developing eczema vaccinatum after smallpox vaccination among either vaccinees or their close contacts (10,(29)(30)(31)(32)(33), but no data exist to predict the absolute risk for this population. Because the majority of primary-care providers do not distinguish between eczema and atopic dermatitis, including when describing chronic exfoliative skin conditions among infants (34,35), ACIP recommends that smallpox vaccine not be administered to persons with a history of eczema or atopic dermatitis, irrespective of disease severity or activity.
Persons with other active acute, chronic, or exfoliative conditions (e.g., burns, impetigo, varicella zoster, herpes, severe acne, severe diaper dermatitis with extensive areas of denuded skin, or psoriasis) are at higher risk for clinically severe inadvertent inoculation and should not be vaccinated until the condition resolves. Additionally, persons with Darier disease (keratosis follicularis) can develop eczema vaccinatum and therefore should not be vaccinated (32,36).
Replication of vaccinia virus can be enhanced among persons with cellular or humoral immunodeficiencies and among those with immunosuppression (e.g., HIV/AIDS, leukemia, lymphoma, generalized malignancy, solid organ transplantation, or therapy with alkylating agents, antimetabolites, radiation, or high-dose corticosteroids [i.e., >2 mg/kg body weight or 20 mg/day of prednisone for >2 weeks]). Persons who are taking or have taken high-dose corticosteroids should not be vaccinated within 1 month of completing corticosteroid therapy, and persons treated with other immunosuppressive drugs within the previous 3 months should not be vaccinated (37). Persons with immunosuppression also include hematopoietic stem cell transplant recipients who are <24 months posttransplant, and hematopoietic stem cell transplant recipients who are >24 months posttransplant, but have graftversus-host disease or disease relapse. Patients with severe clinical manifestations of certain autoimmune diseases (e.g., systemic lupus erythematosis) might have a degree of immunocompromise as a component of the disease (38). Although no data exist to indicate that a person is at risk from live-virus vaccines because of severe autoimmune disease in the absence of immunosuppressive therapy, persons with immunodeficiency as a clinical component of their autoimmune disease should not receive smallpox vaccine during the pre-event vaccination program.
According to product labeling, smallpox vaccine is not recommended for use among breastfeeding women (Wyeth Laboratories. Dryvax [Package insert]. Marietta, PA: Wyeth Laboratories, 1994); whether vaccine virus or antibodies are excreted in human milk is unknown. ACIP does not recommend smallpox vaccination of children and adolescents aged <18 years in the pre-event vaccination program, and smallpox vaccine is contraindicated for infants aged <1 year.
Pre-event vaccination is also contraindicated among persons with household contacts who have a history or presence of eczema or atopic dermatitis, irrespective of disease severity or activity; who have other acute, chronic, or exfoliative skin conditions; who have conditions associated with immunosuppression (see previous discussion); or who are pregnant. For purposes of screening for contraindications for pre-event vaccination, household contacts include persons with prolonged intimate contact with the potential vaccinee (e.g., sexual contacts) and others who might have direct contact with the vaccination site.
The presence of an adolescent or child (including an infant) in the household is not a contraindication to vaccination of adult members of the household; the risk for serious complications from transmission from an adult to a child is limited. Nonetheless, ACIP recognizes that programs might defer vaccination of household contacts of infants aged <1 year because of data indicating a higher risk for adverse events among primary vaccinees in this age group, compared with that among older children (31). The presence of a breastfeeding woman or a person with a vaccine component allergy in the household is also not a contraindication to vaccination of other household members (Table ).
# Precautions for Smallpox Vaccination
Persons with inflammatory eye diseases can be at increased risk for inadvertent inoculation as a result of touching or rubbing the eye. Therefore, deferring vaccination of persons with inflammatory eye diseases requiring steroid treatment is prudent until the condition resolves and the course of therapy is complete.
# Screening for Atopic Dermatitis as a Contraindication for Vaccination
To assist providers in identifying persons who should defer smallpox vaccination, ACIP recommends using two screening questions (Figure). Although sensitive, this approach to screening might preclude vaccination of persons who could otherwise be safely vaccinated. Certain organizations (e.g., the military or CDC) might elect to develop more precise screening tools for persons among whom the dermatologic risk factor or diagnosis is uncertain. These secondary screening tools should weigh the person's risk of developing an adverse event with the requirement of occupational readiness through safe smallpox vaccination.
# Screening for Pregnancy as a Contraindication for Vaccination
Fetal vaccinia is a rare, but serious, complication of smallpox vaccination during pregnancy or immediately before conception. Infection, which can spread to the fetus if viremia
# TABLE. Contraindications to using smallpox vaccine among vaccinees and their household contacts in the pre-event vaccination program
# Household Contraindication
Vaccinees contacts* History or presence of eczema or atopic dermatitis X X Other acute, chronic, or exfoliative skin conditions † X X Immunosuppression § X X Pregnancy X X Breastfeeding X Aged <1 year ¶ X Vaccine component allergy X * For purposes of screening for contraindications for pre-event vaccination, household contacts include persons with prolonged intimate contact with the potential vaccinee (e.g., sexual contacts) and others who might have direct contact with the vaccination site. † Conditions include burns, impetigo, varicella zoster, herpes, severe acne, or psoriasis. Persons with these conditions should not be vaccinated until the dermatologic condition resolves. § Conditions include human immunodeficiency virus, acquired immunodeficiency syndrome, leukemia, lymphoma, generalized malignancy, solid organ transplantation, cellular or humoral immunodeficiencies, or therapy with alkylating agents, antimetabolites, radiation, or high-dose corticosteroids. ¶ Vaccination of infants aged <1 year is contraindicated. Additionally, the Advisory Committee on Immunization Practices does not recommend vaccinating children and adolescents aged <18 years in the pre-event smallpox vaccination program.
occurs after vaccination, is manifested by typical skin lesions, organ involvement, and fetal or early neonatal death (39). During 1932During -1972, of 20 affected pregnancies, 18 occurred when the pregnant woman was vaccinated, and two occurred among pregnant contacts; 13 occurred among primary vaccinees, and three among those being revaccinated. Seven occurred during the first trimester, and 13 in the second trimester. Only one of 20 pregnancies was maintained until term, and of 21 affected births (one birth was of twins), three infants survived (39). A cohort study of pregnant women vaccinated during a mass campaign in Sweden in 1963 demonstrated a higher than expected rate of fetal loss (40); however, pathology was not performed to evaluate causation, and vaccinees might have been at higher risk for adverse outcomes of pregnancy. Smallpox vaccination of pregnant women has not been associated with an increased risk for congenital malformations (41).
Because of the limited risk but severe consequences of fetal infection, smallpox vaccine should not be administered in a pre-event setting to pregnant women or to women who are trying to become pregnant. Before vaccination, women of childbearing age should be asked if they are pregnant or intend to become pregnant in the next 4 weeks; women who respond positively should not be vaccinated. To further reduce the risk for inadvertently vaccinating a woman who is pregnant, at the time of prescreening women of childbearing age should be educated regarding what is known about fetal vaccinia. Women should be counseled to avoid becoming pregnant until >4 weeks after vaccination, and abstinence or highly effective contraceptive measures should be recommended to reduce the risk of pregnancy before or within 4 weeks after vaccination. Any woman who believes she might be pregnant or who wants additional assurance that she is not pregnant should perform a urine pregnancy test by using her firstmorning-void urine on the day scheduled for vaccination. Such tests could be made available at the prescreening and vaccination sites to avoid cost or other barriers to testing. However, women should be informed that a negative urine pregnancy test cannot exclude a very early pregnancy, and therefore, they and their health-care providers should not base a decision regarding their pregnancy status solely on a urine pregnancy test result (42).
If a pregnant woman is inadvertently vaccinated or if she becomes pregnant within 4 weeks after smallpox vaccination, she should be counseled regarding concern for the fetus. Smallpox vaccination during pregnancy should not ordinarily be a reason to terminate pregnancy. To expand understanding of the risk for fetal vaccinia and to document whether other adverse pregnancy outcomes might be associated with vaccination, CDC has established a pregnancy registry to prospectively follow the outcome of such pregnancies and facilitate the investigation of any adverse pregnancy outcome among pregnant women who were inadvertently vaccinated. For enrollment in the registry, contact CDC at 404-639-8253.
# Screening for HIV Infection as a Contraindication for Vaccination
Persons with HIV infection or AIDS might have an increased risk for severe adverse reactions resulting from live-virus vaccines. Because the HIV epidemic began after the cessation of routine smallpox vaccination, data are limited regarding the risks from vaccination among HIV-infected persons. A single case report has been published of a U.S. military recruit who developed disseminated vaccinia after smallpox vaccination and who was successfully treated with VIG, but later died from complications of AIDS (43). Although the exact number of HIV-infected persons who were vaccinated in the military program is unclear, 732 recruits who were in the service during 1981-1985, when vaccinations were administered, tested HIV-positive during 1985-1988, for an estimated fre-FIGURE. Questions used to screen for eczema and atopic dermatitis among potential recipients of smallpox vaccine.
# Question 1:
Have you or a member of your household ever been diagnosed with eczema or atopic dermatitis? Do not vaccinate. Question 2: Eczema or atopic dermatitis is an itchy, red, scaly rash that comes and goes but usually lasts >2 weeks. Have you or a member of your household ever had a rash like that? Continue screening process for other contraindications.
Do not vaccinate unless the vaccinee and his or her health-care provider are certain that the rash is not eczema or atopic dermatitis.
# No
No Yes Yes quency of serious adverse events among HIV-positive persons of 1/732, or 0.137% (95% confidence interval [CI] = 0.084%-0.22%); if only half were HIV-positive at the time of vaccination, the frequency increases to 1/366, or 0.273% (95% CI = 0.17%-0.44%) (Col. Deborah L. Birx, M.D., Walter Reed Army Institute of Medicine, personal communication, September 2002). Because the immunologic status of an HIVinfected person is probably the key to the risk from vaccination and the immunologic status of the recruits at the time of vaccination was unknown, these estimated rates might not apply to other groups of HIV-infected persons.
An estimated 850,000-950,000 HIV-infected persons are living in the United States (prevalence: 0.3%), and of these, an estimated 180,000-280,000 are unaware that they are infected (44). Estimates of the number of HIV-infected healthcare workers range from approximately 21,000 to 48,000 (CDC, Division of Health Care Quality Promotion, unpublished data, 2002), and the proportion of these infected healthcare workers who remain undiagnosed is unknown. Risk assessment followed by counseling and testing is useful in identifying persons with HIV infection. However, substantial numbers of HIV-infected persons might not recognize or acknowledge their risk during risk-assessment screening (45).
Smallpox vaccine should not be administered to persons with HIV infection or AIDS as part of a pre-event program because of their increased risk for progressive vaccinia (vaccinia necrosum). Before vaccination, potential vaccinees should be educated regarding the risk for severe vaccinial complications among persons with HIV infection or other immunosuppressive conditions; persons who think they might have one of these conditions should not be vaccinated.
ACIP does not recommend mandatory HIV testing before smallpox vaccination, but recommends that HIV testing should be readily available to all persons considering smallpox vaccination. HIV testing is recommended for persons who have any history of a risk factor for HIV infection and who are unsure of their HIV infection status. Because known risk factors cannot be identified for certain persons with HIV infection, anyone who is concerned that they could have HIV infection also should be tested. HIV testing should be available in a confidential or anonymous setting, as allowed by local laws and regulations, with results communicated to the potential vaccinee before the planned date of vaccination. Persons with a positive test result should be advised not to be vaccinated. Information regarding local testing options should be provided to all potential vaccinees, including sites where testing is performed at no cost. The recently licensed rapid HIV test might facilitate availability of HIV testing to potential vaccinees (46).
# Simultaneous Administration of Smallpox Vaccine with Other Vaccines
Simultaneously administering the most widely used live and inactivated vaccines has produced seroconversion rates and rates of adverse reactions similar to those observed when the vaccines are administered separately (47)(48)(49)(50). Inactivated vaccines do not interfere with the immune response to other inactivated vaccines or to live vaccines. An inactivated vaccine can be administered either simultaneously or at any time before or after a different inactivated vaccine or live vaccine. The immune response to one live-virus vaccine might be impaired if administered within 30 days of another live-virus vaccine, if not administered simultaneously (51,52). To minimize the potential risk for interference, parenterally administered live vaccines not administered on the same day should be administered >4 weeks apart, whenever possible. If parenterally administered live vaccines are separated by <4 weeks, the vaccine administered second should not be counted as a valid dose and should be repeated. The repeat dose should be administered >4 weeks after the last, invalid dose (37).
Smallpox vaccine can be administered at the same time as certain other vaccines, with levels of safety and efficacy comparable to those observed when the vaccines are administered separately (53). Vaccines that have been documented to be effective when administered simultaneously with smallpox vaccine include oral polio vaccine, bacille of Calmette-Guérin (BCG) vaccine, yellow fever vaccine, measles vaccine, and diphtheria and tetanus toxoids and whole-cell pertussis vaccine (53). However, no data exist regarding simultaneous administration of smallpox vaccine with other vaccines now routinely administered to children and adults in the United States.
Varicella vaccine virus lesions might be confused with vaccinia lesions if the vaccines were administered simultaneously. In uncontrolled trials of persons aged >13 years, approximately 1,600 vaccinees who received 1 dose and 955 who received 2 doses of varicella vaccine were monitored for 42 days for adverse events (Merck and Co., Inc. Varivax [Package insert]. West Point, PA: Merck and Co., 1995). After the first and second doses, a nonlocalized rash consisting of a median number of five lesions developed in 5.5% and 0.9% of vaccinees, respectively, and occurred at a peak of 7-21 days and 0-23 days postvaccination, respectively (54).
Smallpox vaccine can be administered simultaneously with any inactivated vaccine (e.g., influenza vaccine) to encourage appropriate receipt of all indicated vaccines (e.g., among such populations as health-care workers). With the exception of varicella vaccine, smallpox vaccine can be administered simultaneously with other live-virus vaccines. To avoid confusion in ascertaining which vaccine might have caused postvaccination skin lesions or other adverse events, and facilitate managing such events, varicella vaccine and smallpox vaccine should only be administered >4 weeks apart.
# Timing of Tuberculosis Screening and Smallpox Vaccination
Suppression of tuberculin skin test (purified protein derivative [PPD]) reactivity has been demonstrated after administration of smallpox vaccine (55), as has been observed after administration of other parenteral live-virus vaccines (37). Health-care workers scheduled to receive an annual PPD skin test should not receive the skin test for 1 month after smallpox vaccination to prevent possible false-negative reactions.
# Reporting and Managing Adverse Events
Persons with progressive vaccinia, eczema vaccinatum, and severe generalized vaccinia or inadvertent inoculation might benefit from therapy with VIG or cidofovir, although the latter has not been approved by FDA for this indication. Suspected cases of these illnesses or other serious adverse events after smallpox vaccination should be reported immediately to state health departments. VIG and cidofovir are available from CDC for treatment of adverse events among smallpox vaccine recipients and their contacts under IND protocols. Recommendations regarding treatment of adverse events have been published recently (56).
Additionally, serious adverse events after smallpox vaccination should be reported to the Vaccine Adverse Event Reporting System (VAERS). Reports can be submitted through a secure Internet-based system at https://secure.vaers.org/ VaersDataEntryintro.htm. Printable VAERS forms are located online at http://www.vaers.org/pdf/vaers_form.pdf, or postagepaid forms can be obtained by calling 800-822-7967 (tollfree). Submission of VAERS reports by Internet is encouraged to expedite processing and data entry. Completed forms can be faxed to 877-721-0366 (toll-free) or mailed to P.O. Box 1100, Rockville, MD 20894-1100. Additional information related to VAERS reporting can be obtained by calling 800-822-7967 or by e-mail at [email protected].
# Future Directions
ACIP will review these recommendations periodically or more urgently, if necessary. These reviews will include new information or developments related to smallpox disease, smallpox vaccines (including licensure of additional smallpox vaccines), risk of smallpox attack, smallpox vaccine adverse events, and the experience gained in the implementation of these recommendations. Revised recommendations will be developed as needed.
# Acknowledgments
The preparers of this report are grateful for the assistance of the following persons: | None | None |
2029ac98c93ed4e48fb3022108bba292fd65f016 | cdc | None | Metalworking Fluids exposure to MWF aerosol at 1 mg/m 3 (thoracic fraction). This may be an underestimate of effect, as only current workers were included in the study; workers who may have left these three plants as a result of their asthma would not have been included in the study.
Basing an analysis on the same population reported on previously by Greaves et al. , Eisen et al. used a cohort approach and proportional hazards model to evaluate the association of post-hire asthma to MWF aerosol exposures. Among 1,788 active workers (including assembly workers) in the analysis, 29 reported asthma initially diagnosed after hire. Based on MWF exposures during the 2-year period preceding diagnosis (to correlate with likely time of asthma onset), incidence rate ratios (RRs) were calculated. With adjustment for age and period of hire (before or after 1970), RRs were as follows: 2.0 (95% CI=0.9-4.6) for straight MWF; 0.5 (95% CI=0.2-1.1) for soluble MWF; and 3.2 (95% CI=1.2-8.3) for synthetic MWF. Aerosol exposures for the six asthmatics who worked with synthetic MWFs during the 2 years before diagnosis averaged 0.6 mg/m 3 (inhalable fraction); the range was 0.36 to 0.91 mg/m 3 , and the median was 0.58 mg/m 3 . Kriebel et al. found that the association was stronger for asthma with onset following employment than for asthma predating employment as a machinist. Aerosol exposure measurements were made using samplers with a seven-hole cassette inlet face selected to approximate collection efficiencies of the American Conference of Governmental Industrial Hygienists/International Standards Organization (ACGIH/ISO) size-selective criteria for inhalable mass . At the time of the questionnaire survey, machinists at this facility who worked with straight oil MWF had a mean aerosol exposure of 0.24 mg/m 3 (inhalable fraction), and those who worked with soluble oil MWF had a mean exposure of 0.22 mg/m 3 (inhalable fraction).
Robins et al. provided relevant data from a study of machinists exposed to aerosols of soluble MWF and relatively unexposed assembly workers at an automotive transmission manufacturing plant. Among workers who reported not having pre-existing asthma, current asthma was reported and/or a clinically significant cross-shift FEV 1 decrement (of at least 12%) was experienced by 11 of 83 machinists compared with 3 of 44 assembly workers (calculated unadjusted OR=2.1; 95% CI=0.5-12.3).
# RESPIRATORY PROTECTION REQUIRED IN THIS AREA
# CHAPTER 9: Recommendations for an Occupational Safety and Health Program
Good housekeeping includes keeping the floors, equipment, and general work environ-ment clean. Wastes (including floor wash water) should not be dumped or swept into MWF sumps or coolant return trenches.
# Labeling and Posting
Workers should be trained to be aware of labeling practices in accordance with the OSHA hazard communication standards [29 CFR 1910.1200and 29 CFR 1926. Warning labels and signs should be posted on or near hazardous metalworking processes. Depending on the process and MWF exposure concentration, warning signs should state the need to wear protective clothing or an appropriate respirator for exposure to MWF aerosol concentrations exceeding the REL. If respiratory protection is required, the following statement should be posted:
All labels and warning signs should be printed in both English and the predominant language of workers who do not read English. Workers unable to read the labels and signs should be informed verbally about the hazards and instructions printed on the labels and signs.
# Engineering Controls
# Isolation
Skin and inhalation exposures to MWF and MWF aerosol can be minimized by using mechanical parts handling equipment and machine enclosures to isolate the workers. Simple splash-guarding may suffice for low-production machines, but complete enclosure (with ventilation) is required for high-production machines. Plant layouts should be such that transfer machines are isolated from other operations. Workers should be provided with isolation booths or fresh air showers.
Machine enclosures are an effective method of reducing worker exposures. Johnston and White have described the features that are important in designing effective enclosures. ANSI B11 contains detailed enclosure and mist control designs as well as considerations for installation and use. Hands examined exposure data collected at an automobile parts manufacturing plant to determine the effect of enclosures on MWF aerosol exposures. This study suggests that enclosures (particularly manufacturer's enclosures that are original equipment) effectively reduce MWF exposures. Retrofitting enclosure structures may also reduce exposures. | #
Metalworking Fluids exposure to MWF aerosol at 1 mg/m 3 (thoracic fraction). This may be an underestimate of effect, as only current workers were included in the study; workers who may have left these three plants as a result of their asthma would not have been included in the study.
Basing an analysis on the same population reported on previously by Greaves et al. [1995b], Eisen et al. [1997] used a cohort approach and proportional hazards model to evaluate the association of post-hire asthma to MWF aerosol exposures. Among 1,788 active workers (including assembly workers) in the analysis, 29 reported asthma initially diagnosed after hire. Based on MWF exposures during the 2-year period preceding diagnosis (to correlate with likely time of asthma onset), incidence rate ratios (RRs) were calculated. With adjustment for age and period of hire (before or after 1970), RRs were as follows: 2.0 (95% CI=0.9-4.6) for straight MWF; 0.5 (95% CI=0.2-1.1) for soluble MWF; and 3.2 (95% CI=1.2-8.3) for synthetic MWF. Aerosol exposures for the six asthmatics who worked with synthetic MWFs during the 2 years before diagnosis averaged 0.6 mg/m 3 (inhalable fraction); the range was 0.36 to 0.91 mg/m 3 , and the median was 0.58 mg/m 3 . Kriebel et al. [1994Kriebel et al. [ , 1997 studied workers exposed to soluble oil MWFs (142 workers) and straight oil MWFs (74 workers) along with less exposed assembly workers in a major machine shop complex manufacturing automobile transmissions. These investigators found evidence for an association between self-reported physician-diagnosed asthma and work as a machinist. After controlling for age, race, gender, and smoking, machinists exposed to soluble oil MWF reported asthma twice as often as nonmachinists (OR=2.1; 95% CI=0.9-4.6; P<0.10); those exposed to straight MWF also reported more asthma (OR=1.4), but this latter finding was more likely than the former to be due to chance (P>0.10). In an analysis stratified by whether the asthma diagnosis predated employment as a machinist, Kriebel et al. [1994,1997] found that the association was stronger for asthma with onset following employment than for asthma predating employment as a machinist. Aerosol exposure measurements were made using samplers with a seven-hole cassette inlet face selected to approximate collection efficiencies of the American Conference of Governmental Industrial Hygienists/International Standards Organization (ACGIH/ISO) size-selective criteria for inhalable mass [Kriebel et al. 1994]. At the time of the questionnaire survey, machinists at this facility who worked with straight oil MWF had a mean aerosol exposure of 0.24 mg/m 3 (inhalable fraction), and those who worked with soluble oil MWF had a mean exposure of 0.22 mg/m 3 (inhalable fraction).
Robins et al. [1997] provided relevant data from a study of machinists exposed to aerosols of soluble MWF and relatively unexposed assembly workers at an automotive transmission manufacturing plant. Among workers who reported not having pre-existing asthma, current asthma was reported and/or a clinically significant cross-shift FEV 1 decrement (of at least 12%) was experienced by 11 of 83 machinists compared with 3 of 44 assembly workers (calculated unadjusted OR=2.1; 95% CI=0.5-12.3).
# RESPIRATORY PROTECTION REQUIRED IN THIS AREA
# CHAPTER 9: Recommendations for an Occupational Safety and Health Program
Good housekeeping includes keeping the floors, equipment, and general work environ-ment clean. Wastes (including floor wash water) should not be dumped or swept into MWF sumps or coolant return trenches.
# Labeling and Posting
Workers should be trained to be aware of labeling practices in accordance with the OSHA hazard communication standards [29 CFR 1910.1200and 29 CFR 1926. Warning labels and signs should be posted on or near hazardous metalworking processes. Depending on the process and MWF exposure concentration, warning signs should state the need to wear protective clothing or an appropriate respirator for exposure to MWF aerosol concentrations exceeding the REL. If respiratory protection is required, the following statement should be posted:
All labels and warning signs should be printed in both English and the predominant language of workers who do not read English. Workers unable to read the labels and signs should be informed verbally about the hazards and instructions printed on the labels and signs.
# Engineering Controls
# Isolation
Skin and inhalation exposures to MWF and MWF aerosol can be minimized by using mechanical parts handling equipment and machine enclosures to isolate the workers. Simple splash-guarding may suffice for low-production machines, but complete enclosure (with ventilation) is required for high-production machines. Plant layouts should be such that transfer machines are isolated from other operations. Workers should be provided with isolation booths or fresh air showers.
Machine enclosures are an effective method of reducing worker exposures. Johnston and White [1995] have described the features that are important in designing effective enclosures. ANSI B11 [1997] contains detailed enclosure and mist control designs as well as considerations for installation and use. Hands [1995] examined exposure data collected at an automobile parts manufacturing plant to determine the effect of enclosures on MWF aerosol exposures. This study suggests that enclosures (particularly manufacturer's enclosures that are original equipment) effectively reduce MWF exposures. Retrofitting enclosure structures may also reduce exposures. | None | None |
d578e13b9c7c1cc1128125dd4ace033985d5b4df | cdc | None | Insecticide Cadmium Batteries ▶ SHS can worsen pre-existing conditions such as heart Arsenic Toluene Poison disease and respiratory problems. 4 Industrial solvent ▶ Because children breathe faster than adults, have smaller Carbon monoxide Ammonia Exhaust gas Detergent#
This publication is available at .
# II. INTRODUCTION
This manual is designed for state and local Healthy Homes programs that are working to reduce secondhand smoke exposure in multiunit housing. The manual provides field-tested strategies, recom mendations, best practices, and tools. The content draws on peer-reviewed research and interviews with practitioners. The manual is intended to frame issues and provide guidance for programs. Read ers should feel free to pick and choose among the strategies described-but should also understand that the strategies are interconnected and mutually supportive.
General disclaimer: This manual contains general information about legal matters; the information is not advice, and should not be treated as such.
# III. SECONDHAND SMOKE: WHAT IS IT AND WHY IS IT A PROBLEM?
Secondhand smoke (SHS), also known as environmental tobacco smoke, is defined as a mixture of sidestream smoke from the tip of the cigarette and mainstream smoke exhaled by the smoker. 1, SHS contains more than 4,000 chemicals (Figure 1), 5 of which at least 250 are known to be harmful, and more than 50 are known to cause cancer. 2,3,6 Major medical and scientific organizations agree that SHS exposure can cause disease and premature death in nonsmok ers. These include heart disease and lung cancer in nonsmoking bodies and lungs, and are still developing, they are espe cially vulnerable to the health effects of SHS. 4,15 ▶ Exposure to secondhand smoke increases the risk for FIGURE 1: SHS COMPONENTS Sudden Infant Death Syndrome. 4 In response to growing evidence that SHS poses serious health risks to nonsmokers and that only eliminating smoking in indoor settings fully protect nonsmokers 4,16 a growing number of states, communities, and businesses have adopted smoke-free laws and policies that eliminate smoking in workplaces and in public places, including restaurants and bars, to protect nonsmokers from SHS. 31 Smoke-free laws have been shown to reduce SHS exposure among nonsmokers, to reduce heart attack hospitalizations, and to help smokers quit. 4,7,22 Several recent studies have also suggested that smokefree laws may reduce asthma hospitalizations and emergency room visits. Smoke-free laws typically receive high levels of public support and compliance, with the level of support increasing over time after the laws are implemented, especially among smokers. 4,22 Smoke-free policies also educate the public about the health effects of SHS and change social norms. 4,22 This leads to a number of second ary options, including increased adoption of voluntary smoke-free home rules. 2,4,22,23 However, nonsmoking residents of multiunit housing complexes who choose to make their units smoke-free may still be exposed to SHS that infiltrates their units from other units or common areas, potentially endangering their health. 24
# "The connection between the health and the dwelling of the population is one of the most important that exists." -Florence Nightingale
# IV. SMOKE-FREE POLICIES IN MULTIUNIT HOMES
The proportion of U.S. households with smoke-free home rules increased from 43 percent in 1992-93 to 77.6 percent in 2006-2007. 16 The proportion of households with at least one smoker which had adopted smoke-free home rules increased from 10 percent in 1992-93 to 32 percent in 2003, while the proportion of households with no smokers with such rules in place increased from 57 percent to 84 percent over this period. 17 Smoke-free homes were defined as homes where no one is allowed to smoke inside. 17 Additionally, smoke-free home policies are associated with greater use of medications that assist in cessation among current smokers and lower rates of relapse among former smokers. 18,19 However, smoking still occurs in many households. 16 For this reason, and because people spend much of their time in their homes, the home remains a major source of SHS exposure. 4 This is especially true for young children, who tend to spend espe cially large amounts of time in the home and who have little control over their exposure to SHS. 4,17 More than half of U.S. children are exposed to SHS 20 Almost all children and nonsmoking adults who live with smokers who smoke in the home are exposed to SHS. 17,20 Because private single-family homes cannot be re quired to go smoke-free, clinical and educational ini tiatives are typically the only viable direct approach for reducing SHS exposure in this setting. 21 As noted above, laws making workplaces and public places smoke-free can contribute indirectly to increased adoption of smoke-free home rules by private house holds. 22,23 These initiatives can encourage households to adopt voluntary smoke-free home rules, motivate smokers to quit, and guide smokers who want to quit to proven cessation treatments and services. 4,22 However, in multiunit housing facilities, smoke-free policies can potentially play an important role in protecting residents from SHS. SHS can infiltrate from units where smoking occurs into common areas and other units where residents have adopted voluntary smoke-free home rules. SHS can infil trate into these areas through air ducts, cracks in floors and walls, stairwells, hallways, elevator shafts, plumbing, electrical lines, and open windows, among other routes. 24 In fact, as much as 60 percent of airflow in multi-unit housing facilities can come from other units. 20,24 Nearly 50 percent of multiunit housing residents report that they have experienced SHS infiltrating their unit. Smoke-free policies in multiunit housing can protect all occupants from SHS infiltration in individual units and common areas. Smoke-free policies can apply to indoor common areas (e.g., lobbies, laundry rooms, corridors), outdoor common areas (e.g., swimming pools and picnic and barbecue areas), and individual units, and to some or all buildings. Whatever areas such policies cover, they should apply to all residents and visitors at all times. This is necessary for the policies to be effective in protecting multiunit hous ing residents from SHS, since SHS constituents can linger in indoor settings long after smoking has ceased. 28 In some cases, management may need or choose to grandfather existing tenants who smoke for a certain period, such as the time until next lease renewal.
Apartment owners, managers, condominium associations, and public housing authority boards may all adopt policies eliminating or restricting smoking in multiunit housing facilities under their control. 29 A number of communities in California have adopted ordinances restricting smoking in multiunit housing, including several ordinances that eliminate smoking in individual units in certain types of multiunit housing. 30 Several communities in California and a number of states have enacted laws eliminating smoking in common areas, requiring disclosure of smoking policies and status, or establishing that SHS is a nuisance. As with smoke-free policies in workplaces, public places, and other settings, smoke-free policies in multi-unit housing do not ban smokers from using the smokefree facilities, but simply prevent smokers from smoking in settings where SHS affects others-in this case, primarily through SHS infiltration. In other words, smokers are not precluded from living in smoke-free multiunit housing, as long as they adhere to the smoke-free policy.
Although there is limited information available, surveys and focus groups indicate that, while many multiunit housing owners and managers are interested in adopting smoke-free policies, some ex press concerns about doing so. 36 These concerns typically fall into three major categories. First, many multiunit housing proprietors believe that it is illegal for them to bar tenants from smoking in their units. 36 Second, they fear that a smoke-free policy would make it difficult to attract new tenants or retain current tenants. 36 Finally, they are concerned that enforcing the policy could prove difficult, time-consuming, and expensive. 36 However, with regard to the first concern, no legal barrier prevents owners or managers of multiunit housing complexes from adopting smoke-free policies, including policies that apply to individual units. 29,37 The second concern is also unwarranted, with surveys finding that most tenants prefer smokefree policies. 32 Finally, in terms of the third concern, no evidence exists that smoke-free multiunit housing policies would be difficult to implement and enforce. In fact, operators of multiunit housing with existing smoke-free policies indicated that they are more likely to keep the polices in place. 36 Smoke-free-policies in multiunit housing may also potentially have significant economic benefits for owners. Most important, preparing a smoker's unit for occupancy by a new tenant often requires substantially greater time and money than readying a nonsmoker's unit. For example, smokers' units may require extensive repainting, repair of burn damage, and replacement of carpeting, draperies, and upholstered furniture. Secondly, smoking is also a major cause of residential fires and the lead ing cause of fatal residential fires. 40 Finally, owners and managers could potentially be subject to legal action by tenants who experience health problems as a result of SHS infiltration. 29 Multiunit housing residents in several states have brought such legal action in recent years, with mixed results. 29,33 Educational outreach can provide multiunit housing operators with this information. In recent years, as more multiunit housing operators have become aware of the benefits of smoke-free policies and rec ognized that they can be implemented successfully, an increasing number of private multiunit com plexes and public housing authorities have opted to go smoke-free. The U.S. Department of Housing and Urban Development has issued notices encouraging housing authorities and Section 8 housing facilities to adopt smoke-free policies voluntarily, including in individual units. Smoke-free policies in multiunit housing are a win-win -protecting tenants' health while also helping protect owners' investment. r
# V. FRAMEWORK FOR IMPLEMENTATION WITH HEALTHY HOMES PROGRAMS
Initiatives to reduce SHS exposure in multiunit housing offer an attractive opportunity for newly created or transitioning Healthy Homes programs. These initiatives offer Healthy Homes programs a chance to address a potential residential source of indoor air pollution and poor health (See Figure 2). 4,22,43 Unlike some other home health hazards, SHS exposure is preventable; adopting and enforcing a 100 percent smoke-free policy should eliminate most SHS exposure in the home. In addition, because of the growing interest in and demand for smoke-free multiunit housing policies, work in this area may open partnership and funding opportunities. Moreover, because smoke-free multiunit housing policies are relatively simple to adopt, addressing this issue could potentially yield early victories, generating further momentum.
# HEALTHY HOMES
- Secondhand smoke
- Radon - Fire hazards - Fall hazards - Allergens - Lead - Pesticides - Moisture - Volatile
# FIGURE 2: COMPONENTS OF A HEALTHY HOME
Moreover, Healthy Homes programs enjoy ready access to multiunit managers and tenants that state tobacco control programs, typically do not possess. Thus, Healthy Homes programs are therefore in a uniquely favorable position to build relationships with key stakeholders in order to lay the ground work for policy change.
The only way to fully protect nonsmokers from SHS is to eliminate smoking in indoor settings. 4 In a single-family home, this can be accomplished through a voluntary household rule which prohibits anyone from smoking inside the home at any time. However, residents of multiunit housing facilities who adopt such household rules can still be exposed to SHS through infiltration from other units or common areas. 24 Therefore, only a policy making, at a minimum, all units and indoor common areas in a building smoke-free, can effectively protect tenants from SHS. Thus Healthy Homes programs' educational and outreach activities will be most effective if they are directed to ultimately achieving implementation of such policies by convincing owners, managers, and tenants of their importance and benefits. In addition to informing managers and tenants about the health effects of SHS, it is also important to provide managers and tenants who smoke with support and assistance in their efforts to quit, including information on available cessation resources.
It is important for smoke-free policies in multiunit housing to be implemented in a nonpunitive man ner that does not stigmatize residents who smoke or refuse housing to applicants who smoke. Poli cies should be written and implemented in a way that minimizes the chances that multiunit housing residents are evicted for violations. Efforts should also be made to ensure that residents who do smoke have access to smoking cessation resources should they choose to take this opportunity to quit.
The following table provides a menu of resources that Healthy Homes programs can draw on to promote smoke-free policies in multiunit housing facilities. The table is based on a review of current best practices by state and local health departments, tobacco control agencies, public housing authori ties, nonprofit organizations, and community organizations. The framework is structured around four broad strategic activity areas: coordination, communication, collaboration, and capacity building. The table also includes a list of tools and resources for each activity. The goal of this framework is to enable Healthy Homes programs to select and implement strategies to effectively reduce SHS exposure in multiunit housing. The specific approach a program selects will depend on its organizational capacity, resources, existing projects, and the characteristics and circumstances of the community in question.
# Coordination
Research and analyze current smokefree programs and policies.
Review state and local demographics.
Use information to target initial efforts and highlight existing efforts.
Identify key gaps in resources that need to be addressed to support current efforts and develop a work plan.
Conduct a community assessment to identify community needs, characteristics, and cultural identity, and target outreach accordingly.
# VI. ADDENDUM
In addition to the resources listed above, a number of other helpful materials are available for Healthy Homes programs that are interested in working to reduce SHS exposure in multiunit housing. The following addendum provides an in-depth listing of research findings, best practices, web sites, and other information, including both online and print resources. Many resources were identified through interviews with smoke-free practitioners. Healthy Homes programs are free to use or adapt any of these materials.
# AddEndum conTEnTS
▶ Toolkits
- Multiunit housing operators' concerns about the legality of requiring individual units to go smokefree can pose a major barrier to adoption of smoke-free multiunit housing policies. A number of nongovernmental legal organizations have responded to these concerns by providing analyses of the relevant legal issues. While these resources provide an overview of these issues, they do not consti tute legal advice. The language of all smoke-free policies should be based on model language that has withstood legal scrutiny, and should be reviewed by an attorney knowledgeable about local and state ordinances before the policy is adopted.
Corresponding URL's for this table are listed in the Reference section of this manual.
# Federal Law
Federal Statutes: American with Disabilities Act Federal Statutes: Fair Housing Act
# State Statute Designation
There is no constitutional right to smoke, and no law precludes adoption of smoke-free policies in multiunit housing, including policies that make individual units smoke-free. Smoke-free policies are not discriminatory, since smoking is not a protected act and smokers are not a protected class. In some cases, it may be necessary to grandfather for a limited amount of time (e.g., until their leases come up for renewal). For analysis, see Tobacco Control Legal Consortium's There is No Constitutional Right to Smoke. a
The Americans with Disabilities Act permits smoke-free policies. Because smoking is not considered a disability, smokers are not protected under the Fair Housing Act or the Rehabilitation Act. 44 Some health conditions affected by SHS could be considered a disability (e.g., emphysema, heart conditions, asthma, COPD). Multiunit housing facilities may be required to provide some nonsmoking tenants who are affected by SHS infiltration some accommodation for these conditions on a case-by-case basis. Most state smoking restrictions focus on workplaces and public places rather than multiunit housing. Some state laws restrict smoking in common areas in multiunit housing complexes. Utah e law establishes SHS as a potential nuisance, giving tenants grounds for legal action. 46 In addition, Utah law also specifically allows condominium associations to restrict smoking in units, common areas, and facilities. 34 In Oregon, f a disclosure law requires a property owner to notify prospective tenants of a multiunit housing facility's smoking policy and the areas where smoking is permitted. 47
# Local City/ County
A number of communities in California have adopted ordinances addressing SHS infiltration in multiunit housing. These ordinances range from requirements that apartment managers disclose units where smoking is occurring to policies making indoor and/or outdoor common areas smoke-free to policies making individual units in some or all buildings smoke-free. These policies may initially apply only to new properties or may cover existing properties as well. Communities and states can also use tax credits, bonus points in competitive grant proposals, and other financial incentives to encourage the adoption of smoke-free multiunit housing policies (California Tax Credits. g Also, local Ordinances are effective (Oakland, CA; Buffalo, NY). For sample ordinance provisions that provide an overview of the available policy options, see the
# Lower Insurance Costs
Surveys of owners find that staff time spent dealing with smoking complaints was reduced following implementation of a smoke-free policy. 25 Maine's Sanford Housing Authority found that the cost of renovating smokers' units ranged from $1,070-1,670 versus $550 for a non-smoking unit. 39 Starting smoke-free home rules in single-family homes leads to reduced SHS exposure, increased smoking cessation, and reduced smoking among adult and adolescent smokers. 22 High preference and demand for smoke-free housing, as documented by renter surveys. 26 See Smoke-Free Environments Law Project p website for more surveys.
New York realtors have reported that smokers' residences are harder to sell than nonsmokers' residences. 67 Nonsmoking restaurants have on average a 16 percent higher resale value. 68 Cigarettes are a major cause of residential fires and the leading cause of fatal residential fires. 40 Some insurance companies offer discounts on fire, life, liability, and property insurance to multi-unit housing complexes that have adopted smoke-free policies. 71
# SAmPLE imPLEmEnTATion guidE For ownErS And mAnAgEr
Adopting a smoke-free policy in new properties should be relatively straightforward becausemanagement can establish a smoke-free norm from the start.
1. Establish a 100 percent smoke-free policy in all buildings, including individual units and common areas.
2. Include smoke-free provisions in lease/rental agreements.
3. Prominently post "No smoking" signs at entrances, on bulletin boards, in stairwells, and in other locations.
4. Highlight the smoke-free policy as an amenity in listings, ads, and other promotions.
5. Continually remind managers, staff, and tenants about the smoke-free policy. Educate them about the reasons for the policy and what to do if they see a violation. Prepare sup porting evidence, FAQs, and other relevant information.
Adopting a smoke-free policy in existing properties may require more intensive planning and educa tion, and could involve a phased-in approach to provide a transition period for tenants who are accustomed to smoking in their units.
1. Decide on the policy's scope and provisions and on the timeline for implementing it. For example, will the policy apply to individual units as well as common areas, and will it apply to some or all buildings? Also explain how the policy will handle existing tenants who smoke in their units (e.g., they may be grandfathered in until their leases come up for renewal, and, then be required to comply). Use building meetings, notices, and signs to let tenants know that the smoke-free policy is coming. This process should begin several months before the policy's effective date. Use this opportunity to educate tenants on the dangers of SHS and the issue of SHS infiltration. Tell tenants when the policy will take effect and explain how it will be enforced. Ask tenants for ideas on how to implement the policy, but do not give them veto power over its provisions. If necessary, conduct a small survey to gauge tenant response to and readiness for the policy. During the policy phasein, consider clustering nonsmokers and smokers in separate buildings. Tenants who smoke can be offered incentives to move to these buildings.
2. Publicize available smoking-cessation services. Provide support and encouragement to smokers who choose to take this opportunity to quit. Make sure to identify SHS and SHS infiltration, not smokers, as the problem. Don't use language or take steps that could make smoking tenants feel stigmatized.
3. Prominently post "No smoking" signs.
4. Remove ashtrays or relocate them to more appropriate locations.
5. Send tenants a letter formally notifying them of the new policy. Require all residents to sign a statement that they agree to comply with the policy. Enforcement of the policy for current tenants can begin on renewal of the tenant/renter lease, updated with the new smoke-free policy addendum.
rEFErEncES For HyPErLinkS : | Insecticide Cadmium Batteries ▶ SHS can worsen pre-existing conditions such as heart Arsenic Toluene Poison disease and respiratory problems. 4 Industrial solvent ▶ Because children breathe faster than adults, have smaller Carbon monoxide Ammonia Exhaust gas Detergent#
This publication is available at http://www.cdc.gov/healthyhomes.
# II. INTRODUCTION
This manual is designed for state and local Healthy Homes programs that are working to reduce secondhand smoke exposure in multiunit housing. The manual provides field-tested strategies, recom mendations, best practices, and tools. The content draws on peer-reviewed research and interviews with practitioners. The manual is intended to frame issues and provide guidance for programs. Read ers should feel free to pick and choose among the strategies described-but should also understand that the strategies are interconnected and mutually supportive.
General disclaimer: This manual contains general information about legal matters; the information is not advice, and should not be treated as such.
# III. SECONDHAND SMOKE: WHAT IS IT AND WHY IS IT A PROBLEM?
Secondhand smoke (SHS), also known as environmental tobacco smoke, is defined as a mixture of sidestream smoke from the tip of the cigarette and mainstream smoke exhaled by the smoker. 1,[2][3][4] SHS contains more than 4,000 chemicals (Figure 1), 5 of which at least 250 are known to be harmful, and more than 50 are known to cause cancer. 2,3,6 Major medical and scientific organizations agree that SHS exposure can cause disease and premature death in nonsmok ers. These include heart disease and lung cancer in nonsmoking bodies and lungs, and are still developing, they are espe cially vulnerable to the health effects of SHS. 4,15 ▶ Exposure to secondhand smoke increases the risk for FIGURE 1: SHS COMPONENTS Sudden Infant Death Syndrome. 4 In response to growing evidence that SHS poses serious health risks to nonsmokers and that only eliminating smoking in indoor settings fully protect nonsmokers 4,16 a growing number of states, communities, and businesses have adopted smoke-free laws and policies that eliminate smoking in workplaces and in public places, including restaurants and bars, to protect nonsmokers from SHS. 31 Smoke-free laws have been shown to reduce SHS exposure among nonsmokers, to reduce heart attack hospitalizations, and to help smokers quit. 4,7,22 Several recent studies have also suggested that smokefree laws may reduce asthma hospitalizations and emergency room visits. [48][49][50][51] Smoke-free laws typically receive high levels of public support and compliance, with the level of support increasing over time after the laws are implemented, especially among smokers. 4,22 Smoke-free policies also educate the public about the health effects of SHS and change social norms. 4,22 This leads to a number of second ary options, including increased adoption of voluntary smoke-free home rules. 2,4,22,23 However, nonsmoking residents of multiunit housing complexes who choose to make their units smoke-free may still be exposed to SHS that infiltrates their units from other units or common areas, potentially endangering their health. 24
# "The connection between the health and the dwelling of the population is one of the most important that exists." -Florence Nightingale
# IV. SMOKE-FREE POLICIES IN MULTIUNIT HOMES
The proportion of U.S. households with smoke-free home rules increased from 43 percent in 1992-93 to 77.6 percent in 2006-2007. 16 The proportion of households with at least one smoker which had adopted smoke-free home rules increased from 10 percent in 1992-93 to 32 percent in 2003, while the proportion of households with no smokers with such rules in place increased from 57 percent to 84 percent over this period. 17 Smoke-free homes were defined as homes where no one is allowed to smoke inside. 17 Additionally, smoke-free home policies are associated with greater use of medications that assist in cessation among current smokers and lower rates of relapse among former smokers. 18,19 However, smoking still occurs in many households. 16 For this reason, and because people spend much of their time in their homes, the home remains a major source of SHS exposure. 4 This is especially true for young children, who tend to spend espe cially large amounts of time in the home and who have little control over their exposure to SHS. 4,17 More than half of U.S. children are exposed to SHS 20 Almost all children and nonsmoking adults who live with smokers who smoke in the home are exposed to SHS. 17,20 Because private single-family homes cannot be re quired to go smoke-free, clinical and educational ini tiatives are typically the only viable direct approach for reducing SHS exposure in this setting. 21 As noted above, laws making workplaces and public places smoke-free can contribute indirectly to increased adoption of smoke-free home rules by private house holds. 22,23 These initiatives can encourage households to adopt voluntary smoke-free home rules, motivate smokers to quit, and guide smokers who want to quit to proven cessation treatments and services. 4,22 However, in multiunit housing facilities, smoke-free policies can potentially play an important role in protecting residents from SHS. SHS can infiltrate from units where smoking occurs into common areas and other units where residents have adopted voluntary smoke-free home rules. SHS can infil trate into these areas through air ducts, cracks in floors and walls, stairwells, hallways, elevator shafts, plumbing, electrical lines, and open windows, among other routes. 24 In fact, as much as 60 percent of airflow in multi-unit housing facilities can come from other units. 20,24 Nearly 50 percent of multiunit housing residents report that they have experienced SHS infiltrating their unit. [25][26][27] Smoke-free policies in multiunit housing can protect all occupants from SHS infiltration in individual units and common areas. Smoke-free policies can apply to indoor common areas (e.g., lobbies, laundry rooms, corridors), outdoor common areas (e.g., swimming pools and picnic and barbecue areas), and individual units, and to some or all buildings. Whatever areas such policies cover, they should apply to all residents and visitors at all times. This is necessary for the policies to be effective in protecting multiunit hous ing residents from SHS, since SHS constituents can linger in indoor settings long after smoking has ceased. 28 In some cases, management may need or choose to grandfather existing tenants who smoke for a certain period, such as the time until next lease renewal.
Apartment owners, managers, condominium associations, and public housing authority boards may all adopt policies eliminating or restricting smoking in multiunit housing facilities under their control. 29 A number of communities in California have adopted ordinances restricting smoking in multiunit housing, including several ordinances that eliminate smoking in individual units in certain types of multiunit housing. 30 Several communities in California and a number of states have enacted laws eliminating smoking in common areas, requiring disclosure of smoking policies and status, or establishing that SHS is a nuisance. [31][32][33][34][35] As with smoke-free policies in workplaces, public places, and other settings, smoke-free policies in multi-unit housing do not ban smokers from using the smokefree facilities, but simply prevent smokers from smoking in settings where SHS affects others-in this case, primarily through SHS infiltration. In other words, smokers are not precluded from living in smoke-free multiunit housing, as long as they adhere to the smoke-free policy.
Although there is limited information available, surveys and focus groups indicate that, while many multiunit housing owners and managers are interested in adopting smoke-free policies, some ex press concerns about doing so. 36 These concerns typically fall into three major categories. First, many multiunit housing proprietors believe that it is illegal for them to bar tenants from smoking in their units. 36 Second, they fear that a smoke-free policy would make it difficult to attract new tenants or retain current tenants. 36 Finally, they are concerned that enforcing the policy could prove difficult, time-consuming, and expensive. 36 However, with regard to the first concern, no legal barrier prevents owners or managers of multiunit housing complexes from adopting smoke-free policies, including policies that apply to individual units. 29,37 The second concern is also unwarranted, with surveys finding that most tenants prefer smokefree policies. [25][26][27]32 Finally, in terms of the third concern, no evidence exists that smoke-free multiunit housing policies would be difficult to implement and enforce. In fact, operators of multiunit housing with existing smoke-free policies indicated that they are more likely to keep the polices in place. 36 Smoke-free-policies in multiunit housing may also potentially have significant economic benefits for owners. Most important, preparing a smoker's unit for occupancy by a new tenant often requires substantially greater time and money than readying a nonsmoker's unit. For example, smokers' units may require extensive repainting, repair of burn damage, and replacement of carpeting, draperies, and upholstered furniture. [38][39] Secondly, smoking is also a major cause of residential fires and the lead ing cause of fatal residential fires. 40 Finally, owners and managers could potentially be subject to legal action by tenants who experience health problems as a result of SHS infiltration. 29 Multiunit housing residents in several states have brought such legal action in recent years, with mixed results. 29,33 Educational outreach can provide multiunit housing operators with this information. In recent years, as more multiunit housing operators have become aware of the benefits of smoke-free policies and rec ognized that they can be implemented successfully, an increasing number of private multiunit com plexes and public housing authorities have opted to go smoke-free. The U.S. Department of Housing and Urban Development has issued notices encouraging housing authorities and Section 8 housing facilities to adopt smoke-free policies voluntarily, including in individual units. [41][42] Smoke-free policies in multiunit housing are a win-win -protecting tenants' health while also helping protect owners' investment. r
# V. FRAMEWORK FOR IMPLEMENTATION WITH HEALTHY HOMES PROGRAMS
Initiatives to reduce SHS exposure in multiunit housing offer an attractive opportunity for newly created or transitioning Healthy Homes programs. These initiatives offer Healthy Homes programs a chance to address a potential residential source of indoor air pollution and poor health (See Figure 2). 4,22,43 Unlike some other home health hazards, SHS exposure is preventable; adopting and enforcing a 100 percent smoke-free policy should eliminate most SHS exposure in the home. In addition, because of the growing interest in and demand for smoke-free multiunit housing policies, work in this area may open partnership and funding opportunities. Moreover, because smoke-free multiunit housing policies are relatively simple to adopt, addressing this issue could potentially yield early victories, generating further momentum.
# HEALTHY HOMES
• Secondhand smoke
• Radon • Fire hazards • Fall hazards • Allergens • Lead • Pesticides • Moisture • Volatile
# FIGURE 2: COMPONENTS OF A HEALTHY HOME
Moreover, Healthy Homes programs enjoy ready access to multiunit managers and tenants that state tobacco control programs, typically do not possess. Thus, Healthy Homes programs are therefore in a uniquely favorable position to build relationships with key stakeholders in order to lay the ground work for policy change.
The only way to fully protect nonsmokers from SHS is to eliminate smoking in indoor settings. 4 In a single-family home, this can be accomplished through a voluntary household rule which prohibits anyone from smoking inside the home at any time. However, residents of multiunit housing facilities who adopt such household rules can still be exposed to SHS through infiltration from other units or common areas. 24 Therefore, only a policy making, at a minimum, all units and indoor common areas in a building smoke-free, can effectively protect tenants from SHS. Thus Healthy Homes programs' educational and outreach activities will be most effective if they are directed to ultimately achieving implementation of such policies by convincing owners, managers, and tenants of their importance and benefits. In addition to informing managers and tenants about the health effects of SHS, it is also important to provide managers and tenants who smoke with support and assistance in their efforts to quit, including information on available cessation resources.
It is important for smoke-free policies in multiunit housing to be implemented in a nonpunitive man ner that does not stigmatize residents who smoke or refuse housing to applicants who smoke. Poli cies should be written and implemented in a way that minimizes the chances that multiunit housing residents are evicted for violations. Efforts should also be made to ensure that residents who do smoke have access to smoking cessation resources should they choose to take this opportunity to quit.
The following table provides a menu of resources that Healthy Homes programs can draw on to promote smoke-free policies in multiunit housing facilities. The table is based on a review of current best practices by state and local health departments, tobacco control agencies, public housing authori ties, nonprofit organizations, and community organizations. The framework is structured around four broad strategic activity areas: coordination, communication, collaboration, and capacity building. The table also includes a list of tools and resources for each activity. The goal of this framework is to enable Healthy Homes programs to select and implement strategies to effectively reduce SHS exposure in multiunit housing. The specific approach a program selects will depend on its organizational capacity, resources, existing projects, and the characteristics and circumstances of the community in question.
# Coordination
Research and analyze current smokefree programs and policies.
Review state and local demographics.
Use information to target initial efforts and highlight existing efforts.
Identify key gaps in resources that need to be addressed to support current efforts and develop a work plan.
Conduct a community assessment to identify community needs, characteristics, and cultural identity, and target outreach accordingly.
# VI. ADDENDUM
In addition to the resources listed above, a number of other helpful materials are available for Healthy Homes programs that are interested in working to reduce SHS exposure in multiunit housing. The following addendum provides an in-depth listing of research findings, best practices, web sites, and other information, including both online and print resources. Many resources were identified through interviews with smoke-free practitioners. Healthy Homes programs are free to use or adapt any of these materials.
# AddEndum conTEnTS
▶ Toolkits
• Multiunit housing operators' concerns about the legality of requiring individual units to go smokefree can pose a major barrier to adoption of smoke-free multiunit housing policies. A number of nongovernmental legal organizations have responded to these concerns by providing analyses of the relevant legal issues. While these resources provide an overview of these issues, they do not consti tute legal advice. The language of all smoke-free policies should be based on model language that has withstood legal scrutiny, and should be reviewed by an attorney knowledgeable about local and state ordinances before the policy is adopted.
Corresponding URL's for this table are listed in the Reference section of this manual.
# Federal Law
Federal Statutes: American with Disabilities Act Federal Statutes: Fair Housing Act
# State Statute Designation
There is no constitutional right to smoke, and no law precludes adoption of smoke-free policies in multiunit housing, including policies that make individual units smoke-free. Smoke-free policies are not discriminatory, since smoking is not a protected act and smokers are not a protected class. In some cases, it may be necessary to grandfather for a limited amount of time (e.g., until their leases come up for renewal). For analysis, see Tobacco Control Legal Consortium's There is No Constitutional Right to Smoke. a
The Americans with Disabilities Act permits smoke-free policies. Because smoking is not considered a disability, smokers are not protected under the Fair Housing Act or the Rehabilitation Act. 44 Some health conditions affected by SHS could be considered a disability (e.g., emphysema, heart conditions, asthma, COPD). Multiunit housing facilities may be required to provide some nonsmoking tenants who are affected by SHS infiltration some accommodation for these conditions on a case-by-case basis. Most state smoking restrictions focus on workplaces and public places rather than multiunit housing. Some state laws restrict smoking in common areas in multiunit housing complexes. Utah e law establishes SHS as a potential nuisance, giving tenants grounds for legal action. 46 In addition, Utah law also specifically allows condominium associations to restrict smoking in units, common areas, and facilities. 34 In Oregon, f a disclosure law requires a property owner to notify prospective tenants of a multiunit housing facility's smoking policy and the areas where smoking is permitted. 47
# Local City/ County
A number of communities in California have adopted ordinances addressing SHS infiltration in multiunit housing. These ordinances range from requirements that apartment managers disclose units where smoking is occurring to policies making indoor and/or outdoor common areas smoke-free to policies making individual units in some or all buildings smoke-free. These policies may initially apply only to new properties or may cover existing properties as well. Communities and states can also use tax credits, bonus points in competitive grant proposals, and other financial incentives to encourage the adoption of smoke-free multiunit housing policies (California Tax Credits. g Also, local Ordinances are effective (Oakland, CA; Buffalo, NY). For sample ordinance provisions that provide an overview of the available policy options, see the
# Lower Insurance Costs
Surveys of owners find that staff time spent dealing with smoking complaints was reduced following implementation of a smoke-free policy. 25 Maine's Sanford Housing Authority found that the cost of renovating smokers' units ranged from $1,070-1,670 versus $550 for a non-smoking unit. 39 Starting smoke-free home rules in single-family homes leads to reduced SHS exposure, increased smoking cessation, and reduced smoking among adult and adolescent smokers. [52][53][54][55][56][57][58][59][60][61][62][63][64][65][66]22 High preference and demand for smoke-free housing, as documented by renter surveys. 26 See Smoke-Free Environments Law Project p website for more surveys.
New York realtors have reported that smokers' residences are harder to sell than nonsmokers' residences. 67 Nonsmoking restaurants have on average a 16 percent higher resale value. 68 Cigarettes are a major cause of residential fires and the leading cause of fatal residential fires. [69][70]40 Some insurance companies offer discounts on fire, life, liability, and property insurance to multi-unit housing complexes that have adopted smoke-free policies. 71
# SAmPLE imPLEmEnTATion guidE For ownErS And mAnAgEr
Adopting a smoke-free policy in new properties should be relatively straightforward becausemanagement can establish a smoke-free norm from the start.
1. Establish a 100 percent smoke-free policy in all buildings, including individual units and common areas.
2. Include smoke-free provisions in lease/rental agreements.
3. Prominently post "No smoking" signs at entrances, on bulletin boards, in stairwells, and in other locations.
4. Highlight the smoke-free policy as an amenity in listings, ads, and other promotions.
5. Continually remind managers, staff, and tenants about the smoke-free policy. Educate them about the reasons for the policy and what to do if they see a violation. Prepare sup porting evidence, FAQs, and other relevant information.
Adopting a smoke-free policy in existing properties may require more intensive planning and educa tion, and could involve a phased-in approach to provide a transition period for tenants who are accustomed to smoking in their units.
1. Decide on the policy's scope and provisions and on the timeline for implementing it. For example, will the policy apply to individual units as well as common areas, and will it apply to some or all buildings? Also explain how the policy will handle existing tenants who smoke in their units (e.g., they may be grandfathered in until their leases come up for renewal, and, then be required to comply). Use building meetings, notices, and signs to let tenants know that the smoke-free policy is coming. This process should begin several months before the policy's effective date. Use this opportunity to educate tenants on the dangers of SHS and the issue of SHS infiltration. Tell tenants when the policy will take effect and explain how it will be enforced. Ask tenants for ideas on how to implement the policy, but do not give them veto power over its provisions. If necessary, conduct a small survey to gauge tenant response to and readiness for the policy. During the policy phasein, consider clustering nonsmokers and smokers in separate buildings. Tenants who smoke can be offered incentives to move to these buildings.
2. Publicize available smoking-cessation services. Provide support and encouragement to smokers who choose to take this opportunity to quit. Make sure to identify SHS and SHS infiltration, not smokers, as the problem. Don't use language or take steps that could make smoking tenants feel stigmatized.
3. Prominently post "No smoking" signs.
4. Remove ashtrays or relocate them to more appropriate locations.
5. Send tenants a letter formally notifying them of the new policy. Require all residents to sign a statement that they agree to comply with the policy. Enforcement of the policy for current tenants can begin on renewal of the tenant/renter lease, updated with the new smoke-free policy addendum.
#
rEFErEncES For HyPErLinkS : | None | None |
b5fd829035743ad66a14e084a3e116aef71c3699 | cdc | None | The following CDC staff members prepared this report:
Dalya
# Pertussis Vaccination: Use of Acellular Pertussis Vaccines Among Infants and Young Children
Recommendations of the Advisory Committee on Immunization Practices (ACIP) Summary Concerns about the safety of whole-cell pertussis vaccines prompted development of acellular vaccines that are less likely to provoke adverse events because they contain purified antigenic components of Bordetella pertussis. Two diphtheria and tetanus toxoids and acellular pertussis (DTaP) vaccines-ACEL-IMUNE ® - and Tripedia ® † -have been licensed for several years, but (until recently) only for administration of the fourth and fifth doses in the series to children aged 15 months-6 years who previously had received three or more doses of diphtheria and tetanus toxoids and whole-cell pertussis (DTP) vaccine. Published reports indicate that, when administered to infants aged 2, 4, and 6 months, acellular pertussis vaccines are effective in preventing pertussis disease and associated with fewer local, systemic, and certain more serious adverse events than whole-cell pertussis vaccines. On the basis of these data, the Food and Drug Administration (FDA) has licensed three DTaP vaccines for use among children aged 6 weeks-6 years. Tripedia ® is now licensed for the initial four doses, and ACEL-IMUNE ® for all five doses of the diphtheria, tetanus and pertussis vaccination series. A third DTaP vaccine (Infanrix™ ) § was licensed in January 1997 for the initial four doses of the series. Tripedia ® , ACEL-IMUNE ® , and Infanrix™ are now recommended for routine vaccination of infants and young children, although whole-cell pertussis vaccines remain acceptable alternatives. Tripedia ® , ACEL-IMUNE ® , and Infanrix™ are recommended for all remaining doses in the schedule for children who have started the vaccination series with one, two, three, or four doses of whole-cell pertussis vaccines. In September 1996, FDA licensed the use of TriHIBit™ (ActHIB ® reconstituted with Tripedia ® ) ¶ for the fourth dose in the series of vaccinations against diphtheria, tetanus, pertussis, and Haemophilus influenzae type b disease. This statement a) provides general information regarding whole-cell pertussis vaccines currently licensed in the United States; b) summarizes results of recent studies of the immunogenicity, efficacy, and safety of acellular pertussis vaccines administered to infants and young children; c) presents recommendations for the use of Tripedia ® , TriHIBit™ , ACEL-IMUNE ® , and Infanrix™ vaccines; and d) supplements previous recommendations on pertussis vaccination.
# INTRODUCTION Whole-Cell Pertussis Vaccines
Four diphtheria and tetanus toxoids combined with whole-cell pertussis (DTP) vaccines are presently licensed for use in the United States.- Vaccines of this type, prepared from suspensions of inactivated Bordetella pertussis bacterial cells, have been licensed for routine vaccination of infants since the mid-1940s. Based on controlled efficacy trials conducted in the 1940s and on subsequent observational efficacy studies, a primary series comprising four doses of whole-cell DTP vaccine is considered 70%-90% effective in preventing serious pertussis disease (1)(2)(3)(4).
Whole-cell DTP vaccines are commonly associated with several local adverse events (e.g., erythema, swelling, and pain at the injection site), fever, and other mild systemic events (e.g., drowsiness, fretfulness, and anorexia) (5,6 ). More severe systemic events (e.g., convulsions and hypotonic hyporesponsive episodes) occur less frequently (ratio of one case to 1,750 doses administered) among children who receive whole-cell DTP vaccine (5 ). Acute encephalopathy occurs even more rarely (ratio of 0-10.5 cases to one million doses administered) (7 ). Experts disagree on whether whole-cell pertussis vaccine causes lasting brain damage, but agree that if the vaccine causes such damage it does so only rarely (7 ). Concerns about safety prompted the development of more purified (acellular) pertussis vaccines that are associated with a lower frequency of adverse events and are effective in preventing pertussis disease.
# Trends in Pertussis Disease in the United States
In the United States, the highest recorded annual incidence of pertussis occurred in 1934 when >260,000 cases were reported. The incidence of reported pertussis disease declined substantially as use of whole-cell DTP vaccines became widespread. By 1970, the reported incidence had declined >99%; the fewest cases (1,010) were reported in 1976. However, since the early 1980s reported pertussis incidence has increased steadily. Cyclical peaks in incidence occurred in 1983,1986,1990, and in 1993 when 6,586 cases were reported-more than in any year since 1976 (8 ). The number of reported cases has increased in all age groups, but the increase is greatest among persons aged ≥5 years (9 ). Nevertheless, infants and young children continue to have the highest risk for pertussis and its complications (4,8,10 The increase in reported pertussis cases has occurred despite pertussis vaccination coverage levels that are higher than at any time in the past. The proportion of children aged 19-35 months who had received three or more doses of whole-cell DTP or diphtheria and tetanus toxoids vaccine (DT) reached 93% in 1994 (11 ). (Of those vaccinated, <2% are estimated to have received DT .) Possible explanations of this increase in disease include a) decreased vaccine efficacy, b) waning immunity among adolescents and adults vaccinated during childhood, c) increased diagnosis and reporting of pertussis because of greater awareness among physicians about the disease, and d) enhanced surveillance and more complete reporting in some states (12,13 ).
Recent randomized controlled trials in Sweden and in Italy with one of the wholecell DTP vaccines presently licensed in the United States (manufactured by Connaught Laboratories, Inc.) yielded estimates of low clinical efficacy-60% in the 6 months immediately following administration of the third dose. Estimates of vaccine efficacy for the total followup period were even lower-48% in Sweden and 36% in Italy (14,15 ). These estimates were substantially lower than expected on the basis of estimates obtained from observational studies in the United States. One possible explanation for the disparity is the number of doses administered-three in the trials in Sweden and Italy versus five in the United States (doses at ages 2, 4, 6, and 12-18 months and 4-6 years). A recent study in Germany with another whole-cell DTP vaccine currently in use in the United States (distributed by Wyeth-Lederle Vaccines and Pediatrics) demonstrated 83% protective efficacy after the third dose and before administration of the fourth dose and 94% efficacy after four doses (Wyeth-Lederle Vaccines and Pediatrics, ACEL-IMUNE ® package insert). The effectiveness of the current pertussis vaccination program in the United States, which has relied on four different whole-cell DTP vaccines for primary vaccination, remains high (3,4 ).
# Acellular Pertussis Vaccines
Acellular pertussis vaccines contain inactivated pertussis toxin (PT) and may contain one or more other bacterial components (e.g., filamentous hemagglutinin , a 69-kilodalton outer-membrane protein-pertactin , and fimbriae types 2 and 3). PT is detoxified either by treatment with a chemical (e.g., hydrogen peroxide, formalin and/or glutaraldehyde) or by using molecular genetic techniques. Acellular pertussis vaccines contain substantially less endotoxin than whole-cell pertussis vaccines.
Since 1991, two acellular pertussis vaccines (Tripedia ® and ACEL-IMUNE ® ) have been licensed for use in the United States. Until recently, both vaccines were licensed for use only as the fourth and fifth doses of the diphtheria, tetanus, and pertussis vaccination series among children aged 15 months-6 years who had received three primary doses of whole-cell DTP (16,17 ). This licensure was based on findings of studies conducted in Sweden and Japan. These studies did not evaluate the efficacy of acellular pertussis vaccines administered to infants on a schedule similar to the one used in the United States and did not directly compare the efficacy of DTaP vaccines with that of whole-cell DTP vaccines (18)(19)(20)(21)(22).
# Studies of the Efficacy of DTaP Vaccines in Infants
Since 1991, seven studies conducted in Europe and Africa have evaluated the efficacy of eight DTaP vaccines administered to infants. The vaccines, produced by different manufacturers, contained a varying number and quantity of antigens. The derivation and formulation of the individual antigens also varied among vaccines (Table 1). Four doses of vaccine were administered in one study (Wyeth-Lederle Vaccines and Pediatrics, ACEL-IMUNE ® package insert); the other six studies involved three doses (14,15,(23)(24)(25). These studies also differed in other ways (Table 2):
- Design. Three studies were randomized placebo-controlled clinical trials; such studies usually provide the most accurate measure of a treatment effect and are less subject to biases than observational studies.
- Case definition. Estimates of vaccine efficacy tend to be higher when the case definition excludes mild clinical cases.
- Laboratory method used to confirm the diagnosis of pertussis.
Because of these differences, comparisons among studies should be made with caution. Within individual studies, however, the efficacy of acellular pertussis vaccines can be compared directly with that of whole-cell DTP.
The efficacy of three doses of acellular pertussis vaccines in preventing moderate to severe pertussis disease was within the range expected for most whole-cell DTP vaccines. Point estimates of efficacy ranged from 59% to 89%. Mild local and systemic adverse events occurred less frequently among infants vaccinated with acellular pertussis vaccines for the first three or four doses than among those vaccinated with whole-cell DTP. More serious adverse events (e.g., fever ≥105 F , persistent crying of ≥3 hours duration, hypotonic hyporesponsive episodes, and seizures) generally occurred less frequently among infants who received acellular pertussis vaccines than among those vaccinated with whole-cell DTP. The number of subjects included in these studies was insufficient to estimate the risk for rare severe reactions (i.e., encephalopathy or anaphylactic shock). Surveillance for these rare adverse events will be needed as acellular pertussis vaccines are used more widely.
# Interpretation of Immunogenicity Data
The findings of efficacy studies have not demonstrated a direct correlation between antibody responses and protection against pertussis disease. However, antibody studies are useful to compare immune responses elicited by a single vaccine under different conditions or in different studies. Thus, efficacy studies are required to measure clinical protection conferred by each pertussis vaccine.
# TRIPEDIA ®
On July 31, 1996, the Food and Drug Administration (FDA) licensed Tripedia® for use as the initial four doses of the recommended diphtheria, tetanus, and pertussis vaccination series among children aged 6 weeks-6 years. The acellular pertussis vaccine components are purified from B. pertussis by salt precipitation, ultracentrifugation, and ultrafiltration. After purification, fractions containing PT and FHA are combined to obtain a 1:1 ratio and are treated with formaldehyde to inactivate PT. Each dose of Tripedia ® contains approximately 23.4 µg protein of inactivated PT (toxoid) and 23.4 µg protein of FHA, as well as 6.7 limit of flocculation units (Lf) of diphtheria toxoid and 5.0 Lf of tetanus toxoid. The combined components are adsorbed using aluminum potassium sulfate and preserved with 1:10,000 thimerosal (Table 1).
# Immunogenicity
The Multicenter Acellular Pertussis Trial, an immunogenicity and safety study conducted in six centers in the United States and sponsored by the National Institutes of Health (NIH), compared antibody responses of infants vaccinated at ages 2, 4, and 6 months with whole-cell DTP or with one of 13 different acellular pertussis vaccines, including Tripedia ® . Antibody to pertussis antigens was measured in serum samples taken before administration of the first dose and 1 month after administration of the third dose of Tripedia ® ; 99% and 86% of children had fourfold or greater increases in titers of antibody to PT and FHA, respectively. More than 90% of children administered Tripedia ® developed diphtheria and tetanus antibody levels indicative of immunity to these diseases (i.e., >0.1 antitoxin units per mL and >0.01 u/mL, respectively), as did ≥90% of those administered whole-cell DTP (26 ). The immunogenicity of Tripedia ® when administered as a fourth dose to children aged 12-14 months has not been studied.
# Clinical Efficacy
Two studies conducted in Sweden and Germany provide data concerning the clinical efficacy of Tripedia ® . During 1985-1987, a randomized, placebo-controlled clinical trial in Sweden examined the efficacy of two doses of two acellular pertussis vaccines. The acellular pertussis component of one vaccine was comparable to the acellular pertussis component of Tripedia ® (17,18 ). The first dose was administered at age 5-11 months, the second dose 8-12 weeks later. For culture-confirmed disease with cough of any duration, the vaccine's efficacy after two doses was 69% (95% confidence interval =47%-82%) (18 ). Using a more stringent case definition (i.e., ≥21 days paroxysmal cough and confirmation by culture) resulted in an efficacy estimate of 81% (95% CI=61%-90%) (27 ). A non-blinded follow-up study conducted during the 42-month period following the clinical trial yielded similar results (28 ).
A case-control study in Germany evaluated the efficacy of three doses of Tripedia ® administered to children aged approximately 3, 5, and 7 months (Connaught Laboratories, Inc.,Tripedia ® package insert). Comparison groups received whole-cell DTP (manufactured by Behringwerke, A.G.), DT, or no vaccine. A case of pertussis was defined as an illness with cough of ≥21 days duration and confirmation by positive culture for B. pertussis or household contact with a culture-proven case. The estimated clinical efficacy of three doses of Tripedia ® compared with DT was 80% (95% CI=59%-90%). For infants who received three doses of whole-cell DTP, the vaccine efficacy estimate was 95% (95% CI=81%-99%) (25 ). However, the two efficacy estimates are not directly comparable because of differences in the way infants were enrolled in the two groups.
# Safety
The safety of Tripedia ® was assessed in studies conducted in the United States and Germany. Local reactions (e.g., erythema, swelling, or pain), fever, and other common systemic symptoms (e.g., anorexia, vomiting, drowsiness, or fussiness) occurred less frequently among infants administered Tripedia ® than among those who received whole-cell DTP (Connaught Laboratories, Inc., Tripedia ® package insert). In the Multicenter Acellular Pertussis Trial, local and common systemic events occurred less frequently among Tripedia ® recipients than among recipients of whole-cell DTP (Table 3) ( 29). Among recipients of 41,615 doses of Tripedia ® in the trial in Germany, few moderate to severe adverse events occurred within 7 days after vaccination (Connaught Laboratories, Inc., Tripedia ® package insert). The following events and rates of occurrence (per 1,000 doses administered) were reported: persistent crying for ≥3 hours, 0.12; febrile seizures, 0.05; afebrile seizures, 0.02; and hypotonic hyporesponsive episodes, 0.05. Rates of invasive bacterial infections, hospitalizations, and deaths among infants vaccinated with Tripedia ® were similar to those observed among recipients of DT. None of the deaths or invasive bacterial infections was vaccine related.
In a study conducted in the United States, children aged 15-20 months who had received Tripedia ® (n=109) or whole-cell DTP (n=30) for the first three doses were administered Tripedia ® as the fourth dose (30 ). Although the differences were not statistically significant, the percentages of children who had local adverse events (e.g., erythema, swelling, or pain) or certain systemic adverse events (i.e., temperature >101 F or irritability) within 72 hours after administration of the fourth dose was higher among children who had received Tripedia ® for the first three doses. However, the frequency of adverse events was lower than that observed in previous studies in which a fourth dose of whole-cell DTP followed three previous doses of whole-cell DTP.
Limited data are available to evaluate the safety of Tripedia ® when administered as a fifth dose to children aged 4-6 years who have received four previous doses of Tripedia ® . The frequency of local and mild systemic reactions after the last of five doses was no greater among children administered Tripedia ® (n=18) than among children in the same study who were administered five doses of whole-cell DTP (n=10) (M.E. Pichichero, unpublished data). More data concerning the safety of Tripedia ® in such circumstances are being collected and will be available before infants who receive Tripedia ® for the first four doses require a fifth dose at age 4-6 years. Data are insufficient to assess the safety of Tripedia ® administered to persons aged ≥7 years.
# Simultaneous Administration
# Immunogenicity
In a randomized clinical trial, children aged 15-20 months were administered either Tripedia ® and ActHIB ® vaccines at separate sites (n=98) or combined as a single dose (n=93) (Connaught Laboratories, Inc., Tripedia ® package insert). Before the study began, these children all had received three doses of a Hib conjugate vaccine and three doses of whole-cell DTP at approximately ages 2, 4, and 6 months. One month after administration of the fourth dose, 100% of the children in both groups had anti-PRP antibody concentrations ≥1 µg/mL, an indication of long-term protection against invasive H. influenzae type b disease. The proportions of children with protective antibody responses to diphtheria and tetanus toxoids were also high and similar in the two groups. The proportions of children who had fourfold or greater serum antibody responses to PT (measured by enzyme-linked immunosorbent assay or Chinese hamster ovary cell assay) were >85% in both groups. Among children who received TriHIBit™ , the proportion with fourfold or greater antibody responses to FHA was slightly lower. The clinical importance of this difference is not known.
# Clinical Efficacy
TriHIBit™ has been licensed for use as the fourth dose of the two vaccination series on the basis of immunogenicity and safety data. Its protective efficacy when used for this purpose has not been evaluated.
# Safety
The safety of TriHIBit™ was evaluated in two studies involving a total of 960 children who had each received three doses of a Hib vaccine and three doses of whole-cell DTP vaccine at approximately ages 2, 4, and 6 months (Connaught Laboratories, Inc., Tripedia ® package insert). At age 15-20 months, these children were administered the fourth dose of Tripedia ® and ActHIB ® vaccines either combined by reconstitution as a single injection or as two injections at separate sites. Rates of local and systemic reactions were similar in the two groups. Local reactions were mild and resolved within 48 hours following vaccination. The most common local reaction was pain at the injection site.
# Simultaneous Administration
When TriHIBit™ was administered to children aged 15-20 months (n=47) simultaneously with MMR vaccine, >95% developed serum antibody to measles, mumps, and rubella at levels indicative of protection against these diseases (Connaught Laboratories, Inc., Tripedia ® package insert). Immune responses to OPV or IPV and hepatitis B vaccine when administered simultaneously with TriHIBit™ have not been studied.
# ACEL-IMUNE ®
On December 30, 1996, FDA licensed ACEL-IMUNE ® for all five doses of the recommended diphtheria, tetanus, and pertussis vaccination series among children aged 6 weeks-6 years. Each dose of the acellular pertussis component of ACEL-IMUNE ® contains approximately 34.4 µg of FHA, 3.2 µg of inactivated PT, 1.6 µg of Pn, and 0.8 µg of Fim type 2. The acellular pertussis vaccine components are purified by ammonium sulfate fractionation and sucrose density gradient centrifugation. PT is detoxified by treatment with formaldehyde. Each dose of ACEL-IMUNE ® contains 9.0 Lf units of diphtheria toxoid, 5.0 Lf units of tetanus toxoid, and 300 hemagglutinating units of acellular pertussis vaccine. The FHA and PT components both exhibit hemagglutinating activity. The combined components are adsorbed to aluminum hydroxide and aluminum phosphate and preserved with 1:10,000 thimerosal (Table 1).
# Immunogenicity
Data from the Multicenter Acellular Pertussis Trial provide evidence of the immunogenicity of ACEL-IMUNE ® (26). Investigators measured levels of serum antibody to each of the four vaccine antigens after administration of three doses. The percentages of vaccinees with fourfold or greater increases in antibody titer (compared with prevaccination levels) were: PT, 67%; FHA, 80%; Pn, 71%; and Fim, 59%. The percentages of these children who developed diphtheria antibody levels of ≥0.1 u/mL and tetanus antibody levels of ≥0.01 u/mL (i.e., indications of immunity against these diseases) were 86% and 100%, respectively. Antibody responses observed among children in the United States were similar to those observed among children in the study in Germany that demonstrated the efficacy of ACEL-IMUNE ® .
Antibody response to ACEL-IMUNE ® when administered to children aged 12-14 months was evaluated in a clinical trial (Wyeth-Lederle Vaccines and Pediatrics, unpublished data). ACEL-IMUNE ® was administered as a fourth dose to children aged 12-14 months (n=58) or 15-18 months (n=50) who had previously received three doses of whole-cell DTP. In both age groups, >85% of the children had twofold or greater antibody responses to PT, FHA, Pn, and Fim.
# Clinical Efficacy
Efficacy of ACEL-IMUNE ® was assessed in a prospective study in Erlangen, Germany (Wyeth-Lederle Vaccines and Pediatrics, ACEL-IMUNE ® package insert). Infants were randomly assigned to groups that were administered either ACEL-IMUNE ® or whole-cell DTP (distributed by Wyeth-Lederle Vaccines and Pediatrics) at a mean age of 3, 5, 7, and 17 months. A third group of infants (not selected randomly) received DT at ages 3, 5, and 17 months. In this study, pertussis was defined as cough illness lasting ≥21 days with at least one pertussis-associated symptom (paroxysms, whoop, or post-tussive vomiting) confirmed by culture, serology, or epidemiologic link to a culture-positive household contact. Between the third and fourth doses, the efficacy of ACEL-IMUNE ® (compared with DT) was 73% (95% CI=51%-86%) and the efficacy of whole-cell DTP 83% (95% CI=65%-92%). After four doses, the efficacy of ACEL-IMUNE ® was 85% (95% CI=76%-90%), and that of whole-cell DTP was 94% (95% CI=89%-97%). Considering the full observation period after the third and fourth doses, the adjusted efficacy of ACEL-IMUNE ® was 81% (95% CI=73%-87%) compared with 91% (95% CI=85%-95%) for whole-cell DTP.
# Safety
Studies from the United States and Germany provide data concerning the frequency and nature of adverse events that occur after administration of ACEL-IMUNE ® . In the Multicenter Acellular Pertussis Trial, children who were administered ACEL-IMUNE ® experienced fewer local adverse events (e.g., pain, redness, or swelling at the injection site) and systemic adverse events (e.g., temperature >101 F , or fussiness) after any of the first three doses than children who were administered whole-cell DTP (Table 3) (29 ). Similarly, in other studies conducted in the United States and Germany, adverse events (local and systemic) after any of the initial four doses occurred less frequently among children who received ACEL-IMUNE ® than among children administered whole-cell DTP (Wyeth-Lederle Vaccines and Pediatrics, ACEL-IMUNE ® package insert). Rates of adverse events increased with the number of previous doses of ACEL-IMUNE ® administered, but were lower than rates for children who received the same number of doses of whole-cell DTP. Among 357 children who were administered five doses of ACEL-IMUNE ® , adverse events occurred no more frequently than among children in previous studies (historical controls) who received five doses of whole-cell DTP (Wyeth-Lederle Vaccines and Pediatrics, ACEL-IMUNE ® package insert).
In the efficacy trial in Germany (n=16,642 doses of ACEL-IMUNE ® ), the following rates of moderate to severe adverse events (per 1,000 doses administered) were observed within 72 hours after administration of the vaccine: persistent or unusual cry, 1.14; temperature ≥105 F (≥40.5 C), 0.06; febrile seizures (no other type of seizure occurred), 0.06; and hypotonic hyporesponsive episodes, 0 (Wyeth-Lederle Vaccines and Pediatrics, ACEL-IMUNE ® package insert). Rates of all these adverse events were higher among children who received whole-cell DTP.
A clinical trial examined the frequency of local reactions (e.g., erythema, induration, or tenderness) and systemic reactions (e.g., fever, fussiness, drowsiness, or anorexia) among children aged 12-14 months or 15-18 months, all of whom had previously received three doses of whole-cell DTP. Differences in the frequency of adverse reactions in the two age groups were not statistically significant (Wyeth-Lederle Vaccines and Pediatrics, unpublished data).
Neither anaphylaxis nor encephalopathy occurred during clinical trials that involved administration of 25,899 doses of ACEL-IMUNE ® . Six deaths of infants or young children who participated in these trials were reported to study investigators; none was vaccine-related and all occurred >4 weeks after vaccination (Wyeth-Lederle Vaccines and Pediatrics, ACEL-IMUNE ® package insert). The reactogenicity of ACEL-IMUNE ® among persons aged ≥7 years has not been evaluated.
# Simultaneous Administration
The immunogenicity of ACEL-IMUNE ® when administered simultaneously with other recommended childhood vaccines was evaluated in three studies. ACEL-IMUNE ® , Hib vaccine, and hepatitis B vaccine were administered simultaneously to 77 infants at ages 2, 4, and 6 months. After administration of the third dose, serum samples from 94% of the infants demonstrated anti-PRP antibodies indicative of clinical protection (≥1 µg/mL), and all of the infants evaluated (n=74) had antibody levels indicative of protection against hepatitis B (i.e., anti-HBs titers of >10 mIU/mL) (Wyeth-Lederle Vaccines and Pediatrics, ACEL-IMUNE ® package insert). In another clinical study, 30 infants were administered OPV simultaneously with ACEL-IMUNE ® at ages 2 and 4 months; ≥90% had protective neutralizing antibody to all three poliovirus types at age 6 months. When MMR vaccine was administered simultaneously with ACEL-IMUNE ® to children aged 15-18 months (n=48), ≥92% developed serum antibody titers indicative of protection against measles, mumps, and rubella. Similar results were obtained when whole-cell DTP was administered simultaneously with OPV or MMR vaccine (31 ). Simultaneous administration of ACEL-IMUNE ® and IPV or varicella vaccine has not been evaluated.
# INFANRIX™ ™
On January 29, 1997, FDA licensed Infanrix™ for use as the initial four doses of the recommended diphtheria, tetanus, and pertussis vaccination series among children aged 6 weeks-6 years. Infanrix™ is also licensed for all remaining doses in the schedule for children who have received one or more doses of whole-cell DTP vaccine. Each dose of Infanrix™ contains 25 µg PT, 25 µg FHA, 8 µg Pn, 25 Lf of diphtheria toxoid, and 10 Lf of tetanus toxoid (Table 1). The three antigens in the acellular pertussis vaccine component are separately purified in successive chromatographic steps (hydrophobic, affinity, ion exchange, and size exclusion processes). Formalin and glutaraldehyde are used to detoxify PT; FHA and Pn are treated with formalin. The combined components are adsorbed onto ≤0.625 mg of aluminum (as aluminum hydroxide) and preserved with 2-phenoxyethanol.
# Immunogenicity
In the Multicenter Acellular Pertussis Trial, three doses of Infanrix™ were administered to children at ages 2, 4, and 6 months. One month after the third dose, investigators measured fourfold or greater antibody responses to PT, FHA, and Pn in ≥83% of children who received Infanrix™ , a higher proportion than observed among recipients of whole-cell DTP (26 ). All the children who were administered Infanrix™ developed diphtheria antibody titers of ≥0.1 u/mL and tetanus antibody titers of ≥0.01 u/mL (i.e., indications of immunity against these diseases). Whether their primary vaccination was with Infanrix™ or whole-cell DTP, >86% of children aged 15-20 months had a fourfold or greater rise in serum antibody to each of the pertussis antigens in the vaccine after administration of Infanrix™ as the fourth dose (M. E. Pichichero, unpublished data). The immunogenicity of Infanrix™ administered as a fourth dose to children aged 12-14 months has not been studied.
# Efficacy
The efficacy of Infanrix™ was evaluated in two separate studies (Table 2). In Italy, researchers compared the efficacy of Infanrix™ , DTaP manufactured by Chiron Biocine, whole-cell DTP manufactured by Connaught Laboratories, and DT in a randomized controlled trial that enrolled more than 15,000 children (15 ). Participants received three doses of one of the vaccines at ages 2, 4, and 6 months. The efficacy of Infanrix™ in preventing pertussis disease (defined as paroxysmal cough ≥21 days duration, with culture or serologic confirmation of infection with B. pertussis) was 84% (95% CI=76%-89%). The efficacy of whole-cell DTP was 36% (95% CI=14%-52%). After the trial, children were followed in an observational study to an average age of 33 months (range: 20-39 months); the efficacy of Infanrix™ remained high throughout this followup period (78%, 95% CI=62%-87%) (SmithKline Beecham Pharmaceuticals, Infanrix™ package insert).
The second study, conducted in six areas in Germany, was a household contact study. In preparation for this study, three doses of Infanrix™ were administered at ages 3, 4, and 5 months to more than 22,000 infants as part of a large immunogenicity and safety study (23 ). Infants who did not participate in this study could have received whole-cell DTP vaccine (manufactured by Behringwerke, A.G.) or DT vaccine. The efficacy study included 453 households with confirmed cases of pertussis in which 360 contact children aged 6-47 months were eligible for inclusion in the vaccine efficacy calculations. A case of pertussis was defined as ≥21 days of paroxysmal cough illness plus confirmation of B. pertussis infection by culture and/or serologic testing. The efficacy of Infanrix™ was 89% (95% CI=77%-95%); the efficacy of whole-cell DTP was 98% (95% CI=83%-100%).
# Safety
The occurrence of adverse events following vaccination with Infanrix™ was evaluated in clinical studies involving approximately 30,000 children. In these studies, 28,749 infants received Infanrix™ as a three dose primary series, 5,830 children received Infanrix™ as a fourth dose following three doses of Infanrix™ , and 22 children received Infanrix™ as a fifth dose following four doses of Infanrix™ . In addition, 439 children and 169 children received Infanrix™ as a fourth or fifth dose following three or four doses of whole-cell DTP vaccine, respectively. In comparative studies, administration of Infanrix™ was followed by fewer of the local and systemic adverse reactions commonly associated with whole-cell DTP vaccination (15,29,(32)(33)(34). However, results of these studies demonstrated that the rates of erythema, swelling, and fever increased with each successive dose of Infanrix™ (SmithKline Beecham Pharmaceuticals, Infanrix™ package insert). In the Multicenter Acellular Pertussis Trial, local and common systemic adverse events occurred less frequently following any dose of Infanrix™ in the primary series than following any dose of whole-cell DTP (Table 3) (29 ).
The efficacy study conducted in Italy monitored the frequency of moderate to severe adverse events occurring after administration of any of the primary doses of Infanrix™ . Rates (per 1,000 doses administered) of adverse events occurring ≤48 hours after administration were: persistent crying ≥3 hours duration, 0.44; seizures, 0.07; and temperature ≥104 F(≥40.0 C), 0.36. These rates were similar to or slightly higher than the rates reported among children who were administered DT, but lower than those for children who received whole-cell DTP. In this trial, no hypotonic hyporesponsive episodes occurred among children to whom Infanrix™ was administered.
In the safety study in Germany, data were available regarding 1,809 children who received three doses of Infanrix™ at ages 3, 4, and 5 months and a fourth dose at a mean age of 20 months. The percentages of children who experienced each of the adverse events ≤3 days after administration of the fourth dose were: redness, 46%; swelling, 35%; pain, 26%; fever ≥100.4 F (≥38 C), 26%; and restlessness, 16%. In this study the rates of redness, swelling, pain, and fever increased with successive doses of Infanrix™ (SmithKline Beecham Pharmaceuticals, Inc., Infanrix™ package insert).
Additional safety data are available from another study conducted in Germany (SmithKline Beecham Pharmaceuticals, Inc., Infanrix™ package insert). Children aged 13-27 months received Infanrix™ or whole-cell DTP (manufactured by Behringwerke, A.G.) as a fourth dose. These children had previously received three doses of the same vaccine. Among children administered Infanrix™ as the fourth dose, the incidence of redness, swelling, pain, fever, and restlessness was lower than among children administered whole-cell DTP as the fourth dose.
Infanrix™ has not been licensed previously for administration of the fourth or fifth dose to children who have received three or four doses of whole-cell DTP. Two studies conducted in the United States examined the frequency of adverse events among children who had previously received three or four doses of whole-cell DTP vaccine at approximately ages 2, 4, 6, and 15-18 months (Table 4). Children aged 15-20 months received Infanrix™ or whole-cell DTP vaccine as the fourth dose; children aged 4-6 years were administered Infanrix™ or whole-cell DTP as the fifth dose (33,34 ). Significantly fewer local and systemic adverse events were reported following administration of Infanrix™ than following whole-cell DTP vaccine.
In the safety study in Germany, edematous swelling of the entire thigh into which the vaccine was injected was reported spontaneously by parents or care-givers of 62 of 5,361 vaccinees (1.2%) after administration of the fourth dose. The swelling generally began within 48 hours of vaccination and resolved spontaneously without sequelae during an average of 4 days. In other countries where Infanrix™ has been licensed, this type swelling has been reported rarely following administration of Infan-rix™ for any dose, including the primary series (SmithKline Beecham Pharmaceuticals, Infanrix™ package insert). Edematous swelling has also been reported following administration of other DTaP vaccines, acellular pertussis vaccine alone (without DT), whole-cell DTP vaccine and other vaccines (19,(35)(36)(37). However, the precise frequency of these reactions among vaccinated children is unknown.
Data are insufficient to evaluate the safety of administration of a fifth dose of Infan-rix™ to children aged 4-6 years who have received Infanrix™ for the previous four doses. Additional information regarding the immunogenicity and safety of a fifth dose of Infanrix™ administered to children who have received four prior doses of the same vaccine is being collected. This information is expected to be available before infants who receive Infanrix™ for the first four doses require a fifth dose at age 4-6 years. The safety of Infanrix™ when administered to persons aged ≥7 years has not been assessed.
≥10 mIU/mL and 90% of infants (n=72) who received Hib vaccine simultaneously with Infanrix™ achieved anti-PRP antibodies ≥1 µg/mL (i.e., antibody levels indicative of protection against these diseases). The percentage of infants who were administered OPV simultaneously with Infanrix™ (n=60-61) who developed protective neutralizing antibody to poliovirus types 1, 2, and 3 ranged from 96% to 100% (38 ). No data are available regarding antibody responses to MMR vaccine, varicella vaccine, or IPV when administered simultaneously with Infanrix™ .
# VACCINE USE
# Recommended Childhood Vaccination Schedule
The routine diphtheria, tetanus, and pertussis vaccination schedule for children aged <7 years comprises five doses of vaccine containing diphtheria, tetanus, and pertussis antigens (Table 5). Three (primary) doses should be administered during the first year of life, generally at ages 2, 4, and 6 months. To maintain adequate immunity during preschool years, the fourth (first booster) dose is recommended for children *Diphtheria and tetanus toxoids and acellular pertussis vaccine (DTaP); diphtheria and tetanus toxoids and whole-cell pertussis vaccine (DTP) is an acceptable alternative to DTaP for any of the five doses. † Use diphtheria and tetanus toxoids, adsorbed (DT) if encephalopathy has occurred after administration of a previous dose of pertussis-containing vaccine. If the child is age ≥1 year at the time the first dose of DT is administered, a third dose administered 6-12 months after the second dose completes primary vaccination with DT. § Whenever possible, the same DTaP product should be used for all doses. If the same product is not available, Tripedia ® , ACEL-IMUNE ® , and Infanrix™ can be used interchangeably. ¶ Prolonging the interval does not require restarting the series. If the interval between the third and fourth doses is ≥6 months and the child is not likely to return for a visit at the recommended age, the fourth dose of either DTaP or DTP may be administered as early as age 12 months. † † TriHIBit™ can be administered as the fourth dose following a primary series with either DTaP or whole-cell DTP and a primary series with any Haemophilus influenzae type b conjugate vaccine. § § Tetanus-diphtheria toxoids absorbed (Td) (for adult use). aged 15-18 months. The fourth dose should be administered ≥6 months after the third. If the interval between the third and fourth doses is ≥6 months and the child is not likely to return for a visit at the recommended age, the fourth dose of either DTaP or whole-cell DTP may be administered as early as age 12 months. The fifth (second booster) dose is recommended for children aged 4-6 years to confer continued protection against disease during the early years of schooling. A fifth dose is not necessary if the fourth dose in the series is administered on or after the fourth birthday.
# Vaccine Preference
DTaP vaccines are efficacious when administered to infants as the primary series (i.e., doses 1-3). In addition, local reactions, fever, and other systemic events occur substantially less often after DTaP administration than after administration of wholecell DTP. Therefore, DTaP vaccines are recommended for all five doses in the vaccination schedule. For children who have started the vaccination series with one, two, three, or four doses of whole-cell DTP, DTaP is also recommended for all remaining doses in the schedule. During the period of transition from use of whole-cell DTP to DTaP, whole-cell DTP is an acceptable alternative to DTaP for any of the five doses. For the first four doses, whole-cell DTP combined with Hib vaccine (DTP-Hib vaccine) is an acceptable alternative to DTaP and Hib vaccine administered at separate sites.
# Licensed Products
Three acellular pertussis vaccines (Tripedia ® and Infanrix™ for the first four doses and ACEL-IMUNE ® for all five doses) are licensed for the diphtheria, tetanus, and pertussis vaccination series. FDA has not approved Tripedia ® or Infanrix™ as the fifth dose among persons who have received only Tripedia ® or only Infanrix™ for the first four doses in the vaccination series, because data are insufficient to evaluate their safety in this situation. However, such data should be available before infants vaccinated with four doses of these vaccines require a fifth dose at age 4-6 years.
TriHIBit™ (ActHIB ® reconstituted with Tripedia ® ) is licensed only for the fourth dose of the vaccination series, and is not licensed for the first three doses. TriHIBit™ can be used for the fourth dose following three doses of either DTaP or whole-cell DTP and a primary series of any Hib vaccine.
- Inject Tripedia ® into the vial of lyophilized ActHIB ® . Agitate vial thoroughly; the combined reconstituted vaccines should appear whitish in color.
- Withdraw 0.5 mL dose of the combined vaccines; administer intramuscularly within 30 minutes of reconstitution.
# Interchangeable Use of Acellular Pertussis Vaccines
Whenever feasible, the same brand of DTaP vaccine should be used for all doses of the vaccination series. Data do not exist regarding the safety, immunogenicity, and efficacy of using DTaP vaccines from different manufacturers for successive doses of the primary or booster vaccination series. However, the vaccine provider may not know or may not have available the type of DTaP vaccine previously administered to a child. Neither circumstance should present a barrier to administration of the vaccine and any of the licensed DTaP vaccines may be used to complete the vaccination series.
# Simultaneous Administration of Vaccines
Limited data regarding simultaneous administration of the first three doses of DTaP with other childhood vaccines indicate no interference with response to any of these other antigens. Data are available regarding administration of DTaP with the other vaccines recommended at the same time as the fourth and fifth doses of the diphtheria, tetanus, and pertussis series (i.e., Hib vaccine, OPV, MMR vaccine, and varicella vaccine), and regarding administration of whole-cell DTP (all doses in the series) with these vaccines (40 ). On the basis of this experience, DTaP may be administered simultaneously with hepatitis B vaccine, Hib vaccine, and IPV or OPV to infants at ages 2, 4, or 6 months as indicated in the recommended childhood vaccination schedule (41 ). All vaccines appropriate to the age and previous vaccination status of the child should be administered simultaneously including DTaP, Hib vaccine, IPV or OPV, hepatitis B vaccine, MMR vaccine, and varicella vaccine.
# Special Considerations
# Vaccination of Infants and Young Children Who Have a Personal or Family History of Seizures
Infants and young children who have had previous seizures (whether febrile or nonfebrile) are at greater risk for seizures after administration of whole-cell pertussis vaccination than are infants who do not have such a history (42 ). Because these reactions may be caused by the fever induced by whole-cell DTP and because DTaP is less frequently associated with moderate to high fever, DTaP is the vaccine of choice when pertussis vaccination is considered for these children.
Among infants and children with a history of previous seizures, it is prudent to delay pertussis vaccination until the child's neurologic status has been assessed. Infants and children with a stable neurologic condition, including well-controlled seizures, may be vaccinated with DTaP. Infants with evolving neurologic conditions should not be vaccinated until a treatment regimen has been established and the condition has stabilized. Acetaminophen or ibuprofen may be administered to these children at the time of DTaP vaccination and every 4 hours for 24 hours thereafter to reduce the possibility of postvaccination fever.
Data from one study indicate that infants and young children who have a parent or sibling with a history of convulsions are more likely to have seizures following wholecell DTP vaccination than those without such histories (43 ). However, seizures occur infrequently after administration of whole-cell DTP, are usually febrile in nature, and generally have a benign outcome (44 ). An estimated 5%-7% of children have parents or siblings with a history of convulsions (43 ). If these children were exempted from pertussis vaccination, unvaccinated persons and the general population might face an increased risk for pertussis. Therefore, a family history of convulsions or other central nervous system disorders is not a contraindication to pertussis vaccination. Acetaminophen or ibuprofen may be administered to these children at the time of DTaP vaccination and every 4 hours for 24 hours thereafter to reduce the possibility of postvaccination fever.
# Children Who Have Had Pertussis Disease
Although pertussis disease is likely to confer immunity against pertussis, the duration of such immunity is unknown. Children with well-documented pertussis disease (i.e., positive culture for B. pertussis or epidemiologic linkage to a culture-positive case) should be administered DT vaccine for the remaining doses of the vaccination series to ensure that they are protected against diphtheria and tetanus. Some experts recommend including the pertussis component for subsequent vaccination of infants who have had culture-proven pertussis because infants may have a suboptimal immune response following B. pertussis infection (45 ).
# Pertussis Vaccination for Persons Aged ≥7 Years
Pertussis vaccines are presently licensed for use only among children aged 6 weeks-6 years. In the United States, adolescents and adults whose immunity has waned are an important reservoir for B. pertussis and may infect unvaccinated young children. In the future, booster doses of adult formulations of acellular pertussis vaccines may be recommended to prevent the occurrence and spread of the disease among these older persons. However, acellular pertussis vaccines combined with diphtheria and tetanus toxoids will need to be reformulated for use in adults because all infant formulations contain more diphtheria toxoid than is recommended for persons aged ≥7 years. Recommendations regarding routine vaccination of adults will require additional research (e.g., studies of the incidence, severity, and cost of pertussis among adolescents and adults; studies of the effectiveness and safety of adult formulations of DTaP; and studies of the cost-effectiveness of a strategy of adult vaccination).
# ADVERSE REACTIONS
Mild systemic reactions such as fever, drowsiness, fretfulness, and anorexia may occur after both whole-cell DTP vaccination and DTaP vaccination. However, data concerning adverse reactions following the first four doses indicate that mild reactions are less common among children who receive DTaP. These reactions are self-limited and can be managed safely with symptomatic treatment.- *For a complete discussion, see the general ACIP statement on diphtheria, tetanus, and pertussis and the supplementary statements on DTaP (16,17,42 ).
- Persistent crying lasting ≥3 hours, occurring within 48 hours.
- Convulsions with or without fever, occurring within 3 days.
In circumstances in which the benefits of further pertussis vaccination outweigh the possible risks (e.g., during an outbreak of pertussis), DTaP should be administered for the subsequent doses.
# REPORTING OF ADVERSE EVENTS AFTER VACCINATION
As with any newly licensed vaccine, surveillance for rare adverse events potentially associated with administration of DTaP is important for assessing its safety in largescale use. The National Childhood Vaccine Injury Act of 1986 requires health-care providers to report serious adverse events that follow pertussis vaccination (47 ). The events that must be reported are detailed in the Reportable Events Table within this Act, and include anaphylaxis or anaphylactic shock, encephalopathy (or encephalitis), shock collapse or hypotonic hyporesponsive collapse, and any acute complication or sequela (including death) of these events. Adverse reactions should be reported to VAERS (48 ). VAERS reporting forms and information are available 24 hours a day by calling (800) 822-7967.
# VACCINE INJURY COMPENSATION
The National Vaccine Injury Compensation Program, established by the National Childhood Vaccine Injury Act of 1986, provides a mechanism through which compensation can be paid on behalf of a person thought to have been injured or to have died as a result of receiving a vaccine covered by the program (49,50 ).
A Vaccine Injury Compensation Table in the Act lists the vaccines covered by the program and the injuries, disabilities, and conditions (including death) for which compensation may be paid. Development or onset of anaphylaxis or anaphylactic shock ≤4 hours or encephalopathy with onset ≤72 hours after administration of pertussis vaccine (or sequelae of these conditions) are potentially compensable under this law. Persons may be compensated for an injury listed in the established table or The Morbidity and Mortality Weekly Report (MMWR) Series is prepared by the Centers for Disease Control and Prevention (CDC) and is available free of charge in electronic format and on a paid subscription basis for paper copy. To receive an electronic copy on Friday of each week, send an e-mail message to [email protected]. The body content should read SUBscribe mmwr-toc. Electronic copy also is available from CDC's World-Wide Web server at / or from CDC's file transfer protocol server at ftp.cdc.gov. To subscribe for paper copy, contact Superintendent of Documents, U.S. Government Printing Office, Washington, DC 20402; telephone (202) 512-1800.
Data in the weekly MMWR are provisional, based on weekly reports to CDC by state health departments. The reporting week concludes at close of business on Friday; compiled data on a national basis are officially released to the public on the following Friday. Address inquiries about the MMWR Series, including material to be considered for publication, to: Editor, MMWR Series, Mailstop C-08, CDC, 1600 Clifton Rd., N.E., Atlanta, GA 30333; telephone (404) 332-4555.
All material in the MMWR Series is in the public domain and may be used and reprinted without permission; citation as to source, however, is appreciated.
# 6U.S. Government Printing Office: 1997-532-228/47066 Region IV
# Simultaneous Administration
In a clinical trial in the United States, Infanrix™ was administered simultaneously, at separate sites, with hepatitis B vaccine, Hib vaccine, and OPV to children aged 2, 4, and 6 months. One month after the third dose, 100% of infants (n=64) administered hepatitis B vaccine simultaneously with Infanrix™ demonstrated anti-HBs antibodies
# Dosage and Administration
The dose of all four vaccines-Tripedia ® , TriHIBit™ , ACEL-IMUNE ® , and Infanrix™ -is 0.5 mL, administered intramuscularly. Fractional doses (<0.5 mL) should not be administered. The preferred injection sites are the anterolateral aspect of the thigh and the deltoid muscle of the upper arm (39 ).
To administer TriHIBit™ (ActHIB ® reconstituted with Tripedia ® ) (Connaught Laboratories, Inc., ActHIB ® package insert):
- Cleanse the rubber stoppers of both vials with a suitable germicide.
- Thoroughly agitate the vial of Tripedia ® . Insert the needle of a syringe through the vial's rubber stopper and withdraw 0.6 mL of Tripedia ® .
Moderate-to-severe systemic events (e.g., temperature of ≥105 F ; febrile seizures; persistent, crying lasting ≥3 hours; and hypotonic hyporesponsive episodes) have been reported rarely after administration of DTaP, and occur less frequently among children administered DTaP than among children administered whole-cell DTP.
Data from the Vaccine Adverse Event Reporting System (VAERS)- were used to compare rates of fever, seizures, and hospitalizations among children who, having had ≥3 previous doses of whole-cell DTP, were administered either DTaP or whole-cell DTP vaccines for the fourth or fifth doses (46 ). During 1991-1993, approximately 5 million doses of DTaP (distributed by Connaught Laboratories, Inc., or Wyeth-Lederle Vaccines and Pediatrics) and 27 million doses of whole-cell DTP were distributed for use among children aged 15 months-6 years. Adverse events were reported significantly less commonly among the children who received DTaP. VAERS is a passive surveillance system and these data should be interpreted with caution because the events reported may be linked to vaccine administration only by temporal coincidence.
# CONTRAINDICATIONS
If either of the following events occurs after administration of DTaP or whole-cell DTP, subsequent vaccination with DTaP or whole-cell DTP is contraindicated:
- An immediate anaphylactic reaction. Further vaccination with any of the three components of DTaP or whole-cell DTP should be deferred because of uncertainty as to which component of the vaccine might be responsible. Because of the importance of tetanus vaccination, persons who experience anaphylactic reactions may be referred to an allergist for evaluation and (if specific allergy can be demonstrated) desensitized to tetanus toxoid.
- Encephalopathy not attributable to another identifiable cause (e.g., an acute, severe central nervous system disorder occurring within 7 days after vaccination and generally consisting of major alterations in consciousness, unresponsiveness, or generalized or focal seizures that persist more than a few hours, without recovery within 24 hours.) In such cases, DT vaccine should be administered for the remaining doses in the vaccination schedule to ensure protection against diphtheria and tetanus.
# PRECAUTIONS
If any of the following events occurs within the specified period after administration of either whole-cell DTP or DTaP, vaccine providers and parents should evaluate the risks and benefits of administering subsequent doses of a pertussis-containing vaccine:
- Temperature of ≥105 F (≥40.5 C) within 48 hours, not attributable to another identifiable cause.
- Collapse or shock-like state (hypotonic hyporesponsive episode) within 48 hours. *VAERS is a passive surveillance system for reporting of adverse events temporally associated with administration of vaccines. | #
The following CDC staff members prepared this report:
Dalya
# Pertussis Vaccination: Use of Acellular Pertussis Vaccines Among Infants and Young Children
Recommendations of the Advisory Committee on Immunization Practices (ACIP) Summary Concerns about the safety of whole-cell pertussis vaccines prompted development of acellular vaccines that are less likely to provoke adverse events because they contain purified antigenic components of Bordetella pertussis. Two diphtheria and tetanus toxoids and acellular pertussis (DTaP) vaccines-ACEL-IMUNE ® * and Tripedia ® † -have been licensed for several years, but (until recently) only for administration of the fourth and fifth doses in the series to children aged 15 months-6 years who previously had received three or more doses of diphtheria and tetanus toxoids and whole-cell pertussis (DTP) vaccine. Published reports indicate that, when administered to infants aged 2, 4, and 6 months, acellular pertussis vaccines are effective in preventing pertussis disease and associated with fewer local, systemic, and certain more serious adverse events than whole-cell pertussis vaccines. On the basis of these data, the Food and Drug Administration (FDA) has licensed three DTaP vaccines for use among children aged 6 weeks-6 years. Tripedia ® is now licensed for the initial four doses, and ACEL-IMUNE ® for all five doses of the diphtheria, tetanus and pertussis vaccination series. A third DTaP vaccine (Infanrix™ ) § was licensed in January 1997 for the initial four doses of the series. Tripedia ® , ACEL-IMUNE ® , and Infanrix™ are now recommended for routine vaccination of infants and young children, although whole-cell pertussis vaccines remain acceptable alternatives. Tripedia ® , ACEL-IMUNE ® , and Infanrix™ are recommended for all remaining doses in the schedule for children who have started the vaccination series with one, two, three, or four doses of whole-cell pertussis vaccines. In September 1996, FDA licensed the use of TriHIBit™ (ActHIB ® reconstituted with Tripedia ® ) ¶ for the fourth dose in the series of vaccinations against diphtheria, tetanus, pertussis, and Haemophilus influenzae type b disease. This statement a) provides general information regarding whole-cell pertussis vaccines currently licensed in the United States; b) summarizes results of recent studies of the immunogenicity, efficacy, and safety of acellular pertussis vaccines administered to infants and young children; c) presents recommendations for the use of Tripedia ® , TriHIBit™ , ACEL-IMUNE ® , and Infanrix™ vaccines; and d) supplements previous recommendations on pertussis vaccination.
# INTRODUCTION Whole-Cell Pertussis Vaccines
Four diphtheria and tetanus toxoids combined with whole-cell pertussis (DTP) vaccines are presently licensed for use in the United States.* Vaccines of this type, prepared from suspensions of inactivated Bordetella pertussis bacterial cells, have been licensed for routine vaccination of infants since the mid-1940s. Based on controlled efficacy trials conducted in the 1940s and on subsequent observational efficacy studies, a primary series comprising four doses of whole-cell DTP vaccine is considered 70%-90% effective in preventing serious pertussis disease (1)(2)(3)(4).
Whole-cell DTP vaccines are commonly associated with several local adverse events (e.g., erythema, swelling, and pain at the injection site), fever, and other mild systemic events (e.g., drowsiness, fretfulness, and anorexia) (5,6 ). More severe systemic events (e.g., convulsions [with or without fever] and hypotonic hyporesponsive episodes) occur less frequently (ratio of one case to 1,750 doses administered) among children who receive whole-cell DTP vaccine (5 ). Acute encephalopathy occurs even more rarely (ratio of 0-10.5 cases to one million doses administered) (7 ). Experts disagree on whether whole-cell pertussis vaccine causes lasting brain damage, but agree that if the vaccine causes such damage it does so only rarely (7 ). Concerns about safety prompted the development of more purified (acellular) pertussis vaccines that are associated with a lower frequency of adverse events and are effective in preventing pertussis disease.
# Trends in Pertussis Disease in the United States
In the United States, the highest recorded annual incidence of pertussis occurred in 1934 when >260,000 cases were reported. The incidence of reported pertussis disease declined substantially as use of whole-cell DTP vaccines became widespread. By 1970, the reported incidence had declined >99%; the fewest cases (1,010) were reported in 1976. However, since the early 1980s reported pertussis incidence has increased steadily. Cyclical peaks in incidence occurred in 1983,1986,1990, and in 1993 when 6,586 cases were reported-more than in any year since 1976 (8 ). The number of reported cases has increased in all age groups, but the increase is greatest among persons aged ≥5 years (9 ). Nevertheless, infants and young children continue to have the highest risk for pertussis and its complications (4,8,10 The increase in reported pertussis cases has occurred despite pertussis vaccination coverage levels that are higher than at any time in the past. The proportion of children aged 19-35 months who had received three or more doses of whole-cell DTP or diphtheria and tetanus toxoids vaccine (DT) reached 93% in 1994 (11 ). (Of those vaccinated, <2% are estimated to have received DT [CDC, unpublished data].) Possible explanations of this increase in disease include a) decreased vaccine efficacy, b) waning immunity among adolescents and adults vaccinated during childhood, c) increased diagnosis and reporting of pertussis because of greater awareness among physicians about the disease, and d) enhanced surveillance and more complete reporting in some states (12,13 ).
Recent randomized controlled trials in Sweden and in Italy with one of the wholecell DTP vaccines presently licensed in the United States (manufactured by Connaught Laboratories, Inc.) yielded estimates of low clinical efficacy-60% in the 6 months immediately following administration of the third dose. Estimates of vaccine efficacy for the total followup period were even lower-48% in Sweden and 36% in Italy (14,15 ). These estimates were substantially lower than expected on the basis of estimates obtained from observational studies in the United States. One possible explanation for the disparity is the number of doses administered-three in the trials in Sweden and Italy versus five in the United States (doses at ages 2, 4, 6, and 12-18 months and 4-6 years). A recent study in Germany with another whole-cell DTP vaccine currently in use in the United States (distributed by Wyeth-Lederle Vaccines and Pediatrics) demonstrated 83% protective efficacy after the third dose and before administration of the fourth dose and 94% efficacy after four doses (Wyeth-Lederle Vaccines and Pediatrics, ACEL-IMUNE ® package insert). The effectiveness of the current pertussis vaccination program in the United States, which has relied on four different whole-cell DTP vaccines for primary vaccination, remains high (3,4 ).
# Acellular Pertussis Vaccines
Acellular pertussis vaccines contain inactivated pertussis toxin (PT) and may contain one or more other bacterial components (e.g., filamentous hemagglutinin [FHA], a 69-kilodalton outer-membrane protein-pertactin [Pn], and fimbriae [Fim] types 2 and 3). PT is detoxified either by treatment with a chemical (e.g., hydrogen peroxide, formalin and/or glutaraldehyde) or by using molecular genetic techniques. Acellular pertussis vaccines contain substantially less endotoxin than whole-cell pertussis vaccines.
Since 1991, two acellular pertussis vaccines (Tripedia ® and ACEL-IMUNE ® ) have been licensed for use in the United States. Until recently, both vaccines were licensed for use only as the fourth and fifth doses of the diphtheria, tetanus, and pertussis vaccination series among children aged 15 months-6 years who had received three primary doses of whole-cell DTP (16,17 ). This licensure was based on findings of studies conducted in Sweden and Japan. These studies did not evaluate the efficacy of acellular pertussis vaccines administered to infants on a schedule similar to the one used in the United States and did not directly compare the efficacy of DTaP vaccines with that of whole-cell DTP vaccines (18)(19)(20)(21)(22).
# Studies of the Efficacy of DTaP Vaccines in Infants
Since 1991, seven studies conducted in Europe and Africa have evaluated the efficacy of eight DTaP vaccines administered to infants. The vaccines, produced by different manufacturers, contained a varying number and quantity of antigens. The derivation and formulation of the individual antigens also varied among vaccines (Table 1). Four doses of vaccine were administered in one study (Wyeth-Lederle Vaccines and Pediatrics, ACEL-IMUNE ® package insert); the other six studies involved three doses (14,15,(23)(24)(25). These studies also differed in other ways (Table 2):
• Design. Three studies were randomized placebo-controlled clinical trials; such studies usually provide the most accurate measure of a treatment effect and are less subject to biases than observational studies.
• Case definition. Estimates of vaccine efficacy tend to be higher when the case definition excludes mild clinical cases.
• Laboratory method used to confirm the diagnosis of pertussis.
Because of these differences, comparisons among studies should be made with caution. Within individual studies, however, the efficacy of acellular pertussis vaccines can be compared directly with that of whole-cell DTP.
The efficacy of three doses of acellular pertussis vaccines in preventing moderate to severe pertussis disease was within the range expected for most whole-cell DTP vaccines. Point estimates of efficacy ranged from 59% to 89%. Mild local and systemic adverse events occurred less frequently among infants vaccinated with acellular pertussis vaccines for the first three or four doses than among those vaccinated with whole-cell DTP. More serious adverse events (e.g., fever ≥105 F [≥40.5 C], persistent crying of ≥3 hours duration, hypotonic hyporesponsive episodes, and seizures) generally occurred less frequently among infants who received acellular pertussis vaccines than among those vaccinated with whole-cell DTP. The number of subjects included in these studies was insufficient to estimate the risk for rare severe reactions (i.e., encephalopathy or anaphylactic shock). Surveillance for these rare adverse events will be needed as acellular pertussis vaccines are used more widely.
# Interpretation of Immunogenicity Data
The findings of efficacy studies have not demonstrated a direct correlation between antibody responses and protection against pertussis disease. However, antibody studies are useful to compare immune responses elicited by a single vaccine under different conditions or in different studies. Thus, efficacy studies are required to measure clinical protection conferred by each pertussis vaccine.
# TRIPEDIA ®
On July 31, 1996, the Food and Drug Administration (FDA) licensed Tripedia® for use as the initial four doses of the recommended diphtheria, tetanus, and pertussis vaccination series among children aged 6 weeks-6 years. The acellular pertussis vaccine components are purified from B. pertussis by salt precipitation, ultracentrifugation, and ultrafiltration. After purification, fractions containing PT and FHA are combined to obtain a 1:1 ratio and are treated with formaldehyde to inactivate PT. Each dose of Tripedia ® contains approximately 23.4 µg protein of inactivated PT (toxoid) and 23.4 µg protein of FHA, as well as 6.7 limit of flocculation units (Lf) of diphtheria toxoid and 5.0 Lf of tetanus toxoid. The combined components are adsorbed using aluminum potassium sulfate and preserved with 1:10,000 thimerosal (Table 1).
# Immunogenicity
The Multicenter Acellular Pertussis Trial, an immunogenicity and safety study conducted in six centers in the United States and sponsored by the National Institutes of Health (NIH), compared antibody responses of infants vaccinated at ages 2, 4, and 6 months with whole-cell DTP or with one of 13 different acellular pertussis vaccines, including Tripedia ® . Antibody to pertussis antigens was measured in serum samples taken before administration of the first dose and 1 month after administration of the third dose of Tripedia ® ; 99% and 86% of children had fourfold or greater increases in titers of antibody to PT and FHA, respectively. More than 90% of children administered Tripedia ® developed diphtheria and tetanus antibody levels indicative of immunity to these diseases (i.e., >0.1 antitoxin units [u] per mL and >0.01 u/mL, respectively), as did ≥90% of those administered whole-cell DTP (26 ). The immunogenicity of Tripedia ® when administered as a fourth dose to children aged 12-14 months has not been studied.
# Clinical Efficacy
Two studies conducted in Sweden and Germany provide data concerning the clinical efficacy of Tripedia ® . During 1985-1987, a randomized, placebo-controlled clinical trial in Sweden examined the efficacy of two doses of two acellular pertussis vaccines. The acellular pertussis component of one vaccine was comparable to the acellular pertussis component of Tripedia ® (17,18 ). The first dose was administered at age 5-11 months, the second dose 8-12 weeks later. For culture-confirmed disease with cough of any duration, the vaccine's efficacy after two doses was 69% (95% confidence interval [CI]=47%-82%) (18 ). Using a more stringent case definition (i.e., ≥21 days paroxysmal cough and confirmation by culture) resulted in an efficacy estimate of 81% (95% CI=61%-90%) (27 ). A non-blinded follow-up study conducted during the 42-month period following the clinical trial yielded similar results (28 ).
A case-control study in Germany evaluated the efficacy of three doses of Tripedia ® administered to children aged approximately 3, 5, and 7 months (Connaught Laboratories, Inc.,Tripedia ® package insert). Comparison groups received whole-cell DTP (manufactured by Behringwerke, A.G.), DT, or no vaccine. A case of pertussis was defined as an illness with cough of ≥21 days duration and confirmation by positive culture for B. pertussis or household contact with a culture-proven case. The estimated clinical efficacy of three doses of Tripedia ® compared with DT was 80% (95% CI=59%-90%). For infants who received three doses of whole-cell DTP, the vaccine efficacy estimate was 95% (95% CI=81%-99%) (25 ). However, the two efficacy estimates are not directly comparable because of differences in the way infants were enrolled in the two groups.
# Safety
The safety of Tripedia ® was assessed in studies conducted in the United States and Germany. Local reactions (e.g., erythema, swelling, or pain), fever, and other common systemic symptoms (e.g., anorexia, vomiting, drowsiness, or fussiness) occurred less frequently among infants administered Tripedia ® than among those who received whole-cell DTP (Connaught Laboratories, Inc., Tripedia ® package insert). In the Multicenter Acellular Pertussis Trial, local and common systemic events occurred less frequently among Tripedia ® recipients than among recipients of whole-cell DTP (Table 3) ( 29). Among recipients of 41,615 doses of Tripedia ® in the trial in Germany, few moderate to severe adverse events occurred within 7 days after vaccination (Connaught Laboratories, Inc., Tripedia ® package insert). The following events and rates of occurrence (per 1,000 doses administered) were reported: persistent crying for ≥3 hours, 0.12; febrile seizures, 0.05; afebrile seizures, 0.02; and hypotonic hyporesponsive episodes, 0.05. Rates of invasive bacterial infections, hospitalizations, and deaths among infants vaccinated with Tripedia ® were similar to those observed among recipients of DT. None of the deaths or invasive bacterial infections was vaccine related.
In a study conducted in the United States, children aged 15-20 months who had received Tripedia ® (n=109) or whole-cell DTP (n=30) for the first three doses were administered Tripedia ® as the fourth dose (30 ). Although the differences were not statistically significant, the percentages of children who had local adverse events (e.g., erythema, swelling, or pain) or certain systemic adverse events (i.e., temperature >101 F [>38.3 C] or irritability) within 72 hours after administration of the fourth dose was higher among children who had received Tripedia ® for the first three doses. However, the frequency of adverse events was lower than that observed in previous studies in which a fourth dose of whole-cell DTP followed three previous doses of whole-cell DTP.
Limited data are available to evaluate the safety of Tripedia ® when administered as a fifth dose to children aged 4-6 years who have received four previous doses of Tripedia ® . The frequency of local and mild systemic reactions after the last of five doses was no greater among children administered Tripedia ® (n=18) than among children in the same study who were administered five doses of whole-cell DTP (n=10) (M.E. Pichichero, unpublished data). More data concerning the safety of Tripedia ® in such circumstances are being collected and will be available before infants who receive Tripedia ® for the first four doses require a fifth dose at age 4-6 years. Data are insufficient to assess the safety of Tripedia ® administered to persons aged ≥7 years.
# Simultaneous Administration
# Immunogenicity
In a randomized clinical trial, children aged 15-20 months were administered either Tripedia ® and ActHIB ® vaccines at separate sites (n=98) or combined as a single dose (n=93) (Connaught Laboratories, Inc., Tripedia ® package insert). Before the study began, these children all had received three doses of a Hib conjugate vaccine and three doses of whole-cell DTP at approximately ages 2, 4, and 6 months. One month after administration of the fourth dose, 100% of the children in both groups had anti-PRP antibody concentrations ≥1 µg/mL, an indication of long-term protection against invasive H. influenzae type b disease. The proportions of children with protective antibody responses to diphtheria and tetanus toxoids were also high and similar in the two groups. The proportions of children who had fourfold or greater serum antibody responses to PT (measured by enzyme-linked immunosorbent assay [ELISA] or Chinese hamster ovary [CHO] cell assay) were >85% in both groups. Among children who received TriHIBit™ , the proportion with fourfold or greater antibody responses to FHA was slightly lower. The clinical importance of this difference is not known.
# Clinical Efficacy
TriHIBit™ has been licensed for use as the fourth dose of the two vaccination series on the basis of immunogenicity and safety data. Its protective efficacy when used for this purpose has not been evaluated.
# Safety
The safety of TriHIBit™ was evaluated in two studies involving a total of 960 children who had each received three doses of a Hib vaccine and three doses of whole-cell DTP vaccine at approximately ages 2, 4, and 6 months (Connaught Laboratories, Inc., Tripedia ® package insert). At age 15-20 months, these children were administered the fourth dose of Tripedia ® and ActHIB ® vaccines either combined by reconstitution as a single injection or as two injections at separate sites. Rates of local and systemic reactions were similar in the two groups. Local reactions were mild and resolved within 48 hours following vaccination. The most common local reaction was pain at the injection site.
# Simultaneous Administration
When TriHIBit™ was administered to children aged 15-20 months (n=47) simultaneously with MMR vaccine, >95% developed serum antibody to measles, mumps, and rubella at levels indicative of protection against these diseases (Connaught Laboratories, Inc., Tripedia ® package insert). Immune responses to OPV or IPV and hepatitis B vaccine when administered simultaneously with TriHIBit™ have not been studied.
# ACEL-IMUNE ®
On December 30, 1996, FDA licensed ACEL-IMUNE ® for all five doses of the recommended diphtheria, tetanus, and pertussis vaccination series among children aged 6 weeks-6 years. Each dose of the acellular pertussis component of ACEL-IMUNE ® contains approximately 34.4 µg of FHA, 3.2 µg of inactivated PT, 1.6 µg of Pn, and 0.8 µg of Fim type 2. The acellular pertussis vaccine components are purified by ammonium sulfate fractionation and sucrose density gradient centrifugation. PT is detoxified by treatment with formaldehyde. Each dose of ACEL-IMUNE ® contains 9.0 Lf units of diphtheria toxoid, 5.0 Lf units of tetanus toxoid, and 300 hemagglutinating units of acellular pertussis vaccine. The FHA and PT components both exhibit hemagglutinating activity. The combined components are adsorbed to aluminum hydroxide and aluminum phosphate and preserved with 1:10,000 thimerosal (Table 1).
# Immunogenicity
Data from the Multicenter Acellular Pertussis Trial provide evidence of the immunogenicity of ACEL-IMUNE ® (26). Investigators measured levels of serum antibody to each of the four vaccine antigens after administration of three doses. The percentages of vaccinees with fourfold or greater increases in antibody titer (compared with prevaccination levels) were: PT, 67%; FHA, 80%; Pn, 71%; and Fim, 59%. The percentages of these children who developed diphtheria antibody levels of ≥0.1 u/mL and tetanus antibody levels of ≥0.01 u/mL (i.e., indications of immunity against these diseases) were 86% and 100%, respectively. Antibody responses observed among children in the United States were similar to those observed among children in the study in Germany that demonstrated the efficacy of ACEL-IMUNE ® .
Antibody response to ACEL-IMUNE ® when administered to children aged 12-14 months was evaluated in a clinical trial (Wyeth-Lederle Vaccines and Pediatrics, unpublished data). ACEL-IMUNE ® was administered as a fourth dose to children aged 12-14 months (n=58) or 15-18 months (n=50) who had previously received three doses of whole-cell DTP. In both age groups, >85% of the children had twofold or greater antibody responses to PT, FHA, Pn, and Fim.
# Clinical Efficacy
Efficacy of ACEL-IMUNE ® was assessed in a prospective study in Erlangen, Germany (Wyeth-Lederle Vaccines and Pediatrics, ACEL-IMUNE ® package insert). Infants were randomly assigned to groups that were administered either ACEL-IMUNE ® or whole-cell DTP (distributed by Wyeth-Lederle Vaccines and Pediatrics) at a mean age of 3, 5, 7, and 17 months. A third group of infants (not selected randomly) received DT at ages 3, 5, and 17 months. In this study, pertussis was defined as cough illness lasting ≥21 days with at least one pertussis-associated symptom (paroxysms, whoop, or post-tussive vomiting) confirmed by culture, serology, or epidemiologic link to a culture-positive household contact. Between the third and fourth doses, the efficacy of ACEL-IMUNE ® (compared with DT) was 73% (95% CI=51%-86%) and the efficacy of whole-cell DTP 83% (95% CI=65%-92%). After four doses, the efficacy of ACEL-IMUNE ® was 85% (95% CI=76%-90%), and that of whole-cell DTP was 94% (95% CI=89%-97%). Considering the full observation period after the third and fourth doses, the adjusted efficacy of ACEL-IMUNE ® was 81% (95% CI=73%-87%) compared with 91% (95% CI=85%-95%) for whole-cell DTP.
# Safety
Studies from the United States and Germany provide data concerning the frequency and nature of adverse events that occur after administration of ACEL-IMUNE ® . In the Multicenter Acellular Pertussis Trial, children who were administered ACEL-IMUNE ® experienced fewer local adverse events (e.g., pain, redness, or swelling at the injection site) and systemic adverse events (e.g., temperature >101 F [>38.3 C], or fussiness) after any of the first three doses than children who were administered whole-cell DTP (Table 3) (29 ). Similarly, in other studies conducted in the United States and Germany, adverse events (local and systemic) after any of the initial four doses occurred less frequently among children who received ACEL-IMUNE ® than among children administered whole-cell DTP (Wyeth-Lederle Vaccines and Pediatrics, ACEL-IMUNE ® package insert). Rates of adverse events increased with the number of previous doses of ACEL-IMUNE ® administered, but were lower than rates for children who received the same number of doses of whole-cell DTP. Among 357 children who were administered five doses of ACEL-IMUNE ® , adverse events occurred no more frequently than among children in previous studies (historical controls) who received five doses of whole-cell DTP (Wyeth-Lederle Vaccines and Pediatrics, ACEL-IMUNE ® package insert).
In the efficacy trial in Germany (n=16,642 doses of ACEL-IMUNE ® ), the following rates of moderate to severe adverse events (per 1,000 doses administered) were observed within 72 hours after administration of the vaccine: persistent or unusual cry, 1.14; temperature ≥105 F (≥40.5 C), 0.06; febrile seizures (no other type of seizure occurred), 0.06; and hypotonic hyporesponsive episodes, 0 (Wyeth-Lederle Vaccines and Pediatrics, ACEL-IMUNE ® package insert). Rates of all these adverse events were higher among children who received whole-cell DTP.
A clinical trial examined the frequency of local reactions (e.g., erythema, induration, or tenderness) and systemic reactions (e.g., fever, fussiness, drowsiness, or anorexia) among children aged 12-14 months or 15-18 months, all of whom had previously received three doses of whole-cell DTP. Differences in the frequency of adverse reactions in the two age groups were not statistically significant (Wyeth-Lederle Vaccines and Pediatrics, unpublished data).
Neither anaphylaxis nor encephalopathy occurred during clinical trials that involved administration of 25,899 doses of ACEL-IMUNE ® . Six deaths of infants or young children who participated in these trials were reported to study investigators; none was vaccine-related and all occurred >4 weeks after vaccination (Wyeth-Lederle Vaccines and Pediatrics, ACEL-IMUNE ® package insert). The reactogenicity of ACEL-IMUNE ® among persons aged ≥7 years has not been evaluated.
# Simultaneous Administration
The immunogenicity of ACEL-IMUNE ® when administered simultaneously with other recommended childhood vaccines was evaluated in three studies. ACEL-IMUNE ® , Hib vaccine, and hepatitis B vaccine were administered simultaneously to 77 infants at ages 2, 4, and 6 months. After administration of the third dose, serum samples from 94% of the infants demonstrated anti-PRP antibodies indicative of clinical protection (≥1 µg/mL), and all of the infants evaluated (n=74) had antibody levels indicative of protection against hepatitis B (i.e., anti-HBs titers of >10 mIU/mL) (Wyeth-Lederle Vaccines and Pediatrics, ACEL-IMUNE ® package insert). In another clinical study, 30 infants were administered OPV simultaneously with ACEL-IMUNE ® at ages 2 and 4 months; ≥90% had protective neutralizing antibody to all three poliovirus types at age 6 months. When MMR vaccine was administered simultaneously with ACEL-IMUNE ® to children aged 15-18 months (n=48), ≥92% developed serum antibody titers indicative of protection against measles, mumps, and rubella. Similar results were obtained when whole-cell DTP was administered simultaneously with OPV or MMR vaccine (31 ). Simultaneous administration of ACEL-IMUNE ® and IPV or varicella vaccine has not been evaluated.
# INFANRIX™ ™
On January 29, 1997, FDA licensed Infanrix™ for use as the initial four doses of the recommended diphtheria, tetanus, and pertussis vaccination series among children aged 6 weeks-6 years. Infanrix™ is also licensed for all remaining doses in the schedule for children who have received one or more doses of whole-cell DTP vaccine. Each dose of Infanrix™ contains 25 µg PT, 25 µg FHA, 8 µg Pn, 25 Lf of diphtheria toxoid, and 10 Lf of tetanus toxoid (Table 1). The three antigens in the acellular pertussis vaccine component are separately purified in successive chromatographic steps (hydrophobic, affinity, ion exchange, and size exclusion processes). Formalin and glutaraldehyde are used to detoxify PT; FHA and Pn are treated with formalin. The combined components are adsorbed onto ≤0.625 mg of aluminum (as aluminum hydroxide) and preserved with 2-phenoxyethanol.
# Immunogenicity
In the Multicenter Acellular Pertussis Trial, three doses of Infanrix™ were administered to children at ages 2, 4, and 6 months. One month after the third dose, investigators measured fourfold or greater antibody responses to PT, FHA, and Pn in ≥83% of children who received Infanrix™ , a higher proportion than observed among recipients of whole-cell DTP (26 ). All the children who were administered Infanrix™ developed diphtheria antibody titers of ≥0.1 u/mL and tetanus antibody titers of ≥0.01 u/mL (i.e., indications of immunity against these diseases). Whether their primary vaccination was with Infanrix™ or whole-cell DTP, >86% of children aged 15-20 months had a fourfold or greater rise in serum antibody to each of the pertussis antigens in the vaccine after administration of Infanrix™ as the fourth dose (M. E. Pichichero, unpublished data). The immunogenicity of Infanrix™ administered as a fourth dose to children aged 12-14 months has not been studied.
# Efficacy
The efficacy of Infanrix™ was evaluated in two separate studies (Table 2). In Italy, researchers compared the efficacy of Infanrix™ , DTaP manufactured by Chiron Biocine, whole-cell DTP manufactured by Connaught Laboratories, and DT in a randomized controlled trial that enrolled more than 15,000 children (15 ). Participants received three doses of one of the vaccines at ages 2, 4, and 6 months. The efficacy of Infanrix™ in preventing pertussis disease (defined as paroxysmal cough ≥21 days duration, with culture or serologic confirmation of infection with B. pertussis) was 84% (95% CI=76%-89%). The efficacy of whole-cell DTP was 36% (95% CI=14%-52%). After the trial, children were followed in an observational study to an average age of 33 months (range: 20-39 months); the efficacy of Infanrix™ remained high throughout this followup period (78%, 95% CI=62%-87%) (SmithKline Beecham Pharmaceuticals, Infanrix™ package insert).
The second study, conducted in six areas in Germany, was a household contact study. In preparation for this study, three doses of Infanrix™ were administered at ages 3, 4, and 5 months to more than 22,000 infants as part of a large immunogenicity and safety study (23 ). Infants who did not participate in this study could have received whole-cell DTP vaccine (manufactured by Behringwerke, A.G.) or DT vaccine. The efficacy study included 453 households with confirmed cases of pertussis in which 360 contact children aged 6-47 months were eligible for inclusion in the vaccine efficacy calculations. A case of pertussis was defined as ≥21 days of paroxysmal cough illness plus confirmation of B. pertussis infection by culture and/or serologic testing. The efficacy of Infanrix™ was 89% (95% CI=77%-95%); the efficacy of whole-cell DTP was 98% (95% CI=83%-100%).
# Safety
The occurrence of adverse events following vaccination with Infanrix™ was evaluated in clinical studies involving approximately 30,000 children. In these studies, 28,749 infants received Infanrix™ as a three dose primary series, 5,830 children received Infanrix™ as a fourth dose following three doses of Infanrix™ , and 22 children received Infanrix™ as a fifth dose following four doses of Infanrix™ . In addition, 439 children and 169 children received Infanrix™ as a fourth or fifth dose following three or four doses of whole-cell DTP vaccine, respectively. In comparative studies, administration of Infanrix™ was followed by fewer of the local and systemic adverse reactions commonly associated with whole-cell DTP vaccination (15,29,(32)(33)(34). However, results of these studies demonstrated that the rates of erythema, swelling, and fever increased with each successive dose of Infanrix™ (SmithKline Beecham Pharmaceuticals, Infanrix™ package insert). In the Multicenter Acellular Pertussis Trial, local and common systemic adverse events occurred less frequently following any dose of Infanrix™ in the primary series than following any dose of whole-cell DTP (Table 3) (29 ).
The efficacy study conducted in Italy monitored the frequency of moderate to severe adverse events occurring after administration of any of the primary doses of Infanrix™ . Rates (per 1,000 doses administered) of adverse events occurring ≤48 hours after administration were: persistent crying ≥3 hours duration, 0.44; seizures, 0.07; and temperature ≥104 F(≥40.0 C), 0.36. These rates were similar to or slightly higher than the rates reported among children who were administered DT, but lower than those for children who received whole-cell DTP. In this trial, no hypotonic hyporesponsive episodes occurred among children to whom Infanrix™ was administered.
In the safety study in Germany, data were available regarding 1,809 children who received three doses of Infanrix™ at ages 3, 4, and 5 months and a fourth dose at a mean age of 20 months. The percentages of children who experienced each of the adverse events ≤3 days after administration of the fourth dose were: redness, 46%; swelling, 35%; pain, 26%; fever ≥100.4 F (≥38 C), 26%; and restlessness, 16%. In this study the rates of redness, swelling, pain, and fever increased with successive doses of Infanrix™ (SmithKline Beecham Pharmaceuticals, Inc., Infanrix™ package insert).
Additional safety data are available from another study conducted in Germany (SmithKline Beecham Pharmaceuticals, Inc., Infanrix™ package insert). Children aged 13-27 months received Infanrix™ or whole-cell DTP (manufactured by Behringwerke, A.G.) as a fourth dose. These children had previously received three doses of the same vaccine. Among children administered Infanrix™ as the fourth dose, the incidence of redness, swelling, pain, fever, and restlessness was lower than among children administered whole-cell DTP as the fourth dose.
Infanrix™ has not been licensed previously for administration of the fourth or fifth dose to children who have received three or four doses of whole-cell DTP. Two studies conducted in the United States examined the frequency of adverse events among children who had previously received three or four doses of whole-cell DTP vaccine at approximately ages 2, 4, 6, and 15-18 months (Table 4). Children aged 15-20 months received Infanrix™ or whole-cell DTP vaccine as the fourth dose; children aged 4-6 years were administered Infanrix™ or whole-cell DTP as the fifth dose (33,34 ). Significantly fewer local and systemic adverse events were reported following administration of Infanrix™ than following whole-cell DTP vaccine.
In the safety study in Germany, edematous swelling of the entire thigh into which the vaccine was injected was reported spontaneously by parents or care-givers of 62 of 5,361 vaccinees (1.2%) after administration of the fourth dose. The swelling generally began within 48 hours of vaccination and resolved spontaneously without sequelae during an average of 4 days. In other countries where Infanrix™ has been licensed, this type swelling has been reported rarely following administration of Infan-rix™ for any dose, including the primary series (SmithKline Beecham Pharmaceuticals, Infanrix™ package insert). Edematous swelling has also been reported following administration of other DTaP vaccines, acellular pertussis vaccine alone (without DT), whole-cell DTP vaccine and other vaccines (19,(35)(36)(37). However, the precise frequency of these reactions among vaccinated children is unknown.
Data are insufficient to evaluate the safety of administration of a fifth dose of Infan-rix™ to children aged 4-6 years who have received Infanrix™ for the previous four doses. Additional information regarding the immunogenicity and safety of a fifth dose of Infanrix™ administered to children who have received four prior doses of the same vaccine is being collected. This information is expected to be available before infants who receive Infanrix™ for the first four doses require a fifth dose at age 4-6 years. The safety of Infanrix™ when administered to persons aged ≥7 years has not been assessed.
≥10 mIU/mL and 90% of infants (n=72) who received Hib vaccine simultaneously with Infanrix™ achieved anti-PRP antibodies ≥1 µg/mL (i.e., antibody levels indicative of protection against these diseases). The percentage of infants who were administered OPV simultaneously with Infanrix™ (n=60-61) who developed protective neutralizing antibody to poliovirus types 1, 2, and 3 ranged from 96% to 100% (38 ). No data are available regarding antibody responses to MMR vaccine, varicella vaccine, or IPV when administered simultaneously with Infanrix™ .
# VACCINE USE
# Recommended Childhood Vaccination Schedule
The routine diphtheria, tetanus, and pertussis vaccination schedule for children aged <7 years comprises five doses of vaccine containing diphtheria, tetanus, and pertussis antigens (Table 5). Three (primary) doses should be administered during the first year of life, generally at ages 2, 4, and 6 months. To maintain adequate immunity during preschool years, the fourth (first booster) dose is recommended for children *Diphtheria and tetanus toxoids and acellular pertussis vaccine (DTaP); diphtheria and tetanus toxoids and whole-cell pertussis vaccine (DTP) is an acceptable alternative to DTaP for any of the five doses. † Use diphtheria and tetanus toxoids, adsorbed (DT) if encephalopathy has occurred after administration of a previous dose of pertussis-containing vaccine. If the child is age ≥1 year at the time the first dose of DT is administered, a third dose administered 6-12 months after the second dose completes primary vaccination with DT. § Whenever possible, the same DTaP product should be used for all doses. If the same product is not available, Tripedia ® , ACEL-IMUNE ® , and Infanrix™ can be used interchangeably. ¶ Prolonging the interval does not require restarting the series. ** If the interval between the third and fourth doses is ≥6 months and the child is not likely to return for a visit at the recommended age, the fourth dose of either DTaP or DTP may be administered as early as age 12 months. † † TriHIBit™ can be administered as the fourth dose following a primary series with either DTaP or whole-cell DTP and a primary series with any Haemophilus influenzae type b conjugate vaccine. § § Tetanus-diphtheria toxoids absorbed (Td) (for adult use). aged 15-18 months. The fourth dose should be administered ≥6 months after the third. If the interval between the third and fourth doses is ≥6 months and the child is not likely to return for a visit at the recommended age, the fourth dose of either DTaP or whole-cell DTP may be administered as early as age 12 months. The fifth (second booster) dose is recommended for children aged 4-6 years to confer continued protection against disease during the early years of schooling. A fifth dose is not necessary if the fourth dose in the series is administered on or after the fourth birthday.
# Vaccine Preference
DTaP vaccines are efficacious when administered to infants as the primary series (i.e., doses 1-3). In addition, local reactions, fever, and other systemic events occur substantially less often after DTaP administration than after administration of wholecell DTP. Therefore, DTaP vaccines are recommended for all five doses in the vaccination schedule. For children who have started the vaccination series with one, two, three, or four doses of whole-cell DTP, DTaP is also recommended for all remaining doses in the schedule. During the period of transition from use of whole-cell DTP to DTaP, whole-cell DTP is an acceptable alternative to DTaP for any of the five doses. For the first four doses, whole-cell DTP combined with Hib vaccine (DTP-Hib vaccine) is an acceptable alternative to DTaP and Hib vaccine administered at separate sites.
# Licensed Products
Three acellular pertussis vaccines (Tripedia ® and Infanrix™ for the first four doses and ACEL-IMUNE ® for all five doses) are licensed for the diphtheria, tetanus, and pertussis vaccination series. FDA has not approved Tripedia ® or Infanrix™ as the fifth dose among persons who have received only Tripedia ® or only Infanrix™ for the first four doses in the vaccination series, because data are insufficient to evaluate their safety in this situation. However, such data should be available before infants vaccinated with four doses of these vaccines require a fifth dose at age 4-6 years.
TriHIBit™ (ActHIB ® reconstituted with Tripedia ® ) is licensed only for the fourth dose of the vaccination series, and is not licensed for the first three doses. TriHIBit™ can be used for the fourth dose following three doses of either DTaP or whole-cell DTP and a primary series of any Hib vaccine.
• Inject Tripedia ® into the vial of lyophilized ActHIB ® . Agitate vial thoroughly; the combined reconstituted vaccines should appear whitish in color.
• Withdraw 0.5 mL dose of the combined vaccines; administer intramuscularly within 30 minutes of reconstitution.
# Interchangeable Use of Acellular Pertussis Vaccines
Whenever feasible, the same brand of DTaP vaccine should be used for all doses of the vaccination series. Data do not exist regarding the safety, immunogenicity, and efficacy of using DTaP vaccines from different manufacturers for successive doses of the primary or booster vaccination series. However, the vaccine provider may not know or may not have available the type of DTaP vaccine previously administered to a child. Neither circumstance should present a barrier to administration of the vaccine and any of the licensed DTaP vaccines may be used to complete the vaccination series.
# Simultaneous Administration of Vaccines
Limited data regarding simultaneous administration of the first three doses of DTaP with other childhood vaccines indicate no interference with response to any of these other antigens. Data are available regarding administration of DTaP with the other vaccines recommended at the same time as the fourth and fifth doses of the diphtheria, tetanus, and pertussis series (i.e., Hib vaccine, OPV, MMR vaccine, and varicella vaccine), and regarding administration of whole-cell DTP (all doses in the series) with these vaccines (40 ). On the basis of this experience, DTaP may be administered simultaneously with hepatitis B vaccine, Hib vaccine, and IPV or OPV to infants at ages 2, 4, or 6 months as indicated in the recommended childhood vaccination schedule (41 ). All vaccines appropriate to the age and previous vaccination status of the child should be administered simultaneously including DTaP, Hib vaccine, IPV or OPV, hepatitis B vaccine, MMR vaccine, and varicella vaccine.
# Special Considerations
# Vaccination of Infants and Young Children Who Have a Personal or Family History of Seizures
Infants and young children who have had previous seizures (whether febrile or nonfebrile) are at greater risk for seizures after administration of whole-cell pertussis vaccination than are infants who do not have such a history (42 ). Because these reactions may be caused by the fever induced by whole-cell DTP and because DTaP is less frequently associated with moderate to high fever, DTaP is the vaccine of choice when pertussis vaccination is considered for these children.
Among infants and children with a history of previous seizures, it is prudent to delay pertussis vaccination until the child's neurologic status has been assessed. Infants and children with a stable neurologic condition, including well-controlled seizures, may be vaccinated with DTaP. Infants with evolving neurologic conditions should not be vaccinated until a treatment regimen has been established and the condition has stabilized. Acetaminophen or ibuprofen may be administered to these children at the time of DTaP vaccination and every 4 hours for 24 hours thereafter to reduce the possibility of postvaccination fever.
Data from one study indicate that infants and young children who have a parent or sibling with a history of convulsions are more likely to have seizures following wholecell DTP vaccination than those without such histories (43 ). However, seizures occur infrequently after administration of whole-cell DTP, are usually febrile in nature, and generally have a benign outcome (44 ). An estimated 5%-7% of children have parents or siblings with a history of convulsions (43 ). If these children were exempted from pertussis vaccination, unvaccinated persons and the general population might face an increased risk for pertussis. Therefore, a family history of convulsions or other central nervous system disorders is not a contraindication to pertussis vaccination. Acetaminophen or ibuprofen may be administered to these children at the time of DTaP vaccination and every 4 hours for 24 hours thereafter to reduce the possibility of postvaccination fever.
# Children Who Have Had Pertussis Disease
Although pertussis disease is likely to confer immunity against pertussis, the duration of such immunity is unknown. Children with well-documented pertussis disease (i.e., positive culture for B. pertussis or epidemiologic linkage to a culture-positive case) should be administered DT vaccine for the remaining doses of the vaccination series to ensure that they are protected against diphtheria and tetanus. Some experts recommend including the pertussis component for subsequent vaccination of infants who have had culture-proven pertussis because infants may have a suboptimal immune response following B. pertussis infection (45 ).
# Pertussis Vaccination for Persons Aged ≥7 Years
Pertussis vaccines are presently licensed for use only among children aged 6 weeks-6 years. In the United States, adolescents and adults whose immunity has waned are an important reservoir for B. pertussis and may infect unvaccinated young children. In the future, booster doses of adult formulations of acellular pertussis vaccines may be recommended to prevent the occurrence and spread of the disease among these older persons. However, acellular pertussis vaccines combined with diphtheria and tetanus toxoids will need to be reformulated for use in adults because all infant formulations contain more diphtheria toxoid than is recommended for persons aged ≥7 years. Recommendations regarding routine vaccination of adults will require additional research (e.g., studies of the incidence, severity, and cost of pertussis among adolescents and adults; studies of the effectiveness and safety of adult formulations of DTaP; and studies of the cost-effectiveness of a strategy of adult vaccination).
# ADVERSE REACTIONS
Mild systemic reactions such as fever, drowsiness, fretfulness, and anorexia may occur after both whole-cell DTP vaccination and DTaP vaccination. However, data concerning adverse reactions following the first four doses indicate that mild reactions are less common among children who receive DTaP. These reactions are self-limited and can be managed safely with symptomatic treatment.* *For a complete discussion, see the general ACIP statement on diphtheria, tetanus, and pertussis and the supplementary statements on DTaP (16,17,42 ).
• Persistent crying lasting ≥3 hours, occurring within 48 hours.
• Convulsions with or without fever, occurring within 3 days.
In circumstances in which the benefits of further pertussis vaccination outweigh the possible risks (e.g., during an outbreak of pertussis), DTaP should be administered for the subsequent doses.
# REPORTING OF ADVERSE EVENTS AFTER VACCINATION
As with any newly licensed vaccine, surveillance for rare adverse events potentially associated with administration of DTaP is important for assessing its safety in largescale use. The National Childhood Vaccine Injury Act of 1986 requires health-care providers to report serious adverse events that follow pertussis vaccination (47 ). The events that must be reported are detailed in the Reportable Events Table within this Act, and include anaphylaxis or anaphylactic shock, encephalopathy (or encephalitis), shock collapse or hypotonic hyporesponsive collapse, and any acute complication or sequela (including death) of these events. Adverse reactions should be reported to VAERS (48 ). VAERS reporting forms and information are available 24 hours a day by calling (800) 822-7967.
# VACCINE INJURY COMPENSATION
The National Vaccine Injury Compensation Program, established by the National Childhood Vaccine Injury Act of 1986, provides a mechanism through which compensation can be paid on behalf of a person thought to have been injured or to have died as a result of receiving a vaccine covered by the program (49,50 ).
A Vaccine Injury Compensation Table in the Act lists the vaccines covered by the program and the injuries, disabilities, and conditions (including death) for which compensation may be paid. Development or onset of anaphylaxis or anaphylactic shock ≤4 hours or encephalopathy with onset ≤72 hours after administration of pertussis vaccine (or sequelae of these conditions) are potentially compensable under this law. Persons may be compensated for an injury listed in the established table or The Morbidity and Mortality Weekly Report (MMWR) Series is prepared by the Centers for Disease Control and Prevention (CDC) and is available free of charge in electronic format and on a paid subscription basis for paper copy. To receive an electronic copy on Friday of each week, send an e-mail message to [email protected]. The body content should read SUBscribe mmwr-toc. Electronic copy also is available from CDC's World-Wide Web server at http://www.cdc.gov/ or from CDC's file transfer protocol server at ftp.cdc.gov. To subscribe for paper copy, contact Superintendent of Documents, U.S. Government Printing Office, Washington, DC 20402; telephone (202) 512-1800.
Data in the weekly MMWR are provisional, based on weekly reports to CDC by state health departments. The reporting week concludes at close of business on Friday; compiled data on a national basis are officially released to the public on the following Friday. Address inquiries about the MMWR Series, including material to be considered for publication, to: Editor, MMWR Series, Mailstop C-08, CDC, 1600 Clifton Rd., N.E., Atlanta, GA 30333; telephone (404) 332-4555.
All material in the MMWR Series is in the public domain and may be used and reprinted without permission; citation as to source, however, is appreciated.
# 6U.S. Government Printing Office: 1997-532-228/47066 Region IV
# Simultaneous Administration
In a clinical trial in the United States, Infanrix™ was administered simultaneously, at separate sites, with hepatitis B vaccine, Hib vaccine, and OPV to children aged 2, 4, and 6 months. One month after the third dose, 100% of infants (n=64) administered hepatitis B vaccine simultaneously with Infanrix™ demonstrated anti-HBs antibodies
# Dosage and Administration
The dose of all four vaccines-Tripedia ® , TriHIBit™ , ACEL-IMUNE ® , and Infanrix™ -is 0.5 mL, administered intramuscularly. Fractional doses (<0.5 mL) should not be administered. The preferred injection sites are the anterolateral aspect of the thigh and the deltoid muscle of the upper arm (39 ).
To administer TriHIBit™ (ActHIB ® reconstituted with Tripedia ® ) (Connaught Laboratories, Inc., ActHIB ® package insert):
• Cleanse the rubber stoppers of both vials with a suitable germicide.
• Thoroughly agitate the vial of Tripedia ® . Insert the needle of a syringe through the vial's rubber stopper and withdraw 0.6 mL of Tripedia ® .
Moderate-to-severe systemic events (e.g., temperature of ≥105 F [≥40.5 C]; febrile seizures; persistent, crying lasting ≥3 hours; and hypotonic hyporesponsive episodes) have been reported rarely after administration of DTaP, and occur less frequently among children administered DTaP than among children administered whole-cell DTP.
Data from the Vaccine Adverse Event Reporting System (VAERS)* were used to compare rates of fever, seizures, and hospitalizations among children who, having had ≥3 previous doses of whole-cell DTP, were administered either DTaP or whole-cell DTP vaccines for the fourth or fifth doses (46 ). During 1991-1993, approximately 5 million doses of DTaP (distributed by Connaught Laboratories, Inc., or Wyeth-Lederle Vaccines and Pediatrics) and 27 million doses of whole-cell DTP were distributed for use among children aged 15 months-6 years. Adverse events were reported significantly less commonly among the children who received DTaP. VAERS is a passive surveillance system and these data should be interpreted with caution because the events reported may be linked to vaccine administration only by temporal coincidence.
# CONTRAINDICATIONS
If either of the following events occurs after administration of DTaP or whole-cell DTP, subsequent vaccination with DTaP or whole-cell DTP is contraindicated:
• An immediate anaphylactic reaction. Further vaccination with any of the three components of DTaP or whole-cell DTP should be deferred because of uncertainty as to which component of the vaccine might be responsible. Because of the importance of tetanus vaccination, persons who experience anaphylactic reactions may be referred to an allergist for evaluation and (if specific allergy can be demonstrated) desensitized to tetanus toxoid.
• Encephalopathy not attributable to another identifiable cause (e.g., an acute, severe central nervous system disorder occurring within 7 days after vaccination and generally consisting of major alterations in consciousness, unresponsiveness, or generalized or focal seizures that persist more than a few hours, without recovery within 24 hours.) In such cases, DT vaccine should be administered for the remaining doses in the vaccination schedule to ensure protection against diphtheria and tetanus.
# PRECAUTIONS
If any of the following events occurs within the specified period after administration of either whole-cell DTP or DTaP, vaccine providers and parents should evaluate the risks and benefits of administering subsequent doses of a pertussis-containing vaccine:
• Temperature of ≥105 F (≥40.5 C) within 48 hours, not attributable to another identifiable cause.
• Collapse or shock-like state (hypotonic hyporesponsive episode) within 48 hours. *VAERS is a passive surveillance system for reporting of adverse events temporally associated with administration of vaccines. | None | None |
3e8a177b4c6ecbdd4829e4573c228981dc6b182a | cdc | None | # Introduction
Group B streptococcus (GBS) emerged as the leading infectious cause of neonatal morbidity and mortality in the United States in the 1970s (1)(2)(3)(4). Initial case series reported casefatality ratios as high as 50%. In the early 1980s, clinical trials demonstrated that administering antibiotics during labor to women at risk of transmitting GBS to their newborns could prevent invasive disease in the first week of life (i.e., earlyonset disease) (5). As a result of the collaborative efforts of clinicians, researchers, professional organizations, parent advocacy groups, and the public health community in the 1990s, recommendations for intrapartum prophylaxis to prevent perinatal GBS disease were issued in 1996 by the American College of Obstetricians and Gynecologists (ACOG) (6) and CDC (7), and in 1997 by the American Academy of Pediatrics (8).
Those guidelines recommended the use of one of two prevention methods, a risk-based approach or a culture-based screening approach. Providers using the risk-based method identify candidates for intrapartum chemoprophylaxis according to the presence of any of the following intrapartum risk factors associated with early-onset disease: delivering at 100.4 º F (>38.0 º C), or rupture of membranes for >18 hours. The screening-based method recommends screening of all pregnant women for vaginal and rectal GBS colonization between 35 and 37 weeks' gestation. Colonized women are then offered intrapartum antibiotics at the time of labor. Under both strategies, women with GBS bacteriuria during their current
# Summary
Group B streptococcus (GBS) remains a leading cause of serious neonatal infection despite great progress in perinatal GBS disease prevention in the 1990s. In 1996, CDC, in collaboration with other agencies, published guidelines for the prevention of perinatal group B streptococcal disease (CDC. Prevention of perinatal group B streptococcal disease: a public health perspective. MMWR 1996;45:1-24). Data collected after the issuance of the 1996 guidelines prompted reevaluation of prevention strategies at a meeting of clinical and public health representatives in November 2001. This report replaces CDC's 1996 guidelines. The recommendations are based on available evidence and expert opinion where sufficient evidence was lacking. Although many of the recommendations in the 2002 guidelines are the same as those in 1996, they include some key changes:
- Recommendation of universal prenatal screening for vaginal and rectal GBS colonization of all pregnant women at 35-37 weeks' gestation, based on recent documentation in a large retrospective cohort study of a strong protective effect of this culture-based screening strategy relative to the risk-based strategy - Updated prophylaxis regimens for women with penicillin allergy - Detailed instruction on prenatal specimen collection and expanded methods of GBS culture processing, including instructions on antimicrobial susceptibility testing - Recommendation against routine intrapartum antibiotic prophylaxis for GBS-colonized women undergoing planned cesarean deliveries who have not begun labor or had rupture of membranes - A suggested algorithm for management of patients with threatened preterm delivery - An updated algorithm for management of newborns exposed to intrapartum antibiotic prophylaxis Although universal screening for GBS colonization is anticipated to result in further reductions in the burden of GBS disease, the need to monitor for potential adverse consequences of intrapartum antibiotic use, such as emergence of bacterial antimicrobial resistance or increased incidence or severity of non-GBS neonatal pathogens, continues, and intrapartum antibiotics are still viewed as an interim strategy until GBS vaccines achieve licensure.
pregnancy, or who previously gave birth to an infant with earlyonset GBS disease are candidates for intrapartum antibiotic prophylaxis.
Before active prevention was initiated, an estimated 7,500 cases of neonatal GBS disease occurred annually (9). Despite striking declines in disease incidence coinciding with increased prevention activities in the 1990s, GBS disease remains a leading infectious cause of morbidity and mortality among newborns in the United States (10,11). Moreover, since the release of the 1996 guidelines, new data are available to evaluate the effectiveness of the screening approach relative to the risk-based approach and to resolve some of the clinical challenges of implementing prevention.
In light of these new data, in November 2001, CDC consulted with multiple partners to revise the 1996 guidelines for the prevention of perinatal group B streptococcal disease, using an evidence-based approach where possible and scientific opinion when sufficient data were lacking (Table 1). These updated guidelines replace CDC's 1996 guidelines. They are intended for the following groups: providers of prenatal, obstetric, and pediatric care; supporting microbiology laboratories, hospital administrators and managed care organizations; childbirth educators; public health authorities; and expectant parents and their advocates.
# Differences and similarities between current and previous guidelines
Following are major differences in the new guidelines: - Recommendation of universal prenatal culture-based screening for vaginal and rectal GBS colonization of all pregnant women at 35-37 weeks' gestation - Updated prophylaxis regimens for women with penicillin allergy Evidence from at least one well-executed randomized, controlled trial or one rigorously designed laboratory-based experimental study that has been replicated by an independent investigator II Evidence from at least one well-designed clinical trial without randomization; cohort or case-controlled analytic studies (preferably from more than one center); multiple time-series studies; dramatic results from uncontrolled studies; or some evidence from laboratory experiments III Evidence from opinions of respected authorities based on clinical or laboratory experience, descriptive studies, or reports of expert committees Source: Adapted from CDC, 1999 USPHS/IDSA guidelines for the prevention of opportunistic infections in persons infected with human immunodeficiency virus. MMWR 1999; 48(RR-10):1-66.
- Detailed instruction on prenatal specimen collection and expanded methods of GBS culture processing, including instructions on susceptibility testing - Recommendation against routine intrapartum antibiotic prophylaxis for GBS-colonized women undergoing planned cesarean deliveries who have not begun labor or had rupture of membranes - A suggested algorithm for management of patients with threatened preterm delivery - An updated algorithm for management of newborns exposed to intrapartum antibiotic prophylaxis Although important changes have been instituted, many recommendations remain the same:
- Penicillin remains the first-line agent for intrapartum antibiotic prophylaxis, with ampicillin an acceptable alternative. - Women whose culture results are unknown at the time of delivery should be managed according to the risk-based approach; the obstetric risk factors remain unchanged (i.e., delivery at 18 hours, or temperature >100.4 º F ). - Women with negative vaginal and rectal GBS screening cultures within 5 weeks of delivery do not require intrapartum antimicrobial prophylaxis for GBS even if obstetric risk factors develop (i.e., delivery at 18 hours, or temperature >100.4 º F ). - Women with GBS bacteriuria in any concentration during their current pregnancy or who previously gave birth to an infant with GBS disease should receive intrapartum antimicrobial prophylaxis. - In the absence of GBS urinary tract infection, antimicrobial agents should not be used before the intrapartum period to treat asymptomatic GBS colonization.
# Background Early Infancy and Pregnancy-Related Infections
GBS causes severe invasive disease in young infants. The majority of infections in newborns occur within the first week of life and are designated early-onset disease. Late-onset infections occur in infants aged >1 week, with most infections evident in the first 3 months of life. Young infants with invasive GBS disease usually present with sepsis or pneumonia, and less often contract meningitis, osteomyelitis, or septic arthritis. The proportion of infants with meningitis is higher among those with late-onset infections. When neonatal infections caused by GBS appeared in the 1970s, as many as 50% of patients died. During the 1990s, the case-fatality ratio of earlyand late-onset disease was 4% (10) because of advances in neonatal care.
Intrauterine infection of the fetus results from ascending spread of GBS from the vagina of a colonized woman who is typically asymptomatic. Fetal aspiration of infected amniotic fluid can lead to stillbirth, neonatal pneumonia, or sepsis. Infants can also become infected with GBS during passage through the birth canal, although the majority of infants who are exposed to the organism through this route become colonized on skin or mucous membranes but remain asymptomatic.
In pregnant women, GBS can cause clinical infections, but most women have no symptoms associated with genital tract colonization. Urinary tract infections caused by GBS complicate 2%-4% of pregnancies (12,13). During pregnancy or the postpartum period, women can contract amnionitis, endometritis, sepsis, or rarely, meningitis caused by GBS (14)(15)(16)(17)(18)(19). Fatalities among women with pregnancy-associated GBS disease are extremely rare.
# GBS Colonization
The gastrointestinal tract serves as the natural reservoir for GBS and is the likely source of vaginal colonization. Vaginal colonization is unusual in childhood but becomes more common in late adolescence (20). Approximately 10% to 30% of pregnant women are colonized with GBS in the vagina or rectum (21). GBS colonization can be transient, chronic, or intermittent. Maternal intrapartum GBS colonization is a major risk factor for early-onset disease in infants, and vertical transmission of GBS from mother to fetus primarily occurs after the onset of labor or membrane rupture. However, colonization early in pregnancy is not predictive of neonatal sepsis (22). Culture screening of both the vagina and rectum for GBS late in gestation during prenatal care can detect women who are likely to be colonized with GBS at the time of delivery and are thus at higher risk of perinatal transmission of the organism (23).
Classic epidemiologic studies conducted during the 1980s revealed that women with prenatal GBS colonization were >25 times more likely than women with negative prenatal cultures to deliver infants with early-onset GBS disease (24). Researchers used prenatal cultures as the basis for identifying candidates for intrapartum antimicrobial chemoprophylaxis; clinical trials identified reductions in vertical transmission of the organism, as measured by infant colonization (25,26) or by protection against early-onset disease (5,27). Heavy colonization, defined as culture of GBS from direct plating rather than only from selective broth, is associated with higher risk for early-onset disease. GBS identified in clean-catch urine specimens is considered a surrogate for heavy maternal colonization and also is associated with a higher risk for early-onset GBS disease (12,13); it has been included among indications for intrapartum antibiotic prophylaxis.
# GBS Culture-Based Screening Methods
Numerous studies have documented that the accuracy of prenatal screening cultures in identifying intrapartum colonization status can be enhanced by careful attention to the timing of cultures, the anatomic sites swabbed, and the precise microbiologic methods used for culture and detection of organisms (Box 1). Collection of cultures between 35 and 37 weeks' gestation is recommended to improve the sensitivity and specificity of detection of women who remain colonized at the time of delivery (23,28). Swabbing both the lower vagina and rectum (i.e., through the anal sphincter) increases the yield substantially compared with sampling the cervix or sampling the vagina without also swabbing the rectum (29). Studies have indicated that when women in the outpatient clinic setting collect their own screening specimens, with appropriate instruction, GBS yield is similar to when specimens are collected by a health-care provider (30). Although swabbing both sites is recommended and use of two swabs can be justified, both swabs should be placed in a single broth culture medium because the site of isolation is not important for clinical management and laboratory costs can thereby be minimized. Because vaginal and rectal swabs are likely to yield diverse bacteria, use of selective enrichment broth is recommended (Box 1) to maximize the isolation of GBS and avoid overgrowth of other organisms. When direct agar plating is used instead of selective enrichment broth, as many as 50% of women who are GBS carriers have false-negative culture results (31).
# Additional Risk Factors for Perinatal GBS Disease
In addition to colonization with GBS, other factors increase the risk for early-onset disease. These include gestational age 12 hours, or intrapartum temperature >99.5 º F (37.5 º C) had 6.5 times the risk of having an infant with earlyonset GBS disease compared with women with none of those factors. Of note, women who had one of these risk factors but who had negative prenatal screening cultures were at relatively low risk for early-onset GBS disease (attack rate 0.9 per 1,000 births) compared with women who were colonized prenatally but had none of the risk factors (attack rate 5.1 per 1,000 births) (24). In a risk-based strategy promoted during the 1990s as an alternative to prenatal culture-based screening approaches, prematurity (gestation 100.4 º F or 38 º C), or duration of membrane rupture >18 hours were used as clinical indications for intrapartum prophylaxis. Previous delivery of an infant with invasive GBS disease may increase the risk of early-onset disease in subsequent deliveries (38,39), and intrapartum treatment of such women in subsequent pregnancies has been promoted. By contrast, colonization with GBS in a previous pregnancy is not considered an indication for intrapartum prophylaxis in subsequent pregnancies; rather, women require evaluation for prenatal colonization in each pregnancy. Because colonization is transient, the predictive value of culture-based screening is too low to be clinically useful when performed more than 5 weeks before delivery (28); thus, many women with GBS colonization during one pregnancy will no longer be colonized during subsequent pregnancies.
# Impact and Implementation of the 1996 Guidelines
# Declines in Perinatal GBS Disease Incidence in the Era of Chemoprophylaxis
Before the widespread use of intrapartum antibiotics, the incidence of invasive neonatal GBS disease ranged from 2 to 3 cases per 1,000 live births (9,40). Active, population-based surveillance in selected states in 1990, when GBS prevention was still rarely implemented, projected an incidence of 1.8 cases per 1,000 live births in the United States (early-onset disease: 1.5/1,000; late-onset: 0.35/1,000) (9).
Coinciding with active prevention efforts in the 1990s, the incidence of early-onset disease declined by 70% to 0.5 cases per 1,000 live births in 1999 (Figure 1). Projections from active surveillance data for 1999 from the Active Bacterial Core surveillance/Emerging Infections Program Network (ABCs)(41) estimate that intrapartum antibiotics prevented nearly 4,500 early-onset cases and 225 deaths that year (10,11). Other countries that have adopted perinatal GBS disease prevention guidelines similar to the United States have seen comparable declines in early-onset disease incidence (42)(43)(44). Recent estimates of early-onset disease incidence in the United States suggest a slight increase in incidence from 1999 to 2000, consistent with a plateau in the impact of prevention efforts (Figure 1).
The incidence of invasive GBS infections among pregnant women in the United States declined by 21% from 0.29 per 1,000 live births in 1993 to 0.23 in 1998 ( 10), suggesting that increased use of intrapartum antibiotics also prevented some cases of maternal GBS amnionitis and endometritis. In contrast, the rate of late-onset disease remained fairly constant throughout the 1990s (Figure 1). Although intrapartum chemoprophylaxis for women with heavy GBS colonization may prevent a portion of late-onset disease, the stable incidence of late-onset disease during a period when use of intrapartum antibiotics was increasing suggests that this intervention is not effective against late-onset disease. 1989 1990 1991 1992 1993 1994 1995 1996 1997 1998 1999
# Implementation of Chemoprophylaxis Strategies After the Release of the 1996 Guidelines
Declines in perinatal GBS disease incidence in the 1990s suggest that prevention strategies have been implemented successfully. Several studies have explored directly the challenges of implementation and extent of compliance with recommendations. Surveys of prenatal care providers in Connecticut and Minnesota in 1998 found that over 80% had a GBS prevention policy (Connecticut, 95%; Minnesota, 85%) (45). In Minnesota, family physicians were less likely to have a policy than were obstetrician/gynecologists and certified nurse midwives (45). A national survey of ACOG members in 2000 found that 98% of respondents had a GBS prevention policy; 75% of respondents reported using a version of the culture-based screening approach (46). Providers in all three surveys scored well on questions about their knowledge of the screening and risk-based strategies (45,46).
In hospitals that established or revised policies for GBS prevention shortly after the release of the 1996 guidelines, rates of early-onset GBS disease declined by 1997 (47). By 1999, although only 63% of hospitals in a multistate survey of hospitals in the ABCs areas had a formal GBS prevention policy (48), having a hospital policy was no longer associated with changes in incidence of GBS disease, likely because a high proportion of individual practitioners had adopted policies by this time. Several studies of single institutions or health maintenance organizations have evaluated adherence of hospital personnel to GBS guidelines (Table 2). Among hospitals with a riskbased policy, intrapartum antibiotics were administered in 40%-80% of preterm deliveries or deliveries with prolonged rupture of membranes (Table 2) (49)(50)(51)(52)(53). Among hospitals with a culture-based screening policy, close to 90% of delivering women had documented GBS screening, and close to 90% of GBS-positive women received intrapartum antibiotics (Table 2) (42,51,(54)(55)(56)(57)(58)(59).
Correct laboratory processing of culture specimens (Box 1) plays a critical role in successful implementation of the screening policy. A survey of clinical laboratories in selected counties of three states in 1997-1998 found that only a proportion of laboratories were using the recommended selective broth media to process GBS cultures (Georgia, 39% of laboratories; Minnesota, 42%; Connecticut, 62%), suggesting that this may be an area in need of improvement (31).
Although surveys of practitioners and laboratories and reports from single hospitals help monitor implementation of GBS prevention guidelines, a recent CDC-sponsored review of labor and delivery records in selected counties of eight states in the ABCs areas in 1998 and 1999 sheds light on actual provider practices 2 to 3 years after the release of the 1996 guidelines (60). In this population, GBS screening was documented in 52% of deliveries, although this varied widely, from 24% in selected counties of Oregon to 70% in Maryland. Among screened women, 24% were GBS positive, consistent with carriage rates reported in earlier studies; 89% of GBSpositive women received intrapartum antibiotics. The median time of GBS culture collection was at 35.6 weeks' gestation, consistent with the recommendation of 35-37 weeks' gestation. Among unscreened women, 24% had at least one intrapartum risk factor; however, only 61% of women with at least one risk factor received intrapartum antibiotics. Preterm delivery (<37 weeks' gestation) was the most common indication for which intrapartum antibiotics were not administered. Thus, this multistate record review confirmed trends in adherence identified in reports from single hospitals (Table 2).
# Maximizing Prevention by Chemoprophylaxis Effectiveness of the Risk-Based Approach Versus the Screening Approach
Despite dramatic declines in GBS incidence in the United States in the 1990s, GBS remains a leading cause of newborn morbidity and mortality, resulting in an estimated 1,600 earlyonset cases and 80 deaths annually. Although alternatives to intrapartum antibiotics such as a vaccine may become available in the future, intrapartum chemoprophylaxis remains the most effective available intervention against perinatal GBS disease. However, debate about the most effective strategy for identifying candidates for intrapartum chemoprophylaxis continues.
When the 1996 guidelines were issued, data regarding the relative effectiveness of the risk-based and screening approaches were not available. Theoretical predictions based on population estimates of the proportion of early-onset GBS cases without obstetric risk factors (approximately 45% in the preprevention era ) suggested that the screening-based approach would lead to greater declines in disease incidence than the risk-based approach (61,62). However, because implementation of the risk-based approach has been viewed as simpler than the screening-based approach, which requires correct specimen collection at the prenatal clinic, appropriate laboratory processing, and timely reporting of results to delivery staff, the actual effectiveness of these strategies is unknown. Consequently, since 1996, both approaches have been recommended as equally acceptable pending further data (6)(7)(8).
Although observational data are now available suggesting that each strategy can lead to reduced incidence of early-onset GBS disease (49,50,(63)(64)(65), the strategies have not been directly compared by clinical trial because of the large sample size required. A series of single hospital analyses finding benefits of screening over the risk-based approach (51,56,59,66) were limited by sequential use of the strategies and inability to control for potential confounders. A recent CDC-sponsored multistate study provided the first large-scale direct comparison of the strategies (60). By incorporating population-based surveillance for early-onset GBS disease into a sample survey of a population of over 600,000 live births, this analysis found that the screening approach was >50% more effective than the risk-based approach at preventing perinatal GBS disease.
The protective effect of the screening approach was robust and persisted after controlling for risk factors associated with early-onset GBS disease (e.g., preterm delivery, prolonged membrane rupture, young maternal age, black race). The benefit of screening stemmed from two main factors. First, by identifying GBS-colonized women who did not present with obstetric risk factors, screening reached more of the population at risk than did the risk-based approach. Among the cohort of screened women, 18% of all deliveries were to mothers who were colonized with GBS but did not have obstetric risk factors. The efficacy of intrapartum antibiotics in preventing early-onset GBS disease among infants in this cohort was close to 90%, suggesting that chemoprophylaxis of GBS-positive women without obstetric risk factors resulted in significant prevention of early-onset disease.
Women who were GBS positive in the screening cohort were also more likely to receive intrapartum antibiotics than were women with obstetric risk factors in the risk cohort. Although improvements in implementation of the risk-based approach would lead to further decline in disease, this would not be as great as with universal screening (60).
Finally, because the effectiveness of screening in this study was based on actual implementation of this strategy in clinical practice in 1998 and 1999, further improvements in screening implementation (e.g., improvements in specimen collection and the methods used for processing cultures) are expected to result in further benefits.
# Rationale for a Universal Prenatal Screening Strategy to Detect GBS Status
The new availability of category II evidence (Table 1) for a large protective effect of prenatal GBS screening compared with the risk-based approach provides the foundation for a recommendation of universal prenatal GBS screening (Figure 2). Statewide prevention activities in some ABCs areas further demonstrate that culture-based screening can be successfully implemented in a variety of settings and institutions. For example, a health department-led survey of clinical laboratories in Connecticut followed by rapid feedback of survey results found that the proportion of laboratories in Connecticut using the correct media for processing GBS screening cultures increased from 62% in 1997 to 92% in 1998 (67) and 100% in 2000. Moreover, coinciding with an active prevention campaign launched by the state health department that advocated the screening-based approach, the incidence of early-onset GBS disease in Connecticut declined from 0.6 cases per 1,000 live births in 1996 (68) to 0.2 cases per 1,000 live births in 1999.
From the standpoint of implementation, universal screening has two additional benefits over the dual recommendations of 1996. Communication of the public health messages associated with a single strategy is simpler than communicating and educating about multiple strategies. Additionally, screening has clear indicators that facilitate evaluation of implementation (e.g., documentation of GBS test, timing of test, rates of GBS positivity) (58) compared with the risk-based approach, in which evidence of prevention implementation cannot be assessed for approximately 75% of deliveries because they have no intrapartum risk factors.
Cost-effectiveness analyses of the screening-and risk-based strategies (62,(69)(70)(71)(72)(73) have indicated that although the initial costs associated with specimen collection and processing make the screening strategy more expensive than the risk-based approach, the overall cost savings due to disease prevention do not differ importantly between strategies. Additionally, multistate review of labor and delivery records in 1998 and 1999 suggests that perfect implementation of the screeningor risk-based strategies will result in a comparable proportion of deliveries in which women receive intrapartum antibiotic prophylaxis for GBS (24% for both strategies) (60,74). Thus, the strategies cannot be distinguished in terms of the proportion of deliveries that will be exposed to intrapartum antibiotics.
# Adverse Effects and Unintended Consequences of Chemoprophylaxis
Potential adverse or unintended effects of GBS prevention efforts that have raised concern include allergic or anaphylactic reactions to agents used for intrapartum antibiotic prophylaxis, emergence of GBS strains resistant to standard therapies, and increasing incidence of serious neonatal infections caused by pathogens other than GBS, including antimicrobial-resistant strains. Because of the increasing emergence of bacterial resistance to antimicrobial agents in both nosocomial and community settings, assessment of the impact and continued effectiveness of interventions based on antimicrobial prophylaxis is critical.
# FIGURE 2. Indications for intrapartum antibiotic prophylaxis to prevent perinatal GBS disease under a universal prenatal screening strategy based on combined vaginal and rectal cultures collected at 35-37 weeks' gestation from all pregnant women
- If onset of labor or rupture of amniotic membranes occurs at <37 weeks' gestation and there is a significant risk for preterm delivery (as assessed by the clinician), a suggested algorithm for GBS prophylaxis management is provided (Figure 3). † If amnionitis is suspected, broad-spectrum antibiotic therapy that includes an agent known to be active against GBS should replace GBS prophylaxis.
Vaginal and rectal GBS screening cultures at 35-37 weeks' gestation for pregnant women (unless patient had GBS bacteriuria during the current pregnancy or a previous infant with invasive GBS disease)
# ALL
# Intrapartum prophylaxis indicated
- Previous infant with invasive GBS disease - GBS bacteriuria during current pregnancy - Positive GBS screening culture during current pregnancy (unless a planned cesarean delivery, in the absence of labor or amniotic membrane rupture, is performed)
- Unknown GBS status (culture not done, incomplete, or results unknown) and any of the following:
- Delivery at - Intrapartum temperature 100.4°F ( 38.0°C) > > †
# Intrapartum prophylaxis not indicated
- Previous pregnancy with a positive GBS screening culture (unless a culture was also positive during the current pregnancy)
- Planned cesarean delivery performed in the absence of labor or membrane rupture (regardless of maternal GBS culture status)
- Negative vaginal and rectal GBS screening culture in late gestation during the current pregnancy, regardless of intrapartum risk factors
# Antibiotic Allergies Including Anaphylaxis
Anaphylaxis associated with GBS chemoprophylaxis occurs but is sufficiently rare that any morbidity associated with anaphylaxis is greatly offset by reductions in the incidence of maternal and neonatal invasive GBS disease. Anaphylaxisrelated mortality is likely to be a rare event since women receiving intrapartum antibiotics will be in hospital settings where rapid intervention is readily available. Estimates of the rate of anaphylaxis caused by penicillin range from 4/10,000 to 4/100,000 recipients. Additionally, as many as 10% of the adult population have less severe allergic reactions to penicillin (75). Anaphylaxis associated with GBS prophylaxis was reported in the early 1990s (76); since the release of the 1996 guidelines, an additional report of a nonfatal case of anaphylaxis associated with GBS chemoprophylaxis has been published (77). In a CDC multistate sample of over 5,000 live births, a single, nonfatal anaphylactic reaction was noted among the 27% of deliveries in which intrapartum antibiotics were administered (60). In that case, a single dose of penicillin was administered approximately 4 hours before a preterm cesarean delivery, and an anaphylactic reaction occurred shortly after the mother received a single dose of a cephalosporin following umbilical cord clamping.
# Resistance in GBS
GBS isolates with confirmed resistance to penicillin or ampicillin have not been observed to date (78)(79)(80)(81)(82)(83). Penicillin remains the agent of choice for intrapartum antibiotic prophylaxis. Ampicillin is an acceptable alternative, but penicillin is preferred because it has a narrower spectrum of antimicrobial activity and may be less likely to select for resistant organisms. The efficacy of both penicillin (27) and ampicillin (5) as intrapartum agents for the prevention of early-onset neonatal GBS disease has been demonstrated in clinical trials. Although the intramuscular route of administration for penicillin has been evaluated (25), intravenous administration is the only route of administration recommended for intrapartum chemoprophylaxis to prevent perinatal GBS disease, regardless of the antimicrobial agent used, because of the higher intraamniotic concentrations achieved with this method.
In contrast, the proportions of GBS isolates with in vitro resistance to clindamycin and erythromycin have increased since 1996. The prevalence of resistance among invasive GBS isolates in the United States and Canada ranged from 7% to 25% for erythromycin and from 3% to 15% for clindamycin in reports published between 1998 and 2001 (79)(80)(81)84). Resistance to erythromycin is frequently but not always associated with clindamycin resistance. Resistance of GBS isolates to cefoxitin, a second-generation cephalosporin sometimes used as a component of broad-spectrum coverage for chorioamnionitis, has also been reported (85); cefoxitin resistance has similarly been observed among invasive GBS isolates collected from 1996 to 2000 as part of CDC's active surveillance. Whether in vitro resistance of GBS has direct clinical implications remains unclear (86). Despite emerging resistance to some drug classes, minimum inhibitory concentrations of cefazolin, a first-generation cephalosporin available in an intravenous formulation, were low (<0.5 µg/ml) among a sample of invasive U.S. isolates from 1996 to 2000 (87), suggesting that GBS isolates are currently susceptible to this agent. Although NCCLS guidelines do not specify susceptibility breakpoints for cefazolin, they recommend that all isolates susceptible to penicillin be considered susceptible to cefazolin (88).
In light of the increasing prevalence of resistance to clindamycin, erythromycin, or both, recommended strategies for providing intrapartum antibiotic prophylaxis to penicillinallergic women are updated (Box 2). Because the efficacy of recommended alternatives to penicillin or ampicillin has not been measured in controlled trials, and because some of the recommended alternatives have a broad spectrum of activity and may be more complicated and costly to administer, verification of a reported history of penicillin allergy is important. Patients with reported penicillin allergy should then be assessed to determine their risk for anaphylaxis. Persons at high risk for anaphylaxis are those who have had immediate hypersensitivity reactions to penicillin (e.g., anaphylaxis, angioedema, or urticaria) or who have a history of asthma or other conditions that would make anaphylaxis more dangerous (89,90). An estimated 10% of persons with penicillin allergy also have immediate hypersensitivity reactions to cephalosporins (90). Among penicillin-allergic women not at high risk for anaphylaxis, cefazolin, because of its narrow spectrum of activity and ability to achieve high intraamniotic concentrations, is the agent of choice for intrapartum chemoprophylaxis.
For penicillin-allergic women at high risk for anaphylaxis, testing of GBS isolates from prenatal screening for susceptibility to clindamycin and erythromycin is recommended if feasible (Box 1). One of these agents should be employed for intrapartum GBS prophylaxis if the screening isolate is susceptible to both agents.
Vancomycin should be reserved for penicillin-allergic women at high risk for beta-lactam anaphylaxis when clindamycin or erythromycin are not options because of in vitro resistance or unknown susceptibility of a prenatal isolate. Vancomycin use is generally restricted because of emerging vancomycin resistance among some gram-positive organisms (e.g., vancomycinresistant enterococcus and vancomycin-resistant Staphylococcus
MMWR August 16, aureus
). An estimated 13.8 million hospitalized patients received vancomycin therapy in 1998 (91). If penicillin allergy occurs in approximately 10% of adults, and 25% of parturients are colonized with GBS prenatally, approximately 100,000 of the 4 million annual deliveries would require prophylaxis with vancomycin in the absence of clindamycin and erythromycin susceptibility testing of GBS prenatal isolates. This represents a 7% increase in the number of patients exposed to vancomycin. The total grams of vancomycin used annually would increase by less than 1% if all penicillinallergic colonized women received vancomycin prophylaxis.
# Increased Incidence or Resistance in Non-GBS Pathogens
Decreases in the incidence of early-onset GBS sepsis have not usually been accompanied by increases in incidence of early-onset sepsis caused by other pathogens, including those that are antibiotic resistant. Most studies, including population-based multicenter studies, have found stable (59,92,93) or decreasing (43) rates of non-GBS early-onset sepsis during a period of increasing use of intrapartum antibiotic prophylaxis for GBS (Table 3). This is true both for overall non-GBS sepsis and for neonatal sepsis caused by Escherichia coli, the second leading bacterial cause of neonatal sepsis after GBS (93,94). Some single hospital studies have found increased rates or case counts of neonatal sepsis caused by E. coli, gramnegative organisms in general, or ampicillin-resistant pathogens (64,94,95), but these increases appear to be limited to preterm or low-birth-weight infants. An increasing proportion of E. coli neonatal sepsis cases caused by ampicillinresistant organisms was observed in two studies (92,94), but again was limited to preterm or low-birth-weight infants. Furthermore, the proportion of community-acquired E. coli infections that are ampicillin resistant has been increasing (96), suggesting that trends in antimicrobial resistance should not be attributed to GBS prophylaxis.
An association between intrapartum antibiotic exposure and ampicillin resistance in cases of E. coli or other non-GBS earlyonset sepsis has been observed in several studies (36,94,95,97,98). These reports established that infections caused by antibiotic-resistant organisms were more frequently preceded by antibiotic use than were infections caused by susceptible organisms, and that more doses or longer duration of antibiotics before delivery increased the chance that a neonatal infection, if it occurred, would be caused by an antibioticresistant organism. These studies, however, were not designed to assess whether intrapartum antibiotic use increased the rate of antibiotic-resistant infections. Moreover, findings from these studies are consistent with intrapartum antibiotics inducing
# BOX 2. Recommended regimens for intrapartum antimicrobial prophylaxis for perinatal GBS disease prevention*
# Recommended
Penicillin G, 5 million units IV initial dose, then 2.5 million units IV every 4 hours until delivery Alternative Ampicillin, 2 g IV initial dose, then 1 g IV every 4 hours until delivery If penicillin allergic † Patients not at high Cefazolin, 2 g IV initial dose, risk for anaphylaxis then 1 g IV every 8 hours until delivery resistance among initially susceptible organisms, but also with intrapartum antibiotics preventing antibiotic-susceptible infections and having no impact on antibiotic-resistant infections, resulting in a net decrease in the total rate of infection. The reported increases in antibiotic-resistant early-onset infections in a few studies are not of sufficient magnitude to outweigh the benefits of intrapartum antibiotic prophylaxis to prevent perinatal GBS disease. However, to assure early detection of increases in the rate of disease or deaths caused by organisms other than GBS, continued surveillance of neonatal sepsis caused by organisms other than GBS is needed.
# Clinical Challenges
# GBS Bacteriuria During Pregnancy
The presence of GBS bacteriuria in any concentration in a pregnant woman is a marker for heavy genital tract colonization. Therefore, women with any quantity of GBS bacteriuria during pregnancy should receive intrapartum chemoprophylaxis. Vaginal and rectal screening at 35-37 weeks is not necessary for these women. GBS can cause both symptomatic and asymptomatic urinary tract infections, which should be diagnosed and treated according to current standards of care for urinary tract infections in pregnancy. Women with GBS urinary tract infections during pregnancy should receive appropriate treatment at the time of diagnosis as well as intrapartum GBS prophylaxis. Laboratory personnel should report any presence of GBS bacteriuria in specimens obtained from pregnant women. For this to occur, labeling of urine specimens to indicate that they were obtained from a pregnant woman is imperative.
# Planned Cesarean Delivery
Because GBS can cross intact amniotic membranes, a cesarean delivery does not prevent mother-to-child transmission of GBS. Moreover, because cesarean delivery itself is associated with health risks for mother and newborn, GBS colonization of the mother is not an indication for cesarean delivery, and cesarean delivery should not be used as an alternative to intrapartum antibiotic prophylaxis for GBS prevention. However, although a risk does exist for transmission of GBS from a colonized mother to her infant during a planned cesarean delivery performed before onset of labor in a woman with intact amniotic membranes, it is extremely low, based on a retrospective study at a single hospital (99) and a review of CDC active, population-based surveillance data from the 1990s. Thus, in this specific circumstance, in which the risk for disease is extremely low, the individual risks to a mother and her infant from receiving intrapartum antibiotic prophylaxis may balance or outweigh the benefits. Intrapartum antibiotic prophylaxis to prevent perinatal GBS disease is, therefore, not recommended as a routine practice for women undergoing planned cesarean deliveries in the absence of labor or amniotic membrane rupture, regardless of the GBS colonization status of the mother. Patients expected to undergo planned cesarean deliveries should nonetheless still undergo routine vaginal and rectal screening for GBS at 35-37 weeks because onset of labor or rupture of membranes may occur before the planned cesarean delivery. In rare situations in which patients or providers opt for intrapartum prophylaxis before planned cesarean deliveries, administration of antibiotics at the time of incision rather than at least 4 hours before delivery may be reasonable (100).
# Threatened Preterm Delivery
Because preterm (at <37 weeks' gestation) delivery is an important risk factor for early-onset GBS disease, and because timing of delivery can be difficult to assess, management of intrapartum prophylaxis for women with threatened preterm delivery can be challenging. Assessing the need for intrapartum prophylaxis for these women can also be difficult because GBS screening is recommended at 35 to 37 weeks' gestation, and culture results are not always available when labor or rupture of membranes occur preterm.
A suggested approach to GBS chemoprophylaxis in the context of threatened preterm delivery is outlined (Figure 3). Because insufficient data are available to suggest a single course of management, other management strategies developed by individual physicians or institutions may be appropriate alternatives. The algorithm suggests that if GBS screening culture results from the current pregnancy are not available and if onset of labor or rupture of membranes occurs before 37 weeks' gestation with a substantial risk for preterm delivery (as assessed by the woman's health-care provider), intrapartum antibiotic prophylaxis for GBS should be provided pending culture results. For women not yet screened for GBS, a vaginal and rectal specimen for GBS culture should be obtained if time permits. If a negative culture result within the previous 4 weeks is on record, or if the clinician determines that labor can be successfully arrested and preterm delivery averted, antibiotics for GBS prophylaxis should not be initiated. Because recent clinical trials suggest that antibiotics administered during pregnancy may be associated with adverse neonatal outcomes, such as necrotizing enterocolitis or increased need for supplementary oxygen, without evident benefit for preterm labor or preterm premature rupture of membranes (101,102), antibiotics should be reserved for instances in which a significant risk for preterm delivery is present.
No data are available on which to recommend a specific duration of antibiotic administration for GBS-positive women with threatened preterm delivery when delivery is successfully postponed. Management strategies based on scientific opinion have been proposed (100); without further data, the management approach is left to the discretion of the individual provider. Regardless of management strategy chosen, these women should also receive intrapartum antibiotic chemoprophylaxis for GBS when labor likely to proceed to delivery occurs or recurs.
Previous data (28) suggest that the accuracy of GBS screening cultures in predicting colonization status at delivery is greatest if the cultures are collected within 5 weeks of delivery. Therefore, if a woman is screened early for GBS because of threatened preterm delivery but does not deliver within 4 weeks, she should be screened again for GBS colonization and managed according to the result of the repeated screening culture (Figure 3).
# Obstetric Procedures for GBS-Colonized Women
Questions have arisen regarding whether certain obstetric procedures, such as digital vaginal examinations, intrauterine fetal monitoring, and membrane stripping or sweeping to hasten the onset of labor, should be performed on GBScolonized women. Asymptomatic GBS colonization is not an indication to perform any of these procedures. When such procedures are indicated for other reasons, evidence is currently not sufficient to recommend that particular procedures should be avoided because of increased risk of peripartum or perinatal infection. Although some obstetric procedures (frequent vaginal examinations after onset of labor or membrane rupture , intrauterine fetal monitoring , and mechanical cervical ripening devices ) have been significantly associated with peripartum or perinatal infectious outcomes, most studies to date have been limited by an inability to randomly allocate women to treatment groups and have yielded conflicting results. Moreover, because many studies were performed before GBS prevention was widely implemented, GBS colonization status was often not known and intrapartum chemoprophylaxis was less common. A meta-analysis of available studies examining the use of membrane stripping among women of undetermined GBS colonization status (109) found no significant increases in overall peripartum or perinatal infection rates among women who underwent this procedure and their infants compared with those who did not.
# Management of Newborns Exposed to Intrapartum Prophylaxis
On the basis of information available since the publication of the 1996 guidelines, a modified approach for empiric management of newborns born to women who receive intrapartum antibiotics to prevent early-onset GBS disease or to treat suspected chorioamnionitis is provided (Figure 4). Variations in the algorithm that incorporate individual circumstances or institutional preferences may be appropriate. The modified approach contains the following changes:
- If a woman receives intrapartum antibiotics for treatment of suspected chorioamnionitis, her newborn should have a full diagnostic evaluation and empiric therapy pending - If no maternal intrapartum prophylaxis for GBS was administered despite an indication being present, data are insufficient on which to recommend a single management strategy. † Includes complete blood cell count and differential, blood culture, and chest radiograph if respiratory abnormalities are present. When signs of sepsis are present, a lumbar puncture, if feasible, should be performed. § Duration of therapy varies depending on results of blood culture, cerebrospinal fluid findings, if obtained, and the clinical course of the infant.
If laboratory results and clinical course do not indicate bacterial infection, duration may be as short as 48 hours. ¶ CBC with differential and blood culture. Applies only to penicillin, ampicillin, or cefazolin and assumes recommended dosing regimens (Box 2) † † A healthy-appearing infant who was >38 weeks' gestation at delivery and whose mother received >4 hours of intrapartum prophylaxis before delivery may be discharged home after 24 hours if other discharge criteria have been met and a person able to comply fully with instructions for home observation will be present. If any one of these conditions is not met, the infant should be observed in the hospital for at least 48 hours and until criteria for discharge are achieved. culture results, regardless of clinical condition at birth, duration of maternal antibiotic therapy before delivery, or gestational age at delivery (110). Empiric therapy for the infant should include antimicrobial agents active against GBS as well as other organisms that might cause neonatal sepsis (e.g., ampicillin and gentamicin).
- When clinical signs in the infant suggest sepsis, a full diagnostic evaluation should include a lumbar puncture, if feasible. Blood cultures can be sterile in as many as 15% of newborns with meningitis (111)(112)(113), and the clinical management of an infant with abnormal cerebrospinal fluid (CSF) findings differs from that of an infant with normal CSF. If a lumbar puncture has been deferred for a neonate receiving empiric antibiotic therapy, and the therapy is continued beyond 48 hours because of clinical instability, CSF should be obtained for cell count, glucose, protein, and culture. - In addition to penicillin or ampicillin, initiation of intrapartum antibiotic prophylaxis with cefazolin at least 4 hours before delivery can be considered adequate, based on achievable amniotic fluid concentrations of cefazolin (114). Although other agents may be substituted for penicillin if the woman has a history of penicillin allergy (Box 2), the effectiveness of these agents in preventing early-onset GBS disease has not been studied and no data are available to suggest the durations before delivery of these regimens that can be considered adequate. - Based on the demonstrated effectiveness of intrapartum antibiotic prophylaxis at preventing early-onset GBS disease (65) and data indicating that clinical onset occurs within the first 24 hours of life in over 90% of infants who contract early-onset GBS disease (115), hospital discharge as early as 24 hours after delivery may be reasonable under certain circumstances. Specifically, a healthy-appearing infant who is >38 weeks' gestation at delivery and whose mother received >4 hours of intrapartum antibiotic prophylaxis before delivery may be discharged home as early as 24 hours after delivery, assuming that other discharge criteria have been met and that a person able to comply fully with instructions for home observation will be present. A key component of following instructions is the ability of the person observing to communicate with health-care providers by telephone and to transport the child promptly to an appropriate healthcare facility if clinical signs of sepsis develop. If these conditions are not met, the infant should remain in the hospital for at least 48 hours of observation and until criteria for discharge are achieved.
Investigations since 1996 lend additional support to several components of the algorithm. A retrospective study of over 250,000 live births (115) found that administration of intrapartum antibiotic prophylaxis did not change the clinical spectrum of neonatal illness or delay the onset of clinical signs among infants who contracted GBS disease despite prophylaxis. Thus, the algorithm targets infants born to mothers with suspected chorioamnionitis and infants with signs of sepsis for full diagnostic evaluation and empiric therapy. Also, new evidence indicates that 4 or more hours of intrapartum ampicillin or penicillin administered according to recommended dosing intervals (Box 2) significantly reduces vertical transmission of GBS (116) and risk of early-onset GBS disease (65). Thus, although the American Academy of Pediatrics 1997 guidelines suggested 2 or more doses as a threshold for prophylaxis adequacy for infants >35 weeks' gestation (8), the revised algorithm continues to use >4 hours, administered according to recommended dosing intervals, as the benchmark for optimal prevention of early-onset GBS disease. Moreover, a review of pregnancies at a West Coast health maintenance organization using the GBS culture-based screening strategy found that among women who received intrapartum antibiotic prophylaxis, 50% received prophylaxis at least 4 hours before delivery, whereas only 14% received at least 2 doses of intrapartum antibiotics (58); this indicates that duration of prophylaxis is a more practical target than number of doses, in addition to being associated with efficacy.
One objective of developing an algorithm for management of newborns was to minimize unnecessary evaluation and antimicrobial treatment of infants whose mothers received intrapartum prophylaxis. Although early provider surveys indicated that pediatricians and neonatologists were more likely to conduct diagnostic evaluations and initiate empiric antibiotics for an infant whose mother received intrapartum antibiotic prophylaxis (117)(118)(119), more recent data indicate that implementation of GBS prevention strategies has not resulted in increased use of health services for neonates (120), and in some circumstances, when GBS prophylaxis increased a decrease occurred in the proportion of neonates who received laboratory evaluations (58).
Intrapartum antibiotic prophylaxis is the method of choice for preventing neonatal early-onset GBS disease. In the event that intrapartum antibiotics are not given despite an indication (e.g., delivery occurred precipitously before antibiotics could be administered to a GBS-positive woman), sufficient data are not available on which to recommend a single management strategy for the newborn. Some centers provide intramuscular penicillin to asymptomatic infants within 1 hour of birth, based on results of observational studies showing declines in early-onset GBS disease coincident with a policy of universal administration of intramuscular penicillin to all newborns (121).
# Future Prevention Technology
# Rapid Tests to Detect GBS Colonization Status
Rapid tests for detection of GBS colonization at the time of onset of labor or rupture of amniotic membranes might obviate the need for prenatal culture-based screening if their sensitivity and specificity are comparable to culture in selective broth media and they yield results rapidly enough to permit administration of adequate intrapartum antibiotic prophylaxis to women detected as carriers. Currently available rapid tests detect GBS antigen from swab specimens. These tests are insufficiently sensitive to detect light colonization, and therefore are not adequate to replace culture-based prenatal screening (122,123) or to use in place of the risk-based approach when culture results are unknown at the time of labor. An adequate rapid intrapartum test must be as sensitive as culture (minimally 85% compared with culture of vaginal and rectal swabs inoculated into selective broth media), rapid so that results are available to clinicians in time for antibiotics to be given before delivery, and convenient for integration into routine laboratory use. Even a highly sensitive rapid detection test would not be adequate if results were not available to clinicians 24 hours a day, 7 days a week. Alternatives to culturing vaginal and rectal swab specimens at 35-37 weeks' gestation using recommended procedures should be validated to show sensitivity similar to recommended culture methods.
A rapid intrapartum test possessing the attributes described above offers the advantage of ascertaining GBS colonization status before delivery among women who have had no prenatal care. Although such tests might initially be introduced selectively in certain facilities with sufficient demand and capability, a general recommendation for their use would require the capacity for effective implementation in a wide range of hospital settings. Drawbacks of rapid tests include delays in administration of intrapartum antibiotic prophylaxis while test results are pending and lack of an isolate for susceptibility testing, which is of particular concern for penicillinallergic women. Additionally, until rapid tests are universally used, missed opportunities for GBS screening may occur among women who receive prenatal care at institutions relying on intrapartum rapid tests but who deliver at institutions where such tests are not yet available.
In a study of 112 pregnant women at an academic hospital in Quebec, a new, not yet commercially available fluorogenic polymerase chain reaction assay was 97% sensitive and 100% specific when compared with vaginal and rectal cultures collected at admission for delivery. Test results in this study were available within 45 minutes of specimen collection (124). Further studies are needed to determine whether this type of test can be adapted for use outside the research setting. If appropriate techniques for rapid detection of GBS become commercially available, they may be integrated into the currently recommended screening strategy.
# Vaccines To Prevent GBS Disease
Improved use of intrapartum antimicrobial prophylaxis has resulted in a substantial reduction in early-onset GBS disease, but it is unlikely to prevent most late-onset neonatal infections, GBS-related stillbirths, or prematurity, and does not address GBS disease in nonpregnant adults. Immunization of women during or before pregnancy could prevent peripartum maternal disease and protect infants from perinatally acquired infection by transplacental transfer of protective IgG antibodies (125,126). This would eliminate the need for prenatal GBS screening and intrapartum antimicrobial prophylaxis, along with associated costs and concerns regarding the potential adverse effects of intrapartum antibiotic use discussed previously.
Serotype-specific antibodies to GBS capsular polysaccharide, although rare in populations of unvaccinated women, have been shown to protect against disease (32,127). Phase 1 and 2 clinical trials among healthy, nonpregnant adults of monovalent protein-conjugate vaccines containing capsular polysaccharide antigens of GBS disease-associated serotypes have shown these vaccines to be well tolerated and immunogenic (128)(129)(130). One challenge of demonstrating vaccine efficacy in preventing early-onset GBS disease is that the sample size required for clinical trials may be prohibitively large. Identification of surrogate immunologic measures of clinical efficacy may thus be important (131,132). Surrogate information on clinical vaccine efficacy may also be gained by measuring the impact of multivalent conjugate vaccines on vaginal GBS colonization (132,133).
Anticipated difficulties in making vaccine available to pregnant women have resulted in consideration of other target populations for vaccine administration, including adolescent girls (134), women of childbearing age, and infants (135). The duration of protection that could be afforded by vaccination is unknown; one or more booster doses might be required, potentially complicating vaccine delivery. Shifts in the GBS serotypes causing disease have provided an additional
# Research Priorities and Tools To Aid Prevention
Technological advances that aid the implementation of a universal screening strategy will further prevention efforts. In addition to development of reliable rapid tests that can be performed in a wide range of labor and delivery settings, methods of simplifying prenatal culture procedures, e.g., the development of media with a reliable color indicator to signal presence of GBS, might improve accuracy of prenatal culture results and facilitate prenatal culture processing at clinical laboratories with limited technical capacity. Media that have been developed for this purpose, such as Granada (136,137) or GBS medium (138), should be further evaluated to determine if sensitivity and specificity are comparable to recommended methods, which consist of culture in selective broth media followed by GBS-specific identification.
Although universal prenatal GBS culture-based screening is likely to result in substantial further declines in the incidence of early-onset disease, intrapartum chemoprophylaxis is not a permanent or comprehensive strategy for GBS disease prevention. Because vaccines under development hold promise to prevent a larger portion of the burden of GBS disease with a simpler and sustainable intervention, further work on GBS vaccine development and support of phase 3 clinical trials are warranted (139).
Until a safe, effective, and economical vaccine achieves licensure, it will be important to continue to monitor for potential adverse effects of chemoprophylaxis, with an emphasis on tracking key sentinel events signaling a need for revision of the guidelines. Such sentinel events include the emergence of penicillin resistance among GBS, which to date has not been detected, and an increase in the incidence of disease or deaths due to neonatal pathogens other than GBS that offsets the burden of early-onset disease prevented by chemoprophylaxis. Monitoring for the latter will require longterm surveillance of a large population of term and preterm births (140).
Because GBS carriage is common among delivering women in the United States, continued surveillance for GBS disease and evaluation of prevention implementation remains important to minimize missed opportunities for prevention. States are encouraged to monitor incidence of GBS disease, to promote activities that enhance perinatal GBS disease prevention and education, and to assess progress toward national objectives for disease reduction, such as Healthy People 2010, which sets a target of reducing the incidence of early-onset GBS disease in all racial and ethnic groups to 0.5 cases per 1,000 live births (141). Practical tools to assist with monitoring for missed opportunities for perinatal GBS prevention within hospitals have been published (142); additional prevention information and tools for providers, patients and clinical microbiologists are available at / groupbstrep, , , , and / dpc/ades/invbact/strepb.htm.
# Recommendations
The following updated recommendations for the prevention of GBS disease are based on critical appraisal of multistate population-based observational data and several studies from individual institutions that have been completed since publication of previous CDC ( 7), ACOG (6), and AAP (8) recommendations. They replace previous recommendations from CDC. The strength (indicated by a letter) and quality (indicated by a roman numeral) of evidence supporting each recommendation are shown in parentheses, according to the evidence-based rating system outlined in Table 1.
Obstetric-care practitioners, in conjunction with supporting laboratories and labor and delivery facilities, should adopt the following strategy for the prevention of perinatal GBS disease based on prenatal screening for GBS colonization. The risk-based approach is no longer an acceptable alternative except for circumstances in which screening results are not available before delivery (AII).
- All pregnant women should be screened at 35-37 weeks' gestation for vaginal and rectal GBS colonization (Figure 2) (AII). At the time of labor or rupture of membranes, intrapartum chemoprophylaxis should be given to all pregnant women identified as GBS carriers (AII). Colonization during a previous pregnancy is not an indication for intrapartum prophylaxis in subsequent deliveries. Screening to detect GBS colonization in each pregnancy will determine the need for prophylaxis in that pregnancy. - Women with GBS isolated from the urine in any concentration (e.g., 10 3 ) during their current pregnancy should receive intrapartum chemoprophylaxis because such women usually are heavily colonized with GBS and are at increased risk of delivering an infant with early-onset GBS disease (BII). Labels on urine specimens from prenatal patients should clearly state the patient's pregnancy status to assist laboratory processing and reporting of results. Prenatal culture-based screening at 35-37 weeks' gestation is not necessary for women with GBS bacteriuria. Women with symptomatic or asymptomatic GBS urinary tract infection detected during pregnancy should be treated according to current standards of care for urinary tract infection during pregnancy. - Women who have previously given birth to an infant with invasive GBS disease should receive intrapartum chemoprophylaxis; prenatal culture-based screening is not necessary for these women (BII). - If the result of GBS culture is not known at the onset of labor, intrapartum chemoprophylaxis should be administered to women with any of the following risk factors: gestation 18 hours, or a temperature of >100.4 º F (>38.0 º C) (AII). Women with known negative results from vaginal and rectal GBS screening cultures within 5 weeks of delivery do not require prophylaxis to prevent GBS disease even if any of the intrapartum risk factors develop. - Women with threatened preterm (<37 weeks' gestation) delivery should be assessed for need for intrapartum prophylaxis to prevent perinatal GBS disease. An algorithm for management of women with threatened preterm delivery is provided (Figure 3). Other management approaches, developed by individual physicians or institutions, may be appropriate (CIII). - Culture techniques that maximize the likelihood of GBS recovery are required for prenatal screening (Box 1). Collection of specimens for culture may be conducted in the outpatient clinic setting by either the patient, with appropriate instruction, or health-care provider (BII). This involves swabbing the lower vagina and rectum (i.e., through the anal sphincter). Because lower vaginal as opposed to cervical cultures are recommended, cultures should not be collected by speculum examination. Specimens should be placed in a nonnutritive transport medium (e.g., Amies or Stuart's without charcoal). Specimen labels should clearly identify that specimens are for group B streptococcal culture. If susceptibility testing is ordered for penicillin-allergic women (Box 2), specimen labels should also identify the patient as penicillin allergic and should specify that if GBS is isolated, it should be tested for susceptibility to clindamycin and erythromycin. Specimens should be inoculated into a selective broth medium (examples of appropriate commercially available media include Trans-Vag Broth supplemented with 5% defibrinated sheep blood or LIM broth), incubated overnight, and subcultured onto solid blood agar medium (AII). Methods of testing prenatal isolates from penicillinallergic women for susceptibility to clindamycin and erythromycin are outlined (Box 1). Laboratories should report culture results (positive and negative) and susceptibility testing results to the anticipated site of delivery (when known) and to the health-care provider who ordered the test. - Health-care providers should inform women of their GBS screening test result and the recommended interventions.
In the absence of GBS urinary tract infection, antimicrobial agents should not be used before the intrapartum period to treat GBS colonization. Such treatment is not effective in eliminating carriage or preventing neonatal disease and may cause adverse consequences (DI). - GBS-colonized women who have a planned cesarean delivery performed before rupture of membranes and onset of labor are at low risk for having an infant with early-onset GBS disease. These women should not routinely receive intrapartum chemoprophylaxis for perinatal GBS disease prevention (CII). - For intrapartum chemoprophylaxis, the following regimen is recommended for women without penicillin allergy (Box 2): penicillin G, 5 million units intravenously initial dose, then 2.5 million units intravenously every 4 hours until delivery (AII). Because of its narrow spectrum of activity, penicillin is the preferred agent. An alternative regimen is ampicillin, 2 g intravenously initial dose, then 1 g intravenously every 4 hours until delivery (AI). - Intrapartum chemoprophylaxis for penicillin-allergic women takes into account increasing resistance to clindamycin and erythromycin among GBS isolates (Box 2). During prenatal care, history of penicillin allergy should be assessed to determine whether a patient is at high risk for anaphylaxis, i.e., has a history of immediate hypersensitivity reactions to penicillin (e.g., anaphylaxis, angioedema, or urticaria) or history of asthma or other conditions that would make anaphylaxis more dangerous (89). Women who are not at high risk for anaphylaxis should be given cefazolin, 2 g intravenously initial dose, then 1 g intravenously every 8 hours until delivery (BIII). For women at high risk for anaphylaxis, clindamycin and erythromycin susceptibility testing, if available, should be performed on isolates obtained during GBS prenatal carriage screening. Women with clindamycin-and erythromycin-susceptible isolates should be given either clindamycin, 900 mg intravenously every 8 hours until delivery; OR erythromycin, 500 mg intravenously every 6 hours until delivery. If susceptibility testing is not possible, susceptibility results are not known, or isolates are resistant to erythromycin or clindamycin, the following regimen can be used for women with immediate penicillin hypersensitivity: vancomycin, 1 g intravenously every 12 hours until delivery (CIII).
- Routine use of antimicrobial prophylaxis for newborns whose mothers received intrapartum chemoprophylaxis for GBS infection is not recommended. However, therapeutic use of these agents is appropriate for infants with clinically suspected sepsis. An updated algorithm for management of infants born to mothers who received intrapartum chemoprophylaxis for GBS infection is provided (Figure 4). This revised algorithm is not an exclusive approach to management; variation that incorporates individual circumstances or institutional preferences may be appropriate (CIII). - Local and state public health agencies, in conjunction with appropriate groups of hospitals, are encouraged to establish surveillance for early-onset GBS disease and to take other steps to promote perinatal GBS disease prevention and education to reduce the incidence of early-onset GBS disease in their states. Efforts to monitor the emergence of perinatal infections caused by other organisms are also encouraged. Before full implementation of this strategy can be expected in all health-care settings, all members of the health-care team will need to improve protocols for isolation and reporting of GBS culture results, to improve information management to ensure communication of screening results, and to educate medical and nursing staff responsible for prenatal and intrapartum care. Within institutions, such efforts may take several months.
Even with ideal implementation, cases of early-onset GBS disease will continue to occur. Tools to help promote prevention and educate parents of infants with early-onset GBS disease are available at . Additional tools available to assist with prevention implementation are available at , , and / dpc/ades/invbact/strepb.htm Multiple copies of educational materials published by CDC are available at the Public Health Foundation, 1220 L St., NW Suite 350, Washington, DC 20005, telephone 877-252-1200, or online at http:// www.phf.org. | # Introduction
Group B streptococcus (GBS) emerged as the leading infectious cause of neonatal morbidity and mortality in the United States in the 1970s (1)(2)(3)(4). Initial case series reported casefatality ratios as high as 50%. In the early 1980s, clinical trials demonstrated that administering antibiotics during labor to women at risk of transmitting GBS to their newborns could prevent invasive disease in the first week of life (i.e., earlyonset disease) (5). As a result of the collaborative efforts of clinicians, researchers, professional organizations, parent advocacy groups, and the public health community in the 1990s, recommendations for intrapartum prophylaxis to prevent perinatal GBS disease were issued in 1996 by the American College of Obstetricians and Gynecologists (ACOG) (6) and CDC (7), and in 1997 by the American Academy of Pediatrics (8).
Those guidelines recommended the use of one of two prevention methods, a risk-based approach or a culture-based screening approach. Providers using the risk-based method identify candidates for intrapartum chemoprophylaxis according to the presence of any of the following intrapartum risk factors associated with early-onset disease: delivering at <37 weeks' gestation, having an intrapartum temperature >100.4 º F (>38.0 º C), or rupture of membranes for >18 hours. The screening-based method recommends screening of all pregnant women for vaginal and rectal GBS colonization between 35 and 37 weeks' gestation. Colonized women are then offered intrapartum antibiotics at the time of labor. Under both strategies, women with GBS bacteriuria during their current
# Summary
Group B streptococcus (GBS) remains a leading cause of serious neonatal infection despite great progress in perinatal GBS disease prevention in the 1990s. In 1996, CDC, in collaboration with other agencies, published guidelines for the prevention of perinatal group B streptococcal disease (CDC. Prevention of perinatal group B streptococcal disease: a public health perspective. MMWR 1996;45[RR-7]:1-24). Data collected after the issuance of the 1996 guidelines prompted reevaluation of prevention strategies at a meeting of clinical and public health representatives in November 2001. This report replaces CDC's 1996 guidelines. The recommendations are based on available evidence and expert opinion where sufficient evidence was lacking. Although many of the recommendations in the 2002 guidelines are the same as those in 1996, they include some key changes:
• Recommendation of universal prenatal screening for vaginal and rectal GBS colonization of all pregnant women at 35-37 weeks' gestation, based on recent documentation in a large retrospective cohort study of a strong protective effect of this culture-based screening strategy relative to the risk-based strategy • Updated prophylaxis regimens for women with penicillin allergy • Detailed instruction on prenatal specimen collection and expanded methods of GBS culture processing, including instructions on antimicrobial susceptibility testing • Recommendation against routine intrapartum antibiotic prophylaxis for GBS-colonized women undergoing planned cesarean deliveries who have not begun labor or had rupture of membranes • A suggested algorithm for management of patients with threatened preterm delivery • An updated algorithm for management of newborns exposed to intrapartum antibiotic prophylaxis Although universal screening for GBS colonization is anticipated to result in further reductions in the burden of GBS disease, the need to monitor for potential adverse consequences of intrapartum antibiotic use, such as emergence of bacterial antimicrobial resistance or increased incidence or severity of non-GBS neonatal pathogens, continues, and intrapartum antibiotics are still viewed as an interim strategy until GBS vaccines achieve licensure.
pregnancy, or who previously gave birth to an infant with earlyonset GBS disease are candidates for intrapartum antibiotic prophylaxis.
Before active prevention was initiated, an estimated 7,500 cases of neonatal GBS disease occurred annually (9). Despite striking declines in disease incidence coinciding with increased prevention activities in the 1990s, GBS disease remains a leading infectious cause of morbidity and mortality among newborns in the United States (10,11). Moreover, since the release of the 1996 guidelines, new data are available to evaluate the effectiveness of the screening approach relative to the risk-based approach and to resolve some of the clinical challenges of implementing prevention.
In light of these new data, in November 2001, CDC consulted with multiple partners to revise the 1996 guidelines for the prevention of perinatal group B streptococcal disease, using an evidence-based approach where possible and scientific opinion when sufficient data were lacking (Table 1). These updated guidelines replace CDC's 1996 guidelines. They are intended for the following groups: providers of prenatal, obstetric, and pediatric care; supporting microbiology laboratories, hospital administrators and managed care organizations; childbirth educators; public health authorities; and expectant parents and their advocates.
# Differences and similarities between current and previous guidelines
Following are major differences in the new guidelines: • Recommendation of universal prenatal culture-based screening for vaginal and rectal GBS colonization of all pregnant women at 35-37 weeks' gestation • Updated prophylaxis regimens for women with penicillin allergy Evidence from at least one well-executed randomized, controlled trial or one rigorously designed laboratory-based experimental study that has been replicated by an independent investigator II Evidence from at least one well-designed clinical trial without randomization; cohort or case-controlled analytic studies (preferably from more than one center); multiple time-series studies; dramatic results from uncontrolled studies; or some evidence from laboratory experiments III Evidence from opinions of respected authorities based on clinical or laboratory experience, descriptive studies, or reports of expert committees Source: Adapted from CDC, 1999 USPHS/IDSA guidelines for the prevention of opportunistic infections in persons infected with human immunodeficiency virus. MMWR 1999; 48(RR-10):1-66.
• Detailed instruction on prenatal specimen collection and expanded methods of GBS culture processing, including instructions on susceptibility testing • Recommendation against routine intrapartum antibiotic prophylaxis for GBS-colonized women undergoing planned cesarean deliveries who have not begun labor or had rupture of membranes • A suggested algorithm for management of patients with threatened preterm delivery • An updated algorithm for management of newborns exposed to intrapartum antibiotic prophylaxis Although important changes have been instituted, many recommendations remain the same:
• Penicillin remains the first-line agent for intrapartum antibiotic prophylaxis, with ampicillin an acceptable alternative. • Women whose culture results are unknown at the time of delivery should be managed according to the risk-based approach; the obstetric risk factors remain unchanged (i.e., delivery at <37 weeks' gestation, duration of membrane rupture >18 hours, or temperature >100.4 º F [>38.0 º C]). • Women with negative vaginal and rectal GBS screening cultures within 5 weeks of delivery do not require intrapartum antimicrobial prophylaxis for GBS even if obstetric risk factors develop (i.e., delivery at <37 weeks' gestation, duration of membrane rupture >18 hours, or temperature >100.4 º F [>38.0 º C]). • Women with GBS bacteriuria in any concentration during their current pregnancy or who previously gave birth to an infant with GBS disease should receive intrapartum antimicrobial prophylaxis. • In the absence of GBS urinary tract infection, antimicrobial agents should not be used before the intrapartum period to treat asymptomatic GBS colonization.
# Background Early Infancy and Pregnancy-Related Infections
GBS causes severe invasive disease in young infants. The majority of infections in newborns occur within the first week of life and are designated early-onset disease. Late-onset infections occur in infants aged >1 week, with most infections evident in the first 3 months of life. Young infants with invasive GBS disease usually present with sepsis or pneumonia, and less often contract meningitis, osteomyelitis, or septic arthritis. The proportion of infants with meningitis is higher among those with late-onset infections. When neonatal infections caused by GBS appeared in the 1970s, as many as 50% of patients died. During the 1990s, the case-fatality ratio of earlyand late-onset disease was 4% (10) because of advances in neonatal care.
Intrauterine infection of the fetus results from ascending spread of GBS from the vagina of a colonized woman who is typically asymptomatic. Fetal aspiration of infected amniotic fluid can lead to stillbirth, neonatal pneumonia, or sepsis. Infants can also become infected with GBS during passage through the birth canal, although the majority of infants who are exposed to the organism through this route become colonized on skin or mucous membranes but remain asymptomatic.
In pregnant women, GBS can cause clinical infections, but most women have no symptoms associated with genital tract colonization. Urinary tract infections caused by GBS complicate 2%-4% of pregnancies (12,13). During pregnancy or the postpartum period, women can contract amnionitis, endometritis, sepsis, or rarely, meningitis caused by GBS (14)(15)(16)(17)(18)(19). Fatalities among women with pregnancy-associated GBS disease are extremely rare.
# GBS Colonization
The gastrointestinal tract serves as the natural reservoir for GBS and is the likely source of vaginal colonization. Vaginal colonization is unusual in childhood but becomes more common in late adolescence (20). Approximately 10% to 30% of pregnant women are colonized with GBS in the vagina or rectum (21). GBS colonization can be transient, chronic, or intermittent. Maternal intrapartum GBS colonization is a major risk factor for early-onset disease in infants, and vertical transmission of GBS from mother to fetus primarily occurs after the onset of labor or membrane rupture. However, colonization early in pregnancy is not predictive of neonatal sepsis (22). Culture screening of both the vagina and rectum for GBS late in gestation during prenatal care can detect women who are likely to be colonized with GBS at the time of delivery and are thus at higher risk of perinatal transmission of the organism (23).
Classic epidemiologic studies conducted during the 1980s revealed that women with prenatal GBS colonization were >25 times more likely than women with negative prenatal cultures to deliver infants with early-onset GBS disease (24). Researchers used prenatal cultures as the basis for identifying candidates for intrapartum antimicrobial chemoprophylaxis; clinical trials identified reductions in vertical transmission of the organism, as measured by infant colonization (25,26) or by protection against early-onset disease (5,27). Heavy colonization, defined as culture of GBS from direct plating rather than only from selective broth, is associated with higher risk for early-onset disease. GBS identified in clean-catch urine specimens is considered a surrogate for heavy maternal colonization and also is associated with a higher risk for early-onset GBS disease (12,13); it has been included among indications for intrapartum antibiotic prophylaxis.
# GBS Culture-Based Screening Methods
Numerous studies have documented that the accuracy of prenatal screening cultures in identifying intrapartum colonization status can be enhanced by careful attention to the timing of cultures, the anatomic sites swabbed, and the precise microbiologic methods used for culture and detection of organisms (Box 1). Collection of cultures between 35 and 37 weeks' gestation is recommended to improve the sensitivity and specificity of detection of women who remain colonized at the time of delivery (23,28). Swabbing both the lower vagina and rectum (i.e., through the anal sphincter) increases the yield substantially compared with sampling the cervix or sampling the vagina without also swabbing the rectum (29). Studies have indicated that when women in the outpatient clinic setting collect their own screening specimens, with appropriate instruction, GBS yield is similar to when specimens are collected by a health-care provider (30). Although swabbing both sites is recommended and use of two swabs can be justified, both swabs should be placed in a single broth culture medium because the site of isolation is not important for clinical management and laboratory costs can thereby be minimized. Because vaginal and rectal swabs are likely to yield diverse bacteria, use of selective enrichment broth is recommended (Box 1) to maximize the isolation of GBS and avoid overgrowth of other organisms. When direct agar plating is used instead of selective enrichment broth, as many as 50% of women who are GBS carriers have false-negative culture results (31).
# Additional Risk Factors for Perinatal GBS Disease
In addition to colonization with GBS, other factors increase the risk for early-onset disease. These include gestational age <37 completed weeks, longer duration of membrane rupture, intraamniotic infection, young maternal age, black race, Hispanic ethnicity, and low maternal levels of anticapsular antibody (32)(33)(34)(35)(36)(37). In a 1985 report of predictors of early-onset disease (24), women with gestation <37 weeks, membrane rupture of >12 hours, or intrapartum temperature >99.5 º F (37.5 º C) had 6.5 times the risk of having an infant with earlyonset GBS disease compared with women with none of those factors. Of note, women who had one of these risk factors but who had negative prenatal screening cultures were at relatively low risk for early-onset GBS disease (attack rate 0.9 per 1,000 births) compared with women who were colonized prenatally but had none of the risk factors (attack rate 5.1 per 1,000 births) (24). In a risk-based strategy promoted during the 1990s as an alternative to prenatal culture-based screening approaches, prematurity (gestation <37 weeks), intrapartum fever (temperature >100.4 º F or 38 º C), or duration of membrane rupture >18 hours were used as clinical indications for intrapartum prophylaxis. Previous delivery of an infant with invasive GBS disease may increase the risk of early-onset disease in subsequent deliveries (38,39), and intrapartum treatment of such women in subsequent pregnancies has been promoted. By contrast, colonization with GBS in a previous pregnancy is not considered an indication for intrapartum prophylaxis in subsequent pregnancies; rather, women require evaluation for prenatal colonization in each pregnancy. Because colonization is transient, the predictive value of culture-based screening is too low to be clinically useful when performed more than 5 weeks before delivery (28); thus, many women with GBS colonization during one pregnancy will no longer be colonized during subsequent pregnancies.
# Impact and Implementation of the 1996 Guidelines
# Declines in Perinatal GBS Disease Incidence in the Era of Chemoprophylaxis
Before the widespread use of intrapartum antibiotics, the incidence of invasive neonatal GBS disease ranged from 2 to 3 cases per 1,000 live births (9,40). Active, population-based surveillance in selected states in 1990, when GBS prevention was still rarely implemented, projected an incidence of 1.8 cases per 1,000 live births in the United States (early-onset disease: 1.5/1,000; late-onset: 0.35/1,000) (9).
Coinciding with active prevention efforts in the 1990s, the incidence of early-onset disease declined by 70% to 0.5 cases per 1,000 live births in 1999 (Figure 1). Projections from active surveillance data for 1999 from the Active Bacterial Core surveillance/Emerging Infections Program Network (ABCs)(41) estimate that intrapartum antibiotics prevented nearly 4,500 early-onset cases and 225 deaths that year (10,11). Other countries that have adopted perinatal GBS disease prevention guidelines similar to the United States have seen comparable declines in early-onset disease incidence (42)(43)(44). Recent estimates of early-onset disease incidence in the United States suggest a slight increase in incidence from 1999 to 2000, consistent with a plateau in the impact of prevention efforts (Figure 1).
The incidence of invasive GBS infections among pregnant women in the United States declined by 21% from 0.29 per 1,000 live births in 1993 to 0.23 in 1998 ( 10), suggesting that increased use of intrapartum antibiotics also prevented some cases of maternal GBS amnionitis and endometritis. In contrast, the rate of late-onset disease remained fairly constant throughout the 1990s (Figure 1). Although intrapartum chemoprophylaxis for women with heavy GBS colonization may prevent a portion of late-onset disease, the stable incidence of late-onset disease during a period when use of intrapartum antibiotics was increasing suggests that this intervention is not effective against late-onset disease. 1989 1990 1991 1992 1993 1994 1995 1996 1997 1998 1999
# Implementation of Chemoprophylaxis Strategies After the Release of the 1996 Guidelines
Declines in perinatal GBS disease incidence in the 1990s suggest that prevention strategies have been implemented successfully. Several studies have explored directly the challenges of implementation and extent of compliance with recommendations. Surveys of prenatal care providers in Connecticut and Minnesota in 1998 found that over 80% had a GBS prevention policy (Connecticut, 95%; Minnesota, 85%) (45). In Minnesota, family physicians were less likely to have a policy than were obstetrician/gynecologists and certified nurse midwives (45). A national survey of ACOG members in 2000 found that 98% of respondents had a GBS prevention policy; 75% of respondents reported using a version of the culture-based screening approach (46). Providers in all three surveys scored well on questions about their knowledge of the screening and risk-based strategies (45,46).
In hospitals that established or revised policies for GBS prevention shortly after the release of the 1996 guidelines, rates of early-onset GBS disease declined by 1997 (47). By 1999, although only 63% of hospitals in a multistate survey of hospitals in the ABCs areas had a formal GBS prevention policy (48), having a hospital policy was no longer associated with changes in incidence of GBS disease, likely because a high proportion of individual practitioners had adopted policies by this time. Several studies of single institutions or health maintenance organizations have evaluated adherence of hospital personnel to GBS guidelines (Table 2). Among hospitals with a riskbased policy, intrapartum antibiotics were administered in 40%-80% of preterm deliveries or deliveries with prolonged rupture of membranes (Table 2) (49)(50)(51)(52)(53). Among hospitals with a culture-based screening policy, close to 90% of delivering women had documented GBS screening, and close to 90% of GBS-positive women received intrapartum antibiotics (Table 2) (42,51,(54)(55)(56)(57)(58)(59).
Correct laboratory processing of culture specimens (Box 1) plays a critical role in successful implementation of the screening policy. A survey of clinical laboratories in selected counties of three states in 1997-1998 found that only a proportion of laboratories were using the recommended selective broth media to process GBS cultures (Georgia, 39% of laboratories; Minnesota, 42%; Connecticut, 62%), suggesting that this may be an area in need of improvement (31).
Although surveys of practitioners and laboratories and reports from single hospitals help monitor implementation of GBS prevention guidelines, a recent CDC-sponsored review of labor and delivery records in selected counties of eight states in the ABCs areas in 1998 and 1999 sheds light on actual provider practices 2 to 3 years after the release of the 1996 guidelines (60). In this population, GBS screening was documented in 52% of deliveries, although this varied widely, from 24% in selected counties of Oregon to 70% in Maryland. Among screened women, 24% were GBS positive, consistent with carriage rates reported in earlier studies; 89% of GBSpositive women received intrapartum antibiotics. The median time of GBS culture collection was at 35.6 weeks' gestation, consistent with the recommendation of 35-37 weeks' gestation. Among unscreened women, 24% had at least one intrapartum risk factor; however, only 61% of women with at least one risk factor received intrapartum antibiotics. Preterm delivery (<37 weeks' gestation) was the most common indication for which intrapartum antibiotics were not administered. Thus, this multistate record review confirmed trends in adherence identified in reports from single hospitals (Table 2).
# Maximizing Prevention by Chemoprophylaxis Effectiveness of the Risk-Based Approach Versus the Screening Approach
Despite dramatic declines in GBS incidence in the United States in the 1990s, GBS remains a leading cause of newborn morbidity and mortality, resulting in an estimated 1,600 earlyonset cases and 80 deaths annually. Although alternatives to intrapartum antibiotics such as a vaccine may become available in the future, intrapartum chemoprophylaxis remains the most effective available intervention against perinatal GBS disease. However, debate about the most effective strategy for identifying candidates for intrapartum chemoprophylaxis continues.
When the 1996 guidelines were issued, data regarding the relative effectiveness of the risk-based and screening approaches were not available. Theoretical predictions based on population estimates of the proportion of early-onset GBS cases without obstetric risk factors (approximately 45% in the preprevention era [61]) suggested that the screening-based approach would lead to greater declines in disease incidence than the risk-based approach (61,62). However, because implementation of the risk-based approach has been viewed as simpler than the screening-based approach, which requires correct specimen collection at the prenatal clinic, appropriate laboratory processing, and timely reporting of results to delivery staff, the actual effectiveness of these strategies is unknown. Consequently, since 1996, both approaches have been recommended as equally acceptable pending further data (6)(7)(8).
Although observational data are now available suggesting that each strategy can lead to reduced incidence of early-onset GBS disease (49,50,(63)(64)(65), the strategies have not been directly compared by clinical trial because of the large sample size required. A series of single hospital analyses finding benefits of screening over the risk-based approach (51,56,59,66) were limited by sequential use of the strategies and inability to control for potential confounders. A recent CDC-sponsored multistate study provided the first large-scale direct comparison of the strategies (60). By incorporating population-based surveillance for early-onset GBS disease into a sample survey of a population of over 600,000 live births, this analysis found that the screening approach was >50% more effective than the risk-based approach at preventing perinatal GBS disease.
The protective effect of the screening approach was robust and persisted after controlling for risk factors associated with early-onset GBS disease (e.g., preterm delivery, prolonged membrane rupture, young maternal age, black race). The benefit of screening stemmed from two main factors. First, by identifying GBS-colonized women who did not present with obstetric risk factors, screening reached more of the population at risk than did the risk-based approach. Among the cohort of screened women, 18% of all deliveries were to mothers who were colonized with GBS but did not have obstetric risk factors. The efficacy of intrapartum antibiotics in preventing early-onset GBS disease among infants in this cohort was close to 90%, suggesting that chemoprophylaxis of GBS-positive women without obstetric risk factors resulted in significant prevention of early-onset disease.
Women who were GBS positive in the screening cohort were also more likely to receive intrapartum antibiotics than were women with obstetric risk factors in the risk cohort. Although improvements in implementation of the risk-based approach would lead to further decline in disease, this would not be as great as with universal screening (60).
Finally, because the effectiveness of screening in this study was based on actual implementation of this strategy in clinical practice in 1998 and 1999, further improvements in screening implementation (e.g., improvements in specimen collection and the methods used for processing cultures) are expected to result in further benefits.
# Rationale for a Universal Prenatal Screening Strategy to Detect GBS Status
The new availability of category II evidence (Table 1) for a large protective effect of prenatal GBS screening compared with the risk-based approach provides the foundation for a recommendation of universal prenatal GBS screening (Figure 2). Statewide prevention activities in some ABCs areas further demonstrate that culture-based screening can be successfully implemented in a variety of settings and institutions. For example, a health department-led survey of clinical laboratories in Connecticut followed by rapid feedback of survey results found that the proportion of laboratories in Connecticut using the correct media for processing GBS screening cultures increased from 62% in 1997 to 92% in 1998 (67) and 100% in 2000. Moreover, coinciding with an active prevention campaign launched by the state health department that advocated the screening-based approach, the incidence of early-onset GBS disease in Connecticut declined from 0.6 cases per 1,000 live births in 1996 (68) to 0.2 cases per 1,000 live births in 1999.
From the standpoint of implementation, universal screening has two additional benefits over the dual recommendations of 1996. Communication of the public health messages associated with a single strategy is simpler than communicating and educating about multiple strategies. Additionally, screening has clear indicators that facilitate evaluation of implementation (e.g., documentation of GBS test, timing of test, rates of GBS positivity) (58) compared with the risk-based approach, in which evidence of prevention implementation cannot be assessed for approximately 75% of deliveries because they have no intrapartum risk factors.
Cost-effectiveness analyses of the screening-and risk-based strategies (62,(69)(70)(71)(72)(73) have indicated that although the initial costs associated with specimen collection and processing make the screening strategy more expensive than the risk-based approach, the overall cost savings due to disease prevention do not differ importantly between strategies. Additionally, multistate review of labor and delivery records in 1998 and 1999 suggests that perfect implementation of the screeningor risk-based strategies will result in a comparable proportion of deliveries in which women receive intrapartum antibiotic prophylaxis for GBS (24% for both strategies) (60,74). Thus, the strategies cannot be distinguished in terms of the proportion of deliveries that will be exposed to intrapartum antibiotics.
# Adverse Effects and Unintended Consequences of Chemoprophylaxis
Potential adverse or unintended effects of GBS prevention efforts that have raised concern include allergic or anaphylactic reactions to agents used for intrapartum antibiotic prophylaxis, emergence of GBS strains resistant to standard therapies, and increasing incidence of serious neonatal infections caused by pathogens other than GBS, including antimicrobial-resistant strains. Because of the increasing emergence of bacterial resistance to antimicrobial agents in both nosocomial and community settings, assessment of the impact and continued effectiveness of interventions based on antimicrobial prophylaxis is critical.
# FIGURE 2. Indications for intrapartum antibiotic prophylaxis to prevent perinatal GBS disease under a universal prenatal screening strategy based on combined vaginal and rectal cultures collected at 35-37 weeks' gestation from all pregnant women
* If onset of labor or rupture of amniotic membranes occurs at <37 weeks' gestation and there is a significant risk for preterm delivery (as assessed by the clinician), a suggested algorithm for GBS prophylaxis management is provided (Figure 3). † If amnionitis is suspected, broad-spectrum antibiotic therapy that includes an agent known to be active against GBS should replace GBS prophylaxis.
Vaginal and rectal GBS screening cultures at 35-37 weeks' gestation for pregnant women (unless patient had GBS bacteriuria during the current pregnancy or a previous infant with invasive GBS disease)
# ALL
# Intrapartum prophylaxis indicated
• Previous infant with invasive GBS disease • GBS bacteriuria during current pregnancy • Positive GBS screening culture during current pregnancy (unless a planned cesarean delivery, in the absence of labor or amniotic membrane rupture, is performed)
• Unknown GBS status (culture not done, incomplete, or results unknown) and any of the following:
• Delivery at <37 weeks' gestation* • Amniotic membrane rupture 18 hours > • Intrapartum temperature 100.4°F ( 38.0°C) > > †
# Intrapartum prophylaxis not indicated
• Previous pregnancy with a positive GBS screening culture (unless a culture was also positive during the current pregnancy)
• Planned cesarean delivery performed in the absence of labor or membrane rupture (regardless of maternal GBS culture status)
• Negative vaginal and rectal GBS screening culture in late gestation during the current pregnancy, regardless of intrapartum risk factors
# Antibiotic Allergies Including Anaphylaxis
Anaphylaxis associated with GBS chemoprophylaxis occurs but is sufficiently rare that any morbidity associated with anaphylaxis is greatly offset by reductions in the incidence of maternal and neonatal invasive GBS disease. Anaphylaxisrelated mortality is likely to be a rare event since women receiving intrapartum antibiotics will be in hospital settings where rapid intervention is readily available. Estimates of the rate of anaphylaxis caused by penicillin range from 4/10,000 to 4/100,000 recipients. Additionally, as many as 10% of the adult population have less severe allergic reactions to penicillin (75). Anaphylaxis associated with GBS prophylaxis was reported in the early 1990s (76); since the release of the 1996 guidelines, an additional report of a nonfatal case of anaphylaxis associated with GBS chemoprophylaxis has been published (77). In a CDC multistate sample of over 5,000 live births, a single, nonfatal anaphylactic reaction was noted among the 27% of deliveries in which intrapartum antibiotics were administered (60). In that case, a single dose of penicillin was administered approximately 4 hours before a preterm cesarean delivery, and an anaphylactic reaction occurred shortly after the mother received a single dose of a cephalosporin following umbilical cord clamping.
# Resistance in GBS
GBS isolates with confirmed resistance to penicillin or ampicillin have not been observed to date (78)(79)(80)(81)(82)(83). Penicillin remains the agent of choice for intrapartum antibiotic prophylaxis. Ampicillin is an acceptable alternative, but penicillin is preferred because it has a narrower spectrum of antimicrobial activity and may be less likely to select for resistant organisms. The efficacy of both penicillin (27) and ampicillin (5) as intrapartum agents for the prevention of early-onset neonatal GBS disease has been demonstrated in clinical trials. Although the intramuscular route of administration for penicillin has been evaluated (25), intravenous administration is the only route of administration recommended for intrapartum chemoprophylaxis to prevent perinatal GBS disease, regardless of the antimicrobial agent used, because of the higher intraamniotic concentrations achieved with this method.
In contrast, the proportions of GBS isolates with in vitro resistance to clindamycin and erythromycin have increased since 1996. The prevalence of resistance among invasive GBS isolates in the United States and Canada ranged from 7% to 25% for erythromycin and from 3% to 15% for clindamycin in reports published between 1998 and 2001 (79)(80)(81)84). Resistance to erythromycin is frequently but not always associated with clindamycin resistance. Resistance of GBS isolates to cefoxitin, a second-generation cephalosporin sometimes used as a component of broad-spectrum coverage for chorioamnionitis, has also been reported (85); cefoxitin resistance has similarly been observed among invasive GBS isolates collected from 1996 to 2000 as part of CDC's active surveillance. Whether in vitro resistance of GBS has direct clinical implications remains unclear (86). Despite emerging resistance to some drug classes, minimum inhibitory concentrations of cefazolin, a first-generation cephalosporin available in an intravenous formulation, were low (<0.5 µg/ml) among a sample of invasive U.S. isolates from 1996 to 2000 (87), suggesting that GBS isolates are currently susceptible to this agent. Although NCCLS guidelines do not specify susceptibility breakpoints for cefazolin, they recommend that all isolates susceptible to penicillin be considered susceptible to cefazolin (88).
In light of the increasing prevalence of resistance to clindamycin, erythromycin, or both, recommended strategies for providing intrapartum antibiotic prophylaxis to penicillinallergic women are updated (Box 2). Because the efficacy of recommended alternatives to penicillin or ampicillin has not been measured in controlled trials, and because some of the recommended alternatives have a broad spectrum of activity and may be more complicated and costly to administer, verification of a reported history of penicillin allergy is important. Patients with reported penicillin allergy should then be assessed to determine their risk for anaphylaxis. Persons at high risk for anaphylaxis are those who have had immediate hypersensitivity reactions to penicillin (e.g., anaphylaxis, angioedema, or urticaria) or who have a history of asthma or other conditions that would make anaphylaxis more dangerous (89,90). An estimated 10% of persons with penicillin allergy also have immediate hypersensitivity reactions to cephalosporins (90). Among penicillin-allergic women not at high risk for anaphylaxis, cefazolin, because of its narrow spectrum of activity and ability to achieve high intraamniotic concentrations, is the agent of choice for intrapartum chemoprophylaxis.
For penicillin-allergic women at high risk for anaphylaxis, testing of GBS isolates from prenatal screening for susceptibility to clindamycin and erythromycin is recommended if feasible (Box 1). One of these agents should be employed for intrapartum GBS prophylaxis if the screening isolate is susceptible to both agents.
Vancomycin should be reserved for penicillin-allergic women at high risk for beta-lactam anaphylaxis when clindamycin or erythromycin are not options because of in vitro resistance or unknown susceptibility of a prenatal isolate. Vancomycin use is generally restricted because of emerging vancomycin resistance among some gram-positive organisms (e.g., vancomycinresistant enterococcus and vancomycin-resistant Staphylococcus
MMWR August 16, aureus
). An estimated 13.8 million hospitalized patients received vancomycin therapy in 1998 (91). If penicillin allergy occurs in approximately 10% of adults, and 25% of parturients are colonized with GBS prenatally, approximately 100,000 of the 4 million annual deliveries would require prophylaxis with vancomycin in the absence of clindamycin and erythromycin susceptibility testing of GBS prenatal isolates. This represents a 7% increase in the number of patients exposed to vancomycin. The total grams of vancomycin used annually would increase by less than 1% if all penicillinallergic colonized women received vancomycin prophylaxis.
# Increased Incidence or Resistance in Non-GBS Pathogens
Decreases in the incidence of early-onset GBS sepsis have not usually been accompanied by increases in incidence of early-onset sepsis caused by other pathogens, including those that are antibiotic resistant. Most studies, including population-based multicenter studies, have found stable (59,92,93) or decreasing (43) rates of non-GBS early-onset sepsis during a period of increasing use of intrapartum antibiotic prophylaxis for GBS (Table 3). This is true both for overall non-GBS sepsis and for neonatal sepsis caused by Escherichia coli, the second leading bacterial cause of neonatal sepsis after GBS (93,94). Some single hospital studies have found increased rates or case counts of neonatal sepsis caused by E. coli, gramnegative organisms in general, or ampicillin-resistant pathogens (64,94,95), but these increases appear to be limited to preterm or low-birth-weight infants. An increasing proportion of E. coli neonatal sepsis cases caused by ampicillinresistant organisms was observed in two studies (92,94), but again was limited to preterm or low-birth-weight infants. Furthermore, the proportion of community-acquired E. coli infections that are ampicillin resistant has been increasing (96), suggesting that trends in antimicrobial resistance should not be attributed to GBS prophylaxis.
An association between intrapartum antibiotic exposure and ampicillin resistance in cases of E. coli or other non-GBS earlyonset sepsis has been observed in several studies (36,94,95,97,98). These reports established that infections caused by antibiotic-resistant organisms were more frequently preceded by antibiotic use than were infections caused by susceptible organisms, and that more doses or longer duration of antibiotics before delivery increased the chance that a neonatal infection, if it occurred, would be caused by an antibioticresistant organism. These studies, however, were not designed to assess whether intrapartum antibiotic use increased the rate of antibiotic-resistant infections. Moreover, findings from these studies are consistent with intrapartum antibiotics inducing
# BOX 2. Recommended regimens for intrapartum antimicrobial prophylaxis for perinatal GBS disease prevention*
# Recommended
Penicillin G, 5 million units IV initial dose, then 2.5 million units IV every 4 hours until delivery Alternative Ampicillin, 2 g IV initial dose, then 1 g IV every 4 hours until delivery If penicillin allergic † Patients not at high Cefazolin, 2 g IV initial dose, risk for anaphylaxis then 1 g IV every 8 hours until delivery resistance among initially susceptible organisms, but also with intrapartum antibiotics preventing antibiotic-susceptible infections and having no impact on antibiotic-resistant infections, resulting in a net decrease in the total rate of infection. The reported increases in antibiotic-resistant early-onset infections in a few studies are not of sufficient magnitude to outweigh the benefits of intrapartum antibiotic prophylaxis to prevent perinatal GBS disease. However, to assure early detection of increases in the rate of disease or deaths caused by organisms other than GBS, continued surveillance of neonatal sepsis caused by organisms other than GBS is needed.
# Clinical Challenges
# GBS Bacteriuria During Pregnancy
The presence of GBS bacteriuria in any concentration in a pregnant woman is a marker for heavy genital tract colonization. Therefore, women with any quantity of GBS bacteriuria during pregnancy should receive intrapartum chemoprophylaxis. Vaginal and rectal screening at 35-37 weeks is not necessary for these women. GBS can cause both symptomatic and asymptomatic urinary tract infections, which should be diagnosed and treated according to current standards of care for urinary tract infections in pregnancy. Women with GBS urinary tract infections during pregnancy should receive appropriate treatment at the time of diagnosis as well as intrapartum GBS prophylaxis. Laboratory personnel should report any presence of GBS bacteriuria in specimens obtained from pregnant women. For this to occur, labeling of urine specimens to indicate that they were obtained from a pregnant woman is imperative.
# Planned Cesarean Delivery
Because GBS can cross intact amniotic membranes, a cesarean delivery does not prevent mother-to-child transmission of GBS. Moreover, because cesarean delivery itself is associated with health risks for mother and newborn, GBS colonization of the mother is not an indication for cesarean delivery, and cesarean delivery should not be used as an alternative to intrapartum antibiotic prophylaxis for GBS prevention. However, although a risk does exist for transmission of GBS from a colonized mother to her infant during a planned cesarean delivery performed before onset of labor in a woman with intact amniotic membranes, it is extremely low, based on a retrospective study at a single hospital (99) and a review of CDC active, population-based surveillance data from the 1990s. Thus, in this specific circumstance, in which the risk for disease is extremely low, the individual risks to a mother and her infant from receiving intrapartum antibiotic prophylaxis may balance or outweigh the benefits. Intrapartum antibiotic prophylaxis to prevent perinatal GBS disease is, therefore, not recommended as a routine practice for women undergoing planned cesarean deliveries in the absence of labor or amniotic membrane rupture, regardless of the GBS colonization status of the mother. Patients expected to undergo planned cesarean deliveries should nonetheless still undergo routine vaginal and rectal screening for GBS at 35-37 weeks because onset of labor or rupture of membranes may occur before the planned cesarean delivery. In rare situations in which patients or providers opt for intrapartum prophylaxis before planned cesarean deliveries, administration of antibiotics at the time of incision rather than at least 4 hours before delivery may be reasonable (100).
# Threatened Preterm Delivery
Because preterm (at <37 weeks' gestation) delivery is an important risk factor for early-onset GBS disease, and because timing of delivery can be difficult to assess, management of intrapartum prophylaxis for women with threatened preterm delivery can be challenging. Assessing the need for intrapartum prophylaxis for these women can also be difficult because GBS screening is recommended at 35 to 37 weeks' gestation, and culture results are not always available when labor or rupture of membranes occur preterm.
A suggested approach to GBS chemoprophylaxis in the context of threatened preterm delivery is outlined (Figure 3). Because insufficient data are available to suggest a single course of management, other management strategies developed by individual physicians or institutions may be appropriate alternatives. The algorithm suggests that if GBS screening culture results from the current pregnancy are not available and if onset of labor or rupture of membranes occurs before 37 weeks' gestation with a substantial risk for preterm delivery (as assessed by the woman's health-care provider), intrapartum antibiotic prophylaxis for GBS should be provided pending culture results. For women not yet screened for GBS, a vaginal and rectal specimen for GBS culture should be obtained if time permits. If a negative culture result within the previous 4 weeks is on record, or if the clinician determines that labor can be successfully arrested and preterm delivery averted, antibiotics for GBS prophylaxis should not be initiated. Because recent clinical trials suggest that antibiotics administered during pregnancy may be associated with adverse neonatal outcomes, such as necrotizing enterocolitis or increased need for supplementary oxygen, without evident benefit for preterm labor or preterm premature rupture of membranes (101,102), antibiotics should be reserved for instances in which a significant risk for preterm delivery is present.
No data are available on which to recommend a specific duration of antibiotic administration for GBS-positive women with threatened preterm delivery when delivery is successfully postponed. Management strategies based on scientific opinion have been proposed (100); without further data, the management approach is left to the discretion of the individual provider. Regardless of management strategy chosen, these women should also receive intrapartum antibiotic chemoprophylaxis for GBS when labor likely to proceed to delivery occurs or recurs.
Previous data (28) suggest that the accuracy of GBS screening cultures in predicting colonization status at delivery is greatest if the cultures are collected within 5 weeks of delivery. Therefore, if a woman is screened early for GBS because of threatened preterm delivery but does not deliver within 4 weeks, she should be screened again for GBS colonization and managed according to the result of the repeated screening culture (Figure 3).
# Obstetric Procedures for GBS-Colonized Women
Questions have arisen regarding whether certain obstetric procedures, such as digital vaginal examinations, intrauterine fetal monitoring, and membrane stripping or sweeping to hasten the onset of labor, should be performed on GBScolonized women. Asymptomatic GBS colonization is not an indication to perform any of these procedures. When such procedures are indicated for other reasons, evidence is currently not sufficient to recommend that particular procedures should be avoided because of increased risk of peripartum or perinatal infection. Although some obstetric procedures (frequent vaginal examinations after onset of labor or membrane rupture [17,36,[103][104][105], intrauterine fetal monitoring [104,106,107], and mechanical cervical ripening devices [108]) have been significantly associated with peripartum or perinatal infectious outcomes, most studies to date have been limited by an inability to randomly allocate women to treatment groups and have yielded conflicting results. Moreover, because many studies were performed before GBS prevention was widely implemented, GBS colonization status was often not known and intrapartum chemoprophylaxis was less common. A meta-analysis of available studies examining the use of membrane stripping among women of undetermined GBS colonization status (109) found no significant increases in overall peripartum or perinatal infection rates among women who underwent this procedure and their infants compared with those who did not.
# Management of Newborns Exposed to Intrapartum Prophylaxis
On the basis of information available since the publication of the 1996 guidelines, a modified approach for empiric management of newborns born to women who receive intrapartum antibiotics to prevent early-onset GBS disease or to treat suspected chorioamnionitis is provided (Figure 4). Variations in the algorithm that incorporate individual circumstances or institutional preferences may be appropriate. The modified approach contains the following changes:
• If a woman receives intrapartum antibiotics for treatment of suspected chorioamnionitis, her newborn should have a full diagnostic evaluation and empiric therapy pending * If no maternal intrapartum prophylaxis for GBS was administered despite an indication being present, data are insufficient on which to recommend a single management strategy. † Includes complete blood cell count and differential, blood culture, and chest radiograph if respiratory abnormalities are present. When signs of sepsis are present, a lumbar puncture, if feasible, should be performed. § Duration of therapy varies depending on results of blood culture, cerebrospinal fluid findings, if obtained, and the clinical course of the infant.
If laboratory results and clinical course do not indicate bacterial infection, duration may be as short as 48 hours. ¶ CBC with differential and blood culture. ** Applies only to penicillin, ampicillin, or cefazolin and assumes recommended dosing regimens (Box 2) † † A healthy-appearing infant who was >38 weeks' gestation at delivery and whose mother received >4 hours of intrapartum prophylaxis before delivery may be discharged home after 24 hours if other discharge criteria have been met and a person able to comply fully with instructions for home observation will be present. If any one of these conditions is not met, the infant should be observed in the hospital for at least 48 hours and until criteria for discharge are achieved. culture results, regardless of clinical condition at birth, duration of maternal antibiotic therapy before delivery, or gestational age at delivery (110). Empiric therapy for the infant should include antimicrobial agents active against GBS as well as other organisms that might cause neonatal sepsis (e.g., ampicillin and gentamicin).
• When clinical signs in the infant suggest sepsis, a full diagnostic evaluation should include a lumbar puncture, if feasible. Blood cultures can be sterile in as many as 15% of newborns with meningitis (111)(112)(113), and the clinical management of an infant with abnormal cerebrospinal fluid (CSF) findings differs from that of an infant with normal CSF. If a lumbar puncture has been deferred for a neonate receiving empiric antibiotic therapy, and the therapy is continued beyond 48 hours because of clinical instability, CSF should be obtained for cell count, glucose, protein, and culture. • In addition to penicillin or ampicillin, initiation of intrapartum antibiotic prophylaxis with cefazolin at least 4 hours before delivery can be considered adequate, based on achievable amniotic fluid concentrations of cefazolin (114). Although other agents may be substituted for penicillin if the woman has a history of penicillin allergy (Box 2), the effectiveness of these agents in preventing early-onset GBS disease has not been studied and no data are available to suggest the durations before delivery of these regimens that can be considered adequate. • Based on the demonstrated effectiveness of intrapartum antibiotic prophylaxis at preventing early-onset GBS disease (65) and data indicating that clinical onset occurs within the first 24 hours of life in over 90% of infants who contract early-onset GBS disease (115), hospital discharge as early as 24 hours after delivery may be reasonable under certain circumstances. Specifically, a healthy-appearing infant who is >38 weeks' gestation at delivery and whose mother received >4 hours of intrapartum antibiotic prophylaxis before delivery may be discharged home as early as 24 hours after delivery, assuming that other discharge criteria have been met and that a person able to comply fully with instructions for home observation will be present. A key component of following instructions is the ability of the person observing to communicate with health-care providers by telephone and to transport the child promptly to an appropriate healthcare facility if clinical signs of sepsis develop. If these conditions are not met, the infant should remain in the hospital for at least 48 hours of observation and until criteria for discharge are achieved.
Investigations since 1996 lend additional support to several components of the algorithm. A retrospective study of over 250,000 live births (115) found that administration of intrapartum antibiotic prophylaxis did not change the clinical spectrum of neonatal illness or delay the onset of clinical signs among infants who contracted GBS disease despite prophylaxis. Thus, the algorithm targets infants born to mothers with suspected chorioamnionitis and infants with signs of sepsis for full diagnostic evaluation and empiric therapy. Also, new evidence indicates that 4 or more hours of intrapartum ampicillin or penicillin administered according to recommended dosing intervals (Box 2) significantly reduces vertical transmission of GBS (116) and risk of early-onset GBS disease (65). Thus, although the American Academy of Pediatrics 1997 guidelines suggested 2 or more doses as a threshold for prophylaxis adequacy for infants >35 weeks' gestation (8), the revised algorithm continues to use >4 hours, administered according to recommended dosing intervals, as the benchmark for optimal prevention of early-onset GBS disease. Moreover, a review of pregnancies at a West Coast health maintenance organization using the GBS culture-based screening strategy found that among women who received intrapartum antibiotic prophylaxis, 50% received prophylaxis at least 4 hours before delivery, whereas only 14% received at least 2 doses of intrapartum antibiotics (58); this indicates that duration of prophylaxis is a more practical target than number of doses, in addition to being associated with efficacy.
One objective of developing an algorithm for management of newborns was to minimize unnecessary evaluation and antimicrobial treatment of infants whose mothers received intrapartum prophylaxis. Although early provider surveys indicated that pediatricians and neonatologists were more likely to conduct diagnostic evaluations and initiate empiric antibiotics for an infant whose mother received intrapartum antibiotic prophylaxis (117)(118)(119), more recent data indicate that implementation of GBS prevention strategies has not resulted in increased use of health services for neonates (120), and in some circumstances, when GBS prophylaxis increased a decrease occurred in the proportion of neonates who received laboratory evaluations (58).
Intrapartum antibiotic prophylaxis is the method of choice for preventing neonatal early-onset GBS disease. In the event that intrapartum antibiotics are not given despite an indication (e.g., delivery occurred precipitously before antibiotics could be administered to a GBS-positive woman), sufficient data are not available on which to recommend a single management strategy for the newborn. Some centers provide intramuscular penicillin to asymptomatic infants within 1 hour of birth, based on results of observational studies showing declines in early-onset GBS disease coincident with a policy of universal administration of intramuscular penicillin to all newborns (121).
# Future Prevention Technology
# Rapid Tests to Detect GBS Colonization Status
Rapid tests for detection of GBS colonization at the time of onset of labor or rupture of amniotic membranes might obviate the need for prenatal culture-based screening if their sensitivity and specificity are comparable to culture in selective broth media and they yield results rapidly enough to permit administration of adequate intrapartum antibiotic prophylaxis to women detected as carriers. Currently available rapid tests detect GBS antigen from swab specimens. These tests are insufficiently sensitive to detect light colonization, and therefore are not adequate to replace culture-based prenatal screening (122,123) or to use in place of the risk-based approach when culture results are unknown at the time of labor. An adequate rapid intrapartum test must be as sensitive as culture (minimally 85% compared with culture of vaginal and rectal swabs inoculated into selective broth media), rapid so that results are available to clinicians in time for antibiotics to be given before delivery, and convenient for integration into routine laboratory use. Even a highly sensitive rapid detection test would not be adequate if results were not available to clinicians 24 hours a day, 7 days a week. Alternatives to culturing vaginal and rectal swab specimens at 35-37 weeks' gestation using recommended procedures should be validated to show sensitivity similar to recommended culture methods.
A rapid intrapartum test possessing the attributes described above offers the advantage of ascertaining GBS colonization status before delivery among women who have had no prenatal care. Although such tests might initially be introduced selectively in certain facilities with sufficient demand and capability, a general recommendation for their use would require the capacity for effective implementation in a wide range of hospital settings. Drawbacks of rapid tests include delays in administration of intrapartum antibiotic prophylaxis while test results are pending and lack of an isolate for susceptibility testing, which is of particular concern for penicillinallergic women. Additionally, until rapid tests are universally used, missed opportunities for GBS screening may occur among women who receive prenatal care at institutions relying on intrapartum rapid tests but who deliver at institutions where such tests are not yet available.
In a study of 112 pregnant women at an academic hospital in Quebec, a new, not yet commercially available fluorogenic polymerase chain reaction assay was 97% sensitive and 100% specific when compared with vaginal and rectal cultures collected at admission for delivery. Test results in this study were available within 45 minutes of specimen collection (124). Further studies are needed to determine whether this type of test can be adapted for use outside the research setting. If appropriate techniques for rapid detection of GBS become commercially available, they may be integrated into the currently recommended screening strategy.
# Vaccines To Prevent GBS Disease
Improved use of intrapartum antimicrobial prophylaxis has resulted in a substantial reduction in early-onset GBS disease, but it is unlikely to prevent most late-onset neonatal infections, GBS-related stillbirths, or prematurity, and does not address GBS disease in nonpregnant adults. Immunization of women during or before pregnancy could prevent peripartum maternal disease and protect infants from perinatally acquired infection by transplacental transfer of protective IgG antibodies (125,126). This would eliminate the need for prenatal GBS screening and intrapartum antimicrobial prophylaxis, along with associated costs and concerns regarding the potential adverse effects of intrapartum antibiotic use discussed previously.
Serotype-specific antibodies to GBS capsular polysaccharide, although rare in populations of unvaccinated women, have been shown to protect against disease (32,127). Phase 1 and 2 clinical trials among healthy, nonpregnant adults of monovalent protein-conjugate vaccines containing capsular polysaccharide antigens of GBS disease-associated serotypes have shown these vaccines to be well tolerated and immunogenic (128)(129)(130). One challenge of demonstrating vaccine efficacy in preventing early-onset GBS disease is that the sample size required for clinical trials may be prohibitively large. Identification of surrogate immunologic measures of clinical efficacy may thus be important (131,132). Surrogate information on clinical vaccine efficacy may also be gained by measuring the impact of multivalent conjugate vaccines on vaginal GBS colonization (132,133).
Anticipated difficulties in making vaccine available to pregnant women have resulted in consideration of other target populations for vaccine administration, including adolescent girls (134), women of childbearing age, and infants (135). The duration of protection that could be afforded by vaccination is unknown; one or more booster doses might be required, potentially complicating vaccine delivery. Shifts in the GBS serotypes causing disease have provided an additional
# Research Priorities and Tools To Aid Prevention
Technological advances that aid the implementation of a universal screening strategy will further prevention efforts. In addition to development of reliable rapid tests that can be performed in a wide range of labor and delivery settings, methods of simplifying prenatal culture procedures, e.g., the development of media with a reliable color indicator to signal presence of GBS, might improve accuracy of prenatal culture results and facilitate prenatal culture processing at clinical laboratories with limited technical capacity. Media that have been developed for this purpose, such as Granada (136,137) or GBS medium (138), should be further evaluated to determine if sensitivity and specificity are comparable to recommended methods, which consist of culture in selective broth media followed by GBS-specific identification.
Although universal prenatal GBS culture-based screening is likely to result in substantial further declines in the incidence of early-onset disease, intrapartum chemoprophylaxis is not a permanent or comprehensive strategy for GBS disease prevention. Because vaccines under development hold promise to prevent a larger portion of the burden of GBS disease with a simpler and sustainable intervention, further work on GBS vaccine development and support of phase 3 clinical trials are warranted (139).
Until a safe, effective, and economical vaccine achieves licensure, it will be important to continue to monitor for potential adverse effects of chemoprophylaxis, with an emphasis on tracking key sentinel events signaling a need for revision of the guidelines. Such sentinel events include the emergence of penicillin resistance among GBS, which to date has not been detected, and an increase in the incidence of disease or deaths due to neonatal pathogens other than GBS that offsets the burden of early-onset disease prevented by chemoprophylaxis. Monitoring for the latter will require longterm surveillance of a large population of term and preterm births (140).
Because GBS carriage is common among delivering women in the United States, continued surveillance for GBS disease and evaluation of prevention implementation remains important to minimize missed opportunities for prevention. States are encouraged to monitor incidence of GBS disease, to promote activities that enhance perinatal GBS disease prevention and education, and to assess progress toward national objectives for disease reduction, such as Healthy People 2010, which sets a target of reducing the incidence of early-onset GBS disease in all racial and ethnic groups to 0.5 cases per 1,000 live births (141). Practical tools to assist with monitoring for missed opportunities for perinatal GBS prevention within hospitals have been published (142); additional prevention information and tools for providers, patients and clinical microbiologists are available at http://www.cdc.gov/ groupbstrep, http://www.acog.org, http://sales.acog.com, http://www.aap.org, and http://www.health.state.mn.us/divs/ dpc/ades/invbact/strepb.htm.
# Recommendations
The following updated recommendations for the prevention of GBS disease are based on critical appraisal of multistate population-based observational data and several studies from individual institutions that have been completed since publication of previous CDC ( 7), ACOG (6), and AAP (8) recommendations. They replace previous recommendations from CDC. The strength (indicated by a letter) and quality (indicated by a roman numeral) of evidence supporting each recommendation are shown in parentheses, according to the evidence-based rating system outlined in Table 1.
Obstetric-care practitioners, in conjunction with supporting laboratories and labor and delivery facilities, should adopt the following strategy for the prevention of perinatal GBS disease based on prenatal screening for GBS colonization. The risk-based approach is no longer an acceptable alternative except for circumstances in which screening results are not available before delivery (AII).
• All pregnant women should be screened at 35-37 weeks' gestation for vaginal and rectal GBS colonization (Figure 2) (AII). At the time of labor or rupture of membranes, intrapartum chemoprophylaxis should be given to all pregnant women identified as GBS carriers (AII). Colonization during a previous pregnancy is not an indication for intrapartum prophylaxis in subsequent deliveries. Screening to detect GBS colonization in each pregnancy will determine the need for prophylaxis in that pregnancy. • Women with GBS isolated from the urine in any concentration (e.g., 10 3 ) during their current pregnancy should receive intrapartum chemoprophylaxis because such women usually are heavily colonized with GBS and are at increased risk of delivering an infant with early-onset GBS disease (BII). Labels on urine specimens from prenatal patients should clearly state the patient's pregnancy status to assist laboratory processing and reporting of results. Prenatal culture-based screening at 35-37 weeks' gestation is not necessary for women with GBS bacteriuria. Women with symptomatic or asymptomatic GBS urinary tract infection detected during pregnancy should be treated according to current standards of care for urinary tract infection during pregnancy. • Women who have previously given birth to an infant with invasive GBS disease should receive intrapartum chemoprophylaxis; prenatal culture-based screening is not necessary for these women (BII). • If the result of GBS culture is not known at the onset of labor, intrapartum chemoprophylaxis should be administered to women with any of the following risk factors: gestation <37 weeks, duration of membrane rupture >18 hours, or a temperature of >100.4 º F (>38.0 º C) (AII). Women with known negative results from vaginal and rectal GBS screening cultures within 5 weeks of delivery do not require prophylaxis to prevent GBS disease even if any of the intrapartum risk factors develop. • Women with threatened preterm (<37 weeks' gestation) delivery should be assessed for need for intrapartum prophylaxis to prevent perinatal GBS disease. An algorithm for management of women with threatened preterm delivery is provided (Figure 3). Other management approaches, developed by individual physicians or institutions, may be appropriate (CIII). • Culture techniques that maximize the likelihood of GBS recovery are required for prenatal screening (Box 1). Collection of specimens for culture may be conducted in the outpatient clinic setting by either the patient, with appropriate instruction, or health-care provider (BII). This involves swabbing the lower vagina and rectum (i.e., through the anal sphincter). Because lower vaginal as opposed to cervical cultures are recommended, cultures should not be collected by speculum examination. Specimens should be placed in a nonnutritive transport medium (e.g., Amies or Stuart's without charcoal). Specimen labels should clearly identify that specimens are for group B streptococcal culture. If susceptibility testing is ordered for penicillin-allergic women (Box 2), specimen labels should also identify the patient as penicillin allergic and should specify that if GBS is isolated, it should be tested for susceptibility to clindamycin and erythromycin. Specimens should be inoculated into a selective broth medium (examples of appropriate commercially available media include Trans-Vag Broth supplemented with 5% defibrinated sheep blood or LIM broth), incubated overnight, and subcultured onto solid blood agar medium (AII). Methods of testing prenatal isolates from penicillinallergic women for susceptibility to clindamycin and erythromycin are outlined (Box 1). Laboratories should report culture results (positive and negative) and susceptibility testing results to the anticipated site of delivery (when known) and to the health-care provider who ordered the test. • Health-care providers should inform women of their GBS screening test result and the recommended interventions.
In the absence of GBS urinary tract infection, antimicrobial agents should not be used before the intrapartum period to treat GBS colonization. Such treatment is not effective in eliminating carriage or preventing neonatal disease and may cause adverse consequences (DI). • GBS-colonized women who have a planned cesarean delivery performed before rupture of membranes and onset of labor are at low risk for having an infant with early-onset GBS disease. These women should not routinely receive intrapartum chemoprophylaxis for perinatal GBS disease prevention (CII). • For intrapartum chemoprophylaxis, the following regimen is recommended for women without penicillin allergy (Box 2): penicillin G, 5 million units intravenously initial dose, then 2.5 million units intravenously every 4 hours until delivery (AII). Because of its narrow spectrum of activity, penicillin is the preferred agent. An alternative regimen is ampicillin, 2 g intravenously initial dose, then 1 g intravenously every 4 hours until delivery (AI). • Intrapartum chemoprophylaxis for penicillin-allergic women takes into account increasing resistance to clindamycin and erythromycin among GBS isolates (Box 2). During prenatal care, history of penicillin allergy should be assessed to determine whether a patient is at high risk for anaphylaxis, i.e., has a history of immediate hypersensitivity reactions to penicillin (e.g., anaphylaxis, angioedema, or urticaria) or history of asthma or other conditions that would make anaphylaxis more dangerous (89). Women who are not at high risk for anaphylaxis should be given cefazolin, 2 g intravenously initial dose, then 1 g intravenously every 8 hours until delivery (BIII). For women at high risk for anaphylaxis, clindamycin and erythromycin susceptibility testing, if available, should be performed on isolates obtained during GBS prenatal carriage screening. Women with clindamycin-and erythromycin-susceptible isolates should be given either clindamycin, 900 mg intravenously every 8 hours until delivery; OR erythromycin, 500 mg intravenously every 6 hours until delivery. If susceptibility testing is not possible, susceptibility results are not known, or isolates are resistant to erythromycin or clindamycin, the following regimen can be used for women with immediate penicillin hypersensitivity: vancomycin, 1 g intravenously every 12 hours until delivery (CIII).
• Routine use of antimicrobial prophylaxis for newborns whose mothers received intrapartum chemoprophylaxis for GBS infection is not recommended. However, therapeutic use of these agents is appropriate for infants with clinically suspected sepsis. An updated algorithm for management of infants born to mothers who received intrapartum chemoprophylaxis for GBS infection is provided (Figure 4). This revised algorithm is not an exclusive approach to management; variation that incorporates individual circumstances or institutional preferences may be appropriate (CIII). • Local and state public health agencies, in conjunction with appropriate groups of hospitals, are encouraged to establish surveillance for early-onset GBS disease and to take other steps to promote perinatal GBS disease prevention and education to reduce the incidence of early-onset GBS disease in their states. Efforts to monitor the emergence of perinatal infections caused by other organisms are also encouraged. Before full implementation of this strategy can be expected in all health-care settings, all members of the health-care team will need to improve protocols for isolation and reporting of GBS culture results, to improve information management to ensure communication of screening results, and to educate medical and nursing staff responsible for prenatal and intrapartum care. Within institutions, such efforts may take several months.
Even with ideal implementation, cases of early-onset GBS disease will continue to occur. Tools to help promote prevention and educate parents of infants with early-onset GBS disease are available at http://www.cdc.gov/groupbstrep. Additional tools available to assist with prevention implementation are available at http://www.acog.org, http://sales.acog.com, http://www.aap.org and http://www.health.state.mn.us/divs/ dpc/ades/invbact/strepb.htm Multiple copies of educational materials published by CDC are available at the Public Health Foundation, 1220 L St., NW Suite 350, Washington, DC 20005, telephone 877-252-1200, or online at http:// www.phf.org. | None | None |
0ea76588f36aeafb199d2f30e8262a47a3b7e57e | cdc | None | depar depar depar depar department of health and human ser tment of health and human ser tment of health and human ser tment of health and human ser tment of health and human services vices vices vices vices#
All vaccines must be administered in accordance with the specifications of the product label or package insert. B. Vaccine Selection. Part III lists all vaccines licensed by USDA and marketed in the United States at the time of publication. New vaccine approvals or changes in label specifications made subsequent to publication should be considered as part of this list. Any of the listed vaccines can be used for revaccination, even if the product is not the same brand as previously administered vaccines. Vaccines used in state and local rabies control programs should have a 3-year duration of immunity. This constitutes the most effective method of increasing the proportion of immunized dogs and cats in any population (3). No laboratory or epidemiologic data exist to support the annual or biennial administration of 3-year vaccines following the initial series.
C. Adverse Events. Currently, no epidemiologic association exists between a particular licensed vaccine product and adverse events including vaccine failure (4,5). Adverse events should be reported to the vaccine manufacturer and to USDA, Animal and Plant Health Inspection Service, Center for Veterinary Biologics (Internet: . aphis.usda.gov/vs/cvb/ic/adverseeventreport.htm; telephone: 800-752-6255; or e-mail: [email protected]). D. Wildlife and Hybrid Animal Vaccination. The efficacy of parenteral rabies vaccination of wildlife and hybrids (the offspring of wild animals crossbred to domestic animals) has not been established, and no such vaccine is licensed for these animals. Zoos or research institutions may establish vaccination programs, which attempt to protect valuable animals, but these should not replace appropriate public health activities that protect humans. animals or by providing exposed persons with prompt local treatment of wounds combined with the administration of human rabies immune globulin and vaccine. The rationale for recommending preexposure and postexposure rabies prophylaxis and details of their administration can be found in the current recommendations of the Advisory Committee on Immunization Practices (ACIP) (7). These recommendations, with information concerning the current local and regional status of animal rabies and the availability of human rabies biologics, are available from state health departments. Rabies vaccinations may also be administered under the supervision of a veterinarian to animals held in animal control shelters before release. Any veterinarian signing a rabies certificate should ensure that the person administering vaccine is identified on the certificate and is appropriately trained in vaccine storage, handling, administration, management of adverse events, etc. This practice ensures that a qualified and responsible person can be held accountable to ensure that the animal has been properly vaccinated. Within 28 days after primary vaccination, a peak rabies antibody titer is reached, and the animal can be considered immunized. An animal is currently vaccinated and is considered immunized if the primary vaccination was administered at least 28 days previously and vaccinations have been administered in accordance with this compendium.
# E. Accidental Human
Regardless of the age of the animal at initial vaccination, a booster vaccination should be administered 1 year later (see Parts I and III for vaccines and procedures). No laboratory or epidemiologic data exist to support the annual or biennial administration of 3-year vaccines following the initial series. Because a rapid anamnestic response is expected, an animal is considered currently vaccinated immediately after a booster vaccination. Protocols for the postexposure vaccination of previously unvaccinated domestic animals have not been validated, and evidence exists that use of vaccine alone will not prevent the disease (19). Dogs, cats, and ferrets that are currently vaccinated should be revaccinated immediately, kept under the owner's control, and observed for 45 days. b. Livestock. All species of livestock are susceptible to rabies; cattle and horses are among the most frequently infected. Livestock exposed to a rabid animal and currently vaccinated with a vaccine approved by USDA for that species should be revaccinated immediately and observed for 45 days. Unvaccinated livestock should be slaughtered immediately. If the owner is unwilling to have this done, the animal should be kept under close observation for 6 months. The following are recommendations for owners of unvaccinated livestock exposed to rabid animals: 1) If the animal is slaughtered within 7 days of being bitten, its tissues may be eaten without risk of infection, provided that liberal portions of the exposed area are discarded. Federal guidelines for meat inspectors require that any animal known to have been exposed to rabies within 8 months be rejected for slaughter. 2) Neither tissues nor milk from a rabid animal should be used for human or animal consumption (20). Pasteurization temperatures will inactivate rabies virus; therefore, drinking pasteurized milk or eating cooked meat does not constitute a rabies exposure.
3) Having more than one rabid animal in a herd or having herbivore-to-herbivore transmission is uncommon; therefore, restricting the rest of the herd if a single animal has been exposed to or infected by rabies might not be necessary. (24,25); therefore, the translocation of known terrestrial rabies reservoir species should be prohibited.
1. Terrestrial Mammals. The use of licensed oral vaccines for the mass vaccination of free-ranging wildlife should be considered in selected situations, with the approval of the state agency responsible for animal rabies control (9). The distribution of oral rabies vaccine should be based on scientific assessments of the target species and followed by timely and appropriate analysis of surveillance data; such results should be provided to all stakeholders. Continuous and persistent programs for trapping or poisoning wildlife are not effective in reducing wildlife rabies reservoirs on a statewide basis. However, limited control in high-contact areas (e.g., picnic grounds, camps, or suburban areas) may be indicated for the removal of selected high-risk species of wildlife (9). State agriculture, public health, and wildlife agencies should be consulted for planning, coordination, and evaluation of vaccination or populationreduction programs. 2. Bats. Indigenous rabid bats have been reported from every state except Hawaii, and have caused rabies in at least 40 humans in the United States (26)(27)(28)(29). Bats should be excluded from houses, public buildings, and adjacent structures to prevent direct association with humans (30,31). Such structures should then be made bat-proof by sealing entrances used by bats. Controlling rabies in bats through programs designed to reduce bat populations is neither feasible nor desirable. | depar depar depar depar department of health and human ser tment of health and human ser tment of health and human ser tment of health and human ser tment of health and human services vices vices vices vices#
All vaccines must be administered in accordance with the specifications of the product label or package insert. B. Vaccine Selection. Part III lists all vaccines licensed by USDA and marketed in the United States at the time of publication. New vaccine approvals or changes in label specifications made subsequent to publication should be considered as part of this list. Any of the listed vaccines can be used for revaccination, even if the product is not the same brand as previously administered vaccines. Vaccines used in state and local rabies control programs should have a 3-year duration of immunity. This constitutes the most effective method of increasing the proportion of immunized dogs and cats in any population (3). No laboratory or epidemiologic data exist to support the annual or biennial administration of 3-year vaccines following the initial series.
C. Adverse Events. Currently, no epidemiologic association exists between a particular licensed vaccine product and adverse events including vaccine failure (4,5). Adverse events should be reported to the vaccine manufacturer and to USDA, Animal and Plant Health Inspection Service, Center for Veterinary Biologics (Internet: http://www. aphis.usda.gov/vs/cvb/ic/adverseeventreport.htm; telephone: 800-752-6255; or e-mail: [email protected]). D. Wildlife and Hybrid Animal Vaccination. The efficacy of parenteral rabies vaccination of wildlife and hybrids (the offspring of wild animals crossbred to domestic animals) has not been established, and no such vaccine is licensed for these animals. Zoos or research institutions may establish vaccination programs, which attempt to protect valuable animals, but these should not replace appropriate public health activities that protect humans. animals or by providing exposed persons with prompt local treatment of wounds combined with the administration of human rabies immune globulin and vaccine. The rationale for recommending preexposure and postexposure rabies prophylaxis and details of their administration can be found in the current recommendations of the Advisory Committee on Immunization Practices (ACIP) (7). These recommendations, with information concerning the current local and regional status of animal rabies and the availability of human rabies biologics, are available from state health departments. Rabies vaccinations may also be administered under the supervision of a veterinarian to animals held in animal control shelters before release. Any veterinarian signing a rabies certificate should ensure that the person administering vaccine is identified on the certificate and is appropriately trained in vaccine storage, handling, administration, management of adverse events, etc. This practice ensures that a qualified and responsible person can be held accountable to ensure that the animal has been properly vaccinated. Within 28 days after primary vaccination, a peak rabies antibody titer is reached, and the animal can be considered immunized. An animal is currently vaccinated and is considered immunized if the primary vaccination was administered at least 28 days previously and vaccinations have been administered in accordance with this compendium.
# E. Accidental Human
Regardless of the age of the animal at initial vaccination, a booster vaccination should be administered 1 year later (see Parts I and III for vaccines and procedures). No laboratory or epidemiologic data exist to support the annual or biennial administration of 3-year vaccines following the initial series. Because a rapid anamnestic response is expected, an animal is considered currently vaccinated immediately after a booster vaccination. Protocols for the postexposure vaccination of previously unvaccinated domestic animals have not been validated, and evidence exists that use of vaccine alone will not prevent the disease (19). Dogs, cats, and ferrets that are currently vaccinated should be revaccinated immediately, kept under the owner's control, and observed for 45 days. b. Livestock. All species of livestock are susceptible to rabies; cattle and horses are among the most frequently infected. Livestock exposed to a rabid animal and currently vaccinated with a vaccine approved by USDA for that species should be revaccinated immediately and observed for 45 days. Unvaccinated livestock should be slaughtered immediately. If the owner is unwilling to have this done, the animal should be kept under close observation for 6 months. The following are recommendations for owners of unvaccinated livestock exposed to rabid animals: 1) If the animal is slaughtered within 7 days of being bitten, its tissues may be eaten without risk of infection, provided that liberal portions of the exposed area are discarded. Federal guidelines for meat inspectors require that any animal known to have been exposed to rabies within 8 months be rejected for slaughter. 2) Neither tissues nor milk from a rabid animal should be used for human or animal consumption (20). Pasteurization temperatures will inactivate rabies virus; therefore, drinking pasteurized milk or eating cooked meat does not constitute a rabies exposure.
3) Having more than one rabid animal in a herd or having herbivore-to-herbivore transmission is uncommon; therefore, restricting the rest of the herd if a single animal has been exposed to or infected by rabies might not be necessary. (24,25); therefore, the translocation of known terrestrial rabies reservoir species should be prohibited.
1. Terrestrial Mammals. The use of licensed oral vaccines for the mass vaccination of free-ranging wildlife should be considered in selected situations, with the approval of the state agency responsible for animal rabies control (9). The distribution of oral rabies vaccine should be based on scientific assessments of the target species and followed by timely and appropriate analysis of surveillance data; such results should be provided to all stakeholders. Continuous and persistent programs for trapping or poisoning wildlife are not effective in reducing wildlife rabies reservoirs on a statewide basis. However, limited control in high-contact areas (e.g., picnic grounds, camps, or suburban areas) may be indicated for the removal of selected high-risk species of wildlife (9). State agriculture, public health, and wildlife agencies should be consulted for planning, coordination, and evaluation of vaccination or populationreduction programs. 2. Bats. Indigenous rabid bats have been reported from every state except Hawaii, and have caused rabies in at least 40 humans in the United States (26)(27)(28)(29). Bats should be excluded from houses, public buildings, and adjacent structures to prevent direct association with humans (30,31). Such structures should then be made bat-proof by sealing entrances used by bats. Controlling rabies in bats through programs designed to reduce bat populations is neither feasible nor desirable. | None | None |
90144552bbf33ea849d74f48675efc94fa9fc290 | cdc | None | In 2008, a total of 12,898 incident tuberculosis (TB) cases were reported in the United States; the TB rate declined 3.8% from 2007 to 4.2 cases per 100,000 population, the lowest rate recorded since national reporting began in 1953. This report summarizes provisional 2008 data from the National TB Surveillance System and describes trends since 1993. Despite this overall improvement, progress has slowed in recent years; the average annual percentage decline in the TB rate decreased from 7.3% per year during 1993-2000 to 3.8% during 2000-2008.- Foreign-born persons and racial/ethnic minorities continued to bear a disproportionate burden of TB disease in the United States. In 2008, the TB rate in foreignborn persons in the United States was 10 times higher than in U.S.-born persons. TB rates among Hispanics and blacks were nearly eight times higher than among non-Hispanic whites, and rates among Asians were nearly 23 times higher than among non-Hispanic whites. In 2008, among persons with TB whose country of origin was known, approximately 95% of Asians, 76% of Hispanics, 32% of blacks, and 18% of#
whites were foreign born. Among U.S.-born racial and ethnic groups, the greatest racial disparity in TB rates was for U.S.born blacks, whose rate was seven times higher than the rate for U.S.-born whites. Intensified efforts are needed to address the slowing decline in TB incidence and the persistent disparities that exist between U.S.-born and foreign-born persons and between whites and minorities in the United States.
Health departments in the 50 states and the District of Columbia (DC) electronically report to CDC verified TB cases that meet the CDC/Council of State and Territorial Epidemiologists case definition. † Reports include the patient's race, ethnicity (i.e., Hispanic or non-Hispanic), treatment information, and, whenever available, drug-susceptibility test results. CDC calculates national and state TB rates overall and by racial/ethnic group using current U.S. Census population estimates. U.S. Census annual estimates were used to calculate the national TB rate and the percentage change from 2007 to 2008. Population denominators used to calculate TB rates and percentage changes over time according to national origin (U.S.-born versus foreign-born persons) were from the U.S. Census Current Population Survey. A U.S.-born person was defined as someone born in the United States or its associated jurisdictions or someone born in a foreign country but having at least one U.S.-born parent. Persons not meeting this definition were classified as foreign born. For 2008, patients with unknown origin of birth represented 0.6% (74 of 12,898) of total cases. For this report, persons identified as white, black, Asian, American Indian/Alaska Native, native Hawaiian or other Pacific Islander, or of multiple races were all classified as non-Hispanic. Persons identified as Hispanic might be of any race.
In 2008, TB rates in the 51 reporting areas ranged from 0.5 (North Dakota) to 9.6 (Hawaii) cases per 100,000 population (median: 3.0 cases per 100,000 population) (Figure 1). Thirtythree states and DC had lower rates in 2008 than in 2007; however, 17 states had higher rates. Four states (California, Florida, New York, and Texas) reported more than 500 cases each for 2008, a decline from seven states with at least 500 cases in 2006 and five states in 2007. Combined, these four states accounted for approximately half (49.2% ) of all TB cases in 2008.
Among U.S.-born persons, the number and rate of TB cases continued to decline in 2008. The number of TB cases in U.S.-born persons (5,283 ) declined 3.9% compared with 2007 and 69.7% compared with 1993 (Figure 2). In 2008, the TB rate among U.S.-born persons was 2.0 per 100,000 population, § TB rate cutoff points were based on terciles: 18 states had TB case rates of 4.0 (range: 4.02-9.63) per 100,000. DC 4.0 § Editorial Note: In 2008, the number of TB cases and annual TB rate reached all-time lows in the United States. After the resurgence of TB during 1985-1992, the annual TB rate has steadily decreased. However, since 2000, the pace of that decline has slowed. To hasten the decline of TB in the United States, intensified efforts are required to address the disproportionately high rates of TB that persist among foreign-born persons and racial/ethnic minorities. The proportion of TB cases contributed by foreign-born persons has increased each year since 1993. This is a reflection of high rates of TB in countries of origin for U.S. immigrants. To help address this, in 2007, CDC issued revised technical instructions for TB screening and treatment among persons applying for immigration to the United States (3). The revision included instructions for 1) more comprehensive diagnostic testing among applicants (e.g., cultures and drug-susceptibility testing for persons with suspected TB); 2) the administration of directly observed therapy overseas, before entry into the United States; and 3) targeted tuberculin skin testing (before entry into the United States) of children from high-incidence countries and contacts of persons known to have TB. In addition, CDC continues to work with international partners, including the Stop TB Partnership, to strengthen TB control in countries with high TB incidence. For example, to facilitate patient referral and treatment among persons who cross the U.S.-Mexico border, bilateral initiatives (e.g., CureTB) are improving coordination of TB care between U.S. TB programs and Mexican counterparts. Modeling has suggested that U.S.-funded expansion of the directly observed treatment (short course) strategy in selected high-incidence countries (e.g., Mexico) might be a cost-saving approach to reducing TB-related morbidity and mortality among U.S. immigrants (4).
The proportion of TB cases that are multidrug resistant has remained approximately 1% of culture-positive cases since 1997; however, MDR TB has continued to disproportionately affect foreign-born persons in the United States. CDC continues to provide technical assistance to domestic and international partners to increase detection of MDR TB and improve access to second-line TB drugs (5). In 2008, TB rates declined for all racial/ethnic minorities, yet among the U.S. born, blacks continue to experience a disproportionately high rate of TB. CDC's TB Epidemiologic Studies Consortium currently is conducting studies to understand how to reduce TB in blacks effectively, including a study to identify barriers to treatment adherence for latent TB infection and TB disease and a study examining the determinants of early diagnosis, prevention, and treatment of TB.
The findings in this report are subject to at least two limitations. First, the analysis was based on provisional 2008 data that are subject to change. This applies to TB case counts and HIV testing results data, both of which were incomplete. Additional data might change the results marginally. Second, population denominator data were drawn from multiple U.S. census sources and are subject to periodic adjustment. CDC's annual TB surveillance summary, due to be published in fall 2009, will provide updated data.
To ensure that TB rates decline further in the United States, especially among foreign-born persons and minority populations, TB prevention and control capacity should be increased (6)(7)(8). Additional capacity should be used to 1) improve case management and contact investigations; 2) intensify outreach, testing, and treatment of high-risk and hard-to-reach populations; 3) enhance treatment and diagnostic tools; 4) increase scientific research to better understand TB transmission; and 5) continue collaboration with other nations to reduce TB globally. FSM comprises four states and more than 600 islands spread across 1 million square miles in the western Pacific Ocean. Half of the population of 108,000 lives in Chuuk, the largest state (2). TB is endemic in Chuuk, where 70 cases of TB were recorded in 2007. The 2007 incidence rate (127 TB cases per 100,000) is 29 times higher than the 2007 U.S. rate (3).
# Two Simultaneous
# Limited transportation hinders access to the only hospital in
Chuuk, which provides chest radiography and smear microscopy services to help diagnose TB. Culture confirmation, drug-susceptibility testing, and genotyping were not available routinely for TB cases in FSM until January 2006, when referral laboratories in Hawaii and California began to offer these services. Before 2008, the state's geography, combined with limited TB program staffing, precluded active case-finding via routine contact investigations or the administration of DOT, a cornerstone of TB treatment that improves completion of therapy and prevents the emergence of drug resistance. Before July 2008, TB patients were identified as they showed signs or symptoms of TB disease at the local clinic or hospital; all received self-administered therapy. FSM's National TB Program has an annual budget of $170,000, and second-line drugs for treating MDR TB were not available because of funding constraints.
In June 2007, pulmonary TB was diagnosed in a Chuuk resident aged 37 years. Sputum-smear microscopy detected acid-fast bacilli, and a chest radiograph showed lung cavitation, both indicators of contagiousness. In November 2007, drug-susceptibility test results confirmed multidrug resistance. The patient did not have access to second-line drugs and died. During December 2007-June 2008, four additional patients with MDR TB disease came to the local clinic or hospital. None of the four patients were treated with second-line drugs; three died, including a child aged 2 years. In May 2008, FSM authorities requested CDC assistance because of the 80% fatality rate and evidence of recent MDR TB transmission.
A confirmed case was defined as laboratory-confirmed MDR TB disease in a Chuuk resident during January 2006-June 2008. A suspected case of MDR TB disease was defined as exposure (based on intensity and duration of contact) to a patient with confirmed TB and clinical findings of TB disease (i.e., laboratory confirmation pending). Patients (or proxies for deceased patients) were interviewed and laboratory and medical records reviewed.
The July 2008 investigation focused on the initial five confirmed MDR TB cases. All patients were born in Chuuk; their median age was 16 years (range: 2-37 years), and four were female. None of the patients had a history of TB disease or treatment with TB drugs. All five patients had pulmonary TB, two with cavitation on chest radiograph and hemoptysis. None of the four patients who died before the investigation had been tested for human immunodeficiency virus (HIV) infection; the surviving patient had a negative HIV test result in July 2008. Two distinct clusters, associated with two different villages, were identified based on genotypes and drug-susceptibility patterns (Figure).
In the first cluster of three cases, Mycobacterium tuberculosis isolates had a matching genotype and resistance to five drugs: isoniazid, rifampin, pyrazinamide, ethambutol, and streptomycin. This drug-susceptibility pattern had not been seen in Chuuk since routine drug-susceptibility testing became available in January 2006. The index patient in this cluster had worked during 1987-2000 in the garment industry in the Commonwealth of the Northern Mariana Islands (Saipan), which employs migrants from Southeast Asian countries (4) where MDR TB is common (5).
In the second cluster of two cases, the isolates had a matching genotype and resistance to three drugs: isoniazid, rifampin, and ethionamide. The two patients were cousins whose extended family included five persons who previously had TB disease with isolates genotypically matched to those of the outbreak patients. However, the earlier isolates had resistance to isoniazid and ethionamide only. These five previous cases of non-MDR TB were diagnosed from January 2006, when genotyping became routinely available in Chuuk, to October 2007. Household caregivers reported that the five patients had self-administered therapy inconsistently or incompletely.
During investigations of the five initial cases of MDR TB disease, a standardized clinical examination, chest radiography, and tuberculin skin testing were used to evaluate contacts for TB disease and latent TB infection (6). The 205 named contacts, of whom 163 (80%) were household members and 42 (20%) were health-care workers, had a median age of 20 years (range: 4 months-62 years), and 117 (57%) were female. During July 1, 2008-March 13, 2009, three additional MDR TB cases were confirmed among household members (Figure ), including a household contact aged 4 years who in November 2008 died of meningitis later confirmed to be caused by MDR TB. Based on history of household exposure to a patient with confirmed TB and clinical findings (e.g., chest radiography consistent with TB disease), 13 other suspected cases of MDR TB disease were identified; all 13 patients began treatment based on the drug-susceptibility results of the respective source case (Table ). Although fewer than one third of the contacts were aged <15 years (60 of 205), they accounted for more than half of the suspected and confirmed MDR TB cases since July 2008 (nine of 16). Latent TB infection was diagnosed in 124 (60%) contacts, although many of the adults were probably infected before this documented emergence of MDR TB in Chuuk. Among contacts aged <15 years, 20 (33%) of 60 had latent TB infection. All household contacts with latent TB infection have begun receiving second-line drugs based on the drug-susceptibility results of the respective source case (1,7).
Multiple (9) have resulted in the following actions: 1) a consistent supply of fluoroquinolones, aminoglycosides, and other second-line drugs was procured; 2) Chuuk State Hospital added a separate ward for inpatient treatment of patients with TB; 3) TB program staff members received on-site training on providing DOT and conducting contact investigations; 4) nine new outreach workers were hired to administer DOT, and three vehicles were acquired to help workers investigate contacts; 5) the hospital laboratory was equipped for processing specimens for smear microscopy daily and shipping specimens for culture and drug-susceptibility testing weekly. For 2008, the improved case-detection capacity increased the recorded TB incidence to 204 cases per 100,000 persons. The Chuuk TB program is consulting with U.S. MDR TB experts by telephone and e-mail for assistance with complex treatment decisions, and implementing measures to prevent the selection of drug-resistant strains and reduce all TB transmission. Editorial Note: These two clusters of MDR TB represent two distinct outbreaks and illustrate two mechanisms for the emergence of drug resistance. In the first outbreak, the index patient had not been treated previously for TB and probably became infected with a MDR TB strain before returning to Chuuk in 2000 from Saipan; this case illustrates primary (i.e., initial) drug resistance. In the second outbreak, lack of DOT for the five family members with TB disease initially resistant to only isoniazid and ethionamide probably led to secondary (i.e., acquired) rifampin resistance. At least one of these five previous patients thus acquired multidrug resistance and transmitted MDR TB to the index case in the second outbreak.
The emergence and transmission of MDR TB in these outbreaks were caused by the inability to follow standard TB control practices or to provide appropriate drugs. The findings also highlight the vulnerability of pediatric contacts and the challenges of diagnosing and treating MDR TB in resource-limited settings. Laboratory capacity and access to second-line TB drugs are fundamental to controlling MDR TB (1), and finding and curing all persons with TB is critical for interrupting transmission (8). Contact investigations enable active case-finding and early identification of recently infected contacts at highest risk for developing TB disease. Infection control practices (e.g., isolating contagious patients initially during treatment and wearing appropriate personal protective equipment) can prevent transmission of susceptible and drug-resistant TB, and are particularly important in congregate settings such as clinics, hospitals, and prisons. Uniform DOT for patients with TB disease prevents acquired drug resistance (5) and, where feasible, DOT should be offered for contacts with latent TB infection as well.
The measures implemented in response to the MDR TB outbreaks in Chuuk have reflected all five aspects of the WHO global response plan for drug-resistant TB (10), which calls for augmenting the public health infrastructure to control TB, strengthening laboratory services for early diagnosis, improving surveillance to better understand drug resistance, implementing infection control to prevent transmission, and enhancing management of drug-resistant TB cases to reach the Global Plan to Stop TB 2006-2015 goals. † Tangible progress in treating and preventing the spread of TB has been made in Chuuk as recommendations from the investigation have been implemented.
In 2008, an estimated 500,000 persons in the world developed MDR TB, largely as a result of inadequate TB control activities (5). In many countries where TB is endemic, ongoing transmission of multiple strains of MDR TB probably will be discovered as access to laboratory services improves (10). The challenge of primary drug resistance is likely to be exacerbated further by the increasing numbers of migratory and displaced populations (4). Many developing countries provide free firstline TB drugs through TB control programs. However, effective and sustainable mechanisms for access to expensive second-line TB drugs are needed for timely treatment of patients with drug-resistant TB. The multiagency response to the MDR TB outbreaks in Chuuk is a good example of the coordinated efforts that are needed to control MDR TB in many developing countries. As in Chuuk, a concerted focus on improving access to enhanced laboratory services and second-line TB drugs, and building local capacity for finding, diagnosing, and curing all forms of TB is necessary to address the global threat of MDR TB.
# Guidance for Control of Infections with Carbapenem-Resistant or Carbapenemase-Producing Enterobacteriaceae in Acute Care Facilities
Infection with carbapenem-resistant Enterobacteriaceae (CRE) or carbapenemase-producing Enterobacteriaceae is emerging as an important challenge in health-care settings (1). Currently, carbapenem-resistant Klebsiella pneumoniae (CRKP) is the species of CRE most commonly encountered in the United States. CRKP is resistant to almost all available antimicrobial agents, and infections with CRKP have been associated with high rates of morbidity and mortality, particularly among persons with prolonged hospitalization and those who are critically ill and exposed to invasive devices (e.g., ventilators or central venous catheters). This report provides updated recommendations from CDC and the Healthcare Infection Control Practices Advisory Committee (HICPAC) for the control of CRE or carbapenemase-producing Enterobacteriaceae in acute care (inpatient) facilities. For all acute care facilities, CDC and HICPAC recommend an aggressive infection control strategy, including managing all patients with CRE using contact precautions and implementing Clinical and Laboratory Standards Institute (CLSI) guidelines for detection of carbapenemase production. In areas where CRE are not endemic, acute care facilities should 1) review microbiology records for the preceding 6-12 months to determine whether CRE have been recovered at the facility, 2) if the review finds previously unrecognized CRE, perform a point prevalence culture survey in high-risk units to look for other cases of CRE, and 3) perform active surveillance cultures of patients with epidemiologic links to persons from whom CRE have been recovered. In areas where CRE are endemic, an increased likelihood exists for imporation of CRE, and facilities should consider additional strategies to reduce rates of CRE (2). Acute care facilities should review these recommendations and implement appropriate strategies to limit the spread of these pathogens.
For CRKP, the most important mechanism of resistance is the production of a carbapenemase enzyme, bla kpc . The gene that encodes the bla kpc enzyme is carried on a mobile piece of genetic material (transposon), which increases the risk for dissemination. Since first described in North Carolina in 1999, CRKP has been identified in 24 states and is recovered routinely in certain hospitals in New York and New Jersey (3). Analysis of 2007 data regarding health-care-associated infections reported to CDC indicated that 8% of all Klebsiella isolates were CRKP, compared with fewer than 1% in 2000 (CDC, unpublished data, 2008). CRKP poses significant treatment challenges, and CRKP infections have been associated with increased mortality, length of stay, and increased cost (4). The emergence and spread of CRKP and other types of CRE is another in a series of worrisome public health developments regarding antimicrobial resistance among gram-negative bacteria and underscores the immediate need for aggressive detection and control strategies (5).
A difficulty in detecting CRE is the fact that some strains that harbor bla kpc have minimal inhibitory concentrations (MICs) that are elevated but still within the susceptible range for carbapenems. Because these strains are susceptible to carbapenems, they are not identified as potential clinical or infection control risks using current susceptibility testing guidelines. To address this challenge, in January 2009, CLSI published a recommendation that carbapenem-susceptible Enterobacteriaceae with elevated MICs or reduced disk diffusion zone sizes be tested for the presence of carbapenemases using the modified Hodge test (MHT) (6). The MHT is a phenotypic test used to detect carbapenemases in isolates demonstrating elevated but susceptible carbapenem MICs and has demonstrated sensitivity and specificity exceeding 90% in identifying carbapenemase-producing Enterobacteriaceae (6). If the MHT reveals the presence of a carbapenemase, CLSI recommends that a comment be added to the microbiology report to inform clinicians and infection preventionists. Because treatment information on MHT-positive, carbapenem-susceptible isolates is limited, CLSI guidelines do not recommend any changes regarding the reporting of susceptibility results themselves. Strains of Enterobacteriaceae that test intermediate or resistant to carbapenems should be reported as such and do not need to be subjected to the MHT.
Patients with unrecognized CRKP colonization have served as reservoirs for transmission during health-care-associated outbreaks (7). For example, during an outbreak of 39 cases of CRKP infection in a hospital in Puerto Rico in 2008, in addition to a review of infection control practices, active surveillance cultures were performed on patients in the same units as persons with confirmed CRKP infection. Cultures performed on 30 patients in the intensive care unit revealed two colonized patients who were not previously known to harbor CRKP and were not placed in contact precautions (CDC, unpublished data, 2008). Control of the outbreak was hindered by lack of compliance with infection control practices. Health-care personnel adherence to recommendations for gown and glove use was low (62%) at the hospital, and appropriate hand hygiene (i.e., hand washing or using a waterless alcohol-based hand rub before and after patient contact) was observed in only 48% of patient encounters. The hospital eventually was able to control the outbreak through enhanced infection control compliance, patient cohorting, and weekly perirectal surveillance cultures of patients in the outbreak units until no new cases were identified.
Experience from the outbreak in Puerto Rico and elsewhere (notably Israel) suggests that early detection through use of targeted surveillance and introduction of strict infection control measures (including reinforcement of hand hygiene and contact precautions) can help control the spread of CRKP (7). Other recent reports have demonstrated that microbiologic surveillance for CRKP can be accomplished using brothbased culture techniques that are widely available and also by in-house prepared molecular techniques and a commercial chromogenic agar (4,7-9); however, the latter two methods are not currently approved by the Food and Drug Administration. The screening tests used in several studies were performed on rectal or perirectal swabs; limited data indicate that surveillance screening of stool specimens, rectal swabs, or perirectal swabs might produce higher yield than testing of other body sites (e.g., nares or skin) (9).
# CDC and HICPAC Recommendations
In light of the clinical and infection control challenges posed by CRE and advances in the ability to detect these pathogens, CDC and HICPAC have developed new guidance for CRE infection prevention and control in an effort to limit the further emergence of these organisms (Box). These recommendations are based on strategies outlined in the 2006 HICPAC guidelines for management of multidrug-resistant organisms in health-care settings (2).
All patients colonized or infected with CRE or carbapenemase-producing Enterobacteriaceae should be placed on contact precautions. Acute care facilities should establish a protocol, in conjunction with CLSI guidelines, to detect nonsusceptibility and carbapenemase production in Enterobacteriaceae, particularly Klebsiella spp. and Escherichia coli, and immediately alert epidemiology and infection control staff members if identified. All acute care facilities should review microbiology records for the preceding 6-12 months to ensure that previously unrecognized CRE cases have not occurred. If previously unrecognized cases are identified, facilities should conduct a point prevalence survey (a single round of active surveillance cultures) in units with patients at high risk (e.g., intensive care units, units where previous cases have been identified, and units where many patients are exposed to broad-spectrum antimicrobials) to identify any additional patients colonized with carbapenemresistant or carbapenemase-producing Klebsiella spp. and E. coli. The recommended surveillance culture methodology is aimed at detecting carbapenem resistance or carbapenemase production in Klebsiella spp. and E. coli only, because 1) this method facilitates performing the test in the microbiology laboratory without the use of molecular methods and 2) these organisms represent the majority of CRE encountered in the United States. When a case of hospital-associated CRE is identified, facilities should conduct a single round of active surveillance testing of patients with epidemiologic links to the CRE case (e.g., those patients in the same unit or patients who have been cared for by the same health-care personnel).
The goal of active surveillance is to identify undetected carriers of carbapenem-resistant or carbapenemase-producing Klebsiella spp. and E. coli. Identification of other cases among patients with epidemiologic links to persons with confirmed infection suggests patient-to-patient transmission (7); in such instances, infection prevention measures should be vigorously reinforced, and surveillance cultures repeated periodically (e.g., weekly) until no new cases are identified. Situations where periodic point prevalence surveys repeatedly fail to identify other colonized patients suggest that infection control measures at the facility are effective in controlling transmission.
In such instances, consideration should be given to halting active surveillance cultures in response to clinical cases and replacing them with periodic point prevalence surveys in units with patients at high risk to ensure that carbapenem-resistant or carbapenemase-producing Klebsiella spp. and E. coli do not reemerge.
Because the prevalence of CRE is low in the majority of U.S. hospitals, routine microbiologic surveillance of persons admitted, such as that performed in some facilities to detect carriage of methicillin-resistant Staphylococcus aureus, is not recommended. However, in some areas of the United States, notably New York City, CRE are routinely recovered, including from many patients who are admitted from the community. In these settings, point prevalence surveys in response to detected clinical cases might be less useful in controlling transmission of CRE. Facilities in regions where CRE are endemic should monitor clinical cases of CRE and implement the intensified (i.e., Tier 2) infection control strategies outlined in the 2006 HICPAC guidelines if rates of CRE are not decreasing (2). The challenges to hospitals of allocating additional resources to prevent and control CRE are balanced by the fact that an aggressive infection control strategy, such as that recommended in this report, offers an opportunity to limit the impact of these problematic pathogens while CRE prevalence remains low in most U.S. hospitals.
# Infection Prevention and Control
- All acute care facilities should implement contact precautions for patients colonized or infected with carbapenemresistant Enterobacteriaceae (CRE) or carbapenemase-producing Enterobacteriaceae. No recommendation can be made regarding when to discontinue contact precautions.
# Laboratory
- Clinical microbiology laboratories should follow Clinical and Laboratory Standards Institute guidelines for susceptibility testing (1) and establish a protocol for detection of carbapenemase production (e.g., performance of the modified Hodge test).
- Clinical microbiology laboratories should establish systems to ensure prompt notification of infection prevention staff of all Enterobacteriaceae isolates that are nonsusceptible to carbapenems or Klebsiella spp. or Escherichia coli isolates that test positive for a carbapenemase.
# Surveillance
- All acute care facilities should review clinical culture results for the preceding 6-12 months to determine whether previously unrecognized CRE have been present in the facility.
-If this review identifies previously unrecognized CRE, a point prevalence survey (a single round of active surveillance cultures) should be performed to look for CRE in high-risk units (e.g., intensive care units, units where previous cases have been identified, and units where many patients are exposed to broad-spectrum antimicrobials).
-If this review does not identify previously unrecognized CRE, monitoring for clinical infections should be continued.
- If CRE or carbapenemase-producing Klebsiella spp. or E. coli are detected from one or more clinical cultures OR if the point prevalence survey reveals unrecognized colonization, the facility should investigate for possible transmission by:
-Conducting active surveillance testing of patients with epidemiologic links to a patient with CRE infection (e.g., patients in the same unit or who have been cared for by the same health-care personnel).
Continue active surveillance periodically (e.g., weekly) until no new cases of colonization or infection suggesting cross-transmission are identified.
If transmission of CRE is not identified after repeated active surveillance testing, consider altering the surveillance strategy by performing periodic point prevalence surveys in high-risk units.
-In areas where CRE are endemic, an increased likelihood exists for importation of CRE, and the procedures outlined might not be sufficient to prevent transmission. Facilities in such areas should monitor clinical cases and consider additional strategies to reduce rates of CRE as described in the 2006 Tier 2 guidelines for management of multidrug-resistant organisms in health-care settings (2). Recommendations for rate calculations have been described previously (3).
# Notice to Readers
# World Water Day -March 22, 2009
Each year on March 22, World Water Day attracts international attention to the need to conserve and develop water resources. Shared Waters-Shared Opportunities, the theme for World Water Day 2009, focuses on issues associated with 263 lakes and river basins that cross the borders of two or more countries.
Worldwide, nearly one third of those 263 water basins are shared by three or more countries, and 19 are shared by five or more countries (1). Despite the complexity of these boundaries, hundreds of successful international transboundary agreements have been negotiated. The United Nations Educational, Scientific and Cultural Organization (UNESCO), the United Nations Economic Commission for Europe, and other organizations are working to ensure the peaceful collaboration of countries who share water systems (1).
Many countries lack resources to provide their inhabitants with safe drinking water and adequate sanitation. Approximately 880 million people still lack access to improved sources of drinking water (2), leaving them at risk for water-, sanitation-, and hygiene-related diseases. Worldwide, 1.6 million deaths per year result from unsafe water, poor sanitation, and lack of hygiene (3). Most of these deaths occur among children aged <5 years. The ongoing cholera epidemic in Zimbabwe (4), which has affected approximately 91,000 persons and caused more than 4,000 deaths (5) since it began in August 2008, is an example of the health risks of waterborne diseases, although most cases and fatalities resulting from waterborne diseases are never reported.
# Notice to Readers
# State Reportable Condition Assessment Results
The Council of State and Territorial Epidemiologists (CSTE) recently completed work on an assessment that captured information regarding which public health conditions were reportable by clinicians, laboratories, hospitals, or other public health reporters, as mandated by law or regulation in 50 U.S. states, four U.S. territories, and two autonomous reporting jurisdictions (New York City and the District of Columbia). A total of 255 conditions, including infectious conditions and noninfectious conditions (e.g., injuries, cancer, and workrelated conditions) were included in the assessment. Results for both the 2008 and 2007 assessments are available, using a web query tool, at / publichealthinformatics/statereportableconditionsqueryresults/tabid/261/default.aspx.
Feedback concerning the 2008 assessment or the web query tool should be directed to CSTE via e-mail ([email protected]). Subject matter experts at CDC or local or state health departments who are interested in helping CSTE develop requirements for the 2009 assessment may also notify CSTE at the same e-mail address. † Calculated by summing the incidence counts for the current week, the 2 weeks preceding the current week, and the 2 weeks following the current week, for a total of 5 preceding years. Additional information is available at . § Not notifiable in all states. Data from states where the condition is not notifiable are excluded from this table, except starting in 2007 for the domestic arboviral diseases and influenza-associated pediatric mortality, and in 2003 for SARS-CoV. Reporting exceptions are available at . ¶ Includes both neuroinvasive and nonneuroinvasive. Updated weekly from reports to the Division of Vector-Borne Infectious Diseases, National Center for Zoonotic, Vector-Borne, and Enteric Diseases (ArboNET Surveillance). Data for West Nile virus are available in Table II. The names of the reporting categories changed in 2008 as a result of revisions to the case definitions. Cases reported prior to 2008 were reported in the categories: Ehrlichiosis, human monocytic (analogous to E. chaffeensis); Ehrlichiosis, human granulocytic (analogous to Anaplasma phagocytophilum), and Ehrlichiosis, unspecified, or other agent (which included cases unable to be clearly placed in other categories, as well as possible cases of E. ewingii). † † Data for H. influenzae (all ages, all serotypes) are available in Table II. § § Updated monthly from reports to the Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. Implementation of HIV reporting influences the number of cases reported. Updates of pediatric HIV data have been temporarily suspended until upgrading of the national HIV/AIDS surveillance data management system is completed. Data for HIV/AIDS, when available, are displayed in Table IV
# QuickStats
- 1 0 - - 1 1 - SARS-CoV § , - - - - - - - - Smallpox § - - - - - - - - Streptococcal | In 2008, a total of 12,898 incident tuberculosis (TB) cases were reported in the United States; the TB rate declined 3.8% from 2007 to 4.2 cases per 100,000 population, the lowest rate recorded since national reporting began in 1953. This report summarizes provisional 2008 data from the National TB Surveillance System and describes trends since 1993. Despite this overall improvement, progress has slowed in recent years; the average annual percentage decline in the TB rate decreased from 7.3% per year during 1993-2000 to 3.8% during 2000-2008.* Foreign-born persons and racial/ethnic minorities continued to bear a disproportionate burden of TB disease in the United States. In 2008, the TB rate in foreignborn persons in the United States was 10 times higher than in U.S.-born persons. TB rates among Hispanics and blacks were nearly eight times higher than among non-Hispanic whites, and rates among Asians were nearly 23 times higher than among non-Hispanic whites. In 2008, among persons with TB whose country of origin was known, approximately 95% of Asians, 76% of Hispanics, 32% of blacks, and 18% of#
whites were foreign born. Among U.S.-born racial and ethnic groups, the greatest racial disparity in TB rates was for U.S.born blacks, whose rate was seven times higher than the rate for U.S.-born whites. Intensified efforts are needed to address the slowing decline in TB incidence and the persistent disparities that exist between U.S.-born and foreign-born persons and between whites and minorities in the United States.
Health departments in the 50 states and the District of Columbia (DC) electronically report to CDC verified TB cases that meet the CDC/Council of State and Territorial Epidemiologists case definition. † Reports include the patient's race, ethnicity (i.e., Hispanic or non-Hispanic), treatment information, and, whenever available, drug-susceptibility test results. CDC calculates national and state TB rates overall and by racial/ethnic group using current U.S. Census population estimates. U.S. Census annual estimates were used to calculate the national TB rate and the percentage change from 2007 to 2008. Population denominators used to calculate TB rates and percentage changes over time according to national origin (U.S.-born versus foreign-born persons) were from the U.S. Census Current Population Survey. A U.S.-born person was defined as someone born in the United States or its associated jurisdictions or someone born in a foreign country but having at least one U.S.-born parent. Persons not meeting this definition were classified as foreign born. For 2008, patients with unknown origin of birth represented 0.6% (74 of 12,898) of total cases. For this report, persons identified as white, black, Asian, American Indian/Alaska Native, native Hawaiian or other Pacific Islander, or of multiple races were all classified as non-Hispanic. Persons identified as Hispanic might be of any race.
In 2008, TB rates in the 51 reporting areas ranged from 0.5 (North Dakota) to 9.6 (Hawaii) cases per 100,000 population (median: 3.0 cases per 100,000 population) (Figure 1). Thirtythree states and DC had lower rates in 2008 than in 2007; however, 17 states had higher rates. Four states (California, Florida, New York, and Texas) reported more than 500 cases each for 2008, a decline from seven states with at least 500 cases in 2006 and five states in 2007. Combined, these four states accounted for approximately half (49.2% [6,349]) of all TB cases in 2008.
Among U.S.-born persons, the number and rate of TB cases continued to decline in 2008. The number of TB cases in U.S.-born persons (5,283 [or 41.2% of all cases in persons with known origin]) declined 3.9% compared with 2007 and 69.7% compared with 1993 (Figure 2). In 2008, the TB rate among U.S.-born persons was 2.0 per 100,000 population, § TB rate cutoff points were based on terciles: 18 states had TB case rates of <2.0 (range: 0.46-1.99) per 100,000, 17 states had TB case rates of 2.0-4.0 (range: 2.03-3.92) per 100,000, and 15 states and the District of Columbia had TB case rates of >4.0 (range: 4.02-9.63) per 100,000. DC <2.0 2.0-4.0 >4.0 § Editorial Note: In 2008, the number of TB cases and annual TB rate reached all-time lows in the United States. After the resurgence of TB during 1985-1992, the annual TB rate has steadily decreased. However, since 2000, the pace of that decline has slowed. To hasten the decline of TB in the United States, intensified efforts are required to address the disproportionately high rates of TB that persist among foreign-born persons and racial/ethnic minorities. The proportion of TB cases contributed by foreign-born persons has increased each year since 1993. This is a reflection of high rates of TB in countries of origin for U.S. immigrants. To help address this, in 2007, CDC issued revised technical instructions for TB screening and treatment among persons applying for immigration to the United States (3). The revision included instructions for 1) more comprehensive diagnostic testing among applicants (e.g., cultures and drug-susceptibility testing for persons with suspected TB); 2) the administration of directly observed therapy overseas, before entry into the United States; and 3) targeted tuberculin skin testing (before entry into the United States) of children from high-incidence countries and contacts of persons known to have TB. In addition, CDC continues to work with international partners, including the Stop TB Partnership, to strengthen TB control in countries with high TB incidence. For example, to facilitate patient referral and treatment among persons who cross the U.S.-Mexico border, bilateral initiatives (e.g., CureTB) are improving coordination of TB care between U.S. TB programs and Mexican counterparts. Modeling has suggested that U.S.-funded expansion of the directly observed treatment (short course) strategy in selected high-incidence countries (e.g., Mexico) might be a cost-saving approach to reducing TB-related morbidity and mortality among U.S. immigrants (4).
The proportion of TB cases that are multidrug resistant has remained approximately 1% of culture-positive cases since 1997; however, MDR TB has continued to disproportionately affect foreign-born persons in the United States. CDC continues to provide technical assistance to domestic and international partners to increase detection of MDR TB and improve access to second-line TB drugs (5). In 2008, TB rates declined for all racial/ethnic minorities, yet among the U.S. born, blacks continue to experience a disproportionately high rate of TB. CDC's TB Epidemiologic Studies Consortium currently is conducting studies to understand how to reduce TB in blacks effectively, including a study to identify barriers to treatment adherence for latent TB infection and TB disease and a study examining the determinants of early diagnosis, prevention, and treatment of TB.
The findings in this report are subject to at least two limitations. First, the analysis was based on provisional 2008 data that are subject to change. This applies to TB case counts and HIV testing results data, both of which were incomplete. Additional data might change the results marginally. Second, population denominator data were drawn from multiple U.S. census sources and are subject to periodic adjustment. CDC's annual TB surveillance summary, due to be published in fall 2009, will provide updated data.
To ensure that TB rates decline further in the United States, especially among foreign-born persons and minority populations, TB prevention and control capacity should be increased (6)(7)(8). Additional capacity should be used to 1) improve case management and contact investigations; 2) intensify outreach, testing, and treatment of high-risk and hard-to-reach populations; 3) enhance treatment and diagnostic tools; 4) increase scientific research to better understand TB transmission; and 5) continue collaboration with other nations to reduce TB globally. FSM comprises four states and more than 600 islands spread across 1 million square miles in the western Pacific Ocean. Half of the population of 108,000 lives in Chuuk, the largest state (2). TB is endemic in Chuuk, where 70 cases of TB were recorded in 2007. The 2007 incidence rate (127 TB cases per 100,000) is 29 times higher than the 2007 U.S. rate (3).
# Two Simultaneous
# Limited transportation hinders access to the only hospital in
Chuuk, which provides chest radiography and smear microscopy services to help diagnose TB. Culture confirmation, drug-susceptibility testing, and genotyping were not available routinely for TB cases in FSM until January 2006, when referral laboratories in Hawaii and California began to offer these services. Before 2008, the state's geography, combined with limited TB program staffing, precluded active case-finding via routine contact investigations or the administration of DOT, a cornerstone of TB treatment that improves completion of therapy and prevents the emergence of drug resistance. Before July 2008, TB patients were identified as they showed signs or symptoms of TB disease at the local clinic or hospital; all received self-administered therapy. FSM's National TB Program has an annual budget of $170,000, and second-line drugs for treating MDR TB were not available because of funding constraints.
In June 2007, pulmonary TB was diagnosed in a Chuuk resident aged 37 years. Sputum-smear microscopy detected acid-fast bacilli, and a chest radiograph showed lung cavitation, both indicators of contagiousness. In November 2007, drug-susceptibility test results confirmed multidrug resistance. The patient did not have access to second-line drugs and died. During December 2007-June 2008, four additional patients with MDR TB disease came to the local clinic or hospital. None of the four patients were treated with second-line drugs; three died, including a child aged 2 years. In May 2008, FSM authorities requested CDC assistance because of the 80% fatality rate and evidence of recent MDR TB transmission.
A confirmed case was defined as laboratory-confirmed MDR TB disease in a Chuuk resident during January 2006-June 2008. A suspected case of MDR TB disease was defined as exposure (based on intensity and duration of contact) to a patient with confirmed TB and clinical findings of TB disease (i.e., laboratory confirmation pending). Patients (or proxies for deceased patients) were interviewed and laboratory and medical records reviewed.
The July 2008 investigation focused on the initial five confirmed MDR TB cases. All patients were born in Chuuk; their median age was 16 years (range: 2-37 years), and four were female. None of the patients had a history of TB disease or treatment with TB drugs. All five patients had pulmonary TB, two with cavitation on chest radiograph and hemoptysis. None of the four patients who died before the investigation had been tested for human immunodeficiency virus (HIV) infection; the surviving patient had a negative HIV test result in July 2008. Two distinct clusters, associated with two different villages, were identified based on genotypes and drug-susceptibility patterns (Figure).
In the first cluster of three cases, Mycobacterium tuberculosis isolates had a matching genotype and resistance to five drugs: isoniazid, rifampin, pyrazinamide, ethambutol, and streptomycin. This drug-susceptibility pattern had not been seen in Chuuk since routine drug-susceptibility testing became available in January 2006. The index patient in this cluster had worked during 1987-2000 in the garment industry in the Commonwealth of the Northern Mariana Islands (Saipan), which employs migrants from Southeast Asian countries (4) where MDR TB is common (5).
In the second cluster of two cases, the isolates had a matching genotype and resistance to three drugs: isoniazid, rifampin, and ethionamide. The two patients were cousins whose extended family included five persons who previously had TB disease with isolates genotypically matched to those of the outbreak patients. However, the earlier isolates had resistance to isoniazid and ethionamide only. These five previous cases of non-MDR TB were diagnosed from January 2006, when genotyping became routinely available in Chuuk, to October 2007. Household caregivers reported that the five patients had self-administered therapy inconsistently or incompletely.
During investigations of the five initial cases of MDR TB disease, a standardized clinical examination, chest radiography, and tuberculin skin testing were used to evaluate contacts for TB disease and latent TB infection (6). The 205 named contacts, of whom 163 (80%) were household members and 42 (20%) were health-care workers, had a median age of 20 years (range: 4 months-62 years), and 117 (57%) were female. During July 1, 2008-March 13, 2009, three additional MDR TB cases were confirmed among household members (Figure ), including a household contact aged 4 years who in November 2008 died of meningitis later confirmed to be caused by MDR TB. Based on history of household exposure to a patient with confirmed TB and clinical findings (e.g., chest radiography consistent with TB disease), 13 other suspected cases of MDR TB disease were identified; all 13 patients began treatment based on the drug-susceptibility results of the respective source case (Table ). Although fewer than one third of the contacts were aged <15 years (60 of 205), they accounted for more than half of the suspected and confirmed MDR TB cases since July 2008 (nine of 16). Latent TB infection was diagnosed in 124 (60%) contacts, although many of the adults were probably infected before this documented emergence of MDR TB in Chuuk. Among contacts aged <15 years, 20 (33%) of 60 had latent TB infection. All household contacts with latent TB infection have begun receiving second-line drugs based on the drug-susceptibility results of the respective source case (1,7).
Multiple (9) have resulted in the following actions: 1) a consistent supply of fluoroquinolones, aminoglycosides, and other second-line drugs was procured; 2) Chuuk State Hospital added a separate ward for inpatient treatment of patients with TB; 3) TB program staff members received on-site training on providing DOT and conducting contact investigations; 4) nine new outreach workers were hired to administer DOT, and three vehicles were acquired to help workers investigate contacts; 5) the hospital laboratory was equipped for processing specimens for smear microscopy daily and shipping specimens for culture and drug-susceptibility testing weekly. For 2008, the improved case-detection capacity increased the recorded TB incidence to 204 cases per 100,000 persons. The Chuuk TB program is consulting with U.S. MDR TB experts by telephone and e-mail for assistance with complex treatment decisions, and implementing measures to prevent the selection of drug-resistant strains and reduce all TB transmission. Editorial Note: These two clusters of MDR TB represent two distinct outbreaks and illustrate two mechanisms for the emergence of drug resistance. In the first outbreak, the index patient had not been treated previously for TB and probably became infected with a MDR TB strain before returning to Chuuk in 2000 from Saipan; this case illustrates primary (i.e., initial) drug resistance. In the second outbreak, lack of DOT for the five family members with TB disease initially resistant to only isoniazid and ethionamide probably led to secondary (i.e., acquired) rifampin resistance. At least one of these five previous patients thus acquired multidrug resistance and transmitted MDR TB to the index case in the second outbreak.
The emergence and transmission of MDR TB in these outbreaks were caused by the inability to follow standard TB control practices or to provide appropriate drugs. The findings also highlight the vulnerability of pediatric contacts and the challenges of diagnosing and treating MDR TB in resource-limited settings. Laboratory capacity and access to second-line TB drugs are fundamental to controlling MDR TB (1), and finding and curing all persons with TB is critical for interrupting transmission (8). Contact investigations enable active case-finding and early identification of recently infected contacts at highest risk for developing TB disease. Infection control practices (e.g., isolating contagious patients initially during treatment and wearing appropriate personal protective equipment) can prevent transmission of susceptible and drug-resistant TB, and are particularly important in congregate settings such as clinics, hospitals, and prisons. Uniform DOT for patients with TB disease prevents acquired drug resistance (5) and, where feasible, DOT should be offered for contacts with latent TB infection as well.
The measures implemented in response to the MDR TB outbreaks in Chuuk have reflected all five aspects of the WHO global response plan for drug-resistant TB (10), which calls for augmenting the public health infrastructure to control TB, strengthening laboratory services for early diagnosis, improving surveillance to better understand drug resistance, implementing infection control to prevent transmission, and enhancing management of drug-resistant TB cases to reach the Global Plan to Stop TB 2006-2015 goals. † Tangible progress in treating and preventing the spread of TB has been made in Chuuk as recommendations from the investigation have been implemented.
In 2008, an estimated 500,000 persons in the world developed MDR TB, largely as a result of inadequate TB control activities (5). In many countries where TB is endemic, ongoing transmission of multiple strains of MDR TB probably will be discovered as access to laboratory services improves (10). The challenge of primary drug resistance is likely to be exacerbated further by the increasing numbers of migratory and displaced populations (4). Many developing countries provide free firstline TB drugs through TB control programs. However, effective and sustainable mechanisms for access to expensive second-line TB drugs are needed for timely treatment of patients with drug-resistant TB. The multiagency response to the MDR TB outbreaks in Chuuk is a good example of the coordinated efforts that are needed to control MDR TB in many developing countries. As in Chuuk, a concerted focus on improving access to enhanced laboratory services and second-line TB drugs, and building local capacity for finding, diagnosing, and curing all forms of TB is necessary to address the global threat of MDR TB.
# Guidance for Control of Infections with Carbapenem-Resistant or Carbapenemase-Producing Enterobacteriaceae in Acute Care Facilities
Infection with carbapenem-resistant Enterobacteriaceae (CRE) or carbapenemase-producing Enterobacteriaceae is emerging as an important challenge in health-care settings (1). Currently, carbapenem-resistant Klebsiella pneumoniae (CRKP) is the species of CRE most commonly encountered in the United States. CRKP is resistant to almost all available antimicrobial agents, and infections with CRKP have been associated with high rates of morbidity and mortality, particularly among persons with prolonged hospitalization and those who are critically ill and exposed to invasive devices (e.g., ventilators or central venous catheters). This report provides updated recommendations from CDC and the Healthcare Infection Control Practices Advisory Committee (HICPAC) for the control of CRE or carbapenemase-producing Enterobacteriaceae in acute care (inpatient) facilities. For all acute care facilities, CDC and HICPAC recommend an aggressive infection control strategy, including managing all patients with CRE using contact precautions and implementing Clinical and Laboratory Standards Institute (CLSI) guidelines for detection of carbapenemase production. In areas where CRE are not endemic, acute care facilities should 1) review microbiology records for the preceding 6-12 months to determine whether CRE have been recovered at the facility, 2) if the review finds previously unrecognized CRE, perform a point prevalence culture survey in high-risk units to look for other cases of CRE, and 3) perform active surveillance cultures of patients with epidemiologic links to persons from whom CRE have been recovered. In areas where CRE are endemic, an increased likelihood exists for imporation of CRE, and facilities should consider additional strategies to reduce rates of CRE (2). Acute care facilities should review these recommendations and implement appropriate strategies to limit the spread of these pathogens.
For CRKP, the most important mechanism of resistance is the production of a carbapenemase enzyme, bla kpc . The gene that encodes the bla kpc enzyme is carried on a mobile piece of genetic material (transposon), which increases the risk for dissemination. Since first described in North Carolina in 1999, CRKP has been identified in 24 states and is recovered routinely in certain hospitals in New York and New Jersey (3). Analysis of 2007 data regarding health-care-associated infections reported to CDC indicated that 8% of all Klebsiella isolates were CRKP, compared with fewer than 1% in 2000 (CDC, unpublished data, 2008). CRKP poses significant treatment challenges, and CRKP infections have been associated with increased mortality, length of stay, and increased cost (4). The emergence and spread of CRKP and other types of CRE is another in a series of worrisome public health developments regarding antimicrobial resistance among gram-negative bacteria and underscores the immediate need for aggressive detection and control strategies (5).
A difficulty in detecting CRE is the fact that some strains that harbor bla kpc have minimal inhibitory concentrations (MICs) that are elevated but still within the susceptible range for carbapenems. Because these strains are susceptible to carbapenems, they are not identified as potential clinical or infection control risks using current susceptibility testing guidelines. To address this challenge, in January 2009, CLSI published a recommendation that carbapenem-susceptible Enterobacteriaceae with elevated MICs or reduced disk diffusion zone sizes be tested for the presence of carbapenemases using the modified Hodge test (MHT) (6). The MHT is a phenotypic test used to detect carbapenemases in isolates demonstrating elevated but susceptible carbapenem MICs and has demonstrated sensitivity and specificity exceeding 90% in identifying carbapenemase-producing Enterobacteriaceae (6). If the MHT reveals the presence of a carbapenemase, CLSI recommends that a comment be added to the microbiology report to inform clinicians and infection preventionists. Because treatment information on MHT-positive, carbapenem-susceptible isolates is limited, CLSI guidelines do not recommend any changes regarding the reporting of susceptibility results themselves. Strains of Enterobacteriaceae that test intermediate or resistant to carbapenems should be reported as such and do not need to be subjected to the MHT.
Patients with unrecognized CRKP colonization have served as reservoirs for transmission during health-care-associated outbreaks (7). For example, during an outbreak of 39 cases of CRKP infection in a hospital in Puerto Rico in 2008, in addition to a review of infection control practices, active surveillance cultures were performed on patients in the same units as persons with confirmed CRKP infection. Cultures performed on 30 patients in the intensive care unit revealed two colonized patients who were not previously known to harbor CRKP and were not placed in contact precautions (CDC, unpublished data, 2008). Control of the outbreak was hindered by lack of compliance with infection control practices. Health-care personnel adherence to recommendations for gown and glove use was low (62%) at the hospital, and appropriate hand hygiene (i.e., hand washing or using a waterless alcohol-based hand rub before and after patient contact) was observed in only 48% of patient encounters. The hospital eventually was able to control the outbreak through enhanced infection control compliance, patient cohorting, and weekly perirectal surveillance cultures of patients in the outbreak units until no new cases were identified.
Experience from the outbreak in Puerto Rico and elsewhere (notably Israel) suggests that early detection through use of targeted surveillance and introduction of strict infection control measures (including reinforcement of hand hygiene and contact precautions) can help control the spread of CRKP (7). Other recent reports have demonstrated that microbiologic surveillance for CRKP can be accomplished using brothbased culture techniques that are widely available and also by in-house prepared molecular techniques and a commercial chromogenic agar (4,7-9); however, the latter two methods are not currently approved by the Food and Drug Administration. The screening tests used in several studies were performed on rectal or perirectal swabs; limited data indicate that surveillance screening of stool specimens, rectal swabs, or perirectal swabs might produce higher yield than testing of other body sites (e.g., nares or skin) (9).
# CDC and HICPAC Recommendations
In light of the clinical and infection control challenges posed by CRE and advances in the ability to detect these pathogens, CDC and HICPAC have developed new guidance for CRE infection prevention and control in an effort to limit the further emergence of these organisms (Box). These recommendations are based on strategies outlined in the 2006 HICPAC guidelines for management of multidrug-resistant organisms in health-care settings (2).
All patients colonized or infected with CRE or carbapenemase-producing Enterobacteriaceae should be placed on contact precautions. Acute care facilities should establish a protocol, in conjunction with CLSI guidelines, to detect nonsusceptibility and carbapenemase production in Enterobacteriaceae, particularly Klebsiella spp. and Escherichia coli, and immediately alert epidemiology and infection control staff members if identified. All acute care facilities should review microbiology records for the preceding 6-12 months to ensure that previously unrecognized CRE cases have not occurred. If previously unrecognized cases are identified, facilities should conduct a point prevalence survey (a single round of active surveillance cultures) in units with patients at high risk (e.g., intensive care units, units where previous cases have been identified, and units where many patients are exposed to broad-spectrum antimicrobials) to identify any additional patients colonized with carbapenemresistant or carbapenemase-producing Klebsiella spp. and E. coli. The recommended surveillance culture methodology is aimed at detecting carbapenem resistance or carbapenemase production in Klebsiella spp. and E. coli only, because 1) this method facilitates performing the test in the microbiology laboratory without the use of molecular methods and 2) these organisms represent the majority of CRE encountered in the United States. When a case of hospital-associated CRE is identified, facilities should conduct a single round of active surveillance testing of patients with epidemiologic links to the CRE case (e.g., those patients in the same unit or patients who have been cared for by the same health-care personnel).
The goal of active surveillance is to identify undetected carriers of carbapenem-resistant or carbapenemase-producing Klebsiella spp. and E. coli. Identification of other cases among patients with epidemiologic links to persons with confirmed infection suggests patient-to-patient transmission (7); in such instances, infection prevention measures should be vigorously reinforced, and surveillance cultures repeated periodically (e.g., weekly) until no new cases are identified. Situations where periodic point prevalence surveys repeatedly fail to identify other colonized patients suggest that infection control measures at the facility are effective in controlling transmission.
In such instances, consideration should be given to halting active surveillance cultures in response to clinical cases and replacing them with periodic point prevalence surveys in units with patients at high risk to ensure that carbapenem-resistant or carbapenemase-producing Klebsiella spp. and E. coli do not reemerge.
Because the prevalence of CRE is low in the majority of U.S. hospitals, routine microbiologic surveillance of persons admitted, such as that performed in some facilities to detect carriage of methicillin-resistant Staphylococcus aureus, is not recommended. However, in some areas of the United States, notably New York City, CRE are routinely recovered, including from many patients who are admitted from the community. In these settings, point prevalence surveys in response to detected clinical cases might be less useful in controlling transmission of CRE. Facilities in regions where CRE are endemic should monitor clinical cases of CRE and implement the intensified (i.e., Tier 2) infection control strategies outlined in the 2006 HICPAC guidelines if rates of CRE are not decreasing (2). The challenges to hospitals of allocating additional resources to prevent and control CRE are balanced by the fact that an aggressive infection control strategy, such as that recommended in this report, offers an opportunity to limit the impact of these problematic pathogens while CRE prevalence remains low in most U.S. hospitals.
# Infection Prevention and Control
• All acute care facilities should implement contact precautions for patients colonized or infected with carbapenemresistant Enterobacteriaceae (CRE) or carbapenemase-producing Enterobacteriaceae. No recommendation can be made regarding when to discontinue contact precautions.
# Laboratory
• Clinical microbiology laboratories should follow Clinical and Laboratory Standards Institute guidelines for susceptibility testing (1) and establish a protocol for detection of carbapenemase production (e.g., performance of the modified Hodge test).
• Clinical microbiology laboratories should establish systems to ensure prompt notification of infection prevention staff of all Enterobacteriaceae isolates that are nonsusceptible to carbapenems or Klebsiella spp. or Escherichia coli isolates that test positive for a carbapenemase.
# Surveillance
• All acute care facilities should review clinical culture results for the preceding 6-12 months to determine whether previously unrecognized CRE have been present in the facility.
-If this review identifies previously unrecognized CRE, a point prevalence survey (a single round of active surveillance cultures) should be performed to look for CRE in high-risk units (e.g., intensive care units, units where previous cases have been identified, and units where many patients are exposed to broad-spectrum antimicrobials).
-If this review does not identify previously unrecognized CRE, monitoring for clinical infections should be continued.
• If CRE or carbapenemase-producing Klebsiella spp. or E. coli are detected from one or more clinical cultures OR if the point prevalence survey reveals unrecognized colonization, the facility should investigate for possible transmission by:
-Conducting active surveillance testing of patients with epidemiologic links to a patient with CRE infection (e.g., patients in the same unit or who have been cared for by the same health-care personnel).
Continue active surveillance periodically (e.g., weekly) until no new cases of colonization or infection suggesting cross-transmission are identified.
If transmission of CRE is not identified after repeated active surveillance testing, consider altering the surveillance strategy by performing periodic point prevalence surveys in high-risk units.
-In areas where CRE are endemic, an increased likelihood exists for importation of CRE, and the procedures outlined might not be sufficient to prevent transmission. Facilities in such areas should monitor clinical cases and consider additional strategies to reduce rates of CRE as described in the 2006 Tier 2 guidelines for management of multidrug-resistant organisms in health-care settings (2). Recommendations for rate calculations have been described previously (3).
# Notice to Readers
# World Water Day -March 22, 2009
Each year on March 22, World Water Day attracts international attention to the need to conserve and develop water resources. Shared Waters-Shared Opportunities, the theme for World Water Day 2009, focuses on issues associated with 263 lakes and river basins that cross the borders of two or more countries.
Worldwide, nearly one third of those 263 water basins are shared by three or more countries, and 19 are shared by five or more countries (1). Despite the complexity of these boundaries, hundreds of successful international transboundary agreements have been negotiated. The United Nations Educational, Scientific and Cultural Organization (UNESCO), the United Nations Economic Commission for Europe, and other organizations are working to ensure the peaceful collaboration of countries who share water systems (1).
Many countries lack resources to provide their inhabitants with safe drinking water and adequate sanitation. Approximately 880 million people still lack access to improved sources of drinking water (2), leaving them at risk for water-, sanitation-, and hygiene-related diseases. Worldwide, 1.6 million deaths per year result from unsafe water, poor sanitation, and lack of hygiene (3). Most of these deaths occur among children aged <5 years. The ongoing cholera epidemic in Zimbabwe (4), which has affected approximately 91,000 persons and caused more than 4,000 deaths (5) since it began in August 2008, is an example of the health risks of waterborne diseases, although most cases and fatalities resulting from waterborne diseases are never reported.
# Notice to Readers
# State Reportable Condition Assessment Results
The Council of State and Territorial Epidemiologists (CSTE) recently completed work on an assessment that captured information regarding which public health conditions were reportable by clinicians, laboratories, hospitals, or other public health reporters, as mandated by law or regulation in 50 U.S. states, four U.S. territories, and two autonomous reporting jurisdictions (New York City and the District of Columbia). A total of 255 conditions, including infectious conditions and noninfectious conditions (e.g., injuries, cancer, and workrelated conditions) were included in the assessment. Results for both the 2008 and 2007 assessments are available, using a web query tool, at http://www.cste.org/dnn/programsandactivities/ publichealthinformatics/statereportableconditionsqueryresults/tabid/261/default.aspx.
Feedback concerning the 2008 assessment or the web query tool should be directed to CSTE via e-mail ([email protected]). Subject matter experts at CDC or local or state health departments who are interested in helping CSTE develop requirements for the 2009 assessment may also notify CSTE at the same e-mail address. † Calculated by summing the incidence counts for the current week, the 2 weeks preceding the current week, and the 2 weeks following the current week, for a total of 5 preceding years. Additional information is available at http://www.cdc.gov/epo/dphsi/phs/files/5yearweeklyaverage.pdf. § Not notifiable in all states. Data from states where the condition is not notifiable are excluded from this table, except starting in 2007 for the domestic arboviral diseases and influenza-associated pediatric mortality, and in 2003 for SARS-CoV. Reporting exceptions are available at http://www.cdc.gov/epo/dphsi/phs/infdis.htm. ¶ Includes both neuroinvasive and nonneuroinvasive. Updated weekly from reports to the Division of Vector-Borne Infectious Diseases, National Center for Zoonotic, Vector-Borne, and Enteric Diseases (ArboNET Surveillance). Data for West Nile virus are available in Table II. ** The names of the reporting categories changed in 2008 as a result of revisions to the case definitions. Cases reported prior to 2008 were reported in the categories: Ehrlichiosis, human monocytic (analogous to E. chaffeensis); Ehrlichiosis, human granulocytic (analogous to Anaplasma phagocytophilum), and Ehrlichiosis, unspecified, or other agent (which included cases unable to be clearly placed in other categories, as well as possible cases of E. ewingii). † † Data for H. influenzae (all ages, all serotypes) are available in Table II. § § Updated monthly from reports to the Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. Implementation of HIV reporting influences the number of cases reported. Updates of pediatric HIV data have been temporarily suspended until upgrading of the national HIV/AIDS surveillance data management system is completed. Data for HIV/AIDS, when available, are displayed in Table IV
# QuickStats
- 1 0 - - 1 1 - SARS-CoV § , **** - - - - - - - - Smallpox § - - - - - - - - Streptococcal
# Acknowledgments
The findings in this report are based, in part, on data contributed by state and local TB control officials.
# Acknowledgments
The findings in this report are based, in part, on contributions by M Kawamura, MD, Francis J.
#
in the United States, most of which have populations of >100,000. A death is reported by the place of its occurrence and by the week that the death certificate was filed. Fetal deaths are not included. † Pneumonia and influenza. § Because of changes in reporting methods in this Pennsylvania city, these numbers are partial counts for the current week. Complete counts will be available in 4 to 6 weeks. ¶ Total includes unknown ages. | None | None |
8c25cc5615b9ca3feaeae48adb7020f4f9c2cf82 | cdc | None | Reviewer No. 1: COMMENT: I have reviewed both documents and agree with the recommendations. I don't have substantive changes to suggest. Please see the attached for a suggestion about removing two comma splices.Thanks for taking the time to review the documents. The suggested edits were made to the policy document.COMMENT: I've reviewed the documents and recommendations, and I find them to be fair, well crafted, and appropriately extensive. I support them in their current form and in their entirety, and I do not have edits to recommend. From the perspective of a practicing urologist, I would say that great benefit will be derived from such a clear statement indicating efficacy not only in potentially preventing HIV but also of other STDs and health conditions likely related to STDs in a care environment that is increasingly limiting. Another great potential benefit to be derived will be in increasing acceptance of male circumcision in a historical era of increasing opposition.Thanks for taking the time to review the documents and provide comments.Note from CDC: Reviewer No. 3 has provided three sections of commentary: (1) general comments regarding the CDC recommendations, (2) comments pertaining to specific text of the CDC recommendations, and (3) summary comments about each section of the CDC background document. A response has been provided to each main point in the general comments on the CDC recommendations (1) and to each comment about specific text in the draft recommendations (2). A summary response has been provided at the beginning commentary on the CDC background document (3). Citations pertaining to comments from peer reviewer No. 3 are located on pages 140 -208. Citations pertaining to responses from CDC are located on pages 209-212. CDC thanks the reviewer for taking the time to review the documents and providing extensive comments.COMMENT: This peer-review of the Centers for Disease Control and Prevention's (CDC's) Draft Recommendations and Background Documents was generated after December 2, 2014 when the documents first became available. Because of the limited time in which to review and comment on these documents, there may be some topics that could have been addressed more completely, some topics that were addressed more than once, and some citations that may be missing. In the interest of time, the citations given in the review may not be sequenced properly, but each citation should be properly identified. There may be some grammatical and typographical errors because there was insufficient time to identify and correct them. The comments addressing the Recommendations draft are made in direct response to the statements in that draft and appear in italics. The evaluation of the Background draft does not use the statement-bystatement format. This is a peer-review of draft documents and the comments are directed at these documents. It may be helpful for the reader to have copies of the drafts available. Several things are remarkable about this draft.The CDC recommendations are intended to assist medical providers in the United States in counseling individuals on the health risks and benefits of medical male circumcision. Male circumcision policy in non-US settings is outside the scope of the CDC recommendations. COMMENT: Sixth, it took over seven years for the CDC to produce a substandard, scientifically unacceptable product, nearly identical in content to what was presented at the 2007 consultation.No response. This comment does not address the content of the CDC recommendations or background document. COMMENT: Finally, the most remarkable thing is that the CDC is recommending clinicians and health care providers relay information that is counterfactual, incomplete, and biased to medical decision makers. In essence, they are deliberately encouraging health care providers to misinform their patients and thus commit medical malpractice.See RESPONSE 1 and RESPONSE 6.The CDC needs to throw out this draft and start again from scratch, this time without a preconceived conclusion in mind.No response. This comment does not address the content of the CDC recommendations or background document. COMMENT: They need to review the entire medical literature, thoroughly scrutinize the studies in the literature, and properly apply basic epidemiological principles.See RESPONSES 1, 2, 4, and 6. COMMENT: When they have done so, they need to consult with experts from around the world to make sure their findings are not culturally biased. They also need to focus on the United States, not Africa.These recommendations are for U.S. providers. Data from Africa is pertinent to the discussion in these recommendations.The following comments are made in response to incorrect and/or misleading statements contained in the "Recommendations" section of the draft by the CDC. In most cases, these issues are discussed in further detail in the review of the "Background" document. CDC draft: These recommendations are intended to assist health care providers in the United States who are counseling men and parents of male infants in decision making about male circumcision conducted by health care providers (i.e. medically performed) as it relates to the prevention of human immunodeficiency virus (HIV) infection, sexually transmitted infections (STIs), and other health outcomes. Reviewer Comment: If the target audience is health care providers in the United States, why is so much of the Background Draft directed at what is happening in Africa? RESPONSE 10: A majority of research on the health risks and benefits of medical male circumcision, including the 3 randomized controlled trials, has been carried out in sub-Saharan Africa due to a high prevalence of HIV, low prevalence of male circumcision in some areas, and a generalized epidemic largely driven by heterosexual transmission. The few studies on the effect of male circumcision on HIV and other STIs in the United States are also included in the CDC background document. The benefits and drawbacks of applying evidence from African settings to the HIV epidemic in the United States are also addressed in the CDC background document. CDC draft: Such decision making is made in the context of not only health considerations, but also other social, cultural, ethical, and religious factors. Reviewer Comment: Why should these factors be a consideration of the CDC or health care providers? Is the CDC suggesting that health care providers take on the role of shaman or cultural broker? Are these other considerations the real impetus for promoting male circumcision? RESPONSE 11: CDC is not suggesting that "healthcare providers should take on the role of shaman or health broker." The CDC recommendations provide counseling messages on health risks and benefits of medical male circumcision for healthcare providers to use when discussing male circumcision with patients and parents of male children. The recommendations acknowledge that decisions whether to circumcise are made by the individuals, not the health providers. Individuals may consider social, cultural, ethical, and religious factors in addition to the health risks and benefits that they have discussed with their provider when considering male circumcision. COMMENT: CDC draft: Although data have been accumulating about infant male circumcision for many years, clinical trials conducted in Africa between 2005-2010 have demonstrated safety and significant efficacy of voluntary adult male circumcision performed by clinicians for reducing the risk of acquisition of human immunodeficiency virus (HIV) by a male during penile-vaginal sex ("heterosexual sex"). Reviewer Comment: The clinical trials referred to did not assess the risk of acquisition of HIV by a male during penile-vaginal sex as these trials made no effort to determine the source of the infections they diagnosed during the course of the trials. These infections could have been from male-to-male sexual contact or from iatrogenic sources. Data from within these trials indicate that about 1/3 to 1/2 of the infections diagnosed during the trials were transmitted through non-sexual means. RESPONSE 12: Heterosexual transmission of HIV is the primary route of transmission in Kenya, South Africa, and Uganda, the 3 countries where the RCTs were conducted_ENREF_2. Due to the nature of the epidemics in these locations, there is no indication that a substantial number of HIV infections was caused by non-heterosexual means. Random assignment to the study arms in each of the trials would also ensure that populations in each arm were comparable, and that risk of exposure to HIV through male-male sexual intercourse or other sources would be equally distributed between the groups. Reported sexual history and risk behavior was similar in experimental and control arms of each RCT at baseline. COMMENT: Furthermore, these trials have nothing to do with infants, and infant male circumcision is never voluntary because the infant cannot give consent. RESPONSE 13: Parents or guardians are able to provide consent on behalf of infants. COMMENT: CDC draft: Three randomized clinical trials showed that adult male circumcision reduced HIV infection risk by 50-60% over time. Reviewer Comment: Reporting the results in this manner is misleading. It needs to be stated that the reduction reported here is the relative risk reduction. What is of clinical importance is the absolute risk reduction, which in the case of these trials overall was 1.3%. This is the number that should be reported instead of the relative risk reduction. As the incidence of HIV infection in the United States is much smaller than in Africa, one would expect that if male circumcision were effective in the United States, which has never been demonstrated, the absolute risk reduction would be quite a bit smaller. Again, the source of infection was not determined in the African studies making the results suspect and likely meaningless. RESPONSE 14: Relationships between exposures and health outcomes are commonly presented as relative risks. An example is provided in the methods section in the CDC recommendations to demonstrate how to interpret relative risk reductions. Individual, absolute risk is dependent on a number of factors, and appropriate denominators are not always available to establish an absolute risk for HIV and other STIs in specific subpopulations. See RESPONSE 12 for discussion to source of HIV infection. COMMENT: CDC draft: These trials also found that medically performed adult male circumcision reduced the risk of men acquiring two common sexually transmitted infections (STIs), herpes simplex virus type-2 (HSV-2) and types of human papilloma virus (HPV) that can cause penile and other anogenital cancers, by 30%. Reviewer Comment: These trials were methodologically flawed. For both HSV-2 and HPV, the trials failed to adjust for lead-time bias. By doing so, the findings for HSV-2 are no longer statistically significant. For HPV, the two trials only sampled the head of the RESPONSE 16: See RESPONSE 9. The fact that some western national medical organizations outside of the U.S. have differing views of infant male circumcision from similar organizations in the United States may be a result of cultural differences in how male circumcision is viewed. 10 COMMENT: CDC draft: Much of the data related to HIV and STI prevention are from randomized clinical trials (RCTs) conducted among men in sub-Saharan Africa in regions with high rates of heterosexually acquired HIV infection. Reviewer Comment: Three randomized clinical trials have been performed, which were basically one trial in three locations of Africa. There are over 100 other populations in which the association between HIV incidence or prevalence and male circumcision status has been assessed. Consequently, very little of the data available on HIV and STI prevention has come from the RCTs. As mentioned above, it is not known whether the infections in the RCTs were heterosexually acquired because the source of infection in these men was not determined. There is much more to this issue than is being presented here by the CDC. Some have argued that the randomized clinical trials were unnecessary since it was known prior to the trials that male circumcision did not have an impact on HIV prevalence at the country level in several countries in Africa. Please read the response in the Background document.See RESPONSE 1 and RESPONSE 6. COMMENT: CDC draft: While such factors limit the impact of medically performed male circumcision in reducing the overall HIV epidemic in the U.S., there is epidemiological data to suggest that some subpopulations in the U.S. are likely to benefit.The data indicate that the only subpopulation in the United States that has seen an association between male circumcision and HIV prevalence were the males whose regular female sexual partners were HIV-positive. These data were from a very small subpopulation from a single study, the results of which were not robust and have not been confirmed by other studies. Without such confirmation, the benefit for HIV-negative men who have HIV-positive female sexual partners remains to be seen.See RESPONSE 4.Modeling by the CDC indicates that such men are unlikely to benefit from male circumcision, RESPONSE: See RESPONSE 3. COMMENT: ….and the standard recommendation for these men is to always use condoms, consider pre-exposure prophylaxis, and to have the female partner lower her HIV viral load with anti-retroviral medications. RESPONSE 17: Evidence from randomized controlled trials, ecological studies, crosssectional studies, and systematic reviews has demonstrated the protective effects of male circumcision against female-to-male sexual transmission of HIV and other STIs. A circumcised man who has sexual intercourse with a woman who is infected with HIV is less likely to acquire HIV than an uncircumcised man, but he is not completely protected from HIV. The CDC recommendations discuss counseling on male circumcision in addition to, not in place of, other evidence-based HIV prevention interventions for individuals who engage in high-risk sexual behavior. Because no HIV prevention intervention is 100% effective, utilizing a combination of interventions is the most successful approach to prevent HIV transmission. Male circumcision is unique among HIV prevention interventions in that it is a single procedure that confers lifelong protection against HIV, and is a valuable addition to the HIV prevention portfolio. COMMENT: Therefore, it appears that this CDC draft is not actually about decreasing HIV infection, but about some other underlying premise or other motivation. RESPONSE: See RESPONSE 6. COMMENT: CDC draft: In addition, African-American and Hispanic men have higher risk of HIV infection and lower male circumcision rates than men of other race/ethnicities. Reviewer Comment: African-American men have a higher prevalence of HIV than Hispanic men and also a much higher male circumcision rate. In several studies, the male circumcision rate in African-American men is similar or higher than the male circumcision rate in non-Hispanic Caucasian men. RESPONSE 18: Several studies conducted in the United States have demonstrated an association between male circumcision and lower HIV prevalence. A study of heterosexual African-American men attending an STI clinic in the United States observed male circumcision status was associated with a substantial and significant reduction in HIV prevalence. As stated in the CDC recommendations introduction section, African-American and Hispanic men have higher risk of HIV infection and lower male circumcision rates than men of other race/ethnicities. Because of this, the public health benefit of male circumcision may be greatest in these subpopulations. COMMENT: CDC draft: Although similar randomized clinical trials have not been conducted in the United States, based on evidence from the African trials, uncircumcised heterosexual men living in areas with high HIV prevalence are likely to experience the most public health risk-reduction benefit from elective male circumcision. Reviewer Comment: There is no evidence that any males in the United States would RESPONSE 19: Evidence from randomized controlled trials, observational cohorts, cross-sectional studies, and ecological studies in the United States and globally demonstrate the protective effects of male circumcision. In addition, findings from research conducted in other settings, including evidence from the RCTs, can be applied to US populations.Methods: CDC draft: A CDC consultation was held in April 2007 to obtain input on the potential role of male circumcision in preventing transmission of HIV in the United States. A summary of the consultation, including a list of the participants has been previously published and helped define key issues for inclusion in this document. Reviewer Comment: The list of participants reads like a Who's Who of Circumcision Advocates. No group opposing male circumcision was allowed any input. Only one physician was in attendance who had any record of publishing studies unsupportive of male circumcision. RESPONSE 20: Dr. Robert Van Howe was a presenter and attendee at the meeting selected to represent the intactivist viewpoint.CDC draft: These recommendations are based on an evaluation of available information on the health risks and benefits associated with high-quality, medically performed male circumcision and were developed to pertain to men and male newborns in the United States. Reviewer Comment: If one reads the Background Draft, it becomes abundantly clear that only the available information on the health risks and benefits favorable to male circumcision were considered. The evaluation basically used a selective bibliography to cherry-pick the studies that supported male circumcision.See RESPONSE 1 and RESPONSE 4. COMMENT: CDC draft: In these recommendations, the preventive benefits of male circumcision are generally expressed as relative-risk reductions (e.g., a 50% reduction from a 2% risk of an STI to a 1% risk), whereas any associated harm is expressed as an absolute risk (e.g., a 2-4% risk of adverse events). Reviewer Comment: While it is refreshing that the CDC admits to using this deceptive practice, it would have been more appropriate to express those factors in terms of number needed to treat and number needed to harm. Readers of this draft will be unable to convert relative risk to absolute risk unless the absolute percentages or incidence rates are given. By giving only the relative risks, the CDC is guaranteeing that their readers will be deceived and unable to make an accurate comparison. This is unprofessional and unscientific. Health care providers realize that their patients are confused by relative risk, but patients can understand data when it is presented in terms of "number needed to treat-NNT" and "number needed to harm-NNH." By taking this step, the CDC is preventing health care providers from being able to present information to their patients in a manner which can be most easily and accurately assimilated. RESPONSE: See RESPONSE 14. COMMENT: CDC draft: Appropriate denominators are not available in many cases to establish an absolute risk for HIV and other STIs in higher-risk populations, e.g., heterosexual males at increased risk for infection. Reviewer Comment: This is not true. The CDC has gone to great lengths to generate models and analyses to prove that male circumcision is cost effective and will save lives. These models are based on estimates of the absolute risks that would be considered realistic in the population of interest. But, when it comes to having these estimates available so that health care providers can deliver useful information to their patients, all of sudden these estimates do not exist?! This selectivity in availability of estimates may indicate the presence of a very low absolute risk, which would make the number needed to treat so high that no one would consider cutting off the most sensitive portion of their penis for such a minuscule possibility of a benefit.See RESPONSE 14.Recommendations:CDC draft: Health benefits and risks of elective neonatal, adolescent, or adult medically performed male circumcision should be considered in consultation with medical providers while taking into account factors associated with decision-making around male circumcision including religion, societal norms and social customs, hygiene, complication and may be more expensive than male circumcision conducted before one year of age.2. Counseling sexually active adolescent and adult males regardless of circumcision status CDC draft: All sexually active adolescent and adult males should continue to use other proven HIV and STI risk-reduction strategies such as reducing the number of partners, and correct and consistent use of male latex condoms, and HIV preexposure or postexposure prophylaxis among others. Reviewer Comment: If these steps are followed, there is no need to circumcise. Consistent condom use is over 99% effective in preventing HIV infection. Adding male circumcision is unnecessary, and encourages males to avoid using condoms in the belief that male circumcision protects against HIV.COMMENT: This is known as risk compensation, which is already occurring in Africa with negative consequences. RESPONSE 23: While risk compensation has been a potential concern following the male circumcision RCTs and subsequent programmatic scale-up, studies evaluating risk compensation following voluntary medical male circumcision have not presented compelling evidence that there is any real increased frequency of sexual risk behavior that would undermine the protective effect of male circumcision.3. Counseling uncircumcised sexually active adolescent and adult males CDC draft: Prior to counseling uncircumcised sexually active adolescent and adult males about medically performed male circumcision, their HIV risk behaviors, HIV infection status, and the gender of their sexual partner should be assessed. The results of these assessments will inform the discussion with men about the risks and benefits of male circumcision. Reviewer Comment: The term "uncircumcised," while widely used, is a pejorative term. One definition of the word "uncircumcised" is "spiritually impure: heathen: unregenerate." It is also a term that is technically inaccurate. For a man to be "uncircumcised," he would need to first be circumcised and then have the process reversed. By using the term "uncircumcised" or "non-circumcised," the CDC is making the underlying value-laden assumption that being circumcised is the preferred condition, when there is no evidence, other than cultural pressure, to support this. The most Reviewer Comment: There is no evidence in North America that male circumcision reduces the risk of acquiring HIV in the general population.See RESPONSE 2 and RESPONSE 10. COMMENT: If male circumcision reduced the risk of HIV in the United States, why is the prevalence of heterosexually-transmitted HIV three times higher in the United States, where about 70% of sexually active men are circumcised, than it is in Europe, where less than 2% of sexually active men are circumcised? RESPONSE 25: The ecological evidence that the reviewer has chosen to support their point is insufficient to refute the large body of high-quality scientific evidence demonstrating the protective effect of male circumcision against HIV. HIV transmission is affected by many factors that differ between the United States and Europe, which include but are not limited to extent of access to healthcare, promotion of HIV testing, access to HIV treatment, sex education, condom usage, and primary modes of HIV transmission. COMMENT: There is evidence that male circumcision increases the overall risk of sexually transmitted infections through heterosexual sex. RESPONSE 26: The reviewer's conclusion that male circumcision 'increases the overall risk of sexually transmitted infections through heterosexual sex" is based on a scientific analysis with extensive methodological problems that have been discussed elsewhere 11,12 There is a large body of high-quality scientific evidence that demonstrates male circumcision protects men from acquiring HIV and other STIs through heterosexual intercourse. COMMENT: The premise of this section is incorrect, so what follows is of little or no value. If male circumcision is of only "partial efficacy," but other measures are almost completely effective at preventing transmission of HIV, then why bother with male circumcision at all? RESPONSE: See RESPONSE 17.o CDC draft: Men and male adolescents being counseled about male circumcision should be told that (see Box 1): Male circumcision reduces, but does not eliminate, the risk of acquiring HIV and some STIs during penile-vaginal sex. In clinical trials, medically performed male circumcision was associated with reduced number of new herpes simplex virus type 2 (HSV-2) infections and reduced number of oncogenic types of human papilloma virus (HPV) among circumcised men. Reviewer Comment: As mentioned above, the medical literature demonstrates that male circumcision is not effective as a primary preventive measure for HIV infection.See RESPONSE 2. COMMENT: Also, male circumcision does not reduce the risk of infections with HSV-2 or HPV. RESPONSE: See RESPONSE 15. COMMENT: In fact, male circumcision may actually increase the risk of such infections. RESPONSE: See RESPONSE 26.The CDC is selectively citing methodologically flawed studies from Africa to make a claim that is not supported by the full body of research currently available.See RESPONSE 1 and RESPONSE 4.o CDC draft: Uncircumcised, HIV-uninfected men and male adolescents at increased risk for HIV acquisition through heterosexual sex should be counseled about the risk and benefits of male circumcision (See Box 1). When a decision is made to undergo male circumcision, a referral for surgical consultation and access to high-quality male circumcision surgical services should be provided. Reviewer Comment: Soliciting male circumcision to males is not supported by the medical evidence and is unethical.See RESPONSE 21. The reviewer's statement that the CDC recommendations imply that health providers should "solicit male circumcision" to males is inaccurate. COMMENT: Given the highly effective measures of secondary prevention, there is no need for a health care provider to mention male circumcision. RESPONSE: See RESPONSE 17.3B. Counseling men who have sex with men (exclusively) CDC draft: Although it is biologically plausible that male circumcision could benefit MSM during insertive sex, no definitive data exist. Reviewer Comment: That it is "biologically plausible" male circumcision may be a benefit is highly speculative and unsupported by any evidence in the medical research, either biologically or epidemiologically. Wishes and hopes are not data. There is no strong biological evidence to support the claim that male circumcision could benefit MSM during insertive sex. RESPONSE 27: While removal of the foreskin provides is protective for men against HIV transmission through insertive vaginal sex, the role of the foreskin in acquiring HIV infection is not fully understood. One likely reason that male circumcision provides partial protection from HIV and some other STIs is that the foreskin is more susceptible to these infections than are other parts of the penis. It is therefore plausible that male circumcision would protect men from acquiring HIV and some other STIs during both insertive vaginal and insertive anal sex; however, there is no definitive data at present that indicates the mechanism that protects men from acquiring HIV through insertive vaginal sex is also protective during insertive anal sex. There is no evidence that male circumcision protects against HIV during receptive anal intercourse. COMMENT: CDC draft: Currently, there are no study results from RCTs including large enough numbers of MSM and results from observational studies are not conclusive among MSM overall or among MSM who practice exclusively insertive anal sex. Reviewer Comment: This statement reveals that those within the CDC who generated this document do not understand basic statistics and research study design principles. Just because a study is larger does not mean that it will provide a statistically significant result to one's liking. Remember the Women's Health Initiative Study? It had the exact opposite result of what was predicted. The results of a study are not known until the study is performed. The current available data do not support the CDC's wish that male circumcision would provide some benefit among MSM. RESPONSE 28: The CDC recommendations state that medical providers should counsel MSM that: o "Based on clinical trials, the demonstrated benefits of male circumcision for HIV risk reduction apply to heterosexual (penile-vaginal) sex only. o In the absence of clinical trial data for MSM related to male circumcision, definitive statements about whether male circumcision can reduce the risk of acquiring HIV and other STIs cannot be made. However, in observational studies, pooled data indicate that among MSM who practiced mainly insertive anal sex, male circumcision was associated with a decrease in acquiring new HIV infections. One observational study also found that new infection with one oncogenic type of HPV type (HPV-16) was reduced among circumcised MSM who practiced mainly insertive anal sex. Data from observational studies are considered weaker compared to data from clinical trials. However, it is biologically plausible that MSM who practice mainly insertive anal sex may experience a reduction in the risk for acquiring HIV and STIs like that among heterosexuals in clinical trials during penile-vaginal sex. o While some MSM may choose to be circumcised because of the potential to decrease risk for the insertive anal sex partner, male circumcision involves potential risks (see Adverse Events section of Box 1) and costs."3B-1. CDC draft: Men who have sex with men should be informed that: o The demonstrated benefits of male circumcision for HIV risk reduction apply to heterosexual (penile-vaginal) sex only. Reviewer Comment: Several studies, two of which included more than 30,000 subjects, in the United States have failed to a find a risk reduction from male circumcision in heterosexual men. Therefore, the CDC's statement is misleading and, in the US, false.See RESPONSE 2.4. Counseling parents of male newborns, children, or adolescents CDC draft: Health benefits and risks of elective neonatal, pediatric, or adolescent male circumcision should be considered in consultation with medical providers. In the case of discussion about neonatal male circumcision, ideally such discussion should occur prior to the birth of the child. Ultimately, whether to circumcise a male neonate or child is a decision made by parents or guardians on behalf of their newborn son or dependent child. Reviewer Comment: Since neonatal male circumcision is a non-therapeutic, purely cosmetic procedure, solicitation of the procedure is unethical according to the standards of the American Medical Association. RESPONSE 29: The reviewer's statement that neonatal male circumcision is a "nontherapeutic, purely cosmetic procedure" is inaccurate. There is strong scientific evidence that demonstrates several health benefits of male circumcision, which has been discussed in previous responses and outlined in the CDC background document. Adverse events are rare and are generally easily managed, particularly in children under one year of age. The background document provides evidence that the benefits of neonatal male circumcision outweigh the risks by 100 to 1, and include benefits such as reduced risk for HIV and STD acquisition, urinary tract infections, penile cancer, prostate cancer, Reviewer Comment: Whether parents can legally and ethically make a decision on the child's behalf to undergo a non-therapeutic, purely cosmetic procedure has not been clearly decided. The current ethical standard is that procedures in children that can safely wait until the child can provide his own informed consent should be delayed until Concerns about the CDC background document are similar to those that have been addressed in responses to the CDC recommendations, so we refer the reviewer to our prior responses on these issues. The literature review has been updated through October 2015, and in doing so we have added reductions among heterosexual men in the incidence and prevalence of genitourinary disease, prevalence and incidence of high-risk oncogenic human papillomavirus (HR-HPV), prevalence of Trichomonas vaginalis (T. vaginalis), incidence of syphilis, and prevalence of Mycoplasma genitalium ( M. genitalium) We also added a discussion of reductions in the following infections among female sexual partners of circumcised men based on RCTs: prevalence of GUD, prevalence of HR-HPV, prevalence of T. vaginalis, prevalence of bacterial vaginosis, and incidence of syphilis. There was also evidence of increased clearance of HR-HPV infection among circumcised heterosexual men and their female sexual partners in the RCTs. In the absence of RCTs in MSM, we also summarized data from observational studies showing that among MSM who practiced mainly or exclusively insertive anal sex, circumcision was associated with a decrease in acquiring new infections with HIV and with one oncogenic HPV type (HPV-16).#
First, is the obvious lack of scientific and scholarly rigor that went into preparing this draft. While it is stated that the writers of the draft performed a search of the medical literature, the evidence (in the form of the draft itself) indicates that their search was far from complete. Instead of collecting and analyzing data, they relied on review articles to do the work for them. One review article was published in 1983 -a bit dated to say the least. In some sections, the draft relied on opinion pieces as their sources of information. In areas where review articles were not available, the information provided was far from complete. For example, in reviewing the medical literature on the impact of male circumcision in North America, which is a major thrust of the draft, only two of the eight available studies are mentioned. Similarly, no serious attempt was made to review the harms, risks, complications, or pain associated with male circumcision. The draft has only 255 references, some of which are redundant, which are only a small sampling of the material available in the literature. A PUBMED search using the search word "circumcision" on January 12, 2015 identified 6338 publications.
# RESPONSE 1:
The CDC background document summarizes findings from a systematic literature review that was conducted in order to assess evidence on the association of male circumcision with medical benefits and adverse effects. Systematic reviews were conducted for the following outcomes related to medically attended male circumcision: HIV acquisition and transmission (female-to-male, male-to-female, and male-to-male); other STIs; penile cancer; cervical cancer; infant UTIs; risks and adverse events; sexual function and penile sensation. All studies of outcomes of male circumcision up to the end of November 2012 in Medline, Embase and Cochrane Library, as well as citation lists were included in the draft recommendations for public comment and peer review. More recent data through March 2013 were included in updating data related to the HIV epidemic in the United States. Studies were restricted to those published in English after 1950, presenting original data, including RCTs, cohort studies, case-control studies, cross-sectional studies, case series and case reports. Study design was classified according to guidelines used for collecting scientific data in reports published in the Guide to Community Preventive Services (the Guide). The evidence was assessed according to strength of association, consistency of findings across studies and the methodologic rigor of study designs. Because they minimize considerably the risk of spurious causality and bias, randomized controlled trails (RCTs) are considered the most rigorous method for determining whether a cause-effect relationship exists between a treatment and an outcome. Our literature review through November 2012 also included a broad, non-systematic narrative review for the section "Considerations related to male circumcision in the United States," because this section did not evaluate clinical outcomes. Since the time of the initial review, an updated literature review was conducted through October 2015 which added more evidence to the already strong field of evidence indicating that male circumcision is associated not only with a reduction in transmission of HIV, HSV-2, and oncogenic forms of HPV, but also decreased transmission of other STDs including genital ulcer disease, syphilis, m. genitalium, t. vaginalis, bacterial vaginosis, and trichomoniasis.
# COMMENT:
The draft also ignores basic epidemiological principles. It fails to apply the standards that are needed to identify when an intervention should be applied. Throughout the draft, it is assumed that male circumcision will be successful as a primary prevention for HIV, when the data clearly demonstrate that it is ineffective as primary prevention.
# RESPONSE 2:
Male circumcision is an effective primary prevention strategy, preventing transmission of HIV infections to men during penile-vaginal intercourse. Three large, well-designed RCTs have demonstrated that men who were circumcised are 50-60% less likely to acquire HIV through heterosexual intercourse than men who were not circumcised. The findings from the RCTs are also consistent with many other observational studies of the effect of male circumcision on HIV transmission. In 2007, a panel of consultants convened by CDC concluded that conducting a trial in the United States to evaluate efficacy of male circumcision for HIV prevention would not satisfy the criteria of clinical equipoise, given the weight of evidence from existing studies that male circumcision is protective against HIV. 1 COMMENT: Even its role as a secondary preventive measure has only been evaluated in one study in the United States, which included a very small, limited population. For this very small population, modeling by the CDC has estimated that male circumcision's impact on infection risk is nearly inconsequential.
# RESPONSE 3:
The CDC recommendations state that while the impact of male circumcision on HIV in the United States is limited by relatively low HIV prevalence and high male circumcision rates, there is epidemiologic data to suggest that some subpopulations in the U.S. are likely to benefit. Sansom and colleagues modelled the impact of male circumcision on lifetime risk of HIV infection in males in the United States, demonstrating that male circumcision reduced the 1.87% lifetime risk of HIV among all males by about 16% but that the effect varied by racial group. The effect was greatest among black males, where the 6.23% lifetime risk of HIV was reduced by about 21%. 2 It is also important to note that male circumcision confers health benefits in addition to protection against HIV, including protection against oncogenic forms of HPV, HSV-2, and infant urinary tract infections.
COMMENT: Policy should be based on more than one small subset of patients from a single study when several other studies fail to support this conclusion. It is clear that both the investigators of the randomized clinical trials and the CDC draft authors do not understand the epidemiological difference between efficacy (a positive finding in a research setting) and effectiveness (positive results in the real world).
# RESPONSE 4:
The CDC recommendations are not based on "one small subset of patients from a single study." The CDC recommendations are based on a thorough review of the large body evidence demonstrating certain health benefits of male circumcision, as well as on careful consideration of the potential public health implications of these findings in the United States. See RESPONSE 1 for a description of literature review methods.
# COMMENT:
The draft fails to adequately scrutinize the validity of the few studies it identified. It assumed the randomized clinical trials could not harbor any bias (the draft actually states this!) and did not question the methodology of these studies, although their methodology has been questioned extensively. Instead of accepting the study results at face value, the expectation of scholarly rigor would demand that these studies be carefully scrutinized, and a determination made as to whether the studies generated valid results and/or if the criticisms raised about these studies were convincing. The writers of the draft made no effort to question or analyze these studies.
# RESPONSE 5:
In 2009, a Cochrane committee conducted a review of the findings from the 3 male circumcision RCTs. The review evaluated the quality of the scientific evidence and potential impact of bias on the results for each trial. The review authors reported that the potential for significant biases affecting the trial results was low to moderate, and concluded that in spite of any potential bias there is "strong evidence" that male circumcision reduces the likelihood of HIV acquisition in men through heterosexual transmission. Authors concluded "male circumcision can be considered as an effective measure to partly prevent HIV acquisition in heterosexual men." 3 A sentence in the "Methods to gather, synthesize, and interpret information" section of the background document was amended to read: "Because they reduce spurious causality and bias, RCTs were considered the most rigorous method for determining whether a cause-effect relationship exists between a treatment and an outcome."
COMMENT: If a student were to submit these drafts for consideration as a senior undergraduate or master's thesis, they would fail based on their lack of scholarship. It appears the CDC was only going through the motions in preparing this draft. If the CDC had performed an adequate search of the medical literature and applied the expected level of scholarly rigor, their conclusions and recommendations would have been different. Perhaps that was the point. Perhaps the hope was, by releasing the draft with a selective bibliography, no one would recognize the lack of scholarly effort or call the CDC out on doing a subpar job. It worked for the American Academy of Pediatrics, and they seemed to get away with it. The difference is that CDC documents are open for public comment because it is a government agency. One would think that, after all of the embarrassment the CDC has endured in the recent past, they would want to put their best foot forward by publishing a rigorous, balanced, evidence-based assessment of male circumcision. That obviously did not happen.
# RESPONSE 6:
The background document is inclusive of research that both supports and refutes the conclusions shared in the CDC recommendations, including multiple documents authored and co-authored by the reviewer. Commentary within the CDC background document that pertains to the quality of the individual findings analyses is based on an objective evaluation of scientific merit. Also see RESPONSE 1 for a description of methods used to literature search.
COMMENT: Second, is the lack of attention to detail. Many of the citations given have the authors and journals incorrectly listed. Several of the citations require updating, while several of the citations were redundant. There are several misspellings in the manuscript. This indicates the CDC did not expend sufficient effort putting forth this piece of work, which is consistent with its lack of scholarly rigor.
# RESPONSE 7:
Peer reviewers were provided with the latest available draft of the CDC recommendations and background documents. These documents were working drafts, not a final version for publication. Any errors in spelling, grammar, or punctuation will be addressed prior to dissemination of the final documents.
COMMENT: Third, is the wanton disregard for the medical evidence. It is clear throughout that the writers of the CDC draft believe absolutely in the presumption that infant male circumcision can reduce HIV and sexually transmitted infections beyond a shadow of a doubt. As a consequence, the draft goes about finding evidence to support their presumption and primarily presents evidence supportive of this presumption, despite evidence to the contrary. The quality of the evidence supporting the presumption is never questioned. Any evidence that does not support their presumption is either ignored, criticized, or dismissed. As a consequence, the draft is laughably biased and reflects the expectation bias of its writers.
RESPONSE: See RESPONSE 6.
COMMENT: Fourth, is the lack of a thorough discussion of the foreskin and its anatomy, histology, physiology, and function. It is standard procedure for review articles of this type to review these topics to provide a basic science foundation. How can the CDC discuss the biological plausibility of sexually transmitted infections without a knowledge of the basic anatomy, histology, physiology, and function? This information must be included since health care providers must understand what is lost by removing the normal foreskin/prepuce. How else can they explain the impact of its removal to patients? This information is also an essential element of the disclosure given during the informed consent process.
# RESPONSE 8:
The CDC background document addresses concerns surrounding the role of the foreskin in sexual sensation and discusses research on the impact of male circumcision on sexual function and penile sensation. The background document also includes a section on biologic plausibility which describes the biology of the foreskin and the basis for HIV acquisition.
COMMENT: Fifth, is how out of step the CDC is with the rest of the world. National medical organizations and human rights groups throughout the world, including the Council of Europe, are, in increasing numbers, denouncing infant male circumcision as being medically unnecessary and a blatant human rights violation. At this point in time, the CDC and the American Academy of Pediatrics are the last stronghold in the defense of infant male circumcision. Remarkably, the draft fails to mention all the medical organizations outside of the United States who have weighed in with an opposing opinion on male circumcision. Is there some source of special knowledge the CDC has in its possession that allowed them to reach conclusions that are diametrically opposed to every other national medical organization (other than the American Academy of Pediatrics)? If it exists, why is it missing from the draft? Please provide enlightenment. If the CDC has a clue, they could at least share it. penis, which would result in intact men being over-diagnosed with HPV because circumcised men are more likely to have HPV on the shaft of the penis, which these researchers did not sample. As a consequence, their results can be completely explained on the basis of inadequate sampling. Subsequent large cohort studies have failed to find an association between male circumcision status and genital HPV infections. The CDC is selectively citing studies that promote male circumcision while ignoring studies, without a sampling bias, that do not support the practice of male circumcision. In other words, the CDC is using a selective bibliography to cherry-pick the studies to support male circumcision.
# RESPONSE 15:
The findings from the randomized controlled trials present high-quality evidence that male circumcision is protective against HSV-2 and high-risk oncogenic types of HPV.
Claims that the cause of lower STI incidence measured in the male circumcision arm of the RCTs was due to sexual abstinence during the 6-week healing period, referred to by the reviewer here as "lead-time bias", not to the intervention itself, have been discredited. The protective effect of male circumcision against HPV in the first 12 months has been observed during the months 12-24, well after the initial period of abstinence ended. In addition, authors of one RCT provided calculations that demonstrate that male circumcision is protective against HSV-2 even when abstinence during healing time was accounted for in the male circumcision arm. 7 Concerns that sampling site impacted the findings for HPV have also been discredited previously. In the South Africa RCT, authors intentionally sampled the urethra for HPV because it was unlikely detection of HPV or other lesions would be affected by male circumcision status at this site. 8 In addition, authors of the Uganda RCT conducted a follow-up analysis on prevalence of HPV on the coronal sulcus and shaft of the penis, and reported that men in the male circumcision arm men had lower prevalence in both areas 12 months after the procedure than those in the control (uncircumcised) arm. A 2011 meta-analysis of 23 RCTs and cross-sectional studies investigated the effect of the anatomical sampling site on relationship between male circumcision and HPV. Authors reported a strong protective effect of male circumcision against HPV when sampling was done at each of glans/corona, penile shaft, and scrotum (OR, 0.58; 95% CI, 0.40-0.82; n = 10 studies), and also that this protective effect was observed when sampling was done at the glans/corona only (OR, 0.47, 95% CI, .37-.60; n=2 studies) and at the urethra only (OR, 0.35; 95% CI, 0.12-1.05; n=5 studies). 9 COMMENT: CDC draft: Since the release of these trial data, various organizations have updated their recommendations about adult male 8 and infant male circumcision.
Reviewer Comment: The CDC lists only organizations from the United States that have leaned in favor of male circumcision. They fail to mention that national medical organizations from Norway, Sweden, Germany, Denmark, the Netherlands, Slovenia, Finland and others have condemned the practice of infant male circumcision, both on medical and on human rights grounds. The Council of Europe also considers infant male circumcision a human rights violation. _ENREF_8 benefit from elective male circumcision. When one looks at the impact of male circumcision on HIV prevalence in African countries, in at least eight countries the prevalence of HIV infection is higher in circumcised men than it is in intact men. This suggests that the results of the randomized trials from Africa do not even apply to Africa, let alone the United States. There is not a single study of infant male circumcision that has found a significant protective effect against HIV. Most male circumcisions in the United States are performed on infants. There have been eight studies looking at the impact of male circumcision on HIV prevalence in North America. None of them have found a significant protective effect, and one found that circumcised men were at significantly greater risk of HIV infection. The preponderance of evidence indicates that the results of the trials in Africa do not apply to the United States. aesthetic preference, and ethical considerations.
Reviewer Comment: The Council of Europe and national medical organizations from a number of European countries consider neonatal male circumcision to be a human rights violation, so this recommendation does not apply to neonatal male circumcision, as the proxy consent provided for the procedure may not be valid.
# RESPONSE: See RESPONSE 9.
COMMENT: Regarding male circumcisions for males who are able to provide their own consent, the disclosure process needs to be extensive and exhaustive since this is usually an elective, cosmetic procedure. Because it is usually an elective, cosmetic procedure, such a discussion should only take place after the male inquires regarding the procedure. Solicitation of male circumcision without a clear immediate medical indication is considered unethical according to the American Medical Association.
# RESPONSE 21:
The reviewer is correct in stating that male circumcision is usually an elective procedure, but the implication that the choice to circumcise is only "cosmetic" and that CDC recommendations encourage health providers to "solicit" male circumcision is inaccurate. The CDC recommendations outline counseling topics to assist health providers in discussing medical male circumcision with individuals who are considering male circumcision for themselves or for their male child. The counseling topics contain information on potential health risks and benefits of male circumcision at different ages and within different subpopulations. All statements about health risks and benefits in the document are based on sound scientific evidence and were informed by an objective and comprehensive review of scientific data from studies conducted in the United States and in international settings. The CDC recommendations suggest that individuals consider these messages on health risks and benefits in conjunction with other non-medical factors in the decision, which may include aesthetics, religion, or cultural considerations.
COMMENT: Performance of a procedure on a child, by a physician or health care provider, should be done based on medical need, not based on religion, societal norms or customs, vague notions of hygiene, or the aesthetic preference of an adult. To do otherwise, violates the child's basic human rights. Physicians are not cultural brokers. They have taken an oath to "Do no harm" and to do what is in the patient's best interest. In no respect is the removal of normal, healthy genital tissue in a child's best interest. Physicians do not routinely remove normal tissue from children for any other reason, so why would removal of the foreskin be the exception? RESPONSE 22: Because medical male circumcision confers a number of health benefits and has a low risk of adverse events, the decision whether to circumcise an infant or child is considered an appropriate exercise of parental or guardian authority. If a child's preference is of particular importance to parents or guardians, they may opt to delay male circumcision until a time when the child can make a decision for himself. Delaying medical male circumcision to adolescence or adulthood has a higher risk of accurate, value-neutral term for a man with all of his original genital tissue is "intact" or "normal" or "natural." By continuing to use the term "uncircumcised," the CDC is identifying its pro-circumcision bias to anyone who is familiar with the semantics on this issue. Males who are indeed "intact" find use of the term "uncircumcised" to be hate speech because they are singled out as "different," supposedly "abnormal" and/or possibly "unclean." Nothing could be further from the truth. Profiling a group of people in this way is discriminatory, hateful rhetoric. Furthermore, counseling any sexually active intact adolescent about male circumcision without provocation is malicious sadism. Teens, by their very state of emotional development, have self-image and self-esteem issues. This is especially true in regards to their primary and secondary sex organs. For a health care provider to engage in an unsolicited discussion of male circumcision with an intact adolescent male, only sends the message to the patient that something is seriously wrong with their genitals and, by extension, there is something wrong with them and with their parents. Given that Hispanics are less likely to be circumcised than other ethnic groups in the United States, would such a discussion be interpreted as racist, anti-immigrant hate speech? What self-respecting health care provider would want to impose such emotional trauma on their patient when there is no benefit in doing so. It is important to obtain a good sexual history on patients, but extraordinarily few adolescents would fall into a category that might possibly impact their risk of HIV infection. Furthermore, the gender of an adolescent's sexual partner may, and likely will, change frequently over the years, so determining this information seems of little value. The limited time during an office visit with an adolescent male would be better spent discussing how to properly apply a condom.
# RESPONSE 24:
The terms "circumcised" and "uncircumcised" are used to describe whether a male has undergone a procedure to remove the foreskin. The CDC recommendations in no way encourage providers to place a value judgement on either status.
The CDC recommends that health providers discuss sexual risk behaviors and risk reduction strategies with all sexually active adolescent and adult males. The CDC also recommends health providers ascertain whether an adolescent or adult male is at risk for acquiring HIV through heterosexual intercourse prior to discussing male circumcision. Neither recommendation is discriminatory towards male circumcision status.
# COMMENT:
3A. Counseling uncircumcised heterosexually and bisexually active adolescent and adult males (i.e., men who have sex with women) 3A-2. CDC draft: All uncircumcised adolescent and adult males who engage in heterosexual sex should be informed about the significant, but partial, efficacy of male circumcision in reducing the risk of acquiring HIV and some STIs through heterosexual sex, as well as the potential harms of male circumcision. the child can provide that consent. See also RESPONSE 22.
# COMMENT:
CDC draft: When counseling parents about male circumcision for an adolescent minor, the adolescent should be included in the decision-making process about undergoing elective male circumcision. When counseling an adolescent inquiring about male circumcision, parents should be engaged in the discussion, unless the adolescent is legally emancipated.
Reviewer Comment: Such counseling should only occur when the patient inquires about the procedure. To offer this information without an inquiry would be unethical, and potentially harm the adolescent's self-esteem and body image.
# RESPONSE 30:
The CDC recommendations state that male adolescent minors and their legal guardians should be included in the decision surrounding elective male circumcision, and that medical providers should inform the adolescent and guardians of health benefits and risks associated with the procedure. The CDC recommendations do not restrict counseling about male circumcision to inquiries from adolescents. Providers may also counsel on male circumcision if parents or guardians inquire and in cases where the provider believes the adolescent may be at risk of acquiring HIV through heterosexual intercourse. Counseling messages on elective male circumcision discuss the health benefits and risks associated with the procedure, and are not discriminatory toward uncircumcised males. See also RESPONSE 21.
# COMMENT:
4-A. CDC draft: Parents and guardians should be informed about the medical benefits and risks of neonatal, pediatric, or adolescent medically performed male circumcision (see Box):
- During infancy, circumcised infants are less likely than uncircumcised infants to experience urinary tract infections (UTIs), although UTIs are uncommon during infancy.
Reviewer Comment: To be accurate, this statement should state that intact boys are more likely to be diagnosed with urinary tract infections, but they may not necessarily have more actual UTIs. Whether or not they actually have more urinary tract infections is unclear. It needs to be added that between 110 and 190 boys need to be circumcised to avoid one additional boy being diagnosed with a urinary tract infection. Parents and guardians should be reassured that urinary tract infections can be treated with oral antibiotics and rarely, if ever, lead to long-term kidney problems or hypertension. It should be added that multiple studies from Israel have found that urinary tract infections increase in boys following ritual male circumcision.
# RESPONSE 31:
The absolute risk of a male infant developing a urinary tract infection and relative risk reduction of infant urinary tract infections (UTIs) associated with male circumcision is provided in the CDC recommendations. There is a strong evidence base that male circumcision protects against infant UTIs. Typical treatments and long-term impact of infant UTIs vary with severity of infection; infant UTIs may require more invasive treatment and diagnosis beyond oral antibiotics. Ritual male circumcision is outside the scope of these guidelines.
Reviewer Comment: The bandaging used following a ritual male circumcision may obstruct urine flow, leading to the urinary tract infection.
# RESPONSE 32:
The CDC recommendations address medical male circumcision only. Discussion of adverse events caused by ritual male circumcision is outside of the scope of the recommendations.
# COMMENT:
- CDC draft: Circumcised boys are less likely than uncircumcised males to experience balanitis and balanoposthitis.
Reviewer Comment: This statement needs to be deleted as it is factually incorrect.
There is no evidence to support this. Two studies found that circumcised boys under the age of three years were more likely to have penile inflammation than their intact counterparts. By providing health care providers with recommendations that are not factually accurate, the CDC is encouraging health care providers to provide parents and guardians with information that is not true. In other words, they are encouraging health care providers to violate the trust patients have in them and to engage in malpractice. If the provider is sued on the basis of providing the false information the CDC is encouraging, who is liable? The CDC should not put health care providers in the position of lying to their patients. (However, the entire CDC draft document is putting health care providers at risk for medical malpractice because of the fallacies it contains.) RESPONSE 33: As stated in the CDC background document, findings from a retrospective cohort and a prospective cohort study indicate that inflammation such as balanitis and balanoposthitis were less likely to occur in circumcised boys than in uncircumcised boys. Male circumcision may also be recommended as a treatment for balanitis or balanoposthitis that does not respond to other treatments.
# COMMENT:
- CDC draft: During adulthood, circumcised males are less likely than uncircumcised males to experience penile or possibly prostate cancer.
Reviewer Comment: The incidence of penile cancer is quite low, and it should be mentioned that the number needed to treat is between 4237 and 7184. Despite having a much higher male circumcision rate in the United States, the penile cancer incidence rate in the United States is no different than what is seen in Europe among primarily intact males. The evidence on prostate cancer is so weak, inconsistent, and inconclusive, that it should not be mentioned, especially when the incidence in the United States is quite high as is the male circumcision rate. Pathological studies indicate that many males, up to 70-80% by the seventh and eighth decades, have microscopic prostate cancer at autopsy, which was not clinically detected. So, where is the benefit of being circumcised? RESPONSE 34: As stated in the CDC background document, penile cancer is rare in developed countries, accounting for <1% of malignancies among men. Several observational studies demonstrate penile cancer strongly associated with a lack of male circumcision, and a case control study has demonstrated the odds of invasive penile cancer are greater in uncircumcised men than in circumcised men. See the CDC background document "Penile and prostate cancers" section for additional information.
The lifetime risk of prostate cancer among men in the U.S. during 2008-1010 was about 15%. 13 Male circumcision before first sexual intercourse was associated with a 15% reduction in risk of prostate cancer compared to that of uncircumcised men in a combined analysis using pooled data from 1754 cases and 1645 controls in 2 population-based case-control studies (95% confidence interval , 0.73-0.99). 14
# COMMENT:
- CDC draft: Other anticipated health benefits derive in part from future prevention of HIV and some STIs acquired through heterosexual sex. The risk for any individual neonate, child, or adolescent cannot be definitively defined at the time that a male circumcision decision is made; for example, current risks for HIV and STIs, such as those for a particular individual's racial/ethnic group or gender, may not remain constant in the future.
Reviewer Comment: Circumcised men have an overall STI risk that is greater than for intact men.
RESPONSE: See RESPONSE 26.
# COMMENT:
Is this stating that infants are not at risk for sexually transmitted infections, including HIV? If this is the case, that would favor waiting until the child is old enough to provide his own consent. Since when do we remove healthy normal tissue from a baby to possibly prevent some unknown future risk of disease? There are other more pressing diseases to contend with, if this is the focus of the CDC.
# RESPONSE 35:
Persons are not at risk of acquiring HIV and other STIs through sexual transmission until sexual debut. Individual lifetime risk of acquiring HIV and other STIs is not known at the time of birth, and may change from the time of birth to the time of sexual debut. A benefit of male circumcision prior to sexual debut is that it ensures the protective effects of male circumcision against sexually transmitted infections, including HIV, are present before commencement of sexual activity that put men at risk for these infections.
# COMMENT:
- CDC draft: Considerations for the timing of male circumcision:
- Neonatal male circumcision is, safer, and heals more rapidly than male circumcision performed on older boys, adolescent males, and men, and is less expensive.
Reviewer Comment: It is patently false that neonatal male circumcision is safer. This statement is based on myth, not on facts. The few studies that have made the appropriate comparison do not support this conclusion. There is no evidence that the wound heals more rapidly. There have been no studies in the medical literature that address wound healing and the Background draft does not address this claim. Since the foreskin has not separated from the glans in neonates, it is more likely that neonatal male circumcision takes longer to heal and is more painful.
# RESPONSE 36:
Complications occur in less than 0.5% of infants, and in approximately 9% of children age 1 -9 years. Among newborns and children age 1 -9 years, the most frequently reported complications include bleeding and inflammation of the penis and the need for corrective procedures. Delaying age of male circumcision from infancy to one year of age or older can increase the risk of some complications associated with the procedure, which include correctional procedures, bleeding, and inflammation. 15 In patient-oriented health educational materials in the U.S., healing time after infant male circumcision is reported to be about 7 to 14 days 18 19-21 and to be about 2 -6 weeks in older children, adolescent, and adults. 19,22 COMMENT: Neonatal male circumcision is less expensive because it is not performed under general anesthesia, the only adequate anesthesia besides a caudal block.
Neonates also are much easier to strap down without a major fight ensuing. The topical and local anesthetics that are used for neonatal male circumcision do not provide adequate anesthesia, as has been demonstrated in multiple studies. The procedure is still quite painful when these are used. The pain associated with neonatal male circumcision, even when topical and local anesthetics are used, has been linked to circumcised boys crying longer and louder when given vaccinations at four to six months of age and circumcised boys having a significantly greater risk of developing infantile autism, autism spectrum disorder, and hyperactivity. The availability of general anesthesia for male circumcision performed in older males is another advantage of waiting until the male can provide his own consent.
# RESPONSE 37:
Minimizing pain is an important consideration for medical male circumcision. Appropriate use of analgesia is considered standard of care for medical male circumcision at all ages, and appropriate analgesia can substantially control pain for infants, children, and adults during and after the procedure. As demonstrated by Banieghbal and colleagues, appropriate analgesia can substantially control pain. In their study, 93.5% of neonates circumcised in the first week of life with appropriate analgesia gave no indication of pain on an objective, standardized neonatal pain rating system. 23 The study which found an association with autism and male circumcision focused only on ritual male circumcision which is outside the scope of these guidelines and has been critiqued as being methodologically unsound and biased. 16,17 COMMENT:
- CDC draft: Male circumcision can also be conducted in adulthood when the individual can make the decision for himself. However, male circumcision after sexual debut could result in missed opportunities for: HIV and STI prevention during the window period between sexual debut and male circumcision
Reviewer Comment: This a cheap scare tactic designed to influence parents and teens into accepting male circumcision before full adulthood. According to the CDC's own numbers, the risk of HIV infection under the age of 15 years is very low. How many 15 year olds are having unprotected sex with female partners who are HIV-infected? RESPONSE 38: Prevention interventions work best when implemented prior to exposure. In the case of sexually-transmitted infections such as HIV, the time period prior to exposure occurs prior to sexual debut. In addition, male circumcision prior to sexual debut is more effective at protecting against prostate and penile cancer 14,24 . Uptake of the procedure after the neonatal period is also likely to be lower due to the increased cost, greater likelihood of complications, and other barriers to male circumcision at a later age.
Similarly, the only STI that might be associated with male circumcision status is syphilis, which is also very rare and easily treated with antibiotics. This risk is so low that there is no need to mention it. The only people who do mention it are the pro-circumcision lobbyists, who believe it may have some rhetorical value. STIs, HPV, HIV have been shown to be more common in circumcised males in North American studies.
# RESPONSE 39:
Several STIs are associated with lack of male circumcision. In randomized controlled trials for which data are available, reductions in the 1) prevalence of genitourinary disease (GUD) , 2) incidence of herpes simplex virus type 2 (HSV-2), 4,28 3) prevalence, 29 _ENREF_9 incidence, 30,31 and clearance 29,31 of high-risk oncogenic human papillomavirus (HR-HPV)_ENREF_7, 4) prevalence of Trichomonas vaginalis, 27,32 5) incidence of syphilis, 33 6) prevalence of bacterial vaginosis, 27 and 7) prevalence of mycoplasma genitalium 34 were also demonstrated._ENREF_19
See also RESPONSE 15.
# COMMENT:
CDC draft: Prevention of UTIs during infancy.
# Reviewer Comment:
The risk of UTI is small and none of the analyses that have been published believe that male circumcision is a cost-effective method to address this small risk. If an infant male circumcision costs $285 (according to the CDC) and the number needed to treat is 195, then it would cost over $50,000 to prevent one urinary tract infection that can easily be treated with an antibiotic that costs less than $20. So, this is also a cheap scare tactic.
# RESPONSE 39a:
See RESPONSE 31. The cost-effectiveness of treatment of UTIs is not relevant to the statement in the CDC recommendations that male circumcision prevents UTIs during infancy. In addition, In a meta-analysis of 18 studies mainly from the U.S., the prevalence of UTI in infants presenting with fever in outpatient clinics and emergency departments was 7.0% (95% CI = 5/5 -8.4), but as high as 20.1% (95% CI = 16.8 -23.4) among febrile uncircumcised males aged < 3 months compared with 2.4% (95% CI = 1.4 -3.5) among febrile circumcised males aged < 3 months, and 7.8% (95% CI = 6.6 -8.9) among both febrile and afebrile older children aged < 19 years. 35
# COMMENT:
- CDC draft: The most commonly described complications of medically performed male circumcision in the United States are typically uncommon and easily managed.
Reviewer Comment: The most commonly described complications of medically performed male circumcision are the loss of the most sensitive portion of the penis (100%) and meatal stenosis (5% to 20%). Both are common and not easily managed.
Once the majority of the fine-touch neuroreceptors are removed from the penis via male circumcision, there is no way to grow them back. While there are thousands of circumcised men who spend years trying to stretch their remaining shaft skin so the glans of the penis can once again be covered, there is no way to restore the fine-touch neuroreceptors.
# RESPONSE 40:
Many studies have evaluated the impact of male circumcision on sexual satisfaction or function and have found little evidence of adverse effect on penile sensitivity, sensation, or sexual satisfaction. The randomized controlled trials in Kenya and Uganda reported no adverse effects of male circumcision on sexual satisfaction. 38,43 COMMENT: Meatal stenosis (narrowing of the opening of the urethra) usually requires surgical enlargement of the urethral opening done under general anesthesia (the child might as well have waited to be circumcised to partake of such pain control). Consequently, neither of these complications is easily managed. Either the writers of this set of recommendations are intellectually obtuse, or they are purposely covering up the side effects of male circumcision to portray the procedure in the most positive light possible. By ignoring the harms and complications of male circumcision, of which there are hundreds, they are doing a disservice to the health care professionals, parents and patients who might rely on this information, and ultimately it is a disservice to society as a whole.
RESPONSE 41: Meatal stenosis may occur very rarely as a result of medical male circumcision, but there is no high quality study that links meatal stenosis to medical male circumcision. See also RESPONSE 35.
# COMMENT:
- CDC draft: Severe complications are rare in all age groups.
Reviewer Comment: It all depends on how "rare" and how "severe" and how "complication" is defined. But perhaps a more important discussion is whether any severe complications, regardless of their rarity, are acceptable following a nontherapeutic, purely cosmetic procedure performed on an individual who is unable to give his own consent? RESPONSE 42: Potential complications from male circumcision are addressed in the CDC background document. Severe complications from the procedure include severe bleeding, partial or complete amputation, laceration repair, or other correctional procedures.
See also RESPONSE 35 and RESPONSE 29.
# COMMENT:
- CDC draft: Among newborns and children age 1 to 9 years, most frequently reported complications include bleeding and inflammation of the penis or the need for corrective procedures. Complications occur in less than ½ % of infants, and in approximately 9% of children age 1 to 9 years.
# Reviewer Comment:
The complication rates in this statement come from a study based on data collected from a database. This study design typically misses between 90% and 95% of the complications when compared to the number of complications identified when performing a chart review. This statement needs to be deleted and the complication rate from charts reviewed by the CDC, which revealed a complication rate of 3.1%, should be put in its place. Similarly, there are studies in which the complication rates of male circumcisions performed in neonates were compared to the complication rates of male circumcisions on older boys at the same time in the same place using the same criteria. The results have been mixed. In some, the complication rates were higher in newborns or there was no difference between the two groups. None showed a lower rate of complications in newborns. This effort to paint neonatal male circumcision as having lower complication rates is purely a propaganda tool with insufficient quality evidence to support it.
# RESPONSE 43:
The statement that there is "insufficient quality evidence to support" the cited complication rates of male circumcision is inaccurate. Several large studies of medically attended male circumcision in the neonatal period in the United States estimate the rate of adverse events at less than 0.5% (ref: Cristakis, Wiswell, Gee). See also RESPONSE 36.
# COMMENT:
- CDC draft: Among persons 10 years of age and older, the most frequently reported complications include those complications reported in younger children as well as wounds of the penis. Complications occur in approximately 5% of persons in this age group 15 .
Reviewer Comment: The immediate complication rate for neonatal male circumcision ranges from 2% to about 6%, with delayed complications being much higher. For example, meatitis (inflammation of the urethral opening) occurs in 20%, meatal stenosis in 5% to 20%, adhesions in 25%, skin bridges in 4.1% to 12.7%, subcutaneous granuloma in 4.97%, phimosis in up to 2.9%, hidden penis in 1%, and 1% of parents who insist on the male circumcision being redone because they do not like the cosmetic outcome. The point is that neonatal male circumcision may have a higher complication rate than when it is performed on boys 10 years and older.
# RESPONSE:
See RESPONSE 36, RESPONSE 41, RESPONSE 43.
# COMMENT:
- CDC draft: The American Academy of Pediatrics Taskforce on Circumcision states that the health benefits of newborn male circumcision outweigh the risks and that the benefits of newborn male circumcision justify access to this procedure for families who choose it.
Reviewer Comment: This appeal to authority is inappropriate. The American Academy of Pediatrics Task Force on Circumcision in their report stated several times that they did not know the rate of complications following male circumcision. This may be related to the refusal of the Task Force to consider any case reports or case series in their limited analysis of the medical literature. Most reports in the medical literature of complications are in the form of case reports and case series. The Task Force also did not quantify the rate at which a male who was circumcised would reap any benefit from the procedure. Yet, with the rates of the benefits undefined and the rates of complications unknown, somehow the Task Force was able to say that the benefits outweighed the risks. Making such a statement defies the basic principles of mathematics. When pressed on how they reached their conclusion, the Task Force stated that they felt the benefits outweighed the risks. So, their conclusion was not evidence-based but feelings-based. This conclusion was also criticized by thirty-eight well-regarded medical experts, primarily from Europe, who argued that this conclusion was culturally biased. Why does the CDC mention the Task Force report, which suffers from the same biases and lack of scholarly rigor as the Background Draft? Is it thought that reference to an equally pathetic effort will give the CDC's efforts some unearned credibility?
# RESPONSE 44:
In the United States, reported rates of complications in large studies of medically attended male circumcision in the neonatal period, including infants from birth to age 1 month, are approximately 0.2%, 44,45,46 and vary by type of study, setting, operator and surgical technique. Similarly, the reported rate of complications of medically attended male circumcisions occurring at any age in the United States is 0.23%. 15 In a comprehensive risk-benefit analysis of infant male circumcision based on reviews of the literature and meta-analyses, it is estimated that over a lifetime, benefits exceed risks by a factor of 100:1. 47 Based on a meta-analysis of 22
# RESPONSE 45:
The AAP states that "Trained and competent practitioners, by using sterile techniques and effective pain management, should perform male circumcision. Analgesia is safe and effective in reducing the procedural pain associated with newborn male circumcision; thus, adequate analgesia should be provided whenever newborn male circumcision is performed." See also RESPONSE 37.
Typically in the U.S., providers who perform male circumcision include obstetricians, pediatricians, family practitioners, midwives, and urologists. Also, the AAP notes that "most residency training programs in the respective specialties teach techniques, including the Gomco clamp, Mogen clamp, and Plastibell device." In the U.S., accepted standards of clinical care have been put into place for surgical procedures regardless of the individual procedure, such as pre-op screening of the patient to rule out conditions that might rule out the patient as a surgical candidate. Infection control procedures are also in place. Regarding the technical aspects of conducting male circumcision, medical textbooks describe the various surgical procedures for conducting male circumcision. Typically, residents in training read about a procedure and then observe an experienced surgeon perform the procedure. They may assist an experienced surgeon conduct a surgery until they are deemed ready to take the lead in conducting such a surgery. Routinely, hospitals conduct periodic reviews of morbidity and mortality associated with individual practitioners to determine if a higher level of adverse events is occurring than what is anticipated.
# COMMENT:
Box: CDC draft: Health Benefits and Risks of Elective Medically Performed Male Circumcision - CDC draft: Health benefits of elective male circumcision in adults and adolescents: o Male circumcision reduces the risk of acquiring HIV infection through penilevaginal sex by 50-60%, as demonstrated in three well-conducted clinical trials among adult men living in sub-Saharan Africa.
Reviewer Comment: There is no evidence that the findings of the clinical trials in Africa, which by several objective standards were not "well conducted," apply to male infants or to males living in North America, and there is ample evidence they do not apply. The existence of this "health benefit" is highly speculative. There is no evidence to suggest that any benefit has been demonstrated for infant male circumcision or for heterosexual men in North America.
# COMMENT:
The reduction should be identified as a relative risk reduction. The absolute risk reduction in these trials should be mentioned to provide a true comparison. For example, in the Ugandan study the absolute risk reduction was 0.67% with a number needed to treat of 149. These numbers need to be adjusted for the lower incidence seen in the United States. If one assumes the African results apply to the United States, and there is no evidence to support this assumption, then the absolute risk reduction would be 0.02% with a number needed to treat of 5000. At $285 per male circumcision, this would cost $1.425 million to avoid one HIV infection. Not a good use of resources, especially when this is based on an assumption that is not consistent with the medical evidence. Even if the relative risk reduction is 10%, the number needed to treat would be 25,000 and cost would be $7.125 million. The CDC, by only mentioning the relative risk reduction, is hoping that readers will forget that 50% of a very small number is still a very small number.
# RESPONSE 45b:
See RESPONSE 14. The reviewer's comment on cost-effectiveness is not relevant to the statement in the CDC recommendations that male circumcision reduces the risk of acquiring HIV infection through penile-vaginal sex in men.
- CDC draft: In clinical trials involving heterosexual males living in sub-Saharan Africa, male circumcision reduces the risk of some sexually transmitted infections. Male circumcision reduces the risk of circumcised men acquiring infections with:
- Genital ulcer disease (GUD) (by 48%)
- Herpes simplex virus type-2 (HSV-2) (by 28% -45%)
- Oncogenic types of human papilloma virus (HPV) (by 24% -47%)
- Syphilis (by 42% -62%): Male circumcision reduces the risk of circumcised men having existing infections with:
- Oncogenic types of HPV (by 25% -47%)
- Trichomonas vaginalis (by 53%)
- Mycoplasms genitalium (by 46%)
# COMMENT:
Reviewer Comment: This statement is selective in the results provided and fails to note that these trials did not adjust their results for lead-time bias. Of the three randomized trials, one found virtually no difference (RR 1.06), and in only one was the difference statistically significant. When adjusted for lead-time bias, none of the trials had a result that was statistically significant. When the results of prospective studies on the incidence of HSV-2 infections by male circumcision status are combined in a metaanalysis, and the studies are adjusted for lead-time bias, the results are not statistically significant. This finding is consistent with the meta-analysis results of observational studies that have looked at HSV-2 prevalence by male circumcision status: no statistically significant difference. The CDC markedly overstates this difference. Their draft should also list the number needed to treat for these differences. For the study in Uganda, the NNT was 93, in South Africa 98.6, and in Kenya 261. If the incidence of HSV-2 is lower in the United States, the numbers needed to treat would be greater.
# RESPONSE 45c:
See RESPONSE 15.
# COMMENT:
- CDC draft: HPV: circumcised men were approximately 30% less likely to be infected with high-risk strains of HPV associated with cancers than were uncircumcised men.
Reviewer Comment: The 30% reductions were only reported in two of the prospective studies, where only the glans was sampled. In multiple studies, it has been demonstrated that intact men who have HPV on their genitals are more likely to have the virus primarily on the glans, whereas circumcised men who have genital HPV are more likely to have the virus primarily on the shaft of the penis. By not sampling the shaft of the penis, these studies guaranteed that HPV would be detected 30% more often in intact men, even if the infection rate on the genitals was the same in both circumcised and intact men. In other words, the 30% reduction can be completely attributed to their decision to only sample the glans of the penis, or to only report the results of the samples taken from the glans of the penis. The largest prospective study of HPV and male circumcision was published in 2014. This study sampled the male genitals properly, finding that circumcised men were at greater risk for genital HPV infections, but the difference was not statistically significant. It also found that HPV cleared significantly faster in intact men. The medical literature does not support the hypothesis that intact men are at greater risk for HPV infection. This myth evolved out of methodologically flawed studies that did not properly sample the penis.
# RESPONSE 45d:
See RESPONSE 15.
# COMMENT:
- CDC draft: Adverse events and risks associated with elective male circumcision of adults: o For adult male circumcision performed by clinicians, the rate of adverse events is up to 5%, with pain, bleeding, infection and unsatisfactory postsurgical appearance most commonly reported. While severe and/or long-term complications have been reported, they are so rare that they have not been precisely established.
# Reviewer Comment:
The low percentages reported in these studies indicate that, if a male circumcision is to be performed, it should be performed during adulthood to reduce the risk of complications. At least in adulthood, the male can understand and accept the risks involved. Infant male circumcision has much higher rates of adverse events. It is time studies were done to precisely establish all the complications from male circumcision because it is doubtful they are rare.
# RESPONSE 45d:
See RESPONSE 36.
# COMMENT:
- CDC draft: Adult men who undergo male circumcision generally report minimal or no change in sexual satisfaction or function.
Reviewer Comment: This statement is based primarily on wishful thinking supported by two studies with serious/fatal methodological flaws. The medical literature is replete with studies of circumcised adults who report decreased penile sensitivity, erectile problems, difficulty with insertion during coitus, and difficulty reaching orgasm. Two studies out of Africa used questionnaires whose questions would not have been able to detect a difference if one existed. The men in these studies, if the results are to be believed, are having the best sexual experiences on the planet as their rates of sexual dysfunction were 6 to 30 times lower than reported in other countries. The participants in these studies were, by African standards, extremely well paid for their participation, so it is unknown if this had an undue influence on their answers. There are several studies, including a representative national survey from Denmark, indicating that male circumcision has a negative impact on sexual function. There are several studies that have found circumcised men suffer from premature ejaculation significantly more frequently than intact men. Studies have also indicated that the female partners of circumcised men are significantly more likely to report a lack of sexual fulfillment and pain with intercourse. This statement needs to be changed to fit the currently available evidence.
# RESPONSE 45e:
See RESPONSE 40.
# COMMENT:
- CDC draft: Health benefits of neonatal male circumcision: o The estimated annual rate of urinary tract infections (UTIs) in uncircumcised male infants is 0.70%. Male circumcision reduces the risk for infant UTIs by about 80%.
# Reviewer Comment:
The CDC needs to make a simple calculation to provide the number needed to treat using the numbers provided above: NNT=178.6. At $285 per male circumcision, it will cost over $50,000 to avoid one urinary tract infection that can be treated with an antibiotic that costs less than $20. (Another example of: a large percentage of a small number is still a small number.) It should also be mentioned that urinary tract infections in children are not associated with later development of renal failure or hypertension. Recent recommendations from the American Academy of Pediatrics are that extensive work-ups following urinary tract infections are no longer needed.
# RESPONSE 45f:
The reviewer's comment on cost-effectiveness is not relevant to the statement in the CDC recommendations that male circumcision reduces the risk of infant UTIs. See also response 31.
# COMMENT:
- CDC draft: In the U.S., the estimated lifetime risk of penile cancer for males is about 1 in 1,400 (0.07%) and that of prostate cancer is about 15%. Neonatal male circumcision reduces the risk of penile carcinoma by about 90% and may reduce the risk of prostate cancer by 15% compared to men who are uncircumcised.
# Reviewer Comment
# COMMENT:
- CDC draft: Adverse events and risks associated with neonatal male circumcision: o Adverse events: For male circumcision performed by clinicians,
- the rate of reported adverse events is as follows 0.4% in infants (age through 12 mo.)
Reviewer Comment: This estimate is from a study that collected its data from databases, which have been shown to only identify 5% to 10% of the complications, as compared to those that can be identified from a chart review. As a consequence, this number has no basis in reality, and it grossly underestimates the actual rates for adverse events and risks in neonates. Percentages for adverse events/complications are listed later in this review.
# RESPONSE 45h:
See RESPONSE 36, RESPONSE 41.
# COMMENT:
CDC draft: 9.1% in children (age 1-9 years) CDC draft: 5.3% in persons (age 10 years and older)
Reviewer Comment: Older children and their parents are more likely to identify and complain about complications. Consequently, this number may be an overestimate. Yet, when compared to the well documented rates of complications following infant male circumcision, older children may have lower complication rates.
# RESPONSE 46:
Estimates reported for children aged 1-9 years and children aged 10 years and older are from a study using data from a large longitudinal healthcare reimbursement dataset that estimated the incidence of adverse events (AEs) from 2001-2010 that were attributable to male circumcision. 15 These numbers are consistent with data from other prospective and retrospective studies.
# COMMENT:
- CDC draft: Most commonly reported complications in all age groups include bleeding and inflammation of the penis, and correctional procedures. - CDC draft: The incidence of severe adverse events associated with male circumcision performed by clinicians, such as permanent disabilities, disfigurements, and death, is so low that rates have not been precisely established; these events have occurred, but are rare.
Other major complications requiring intervention including major bleeding, and severe infection are uncommon.
Reviewer Comment: The disclosure of information to decision makers during the informed consent process for a non-therapeutic, cosmetic procedure needs to be exhaustive and complete. Male circumcisions are performed primarily for cultural and religious reasons. Therefore, from a medical perspective, the consequences are much more likely to be negative than positive. Health care providers who perform male circumcisions would be well advised to inform decision makers of all of the known complications/consequences because these may occur despite the skill of the provider.
If an adverse or serious complication occurs, the health care provider will be able to document that such a complication was understood by the patient and signed off on. Some of the complications are so common following male circumcision that they are not recognized as complications. Health care providers, when providing disclosure, also must discuss the normal anatomy, histology, and function of the foreskin so the decision maker is informed of what harm/loss results from every male circumcision. The CDC drafts do not mention the normal anatomy, histology, or function of the foreskin, thus disadvantaging the health care provider who is reliant on these documents to properly inform decision makers. This major oversight on the part of the CDC requires attention.
# RESPONSE 47:
The CDC recommendations describe the most common complications of the procedure in all age groups in order to assist medical providers in counseling individuals considering male circumcision for themselves or their child. This document is not intended to take the place the place of a consent form.
# COMMENT:
Here is a list of consequences/complications: Behavioral changes -Newborn male circumcision interferes with breastfeeding -Newborn male circumcision interferes with maternal-infant bonding -Newborn male circumcision interferes with normal sleep patterns -Following male circumcision, with or without anesthetic, boys cry longer and louder when given their vaccinations at 4 to 6 months of age suggesting that male circumcision may permanently alter pain perception.
-Circumcised boys have been found to have a significant association with an increased risk of autism in two studies. There are no contrary data.
-Circumcised boys are at a significantly greater risk of being diagnosed with hyperactivity disorder (attention deficit hyperactivity disorder).
-Circumcised men have a greater risk of having alexithymia (the inability to express emotions) -Circumcised men have been found in two studies to identify themselves as gay/bisexual significantly more frequently than intact men Complications of topical/local anesthesia:
# Hematoma and bruising Methemoglobinemia
Gangrene RESPONSE 48: A thorough discussion of adverse events associated with male circumcision in all age groups is included in the CDC background document. The line listing of adverse events provided by the reviewer is not helpful without citations indicating the source of the information, the proportion of patients who had a male circumcision who experienced such an adverse event, and a comparison of the proportions of uncircumcised and circumcised boys who have experienced these adverse events, and where possible, information about whether the adverse event was associated with medical male circumcision or ritual male circumcision. As earlier noted, ritual male circumcision is outside the scope of the CDC male circumcision counseling recommendations.
# COMMENT:
Reviewer Conclusions:
The CDC recommendations are counterfactual and not evidence-based. The supporting evidence provided is extremely selective and biased. If the CDC had carefully scrutinized much of the supportive evidence they provided, they would have identified methodological weaknesses that would, if they were to act on the quality of the evidence, change their recommendations. Acknowledgement of the vast majority of the medical literature that the CDC ignored would have also altered their recommendations. There are significant oversights, omissions, and inconsistencies throughout that are critical knowledge for the intended audience of clinicians. By using a selective bibliography and by depending on speculation and hype, rather than science, to develop these recommendations, the CDC has placed clinicians and health care providers in an untenable position. In effect, the CDC, by making the recommendations it has, is asking clinicians and health care providers to misinform their patients, and by doing so, commit medical malpractice. As a consequence, the recommendations for the intended audience of health care providers are inconsistent with the medical evidence, reckless, and dangerous. The CDC should eliminate this draft and approach the topic using an evidence-based approach, hopefully with the involvement of experts from around the world on both sides of the discussion.
# RESPONSE 48a: CDC RESPONSE TO REVIEWER CONCLUSIONS:
As stated in previous comments, the recommendations on the health risks and benefits of male circumcision were informed by a careful consideration of high-quality scientific literature, the epidemiologic context of the United States, as well as cultural and ethical considerations. As such, we do not agree with the reviewer's statements that the CDC recommendations are counterfactual and reckless.
The reviewer implies in the conclusion throughout the comments that the CDC recommendations are meant to advocate for male circumcision, which is an inaccurate characterization of the CDC recommendations. The CDC recommendations outline counseling topics to assist medical providers in discussing medical male circumcision with individuals who are considering male circumcision for themselves or for their male child. The counseling topics contain information on potential health risks and benefits of male circumcision at different ages and within different subpopulations. All statements about health risks and benefits in the document are based on sound scientific evidence and were informed by an objective and comprehensive review of scientific data from studies conducted in the United States and in international settings in consultation with subject matter experts. The CDC recommendations suggest that individuals consider this information on health risks and benefits in conjunction with other non-medical factors in the decision. The document does not contain a direct recommendation in support of or in opposition to medical male circumcision for any age group or any demographic.
COMMENT: Reviewer Commentary on CDC Background Draft:
Overall RESPONSE 48b: CDC RESPONSE TO BACKGROUND DRAFT COMMENTARY: We recognize and acknowledge the effort the reviewer has put into the lengthy discussion of the CDC background draft that follows. The citations provided by the reviewer were evaluated for possible inclusion in the most recent update to the CDC background document. Introduction
The material presented in this section of the background document is riddled with inaccurate statements and misrepresentations.
# RESPONSE 48c:
See Responses 1 and 6.
# COMMENT:
Male circumcision performed on an infant is not "voluntary." The infant does not give consent. (Male circumcision campaigns in Africa have become less and less "voluntary" and some adult males are being forcibly circumcised.) Consequently, this statement is false and needs to be revised.
# RESPONSE 49:
Parents provide "voluntary" consent for the infant. See Responses 13 and 22.
# COMMENT:
It is not clear why reference CDC3 was chosen as it is a book written by a known male circumcision advocate. There are basic research articles that should be cited instead.
Prevention of HIV continues to be an unlikely consideration in the decision to circumcise despite pressure by the CDC to make it so (see discussion below). Infants are not sexually active, so HIV prevention is not a concern for them, nor has infant male circumcision been shown to have any impact on HIV acquisition or prevention. Prevention of HIV in adults can be obtained more effectively through non-surgical methods, primarily with the use of condoms.
RESPONSE 50: Upon hearing information about the risks and benefits of male circumcision, including that of reducing a heterosexual male's risk of acquiring HIV infection from an HIV-infected female partner, parents will make a decision as to whether they think this information is pertinent in deciding whether to circumcise their child. A reduction in the future risk of acquiring HIV infection is part of any HIV prevention strategy. A parental decision to circumcise their infant to reduce his future risk of HIV acquisition based on such evidence, is by definition a prevention strategy.
# COMMENT:
When the draft states that male circumcision reduces the risk of male HIV acquisition through penile-vaginal sex, it relies on the results of the randomized clinical trials to make this claim. The problem is that these trials did not make any effort to determine the source of the infections they diagnosed during their course, so it is unknown whether these infections were the results of penile-vaginal sex, male-to-male sexual contact, or iatrogenic infections. Without knowing where the infections came from, the claim that male circumcision reduces the risk of male HIV acquisition through penilevaginal sex cannot be made.
RESPONSE: See response 12.
# COMMENT:
The CDC draft portrays the perceived benefits in terms of relative risk reduction, but the risks are presented in terms of absolute risk. For example, the 50% to 60% relative risk reduction in HIV infections in the randomized clinical trials sounds like a big deal, but the absolute risk reduction was only 1.3%, which is a difference that many would not consider clinically of any value. It would be best if this draft presented the perceived benefits in terms of the number needed to treat (NNT), and presented the risks in terms of the number needed to harm (NNH) in order to compare them fairly.
RESPONSE: See response 14.
# COMMENT:
In reporting on the 2007 recommendations of the WHO/UNAIDS, it should be explicitly stated that their recommendations did not apply to infant male circumcision. Nor was there a consensus of opinion. In fact, those present describe the measure as being "railroaded through." 4,5 RESPONSE 51: The 2007 recommendations states the following: "Since neonatal male circumcision is a less complicated and risky procedure than male circumcision performed in young boys, adolescents or adults, such countries should consider how to promote neonatal male circumcision in a safe, culturally acceptable and sustainable manner."
# COMMENT:
The statement, "Despite these overall differences, the results of the African trials are likely to have application to HIV prevention efforts in the United States," is completely without foundation. While this may be what the CDC authors want everyone reading it to believe, it has no basis in fact. (The situation in the United States is quite different from that in Africa, including having a first-class medical system in place.) Making such an unsubstantiated statement is unscientific and should be left to the male circumcision lobbyists.
RESPONSE: See responses 2, 19.
# COMMENT:
The statement that African-American men "are known to be significantly less likely to be circumcised compared to white, non-Hispanic men," is, as discussed below, also untrue. African-Americans in several studies have higher, or the same, overall male circumcision rates in the US, as compared to whites. Hispanics have lower male circumcision rates than either of these groups.
RESPONSE 52: CDC used the most recent nationally representative data available at the time the document was written. See responses 18.
# COMMENT:
It is unclear why the CDC draft questions "whether parents would be willing to have their newborns circumcised to reduce possible future HIV and sexually transmitted infection (STI) risk," when there is no strong evidence that circumcising a newborn will reduce the risk of these infections. To date, not a single study has found neonatal male circumcision to significantly reduce the risk of HIV. (Not to mention, the adult studies fail to show a significant reduction in any risk.) RESPONSE 53: Ecologic studies demonstrate a strong association between lack of male circumcision and HIV infection at the population level. Although links between male circumcision, culture, religion, and risk behavior likely account for some of the differences in HIV infection prevalence, the countries in Africa and Asia with prevalence of male circumcision of less than 20% have HIV-infection prevalence several times as high (seroprevalence range: 0.24 -25.84) than countries in those regions where more than 80% of men are circumcised (seroprevalence range: 0.03-11.64). 49 In addition, based on data from an HIV transmission model fitted to data from the Four Cities Study, including 2 cities in sub-Saharan Africa with relatively low HIV prevalence (Cotonou and Yaoundé) and 2 with high HIV prevalence (Kisumu and Ndola), investigators concluded that differences in rates of male circumcision likely played an important role in differing rates of HIV transmission across Africa. 50 Results from such ecologic studies are important as most male circumcisions globally are thought to occur during infancy, childhood, or adolescence, suggesting that male circumcision at an earlier age confers a long term reduction in risk for HIV acquisition. The fact that male circumcision performed during the neonatal period is associated with fewer and less severe side effects compared to male circumcision performed during adulthood is one of the most important reasons that most male circumcisions are performed neonatally in the U.S. See response 35.
# COMMENT:
This background document presents a very biased, one-sided summary of the data that support the practice of male circumcision while ignoring most of the medical literature that does not support the practice. When the medical literature is looked at in its entirety, male circumcision is not a medically sound intervention. While this background document is supposed to focus on the data in the context of the United States, it only considers two of the eight studies that have looked at the impact of male circumcision on the risk of HIV infection. None of these eight studies found a statistically significant positive effect for the intervention, and one found that circumcised men had a statistically significant higher prevalence of HIV than intact men. 14 Likewise, much of this background document is allocated to a discussion about male circumcisions performed in Africa, which are of little interest and irrelevant to the target audience of health care professionals in the United States and not within the scope of the charge the CDC was given in developing these drafts. The effort that went into providing the minute details regarding male circumcision in Africa would have been better spent researching the anatomy, histology, physiology, and function of the foreskin (which this document completely ignores), researching the complications associated with male circumcision, updating information on the risk of sexually transmitted infections, and analyzing the data in the literature rather than relying on the often misguided analysis of others in review articles and opinion pieces.
# COMMENT: Methods to gather, synthesize, and interpret information
The material presented in this section of the background document is fairly straightforward, but the question remains as to whether the CDC followed their listed methodology in generating this report. The evidence, in the form of the final product, indicates they did not.
RESPONSE 54: CDC conducted a systematic review of the scientific literature and updated the review after the public comment period. The newer data supports our previous conclusions and includes data that male circumcision is associated with reduction in the incidence and/or prevalence of more STDs than previously thought based on RCTs. See responses 39 and 48b
# COMMENT:
The two-day consultation convened by the CDC on April 26-27, 2007 brought together a virtual Who's Who of Circumcision Advocates and Lobbyists. 16 Given the likemindedness of nearly all the participants in attendance, it is not surprising they managed to produce a massive "group think" phenomenon. Their conclusions were more radical and less scientific than what the participants would have likely considered acceptable, if left to their own devices. 17 This experiment in "group think" resulted in what will be referred to as the "CDC group think presumption:" namely that findings of the randomized clinical trials of adult male volunteers in Africa would apply to infant males circumcised against their will in the United States. In reading the CDC draft, this presumption is presented as gospel truth, when the reality is quite the opposite, with the data currently available not in support of this presumption. It appears the CDC has adopted the attitude seen with other male circumcision enthusiasts, in that the issue was not open for discussion or questioning. 18 RESPONSE 55: CDC's recommendations related to counseling around the issue of male circumcision is based on a systematic review of the scientific literature.
# COMMENT:
While the CDC draft states that "a systematic review was conducted" there is little or no evidence that such a review was conducted. Instead, the CDC draft relies on the information published in non-systematic review articles from 1983, 19 and 1998; 20 systematic reviews from 2000, 21 2003, 22 2005, 23 2006, 24 2008, 25,26 2009, 27,28 2010, 30 and 2011; 30 and opinion pieces from 1999, 31 , 2000, 32 and 2014. 33 Beyond reporting what was found in these articles, there is little, or no, evidence of a literature search being performed. The small number of citations (255,
# COMMENT:
The statement "Because they eliminate spurious causality and bias, RCTs are considered the most rigorous method for determining whether a cause-effect relationship exists between a treatment and an outcome," is clearly an overstatement. No research method can completely "eliminate" bias. The elevation of randomized controlled trials to the status of the gold standard is misplaced, as they often deliver results that are invalid. Throughout this draft, the CDC reflexively genuflects in the face of any results from a randomized trial. But every study, regardless of its methodology, requires careful scrutiny. The CDC did not scrutinize these studies. In fact, as will be discussed below, the randomized clinical trials cited in the CDC draft have multiple sources of bias, which rendered their findings meaningless. Randomized clinical trials, such as these, with serious methodological flaws are less rigorous in determining cause and effect than well-designed observation studies. Just because a randomized clinical trial format was employed does not mean that its findings are valid.
# RESPONSE 57:
Agree that RCTs do not eliminate all bias, therefore the word "eliminate" has been replaced with the word "reduce". See response 5.
# COMMENT:
When the draft states that "None of the primary authors of these recommendations reported a financial or other conflict of interest," does this include any conflicts from being an adherent of a religion that requires male circumcision, being from a cultural background that has a high male circumcision rate, being circumcised themselves, being married to someone who is circumcised, and/or having circumcised one's children? Male circumcision status in participants is considered by many as a clear bias and a conflict that should be declared. 38 Such a declaration is important, as male circumcision status or having a circumcised son clearly impacts what advice physicians give to parents regarding infant male circumcision. 39 The conflict of interest on this issue goes well beyond financial considerations. Where is the list of the primary authors of these recommendations, or a list of those who served on the subcommittee of the CDC Public Health Ethics Committee? The makeup of these groups will be an important factor by many, when looked at in conjunction with the obvious lack of scholarship displayed in this draft, in determining how seriously to take the recommendations.
RESPONSE 58: CDC did not ask for reporting of nontraditional forms conflict of interest such as "personal male circumcision status", or religious beliefs. However, in this CDC consultation, consultants were asked to review the merits of the scientific evidence at hand.
# COMMENT:
# Summary of evidence
Conspicuously absent from the CDC draft is a discussion of the normal anatomy, histology, physiology and function of the male foreskin or prepuce. Nearly every review article on any medical topic begins with a discussion of the basic anatomy, histology, physiology, and function of the organs and tissues involved. The recent Task Force report of the American Academy of Pediatrics also failed to address this, 40 and members of the Task Force had to admit ignorance on this topic. 41 It is impossible to understand the impact of amputating a healthy structure from the body, if these characteristics are not understood. The vast majority of physicians in the United States do not have a working knowledge of the anatomy, histology, physiology, or function of the foreskin because they were never taught it in medical school, and medical textbooks contain little or no information on these topics.
The prepuce is a common anatomic structure of the male 42 and female 43 external genitalia of all human and non-human primates. The prepuce has been present in primates for at least 65 million years, and is likely over 100 million years old based on its commonality as an anatomical feature in mammals. 44 The prepuce is best understood not as a separate structure of the penis, but rather as an integral part of the penile skin system.
As a modified extension of the penile shaft skin, representing 22 to 33% of the overall length of the flaccid penis, the prepuce covers the glans, extends beyond it, folds back upon itself, and attaches just behind the corona glandis, providing adequate mucocutaneous tissue to cover the entire penis during erection. There is variability in the preputial coverage of the glans penis ranging from complete coverage to only partial coverage. 45 The portion of the prepuce extending beyond the glans can be quite long in children, while those of adults can be shorter. In many boys, the "redundant foreskin" can be longer than the penile shaft. Based on measurements available in the medical literature, the average surface area can be calculated to be between 50 to 62 square centimeters. 46,47 In a randomized clinical trial in Rakai, Uganda, the surface area was calculated by "multiplying the length by the width of the foreskin," 48 but their calculations would underestimate the surface area by half as it only accounts for one side of the prepuce. Correcting for the prepuce having two sides, the average surface area in this study was 74.2 square centimeters. 48 The prepuce is perfectly designed to protect the glans, an internal organ. Tapered and double layered, it extends beyond the glans in a long, narrow, tube-like structure, terminating in the preputial orifice. The peripenic muscle sheet lines the skin, is continuous with the dartos muscle of the scrotum, 49 and lines the mucosal layer allowing the prepuce to maintain its close fit over the glans. 50 At the preputial orifice, the muscle fibers are arranged in a whorled manner and form a sphincter that keeps unwanted contaminants away from the sensitive mucosa. 51 This is most evident in the prepubescent male in whom the portion of the prepuce extending beyond the tip of the glans has a characteristic puckered appearance.
The preputial orifice is able to dilate 15 to 20 times its normal size to allow the glans to pass through without entrapment. This expandability increases with age and sexual maturity but may be negligible during infancy. 52 Premature and inappropriate attempts to retract and dilate the preputial opening of infants and children can damage and scar the prepuce, reducing elasticity and impairing sexual function. 53 While the outer surface of the prepuce is similar to skin, the inner surface of the prepuce can be subdivided into two zones of mucosa. One consists of a prominent band of ridged mucosa, with several (8-12) transverse mucosal ridges or pleats, just inside the tip of the prepuce. This band merges with the frenulum on the ventral aspect of the penis. When the prepuce is fully retracted, the ridged band lies across the upper surface and sides of the shaft of the middle third of the penis. Histologically, the ridged band has a rich vascular supply, explaining its deep red color, and a high concentration of fine-touch neuroreceptors (such as Meissner's corpuscles, Pacinian corpuscles, genital corpuscles, and mucocutaneous corpuscles) that transmit fine touch, pressure, proprioception, and temperature. 55, The other zone is the smooth, non-ridged, preputial mucosa, which does not have a high concentration of fine-touch neuroreceptors.
The frenulum, in conjunction with the smooth muscle fibers of the prepuce, helps return the everted prepuce to its forward position. The frenulum, like the ridged band, also contains a dense concentration of erotogenic nerve endings and is a primary orgasmic trigger. Along with the prepuce, also the site of erogenous triggers, stimulation of the frenulum is particularly effective at producing erections. Retraction, rolling, and stretching of the prepuce triggers erotogenic stretch receptors, which comprise the bulk of the sexual sensations of the erect penis. 69 Blood enters the penis via two principal arteries -the pudendal artery, which carries blood down from the pelvic region, and the femoral artery, which also supplies blood to the legs. Neither of these arteries is superficial, instead lying close to the corpus cavernosa/corpus spongiosa. They flow directly to and alongside the glans, supplying it with blood. Then, they continue down to the underside of the glans to the forward-most point of the frenulum where the arteries meet up with the venous system.
The primary route for venous return from the penis is through the foreskin. The superficial veins drain the skin of the prepuce and glans via a complex vascular plexus that traverses the inner prepuce. These superficial veins drain into larger veins that run up through the frenulum and up the sides through the ridged band. From the ridged band, the veins continue their route back through the skin and Buck's fascia along the corpus cavernosa/corpus spongiosa.
The male prepuce receives its somatosensory innervation via the dorsal nerve of the penis and branches of the perineal nerve (including the posterior scrotal nerves). 70,71 The dorsal penile nerve of the penis supplies sensory axons to the penile shaft and glans. One axon innervates the penile shaft and the urethra, while the other innervates the glans. Stimulation of the urethra results in contraction of the bulbocavernosus muscles enhancing penile rigidity. Impulses from the dorsal penile nerve also initiate reflex semen emission and power the contractions of the bulbospongiosum muscle that results in external ejaculation. There are portions of the penis, particularly the ventral side and the frenulum, that are partially or completely innervated by a branch of the perineal nerve, 75 which also can induce contractions of the bulbocavernosus muscle. 73 A portion of the fibers within the dorsal nerve carries autonomic branches and is responsible for the hemodynamic events of the distal corpus cavernosum and the glans penis." 72 Autonomic innervation of the prepuce arises from the pelvic plexus. The parasympathetic visceral efferent and afferent fibers arise from the sacral center (S2-S4), and sympathetic preganglionic afferent and visceral afferent fibers arise from the thoracolumbar center (T11-L2). The parasympathetic nerves run adjacent to, and through the wall of, the membranous urethra. 70 Histologically, the foreskin is a specialized, junctional, pentalaminar structure. The prepuce is considered a specialized tissue because it contains elements that are present only in select portions of the body.
It is a junctional tissue because it the junction where the transition from skin to mucosa takes place. Analogous tissues include the eyelids, oral labia and the anus, which are also transitional between skin and mucosa. All of these transitional zones contain a high concentration of fine-touch neuroreceptors. In the oral labia, the absence of these neuroreceptors would result in constant drooling, and kissing would lose most of its erotic appeal. In the eyelid, constant tearing would be the rule. Likewise, the protective function of the eyelids would be severely handicapped if unable to sense the presence of contaminants. The function of these specialized, junctional tissues is remarkably similar: keep moisture on the internal mucosal surfaces and keep contaminants out.
It is pentalaminar in that it has five layers, with each layer having its own unique histological and functional features:
1. The external skin has already been described.
2. The dermis of the prepuce consists of vascular tissue, dense nerve trunks, Meissner corpuscles within the papillae, and scattered sebaceous glands. The dermis of the male prepuce appears to have more elastic fibers than the lamina propria of the prepuce. The elastic tissue of the prepuce dermis, along with the dartos muscle and frenulum, tether the prepuce and help return it to its anatomically correct position after erection.
3. The dartos layer is specific to the male prepuce and is not found in the female prepuce. It consists of smooth muscle fibers invested with elastic fibers. The delicate, attenuated penile dartos muscle surrounds the shaft of the penis and is continuous with the scrotal dartos muscle. 49 This layer's elasticity allows for the volume changes required for erection, 49 while the muscular component is responsible for the prepuce fitting closely over the glans. 50 In the distal prepuce (acroposthion), the muscle fibers are intertwined and arranged in a mosaic-like pattern in the infant, 50 causing the distal prepuce to pucker and close, acting like a one-way valve. 51 This is most notable when a young boy voids. As the urine is expelled from the bladder it must first build up enough pressure to overcome the preputial valve. Because of the elasticity of the prepuce, it is not unusual for the prepuce to balloon before enough pressure is generated and a urinary stream results. As a male ages and passes through puberty, the ratio of muscle fibers to elastic fibers decreases, explaining why, on gross inspection, the acroposthion is puckered in the infant and more relaxed appearing in the adult. 50 The increase in elastic fibers may be necessary for the uncomplicated eversion of the glans in the adult. 4. The lamina propria of the prepuce is highly vascular and has looser collagen than the dense collagenous lamina propria of the glans penis. The ridged band of the prepuce is near the tip (acroposthion) of the male prepuce and, in the unretracted prepuce, usually lies against the glans. It is in the lamina propria of the ridged band that there is a high concentration of specialized neuroreceptors. All of these receptors have a capsule and an inner core composed of both neural and nonneural elements. The capsule is a continuation of the perineurium and the core includes preterminal and terminal portions of the nerve fibers surrounded by laminated layers of modified Schwann cells (laminar cells). 68 The Meissner corpuscles, genital corpuscles, and mucocutaneous receptors are similar in that there is a complex branching of the nerves within the corpuscular core, while the Pacinian corpuscle has a single nerve through the core that is surrounded by laminar cells to form an onion bulb configuration. The prepuce possesses a richer variety and a greater number of nerve endings than any other part of the penis. 76,77 These corpuscular receptors represent one of the two primary somatosensory receptors in skin, the other being free nerve endings or nocioceptors. 67 While free nerve endings (pain, itch, and touch receptors) are found in most skin, the encapsulated receptors are concentrated in regions that require specialized sensitivity, such as at the fingertips, eyelids, lips, external genitalia, perianal skin, and transition areas between skin and mucous membranes. 68 The glans penis is primarily innervated by free nerve endings and has primarily protopathic sensitivity. 78,79 Protopathic sensibility refers to cruder, poorly localized feelings (including pain, some temperature sensations, and certain perceptions of mechanical contact such as rubbing). 78,80 In the glans penis, encapsulated end organs are found in much lower concentrations and are found mainly along the glans corona and the frenulum. 78 The glans is best stimulated by the mechanical rolling pressure of the prepuce over its surface. By comparison to the prepuce, the glans is a neurologically "dumb" organ. 56 [ The only portion of the body with less fine touch than the glans penis is the heel of the foot. 81 The mucosal lamina propria is devoid of lanugo hair follicles, sweat, or sebaceous glands. The lamina propria is highly vascular.
5. The mucosal epithelium of the prepuce is the same as the squamous mucosal epithelium that covers the glans penis. 82 The mucosal epithelium contains Langerhan's cells, but does not contain melanocytes. It provides the moist lining necessary for the preputial sac to function properly.
It is also important to recognize that separation of the foreskin from the glans of the penis is a gradual process. The glans penis and the inner prepuce share a common, fused mucosal epithelium at birth. The two opposing fused epithelial surfaces separate gradually over years as desquamated cells build up between the two layers when the proper hormonal and growth factors are present. 83 While the separation of the prepuce from the glans has been shown to be androgen dependent in rats, 84 the hormones and/or growth factors responsible for this separation are poorly understood in humans. The process of keratinization of the intervening epithelium begins anteriorly and posteriorly at approximately the same time and proceeds toward the center. Anterior desquamation, because it is confined, can result in pearls of desquamated skin cells.
Øster demonstrated that preputial non-separation is very common in children and teenagers. The separation of the mucosa is usually complete by about age 17 years, with the median age being 10 years of age. 52,86,86 The newborn penis is in a state of evolution that may take many years until the common prepuce/glans mucosa separates, and the preputial orifice enlarges to allow complete exposure of the glans. Ignorant of the normal development of the penis, some physicians advocate childhood male circumcision as a treatment of normal anatomy. 87 Even the 2012 Task Force report of the American Academy of Pediatrics incorrectly reported that "Most adhesions present at birth spontaneously resolve by age 2 to 4 months." 40 Lysis of preputial adhesions in childhood is ill-advised, since this process resolves spontaneously and forcible manipulation and retraction of the immature prepuce can lead to scarring, bleeding, phimosis, and psychological trauma. 88,89 The foreskin plays a protective and erogenous role. Animal studies have found that surgically removing the prepuce disturbs normal copulatory behavior, the ability to attract female sexual partners, and it increases aggressive behavior. 103,104 The foreskin keeps the surface of the glans penis clean, free of infection, smooth, moist, supple, and sensitive. 105 The prepuce protects and preserves the sensitivity of the glans by maintaining optimal moisture, warmth, pH, and cleanliness. The foreskin may have a role in keeping the glans warm, much the way the dartos muscle in the scrotum helps regulate the temperature of the testes. 106 There are temperature sensors in the foreskin that regulate the blood flow to the penis and thus regulate the temperature of the glans penis. These sensors appear to also impact the positioning of the scrotum, which, in turn, affects how close the testicles are to the torso, how warm the testicles are, and how fertile the male is.
The foreskin also provides a protective covering over the glans. Without the foreskin, the glans becomes exposed to the elements and dries out. The surface of the glans goes from a shiny, smooth, wet mucosa to a desiccated, rough surface. There is debate whether the exposed glans seen in circumcised men becomes keratinized or not. 32,107 Men who have foreskins report that having the glans exposed for prolonged periods is often quite uncomfortable because the surface is more sensitive.
The decreased sensitivity of the glans in circumcised male adults has been documented in three studies that objectively measured fine-touch pressure thresholds of the glans in circumcised and intact men, which are discussed in further detail later in this review. Two studies have compared the vibratory perception thresholds of the glans in circumcised and normal men. Bleustein et al. in a study in which 76.8% of the men in the study had erectile dysfunction, found that vibratory perception thresholds were significantly higher in intact men using the raw data, but the difference was no longer statistically significant when adjusted for age, hypertension, and diabetes. 109 A study in China looking at vibratory perception thresholds before and at one, two, and three months after male circumcision in 96 men found that the vibratory perception threshold increased significantly following the procedure. 111 Intromission in the circumcised man is akin to thrusting the foot into a sock held open at the top. By contrast, the intact counterpart is like slipping the foot into a sock that had previously been rolled up. 112,113 Consequently, during coitus the complete phallus penetrates smoothly with the prepuce retracting as the glans advances; 114 however, when the circumcised penis is introduced, friction and chafing develop. The double-surfaced prepuce provides the skin necessary to accommodate the expanded erect organ and to allow the penile skin to slide freely, smoothly, and pleasurably over the shaft and glans. This also facilitates smooth, gentle movement between the mucosal surfaces of the two partners during intercourse. The female is stimulated by moving pressure rather than by the friction from a penis with the prepuce missing. 50,118 O'Hara and O'Hara, from their survey of women who reported having had both intact and circumcised male sexual partners, determined that intact men provide shorter penile thrusts during coitus that resulted in more clitoral stimulation for the woman. By contrast, circumcised men used longer, deeper thrusts to provide themselves with enough stimulation to maintain erection and reach orgasm. 115 Because the foreskin is designed to feel fine-touch, only small movements are needed for adequate stimulation. When the exposed glans is in the vagina, the foreskin is bunched behind the corona with the ridged band juxtaposed against the corona, which is the most sensitive portion of the glans. With this juxtaposition, small movements are all that are needed to keep an intact male aroused and tumescent.
The unique innervation of the prepuce establishes its function as erogenous tissue. 58 Fine-touch pressure threshold mapping has demonstrated that parts of the foreskin and frenulum are the most sensitive portions of the penis. The foreskin sends signals to the bulbocavernosus muscle that results in arousal and tumescence of the penis. Therefore, the foreskin may have a key role in facilitating a normal penilo-cavernosus reflex.
McGrath's research has emphasized the important role of the frenular delta, the triangular area where the ridged band attaches to the frenulum, 119 the frenulum, and the ridged band in providing possibly 80% of the sensory input from the penis, and their contribution in orchestrating signals to the bulbocavernosus muscle, which plays a key role in tumescence. The stimulation from these structures also provides an inhibitory function in dampening the signal of pressure and pain coming from the free nerve endings that make up nearly all of the sensory data from the glans. Without inhibiting the pain and pressure signals from the glans during coitus, the activity would be less enjoyable.
While the penilo-cavernosus reflex has not been fully studied, it is a neurological reflex at the sacral level that has a role in the ejaculatory process. Podnar found clinically this reflex could not be elicited in 22 (73.3%) of 30 circumcised men, but was absent in only 2 (6.9%) of 29 intact controls. 120 Podnar speculates that this missing reflex in circumcised men may explain the higher rate of premature ejaculation seen in circumcised men. The impact of male circumcision on sexual function is discussed in detail later in this review.
As a mucosal surface, similar to the inside of the mouth, the lining of the alimentary canal, or the conjunctiva of the eye, the inner surface of the foreskin is an immunological organ.
The mucosal surface of the inner prepuce and the glans, like all mucosal tissues, requires constant lubrication. Because the glans does not contain any sebaceous glands, it relies on the prepuce for production, distribution and maintenance of proper lubrication. The male preputial sac is moistened by secretions from the prostate, seminal vesicle, and urethral glands of Liftre. 121 Urine is not a normal component of subpreputial wetness. The rich vascular plexus of the prepuce mucosa facilitates production of a fluid transudate similar to that of the vaginal mucosa. 122 Animal experiments reveal that, in the presence of hydrogen peroxide and halide or pseudohalides, soluble peroxidase in the prepuce has an antimicrobial activity. 123 Antibodies present in breastmilk supplement genital mucosal immunity in infants. Oligosaccharides in breastmilk are ingested, then excreted in the urine, where they prevent E. coli from adhering to the urinary tract and inner lining of the prepuce. 124 The inner prepuce secretes cathepsin B, lysozyme, chymotrypsin, neutrophil elastase, 125 cytokine (a non-antibody protein that generates an immune response on contact with specific antigens), 126 langerin, 127 and pheromones such as androsterone. 128 Lysozyme, which is also found in tears, human milk, and other body fluids, destroys bacterial cell walls as well as inhibits and destroys Candidal species (yeast). 129 The prostatic and seminal vesicle secretions that provide the subpreputial moisture are known to be rich in lytic material. 121 Langerin, which is a C-type lectin, is specifically expressed by Langerhans cells and induces the formation of Birbeck granules. The langerin on the surface of the Langerhans cell captures the HIV viron and internalizes it to the Birbeck granules where it is destroyed. In this way, langerin keeps Langerhans cells from internalizing HIV and activating T-cells by clearing the virus before getting the T-cells involved. 127 Like other exposed mucosal surfaces, the inner lining of the prepuce and the surface of the glans are covered with bacteria. The composition of the normal flora can impact whether a disease takes place. For example, the presence of one microorganism can inhibit the growth of another organism. The subpreputial flora has been known to be affected by a number of factors such as a patient's age, general hygiene, medical history, sexual activity, and sexual predilections. 138,139 The role of the diversity in subpreputial flora has not been explored in terms of preventing infection, but there is a growing amount of information that allows us to understand the flora in the subpreputial space. Earlier studies had documented that the preputial sac is colonized by cornybacterium, gram negative anaerobes (especially bacteroides melaninogenicus), enterococci, enterobacteria, and coagulasepositive staphylococci. 140 The impetus to study the subpreputial flora in recent decades has been resurrected by male circumcision enthusiasts in hopes of providing evidence of a biologic mechanism to support their theories that the foreskin increases the risk of urinary tract infections and HIV infections. The authors of these studies try to spin the changes following male circumcision as beneficial, but without understanding the role of normal flora prior to male circumcision there is no way to know if the change is beneficial. The latest speculation is that genital inflammation might be associated with bacterial antigens from bacteria that are not associated with sexually transmitted infections, and that this inflammation might activate T-cells, which might be necessary for the transmission of HIV through the mucosal surface. Therefore, they conjecture that changing the flora at the end of the penis is why circumcised men are at lower risk of HIV infections. There is no evidence that normal flora in the subpreputial space is associated with penile inflammation. One could more convincingly argue that the presence of a variety of anaerobes and a microbiota with more major players is more protective against infection and inflammation. It is when the spectrum of bacteria narrows, which is what occurs following male circumcision, that infection is more likely to occur. Certainly, developed countries with low male circumcision rates do not seem to suffer from higher rates of HIV or other pathologic infections of the genitals.
The problem with the conclusions reached by these male circumcision enthusiasts, including the writers of the CDC draft, is that they are too simplistic, agenda-driven, and reek of confirmation bias. 18 Gram-negative organisms are not all bad. Colonic flora is primarily gram-negatives, yet considered normal. The assessment of microbiological findings and their correlation to clinical findings is difficult, in particular when quantitative determinations have not been done. 150 The presence of normal flora is not a disease state. The most common bacteria responsible for otitis media, pneumonia, and acute sinusitis are normal flora in the nose, pharynx, and mouth. Rather than blame normal flora in a healthy individual and use this in an attempt to justify amputating healthy body parts, a better approach may be to ensure healthy flora in the subpreputial space by lowering the rate of Cesarean sections and perinatal antibiotic usage, but calls to do this have been largely ignored. The understanding of mucosal immunity is in its infancy. While the mucosa in our mouths, noses, and genitalia encounter pathogens constantly, we rarely are infected. The mechanisms of mucosal immunity are complex and poorly understood. The mucosal immune system protects against potentially invasive microorganisms using antigen-presenting Langerhans cells, dermal and epidermal T lymphocytes, cytokineproducing keratinocytes, and draining peripheral lymph nodes. 154 Most of the "heavy lifting" is performed by Langerhans cells that hang out on the surface of the epithelium.
Langerhans cells are a specific type of dendritic cell. On electron microscopic examination, they have a lobulated nucleus with a clear cytoplasm, rough endoplasmic reticulum, and a well-developed Golgi apparatus. 155 They possess a unique granule in the cytoplasm, which has a "tennis racket"-like appearance, that is responsible for the internalization and processing of antigens. 156 Langerhans cells are the first line of defense to help the body recognize and process antigens, directing them towards lymphocytes or macrophages. 157,158 To understand how this happens, it may be helpful to follow a Langerhans cell through its life cycle. The Langerhans cell begins life in the bone marrow. It is released into the blood stream and is circulated to the dermal blood vessels where it finds its way to the surface. 159,160 Here the Langerhans cell takes up a suprabasal position with its processes extending between neighboring keratinocytes and joins a web of interconnected Langerhans cells that surveys the epithelial surface for antigens. They make up 2 to 5% of all epidermal cells, 164,165 yet their long processes allow them to cover broad expanses of the epithelial surface. Once an antigen is identified, it is captured by the Langerhans cell. Following antigen uptake, the major histocompatibility complex and costimulatory molecules are up-regulated on the surface of the Langerhans cells. 169 The Langerhans cell then migrates from the epithelial surface to the paracortex of the nearest draining lymph node where it activates T-cells by producing cytokines and by presenting the major histocompatibility complex-restricted antigen-specific molecules. 166, This in turn begins an antigen-specific immune response by the activated T-cell. 166 The Langerhans cell then will return to the epithelial surface and repeat the process. 172 Perhaps the most studied example of Langerhans cell activity is in antigen-specific delayed-type hypersensitivity resulting from contact with substances containing nickel that leads to T-cell responses. 165,167,173 Langerhans cells have also been documented fighting infections of human papillomavirus in the female genital tract and of herpes simplex virus on the lips. 167,168, They interfere with skin graft rejection from foreign donors, 167 and suppress tumor growth in mice. 177 Langerhans cells have been known to act like macrophages both in the allo-activating and in the antigen-presenting function. 168,178,179 It has been shown that smoking decreases the number of Langerhans cells. 180 The location and densities of Langerhans cell populations have been mapped. 164,170, Langerhans cells are found in the normal dermis, the lymphatics and in draining lymph nodes, in mucous membranes of tongue and tonsils, esophagus and gastric mucosa, as well as in the mucocutaneous junctions of the vagina, rectum, uterine cervix, prepuce, and urethra. 168,184 Much of the controversy about the purported role of male circumcision in reducing the number of heterosexually transmitted HIV infections surrounds the theory that Langerhans cells act as the mode of HIV entry into the body. The bottom line is that Langerhans cells in the prepuce should be considered normal, rather than a pathologic entity requiring excision. 165 A review of the scientific literature reveals that the actual effect of male circumcision is the destruction of the clinically-demonstrated hygienic and immunological properties of the prepuce and intact penis. There are no histological studies to validate the claim that the sclerotic keratinization of the epithelium of the surgically externalized, desiccated glans penis, meatus, or scar of the circumcised penis creates a barrier against infection. The higher rate of sexually transmitted infections in circumcised males might well be the result of the loss of preputial immuno-protective structures. 185 The loss of the protective, self-lubricating, mobile, double-layered prepuce exposes the glans and meatus to direct friction, abrasion, and trauma. The surgically externalized and unprotected glans and meatus of the circumcised penis are constantly exposed to abrasion and dirt, making the circumcised penis less hygienic and prone to meatal stenosis. 186 The circumcised penis is more prone to infection in the first years of life than the intact penis. RESPONSE 59: CDC's view of the biologic evidence differs from that of the peer reviewer. The scientific evidence from the literature supports the view that lymphocytic cells in the prepuce serve as a portal for HIV and other infections as documented in the background document.
# COMMENT:
# Effect of male circumcision on health outcomes
The material presented in this section of the background document does not adequately represent the medical evidence currently available. In most areas discussed in the CDC draft, the medical evidence taken as a whole does not support the conclusions reached by the writers of the CDC draft.
# RESPONSE:
See response 1 and 6.
# COMMENT:
# Biological plausibility
The material presented in this section of the background document is highly speculative and based on conjecture rather than actual data. The speculations presented suggest that the writers were given the outcome of interest, namely the "CDC group think presumption" that male circumcision of infants will reduce the risk of HIV infection in adults, and then they were instructed to find any data that supported this conclusion: a classic example of confirmation bias. When the scientific process is followed properly, conclusions are data-driven instead of data being conclusion-driven.
# RESPONSE: See responses 1 and 6
# COMMENT:
This section begins with the statement, "The foreskin can serve as a portal of entry for STIs (including HIV), lending biological credibility to the role of male circumcision in preventing STI and HIV acquisition through insertive sexual intercourse," which cites an opinion piece as its source. 32 As any part of the body can be a portal for infection, it does not follow that removal of that body part will decrease the risk of infections, nor should removal of normal tissue be given any serious consideration. This is a circular argument that begins with assuming the "CDC group think presumption" is true.
# COMMENT:
The statement, "Compared to the dry external skin surface of the glans penis and the penile shaft, the inner surface of the foreskin is less keratinized. This may allow easier access to the epithelial cells of the epidermis and dermis (in which STIs such as HPV and HSV-2 replicate) as well as access to target cells for HIV infection," uses citations from an opinion piece and a review article on an unrelated topic. 32,191 Interestingly, the opinion piece cited states that in a series of seven circumcised and six intact men, the glans was equally keratinized in both groups. Studies have found that the thickness of the epithelial layer of inner and outer foreskin are similar. 191,192 Therefore, the underlying premise of this statement has been demonstrated to be untrue. For the same reason the statement, "Because the inner surface of the foreskin is lightly keratinized, it may be relatively susceptible to traumatic epithelial disruptions during intercourse, providing a portal of entry for pathogens," which is also referenced to an opinion piece, 32 is unsubstantiated conjecture.
The importance of the statement, "Furthermore, the foreskin retracts away from the glans and over the shaft of the penis during intercourse, which exposes this surface to the body fluids of the sex partner," is unclear. The circumcised penis is also exposed to the body fluids of the sex partner. The only way to avoid this is to avoid sex or wear a condom.
While it has been "postulated" that the foreskin may serve as a reservoir of sexually transmitted pathogens, there is no evidence that the preputial sac is conducive to viral survival. The facts speak against this. For example, there is no evidence that herpes simplex virus type 2 or human papillomavirus infections are more common in intact men (see discussion elsewhere). A large prospective study recently demonstrated that human papillomavirus (any type, oncogenic, HPV-16) are shed significantly faster from the penis of intact men. 193 With evidence to the contrary, it is time to end this type of speculation. That normal flora anywhere in or on the body, let alone in the preputial sac, would have an inflammatory impact that would increase the risk of HIV infection is ludicrous.
Level of penile wetness has been shown to be a factor in one study, but, in the randomized clinical trial in Uganda, men who did not clean their genitals for the first ten minutes following intercourse had significantly lower rates of HIV infection than men who washed in the first three minutes. 194 This suggests that there may be something in the preputial wetness or in vaginal secretions that interferes with the infectiveness of HIV. Furthermore, women have constant vaginal wetness and the CDC is not speculating about their need to be circumcised.
The suggestion that higher numbers of immune cells on the inner foreskin that can more easily respond to infections, and other exposures, will result in an increase in viral susceptibility of the inner foreskin is counterintuitive. Mucosal immunity is based on immune cells doing their job. If they are responding to infections, this would suggest they are more effective at repelling infection. This is borne out by the fact that sexually transmitted infections overall (as discussed elsewhere) are more common in circumcised men. 185 The increased risk of HIV infection in those with genital ulcers makes sense as the ulcers compromise the barrier that is effective in keeping infections out and activates the T-cells, which is considered part of the HIV infection process. The mucosal immune system is quite effective in preventing HIV infections, as indicated by the low rate of transmission through penile-vaginal intercourse (1 per 1000 acts of unprotected coitus). It is only when high viral loads are present that infection is more likely to occur. The speculation surrounding the biological plausibility of the foreskin increasing the likelihood of HIV acquisition is strained and depends on the lining of the foreskin being thinner (which it is not), the preputial sac being more likely to harbor viruses (which it does not), and functional immune cells on the surface (which actually reduces the likelihood of infection). This theory is so farfetched and counterfactual, why would anyone believe it?
The statements made in this section are based purely on speculations that directly contradict the facts. Although these speculative claims have been repeated, ad nauseam, in the medical literature, there is no science to support them. RESPONSE: See response 60.
# COMMENT:
# Male circumcision and the risk of HIV infection acquisition
# Male acquisition of HIV infection from female partners
The material presented in this section of the background document is a confusing regurgitation of review articles that are incomplete and out of date. 21,22,24,27 More importantly, this section fails to address several key questions, namely whether the results of the randomized clinical trials from Africa 1-3 are valid, whether they apply in the United States, and, if applicable, to whom should they be applied.
# RESPONSE:
See Responses 1, 6 and 19.
# COMMENT:
Three randomized clinical trials were undertaken simultaneously in Africa with nearly identical methodology. This lack of methodological variation is not a sign that the best methodology was used, but instead undermines the robustness of their findings. Because of this lack of variation, one might think of the trials collectively as one trial performed at three sites. 195 The results of the trials were remarkably consistent, to the point that some would consider the similarity of the results to be mathematically improbable. Because of the similarity in the results, one could argue that the studies were precise in their estimates, but with a lack of methodological variability the accuracy of their estimates cannot be assessed. More studies using a variety of methods reaching consistent results would provide a stronger testament to their accuracy. The accuracy of their estimates can be called into question because of the internal validity issues these trials share (discussed below) and the fact that their estimates of the treatment effect were greater than seen in observational studies. This is quite atypical as the treatment effect in randomized trials are typically about 25% to 30% smaller than seen in observational studies.
# RESPONSE 61:
The similarity in methodology of the 3 randomized clinical trials is a strength in that it allows for comparison and validation of results. The fact that 3 such trials in 3 different regions of Africa had similar results represents the best and highest level of scientific evidence. See response 5. Cochrane reviews point to RCTs as the gold standard as do most scientific bodies tasked with evaluating scientific rigor.
# COMMENT:
The methodology of these trials undermine the internal validity (how well the estimates generated by the trial reflect reality) in a number of ways. Perhaps the most important methodological flaw is that no effort was made to identify the source of the infections that were diagnosed during the course of the trial. By failing to do so, these trials cannot answer their research question of determining the impact of male circumcision on the heterosexual transmission of HIV from females to males because it not known how the infection was transmitted. Consequently, the CDC draft is incorrect throughout by suggesting these trials measured this form of transmission, when they clearly did not. This is important because some of the infections may have resulted from male-to-male transmission and some may have been transmitted through iatrogenic means. In the trial in Kenya, only 0.2% of the participants reporting having had male-to-male sexual contact. 2 For many in developed nations this would be considered an extremely low percentage, as male-to-male sexual contact is seen in the range of 5% to 10%. The low rate of men reporting male-to-male contact may reflect the extreme homophobia in sub-Saharan Africa. In Uganda, for example, their Anti-Homosexuality Act of 2014 will punish homosexual activity with life imprisonment (they were considering making it a capital offense). Given the extreme penalties and social stigmatization, admitting homosexual activity to researchers could result in dreadful consequences. Therefore, it is reasonable to assume that, among the thousands of participants in these trials, many were having male-to-male contact. Consequently, the role of anal intercourse in transmitting HIV in this population is unknown. 196 Given that transmission rates between two men is more efficient and that this mode of transmission is not impacted by male circumcision, 25 the failure to identify the source of infection would likely impact their final estimates.
A surprising number of participants in these trials became HIV infected despite not being sexually active or always using condoms. Consequently, it is unlikely that their infections were sexually transmitted. Iatrogenic transmission of HIV is well documented in Africa typically from procedures in which the skin is punctured with instruments or needles that have not been properly sterilized. This possibility should not have been a surprise to the trial investigators. In one African study, female and male virgins who were circumcised were more likely to be HIV-infected. 209 Some have argued that the iatrogenic spread of HIV in Africa is better able to explain the high prevalence of HIV rather than convoluted models that rely on multiple concomitant sexual partners and a high burden of sexually transmitted infections. 200,210 In each of the trials, there were infections that could not be accounted for on the basis of sexual transmission alone. For example, in the South African trial 23 men, who accounted for 2076 person years, became HIV positive with either having no sexual contact or always using a condom (infection rate 1.11/100 person-years) compared to 46 infections in 2498 person-years among men who at least one episode of unprotected sex during the trial (1.84/100 person-years). 1 Assuming that all of the men in the trial had the same risk of infection through non-sexual transmission only, only 18 of the 69 infections can be attributed to sexual transmission (1.84 minus 1.11 per 100 personyears times 2498 person-years). In the Ugandan trial, 1252.1 person years and 6 infections can be attributed to men who reported no sexual partners for the duration of the trial (0.48/100 person-years). 3 When this baseline rate of infections in those who were not sexually active is subtracted from the total rate in the men who were sexually active, 35 of the 67 infections can be attributed to sexual transmission.
In the Kenyan trial, there were five men reporting no sexual activity in the first three months of the trial who subsequently seroconverted (0.73/100 person-years). 2 When this rate is subtracted from the rate seen in those who were sexually active, only 36 of the 69 total infections can be attributed to sexual transmission.
Without knowing the source of the infections they diagnosed, it is hard to determine what actually was measured in these trials and even harder to extrapolate their findings across the ocean to infants. How can the CDC base policy on trials that did not measure what they set out to measure?
The study methodology, which was nearly identical in each of the trials, had several built-in forms of bias, all of which would be likely to overestimate the treatment effect.
RESPONSE: See Response 12.
# COMMENT:
Expectation bias: At least one primary investigator was on record prior to execution of his trial expressing his impatience and stating that it was time "to begin investigations of the feasibility of acceptable male circumcision interventions in communities with high HIV and STD seroprevalence where male circumcision has traditionally not been practiced." 31 So, it would appear that Bailey believed a randomized clinical trial was unnecessary, as the issue was already settled for him. Similarly, in the Ugandan trial, the researchers from Johns Hopkins dismissed the results of the six men who became infected despite no sexual partners noting, "these participants probably under-reported their sexual activity." 3 Infection in men who were not sexually active did not agree with their expectations, so the results were summarily dismissed. How many other unwanted results were similarly dismissed because they did not agree with the investigators' expectations. Furthermore, there is evidence of expectation bias on the part of the participants. These men agreed to participate because they believed that male circumcision would lower their risk of HIV. Even after the informed consent process, more than half (57%) believed that male circumcision would reduce their risk of infections. 211,212 Since the researchers and participants could not be blinded to which group a participant was assigned to, one would expect that participants would act differently based on their assignment and be treated differently by the researchers. Both researchers and those assigned to the intervention group would be expected to change their behavior to make the intervention pay off.
Selection bias: The men in these trials were those who were interested in undergoing male circumcision. After the propaganda sessions in the roll-out before the trials, many men were convinced they wanted a male circumcision in order to reduce their risk of HIV. When compared to the general population, one would expect that at least some of these men viewed themselves as, or were in reality, at greater risk for HIV infection. The percentage of men interested in a free male circumcision, as evidenced by the current voluntary medical male circumcision programs, is less than 5% in most countries. So, the participants in these trials are representative of only a small subset of the general population. As noted above, the motivation of the participants in these trials would be expected to alter their behavior.
Lead-time bias: The men who were randomized to be immediately circumcised were instructed to abstain from sexual relations or to always use condoms for the first six weeks following the procedure to allow for proper healing. The data reported in these trials was number of infections per time of potential exposure. Since those in the intervention group each had six weeks less of potential exposure, one would expect them to have a smaller number of infections. Avoiding lead-time bias is a fundamental principle of study design that is taught in the most rudimentary of courses on clinical study design. None of the randomized clinical trials adjusted for this bias in their study design, and only one made an adjustment in their post hoc analysis. 1 This indicates either incompetence or a conscious omission that would increase the likelihood of producing data favorable to male circumcision. Intervention bias: The men who were randomized to the intervention group had more visits and exposure to the research team. This would give researchers additional opportunities to provide education on safe-sex practices and to emphasize how important it was for the trial participants to follow-up as requested.
Attrition bias: These trials had a substantial number of participants who were lost to follow-up. The number lost was 251 (8.0%) in South Africa, 1 240 (8.6%) in Kenya, 2 and 493 (9.9%) in Uganda. 3 Those who were assigned to the intervention group were significantly less likely to be lost to follow-up (OR 0.83; 95%CI 0.73-0.95). One possible explanation is that men who were hoping for a free male circumcision but assigned to the control group would see no purpose in staying in the study. Participants who are lost to follow-up are not the same as those who continue to participate. In the Kenyan study, they had a greater number of lifetime sexual partners and a higher prevalence of being seropositive for herpes simplex type 2 virus (Robert Bailey, personal communication). What is more concerning is that for every participant who become infected with HIV during these trials, there were 4.8 who were lost to follow-up. This is a serious missingdata problem.
Duration bias: The trials involved 24 or fewer months of follow-up. The shape of the trajectory following 24 months is unknown. It could very well be that over time the number of infections will be the same in both groups and male circumcision may only slightly delay the time to infection. Several of the models have assumed that the trajectory seen in the first two years will continue for 20 years, based on faith more than science. There is also growing evidence that HIV is losing its virulence. 233 Early termination bias: All three of the trials were terminated early. Early termination, in and of itself, is more likely to result in an overestimate of the treatment effect. 234 It also amplifies any impact of the lead-time bias. Of interest, the Ugandan study had a Fragility Index 235 of 4, which suggests that findings of the study were not particularly robust. How can a study that is terminated early, have such a low Fragility Index?
Overpowered studies: These studies were powered to detect a 1% ARR difference in HIV incidence between the intervention group and the control group. 236,237 This explains the high number of participants in each trial. The important question is whether a 1% difference is clinically important, not whether the difference is statistically significant. If a 1% difference is not important, then demonstrating that this difference is statistically significant misses the point of doing the studies. Studies with a large number of participants, such as these randomized clinical trials, are able to demonstrate a statistically significant difference for very small absolute differences, but when the absolute differences are so small, these studies can also have trouble distinguishing between real findings and background noise. With these trials, even though each source of bias may not be enough alone to explain the difference seen, their cumulative effects, since they all would work to overestimate the treatment effect, would be enough to explain the 1.3% absolute difference seen.
The randomized clinical trials, especially the Ugandan trial, have a number of unexplained anomalies. For example, in the Ugandan trial, those who reported consistent use of condoms had a trend toward a higher rate of HIV infection than in those who reported never using condoms (consistent condom use: 1.03/100 personyears; No condom use 0.91/100 person-years; RR 1.13; 95%CI=0.54-2.38, p=0.74). 3 Given all of the problems with how the data in these studies were handled, it would be helpful if these data could be analyzed by independent experts, rather than researchers who have careers that depend on generating positive results. Even though the National Institutes of Health used our tax dollars to fund two of the randomized clinical trials, the data are not available to the public and are not subject to the Freedom of Information Act. Some have called on these data to become available, 238 but researchers of the studies from Kenya and Uganda have not complied. There were several ethical concerns regarding the trials, 239,240 including that the financial incentives to participate (a free male circumcision, money equivalent to twoweeks employment, cash for recruiting additional subjects, unlimited access to free condoms, and free health care for 21 to 24 months) were coercive. There is a lack of equipoise seen in both researchers and participants. 211,212 Based on the extremely promale circumcision bias of the researchers, it is unlikely that participants were given full disclosure, particularly regarding the risks and long-term harms of the procedure, while obtaining informed consent. Furthermore, going into these trials, the researchers knew that male circumcision would be less effective, more expensive, and more invasive compared to other interventions already available at that time (most notably condoms). Typically, trials that evaluate interventions that are known to be inferior to current therapies are not pursued because they violate the Helsinki Declaration. 239,241 Finally, it is unclear whether these trials were necessary as demographic information was available prior to the initiation of these trials showing that, even if they generated a positive result, their results would not have external validity. Typically, when a new drug is developed it is subjected to a Phase III trial in a closely defined and monitored population. Phase IV studies take place once the medication is being used in the general population. In the case of male circumcision and its impact on HIV infection, the Phase IV type data were available before the Phase III studies were designed. The Phase IV type data indicated that male circumcision did not have any impact on a demographic level. For example, in South Africa HIV spread had similar dynamics of spread in the Shangaau and Xhosa tribes that are circumcised and the Zulu and Tswana tribes that do not circumcise. The fact that the researchers who performed the randomized clinical trials went ahead with the trials, despite the availability of this Phase IV type data, suggests that they were not properly educated in basic epidemiological methods, such as the difference between efficacious and effective, or that they chose to ignore basic principles of epidemiology when moving forward with these trials.
While randomized double-blinded placebo-controlled trials are considered the gold standard for testing a hypothesis, the quality of the information garnered from poorly designed randomized trials, such as the randomized clinical trials undertaken in Africa, can be below that of a well-designed observational study. The CDC draft places unearned importance on the results of these trials. While there are serious concerns about the internal validity of these trials, there is ample evidence that the trials lack external validity. While some male circumcision advocates, including the writers of the CDC draft, have suggested that data collected from the participants in the trials after the completion of the trials indicates that male circumcision is effective (in addition to being efficacious), and thus has external validity, these participants would still be subject to the Hawthorne effect and the undue influence of the large financial advantages of having participated in the trials. These people should still be considered to be acting within a research setting as they likely received far more attention and education than men who would be getting circumcised outside a research setting, but the results should not be considered on the same quality level as a randomized trial.
The randomized clinical trials lack external validity. When there is a treatment effect in a clinical trial, it would be expected that such a treatment effect would be seen outside of research settings and in the population at large. This has not been seen. There are eight or more countries within Africa where the prevalence of HIV infection is greater in circumcised men than in intact men. 13, When the national survey data are included in a meta-analysis, no difference in HIV prevalence is noted by male circumcision status (intact versus circumcised men random-effects summary OR 1.10; 95%CI 0.81-1.50). 251 If the results from the three randomized clinical trials do not apply to the countries in Africa, do they apply to countries outside of Africa? While some ecological studies within Africa have suggested a correlation between male circumcision prevalence and HIV prevalence, other analyses have not found male circumcision to be a factor. 256 When these methods are applied to developed countries, there is a significant positive correlation between male circumcision prevalence and the prevalence of heterosexually-transmitted HIV infections. 257 When only English-speaking countries are considered, there is a strong linear relationship between a country's male circumcision rate and its rate of heterosexually-transmitted HIV (r 2 =.9756). 258 If the writers of the CDC draft want to accept the results of those ecological studies in Africa showing that increasing male circumcision rates correlate to decreasing rates of HIV infection, then they also need to accept the results of the recent study that found a statistically significant correlation between the prevalence of infant male circumcision and the prevalence of autism. 259 Before accepting the "CDC group think presumption" that the findings of the methodologically flawed randomized clinical trials of adult males in Africa would apply to infants circumcised in the United States, it is important to look at the evidence available. One approach would be to look at the entire body of literature on the association between HIV incidence and prevalence and male circumcision status. This has been assessed in over 100 populations. 246, These include randomized clinical trials, prospective cohort studies, national surveys, and case-control studies and all of these study types can be informative. When study characteristics of the various populations are adjusted for, meta-regression 324 reveals that studies of general populations broadly, and outside of Africa in particular, do not support the hypothesis that male circumcision lowers the risk of HIV infection. Meta-regression also indicates that as the prevalence of male circumcision in a community increases the association between being intact and HIV infection increases. 325 This would indicate that male circumcision has no role as primary prevention either in Africa or outside Africa.
A second approach would be to look at the studies that have been performed in North America on heterosexual men. None of them support the "CDC's group think presumption," and none of their findings in favor of male circumcision are statistically significant. A 1991 study of men at high risk for HIV infection had an odds ratio (intact versus circumcised men) of 1.75 (95%CI 0.93-3.27). 11 A 1993 study by the same researchers found an odds ratio of 4.25 (95%CI 0.94-19.13). 15 A representative national survey found an odds ratio of 2.60 (95%CI 0.65-10.42). 9 A 2004 study from the US Navy found a slight decrease in risk for intact men with an odds ratio of 0.80 (95%CI 0.52-1.22). 10 A national survey in Haiti found a similar trend with an odds ratio of 0.67 (95%CI 0.33-1.35). 13 A very large study from an STD clinic in San Francisco found no difference with an odds ratio of 0.93 (95%CI 0.33-1.05). 8 Another large STD clinic study from Baltimore found the raw data had an adjusted odds ratio of 1.00 (95CI 0.86-1.15). 12 None of these studies found a statistically significant difference. Finally, a study from a STD clinic in Puerto Rico found that circumcised men had a significantly higher prevalence of HIV infection (OR 0.68; 95%CI 0.49-0.95). 14 When these studies are combined in a meta-analysis, the random-effects summary odds ratio was 1.21 (95%CI 0.78-1.88, between-study heterogeneity chi-square (df=7) = 91.64, p <.0001, I 2 = 91.3%) when raw numbers are used and 0.94 (95%CI 0.79-1.13, between-study heterogeneity chi-square (df=7) = 15.56 p=.0295, I2 = 48.7%) when the adjusted odds ratio for the Baltimore study is used. Most of these studies were performed in high-risk men and no difference was documented. One would expect there to be even less of an association in general populations. Consequently, these data do not support the "CDC group think presumption." Finally, the target population for male circumcision needs to be delineated. The data clearly show that male circumcision is unlikely to be effective if targeted at the general population. The US data, which is derived primarily from patients seeking care at STD clinics, indicates that male circumcision would not be effective for high risk populations either, such as attendees of STD clinics. The sub-strata data from the Baltimore study, which made up only 1.4% of men seeking care at an STD clinic, suggest that there may be a slight role for male circumcision in the subpopulation of men who are at imminent risk of infection, such as those who have a regular female sexual partner who is known to be HIV-infected. In this subpopulation, only 11 intact men were HIV infected and their findings had a Fragility Index 235 of 1, indicating results that are far from robust. 12 Policy decisions should be delayed until this association is replicated in multiple studies with sufficient robustness. Consequently, any discussion of male circumcision related to the risk of HIV infection in the United States, if they should occur at all, should only be directed toward discordant couples with HIV-negative men who have regular sexual relations with known HIV-positive female sexual partners. There is no evidence to support suggesting male circumcision for any other populations. For this small subpopulation, there are a number of far more effective options such as condoms, preexposure prophylaxis, and anti-retroviral therapy for the infected sexual partner. Even a model developed by the CDC, that assumes the "CDC group think presumption" is true, has determined that male circumcision would have minimal impact in preventing HIV infection in this population. So, why is the CDC contradicting its own findings by bringing forth the recommendations in this draft?
The bottom line is that data does not support the use of male circumcision to reduce the risk of heterosexual transmission of HIV in the United States.
The material given in this section by the CDC is counterfactual, biased, and dangerous. The medical literature suggests that male circumcision might have a minimal impact on the risk of HIV infection in a very small sub-population, but this needs further study before implementation. To extend the discussion of male circumcision beyond this easily identifiable sub-population is reckless and would result in unnecessary physical and psychological harm. The fear-mongering implicit in this section makes the CDC look foolish and desperate. In the seven years since the CDC held its consultation, several things have happened that have taken male circumcision out of consideration as an HIV preventive measure. AIDS researchers have adopted secondary prevention methods such as "treatment as prevention" that has changed infection with HIV from a death sentence into a chronic disease. 326 Similarly, the virulence of the HIV virus is weakening. 233 Finally, the roll-out of male circumcision in Uganda and Kenya has resulted in increases in the incidence of HIV in men in those countries. Not to mention the number of men and boys who have died as a direct result of being circumcised in Africa, some forcibly against their will. The CDC would be better off expending its energies, and US taxpayers' money, promoting interventions that are not ineffective and harmful. RESPONSE 62: See response 5. The concerns presented by the reviewer have been previously addressed and adequately refuted in the literature. 51,52
# COMMENT: HIV infection transmission from circumcised men to female partners
The material presented in this section of the background document is incomplete with some of the material being misrepresented.
# RESPONSE:
See Responses 1 and 5.
# COMMENT:
The early studies, which looked at whether the male circumcision status of a woman's male sexual partner was a risk factor for women becoming infected with HIV, showed mixed results. 287,317, Since then, the evidence emerging fails to support the theory of male circumcision directly reducing the male-to-female transmission of HIV. The only randomized clinical trial addressing this issue found a marked increase in HIV infections in the female partners of men who had been circumcised. 338 The writers of the CDC draft give a very pro-male circumcision spin to these results. The absolute risk increase for these women was 6%, which translates to a number needed to harm of almost 17. So, for every 17 male circumcisions performed on an HIV-infected man with a female partner that was not infected, one would expect one additional female partner to become infected. This study was terminated early, and rightly so, because early looks at the data indicated that the practice was too dangerous to continue. To state that the study was terminated because it was unlikely to show a favorable result may be technically accurate, but it belies the 50% relative increase in HIV infections. The promale circumcision spin stating the study failed to show a difference is also true, but disingenuous since the trial was rightly terminated before the study had enough power to show a statistically significant difference if one existed. The study was also profoundly unethical because the women were not told their sexual partners had HIVvery reminiscent of Tuskegee. Shockingly, the authors of the study recommended that HIV-infected men undergo male circumcision, with a total disregard for the increased risk of HIV infection the procedure foisted on female partners, because of the fear that these men would feel stigmatized if they were not circumcised. 338 Too bizarre to have been made up.
The two models that have assessed the impact of male circumcision on the incidence of HIV infections in women assumes the findings of the randomized clinical trials have both internal and external validity, both of which are risky assumptions. 223,339 The extremely speculative nature of these models should exclude them from being considered in formulating policy.
# RESPONSE 63:
The CDC background document provides an unbiased and accurate summary of the available data indicating that male circumcision does not significantly reduce heterosexual male-to-female HIV transmission.
# COMMENT: Male acquisition of HIV infection and other STIs from male partners
The material presented in this section of the background document is generally accurate, incomplete in a few areas, but needs to be more explicit in its conclusion, namely that male circumcision is not a reasonable intervention in the prevention of HIV infection that might be acquired by men from their male sexual partners. A recent model published by the CDC assessing the effectiveness of various interventions in the prevention of HIV infection in discordant couples found that, for a man with a male partner who was HIV-infected, over a 10-year period, reliance on male circumcision alone would nearly guarantee the man would become infected. 340 A major thrust that resulted from the CDC's 2007 consultation was an effort to find a link between male circumcision and the risk of HIV infection in men having sex with men. 16 One opinion as to why the CDC took over seven years from the time of the consultation to the release of this draft was the hope of a breakthrough study that would demonstrate that male circumcision reduced the risk of HIV infection in men having sex with men. Many at the consultation believed that such a finding would secure the practice of infant male circumcision in the United States for decades to come, thus worth holding out for. The many studies on men having sex with men have overcome researcher expectation bias and failed to generate the results hoped for.
RESPONSE 64: See response 27 and 39. A summary of the findings of the 2007 CDC male circumcision consultation has been previously reported. 1 The Cochrane review provides evidence from a meta-analysis of 21 observational studies indicating that circumcised insertive men who have sex with men (MSM) experienced a significant reduction in HIV acquisition compared with uncircumcised insertive MSM; circumcised receptive MSM didn't experience a significant reduction in HIV acquisition compared to their uncircumcised receptive MSM counterparts. Because these results did not include results from RCTs, the Cochrane review did not conclude that male circumcision conclusively protected insertive MSMs from acquiring HIV infection. Nevertheless, biological plausibility would argue that insertive MSM should experience a protective benefit against acquiring HIV just as circumcised heterosexual men do. The CDC recommendations explicitly state that due to the lack of RCTs, it cannot definitively conclude that HIV acquisition is reduced among circumcised insertive MSM compared to their uncircumcised insertive counterparts.
# COMMENT: HIV transmission in other populations at high risk for HIV acquisition
The material presented in this section of the background document is appropriate.
# RESPONSE 64a:
No response required.
# COMMENT:
# Male circumcision and other health conditions
The material presented in this section of the background document is misleading. The medical literature does not support the claims that male circumcision has a positive impact on the incidence or prevalence of penile, prostate, or cervical cancer. Likewise, it has no positive impact on the incidence of any of the sexually transmitted infections. It has no impact on the prevalence of any of the individual sexually transmitted infections, with the exception of syphilis, which fortunately is rare in the United States. 341 To mention these diseases and devote substantial discussion to them gives the false impression that male circumcision in reality has an impact on these diseases.
# RESPONSE 65:
See responses 1 and 6. While the meta-analysis of STDs and male circumcision cited by the reviewer failed to find a significant association between the two 11 , a careful review of the methods used to conduct this review render the results of that meta-analysis to be scientifically biased and lacking scientific validity. 12 COMMENT:
# Sexually transmitted infections (STIs)
The material presented in this section of the background document is biased, incomplete, and inaccurate.
RESPONSE: See response 65.
# COMMENT:
This section is markedly incomplete. Instead of searching the medical literature, or even relying on recently published meta-analyses 185, as a starting point, this draft relies on non-systematic reviews/opinion pieces 20 and a meta-analysis that is over a decade old 24 as the source of information. Consequently, the sections addressing the various sexually transmitted infections are woefully incomplete, inaccurate, and misleading. It has been over seven years since the CDC held a "consultation" on male circumcision 16 where it was decided to release recommendations concerning male circumcision. That should have provided enough time for their staff to search the medical literature, examine the data, and perform meta-analyses (although the only meta-analysis generated on the topic of male circumcision proved to have erroneous calculations requiring a three-page erratum in the Journal of the American Medical Association 25 The summary effects odds ratio, when properly calculated, was 0.95. If the staff was going to rely on the work of others, they could have at least referenced the most up-to-date systematic reviews and metaanalyses. But several sexually transmitted infections, for which there are multiple studies in the medical literature, were nearly completely ignored, yet there are extensive discussions of chancroid, Trichomoniasis vaginalis, and the transfer of various infections to female partners, all based on a small number of studies. What explains such a low quality of scholarship? Laziness? Insufficient time? Preconceived bias? The CDC has had over 7 years to produce this draft, yet this response, written in less than 45 days, has more references and more detail covering ALL the evidence in the medical literature. Were there directives from leadership to present male circumcision in the best light possible and to bury, ignore, or omit any studies to the contrary? Apparently, not out of the question. Given the poor quality of the effort to find (let alone evaluate) the evidence, how can this draft of the CDC be taken seriously by scientists, epidemiologists, or health care providers? This entire section needs to be scrapped, the evidence found and properly evaluated, and accurate information provided.
# RESPONSE:
See responses 1 and 6.
# COMMENT:
The statement, "Male circumcision has been shown to reduce the risk for some other STIs in addition to HIV," is factually inaccurate. The only STI that the medical literature may support as male circumcision having a minimal reductive impact is in the prevalence of syphilis (see discussion below), but male circumcision has not been shown to impact the incidence of syphilis. Consequently, the word "some" should be replaced with "possibly one."
RESPONSE 66: See response 39. Based on the update of the review of the literature during the response process, more benefits for reduction in various STDs have accrued since the initial review. In randomized controlled trials for which data are available, reductions in the 1) prevalence of genitourinary disease (GUD) , 2) incidence of herpes simplex virus type 2 (HSV-2), 4,28 3) prevalence, 29 _ENREF_9 incidence, 30,31 and clearance 29,31 of high-risk oncogenic human papillomavirus (HR-HPV)_ENREF_7, 4) prevalence of Trichomonas vaginalis, 27,32 5) incidence of syphilis, 33 6) prevalence of bacterial vaginosis, 27 and 7) prevalence of mycoplasma genitalium 34 were also demonstrated._ENREF_19
# COMMENT:
It is clear that the writers of the CDC draft did not look carefully at, or critically evaluate, the sexually transmitted infection data from the African randomized clinical trials. Even a cursory reading of the methodology of these trials would reveal that these trials made no attempt to minimize or provide any post hoc adjustment for lead-time bias. The men who were randomized to immediate male circumcision were instructed to abstain from sexual relations or always use condoms for the first six weeks following the procedure to allow for proper healing. The data reported in these trials was: "number of infections per time of potential exposure." Since those in the intervention group each had six weeks less of potential exposure, one would expect them to have a smaller number of infections. Avoiding lead-time bias is a fundamental principle of study design that is taught in the most rudimentary of courses on clinical study design. The fact that all three randomized clinical trials did not adjust for this bias, either in the study design or post hoc analysis, indicates either incompetence or a deliberate omission that would increase the likelihood of producing data favorable to male circumcision. As will be shown in the sections below, adjusting for lead-time bias changes the outcomes of these studies. If one looks carefully at the prospective studies of genital human papillomavirus and male circumcision, the studies suffer from incomplete sampling to the point, as discussed below, that the treatment effect in these trials can be completely attributed to sampling bias. RESPONSE: See response 15 and 65.
# COMMENT:
The statement, "Although rarely fatal, STIs other than HIV are among the most common communicable diseases in the United States, and interventions that prevent STIs would result in substantial reductions in morbidity and cost of health services," while true, is misplaced hyperbole. As will be discussed in the sections below, the incidence and prevalence of none of the common sexually transmitted infections are impacted by male circumcision. Only the prevalence of syphilis may be minimally impacted, but syphilis is very rare in the United States infecting only 9.8 per 100,000. 341 Consequently, the CDC draft is trying to jack up the importance of male circumcision through thinly veiled fear mongering, when the medical literature totally undercuts their message.
RESPONSE: See responses 65 and 66
# COMMENT:
While the CDC draft discusses several of the sexually transmitted infections individually, it fails to address the impact of male circumcision on the overall risk of contracting a sexually transmitted infection of any type. In other words, the risk of any sexually transmitted infection versus no sexually transmitted infections. There have been 20 publications that have looked at the prevalence of any sexually transmitted infection by male circumcision status, 9,10,14,248,260,271,275, and four prospective studies that have looked at the incidence of any sexually transmitted infection. 358, A meta-analysis of the studies of prevalence, in which the data in one study was stratified by race, 362 by number of life-time sexual partners in another, 9 and by the five populations in which data were collected in another, 260 yields a random-effects summary odds ratio (intact men versus circumcised men) of 0.86 (95%CI 0.74-1.01, between-study heterogeneity chi-square (df=26) = 303.00, p<.0001, I 2 = 91.1%). In the analysis, there was one clear outlier that reported an odds ratio of 1.51 (95%CI 1.41-1.62). 368 When this outlier is removed from the analysis, the between-study heterogeneity chi-square drops by 203.41, and the random-effects odds ratio is 0.82 (95%CI 0.74-0.92, I 2 = 73.9%). 185 This would indicate that when all sexually transmitted infections are considered together, male circumcision significantly increases the risk of contracting a sexually transmitted infection. When the studies of incidence are stratified by study, the fixed-effect of the summary relative risk ratio is 0.91 (95%CI 0.78-1.07) 185 which, while not statistically significant, trends in the same direction of the studies of prevalence. Therefore, an intact male is at lower overall risk of contracting a sexually transmitted infection.
RESPONSE 67: The category of "any STD" is an artificial construct. Our background document provides clear evidence of decreased prevalence of HSV, HPV, syphilis, and others associated with male circumcision.
# COMMENT:
(Continued from comment before Response 67). This finding should not be surprising as there have been several studies comparing the risk of genital discharge syndrome versus genital ulcerative disease by male circumcision status, 12,185,265,372,373 which have been ignored in the CDC draft. Those studies on meta-analysis have found the risk of genital ulcerative disease versus genital discharge syndrome in intact men had a random-effects summary odds ratio of 2.24 (95%CI 1.63-2.24, between-study heterogeneity chi-square (df=4) = 17.94, p=.0013, I 2 = 72.1%) 185 Conversely, circumcised men would be twice as likely to have genital discharge syndrome versus genital ulcerative disease. Since genital discharge syndrome is far more common than genital ulcer disease, it makes sense that the overall risk of sexually transmitted infections may be higher in circumcised men. The data may not have been precisely collected in these studies, but they were not collected any less precisely than in the studies the CDC draft has elected to include.
This finding also makes sense on a biological level. Mucosal immunity is quite efficient in keeping invasive organisms at bay. By removing much of the penile mucosa and drying out the remaining mucosal surfaces, the natural immune system is disrupted. For example, the first line of defense on the mucosal surface are the dendritic (Langerhans) cells. With these cells removed by male circumcision, the penis has fewer defenses against the garden-variety sexually transmitted infections, thus making them more prone, overall, to sexually transmitted infections. This may explain why, in a large prospective study, clearance of human papillomavirus occurred significantly more quickly in intact men than in circumcised men. 193 Consequently, the recommendations for the intended audience of health care providers are biased, hyperbolic, and are missing essential information. Health care providers need to be told that male circumcision may increase the overall risk of sexually transmitted infections.
RESPONSE: See responses 65, 66, and 67.
# COMMENT:
Note: There are number of redundant citations in this section. For example, citations 74, 75, and 76, are the same as citations 4, 5, and 6.
# RESPONSE 67a:
We have corrected this duplication of citations.
# COMMENT: Genital Ulcer Disease (GUD)
The only sentence under this heading is factually inaccurate and reflects a misinterpretation of the data. As will be discussed in the sections below, while GUD incidence was decreased in the only prospective studies to explore it, 347,350 the studies that looked at herpes simplex virus, after adjustment for lead-time bias, were not statistically significant. 347, It is not clear why this sentence fails to mention that the randomized clinical trials failed to find an association between male circumcision and syphilis. 347,350 Is such an oversight because of a lack of attention to details or to give this section the proper pro-circumcision spin?
# GUD (various types)
The material presented in this section of the background document is incomplete and confusing. One would expect the section to address GUD generally, but the discussion is quite specific about herpes simplex virus, which has its own subsection. The section fails to mention the 15 observational studies that have assessed the prevalence of genital ulcer disease by male circumcision status. 12,15, When one of the studies with redundant data is excluded, 261 there is a positive association between having a foreskin and clinical presence of genital ulcers (random-effects summary odds ratio 1.60; 95%CI 1.34-1.92, between-study heterogeneity chi-square (df=13) = 31.09, p<.0001, I 2 = 66.8%). 185 Other meta-analyses have yielded similar results. 24,342 The data from both of the prospective studies need to be adjusted for lead-time bias. 349,379 When the data are adjusted, the fixed-effect summary relative risk ratio is 1.62 (95%CI 1.27-2.07). 185 Part of the reason ulcers are more commonly seen in intact men is that ulcers have a propensity for mucosal surfaces and mucocutaneous junctions. This is why cold sores are seen most commonly on the lips around the mouth, as this is a mucocutaneous junction. One could speculate that if the lips were surgically removed, the number of cold sore eruptions would also decrease. Similarly, the removal of much of the mucosal surface and the mucocutaneous junction from the penis may explain the decrease in prevalence.
# Herpes Simplex Virus (HSV-2)
The material presented in this section of the background document is hyperbolic, incomplete, and misleading.
The authors of this section boast of "ompelling evidence of the protective effect of HSV-2 acquisition from male circumcision is available from two of the three RCTs." The data from these studies tell a different story. 349,350,380 Two of the studies have results that were not statistically significant. 349,351 All three of these reports failed to adjust for lead-time bias. When the only study to show a statistically significant finding 350 is adjusted for lead-time bias, the difference is no longer statistically significant. 352 Even before making the adjustment for lead-time bias, the fragility index 235 for the study was 1, indicating that findings were not robust. The section fails to mention the cohort study by Dickson et al, which followed children from birth until 26 years of age and found no difference in herpes simplex type 2 virus serology (intact men versus circumcised men RR 0.99; 95%CI 0.49-2.00). When the data for the four prospective studies are combined (stratifying by study), the fixed-effect summary relative risk ratio (intact men versus circumcised men) is 1.23 (95%CI 1.04-1.46). When the data are adjusted for lead-time bias, the fixed-effect summary relative risk ratio is 1.15 (95%CI 0.97-1.36). 185 The large impact on the summary relative risk ratio by a six-week adjustment to compensate for the lead-time bias suggests the data are neither robust nor "compelling."
Regarding observational studies, the CDC draft relies on a 1998 non-systematic review/opinion piece as a source of reliable information. 20 That "review" noted only six observational studies available at that time and was obviously missing several studies. The more recent 2006 review cited in the draft noted only 10 observational studies, but excluded two populations that had been reported previously 381 by the lead author of the review article. 24 Since this review was published, a study of 6187 men in India found that the seroprevalence for herpes simplex type 2 virus was significantly lower in intact men (OR 0.66; 95%CI 0.51-0.86). 382 There have been 29 publications of observational studies addressing the association between genital herpes and male circumcision status in men. 9,14,262,263,267,274,356,357,363,377,378, While one publication reported on four populations, 381 another stratified the data by age, 393 and another by country of origin. 363 When a meta-analysis is performed on these studies, the random-effects odds ratio is 1.18 (95%CI 0.998-1.39 , between-study heterogeneity chi-square (df=35) = 170.62 , p < .0001, I 2 = 78.9%). The difference is not statistically significant.
Based on the data that currently appear in the medical literature, no position should be taken on the impact of male circumcision on the risk of infection with herpes simplex type 2 virus. The data are inconsistent, poorly collected, and meta-analyses do not show a significant difference.
# Treponema pallidum (Syphilis)
The material presented in this section of the background document is also confusing as the authors refer to genital ulcer disease when this section should focus on syphilis. The 1998 non-systematic review/opinion piece 20 and the 2006 meta-analysis 24 cited in this section as the source for information on syphilis and male circumcision are out of date, and they do not come close to addressing the 29 observational studies in the medical literature that assess the association between the prevalence of syphilis and male circumcision status. 8,9,271,273,360,362,374,376,377,382,384, One study looked at two populations 384 and one study was stratified by race. 362 A meta-analysis of these studies estimated the random-effects summary odds ratio (intact men versus circumcised men) to be 1.31 (95%CI 1.13-1.52, between-study heterogeneity chisquare (df=30) = 70.67, p < .0001, I 2 = 56.1%). This is a drop in the summary odds ratio reported in the 2006 meta-analysis of 1.45. 24 The incidence of syphilis in men not infected with HIV in Kenya and Uganda is 1.09 per 100 person-years, which is about the same incidence rate as HIV infections in the randomized clinical trials that were performed in those countries. The absolute risk reduction for a circumcised man in this trial was 0.49 per 100 person-years at the ages when someone is most-likely to contract syphilis. 402 Given that the sexual transmission of syphilis is far more efficient than the rate of 1 infection in 1000 sexual encounters for HIV, 403 this would suggest that a substantial proportion of HIV infections are not spread through heterosexual contact alone.
The incidence of syphilis has been addressed in four studies. 349,350,358,402 In two of the studies, no adjustment was made for lead-time bias. 349,350 When the data are stratified by study, and adjusted for lead time bias, the fixed-effect relative risk ratio (intact men versus circumcised men is 1.09 (95%CI=0.82-1.45), and therefore, not statistically significant.
This section is little more than fear-mongering. The incidence of syphilis in men in the United States is low (9.8 per 100,000 in 2013). 341 Based on the prospective studies, there is no significant difference in the incidence of syphilis between intact and circumcised men.
# Haemophilus ducreyi (Chancroid)
The material presented in this section of the background document is inaccurate and misinterpreted. The CDC draft cites a meta-analysis of six studies looking at chancroid, which found circumcised men had a reduced relative risk. 24 If the authors of this draft had looked at the meta-analysis, they would have found that three of the six studies included in their analysis did not assess chancroid directly 265,266,374 and nearly all of the between-study heterogeneity could be attributed to a single study. 404 Weiss et al. 24 included several studies in their meta-analysis that were not strictly studies of chancroid and did not meet basic inclusion criteria because they lacked a direct comparison between intact and circumcised men for a specific diagnosis of chancroid. 265,266,374 In two studies, men with genital ulcers were not tested for chancroid but merely presumed to have chancroid. 265,266 In the third study, 31.4% had herpes simplex virus type 2 and only 22.9% had a positive culture for Haemophilus ducreyi. 374 Some of the remaining studies are now quite dated having been published in 1934, 397 1949, 396 and 1975. 404 When the remaining studies of chancroid are included, 263,264,396,397,404 and the results of the study by Hand 396 are stratified by race, meta-analysis yields a random-effects summary odds ratio of intact men versus circumcised men of 1.33 (95%CI 0.52-1.33). 185 How much weight to give to these findings needs to be tempered by the high degree of between-study heterogeneity (chisquare (df=5) = 59.71, p<.0001, I 2 = 91.4%), the reliability of the clinical diagnosis in several of the studies, and the age of the studies. With the current data, it is not possible to say conclusively that circumcision has an impact on genital infections with Haemophilus ducreyi. It is not clear why this was included in the CDC draft when it does not really apply in the United States as chancroid is extremely rare, and the evidence gathered to date is of such poor quality.
# Other STIs.
The material presented in this section of the background document is misleading. While randomized clinical trials in Africa reported a reduction in high risk HPV infections following male circumcision, nearly all of this perceived reduction can be attributed to the researchers selective sampling practices. This will be discussed further in the section below.
# Human Papilloma Virus (HPV)
The material presented in this section of the background document is riddled with factual errors, is incomplete, and is a misinterpretation of the medical literature.
The statement, "Penile squamous carcinoma (caused by carcinogenic HPV subtypes) has been strongly and consistently associated with lack of male circumcision," is supported by a citation of a non-systematic review/opinion piece written by authors with a known pro-male circumcision bias. 20 As will be discussed below, the medical literature does not support this statement, and the writers of the CDC draft should not rely on opinion pieces as though they are evidence-based citations.
The statement, "Cervical cancer has been associated with lack of male circumcision in male partners of women in several case-control studies," can easily be demonstrated to be false. As discussed below, there are 16 studies that have looked for an association between cervical cancer and the male circumcision status of a woman's male sexual partner and none have found a statistically significant association. The citation given for this statement also did not find a statistically significant association. 405 To be factually accurate and reflect the information that is currently available in the medical literature, this statement should read: "A significant association between cervical cancer and the lack of male circumcision in male partners of women has never been demonstrated despite evaluation of this association in multiple case-control studies."
The CDC draft relies on a 1998 non-systematic review/opinion piece 20 as its source of information on genital warts, which noted only three studies had been published. To date, there have been 15 observational studies in 14 publications that have assessed the prevalence of genital warts in men based on their male circumcision status. 14,263,356,357,360,361,394,398, When a meta-analysis is performed on these studies, the random-effects summary odds ratio (intact men versus circumcised men) is 0.82 (95%CI 0.65-1.04, between-study heterogeneity chi-square (df=14) = 37.07 , p=.0007 , I 2 = 59.5%). 185 This indicates that there may be a trend indicating that circumcised men are at greater risk for genital warts. When only studies assessing general populations are evaluated, the between-study heterogeneity is not statistically significant (chi-square (df=6) = 8.61, p=.1969, I 2 = 18.7%), which is rarely seen in studies of sexually transmitted infections and male circumcision status, and the randomeffects summary odds ratio is 0.78 (95%CI 0.63-0.96), a statistically significant difference. 185 These studies noted that genital warts in circumcised men were more likely to be found on the penile shaft. 356 Why would the writers of the CDC draft rely on a non-systematic review/opinion piece 20 that is 16 years old as a source of its information when several systematic reviews have addressed this topic more recently? 24,185,342 Was the goal of the CDC draft to be out of date and incomplete, or just to make headlines assuming no one would read the draft and see through the coverup?
The CDC draft makes no mention of the 20 observational studies that have assessed the prevalence rates of genital HPV infection in men based on male circumcision status, 355,405,406, or the three meta-analyses that have looked at these studies. 185, The draft may have avoided discussion of these studies because the results of several of the studies were biased by either sampling bias, 412 misclassification bias, 410,422,423 or both. 405 The type of HPV also varied from study to study with some reporting all HPV types, others only HPV types known to be carcinogenic/oncogenic, and other studies reporting their findings by all types, non-oncogenic and oncogenic. 414,416,418,419,426 It should also be noted that most genital HPV infections are transient and clear spontaneously.
Misclassification bias occurred in the studies where researchers relied on men to properly identify their male circumcision status, but the men did so incorrectly. The most egregious example of this is the study by Lajous et al. out of Mexico in which 95 men reported being circumcised yet only 8.3% of them were noted to be circumcised on physical examination. 410 While the authors of this study had determined the male circumcision status of the study participants based on physical examination, they reported their results based on the male circumcision status as reported by the men. In effect, the study demonstrated that HPV risk was lower in men who thought they were circumcised rather than whether they were actually circumcised or not. The results using physical examination to determine male circumcision status were not provided. 427 Evaluating all of the studies of prevalence using meta-regression 324 has demonstrated that studies that relied on patient report to determine male circumcision status consistently and systematically significantly overestimated the association between having a foreskin and genital HPV. 185,343 The impact of sampling bias is more easily quantified. Sampling bias occurs when only selected portions of the genitals are sampled for the presence of HPV. Selective sampling would not be a problem if doing so provided similar results to comprehensive sampling. For HPV on the male genitals, however, this is not the case. Several studies have shown that circumcised men who have HPV somewhere on their genitals are more likely to harbor the virus on the shaft of the penis. 355,411,415,420,426,428 Other studies have shown that genital warts are more likely to be found on the shaft of the penis in circumcised men as compared to the glans in intact men. 429 Two studies out of the University of Washington found that, if only the glans is sampled, 45 to 47% of circumcised men with genital HPV will be detected. 365,429 In contrast, sampling only the glans of intact men will identify 65 to 66% of intact men who have HPV on their genitals. As a consequence, sampling only the glans of the penis will miss more HPV infections in circumcised men than it will in intact men. If the numbers from Van Buskirk et al. 428 are correct, the number of intact men expected to be infected with HPV infection would be the number of men identified by sampling only the glans increased by a factor of 1.514. Similarly, for the men who underwent male circumcision, the number identified in the trial would be increased by a factor of 2.212. When an analysis of the entire medical literature is performed using meta-regression, 185,343 studies that sampled only the glans were demonstrated to have stronger associations between having a foreskin and having HPV infections. This finding was statistically significant, suggesting that sampling only the glans of the penis consistently overestimates the association between having a foreskin and genital HPV.
An added wrinkle to the finding that circumcised men are more prone to have HPV lesions on the shaft of their penis is that the penile shaft is the portion of the penis with the highest viral loads and the preferred location for HPV-16, which is the most oncogenic HPV type. 430 This would suggest that circumcised men might be more likely to pass HPV-16 to their sexual partners, thereby leading to an increase in cervical cancer.
The dilemma is: what to do with studies containing these obvious methodological flaws, which will have a significant impact on the odds ratios reported by these studies. One approach would be to adjust for these factors by adjusting the odds ratios in studies with sampling bias. Another, would be to adjust using meta-regression. And, the last would be to exclude studies with these methodological problems when performing a metaanalysis.
Twenty publications reported prevalence data on 25 separate populations. Five of these studies provided data on any type of HPV being isolated, as well as high risk HPV. Since high-risk HPV is of more clinical interest, these data were used in the metaanalysis with a random-effects summary odds ratio (intact men versus circumcised men) of 1.16 (95%CI 0.94-1.45, between-study heterogeneity chi-square (df=24) = 45.27, p = .0054, I 2 = 44.7%), which was not statistically significantly different. 185 This analysis included studies that were known to have either sampling bias or misclassification bias for which no adjustment was made. When adjusted for sampling bias using meta-regression, the random-effects summary odds ratio was 1.10 (95%CI=0.88-1.37). For studies that sampled only the glans, the random-effects summary odds ratio is much greater (OR=1.86, 0.99-3.46). When adjusted for misclassification bias using meta-regression, studies that relied on physical examination to determine male circumcision status had a random-effects summary odds ratio of 1.08 (95%CI=0.88-1.32), which was not statistically significant. Studies that relied on patient report had a much greater random-effects summary odds ratio (OR=2.16, 95%CI=1.18-3.99). When studies with known sampling bias or misclassification bias were excluded, the random-effects summary odds ratio was 1.01 (95%CI 0.80-1.28, between-study heterogeneity chi-square (df=15) = 28.82, p = .0164, I 2 = 44.5%). 185 This indicates that observational studies not tainted with methodological flaws have failed to establish an association between genital HPV infection prevalence and circumcision status in men. Is this lack of association why the CDC ignored these 20 publications?
There have been eight prospective studies that looked at the incidence of HPV infection in men by circumcision status, 193,348,350,410,428, but this CDC draft only mentions two of them. The two studies identified in the CDC draft are also the only two studies to find a statistically significant difference, the only two studies to find the greatest treatment effect (relative risk ratios of 1.51 and 1.54, with next highest being 1.19, 433 and the only two studies that reported only the results of samples taken from the glans without including samples taken from the penile shaft. 348,350 Clearly, the results of these two outlying studies were impacted by sampling bias. For example, in the Ugandan trial, 350 when an adjustment for sampling bias is made, the relative risk ratio (intact men versus circumcised men) was reduced from 1.54 (95%CI 1.11-2.17) to 1.09 (95CI 0.83-1.43), with the difference no longer being statistically significant. As a consequence, the difference in incidence between intact and circumcised men reported by the Johns Hopkins team can be completely explained by their failure to sample beyond the glans of the penis. 352 The story on sampling bias, however, goes deeper. In 2007, researchers from Johns Hopkins reported at the beginning of their randomized clinical trial that, "Two subpreputial and shaft swabs were also obtained for future testing of human papillomavirus infection." 3 However, in the 2009 report of their findings, only the results from swabbing the glans were reported. The results from swabbing the shaft of the penis were not included in their report. 350 In 2011, the same team reported the results of HPV cultures from the glans and the penile shaft collected at the 12 month follow-up visit of the randomized clinical controlled trial participants. 434 It remains unclear why the researchers from Johns Hopkins would selectively report the results in this fashion, especially given the fact that Weaver at al. had published their findings of a differential in HPV acquisition based on the site of sampling on male genitals in 2004. 429 When the prospective data are stratified by study, the fixed-effect summary relative risk ratio is 1.05 (95%CI 0.88-1.25), which indicates that circumcision has no effect on the incidence of genital HPV infections in men. When the Ugandan and South African data, which account for nearly all of the between-study heterogeneity, are corrected for sampling bias and lead-time bias, the summary relative risk reduction is 0.97 (95%CI 0.91-1.04).
The CDC draft must include the results of the "HPV Infection in Men" (HIM) study: a prospective study of HPV in men that looked at the risk of new HPV infections by circumcision status. 193 This study was to be the ultimate prospective cohort study on the topic. Preliminary reports from the study appeared in such high-profile journals as the International Journal of Cancer and The Lancet. 414,435 The study included 4033 participants aged 18 to 70 years. In the study, they sampled the glans, the penile shaft, and the scrotum. Men were evaluated every six months for a median of 17.5 months.
Participants came from Florida, Mexico, and Brazil, and the results were stratified by country of origin. The hazard ratio for oncogenic HPV was 0.90 (95%CI%=0.76-1.06) indicating a non-significant trend for circumcised men to have a higher incidence overall of HPV infections. No difference was seen for HPV-16. HPV of any type, oncogenic HPV, and HPV-16, cleared significantly more quickly from the intact penis then the circumcised penis (any HPV: hazard ratio (HR) 0.85; 95%CI 0.80-0.91, oncogenic HPV: HR 0.83; 95%CI 0.75-0.92, HPV-16: HR 0.56; 95%CI 0.42-0.75). 193 This significantly faster clearance of HPV from the intact penis is the opposite finding seen in other smaller studies. 370,432, Two additional comments:
First, the study by Castellsequé et al. combined the data from seven studies in five countries on three continents. 405 Analysis of the data from this study presented several statistical challenges that the authors of the study did not correctly deal with, and the editors of the New England Journal of Medicine let slide by. The challenge was the small number of circumcised men in four of the five countries and a small number of intact men in the fifth country. In order for asymptotic statistical methods, which rely on the assumption that values follow a normal distribution, to provide accurate results there needs to be more than 5 (some say more than 10) subjects who conform to each classification. Of the twenty classifications (five countries by 4 outcomes), seven have 5 or fewer subjects in them. The authors used asymptotic statistical methods, even though this would not yield valid results. They should have used exact statistical methods instead. In other words, the small number of circumcised men in Brazil, Columbia, Spain, and Thailand, and the small number of intact men in the Philippines made for an unstable statistical model. Furthermore, it renders stratified analysis nearly impossible, if the analysis wants to control for the country from which the data was collected. For example, if the prevalence is much greater in one country that has a very low circumcision rate, results may be attributed to male circumcision that should instead be attributed to the country of origin.
Second, the data from the randomized trial in Kisumu, Kenya has never been clearly presented. In 2012, Bailey and Moses's group published the results of their data on high-risk HPV, but they did not report the number of circumcised men or intact men who became infected with high-risk HPV. Instead, they reported that intact men developed more flat lesions that were more likely to harbor high-risk HPV. 439 On the face of it, and from the title of their publication, it may sound as though intact men were at greater risk for an infection with high-risk HPV, but this is not the case. While intact men were at greater risk for flat lesions, circumcised men were at greater risk for papular and pearly lesions. While the papular and pearly lesions are less likely to harbor high-risk HPV, they are much more common than the flat lesions and more common in circumcised men. For example, 33 men in the study had flat lesions, while 133 and 187 men had papular and pearly lesions, respectively. Of the men with flat lesions, one was circumcised and 32 were intact. Of the flat lesions 22 were found to harbor high-risk HPV. Papular lesions were found in 91 circumcised men and 42 intact men. Of the 133 papular lesions, 28 harbored high-risk HPV. Pearly lesions were found in 112 circumcised men and 75 intact men. Of the 187 pearly lesions, 49 harbored high-risk HPV. Based on these numbers, one can back-calculate and estimate the number of men expected to have been infected with high-risk HPV based on male circumcision status. Considering there were 124 intact men and 151 circumcised men, the odds ratio was 1.45 (95%CI=0.89-2.38), a difference that is not statistically significant. This should not be a surprise as this study sampled both the glans and penile shaft of the study participants and reported the results on all of the samples they collected. It is not clear why the straight-forward number of intact and circumcised men who became infected with high-risk HPV has never been revealed publicly.
The CDC has placed its entire wager behind two outlier studies with serious methodological flaws whose results are not consistent with the rest of the medical literature. The analysis is incomplete, biased, and misinterpreted the small fraction of the data in the medical literature that the CDC considered.
# Trichomonas vaginalis
The material presented in this section of the background document does not contribute adequately to the discussion to even merit inclusion. The entire section could be tersely reduced to one sentence: The impact of male circumcision on trichomoniasis in men and their female sexual partners has received limited study with conflicting results. 346,347,440 There are no studies outside of Africa by which to gauge the importance of these infections.
In reporting the results by Mehta et al., 347 the writers of the draft give results of the "astreated" analysis as being statistically significant and the "intention-to-treat" results as having "borderline statistical significance." The standard is to report only intention-totreat results. Doing otherwise undermines the whole purpose of a randomized trial. Crossover, which in these trials would entail men randomized to be circumcised not undergoing the procedure and men randomized to not be circumcised undergoing the procedure, does not in most cases happen randomly. By reporting the as-treated results, the writers of the CDC draft knowingly reported potentially biased results. While they may believe they are justified in doing so because it furthers their cause of promoting male circumcision, they should know better on an epidemiological level. Intention-to-treat analysis may be more conservative in estimating treatment effects, but it does not introduce the bias of differential crossover and it is more reflective of the reality of patient non-compliance. The writers should also know better than to use the phrase "borderline statistical significance." This phrase is similar to being "kind of pregnant." While the statistical significance has been somewhat arbitrarily set at a pvalue of .05 by Ronald A. Fisher, it is the standard everyone abides by. In this case statement, the as-treated results should not have been presented, and the intention-totreat results should have been described as showing a trend that is not statistically significant. Once again, the writers of this draft are either improperly trained in statistics and epidemiology, or they are trying to promote male circumcision unjustifiably. These epidemiologically inappropriate phrases were used by the authors of the studies in an effort to spin their results in the most favorable fashion. The fact that writers of the CDC draft accepted this language without question also indicates that they did not read these studies carefully enough to properly evaluate the methodology and data generated in order to develop their own conclusions. The CDC had over seven years to carefully read the small percentage of studies in the medical literature they decided to include in this draft. This should have taken a matter of weeks. What did the CDC with the rest of the time?
# Chlamydia trachomatis
The material presented in this section of the background document is very confusing. It is not clear if the authors of this section were purposely being obtuse. The statement that "chlamydial infection in men was often diagnosed syndromically as 'non-gonococcal urethritis,' after exclusion of gonorrhea by Gram stain" is an oversimplification. Several studies collected data on both chlamydia and non-specific urethritis, 9,263, which in the era of testing for both chlamydia and gonorrhea, is its own entity. This section would be best if divided up into sections of 1) genital discharge syndrome, 2) non-specific urethritis, and 3) Chlamydia trachomatis.
Several studies examined the association between male circumcision status and the prevalence of genital discharge syndrome, which includes any genital infection that results in a urethral discharge, such as gonorrhea, chlamydia, and non-specific urethritis. The CDC draft makes no mention of the studies that assessed men for genital discharge syndrome except to mention the single study that looked at its incidence in Table 2. The draft fails to mention the eleven studies that have compared the prevalence of genital discharge syndrome in men by circumcision status. 12,248,442 When the results of these studies are combined in a meta-analysis, the random-effects summary odds ratio (intact men versus circumcised men) shows a trend toward genital discharge syndrome being more common in circumcised men (summary OR 0.92; 95%CI 0.78-1.09, between-study heterogeneity chi-square (df=10) = 52.13, p < .0001, I 2 = 78.9%). It is not clear why the CDC draft failed to consider this information.
The one study that measured incidence failed to adjust for lead-time bias. 350 When this adjustment is made, the relative risk ratio (intact men versus circumcised men) is reduced from 1.11 (95%CI 0.77-1.61) to 0.98 (95%CI 0.68-1.42).
The CDC draft relies on a 1998 non-systematic review/opinion piece for its information on non-specific urethritis and tallies the results of the studies rather than performs a meta-analysis. 20 A systematic review of the medical literature will uncover 12 studies on the prevalence of non-specific urethritis. 9,263,266,355,357,363,383,398,442 When the data from these studies are combined in a meta-analysis, the random-effects summary odds ratio (intact men versus circumcised men) is 0.76 (95%CI 0.63-0.92, between-study heterogeneity chi-square (df=11) = 39.78, p<.0001, I 2 = 69.8%.) 185 This result indicates that circumcised men are at a statistically significantly increased risk for nonspecific urethritis.
This section on Chlamydia trachomatis makes no mention of the 16 observational studies that looked for an association between prevalence of Chlamydia and circumcision status in men. 9,14,263,364,369,377, If one of the studies that presented redundant data is excluded, 261 the random-effects summary odds ratio for these studies (intact men versus circumcised men) is 0.94 (95%CI 0.76-1.17, betweenstudy heterogeneity chi-square (df=14) = 36.16, p=.0010, I 2 = 58.5%). It is unclear what harm there would be in the CDC reporting these results, except that the meta-analysis indicates a non-significant trend that circumcised men are at greater risk for Chlamydia.
There have been three studies published, which looked at the incidence of Chlamydia by circumcision status in men. 346,347,358 The two studies identified by the CDC failed to correct for lead-time bias. The fixed-effect summary relative risk ratio for the three studies (intact men versus circumcised men) is 1.26 (95%CI 1.02-1.57); however, when the two studies are adjusted for lead-time bias the result is no longer statistically significant (RR 1.19; 95%CI 0.96-1.49). 185 The CDC did not make the effort to gather or properly interpret the evidence that is currently available in the medical literature. Instead, it wasted its time and space giving the details of the two conflicting studies regarding the risk of Chlamydia in women based on the circumcision status of their regular male partner. 446,447 The conclusion that would be most accurate and helpful for the intended audience of health care providers is that male circumcision may increase the likelihood of urethritis, including Chlamydia and non-specific urethritis.
# Neisseria gonorrhea
The material presented in this section of the background document is woefully out of date and incomplete. The CDC draft cites a 1998 non-systematic review article as the source of its material, 20 which notes that five of seven observational studies list a statistically significant decrease in gonorrhea prevalence in circumcised men. This review was incomplete at the time it was published. There have been 24 studies that have assessed the association between male circumcision status and gonococcal infections. 9,14,267,268,377,383, Two of the studies presented redundant data 261,262 and only four had associations that were statistically significant. 267,356,360,446 But a tally of positive studies, a much used rhetorical device, 20,31 is not the proper method of determining the overall findings in the medical literature. When one of the redundant studies is excluded, 261 the data reported by Hand 396 and Schrek 362 are stratified by race and the data reported by Laumann et al. 9 are stratified by the number of lifetime sexual partners, the random-effects summary odds ratio of intact men versus circumcised men was 1.03 (95%CI 0.88-1.21, between-study heterogeneity chi-square (df=27) = 95.97, p<.0001, I 2 = 70.8%). Since an odds ratio is 1.00 when two groups have identical risks, there is no difference in the risk of gonorrhea based on male circumcision status.
This holds up in studies on the incidence of gonorrhea. Three studies have looked at this issue. 346,347,358 Two of them suffered from lead-time bias. 346,347 None of them found a statistically significant difference. The fixed-effect summary relative risk ratio (intact men versus circumcised men) for the three studies was 1.10 (95%CI 0.91-1.34). When the two studies with lead-time bias are adjusted for, the summary relative risk ratio is 1.04 (95%CI 0.86-1.27). 185 The data from the medical literature clearly demonstrates that male circumcision does not impact the risk of gonorrhea.
Based on what is presented in the CDC draft, the authors of this draft are either incompetent reviewers of the medical literature or are purposely trying to deceive the public and their intended audience of health care professionals. Reliance on a nonsystematic review that is little more than an opinion piece, in which only seven observational studies were identified, when a simple PUBMED search would have quickly identified many of the 23 observational studies and two systematic reviews with meta-analyses, 185,342 is inexcusable. Is this just willful incompetence, or is there an institutional directive to misrepresent the evidence in the medical literature? COMMENT:
# Penile and prostate cancers
The material presented in this section of the background document is incomplete, misleading, and contains inappropriate citations.
# RESPONSE:
See responses 1, 6, and 39.
# COMMENT:
Penile cancer is extremely rare (0.6 to 0.8 per 100,000 person years), less common than breast cancer in men. In the United States, the incidence of penile cancer occurs at rates that are similar to or lower than rates in other developed countries where male circumcision is rarely practiced, such as in Japan, Germany, Iceland, Spain, Sweden, Switzerland, United Kingdom, Yugoslavia, 448 Denmark, 448,449 Finland, 448,450 and Norway. 448,451 Also, as the percentage of circumcised septuagenarian and octogenarian men has increased, there has been no corresponding decrease in the incidence of penile cancer in the United States. Both of these findings suggest that, on a population level, male circumcision has little or no impact on penile cancer. This information needs to be included in the CDC draft discussion.
The discussions of any case series or reviews of case series should be excluded 452,453 because, without control groups and with a changing prevalence of circumcision in men at the age at which penile cancer is likely to occur, the numbers from these publications have little or no epidemiological value. yielded similar results to that of Daling et al. 454 For Tseng et al., the presence of phimosis increased the risk of penile cancer 16-fold. When adjusted for phimosis, lack of neonatal male circumcision was not a significant risk factor. 408 All three studies emphasize that phimosis, rather than neonatal male circumcision, is the more important risk factor. Half of the cases of invasive penile cancer can be attributed to oncogenic HPV viruses. 456 As is discussed elsewhere in this response, there is no significant association between male circumcision and carriage of oncogenic HPV. The link between phimosis and penile cancer may be balanitis xerotica obliterans, the most common cause of pathologic phimosis with a cumulative incidence of 0.6% by 15 years of age, 457 which is increasingly being recognized as a precancerous condition. Consequently, the focus should be shifted to efforts that minimize infections with oncogenic HPV (such as use of condoms and use of the HPV vaccines) and early recognition and treatment of balanitis xerotica obliterans.
The section should also include a realistic discussion of the risk of penile cancer. For example, the 2012 American Academy of Pediatric Task Force on Circumcision noted that the incidence of penile cancer was 0.58 per 100,000 person-years. 40 Using this incidence for penile cancer in the United States, the lifetime risk (average life span 72 years) would be 0.000417512, or a lifetime risk of 1 in 2395. The Task Force report noted that the relative risk reduction for penile cancer by circumcision was between 1.5 and 2.3. If you take the lifetime risk of penile cancer and reduce this incidence rate by a factor of 2.3, the result, 0.0001815, would be the expected lifetime risk for penile cancer in circumcised men. The absolute risk reduction would be the difference between the two rates: 0.0004176 minus 0.0001815 or 0.0002360, so the number needed to treat would be 4237. If, however, the relative risk reduction is 1.5, the number needed to treat is 7184. If it takes 7184 male circumcisions to prevent one case of penile cancer and each male circumcision costs an average of $285 paid at the time of the procedure, 472 the cost to avoid one case of cancer is $2,047,440. However, the money for the male circumcision was spent at the time the male was circumcised not at the time the male developed penile cancer, which is usually around 80 years of age. Therefore, for 80 years, the opportunity of having that cash available, which was spent at the time of the procedure, has been lost. If that money was put out at 3% interest for 80 years, the opportunity costs would be $21,786,584. If the money were to earn 5% interest for 80 years, the cost of preventing one case of penile cancer would be$101,474,076. This is the true cost of preventing one case of penile cancer. Obviously, neonatal male circumcision to prevent penile cancer is NOT cost-effective nor justifiable from a public health standpoint.
The discussion of male circumcision and prostate cancer should be deleted. The argument put forth by the writers of the CDC draft borrows from that proposed by Morris and colleagues, 473 which is based on several tenuous assumptions. The first is that the risk of prostate cancer is increased by sexually transmitted infections. As the writers of the CDC draft note, the medical literature on this point is mixed, showing populations at low risk for sexually transmitted infections being sometimes at greater risk for development of prostate cancer. 474 Even if one accepts this contentious assumption, one would need to demonstrate that circumcised men are at lower risk of sexually transmitted infections. Instead, the medical literature indicates circumcised males are at an overall greater risk of sexually transmitted infections. Since a single infectious agent has not been identified as being associated with a greater risk of prostate cancer, it is more likely that infectious agents associated with urethritis would impact the health of the prostate. Urethritis is not reduced, and may be increased, with male circumcision.
The CDC draft mentions only one observational case-control study, of the many that have been published, on the topic of prostate cancer as associated with male circumcision. 475 The writers of the CDC draft fail to mention several important aspects of this study. Male circumcision status was determined by self report, which is known to be notoriously inaccurate. The study did not find a significant association between prostate cancer and a history of sexually transmitted infections (OR 1.05; 95%CI 0.87-1.27), which undermines their working hypothesis. The adjusted odds ratio for the risk of prostate cancer (circumcised versus intact men) reported in the body of the study was 0.87 (95%CI 0.74-1.02), which was not statistically significant. Therefore, as a whole, this study does not support their contention. Other concerns about the validity of this study have been raised. 476 Isolating the impact of male circumcision on the risk of prostate cancer has been difficult. For example, race and ethnicity are important factors. When compared to controls with benign prostatic hypertrophy, circumcised non-Jews had a significantly greater risk of prostate cancer than Jews (OR 3.23; 95% CI 1.56-6.69). This would indicate that race/ethnicity are more important than male circumcision. 477 A British study failed to consider race or ethnicity, so male circumcision status may have been a marker of race and/or socioeconomic status. 478 In an American study, there was an interaction between race and male circumcision status. 479 When Jews are excluded, several studies have failed to find a significant association between male circumcision status and prostate cancer. 480,481 Also, no association has been demonstrated between male circumcision status and PSA levels. 482 On a population level, if male circumcision decreased the risk of prostate cancer, one would expect as the male circumcision prevalence increased in the United States, the incidence of prostate cancer would decrease, but the opposite has occurred. 483 One would also expect the age-adjusted incidence of prostate cancer in European countries to be higher than that in the United States, but it is lower in Denmark, Finland, Iceland, Norway, and Sweden, 484 as compared to the United States. 483 Several of the studies relied on patient report to determine male circumcision status 475,478,479 and failed to adjust for risk factors known to influence prostate cancer risk. The combination of poorly executed studies, along with an unproven theory linking prostate cancer to sexually transmitted infections, the lack of evidence linking sexually transmitted infections to male circumcision status, and the lack of evidence linking male circumcision to prostate cancer on a population level should have indicated to the writers of the CDC draft that this topic was not worthy of inclusion in the draft.
In summary, penile cancer is very rare, more rare than male breast cancer, and its link to neonatal male circumcision, based on recent studies, is tenuous. An evidence-based discussion of male circumcision should not include any discussion of prostate cancer.
# RESPONSE 69:
See responses 1 and 6. We have updated the literature review and it provides more evidence indicating the male circumcision if protective against penile and prostate cancers.
# COMMENT:
# Cervical cancer in female partners of circumcised men
The material presented in this section of the background document is limited to one select substrata of a single study. 405 The study from which this substrata was extracted did not properly analyze the data. The data were collected in studies from five different countries, yet were not stratified by country. In four of the countries, only a small number of men were circumcised. In the fifth country, only a small number of men were not circumcised. Since cervical cancer rates can vary by geography, it is important to stratify the data by geography. The analysis in this study failed to do this. If they had performed the analysis properly, this selected substrata when further stratified by geography would have necessitated the use of exact statistics, which the authors of the study did not use. Exact statistics revealed much wider confidence intervals. Even with the stratification they performed (monogamous women with male partner with 6 or more lifetime sexual partners), it is interesting to note that the raw numbers found little or no difference (OR 1.02; 0.71-1.47). Furthermore, with reporting the results of the selected substrata the finding should have been subjected to a Bonferroni adjustment, but was not. By doing so, the threshold p-value would be divided by 3. Consequently, this statement is based on evidence that was misinterpreted.
This section also exhibits significant omissions that are critical for the intended audience of clinicians. The single study cited in the background document on this topic did not find a statistically significant association between cervical cancer in women and the circumcision status of their male sexual partners. 405 There have been 15 other studies that have reported on the association between cervical cancer and the circumcision status of a woman's male sexual partner. None of them found an association that was statistically significant. 405, (One study reported a p-value of .045, 495 but this was not properly calculated. Using Fisher's two-sided exact test, the p-value is .0733.)
The CDC has focused on a substratum of one of 16 studies while ignoring the other 15 studies in order to find a statement that supported their conclusion. This is a clear case of confirmation bias.
# RESPONSE:
See responses 1 and 6.
# COMMENT:
Urinary tract infections in male infants
# COMMENT:
The material presented in this section of the background document is overly optimistic and misinterpreted. The data on which the report relies have been extracted from observational studies that contain a number of methodological flaws that make it difficult to ascertain whether urinary tract infections were properly diagnosed in these studies.
For example, many studies use only bacteriuria as a diagnostic criterion, which would include the 1% of children who, at any given time, will have asymptomatic bacteriuria.
To properly make the diagnosis of urinary tract infection, there must be evidence of inflammation. 500 Similarly, urine specimens collected in bags placed over the genitals are often used to screen for urinary tract infection. This method has a high false positive rate, especially in girls and normal boys, with a contamination rate of 65% to 70%. This may lead to an oversampling of intact boys. There may also be a differential in health care seeking behaviors. 504 For example, Hispanic boys, who are more likely to have normal genitals, seek health care more frequently, 505 and therefore are more likely to be diagnosed, often incorrectly, with a urinary tract infection.
# RESPONSE 71:
The reviewer fails to provide evidence that the UTI studies used in the CDC background analysis were methodologically flawed. The statement that bagged urine specimens may have a high false positive rate and may lead to "an oversampling of intact boys" is unclear. The argument that Hispanic boys seek care more frequently and are more likely to be diagnosed, often incorrectly, with a UTI is the reviewer's opinion rather than a scientific finding.
# COMMENT:
The reference to the 1987 study of US Army hospitals worldwide 506 that noted an increase in the total number of urinary tract infections as the male circumcision rate declined overlooks the fact that the data collected by the authors were not consistent over time. 507 For example, the rate of diagnosing urinary tract infection decreased significantly from 0.16% in the first three years of the study to 0.07% in the last three years of the study. (RR 0.462; 95%CI 0.338-0.633). 504 The yearly rates of urinary tract infections in circumcised boys ranged from 0.07% to 0.23%, which the authors characterized as being "relatively consistent." 506 The rate of urinary tract infections in boys with normal genitals increased from 0.87% to 1.09% between the two time spans (OR 1.25; 95%CI 0.96-1.61). The association between male circumcision and urinary tract infection was not consistent over time. The odds ratio for intact boys being diagnosed with a urinary tract infection in the first three years of the study was 5.51 (95%CI 4.08-7.44) and in the last three years of the study was 14.91 (95%CI 10.48-21.21). Both of these estimates are outside the 95% confidence interval for the odds ratio estimated for the entire time span of the study (8.69-12.15). This undermines the internal validity of the study. 507
Response 72: Any supposed change in rates of diagnosing UTIs would likely be the same for both circumcised and uncircumcised boys, however, the important fact here is that uncircumcised boys had a higher risk of UTIs compared with circumcised boys.
# COMMENT:
Several studies suffered from misclassification bias in that the male circumcision status could not be correctly identified. 508,509 The studies generated from the database of US Army hospitals worldwide also made no attempt to determine if there was the possibility of misclassification bias. In a chart review performed by the Centers for Disease Control, 15.7% of the boys circumcised neonatally did not have it documented on the hospital chart's face sheet, which is the source of database information. 6 In the US Army studies, if 15% of the boys circumcised did not have it documented on the face sheet, as many as 78.1% of the boys thought to be intact may have actually been circumcised. If one adjusts for this possible non-differential misclassification, the US Army data from 1974 to 1983 would yield an odds ratio (intact males versus circumcised males) of 4.13 (95%CI 3.34-5.11), while the data from 1984-88 would yield an odds ratio of 4.07 (95%CI 3.28-5.05). These odds ratios are more in line with those estimated in other studies.
Response 73: Once again, despite the reviewer's adjustment for "possible nondifferential misclassification", the odds ratio indicates that uncircumcised boys had a higher risk of UTIs compared with circumcised boys.
# COMMENT:
One model has been published that estimated the impact of confounding on the association between male circumcision and urinary tract infections. If one begins with the assumption that the rate of true urinary traction infections is the same in intact and circumcised boys, modeling of confounding factors -such as frequency of medical visits, likelihood of collecting a urine sample, urine collection method, et cetera -will result in making a diagnosis of urinary tract infection (a combination of true positives and false positives) 4.27 times more frequently in intact boys. 510 Consequently, the associations that have been measured between male circumcision and urinary tract infection may have been largely the result of confounding factors rather than a true association.
This is consistent with the HMO data collected by Altschul who found a high rate of misdiagnosis of urinary tract infection when he compared information garnered from the medical chart as opposed to the HMO's database. When proper diagnostic criteria are applied, the urinary tract infection was much lower than reported from the US Army data. 511 In a study of 603 intact Japanese boys aged 0 to 15 years, none had ever reported having had a urinary tract infection. 85 An important omission in the background report is that at least seven studies out of Israel indicated that urinary tract infections occur at a higher rate following infant male circumcision. This increased risk of urinary tract infection may be related to techniques used in ritual male circumcision to control the bleeding that may restrict urine flow, thus leading to the urinary tract infection. Parents who desire a ritual male circumcision for their son need to be aware of this risk.
# COMMENT:
The increase in diagnosis of urinary tract infections may be because parents are instructed to retract the foreskin on a regular basis in order to clean the head of the penis. This is inappropriate advice resulting in manipulation of the urethra and the equivalent of "honeymoon cystitis." Consequently, these infections may be iatrogenic.
An important omission in this section is that the long-term risks associated with urinary tract infections in infants are less than previously believed. For example, it has been demonstrated that treatment with oral antibiotics is as effective as treatment with intravenous antibiotics. 519 Urinary tract infections that occur in the first twelve months of life are less likely to result in renal parenchymal involvement. 520 There is now a strong body of evidence that urinary tract infections rarely, if ever, lead to hypertension or persistent renal dysfunction. While males are more likely to have vesicoureteral reflux noted on prenatal ultrasound, most cases resolve spontaneously. This temporarily predisposes males to urinary tract infection, 529,530 but the risk is quite low after six months of age, by which time the reflux has resolved. The recommended evaluation for infants with urinary tract infection is less rigorous than previously recommended. 531 Urinary tract infections should not be mischaracterized as an infection with life-long serious consequences, because the medical literature does not support such a characterization.
# RESPONSE 75:
While UTIs can be treated with antibiotics, some children who are treated for UTIs may be resistant to antibiotics while children with UTIs may not be symptomatic or may not be diagnosed in a timely fashion or may not be diagnosed at all if they don't have adequate access to a medical doctor. While UTIs do not always have life-long consequences, they may have such consequences. 53
# COMMENT:
Comparing the rate of urinary tract infections to the rate of immediate complications associated with infant male circumcision drawn from database sources is inappropriate and can be easily misinterpreted. Doing so also deviates from standard epidemiological practices and is misleading. As discussed elsewhere, the rates of complications following infant male circumcision have not been well or consistently measured. Consequently, any comparisons would have little meaning. Citing a study with one of the lowest reported complication rates (0.2% 532 ) to be used for comparison reflects a potential bias of those generating this report. A more apt comparison would involve comparing the rate of urinary tract infection with the rate of meatal stenosis following male circumcision. Meatal stenosis rates range from 5% to 20% and often require surgical correction (meatotomy), 186, while the rate of urinary tract infection is 0.7%. 538 In this comparison, there would be approximately 3 to 15 meatotomies performed for every urinary tract infection. Yet, this is not a standard epidemiological approach. The most appropriate approach is to calculate the number needed to treat. This number has been estimated to be between 111 23 and 195. 538 The average cost of an infant male circumcision, according to investigators at the CDC, is $285. 472 Consequently, one would need to spend between $31,635 and $55,575 to prevent one urinary tract infection that can be treated with a course of oral antibiotics that cost less than $20.
# RESPONSE 76:
The neonatal complication rate in the first month of life of 0.2% has been consistently found across several studies indicating strong reliability of results. COMMENT:
# Other health conditions
The material presented in this section of the background document is highly selective, omits several important studies, and gives credence to studies with serious methodological flaws.
# RESPONSE:
See responses 1, 6, 33, and 41 for all sections in "other health conditions".
# COMMENT:
The authors of the draft rely heavily on the 2000 study of Mallon et al. 394 This study has two fatal methodological flaws. The first is that it was undertaken in a dermatology practice, thus is subject to referral bias. If primary care physicians are capable of taking care of penile dermatoses in circumcised males, they may be less likely to refer them for specialty care. Therefore, penile dermatoses in circumcised men would be underrepresented in a dermatology practice. Consequently, it is impossible to say whether this referred population is representative of the general population. The second fatal flaw is that the study had a control group of men seen in the dermatology clinic who did not have penile problems. The control group had a male circumcision rate of 47.8%. Britain has a national male circumcision rate of 21%. 539 If one had a control group with a male circumcision rate of 21%, the positive findings of the study are negated.
There are a number of important oversights in this section of the draft. For example, in the 1986 study by Herzog and Alvarez, the differences in prevalence of balanitis, penile irritation, and phimosis based on male circumcision status were not statistically significant. 505 In the 1988 study by Fergusson et al., penile inflammation was more common in circumcised boys in the first three years of life and overall there was no statistically significant difference. 190 For reasons that are unclear, the authors of this draft cite an opinion piece written by a known male circumcision advocate to support their assertions. 540 Citing review articles and opinion pieces is inappropriate and not considered scientifically valid or evidence-based.
Regarding the risk of balanitis (which includes balanitis, posthitis, and balanoposthitis), this section of the CDC draft has several important omissions. First, in a 1982 study of over 1000 intact Chinese boys only 0.08% (95%CI 0%-0.24%) had signs of active balanitis, while only 0.65% (95%CI 0.20%-1.10%) had ever had balanitis. 541 Second, in a 1997 study of Japanese boys, they found one case of balanitis in 1283 (0.08%) three year old boys. 542 Third, is a 1989 study in Britain that found the cumulative risk of balanitis by age 7 to 14 years of age to be 4%, with most patients having a single episode easily treated with topical agents. 543 Finally, a 2007 report, 187 which updated a 1997 study 186 of 468 boys, found that among 473 boys under three years of age, intact boys were significantly less likely to have penile inflammation than circumcised boys (OR 8.01; 95%CI 1.31-329.15). After three years of age, there was no difference.
Regarding the risk of pathologic phimosis, this section fails to mention that the cumulative risk of phimosis in intact English boys is 0.6% in the first 15 years of life 457 and 0.42% in Chinese boys, 541 while the risk of phimosis following male circumcision ranges from 0.3% to 2.9%. There have been three studies directly comparing the rates of phimosis in normal and circumcised boys and none have found a statistically significant difference. 186,190,505 The section fails to mention that meatitis/meatal ulceration is common in circumcised males and rare in intact males. It is most commonly seen in the first few months of life. The inflammation is thought to be the result of constant irritation from urine, stool, and friction from rubbing against a diaper. 547 One report noted that meatal ulcers were seen in 20% of newborns in the first 35 days following male circumcision. 548 In 219 circumcised boys under 3 years of age, 19.1% had meatitis, a rate significantly higher than in intact boys in whom it was not seen (p=.030). 186 A review of the entire medical literature does not support the contention that male circumcision has a positive impact on phimosis, balanitis, and meatitis. Consequently, the recommendation for the intended audience of health providers is misleading, not justified, and not appropriate.
# Health conditions for which male circumcision is indicated
The material presented in this section of the background document is, for the most part, somewhat accurate. However, the statement that male circumcision is the "definitive treatment" for phimosis is confusing. Phimosis can be physiologic, which requires no treatment, or it can be pathologic, which requires treatment. Circumcision should not be considered first line therapy for pathologic phimosis. Balanitis xerotica obliterans (BXO) is the most common cause of pathologic phimosis. Fortunately, it is rare. Some, but not all, cases of BXO will respond to topical steroid application. A high response rate of phimosis to topical steroid application has been repeatedly demonstrated. Likewise, there have been many reports of surgical techniques that correct phimosis without removing any tissue. Several systematic reviews and cost-benefit analyses have indicated that male circumcision is the least favorable method of treating phimosis and the standard of care is shifting to topical steroids as the first line of therapy followed by surgery, if topical therapy fails. The language of the draft needs to reflect this shift.
# RESPONSE 77:
We have clarified that there is a distinction between physiologic and pathologic phimosis in the text and changed the text to read "In the absence of a response to topical steroids, or when the child is not a candidate for steroid use, male circumcision is the definitive treatment."
# COMMENT:
# Safety and risks associated with male circumcision
The material presented in this section of the background document is highly selective and ignores studies that do not agree with the CDC's apparent goal of presenting infant male circumcision as being safer than it actually is. Most of this section is spent reviewing studies that derived their data from databases, 532,591,592 which will underestimate the rate of complications by at least 10-fold, if not more. When assessing the rate of complications reported in the medical literature, several factors are important. Some immediate complications are common and their frequency can be easily estimated. Others have been reported in case series, where the authors report their experiences with several patient episodes. Many of the more uncommon complications have been reported as case reports. From case series and case reports, it is hard to estimate the frequency of a particular complication. Certainly, not every complication is reported in the medical literature, and a number of barriers keep unusual complications from being reported. The complication needs to be recognized as related to, associated with, or caused by the procedure, and authors need to be willing to take responsibility for the complication. Next, the person identifying the complication has to decide whether to pursue reporting the complication, and they must have the time and resources to perform the task. Once the case report or case series is written and submitted, it is unlikely to get published unless the new report adds something to what has already been published. Medical journals are publishing fewer case reports, so a case report often needs to be shopped around to several journals before it finds a home. Most authors will give up submitting after a couple of rejections. Consequently, some have estimated that for every case report published in the medical literature, there may be 100 to 1000 unreported cases.
Imprecise and inconsistent definitions for what constitutes a complication, such as how much post-operative bleeding is permissible, also muddies the waters. Definitions may be more or less inclusive, often depending on what message the author wants to convey. This expectation bias is blatant in some studies. For example, in the African randomized clinical trials of adult male circumcision, very low complication rates (1.3% to 3.6%), lower than those commonly reported for infant male circumcision, were reported for the procedure and delayed complications were not assessed. It would appear that the aim was to present adult male circumcision as a low-risk procedure in advance of the planned male circumcision roll-out. Because the definitions and criteria for inclusion of complications vary so widely, any attempt to perform a systematic review and meta-analysis of the medical literature on this topic would be a fool's errand, and assigning any worth to conclusions reached in the process would be pointless. 29 Any such analyses are not worthy of mention. If mentioned at all, the extreme limitations in studying this topic need to be stressed.
What constitutes a complication by a researcher's definition also affects the reported incidence of that complication. If bleeding complications included those patients who had any oozing of blood following male circumcision, then the complication rate would be much higher than if bleeding complications included only those who required sutures. For example, in the study by Gee and Ansell the definition of "really significant" is arbitrary. One could easily include all of the hemorrhages requiring sutures (15), all of the denudation patients (2), half of the dehiscence patients (4), and all of the Plastibell being too tight (7). Instead of 14 patients who had "really significant" complications, the number tripled to 42. 593 Many studies are limited by how long they follow their subjects. As a consequence, many of the delayed complications will be missed. For example, the database study by Christakis et al. only considered complications noted during the perinatal admission. As expected, they saw virtually no infectious complications. 532 Infections resulting from male circumcision would be expected to occur days after the procedure, a time when nearly all these patients would have been discharged from the hospital. Likewise, the database study by Wiswell and Geschke looked only at the complications occurring during the first month of age. 591 This study, by design, would miss nearly all the cases of skin bridging and adhesion formation, buried penis, meatal stenosis, and inadequate or cosmetically inferior results.
Pediatric urologists are faced on a daily basis with the complications resulting from infant male circumcision. Nearly all of these complications are not seen in the immediate post-operative period. One pediatric urologist noted that of 235 boys referred to him in a 24-month period with male circumcision complications, about half of them required additional surgery. His experience is typical for his surgical sub-specialty. In the United States, a third of pediatric urologists report having served as an expert witness in male circumcision injury cases. Substantial malpractice claims have been paid for male circumcision-related injuries. 594 The study design and method of data collection can also have an impact on estimating the rates of complications. Higher complication rates will be documented in a group followed prospectively over a short period of time with scheduled follow-up examinations, as compared to a group followed retrospectively over a decade. When looking for complications prospectively, the complications are proactively observed and recorded. For example, a prospective study found an excessive bleeding rate of 8.9% to 9.9% following infant male circumcision. 595 Retrospective studies typically see excessive bleeding following 1% to 2% of male circumcisions.
In a retrospective study, only those complications recorded in the chart, usually in the nurses' notes, are available. Complications not documented in the chart would be missed. Therefore, the complication rates in chart reviews would be lower than in a prospective study. Chart reviews, including one published by the CDC, have documented complication rates of 2% to 6%. 6,593,596 Still, a chart review will uncover more complications than searching a database for diagnostic and procedure codes. For a complication to be tallied in a database, it not only must be recorded in the medical record, but it also must be listed as a discharge diagnosis. Only the most severe, lifethreatening complications will be picked up in a database study. This does not mean that severe complications will not also be missed in a database. For example, an infant who had a third of his glans amputated using a Mogen clamp, resulting in a $2.3 million malpractice judgment awarded in 2009, did not have this complication listed on the medical record's face-sheet, so it would not have been entered into the database. 597 As a consequence, the complication rates for the database studies, which are in the range of 0.1% to 0.2%, 532,591 are ten times lower than the complication rates in chart review studies.
RESPONSE 78: : CDC stands by the accuracy and scientific rigor used to conduct its study on adverse events associated with male circumcision 15 and represents the first study of its kind in the U.S. which allows a comparison in adverse events reported among circumcised and uncircumcised males during three age ranges (age < 1 year, 1-9 years, ≥10 years). In the absence of longitudinal data on circumcised versus uncircumcised males comparing rates of adverse events related to male circumcision, a database study provides a good source of data to describe complications reported at discharge. No study is without limitations. Longitudinal chart review studies may only provide data that is representative for those geographic sites where the studies are located.
# COMMENT:
If studies whose data are mined from databases miss approximately 90% to 95% of the complications, do they serve any purpose? They would if their results can be extrapolated to accurately reflect reality. To demonstrate this, one would need to perform either a blinded prospective data collection or a chart review data collection in which information for the database is simultaneously generated to assess how well these sources of information correlate. To date, such a study has not been published.
Consequently, the studies of complication rates that are based on databases do not provide useful information and should not be taken seriously when developing policy.
While the CDC draft elaborates on the numbers generated by one such study, 592 the time spent by these researchers would have been better spent collecting useful information.
RESPONSE 79: The reviewer's allegation that database studies miss approximately 90% to 95% of the complications is conjecture.
# COMMENT:
This study, with its markedly flawed data, makes the claim that complication rates are greater if male circumcision is delayed beyond the newborn period. The problem is that data collection and reporting methods differ in the two age groups, which alone could explain the difference. The only reliable studies to assess this question are those that compared two age groups using the same evaluation tools, the same skill in practitioners, in the same environment, at the same time. Only a handful of studies have done so, and they do not support the authors' claim. In one study, complications were only seen in those who were circumcised at under 72 hours of life. 544 In the second, the Gomco clamp was found to have more bleeding complications in older boys than in neonates. 598 In a third study from Iran, no difference in the complication rate was found between age groups. 599 In a fourth study from Saudi Arabia, a greater rate of complications was seen in male circumcisions performed in the neonatal period. 600 Several studies have indicated that the Plastibell should not be used after the neonatal period. 601,602 RESPONSE: See response 78.
# COMMENT:
The CDC draft, citing a 1983 review article, 19 provides an incomplete list of complications following infant male circumcision. The CDC draft should have included a complete list of complications and, where available, estimates of their likelihood. While this information is not available in the CDC draft, this information is essential for the intended audience of health care providers, so they can provide adequate disclosure to patients or their proxies for the fully informed consent process to be valid. Considering that infant male circumcision is a purely cosmetic procedure performed primarily for cultural reasons, the required level of disclosure is higher than for procedures for which there is a clear medical indication. For this reason, providing complete disclosure should be the standard of care prior to infant male circumcision. This would include a listing of all the known complications resulting from infant male circumcision. Doing so not only fully informs the person providing consent/permission, but it also protects the health care provider performing the procedure should a complication develop as a result of the procedure.
Bleeding: Bleeding can be minor or require the application of clotting enhancers, suturing, and/or blood transfusions. 591,603,604 It can result in cardiac arrest, 605 or exsanguination. 606 Some patients will lose enough blood that a blood transfusion is needed. 591,593,596, In male circumcisions performed on older children, postoperative bleeding is often the reason for hospital admission following the outpatient procedure. 611,612 The penis and the foreskin, which is fed by the frenular artery and is a frequent source of bleeding, are highly vascularized structures. Bleeding complications can occur with any of the techniques used without regard for the experience or expertise of the operator. 613,614 The complication rate from bleeding varies widely with study design, the definition of excessive bleeding, and the attitude of the researcher toward male circumcision. For example, in a prospective study designed to determine the incidence of hemorrhagic diseases and the impact of vitamin K, 9.87% of male circumcisions resulted in abnormal bleeding. 595 A chart review by Gee and Ansell found a bleeding rate of 1.0%, 593 while data from a database noted excessive bleeding in 0.083% with 0.028% needing ligatures applied and 0.003% requiring transfusion. 591 Health care providers also need to recognize that excessive bleeding following male circumcision may be the first sign of an undiagnosed bleeding disorder. Infection: Following male circumcision, the newborn is at greater risk for infections because of the open wound involving the entire surface of the glans, which then sits in a diaper exposed to urine and feces. For several days following male circumcision, a greenish-white, fibrinous discharge forms over the male circumcision wound, which will exhibit a mixture of flora, including Klebsiella, Enterobacter, and Acinetobacter. 625 Infections can also be caused by Staphylococcus aureus, 626 Escherichia coli, 627 Group A ß-hemolytic Streptococcus. 628,629 A positive bacterial culture cannot differentiate between colonization and tissue invasion. 625 Because of the high frequency of purulentappearing exudate from the wound, it is difficult to differentiate this exudate and erythema, which results from an open wound, from that of an infection. Estimates of the frequency of infections following male circumcision vary considerably as there is a tendency not to ascribe a poor outcome to an elective procedure. 629 The Plastibell, because it involves necrotic tissue adhering to the wound, may be associated with more infections and is linked to tissue necrosis and gangrene.
Staphylococcal infections (including MRSA): Several studies have found a higher rate of Staphylococcal skin infections in the first weeks of life in males, especially among those circumcised, as compared to females. 188,189, More recently, several outbreaks of neonatal cutaneous MRSA infections have been reported, primarily in circumcised boys. In only one outbreak reported had none of the infected boys been circumcised. 650 One case-control study was able to document that a circumcised newborn boy was at 12 times the risk of developing a MRSA infection compared to a newborn boy that was not circumcised. 651 In describing this study, the CDC mischaracterizes and downplays the results as the "hospital identified male circumcision as a potential risk factor," when the study found a statistically significant association. It is revealing that in instances where studies are favorable to male circumcision the CDC draft does not downplay these associations. In one case report, MRSA was recovered from the male circumcision wound of a newborn infant whose mother had staphylococcal toxic shock syndrome. 652 The frequency of staphylococcal infections varies from study to study, but in one series of male circumcisions performed with a Plastibell, 10.7% developed impetigo. 653 The increase in staphylococcal infections following male circumcision is not unexpected. Studies have shown that male circumcision alters the normal flora from primarily gram-negative organisms to grampositive organisms, including staphylococci. Staphylococcal scalded skin syndrome: Case reports and cases series of staphylococcal scalded skin syndrome following neonatal male circumcision have been reported. In one series of 75 male circumcisions performed with a Plastibell, 2.7% developed staphylococcal scalded skin syndrome. 653 Abscesses of the penis and scrotum following male circumcision have been reported in a number of case reports. 628, Erysipelas, a skin infection usually caused by Streptococcus that can lead to Fornier's gangrene, has been reported following male circumcision. 661,662 Group A ß-hemolytic Streptococcus infections have been reported following infant male circumcision during outbreaks in neonatal nurseries. 663,664 Acute post-streptococcal glomerulonephritis has been reported following an infected male circumcision. 665 Diphtheria infections, before widespread vaccination programs, were reported following both ritual and medical male circumcisions. 666,667 Syphilis: In the late 1800s, there were many reports of syphilis following neonatal male circumcisions from oral-genital contact during the procedure performed by infected mohelim. 668 Tuberculous: Reports of penile tuberculosis following ritual male circumcision were commonplace in the first half of the twentieth century. Most often, the history involved the wound being sucked by the mohel, who would invariably be found to have tuberculosis. 674,675 Cases continued to be reported well into the twentieth century. Herpes simplex virus is also spread via the oral-genital contact that can occur during ritual male circumcision with some cases resulting in death or brain damage. When these infections were discovered in New York City, Tom Frieden, current director of the CDC and the Commissioner of the New York City Department of Health and Mental Hygiene at the time of the herpes outbreaks, and Susan Blank, the chair of the American Academy of Pediatrics Task Force on Circumcision, did nothing to stop these easily preventable infections.
Tetanus following ritual male circumcision has been reported in multiple case series. Septicemia, which is an overwhelming, systemic, life-threatening infection can follow male circumcision. 660, Once the bacteria have entered the bloodstream, the infection can spread throughout the body. Reports have noted pneumonia, 698,699 empyema, 660 soft tissue abscesses, 660 osteomyelitis, 694,698,700,701 septic arthritis, 660,694,701,702 pyelonephritis, 698 peritonitis, 703 bilateral femoral head necrosis, 694 umbilical arteritis, 628 gangrene, 702,704,705 suppurative inguinal lymphadenitis, 694 and meningitis. 627,629,694,705,706 Sepsis following male circumcision can also lead to disseminated intravascular coagulopathy, jaundice, congestive heart failure, 697 peripheral circulatory collapse, 698 hypothermia, 697 and death. 654,693,696,699,707,708 Fornier's gangrene, which is necrotizing fasciitis of the perirectal, perineal or genital area, resulting in gangrene of the overlying skin, 709 has been repeatedly reported in the medical literature, following both tribal male circumcisions 722 and male circumcisions performed in a medical setting. 704 These serious, life-threatening cases emphasize the necessity of informing parents of the uncommon, but potentially serious, risks of neonatal male circumcision. 723 Surgical complications include total denudation of the penis 718, and the removal of too much shaft skin. 660, Even with proper technique, especially with the clamp techniques, it may be difficult to estimate how much skin is removed. The removal of too much skin is so common that many practitioners may view the results as normal.
Urethral fistula following male circumcision has been reported in a number of case reports and case series. 83,720,732, This complication requires careful repair by experienced specialists. 757 Other surgical complications, such as multiple pyogenic granulomas, 758,759 subglandular stricture, 760 and scrotal trauma have been reported following male circumcision.
Plastibell retention/pseudoparaphimosis: If the Plastibell ring does not fall off within eight days, a complication is likely to result. The Plastibell ring can dislocate proximal to the glans, where it can mimic paraphimosis, also known as pseudoparaphimosis. The dislocated ring can result in compression damage, ulceration of the corona and proximal glans, and edema and vascular congestion distal to the ring. Removal of the ring with a wire cutter is often needed. Reports in the medical literature have included significant long-term penile deformities, 732, signs of urinary obstruction, 770 pseudoparaphimosis, and strangulation of the penis. 774 The incidence of pseudoparaphimosis following use of a plastic bell male circumcision device has been reported to range between 0.27% 593 to 1% 765 to 1.6%. 596 The risk of a Plastibell tracking back onto the shaft and needing to be removed using a ring cutter is 3.6% and incomplete separation is seen in 5.9% of patients. 775 Another study found ring retention in 2.1%, with 0.8% developing necrosis and 0.9% developing pseudoparaphimosis. 776 In one series, primarily in neonates, there was an 11% retention rate. 614 Bivalving: Inadvertent placement of scissors into the urethra while attempting a dorsal slit resulted in surgical bivalving of the glans. 731,777 Penile necrosis/ischemia is a serious complication that has been noted in a number of case reports and case series. 6,660,704,718,746,763,776, In one series the rate of necrosis was 0.8%. 776 Amputation of the penis and glans: Since several of the devices used to perform male circumcision involve a "blind" amputation of the foreskin, there are multiple case reports and case series reported in the medical literature related to partial or complete amputations of the glans. 628,696,705,731,741,750,755,762, Since many of these reports are in the form of describing techniques to reattach the inadvertently amputated tissues, the number of actual cases might be much greater. These amputations are often the source of malpractice cases. In some instances, it was decided to raise these boys as girls. 801 Acute urinary retention, typically from bandages that are too tightly wrapped around the wound in ritual male circumcisions, or a Plastibell ring obstructing the meatus, has also been reported. 593,705,762, In a series of older boys circumcised with a Plastibell, 0.35% complained of urinary retention. 826 In follow-up of 99 boys circumcised at a mean age of 4.3 years, 19 did not pass urine for more than 12 hours. Five boys held out for several days (maximum 3 days) with one requiring readmission. 533 In a study of older boys circumcised with a Plastibell, 56.3% had difficulty with micturition. 827 In a study of healthy male neonates, the mean time to voiding was 5.3 (SD=2.5) hours after the procedure with the longest duration to post-male circumcision voiding being 11.5 hours. 828 In another study of circumcised newborns, the mean time to post-male circumcision voiding was 4.97 hours (SD=3.35). A few (0.38%) took more than eighteen hours after male circumcision to void. 829 Other complications from urinary retention, such as bladder rupture, 830 obstructive uropathy, 831 acute renal failure, and urine advancing in subcutaneous fascial planes 834 have also been reported.
The tight bandaging technique used in ritual male circumcision also places the boy at greater risk for urinary tract infections. Leg cyanosis, both unilateral 835 and bilateral, 836 gastric rupture from air swallowed while crying during the procedure, 837 pulmonary embolism, 838 pneumothorax, 839 erythema multiforme, 840,841 myocardial injury, tachycardia, heart failure, 842,843 and impotence (in adult men) 844,845 have all been reported following male circumcision.
Apnea/Apparent life-threatening events have been reported, 846,847 with a rate of 3.85% of prolonged apnea following the procedure. 847 Chilling was noted to be a problem when male circumcision was performed just after delivery. 848 Hyperbilirubinemia (jaundice). Since it has been shown that breastfeeding and bottle feeding are adversely affected by neonatal male circumcision, one would expect that circumcised boys might be at greater risk for hyperbilirubinemia. While not studied directly, two studies in American infants have found boys to be at greater risk for hyperbilirubinemia. 849,850 In the Canadian database used to determine the rate of urinary tract infection based on male circumcision status, it was discovered that circumcised boys were significantly more likely to require hospitalization (excluding hospitalizations for urinary tract infection) during the first year of life. 538 This differential could be due to hospitalizations for hyperbilirubinemia. This is an area open for future research.
The presence of a hypospadias is an absolute contraindication to male circumcision, yet circumcisions have been reported being performed on boys with a hypospadias. 593,851 There have been reports of techniques to correct hypospadias in circumcised patients, and techniques to repair hypospadias without a male circumcision leaving the penis with a fully intact appearance. 856 Hematoma following male circumcision is fairly common. 753,857 The rates have been reported as 0.46%, 776 0.98%, 858 6.1%, 827 and 7.7%. 695 It is one of those complications so common that it is not usually considered out of the ordinary, and therefore, is not likely to be identified as a "complication."
Delayed complications: Most studies attempting to compile the complication rates for male circumcision do not collect data long enough to capture the long-term complications.
Meatitis is a common finding as most circumcised boys shortly after the procedure will have erythematous meatal openings. Most physicians unaccustomed to examining the meatus in intact males would consider the inflamed meatus to be a normal feature of the circumcised penis. 547,548 The inflammation is thought to be the result of constant irritation from urine, stool, and friction from rubbing against a diaper. 859 The rates of meatitis are approximately 20%. 186,548 Meatal stenosis, which has been recognized as a complication of male circumcision for some time, may be the most common complication following male circumcision. 186,533,535,536,545,604,614,741, In 1881, Mastin stated that narrowing of the meatus was the rule for Jews, not the exception, and meatotomy (the surgical correction of meatal stenosis) was designated by many Jews as their "Second Circumcision." 885 Symptoms associated with meatal stenosis include penile pain at the initiation of micturition, narrow high velocity stream, the need to sit or stand back from the toilet bowl to urinate, abdominal pain, enuresis, dysuria, urinary urgency, urinary frequency, straining to urinate, urinary dribbling, and urinary retention. 535,870,879,886,887,888 The meatal slit at the urethral opening should be 25% to 30% of the diameter of the glans. 860 The meatal opening is significantly smaller in circumcised males and meatal stenosis occurs almost exclusively in the circumcised penis. 46,538,873,889 (Most physicians do not know what constitutes a normal meatal opening, if they have never examined an intact male or been educated about the normal penis. The CDC should focus its efforts on educating health care providers about normal penile anatomy, care of the normal intact penis, and on diagnosing and appropriately treating the complications of male circumcision.)
The incidence of meatal stenosis following infant male circumcision is found in 2.8% (requiring meatotomy), 533 7.3%, 186,536 32.1%, 871 3.55%, 614 and 20.4%. 537 For boys circumcised later in life, the incidence is 11.1% (necessitating meatotomy) 545 and 7.95%. 538 A report of 58 meatotomies performed on circumcised boys on an outpatient basis in one year's time in a single practice 874 suggests that urethral meatotomy is a very common procedure in the United States. The writers of the CDC draft need to be congratulated on finding the study with the lowest reported rate (0.9%) of meatal stenosis following male circumcision in the literature 599 while turning a blind eye to the remainder of the medical literature. They accept this outlying study without question, yet take a cheap shot at the methodology of a study whose results have repeatedly been verified. 536 Such behavior is both unscientific and unprofessional. One cannot help but notice that the CDC draft is only critical of studies that show male circumcision in a neutral or negative light. It gives the impression, either rightly or wrongly, that the CDC is pursuing a specific pro-male circumcision agenda with this draft.
Meatal stenosis obstructs the flow of urine and can lead to urinary tract infections, vesicoureteral reflux, hydronephrosis, obstructive uropathy, and renal failure. 880,881,887, Hidden Penis, Buried Penis, Concealed Penis, Trapped Penis, Webbed Penis, Inconspicuous Penis: These conditions have generated much discussion on how to define them and how to treat them.
A concealed penis is a penis that is inconspicuous because of an overlying fold of abdominal fat. A buried penis refers to a penile shaft that is buried below the surface of the prepubic skin and has also been used to describe a partially or totally obscured penis caused by obesity or by a radical male circumcision. A true buried penis is a congenital anomaly that includes an abnormally large suprapubic fat pad and dense dysgenetic dartos fascial bands that tether the penis inward. This requires surgical intervention.
A webbed penis consists of midline skin webs which bind the ventrum of the penis to the scrotum with an abnormal insertion of the scrotum onto the ventral aspect of the penis. Because the skin and dartos fascia are inadequately attached to the underlying Buck's fascia, the corporeal bodies telescope proximally without the skin and dartos fascia covering. Because the penis is suspended from the pubis by the suspensory ligament, it remains fixed, but the fat does not. Fat descends over the penis and covers it. Many intact boys have baby fat surrounding the undeveloped penile shaft. Most of these patients will develop normally, with the excessive baby fat in the pubic area regressing and the penis lengthening under the influence of endogenous testosterone. 897,901,904 Failing to recognize a "hidden or buried penis" at birth makes the condition worse and more difficult to correct down the road if the boy is circumcised. There are multiple case reports of buried penis following male circumcision, 752,762, and most case series of patients undergoing repairs for this problem are populated with boys who were circumcised as infants. 546,894,899,911 This has also been reported as a problem in circumcised adults. 912 Male circumcision is a problem for these patients, with buried penis, because the base of the shaft skin is not properly attached to the base of the tunica albuginea, so the shaft skin will be bunched up around, and distal to, the sulcus of the glans. Because nearly all of the shaft skin is in a location where it is typically removed by a clamp device, nearly all of the shaft skin is at risk for removal. 893 Since the synechiae that fuses the glans to the inner surface of the foreskin is removed, there is nothing to hold the penis away from the body, so the penis becomes buried in the scrotum and fat pad. 893,910 With the penis completely buried, the circular scar from the male circumcision can constrict resulting in phimosis. 893 This often gives the appearance of "redundant foreskin." 83,893,903,908 This leads the parents to blame the physician for an "inadequate" male circumcision. Despite reassurance from the physician, 899 some parents will demand that the child be re-circumcised, and indeed many of these children will be referred to the urologist for recircumcision. 913 Attempts to re-circumcise, which entails removal of more penile skin, often makes the condition worse, by further burying of the penis, and it makes reconstruction more difficult. 893, The repair is a complex procedure, which is only made more difficult if the patient is circumcised.
The consensus among pediatric urologists is that infants with buried penis should not be circumcised as it can result in serious consequences. 893,913,916 The take home lesson from all of this is: if the penis appears too small, it should not be circumcised unless it can be demonstrated that it is not a buried penis. 893 It is difficult to estimate the incidence of buried penis. In a series of 313 neonatal circumcisions performed with a Mogen clamp, one developed hidden penis. 544 It is not known if this rate is low because the incidence is low or because researchers did not successfully identify those for whom male circumcision was contraindicated. In one series of healthy boys, 20.1% of boys in the first year of life had a glans that was completely covered, but only 0.9% would be considered to have a buried penis/preputial stenosis. 186 Iatrogenic phimosis/preputial stenosis: Iatrogenic phimosis occurs when the head of the penis is trapped behind the male circumcision scar. The skin remaining after male circumcision can develop a circular cicatrix that contracts and draws the proximal skin over the glans forming a resistant phimosis. Since 1895, multiple case reports have appeared in the literature. 544,917 The incidence has been reported as 1.7% in older boys, 534 0.3% in infants using the Mogen clamp, 544 2.9% using the Gomco clamp, 546 and 0.9% using a variety of other male circumcision techniques. 186 Given that the cumulative incidence of pathological phimosis in intact boys by 15 years of age is 0.6%, 457 phimosis following male circumcision occurs with equal frequency as in boys who are not circumcised.
Cosmetic concerns: Parents, to a large degree, have their infant sons circumcised for cosmetic reasons: primarily so the boy's genitals will look like the father's genitals.
Since there is a wide variety to be had in the appearance of the circumcised penis, both in children 186 and adults, 46 the intended outcome is unlikely to occur. 918 The desired outcome of a fully exposed glans on an infant in the first year of age is the exception, 186 and parents and older boys are often not pleased with the cosmetic outcome. 776,919 In a series of boys circumcised with a Plastibell, 33.1% of patients experienced cosmetic complications, and 20.8% claimed to have experienced psycho-social problems because of the appearance of the penis after the operation. 920 In a comparison of the Plastibell versus standard free-hand technique in older boys, favorable cosmesis was seen in 60.9% with the Plastibell and 44.9% with standard technique. 827 Consequently, the primary care physician is bombarded with parental concerns that not enough skin was removed. While reassurance is warranted in nearly all cases, there are a substantial number of patients who will doctor-shop until they find someone willing to recircumcise their infant. 921 Re-circumcision to address cosmetic concerns is a commonly performed procedure, 607,922 but, in the case of a buried penis, it will make the situation worse. 893, In one study, the rate of inadequate male circumcision prompting a surgical revision was 2.8%. 190 In other studies the rate of re-circumcision ran about 1%. Adhesions: There is some debate whether the adhesions are the result of inadequate stripping of the inner prepuce away from the glans at the time of male circumcision 926 or the reattachment of the epithelium of the inner prepuce to the epithelium of the glans. 927,928 Adhesions have been noted in 15.3% of newborns at their first office visit, 929 10% at the one-month well-child visit, 927 and in 25.6% to 27.6% of circumcised boys overall. Fortunately, with age the prevalence decreases. 186,930 The adhesions which form following male circumcision are more dense than the connections normally found between the inner prepuce and the glans. 927 Parents must be taught how to care for the circumcised penis by pulling back on the penile skin and exposing the glans on a regular basis, so adhesion formation can be avoided. 929 It has been suggested that daily application of petroleum jelly for three weeks following the procedure may decrease the rate of adhesion formation.
Many physicians wrongly believe the proper treatment is to tear the adhesions apart, but this can lead to skin bridges and further scar tissue formation. Most adhesions will resolve spontaneously.
Skin bridges: Some adhesions will form a permanent bridge from the male circumcision wound to the surface of the glans. Skin bridges can cause tethering of the penis, entrapment of debris, curvature of the penis, and pain on erection. 927,929 Several case reports have appeared in the medical literature describing this complication. Skin bridges are commonly seen by urologic practices. 933 The prevalence of skin bridges was 4.1% in circumcised boys under 3 year of age, 186 Among adult circumcised males, skin bridges were noted in 12.7%. 46 Keloid formation: Keloids are hypertrophic scars that do not decrease in size over time.
Although penile keloid formation is rare, it has been reported following male circumcision. The treatment consists of intralesional steroid injections, surgical excision, or a combination of the two. 934,939,940 Subcutaneous granuloma: A subcutaneous granuloma following male circumcision has been described as an "indurated, confluent, red-violet plaque, freely movable over the underlying tissue, 0.3-1.0 cm wide of firm consistence, surrounding the penis in the neighborhood of the coronal sulcus. Its surface is smooth and the borders are distinctly defined." 941 Penile edema: Acquired penile edema in adult males has been reported since 1928 under a wide variety of names. The entity has been described as "a painful, hard, nodular, translucent cord that suddenly appears in the penis and is usually confined to the coronal sulcus," 822 or as a "hard worm-shaped lesion" on the dorsum of the coronal sulcus. 956 The edema comes on suddenly and is self-limited. It is typically seen in circumcised, sexually active men often after vigorous, frequent, or prolonged sexual intercourse. 948,950,952,954,956,957, In a series of genital dermatoses presenting to a dermatological referral practice, "idiopathic penile edema" was seen only in circumcised men (p<.01). 394 In most series, the circumcised penis appears predisposed to this condition. 948,955, It has been postulated that the male circumcision scar interferes with normal lymphatic drainage. 948,955 Alternatively, penile edema has also been attributed to decreased vaginal lubrication, 961 which is a common condition in vaginal intercourse involving a circumcised penis. 115 Inadequate lubrication leads to abrasions of the penile skin, which, in turn, can result in antigen transfer and subsequent hypersensitivity. 963 The uniform success of a variety of interventions 950,951,954 suggests that this condition is benign and self-limited. Acquired penile edema affecting pediatric or adolescent males has been reported less frequently. 963, Based on one prospective series, the incidence in pediatric patients was estimated to be 0.62%. 186 Following adult male circumcisions, penile cutaneous horns can develop. Many of these may harbor malignancies. Hair strangulation occurs when a human hair becomes inadvertently wrapped around an appendage, usually a finger or a toe. Once the hair gets wet it contracts and cuts into the appendage. There have been multiple case reports of penile strangulation by a hair. 865, Some cases have resulted in urethral fistulas and partial or complete amputation of the penis. 975,976, The hair typically becomes entrapped in the coronal groove. 979 Of the more than 70 cases reported in the medical literature, all but one case occurred in circumcised males.
Two studies determined that the size of the adult penis is significantly smaller in circumcised men. 46,47 This is important information that needs to be disclosed as part of the informed consent process.
Psychological sequelae: The aftermath of infant male circumcision shares many of the attributes of post-traumatic stress disorder; 984 however, there has been little study to confirm or deny this hypothesis. There is solid evidence to indicate that imprinting happens in the perinatal period, which can have long-term consequences when these infants become adults. Given that male circumcision is more traumatic (in terms of provoking a cortisol surge) than gastric suctioning, one would expect that it might have long-term consequences. This has been seen in two studies in which it was found that male infants who had been circumcised shortly after birth cried longer and louder than girls and intact boys when given vaccinations at 4 to 6 months of age. 993,994 The studies concluded, "Because memory of pain is believed to be important in subsequent pain perception, and the main structures for memory are functional in the neonatal period, it is conceivable that pain from male circumcision may have long-lasting effects on pain response and/or perception." 993 Subsequently, it has been demonstrated that inadequate analgesia for initial procedures in young children may reduce the effectiveness of analgesia in subsequent procedures. 995 One study found a positive statistically significant association between male circumcision rates and the rates of autism in boys. 259 A recent national, register-based cohort study from Denmark found that circumcised boys were at significant risk for developing autism spectrum disorder by ten years of age (hazard risk (HR) 1.46; 95%CI 1.11-1.93) and at greater relative risk for infantile autism before five years age (HR 2.06; 95%CI 1. 36-3.13). This same study found that circumcised boys were at greater risk for developing hyperactivity disorder (attention deficit disorder) (HR 1.81; 95%CI1.11-2.96). 996 The link between attention deficit disorder and male circumcision has been suspected for some time given that it has a higher rate in boys and it is diagnosed more frequently in the United States than in Europe. Another preliminary study indicated that circumcised adults are more likely to have alexithymia (difficulty in identifying and expressing feelings). 997 Further study is needed in each of these areas.
Cansever performed psychological testing on Turkish boys before and after ritual male circumcision. Following male circumcision, there was a decrease in IQ, a decrease in body image, disturbance in sexual identification, an increase in regressive traits, and an increase in aggressive behavior, especially toward their mothers. 998 While there has been little study of the psychological sequelae of infant male circumcision, there is no evidence to suggest there is no harm. 999 A potential impact on sexual identification following infant male circumcision needs further study. In a study of men seeking care at a sexually transmitted disease clinic in San Francisco, circumcised men were statistically significantly more likely to identify themselves as men having sex with men (OR 1.13; 95%CI 1.10-1.16). 8 The same lead author collected similar information in a sexually transmitted disease clinic in Tel Aviv with similar results (OR 1.57; 95%CI 1.11-2.22). 1000 This finding needs further research.
Based on these studies, part of the disclosure in the informed consent process needs to include the statement that there are currently preliminary findings indicating that male circumcision is associated with a higher rate of autism, attention deficit disorder, and identifying oneself as gay/bisexual.
Behavioral changes: Richards et al. present both circumstantial and direct evidence that circumcision of male infants leads to behavioral changes. 1001 Several early behavioral gender differences, noted in studies performed in the United States, have not been noted in similar studies performed in Britain or The Netherlands. Changes in Sleep Pattern: When circumcised males were compared to genitally intact boys and girls, they showed less active sleep time, more time awake and agitated (active awake and crying awake), longer latencies to sleep and more extreme long non-REM sleep periods. 1012 Sleep patterns were correlated with rapidity of drops in cortisol levels. 1014 Sleep changes have not been documented in newborns with prolonged crying. 1012 These findings need to be placed in context. Changes in the amount and type of sleep and the latency to sleep are indicative of stress. The immature human infant has a limited capacity to actively avoid stressful stimulation and responds to such stimulation with the "conservation-withdrawal" pattern. This leads to increases in non-rapid-eyemovement (non-REM) sleep, which is the low point on an arousal continuum, where thresholds to sensory stimulation are high and motor activity is low. 1015 REM states probably represent the operation of maturational processes in the central nervous system of the neonate, which are primarily related to physiological processes not yet influenced by experience. These maturational processes are part of an unfolding genetic progression, phylogenetically preformed for an average expectable environment. The processes involve the establishment of the necessary connections within the central nervous system as well as in behavioral integration. By comparison with adult sleep, prototype REM sleep is poorly organized. But, in the neonate, it only takes three months of development to organize it. 1016 An increase in non-REM sleep has been observed following heel lancing. 1016 Male circumcision without anesthesia in a newborn is followed by prolonged non-REM sleep, which is consistent with the "conservation-withdrawal" theory. Newborns usually begin their sleep cycle with REM sleep, but following heel lancing, they began sleep with a lengthy period of non-REM sleep. Following either selective interruption of REM or non-REM sleep or deprivation of total sleep, neonates exhibit a propensity to recover quiet non-REM sleep rather than active REM sleep. The quiet sleep priority may be related to "stress" or wakefulness and fatigue. 1017 Consequently, an inborn adaptive response to stress is to produce a quiescent state with high sensory thresholds. 1016 A "common sense" guess about the effects of a continual disruptive stimulation for a newborn would be that an infant would sleep less and cry more; however, in the period following male circumcision infants have an increase in light sleep and a decrease in deep sleep, 1018,1019 but they cried the same amount of time as before circumcision. Consequently, these changes in sleep pattern following male circumcision are a much more accurate measure of the stress of male circumcision than is crying.
Interruption of maternal-infant bonding and changes in breastfeeding: A study of the effects of male circumcision on maternal-infant interactions noted a trend toward fewer intervals of uninterrupted feeding, with infants who were circumcised sucking on their bottles harder, faster, and more concertedly than those not circumcised. This, in turn, made them less available to their surroundings and less able to interact with their mother. This finding lasted for approximately twenty-four hours following the procedure. 1020 Dixon et al. also established that male circumcision disrupts feeding and impairs infant/maternal attachment. 1021 In babies who breastfeed, feeding deteriorates following male circumcision. 1022 Lactation consultants noted that boys circumcised before breastfeeding has been established subsequently have more problems establishing breastfeeding. However, boys recovering from traumatic birth, but not circumcised, have fewer breastfeeding difficulties. 1023 Death: Deaths following male circumcisions have been acknowledged for a long time, as noted in the Talmud, and unfortunately they continue today. Reports of death following male circumcision have been related to exsanguination, 1028,1029 bronchopneumonia, 1030 secondary pulmonary tuberculosis, 672, secondary sepsis, 660 secondary meningitis, 629 and undisclosed reasons. 691 The incidence of death following male circumcision is unknown. Each year there are reports of multiple deaths in Africa of boys following their ritual male circumcision that initiates them into manhood. In developed nations, the most common estimate, approximately 1 in 500,000, 1048 is at best a guess. Gairdner reported between 9 and 12 deaths out of 90,000 male circumcisions performed each year in the United Kingdom for an incidence of 1 in 7,500 to 1 in 10,000. 181 The primary obstacle to obtaining an accurate estimate of the incidence of death from male circumcision is the underreporting of male circumcision as a cause or contributor to death. Instead of listing male circumcision as a cause of death, the infection or hemorrhage/exsanguination that led to the baby's demise is listed. Incomplete and inaccurate death certificates for pediatric deaths are not uncommon. In a study of children with heritable disorders who died while in a pediatric intensive care unit, the underlying disorder was not listed on the death certificate 41% of the time. 1049 An example of this was a clinical-pathological conference published in The Journal of Pediatrics involving a newborn who died of an overwhelming echovirus infection. For reasons that are unclear, the patient was circumcised at 4 days of age, which "was complicated by persistent oozing of blood." While this was mentioned in the case report, the authors did not discuss the role the male circumcision may have played in the patient's fatal outcome. 1050 This struck some readers as odd that "an infant with respiratory distress and suspected of sepsis would be subjected to a stressful procedure such as a male circumcision." 1051 The authors of the case report responded that "it was the attending pediatrician's judgment that the infant had improved to the point where he did not interfere with the obstetrician's and parent's decision to go ahead with this procedure, but following the male circumcision, the clinical course rapidly deteriorated." 1052 Did the sudden deterioration in this patient coincide with the male circumcision or did the male circumcision contribute to the patient's demise? Without mention during the clinical-pathological conference of male circumcision contributing to his death, it can be assumed that male circumcision was not mentioned on the death certificate.
Of note, in England and Wales, the Registrar-General's tabulations for deaths in children under 5 years from "circumcision or phimosis" showed a dramatic drop with the decrease in the number of male circumcisions performed. During 1942-49, between 11 to 19 deaths occurred each year, while in 1950 and 1951 the number of deaths were six and one, respectively. 1053 One of the hardest comparisons for commentators on this topic to resist is that between the risk of death from male circumcision and the risk of death from penile cancer. Gellis, a highly respected pediatrician, noted that, "It is an uncontestable fact at this point that there are more deaths from complications of male circumcision than from cancer of the penis." 1054 Others have estimated that at least 41 children will die from male circumcision for each case of penile cancer prevented. 1055 If the incidence of death following male circumcision and the incidence of death following penile cancer are roughly equal, then they should be given equal weight during the disclosure portion of the informed consent procedure. Since the risk of death from male circumcision is on par with the risk of penile cancer, this deserves a prominent place in the discussion of risks, benefits, and harms.
Bollinger estimated there may be approximately 117 deaths per year in the United States that can be attributed to infant male circumcision (9.01 per 100,000). 1056 These death rates are on par with those reported in Brazil. 1057 The studies relying on data collected from databases 532,591,592 are only picking the lowhanging fruit, so to speak. Thus, they do not provide a valid picture of the true rates of complications. Their results are only useful as a rhetorical device for those who want to promote male circumcision, such as the American Academy of Pediatrics 40,1058,1059 and the writers of the CDC draft. Any discussion of their results should focus on the unreliability of this data collection method for this purpose and their role in distorting the discussion.
Throughout the CDC draft, pain is cited as a major concern by those considering the procedure. Yet, the draft glosses over the issue of pain in a brief paragraph citing a methodologically incomplete study with perhaps the highest efficacy for infant male circumcision anesthesia in the entire medical literature. 1060 As will become clear from the discussion below, the writers of the CDC draft had to dismiss a broad swath of studies in order to isolate this outlying study.
It is important to make clear that noxious stimuli are perceived as more painful in newborns compared to older children and adults. 1061 There are several reasons for this. First, the human brain learns following a noxious stimulus and compensates for the stimulus. With novel noxious stimuli, such as tearing the prepuce from the surface of the glans and crushing the prepuce, the brain does not know how to filter or tolerate it, so consequently the stimulus is more raw and intense in an infant. For example, an infant's spinal sensory nerve cells are more excitable than an adult's, making their spinal reflex response to a harmful stimulus more intense and prolonged. 1062 Second, infants do not have fully developed, fully functioning descending inhibitory nerve fibers that attenuate noxious stimuli from the periphery. Consequently, noxious stimuli that reach the brain are more intense. Third, endogenous opioids, which are responsible for postsynaptic modulation of pain signal transmission, have levels in neonates several logarithms in magnitude lower than reported in adults. Consequently, endorphin release is unlikely to provide the neonate relief from many sort of pain. 1062 Researchers typically do not study a complete evaluation of pain in newborns. For example, the study cited in the CDC draft 1060 used only the Neonatal/Infant Pain Scale 1065 to assess pain. The Neonatal/Infant Pain Scale gives a score of 0 to 2 for six factors: facial expression, crying, breathing, arm positioning, leg positioning, and alertness. Given that part of the study's protocol was to give formula, breastmilk or a 20% sucrose solution ad libitum, to restrain the arms and legs during the procedure, and to use of a pacifier, these interfered with interpretation of facial expressions and the ability to accurately assess three of the six factors of the scale. In general, scales that rely only on behavioral signs can be misleading. A pacifier can reduce crying, but will have no impact on cortisol levels. 1066 A lack of behavioral responses (including crying and movement) does not necessarily indicate a lack of pain. 1067 For example, Johnston and Stevens found strong correlations between three facial scores, but they were not related to the physiological variables, and the physiological variables did not correlate with each other. 1068 Slater and colleagues, after directly measuring spinal nociceptive reflex withdrawal activity and nociceptive brain activity, concluded that the reduction in clinical observational scores following noxious events in newborns should not be interpreted as pain relief. 1069 Raw noxious stimuli are relayed to the brain via small myelinated (A delta) fibers and unmyelinated C fibers. 1062 Simultaneously, the hypothalamus triggers a chain of events that results in the adrenal glands secreting cortisol, epinephrine, and norepinephrine. Epinephrine in turn accelerates the respiratory rate, dilates the bronchi and bronchioles, potentiates muscle contraction, and increases blood pressure and heart rate. 1070 The pain message and its response are wired through a complicated, redundant, widespread neurologic information processing system with both conscious and emotive components. This network is part of the phylogenetically most primitive nervous system, and as such, is functional early in development. The average newborn can differentiate the intensity or invasiveness of stimuli with the magnitude of their physiologic and behavioral responses reflecting the intensity of the stimulation. 1075 Pain is also largely a subjective experience, which makes assessment of pain in newborns more difficult and comparisons of pain levels in neonates with older children nearly impossible. Performing male circumcisions without anesthesia has allowed researchers to study the parameters of extreme pain in experiments that would not have been allowed on laboratory animals. Some have argued that the placebo-controlled trials of various topical and local anesthetics for infant male circumcision violated the Helsinki Declaration. 1080 Because pain in the newborn is expressed in a number of ways and focusing on one modality of expression provides a limited view, studies of pain in newborns should make a broad assessment of all pain parameters in order to get a complete picture. Studies should assess all of the following. 1081 1. Crying: The duration and pitch of crying can give an indication of the degree of pain and stress. 1082 There is a direct relationship between cry acoustics and vagal tone. 1083 Cry duration, as opposed to cry acoustics, is not as reliable a measure of stress and pain as compared to vagal tone and cortisol levels. There is a positive correlation between cry duration and both cortisol levels and behavior state following male circumcision, except when a pacifier is used. 1018,1066 2. Facial expressions: A variety of facial expression and behavior state scores have been used to quantify neonatal pain, with inter-observer scores showing reasonable reproducibility. Average behavioral state scores during male circumcision are positively correlated with increases in serum cortisol levels. 1019 3. Vital signs: Pain is associated with drops in blood oxygen levels and increases in heart rate, respiratory rate, and blood pressure.
4. Vagal tone: Reactivity and regulation of the autonomic nervous system, as measured by vagal tone, is a very sensitive measure of stress. A decrease in vagal tone is a quantitative indicator of the central nervous system's response to pain that parallels other measures of neonatal pain. 1062,1081,1083 Decreases in vagal tone are proportional to the invasiveness of a procedure. 1062,1083 5. Cortisol levels: Activity in the hypothalamic-pituitary-adrenocortical axis has long been linked with the concept of stress and arousal. Cortisol levels, which can now be measured in the saliva thus avoiding the stress and pain of drawing blood, will surge as a result of pain. The rise in cortisol levels, often seen hours after the stressful event, may be the most sensitive measure of pain in a newborn. 1084 There is increasing evidence that cortisol surges may impact long-term aspects of infant development. 1016, 6. One group of investigators was able to measure pain-specific brain activity recorded by electroencephalography and identified by principle component analysis. They also measured the magnitude and latency of the spinal nociceptive reflex withdrawal. This direct measure of nociceptive spinal cord and brain activity was found to be more accurate than observational pain scores and changes in facial expressions. 1069 Infant male circumcision is very painful and needs to be placed within the same context as all other painful procedures performed on neonates. Gunnar et al. found male circumcision elicited more behavioral distress and evoked a larger cortisol response than blood sampling, weighing, or physical examination. 1089 In a study of post-operative pain following "minor" surgery, the pain of male circumcision was behind only tonsillectomy and orchidopexy, making it more painful than sinus surgery, otoplasty, strabismus repair, dental extraction, urethral repair, hernia repair, reset of limb fracture, and revision of the thumb. 1090 In a study of the magnitude of an infant's response to procedures, such procedures as the insertion of a gavage tube, physical examinations, nose cultures, and insertion of an umbilical arterial catheter were considered mildly invasive procedures. Arterial punctures, venous punctures, and heel sticks were considered moderately invasive procedures. Male circumcision, lumbar punctures, and eye examinations for retinopathy of prematurity were considered highly invasive procedures. 1075 In a survey of 467 clinicians (nurses and physicians) working in level II and level III nurseries asked to rate the painfulness of 12 common bedside nursery procedures, male circumcision was considered the most painful procedure (tied with chest tube insertion). Male circumcision was considered more painful than endotracheal intubation, insertion of gavage tube, tracheal suctioning, arterial or venous cutdown, lumbar puncture, intramuscular injections, insertion of an umbilical artery catheter, insertion of peripheral intravenous line, heel stick, and insertion of radial or tibial arterial catheter. 1091 The signs of pain seen during infant male circumcision include surprisingly high-pitched crying, 1082,1083 changes in facial expressions, 1019 a drop in blood oxygenation with hypoxemia, significant increases in heart rate, respiratory rate, and blood pressure, 1014,1018,1019,1081,1200 and a significant decrease in vagal tone. 1083 Direct measures of nociceptive spinal cord and brain activity during infant male circumcisions have not been reported in the medical literature. To properly assess the pain of infant male circumcision, all of these need to be measured.
Because of the highly invasive nature of infant male circumcision, providing adequate anesthesia is indicated. While United States law requires that effective anesthesia and analgesia be provided for veterinary and laboratory animals, it appears this does not apply to human newborns. In an effort to alleviate the pain of male circumcision, a number of interventions have been implemented and assessed. These include comforting measures, sucrose nipple, acetaminophen, dorsal penile nerve block, topical anesthesia, injection of local anesthesia, alternative restraints, and different male circumcision methods.
Despite improvements, compared to placebo and dorsal penile nerve block, studies looking at these interventions still showed significant departures from baseline status in regards to vital signs, vagal tone, and cortisol levels, indicating that the procedure was not pain-free. Therefore, none of these methods have been shown to provide adequate anesthesia. 847,1018,1019,1022,1066,1089, A cynic might note that topical and local anesthetics are used in infant male circumcisions more to benefit the parents than the child.
The complications of topical and local anesthesia include bruising and hematoma formation, 847,1114, gangrene of the penis, 1119 and methemoglobinemia. More effective methods of anesthesia, such as general anesthesia and caudal blocks, are not used because of the difficulty, and the associated risks, of using them in infants. According to the standards established by the American Academy of Pediatrics, neonates should receive the same pain relief measures as those afforded to older children and adults. 1151 To accomplish this, male circumcision would need to be delayed until general anesthesia can be more safely delivered. In keeping with this recommendation, the Australasian Association of Paediatric Surgeons recommends deferring the procedure until at least six months of age. 1152 Claims that male circumcision is less painful when performed on an infant have not been substantiated with any evidence. The fact that noxious stimuli are more painful for the neonate, along with the known inadequacy of topical and local anesthesia, provides evidence to the contrary. There are also differences in the procedure between infancy and later in life that make it more uncomfortable for the neonate. For the majority of males older than fifteen years of age, the inner surface of the foreskin is no longer attached to the surface of the glans. 52,85,86,1153 In newborns, nearly all of the glans is attached to the foreskin. Unlike circumcision of an older male, infant male circumcision requires tearing the two structures apart, which is akin to pulling a fingernail from the nail bed. This open wound is exposed until it heals within a few weeks. For an older individual, there is no open wound on the surface of the glans.
Health care providers need to include, as part of the disclosure element of the informed consent process, that currently used methods of anesthetics do not provide adequate anesthesia for the procedure, and that the procedure is still unacceptably painful when these agents are used.
Missing from this section is a recognition of the harm that accompanies removal of the foreskin, which contains nearly all of the fine touch neuroreceptors of the penis, and thus deprives the male of the functions the foreskin provides. The normal anatomy, histology, physiology, and function of the foreskin are discussed earlier in this response, but they were completely left out of the CDC's draft. Removal of this specialized tissue would be expected to result in changes in function. Harm also comes in the form of pain, and in the form of no longer being whole or feeling whole. By ignoring the harms of the intervention, the writers of the CDC draft are ignoring medical evidence and aligning themselves with the "harm denialists" on this issue.
While the sections outlining the complication rates of circumcisions performed on adults and infants in Africa are interesting, this information is peripheral and unlikely to be of interest to health care providers in the United States. As noted above, the low complication rates seen in the randomized clinical trials might indicate that complication rates are lower for male circumcisions performed on adults than on male circumcisions performed on infants. 1154 Finally, one specific comment. The CDC draft includes the following statement: "In a comprehensive risk-benefit analysis of infant male circumcision based on reviews of the literature and meta-analyses it is estimated that over a lifetime, benefits exceed risks by a factor of 100." It gives as its citation an opinion piece, 33 which based its calculations on a selective bibliography and a number of other like-minded opinion pieces written by the same author. 473, To accept this ratio, one must live in a fantasy world where the incidence of phimosis is 10% (instead of 0.6% 457 ), where the incidence of balanitis is 10%(instead of 0.65% to 4% 541,543 ), where circumcision is a risk factor for urinary tract infection in elderly men in their dotage (it is not one), where hypertension and end-stage renal disease are associated with urinary tract infections (they are not), where prostate cancer risk is lower in circumcised men (it is not), where penile cancer is 20 times more common in intact males (instead of at most 3 times 455 ), where HPV and herpes risk is reduced by male circumcision (it is not), where cervical cancer risk is associated with the circumcision status of the male sexual partner (no studies have found such an association), where risk of infection is 0.2% (instead of 1% to 2%), where the risk of bleeding is 0.1% (instead of 1% to 2%), where the risk of repeated surgery/skin bridges is 0.1% (instead of 4% to 12% 46,186 ), where meatal stenosis never happens (instead of 5% to 20%, 186, and where there is never a loss of sensitivity or any sexual dysfunction following male circumcision. If one takes the complication rate compiled reviewing the charts of newborn males by the CDC (3.1%) 6 as a baseline and applies the 100:1 ratio, then every circumcised man should reap, on average, 3.1 benefits being circumcised. This is patently absurd. So, why would the writers of the CDC draft accept and propagate a ratio, from an opinion piece written by an individual whose scientific rigor in these matters has been called into question repeatedly, 1160 that is clearly implausible? Why did they not perform a comprehensive literature review of their own? What has the CDC been doing on this topic for the past seven years? Clearly, reference to this preposterous "ratio," and the opinion piece that generated it, needs to be deleted from the final draft. Any health care provider that informs a parent or patient that the ratio of benefits to risk exceeds 100:1 is putting themselves at risk of a lawsuit for making such a wildly unsubstantiated claim. It has been argued that, by taking the scientifically unsupported position it has, the American Academy of Pediatrics is susceptible to successful litigation for misleading health care providers. 1161
# RESPONSE 80:
See responses 1, 6 and 48. The reviewer's listing of reported adverse events is in isolation and does not describe the proportion of circumcised males that experience such an adverse event, or how the rate of adverse events differs between circumcised and uncircumcised males or whether such events occurred as a result of medical or ritual male circumcision. Based on a meta-analysis of 22 studies, most of which were based in the U.S., it is estimated that 32.1% (95% CI = 15.6 -49.8) of uncircumcised men compared with 8.8% (95% CI = 4.15 -13.2) of circumcised men will experience a UTI in their lifetime, suggesting that lack of male circumcision is associated with a 23.3% increased risk of UTI during a man's lifetime. 48 COMMENT:
# Effect of male circumcision on sexual function and penile sensation
The material presented in this section of the background document is highly selective and ignores studies indicating male circumcision has a negative impact on sexual function and penile sensation. It also misrepresents the findings of some of the studies cited.
There are a number of important omissions. For example, the 2007 study by Sorrells et al. "expressed concern that its removal may compromise sexual sensation or function," based on their mapping of the fine-touch thresholds of the penile surface in 68 circumcised men and 91 men with normal, intact genitals. Mapping revealed that the most sensitive portion of the penis is that which is removed by circumcision, the circumcision scar is the most sensitive location on the circumcised penis, and the sensitivity of the glans (head) of the penis is significantly less in circumcised men. 108 Decreased sensitivity in the glans when flaccid in circumcised men has been documented in two other studies that the CDC draft has omitted. 109,110 In one study, the difference was statistically significant using the raw data, but was no longer statistically significant when adjusted for age, hypertension, and diabetes. 109 In the other study with only 20 men in each group, the difference is shown in Figure 2, but the data are not provided and the significance of the difference is not assessed. 110 The section fails to mention that the penilo-cavernosus reflex, which is related to the ejaculation process, is significantly more difficult to elicit in circumcised men than in men with normal genitals. 120 This may contribute to the higher rates of sexual dysfunction seen in circumcised men.
In addressing studies that looked at penile problems in men before and after circumcision, the CDC draft demonstrates several important oversights. For example, in the 2002 study by Fink et al., they fail to mention that men in this study reported a significant reduction in erectile function (p=.01) and decreased penile sensitivity (p=.08).
A perceived problem or difficulty as a result of the procedure was reported by 38% of the men studied. 1162 The 2002 study by Collins et al. would, because of its small size, not be expected to provide any results that were statistically significant. This is unfortunate because, of the 15 men who were circumcised as adults, all but one had a penile problem. The fact that there was no measured improvement in sex drive, erection, ejaculation, problem assessment, or overall satisfaction suggests that the procedure was a failure. 1163 There are a number of similar studies the draft has omitted. For example, Coursey and colleagues included a control group of men who were circumcised for "phimosis or other benign indication" in a study designed to measure the impact of anterior urethroplasty on erectile function. Of the men who underwent circumcision, 27% reported worsening of their erectile function after the procedure. 1164 In a study of 95 men undergoing circumcision in China, erectile dysfunction increased following the procedure (p=.001). These men also reported increased problems with weakened erectile confidence (p=.04), and difficult insertion during coitus (p=. 03). Improved satisfaction following the male circumcision was reported in only 34 patients (p=.04). 116 Similarly, a study from Portugal of 62 men circumcised for medical reasons reported a significant increase in erectile dysfunction and difficulty reaching orgasm following male circumcision. 1165 The CDC draft mentions two other studies in passing, 1166,1167 without providing details.
The first study was performed in Turkey where most men undergo circumcision to satisfy a religious requirement, making it difficult to properly interpret the results. 1166 In the second study, while there was no difference in the overall mean of the International Index of Erectile Function, satisfaction was only 61% following the procedure. 1167 The draft mentions the results of two studies that assessed sexual function before and after circumcision in men who were enrolled in the randomized clinical trials in Kenya and Uganda. 1168,1169 Because these studies were large and part of a randomized clinical trial, the results have been given more weight than they deserve. There are several reasons to distrust their conclusions. The studies from Africa show rates of sexual dysfunction that were orders of magnitude lower than studies performed outside of Africa. For example, in the study by Krieger et al. 1168 the prevalence of premature ejaculation was 4.27% (95%CI 3.12%-5.41%) and the prevalence of trouble achieving orgasm was 1.26% (95%CI 0.62%-1.89%) while the prevalence in the other studies performed outside Africa were 30.59% (95%CI=29.74%-31.43%) and 11.19% (95%CI=10.61%-11.77%), respectively. In the study by Kigozi et al., 1169 the prevalence of lack of sexual desire was 0.80% (95%CI 0.35%-1.25%) while the prevalence in the other studies was 28.83% (95%CI 27.99%-29.66%). Similarly, the two African studies together had a prevalence of erectile dysfunction of 0.93% (95%CI 0.57%-1.29%) and prevalence of dyspareunia of 1.13% (95%CI 0.72%-1.54%), while the prevalence in other studies was 18.16% (95%CI 17.47%-18.88%) and 3.47% (95%CI 3.13%-3.81%), respectively. These vast differences suggest either cultural differences in what these conditions entail, unwillingness to disclose the presence of sexual dysfunction, or the coercive impact of the large subsidies men received for their participation in the studies. These subsidies could explain their eagerness to tell the researchers what the researchers wanted to hear. Of course, it could be that these sexual problems occur 3 to 36 times less frequently in Africa. If that is the case, as someone jokingly suggested, Uganda and Kenya should consider developing tourism campaigns that would tout coming to these countries for the "best sexual experiences on the planet."
The extremely low rates of sexual problems that were documented in Africa are examples of both the element of ceiling effect 1170 and of asking non-differentiating questions. With sexual satisfaction measured at rates exceeding 98% when surveyed both before and after circumcision, there is no room to move up (thus pinned against the ceiling). It is also not known how high the level of satisfaction actually is because the ceiling (the limitation of the assessment tool) acts as a barrier. For example, if the ceiling score is set at 100 and the average score before male circumcision was 125, the best one could score would be 100 because of the ceiling in place. The few scores below 100 would bring the average to slightly below this. If the average score after male circumcision was 112 (a 10% decrease), the best one could score would be 100, so the score after male circumcision would be similar and this 10% decrease would not be detected. Similarly, a 10% increase in the score following male circumcision would also be missed using the tools these researchers employed. Consequently, the negative findings of these studies are meaningless.
The questions asked in the survey were also so vague that they would not have been able to demonstrate a difference in sexual function, if one existed. As Morten Frisch, MD, has noted, "I am not surprised that these studies provided little evidence of a link between male circumcision and various sexual difficulties. Several questions were too vague to capture possible differences between circumcised and not-yet circumcised participants (e.g. lack of a clear distinction between intercourse and masturbationrelated sexual problems and no distinction between premature ejaculation and trouble or inability to reach orgasm). Thus, non-differential misclassification of sexual outcomes in these African trials probably favoured the null hypothesis of no difference, whether an association was truly present or not." 1171 The draft omits mention of several studies that have addressed the impact of male circumcision on sexual function and how it impacts the female sexual partner. A 1999 study of women who had sexual experiences with both intact and circumcised men found that they strongly preferred sex with an intact penis. 115 While this study may have suffered from selection bias, as the participants were volunteers who responded to an announcement in an anti-male circumcision newsletter and classified advertisements in magazines, its results were replicated in a cross-sectional national survey in Denmark.
The Danish survey demonstrated that the female sexual partners of circumcised men were significantly less likely to have their sexual needs fulfilled (adjusted OR 2. This Danish study also documented that circumcised men were more likely to report frequent orgasm difficulties (adjusted OR 3.26; 95%CI 1.42-7.47). 1172 In a survey of 1059 normal and 310 circumcised men, Bronselaer and colleagues reported that circumcised men were significantly more likely to report decreased sexual pleasure, lower orgasm intensity, more effort required to achieve orgasm, unusual sensations on their glans (burning, prickling, itching, or tingling and numbness), and discomfort and pain on the penile shaft. 1173 The draft does not address the issue of premature ejaculation. One Turkish study found that following male circumcision, the intra-vaginal ejaculation latency time increased by 20 seconds (a statistically significant difference), which certainly should be enough extra time to help their female partners achieve orgasm. 1174 While several studies have shown no difference in the rates of premature ejaculation between normal and circumcised men, 1175,1176 this does not mean that studies in which a statistically significant difference is found can be ignored. For example, a study by Tang et al. found a four-fold increase in premature ejaculation in circumcised men (adjusted OR 4.881; 95%CI 2.346-10.153). 1177 In a representative household sample of Australian men, circumcised men were significantly more likely to report premature ejaculation (OR 1.41; 95%CI 1.14-1.75) and erectile dysfunction (OR 1.39; 95%CI 1.08-1.79). 1178 This was consistent with an earlier Australian survey that found circumcised males were more likely to report premature ejaculation (OR 1.28; 95%CI1.15-1.42). 1179 The studies of the effect of male circumcision on sexual function indicate a negative impact. 1180 It also warrants mention in the informed consent discussion that male circumcision may have a deleterious impact on sexual function, but further study is needed to fully evaluate the impact.
The CDC draft only performed a cursory exploration of whether male circumcision impacts sexual function or penile sensitivity and only cited negative studies while ignoring the many positive studies. Their discussion is inadequate and not evidencebased.
# COMMENT:
Considerations related to male circumcision in the United States
# HIV infection in the United States
The material presented in this section of the background document is incomplete and somewhat misleading.
It should be noted that while the HIV prevalence is high in several cities, the male circumcision prevalence, especially among African-Americans, is high as well.
The statement, "Circumcision is likely to play a role in preventing HIV among men who engage in unprotected heterosexual vaginal sex, especially in communities where prevalence of HIV infection among women is high or among men with multiple sex partners," is another restatement of the CDC "group think" presumption, and has no factual foundation.
The discussion about which ethnic and racial groups should be targeted for male circumcision is moot. As discussed elsewhere, the medical evidence indicates that the only population that should be targeted for possible discussion of male circumcision are HIV-negative men who have regular sexual contact with an HIV-positive female sexual partner. And, as modeling by the CDC has demonstrated, male circumcision has very little impact over the long term in how frequently these men will become infected. 340 While HIV infections continue to occur in the United States, most infections are in men having sex with men and intravenous drug users, groups that will not benefit from male circumcision. If male circumcision was to have a protective effect against female-tomale transmission of HIV, one would have expected the United States to have a lower prevalence of heterosexually-transmitted HIV than similarly situated developed countries with low male circumcision rates. The prevalence of heterosexuallytransmitted HIV is several times higher in the United States than in Europe. The United States has already completed the male circumcision experiment, and the results show it has failed to protect its population from HIV infections. Our experience in the United States indicates that male circumcision is a factor that is not worthy of the attention that CDC has expended on promoting it. This is a complete waste of taxpayers' money both here and in Africa. Taxpayers would be astounded at the amount of their money being used to fund programs in Africa involving mass male circumcisions promoted by propaganda campaigns, unethical solicitation, coercion, and misinformation.
RESPONSE 82: See responses 2, 18, 19, In addition, responses to these concerns have been adequately addressed previously. 55,56 COMMENT:
# Rates of male circumcision in the United States
The material presented in this section of the background document is fairly straight forward, but there are some additions and corrections that need to be made.
While it is true that male circumcision unrelated to religious beliefs was introduced into the United States in the late 1800s, it needs to be added that male circumcision was introduced as a "cure" for masturbation. A more appropriate citation for this is also needed. The current citation, 1181 does not give the complete title of the book (Circumcision: Timely Information for Parents and Professionals from America's #1 Expert on Circumcision) and is not written by a medical historian, but rather an unabashed circumcision advocate. Several other citations, written by medical historians would be more appropriate. RESPONSE 83: The citation has been edited to read the full title: Schoen EJ. On circumcision: Timely Information for Parents and Professionals from America's #1 Expert on Circumcision. Berkley: RBR Books; 2005.
# COMMENT:
There needs to be an acknowledgement that we do not have a mechanism in place in this country to accurately determine the number of infant males being circumcised here.
For example, one 1968 study found that 30% of circumcisions were not documented in hospital discharge summaries, 1186 and another extensive chart review performed by the CDC found that 15.7% of male circumcisions that are documented in medical charts were not documented on the facesheet, from which data are collected into databases. 6 Likewise, self-report of male circumcision status is often unreliable. 260, It should also be noted that several studies have indicated that the male circumcision rate in blacks is similar or higher than in non-Hispanic whites. For example, data from Atlanta from 1985 to 1986 by the CDC found that 95.9% of blacks were circumcised as opposed to 86.7% of whites (OR 3.75; 95%CI 1.58-10.25). 6 Mor et al., in a study of 58,598 male patients in San Francisco, found that, in males born in 1960 or after, blacks were more likely to be circumcised than non-Hispanic whites. 8 Similarly, Mansfield et al. found 86.8% of blacks were circumcised as opposed to 89.6% of whites (OR 1.30; 95%CI 0.95-1.79). 7 The assertion that male circumcision is more common among newborns born to families of higher socioeconomic status may no longer be true. It may have been true when data were collected in 1988 to 2000, 1193 but there is increasing evidence that as maternal education levels increase male circumcision rates decrease. With the advent of the internet and medical literature searches available to the public, parents with higher levels of education are increasingly choosing not to circumcise their sons. This is consistent with the fact that physicians are less likely to circumcise their sons as compared to the populations they serve. 112 The purpose of this section is unclear. The reader should take away two clear conclusions: first, that the rate of infant male circumcision in United States is declining; second, that the method of collecting male circumcision prevalence data is highly flawed and unreliable. It is unclear whether the purpose of the section was to raise alarm over the falling male circumcision rates or to reassure male circumcision advocates that all is not lost. In either case, the inclusion of this section in the draft needs further justification.
RESPONSE 84: Scientifically rigourous methods have been used to describe the prevalence of neonatal male circumcision in the U.S. In a study using hospital discharge data from the 2000 -2010 Nationwide Inpatient Sample, male circumcision incidence decreased significantly from 61.3% in 2000 to 56.9% in 2010 and overall remained higher for newborn hospitalizations covered by private insurance compared with Medicaid (66.9% vs 44.0%). 57 During this same time period, the proportion of male newborn hospitalizations nationwide with Medicaid coverage increased from 36.0% in 2000 to 50.1% in 2010. 57 COMMENT:
# Acceptability of adult male circumcision in the United States
The material presented in this section of the background document is tainted by an underlying false assumption: that American men and adolescent males who have normal genitals are at increased risk for heterosexual acquisition of HIV. As discussed elsewhere, the data do not support this assumption. With that in mind, one has to assess whether the data collection documented in this section was based on their faulty premise. The authors of the 2008 CDC study by Begley et al. asked gay men, "If Scientific studies in the United States among men who have sex with men showed that circumcision reduced the risk of HIV infection, would you be willing to be circumcised as an adult?" 1194 Given that, as discussed elsewhere, there is no evidence of male circumcision being a risk factor for HIV infection in men having sex with men, the question carries as much validity as asking, "If the moon is made of cheese, would you prefer that it be cheddar or gouda?" The authors in the CDC 2011 study by Gust et al. also clearly begin with an unproven assumption. 1195 The question asked in the survey was, "If your health care provider told you that getting circumcised would reduce your risk of becoming infected with HIV, how likely would you be to get circumcised?" The study did not include a control question which would be, "If your health care provider told you that there is no evidence in the United States to suggest that circumcision reduces the risk of HIV in United States how likely would you be to get circumcised?" By not including this alternative question, it is impossible to know how much of the response is based on scare tactics alone. It would appear that the scare tactics have continued and are now extended to this draft. The low response rate of normal men willing to undergo circumcision, even in the face of the CDC's scare tactics, reflects that men with normal genitals recognize the value of having normal genitals and would be willing to pursue other, more effective, avenues of decreasing their risk of HIV infection.
The statement, "Adult and adolescent male circumcision potentially has the largest impact on HIV acquisition in populations in which a low percentage of males are circumcised and there is a high risk for HIV transmission through penile-vaginal sex," is not applicable in the United States for several reasons. There is no evidence that male circumcision has an impact on risk of HIV transmission through penile-vaginal sex, as the randomized controlled trials in Africa did not assess the origins or mode of transmission of the infections they documented. As discussed elsewhere, none of the studies in North America of heterosexually-transmitted HIV infections have found male circumcision to be a significant risk factor. Finally, the United States has, by developed-nation standards, a very high prevalence of male circumcision and a very high prevalence of heterosexually-transmitted HIV. As noted in this section of the draft, African-Americans have the highest prevalence of heterosexually-transmitted HIV, but the CDC neglects to mention that African-Americans also have the highest prevalence of male circumcision, on par with non-Hispanic whites. If anything, this would indicate that male circumcision is either a marker for other socio-behavioral or ethnic factors, or, if it has an impact on HIV risk, it is clinically inconsequential and, therefore, not worthy of pursuit. It appears as though the CDC is trying to create additional demand for male circumcision in an unreceptive market. Consequently, the recommendations for the intended audience of health care providers are unjustified and inappropriate.
# RESPONSE 84a:
See responses 1, 2, 3, 18, 19, 28, 64. While the authors of the article by Begley, et al, note that one of their limitations was that " overall willingness to be circumcised was not assessed separately from willingness to be circumcised if scientific evidence demonstrated a reduced risk of HIV acquisition" and thus they "were not able to compare whether the decision to be circumcised would be influenced by the evidence to support the effectiveness of male circumcision in the reduction in risk of HIV acquisition." they were able to show that "despite these complexities, we have shown that the majority of uncircumcised MSM may be willing to be circumcised as adults if this was recommended as an HIV prevention intervention in the United States". While the MSM who participated in the survey by Begley et al. represented a convenience sample and were not necessarily representative of all MSM attending the gay pride events, the response rate was high; 1127 (77%) of 1457 men approached to participate in the survey at the seven gay pride events, agreed to be surveyed. One hundred and twenty-seven of 133 (95%) men who reported being uncircumcised provided complete responses to the questions related to the risk and benefits of male circumcision and were able to be included in the final multivariable analysis. In addition, in a crosssectional study of heterosexual African American men attending an STD clinic in Baltimore, with an overall HIV seroprevalence of 3%, among 394 visits by men who had female sexual partners who were known to be infected with HIV, male circumcision was significantly associated with a 51% reduced relative prevalence of HIV infection (10.2% among circumcised men vs. 22.0% among uncircumcised men). 58 CDC's background document indicates that "the overall estimated prevalence of male circumcision among men and adolescents aged 60 uncircumcised heterosexual males and parents of male infants should be counseled about the evidence at hand and allowed to make their own decision regarding the decision to undergo male circumcision to have their male infant undergo male circumcision.
# COMMENT:
# Acceptability of adult male circumcision in sub-Saharan Africa
The material presented in this section of the background document has little or nothing to do with how male circumcision relates to HIV infection in North America. Since when is the CDC the arbitrator of health care in Africa? And, why is our tax money being used to promote a surgery of unproven benefit in Africa? How is this part of the charge that was given to the CDC by the "consultation" in 2007?
A little history lesson: generating acceptability of adult male circumcision in sub-Saharan Africa began as an important precursor to the randomized clinical trials. While male circumcision advocates believed that they made a legitimate case based on a handful of observational studies for using male circumcision as a preventive measure for HIV infection, 31, mainstream HIV researchers demanded randomized clinical trials. 1199 For a randomized clinical trial in Africa to demonstrate a statistically significant difference, it needed to be powered to document a 1% absolute risk reduction. Consequently, several thousand participants would need to be recruited. 236,237 In order to garner enough participants, the investigators for the randomized clinic trials implemented sessions within the communities in which the trials were to take place that disseminated pro-male circumcision propaganda under the guise of assessing acceptability of male circumcision as a strategy to reduce sexually transmitted diseases and HIV infection. These propaganda sessions had three effects: they convinced enough men to enroll in the overpowered clinical trials, they introduced an expectation bias on the part of the participants, and they undermined the validity of the informed consent process in the trials. Given the pro-male circumcision bias of the researchers, it is unlikely that participants were given full disclosure, particularly regarding the harms of the procedure. This is evident in the consent form used in the trial undertaken in South Africa, in which none of the adverse effects of male circumcision are listed. 1 There is direct evidence that participants did not show understanding of what was told to them as most (57%) believed, even after disclosure, that male circumcision would reduce their risk of infections. 211,212 This would certainly affect the behavior of the participants and contribute to participant expectation bias. So much for equipoise. 1208 The effectiveness of the propaganda campaign was based on illusory or fabricated factors designed to increase the acceptability of male circumcision. For example, there is no evidence that male circumcision improves hygiene. There is no evidence that male circumcision improves the use of condoms, but there is evidence that condoms slip off more frequently in circumcised men. 1209 There is no evidence that male circumcision increases sexual pleasure, but, as discussed above, ample evidence to suggest that male circumcision interferes with the sexual pleasure of both the male and his female partner. 115,1165,1172,1173 The evidence that male circumcision protects against sexually transmitted infections is, as discussed elsewhere, also lacking.
The propaganda campaign had an interesting unexpected impact on women. For example, while women in Tanzania had heard the expression "partial protection," they had no idea what it meant. 1210 In a South African study, it was found that women who perceived male circumcision as reducing the risk of HIV infection were less likely to use condoms in their last sexual encounter, generally, and with circumcised partners of positive or unknown HIV status. Men were more likely to use condoms. 1211 Similar findings have been reported from Kenya. 1212 There is also the belief among women in some parts of Africa that male circumcision reduces the male-to-female transmission of HIV, 1213 where the opposite may be the case. 338 This indicates that the impact of male circumcision on risk compensation in Africa may be driven more by the attitudes and misperceptions of women than those of men. Women may be the ones more susceptible to, or aware of, the advertising and marketing endeavors of those promoting male circumcision.
A major barrier to the rollout of adult male circumcision in Africa was that acceptability of the intervention for HIV prevention was much lower than the male circumcision advocates had anticipated. They believed that, if it could be demonstrated in randomized clinical trials that male circumcision reduced the risk of HIV infection, normal African men would swarm to have their foreskins removed. This did not happen.
There was some initial interest in male circumcision programs from men who, likely for religious or cultural reasons, would have requested male circumcision anyway and saw this as an opportunity to obtain a free male circumcision performed under more sterile conditions. By 2012, with the exception of Kenya, the roll out of adult male circumcision programs has been an abysmal failure. For example, of the men targeted to be circumcised only 4.8% have been in Uganda, 0.7% in Rwanda, 11.1% in Zambia, 1.5% in Namibia, 6.5% in Botswana, 7.0% in South Africa, 12.7% in Tanzania, 0.4% in Malawi, 2.9% in Zimbabwe, 4.7% in Mozambique, and 0.2% in Lesotho. Only Kenya, Swaziland, and Ethiopia had a response rate over 20%. 1214 In response to the poor uptake, male circumcision advocates held sessions at the 2012 XIX International AIDS Conference in Washington, DC, to announce that male medical circumcision was being rebranded as a way of building intimacy and improving one's sex life with the phrase "Reshape your Relationship." Since women tend to take responsibility for "relationships," the advertising is shifting towards women, who ironically are more likely than men to encourage risk compensation, and women are more at risk of becoming infected with HIV from their male partners. 1212,1213 Over 100 articles have been published assessing the rollout of adult male circumcision in Africa. Nearly all of them have focused on the wrong outcome: increasing the number of men circumcised. Instead, the focus should be on looking for the most effective and efficient way of reducing the number of people who become infected with HIV.
To give you an example of how pathetically desperate male circumcision advocates are to increase the acceptability of adult male circumcision in Africa, the Journal of the American Medical Association in 2014 published a study to determine what impact bribing African men would have on the acceptability of male circumcision in Kenya.
When offered a free male circumcision without any bribe, only 1.6% of intact men were interested. When a bribe worth $15 was offered, the number of men accepting the bribe increased the percentage to 9.0%. 1214 Keep in mind that Gross National Income per capita in Kenya in 2013 was $1160, 1215 this would be equivalent to a $691 bribe in the United States ($53,470 GNI per capita in 2013). 1216 Models of the impact of male circumcision on overall HIV incidence in Africa reported their results based on reaching compliance levels of 55%, 229 60%, 220 70%, 230 80%, 222,225,228 95%, 224 and 100%. 221,223,226,227,231,232 If one assumes that the increase in compliance has a linear relationship to an increase in the amount of the bribe offered, then the bribe amount needed for the percentage to increase from 59% to 60% would be $147.81 and to increase from 79% to 80% would be $199.89. The average bribe needed to get to 60% compliance would be $71.60 and to get to 80% would be $97.49. The cost of these inducements would more than double the marginal costs of the male circumcision programs. If the relationship between compliance and the amount of bribe is non-linear, the cost to bribe men to get circumcised might be even greater. Other adult male circumcision programs in Africa have resorted to bribery to get men to participate. 1217 Bribery and coercion tactics violate basic research ethics and would not be allowed in the US, so how is this allowable in Africa?
The call for African men to become circumcised has also led to a number of men and boys being forcibly circumcised. Given tribal tensions, between tribes that traditionally circumcise and those that do not, this was a predictable consequence of the widespread propaganda encouraging male circumcision. There have also been reports of boys being told they would not be allowed to play football (soccer) unless they were circumcised.
Efforts to increase the acceptability of adult male circumcision in sub-Saharan Africa are based on misinformation and deception, consequently, the material in this section is inappropriate, and fraudulent. African male circumcision has little or nothing to do with the United States and other developed countries.
RESPONSE: See responses 10, 18, 19, 23 COMMENT:
# Acceptability of newborn male circumcision in the United States
The material presented in this section of the background document misses several key points. The CDC draft fails to mention that the acceptability of newborn male circumcision in the United States may be, in part, driven by the fact that the procedure is solicited by physicians, nurses, and hospitals. At the first prenatal visit, mothers are routinely asked whether they would want a son circumcised. The question is repeated upon admission for the perinatal hospitalization. For parents who have done little or no research on the topic of infant circumcision, this can be interpreted as a recommendation to have the procedure performed on their son. Parents who do not want their sons circumcised have often reported that they are asked multiple times during the hospitalization whether they want their son circumcised, with many of them reporting that they are harassed and outright bullied by the hospital staff. The degree to which parents are intimidated into circumcising their sons has received little study. 1228 Such solicitation is considered unethical under the guidelines of the American Medical Association because the procedure removes healthy tissue, and male circumcision will benefit the physician's and hospital's pocketbook more than it will benefit the patient. 1229
# RESPONSE 85:
The CDC recommendations provide added unbiased scientific information that assists parents in making a decision about whether to circumcise their child. The counseling recommendations state that the decision to circumcise is that of the parents of the male infant or the adults considering male circumcision.
# COMMENT:
This CDC section fails to address the impact of the physician's male circumcision status on the advice delivered to parents. In a survey of Canadian physicians, circumcised male physicians were almost five times as likely to recommend male circumcision (OR 4.76; 95%CI 3.00-7.55) and those physicians with circumcised sons were six times more likely to recommend male circumcision to the parents of their male patients (OR 6.22; 95%CI 3.83-10.10). Those who said they based their recommendation on the medical evidence were twice as likely to recommend against male circumcision (OR 1.95; 95%CI 1.29-2.95). 39 One can only speculate whether this CDC draft has been influenced similarly. It is reasonable to question whether the male circumcision status of a physician or the physician's children, and the associated bias thereof, should be disclosed to parents. The same could be said regarding the authors of this draft and whether their inherent biases should be disclosed to the public.
RESPONSE: See response 85.
# COMMENT:
Whether parents have the moral or legal authority to choose circumcision on behalf of their sons will be discussed in a later section. 1230 Parents do not have to provide a justification in order to direct the health care provider to circumcise their son, unlike the removal of any other healthy body part. Likewise, physicians would not agree to blithely removing any other healthy normal body part from an infant or child without a disease being present. As noted in the citations given in the draft report, studies of the reasons parents choose circumcision for their sons have not been updated since the 1980s. 923,1231 If these studies were to be repeated today, cultural conformity would likely be the most common justification.
RESPONSE: See response 22.
# COMMENT:
The authors of this section accept the interpretation provided by Adler et al. of their survey data, which reflects the bias of the study's authors more than the data they collected. 1232 The study indicates that physicians were not supportive of parents deciding not to circumcise their sons and perhaps berated them for not doing so. The conclusions reached by the authors is not surprising. The parents of intact boys, by virtue of being asked so many questions about circumcision, would have to wonder if there was something about male circumcision they were not told. If, however, complete disclosure, consistent with the current standard applied to other procedures, were provided, parents who had already chosen to circumcise their sons would not want to be confronted with the litany of complications and harms associated with the procedure.
Their minds are already made up and providing information has little impact. 1233 For these parents, any information is too much. It would have been more appropriate for the survey to have asked if too much information was provided. This is a clear example of expectation bias on the part of researchers impacting the methodology of a study to ensure the preconceived outcome was obtained.
RESPONSE 85a: See response 6. The citation by Wang. Et al. 2010 has been updated in the CDC background document.
# COMMENT:
The study by Gust et al. is perhaps more contrived. 1195 The study collected data based on an unproven premise: that infant male circumcision would have an impact on HIV risk in the United States. As noted elsewhere, there are no studies of infant male circumcision that have demonstrated a significant association with HIV prevalence or incidence, and no studies in North America that have found male circumcision to be protective against HIV infection. The study by Gust et al. 61 cited by the reviewer focuses on adult male circumcision, not infant male circumcision. (note: See CDC citation 59; same as reviewer citation 1195).
While there are no longitudinal studies demonstrating a significant association with infant male circumcision and HIV prevalence or incidence, ecologic studies demonstrate a strong association between lack of male circumcision and HIV infection at the population level. Although links between male circumcision, culture, religion, and risk behavior likely account for some of the differences in HIV infection prevalence, the countries in Africa and Asia with prevalence of male circumcision of less than 20% have HIV-infection prevalence several times as high (seroprevalence range: 0.24 -25.84) than countries in those regions where more than 80% of men are circumcised (seroprevalence range: 0.03-11.64). 49 Based on data from an HIV transmission model fitted to data from the Four Cities Study, including 2 cities in sub-Saharan Africa with relatively low HIV prevalence (Cotonou and Yaoundé) and 2 with high HIV prevalence (Kisumu and Ndola), investigators concluded that differences in rates of male circumcision likely played an important role in differing rates of HIV transmission across Africa. 50 _ENREF_62 Results from such ecologic studies are important as most male circumcisions globally are thought to occur during infancy, childhood, or adolescence, suggesting that male circumcision at an earlier age confers a long term reduction in risk for HIV acquisition. The fact that male circumcision performed during the neonatal period is associated with fewer and less severe side effects compared to male circumcision performed during adulthood is one of the most important reasons that most male circumcisions are performed neonatally in the U.S.
One of the studies 58 reported by the reviewer as evidence that no studies in North America have found male circumcision to be protective against HIV infection actually did find that among visits of heterosexual African American men attending an STD clinic in Baltimore who had female sexual partners who were known to be infected with HIV, male circumcision was significantly associated with a 51% reduced relative prevalence of HIV infection (10.2% among circumcised men vs. 22.0% among uncircumcised men). Another two of the studies cited by the reviewer as lack of evidence of the protective effect of male circumcision against HIV infection did not adequately address this question. Although a study of male circumcision and HIV in an urban STI/HIV prevention treatment center found that circumcised men were more likely than uncircumcised men to have HIV infection (circumcised men = 43% vs uncircumcised men= 33.9% , p = 0.23), they also noted that at last sexual intercourse, circumcised men were also more likely to report unprotected receptive anal intercourse (circumcised men = 43.8% vs uncircumcised men = 20.4%, P = 0.025) 62 . In a naval study of male circumcision and HIV status, HIV-infected case participants identified through HIV testing in medical referral centers were compared to control participants from a general aircraft carrier population who were assumed to be HIV-uninfected due to negative results on a predeployment HIV screening test. 63 Because enlisted men can seroconvert during deployment, the results of the study may have compromised if controls included both HIV-uninfected and men who HIV-seroconverted after the predeployment evaluation. Although the authors of the naval study found no significant association between HIV and male circumcision status, they underscored the importance of results from randomized clinical trials.
# COMMENT:
The inclusion in this section of whether or not there is state Medicaid coverage of infant male circumcision is inappropriate and irrelevant. The only reason to include this topic would be because the CDC has an underlying motivation to promote male circumcision in order to increase demand for male circumcisions, thereby increasing physician reimbursement. It has been argued that under the current federal statute, it is illegal for states to reimburse physicians for performing male circumcisions on infants as it is an "unnecessary, elective, cosmetic surgery on healthy boys, usually performed for cultural, personal or religious reasons." 1234 While there is an association between Medicaid coverage and infant male circumcision rates, it does not follow, as Leibowitz et al. suggest, 1235 that providing Medicaid coverage would increase the male circumcision rates in these states where the rates have been historically low.
RESPONSE 86: Because of the benefits associated with male circumcision outweigh the risks of male circumcision, parents should have financial access to this procedure. (AAP 2013) For this reason, a discussion of Medicaid coverage is appropriate.
# COMMENT:
# Acceptability of newborn male circumcision in sub-Saharan Africa
The material presented in this section is totally ludicrous. Why should the United States care about uninformed opinions regarding infant circumcision from propagandized Africans?
The material in this section is not evidence-based, but based on uninformed opinions of populations that are vulnerable to false propaganda.
# RESPONSE:
See responses 1, 6, 18, and 19.
# COMMENT:
# Provider attitudes and practices regarding male circumcision in the United States
The material presented in this section is incomplete with multiple omissions. For example, it is stated that "many medical societies have addressed neonatal male circumcision," yet only the American Medical Association, the American Academy of Pediatrics, the American Academy of Family Physicians, and American Urological Association are cited. Many medical societies outside of the United States have addressed neonatal male circumcision. It is odd that the draft report is taking a global perspective when assessing the acceptability of adult and infant male circumcision in Africa, yet is provincial when it comes to the opinions of medical societies. Is there something in the opinions of medical societies outside of the United States that authors of this draft find troublesome? The draft needs to include the opinions of medical societies outside of the United States. More importantly, the CDC needs to provide insight on how they have access to "special knowledge" that the rest of world is missing, which led them to reach such a discordant conclusion.
The Royal Dutch Medical Association in 2010 noted that there is no convincing evidence that infant male circumcision, which constitutes a human rights violation, is useful or necessary, and there are good reasons for legal prohibition of the practice, consequently "it is reasonable to put off circumcision until the age at which such a risk is relevant and the boy himself can decide about the intervention, or can opt for any available alternatives." 1236 The Swedish Medical Association recommends a minimum age of 12 years for performing a circumcision as it requires fully informed consent from the boy. 1237 The Finnish Union of Medical Doctors (Suomen Lääkäriliitto) is opposed to infant male circumcision because of its risk, pain, and the injury inflicted. 1238 The Swedish Pediatric Society came out against infant male circumcision characterizing it as an "assault on boys." 1239 The Danish College of General Practitioners has stated that infant male circumcision is tantamount to abuse and mutilation. 1240 In 2012, the Berufsverbands der Kinder-und Jugendärzte (the German national organization of Pediatrics) condemned the practice of infant male circumcision. 1241 Medical organizations in British Columbia and Saskatchewan have come out against infant male circumcision. 1242,1243 As noted below, several national medical associations consider infant male circumcision a human rights violation. 1244,1245 Other medical organizations from Canada, Britain, and Australia have adopted a position where the practice is tolerated, but not endorsed, encouraged, or recommended. Having taken an exceptional position, the CDC needs to provide an exceptional justification: one that should take our breath away. They need to defend their position on an international stage, something the American Academy of Pediatrics had trouble doing in 2012 when they did not recommend male circumcision, but stated they "felt" that the benefits outweighed the risks. So, instead of providing an evidencebased evaluation, the American Academy of Pediatrics provided a feelings-based evaluation. The CDC has taken a more extreme position and runs the risk of embarrassing itself and the United States once again.
The studies cited by the CDC in this section give a mixed message. On one side, it is well-documented that physicians are very poorly educated regarding normal male anatomy and infant male circumcision, 1253 and on the other, physicians are encouraged to act on their clearly uninformed opinions. 1254 The surveys conducted of physicians are reminiscent of push-polls used by politicians, where conducting a survey is a premise for propagandizing. These "studies" contain those elements. At a conference held in the Fall of 2013 in South Carolina at the Pitts Lectureship in Medical Ethics, members of the 2012 American Academy of Pediatrics Task Force on Circumcision confessed ignorance regarding the function of the foreskin. 41 If policy-makers on this issue are ignorant, what can be expected of the average medical professional? Education is sadly needed, but it should not take the form of clearly subjective, biased pro-male circumcision propaganda peddled by the misguided American Academy of Pediatrics task force on circumcision, or what is currently proposed by the CDC. It has to be evidence-based, not culture-based. This may be difficult, as the male circumcision status of the physicians and their children has a substantial impact on whether a physician recommends male circumcision. 39,1254 It is not surprising that European physicians, where there is no cultural pressure to be circumcised, have different attitudes towards protecting newborn males from harm.
The material presented in this section is the result of a very narrow ideological focus.
RESPONSE: See response 9 and 16 COMMENT:
# Cost-effectiveness
The material presented in this section is selective in favor of male circumcision. It presents findings in a biased manner where the positive aspects of male circumcision are emphasized, while studies that expose the weaknesses of male circumcision are dismissed, omitted, or ignored. Some statements are factually untrue. For example, the statement, "While male circumcision has been shown to be a cost-saving HIV prevention intervention in sub-Saharan Africa" is not supported by the citations provided. 227,232 These references are mathematical models based on assumptions. The models are only as good as the assumptions and do not measure costs in the real world. They only provide conjecture as to what might happen in the real world if the assumptions turn out to be true. As far as these models are concerned, the calculations are based on reaching universal male circumcision within the targeted populations. As noted earlier, the efforts to roll out adult male circumcision are far below this goal. Until actual, real-life data are collected, this statement is inaccurate. Furthermore, the randomized clinical trials have multiple biases and flaws, which discount any perceived benefits.
Several of the cost-effectiveness and cost-utility analyses published prior to the release of the results from the randomized clinical trials focused on male circumcision's impact on urinary tract infections and they found the procedure wanting. The 2004 analysis by Van Howe, 1258 which used a Markov analysis and estimated the variability of its findings using Monte Carlo simulations, provided a comprehensive analysis of the costs and health states that may be impacted by infant male circumcision. It included the baseline assumption that an intact male had, based on published meta-analyses available at the time, an odds ratio of 1.78 (95%CI 1.33-2.37) of being more likely to become infected with HIV through heterosexual transmission. This assumption is consistent with the results of the randomized clinical trials, yet the cost-utility analysis found that infant male circumcision resulted in a lifetime increase in costs ($828. 42 per patient) and a decrease in health (15.30 quality adjusted life-years per 1000 males), results that were ignored by the CDC in this draft.
By contrast, the CDC draft propagates the misrepresentation of the findings of a costanalysis published by Schoen et al. 1259 A cost-analysis calculates the difference between the costs incurred by an intervention and costs that are saved as a result of the intervention. The benefits and risks are reflected in their respective monetary costs. In the cost analysis by Schoen et al., infant male circumcision resulted in more costs than it was able to recoup in benefits ($27 per circumcision). In other words, male circumcision cost more money than it saved. To conclude that "the expected lifetime cost of male circumcision was small, compared with larger expected benefits" reveals that the authors of the cost-analysis and the authors of this section do not understand that any benefits are already included in the analysis (in monetary form) and their conclusion is, in effect, an inappropriate attempt to count the benefits twice, which is beyond the scope of a cost-analysis. This indicates a bias, or incompetence, on the part of the CDC.
The statement, "Much of the benefit of neonatal male circumcision in that analysis derived from pre-empting the need for post-neonatal male circumcision, which is substantially more costly," is made without reference or citation. Where is the evidence? Post-neonatal male circumcision, which a recent study published by the CDC estimates as costing on average $1885, is more expensive than neonatal male circumcision (average cost $285). 472 Most of this expense is related to the use of general anesthesia. Considering, as discussed earlier, that local and topical anesthesia do not provide adequate anesthesia for the procedure, this may be money well spent. Post-neonatal male circumcision is rarely indicated, and it is never indicated in the healthy neonate. For example, the cumulative risk by age 15 of pathological phimosis is 0.6% 457 and the cumulative incidence of balanitis is 0.65%. 541 Consequently we would expect that only 1.3% of boys would have a medical indication for a post-neonatal male circumcision. This is consistent with the experience in Denmark were 1.6% of boys are circumcised by age 15 years. 449 This translates into a number needed to treat of between 63 472,457 This indicates that either physicians in the United States do not know how to properly diagnose phimosis requiring male circumcision, or they use the diagnosis of phimosis to secure reimbursement for elective male circumcisions, or both. Since true pathologic phimosis is rare under five years of age, it might be more cost effective for insurance companies to not pay for the procedure unless the child is over five years of age, failed a course of steroids, and had the diagnosis of balanitis xerotica obliterans confirmed.
This section of the draft report pays extensive attention to a cost-effectiveness analysis generated from within the CDC. 1260 As can be the case with secondary analysis, this analysis has a "garbage-in:garbage-out" problem. It almost appears as if the conclusion was determined first, and then the assumptions were sought out to justify the conclusion. To construct a cost-utility model that is most favorable to infant male circumcision, the model would assume the highest efficacy rate, the highest prevalence of HIV, no complications from male circumcision, and the lowest discount rate; this costutility did all these things. The basic assumptions, upon which the analysis is based, are each suspect.
First, it was assumed in the model that the lifetime risk of HIV infection for a male in the United States is several orders of magnitude higher than reported by other studies.
Based on the numbers used in the model, 1 in 16 African-American males in the United States will become HIV infected in his lifetime. So, for every two women that get breast cancer there will be one African-American male who will become HIV-infected. This is inconsistent with data collected in a national probability sample by the University of Chicago in which 0.35% (9 of 2577) of men 18 to 59 years of age were HIV-infected. 9 Why the five-fold difference?
Second, the model assumed a 60% efficacy in preventing heterosexually transmitted HIV for male circumcision over a lifetime. There are several reasons to doubt the validity of applying 60% to populations in the United States. The first, as discussed earlier, are questions regarding the internal validity of the three randomized clinical trials. It is also unlikely that a 60% reduction in risk would be seen over a lifetime. The trials followed their subjects for, at most, 24 months. There is nothing to suggest the same linear trajectory would continue over 40 years. It is impossible to know whether the pattern would continue as linear, exponential, or whether it reaches a ceiling and stops. It could easily be that male circumcision merely delays infection and the overall prevalence is the same over a lifetime. In the African randomized clinical trials, 1% of circumcised men became infected each year. So, if one assumes a linear model, between ages 20 and 80, one would expect approximately 40% of the men circumcised in these trials to become infected with HIV. Given that the prevalence of HIV in South Africa is slightly higher in circumcised men, this may be the case. 246 The second reason to doubt the 60% efficacy is that the results in Africa, which involved high-risk, well-compensated men who were willing to be circumcised, may not apply to a program of circumcising all males, regardless of their risk of HIV-infection, in the United States. Sansom et al., argue that data collected from people at highest risk for HIV infection (such as regular sexual partners of HIV-infected individuals) should be the basis for a program of circumcising regardless of risk profile. There is no evidence that 60% efficacy applies to males at low risk, and plenty of evidence to the contrary. 325 Finally, results from a study of adults may not apply to infants. To date, there have been no observational studies to indicate that infant male circumcision has any significant impact in reducing HIVinfection rates.
Third, the model assumed that African-Americans have a lower male circumcision rate than whites, yet there is ample evidence to contradict this, as is mentioned earlier. If African-Americans have a risk of heterosexually transmitted HIV infection five times higher than non-Hispanic whites, this would indicate that male circumcision is not an important factor in HIV-prevention and African-Americans do not benefit from the supposed 60% protective effects of male circumcision. Before contemplating a model of infant male circumcision, the lack of correlation between male circumcision rates and heterosexually transmitted HIV-infection rates between ethnic groups needs explanation.
Fourth, it was assumed that infant male circumcision had no impact on the length of stay of the perinatal hospitalization. It has been demonstrated that one in six males circumcised as newborns will spend an extra day in the hospital. 7 Sixth, as for other "harm-denialists," the CDC assumed that infant male circumcision had no complications. Previous cost-utility analyses have found that the more common adverse events have the most impact on the cost-utility of infant male circumcision. 1257,1258 For example, at least 5% of circumcised boys develop meatal stenosis that requires a meatotomy. 186, At $1500 per procedure, this adds $64.41 (3% discount for 5 years) to the cost of each male circumcision. Another 1-2% end up having a male circumcision revision, at substantial increased costs. MRSA infections are 12 times more common in infants that are circumcised. 651,1251 While heterosexually transmitted HIV infection is a relatively rare event, it may be of similar frequency as the severely botched male circumcisions in which part of the glans is amputated, or there is a serious, life-threatening infection or hemorrhage. The analysis needs to consider the cost of treating these complications, the multi-million dollar malpractice settlements, and the devastating impact on health. Death is another well-documented complication of male circumcision. 1262 While the exact number is unknown, some have estimated that between 100 and 200 deaths are related to infant male circumcisions each year in the United States. 1056 If rare catastrophic events are to be considered on one side of the ledger, they need to be considered on the other.
The CDC also failed to compare infant male circumcision to other interventions such as limiting the number of sexual partners, using condoms, early treatment of sexually transmitted infections, and secondary prevention measures such as treating HIVpositive individuals with anti-retroviral therapy. All of these options are known to be more effective, less invasive, and less expensive than circumcising all infants.
High-risk behavior will not manifest itself in infancy, so interventions should be directed at those who are sexually active. With all of these serious flaws in this model, it makes it looks like the CDC is trying too hard and is willing to say anything to make the hard sell for infant male circumcision. Consequently, the results of this model cannot be taken seriously.
The model developed by Kacker et al. is equally unjustifiable as it is based on assumptions gleaned from outlier studies that are methodologically unsound when compared to the entire body of the medical literature. 1263 To the researchers from Johns Hopkins these numbers may ring true; to others, their analysis is unabashedly onesided and biased. The analysis presents the most extreme case. That the CDC presented the results of this analysis indicates their lack of respect for the scientific method and their underlying pro-male circumcision bias.
The models for MSM are also based on wildly unrealistic protection rates for the insertive circumcised partner. It is unclear why this section gives so much space to wildly speculative, non-reality based models and little or no space to models that are evidence-based.
As mentioned earlier, the models predicting the impact of adult male circumcision on the HIV epidemic in Africa is thwarted by the lack of internal and external validity of the randomized clinical trials performed in Africa, the assumption that the effect remains linear over decades, and the incredibly limited response to the various male circumcision roll-out programs. The poor response is not a surprise. First of all, when men learn they still need to wear condoms, they will see no point in getting circumcised (male circumcision is either worthless or redundant). Second, HIV research has moved far beyond male circumcision to the point where male circumcision as prevention is rapidly becoming a footnote in the history of the HIV pandemic: an interesting historical oddity that popped up along the way. Third, treatment as prevention makes so much more sense. It works better, it is cheaper, it protects those who might be exposed through unclean medical equipment, it protects women, and it is not ultimately dependent on wearing condoms. Fourth, there is evidence that HIV is losing its virulence. 233 In the seven years since male circumcision exploded onto the scene, its flame is flickering and about to be extinguished.
# RESPONSE:
See responses 1, and 6.
# COMMENT:
Other considerations
# Risk compensation
The material in this section is incomplete and fails to place the results of studies in proper perspective. The CDC draft does not properly emphasize how important risk compensation is in the whole scheme of HIV prevention. In 1994, Blower and McLean formulated a model showing how the implementation of an HIV vaccination program with a vaccine of only 60% efficacy could easily increase the incidence of HIV infections, if risky behaviors are only slightly increased. 1264 Similar failures have been seen with vaccine programs using vaccines with efficacy in this range, such as the cholera vaccine. 1265 Another analogy is relying on birth control that is only 60% effective. 1266 Even with the most rudimentary modeling, it can be demonstrated that small changes in condom use can undermine any possible advantages of large-scale male circumcision programs, resulting in more infections following implementation of a male circumcision roll-out and billions of dollars spent. 251 The measurements of risk compensation in the men who participated in the randomized clinical trials 2,211,242,1267,1268 need to be interpreted with caution.
First, the results may reflect the Hawthorne effect: participants knew they were being watched, so this fact alone likely altered their behavior.
Second, the participants in these studies were highly compensated for their participation. For example, in the Kenya study, in addition to the equivalent in the United States of about $12,000 in goods and services for participating in the randomized clinical trial, participants were paid the equivalent in the United States of about $800 more to be in the study assessing risk compensation. This may have motivated the participants to tell the researchers what they wanted to hear.
Third, defining risk compensation as only applying to those who believe there is a change in the risk of becoming infected with HIV after male circumcision is atypical. Risk compensation has to do with changes in behavior, whether people are conscious of the changes or not. In the example of wearing seat belts, risk compensation applies equally to those who consciously think they can drive faster because they have a seat belt on and also to those who drive faster on an unconscious level because they have a seat belt on.
Their working hypothesis, that the belief in the power of circumcision makes a man less fatalistic, thus more cautious, is counter-intuitive. If men think circumcision will make them live longer since they are less likely to be infected with HIV, they will likely live a bit more recklessly from a sexual standpoint. If the fatalism theory were true, we would expect to see intact men, who believe in the power of male circumcision, be more cautious than the circumcised believers because they would perceive themselves at higher risk.
A much more likely hypothesis is that people who are risk-averse are more likely to pursue whatever they think will decrease their risk. They are more likely to believe that male circumcision will help them and undergo circumcision for this reason. They are also more likely to have fewer partners and not engage in other risky behaviors.
This has implications for men in Africa who become circumcised as part of "voluntary" male medical circumcision campaigns. Early adopters were more likely to be those who believed in the power of circumcision. These men may account for the 2% to 5% who participated before March 2012. 213 The rest of the men are less likely to believe in the power of circumcision and need further persuasion, including bribes, 1215,1217 to consider participation. These are the men who will be less risk-averse. Consequently, one would expect a slight delay in detecting the impact of risk compensation. This is not to say that risk compensation is not already having an effect on national levels. For example, Uganda, which saw dramatic drops in the incidence of HIV infections using a program of "Abstinence, Be Faithful, Condoms," 1269 has seen an increase in the incidence of HIV infections. 327 Kenya, which has seen the largest uptake in its male circumcision roll-out has also seen an increase in HIV incidence since the roll-out. 328,329 This has occurred despite evidence that the incidence of HIV infections peaked globally in the late 1990's and has been gradually decreasing since then. 625 This section omitted a few relevant studies. For example, Limburgh et al. found that participants in South Africa did not have a complete understanding of how male circumcision is protective and, while they expected to continue using condoms following circumcision, they did not expect others in the community who underwent circumcision to do so. 1270 In a study by Grund and Hennick in Swaziland, most men had more responsible attitudes in the first 12 months following male circumcision, but a minority exhibited increased sexual risk-taking, especially during a brief period of sexual experimentation shortly after circumcision. 1270 The problem is that small overall changes in risk taking is all that is needed to increase HIV infection rates. Reiss et al. also reported a minority of men (16%) who abandoned condom use and increased the number of sexual partners following male circumcision. 1271 In a study from South Africa by Nkosi, they found that males who had traditional circumcisions were associated with the greatest level of risky behavior; intact men had less risky behavior than men who were medically circumcised (adjusted OR 0.71; 95%CI 0.40-1.25). 1272 Westercamp, and the team responsible for the Kenyan randomized clinic trial, somehow have found no evidence of risk compensation. 1273 One cannot help but note the conflict of interest here on the part of the investigators. For a research group, any finding of risk compensation would undermine the importance and relevance of their randomized clinical trial, the pinnacle of their career. These results also conflict with a survey published of men and women in Kisumu, Kenya. Intact men were divided into those who preferred to get circumcised and those who did not. The intact men who preferred to get circumcised were significantly more likely to never use, or inconsistently use, a condom (OR 2.7; 95%CI 1.6-4.7) and to have one or more casual sexual partners (OR 1.9; 1.03-3.6). 378 This would indicate that men who were interested in male circumcision were those who were exhibiting more high risk behaviors than those not interested in circumcision. There are multiple reports outside of the medical literature to indicate that risk compensation is a concerning issue. Two studies have indicated that women may have more influence on how much risk compensation takes place. 1211,1212 These were unexpected findings, which could further derail the male circumcision roll-out in Africa. The women told their male sexual partners they did not have to use condoms if the men were circumcised. Nothing less would be expected considering the propaganda campaign going on in Africa.
Because the incidence of heterosexually transmitted HIV is much lower in the United States than in Africa, infant male circumcision has never been shown to be associated with a lower risk of HIV, and none of the studies from North America have found that male circumcision significantly lowers the risk of HIV, a discussion about risk compensation in the United States is about as important as debating whether pigs can fly.
An excellent discussion on the issue of risk compensation as it relates to male circumcision and HIV infection in Africa appears in a Nature article by de Lange, 1280 in which it is noted that a change in risky behaviors, such as a decrease in condom use following male circumcision, could mean that male circumcision "could have the opposite effect in the long run. People might be more likely to get HIV than if they were not circumcised at all." (Quoting Michel Garenne). The other problem is that Africans, both men and women, are getting a mixed message. On the one hand, male circumcision is supposedly the "breakthrough that will end the AIDS pandemic in Africa," but on the other hand, "everyone still needs to wear condoms." Another factor that could develop with time is that, as the sensitivity of the glans is lost following male circumcision, 108 the willingness to further decrease the sensitivity of the glans by wearing a condom may drop even more. It is also unclear whether the counseling, which supposedly accompanied the procedure, will impact risky behaviors in the long run.
The materials in this section are irrelevant for health care providers in the United States.
For health care providers in Africa, it is important to emphasize that small changes in behavior, or a big change in behavior by a few, can have a huge impact, negating any gains.
# COMMENT:
# Policy considerations regarding reimbursement
The material presented in this section of the background document is off point. Why should the CDC be concerned about physician reimbursement? Professional organizations, such as the American Academy of Pediatrics, the American Academy of Family Physicians, and the American Urological Association, may have an interest in lobbying for physician reimbursement, but it is not clear why the CDC would be interested in this topic.
# RESPONSE: See Response 86
# COMMENT:
This section of the draft fails to note the trend that is taking place among obstetricians. In a 1998 report, 70% of obstetricians reported performing at least one male circumcision per month (as opposed to 35% of pediatricians), 445 although their scope of practice includes only female reproductive organs. A 1994 article indicated that pediatricians are happy to have obstetricians perform infant male circumcisions and obstetricians are happy to have pediatricians perform infant male circumcisions. 1281 The shift away from obstetricians/gynecologists performing male circumcisions has become more formalized in recent years when Intact America was refused a booth at the national meeting of ACOG (American College of Obstetricians/Gynecologists) because male circumcision is not considered within the scope of obstetrics. Opinion pieces have been published supporting this position. 1282 Other obstetricians have published their success in shifting the burden of performing male circumcisions away from them and onto the pediatricians or family medicine physicians in the community. 443 While national medical organizations within the United States may have taken a position on infant male circumcision, it does not mean that their positions are evidence-based. In fact, the American Academy of Pediatrics' position has been criticized as being based on culture. 1249 This section also misrepresents the position taken by the American Academy of Pediatrics. Instead of "concluding that new evidence indicates" that the benefits outweigh the risks, the Academy's Task Force has taken the position that "These benefits were felt to outweigh the risks of the procedure."(emphasis added) 1237 So, the conclusions of the American Academy of Pediatrics are based on feelings rather than evidence. This may explain why none of the other national pediatric organizations in the world have reached a similar conclusion. One of the Task Force members has recently noted he hopes the CDC report is not viewed as being as biased as their report. 1283 The fallacy in this discussion is an appeal to authority: in this case, the authorities are themselves culturally biased.
# RESPONSE 87:
The position statement by the American Academy of Pediatrics is evidence based.
# COMMENT:
It is not surprising that male circumcision rates are higher when parents do not need to pay out of pocket. However, the Midwest has a high male circumcision rate because of high demand. This may explain why the study in the Midwest, where demand is the highest, found that insurance coverage did not affect the male circumcision rates. 1284 Given that infant male circumcision is a purely cosmetic procedure, one would expect that it would not be paid for by third party payers. Furthermore, it is not the CDC's role to be in the business of justifying financial reimbursement for physicians.
RESPONSE 87a: See response 86. The duplicate citation has been corrected.
# COMMENT:
The material in this section is relevant for health care providers who depend on the income they generate from infant male circumcision and would like to see higher reimbursement rates from programs such as Medicaid. The problem is that the CDC should not be involved in efforts to improve physician reimbursement especially when it is not clear whether Medicaid can legally pay health care providers for performing male circumcision, a cosmetic surgery, on non-consenting infants. 1234 RESPONSE: See response 86.
# COMMENT:
# Ethical considerations GENERAL RESPONSE TO COMMENTS ABOUT ETHICAL CONSIDERATIONS -RESPONSE 88:
From its first consultation on male circumcision and as a part of writing of the background document, CDC carefully considered the ethical issues associated with male circumcision, including neonatal male circumcision. See ethical considerations section of background document. See responses 22, 24.
# COMMENT:
The material presented in this section of the background document is markedly incomplete, and reflects a socio-cultural bias in favor of male circumcision because of its normalized status as a birth ritual in the US, in contrast to most other nations with advanced health care systems.
For example, the Royal Dutch Medical Association, 1236 the South African Medical Association, 1244 the Finnish Medical Association, 1238 the Tasmanian Law Reform Institute, 1285 and representatives of four leading Swedish physician organizations 1237 have all concluded that infant male circumcision is a human rights violation and should be legally restricted. In addition, on October 1, 2013, the Council of Europe passed a recommendation endorsing a child's right to physical integrity and a resolution discussing the right to physical integrity in more detail. The Council specifically supported genital autonomy for children by opposing several practices including male circumcision, female genital mutilation, and early childhood medical interventions in the case of inter-sex children. 1286 If the CDC wishes to advance a moral viewpoint that stands in contrast to those adopted by peer organizations in other Western countries, it would do well to engage directly with the arguments and analyses that have been presented by those peer organizations, and attempt to show, systematically, why those arguments are not convincing. To ignore the published viewpoints of distinguished medical organizations in peer nations, all of which have gone to great lengths to assess the moral permissibility of male circumcision in light of widely-accepted ethical standards, gives the impression that the CDC is not concerned with the pressing moral issues raised by this controversial surgery.
# RESPONSE: See Response 16:
COMMENT:
Consistent with this impression is further concern about the composition of consultants at the CDC 2007 consultation. It reads, to put the point bluntly, like a Who's Who of Male Circumcision Lobbyists. 16 In the reporting on the consultation, it is stated, "Invited participants included epidemiologists; researchers; health economists; ethicists; physicians; and representatives of practitioner associations, community-based organizations, and groups objecting to elective circumcision." However, no one from any of the major groups objecting to elective infant/child male circumcision was in fact invited to the consultation (correspondence with Georganne Chapin, JD, Founding Executive Director of Intact America; Marilyn Milos, RN, Co-founder and Director of the National Organization of Circumcision Information Resource Centers (NOCIRC); John Geisheker, JD, Director and General Counsel of Doctors Opposing Circumcision (DOC); J. Steven Svoboda, MS, JD, Founder of Attorneys for the Rights of the Child). Also, no one from a group objecting to elective circumcision was invited to participate in, or provide materials for, the subcommittee of the CDC Public Health Ethics Committee. The draft does not provide a citation for the findings of the subcommittee. Nor does it disclose any cultural or religious affiliations of committee members that might have bearing upon the question of non-financial conflicts of interest. Finally, given the same reasoning for deeming male circumcision of non-consenting minors justifiable, would the subcommittee agree with the 2010 American Academy of Pediatric policy statement on female genital cutting, 1287 -later retracted-which stated some forms of female genital cutting are permissible? Is there a compelling reason why females should be protected and not males?
This section provides only cursory treatment of the many important ethical issues that are raised by the male circumcision of non-consenting minors.
Regarding the five major principles of bioethics, 1288 it has been argued that male circumcision fails to pass any of them. For infant male circumcision to be morally permissible, it must pass all five. This section of the draft only included three of the five principles.
1. Beneficence (maximizing benefit and minimizing harm, both at the individual and society level): This has been addressed in the cost-utility analyses that have been published. In the analysis that included complications, impact on urinary tract infections, impact on sexually transmitted infections (including HIV), and was properly discounted for time, it concluded that male circumcision wasted money and resulted in an average decrease in quality-adjusted life years. 1258 To conjure up a rare benefit, another analysis needed to overestimate the incidence of HIV five-fold, fail to consider any complications, and make a number of unjustifiable assumptions. 1260 The differences in these analyses can be explained on the basis of what Sarah Waldeck, a law professor at Seton Hall University School of Law, calls the "multiplier effect." 1289 Simply put, those who have accepted the social norm of infant male circumcision will overemphasize the importance of studies documenting a benefit regardless of their methodological weaknesses, and will ignore or minimize the importance of studies showing evidence of a neutral or negative impact from infant male circumcision. Considering that this draft does not address the function of the foreskin and does not adequately address the multiple harms associated with its amputation, how can the CDC acknowledge any negative consequences related to male circumcision? This draft also selectively cites studies, regardless of their methodological weaknesses, that support male circumcision. This indicates that the draft is strongly influenced by social normality and its recommendations are strongly influenced by cultural, or other, factors.
# Autonomy (respect for individual values and choices):
Infant male circumcision fails to satisfy this principle. There is no compelling medical reason to circumcise an infant. In such a situation, the Committee on Bioethics of the American Academy of Pediatrics recommends waiting until the child can provide his own fully informed consent. 1290 Male circumcision, by virtue of the fact that it breaks the skin, violates the infant's bodily integrity. One of the most universally accepted basic human rights is the right to bodily integrity and security of person. 1283,1291,1292 As a result, it is not very difficult to make a cogent argument that infant male circumcision is a human rights violation. 1293 It is widely held that no one has the right to violate the human rights of another human except in extreme circumstances. 1294 Consequently, the child's right to self-determination should be respected. There are two ways to approach an infant's autonomy when it comes to infant male circumcision. The first is to decide for the child on the basis of what he would choose, if he was able to provide his own fully informed consent, without parents projecting their value system on the child. 1294 Given that adult males rarely 1295 chose to undergo circumcision without a medical indication, the substitute judgment test requires that it not be performed on an infant (who cannot effectively resist). The second approach is based on Joel Feinberg's concept of the right to an open future. Briefly, a child should have rights that should be saved for the child until he is an adult, or what he calls "rights in trust." These are the sort of rights an autonomous adult would have, but a child would be too young to exercise them. They are "rights that are to be saved for the child until he is an adult, but which can be violated 'in advance' before the child is even in a position to exercise them." Following such violations, a child upon reaching adulthood would find that certain options would already be closed. 1296 The concept of a right to an open future has been adopted by subsequent ethicists. 1297 Certainly, infants, whether male or female, have a right to their complete genitals coming into adulthood.
The right to bodily integrity should be a "right in trust" that Feinberg envisioned. Consequently, it has been argued that infant male circumcision violates an infant's right to an open future. 1298 Subsequent analysis has determined that physical violations do carry more moral weight than non-physical violations. 1299 In either case, violating the infant's developing/future autonomy by cutting off the most sensitive portion of his penis without his permission is a matter for great moral concern. Since autonomy is considered by some to be the primary principle of modern bioethics, 1300 there needs to be a compelling reason to violate anyone's autonomy, especially someone who is vulnerable. No such reason has been provided in this draft.
3. Justice (the obligation to fairly distribute risks, burdens, and benefits, to minimize stigmatization, and to make decisions in a transparent fashion): When male circumcision is performed on an infant at the parents' behest, the parents do not assume any of the risks, the infant does. The infant has no say in the matter, yet takes on all of the harms and risks associated with the procedure. Such a shift of risk onto someone who cannot consent is inconsistent with the concept of justice. Obviously the risks are not fairly distributed. Infants who are circumcised for religious or cultural reasons or for misguided beliefs that it improves hygiene, which covers the vast majority of male circumcisions, undergo the procedure for what parents believe is their religious or cultural obligation. Consequently, the infants are being used instrumentally as a means to satisfy ends determined by their parents. 1299 In Kantian ethics, anyone of moral worth should not be treated as a means to an end, but always as an end in themselves. 1301 Treating a human being instrumentally in this fashion is in direct opposition with our modern concept of justice. 1302 Likewise, the randomized clinical trial which purported to find that circumcision of HIVinfected men increased the relative risk of infection in female sexual partners by 50% placed an increased risk of HIV infection on women who were unaware of their partner's HIV status. 338 This abuse of the principle of justice was one of several reasons why this study was perhaps the most unethical study since Tuskegee. If the CDC was interested in minimizing stigmatization, it would abandon the use of the term "uncircumcised," which is now considered by many to be pejorative. One definition of the word "uncircumcised" is "spiritually impure: heathen: unregenerate." It is also a term that is technically inaccurate. For a man to be "uncircumcised," he would need to first be circumcised and then have the process reversed. By using the term "uncircumcised" or "non-circumcised," the authors of this draft are making the underlying value-laden assumption that being circumcised is the preferred condition, when there is no evidence, other than cultural pressure, to support this. The most accurate, value-neutral term for a man with all of his original genital tissue is "intact." By continuing to use the term "uncircumcised," the CDC is identifying its pro-circumcision bias to anyone who is familiar with the semantics on this issue. Males who are indeed "intact" find use of the word "uncircumcised" to be akin to hate speech because they are singled out as "different," supposedly "abnormal," and/or possibly unclean." 1181 Nothing could be further from the truth. Profiling a group of people in this way is unjustified, discriminatory rhetoric.
The use of this terminology has racist and anti-immigrant overtones. With the exception of a few immigrants who come from circumcising cultures, most immigrant males have intact genitals. The overall tone of this draft unnecessarily and counterfactually characterizes normal, intact males as inferior and disease-laden. The draft also places more credence with investigators who focus on certain racial and ethnic groups for increasing male circumcision rates. 345 Less than a third of the world's men are circumcised, and nearly all of them are circumcised for religious or cultural reasons. Why would the CDC want to stigmatize the majority of males on the planet? Many intact males who read the American Academy of Pediatrics 2012 Task Force report 1306 interpreted the Academy's position as thinly veiled hate speech (personal communications). The CDC's recommendation may be interpreted as even more insulting.
If justice requires that decisions be made in a transparent fashion, then major reform is needed in the informed consent process that accompanies infant male circumcision. This is needed to ensure full disclosure is provided, that those providing proxy consent understand what they are providing consent to, and that those providing consent do so voluntarily without being coerced or solicited. Currently, the level of disclosure provided is far below the standard expected for similar elective procedures. 1228,1231,1310 One study in which full disclosure was provided resulted in parents becoming very upset with the physicians providing the disclosure. 1311 This may reflect that many parents are unaware male circumcision leads to any harm or complications, and parents have usually made up their minds about male circumcision based on social or cultural factors. They may not want to hear about any untoward effects because this creates cognitive dissonance. But, this does not excuse physicians from their duty to provide full disclosure. Sometimes, this information will dissuade parents from agreeing to a circumcision for their son. Full informed consent also protects the health care provider in the event of an adverse outcome. Even in the adult male circumcision roll out in Africa, the men are not given full disclosure regarding the harms and complications of male circumcision. The fact that bribes are becoming necessary to recruit adult males to undergo a free male circumcision 1214 is an evident sign that the decision process is less than transparent.
Is it justifiable for parents to impose male circumcision on their sons when there are more effective, less expensive, less invasive methods of preventing urinary tract infections, sexually transmitted infections, HIV infections, and penile cancer? Imposing such inefficiencies in a nonconsensual fashion onto an infant in the name of parental convenience is both unfair and unjust. If an infant cannot choose his preferred method of prevention, the parent at least should choose a more efficient, less expensive, less invasive measure.
The two principles omitted in this section of the draft are:
4. Non-maleficence (does the procedure avoid permanently diminishing the patient in any way that can be prevented?): Male circumcision permanently removes the most sensitive portion of the penis. 54,55,108 Some would argue this is the intent and purpose of the procedure, 1312,1313 and certainly it was the intent when male circumcision was first introduced in the United States and Britain as a "cure" for masturbation. 5. Proportionality (will the final result provide a net benefit to the patient in proportion to the risk undertaken and the losses sustained?): Decisions are made in everyday life based on proportionality. If a shop is asking too much money for an item, they may have trouble selling it because the price is out of proportion to the value the customer has assigned to the item. For infant male circumcision proportionality works on two levels: the physical and the moral. It fails on both levels.
The measure of proportionality on the physical level has already been assessed with the roll-out of adult male circumcision in Africa. Men who live in countries with some of the highest prevalence levels of HIV infection in the world have been subjected to wellfinanced advertising and have been offered a free male circumcision, but they are only agreeing to undergo the procedure 1.6% of the time unless they are given an additional bribe. 1214 The advertising programs have informed these men regarding the ease and simplicity of the procedure, the lack of complications, and the overwhelming benefits in protecting them from sexually transmitted infections and HIV, yet only 1.6% are interested in a male circumcision paid for by the Bill and Melinda Gates Foundation, the Clinton Foundation, and PEPFAR. How could this be explained? These men have a foreskin. They know how it works, what it does, and how it feels. It seems that they recognize on a physical, biological level that the resultant harm of removing the foreskin is out of proportion to the unlikely benefits, especially when the same benefits can be more easily and effectively obtained using methods that do not involve the removal of sensitive, functional tissue. Instead of recognizing the value that men have assigned to their foreskins, advocates of mass male circumcision spend their time trying to discover the inducement that will entice these men to get on the male circumcision bandwagon.
On the moral level, the value of one's wholeness and the ability to exercise one's autonomy are important elements in the equation. David Lang 1314 and Wim Dekkers 1315,1316 have identified totality and wholeness as important issues in the ethical debate over male circumcision. Lang applies the principle of totality to argue that "the good of the whole overrides the good of a part if that part is truly (not merely hypothetically or speculatively) a threat to the well-being of the whole." 1317 In other words, all parts of the body form a cohesive, integrated unit. 1314 This principle complements the principle of bodily integrity. Lang argues that, since male circumcision disrupts normal sexual function, the principle of bodily totality is violated.
For Dekkers, "wholeness" has four aspects: biological, experiential, intact, and inviolable. 1315,1316 Biological wholeness refers to anatomical and functional integrity, which is conceptually similar to Lang's notion of totality. Excising erogenous genital tissue violates this sense of wholeness. Experiential wholeness is not dependent on biological wholeness, but is a phenomenological view of the human body in which the body is a "lived body." By altering responses to subsequent painful stimuli 993,994 and altering normal penile reflexes, 120 removal of the foreskin may negatively impact experiential wholeness. One aim of medicine is, or should be, to restore this sense of intactness and completeness -to make the body whole again, not to introduce deficiency. For medical practitioners to remove functional tissue runs against this aspect of wholeness. Inviolable wholeness is an outgrowth of a Kantian principle that violating the body also violates the person's dignity. 1299 According to this principle, the integrity of the body is a necessary condition for the fulfillment of human moral purposes, and respect for the integrity of the body is necessary for proper moral sensibility.
Male circumcision also violates an infant's sense of wholeness without consideration. On a contractual level, such a one-sided transaction would not be binding. Proportionality is not achieved as the infant is not compensated for this loss. The loss of the protection of bodily integrity, security of person, and self-determination (autonomy) are also not adequately compensated for. According to John Rawls, depriving one of a basic human liberty is only morally permissible if doing so enriches or enhances one of the other basic human liberties. 1302 During infant male circumcision, the basic human right to bodily integrity and security of person is violated without compensation. It is thus not proportional.
The possibility of death, although rare, following infant male circumcision, which has not been reported following circumcision in older boys and adults, also violates the principle of proportionality. This potential outcome may be grounds enough for delaying the procedure until the patient is old enough to grant his own fully informed consent.
This section states that "Others argue that it is a choice that parents should be able to make on behalf of their male children because of the strong evidence showing that the procedure is beneficial and the risks are minimal if performed competently." This statement has several problems. First, at least one of the citations given for this statement does not make this assertion. The 2003 article by Benatar and Benatar does not contend that there is strong evidence favoring male circumcision or a minimal risk, but rather that the benefits and risks are balanced and given the non-medical benefits, which they fail to identify, male circumcision is morally permissible. 1318 Second, there is clear debate over the value of the evidence. As noted by Waldeck, male circumcision status and the prevalence of circumcision within a culture will impact how evidence is prioritized and interpreted. 1289 So, it is telling that the CDC cites the opinion piece in favor of male circumcision published in the British Medical Journal, 1319 but failed to cite the opinion piece arguing the opposing view that accompanied it. 1320 Others have put forth such utilitarian arguments, but such arguments have been challenged because of their dependence on false analogies, speculation, selective bibliographies, being oblivious to the harms and risks of the procedure, and fallacious reasoning. 1299,1317, The importance of unproven benefits and ignored harms needs to be part of the debate and not just accepted because it makes one feel better about being circumcised. Furthermore, many male circumcisions are performed by those least competent to be doing the procedure: medical students, interns, residents, physician assistants, etc. And, few, if any, health care providers are adequately educated about the anatomy of the foreskin, which explains the high number of complications surrounding its removal.
Second, it is merely assumed that parents have the authority or "right" to have parts of the genitals of their children amputated. The concept of parental rights is a legal fiction that has outlasted its usefulness. When women and children were considered property/chattel, such property rights made sense. As the moral worth and status of children is increasingly being recognized, treating children as property/chattel is becoming more difficult to rationalize. One legal scholar has noted that parental rights are only invoked when the parents are doing something that is not in the child's best interests. 1328 It has been argued that parents do not have the "right" or the authority to violate their child's basic human rights and that this prohibition extends to infant male circumcision. 1329 One could argue that the onus is on those who want to encourage or defend infant male circumcision to make a positive argument to justify violating an infant's right to bodily integrity and security of person based primarily on parental judgment.
While parents are given the authority to vaccinate their children, infant male circumcision has little in common with vaccination other than that they are both implemented on infants or children. Male circumcision removes tissue that is irreplaceable and that serves specific functions; vaccines stimulate the production of antibodies by the immune system to fight off infections.
The claim that infant male circumcision acts like a vaccine has been made by a number of male circumcision enthusiasts. 1, They use this analogy because the average person understands the concept of vaccination and has seen the ability of vaccines to greatly reduce the incidence and prevalence of a number of serious and non-serious illnesses. A highly effective vaccine against a life-threatening infection can have an almost miraculous impact, but most are not aware that a vaccination program using a vaccine with only 40% to 60% effectiveness will ultimately increase the number of infections. 1265 Male circumcision enthusiasts use the vaccine analogy because they want people to associate the miracles brought about by vaccines to also be associated with infant male circumcision, in the hope that those opposing infant male circumcision would then be thought of as irrational and unwilling to do what is in their child's best interest.
The analogy between vaccination and male circumcision is spurious:
1. Vaccines target specific illnesses that are either common, infectious, or carry significant personal or public health consequences. Male circumcision does not.
2. Only vaccines that have been demonstrated to be effective in decreasing the risk of severity of the targeted illness are released for use on the public. Nearly all of the vaccines that are commonly used are effective in more than 85% of those vaccinated (an exception is the influenza vaccine). Typically, vaccines that only reduce the risk by 40% to 50% are often not used. 247,1265,1340,1341 Male circumcision has not been clearly demonstrated to be effective, let alone provide more than 85% protection. By making the analogy, male circumcision enthusiasts are trying to get people to believe that circumcision has these high levels of protection.
3. Vaccines do not permanently remove any body parts. Male circumcision does. As Wayne Hampton notes, "Circumcision is a subtraction whereas vaccination is the addition of immunizing agents to the bloodstream. Circumcision is a loss while a vaccine is a gain." 1342 Removing the foreskin, with its functioning mucosal immunity, subtracts from the value of the body as a working system. A vaccination adds to the value of the body as a working system by boosting the immune system. This is morally interesting, especially from a utilitarian standpoint, because the net effect of a vaccination is improved function both on an individual and a societal level, while this is not true for male circumcision. It is also interesting from a Rawlsian perspective because a vaccine program serves the purpose of justice as it improves life, especially for those who are the most vulnerable.
In a similar vein, male circumcision is more invasive than vaccination. To make the analogy of male circumcision being similar to vaccination plausible, male circumcision enthusiasts would need to demonstrate that male circumcision is not excessively invasive, but this cannot be demonstrated.
4. Vaccines typically have been shown to have a positive cost-effectiveness or a reasonable cost-utility. Male circumcision has not. 1258 5. The long-term effects of vaccinations have been well studied and documented. This has not happened with male circumcision. Even the 2012 Task Force report from the American Academy of Pediatrics acknowledges that the long-term risks of male circumcision are unknown. A registry and compensation system exists to address unfortunate outcomes of vaccination, yet no such system exists for male circumcision. 1342 6. Vaccination programs have decreased the incidence/prevalence of the targeted diseases. The illnesses associated with male circumcision have not decreased and in several instances have increased. The diseases that have been targeted by vaccination programs, for the most part, have been either illnesses with a high incidence and/or with associated significant morbidity/mortality. 1340 While vaccination programs have clear public health benefits, both for the individual and society overall, any such benefits for male circumcision, if they exist at all, are miniscule by comparison. 1344 7. The level of acceptable risk for the public for vaccinations is very low and well below the risks associated with infant male circumcision.
8. The diseases targeted by vaccines typically have a high incidence, often the majority of the population is at risk, otherwise a vaccination program would not be worth pursuing. By contrast, the illnesses male circumcision is presumed to prevent are uncommon, rare, or nonexistent. 1348 9. When male circumcision apologists and enthusiasts link male circumcision and vaccination, they need to be aware that by doing so they may undermine the efforts of vaccination programs. Clearly, parents who do their due diligence will discover male circumcision is questionably effective at best. By linking male circumcision and vaccination, parents may be given the false impression that vaccinations are as ineffective as male circumcision. Claims of a public health benefit should be limited to interventions that actually have a positive impact on the health of the public.
The argument provided by Benatar and Benatar posits that the legitimacy of parental authorization of infant male circumcision is based on the vaccine analogy. 1318 The points of their argument can be summarized as follows:
1) There are parts of the world where diseases against which children are frequently vaccinated are now uncommon.
2) The necessity of such vaccination for the individual child is neither clear nor immediate.
3) There are small but real risks from vaccination (including death).
4) The child is unable to give consent for vaccination.
5) The power to consent can be deferred to proxy decision makers or delayed until the child is old enough to give consent himself.
6) Delaying vaccination can undermine its benefit.
7) It is reasonable for parents or other guardians to make decisions on behalf of a child that are in the child's best interests.
8) "The role of a parent is not simply to save children from immediate catastrophe, but is to protect and foster a child's long-term best interests." 9) Therefore, "parents may consent on behalf of their children not only to vaccination but also to such procedures as orthodontics and various non-medical interventions, including schooling."
A point by point rebuttal follows:
1) Not only is this true, but vaccination programs are effective. (Although, it translates into fewer sick visits at our office and less revenue for physicians. If the CDC translated their interest in increasing physician income generated from male circumcision, they would also come out against vaccinations.)
2) The presumption that vaccinations have no clear necessity for the individual is unsubstantiated. If a vaccine did have not a clear indication, it would no longer be given. This is the case for small pox. Vaccination programs against smallpox were discontinued after it was determined that smallpox had been eradicated. Vaccines can also be justified on the basis of public health considerations. 1343 To say that vaccines have no clear indication for the individual is foolhardy. Herd immunity may reduce some risk, but does not eliminate risk. If it did, the pertussis and measles outbreaks in unvaccinated children that emerge on a fairly regular basis would not take place. Consequently, there is always a potential advantage to the individual to be vaccinated. This presumption is not only wrong but extremely dangerous. If this erroneous position was adopted by a sufficient number of people, even the positive impact of herd immunity could be lost, leading to a public and personal health disaster.
The Benatars's entire argument is dependent on this false assumption. If vaccines had no benefits, then parents would not be allowed to authorize their use. It is only because they have benefits that parents can direct medical personnel to administer the vaccines. People are allowed choices and parents can forgo vaccinating their children. When they do so, it is common practice to have parents sign a waiver indicating they are aware of the benefits of the vaccine, yet they wish to forgo its administration to their children.
3) Agreed.
4) Agreed, but given the benefits of the vaccine, it is both in the child's best interest and also something the child would choose for himself if able to.
5) Agreed.
6) Agreed.
7) Partially agreed. The language should be altered to state it is reasonable for parents to consider making some decisions on behalf of the child that are believed to be in the child's best interests. For example, a girl with a gene that puts her at high risk for breast cancer, one could argue that a prophylactic double mastectomy would be in her best interests, but not a decision that the parents should make on her behalf. The American Academy of Pediatrics Committee on Bioethics notes that: parental decisions are limited to those where there is an immediate danger, and that decisions which can safely wait should be delayed until the child can have input into the decision. 1238 8) Agreed. But parents also have the responsibility to be the child's guardian, which includes the duty to protect the child's basic human rights, 1318 protect the child's right to an open future, and not treat the child instrumentally. Comparing choices for education has no discernible connection to making medical choices for a child who cannot choose for himself. At the age where education outside the home is offered, the child can have a varied amount of input. There is also disagreement about the authority of parents to force children to undergo education that is not in their best interests 1346 This is also a false analogy that does not apply to infant male circumcision because, as a society, we consider education necessary to become a good citizen 1347 and we believe delaying education will undermine its effectiveness. Education is clearly in the child's best interests, and it is something the child would have chosen for himself once he becomes competent.
While, in the opinion of the undefined, unpublished findings of the subcommittee of the CDC Public Health Ethics Committee, the decision either to or not to circumcise is an appropriate exercise of parental authority, the CDC draft fails to recognize that many disagree with this opinion. For example, all of the national medical organizations who have come out against infant male circumcision and have characterized it as a human rights violation are not mentioned by the CDC. 1236,1238,1240,1241,1244,1245,1250 Legal scholars have questioned the legitimacy of parents violating their child's human rights and best interests under the rubric of "parental rights" because such actions only result in harming children. 1293,1327,1346,1347 It has been argued, given the moral status of infants being increasingly recognized, 1292,1347 that infant male circumcision may be the last holdout in which parental rights are recognized. 1329 The rest of the Western world recognizes that parents do not have the authority to violate their child's basic human right to bodily integrity and security of person.
Did this CDC subcommittee consider whether this same parental authority would allow parents to direct health care professionals to cut the genitals of their daughters? The same ethical principles would apply. There is some evidence that female genital cutting has medical benefits in decreasing the risk of HIV infection 1348 and a significantly shortened second stage of labor. 1349 Proponents of female genital cutting maintain the procedure also decreases a woman's risk of sexually transmitted diseases. At least one study has documented that female genital cutting has no impact on sexual fulfillment or the ability to have an orgasm. 1350 In 2010, the American Academy of Pediatrics Committee on Bioethics released a statement, in an effort to acknowledge cultural diversity while ignoring the moral status and human rights of children, stating some forms of female genital cutting are morally permissible. 1287 The report generated such a negative response that the Academy was forced to "retire" the statement 31 days later. 1351,1352 It would certainly be unfair and unjust if the subcommittee were to treat males and females differently.
The justification for the moral permissibility of infant male circumcision in the CDC draft, and as argued by other male circumcision apologists, 1340 is based on the presumption that the procedure is safer and simpler when performed on newborns and infants. Unfortunately, presumptions are not data. 1353 As addressed earlier, the evidence does not support the contention that there is an advantage to male circumcision being performed in infancy, other than the ease with which the boy can be restrained.
The CDC draft should also refrain from fear-mongering. Apparently, those who wrote the draft must be concerned over the remote possibility of missing an opportunity to prevent an HIV infection in a male who becomes sexually active before he has the chance to get circumcised. How many 14-year-old males are going to get HIV from their 14-year-old girlfriends? While the age of sexual debut may be getting younger, the rate of heterosexually transmitted HIV infection is extremely rare through sexual contact with other young people. There is no evidence in North America that any HIV infections are prevented by male circumcision, 8-14 so there is no reason to lose sleep over the number of HIV infections potentially caused by a delay in male circumcision. Likewise, neonates are not sexually active.
The statement, "Uptake of the procedure after the neonatal period is also likely to be lower due to the increased cost, greater likelihood of complications, and other barriers to male circumcision at a later age," contains several inaccuracies. First, as discussed in detail earlier, there is no properly controlled experimental evidence that later male circumcision has a greater likelihood of complications. There are numerous case reports of infant deaths resulting from male circumcision in the medical literature in the United States, but none known of adolescent or adult deaths as a consequence of male circumcision. Adolescents and adults are capable, unlike neonates, of expressing pain and requesting adequate pain relief, of noting excessive bleeding and infection. They would also have undergone a thorough pre-operative history and physical exam noting any possible reasons to not have surgery. Neonates undergo male circumcision surgery without knowing whether they have any underlying medical problems such as hemophilia, and many premature neonates are circumcised while still undergoing care in the NICU. If surgery under general anesthesia is unacceptable for neonates, then any surgery should be postponed until adequate pain relief can be provided. Male circumcision is done to infants because it can be done, not because it is safer with fewer complications. (see complications section.)
It is also unclear what the other barriers to male circumcision might be in adolescents or adults. Somehow, teenagers are able to undergo orthodontia, which is much more time consuming than male circumcision. Some teenagers manage to undergo cosmetic surgery during school vacations. It is unclear how there would be significant barriers, if male circumcision would be considered so terribly important. If the CDC and American Academy of Pediatrics have their way, there should be no financial barriers to this cosmetic surgery. What this statement is missing are the real reasons that uptake is lower after the neonatal period. After several weeks of bonding with their baby, parents are less likely to put their baby through a painful procedure. The older boy, who has experience with his foreskin, would consider the suggestion of cutting off his foreskin, which at that point may have acquired a distinct value to him as sensitive tissue, as imprudent. "Why would anybody want to do that?" is a typical response. The foreskin is a valued possession that even a young boy knows enough not to relinquish.
The subcommittee recommended that male circumcision be an "informed choice" but fails to consider that informed consent is impossible for infant male circumcision. 1231 This is an important issue that warrants debate, but it was apparently not addressed by the subcommittee. The Europeans do not think parents can provide informed consent, and certainly the infant cannot either. Many would contend that adolescents are also unable to give consent.
Finally, the lack of health insurance coverage for male circumcision is not an issue of justice because male circumcision is a cultural practice. It is typically not the role of government, and definitely not the role of Medicaid, 1234 to support cultural practices. By supporting one cultural practice, those who do not participate in that practice are discriminated against. If, as appears to be the case with this draft, the CDC is applying pressure on ethnic groups that have traditionally kept their infants genitally intact, then they are enforcing an unwanted hegemony. The reduction in risk of HIV infection and other adverse health conditions is illusory. This leads to the question of why the CDC is so interested in implementing this hegemony.
# RESPONSE 89:
The CDC adequately bases its analysis on the best quality scientific evidence available, mainly the RCTs, which are consistent in their findings around prevention of HIV acquisition.
The CDC Public Health Ethics Committee (PHEC) concluded that newborns cannot provide informed consent and so must rely on their parents or caretakers to determine and act in their best interests, raising the issue of autonomy in discussions of circumcision of male newborns. They took into account varying opinions about the decision-making process including that the decision about whether to be circumcised should be made by individuals when they are old enough to make their own informed decisions. It has been pointed out that a man with a foreskin can elect to be circumcised but if circumcised as a newborn, cannot easily reverse the decision. Others argue that it is a choice that parents should be able to make on behalf of their male children because of the strong evidence showing that the procedure is beneficial and the risks are minimal if performed competently. Parents are generally given the authority to make decisions, such as vaccination, for their minor children based on their evaluative consideration of the child's best interests. Appropriately, this consideration takes into account social, cultural, and religious perspectives, as well as objective, scientific information about preventive health benefits and risks. Thus, in the opinion of the PHEC, both a decision to circumcise and a decision to not circumcise are legitimate decisions, and either decision is an appropriate exercise of parental authority on behalf of a minor child.
# COMMENT: Tables
Both tables are highly selective in the data presented and need to be completely revised. Results for which there was clear sampling bias and/or lead-time bias need to be adjusted accordingly. The results of meta-analysis of observational studies need to be included. All of the prospective studies of incidence need to be included and updated.
# RESPONSE 90:
The data selected for presentation in the tables represent the best quality scientific evidence available (RCTs) at the time of the review.
# COMMENT:
Closing Comments
What is going on at the CDC? After taking over seven years, the CDC finally generates recommendations that mimic the talking points propagated by male circumcision enthusiasts. But, this is only the latest in a string of bizarre actions taken by people within the CDC who have been addressing the issue of male circumcision. The first action was taking up the issue at all. Heterosexually-transmitted HIV infection is only 10% of the HIV infections seen in the United States and 70% or more of the sexually active males in the United States are already circumcised. Many of those males with HIV are/were circumcised, so how did circumcision help them? Why is "circumcision to prevent HIV" even an issue in the United States? It does not make sense to expend the energy on such a highly circumcised population unless the action was intended to maintain a high percentage of male circumcision for some other reason.
The next action was to convene the consultation in 2007, inviting nearly every prominent male circumcision enthusiast on the planet. Of the 50 or so people from outside the CDC invited to attend, only one had ever published studies that were not favorable to the practice of male circumcision. Not much diversity represented there. This would make it sound as though there is only one scientist in the world who has published such studies. Clearly, there are plenty of scientists who could have voiced an alternative viewpoint and who would have been willing to attend the consultation, but they were not invited. Only one was invited, as the token dissenting voice. A similar tactic was used when the WHO/UNAIDS rammed through its approval of male circumcision in Montreux in 2007, where Gary Dowsett was the token voice of opposition. 5 It is not surprising that this experiment in "group think" provided the CDC with all the ammunition it needed to move forward. In 2009, the CDC held a conference in Atlanta on male circumcision and HIV. They invited Inon Schenker of Operation Abraham and the Jerusalem AIDS Project to give a presentation. The last slide in his presentation was a photograph of a completely naked, genitally intact male on whom the figure of an elephant had been drawn around the penis so that the intact penis looked like an elephant's trunk. The words "Yes! A circumcision please!" had been added to the photo. Such a crass insult to every intact male was uncalled for. Apologies have obviously been in order, and requested, but never granted. It is not apparent why the CDC would tolerate what was clearly intended to be hate speech.
It is not clear why the CDC would purposely publish recommendations and a supporting background document that they must know is not evidence-based. By doing so, the CDC has placed health care providers in the untenable situation of committing malpractice, by disseminating false information, thereby placing their patients at unnecessary risk. Why would they want to embarrass themselves in this fashion? Is the CDC so infiltrated and controlled with male circumcision advocates that producing something this biased and unscientific was mandated from the top? There is evidence that Peter Kilmarx, who initially headed up this project, was part of an email mailing list of male circumcision advocates in 2006. How much contact between officials at the CDC and pro-male circumcision lobbyists would a freedom of information request reveal? Is the CDC somehow beholden to the pro-male circumcision lobby? Is this draft a concession to the lobby to demonstrate that the CDC was willing to do their bidding? One has to wonder how much of the effort to "prove" that male circumcision prevented HIV and other sexually transmitted diseases in Africa was actually not about helping those in Africa, but more about maintaining the current rates of male circumcision in the United States, keeping them from going into free fall. The narrow, single-minded focus of the CDC in this draft supports this contention.
What will the CDC do now that their biased, culturally-based position has been exposed as being scientifically fraudulent? How can anything the CDC says or does be taken seriously after one has followed their subjective handling of this issue over the years? It is time to save face. Trash this draft and start over. | Reviewer No. 1: COMMENT: I have reviewed both documents and agree with the recommendations. I don't have substantive changes to suggest. Please see the attached for a suggestion about removing two comma splices.Thanks for taking the time to review the documents. The suggested edits were made to the policy document.COMMENT: I've reviewed the documents and recommendations, and I find them to be fair, well crafted, and appropriately extensive. I support them in their current form and in their entirety, and I do not have edits to recommend. From the perspective of a practicing urologist, I would say that great benefit will be derived from such a clear statement indicating efficacy not only in potentially preventing HIV but also of other STDs and health conditions likely related to STDs in a care environment that is increasingly limiting. Another great potential benefit to be derived will be in increasing acceptance of male circumcision in a historical era of increasing opposition.Thanks for taking the time to review the documents and provide comments.Note from CDC: Reviewer No. 3 has provided three sections of commentary: (1) general comments regarding the CDC recommendations, (2) comments pertaining to specific text of the CDC recommendations, and (3) summary comments about each section of the CDC background document. A response has been provided to each main point in the general comments on the CDC recommendations (1) and to each comment about specific text in the draft recommendations (2). A summary response has been provided at the beginning commentary on the CDC background document (3). Citations pertaining to comments from peer reviewer No. 3 are located on pages 140 -208. Citations pertaining to responses from CDC are located on pages 209-212. CDC thanks the reviewer for taking the time to review the documents and providing extensive comments.COMMENT: This peer-review of the Centers for Disease Control and Prevention's (CDC's) Draft Recommendations and Background Documents was generated after December 2, 2014 when the documents first became available. Because of the limited time in which to review and comment on these documents, there may be some topics that could have been addressed more completely, some topics that were addressed more than once, and some citations that may be missing. In the interest of time, the citations given in the review may not be sequenced properly, but each citation should be properly identified. There may be some grammatical and typographical errors because there was insufficient time to identify and correct them. The comments addressing the Recommendations draft are made in direct response to the statements in that draft and appear in italics. The evaluation of the Background draft does not use the statement-bystatement format. This is a peer-review of draft documents and the comments are directed at these documents. It may be helpful for the reader to have copies of the drafts available. Several things are remarkable about this draft.The CDC recommendations are intended to assist medical providers in the United States in counseling individuals on the health risks and benefits of medical male circumcision. Male circumcision policy in non-US settings is outside the scope of the CDC recommendations. COMMENT: Sixth, it took over seven years for the CDC to produce a substandard, scientifically unacceptable product, nearly identical in content to what was presented at the 2007 consultation.No response. This comment does not address the content of the CDC recommendations or background document. COMMENT: Finally, the most remarkable thing is that the CDC is recommending clinicians and health care providers relay information that is counterfactual, incomplete, and biased to medical decision makers. In essence, they are deliberately encouraging health care providers to misinform their patients and thus commit medical malpractice.See RESPONSE 1 and RESPONSE 6.The CDC needs to throw out this draft and start again from scratch, this time without a preconceived conclusion in mind.No response. This comment does not address the content of the CDC recommendations or background document. COMMENT: They need to review the entire medical literature, thoroughly scrutinize the studies in the literature, and properly apply basic epidemiological principles.See RESPONSES 1, 2, 4, and 6. COMMENT: When they have done so, they need to consult with experts from around the world to make sure their findings are not culturally biased. They also need to focus on the United States, not Africa.These recommendations are for U.S. providers. Data from Africa is pertinent to the discussion in these recommendations.The following comments are made in response to incorrect and/or misleading statements contained in the "Recommendations" section of the draft by the CDC. In most cases, these issues are discussed in further detail in the review of the "Background" document. [CDC note: Excerpts from the CDC draft, as well as the CDC responses to the reviewer's comments are in regular print. The reviewer's comments are in italics.]CDC draft: These recommendations are intended to assist health care providers in the United States who are counseling men and parents of male infants in decision making about male circumcision conducted by health care providers (i.e. medically performed) as it relates to the prevention of human immunodeficiency virus (HIV) infection, sexually transmitted infections (STIs), and other health outcomes. Reviewer Comment: If the target audience is health care providers in the United States, why is so much of the Background Draft directed at what is happening in Africa? RESPONSE 10: A majority of research on the health risks and benefits of medical male circumcision, including the 3 randomized controlled trials, has been carried out in sub-Saharan Africa due to a high prevalence of HIV, low prevalence of male circumcision in some areas, and a generalized epidemic largely driven by heterosexual transmission. The few studies on the effect of male circumcision on HIV and other STIs in the United States are also included in the CDC background document. The benefits and drawbacks of applying evidence from African settings to the HIV epidemic in the United States are also addressed in the CDC background document. CDC draft: Such decision making is made in the context of not only health considerations, but also other social, cultural, ethical, and religious factors. Reviewer Comment: Why should these factors be a consideration of the CDC or health care providers? Is the CDC suggesting that health care providers take on the role of shaman or cultural broker? Are these other considerations the real impetus for promoting male circumcision? RESPONSE 11: CDC is not suggesting that "healthcare providers should take on the role of shaman or health broker." The CDC recommendations provide counseling messages on health risks and benefits of medical male circumcision for healthcare providers to use when discussing male circumcision with patients and parents of male children. The recommendations acknowledge that decisions whether to circumcise are made by the individuals, not the health providers. Individuals may consider social, cultural, ethical, and religious factors in addition to the health risks and benefits that they have discussed with their provider when considering male circumcision. COMMENT: CDC draft: Although data have been accumulating about infant male circumcision for many years, clinical trials conducted in Africa between 2005-2010 have demonstrated safety and significant efficacy of voluntary adult male circumcision performed by clinicians for reducing the risk of acquisition of human immunodeficiency virus (HIV) by a male during penile-vaginal sex ("heterosexual sex"). Reviewer Comment: The clinical trials referred to did not assess the risk of acquisition of HIV by a male during penile-vaginal sex as these trials made no effort to determine the source of the infections they diagnosed during the course of the trials. These infections could have been from male-to-male sexual contact or from iatrogenic sources. Data from within these trials indicate that about 1/3 to 1/2 of the infections diagnosed during the trials were transmitted through non-sexual means. RESPONSE 12: Heterosexual transmission of HIV is the primary route of transmission in Kenya, South Africa, and Uganda, the 3 countries where the RCTs were conducted_ENREF_2. Due to the nature of the epidemics in these locations, there is no indication that a substantial number of HIV infections was caused by non-heterosexual means. Random assignment to the study arms in each of the trials would also ensure that populations in each arm were comparable, and that risk of exposure to HIV through male-male sexual intercourse or other sources would be equally distributed between the groups. Reported sexual history and risk behavior was similar in experimental and control arms of each RCT at baseline. COMMENT: Furthermore, these trials have nothing to do with infants, and infant male circumcision is never voluntary because the infant cannot give consent. RESPONSE 13: Parents or guardians are able to provide consent on behalf of infants. COMMENT: CDC draft: Three randomized clinical trials showed that adult male circumcision reduced HIV infection risk by 50-60% over time. Reviewer Comment: Reporting the results in this manner is misleading. It needs to be stated that the reduction reported here is the relative risk reduction. What is of clinical importance is the absolute risk reduction, which in the case of these trials overall was 1.3%. This is the number that should be reported instead of the relative risk reduction. As the incidence of HIV infection in the United States is much smaller than in Africa, one would expect that if male circumcision were effective in the United States, which has never been demonstrated, the absolute risk reduction would be quite a bit smaller. Again, the source of infection was not determined in the African studies making the results suspect and likely meaningless. RESPONSE 14: Relationships between exposures and health outcomes are commonly presented as relative risks. An example is provided in the methods section in the CDC recommendations to demonstrate how to interpret relative risk reductions. Individual, absolute risk is dependent on a number of factors, and appropriate denominators are not always available to establish an absolute risk for HIV and other STIs in specific subpopulations. See RESPONSE 12 for discussion to source of HIV infection. COMMENT: CDC draft: These trials also found that medically performed adult male circumcision reduced the risk of men acquiring two common sexually transmitted infections (STIs), herpes simplex virus type-2 (HSV-2) and types of human papilloma virus (HPV) that can cause penile and other anogenital cancers, by 30%. Reviewer Comment: These trials were methodologically flawed. For both HSV-2 and HPV, the trials failed to adjust for lead-time bias. By doing so, the findings for HSV-2 are no longer statistically significant. For HPV, the two trials only sampled the head of the RESPONSE 16: See RESPONSE 9. The fact that some western national medical organizations outside of the U.S. have differing views of infant male circumcision from similar organizations in the United States may be a result of cultural differences in how male circumcision is viewed. 10 COMMENT: CDC draft: Much of the data related to HIV and STI prevention are from randomized clinical trials (RCTs) conducted among men in sub-Saharan Africa in regions with high rates of heterosexually acquired HIV infection. Reviewer Comment: Three randomized clinical trials have been performed, which were basically one trial in three locations of Africa. There are over 100 other populations in which the association between HIV incidence or prevalence and male circumcision status has been assessed. Consequently, very little of the data available on HIV and STI prevention has come from the RCTs. As mentioned above, it is not known whether the infections in the RCTs were heterosexually acquired because the source of infection in these men was not determined. There is much more to this issue than is being presented here by the CDC. Some have argued that the randomized clinical trials were unnecessary since it was known prior to the trials that male circumcision did not have an impact on HIV prevalence at the country level in several countries in Africa. Please read the response in the Background document.See RESPONSE 1 and RESPONSE 6. COMMENT: CDC draft: While such factors limit the impact of medically performed male circumcision in reducing the overall HIV epidemic in the U.S., there is epidemiological data to suggest that some subpopulations in the U.S. are likely to benefit.The data indicate that the only subpopulation in the United States that has seen an association between male circumcision and HIV prevalence were the males whose regular female sexual partners were HIV-positive. These data were from a very small subpopulation from a single study, the results of which were not robust and have not been confirmed by other studies. Without such confirmation, the benefit for HIV-negative men who have HIV-positive female sexual partners remains to be seen.See RESPONSE 4.Modeling by the CDC indicates that such men are unlikely to benefit from male circumcision, RESPONSE: See RESPONSE 3. COMMENT: ….and the standard recommendation for these men is to always use condoms, consider pre-exposure prophylaxis, and to have the female partner lower her HIV viral load with anti-retroviral medications. RESPONSE 17: Evidence from randomized controlled trials, ecological studies, crosssectional studies, and systematic reviews has demonstrated the protective effects of male circumcision against female-to-male sexual transmission of HIV and other STIs. A circumcised man who has sexual intercourse with a woman who is infected with HIV is less likely to acquire HIV than an uncircumcised man, but he is not completely protected from HIV. The CDC recommendations discuss counseling on male circumcision in addition to, not in place of, other evidence-based HIV prevention interventions for individuals who engage in high-risk sexual behavior. Because no HIV prevention intervention is 100% effective, utilizing a combination of interventions is the most successful approach to prevent HIV transmission. Male circumcision is unique among HIV prevention interventions in that it is a single procedure that confers lifelong protection against HIV, and is a valuable addition to the HIV prevention portfolio. COMMENT: Therefore, it appears that this CDC draft is not actually about decreasing HIV infection, but about some other underlying premise or other motivation. RESPONSE: See RESPONSE 6. COMMENT: CDC draft: In addition, African-American and Hispanic men have higher risk of HIV infection and lower male circumcision rates than men of other race/ethnicities. Reviewer Comment: African-American men have a higher prevalence of HIV than Hispanic men and also a much higher male circumcision rate. In several studies, the male circumcision rate in African-American men is similar or higher than the male circumcision rate in non-Hispanic Caucasian men. RESPONSE 18: Several studies conducted in the United States have demonstrated an association between male circumcision and lower HIV prevalence. A study of heterosexual African-American men attending an STI clinic in the United States observed male circumcision status was associated with a substantial and significant reduction in HIV prevalence. As stated in the CDC recommendations introduction section, African-American and Hispanic men have higher risk of HIV infection and lower male circumcision rates than men of other race/ethnicities. Because of this, the public health benefit of male circumcision may be greatest in these subpopulations. COMMENT: CDC draft: Although similar randomized clinical trials have not been conducted in the United States, based on evidence from the African trials, uncircumcised heterosexual men living in areas with high HIV prevalence are likely to experience the most public health risk-reduction benefit from elective male circumcision. Reviewer Comment: There is no evidence that any males in the United States would RESPONSE 19: Evidence from randomized controlled trials, observational cohorts, cross-sectional studies, and ecological studies in the United States and globally demonstrate the protective effects of male circumcision. In addition, findings from research conducted in other settings, including evidence from the RCTs, can be applied to US populations.Methods: CDC draft: A CDC consultation was held in April 2007 to obtain input on the potential role of male circumcision in preventing transmission of HIV in the United States. A summary of the consultation, including a list of the participants has been previously published and helped define key issues for inclusion in this document. Reviewer Comment: The list of participants reads like a Who's Who of Circumcision Advocates. No group opposing male circumcision was allowed any input. Only one physician was in attendance who had any record of publishing studies unsupportive of male circumcision. RESPONSE 20: Dr. Robert Van Howe was a presenter and attendee at the meeting selected to represent the intactivist viewpoint.CDC draft: These recommendations are based on an evaluation of available information on the health risks and benefits associated with high-quality, medically performed male circumcision and were developed to pertain to men and male newborns in the United States. Reviewer Comment: If one reads the Background Draft, it becomes abundantly clear that only the available information on the health risks and benefits favorable to male circumcision were considered. The evaluation basically used a selective bibliography to cherry-pick the studies that supported male circumcision.See RESPONSE 1 and RESPONSE 4. COMMENT: CDC draft: In these recommendations, the preventive benefits of male circumcision are generally expressed as relative-risk reductions (e.g., a 50% reduction from a 2% risk of an STI to a 1% risk), whereas any associated harm is expressed as an absolute risk (e.g., a 2-4% risk of adverse events). Reviewer Comment: While it is refreshing that the CDC admits to using this deceptive practice, it would have been more appropriate to express those factors in terms of number needed to treat and number needed to harm. Readers of this draft will be unable to convert relative risk to absolute risk unless the absolute percentages or incidence rates are given. By giving only the relative risks, the CDC is guaranteeing that their readers will be deceived and unable to make an accurate comparison. This is unprofessional and unscientific. Health care providers realize that their patients are confused by relative risk, but patients can understand data when it is presented in terms of "number needed to treat-NNT" and "number needed to harm-NNH." By taking this step, the CDC is preventing health care providers from being able to present information to their patients in a manner which can be most easily and accurately assimilated. RESPONSE: See RESPONSE 14. COMMENT: CDC draft: Appropriate denominators are not available in many cases to establish an absolute risk for HIV and other STIs in higher-risk populations, e.g., heterosexual males at increased risk for infection. Reviewer Comment: This is not true. The CDC has gone to great lengths to generate models and analyses to prove that male circumcision is cost effective and will save lives. These models are based on estimates of the absolute risks that would be considered realistic in the population of interest. But, when it comes to having these estimates available so that health care providers can deliver useful information to their patients, all of sudden these estimates do not exist?! This selectivity in availability of estimates may indicate the presence of a very low absolute risk, which would make the number needed to treat so high that no one would consider cutting off the most sensitive portion of their penis for such a minuscule possibility of a benefit.See RESPONSE 14.Recommendations:CDC draft: Health benefits and risks of elective neonatal, adolescent, or adult medically performed male circumcision should be considered in consultation with medical providers while taking into account factors associated with decision-making around male circumcision including religion, societal norms and social customs, hygiene, complication and may be more expensive than male circumcision conducted before one year of age.2. Counseling sexually active adolescent and adult males regardless of circumcision status CDC draft: All sexually active adolescent and adult males should continue to use other proven HIV and STI risk-reduction strategies such as reducing the number of partners, and correct and consistent use of male latex condoms, and HIV preexposure or postexposure prophylaxis among others. Reviewer Comment: If these steps are followed, there is no need to circumcise. Consistent condom use is over 99% effective in preventing HIV infection. Adding male circumcision is unnecessary, and encourages males to avoid using condoms in the belief that male circumcision protects against HIV.COMMENT: This is known as risk compensation, which is already occurring in Africa with negative consequences. RESPONSE 23: While risk compensation has been a potential concern following the male circumcision RCTs and subsequent programmatic scale-up, studies evaluating risk compensation following voluntary medical male circumcision have not presented compelling evidence that there is any real increased frequency of sexual risk behavior that would undermine the protective effect of male circumcision.3. Counseling uncircumcised sexually active adolescent and adult males CDC draft: Prior to counseling uncircumcised sexually active adolescent and adult males about medically performed male circumcision, their HIV risk behaviors, HIV infection status, and the gender of their sexual partner should be assessed. The results of these assessments will inform the discussion with men about the risks and benefits of male circumcision. Reviewer Comment: The term "uncircumcised," while widely used, is a pejorative term. One definition of the word "uncircumcised" is "spiritually impure: heathen: unregenerate." It is also a term that is technically inaccurate. For a man to be "uncircumcised," he would need to first be circumcised and then have the process reversed. By using the term "uncircumcised" or "non-circumcised," the CDC is making the underlying value-laden assumption that being circumcised is the preferred condition, when there is no evidence, other than cultural pressure, to support this. The most Reviewer Comment: There is no evidence in North America that male circumcision reduces the risk of acquiring HIV in the general population.See RESPONSE 2 and RESPONSE 10. COMMENT: If male circumcision reduced the risk of HIV in the United States, why is the prevalence of heterosexually-transmitted HIV three times higher in the United States, where about 70% of sexually active men are circumcised, than it is in Europe, where less than 2% of sexually active men are circumcised? RESPONSE 25: The ecological evidence that the reviewer has chosen to support their point is insufficient to refute the large body of high-quality scientific evidence demonstrating the protective effect of male circumcision against HIV. HIV transmission is affected by many factors that differ between the United States and Europe, which include but are not limited to extent of access to healthcare, promotion of HIV testing, access to HIV treatment, sex education, condom usage, and primary modes of HIV transmission. COMMENT: There is evidence that male circumcision increases the overall risk of sexually transmitted infections through heterosexual sex. RESPONSE 26: The reviewer's conclusion that male circumcision 'increases the overall risk of sexually transmitted infections through heterosexual sex" is based on a scientific analysis with extensive methodological problems that have been discussed elsewhere 11,12 There is a large body of high-quality scientific evidence that demonstrates male circumcision protects men from acquiring HIV and other STIs through heterosexual intercourse. COMMENT: The premise of this section is incorrect, so what follows is of little or no value. If male circumcision is of only "partial efficacy," but other measures are almost completely effective at preventing transmission of HIV, then why bother with male circumcision at all? RESPONSE: See RESPONSE 17.o CDC draft: Men and male adolescents being counseled about male circumcision should be told that (see Box 1): ▪ Male circumcision reduces, but does not eliminate, the risk of acquiring HIV and some STIs during penile-vaginal sex. In clinical trials, medically performed male circumcision was associated with reduced number of new herpes simplex virus type 2 (HSV-2) infections and reduced number of oncogenic types of human papilloma virus (HPV) among circumcised men. Reviewer Comment: As mentioned above, the medical literature demonstrates that male circumcision is not effective as a primary preventive measure for HIV infection.See RESPONSE 2. COMMENT: Also, male circumcision does not reduce the risk of infections with HSV-2 or HPV. RESPONSE: See RESPONSE 15. COMMENT: In fact, male circumcision may actually increase the risk of such infections. RESPONSE: See RESPONSE 26.The CDC is selectively citing methodologically flawed studies from Africa to make a claim that is not supported by the full body of research currently available.See RESPONSE 1 and RESPONSE 4.o CDC draft: Uncircumcised, HIV-uninfected men and male adolescents at increased risk for HIV acquisition through heterosexual sex should be counseled about the risk and benefits of male circumcision (See Box 1). When a decision is made to undergo male circumcision, a referral for surgical consultation and access to high-quality male circumcision surgical services should be provided. Reviewer Comment: Soliciting male circumcision to males is not supported by the medical evidence and is unethical.See RESPONSE 21. The reviewer's statement that the CDC recommendations imply that health providers should "solicit male circumcision" to males is inaccurate. COMMENT: Given the highly effective measures of secondary prevention, there is no need for a health care provider to mention male circumcision. RESPONSE: See RESPONSE 17.3B. Counseling men who have sex with men (exclusively) CDC draft: Although it is biologically plausible that male circumcision could benefit MSM during insertive sex, no definitive data exist. Reviewer Comment: That it is "biologically plausible" male circumcision may be a benefit is highly speculative and unsupported by any evidence in the medical research, either biologically or epidemiologically. Wishes and hopes are not data. There is no strong biological evidence to support the claim that male circumcision could benefit MSM during insertive sex. RESPONSE 27: While removal of the foreskin provides is protective for men against HIV transmission through insertive vaginal sex, the role of the foreskin in acquiring HIV infection is not fully understood. One likely reason that male circumcision provides partial protection from HIV and some other STIs is that the foreskin is more susceptible to these infections than are other parts of the penis. It is therefore plausible that male circumcision would protect men from acquiring HIV and some other STIs during both insertive vaginal and insertive anal sex; however, there is no definitive data at present that indicates the mechanism that protects men from acquiring HIV through insertive vaginal sex is also protective during insertive anal sex. There is no evidence that male circumcision protects against HIV during receptive anal intercourse. COMMENT: CDC draft: Currently, there are no study results from RCTs including large enough numbers of MSM and results from observational studies are not conclusive among MSM overall or among MSM who practice exclusively insertive anal sex. Reviewer Comment: This statement reveals that those within the CDC who generated this document do not understand basic statistics and research study design principles. Just because a study is larger does not mean that it will provide a statistically significant result to one's liking. Remember the Women's Health Initiative Study? It had the exact opposite result of what was predicted. The results of a study are not known until the study is performed. The current available data do not support the CDC's wish that male circumcision would provide some benefit among MSM. RESPONSE 28: The CDC recommendations state that medical providers should counsel MSM that: o "Based on clinical trials, the demonstrated benefits of male circumcision for HIV risk reduction apply to heterosexual (penile-vaginal) sex only. o In the absence of clinical trial data for MSM related to male circumcision, definitive statements about whether male circumcision can reduce the risk of acquiring HIV and other STIs cannot be made. However, in observational studies, pooled data indicate that among MSM who practiced mainly insertive anal sex, male circumcision was associated with a decrease in acquiring new HIV infections. One observational study also found that new infection with one oncogenic type of HPV type (HPV-16) was reduced among circumcised MSM who practiced mainly insertive anal sex. Data from observational studies are considered weaker compared to data from clinical trials. However, it is biologically plausible that MSM who practice mainly insertive anal sex may experience a reduction in the risk for acquiring HIV and STIs like that among heterosexuals in clinical trials during penile-vaginal sex. o While some MSM may choose to be circumcised because of the potential to decrease risk for the insertive anal sex partner, male circumcision involves potential risks (see Adverse Events section of Box 1) and costs."3B-1. CDC draft: Men who have sex with men should be informed that: o The demonstrated benefits of male circumcision for HIV risk reduction apply to heterosexual (penile-vaginal) sex only. Reviewer Comment: Several studies, two of which included more than 30,000 subjects, in the United States have failed to a find a risk reduction from male circumcision in heterosexual men. Therefore, the CDC's statement is misleading and, in the US, false.See RESPONSE 2.4. Counseling parents of male newborns, children, or adolescents CDC draft: Health benefits and risks of elective neonatal, pediatric, or adolescent male circumcision should be considered in consultation with medical providers. In the case of discussion about neonatal male circumcision, ideally such discussion should occur prior to the birth of the child. Ultimately, whether to circumcise a male neonate or child is a decision made by parents or guardians on behalf of their newborn son or dependent child. Reviewer Comment: Since neonatal male circumcision is a non-therapeutic, purely cosmetic procedure, solicitation of the procedure is unethical according to the standards of the American Medical Association. RESPONSE 29: The reviewer's statement that neonatal male circumcision is a "nontherapeutic, purely cosmetic procedure" is inaccurate. There is strong scientific evidence that demonstrates several health benefits of male circumcision, which has been discussed in previous responses and outlined in the CDC background document. Adverse events are rare and are generally easily managed, particularly in children under one year of age. The background document provides evidence that the benefits of neonatal male circumcision outweigh the risks by 100 to 1, and include benefits such as reduced risk for HIV and STD acquisition, urinary tract infections, penile cancer, prostate cancer, Reviewer Comment: Whether parents can legally and ethically make a decision on the child's behalf to undergo a non-therapeutic, purely cosmetic procedure has not been clearly decided. The current ethical standard is that procedures in children that can safely wait until the child can provide his own informed consent should be delayed until Concerns about the CDC background document are similar to those that have been addressed in responses to the CDC recommendations, so we refer the reviewer to our prior responses on these issues. The literature review has been updated through October 2015, and in doing so we have added reductions among heterosexual men in the incidence and prevalence of genitourinary disease, prevalence and incidence of high-risk oncogenic human papillomavirus (HR-HPV), prevalence of Trichomonas vaginalis (T. vaginalis), incidence of syphilis, and prevalence of Mycoplasma genitalium ( M. genitalium) We also added a discussion of reductions in the following infections among female sexual partners of circumcised men based on RCTs: prevalence of GUD, prevalence of HR-HPV, prevalence of T. vaginalis, prevalence of bacterial vaginosis, and incidence of syphilis. There was also evidence of increased clearance of HR-HPV infection among circumcised heterosexual men and their female sexual partners in the RCTs. In the absence of RCTs in MSM, we also summarized data from observational studies showing that among MSM who practiced mainly or exclusively insertive anal sex, circumcision was associated with a decrease in acquiring new infections with HIV and with one oncogenic HPV type (HPV-16).#
First, is the obvious lack of scientific and scholarly rigor that went into preparing this draft. While it is stated that the writers of the draft performed a search of the medical literature, the evidence (in the form of the draft itself) indicates that their search was far from complete. Instead of collecting and analyzing data, they relied on review articles to do the work for them. One review article was published in 1983 -a bit dated to say the least. In some sections, the draft relied on opinion pieces as their sources of information. In areas where review articles were not available, the information provided was far from complete. For example, in reviewing the medical literature on the impact of male circumcision in North America, which is a major thrust of the draft, only two of the eight available studies are mentioned. Similarly, no serious attempt was made to review the harms, risks, complications, or pain associated with male circumcision. The draft has only 255 references, some of which are redundant, which are only a small sampling of the material available in the literature. A PUBMED search using the search word "circumcision" on January 12, 2015 identified 6338 publications.
# RESPONSE 1:
The CDC background document summarizes findings from a systematic literature review that was conducted in order to assess evidence on the association of male circumcision with medical benefits and adverse effects. Systematic reviews were conducted for the following outcomes related to medically attended male circumcision: HIV acquisition and transmission (female-to-male, male-to-female, and male-to-male); other STIs; penile cancer; cervical cancer; infant UTIs; risks and adverse events; sexual function and penile sensation. All studies of outcomes of male circumcision up to the end of November 2012 in Medline, Embase and Cochrane Library, as well as citation lists were included in the draft recommendations for public comment and peer review. More recent data through March 2013 were included in updating data related to the HIV epidemic in the United States. Studies were restricted to those published in English after 1950, presenting original data, including RCTs, cohort studies, case-control studies, cross-sectional studies, case series and case reports. Study design was classified according to guidelines used for collecting scientific data in reports published in the Guide to Community Preventive Services (the Guide). The evidence was assessed according to strength of association, consistency of findings across studies and the methodologic rigor of study designs. Because they minimize considerably the risk of spurious causality and bias, randomized controlled trails (RCTs) are considered the most rigorous method for determining whether a cause-effect relationship exists between a treatment and an outcome. Our literature review through November 2012 also included a broad, non-systematic narrative review for the section "Considerations related to male circumcision in the United States," because this section did not evaluate clinical outcomes. Since the time of the initial review, an updated literature review was conducted through October 2015 which added more evidence to the already strong field of evidence indicating that male circumcision is associated not only with a reduction in transmission of HIV, HSV-2, and oncogenic forms of HPV, but also decreased transmission of other STDs including genital ulcer disease, syphilis, m. genitalium, t. vaginalis, bacterial vaginosis, and trichomoniasis.
# COMMENT:
The draft also ignores basic epidemiological principles. It fails to apply the standards that are needed to identify when an intervention should be applied. Throughout the draft, it is assumed that male circumcision will be successful as a primary prevention for HIV, when the data clearly demonstrate that it is ineffective as primary prevention.
# RESPONSE 2:
Male circumcision is an effective primary prevention strategy, preventing transmission of HIV infections to men during penile-vaginal intercourse. Three large, well-designed RCTs have demonstrated that men who were circumcised are 50-60% less likely to acquire HIV through heterosexual intercourse than men who were not circumcised. The findings from the RCTs are also consistent with many other observational studies of the effect of male circumcision on HIV transmission. In 2007, a panel of consultants convened by CDC concluded that conducting a trial in the United States to evaluate efficacy of male circumcision for HIV prevention would not satisfy the criteria of clinical equipoise, given the weight of evidence from existing studies that male circumcision is protective against HIV. 1 COMMENT: Even its role as a secondary preventive measure has only been evaluated in one study in the United States, which included a very small, limited population. For this very small population, modeling by the CDC has estimated that male circumcision's impact on infection risk is nearly inconsequential.
# RESPONSE 3:
The CDC recommendations state that while the impact of male circumcision on HIV in the United States is limited by relatively low HIV prevalence and high male circumcision rates, there is epidemiologic data to suggest that some subpopulations in the U.S. are likely to benefit. Sansom and colleagues modelled the impact of male circumcision on lifetime risk of HIV infection in males in the United States, demonstrating that male circumcision reduced the 1.87% lifetime risk of HIV among all males by about 16% but that the effect varied by racial group. The effect was greatest among black males, where the 6.23% lifetime risk of HIV was reduced by about 21%. 2 It is also important to note that male circumcision confers health benefits in addition to protection against HIV, including protection against oncogenic forms of HPV, HSV-2, and infant urinary tract infections.
COMMENT: Policy should be based on more than one small subset of patients from a single study when several other studies fail to support this conclusion. It is clear that both the investigators of the randomized clinical trials and the CDC draft authors do not understand the epidemiological difference between efficacy (a positive finding in a research setting) and effectiveness (positive results in the real world).
# RESPONSE 4:
The CDC recommendations are not based on "one small subset of patients from a single study." The CDC recommendations are based on a thorough review of the large body evidence demonstrating certain health benefits of male circumcision, as well as on careful consideration of the potential public health implications of these findings in the United States. See RESPONSE 1 for a description of literature review methods.
# COMMENT:
The draft fails to adequately scrutinize the validity of the few studies it identified. It assumed the randomized clinical trials could not harbor any bias (the draft actually states this!) and did not question the methodology of these studies, although their methodology has been questioned extensively. Instead of accepting the study results at face value, the expectation of scholarly rigor would demand that these studies be carefully scrutinized, and a determination made as to whether the studies generated valid results and/or if the criticisms raised about these studies were convincing. The writers of the draft made no effort to question or analyze these studies.
# RESPONSE 5:
In 2009, a Cochrane committee conducted a review of the findings from the 3 male circumcision RCTs. The review evaluated the quality of the scientific evidence and potential impact of bias on the results for each trial. The review authors reported that the potential for significant biases affecting the trial results was low to moderate, and concluded that in spite of any potential bias there is "strong evidence" that male circumcision reduces the likelihood of HIV acquisition in men through heterosexual transmission. Authors concluded "male circumcision can be considered as an effective measure to partly prevent HIV acquisition in heterosexual men." 3 A sentence in the "Methods to gather, synthesize, and interpret information" section of the background document was amended to read: "Because they reduce spurious causality and bias, RCTs were considered the most rigorous method for determining whether a cause-effect relationship exists between a treatment and an outcome."
COMMENT: If a student were to submit these drafts for consideration as a senior undergraduate or master's thesis, they would fail based on their lack of scholarship. It appears the CDC was only going through the motions in preparing this draft. If the CDC had performed an adequate search of the medical literature and applied the expected level of scholarly rigor, their conclusions and recommendations would have been different. Perhaps that was the point. Perhaps the hope was, by releasing the draft with a selective bibliography, no one would recognize the lack of scholarly effort or call the CDC out on doing a subpar job. It worked for the American Academy of Pediatrics, and they seemed to get away with it. The difference is that CDC documents are open for public comment because it is a government agency. One would think that, after all of the embarrassment the CDC has endured in the recent past, they would want to put their best foot forward by publishing a rigorous, balanced, evidence-based assessment of male circumcision. That obviously did not happen.
# RESPONSE 6:
The background document is inclusive of research that both supports and refutes the conclusions shared in the CDC recommendations, including multiple documents authored and co-authored by the reviewer. Commentary within the CDC background document that pertains to the quality of the individual findings analyses is based on an objective evaluation of scientific merit. Also see RESPONSE 1 for a description of methods used to literature search.
COMMENT: Second, is the lack of attention to detail. Many of the citations given have the authors and journals incorrectly listed. Several of the citations require updating, while several of the citations were redundant. There are several misspellings in the manuscript. This indicates the CDC did not expend sufficient effort putting forth this piece of work, which is consistent with its lack of scholarly rigor.
# RESPONSE 7:
Peer reviewers were provided with the latest available draft of the CDC recommendations and background documents. These documents were working drafts, not a final version for publication. Any errors in spelling, grammar, or punctuation will be addressed prior to dissemination of the final documents.
COMMENT: Third, is the wanton disregard for the medical evidence. It is clear throughout that the writers of the CDC draft believe absolutely in the presumption that infant male circumcision can reduce HIV and sexually transmitted infections beyond a shadow of a doubt. As a consequence, the draft goes about finding evidence to support their presumption and primarily presents evidence supportive of this presumption, despite evidence to the contrary. The quality of the evidence supporting the presumption is never questioned. Any evidence that does not support their presumption is either ignored, criticized, or dismissed. As a consequence, the draft is laughably biased and reflects the expectation bias of its writers.
RESPONSE: See RESPONSE 6.
COMMENT: Fourth, is the lack of a thorough discussion of the foreskin and its anatomy, histology, physiology, and function. It is standard procedure for review articles of this type to review these topics to provide a basic science foundation. How can the CDC discuss the biological plausibility of sexually transmitted infections without a knowledge of the basic anatomy, histology, physiology, and function? This information must be included since health care providers must understand what is lost by removing the normal foreskin/prepuce. How else can they explain the impact of its removal to patients? This information is also an essential element of the disclosure given during the informed consent process.
# RESPONSE 8:
The CDC background document addresses concerns surrounding the role of the foreskin in sexual sensation and discusses research on the impact of male circumcision on sexual function and penile sensation. The background document also includes a section on biologic plausibility which describes the biology of the foreskin and the basis for HIV acquisition.
COMMENT: Fifth, is how out of step the CDC is with the rest of the world. National medical organizations and human rights groups throughout the world, including the Council of Europe, are, in increasing numbers, denouncing infant male circumcision as being medically unnecessary and a blatant human rights violation. At this point in time, the CDC and the American Academy of Pediatrics are the last stronghold in the defense of infant male circumcision. Remarkably, the draft fails to mention all the medical organizations outside of the United States who have weighed in with an opposing opinion on male circumcision. Is there some source of special knowledge the CDC has in its possession that allowed them to reach conclusions that are diametrically opposed to every other national medical organization (other than the American Academy of Pediatrics)? If it exists, why is it missing from the draft? Please provide enlightenment. If the CDC has a clue, they could at least share it. penis, which would result in intact men being over-diagnosed with HPV because circumcised men are more likely to have HPV on the shaft of the penis, which these researchers did not sample. As a consequence, their results can be completely explained on the basis of inadequate sampling. Subsequent large cohort studies have failed to find an association between male circumcision status and genital HPV infections. The CDC is selectively citing studies that promote male circumcision while ignoring studies, without a sampling bias, that do not support the practice of male circumcision. In other words, the CDC is using a selective bibliography to cherry-pick the studies to support male circumcision.
# RESPONSE 15:
The findings from the randomized controlled trials present high-quality evidence that male circumcision is protective against HSV-2 and high-risk oncogenic types of HPV.
Claims that the cause of lower STI incidence measured in the male circumcision arm of the RCTs was due to sexual abstinence during the 6-week healing period, referred to by the reviewer here as "lead-time bias", not to the intervention itself, have been discredited. The protective effect of male circumcision against HPV in the first 12 months has been observed during the months 12-24, well after the initial period of abstinence ended. [4][5][6] In addition, authors of one RCT provided calculations that demonstrate that male circumcision is protective against HSV-2 even when abstinence during healing time was accounted for in the male circumcision arm. 7 Concerns that sampling site impacted the findings for HPV have also been discredited previously. In the South Africa RCT, authors intentionally sampled the urethra for HPV because it was unlikely detection of HPV or other lesions would be affected by male circumcision status at this site. 8 In addition, authors of the Uganda RCT conducted a follow-up analysis on prevalence of HPV on the coronal sulcus and shaft of the penis, and reported that men in the male circumcision arm men had lower prevalence in both areas 12 months after the procedure than those in the control (uncircumcised) arm. A 2011 meta-analysis of 23 RCTs and cross-sectional studies investigated the effect of the anatomical sampling site on relationship between male circumcision and HPV. Authors reported a strong protective effect of male circumcision against HPV when sampling was done at each of glans/corona, penile shaft, and scrotum (OR, 0.58; 95% CI, 0.40-0.82; n = 10 studies), and also that this protective effect was observed when sampling was done at the glans/corona only (OR, 0.47, 95% CI, .37-.60; n=2 studies) and at the urethra only (OR, 0.35; 95% CI, 0.12-1.05; n=5 studies). 9 COMMENT: CDC draft: Since the release of these trial data, various organizations have updated their recommendations about adult male 8 and infant male circumcision.
Reviewer Comment: The CDC lists only organizations from the United States that have leaned in favor of male circumcision. They fail to mention that national medical organizations from Norway, Sweden, Germany, Denmark, the Netherlands, Slovenia, Finland and others have condemned the practice of infant male circumcision, both on medical and on human rights grounds. The Council of Europe also considers infant male circumcision a human rights violation. _ENREF_8 benefit from elective male circumcision. When one looks at the impact of male circumcision on HIV prevalence in African countries, in at least eight countries the prevalence of HIV infection is higher in circumcised men than it is in intact men. This suggests that the results of the randomized trials from Africa do not even apply to Africa, let alone the United States. There is not a single study of infant male circumcision that has found a significant protective effect against HIV. Most male circumcisions in the United States are performed on infants. There have been eight studies looking at the impact of male circumcision on HIV prevalence in North America. None of them have found a significant protective effect, and one found that circumcised men were at significantly greater risk of HIV infection. The preponderance of evidence indicates that the results of the trials in Africa do not apply to the United States. aesthetic preference, and ethical considerations.
Reviewer Comment: The Council of Europe and national medical organizations from a number of European countries consider neonatal male circumcision to be a human rights violation, so this recommendation does not apply to neonatal male circumcision, as the proxy consent provided for the procedure may not be valid.
# RESPONSE: See RESPONSE 9.
COMMENT: Regarding male circumcisions for males who are able to provide their own consent, the disclosure process needs to be extensive and exhaustive since this is usually an elective, cosmetic procedure. Because it is usually an elective, cosmetic procedure, such a discussion should only take place after the male inquires regarding the procedure. Solicitation of male circumcision without a clear immediate medical indication is considered unethical according to the American Medical Association.
# RESPONSE 21:
The reviewer is correct in stating that male circumcision is usually an elective procedure, but the implication that the choice to circumcise is only "cosmetic" and that CDC recommendations encourage health providers to "solicit" male circumcision is inaccurate. The CDC recommendations outline counseling topics to assist health providers in discussing medical male circumcision with individuals who are considering male circumcision for themselves or for their male child. The counseling topics contain information on potential health risks and benefits of male circumcision at different ages and within different subpopulations. All statements about health risks and benefits in the document are based on sound scientific evidence and were informed by an objective and comprehensive review of scientific data from studies conducted in the United States and in international settings. The CDC recommendations suggest that individuals consider these messages on health risks and benefits in conjunction with other non-medical factors in the decision, which may include aesthetics, religion, or cultural considerations.
COMMENT: Performance of a procedure on a child, by a physician or health care provider, should be done based on medical need, not based on religion, societal norms or customs, vague notions of hygiene, or the aesthetic preference of an adult. To do otherwise, violates the child's basic human rights. Physicians are not cultural brokers. They have taken an oath to "Do no harm" and to do what is in the patient's best interest. In no respect is the removal of normal, healthy genital tissue in a child's best interest. Physicians do not routinely remove normal tissue from children for any other reason, so why would removal of the foreskin be the exception? RESPONSE 22: Because medical male circumcision confers a number of health benefits and has a low risk of adverse events, the decision whether to circumcise an infant or child is considered an appropriate exercise of parental or guardian authority. If a child's preference is of particular importance to parents or guardians, they may opt to delay male circumcision until a time when the child can make a decision for himself. Delaying medical male circumcision to adolescence or adulthood has a higher risk of accurate, value-neutral term for a man with all of his original genital tissue is "intact" or "normal" or "natural." By continuing to use the term "uncircumcised," the CDC is identifying its pro-circumcision bias to anyone who is familiar with the semantics on this issue. Males who are indeed "intact" find use of the term "uncircumcised" to be hate speech because they are singled out as "different," supposedly "abnormal" and/or possibly "unclean." Nothing could be further from the truth. Profiling a group of people in this way is discriminatory, hateful rhetoric. Furthermore, counseling any sexually active intact adolescent about male circumcision without provocation is malicious sadism. Teens, by their very state of emotional development, have self-image and self-esteem issues. This is especially true in regards to their primary and secondary sex organs. For a health care provider to engage in an unsolicited discussion of male circumcision with an intact adolescent male, only sends the message to the patient that something is seriously wrong with their genitals and, by extension, there is something wrong with them and with their parents. Given that Hispanics are less likely to be circumcised than other ethnic groups in the United States, would such a discussion be interpreted as racist, anti-immigrant hate speech? What self-respecting health care provider would want to impose such emotional trauma on their patient when there is no benefit in doing so. It is important to obtain a good sexual history on patients, but extraordinarily few adolescents would fall into a category that might possibly impact their risk of HIV infection. Furthermore, the gender of an adolescent's sexual partner may, and likely will, change frequently over the years, so determining this information seems of little value. The limited time during an office visit with an adolescent male would be better spent discussing how to properly apply a condom.
# RESPONSE 24:
The terms "circumcised" and "uncircumcised" are used to describe whether a male has undergone a procedure to remove the foreskin. The CDC recommendations in no way encourage providers to place a value judgement on either status.
The CDC recommends that health providers discuss sexual risk behaviors and risk reduction strategies with all sexually active adolescent and adult males. The CDC also recommends health providers ascertain whether an adolescent or adult male is at risk for acquiring HIV through heterosexual intercourse prior to discussing male circumcision. Neither recommendation is discriminatory towards male circumcision status.
# COMMENT:
3A. Counseling uncircumcised heterosexually and bisexually active adolescent and adult males (i.e., men who have sex with women) 3A-2. CDC draft: All uncircumcised adolescent and adult males who engage in heterosexual sex should be informed about the significant, but partial, efficacy of male circumcision in reducing the risk of acquiring HIV and some STIs through heterosexual sex, as well as the potential harms of male circumcision. the child can provide that consent. See also RESPONSE 22.
# COMMENT:
CDC draft: When counseling parents about male circumcision for an adolescent minor, the adolescent should be included in the decision-making process about undergoing elective male circumcision. When counseling an adolescent inquiring about male circumcision, parents should be engaged in the discussion, unless the adolescent is legally emancipated.
Reviewer Comment: Such counseling should only occur when the patient inquires about the procedure. To offer this information without an inquiry would be unethical, and potentially harm the adolescent's self-esteem and body image.
# RESPONSE 30:
The CDC recommendations state that male adolescent minors and their legal guardians should be included in the decision surrounding elective male circumcision, and that medical providers should inform the adolescent and guardians of health benefits and risks associated with the procedure. The CDC recommendations do not restrict counseling about male circumcision to inquiries from adolescents. Providers may also counsel on male circumcision if parents or guardians inquire and in cases where the provider believes the adolescent may be at risk of acquiring HIV through heterosexual intercourse. Counseling messages on elective male circumcision discuss the health benefits and risks associated with the procedure, and are not discriminatory toward uncircumcised males. See also RESPONSE 21.
# COMMENT:
4-A. CDC draft: Parents and guardians should be informed about the medical benefits and risks of neonatal, pediatric, or adolescent medically performed male circumcision (see Box):
o During infancy, circumcised infants are less likely than uncircumcised infants to experience urinary tract infections (UTIs), although UTIs are uncommon during infancy.
Reviewer Comment: To be accurate, this statement should state that intact boys are more likely to be diagnosed with urinary tract infections, but they may not necessarily have more actual UTIs. Whether or not they actually have more urinary tract infections is unclear. It needs to be added that between 110 and 190 boys need to be circumcised to avoid one additional boy being diagnosed with a urinary tract infection. Parents and guardians should be reassured that urinary tract infections can be treated with oral antibiotics and rarely, if ever, lead to long-term kidney problems or hypertension. It should be added that multiple studies from Israel have found that urinary tract infections increase in boys following ritual male circumcision.
# RESPONSE 31:
The absolute risk of a male infant developing a urinary tract infection and relative risk reduction of infant urinary tract infections (UTIs) associated with male circumcision is provided in the CDC recommendations. There is a strong evidence base that male circumcision protects against infant UTIs. Typical treatments and long-term impact of infant UTIs vary with severity of infection; infant UTIs may require more invasive treatment and diagnosis beyond oral antibiotics. Ritual male circumcision is outside the scope of these guidelines.
Reviewer Comment: The bandaging used following a ritual male circumcision may obstruct urine flow, leading to the urinary tract infection.
# RESPONSE 32:
The CDC recommendations address medical male circumcision only. Discussion of adverse events caused by ritual male circumcision is outside of the scope of the recommendations.
# COMMENT:
o CDC draft: Circumcised boys are less likely than uncircumcised males to experience balanitis and balanoposthitis.
Reviewer Comment: This statement needs to be deleted as it is factually incorrect.
There is no evidence to support this. Two studies found that circumcised boys under the age of three years were more likely to have penile inflammation than their intact counterparts. By providing health care providers with recommendations that are not factually accurate, the CDC is encouraging health care providers to provide parents and guardians with information that is not true. In other words, they are encouraging health care providers to violate the trust patients have in them and to engage in malpractice. If the provider is sued on the basis of providing the false information the CDC is encouraging, who is liable? The CDC should not put health care providers in the position of lying to their patients. (However, the entire CDC draft document is putting health care providers at risk for medical malpractice because of the fallacies it contains.) RESPONSE 33: As stated in the CDC background document, findings from a retrospective cohort and a prospective cohort study indicate that inflammation such as balanitis and balanoposthitis were less likely to occur in circumcised boys than in uncircumcised boys. Male circumcision may also be recommended as a treatment for balanitis or balanoposthitis that does not respond to other treatments.
# COMMENT:
o CDC draft: During adulthood, circumcised males are less likely than uncircumcised males to experience penile or possibly prostate cancer.
Reviewer Comment: The incidence of penile cancer is quite low, and it should be mentioned that the number needed to treat is between 4237 and 7184. Despite having a much higher male circumcision rate in the United States, the penile cancer incidence rate in the United States is no different than what is seen in Europe among primarily intact males. The evidence on prostate cancer is so weak, inconsistent, and inconclusive, that it should not be mentioned, especially when the incidence in the United States is quite high as is the male circumcision rate. Pathological studies indicate that many males, up to 70-80% by the seventh and eighth decades, have microscopic prostate cancer at autopsy, which was not clinically detected. So, where is the benefit of being circumcised? RESPONSE 34: As stated in the CDC background document, penile cancer is rare in developed countries, accounting for <1% of malignancies among men. Several observational studies demonstrate penile cancer strongly associated with a lack of male circumcision, and a case control study has demonstrated the odds of invasive penile cancer are greater in uncircumcised men than in circumcised men. See the CDC background document "Penile and prostate cancers" section for additional information.
The lifetime risk of prostate cancer among men in the U.S. during 2008-1010 was about 15%. 13 Male circumcision before first sexual intercourse was associated with a 15% reduction in risk of prostate cancer compared to that of uncircumcised men in a combined analysis using pooled data from 1754 cases and 1645 controls in 2 population-based case-control studies (95% confidence interval [CI], 0.73-0.99). 14
# COMMENT:
o CDC draft: Other anticipated health benefits derive in part from future prevention of HIV and some STIs acquired through heterosexual sex. The risk for any individual neonate, child, or adolescent cannot be definitively defined at the time that a male circumcision decision is made; for example, current risks for HIV and STIs, such as those for a particular individual's racial/ethnic group or gender, may not remain constant in the future.
Reviewer Comment: Circumcised men have an overall STI risk that is greater than for intact men.
RESPONSE: See RESPONSE 26.
# COMMENT:
Is this stating that infants are not at risk for sexually transmitted infections, including HIV? If this is the case, that would favor waiting until the child is old enough to provide his own consent. Since when do we remove healthy normal tissue from a baby to possibly prevent some unknown future risk of disease? There are other more pressing diseases to contend with, if this is the focus of the CDC.
# RESPONSE 35:
Persons are not at risk of acquiring HIV and other STIs through sexual transmission until sexual debut. Individual lifetime risk of acquiring HIV and other STIs is not known at the time of birth, and may change from the time of birth to the time of sexual debut. A benefit of male circumcision prior to sexual debut is that it ensures the protective effects of male circumcision against sexually transmitted infections, including HIV, are present before commencement of sexual activity that put men at risk for these infections.
# COMMENT:
o CDC draft: Considerations for the timing of male circumcision:
• Neonatal male circumcision is, safer, and heals more rapidly than male circumcision performed on older boys, adolescent males, and men, and is less expensive.
Reviewer Comment: It is patently false that neonatal male circumcision is safer. This statement is based on myth, not on facts. The few studies that have made the appropriate comparison do not support this conclusion. There is no evidence that the wound heals more rapidly. There have been no studies in the medical literature that address wound healing and the Background draft does not address this claim. Since the foreskin has not separated from the glans in neonates, it is more likely that neonatal male circumcision takes longer to heal and is more painful.
# RESPONSE 36:
Complications occur in less than 0.5% of infants, and in approximately 9% of children age 1 -9 years. Among newborns and children age 1 -9 years, the most frequently reported complications include bleeding and inflammation of the penis and the need for corrective procedures. Delaying age of male circumcision from infancy to one year of age or older can increase the risk of some complications associated with the procedure, which include correctional procedures, bleeding, and inflammation. 15 In patient-oriented health educational materials in the U.S., healing time after infant male circumcision is reported to be about 7 to 14 days 18 19-21 and to be about 2 -6 weeks in older children, adolescent, and adults. 19,22 COMMENT: Neonatal male circumcision is less expensive because it is not performed under general anesthesia, the only adequate anesthesia besides a caudal block.
Neonates also are much easier to strap down without a major fight ensuing. The topical and local anesthetics that are used for neonatal male circumcision do not provide adequate anesthesia, as has been demonstrated in multiple studies. The procedure is still quite painful when these are used. The pain associated with neonatal male circumcision, even when topical and local anesthetics are used, has been linked to circumcised boys crying longer and louder when given vaccinations at four to six months of age and circumcised boys having a significantly greater risk of developing infantile autism, autism spectrum disorder, and hyperactivity. The availability of general anesthesia for male circumcision performed in older males is another advantage of waiting until the male can provide his own consent.
# RESPONSE 37:
Minimizing pain is an important consideration for medical male circumcision. Appropriate use of analgesia is considered standard of care for medical male circumcision at all ages, and appropriate analgesia can substantially control pain for infants, children, and adults during and after the procedure. As demonstrated by Banieghbal and colleagues, appropriate analgesia can substantially control pain. In their study, 93.5% of neonates circumcised in the first week of life with appropriate analgesia gave no indication of pain on an objective, standardized neonatal pain rating system. 23 The study which found an association with autism and male circumcision focused only on ritual male circumcision which is outside the scope of these guidelines and has been critiqued as being methodologically unsound and biased. 16,17 COMMENT:
• CDC draft: Male circumcision can also be conducted in adulthood when the individual can make the decision for himself. However, male circumcision after sexual debut could result in missed opportunities for: ▪ HIV and STI prevention during the window period between sexual debut and male circumcision
Reviewer Comment: This a cheap scare tactic designed to influence parents and teens into accepting male circumcision before full adulthood. According to the CDC's own numbers, the risk of HIV infection under the age of 15 years is very low. How many 15 year olds are having unprotected sex with female partners who are HIV-infected? RESPONSE 38: Prevention interventions work best when implemented prior to exposure. In the case of sexually-transmitted infections such as HIV, the time period prior to exposure occurs prior to sexual debut. In addition, male circumcision prior to sexual debut is more effective at protecting against prostate and penile cancer 14,24 . Uptake of the procedure after the neonatal period is also likely to be lower due to the increased cost, greater likelihood of complications, and other barriers to male circumcision at a later age.
Similarly, the only STI that might be associated with male circumcision status is syphilis, which is also very rare and easily treated with antibiotics. This risk is so low that there is no need to mention it. The only people who do mention it are the pro-circumcision lobbyists, who believe it may have some rhetorical value. STIs, HPV, HIV have been shown to be more common in circumcised males in North American studies.
# RESPONSE 39:
Several STIs are associated with lack of male circumcision. In randomized controlled trials for which data are available, reductions in the 1) prevalence of genitourinary disease (GUD) [25][26][27] , 2) incidence of herpes simplex virus type 2 (HSV-2), 4,28 3) prevalence, [4][5][6]29 _ENREF_9 incidence, 30,31 and clearance 29,31 of high-risk oncogenic human papillomavirus (HR-HPV)_ENREF_7, 4) prevalence of Trichomonas vaginalis, 27,32 5) incidence of syphilis, 33 6) prevalence of bacterial vaginosis, 27 and 7) prevalence of mycoplasma genitalium 34 were also demonstrated._ENREF_19
See also RESPONSE 15.
# COMMENT:
▪ CDC draft: Prevention of UTIs during infancy.
# Reviewer Comment:
The risk of UTI is small and none of the analyses that have been published believe that male circumcision is a cost-effective method to address this small risk. If an infant male circumcision costs $285 (according to the CDC) and the number needed to treat is 195, then it would cost over $50,000 to prevent one urinary tract infection that can easily be treated with an antibiotic that costs less than $20. So, this is also a cheap scare tactic.
# RESPONSE 39a:
See RESPONSE 31. The cost-effectiveness of treatment of UTIs is not relevant to the statement in the CDC recommendations that male circumcision prevents UTIs during infancy. In addition, In a meta-analysis of 18 studies mainly from the U.S., the prevalence of UTI in infants presenting with fever in outpatient clinics and emergency departments was 7.0% (95% CI = 5/5 -8.4), but as high as 20.1% (95% CI = 16.8 -23.4) among febrile uncircumcised males aged < 3 months compared with 2.4% (95% CI = 1.4 -3.5) among febrile circumcised males aged < 3 months, and 7.8% (95% CI = 6.6 -8.9) among both febrile and afebrile older children aged < 19 years. 35
# COMMENT:
o CDC draft: The most commonly described complications of medically performed male circumcision in the United States are typically uncommon and easily managed.
Reviewer Comment: The most commonly described complications of medically performed male circumcision are the loss of the most sensitive portion of the penis (100%) and meatal stenosis (5% to 20%). Both are common and not easily managed.
Once the majority of the fine-touch neuroreceptors are removed from the penis via male circumcision, there is no way to grow them back. While there are thousands of circumcised men who spend years trying to stretch their remaining shaft skin so the glans of the penis can once again be covered, there is no way to restore the fine-touch neuroreceptors.
# RESPONSE 40:
Many studies have evaluated the impact of male circumcision on sexual satisfaction or function and have found little evidence of adverse effect on penile sensitivity, sensation, or sexual satisfaction. [36][37][38][39][40][41][42] The randomized controlled trials in Kenya and Uganda reported no adverse effects of male circumcision on sexual satisfaction. 38,43 COMMENT: Meatal stenosis (narrowing of the opening of the urethra) usually requires surgical enlargement of the urethral opening done under general anesthesia (the child might as well have waited to be circumcised to partake of such pain control). Consequently, neither of these complications is easily managed. Either the writers of this set of recommendations are intellectually obtuse, or they are purposely covering up the side effects of male circumcision to portray the procedure in the most positive light possible. By ignoring the harms and complications of male circumcision, of which there are hundreds, they are doing a disservice to the health care professionals, parents and patients who might rely on this information, and ultimately it is a disservice to society as a whole.
RESPONSE 41: Meatal stenosis may occur very rarely as a result of medical male circumcision, but there is no high quality study that links meatal stenosis to medical male circumcision. See also RESPONSE 35.
# COMMENT:
o CDC draft: Severe complications are rare in all age groups.
Reviewer Comment: It all depends on how "rare" and how "severe" and how "complication" is defined. But perhaps a more important discussion is whether any severe complications, regardless of their rarity, are acceptable following a nontherapeutic, purely cosmetic procedure performed on an individual who is unable to give his own consent? RESPONSE 42: Potential complications from male circumcision are addressed in the CDC background document. Severe complications from the procedure include severe bleeding, partial or complete amputation, laceration repair, or other correctional procedures.
See also RESPONSE 35 and RESPONSE 29.
# COMMENT:
• CDC draft: Among newborns and children age 1 to 9 years, most frequently reported complications include bleeding and inflammation of the penis or the need for corrective procedures. Complications occur in less than ½ % of infants, and in approximately 9% of children age 1 to 9 years.
# Reviewer Comment:
The complication rates in this statement come from a study based on data collected from a database. This study design typically misses between 90% and 95% of the complications when compared to the number of complications identified when performing a chart review. This statement needs to be deleted and the complication rate from charts reviewed by the CDC, which revealed a complication rate of 3.1%, should be put in its place. Similarly, there are studies in which the complication rates of male circumcisions performed in neonates were compared to the complication rates of male circumcisions on older boys at the same time in the same place using the same criteria. The results have been mixed. In some, the complication rates were higher in newborns or there was no difference between the two groups. None showed a lower rate of complications in newborns. This effort to paint neonatal male circumcision as having lower complication rates is purely a propaganda tool with insufficient quality evidence to support it.
# RESPONSE 43:
The statement that there is "insufficient quality evidence to support" the cited complication rates of male circumcision is inaccurate. Several large studies of medically attended male circumcision in the neonatal period in the United States estimate the rate of adverse events at less than 0.5% (ref: Cristakis, Wiswell, Gee). See also RESPONSE 36.
# COMMENT:
• CDC draft: Among persons 10 years of age and older, the most frequently reported complications include those complications reported in younger children as well as wounds of the penis. Complications occur in approximately 5% of persons in this age group 15 .
Reviewer Comment: The immediate complication rate for neonatal male circumcision ranges from 2% to about 6%, with delayed complications being much higher. For example, meatitis (inflammation of the urethral opening) occurs in 20%, meatal stenosis in 5% to 20%, adhesions in 25%, skin bridges in 4.1% to 12.7%, subcutaneous granuloma in 4.97%, phimosis in up to 2.9%, hidden penis in 1%, and 1% of parents who insist on the male circumcision being redone because they do not like the cosmetic outcome. The point is that neonatal male circumcision may have a higher complication rate than when it is performed on boys 10 years and older.
# RESPONSE:
See RESPONSE 36, RESPONSE 41, RESPONSE 43.
# COMMENT:
o CDC draft: The American Academy of Pediatrics Taskforce on Circumcision states that the health benefits of newborn male circumcision outweigh the risks and that the benefits of newborn male circumcision justify access to this procedure for families who choose it.
Reviewer Comment: This appeal to authority is inappropriate. The American Academy of Pediatrics Task Force on Circumcision in their report stated several times that they did not know the rate of complications following male circumcision. This may be related to the refusal of the Task Force to consider any case reports or case series in their limited analysis of the medical literature. Most reports in the medical literature of complications are in the form of case reports and case series. The Task Force also did not quantify the rate at which a male who was circumcised would reap any benefit from the procedure. Yet, with the rates of the benefits undefined and the rates of complications unknown, somehow the Task Force was able to say that the benefits outweighed the risks. Making such a statement defies the basic principles of mathematics. When pressed on how they reached their conclusion, the Task Force stated that they felt the benefits outweighed the risks. So, their conclusion was not evidence-based but feelings-based. This conclusion was also criticized by thirty-eight well-regarded medical experts, primarily from Europe, who argued that this conclusion was culturally biased. Why does the CDC mention the Task Force report, which suffers from the same biases and lack of scholarly rigor as the Background Draft? Is it thought that reference to an equally pathetic effort will give the CDC's efforts some unearned credibility?
# RESPONSE 44:
In the United States, reported rates of complications in large studies of medically attended male circumcision in the neonatal period, including infants from birth to age 1 month, are approximately 0.2%, 44,45,46 and vary by type of study, setting, operator and surgical technique. Similarly, the reported rate of complications of medically attended male circumcisions occurring at any age in the United States is 0.23%. 15 In a comprehensive risk-benefit analysis of infant male circumcision based on reviews of the literature and meta-analyses, it is estimated that over a lifetime, benefits exceed risks by a factor of 100:1. 47 Based on a meta-analysis of 22
# RESPONSE 45:
The AAP states that "Trained and competent practitioners, by using sterile techniques and effective pain management, should perform male circumcision. Analgesia is safe and effective in reducing the procedural pain associated with newborn male circumcision; thus, adequate analgesia should be provided whenever newborn male circumcision is performed." See also RESPONSE 37.
Typically in the U.S., providers who perform male circumcision include obstetricians, pediatricians, family practitioners, midwives, and urologists. Also, the AAP notes that "most residency training programs in the respective specialties teach techniques, including the Gomco clamp, Mogen clamp, and Plastibell device." In the U.S., accepted standards of clinical care have been put into place for surgical procedures regardless of the individual procedure, such as pre-op screening of the patient to rule out conditions that might rule out the patient as a surgical candidate. Infection control procedures are also in place. Regarding the technical aspects of conducting male circumcision, medical textbooks describe the various surgical procedures for conducting male circumcision. Typically, residents in training read about a procedure and then observe an experienced surgeon perform the procedure. They may assist an experienced surgeon conduct a surgery until they are deemed ready to take the lead in conducting such a surgery. Routinely, hospitals conduct periodic reviews of morbidity and mortality associated with individual practitioners to determine if a higher level of adverse events is occurring than what is anticipated.
# COMMENT:
Box: CDC draft: Health Benefits and Risks of Elective Medically Performed Male Circumcision • CDC draft: Health benefits of elective male circumcision in adults and adolescents: o Male circumcision reduces the risk of acquiring HIV infection through penilevaginal sex by 50-60%, as demonstrated in three well-conducted clinical trials among adult men living in sub-Saharan Africa.
Reviewer Comment: There is no evidence that the findings of the clinical trials in Africa, which by several objective standards were not "well conducted," apply to male infants or to males living in North America, and there is ample evidence they do not apply. The existence of this "health benefit" is highly speculative. There is no evidence to suggest that any benefit has been demonstrated for infant male circumcision or for heterosexual men in North America.
# COMMENT:
The reduction should be identified as a relative risk reduction. The absolute risk reduction in these trials should be mentioned to provide a true comparison. For example, in the Ugandan study the absolute risk reduction was 0.67% with a number needed to treat of 149. These numbers need to be adjusted for the lower incidence seen in the United States. If one assumes the African results apply to the United States, and there is no evidence to support this assumption, then the absolute risk reduction would be 0.02% with a number needed to treat of 5000. At $285 per male circumcision, this would cost $1.425 million to avoid one HIV infection. Not a good use of resources, especially when this is based on an assumption that is not consistent with the medical evidence. Even if the relative risk reduction is 10%, the number needed to treat would be 25,000 and cost would be $7.125 million. The CDC, by only mentioning the relative risk reduction, is hoping that readers will forget that 50% of a very small number is still a very small number.
# RESPONSE 45b:
See RESPONSE 14. The reviewer's comment on cost-effectiveness is not relevant to the statement in the CDC recommendations that male circumcision reduces the risk of acquiring HIV infection through penile-vaginal sex in men.
o CDC draft: In clinical trials involving heterosexual males living in sub-Saharan Africa, male circumcision reduces the risk of some sexually transmitted infections. Male circumcision reduces the risk of circumcised men acquiring infections with:
• Genital ulcer disease (GUD) (by 48%)
• Herpes simplex virus type-2 (HSV-2) (by 28% -45%)
• Oncogenic types of human papilloma virus (HPV) (by 24% -47%)
• Syphilis (by 42% -62%): Male circumcision reduces the risk of circumcised men having existing infections with:
• Oncogenic types of HPV (by 25% -47%)
• Trichomonas vaginalis (by 53%)
• Mycoplasms genitalium (by 46%)
# COMMENT:
Reviewer Comment: This statement is selective in the results provided and fails to note that these trials did not adjust their results for lead-time bias. Of the three randomized trials, one found virtually no difference (RR 1.06), and in only one was the difference statistically significant. When adjusted for lead-time bias, none of the trials had a result that was statistically significant. When the results of prospective studies on the incidence of HSV-2 infections by male circumcision status are combined in a metaanalysis, and the studies are adjusted for lead-time bias, the results are not statistically significant. This finding is consistent with the meta-analysis results of observational studies that have looked at HSV-2 prevalence by male circumcision status: no statistically significant difference. The CDC markedly overstates this difference. Their draft should also list the number needed to treat for these differences. For the study in Uganda, the NNT was 93, in South Africa 98.6, and in Kenya 261. If the incidence of HSV-2 is lower in the United States, the numbers needed to treat would be greater.
# RESPONSE 45c:
See RESPONSE 15.
# COMMENT:
• CDC draft: HPV: circumcised men were approximately 30% less likely to be infected with high-risk strains of HPV associated with cancers than were uncircumcised men.
Reviewer Comment: The 30% reductions were only reported in two of the prospective studies, where only the glans was sampled. In multiple studies, it has been demonstrated that intact men who have HPV on their genitals are more likely to have the virus primarily on the glans, whereas circumcised men who have genital HPV are more likely to have the virus primarily on the shaft of the penis. By not sampling the shaft of the penis, these studies guaranteed that HPV would be detected 30% more often in intact men, even if the infection rate on the genitals was the same in both circumcised and intact men. In other words, the 30% reduction can be completely attributed to their decision to only sample the glans of the penis, or to only report the results of the samples taken from the glans of the penis. The largest prospective study of HPV and male circumcision was published in 2014. This study sampled the male genitals properly, finding that circumcised men were at greater risk for genital HPV infections, but the difference was not statistically significant. It also found that HPV cleared significantly faster in intact men. The medical literature does not support the hypothesis that intact men are at greater risk for HPV infection. This myth evolved out of methodologically flawed studies that did not properly sample the penis.
# RESPONSE 45d:
See RESPONSE 15.
# COMMENT:
• CDC draft: Adverse events and risks associated with elective male circumcision of adults: o For adult male circumcision performed by clinicians, the rate of adverse events is up to 5%, with pain, bleeding, infection and unsatisfactory postsurgical appearance most commonly reported. While severe and/or long-term complications have been reported, they are so rare that they have not been precisely established.
# Reviewer Comment:
The low percentages reported in these studies indicate that, if a male circumcision is to be performed, it should be performed during adulthood to reduce the risk of complications. At least in adulthood, the male can understand and accept the risks involved. Infant male circumcision has much higher rates of adverse events. It is time studies were done to precisely establish all the complications from male circumcision because it is doubtful they are rare.
# RESPONSE 45d:
See RESPONSE 36.
# COMMENT:
o CDC draft: Adult men who undergo male circumcision generally report minimal or no change in sexual satisfaction or function.
Reviewer Comment: This statement is based primarily on wishful thinking supported by two studies with serious/fatal methodological flaws. The medical literature is replete with studies of circumcised adults who report decreased penile sensitivity, erectile problems, difficulty with insertion during coitus, and difficulty reaching orgasm. Two studies out of Africa used questionnaires whose questions would not have been able to detect a difference if one existed. The men in these studies, if the results are to be believed, are having the best sexual experiences on the planet as their rates of sexual dysfunction were 6 to 30 times lower than reported in other countries. The participants in these studies were, by African standards, extremely well paid for their participation, so it is unknown if this had an undue influence on their answers. There are several studies, including a representative national survey from Denmark, indicating that male circumcision has a negative impact on sexual function. There are several studies that have found circumcised men suffer from premature ejaculation significantly more frequently than intact men. Studies have also indicated that the female partners of circumcised men are significantly more likely to report a lack of sexual fulfillment and pain with intercourse. This statement needs to be changed to fit the currently available evidence.
# RESPONSE 45e:
See RESPONSE 40.
# COMMENT:
• CDC draft: Health benefits of neonatal male circumcision: o The estimated annual rate of urinary tract infections (UTIs) in uncircumcised male infants is 0.70%. Male circumcision reduces the risk for infant UTIs by about 80%.
# Reviewer Comment:
The CDC needs to make a simple calculation to provide the number needed to treat using the numbers provided above: NNT=178.6. At $285 per male circumcision, it will cost over $50,000 to avoid one urinary tract infection that can be treated with an antibiotic that costs less than $20. (Another example of: a large percentage of a small number is still a small number.) It should also be mentioned that urinary tract infections in children are not associated with later development of renal failure or hypertension. Recent recommendations from the American Academy of Pediatrics are that extensive work-ups following urinary tract infections are no longer needed.
# RESPONSE 45f:
The reviewer's comment on cost-effectiveness is not relevant to the statement in the CDC recommendations that male circumcision reduces the risk of infant UTIs. See also response 31.
# COMMENT:
o CDC draft: In the U.S., the estimated lifetime risk of penile cancer for males is about 1 in 1,400 (0.07%) and that of prostate cancer is about 15%. Neonatal male circumcision reduces the risk of penile carcinoma by about 90% and may reduce the risk of prostate cancer by 15% compared to men who are uncircumcised.
# Reviewer Comment
# COMMENT:
• CDC draft: Adverse events and risks associated with neonatal male circumcision: o Adverse events: For male circumcision performed by clinicians,
• the rate of reported adverse events is as follows ▪ 0.4% in infants (age through 12 mo.)
Reviewer Comment: This estimate is from a study that collected its data from databases, which have been shown to only identify 5% to 10% of the complications, as compared to those that can be identified from a chart review. As a consequence, this number has no basis in reality, and it grossly underestimates the actual rates for adverse events and risks in neonates. Percentages for adverse events/complications are listed later in this review.
# RESPONSE 45h:
See RESPONSE 36, RESPONSE 41.
# COMMENT:
▪ CDC draft: 9.1% in children (age 1-9 years) ▪ CDC draft: 5.3% in persons (age 10 years and older)
Reviewer Comment: Older children and their parents are more likely to identify and complain about complications. Consequently, this number may be an overestimate. Yet, when compared to the well documented rates of complications following infant male circumcision, older children may have lower complication rates.
# RESPONSE 46:
Estimates reported for children aged 1-9 years and children aged 10 years and older are from a study using data from a large longitudinal healthcare reimbursement dataset that estimated the incidence of adverse events (AEs) from 2001-2010 that were attributable to male circumcision. 15 These numbers are consistent with data from other prospective and retrospective studies.
# COMMENT:
• CDC draft: Most commonly reported complications in all age groups include bleeding and inflammation of the penis, and correctional procedures. • CDC draft: The incidence of severe adverse events associated with male circumcision performed by clinicians, such as permanent disabilities, disfigurements, and death, is so low that rates have not been precisely established; these events have occurred, but are rare.
Other major complications requiring intervention including major bleeding, and severe infection are uncommon.
Reviewer Comment: The disclosure of information to decision makers during the informed consent process for a non-therapeutic, cosmetic procedure needs to be exhaustive and complete. Male circumcisions are performed primarily for cultural and religious reasons. Therefore, from a medical perspective, the consequences are much more likely to be negative than positive. Health care providers who perform male circumcisions would be well advised to inform decision makers of all of the known complications/consequences because these may occur despite the skill of the provider.
If an adverse or serious complication occurs, the health care provider will be able to document that such a complication was understood by the patient and signed off on. Some of the complications are so common following male circumcision that they are not recognized as complications. Health care providers, when providing disclosure, also must discuss the normal anatomy, histology, and function of the foreskin so the decision maker is informed of what harm/loss results from every male circumcision. The CDC drafts do not mention the normal anatomy, histology, or function of the foreskin, thus disadvantaging the health care provider who is reliant on these documents to properly inform decision makers. This major oversight on the part of the CDC requires attention.
# RESPONSE 47:
The CDC recommendations describe the most common complications of the procedure in all age groups in order to assist medical providers in counseling individuals considering male circumcision for themselves or their child. This document is not intended to take the place the place of a consent form.
# COMMENT:
Here is a list of consequences/complications: Behavioral changes -Newborn male circumcision interferes with breastfeeding -Newborn male circumcision interferes with maternal-infant bonding -Newborn male circumcision interferes with normal sleep patterns -Following male circumcision, with or without anesthetic, boys cry longer and louder when given their vaccinations at 4 to 6 months of age suggesting that male circumcision may permanently alter pain perception.
-Circumcised boys have been found to have a significant association with an increased risk of autism in two studies. There are no contrary data.
-Circumcised boys are at a significantly greater risk of being diagnosed with hyperactivity disorder (attention deficit hyperactivity disorder).
-Circumcised men have a greater risk of having alexithymia (the inability to express emotions) -Circumcised men have been found in two studies to identify themselves as gay/bisexual significantly more frequently than intact men Complications of topical/local anesthesia:
# Hematoma and bruising Methemoglobinemia
Gangrene RESPONSE 48: A thorough discussion of adverse events associated with male circumcision in all age groups is included in the CDC background document. The line listing of adverse events provided by the reviewer is not helpful without citations indicating the source of the information, the proportion of patients who had a male circumcision who experienced such an adverse event, and a comparison of the proportions of uncircumcised and circumcised boys who have experienced these adverse events, and where possible, information about whether the adverse event was associated with medical male circumcision or ritual male circumcision. As earlier noted, ritual male circumcision is outside the scope of the CDC male circumcision counseling recommendations.
# COMMENT:
Reviewer Conclusions:
The CDC recommendations are counterfactual and not evidence-based. The supporting evidence provided is extremely selective and biased. If the CDC had carefully scrutinized much of the supportive evidence they provided, they would have identified methodological weaknesses that would, if they were to act on the quality of the evidence, change their recommendations. Acknowledgement of the vast majority of the medical literature that the CDC ignored would have also altered their recommendations. There are significant oversights, omissions, and inconsistencies throughout that are critical knowledge for the intended audience of clinicians. By using a selective bibliography and by depending on speculation and hype, rather than science, to develop these recommendations, the CDC has placed clinicians and health care providers in an untenable position. In effect, the CDC, by making the recommendations it has, is asking clinicians and health care providers to misinform their patients, and by doing so, commit medical malpractice. As a consequence, the recommendations for the intended audience of health care providers are inconsistent with the medical evidence, reckless, and dangerous. The CDC should eliminate this draft and approach the topic using an evidence-based approach, hopefully with the involvement of experts from around the world on both sides of the discussion.
# RESPONSE 48a: CDC RESPONSE TO REVIEWER CONCLUSIONS:
As stated in previous comments, the recommendations on the health risks and benefits of male circumcision were informed by a careful consideration of high-quality scientific literature, the epidemiologic context of the United States, as well as cultural and ethical considerations. As such, we do not agree with the reviewer's statements that the CDC recommendations are counterfactual and reckless.
The reviewer implies in the conclusion throughout the comments that the CDC recommendations are meant to advocate for male circumcision, which is an inaccurate characterization of the CDC recommendations. The CDC recommendations outline counseling topics to assist medical providers in discussing medical male circumcision with individuals who are considering male circumcision for themselves or for their male child. The counseling topics contain information on potential health risks and benefits of male circumcision at different ages and within different subpopulations. All statements about health risks and benefits in the document are based on sound scientific evidence and were informed by an objective and comprehensive review of scientific data from studies conducted in the United States and in international settings in consultation with subject matter experts. The CDC recommendations suggest that individuals consider this information on health risks and benefits in conjunction with other non-medical factors in the decision. The document does not contain a direct recommendation in support of or in opposition to medical male circumcision for any age group or any demographic.
COMMENT: Reviewer Commentary on CDC Background Draft:
Overall RESPONSE 48b: CDC RESPONSE TO BACKGROUND DRAFT COMMENTARY: We recognize and acknowledge the effort the reviewer has put into the lengthy discussion of the CDC background draft that follows. The citations provided by the reviewer were evaluated for possible inclusion in the most recent update to the CDC background document. Introduction
The material presented in this section of the background document is riddled with inaccurate statements and misrepresentations.
# RESPONSE 48c:
See Responses 1 and 6.
# COMMENT:
Male circumcision performed on an infant is not "voluntary." The infant does not give consent. (Male circumcision campaigns in Africa have become less and less "voluntary" and some adult males are being forcibly circumcised.) Consequently, this statement is false and needs to be revised.
# RESPONSE 49:
Parents provide "voluntary" consent for the infant. See Responses 13 and 22.
# COMMENT:
It is not clear why reference CDC3 was chosen as it is a book written by a known male circumcision advocate. There are basic research articles that should be cited instead.
Prevention of HIV continues to be an unlikely consideration in the decision to circumcise despite pressure by the CDC to make it so (see discussion below). Infants are not sexually active, so HIV prevention is not a concern for them, nor has infant male circumcision been shown to have any impact on HIV acquisition or prevention. Prevention of HIV in adults can be obtained more effectively through non-surgical methods, primarily with the use of condoms.
RESPONSE 50: Upon hearing information about the risks and benefits of male circumcision, including that of reducing a heterosexual male's risk of acquiring HIV infection from an HIV-infected female partner, parents will make a decision as to whether they think this information is pertinent in deciding whether to circumcise their child. A reduction in the future risk of acquiring HIV infection is part of any HIV prevention strategy. A parental decision to circumcise their infant to reduce his future risk of HIV acquisition based on such evidence, is by definition a prevention strategy.
# COMMENT:
When the draft states that male circumcision reduces the risk of male HIV acquisition through penile-vaginal sex, it relies on the results of the randomized clinical trials to make this claim. [1][2][3] The problem is that these trials did not make any effort to determine the source of the infections they diagnosed during their course, so it is unknown whether these infections were the results of penile-vaginal sex, male-to-male sexual contact, or iatrogenic infections. Without knowing where the infections came from, the claim that male circumcision reduces the risk of male HIV acquisition through penilevaginal sex cannot be made.
RESPONSE: See response 12.
# COMMENT:
The CDC draft portrays the perceived benefits in terms of relative risk reduction, but the risks are presented in terms of absolute risk. For example, the 50% to 60% relative risk reduction in HIV infections in the randomized clinical trials sounds like a big deal, but the absolute risk reduction was only 1.3%, which is a difference that many would not consider clinically of any value. It would be best if this draft presented the perceived benefits in terms of the number needed to treat (NNT), and presented the risks in terms of the number needed to harm (NNH) in order to compare them fairly.
RESPONSE: See response 14.
# COMMENT:
In reporting on the 2007 recommendations of the WHO/UNAIDS, it should be explicitly stated that their recommendations did not apply to infant male circumcision. Nor was there a consensus of opinion. In fact, those present describe the measure as being "railroaded through." 4,5 RESPONSE 51: The 2007 recommendations states the following: "Since neonatal male circumcision is a less complicated and risky procedure than male circumcision performed in young boys, adolescents or adults, such countries should consider how to promote neonatal male circumcision in a safe, culturally acceptable and sustainable manner."
# COMMENT:
The statement, "Despite these overall differences, the results of the African trials are likely to have application to HIV prevention efforts in the United States," is completely without foundation. While this may be what the CDC authors want everyone reading it to believe, it has no basis in fact. (The situation in the United States is quite different from that in Africa, including having a first-class medical system in place.) Making such an unsubstantiated statement is unscientific and should be left to the male circumcision lobbyists.
RESPONSE: See responses 2, 19.
# COMMENT:
The statement that African-American men "are known to be significantly less likely to be circumcised compared to white, non-Hispanic men," is, as discussed below, also untrue. [6][7][8] African-Americans in several studies have higher, or the same, overall male circumcision rates in the US, as compared to whites. Hispanics have lower male circumcision rates than either of these groups.
RESPONSE 52: CDC used the most recent nationally representative data available at the time the document was written. See responses 18.
# COMMENT:
It is unclear why the CDC draft questions "whether parents would be willing to have their newborns circumcised to reduce possible future HIV and sexually transmitted infection (STI) risk," when there is no strong evidence that circumcising a newborn will reduce the risk of these infections. To date, not a single study has found neonatal male circumcision to significantly reduce the risk of HIV. (Not to mention, the adult studies fail to show a significant reduction in any risk.) RESPONSE 53: Ecologic studies demonstrate a strong association between lack of male circumcision and HIV infection at the population level. Although links between male circumcision, culture, religion, and risk behavior likely account for some of the differences in HIV infection prevalence, the countries in Africa and Asia with prevalence of male circumcision of less than 20% have HIV-infection prevalence several times as high (seroprevalence range: 0.24 -25.84) than countries in those regions where more than 80% of men are circumcised (seroprevalence range: 0.03-11.64). 49 In addition, based on data from an HIV transmission model fitted to data from the Four Cities Study, including 2 cities in sub-Saharan Africa with relatively low HIV prevalence (Cotonou and Yaoundé) and 2 with high HIV prevalence (Kisumu and Ndola), investigators concluded that differences in rates of male circumcision likely played an important role in differing rates of HIV transmission across Africa. 50 Results from such ecologic studies are important as most male circumcisions globally are thought to occur during infancy, childhood, or adolescence, suggesting that male circumcision at an earlier age confers a long term reduction in risk for HIV acquisition. The fact that male circumcision performed during the neonatal period is associated with fewer and less severe side effects compared to male circumcision performed during adulthood is one of the most important reasons that most male circumcisions are performed neonatally in the U.S. See response 35.
# COMMENT:
This background document presents a very biased, one-sided summary of the data that support the practice of male circumcision while ignoring most of the medical literature that does not support the practice. When the medical literature is looked at in its entirety, male circumcision is not a medically sound intervention. While this background document is supposed to focus on the data in the context of the United States, it only considers two of the eight studies that have looked at the impact of male circumcision on the risk of HIV infection. [8][9][10][11][12][13][14][15] None of these eight studies found a statistically significant positive effect for the intervention, and one found that circumcised men had a statistically significant higher prevalence of HIV than intact men. 14 Likewise, much of this background document is allocated to a discussion about male circumcisions performed in Africa, which are of little interest and irrelevant to the target audience of health care professionals in the United States and not within the scope of the charge the CDC was given in developing these drafts. The effort that went into providing the minute details regarding male circumcision in Africa would have been better spent researching the anatomy, histology, physiology, and function of the foreskin (which this document completely ignores), researching the complications associated with male circumcision, updating information on the risk of sexually transmitted infections, and analyzing the data in the literature rather than relying on the often misguided analysis of others in review articles and opinion pieces.
# COMMENT: Methods to gather, synthesize, and interpret information
The material presented in this section of the background document is fairly straightforward, but the question remains as to whether the CDC followed their listed methodology in generating this report. The evidence, in the form of the final product, indicates they did not.
RESPONSE 54: CDC conducted a systematic review of the scientific literature and updated the review after the public comment period. The newer data supports our previous conclusions and includes data that male circumcision is associated with reduction in the incidence and/or prevalence of more STDs than previously thought based on RCTs. See responses 39 and 48b
# COMMENT:
The two-day consultation convened by the CDC on April 26-27, 2007 brought together a virtual Who's Who of Circumcision Advocates and Lobbyists. 16 Given the likemindedness of nearly all the participants in attendance, it is not surprising they managed to produce a massive "group think" phenomenon. Their conclusions were more radical and less scientific than what the participants would have likely considered acceptable, if left to their own devices. 17 This experiment in "group think" resulted in what will be referred to as the "CDC group think presumption:" namely that findings of the randomized clinical trials of adult male volunteers in Africa would apply to infant males circumcised against their will in the United States. In reading the CDC draft, this presumption is presented as gospel truth, when the reality is quite the opposite, with the data currently available not in support of this presumption. It appears the CDC has adopted the attitude seen with other male circumcision enthusiasts, in that the issue was not open for discussion or questioning. 18 RESPONSE 55: CDC's recommendations related to counseling around the issue of male circumcision is based on a systematic review of the scientific literature.
# COMMENT:
While the CDC draft states that "a systematic review was conducted" there is little or no evidence that such a review was conducted. Instead, the CDC draft relies on the information published in non-systematic review articles from 1983, 19 and 1998; 20 systematic reviews from 2000, 21 2003, 22 2005, 23 2006, 24 2008, 25,26 2009, 27,28 2010, 30 and 2011; 30 and opinion pieces from 1999, 31 , 2000, 32 and 2014. 33 Beyond reporting what was found in these articles, there is little, or no, evidence of a literature search being performed. The small number of citations (255,
# COMMENT:
The statement "Because they eliminate spurious causality and bias, RCTs are considered the most rigorous method for determining whether a cause-effect relationship exists between a treatment and an outcome," is clearly an overstatement. No research method can completely "eliminate" bias. The elevation of randomized controlled trials to the status of the gold standard is misplaced, as they often deliver results that are invalid. [34][35][36][37] Throughout this draft, the CDC reflexively genuflects in the face of any results from a randomized trial. But every study, regardless of its methodology, requires careful scrutiny. The CDC did not scrutinize these studies. In fact, as will be discussed below, the randomized clinical trials cited in the CDC draft have multiple sources of bias, which rendered their findings meaningless. Randomized clinical trials, such as these, with serious methodological flaws are less rigorous in determining cause and effect than well-designed observation studies. Just because a randomized clinical trial format was employed does not mean that its findings are valid.
# RESPONSE 57:
Agree that RCTs do not eliminate all bias, therefore the word "eliminate" has been replaced with the word "reduce". See response 5.
# COMMENT:
When the draft states that "None of the primary authors of these recommendations reported a financial or other conflict of interest," does this include any conflicts from being an adherent of a religion that requires male circumcision, being from a cultural background that has a high male circumcision rate, being circumcised themselves, being married to someone who is circumcised, and/or having circumcised one's children? Male circumcision status in participants is considered by many as a clear bias and a conflict that should be declared. 38 Such a declaration is important, as male circumcision status or having a circumcised son clearly impacts what advice physicians give to parents regarding infant male circumcision. 39 The conflict of interest on this issue goes well beyond financial considerations. Where is the list of the primary authors of these recommendations, or a list of those who served on the subcommittee of the CDC Public Health Ethics Committee? The makeup of these groups will be an important factor by many, when looked at in conjunction with the obvious lack of scholarship displayed in this draft, in determining how seriously to take the recommendations.
RESPONSE 58: CDC did not ask for reporting of nontraditional forms conflict of interest such as "personal male circumcision status", or religious beliefs. However, in this CDC consultation, consultants were asked to review the merits of the scientific evidence at hand.
# COMMENT:
# Summary of evidence
Conspicuously absent from the CDC draft is a discussion of the normal anatomy, histology, physiology and function of the male foreskin or prepuce. Nearly every review article on any medical topic begins with a discussion of the basic anatomy, histology, physiology, and function of the organs and tissues involved. The recent Task Force report of the American Academy of Pediatrics also failed to address this, 40 and members of the Task Force had to admit ignorance on this topic. 41 It is impossible to understand the impact of amputating a healthy structure from the body, if these characteristics are not understood. The vast majority of physicians in the United States do not have a working knowledge of the anatomy, histology, physiology, or function of the foreskin because they were never taught it in medical school, and medical textbooks contain little or no information on these topics.
The prepuce is a common anatomic structure of the male 42 and female 43 external genitalia of all human and non-human primates. The prepuce has been present in primates for at least 65 million years, and is likely over 100 million years old based on its commonality as an anatomical feature in mammals. 44 The prepuce is best understood not as a separate structure of the penis, but rather as an integral part of the penile skin system.
As a modified extension of the penile shaft skin, representing 22 to 33% of the overall length of the flaccid penis, the prepuce covers the glans, extends beyond it, folds back upon itself, and attaches just behind the corona glandis, providing adequate mucocutaneous tissue to cover the entire penis during erection. There is variability in the preputial coverage of the glans penis ranging from complete coverage to only partial coverage. 45 The portion of the prepuce extending beyond the glans can be quite long in children, while those of adults can be shorter. In many boys, the "redundant foreskin" can be longer than the penile shaft. Based on measurements available in the medical literature, the average surface area can be calculated to be between 50 to 62 square centimeters. 46,47 In a randomized clinical trial in Rakai, Uganda, the surface area was calculated by "multiplying the length by the width of the foreskin," 48 but their calculations would underestimate the surface area by half as it only accounts for one side of the prepuce. Correcting for the prepuce having two sides, the average surface area in this study was 74.2 square centimeters. 48 The prepuce is perfectly designed to protect the glans, an internal organ. Tapered and double layered, it extends beyond the glans in a long, narrow, tube-like structure, terminating in the preputial orifice. The peripenic muscle sheet lines the skin, is continuous with the dartos muscle of the scrotum, 49 and lines the mucosal layer allowing the prepuce to maintain its close fit over the glans. 50 At the preputial orifice, the muscle fibers are arranged in a whorled manner and form a sphincter that keeps unwanted contaminants away from the sensitive mucosa. 51 This is most evident in the prepubescent male in whom the portion of the prepuce extending beyond the tip of the glans has a characteristic puckered appearance.
The preputial orifice is able to dilate 15 to 20 times its normal size to allow the glans to pass through without entrapment. This expandability increases with age and sexual maturity but may be negligible during infancy. 52 Premature and inappropriate attempts to retract and dilate the preputial opening of infants and children can damage and scar the prepuce, reducing elasticity and impairing sexual function. 53 While the outer surface of the prepuce is similar to skin, the inner surface of the prepuce can be subdivided into two zones of mucosa. One consists of a prominent band of ridged mucosa, with several (8-12) transverse mucosal ridges or pleats, just inside the tip of the prepuce. This band merges with the frenulum on the ventral aspect of the penis. When the prepuce is fully retracted, the ridged band lies across the upper surface and sides of the shaft of the middle third of the penis. [54][55][56] Histologically, the ridged band has a rich vascular supply, explaining its deep red color, and a high concentration of fine-touch neuroreceptors (such as Meissner's corpuscles, Pacinian corpuscles, genital corpuscles, and mucocutaneous corpuscles) that transmit fine touch, pressure, proprioception, and temperature. 55,[57][58][59][60][61][62][63][64][65][66][67][68] The other zone is the smooth, non-ridged, preputial mucosa, which does not have a high concentration of fine-touch neuroreceptors.
The frenulum, in conjunction with the smooth muscle fibers of the prepuce, helps return the everted prepuce to its forward position. The frenulum, like the ridged band, also contains a dense concentration of erotogenic nerve endings and is a primary orgasmic trigger. Along with the prepuce, also the site of erogenous triggers, stimulation of the frenulum is particularly effective at producing erections. Retraction, rolling, and stretching of the prepuce triggers erotogenic stretch receptors, which comprise the bulk of the sexual sensations of the erect penis. 69 Blood enters the penis via two principal arteries -the pudendal artery, which carries blood down from the pelvic region, and the femoral artery, which also supplies blood to the legs. Neither of these arteries is superficial, instead lying close to the corpus cavernosa/corpus spongiosa. They flow directly to and alongside the glans, supplying it with blood. Then, they continue down to the underside of the glans to the forward-most point of the frenulum where the arteries meet up with the venous system.
The primary route for venous return from the penis is through the foreskin. The superficial veins drain the skin of the prepuce and glans via a complex vascular plexus that traverses the inner prepuce. These superficial veins drain into larger veins that run up through the frenulum and up the sides through the ridged band. From the ridged band, the veins continue their route back through the skin and Buck's fascia along the corpus cavernosa/corpus spongiosa.
The male prepuce receives its somatosensory innervation via the dorsal nerve of the penis and branches of the perineal nerve (including the posterior scrotal nerves). 70,71 The dorsal penile nerve of the penis supplies sensory axons to the penile shaft and glans. One axon innervates the penile shaft and the urethra, while the other innervates the glans. Stimulation of the urethra results in contraction of the bulbocavernosus muscles enhancing penile rigidity. Impulses from the dorsal penile nerve also initiate reflex semen emission and power the contractions of the bulbospongiosum muscle that results in external ejaculation. [72][73][74] There are portions of the penis, particularly the ventral side and the frenulum, that are partially or completely innervated by a branch of the perineal nerve, 75 which also can induce contractions of the bulbocavernosus muscle. 73 A portion of the fibers within the dorsal nerve carries autonomic branches and is responsible for the hemodynamic events of the distal corpus cavernosum and the glans penis." 72 Autonomic innervation of the prepuce arises from the pelvic plexus. The parasympathetic visceral efferent and afferent fibers arise from the sacral center (S2-S4), and sympathetic preganglionic afferent and visceral afferent fibers arise from the thoracolumbar center (T11-L2). The parasympathetic nerves run adjacent to, and through the wall of, the membranous urethra. 70 Histologically, the foreskin is a specialized, junctional, pentalaminar structure. The prepuce is considered a specialized tissue because it contains elements that are present only in select portions of the body.
It is a junctional tissue because it the junction where the transition from skin to mucosa takes place. Analogous tissues include the eyelids, oral labia and the anus, which are also transitional between skin and mucosa. All of these transitional zones contain a high concentration of fine-touch neuroreceptors. In the oral labia, the absence of these neuroreceptors would result in constant drooling, and kissing would lose most of its erotic appeal. In the eyelid, constant tearing would be the rule. Likewise, the protective function of the eyelids would be severely handicapped if unable to sense the presence of contaminants. The function of these specialized, junctional tissues is remarkably similar: keep moisture on the internal mucosal surfaces and keep contaminants out.
It is pentalaminar in that it has five layers, with each layer having its own unique histological and functional features:
1. The external skin has already been described.
2. The dermis of the prepuce consists of vascular tissue, dense nerve trunks, Meissner corpuscles within the papillae, and scattered sebaceous glands. The dermis of the male prepuce appears to have more elastic fibers than the lamina propria of the prepuce. The elastic tissue of the prepuce dermis, along with the dartos muscle and frenulum, tether the prepuce and help return it to its anatomically correct position after erection.
3. The dartos layer is specific to the male prepuce and is not found in the female prepuce. It consists of smooth muscle fibers invested with elastic fibers. The delicate, attenuated penile dartos muscle surrounds the shaft of the penis and is continuous with the scrotal dartos muscle. 49 This layer's elasticity allows for the volume changes required for erection, 49 while the muscular component is responsible for the prepuce fitting closely over the glans. 50 In the distal prepuce (acroposthion), the muscle fibers are intertwined and arranged in a mosaic-like pattern in the infant, 50 causing the distal prepuce to pucker and close, acting like a one-way valve. 51 This is most notable when a young boy voids. As the urine is expelled from the bladder it must first build up enough pressure to overcome the preputial valve. Because of the elasticity of the prepuce, it is not unusual for the prepuce to balloon before enough pressure is generated and a urinary stream results. As a male ages and passes through puberty, the ratio of muscle fibers to elastic fibers decreases, explaining why, on gross inspection, the acroposthion is puckered in the infant and more relaxed appearing in the adult. 50 The increase in elastic fibers may be necessary for the uncomplicated eversion of the glans in the adult. 4. The lamina propria of the prepuce is highly vascular and has looser collagen than the dense collagenous lamina propria of the glans penis. The ridged band of the prepuce is near the tip (acroposthion) of the male prepuce and, in the unretracted prepuce, usually lies against the glans. It is in the lamina propria of the ridged band that there is a high concentration of specialized neuroreceptors. All of these receptors have a capsule and an inner core composed of both neural and nonneural elements. The capsule is a continuation of the perineurium and the core includes preterminal and terminal portions of the nerve fibers surrounded by laminated layers of modified Schwann cells (laminar cells). 68 The Meissner corpuscles, genital corpuscles, and mucocutaneous receptors are similar in that there is a complex branching of the nerves within the corpuscular core, while the Pacinian corpuscle has a single nerve through the core that is surrounded by laminar cells to form an onion bulb configuration. The prepuce possesses a richer variety and a greater number of nerve endings than any other part of the penis. 76,77 These corpuscular receptors represent one of the two primary somatosensory receptors in skin, the other being free nerve endings or nocioceptors. 67 While free nerve endings (pain, itch, and touch receptors) are found in most skin, the encapsulated receptors are concentrated in regions that require specialized sensitivity, such as at the fingertips, eyelids, lips, external genitalia, perianal skin, and transition areas between skin and mucous membranes. 68 The glans penis is primarily innervated by free nerve endings and has primarily protopathic sensitivity. 78,79 Protopathic sensibility refers to cruder, poorly localized feelings (including pain, some temperature sensations, and certain perceptions of mechanical contact such as rubbing). 78,80 In the glans penis, encapsulated end organs are found in much lower concentrations and are found mainly along the glans corona and the frenulum. 78 The glans is best stimulated by the mechanical rolling pressure of the prepuce over its surface. By comparison to the prepuce, the glans is a neurologically "dumb" organ. 56 [ The only portion of the body with less fine touch than the glans penis is the heel of the foot. 81 The mucosal lamina propria is devoid of lanugo hair follicles, sweat, or sebaceous glands. The lamina propria is highly vascular.
5. The mucosal epithelium of the prepuce is the same as the squamous mucosal epithelium that covers the glans penis. 82 The mucosal epithelium contains Langerhan's cells, but does not contain melanocytes. It provides the moist lining necessary for the preputial sac to function properly.
It is also important to recognize that separation of the foreskin from the glans of the penis is a gradual process. The glans penis and the inner prepuce share a common, fused mucosal epithelium at birth. The two opposing fused epithelial surfaces separate gradually over years as desquamated cells build up between the two layers when the proper hormonal and growth factors are present. 83 While the separation of the prepuce from the glans has been shown to be androgen dependent in rats, 84 the hormones and/or growth factors responsible for this separation are poorly understood in humans. The process of keratinization of the intervening epithelium begins anteriorly and posteriorly at approximately the same time and proceeds toward the center. Anterior desquamation, because it is confined, can result in pearls of desquamated skin cells.
Øster demonstrated that preputial non-separation is very common in children and teenagers. The separation of the mucosa is usually complete by about age 17 years, with the median age being 10 years of age. 52,86,86 The newborn penis is in a state of evolution that may take many years until the common prepuce/glans mucosa separates, and the preputial orifice enlarges to allow complete exposure of the glans. Ignorant of the normal development of the penis, some physicians advocate childhood male circumcision as a treatment of normal anatomy. 87 Even the 2012 Task Force report of the American Academy of Pediatrics incorrectly reported that "Most adhesions present at birth spontaneously resolve by age 2 to 4 months." 40 Lysis of preputial adhesions in childhood is ill-advised, since this process resolves spontaneously and forcible manipulation and retraction of the immature prepuce can lead to scarring, bleeding, phimosis, and psychological trauma. 88,89 The foreskin plays a protective and erogenous role. Animal studies have found that surgically removing the prepuce disturbs normal copulatory behavior, [90][91][92][93][94] the ability to attract female sexual partners, [95][96][97][98][99][100][101][102] and it increases aggressive behavior. 103,104 The foreskin keeps the surface of the glans penis clean, free of infection, smooth, moist, supple, and sensitive. 105 The prepuce protects and preserves the sensitivity of the glans by maintaining optimal moisture, warmth, pH, and cleanliness. The foreskin may have a role in keeping the glans warm, much the way the dartos muscle in the scrotum helps regulate the temperature of the testes. 106 There are temperature sensors in the foreskin that regulate the blood flow to the penis and thus regulate the temperature of the glans penis. These sensors appear to also impact the positioning of the scrotum, which, in turn, affects how close the testicles are to the torso, how warm the testicles are, and how fertile the male is.
The foreskin also provides a protective covering over the glans. Without the foreskin, the glans becomes exposed to the elements and dries out. The surface of the glans goes from a shiny, smooth, wet mucosa to a desiccated, rough surface. There is debate whether the exposed glans seen in circumcised men becomes keratinized or not. 32,107 Men who have foreskins report that having the glans exposed for prolonged periods is often quite uncomfortable because the surface is more sensitive.
The decreased sensitivity of the glans in circumcised male adults has been documented in three studies that objectively measured fine-touch pressure thresholds of the glans in circumcised and intact men, which are discussed in further detail later in this review. [108][109][110] Two studies have compared the vibratory perception thresholds of the glans in circumcised and normal men. Bleustein et al. in a study in which 76.8% of the men in the study had erectile dysfunction, found that vibratory perception thresholds were significantly higher in intact men using the raw data, but the difference was no longer statistically significant when adjusted for age, hypertension, and diabetes. 109 A study in China looking at vibratory perception thresholds before and at one, two, and three months after male circumcision in 96 men found that the vibratory perception threshold increased significantly following the procedure. 111 Intromission in the circumcised man is akin to thrusting the foot into a sock held open at the top. By contrast, the intact counterpart is like slipping the foot into a sock that had previously been rolled up. 112,113 Consequently, during coitus the complete phallus penetrates smoothly with the prepuce retracting as the glans advances; 114 however, when the circumcised penis is introduced, friction and chafing develop. [113][114][115][116][117][118] The double-surfaced prepuce provides the skin necessary to accommodate the expanded erect organ and to allow the penile skin to slide freely, smoothly, and pleasurably over the shaft and glans. This also facilitates smooth, gentle movement between the mucosal surfaces of the two partners during intercourse. The female is stimulated by moving pressure rather than by the friction from a penis with the prepuce missing. 50,118 O'Hara and O'Hara, from their survey of women who reported having had both intact and circumcised male sexual partners, determined that intact men provide shorter penile thrusts during coitus that resulted in more clitoral stimulation for the woman. By contrast, circumcised men used longer, deeper thrusts to provide themselves with enough stimulation to maintain erection and reach orgasm. 115 Because the foreskin is designed to feel fine-touch, only small movements are needed for adequate stimulation. When the exposed glans is in the vagina, the foreskin is bunched behind the corona with the ridged band juxtaposed against the corona, which is the most sensitive portion of the glans. With this juxtaposition, small movements are all that are needed to keep an intact male aroused and tumescent.
The unique innervation of the prepuce establishes its function as erogenous tissue. 58 Fine-touch pressure threshold mapping has demonstrated that parts of the foreskin and frenulum are the most sensitive portions of the penis. [108][109][110] The foreskin sends signals to the bulbocavernosus muscle that results in arousal and tumescence of the penis. Therefore, the foreskin may have a key role in facilitating a normal penilo-cavernosus reflex.
McGrath's research has emphasized the important role of the frenular delta, the triangular area where the ridged band attaches to the frenulum, 119 the frenulum, and the ridged band in providing possibly 80% of the sensory input from the penis, and their contribution in orchestrating signals to the bulbocavernosus muscle, which plays a key role in tumescence. The stimulation from these structures also provides an inhibitory function in dampening the signal of pressure and pain coming from the free nerve endings that make up nearly all of the sensory data from the glans. Without inhibiting the pain and pressure signals from the glans during coitus, the activity would be less enjoyable.
While the penilo-cavernosus reflex has not been fully studied, it is a neurological reflex at the sacral level that has a role in the ejaculatory process. Podnar found clinically this reflex could not be elicited in 22 (73.3%) of 30 circumcised men, but was absent in only 2 (6.9%) of 29 intact controls. 120 Podnar speculates that this missing reflex in circumcised men may explain the higher rate of premature ejaculation seen in circumcised men. The impact of male circumcision on sexual function is discussed in detail later in this review.
As a mucosal surface, similar to the inside of the mouth, the lining of the alimentary canal, or the conjunctiva of the eye, the inner surface of the foreskin is an immunological organ.
The mucosal surface of the inner prepuce and the glans, like all mucosal tissues, requires constant lubrication. Because the glans does not contain any sebaceous glands, it relies on the prepuce for production, distribution and maintenance of proper lubrication. The male preputial sac is moistened by secretions from the prostate, seminal vesicle, and urethral glands of Liftre. 121 Urine is not a normal component of subpreputial wetness. The rich vascular plexus of the prepuce mucosa facilitates production of a fluid transudate similar to that of the vaginal mucosa. 122 Animal experiments reveal that, in the presence of hydrogen peroxide and halide or pseudohalides, soluble peroxidase in the prepuce has an antimicrobial activity. 123 Antibodies present in breastmilk supplement genital mucosal immunity in infants. Oligosaccharides in breastmilk are ingested, then excreted in the urine, where they prevent E. coli from adhering to the urinary tract and inner lining of the prepuce. 124 The inner prepuce secretes cathepsin B, lysozyme, chymotrypsin, neutrophil elastase, 125 cytokine (a non-antibody protein that generates an immune response on contact with specific antigens), 126 langerin, 127 and pheromones such as androsterone. 128 Lysozyme, which is also found in tears, human milk, and other body fluids, destroys bacterial cell walls as well as inhibits and destroys Candidal species (yeast). 129 The prostatic and seminal vesicle secretions that provide the subpreputial moisture are known to be rich in lytic material. 121 Langerin, which is a C-type lectin, is specifically expressed by Langerhans cells and induces the formation of Birbeck granules. The langerin on the surface of the Langerhans cell captures the HIV viron and internalizes it to the Birbeck granules where it is destroyed. In this way, langerin keeps Langerhans cells from internalizing HIV and activating T-cells by clearing the virus before getting the T-cells involved. 127 Like other exposed mucosal surfaces, the inner lining of the prepuce and the surface of the glans are covered with bacteria. The composition of the normal flora can impact whether a disease takes place. For example, the presence of one microorganism can inhibit the growth of another organism. [130][131][132][133][134][135][136][137] The subpreputial flora has been known to be affected by a number of factors such as a patient's age, general hygiene, medical history, sexual activity, and sexual predilections. 138,139 The role of the diversity in subpreputial flora has not been explored in terms of preventing infection, but there is a growing amount of information that allows us to understand the flora in the subpreputial space. Earlier studies had documented that the preputial sac is colonized by cornybacterium, gram negative anaerobes (especially bacteroides melaninogenicus), enterococci, enterobacteria, and coagulasepositive staphylococci. 140 The impetus to study the subpreputial flora in recent decades has been resurrected by male circumcision enthusiasts in hopes of providing evidence of a biologic mechanism to support their theories that the foreskin increases the risk of urinary tract infections and HIV infections. [141][142][143][144][145][146][147][148][149] The authors of these studies try to spin the changes following male circumcision as beneficial, but without understanding the role of normal flora prior to male circumcision there is no way to know if the change is beneficial. The latest speculation is that genital inflammation might be associated with bacterial antigens from bacteria that are not associated with sexually transmitted infections, and that this inflammation might activate T-cells, which might be necessary for the transmission of HIV through the mucosal surface. Therefore, they conjecture that changing the flora at the end of the penis is why circumcised men are at lower risk of HIV infections. There is no evidence that normal flora in the subpreputial space is associated with penile inflammation. One could more convincingly argue that the presence of a variety of anaerobes and a microbiota with more major players is more protective against infection and inflammation. It is when the spectrum of bacteria narrows, which is what occurs following male circumcision, that infection is more likely to occur. Certainly, developed countries with low male circumcision rates do not seem to suffer from higher rates of HIV or other pathologic infections of the genitals.
The problem with the conclusions reached by these male circumcision enthusiasts, including the writers of the CDC draft, is that they are too simplistic, agenda-driven, and reek of confirmation bias. 18 Gram-negative organisms are not all bad. Colonic flora is primarily gram-negatives, yet considered normal. The assessment of microbiological findings and their correlation to clinical findings is difficult, in particular when quantitative determinations have not been done. 150 The presence of normal flora is not a disease state. The most common bacteria responsible for otitis media, pneumonia, and acute sinusitis are normal flora in the nose, pharynx, and mouth. Rather than blame normal flora in a healthy individual and use this in an attempt to justify amputating healthy body parts, a better approach may be to ensure healthy flora in the subpreputial space by lowering the rate of Cesarean sections and perinatal antibiotic usage, but calls to do this have been largely ignored. [151][152][153] The understanding of mucosal immunity is in its infancy. While the mucosa in our mouths, noses, and genitalia encounter pathogens constantly, we rarely are infected. The mechanisms of mucosal immunity are complex and poorly understood. The mucosal immune system protects against potentially invasive microorganisms using antigen-presenting Langerhans cells, dermal and epidermal T lymphocytes, cytokineproducing keratinocytes, and draining peripheral lymph nodes. 154 Most of the "heavy lifting" is performed by Langerhans cells that hang out on the surface of the epithelium.
Langerhans cells are a specific type of dendritic cell. On electron microscopic examination, they have a lobulated nucleus with a clear cytoplasm, rough endoplasmic reticulum, and a well-developed Golgi apparatus. 155 They possess a unique granule in the cytoplasm, which has a "tennis racket"-like appearance, that is responsible for the internalization and processing of antigens. 156 Langerhans cells are the first line of defense to help the body recognize and process antigens, directing them towards lymphocytes or macrophages. 157,158 To understand how this happens, it may be helpful to follow a Langerhans cell through its life cycle. The Langerhans cell begins life in the bone marrow. It is released into the blood stream and is circulated to the dermal blood vessels where it finds its way to the surface. 159,160 Here the Langerhans cell takes up a suprabasal position with its processes extending between neighboring keratinocytes and joins a web of interconnected Langerhans cells that surveys the epithelial surface for antigens. [161][162][163] They make up 2 to 5% of all epidermal cells, 164,165 yet their long processes allow them to cover broad expanses of the epithelial surface. Once an antigen is identified, it is captured by the Langerhans cell. [166][167][168] Following antigen uptake, the major histocompatibility complex and costimulatory molecules are up-regulated on the surface of the Langerhans cells. 169 The Langerhans cell then migrates from the epithelial surface to the paracortex of the nearest draining lymph node where it activates T-cells by producing cytokines and by presenting the major histocompatibility complex-restricted antigen-specific molecules. 166,[169][170][171] This in turn begins an antigen-specific immune response by the activated T-cell. 166 The Langerhans cell then will return to the epithelial surface and repeat the process. 172 Perhaps the most studied example of Langerhans cell activity is in antigen-specific delayed-type hypersensitivity resulting from contact with substances containing nickel that leads to T-cell responses. 165,167,173 Langerhans cells have also been documented fighting infections of human papillomavirus in the female genital tract and of herpes simplex virus on the lips. 167,168,[174][175][176] They interfere with skin graft rejection from foreign donors, 167 and suppress tumor growth in mice. 177 Langerhans cells have been known to act like macrophages both in the allo-activating and in the antigen-presenting function. 168,178,179 It has been shown that smoking decreases the number of Langerhans cells. 180 The location and densities of Langerhans cell populations have been mapped. 164,170,[181][182][183] Langerhans cells are found in the normal dermis, the lymphatics and in draining lymph nodes, in mucous membranes of tongue and tonsils, esophagus and gastric mucosa, as well as in the mucocutaneous junctions of the vagina, rectum, uterine cervix, prepuce, and urethra. 168,184 Much of the controversy about the purported role of male circumcision in reducing the number of heterosexually transmitted HIV infections surrounds the theory that Langerhans cells act as the mode of HIV entry into the body. The bottom line is that Langerhans cells in the prepuce should be considered normal, rather than a pathologic entity requiring excision. 165 A review of the scientific literature reveals that the actual effect of male circumcision is the destruction of the clinically-demonstrated hygienic and immunological properties of the prepuce and intact penis. There are no histological studies to validate the claim that the sclerotic keratinization of the epithelium of the surgically externalized, desiccated glans penis, meatus, or scar of the circumcised penis creates a barrier against infection. The higher rate of sexually transmitted infections in circumcised males might well be the result of the loss of preputial immuno-protective structures. 185 The loss of the protective, self-lubricating, mobile, double-layered prepuce exposes the glans and meatus to direct friction, abrasion, and trauma. The surgically externalized and unprotected glans and meatus of the circumcised penis are constantly exposed to abrasion and dirt, making the circumcised penis less hygienic and prone to meatal stenosis. 186 The circumcised penis is more prone to infection in the first years of life than the intact penis. [187][188][189][190] RESPONSE 59: CDC's view of the biologic evidence differs from that of the peer reviewer. The scientific evidence from the literature supports the view that lymphocytic cells in the prepuce serve as a portal for HIV and other infections as documented in the background document.
# COMMENT:
# Effect of male circumcision on health outcomes
The material presented in this section of the background document does not adequately represent the medical evidence currently available. In most areas discussed in the CDC draft, the medical evidence taken as a whole does not support the conclusions reached by the writers of the CDC draft.
# RESPONSE:
See response 1 and 6.
# COMMENT:
# Biological plausibility
The material presented in this section of the background document is highly speculative and based on conjecture rather than actual data. The speculations presented suggest that the writers were given the outcome of interest, namely the "CDC group think presumption" that male circumcision of infants will reduce the risk of HIV infection in adults, and then they were instructed to find any data that supported this conclusion: a classic example of confirmation bias. When the scientific process is followed properly, conclusions are data-driven instead of data being conclusion-driven.
# RESPONSE: See responses 1 and 6
# COMMENT:
This section begins with the statement, "The foreskin can serve as a portal of entry for STIs (including HIV), lending biological credibility to the role of male circumcision in preventing STI and HIV acquisition through insertive sexual intercourse," which cites an opinion piece as its source. 32 As any part of the body can be a portal for infection, it does not follow that removal of that body part will decrease the risk of infections, nor should removal of normal tissue be given any serious consideration. This is a circular argument that begins with assuming the "CDC group think presumption" is true.
# COMMENT:
The statement, "Compared to the dry external skin surface of the glans penis and the penile shaft, the inner surface of the foreskin is less keratinized. This may allow easier access to the epithelial cells of the epidermis and dermis (in which STIs such as HPV and HSV-2 replicate) as well as access to target cells for HIV infection," uses citations from an opinion piece and a review article on an unrelated topic. 32,191 Interestingly, the opinion piece cited states that in a series of seven circumcised and six intact men, the glans was equally keratinized in both groups. Studies have found that the thickness of the epithelial layer of inner and outer foreskin are similar. 191,192 [Note: these references should replace CDC20, which listed the author's name incorrectly, as these studies have been published subsequent to the 2009 abstract cited.] Therefore, the underlying premise of this statement has been demonstrated to be untrue. For the same reason the statement, "Because the inner surface of the foreskin is lightly keratinized, it may be relatively susceptible to traumatic epithelial disruptions during intercourse, providing a portal of entry for pathogens," which is also referenced to an opinion piece, 32 is unsubstantiated conjecture.
The importance of the statement, "Furthermore, the foreskin retracts away from the glans and over the shaft of the penis during intercourse, which exposes this surface to the body fluids of the sex partner," is unclear. The circumcised penis is also exposed to the body fluids of the sex partner. The only way to avoid this is to avoid sex or wear a condom.
While it has been "postulated" that the foreskin may serve as a reservoir of sexually transmitted pathogens, there is no evidence that the preputial sac is conducive to viral survival. The facts speak against this. For example, there is no evidence that herpes simplex virus type 2 or human papillomavirus infections are more common in intact men (see discussion elsewhere). A large prospective study recently demonstrated that human papillomavirus (any type, oncogenic, HPV-16) are shed significantly faster from the penis of intact men. 193 With evidence to the contrary, it is time to end this type of speculation. That normal flora anywhere in or on the body, let alone in the preputial sac, would have an inflammatory impact that would increase the risk of HIV infection is ludicrous.
Level of penile wetness has been shown to be a factor in one study, but, in the randomized clinical trial in Uganda, men who did not clean their genitals for the first ten minutes following intercourse had significantly lower rates of HIV infection than men who washed in the first three minutes. 194 This suggests that there may be something in the preputial wetness or in vaginal secretions that interferes with the infectiveness of HIV. Furthermore, women have constant vaginal wetness and the CDC is not speculating about their need to be circumcised.
The suggestion that higher numbers of immune cells on the inner foreskin that can more easily respond to infections, and other exposures, will result in an increase in viral susceptibility of the inner foreskin is counterintuitive. Mucosal immunity is based on immune cells doing their job. If they are responding to infections, this would suggest they are more effective at repelling infection. This is borne out by the fact that sexually transmitted infections overall (as discussed elsewhere) are more common in circumcised men. 185 The increased risk of HIV infection in those with genital ulcers makes sense as the ulcers compromise the barrier that is effective in keeping infections out and activates the T-cells, which is considered part of the HIV infection process. The mucosal immune system is quite effective in preventing HIV infections, as indicated by the low rate of transmission through penile-vaginal intercourse (1 per 1000 acts of unprotected coitus). It is only when high viral loads are present that infection is more likely to occur. The speculation surrounding the biological plausibility of the foreskin increasing the likelihood of HIV acquisition is strained and depends on the lining of the foreskin being thinner (which it is not), the preputial sac being more likely to harbor viruses (which it does not), and functional immune cells on the surface (which actually reduces the likelihood of infection). This theory is so farfetched and counterfactual, why would anyone believe it?
The statements made in this section are based purely on speculations that directly contradict the facts. Although these speculative claims have been repeated, ad nauseam, in the medical literature, there is no science to support them. RESPONSE: See response 60.
# COMMENT:
# Male circumcision and the risk of HIV infection acquisition
# Male acquisition of HIV infection from female partners
The material presented in this section of the background document is a confusing regurgitation of review articles that are incomplete and out of date. 21,22,24,27 More importantly, this section fails to address several key questions, namely whether the results of the randomized clinical trials from Africa 1-3 are valid, whether they apply in the United States, and, if applicable, to whom should they be applied.
# RESPONSE:
See Responses 1, 6 and 19.
# COMMENT:
Three randomized clinical trials were undertaken simultaneously in Africa with nearly identical methodology. [1][2][3] This lack of methodological variation is not a sign that the best methodology was used, but instead undermines the robustness of their findings. Because of this lack of variation, one might think of the trials collectively as one trial performed at three sites. 195 The results of the trials were remarkably consistent, to the point that some would consider the similarity of the results to be mathematically improbable. Because of the similarity in the results, one could argue that the studies were precise in their estimates, but with a lack of methodological variability the accuracy of their estimates cannot be assessed. More studies using a variety of methods reaching consistent results would provide a stronger testament to their accuracy. The accuracy of their estimates can be called into question because of the internal validity issues these trials share (discussed below) and the fact that their estimates of the treatment effect were greater than seen in observational studies. This is quite atypical as the treatment effect in randomized trials are typically about 25% to 30% smaller than seen in observational studies.
# RESPONSE 61:
The similarity in methodology of the 3 randomized clinical trials is a strength in that it allows for comparison and validation of results. The fact that 3 such trials in 3 different regions of Africa had similar results represents the best and highest level of scientific evidence. See response 5. Cochrane reviews point to RCTs as the gold standard as do most scientific bodies tasked with evaluating scientific rigor.
# COMMENT:
The methodology of these trials undermine the internal validity (how well the estimates generated by the trial reflect reality) in a number of ways. Perhaps the most important methodological flaw is that no effort was made to identify the source of the infections that were diagnosed during the course of the trial. By failing to do so, these trials cannot answer their research question of determining the impact of male circumcision on the heterosexual transmission of HIV from females to males because it not known how the infection was transmitted. Consequently, the CDC draft is incorrect throughout by suggesting these trials measured this form of transmission, when they clearly did not. This is important because some of the infections may have resulted from male-to-male transmission and some may have been transmitted through iatrogenic means. In the trial in Kenya, only 0.2% of the participants reporting having had male-to-male sexual contact. 2 For many in developed nations this would be considered an extremely low percentage, as male-to-male sexual contact is seen in the range of 5% to 10%. The low rate of men reporting male-to-male contact may reflect the extreme homophobia in sub-Saharan Africa. In Uganda, for example, their Anti-Homosexuality Act of 2014 will punish homosexual activity with life imprisonment (they were considering making it a capital offense). Given the extreme penalties and social stigmatization, admitting homosexual activity to researchers could result in dreadful consequences. Therefore, it is reasonable to assume that, among the thousands of participants in these trials, many were having male-to-male contact. Consequently, the role of anal intercourse in transmitting HIV in this population is unknown. 196 Given that transmission rates between two men is more efficient and that this mode of transmission is not impacted by male circumcision, 25 the failure to identify the source of infection would likely impact their final estimates.
A surprising number of participants in these trials became HIV infected despite not being sexually active or always using condoms. Consequently, it is unlikely that their infections were sexually transmitted. Iatrogenic transmission of HIV is well documented in Africa typically from procedures in which the skin is punctured with instruments or needles that have not been properly sterilized. [197][198][199][200][201][202][203][204][205][206][207][208] This possibility should not have been a surprise to the trial investigators. In one African study, female and male virgins who were circumcised were more likely to be HIV-infected. 209 Some have argued that the iatrogenic spread of HIV in Africa is better able to explain the high prevalence of HIV rather than convoluted models that rely on multiple concomitant sexual partners and a high burden of sexually transmitted infections. 200,210 In each of the trials, there were infections that could not be accounted for on the basis of sexual transmission alone. For example, in the South African trial 23 men, who accounted for 2076 person years, became HIV positive with either having no sexual contact or always using a condom (infection rate 1.11/100 person-years) compared to 46 infections in 2498 person-years among men who at least one episode of unprotected sex during the trial (1.84/100 person-years). 1 Assuming that all of the men in the trial had the same risk of infection through non-sexual transmission only, only 18 of the 69 infections can be attributed to sexual transmission (1.84 minus 1.11 per 100 personyears times 2498 person-years). In the Ugandan trial, 1252.1 person years and 6 infections can be attributed to men who reported no sexual partners for the duration of the trial (0.48/100 person-years). 3 When this baseline rate of infections in those who were not sexually active is subtracted from the total rate in the men who were sexually active, 35 of the 67 infections can be attributed to sexual transmission.
In the Kenyan trial, there were five men reporting no sexual activity in the first three months of the trial who subsequently seroconverted (0.73/100 person-years). 2 When this rate is subtracted from the rate seen in those who were sexually active, only 36 of the 69 total infections can be attributed to sexual transmission.
Without knowing the source of the infections they diagnosed, it is hard to determine what actually was measured in these trials and even harder to extrapolate their findings across the ocean to infants. How can the CDC base policy on trials that did not measure what they set out to measure?
The study methodology, which was nearly identical in each of the trials, had several built-in forms of bias, all of which would be likely to overestimate the treatment effect.
RESPONSE: See Response 12.
# COMMENT:
Expectation bias: At least one primary investigator was on record prior to execution of his trial expressing his impatience and stating that it was time "to begin investigations of the feasibility of acceptable male circumcision interventions in communities with high HIV and STD seroprevalence where male circumcision has traditionally not been practiced." 31 So, it would appear that Bailey believed a randomized clinical trial was unnecessary, as the issue was already settled for him. Similarly, in the Ugandan trial, the researchers from Johns Hopkins dismissed the results of the six men who became infected despite no sexual partners noting, "these participants probably under-reported their sexual activity." 3 Infection in men who were not sexually active did not agree with their expectations, so the results were summarily dismissed. How many other unwanted results were similarly dismissed because they did not agree with the investigators' expectations. Furthermore, there is evidence of expectation bias on the part of the participants. These men agreed to participate because they believed that male circumcision would lower their risk of HIV. Even after the informed consent process, more than half (57%) believed that male circumcision would reduce their risk of infections. 211,212 Since the researchers and participants could not be blinded to which group a participant was assigned to, one would expect that participants would act differently based on their assignment and be treated differently by the researchers. Both researchers and those assigned to the intervention group would be expected to change their behavior to make the intervention pay off.
Selection bias: The men in these trials were those who were interested in undergoing male circumcision. After the propaganda sessions in the roll-out before the trials, many men were convinced they wanted a male circumcision in order to reduce their risk of HIV. When compared to the general population, one would expect that at least some of these men viewed themselves as, or were in reality, at greater risk for HIV infection. The percentage of men interested in a free male circumcision, as evidenced by the current voluntary medical male circumcision programs, is less than 5% in most countries. [213][214][215][216][217][218][219] So, the participants in these trials are representative of only a small subset of the general population. As noted above, the motivation of the participants in these trials would be expected to alter their behavior.
Lead-time bias: The men who were randomized to be immediately circumcised were instructed to abstain from sexual relations or to always use condoms for the first six weeks following the procedure to allow for proper healing. The data reported in these trials was number of infections per time of potential exposure. Since those in the intervention group each had six weeks less of potential exposure, one would expect them to have a smaller number of infections. Avoiding lead-time bias is a fundamental principle of study design that is taught in the most rudimentary of courses on clinical study design. None of the randomized clinical trials adjusted for this bias in their study design, and only one made an adjustment in their post hoc analysis. 1 This indicates either incompetence or a conscious omission that would increase the likelihood of producing data favorable to male circumcision. Intervention bias: The men who were randomized to the intervention group had more visits and exposure to the research team. This would give researchers additional opportunities to provide education on safe-sex practices and to emphasize how important it was for the trial participants to follow-up as requested.
Attrition bias: These trials had a substantial number of participants who were lost to follow-up. The number lost was 251 (8.0%) in South Africa, 1 240 (8.6%) in Kenya, 2 and 493 (9.9%) in Uganda. 3 Those who were assigned to the intervention group were significantly less likely to be lost to follow-up (OR 0.83; 95%CI 0.73-0.95). One possible explanation is that men who were hoping for a free male circumcision but assigned to the control group would see no purpose in staying in the study. Participants who are lost to follow-up are not the same as those who continue to participate. In the Kenyan study, they had a greater number of lifetime sexual partners and a higher prevalence of being seropositive for herpes simplex type 2 virus (Robert Bailey, personal communication). What is more concerning is that for every participant who become infected with HIV during these trials, there were 4.8 who were lost to follow-up. This is a serious missingdata problem.
Duration bias: The trials involved 24 or fewer months of follow-up. The shape of the trajectory following 24 months is unknown. It could very well be that over time the number of infections will be the same in both groups and male circumcision may only slightly delay the time to infection. Several of the models have assumed that the trajectory seen in the first two years will continue for 20 years, based on faith more than science. [220][221][222][223][224][225][226][227][228][229][230][231][232] There is also growing evidence that HIV is losing its virulence. 233 Early termination bias: All three of the trials were terminated early. Early termination, in and of itself, is more likely to result in an overestimate of the treatment effect. 234 It also amplifies any impact of the lead-time bias. Of interest, the Ugandan study had a Fragility Index 235 of 4, which suggests that findings of the study were not particularly robust. How can a study that is terminated early, have such a low Fragility Index?
Overpowered studies: These studies were powered to detect a 1% ARR difference in HIV incidence between the intervention group and the control group. 236,237 This explains the high number of participants in each trial. The important question is whether a 1% difference is clinically important, not whether the difference is statistically significant. If a 1% difference is not important, then demonstrating that this difference is statistically significant misses the point of doing the studies. Studies with a large number of participants, such as these randomized clinical trials, are able to demonstrate a statistically significant difference for very small absolute differences, but when the absolute differences are so small, these studies can also have trouble distinguishing between real findings and background noise. With these trials, even though each source of bias may not be enough alone to explain the difference seen, their cumulative effects, since they all would work to overestimate the treatment effect, would be enough to explain the 1.3% absolute difference seen.
The randomized clinical trials, especially the Ugandan trial, have a number of unexplained anomalies. For example, in the Ugandan trial, those who reported consistent use of condoms had a trend toward a higher rate of HIV infection than in those who reported never using condoms (consistent condom use: 1.03/100 personyears; No condom use 0.91/100 person-years; RR 1.13; 95%CI=0.54-2.38, p=0.74). 3 Given all of the problems with how the data in these studies were handled, it would be helpful if these data could be analyzed by independent experts, rather than researchers who have careers that depend on generating positive results. Even though the National Institutes of Health used our tax dollars to fund two of the randomized clinical trials, the data are not available to the public and are not subject to the Freedom of Information Act. Some have called on these data to become available, 238 but researchers of the studies from Kenya and Uganda have not complied. There were several ethical concerns regarding the trials, 239,240 including that the financial incentives to participate (a free male circumcision, money equivalent to twoweeks employment, cash for recruiting additional subjects, unlimited access to free condoms, and free health care for 21 to 24 months) were coercive. There is a lack of equipoise seen in both researchers and participants. 211,212 Based on the extremely promale circumcision bias of the researchers, it is unlikely that participants were given full disclosure, particularly regarding the risks and long-term harms of the procedure, while obtaining informed consent. Furthermore, going into these trials, the researchers knew that male circumcision would be less effective, more expensive, and more invasive compared to other interventions already available at that time (most notably condoms). Typically, trials that evaluate interventions that are known to be inferior to current therapies are not pursued because they violate the Helsinki Declaration. 239,241 Finally, it is unclear whether these trials were necessary as demographic information was available prior to the initiation of these trials showing that, even if they generated a positive result, their results would not have external validity. Typically, when a new drug is developed it is subjected to a Phase III trial in a closely defined and monitored population. Phase IV studies take place once the medication is being used in the general population. In the case of male circumcision and its impact on HIV infection, the Phase IV type data were available before the Phase III studies were designed. The Phase IV type data indicated that male circumcision did not have any impact on a demographic level. For example, in South Africa HIV spread had similar dynamics of spread in the Shangaau and Xhosa tribes that are circumcised and the Zulu and Tswana tribes that do not circumcise. The fact that the researchers who performed the randomized clinical trials went ahead with the trials, despite the availability of this Phase IV type data, suggests that they were not properly educated in basic epidemiological methods, such as the difference between efficacious and effective, or that they chose to ignore basic principles of epidemiology when moving forward with these trials.
While randomized double-blinded placebo-controlled trials are considered the gold standard for testing a hypothesis, the quality of the information garnered from poorly designed randomized trials, such as the randomized clinical trials undertaken in Africa, can be below that of a well-designed observational study. The CDC draft places unearned importance on the results of these trials. While there are serious concerns about the internal validity of these trials, there is ample evidence that the trials lack external validity. While some male circumcision advocates, including the writers of the CDC draft, have suggested that data collected from the participants in the trials after the completion of the trials [242][243][244][245] indicates that male circumcision is effective (in addition to being efficacious), and thus has external validity, these participants would still be subject to the Hawthorne effect and the undue influence of the large financial advantages of having participated in the trials. These people should still be considered to be acting within a research setting as they likely received far more attention and education than men who would be getting circumcised outside a research setting, but the results should not be considered on the same quality level as a randomized trial.
The randomized clinical trials lack external validity. When there is a treatment effect in a clinical trial, it would be expected that such a treatment effect would be seen outside of research settings and in the population at large. This has not been seen. There are eight or more countries within Africa where the prevalence of HIV infection is greater in circumcised men than in intact men. 13,[246][247][248][249][250] When the national survey data are included in a meta-analysis, no difference in HIV prevalence is noted by male circumcision status (intact versus circumcised men random-effects summary OR 1.10; 95%CI 0.81-1.50). 251 If the results from the three randomized clinical trials do not apply to the countries in Africa, do they apply to countries outside of Africa? While some ecological studies within Africa have suggested a correlation between male circumcision prevalence and HIV prevalence, [252][253][254][255] [Note: citation CDC57 is an opinion piece and should not be cited in this context. The authors need to cite the original studies as included above.] other analyses have not found male circumcision to be a factor. 256 When these methods are applied to developed countries, there is a significant positive correlation between male circumcision prevalence and the prevalence of heterosexually-transmitted HIV infections. 257 When only English-speaking countries are considered, there is a strong linear relationship between a country's male circumcision rate and its rate of heterosexually-transmitted HIV (r 2 =.9756). 258 If the writers of the CDC draft want to accept the results of those ecological studies in Africa showing that increasing male circumcision rates correlate to decreasing rates of HIV infection, then they also need to accept the results of the recent study that found a statistically significant correlation between the prevalence of infant male circumcision and the prevalence of autism. 259 Before accepting the "CDC group think presumption" that the findings of the methodologically flawed randomized clinical trials of adult males in Africa would apply to infants circumcised in the United States, it is important to look at the evidence available. One approach would be to look at the entire body of literature on the association between HIV incidence and prevalence and male circumcision status. This has been assessed in over 100 populations. [1][2][3][8][9][10][11][12][13][14][15]246,[248][249][250] These include randomized clinical trials, prospective cohort studies, national surveys, and case-control studies and all of these study types can be informative. When study characteristics of the various populations are adjusted for, meta-regression 324 reveals that studies of general populations broadly, and outside of Africa in particular, do not support the hypothesis that male circumcision lowers the risk of HIV infection. Meta-regression also indicates that as the prevalence of male circumcision in a community increases the association between being intact and HIV infection increases. 325 This would indicate that male circumcision has no role as primary prevention either in Africa or outside Africa.
A second approach would be to look at the studies that have been performed in North America on heterosexual men. None of them support the "CDC's group think presumption," and none of their findings in favor of male circumcision are statistically significant. A 1991 study of men at high risk for HIV infection had an odds ratio (intact versus circumcised men) of 1.75 (95%CI 0.93-3.27). 11 A 1993 study by the same researchers found an odds ratio of 4.25 (95%CI 0.94-19.13). 15 A representative national survey found an odds ratio of 2.60 (95%CI 0.65-10.42). 9 A 2004 study from the US Navy found a slight decrease in risk for intact men with an odds ratio of 0.80 (95%CI 0.52-1.22). 10 A national survey in Haiti found a similar trend with an odds ratio of 0.67 (95%CI 0.33-1.35). 13 A very large study from an STD clinic in San Francisco found no difference with an odds ratio of 0.93 (95%CI 0.33-1.05). 8 Another large STD clinic study from Baltimore found the raw data had an adjusted odds ratio of 1.00 (95CI 0.86-1.15). 12 None of these studies found a statistically significant difference. Finally, a study from a STD clinic in Puerto Rico found that circumcised men had a significantly higher prevalence of HIV infection (OR 0.68; 95%CI 0.49-0.95). 14 When these studies are combined in a meta-analysis, the random-effects summary odds ratio was 1.21 (95%CI 0.78-1.88, between-study heterogeneity chi-square (df=7) = 91.64, p <.0001, I 2 = 91.3%) when raw numbers are used and 0.94 (95%CI 0.79-1.13, between-study heterogeneity chi-square (df=7) = 15.56 p=.0295, I2 = 48.7%) when the adjusted odds ratio for the Baltimore study is used. Most of these studies were performed in high-risk men and no difference was documented. One would expect there to be even less of an association in general populations. Consequently, these data do not support the "CDC group think presumption." Finally, the target population for male circumcision needs to be delineated. The data clearly show that male circumcision is unlikely to be effective if targeted at the general population. The US data, which is derived primarily from patients seeking care at STD clinics, indicates that male circumcision would not be effective for high risk populations either, such as attendees of STD clinics. The sub-strata data from the Baltimore study, which made up only 1.4% of men seeking care at an STD clinic, suggest that there may be a slight role for male circumcision in the subpopulation of men who are at imminent risk of infection, such as those who have a regular female sexual partner who is known to be HIV-infected. In this subpopulation, only 11 intact men were HIV infected and their findings had a Fragility Index 235 of 1, indicating results that are far from robust. 12 Policy decisions should be delayed until this association is replicated in multiple studies with sufficient robustness. Consequently, any discussion of male circumcision related to the risk of HIV infection in the United States, if they should occur at all, should only be directed toward discordant couples with HIV-negative men who have regular sexual relations with known HIV-positive female sexual partners. There is no evidence to support suggesting male circumcision for any other populations. For this small subpopulation, there are a number of far more effective options such as condoms, preexposure prophylaxis, and anti-retroviral therapy for the infected sexual partner. Even a model developed by the CDC, that assumes the "CDC group think presumption" is true, has determined that male circumcision would have minimal impact in preventing HIV infection in this population. So, why is the CDC contradicting its own findings by bringing forth the recommendations in this draft?
The bottom line is that data does not support the use of male circumcision to reduce the risk of heterosexual transmission of HIV in the United States.
The material given in this section by the CDC is counterfactual, biased, and dangerous. The medical literature suggests that male circumcision might have a minimal impact on the risk of HIV infection in a very small sub-population, but this needs further study before implementation. To extend the discussion of male circumcision beyond this easily identifiable sub-population is reckless and would result in unnecessary physical and psychological harm. The fear-mongering implicit in this section makes the CDC look foolish and desperate. In the seven years since the CDC held its consultation, several things have happened that have taken male circumcision out of consideration as an HIV preventive measure. AIDS researchers have adopted secondary prevention methods such as "treatment as prevention" that has changed infection with HIV from a death sentence into a chronic disease. 326 Similarly, the virulence of the HIV virus is weakening. 233 Finally, the roll-out of male circumcision in Uganda and Kenya has resulted in increases in the incidence of HIV in men in those countries. [327][328][329] Not to mention the number of men and boys who have died as a direct result of being circumcised in Africa, some forcibly against their will. The CDC would be better off expending its energies, and US taxpayers' money, promoting interventions that are not ineffective and harmful. RESPONSE 62: See response 5. The concerns presented by the reviewer have been previously addressed and adequately refuted in the literature. 51,52
# COMMENT: HIV infection transmission from circumcised men to female partners
The material presented in this section of the background document is incomplete with some of the material being misrepresented.
# RESPONSE:
See Responses 1 and 5.
# COMMENT:
The early studies, which looked at whether the male circumcision status of a woman's male sexual partner was a risk factor for women becoming infected with HIV, showed mixed results. 287,317,[330][331][332][333][334][335][336][337] Since then, the evidence emerging fails to support the theory of male circumcision directly reducing the male-to-female transmission of HIV. The only randomized clinical trial addressing this issue found a marked increase in HIV infections in the female partners of men who had been circumcised. 338 The writers of the CDC draft give a very pro-male circumcision spin to these results. The absolute risk increase for these women was 6%, which translates to a number needed to harm of almost 17. So, for every 17 male circumcisions performed on an HIV-infected man with a female partner that was not infected, one would expect one additional female partner to become infected. This study was terminated early, and rightly so, because early looks at the data indicated that the practice was too dangerous to continue. To state that the study was terminated because it was unlikely to show a favorable result may be technically accurate, but it belies the 50% relative increase in HIV infections. The promale circumcision spin stating the study failed to show a difference is also true, but disingenuous since the trial was rightly terminated before the study had enough power to show a statistically significant difference if one existed. The study was also profoundly unethical because the women were not told their sexual partners had HIVvery reminiscent of Tuskegee. Shockingly, the authors of the study recommended that HIV-infected men undergo male circumcision, with a total disregard for the increased risk of HIV infection the procedure foisted on female partners, because of the fear that these men would feel stigmatized if they were not circumcised. 338 Too bizarre to have been made up.
The two models that have assessed the impact of male circumcision on the incidence of HIV infections in women assumes the findings of the randomized clinical trials have both internal and external validity, both of which are risky assumptions. 223,339 The extremely speculative nature of these models should exclude them from being considered in formulating policy.
# RESPONSE 63:
The CDC background document provides an unbiased and accurate summary of the available data indicating that male circumcision does not significantly reduce heterosexual male-to-female HIV transmission.
# COMMENT: Male acquisition of HIV infection and other STIs from male partners
The material presented in this section of the background document is generally accurate, incomplete in a few areas, but needs to be more explicit in its conclusion, namely that male circumcision is not a reasonable intervention in the prevention of HIV infection that might be acquired by men from their male sexual partners. A recent model published by the CDC assessing the effectiveness of various interventions in the prevention of HIV infection in discordant couples found that, for a man with a male partner who was HIV-infected, over a 10-year period, reliance on male circumcision alone would nearly guarantee the man would become infected. 340 A major thrust that resulted from the CDC's 2007 consultation was an effort to find a link between male circumcision and the risk of HIV infection in men having sex with men. 16 One opinion as to why the CDC took over seven years from the time of the consultation to the release of this draft was the hope of a breakthrough study that would demonstrate that male circumcision reduced the risk of HIV infection in men having sex with men. Many at the consultation believed that such a finding would secure the practice of infant male circumcision in the United States for decades to come, thus worth holding out for. The many studies on men having sex with men have overcome researcher expectation bias and failed to generate the results hoped for.
RESPONSE 64: See response 27 and 39. A summary of the findings of the 2007 CDC male circumcision consultation has been previously reported. 1 The Cochrane review provides evidence from a meta-analysis of 21 observational studies indicating that circumcised insertive men who have sex with men (MSM) experienced a significant reduction in HIV acquisition compared with uncircumcised insertive MSM; circumcised receptive MSM didn't experience a significant reduction in HIV acquisition compared to their uncircumcised receptive MSM counterparts. Because these results did not include results from RCTs, the Cochrane review did not conclude that male circumcision conclusively protected insertive MSMs from acquiring HIV infection. Nevertheless, biological plausibility would argue that insertive MSM should experience a protective benefit against acquiring HIV just as circumcised heterosexual men do. The CDC recommendations explicitly state that due to the lack of RCTs, it cannot definitively conclude that HIV acquisition is reduced among circumcised insertive MSM compared to their uncircumcised insertive counterparts.
# COMMENT: HIV transmission in other populations at high risk for HIV acquisition
The material presented in this section of the background document is appropriate.
# RESPONSE 64a:
No response required.
# COMMENT:
# Male circumcision and other health conditions
The material presented in this section of the background document is misleading. The medical literature does not support the claims that male circumcision has a positive impact on the incidence or prevalence of penile, prostate, or cervical cancer. Likewise, it has no positive impact on the incidence of any of the sexually transmitted infections. It has no impact on the prevalence of any of the individual sexually transmitted infections, with the exception of syphilis, which fortunately is rare in the United States. 341 To mention these diseases and devote substantial discussion to them gives the false impression that male circumcision in reality has an impact on these diseases.
# RESPONSE 65:
See responses 1 and 6. While the meta-analysis of STDs and male circumcision cited by the reviewer failed to find a significant association between the two 11 , a careful review of the methods used to conduct this review render the results of that meta-analysis to be scientifically biased and lacking scientific validity. 12 COMMENT:
# Sexually transmitted infections (STIs)
The material presented in this section of the background document is biased, incomplete, and inaccurate.
RESPONSE: See response 65.
# COMMENT:
This section is markedly incomplete. Instead of searching the medical literature, or even relying on recently published meta-analyses 185,[342][343][344][345] as a starting point, this draft relies on non-systematic reviews/opinion pieces 20 and a meta-analysis that is over a decade old 24 as the source of information. Consequently, the sections addressing the various sexually transmitted infections are woefully incomplete, inaccurate, and misleading. It has been over seven years since the CDC held a "consultation" on male circumcision 16 where it was decided to release recommendations concerning male circumcision. That should have provided enough time for their staff to search the medical literature, examine the data, and perform meta-analyses (although the only meta-analysis generated on the topic of male circumcision proved to have erroneous calculations requiring a three-page erratum in the Journal of the American Medical Association 25 [NOTE: The citation given in the CDC draft fails to include the reference to an extensive erratum published at: JAMA 2009; 301: 1126-9.] The summary effects odds ratio, when properly calculated, was 0.95. If the staff was going to rely on the work of others, they could have at least referenced the most up-to-date systematic reviews and metaanalyses. But several sexually transmitted infections, for which there are multiple studies in the medical literature, were nearly completely ignored, yet there are extensive discussions of chancroid, Trichomoniasis vaginalis, and the transfer of various infections to female partners, all based on a small number of studies. What explains such a low quality of scholarship? Laziness? Insufficient time? Preconceived bias? The CDC has had over 7 years to produce this draft, yet this response, written in less than 45 days, has more references and more detail covering ALL the evidence in the medical literature. Were there directives from leadership to present male circumcision in the best light possible and to bury, ignore, or omit any studies to the contrary? Apparently, not out of the question. Given the poor quality of the effort to find (let alone evaluate) the evidence, how can this draft of the CDC be taken seriously by scientists, epidemiologists, or health care providers? This entire section needs to be scrapped, the evidence found and properly evaluated, and accurate information provided.
# RESPONSE:
See responses 1 and 6.
# COMMENT:
The statement, "Male circumcision has been shown to reduce the risk for some other STIs in addition to HIV," is factually inaccurate. The only STI that the medical literature may support as male circumcision having a minimal reductive impact is in the prevalence of syphilis (see discussion below), but male circumcision has not been shown to impact the incidence of syphilis. Consequently, the word "some" should be replaced with "possibly one."
RESPONSE 66: See response 39. Based on the update of the review of the literature during the response process, more benefits for reduction in various STDs have accrued since the initial review. In randomized controlled trials for which data are available, reductions in the 1) prevalence of genitourinary disease (GUD) [25][26][27] , 2) incidence of herpes simplex virus type 2 (HSV-2), 4,28 3) prevalence, [4][5][6]29 _ENREF_9 incidence, 30,31 and clearance 29,31 of high-risk oncogenic human papillomavirus (HR-HPV)_ENREF_7, 4) prevalence of Trichomonas vaginalis, 27,32 5) incidence of syphilis, 33 6) prevalence of bacterial vaginosis, 27 and 7) prevalence of mycoplasma genitalium 34 were also demonstrated._ENREF_19
# COMMENT:
It is clear that the writers of the CDC draft did not look carefully at, or critically evaluate, the sexually transmitted infection data from the African randomized clinical trials. [346][347][348][349][350][351] Even a cursory reading of the methodology of these trials would reveal that these trials made no attempt to minimize or provide any post hoc adjustment for lead-time bias. The men who were randomized to immediate male circumcision were instructed to abstain from sexual relations or always use condoms for the first six weeks following the procedure to allow for proper healing. The data reported in these trials was: "number of infections per time of potential exposure." Since those in the intervention group each had six weeks less of potential exposure, one would expect them to have a smaller number of infections. Avoiding lead-time bias is a fundamental principle of study design that is taught in the most rudimentary of courses on clinical study design. The fact that all three randomized clinical trials did not adjust for this bias, either in the study design or post hoc analysis, indicates either incompetence or a deliberate omission that would increase the likelihood of producing data favorable to male circumcision. As will be shown in the sections below, adjusting for lead-time bias changes the outcomes of these studies. If one looks carefully at the prospective studies of genital human papillomavirus and male circumcision, the studies suffer from incomplete sampling to the point, as discussed below, that the treatment effect in these trials can be completely attributed to sampling bias. [352][353][354] RESPONSE: See response 15 and 65.
# COMMENT:
The statement, "Although rarely fatal, STIs other than HIV are among the most common communicable diseases in the United States, and interventions that prevent STIs would result in substantial reductions in morbidity and cost of health services," while true, is misplaced hyperbole. As will be discussed in the sections below, the incidence and prevalence of none of the common sexually transmitted infections are impacted by male circumcision. Only the prevalence of syphilis may be minimally impacted, but syphilis is very rare in the United States infecting only 9.8 per 100,000. 341 Consequently, the CDC draft is trying to jack up the importance of male circumcision through thinly veiled fear mongering, when the medical literature totally undercuts their message.
RESPONSE: See responses 65 and 66
# COMMENT:
While the CDC draft discusses several of the sexually transmitted infections individually, it fails to address the impact of male circumcision on the overall risk of contracting a sexually transmitted infection of any type. In other words, the risk of any sexually transmitted infection versus no sexually transmitted infections. There have been 20 publications that have looked at the prevalence of any sexually transmitted infection by male circumcision status, 9,10,14,248,260,271,275,[355][356][357][358][359][360][361][362][363][364][365][366][367][368] and four prospective studies that have looked at the incidence of any sexually transmitted infection. 358,[369][370][371] A meta-analysis of the studies of prevalence, in which the data in one study was stratified by race, 362 by number of life-time sexual partners in another, 9 and by the five populations in which data were collected in another, 260 yields a random-effects summary odds ratio (intact men versus circumcised men) of 0.86 (95%CI 0.74-1.01, between-study heterogeneity chi-square (df=26) = 303.00, p<.0001, I 2 = 91.1%). In the analysis, there was one clear outlier that reported an odds ratio of 1.51 (95%CI 1.41-1.62). 368 When this outlier is removed from the analysis, the between-study heterogeneity chi-square drops by 203.41, and the random-effects odds ratio is 0.82 (95%CI 0.74-0.92, I 2 = 73.9%). 185 This would indicate that when all sexually transmitted infections are considered together, male circumcision significantly increases the risk of contracting a sexually transmitted infection. When the studies of incidence are stratified by study, the fixed-effect of the summary relative risk ratio is 0.91 (95%CI 0.78-1.07) 185 which, while not statistically significant, trends in the same direction of the studies of prevalence. Therefore, an intact male is at lower overall risk of contracting a sexually transmitted infection.
RESPONSE 67: The category of "any STD" is an artificial construct. Our background document provides clear evidence of decreased prevalence of HSV, HPV, syphilis, and others associated with male circumcision.
# COMMENT:
(Continued from comment before Response 67). This finding should not be surprising as there have been several studies comparing the risk of genital discharge syndrome versus genital ulcerative disease by male circumcision status, 12,185,265,372,373 which have been ignored in the CDC draft. Those studies on meta-analysis have found the risk of genital ulcerative disease versus genital discharge syndrome in intact men had a random-effects summary odds ratio of 2.24 (95%CI 1.63-2.24, between-study heterogeneity chi-square (df=4) = 17.94, p=.0013, I 2 = 72.1%) 185 Conversely, circumcised men would be twice as likely to have genital discharge syndrome versus genital ulcerative disease. Since genital discharge syndrome is far more common than genital ulcer disease, it makes sense that the overall risk of sexually transmitted infections may be higher in circumcised men. The data may not have been precisely collected in these studies, but they were not collected any less precisely than in the studies the CDC draft has elected to include.
This finding also makes sense on a biological level. Mucosal immunity is quite efficient in keeping invasive organisms at bay. By removing much of the penile mucosa and drying out the remaining mucosal surfaces, the natural immune system is disrupted. For example, the first line of defense on the mucosal surface are the dendritic (Langerhans) cells. With these cells removed by male circumcision, the penis has fewer defenses against the garden-variety sexually transmitted infections, thus making them more prone, overall, to sexually transmitted infections. This may explain why, in a large prospective study, clearance of human papillomavirus occurred significantly more quickly in intact men than in circumcised men. 193 Consequently, the recommendations for the intended audience of health care providers are biased, hyperbolic, and are missing essential information. Health care providers need to be told that male circumcision may increase the overall risk of sexually transmitted infections.
RESPONSE: See responses 65, 66, and 67.
# COMMENT:
Note: There are number of redundant citations in this section. For example, citations 74, 75, and 76, are the same as citations 4, 5, and 6.
# RESPONSE 67a:
We have corrected this duplication of citations.
# COMMENT: Genital Ulcer Disease (GUD)
The only sentence under this heading is factually inaccurate and reflects a misinterpretation of the data. As will be discussed in the sections below, while GUD incidence was decreased in the only prospective studies to explore it, 347,350 the studies that looked at herpes simplex virus, after adjustment for lead-time bias, were not statistically significant. 347,[350][351][352] It is not clear why this sentence fails to mention that the randomized clinical trials failed to find an association between male circumcision and syphilis. 347,350 Is such an oversight because of a lack of attention to details or to give this section the proper pro-circumcision spin?
# GUD (various types)
The material presented in this section of the background document is incomplete and confusing. One would expect the section to address GUD generally, but the discussion is quite specific about herpes simplex virus, which has its own subsection. The section fails to mention the 15 observational studies that have assessed the prevalence of genital ulcer disease by male circumcision status. 12,15,[261][262][263][269][270][271][272][374][375][376][377][378] When one of the studies with redundant data is excluded, 261 there is a positive association between having a foreskin and clinical presence of genital ulcers (random-effects summary odds ratio 1.60; 95%CI 1.34-1.92, between-study heterogeneity chi-square (df=13) = 31.09, p<.0001, I 2 = 66.8%). 185 Other meta-analyses have yielded similar results. 24,342 The data from both of the prospective studies need to be adjusted for lead-time bias. 349,379 When the data are adjusted, the fixed-effect summary relative risk ratio is 1.62 (95%CI 1.27-2.07). 185 Part of the reason ulcers are more commonly seen in intact men is that ulcers have a propensity for mucosal surfaces and mucocutaneous junctions. This is why cold sores are seen most commonly on the lips around the mouth, as this is a mucocutaneous junction. One could speculate that if the lips were surgically removed, the number of cold sore eruptions would also decrease. Similarly, the removal of much of the mucosal surface and the mucocutaneous junction from the penis may explain the decrease in prevalence.
# Herpes Simplex Virus (HSV-2)
The material presented in this section of the background document is hyperbolic, incomplete, and misleading.
The authors of this section boast of "[c]ompelling evidence of the protective effect of HSV-2 acquisition from male circumcision is available from two of the three RCTs." The data from these studies tell a different story. 349,350,380 Two of the studies have results that were not statistically significant. 349,351 All three of these reports failed to adjust for lead-time bias. When the only study to show a statistically significant finding 350 is adjusted for lead-time bias, the difference is no longer statistically significant. 352 Even before making the adjustment for lead-time bias, the fragility index 235 for the study was 1, indicating that findings were not robust. The section fails to mention the cohort study by Dickson et al, which followed children from birth until 26 years of age and found no difference in herpes simplex type 2 virus serology (intact men versus circumcised men RR 0.99; 95%CI 0.49-2.00). When the data for the four prospective studies are combined (stratifying by study), the fixed-effect summary relative risk ratio (intact men versus circumcised men) is 1.23 (95%CI 1.04-1.46). When the data are adjusted for lead-time bias, the fixed-effect summary relative risk ratio is 1.15 (95%CI 0.97-1.36). 185 The large impact on the summary relative risk ratio by a six-week adjustment to compensate for the lead-time bias suggests the data are neither robust nor "compelling."
Regarding observational studies, the CDC draft relies on a 1998 non-systematic review/opinion piece as a source of reliable information. 20 That "review" noted only six observational studies available at that time and was obviously missing several studies. The more recent 2006 review cited in the draft noted only 10 observational studies, but excluded two populations that had been reported previously 381 by the lead author of the review article. 24 Since this review was published, a study of 6187 men in India found that the seroprevalence for herpes simplex type 2 virus was significantly lower in intact men (OR 0.66; 95%CI 0.51-0.86). 382 There have been 29 publications of observational studies addressing the association between genital herpes and male circumcision status in men. 9,14,262,263,267,274,356,357,[359][360][361]363,377,378,[381][382][383][384][385][386][387][388][389][390][391][392][393][394][395] While one publication reported on four populations, 381 another stratified the data by age, 393 and another by country of origin. 363 When a meta-analysis is performed on these studies, the random-effects odds ratio is 1.18 (95%CI 0.998-1.39 , between-study heterogeneity chi-square (df=35) = 170.62 , p < .0001, I 2 = 78.9%). The difference is not statistically significant.
Based on the data that currently appear in the medical literature, no position should be taken on the impact of male circumcision on the risk of infection with herpes simplex type 2 virus. The data are inconsistent, poorly collected, and meta-analyses do not show a significant difference.
# Treponema pallidum (Syphilis)
The material presented in this section of the background document is also confusing as the authors refer to genital ulcer disease when this section should focus on syphilis. The 1998 non-systematic review/opinion piece 20 and the 2006 meta-analysis 24 cited in this section as the source for information on syphilis and male circumcision are out of date, and they do not come close to addressing the 29 observational studies in the medical literature that assess the association between the prevalence of syphilis and male circumcision status. 8,9,[260][261][262][263][267][268][269]271,273,[356][357][358]360,362,374,376,377,382,384,[396][397][398][399][400][401][402] One study looked at two populations 384 and one study was stratified by race. 362 A meta-analysis of these studies estimated the random-effects summary odds ratio (intact men versus circumcised men) to be 1.31 (95%CI 1.13-1.52, between-study heterogeneity chisquare (df=30) = 70.67, p < .0001, I 2 = 56.1%). This is a drop in the summary odds ratio reported in the 2006 meta-analysis of 1.45. 24 The incidence of syphilis in men not infected with HIV in Kenya and Uganda is 1.09 per 100 person-years, which is about the same incidence rate as HIV infections in the randomized clinical trials that were performed in those countries. The absolute risk reduction for a circumcised man in this trial was 0.49 per 100 person-years at the ages when someone is most-likely to contract syphilis. 402 Given that the sexual transmission of syphilis is far more efficient than the rate of 1 infection in 1000 sexual encounters for HIV, 403 this would suggest that a substantial proportion of HIV infections are not spread through heterosexual contact alone.
The incidence of syphilis has been addressed in four studies. 349,350,358,402 In two of the studies, no adjustment was made for lead-time bias. 349,350 When the data are stratified by study, and adjusted for lead time bias, the fixed-effect relative risk ratio (intact men versus circumcised men is 1.09 (95%CI=0.82-1.45), and therefore, not statistically significant.
This section is little more than fear-mongering. The incidence of syphilis in men in the United States is low (9.8 per 100,000 in 2013). 341 Based on the prospective studies, there is no significant difference in the incidence of syphilis between intact and circumcised men.
# Haemophilus ducreyi (Chancroid)
The material presented in this section of the background document is inaccurate and misinterpreted. The CDC draft cites a meta-analysis of six studies looking at chancroid, which found circumcised men had a reduced relative risk. 24 If the authors of this draft had looked at the meta-analysis, they would have found that three of the six studies included in their analysis did not assess chancroid directly 265,266,374 and nearly all of the between-study heterogeneity could be attributed to a single study. 404 Weiss et al. 24 included several studies in their meta-analysis that were not strictly studies of chancroid and did not meet basic inclusion criteria because they lacked a direct comparison between intact and circumcised men for a specific diagnosis of chancroid. 265,266,374 In two studies, men with genital ulcers were not tested for chancroid but merely presumed to have chancroid. 265,266 In the third study, 31.4% had herpes simplex virus type 2 and only 22.9% had a positive culture for Haemophilus ducreyi. 374 Some of the remaining studies are now quite dated having been published in 1934, 397 1949, 396 and 1975. 404 When the remaining studies of chancroid are included, 263,264,396,397,404 and the results of the study by Hand 396 are stratified by race, meta-analysis yields a random-effects summary odds ratio of intact men versus circumcised men of 1.33 (95%CI 0.52-1.33). 185 How much weight to give to these findings needs to be tempered by the high degree of between-study heterogeneity (chisquare (df=5) = 59.71, p<.0001, I 2 = 91.4%), the reliability of the clinical diagnosis in several of the studies, and the age of the studies. With the current data, it is not possible to say conclusively that circumcision has an impact on genital infections with Haemophilus ducreyi. It is not clear why this was included in the CDC draft when it does not really apply in the United States as chancroid is extremely rare, and the evidence gathered to date is of such poor quality.
# Other STIs.
The material presented in this section of the background document is misleading. While randomized clinical trials in Africa reported a reduction in high risk HPV infections following male circumcision, nearly all of this perceived reduction can be attributed to the researchers selective sampling practices. [352][353][354] This will be discussed further in the section below.
# Human Papilloma Virus (HPV)
The material presented in this section of the background document is riddled with factual errors, is incomplete, and is a misinterpretation of the medical literature.
The statement, "Penile squamous carcinoma (caused by carcinogenic HPV subtypes) has been strongly and consistently associated with lack of male circumcision," is supported by a citation of a non-systematic review/opinion piece written by authors with a known pro-male circumcision bias. 20 As will be discussed below, the medical literature does not support this statement, and the writers of the CDC draft should not rely on opinion pieces as though they are evidence-based citations.
The statement, "Cervical cancer has been associated with lack of male circumcision in male partners of women in several case-control studies," can easily be demonstrated to be false. As discussed below, there are 16 studies that have looked for an association between cervical cancer and the male circumcision status of a woman's male sexual partner and none have found a statistically significant association. The citation given for this statement also did not find a statistically significant association. 405 To be factually accurate and reflect the information that is currently available in the medical literature, this statement should read: "A significant association between cervical cancer and the lack of male circumcision in male partners of women has never been demonstrated despite evaluation of this association in multiple case-control studies."
The CDC draft relies on a 1998 non-systematic review/opinion piece 20 as its source of information on genital warts, which noted only three studies had been published. To date, there have been 15 observational studies in 14 publications that have assessed the prevalence of genital warts in men based on their male circumcision status. 14,263,356,357,360,361,394,398,[406][407][408][409] When a meta-analysis is performed on these studies, the random-effects summary odds ratio (intact men versus circumcised men) is 0.82 (95%CI 0.65-1.04, between-study heterogeneity chi-square (df=14) = 37.07 , p=.0007 , I 2 = 59.5%). 185 This indicates that there may be a trend indicating that circumcised men are at greater risk for genital warts. When only studies assessing general populations are evaluated, the between-study heterogeneity is not statistically significant (chi-square (df=6) = 8.61, p=.1969, I 2 = 18.7%), which is rarely seen in studies of sexually transmitted infections and male circumcision status, and the randomeffects summary odds ratio is 0.78 (95%CI 0.63-0.96), a statistically significant difference. 185 These studies noted that genital warts in circumcised men were more likely to be found on the penile shaft. 356 Why would the writers of the CDC draft rely on a non-systematic review/opinion piece 20 that is 16 years old as a source of its information when several systematic reviews have addressed this topic more recently? 24,185,342 Was the goal of the CDC draft to be out of date and incomplete, or just to make headlines assuming no one would read the draft and see through the coverup?
The CDC draft makes no mention of the 20 observational studies that have assessed the prevalence rates of genital HPV infection in men based on male circumcision status, 355,405,406,[410][411][412][413][414][415][416][417][418][419][420][421][422][423][424][425][426] or the three meta-analyses that have looked at these studies. 185,[343][344][345] The draft may have avoided discussion of these studies because the results of several of the studies were biased by either sampling bias, 412 misclassification bias, 410,422,423 or both. 405 The type of HPV also varied from study to study with some reporting all HPV types, others only HPV types known to be carcinogenic/oncogenic, and other studies reporting their findings by all types, non-oncogenic and oncogenic. 414,416,418,419,426 It should also be noted that most genital HPV infections are transient and clear spontaneously.
Misclassification bias occurred in the studies where researchers relied on men to properly identify their male circumcision status, but the men did so incorrectly. The most egregious example of this is the study by Lajous et al. out of Mexico in which 95 men reported being circumcised yet only 8.3% of them were noted to be circumcised on physical examination. 410 While the authors of this study had determined the male circumcision status of the study participants based on physical examination, they reported their results based on the male circumcision status as reported by the men. In effect, the study demonstrated that HPV risk was lower in men who thought they were circumcised rather than whether they were actually circumcised or not. The results using physical examination to determine male circumcision status were not provided. 427 Evaluating all of the studies of prevalence using meta-regression 324 has demonstrated that studies that relied on patient report to determine male circumcision status consistently and systematically significantly overestimated the association between having a foreskin and genital HPV. 185,343 The impact of sampling bias is more easily quantified. Sampling bias occurs when only selected portions of the genitals are sampled for the presence of HPV. Selective sampling would not be a problem if doing so provided similar results to comprehensive sampling. For HPV on the male genitals, however, this is not the case. Several studies have shown that circumcised men who have HPV somewhere on their genitals are more likely to harbor the virus on the shaft of the penis. 355,411,415,420,426,428 Other studies have shown that genital warts are more likely to be found on the shaft of the penis in circumcised men as compared to the glans in intact men. 429 Two studies out of the University of Washington found that, if only the glans is sampled, 45 to 47% of circumcised men with genital HPV will be detected. 365,429 In contrast, sampling only the glans of intact men will identify 65 to 66% of intact men who have HPV on their genitals. As a consequence, sampling only the glans of the penis will miss more HPV infections in circumcised men than it will in intact men. If the numbers from Van Buskirk et al. 428 are correct, the number of intact men expected to be infected with HPV infection would be the number of men identified by sampling only the glans increased by a factor of 1.514. Similarly, for the men who underwent male circumcision, the number identified in the trial would be increased by a factor of 2.212. When an analysis of the entire medical literature is performed using meta-regression, 185,343 studies that sampled only the glans were demonstrated to have stronger associations between having a foreskin and having HPV infections. This finding was statistically significant, suggesting that sampling only the glans of the penis consistently overestimates the association between having a foreskin and genital HPV.
An added wrinkle to the finding that circumcised men are more prone to have HPV lesions on the shaft of their penis is that the penile shaft is the portion of the penis with the highest viral loads and the preferred location for HPV-16, which is the most oncogenic HPV type. 430 This would suggest that circumcised men might be more likely to pass HPV-16 to their sexual partners, thereby leading to an increase in cervical cancer.
The dilemma is: what to do with studies containing these obvious methodological flaws, which will have a significant impact on the odds ratios reported by these studies. One approach would be to adjust for these factors by adjusting the odds ratios in studies with sampling bias. Another, would be to adjust using meta-regression. And, the last would be to exclude studies with these methodological problems when performing a metaanalysis.
Twenty publications reported prevalence data on 25 separate populations. Five of these studies provided data on any type of HPV being isolated, as well as high risk HPV. Since high-risk HPV is of more clinical interest, these data were used in the metaanalysis with a random-effects summary odds ratio (intact men versus circumcised men) of 1.16 (95%CI 0.94-1.45, between-study heterogeneity chi-square (df=24) = 45.27, p = .0054, I 2 = 44.7%), which was not statistically significantly different. 185 This analysis included studies that were known to have either sampling bias or misclassification bias for which no adjustment was made. When adjusted for sampling bias using meta-regression, the random-effects summary odds ratio was 1.10 (95%CI=0.88-1.37). For studies that sampled only the glans, the random-effects summary odds ratio is much greater (OR=1.86, 0.99-3.46). When adjusted for misclassification bias using meta-regression, studies that relied on physical examination to determine male circumcision status had a random-effects summary odds ratio of 1.08 (95%CI=0.88-1.32), which was not statistically significant. Studies that relied on patient report had a much greater random-effects summary odds ratio (OR=2.16, 95%CI=1.18-3.99). When studies with known sampling bias or misclassification bias were excluded, the random-effects summary odds ratio was 1.01 (95%CI 0.80-1.28, between-study heterogeneity chi-square (df=15) = 28.82, p = .0164, I 2 = 44.5%). 185 This indicates that observational studies not tainted with methodological flaws have failed to establish an association between genital HPV infection prevalence and circumcision status in men. Is this lack of association why the CDC ignored these 20 publications?
There have been eight prospective studies that looked at the incidence of HPV infection in men by circumcision status, 193,348,350,410,428,[431][432][433] but this CDC draft only mentions two of them. The two studies identified in the CDC draft are also the only two studies to find a statistically significant difference, the only two studies to find the greatest treatment effect (relative risk ratios of 1.51 and 1.54, with next highest being 1.19, 433 and the only two studies that reported only the results of samples taken from the glans without including samples taken from the penile shaft. 348,350 Clearly, the results of these two outlying studies were impacted by sampling bias. For example, in the Ugandan trial, 350 when an adjustment for sampling bias is made, the relative risk ratio (intact men versus circumcised men) was reduced from 1.54 (95%CI 1.11-2.17) to 1.09 (95CI 0.83-1.43), with the difference no longer being statistically significant. As a consequence, the difference in incidence between intact and circumcised men reported by the Johns Hopkins team can be completely explained by their failure to sample beyond the glans of the penis. 352 The story on sampling bias, however, goes deeper. In 2007, researchers from Johns Hopkins reported at the beginning of their randomized clinical trial that, "Two subpreputial and shaft swabs were also obtained for future testing of human papillomavirus infection." 3 However, in the 2009 report of their findings, only the results from swabbing the glans were reported. The results from swabbing the shaft of the penis were not included in their report. 350 In 2011, the same team reported the results of HPV cultures from the glans and the penile shaft collected at the 12 month follow-up visit of the randomized clinical controlled trial participants. 434 It remains unclear why the researchers from Johns Hopkins would selectively report the results in this fashion, especially given the fact that Weaver at al. had published their findings of a differential in HPV acquisition based on the site of sampling on male genitals in 2004. 429 When the prospective data are stratified by study, the fixed-effect summary relative risk ratio is 1.05 (95%CI 0.88-1.25), which indicates that circumcision has no effect on the incidence of genital HPV infections in men. When the Ugandan and South African data, which account for nearly all of the between-study heterogeneity, are corrected for sampling bias and lead-time bias, the summary relative risk reduction is 0.97 (95%CI 0.91-1.04).
The CDC draft must include the results of the "HPV Infection in Men" (HIM) study: a prospective study of HPV in men that looked at the risk of new HPV infections by circumcision status. 193 This study was to be the ultimate prospective cohort study on the topic. Preliminary reports from the study appeared in such high-profile journals as the International Journal of Cancer and The Lancet. 414,435 The study included 4033 participants aged 18 to 70 years. In the study, they sampled the glans, the penile shaft, and the scrotum. Men were evaluated every six months for a median of 17.5 months.
Participants came from Florida, Mexico, and Brazil, and the results were stratified by country of origin. The hazard ratio for oncogenic HPV was 0.90 (95%CI%=0.76-1.06) indicating a non-significant trend for circumcised men to have a higher incidence overall of HPV infections. No difference was seen for HPV-16. HPV of any type, oncogenic HPV, and HPV-16, cleared significantly more quickly from the intact penis then the circumcised penis (any HPV: hazard ratio (HR) 0.85; 95%CI 0.80-0.91, oncogenic HPV: HR 0.83; 95%CI 0.75-0.92, HPV-16: HR 0.56; 95%CI 0.42-0.75). 193 This significantly faster clearance of HPV from the intact penis is the opposite finding seen in other smaller studies. 370,432,[436][437][438] Two additional comments:
First, the study by Castellsequé et al. combined the data from seven studies in five countries on three continents. 405 Analysis of the data from this study presented several statistical challenges that the authors of the study did not correctly deal with, and the editors of the New England Journal of Medicine let slide by. The challenge was the small number of circumcised men in four of the five countries and a small number of intact men in the fifth country. In order for asymptotic statistical methods, which rely on the assumption that values follow a normal distribution, to provide accurate results there needs to be more than 5 (some say more than 10) subjects who conform to each classification. Of the twenty classifications (five countries by 4 outcomes), seven have 5 or fewer subjects in them. The authors used asymptotic statistical methods, even though this would not yield valid results. They should have used exact statistical methods instead. In other words, the small number of circumcised men in Brazil, Columbia, Spain, and Thailand, and the small number of intact men in the Philippines made for an unstable statistical model. Furthermore, it renders stratified analysis nearly impossible, if the analysis wants to control for the country from which the data was collected. For example, if the prevalence is much greater in one country that has a very low circumcision rate, results may be attributed to male circumcision that should instead be attributed to the country of origin.
Second, the data from the randomized trial in Kisumu, Kenya has never been clearly presented. In 2012, Bailey and Moses's group published the results of their data on high-risk HPV, but they did not report the number of circumcised men or intact men who became infected with high-risk HPV. Instead, they reported that intact men developed more flat lesions that were more likely to harbor high-risk HPV. 439 On the face of it, and from the title of their publication, it may sound as though intact men were at greater risk for an infection with high-risk HPV, but this is not the case. While intact men were at greater risk for flat lesions, circumcised men were at greater risk for papular and pearly lesions. While the papular and pearly lesions are less likely to harbor high-risk HPV, they are much more common than the flat lesions and more common in circumcised men. For example, 33 men in the study had flat lesions, while 133 and 187 men had papular and pearly lesions, respectively. Of the men with flat lesions, one was circumcised and 32 were intact. Of the flat lesions 22 were found to harbor high-risk HPV. Papular lesions were found in 91 circumcised men and 42 intact men. Of the 133 papular lesions, 28 harbored high-risk HPV. Pearly lesions were found in 112 circumcised men and 75 intact men. Of the 187 pearly lesions, 49 harbored high-risk HPV. Based on these numbers, one can back-calculate and estimate the number of men expected to have been infected with high-risk HPV based on male circumcision status. Considering there were 124 intact men and 151 circumcised men, the odds ratio was 1.45 (95%CI=0.89-2.38), a difference that is not statistically significant. This should not be a surprise as this study sampled both the glans and penile shaft of the study participants and reported the results on all of the samples they collected. It is not clear why the straight-forward number of intact and circumcised men who became infected with high-risk HPV has never been revealed publicly.
The CDC has placed its entire wager behind two outlier studies with serious methodological flaws whose results are not consistent with the rest of the medical literature. The analysis is incomplete, biased, and misinterpreted the small fraction of the data in the medical literature that the CDC considered.
# Trichomonas vaginalis
The material presented in this section of the background document does not contribute adequately to the discussion to even merit inclusion. The entire section could be tersely reduced to one sentence: The impact of male circumcision on trichomoniasis in men and their female sexual partners has received limited study with conflicting results. 346,347,440 There are no studies outside of Africa by which to gauge the importance of these infections.
In reporting the results by Mehta et al., 347 the writers of the draft give results of the "astreated" analysis as being statistically significant and the "intention-to-treat" results as having "borderline statistical significance." The standard is to report only intention-totreat results. Doing otherwise undermines the whole purpose of a randomized trial. Crossover, which in these trials would entail men randomized to be circumcised not undergoing the procedure and men randomized to not be circumcised undergoing the procedure, does not in most cases happen randomly. By reporting the as-treated results, the writers of the CDC draft knowingly reported potentially biased results. While they may believe they are justified in doing so because it furthers their cause of promoting male circumcision, they should know better on an epidemiological level. Intention-to-treat analysis may be more conservative in estimating treatment effects, but it does not introduce the bias of differential crossover and it is more reflective of the reality of patient non-compliance. The writers should also know better than to use the phrase "borderline statistical significance." This phrase is similar to being "kind of pregnant." While the statistical significance has been somewhat arbitrarily set at a pvalue of .05 by Ronald A. Fisher, it is the standard everyone abides by. In this case statement, the as-treated results should not have been presented, and the intention-totreat results should have been described as showing a trend that is not statistically significant. Once again, the writers of this draft are either improperly trained in statistics and epidemiology, or they are trying to promote male circumcision unjustifiably. These epidemiologically inappropriate phrases were used by the authors of the studies in an effort to spin their results in the most favorable fashion. The fact that writers of the CDC draft accepted this language without question also indicates that they did not read these studies carefully enough to properly evaluate the methodology and data generated in order to develop their own conclusions. The CDC had over seven years to carefully read the small percentage of studies in the medical literature they decided to include in this draft. This should have taken a matter of weeks. What did the CDC with the rest of the time?
# Chlamydia trachomatis
The material presented in this section of the background document is very confusing. It is not clear if the authors of this section were purposely being obtuse. The statement that "chlamydial infection in men was often diagnosed syndromically as 'non-gonococcal urethritis,' after exclusion of gonorrhea by Gram stain" is an oversimplification. Several studies collected data on both chlamydia and non-specific urethritis, 9,263,[355][356][357][359][360][361] which in the era of testing for both chlamydia and gonorrhea, is its own entity. This section would be best if divided up into sections of 1) genital discharge syndrome, 2) non-specific urethritis, and 3) Chlamydia trachomatis.
Several studies examined the association between male circumcision status and the prevalence of genital discharge syndrome, which includes any genital infection that results in a urethral discharge, such as gonorrhea, chlamydia, and non-specific urethritis. The CDC draft makes no mention of the studies that assessed men for genital discharge syndrome except to mention the single study that looked at its incidence in Table 2. The draft fails to mention the eleven studies that have compared the prevalence of genital discharge syndrome in men by circumcision status. 12,248,[261][262][263][269][270][271][375][376][377]442 When the results of these studies are combined in a meta-analysis, the random-effects summary odds ratio (intact men versus circumcised men) shows a trend toward genital discharge syndrome being more common in circumcised men (summary OR 0.92; 95%CI 0.78-1.09, between-study heterogeneity chi-square (df=10) = 52.13, p < .0001, I 2 = 78.9%). It is not clear why the CDC draft failed to consider this information.
The one study that measured incidence failed to adjust for lead-time bias. 350 When this adjustment is made, the relative risk ratio (intact men versus circumcised men) is reduced from 1.11 (95%CI 0.77-1.61) to 0.98 (95%CI 0.68-1.42).
The CDC draft relies on a 1998 non-systematic review/opinion piece for its information on non-specific urethritis and tallies the results of the studies rather than performs a meta-analysis. 20 A systematic review of the medical literature will uncover 12 studies on the prevalence of non-specific urethritis. 9,263,266,355,357,[359][360][361]363,383,398,442 When the data from these studies are combined in a meta-analysis, the random-effects summary odds ratio (intact men versus circumcised men) is 0.76 (95%CI 0.63-0.92, between-study heterogeneity chi-square (df=11) = 39.78, p<.0001, I 2 = 69.8%.) 185 [353] This result indicates that circumcised men are at a statistically significantly increased risk for nonspecific urethritis.
This section on Chlamydia trachomatis makes no mention of the 16 observational studies that looked for an association between prevalence of Chlamydia and circumcision status in men. 9,14,263,[355][356][357][358][359][360][361]364,369,377,[443][444][445] If one of the studies that presented redundant data is excluded, 261 the random-effects summary odds ratio for these studies (intact men versus circumcised men) is 0.94 (95%CI 0.76-1.17, betweenstudy heterogeneity chi-square (df=14) = 36.16, p=.0010, I 2 = 58.5%). It is unclear what harm there would be in the CDC reporting these results, except that the meta-analysis indicates a non-significant trend that circumcised men are at greater risk for Chlamydia.
There have been three studies published, which looked at the incidence of Chlamydia by circumcision status in men. 346,347,358 The two studies identified by the CDC failed to correct for lead-time bias. The fixed-effect summary relative risk ratio for the three studies (intact men versus circumcised men) is 1.26 (95%CI 1.02-1.57); however, when the two studies are adjusted for lead-time bias the result is no longer statistically significant (RR 1.19; 95%CI 0.96-1.49). 185 The CDC did not make the effort to gather or properly interpret the evidence that is currently available in the medical literature. Instead, it wasted its time and space giving the details of the two conflicting studies regarding the risk of Chlamydia in women based on the circumcision status of their regular male partner. 446,447 The conclusion that would be most accurate and helpful for the intended audience of health care providers is that male circumcision may increase the likelihood of urethritis, including Chlamydia and non-specific urethritis.
# Neisseria gonorrhea
The material presented in this section of the background document is woefully out of date and incomplete. The CDC draft cites a 1998 non-systematic review article as the source of its material, 20 which notes that five of seven observational studies list a statistically significant decrease in gonorrhea prevalence in circumcised men. This review was incomplete at the time it was published. There have been 24 studies that have assessed the association between male circumcision status and gonococcal infections. 9,14,[261][262][263]267,268,[355][356][357][358][359][360][361][362][363]377,383,[396][397][398][441][442][443][444][445] Two of the studies presented redundant data 261,262 and only four had associations that were statistically significant. 267,356,360,446 But a tally of positive studies, a much used rhetorical device, 20,31 is not the proper method of determining the overall findings in the medical literature. When one of the redundant studies is excluded, 261 the data reported by Hand 396 and Schrek 362 are stratified by race and the data reported by Laumann et al. 9 are stratified by the number of lifetime sexual partners, the random-effects summary odds ratio of intact men versus circumcised men was 1.03 (95%CI 0.88-1.21, between-study heterogeneity chi-square (df=27) = 95.97, p<.0001, I 2 = 70.8%). Since an odds ratio is 1.00 when two groups have identical risks, there is no difference in the risk of gonorrhea based on male circumcision status.
This holds up in studies on the incidence of gonorrhea. Three studies have looked at this issue. 346,347,358 Two of them suffered from lead-time bias. 346,347 None of them found a statistically significant difference. The fixed-effect summary relative risk ratio (intact men versus circumcised men) for the three studies was 1.10 (95%CI 0.91-1.34). When the two studies with lead-time bias are adjusted for, the summary relative risk ratio is 1.04 (95%CI 0.86-1.27). 185 The data from the medical literature clearly demonstrates that male circumcision does not impact the risk of gonorrhea.
Based on what is presented in the CDC draft, the authors of this draft are either incompetent reviewers of the medical literature or are purposely trying to deceive the public and their intended audience of health care professionals. Reliance on a nonsystematic review that is little more than an opinion piece, in which only seven observational studies were identified, when a simple PUBMED search would have quickly identified many of the 23 observational studies and two systematic reviews with meta-analyses, 185,342 is inexcusable. Is this just willful incompetence, or is there an institutional directive to misrepresent the evidence in the medical literature? COMMENT:
# Penile and prostate cancers
The material presented in this section of the background document is incomplete, misleading, and contains inappropriate citations.
# RESPONSE:
See responses 1, 6, and 39.
# COMMENT:
Penile cancer is extremely rare (0.6 to 0.8 per 100,000 person years), less common than breast cancer in men. In the United States, the incidence of penile cancer occurs at rates that are similar to or lower than rates in other developed countries where male circumcision is rarely practiced, such as in Japan, Germany, Iceland, Spain, Sweden, Switzerland, United Kingdom, Yugoslavia, 448 Denmark, 448,449 Finland, 448,450 and Norway. 448,451 Also, as the percentage of circumcised septuagenarian and octogenarian men has increased, there has been no corresponding decrease in the incidence of penile cancer in the United States. Both of these findings suggest that, on a population level, male circumcision has little or no impact on penile cancer. This information needs to be included in the CDC draft discussion.
The discussions of any case series or reviews of case series should be excluded 452,453 because, without control groups and with a changing prevalence of circumcision in men at the age at which penile cancer is likely to occur, the numbers from these publications have little or no epidemiological value. [Please note that reference CDC121 lists the wrong study. Instead of Schoen EJ, Colby CJ, Ray GT. Newborn male circumcision decreases incidence and cost of urinary tract infections during the first year of life. 454 it should also include the results of the other two case control studies. 408,455 The study by Maden et al. found that men who had never been circumcised were at about three times greater risk for penile cancer (OR 3.04; 95%CI 1.79-5.15), while intact men with pathologic phimosis were at six times greater risk (OR 6.23; 95%CI 3. 18-12.19). 455 But, when the control group is age adjusted, the findings are less spectacular and not statistically significant (OR 1.19; 95%CI 0.77-1.85). This study did not adjust for phimosis in its analysis. A case-control study by Tseng et al. 408 [440] yielded similar results to that of Daling et al. 454 For Tseng et al., the presence of phimosis increased the risk of penile cancer 16-fold. When adjusted for phimosis, lack of neonatal male circumcision was not a significant risk factor. 408 All three studies emphasize that phimosis, rather than neonatal male circumcision, is the more important risk factor. Half of the cases of invasive penile cancer can be attributed to oncogenic HPV viruses. 456 As is discussed elsewhere in this response, there is no significant association between male circumcision and carriage of oncogenic HPV. The link between phimosis and penile cancer may be balanitis xerotica obliterans, the most common cause of pathologic phimosis with a cumulative incidence of 0.6% by 15 years of age, 457 which is increasingly being recognized as a precancerous condition. [458][459][460][461][462][463][464][465][466][467][468][469][470][471] Consequently, the focus should be shifted to efforts that minimize infections with oncogenic HPV (such as use of condoms and use of the HPV vaccines) and early recognition and treatment of balanitis xerotica obliterans.
The section should also include a realistic discussion of the risk of penile cancer. For example, the 2012 American Academy of Pediatric Task Force on Circumcision noted that the incidence of penile cancer was 0.58 per 100,000 person-years. 40 Using this incidence for penile cancer in the United States, the lifetime risk (average life span 72 years) would be 0.000417512, or a lifetime risk of 1 in 2395. The Task Force report noted that the relative risk reduction for penile cancer by circumcision was between 1.5 and 2.3. If you take the lifetime risk of penile cancer and reduce this incidence rate by a factor of 2.3, the result, 0.0001815, would be the expected lifetime risk for penile cancer in circumcised men. The absolute risk reduction would be the difference between the two rates: 0.0004176 minus 0.0001815 or 0.0002360, so the number needed to treat would be 4237. If, however, the relative risk reduction is 1.5, the number needed to treat is 7184. If it takes 7184 male circumcisions to prevent one case of penile cancer and each male circumcision costs an average of $285 paid at the time of the procedure, 472 the cost to avoid one case of cancer is $2,047,440. However, the money for the male circumcision was spent at the time the male was circumcised not at the time the male developed penile cancer, which is usually around 80 years of age. Therefore, for 80 years, the opportunity of having that cash available, which was spent at the time of the procedure, has been lost. If that money was put out at 3% interest for 80 years, the opportunity costs would be $21,786,584. If the money were to earn 5% interest for 80 years, the cost of preventing one case of penile cancer would be$101,474,076. This is the true cost of preventing one case of penile cancer. Obviously, neonatal male circumcision to prevent penile cancer is NOT cost-effective nor justifiable from a public health standpoint.
The discussion of male circumcision and prostate cancer should be deleted. The argument put forth by the writers of the CDC draft borrows from that proposed by Morris and colleagues, 473 which is based on several tenuous assumptions. The first is that the risk of prostate cancer is increased by sexually transmitted infections. As the writers of the CDC draft note, the medical literature on this point is mixed, showing populations at low risk for sexually transmitted infections being sometimes at greater risk for development of prostate cancer. 474 Even if one accepts this contentious assumption, one would need to demonstrate that circumcised men are at lower risk of sexually transmitted infections. Instead, the medical literature indicates circumcised males are at an overall greater risk of sexually transmitted infections. Since a single infectious agent has not been identified as being associated with a greater risk of prostate cancer, it is more likely that infectious agents associated with urethritis would impact the health of the prostate. Urethritis is not reduced, and may be increased, with male circumcision.
The CDC draft mentions only one observational case-control study, of the many that have been published, on the topic of prostate cancer as associated with male circumcision. 475 The writers of the CDC draft fail to mention several important aspects of this study. Male circumcision status was determined by self report, which is known to be notoriously inaccurate. The study did not find a significant association between prostate cancer and a history of sexually transmitted infections (OR 1.05; 95%CI 0.87-1.27), which undermines their working hypothesis. The adjusted odds ratio for the risk of prostate cancer (circumcised versus intact men) reported in the body of the study was 0.87 (95%CI 0.74-1.02), which was not statistically significant. Therefore, as a whole, this study does not support their contention. Other concerns about the validity of this study have been raised. 476 Isolating the impact of male circumcision on the risk of prostate cancer has been difficult. For example, race and ethnicity are important factors. When compared to controls with benign prostatic hypertrophy, circumcised non-Jews had a significantly greater risk of prostate cancer than Jews (OR 3.23; 95% CI 1.56-6.69). This would indicate that race/ethnicity are more important than male circumcision. 477 A British study failed to consider race or ethnicity, so male circumcision status may have been a marker of race and/or socioeconomic status. 478 In an American study, there was an interaction between race and male circumcision status. 479 When Jews are excluded, several studies have failed to find a significant association between male circumcision status and prostate cancer. 480,481 Also, no association has been demonstrated between male circumcision status and PSA levels. 482 On a population level, if male circumcision decreased the risk of prostate cancer, one would expect as the male circumcision prevalence increased in the United States, the incidence of prostate cancer would decrease, but the opposite has occurred. 483 One would also expect the age-adjusted incidence of prostate cancer in European countries to be higher than that in the United States, but it is lower in Denmark, Finland, Iceland, Norway, and Sweden, 484 as compared to the United States. 483 Several of the studies relied on patient report to determine male circumcision status 475,478,479 and failed to adjust for risk factors known to influence prostate cancer risk. The combination of poorly executed studies, along with an unproven theory linking prostate cancer to sexually transmitted infections, the lack of evidence linking sexually transmitted infections to male circumcision status, and the lack of evidence linking male circumcision to prostate cancer on a population level should have indicated to the writers of the CDC draft that this topic was not worthy of inclusion in the draft.
In summary, penile cancer is very rare, more rare than male breast cancer, and its link to neonatal male circumcision, based on recent studies, is tenuous. An evidence-based discussion of male circumcision should not include any discussion of prostate cancer.
# RESPONSE 69:
See responses 1 and 6. We have updated the literature review and it provides more evidence indicating the male circumcision if protective against penile and prostate cancers.
# COMMENT:
# Cervical cancer in female partners of circumcised men
The material presented in this section of the background document is limited to one select substrata of a single study. 405 The study from which this substrata was extracted did not properly analyze the data. The data were collected in studies from five different countries, yet were not stratified by country. In four of the countries, only a small number of men were circumcised. In the fifth country, only a small number of men were not circumcised. Since cervical cancer rates can vary by geography, it is important to stratify the data by geography. The analysis in this study failed to do this. If they had performed the analysis properly, this selected substrata when further stratified by geography would have necessitated the use of exact statistics, which the authors of the study did not use. Exact statistics revealed much wider confidence intervals. Even with the stratification they performed (monogamous women with male partner with 6 or more lifetime sexual partners), it is interesting to note that the raw numbers found little or no difference (OR 1.02; 0.71-1.47). Furthermore, with reporting the results of the selected substrata the finding should have been subjected to a Bonferroni adjustment, but was not. By doing so, the threshold p-value would be divided by 3. Consequently, this statement is based on evidence that was misinterpreted.
This section also exhibits significant omissions that are critical for the intended audience of clinicians. The single study cited in the background document on this topic did not find a statistically significant association between cervical cancer in women and the circumcision status of their male sexual partners. 405 There have been 15 other studies that have reported on the association between cervical cancer and the circumcision status of a woman's male sexual partner. None of them found an association that was statistically significant. 405,[485][486][487][488][489][490][491][492][493][494][495][496][497][498][499] (One study reported a p-value of .045, 495 but this was not properly calculated. Using Fisher's two-sided exact test, the p-value is .0733.)
The CDC has focused on a substratum of one of 16 studies while ignoring the other 15 studies in order to find a statement that supported their conclusion. This is a clear case of confirmation bias.
# RESPONSE:
See responses 1 and 6.
# COMMENT:
Urinary tract infections in male infants
# COMMENT:
The material presented in this section of the background document is overly optimistic and misinterpreted. The data on which the report relies have been extracted from observational studies that contain a number of methodological flaws that make it difficult to ascertain whether urinary tract infections were properly diagnosed in these studies.
For example, many studies use only bacteriuria as a diagnostic criterion, which would include the 1% of children who, at any given time, will have asymptomatic bacteriuria.
To properly make the diagnosis of urinary tract infection, there must be evidence of inflammation. 500 Similarly, urine specimens collected in bags placed over the genitals are often used to screen for urinary tract infection. This method has a high false positive rate, especially in girls and normal boys, with a contamination rate of 65% to 70%. [501][502][503] This may lead to an oversampling of intact boys. There may also be a differential in health care seeking behaviors. 504 For example, Hispanic boys, who are more likely to have normal genitals, seek health care more frequently, 505 and therefore are more likely to be diagnosed, often incorrectly, with a urinary tract infection.
# RESPONSE 71:
The reviewer fails to provide evidence that the UTI studies used in the CDC background analysis were methodologically flawed. The statement that bagged urine specimens may have a high false positive rate and may lead to "an oversampling of intact boys" is unclear. The argument that Hispanic boys seek care more frequently and are more likely to be diagnosed, often incorrectly, with a UTI is the reviewer's opinion rather than a scientific finding.
# COMMENT:
The reference to the 1987 study of US Army hospitals worldwide 506 that noted an increase in the total number of urinary tract infections as the male circumcision rate declined overlooks the fact that the data collected by the authors were not consistent over time. 507 For example, the rate of diagnosing urinary tract infection decreased significantly from 0.16% in the first three years of the study to 0.07% in the last three years of the study. (RR 0.462; 95%CI 0.338-0.633). 504 The yearly rates of urinary tract infections in circumcised boys ranged from 0.07% to 0.23%, which the authors characterized as being "relatively consistent." 506 The rate of urinary tract infections in boys with normal genitals increased from 0.87% to 1.09% between the two time spans (OR 1.25; 95%CI 0.96-1.61). The association between male circumcision and urinary tract infection was not consistent over time. The odds ratio for intact boys being diagnosed with a urinary tract infection in the first three years of the study was 5.51 (95%CI 4.08-7.44) and in the last three years of the study was 14.91 (95%CI 10.48-21.21). Both of these estimates are outside the 95% confidence interval for the odds ratio estimated for the entire time span of the study (8.69-12.15). This undermines the internal validity of the study. 507
Response 72: Any supposed change in rates of diagnosing UTIs would likely be the same for both circumcised and uncircumcised boys, however, the important fact here is that uncircumcised boys had a higher risk of UTIs compared with circumcised boys.
# COMMENT:
Several studies suffered from misclassification bias in that the male circumcision status could not be correctly identified. 508,509 The studies generated from the database of US Army hospitals worldwide also made no attempt to determine if there was the possibility of misclassification bias. In a chart review performed by the Centers for Disease Control, 15.7% of the boys circumcised neonatally did not have it documented on the hospital chart's face sheet, which is the source of database information. 6 In the US Army studies, if 15% of the boys circumcised did not have it documented on the face sheet, as many as 78.1% of the boys thought to be intact may have actually been circumcised. If one adjusts for this possible non-differential misclassification, the US Army data from 1974 to 1983 would yield an odds ratio (intact males versus circumcised males) of 4.13 (95%CI 3.34-5.11), while the data from 1984-88 would yield an odds ratio of 4.07 (95%CI 3.28-5.05). These odds ratios are more in line with those estimated in other studies.
Response 73: Once again, despite the reviewer's adjustment for "possible nondifferential misclassification", the odds ratio indicates that uncircumcised boys had a higher risk of UTIs compared with circumcised boys.
# COMMENT:
One model has been published that estimated the impact of confounding on the association between male circumcision and urinary tract infections. If one begins with the assumption that the rate of true urinary traction infections is the same in intact and circumcised boys, modeling of confounding factors -such as frequency of medical visits, likelihood of collecting a urine sample, urine collection method, et cetera -will result in making a diagnosis of urinary tract infection (a combination of true positives and false positives) 4.27 times more frequently in intact boys. 510 Consequently, the associations that have been measured between male circumcision and urinary tract infection may have been largely the result of confounding factors rather than a true association.
This is consistent with the HMO data collected by Altschul who found a high rate of misdiagnosis of urinary tract infection when he compared information garnered from the medical chart as opposed to the HMO's database. When proper diagnostic criteria are applied, the urinary tract infection was much lower than reported from the US Army data. 511 In a study of 603 intact Japanese boys aged 0 to 15 years, none had ever reported having had a urinary tract infection. 85 An important omission in the background report is that at least seven studies out of Israel indicated that urinary tract infections occur at a higher rate following infant male circumcision. [512][513][514][515][516][517][518] This increased risk of urinary tract infection may be related to techniques used in ritual male circumcision to control the bleeding that may restrict urine flow, thus leading to the urinary tract infection. Parents who desire a ritual male circumcision for their son need to be aware of this risk.
# COMMENT:
The increase in diagnosis of urinary tract infections may be because parents are instructed to retract the foreskin on a regular basis in order to clean the head of the penis. This is inappropriate advice resulting in manipulation of the urethra and the equivalent of "honeymoon cystitis." Consequently, these infections may be iatrogenic.
An important omission in this section is that the long-term risks associated with urinary tract infections in infants are less than previously believed. For example, it has been demonstrated that treatment with oral antibiotics is as effective as treatment with intravenous antibiotics. 519 Urinary tract infections that occur in the first twelve months of life are less likely to result in renal parenchymal involvement. 520 There is now a strong body of evidence that urinary tract infections rarely, if ever, lead to hypertension or persistent renal dysfunction. [521][522][523][524][525][526][527][528] [38][39][40][41][42][43][44][45] While males are more likely to have vesicoureteral reflux noted on prenatal ultrasound, most cases resolve spontaneously. This temporarily predisposes males to urinary tract infection, 529,530 but the risk is quite low after six months of age, by which time the reflux has resolved. The recommended evaluation for infants with urinary tract infection is less rigorous than previously recommended. 531 Urinary tract infections should not be mischaracterized as an infection with life-long serious consequences, because the medical literature does not support such a characterization.
# RESPONSE 75:
While UTIs can be treated with antibiotics, some children who are treated for UTIs may be resistant to antibiotics while children with UTIs may not be symptomatic or may not be diagnosed in a timely fashion or may not be diagnosed at all if they don't have adequate access to a medical doctor. While UTIs do not always have life-long consequences, they may have such consequences. 53
# COMMENT:
Comparing the rate of urinary tract infections to the rate of immediate complications associated with infant male circumcision drawn from database sources is inappropriate and can be easily misinterpreted. Doing so also deviates from standard epidemiological practices and is misleading. As discussed elsewhere, the rates of complications following infant male circumcision have not been well or consistently measured. Consequently, any comparisons would have little meaning. Citing a study with one of the lowest reported complication rates (0.2% 532 ) to be used for comparison reflects a potential bias of those generating this report. A more apt comparison would involve comparing the rate of urinary tract infection with the rate of meatal stenosis following male circumcision. Meatal stenosis rates range from 5% to 20% and often require surgical correction (meatotomy), 186,[533][534][535][536][537] while the rate of urinary tract infection is 0.7%. 538 In this comparison, there would be approximately 3 to 15 meatotomies performed for every urinary tract infection. Yet, this is not a standard epidemiological approach. The most appropriate approach is to calculate the number needed to treat. This number has been estimated to be between 111 23 and 195. 538 The average cost of an infant male circumcision, according to investigators at the CDC, is $285. 472 Consequently, one would need to spend between $31,635 and $55,575 to prevent one urinary tract infection that can be treated with a course of oral antibiotics that cost less than $20.
# RESPONSE 76:
The neonatal complication rate in the first month of life of 0.2% has been consistently found across several studies indicating strong reliability of results. [44][45][46] COMMENT:
# Other health conditions
The material presented in this section of the background document is highly selective, omits several important studies, and gives credence to studies with serious methodological flaws.
# RESPONSE:
See responses 1, 6, 33, and 41 for all sections in "other health conditions".
# COMMENT:
The authors of the draft rely heavily on the 2000 study of Mallon et al. 394 This study has two fatal methodological flaws. The first is that it was undertaken in a dermatology practice, thus is subject to referral bias. If primary care physicians are capable of taking care of penile dermatoses in circumcised males, they may be less likely to refer them for specialty care. Therefore, penile dermatoses in circumcised men would be underrepresented in a dermatology practice. Consequently, it is impossible to say whether this referred population is representative of the general population. The second fatal flaw is that the study had a control group of men seen in the dermatology clinic who did not have penile problems. The control group had a male circumcision rate of 47.8%. Britain has a national male circumcision rate of 21%. 539 If one had a control group with a male circumcision rate of 21%, the positive findings of the study are negated.
There are a number of important oversights in this section of the draft. For example, in the 1986 study by Herzog and Alvarez, the differences in prevalence of balanitis, penile irritation, and phimosis based on male circumcision status were not statistically significant. 505 In the 1988 study by Fergusson et al., penile inflammation was more common in circumcised boys in the first three years of life and overall there was no statistically significant difference. 190 For reasons that are unclear, the authors of this draft cite an opinion piece written by a known male circumcision advocate to support their assertions. 540 Citing review articles and opinion pieces is inappropriate and not considered scientifically valid or evidence-based.
Regarding the risk of balanitis (which includes balanitis, posthitis, and balanoposthitis), this section of the CDC draft has several important omissions. First, in a 1982 study of over 1000 intact Chinese boys only 0.08% (95%CI 0%-0.24%) had signs of active balanitis, while only 0.65% (95%CI 0.20%-1.10%) had ever had balanitis. 541 Second, in a 1997 study of Japanese boys, they found one case of balanitis in 1283 (0.08%) three year old boys. 542 Third, is a 1989 study in Britain that found the cumulative risk of balanitis by age 7 to 14 years of age to be 4%, with most patients having a single episode easily treated with topical agents. 543 Finally, a 2007 report, 187 which updated a 1997 study 186 of 468 boys, found that among 473 boys under three years of age, intact boys were significantly less likely to have penile inflammation than circumcised boys (OR 8.01; 95%CI 1.31-329.15). After three years of age, there was no difference.
Regarding the risk of pathologic phimosis, this section fails to mention that the cumulative risk of phimosis in intact English boys is 0.6% in the first 15 years of life 457 and 0.42% in Chinese boys, 541 while the risk of phimosis following male circumcision ranges from 0.3% to 2.9%. [544][545][546] There have been three studies directly comparing the rates of phimosis in normal and circumcised boys and none have found a statistically significant difference. 186,190,505 The section fails to mention that meatitis/meatal ulceration is common in circumcised males and rare in intact males. It is most commonly seen in the first few months of life. The inflammation is thought to be the result of constant irritation from urine, stool, and friction from rubbing against a diaper. 547 One report noted that meatal ulcers were seen in 20% of newborns in the first 35 days following male circumcision. 548 In 219 circumcised boys under 3 years of age, 19.1% had meatitis, a rate significantly higher than in intact boys in whom it was not seen (p=.030). 186 A review of the entire medical literature does not support the contention that male circumcision has a positive impact on phimosis, balanitis, and meatitis. Consequently, the recommendation for the intended audience of health providers is misleading, not justified, and not appropriate.
# Health conditions for which male circumcision is indicated
The material presented in this section of the background document is, for the most part, somewhat accurate. However, the statement that male circumcision is the "definitive treatment" for phimosis is confusing. Phimosis can be physiologic, which requires no treatment, or it can be pathologic, which requires treatment. Circumcision should not be considered first line therapy for pathologic phimosis. Balanitis xerotica obliterans (BXO) is the most common cause of pathologic phimosis. Fortunately, it is rare. Some, but not all, cases of BXO will respond to topical steroid application. A high response rate of phimosis to topical steroid application has been repeatedly demonstrated. Likewise, there have been many reports of surgical techniques that correct phimosis without removing any tissue. [572][573][574][575][576][577][578][579][580][581][582][583][584][585][586][587] Several systematic reviews and cost-benefit analyses have indicated that male circumcision is the least favorable method of treating phimosis and the standard of care is shifting to topical steroids as the first line of therapy followed by surgery, if topical therapy fails. [588][589][590] The language of the draft needs to reflect this shift.
# RESPONSE 77:
We have clarified that there is a distinction between physiologic and pathologic phimosis in the text and changed the text to read "In the absence of a response to topical steroids, or when the child is not a candidate for steroid use, male circumcision is the definitive treatment."
# COMMENT:
# Safety and risks associated with male circumcision
The material presented in this section of the background document is highly selective and ignores studies that do not agree with the CDC's apparent goal of presenting infant male circumcision as being safer than it actually is. Most of this section is spent reviewing studies that derived their data from databases, 532,591,592 which will underestimate the rate of complications by at least 10-fold, if not more. When assessing the rate of complications reported in the medical literature, several factors are important. Some immediate complications are common and their frequency can be easily estimated. Others have been reported in case series, where the authors report their experiences with several patient episodes. Many of the more uncommon complications have been reported as case reports. From case series and case reports, it is hard to estimate the frequency of a particular complication. Certainly, not every complication is reported in the medical literature, and a number of barriers keep unusual complications from being reported. The complication needs to be recognized as related to, associated with, or caused by the procedure, and authors need to be willing to take responsibility for the complication. Next, the person identifying the complication has to decide whether to pursue reporting the complication, and they must have the time and resources to perform the task. Once the case report or case series is written and submitted, it is unlikely to get published unless the new report adds something to what has already been published. Medical journals are publishing fewer case reports, so a case report often needs to be shopped around to several journals before it finds a home. Most authors will give up submitting after a couple of rejections. Consequently, some have estimated that for every case report published in the medical literature, there may be 100 to 1000 unreported cases.
Imprecise and inconsistent definitions for what constitutes a complication, such as how much post-operative bleeding is permissible, also muddies the waters. Definitions may be more or less inclusive, often depending on what message the author wants to convey. This expectation bias is blatant in some studies. For example, in the African randomized clinical trials of adult male circumcision, very low complication rates (1.3% to 3.6%), lower than those commonly reported for infant male circumcision, were reported for the procedure and delayed complications were not assessed. [1][2][3] It would appear that the aim was to present adult male circumcision as a low-risk procedure in advance of the planned male circumcision roll-out. Because the definitions and criteria for inclusion of complications vary so widely, any attempt to perform a systematic review and meta-analysis of the medical literature on this topic would be a fool's errand, and assigning any worth to conclusions reached in the process would be pointless. 29 [Note: citation CDC157 does not properly list the authors of this study.] Any such analyses are not worthy of mention. If mentioned at all, the extreme limitations in studying this topic need to be stressed.
What constitutes a complication by a researcher's definition also affects the reported incidence of that complication. If bleeding complications included those patients who had any oozing of blood following male circumcision, then the complication rate would be much higher than if bleeding complications included only those who required sutures. For example, in the study by Gee and Ansell the definition of "really significant" is arbitrary. One could easily include all of the hemorrhages requiring sutures (15), all of the denudation patients (2), half of the dehiscence patients (4), and all of the Plastibell being too tight (7). Instead of 14 patients who had "really significant" complications, the number tripled to 42. 593 Many studies are limited by how long they follow their subjects. As a consequence, many of the delayed complications will be missed. For example, the database study by Christakis et al. only considered complications noted during the perinatal admission. As expected, they saw virtually no infectious complications. 532 Infections resulting from male circumcision would be expected to occur days after the procedure, a time when nearly all these patients would have been discharged from the hospital. Likewise, the database study by Wiswell and Geschke looked only at the complications occurring during the first month of age. 591 This study, by design, would miss nearly all the cases of skin bridging and adhesion formation, buried penis, meatal stenosis, and inadequate or cosmetically inferior results.
Pediatric urologists are faced on a daily basis with the complications resulting from infant male circumcision. Nearly all of these complications are not seen in the immediate post-operative period. One pediatric urologist noted that of 235 boys referred to him in a 24-month period with male circumcision complications, about half of them required additional surgery. His experience is typical for his surgical sub-specialty. In the United States, a third of pediatric urologists report having served as an expert witness in male circumcision injury cases. Substantial malpractice claims have been paid for male circumcision-related injuries. 594 The study design and method of data collection can also have an impact on estimating the rates of complications. Higher complication rates will be documented in a group followed prospectively over a short period of time with scheduled follow-up examinations, as compared to a group followed retrospectively over a decade. When looking for complications prospectively, the complications are proactively observed and recorded. For example, a prospective study found an excessive bleeding rate of 8.9% to 9.9% following infant male circumcision. 595 Retrospective studies typically see excessive bleeding following 1% to 2% of male circumcisions.
In a retrospective study, only those complications recorded in the chart, usually in the nurses' notes, are available. Complications not documented in the chart would be missed. Therefore, the complication rates in chart reviews would be lower than in a prospective study. Chart reviews, including one published by the CDC, have documented complication rates of 2% to 6%. 6,593,596 Still, a chart review will uncover more complications than searching a database for diagnostic and procedure codes. For a complication to be tallied in a database, it not only must be recorded in the medical record, but it also must be listed as a discharge diagnosis. Only the most severe, lifethreatening complications will be picked up in a database study. This does not mean that severe complications will not also be missed in a database. For example, an infant who had a third of his glans amputated using a Mogen clamp, resulting in a $2.3 million malpractice judgment awarded in 2009, did not have this complication listed on the medical record's face-sheet, so it would not have been entered into the database. 597 As a consequence, the complication rates for the database studies, which are in the range of 0.1% to 0.2%, 532,591 are ten times lower than the complication rates in chart review studies.
RESPONSE 78: : CDC stands by the accuracy and scientific rigor used to conduct its study on adverse events associated with male circumcision 15 and represents the first study of its kind in the U.S. which allows a comparison in adverse events reported among circumcised and uncircumcised males during three age ranges (age < 1 year, 1-9 years, ≥10 years). In the absence of longitudinal data on circumcised versus uncircumcised males comparing rates of adverse events related to male circumcision, a database study provides a good source of data to describe complications reported at discharge. No study is without limitations. Longitudinal chart review studies may only provide data that is representative for those geographic sites where the studies are located.
# COMMENT:
If studies whose data are mined from databases miss approximately 90% to 95% of the complications, do they serve any purpose? They would if their results can be extrapolated to accurately reflect reality. To demonstrate this, one would need to perform either a blinded prospective data collection or a chart review data collection in which information for the database is simultaneously generated to assess how well these sources of information correlate. To date, such a study has not been published.
Consequently, the studies of complication rates that are based on databases do not provide useful information and should not be taken seriously when developing policy.
While the CDC draft elaborates on the numbers generated by one such study, 592 the time spent by these researchers would have been better spent collecting useful information.
RESPONSE 79: The reviewer's allegation that database studies miss approximately 90% to 95% of the complications is conjecture.
# COMMENT:
This study, with its markedly flawed data, makes the claim that complication rates are greater if male circumcision is delayed beyond the newborn period. The problem is that data collection and reporting methods differ in the two age groups, which alone could explain the difference. The only reliable studies to assess this question are those that compared two age groups using the same evaluation tools, the same skill in practitioners, in the same environment, at the same time. Only a handful of studies have done so, and they do not support the authors' claim. In one study, complications were only seen in those who were circumcised at under 72 hours of life. 544 In the second, the Gomco clamp was found to have more bleeding complications in older boys than in neonates. 598 In a third study from Iran, no difference in the complication rate was found between age groups. 599 In a fourth study from Saudi Arabia, a greater rate of complications was seen in male circumcisions performed in the neonatal period. 600 Several studies have indicated that the Plastibell should not be used after the neonatal period. 601,602 RESPONSE: See response 78.
# COMMENT:
The CDC draft, citing a 1983 review article, 19 provides an incomplete list of complications following infant male circumcision. The CDC draft should have included a complete list of complications and, where available, estimates of their likelihood. While this information is not available in the CDC draft, this information is essential for the intended audience of health care providers, so they can provide adequate disclosure to patients or their proxies for the fully informed consent process to be valid. Considering that infant male circumcision is a purely cosmetic procedure performed primarily for cultural reasons, the required level of disclosure is higher than for procedures for which there is a clear medical indication. For this reason, providing complete disclosure should be the standard of care prior to infant male circumcision. This would include a listing of all the known complications resulting from infant male circumcision. Doing so not only fully informs the person providing consent/permission, but it also protects the health care provider performing the procedure should a complication develop as a result of the procedure.
Bleeding: Bleeding can be minor or require the application of clotting enhancers, suturing, and/or blood transfusions. 591,603,604 It can result in cardiac arrest, 605 or exsanguination. 606 Some patients will lose enough blood that a blood transfusion is needed. 591,593,596,[607][608][609][610] In male circumcisions performed on older children, postoperative bleeding is often the reason for hospital admission following the outpatient procedure. 611,612 The penis and the foreskin, which is fed by the frenular artery and is a frequent source of bleeding, are highly vascularized structures. Bleeding complications can occur with any of the techniques used without regard for the experience or expertise of the operator. 613,614 The complication rate from bleeding varies widely with study design, the definition of excessive bleeding, and the attitude of the researcher toward male circumcision. For example, in a prospective study designed to determine the incidence of hemorrhagic diseases and the impact of vitamin K, 9.87% of male circumcisions resulted in abnormal bleeding. 595 A chart review by Gee and Ansell found a bleeding rate of 1.0%, 593 while data from a database noted excessive bleeding in 0.083% with 0.028% needing ligatures applied and 0.003% requiring transfusion. 591 Health care providers also need to recognize that excessive bleeding following male circumcision may be the first sign of an undiagnosed bleeding disorder. [615][616][617][618][619][620][621][622][623][624] Infection: Following male circumcision, the newborn is at greater risk for infections because of the open wound involving the entire surface of the glans, which then sits in a diaper exposed to urine and feces. For several days following male circumcision, a greenish-white, fibrinous discharge forms over the male circumcision wound, which will exhibit a mixture of flora, including Klebsiella, Enterobacter, and Acinetobacter. 625 Infections can also be caused by Staphylococcus aureus, 626 Escherichia coli, 627 Group A ß-hemolytic Streptococcus. 628,629 A positive bacterial culture cannot differentiate between colonization and tissue invasion. 625 Because of the high frequency of purulentappearing exudate from the wound, it is difficult to differentiate this exudate and erythema, which results from an open wound, from that of an infection. Estimates of the frequency of infections following male circumcision vary considerably as there is a tendency not to ascribe a poor outcome to an elective procedure. 629 The Plastibell, because it involves necrotic tissue adhering to the wound, may be associated with more infections and is linked to tissue necrosis and gangrene.
Staphylococcal infections (including MRSA): Several studies have found a higher rate of Staphylococcal skin infections in the first weeks of life in males, especially among those circumcised, as compared to females. 188,189,[630][631][632][633][634][635][636][637][638] More recently, several outbreaks of neonatal cutaneous MRSA infections have been reported, primarily in circumcised boys. [639][640][641][642][643][644][645][646][647][648][649] In only one outbreak reported had none of the infected boys been circumcised. 650 One case-control study was able to document that a circumcised newborn boy was at 12 times the risk of developing a MRSA infection compared to a newborn boy that was not circumcised. 651 In describing this study, the CDC mischaracterizes and downplays the results as the "hospital identified male circumcision as a potential risk factor," when the study found a statistically significant association. It is revealing that in instances where studies are favorable to male circumcision the CDC draft does not downplay these associations. In one case report, MRSA was recovered from the male circumcision wound of a newborn infant whose mother had staphylococcal toxic shock syndrome. 652 The frequency of staphylococcal infections varies from study to study, but in one series of male circumcisions performed with a Plastibell, 10.7% developed impetigo. 653 The increase in staphylococcal infections following male circumcision is not unexpected. Studies have shown that male circumcision alters the normal flora from primarily gram-negative organisms to grampositive organisms, including staphylococci. [141][142][143][144] Staphylococcal scalded skin syndrome: Case reports and cases series of staphylococcal scalded skin syndrome following neonatal male circumcision have been reported. [653][654][655][656] In one series of 75 male circumcisions performed with a Plastibell, 2.7% developed staphylococcal scalded skin syndrome. 653 Abscesses of the penis and scrotum following male circumcision have been reported in a number of case reports. 628,[657][658][659][660] Erysipelas, a skin infection usually caused by Streptococcus that can lead to Fornier's gangrene, has been reported following male circumcision. 661,662 Group A ß-hemolytic Streptococcus infections have been reported following infant male circumcision during outbreaks in neonatal nurseries. 663,664 Acute post-streptococcal glomerulonephritis has been reported following an infected male circumcision. 665 Diphtheria infections, before widespread vaccination programs, were reported following both ritual and medical male circumcisions. 666,667 Syphilis: In the late 1800s, there were many reports of syphilis following neonatal male circumcisions from oral-genital contact during the procedure performed by infected mohelim. 668 Tuberculous: Reports of penile tuberculosis following ritual male circumcision were commonplace in the first half of the twentieth century. [669][670][671][672][673] Most often, the history involved the wound being sucked by the mohel, who would invariably be found to have tuberculosis. 674,675 Cases continued to be reported well into the twentieth century. [676][677][678] Herpes simplex virus is also spread via the oral-genital contact that can occur during ritual male circumcision with some cases resulting in death or brain damage. [679][680][681][682] When these infections were discovered in New York City, Tom Frieden, current director of the CDC and the Commissioner of the New York City Department of Health and Mental Hygiene at the time of the herpes outbreaks, and Susan Blank, the chair of the American Academy of Pediatrics Task Force on Circumcision, did nothing to stop these easily preventable infections.
Tetanus following ritual male circumcision has been reported in multiple case series. [682][683][684][685][686][687][688][689] Septicemia, which is an overwhelming, systemic, life-threatening infection can follow male circumcision. 660,[690][691][692][693][694][695][696][697] Once the bacteria have entered the bloodstream, the infection can spread throughout the body. Reports have noted pneumonia, 698,699 empyema, 660 soft tissue abscesses, 660 osteomyelitis, 694,698,700,701 septic arthritis, 660,694,701,702 pyelonephritis, 698 peritonitis, 703 bilateral femoral head necrosis, 694 umbilical arteritis, 628 gangrene, 702,704,705 suppurative inguinal lymphadenitis, 694 and meningitis. 627,629,694,705,706 Sepsis following male circumcision can also lead to disseminated intravascular coagulopathy, jaundice, congestive heart failure, 697 peripheral circulatory collapse, 698 hypothermia, 697 and death. 654,693,696,699,707,708 Fornier's gangrene, which is necrotizing fasciitis of the perirectal, perineal or genital area, resulting in gangrene of the overlying skin, 709 has been repeatedly reported in the medical literature, [710][711][712][713][714][715][716][717][718][719][720][721] following both tribal male circumcisions 722 and male circumcisions performed in a medical setting. 704 These serious, life-threatening cases emphasize the necessity of informing parents of the uncommon, but potentially serious, risks of neonatal male circumcision. 723 Surgical complications include total denudation of the penis 718,[724][725][726][727][728][729][730][731][732] and the removal of too much shaft skin. 660,[733][734][735][736] Even with proper technique, especially with the clamp techniques, it may be difficult to estimate how much skin is removed. The removal of too much skin is so common that many practitioners may view the results as normal.
Urethral fistula following male circumcision has been reported in a number of case reports and case series. 83,720,732,[737][738][739][740][741][742][743][744][745][746][747][748][749][750][751][752][753][754][755][756] This complication requires careful repair by experienced specialists. 757 Other surgical complications, such as multiple pyogenic granulomas, 758,759 subglandular stricture, 760 and scrotal trauma [761][762][763] have been reported following male circumcision.
Plastibell retention/pseudoparaphimosis: If the Plastibell ring does not fall off within eight days, a complication is likely to result. The Plastibell ring can dislocate proximal to the glans, where it can mimic paraphimosis, also known as pseudoparaphimosis. The dislocated ring can result in compression damage, ulceration of the corona and proximal glans, and edema and vascular congestion distal to the ring. Removal of the ring with a wire cutter is often needed. Reports in the medical literature have included significant long-term penile deformities, 732,[764][765][766][767][768][769] signs of urinary obstruction, 770 pseudoparaphimosis, [765][766][767][768][771][772][773] and strangulation of the penis. 774 The incidence of pseudoparaphimosis following use of a plastic bell male circumcision device has been reported to range between 0.27% 593 to 1% 765 to 1.6%. 596 The risk of a Plastibell tracking back onto the shaft and needing to be removed using a ring cutter is 3.6% and incomplete separation is seen in 5.9% of patients. 775 Another study found ring retention in 2.1%, with 0.8% developing necrosis and 0.9% developing pseudoparaphimosis. 776 In one series, primarily in neonates, there was an 11% retention rate. 614 Bivalving: Inadvertent placement of scissors into the urethra while attempting a dorsal slit resulted in surgical bivalving of the glans. 731,777 Penile necrosis/ischemia is a serious complication that has been noted in a number of case reports and case series. 6,660,704,718,746,763,776,[778][779][780][781][782][783][784][785][786][787][788][789][790][791][792][793][794][795] In one series the rate of necrosis was 0.8%. 776 Amputation of the penis and glans: Since several of the devices used to perform male circumcision involve a "blind" amputation of the foreskin, there are multiple case reports and case series reported in the medical literature related to partial or complete amputations of the glans. 628,696,705,731,741,750,755,762, Since many of these reports are in the form of describing techniques to reattach the inadvertently amputated tissues, the number of actual cases might be much greater. These amputations are often the source of malpractice cases. In some instances, it was decided to raise these boys as girls. 801 Acute urinary retention, typically from bandages that are too tightly wrapped around the wound in ritual male circumcisions, or a Plastibell ring obstructing the meatus, has also been reported. 593,705,762,[823][824][825][826] In a series of older boys circumcised with a Plastibell, 0.35% complained of urinary retention. 826 In follow-up of 99 boys circumcised at a mean age of 4.3 years, 19 did not pass urine for more than 12 hours. Five boys held out for several days (maximum 3 days) with one requiring readmission. 533 In a study of older boys circumcised with a Plastibell, 56.3% had difficulty with micturition. 827 In a study of healthy male neonates, the mean time to voiding was 5.3 (SD=2.5) hours after the procedure with the longest duration to post-male circumcision voiding being 11.5 hours. 828 In another study of circumcised newborns, the mean time to post-male circumcision voiding was 4.97 hours (SD=3.35). A few (0.38%) took more than eighteen hours after male circumcision to void. 829 Other complications from urinary retention, such as bladder rupture, 830 obstructive uropathy, 831 acute renal failure, [831][832][833] and urine advancing in subcutaneous fascial planes 834 have also been reported.
The tight bandaging technique used in ritual male circumcision also places the boy at greater risk for urinary tract infections. [512][513][514][515][516][517][518] Leg cyanosis, both unilateral 835 and bilateral, 836 gastric rupture from air swallowed while crying during the procedure, 837 pulmonary embolism, 838 pneumothorax, 839 erythema multiforme, 840,841 myocardial injury, tachycardia, heart failure, 842,843 and impotence (in adult men) 844,845 have all been reported following male circumcision.
Apnea/Apparent life-threatening events have been reported, 846,847 with a rate of 3.85% of prolonged apnea following the procedure. 847 Chilling was noted to be a problem when male circumcision was performed just after delivery. 848 Hyperbilirubinemia (jaundice). Since it has been shown that breastfeeding and bottle feeding are adversely affected by neonatal male circumcision, one would expect that circumcised boys might be at greater risk for hyperbilirubinemia. While not studied directly, two studies in American infants have found boys to be at greater risk for hyperbilirubinemia. 849,850 In the Canadian database used to determine the rate of urinary tract infection based on male circumcision status, it was discovered that circumcised boys were significantly more likely to require hospitalization (excluding hospitalizations for urinary tract infection) during the first year of life. 538 This differential could be due to hospitalizations for hyperbilirubinemia. This is an area open for future research.
The presence of a hypospadias is an absolute contraindication to male circumcision, yet circumcisions have been reported being performed on boys with a hypospadias. 593,851 There have been reports of techniques to correct hypospadias in circumcised patients, [852][853][854][855] and techniques to repair hypospadias without a male circumcision leaving the penis with a fully intact appearance. 856 Hematoma following male circumcision is fairly common. 753,857 The rates have been reported as 0.46%, 776 0.98%, 858 6.1%, 827 and 7.7%. 695 It is one of those complications so common that it is not usually considered out of the ordinary, and therefore, is not likely to be identified as a "complication."
Delayed complications: Most studies attempting to compile the complication rates for male circumcision do not collect data long enough to capture the long-term complications.
Meatitis is a common finding as most circumcised boys shortly after the procedure will have erythematous meatal openings. Most physicians unaccustomed to examining the meatus in intact males would consider the inflamed meatus to be a normal feature of the circumcised penis. 547,548 The inflammation is thought to be the result of constant irritation from urine, stool, and friction from rubbing against a diaper. 859 The rates of meatitis are approximately 20%. 186,548 Meatal stenosis, which has been recognized as a complication of male circumcision for some time, may be the most common complication following male circumcision. 186,533,535,536,545,604,614,741, In 1881, Mastin stated that narrowing of the meatus was the rule for Jews, not the exception, and meatotomy (the surgical correction of meatal stenosis) was designated by many Jews as their "Second Circumcision." 885 Symptoms associated with meatal stenosis include penile pain at the initiation of micturition, narrow high velocity stream, the need to sit or stand back from the toilet bowl to urinate, abdominal pain, enuresis, dysuria, urinary urgency, urinary frequency, straining to urinate, urinary dribbling, and urinary retention. 535,870,879,886,887,888 The meatal slit at the urethral opening should be 25% to 30% of the diameter of the glans. 860 The meatal opening is significantly smaller in circumcised males and meatal stenosis occurs almost exclusively in the circumcised penis. 46,538,873,889 (Most physicians do not know what constitutes a normal meatal opening, if they have never examined an intact male or been educated about the normal penis. The CDC should focus its efforts on educating health care providers about normal penile anatomy, care of the normal intact penis, and on diagnosing and appropriately treating the complications of male circumcision.)
The incidence of meatal stenosis following infant male circumcision is found in 2.8% (requiring meatotomy), 533 7.3%, 186,536 32.1%, 871 3.55%, 614 and 20.4%. 537 For boys circumcised later in life, the incidence is 11.1% (necessitating meatotomy) 545 and 7.95%. 538 A report of 58 meatotomies performed on circumcised boys on an outpatient basis in one year's time in a single practice 874 suggests that urethral meatotomy is a very common procedure in the United States. The writers of the CDC draft need to be congratulated on finding the study with the lowest reported rate (0.9%) of meatal stenosis following male circumcision in the literature 599 while turning a blind eye to the remainder of the medical literature. They accept this outlying study without question, yet take a cheap shot at the methodology of a study whose results have repeatedly been verified. 536 Such behavior is both unscientific and unprofessional. One cannot help but notice that the CDC draft is only critical of studies that show male circumcision in a neutral or negative light. It gives the impression, either rightly or wrongly, that the CDC is pursuing a specific pro-male circumcision agenda with this draft.
Meatal stenosis obstructs the flow of urine and can lead to urinary tract infections, vesicoureteral reflux, hydronephrosis, obstructive uropathy, and renal failure. 880,881,887,[890][891][892] Hidden Penis, Buried Penis, Concealed Penis, Trapped Penis, Webbed Penis, Inconspicuous Penis: These conditions have generated much discussion on how to define them and how to treat them.
A concealed penis is a penis that is inconspicuous because of an overlying fold of abdominal fat. A buried penis refers to a penile shaft that is buried below the surface of the prepubic skin and has also been used to describe a partially or totally obscured penis caused by obesity or by a radical male circumcision. A true buried penis is a congenital anomaly that includes an abnormally large suprapubic fat pad and dense dysgenetic dartos fascial bands that tether the penis inward. This requires surgical intervention.
A webbed penis consists of midline skin webs which bind the ventrum of the penis to the scrotum with an abnormal insertion of the scrotum onto the ventral aspect of the penis. [893][894][895][896][897][898][899][900][901][902] Because the skin and dartos fascia are inadequately attached to the underlying Buck's fascia, the corporeal bodies telescope proximally without the skin and dartos fascia covering. Because the penis is suspended from the pubis by the suspensory ligament, it remains fixed, but the fat does not. Fat descends over the penis and covers it. [900][901][902][903] Many intact boys have baby fat surrounding the undeveloped penile shaft. Most of these patients will develop normally, with the excessive baby fat in the pubic area regressing and the penis lengthening under the influence of endogenous testosterone. 897,901,904 Failing to recognize a "hidden or buried penis" at birth makes the condition worse and more difficult to correct down the road if the boy is circumcised. There are multiple case reports of buried penis following male circumcision, 752,762,[905][906][907][908][909][910] and most case series of patients undergoing repairs for this problem are populated with boys who were circumcised as infants. 546,894,899,[901][902][903][904]911 This has also been reported as a problem in circumcised adults. 912 Male circumcision is a problem for these patients, with buried penis, because the base of the shaft skin is not properly attached to the base of the tunica albuginea, so the shaft skin will be bunched up around, and distal to, the sulcus of the glans. Because nearly all of the shaft skin is in a location where it is typically removed by a clamp device, nearly all of the shaft skin is at risk for removal. 893 Since the synechiae that fuses the glans to the inner surface of the foreskin is removed, there is nothing to hold the penis away from the body, so the penis becomes buried in the scrotum and fat pad. 893,910 With the penis completely buried, the circular scar from the male circumcision can constrict resulting in phimosis. 893 This often gives the appearance of "redundant foreskin." 83,893,903,908 This leads the parents to blame the physician for an "inadequate" male circumcision. Despite reassurance from the physician, 899 some parents will demand that the child be re-circumcised, and indeed many of these children will be referred to the urologist for recircumcision. 913 Attempts to re-circumcise, which entails removal of more penile skin, often makes the condition worse, by further burying of the penis, and it makes reconstruction more difficult. 893,[913][914][915] The repair is a complex procedure, which is only made more difficult if the patient is circumcised.
The consensus among pediatric urologists is that infants with buried penis should not be circumcised as it can result in serious consequences. 893,913,916 The take home lesson from all of this is: if the penis appears too small, it should not be circumcised unless it can be demonstrated that it is not a buried penis. 893 It is difficult to estimate the incidence of buried penis. In a series of 313 neonatal circumcisions performed with a Mogen clamp, one developed hidden penis. 544 It is not known if this rate is low because the incidence is low or because researchers did not successfully identify those for whom male circumcision was contraindicated. In one series of healthy boys, 20.1% of boys in the first year of life had a glans that was completely covered, but only 0.9% would be considered to have a buried penis/preputial stenosis. 186 Iatrogenic phimosis/preputial stenosis: Iatrogenic phimosis occurs when the head of the penis is trapped behind the male circumcision scar. The skin remaining after male circumcision can develop a circular cicatrix that contracts and draws the proximal skin over the glans forming a resistant phimosis. Since 1895, multiple case reports have appeared in the literature. 544,917 The incidence has been reported as 1.7% in older boys, 534 0.3% in infants using the Mogen clamp, 544 [67] 2.9% using the Gomco clamp, 546 and 0.9% using a variety of other male circumcision techniques. 186 Given that the cumulative incidence of pathological phimosis in intact boys by 15 years of age is 0.6%, 457 phimosis following male circumcision occurs with equal frequency as in boys who are not circumcised.
Cosmetic concerns: Parents, to a large degree, have their infant sons circumcised for cosmetic reasons: primarily so the boy's genitals will look like the father's genitals.
Since there is a wide variety to be had in the appearance of the circumcised penis, both in children 186 and adults, 46 the intended outcome is unlikely to occur. 918 The desired outcome of a fully exposed glans on an infant in the first year of age is the exception, 186 and parents and older boys are often not pleased with the cosmetic outcome. 776,919 In a series of boys circumcised with a Plastibell, 33.1% of patients experienced cosmetic complications, and 20.8% claimed to have experienced psycho-social problems because of the appearance of the penis after the operation. 920 In a comparison of the Plastibell versus standard free-hand technique in older boys, favorable cosmesis was seen in 60.9% with the Plastibell and 44.9% with standard technique. 827 Consequently, the primary care physician is bombarded with parental concerns that not enough skin was removed. While reassurance is warranted in nearly all cases, there are a substantial number of patients who will doctor-shop until they find someone willing to recircumcise their infant. 921 Re-circumcision to address cosmetic concerns is a commonly performed procedure, 607,922 but, in the case of a buried penis, it will make the situation worse. 893,[913][914][915] In one study, the rate of inadequate male circumcision prompting a surgical revision was 2.8%. 190 In other studies the rate of re-circumcision ran about 1%. [923][924][925] Adhesions: There is some debate whether the adhesions are the result of inadequate stripping of the inner prepuce away from the glans at the time of male circumcision 926 or the reattachment of the epithelium of the inner prepuce to the epithelium of the glans. 927,928 Adhesions have been noted in 15.3% of newborns at their first office visit, 929 10% at the one-month well-child visit, 927 and in 25.6% to 27.6% of circumcised boys overall. Fortunately, with age the prevalence decreases. 186,930 The adhesions which form following male circumcision are more dense than the connections normally found between the inner prepuce and the glans. 927 Parents must be taught how to care for the circumcised penis by pulling back on the penile skin and exposing the glans on a regular basis, so adhesion formation can be avoided. 929 It has been suggested that daily application of petroleum jelly for three weeks following the procedure may decrease the rate of adhesion formation.
Many physicians wrongly believe the proper treatment is to tear the adhesions apart, but this can lead to skin bridges and further scar tissue formation. Most adhesions will resolve spontaneously.
Skin bridges: Some adhesions will form a permanent bridge from the male circumcision wound to the surface of the glans. Skin bridges can cause tethering of the penis, entrapment of debris, curvature of the penis, and pain on erection. 927,929 Several case reports have appeared in the medical literature describing this complication. [931][932][933] Skin bridges are commonly seen by urologic practices. 933 The prevalence of skin bridges was 4.1% in circumcised boys under 3 year of age, 186 Among adult circumcised males, skin bridges were noted in 12.7%. 46 Keloid formation: Keloids are hypertrophic scars that do not decrease in size over time.
Although penile keloid formation is rare, it has been reported following male circumcision. [934][935][936][937][938][939][940] The treatment consists of intralesional steroid injections, surgical excision, or a combination of the two. 934,939,940 Subcutaneous granuloma: A subcutaneous granuloma following male circumcision has been described as an "indurated, confluent, red-violet plaque, freely movable over the underlying tissue, 0.3-1.0 cm wide of firm consistence, surrounding the penis in the neighborhood of the coronal sulcus. Its surface is smooth and the borders are distinctly defined." 941 [These lesions are found on the penis in 4.97% of circumcised boys. 942 Epidermal cysts have been reported following male circumcision. 771,[943][944][945][946] Penile edema: Acquired penile edema in adult males has been reported since 1928 under a wide variety of names. [947][948][949][950][951][952][953][954][955][956][957][958][959][960][961][962] The entity has been described as "a painful, hard, nodular, translucent cord that suddenly appears in the penis and is usually confined to the coronal sulcus," 822 [835] or as a "hard worm-shaped lesion" on the dorsum of the coronal sulcus. 956 The edema comes on suddenly and is self-limited. [960][961][962] It is typically seen in circumcised, sexually active men often after vigorous, frequent, or prolonged sexual intercourse. 948,950,952,954,956,957,[960][961][962] In a series of genital dermatoses presenting to a dermatological referral practice, "idiopathic penile edema" was seen only in circumcised men (p<.01). 394 In most series, the circumcised penis appears predisposed to this condition. 948,955,[959][960][961][962][963][964][965][966][967] It has been postulated that the male circumcision scar interferes with normal lymphatic drainage. 948,955 Alternatively, penile edema has also been attributed to decreased vaginal lubrication, 961 which is a common condition in vaginal intercourse involving a circumcised penis. 115 Inadequate lubrication leads to abrasions of the penile skin, which, in turn, can result in antigen transfer and subsequent hypersensitivity. 963 The uniform success of a variety of interventions 950,951,954 suggests that this condition is benign and self-limited. Acquired penile edema affecting pediatric or adolescent males has been reported less frequently. 963,[965][966][967][968] Based on one prospective series, the incidence in pediatric patients was estimated to be 0.62%. 186 Following adult male circumcisions, penile cutaneous horns can develop. Many of these may harbor malignancies. [969][970][971] Hair strangulation occurs when a human hair becomes inadvertently wrapped around an appendage, usually a finger or a toe. Once the hair gets wet it contracts and cuts into the appendage. There have been multiple case reports of penile strangulation by a hair. 865,[972][973][974][975][976][977][978][979][980][981] Some cases have resulted in urethral fistulas and partial or complete amputation of the penis. 975,976,[981][982][983] The hair typically becomes entrapped in the coronal groove. 979 Of the more than 70 cases reported in the medical literature, all but one case occurred in circumcised males.
Two studies determined that the size of the adult penis is significantly smaller in circumcised men. 46,47 This is important information that needs to be disclosed as part of the informed consent process.
Psychological sequelae: The aftermath of infant male circumcision shares many of the attributes of post-traumatic stress disorder; 984 however, there has been little study to confirm or deny this hypothesis. There is solid evidence to indicate that imprinting happens in the perinatal period, which can have long-term consequences when these infants become adults. [985][986][987][988][989][990][991][992] Given that male circumcision is more traumatic (in terms of provoking a cortisol surge) than gastric suctioning, one would expect that it might have long-term consequences. This has been seen in two studies in which it was found that male infants who had been circumcised shortly after birth cried longer and louder than girls and intact boys when given vaccinations at 4 to 6 months of age. 993,994 The studies concluded, "Because memory of pain is believed to be important in subsequent pain perception, and the main structures for memory are functional in the neonatal period, it is conceivable that pain from male circumcision may have long-lasting effects on pain response and/or perception." 993 Subsequently, it has been demonstrated that inadequate analgesia for initial procedures in young children may reduce the effectiveness of analgesia in subsequent procedures. 995 One study found a positive statistically significant association between male circumcision rates and the rates of autism in boys. 259 A recent national, register-based cohort study from Denmark found that circumcised boys were at significant risk for developing autism spectrum disorder by ten years of age (hazard risk (HR) 1.46; 95%CI 1.11-1.93) and at greater relative risk for infantile autism before five years age (HR 2.06; 95%CI 1. 36-3.13). This same study found that circumcised boys were at greater risk for developing hyperactivity disorder (attention deficit disorder) (HR 1.81; 95%CI1.11-2.96). 996 The link between attention deficit disorder and male circumcision has been suspected for some time given that it has a higher rate in boys and it is diagnosed more frequently in the United States than in Europe. Another preliminary study indicated that circumcised adults are more likely to have alexithymia (difficulty in identifying and expressing feelings). 997 Further study is needed in each of these areas.
Cansever performed psychological testing on Turkish boys before and after ritual male circumcision. Following male circumcision, there was a decrease in IQ, a decrease in body image, disturbance in sexual identification, an increase in regressive traits, and an increase in aggressive behavior, especially toward their mothers. 998 While there has been little study of the psychological sequelae of infant male circumcision, there is no evidence to suggest there is no harm. 999 A potential impact on sexual identification following infant male circumcision needs further study. In a study of men seeking care at a sexually transmitted disease clinic in San Francisco, circumcised men were statistically significantly more likely to identify themselves as men having sex with men (OR 1.13; 95%CI 1.10-1.16). 8 The same lead author collected similar information in a sexually transmitted disease clinic in Tel Aviv with similar results (OR 1.57; 95%CI 1.11-2.22). 1000 This finding needs further research.
Based on these studies, part of the disclosure in the informed consent process needs to include the statement that there are currently preliminary findings indicating that male circumcision is associated with a higher rate of autism, attention deficit disorder, and identifying oneself as gay/bisexual.
Behavioral changes: Richards et al. present both circumstantial and direct evidence that circumcision of male infants leads to behavioral changes. 1001 Several early behavioral gender differences, noted in studies performed in the United States, [1002][1003][1004][1005][1006] have not been noted in similar studies performed in Britain or The Netherlands. [1007][1008][1009][1010] Changes in Sleep Pattern: When circumcised males were compared to genitally intact boys and girls, they showed less active sleep time, more time awake and agitated (active awake and crying awake), longer latencies to sleep [1011][1012][1013] and more extreme long non-REM sleep periods. 1012 Sleep patterns were correlated with rapidity of drops in cortisol levels. 1014 Sleep changes have not been documented in newborns with prolonged crying. 1012 These findings need to be placed in context. Changes in the amount and type of sleep and the latency to sleep are indicative of stress. The immature human infant has a limited capacity to actively avoid stressful stimulation and responds to such stimulation with the "conservation-withdrawal" pattern. This leads to increases in non-rapid-eyemovement (non-REM) sleep, which is the low point on an arousal continuum, where thresholds to sensory stimulation are high and motor activity is low. 1015 REM states probably represent the operation of maturational processes in the central nervous system of the neonate, which are primarily related to physiological processes not yet influenced by experience. These maturational processes are part of an unfolding genetic progression, phylogenetically preformed for an average expectable environment. The processes involve the establishment of the necessary connections within the central nervous system as well as in behavioral integration. By comparison with adult sleep, prototype REM sleep is poorly organized. But, in the neonate, it only takes three months of development to organize it. 1016 An increase in non-REM sleep has been observed following heel lancing. 1016 Male circumcision without anesthesia in a newborn is followed by prolonged non-REM sleep, which is consistent with the "conservation-withdrawal" theory. Newborns usually begin their sleep cycle with REM sleep, but following heel lancing, they began sleep with a lengthy period of non-REM sleep. Following either selective interruption of REM or non-REM sleep or deprivation of total sleep, neonates exhibit a propensity to recover quiet non-REM sleep rather than active REM sleep. The quiet sleep priority may be related to "stress" or wakefulness and fatigue. 1017 Consequently, an inborn adaptive response to stress is to produce a quiescent state with high sensory thresholds. 1016 A "common sense" guess about the effects of a continual disruptive stimulation for a newborn would be that an infant would sleep less and cry more; however, in the period following male circumcision infants have an increase in light sleep and a decrease in deep sleep, [1012][1013][1014][1015][1016]1018,1019 but they cried the same amount of time as before circumcision. Consequently, these changes in sleep pattern following male circumcision are a much more accurate measure of the stress of male circumcision than is crying.
Interruption of maternal-infant bonding and changes in breastfeeding: A study of the effects of male circumcision on maternal-infant interactions noted a trend toward fewer intervals of uninterrupted feeding, with infants who were circumcised sucking on their bottles harder, faster, and more concertedly than those not circumcised. This, in turn, made them less available to their surroundings and less able to interact with their mother. This finding lasted for approximately twenty-four hours following the procedure. 1020 Dixon et al. also established that male circumcision disrupts feeding and impairs infant/maternal attachment. 1021 In babies who breastfeed, feeding deteriorates following male circumcision. 1022 Lactation consultants noted that boys circumcised before breastfeeding has been established subsequently have more problems establishing breastfeeding. However, boys recovering from traumatic birth, but not circumcised, have fewer breastfeeding difficulties. 1023 Death: Deaths following male circumcisions have been acknowledged for a long time, as noted in the Talmud, and unfortunately they continue today. [1024][1025][1026][1027] Reports of death following male circumcision have been related to exsanguination, 1028,1029 bronchopneumonia, 1030 secondary pulmonary tuberculosis, 672,[1031][1032][1033] secondary sepsis, 660 secondary meningitis, 629 and undisclosed reasons. 691 The incidence of death following male circumcision is unknown. Each year there are reports of multiple deaths in Africa of boys following their ritual male circumcision that initiates them into manhood. [1034][1035][1036][1037][1038][1039][1040][1041][1042][1043][1044][1045][1046][1047] In developed nations, the most common estimate, approximately 1 in 500,000, 1048 is at best a guess. Gairdner reported between 9 and 12 deaths out of 90,000 male circumcisions performed each year in the United Kingdom for an incidence of 1 in 7,500 to 1 in 10,000. 181 The primary obstacle to obtaining an accurate estimate of the incidence of death from male circumcision is the underreporting of male circumcision as a cause or contributor to death. Instead of listing male circumcision as a cause of death, the infection or hemorrhage/exsanguination that led to the baby's demise is listed. Incomplete and inaccurate death certificates for pediatric deaths are not uncommon. In a study of children with heritable disorders who died while in a pediatric intensive care unit, the underlying disorder was not listed on the death certificate 41% of the time. 1049 An example of this was a clinical-pathological conference published in The Journal of Pediatrics involving a newborn who died of an overwhelming echovirus infection. For reasons that are unclear, the patient was circumcised at 4 days of age, which "was complicated by persistent oozing of blood." While this was mentioned in the case report, the authors did not discuss the role the male circumcision may have played in the patient's fatal outcome. 1050 This struck some readers as odd that "an infant with respiratory distress and suspected of sepsis would be subjected to a stressful procedure such as a male circumcision." 1051 The authors of the case report responded that "it was the attending pediatrician's judgment that the infant had improved to the point where he did not interfere with the obstetrician's and parent's decision to go ahead with this procedure, but following the male circumcision, the clinical course rapidly deteriorated." 1052 Did the sudden deterioration in this patient coincide with the male circumcision or did the male circumcision contribute to the patient's demise? Without mention during the clinical-pathological conference of male circumcision contributing to his death, it can be assumed that male circumcision was not mentioned on the death certificate.
Of note, in England and Wales, the Registrar-General's tabulations for deaths in children under 5 years from "circumcision or phimosis" showed a dramatic drop with the decrease in the number of male circumcisions performed. During 1942-49, between 11 to 19 deaths occurred each year, while in 1950 and 1951 the number of deaths were six and one, respectively. 1053 One of the hardest comparisons for commentators on this topic to resist is that between the risk of death from male circumcision and the risk of death from penile cancer. Gellis, a highly respected pediatrician, noted that, "It is an uncontestable fact at this point that there are more deaths from complications of male circumcision than from cancer of the penis." 1054 Others have estimated that at least 41 children will die from male circumcision for each case of penile cancer prevented. 1055 If the incidence of death following male circumcision and the incidence of death following penile cancer are roughly equal, then they should be given equal weight during the disclosure portion of the informed consent procedure. Since the risk of death from male circumcision is on par with the risk of penile cancer, this deserves a prominent place in the discussion of risks, benefits, and harms.
Bollinger estimated there may be approximately 117 deaths per year in the United States that can be attributed to infant male circumcision (9.01 per 100,000). 1056 These death rates are on par with those reported in Brazil. 1057 The studies relying on data collected from databases 532,591,592 are only picking the lowhanging fruit, so to speak. Thus, they do not provide a valid picture of the true rates of complications. Their results are only useful as a rhetorical device for those who want to promote male circumcision, such as the American Academy of Pediatrics 40,1058,1059 and the writers of the CDC draft. Any discussion of their results should focus on the unreliability of this data collection method for this purpose and their role in distorting the discussion.
Throughout the CDC draft, pain is cited as a major concern by those considering the procedure. Yet, the draft glosses over the issue of pain in a brief paragraph citing a methodologically incomplete study with perhaps the highest efficacy for infant male circumcision anesthesia in the entire medical literature. 1060 As will become clear from the discussion below, the writers of the CDC draft had to dismiss a broad swath of studies in order to isolate this outlying study.
It is important to make clear that noxious stimuli are perceived as more painful in newborns compared to older children and adults. 1061 There are several reasons for this. First, the human brain learns following a noxious stimulus and compensates for the stimulus. With novel noxious stimuli, such as tearing the prepuce from the surface of the glans and crushing the prepuce, the brain does not know how to filter or tolerate it, so consequently the stimulus is more raw and intense in an infant. For example, an infant's spinal sensory nerve cells are more excitable than an adult's, making their spinal reflex response to a harmful stimulus more intense and prolonged. 1062 Second, infants do not have fully developed, fully functioning descending inhibitory nerve fibers that attenuate noxious stimuli from the periphery. Consequently, noxious stimuli that reach the brain are more intense. [1062][1063][1064] Third, endogenous opioids, which are responsible for postsynaptic modulation of pain signal transmission, have levels in neonates several logarithms in magnitude lower than reported in adults. Consequently, endorphin release is unlikely to provide the neonate relief from many sort of pain. 1062 Researchers typically do not study a complete evaluation of pain in newborns. For example, the study cited in the CDC draft 1060 used only the Neonatal/Infant Pain Scale 1065 to assess pain. The Neonatal/Infant Pain Scale gives a score of 0 to 2 for six factors: facial expression, crying, breathing, arm positioning, leg positioning, and alertness. Given that part of the study's protocol was to give formula, breastmilk or a 20% sucrose solution ad libitum, to restrain the arms and legs during the procedure, and to use of a pacifier, these interfered with interpretation of facial expressions and the ability to accurately assess three of the six factors of the scale. In general, scales that rely only on behavioral signs can be misleading. A pacifier can reduce crying, but will have no impact on cortisol levels. 1066 A lack of behavioral responses (including crying and movement) does not necessarily indicate a lack of pain. 1067 For example, Johnston and Stevens found strong correlations between three facial scores, but they were not related to the physiological variables, and the physiological variables did not correlate with each other. 1068 Slater and colleagues, after directly measuring spinal nociceptive reflex withdrawal activity and nociceptive brain activity, concluded that the reduction in clinical observational scores following noxious events in newborns should not be interpreted as pain relief. 1069 Raw noxious stimuli are relayed to the brain via small myelinated (A delta) fibers and unmyelinated C fibers. 1062 Simultaneously, the hypothalamus triggers a chain of events that results in the adrenal glands secreting cortisol, epinephrine, and norepinephrine. Epinephrine in turn accelerates the respiratory rate, dilates the bronchi and bronchioles, potentiates muscle contraction, and increases blood pressure and heart rate. 1070 The pain message and its response are wired through a complicated, redundant, widespread neurologic information processing system with both conscious and emotive components. This network is part of the phylogenetically most primitive nervous system, and as such, is functional early in development. [1071][1072][1073][1074] The average newborn can differentiate the intensity or invasiveness of stimuli with the magnitude of their physiologic and behavioral responses reflecting the intensity of the stimulation. 1075 Pain is also largely a subjective experience, which makes assessment of pain in newborns more difficult and comparisons of pain levels in neonates with older children nearly impossible. Performing male circumcisions without anesthesia has allowed researchers to study the parameters of extreme pain in experiments that would not have been allowed on laboratory animals. [1076][1077][1078][1079] Some have argued that the placebo-controlled trials of various topical and local anesthetics for infant male circumcision violated the Helsinki Declaration. 1080 Because pain in the newborn is expressed in a number of ways and focusing on one modality of expression provides a limited view, studies of pain in newborns should make a broad assessment of all pain parameters in order to get a complete picture. Studies should assess all of the following. 1081 1. Crying: The duration and pitch of crying can give an indication of the degree of pain and stress. 1082 There is a direct relationship between cry acoustics and vagal tone. 1083 Cry duration, as opposed to cry acoustics, is not as reliable a measure of stress and pain as compared to vagal tone and cortisol levels. There is a positive correlation between cry duration and both cortisol levels and behavior state following male circumcision, except when a pacifier is used. 1018,1066 2. Facial expressions: A variety of facial expression and behavior state scores have been used to quantify neonatal pain, with inter-observer scores showing reasonable reproducibility. Average behavioral state scores during male circumcision are positively correlated with increases in serum cortisol levels. 1019 3. Vital signs: Pain is associated with drops in blood oxygen levels and increases in heart rate, respiratory rate, and blood pressure.
4. Vagal tone: Reactivity and regulation of the autonomic nervous system, as measured by vagal tone, is a very sensitive measure of stress. A decrease in vagal tone is a quantitative indicator of the central nervous system's response to pain that parallels other measures of neonatal pain. 1062,1081,1083 Decreases in vagal tone are proportional to the invasiveness of a procedure. 1062,1083 5. Cortisol levels: Activity in the hypothalamic-pituitary-adrenocortical axis has long been linked with the concept of stress and arousal. Cortisol levels, which can now be measured in the saliva thus avoiding the stress and pain of drawing blood, will surge as a result of pain. The rise in cortisol levels, often seen hours after the stressful event, may be the most sensitive measure of pain in a newborn. 1084 There is increasing evidence that cortisol surges may impact long-term aspects of infant development. 1016,[1085][1086][1087] 6. One group of investigators was able to measure pain-specific brain activity recorded by electroencephalography and identified by principle component analysis. They also measured the magnitude and latency of the spinal nociceptive reflex withdrawal. This direct measure of nociceptive spinal cord and brain activity was found to be more accurate than observational pain scores and changes in facial expressions. 1069 Infant male circumcision is very painful and needs to be placed within the same context as all other painful procedures performed on neonates. Gunnar et al. found male circumcision elicited more behavioral distress and evoked a larger cortisol response than blood sampling, weighing, or physical examination. 1089 In a study of post-operative pain following "minor" surgery, the pain of male circumcision was behind only tonsillectomy and orchidopexy, making it more painful than sinus surgery, otoplasty, strabismus repair, dental extraction, urethral repair, hernia repair, reset of limb fracture, and revision of the thumb. 1090 In a study of the magnitude of an infant's response to procedures, such procedures as the insertion of a gavage tube, physical examinations, nose cultures, and insertion of an umbilical arterial catheter were considered mildly invasive procedures. Arterial punctures, venous punctures, and heel sticks were considered moderately invasive procedures. Male circumcision, lumbar punctures, and eye examinations for retinopathy of prematurity were considered highly invasive procedures. 1075 In a survey of 467 clinicians (nurses and physicians) working in level II and level III nurseries asked to rate the painfulness of 12 common bedside nursery procedures, male circumcision was considered the most painful procedure (tied with chest tube insertion). Male circumcision was considered more painful than endotracheal intubation, insertion of gavage tube, tracheal suctioning, arterial or venous cutdown, lumbar puncture, intramuscular injections, insertion of an umbilical artery catheter, insertion of peripheral intravenous line, heel stick, and insertion of radial or tibial arterial catheter. 1091 The signs of pain seen during infant male circumcision include surprisingly high-pitched crying, 1082,1083 changes in facial expressions, 1019 a drop in blood oxygenation with hypoxemia, [1092][1093][1094][1095][1096][1097][1098][1099] significant increases in heart rate, respiratory rate, and blood pressure, 1014,1018,1019,1081,1200 and a significant decrease in vagal tone. 1083 Direct measures of nociceptive spinal cord and brain activity during infant male circumcisions have not been reported in the medical literature. To properly assess the pain of infant male circumcision, all of these need to be measured.
Because of the highly invasive nature of infant male circumcision, providing adequate anesthesia is indicated. While United States law requires that effective anesthesia and analgesia be provided for veterinary and laboratory animals, [1077][1078][1079] it appears this does not apply to human newborns. In an effort to alleviate the pain of male circumcision, a number of interventions have been implemented and assessed. These include comforting measures, sucrose nipple, acetaminophen, dorsal penile nerve block, topical anesthesia, injection of local anesthesia, alternative restraints, and different male circumcision methods.
Despite improvements, compared to placebo and dorsal penile nerve block, studies looking at these interventions still showed significant departures from baseline status in regards to vital signs, vagal tone, and cortisol levels, indicating that the procedure was not pain-free. Therefore, none of these methods have been shown to provide adequate anesthesia. 847,1018,1019,1022,1066,1089,[1093][1094][1095][1096][1097][1098][1099][1101][1102][1103][1104][1105][1106][1107][1108][1109][1110][1111][1112][1113][1114][1115] A cynic might note that topical and local anesthetics are used in infant male circumcisions more to benefit the parents than the child.
The complications of topical and local anesthesia include bruising and hematoma formation, 847,1114,[1116][1117][1118] gangrene of the penis, 1119 and methemoglobinemia. [1119][1120][1121][1122][1123][1124][1125][1126][1127][1128][1129][1130][1131][1132][1133] More effective methods of anesthesia, such as general anesthesia and caudal blocks, [1134][1135][1136][1137][1138][1139][1140][1141][1142][1143][1144][1145][1146][1147][1148][1149][1150] are not used because of the difficulty, and the associated risks, of using them in infants. According to the standards established by the American Academy of Pediatrics, neonates should receive the same pain relief measures as those afforded to older children and adults. 1151 To accomplish this, male circumcision would need to be delayed until general anesthesia can be more safely delivered. In keeping with this recommendation, the Australasian Association of Paediatric Surgeons recommends deferring the procedure until at least six months of age. 1152 Claims that male circumcision is less painful when performed on an infant have not been substantiated with any evidence. The fact that noxious stimuli are more painful for the neonate, along with the known inadequacy of topical and local anesthesia, provides evidence to the contrary. There are also differences in the procedure between infancy and later in life that make it more uncomfortable for the neonate. For the majority of males older than fifteen years of age, the inner surface of the foreskin is no longer attached to the surface of the glans. 52,85,86,1153 In newborns, nearly all of the glans is attached to the foreskin. Unlike circumcision of an older male, infant male circumcision requires tearing the two structures apart, which is akin to pulling a fingernail from the nail bed. This open wound is exposed until it heals within a few weeks. For an older individual, there is no open wound on the surface of the glans.
Health care providers need to include, as part of the disclosure element of the informed consent process, that currently used methods of anesthetics do not provide adequate anesthesia for the procedure, and that the procedure is still unacceptably painful when these agents are used.
Missing from this section is a recognition of the harm that accompanies removal of the foreskin, which contains nearly all of the fine touch neuroreceptors of the penis, and thus deprives the male of the functions the foreskin provides. The normal anatomy, histology, physiology, and function of the foreskin are discussed earlier in this response, but they were completely left out of the CDC's draft. Removal of this specialized tissue would be expected to result in changes in function. Harm also comes in the form of pain, and in the form of no longer being whole or feeling whole. By ignoring the harms of the intervention, the writers of the CDC draft are ignoring medical evidence and aligning themselves with the "harm denialists" on this issue.
While the sections outlining the complication rates of circumcisions performed on adults and infants in Africa are interesting, this information is peripheral and unlikely to be of interest to health care providers in the United States. As noted above, the low complication rates seen in the randomized clinical trials might indicate that complication rates are lower for male circumcisions performed on adults than on male circumcisions performed on infants. [1][2][3]1154 Finally, one specific comment. The CDC draft includes the following statement: "In a comprehensive risk-benefit analysis of infant male circumcision based on reviews of the literature and meta-analyses it is estimated that over a lifetime, benefits exceed risks by a factor of 100." It gives as its citation an opinion piece, 33 which based its calculations on a selective bibliography and a number of other like-minded opinion pieces written by the same author. 473,[1155][1156][1157][1158][1159] To accept this ratio, one must live in a fantasy world where the incidence of phimosis is 10% (instead of 0.6% 457 ), where the incidence of balanitis is 10%(instead of 0.65% to 4% 541,543 ), where circumcision is a risk factor for urinary tract infection in elderly men in their dotage (it is not one), where hypertension and end-stage renal disease are associated with urinary tract infections (they are not), where prostate cancer risk is lower in circumcised men (it is not), where penile cancer is 20 times more common in intact males (instead of at most 3 times 455 ), where HPV and herpes risk is reduced by male circumcision (it is not), where cervical cancer risk is associated with the circumcision status of the male sexual partner (no studies have found such an association), where risk of infection is 0.2% (instead of 1% to 2%), where the risk of bleeding is 0.1% (instead of 1% to 2%), where the risk of repeated surgery/skin bridges is 0.1% (instead of 4% to 12% 46,186 ), where meatal stenosis never happens (instead of 5% to 20%, 186,[533][534][535][536][537] and where there is never a loss of sensitivity or any sexual dysfunction following male circumcision. If one takes the complication rate compiled reviewing the charts of newborn males by the CDC (3.1%) 6 as a baseline and applies the 100:1 ratio, then every circumcised man should reap, on average, 3.1 benefits being circumcised. This is patently absurd. So, why would the writers of the CDC draft accept and propagate a ratio, from an opinion piece written by an individual whose scientific rigor in these matters has been called into question repeatedly, 1160 that is clearly implausible? Why did they not perform a comprehensive literature review of their own? What has the CDC been doing on this topic for the past seven years? Clearly, reference to this preposterous "ratio," and the opinion piece that generated it, needs to be deleted from the final draft. Any health care provider that informs a parent or patient that the ratio of benefits to risk exceeds 100:1 is putting themselves at risk of a lawsuit for making such a wildly unsubstantiated claim. It has been argued that, by taking the scientifically unsupported position it has, the American Academy of Pediatrics is susceptible to successful litigation for misleading health care providers. 1161
# RESPONSE 80:
See responses 1, 6 and 48. The reviewer's listing of reported adverse events is in isolation and does not describe the proportion of circumcised males that experience such an adverse event, or how the rate of adverse events differs between circumcised and uncircumcised males or whether such events occurred as a result of medical or ritual male circumcision. Based on a meta-analysis of 22 studies, most of which were based in the U.S., it is estimated that 32.1% (95% CI = 15.6 -49.8) of uncircumcised men compared with 8.8% (95% CI = 4.15 -13.2) of circumcised men will experience a UTI in their lifetime, suggesting that lack of male circumcision is associated with a 23.3% increased risk of UTI during a man's lifetime. 48 COMMENT:
# Effect of male circumcision on sexual function and penile sensation
The material presented in this section of the background document is highly selective and ignores studies indicating male circumcision has a negative impact on sexual function and penile sensation. It also misrepresents the findings of some of the studies cited.
There are a number of important omissions. For example, the 2007 study by Sorrells et al. "expressed concern that its [the foreskin's] removal may compromise sexual sensation or function," based on their mapping of the fine-touch thresholds of the penile surface in 68 circumcised men and 91 men with normal, intact genitals. Mapping revealed that the most sensitive portion of the penis is that which is removed by circumcision, the circumcision scar is the most sensitive location on the circumcised penis, and the sensitivity of the glans (head) of the penis is significantly less in circumcised men. 108 Decreased sensitivity in the glans when flaccid in circumcised men has been documented in two other studies that the CDC draft has omitted. 109,110 In one study, the difference was statistically significant using the raw data, but was no longer statistically significant when adjusted for age, hypertension, and diabetes. 109 In the other study with only 20 men in each group, the difference is shown in Figure 2, but the data are not provided and the significance of the difference is not assessed. 110 The section fails to mention that the penilo-cavernosus reflex, which is related to the ejaculation process, is significantly more difficult to elicit in circumcised men than in men with normal genitals. 120 This may contribute to the higher rates of sexual dysfunction seen in circumcised men.
In addressing studies that looked at penile problems in men before and after circumcision, the CDC draft demonstrates several important oversights. For example, in the 2002 study by Fink et al., they fail to mention that men in this study reported a significant reduction in erectile function (p=.01) and decreased penile sensitivity (p=.08).
A perceived problem or difficulty as a result of the procedure was reported by 38% of the men studied. 1162 The 2002 study by Collins et al. would, because of its small size, not be expected to provide any results that were statistically significant. This is unfortunate because, of the 15 men who were circumcised as adults, all but one had a penile problem. The fact that there was no measured improvement in sex drive, erection, ejaculation, problem assessment, or overall satisfaction suggests that the procedure was a failure. 1163 There are a number of similar studies the draft has omitted. For example, Coursey and colleagues included a control group of men who were circumcised for "phimosis or other benign indication" in a study designed to measure the impact of anterior urethroplasty on erectile function. Of the men who underwent circumcision, 27% reported worsening of their erectile function after the procedure. 1164 In a study of 95 men undergoing circumcision in China, erectile dysfunction increased following the procedure (p=.001). These men also reported increased problems with weakened erectile confidence (p=.04), and difficult insertion during coitus (p=. 03). Improved satisfaction following the male circumcision was reported in only 34 patients (p=.04). 116 Similarly, a study from Portugal of 62 men circumcised for medical reasons reported a significant increase in erectile dysfunction and difficulty reaching orgasm following male circumcision. 1165 The CDC draft mentions two other studies in passing, 1166,1167 without providing details.
The first study was performed in Turkey where most men undergo circumcision to satisfy a religious requirement, making it difficult to properly interpret the results. 1166 In the second study, while there was no difference in the overall mean of the International Index of Erectile Function, satisfaction was only 61% following the procedure. 1167 The draft mentions the results of two studies that assessed sexual function before and after circumcision in men who were enrolled in the randomized clinical trials in Kenya and Uganda. 1168,1169 Because these studies were large and part of a randomized clinical trial, the results have been given more weight than they deserve. There are several reasons to distrust their conclusions. The studies from Africa show rates of sexual dysfunction that were orders of magnitude lower than studies performed outside of Africa. For example, in the study by Krieger et al. 1168 the prevalence of premature ejaculation was 4.27% (95%CI 3.12%-5.41%) and the prevalence of trouble achieving orgasm was 1.26% (95%CI 0.62%-1.89%) while the prevalence in the other studies performed outside Africa were 30.59% (95%CI=29.74%-31.43%) and 11.19% (95%CI=10.61%-11.77%), respectively. In the study by Kigozi et al., 1169 the prevalence of lack of sexual desire was 0.80% (95%CI 0.35%-1.25%) while the prevalence in the other studies was 28.83% (95%CI 27.99%-29.66%). Similarly, the two African studies together had a prevalence of erectile dysfunction of 0.93% (95%CI 0.57%-1.29%) and prevalence of dyspareunia of 1.13% (95%CI 0.72%-1.54%), while the prevalence in other studies was 18.16% (95%CI 17.47%-18.88%) and 3.47% (95%CI 3.13%-3.81%), respectively. These vast differences suggest either cultural differences in what these conditions entail, unwillingness to disclose the presence of sexual dysfunction, or the coercive impact of the large subsidies men received for their participation in the studies. These subsidies could explain their eagerness to tell the researchers what the researchers wanted to hear. Of course, it could be that these sexual problems occur 3 to 36 times less frequently in Africa. If that is the case, as someone jokingly suggested, Uganda and Kenya should consider developing tourism campaigns that would tout coming to these countries for the "best sexual experiences on the planet."
The extremely low rates of sexual problems that were documented in Africa are examples of both the element of ceiling effect 1170 and of asking non-differentiating questions. With sexual satisfaction measured at rates exceeding 98% when surveyed both before and after circumcision, there is no room to move up (thus pinned against the ceiling). It is also not known how high the level of satisfaction actually is because the ceiling (the limitation of the assessment tool) acts as a barrier. For example, if the ceiling score is set at 100 and the average score before male circumcision was 125, the best one could score would be 100 because of the ceiling in place. The few scores below 100 would bring the average to slightly below this. If the average score after male circumcision was 112 (a 10% decrease), the best one could score would be 100, so the score after male circumcision would be similar and this 10% decrease would not be detected. Similarly, a 10% increase in the score following male circumcision would also be missed using the tools these researchers employed. Consequently, the negative findings of these studies are meaningless.
The questions asked in the survey were also so vague that they would not have been able to demonstrate a difference in sexual function, if one existed. As Morten Frisch, MD, has noted, "I am not surprised that these studies provided little evidence of a link between male circumcision and various sexual difficulties. Several questions were too vague to capture possible differences between circumcised and not-yet circumcised participants (e.g. lack of a clear distinction between intercourse and masturbationrelated sexual problems and no distinction between premature ejaculation and trouble or inability to reach orgasm). Thus, non-differential misclassification of sexual outcomes in these African trials probably favoured the null hypothesis of no difference, whether an association was truly present or not." 1171 The draft omits mention of several studies that have addressed the impact of male circumcision on sexual function and how it impacts the female sexual partner. A 1999 study of women who had sexual experiences with both intact and circumcised men found that they strongly preferred sex with an intact penis. 115 While this study may have suffered from selection bias, as the participants were volunteers who responded to an announcement in an anti-male circumcision newsletter and classified advertisements in magazines, its results were replicated in a cross-sectional national survey in Denmark.
The Danish survey demonstrated that the female sexual partners of circumcised men were significantly less likely to have their sexual needs fulfilled (adjusted OR 2. This Danish study also documented that circumcised men were more likely to report frequent orgasm difficulties (adjusted OR 3.26; 95%CI 1.42-7.47). 1172 In a survey of 1059 normal and 310 circumcised men, Bronselaer and colleagues reported that circumcised men were significantly more likely to report decreased sexual pleasure, lower orgasm intensity, more effort required to achieve orgasm, unusual sensations on their glans (burning, prickling, itching, or tingling and numbness), and discomfort and pain on the penile shaft. 1173 The draft does not address the issue of premature ejaculation. One Turkish study found that following male circumcision, the intra-vaginal ejaculation latency time increased by 20 seconds (a statistically significant difference), which certainly should be enough extra time to help their female partners achieve orgasm. 1174 While several studies have shown no difference in the rates of premature ejaculation between normal and circumcised men, 1175,1176 this does not mean that studies in which a statistically significant difference is found can be ignored. For example, a study by Tang et al. found a four-fold increase in premature ejaculation in circumcised men (adjusted OR 4.881; 95%CI 2.346-10.153). 1177 In a representative household sample of Australian men, circumcised men were significantly more likely to report premature ejaculation (OR 1.41; 95%CI 1.14-1.75) and erectile dysfunction (OR 1.39; 95%CI 1.08-1.79). 1178 This was consistent with an earlier Australian survey that found circumcised males were more likely to report premature ejaculation (OR 1.28; 95%CI1.15-1.42). 1179 The studies of the effect of male circumcision on sexual function indicate a negative impact. 1180 It also warrants mention in the informed consent discussion that male circumcision may have a deleterious impact on sexual function, but further study is needed to fully evaluate the impact.
The CDC draft only performed a cursory exploration of whether male circumcision impacts sexual function or penile sensitivity and only cited negative studies while ignoring the many positive studies. Their discussion is inadequate and not evidencebased.
# COMMENT:
Considerations related to male circumcision in the United States
# HIV infection in the United States
The material presented in this section of the background document is incomplete and somewhat misleading.
It should be noted that while the HIV prevalence is high in several cities, the male circumcision prevalence, especially among African-Americans, is high as well.
The statement, "Circumcision is likely to play a role in preventing HIV among men who engage in unprotected heterosexual vaginal sex, especially in communities where prevalence of HIV infection among women is high or among men with multiple sex partners," is another restatement of the CDC "group think" presumption, and has no factual foundation.
The discussion about which ethnic and racial groups should be targeted for male circumcision is moot. As discussed elsewhere, the medical evidence indicates that the only population that should be targeted for possible discussion of male circumcision are HIV-negative men who have regular sexual contact with an HIV-positive female sexual partner. And, as modeling by the CDC has demonstrated, male circumcision has very little impact over the long term in how frequently these men will become infected. 340 While HIV infections continue to occur in the United States, most infections are in men having sex with men and intravenous drug users, groups that will not benefit from male circumcision. If male circumcision was to have a protective effect against female-tomale transmission of HIV, one would have expected the United States to have a lower prevalence of heterosexually-transmitted HIV than similarly situated developed countries with low male circumcision rates. The prevalence of heterosexuallytransmitted HIV is several times higher in the United States than in Europe. The United States has already completed the male circumcision experiment, and the results show it has failed to protect its population from HIV infections. Our experience in the United States indicates that male circumcision is a factor that is not worthy of the attention that CDC has expended on promoting it. This is a complete waste of taxpayers' money both here and in Africa. Taxpayers would be astounded at the amount of their money being used to fund programs in Africa involving mass male circumcisions promoted by propaganda campaigns, unethical solicitation, coercion, and misinformation.
RESPONSE 82: See responses 2, 18, 19, In addition, responses to these concerns have been adequately addressed previously. 55,56 COMMENT:
# Rates of male circumcision in the United States
The material presented in this section of the background document is fairly straight forward, but there are some additions and corrections that need to be made.
While it is true that male circumcision unrelated to religious beliefs was introduced into the United States in the late 1800s, it needs to be added that male circumcision was introduced as a "cure" for masturbation. A more appropriate citation for this is also needed. The current citation, 1181 does not give the complete title of the book (Circumcision: Timely Information for Parents and Professionals from America's #1 Expert on Circumcision) and is not written by a medical historian, but rather an unabashed circumcision advocate. Several other citations, written by medical historians would be more appropriate. [1182][1183][1184][1185] RESPONSE 83: The citation has been edited to read the full title: Schoen EJ. On circumcision: Timely Information for Parents and Professionals from America's #1 Expert on Circumcision. Berkley: RBR Books; 2005.
# COMMENT:
There needs to be an acknowledgement that we do not have a mechanism in place in this country to accurately determine the number of infant males being circumcised here.
For example, one 1968 study found that 30% of circumcisions were not documented in hospital discharge summaries, 1186 and another extensive chart review performed by the CDC found that 15.7% of male circumcisions that are documented in medical charts were not documented on the facesheet, from which data are collected into databases. 6 Likewise, self-report of male circumcision status is often unreliable. 260,[1187][1188][1189][1190][1191][1192] It should also be noted that several studies have indicated that the male circumcision rate in blacks is similar or higher than in non-Hispanic whites. For example, data from Atlanta from 1985 to 1986 by the CDC found that 95.9% of blacks were circumcised as opposed to 86.7% of whites (OR 3.75; 95%CI 1.58-10.25). 6 Mor et al., in a study of 58,598 male patients in San Francisco, found that, in males born in 1960 or after, blacks were more likely to be circumcised than non-Hispanic whites. 8 Similarly, Mansfield et al. found 86.8% of blacks were circumcised as opposed to 89.6% of whites (OR 1.30; 95%CI 0.95-1.79). 7 The assertion that male circumcision is more common among newborns born to families of higher socioeconomic status may no longer be true. It may have been true when data were collected in 1988 to 2000, 1193 [Note that CDC185 reference lists the authors of the study incorrectly] but there is increasing evidence that as maternal education levels increase male circumcision rates decrease. With the advent of the internet and medical literature searches available to the public, parents with higher levels of education are increasingly choosing not to circumcise their sons. This is consistent with the fact that physicians are less likely to circumcise their sons as compared to the populations they serve. 112 The purpose of this section is unclear. The reader should take away two clear conclusions: first, that the rate of infant male circumcision in United States is declining; second, that the method of collecting male circumcision prevalence data is highly flawed and unreliable. It is unclear whether the purpose of the section was to raise alarm over the falling male circumcision rates or to reassure male circumcision advocates that all is not lost. In either case, the inclusion of this section in the draft needs further justification.
RESPONSE 84: Scientifically rigourous methods have been used to describe the prevalence of neonatal male circumcision in the U.S. In a study using hospital discharge data from the 2000 -2010 Nationwide Inpatient Sample, male circumcision incidence decreased significantly from 61.3% in 2000 to 56.9% in 2010 and overall remained higher for newborn hospitalizations covered by private insurance compared with Medicaid (66.9% vs 44.0%). 57 During this same time period, the proportion of male newborn hospitalizations nationwide with Medicaid coverage increased from 36.0% in 2000 to 50.1% in 2010. 57 COMMENT:
# Acceptability of adult male circumcision in the United States
The material presented in this section of the background document is tainted by an underlying false assumption: that American men and adolescent males who have normal genitals are at increased risk for heterosexual acquisition of HIV. As discussed elsewhere, the data do not support this assumption. With that in mind, one has to assess whether the data collection documented in this section was based on their faulty premise. The authors of the 2008 CDC study by Begley et al. asked gay men, "If Scientific studies in the United States among men who have sex with men showed that circumcision reduced the risk of HIV infection, would you be willing to be circumcised as an adult?" 1194 Given that, as discussed elsewhere, there is no evidence of male circumcision being a risk factor for HIV infection in men having sex with men, the question carries as much validity as asking, "If the moon is made of cheese, would you prefer that it be cheddar or gouda?" The authors in the CDC 2011 study by Gust et al. also clearly begin with an unproven assumption. 1195 [The citation as given in the draft does not list the authors correctly.] The question asked in the survey was, "If your health care provider told you that getting circumcised would reduce your risk of becoming infected with HIV, how likely would you be to get circumcised?" The study did not include a control question which would be, "If your health care provider told you that there is no evidence in the United States to suggest that circumcision reduces the risk of HIV in United States how likely would you be to get circumcised?" By not including this alternative question, it is impossible to know how much of the response is based on scare tactics alone. It would appear that the scare tactics have continued and are now extended to this draft. The low response rate of normal men willing to undergo circumcision, even in the face of the CDC's scare tactics, reflects that men with normal genitals recognize the value of having normal genitals and would be willing to pursue other, more effective, avenues of decreasing their risk of HIV infection.
The statement, "Adult and adolescent male circumcision potentially has the largest impact on HIV acquisition in populations in which a low percentage of males are circumcised and there is a high risk for HIV transmission through penile-vaginal sex," is not applicable in the United States for several reasons. There is no evidence that male circumcision has an impact on risk of HIV transmission through penile-vaginal sex, as the randomized controlled trials in Africa did not assess the origins or mode of transmission of the infections they documented. [1][2][3] As discussed elsewhere, none of the studies in North America of heterosexually-transmitted HIV infections have found male circumcision to be a significant risk factor. [8][9][10][11][12][13][14][15] Finally, the United States has, by developed-nation standards, a very high prevalence of male circumcision and a very high prevalence of heterosexually-transmitted HIV. As noted in this section of the draft, African-Americans have the highest prevalence of heterosexually-transmitted HIV, but the CDC neglects to mention that African-Americans also have the highest prevalence of male circumcision, on par with non-Hispanic whites. If anything, this would indicate that male circumcision is either a marker for other socio-behavioral or ethnic factors, or, if it has an impact on HIV risk, it is clinically inconsequential and, therefore, not worthy of pursuit. It appears as though the CDC is trying to create additional demand for male circumcision in an unreceptive market. Consequently, the recommendations for the intended audience of health care providers are unjustified and inappropriate.
# RESPONSE 84a:
See responses 1, 2, 3, 18, 19, 28, 64. While the authors of the article by Begley, et al, note that one of their limitations was that " overall willingness to be circumcised was not assessed separately from willingness to be circumcised if scientific evidence demonstrated a reduced risk of HIV acquisition" and thus they "were not able to compare whether the decision to be circumcised would be influenced by the evidence to support the effectiveness of male circumcision in the reduction in risk of HIV acquisition." they were able to show that "despite these complexities, we have shown that the majority of uncircumcised MSM may be willing to be circumcised as adults if this was recommended as an HIV prevention intervention in the United States". While the MSM who participated in the survey by Begley et al. represented a convenience sample and were not necessarily representative of all MSM attending the gay pride events, the response rate was high; 1127 (77%) of 1457 men approached to participate in the survey at the seven gay pride events, agreed to be surveyed. One hundred and twenty-seven of 133 (95%) men who reported being uncircumcised provided complete responses to the questions related to the risk and benefits of male circumcision and were able to be included in the final multivariable analysis. In addition, in a crosssectional study of heterosexual African American men attending an STD clinic in Baltimore, with an overall HIV seroprevalence of 3%, among 394 visits by men who had female sexual partners who were known to be infected with HIV, male circumcision was significantly associated with a 51% reduced relative prevalence of HIV infection (10.2% among circumcised men vs. 22.0% among uncircumcised men). 58 CDC's background document indicates that "the overall estimated prevalence of male circumcision among men and adolescents aged 60 uncircumcised heterosexual males and parents of male infants should be counseled about the evidence at hand and allowed to make their own decision regarding the decision to undergo male circumcision to have their male infant undergo male circumcision.
# COMMENT:
# Acceptability of adult male circumcision in sub-Saharan Africa
The material presented in this section of the background document has little or nothing to do with how male circumcision relates to HIV infection in North America. Since when is the CDC the arbitrator of health care in Africa? And, why is our tax money being used to promote a surgery of unproven benefit in Africa? How is this part of the charge that was given to the CDC by the "consultation" in 2007?
A little history lesson: generating acceptability of adult male circumcision in sub-Saharan Africa began as an important precursor to the randomized clinical trials. While male circumcision advocates believed that they made a legitimate case based on a handful of observational studies for using male circumcision as a preventive measure for HIV infection, 31,[1196][1197][1198] mainstream HIV researchers demanded randomized clinical trials. 1199 For a randomized clinical trial in Africa to demonstrate a statistically significant difference, it needed to be powered to document a 1% absolute risk reduction. Consequently, several thousand participants would need to be recruited. 236,237 In order to garner enough participants, the investigators for the randomized clinic trials implemented sessions within the communities in which the trials were to take place that disseminated pro-male circumcision propaganda under the guise of assessing acceptability of male circumcision as a strategy to reduce sexually transmitted diseases and HIV infection. [1200][1201][1202][1203][1204][1205][1206][1207] These propaganda sessions had three effects: they convinced enough men to enroll in the overpowered clinical trials, they introduced an expectation bias on the part of the participants, and they undermined the validity of the informed consent process in the trials. Given the pro-male circumcision bias of the researchers, it is unlikely that participants were given full disclosure, particularly regarding the harms of the procedure. This is evident in the consent form used in the trial undertaken in South Africa, in which none of the adverse effects of male circumcision are listed. 1 There is direct evidence that participants did not show understanding of what was told to them as most (57%) believed, even after disclosure, that male circumcision would reduce their risk of infections. 211,212 This would certainly affect the behavior of the participants and contribute to participant expectation bias. So much for equipoise. 1208 The effectiveness of the propaganda campaign was based on illusory or fabricated factors designed to increase the acceptability of male circumcision. For example, there is no evidence that male circumcision improves hygiene. There is no evidence that male circumcision improves the use of condoms, but there is evidence that condoms slip off more frequently in circumcised men. 1209 There is no evidence that male circumcision increases sexual pleasure, but, as discussed above, ample evidence to suggest that male circumcision interferes with the sexual pleasure of both the male and his female partner. 115,1165,1172,1173 The evidence that male circumcision protects against sexually transmitted infections is, as discussed elsewhere, also lacking.
The propaganda campaign had an interesting unexpected impact on women. For example, while women in Tanzania had heard the expression "partial protection," they had no idea what it meant. 1210 In a South African study, it was found that women who perceived male circumcision as reducing the risk of HIV infection were less likely to use condoms in their last sexual encounter, generally, and with circumcised partners of positive or unknown HIV status. Men were more likely to use condoms. 1211 Similar findings have been reported from Kenya. 1212 There is also the belief among women in some parts of Africa that male circumcision reduces the male-to-female transmission of HIV, 1213 where the opposite may be the case. 338 This indicates that the impact of male circumcision on risk compensation in Africa may be driven more by the attitudes and misperceptions of women than those of men. Women may be the ones more susceptible to, or aware of, the advertising and marketing endeavors of those promoting male circumcision.
A major barrier to the rollout of adult male circumcision in Africa was that acceptability of the intervention for HIV prevention was much lower than the male circumcision advocates had anticipated. They believed that, if it could be demonstrated in randomized clinical trials that male circumcision reduced the risk of HIV infection, normal African men would swarm to have their foreskins removed. This did not happen.
There was some initial interest in male circumcision programs from men who, likely for religious or cultural reasons, would have requested male circumcision anyway and saw this as an opportunity to obtain a free male circumcision performed under more sterile conditions. By 2012, with the exception of Kenya, the roll out of adult male circumcision programs has been an abysmal failure. For example, of the men targeted to be circumcised only 4.8% have been in Uganda, 0.7% in Rwanda, 11.1% in Zambia, 1.5% in Namibia, 6.5% in Botswana, 7.0% in South Africa, 12.7% in Tanzania, 0.4% in Malawi, 2.9% in Zimbabwe, 4.7% in Mozambique, and 0.2% in Lesotho. Only Kenya, Swaziland, and Ethiopia had a response rate over 20%. 1214 In response to the poor uptake, male circumcision advocates held sessions at the 2012 XIX International AIDS Conference in Washington, DC, to announce that male medical circumcision was being rebranded as a way of building intimacy and improving one's sex life with the phrase "Reshape your Relationship." Since women tend to take responsibility for "relationships," the advertising is shifting towards women, who ironically are more likely than men to encourage risk compensation, and women are more at risk of becoming infected with HIV from their male partners. 1212,1213 Over 100 articles have been published assessing the rollout of adult male circumcision in Africa. Nearly all of them have focused on the wrong outcome: increasing the number of men circumcised. Instead, the focus should be on looking for the most effective and efficient way of reducing the number of people who become infected with HIV.
To give you an example of how pathetically desperate male circumcision advocates are to increase the acceptability of adult male circumcision in Africa, the Journal of the American Medical Association in 2014 published a study to determine what impact bribing African men would have on the acceptability of male circumcision in Kenya.
When offered a free male circumcision without any bribe, only 1.6% of intact men were interested. When a bribe worth $15 was offered, the number of men accepting the bribe increased the percentage to 9.0%. 1214 Keep in mind that Gross National Income per capita in Kenya in 2013 was $1160, 1215 this would be equivalent to a $691 bribe in the United States ($53,470 GNI per capita in 2013). 1216 Models of the impact of male circumcision on overall HIV incidence in Africa reported their results based on reaching compliance levels of 55%, 229 60%, 220 70%, 230 80%, 222,225,228 95%, 224 and 100%. 221,223,226,227,231,232 If one assumes that the increase in compliance has a linear relationship to an increase in the amount of the bribe offered, then the bribe amount needed for the percentage to increase from 59% to 60% would be $147.81 and to increase from 79% to 80% would be $199.89. The average bribe needed to get to 60% compliance would be $71.60 and to get to 80% would be $97.49. The cost of these inducements would more than double the marginal costs of the male circumcision programs. If the relationship between compliance and the amount of bribe is non-linear, the cost to bribe men to get circumcised might be even greater. Other adult male circumcision programs in Africa have resorted to bribery to get men to participate. 1217 Bribery and coercion tactics violate basic research ethics and would not be allowed in the US, so how is this allowable in Africa?
The call for African men to become circumcised has also led to a number of men and boys being forcibly circumcised. [1218][1219][1220][1221][1222][1223][1224][1225][1226][1227] Given tribal tensions, between tribes that traditionally circumcise and those that do not, this was a predictable consequence of the widespread propaganda encouraging male circumcision. There have also been reports of boys being told they would not be allowed to play football (soccer) unless they were circumcised.
Efforts to increase the acceptability of adult male circumcision in sub-Saharan Africa are based on misinformation and deception, consequently, the material in this section is inappropriate, and fraudulent. African male circumcision has little or nothing to do with the United States and other developed countries.
RESPONSE: See responses 10, 18, 19, 23 COMMENT:
# Acceptability of newborn male circumcision in the United States
The material presented in this section of the background document misses several key points. The CDC draft fails to mention that the acceptability of newborn male circumcision in the United States may be, in part, driven by the fact that the procedure is solicited by physicians, nurses, and hospitals. At the first prenatal visit, mothers are routinely asked whether they would want a son circumcised. The question is repeated upon admission for the perinatal hospitalization. For parents who have done little or no research on the topic of infant circumcision, this can be interpreted as a recommendation to have the procedure performed on their son. Parents who do not want their sons circumcised have often reported that they are asked multiple times during the hospitalization whether they want their son circumcised, with many of them reporting that they are harassed and outright bullied by the hospital staff. The degree to which parents are intimidated into circumcising their sons has received little study. 1228 Such solicitation is considered unethical under the guidelines of the American Medical Association because the procedure removes healthy tissue, and male circumcision will benefit the physician's and hospital's pocketbook more than it will benefit the patient. 1229
# RESPONSE 85:
The CDC recommendations provide added unbiased scientific information that assists parents in making a decision about whether to circumcise their child. The counseling recommendations state that the decision to circumcise is that of the parents of the male infant or the adults considering male circumcision.
# COMMENT:
This CDC section fails to address the impact of the physician's male circumcision status on the advice delivered to parents. In a survey of Canadian physicians, circumcised male physicians were almost five times as likely to recommend male circumcision (OR 4.76; 95%CI 3.00-7.55) and those physicians with circumcised sons were six times more likely to recommend male circumcision to the parents of their male patients (OR 6.22; 95%CI 3.83-10.10). Those who said they based their recommendation on the medical evidence were twice as likely to recommend against male circumcision (OR 1.95; 95%CI 1.29-2.95). 39 One can only speculate whether this CDC draft has been influenced similarly. It is reasonable to question whether the male circumcision status of a physician or the physician's children, and the associated bias thereof, should be disclosed to parents. The same could be said regarding the authors of this draft and whether their inherent biases should be disclosed to the public.
RESPONSE: See response 85.
# COMMENT:
Whether parents have the moral or legal authority to choose circumcision on behalf of their sons will be discussed in a later section. 1230 Parents do not have to provide a justification in order to direct the health care provider to circumcise their son, unlike the removal of any other healthy body part. Likewise, physicians would not agree to blithely removing any other healthy normal body part from an infant or child without a disease being present. As noted in the citations given in the draft report, studies of the reasons parents choose circumcision for their sons have not been updated since the 1980s. 923,1231 If these studies were to be repeated today, cultural conformity would likely be the most common justification.
RESPONSE: See response 22.
# COMMENT:
The authors of this section accept the interpretation provided by Adler et al. of their survey data, which reflects the bias of the study's authors more than the data they collected. 1232 The study indicates that physicians were not supportive of parents deciding not to circumcise their sons and perhaps berated them for not doing so. The conclusions reached by the authors is not surprising. The parents of intact boys, by virtue of being asked so many questions about circumcision, would have to wonder if there was something about male circumcision they were not told. If, however, complete disclosure, consistent with the current standard applied to other procedures, were provided, parents who had already chosen to circumcise their sons would not want to be confronted with the litany of complications and harms associated with the procedure.
Their minds are already made up and providing information has little impact. 1233 [This is another citation that has not been updated. The article was published in 2010.] For these parents, any information is too much. It would have been more appropriate for the survey to have asked if too much information was provided. This is a clear example of expectation bias on the part of researchers impacting the methodology of a study to ensure the preconceived outcome was obtained.
RESPONSE 85a: See response 6. The citation by Wang. Et al. 2010 has been updated in the CDC background document.
# COMMENT:
The study by Gust et al. is perhaps more contrived. 1195 The study collected data based on an unproven premise: that infant male circumcision would have an impact on HIV risk in the United States. As noted elsewhere, there are no studies of infant male circumcision that have demonstrated a significant association with HIV prevalence or incidence, and no studies in North America that have found male circumcision to be protective against HIV infection. The study by Gust et al. 61 cited by the reviewer focuses on adult male circumcision, not infant male circumcision. (note: See CDC citation 59; same as reviewer citation 1195).
While there are no longitudinal studies demonstrating a significant association with infant male circumcision and HIV prevalence or incidence, ecologic studies demonstrate a strong association between lack of male circumcision and HIV infection at the population level. Although links between male circumcision, culture, religion, and risk behavior likely account for some of the differences in HIV infection prevalence, the countries in Africa and Asia with prevalence of male circumcision of less than 20% have HIV-infection prevalence several times as high (seroprevalence range: 0.24 -25.84) than countries in those regions where more than 80% of men are circumcised (seroprevalence range: 0.03-11.64). 49 Based on data from an HIV transmission model fitted to data from the Four Cities Study, including 2 cities in sub-Saharan Africa with relatively low HIV prevalence (Cotonou and Yaoundé) and 2 with high HIV prevalence (Kisumu and Ndola), investigators concluded that differences in rates of male circumcision likely played an important role in differing rates of HIV transmission across Africa. 50 _ENREF_62 Results from such ecologic studies are important as most male circumcisions globally are thought to occur during infancy, childhood, or adolescence, suggesting that male circumcision at an earlier age confers a long term reduction in risk for HIV acquisition. The fact that male circumcision performed during the neonatal period is associated with fewer and less severe side effects compared to male circumcision performed during adulthood is one of the most important reasons that most male circumcisions are performed neonatally in the U.S.
One of the studies 58 reported by the reviewer as evidence that no studies in North America have found male circumcision to be protective against HIV infection actually did find that among visits of heterosexual African American men attending an STD clinic in Baltimore who had female sexual partners who were known to be infected with HIV, male circumcision was significantly associated with a 51% reduced relative prevalence of HIV infection (10.2% among circumcised men vs. 22.0% among uncircumcised men). Another two of the studies cited by the reviewer as lack of evidence of the protective effect of male circumcision against HIV infection did not adequately address this question. Although a study of male circumcision and HIV in an urban STI/HIV prevention treatment center found that circumcised men were more likely than uncircumcised men to have HIV infection (circumcised men = 43% vs uncircumcised men= 33.9% , p = 0.23), they also noted that at last sexual intercourse, circumcised men were also more likely to report unprotected receptive anal intercourse (circumcised men = 43.8% vs uncircumcised men = 20.4%, P = 0.025) 62 . In a naval study of male circumcision and HIV status, HIV-infected case participants identified through HIV testing in medical referral centers were compared to control participants from a general aircraft carrier population who were assumed to be HIV-uninfected due to negative results on a predeployment HIV screening test. 63 Because enlisted men can seroconvert during deployment, the results of the study may have compromised if controls included both HIV-uninfected and men who HIV-seroconverted after the predeployment evaluation. Although the authors of the naval study found no significant association between HIV and male circumcision status, they underscored the importance of results from randomized clinical trials.
# COMMENT:
The inclusion in this section of whether or not there is state Medicaid coverage of infant male circumcision is inappropriate and irrelevant. The only reason to include this topic would be because the CDC has an underlying motivation to promote male circumcision in order to increase demand for male circumcisions, thereby increasing physician reimbursement. It has been argued that under the current federal statute, it is illegal for states to reimburse physicians for performing male circumcisions on infants as it is an "unnecessary, elective, cosmetic surgery on healthy boys, usually performed for cultural, personal or religious reasons." 1234 While there is an association between Medicaid coverage and infant male circumcision rates, it does not follow, as Leibowitz et al. suggest, 1235 [Again the citation in the draft fails to include all of the authors.] that providing Medicaid coverage would increase the male circumcision rates in these states where the rates have been historically low.
RESPONSE 86: Because of the benefits associated with male circumcision outweigh the risks of male circumcision, parents should have financial access to this procedure. (AAP 2013) For this reason, a discussion of Medicaid coverage is appropriate.
# COMMENT:
# Acceptability of newborn male circumcision in sub-Saharan Africa
The material presented in this section is totally ludicrous. Why should the United States care about uninformed opinions regarding infant circumcision from propagandized Africans?
The material in this section is not evidence-based, but based on uninformed opinions of populations that are vulnerable to false propaganda.
# RESPONSE:
See responses 1, 6, 18, and 19.
# COMMENT:
# Provider attitudes and practices regarding male circumcision in the United States
The material presented in this section is incomplete with multiple omissions. For example, it is stated that "many medical societies have addressed neonatal male circumcision," yet only the American Medical Association, the American Academy of Pediatrics, the American Academy of Family Physicians, and American Urological Association are cited. Many medical societies outside of the United States have addressed neonatal male circumcision. It is odd that the draft report is taking a global perspective when assessing the acceptability of adult and infant male circumcision in Africa, yet is provincial when it comes to the opinions of medical societies. Is there something in the opinions of medical societies outside of the United States that authors of this draft find troublesome? The draft needs to include the opinions of medical societies outside of the United States. More importantly, the CDC needs to provide insight on how they have access to "special knowledge" that the rest of world is missing, which led them to reach such a discordant conclusion.
The Royal Dutch Medical Association in 2010 noted that there is no convincing evidence that infant male circumcision, which constitutes a human rights violation, is useful or necessary, and there are good reasons for legal prohibition of the practice, consequently "it is reasonable to put off circumcision until the age at which such a risk is relevant and the boy himself can decide about the intervention, or can opt for any available alternatives." 1236 The Swedish Medical Association recommends a minimum age of 12 years for performing a circumcision as it requires fully informed consent from the boy. 1237 The Finnish Union of Medical Doctors (Suomen Lääkäriliitto) is opposed to infant male circumcision because of its risk, pain, and the injury inflicted. 1238 The Swedish Pediatric Society came out against infant male circumcision characterizing it as an "assault on boys." 1239 The Danish College of General Practitioners has stated that infant male circumcision is tantamount to abuse and mutilation. 1240 In 2012, the Berufsverbands der Kinder-und Jugendärzte (the German national organization of Pediatrics) condemned the practice of infant male circumcision. 1241 Medical organizations in British Columbia and Saskatchewan have come out against infant male circumcision. 1242,1243 As noted below, several national medical associations consider infant male circumcision a human rights violation. [1236][1237][1238]1244,1245 Other medical organizations from Canada, Britain, and Australia have adopted a position where the practice is tolerated, but not endorsed, encouraged, or recommended. [1246][1247][1248] Having taken an exceptional position, the CDC needs to provide an exceptional justification: one that should take our breath away. They need to defend their position on an international stage, something the American Academy of Pediatrics had trouble doing in 2012 when they did not recommend male circumcision, but stated they "felt" that the benefits outweighed the risks. [1249][1250][1251][1252] So, instead of providing an evidencebased evaluation, the American Academy of Pediatrics provided a feelings-based evaluation. The CDC has taken a more extreme position and runs the risk of embarrassing itself and the United States once again.
The studies cited by the CDC in this section give a mixed message. On one side, it is well-documented that physicians are very poorly educated regarding normal male anatomy and infant male circumcision, 1253 and on the other, physicians are encouraged to act on their clearly uninformed opinions. 1254 The surveys conducted of physicians are reminiscent of push-polls used by politicians, where conducting a survey is a premise for propagandizing. These "studies" contain those elements. At a conference held in the Fall of 2013 in South Carolina at the Pitts Lectureship in Medical Ethics, members of the 2012 American Academy of Pediatrics Task Force on Circumcision confessed ignorance regarding the function of the foreskin. 41 If policy-makers on this issue are ignorant, what can be expected of the average medical professional? Education is sadly needed, but it should not take the form of clearly subjective, biased pro-male circumcision propaganda peddled by the misguided American Academy of Pediatrics task force on circumcision, or what is currently proposed by the CDC. It has to be evidence-based, not culture-based. This may be difficult, as the male circumcision status of the physicians and their children has a substantial impact on whether a physician recommends male circumcision. 39,1254 It is not surprising that European physicians, where there is no cultural pressure to be circumcised, have different attitudes towards protecting newborn males from harm.
The material presented in this section is the result of a very narrow ideological focus.
[Note: The American Pediatric Association (Does this organization even exist? There is an American Pediatric Society that is populated with pediatric researchers and the Academic Pediatric Association that is populated by academic pediatricians who teach general pediatrics) does not have guidelines on male circumcision, but the American Academy of Pediatrics has published several Task Force reports on male circumcision.] RESPONSE: See response 9 and 16 COMMENT:
# Cost-effectiveness
The material presented in this section is selective in favor of male circumcision. It presents findings in a biased manner where the positive aspects of male circumcision are emphasized, while studies that expose the weaknesses of male circumcision are dismissed, omitted, or ignored. Some statements are factually untrue. For example, the statement, "While male circumcision has been shown to be a cost-saving HIV prevention intervention in sub-Saharan Africa" is not supported by the citations provided. 227,232 These references are mathematical models based on assumptions. The models are only as good as the assumptions and do not measure costs in the real world. They only provide conjecture as to what might happen in the real world if the assumptions turn out to be true. As far as these models are concerned, the calculations are based on reaching universal male circumcision within the targeted populations. As noted earlier, the efforts to roll out adult male circumcision are far below this goal. [213][214][215][216][217][218][219] Until actual, real-life data are collected, this statement is inaccurate. Furthermore, the randomized clinical trials have multiple biases and flaws, which discount any perceived benefits.
Several of the cost-effectiveness and cost-utility analyses published prior to the release of the results from the randomized clinical trials focused on male circumcision's impact on urinary tract infections and they found the procedure wanting. [1255][1256][1257] The 2004 analysis by Van Howe, 1258 which used a Markov analysis and estimated the variability of its findings using Monte Carlo simulations, provided a comprehensive analysis of the costs and health states that may be impacted by infant male circumcision. It included the baseline assumption that an intact male had, based on published meta-analyses available at the time, an odds ratio of 1.78 (95%CI 1.33-2.37) of being more likely to become infected with HIV through heterosexual transmission. This assumption is consistent with the results of the randomized clinical trials, yet the cost-utility analysis found that infant male circumcision resulted in a lifetime increase in costs ($828. 42 per patient) and a decrease in health (15.30 quality adjusted life-years per 1000 males), results that were ignored by the CDC in this draft.
By contrast, the CDC draft propagates the misrepresentation of the findings of a costanalysis published by Schoen et al. 1259 A cost-analysis calculates the difference between the costs incurred by an intervention and costs that are saved as a result of the intervention. The benefits and risks are reflected in their respective monetary costs. In the cost analysis by Schoen et al., infant male circumcision resulted in more costs than it was able to recoup in benefits ($27 per circumcision). In other words, male circumcision cost more money than it saved. To conclude that "the expected lifetime cost of male circumcision was small, compared with larger expected benefits" reveals that the authors of the cost-analysis and the authors of this section do not understand that any benefits are already included in the analysis (in monetary form) and their conclusion is, in effect, an inappropriate attempt to count the benefits twice, which is beyond the scope of a cost-analysis. This indicates a bias, or incompetence, on the part of the CDC.
The statement, "Much of the benefit of neonatal male circumcision in that analysis derived from pre-empting the need for post-neonatal male circumcision, which is substantially more costly," is made without reference or citation. Where is the evidence? Post-neonatal male circumcision, which a recent study published by the CDC estimates as costing on average $1885, is more expensive than neonatal male circumcision (average cost $285). 472 Most of this expense is related to the use of general anesthesia. Considering, as discussed earlier, that local and topical anesthesia do not provide adequate anesthesia for the procedure, this may be money well spent. Post-neonatal male circumcision is rarely indicated, and it is never indicated in the healthy neonate. For example, the cumulative risk by age 15 of pathological phimosis is 0.6% 457 and the cumulative incidence of balanitis is 0.65%. 541 Consequently we would expect that only 1.3% of boys would have a medical indication for a post-neonatal male circumcision. This is consistent with the experience in Denmark were 1.6% of boys are circumcised by age 15 years. 449 This translates into a number needed to treat of between 63 472,457 This indicates that either physicians in the United States do not know how to properly diagnose phimosis requiring male circumcision, or they use the diagnosis of phimosis to secure reimbursement for elective male circumcisions, or both. Since true pathologic phimosis is rare under five years of age, it might be more cost effective for insurance companies to not pay for the procedure unless the child is over five years of age, failed a course of steroids, and had the diagnosis of balanitis xerotica obliterans confirmed.
This section of the draft report pays extensive attention to a cost-effectiveness analysis generated from within the CDC. 1260 As can be the case with secondary analysis, this analysis has a "garbage-in:garbage-out" problem. It almost appears as if the conclusion was determined first, and then the assumptions were sought out to justify the conclusion. To construct a cost-utility model that is most favorable to infant male circumcision, the model would assume the highest efficacy rate, the highest prevalence of HIV, no complications from male circumcision, and the lowest discount rate; this costutility did all these things. The basic assumptions, upon which the analysis is based, are each suspect.
First, it was assumed in the model that the lifetime risk of HIV infection for a male in the United States is several orders of magnitude higher than reported by other studies.
Based on the numbers used in the model, 1 in 16 African-American males in the United States will become HIV infected in his lifetime. So, for every two women that get breast cancer there will be one African-American male who will become HIV-infected. This is inconsistent with data collected in a national probability sample by the University of Chicago in which 0.35% (9 of 2577) of men 18 to 59 years of age were HIV-infected. 9 Why the five-fold difference?
Second, the model assumed a 60% efficacy in preventing heterosexually transmitted HIV for male circumcision over a lifetime. There are several reasons to doubt the validity of applying 60% to populations in the United States. The first, as discussed earlier, are questions regarding the internal validity of the three randomized clinical trials. It is also unlikely that a 60% reduction in risk would be seen over a lifetime. The trials followed their subjects for, at most, 24 months. There is nothing to suggest the same linear trajectory would continue over 40 years. It is impossible to know whether the pattern would continue as linear, exponential, or whether it reaches a ceiling and stops. It could easily be that male circumcision merely delays infection and the overall prevalence is the same over a lifetime. In the African randomized clinical trials, 1% of circumcised men became infected each year. So, if one assumes a linear model, between ages 20 and 80, one would expect approximately 40% of the men circumcised in these trials to become infected with HIV. Given that the prevalence of HIV in South Africa is slightly higher in circumcised men, this may be the case. 246 The second reason to doubt the 60% efficacy is that the results in Africa, which involved high-risk, well-compensated men who were willing to be circumcised, may not apply to a program of circumcising all males, regardless of their risk of HIV-infection, in the United States. Sansom et al., argue that data collected from people at highest risk for HIV infection (such as regular sexual partners of HIV-infected individuals) should be the basis for a program of circumcising regardless of risk profile. There is no evidence that 60% efficacy applies to males at low risk, and plenty of evidence to the contrary. 325 Finally, results from a study of adults may not apply to infants. To date, there have been no observational studies to indicate that infant male circumcision has any significant impact in reducing HIVinfection rates.
Third, the model assumed that African-Americans have a lower male circumcision rate than whites, yet there is ample evidence to contradict this, as is mentioned earlier. [6][7][8] If African-Americans have a risk of heterosexually transmitted HIV infection five times higher than non-Hispanic whites, this would indicate that male circumcision is not an important factor in HIV-prevention and African-Americans do not benefit from the supposed 60% protective effects of male circumcision. Before contemplating a model of infant male circumcision, the lack of correlation between male circumcision rates and heterosexually transmitted HIV-infection rates between ethnic groups needs explanation.
Fourth, it was assumed that infant male circumcision had no impact on the length of stay of the perinatal hospitalization. It has been demonstrated that one in six males circumcised as newborns will spend an extra day in the hospital. 7 Sixth, as for other "harm-denialists," the CDC assumed that infant male circumcision had no complications. Previous cost-utility analyses have found that the more common adverse events have the most impact on the cost-utility of infant male circumcision. 1257,1258 For example, at least 5% of circumcised boys develop meatal stenosis that requires a meatotomy. 186,[533][534][535][536][537] At $1500 per procedure, this adds $64.41 (3% discount for 5 years) to the cost of each male circumcision. Another 1-2% end up having a male circumcision revision, at substantial increased costs. MRSA infections are 12 times more common in infants that are circumcised. 651,1251 While heterosexually transmitted HIV infection is a relatively rare event, it may be of similar frequency as the severely botched male circumcisions in which part of the glans is amputated, or there is a serious, life-threatening infection or hemorrhage. The analysis needs to consider the cost of treating these complications, the multi-million dollar malpractice settlements, and the devastating impact on health. Death is another well-documented complication of male circumcision. 1262 While the exact number is unknown, some have estimated that between 100 and 200 deaths are related to infant male circumcisions each year in the United States. 1056 If rare catastrophic events are to be considered on one side of the ledger, they need to be considered on the other.
The CDC also failed to compare infant male circumcision to other interventions such as limiting the number of sexual partners, using condoms, early treatment of sexually transmitted infections, and secondary prevention measures such as treating HIVpositive individuals with anti-retroviral therapy. All of these options are known to be more effective, less invasive, and less expensive than circumcising all infants.
High-risk behavior will not manifest itself in infancy, so interventions should be directed at those who are sexually active. With all of these serious flaws in this model, it makes it looks like the CDC is trying too hard and is willing to say anything to make the hard sell for infant male circumcision. Consequently, the results of this model cannot be taken seriously.
The model developed by Kacker et al. is equally unjustifiable as it is based on assumptions gleaned from outlier studies that are methodologically unsound when compared to the entire body of the medical literature. 1263 To the researchers from Johns Hopkins these numbers may ring true; to others, their analysis is unabashedly onesided and biased. The analysis presents the most extreme case. That the CDC presented the results of this analysis indicates their lack of respect for the scientific method and their underlying pro-male circumcision bias.
The models for MSM are also based on wildly unrealistic protection rates for the insertive circumcised partner. It is unclear why this section gives so much space to wildly speculative, non-reality based models and little or no space to models that are evidence-based.
As mentioned earlier, the models predicting the impact of adult male circumcision on the HIV epidemic in Africa is thwarted by the lack of internal and external validity of the randomized clinical trials performed in Africa, the assumption that the effect remains linear over decades, and the incredibly limited response to the various male circumcision roll-out programs. The poor response is not a surprise. First of all, when men learn they still need to wear condoms, they will see no point in getting circumcised (male circumcision is either worthless or redundant). Second, HIV research has moved far beyond male circumcision to the point where male circumcision as prevention is rapidly becoming a footnote in the history of the HIV pandemic: an interesting historical oddity that popped up along the way. Third, treatment as prevention makes so much more sense. It works better, it is cheaper, it protects those who might be exposed through unclean medical equipment, it protects women, and it is not ultimately dependent on wearing condoms. Fourth, there is evidence that HIV is losing its virulence. 233 In the seven years since male circumcision exploded onto the scene, its flame is flickering and about to be extinguished.
# RESPONSE:
See responses 1, and 6.
# COMMENT:
Other considerations
# Risk compensation
The material in this section is incomplete and fails to place the results of studies in proper perspective. The CDC draft does not properly emphasize how important risk compensation is in the whole scheme of HIV prevention. In 1994, Blower and McLean formulated a model showing how the implementation of an HIV vaccination program with a vaccine of only 60% efficacy could easily increase the incidence of HIV infections, if risky behaviors are only slightly increased. 1264 Similar failures have been seen with vaccine programs using vaccines with efficacy in this range, such as the cholera vaccine. 1265 Another analogy is relying on birth control that is only 60% effective. 1266 Even with the most rudimentary modeling, it can be demonstrated that small changes in condom use can undermine any possible advantages of large-scale male circumcision programs, resulting in more infections following implementation of a male circumcision roll-out and billions of dollars spent. 251 The measurements of risk compensation in the men who participated in the randomized clinical trials 2,211,242,1267,1268 need to be interpreted with caution.
First, the results may reflect the Hawthorne effect: participants knew they were being watched, so this fact alone likely altered their behavior.
Second, the participants in these studies were highly compensated for their participation. For example, in the Kenya study, in addition to the equivalent in the United States of about $12,000 in goods and services for participating in the randomized clinical trial, participants were paid the equivalent in the United States of about $800 more to be in the study assessing risk compensation. This may have motivated the participants to tell the researchers what they wanted to hear.
Third, defining risk compensation as only applying to those who believe there is a change in the risk of becoming infected with HIV after male circumcision is atypical. Risk compensation has to do with changes in behavior, whether people are conscious of the changes or not. In the example of wearing seat belts, risk compensation applies equally to those who consciously think they can drive faster because they have a seat belt on and also to those who drive faster on an unconscious level because they have a seat belt on.
Their working hypothesis, that the belief in the power of circumcision makes a man less fatalistic, thus more cautious, is counter-intuitive. If men think circumcision will make them live longer since they are less likely to be infected with HIV, they will likely live a bit more recklessly from a sexual standpoint. If the fatalism theory were true, we would expect to see intact men, who believe in the power of male circumcision, be more cautious than the circumcised believers because they would perceive themselves at higher risk.
A much more likely hypothesis is that people who are risk-averse are more likely to pursue whatever they think will decrease their risk. They are more likely to believe that male circumcision will help them and undergo circumcision for this reason. They are also more likely to have fewer partners and not engage in other risky behaviors.
This has implications for men in Africa who become circumcised as part of "voluntary" male medical circumcision campaigns. Early adopters were more likely to be those who believed in the power of circumcision. These men may account for the 2% to 5% who participated before March 2012. 213 The rest of the men are less likely to believe in the power of circumcision and need further persuasion, including bribes, 1215,1217 to consider participation. These are the men who will be less risk-averse. Consequently, one would expect a slight delay in detecting the impact of risk compensation. This is not to say that risk compensation is not already having an effect on national levels. For example, Uganda, which saw dramatic drops in the incidence of HIV infections using a program of "Abstinence, Be Faithful, Condoms," 1269 has seen an increase in the incidence of HIV infections. 327 Kenya, which has seen the largest uptake in its male circumcision roll-out has also seen an increase in HIV incidence since the roll-out. 328,329 This has occurred despite evidence that the incidence of HIV infections peaked globally in the late 1990's and has been gradually decreasing since then. 625 This section omitted a few relevant studies. For example, Limburgh et al. found that participants in South Africa did not have a complete understanding of how male circumcision is protective and, while they expected to continue using condoms following circumcision, they did not expect others in the community who underwent circumcision to do so. 1270 In a study by Grund and Hennick in Swaziland, most men had more responsible attitudes in the first 12 months following male circumcision, but a minority exhibited increased sexual risk-taking, especially during a brief period of sexual experimentation shortly after circumcision. 1270 The problem is that small overall changes in risk taking is all that is needed to increase HIV infection rates. Reiss et al. also reported a minority of men (16%) who abandoned condom use and increased the number of sexual partners following male circumcision. 1271 In a study from South Africa by Nkosi, they found that males who had traditional circumcisions were associated with the greatest level of risky behavior; intact men had less risky behavior than men who were medically circumcised (adjusted OR 0.71; 95%CI 0.40-1.25). 1272 Westercamp, and the team responsible for the Kenyan randomized clinic trial, somehow have found no evidence of risk compensation. 1273 One cannot help but note the conflict of interest here on the part of the investigators. For a research group, any finding of risk compensation would undermine the importance and relevance of their randomized clinical trial, the pinnacle of their career. These results also conflict with a survey published of men and women in Kisumu, Kenya. Intact men were divided into those who preferred to get circumcised and those who did not. The intact men who preferred to get circumcised were significantly more likely to never use, or inconsistently use, a condom (OR 2.7; 95%CI 1.6-4.7) and to have one or more casual sexual partners (OR 1.9; 1.03-3.6). 378 This would indicate that men who were interested in male circumcision were those who were exhibiting more high risk behaviors than those not interested in circumcision. There are multiple reports outside of the medical literature to indicate that risk compensation is a concerning issue. [1274][1275][1276][1277][1278][1279] Two studies have indicated that women may have more influence on how much risk compensation takes place. 1211,1212 These were unexpected findings, which could further derail the male circumcision roll-out in Africa. The women told their male sexual partners they did not have to use condoms if the men were circumcised. Nothing less would be expected considering the propaganda campaign going on in Africa.
Because the incidence of heterosexually transmitted HIV is much lower in the United States than in Africa, infant male circumcision has never been shown to be associated with a lower risk of HIV, and none of the studies from North America have found that male circumcision significantly lowers the risk of HIV, a discussion about risk compensation in the United States is about as important as debating whether pigs can fly.
An excellent discussion on the issue of risk compensation as it relates to male circumcision and HIV infection in Africa appears in a Nature article by de Lange, 1280 in which it is noted that a change in risky behaviors, such as a decrease in condom use following male circumcision, could mean that male circumcision "could have the opposite effect in the long run. People might be more likely to get HIV than if they were not circumcised at all." (Quoting Michel Garenne). The other problem is that Africans, both men and women, are getting a mixed message. On the one hand, male circumcision is supposedly the "breakthrough that will end the AIDS pandemic in Africa," but on the other hand, "everyone still needs to wear condoms." Another factor that could develop with time is that, as the sensitivity of the glans is lost following male circumcision, 108 the willingness to further decrease the sensitivity of the glans by wearing a condom may drop even more. It is also unclear whether the counseling, which supposedly accompanied the procedure, will impact risky behaviors in the long run.
The materials in this section are irrelevant for health care providers in the United States.
For health care providers in Africa, it is important to emphasize that small changes in behavior, or a big change in behavior by a few, can have a huge impact, negating any gains.
[
# COMMENT:
# Policy considerations regarding reimbursement
The material presented in this section of the background document is off point. Why should the CDC be concerned about physician reimbursement? Professional organizations, such as the American Academy of Pediatrics, the American Academy of Family Physicians, and the American Urological Association, may have an interest in lobbying for physician reimbursement, but it is not clear why the CDC would be interested in this topic.
# RESPONSE: See Response 86
# COMMENT:
This section of the draft fails to note the trend that is taking place among obstetricians. In a 1998 report, 70% of obstetricians reported performing at least one male circumcision per month (as opposed to 35% of pediatricians), 445 although their scope of practice includes only female reproductive organs. A 1994 article indicated that pediatricians are happy to have obstetricians perform infant male circumcisions and obstetricians are happy to have pediatricians perform infant male circumcisions. 1281 The shift away from obstetricians/gynecologists performing male circumcisions has become more formalized in recent years when Intact America was refused a booth at the national meeting of ACOG (American College of Obstetricians/Gynecologists) because male circumcision is not considered within the scope of obstetrics. Opinion pieces have been published supporting this position. 1282 Other obstetricians have published their success in shifting the burden of performing male circumcisions away from them and onto the pediatricians or family medicine physicians in the community. 443 While national medical organizations within the United States may have taken a position on infant male circumcision, it does not mean that their positions are evidence-based. In fact, the American Academy of Pediatrics' position has been criticized as being based on culture. 1249 This section also misrepresents the position taken by the American Academy of Pediatrics. Instead of "concluding that new evidence indicates" that the benefits outweigh the risks, the Academy's Task Force has taken the position that "These benefits were felt to outweigh the risks of the procedure."(emphasis added) 1237 So, the conclusions of the American Academy of Pediatrics are based on feelings rather than evidence. This may explain why none of the other national pediatric organizations in the world have reached a similar conclusion. One of the Task Force members has recently noted he hopes the CDC report is not viewed as being as biased as their report. 1283 The fallacy in this discussion is an appeal to authority: in this case, the authorities are themselves culturally biased.
# RESPONSE 87:
The position statement by the American Academy of Pediatrics is evidence based.
# COMMENT:
It is not surprising that male circumcision rates are higher when parents do not need to pay out of pocket. However, the Midwest has a high male circumcision rate because of high demand. This may explain why the study in the Midwest, where demand is the highest, found that insurance coverage did not affect the male circumcision rates. 1284 Given that infant male circumcision is a purely cosmetic procedure, one would expect that it would not be paid for by third party payers. Furthermore, it is not the CDC's role to be in the business of justifying financial reimbursement for physicians.
[Note: Reference CDC246 is the same as CDC209. In CDC246, the first authors last name is misspelled.] RESPONSE 87a: See response 86. The duplicate citation has been corrected.
# COMMENT:
The material in this section is relevant for health care providers who depend on the income they generate from infant male circumcision and would like to see higher reimbursement rates from programs such as Medicaid. The problem is that the CDC should not be involved in efforts to improve physician reimbursement especially when it is not clear whether Medicaid can legally pay health care providers for performing male circumcision, a cosmetic surgery, on non-consenting infants. 1234 RESPONSE: See response 86.
# COMMENT:
# Ethical considerations GENERAL RESPONSE TO COMMENTS ABOUT ETHICAL CONSIDERATIONS -RESPONSE 88:
From its first consultation on male circumcision and as a part of writing of the background document, CDC carefully considered the ethical issues associated with male circumcision, including neonatal male circumcision. See ethical considerations section of background document. See responses 22, 24.
# COMMENT:
The material presented in this section of the background document is markedly incomplete, and reflects a socio-cultural bias in favor of male circumcision because of its normalized status as a birth ritual in the US, in contrast to most other nations with advanced health care systems.
For example, the Royal Dutch Medical Association, 1236 the South African Medical Association, 1244 the Finnish Medical Association, 1238 the Tasmanian Law Reform Institute, 1285 and representatives of four leading Swedish physician organizations 1237 have all concluded that infant male circumcision is a human rights violation and should be legally restricted. In addition, on October 1, 2013, the Council of Europe passed a recommendation endorsing a child's right to physical integrity and a resolution discussing the right to physical integrity in more detail. The Council specifically supported genital autonomy for children by opposing several practices including male circumcision, female genital mutilation, and early childhood medical interventions in the case of inter-sex children. 1286 If the CDC wishes to advance a moral viewpoint that stands in contrast to those adopted by peer organizations in other Western countries, it would do well to engage directly with the arguments and analyses that have been presented by those peer organizations, and attempt to show, systematically, why those arguments are not convincing. To ignore the published viewpoints of distinguished medical organizations in peer nations, all of which have gone to great lengths to assess the moral permissibility of male circumcision in light of widely-accepted ethical standards, gives the impression that the CDC is not concerned with the pressing moral issues raised by this controversial surgery.
# RESPONSE: See Response 16:
COMMENT:
Consistent with this impression is further concern about the composition of consultants at the CDC 2007 consultation. It reads, to put the point bluntly, like a Who's Who of Male Circumcision Lobbyists. 16 In the reporting on the consultation, it is stated, "Invited participants included epidemiologists; researchers; health economists; ethicists; physicians; and representatives of practitioner associations, community-based organizations, and groups objecting to elective circumcision." However, no one from any of the major groups objecting to elective infant/child male circumcision was in fact invited to the consultation (correspondence with Georganne Chapin, JD, Founding Executive Director of Intact America; Marilyn Milos, RN, Co-founder and Director of the National Organization of Circumcision Information Resource Centers (NOCIRC); John Geisheker, JD, Director and General Counsel of Doctors Opposing Circumcision (DOC); J. Steven Svoboda, MS, JD, Founder of Attorneys for the Rights of the Child). Also, no one from a group objecting to elective circumcision was invited to participate in, or provide materials for, the subcommittee of the CDC Public Health Ethics Committee. The draft does not provide a citation for the findings of the subcommittee. Nor does it disclose any cultural or religious affiliations of committee members that might have bearing upon the question of non-financial conflicts of interest. Finally, given the same reasoning for deeming male circumcision of non-consenting minors justifiable, would the subcommittee agree with the 2010 American Academy of Pediatric policy statement on female genital cutting, 1287 -later retracted-which stated some forms of female genital cutting are permissible? Is there a compelling reason why females should be protected and not males?
This section provides only cursory treatment of the many important ethical issues that are raised by the male circumcision of non-consenting minors.
Regarding the five major principles of bioethics, 1288 it has been argued that male circumcision fails to pass any of them. For infant male circumcision to be morally permissible, it must pass all five. This section of the draft only included three of the five principles.
1. Beneficence (maximizing benefit and minimizing harm, both at the individual and society level): This has been addressed in the cost-utility analyses that have been published. In the analysis that included complications, impact on urinary tract infections, impact on sexually transmitted infections (including HIV), and was properly discounted for time, it concluded that male circumcision wasted money and resulted in an average decrease in quality-adjusted life years. 1258 To conjure up a rare benefit, another analysis needed to overestimate the incidence of HIV five-fold, fail to consider any complications, and make a number of unjustifiable assumptions. 1260 The differences in these analyses can be explained on the basis of what Sarah Waldeck, a law professor at Seton Hall University School of Law, calls the "multiplier effect." 1289 Simply put, those who have accepted the social norm of infant male circumcision will overemphasize the importance of studies documenting a benefit regardless of their methodological weaknesses, and will ignore or minimize the importance of studies showing evidence of a neutral or negative impact from infant male circumcision. Considering that this draft does not address the function of the foreskin and does not adequately address the multiple harms associated with its amputation, how can the CDC acknowledge any negative consequences related to male circumcision? This draft also selectively cites studies, regardless of their methodological weaknesses, that support male circumcision. This indicates that the draft is strongly influenced by social normality and its recommendations are strongly influenced by cultural, or other, factors.
# Autonomy (respect for individual values and choices):
Infant male circumcision fails to satisfy this principle. There is no compelling medical reason to circumcise an infant. In such a situation, the Committee on Bioethics of the American Academy of Pediatrics recommends waiting until the child can provide his own fully informed consent. 1290 Male circumcision, by virtue of the fact that it breaks the skin, violates the infant's bodily integrity. One of the most universally accepted basic human rights is the right to bodily integrity and security of person. 1283,1291,1292 As a result, it is not very difficult to make a cogent argument that infant male circumcision is a human rights violation. 1293 It is widely held that no one has the right to violate the human rights of another human except in extreme circumstances. 1294 Consequently, the child's right to self-determination should be respected. There are two ways to approach an infant's autonomy when it comes to infant male circumcision. The first is to decide for the child on the basis of what he would choose, if he was able to provide his own fully informed consent, without parents projecting their value system on the child. 1294 Given that adult males rarely 1295 chose to undergo circumcision without a medical indication, the substitute judgment test requires that it not be performed on an infant (who cannot effectively resist). The second approach is based on Joel Feinberg's concept of the right to an open future. Briefly, a child should have rights that should be saved for the child until he is an adult, or what he calls "rights in trust." These are the sort of rights an autonomous adult would have, but a child would be too young to exercise them. They are "rights that are to be saved for the child until he is an adult, but which can be violated 'in advance' before the child is even in a position to exercise them." Following such violations, a child upon reaching adulthood would find that certain options would already be closed. 1296 The concept of a right to an open future has been adopted by subsequent ethicists. 1297 Certainly, infants, whether male or female, have a right to their complete genitals coming into adulthood.
The right to bodily integrity should be a "right in trust" that Feinberg envisioned. Consequently, it has been argued that infant male circumcision violates an infant's right to an open future. 1298 Subsequent analysis has determined that physical violations do carry more moral weight than non-physical violations. 1299 In either case, violating the infant's developing/future autonomy by cutting off the most sensitive portion of his penis without his permission is a matter for great moral concern. Since autonomy is considered by some to be the primary principle of modern bioethics, 1300 there needs to be a compelling reason to violate anyone's autonomy, especially someone who is vulnerable. No such reason has been provided in this draft.
3. Justice (the obligation to fairly distribute risks, burdens, and benefits, to minimize stigmatization, and to make decisions in a transparent fashion): When male circumcision is performed on an infant at the parents' behest, the parents do not assume any of the risks, the infant does. The infant has no say in the matter, yet takes on all of the harms and risks associated with the procedure. Such a shift of risk onto someone who cannot consent is inconsistent with the concept of justice. Obviously the risks are not fairly distributed. Infants who are circumcised for religious or cultural reasons or for misguided beliefs that it improves hygiene, which covers the vast majority of male circumcisions, undergo the procedure for what parents believe is their religious or cultural obligation. Consequently, the infants are being used instrumentally as a means to satisfy ends determined by their parents. 1299 In Kantian ethics, anyone of moral worth should not be treated as a means to an end, but always as an end in themselves. 1301 Treating a human being instrumentally in this fashion is in direct opposition with our modern concept of justice. 1302 Likewise, the randomized clinical trial which purported to find that circumcision of HIVinfected men increased the relative risk of infection in female sexual partners by 50% placed an increased risk of HIV infection on women who were unaware of their partner's HIV status. 338 This abuse of the principle of justice was one of several reasons why this study was perhaps the most unethical study since Tuskegee. [1303][1304][1305] If the CDC was interested in minimizing stigmatization, it would abandon the use of the term "uncircumcised," which is now considered by many to be pejorative. One definition of the word "uncircumcised" is "spiritually impure: heathen: unregenerate." It is also a term that is technically inaccurate. For a man to be "uncircumcised," he would need to first be circumcised and then have the process reversed. By using the term "uncircumcised" or "non-circumcised," the authors of this draft are making the underlying value-laden assumption that being circumcised is the preferred condition, when there is no evidence, other than cultural pressure, to support this. The most accurate, value-neutral term for a man with all of his original genital tissue is "intact." By continuing to use the term "uncircumcised," the CDC is identifying its pro-circumcision bias to anyone who is familiar with the semantics on this issue. Males who are indeed "intact" find use of the word "uncircumcised" to be akin to hate speech because they are singled out as "different," supposedly "abnormal," and/or possibly unclean." 1181 Nothing could be further from the truth. Profiling a group of people in this way is unjustified, discriminatory rhetoric.
The use of this terminology has racist and anti-immigrant overtones. With the exception of a few immigrants who come from circumcising cultures, most immigrant males have intact genitals. The overall tone of this draft unnecessarily and counterfactually characterizes normal, intact males as inferior and disease-laden. The draft also places more credence with investigators who focus on certain racial and ethnic groups for increasing male circumcision rates. 345 Less than a third of the world's men are circumcised, and nearly all of them are circumcised for religious or cultural reasons. Why would the CDC want to stigmatize the majority of males on the planet? Many intact males who read the American Academy of Pediatrics 2012 Task Force report 1306 interpreted the Academy's position as thinly veiled hate speech (personal communications). The CDC's recommendation may be interpreted as even more insulting.
If justice requires that decisions be made in a transparent fashion, then major reform is needed in the informed consent process that accompanies infant male circumcision. This is needed to ensure full disclosure is provided, that those providing proxy consent understand what they are providing consent to, and that those providing consent do so voluntarily without being coerced or solicited. [1307][1308][1309] Currently, the level of disclosure provided is far below the standard expected for similar elective procedures. 1228,1231,1310 One study in which full disclosure was provided resulted in parents becoming very upset with the physicians providing the disclosure. 1311 This may reflect that many parents are unaware male circumcision leads to any harm or complications, and parents have usually made up their minds about male circumcision based on social or cultural factors. They may not want to hear about any untoward effects because this creates cognitive dissonance. But, this does not excuse physicians from their duty to provide full disclosure. Sometimes, this information will dissuade parents from agreeing to a circumcision for their son. Full informed consent also protects the health care provider in the event of an adverse outcome. Even in the adult male circumcision roll out in Africa, the men are not given full disclosure regarding the harms and complications of male circumcision. The fact that bribes are becoming necessary to recruit adult males to undergo a free male circumcision 1214 is an evident sign that the decision process is less than transparent.
Is it justifiable for parents to impose male circumcision on their sons when there are more effective, less expensive, less invasive methods of preventing urinary tract infections, sexually transmitted infections, HIV infections, and penile cancer? Imposing such inefficiencies in a nonconsensual fashion onto an infant in the name of parental convenience is both unfair and unjust. If an infant cannot choose his preferred method of prevention, the parent at least should choose a more efficient, less expensive, less invasive measure.
The two principles omitted in this section of the draft are:
4. Non-maleficence (does the procedure avoid permanently diminishing the patient in any way that can be prevented?): Male circumcision permanently removes the most sensitive portion of the penis. 54,55,108 Some would argue this is the intent and purpose of the procedure, 1312,1313 and certainly it was the intent when male circumcision was first introduced in the United States and Britain as a "cure" for masturbation. [1183][1184][1185] 5. Proportionality (will the final result provide a net benefit to the patient in proportion to the risk undertaken and the losses sustained?): Decisions are made in everyday life based on proportionality. If a shop is asking too much money for an item, they may have trouble selling it because the price is out of proportion to the value the customer has assigned to the item. For infant male circumcision proportionality works on two levels: the physical and the moral. It fails on both levels.
The measure of proportionality on the physical level has already been assessed with the roll-out of adult male circumcision in Africa. Men who live in countries with some of the highest prevalence levels of HIV infection in the world have been subjected to wellfinanced advertising and have been offered a free male circumcision, but they are only agreeing to undergo the procedure 1.6% of the time unless they are given an additional bribe. 1214 The advertising programs have informed these men regarding the ease and simplicity of the procedure, the lack of complications, and the overwhelming benefits in protecting them from sexually transmitted infections and HIV, yet only 1.6% are interested in a male circumcision paid for by the Bill and Melinda Gates Foundation, the Clinton Foundation, and PEPFAR. How could this be explained? These men have a foreskin. They know how it works, what it does, and how it feels. It seems that they recognize on a physical, biological level that the resultant harm of removing the foreskin is out of proportion to the unlikely benefits, especially when the same benefits can be more easily and effectively obtained using methods that do not involve the removal of sensitive, functional tissue. Instead of recognizing the value that men have assigned to their foreskins, advocates of mass male circumcision spend their time trying to discover the inducement that will entice these men to get on the male circumcision bandwagon.
On the moral level, the value of one's wholeness and the ability to exercise one's autonomy are important elements in the equation. David Lang 1314 and Wim Dekkers 1315,1316 have identified totality and wholeness as important issues in the ethical debate over male circumcision. Lang applies the principle of totality to argue that "the good of the whole overrides the good of a part if [the loss of] that part is truly (not merely hypothetically or speculatively) a threat to the well-being of the whole." 1317 In other words, all parts of the body form a cohesive, integrated unit. 1314 This principle complements the principle of bodily integrity. Lang argues that, since male circumcision disrupts normal sexual function, the principle of bodily totality is violated.
For Dekkers, "wholeness" has four aspects: biological, experiential, intact, and inviolable. 1315,1316 Biological wholeness refers to anatomical and functional integrity, which is conceptually similar to Lang's notion of totality. Excising erogenous genital tissue violates this sense of wholeness. Experiential wholeness is not dependent on biological wholeness, but is a phenomenological view of the human body in which the body is a "lived body." By altering responses to subsequent painful stimuli 993,994 and altering normal penile reflexes, 120 removal of the foreskin may negatively impact experiential wholeness. One aim of medicine is, or should be, to restore this sense of intactness and completeness -to make the body whole again, not to introduce deficiency. For medical practitioners to remove functional tissue runs against this aspect of wholeness. Inviolable wholeness is an outgrowth of a Kantian principle that violating the body also violates the person's dignity. 1299 According to this principle, the integrity of the body is a necessary condition for the fulfillment of human moral purposes, and respect for the integrity of the body is necessary for proper moral sensibility.
Male circumcision also violates an infant's sense of wholeness without consideration. On a contractual level, such a one-sided transaction would not be binding. Proportionality is not achieved as the infant is not compensated for this loss. The loss of the protection of bodily integrity, security of person, and self-determination (autonomy) are also not adequately compensated for. According to John Rawls, depriving one of a basic human liberty is only morally permissible if doing so enriches or enhances one of the other basic human liberties. 1302 During infant male circumcision, the basic human right to bodily integrity and security of person is violated without compensation. It is thus not proportional.
The possibility of death, although rare, following infant male circumcision, which has not been reported following circumcision in older boys and adults, also violates the principle of proportionality. This potential outcome may be grounds enough for delaying the procedure until the patient is old enough to grant his own fully informed consent.
This section states that "Others argue that it is a choice that parents should be able to make on behalf of their male children because of the strong evidence showing that the procedure is beneficial and the risks are minimal if performed competently." This statement has several problems. First, at least one of the citations given for this statement does not make this assertion. The 2003 article by Benatar and Benatar does not contend that there is strong evidence favoring male circumcision or a minimal risk, but rather that the benefits and risks are balanced and given the non-medical benefits, which they fail to identify, male circumcision is morally permissible. 1318 Second, there is clear debate over the value of the evidence. As noted by Waldeck, male circumcision status and the prevalence of circumcision within a culture will impact how evidence is prioritized and interpreted. 1289 So, it is telling that the CDC cites the opinion piece in favor of male circumcision published in the British Medical Journal, 1319 but failed to cite the opinion piece arguing the opposing view that accompanied it. 1320 Others have put forth such utilitarian arguments, [1321][1322][1323] but such arguments have been challenged because of their dependence on false analogies, speculation, selective bibliographies, being oblivious to the harms and risks of the procedure, and fallacious reasoning. 1299,1317,[1324][1325][1326][1327] The importance of unproven benefits and ignored harms needs to be part of the debate and not just accepted because it makes one feel better about being circumcised. Furthermore, many male circumcisions are performed by those least competent to be doing the procedure: medical students, interns, residents, physician assistants, etc. And, few, if any, health care providers are adequately educated about the anatomy of the foreskin, which explains the high number of complications surrounding its removal.
Second, it is merely assumed that parents have the authority or "right" to have parts of the genitals of their children amputated. The concept of parental rights is a legal fiction that has outlasted its usefulness. When women and children were considered property/chattel, such property rights made sense. As the moral worth and status of children is increasingly being recognized, treating children as property/chattel is becoming more difficult to rationalize. One legal scholar has noted that parental rights are only invoked when the parents are doing something that is not in the child's best interests. 1328 It has been argued that parents do not have the "right" or the authority to violate their child's basic human rights and that this prohibition extends to infant male circumcision. 1329 One could argue that the onus is on those who want to encourage or defend infant male circumcision to make a positive argument to justify violating an infant's right to bodily integrity and security of person based primarily on parental judgment.
While parents are given the authority to vaccinate their children, infant male circumcision has little in common with vaccination other than that they are both implemented on infants or children. Male circumcision removes tissue that is irreplaceable and that serves specific functions; vaccines stimulate the production of antibodies by the immune system to fight off infections.
The claim that infant male circumcision acts like a vaccine has been made by a number of male circumcision enthusiasts. 1,[1330][1331][1332][1333][1334][1335][1336][1337][1338][1339] They use this analogy because the average person understands the concept of vaccination and has seen the ability of vaccines to greatly reduce the incidence and prevalence of a number of serious and non-serious illnesses. A highly effective vaccine against a life-threatening infection can have an almost miraculous impact, but most are not aware that a vaccination program using a vaccine with only 40% to 60% effectiveness will ultimately increase the number of infections. 1265 Male circumcision enthusiasts use the vaccine analogy because they want people to associate the miracles brought about by vaccines to also be associated with infant male circumcision, in the hope that those opposing infant male circumcision would then be thought of as irrational and unwilling to do what is in their child's best interest.
The analogy between vaccination and male circumcision is spurious:
1. Vaccines target specific illnesses that are either common, infectious, or carry significant personal or public health consequences. Male circumcision does not.
2. Only vaccines that have been demonstrated to be effective in decreasing the risk of severity of the targeted illness are released for use on the public. Nearly all of the vaccines that are commonly used are effective in more than 85% of those vaccinated (an exception is the influenza vaccine). Typically, vaccines that only reduce the risk by 40% to 50% are often not used. 247,1265,1340,1341 Male circumcision has not been clearly demonstrated to be effective, let alone provide more than 85% protection. By making the analogy, male circumcision enthusiasts are trying to get people to believe that circumcision has these high levels of protection.
3. Vaccines do not permanently remove any body parts. Male circumcision does. As Wayne Hampton notes, "Circumcision is a subtraction whereas vaccination is the addition of immunizing agents to the bloodstream. Circumcision is a loss while a vaccine is a gain." 1342 Removing the foreskin, with its functioning mucosal immunity, subtracts from the value of the body as a working system. A vaccination adds to the value of the body as a working system by boosting the immune system. This is morally interesting, especially from a utilitarian standpoint, because the net effect of a vaccination is improved function both on an individual and a societal level, while this is not true for male circumcision. It is also interesting from a Rawlsian perspective because a vaccine program serves the purpose of justice as it improves life, especially for those who are the most vulnerable.
In a similar vein, male circumcision is more invasive than vaccination. To make the analogy of male circumcision being similar to vaccination plausible, male circumcision enthusiasts would need to demonstrate that male circumcision is not excessively invasive, but this cannot be demonstrated.
4. Vaccines typically have been shown to have a positive cost-effectiveness or a reasonable cost-utility. Male circumcision has not. 1258 5. The long-term effects of vaccinations have been well studied and documented. This has not happened with male circumcision. Even the 2012 Task Force report from the American Academy of Pediatrics acknowledges that the long-term risks of male circumcision are unknown. A registry and compensation system exists to address unfortunate outcomes of vaccination, yet no such system exists for male circumcision. 1342 6. Vaccination programs have decreased the incidence/prevalence of the targeted diseases. The illnesses associated with male circumcision have not decreased and in several instances have increased. The diseases that have been targeted by vaccination programs, for the most part, have been either illnesses with a high incidence and/or with associated significant morbidity/mortality. 1340 While vaccination programs have clear public health benefits, both for the individual and society overall, any such benefits for male circumcision, if they exist at all, are miniscule by comparison. 1344 7. The level of acceptable risk for the public for vaccinations is very low and well below the risks associated with infant male circumcision.
8. The diseases targeted by vaccines typically have a high incidence, often the majority of the population is at risk, otherwise a vaccination program would not be worth pursuing. By contrast, the illnesses male circumcision is presumed to prevent are uncommon, rare, or nonexistent. 1348 9. When male circumcision apologists and enthusiasts link male circumcision and vaccination, they need to be aware that by doing so they may undermine the efforts of vaccination programs. Clearly, parents who do their due diligence will discover male circumcision is questionably effective at best. By linking male circumcision and vaccination, parents may be given the false impression that vaccinations are as ineffective as male circumcision. Claims of a public health benefit should be limited to interventions that actually have a positive impact on the health of the public.
The argument provided by Benatar and Benatar posits that the legitimacy of parental authorization of infant male circumcision is based on the vaccine analogy. 1318 The points of their argument can be summarized as follows:
1) There are parts of the world where diseases against which children are frequently vaccinated are now uncommon.
2) The necessity of such vaccination for the individual child is neither clear nor immediate.
3) There are small but real risks from vaccination (including death).
4) The child is unable to give consent for vaccination.
5) The power to consent can be deferred to proxy decision makers or delayed until the child is old enough to give consent himself.
6) Delaying vaccination can undermine its benefit.
7) It is reasonable for parents or other guardians to make decisions on behalf of a child that are in the child's best interests.
8) "The role of a parent is not simply to save children from immediate catastrophe, but is to protect and foster a child's long-term best interests." 9) Therefore, "parents may consent on behalf of their children not only to vaccination but also to such procedures as orthodontics and various non-medical interventions, including schooling."
A point by point rebuttal follows:
1) Not only is this true, but vaccination programs are effective. (Although, it translates into fewer sick visits at our office and less revenue for physicians. If the CDC translated their interest in increasing physician income generated from male circumcision, they would also come out against vaccinations.)
2) The presumption that vaccinations have no clear necessity for the individual is unsubstantiated. If a vaccine did have not a clear indication, it would no longer be given. This is the case for small pox. Vaccination programs against smallpox were discontinued after it was determined that smallpox had been eradicated. Vaccines can also be justified on the basis of public health considerations. 1343 To say that vaccines have no clear indication for the individual is foolhardy. Herd immunity may reduce some risk, but does not eliminate risk. If it did, the pertussis and measles outbreaks in unvaccinated children that emerge on a fairly regular basis would not take place. Consequently, there is always a potential advantage to the individual to be vaccinated. This presumption is not only wrong but extremely dangerous. If this erroneous position was adopted by a sufficient number of people, even the positive impact of herd immunity could be lost, leading to a public and personal health disaster.
The Benatars's entire argument is dependent on this false assumption. If vaccines had no benefits, then parents would not be allowed to authorize their use. It is only because they have benefits that parents can direct medical personnel to administer the vaccines. People are allowed choices and parents can forgo vaccinating their children. When they do so, it is common practice to have parents sign a waiver indicating they are aware of the benefits of the vaccine, yet they wish to forgo its administration to their children.
3) Agreed.
4) Agreed, but given the benefits of the vaccine, it is both in the child's best interest and also something the child would choose for himself if able to.
5) Agreed.
6) Agreed.
7) Partially agreed. The language should be altered to state it is reasonable for parents to consider making some decisions on behalf of the child that are believed to be in the child's best interests. For example, a girl with a gene that puts her at high risk for breast cancer, one could argue that a prophylactic double mastectomy would be in her best interests, but not a decision that the parents should make on her behalf. The American Academy of Pediatrics Committee on Bioethics notes that: parental decisions are limited to those where there is an immediate danger, and that decisions which can safely wait should be delayed until the child can have input into the decision. 1238 8) Agreed. But parents also have the responsibility to be the child's guardian, which includes the duty to protect the child's basic human rights, 1318 protect the child's right to an open future, [1296][1297][1298] and not treat the child instrumentally. Comparing choices for education has no discernible connection to making medical choices for a child who cannot choose for himself. At the age where education outside the home is offered, the child can have a varied amount of input. There is also disagreement about the authority of parents to force children to undergo education that is not in their best interests 1346 This is also a false analogy that does not apply to infant male circumcision because, as a society, we consider education necessary to become a good citizen 1347 and we believe delaying education will undermine its effectiveness. Education is clearly in the child's best interests, and it is something the child would have chosen for himself once he becomes competent.
While, in the opinion of the undefined, unpublished findings of the subcommittee of the CDC Public Health Ethics Committee, the decision either to or not to circumcise is an appropriate exercise of parental authority, the CDC draft fails to recognize that many disagree with this opinion. For example, all of the national medical organizations who have come out against infant male circumcision and have characterized it as a human rights violation are not mentioned by the CDC. 1236,1238,1240,1241,1244,1245,1250 Legal scholars have questioned the legitimacy of parents violating their child's human rights and best interests under the rubric of "parental rights" because such actions only result in harming children. 1293,1327,1346,1347 It has been argued, given the moral status of infants being increasingly recognized, 1292,1347 that infant male circumcision may be the last holdout in which parental rights are recognized. 1329 The rest of the Western world recognizes that parents do not have the authority to violate their child's basic human right to bodily integrity and security of person.
Did this CDC subcommittee consider whether this same parental authority would allow parents to direct health care professionals to cut the genitals of their daughters? The same ethical principles would apply. There is some evidence that female genital cutting has medical benefits in decreasing the risk of HIV infection 1348 and a significantly shortened second stage of labor. 1349 Proponents of female genital cutting maintain the procedure also decreases a woman's risk of sexually transmitted diseases. At least one study has documented that female genital cutting has no impact on sexual fulfillment or the ability to have an orgasm. 1350 In 2010, the American Academy of Pediatrics Committee on Bioethics released a statement, in an effort to acknowledge cultural diversity while ignoring the moral status and human rights of children, stating some forms of female genital cutting are morally permissible. 1287 The report generated such a negative response that the Academy was forced to "retire" the statement 31 days later. 1351,1352 It would certainly be unfair and unjust if the subcommittee were to treat males and females differently.
The justification for the moral permissibility of infant male circumcision in the CDC draft, and as argued by other male circumcision apologists, 1340 is based on the presumption that the procedure is safer and simpler when performed on newborns and infants. Unfortunately, presumptions are not data. 1353 As addressed earlier, the evidence does not support the contention that there is an advantage to male circumcision being performed in infancy, other than the ease with which the boy can be restrained.
The CDC draft should also refrain from fear-mongering. Apparently, those who wrote the draft must be concerned over the remote possibility of missing an opportunity to prevent an HIV infection in a male who becomes sexually active before he has the chance to get circumcised. How many 14-year-old males are going to get HIV from their 14-year-old girlfriends? While the age of sexual debut may be getting younger, the rate of heterosexually transmitted HIV infection is extremely rare through sexual contact with other young people. There is no evidence in North America that any HIV infections are prevented by male circumcision, 8-14 so there is no reason to lose sleep over the number of HIV infections potentially caused by a delay in male circumcision. Likewise, neonates are not sexually active.
The statement, "Uptake of the procedure after the neonatal period is also likely to be lower due to the increased cost, greater likelihood of complications, and other barriers to male circumcision at a later age," contains several inaccuracies. First, as discussed in detail earlier, there is no properly controlled experimental evidence that later male circumcision has a greater likelihood of complications. There are numerous case reports of infant deaths resulting from male circumcision in the medical literature in the United States, but none known of adolescent or adult deaths as a consequence of male circumcision. Adolescents and adults are capable, unlike neonates, of expressing pain and requesting adequate pain relief, of noting excessive bleeding and infection. They would also have undergone a thorough pre-operative history and physical exam noting any possible reasons to not have surgery. Neonates undergo male circumcision surgery without knowing whether they have any underlying medical problems such as hemophilia, and many premature neonates are circumcised while still undergoing care in the NICU. If surgery under general anesthesia is unacceptable for neonates, then any surgery should be postponed until adequate pain relief can be provided. Male circumcision is done to infants because it can be done, not because it is safer with fewer complications. (see complications section.)
It is also unclear what the other barriers to male circumcision might be in adolescents or adults. Somehow, teenagers are able to undergo orthodontia, which is much more time consuming than male circumcision. Some teenagers manage to undergo cosmetic surgery during school vacations. It is unclear how there would be significant barriers, if male circumcision would be considered so terribly important. If the CDC and American Academy of Pediatrics have their way, there should be no financial barriers to this cosmetic surgery. What this statement is missing are the real reasons that uptake is lower after the neonatal period. After several weeks of bonding with their baby, parents are less likely to put their baby through a painful procedure. The older boy, who has experience with his foreskin, would consider the suggestion of cutting off his foreskin, which at that point may have acquired a distinct value to him as sensitive tissue, as imprudent. "Why would anybody want to do that?" is a typical response. The foreskin is a valued possession that even a young boy knows enough not to relinquish.
The subcommittee recommended that male circumcision be an "informed choice" but fails to consider that informed consent is impossible for infant male circumcision. 1231 This is an important issue that warrants debate, but it was apparently not addressed by the subcommittee. The Europeans do not think parents can provide informed consent, and certainly the infant cannot either. Many would contend that adolescents are also unable to give consent.
Finally, the lack of health insurance coverage for male circumcision is not an issue of justice because male circumcision is a cultural practice. It is typically not the role of government, and definitely not the role of Medicaid, 1234 to support cultural practices. By supporting one cultural practice, those who do not participate in that practice are discriminated against. If, as appears to be the case with this draft, the CDC is applying pressure on ethnic groups that have traditionally kept their infants genitally intact, then they are enforcing an unwanted hegemony. The reduction in risk of HIV infection and other adverse health conditions is illusory. This leads to the question of why the CDC is so interested in implementing this hegemony.
# RESPONSE 89:
The CDC adequately bases its analysis on the best quality scientific evidence available, mainly the RCTs, which are consistent in their findings around prevention of HIV acquisition.
The CDC Public Health Ethics Committee (PHEC) concluded that newborns cannot provide informed consent and so must rely on their parents or caretakers to determine and act in their best interests, raising the issue of autonomy in discussions of circumcision of male newborns. They took into account varying opinions about the decision-making process including that the decision about whether to be circumcised should be made by individuals when they are old enough to make their own informed decisions. It has been pointed out that a man with a foreskin can elect to be circumcised but if circumcised as a newborn, cannot easily reverse the decision. Others argue that it is a choice that parents should be able to make on behalf of their male children because of the strong evidence showing that the procedure is beneficial and the risks are minimal if performed competently. Parents are generally given the authority to make decisions, such as vaccination, for their minor children based on their evaluative consideration of the child's best interests. Appropriately, this consideration takes into account social, cultural, and religious perspectives, as well as objective, scientific information about preventive health benefits and risks. Thus, in the opinion of the PHEC, both a decision to circumcise and a decision to not circumcise are legitimate decisions, and either decision is an appropriate exercise of parental authority on behalf of a minor child.
# COMMENT: Tables
Both tables are highly selective in the data presented and need to be completely revised. Results for which there was clear sampling bias and/or lead-time bias need to be adjusted accordingly. The results of meta-analysis of observational studies need to be included. All of the prospective studies of incidence need to be included and updated.
# RESPONSE 90:
The data selected for presentation in the tables represent the best quality scientific evidence available (RCTs) at the time of the review.
# COMMENT:
Closing Comments
What is going on at the CDC? After taking over seven years, the CDC finally generates recommendations that mimic the talking points propagated by male circumcision enthusiasts. But, this is only the latest in a string of bizarre actions taken by people within the CDC who have been addressing the issue of male circumcision. The first action was taking up the issue at all. Heterosexually-transmitted HIV infection is only 10% of the HIV infections seen in the United States and 70% or more of the sexually active males in the United States are already circumcised. Many of those males with HIV are/were circumcised, so how did circumcision help them? Why is "circumcision to prevent HIV" even an issue in the United States? It does not make sense to expend the energy on such a highly circumcised population unless the action was intended to maintain a high percentage of male circumcision for some other reason.
The next action was to convene the consultation in 2007, inviting nearly every prominent male circumcision enthusiast on the planet. Of the 50 or so people from outside the CDC invited to attend, only one had ever published studies that were not favorable to the practice of male circumcision. Not much diversity represented there. This would make it sound as though there is only one scientist in the world who has published such studies. Clearly, there are plenty of scientists who could have voiced an alternative viewpoint and who would have been willing to attend the consultation, but they were not invited. Only one was invited, as the token dissenting voice. A similar tactic was used when the WHO/UNAIDS rammed through its approval of male circumcision in Montreux in 2007, where Gary Dowsett was the token voice of opposition. 5 It is not surprising that this experiment in "group think" provided the CDC with all the ammunition it needed to move forward. In 2009, the CDC held a conference in Atlanta on male circumcision and HIV. They invited Inon Schenker of Operation Abraham and the Jerusalem AIDS Project to give a presentation. The last slide in his presentation was a photograph of a completely naked, genitally intact male on whom the figure of an elephant had been drawn around the penis so that the intact penis looked like an elephant's trunk. The words "Yes! A circumcision please!" had been added to the photo. Such a crass insult to every intact male was uncalled for. Apologies have obviously been in order, and requested, but never granted. It is not apparent why the CDC would tolerate what was clearly intended to be hate speech.
It is not clear why the CDC would purposely publish recommendations and a supporting background document that they must know is not evidence-based. By doing so, the CDC has placed health care providers in the untenable situation of committing malpractice, by disseminating false information, thereby placing their patients at unnecessary risk. Why would they want to embarrass themselves in this fashion? Is the CDC so infiltrated and controlled with male circumcision advocates that producing something this biased and unscientific was mandated from the top? There is evidence that Peter Kilmarx, who initially headed up this project, was part of an email mailing list of male circumcision advocates in 2006. How much contact between officials at the CDC and pro-male circumcision lobbyists would a freedom of information request reveal? Is the CDC somehow beholden to the pro-male circumcision lobby? Is this draft a concession to the lobby to demonstrate that the CDC was willing to do their bidding? One has to wonder how much of the effort to "prove" that male circumcision prevented HIV and other sexually transmitted diseases in Africa was actually not about helping those in Africa, but more about maintaining the current rates of male circumcision in the United States, keeping them from going into free fall. The narrow, single-minded focus of the CDC in this draft supports this contention.
What will the CDC do now that their biased, culturally-based position has been exposed as being scientifically fraudulent? How can anything the CDC says or does be taken seriously after one has followed their subjective handling of this issue over the years? It is time to save face. Trash this draft and start over. | None | None |
4ec67e6602aa503bff944f2c0a289699752b86dd | cdc | None | # CRITERIA DOCUMENT: RECOMMENDATIONS FOR AN OCCUPATIONAL EXPOSURE STANDARD FOR THE DECOMPOSITION PRODUCTS OF FLUOROCARBON POLYMERS
recommends that exposure to the decomposition products of fluorocarbon polymers in the workplace be controlled by adherence to the following sections. The standard is designed to protect the health and provide for the safety of employees for up to a 10-hour work shift, 40-hour workweek, over a working lifetime. The recommended standard for the decomposition products of fluorocarbon polymers emphasizes good work practices and engineering controls and medical management. Since no measurable environmental level of any single decomposition product of fluorocarbon polymers can ensure complete protection of worker health, no occupational exposure limit is recommended in this document. The criteria and standard will be subject to review and revision as necessary.
Fluorocarbon polymers include polymers of substituted polyethylene monomers of the general formula (XCX-XCF)n, where X can be F, H, Cl, CF3, or CF3-CF2-CF2-0. The decomposition products of fluorocarbon polymers are defined as substances which are thermally generated from fluorocarbon polymers.
The greatest danger to workers exposed to the decomposition products of fluorocarbon polymers is from inhalation. Adverse effects could result from exposure to dusts of undecomposed fluorocarbon polymers, from exposure to the decomposition products, or from exposure to a single or several 1 decomposition products. The major concern in occupational exposure to the decomposition products of fluorocarbon polymers is their potential for causing polymer fume fever and damage to the respiratory tract. Polymer fume fever is characterized by headache, aching joints, general malaise, cough, shivering, chills, fever, tachycardia, and possible chest discomfort. The temperature may rise as high as 39.6 C (103.3 F ) .
Adherence to all provisions of the recommended standard is required in work areas in which fluorocarbon polymers are used, regardless of the concentration of airborne decomposition products of fluorocarbon polymers.
Occupational exposure is defined as any exposure to fluorocarbon polymers that may involve the production of decomposition products.
The products liberated from fluorocarbon polymers by the application of heat vary with the polymer, the temperature to which it is exposed, and the humidity of the ambient air. Because there is insufficient information on which to establish a safe workplace environmental concentration, none is recommended.
Both employers and employees should take all steps possible to keep occupational exposure to the decomposition products of fluorocarbon polymers as near to zero as possible. Careful adherence to all sections of this recommended standard will facilitate accomplishment of this aim. Controls which may be appropriate include isolation of a process within a controlled ventilation area, installation of safeguards to prevent thermal excursions, and installation of redundant temperature monitoring systems and associated alarms.
(a) Coveralls, or equivalent clothing, and gloves should be worn by the employee in areas where bulk fluorocarbon polymer dust is handled or where contact of powdered polymer with the skin is likely.
# (b)
Respiratory protective equipment to be used, if necessary, during emergencies or during the performance of nonroutine maintenance or repair activities in which exposure to the decomposition products of fluorocarbon polymers is likely should be provided in accordance with Table 1-1. Applicable regulations for the use of respirators are found in 29 CFR 1910.134.
# (c)
When a respirator is required by paragraph (b) of this section, it shall be selected and used in accordance with Administration (previously by the Bureau of Mines) as specified under the provisions of 30 CFR 11. The employer shall ensure that respirators are adequately cleaned and maintained, and that employees are instructed in the proper use and testing for leakage of respirators assigned to them.
Respirators shall be easily accessible, and employees shall be informed of their locations. (1) Half-mask respirator equipped with combination acid-gas/organic-vapor sorbent and high-efficiency filter cartridge (2) Full-facepiece gas mask equipped with acidgas/organic-vapor sorbent and high-efficiency filter canister, changed every 4 hours Maintenance (Equipment breakdown or cleaning of distillation vessels, etc; no time limit) Type C supplied-air respirator operated in demand, pressure-demand, or continuous-flow mode and equipped with full facepiece, hood, helmet, or suit where there is occupational exposure to the decomposition products of fluorocarbon polymers. As a further precaution, the carrying of smoking materials into such areas shall be prohibited.
Employees shall be instructed to wash their hands before smoking.
# (b)
In sintering or molding operations where fluorocarbon polymer is heated above its melting point, temperatures in excess of the manufacturers' recommended range should be avoided whenever possible. To prevent overheating, ovens shall be fitted with an automatic temperature cutout set at the manufacturers' recommended temperature for the fluorocarbon polymer.
(c) If necessary to prevent accumulation or recirculation of the decomposition products of fluorocarbon polymers in the workplace, ovens shall be fitted with a local exhaust ventilation system. An appropriate alarm shall be incorporated into any exhaust system in case of its failure.
(d) Local exhaust ventilation, located as close as possible to the operation, shall be used whenever welding, cutting, or related hightemperature operations are performed.
(e) Exhaust systems and ductwork shall be kept in good repair so that design airflows and pressures are maintained. Airflow and pressure should be measured at least twice a year. Continuous airflow indicators (oil or water manometers) are recommended. A log shall be kept showing design airflow or pressure and the results of periodic inspection.
(f) Ventilation systems discharging to outside air must be designed to conform to applicable local, state, and federal air pollution regulations and must not constitute a hazard to employees or to the general population.
(g)
General Housekeeping
(1) Spills of fluorocarbon polymers shall be cleaned up, preferably by vacuuming. Care shall be taken that polymer dust is not blown onto steampipes or other heated equipment.
(2) Emphasis shall be placed on prompt and frequent cleanup of dust to prevent accumulation of fluorocarbon polymers.
(3) Equipment shall be maintained regularly, and necessary repairs shall be made promptly.
(4) Fluorocarbon polymer scrap and waste shall be collected in special containers and, if not reused, shall be disposed of by high temperature incineration or by burying. Where excessive contamination of clothing with fluorocarbon polymer dust is likely, employers shall provide employees with launderable clothing for repeated use or disposable outer garments for one-time use.
(e) Laundry personnel should be informed of the hazards and of safe procedures if they are likely to encounter clothing contaminated with fluorocarbon polymers.
# II. INTRODUCTION
This report presents the criteria and the recommended standard that were prepared to meet the need for preventing occupational disease or injury arising from exposure to the decomposition products of fluorocarbon polymers.
The criteria document fulfills the responsibility of the
# III. BIOLOGIC EFFECTS OF EXPOSURE
# Extent of Exposure
Fluorocarbon polymers are made from substituted polyethylene monomers of the general formula (XCF-XCF)n, where X can be H, F, Cl, CF3, or CF3-CF2-CF2-0 , Copolymers, made from two monomers with as little as 10% of the comonomer, and terpolymers, made from three monomers, are additional forms of fluorocarbon polymers . Fluorocarbon telomers are fluorocarbon polymers of low-molecular-weight produced by chemical reactions that limit the degree of polymerization .
Some important commercial fluorocarbon polymers are listed, along with the monomers used in their preparation, in Table III-l .
The preparation of unsaturated fluorocarbon monomers from saturated fluorinated hydrocarbons is normally carried out in closed systems. These processes present a potential hazard because such toxic byproducts as perfluoroisobutylene (PFIB) may be formed . Fluorocarbon polymers are prepared from the monomers by conventional free-radical polymerization techniques, but the preparation of each polymer requires different formulation procedures involving a variety of redox catalyst systems , Because of its high viscosity at temperatures greater than its crystalline melting point (327 C), PTFE must be processed by techniques similar to those used for processing powdered metals or ceramics (eg, compression molding or ram extrusion) . The heat treatments necessary for processing fluorocarbon polymers may result in the generation of toxic decomposition products .
Total estimated production of fluorocarbon polymers in 1974 was approximately 27 million pounds, 67% of which was PTFE. Other fluorocarbon polymers, including fluorocarbon elastomers, accounted for the remaining 9 million pounds . NIOSH estimates that 5,000 workers are exposed to the decomposition products of fluorocarbon polymers.
# Identification of Decomposition Products
The decomposition products of fluorocarbon polymers depend not only on the chemical composition of the intact polymers but also on the conditions under which they are decomposed. The temperature to which the polymer is subjected, the atmosphere in which decomposition occurs, and the material of the vessel used can alter the kinds and quantities of the decomposition products formed.
The studies that discuss the identities of the products of pyrolysis of fluorocarbon polymers that have been found [A, give the following general picture of the pyrolysis products: at temperatures that produce just softening or melting of the polymer, the monomer tends to be the principal pyrolysis product. This is true for PTFE up to a temperature of about 500 C. At the same time, however, perfluoropropene, other perfluoro compounds containing four or five carbon atoms, and a particulate, waxy fume are generated. For PTFE, the principal pyrolysis product within the range of temperatures from 500 to 800 C becomes carbonyl fluoride. This compound hydrolyzes readily to hydrogen fluoride and carbon dioxide, so that, in the presence of moist air, these may appear to be the principal pyrolysis products in this temperature range. At temperatures above 800 C, the principal pyrolysis products of PTFE are tetrafluoromethane, hydrofluoric acid, and carbon dioxide. If pyrolysis occurs in the presence of glass, silicon tetrafluoride may be formed by reaction between the silicon in the glass and hydrofluoric acid.
Pyrolysis of PTFE in a vacuum at 360-700 C has yielded almost 100% of its monomer, tetrafluoroethylene . Zapp et al reported that a fine dust or sublimate was produced at temperatures above 200 C. Harris reported the evolution of a mineral acid when PTFE was pyrolyzed at 140-325 C. Adams found that hydrogen fluoride was released when PTFE was heated above 300 C. Waritz and Kwon found that hydrolyzable fluoride was evolved from PTFE heated at 400 C and suggested that this was carbonyl fluoride or hydrogen fluoride. Zapp et al reported that carbonyl fluoride was not detected by the method of analysis used when PTFE was decomposed at 300-550 C.
Other pyrolysis products of PTFE that have been identified include: octafluorocyclobutane (0FCB) at 300-360 C and at 500-550 C , perfluoroisobutylene (PFIB) at 380-400 C , at 475-480 C , and at 500-550 C , tetrafluoroethylene (TFE) at 450-480 C and at 500-550 C , hexafluoropropylene (HFP) at 450-480 C and at 500-550 C , hexafluoroethane (HFE) at 300-360 C , an unidentified five-carbon olefin at 500-550 C , and a higher-boiling residue consisting of a complex mixture of perfluoroolefins at 500-550 C .
Silicon tetrafluoride has been formed from the pyrolysis of PTFE at temperatures ranging from 300 to 650 C and was probably produced by the reaction of hydrogen fluoride with silicon dioxide from the glass vessel. Table X-2 summarizes these results.
Several investigators have indicated that particulate material or sublimate, with particle size ranging from 0.2 ¿urn to .0.5 /um, was evolved when PTFE was decomposed. Some authors speculated that this particulate material contained absorbed hydrogen fluoride , acidic carboxyl groups , or oxygen difluoride . The short chain represents the primary particle. Difluorocarbene (DFC) would tend to form preferentially. Combination of two DFC moieties would form TFE, and one TFE could combine with one DFC moiety to form HFP.
Although theoretical, Errede*s hypothesis does account for the formation of the pyrolysis products of PTFE that have been identified.
Further evidence of the multiplicity of the pyrolysis products was obtained by mass spectrometric analysis . Typical mass spectra of the products of PTFE pyrolysis in air and of the particles so obtained were reported by Coleman et al and are shown in Tables X-3 and X-4.
The decomposition products of other fluorocarbon polymers have not been so intensively studied as those of PTFE. Polychlorotrifluoroethylene (PCTFE) heated at 347-418 C in a vacuum yielded 27% of the monomer, chlorotrifluoroethylene . Birnbaum et al found that pyrolysis of PCTFE in air at 375 C and at 400 C produced hydrolyzable fluoride, which they thought was carbonyl fluoride. No carbonyl chloride (phosgene) was found.
The authors speculated that fluorocarbonylchloride (C0FC1) and chlorodifluoroacetylchloride (CF2C1C0C1) had been evolved and presented evidence for the formation of a variety of fluorinated, chlorinated compounds with up to three carbon atoms.
The authors also found a particulate with a mean particle size of 0.5 /im.
When a copolymer of vinylidene fluoride (VF2) and hexafluoropropylene (HFP) and a terpolymer of VF2, HFP, and TFE decomposed at 550 C and 800 C, carbon monoxide and carbon dioxide were produced . Clayton has suggested that decomposition of VF2-HFP, VF2-HFP-TFE, and polyvinyl fluoride would produce hydrogen fluoride, but he gave no experimental data to support this theory. Clayton also suggested that the decomposition of fluorinated ethylene propylene (FEP), a copolymer of TFE and HFP, would produce HFP; again, no experimental data were given. Madorsky et al reported that pyrolysis of polyvinyl fluoride and polyvinylidene fluoride in a vacuum at 372-500 C produced hydrogen fluoride and a waxlike material consisting of chain fragments of low volatility.
# Effects on Humans
As early as 1951, Harris described two cases of an influenza like syndrome in workers who had been experimenting with PTFE for an unspecified period. The first worker, 29 years old, was exposed to fumes emitted from PTFE heated in an extruder with a malfunctioning thermostat.
Although the extrusion process was normally carried out at 350 C, the machine in this instance overheated to about 450-500 C. had asthma attacks for many years, although he had been symptom-free for 18 months prior to this incident. Harris noted that the exhaust ventilation system on the oven was subsequently found to be inadequate and that, once that situation was remedied, no further attacks occurred. He called the illness of these workers polymer fume fever, which he proposed was caused by inhalation of fume from heated PTFE, and noted the similarity of this syndrome to metal fume fever.
Harris also noted that the two cases he had diagnosed as polymer fume fever were similar to two cases of illness in PTFE workers described to him by HF Gilbert in a personal communication. Because the symptoms so closely resembled those seen in metal fume fever, Harris analyzed PTFE ash and the sublimate evolved from PTFE heated at 400 C for various metals. The sensitivity of the method of analysis was not reported. From these studies, Harris concluded that the concentrations of metals in the ash and the sublimate could not explain their findings, so that a toxic fume from heated PTFE seemed to be the responsible agent in polymer fume fever from PTFE.
In 1967, Bruton described two cases of illness in aviation employees whose work involved contact with a neoprene door seal that had been sprayed with an aerosol of an unspecified fluorocarbon telomer.
Smoking was not permitted in the hangar; however, toward the end of his shift, the first worker had smoked a cigarette in an office where smoking was allowed. Approximately 30 minutes later, he experienced shivering and chills, which lasted for about 6 hours, but no other effects. The second worker had been handling the polymer spray for approximately 1 year and had become ill once before when he failed to wash his hands before smoking after working with the aerosol. On this occasion, he started to smoke a cigarette during his break and realized by the taste that it was contaminated. He extinguished the cigarette immediately, but, within 30 minutes, he began to shiver and developed a headache and muscular aches, but no respiratory effects. Recovery was complete within 24 hours.
Bruton believed that the polymer-treated surface had contaminated the cigarettes.
To demonstrate the possibility of hand contamination, he conducted an informal experiment in which the aerosol was sprayed onto a clean aluminum surface according to the manufacturer's instructions. When he wiped the surface with his finger, a line across the sprayed surface and a faint white dust on his finger were visible. The author suggested that handling of objects treated with aerosols of fluorocarbon telomers represented a hazard to smokers because of the possibility of contamination of smoking materials. He noted that workers should be required to wash their hands before smoking to avoid contaminating smoking materials. Although Bruton diagnosed this syndrome as polymer fume fever, he did not disprove the possibility that the respiratory symptoms were due to other causes. He was correct in assuming that the temperature of the cigarette was sufficient to cause pyrolysis of the fluorocarbon telomer, however, since the temperature of the burning zone of cigarettes has been shown to range from 854 to 913 C .
In 1964, Nuttall et al reported an incident of in-flight illness that affected 35 passengers, including 2 flight surgeons and 4 of 5 crew members, on a C54 aircraft. The total flight time was 165 minutes, and the authors mentioned a flight altitude of 9,500 feet. The auxiliary power unit (APU) of the aircraft was located in the rear compartment, which "freely communicated" with the main passenger cabin. The crew compartment door was closed. After the passengers and crew members boarded the plane, the APU was started; fume and odor levels within the main cabin were reported to have been "normal." Takeoff was delayed because of magneto trouble, and the passengers debarked after the APU had run for approximately an hour. A few had mild symptoms of respiratory Irritation, and some became nauseated when they smoked. About 1.5 hours later, the passengers reboarded the aircraft and the APU was restarted. The plane took off 45 minutes later and the APU was turned off. Within 1 hour of takeoff, most of the passengers and two of the crew members had chest discomfort and general malaise, including chills, nausea, and respiratory distress in some. One passenger vomited and collapsed and was found 5-10 minutes later in a cyanotic state with a weak and rapid pulse.
A second passenger had severe respiratory distress and moderate collapse. Six passengers were incapacitated, and five were given oxygen. The heating system was suspected of being a source of toxic fumes and was turned off.
Although a fusilage hatch was opened to provide ventilation, some passengers continued to complain. On arrivàl, three passengers required hospitalization, and everyone aboard the plane except one co-pilot had experienced effects, which persisted after the plane landed.
To characterize the illness, Nuttall et al interviewed and gave questionnaires to all crew members and passengers.
The answers to the questionnaire revealed a toxic reaction pattern similar to that of influenza, with onset of symptoms occurring within 2-6 hours after exposure to the unidentified agent. Typical symptoms were chest discomfort, difficulty in breathing deeply, chills, muscular aches, fever, dull headache, and general malaise. Respiratory symptoms were not present in all cases, and nausea and aversion to cigarettes was often reported. The number of smokers aboard the plane was unspecified, and it was not stated whether smoking was permitted during the flight. Recovery was complete within 24 hours in most cases, including those of the three hospitalized patients. The authors noted that examination of these three patients showed elevated temperatures, increased white blood cell counts with a shift to the left (indicative of an increased proportion of young cells), and rapid pulse rates. They emphasized the similarity of the reported symptoms to those of metal or polymer fume fever, characterizing 50% of the cases as "typical" examples of this syndrome. The questionnaire data indicated that 6 cases were severe, 12 were moderate, and 9 were mild.
Although 12 of those aboard the flight did not complete questionnaires because they could not be located, the flight surgeons who had interviewed everyone on the plane at the time of the incident reported that they also had been affected to some extent.
Nuttall and coworkers conducted an extensive investigation to determine the cause of the illness. Air samples were collected in the grounded aircraft and analyzed for total metals and zinc with negative results. The four who collected samples developed a typical fume fever reaction. Six volunteers were exposed to fumes from the APU for 40 minutes. All six developed symptoms similar to those of the affected passengers and crew members 1-3 hours after exposure. All had elevated temperatures and elevated white blood cell counts, with polymorphonuclear leukocytosis and a shift to the left. A trip made by the same plane 2 days later, after a new APU had been installed, was uneventful.
The tape used to wrap the exhaust manifolds of the old APU was subjected to a variety of tests . Five volunteers were exposed to fumes emitted from the APU before the manifold was wrapped with tape. No symptoms were reported after 35 minutes of exposure. Next, the APU exhaust manifolds were wrapped with an unspecified amount of asbestos tape salvaged from the old wrappings of the manifold, and used APU oil was placed on the wrapping.
In this instance, two of six subjects exposed for 35 minutes reported symptoms, and small quantities of uncharacterized fumes were observed around the wrappings. Carbon monoxide levels were below 50 ppm in both these runs. The authors noted elevated temperatures and mild leukocytoses in the two affected subjects, but suggested that the reported effects were questionable. This second run was repeated, whereupon two of the six subjects exposed for 35 minutes developed mildly elevated temperatures and leukocytosis. Subsequent exposure of four subjects to oil fumes alone for 40 minutes failed to produce symptoms. Nuttall et al concluded that the asbestos tape was the source of toxic fumes, although the oil might have been a modifying agent. New asbestos tape of the same type that had been used to wrap the manifolds of the APU was analyzed with an infrared spectrometer. This examination revealed the presence of PTFE, a finding that was later confirmed by the manufacturer.
In a final experiment, one subject was exposed to fumes emitted from an unspecified amount of the tape pyrolyzed in a platinum dish at 800-1,000 In 1967, Barnes and Jones gave the results of an investigation of an outbreak of respiratory illness affecting 4 of 19 workers at a factory that made abrasive wheels. The affected workers were male press operators, aged 20-32 years, whose employment histories were not given.
Their work involved placing by hand a mixture of phenol-formaldehyde resin, furfural, abrasive grain, a small amount of hexamethylenetetramine, and, occasionally, a rectifying oil containing cresylic acid on cold presses in a tray. The wheels thus formed were removed from the press room and placed in batches in an oven heated to 177 C for curing. The investigators noted that the factory consisted of one large shed and that the press room was not physically closed off from the area where the mixture was made. The press room was mechanically ventilated by recirculated, cooled air, and the mixing area was air-conditioned.
In describing these four case histories, Barnes and Jones noted that these workers were moderate to heavy smokers who smoked on the job.
All four had suffered recurrent bouts of illness over a 2-to 4-month period and had experienced respiratory distress characterized as either tightness of the chest or difficulty in breathing deeply. Typical symptoms of these attacks included uncontrollable shivering lasting 1-2 hours in two workers, pain in the retrosternal area in one worker, sore throat in one worker, and severe headache in one worker. Physical examinations at the time of the plant visit revealed scattered rhonchi in the chest of one worker, congested throat and congested soft palate in a second worker who had not complained of a sore throat, congested pharynx in a third, and no signs in a fourth worker who had been transferred to the packing room 2 weeks earlier.
The authors discovered during their investigation of the plant that the use of powdered PTFE as a mold-release agent had been initiated approximately 3 months earlier. They noted that, although the pressing and curing processes were carried out at temperatures below 300 C, all the affected workers handled the PTFE-treated plates and all smoked while working. They further stated that PTFE powder was detected on the hands of the press operators and that there was ample opportunity for the skin to become contaminated in the plant. Smoking on the job was then prohibited. The authors reported that, according to the plant manager, there had been no recurrence of symptoms during the 2 months after the reported illnesses and the prohibition of smoking in the work area.
Although the decomposition products of PTFE may have been the cause of the illness, some of the typical polymer fume fever symptoms were not present.
In 1974, Wegman and Peters reported the investigation of a similar outbreak of influenza-like illness in workers in a textile mill that produced imitation crushed velvet. The fabric was made of nylon and rayon, and the final stage of its production was a flocking process that consisted of the addition of a liquid fluorocarbon polymer to the material, with subsequent dipping, rolling, and squeezing of the mixture, curing at 150-155 C, mechanical crushing and steaming at 135 C, and final static elimination. In an initial interview, the plant manager revealed that a number of workers involved in the flocking process had reported symptoms of weakness, muscle aches, fever, chills, and shortness of breath.
The authors interviewed and examined all workers in the flocking division, 10 men and 3 women, ranging in age from 19 to 61 years. Those complaining of symptoms had been employed in this division for from 2 months to 6 years. Seven of these workers, six men and one woman, described symptoms of cough, muscular aching or weakness, fever, and chills. Four of these seven workers also had experienced shortness of breath.
All had suffered repeated bouts of illness, three of the seven workers having experienced as many as six attacks during an unspecified period of time. In several instances, symptoms were of such severity that affected workers had to leave the plant. Onset of symptoms was generally gradual and illness persisted for 6-72 hours, most workers reporting recovery within 24 hours. Of the six workers who did not report such attacks, one nonsmoking man had experienced headache on five occasions and possibly some coughing; a second had had an isolated bout of cough, fever, and chills, which the authors attributed to a common cold. One woman who did not report typical attacks had an unspecified number of attacks of coughing, fever, chills, and shortness of breath, but these were of rapid onset and short duration. One of the six men experienced severe weakness, chest discomfort, and shortness of breath on one occasion. The affected workers experienced symptoms only when they worked in the area where the fluorocarbon polymer-treated material was cured.
The authors considered four materials as possible causes of the symptoms: ammonia, formaldehyde, nylon, and the fluorocarbon polymer.
Analysis of the air of the workplace found air concentrations of less than 50 ppm of ammonia and less than 1 ppm of formaldehyde.
The nylon was reported to be of nonrespirable size. The authors maintained that exposure could not have resulted from the flocking process itself, since the maximum temperatures at which the fluorocarbon was applied and cured were at or below 165 C. However, the authors noted that all seven workers who had "typical" symptoms of polymer fume fever were cigarette smokers, and that all but two of the other workers experiencing symptoms were also smokers.
They observed that workers engaged in applying the polymer to the material had frequent hand contact with both liquid and cured polymer and that they often smoked during breaks without first washing their hands. The authors concluded that the source of the illness was polymer fume generated by the smoking of PTFE-contaminated tobacco. No further symptoms were reported after smoking in the work area was prohibited and the workers were instructed to wash their hands before smoking or eating.
In 1973, Evans reported a case of respiratory illness in a 49year-old man who had been using an oxyacetylene torch to dismantle a metal table used to hold PTFE-coated molds. The molds had been sprayed with S-143, a dispersion of TFE telomer in unspecified fluorocarbon solvents. In 1975, Blandford et al described a case of nonoccupational respiratory illness in a man who had inhaled fumes from a PTFE-coated pan that had contained only water and had boiled dry when left unattended on an electric stove.
When he removed the pan from the stove, the man noticed that the fumes "took his breath." No smoke was visible. Five cockatiels kept caged in an adjoining room died within 30 minutes after the incident.
The patient's wife, who was in the same room as the birds during the incident, was unaffected. About 60 minutes postexposure, the patient experienced shortness of breath and a paroxysm of coughing when he tried to smoke a cigarette. About 80 minutes after the incident, the man's symptoms included shivering, dizziness, and nausea. He felt cold and noted a painful tightening of the chest. The next day, on awakening after 8 hours of sleep, he had a severe headache, which subsided during the morning. The tightness of the chest persisted for the remainder of the day. The subsequent recovery was complete and uneventful, although the patient had difficulty remembering events following the death of his birds and felt that the fumes had affected his level of consciousness. The authors noted that this was an unusually clearcut case of polymer fume fever, because there had been no smoke and the pan had contained only water. The data as reported by the authors demonstrated that PTFE produced toxic decomposition products that were more lethal to birds than to humans.
In 1967, Clayton published the results of investigations conducted by Kligman for the Haskell Laboratory for Toxicology and
# Industrial
Medicine to determine the effects on humans of smoking cigarettes contaminated with known amounts of a TFE fluorocarbon telomer.
The sex, age, medical and employment histories, and smoking histories of the subjects were not reported, and the author did not specify whether the same or different subjects were exposed at the various dose levels.
The first experiment evaluated the effects of smoking a cigarette to which 0.05, 0.10, 0.20, or 0.40 mg of a TFE fluorocarbon telomer had been added. Ten volunteers smoked one cigarette apiece with each of the added amounts of telomer.
Results indicated that 0.40 mg telomer in each cigarette was necessary to cause an increase in body temperature and pulse rate. No symptoms were reported at the lower levels, although average maximum pulse rates were slightly elevated at an unspecified interval after smoking. At the 0.40 mg dose level, the author reported that 9 of 10 subjects had what he considered to be typical symptoms of polymer fume fever, with cough as the first symptom in 6 subjects. The symptoms reported by the nine affected subjects were headache, muscular aches, chills, malaise, sluggishness, excessive perspiration, and weakness. Onset of symptoms occurred 1-3.5 hours after smoking, with a mean latency period of 2 hours. From 2.5 to 5.5 hours after the volunteers smoked, the average temperature of the nine affected volunteers increased to 100.5 F from a mean preexposure value of 98.1. From 2.5 to 4.5 hours after they smoked, The other four subjects expressed well-defined symptoms of polymer fume fever after smoking six to eight cigarettes; the first symptom to appear was chills.
Other symptoms were the same as those of subjects in the first experiment, except that coughing was not reported by any of the subjects.
Clear symptoms first appeared 3-5 hours (average 3.8) after the subjects smoked. Five to 6 hours after smoking, average temperatures of these four subjects increased from 98.3 to 101.4 F. From 1 to 9.5 hours (average 5.4) after smoking, the average pulse rate of the four affected subjects increased from 87 to 111. Recovery time in the subjects with well-defined attacks was 7.5-12.5 hours (average 9.8), but the author did not explain the criteria for recovery. The cumulative amount of added telomer necessary to elicit signs and symptoms of illness in these four patients was 0.30-0.40 mg.
Clayton noted that the cumulative amount of telomer (0.30-0.40 mg) needed to produce well-defined symptoms in four subjects coincided with the amount of telomer (0.40 mg) needed to produce symptoms in subjects who smoked one cigarette. The sequence of events was similar in subjects given both single and cumulative exposures, but the signs and symptoms differed.
Six of 10 subjects complained about a cough in the first experiment but none of the 4 subjects in the second experiment complained of cough.
Clayton suggested that subjects receiving single large exposures to fluorocarbon telomer had an initial respiratory tract irritation that was not experienced by subjects receiving cumulative exposures because the latter were subjected to irritant substances at lower concentrations. The same amount of telomer, however, produced fever in both experiments.
Clayton concluded that there is no obligatory sequence of effects in polymer fume fever and that the absence of cough does not preclude a diagnosis of this illness. He emphasized that the total clinical picture should be considered by anyone contemplating a diagnosis of polymer fume fever, and that objective measurements such as temperature, pulse rate, and white blood cell counts should be relied on as indices of illness; however, he did not report white blood cell counts. The interval between the smoking of cigarettes was also not specified, and any individual differences in the subjects that might have explained their differing reactions were not discussed. Nevertheless, these experiments indicate that smoking cigarettes contaminated with a TFE-telomer can result in a syndrome commonly referred to as polymer fume fever.
In 1965, Makulova reported five cases of perfluoroisobutylene (PFIB) poisoning in two male and three female laboratory workers. A 34year -old woman had worked with this compound for approximately 2.5 years with no previous ill effects. The ages and employment histories of the other patients were not specified. Four of the five workers reported that exposure to PFIB lasted less than 1 minute, during which time they inhaled two to five times. All patients described symptoms of coughing, difficulty in breathing, and chest pains immediately after exposure. These symptoms became progressively more severe, and by 6-8 hours after exposure, all patients had developed headaches and other symptoms and had begun to expectorate sputum.
Makulova Chest X-rays of all patients showed significant pulmonary changes that came on rapidly 4-6 hours postexposure and became fully developed approximately 48 hours postexposure.
In four patients, these changes consisted of bilateral, confluent pulmonary edema, especially in the middle lobes, with emphysematous lateral borders and segments above the diaphragm. In the other patient, multiple clearly defined small foci of intense opacity were found.
The author noted that treatment was largely symptomatic and consisted of calcium chloride, ascorbic acid, glucose, unspecified cardiac medication, and oxygen administration to combat the pulmonary edema.
Penicillin or streptomycin in combination with sulfonamides was given during the first few hours postexposure. Symptomatic improvement was noted in some patients within 4-6 days postexposure, and complete resolution of breathing difficulties and pulmonary rales occurred 7-10 days after exposure. At 10-13 days postexposure, pulmonary damage observed in X-rays had been resolved, and leukocytosis and eosinopenia improved 15-20 days postexposure. Three patients were discharged from the clinic in good health 13-23 days after exposure, and a followup 2 years later revealed no complications. One patient developed exudative pleurisy and remained in the clinic for more than 2 months.
The fifth patient, the 34-year-old woman, died 2 days after exposure.
Makulova described the last patient's history and illness in detail, noting that she had suffered from influenzal pneumonia 2 months before poisoning. She was unable to give any information on the duration or degree of her exposure to PFIB on the day she became ill. Her symptoms were similar to those already described, and clinical findings were similar to those for the other patients. She was admitted to the clinic with a where gaskets were produced, 0.2-2.9 mg/cu m in the machine shop, and 2.5-2.9 mg/cu m in a sample for a worker who operated the ring-grinding machines.
A questionnaire was completed by 77 workers (about 75% of the workers in the plant) . Sixty of the production workers (86%) said that they had experienced polymer fume fever at some time in the past, but only 50% had experienced polymer fume fever during the past year. Fourteen percent of the workers stated that they had had more than three episodes in the preceding year. Only 10% of those who had experienced polymer fume fever In the fabrication techniques studied by Sherwood , the polymer was pressed into a mold or "pre-form" and sintered at 350-380 C to form a finished product or a material suitable for machining to final specifications. Variations of this technique included prebaking before molding, repressing after sintering, and extrusion. Machining was carried out on standard metal-working machines, and waste was recovered for reuse.
Tape was produced by veneering followed by a heat treatment, which is known as tensilating. In 1963, Adams conducted an investigation to determine the cause of polymer fume fever in employees in a plant where PTFE was processed.
Altogether, 30 wage and 8 staff employees were interviewed by a medical
-fficer. An investigation of the plant was also conducted. Of the 30 wage employees, 14 had experienced symptoms of polymer fume fever in the 2 months previous to the interview. A total of 32 incidents of polymer fume fever were reported by these 14 workers. Only employees working in the finishing room had been affected.
Of the 18 men who worked in the finishing room, 12 who were smokers accounted for 30 incidents and 2 nonsmokers accounted for the other 2 attacks.
A detailed investigation showed that 6 men who rolled their own cigarettes had had 21 of the attacks of polymer fume fever. Of the eight staff employees, only one, a pipe smoker, had had an attack of polymer fume fever.
In the finishing room, PTFE was dried, sifted, and packed . In an unspecified drying operation, a small amount of PTFE was occasionally heated beyond the normal drying temperatures. Air samples were taken by an unidentified method at points close to the drying ovens and the ovens where the polymer was further heated when required. Adams found concentrations of hydrogen chloride as high as 35 ppm on occasions when PTFE was heated only to normal drying temperatures. When oven temperatures exceeded 300 C , the author found up to 6 ppm of hydrogen fluoride. Although acetic acid is usually used to coagulate PTFE latex, it is possible that hydrogen chloride was used and that residues of this acid provided the HC1. HC1 boils at 110 C whereas something like 250 C is required to liberate HF from PTFE.
Adams concluded that the majority of incidents of polymer fume fever resulted from the smoking of PTFE-contaminated tobacco. He noted that precautions must be taken to prevent particles of polymer from lodging beneath nails, in hair, or on clothing. Adams did not report the method of analysis used to detect hydrogen fluoride. That the hydrogen chloride in the vicinity of the drying ovens came from PTFE per se is highly unlikely because this polymer contains no chlorine atoms.
# Animal Toxicity
A list of compounds that have been identified as pyrolysis products of fluorine-containing polymers, as stated previously in the section on In addition to the various molecular species mentioned in the preceding paragraph, there is the particulate material that may be the principal cause of polymer fume fever . Harris had found in 1957 that heating PTFE at temperatures above 300 C produced the deposition of a solid material within his exposure chamber and also liberated an acid into the air of the chamber. Four rats exposed to such atmospheres developed congested or hemorrhagic lungs and pulmonary edema. Harris concluded that PTFE heated to 300 C or more produced a sublimate or an acid that induced pulmonary edema and killed rats thereby.
In 1968, Waritz and Kwon and Birnbaum et al suggested that the particulate material may carry adsorbed toxic materials (perhaps hydrofluoric acid, carbonyl fluoride, octafluoroisobutene, or chlorotrifluoroethylene) into the alveoli, the latter group of researchers having found that the mean particle size of this material was 0.5 jum and that 99% of the particles had diameters of less than 2 ¡m. These dimensions place the polymer fume in the category of inhalable dusts.
Waritz and Kwon found that removal of the particulate material by produced minimal mortality in rabbits and rats, respectively. Hyperemia of the liver, hemorrhage in spleen and lungs, dystrophic changes in the epithelium of the renal tubules, atelectasis and emphysema in the lungs, and desquamation of the bronchial epithelium were the principal changes attributed to the monomer. Clayton reported that the LC50 for the rat exposed to tetrafluoroethylene for 4 hours was 163,600 mg/cu m.
For CTFE, the LC50 for rabbits and white rats exposed for 2 hours was reported to be 24,000 mg/cu m .
The "absolutnaya smertelyenya kontsentratsiya," meaning probably the LC100, was said to be 26,400 mg/cu m for the rabbit and 36,000 mg/cu m for the white rat. No actual data on the numbers of deaths after exposure at any concentration were provided.
Clayton, in a series of papers all probably referring to a single estimation of the inhalation toxicity of CTFE, has reported that the LC50 for the rat exposed for 4 hours was 1,000 ppm (4,770 mg/cu m ) .
More recently, Hood et al have exposed rats, guinea pigs, rabbits, and dogs to chlorotrifluoroethylene at concentrations of 300 ppm
(1,431 mg/cu m) for 4 hours/day, 5 days/week, for a total of 18 exposures.
One of 10 male guinea pigs died after the sixth exposure. One of 10 male rabbits died after 4 exposures and another after 5. None of 10 rats of to have increased more than that of the control animals; the increase was stated to have become progressively larger throughout exposure in the exposed rabbits. The exposed animals also were said to have recovered from the orthostatic tachycardia more slowly than the control animals. These observations suggest that exposure to CTFE altered the properties of the sympathetic nervous system, including possibly such centers in the brain stem as the bulbar vasomotor mechanisms. The exposed rats were reported to have undergone a significant decrease in the ability to summate subthreshold stimuli (presumably applied to the motor nerve of some unidentified effector).
Hood et al exposed rats of both sexes, male guinea pigs, male rabbits, and dogs for 6 hours/day, 5 days/week, for 14 months to CTFE at concentrations starting at 15 ppm (about 71.6 mg/cu m) and increasing progressively, at irregular intervals of time, to 30, 50, 100, and 150 ppm (715.5 mg/cu m ) . These exposures produced no significant pathologic effects in rabbits and guinea pigs but produced severe tubular necrosis in rats.
Two of four exposed dogs began to exhibit signs of neurologic disturbances after 27 and 64 exposures, respectively, at 150 ppm. These consisted of stiffness and weakness of the legs and unsteadiness in standing. One of two other dogs that were added to the exposed group at the beginning of exposure at 100 ppm (477 mg/cu m) died after 56 exposures at that concentration followed by 54 exposures at 150 ppm. The second of these dogs was reported to have become very irritable at this same time.
Degenerative changes in the central and peripheral portions of the somatic nervous system were found, most severe in samples of nerve tissue from the dog that had exhibited the most marked neurologic signs (temporary prostration at the end of each period of exposure, ataxia, and difficulty in swallowing). This dog was found to have atrophy of the muscles of the hindlegs.
Clayton reported that a mixture of 80% hexafluoroethane with 20% oxygen (about 4,515,000 mg/cu m of hexafluoroethane) was an approximate lethal concentration for the rat exposed to it for 4 hours. The data in these paragraphs allow arrangement of the compounds on which information is available in a hierarchy of decreasing toxicity, albeit with some uncertainty.
There is little doubt that perfluoro isobutylene is the most toxic compound and that octafluorocyclobutane and hexafluoroethane are the least toxic. The ranking of inhalation toxicity for the rat, based largely on single exposures, that NIOSH has derived from the information stated above is as follows, going from the most toxic to the least: perfluoroisobutylene, hydrofluoric acid, carbonyl fluoride, silicon tetrafluoride, chlorotrifluoroethylene, hexafluoropropene, tetrafluoroethylene, tetrafluoromethane, hexafluoroethane, and octafluorocyclobutane.
In addition to the information summarized above on the breakdown The other general approach to assessing the toxicity of the pyrolysis products of fluorinated polymers, ie, exposing experimental animals to mixed decomposition products of polymers heated to various temperatures, has been used by a number of investigators.
In 1955, Zapp et al pointed out that the intact PTFE polymer is nearly inert but that products of its thermal decomposition are not. Polymer fume fever has been recognized to be a consequence of exposure to heated PTFE since its description in 1951 by Harris .
Studies of the toxicity of the pyrolysis products of PTFE had been started at the Haskell Laboratory in 1943, but polymer fume fever had not been reproduced in experimental animals. Lethal activity had been demonstrated, however .
Strips of PTFE subjected to temperatures of 200 and 250 C in a stream of air passing into an exposure chamber containing 2 rats caused no deaths of the rats after a 6-hour exposure , Similar exposures to air passing over strips of PTFE heated to 300 and 350 C did result in the death of rats, the higher temperature having a more marked effect with "Teflon 6," described as a low-molecular-weight polymer, than with "Teflon 1," a highmolecular-weight polymer.
Clayton et al reported that, when "Teflon 1" and "Teflon 6" were subjected to temperatures of 300, 325, and 350 C in tubes of either glass or stainless steel, the materials heated in glass tubes yielded more toxic pyrolysis products than those heated in the stainless steel tubes. The differences were most marked for "Teflon 6" at 300 C and for "Teflon 1" at 350 C. Samples of "Teflon 6" that yielded comparatively large amounts of particulate material were more toxic than those that yielded less.
Filtration of the pyrolysis products with a filter having a pore size of 0.45 j i r n i lowered the mortality of rats exposed to the pyrolysis products from 43/48 to 7/48.
"Teflon 6" manufactured before 1958 was reported to yield toxic breakdown products at 350 C, whereas "Teflon 6" manufactured "currently"
(1959 and thereafter) yielded pyrolysis products of approximately equal toxicity only when the temperature was raised to 425 C .
# Cavagna et al
reported they had been able to produce attacks of fever in rabbits subjected to inhalation of aerosolized 20% acetic acid, in an undisclosed concentration in the inspired air, for 10 minutes, followed 16 hours later by exposure for 30 minutes to an atmosphere containing 10-12 mg/cu m of hydrogen fluoride and 1.0-1.7 billion particles/cu m with diameters greater than 0.7 jum, which had been generated by heating PTFE in a tube furnace at 400-500 C. Seven of 11 rabbits had temperature increases of 0.5-1.5 C. These appeared after a latency period of about 5 hours, during which a decrease in body temperature, leukopenia, and cough and rhinorrhea were observed. The fever lasted 6-7 hours and coincided approximately in onset, but not in duration, with leukocytosis. Exposures of naive rabbits to fumes from heated PTFE produced initial hypothermia and irritation of the respiratory tract but no fever. the particles produced. Some of this powder was used at once, another aliquot was washed with water to remove the gaseous products of decomposition, and a third portion was stored for 6 months before being used. These three samples of powder were compared with a powder produced by grinding PTFE that had not been pyrolyzed and with powdered chalk.
The powders were administered to rabbits by iv injection of 1-1.5 mg/kg in suspension in sterile, apyrogenic saline. Control rabbits received only saline.
Only the unwashed pyrolyzed particles produced a febrile reaction in the rabbits. This was preceded by leukopenia, which was frequently succeeded by leukocytosis.
A similar response was induced in rabbits by inhalation exposure to the unwashed pyrolyzed particles at a concentration of 122.8 mg/cu m for 2.5 hours.
The succession of leukopenia, pyrexia, and leukocytosis reported by Blagodarnaya in the rabbits exposed to unwashed pyrolyzed particles from PTFE is reminiscent of the febrile response to gram-positive bacteria injected iv into rabbits . The failure of washed pyrolyzed particles to produce fever in these experiments indicates that the response is not to particulate agents alone. The presumption is that some water-soluble and volatile component of pyrolyzed PTFE adsorbed on the surfaces of the particulate material render the particles capable of interacting with the leukocytes of the blood and releasing the leukocytic pyrogen as suggested by Cavagna et al . Some further study of the pyrogenic process after exposure to pyrolyzed fluorocarbon polymers seems desirable.
Treon et al compared the toxicities of the pyrolysis products of PTFE and of two polymers of PCTFE differing in extent of polymerization, so that one (FL) was a liquid and the other (KF) was a solid. The liquid polymer (FL) was dropped into an Inconel tube heated by an electric current through resistance wire wound around the tube. The solid polymers (PTFE and KF) were prepared as strips which were inserted into the cold Inconel tube.
The tube was then raised to the planned temperature as rapidly as possible. Air or nitrogen (PTFE only) was passed through the furnace at a rate of 31.8 liters/minute and into the 800 liter exposure chamber. PTFE was pyrolyzed at temperatures of 375-878 C. FL was pyrolyzed at either 371 or 482 C, whereas KF was heated to temperatures of 803-813 C.
Groups of five mice, six rats, four guinea pigs, four rabbits, one cat, and one dog (PTFE only) were exposed in the chamber to various concentrations of pyrolysis products (graded by the rate at which the polymer was fed into the furnace) and for different spans of time .
The exposures to pyrolysis products of PTFE lasted for 30-180 minutes, most being less than 60 minutes in duration.
Exposures to the pyrolysis products of FL were for 2, 7, or 24 hours, whereas those to the pyrolysis products of KF were for 32-34 minutes.
Dogs, mice, and rabbits were the most resistant species to PTFE pyrolyzed at temperatures of 739-813 C in the presence of air. When PTFE was pyrolyzed at temperatures of 811-878 in nitrogen, rabbits, guinea pigs, and rats were more resistant than mice. Cats and dogs were not used in these last tests. When the temperature of pyrolysis was 491-527 C in the presence of air, rats and rabbits were more resistant to a lethal effect than mice and guinea pigs. Cats and dogs were not included in these studies either. Pyrolysis of PTFE in the presence of air yielded pyrolysis products of greater toxicity than those produced in nitrogen. Lowering the temperature of the pyrolysis apparatus from 739-813 to 491-527 C decreased the toxicity of the pyrolysis products to rats, rabbits, and mice, but slightly increased the toxicity to guinea pigs.
Cats and rats were the most resistant species to the lethal effect of the pyrolysis products of FL heated at 482 C . When the pyrolysis temperature of this polymer was lowered to 371 C, no animals were killed during exposures of 2 or 7 hours. Mice, cats, and rabbits were more resistant to the lethal action of the pyrolysis products of KF than were guinea pigs and rats.
When PTFE was pyrolyzed in the presence of nitrogen, pyrolysis at a rate of 1.99 g/hour produced no fatalities in any of the four species exposed . When PTFE was pyrolyzed in air, pyrolysis at a rate of 2.60
g/hour at 506 C produced death of only 1/6 rats, 1/4 rabbits, 0/5 mice, and 0/4 guinea pigs after an exposure of 36 minutes. Pyrolysis at a rate of 1.67 g/hour at 805 C produced death of 3/6 rats, 2/4 rabbits, 2/5 mice, and 0/4 guinea pigs after an exposure of 33 minutes.
Pyrolysis of FL at 482 C at rates of 3.18 g/hour or 1.02 g/hour killed no animals after exposures of 2 and 7 hours, respectively .
Pyrolysis of KF at 805 C at a rate of 0.88 g/hour killed no mice, rats, guinea pigs or rabbits after an exposure of 34 minutes .
The Treon et al data are difficult to interpret in a comparative way because of the various conditions of pyrolysis and exposure of the experimental animals. A higher temperature of pyrolysis seems generally to produce more toxic pyrolysis products. The observations that species sensitivity to the pyrolysis products of the three polymers varies not only with the polymer but also with the conditions of pyrolysis indicate that, under similiar conditions, the two polymers of PCTFE probably yield different pyrolytic products, despite their monomeric identity, and that a single polymer yields different products under different conditions of pyrolysis. Pyrolysis in the presence of an inert gas seems to be less hazardous than that in the presence of air. The pyrolysis products from FL may be less hazardous than those from either PTFE or K F , but this conclusion cannot be supported satisfactorily by the data provided. Good comparative data would be useful.
Zapp gave a little further information about the pyrolysis of PCTFE, finding that it, like PTFE, undergoes degradation when exposed to a temperature of 300 C but not when exposed to one of 250 C.
Birnbaum et al exposed rats to the products of pyrolysis of PCTFE heated to temperatures of either 375 C or 400 C, determining the rate at which a rod of PCTFE had to be fed into a pipe heated to the desired temperature in an electric furnace to maintain an LC50 of pyrolysis products within an exposure chamber fed with air passed through the furnace at a rate of 4 liters/minute. The exposure periods were either 1 or 3 hours.
One-hour exposures at 375 C did not result in sufficient mortality to yield valid estimates of the LC50 at the highest rate of feed of the PCTFE rod into the heated tube. The 3-hour exposure to the products of pyrolysis at this temperature yielded an estimate that 31.5 g/hr of the polymer had to be subjected to pyrolysis to maintain an LC50 of the pyrolysis products within the chamber. Exposure for 1 hour at the higher temperature of pyrolysis (400 C) yielded an estimate that 23.5 g/hr of the polymer had to be pyrolyzed at this temperature to maintain an LC50 of the pyrolysis products within the chamber. The particles in the pyrolysis products ranged in diameter from about 0.15 to 3.0 jiim, 85% of the particles being less than 1 /nm in diameter and 99% less than 2 /um. Infrared and mass spectrometers were used to obtain some idea of the molecular species present in the exposure atmosphere; these two techniques indicated the presence of perhaps as many as 13 different materials in the pyrolysis products.
Comparatively little information about pyrolysis products of fluorocarbon polymers other than PTFE and PCTFE has been found. Clayton reported studies of the inhalation toxicities of two samples of a copolymer of vinylidene fluoride and hexafluoropropylene for the rat. One Hydrogen fluoride was the only pyrolysis product whose concentration in the exposure chamber seemed to be related to mortality in the exposed rats. The principal effects of the exposure on rats were irritation of the respiratory tract, pulmonary edema, hemorrhage in the lungs, congestion of the liver, vacuolation of hepatocytes, tubular necrosis in the kidneys, and proteinaceous material in the renal tubules.
Ehrsam has shown that the pyrolysis products of PTFE are more toxic to birds than to mice or guinea pigs. Similarly, Griffith et al has reported that Japanese quail and parakeets were killed by effluvia from a frying pan coated with PTFE and heated to 330 C and 280 C, respectively, whereas rats appeared not to be harmed until the pan was heated to 450 C . Some investigators have reported that subcutaneous implantation of PTFE into rats resulted in the formation of fibrosarcomas.
However, Bryson and Bischoff were unable to duplicate these results.
# Correlation of Exposure and Effects
The most frequently reported effect of workplace exposure to the pyrolysis products of PTFE is an influenza-like syndrome designated polymer fume fever .
No effects of workplace exposure to the pyrolysis products of other fluorocarbon polymers were found in the literature.
The major signs and symptoms associated with polymer fume fever are chest discomfort , fever , leukocytosis , headache , chills 40,41], achy feeling , and weakness .
Complete recovery usually occurred within 12-48 hours after the exposure ended .
Other effects reported in humans exposed to the pyrolysis products of PTFE were nausea , malaise , congested throat and pharynx , basal rales of the lungs , pulmonary edema , hyperpnea , and increased pulse rate ,
Damage to the respiratory tract, occasionally severe enough to result in pulmonary edema, was found in humans exposed to the pyrolysis products of PTFE and in animals exposed to the pyrolysis products of PTFE , PCTFE , VF2-HFP , VF2-HFP-TFE , and E-CTFE . Effects such as leukocytosis and elevated temperature were difficult to produce in animals .
Polymer fume fever has resulted when there was an insufficient amount of ventilation in molding operations and when PTFE processing temperatures were not controlled because of malfunctioning thermostats . Polymer fume fever has also resulted from the smoking of PTFEcontaminated tobacco . As little as 0.3 mg of a TFE fluorocarbon telomer added to the cigarettes of volunteers produced polymer fume fever Without these data, it is difficult to determine whether the authors' conclusions were justified.
Clayton et al also concluded that the toxicity of the pyrolysis products of PTFE heated at 350 C was caused by a particulate. Seven of 36 (19.4%) rats were killed when the pyrolysis products of PTFE heated at 350 C were filtered (Millipore filter, 0.45 jum pore size). The expected mortality was 100%. When PTFE was pyrolyzed at 325 C, the unfiltered fume killed 6/16 rats (37.5%). The same pyrolysis products after filtration through a filter of 0.45 ¡m. pore size killed 0/8 rats. These results are in agreement with the findings of Waritz and Kwon , since filtration of the pyrolysis products reduced mortality. However, Waritz and Kwon reported that the unfiltered pyrolysis products of PTFE heated at 400 C were not lethal to rats. This discrepancy may be related to the finding of Clayton et al that low-molecular-weight PTFE yielded pyrolysis products more toxic than those from high-molecular-weight PTFE; Clayton et al and Waritz and Kwon perhaps used samples of PTFE of different molecular weights.
In animal studies, Scheel found a correlation of lethality with the amount of hydrolyzable fluoride produced when E-CTFE was pyrolyzed at 550 C, but the amount of hydrolyzable fluoride produced was not correlated with the amount of E-CTFE pyrolyzed.
Other investigators found no correlation of lethality with the amount of hydrolyzable fluoride produced by pyrolysis of PCTFE , VF2-HFP , or VF2-HFP-TFE .
Waritz and Kwon reported that traces of perfluoroisobutylene (PFIB) were produced when PTFE was pyrolyzed at 475 C and that pyrolysis at 480 C produced 5 ppm of PFIB. Clayton has reported that the LC50 for PFIB in rats after a 6-hour exposure was 0.5 ppm. Although PFIB appears to be the most toxic gas produced by the pyrolysis of PTFE, no studies correlating the concentration of PFIB with the toxicity of the pyrolysis products of PTFE were found in the literature.
In the absence of pertinent data, no useful correlation can be made between the type and extent of exposure and the degree of human intoxication produced by the decomposition products of fluorocarbon polymers. However, compiling and summarizing the signs and symptoms reported in humans is a useful first step in the attempt to understand the adverse effects of these substances. dust counts were of the order of 1,000 particles/cc with diameters smaller than 5 ¡m , 15 particles/cc with diameters between 0.5 and 1.0 ¿urn, and 1 particle/cc with a diameter greater than 1 jum.
# Carcinogenicity, Mutagenicity, Teratogenicity, and Effects on Reproduction
Adams sampled air in a finishing room where PTFE was dried, sifted, and packed. At collection sites close to ovens which were heated occasionally to above 300 C, he found concentrations of hydrogen fluoride up to 6 ppm. This assumption was used because the toxic effects of decomposition products of PTFE are associated with a particulate substance which is a small fraction of the total decomposition products. Waritz and Kwon observed that test animals died after being exposed to the particles at a concentration of 1.4 mg/cu m (equivalent to 1.2 ppm by weight at ambient conditions). NIOSH maintains that the most important feature of an exhaust ventilation system is its design. Guidance for designing a local exhaust ventilation system can be found in Industrial Ventilation-A Manual of Recommended Practice and in Fundamentals Governing the Design and Operation of Local Exhaust Systems . Ventilation systems of this type require regular inspection and maintenance to ensure effective operation.
Regularly scheduled inspections should include face-velocity measurements of the collecting hood and inspection of the air mover and collector.
In addition to providing adequate ventilation, it may be appropriate, under certain circumstances, to isolate a process or system in an especially designed enclosure to minimize exposure. Other control measures may be intentionally redundant temperature monitoring systems and alarms to signal harmful thermal excursions. In all extrusion processes, the handling precautions described above must be observed. As in sintering operations, the temperature to which the fluorocarbon polymer is subjected must not be allowed to exceed the manufacturer's recommended processing temperature, and an appropriate temperature cutout system must be used. Local exhaust ventilation must be installed at the orifice from which the melt is extruded to keep decomposition products from entering the work area. An appropriate alarm system must be incorporated into the exhaust ventilation system.
# Biologic Evaluation
In thermoforming, compression molding, and coining, and in all processes in which the temperature of the fluorocarbon polymer approaches its melting point, ovens must be fitted with exhaust ventilation and temperature-regulating systems. These systems must be equipped with appropriate alarms and must be serviced at regular intervals.
Coagulated dispersion polymers are usually processed by "paste extrusion." This involves mixing the fluorocarbon polymer with a lubricant, generally a volatile petroleum fraction. This use of flammable liquids adds a potential hazard. The lubricant may be removed in a drying oven or in a continuous oven constructed in series with the extruder and a sintering oven. Precautions must be taken to minimize the risk of forming explosive mixtures of vapor and air and to prevent their ignition if they should form. These precautions might include controlling the rate of solvent removal, increasing the exhaust ventilation in the solvent-removal area, and locating the solvent-removal zone apart from the sintering area.
If flammable vapor enters the sintering oven, it probably will ignite.
Removal of all traces of the lubricant before sintering is necessary. As in sintering operations, appropriate temperature-regulating and exhaustventilation systems should be used on ovens where solvent removal takes place. Fire-extinguishing equipment should also be readily available. (29 CFR 1910(29 CFR .1000).
# Basis for the Recommended Standard
The most frequently reported effect of exposure in the workplace to the pyrolysis products of fluorocarbon polymers has been an influenza-like syndrome, polymer fume fever, which was described first by Harris in 1951 and subsequently by several other investigators . The major signs and symptoms associated with polymer fume fever are chest discomfort , fever , leukocytosis , Other effects found in humans exposed to the pyrolysis products of fluorocarbon polymers were nausea , malaise , congested throat and pharynx , rales in the bases of the lungs , pulmonary edema , hyperpnea , and increased pulse rate . Respiratory irritation and pulmonary edema have been reported in humans and animals exposed to the pyrolysis products of fluorocarbon polymers.
No reports of serious injury or of long-term effects of polymer fume fever were found in the literature.
The syndrome outlined above has been described most frequently as a result of exposure to fumes from heated PTFE. Since there are now a number of other fluorinated polymers whose breakdown products are almost entirely unidentified and untested for toxicity, there seems to be no basis for attempting to set an occupational exposure limit that will apply to breakdown products of fluorinated polymers in general. Accordingly, NIOSH suggests that exposure of employees to breakdown products of polymers of fluorinated monomers be limited to the greatest extent possible by designing production processes to restrict heating of these polymers to the lowest temperature that permits the desired operation, to limit access of air and oxygen to heated polymers to the greatest extent feasible, and to take the greatest possible advantage of local ventilation of sites from which polymer fumes may enter the occupational environment. Such steps, in conjunction with effective general ventilation of the workplace and good work practices, should go far toward protecting employees from deleterious effects from breakdown products of the materials with which they work.
Although these deleterious effects are more likely to be incapacitating than dangerous, their avoidance is certainly desirable.
# (c) Medical
Several studies on humans and animals showed that exposure to fluorocarbon polymer decomposition products produced respiratory irritation and pulmonary edema. Chemical substances should be listed according to their complete name derived from a recognized system of nomenclature.
Where possible, avoid using common names and general class names such as "aromatic amine,"
"safety solvent," or "aliphatic hydrocarbon" when the specific name is known.
The "%" may be the approximate percentage by weight or volume (indicate basis) which each hazardous ingredient of the mixture bears to the whole mixture. This may be indicated as a range or maximum amount, ie, "10-40% vol" or "10% max wt" to avoid disclosure of trade secrets.
Toxic hazard data shall be stated in terms of concentration, mode of exposure or test, and animal used, eg, "100 ppm LC50-rat," "25 mg/kg LD50skin-rabbit," "75 ppm LC man," or "permissible exposure from 29 CFR The "Health Hazard Data" should be a combined estimate of the hazard of the total product. This can be expressed as a TWA concentration, as a permissible exposure, or by some other indication of an acceptable standard. Other data are acceptable, such as lowest LD50 if multiple components are involved.
Under "Routes of Exposure," comments in each category should reflect the potential hazard from absorption by the route in question. Comments should indicate the severity of the effect and the basis for the statement if possible. The basis might be animal studies, analogy with similar products, or human experiences. Comments such as "yes" or "possible" are not helpful. Typical comments might be:
Skin Contact-single short contact, no adverse effects likely; prolonged or repeated contact, possibly mild irritation.
Eye Contact-some pain and mild transient irritation; no corneal scarring.
"Emergency and First Aid Procedures" should be written in lay language and should primarily represent first-aid treatment that could be provided by paramedical personnel or individuals trained in first aid.
Information in the "Notes to Physician" section should include any special medical information which would be of assistance to an attending physician including required or recommended preplacement and periodic medical examinations, diagnostic procedures, and medical management of overexposed employees. Respirators shall be specified as to type and NIOSH or US Bureau of Mines approval class, ie, "Supplied air," "Organic vapor canister," etc.
Protective equipment must be specified as to type and materials of construction.
# C E N T E R F O R D I S E A S E C O N T R O L N A T ' O N A L I N S T I T U T E F O R O C C U P A T I O N A L S A F E T Y A N D H E A L T H R O B E R T A T A F T L A B O R
# MATERIAL SAFETY DATA SHEET 1 PRODUCT IDENTIFICATION M A N U F A C T U R E R S N A M E R E G U L A R T E LE P H O N E NO
# % V O L A T IL E S BY V O L E V A P O R A T IO N R A TE »BUTYL A C E T A T E 11 A P P E A R A N C E A N O ODOR
# IV FIRE AND EXPLOSION DATA | # CRITERIA DOCUMENT: RECOMMENDATIONS FOR AN OCCUPATIONAL EXPOSURE STANDARD FOR THE DECOMPOSITION PRODUCTS OF FLUOROCARBON POLYMERS
recommends that exposure to the decomposition products of fluorocarbon polymers in the workplace be controlled by adherence to the following sections. The standard is designed to protect the health and provide for the safety of employees for up to a 10-hour work shift, 40-hour workweek, over a working lifetime. The recommended standard for the decomposition products of fluorocarbon polymers emphasizes good work practices and engineering controls and medical management. Since no measurable environmental level of any single decomposition product of fluorocarbon polymers can ensure complete protection of worker health, no occupational exposure limit is recommended in this document. The criteria and standard will be subject to review and revision as necessary.
Fluorocarbon polymers include polymers of substituted polyethylene monomers of the general formula (XCX-XCF)n, where X can be F, H, Cl, CF3, or CF3-CF2-CF2-0. The decomposition products of fluorocarbon polymers are defined as substances which are thermally generated from fluorocarbon polymers.
The greatest danger to workers exposed to the decomposition products of fluorocarbon polymers is from inhalation. Adverse effects could result from exposure to dusts of undecomposed fluorocarbon polymers, from exposure to the decomposition products, or from exposure to a single or several 1 decomposition products. The major concern in occupational exposure to the decomposition products of fluorocarbon polymers is their potential for causing polymer fume fever and damage to the respiratory tract. Polymer fume fever is characterized by headache, aching joints, general malaise, cough, shivering, chills, fever, tachycardia, and possible chest discomfort. The temperature may rise as high as 39.6 C (103.3 F ) .
Adherence to all provisions of the recommended standard is required in work areas in which fluorocarbon polymers are used, regardless of the concentration of airborne decomposition products of fluorocarbon polymers.
Occupational exposure is defined as any exposure to fluorocarbon polymers that may involve the production of decomposition products.
The products liberated from fluorocarbon polymers by the application of heat vary with the polymer, the temperature to which it is exposed, and the humidity of the ambient air. Because there is insufficient information on which to establish a safe workplace environmental concentration, none is recommended.
Both employers and employees should take all steps possible to keep occupational exposure to the decomposition products of fluorocarbon polymers as near to zero as possible. Careful adherence to all sections of this recommended standard will facilitate accomplishment of this aim. Controls which may be appropriate include isolation of a process within a controlled ventilation area, installation of safeguards to prevent thermal excursions, and installation of redundant temperature monitoring systems and associated alarms.
(a) Coveralls, or equivalent clothing, and gloves should be worn by the employee in areas where bulk fluorocarbon polymer dust is handled or where contact of powdered polymer with the skin is likely.
# (b)
Respiratory protective equipment to be used, if necessary, during emergencies or during the performance of nonroutine maintenance or repair activities in which exposure to the decomposition products of fluorocarbon polymers is likely should be provided in accordance with Table 1-1. Applicable regulations for the use of respirators are found in 29 CFR 1910.134.
# (c)
When a respirator is required by paragraph (b) of this section, it shall be selected and used in accordance with Administration (previously by the Bureau of Mines) as specified under the provisions of 30 CFR 11. The employer shall ensure that respirators are adequately cleaned and maintained, and that employees are instructed in the proper use and testing for leakage of respirators assigned to them.
Respirators shall be easily accessible, and employees shall be informed of their locations. (1) Half-mask respirator equipped with combination acid-gas/organic-vapor sorbent and high-efficiency filter cartridge (2) Full-facepiece gas mask equipped with acidgas/organic-vapor sorbent and high-efficiency filter canister, changed every 4 hours Maintenance (Equipment breakdown or cleaning of distillation vessels, etc; no time limit) Type C supplied-air respirator operated in demand, pressure-demand, or continuous-flow mode and equipped with full facepiece, hood, helmet, or suit where there is occupational exposure to the decomposition products of fluorocarbon polymers. As a further precaution, the carrying of smoking materials into such areas shall be prohibited.
Employees shall be instructed to wash their hands before smoking.
# (b)
In sintering or molding operations where fluorocarbon polymer is heated above its melting point, temperatures in excess of the manufacturers' recommended range should be avoided whenever possible. To prevent overheating, ovens shall be fitted with an automatic temperature cutout set at the manufacturers' recommended temperature for the fluorocarbon polymer.
(c) If necessary to prevent accumulation or recirculation of the decomposition products of fluorocarbon polymers in the workplace, ovens shall be fitted with a local exhaust ventilation system. An appropriate alarm shall be incorporated into any exhaust system in case of its failure.
(d) Local exhaust ventilation, located as close as possible to the operation, shall be used whenever welding, cutting, or related hightemperature operations are performed.
(e) Exhaust systems and ductwork shall be kept in good repair so that design airflows and pressures are maintained. Airflow and pressure should be measured at least twice a year. Continuous airflow indicators (oil or water manometers) are recommended. A log shall be kept showing design airflow or pressure and the results of periodic inspection.
(f) Ventilation systems discharging to outside air must be designed to conform to applicable local, state, and federal air pollution regulations and must not constitute a hazard to employees or to the general population.
(g)
General Housekeeping
(1) Spills of fluorocarbon polymers shall be cleaned up, preferably by vacuuming. Care shall be taken that polymer dust is not blown onto steampipes or other heated equipment.
(2) Emphasis shall be placed on prompt and frequent cleanup of dust to prevent accumulation of fluorocarbon polymers.
(3) Equipment shall be maintained regularly, and necessary repairs shall be made promptly.
(4) Fluorocarbon polymer scrap and waste shall be collected in special containers and, if not reused, shall be disposed of by high temperature incineration or by burying. Where excessive contamination of clothing with fluorocarbon polymer dust is likely, employers shall provide employees with launderable clothing for repeated use or disposable outer garments for one-time use.
(e) Laundry personnel should be informed of the hazards and of safe procedures if they are likely to encounter clothing contaminated with fluorocarbon polymers.
# II. INTRODUCTION
This report presents the criteria and the recommended standard that were prepared to meet the need for preventing occupational disease or injury arising from exposure to the decomposition products of fluorocarbon polymers.
The criteria document fulfills the responsibility of the
# III. BIOLOGIC EFFECTS OF EXPOSURE
# Extent of Exposure
Fluorocarbon polymers are made from substituted polyethylene monomers of the general formula (XCF-XCF)n, where X can be H, F, Cl, CF3, or CF3-CF2-CF2-0 [1], Copolymers, made from two monomers with as little as 10% of the comonomer, and terpolymers, made from three monomers, are additional forms of fluorocarbon polymers [1]. Fluorocarbon telomers are fluorocarbon polymers of low-molecular-weight produced by chemical reactions that limit the degree of polymerization [2].
Some important commercial fluorocarbon polymers are listed, along with the monomers used in their preparation, in Table III-l [1].
The preparation of unsaturated fluorocarbon monomers from saturated fluorinated hydrocarbons is normally carried out in closed systems. These processes present a potential hazard because such toxic byproducts as perfluoroisobutylene (PFIB) may be formed [3]. Fluorocarbon polymers are prepared from the monomers by conventional free-radical polymerization techniques, but the preparation of each polymer requires different formulation procedures involving a variety of redox catalyst systems [1], Because of its high viscosity at temperatures greater than its crystalline melting point (327 C), PTFE must be processed by techniques similar to those used for processing powdered metals or ceramics (eg, compression molding or ram extrusion) [1]. The heat treatments necessary for processing fluorocarbon polymers may result in the generation of toxic decomposition products [4,5].
Total estimated production of fluorocarbon polymers in 1974 was approximately 27 million pounds, 67% of which was PTFE. Other fluorocarbon polymers, including fluorocarbon elastomers, accounted for the remaining 9 million pounds [1]. NIOSH estimates that 5,000 workers are exposed to the decomposition products of fluorocarbon polymers.
# Identification of Decomposition Products
The decomposition products of fluorocarbon polymers depend not only on the chemical composition of the intact polymers but also on the conditions under which they are decomposed. The temperature to which the polymer is subjected, the atmosphere in which decomposition occurs, and the material of the vessel used can alter the kinds and quantities of the decomposition products formed.
The studies that discuss the identities of the products of pyrolysis of fluorocarbon polymers that have been found [A, give the following general picture of the pyrolysis products: at temperatures that produce just softening or melting of the polymer, the monomer tends to be the principal pyrolysis product. This is true for PTFE up to a temperature of about 500 C. At the same time, however, perfluoropropene, other perfluoro compounds containing four or five carbon atoms, and a particulate, waxy fume are generated. For PTFE, the principal pyrolysis product within the range of temperatures from 500 to 800 C becomes carbonyl fluoride. This compound hydrolyzes readily to hydrogen fluoride and carbon dioxide, so that, in the presence of moist air, these may appear to be the principal pyrolysis products in this temperature range. At temperatures above 800 C, the principal pyrolysis products of PTFE are tetrafluoromethane, hydrofluoric acid, and carbon dioxide. If pyrolysis occurs in the presence of glass, silicon tetrafluoride may be formed by reaction between the silicon in the glass and hydrofluoric acid.
Pyrolysis of PTFE in a vacuum at 360-700 C has yielded almost 100% of its monomer, tetrafluoroethylene [16,17,26]. Zapp et al [19] reported that a fine dust or sublimate was produced at temperatures above 200 C. Harris [10] reported the evolution of a mineral acid when PTFE was pyrolyzed at 140-325 C. Adams [22] found that hydrogen fluoride was released when PTFE was heated above 300 C. Waritz and Kwon [7] found that hydrolyzable fluoride was evolved from PTFE heated at 400 C and suggested that this was carbonyl fluoride or hydrogen fluoride. Zapp et al [19] reported that carbonyl fluoride was not detected by the method of analysis used when PTFE was decomposed at 300-550 C.
Other pyrolysis products of PTFE that have been identified include: octafluorocyclobutane (0FCB) at 300-360 C and at 500-550 C [19], perfluoroisobutylene (PFIB) at 380-400 C [19], at 475-480 C [7], and at 500-550 C [19], tetrafluoroethylene (TFE) at 450-480 C [7] and at 500-550 C [19], hexafluoropropylene (HFP) at 450-480 C [7] and at 500-550 C [19], hexafluoroethane (HFE) at 300-360 C [19], an unidentified five-carbon olefin at 500-550 C [19], and a higher-boiling residue consisting of a complex mixture of perfluoroolefins at 500-550 C [19].
Silicon tetrafluoride has been formed from the pyrolysis of PTFE at temperatures ranging from 300 to 650 C [8,19] and was probably produced by the reaction of hydrogen fluoride with silicon dioxide from the glass vessel. Table X-2 summarizes these results.
Several investigators [7,9,19] have indicated that particulate material or sublimate, with particle size ranging from 0.2 ¿urn to .0.5 /um, was evolved when PTFE was decomposed. Some authors speculated that this particulate material contained absorbed hydrogen fluoride [19], acidic carboxyl groups [13], or oxygen difluoride [9]. The short chain represents the primary particle. Difluorocarbene (DFC) would tend to form preferentially. Combination of two DFC moieties would form TFE, and one TFE could combine with one DFC moiety to form HFP.
Although theoretical, Errede*s hypothesis [21] does account for the formation of the pyrolysis products of PTFE that have been identified.
Further evidence of the multiplicity of the pyrolysis products was obtained by mass spectrometric analysis [8,13]. Typical mass spectra of the products of PTFE pyrolysis in air [8] and of the particles so obtained were reported by Coleman et al [13] and are shown in Tables X-3 and X-4.
The decomposition products of other fluorocarbon polymers have not been so intensively studied as those of PTFE. Polychlorotrifluoroethylene (PCTFE) heated at 347-418 C in a vacuum yielded 27% of the monomer, chlorotrifluoroethylene [32]. Birnbaum et al [14] found that pyrolysis of PCTFE in air at 375 C and at 400 C produced hydrolyzable fluoride, which they thought was carbonyl fluoride. No carbonyl chloride (phosgene) was found.
The authors speculated that fluorocarbonylchloride (C0FC1) and chlorodifluoroacetylchloride (CF2C1C0C1) had been evolved and presented evidence for the formation of a variety of fluorinated, chlorinated compounds with up to three carbon atoms.
The authors also found a particulate with a mean particle size of 0.5 /im.
When a copolymer of vinylidene fluoride (VF2) and hexafluoropropylene (HFP) and a terpolymer of VF2, HFP, and TFE decomposed at 550 C and 800 C, carbon monoxide and carbon dioxide were produced [6]. Clayton [23] has suggested that decomposition of VF2-HFP, VF2-HFP-TFE, and polyvinyl fluoride would produce hydrogen fluoride, but he gave no experimental data to support this theory. Clayton [23] also suggested that the decomposition of fluorinated ethylene propylene (FEP), a copolymer of TFE and HFP, would produce HFP; again, no experimental data were given. Madorsky et al [26] reported that pyrolysis of polyvinyl fluoride and polyvinylidene fluoride in a vacuum at 372-500 C produced hydrogen fluoride and a waxlike material consisting of chain fragments of low volatility.
# Effects on Humans
As early as 1951, Harris [10] described two cases of an influenza like syndrome in workers who had been experimenting with PTFE for an unspecified period. The first worker, 29 years old, was exposed to fumes emitted from PTFE heated in an extruder with a malfunctioning thermostat.
Although the extrusion process was normally carried out at 350 C, the machine in this instance overheated to about 450-500 C. had asthma attacks for many years, although he had been symptom-free for 18 months prior to this incident. Harris noted that the exhaust ventilation system on the oven was subsequently found to be inadequate and that, once that situation was remedied, no further attacks occurred. He called the illness of these workers polymer fume fever, which he proposed was caused by inhalation of fume from heated PTFE, and noted the similarity of this syndrome to metal fume fever.
Harris [10] also noted that the two cases he had diagnosed as polymer fume fever were similar to two cases of illness in PTFE workers described to him by HF Gilbert in a personal communication. Because the symptoms so closely resembled those seen in metal fume fever, Harris [10] analyzed PTFE ash and the sublimate evolved from PTFE heated at 400 C for various metals. The sensitivity of the method of analysis was not reported. From these studies, Harris concluded that the concentrations of metals in the ash and the sublimate could not explain their findings, so that a toxic fume from heated PTFE seemed to be the responsible agent in polymer fume fever from PTFE.
In 1967, Bruton [34] described two cases of illness in aviation employees whose work involved contact with a neoprene door seal that had been sprayed with an aerosol of an unspecified fluorocarbon telomer.
Smoking was not permitted in the hangar; however, toward the end of his shift, the first worker had smoked a cigarette in an office where smoking was allowed. Approximately 30 minutes later, he experienced shivering and chills, which lasted for about 6 hours, but no other effects. The second worker had been handling the polymer spray for approximately 1 year and had become ill once before when he failed to wash his hands before smoking after working with the aerosol. On this occasion, he started to smoke a cigarette during his break and realized by the taste that it was contaminated. He extinguished the cigarette immediately, but, within 30 minutes, he began to shiver and developed a headache and muscular aches, but no respiratory effects. Recovery was complete within 24 hours.
Bruton [34] believed that the polymer-treated surface had contaminated the cigarettes.
To demonstrate the possibility of hand contamination, he conducted an informal experiment in which the aerosol was sprayed onto a clean aluminum surface according to the manufacturer's instructions. When he wiped the surface with his finger, a line across the sprayed surface and a faint white dust on his finger were visible. The author suggested that handling of objects treated with aerosols of fluorocarbon telomers represented a hazard to smokers because of the possibility of contamination of smoking materials. He noted that workers should be required to wash their hands before smoking to avoid contaminating smoking materials. Although Bruton diagnosed this syndrome as polymer fume fever, he did not disprove the possibility that the respiratory symptoms were due to other causes. He was correct in assuming that the temperature of the cigarette was sufficient to cause pyrolysis of the fluorocarbon telomer, however, since the temperature of the burning zone of cigarettes has been shown to range from 854 to 913 C [35].
In 1964, Nuttall et al [36] reported an incident of in-flight illness that affected 35 passengers, including 2 flight surgeons and 4 of 5 crew members, on a C54 aircraft. The total flight time was 165 minutes, and the authors mentioned a flight altitude of 9,500 feet. The auxiliary power unit (APU) of the aircraft was located in the rear compartment, which "freely communicated" with the main passenger cabin. The crew compartment door was closed. After the passengers and crew members boarded the plane, the APU was started; fume and odor levels within the main cabin were reported to have been "normal." Takeoff was delayed because of magneto trouble, and the passengers debarked after the APU had run for approximately an hour. A few had mild symptoms of respiratory Irritation, and some became nauseated when they smoked. About 1.5 hours later, the passengers reboarded the aircraft and the APU was restarted. The plane took off 45 minutes later and the APU was turned off. Within 1 hour of takeoff, most of the passengers and two of the crew members had chest discomfort and general malaise, including chills, nausea, and respiratory distress in some. One passenger vomited and collapsed and was found 5-10 minutes later in a cyanotic state with a weak and rapid pulse.
A second passenger had severe respiratory distress and moderate collapse. Six passengers were incapacitated, and five were given oxygen. The heating system was suspected of being a source of toxic fumes and was turned off.
Although a fusilage hatch was opened to provide ventilation, some passengers continued to complain. On arrivàl, three passengers required hospitalization, and everyone aboard the plane except one co-pilot had experienced effects, which persisted after the plane landed.
To characterize the illness, Nuttall et al [36] interviewed and gave questionnaires to all crew members and passengers.
The answers to the questionnaire revealed a toxic reaction pattern similar to that of influenza, with onset of symptoms occurring within 2-6 hours after exposure to the unidentified agent. Typical symptoms were chest discomfort, difficulty in breathing deeply, chills, muscular aches, fever, dull headache, and general malaise. Respiratory symptoms were not present in all cases, and nausea and aversion to cigarettes was often reported. The number of smokers aboard the plane was unspecified, and it was not stated whether smoking was permitted during the flight. Recovery was complete within 24 hours in most cases, including those of the three hospitalized patients. The authors noted that examination of these three patients showed elevated temperatures, increased white blood cell counts with a shift to the left (indicative of an increased proportion of young cells), and rapid pulse rates. They emphasized the similarity of the reported symptoms to those of metal or polymer fume fever, characterizing 50% of the cases as "typical" examples of this syndrome. The questionnaire data indicated that 6 cases were severe, 12 were moderate, and 9 were mild.
Although 12 of those aboard the flight did not complete questionnaires because they could not be located, the flight surgeons who had interviewed everyone on the plane at the time of the incident reported that they also had been affected to some extent.
Nuttall and coworkers [36] conducted an extensive investigation to determine the cause of the illness. Air samples were collected in the grounded aircraft and analyzed for total metals and zinc with negative results. The four who collected samples developed a typical fume fever reaction. Six volunteers were exposed to fumes from the APU for 40 minutes. All six developed symptoms similar to those of the affected passengers and crew members 1-3 hours after exposure. All had elevated temperatures and elevated white blood cell counts, with polymorphonuclear leukocytosis and a shift to the left. A trip made by the same plane 2 days later, after a new APU had been installed, was uneventful.
The tape used to wrap the exhaust manifolds of the old APU was subjected to a variety of tests [36] . Five volunteers were exposed to fumes emitted from the APU before the manifold was wrapped with tape. No symptoms were reported after 35 minutes of exposure. Next, the APU exhaust manifolds were wrapped with an unspecified amount of asbestos tape salvaged from the old wrappings of the manifold, and used APU oil was placed on the wrapping.
In this instance, two of six subjects exposed for 35 minutes reported symptoms, and small quantities of uncharacterized fumes were observed around the wrappings. Carbon monoxide levels were below 50 ppm in both these runs. The authors noted elevated temperatures and mild leukocytoses in the two affected subjects, but suggested that the reported effects were questionable. This second run was repeated, whereupon two of the six subjects exposed for 35 minutes developed mildly elevated temperatures and leukocytosis. Subsequent exposure of four subjects to oil fumes alone for 40 minutes failed to produce symptoms. Nuttall et al [36] concluded that the asbestos tape was the source of toxic fumes, although the oil might have been a modifying agent. New asbestos tape of the same type that had been used to wrap the manifolds of the APU was analyzed with an infrared spectrometer. This examination revealed the presence of PTFE, a finding that was later confirmed by the manufacturer.
In a final experiment, one subject was exposed to fumes emitted from an unspecified amount of the tape pyrolyzed in a platinum dish at 800-1,000 In 1967, Barnes and Jones [37] gave the results of an investigation of an outbreak of respiratory illness affecting 4 of 19 workers at a factory that made abrasive wheels. The affected workers were male press operators, aged 20-32 years, whose employment histories were not given.
Their work involved placing by hand a mixture of phenol-formaldehyde resin, furfural, abrasive grain, a small amount of hexamethylenetetramine, and, occasionally, a rectifying oil containing cresylic acid on cold presses in a tray. The wheels thus formed were removed from the press room and placed in batches in an oven heated to 177 C for curing. The investigators noted that the factory consisted of one large shed and that the press room was not physically closed off from the area where the mixture was made. The press room was mechanically ventilated by recirculated, cooled air, and the mixing area was air-conditioned.
In describing these four case histories, Barnes and Jones [37] noted that these workers were moderate to heavy smokers who smoked on the job.
All four had suffered recurrent bouts of illness over a 2-to 4-month period and had experienced respiratory distress characterized as either tightness of the chest or difficulty in breathing deeply. Typical symptoms of these attacks included uncontrollable shivering lasting 1-2 hours in two workers, pain in the retrosternal area in one worker, sore throat in one worker, and severe headache in one worker. Physical examinations at the time of the plant visit revealed scattered rhonchi in the chest of one worker, congested throat and congested soft palate in a second worker who had not complained of a sore throat, congested pharynx in a third, and no signs in a fourth worker who had been transferred to the packing room 2 weeks earlier.
The authors discovered during their investigation of the plant that the use of powdered PTFE as a mold-release agent had been initiated approximately 3 months earlier. They noted that, although the pressing and curing processes were carried out at temperatures below 300 C, all the affected workers handled the PTFE-treated plates and all smoked while working. They further stated that PTFE powder was detected on the hands of the press operators and that there was ample opportunity for the skin to become contaminated in the plant. Smoking on the job was then prohibited. The authors reported that, according to the plant manager, there had been no recurrence of symptoms during the 2 months after the reported illnesses and the prohibition of smoking in the work area.
Although the decomposition products of PTFE may have been the cause of the illness, some of the typical polymer fume fever symptoms were not present.
In 1974, Wegman and Peters [38] reported the investigation of a similar outbreak of influenza-like illness in workers in a textile mill that produced imitation crushed velvet. The fabric was made of nylon and rayon, and the final stage of its production was a flocking process that consisted of the addition of a liquid fluorocarbon polymer to the material, with subsequent dipping, rolling, and squeezing of the mixture, curing at 150-155 C, mechanical crushing and steaming at 135 C, and final static elimination. In an initial interview, the plant manager revealed that a number of workers involved in the flocking process had reported symptoms of weakness, muscle aches, fever, chills, and shortness of breath.
The authors [38] interviewed and examined all workers in the flocking division, 10 men and 3 women, ranging in age from 19 to 61 years. Those complaining of symptoms had been employed in this division for from 2 months to 6 years. Seven of these workers, six men and one woman, described symptoms of cough, muscular aching or weakness, fever, and chills. Four of these seven workers also had experienced shortness of breath.
All had suffered repeated bouts of illness, three of the seven workers having experienced as many as six attacks during an unspecified period of time. In several instances, symptoms were of such severity that affected workers had to leave the plant. Onset of symptoms was generally gradual and illness persisted for 6-72 hours, most workers reporting recovery within 24 hours. Of the six workers who did not report such attacks, one nonsmoking man had experienced headache on five occasions and possibly some coughing; a second had had an isolated bout of cough, fever, and chills, which the authors attributed to a common cold. One woman who did not report typical attacks had an unspecified number of attacks of coughing, fever, chills, and shortness of breath, but these were of rapid onset and short duration. One of the six men experienced severe weakness, chest discomfort, and shortness of breath on one occasion. The affected workers experienced symptoms only when they worked in the area where the fluorocarbon polymer-treated material was cured.
The authors [38] considered four materials as possible causes of the symptoms: ammonia, formaldehyde, nylon, and the fluorocarbon polymer.
Analysis of the air of the workplace found air concentrations of less than 50 ppm of ammonia and less than 1 ppm of formaldehyde.
The nylon was reported to be of nonrespirable size. The authors maintained that exposure could not have resulted from the flocking process itself, since the maximum temperatures at which the fluorocarbon was applied and cured were at or below 165 C. However, the authors noted that all seven workers who had "typical" symptoms of polymer fume fever were cigarette smokers, and that all but two of the other workers experiencing symptoms were also smokers.
They observed that workers engaged in applying the polymer to the material had frequent hand contact with both liquid and cured polymer and that they often smoked during breaks without first washing their hands. The authors concluded that the source of the illness was polymer fume generated by the smoking of PTFE-contaminated tobacco. No further symptoms were reported after smoking in the work area was prohibited and the workers were instructed to wash their hands before smoking or eating.
In 1973, Evans [39] reported a case of respiratory illness in a 49year-old man who had been using an oxyacetylene torch to dismantle a metal table used to hold PTFE-coated molds. The molds had been sprayed with S-143, a dispersion of TFE telomer in unspecified fluorocarbon solvents. In 1975, Blandford et al [41] described a case of nonoccupational respiratory illness in a man who had inhaled fumes from a PTFE-coated pan that had contained only water and had boiled dry when left unattended on an electric stove.
When he removed the pan from the stove, the man noticed that the fumes "took his breath." No smoke was visible. Five cockatiels kept caged in an adjoining room died within 30 minutes after the incident.
The patient's wife, who was in the same room as the birds during the incident, was unaffected. About 60 minutes postexposure, the patient experienced shortness of breath and a paroxysm of coughing when he tried to smoke a cigarette. About 80 minutes after the incident, the man's symptoms included shivering, dizziness, and nausea. He felt cold and noted a painful tightening of the chest. The next day, on awakening after 8 hours of sleep, he had a severe headache, which subsided during the morning. The tightness of the chest persisted for the remainder of the day. The subsequent recovery was complete and uneventful, although the patient had difficulty remembering events following the death of his birds and felt that the fumes had affected his level of consciousness. The authors noted that this was an unusually clearcut case of polymer fume fever, because there had been no smoke and the pan had contained only water. The data as reported by the authors demonstrated that PTFE produced toxic decomposition products that were more lethal to birds than to humans.
In 1967, Clayton [23] published the results of investigations conducted by Kligman for the Haskell Laboratory for Toxicology and
# Industrial
Medicine to determine the effects on humans of smoking cigarettes contaminated with known amounts of a TFE fluorocarbon telomer.
The sex, age, medical and employment histories, and smoking histories of the subjects were not reported, and the author did not specify whether the same or different subjects were exposed at the various dose levels.
The first experiment evaluated the effects of smoking a cigarette to which 0.05, 0.10, 0.20, or 0.40 mg of a TFE fluorocarbon telomer had been added. Ten volunteers smoked one cigarette apiece with each of the added amounts of telomer.
Results indicated that 0.40 mg telomer in each cigarette was necessary to cause an increase in body temperature and pulse rate. No symptoms were reported at the lower levels, although average maximum pulse rates were slightly elevated at an unspecified interval after smoking. At the 0.40 mg dose level, the author reported that 9 of 10 subjects had what he considered to be typical symptoms of polymer fume fever, with cough as the first symptom in 6 subjects. The symptoms reported by the nine affected subjects were headache, muscular aches, chills, malaise, sluggishness, excessive perspiration, and weakness. Onset of symptoms occurred 1-3.5 hours after smoking, with a mean latency period of 2 hours. From 2.5 to 5.5 hours after the volunteers smoked, the average temperature of the nine affected volunteers increased to 100.5 F from a mean preexposure value of 98.1. From 2.5 to 4.5 hours after they smoked, The other four subjects expressed well-defined symptoms of polymer fume fever after smoking six to eight cigarettes; the first symptom to appear was chills.
Other symptoms were the same as those of subjects in the first experiment, except that coughing was not reported by any of the subjects.
Clear symptoms first appeared 3-5 hours (average 3.8) after the subjects smoked. Five to 6 hours after smoking, average temperatures of these four subjects increased from 98.3 to 101.4 F. From 1 to 9.5 hours (average 5.4) after smoking, the average pulse rate of the four affected subjects increased from 87 to 111. Recovery time in the subjects with well-defined attacks was 7.5-12.5 hours (average 9.8), but the author did not explain the criteria for recovery. The cumulative amount of added telomer necessary to elicit signs and symptoms of illness in these four patients was 0.30-0.40 mg.
Clayton [23] noted that the cumulative amount of telomer (0.30-0.40 mg) needed to produce well-defined symptoms in four subjects coincided with the amount of telomer (0.40 mg) needed to produce symptoms in subjects who smoked one cigarette. The sequence of events was similar in subjects given both single and cumulative exposures, but the signs and symptoms differed.
Six of 10 subjects complained about a cough in the first experiment but none of the 4 subjects in the second experiment complained of cough.
Clayton suggested that subjects receiving single large exposures to fluorocarbon telomer had an initial respiratory tract irritation that was not experienced by subjects receiving cumulative exposures because the latter were subjected to irritant substances at lower concentrations. The same amount of telomer, however, produced fever in both experiments.
Clayton concluded that there is no obligatory sequence of effects in polymer fume fever and that the absence of cough does not preclude a diagnosis of this illness. He emphasized that the total clinical picture should be considered by anyone contemplating a diagnosis of polymer fume fever, and that objective measurements such as temperature, pulse rate, and white blood cell counts should be relied on as indices of illness; however, he did not report white blood cell counts. The interval between the smoking of cigarettes was also not specified, and any individual differences in the subjects that might have explained their differing reactions were not discussed. Nevertheless, these experiments indicate that smoking cigarettes contaminated with a TFE-telomer can result in a syndrome commonly referred to as polymer fume fever.
In 1965, Makulova [42] reported five cases of perfluoroisobutylene (PFIB) poisoning in two male and three female laboratory workers. A 34year -old woman had worked with this compound for approximately 2.5 years with no previous ill effects. The ages and employment histories of the other patients were not specified. Four of the five workers reported that exposure to PFIB lasted less than 1 minute, during which time they inhaled two to five times. All patients described symptoms of coughing, difficulty in breathing, and chest pains immediately after exposure. These symptoms became progressively more severe, and by 6-8 hours after exposure, all patients had developed headaches and other symptoms and had begun to expectorate sputum.
Makulova [42] Chest X-rays of all patients showed significant pulmonary changes that came on rapidly 4-6 hours postexposure and became fully developed approximately 48 hours postexposure.
In four patients, these changes consisted of bilateral, confluent pulmonary edema, especially in the middle lobes, with emphysematous lateral borders and segments above the diaphragm. In the other patient, multiple clearly defined small foci of intense opacity were found.
The author [42] noted that treatment was largely symptomatic and consisted of calcium chloride, ascorbic acid, glucose, unspecified cardiac medication, and oxygen administration to combat the pulmonary edema.
Penicillin or streptomycin in combination with sulfonamides was given during the first few hours postexposure. Symptomatic improvement was noted in some patients within 4-6 days postexposure, and complete resolution of breathing difficulties and pulmonary rales occurred 7-10 days after exposure. At 10-13 days postexposure, pulmonary damage observed in X-rays had been resolved, and leukocytosis and eosinopenia improved 15-20 days postexposure. Three patients were discharged from the clinic in good health 13-23 days after exposure, and a followup 2 years later revealed no complications. One patient developed exudative pleurisy and remained in the clinic for more than 2 months.
The fifth patient, the 34-year-old woman, died 2 days after exposure.
Makulova [42] described the last patient's history and illness in detail, noting that she had suffered from influenzal pneumonia 2 months before poisoning. She was unable to give any information on the duration or degree of her exposure to PFIB on the day she became ill. Her symptoms were similar to those already described, and clinical findings were similar to those for the other patients. She was admitted to the clinic with a where gaskets were produced, 0.2-2.9 mg/cu m in the machine shop, and 2.5-2.9 mg/cu m in a sample for a worker who operated the ring-grinding machines.
A questionnaire was completed by 77 workers (about 75% of the workers in the plant) [46] . Sixty of the production workers (86%) said that they had experienced polymer fume fever at some time in the past, but only 50% had experienced polymer fume fever during the past year. Fourteen percent of the workers stated that they had had more than three episodes in the preceding year. Only 10% of those who had experienced polymer fume fever In the fabrication techniques studied by Sherwood [47], the polymer was pressed into a mold or "pre-form" and sintered at 350-380 C to form a finished product or a material suitable for machining to final specifications. Variations of this technique included prebaking before molding, repressing after sintering, and extrusion. Machining was carried out on standard metal-working machines, and waste was recovered for reuse.
Tape was produced by veneering followed by a heat treatment, which is known as tensilating. In 1963, Adams [22] conducted an investigation to determine the cause of polymer fume fever in employees in a plant where PTFE was processed.
Altogether, 30 wage and 8 staff employees were interviewed by a medical
officer. An investigation of the plant was also conducted. Of the 30 wage employees, 14 had experienced symptoms of polymer fume fever in the 2 months previous to the interview. A total of 32 incidents of polymer fume fever were reported by these 14 workers. Only employees working in the finishing room had been affected.
Of the 18 men who worked in the finishing room, 12 who were smokers accounted for 30 incidents and 2 nonsmokers accounted for the other 2 attacks.
A detailed investigation showed that 6 men who rolled their own cigarettes had had 21 of the attacks of polymer fume fever. Of the eight staff employees, only one, a pipe smoker, had had an attack of polymer fume fever.
In the finishing room, PTFE was dried, sifted, and packed [22]. In an unspecified drying operation, a small amount of PTFE was occasionally heated beyond the normal drying temperatures. Air samples were taken by an unidentified method at points close to the drying ovens and the ovens where the polymer was further heated when required. Adams found concentrations of hydrogen chloride as high as 35 ppm on occasions when PTFE was heated only to normal drying temperatures. When oven temperatures exceeded 300 C , the author found up to 6 ppm of hydrogen fluoride. Although acetic acid is usually used to coagulate PTFE latex, it is possible that hydrogen chloride was used and that residues of this acid provided the HC1. HC1 boils at 110 C whereas something like 250 C is required to liberate HF from PTFE.
Adams [22] concluded that the majority of incidents of polymer fume fever resulted from the smoking of PTFE-contaminated tobacco. He noted that precautions must be taken to prevent particles of polymer from lodging beneath nails, in hair, or on clothing. Adams did not report the method of analysis used to detect hydrogen fluoride. That the hydrogen chloride in the vicinity of the drying ovens came from PTFE per se is highly unlikely because this polymer contains no chlorine atoms.
# Animal Toxicity
A list of compounds that have been identified as pyrolysis products of fluorine-containing polymers, as stated previously in the section on In addition to the various molecular species mentioned in the preceding paragraph, there is the particulate material that may be the principal cause of polymer fume fever [49]. Harris [10] had found in 1957 that heating PTFE at temperatures above 300 C produced the deposition of a solid material within his exposure chamber and also liberated an acid into the air of the chamber. Four rats exposed to such atmospheres developed congested or hemorrhagic lungs and pulmonary edema. Harris concluded that PTFE heated to 300 C or more produced a sublimate or an acid that induced pulmonary edema and killed rats thereby.
In 1968, Waritz and Kwon [7] and Birnbaum et al [14] suggested that the particulate material may carry adsorbed toxic materials (perhaps hydrofluoric acid, carbonyl fluoride, octafluoroisobutene, or chlorotrifluoroethylene) into the alveoli, the latter group of researchers [14] having found that the mean particle size of this material was 0.5 jum and that 99% of the particles had diameters of less than 2 ¡m. These dimensions place the polymer fume in the category of inhalable dusts.
Waritz and Kwon [7] found that removal of the particulate material by produced minimal mortality in rabbits and rats, respectively. Hyperemia of the liver, hemorrhage in spleen and lungs, dystrophic changes in the epithelium of the renal tubules, atelectasis and emphysema in the lungs, and desquamation of the bronchial epithelium were the principal changes attributed to the monomer. Clayton [54,57] reported that the LC50 for the rat exposed to tetrafluoroethylene for 4 hours was 163,600 mg/cu m.
For CTFE, the LC50 for rabbits and white rats exposed for 2 hours was reported to be 24,000 mg/cu m [58].
The "absolutnaya smertelyenya kontsentratsiya," meaning probably the LC100, was said to be 26,400 mg/cu m for the rabbit and 36,000 mg/cu m for the white rat. No actual data on the numbers of deaths after exposure at any concentration were provided.
Clayton, in a series of papers [23,54,57] all probably referring to a single estimation of the inhalation toxicity of CTFE, has reported that the LC50 for the rat exposed for 4 hours was 1,000 ppm (4,770 mg/cu m ) .
More recently, Hood et al [59] have exposed rats, guinea pigs, rabbits, and dogs to chlorotrifluoroethylene at concentrations of 300 ppm
(1,431 mg/cu m) for 4 hours/day, 5 days/week, for a total of 18 exposures.
One of 10 male guinea pigs died after the sixth exposure. One of 10 male rabbits died after 4 exposures and another after 5. None of 10 rats of to have increased more than that of the control animals; the increase was stated to have become progressively larger throughout exposure in the exposed rabbits. The exposed animals also were said to have recovered from the orthostatic tachycardia more slowly than the control animals. These observations suggest that exposure to CTFE altered the properties of the sympathetic nervous system, including possibly such centers in the brain stem as the bulbar vasomotor mechanisms. The exposed rats were reported to have undergone a significant decrease in the ability to summate subthreshold stimuli (presumably applied to the motor nerve of some unidentified effector).
Hood et al [59] exposed rats of both sexes, male guinea pigs, male rabbits, and dogs for 6 hours/day, 5 days/week, for 14 months to CTFE at concentrations starting at 15 ppm (about 71.6 mg/cu m) and increasing progressively, at irregular intervals of time, to 30, 50, 100, and 150 ppm (715.5 mg/cu m ) . These exposures produced no significant pathologic effects in rabbits and guinea pigs but produced severe tubular necrosis in rats.
Two of four exposed dogs began to exhibit signs of neurologic disturbances after 27 and 64 exposures, respectively, at 150 ppm. These consisted of stiffness and weakness of the legs and unsteadiness in standing. One of two other dogs that were added to the exposed group at the beginning of exposure at 100 ppm (477 mg/cu m) died after 56 exposures at that concentration followed by 54 exposures at 150 ppm. The second of these dogs was reported to have become very irritable at this same time.
Degenerative changes in the central and peripheral portions of the somatic nervous system were found, most severe in samples of nerve tissue from the dog that had exhibited the most marked neurologic signs (temporary prostration at the end of each period of exposure, ataxia, and difficulty in swallowing). This dog was found to have atrophy of the muscles of the hindlegs.
Clayton [54] reported that a mixture of 80% hexafluoroethane with 20% oxygen (about 4,515,000 mg/cu m of hexafluoroethane) was an approximate lethal concentration for the rat exposed to it for 4 hours. The data in these paragraphs allow arrangement of the compounds on which information is available in a hierarchy of decreasing toxicity, albeit with some uncertainty.
There is little doubt that perfluoro isobutylene is the most toxic compound and that octafluorocyclobutane and hexafluoroethane are the least toxic. The ranking of inhalation toxicity for the rat, based largely on single exposures, that NIOSH has derived from the information stated above is as follows, going from the most toxic to the least: perfluoroisobutylene, hydrofluoric acid, carbonyl fluoride, silicon tetrafluoride, chlorotrifluoroethylene, hexafluoropropene, tetrafluoroethylene, tetrafluoromethane, hexafluoroethane, and octafluorocyclobutane.
In addition to the information summarized above on the breakdown The other general approach to assessing the toxicity of the pyrolysis products of fluorinated polymers, ie, exposing experimental animals to mixed decomposition products of polymers heated to various temperatures, has been used by a number of investigators.
In 1955, Zapp et al [19] pointed out that the intact PTFE polymer is nearly inert but that products of its thermal decomposition are not. Polymer fume fever has been recognized to be a consequence of exposure to heated PTFE since its description in 1951 by Harris [10].
Studies of the toxicity of the pyrolysis products of PTFE had been started at the Haskell Laboratory in 1943, but polymer fume fever had not been reproduced in experimental animals. Lethal activity had been demonstrated, however [19].
Strips of PTFE subjected to temperatures of 200 and 250 C in a stream of air passing into an exposure chamber containing 2 rats caused no deaths of the rats after a 6-hour exposure [19], Similar exposures to air passing over strips of PTFE heated to 300 and 350 C did result in the death of rats, the higher temperature having a more marked effect with "Teflon 6," described as a low-molecular-weight polymer, than with "Teflon 1," a highmolecular-weight polymer.
Clayton et al [64] reported that, when "Teflon 1" and "Teflon 6" were subjected to temperatures of 300, 325, and 350 C in tubes of either glass or stainless steel, the materials heated in glass tubes yielded more toxic pyrolysis products than those heated in the stainless steel tubes. The differences were most marked for "Teflon 6" at 300 C and for "Teflon 1" at 350 C. Samples of "Teflon 6" that yielded comparatively large amounts of particulate material were more toxic than those that yielded less.
Filtration of the pyrolysis products with a filter having a pore size of 0.45 j i r n i lowered the mortality of rats exposed to the pyrolysis products from 43/48 to 7/48.
"Teflon 6" manufactured before 1958 was reported [57] to yield toxic breakdown products at 350 C, whereas "Teflon 6" manufactured "currently"
(1959 and thereafter) yielded pyrolysis products of approximately equal toxicity only when the temperature was raised to 425 C .
# Cavagna et al
[49] reported they had been able to produce attacks of fever in rabbits subjected to inhalation of aerosolized 20% acetic acid, in an undisclosed concentration in the inspired air, for 10 minutes, followed 16 hours later by exposure for 30 minutes to an atmosphere containing 10-12 mg/cu m of hydrogen fluoride and 1.0-1.7 billion particles/cu m with diameters greater than 0.7 jum, which had been generated by heating PTFE in a tube furnace at 400-500 C. Seven of 11 rabbits had temperature increases of 0.5-1.5 C. These appeared after a latency period of about 5 hours, during which a decrease in body temperature, leukopenia, and cough and rhinorrhea were observed. The fever lasted 6-7 hours and coincided approximately in onset, but not in duration, with leukocytosis. Exposures of naive rabbits to fumes from heated PTFE produced initial hypothermia and irritation of the respiratory tract but no fever. the particles produced. Some of this powder was used at once, another aliquot was washed with water to remove the gaseous products of decomposition, and a third portion was stored for 6 months before being used. These three samples of powder were compared with a powder produced by grinding PTFE that had not been pyrolyzed and with powdered chalk.
The powders were administered to rabbits by iv injection of 1-1.5 mg/kg in suspension in sterile, apyrogenic saline. Control rabbits received only saline.
Only the unwashed pyrolyzed particles produced a febrile reaction in the rabbits. This was preceded by leukopenia, which was frequently succeeded by leukocytosis.
A similar response was induced in rabbits by inhalation exposure to the unwashed pyrolyzed particles at a concentration of 122.8 mg/cu m for 2.5 hours.
The succession of leukopenia, pyrexia, and leukocytosis reported by Blagodarnaya [65] in the rabbits exposed to unwashed pyrolyzed particles from PTFE is reminiscent of the febrile response to gram-positive bacteria injected iv into rabbits [66] . The failure of washed pyrolyzed particles to produce fever in these experiments indicates that the response is not to particulate agents alone. The presumption is that some water-soluble and volatile component of pyrolyzed PTFE adsorbed on the surfaces of the particulate material render the particles capable of interacting with the leukocytes of the blood and releasing the leukocytic pyrogen as suggested by Cavagna et al [49] . Some further study of the pyrogenic process after exposure to pyrolyzed fluorocarbon polymers seems desirable.
Treon et al [67] compared the toxicities of the pyrolysis products of PTFE and of two polymers of PCTFE differing in extent of polymerization, so that one (FL) was a liquid and the other (KF) was a solid. The liquid polymer (FL) was dropped into an Inconel tube heated by an electric current through resistance wire wound around the tube. The solid polymers (PTFE and KF) were prepared as strips which were inserted into the cold Inconel tube.
The tube was then raised to the planned temperature as rapidly as possible. Air or nitrogen (PTFE only) was passed through the furnace at a rate of 31.8 liters/minute and into the 800 liter exposure chamber. PTFE was pyrolyzed at temperatures of 375-878 C. FL was pyrolyzed at either 371 or 482 C, whereas KF was heated to temperatures of 803-813 C.
Groups of five mice, six rats, four guinea pigs, four rabbits, one cat, and one dog (PTFE only) were exposed in the chamber to various concentrations of pyrolysis products (graded by the rate at which the polymer was fed into the furnace) and for different spans of time [67].
The exposures to pyrolysis products of PTFE lasted for 30-180 minutes, most being less than 60 minutes in duration.
Exposures to the pyrolysis products of FL were for 2, 7, or 24 hours, whereas those to the pyrolysis products of KF were for 32-34 minutes.
Dogs, mice, and rabbits were the most resistant species to PTFE pyrolyzed at temperatures of 739-813 C in the presence of air. When PTFE was pyrolyzed at temperatures of 811-878 in nitrogen, rabbits, guinea pigs, and rats were more resistant than mice. Cats and dogs were not used in these last tests. When the temperature of pyrolysis was 491-527 C in the presence of air, rats and rabbits were more resistant to a lethal effect than mice and guinea pigs. Cats and dogs were not included in these studies either. Pyrolysis of PTFE in the presence of air yielded pyrolysis products of greater toxicity than those produced in nitrogen. Lowering the temperature of the pyrolysis apparatus from 739-813 to 491-527 C decreased the toxicity of the pyrolysis products to rats, rabbits, and mice, but slightly increased the toxicity to guinea pigs.
Cats and rats were the most resistant species to the lethal effect of the pyrolysis products of FL heated at 482 C [67] . When the pyrolysis temperature of this polymer was lowered to 371 C, no animals were killed during exposures of 2 or 7 hours. Mice, cats, and rabbits were more resistant to the lethal action of the pyrolysis products of KF than were guinea pigs and rats.
When PTFE was pyrolyzed in the presence of nitrogen, pyrolysis at a rate of 1.99 g/hour produced no fatalities in any of the four species exposed [67]. When PTFE was pyrolyzed in air, pyrolysis at a rate of 2.60
g/hour at 506 C produced death of only 1/6 rats, 1/4 rabbits, 0/5 mice, and 0/4 guinea pigs after an exposure of 36 minutes. Pyrolysis at a rate of 1.67 g/hour at 805 C produced death of 3/6 rats, 2/4 rabbits, 2/5 mice, and 0/4 guinea pigs after an exposure of 33 minutes.
Pyrolysis of FL at 482 C at rates of 3.18 g/hour or 1.02 g/hour killed no animals after exposures of 2 and 7 hours, respectively [67].
Pyrolysis of KF at 805 C at a rate of 0.88 g/hour killed no mice, rats, guinea pigs or rabbits after an exposure of 34 minutes [67].
The Treon et al [67] data are difficult to interpret in a comparative way because of the various conditions of pyrolysis and exposure of the experimental animals. A higher temperature of pyrolysis seems generally to produce more toxic pyrolysis products. The observations that species sensitivity to the pyrolysis products of the three polymers varies not only with the polymer but also with the conditions of pyrolysis indicate that, under similiar conditions, the two polymers of PCTFE probably yield different pyrolytic products, despite their monomeric identity, and that a single polymer yields different products under different conditions of pyrolysis. Pyrolysis in the presence of an inert gas seems to be less hazardous than that in the presence of air. The pyrolysis products from FL may be less hazardous than those from either PTFE or K F , but this conclusion cannot be supported satisfactorily by the data provided. Good comparative data would be useful.
Zapp [68] gave a little further information about the pyrolysis of PCTFE, finding that it, like PTFE, undergoes degradation when exposed to a temperature of 300 C but not when exposed to one of 250 C.
Birnbaum et al [14] exposed rats to the products of pyrolysis of PCTFE heated to temperatures of either 375 C or 400 C, determining the rate at which a rod of PCTFE had to be fed into a pipe heated to the desired temperature in an electric furnace to maintain an LC50 of pyrolysis products within an exposure chamber fed with air passed through the furnace at a rate of 4 liters/minute. The exposure periods were either 1 or 3 hours.
One-hour exposures at 375 C did not result in sufficient mortality to yield valid estimates of the LC50 at the highest rate of feed of the PCTFE rod into the heated tube. The 3-hour exposure to the products of pyrolysis at this temperature yielded an estimate that 31.5 g/hr of the polymer had to be subjected to pyrolysis to maintain an LC50 of the pyrolysis products within the chamber. Exposure for 1 hour at the higher temperature of pyrolysis (400 C) yielded an estimate that 23.5 g/hr of the polymer had to be pyrolyzed at this temperature to maintain an LC50 of the pyrolysis products within the chamber. The particles in the pyrolysis products ranged in diameter from about 0.15 to 3.0 jiim, 85% of the particles being less than 1 /nm in diameter and 99% less than 2 /um. Infrared and mass spectrometers were used to obtain some idea of the molecular species present in the exposure atmosphere; these two techniques indicated the presence of perhaps as many as 13 different materials in the pyrolysis products.
Comparatively little information about pyrolysis products of fluorocarbon polymers other than PTFE and PCTFE has been found. Clayton [57] reported studies of the inhalation toxicities of two samples of a copolymer of vinylidene fluoride and hexafluoropropylene for the rat. One Hydrogen fluoride was the only pyrolysis product whose concentration in the exposure chamber seemed to be related to mortality in the exposed rats. The principal effects of the exposure on rats were irritation of the respiratory tract, pulmonary edema, hemorrhage in the lungs, congestion of the liver, vacuolation of hepatocytes, tubular necrosis in the kidneys, and proteinaceous material in the renal tubules.
Ehrsam [70] has shown that the pyrolysis products of PTFE are more toxic to birds than to mice or guinea pigs. Similarly, Griffith et al [71] has reported that Japanese quail and parakeets were killed by effluvia from a frying pan coated with PTFE and heated to 330 C and 280 C, respectively, whereas rats appeared not to be harmed until the pan was heated to 450 C . Some investigators [72,73] have reported that subcutaneous implantation of PTFE into rats resulted in the formation of fibrosarcomas.
However, Bryson and Bischoff [74] were unable to duplicate these results.
# Correlation of Exposure and Effects
The most frequently reported effect of workplace exposure to the pyrolysis products of PTFE is an influenza-like syndrome designated polymer fume fever [10,34,37,[39][40][41].
No effects of workplace exposure to the pyrolysis products of other fluorocarbon polymers were found in the literature.
The major signs and symptoms associated with polymer fume fever are chest discomfort [10,23,34,[36][37][38][39][40][41], fever [10,23,36,39,40], leukocytosis [10,36], headache [23,34,36,37,40,41], chills [10,23,34,[36][37][38]40,41], achy feeling [10,23,34,36,38], and weakness [10,23,36].
Complete recovery usually occurred within 12-48 hours after the exposure ended [10,23,34].
Other effects reported in humans exposed to the pyrolysis products of PTFE were nausea [40], malaise [10,36], congested throat and pharynx [37], basal rales of the lungs [39,40], pulmonary edema [39,40], hyperpnea [10,40], and increased pulse rate [40],
Damage to the respiratory tract, occasionally severe enough to result in pulmonary edema, was found in humans exposed to the pyrolysis products of PTFE [10,34,39,40] and in animals exposed to the pyrolysis products of PTFE [7,55], PCTFE [14], VF2-HFP [6,23], VF2-HFP-TFE [6,23], and E-CTFE [69]. Effects such as leukocytosis and elevated temperature were difficult to produce in animals [49,57,65].
Polymer fume fever has resulted when there was an insufficient amount of ventilation in molding operations [10,47] and when PTFE processing temperatures were not controlled because of malfunctioning thermostats [10]. Polymer fume fever has also resulted from the smoking of PTFEcontaminated tobacco [22,23,34]. As little as 0.3 mg of a TFE fluorocarbon telomer added to the cigarettes of volunteers produced polymer fume fever Without these data, it is difficult to determine whether the authors' conclusions were justified.
Clayton et al [64] also concluded that the toxicity of the pyrolysis products of PTFE heated at 350 C was caused by a particulate. Seven of 36 (19.4%) rats were killed when the pyrolysis products of PTFE heated at 350 C were filtered (Millipore filter, 0.45 jum pore size). The expected mortality was 100%. When PTFE was pyrolyzed at 325 C, the unfiltered fume killed 6/16 rats (37.5%). The same pyrolysis products after filtration through a filter of 0.45 ¡m. pore size killed 0/8 rats. These results are in agreement with the findings of Waritz and Kwon [7], since filtration of the pyrolysis products reduced mortality. However, Waritz and Kwon [7] reported that the unfiltered pyrolysis products of PTFE heated at 400 C were not lethal to rats. This discrepancy may be related to the finding of Clayton et al [64] that low-molecular-weight PTFE yielded pyrolysis products more toxic than those from high-molecular-weight PTFE; Clayton et al and Waritz and Kwon perhaps used samples of PTFE of different molecular weights.
In animal studies, Scheel [69] found a correlation of lethality with the amount of hydrolyzable fluoride produced when E-CTFE was pyrolyzed at 550 C, but the amount of hydrolyzable fluoride produced was not correlated with the amount of E-CTFE pyrolyzed.
Other investigators found no correlation of lethality with the amount of hydrolyzable fluoride produced by pyrolysis of PCTFE [14], VF2-HFP [6], or VF2-HFP-TFE [6].
Waritz and Kwon [7] reported that traces of perfluoroisobutylene (PFIB) were produced when PTFE was pyrolyzed at 475 C and that pyrolysis at 480 C produced 5 ppm of PFIB. Clayton [57] has reported that the LC50 for PFIB in rats after a 6-hour exposure was 0.5 ppm. Although PFIB appears to be the most toxic gas produced by the pyrolysis of PTFE, no studies correlating the concentration of PFIB with the toxicity of the pyrolysis products of PTFE were found in the literature.
In the absence of pertinent data, no useful correlation can be made between the type and extent of exposure and the degree of human intoxication produced by the decomposition products of fluorocarbon polymers. However, compiling and summarizing the signs and symptoms reported in humans is a useful first step in the attempt to understand the adverse effects of these substances. dust counts were of the order of 1,000 particles/cc with diameters smaller than 5 ¡m , 15 particles/cc with diameters between 0.5 and 1.0 ¿urn, and 1 particle/cc with a diameter greater than 1 jum.
# Carcinogenicity, Mutagenicity, Teratogenicity, and Effects on Reproduction
Adams [22] sampled air in a finishing room where PTFE was dried, sifted, and packed. At collection sites close to ovens which were heated occasionally to above 300 C, he found concentrations of hydrogen fluoride up to 6 ppm. This assumption was used because the toxic effects of decomposition products of PTFE are associated with a particulate substance which is a small fraction of the total decomposition products. Waritz and Kwon [7] observed that test animals died after being exposed to the particles at a concentration of 1.4 mg/cu m (equivalent to 1.2 ppm by weight at ambient conditions). NIOSH maintains that the most important feature of an exhaust ventilation system is its design. Guidance for designing a local exhaust ventilation system can be found in Industrial Ventilation-A Manual of Recommended Practice [78] and in Fundamentals Governing the Design and Operation of Local Exhaust Systems [79]. Ventilation systems of this type require regular inspection and maintenance to ensure effective operation.
Regularly scheduled inspections should include face-velocity measurements of the collecting hood and inspection of the air mover and collector.
In addition to providing adequate ventilation, it may be appropriate, under certain circumstances, to isolate a process or system in an especially designed enclosure to minimize exposure. Other control measures may be intentionally redundant temperature monitoring systems and alarms to signal harmful thermal excursions. In all extrusion processes, the handling precautions described above must be observed. As in sintering operations, the temperature to which the fluorocarbon polymer is subjected must not be allowed to exceed the manufacturer's recommended processing temperature, and an appropriate temperature cutout system must be used. Local exhaust ventilation must be installed at the orifice from which the melt is extruded to keep decomposition products from entering the work area. An appropriate alarm system must be incorporated into the exhaust ventilation system.
# Biologic Evaluation
In thermoforming, compression molding, and coining, and in all processes in which the temperature of the fluorocarbon polymer approaches its melting point, ovens must be fitted with exhaust ventilation and temperature-regulating systems. These systems must be equipped with appropriate alarms and must be serviced at regular intervals.
Coagulated dispersion polymers are usually processed by "paste extrusion." This involves mixing the fluorocarbon polymer with a lubricant, generally a volatile petroleum fraction. This use of flammable liquids adds a potential hazard. The lubricant may be removed in a drying oven or in a continuous oven constructed in series with the extruder and a sintering oven. Precautions must be taken to minimize the risk of forming explosive mixtures of vapor and air and to prevent their ignition if they should form. These precautions might include controlling the rate of solvent removal, increasing the exhaust ventilation in the solvent-removal area, and locating the solvent-removal zone apart from the sintering area.
If flammable vapor enters the sintering oven, it probably will ignite.
Removal of all traces of the lubricant before sintering is necessary. As in sintering operations, appropriate temperature-regulating and exhaustventilation systems should be used on ovens where solvent removal takes place. Fire-extinguishing equipment should also be readily available. (29 CFR 1910(29 CFR .1000).
# Basis for the Recommended Standard
The most frequently reported effect of exposure in the workplace to the pyrolysis products of fluorocarbon polymers has been an influenza-like syndrome, polymer fume fever, which was described first by Harris [10] in 1951 and subsequently by several other investigators [34,37,[39][40][41]. The major signs and symptoms associated with polymer fume fever are chest discomfort [10,23,34,[36][37][38][39][40][41], fever [10,23,36,[38][39][40], leukocytosis [10,36], Other effects found in humans exposed to the pyrolysis products of fluorocarbon polymers were nausea [40], malaise [10,23,36], congested throat and pharynx [37], rales in the bases of the lungs [39,40], pulmonary edema [39,40], hyperpnea [40], and increased pulse rate [40]. Respiratory irritation and pulmonary edema have been reported in humans [34,37,39,40] and animals [6,7,14,23,55,69] exposed to the pyrolysis products of fluorocarbon polymers.
No reports of serious injury or of long-term effects of polymer fume fever were found in the literature.
The syndrome outlined above has been described most frequently as a result of exposure to fumes from heated PTFE. Since there are now a number of other fluorinated polymers whose breakdown products are almost entirely unidentified and untested for toxicity, there seems to be no basis for attempting to set an occupational exposure limit that will apply to breakdown products of fluorinated polymers in general. Accordingly, NIOSH suggests that exposure of employees to breakdown products of polymers of fluorinated monomers be limited to the greatest extent possible by designing production processes to restrict heating of these polymers to the lowest temperature that permits the desired operation, to limit access of air and oxygen to heated polymers to the greatest extent feasible, and to take the greatest possible advantage of local ventilation of sites from which polymer fumes may enter the occupational environment. Such steps, in conjunction with effective general ventilation of the workplace and good work practices, should go far toward protecting employees from deleterious effects from breakdown products of the materials with which they work.
Although these deleterious effects are more likely to be incapacitating than dangerous, their avoidance is certainly desirable.
# (c) Medical
Several studies on humans [34,37,39,40] and animals [6,7,14,23,55,69] showed that exposure to fluorocarbon polymer decomposition products produced respiratory irritation and pulmonary edema. Chemical substances should be listed according to their complete name derived from a recognized system of nomenclature.
Where possible, avoid using common names and general class names such as "aromatic amine,"
"safety solvent," or "aliphatic hydrocarbon" when the specific name is known.
The "%" may be the approximate percentage by weight or volume (indicate basis) which each hazardous ingredient of the mixture bears to the whole mixture. This may be indicated as a range or maximum amount, ie, "10-40% vol" or "10% max wt" to avoid disclosure of trade secrets.
Toxic hazard data shall be stated in terms of concentration, mode of exposure or test, and animal used, eg, "100 ppm LC50-rat," "25 mg/kg LD50skin-rabbit," "75 ppm LC man," or "permissible exposure from 29 CFR The "Health Hazard Data" should be a combined estimate of the hazard of the total product. This can be expressed as a TWA concentration, as a permissible exposure, or by some other indication of an acceptable standard. Other data are acceptable, such as lowest LD50 if multiple components are involved.
Under "Routes of Exposure," comments in each category should reflect the potential hazard from absorption by the route in question. Comments should indicate the severity of the effect and the basis for the statement if possible. The basis might be animal studies, analogy with similar products, or human experiences. Comments such as "yes" or "possible" are not helpful. Typical comments might be:
Skin Contact-single short contact, no adverse effects likely; prolonged or repeated contact, possibly mild irritation.
Eye Contact-some pain and mild transient irritation; no corneal scarring.
"Emergency and First Aid Procedures" should be written in lay language and should primarily represent first-aid treatment that could be provided by paramedical personnel or individuals trained in first aid.
Information in the "Notes to Physician" section should include any special medical information which would be of assistance to an attending physician including required or recommended preplacement and periodic medical examinations, diagnostic procedures, and medical management of overexposed employees. Respirators shall be specified as to type and NIOSH or US Bureau of Mines approval class, ie, "Supplied air," "Organic vapor canister," etc.
Protective equipment must be specified as to type and materials of construction.
# C E N T E R F O R D I S E A S E C O N T R O L N A T ' O N A L I N S T I T U T E F O R O C C U P A T I O N A L S A F E T Y A N D H E A L T H R O B E R T A T A F T L A B O R
# MATERIAL SAFETY DATA SHEET 1 PRODUCT IDENTIFICATION M A N U F A C T U R E R S N A M E R E G U L A R T E LE P H O N E NO
# % V O L A T IL E S BY V O L E V A P O R A T IO N R A TE »BUTYL A C E T A T E 11 A P P E A R A N C E A N O ODOR
# IV FIRE AND EXPLOSION DATA
| None | None |
583b2895e35a5394ceaaad64724eb99bebd5aa60 | cdc | None | department of health and human services department of health and human services department of health and human services department of health and human services department of health and human services Centers for Disease Control and Prevention Centers for Disease Control and Prevention Centers for Disease Control and Prevention Centers for Disease Control and Prevention Centers for Disease Control and Prevention INSIDE 789 Update: Influenza Activity -United States and Worldwide, 2006-07 Season, and Composition of the 2007-08 Influenza Vaccine 794 Notices to Readers 796 QuickStats - <100,000 platelets/mm 3 . FIGURE 1. Jurisdictions affected by dengue fever outbreak -Texas-Mexico border,# Dengue Hemorrhagic Fever -U.S.-Mexico Border, 2005
Dengue fever is a mosquito-transmitted disease caused by any of four closely related virus serotypes (DEN-1, DEN-2, DEN-3, and DEN-4) of the genus Flavivirus. Infection with one of these serotypes provides lifelong immunity to the infecting serotype only. Therefore, persons can acquire a second dengue infection from a different serotype, and second infections place them at greater risk for dengue hemorrhagic fever (DHF), the more severe form of the disease (1). DHF is characterized by bleeding manifestations, thrombocytopenia,- and increased vascular permeability that can lead to life-threatening shock (2). In south Texas, near the border with Mexico, sporadic, locally acquired outbreaks of dengue fever have been reported previously; however, on the Texas side of the border, these outbreaks have not included recognized cases of locally acquired DHF in persons native to the area. In July 2005, a case of DHF was reported in a resident of Brownsville, Texas (Figure 1). In August 2005, health authorities in the neigh-boring state of Tamaulipas, Mexico, reported an ongoing dengue outbreak with 1,251 cases of dengue fever, including 223 cases (17.8%) of DHF. To characterize this dengue outbreak, the Texas Department of State Health Services (TDSHS), Mexican health authorities, and CDC conducted a clinical and epidemiologic investigation. This report summarizes the results of that investigation, which determined that the percentage of DHF cases associated with dengue fever outbreaks at the Texas-Tamaulipas border has increased. Health-care providers along the U.S. border with Mexico should be vigilant for DHF and familiar with its diagnosis and management to reduce the number of severe illnesses and deaths associated with outbreaks of dengue fever.
# Autochthonous DHF Case Report
On June 24, 2005, a woman from Brownsville, Texas, had acute onset of fever, chills, headache, nausea, vomiting, abdominal pain, arthralgia, and myalgia. As a youth, the patient had resided across the border in the city of Matamoros in Tamaulipas, Mexico; however, she had been a Brownsville resident for 16 years with the exception of 1 year in Houston, Texas. After she became ill, the woman crossed the border into Matamoros for the first time in approximately 2 months, where she visited a clinician and was given antibiotics. On June 28, the woman was hospitalized in Matamoros with a diagnosis of probable dengue fever and urinary tract infection. During her 3-day hospitalization in Mexico, she had thrombocytopenia (62,000 platelets/mm 3 ) but no hemorrhagic manifestations; she was treated with fluids and antibiotics and discharged.
On July 1, the woman reentered the United States and sought treatment for continued fever, chills, vomiting, and abdominal pain. She was admitted to a hospital in Brownsville, Texas, where her blood pressure was 94/70 mm Hg, and laboratory testing indicated proteinuria, hematuria, and a further decrease in platelet count (43,000/mm 3 ). She was given antibiotics for suspected partially treated urinary tract infection and fluids for dehydration. During her hospital stay, the patient's platelet count dropped to 39,000/ mm 3 and albumin to 2.9 g/100 mL; a fecal occult blood test was positive, and pleural effusion was noted on ultrasound. Upon discharge on July 4, her platelet count had increased to 118,000/mm 3 . The woman was discharged with a diagnosis of possible murine typhus or viral infection and instructions to take a course of doxycycline.
Although the woman's clinical characteristics (i.e., acute fever, platelet count <100,000/mm 3 , evidence of bleeding and plasma leakage) were consistent with World Health Organization (WHO) criteria for DHF (Box) (2), dengue was not diagnosed at the Brownsville hospital. Subsequently, results from a July 3
# BOX. World Health Organization case definition for dengue hemorrhagic fever
The following must all be present: - Fever, or history of acute fever, lasting 2-7 days, occasionally biphasic. - Hemorrhagic tendencies, evidenced by at least one of the following: -a positive tourniquet test; -petechiae, ecchymoses, or purpura; -bleeding from the mucosa, gastrointestinal tract, injection sites, or other locations; -hematemesis or melena.
- Thrombocytopenia (<100,000 platelets/mm 3 ).
- Evidence of plasma leakage because of increased vascular permeability, manifested by at least one of the following: -an increase in the hematocrit >20% above average for age, sex, and population; -a decrease in the hematocrit following volumereplacement treatment >20% of baseline; -signs of plasma leakage such as pleural effusion, ascites, and hypoproteinemia.
treated at three hospitals in Matamoros. Fifty-nine percent of the patients were female. Ages ranged from 30 to 76 years (median 47.5 years) among the Cameron County cases and from 7 to 70 years (median 36.0 years) among the Matamoros cases. In addition to fever, 82% had myalgia, 78% headache, 41% abdominal pain, 23% rash, and 19% had underlying chronic diseases. No fatalities were recorded. A total of 16 (64.0%) of the 25 dengue cases from Cameron County and 34 (32.7%) of the 104 cases from Matamoros met WHO criteria for DHF (Box). Eleven of the 50 DHF cases, including one from Cameron County, were classified as WHO grade III, or dengue shock syndrome, with early or mild evidence of hypotension or shock. The remaining 39 DHF cases were classified as WHO grade II. ¶ Serosurveys. Because many dengue infections are asymptomatic, and most ill persons likely do not seek medical attention, investigators conducted serosurveys to assess the incidence of dengue infection in the populations of Matamoros and Brownsville. Serosurveys also enable estimation of the population susceptible to second dengue infections and DHF. For the serosurveys, a two-stage cluster design was used to obtain a representative sample of households from Brownsville and Matamoros (6). Thirty census tracts were selected systematically from each city after stratifying by income. Four households were selected from each census tract after mapping and selecting a random start point and random direction for sampling.
At each participating household, all residents present and aged >5 years were asked to provide a blood sample and demographic information. Serum samples were tested for IgM and IgG antibodies to dengue virus by ELISA. The seroincidence of recent dengue infection was defined by IgM antibodies >0.2 optical density (OD). Seroprevalence was defined as the presence of IgG antibodies >1:40. Data were weighted to reflect probability of selection, taking into account the population and numbers of households per census tract and size of household.
In Matamoros, 240 households were visited during December 5-10, and 143 (59.6%) had residents at home. Blood samples were obtained from 131 persons in 111 homes. Of these samples, 30 were anti-dengue IgM posi-serum sample from the woman obtained by the regional Texas Border Infectious Disease Surveillance (BIDS) project tested positive for dengue immunoglobulin M (IgM) by enzyme-linked immunosorbent assay (ELISA) and had an elevated titer of immunoglobulin G (IgG) antibodies to dengue fever (1:655,350); this was interpreted as indicative of a secondary dengue infection (1).
# Outbreak Investigation and Response
Dengue fever case finding. On August 27, 2005, Tamaulipas State Health Services reported to TDSHS that an outbreak of dengue fever in the border state had grown to 1,251 cases that met the Mexico case definition (i.e., fever and at least two of the following symptoms: headache, myalgia, arthralgia, and rash). Using WHO criteria for DHF, Tamaulipas health authorities had classified 223 (17.8%) of the cases as DHF, an increase in the percentage classified as DHF from 2000-2004, when 541 dengue fever cases were reported, including 20 cases (3.7%) classified as DHF. † In October, investigators in Texas and Tamaulipas began conducting expanded outbreak case finding, including active surveillance in local hospitals, with laboratory testing encouraged for patients with undifferentiated fever as part of the BIDS project. In Cameron County, Texas, where Brownsville is the county seat, TDSHS identified 24 additional cases of laboratory-confirmed dengue fever § , including two additional cases of locally transmitted dengue fever and 22 cases associated with travel to Mexico; the cases had been reported during August-November (Figure 2). The serotype most commonly associated with the outbreak was identified as DEN-2 (i.e., 27 of 28 viral isolates in Tamaulipas). Molecular analysis of isolates at CDC indicated that the circulating strain of DEN-2 was one previously associated with DHF in the Americas region (4,5). Plotting reports of cases by week determined that the border outbreak peaked in October and substantially subsided by December (Figure 2). DHF case finding. In December, investigators reviewed medical records of 129 patients who had been hospitalized and reported to public health authorities with both clinical and laboratory evidence of dengue fever, including 25 persons treated at three Cameron County hospitals and 104 ¶ DHF is classified into four grades of severity; grades III and IV are considered to be dengue shock syndrome. Grade I: Fever accompanied by nonspecific constitutional symptoms; the only hemorrhagic manifestation is a positive tourniquet test and/or easy bruising. Grade II: Spontaneous bleeding in addition to the manifestations of Grade I patients, usually in the forms of skin or other hemorrhages. Grade III: Circulatory failure manifested by a rapid, weak pulse and narrowing of pulse pressure or hypotension, with the presence of cold, clammy skin and restlessness. Grade IV: Profound shock with undetectable blood pressure or pulse (2). (3,8), but locally acquired DHF has been reported only recently (9). The first report of locally acquired DHF in Texas, published in 2004, described a fatal case involving a woman originally from Southeast Asia (9). She presumably had acquired her first dengue infection in Asia and her second dengue infection in Val Verde, Texas, near the U.S.-Mexico border. However, the DHF case described in this report is the first in a Texas resident who was native to the U.S.-Mexico border area. Case-finding activities during the dengue outbreak identified 15 additional DHF cases on the Texas side of the border.
Entomologic, serologic and virologic conditions are now such that locally acquired DHF can occur in south Texas. The principal dengue vector, the Aedes aegypti mosquito, is well established in south Texas, as is Aedes albopictus, which also is capable of transmitting dengue (7,10;TDSHS, unpublished data, 2007). The finding that 38% of surveyed Brownsville residents have IgG antibodies to dengue indicates that a substantial proportion of the city population has been infected with the dengue virus and might be more susceptible to DHF if they receive a second infection with a heterologous dengue serotype. The presence in Brownsville of multiple dengue serotypes since 1980 might increase the likelihood for secondary dengue infections from a different serotype and increase the risk for DHF.
The findings in this report are subject to at least two limitations. First, more comprehensive laboratory testing
# United States
The national percentage of respiratory specimens testing positive for influenza and the proportion of outpatient visits to sentinel providers for influenza-like illness (ILI)- peaked in mid-February. Although influenza A (H1) viruses were most commonly isolated overall, influenza A (H3) viruses were more frequently identified than influenza A (H1) viruses from early March through May. A small number of influenza B viruses also were identified. 1). Of these, 18,817 (79.2%) were influenza A viruses and 4,936 (20.8%) were influenza B viruses. Among the influenza A viruses, 6,280 (33.4%) were subtyped; 3,912 (62.3%) were influenza A (H1) viruses and 2,368 (37.7%) were influenza A (H3) viruses. The proportion of specimens testing positive for influenza first exceeded 10% during the week ending December 23, 2006 (week 51), peaked at 28.0% during the week ending February 10, 2007 (week 6), and declined to less than 10% during the week ending April 28, 2007 (week 17). The proportion was above 10% positive for 14 consecutive weeks. The peak percentage of specimens testing positive for influenza during the previous three seasons ranged from 22.6% to 34.7%, and the peak occurred during early December to early March (1;CDC, unpublished data, 2007). During the previous three influenza seasons, the number of consecutive weeks during which more than 10% of specimens tested positive for influenza ranged from 13 to 17 weeks (1;CDC, unpublished data, 2007).
# Viral Surveillance
# Composition of the Influenza Vaccine for the 2007-08 Season
# Antigenic Characterization
# Influenza-Like Illness (ILI) Surveillance
The weekly percentage of patient visits to U.S. sentinel providers for ILI exceeded or was at baseline levels (2.1%) † during the weeks ending December 16, 2006-March 24, 2007 (weeks 50-12) and peaked twice, once at 3.0% for the week ending December 30, 2006 (week 52), and again at 3.5% for the week ending February 17, 2007 (week 7) (Figure 2). The increase in the percentage of patient visits for ILI during the week ending December 30, 2006 (week 52) might have been influenced by a reduction in routine health-care visits during the holiday season, as has occurred in previous seasons. During the previous three influenza seasons, the peak percentage of patient visits for ILI has ranged from 3.3% to 7.6% and the peak occurred during late December to mid-February (1; CDC, unpublished data, 2007).
# State-Specific Activity Levels
State and territorial epidemiologists report the geographic distribution of influenza in their state through a weekly influenza activity code. The geographic distribution of influenza activity peaked during the week ending February 24, 2007 (week 8), when 25 states reported widespread activity and 19 states reported regional activity. § Forty-one states reported widespread influenza activity at least once during the 2006-07 season. No states reported widespread influenza activity during the weeks ending April 21-May 19, 2007 (weeks 16-20). The peak number of states reporting widespread or regional activity during the previous three seasons ranged from 41 to 50 states (1; CDC, unpublished data, 2007). Percentage † The national baseline is the mean percentage of visits for ILI during noninfluenza weeks for the previous three seasons plus two standard deviations. Noninfluenza weeks are those in which less than 10% of laboratory specimens are positive for influenza. National percentages of patient visits for ILI are weighted on the basis of state population. § Levels of activity are 1) no activity; 2) sporadic: isolated laboratory-confirmed influenza cases or a laboratory-confirmed outbreak in one institution, with no increase in ILI activity; 3) local: increased ILI , or at least two institutional outbreaks (ILI or laboratory-confirmed influenza) in one region with recent laboratory evidence of influenza in that region; virus activity no greater than sporadic in other regions; 4) regional: increased ILI activity or institutional outbreaks (ILI or laboratory-confirmed influenza) in at least two but less than half of the regions in the state with recent laboratory evidence of influenza in those regions; and 5) widespread: increased ILI activity or institutional outbreaks (ILI or laboratory-confirmed influenza) in at least half the regions in the state with recent laboratory evidence of influenza in the state.
# Influenza-Associated Pediatric Hospitalization
# MMWR August 10, 2007
systems likely result from different case-finding methods, the diagnostic tests used, and the populations monitored. ¶
# Pneumonia-and Influenza-Related Mortality
During the 2006-07 influenza season, the percentage of deaths attributed to pneumonia and influenza (P&I) did not exceed the epidemic threshold in the 122 Cities Mortality Reporting System (Figure 3). The percentage of P&I deaths peaked three times, once at 7.5% during the week ending January 20, 2007 (week 3), once at 7.7% during the week ending February 24, 2007 (week 8), and again at 7.5% during the week ending March 24, 2007 (week 12). During the previous three influenza seasons, the peak percentage of P&I deaths ranged from 7.8% to 10.4%, and the total number of weeks above the epidemic threshold ranged from one to 16 (1; CDC, unpublished data, 2007).
# Influenza-Associated Pediatric Mortality
As of August 6, 2007, among persons aged 6 months for whom vaccination status was known, 50 (94%) had not been vaccinated against influenza. These data are provisional.
# Worldwide
During the 2006-07 influenza season, influenza A (H1), A (H3), and B viruses cocirculated worldwide. In Africa, small numbers of influenza A and B viruses were reported. In Europe and Asia, influenza A (H3) viruses were identified most frequently, but influenza A (H1) viruses circulated at low levels. Influenza B viruses circulated at lower levels overall in Asia and Europe but predominated in some countries.
# Human Infections with Avian Influenza A (H5N1) Viruses
From December 1, 2003, through July 25, 2007, a total of 319 human cases of avian influenza A (H5N1) infection were reported to WHO (2). Of these, 192 (60%) were fatal (Table ). All cases were reported from Asia (Azerbaijan, Cambodia, China, Indonesia, Iraq, Laos, Thailand, Turkey, and Viet Nam) and Africa (Djibouti, Egypt, and Nigeria). To date, no human case of avian influenza A (H5N1) virus infection has been identified in the United States. At the June 2007 Annual Meeting of the Council of State and Territorial Epidemiologists (CSTE), members voted to ratify a position statement adopted by the CSTE Executive Committee in January 2007 that adds human infections with novel influenza A viruses to the list of nationally notifiable diseases and conditions reportable to the National Notifiable Disease Surveillance System. Novel influenza A viruses are defined as those isolated from a human but subtyped as nonhuman, or those that cannot be subtyped by standard methods. Human infections with novel influenza A viruses that can be transmitted from person-toperson might signal the beginning of an influenza pandemic. Rapid reporting of human infections with novel influenza A viruses will facilitate prompt detection and characterization of influenza A viruses with pandemic potential and accelerate implementation of effective public health responses. In addition, influenza-associated pediatric deaths were maintained as a nationally notifiable disease reportable to the National Notifiable Disease Surveillance System.
In May 2007, health authorities in the United Kingdom identified four persons, two in Wales and two in northwest England, who were infected with a low pathogenic avian influenza A (H7N2) virus (4). All four persons had been exposed to infected poultry at a farm in Wales; limited evidence of human-to-human transmission has been associated with low pathogenic avian influenza viruses such as influenza A (H7N2) virus (4). The United Kingdom inci- (1). Background information regarding meningococcal disease and the vaccine, including a discussion of duration of protection and use of the vaccine for outbreak control, has been published previously (1).
In June 2007, ACIP revised its recommendation to include routine vaccination of all persons aged 11-18 years with 1 dose of MCV4 at the earliest opportunity. Persons aged 11-12 years should be routinely vaccinated at the 11-12 years health-care visit as recommended by ACIP (2). ACIP continues to recommend routine vaccination for persons aged 19-55 years who are at increased risk for meningococcal disease: college freshmen living in dormitories, microbiologists routinely exposed to isolates of Neisseria meningitidis, military recruits, travelers to or residents of countries in which N. meningitidis meningitis is hyperendemic or epidemic, persons with terminal complement component deficiencies, and persons with anatomic or functional asplenia.
The ACIP goal is routine vaccination of all adolescents with MCV4 beginning at age 11 years. ACIP and partner organizations, including the American Academy of Pediatrics, American Academy of Family Physicians, American Medical Association, and Society for Adolescent Medicine, recommend a health-care visit for children aged 11-12 years to receive recommended vaccinations and indicated preventive services. This visit is the optimal time for adolescents to receive MCV4. In addition, because the incidence of meningococcal disease increases during adolescence, health-care providers should vaccinate previously unvaccinated persons aged 11-18 years with MCV4 at the earliest possible health-care visit. College freshmen living in dormitories are at increased risk for meningococcal disease and should be vaccinated with MCV4 before college entry if they have not been vaccinated previously. Because of difficulties in targeting freshmen in dormitories, colleges may elect to target their vaccination campaigns to all matriculating freshmen (1).
The ACIP meningococcal vaccine workgroup reviewed updated data on MCV4 use and supply projections and data presented previously on the epidemiology of meningococcal disease, safety, and the cost-effectiveness of MCV vaccination strategies. On the basis of these data, expert opinion of the workgroup members, and feedback from partner organizations, the workgroup revised the MCV4 recommendations, which were approved by ACIP at the June 2007 meeting.
The 2005 ACIP MCV4 recommendation was influenced by concern that implementation of MCV4 recommendations might be hindered by reduced vaccine supply during the first few years of production. In 2005 and 2006, peaks in demand were observed during the months when children were returning to school after summer vacation, leading to limited vaccine availability (3,4). However, as of June 2007, ACIP expects supply of MCV4 to be sufficient to meet increased vaccine demand resulting from the revised recommendations. ACIP anticipates that recommending vaccination of all persons aged 11-18 years will improve MCV4 vaccination coverage in this age group and simplify provider decisions to vaccinate.
ACIP encourages health-care providers to vaccinate with MCV4 throughout the year to minimize seasonal increases in demand during July and August when students prepare to return to school from summer vacation. Vaccine providers should administer MCV4 and Tdap (tetanus toxoid, reduced diphtheria toxoid and acellular pertussis) vaccine to persons aged 11-18 years during the same visit if both vaccines are indicated and available. If simultaneous vaccination is not feasible (e.g., a vaccine is not available), MCV4 and Tdap can be administered using any order of administration (5). When making decisions about timing of vaccination, providers should consider that eligibility for the Vaccines for Children Program ends at age 19 years.
Guillain-Barré syndrome (GBS) has been associated with receipt of MCV4 (6). Persons with a history of GBS might be at increased risk for postvaccination GBS; therefore, a history of GBS is a relative contraindication to receiving MCV4. Persons recommended to receive meningococcal vaccination who have a history of GBS (or their parents) should discuss the decision to be vaccinated with their health-care provider (6). Meningococcal polysaccharide vaccine (MPSV4) is an acceptable alternative for short-term protection against meningococcal disease (3-5 years). Providers who have questions about ordering MCV4 or MPSV4 may contact Sanofi Pasteur by telephone at 1-800-VAC-CINE or online at . Organizations are responsible for setting up their own viewing locations and are encouraged to register their locations as soon as possible so that potential viewers can access information online. Additional information regarding the broadcast and directions for establishing and registering a viewing location are available at npin-broadcast.org. The broadcast will be available for 3 years after its initial airing at . DVDs can be ordered by telephone, 800-458-5231. Among both men and women, non-Hispanic blacks (51.6% of men and 53.5% of women) were more likely to report ever being tested for HIV than Hispanics (35.7% of men and 46.1% of women) and non-Hispanic whites (30.5% of men and 33.5% of women). Overall, women (37.8%) were more likely than men (33.7%) to report ever being tested for HIV.
# Notice to Readers
# Satellite Broadcast and Webcast: Current Challenges and Successes in HIV Prevention with Hispanics/Latinos
2 0 2 7 1 2 0 1 2 - - 0 1 3 1 Montana § - 0 1 1 - - 0 1 3 1 - 0 1 1 3 Nevada § - 0 2 5 1 - 0 1 2 2 - 0 1 3 4 New Mexico § - 0 0 - 3 - 0 1 1 4 - 0 1 2 2 Utah - 0 1 2 2 - 0 3 9 8 - 0 2 8 5 Wyoming § - 0 0 - 1 - 0 0 - - - 0 2 2 4 | department of health and human services department of health and human services department of health and human services department of health and human services department of health and human services Centers for Disease Control and Prevention Centers for Disease Control and Prevention Centers for Disease Control and Prevention Centers for Disease Control and Prevention Centers for Disease Control and Prevention INSIDE 789 Update: Influenza Activity -United States and Worldwide, 2006-07 Season, and Composition of the 2007-08 Influenza Vaccine 794 Notices to Readers 796 QuickStats * <100,000 platelets/mm 3 . FIGURE 1. Jurisdictions affected by dengue fever outbreak -Texas-Mexico border,# Dengue Hemorrhagic Fever -U.S.-Mexico Border, 2005
Dengue fever is a mosquito-transmitted disease caused by any of four closely related virus serotypes (DEN-1, DEN-2, DEN-3, and DEN-4) of the genus Flavivirus. Infection with one of these serotypes provides lifelong immunity to the infecting serotype only. Therefore, persons can acquire a second dengue infection from a different serotype, and second infections place them at greater risk for dengue hemorrhagic fever (DHF), the more severe form of the disease (1). DHF is characterized by bleeding manifestations, thrombocytopenia,* and increased vascular permeability that can lead to life-threatening shock (2). In south Texas, near the border with Mexico, sporadic, locally acquired outbreaks of dengue fever have been reported previously; however, on the Texas side of the border, these outbreaks have not included recognized cases of locally acquired DHF in persons native to the area. In July 2005, a case of DHF was reported in a resident of Brownsville, Texas (Figure 1). In August 2005, health authorities in the neigh-boring state of Tamaulipas, Mexico, reported an ongoing dengue outbreak with 1,251 cases of dengue fever, including 223 cases (17.8%) of DHF. To characterize this dengue outbreak, the Texas Department of State Health Services (TDSHS), Mexican health authorities, and CDC conducted a clinical and epidemiologic investigation. This report summarizes the results of that investigation, which determined that the percentage of DHF cases associated with dengue fever outbreaks at the Texas-Tamaulipas border has increased. Health-care providers along the U.S. border with Mexico should be vigilant for DHF and familiar with its diagnosis and management to reduce the number of severe illnesses and deaths associated with outbreaks of dengue fever.
# Autochthonous DHF Case Report
On June 24, 2005, a woman from Brownsville, Texas, had acute onset of fever, chills, headache, nausea, vomiting, abdominal pain, arthralgia, and myalgia. As a youth, the patient had resided across the border in the city of Matamoros in Tamaulipas, Mexico; however, she had been a Brownsville resident for 16 years with the exception of 1 year in Houston, Texas. After she became ill, the woman crossed the border into Matamoros for the first time in approximately 2 months, where she visited a clinician and was given antibiotics. On June 28, the woman was hospitalized in Matamoros with a diagnosis of probable dengue fever and urinary tract infection. During her 3-day hospitalization in Mexico, she had thrombocytopenia (62,000 platelets/mm 3 ) but no hemorrhagic manifestations; she was treated with fluids and antibiotics and discharged.
On July 1, the woman reentered the United States and sought treatment for continued fever, chills, vomiting, and abdominal pain. She was admitted to a hospital in Brownsville, Texas, where her blood pressure was 94/70 mm Hg, and laboratory testing indicated proteinuria, hematuria, and a further decrease in platelet count (43,000/mm 3 ). She was given antibiotics for suspected partially treated urinary tract infection and fluids for dehydration. During her hospital stay, the patient's platelet count dropped to 39,000/ mm 3 and albumin to 2.9 g/100 mL; a fecal occult blood test was positive, and pleural effusion was noted on ultrasound. Upon discharge on July 4, her platelet count had increased to 118,000/mm 3 . The woman was discharged with a diagnosis of possible murine typhus or viral infection and instructions to take a course of doxycycline.
Although the woman's clinical characteristics (i.e., acute fever, platelet count <100,000/mm 3 , evidence of bleeding [hematuria and fecal occult blood] and plasma leakage) were consistent with World Health Organization (WHO) criteria for DHF (Box) (2), dengue was not diagnosed at the Brownsville hospital. Subsequently, results from a July 3
# BOX. World Health Organization case definition for dengue hemorrhagic fever
The following must all be present: • Fever, or history of acute fever, lasting 2-7 days, occasionally biphasic. • Hemorrhagic tendencies, evidenced by at least one of the following: -a positive tourniquet test; -petechiae, ecchymoses, or purpura; -bleeding from the mucosa, gastrointestinal tract, injection sites, or other locations; -hematemesis or melena.
• Thrombocytopenia (<100,000 platelets/mm 3 ).
• Evidence of plasma leakage because of increased vascular permeability, manifested by at least one of the following: -an increase in the hematocrit >20% above average for age, sex, and population; -a decrease in the hematocrit following volumereplacement treatment >20% of baseline; -signs of plasma leakage such as pleural effusion, ascites, and hypoproteinemia.
treated at three hospitals in Matamoros. Fifty-nine percent of the patients were female. Ages ranged from 30 to 76 years (median 47.5 years) among the Cameron County cases and from 7 to 70 years (median 36.0 years) among the Matamoros cases. In addition to fever, 82% had myalgia, 78% headache, 41% abdominal pain, 23% rash, and 19% had underlying chronic diseases. No fatalities were recorded. A total of 16 (64.0%) of the 25 dengue cases from Cameron County and 34 (32.7%) of the 104 cases from Matamoros met WHO criteria for DHF (Box). Eleven of the 50 DHF cases, including one from Cameron County, were classified as WHO grade III, or dengue shock syndrome, with early or mild evidence of hypotension or shock. The remaining 39 DHF cases were classified as WHO grade II. ¶ Serosurveys. Because many dengue infections are asymptomatic, and most ill persons likely do not seek medical attention, investigators conducted serosurveys to assess the incidence of dengue infection in the populations of Matamoros and Brownsville. Serosurveys also enable estimation of the population susceptible to second dengue infections and DHF. For the serosurveys, a two-stage cluster design was used to obtain a representative sample of households from Brownsville and Matamoros (6). Thirty census tracts were selected systematically from each city after stratifying by income. Four households were selected from each census tract after mapping and selecting a random start point and random direction for sampling.
At each participating household, all residents present and aged >5 years were asked to provide a blood sample and demographic information. Serum samples were tested for IgM and IgG antibodies to dengue virus by ELISA. The seroincidence of recent dengue infection was defined by IgM antibodies >0.2 optical density (OD). Seroprevalence was defined as the presence of IgG antibodies >1:40. Data were weighted to reflect probability of selection, taking into account the population and numbers of households per census tract and size of household.
In Matamoros, 240 households were visited during December 5-10, and 143 (59.6%) had residents at home. Blood samples were obtained from 131 persons in 111 homes. Of these samples, 30 were anti-dengue IgM posi-serum sample from the woman obtained by the regional Texas Border Infectious Disease Surveillance (BIDS) project tested positive for dengue immunoglobulin M (IgM) by enzyme-linked immunosorbent assay (ELISA) and had an elevated titer of immunoglobulin G (IgG) antibodies to dengue fever (1:655,350); this was interpreted as indicative of a secondary dengue infection (1).
# Outbreak Investigation and Response
Dengue fever case finding. On August 27, 2005, Tamaulipas State Health Services reported to TDSHS that an outbreak of dengue fever in the border state had grown to 1,251 cases that met the Mexico case definition (i.e., fever and at least two of the following symptoms: headache, myalgia, arthralgia, and rash). Using WHO criteria for DHF, Tamaulipas health authorities had classified 223 (17.8%) of the cases as DHF, an increase in the percentage classified as DHF from 2000-2004, when 541 dengue fever cases were reported, including 20 cases (3.7%) classified as DHF. † In October, investigators in Texas and Tamaulipas began conducting expanded outbreak case finding, including active surveillance in local hospitals, with laboratory testing encouraged for patients with undifferentiated fever as part of the BIDS project. In Cameron County, Texas, where Brownsville is the county seat, TDSHS identified 24 additional cases of laboratory-confirmed dengue fever § , including two additional cases of locally transmitted dengue fever and 22 cases associated with travel to Mexico; the cases had been reported during August-November (Figure 2). The serotype most commonly associated with the outbreak was identified as DEN-2 (i.e., 27 of 28 viral isolates in Tamaulipas). Molecular analysis of isolates at CDC indicated that the circulating strain of DEN-2 was one previously associated with DHF in the Americas region (4,5). Plotting reports of cases by week determined that the border outbreak peaked in October and substantially subsided by December (Figure 2). DHF case finding. In December, investigators reviewed medical records of 129 patients who had been hospitalized and reported to public health authorities with both clinical and laboratory evidence of dengue fever, including 25 persons treated at three Cameron County hospitals and 104 ¶ DHF is classified into four grades of severity; grades III and IV are considered to be dengue shock syndrome. Grade I: Fever accompanied by nonspecific constitutional symptoms; the only hemorrhagic manifestation is a positive tourniquet test and/or easy bruising. Grade II: Spontaneous bleeding in addition to the manifestations of Grade I patients, usually in the forms of skin or other hemorrhages. Grade III: Circulatory failure manifested by a rapid, weak pulse and narrowing of pulse pressure or hypotension, with the presence of cold, clammy skin and restlessness. Grade IV: Profound shock with undetectable blood pressure or pulse (2). (3,8), but locally acquired DHF has been reported only recently (9). The first report of locally acquired DHF in Texas, published in 2004, described a fatal case involving a woman originally from Southeast Asia (9). She presumably had acquired her first dengue infection in Asia and her second dengue infection in Val Verde, Texas, near the U.S.-Mexico border. However, the DHF case described in this report is the first in a Texas resident who was native to the U.S.-Mexico border area. Case-finding activities during the dengue outbreak identified 15 additional DHF cases on the Texas side of the border.
Entomologic, serologic and virologic conditions are now such that locally acquired DHF can occur in south Texas. The principal dengue vector, the Aedes aegypti mosquito, is well established in south Texas, as is Aedes albopictus, which also is capable of transmitting dengue (7,10;TDSHS, unpublished data, 2007). The finding that 38% of surveyed Brownsville residents have IgG antibodies to dengue indicates that a substantial proportion of the city population has been infected with the dengue virus and might be more susceptible to DHF if they receive a second infection with a heterologous dengue serotype. The presence in Brownsville of multiple dengue serotypes since 1980 might increase the likelihood for secondary dengue infections from a different serotype and increase the risk for DHF.
The findings in this report are subject to at least two limitations. First, more comprehensive laboratory testing
# United States
The national percentage of respiratory specimens testing positive for influenza and the proportion of outpatient visits to sentinel providers for influenza-like illness (ILI)* peaked in mid-February. Although influenza A (H1) viruses were most commonly isolated overall, influenza A (H3) viruses were more frequently identified than influenza A (H1) viruses from early March through May. A small number of influenza B viruses also were identified. 1). Of these, 18,817 (79.2%) were influenza A viruses and 4,936 (20.8%) were influenza B viruses. Among the influenza A viruses, 6,280 (33.4%) were subtyped; 3,912 (62.3%) were influenza A (H1) viruses and 2,368 (37.7%) were influenza A (H3) viruses. The proportion of specimens testing positive for influenza first exceeded 10% during the week ending December 23, 2006 (week 51), peaked at 28.0% during the week ending February 10, 2007 (week 6), and declined to less than 10% during the week ending April 28, 2007 (week 17). The proportion was above 10% positive for 14 consecutive weeks. The peak percentage of specimens testing positive for influenza during the previous three seasons ranged from 22.6% to 34.7%, and the peak occurred during early December to early March (1;CDC, unpublished data, 2007). During the previous three influenza seasons, the number of consecutive weeks during which more than 10% of specimens tested positive for influenza ranged from 13 to 17 weeks (1;CDC, unpublished data, 2007).
# Viral Surveillance
# Composition of the Influenza Vaccine for the 2007-08 Season
# Antigenic Characterization
# Influenza-Like Illness (ILI) Surveillance
The weekly percentage of patient visits to U.S. sentinel providers for ILI exceeded or was at baseline levels (2.1%) † during the weeks ending December 16, 2006-March 24, 2007 (weeks 50-12) and peaked twice, once at 3.0% for the week ending December 30, 2006 (week 52), and again at 3.5% for the week ending February 17, 2007 (week 7) (Figure 2). The increase in the percentage of patient visits for ILI during the week ending December 30, 2006 (week 52) might have been influenced by a reduction in routine health-care visits during the holiday season, as has occurred in previous seasons. During the previous three influenza seasons, the peak percentage of patient visits for ILI has ranged from 3.3% to 7.6% and the peak occurred during late December to mid-February (1; CDC, unpublished data, 2007).
# State-Specific Activity Levels
State and territorial epidemiologists report the geographic distribution of influenza in their state through a weekly influenza activity code. The geographic distribution of influenza activity peaked during the week ending February 24, 2007 (week 8), when 25 states reported widespread activity and 19 states reported regional activity. § Forty-one states reported widespread influenza activity at least once during the 2006-07 season. No states reported widespread influenza activity during the weeks ending April 21-May 19, 2007 (weeks 16-20). The peak number of states reporting widespread or regional activity during the previous three seasons ranged from 41 to 50 states (1; CDC, unpublished data, 2007). Percentage † The national baseline is the mean percentage of visits for ILI during noninfluenza weeks for the previous three seasons plus two standard deviations. Noninfluenza weeks are those in which less than 10% of laboratory specimens are positive for influenza. National percentages of patient visits for ILI are weighted on the basis of state population. § Levels of activity are 1) no activity; 2) sporadic: isolated laboratory-confirmed influenza cases or a laboratory-confirmed outbreak in one institution, with no increase in ILI activity; 3) local: increased ILI , or at least two institutional outbreaks (ILI or laboratory-confirmed influenza) in one region with recent laboratory evidence of influenza in that region; virus activity no greater than sporadic in other regions; 4) regional: increased ILI activity or institutional outbreaks (ILI or laboratory-confirmed influenza) in at least two but less than half of the regions in the state with recent laboratory evidence of influenza in those regions; and 5) widespread: increased ILI activity or institutional outbreaks (ILI or laboratory-confirmed influenza) in at least half the regions in the state with recent laboratory evidence of influenza in the state.
# Influenza-Associated Pediatric Hospitalization
# MMWR August 10, 2007
systems likely result from different case-finding methods, the diagnostic tests used, and the populations monitored. ¶
# Pneumonia-and Influenza-Related Mortality
During the 2006-07 influenza season, the percentage of deaths attributed to pneumonia and influenza (P&I) did not exceed the epidemic threshold** in the 122 Cities Mortality Reporting System (Figure 3). The percentage of P&I deaths peaked three times, once at 7.5% during the week ending January 20, 2007 (week 3), once at 7.7% during the week ending February 24, 2007 (week 8), and again at 7.5% during the week ending March 24, 2007 (week 12). During the previous three influenza seasons, the peak percentage of P&I deaths ranged from 7.8% to 10.4%, and the total number of weeks above the epidemic threshold ranged from one to 16 (1; CDC, unpublished data, 2007).
# Influenza-Associated Pediatric Mortality
As of August 6, 2007, among persons aged <18 years, a total of 68 deaths associated with influenza infection occurring during October 1, 2006-May 19, 2007, were reported to CDC. These deaths were reported from 26 states (Alabama, Alaska, Arizona, California, Colorado, Connecticut, Florida, Georgia, Illinois, Indiana, Kansas, Louisiana, Minnesota, North Carolina, Nebraska, Nevada, New Mexico, New York, Ohio, Oklahoma, South Dakota, Tennessee, Texas, Virginia, Washington, and Wisconsin). All patients had laboratory-confirmed influenza virus infection. Age-specific information was available for all 68 persons; 10 were aged <6 months, 10 were aged 6-23 months, nine were aged 2-4 years, and 39 were aged 5-17 years. Of the 63 patients for whom influenza virus type was known, 47 had influenza A and 16 had influenza B viruses. Of the 53 patients aged >6 months for whom vaccination status was known, 50 (94%) had not been vaccinated against influenza. These data are provisional.
# Worldwide
During the 2006-07 influenza season, influenza A (H1), A (H3), and B viruses cocirculated worldwide. In Africa, small numbers of influenza A and B viruses were reported. In Europe and Asia, influenza A (H3) viruses were identified most frequently, but influenza A (H1) viruses circulated at low levels. Influenza B viruses circulated at lower levels overall in Asia and Europe but predominated in some countries.
# Human Infections with Avian Influenza A (H5N1) Viruses
From December 1, 2003, through July 25, 2007, a total of 319 human cases of avian influenza A (H5N1) infection were reported to WHO (2). Of these, 192 (60%) were fatal (Table ). All cases were reported from Asia (Azerbaijan, Cambodia, China, Indonesia, Iraq, Laos, Thailand, Turkey, and Viet Nam) and Africa (Djibouti, Egypt, and Nigeria). To date, no human case of avian influenza A (H5N1) virus infection has been identified in the United States. At the June 2007 Annual Meeting of the Council of State and Territorial Epidemiologists (CSTE), members voted to ratify a position statement adopted by the CSTE Executive Committee in January 2007 that adds human infections with novel influenza A viruses to the list of nationally notifiable diseases and conditions reportable to the National Notifiable Disease Surveillance System. Novel influenza A viruses are defined as those isolated from a human but subtyped as nonhuman, or those that cannot be subtyped by standard methods. Human infections with novel influenza A viruses that can be transmitted from person-toperson might signal the beginning of an influenza pandemic. Rapid reporting of human infections with novel influenza A viruses will facilitate prompt detection and characterization of influenza A viruses with pandemic potential and accelerate implementation of effective public health responses. In addition, influenza-associated pediatric deaths were maintained as a nationally notifiable disease reportable to the National Notifiable Disease Surveillance System.
In May 2007, health authorities in the United Kingdom identified four persons, two in Wales and two in northwest England, who were infected with a low pathogenic avian influenza A (H7N2) virus (4). All four persons had been exposed to infected poultry at a farm in Wales; limited evidence of human-to-human transmission has been associated with low pathogenic avian influenza viruses such as influenza A (H7N2) virus (4). The United Kingdom inci- (1). Background information regarding meningococcal disease and the vaccine, including a discussion of duration of protection and use of the vaccine for outbreak control, has been published previously (1).
In June 2007, ACIP revised its recommendation to include routine vaccination of all persons aged 11-18 years with 1 dose of MCV4 at the earliest opportunity. Persons aged 11-12 years should be routinely vaccinated at the 11-12 years health-care visit as recommended by ACIP (2). ACIP continues to recommend routine vaccination for persons aged 19-55 years who are at increased risk for meningococcal disease: college freshmen living in dormitories, microbiologists routinely exposed to isolates of Neisseria meningitidis, military recruits, travelers to or residents of countries in which N. meningitidis meningitis is hyperendemic or epidemic, persons with terminal complement component deficiencies, and persons with anatomic or functional asplenia.
The ACIP goal is routine vaccination of all adolescents with MCV4 beginning at age 11 years. ACIP and partner organizations, including the American Academy of Pediatrics, American Academy of Family Physicians, American Medical Association, and Society for Adolescent Medicine, recommend a health-care visit for children aged 11-12 years to receive recommended vaccinations and indicated preventive services. This visit is the optimal time for adolescents to receive MCV4. In addition, because the incidence of meningococcal disease increases during adolescence, health-care providers should vaccinate previously unvaccinated persons aged 11-18 years with MCV4 at the earliest possible health-care visit. College freshmen living in dormitories are at increased risk for meningococcal disease and should be vaccinated with MCV4 before college entry if they have not been vaccinated previously. Because of difficulties in targeting freshmen in dormitories, colleges may elect to target their vaccination campaigns to all matriculating freshmen (1).
The ACIP meningococcal vaccine workgroup reviewed updated data on MCV4 use and supply projections and data presented previously on the epidemiology of meningococcal disease, safety, and the cost-effectiveness of MCV vaccination strategies. On the basis of these data, expert opinion of the workgroup members, and feedback from partner organizations, the workgroup revised the MCV4 recommendations, which were approved by ACIP at the June 2007 meeting.
The 2005 ACIP MCV4 recommendation was influenced by concern that implementation of MCV4 recommendations might be hindered by reduced vaccine supply during the first few years of production. In 2005 and 2006, peaks in demand were observed during the months when children were returning to school after summer vacation, leading to limited vaccine availability (3,4). However, as of June 2007, ACIP expects supply of MCV4 to be sufficient to meet increased vaccine demand resulting from the revised recommendations. ACIP anticipates that recommending vaccination of all persons aged 11-18 years will improve MCV4 vaccination coverage in this age group and simplify provider decisions to vaccinate.
ACIP encourages health-care providers to vaccinate with MCV4 throughout the year to minimize seasonal increases in demand during July and August when students prepare to return to school from summer vacation. Vaccine providers should administer MCV4 and Tdap (tetanus toxoid, reduced diphtheria toxoid and acellular pertussis) vaccine to persons aged 11-18 years during the same visit if both vaccines are indicated and available. If simultaneous vaccination is not feasible (e.g., a vaccine is not available), MCV4 and Tdap can be administered using any order of administration (5). When making decisions about timing of vaccination, providers should consider that eligibility for the Vaccines for Children Program ends at age 19 years.
Guillain-Barré syndrome (GBS) has been associated with receipt of MCV4 (6). Persons with a history of GBS might be at increased risk for postvaccination GBS; therefore, a history of GBS is a relative contraindication to receiving MCV4. Persons recommended to receive meningococcal vaccination who have a history of GBS (or their parents) should discuss the decision to be vaccinated with their health-care provider (6). Meningococcal polysaccharide vaccine (MPSV4) is an acceptable alternative for short-term protection against meningococcal disease (3-5 years). Providers who have questions about ordering MCV4 or MPSV4 may contact Sanofi Pasteur by telephone at 1-800-VAC-CINE or online at http://www.vaccineshoppe.com. Organizations are responsible for setting up their own viewing locations and are encouraged to register their locations as soon as possible so that potential viewers can access information online. Additional information regarding the broadcast and directions for establishing and registering a viewing location are available at http://www.cdc npin-broadcast.org. The broadcast will be available for 3 years after its initial airing at http://www2a.cdc.gov/phtn. DVDs can be ordered by telephone, 800-458-5231. Among both men and women, non-Hispanic blacks (51.6% of men and 53.5% of women) were more likely to report ever being tested for HIV than Hispanics (35.7% of men and 46.1% of women) and non-Hispanic whites (30.5% of men and 33.5% of women). Overall, women (37.8%) were more likely than men (33.7%) to report ever being tested for HIV.
# Notice to Readers
# Satellite Broadcast and Webcast: Current Challenges and Successes in HIV Prevention with Hispanics/Latinos
2 0 2 7 1 2 0 1 2 - - 0 1 3 1 Montana § - 0 1 1 - - 0 1 3 1 - 0 1 1 3 Nevada § - 0 2 5 1 - 0 1 2 2 - 0 1 3 4 New Mexico § - 0 0 - 3 - 0 1 1 4 - 0 1 2 2 Utah - 0 1 2 2 - 0 3 9 8 - 0 2 8 5 Wyoming § - 0 0 - 1 - 0 0 - - - 0 2 2 4
# Acknowledgments
This report is based, in part, on contributions from DJ | None | None |
46752eaa6cc857196619e74fa121cefd8c3f1800 | cdc | None | This document is in the public domain and may be freely copied or reprinted. Disclaimer: Mention of any company, product, policy, or the inclusion of any reference does not constitute endorsement by NIOSH. Prevention is the cornerstone of public and occupational health. This document provides preventive measures that building owners and managers can implement promptly to protect building air environments from a terrorist release of chemical, biological, or radiological contaminants. These recommendations, focusing on shortterm actions, are only the beginning of a process to develop more comprehensive guidance. Working with the Building Air Protection Workgroup, as well as partners in the public and private sectors, NIOSH will continue to build on this effort. This document is a useful first step in the process.# Foreword
The Occupational Safety and Health Act of 1970 assures so far as possible every working man and woman in the Nation safe and healthful working conditions. The Act charges the National Institute for Occupational Safety and Health (NIOSH) with conducting research and making science-based recommendations to prevent work-related illness, injury, disability, and death.
On October 8, 2001, the President of the United States established by executive order the Office of Homeland Security (OHS), which is mandated "to develop and coordinate the implementation of a comprehensive national strategy to secure the United States from terrorist threats or attacks." In January 2002, the OHS formed the Interagency Workgroup on Building Air Protection under the Medical and Public Health Preparedness Policy Coordinating Committee of the OHS. The Workgroup includes representatives from agencies throughout the Federal government, including NIOSH, which is part of the Centers for Disease Control and Prevention.
With U.S. workers facing potential hazards associated with chemical, biological, or radiological terrorism, the missions of the OHS and NIOSH overlap. As with most hazards, there are preventive steps that can reduce the likelihood and mitigate the impact of terrorist threats. Tried and proven principles in the control of airborne contaminants can be joined with similarly focused safety and security principles to provide guidance on how we design and operate our building environments. This document is the result of recent building vulnerability assessments conducted by NIOSH, as well as significant content and review recommendations provided by Workgroup members. . The Workgroup's purpose is to focus on building air protection issues associated with an airborne chemical, biological, or radiological (CBR) attack. Workgroup participants provided guidance and direction at several points during this document's development. Their diverse expertise and perspectives resulted in a set of real-world recommendations intended to increase protection of building environments from a terrorist's chemical, biological, or radiological attack. Participants on the Workgroup and their agency affiliations may be found in Appendix A.
In addition to the efforts of the Workgroup, the contributions of the NIOSH Research Team on Building Vulnerabilities are greatly appreciated. This team was augmented by representatives from Sandia National Laboratories and the Agency for Toxic Substances and Disease Registry (ATSDR). Many of the recommendations found in this document originated from the numerous vulnerability assessments conducted by this team. Members of the team are listed in Appendix B.
Anne Votaw, Pauline Elliott, Anne Stirnkorb, and Dick Carlson (NIOSH) provided editorial support, produced the camera-ready copy, and prepared the graphics. Review and preparation for printing were performed by Penny Arthur.
# vii
# SCOPE
T HIS DOCUMENT IDENTIFIES ACTIONS that a building owner or manager can implement without undue delay to enhance occupant protection from an airborne chemical, biological, or radiological (CBR) attack. The intended audience includes building owners, managers, and maintenance personnel of public, private, and governmental buildings, including offices, laboratories, hospitals, retail facilities, schools, transportation terminals, and public venues (for example, sports arenas, malls, coliseums). This document is not intended to address single-family or low-occupancy residential housing (less than five family units). Higher risk facilities such as industrial facilities, military facilities, subway systems, and law enforcement facilities require special considerations that are beyond the scope of this guide.
# Guidance for
# P rotecting B uilding E nvironments from Airborne Chemical, Biological, or Radiological Attacks
The likelihood of a specific building being targeted for terrorist activity is generally difficult to predict. As such, there is no specific formula that will determine a certain building's level of risk. Building owners must make their own decisions about how to reduce their building's risk to a CBR attack. These decisions may be aided by a comprehensive building security assessment. Many government and private organizations have identified resources that provide insight into building security assessments. The reference list at the end of this document will help the reader obtain this information.
No building can be fully protected from a determined individual who is intent on releasing a CBR agent. The recommendations in this guide will not preclude injuries or fatalities in the event of a CBR release. However, facility owners and managers can transform their buildings into less attractive targets by increasing the difficulty of introducing a CBR agent, by increasing the ability to detect terrorists before they carry out an intended release, and by incorporating plans and procedures to mitigate the effects of a CBR release. Some of the references listed in the back of this document can provide information on how to recognize if a CBR release has occurred. These recommendations focus on airborne releases of CBR agents- in quantities capable of being easily transported by a few individuals. Protection from other types of attacks such as explosions, building collapses, and water supply contamination require much different measures and are not addressed in this document.
The recommendations set forth in this document are not intended to be a minimum requirement that every building owner and manager should implement for every building. Rather, the decisions concerning which protective measures should be implemented for any building should be based on several factors, including the perceived risk associated with the building and its tenants, engineering and architectural feasibility, and cost. *Note: References to a release of CBR agent in this document will always refer to an airborne CBR release.
# BACKGROUND
Terrorism events have increased interest in the vulnerability of U.S. workplaces, schools, and other occupied buildings to CBR threats. Of particular concern are the airflow patterns and dynamics in buildings, specifically in the building heating, ventilating, and air-conditioning (HVAC) systems. These systems can become an entry point and a distribution system for hazardous contaminants, particularly CBR agents. Building owners need reliable information about how they can (1) modify their buildings to decrease the likelihood or effects of a CBR incident and (2) respond quickly and appropriately should a CBR incident occur. Comprehensive guidance is needed in several areas, including: p How to modify existing buildings for better air protection and security.
p How to design new buildings to be more secure.
p What plans building managers should prepare in advance to help them make effective decisions in the midst of a CBR incident.
# PREPARATORY RECOMMENDATION-KNOW YOUR BUILDING
While more comprehensive guidance is being developed, this document focuses on the shorter-term goals of identifying those protective actions that you can take immediately. But it recognizes that some recommendations may not be feasible for you or in all situations.
In initiating any plan to modify building system design or operation, an important first step is to understand these systems: How were they intended to operate? How do they currently operate?
Getting to know your building may best be handled by conducting a walk-through inspection of the building and its systems, including the HVAC, fire protection, and life-safety systems. During this inspection, compare the most up-to-date design drawings available to the operation of the current systems.- This step may require, or benefit from, the assistance of qualified outside professionals. Without this baseline knowledge, it is difficult to accurately identify what impact a particular security modification may have on building operation. While it is important to understand how the existing building systems function, the systems need not operate per design before you implement security measures. A partial list of items to consider during your building walk-through includes:
p What is the mechanical condition of the equipment?
# SPECIFIC RECOMMENDATIONS
The recommendations can be divided into four general categories: (1) things not to do; (2) physical security; (3) ventilation and filtration; and (4) maintenance, administration, and training. Some of these items, such as securing mechanical rooms, may be started prior to your completing the recommendations in the "Know your building" section. Items within each of the four categories are listed in the order of priority. Items considered to be highly critical are identified by "*" next to the number. As you review these recommendations, consider their potential implications upon the contract language necessary for existing and future service contracts. A brief discussion of the four categories and some commonly considered recommendations follow.
# Things not to do
More than anything else, building owners and managers should ensure that any actions they take do not have a detrimental effect on the building systems (HVAC, fire protection, life safety, etc.) or the building occupants under normal building operation. Some efforts to protect the building from a CBR attack could have adverse effects on the building's indoor environmental quality. Building owners and managers should understand how the building systems operate and assess the impact of security measures on those systems. This caution directly relates to the recommendation that building owners and managers should understand the operation of their building systems. If there is uncertainty about the effects of a proposed modification, a qualified professional should be consulted.
# *3. DO NOT INTERFERE WITH FIRE PROTECTION AND LIFE SAFETY
SYSTEMS. These systems provide protection in the event of fire or other types of events. They should not be altered without guidance from a professional specifically qualified in fire protection and life safety systems.
# Physical Security
Preventing terrorist access to a targeted facility requires physical security of entry, storage, roof, and mechanical areas, as well as securing access to the outdoor air intakes of the building HVAC system. The physical security needs of each building should be assessed, as the threat of a CBR attack will vary considerably from building to building. For example, the threat to a large corporate headquarters may be considered greater than the threat to a small retail establishment. Some physical security measures, such as locking doors to mechanical rooms, are low cost and will not inconvenience the users of the building. These types of measures can be implemented in most buildings. Other physical security measures, such as increased security personnel or package x-ray equipment, are more costly or may inconvenience users substantially. These measures should be implemented when merited after consideration of the threat and consequences of a terrorist attack. Building owners and managers should be familiar with their buildings and understand what assets require protection and what characteristics about the building or its occupants make it a potential target. By first assessing the vulnerabilities of facilities, building owners and managers can address physical security in an effective manner. While the identification and resolution of building vulnerabilities will be specific to each building, some physical security actions are applicable to many building types. These include: *1. PREVENT ACCESS TO OUTDOOR AIR INTAKES. One of the most important steps in protecting a building's indoor environment is the security of the outdoor air intakes. Outdoor air enters the building through these intakes and is distributed throughout the building by the HVAC system. Introducing CBR agents into the outdoor air intakes allows a terrorist to use the HVAC system as a means of dispersing the agent throughout a building. Publicly accessible outdoor air intakes located at or below ground level are at most risk-due partly to their accessibility (which also makes visual or audible identification easier) and partly because most CBR agent releases near a building will be close to the ground and may remain there. Securing the outdoor air intakes is a critical line of defense in limiting an external CBR attack on a building.
Relocate outdoor air intake vents. Relocating accessible air intakes to a publicly inaccessible location is preferable. Ideally, the intake should be located on a secure roof or high sidewall. The lowest edge of the outdoor air intakes should be placed at the highest feasible level above the ground or above any nearby accessible level (i.e., adjacent retaining walls, loading docks, handrail). These measures are also beneficial in limiting the inadvertent introduction of other types of contaminants, such as landscaping chemicals, into the building.
Extend outdoor air intakes. If relocation of outdoor air intakes is not feasible, intake extensions can be constructed without creating adverse effects on HVAC performance. Depending upon budget, time, or the perceived threat, the intake extensions may be temporary or constructed in a permanent, architecturally compatible design. The goal is to minimize public accessibility. In general, this means the higher the extensions, the better-as long as other design constraints (excessive pressure loss, dynamic and static loads on structure) are appropriately considered. An extension height of 12 feet (3.7 m) will place the intake out of reach of individuals without some assistance. Also, the entrance to the intake should be covered with a sloped metal mesh to reduce the threat of objects being tossed into the intake. A minimum slope of 45˚is generally adequate. Extension height should be increased where existing platforms or building features (i.e., loading docks, retaining walls) might provide access to the outdoor air intakes.
# Establish a security zone around outdoor air intakes.
Physically inaccessible outdoor air intakes are the preferred protection strategy. When outdoor air intakes are publicly accessible and relocation or physical extensions are not viable options, perimeter barriers that prevent public access to outdoor air intake areas may be an effective alternative. Iron fencing or similar see-through barriers that will not obscure visual detection of terrorist activities or a deposited CBR source are preferred. The restricted area should also include an open buffer zone between the public areas and the intake louvers. Thus, individuals attempting to enter these protected areas will be more conspicuous to security personnel and the public. Monitoring the buffer zone by physical security, closedcircuit television (CCTV), security lighting, or intrusion detection sensors will enhance this protective approach. To prevent widespread dispersion of a contaminant released within lobbies, mailrooms, and loading docks, their HVAC systems should be isolated and the areas maintained at a negative pressure relative to the rest of the building, but at positive pressure relative to the outdoors. Physical isolation of these areas (well-sealed floor to roof-deck walls, sealed wall penetrations) is critical to maintaining the pressure differential and requires special attention to ensure airtight boundaries between these areas and adjacent spaces. In some building designs (those having lobbies with elevator access, for example), establishing a negative pressure differential will present a challenge. A qualified HVAC professional can assist in determining if the recommended isolation is feasible for a given building. In addition, lobbies, mailrooms, and loading docks should not share a return-air system or return pathway (e.g., ceiling plenum) with other areas of the building. Some of these measures are more feasible for new construction or buildings undergoing major renovation.
Building access from lobby areas should be limited by security checks of individuals and packages prior to their entry into secure areas. Lobby isolation is particularly critical in buildings where the main lobbies are open to the public. Similar checks of incoming mail should also occur before its conveyance into the secure building areas. Side entry doors that circumvent established security checkpoints should be strictly controlled. 9. GENERAL BUILDING PHYSICAL SECURITY UPGRADES. In addition to the security measures for HVAC and other building operations described earlier, physical security upgrades can enhance the overall security of a building. A building or building complex might have security fencing and controlled access points. Some buildings such as museums are, by their very nature, openly accessible to the public. However, even in these buildings, areas such as mechanical rooms need to remain off-limits to unauthorized individuals. Unless the building is regarded as open to the general public, owners and managers should consider not allowing visitors outside the lobby area without an escort. Layered levels of security access should be considered. For example, entry to a hospital's patient care areas could be less strict than to hospital laboratories, and successively more strict for other areas, such as ventilation control rooms. Physical security is of prime concern in lobby areas.
# Ventilation and Filtration
HVAC systems and their components should be evaluated with respect to how they impact vulnerability to the introduction of CBR agents. Relevant issues include the HVAC system controls, the ability of the HVAC system to purge the building, the efficiency of installed filters, the capacity of the system relative to potential filter upgrades, and the significance of uncontrolled leakage into the building. Another consideration is the vulnerability of the HVAC system and components themselves, particularly when the facility is open to the public. For buildings under secure access, interior components may be considered less vulnerable, depending upon the perceived threat and the confidence in the level of security. Increasing filter efficiency is one of the few measures that can be implemented in advance to reduce the consequences of both an interior and exterior release of a particulate CBR agent. However, the decision to increase efficiency should be made cautiously, with a careful understanding of the protective limitations resulting from the upgrade. The filtration needs of a building should be assessed with a view to implementing the highest filtration efficiency that is compatible with the installed HVAC system and its required operating parameters. In general, increased filter efficiency will provide benefits to the indoor environmental quality of the building. However, the increased protection from CBR aerosols will occur only if the filtration efficiency increase applies to the particle size range and physical state of the CBR contaminant. It is important to note that particulate air filters are used for biological and radiological particles and are not effective for gases and vapors typical of chemical attacks. These types of compounds require adsorbent filters (i.e., activated carbon or other sorbent-type media) and result in substantial initial and recurring costs.
Upgrading filtration is not as simple as merely replacing a low-efficiency filter with a higher efficiency one. Typically, higher efficiency filters have a higher pressure loss, which will result in some airflow reduction through the system. The magnitude of the reduction is dependent on the design and capacity of the HVAC system. If the airflow reduction is substantial, it may result in inadequate ventilation, reductions in heating and cooling capacity, or potentially frozen coils. To minimize pressure loss, deep pleated filters or filter banks having a larger nominal inlet area might be feasible alternatives, if space allows. Also, high-pressure losses can sometimes be avoided by using prefilters or more frequent filter changeouts. Pressure loss associated with adsorbent filters can be even greater.
The integrity of the HVAC system's filter rack or frame system has a major impact upon the installed filtration efficiency.
Reducing the leakage of unfiltered air around filters, caused by a poor seal between the filter and the frame, may be as important as increasing filter efficiency. If filter bypass proves to be significant, corrective actions will be needed. Some highefficiency filter systems have better seals and frames constructed to reduce bypass. During an upgrade to higher efficiency filters, the HVAC and filtration systems should be evaluated by a qualified HVAC professional to verify proper performance.
While higher filtration efficiency is encouraged and should provide indoor air quality benefits beyond an increased protection from CBR terrorist events, the overall cost of filtration should be evaluated. Filtration costs include the periodic cost of the filter media, the labor cost to remove and replace filters, and the fan energy cost required to overcome the pressure loss of the filters. While higher efficiency filters tend to have a higher life cycle cost than lower efficiency filters, this is not always the case. With some higher efficiency filter systems, higher acquisition and energy costs can be offset by longer filter life and a reduced labor cost for filter replacements. Also, improved filtration generally keeps heating and cooling coils cleaner and, thus, may reduce energy costs through improvements in heat transfer efficiency. However, when high efficiency particulate air (HEPA) filters and/or activated carbon adsorbers are used, the overall costs will generally increase substantially.
3. DUCTED AND NON-DUCTED RETURN AIR SYSTEMS. Ducted returns offer limited access points to introduce a CBR agent. The return vents can be placed in conspicuous locations, reducing the risk of an agent being secretly introduced into the return system. Non-ducted return air systems commonly use hallways or spaces above dropped ceilings as a return-air path or plenum. CBR agents introduced at any location above the dropped ceiling in a ceiling plenum return system will most likely migrate back to the HVAC unit and, without highly efficient filtration for the particular agent, redistribute to occupied areas. Buildings should be designed to minimize mixing between air-handling zones, which can be partially accomplished by limiting shared returns. Where ducted returns are not feasible or warranted, hold-down clips may be used for accessible areas of dropped ceilings that serve as the return plenum. This issue is closely related to the isolation of lobbies and mailrooms, as shared returns are a common way for contaminants from these areas to disperse into the rest of the building. These modifications may be more feasible for new building construction or those undergoing major renovation.
4. LOW-LEAKAGE, FAST-ACTING DAMPERS. Rapid response, such as shutting down an HVAC system, may also involve closing various dampers, especially those controlling the flow of outdoor air (in the event of an exterior CBR release). When the HVAC system is turned off, the building pressure compared to outdoors may still be negative, drawing outdoor air into the building via many leakage pathways, including the HVAC system. Consideration should be given to installing low leakage dampers to minimize this flow pathway. Damper leakage ratings are available as part of the manufacturer's specifications and range from ultra-low to normal categories. Assuming that you have some warning prior to a direct CBR release, the speed with which these dampers respond to a "close" instruction can also be important. From a protective standpoint, dampers that respond quickly are preferred over dampers that might take 30 seconds or more to respond.
5. BUILDING AIR TIGHTNESS. Significant quantities of air can enter a building by means of infiltration through unintentional leakage paths in the building envelope. Such leakage is of more concern for an exterior CBR release at some distance from a building, such as a large-scale attack, than for a directed terrorist act. The reduction of air leakage is a matter of tight building construction in combination with building pressurization. While building pressurization may be a valuable CBR-protection strategy in any building, it is much more likely to be effective in a tight building. However, to be effective, filtration of building supply air must be appropriate for the CBR agent introduced. Although increasing the air tightness of an existing building can be more challenging than during new construction, it should still be seriously considered.
# Maintenance, Administration, and Training
# CONCLUSIONS
Reducing a building's vulnerability to an airborne chemical, biological, or radiological attack requires a comprehensive approach. Decisions concerning which protective measures to implement should be based upon the threat profile and a security assessment of the building and its occupants. While physical security is the first layer of defense, other issues must also be addressed. Preventing possible terrorist access to outdoor air intakes and mechanical rooms and developing CBR-contingent emergency response plans should be addressed as soon as possible. Additional measures can provide further protection. A building security assessment should be done to determine the necessity of additional measures. Some items, such as improved maintenance and HVAC system controls, may also provide a payback in operating costs and/or improved building air quality. As new building designs or modifications are considered, designers should consider that practical CBR sensors may soon become available. Building system design features that are capable of incorporating this rapidly evolving technology will most likely offer a greater level of protection. While it is not possible to completely eliminate the risk of a CBR terrorist attack, several measures can be taken to reduce the likelihood and consequences of such an attack. Many of the recommendations presented here are ones that can be implemented reasonably quickly and cost effectively. Many are applicable to both new construction and existing buildings, although some may be more feasible than others. Building owners and managers should assess buildings by looking first for those items that are most vulnerable and can be addressed easily. Additional measures should be implemented as feasible. The goals are to make your building an unattractive target for a CBR attack and to maximize occupant protection in the event that such an attack occurs.
# For Additional Information
Several organizations have developed guidance to assist building owners and operators in addressing issues related to building security and CBR terrorist attacks. Many other organizations have guidance that addresses security needs and disaster response plans for events such as fire, natural disasters, and bomb threats. While this latter guidance may not specifically address the terrorist threat to HVAC systems, readers may find portions of the information beneficial in establishing their own building's emergency response plans.
The following list is not all-inclusive. Available guidance is updated regularly as additional organizations and evolving technologies identify new protective recommendations.
# Organization
Reference or Link Description | This document is in the public domain and may be freely copied or reprinted. Disclaimer: Mention of any company, product, policy, or the inclusion of any reference does not constitute endorsement by NIOSH. Prevention is the cornerstone of public and occupational health. This document provides preventive measures that building owners and managers can implement promptly to protect building air environments from a terrorist release of chemical, biological, or radiological contaminants. These recommendations, focusing on shortterm actions, are only the beginning of a process to develop more comprehensive guidance. Working with the Building Air Protection Workgroup, as well as partners in the public and private sectors, NIOSH will continue to build on this effort. This document is a useful first step in the process.# Foreword
The Occupational Safety and Health Act of 1970 [Public Law 91-596] assures so far as possible every working man and woman in the Nation safe and healthful working conditions. The Act charges the National Institute for Occupational Safety and Health (NIOSH) with conducting research and making science-based recommendations to prevent work-related illness, injury, disability, and death.
On October 8, 2001, the President of the United States established by executive order the Office of Homeland Security (OHS), which is mandated "to develop and coordinate the implementation of a comprehensive national strategy to secure the United States from terrorist threats or attacks." In January 2002, the OHS formed the Interagency Workgroup on Building Air Protection under the Medical and Public Health Preparedness Policy Coordinating Committee of the OHS. The Workgroup includes representatives from agencies throughout the Federal government, including NIOSH, which is part of the Centers for Disease Control and Prevention.
With U.S. workers facing potential hazards associated with chemical, biological, or radiological terrorism, the missions of the OHS and NIOSH overlap. As with most hazards, there are preventive steps that can reduce the likelihood and mitigate the impact of terrorist threats. Tried and proven principles in the control of airborne contaminants can be joined with similarly focused safety and security principles to provide guidance on how we design and operate our building environments. This document is the result of recent building vulnerability assessments conducted by NIOSH, as well as significant content and review recommendations provided by Workgroup members. . The Workgroup's purpose is to focus on building air protection issues associated with an airborne chemical, biological, or radiological (CBR) attack. Workgroup participants provided guidance and direction at several points during this document's development. Their diverse expertise and perspectives resulted in a set of real-world recommendations intended to increase protection of building environments from a terrorist's chemical, biological, or radiological attack. Participants on the Workgroup and their agency affiliations may be found in Appendix A.
In addition to the efforts of the Workgroup, the contributions of the NIOSH Research Team on Building Vulnerabilities are greatly appreciated. This team was augmented by representatives from Sandia National Laboratories and the Agency for Toxic Substances and Disease Registry (ATSDR). Many of the recommendations found in this document originated from the numerous vulnerability assessments conducted by this team. Members of the team are listed in Appendix B.
Anne Votaw, Pauline Elliott, Anne Stirnkorb, and Dick Carlson (NIOSH) provided editorial support, produced the camera-ready copy, and prepared the graphics. Review and preparation for printing were performed by Penny Arthur.
# vii
# SCOPE
T HIS DOCUMENT IDENTIFIES ACTIONS that a building owner or manager can implement without undue delay to enhance occupant protection from an airborne chemical, biological, or radiological (CBR) attack. The intended audience includes building owners, managers, and maintenance personnel of public, private, and governmental buildings, including offices, laboratories, hospitals, retail facilities, schools, transportation terminals, and public venues (for example, sports arenas, malls, coliseums). This document is not intended to address single-family or low-occupancy residential housing (less than five family units). Higher risk facilities such as industrial facilities, military facilities, subway systems, and law enforcement facilities require special considerations that are beyond the scope of this guide.
# Guidance for
# P rotecting B uilding E nvironments from Airborne Chemical, Biological, or Radiological Attacks
The likelihood of a specific building being targeted for terrorist activity is generally difficult to predict. As such, there is no specific formula that will determine a certain building's level of risk. Building owners must make their own decisions about how to reduce their building's risk to a CBR attack. These decisions may be aided by a comprehensive building security assessment. Many government and private organizations have identified resources that provide insight into building security assessments. The reference list at the end of this document will help the reader obtain this information.
No building can be fully protected from a determined individual who is intent on releasing a CBR agent. The recommendations in this guide will not preclude injuries or fatalities in the event of a CBR release. However, facility owners and managers can transform their buildings into less attractive targets by increasing the difficulty of introducing a CBR agent, by increasing the ability to detect terrorists before they carry out an intended release, and by incorporating plans and procedures to mitigate the effects of a CBR release. Some of the references listed in the back of this document can provide information on how to recognize if a CBR release has occurred. These recommendations focus on airborne releases of CBR agents* in quantities capable of being easily transported by a few individuals. Protection from other types of attacks such as explosions, building collapses, and water supply contamination require much different measures and are not addressed in this document.
The recommendations set forth in this document are not intended to be a minimum requirement that every building owner and manager should implement for every building. Rather, the decisions concerning which protective measures should be implemented for any building should be based on several factors, including the perceived risk associated with the building and its tenants, engineering and architectural feasibility, and cost. *Note: References to a release of CBR agent in this document will always refer to an airborne CBR release.
# BACKGROUND
Terrorism events have increased interest in the vulnerability of U.S. workplaces, schools, and other occupied buildings to CBR threats. Of particular concern are the airflow patterns and dynamics in buildings, specifically in the building heating, ventilating, and air-conditioning (HVAC) systems. These systems can become an entry point and a distribution system for hazardous contaminants, particularly CBR agents. Building owners need reliable information about how they can (1) modify their buildings to decrease the likelihood or effects of a CBR incident and (2) respond quickly and appropriately should a CBR incident occur. Comprehensive guidance is needed in several areas, including: p How to modify existing buildings for better air protection and security.
p How to design new buildings to be more secure.
p What plans building managers should prepare in advance to help them make effective decisions in the midst of a CBR incident.
# PREPARATORY RECOMMENDATION-KNOW YOUR BUILDING
While more comprehensive guidance is being developed, this document focuses on the shorter-term goals of identifying those protective actions that you can take immediately. But it recognizes that some recommendations may not be feasible for you or in all situations.
In initiating any plan to modify building system design or operation, an important first step is to understand these systems: How were they intended to operate? How do they currently operate?
Getting to know your building may best be handled by conducting a walk-through inspection of the building and its systems, including the HVAC, fire protection, and life-safety systems. During this inspection, compare the most up-to-date design drawings available to the operation of the current systems.* This step may require, or benefit from, the assistance of qualified outside professionals. Without this baseline knowledge, it is difficult to accurately identify what impact a particular security modification may have on building operation. While it is important to understand how the existing building systems function, the systems need not operate per design before you implement security measures. A partial list of items to consider during your building walk-through includes:
p What is the mechanical condition of the equipment?
# SPECIFIC RECOMMENDATIONS
The recommendations can be divided into four general categories: (1) things not to do; (2) physical security; (3) ventilation and filtration; and (4) maintenance, administration, and training. Some of these items, such as securing mechanical rooms, may be started prior to your completing the recommendations in the "Know your building" section. Items within each of the four categories are listed in the order of priority. Items considered to be highly critical are identified by "***" next to the number. As you review these recommendations, consider their potential implications upon the contract language necessary for existing and future service contracts. A brief discussion of the four categories and some commonly considered recommendations follow.
# Things not to do
More than anything else, building owners and managers should ensure that any actions they take do not have a detrimental effect on the building systems (HVAC, fire protection, life safety, etc.) or the building occupants under normal building operation. Some efforts to protect the building from a CBR attack could have adverse effects on the building's indoor environmental quality. Building owners and managers should understand how the building systems operate and assess the impact of security measures on those systems. This caution directly relates to the recommendation that building owners and managers should understand the operation of their building systems. If there is uncertainty about the effects of a proposed modification, a qualified professional should be consulted.
# ***3. DO NOT INTERFERE WITH FIRE PROTECTION AND LIFE SAFETY
SYSTEMS. These systems provide protection in the event of fire or other types of events. They should not be altered without guidance from a professional specifically qualified in fire protection and life safety systems.
# Physical Security
Preventing terrorist access to a targeted facility requires physical security of entry, storage, roof, and mechanical areas, as well as securing access to the outdoor air intakes of the building HVAC system. The physical security needs of each building should be assessed, as the threat of a CBR attack will vary considerably from building to building. For example, the threat to a large corporate headquarters may be considered greater than the threat to a small retail establishment. Some physical security measures, such as locking doors to mechanical rooms, are low cost and will not inconvenience the users of the building. These types of measures can be implemented in most buildings. Other physical security measures, such as increased security personnel or package x-ray equipment, are more costly or may inconvenience users substantially. These measures should be implemented when merited after consideration of the threat and consequences of a terrorist attack. Building owners and managers should be familiar with their buildings and understand what assets require protection and what characteristics about the building or its occupants make it a potential target. By first assessing the vulnerabilities of facilities, building owners and managers can address physical security in an effective manner. While the identification and resolution of building vulnerabilities will be specific to each building, some physical security actions are applicable to many building types. These include: ***1. PREVENT ACCESS TO OUTDOOR AIR INTAKES. One of the most important steps in protecting a building's indoor environment is the security of the outdoor air intakes. Outdoor air enters the building through these intakes and is distributed throughout the building by the HVAC system. Introducing CBR agents into the outdoor air intakes allows a terrorist to use the HVAC system as a means of dispersing the agent throughout a building. Publicly accessible outdoor air intakes located at or below ground level are at most risk-due partly to their accessibility (which also makes visual or audible identification easier) and partly because most CBR agent releases near a building will be close to the ground and may remain there. Securing the outdoor air intakes is a critical line of defense in limiting an external CBR attack on a building.
Relocate outdoor air intake vents. Relocating accessible air intakes to a publicly inaccessible location is preferable. Ideally, the intake should be located on a secure roof or high sidewall. The lowest edge of the outdoor air intakes should be placed at the highest feasible level above the ground or above any nearby accessible level (i.e., adjacent retaining walls, loading docks, handrail). These measures are also beneficial in limiting the inadvertent introduction of other types of contaminants, such as landscaping chemicals, into the building.
Extend outdoor air intakes. If relocation of outdoor air intakes is not feasible, intake extensions can be constructed without creating adverse effects on HVAC performance. Depending upon budget, time, or the perceived threat, the intake extensions may be temporary or constructed in a permanent, architecturally compatible design. The goal is to minimize public accessibility. In general, this means the higher the extensions, the better-as long as other design constraints (excessive pressure loss, dynamic and static loads on structure) are appropriately considered. An extension height of 12 feet (3.7 m) will place the intake out of reach of individuals without some assistance. Also, the entrance to the intake should be covered with a sloped metal mesh to reduce the threat of objects being tossed into the intake. A minimum slope of 45˚is generally adequate. Extension height should be increased where existing platforms or building features (i.e., loading docks, retaining walls) might provide access to the outdoor air intakes.
# Establish a security zone around outdoor air intakes.
Physically inaccessible outdoor air intakes are the preferred protection strategy. When outdoor air intakes are publicly accessible and relocation or physical extensions are not viable options, perimeter barriers that prevent public access to outdoor air intake areas may be an effective alternative. Iron fencing or similar see-through barriers that will not obscure visual detection of terrorist activities or a deposited CBR source are preferred. The restricted area should also include an open buffer zone between the public areas and the intake louvers. Thus, individuals attempting to enter these protected areas will be more conspicuous to security personnel and the public. Monitoring the buffer zone by physical security, closedcircuit television (CCTV), security lighting, or intrusion detection sensors will enhance this protective approach. To prevent widespread dispersion of a contaminant released within lobbies, mailrooms, and loading docks, their HVAC systems should be isolated and the areas maintained at a negative pressure relative to the rest of the building, but at positive pressure relative to the outdoors. Physical isolation of these areas (well-sealed floor to roof-deck walls, sealed wall penetrations) is critical to maintaining the pressure differential and requires special attention to ensure airtight boundaries between these areas and adjacent spaces. In some building designs (those having lobbies with elevator access, for example), establishing a negative pressure differential will present a challenge. A qualified HVAC professional can assist in determining if the recommended isolation is feasible for a given building. In addition, lobbies, mailrooms, and loading docks should not share a return-air system or return pathway (e.g., ceiling plenum) with other areas of the building. Some of these measures are more feasible for new construction or buildings undergoing major renovation.
Building access from lobby areas should be limited by security checks of individuals and packages prior to their entry into secure areas. Lobby isolation is particularly critical in buildings where the main lobbies are open to the public. Similar checks of incoming mail should also occur before its conveyance into the secure building areas. Side entry doors that circumvent established security checkpoints should be strictly controlled. 9. GENERAL BUILDING PHYSICAL SECURITY UPGRADES. In addition to the security measures for HVAC and other building operations described earlier, physical security upgrades can enhance the overall security of a building. A building or building complex might have security fencing and controlled access points. Some buildings such as museums are, by their very nature, openly accessible to the public. However, even in these buildings, areas such as mechanical rooms need to remain off-limits to unauthorized individuals. Unless the building is regarded as open to the general public, owners and managers should consider not allowing visitors outside the lobby area without an escort. Layered levels of security access should be considered. For example, entry to a hospital's patient care areas could be less strict than to hospital laboratories, and successively more strict for other areas, such as ventilation control rooms. Physical security is of prime concern in lobby areas.
# Ventilation and Filtration
HVAC systems and their components should be evaluated with respect to how they impact vulnerability to the introduction of CBR agents. Relevant issues include the HVAC system controls, the ability of the HVAC system to purge the building, the efficiency of installed filters, the capacity of the system relative to potential filter upgrades, and the significance of uncontrolled leakage into the building. Another consideration is the vulnerability of the HVAC system and components themselves, particularly when the facility is open to the public. For buildings under secure access, interior components may be considered less vulnerable, depending upon the perceived threat and the confidence in the level of security. Increasing filter efficiency is one of the few measures that can be implemented in advance to reduce the consequences of both an interior and exterior release of a particulate CBR agent. However, the decision to increase efficiency should be made cautiously, with a careful understanding of the protective limitations resulting from the upgrade. The filtration needs of a building should be assessed with a view to implementing the highest filtration efficiency that is compatible with the installed HVAC system and its required operating parameters. In general, increased filter efficiency will provide benefits to the indoor environmental quality of the building. However, the increased protection from CBR aerosols will occur only if the filtration efficiency increase applies to the particle size range and physical state of the CBR contaminant. It is important to note that particulate air filters are used for biological and radiological particles and are not effective for gases and vapors typical of chemical attacks. These types of compounds require adsorbent filters (i.e., activated carbon or other sorbent-type media) and result in substantial initial and recurring costs.
Upgrading filtration is not as simple as merely replacing a low-efficiency filter with a higher efficiency one. Typically, higher efficiency filters have a higher pressure loss, which will result in some airflow reduction through the system. The magnitude of the reduction is dependent on the design and capacity of the HVAC system. If the airflow reduction is substantial, it may result in inadequate ventilation, reductions in heating and cooling capacity, or potentially frozen coils. To minimize pressure loss, deep pleated filters or filter banks having a larger nominal inlet area might be feasible alternatives, if space allows. Also, high-pressure losses can sometimes be avoided by using prefilters or more frequent filter changeouts. Pressure loss associated with adsorbent filters can be even greater.
The integrity of the HVAC system's filter rack or frame system has a major impact upon the installed filtration efficiency.
Reducing the leakage of unfiltered air around filters, caused by a poor seal between the filter and the frame, may be as important as increasing filter efficiency. If filter bypass proves to be significant, corrective actions will be needed. Some highefficiency filter systems have better seals and frames constructed to reduce bypass. During an upgrade to higher efficiency filters, the HVAC and filtration systems should be evaluated by a qualified HVAC professional to verify proper performance.
While higher filtration efficiency is encouraged and should provide indoor air quality benefits beyond an increased protection from CBR terrorist events, the overall cost of filtration should be evaluated. Filtration costs include the periodic cost of the filter media, the labor cost to remove and replace filters, and the fan energy cost required to overcome the pressure loss of the filters. While higher efficiency filters tend to have a higher life cycle cost than lower efficiency filters, this is not always the case. With some higher efficiency filter systems, higher acquisition and energy costs can be offset by longer filter life and a reduced labor cost for filter replacements. Also, improved filtration generally keeps heating and cooling coils cleaner and, thus, may reduce energy costs through improvements in heat transfer efficiency. However, when high efficiency particulate air (HEPA) filters and/or activated carbon adsorbers are used, the overall costs will generally increase substantially.
3. DUCTED AND NON-DUCTED RETURN AIR SYSTEMS. Ducted returns offer limited access points to introduce a CBR agent. The return vents can be placed in conspicuous locations, reducing the risk of an agent being secretly introduced into the return system. Non-ducted return air systems commonly use hallways or spaces above dropped ceilings as a return-air path or plenum. CBR agents introduced at any location above the dropped ceiling in a ceiling plenum return system will most likely migrate back to the HVAC unit and, without highly efficient filtration for the particular agent, redistribute to occupied areas. Buildings should be designed to minimize mixing between air-handling zones, which can be partially accomplished by limiting shared returns. Where ducted returns are not feasible or warranted, hold-down clips may be used for accessible areas of dropped ceilings that serve as the return plenum. This issue is closely related to the isolation of lobbies and mailrooms, as shared returns are a common way for contaminants from these areas to disperse into the rest of the building. These modifications may be more feasible for new building construction or those undergoing major renovation.
4. LOW-LEAKAGE, FAST-ACTING DAMPERS. Rapid response, such as shutting down an HVAC system, may also involve closing various dampers, especially those controlling the flow of outdoor air (in the event of an exterior CBR release). When the HVAC system is turned off, the building pressure compared to outdoors may still be negative, drawing outdoor air into the building via many leakage pathways, including the HVAC system. Consideration should be given to installing low leakage dampers to minimize this flow pathway. Damper leakage ratings are available as part of the manufacturer's specifications and range from ultra-low to normal categories. Assuming that you have some warning prior to a direct CBR release, the speed with which these dampers respond to a "close" instruction can also be important. From a protective standpoint, dampers that respond quickly are preferred over dampers that might take 30 seconds or more to respond.
5. BUILDING AIR TIGHTNESS. Significant quantities of air can enter a building by means of infiltration through unintentional leakage paths in the building envelope. Such leakage is of more concern for an exterior CBR release at some distance from a building, such as a large-scale attack, than for a directed terrorist act. The reduction of air leakage is a matter of tight building construction in combination with building pressurization. While building pressurization may be a valuable CBR-protection strategy in any building, it is much more likely to be effective in a tight building. However, to be effective, filtration of building supply air must be appropriate for the CBR agent introduced. Although increasing the air tightness of an existing building can be more challenging than during new construction, it should still be seriously considered.
# Maintenance, Administration, and Training
# CONCLUSIONS
Reducing a building's vulnerability to an airborne chemical, biological, or radiological attack requires a comprehensive approach. Decisions concerning which protective measures to implement should be based upon the threat profile and a security assessment of the building and its occupants. While physical security is the first layer of defense, other issues must also be addressed. Preventing possible terrorist access to outdoor air intakes and mechanical rooms and developing CBR-contingent emergency response plans should be addressed as soon as possible. Additional measures can provide further protection. A building security assessment should be done to determine the necessity of additional measures. Some items, such as improved maintenance and HVAC system controls, may also provide a payback in operating costs and/or improved building air quality. As new building designs or modifications are considered, designers should consider that practical CBR sensors may soon become available. Building system design features that are capable of incorporating this rapidly evolving technology will most likely offer a greater level of protection. While it is not possible to completely eliminate the risk of a CBR terrorist attack, several measures can be taken to reduce the likelihood and consequences of such an attack. Many of the recommendations presented here are ones that can be implemented reasonably quickly and cost effectively. Many are applicable to both new construction and existing buildings, although some may be more feasible than others. Building owners and managers should assess buildings by looking first for those items that are most vulnerable and can be addressed easily. Additional measures should be implemented as feasible. The goals are to make your building an unattractive target for a CBR attack and to maximize occupant protection in the event that such an attack occurs.
# For Additional Information
Several organizations have developed guidance to assist building owners and operators in addressing issues related to building security and CBR terrorist attacks. Many other organizations have guidance that addresses security needs and disaster response plans for events such as fire, natural disasters, and bomb threats. While this latter guidance may not specifically address the terrorist threat to HVAC systems, readers may find portions of the information beneficial in establishing their own building's emergency response plans.
The following list is not all-inclusive. Available guidance is updated regularly as additional organizations and evolving technologies identify new protective recommendations.
# Organization
Reference or Link Description | None | None |
8a49a817d4419f91ef6706754d94b28c03aace2c | cdc | None | The full-text version of the guidelines appears as a web-based document at the CDC's Division of Healthcare Quality Promotion's Internet site at: www.cdc.gov/ncidod/hip/enviro/guide.htm The full-text version of the guidelines should be cited when reference is made primarily to material in Parts I and IV.#
microorganisms; k) infection-control procedures for health-care laundry; l) use of animals in health care for activities and therapy; m) managing the presence of service animals in health-care facilities; n) infection-control strategies for when animals receive treatment in human health-care facilities; and o) a call to reinstate the practice of inactivating amplified cultures and stocks of microorganisms on-site during medical waste treatment.
Whenever possible, the recommendations in Part II are based on data from well-designed scientific studies. However, certain of these studies were conducted by using narrowly defined patient populations or for specific health-care settings (e.g., hospitals versus long-term care facilities), making generalization of findings potentially problematic. Construction standards for hospitals or other health care facilities may not apply to residential home-care units. Similarly, infection-control measures indicated for immunosuppressed patient care are usually not necessary in those facilities where such patients are not present. Other recommendations were derived from knowledge gained during infectious disease investigations in health-care facilities, where successful termination of the outbreak was often the result of multiple interventions, the majority of which cannot be independently and rigorously evaluated. This is especially true for construction situations involving air or water.
Other recommendations are derived from empiric engineering concepts and may reflect an industry standard rather than an evidence-based conclusion. Where recommendations refer to guidance from the American Institute of Architects (AIA), the statements reflect standards intended for new construction or renovation. Existing structures and engineered systems are expected to be in continued compliance with the standards in effect at the time of construction or renovation. Also, in the absence of scientific confirmation, certain infection-control recommendations that cannot be rigorously evaluated are based on a strong theoretical rationale and suggestive evidence. Finally, certain recommendations are derived from existing federal regulations. The references and the appendices comprise Parts III and IV of this document, respectively.
Infections caused by the microorganisms described in these guidelines are rare events, and the effect of these recommendations on infection rates in a facility may not be readily measurable. Therefore, the following steps to measure performance are suggested to evaluate these recommendations (Box 1): Topics outside the scope of this document include a) noninfectious adverse events (e.g., sick building syndrome); b) environmental concerns in the home; c) home health care; d) bioterrorism; and e) health care-associated foodborne illness. This document includes only limited discussion of a) handwashing/hand hygiene; b) standard precautions; and c) infection-control measures used to prevent instrument or equipment contamination during patient care (e.g., preventing waterborne contamination of nebulizers or ventilator humidifiers). These topics are mentioned only if they are important in minimizing the transfer of pathogens to and from persons or equipment and the environment. Although the document discusses principles of cleaning and disinfection as they are applied to maintenance of environmental surfaces, the full discussion of sterilization and disinfection of medical instruments and direct patient-care devices is deferred for inclusion in the Guideline for Disinfection and Sterilization in Health-Care Facilities, a document currently under development. Similarly, the full discussion of hand hygiene is available as the
# Part I. Background Information: Environmental Infection Control in Health-Care Facilities
# A. Introduction
The health-care environment contains a diverse population of microorganisms, but only a few are significant pathogens for susceptible humans. Microorganisms are present in great numbers in moist, organic environments, but some also can persist under dry conditions. Although pathogenic microorganisms can be detected in air and water and on fomites, assessing their role in causing infection and disease is difficult.11 Only a few reports clearly delineate a "cause and effect" with respect to the environment and in particular, housekeeping surfaces.
Eight criteria are used to evaluate the strength of evidence for an environmental source or means of transmission of infectious agents (Box 2).11, 12 Applying these criteria to disease investigations allows scientists to assess the contribution of the environment to disease transmission. An example of this application is the identification of a pathogen (e.g., vancomycin-resistant enterococci ) on an environmental surface during an outbreak. The presence of the pathogen does not establish its causal role; its transmission from source to host could be through indirect means (e.g., via hand transferral). 11 The surface, therefore, would be considered one of a number of potential reservoirs for the pathogen, but not the "de facto" source of exposure. An understanding of how infection occurs after exposure, based on the principles of the "chain of infection," is also important in evaluating the contribution of the environment to health-care-associated disease. 13 All of the components of the "chain" must be operational for infection to occur (Box 3). The presence of the susceptible host is one of these components that underscores the importance of the health-care environment and opportunistic pathogens on fomites and in air and water. As a result of advances in medical technology and therapies (e.g., cytotoxic chemotherapy and transplantation medicine), more patients are becoming immunocompromised in the course of treatment and are therefore at increased risk for acquiring health-care-associated opportunistic infections. Trends in health-care delivery (e.g., early discharge of patients from acute care facilities) also are changing the distribution of patient populations and increasing the number of immunocompromised persons in non acute-care hospitals. According to the American Hospital Association (AHA), in 1998, the number of hospitals in the United States totaled 6,021; these hospitals had a total of 1,013,000 beds,14 representing a 5.5% decrease in the number of acute-care facilities and a 10.2% decrease in the number of beds over the 5-year period 1994-1998.14 In addition, the total average daily number of patients receiving care in U.S. acute-care hospitals in 1998 was 662,000 (65.4%) -36.5% less than the 1978 average of 1,042,000.14 As the number of acute-care hospitals declines, the length of stay in these facilities is concurrently decreasing, particularly for immunocompetent patients. Those patients remaining in acutecare facilities are likely to be those requiring extensive medical interventions who therefore at high risk for opportunistic infection.
The growing population of severely immunocompromised patients is at odds with demands on the health-care industry to remain viable in the marketplace; to incorporate modern equipment, new diagnostic procedures, and new treatments; and to construct new facilities. Increasing numbers of health-care facilities are likely to be faced with construction in the near future as hospitals consolidate to reduce costs, defer care to ambulatory centers and satellite clinics, and try to create more "home-like" acute-care settings. In 1998, approximately 75% of health-care-associated construction projects focused on renovation of existing outpatient facilities or the building of such facilities;15 the number of projects associated with outpatient health care rose by 17% from 1998 through 1999. 16 An aging population is also creating increasing demand for assisted-living facilities and skilled nursing centers. Construction of assisted-living facilities in 1998 increased 49% from the previous year, with 138 projects completed at a cost of $703 million. 16 Overall, from 1998 to 1999, health-care-associated construction costs increased by 28.5%, from $11.56 billion to $14.86 billion. 16 Environmental disturbances associated with construction activities near health-care facilities pose airborne and waterborne disease threats risks for the substantial number of patients who are at risk for health-care-associated opportunistic infections. The increasing age of hospitals and other health-care facilities is also generating ongoing need for repair and remediation work (e.g., installing wiring for new information systems, removing old sinks, and repairing elevator shafts) that can introduce or increase contamination of the air and water in patient-care environments. Aging equipment, deferred maintenance, and natural disasters provide additional mechanisms for the entry of environmental pathogens into high-risk patient-care areas.
Architects, engineers, construction contractors, environmental health scientists, and industrial hygienists historically have directed the design and function of hospitals' physical plants. Increasingly, however, because of the growth in the number of susceptible patients and the increase in construction projects, the involvement of hospital epidemiologists and infection-control professionals is required. These experts help make plans for building, maintaining, and renovating health-care facilities to ensure that the adverse impact of the environment on the incidence of health-care-associated infections is minimal. The following are examples of adverse outcomes that could have been prevented had such experts been involved in the planning process: a) transmission of infections caused by Mycobacterium tuberculosis, varicella-zoster virus (VZV), and measles (i.e., rubeola) facilitated by inappropriate air-handling systems in health-care facilities;6 b) disease outbreaks caused by Aspergillus spp., 20 and Penicillium spp. associated with the absence of environmental controls during periods of health-care facility-associated construction;21 c) infections and/or colonizations of patients and staff with vancomycin-resistant Enterococcus faecium and Clostridium difficile acquired indirectly from contact with organisms present on environmental surfaces in health-care facilities;22-25 and d) outbreaks and pseudoepidemics of legionellae,26, 27 Pseudomonas aeruginosa383 and the nontuberculous mycobacteria (NTM)31, 32 linked to water and aqueous solutions used in health-care facilities. The purpose of this guideline is to provide useful information for both health-care professionals and engineers in efforts to provide a safe environment in which quality health care may be provided to patients. The recommendations herein provide guidance to minimize the risk for and prevent transmission of pathogens in the indoor environment.
# B. Key Terms Used in this Guideline
Although Appendix A provides definitions for terms discussed in Part I, several terms that pertain to specific patient-care areas and patients who are at risk for health-care-associated opportunistic infections are presented here. Specific engineering parameters for these care areas are discussed more fully in the text. Airborne Infection Isolation (AII) refers to the isolation of patients infected with organisms spread via airborne droplet nuclei 12 ACH for new construction as of 2001; >6 ACH for construction before 2001), and is under negative pressure, such that the direction of the airflow is from the outside adjacent space (e.g., corridor) into the room. The air in an AII room is preferably exhausted to the outside, but may be recirculated provided that the return air is filtered through a high efficiency particulate air (HEPA) filter. The use of personal respiratory protection is also indicated for persons entering these rooms.
Protective Environment (PE) is a specialized patient-care area, usually in a hospital, with a positive airflow relative to the corridor (i.e., air flows from the room to the outside adjacent space). The combination of HEPA filtration, high numbers of air changes per hour (>12 ACH), and minimal leakage of air into the room creates an environment that can safely accommodate patients who have undergone allogeneic hematopoietic stem cell transplant (HSCT).
Immunocompromised patients are those patients whose immune mechanisms are deficient because of immunologic disorders (e.g., human immunodeficiency virus infection, congenital immune deficiency syndrome, chronic diseases ) or immunosuppressive therapy (e.g., radiation, cytotoxic chemotherapy, anti-rejection medication, and steroids). Immunocompromised patients who are identified as high-risk patients have the greatest risk of infection caused by airborne or waterborne microorganisms. Patients in this subset include those who are severely neutropenic for prolonged periods of time (i.e., an absolute neutrophil count of <500 cells/mL), allogeneic HSCT patients, and those who have received intensive chemotherapy (e.g., childhood acute myelogenous leukemia patients).
# C. Air
# Modes of Transmission of Airborne Diseases
A variety of airborne infections in susceptible hosts can result from exposures to clinically significant microorganisms released into the air when environmental reservoirs (i.e., soil, water, dust, and decaying organic matter) are disturbed. Once these materials are brought indoors into a health-care facility by any of a number of vehicles (e.g., people, air currents, water, construction materials, and equipment), the attendant microorganisms can proliferate in various indoor ecological niches and, if subsequently disbursed into the air, serve as a source for airborne health-care-associated infections.
Respiratory infections can be acquired from exposure to pathogens contained either in droplets or droplet nuclei. Exposure to microorganisms in droplets (e.g., through aerosolized oral and nasal secretions from infected patients33) constitutes a form of direct contact transmission. When droplets are produced during a sneeze or cough, a cloud of infectious particles >5 pm in size is expelled, resulting in the potential exposure of susceptible persons within 3 feet of the source person.6 Examples of pathogens spread in this manner are influenza virus, rhinoviruses, adenoviruses, and respiratory syncytial virus (RSV). Because these agents primarily are transmitted directly and because the droplets tend to fall out of the air quickly, measures to control air flow in a health-care facility (e.g., use of negative pressure rooms) generally are not indicated for preventing the spread of diseases caused by these agents. Strategies to control the spread of these diseases are outlined in another guideline. 3 The spread of airborne infectious diseases via droplet nuclei is a form of indirect transmission. 34 Droplet nuclei are the residuals of droplets that, when suspended in air, subsequently dry and produce particles ranging in size from 1-5 pm. These particles can a) contain potentially viable microorganisms, b) be protected by a coat of dry secretions, c) remain suspended indefinitely in air, and d) be transported over long distances. The microorganisms in droplet nuclei persist in favorable conditions (e.g., a dry, cool atmosphere with little or no direct exposure to sunlight or other sources of radiation). Pathogenic microorganisms that can be spread via droplet nuclei include Mycobacterium tuberculosis, VZV, measles virus (i.e., rubeola), and smallpox virus (i.e., variola major).6 Several environmental pathogens have life-cycle forms that are similar in size to droplet nuclei and may exhibit similar behavior in the air. The spores of Aspergillus fumigatus have a diameter of 2-3.5 pm, with a settling velocity estimated at 0.03 cm/second (or about 1 meter/hour) in still air. With this enhanced buoyancy, the spores, which resist desiccation, can remain airborne indefinitely in air currents and travel far from their source.35
# Airborne Infectious Diseases in Health-Care Facilities a. Aspergillosis and Other Fungal Diseases
Aspergillosis is caused by molds belonging to the genus Aspergillus. Aspergillus spp. are prototype health-care-acquired pathogens associated with dusty or moist environmental conditions. Clinical and epidemiologic aspects of aspergillosis (Table 1) are discussed extensively in another guideline.3
# Table 1. Clinical and epidemiologic characteristics of aspergillosis
fungal spores. Increased levels of atmospheric dust and fungal spores have been associated with clusters of health-care-acquired infections in immunocompromised patients. 17' 20, 44, 47, 49, 50, 95-98 Absorbent building materials (e.g., wallboard) serve as an ideal substrate for the proliferation of this organism if they become and remain wet, thereby increasing the numbers of fungal spores in the area. Patient-care items, devices, and equipment can become contaminated with Aspergillus spp. spores and serve as sources of infection if stored in such areas. 57 Most cases of aspergillosis are caused by Aspergillus fumigatus, a thermotolerant/thermophilic fungus capable of growing over a temperature range from 53.6°F-127.4°F (12°C-53°C); optimal growth occurs at approximately 104°F (40°C), a temperature inhibitory to most other saprophytic fungi.99 It can use cellulose or sugars as carbon sources; because its respiratory process requires an ample supply of carbon, decomposing organic matter is an ideal substrate.
Other opportunistic fungi that have been occasionally linked with health-care-associated infections are members of the orderMucorales (e.g., Rhizopus spp.) and miscellaneous moniliaceous molds (e.g., Fusarium spp. and Penicillium spp.) (Table 2). Many of these fungi can proliferate in moist environments (e.g., water-damaged wood and building materials). Some fungi (e.g., Fusarium spp. and Pseudoallescheria spp.) also can be airborne pathogens.100 As with aspergillosis, a major risk factor for disease caused by any of these pathogens is the host's severe immunosuppression from either underlying disease or immunosuppressive therapy.101, 102
# Table 2. Environmental fungal pathogens: entry into and contamination of the health care facility
Infections due Cryptococcus neoformans, Histoplasma capsulatum, or Coccidioides immitis can occur in health-care settings if nearby ground is disturbed and a malfunction of the facility's air-intake components allows these pathogens to enter the ventilation system. C. neoformans is a yeast usually 4 8 pm in size. However, viable particles of <2 pm diameter (and thus permissive to alveolar deposition) have been found in soil contaminated with bird droppings, particularly from pigeons.98, 103, 104, 121 H. capsulatum, with the infectious microconidia ranging in size from 2-5 pm, is endemic in the soil of the central river valleys of the United States. Substantial numbers of these infectious particles have been associated with chicken coops and the roosts of blackbirds.98, 103, 104, 122 Several outbreaks of histoplasmosis have been associated with disruption of the environment; construction activities in an endemic area may be a potential risk factor for health-care-acquired airborne infection.123, 124 C. immitis, with arthrospores of 3-5 pm diameter, has similar potential, especially in the endemic southwestern United States and during seasons of drought followed by heavy rainfall. After the 1994 earthquake centered near Northridge, California, the incidence of coccidioidomycosis in the surrounding area exceeded the historical norm. 125 Emerging evidence suggests that Pneumocystis carinii, now classified as a fungus, may be spread via airborne, person-to-person transmission.126 Controlled studies in animals first demonstrated that P. carinii could be spread through the air. 127 More recent studies in health-care settings have detected nucleic acids of P. carinii in air samples from areas frequented or occupied by P. carinii-infected patients but not in control areas that are not occupied by these patients. , Clusters of cases have been identified among immunocompromised patients who had contact with a source patient and with each other. Recent studies have examined the presence of P. carinii DNA in oropharyngeal washings and the nares of infected patients, their direct contacts, and persons with no direct contact. 130,131 Molecular analysis of the DNA by polymerase chain reaction (PCR) provides evidence for airborne transmission of P. carinii from infected patients to direct contacts, but immunocompetent contacts tend to become transiently colonized rather than infected.131 The role of colonized persons in the spread of P. carinii pneumonia (PCP) remains to be determined. At present, specific modifications to ventilation systems to control spread of PCP in a health-care facility are not indicated. Current recommendations M. tuberculosis is carried by droplet nuclei generated when persons (primarily adults and adolescents) who have pulmonary or laryngeal TB sneeze, cough, speak, or sing;139 normal air currents can keep these particles airborne for prolonged periods and spread them throughout a room or building.142 However, transmission of TB has occurred from mycobacteria aerosolized during provision of care (e.g., wound/lesion care or during handling of infectious peritoneal dialysis fluid) for extrapulmonary TB patients. 135,140 Gram-positive cocci (i.e., Staphylococcus aureus, group A beta-hemolytic streptococci), also important health-care-associated pathogens, are resistant to inactivation by drying and can persist in the environment and on environmental surfaces for extended periods. These organisms can be shed from heavily colonized persons and discharged into the air. Airborne dispersal of S. aureus is directly associated with the concentration of the bacterium in the anterior nares.143 Approximately 10% of healthy carriers will disseminate S. aureus into the air, and some persons become more effective disseminators of S. aureus than others. The dispersal of S. aureus into air can be exacerbated by concurrent viral upper respiratory infection, thereby turning a carrier into a "cloud shedder."149 Outbreaks of surgical site infections (SSIs) caused by group A beta-hemolytic streptococci have been traced to airborne transmission from colonized operating-room personnel to patients.150153 In these situations, the strain causing the outbreak was recovered from the air in the operating room150, 151, 154 or on settle plates in a room in which the carrier exercised.151153 S. aureus and group A streptococci have not been linked to airborne transmission outside of operating rooms, burn units, and neonatal nurseries. 155,156 Transmission of these agents occurs primarily via contact and droplets.
Other gram-positive bacteria linked to airborne transmission include Bacillus spp. which are capable of sporulation as environmental conditions become less favorable to support their growth. Outbreaks and pseudo-outbreaks have been attributed to Bacillus cereus in maternity, pediatric, intensive care, and bronchoscopy units; many of these episodes were secondary to environmental contamination.157160 Gram-negative bacteria rarely are associated with episodes of airborne transmission because they generally require moist environments for persistence and growth. The main exception is Acinetobacter spp., which can withstand the inactivating effects of drying. In one epidemiologic investigation of bloodstream infections among pediatric patients, identical Acinetobacter spp. were cultured from the patients, air, and room air conditioners in a nursery. 161 Aerosols generated from showers and faucets may potentially contain legionellae and other gram negative waterborne bacteria (e.g., Pseudomonas aeruginosa). Exposure to these organisms is through direct inhalation. However, because water is the source of the organisms and exposure occurs in the vicinity of the aerosol, the discussion of the diseases associated with such aerosols and the prevention measures used to curtail their spread is discussed in another section of the Guideline (see Part I: Water).
# c. Airborne Viral Diseases
Some human viruses are transmitted from person to person via droplet aerosols, but very few viruses are consistently airborne in transmission (i.e., are routinely suspended in an infective state in air and capable of spreading great distances), and health-care-associated outbreaks of airborne viral disease are limited to a few agents. Consequently, infection-control measures used to prevent spread of these viral diseases in health-care facilities primarily involve patient isolation, vaccination of susceptible persons, and antiviral therapy as appropriate rather than measures to control air flow or quality. 6 Infections caused by VZV frequently are described in health-care facilities. Health-care-associated airborne outbreaks of VZV infections from patients with primary infection and disseminated zoster have been documented; patients with localized zoster have, on rare occasions, also served as source patients for outbreaks in health-care facilities.162-166 VZV infection can be prevented by vaccination, although patients who develop a rash within 6 weeks of receiving varicella vaccine or who develop breakthrough varicella following exposure should be considered contagious. 167 Viruses whose major mode of transmission is via droplet contact rarely have caused clusters of infections in group settings through airborne routes. The factors facilitating airborne distribution of these viruses in an infective state are unknown, but a presumed requirement is a source patient in the early stage of infection who is shedding large numbers of viral particles into the air. Airborne transmission of measles has been documented in health-care facilities. In addition, institutional outbreaks of influenza virus infections have occurred predominantly in nursing homes,172-176 and less frequently in medical and neonatal intensive care units, chronic-care areas, HSCT units, and pediatric wards.177-180 Some evidence supports airborne transmission of influenza viruses by droplet nuclei,181, 182 and case clusters in pediatric wards suggest that droplet nuclei may play a role in transmitting certain respiratory pathogens (e.g., adenoviruses and respiratory syncytial virus ).177, 183, 184 Some evidence also supports airborne transmission of enteric viruses. An outbreak of a Norwalk-like virus infection involving more than 600 staff personnel over a 3-week period was investigated in a Toronto, Ontario hospital in 1985; common sources (e.g., food and water) were ruled out during the investigation, leaving airborne spread as the most likely mode of transmission.185 Smallpox virus, a potential agent of bioterrorism, is spread predominantly via direct contact with infectious droplets, but it also can be associated with airborne transmission.186, 187 A German hospital study from 1970 documented the ability of this virus to spread over considerable distances and cause infection at low doses in a well-vaccinated population; factors potentially facilitating transmission in this situation included a patient with cough and an extensive rash, indoor air with low relative humidity, and faulty ventilation patterns resulting from hospital design (e.g., open windows).188 Smallpox patients with extensive rash are more likely to have lesions present on mucous membranes and therefore have greater potential to disseminate virus into the air. 188 In addition to the smallpox transmission in Germany, two cases of laboratory-acquired smallpox virus infection in the United Kingdom in 1978 also were thought to be caused by airborne transmission. 189 Airborne transmission may play a role in the natural spread of hantaviruses and certain hemorrhagic fever viruses (e.g., Ebola, Marburg, and Lassa), but evidence for airborne spread of these agents in health-care facilities is inconclusive. 190 Although hantaviruses can be transmitted when aerosolized from rodent excreta ,191, 192 person-to-person spread of hantavirus infection from source patients has not occurred in health-care facilities. Nevertheless, health-care workers are advised to contain potentially infectious aerosols and wear National Institute of Occupational Safety and Health (NIOSH) approved respiratory protection when working with this agent in laboratories or autopsy suites.196 Lassa virus transmission via aerosols has been demonstrated in the laboratory and incriminated in health-care-associated infections in Africa,197-199 but airborne spread of this agent in hospitals in developed nations likely is inefficient. 200,201 Yellow fever is considered to be a viral hemorrhagic fever agent with high aerosol infectivity potential, but health-care-associated transmission of this virus has not been described.202 Viral hemorrhagic fever diseases primarily occur after direct exposure to infected blood and body fluids, and the use of standard and droplet precautions prevents transmission early in the course of these illnesses.203, 204 However, whether these viruses can persist in droplet nuclei that might remain after droplet production from coughs or vomiting in the latter stages of illness is unknown. 205 Although the use of a negative-pressure room is not required during the early stages of illness, its use might be prudent at the time of hospitalization to avoid the need for subsequent patient transfer. Current CDC guidelines recommend negative-pressure rooms with anterooms for patients with hemorrhagic fever and use of HEPA respirators by persons entering these rooms when the patient has prominent cough, vomiting, diarrhea, or hemorrhage.6, 203 Face shields or goggles will help to prevent mucous-membrane exposure to potentially-aerosolized infectious material in these situations. If an anteroom is not available, portable, industrial-grade high efficiency particulate air (HEPA) filter units can be used to provide the equivalent of additional air changes per hour (ACH).
The recommendations in this guideline for Ebola Virus Disease has been superseded by CDC's Infection Prevention and Control Recommendations for Hospitalized Patients with Known or Suspected Ebola Virus Disease in U.S. Hospitals and by CDC's Interim Guidance for Environmental Infection Control in Hospitals for Ebola Virus issued on August 1, 2014. 13 Click here for current information on how Ebola virus is transmitted. Under investigation Pneumocystis cariniilil --- This list excludes microorganisms transmitted from aerosols derived from water. + Refer to the text for references for these disease agents. § Airborne transmission of smallpox is infrequent. Potential for airborne transmission increases with patients who are effective disseminators present in facilities with low relative humidity in the air and faulty ventilation. Documentation of pseudoepidemic during construction. Airborne transmission documented in the laboratory but not in patient-care areas
# Heating, Ventilation, and Air Conditioning Systems in Health-Care Facilities a. Basic Components and Operations
Heating, ventilation, and air conditioning (HVAC) systems in health-care facilities are designed to a) maintain the indoor air temperature and humidity at comfortable levels for staff, patients, and visitors; b) control odors; c) remove contaminated air; d) facilitate air-handling requirements to protect susceptible staff and patients from airborne health-care-associated pathogens; and e) minimize the risk for transmission of airborne pathogens from infected patients.35, 120 An HVAC system includes an outside air inlet or intake; filters; humidity modification mechanisms (i.e., humidity control in summer, humidification in winter); heating and cooling equipment; fans; ductwork; air exhaust or out-takes; and registers, diffusers, or grilles for proper distribution of the air (Figure 1).213, 214 Decreased performance of healthcare facility HVAC systems, filter inefficiencies, improper installation, and poor maintenance can contribute to the spread of health-care-associated airborne infections.
The American Institute of Architects (AIA) has published guidelines for the design and construction of new health-care facilities and for renovation of existing facilities. These AIA guidelines address indoor air-quality standards (e.g., ventilation rates, temperature levels, humidity levels, pressure relationships, and minimum air changes per hour ) specific to each zone or area in health-care facilities (e.g., operating rooms, laboratories, diagnostic areas, patient-care areas, and support departments).120 These guidelines represent a consensus document among authorities having jurisdiction (AHJ), governmental regulatory agencies (i.e., Department of Health and Human Services ; Department of Labor, Occupational Safety and Health Administration ), health-care professionals, professional organizations (e.g., American Society of Heating, Refrigeration, and Air-Conditioning Engineers , American Society for Healthcare Engineering ), and accrediting organizations (i.e., Joint Commission on Accreditation of Healthcare Organizations ). More than 40 state agencies that license health-care facilities have either incorporated or adopted by reference these
# GENERAL R t LJRN AIR EXHAUST
Outdoor air and recirculated air pass through air cleaners (e.g., filter banks) designed to reduce the concentration of airborne contaminants. Air is conditioned for temperature and humidity before it enters the occupied space as supply air. Infiltration is air leakage inward through cracks and interstitial spaces of walls, floors, and ceilings. Exfiltration is air leakage outward through these same cracks and spaces. Return air is largely exhausted from the system, but a portion is recirculated with fresh, incoming air. - Used with permission of the publisher of reference 214 (ASHRAE) Engineering controls to contain or prevent the spread of airborne contaminants center on a) local exhaust ventilation , b) general ventilation, and c) air cleaning. 4 General ventilation encompasses a) dilution and removal of contaminants via well-mixed air distribution of filtered air, b) directing contaminants toward exhaust registers and grilles via uniform, non-mixed airflow patterns, c) pressurization of individual spaces relative to all other spaces, and d) pressurization of buildings relative to the outdoors and other attached buildings.
A centralized HVAC system operates as follows. Outdoor air enters the system, where low-efficiency or "roughing" filters remove large particulate matter and many microorganisms. The air enters the distribution system for conditioning to appropriate temperature and humidity levels, passes through an additional bank of filters for further cleaning, and is delivered to each zone of the building. After the conditioned air is distributed to the designated space, it is withdrawn through a return duct system and delivered back to the HVAC unit. A portion of this "return air" is exhausted to the outside while the remainder is mixed with outdoor air for dilution and filtered for removal of contaminants.215 Air from toilet rooms or other soiled areas is usually exhausted directly to the atmosphere through a separate duct exhaust system. Air from rooms housing tuberculosis patients is exhausted to the outside if possible, or passed through a HEPA filter before recirculation. Ultraviolet germicidal irradiation (UVGI) can be used as an adjunct air-cleaning measure, but it cannot replace HEPA filtration.
# b. Filtration
i. Filter Types and Methods of Filtration Filtration, the physical removal of particulates from air, is the first step in achieving acceptable indoor air quality. Filtration is the primary means of cleaning the air. Five methods of filtration can be used (Table 5). During filtration, outdoor air passes through two filter beds or banks (with efficiencies of 20%-40% and >90%, respectively) for effective removal of particles 1-5 pm in diameter.35, 120 The low-to-medium efficiency filters in the first bank have low resistance to airflow, but this feature allows some small particulates to pass onto heating and air conditioning coils and into the indoor environment.35 Incoming air is mixed with recirculated air and reconditioned for temperature and humidity before being filtered by the second bank of filters. The performance of filters with <90% efficiency is measured using either the dust-spot test or the weight-arrestance test.35, 216 Maintenance costs associated with HEPA filters are high compared with other types of filters, but use of in-line disposable prefilters can increase the life of a HEPA filter by approximately 25%. Alternatively, if a disposable prefilter is followed by a filter that is 90% efficient, the life of the HEPA filter can be extended ninefold. This concept, called progressive filtration, allows HEPA filters in special care areas to be used for 10 years. 213 Although progressive filtering will extend the mechanical ability of the HEPA filter, these filters may absorb chemicals in the environment and later desorb those chemicals, thereby necessitating a more frequent replacement program. HEPA filter efficiency is monitored with the dioctylphthalate (DOP) particle test using particles that are 0.3 pm in diameter.218
HEPA filters are usually framed with metal, although some older versions have wood frames. A metal frame has no advantage over a properly fitted wood frame with respect to performance, but wood can compromise the air quality if it becomes and remains wet, allowing the growth of fungi and bacteria. Hospitals are therefore advised to phase out water-damaged or spent wood-framed filter units and replace them with metal-framed HEPA filters.
HEPA filters are usually fixed into the HVAC system; however, portable, industrial grade HEPA units are available that can filter air at the rate of 300-800 ft3/min. Portable HEPA filters are used to a) temporarily recirculate air in rooms with no general ventilation, b) augment systems that cannot provide adequate airflow, and c) provide increased effectiveness in airflow.4 Portable HEPA units are useful engineering controls that help clean the air when the central HVAC system is undergoing repairs,219 but these units do not satisfy fresh-air requirements.214 The effectiveness of the portable unit for particle removal is dependent on a) the configuration of the room, b) the furniture and persons in the room, c) the placement of the units relative to the contents and layout of the room, and d) the location of the supply and exhaust registers or grilles. If portable, industrial-grade units are used, they should be capable of recirculating all or nearly all of the room air through the HEPA filter, and the unit should be designed to achieve the equivalent of >12 ACH.4 (An average room has approximately 1,600 ft3 of airspace.) The hospital engineering department should be contacted to provide ACH information in the event that a portable HEPA filter unit is necessary to augment the existing fixed HVAC system for air cleaning.
ii. Filter Maintenance Efficiency of the filtration system is dependent on the density of the filters, which can create a drop in pressure unless compensated by stronger and more efficient fans, thus maintaining air flow. For optimal performance, filters require monitoring and replacement in accordance with the manufacturer's recommendations and standard preventive maintenance practices.220 Upon removal, spent filters can be bagged and discarded with the routine solid waste, regardless of their patient-care area location.221 Excess accumulation of dust and particulates increases filter efficiency, requiring more pressure to push the air through. The pressure differential across filters is measured by use of manometers or other gauges. A pressure reading that exceeds specifications indicates the need to change the filter. Filters also require regular inspection for other potential causes of decreased performance. Gaps in and around filter banks and heavy soil and debris upstream of poorly maintained filters have been implicated in health-care-associated outbreaks of aspergillosis, especially when accompanied by construction activities at the facility.17, 18, 106, 222
# c. Ultraviolet Germicidal Irradiation (UVGI)
As a supplemental air-cleaning measure, UVGI is effective in reducing the transmission of airborne bacterial and viral infections in hospitals, military housing, and classrooms, but it has only a minimal inactivating effect on fungal spores. -UVGI is also used in air handling units to prevent or limit the growth of vegetative bacteria and fungi. Most commercially available UV lamps used for germicidal purposes are low-pressure mercury vapor lamps that emit radiant energy predominantly at a wave-length of 253.7 nm. , Two systems of UVGI have been used in health-care settings -duct irradiation and upper-room air irradiation. In duct irradiation systems, UV lamps are placed inside ducts that remove air from rooms to disinfect the air before it is recirculated. When properly designed, installed, and maintained, high levels of UVGI can be attained in the ducts with little or no exposure of persons in the rooms. ,
In upper-room air irradiation, UV lamps are either suspended from the ceiling or mounted on the wall.4 Upper air UVGI units have two basic designs: a) a "pan" fixture with UVGI unshielded above the unit to direct the irradiation upward and b) a fixture with a series of parallel plates to columnize the irradiation outward while preventing the light from getting to the eyes of the room's occupants. The germicidal effect is dependent on air mixing via convection between the room's irradiated upper zone and the lower patient-care zones. 233,234 Bacterial inactivation studies using BCG mycobacteria and Serratia marcescens have estimated the effect of UVGI as equivalent to 10 ACH-39 ACH.235, 236 Another study, however, suggests that UVGI may result in fewer equivalent ACH in the patient-care zone, especially if the mixing of air between zones is insufficient. 234 The use of fans or HVAC systems to generate air movement may increase the effectiveness of UVGI if airborne microorganisms are exposed to the light energy for a sufficient length of time. 233, 235, 237 239 The optimal relationship between ventilation and UVGI is not known.
Because the clinical effectiveness of UV systems may vary, UVGI is not recommended for air management prior to air recirculation from airborne isolation rooms. It is also not recommended as a substitute for HEPA filtration, local exhaust of air to the outside, or negative pressure. 4 The use of UV lamps and HEPA filtration in a single unit offers only minimal infection-control benefits over those provided by the use of a HEPA filter alone.240 Duct systems with UVGI are not recommended as a substitute for HEPA filters if the air from isolation rooms must be recirculated to other areas of the facility.4 Regular maintenance of UVGI systems is crucial and usually consists of keeping the bulbs free of dust and replacing old bulbs as necessary. Safety issues associated with the use of UVGI systems are described in other guidelines.4
# d. Conditioned Air in Occupied Spaces
Temperature and humidity are two essential components of conditioned air. After outside air passes through a low-or medium-efficiency filter, the air undergoes conditioning for temperature and humidity control before it passes through high-efficiency or HEPA filtration. i. Temperature HVAC systems in health-care facilities are often single-duct or dual-duct systems.35, 241 A single-duct system distributes cooled air (55°F ) throughout the building and uses thermostatically controlled reheat boxes located in the terminal ductwork to warm the air for individual or multiple rooms. The dual-duct system consists of parallel ducts, one with a cold air stream and the other with a hot air stream. A mixing box in each room or group of rooms mixes the two air streams to achieve the desired temperature. Temperature standards are given as either a single temperature or a range, depending on the specific health-care zone. Cool temperature standards (68°F-73°F ) usually are associated with operating rooms, clean workrooms, and endoscopy suites.120 A warmer temperature (75°F ) is needed in areas requiring greater degrees of patient comfort. Most other zones use a temperature range of 70°F-75°F (21°C-24°C).120 Temperatures outside of these ranges may be needed occasionally in limited areas depending on individual circumstances during patient care (e.g., cooler temperatures in operating rooms during specialized operations).
ii. Humidity Four measures of humidity are used to quantify different physical properties of the mixture of water vapor and air. The most common of these is relative humidity, which is the ratio of the amount of water vapor in the air to the amount of water vapor air can hold at that temperature. 242 The other measures of humidity are specific humidity, dew point, and vapor pressure. 242 Relative humidity measures the percentage of saturation. At 100% relative humidity, the air is saturated. For most areas within health-care facilities, the designated comfort range is 30%-60% relative humidity. , Relative humidity levels >60%, in addition to being perceived as uncomfortable, promote fungal growth.243 Humidity levels can be manipulated by either of two mechanisms. 244 In a water-wash unit, water is sprayed and drops are taken up by the filtered air; additional heating or cooling of this air sets the humidity levels. The second mechanism is by means of water vapor created from steam and added to filtered air in humidifying boxes. Reservoir-type humidifiers are not allowed in health-care facilities as per AIA guidelines and many state codes.120 Cool-mist humidifiers should be avoided, because they can disseminate aerosols containing allergens and microorganisms.245 Additionally, the small, personal-use versions of this equipment can be difficult to clean.
# iii. Ventilation
The control of air pollutants (e.g., microorganisms, dust, chemicals, and smoke) at the source is the most effective way to maintain clean air. The second most effective means of controlling indoor air pollution is through ventilation. Ventilation rates are voluntary unless a state or local government specifies a standard in health-care licensing or health department requirements. These standards typically apply to only the design of a facility, rather than its operation.220, 246 Health-care facilities without specific ventilation standards should follow the AIA guideline specific to the year in which the building was built or the ANSI/ASHRAE Standard 62, Ventilation for Acceptable Indoor Air Quality .120, 214, 241 Ventilation guidelines are defined in terms of air volume per minute per occupant and are based on the assumption that occupants and their activities are responsible for most of the contaminants in the conditioned space.215 Most ventilation rates for health-care facilities are expressed as room ACH. Peak efficiency for particle removal in the air space occurs between 12 ACH-15 ACH.35, 247, 248 Ventilation rates vary among the different patient-care areas of a health-care facility (Appendix B).120
Health-care facilities generally use recirculated air.35, 120, 241, 249, 250 Fans create sufficient positive pressure to force air through the building duct work and adequate negative pressure to evacuate air from the conditioned space into the return duct work and/or exhaust, thereby completing the circuit in a sealed system (Figure 1). However, because gaseous contaminants tend to accumulate as the air recirculates, a percentage of the recirculated air is exhausted to the outside and replaced by fresh outdoor air. In hospitals, the delivery of filtered air to an occupied space is an engineered system design issue, the full discussion of which is beyond the scope of this document.
Hospitals with areas not served by central HVAC systems often use through-the-wall or fan coil air conditioning units as the sole source of room ventilation. AIA guidelines for newly installed systems stipulate that through-the-wall fan-coil units be equipped with permanent (i.e., cleanable) or replaceable filters with a minimum efficiency of 68% weight arrestance.120 These units may be used only as recirculating units; all outdoor air requirements must be met by a separate central air handling system with proper filtration, with a minimum of two outside air changes in general patient rooms (D. Erickson, ASHE, 2000).120 If a patient room is equipped with an individual through-the-wall fan coil unit, the room should not be used as either AII or as PE.120 These requirements, although directed to new HVAC installations also are appropriate for existing settings. Non-central air-handling systems are prone to problems associated with excess condensation accumulating in drip pans and improper filter maintenance; health-care facilities should clean or replace the filters in these units on a regular basis while the patient is out of the room.
Laminar airflow ventilation systems are designed to move air in a single pass, usually through a bank of HEPA filters either along a wall or in the ceiling, in a one-way direction through a clean zone with parallel streamlines. Laminar airflow can be directed vertically or horizontally; the unidirectional system optimizes airflow and minimizes air turbulence.63, 241 Delivery of air at a rate of 0.5 meters per second (90 + 20 ft/min) helps to minimize opportunities for microorganism proliferation.63, 251, 252 Laminar airflow systems have been used in PE to help reduce the risk for health-care-associated airborne infections (e.g., aspergillosis) in high-risk patients.63, 93, 253, 254 However, data that demonstrate a survival benefit for patients in PE with laminar airflow are lacking. Given the high cost of installation and apparent lack of benefit, the value of laminar airflow in this setting is questionable.9, 37 Few data support the use of laminar airflow systems elsewhere in a hospital.255 iv. Pressurization Positive and negative pressures refer to a pressure differential between two adjacent air spaces (e.g., rooms and hallways). Air flows away from areas or rooms with positive pressure (pressurized), while air flows into areas with negative pressure (depressurized). AII rooms are set at negative pressure to prevent airborne microorganisms in the room from entering hallways and corridors. PE rooms housing severely neutropenic patients are set at positive pressure to keep airborne pathogens in adjacent spaces or corridors from coming into and contaminating the airspace occupied by such high-risk patients. Self closing doors are mandatory for both of these areas to help maintain the correct pressure differential.4, 6 120 Older health-care facilities may have variable pressure rooms (i.e., rooms in which the ventilation can be manually switched between positive and negative pressure). These rooms are no longer permitted in the construction of new facilities or in renovated areas of the facility,120 and their use in existing facilities has been discouraged because of difficulties in assuring the proper pressure differential, especially for the negative pressure setting, and because of the potential for error associated with switching the pressure differentials for the room. Continued use of existing variable pressure rooms depends on a partnership between engineering and infection control. Both positive-and negative-pressure rooms should be maintained according to specific engineering specifications (Table 6).
# Room airflow direction
# Out to the adjacent area
In to the room
# Clean-to-dirty airflow in room
Away from the patient (high-risk patient, immunosuppressed patient) Health-care professionals (e.g., infection control, hospital epidemiologists) must perform a risk assessment to determine the appropriate number of AII rooms (negative pressure) and/or PE rooms (positive pressure) to serve the patient population. The AIA guidelines require a certain number of AII rooms as a minimum, and it is important to refer to the edition under which the building was built for appropriate guidance.120
In large health-care facilities with central HVAC systems, sealed windows help to ensure the efficient operation of the system, especially with respect to creating and maintaining pressure differentials. Sealing the windows in PE areas helps minimize the risk of airborne contamination from the outside. One outbreak of aspergillosis among immunosuppressed patients in a hospital was attributed in part to an open window in the unit during a time when both construction and a fire happened nearby; sealing the window prevented further entry of fungal spores into the unit from the outside air.111 Additionally, all emergency exits (e.g., fire escapes and emergency doors) in PE wards should be kept closed (except during emergencies) and equipped with alarms.
# e. Infection Control Impact of HVAC System Maintenance and Repair
A failure or malfunction of any component of the HVAC system may subject patients and staff to discomfort and exposure to airborne contaminants. Only limited information is available from formal studies on the infection-control implications of a complete air-handling system failure or shutdown for maintenance. Most experience has been derived from infectious disease outbreaks and adverse outcomes among high-risk patients when HVAC systems are poorly maintained. (See Table 7 for potential ventilation hazards, consequences, and correction measures.)
AIA guidelines prohibit U.S. hospitals and surgical centers from shutting down their HVAC systems for purposes other than required maintenance, filter changes, and construction.120 Airflow can be reduced; however, sufficient supply, return, and exhaust must be provided to maintain required pressure relationships when the space is not occupied. Maintaining these relationships can be accomplished with special drives on the air-handling units (i.e., a variable air ventilation system).
Microorganisms proliferate in environments wherever air, dust, and water are present, and air-handling systems can be ideal environments for microbial growth.35 Properly engineered HVAC systems require routine maintenance and monitoring to provide acceptable indoor air quality efficiently and to minimize conditions that favor the proliferation of health-care-associated pathogens.35, 249 Performance monitoring of the system includes determining pressure differentials across filters, regular inspection of system filters, DOP testing of HEPA filters, testing of low-or medium efficiency filters, and manometer tests for positive-and negative-pressure areas in accordance with nationally recognized standards, guidelines, and manufacturers' recommendations. The use of hand-held, calibrated equipment that can provide a numerical reading on a daily basis is preferred for engineering purposes (A.Streifel, University of Minnesota, 2000). 256 Several methods that provide a visual, qualitative measure of pressure differentials (i.e., airflow direction) include smoke-tube tests or placing flutter strips, ping-pong balls, or tissue in the air stream.
Preventive filter and duct maintenance (e.g., cleaning ductwork vents, replacing filters as needed, and properly disposing spent filters into plastic bags immediately upon removal) is important to prevent potential exposures of patients and staff during HVAC system shut-down. The frequency of filter inspection and the parameters of this inspection are established by each facility to meet their unique needs. Ductwork in older health-care facilities may have insulation on the interior surfaces that can trap contaminants. This insulation material tends to break down over time to be discharged from the HVAC system. Additionally, a malfunction of the air-intake system can overburden the filtering system and permit aerosolization of fungal pathogens. Keeping the intakes free from bird droppings, especially those from pigeons, helps to minimize the concentration of fungal spores entering from the outside.98
Accumulation of dust and moisture within HVAC systems increases the risk for spread of health-careassociated environmental fungi and bacteria. Clusters of infections caused by Aspergillus spp., P. aeruginosa, S. aureus, and Acinetobacter spp. have been linked to poorly maintained and/or malfunctioning air conditioning systems.68, 161, 257, 258 Efforts to limit excess humidity and moisture in the infrastructure and on air-stream surfaces in the HVAC system can minimize the proliferation and dispersion of fungal spores and waterborne bacteria throughout indoor air.259-262 Within the HVAC system, water is present in water-wash units, humidifying boxes, or cooling units. The dual-duct system may also create conditions of high humidity and excess moisture that favor fungal growth in drain pans as well as in fibrous insulation material that becomes damp as a result of the humid air passing over the hot stream and condensing.
If moisture is present in the HVAC system, periods of stagnation should be avoided. Bursts of organisms can be released upon system start-up, increasing the risk of airborne infection.206 Proper engineering of the HVAC system is critical to preventing dispersal of airborne organisms. In one hospital, endophthalmitis caused by Acremonium kiliense infection following cataract extraction in an ambulatory surgical center was traced to aerosols derived from the humidifier water in the ventilation system.206 The organism proliferated because the ventilation system was turned off routinely when the center was not in operation; the air was filtered before humidification, but not afterwards.
Most health-care facilities have contingency plans in case of disruption of HVAC services. These plans include back-up power generators that maintain the ventilation system in high-risk areas (e.g., operating rooms, intensive-care units, negative-and positive-pressure rooms, transplantation units, and oncology units). Alternative generators are required to engage within 10 seconds of a loss of main power. If the ventilation system is out of service, rendering indoor air stagnant, sufficient time must be allowed to clean the air and re-establish the appropriate number of ACH once the HVAC system begins to function again. Air filters may also need to be changed, because reactivation of the system can dislodge substantial amounts of dust and create a transient burst of fungal spores.
Duct cleaning in health-care facilities has benefits in terms of system performance, but its usefulness for infection control has not been conclusively determined. Duct cleaning typically involves using specialized tools to dislodge dirt and a high-powered vacuum cleaner to clean out debris.263 Some duct cleaning services also apply chemical biocides or sealants to the inside surfaces of ducts to minimize fungal growth and prevent the release of particulate matter. The U.S. Environmental Protection Agency (EPA), however, has concerns with the use of sanitizers and/or disinfectants to treat the surfaces of ductwork, because the label indications for most of these products may not specifically include the use of the product in HVAC systems.264 Further, EPA has not evaluated the potency of disinfectants in such applications, nor has the agency examined the potential attendant health and safety risks. The EPA recommends that companies use only those chemical biocides that are registered for use in HVAC systems.264 Although infrequent cleaning of the exhaust ducts in AII areas has been documented as a cause of diminishing negative pressure and a decrease in the air exchange rates,214 no data indicate that duct cleaning, beyond what is recommended for optimal performance, improves indoor air quality or reduces the risk of infection. Exhaust return systems should be cleaned as part of routine system maintenance. Duct cleaning has not been shown to prevent any health problems,265 and EPA studies indicate that airborne particulate levels do not increase as a result of dirty air ducts, nor do they diminish after cleaning, presumably because much of the dirt inside air ducts adheres to duct surfaces and does not enter the conditioned space.265 Additional research is needed to determine if air-duct contamination can significantly increase the airborne infection risk in general areas of health-care facilities.
# Construction, Renovation, Remediation, Repair, and Demolition
# a. General Information
Environmental disturbances caused by construction and/or renovation and repair activities (e.g., disruption of the above-ceiling area, running cables through the ceiling, and structural repairs) in and near health-care facilities markedly increase the airborne Aspergillus spp. spore counts in the indoor air of such facilities, thereby increasing the risk for health-care-associated aspergillosis among high-risk patients. Although one case of health-care-associated aspergillosis is often difficult to link to a specific environmental exposure, the occurrence of temporarily clustered cases increase the likelihood that an environmental source within the facility may be identified and corrected. Construction, renovation, repair, and demolition activities in health-care facilities require substantial planning and coordination to minimize the risk for airborne infection both during projects and after their completion. Several organizations and experts have endorsed a multi-disciplinary team approach (Box 4) to coordinate the various stages of construction activities (e.g., project inception, project implementation, final walk-through, and completion).120, 249, 250, 273-276 Environmental services, employee health, engineering, and infection control must be represented in construction planning and design meetings should be convened with architects and design engineers. The number of members and disciplines represented is a function of the complexity of a project. Smaller, less complex projects and maintenance may require a minimal number of members beyond the core representation from engineering, infection control, environmental services, and the directors of the specialized departments.
# b. Preliminary Considerations
The three major topics to consider before initiating any construction or repair activity are as follows: a) design and function of the new structure or area, b) assessment of environmental risks for airborne disease and opportunities for prevention, and c) measures to contain dust and moisture during construction or repairs. A checklist of design and function considerations can help to ensure that a planned structure or area can be easily serviced and maintained for environmental infection control (Box 5) . , , , -Specifications for the construction, renovation, remodeling, and maintenance of health-care facilities are outlined in the AIA document, Guidelines for Design and Construction o f Hospitals and Health Care Facilities.120, 275
# Box 5. Construction design and function considerations for environmental infection control
Location of sinks and dispensers for handwashing products and hand hygiene products Types of faucets (e.g., aerated vs. non-aerated) Air-handling systems engineered for optimal performance, easy maintenance, and repair ACH and pressure differentials to accommodate special patient-care areas Location of fixed sharps containers Types of surface finishes (e.g., porous vs. non-porous) Well-caulked walls with minimal seams Location of adequate storage and supply areas Appropriate location of medicine preparations areas (e.g., >3 ft. from a sink) Appropriate location and type of ice machines (e.g., preferably ice dispensers rather than ice bins) Appropriate materials for sinks and wall coverings Appropriate traffic flow (e.g., no "dirty" movement through "clean" areas) Isolation rooms with anterooms as appropriate Appropriate flooring (e.g., seamless floors in dialysis units) Sensible use carpeting (e.g., avoiding use of carpeting in special care areas or areas likely to become wet)- Convenient location of soiled utility areas Properly engineered areas for linen services and solid waste management Location of main generator to minimize the risk of system failure from flooding or other emergency Installation guidelines for sheetrock Proactive strategies can help prevent environmentally mediated airborne infections in health-care facilities during demolition, construction, and renovation. The potential presence of dust and moisture and their contribution to health-care-associated infections must be critically evaluated early in the planning of any demolition, construction, renovation, and repairs.120, 250, 251, 273, 274, 276-279 Consideration must extend beyond dust generated by major projects to include dust that can become airborne if disturbed during routine maintenance and minor renovation activities (e.g., exposure of ceiling spaces for inspection; installation of conduits, cable, or sprinkler systems; rewiring; and structural repairs or replacement).273, 276, 277 Other projects that can compromise indoor air quality include construction and repair jobs that inadvertently allow substantial amounts of raw, unfiltered outdoor air to enter the facility (e.g., repair of elevators and elevator shafts) and activities that dampen any structure, area, or item made of porous materials or characterized by cracks and crevices (e.g., sink cabinets in need of repair, carpets, ceilings, floors, walls, vinyl wall coverings, upholstery, drapes, and countertops). , , Molds grow and proliferate on these surfaces when they become and remain wet.21, 120, 250, 266, 270, 272, 280 Scrubbable materials are preferred for use in patient-care areas.
Containment measures for dust and/or moisture control are dictated by the location of the construction site. Outdoor demolition and construction require actions to keep dust and moisture out of the facility (e.g., sealing windows and vents and keeping doors closed or sealed). Containment of dust and moisture generated from construction inside a facility requires barrier structures (either pre-fabricated or constructed of more durable materials as needed) and engineering controls to clean the air in and around the construction or repair site.
# c. Infection-Control Risk Assessment
An infection-control risk assessment (ICRA) conducted before initiating repairs, demolition, construction, or renovation activities can identify potential exposures of susceptible patients to dust and moisture and determine the need for dust and moisture containment measures. This assessment centers on the type and extent of the construction or repairs in the work area but may also need to include adjacent patient-care areas, supply storage, and areas on levels above and below the proposed project. An example of designing an ICRA as a matrix, the policy for performing an ICRA and implementing its results, and a sample permit form that streamlines the communication process are available.281 Knowledge of the air flow patterns and pressure differentials helps minimize or eliminate the inadvertent dispersion of dust that could contaminate air space, patient-care items, and surfaces. , , A recent aspergillosis outbreak among oncology patients was attributed to depressurization of the building housing the HSCT unit while construction was underway in an adjacent building. Pressure readings in the affected building (including 12 of 25 HSCT-patient rooms) ranged from 0.1 Pa-5.8 Pa. Unfiltered outdoor air flowed into the building through doors and windows, exposing patients in the HSCT unit to fungal spores.283 During long-term projects, providing temporary essential services (e.g., toilet facilities) and conveniences (e.g., vending machines) to construction workers within the site will help to minimize traffic in and out of the area. The type of barrier systems necessary for the scope of the project must be defined. 12,120,250,279,284 Depending on the location and extent of the construction, patients may need to be relocated to other areas in the facility not affected by construction dust.51, 285 Such relocation might be especially prudent when construction takes place within units housing immunocompromised patients (e.g., severely neutropenic patients and patients on corticosteroid therapy). Advance assessment of high-risk locations and planning for the possible transport of patients to other departments can minimize delays and waiting time in hallways.51 Although hospitals have provided immunocompromised patients with some form of respiratory protection for use outside their rooms, the issue is complex and remains unresolved until more research can be done. Previous guidance on this issue has been inconsistent.9 Protective respirators (i.e., N95) were well tolerated by patients when used to prevent further cases of constructionrelated aspergillosis in a recent outbreak.283 The routine use of the N95 respirator by patients, however, has not been evaluated for preventing exposure to fungal spores during periods of non-construction. Although health-care workers who would be using the N95 respirator for personal respiratory protect must be fit-tested, there is no indication that either patients or visitors should undergo fit-testing.
Surveillance activities should augment preventive strategies during construction projects. 3, 4 20, 110, 286, 287 By determining baseline levels of health-care-acquired airborne and waterborne infections, infectioncontrol staff can monitor changes in infection rates and patterns during and immediately after construction, renovations, or repairs.3
# d. Air Sampling
Air sampling in health-care facilities may be conducted both during periods of construction and on a periodic basis to determine indoor air quality, efficacy of dust-control measures, or air-handling system performance via parametric monitoring. Parametric monitoring consists of measuring the physical performance of the HVAC system in accordance with the system manufacturer's specifications. A periodic assessment of the system (e.g., air flow direction and pressure, ACH, and filter efficiency) can give assurance of proper ventilation, especially for special care areas and operating rooms.288
Air sampling is used to detect aerosols (i.e., particles or microorganisms). Particulate sampling (i.e., total numbers and size range of particulates) is a practical method for evaluating the infection-control performance of the HVAC system, with an emphasis on filter efficiency in removing respirable particles (<5 pm in diameter) or larger particles from the air. Particle size is reported in terms of the mass median aerodynamic diameter (MMAD), whereas count median aerodynamic diameter (CMAD) is useful with respect to particle concentrations.
Particle counts in a given air space within the health-care facility should be evaluated against counts obtained in a comparison area. Particle counts indoors are commonly compared with the particulate levels of the outdoor air. This approach determines the "rank order" air quality from "dirty" (i.e., the outdoor air) to "clean" (i.e., air filtered through high-efficiency filters ) to "cleanest" (i.e., HEPA-filtered air).288 Comparisons from one indoor area to another may also provide useful information about the magnitude of an indoor air-quality problem. Making rank-order comparisons between clean, highly-filtered areas and dirty areas and/or outdoors is one way to interpret sampling results in the absence of air quality and action level standards.35, 289
In addition to verifying filter performance, particle counts can help determine if barriers and efforts to control dust dispersion from construction are effective. This type of monitoring is helpful when performed at various times and barrier perimeter locations during the project. Gaps or breaks in the barriers' joints or seals can then be identified and repaired. The American Conference of Governmental Industrial Hygienists (ACGIH) has set a threshold limit value-time weighted average (TLV®-TWA) of 10 mg/m3 for nuisance dust that contains no asbestos and <1% crystalline silica.290 Alternatively, OSHA has set permissible exposure limits (PELs) for inert or nuisance dust as follows: respirable fraction at 5 mg/m3 and total dust at 15 mg/m3.291 Although these standards are not measures of a bioaerosol, they are used for indoor air quality assessment in occupational settings and may be useful criteria in construction areas. Application of ACGIH guidance to health-care settings has not been standardized, but particulate counts in health-care facilities are likely to be well below this threshold value and approaching clean-room standards in certain care areas (e.g., operating rooms).100 Particle counters and anemometers are used in particulate evaluation. The anemometer measures air flow velocity, which can be used to determine sample volumes. Particulate sampling usually does not require microbiology laboratory services for the reporting of results.
Microbiologic sampling of air in health-care facilities remains controversial because of currently unresolved technical limitations and the need for substantial laboratory support (Box 6). Infectioncontrol professionals, laboratorians, and engineers should determine if microbiologic and/or particle sampling is warranted and assess proposed methods for sampling. The most significant technical limitation of air sampling for airborne fungal agents is the lack of standards linking fungal spore levels with infection rates. Despite this limitation, several health-care institutions have opted to use microbiologic sampling when construction projects are anticipated and/or underway in efforts to assess the safety of the environment for immunocompromised patients.35, 289 Microbiologic air sampling should be limited to assays for airborne fungi; of those, the thermotolerant fungi (i.e., those capable of growing at 95°F-98.6°F ) are of particular concern because of their pathogenicity in immunocompromised hosts.35 Use of selective media (e.g., Sabouraud dextrose agar and inhibitory mold agar) helps with the initial identification of recovered organisms.
Microbiologic sampling for fungal spores performed as part of various airborne disease outbreak investigations has also been problematic. 18, 49, 106, m ' 112, 289 The precise source of a fungus is often difficult to trace with certainty, and sampling conducted after exposure may neither reflect the circumstances that were linked to infection nor distinguish between health-care-acquired and community-acquired infections. Because fungal strains may fluctuate rapidly in the environment, health-care-acquired Aspergillus spp. infection cannot be confirmed or excluded if the infecting strain is not found in the health-care setting.287 Sensitive molecular typing methods (e.g., randomly amplified polymorphic DNA (RAPD) techniques and a more recent DNA fingerprinting technique that detects restriction fragment length polymorphisms in fungal genomic DNA) to identify strain differences among Aspergillus spp., however, are becoming increasingly used in epidemiologic investigations of health-care-acquired fungal infection (A.Streifel, University of Minnesota, 2000).68, 110, 286, 287, 292-296 During case cluster evaluation, microbiologic sampling may provide an isolate from the environment for molecular typing and comparison with patient isolates. Therefore, it may be prudent for the clinical laboratory to save Aspergillus spp. isolated from colonizations and invasive disease cases among patients in PE, oncology, and transplant services for these purposes. Sedimentation methods using settle plates and volumetric sampling methods using solid impactors are commonly employed when sampling air for bacteria and fungi. Settle plates have been used by numerous investigators to detect airborne bacteria or to measure air quality during medical procedures (e.g., surgery - Contamination of water pipes during demolition activities has been associated with health-care-associated transmission of Legionella spp.305 + When health-care facilities have immunosuppressed patients in their census, telephoning the city building department each month to find out if buildings are scheduled for demolition is prudent.
Minimizing the entry of outside dust into the HVAC system is crucial in reducing the risk for airborne contaminants. Facility engineers should be consulted about the potential impact of shutting down the system or increasing the filtration. Selected air handlers, especially those located close to excavation sites, may have to be shut off temporarily to keep from overloading the system with dust and debris.
Care is needed to avoid significant facility-wide reductions in pressure differentials that may cause the building to become negatively pressured relative to the outside. To prevent excessive particulate overload and subsequent reductions in effectiveness of intake air systems that cannot be shut off temporarily, air filters must be inspected frequently for proper installation and function. Excessive dust penetration can be avoided if recirculated air is maximally utilized while outdoor air intakes are shut down. Scheduling demolition and excavation during the winter, when Aspergillus spp. spores may be present in lower numbers, can help, although seasonal variations in spore density differ around the world.92, 287, 303 Dust control can be managed by misting the dirt and debris during heavy dust generating activities. To decrease the amount of aerosols from excavation and demolition projects, nearby windows, especially in areas housing immunocompromised patients, can be sealed and window and door frames caulked or weather-stripped to prevent dust intrusion.50, 301, 306 Monitoring for adherence to these control measures throughout demolition or excavation is crucial. Diverting pedestrian traffic away from the construction sites decreases the amount of dust tracked back into the health-care facility and minimizes exposure of high-risk patients to environmental pathogens. Additionally, closing entrances near construction or demolition sites might be beneficial; if this is not practical, creating an air lock (i.e., pressurizing the entry way) is another option.
# f. Internal Demolition, Construction, Renovations, and Repairs
The focus of a properly implemented infection-control program during interior construction and repairs is containment of dust and moisture. This objective is achieved by a) educating construction workers about the importance of control measures; b) preparing the site; c) notifying and issuing advisories for staff, patients, and visitors; d) moving staff and patients and relocating patients as needed; e) issuing standards of practice and precautions during activities and maintenance; f) monitoring for adherence to control measures during construction and providing prompt feedback about lapses in control; g) monitoring HVAC performance; h) implementing daily clean-up, terminal cleaning and removal of debris upon completion; and i) ensuring the integrity of the water system during and after construction. These activities should be coordinated with engineering staff and infection-control professionals.
Physical barriers capable of containing smoke and dust will confine dispersed fungal spores to the construction zone. , , , The specific type of physical barrier required depends on the project's scope and duration and on local fire codes. Short-term projects that result in minimal dust dispersion (e.g., installation of new cables or wiring above ceiling tiles) require only portable plastic enclosures with negative pressure and HEPA filtration of the exhaust air from the enclosed work area. The placement of a portable industrial-grade HEPA filter device capable of filtration rate of 300-800 ft3/min. adjacent to the work area will help to remove fungal spores, but its efficacy is dependent on the supplied ACH and size of the area. If the project is extensive but short-term, dust-abatement, fire-resistant plastic curtains (e.g., Visqueen®) may be adequate. These should be completely airtight and sealed from ceiling to floor with overlapping curtains;276, 277, 309 holes, tears, or other perforations should be repaired promptly with tape. A portable, industrial-grade HEPA filter unit on continuous operation is needed within the contained area, with the filtered air exhausted to the outside of the work zone. Patients should not remain in the room when dust-generating activities are performed. Tools to assist the decision-making process regarding selection of barriers based on an ICRA approach are available.281 More elaborate barriers are indicated for long-term projects that generate moderate to large amounts of dust. These barrier structures typically consist of rigid, noncombustible walls constructed from sheet rock, drywall, plywood, or plaster board and covered with sheet plastic (e.g., Visqueen®). Barrier requirements to prevent the intrusion of dust into patient-care areas include a) installing a plastic dust abatement curtain before construction of the rigid barrier; b) sealing and taping all joint edges including the top and bottom; c) extending the barrier from floor to floor, which takes into account the space above the finished, lay-down ceiling; and d) fitting or sealing any temporary doors connecting the construction zone to the adjacent area. (See Box 7 for a list of the various construction and repair activities that require the use of some type of barrier.) Dust and moisture abatement and control rely primarily on the impermeable barrier containment approach; as construction continues, numerous opportunities can lead to dispersion of dust to other areas of the health-care facility. Infection-control measures that augment the use of barrier containment should be undertaken (Table 9). Dust-control measures for clinical laboratories are an essential part of the infection-control strategy during hospital construction or renovation. Use of plastic or solid barriers may be needed if the ICRA determines that air flow from construction areas may introduce airborne contaminants into the laboratory space. In one facility, pseudofungemia clusters attributed to Aspergillus spp. and Penicillium spp. were linked to improper air flow patterns and construction projects adjacent to the laboratory; intrusion of dust and spores into a biological safety cabinet from construction activity immediately next to the cabinet resulted in a cluster of cultures contaminated with Aspergillus niger310' 311 Reportedly, no barrier containment was used and the HEPA filtration system was overloaded with dust. In addition, an outbreak of pseudobacteremia caused by Bacillus spp. occurred in another hospital during construction above a storage area for blood culture bottles.207 Airborne spread of Bacillus spp. spores resulted in contamination of the bottles' plastic lids, which were not disinfected or handled with proper aseptic technique prior to collection of blood samples. Control dust in air and on surfaces. 1. Monitor the construction area daily for compliance with the infection-control plan. 2. Protective outer clothing for construction workers should be removed before entering clean areas. 3. Use mats with tacky surfaces within the construction zone at the entry; cover sufficient area so that both feet make contact with the mat while walking through the entry. 4. Construct an anteroom as needed where coveralls can be donned and removed. 5. Clean the construction zone and all areas used by construction workers with a wet mop. 6. If the area is carpeted, vacuum daily with a HEPA-filtered-equipped vacuum. 7. Provide temporary essential services (e.g., toilets) and worker conveniences (e.g, vending machines) in the construction zone as appropriate. 8. Damp-wipe tools if removed from the construction zone or left in the area. 9. Ensure that construction barriers remain well sealed; use particle sampling as needed. 10. Ensure that the clinical laboratory is free from dust contamination.
# Infection-control measure
Steps for implementation
# a. Protective Environments (PE)
Although the exact configuration and specifications of PEs might differ among hospitals, these care areas for high-risk, immunocompromised patients are designed to minimize fungal spore counts in air by maintaining a) filtration of incoming air by using central or point-of-use HEPA filters; b) directed room air flow ; c) positive room air pressure of 2.5 Pa relative to the corridor; d) well-sealed rooms; and e) >12 ACH.44, 120, 251, 254, 316-319 Air flow rates must be adjusted accordingly to ensure sufficient ACH, and these rates vary depending on certain factors (e.g., room air leakage area). For example, to provide >12 ACH in a typical patient room with 0.5 sq. ft. air leakage, the air flow rate will be minimally 125 cubic feet/min (cfm). , Higher air flow rates may be needed. A general ventilation diagram for a positive-pressure room is given in Figure 2. Directed room air flow in PE rooms is not laminar; parallel air streams are not generated. Studies attempting to demonstrate patient benefit from laminar air flow in a PE setting are equivocal.316, 318, 319, 322 " 327
Air flow direction at the entrances to these areas should be maintained and verified, preferably on a daily basis, using either a visual means of indication (e.g., smoke tubes and flutter strips) or manometers. Permanent installation of a visual monitoring device is indicated for new PE construction and renovation.120 Facility service structures can interfere with the proper unidirectional air flow from the patients' rooms to the adjacent corridor. In one outbreak investigation, Aspergillus spp. infections in a critical care unit may have been associated with a pneumatic specimen transport system, a textile disposal duct system, and central vacuum lines for housekeeping, all of which disrupted proper air flow from the patients' rooms to the outside and allowed entry of fungal spores into the unit (M. McNeil, CDC, 2000). Appendix E).
Salient features of engineering controls for AII areas include a) use of negative pressure rooms with close monitoring of air flow direction using manometers or temporary or installed visual indicators placed in the room with the door closed; b) minimum 6 ACH for existing facilities, >12 ACH for areas under renovation or for new construction; and c) air from negative pressure rooms and treatment rooms exhausted directly to the outside if possible.4, 120, 248 As with PE, airflow rates need to be determined to ensure the proper numbers of ACH. , AII rooms can be constructed either with (Figure 3) or without (Figure 4) an anteroom. When the recirculation of air from AII rooms is unavoidable, HEPA filters should be installed in the exhaust duct leading from the room to the general ventilation system. In addition to UVGI fixtures in the room, UVGI can be placed in the ducts as an adjunct measure to HEPA filtration, but it can not replace the HEPA filter. The pressure differential of an anteroom can be positive or negative relative to the patient in the room.120 An anteroom can act as an airlock (Figure 4). If the anteroom is positive relative to the air space in the patient's room, staff members do not have to mask prior to entry into the anteroom if air is directly exhausted to the outside and a minimum of 10 ACH (Figure 4, top diagram).120 When an anteroom is negative relative to both the AII room and the corridor, health-care workers must mask prior to entering the anteroom (Figure 4, bottom diagram). If an AII room with an anteroom is not available, use of a portable, industrial-grade HEPA filter unit may help to increase the number of ACHs while facilitating the removal of fungal spores; however, a fresh air source must be present to achieve the proper air exchange rate. Incoming ambient air should receive HEPA filtration.
# c. Operating Rooms
Operating room air may contain microorganisms, dust, aerosol, lint, skin squamous epithelial cells, and respiratory droplets. The microbial level in operating room air is directly proportional to the number of people moving in the room.351 One study documented lower infection rates with coagulase-negative staphylococci among patients when operating room traffic during the surgical procedure was limited.352 Therefore, efforts should be made to minimize personnel traffic during operations. Outbreaks of SSIs caused by group A beta-hemolytic streptococci have been traced to airborne transmission from colonized operating-room personnel to patients.150154 Several potential health-care-associated pathogens (e.g., Staphylococcus aureus and Staphylococcus epidermidis) and drug-resistant organisms have also been recovered from areas adjacent to the surgical field,353 but the extent to which the presence of bacteria near the surgical field influences the development of postoperative SSIs is not clear. 354 Proper ventilation, humidity (<68%), and temperature control in the operating room is important for the comfort of surgical personnel and patients, but also in preventing environmental conditions that encourage growth and transmission of microorganisms.355 Operating rooms should be maintained at positive pressure with respect to corridors and adjacent areas.356 Operating rooms typically do not have a variable air handling system. Variable air handling systems are permitted for use in operating rooms only if they continue to provide a positive pressure with respect to the corridors and adjacent areas and the proper ACHs are maintained when the room is occupied. Conventional operating-room ventilation systems produce a minimum of about 15 ACH of filtered air for thermal control, three (20%) of which must be fresh air. , , Air should be introduced at the ceiling and exhausted near the floor. , Laminar airflow and UVGI have been suggested as adjunct measures to reduce SSI risk for certain operations. Laminar airflow is designed to move particle-free air over the aseptic operating field at a uniform velocity (0. The portable unit should be turned off while the surgical procedure is underway and turned on following extubation. Portable HEPA filter units previously placed in construction areas may be used in subsequent patient care, provided that all internal and external surfaces are cleaned and the filter's performance is verified with appropriate particle testing and is changed, if needed.
# Other Aerosol Hazards in Health-Care Facilities
In addition to infectious bioaerosols, several crucial non-infectious, indoor air-quality issues must be addressed by health-care facilities. The presence of sensitizing and allergenic agents and irritants in the workplace (e.g., ethylene oxide, glutaraldehyde, formaldehyde, hexachlorophene, and latex allergens375) is increasing. Asthma and dermatologic and systemic reactions often result with exposure to these chemicals. Anesthetic gases and aerosolized medications (e.g., ribavirin, pentamidine, and aminoglycosides) represent some of the emerging potentially hazardous exposures to health-care workers. Containment of the aerosol at the source is the first level of engineering control, but personal protective equipment (e.g., masks, respirators, and glove liners) that distances the worker from the hazard also may be needed.
Laser plumes and surgical smoke represent another potential risk for health-care workers.376-378 Lasers transfer electromagnetic energy into tissues, resulting in the release of a heated plume that includes particles, gases, tissue debris, and offensive smells. One concern is that aerosolized infectious material in the laser plume might reach the nasal mucosa of surgeons and adjacent personnel. Although some viruses (i.e., varicella-zoster virus, pseudorabies virus, and herpes simplex virus) do not aerosolize efficiently, , other viruses and bacteria (e.g., human papilloma virus , HIV, coagulasenegative Staphylococcus, Corynebacterium spp., and Neisseria spp.) have been detected in laser plumes. -The presence of an infectious agent in a laser plume may not, however, be sufficient to cause disease from airborne exposure, especially if the normal mode of transmission for the agent is not airborne. No evidence indicated that HIV or hepatitis B virus (HBV) has been transmitted via aerosolization and inhalation. 388 Although continuing studies are needed to fully evaluate the risk of laser plumes to surgical personnel, the prevention measures in these other guidelines should be followed: a) NIOSH recommendations,378 b) the Recommended Practices for Laser Safety in Practice Settings developed by the Association of periOperative Registered Nurses ,389 c) the assessments of ECRI,390-392 and d) the ANSI standard.393 These guidelines recommend the use of a) respirators (N95 or N100) or full face shields and masks,260 b) central wall-suction units with in-line filters to collect particulate matter from minimal plumes, and c) dedicated mechanical smoke exhaust systems with a high-efficiency filter to remove large amounts of laser plume. Although transmission of TB has occurred as a result of abscess management practices that lacked airborne particulate control measures and respiratory protection, use of a smoke evacuator or needle aspirator and a high degree of clinical awareness can help protect health care workers when excising and draining an extrapulmonary TB abscess.137
# D. Water 1. Modes of Transmission of Waterborne Diseases
Moist environments and aqueous solutions in health-care settings have the potential to serve as reservoirs for waterborne microorganisms. Under favorable environmental circumstances (e.g., warm temperature and the presence of a source of nutrition), many bacterial and some protozoal microorganisms can either proliferate in active growth or remain for long periods in highly stable, environmentally resistant (yet infectious) forms. Modes of transmission for waterborne infections include a) direct contact ; b) ingestion of water ; c) indirect-contact transmission ;6 d) inhalation of aerosols dispersed from water sources;3 and e) aspiration of contaminated water. The first three modes of transmission are commonly associated with infections caused by gram-negative bacteria and nontuberculous mycobacteria (NTM). Aerosols generated from water sources contaminated with Legionella spp. often serve as the vehicle for introducing legionellae to the respiratory tract.
# Waterborne Infectious Diseases in Health-Care Facilities a. Legionellosis
Legionellosis is a collective term describing infection produced by Legionella spp., whereas Legionnaires disease is a multi-system illness with pneumonia.395 The clinical and epidemiologic aspects of these diseases (Table 11) are discussed extensively in another guideline.3 Although Legionnaires disease is a respiratory infection, infection-control measures intended to prevent health care-associated cases center on the quality of water-the principal reservoir for Legionella spp. 12 and 13). Immunocompromised patients are at greatest risk of developing infection. Medical conditions associated with these bacterial agents range from colonization of the respiratory and urinary tracts to deep, disseminated infections that can result in pneumonia and bloodstream bacteremia. Colonization by any of these organisms often precedes the development of infection. The use of tap water in medical care (e.g., in direct patient care, as a diluent for solutions, as a water source for medical instruments and equipment, and during the final stages of instrument disinfection) therefore presents a potential risk for exposure. Colonized patients also can serve as a source of contamination, particularly for moist environments of medical equipment (e.g., ventilators).
In addition to Legionella spp., Pseudomonas aeruginosa and Pseudomonas spp. are among the most clinically relevant, gram-negative, health-care-associated pathogens identified from water. These and other gram-negative, non-fermentative bacteria have minimal nutritional requirements (i.e., these organisms can grow in distilled water) and can tolerate a variety of physical conditions. These attributes are critical to the success of these organisms as health-care-associated pathogens. Measures to prevent the spread of these organisms and other waterborne, gram-negative bacteria include hand hygiene, glove use, barrier precautions, and eliminating potentially contaminated environmental reservoirs.464, 465
# References
# Clinical syndromes and diseases
Septicemia, pneumonia (particularly ventilator-associated), chronic respiratory infections among cystic fibrosis patients, urinary tract infections, skin and soft-tissue infections (e.g., tissue necrosis and hemorrhage), burn-wound infections, folliculitis, endocarditis, central nervous system infections (e.g., meningitis and abscess), eye infections, and bone and joint infections 466-503 Patients and health-care workers contribute significantly to the environmental contamination of surfaces and equipment with Acinetobacter spp. and Enterobacter spp., especially in intensive care areas, because of the nature of the medical equipment (e.g., ventilators) and the moisture associated with this equipment.549, 571, 572, 585 Hand carriage and hand transfer are commonly associated with health-careassociated transmission of these organisms and for S. marcescens.586 Enterobacter spp. are primarily spread in this manner among patients by the hands of health-care workers.567, 587 Acinetobacter spp. have been isolated from the hands of 4%-33% of health-care workers in some studies,585-590 and transfer of an epidemic strain of Acinetobacter from patients' skin to health-care workers' hands has been demonstrated experimentally.591 Acinetobacter infections and outbreaks have also been attributed to medical equipment and materials (e.g., ventilators, cool mist humidifiers, vaporizers, and mist tents) that may have contact with water of uncertain quality (e.g., rinsing a ventilator circuit in tap water).549-556 Strict adherence to hand hygiene helps prevent the spread of both Acinetobacter spp. and 577, 592 Enterobacter spp. , Acinetobacter spp. have also been detected on dry environmental surfaces (e.g., bed rails, counters, sinks, bed cupboards, bedding, floors, telephones, and medical charts) in the vicinity of colonized or infected patients; such contamination is especially problematic for surfaces that are frequently touched.557-564 In two studies, the survival periods of Acinetobacter baumannii and Acinetobacter calcoaceticus on dry surfaces approximated that for S. aureus (e.g., 26-27 days).593, 594 Because Acinetobacter spp. may come from numerous sources at any given time, laboratory investigation of health-care-associated Acinetobacter infections should involve techniques to determine biotype, antibiotype, plasmid profile, and genomic fingerprinting (i.e., macrorestriction analysis) to accurately identify sources and modes of transmission of the organism(s).595 have also demonstrated some resistance to formaldehyde and glutaraldehyde, which has posed problems for reuse of hemodialyzers.31 The ability of NTM to form biofilms at fluid-surface interfaces (e.g., interior surfaces of water pipes) contributes to the organisms' resistance to chemical inactivation and provides a microenvironment for growth and proliferation.636, 637
# Modes of transmission
# c. Infections and Pseudo-Infections Due to Nontuberculous Mycobacteria
# d. Cryptosporidiosis
Cryptosporidium parvum is a protozoan parasite that causes self-limiting gastroenteritis in normal hosts but can cause severe, life-threatening disease in immunocompromised patients. First recognized as a human pathogen in 1976, C. parvum can be present in natural and finished waters after fecal contamination from either human or animal sources.638-641
The health risks associated with drinking potable water contaminated with minimal numbers of C. parvum oocysts are unknown.642 It remains to be determined if immunosuppressed persons are more susceptible to lower doses of oocysts than are immunocompetent persons. One study demonstrated that a median 50% infectious dose (ID50) of 132 oocysts of calf origin was sufficient to cause infection among healthy volunteers. 643 In a second study, the same researchers found that oocysts obtained from infected foals (newborn horses) were infectious for human volunteers at median ID50 of 10 oocysts, indicating that different strains or species of Cryptosporidium may vary in their infectivity for humans.644 In a small study population of 17 healthy adults with pre-existing antibody to C. parvum, the ID50 was determined to be 1,880 oocysts, more than 20-fold higher than in seronegative persons. 645 These data suggest that pre-existing immunity derived from previous exposures to Cryptosporidium offers some protection from infection and illness that ordinarily would result from exposure to low numbers of oocysts.645, 646
Oocysts, particularly those with thick walls, are environmentally resistant, but their survival under natural water conditions is poorly understood. Under laboratory conditions, some oocysts remain viable and infectious in cold (41°F ) for months. 641 The prevalence of Cryptosporidium in the U.S. drinking water supply is notable. Two surveys of approximately 300 surface water supplies revealed that 55%-77% of the water samples contained Cryptosporidium oocysts.647, 648 Because the oocysts are highly resistant to common disinfectants (e.g., chlorine) used to treat drinking water, filtration of the water is important in reducing the risk of waterborne transmission. Coagulation-floculation and sedimentation, when used with filtration, can collectively achieve approximately a 2.5 log10 reduction in the number of oocysts.649 However, outbreaks have been associated with both filtered and unfiltered drinking water systems (e.g., the 1993 outbreak in Milwaukee, Wisconsin that affected 400,000 people).641, 650-652 The presence of oocysts in the water is not an absolute indicator that infection will occur when the water is consumed, nor does the absence of detectable oocysts guarantee that infection will not occur. Health-care-associated outbreaks of cryptosporidiosis primarily have been described among groups of elderly patients and immunocompromised persons.653
# Water Systems in Health-Care Facilities a. Basic Components andPoint-of-Use Fixtures
Treated municipal water enters a health-care facility via the water mains and is distributed throughout the building(s) by a network of pipes constructed of galvanized iron, copper, and polyvinylchloride (PVC). The pipe runs should be as short as is practical. Where recirculation is employed, the pipe runs should be insulated and long dead legs avoided in efforts to minimize the potential for water stagnation, which favors the proliferation of Legionella spp. and NTM. In high-risk applications (e.g., PE areas for severely immunosuppressed patients), insulated recirculation loops should be incorporated as a design feature. Recirculation loops prevent stagnation and insulation maintains return water temperature with minimal loss.
Each water service main, branch main, riser, and branch (to a group of fixtures) has a valve and a means to reach the valves via an access panel.120 Each fixture has a stop valve. Valves permit the isolation of a portion of the water system within a facility during repairs or maintenance. Vacuum breakers and other similar devices in the lines prevent water from back-flowing into the system. All systems that supply water should be evaluated to determine risk for potential back siphonage and cross connections.
Health-care facilities generate hot water from municipal water using a boiler system. Hot water heaters and storage vessels for such systems should have a drainage facility at the lowest point, and the heating element should be located as close as possible to the bottom of the vessel to facilitate mixing and to prevent water temperature stratification. Those hot or cold water systems that incorporate an elevated holding tank should be inspected and cleaned annually. Lids should fit securely to exclude foreign materials.
The most common point-of-use fixtures for water in patient-care areas are sinks, faucets, aerators, showers, and toilets; eye-wash stations are found primarily in laboratories. The potential for these fixtures to serve as a reservoir for pathogenic microorganisms has long been recognized (Table 15). Although aerosols are produced with toilet flushing,662, 663 no epidemiologic evidence suggests that these aerosols pose a direct infection hazard.
Although not considered a standard point-of-use fixture, decorative fountains are being installed in increasing numbers in health-care facilities and other public buildings. Aerosols from a decorative fountain have been associated with transmission of Legionella pneumophila serogroup 1 infection to a small cluster of older adults.664 This hotel lobby fountain had been irregularly maintained, and water in the fountain may have been heated by submersed lighting, all of which favored the proliferation of Legionella in the system.664 Because of the potential for generations of infectious aerosols, a prudent prevention measure is to avoid locating these fixtures in or near high-risk patient-care areas and to adhere to written policies for routine fountain maintenance.120
# b. Water Temperature and Pressure
Hot water temperature is usually measured at the point of use or at the point at which the water line enters equipment requiring hot water for proper operation.120 Generally, the hot water temperature in hospital patient-care areas is no greater than a temperature within the range of 105°F-120°F (40.6°C-49°C), depending on the AIA guidance issued at the year in which the facility was built.120 Hot water temperature in patient-care areas of skilled nursing-care facilities is set within a slightly lower range of 95°F-110°F (35°C-43.3°C) depending on the AIA guidance at the time of facility construction.120 Many states have adopted a temperature setting in these ranges into their health-care regulations and building codes. ASHRAE, however, has recommended higher settings.661 Steam jets or booster heaters are usually needed to meet the hot water temperature requirements in certain service areas of the hospital (e.g., the kitchen or the laundry ).120 Additionally, water lines may need to be heated to a particular temperature specified by manufacturers of specific hospital equipment. Hot-water distribution systems serving patient-care areas are generally operated under constant recirculation to provide continuous hot water at each hot-water outlet.120 If a facility is or has a hemodialysis unit, then continuously circulated, cold treated water is provided to that unit.120
To minimize the growth and persistence of gram-negative waterborne bacteria (e.g., thermophilic NTM and Legionella spp.),627, 703 709 cold water in health-care facilities should be stored and distributed at temperatures below 68°F (20°C); hot water should be stored above 140°F (60°C) and circulated with a minimum return temperature of 124°F (51°C),661 or the highest temperature specified in state regulations and building codes. If the return temperature setting of 124°F (51°C) is permitted, then installation of preset thermostatic mixing valves near the point-of-use can help to prevent scalding.
Valve maintenance is especially important in preventing valve failure, which can result in scalding. New shower systems in large buildings, hospitals, and nursing homes should be designed to permit mixing of hot and cold water near the shower head. The warm water section of pipe between the control valve and shower head should be self-draining. Where buildings can not be retrofitted, other approaches to minimize the growth of Legionella spp. include a) periodically increasing the temperature to at least 150°F at the point of use and b) adding additional chlorine and flushing the water.661, 710, 711 Systems should be inspected annually to ensure that thermostats are functioning properly.
Adequate water pressure ensures sufficient water supplies for a) direct patient care; b) operation of water-cooled instruments and equipment ; c) proper function of vacuum suctioning systems; d) indoor climate control; and e) fire-protection systems. Maintaining adequate pressure also helps to ensure the integrity of the piping system.
# c. Infection-Control Impact of Water System Maintenance and Repair
Corrective measures for water-system failures have not been studied in well-designed experiments; these measures are instead based on empiric engineering and infection-control principles. Health-care facilities can occasionally sustain both intentional cut-offs by the municipal water authority to permit new construction project tie-ins and unintentional disruptions in service when a water main breaks as a result of aging infrastructure or a construction accident. Vacuum breakers or other similar devices can prevent backflow of water in the facility's distribution system during water-disruption emergencies.11 To be prepared for such an emergency, all health-care facilities need contingency plans that identify a) the total demand for potable water, b) the quantity of replacement water required for a minimum of 24 hours when the water system is down, c) mechanisms for emergency water distribution, and 4) procedures for correcting drops in water pressure that affect operation of essential devices and equipment that are driven or cooled by a water system .713 - Arrange to have a contingency provision of these services from another resource, if possible (e.g., another health-care facility or contractor). + Some cooling towers may use a potable water source, but most units use non-potable water. § This item is included in the table under the assumption that electrical power is available during the water emergency.
Detailed, up-to-date plans for hot and cold water piping systems should be readily available for maintenance and repair purposes in case of system problems. Opening potable water systems for repair or construction and subjecting systems to water-pressure changes can result in water discoloration and dramatic increases in the concentrations of Legionella spp. and other gram-negative bacteria. The maintenance of a chlorine residual at all points within the piping system also offers some protection from entry of contamination to the pipes in the event of inadvertent cross-connection between potable and non-potable water lines. As a minimum preventive measure, ASHRAE recommends a thorough flushing of the system.661 High-temperature flushing or hyperchlorination may also be appropriate strategies to decrease potentially high concentrations of waterborne organisms. The decision to pursue either of these remediation strategies, however, should be made on a case-by-case basis. If only a portion of the system is involved, high temperature flushing or chlorination can be used on only that portion of the system.661
When shock decontamination of hot water systems is necessary (e.g., after disruption caused by construction and after cross-connections), the hot water temperature should be raised to 160°F-170°F (71°C-77°C) and maintained at that level while each outlet around the system is progressively flushed.
A minimum flush time of 5 minutes has been recommended;3 the optimal flush time is not known, however, and longer flush times may be necessary.714 The number of outlets that can be flushed simultaneously depends on the capacity of the water heater and the flow capability of the system. Appropriate safety procedures to prevent scalding are essential. When possible, flushing should be performed when the fewest building occupants are present (e.g., during nights and weekends).
When thermal shock treatment is not possible, shock chlorination may serve as an alternative method.661 Experience with this method of decontamination is limited, however, and high levels of free chlorine can corrode metals. Chlorine should be added, preferably overnight, to achieve a free chlorine residual of at least 2 mg/L (2 ppm) throughout the system.661 This may require chlorination of the water heater or tank to levels of 20-50 mg/L (20-50 ppm). The pH of the water should be maintained at 7.0-8.0.661 After completion of the decontamination, recolonization of the hot water system is likely to occur unless proper temperatures are maintained or a procedure such as continuous supplemental chlorination is continued.
Interruptions of the water supply and sewage spills are situations that require immediate recovery and remediation measures to ensure the health and safety of patients and staff.715 When delivery of potable water through the municipal distribution system has been disrupted, the public water supplier must issue a "boil water" advisory if microbial contamination presents an immediate public health risk to customers. The hospital engineer should oversee the restoration of the water system in the facility and clear it for use when appropriate. Hospitals must maintain a high level of surveillance for waterborne disease among patients and staff after the advisory is lifted.642
Flooding from either external (e.g., from a hurricane) or internal sources (e.g., a water system break) usually results in property damage and a temporary loss of water and sanitation.716-718 JCAHO requires all hospitals to have plans that address facility response for recovery from both internal and external disasters. , The plans are required to discuss a) general emergency preparedness, b) staffing, c) regional planning among area hospitals, d) emergency supply of potable water, e) infection control and medical services needs, f) climate control, and g) remediation. The basic principles of structural recovery from flooding are similar to those for recovery from sewage contamination (Box 9 and 10). Following a major event (e.g., flooding), facilities may elect to conduct microbial sampling of water after the system is restored to verify that water quality has been returned to safe levels (<500 CFU/mL, heterotrophic plate count). This approach may help identify point-of-use fixtures that may harbor contamination as a result of design or engineering features.720 Medical records should be allowed to dry and then either photocopied or placed in plastic covers before returning them to the record.
Moisture meters can be used to assess water-damaged structural materials. If porous structural materials for walls have a moisture content of >20% after 72 hours, the affected material should be removed.266, , The management of water-damaged structural materials is not strictly limited to major water catastrophes (e.g., flooding and sewage intrusions); the same principles are used to evaluate the damage from leaking roofs, point-of-use fixtures, and equipment. Additional sources of moisture include condensate on walls from boilers and poorly engineered humidification in HVAC systems.
An exception to these recommendations is made for hemodialysis units where water is further treated either by portable water treatment or large-scale water treatment systems usually involving reverse osmosis (RO). In the United States, >97% of dialysis facilities use RO treatment for their water.721 However, changing pre-treatment filters and disinfecting the system to prevent colonization of the RO membrane and microbial contamination down-stream of the pre-treatment filter are prudent measures.
# Box 10. Contingency planning for flooding G eneral em ergency preparedness
Ensure that emergency electrical generators are not located in flood-prone areas of the facility. Develop alternative strategies for moving patients, water containers, medical records, equipment, and supplies in the event that the elevators are inoperable. Establish in advance a centralized base of operations with batteries, flashlights, and cellular phones. Ensure sufficient supplies of sandbags to place at the entrances and the area around boilers, incinerators, and generators. Establish alternative strategies for bringing core employees to the facility if high water prevents travel.
# Staffing P atterns
Temporarily reassign licensed staff as needed to critical care areas to provide manual ventilation and to perform vital assessments on patients. Designate a core group of employees to remain on site to keep all services operational if the facility remains open. Train all employees in emergency preparedness procedures.
# R egional plan n in g am ong are facilities fo r d isaster m anagem ent
Incorporate community support and involvement (e.g., media alerts, news, and transportation). Develop in advance strategies for transferring patients, as needed. Develop strategies for sharing supplies and providing essential services among participating facilities (e.g., central sterile department services, and laundry services). Identify sources for emergency provisions (e.g., blood, emergency vehicles, and bottled water).
# M edical services and infection control
Use alcohol-based hand rubs in general patient-care areas. Postpone elective surgeries until full services are restored, or transfer these patients to other facilities. Consider using portable dialysis machines.+ Provide an adequate supply of tetanus and hepatitis A immunizations for patients and staff.
# C lim ate control
Provide adequate water for cooling towers. § - Material in this box was compiled from references 713, 716-719. + Portable dialysis machines require less water compared to the larger units situated in dialysis settings.
§ Water for cooling towers may need to be trucked in, especially if the tower uses a potable water source.
# Strategies for Controlling Waterborne Microbial Contamination a. Supplemental Treatment of Water with Heat and/or Chemicals
In addition to using supplemental treatment methods as remediation measures after inadvertent contamination of water systems, health-care facilities sometimes use special measures to control waterborne microorganisms on a sustained basis. This decision is most often associated with outbreaks of legionellosis and subsequent efforts to control legionellae,722 although some facilities have tried supplemental measures to better control thermophilic NTM.627
The primary disinfectant for both cold and hot water systems is chlorine. However, chlorine residuals are expected to be low, and possibly nonexistent, in hot water tanks because of extended retention time in the tank and elevated water temperature. Flushing, especially that which removes sludge from the bottom of the tank, probably provides the most effective treatment of water systems. Unlike the situation for disinfecting cooling towers, no equivalent recommendations have been made for potable water systems, although specific intervention strategies have been published. , The principal approaches to disinfection of potable systems are heat flushing using temperatures 160°F-170°F (71°-77°C), hyperchlorination, and physical cleaning of hot-water tanks.3, 403, 661 Potable systems are easily recolonized and may require continuous intervention (e.g., raising of hot water temperatures or continuous chlorination).403, 711 Chlorine solutions lose potency over time, thereby rendering the stocking of large quantities of chlorine impractical. Some hospitals with hot water systems identified as the source of Legionella spp. have performed emergency decontamination of their systems by pulse (i.e., one-time) thermal disinfection/superheating or hyperchlorination. , , , After either of these procedures, hospitals either maintain their heated water with a minimum return temperature of 124°F (51°C) and cold water at <68°F (<20°C) or chlorinate their hot water to achieve 1-2 mg/L (1-2 ppm) of free residual chlorine at the tap.26, 437, 709-711, 726, 727 Additional measures (e.g., physical cleaning or replacement of hot-water storage tanks, water heaters, faucets, and shower heads) may be required to help eliminate accumulations of scale and sediment that protect organisms from the biocidal effects of heat and chlorine.457, 711 Alternative methods for controlling and eradicating legionellae in water systems (e.g., treating water with chlorine dioxide, heavy metal ions , ozone, and UV light) have limited the growth of legionellae under laboratory and operating conditions.728-742 Further studies on the long-term efficacy of these treatments are needed before these methods can be considered standard applications.
Renewed interest in the use of chloramines stems from concerns about adverse health effects associated with disinfectants and disinfection by-products.743 Monochloramine usage minimizes the formation of disinfection by-products, including trihalomethanes and haloacetic acids. Monochloramine can also reach distal points in a water system and can penetrate into bacterial biofilms more effectively than free chlorine.744 However, monochloramine use is limited to municipal water treatment plants and is currently not available to health-care facilities as a supplemental water-treatment approach. A recent study indicated that 90% of Legionnaires disease outbreaks associated with drinking water could have been prevented if monochloramine rather than free chlorine has been used for residual disinfection.745 In a retrospective comparison of health-care-associated Legionnaires disease incidence in central Texas hospitals, the same research group documented an absence of cases in facilities located in communities with monochloramine-treated municipal water.746 Additional data are needed regarding the effectiveness of using monochloramine before its routine use as a disinfectant in water systems can be recommended. No data have been published regarding the effectiveness of monochloramine installed at the level of the health-care facility.
Additional filtration of potable water systems is not routinely necessary. Filters are used in water lines in dialysis units, however, and may be inserted into the lines for specific equipment (e.g., endoscope washers and disinfectors) for the purpose of providing bacteria-free water for instrument reprocessing. Additionally, an RO unit is usually added to the distribution system leading to PE areas.
# b. Primary Prevention of Legionnaires Disease (No Cases Identified)
The primary and secondary environmental infection-control strategies described in this section on the guideline pertain to health-care facilities without transplant units. Infection-control measures specific to PE or transplant units (i.e., patient-care areas housing patients at the highest risk for morbidity and mortality from Legionella spp. infection) are described in the subsection titled Preventing Legionnaires Disease in Protective Environments.
Health-care facilities use at least two general strategies to prevent health-care-associated legionellosis when no cases or only sporadic cases have been detected. The first is an environmental surveillance approach involving periodic culturing of water samples from the hospital's potable water system to monitor for Legionella spp.747 750 If any sample is culture-positive, diagnostic testing is recommended for all patients with health-care-associated pneumonia.748, 749 In-house testing is recommended for facilities with transplant programs as part of a comprehensive treatment/management program. If >30% of the samples are culture-positive for Legionella spp., decontamination of the facility's potable water system is warranted. 748 The premise for this approach is that no cases of health-care-associated legionellosis can occur if Legionella spp. are not present in the potable water system, and, conversely, cases of health-care-associated legionellosis could potentially occur if Legionella spp. are cultured from the water.26, 751 Physicians who are informed that the hospital's potable water system is culture-positive for Legionella spp. are more likely to order diagnostic tests for legionellosis.
A potential advantage of the environmental surveillance approach is that periodic culturing of water is less costly than routine laboratory diagnostic testing for all patients who have health-care-associated pneumonia. The primary argument against this approach is that, in the absence of cases, the relationship between water-culture results and legionellosis risk remains undefined.3 Legionnella spp. can be present in the water systems of buildings752 without being associated with known cases of disease.437, 707, 753 In a study of 84 hospitals in Québec, 68% of the water systems were found to be colonized with Legionella spp., and 26% were colonized at >30% of sites sampled; cases of Legionnaires disease, however, were infrequently reported from these hospitals.707
Other factors also argue against environmental surveillance. Interpretation of results from periodic water culturing might be confounded by differing results among the sites sampled in a single water system and by fluctuations in the concentration of Legionella spp. at the same site.709, 754 In addition, the risk for illness after exposure to a given source might be influenced by several factors other than the presence or concentration of organisms, including a) the degree to which contaminated water is aerosolized into respirable droplets, b) the proximity of the infectious aerosol to the potential host, c) the susceptibility of the host, and d) the virulence properties of the contaminating strain.755-757 Thus, data are insufficient to assign a level of disease risk even on the basis of the number of colony-forming units detected in samples from areas for immunocompetent patients. Conducting environmental surveillance would obligate hospital administrators to initiate water-decontamination programs if Legionella spp. are identified. Therefore, periodic monitoring of water from the hospital's potable water system and from aerosol-producing devices is not widely recommended in facilities that have not experienced cases of health-care-associated legionellosis.661, 758
The second strategy to prevent and control health-care-associated legionellosis is a clinical approach, in which providers maintain a high index of suspicion for legionellosis and order appropriate diagnostic tests (i.e., culture, urine antigen, and direct fluorescent antibody serology) for patients with health-care-associated pneumonia who are at high risk for legionellosis and its complications.437, 759, 760 The testing of autopsy specimens can be included in this strategy should a death resulting from health care-associated pneumonia occur. Identification of one case of definite or two cases of possible health care-associated Legionnaires disease should prompt an epidemiologic investigation for a hospital source of Legionella spp., which may involve culturing the facility's water for Legionella. Routine maintenance of cooling towers, and use of sterile water for the filling and terminal rinsing of nebulization devices and ventilation equipment can help to minimize potential sources of contamination. Circulating potable water temperatures should match those outlined in the subsection titled Water Temperature and Pressure, as permitted by state code.
# c. Secondary prevention of Legionnaires Disease (With Identified Cases)
The indications for a full-scale environmental investigation to search for and subsequently decontaminate identified sources of Legionella spp. in health-care facilities without transplant units have not been clarified; these indications would likely differ depending on the facility. Case categories for health-care-associated Legionnaires disease in facilities without transplant units include definite cases (i.e., laboratory-confirmed cases of legionellosis that occur in patients who have been hospitalized continuously for >10 days before the onset of illness) and possible cases (i.e., laboratory-confirmed infections that occur 2-9 days after hospital admission). 3 In settings in which as few as one to three health-care-associated cases are recognized over several months, intensified surveillance for Legionnaires disease has frequently identified numerous additional cases.405, 408, 432, 453, 739, 759, 760 This finding suggests the need for a low threshold for initiating an investigation after laboratory confirmation of cases of health-care-associated legionellosis. When developing a strategy for responding to such a finding, however, infection-control personnel should consider the level of risk for health-care-associated acquisition of, and mortality from, Legionella spp. infection at their particular facility.
An epidemiologic investigation conducted to determine the source of Legionella spp. involves several important steps (Box 11). Laboratory assessment is crucial in supporting epidemiologic evidence of a link between human illness and a specific environmental source.761 Strain determination from subtype analysis is most frequently used in these investigations.410, 762-764 Once the environmental source is established and confirmed with laboratory support, supplemental water treatment strategies can be initiated as appropriate.
# Box 11. Steps in an epidemiologic investigation for legionellosis
Review medical and microbiologic records. Initiate active surveillance to identify all recent or ongoing cases. Develop a line listing of cases by time, place, and person. Determine the type of epidemiologic investigation needed for assessing risk factors:
- Case-control study,
- Cohort study. Gather and analyze epidemiologic information:
- Evaluate risk factors associated with potential environmental exposures (e.g., showers, cooling towers, and respiratory-therapy equipment). Collect water samples:
- Sample environmental sources implicated by epidemiologic investigation,
- Sample other potential source of water aerosols. Subtype strains of Legionella spp. cultured from both patients and environmental sources. Review autopsy records and include autopsy specimens in diagnostic testing.
# d. Preventing Legionnaires Disease in Protective Environments
This subsection outlines infection-control measures applicable to those health-care facilities providing care to severely immunocompromised patients. Indigenous microorganisms in the tap water of these facilities may pose problems for such patients. These measures are designed to prevent the generation of potentially infectious aerosols from water and the subsequent exposure of PE patients or other immunocompromised patients (e.g., transplant patients) (Table 17). Infection-control measures that address the use of water with medical equipment (e.g., ventilators, nebulizers, and equipment humidifiers) are described in other guidelines and publications. 3,455 If one case of laboratory-confirmed, health-care-associated Legionnaires disease is identified in a patient in a solid-organ transplant program or in PE (i.e., an inpatient in PE for all or part of the 2-10 days prior to onset of illness) or if two or more laboratory-confirmed cases occur among patients who had visited an outpatient PE setting, the hospital should report the cases to the local and state health departments. The hospital should then initiate a thorough epidemiologic and environmental investigation to determine the likely environmental sources of Legionella spp. 9 The source of Legionella should be decontaminated or removed. Isolated cases may be difficult to investigate. Because transplant recipients are at substantially higher risk for disease and death from legionellosis compared with other hospitalized patients, periodic culturing for Legionella spp. in water samples from the potable water in the solid-organ transplant and/or PE unit can be performed as part of an overall strategy to prevent Legionnaires disease in PE units.9, 431, 710, 769 The optimal methodology (i.e., frequency and number of sites) for environmental surveillance cultures in PE units has not been determined, and the cost-effectiveness of this strategy has not been evaluated. Because transplant recipients are at high risk for Legionnaires disease and because no data are available to determine a safe concentration of legionellae organisms in potable water, the goal of environmental surveillance for Legionella spp. should be to maintain water systems with no detectable organisms.9, 431 Culturing for legionellae may be used to assess the effectiveness of water treatment or decontamination methods, a practice that provides benefits to both patients and health-care workers.767, 770 - Use water that is not contaminated with Legionella spp. for patients' sponge baths.
- 9 - Provide sterile water for drinking, tooth brushing, or for flushing nasogastric tubes.
- 9, 412 - Perform supplemental treatment of the water for the unit.
- 732 - Consider periodic monitoring (i.e., culturing) of the unit water supply for Protecting patient-care devices and instruments from inadvertent tap water contamination during room cleaning procedures is also important in any immunocompromised patient-care area. In a recent outbreak of gram-negative bacteremias among open-heart-surgery patients, pressure-monitoring equipment that was assembled and left uncovered overnight prior to the next day's surgeries was inadvertently contaminated with mists and splashing water from a hose-disinfectant system used for cleaning.771
# Cooling Towers and Evaporative Condensers
Modern health-care facilities maintain indoor climate control during warm weather by use of cooling towers (large facilities) or evaporative condensers (smaller buildings). A cooling tower is a wet-type, evaporative heat transfer device used to discharge to the atmosphere waste heat from a building's air conditioning condensers (Figure 5).772, 773 Warm water from air-conditioning condensers is piped to the cooling tower where it is sprayed downward into a counter-or cross-current air flow. To accelerate heat transfer to the air, the water passes over the fill, which either breaks water into droplets or causes it to spread into a thin film.772, 773 Most systems use fans to move air through the tower, although some large industrial cooling towers rely on natural draft circulation of air. The cooled water from the tower is piped back to the condenser, where it again picks up heat generated during the process of chilling the system's refrigerant. The water is cycled back to the cooling tower to be cooled. Closed-circuit cooling towers and evaporative condensers are also evaporative heat-transfer devices. In these systems, the process fluid (e.g., water, ethylene glycol/water mixture, oil, or a condensing refrigerant) does not directly contact the cooling air, but is contained inside a coil assembly.661
# Figure 5. Diagram of a typical air conditioning (induced draft) cooling tower*
Water temperatures are approximate and may differ substantially according to system use and design. Warm water from the condenser (or chiller) is sprayed downward into a counter-or cross-current air flow. Water passes over the fill (a component of the system designed to increase the surface area of the water exposed to air), and heat from the water is transferred to the air. Some of the water becomes aerosolized during this process, although the volume of aerosol discharged to the air can be reduced by the placement of a drift eliminator. Water cooled in the tower returns to the heat source to cool refrigerant from the air conditioning unit. - This figure is reprinted with permission of the publisher of reference 773 (Plenum Medical).
Cooling towers and evaporative condensers incorporate inertial stripping devices called drift eliminators to remove water droplets generated within the unit. Although the effectiveness of these eliminators varies substantially depending on design and condition, some water droplets in the size range of <5 pm will likely leave the unit, and some larger droplets leaving the unit may be reduced to <5 pm by evaporation. Thus, even with proper operation, a cooling tower or evaporative condenser can generate and expel respirable water aerosols. If either the water in the unit's basin or the make-up water (added to replace water lost to evaporation) contains Legionella spp. or other waterborne microorganisms, these organisms can be aerosolized and dispersed from the unit.774 Clusters of both Legionnaires disease and Pontiac fever have been traced to exposure to infectious water aerosols originating from cooling towers and evaporative condensers contaminated with Legionella spp. Although most of these outbreaks have been community-acquired episodes of pneumonia, -health-care-associated Legionnaires disease has been linked to cooling tower aerosol exposure.404, 405 Contaminated aerosols from cooling towers on hospital premises gained entry to the buildings either through open windows or via air handling system intakes located near the tower equipment.
Cooling towers and evaporative condensers provide ideal ecological niches for Legionella spp. The typical temperature of the water in cooling towers ranges from 85°F-95°F (29°C-35°C), although temperatures can be above 120°F (49°C) and below 70°F (21°C) depending on system heat load, ambient temperature, and operating strategy.661 An Australian study of cooling towers found that legionellae colonized or multiplied in towers with basin temperatures above 60.8°F (16°C), and multiplication became explosive at temperatures above 73.4°F (23°C).783 Water temperature in closedcircuit cooling towers and evaporative condensers is similar to that in cooling towers. Considerable variation in the piping arrangement occurs. In addition, stagnant areas or dead legs may be difficult to clean or penetrate with biocides.
Several documents address the routine maintenance of cooling towers, evaporative condensers, and whirlpool spas.661, 784-787 They suggest following manufacturer's recommendations for cleaning and biocide treatment of these devices; all health-care facilities should ensure proper maintenance for their cooling towers and evaporative condensers, even in the absence of Legionella spp (Appendix C). Because cooling towers and evaporative condensers can be shut down during periods when air conditioning is not needed, this maintenance cleaning and treatment should be performed before starting up the system for the first time in the warm season.782 Emergency decontamination protocols describing cleaning procedures and hyperchlorination for cooling towers have been developed for towers implicated in the transmission of legionellosis.786, 787
# Dialysis Water Quality and Dialysate
# a. Rationale for Water Treatment in Hemodialysis
Hemodialysis, hemofiltration, and hemodiafiltration require special water-treatment processes to prevent adverse patient outcomes of dialysis therapy resulting from improper formulation of dialysate with water containing high levels of certain chemical or biological contaminants. The Association for the Advancement of Medical Instrumentation (AAMI) has established chemical and microbiologic standards for the water used to prepare dialysate, substitution fluid, or to reprocess hemodialyzers for renal replacement therapy. -
The AAMI standards address: a) equipment and processes used to purify water for the preparation of concentrates and dialysate and the reprocessing of dialyzers for multiple use and b) the devices used to store and distribute this water. Future revisions to these standards may include hemofiltration and hemodiafiltration.
Water treatment systems used in hemodialysis employ several physical and/or chemical processes either singly or in combination (Figure 6). These systems may be portable units or large systems that feed several rooms. In the United States, >97% of maintenance hemodialysis facilities use RO alone or in combination with deionization.793 Many acute-care facilities use portable hemodialysis machines with attached portable water treatment systems that use either deionization or RO. These machines were exempted from earlier versions of AAMI recommendations, but given current knowledge about toxic exposures to and inflammatory processes in patients new to dialysis, these machines should now come into compliance with current AAMI recommendations for hemodialysis water and dialysate quality.788, 789 Previous recommendations were based on the assumption that acute-care patients did not experience the same degree of adverse effects from short-term, cumulative exposures to either chemicals or microbiologic agents present in hemodialysis fluids compared with the effects encountered by patients during chronic, maintenance dialysis.788, 789 Additionally, JCAHO is reviewing inpatient practices and record-keeping for dialysis (acute and maintenance) for adherence to AAMI standards and recommended practices. Investigations of adverse outcomes among patients using reprocessed dialyzers have demonstrated a greater risk for developing pyrogenic reactions when the water used to reprocess these devices contained >6 ng/mL endotoxin and > 104 CFU/mL bacteria.820 In addition to the variability in endotoxin assays, host factors also are involved in determining whether a patient will mount a response to endotoxin.803 Outbreak investigations of pyrogenic reactions and bacteremias associated with hemodialyzer reuse have demonstrated that pyrogenic reactions are prevented once the endotoxin level in the water used to reprocess the dialyzers is returned to below the AAMI standard level.821
Reuse of dialyzers and use of bicarbonate dialysate, high-flux dialyzer membranes, or high-flux dialysis may increase the potential for pyrogenic reactions if the water in the dialysis setting does not meet standards.796-798 Although investigators have been unable to demonstrate endotoxin transfer across dialyzer membranes, , , the preponderance of reports now supports the ability of endotoxin to transfer across at least some high-flux membranes under some operating conditions. In addition to the acute risk of pyrogenic reactions, indirect evidence in increasingly demonstrating that chronic exposure to low amounts of endotoxin may play a role in some of the long-term complications of hemodialysis therapy. Patients treated with ultrafiltered dialysate for 5-6 months have demonstrated a decrease in serum p2 microglobulin concentrations and a decrease in markers of an inflammatory response.824-826 In studies of longer duration, use of microbiologically ultrapure dialysate has been associated with a 827, 828 decreased incidence of p2 microglobulin-associated amyloidosis. , Although patient benefit likely is associated with the use of ultrapure dialysate, no consensus has been reached regarding the potential adoption of this as standard in the United States. Debate continues regarding the bacterial and endotoxin limits for dialysate. As advances in water treatment and hemodialysis processes occur, efforts are underway to move improved technology from the manufacturer out into the user community. Cost-benefit studies, however, have not been done, and substantially increased costs to implement newer water treatment modalities are anticipated.
To reconcile AAMI documents with current International Organization for Standardization (ISO) format, AAMI has determined that its hemodialysis standards will be discussed in the following four installments: RD 5 for hemodialysis equipment, RD 62 for product water quality, RD 47 for dialyzer reprocessing, and RD 52 for dialysate quality. The Renal Diseases and Dialysis Committee of AAMI is expected to finalize and promulgated the dialysate standard pertinent to the user community (RD 52), adopting by reference the bacterial and endotoxin limits in product water as currently outlined in the AAMI standard that applies to systems manufacturers (RD 62). At present, the user community should continue to observe water quality and dialysate standards as outlined in AAMI RD 5 (Hemodialysis Systems, 1992) and AAMI RD 47 (Reuse of Hemodialyzers, 1993) until the new RD 52 standard becomes available (Table 18).789, 791 ) now specifies that all product water used to prepare dialysate or to reprocess dialyzers for multiple use should contain <2 endotoxin units per milliliter (EU/mL).792 A level of 2 EU/mL was chosen as the upper limit for endotoxin because this level is easily achieved with contemporary water treatment systems using RO and/or ultrafiltration. CDC has advocated monthly endotoxin testing along with microbiologic assays of water, because endotoxin activity may not correspond to the total heterotrophic plate counts.829 Additionally, the current AAMI standard RD 62 for manufacturers includes action levels for product water. Because 48 hours can elapse between the time of sampling water for microbial contamination and the time when results are received, and because bacterial proliferation can be rapid, action levels for microbial counts and endotoxin concentrations are reported as 50 CFU/mL and 1 EU/mL, respectively, in this revision of the standard.792 These recommendations will allow users to initiate corrective action before levels exceed the maximum levels established by the standard.
In hemodialysis, the net movement of water is from the blood to the dialysate, although within the dialyzer, local movement of water from the dialysate to the blood through the phenomenon of back filtration may occur, particularly in dialyzers with highly permeable membranes.830 In contrast, hemofiltration and hemodiaflltration feature infusion of large volumes of electrolyte solution (20-70 L) into the blood. Increasingly, this electrolyte solution is being prepared on-line from water and concentrate. Because of the large volumes of fluid infused, AAMI considered the necessity of setting more stringent requirements for water to be used in this application, but this organization has not yet established these because of lack of expert consensus and insufficient experience with on-line therapies in the United States. On-line hemofiltration and hemodiafiltration systems use sequential ultrafiltration as the final step in the preparation of infusion fluid. Several experts from AAMI concur that these point-of-use ultrafiltration systems should be capable of further reducing the bacteria and endotoxin burden of solutions prepared from water meeting the requirements of the AAMI standard to a safe level for infusion.
# b. Microbial Control Strategies
The strategy for controlling massive accumulations of gram-negative water bacteria and NTM in dialysis systems primarily involves preventing their growth through proper disinfection of watertreatment systems and hemodialysis machines. Gram-negative water bacteria, their associated lipopolysaccharides (bacterial endotoxins), and NTM ultimately come from the community water supply, and levels of these bacteria can be amplified depending on the water treatment system, dialysate distribution system, type of dialysis machine, and method of disinfection ( piping can act as bacterial reservoirs. Outlet taps should be located at the highest elevation to prevent loss of disinfectant; keep a recirculation loop in the system; flush unused ports routinely. Tanks are undesirable because they act as a reservoir for water bacteria; if tanks are present, they must be routinely scrubbed and disinfected.
# Dialysis machines
# Single-pass
Recirculating single-pass or recirculating (batch)
Disinfectant should have contact with a ll parts of the machine that are exposed to water or dialysis fluid. Recirculating pumps and machine design allow for massive contamination levels if not properly disinfected; overnight chemical germicide treatment is recommended.
Two components of hemodialysis water distribution systems -pipes (particularly those made of polyvinyl chloride ) and storage tanks -can serve as reservoirs of microbial contamination. Hemodialysis systems frequently use pipes that are wider and longer than are needed to handle the required flow, which slows the fluid velocity and increases both the total fluid volume and the wetted surface area of the system. Gram-negative bacteria in fluids remaining in pipes overnight multiply rapidly and colonize the wet surfaces, producing bacterial populations and endotoxin quantities in proportion to the volume and surface area. Such colonization results in formation of protective biofilm that is difficult to remove and protects the bacteria from disinfection.832 Routine (i.e., monthly), lowlevel disinfection of the pipes can help to control bacterial contamination of the distribution system. Additional measures to protect pipes from contaminations include a) situating all outlet taps at equal elevation and at the highest point of the system so that the disinfectant cannot drain from pipes by gravity before adequate contact time has elapsed and b) eliminating rough joints, dead-end pipes, and unused branches and taps that can trap fluid and serve as reservoirs of bacteria capable of continuously inoculating the entire volume of the system.800 Maintain a flow velocity of 3-5 ft/sec.
A storage tank in the distribution system greatly increases the volume of fluid and surface area available and can serve as a niche for water bacteria. Storage tanks are therefore not recommended for use in dialysis systems unless they are frequently drained and adequately disinfected, including scrubbing the sides of the tank to remove bacterial biofilm. An ultrafilter should be used distal to the storage tank.808, 833
Microbiologie sampling of dialysis fluids is recommended because gram-negative bacteria can proliferate rapidly in water and dialysate in hemodialysis systems; high levels of these organisms place patients at risk for pyrogenic reactions or health-care-associated infection.667, 668, 808
Health-care facilities are advised to sample dialysis fluids at least monthly using standard microbiologic assay methods for waterborne microorganisms.788, 793, 799, 834-836 Product water used to prepare dialysate and to reprocess hemodialyzers for reuse on the same patient should also be tested for bacterial endotoxin on a monthly basis. , , (See Appendix C for information about water sampling methods for dialysis.)
Cross-contamination of dialysis machines and inadequate disinfection measures can facilitate the spread of waterborne organisms to patients. Steps should be taken to ensure that dialysis equipment is performing correctly and that all connectors, lines, and other components are specific for the equipment, in good repair, and properly in place. A recent outbreak of gram-negative bacteremias among dialysis patients was attributed to faulty valves in a drain port of the machine that allowed backflow of saline used to flush the dialyzer before patient use.838, 839 This backflow contaminated the drain priming connectors, which contaminated the blood lines and exposed the patients to high concentrations of gram-negative bacteria. Environmental infection control in dialysis settings also includes low-level disinfection of housekeeping surfaces and spot decontamination of spills of blood (see Environmental Services in Part I of this guideline for further information).
# c. Infection-Control Issues in Peritoneal Dialysis
Peritoneal dialysis (PD), most commonly administered as continuous ambulatory peritoneal dialysis (CAPD) and continual cycling peritoneal dialysis (CCPD), is the third most common treatment for end stage renal disease (ESRD) in the United States, accounting for 12% of all dialysis patients.840 Peritonitis is the primary complication of CAPD, with coagulase-negative staphylococci the most clinically significant causative organisms.841 Other organisms that have been found to produce peritonitis include Staphylococcus aureus, Mycobacterium fortuitum, M. mucogenicum, Stenotrophomonas maltophilia, Burkholderia cepacia, Corynebacterium jeikeium, Candida spp., and other fungi.842-850 Substantial morbidity is associated with peritoneal dialysis infections. Removal of peritoneal dialysis catheters usually is required for treatment of peritonitis caused by fungi, NTM, or other bacteria that are not cleared within the first several days of effective antimicrobial treatment. Furthermore, recurrent episodes of peritonitis may lead to fibrosis and loss of the dialysis membrane.
Many reported episodes of peritonitis are associated with exit-site or tunneled catheter infections. Risk factors for the development of peritonitis in PD patients include a) under dialysis, b) immune suppression, c) prolonged antimicrobial treatment, d) patient age , e) length of hospital stay, and f) hypoalbuminemia.844, 851, 852 Concern has been raised about infection risk associated with the use of automated cyclers in both inpatient and outpatient settings; however, studies suggest that PD patients who use automated cyclers have much lower infection rates. 853 One study noted that a closed-drainage system reduced the incidence of system-related peritonitis among intermittent peritoneal dialysis (IPD) patients from 3.6 to 1.5 cases/100 patient days. 854 The association of peritonitis with management of spent dialysate fluids requires additional study. Therefore, ensuring that the tip of the waste line is not submerged beneath the water level in a toilet or in a drain is prudent.
# Ice Machines and Ice
Microorganisms may be present in ice, ice-storage chests, and ice-making machines. The two main sources of microorganisms in ice are the potable water from which it is made and a transferral of organisms from hands (Table 20). Ice from contaminated ice machines has been associated with patient colonization, blood stream infections, pulmonary and gastrointestinal illnesses, and pseudoinfections.602, 603, 683, 684, 854, 855 Microorganisms in ice can secondarily contaminate clinical specimens and medical solutions that require cold temperatures for either transport or holding.601, 620 An outbreak of surgicalsite infections was interrupted when sterile ice was used in place of tap water ice to cool cardioplegia solutions.601 In a study comparing the microbial populations of hospital ice machines with organisms recovered from ice samples gathered from the community, samples from 27 hospital ice machines yielded low numbers (<10 CFU/mL) of several potentially opportunistic microorganisms, mainly gram-negative bacilli.859 During the survey period, no health-care-associated infections were attributed to the use of ice. Ice from community sources had higher levels of microbial contamination (75%-95% of 194 samples had total heterotrophic plate counts <500 CFU/mL, with the proportion of positive cultures dependent on the incubation temperature) and showed evidence of fecal contamination from the source water.859 Thus, ice machines in health-care settings are no more heavily contaminated compared with ice machines in the community. If the source water for ice in a health-care facility is not fecally contaminated, then ice from clean ice machines and chests should pose no increased hazard for immunocompetent patients. Some waterborne bacteria found in ice could potentially be a risk to immunocompromised patients if they consume ice or drink beverages with ice. For example, Burkholderia cepacia in ice could present an infection risk for cystic fibrosis patients.859, 860 Therefore, protecting immunosuppressed and otherwise medically at-risk patients from exposure to tap water and ice potentially contaminated with opportunistic pathogens is prudent.9
No microbiologic standards for ice, ice-making machines, or ice storage equipment have been established, although several investigators have suggested the need for such standards.859, 866 Culturing of ice machines is not routinely recommended, but it may be useful as part of an epidemiologic investigation.867-869 Sampling might also help determine the best schedule for cleaning open ice-storage chests. Recommendations for a regular program of maintenance and disinfection have been published.866-869 Health-care facilities are advised to clean ice-storage chests on a regular basis. Open ice chests may require a more frequent cleaning schedule compared with chests that have covers.
Portable ice chests and containers require cleaning and low-level disinfection before the addition of ice intended for consumption. Ice-making machines may require less frequent cleaning, but their maintenance is important to proper performance. The manufacturer's instructions for both the proper method of cleaning and/or maintenance should be followed. These instructions may also recommend an EPA-registered disinfectant to ensure chemical potency, materials compatibility, and safety. In the event that instructions and suitable EPA-registered disinfectants are not available for this process, then a generic approach to cleaning, disinfecting, and maintaining ice machines and dispensers can be used (Box 12).
Ice and ice-making machines also may be contaminated via improper storage or handling of ice by patients and/or staff.684-686, 855-858, 870 Suggested steps to avoid this means of contamination include a) minimizing or avoiding direct hand contact with ice intended for consumption, b) using a hard-surface scoop to dispense ice, and c) installing machines that dispense ice directly into portable containers at the touch of a control.687, 869
# Hydrotherapy Tanks and Pools
# a. General Information
Hydrotherapy equipment (e.g., pools, whirlpools, whirlpool spas, hot tubs, and physiotherapy tanks) traditionally has been used to treat patients with certain medical conditions (e.g., burns, , septic ulcers, lesions, amputations,873 orthopedic impairments and injuries, arthritis,874 and kidney lithotripsy).654 Wound-care medicine is increasingly moving away from hydrotherapy, however, in favor of bedside pulsed-lavage therapy using sterile solutions for cleaning and irrigation.492, 875-878 Several episodes of health-care-associated infections have been linked to use of hydrotherapy equipment (Table 21). Potential routes of infection include incidental ingestion of the water, sprays and aerosols, and direct contact with wounds and intact skin (folliculitis). Risk factors for infection include a) age and sex of the patient, b) underlying medical conditions, c) length of time spent in the hydrotherapy water, and d) portals of entry.879 Although some facilities have used tub liners to minimize environmental contamination of the tanks, the use of a tub liner does not eliminate the need for cleaning and disinfection. Draining these small pools and tanks after each patient use, thoroughly cleaning with a detergent, and disinfecting according to manufacturers' instructions have reduced bacterial contamination levels in the water from 104 CFU/mL to <10 CFU/mL.892 A chlorine residual of 15 ppm in the water should be obtained prior to the patient's therapy session (e.g., by adding 15 grams of calcium hypochlorite 70% per 100 gallons of water).892 A study of commercial and residential whirlpools found that superchlorination or draining, cleaning, disinfection, and refilling of whirlpools markedly reduced densities of Pseudomonas aeruginosa in whirlpool water. 893 The bacterial populations were rapidly replenished, however, when disinfectant concentrations dropped below recommended levels for recreational use (i.e., chlorine at 3.0 ppm or bromine at 6.0 ppm). When using chlorine, however, knowing whether the community drinking-water system is disinfected with chloramine is important, because municipal utilities adjust the pH of the water to the basic side to enhance chloramine formation. Because chlorine is not very effective at pH levels above 8, it may be necessary to re-adjust the pH of the water to a more acidic level.894
A few reports describe the addition of antiseptic chemicals to hydrotherapy tank water, especially for burn patient therapy.895-897 One study involving a minimal number of participants demonstrated a reduction in the number of Pseudomonas spp. and other gram-negative bacteria from both patients and equipment surfaces when chloramine-T ("chlorazene") was added to the water.898 Chloramine-T has not, however, been approved for water treatment in the United States.
# c. Hydrotherapy Pools
Hydrotherapy pools typically serve large numbers of patients and are usually heated to 91.4°F-98.6°F (31°C-37°C). The temperature range is more narrow (94°F-96.8°F ) for pediatric and geriatric patient use.899 Because the size of hydrotherapy pools precludes draining after patient use, proper management is required to maintain the proper balance of water conditioning (i.e., alkalinity, hardness, and temperature) and disinfection. The most widely used chemicals for disinfection of pools are chlorine and chlorine compounds -calcium hypochlorite, sodium hypochlorite, lithium hypochlorite, chloroisocyanurates, and chlorine gas. Solid and liquid formulations of chlorine chemicals are the easiest and safest to use.900 Other halogenated compounds have also been used for pool-water disinfection, albeit on a limited scale. Bromine, which forms bactericidal bromamines in the presence of ammonia, has limited use because of its association with contact dermatitis.901 Iodine does not bleach hair, swim suits, or cause eye irritation, but when introduced at proper concentrations, it gives water a greenish-yellowish cast.892
In practical terms, maintenance of large hydrotherapy pools (e.g., those used for exercise) is similar to that for indoor public pools (i.e., continuous filtration, chlorine residuals no less than 0.4 ppm, and pH of 7.2-7.6).902, 903 Supply pipes and pumps also need to be maintained to eliminate the possibility of this equipment serving as a reservoir for waterborne organisms.904 Specific standards for chlorine residual and pH of the water are addressed in local and state regulations. Patients who are fecally incontinent or who have draining wounds should refrain from using these pools until their condition improves.
# d. Birthing Tanks and Other Equipment
The use of birthing tanks, whirlpool spas, and whirlpools is a recent addition to obstetrical practice.905 Few studies on the potential risks associated with these pieces of equipment have been conducted. In one study of 32 women, a newborn contracted a Pseudomonas infection after being birthed in such a tank, the strain of which was identical to the organism isolated from the tank water.906 Another report documented identical strains of P. aeruginosa isolates from a newborn with sepsis and on the environmental surfaces of a tub that the mother used for relaxation while in labor. 907 Other studies have shown no significant increases in the rates of post-immersion infections among mothers and infants.908, 909
Because the water and the tub surfaces routinely become contaminated with the mother's skin flora and blood during labor and delivery, birthing tanks and other tub equipment must be drained after each patient use and the surfaces thoroughly cleaned and disinfected. Health-care facilities are advised to follow the manufacturer's instructions for selection of disinfection method and chemical germicide. The range of chlorine residuals for public whirlpools and whirlpool spas is 2-5 ppm.910 Use of an inflatable tub is an alternative solution, but this item must be cleaned and disinfected between patients if it is not considered a single-use unit.
Recreational tanks and whirlpool spas are increasingly being used as hydrotherapy equipment.
Although such home equipment appears to be suitable for hydrotherapy, they are neither designed nor constructed to function in this capacity. Additionally, manufacturers generally are not obligated to provide the health-care facility with cleaning and disinfecting instructions appropriate for medical equipment use, and the U.S. Food and Drug Administration (FDA) does not evaluate recreational equipment. Health-care facilities should therefore carefully evaluate this "off-label" use of home equipment before proceeding with a purchase.
# Miscellaneous Medical/Dental Equipment Connected to Main Water Systems a. Automated Endoscope Reprocessors
The automated endoscopic reprocessor (AER) is classified by the FDA as an accessory for the flexible endoscope.654 A properly operating AER can provide a more consistent, reliable method of decontaminating and terminal reprocessing for endoscopes between patient procedures than manual reprocessing methods alone.911 An endoscope is generally subjected to high-level disinfection using a liquid chemical sterilant or a high-level disinfectant. Because the instrument is a semi-critical device, the optimal rinse fluid for a disinfected endoscope would be sterile water.3 Sterile water, however, is expensive and difficult to produce in sufficient quantities and with adequate quality assurance for instrument rinsing in an AER.912, 913 Therefore, one option to be used for AERs is rinse water that has been passed through filters with a pore size of 0.1-0.2 pm to render the water "bacteria-free." These filters usually are located in the water line at or near the port where the mains water enters the equipment. The product water (i.e., tap water passing through these filters) in these applications is not considered equivalent in microbial quality to that for membrane-filtered water as produced by pharmaceutical firms. Membrane filtration in pharmaceutical applications is intended to ensure the microbial quality of polished product water.
Water has been linked to the contamination of flexible fiberoptic endoscopes in the following two scenarios: a) rinsing a disinfected endoscope with unfiltered tap water, followed by storage of the instrument without drying out the internal channels and b) contamination of AERs from tap water inadvertently introduced into the equipment. In the latter instance, the machine's water reservoirs and fluid circuitry become contaminated with waterborne, heterotrophic bacteria (e.g., Pseudomonas aeruginosa and NTM), which can survive and persist in biofilms attached to these components.914-917 Colonization of the reservoirs and water lines of the AER becomes problematic if the required cleaning, disinfection, and maintenance are not performed on the equipment as recommended by the manufacturer.669, 916, 917 Use of the 0.1-0.2-pm filter in the water line helps to keep bacterial contamination to a minimum,670, 911, 917 but filters may fail and allow bacteria to pass through to the equipment and then to the instrument undergoing reprocessing.671-674, 913, 918 Filters also require maintenance for proper performance.670, 911, 912, 918, 919 Heightened awareness of the proper disinfection of the connectors that hook the instrument to the AER may help to further reduce the potential for contaminating endoscopes during reprocessing.920 An emerging issue in the field of endoscopy is that of the possible role of rinse water monitoring and its potential to help reduce endoscopy/bronchoscopyassociated infections.918
Studies have linked deficiencies in endoscope cleaning and/or disinfecting processes to the incidence of post-endoscopic adverse outcomes.921-924 Several clusters have been traced to AERs of older designs and these were associated with water quality.675, 914-916 Regardless of whether manual or automated terminal reprocessing is used for endoscopes, the internal channels of the instrument should be dried before storage.925 The presence of residual moisture in the internal channels encourages the proliferation of waterborne microorganisms, some of which may be pathogenic. One of the most frequently used methods employs 70% isopropyl alcohol to flush the internal channels, followed by forced air drying of these channels and hanging the endoscope vertically in a protected cabinet; this method ensures internal drying of the endoscope, lessens the potential for proliferation of waterborne microorganisms, 669
# b. Dental Unit Water Lines
Dental unit water lines (DUWLs) consist of small-bore plastic tubing that delivers water used for general, non-surgical irrigation and as a coolant to dental handpieces, sonic and ultrasonic scalers, and air-water syringes; municipal tap water is the source water for these lines. The presence of biofilms of waterborne bacteria and fungi (e.g., Legionella spp., Pseudomonas aeruginosa, and NTM) in DUWLs has been established.636, 637, 694, 695, 932-934 Biofilms continually release planktonic microorganisms into the water, the titers of which can exceed 1x106 CFU/mL.694 However, scientific evidence indicates that immunocompetent persons are only at minimal risk for substantial adverse health effects after contact with water from a dental unit. Nonetheless, exposing patients or dental personnel to water of uncertain microbiological quality is not consistent with universally accepted infection-control principles.935
In 1993, CDC issued guidelines relative to water quality in a dental setting. These guidelines recommend that all dental instruments that use water (including high-speed handpieces) should be run to discharge water for 20-30 seconds after each patient and for several minutes before the start of each clinic day.936 This practice can help to flush out any patient materials that many have entered the turbine, air, or waterlines.937, 938 The 1993 guidance also indicated that waterlines be flushed at the beginning of the clinic day. Although these guidelines are designed to help reduce the number of microorganisms present in treatment water, they do not address the issue of reducing or preventing biofilm formation in the waterlines. Research published subsequent to the 1993 dental infection control guideline suggests that flushing the lines at the beginning of the day has only minimal effect on the status of the biofilm in the lines and does not reliably improve the quality of water during dental treatment.939-941 Updated recommendations on infection-control practices for water line use in dentistry will be available in late 2003.942
The numbers of microorganisms in water used as coolant or irrigant for non-surgical dental treatment should be as low as reasonably achievable and, at a minimum, should meet nationally recognized standards for safe drinking water.935, 943 Only minimal evidence suggests that water meeting drinking water standards poses a health hazard for immunocompetent persons. The EPA, the American Public Health Association (APHA), and the American Water Works Association (AWWA) have set a maximum limit of 500 CFU/mL for aerobic, heterotrophic, mesophilic bacteria in drinking water in municipal distribution systems.944, 945 This standard is achievable, given improvements in water-line technology. Dentists should consult with the manufacturer of their dental unit to determine the best equipment and method for maintaining and monitoring good water quality.935, 946
# E. Environmental Services 1. Principles of Cleaning and Disinfecting Environmental Surfaces
Although microbiologically contaminated surfaces can serve as reservoirs of potential pathogens, these surfaces generally are not directly associated with transmission of infections to either staff or patients. The transferral of microorganisms from environmental surfaces to patients is largely via hand contact with the surface.947, 948 Although hand hygiene is important to minimize the impact of this transfer, cleaning and disinfecting environmental surfaces as appropriate is fundamental in reducing their potential contribution to the incidence of healthcare-associated infections.
The principles of cleaning and disinfecting environmental surfaces take into account the intended use of the surface or item in patient care. CDC retains the Spaulding classification for medical and surgical instruments, which outlines three categories based on the potential for the instrument to transmit infection if the instrument is microbiologically contaminated before use.949, 950 These categories are "critical," "semicritical," and "noncritical." In 1991, CDC proposed an additional category designated "environmental surfaces" to Spaulding's original classification951 to represent surfaces that generally do not come into direct contact with patients during care. Environmental surfaces carry the least risk of disease transmission and can be safely decontaminated using less rigorous methods than those used on medical instruments and devices. Environmental surfaces can be further divided into medical equipment surfaces (e.g., knobs or handles on hemodialysis machines, x-ray machines, instrument carts, and dental units) and housekeeping surfaces (e.g., floors, walls, and tabletops).951
The following factors influence the choice of disinfection procedure for environmental surfaces: a) the nature of the item to be disinfected, b) the number of microorganisms present, c) the innate resistance of those microorganisms to the inactivating effects of the germicide, d) the amount of organic soil present, e) the type and concentration of germicide used, f) duration and temperature of germicide contact, and 952 953 g) if using a proprietary product, other specific indications and directions for use. , Cleaning is the necessary first step of any sterilization or disinfection process. Cleaning is a form of decontamination that renders the environmental surface safe to handle or use by removing organic matter, salts, and visible soils, all of which interfere with microbial inactivation.954-960 The physical action of scrubbing with detergents and surfactants and rinsing with water removes large numbers of microorganisms from surfaces.957 If the surface is not cleaned before the terminal reprocessing procedures are started, the success of the sterilization or disinfection process is compromised.
Spaulding proposed three levels of disinfection for the treatment of devices and surfaces that do not require sterility for safe use. These disinfection levels are "high-level," "intermediate-level," and "lowlevel."949, 950 The basis for these levels is that microorganisms can usually be grouped according to their innate resistance to a spectrum of physical or chemical germicidal agents (Table 22). This information, coupled with the instrument/surface classification, determines the appropriate level of terminal disinfection for an instrument or surface. The process of high-level disinfection, an appropriate standard of treatment for heat-sensitive, semi critical medical instruments (e.g., flexible, fiberoptic endoscopes), inactivates all vegetative bacteria, mycobacteria, viruses, fungi, and some bacterial spores. High-level disinfection is accomplished with powerful, sporicidal chemicals (e.g., glutaraldehyde, peracetic acid, and hydrogen peroxide) that are not appropriate for use on housekeeping surfaces. These liquid chemical sterilants/high-level disinfectants are highly toxic.961-963 Use of these chemicals for applications other than those indicated in their label instructions (i.e., as immersion chemicals for treating heat-sensitive medical instruments) is not appropriate.964 Intermediate-level disinfection does not necessarily kill bacterial spores, but it does inactivate Mycobacterium tuberculosis var. bovis, which is substantially more resistant to chemical germicides than ordinary vegetative bacteria, fungi, and medium to small viruses (with or without lipid envelopes). Chemical germicides with sufficient potency to achieve intermediate-level disinfection include chlorine-containing compounds (e.g., sodium hypochlorite), alcohols, some phenolics, and some iodophors. Low-level disinfection inactivates vegetative bacteria, fungi, enveloped viruses (e.g., human immunodeficiency virus , and influenza viruses), and some non-enveloped viruses (e.g., adenoviruses). Low-level disinfectants include quaternary ammonium compounds, some phenolics, and some iodophors. Sanitizers are agents that reduce the numbers of bacterial contaminants to safe levels as judged by public health requirements, and are used in cleaning operations, particularly in food service and dairy applications. Germicidal chemicals that have been approved by FDA as skin antiseptics are not appropriate for use as environmental surface disinfectants.951
The selection and use of chemical germicides are largely matters ofjudgment, guided by product label instructions, information, and regulations. Liquid sterilant chemicals and high-level disinfectants intended for use on critical and semi-critical medical/dental devices and instruments are regulated exclusively by the FDA as a result of recent memoranda of understanding between FDA and the EPA that delineates agency authority for chemical germicide regulation.965, 966 Environmental surface germicides (i.e., primarily intermediate-and low-level disinfectants) are regulated by the EPA and labeled with EPA registration numbers. The labels and technical data or product literature of these germicides specify indications for product use and provide claims for the range of antimicrobial activity. The EPA requires certain pre-registration laboratory potency tests for these products to support product label claims. EPA verifies (through laboratory testing) manufacturers' claims to inactivate microorganisms for selected products and organisms. Germicides labeled as "hospital disinfectant" have passed the potency tests for activity against three representative microorganisms -Pseudomonas aeruginosa, Staphylococcus aureus, and Salmonella cholerae suis. Low-level disinfectants are often labeled "hospital disinfectant" without a tuberculocidal claim, because they lack the potency to inactivate mycobacteria. Hospital disinfectants with demonstrated potency against mycobacteria (i.e., intermediate-level disinfectants) may list "tuberculocidal" on the label as well. Other claims (e.g., "fungicidal," "pseudomonicidal," and "virucidal") may appear on labels of environmental surface germicides, but the designations of "tuberculocidal hospital disinfectant" and "hospital disinfectant" correlate directly to Spaulding's assessment of intermediate-level disinfectants and low-level disinfectants, respectively.951 A common misconception in the use of surface disinfectants in health-care settings relates to the underlying purpose for use of proprietary products labeled as a "tuberculocidal" germicide. Such products will not interrupt and prevent the transmission of TB in health-care settings because TB is not acquired from environmental surfaces. The tuberculocidal claim is used as a benchmark by which to measure germicidal potency. Because mycobacteria have the highest intrinsic level of resistance among the vegetative bacteria, viruses, and fungi, any germicide with a tuberculocidal claim on the label (i.e., an intermediate-level disinfectant) is considered capable of inactivating a broad spectrum of pathogens, including much less resistant organisms such the bloodborne pathogens (e.g., hepatitis B virus , hepatitis C virus , and HIV). It is this broad spectrum capability, rather than the product's specific potency against mycobacteria, that is the basis for protocols and OSHA regulations indicating the appropriateness of using tuberculocidal chemicals for surface disinfection.967
# General Cleaning Strategies for Patient-Care Areas
The number and types of microorganisms present on environmental surfaces are influenced by the following factors: a) number of people in the environment, b) amount of activity, c) amount of moisture, d) presence of material capable of supporting microbial growth, e) rate at which organisms suspended in the air are removed, and f) type of surface and orientation .968 Strategies for cleaning and disinfecting surfaces in patient-care areas take into account a) potential for direct patient contact, b) degree and frequency of hand contact, and c) potential contamination of the surface with body substances or environmental sources of microorganisms (e.g., soil, dust, and water).
# a. Cleaning of Medical Equipment
Manufacturers of medical equipment should provide care and maintenance instructions specific to their equipment. These instructions should include information about a) the equipments' compatibility with chemical germicides, b) whether the equipment is water-resistant or can be safely immersed for cleaning, and c) how the equipment should be decontaminated if servicing is required.967 In the absence of manufacturers' instructions, non-critical medical equipment (e.g., stethoscopes, blood pressure cuffs, dialysis machines, and equipment knobs and controls) usually only require cleansing followed by low-to intermediate-level disinfection, depending on the nature and degree of contamination. Ethyl alcohol or isopropyl alcohol in concentrations of 60%-90% (v/v) is often used to disinfect small surfaces (e.g., rubber stoppers of multiple-dose medication vials, and thermometers)952, 969 and occasionally external surfaces of equipment (e.g., stethoscopes and ventilators). However, alcohol evaporates rapidly, which makes extended contact times difficult to achieve unless items are immersed, a factor that precludes its practical use as a large-surface disinfectant.951 Alcohol may cause discoloration, swelling, hardening, and cracking of rubber and certain plastics after prolonged and repeated use and may damage the shellac mounting of lenses in medical equipment. 970 Barrier protection of surfaces and equipment is useful, especially if these surfaces are a) touched frequently by gloved hands during the delivery of patient care, b) likely to become contaminated with body substances, or c) difficult to clean. Impervious-backed paper, aluminum foil, and plastic or fluidresistant covers are suitable for use as barrier protection. An example of this approach is the use of plastic wrapping to cover the handle of the operatory light in dental-care settings.936, 942 Coverings should be removed and discarded while the health-care worker is still gloved.936, 942 The health-care worker, after ungloving and performing hand hygiene, must cover these surfaces with clean materials before the next patient encounter.
# b. Cleaning Housekeeping Surfaces
Housekeeping surfaces require regular cleaning and removal of soil and dust. Dry conditions favor the persistence of gram-positive cocci (e.g., coagulase-negative Staphylococcus spp.) in dust and on surfaces, whereas moist, soiled environments favor the growth and persistence of gram-negative bacilli.948, 971, 972 Fungi are also present on dust and proliferate in moist, fibrous material.
Most, if not all, housekeeping surfaces need to be cleaned only with soap and water or a detergent/disinfectant, depending on the nature of the surface and the type and degree of contamination. Cleaning and disinfection schedules and methods vary according to the area of the health-care facility, type of surface to be cleaned, and the amount and type of soil present. Disinfectant/detergent formulations registered by EPA are used for environmental surface cleaning, but the actual physical removal of microorganisms and soil by wiping or scrubbing is probably as important, if not more so, than any antimicrobial effect of the cleaning agent used.973 Therefore, cost, safety, product-surface compatibility, and acceptability by housekeepers can be the main criteria for selecting a registered agent. If using a proprietary detergent/disinfectant, the manufacturers' instructions for appropriate use of the product should be followed.974 Consult the products' material safety data sheets (MSDS) to determine appropriate precautions to prevent hazardous conditions during product application. Personal protective equipment (PPE) used during cleaning and housekeeping procedures should be appropriate to the task.
Housekeeping surfaces can be divided into two groups -those with minimal hand-contact (e.g., floors, and ceilings) and those with frequent hand-contact ("high touch surfaces"). The methods, thoroughness, and frequency of cleaning and the products used are determined by health-care facility policy.6 However, high-touch housekeeping surfaces in patient-care areas (e.g., doorknobs, bedrails, light switches, wall areas around the toilet in the patient's room, and the edges of privacy curtains) should be cleaned and/or disinfected more frequently than surfaces with minimal hand contact. Infection-control practitioners typically use a risk-assessment approach to identify high-touch surfaces and then coordinate an appropriate cleaning and disinfecting strategy and schedule with the housekeeping staff.
Horizontal surfaces with infrequent hand contact (e.g., window sills and hard-surface flooring) in routine patient-care areas require cleaning on a regular basis, when soiling or spills occur, and when a patient is discharged from the facility.6 Regular cleaning of surfaces and decontamination, as needed, is also advocated to protect potentially exposed workers.967 Cleaning of walls, blinds, and window curtains is recommended when they are visibly soiled. , , Disinfectant fogging is not recommended for general infection control in routine patient-care areas.2, 976 Further, paraformaldehyde, which was once used in this application, is no longer registered by EPA for this purpose. Use of paraformaldehyde in these circumstances requires either registration or an exemption issued by EPA under the Federal Insecticide, Fungicide, and Rodenticide Act (FIFRA). Infection control, industrial hygienists, and environmental services supervisors should assess the cleaning procedures, chemicals used, and the safety issues to determine if a temporary relocation of the patient is needed when cleaning in the room.
Extraordinary cleaning and decontamination of floors in health-care settings is unwarranted. Studies have demonstrated that disinfection of floors offers no advantage over regular detergent/water cleaning and has minimal or no impact on the occurrence of health-care-associated infections.947, 948, 977-980 Additionally, newly cleaned floors become rapidly recontaminated from airborne microorganisms and those transferred from shoes, equipment wheels, and body substances.971, 975, 981 Nevertheless, health care institutions or contracted cleaning companies may choose to use an EPA-registered detergent/disinfectant for cleaning low-touch surfaces (e.g., floors) in patient-care areas because of the difficulty that personnel may have in determining if a spill contains blood or body fluids (requiring a detergent/disinfectant for clean-up) or when a multi-drug resistant organism is likely to be in the environment. Methods for cleaning non-porous floors include wet mopping and wet vacuuming, dry dusting with electrostatic materials, and spray buffing.973, 982-984 Methods that produce minimal mists and aerosols or dispersion of dust in patient-care areas are preferred.9, 20, 109, 272 Part of the cleaning strategy is to minimize contamination of cleaning solutions and cleaning tools. Bucket solutions become contaminated almost immediately during cleaning, and continued use of the solution transfers increasing numbers of microorganisms to each subsequent surface to be cleaned.971, 981, 985 Cleaning solutions should be replaced frequently. A variety of "bucket" methods have been devised to address the frequency with which cleaning solutions are replaced.986, 987 Another source of contamination in the cleaning process is the cleaning cloth or mop head, especially if left soaking in dirty cleaning solutions.971, 988-990 Laundering of cloths and mop heads after use and allowing them to dry before re-use can help to minimize the degree of contamination.990 A simplified approach to cleaning involves replacing soiled cloths and mop heads with clean items each time a bucket of detergent/disinfectant is emptied and replaced with fresh, clean solution (B. Stover, Kosair Children's Hospital, 2000). Disposable cleaning cloths and mop heads are an alternative option, if costs permit.
Another reservoir for microorganisms in the cleaning process may be dilute solutions of the detergents or disinfectants, especially if the working solution is prepared in a dirty container, stored for long periods of time, or prepared incorrectly.547 Gram-negative bacilli (e.g., Pseudomonas spp. and Serratia marcescens) have been detected in solutions of some disinfectants (e.g., phenolics and quaternary ammonium compounds).547, 991 Contemporary EPA registration regulations have helped to minimize this problem by asking manufacturers to provide potency data to support label claims for detergent/disinfectant properties under real-use conditions (e.g., diluting the product with tap water instead of distilled water). Application of contaminated cleaning solutions, particularly from smallquantity aerosol spray bottles or with equipment that might generate aerosols during operation, should be avoided, especially in high-risk patient areas.992, 993 Making sufficient fresh cleaning solution for daily cleaning, discarding any remaining solution, and drying out the container will help to minimize the degree of bacterial contamination. Containers that dispense liquid as opposed to spray-nozzle dispensers (e.g., quart-sized dishwashing liquid bottles) can be used to apply detergent/disinfectants to surfaces and then to cleaning cloths with minimal aerosol generation. A pre-mixed, "ready-to-use" detergent/disinfectant solution may be used if available.
# c. Cleaning Special Care Areas
Guidelines have been published regarding cleaning strategies for isolation areas and operating rooms.6, 7
The basic strategies for areas housing immunosuppressed patients include a) wet dusting horizontal surfaces daily with cleaning cloths pre-moistened with detergent or an EPA-registered hospital disinfectant or disinfectant wipes;94, 98463 b) using care when wet dusting equipment and surfaces above the patient to avoid patient contact with the detergent/disinfectant; c) avoiding the use of cleaning equipment that produces mists or aerosols; d) equipping vacuums with HEPA filters, especially for the exhaust, when used in any patient-care area housing immunosuppressed patients;9, 94, 986 and e) regular cleaning and maintenance of equipment to ensure efficient particle removal. When preparing the cleaning cloths for wet-dusting, freshly prepared solutions of detergents or disinfectants should be used rather than cloths that have soaked in such solutions for long periods of time. Dispersal of microorganisms in the air from dust or aerosols is more problematic in these settings than elsewhere in health-care facilities. Vacuum cleaners can serve as dust disseminators if they are not operating properly.994 Doors to immunosuppressed patients' rooms should be closed when nearby areas are being vacuumed.9 Bacterial and fungal contamination of filters in cleaning equipment is inevitable, and these filters should be cleaned regularly or replaced as per equipment manufacturer instructions.
Mats with tacky surfaces placed in operating rooms and other patient-care areas only slightly minimize the overall degree of contamination of floors and have little impact on the incidence rate of health-careassociated infection in general.351, 971, 983 An exception, however, is the use of tacky mats inside the entry ways of cordoned-off construction areas inside the health-care facility; these mats help to minimize the intrusion of dust into patient-care areas.
Special precautions for cleaning incubators, mattresses, and other nursery surfaces have been recommended to address reports of hyperbilirubinemia in newborns linked to inadequately diluted solutions of phenolics and poor ventilation.995-997 These medical conditions have not, however, been associated with the use of properly prepared solutions of phenolics. Non-porous housekeeping surfaces in neonatal units can be disinfected with properly diluted or pre-mixed phenolics, followed by rinsing with clean water.997 However, phenolics are not recommended for cleaning infant bassinets and incubators during the stay of the infant. Infants who remain in the nursery for an extended period should be moved periodically to freshly cleaned and disinfected bassinets and incubators.997 If phenolics are used for cleaning bassinets and incubators after they have been vacated, the surfaces should be rinsed thoroughly with water and dried before either piece of equipment is reused. Cleaning and disinfecting protocols should allow for the full contact time specified for the product used. Bassinet mattresses should be replaced, however, if the mattress cover surface is broken.997
# Cleaning Strategies for Spills of Blood and Body Substances
Neither HBV, HCV, nor HIV has ever been transmitted from a housekeeping surface (i.e., floors, walls, or countertops). Nonetheless, prompt removal and surface disinfection of an area contaminated by either blood or body substances are sound infection-control practices and OSHA requirements.967
Studies have demonstrated that HIV is inactivated rapidly after being exposed to commonly used chemical germicides at concentrations that are much lower than those used in practice.998 1003 HBV is readily inactivated with a variety of germicides, including quaternary ammonium compounds.1004 Embalming fluids (e.g., formaldehyde) are also capable of completely inactivating HIV and HBV.1005, 1006 OSHA has revised its regulation for disinfecting spills of blood or other potentially infectious material to include proprietary products whose label includes inactivation claims for HBV and HIV, provided that such surfaces have not become contaminated with agent(s) or volumes of or concentrations of agent(s) for which a higher level of disinfection is recommended. Sodium hypochlorite solutions are inexpensive and effective broad-spectrum germicidal solutions.1010, 1011 Generic sources of sodium hypochlorite include household chlorine bleach or reagent grade chemical. Concentrations of sodium hypochlorite solutions with a range of 5,000-6,150 ppm (1:10 v/v dilution of household bleaches marketed in the United States) to 500-615 ppm (1:100 v/v dilution) free chlorine are effective depending on the amount of organic material (e.g., blood, mucus, and urine) present on the surface to be cleaned and disinfected.1010, 1011 EPA-registered chemical germicides may be more compatible with certain materials that could be corroded by repeated exposure to sodium hypochlorite, especially the 1:10 dilution. Appropriate personal protective equipment (e.g., gloves and goggles) should be worn when preparing and using hypochlorite solutions or other chemical germicides.967
Despite laboratory evidence demonstrating adequate potency against bloodborne pathogens (e.g., HIV and HBV), many chlorine bleach products available in grocery and chemical-supply stores are not registered by the EPA for use as surface disinfectants. Use of these chlorine products as surface disinfectants is considered by the EPA to be an "unregistered use." EPA encourages the use of registered products because the agency reviews them for safety and performance when the product is used according to label instructions. When unregistered products are used for surface disinfection, users do so at their own risk.
Strategies for decontaminating spills of blood and other body fluids differ based on the setting in which they occur and the volume of the spill.1010 In patient-care areas, workers can manage small spills with cleaning and then disinfecting using an intermediate-level germicide or an EPA-registered germicide from the EPA List D or E.967, 1007 For spills containing large amounts of blood or other body substances, workers should first remove visible organic matter with absorbent material (e.g., disposable paper towels discarded into leak-proof, properly labeled containment) and then clean and decontaminate the area.1002, 1003, 1012 If the surface is nonporous and a generic form of a sodium hypochlorite solution is used (e.g., household bleach), a 1:100 dilution is appropriate for decontamination assuming that a) the worker assigned to clean the spill is wearing gloves and other personal protective equipment appropriate to the task, b) most of the organic matter of the spill has been removed with absorbent material, and c) the surface has been cleaned to remove residual organic matter. A recent study demonstrated that even strong chlorine solutions (i.e., 1:10 dilution of chlorine bleach) may fail to totally inactivate high titers of virus in large quantities of blood, but in the absence of blood these disinfectants can achieve complete viral inactivation.1011 This evidence supports the need to remove most organic matter from a large spill before final disinfection of the surface. Additionally, EPA-registered proprietary disinfectant label claims are based on use on a pre-cleaned surface.951, 954
Managing spills of blood, body fluids, or other infectious materials in clinical, public health, and research laboratories requires more stringent measures because of a) the higher potential risk of disease transmission associated with large volumes of blood and body fluids and b) high numbers of microorganisms associated with diagnostic cultures. The use of an intermediate-level germicide for routine decontamination in the laboratory is prudent.954 Recommended practices for managing large spills of concentrated infectious agents in the laboratory include a) confining the contaminated area, b) flooding the area with a liquid chemical germicide before cleaning, and c) decontaminating with fresh germicidal chemical of at least intermediate-level disinfectant potency.1010 A suggested technique when flooding the spill with germicide is to lay absorbent material down on the spill and apply sufficient germicide to thoroughly wet both the spill and the absorbent material.1013 If using a solution of household chlorine bleach, a 1:10 dilution is recommended for this purpose. EPA-registered germicides should be used according to the manufacturers' instructions for use dilution and contact time. Gloves should be worn during the cleaning and decontamination procedures in both clinical and laboratory settings. PPE in such a situation may include the use of respiratory protection (e.g., an N95 respirator) if clean-up procedures are expected to generate infectious aerosols. Protocols for cleaning spills should be developed and made available on record as part of good laboratory practice.1013 Workers in laboratories and in patient-care areas of the facility should receive periodic training in environmentalsurface infection-control strategies and procedures as part of an overall infection-control and safety curriculum.
# Carpeting and Cloth Furnishings
# a. Carpeting
Carpeting has been used for more than 30 years in both public and patient-care areas of health-care facilities. Advantages of carpeting in patient-care areas include a) its noise-limiting characteristics; b) the "humanizing" effect on health care; and c) its contribution to reductions in falls and resultant injuries, particularly for the elderly.10141016 Compared to hard-surface flooring, however, carpeting is harder to keep clean, especially after spills of blood and body substances. It is also harder to push equipment with wheels (e.g., wheelchairs, carts, and gurneys) on carpeting.
Several studies have documented the presence of diverse microbial populations, primarily bacteria and fungi, in carpeting;111, 10171024 the variety and number of microorganisms tend to stabilize over time. New carpeting quickly becomes colonized, with bacterial growth plateauing after about 4 weeks. 1019 Vacuuming and cleaning the carpeting can temporarily reduce the numbers of bacteria, but these populations soon rebound and return to pre-cleaning levels.1019, 1020, 1023 Bacterial contamination tends to increase with higher levels of activity.10181020, 1025 Soiled carpeting that is or remains damp or wet provides an ideal setting for the proliferation and persistence of gram-negative bacteria and fungi.1026 Carpeting that remains damp should be removed, ideally within 72 hours.
Despite the evidence of bacterial growth and persistence in carpeting, only limited epidemiologic evidence demonstrates that carpets influence health-care-associated infection rates in areas housing immunocompetent patients.1023, 1025, 1027 This guideline, therefore, includes no recommendations against the use of carpeting in these areas. Nonetheless, avoiding the use of carpeting is prudent in areas where spills are likely to occur (e.g., laboratories, areas around sinks, and janitor closets) and where patients may be at greater risk of infection from airborne environmental pathogens (e.g., HSCT units, burn units, ICUs, and ORs).111, 1028 An outbreak of aspergillosis in an HSCT unit was recently attributed to carpet contamination and a particular method of carpet cleaning.111 A window in the unit had been opened repeatedly during the time of a nearby building fire, which allowed fungal spore intrusion into the unit. After the window was sealed, the carpeting was cleaned using a "bonnet buffing" machine, which dispersed Aspergillus spores into the air.111 Wet vacuuming was instituted, replacing the dry cleaning method used previously; no additional cases of invasive aspergillosis were identified.
The care setting and the method of carpet cleaning are important factors to consider when attempting to minimize or prevent production of aerosols and dispersal of carpet microorganisms into the air.94, 111 Both vacuuming and shampooing or wet cleaning with equipment can disperse microorganisms to the air.111, 994 Vacuum cleaners should be maintained to minimize dust dispersal in general, and be equipped with HEPA filters, especially for use in high-risk patient-care areas.9, 94, 986 Some formulations of carpet-cleaning chemicals, if applied or used improperly, can be dispersed into the air as a fine dust capable of causing respiratory irritation in patients and staff.1029 Cleaning equipment, especially those that engage in wet cleaning and extraction, can become contaminated with waterborne organisms (e.g., Pseudomonas aeruginosa) and serve as a reservoir for these organisms if this equipment is not properly maintained. Substantial numbers of bacteria can then be transferred to carpeting during the cleaning process.1030 Therefore, keeping the carpet cleaning equipment in good repair and allowing such equipment to dry between uses is prudent.
Carpet cleaning should be performed on a regular basis determined by internal policy. Although spills of blood and body substances on non-porous surfaces require prompt spot cleaning using standard cleaning procedures and application of chemical germicides,967 similar decontamination approaches to blood and body substance spills on carpeting can be problematic from a regulatory perspective.1031 Most, if not all, modern carpet brands suitable for public facilities can tolerate the activity of a variety of liquid chemical germicides. However, according to OSHA, carpeting contaminated with blood or other potentially infectious materials can not be fully decontaminated.1032 Therefore, facilities electing to use carpeting for high-activity patient-care areas may choose carpet tiles in areas at high risk for spills.967, 1032 In the event of contamination with blood or other body substances, carpet tiles can be removed, discarded, and replaced. OSHA also acknowledges that only minimal direct skin contact occurs with carpeting, and therefore, employers are expected to make reasonable efforts to clean and sanitize carpeting using carpet detergent/cleaner products.1032
Over the last few years, some carpet manufacturers have treated their products with fungicidal and/or bactericidal chemicals. Although these chemicals may help to reduce the overall numbers of bacteria or fungi present in carpet, their use does not preclude the routine care and maintenance of the carpeting. Limited evidence suggests that chemically treated carpet may have helped to keep health-careassociated aspergillosis rates low in one HSCT unit,111 but overall, treated carpeting has not been shown to prevent the incidence of health-care-associated infections in care areas for immunocompetent patients.
# b. Cloth Furnishings
Upholstered furniture and furnishings are becoming increasingly common in patient-care areas. These furnishings range from simple cloth chairs in patients' rooms to a complete decorating scheme that gives the interior of the facility more the look of an elegant hotel.1033 Even though pathogenic microorganisms have been isolated from the surfaces of cloth chairs, no epidemiologic evidence suggests that general patient-care areas with cloth furniture pose increased risks of health-care-associated infection compared with areas that contain hard-surfaced furniture.1034, 1035 Allergens (e.g., dog and cat dander) have been detected in or on cloth furniture in clinics and elsewhere in hospitals in concentrations higher than those found on bed linens.1034, 1035 These allergens presumably are transferred from the clothing of visitors. Researchers have therefore suggested that cloth chairs should be vacuumed regularly to keep the dust and allergen levels to a minimum. This recommendation, however, has generated concerns that aerosols created from vacuuming could place immunocompromised patients or patients with preexisting lung disease (e.g., asthma) at risk for development of health-care-associated, environmental airborne disease.9, 20, 109, 988 Recovering worn, upholstered furniture (especially the seat cushion) with covers that are easily cleaned (e.g., vinyl), or replacing the item is prudent; minimizing the use of upholstered furniture and furnishings in any patientcare areas where immunosuppressed patients are located (e.g., HSCT units) reduces the likelihood of disease.9
# Flowers and Plants in Patient-Care Areas
Fresh flowers, dried flowers, and potted plants are common items in health-care facilities. In 1974, clinicians isolated an Erwinia sp. post mortem from a neonate diagnosed with fulminant septicemia, meningitis, and respiratory distress syndrome.1038 Because Erwinia spp. are plant pathogens, plants brought into the delivery room were suspected to be the source of the bacteria, although the case report did not definitively establish a direct link. Several subsequent studies evaluated the numbers and diversity of microorganisms in the vase water of cut flowers. These studies revealed that high concentrations of bacteria, ranging from 104-1010 CFU/mL, were often present, especially if the water was changed infrequently.515, 702, 1039 The major group of microorganisms in flower vase water was gram-negative bacteria, with Pseudomonas aeruginosa the most frequently isolated organism.515, 702, 1039, 1040 P. aeruginosa was also the primary organism directly isolated from chrysanthemums and other potted plants. 1041, 1042 However, flowers in hospitals were not significantly more contaminated with bacteria compared with flowers in restaurants or in the home.702 Additionally, no differences in the diversity and degree of antibiotic resistance of bacteria have been observed in samples isolated from hospital flowers versus those obtained from flowers elsewhere.702 Despite the diversity and large numbers of bacteria associated with flower-vase water and potted plants, minimal or no evidence indicates that the presence of plants in immunocompetent patient-care areas poses an increased risk of health-care-associated infection.515 In one study involving a limited number of surgical patients, no correlation was observed between bacterial isolates from flowers in the area and the incidence and etiology of postoperative infections among the patients.1040 Similar conclusions were reached in a study that examined the bacteria found in potted plants.1042 Nonetheless, some precautions for general patient-care settings should be implemented, including a) limiting flower and plant care to staff with no direct patient contact, b) advising health-care staff to wear gloves when handling plants, c) washing hands after handling plants, d) changing vase water every 2 days and discharging the water into a sink outside the immediate patient environment, and e) cleaning and disinfecting vases after use.702 Some researchers have examined the possibility of adding a chemical germicide to vase water to control bacterial populations. Certain chemicals (e.g., hydrogen peroxide and chlorhexidine) are well tolerated by plants.1040, 1043, 1044 Use of these chemicals, however, was not evaluated in studies to assess impact on health-care-associated infection rates. Modern florists now have a variety of products available to add to vase water to extend the life of cut flowers and to minimize bacterial clouding of the water.
Flowers (fresh and dried) and ornamental plants, however, may serve as a reservoir of Aspergillus spp., and dispersal of conidiospores into the air from this source can occur.109 Health-care-associated outbreaks of invasive aspergillosis reinforce the importance of maintaining an environment as free of Aspergillus spp. spores as possible for patients with severe, prolonged neutropenia. Potted plants, freshcut flowers, and dried flower arrangements may provide a reservoir for these fungi as well as other fungal species (e.g., Fusarium spp.).109, 1045, Researchers in one study of bacteria and flowers suggested that flowers and vase water should be avoided in areas providing care to medically at-risk patients (e.g., oncology patients and transplant patients), although this study did not attempt to correlate the observations of bacterial populations in the vase water with the incidence of health-care-associated infections.515 Another study using molecular epidemiology techniques demonstrated identical Aspergillus terreus types among environmental and clinical specimens isolated from infected patients with hematological malignancies.1046 Therefore, attempts should be made to exclude flowers and plants from areas where immunosuppressed patients are be located (e.g., HSCT units).9, 1046
# Pest Control
Cockroaches, flies and maggots, ants, mosquitoes, spiders, mites, midges, and mice are among the typical arthropod and vertebrate pest populations found in health-care facilities. Insects can serve as agents for the mechanical transmission of microorganisms, or as active participants in the disease transmission process by serving as a vector.1047-1049 Arthropods recovered from health-care facilities have been shown to carry a wide variety of pathogenic microorganisms.1050-1056 Studies have suggested that the diversity of microorganisms associated with insects reflects the microbial populations present in the indoor health-care environment; some pathogens encountered in insects from hospitals were either absent from or present to a lesser degree in insects trapped from residential settings.1057-1060 Some of the microbial populations associated with insects in hospitals have demonstrated resistance to antibiotics.1048, 1059, 1061-1063 Insect habitats are characterized by warmth, moisture, and availability of food.1064 Insects forage in and feed on substrates, including but not limited to food scraps from kitchens/cafeteria, foods in vending machines, discharges on dressings either in use or discarded, other forms of human detritis, medical wastes, human wastes, and routine solid waste.1057-1061 Cockroaches, in particular, have been known to feed on fixed sputum smears in laboratories.1065, 1066 Both cockroaches and ants are frequently found in the laundry, central sterile supply departments, and anywhere in the facility where water or moisture is present (e.g., sink traps, drains and janitor closets). Ants will often find their way into sterile packs of items as they forage in a warm, moist environment.1057 Cockroaches and other insects frequent loading docks and other areas with direct access to the outdoors.
Although insects carry a wide variety of pathogenic microorganisms on their surfaces and in their gut, the direct association of insects with disease transmission (apart from vector transmission) is limited, especially in health-care settings; the presence of insects in itself likely does not contribute substantially to health-care-associated disease transmission in developed countries. However, outbreaks of infection attributed to microorganisms carried by insects may occur because of infestation coupled with breaks in standard infection-control practices.1063 Studies have been conducted to examine the role of houseflies as possible vectors for shigellosis and other forms of diarrheal disease in non-health-care settings.1046, 1067 When control measures aimed at reducing the fly population density were implemented, a concomitant reduction in the incidence of diarrheal infections, carriage of Shigella organisms, and mortality caused by diarrhea among infants and young children was observed.
Myiasis is defined as a parasitosis in which the larvae of any of a variety of flies use living or necrotic tissue or body substances of the host as a nutritional source.1068 Larvae from health-care-acquired myiasis have been observed in nares, wounds, eyes, ears, sinuses, and the external urogenital structures.1069-1071 Patients with this rare condition are typically older adults with underlying medical conditions (e.g., diabetes, chronic wounds, and alcoholism) who have a decreased capacity to ward off the flies. Persons with underlying conditions who live or travel to tropical regions of the world are especially at risk.1070, 1071 Cases occur in the summer and early fall months in temperate climates when flies are most active.1071 An environmental assessment and review of the patient's history are necessary to verify that the source of the myiasis is health-care-acquired and to identify corrective measures.1069, 1072 Simple prevention measures (e.g., installing screens on windows) are important in reducing the incidence of myiasis.1072 From a public health and hygiene perspective, arthropod and vertebrate pests should be eradicated from all indoor environments, including health-care facilities.1073, 1074 Modern approaches to institutional pest management usually focus on a) eliminating food sources, indoor habitats, and other conditions that attract pests; b) excluding pests from the indoor environments; and c) applying pesticides as needed.1075 Sealing windows in modern health-care facilities helps to minimize insect intrusion. When windows need to be opened for ventilation, ensuring that screens are in good repair and closing doors to the outside can help with pest control. Insects should be kept out of all areas of the health-care facility, especially ORs and any area where immunosuppressed patients are located. A pest-control specialist with appropriate credentials can provide a regular insect-control program that is tailored to the needs of the facility and uses approved chemicals and/or physical methods. Industrial hygienists can provide information on possible adverse reactions of patients and staff to pesticides and suggest alternative methods for pest control, as needed. ) represent crucial and growing concerns for infection control. Although the term GISA is technically a more accurate description of the strains isolated to date (most of which are classified as having intermediate resistance to both vancomycin and teicoplanin), the term "glycopeptide" may not be recognized by many clinicians. Thus, the label of VISA, which emphasizes a change in minimum inhibitory concentration (MICs) to vancomycin, is similar to that of VRE and is more meaningful to clinicians.1076 According to National Nosocomial Infection Surveillance (NNIS) statistics for infections acquired among ICU patients in the United States in 1999, 52.3% of infections resulting from S. aureus were identified as MRSA infections, and 25.2% of enterococcal infections were attributed to VRE. These figures reflect a 37% and a 43% increase, respectively, since 1994-1998.1077
# Special Pathogen Concerns a. Antibiotic-Resistant Gram-Positive Cocci
People represent the primary reservoir of S. aureus.1078 Although S. aureus has been isolated from a variety of environmental surfaces (e.g., stethoscopes, floors, charts, furniture, dry mops, and hydrotherapy tanks), the role of environmental contamination in transmission of this organism in health care appears to be minimal.1079-1082 S. aureus contamination of surfaces and tanks within burn therapy units, however, may be a major factor in the transmission of infection among burn patients.1083
Colonized patients are the principal reservoir of VRE, and patients who are immunosuppressed (e.g., transplant patients) or otherwise medically at-risk (e.g., ICU patients, cardio-thoracic surgical patients, patients previously hospitalized for extended periods, and those having received multi-antimicrobial or vancomycin therapy) are at greatest risk for VRE colonization.1084-1087 The mechanisms by which cross-colonization take place are not well defined, although recent studies have indicated that both MRSA and VRE may be transmitted either a) directly from patient to patient, b) indirectly by transient carriage on the hands of health-care workers,1088-1091 or c) by hand transfer of these gram-positive organisms from contaminated environmental surfaces and patient-care equipment.1084, 1087, 1092-1097 In one survey, hand carriage of VRE in workers in a long-term care facility ranged from 13%-41%.1098 Many of the environmental surfaces found to be contaminated with VRE in outbreak investigations have been those that are touched frequently by the patient or the health-care worker.1099 Such high-touch surfaces include bedrails, doorknobs, bed linens, gowns, overbed tables, blood pressure cuffs, computer table, bedside tables, and various medical equipment.22, 1087, 1094, 1095, 1100-1102 Contamination of environmental surfaces with VRE generally occurs in clinical laboratories and areas where colonized patients are present,1087, 1092, 1094, 1095, 1103 but the potential for contamination increases when such patients have diarrhea1087 or have multiple body-site colonization.1104 Additional factors that can be important in the dispersion of these pathogens to environmental surfaces are misuse of glove techniques by health care workers (especially when cleaning fecal contamination from surfaces) and patient, family, and visitor hygiene.
Interest in the importance of environmental reservoirs of VRE increased when laboratory studies demonstrated that enterococci can persist in a viable state on dry environmental surfaces for extended periods of time (7 days to 4 months)1099, 1105 and multiple strains can be identified during extensive periods of surveillance.1104 VRE can be recovered from inoculated hands of health-care workers (with or without gloves) for up to 60 minutes. 22 The presence of either MRSA, VISA, or VRE on environmental surfaces, however, does not mean that patients in the contaminated areas will become colonized. Strict adherence to hand hygiene/handwashing and the proper use of barrier precautions help to minimize the potential for spread of these pathogens. Published recommendations for preventing the spread of vancomycin resistance address isolation measures, including patient cohorting and management of patient-care items.5 Direct patient-care items (e.g., blood pressure cuffs) should be disposable whenever possible when used in contact isolation settings for patients with multiply resistant microorganisms.1102 Careful cleaning of patient rooms and medical equipment contributes substantially to the overall control of MRSA, VISA, or VRE transmission. The major focus of a control program for either VRE or MRSA should be the prevention of hand transfer of these organisms. Routine cleaning and disinfection of the housekeeping surfaces (e.g., floors and walls) and patient-care surfaces (e.g., bedrails) should be adequate for inactivation of these organisms. Both MRSA and VRE are susceptible to several EPAregistered low-and intermediate-level disinfectants (e.g., alcohols, sodium hypochlorite, quaternary ammonium compounds, phenolics, and iodophors) at recommended use dilutions for environmental surface disinfection.1103, 1106-1109 Additionally, both VRE and vancomycin-sensitive enterococci are equally sensitive to inactivation by chemical germicides,1106, 1107, 1109 and similar observations have been made when comparing the germicidal resistance of MRSA to that of either methicillin-sensitive S. aureus (MSSA) or VISA.1110 The use of stronger solutions of disinfectants for inactivation of either VRE, MRSA, or VISA is not recommended based on the organisms' resistance to antibiotics.1110-1112 VRE from clinical specimens have exhibited some measure of increased tolerance to heat inactivation in temperature ranges <212°F (<100°C);1106, 1113 however, the clinical significance of these observations is unclear because the role of cleaning the surface or item prior to heat treatment was not evaluated. Although routine environmental sampling is not recommended, laboratory surveillance of environmental surfaces during episodes when VRE contamination is suspected can help determine the effectiveness of the cleaning and disinfecting procedures. Environmental culturing should be approved and supervised by the infection-control program in collaboration with the clinical laboratory.1084, 1087, 1088, 1092, 1096 Two cases of wound infections associated with vancomycin-resistant Staphylococcus aureus (VRSA) determined to be resistant by NCCLS standards for sensitivity/resistance testing were identified in Michigan and Pennsylvania in 2002.1114, 1115 These represented isolated cases, and neither the family members nor the health-care providers of these case-patients had evidence of colonization or infection with VRSA. Conventional environmental infection-control measures (i.e., cleaning and then disinfecting surfaces using EPA-registered disinfectants with label claims for S. aureus) were used during the environmental investigation of these two cases;11101112 however, studies have yet to evaluate the potential intrinsic resistance of these VRSA strains to surface disinfectants.
Standard procedures during terminal cleaning and disinfection of surfaces, if performed incorrectly, may be inadequate for the elimination of VRE from patient rooms.1113, 11161118 Given the sensitivity of VRE to hospital disinfectants, current disinfecting protocols should be effective if they are diligently carried out and properly performed. Health-care facilities should be sure that housekeeping staff use correct procedures for cleaning and disinfecting surfaces in VRE-contaminated areas, which include using sufficient amounts of germicide at proper use dilution and allowing adequate contact time.1118
# b. Clostridium difficile
Clostridium difficile is the most frequent etiologic agent for health-care-associated diarrhea.1119, 1120 In one hospital, 30% of adults who developed health-care-associated diarrhea were positive for C. difficile}121 One recent study employing PCR-ribotyping techniques demonstrated that cases of C. difiicile-acquired diarrhea occurring in the hospital included patients whose infections were attributed to endogenous C. difficile strains and patients whose illnesses were considered to be health-careassociated infections.1122 Most patients remain asymptomatic after infection, but the organism continues to be shed in their stools. Risk factors for acquiring C. difficile--associated infection include a) exposure to antibiotic therapy, particularly with beta-lactam agents;1123 b) gastrointestinal procedures and surgery;1124 c) advanced age; and d) indiscriminate use of antibiotics.1125-1128 Of all the measures that have been used to prevent the spread of C. difficile--associated diarrhea, the most successful has been the restriction of the use of antimicrobial agents.1129, 1130 C. difficile is an anaerobic, gram-positive bacterium. Normally fastidious in its vegetative state, it is capable of sporulating when environmental conditions no longer support its continued growth. The capacity to form spores enables the organism to persist in the environment (e.g., in soil and on dry surfaces) for extended periods of time. Environmental contamination by this microorganism is well known, especially in places where fecal contamination may occur. 1131 The environment (especially housekeeping surfaces) rarely serves as a direct source of infection for patients.1024, 1132-1136 However, direct exposure to contaminated patient-care items (e.g., rectal thermometers) and high-touch surfaces in patients' bathrooms (e.g., light switches) have been implicated as sources of infection.1130, 1135,1136,1138 Transfer of the pathogen to the patient via the hands of health-care workers is thought to be the most likely mechanism of exposure. , , Standard isolation techniques intended to minimize enteric contamination of patients, health-care-workers' hands, patient-care items, and environmental surfaces have been published.1140 Handwashing remains the most effective means of reducing hand contamination. Proper use of gloves is an ancillary measure that helps to further minimize transfer of these pathogens from one surface to another.
The degree to which the environment becomes contaminated with C. difficile spores is proportional to the number of patients with C. difficile-associated diarrhea, , , although asymptomatic, colonized patients may also serve as a source of contamination. Few studies have examined the use of specific chemical germicides for the inactivation of C. difficile spores, and no well-controlled trials have been conducted to determine efficacy of surface disinfection and its impact on health-care-associated diarrhea. Some investigators have evaluated the use of chlorine-containing chemicals (e.g., 1,000 ppm hypochlorite at recommended use-dilution, 5,000 ppm sodium hypochlorite , 1:100 v/v dilutions of unbuffered hypochlorite, and phosphate-buffered hypochlorite ). One of the studies demonstrated that the number of contaminated environmental sites was reduced by half,1135 whereas another two studies demonstrated declines in health-care-associated C. difficile infections in a HSCT unit1141 and in two geriatric medical units1142 during a period of hypochlorite use. The presence of confounding factors, however, was acknowledged in one of these studies. 1142 The recommended approach to environmental infection control with respect to C. difficile is meticulous cleaning followed by disinfection using hypochlorite-based germicides as appropriate.952, 1130, 1143 However, because no EPA-registered surface disinfectants with label claims for inactivation of C. difficile spores are available, the recommendation is based on the best available evidence from the scientific literature.
# c. Respiratory and Enteric Viruses in Pediatric-Care Settings
Although the viruses mentioned in this guideline are not unique to the pediatric-care setting in health care facilities, their prevalence in these areas, especially during the winter months, is substantial. Children (particularly neonates) are more likely to develop infection and substantial clinical disease from these agents compared with adults and therefore are more likely to require supportive care during their illness.
Common respiratory viruses in pediatric-care areas include rhinoviruses, respiratory syncytial virus (RSV), adenoviruses, influenza viruses, and parainfluenza viruses. Transmission of these viruses occurs primarily via direct contact with small-particle aerosols or via hand contamination with respiratory secretions that are then transferred to the nose or eyes. Because transmission primarily requires close personal contact, contact precautions are appropriate to interrupt transmission.6 Hand contamination can occur from direct contact with secretions or indirectly from touching high-touch environmental surfaces that have become contaminated with virus from large droplets. The indirect transfer of virus from one persion to other via hand contact with frequently-touched fomites was demonstrated in a study using a bacteriophage whose environmental stability approximated that of human viral pathogens (e.g., poliovirus and parvovirus). 1144 The impact of this mode of transmission with respect to human respiratory-and enteric viruses is dependent on the ability of these agents to survive on environmental surfaces. Infectious RSV has been recovered from skin, porous surfaces, and non-porous surfaces after 30 minutes, 1 hour, and 7 hours, respectively.1145 Parainfluenza viruses are known to persist for up to 4 hours on porous surfaces and up to 10 hours on non-porous surfaces.1146 Rhinoviruses can persist on porous surfaces and non-porous surfaces for approximately 1 and 3 hours respectively; study participants in a controlled environment became infected with rhinoviruses after first touching a surface with dried secretions and then touching their nasal or conjunctival mucosa.1147 Although the efficiency of direct transmission of these viruses from surfaces in uncontrolled settings remains to be defined, these data underscore the basis for maintaining regular protocols for cleaning and disinfecting of high touch surfaces.
The clinically important enteric viruses encountered in pediatric care settings include enteric adenovirus, astroviruses, caliciviruses, and rotavirus. Group A rotavirus is the most common cause of infectious diarrhea in infants and children. Transmission of this virus is primarily fecal-oral, however, the role of fecally contaminated surfaces and fomites in rotavirus transmission is unclear. During one epidemiologic investigation of enteric disease among children attending day care, rotavirus contamination was detected on 19% of inanimate objects in the center. 1148,1149 In an outbreak in a pediatric unit, secondary cases of rotavirus infection clustered in areas where children with rotaviral diarrhea were located.1150 Astroviruses cause gastroenteritis and diarrhea in newborns and young children and can persist on fecally contaminated surfaces for several months during periods of relatively low humidity.1151, 1152 Outbreaks of small round-structured viruses (i.e., caliciviruses ) can affect both patients and staff, with attack rates of >50%.1153 Routes of person-to-person transmission include fecal-oral spread and aerosols generated from vomiting.11541156 Fecal contamination of surfaces in care settings can spread large amounts of virus to the environment. Studies that have attempted to use low-and intermediate-level disinfectants to inactivate rotavirus suspended in feces have demonstrated a protective effect of high concentrations of organic matter.1157, 1158 Intermediate-level disinfectants (e.g., alcoholic quaternary ammonium compounds, and chlorine solutions) can be effective in inactivating enteric viruses provided that a cleaning step to remove most of the organic matter precedes terminal disinfection.1158 These findings underscore the need for proper cleaning and disinfecting procedures where contamination of environmental surfaces with body substances is likely. EPA-registered surface disinfectants with label claims for these viral agents should be used in these settings. Using disposable, protective barrier coverings may help to minimize the degree of surface contamination.936
# d. Severe Acute Respiratory Syndrome (SARS) Virus
In November 2002 an atypical pneumonia of unknown etiology emerged in Asia and subsequently developed into an international outbreak of respiratory illness among persons in 29 countries during the first six months of 2003. "Severe acute respiratory syndrome" (SARS) is a viral upper respiratory infection associated with a newly described coronavirus (SARS-associated Co-V ). SARS-CoV is an enveloped RNA virus. It is present in high titers in respiratory secretions, stool, and blood of infected persons. The modes of transmission determined from epidemiologic investigations were primarily forms of direct contact (i.e., large droplet aerosolization and person-to-person contact). Respiratory secretions were presumed to be the major source of virus in these situations; airborne transmission of virus has not been completely ruled out. Little is known about the impact of fecal-oral transmission and SARS.
The epidemiology of SARS-CoV infection is not completely understood, and therefore recommended infection control and prevention measures to contain the spread of SARS will evolve as new information becomes available.1159 At present there is no indication that established strategies for cleaning (i.e., to remove the majority of bioburden) and disinfecting equipment and environmental surfaces need to be changed for the environmental infection control of SARS. In-patient rooms housing SARS patients should be cleaned and disinfected at least daily and at the time of patient transfer or discharge. More frequent cleaning and disinfection may be indicated for high-touch surfaces and following aerosol-producing procedures (e.g., intubation, bronchoscopy, and sputum production). While there are presently no disinfectant products registered by EPA specifically for inactivation of SARS-CoV, EPA-registered hospital disinfectants that are equivalent to low-and intermediate-level germicides may be used on pre-cleaned, hard, non-porous surfaces in accordance with manufacturer's instructions for environmental surface disinfection. Monitoring adherence to guidelines established for cleaning and disinfection is an important component of environmental infection control to contain the spread of SARS.
# e. Creutzfeldt-Jakob Disease (CJD) in Patient-Care Areas
Creutzfeldt-Jakob disease (CJD) is a rare, invariably fatal, transmissible spongiform encephalopathy (TSE) that occurs worldwide with an average annual incidence of 1 case per million population.11601162 CJD is one of several TSEs affecting humans; other diseases in this group include kuru, fatal familial insomnia, and Gerstmann-Straussler-Scheinker syndrome. A TSE that affects a younger population (compared to the age range of CJD cases) has been described primarily in the United Kingdom since 1996.1163 This variant form of CJD (vCJD) is clinically and neuropathologically distinguishable from classic CJD; epidemiologic and laboratory evidence suggests a causal association for bovine spongiform encephalopathy (BSE ) and vCJD.11631166
The agent associated with CJD is a prion, which is an abnormal isoform of a normal protein constituent of the central nervous system.11671169 The mechanism by which the normal form of the protein is converted to the abnormal, disease-causing prion is unknown. The tertiary conformation of the abnormal prion protein appears to confer a heightened degree of resistance to conventional methods of sterilization and disinfection.1170, 1171
Although about 90% of CJD cases occur sporadically, a limited number of cases are the result of a direct exposure to prion-containing material (usually central nervous system tissue or pituitary hormones) acquired as a result of health care (iatrogenic cases). These cases have been linked to a) pituitary hormone therapy ,11701174 b) transplants of either dura mater or corneas,11751181 and c) neurosurgical instruments and depth electrodes.11821185 In the cases involving instruments and depth electrodes, conventional cleaning and terminal reprocessing methods of the day failed to fully inactivate the contaminating prions and are considered inadequate by today's standards.
Prion inactivation studies involving whole tissues and tissue homogenates have been conducted to determine the parameters of physical and chemical methods of sterilization or disinfection necessary for complete inactivation;1170, 1186 1191 however, the application of these findings to environmental infection control in health-care settings is problematic. No studies have evaluated the effectiveness of medical instrument reprocessing in inactivating prions. Despite a consensus that abnormal prions display some extreme measure of resistance to inactivation by either physical or chemical methods, scientists disagree about the exact conditions needed for sterilization. Inactivation studies utilizing whole tissues present extraordinary challenges to any sterilizing method.1192 Additionally, the experimental designs of these studies preclude the evaluation of surface cleaning as a part of the total approach to pathogen inactivation.951, 1192 Some researchers have recommended the use of either a 1:2 v/v dilution of sodium hypochorite (approximately 20,000 ppm), full-strength sodium hypochlorite (50,000-60,000 ppm), or 1-2 N sodium hydroxide (NaOH) for the inactivation of prions on certain surfaces (e.g., those found in the pathology laboratory).1170, 1188 Although these chemicals may be appropriate for the decontamination of laboratory, operating-room, or autopsy-room surfaces that come into contact with central nervous system tissue from a known or suspected patient, this approach is not indicated for routine or terminal cleaning of a room previously occupied by a CJD patient. Both chemicals pose hazards for the health care worker doing the decontamination. NaOH is caustic and should not make contact with the skin. Sodium hypochlorite solutions (i.e., chlorine bleach) can corrode metals (e.g., aluminum). MSDS information should be consulted when attempting to work with concentrated solutions of either chemical. Currently, no EPA-registered products have label claims for prion inactivation; therefore, this guidance is based on the best available evidence from the scientific literature.
Environmental infection-control strategies must based on the principles of the "chain of infection," regardless of the disease of concern.13 Although CJD is transmissible, it is not highly contagious. All iatrogenic cases of CJD have been linked to a direct exposure to prion-contaminated central nervous system tissue or pituitary hormones. The six documented iatrogenic cases associated with instruments and devices involved neurosurgical instruments and devices that introduced residual contamination directly to the recipient's brain. No evidence suggests that vCJD has been transmitted iatrogenically or that either CJD or vCJD has been transmitted from environmental surfaces (e.g., housekeeping surfaces). Therefore, routine procedures are adequate for terminal cleaning and disinfection of a CJD patient's room. Additionally, in epidemiologic studies involving highly transfused patients, blood was not identified as a source for prion transmission.1193-1198 Routine procedures for containing, decontaminating, and disinfecting surfaces with blood spills should be adequate for proper infection control in these situations. ' Guidance for environmental infection control in ORs and autopsy areas has been published.1197, 1199 Hospitals should develop risk-assessment procedures to identify patients with known or suspected CJD in efforts to implement prion-specific infection-control measures for the OR and for instrument reprocessing.1200 This assessment also should be conducted for older patients undergoing non-lesionous neurosurgery when such procedures are being done for diagnosis. Disposable, impermeable coverings should be used during these autopsies and neurosurgeries to minimize surface contamination. Surfaces that have become contaminated with central nervous system tissue or cerebral spinal fluid should be cleaned and decontaminated by a) removing most of the tissue or body substance with absorbent materials, b) wetting the surface with a sodium hypochlorite solution containing >5,000 ppm or a 1 N NaOH solution, and c) rinsing thoroughly.951, 1197-1199, 1201 The optimum duration of contact exposure in these instances is unclear. Some researchers recommend a 1-hour contact time on the basis of tissueinactivation studies,1197, 1198, 1201 whereas other reviewers of the subject draw no conclusions from this research.1199 Factors to consider before cleaning a potentially contaminated surface are a) the degree to which gross tissue/body substance contamination can be effectively removed and b) the ease with which the surface can be cleaned.
# F. Environmental Sampling
This portion of Part I addresses the basic principles and methods of sampling environmental surfaces and other environmental sources for microorganisms. The applied strategies of sampling with respect to environmental infection control have been discussed in the appropriate preceding subsections.
# General Principles: Microbiologie Sampling of the Environment
Before 1970, U.S. hospitals conducted regularly scheduled culturing of the air and environmental surfaces (e.g., floors, walls, and table tops).1202 By 1970, CDC and the American Hospital Association (AHA) were advocating the discontinuation of routine environmental culturing because rates of health care-associated infection had not been associated with levels of general microbial contamination of air or environmental surfaces, and because meaningful standards for permissible levels of microbial contamination of environmental surfaces or air did not exist. -During 1970-1975, 25% of U.S. hospitals reduced the extent of such routine environmental culturing -a trend that has continued.1206, 1207 Random, undirected sampling (referred to as "routine" in previous guidelines) differs from the current practice of targeted sampling for defined purposes.2, 1204 Previous recommendations against routine sampling were not intended to discourage the use of sampling in which sample collection, culture, and interpretation are conducted in accordance with defined protocols.2 In this guideline, targeted microbiologic sampling connotes a monitoring process that includes a) a written, defined, multidisciplinary protocol for sample collection and culturing; b) analysis and interpretation of results using scientifically determined or anticipatory baseline values for comparison; and c) expected actions based on the results obtained. Infection control, in conjunction with laboratorians, should assess the health-care facility's capability to conduct sampling and determine when expert consultation and/or services are needed.
Microbiologic sampling of air, water, and inanimate surfaces (i.e., environmental sampling) is an expensive and time-consuming process that is complicated by many variables in protocol, analysis, and interpretation. It is therefore indicated for only four situations. 1208 The first is to support an investigation of an outbreak of disease or infections when environmental reservoirs or fomites are implicated epidemiologically in disease transmission.161, 1209, 1210 It is important that such culturing be supported by epidemiologic data. Environmental sampling, as with all laboratory testing, should not be conducted if there is no plan for interpreting and acting on the results obtained. , , Linking microorganisms from environmental samples with clinical isolates by molecular epidemiology is crucial whenever it is possible to do so.
The second situation for which environmental sampling may be warranted is in research. Well-designed and controlled experimental methods and approaches can provide new information about the spread of health-care-associated diseases.126, 129 A classic example is the study of environmental microbial contamination that compared health-care-associated infection rates in an old hospital and a new facility before and shortly after occupancy.947
The third indication for sampling is to monitor a potentially hazardous environmental condition, confirm the presence of a hazardous chemical or biological agent, and validate the successful abatement of the hazard. This type of sampling can be used to: a) detect bioaerosols released from the operation of health-care equipment (e.g., an ultrasonic cleaner) and determine the success of repairs in containing the hazard,1213 b) detect the release of an agent of bioterrorism in an indoor environmental setting and determine its successful removal or inactivation, and c) sample for industrial hygiene or safety purposes (e.g., monitoring a "sick building").
The fourth indication is for quality assurance to evaluate the effects of a change in infection-control practice or to ensure that equipment or systems perform according to specifications and expected outcomes. Any sampling for quality-assurance purposes must follow sound sampling protocols and address confounding factors through the use of properly selected controls. Results from a single environmental sample are difficult to interpret in the absence of a frame of reference or perspective. Evaluations of a change in infection-control practice are based on the assumption that the effect will be measured over a finite period, usually of short duration. Conducting quality-assurance sampling on an extended basis, especially in the absence of an adverse outcome, is usually unjustified. A possible exception might be the use of air sampling during major construction periods to qualitatively detect breaks in environmental infection-control measures. In one study, which began as part of an investigation of an outbreak of health-care-associated aspergillosis, airborne concentrations of Aspergillus spores were measured in efforts to evaluate the effectiveness of sealing hospital doors and windows during a period of construction of a nearby building.50 Other examples of sampling for quality-assurance purposes may include commissioning newly constructed space in special care areas (i.e., ORs and units for immunosuppressed patients) or assessing a change in housekeeping practice. However, the only types of routine environmental microbiologic sampling recommended as part of a quality-assurance program are a) the biological monitoring of sterilization processes by using bacterial spores1214 and b) the monthly culturing of water used in hemodialysis applications and for the final dialysate use dilution. Some experts also advocate periodic environmental sampling to evaluate the microbial/particulate quality for regular maintenance of the air handling system (e.g., filters) and to verify that the components of the system meet manufacturer's specifications (A. Streifel, University of Minnesota, 2000). Certain equipment in health-care settings (e.g., biological safety cabinets) may also be monitored with air flow and particulate sampling to determine performance or as part of adherence to a certification program; results can then be compared with a predetermined standard of performance. These measurements, however, usually do not require microbiologic testing.
# Air Sampling
Biological contaminants occur in the air as aerosols and may include bacteria, fungi, viruses, and pollens.1215, 1216 Aerosols are characterized as solid or liquid particles suspended in air. Talking for 5 minutes and coughing each can produce 3,000 droplet nuclei; sneezing can generate approximately 40,000 droplets which then evaporate to particles in the size range of 0.5-12 pm. , Particles in a biological aerosol usually vary in size from 50 pm. These particles may consist of a single, unattached organism or may occur in the form of clumps composed of a number of bacteria. Clumps can also include dust and dried organic or inorganic material. Vegetative forms of bacterial cells and viruses may be present in the air in a lesser number than bacterial spores or fungal spores. Factors that determine the survival of microorganisms within a bioaerosol include a) the suspending medium, b) temperature, c) relative humidity, d) oxygen sensitivity, and e) exposure to UV or electromagnetic radiation.1215 Many vegetative cells will not survive for lengthy periods of time in the air unless the relative humidity and other factors are favorable for survival and the organism is enclosed within some protective cover (e.g., dried organic or inorganic matter).1216 Pathogens that resist drying (e.g., Staphylococcus spp., Streptococcus spp., and fungal spores) can survive for long periods and can be carried considerable distances via air and still remain viable. They may also settle on surfaces and become airborne again as secondary aerosols during certain activities (e.g., sweeping and bed making). 1216,1218 Microbiologic air sampling is used as needed to determine the numbers and types of microorganisms, or particulates, in indoor air.289 Air sampling for quality control is, however, problematic because of lack of uniform air-quality standards. Although airborne spores of Aspergillus spp. can pose a risk for neutropenic patients, the critical number (i.e., action level) of these spores above which outbreaks of aspergillosis would be expected to occur has not been defined. Health-care professionals considering the use of air sampling should keep in mind that the results represent indoor air quality at singular points in time, and these may be affected by a variety of factors, including a) indoor traffic, b) visitors entering the facility, c) temperature, d) time of day or year, e) relative humidity, f) relative concentration of particles or organisms, and g) the performance of the air-handling system components. To be meaningful, air-sampling results must be compared with those obtained from other defined areas, conditions, or time periods.
Several preliminary concerns must be addressed when designing a microbiologic air sampling strategy (Box 13). Because the amount of particulate material and bacteria retained in the respiratory system is largely dependent on the size of the inhaled particles, particle size should be determined when studying airborne microorganisms and their relation to respiratory infections. Particles >5 pm are efficiently trapped in the upper respiratory tract and are removed primarily by ciliary action.1219 Particles <5 pm in diameter reach the lung, but the greatest retention in the alveoli is of particles 1-2 pm in diameter.1220-1222 Bacteria, fungi, and particulates in air can be identified and quantified with the same methods and equipment (Table 23). The basic methods include a) impingement in liquids, b) impaction on solid surfaces, c) sedimentation, d) filtration, e) centrifugation, f) electrostatic precipitation, and g) thermal precipitation.1218 Of these, impingement in liquids, impaction on solid surfaces, and sedimentation (on settle plates) have been used for various air-sampling purposes in health-care settings.289 Several instruments are available for sampling airborne bacteria and fungi (Box 14). Some of the samplers are self-contained units requiring only a power supply and the appropriate collecting medium, but most require additional auxiliary equipment (e.g., a vacuum pump and an airflow measuring device ). Sedimentation or depositional methods use settle plates and therefore need no special instruments or equipment. Selection of an instrument for air sampling requires a clear understanding of the type of information desired and the particular determinations that must be made (Box 14). Information may be needed regarding a) one particular organism or all organisms that may be present in the air, b) the concentration of viable particles or of viable organisms, c) the change in concentration with time, and d) the size distribution of the collected particles. Before sampling begins, decisions should be made regarding whether the results are to be qualitative or quantitative. Comparing quantities of airborne microorganisms to those of outdoor air is also standard operating procedure. Infection-control professionals, hospital epidemiologists, industrial hygienists, and laboratory supervisors, as part of a multidisciplinary team, should discuss the potential need for microbial air sampling to determine if the capacity and expertise to conduct such sampling exists within the facility and when it is appropriate to enlist the services of an environmental microbiologist consultant.
# Box 14. Selecting an air sampling device*
The following factors must be considered when choosing an air sampling instrument: Liquid impinger and solid impactor samplers are the most practical for sampling bacteria, particles, and fungal spores, because they can sample large volumes of air in relatively short periods of time.289 Solid impactor units are available as either "slit" or "sieve" designs. Slit impactors use a rotating disc as support for the collecting surface, which allows determinations of concentration over time. Sieve impactors commonly use stages with calibrated holes of different diameters. Some impactor-type samplers use centrifugal force to impact particles onto agar surfaces. The interior of either device must be made sterile to avoid inadvertent contamination from the sampler. Results obtained from either sampling device can be expressed as organisms or particles per unit volume of air (CFU/m3).
- V
Sampling for bacteria requires special attention, because bacteria may be present as individual organisms, as clumps, or mixed with or adhering to dust or covered with a protective coating of dried organic or inorganic substances. Reports of bacterial concentrations determined by air sampling therefore must indicate whether the results represent individual organisms or particles bearing multiple cells. Certain types of samplers (e.g., liquid impingers) will completely or partially disintegrate clumps and large particles; the sampling result will therefore reflect the total number of individual organisms present in the air.
The task of sizing a bioaerosol is simplified through the use of sieves or slit impactors because these samplers will separate the particles and microorganisms into size ranges as the sample is collected. These samplers must, however, be calibrated first by sampling aerosols under similar use conditions.1225
The use of settle plates (i.e., the sedimentation or depositional method) is not recommended when sampling air for fungal spores, because single spores can remain suspended in air indefinitely.289 Settle plates have been used mainly to sample for particulates and bacteria either in research studies or during epidemiologic investigations.161, 1226 1229 Results of sedimentation sampling are typically expressed as numbers of viable particles or viable bacteria per unit area per the duration of sampling time (i.e., CFU/area/time); this method can not quantify the volume of air sampled. Because the survival of microorganisms during air sampling is inversely proportional to the velocity at which the air is taken into the sampler,1215 one advantage of using a settle plate is its reliance on gravity to bring organisms and particles into contact with its surface, thus enhancing the potential for optimal survival of collected organisms. This process, however, takes several hours to complete and may be impractical for some situations.
Air samplers are designed to meet differing measurement requirements. Some samplers are better suited for one form of measurement than others. No one type of sampler and assay procedure can be used to collect and enumerate 100% of airborne organisms. The sampler and/or sampling method chosen should, however, have an adequate sampling rate to collect a sufficient number of particles in a reasonable time period so that a representative sample of air is obtained for biological analysis. Newer analytical techniques for assaying air samples include PCR methods and enzyme-linked immunosorbent assays (ELISAs).
# Water Sampling
A detailed discussion of the principles and practices of water sampling has been published.945 Water sampling in health-care settings is used detect waterborne pathogens of clinical significance or to determine the quality of finished water in a facility's distribution system. Routine testing of the water in a health-care facility is usually not indicated, but sampling in support of outbreak investigations can help determine appropriate infection-control measures. Water-quality assessments in dialysis settings have been discussed in this guideline (see Water, Dialysis Water Quality and Dialysate, and Appendix C).
Health-care facilities that conduct water sampling should have their samples assayed in a laboratory that uses established methods and quality-assurance protocols. Water specimens are not "static specimens" at ambient temperature; potential changes in both numbers and types of microbial populations can occur during transport. Consequently, water samples should be sent to the testing laboratory cold (i.e., at approximately 39.2°F ) and testing should be done as soon as practical after collection (preferably within 24 hours).
Because most water sampling in health-care facilities involves the testing of finished water from the facility's distribution system, a reducing agent (i.e., sodium thiosulfate ) needs to be added to neutralize residual chlorine or other halogen in the collected sample. If the water contains elevated levels of heavy metals, then a chelating agent should be added to the specimen. The minimum volume of water to be collected should be sufficient to complete any and all assays indicated; 100 mL is considered a suitable minimum volume. Sterile collection equipment should always be used.
Sampling from a tap requires flushing of the water line before sample collection. If the tap is a mixing faucet, attachments (e.g., screens and aerators) must be removed, and hot and then cold water must be run through the tap before collecting the sample.945 If the cleanliness of the tap is questionable, disinfection with 500-600 ppm sodium hypochlorite (1:100 v/v dilution of chlorine bleach) and flushing the tap should precede sample collection.
Microorganisms in finished or treated water often are physically damaged ("stressed") to the point that growth is limited when assayed under standard conditions. Such situations lead to false-negative readings and misleading assessments of water quality. Appropriate neutralization of halogens and chelation of heavy metals are crucial to the recovery of these organisms. The choice of recovery media and incubation conditions will also affect the assay. Incubation temperatures should be closer to the ambient temperature of the water rather than at 98.6°F (37°C), and recovery media should be formulated to provide appropriate concentrations of nutrients to support organisms exhibiting less than rigorous growth.945 High-nutrient content media (e.g., blood agar and tryptic soy agar ) may actually inhibit the growth of these damaged organisms. Reduced nutrient media (e.g., diluted peptone and R2A) are preferable for recovery of these organisms.945
Use of aerobic, heterotrophic plate counts allows both a qualitative and quantitative measurement for water quality. If bacterial counts in water are expected to be high in number (e.g., during waterborne outbreak investigations), assaying small quantities using pour plates or spread plates is appropriate.945 Membrane filtration is used when low-count specimens are expected and larger sampling volumes are required (>100 mL). The sample is filtered through the membrane, and the filter is applied directly face-up onto the surface of the agar plate and incubated.
Unlike the testing of potable water supplies for coliforms (which uses standardized test and specimen collection parameters and conditions), water sampling to support epidemiologic investigations of disease outbreaks may be subjected to modifications dictated by the circumstances present in the facility. Assay methods for waterborne pathogens may also not be standardized. Therefore, control or comparison samples should be included in the experimental design. Any departure from a standard method should be fully documented and should be considered when interpreting results and developing strategies. Assay methods specific for clinically significant waterborne pathogens (e.g., Legionella spp., Aeromonas spp, Pseudomonas spp., and Acinetobacter spp.) are more complicated and costly compared with both methods used to detect coliforms and other standard indicators of water quality.
# Environmental Surface Sampling
Routine environmental-surface sampling (e.g., surveillance cultures) in health-care settings is neither 951 1225 cost-effective nor warranted. ,
When indicated, surface sampling should be conducted with multidisciplinary approval in adherence to carefully considered plans of action and policy (Box 15).
# Box 15. Undertaking environmental-surface sampling*
The following factors should be considered before engaging in environmental-surface sampling: Surface sampling is used currently for research, as part of an epidemiologic investigation, or as part of a comprehensive approach for specific quality assurance purposes. As a research tool, surface sampling has been used to determine a) potential environmental reservoirs of pathogens,564, 1230 1232 b) survival of microorganisms on surfaces, , and c) the sources of the environmental contamination. Some or all of these approaches can also be used during outbreak investigations.1232 Discussion of surface sampling of medical devices and instruments is beyond the scope of this document and is deferred to future guidelines on sterilization and disinfection issues.
Meaningful results depend on the selection of appropriate sampling and assay techniques.1214 The media, reagents, and equipment required for surface sampling are available from any well-equipped microbiology laboratory and laboratory supplier. For quantitative assessment of surface organisms, non-selective, nutrient-rich agar media and broth (e.g., TSA and brain-heart infusion broth with or without 5% sheep or rabbit blood supplement) are used for the recovery of aerobic bacteria. Broth media are used with membrane-filtration techniques. Further sample work-up may require the use of selective media for the isolation and enumeration of specific groups of microorganisms. Examples of selective media are MacConkey agar (MAC ), Cetrimide agar (selects for Pseudomonas aeruginosa), or Sabouraud dextrose-and malt extract agars and broths (select for fungi). Qualitative determinations of organisms from surfaces require only the use of selective or non-selective broth media.
Effective sampling of surfaces requires moisture, either already present on the surface to be sampled or via moistened swabs, sponges, wipes, agar surfaces, or membrane filters.1214, 1234-1236 Dilution fluids and rinse fluids include various buffers or general purpose broth media (Table 24). If disinfectant residuals are expected on surfaces being sampled, specific neutralizer chemicals should be used in both the growth media and the dilution or rinse fluids. Lists of the neutralizers, the target disinfectant active ingredients, and the use concentrations have been published. , Alternatively, instead of adding neutralizing chemicals to existing culture media (or if the chemical nature of the disinfectant residuals is unknown), the use of either a) commercially available media including a variety of specific and non specific neutralizers or b) double-strength broth media will facilitate optimal recovery of microorganisms. The inclusion of appropriate control specimens should be included to rule out both residual antimicrobial activity from surface disinfectants and potential toxicity caused by the presence of neutralizer chemicals carried over into the assay system.1214 Sample/rinse methods are frequently chosen because of their versatility. However, these sampling methods are the most prone to errors caused by manipulation of the swab, gauze pad, or sponge.1238 Additionally, no microbiocidal or microbiostatic agents should be present in any of these items when used for sampling.1238 Each of the rinse methods requires effective elution of microorganisms from the item used to sample the surface. Thorough mixing of the rinse fluids after elution (e.g., via manual or mechanical mixing using a vortex mixer, shaking with or without glass beads, and ultrasonic bath) will help to remove and suspend material from the sampling device and break up clumps of organisms for a more accurate count.1238 In some instances, the item used to sample the surface (e.g., gauze pad and sponge) may be immersed in the rinse fluids in a sterile bag and subjected to stomaching.1238 This technique, however, is suitable only for soft or absorbent items that will not puncture the bag during the elution process.
If sampling is conducted as part of an epidemiologic investigation of a disease outbreak, identification of isolates to species level is mandatory, and characterization beyond the species level is preferred.1214 When interpreting the results of the sampling, the expected degree of microbial contamination associated with the various categories of surfaces in the Spaulding classification must be considered. Environmental surfaces should be visibly clean; recognized pathogens in numbers sufficient to result in secondary transfer to other animate or inanimate surfaces should be absent from the surface being sampled.1214 Although the interpretation of a sample with positive microbial growth is self-evident, an environmental surface sample, especially that obtained from housekeeping surfaces, that shows no growth does not represent a "sterile" surface. Sensitivities of the sampling and assay methods (i.e., level of detection) must be taken into account when no-growth samples are encountered. Properly collected control samples will help rule out extraneous contamination of the surface sample.
# G. Laundry and Bedding
# General Information
Laundry in a health-care facility may include bed sheets and blankets, towels, personal clothing, patient apparel, uniforms, scrub suits, gowns, and drapes for surgical procedures.1245 Although contaminated textiles and fabrics in health-care facilities can be a source of substantial numbers of pathogenic microorganisms, reports of health-care-associated diseases linked to contaminated fabrics are so few in number that the overall risk of disease transmission during the laundry process likely is negligible.
When the incidence of such events are evaluated in the context of the volume of items laundered in health-care settings (estimated to be 5 billion pounds annually in the United States),1246 existing control measures (e.g., standard precautions) are effective in reducing the risk of disease transmission to patients and staff. Therefore, use of current control measures should be continued to minimize the contribution of contaminated laundry to the incidence of health-care-associated infections. The control measures described in this section of the guideline are based on principles of hygiene, common sense, and consensus guidance; they pertain to laundry services utilized by health-care facilities, either in house or contract, rather than to laundry done in the home.
# Epidemiology and General Aspects of Infection Control
Contaminated textiles and fabrics often contain high numbers of microorganisms from body substances, including blood, skin, stool, urine, vomitus, and other body tissues and fluids. When textiles are heavily contaminated with potentially infective body substances, they can contain bacterial loads of 106-108 CFU/100 cm2 of fabric.1247 Disease transmission attributed to health-care laundry has involved contaminated fabrics that were handled inappropriately (i.e., the shaking of soiled linens). Bacteria (Salmonella spp., Bacillus cereus), viruses (hepatitis B virus ), fungi (Microsporum canis), and ectoparasites (scabies) presumably have been transmitted from contaminated textiles and fabrics to workers via a) direct contact or b) aerosols of contaminated lint generated from sorting and handling contaminated textiles. -In these events, however, investigations could not rule out the possibility that some of these reported infections were acquired from community sources. Through a combination of soil removal, pathogen removal, and pathogen inactivation, contaminated laundry can be rendered hygienically clean. Hygienically clean laundry carries negligible risk to health-care workers and patients, provided that the clean textiles, fabric, and clothing are not inadvertently contaminated before use.
OSHA defines contaminated laundry as "laundry which has been soiled with blood or other potentially infectious materials or may contain sharps."967 The purpose of the laundry portion of the standard is to protect the worker from exposure to potentially infectious materials during collection, handling, and sorting of contaminated textiles through the use of personal protective equipment, proper work practices, containment, labeling, hazard communication, and ergonomics. Experts are divided regarding the practice of transporting clothes worn at the workplace to the health care worker's home for laundering. Although OSHA regulations prohibit home laundering of items that are considered personal protective apparel or equipment (e.g., laboratory coats),967 experts disagree about whether this regulation extends to uniforms and scrub suits that are not contaminated with blood or other potentially infectious material. Health-care facility policies on this matter vary and may be inconsistent with recommendations of professional organizations.1253, 1254 Uniforms without blood or body substance contamination presumably do not differ appreciably from street clothes in the degree and microbial nature of soilage. Home laundering would be expected to remove this level of soil adequately. However, if health-care facilities require the use of uniforms, they should either make provisions to launder them or provide information to the employee regarding infection control and cleaning guidelines for the item based on the tasks being performed at the facility. Health-care facilities should address the need to provide this service and should determine the frequency for laundering these items. In a recent study examining the microbial contamination of medical students' white coats, the students perceived the coats as "clean" as long as the garments were not visibly contaminated with body substances, even after wearing the coats for several weeks.1255 The heaviest bacterial load was found on the sleeves and the pockets of these garments; the organisms most frequently isolated were Staphylococcus aureus, diphtheroids, and Acinetobacter spp.1255 Presumably, the sleeves of the coat may make contact with a patient and potentially serve to transfer environmentally stable microorganisms among patients. In this study, however, surveillance was not conducted among patients to detect new infections or colonizations. The students did, however, report that they would likely replace their coats more frequently and regularly if clean coats were provided.1255 Apart from this study, which documents the presence of pathogenic bacteria on health-care facility clothing, reports of infections attributed to either the contact with such apparel or with home laundering have been rare.1256, 1257 Laundry services for health-care facilities are provided either in-house (i.e., on-premise laundry ), co-operatives (i.e., those entities owned and operated by a group of facilities), or by off-site commercial laundries. In the latter, the textiles may be owned by the health-care facility, in which case the processor is paid for laundering only. Alternatively, the textiles may be owned by the processor who is paid for every piece laundered on a "rental" fee. The laundry facility in a health-care setting should be designed for efficiency in providing hygienically clean textiles, fabrics, and apparel for patients and staff. Guidelines for laundry construction and operation for health-care facilities, including nursing facilities, have been published.120, 1258 The design and engineering standards for existing facilities are those cited in the AIA edition in effect during the time of the facility's construction.120 A laundry facility is usually partitioned into two separate areas -a "dirty" area for receiving and handling the soiled laundry and a "clean" area for processing the washed items.1259 To minimize the potential for recontaminating cleaned laundry with aerosolized contaminated lint, areas receiving contaminated textiles should be at negative air pressure relative to the clean areas.1260 1262 Laundry areas should have handwashing facilities readily available to workers. Laundry workers should wear appropriate personal protective equipment (e.g., gloves and protective garments) while sorting soiled fabrics and textiles.967 Laundry equipment should be used and maintained according to the manufacturer's instructions to prevent microbial contamination of the system.1250, 1263 Damp textiles should not be left in machines overnight.1250
# Collecting, Transporting, and Sorting Contaminated Textiles and Fabrics
The laundry process starts with the removal of used or contaminated textiles, fabrics, and/or clothing from the areas where such contamination occurred, including but not limited to patients' rooms, surgical/operating areas, and laboratories. Handling contaminated laundry with a minimum of agitation can help prevent the generation of potentially contaminated lint aerosols in patient-care areas.967, 1259 Sorting or rinsing contaminated laundry at the location where contamination occurred is prohibited by OSHA.967 Contaminated textiles and fabrics are placed into bags or other appropriate containment in this location; these bags are then securely tied or otherwise closed to prevent leakage.967 Single bags of sufficient tensile strength are adequate for containing laundry, but leak-resistant containment is needed if the laundry is wet and capable of soaking through a cloth bag.1264 Bags containing contaminated laundry must be clearly identified with labels, color-coding, or other methods so that health-care workers handle these items safely, regardless of whether the laundry is transported within the facility or destined for transport to an off-site laundry service.967 Typically, contaminated laundry originating in isolation areas of the hospital is segregated and handled with special practices; however, few, if any, cases of health-care-associated infection have been linked to this source.1265 Single-blinded studies have demonstrated that laundry from isolation areas is no more heavily contaminated with microorganisms than laundry from elsewhere in the hospital.1266 Therefore, adherence to standard precautions when handling contaminated laundry in isolation areas and minimizing agitation of the contaminated items are considered sufficient to prevent the dispersal of potentially infectious aerosols.6 Contaminated textiles and fabrics in bags can be transported by cart or chute.1258, 1262 Laundry chutes require proper design, maintenance, and use, because the piston-like action of a laundry bag traveling in the chute can propel airborne microbial contaminants throughout the facility.1267-1269 Laundry chutes should be maintained under negative air pressure to prevent the spread of microorganisms from floor to floor. Loose, contaminated pieces of laundry should not be tossed into chutes, and laundry bags should be closed or otherwise secured to prevent the contents from falling out into the chute.1270 Health-care facilities should determine the point in the laundry process at which textiles and fabrics should be sorted. Sorting after washing minimizes the exposure of laundry workers to infective material in soiled fabrics, reduces airborne microbial contamination in the laundry area, and helps to prevent potential percutaneous injuries to personnel.1271 Sorting laundry before washing protects both the machinery and fabrics from hard objects (e.g., needles, syringes, and patients' property) and reduces the potential for recontamination of clean textiles.1272 Sorting laundry before washing also allows for customization of laundry formulas based on the mix of products in the system and types of soils encountered. Additionally, if work flow allows, increasing the amount of segregation by specific product types will usually yield the greatest amount of work efficiency during inspection, folding, and pack-making operations.1253 Protective apparel for the workers and appropriate ventilation can minimize these exposures.967, 1258-1260 Gloves used for the task of sorting laundry should be of sufficient thickness to minimize sharps injuries.967 Employee safety personnel and industrial hygienists can help to determine the appropriate glove choice.
# Parameters of the Laundry Process
Fabrics, textiles, and clothing used in health-care settings are disinfected during laundering and generally rendered free of vegetative pathogens (i.e., hygienically clean), but they are not sterile.1273 Laundering cycles consist of flush, main wash, bleaching, rinsing, and souring.1274 Cleaned wet textiles, fabrics, and clothing are then dried, pressed as needed, and prepared (e.g., folded and packaged) for distribution back to the facility. Clean linens provided by an off-site laundry must be packaged prior to transport to prevent inadvertent contamination from dust and dirt during loading, delivery, and unloading. Functional packaging of laundry can be achieved in several ways, including a) placing clean linen in a hamper lined with a previously unused liner, which is then closed or covered; b) placing clean linen in a properly cleaned cart and covering the cart with disposable material or a properly cleaned reusable textile material that can be secured to the cart; and c) wrapping individual bundles of clean textiles in plastic or other suitable material and sealing or taping the bundles.
The antimicrobial action of the laundering process results from a combination of mechanical, thermal, and chemical factors.1271, 1275, 1276 Dilution and agitation in water remove substantial quantities of microorganisms. Soaps and detergents function to suspend soils and also exhibit some microbiocidal properties. Hot water provides an effective means of destroying microorganisms.1277 A temperature of at least 160°F (71°C) for a minimum of 25 minutes is commonly recommended for hot-water washing.2 Water of this temperature can be provided by steam jet or separate booster heater.120 The use of chlorine bleach assures an extra margin of safety. , A total available chlorine residual of 50-150 ppm is usually achieved during the bleach cycle.1277 Chlorine bleach becomes activated at water temperatures of 135°F-145°F (57.2°C-62.7°C). The last of the series of rinse cycles is the addition of a mild acid (i.e., sour) to neutralize any alkalinity in the water supply, soap, or detergent. The rapid shift in pH from approximately 12 to 5 is an effective means to inactivate some microorganisms.1247 Effective removal of residual alkali from fabrics is an important measure in reducing the risk for skin reactions among patients.
Chlorine bleach is an economical, broad-spectrum chemical germicide that enhances the effectiveness of the laundering process. Chlorine bleach is not, however, an appropriate laundry additive for all fabrics. Traditionally, bleach was not recommended for laundering flame-retardant fabrics, linens, and clothing because its use diminished the flame-retardant properties of the treated fabric.1273 However, some modern-day flame retardant fabrics can now tolerate chlorine bleach. Flame-retardant fabrics, whether topically treated or inherently flame retardant, should be thoroughly rinsed during the rinse cycles, because detergent residues are capable of supporting combustion. Chlorine alternatives (e.g., activated oxygen-based laundry detergents) provide added benefits for fabric and color safety in addition to antimicrobial activity. Studies comparing the antimicrobial potencies of chlorine bleach and oxygen-based bleach are needed. Oxygen-based bleach and detergents used in health-care settings should be registered by EPA to ensure adequate disinfection of laundry. Health-care workers should note the cleaning instructions of textiles, fabrics, drapes, and clothing to identify special laundering requirements and appropriate hygienic cleaning options.1278
Although hot-water washing is an effective laundry disinfection method, the cost can be substantial. Laundries are typically the largest users of hot water in hospitals. They consume 50%-75% of the total hot water,1280 representing an average of 10%-15% of the energy used by a hospital. Several studies have demonstrated that lower water temperatures of 71°F-77°F (22°C-25°C) can reduce microbial contamination when the cycling of the washer, the wash detergent, and the amount of laundry additive are carefully monitored and controlled.1247, 1281-1285 Low-temperature laundry cycles rely heavily on the presence of chlorine-or oxygen-activated bleach to reduce the levels of microbial contamination. The selection of hot-or cold-water laundry cycles may be dictated by state health-care facility licensing standards or by other regulation. Regardless of whether hot or cold water is used for washing, the temperatures reached in drying and especially during ironing provide additional significant microbiocidal action.1247 Dryer temperatures and cycle times are dictated by the materials in the fabrics. Man-made fibers (i.e., polyester and polyester blends) require shorter times and lower temperatures.
After washing, cleaned and dried textiles, fabrics, and clothing are pressed, folded, and packaged for transport, distribution, and storage by methods that ensure their cleanliness until use.2 State regulations and/or accrediting standards may dictate the procedures for this activity. Clean/sterile and contaminated textiles should be transported from the laundry to the health-care facility in vehicles (e.g., trucks, vans, and carts) that allow for separation of clean/sterile and contaminated items. Clean/sterile textiles and contaminated textiles may be transported in the same vehicle, provided that the use of physical barriers and/or space separation can be verified to be effective in protecting the clean/sterile items from contamination. Clean, uncovered/unwrapped textiles stored in a clean location for short periods of time (e.g., uncovered and used within a few hours) have not been demonstrated to contribute to increased levels of health-care-acquired infection. Such textiles can be stored in convenient places for use during the provision of care, provided that the textiles can be maintained dry and free from soil and bodysubstance contamination.
In the absence of microbiologic standards for laundered textiles, no rationale exists for routine microbiologic sampling of cleaned health-care textiles and fabrics.1286 Sampling may be used as part of an outbreak investigation if epidemiologic evidence suggests that textiles, fabrics, or clothing are a suspected vehicle for disease transmission. Sampling techniques include aseptically macerating the fabric into pieces and adding these to broth media or using contact plates (RODAC plates) for direct surface sampling.1271, 1286 When evaluating the disinfecting properties of the laundering process specifically, placing pieces of fabric between two membrane filters may help to minimize the contribution of the physical removal of microorganisms.1287
Washing machines and dryers in residential-care settings are more likely to be consumer items rather than the commercial, heavy-duty, large volume units typically found in hospitals and other institutional health-care settings. Although all washing machines and dryers in health-care settings must be properly maintained for performance according to the manufacturer's instructions, questions have been raised about the need to disinfect washers and dryers in residential-care settings. Disinfection of the tubs and tumblers of these machines is unnecessary when proper laundry procedures are followed; these procedures involve a) the physical removal of bulk solids (e.g., feces) before the wash/dry cycle and b) proper use of temperature, detergent, and laundry additives. Infection has not been linked to laundry procedures in residential-care facilities, even when consumer versions of detergents and laundry additives are used.
# Special Laundry Situations
Some textile items (e.g., surgical drapes and reusable gowns) must be sterilized before use and therefore require steam autoclaving after laundering.7 Although the American Academy of Pediatrics in previous guidelines recommended autoclaving for linens in neonatal intensive care units (NICUs), studies on the microbial quality of routinely cleaned NICU linen have not identified any increased risk for infection among the neonates receiving care.1288 Consequently, hygienically clean linens are suitable for use in this setting.997 The use of sterile linens in burn therapy units remains unresolved.
Coated or laminated fabrics are often used in the manufacture of PPE. When these items become contaminated with blood or other body substances, the manufacturer's instructions for decontamination and cleaning take into account the compatibility of the rubber backing with the chemical germicides or detergents used in the process. The directions for decontaminating these items should be followed as indicated; the item should be discarded when the backing develops surface cracks.
Dry cleaning, a cleaning process that utilizes organic solvents (e.g., perchloroethylene) for soil removal, is an alternative means of cleaning fabrics that might be damaged in conventional laundering and detergent washing. Several studies, however, have shown that dry cleaning alone is relatively ineffective in reducing the numbers of bacteria and viruses on contaminated linens;1289, 1290 microbial populations are significantly reduced only when dry-cleaned articles are heat pressed. Dry cleaning should therefore not be considered a routine option for health-care facility laundry and should be reserved for those circumstances in which fabrics can not be safely cleaned with water and detergent.1291
# Surgical Gowns, Drapes, and Disposable Fabrics
An issue of recent concern involves the use of disposable (i.e., single use) versus reusable (i.e., multiple use) surgical attire and fabrics in health-care settings.1292 Regardless of the material used to manufacture gowns and drapes, these items must be resistant to liquid and microbial penetration.7, 1293 1297 Surgical gowns and drapes must be registered with FDA to demonstrate their safety and effectiveness. Repellency and pore size of the fabric contribute to gown performance, but performance capability can be influenced by the item's design and construction.1298, 1299 Reinforced gowns (i.e., gowns with double-layered fabric) generally are more resistant to liquid strike-through.1300, 1301 Reinforced gowns may, however, be less comfortable. Guidelines for selection and use of barrier materials for surgical gowns and drapes have been published.1302 When selecting a barrier product, repellency level and type of barrier should be compatible for the exposure expected.967 However, data are limited regarding the association between gown or drape characteristics and risk for surgical site infections.7, 1303 Health-care facilities must ensure optimal protection of patients and health-care workers. Not all fabric items in health care lend themselves to single-use. Facilities exploring options for gowns and drapes should consider the expense of disposable items and the impact on the facility's waste-management costs once these items are discarded. Costs associated with the use of durable goods involve the fabric or textile items; staff expenses to collect, sort, clean, and package the laundry; and energy costs to operate the laundry if on-site or the costs to contract with an outside service.1304, 1305
# Antimicrobial-Impregnated Articles and Consumer Items Bearing Antimicrobial Labeling
Manufacturers are increasingly incorporating antibacterial or antimicrobial chemicals into consumer and health-care items. Some consumer products bearing labels that indicate treatment with antimicrobial chemicals have included pens, cutting boards, toys, household cleaners, hand lotions, cat litter, soaps, cotton swabs, toothbrushes, and cosmetics. The "antibacterial" label on household cleaning products, in particular, gives consumers the impression that the products perform "better" than comparable products without this labeling, when in fact all household cleaners have antibacterial properties.
In the health-care setting, treated items may include children's pajamas, mattresses, and bed linens with label claims of antimicrobial properties. These claims require careful evaluation to determine whether they pertain to the use of antimicrobial chemicals as preservatives for the fabric or other components or whether they imply a health claim.1306, 1307 No evidence is available to suggest that use of these products will make consumers and patients healthier or prevent disease. No data support the use of these items as part of a sound infection-control strategy, and therefore, the additional expense of replacing a facility's bedding and sheets with these treated products is unwarranted.
EPA has reaffirmed its position that manufacturers who make public health claims for articles containing antimicrobial chemicals must provide evidence to support those claims as part of the registration process.1308 Current EPA regulations outlined in the Treated Articles Exemption of the Federal Insecticide, Fungicide, and Rodenticide Act (FIFRA) require manufacturers to register both the antimicrobial chemical used in or on the product and the finished product itself if a public health claim is maintained for the item. The exemption applies to the use of antimicrobial chemicals for the purpose of preserving the integrity of the product's raw material(s). The U.S. Federal Trade Commission (FTC) is evaluating manufacturer advertising of products with antimicrobial claims.1309
# Standard Mattresses, Pillows, and Air-Fluidized Beds
Standard mattresses and pillows can become contaminated with body substances during patient care if the integrity of the covers of these items is compromised. The practice of sticking needles into the mattress should be avoided. A mattress cover is generally a fitted, protective material, the purpose of which is to prevent the mattress from becoming contaminated with body fluids and substances. A linen sheet placed on the mattress is not considered a mattress cover. Patches for tears and holes in mattress covers do not provide an impermeable surface over the mattress. Mattress covers should be replaced when torn; the mattress should be replaced if it is visibly stained. Wet mattresses, in particular, can be a substantial environmental source of microorganisms. Infections and colonizations caused by Acinetobacter spp., MRSA, and Pseudomonas aeruginosa have been described, especially among burn patients.13101315 In these reports, the removal of wet mattresses was an effective infection-control measure. Efforts were made to ensure that pads and covers were cleaned and disinfected between patients using disinfectant products compatible with mattress-cover materials to ensure that these covers remained impermeable to fluids.13101314 Pillows and their covers should be easily cleanable, preferably in a hot water laundry cycle.1315 These should be laundered between patients or if contaminated with body substances.
Air-fluidized beds are used for the care of patients immobilized for extended periods of time because of therapy or injury (e.g., pain, decubitus ulcers, and burns).1316 These specialized beds consist of a base unit filled with microsphere beads fluidized by warm, dry air flowing upward from a diffuser located at the bottom of the unit. A porous, polyester filter sheet separates the patient from direct contact with the beads but allows body fluids to pass through to the beads. Moist beads aggregate into clumps which settle to the bottom where they are removed as part of routine bed maintenance.
Because the beads become contaminated with the patient's body substances, concerns have been raised about the potential for these beds to serve as an environmental source of pathogens. Certain pathogens (e.g., Enterococcus spp., Serratia marcescens, Staphylococcus aureus, and Streptococcus fecalis) have been recovered either from the microsphere beads or the polyester sheet after cleaning.1317, 1318 Reports of cross-contamination of patients, however, are few.1318 Nevertheless, routine maintenance and between-patient decontamination procedures can minimize potential risks to patients. Regular removal of bead clumps, coupled with the warm, dry air of the bed, can help to minimize bacterial growth in the unit.13191321 Beads are decontaminated between patients by high heat (113°F-194°F , depending on the manufacturer's specifications) for at least 1 hour; this procedure is particularly important for the inactivation of Enterococcus spp. which are relatively resistant to heat. , The polyester filter sheet requires regular changing and thorough cleaning and disinfection, especially between patients.1317, 1318, 1322, 1323 Microbial contamination of the air space in the immediate vicinity of a properly maintained air-fluidized bed is similar to that found in air around conventional bedding, despite the air flow out of the base unit and around the patient. , , An operational air-fluidized bed can, however, interfere with proper pressure differentials, especially in negative-pressure rooms;1326 the effect varies with the location of the bed relative to the room's configuration and supply and exhaust vent locations. Use of an airfluidized bed in a negative-pressure room requires consultation with a facility engineer to determine appropriate placement of the bed.
# H. Animals in Health-Care Facilities I. General Information
Animals in health-care facilities traditionally have been limited to laboratories and research areas. However, their presence in patient-care areas is now more frequent, both in acute-care and long-term care settings, prompting consideration for the potential transmission of zoonotic pathogens from animals to humans in these settings. Although dogs and cats may be commonly encountered in health-care settings, other animals (e.g., fish, birds, non-human primates, rabbits, rodents, and reptiles) also can be present as research, resident, or service animals. These animals can serve as sources of zoonotic pathogens that could potentially infect patients and health-care workers (Table 26). -Animals potentially can serve as reservoirs for antibiotic-resistant microorganisms, which can be introduced to the health-care setting while the animal is present. VRE have been isolated from both farm animals and pets,1341 and a cat in a geriatric care center was found to be colonized with MRSA.1342 - The + symbol indicates that the pathogen associated with the infection has been isolated from animals and is considered to pose potential risk to humans.
Zoonoses can be transmitted from animals to humans either directly or indirectly via bites, scratches, aerosols, ectoparasites, accidental ingestion, or contact with contaminated soil, food, water, or unpasteurized milk. , , -Colonization and hand transferral of pathogens acquired from pets in health-care workers' homes represent potential sources and modes of transmission of zoonotic pathogens in health-care settings. An outbreak of infections caused by a yeast (Malassezia pachydermatis) among newborns was traced to transfer of the yeast from the hands of health-care workers with pet dogs at home.1346 In addition, an outbreak of ringworm in a NICU caused by Microsporum canis was associated with a nurse and her cat,1347 and an outbreak of Rhodococcus (Gordona) bronchialis sternal SSIs after coronary-artery bypass surgery was traced to a colonized nurse whose dogs were culture-positive for the organism.1348 In the latter outbreak, whether the dogs were the sole source of the organism and whether other environmental reservoirs contributed to the outbreak are unknown. Nonetheless, limited data indicate that outbreaks of infectious disease have occurred as a result of contact with animals in areas housing immunocompetent patients. However, the low frequency of outbreaks may result from a) the relatively limited presence of the animals in health-care facilities and b) the immunocompetency of the patients involved in the encounters. Formal scientific studies to evaluate potential risks of transmission of zoonoses in health-care settings outside of the laboratory are lacking.
# Animal-Assisted Activities, Animal-Assisted Therapy, and Resident Animals
Animal-Assisted Activities (AAA) are those programs that enhance the patients' quality of life. These programs allow patients to visit animals in either a common, central location in the facility or in individual patient rooms. A group session with the animals enhances opportunities for ambulatory patients and facility residents to interact with caregivers, family members, and volunteers.1349 1351 Alternatively, allowing the animals access to individual rooms provides the same opportunity to non ambulatory patients and patients for whom privacy or dignity issues are a consideration. The decision to allow this access to patients' rooms should be made on a case-by-case basis, with the consultation and consent of the attending physician and nursing staff.
Animal-Assisted Therapy (AAT) is a goal-directed intervention that incorporates an animal into the 1330, 1331 treatment process provided by a credentialed therapist. ,
The concept for AAT arose from the observation that some patients with pets at home recover from surgical and medical procedures more rapidly than patients without pets. , Contact with animals is considered beneficial for enhancing wellness in certain patient populations (e.g., children, the elderly, and extended-care hospitalized patients).1349, 1354 1357 However, evidence supporting this benefit is largely derived from anecdotal reports and observations of patient/animal interactions. -Guidelines for establishing AAT programs are available for facilities considering this option.1360
The incorporation of non-human primates into an AAA or AAT program is not encouraged because of concerns regarding potential disease transmission from and unpredictable behavior of these animals.1361, 1362 Animals participating in either AAA or AAT sessions should be in good health and up-to-date with recommended immunizations and prophylactic medications (e.g., heartworm prevention) as determined by a licensed veterinarian based on local needs and recommendations. Regular re-evaluation of the animal's health and behavior status is essential.1360 Animals should be routinely screened for enteric parasites and/or have evidence of a recently completed antihelminthic regimen.1363 They should also be free of ectoparasites (e.g., fleas and ticks) and should have no sutures, open wounds, or obvious dermatologic lesions that could be associated with bacterial, fungal, or viral infections or parasitic infestations. Incorporating young animals (i.e., those aged <1 year) into these programs is not encouraged because of issues regarding unpredictable behavior and elimination control. Additionally, the immune systems of very young puppies and kittens is not completely developed, thereby placing the health of these animals at risk. Animals should be clean and well-groomed. The visits must be supervised by persons who know the animals and their behavior. Animal handlers should be trained in these activities and receive site-specific orientation to ensure that they work efficiently with the staff in the specific health-care environment.1360 Additionally, animal handlers should be in good health.1360
The most important infection-control measure to prevent potential disease transmission is strict enforcement of hand-hygiene measures (e.g., using either soap and water or an alcohol-based hand rub) for all patients, staff, and residents after handling the animals.1355, 1364 Care should also be taken to avoid direct contact with animal urine or feces. Clean-up of these substances from environmental surfaces requires gloves and the use of leak-resistant plastic bags to discard absorbent material used in the process.2 The area must be cleaned after visits according to standard cleaning procedures.
The American Academy of Allergy, Asthma, and Immunology estimates that dog or cat allergies occur in approximately 15% of the population.1365 Minimizing contact with animal saliva, dander, and/or urine helps to mitigate allergic responses.1365 1367 Some facilities may not allow animal visitation for patients with a) underlying asthma, b) known allergies to cat or dog hair, c) respiratory allergies of unknown etiology, and d) immunosuppressive disorders. Hair shedding can be minimized by processes that remove dead hair (e.g., grooming) and that prevent the shedding of dead hair (e.g., therapy capes for dogs). Allergens can be minimized by bathing therapy animals within 24 hours of a visit. 1333,1368 Animal therapists and handlers must take precautions to prevent animal bites. Common pathogens associated with animal bites include Capnocytophaga canimorsus, Pasteurella spp., Staphylococcus spp., and Streptococcus spp. Selecting well-behaved and well-trained animals for these programs greatly decreases the incidence of bites. Rodents, exotic species, wild/domestic animals (i.e., wolf-dog hybrids), and wild animals whose behavior is unpredictable should be excluded from AAA or AAT programs. A well-trained animal handler should be able to recognize stress in the animal and to determine when to terminate a session to minimize risk. When an animal bites a person during AAA or AAT, the animal is to be permanently removed from the program. If a bite does occur, the wound must be cleansed immediately and monitored for subsequent infection. Most infections can be treated with antibiotics, and antibiotics often are prescribed prophylactically in these situations.
The health-care facility's infection-control staff should participate actively in planning for and coordinating AAA and AAT sessions. Many facilities do not offer AAA or AAT programs for severely immunocompromised patients (e.g., HSCT patients and patients on corticosteroid therapy).1339 The question of whether family pets or companion animals can visit terminally-ill HSCT patients or other severely immunosuppressed patients is best handled on a case-by-case basis, although animals should not be brought into the HSCT unit or any other unit housing severely immunosuppressed patients. An in-depth discussion of this issue is presented elsewhere.1366 Immunocompromised patients who have been discharged from a health-care facility may be at higher risk for acquiring some pet-related zoonoses. Although guidelines have been developed to minimize the risk of disease transmission to HIV-infected patients,8 these recommendations may be applicable for patients with other immunosuppressive disorders. In addition to handwashing or hand hygiene, these recommendations include avoiding contact with a) animal feces and soiled litter box materials, b) animals with diarrhea, c) very young animals (i.e., dogs <6 months of age and cats <1 year of age), and d) exotic animals and reptiles.8 Pets or companion animals with diarrhea should receive veterinary care to resolve their condition.
Many health-care facilities are adopting more home-like environments for residential-care or extendedstay patients in acute-care settings, and resident animals are one element of this approach.1369 One concept, the "Eden Alternative," incorporates children, plants, and animals (e.g., dogs, cats, fish, birds, rabbits, and rodents) into the daily care setting. ,
The concept of working with resident animals has not been scientifically evaluated. Several issues beyond the benefits of therapy must be considered before embarking on such a program, including a) whether the animals will come into direct contact with patients and/or be allowed to roam freely in the facility; b) how the staff will provide care for the animals; c) the management of patients' or residents' allergies, asthma, and phobias; d) precautionary measures to prevent bites and scratches; and e) measures to properly manage the disposal of animal feces and urine, thereby preventing environmental contamination by zoonotic microorganisms (e.g., Toxoplasma spp., Toxocara spp., and Ancylostoma spp.). , Few data document a link between health-care-acquired infection rates and frequency of cleaning fish tanks or rodent cages. Skin infections caused by Mycobacterium marinum have been described among persons who have fish aquariums at home. , Nevertheless, immunocompromised patients should avoid direct contact with fish tanks and cages and the aerosols that these items produce. Further, fish tanks should be kept clean on a regular basis as determined by facility policy, and this task should be performed by gloved staff members who are not responsible for patient care. The use of the infection-control risk assessment can help determine whether a fish tank poses a risk for patient or resident safety and health in these situations. No evidence, however, links the incidence of health-care-acquired infections among immunocompetent patients or residents with the presence of a properly cleaned and maintained fish tank, even in dining areas. As a general preventive measure, resident animal programs are advised to restrict animals from a) food preparation kitchens, b) laundries, c) central sterile supply and any storage areas for clean supplies, and d) medication preparation areas. Resident-animal programs in acute-care facilities should not allow the animals into the isolation areas, protective environments, ORs, or any area where immunocompromised patients are housed. Patients and staff routinely should wash their hands or use waterless, alcohol-based hand-hygiene products after contact with animals.
# Service Animals
Although this section provides an overview about service animals in health-care settings, it cannot address every situation or question that may arise (see Appendix E -Information Resources). A service animal is any animal individually trained to do work or perform tasks for the benefit of a person with a disability.1366, 1376 A service animal is not considered a pet but rather an animal trained to provide assistance to a person because of a disability. Title III of the "Americans with Disabilities Act" (ADA) of 1990 mandates that persons with disabilities accompanied by service animals be allowed access with their service animals into places of public accommodation, including restaurants, public transportation, schools, and health-care facilities.1366, 1376 In health-care facilities, a person with a disability requiring a service animal may be an employee, a visitor, or a patient.
An overview of the subject of service animals and their presence in health-care facilities has been published.1366 No evidence suggests that animals pose a more significant risk of transmitting infection than people; therefore, service animals should not be excluded from such areas, unless an individual patient's situation or a particular animal poses greater risk that cannot be mitigated through reasonable measures. If health-care personnel, visitors, and patients are permitted to enter care areas (e.g., in patient rooms, some ICUs, and public areas) without taking additional precautions to prevent transmission of infectious agents (e.g., donning gloves, gowns, or masks), a clean, healthy, wellbehaved service animal should be allowed access with its handler.1366 Similarly, if immunocompromised patients are able to receive visitors without using protective garments or equipment, an exclusion of service animals from this area would not be justified.1366
Because health-care facilities are covered by the ADA or the Rehabilitation Act, a person with a disability may be accompanied by a service animal within the facility unless the animal's presence or behavior creates a fundamental alteration in the nature of a facility's services in a particular area or a direct threat to other persons in a particular area.1366 A "direct threat" is defined as a significant risk to the health or safety of others that cannot be mitigated or eliminated by modifying policies, practices, or procedures.1376 The determination that a service animal poses a direct threat in any particular health care setting must be based on an individualized assessment of the service animal, the patient, and the health-care situation. When evaluating risk in such situations, health-care personnel should consider the nature of the risk (including duration and severity); the probability that injury will occur; and whether reasonable modifications of policies, practices, or procedures will mitigate the risk (J. Wodatch, U.S. Department of Justice, 2000). The person with a disability should contribute to the risk-assessment process as part of a pre-procedure health-care provider/patient conference.
Excluding a service animal from an OR or similar special care areas (e.g., burn units, some ICUs, PE units, and any other area containing equipment critical for life support) is appropriate if these areas are considered to have "restricted access" with regards to the general public. General infection-control measures that dictate such limited access include a) the area is required to meet environmental criteria to minimize the risk of disease transmission, b) strict attention to hand hygiene and absence of dermatologic conditions, and c) barrier protective measures are indicated for persons in the affected space. No infection-control measures regarding the use of barrier precautions could be reasonably imposed on the service animal. Excluding a service animal that becomes threatening because of a perceived danger to its handler during treatment also is appropriate; however, exclusion of such an animal must be based on the actual behavior of the particular animal, not on speculation about how the animal might behave.
Another issue regarding service animals is whether to permit persons with disabilities to be accompanied by their service animals during all phases of their stay in the health-care facility. Health care personnel should discuss all aspects of anticipatory care with the patient who uses a service animal. Health-care personnel may not exclude a service animal because health-care staff may be able to perform the same services that the service animal does (e.g., retrieving dropped items and guiding an otherwise ambulatory person to the restroom). Similarly, health-care personnel can not exclude service animals because the health-care staff perceive a lack of need for the service animal during the person's stay in the health-care facility. A person with a disability is entitled to independent access (i.e., to be accompanied by a service animal unless the animal poses a direct threat or a fundamental alteration in the nature of services); "need" for the animal is not a valid factor in either analysis. For some forms of care (e.g., ambulation as physical therapy following total hip replacement or knee replacement), the service animal should not be used in place of a credentialed health-care worker who directly provides therapy. However, service animals need not be restricted from being in the presence of its handler during this time; in addition, rehabilitation and discharge planning should incorporate the patient's future use of the animal. The health-care personnel and the patient with a disability should discuss both the possible need for the service animal to be separated from its handler for a period of time during non emergency care and an alternate plan of care for the service animal in the event the patient is unable or unwilling to provide that care. This plan might include family members taking the animal out of the facility several times a day for exercise and elimination, the animal staying with relatives, or boarding off-site. Care of the service animal, however, remains the obligation of the person with the disability, not the health-care staff.
Although animals potentially carry zoonotic pathogens transmissible to man, the risk is minimal with a healthy, clean, vaccinated, well-behaved, and well-trained service animal, the most common of which are dogs and cats. No reports have been published regarding infectious disease that affects humans originating in service dogs. Standard cleaning procedures are sufficient following occupation of an area by a service animal.1366 Clean-up of spills of animal urine, feces, or other body substances can be accomplished with blood/body substance procedures outlined in the Environmental Services section of this guideline. No special bathing procedures are required prior to a service animal accompanying its handler into a health-care facility.
Providing access to exotic animals (e.g., reptiles and non-human primates) that are used as service animals is problematic. Concerns about these animals are discussed in two published reviews.1331, 1366 Because some of these animals exhibit high-risk behaviors that may increase the potential for zoonotic disease transmission (e.g., herpes B infection), providing health-care facility access to nonhuman primates used as service animals is discouraged, especially if these animals might come into contact with the general public.1361, 1362 Health-care administrators should consult the Americans with Disabilities Act for guidance when developing policies about service animals in their facilities.1366, 1376
Requiring documentation for access of a service animal to an area generally accessible to the public would impose a burden on a person with a disability. When health-care workers are not certain that an animal is a service animal, they may ask the person who has the animal if it is a service animal required because of a disability; however, no certification or other documentation of service animal status can be required.1377
# Animals as Patients in Human Health-Care Facilities
The potential for direct and indirect transmission of zoonoses must be considered when rooms and equipment in human health-care facilities are used for the medical or surgical treatment or diagnosis of animals.1378 Inquiries should be made to veterinary medical professionals to determine an appropriate facility and equipment to care for an animal.
The central issue associated with providing medical or surgical care to animals in human health-care facilities is whether cross-contamination occurs between the animal patient and the human health-care workers and/or human patients. The fundamental principles of infection control and aseptic practice should differ only minimally, if at all, between veterinary medicine and human medicine. Health-careassociated infections can and have occurred in both patients and workers in veterinary medical facilities when lapses in infection-control procedures are evident.1379-1384 Further, veterinary patients can be at risk for acquiring infection from veterinary health-care workers if proper precautions are not taken. 1385 The issue of providing care to veterinary patients in human health-care facilities can be divided into the following three areas of infection-control concerns: a) whether the room/area used for animal care can be made safe for human patients, b) whether the medical/surgical instruments used on animals can be subsequently used on human patients, and c) which disinfecting or sterilizing procedures need to be done for these purposes. Studies addressing these concerns are lacking. However, with respect to disinfection or sterilization in veterinary settings, only minimal evidence suggests that zoonotic microbial pathogens are unusually resistant to inactivation by chemical or physical agents (with the exception of prions). Ample evidence supports the contrary observation (i.e., that pathogens from human-and animal sources are similar in their relative instrinsic resistance to inactivation).1386-1391 Further, no evidence suggests that zoonotic pathogens behave differently from human pathogens with respect to ventilation. Despite this knowledge, an aesthetic and sociologic perception that animal care must remain separate from human care persists. Health-care facilities, however, are increasingly faced with requests from the veterinary medical community for access to human health-care facilities for reasons that are largely economical (e.g., costs of acquiring sophisticated diagnostic technology and complex medical instruments). If hospital guidelines allow treatment of animals, alternate veterinary resources (including veterinary hospitals, clinics, and universities) should be exhausted before using human health-care settings. Additionally, the hospital's public/media relations should be notified of the situation. The goal is to develop policies and procedures to proactively and positively discuss and disclose this activity to the general public.
An infection-control risk assessment (ICRA) must be undertaken to evaluate the circumstances specific to providing care to animals in a human health-care facility. Individual hospital policies and guidelines should be reviewed before any animal treatment is considered in such facilities. Animals treated in human health-care facilities should be under the direct care and supervision of a licensed veterinarian; they also should be free of known infectious diseases, ectoparasites, and other external contaminants (e.g., soil, urine, and feces). Measures should be taken to avoid treating animals with a known or suspected zoonotic disease in a human health-care setting (e.g., lambs being treated for Q fever).
If human health-care facilities must be used for animal treatment or diagnostics, the following general infection-control actions are suggested: a) whenever possible, the use of ORs or other rooms used for invasive procedures should be avoided ; b) when all other space options are exhausted and use of the aforementioned rooms is unavoidable, the procedure should be scheduled late in the day as the last procedure for that particular area such that patients are not present in the department/unit/area; c) environmental surfaces should be thoroughly cleaned and disinfected using procedures discussed in the Environmental Services portion of this guideline after the animal is removed from the care area; d) sufficient time should be allowed for ACH to help prevent allergic reactions by human patients ; e) only disposable equipment or equipment that can be thoroughly and easily cleaned, disinfected, or sterilized should be used; f) when medical or surgical instruments, especially those invasive instruments that are difficult to clean , are used on animals, these instruments should be reserved for future use only on animals; and g) standard precautions should be followed.
# Research Animals in Health-Care Facilities
The risk of acquiring a zoonotic infection from research animals has decreased in recent years because many small laboratory animals (e.g., mice, rats, and rabbits) come from quality stock and have defined microbiologic profiles.1392 Larger animals (e.g., nonhuman primates) are still obtained frequently from the wild and may harbor pathogens transmissible to humans. Primates, in particular, benefit from vaccinations to protect their health during the research period provided the vaccination does not interfere with the study of the particular agent. Animals serving as models for human disease studies pose some risk for transmission of infection to laboratory or health-care workers from percutaneous or mucosal exposure. Exposures can occur either through a) direct contact with an infected animal or its body substances and secretions or b) indirect contact with infectious material on equipment, instruments, surfaces, or supplies.1392 Uncontained aerosols generated during laboratory procedures can also transmit infection.
Infection-control measures to prevent transmission of zoonotic infections from research animals are largely derived from the following basic laboratory safety principles: a) purchasing pathogen-free animals, b) quarantining incoming animals to detect any zoonotic pathogens, c) treating infected animals or removing them from the facility, d) vaccinating animal carriers and high-risk contacts if possible, e) using specialized containment caging or facilities, and f) using protective clothing and equipment .1392 An excellent resource for detailed discussion of these safety measures has been published.1013
The animal research unit within a health-care facility should be engineered to provide a) adequate containment of animals and pathogens; b) daily decontamination and transport of equipment and waste; c) proper ventilation and air filtration, which prevents recirculation of the air in the unit to other areas of the facility; and d) negative air pressure in the animal rooms relative to the corridors. To ensure adequate security and containment, no through traffic to other areas of the health-care facility should flow through this unit; access should be restricted to animal-care staff, researchers, environmental services, maintenance, and security personnel.
Occupational health programs for animal-care staff, researchers, and maintenance staff should take into consideration the animals' natural pathogens and research pathogens. Components of such programs include a) prophylactic vaccines, b) TB skin testing when primates are used, c) baseline serums, and d) hearing and respiratory testing. Work practices, PPE, and engineering controls specific for each of the four animal biosafety levels have been published. , The facility's occupational or employee health clinic should be aware of the appropriate post-exposure procedures involving zoonoses and have available the appropriate post-exposure biologicals and medications.
# I. Regulated Medical Waste
# Epidemiology
No epidemiologic evidence suggests that most of the solid-or liquid wastes from hospitals, other health care facilities, or clinical/research laboratories is any more infective than residential waste. Several studies have compared the microbial load and the diversity of microorganisms in residential wastes and wastes obtained from a variety of health-care settings.1399 1402 Although hospital wastes had a greater number of different bacterial species compared with residential waste, wastes from residences were more heavily contaminated. , Moreover, no epidemiologic evidence suggests that traditional waste-disposal practices of health-care facilities (whereby clinical and microbiological wastes were decontaminated on site before leaving the facility) have caused disease in either the health-care setting or the general community.1400, 1401 This statement excludes, however, sharps injuries sustained during or immediately after the delivery of patient care before the sharp is "discarded." Therefore, identifying wastes for which handling and disposal precautions are indicated is largely a matter of judgment about the relative risk of disease transmission, because no reasonable standards on which to base these determinations have been developed. Aesthetic and emotional considerations (originating during the early years of the HIV epidemic) have, however, figured into the development of treatment and disposal policies, particularly for pathology and anatomy wastes and sharps.1402 1405 Public concerns have resulted in the promulgation of federal, state, and local rules and regulations regarding medical waste management and disposal.1406 1414
# Categories of Medical Waste
Precisely defining medical waste on the basis of quantity and type of etiologic agents present is virtually impossible. The most practical approach to medical waste management is to identify wastes that represent a sufficient potential risk of causing infection during handling and disposal and for which some precautions likely are prudent.2 Health-care facility medical wastes targeted for handling and disposal precautions include microbiology laboratory waste (e.g., microbiologic cultures and stocks of microorganisms), pathology and anatomy waste, blood specimens from clinics and laboratories, blood products, and other body-fluid specimens.2 Moreover, the risk of either injury or infection from certain sharp items (e.g., needles and scalpel blades) contaminated with blood also must be considered. Although any item that has had contact with blood, exudates, or secretions may be potentially infective, treating all such waste as infective is neither practical nor necessary. Federal, state, and local guidelines and regulations specify the categories of medical waste that are subject to regulation and outline the requirements associated with treatment and disposal. The categorization of these wastes has generated the term "regulated medical waste." This term emphasizes the role of regulation in defining the actual material and as an alternative to "infectious waste," given the lack of evidence of this type of waste's infectivity. State regulations also address the degree or amount of contamination (e.g., blood-soaked gauze) that defines the discarded item as a regulated medical waste. The EPA's Manual for Infectious Waste Management identifies and categorizes other specific types of waste generated in health-care facilities with research laboratories that also require handling precautions.1406
# Management of Regulated Medical Waste in Health-Care Facilities
Medical wastes require careful disposal and containment before collection and consolidation for treatment. OSHA has dictated initial measures for discarding regulated medical-waste items. These measures are designed to protect the workers who generate medical wastes and who manage the wastes from point of generation to disposal.967 A single, leak-resistant biohazard bag is usually adequate for containment of regulated medical wastes, provided the bag is sturdy and the waste can be discarded without contaminating the bag's exterior. The contamination or puncturing of the bag requires placement into a second biohazard bag. All bags should be securely closed for disposal. Punctureresistant containers located at the point of use (e.g., sharps containers) are used as containment for discarded slides or tubes with small amounts of blood, scalpel blades, needles and syringes, and unused sterile sharps.967 To prevent needlestick injuries, needles and other contaminated sharps should not be recapped, purposefully bent, or broken by hand. CDC has published general guidelines for handling sharps.6, 1415 Health-care facilities may need additional precautions to prevent the production of aerosols during the handling of blood-contaminated items for certain rare diseases or conditions (e.g.,
# Lassa fever and Ebola virus infection).203
Transporting and storing regulated medical wastes within the health-care facility prior to terminal treatment is often necessary. Both federal and state regulations address the safe transport and storage of on-and off-site regulated medical wastes.1406 1408 Health-care facilities are instructed to dispose medical wastes regularly to avoid accumulation. Medical wastes requiring storage should be kept in labeled, leak-proof, puncture-resistant containers under conditions that minimize or prevent foul odors. The storage area should be well ventilated and be inaccessible to pests. Any facility that generates regulated medical wastes should have a regulated medical waste management plan to ensure health and environmental safety as per federal, state, and local regulations.
# Treatment of Regulated Medical Waste
Regulated medical wastes are treated or decontaminated to reduce the microbial load in or on the waste and to render the by-products safe for further handling and disposal. From a microbiologic standpoint, waste need not be rendered "sterile" because the treated waste will not be deposited in a sterile site. In addition, waste need not be subjected to the same reprocessing standards as are surgical instruments. Historically, treatment methods involved steam-sterilization (i.e., autoclaving), incineration, or interment (for anatomy wastes). Alternative treatment methods developed in recent years include chemical disinfection, grinding/shredding/disinfection methods, energy-based technologies (e.g., microwave or radiowave treatments), and disinfection/encapsulation methods.1409 State medical waste regulations specify appropriate treatment methods for each category of regulated medical waste.
Of all the categories comprising regulated medical waste, microbiologic wastes (e.g., untreated cultures, stocks, and amplified microbial populations) pose the greatest potential for infectious disease transmission, and sharps pose the greatest risk for injuries. Untreated stocks and cultures of microorganisms are subsets of the clinical laboratory or microbiologic waste stream. If the microorganism must be grown and amplified in culture to high concentration to permit work with the specimen, this item should be considered for on-site decontamination, preferably within the laboratory unit. Historically, this was accomplished effectively by either autoclaving (steam sterilization) or incineration. If steam sterilization in the health-care facility is used for waste treatment, exposure of the waste for up to 90 minutes at 250°F (121°C) in a autoclave (depending on the size of the load and type container) may be necessary to ensure an adequate decontamination cycle.14161418 After steam sterilization, the residue can be safely handled and discarded with all other nonhazardous solid waste in accordance with state solid-waste disposal regulations. On-site incineration is another treatment option for microbiologic, pathologic, and anatomic waste, provided the incinerator is engineered to burn these wastes completely and stay within EPA emissions standards.1410 Improper incineration of waste with high moisture and low energy content (e.g., pathology waste) can lead to emission problems. State medical-waste regulatory programs identify acceptable methods for inactivating amplified stocks and cultures of microorganisms, some of which may employ technology rather than steam sterilization or incineration.
Concerns have been raised about the ability of modern health-care facilities to inactivate microbiologic wastes on-site, given that many of these institutions have decommissioned their laboratory autoclaves. Current laboratory guidelines for working with infectious microorganisms at biosafety level (BSL) 3 recommend that all laboratory waste be decontaminated before disposal by an approved method, preferably within the laboratory.1013 These same guidelines recommend that all materials removed from a BSL 4 laboratory (unless they are biological materials that are to remain viable) are to be decontaminated before they leave the laboratory.1013 Recent federal regulations for laboratories that handle certain biological agents known as "select agents" (i.e., those that have the potential to pose a severe threat to public health and safety) require these agents (and those obtained from a clinical specimen intended for diagnostic, reference, or verification purposes) to be destroyed on-site before disposal.1412 Although recommendations for laboratory waste disposal from BSL 1 or 2 laboratories (e.g., most health-care clinical and diagnostic laboratories) allow for these materials to be decontaminated off-site before disposal, on-site decontamination by a known effective method is preferred to reduce the potential of exposure during the handling of infectious material.
A recent outbreak of TB among workers in a regional medical-waste treatment facility in the United States demonstrated the hazards associated with aerosolized microbiologic wastes.1419, 1420 The facility received diagnostic cultures of Mycobacterium tuberculosis from several different health-care facilities before these cultures were chemically disinfected; this facility treated this waste with a grinding/shredding process that generated aerosols from the material. 1419, 1420 Several operational deficiencies facilitated the release of aerosols and exposed workers to airborne M. tuberculosis. Among the suggested control measures was that health-care facilities perform on-site decontamination of laboratory waste containing live cultures of microorganisms before release of the waste to a waste management company.1419, 1420 This measure is supported by recommendations found in the CDC/NIH guideline for laboratory workers.1013 This outbreak demonstrates the need to avoid the use of any medical-waste treatment method or technology that can aerosolize pathogens from live cultures and stocks (especially those of airborne microorganisms) unless aerosols can be effectively contained and workers can be equipped with proper p p e .14191421 Safe laboratory practices, including those addressing waste management, have been published.1013, 1422
In an era when local, state, and federal health-care facilities and laboratories are developing bioterrorism response strategies and capabilities, the need to reinstate in-laboratory capacity to destroy cultures and stocks of microorganisms becomes a relevant issue.1423 Recent federal regulations require health-care facility laboratories to maintain the capability of destroying discarded cultures and stocks on-site if these laboratories isolate from a clinical specimen any microorganism or toxin identified as a "select agent" from a clinical specimen (Table 27).1412, 1413 As an alternative, isolated cultures of select agents can be transferred to a facility registered to accept these agents in accordance with federal regulations.1412 State medical waste regulations can, however, complicate or completely prevent this transfer if these cultures are determined to be medical waste, because most states regulate the inter-facility transfer of untreated medical wastes. Crimean-Congo hemorrhagic fever virus; Ebola viruses; Cercopithecine herpesvirus 1 (herpes B virus); Lassa fever virus; Marburg virus; monkeypox virus; South American hemorrhagic fever viruses (Junin, Machupo, Sabia, Flexal, Guanarito); tick-borne encephalitis complex (flavi) viruses (Central European tick-borne encephalitis, Far Eastern tick-borne encephalitis ); variola major virus (smallpox virus); and variola minor virus (alastrim)
# E x clu sio n s!
Vaccine strain of Junin virus (Candid. #1)
# B acteria
# Rickettsia prowazekii, R. rickettsii, Yersinia pestis
# Fungi
# Coccidioides posadasii T oxins
Abrin; conotoxins; diacetoxyscirpenol; ricin; saxitoxin; Shiga-like ribosome inactivating proteins; tetrodotoxin
# E x clu sio n s!
The following toxins (in purified form or in combinations of pure and impure forms) if the aggregate amount under the control of a principal investigator does not, at any time, exceed the amount specified: 100 mg of abrin; 100 mg of conotoxins; 1,000 mg of diacetoxyscirpenol; 100 mg of ricin; 100 mg of saxitoxin; 100 mg of Shiga-like ribosome inactivating proteins; or 100 mg of tetrodotoxin G enetic elem ents, recom binant nucleic acids, and recom binant o rg a n ism s!
- Select agent viral nucleic acids (synthetic or naturally-derived, contiguous or fragmented, in host chromosomes or in expression vectors) that can encode infectious and/or replication competent forms of any of the select agent viruses; - Nucleic acids (synthetic or naturally-derived) that encode for the functional form(s) of any of the toxins listed in this table if the nucleic acids: a) are in a vector or host chromosome; b) can be expressed in vivo or in vitro; or c) are in a vector or host chromosome and can be expressed in vivo or in vitro;
- Viruses, bacteria, fungi, and toxins listed in this table that have been genetically modified. The following toxins (in purified form or in combinations of pure and impure forms) if the aggregate amount under the control of a principal investigator does not, at any time, exceed the amount specified: 0.5 mg of botulinum neurotoxins; 100 mg of Clostridium perfringens epsilon toxin; 100 mg of Shigatoxin; 5 mg of staphylococcal enterotoxins; or 1,000 mg of T-2 toxin
# High consequence livestock pathogens and toxins/select agents (overlap agents) (42 CFR Part 73 §73.5 and USDA regulation 9 CFR Part 121) (continued)
G enetic elem ents, recom binant nucleic acids, and recom binant organism s^- Select agent viral nuclei acids (synthetic or naturally derived, contiguous or fragmented, in host chromosomes or in expression vectors) thatcan encode infectious and/or replication competent forms of any of the select agent viruses; - Nucleic acids (synthetic or naturally derived) that encode for the functional form(s) of any of the toxins listed in this table if the nucleic acids: a) are in a vector or host chromosome; b) can be expressed in vivo or in vitro; or c) are in a vector or host chromosome and can be expressed in vivo or in vitro;
- Viruses, bacteria, fungi, and toxins listed in this table that have been genetically modified - Material in this table is compiled from references 1412, 1413, and 1424. Reference 1424 also contains lists of select agents that include plant pathogens and pathogens affecting livestock. + 42 CFR 73 § §73.4 and 73.5 do not include any select agent or toxin that is in its naturally-occurring environment, provided it has not been intentionally introduced, cultivated, collected, or otherwise extracted from its natural source. These sections also do not include non-viable select agent organisms or nonfunctional toxins. This list of select agents is current as of 3 October 2003 and is subject to change pending the final adoption of 42 CFR Part 73. These table entries are listed in reference 1412 and 1413, but were not included in reference 1424.
# Discharging Blood, Fluids to Sanitary Sewers or Septic Tanks
The contents of all vessels that contain more than a few milliliters of blood remaining after laboratory procedures, suction fluids, or bulk blood can either be inactivated in accordance with state-approved treatment technologies or carefully poured down a utility sink drain or toilet.1414 State regulations may dictate the maximum volume allowable for discharge of blood/body fluids to the sanitary sewer. No evidence indicates that bloodborne diseases have been transmitted from contact with raw or treated sewage. Many bloodborne pathogens, particularly bloodborne viruses, are not stable in the environment for long periods of time;1425, 1426 therefore, the discharge of small quantities of blood and other body fluids to the sanitary sewer is considered a safe method of disposing of these waste materials.1414 The following factors increase the likelihood that bloodborne pathogens will be inactivated in the disposal process: a) dilution of the discharged materials with water; b) inactivation of pathogens resulting from exposure to cleaning chemicals, disinfectants, and other chemicals in raw sewage; and c) effectiveness of sewage treatment in inactivating any residual bloodborne pathogens that reach the treatment facility. Small amounts of blood and other body fluids should not affect the functioning of a municipal sewer system. However, large quantities of these fluids, with their high protein content, might interfere with the biological oxygen demand (BOD) of the system. Local municipal sewage treatment restrictions may dictate that an alternative method of bulk fluid disposal be selected. State regulations may dictate what quantity constitutes a small amount of blood or body fluids.
Although concerns have been raised about the discharge of blood and other body fluids to a septic tank system, no evidence suggests that septic tanks have transmitted bloodborne infections. A properly functioning septic system is adequate for inactivating bloodborne pathogens. System manufacturers' instructions specify what materials may be discharged to the septic tank without jeopardizing its proper operation.
# Medical Waste and CJD
Concerns also have been raised about the need for special handling and treatment procedures for wastes generated during the care of patients with CJD or other transmissible spongiform encephalopathies (TSEs). Prions, the agents that cause TSEs, have significant resistance to inactivation by a variety of physical, chemical, or gaseous methods.1427 No epidemiologic evidence, however, links acquisition of CJD with medical-waste disposal practices. Although handling neurologic tissue for pathologic examination and autopsy materials with care, using barrier precautions, and following specific procedures for the autopsy are prudent measures,1197 employing extraordinary measures once the materials are discarded is unnecessary. Regulated medical wastes generated during the care of the CJD patient can be managed using the same strategies as wastes generated during the care of other patients. After decontamination, these wastes may then be disposed in a sanitary landfill or discharged to the sanitary sewer, as appropriate.
# Part II. Recommendations for Environmental Infection Control in Health-Care Facilities
# A. Rationale for Recommendations
As in previous CDC guidelines, each recommendation is categorized on the basis of existing scientific data, theoretic rationale, applicability, and possible economic benefit. The recommendations are evidence-based wherever possible. However, certain recommendations are derived from empiric infection-control or engineering principles, theoretic rationale, or from experience gained from events that cannot be readily studied (e.g., floods).
The HICPAC system for categorizing recommendations has been modified to include a category for engineering standards and actions required by state or federal regulations. Guidelines and standards published by the American Institute of Architects (AIA), American Society of Heating, Refrigeration, and Air-Conditioning Engineers (ASHRAE), and the Association for the Advancement in Medical Instrumentation (AAMI) form the basis of certain recommendations. These standards reflect a consensus of expert opinions and extensive consultation with agencies of the U.S. Department of Health and Human Services. Compliance with these standards is usually voluntary. However, state and federal governments often adopt these standards as regulations. For example, the standards from AIA regarding construction and design of new or renovated health-care facilities, have been adopted by reference by >40 states. Certain recommendations have two category ratings (e.g., Categories IA and IC or Categories IB and IC), indicating the recommendation is evidence-based as well as a standard or regulation.
# B. Rating Categories
Recommendations are rated according to the following categories: Seal windows in work zones if practical; use window chutes for disposal of large pieces of debris as needed, but ensure that the negative pressure differential for the area is maintained.20, 120, 273 f.
Direct pedestrian traffic from construction zones away from patient-care areas to minimize the dispersion of dust.20, 49, 97, 109, 111, 120, 273-277 g.
Provide construction crews with 1) designated entrances, corridors, and elevators whenever practical; 2) essential services , and convenience services ; 3) protective clothing for travel to patient-care areas; and 4) a space or anteroom for changing clothing and storing equipment. , ,h.
Clean work zones and their entrances daily by 1) wet-wiping tools and tool carts before their removal from the work zone; 2) placing mats with tacky surfaces inside the entrance; and 3) covering debris and securing this covering before removing debris from the work zone. , ,i.
In patient-care areas, for major repairs that include removal of ceiling tiles and disruption of the space above the false ceiling, use plastic sheets or prefabricated plastic units to contain dust; use a negative pressure system within this enclosure to remove dust; and either pass air through an industrial grade, portable HEPA filter capable of filtration rates ranging from 300-800 ft3/min., or exhaust air directly to the outside. Position the units appropriately so that all room air passes through the filter; obtain engineering consultation to determine the appropriate placement of the unit.4
Category II 2.
Switch the portable unit off during the surgical procedure. Category II 3.
Provide fresh air as per ventilation standards for operating rooms; portable units do not meet the requirements for the number of fresh ACH. , , Category II D.
If possible, schedule infectious TB patients as the last surgical cases of the day to maximize the time available for removal of airborne contamination. Category II E.
No recommendation is offered for performing orthopedic implant operations in rooms supplied with laminar airflow.362, 364 Unresolved issue F.
Maintain backup ventilation equipment (e.g., portable units for fans or filters) for emergency provision of ventilation requirements for operating rooms, and take immediate steps to restore the fixed ventilation system function. Maintain a high level of surveillance for waterborne disease among patients after a boil water advisory is lifted. Category II If the pH of the municipal water is in the basic range (e.g., when chloramine is used as the primary drinking water disinfectant in the community), consult the facility engineer regarding the possible need to adjust the pH of the water to a more acid level before disinfection, to enhance the biocidal activity of chlorine.894 Category II C.
Clean and disinfect hydrotherapy equipment after using tub liners. Category II D.
Clean and disinfect inflatable tubs unless they are single-use equipment.
# Category II E.
No recommendation is offered regarding the use of antiseptic chemicals (e.g., chloramine-T) in the water during hydrotherapy sessions. Unresolved issue F.
Conduct a risk assessment of patients prior to their use of large hydrotherapy pools, deferring patients with draining wounds or fecal incontinence from pool use until their condition resolves. Category II G.
For
# Part III. References
Note: The bold item in parentheses indicated the citation number or the location of this reference listed in the MMWR version of this guideline.
the degree of water pollution. The term is also referred to as Biological Oxygen Demand (BOD). Biological oxygen demand (BOD): an indirect measure of the concentration of biologically degradable material present in organic wastes (pertaining to water quality). It usually reflects the amount of oxygen consumed in five days by biological processes breaking down organic waste (BOD5). Biosafety level: a combination of microbiological practices, laboratory facilities, and safety equipment determined to be sufficient to reduce or prevent occupational exposures of laboratory personnel to the microbiological agents they work with. There are four biosafety levels based on the hazards associated with the various microbiological agents. BOD5: the amount of dissolved oxygen consumed in five days by biological processes breaking down organic matter. Bonneting: a floor cleaning method for either carpeted or hard surface floors that uses a circular motion of a large fibrous disc to lift and remove soil and dust from the surface. Capped spur: a pipe leading from the water recirculating system to an outlet that has been closed off ("capped"). A capped spur cannot be flushed, and it might not be noticed unless the surrounding wall is removed. CFU/m3: colony forming units per cubic meter (of air). Chlamydospores: thick-walled, typically spherical or ovoid resting spores asexually produced by certain types of fungi from cells of the somatic hyphae. Chloramines: compounds containing nitrogen, hydrogen, and chlorine. These are formed by the reaction between hypochlorous acid (HOCl) and ammonia (NH3) and/or organic amines in water. The formation of chloramines in drinking water treatment extends the disinfecting power of chlorine. The term is also referred to as Combined Available Chlorine. Cleaning: the removal of visible soil and organic contamination from a device or surface, using either the physical action of scrubbing with a surfactant or detergent and water, or an energy-based process (e.g., ultrasonic cleaners) with appropriate chemical agents. Coagulation-flocculation: coagulation is the clumping of particles that results in the settling of impurities. It may be induced by coagulants (e.g., lime, alum, and iron salts). Flocculation in water and wastewater treatment is the agglomeration or clustering of colloidal and finely-divided suspended matter after coagulation by gentle stirring by either mechanical or hydraulic means, such that they can be separated from water or sewage. Commissioning (a room): testing a system or device to ensure that it meets the pre-use specifications as indicated by the manufacturer or predetermined standard, or air sampling in a room to establish a pre occupancy baseline standard of microbial or particulate contamination. The term is also referred to as benchmarking at 77°F (25°C). Completely packaged: functionally packaged, as for laundry. Conidia: asexual spores of fungi borne externally. Conidiophores: specialized hyphae that bear conidia in fungi. Conditioned space: that part of a building that is heated or cooled, or both, for the comfort of the occupants.
Contaminant: an unwanted airborne constituent that may reduce the acceptibility of air. Convection: the transfer of heat or other atmospheric properties within the atmosphere or in the airspace of an enclosure by the circulation of currents from one region to another, especially by such motion directed upward.
Cooling tower: a structure engineered to receive accumulated heat from ventilation systems and equipment and transfer this heat to water, which then releases the stored heat to the atmosphere through evaporative cooling.
Critical item (medical instrument): a medical instrument or device that contacts normally sterile areas of the body or enters the vascular system. There is a high risk of infection from such devices if they are microbiologically contaminated prior to use. These devices must be sterilized before use. Dead legs: areas in the water system where water stagnates. A dead leg is a pipe or spur, leading from the water recirculating system to an outlet that is used infrequently, resulting in inadequate flow of water from the recirculating system to the outlet. This inadequate flow reduces the perfusion of heat or chlorine into this part of the water distribution system, thereby adversely affecting the disinfection of the water system in that area. Deionization: removal of ions from water by exchange with other ions associated with fixed charges on a resin bed. Cations are usually removed and H+ ions are exchanged; OH" ions are exchanged for anions. Detritis: particulate matter produced by or remaining after the wearing away or disintegration of a substance or tissue. Dew point: the temperature at which a gas or vapor condenses to form a liquid; the point at which moisture begins to condense out of the air. At dew point, air is cooled to the point where it is at 100% relative humidity or saturation. Dialysate: the aqueous electrolyte solution, usually containing dextrose, used to make a concentration gradient between the solution and blood in the hemodialyzer (dialyzer). Dialyzer: a device that consists of two compartments (blood and dialysate) separated by a semipermeable membrane. A dialyzer is usually referred to as an artificial kidney. Diffuser: the grille plate that disperses the air stream coming into the conditioned air space. Direct transmission: involves direct body surface-to-body surface contact and physical transfer of microorganisms between a susceptible host and an infected/colonized person, or exposure to cloud of infectious particles within 3 feet of the source; the aerosolized particles are >5 pm in size. Disability: as defined by the Americans with Disabilities Act, a disability is any physical or mental impairment that substantially limits one or more major life activities, including but not limited to walking, talking, seeing, breathing, hearing, or caring for oneself. Disinfection: a generally less lethal process of microbial inactivation (compared to sterilization) that eliminates virtually all recognized pathogenic microorganisms but not necessarily all microbial forms (e.g., bacterial spores). Drain pans: pans that collect water within the HVAC system and remove it from the system. Condensation results when air and steam come together. Drift: circulating water lost from the cooling tower in the form as liquid droplets entrained in the exhaust air stream (i.e., exhaust aerosols from a cooling tower). Drift eliminators: an assembly of baffles or labyrinth passages through which the air passes prior to its exit from the cooling tower. The purpose of a drift eliminator is to remove entrained water droplets from the exhaust air. Droplets: particles of moisture, such as are generated when a person coughs or sneezes, or when water is converted to a fine mist by a device such as an aerator or shower head. These particles may contain infectious microorganisms. Intermediate in size between drops and droplet nuclei, these particles tend to quickly settle out from the air so that any risk of disease transmission is generally limited to persons in close proximity to the droplet source. Droplet nuclei: sufficiently small particles (1-5 pm in diameter) that can remain airborne indefinitely and cause infection when a susceptible person is exposed at or beyond 3 feet of the source of these particles.
Dual duct system: an HVAC system that consists of parallel ducts that produce a cold air stream in one and a hot air stream in the other. Dust: an air suspension of particles (aerosol) of any solid material, usually with particle sizes <100 pm in diameter. Dust-spot test: a procedure that uses atmospheric air or a defined dust to measure a filter's ability to remove particles. A photometer is used to measure air samples on either side of the filter, and the difference is expressed as a percentage of particles removed. Effective leakage area: the area through which air can enter or leave the room. This does not include supply, return, or exhaust ducts. The smaller the effective leakage area, the better isolated the room. Endotoxin: the lipopolysaccharides of gram-negative bacteria, the toxic character of which resides in the lipid portion. Endotoxins generally produce pyrogenic reactions in persons exposed to these bacterial components. Enveloped virus: a virus whose outer surface is derived from a membrane of the host cell (either nuclear or the cell's outer membrane) during the budding phase of the maturation process. This membrane-derived material contains lipid, a component that makes these viruses sensitive to the action of chemical germicides. Evaporative condenser: a wet-type, heat-rejection unit that produces large volumes of aerosols during the process of removing heat from conditioned space air. Exhaust air: air removed from a space and not reused therein. Exposure: the condition of being subjected to something (e.g., infectious agents) that could have a harmful effect. Fastidious: having complex nutritional requirements for growth, as in microorganisms.
Fill: that portion of a cooling tower which makes up its primary heat transfer surface. Fill is alternatively known as "packing." Finished water: treated, or potable water. Fixed room-air HEPA recirculation systems: nonmobile devices or systems that remove airborne contaminants by recirculating air through a HEPA filter. These may be built into the room and permanently ducted or may be mounted to the wall or ceiling within the room. In either situation, they are fixed in place and are not easily movable.
Fomite: an inanimate object that may be contaminated with microorganisms and serves in their transmission.
Free and available chlorine: the term applied to the three forms of chlorine that may be found in solution (i.e., chlorine , hypochlorite , and hypochlorous acid ). Germicide: a chemical that destroys microorganisms. Germicides may be used to inactivate microorganisms in or on living tissue (antiseptics) or on environmental surfaces (disinfectants). Health-care-associated: an outcome, usually an infection, that occurs in any health-care facility as a result of medical care. The term "health-care-associated" replaces "nosocomial," the latter term being limited to adverse infectious outcomes occurring only in hospitals. Hemodiafiltration: a form of renal replacement therapy in which waste solutes in the patient's blood are removed by both diffusion and convection through a high-flux membrane. Hemodialysis: a treatment for renal replacement therapy in which waste solutes in the patient's blood are removed by diffusion and/or convection through the semipermeable membrane of an artificial kidney or dialyzer. Hemofiltration: cleansing of waste products or other toxins from the blood by convection across a semipermeable, high-flux membrane where fluid balance is maintained by infusion of sterile, pyrogen free substitution fluid pre-or post-hemodialyzer. HEPA filter: High Efficiency Particulate Air filters capable of removing 99.97% of particles 0.3 pm in diameter and may assist in controlling the transmission of airborne disease agents. These filters may be used in ventilation systems to remove particles from the air or in personal respirators to filter air before it is inhaled by the person wearing the respirator. The use of HEPA filters in ventilation systems requires expertise in installation and maintenance. To test this type of filter, 0.3 pm particles of dioctylphthalate (DOP) are drawn through the filter. Efficiency is calculated by comparing the downstream and upstream particle counts. The optimal HEPA filter allows only three particles to pass through for every 10,000 particles that are fed to the filter. Heterotrophic (heterotroph): that which requires some nutrient components from exogenous sources. Heterotrophic bacteria cannot synthesize all of their metabolites and therefore require certain nutrients from other sources. High-efficiency filter: a filter with a particle-removal efficiency of 90%-95%. High flux: a type of dialyzer or hemodialysis treatment in which large molecules (>8,000 daltons ) are removed from blood. High-level disinfection: a disinfection process that inactivates vegetative bacteria, mycobacteria, fungi, and viruses, but not necessarily high numbers of bacterial spores.
RODAC: Replicate Organism Direct Agar Contact. This term refers to a nutrient agar plate whose convex agar surface is directly pressed onto an environmental surface for the purpose of microbiologic sampling of that surface. Room-air HEPA recirculation systems and units: devices (either fixed or portable) that remove airborne contaminants by recirculating air through a HEPA filter. Routine sampling: environmental sampling conducted without a specific, intended purpose and with no action plan dependent on the results obtained.
Sanitizer: an agent that reduces microbial contamination to safe levels as judged by public health standards or requirements. Saprophytic: a naturally-occurring microbial contaminant. Sedimentation: the act or process of depositing sediment from suspension in water. The term also refers to the process whereby solids settle out of wastewater by gravity during treatment. Semicritical devices: medical devices that come into contact with mucous membranes or non-intact skin.
Service animal: any animal individually trained to do work or perform tasks for the benefit of a person with a disability. Shedding: the generation and dispersion of particles and spores by sources within the patient area, through activities such as patient movement and airflow over surfaces. Single-pass ventilation: ventilation in which 100% of the air supplied to an area is exhausted to the outside. Small, non-enveloped viruses: viruses whose particle diameter is <50 nm and whose outer surface is the protein of the particle itself and not that of host cell membrane components. Examples of small, non-enveloped viruses are polioviruses and hepatitis A virus. Spaulding Classification: the categorization of inanimate medical device surfaces in the medical environment as proposed in 1972 by Dr. Earle Spaulding. Surfaces are divided into three general categories, based on the theoretical risk of infection if the surfaces are contaminated at time of use. The categories are "critical," "semicritical," and "noncritical." Specific humidity: the mass of water vapor per unit mass of moist air. It is expressed as grains of water per pound of dry air, or pounds of water per pound of dry air. The specific humidity changes as moisture is added or removed. However, temperature changes do not change the specific humidity unless the air is cooled below the dew point. Splatter: visible drops of liquid or body fluid that are expelled forcibly into the air and settle out quickly, as distinguished from particles of an aerosol which remain airborne indefinitely. Steady state: the usual state of an area. Sterilization: the use of a physical or chemical procedure to destroy all microbial life, including large numbers of highly-resistant bacterial endospores. Stop valve: a valve that regulates the flow of fluid through a pipe. The term may also refer to a faucet. Substitution fluid: fluid that is used for fluid management of patients receiving hemodiafiltration. This fluid can be prepared on-line at the machine through a series of ultrafilters or with the use of sterile peritoneal dialysis fluid. Supply air: air that is delivered to the conditioned space and used for ventilation, heating, cooling, humidification, or dehumidification. Tensile strength: the resistance of a material to a force tending to tear it apart, measured as the maximum tension the material can withstand without tearing. Therapy animal: an animal (usually a personal pet) that, with their owners or handlers, provide supervised, goal-directed intervention to clients in hospitals, nursing homes, special-population schools, and other treatment sites. Thermophilic: capable of growing in environments warmer than body temperature. Thermotolerant: capable of withstanding high temperature conditions. TLV®: an exposure level under which most people can work consistently for 8 hours a day, day after day, without adverse effects. The term is used by the ACGIH to designate degree of exposure to contaminants. TLV® can be expressed as approximate milligrams of particulate per cubic meter of air (mg/m3). TLVs® are listed as either an 8-hour TWA (time weighted average) or a 15-minute STEL (short term exposure limit). TLV-TWA: Threshold Limit Value-Time Weighted Average. The term refers to the time-weighted average concentration for a normal 8-hour workday and a 40-hour workweek to which nearly all workers may be exposed repeatedly, day after day, without adverse effects. The TLV-TWA for "particulates (insoluble) not otherwise classified" (PNOC) -(sometimes referred to as nuisance dust)are those particulates containing no asbestos and <1% crystalline silica. A TLV-TWA of 10 mg/m3 for inhalable particulates and a TLV-TWA of 3 mg/m3 for respirable particulates (particulates <5 pm in aerodynamic diameter) have been established. Total suspended particulate matter: the mass of particles suspended in a unit of volume of air when collected by a high-volume air sampler.
Transient: a change in the condition of the steady state that takes a very short time compared with the steady state. Opening a door, and shaking bed linens are examples of transient activities.
TWA: average exposure for an individual over a given working period, as determined by sampling at given times during the period. TWA is usually presented as the average concentration over an 8-hour workday for a 40-hour workweek. Ultraclean air: air in laminar flow ventilation that has also passed through a bank of HEPA filters.
Ultrafilter: a membrane filter with a pore size in the range of 0.001-0.05 pm, the performance of which is usually rated in terms of a nominal molecular weight cut-off (defined as the smallest molecular weight species for which the filter membrance has more than 90% rejection).
Ultrafiltered dialysate: the process by which dialysate is passed through a filter having a molecular weight cut-off of approximately 1 kilodalton for the purpose of removing bacteria and endotoxin from the bath. Ultraviolet germicidal irradiation (UVGI): the use of ultraviolet radiation to kill or inactivate microorganisms. Ultraviolet germicidal irradiation lamps: lamps that kill or inactivate microorganisms by emitting ultraviolet germicidal radiation, predominantly at a wavelength of 254 nm. UVGI lamps can be used in ceiling or wall fixtures or within air ducts of ventilation systems.
Vapor pressure: the pressure exerted by free molecules at the surface of a solid or liquid. Vapor pressure is a function of temperature, increasing as the temperature rises.
Vegetative bacteria: bacteria that are actively growing and metabolizing, as opposed to a bacterial state of quiescence that is achieved when certain bacteria (gram-positive bacilli) convert to spores when the environment can no longer support active growth. Vehicle: any object, person, surface, fomite, or media that may carry and transfer infectious microorganisms from one site to another. Ventilation: the process of supplying and removing air by natural or mechanical means to and from any space. Such air may or may not be conditioned. Ventilation air: that portion of the supply air consisting of outdoor air plus any recirculated air that has been treated for the purpose of maintaining acceptable indoor air quality. Ventilation, dilution: an engineering control technique to dilute and remove airborne contaminants by the flow of air into and out of an area. Air that contains droplet nuclei is removed and replaced by contaminant-free air. If the flow is sufficient, droplet nuclei become dispersed, and their concentration in the air is diminished. Ventilation, local exhaust: ventilation used to capture and removed airborne contaminants by enclosing the contaminant source (the patient) or by placing an exhaust hood close to the contaminant source. v/v: volume to volume. This term is an expression of concentration of a percentage solution when the principle component is added as a liquid to the diluent. w/v: weight to volume. This term is an expression of concentration of a percentage solution when the principle component is added as a solid to the diluent.
Weight-arrestance: a measure of filter efficiency, used primarily when describing the performance of low-and medium-efficiency filters. The measurement of weight-arrestance is performed by feeding a standardized synthetic dust to the filter and weighing the fraction of the dust removed. T Values apply to an empty room with no aerosol-generating source. With a person present and generating aerosol, this table would not apply. Other equations are available that include a constant generating source. However, certain diseases (e.g., infectious tuberculosis) are not likely to be aerosolized at a constant rate. The times given assume perfect mixing of the air within the space (i.e., mixing factor = 1). However, perfect mixing usually does not occur. Removal times will be longer in rooms or areas with imperfect mixing or air stagnation.213 Caution should be exercised in using this table in such situations. For booths or other local ventilation enclosures, manufacturers' instructions should be consulted.
# Appendix B. Air 1. Airborne Contaminant Removal
# Air Sampling for Aerosols Containing Legionellae
Air sampling is an insensitive means of detecting Legionella pneumophila, and is of limited practical value in environmental sampling for this pathogen. In certain instances, however, it can be used to a) demonstrate the presence of legionellae in aerosol droplets associated with suspected bacterial reservoirs; b) define the role of certain devices in disease transmission; and c) quantitate and determine the size of the droplets containing legionellae.1436 Stringent controls and calibration are necessary when sampling is used to determine particle size and numbers of viable bacteria.1437 Samplers should be placed in locations where human exposure to aerosols is anticipated, and investigators should wear a NIOSH-approved respirator (e.g., N95 respirator) if sampling involves exposure to potentially infectious aerosols.
Methods used to sample air for legionellae include impingement in liquid, impaction on solid medium, and sedimentation using settle plates.1436 The Chemical Corps.-type all-glass impingers (AGI) with the stem 30 mm from the bottom of the flask have been used successfully to sample for legionellae.1436 Because of the velocity at which air samples are collected, clumps tend to become fragmented, leading to a more accurate count of bacteria present in the air. The disadvantages of this method are a) the velocity of collection tends to destroy some vegetative cells; b) the method does not differentiate particle sizes; and c) AGIs are easily broken in the field. Yeast extract broth (0.25%) is the recommended liquid medium for AGI sampling of legionellae;1437 standard methods for water samples can be used to culture these samples.
Andersen samplers are viable particle samplers in which particles pass through jet orifices of decreasing size in cascade fashion until they impact on an agar surface.1218 The agar plates are then removed and incubated. The stage distribution of the legionellae should indicate the extent to which the bacteria would have penetrated the respiratory system. The advantages of this sampling method are a) the equipment is more durable during use; b) the sampler can cetermine the number and size of droplets containing legionellae; c) the agar plates can be placed directly in an incubator with no further manipulations; and d) both selective and nonselective BCYE agar can be used. If the samples must be shipped to a laboratory, they should be packed and shipped without refrigeration as soon as possible.
# Calculation of Air Sampling Results
Assuming that each colony on the agar plate is the growth from a single bacteria-carrying particle, the contamination of the air being sampled is determined from the number of colonies counted. The airborne microorganisms may be reported in terms of the number per cubic foot of air sampled. The following formulas can be applied to convert colony counts to organisms per cubic foot of air sampled.1218
For solid agar impactor samplers: C / (R x P) = N where N = number of organisms collected per cubic foot of air sampled C = total plate count R = airflow rate in cubic feet per minute P = duration of sampling period in minutes For liquid impingers: (C x V) / (Q x P x R) = N where C = total number of colonies from all aliquots plated V = final volume in mL of collecting media Q = total number of mL plated P, R, and N are defined as above
# Ventilation Specifications for Health-Care Facilities
The 1. The ventilation rates in this table cover ventilation for comfort, as well as for asepsis and odor control in areas of acute care hospitals that directly affect patient care and are determined based on health-care facilities being predominantly "No Smoking" facilities. Where smoking may be allowed, ventilation rates will need adjustment. Areas where specific ventilation rates are not given in the table shall be ventilated in accordance Specialized patient care areas, including organ transplant units, burn units, specialty procedure rooms, etc., shall have additional ventilation provisions for air quality control as may be appropriate. OSHA standards and/or NIOSH criteria require special ventilation requirements for employee health and safety within health-care facilities.
2. Design of the ventilation system shall provide air movement which is generally from clean to less clean areas. If any form of variable air volume or load shedding system is used for energy conservation, it must not compromise the corridor-to-room pressure balancing relationships or the minimum air changes required by the table.
3. To satisfy exhaust needs, replacement air from the outside is necessary. Table B2 does not attempt to describe specific amounts of outside air to be supplied to individual spaces except for certain areas such as those listed. Distribution of the outside air, added to the system to balance required exhaust, shall be as required by good engineering practice. Minimum outside air quantities shall remain constant while the system is in operation.
4. Number of air changes may be reduced when the room is unoccupied if provisions are made to ensure that the number of air changes indicated is reestablished any time the space is being utilized. Adjustments shall include provisions so that the direction of air movement shall remain the same when the number of air changes is reduced. Areas not indicated as having continuous directional control may have ventilation systems shut down when space is unoccupied and ventilation is not otherwise needed, if the maximum infiltration or exfiltration permitted in Note 2 is not exceeded and if adjacent pressure balancing relationships are not compromised. Air quantity calculations must account for filter loading such that the indicated air change rates are provided up until the time of filter change-out.
5. Air change requirements indicated are minimum values. Higher values should be used when required to maintain indicated room conditions (temperature and jumidity), based on the cooling load of the space (lights, equipment, people, exterior walls and windows, etc.).
provided. Rooms with reversible airflow provisions for the purpose of switching between protective environment and airborne infection isolation functions are not acceptable.
18. The infectious disease isolation room described in these guidelines is to be used for isolating the airborne spread of infectious diseases, such as measles, varicella, or tuberculosis. The design of airborne infection isolation (AII) rooms should include the provision for normal patient care during periods not requiring isolation precautions. Supplemental recirculating devices may be used in the patient room to increase the equivalent room air exchanges; however, such recirculating devices do not provide the outside air requirements. Air may be recirculated within individual isolation rooms if HEPA filters are used. Rooms with reversible airflow provisions for the purpose of switching between protective environment and AII functions are not acceptable. 20. Food preparation centers shall have ventilation systems whose air supply mechanisms are interfaced appropriately with exhaust hood controls or relief vents so that exfiltration or infiltration to or from exit corridors does not compromise the exit corridor restrictions of NFPA 90A, the pressure requirements of NFPA 96, or the maximum defined in the table . The number of air changes may be reduced or varied to any extent required for odor control when the space is not in use. See Section 7.31.D1.p in the AIA guideline (reference 120).
# A ppendix I:
A7. Recirculating devices with HEPA filters may have potential uses in existing facilities as interim, supplemental environmental controls to meet requirements for the control of airborne infectious agents. Limitations in design must be recognized. The design of either portable or fixed systems should prevent stagnation and short circuiting of airflow. The supply and exhaust locations should direct clean air to areas where health-care workers are likely to work, across the infectious source, and then to the exhaust, so that the health care worker is not in position between the infectious source and the exhaust location. The design of such systems should also allow for easy access for scheduled preventative maintenance and cleaning.
A11. The verification of airflow direction can include a simple visual method such as smoke trail, ball-in-tube, or flutterstrip. These devices will require a minimum differential air pressure to indicate airflow direction. 1. The ventilation rates in this table cover ventilation for comfort, as well as for asepsis and odor control in areas of nursing facilities that directly affect resident care and are determined based on nursing facilities being predominantly "No Smoking" facilities. Where smoking may be allowed, ventilation rates will need adjustment. Areas where specific ventilation rates are not given in the table shall be ventilated in accordance with ASHRAE Standard 62, 2. Design of the ventilation system shall, insofar as possible, provide that air movement is from clean to less clean areas. However, continuous compliance may be impractical with full utilization of some forms of variable air volume and load shedding systems that may be used for energy conservation. Areas that do require positive and continuous control are noted with "Out" or "In" to indicate the required direction of air movement in relation to the space named. Rate of air movement may, of course, be varied as needed within the limits required for positive control. Where indication of air movement direction is enclosed in parentheses, continuous directional control is required only when the specialized equipment or device is in use or where room use may otherwise compromise the intent of movement from clean to less clean. Air movement for rooms with dashes and nonpatient areas may vary as necessary to satisfy the requirements of those spaces. Additional adjustments may be needed when space is unused or unoccupied and air systems are deenergized or reduced.
3. To satisfy exhaust needs, replacement air from outside is necessary. Table B.3 does not attempt to describe specific amounts of outside air to be supplied to individual spaces except for certain areas such as those listed. Distribution of the outside air, added to the system to balance required exhaust, shall be as required by good engineering practice.
4. Number of air changes may be reduced when the room is unoccupied if provisions are made to ensure that the number of air changes indicated is reestablished any time the space is being utilized. Adjustments shall include provisions so that the direction of air movement shall remain the same when the number of air changes is reduced. Areas not indicated as having continuous directional control may have ventilation systems shut down when space is unoccupied and ventilation is not otherwise needed.
5. Air from areas with contamination and/or odor problems shall be exhausted to the outside and not recirculated to other areas. Note that individual circumstances may require special consideration for air exhaust to outside. 6 7 8 9 1 0 All areas for patient care, treatment, and/or diagnosis, and those areas providing direct service or clean supplies such as sterile and clean processing, etc.
# Appendix C. Water 1. Biofilms
Microorganisms have a tendency to associate with and stick to surfaces. These adherent organisms can initiate and develop biofilms, which are comprised of cells embedded in a matrix of extracellularly produced polymers and associated abiotic particles.1438 It is inevitable that biofilms will form in most water systems. In the health-care facility environment, biofilms may be found in the potable water supply piping, hot water tanks, air conditioning cooling towers, or in sinks, sink traps, aerators, or shower heads. Biofilms, especially in water systems, are not present as a continuous slime or film, but are more often scanty and heterogeneous in nature.1439 Biofilms may form under stagnant as well as flowing conditions, so storage tanks, in addition to water system piping, may be vulnerable to the development of biofilm, especially if water temperatures are low enough to allow the growth of thermophilic bacteria (e.g., Legionella spp.). Favorable conditions for biofilm formation are present if these structures and equipment are not cleaned for extended periods of time.1440
Algae, protozoa, and fungi may be present in biofilms, but the predominant microorganisms of water system biofilms are gram-negative bacteria. Although most of these organisms will not normally pose a problem for healthy individuals, certain biofilm bacteria (e.g., Pseudomonas aeruginosa, Klebsiella spp., Pantoea agglomerans, and Enterobacter cloacae) all may be agents for opportunistic infections for immunocompromised individuals.1441, 1442 These biofilm organisms may easily contaminate indwelling medical devices or intravenous (IV) fluids, and they could be transferred on the hands of health-care workers.14411444 Biofilms may potentially provide an environment for the survival of pathogenic organisms, such as Legionella pneumophila and E. coli O157:H7. Although the association of biofilms and medical devices provides a plausible explanation for a variety of health-care-associated infections, it is not clear how the presence of biofilms in the water system may influence the rates of health-careassociated waterborne infection.
Organisms within biofilms behave quite differently than their planktonic (i.e., free floating) counterparts. Research has shown that biofilm-associated organisms are more resistant to antibiotics and disinfectants than are planktonic organisms, either because the cells are protected by the polymer matrix, or because they are physiologically different.1445-1450 Nevertheless, municipal water utilities attempt to maintain a chlorine residual in the distribution system to discourage microbiological growth.
Though chlorine in its various forms is a proven disinfectant, it has been shown to be less effective against biofilm bacteria.1448 Higher levels of chlorine for longer contact times are necessary to eliminate biofilms.
Routine sampling of health-care facility water systems for biofilms is not warranted. If an epidemiologic investigation points to the water supply system as a possible source of infection, then water sampling for biofilm organisms should be considered so that prevention and control strategies can be developed. An established biofilm is is difficult to remove totally in existing piping. Strategies to remediate biofilms in a water system would include flushing the system piping, hot water tank, dead legs, and those areas of the facility's water system subject to low or intermittent flow. The benefits of this treatment would include a) elimination of corrosion deposits and sludge from the bottom of hot water tanks, b) removal of biofilms from shower heads and sink aerators, and c) circulation of fresh water containing elevated chlorine residuals into the health-care facility water system.
The general strategy for evaluating water system biofilm depends on a comparision of the bacteriological quality of the incoming municipal water and that of water sampled from within facility's distribution system. Heterotrophic plate counts and coliform counts, both of which are routinely run by the municipal water utility, will at least provide in indication of the potential for biofilm formation. Heterotrophic plate count levels in potable water should be 500 CFU/mL would indicate a general decrease in water quality.
A direct correlation between heterotrophic plate count and biofilm levels has been demonstrated.1450 Therefore, an increase in heterotrophic plate count would suggest a greater rate and extent of biofilm formation in a health-care facility water system. The water supplied to the facility should also contain <1 coliform bacteria/100 mL. Coliform bacteria are organisms whose presence in the distribution system could indicate fecal contamination. It has been shown that coliform bacteria can colonize biofilms within drinking water systems. Intermittant contamination of a water system with these organisms could lead to colonization of the system.
Water samples can be collected from throughout the health-care facility system, including both hot and cold water sources; samples should be cultured by standard methods.945 If heterotrophic plate counts in samples from the facility water system are higher than those from samples collected at the point of water entry to the building, it can be concluded that the facility water quality has diminished. If biofilms are detected in the facility water system and determined by an epidemiologic and environmental investigation to be a reservoir for health-care-associated pathogens, the municipal water supplier could be contacted with a request to provide higher chlorine residuals in the distribution system, or the health-care facility could consider installing a supplemental chlorination system.
Sample collection sites for biofilm in health-care facilities include a) hot water tanks; b) shower heads; and c) faucet aerators, especially in immunocompromised patient-care areas. Swabs should be placed into tubes containing phosphate buffered water, pH 7.2 or phosphate buffered saline, shipped to the laboratory under refrigeration and processed within 24 hrs. of collection. Samples are suspended by vortexing with sterile glass beads and plated onto a nonselective medium (e.g., Plate Count Agar or R2A medium) and selective media (e.g., media for Legionella spp. isolation) after serial dilution. If the plate counts are elevated above levels in the water (i.e. comparing the plate count per square centimeter of swabbed surface to the plate count per milliliter of water), then biofilm formation can be suspected.
In the case of an outbreak, it would be advisable to isolate organisms from these plates to determine whether the suspect organisms are present in the biofilm or water samples and compare them to the organisms isolated from patient specimens.
# Water and Dialysate Sampling Strategies in Dialysis
In order to detect the low, total viable heterotrophic plate counts outlined by the current AAMI standards for water and dialysate in dialysis settings, it is necessary to use standard quantitative culture techniques with appropriate sensitivity levels.792, 832, 833 The membrane filter technique is particularly suited for this application because it permits large volumes of water to be assayed.792, 834 Since the membrane filter technique may not be readily available in clinical laboratories, the spread plate assay can be used as an alternative.834 If the spread plate assay is used, however, the standard prohibits the use of a calibrated loop when applying sample to the plate.792 The prohibition is based on the low sensitivity of the calibrated loop. A standard calibrated loop transfers 0.001 mL of sample to the culture medium, so that the minimum sensitivity of the assay is 1,000 CFU/mL. This level of sensitivity is unacceptable when the maximum allowable limit for microorganisms is 200 CFU/mL. Therefore, when the spread plate method is used, a pipette must be used to place 0.1-0.5 mL of water on the culture medium.
The current AAMI standard specifically prohibits the use of nutrient-rich media (e.g., blood agar, and chocolate agar) in dialysis water and dialysate assays because these culture media are too rich for growth of the naturally occurring organisms found in water.792 Debate continues within AAMI, however, as to the most appropriate culture medium and incubation conditions to be used. The original clinical observations on which the microbiological requirements of this standard were based used Standard Methods Agar (SMA), a medium containing relatively few nutrients.666 The use of tryptic soy agar (TSA), a general purpose medium for isolating and cultivating microorganisms was recommended in later versions of the standard because it was thought to be more appropriate for culturing bicarbonatecontaining dialysate.788, 789, 835 Moreover, culturing systems based on TSA are readily available from commercial sources. Several studies, however, have shown that the use of nutrient-poor media, such as R2A, results in an increased recovery of bacteria from water.1451, 1452 The original standard also specified incubation for 48 hours at 95°F-98.6°F (35°C-37°C) before enumeration of bacterial colonies.
Extending the culturing time up to 168 hours, or 7 days and using incubation temperatures of 73.4°F-82.4°F (23°C-28°C) have also been shown to increase the recovery of bacteria.1451, 1452 Other investigators, however, have not found such clear cut differences between culturing techniques.835, 1453 After considerable discussion, the AAMI Committee has not reached a consensus regarding changes in the assay technique, and the use of TSA or its equivalent for 48 hours at 95°F-98.6°F (35°C-37°C) remains the recommended method. It should be recognized, however, that these culturing conditions may underestimate the bacterial burden in the water and fail to identify the presence of some organisms. Specifically, the recommended method may not detect the presence of various NTM that have been associated with several outbreaks of infection in dialysis units.31, 32 In these instances, however, the high numbers of mycobacteria in the water were related to the total heterotrophic plate counts, each of which was significantly greater than that allowable by the AAMI standard. Additionally, the recommended method will not detect fungi and yeast, which have been shown to contaminate water used for hemodialysis applications.1454 Biofilm on the surface of the pipes may hide viable bacterial colonies, even though no viable colonies are detected in the water using sensitive culturing techniques.1455 Many disinfection processes remove biofilm poorly, and a rapid increase in the level of bacteria in the water following disinfection may indicate significant biofilm formation. Therefore, although the results of microbiological surveillance obtained using the test methods outlined above may be useful in guiding disinfection schedules and in demonstrating compliance with AAMI standards, they should not be taken as an indication of the absolute microbiological purity of the water.792
Endotoxin can be tested by one of two types of assays a) a kinetic test method or b) a gel-clot assay. Endotoxin units are assayed by the Limulus Amebocyte Lysate (LAL) method. Because endotoxins differ in their activity on a mass basis, their activity is referred to a standard Escherichia coli endotoxin. The current standard (EC-6) is prepared from E. coli O113:H10. The relationship between mass of endotoxin and its activity varies with both the lot of LAL and the lot of control standard endotoxin used. Since standards for endotoxin were harmonized in 1983 with the introduction of EC-5, the relationship between mass and activity of endotoxin has been approximately 5-10 EU/ng. Studies to harmonize standards have led to the measurement of endotoxin units (EU) where 5 EU is equivalent to 1 ng E. coli O55:B5 endotoxin.1456
In summary, water used to prepare dialysate and to reprocess hemodialyzers should not contain a total microbial count >200 CFU/mL as determined by assay on TSA agar for 48 hrs. at 96.8°F (36°C), and 2,000 CFU/mL.31, 32, 668, 789, 792
# Water Sampling Strategies and Culture Techniques for Detecting Legionellae
Legionella spp. are ubiquitous and can be isolated from 20%-40% of freshwater environments, including man-made water systems.1457, 1458 In health-care facilities, where legionellae in potable water rarely result in disease among immunocompromised patients, courses of remedial action are unclear.
Scheduled microbiologic monitoring for legionellae remains controversial because the presence of legionellae is not necessarily evidence of a potential for causing disease.1459 CDC recommends aggressive disinfection measures for cleaning and maintaining devices known to transmit legionellae, but does not recommend regularly scheduled microbiologic assays for the bacteria.396 However, scheduled monitoring of potable water within a hospital might be considered in certain settings where persons are highly susceptible to illness and mortality from Legionella infection (e.g., hematopoietic stem cell transplantation units and solid organ transplant units).9 Also, after an outbreak of legionellosis, health officials agree monitoring is necessary to identify the source and to evaluate the efficacy of biocides or other prevention measures.
Examination of water samples is the most efficient microbiologic method for identifying sources of legionellae and is an integral part of an epidemiologic investigation into health-care-associated Legionnaires disease. Because of the diversity of plumbing and HVAC systems in health-care facilities, the number and types of sites to be tested must be determined before collection of water samples. One environmental sampling protocol that addresses sampling site selection in hospitals might serve as a prototype for sampling in other institutions.1209 Any water source that might be aerosolized should be considered a potential source for transmission of legionellae. The bacteria are rarely found in municipal water supplies and tend to colonize plumbing systems and point-of-use devices. To colonize, legionellae usually require a temperature range of 77°F-108°F (25°C-42.2°C) and are most commonly located in hot water systems.1460 Legionellae do not survive drying. Therefore, air-conditioning equipment condensate, which frequently evaporates, is not a likely source.1461
Water samples and swabs from point-of-use devices or system surfaces should be collected when sampling for legionellae (Box C.1).1437 Swabs of system surfaces allow sampling of biofilms, which frequently contain legionellae. When culturing faucet aerators and shower heads, swabs of surface areas should be collected first; water samples are collected after aerators or shower heads are removed from their pipes. Collection and culture techniques are outlined (Box C.2). Swabs can be streaked directly onto buffered charcoal yeast extract agar (BCYE) plates if the pates are available at the collection site.
If the swabs and water samples must be transported back to a laboratory for processing, immersing individual swabs in sample water minimizes drying during transit. Place swabs and water samples in insulated coolers to protect specimens from temperature extremes. incoming water main, water softener unit, holding tanks, cisterns, water heater tanks (at the inflows and outflows)
- P otable w ater outlets, especially th ose in o r near patient room s faucets or taps, showers
- C ooling tow ers and evaporative condensers makeup water (e.g., added to replace water lost because of evaporation, drift, or leakage), basin (i.e., area under the tower for collection of cooled water), sump (i.e., section of basin from which cooled water returns to heat source), heat sources (e.g., chillers)
- H um idfiers (e.g., nebullizers)
bubblers for oxygen, water used for respiratory therapy equipment
# Maintenance Procedures Used to Decrease Survival and Multiplications of L e g io n e lla spp. in Potable-Water Distribution Systems
Wherever allowable by state code, provide water at >124°F (>51°C) at all points in the heated water system, including the taps. This requires that water in calorifiers (e.g., water heaters) be maintained at >140°F (>60°C). In the United Kingdom, where maintenance of water temperatures at >122°F (>50°C) in hospitals has been mandated, installation of blending or mixing valves at or near taps to reduce the water temperature to <109.4°F (<63°C) has been recommended in certain settings to reduce the risk for scald injury to patients, visitors, and health care workers.726 However, Legionella spp. can multiply even in short segments of pipe containing water at this temperature. Increasing the flow rate from the hot-water-circulation system may help lessen the likelihood of water stagnation and cooling.711, 1465 Insulation of plumbing to ensure delivery of cold (<68°F ) water to water heaters (and to coldwater outlets) may diminish the opportunity for bacterial multiplication.456 Both dead legs and capped spurs within the plumbing system provide areas of stagnation and cooling to <122°F (<50°C) regardless of the circulating water temperature; these segments may need to be removed to prevent colonization.704 Rubber fittings within plumbing systems have been associated with persistent colonization, and replacement of these fittings may be required for Legionella spp. eradication.1467
Continuous chlorination to maintain concentrations of free residual chlorine at 1-2 mg/L (1-2 ppm) at the tap is an alternative option for treatment. This requires the placement of flow-adjusted, continuous injectors of chlorine throughout the water distribution system. Adverse effects of continuous chlorination can include accelerated corrosion of plumbing (resulting in system leaks) and production of potentially carcinogenic trihalomethanes. However, when levels of free residual chlorine are below 3 mg/L (3 ppm), trihalomethane levels are kept below the maximum safety level recommended by the EPA 727, 1468, 1469
The recommendations in this guideline for Ebola Virus Disease has been superseded by CDC's Infection Prevention and Control Recommendations for Hospitalized Patients with Known or Suspected Ebola Virus Disease in U.S. Hospitals and by CDC's Interim Guidance for Environmental Infection Control in Hospitals for Ebola Virus issued on August 1,2014 Click here for current information on how Ebola virus is transmitted.
# Part IV. Appendices Appendix A. Glossary of Terms
Acceptable indoor air quality: air in which there are no known contaminants at harmful concentrations as determined by knowledgeble authorities and with which a substantial majority (>80%) of the people exposed do not express dissatisfaction. ACGIH: American Conference of Governmental Industrial Hygienists. Action level: the concentration of a contaminant at which steps should be taken to interrupt the trend toward higher, unacceptable levels. Aerosol: particles of respirable size generated by both humans and environmental sources and that have the capability of remaining viable and airborne for extended periods in the indoor environment. AIA: American Institute of Architects, a professional group responsible for publishing the Guidelines for Design and Construction o f Hospitals and Healthcare Facilities, a consensus document for design and construction of health-care facilities endorsed by the U.S. Department of Health and Human Services, health-care professionals, and professional organizations.
Air changes per hour (ACH): the ratio of the volume of air flowing through a space in a certain period of time (the airflow rate) to the volume of that space (the room volume). This ratio is expressed as the number of air changes per hour (ACH).
Air mixing: the degree to which air supplied to a room mixes with the air already in the room, usually expressed as a mixing factor. This factor varies from 1 (for perfect mixing) to 10 (for poor mixing). It is used as a multiplier to determine the actual airflow required (i.e., the recommended ACH multiplied by the mixing factor equals the actual ACH required). Airborne transmission: a means of spreading infection when airborne droplet nuclei (small particle residue of evaporated droplets <5 pm in size containing microorganisms that remain suspended in air for long periods of time) are inhaled by the susceptible host. Air-cleaning system: a device or combination of devices applied to reduce the concentration of airborne contaminants (e.g., microorganisms, dusts, fumes, aerosols, other particulate matter, and gases).
Air conditioning: the process of treating air to meet the requirements of a conditioned space by controlling its temperature, humidity, cleanliness, and distribution. Allogeneic: non-twin, non-self. The term refers to transplanted tissue from a donor closely matched to a recipient but not related to that person. Ambient air: the air surrounding an object. Anemometer: a flow meter which measures the wind force and velocity of air. An anemometer is often used as a means of determining the volume of air being drawn into an air sampler. Anteroom: a small room leading from a corridor into an isolation room. This room can act as an airlock, preventing the escape of contaminants from the isolation room into the corridor. ASHE: American Society for Healthcare Engineering, an association affiliated with the American Hospital Association. ASHRAE: American Society of Heating, Refrigerating, and Air-Conditioning Engineers Inc. Autologous: self. The term refers to transplanted tissue whose source is the same as the recipient, or an identical twin. Automated cycler: a machine used during peritoneal dialysis which pumps fluid into and out of the patient while he/she sleeps. Biochemical oxygen demand (BOD): a measure of the amount of oxygen removed from aquatic environments by aerobic microorganisms for their metabolic requirements. Measurement of BOD is used to determine the level of organic pollution of a stream or lake. The greater the BOD, the greater
# Procedure for Cleaning Cooling Towers and Related Equipment
I. Perform these steps prior to chemical disinfection and mechanical cleaning.
A. Provide protective equipment to workers who perform the disinfection, to prevent their exposure to chemicals used for disinfection and aerosolized water containing Legionella spp. Protective equipment may include full-length protective clothing, boots, gloves, goggles, and a full-or half-face mask that combines a HEPA filter and chemical cartridges to protect against airborne chlorine levels of up to 10 mg/L. B. Shut off cooling tower.
# Appendix D. Insects and Microorganisms
# Appendix E. Information Resources
The following sources of information may be helpful to the reader. Some of these are available at no charge, while others are available for purchase from the publisher.
Air andWater
# Appendix F. Areas of Future Research
# Air
- Standardize the methodology and interpretation of microbiologic air sampling (e.g., determine action levels or minimum infectious dose for aspergillosis, and evaluate the significance of airborne bacteria and fungi in the surgical field and the impact on postoperative SSI). - Develop new molecular typing methods to better define the epidemiology of health-care-associated outbreaks of aspergillosis and to associate isolates recovered from both clinical and environmental sources. - Develop new methods for the diagnosis of aspergillosis that can lead reliably to early recognition of infection. - Assess the value of laminar flow technology for surgeries other than for joint replacement surgery.
- Determine if particulate sampling can be routinely performed in lieu of microbiologic sampling for purposes such as determining air quality of clean environments (e.g., operating rooms, HSCT units).
# Water
- Evaluate new methods of water treatment, both in the facility and at the water utility (e.g., ozone, chlorine dioxide, copper/silver/monochloramine) and perform cost-benefit analyses of treatment in preventing health-care-associated legionellosis. - Evaluate the role of biofilms in overall water quality and determine the impact of water treatments for the control of biofilm in distribution systems. - Determine if the use of ultrapure fluids in dialysis is feasible and warranted, and determine the action level for the final bath. - Develop quality assurance protocols and validated methods for sampling filtered rinse water used with AERs and determine acceptable microbiologic quality of AER rinse water.
# Environmental Services
- Evaluate the innate resistance of microorganisms to the action of chemical germicides, and determine what, if any, linkage there may be between antibiotic resistance and resistance to disinfectants.
# Laundry and Bedding
- Evaluate the microbial inactivation capabilities of new laundry detergents, bleach substitutes, other laundry additives, and new laundry technologies.
# Animals in Health-Care Facilities
- Conduct surveillance to monitor incidence of infections among patients in facilities that use animal programs, and conduct investigations to determine new infection control strategies to prevent these infections. - Evaluate the epidemiologic impact of performing procedures on animals (e.g., surgery or imaging) in human health-care facilities.
# Regulated Medical Waste
- Determine the efficiency of current medical waste treatment technologies to inactivate emerging pathogens that may be present in medical waste (e.g., SARS-coV). - Explore options to enable health-care facilities to reinstate the capacity to inactivate microbiological cultures and stocks on-site. | The full-text version of the guidelines appears as a web-based document at the CDC's Division of Healthcare Quality Promotion's Internet site at: www.cdc.gov/ncidod/hip/enviro/guide.htm The full-text version of the guidelines should be cited when reference is made primarily to material in Parts I and IV.#
microorganisms; k) infection-control procedures for health-care laundry; l) use of animals in health care for activities and therapy; m) managing the presence of service animals in health-care facilities; n) infection-control strategies for when animals receive treatment in human health-care facilities; and o) a call to reinstate the practice of inactivating amplified cultures and stocks of microorganisms on-site during medical waste treatment.
Whenever possible, the recommendations in Part II are based on data from well-designed scientific studies. However, certain of these studies were conducted by using narrowly defined patient populations or for specific health-care settings (e.g., hospitals versus long-term care facilities), making generalization of findings potentially problematic. Construction standards for hospitals or other health care facilities may not apply to residential home-care units. Similarly, infection-control measures indicated for immunosuppressed patient care are usually not necessary in those facilities where such patients are not present. Other recommendations were derived from knowledge gained during infectious disease investigations in health-care facilities, where successful termination of the outbreak was often the result of multiple interventions, the majority of which cannot be independently and rigorously evaluated. This is especially true for construction situations involving air or water.
Other recommendations are derived from empiric engineering concepts and may reflect an industry standard rather than an evidence-based conclusion. Where recommendations refer to guidance from the American Institute of Architects (AIA), the statements reflect standards intended for new construction or renovation. Existing structures and engineered systems are expected to be in continued compliance with the standards in effect at the time of construction or renovation. Also, in the absence of scientific confirmation, certain infection-control recommendations that cannot be rigorously evaluated are based on a strong theoretical rationale and suggestive evidence. Finally, certain recommendations are derived from existing federal regulations. The references and the appendices comprise Parts III and IV of this document, respectively.
Infections caused by the microorganisms described in these guidelines are rare events, and the effect of these recommendations on infection rates in a facility may not be readily measurable. Therefore, the following steps to measure performance are suggested to evaluate these recommendations (Box 1): Topics outside the scope of this document include a) noninfectious adverse events (e.g., sick building syndrome); b) environmental concerns in the home; c) home health care; d) bioterrorism; and e) health care-associated foodborne illness. This document includes only limited discussion of a) handwashing/hand hygiene; b) standard precautions; and c) infection-control measures used to prevent instrument or equipment contamination during patient care (e.g., preventing waterborne contamination of nebulizers or ventilator humidifiers). These topics are mentioned only if they are important in minimizing the transfer of pathogens to and from persons or equipment and the environment. Although the document discusses principles of cleaning and disinfection as they are applied to maintenance of environmental surfaces, the full discussion of sterilization and disinfection of medical instruments and direct patient-care devices is deferred for inclusion in the Guideline for Disinfection and Sterilization in Health-Care Facilities, a document currently under development. Similarly, the full discussion of hand hygiene is available as the
# Part I. Background Information: Environmental Infection Control in Health-Care Facilities
# A. Introduction
The health-care environment contains a diverse population of microorganisms, but only a few are significant pathogens for susceptible humans. Microorganisms are present in great numbers in moist, organic environments, but some also can persist under dry conditions. Although pathogenic microorganisms can be detected in air and water and on fomites, assessing their role in causing infection and disease is difficult.11 Only a few reports clearly delineate a "cause and effect" with respect to the environment and in particular, housekeeping surfaces.
Eight criteria are used to evaluate the strength of evidence for an environmental source or means of transmission of infectious agents (Box 2).11, 12 Applying these criteria to disease investigations allows scientists to assess the contribution of the environment to disease transmission. An example of this application is the identification of a pathogen (e.g., vancomycin-resistant enterococci [VRE]) on an environmental surface during an outbreak. The presence of the pathogen does not establish its causal role; its transmission from source to host could be through indirect means (e.g., via hand transferral). 11 The surface, therefore, would be considered one of a number of potential reservoirs for the pathogen, but not the "de facto" source of exposure. An understanding of how infection occurs after exposure, based on the principles of the "chain of infection," is also important in evaluating the contribution of the environment to health-care-associated disease. 13 All of the components of the "chain" must be operational for infection to occur (Box 3). The presence of the susceptible host is one of these components that underscores the importance of the health-care environment and opportunistic pathogens on fomites and in air and water. As a result of advances in medical technology and therapies (e.g., cytotoxic chemotherapy and transplantation medicine), more patients are becoming immunocompromised in the course of treatment and are therefore at increased risk for acquiring health-care-associated opportunistic infections. Trends in health-care delivery (e.g., early discharge of patients from acute care facilities) also are changing the distribution of patient populations and increasing the number of immunocompromised persons in non acute-care hospitals. According to the American Hospital Association (AHA), in 1998, the number of hospitals in the United States totaled 6,021; these hospitals had a total of 1,013,000 beds,14 representing a 5.5% decrease in the number of acute-care facilities and a 10.2% decrease in the number of beds over the 5-year period 1994-1998.14 In addition, the total average daily number of patients receiving care in U.S. acute-care hospitals in 1998 was 662,000 (65.4%) -36.5% less than the 1978 average of 1,042,000.14 As the number of acute-care hospitals declines, the length of stay in these facilities is concurrently decreasing, particularly for immunocompetent patients. Those patients remaining in acutecare facilities are likely to be those requiring extensive medical interventions who therefore at high risk for opportunistic infection.
The growing population of severely immunocompromised patients is at odds with demands on the health-care industry to remain viable in the marketplace; to incorporate modern equipment, new diagnostic procedures, and new treatments; and to construct new facilities. Increasing numbers of health-care facilities are likely to be faced with construction in the near future as hospitals consolidate to reduce costs, defer care to ambulatory centers and satellite clinics, and try to create more "home-like" acute-care settings. In 1998, approximately 75% of health-care-associated construction projects focused on renovation of existing outpatient facilities or the building of such facilities;15 the number of projects associated with outpatient health care rose by 17% from 1998 through 1999. 16 An aging population is also creating increasing demand for assisted-living facilities and skilled nursing centers. Construction of assisted-living facilities in 1998 increased 49% from the previous year, with 138 projects completed at a cost of $703 million. 16 Overall, from 1998 to 1999, health-care-associated construction costs increased by 28.5%, from $11.56 billion to $14.86 billion. 16 Environmental disturbances associated with construction activities near health-care facilities pose airborne and waterborne disease threats risks for the substantial number of patients who are at risk for health-care-associated opportunistic infections. The increasing age of hospitals and other health-care facilities is also generating ongoing need for repair and remediation work (e.g., installing wiring for new information systems, removing old sinks, and repairing elevator shafts) that can introduce or increase contamination of the air and water in patient-care environments. Aging equipment, deferred maintenance, and natural disasters provide additional mechanisms for the entry of environmental pathogens into high-risk patient-care areas.
Architects, engineers, construction contractors, environmental health scientists, and industrial hygienists historically have directed the design and function of hospitals' physical plants. Increasingly, however, because of the growth in the number of susceptible patients and the increase in construction projects, the involvement of hospital epidemiologists and infection-control professionals is required. These experts help make plans for building, maintaining, and renovating health-care facilities to ensure that the adverse impact of the environment on the incidence of health-care-associated infections is minimal. The following are examples of adverse outcomes that could have been prevented had such experts been involved in the planning process: a) transmission of infections caused by Mycobacterium tuberculosis, varicella-zoster virus (VZV), and measles (i.e., rubeola) facilitated by inappropriate air-handling systems in health-care facilities;6 b) disease outbreaks caused by Aspergillus spp., [17][18][19]20 and Penicillium spp. associated with the absence of environmental controls during periods of health-care facility-associated construction;21 c) infections and/or colonizations of patients and staff with vancomycin-resistant Enterococcus faecium [VRE] and Clostridium difficile acquired indirectly from contact with organisms present on environmental surfaces in health-care facilities;22-25 and d) outbreaks and pseudoepidemics of legionellae,26, 27 Pseudomonas aeruginosa383 and the nontuberculous mycobacteria (NTM)31, 32 linked to water and aqueous solutions used in health-care facilities. The purpose of this guideline is to provide useful information for both health-care professionals and engineers in efforts to provide a safe environment in which quality health care may be provided to patients. The recommendations herein provide guidance to minimize the risk for and prevent transmission of pathogens in the indoor environment.
# B. Key Terms Used in this Guideline
Although Appendix A provides definitions for terms discussed in Part I, several terms that pertain to specific patient-care areas and patients who are at risk for health-care-associated opportunistic infections are presented here. Specific engineering parameters for these care areas are discussed more fully in the text. Airborne Infection Isolation (AII) refers to the isolation of patients infected with organisms spread via airborne droplet nuclei <5 pm in diameter. This isolation area receives numerous air changes per hour (ACH) (>12 ACH for new construction as of 2001; >6 ACH for construction before 2001), and is under negative pressure, such that the direction of the airflow is from the outside adjacent space (e.g., corridor) into the room. The air in an AII room is preferably exhausted to the outside, but may be recirculated provided that the return air is filtered through a high efficiency particulate air (HEPA) filter. The use of personal respiratory protection is also indicated for persons entering these rooms.
Protective Environment (PE) is a specialized patient-care area, usually in a hospital, with a positive airflow relative to the corridor (i.e., air flows from the room to the outside adjacent space). The combination of HEPA filtration, high numbers of air changes per hour (>12 ACH), and minimal leakage of air into the room creates an environment that can safely accommodate patients who have undergone allogeneic hematopoietic stem cell transplant (HSCT).
Immunocompromised patients are those patients whose immune mechanisms are deficient because of immunologic disorders (e.g., human immunodeficiency virus [HIV] infection, congenital immune deficiency syndrome, chronic diseases [such as diabetes, cancer, emphysema, and cardiac failure]) or immunosuppressive therapy (e.g., radiation, cytotoxic chemotherapy, anti-rejection medication, and steroids). Immunocompromised patients who are identified as high-risk patients have the greatest risk of infection caused by airborne or waterborne microorganisms. Patients in this subset include those who are severely neutropenic for prolonged periods of time (i.e., an absolute neutrophil count [ANC] of <500 cells/mL), allogeneic HSCT patients, and those who have received intensive chemotherapy (e.g., childhood acute myelogenous leukemia patients).
# C. Air
# Modes of Transmission of Airborne Diseases
A variety of airborne infections in susceptible hosts can result from exposures to clinically significant microorganisms released into the air when environmental reservoirs (i.e., soil, water, dust, and decaying organic matter) are disturbed. Once these materials are brought indoors into a health-care facility by any of a number of vehicles (e.g., people, air currents, water, construction materials, and equipment), the attendant microorganisms can proliferate in various indoor ecological niches and, if subsequently disbursed into the air, serve as a source for airborne health-care-associated infections.
Respiratory infections can be acquired from exposure to pathogens contained either in droplets or droplet nuclei. Exposure to microorganisms in droplets (e.g., through aerosolized oral and nasal secretions from infected patients33) constitutes a form of direct contact transmission. When droplets are produced during a sneeze or cough, a cloud of infectious particles >5 pm in size is expelled, resulting in the potential exposure of susceptible persons within 3 feet of the source person.6 Examples of pathogens spread in this manner are influenza virus, rhinoviruses, adenoviruses, and respiratory syncytial virus (RSV). Because these agents primarily are transmitted directly and because the droplets tend to fall out of the air quickly, measures to control air flow in a health-care facility (e.g., use of negative pressure rooms) generally are not indicated for preventing the spread of diseases caused by these agents. Strategies to control the spread of these diseases are outlined in another guideline. 3 The spread of airborne infectious diseases via droplet nuclei is a form of indirect transmission. 34 Droplet nuclei are the residuals of droplets that, when suspended in air, subsequently dry and produce particles ranging in size from 1-5 pm. These particles can a) contain potentially viable microorganisms, b) be protected by a coat of dry secretions, c) remain suspended indefinitely in air, and d) be transported over long distances. The microorganisms in droplet nuclei persist in favorable conditions (e.g., a dry, cool atmosphere with little or no direct exposure to sunlight or other sources of radiation). Pathogenic microorganisms that can be spread via droplet nuclei include Mycobacterium tuberculosis, VZV, measles virus (i.e., rubeola), and smallpox virus (i.e., variola major).6 Several environmental pathogens have life-cycle forms that are similar in size to droplet nuclei and may exhibit similar behavior in the air. The spores of Aspergillus fumigatus have a diameter of 2-3.5 pm, with a settling velocity estimated at 0.03 cm/second (or about 1 meter/hour) in still air. With this enhanced buoyancy, the spores, which resist desiccation, can remain airborne indefinitely in air currents and travel far from their source.35
# Airborne Infectious Diseases in Health-Care Facilities a. Aspergillosis and Other Fungal Diseases
Aspergillosis is caused by molds belonging to the genus Aspergillus. Aspergillus spp. are prototype health-care-acquired pathogens associated with dusty or moist environmental conditions. Clinical and epidemiologic aspects of aspergillosis (Table 1) are discussed extensively in another guideline.3
# Table 1. Clinical and epidemiologic characteristics of aspergillosis
fungal spores. Increased levels of atmospheric dust and fungal spores have been associated with clusters of health-care-acquired infections in immunocompromised patients. 17' 20, 44, 47, 49, 50, 95-98 Absorbent building materials (e.g., wallboard) serve as an ideal substrate for the proliferation of this organism if they become and remain wet, thereby increasing the numbers of fungal spores in the area. Patient-care items, devices, and equipment can become contaminated with Aspergillus spp. spores and serve as sources of infection if stored in such areas. 57 Most cases of aspergillosis are caused by Aspergillus fumigatus, a thermotolerant/thermophilic fungus capable of growing over a temperature range from 53.6°F-127.4°F (12°C-53°C); optimal growth occurs at approximately 104°F (40°C), a temperature inhibitory to most other saprophytic fungi.99 It can use cellulose or sugars as carbon sources; because its respiratory process requires an ample supply of carbon, decomposing organic matter is an ideal substrate.
Other opportunistic fungi that have been occasionally linked with health-care-associated infections are members of the orderMucorales (e.g., Rhizopus spp.) and miscellaneous moniliaceous molds (e.g., Fusarium spp. and Penicillium spp.) (Table 2). Many of these fungi can proliferate in moist environments (e.g., water-damaged wood and building materials). Some fungi (e.g., Fusarium spp. and Pseudoallescheria spp.) also can be airborne pathogens.100 As with aspergillosis, a major risk factor for disease caused by any of these pathogens is the host's severe immunosuppression from either underlying disease or immunosuppressive therapy.101, 102
# Table 2. Environmental fungal pathogens: entry into and contamination of the health care facility
Infections due Cryptococcus neoformans, Histoplasma capsulatum, or Coccidioides immitis can occur in health-care settings if nearby ground is disturbed and a malfunction of the facility's air-intake components allows these pathogens to enter the ventilation system. C. neoformans is a yeast usually 4 8 pm in size. However, viable particles of <2 pm diameter (and thus permissive to alveolar deposition) have been found in soil contaminated with bird droppings, particularly from pigeons.98, 103, 104, 121 H. capsulatum, with the infectious microconidia ranging in size from 2-5 pm, is endemic in the soil of the central river valleys of the United States. Substantial numbers of these infectious particles have been associated with chicken coops and the roosts of blackbirds.98, 103, 104, 122 Several outbreaks of histoplasmosis have been associated with disruption of the environment; construction activities in an endemic area may be a potential risk factor for health-care-acquired airborne infection.123, 124 C. immitis, with arthrospores of 3-5 pm diameter, has similar potential, especially in the endemic southwestern United States and during seasons of drought followed by heavy rainfall. After the 1994 earthquake centered near Northridge, California, the incidence of coccidioidomycosis in the surrounding area exceeded the historical norm. 125 Emerging evidence suggests that Pneumocystis carinii, now classified as a fungus, may be spread via airborne, person-to-person transmission.126 Controlled studies in animals first demonstrated that P. carinii could be spread through the air. 127 More recent studies in health-care settings have detected nucleic acids of P. carinii in air samples from areas frequented or occupied by P. carinii-infected patients but not in control areas that are not occupied by these patients. , Clusters of cases have been identified among immunocompromised patients who had contact with a source patient and with each other. Recent studies have examined the presence of P. carinii DNA in oropharyngeal washings and the nares of infected patients, their direct contacts, and persons with no direct contact. 130,131 Molecular analysis of the DNA by polymerase chain reaction (PCR) provides evidence for airborne transmission of P. carinii from infected patients to direct contacts, but immunocompetent contacts tend to become transiently colonized rather than infected.131 The role of colonized persons in the spread of P. carinii pneumonia (PCP) remains to be determined. At present, specific modifications to ventilation systems to control spread of PCP in a health-care facility are not indicated. Current recommendations M. tuberculosis is carried by droplet nuclei generated when persons (primarily adults and adolescents) who have pulmonary or laryngeal TB sneeze, cough, speak, or sing;139 normal air currents can keep these particles airborne for prolonged periods and spread them throughout a room or building.142 However, transmission of TB has occurred from mycobacteria aerosolized during provision of care (e.g., wound/lesion care or during handling of infectious peritoneal dialysis fluid) for extrapulmonary TB patients. 135,140 Gram-positive cocci (i.e., Staphylococcus aureus, group A beta-hemolytic streptococci), also important health-care-associated pathogens, are resistant to inactivation by drying and can persist in the environment and on environmental surfaces for extended periods. These organisms can be shed from heavily colonized persons and discharged into the air. Airborne dispersal of S. aureus is directly associated with the concentration of the bacterium in the anterior nares.143 Approximately 10% of healthy carriers will disseminate S. aureus into the air, and some persons become more effective disseminators of S. aureus than others. [144][145][146][147][148] The dispersal of S. aureus into air can be exacerbated by concurrent viral upper respiratory infection, thereby turning a carrier into a "cloud shedder."149 Outbreaks of surgical site infections (SSIs) caused by group A beta-hemolytic streptococci have been traced to airborne transmission from colonized operating-room personnel to patients.150153 In these situations, the strain causing the outbreak was recovered from the air in the operating room150, 151, 154 or on settle plates in a room in which the carrier exercised.151153 S. aureus and group A streptococci have not been linked to airborne transmission outside of operating rooms, burn units, and neonatal nurseries. 155,156 Transmission of these agents occurs primarily via contact and droplets.
Other gram-positive bacteria linked to airborne transmission include Bacillus spp. which are capable of sporulation as environmental conditions become less favorable to support their growth. Outbreaks and pseudo-outbreaks have been attributed to Bacillus cereus in maternity, pediatric, intensive care, and bronchoscopy units; many of these episodes were secondary to environmental contamination.157160 Gram-negative bacteria rarely are associated with episodes of airborne transmission because they generally require moist environments for persistence and growth. The main exception is Acinetobacter spp., which can withstand the inactivating effects of drying. In one epidemiologic investigation of bloodstream infections among pediatric patients, identical Acinetobacter spp. were cultured from the patients, air, and room air conditioners in a nursery. 161 Aerosols generated from showers and faucets may potentially contain legionellae and other gram negative waterborne bacteria (e.g., Pseudomonas aeruginosa). Exposure to these organisms is through direct inhalation. However, because water is the source of the organisms and exposure occurs in the vicinity of the aerosol, the discussion of the diseases associated with such aerosols and the prevention measures used to curtail their spread is discussed in another section of the Guideline (see Part I: Water).
# c. Airborne Viral Diseases
Some human viruses are transmitted from person to person via droplet aerosols, but very few viruses are consistently airborne in transmission (i.e., are routinely suspended in an infective state in air and capable of spreading great distances), and health-care-associated outbreaks of airborne viral disease are limited to a few agents. Consequently, infection-control measures used to prevent spread of these viral diseases in health-care facilities primarily involve patient isolation, vaccination of susceptible persons, and antiviral therapy as appropriate rather than measures to control air flow or quality. 6 Infections caused by VZV frequently are described in health-care facilities. Health-care-associated airborne outbreaks of VZV infections from patients with primary infection and disseminated zoster have been documented; patients with localized zoster have, on rare occasions, also served as source patients for outbreaks in health-care facilities.162-166 VZV infection can be prevented by vaccination, although patients who develop a rash within 6 weeks of receiving varicella vaccine or who develop breakthrough varicella following exposure should be considered contagious. 167 Viruses whose major mode of transmission is via droplet contact rarely have caused clusters of infections in group settings through airborne routes. The factors facilitating airborne distribution of these viruses in an infective state are unknown, but a presumed requirement is a source patient in the early stage of infection who is shedding large numbers of viral particles into the air. Airborne transmission of measles has been documented in health-care facilities. [168][169][170][171] In addition, institutional outbreaks of influenza virus infections have occurred predominantly in nursing homes,172-176 and less frequently in medical and neonatal intensive care units, chronic-care areas, HSCT units, and pediatric wards.177-180 Some evidence supports airborne transmission of influenza viruses by droplet nuclei,181, 182 and case clusters in pediatric wards suggest that droplet nuclei may play a role in transmitting certain respiratory pathogens (e.g., adenoviruses and respiratory syncytial virus [RSV]).177, 183, 184 Some evidence also supports airborne transmission of enteric viruses. An outbreak of a Norwalk-like virus infection involving more than 600 staff personnel over a 3-week period was investigated in a Toronto, Ontario hospital in 1985; common sources (e.g., food and water) were ruled out during the investigation, leaving airborne spread as the most likely mode of transmission.185 Smallpox virus, a potential agent of bioterrorism, is spread predominantly via direct contact with infectious droplets, but it also can be associated with airborne transmission.186, 187 A German hospital study from 1970 documented the ability of this virus to spread over considerable distances and cause infection at low doses in a well-vaccinated population; factors potentially facilitating transmission in this situation included a patient with cough and an extensive rash, indoor air with low relative humidity, and faulty ventilation patterns resulting from hospital design (e.g., open windows).188 Smallpox patients with extensive rash are more likely to have lesions present on mucous membranes and therefore have greater potential to disseminate virus into the air. 188 In addition to the smallpox transmission in Germany, two cases of laboratory-acquired smallpox virus infection in the United Kingdom in 1978 also were thought to be caused by airborne transmission. 189 Airborne transmission may play a role in the natural spread of hantaviruses and certain hemorrhagic fever viruses (e.g., Ebola, Marburg, and Lassa), but evidence for airborne spread of these agents in health-care facilities is inconclusive. 190 Although hantaviruses can be transmitted when aerosolized from rodent excreta ,191, 192 person-to-person spread of hantavirus infection from source patients has not occurred in health-care facilities. [193][194][195] Nevertheless, health-care workers are advised to contain potentially infectious aerosols and wear National Institute of Occupational Safety and Health (NIOSH) approved respiratory protection when working with this agent in laboratories or autopsy suites.196 Lassa virus transmission via aerosols has been demonstrated in the laboratory and incriminated in health-care-associated infections in Africa,197-199 but airborne spread of this agent in hospitals in developed nations likely is inefficient. 200,201 Yellow fever is considered to be a viral hemorrhagic fever agent with high aerosol infectivity potential, but health-care-associated transmission of this virus has not been described.202 Viral hemorrhagic fever diseases primarily occur after direct exposure to infected blood and body fluids, and the use of standard and droplet precautions prevents transmission early in the course of these illnesses.203, 204 However, whether these viruses can persist in droplet nuclei that might remain after droplet production from coughs or vomiting in the latter stages of illness is unknown. 205 Although the use of a negative-pressure room is not required during the early stages of illness, its use might be prudent at the time of hospitalization to avoid the need for subsequent patient transfer. Current CDC guidelines recommend negative-pressure rooms with anterooms for patients with hemorrhagic fever and use of HEPA respirators by persons entering these rooms when the patient has prominent cough, vomiting, diarrhea, or hemorrhage.6, 203 Face shields or goggles will help to prevent mucous-membrane exposure to potentially-aerosolized infectious material in these situations. If an anteroom is not available, portable, industrial-grade high efficiency particulate air (HEPA) filter units can be used to provide the equivalent of additional air changes per hour (ACH).
The recommendations in this guideline for Ebola Virus Disease has been superseded by CDC's Infection Prevention and Control Recommendations for Hospitalized Patients with Known or Suspected Ebola Virus Disease in U.S. Hospitals and by CDC's Interim Guidance for Environmental Infection Control in Hospitals for Ebola Virus issued on August 1, 2014. 13 Click here for current information on how Ebola virus is transmitted. Under investigation Pneumocystis cariniilil --* This list excludes microorganisms transmitted from aerosols derived from water. + Refer to the text for references for these disease agents. § Airborne transmission of smallpox is infrequent. Potential for airborne transmission increases with patients who are effective disseminators present in facilities with low relative humidity in the air and faulty ventilation. Documentation of pseudoepidemic during construction. ** Airborne transmission documented in the laboratory but not in patient-care areas
# Heating, Ventilation, and Air Conditioning Systems in Health-Care Facilities a. Basic Components and Operations
Heating, ventilation, and air conditioning (HVAC) systems in health-care facilities are designed to a) maintain the indoor air temperature and humidity at comfortable levels for staff, patients, and visitors; b) control odors; c) remove contaminated air; d) facilitate air-handling requirements to protect susceptible staff and patients from airborne health-care-associated pathogens; and e) minimize the risk for transmission of airborne pathogens from infected patients.35, 120 An HVAC system includes an outside air inlet or intake; filters; humidity modification mechanisms (i.e., humidity control in summer, humidification in winter); heating and cooling equipment; fans; ductwork; air exhaust or out-takes; and registers, diffusers, or grilles for proper distribution of the air (Figure 1).213, 214 Decreased performance of healthcare facility HVAC systems, filter inefficiencies, improper installation, and poor maintenance can contribute to the spread of health-care-associated airborne infections.
The American Institute of Architects (AIA) has published guidelines for the design and construction of new health-care facilities and for renovation of existing facilities. These AIA guidelines address indoor air-quality standards (e.g., ventilation rates, temperature levels, humidity levels, pressure relationships, and minimum air changes per hour [ACH]) specific to each zone or area in health-care facilities (e.g., operating rooms, laboratories, diagnostic areas, patient-care areas, and support departments).120 These guidelines represent a consensus document among authorities having jurisdiction (AHJ), governmental regulatory agencies (i.e., Department of Health and Human Services [DHHS]; Department of Labor, Occupational Safety and Health Administration [OSHA]), health-care professionals, professional organizations (e.g., American Society of Heating, Refrigeration, and Air-Conditioning Engineers [ASHRAE], American Society for Healthcare Engineering [ASHE]), and accrediting organizations (i.e., Joint Commission on Accreditation of Healthcare Organizations [JCAHO]). More than 40 state agencies that license health-care facilities have either incorporated or adopted by reference these
# GENERAL R t LJRN AIR EXHAUST
Outdoor air and recirculated air pass through air cleaners (e.g., filter banks) designed to reduce the concentration of airborne contaminants. Air is conditioned for temperature and humidity before it enters the occupied space as supply air. Infiltration is air leakage inward through cracks and interstitial spaces of walls, floors, and ceilings. Exfiltration is air leakage outward through these same cracks and spaces. Return air is largely exhausted from the system, but a portion is recirculated with fresh, incoming air. * Used with permission of the publisher of reference 214 (ASHRAE) Engineering controls to contain or prevent the spread of airborne contaminants center on a) local exhaust ventilation [i.e., source control], b) general ventilation, and c) air cleaning. 4 General ventilation encompasses a) dilution and removal of contaminants via well-mixed air distribution of filtered air, b) directing contaminants toward exhaust registers and grilles via uniform, non-mixed airflow patterns, c) pressurization of individual spaces relative to all other spaces, and d) pressurization of buildings relative to the outdoors and other attached buildings.
A centralized HVAC system operates as follows. Outdoor air enters the system, where low-efficiency or "roughing" filters remove large particulate matter and many microorganisms. The air enters the distribution system for conditioning to appropriate temperature and humidity levels, passes through an additional bank of filters for further cleaning, and is delivered to each zone of the building. After the conditioned air is distributed to the designated space, it is withdrawn through a return duct system and delivered back to the HVAC unit. A portion of this "return air" is exhausted to the outside while the remainder is mixed with outdoor air for dilution and filtered for removal of contaminants.215 Air from toilet rooms or other soiled areas is usually exhausted directly to the atmosphere through a separate duct exhaust system. Air from rooms housing tuberculosis patients is exhausted to the outside if possible, or passed through a HEPA filter before recirculation. Ultraviolet germicidal irradiation (UVGI) can be used as an adjunct air-cleaning measure, but it cannot replace HEPA filtration.
# b. Filtration
i. Filter Types and Methods of Filtration Filtration, the physical removal of particulates from air, is the first step in achieving acceptable indoor air quality. Filtration is the primary means of cleaning the air. Five methods of filtration can be used (Table 5). During filtration, outdoor air passes through two filter beds or banks (with efficiencies of 20%-40% and >90%, respectively) for effective removal of particles 1-5 pm in diameter.35, 120 The low-to-medium efficiency filters in the first bank have low resistance to airflow, but this feature allows some small particulates to pass onto heating and air conditioning coils and into the indoor environment.35 Incoming air is mixed with recirculated air and reconditioned for temperature and humidity before being filtered by the second bank of filters. The performance of filters with <90% efficiency is measured using either the dust-spot test or the weight-arrestance test.35, 216 Maintenance costs associated with HEPA filters are high compared with other types of filters, but use of in-line disposable prefilters can increase the life of a HEPA filter by approximately 25%. Alternatively, if a disposable prefilter is followed by a filter that is 90% efficient, the life of the HEPA filter can be extended ninefold. This concept, called progressive filtration, allows HEPA filters in special care areas to be used for 10 years. 213 Although progressive filtering will extend the mechanical ability of the HEPA filter, these filters may absorb chemicals in the environment and later desorb those chemicals, thereby necessitating a more frequent replacement program. HEPA filter efficiency is monitored with the dioctylphthalate (DOP) particle test using particles that are 0.3 pm in diameter.218
HEPA filters are usually framed with metal, although some older versions have wood frames. A metal frame has no advantage over a properly fitted wood frame with respect to performance, but wood can compromise the air quality if it becomes and remains wet, allowing the growth of fungi and bacteria. Hospitals are therefore advised to phase out water-damaged or spent wood-framed filter units and replace them with metal-framed HEPA filters.
HEPA filters are usually fixed into the HVAC system; however, portable, industrial grade HEPA units are available that can filter air at the rate of 300-800 ft3/min. Portable HEPA filters are used to a) temporarily recirculate air in rooms with no general ventilation, b) augment systems that cannot provide adequate airflow, and c) provide increased effectiveness in airflow.4 Portable HEPA units are useful engineering controls that help clean the air when the central HVAC system is undergoing repairs,219 but these units do not satisfy fresh-air requirements.214 The effectiveness of the portable unit for particle removal is dependent on a) the configuration of the room, b) the furniture and persons in the room, c) the placement of the units relative to the contents and layout of the room, and d) the location of the supply and exhaust registers or grilles. If portable, industrial-grade units are used, they should be capable of recirculating all or nearly all of the room air through the HEPA filter, and the unit should be designed to achieve the equivalent of >12 ACH.4 (An average room has approximately 1,600 ft3 of airspace.) The hospital engineering department should be contacted to provide ACH information in the event that a portable HEPA filter unit is necessary to augment the existing fixed HVAC system for air cleaning.
ii. Filter Maintenance Efficiency of the filtration system is dependent on the density of the filters, which can create a drop in pressure unless compensated by stronger and more efficient fans, thus maintaining air flow. For optimal performance, filters require monitoring and replacement in accordance with the manufacturer's recommendations and standard preventive maintenance practices.220 Upon removal, spent filters can be bagged and discarded with the routine solid waste, regardless of their patient-care area location.221 Excess accumulation of dust and particulates increases filter efficiency, requiring more pressure to push the air through. The pressure differential across filters is measured by use of manometers or other gauges. A pressure reading that exceeds specifications indicates the need to change the filter. Filters also require regular inspection for other potential causes of decreased performance. Gaps in and around filter banks and heavy soil and debris upstream of poorly maintained filters have been implicated in health-care-associated outbreaks of aspergillosis, especially when accompanied by construction activities at the facility.17, 18, 106, 222
# c. Ultraviolet Germicidal Irradiation (UVGI)
As a supplemental air-cleaning measure, UVGI is effective in reducing the transmission of airborne bacterial and viral infections in hospitals, military housing, and classrooms, but it has only a minimal inactivating effect on fungal spores. -UVGI is also used in air handling units to prevent or limit the growth of vegetative bacteria and fungi. Most commercially available UV lamps used for germicidal purposes are low-pressure mercury vapor lamps that emit radiant energy predominantly at a wave-length of 253.7 nm. , Two systems of UVGI have been used in health-care settings -duct irradiation and upper-room air irradiation. In duct irradiation systems, UV lamps are placed inside ducts that remove air from rooms to disinfect the air before it is recirculated. When properly designed, installed, and maintained, high levels of UVGI can be attained in the ducts with little or no exposure of persons in the rooms. ,
In upper-room air irradiation, UV lamps are either suspended from the ceiling or mounted on the wall.4 Upper air UVGI units have two basic designs: a) a "pan" fixture with UVGI unshielded above the unit to direct the irradiation upward and b) a fixture with a series of parallel plates to columnize the irradiation outward while preventing the light from getting to the eyes of the room's occupants. The germicidal effect is dependent on air mixing via convection between the room's irradiated upper zone and the lower patient-care zones. 233,234 Bacterial inactivation studies using BCG mycobacteria and Serratia marcescens have estimated the effect of UVGI as equivalent to 10 ACH-39 ACH.235, 236 Another study, however, suggests that UVGI may result in fewer equivalent ACH in the patient-care zone, especially if the mixing of air between zones is insufficient. 234 The use of fans or HVAC systems to generate air movement may increase the effectiveness of UVGI if airborne microorganisms are exposed to the light energy for a sufficient length of time. 233, 235, 237 239 The optimal relationship between ventilation and UVGI is not known.
Because the clinical effectiveness of UV systems may vary, UVGI is not recommended for air management prior to air recirculation from airborne isolation rooms. It is also not recommended as a substitute for HEPA filtration, local exhaust of air to the outside, or negative pressure. 4 The use of UV lamps and HEPA filtration in a single unit offers only minimal infection-control benefits over those provided by the use of a HEPA filter alone.240 Duct systems with UVGI are not recommended as a substitute for HEPA filters if the air from isolation rooms must be recirculated to other areas of the facility.4 Regular maintenance of UVGI systems is crucial and usually consists of keeping the bulbs free of dust and replacing old bulbs as necessary. Safety issues associated with the use of UVGI systems are described in other guidelines.4
# d. Conditioned Air in Occupied Spaces
Temperature and humidity are two essential components of conditioned air. After outside air passes through a low-or medium-efficiency filter, the air undergoes conditioning for temperature and humidity control before it passes through high-efficiency or HEPA filtration. i. Temperature HVAC systems in health-care facilities are often single-duct or dual-duct systems.35, 241 A single-duct system distributes cooled air (55°F [12.8°C]) throughout the building and uses thermostatically controlled reheat boxes located in the terminal ductwork to warm the air for individual or multiple rooms. The dual-duct system consists of parallel ducts, one with a cold air stream and the other with a hot air stream. A mixing box in each room or group of rooms mixes the two air streams to achieve the desired temperature. Temperature standards are given as either a single temperature or a range, depending on the specific health-care zone. Cool temperature standards (68°F-73°F [20°C-23°C]) usually are associated with operating rooms, clean workrooms, and endoscopy suites.120 A warmer temperature (75°F [24°C]) is needed in areas requiring greater degrees of patient comfort. Most other zones use a temperature range of 70°F-75°F (21°C-24°C).120 Temperatures outside of these ranges may be needed occasionally in limited areas depending on individual circumstances during patient care (e.g., cooler temperatures in operating rooms during specialized operations).
ii. Humidity Four measures of humidity are used to quantify different physical properties of the mixture of water vapor and air. The most common of these is relative humidity, which is the ratio of the amount of water vapor in the air to the amount of water vapor air can hold at that temperature. 242 The other measures of humidity are specific humidity, dew point, and vapor pressure. 242 Relative humidity measures the percentage of saturation. At 100% relative humidity, the air is saturated. For most areas within health-care facilities, the designated comfort range is 30%-60% relative humidity. , Relative humidity levels >60%, in addition to being perceived as uncomfortable, promote fungal growth.243 Humidity levels can be manipulated by either of two mechanisms. 244 In a water-wash unit, water is sprayed and drops are taken up by the filtered air; additional heating or cooling of this air sets the humidity levels. The second mechanism is by means of water vapor created from steam and added to filtered air in humidifying boxes. Reservoir-type humidifiers are not allowed in health-care facilities as per AIA guidelines and many state codes.120 Cool-mist humidifiers should be avoided, because they can disseminate aerosols containing allergens and microorganisms.245 Additionally, the small, personal-use versions of this equipment can be difficult to clean.
# iii. Ventilation
The control of air pollutants (e.g., microorganisms, dust, chemicals, and smoke) at the source is the most effective way to maintain clean air. The second most effective means of controlling indoor air pollution is through ventilation. Ventilation rates are voluntary unless a state or local government specifies a standard in health-care licensing or health department requirements. These standards typically apply to only the design of a facility, rather than its operation.220, 246 Health-care facilities without specific ventilation standards should follow the AIA guideline specific to the year in which the building was built or the ANSI/ASHRAE Standard 62, Ventilation for Acceptable Indoor Air Quality .120, 214, 241 Ventilation guidelines are defined in terms of air volume per minute per occupant and are based on the assumption that occupants and their activities are responsible for most of the contaminants in the conditioned space.215 Most ventilation rates for health-care facilities are expressed as room ACH. Peak efficiency for particle removal in the air space occurs between 12 ACH-15 ACH.35, 247, 248 Ventilation rates vary among the different patient-care areas of a health-care facility (Appendix B).120
Health-care facilities generally use recirculated air.35, 120, 241, 249, 250 Fans create sufficient positive pressure to force air through the building duct work and adequate negative pressure to evacuate air from the conditioned space into the return duct work and/or exhaust, thereby completing the circuit in a sealed system (Figure 1). However, because gaseous contaminants tend to accumulate as the air recirculates, a percentage of the recirculated air is exhausted to the outside and replaced by fresh outdoor air. In hospitals, the delivery of filtered air to an occupied space is an engineered system design issue, the full discussion of which is beyond the scope of this document.
Hospitals with areas not served by central HVAC systems often use through-the-wall or fan coil air conditioning units as the sole source of room ventilation. AIA guidelines for newly installed systems stipulate that through-the-wall fan-coil units be equipped with permanent (i.e., cleanable) or replaceable filters with a minimum efficiency of 68% weight arrestance.120 These units may be used only as recirculating units; all outdoor air requirements must be met by a separate central air handling system with proper filtration, with a minimum of two outside air changes in general patient rooms (D. Erickson, ASHE, 2000).120 If a patient room is equipped with an individual through-the-wall fan coil unit, the room should not be used as either AII or as PE.120 These requirements, although directed to new HVAC installations also are appropriate for existing settings. Non-central air-handling systems are prone to problems associated with excess condensation accumulating in drip pans and improper filter maintenance; health-care facilities should clean or replace the filters in these units on a regular basis while the patient is out of the room.
Laminar airflow ventilation systems are designed to move air in a single pass, usually through a bank of HEPA filters either along a wall or in the ceiling, in a one-way direction through a clean zone with parallel streamlines. Laminar airflow can be directed vertically or horizontally; the unidirectional system optimizes airflow and minimizes air turbulence.63, 241 Delivery of air at a rate of 0.5 meters per second (90 + 20 ft/min) helps to minimize opportunities for microorganism proliferation.63, 251, 252 Laminar airflow systems have been used in PE to help reduce the risk for health-care-associated airborne infections (e.g., aspergillosis) in high-risk patients.63, 93, 253, 254 However, data that demonstrate a survival benefit for patients in PE with laminar airflow are lacking. Given the high cost of installation and apparent lack of benefit, the value of laminar airflow in this setting is questionable.9, 37 Few data support the use of laminar airflow systems elsewhere in a hospital.255 iv. Pressurization Positive and negative pressures refer to a pressure differential between two adjacent air spaces (e.g., rooms and hallways). Air flows away from areas or rooms with positive pressure (pressurized), while air flows into areas with negative pressure (depressurized). AII rooms are set at negative pressure to prevent airborne microorganisms in the room from entering hallways and corridors. PE rooms housing severely neutropenic patients are set at positive pressure to keep airborne pathogens in adjacent spaces or corridors from coming into and contaminating the airspace occupied by such high-risk patients. Self closing doors are mandatory for both of these areas to help maintain the correct pressure differential.4, 6 120 Older health-care facilities may have variable pressure rooms (i.e., rooms in which the ventilation can be manually switched between positive and negative pressure). These rooms are no longer permitted in the construction of new facilities or in renovated areas of the facility,120 and their use in existing facilities has been discouraged because of difficulties in assuring the proper pressure differential, especially for the negative pressure setting, and because of the potential for error associated with switching the pressure differentials for the room. Continued use of existing variable pressure rooms depends on a partnership between engineering and infection control. Both positive-and negative-pressure rooms should be maintained according to specific engineering specifications (Table 6).
# Room airflow direction
# Out to the adjacent area
In to the room
# Clean-to-dirty airflow in room
Away from the patient (high-risk patient, immunosuppressed patient) Health-care professionals (e.g., infection control, hospital epidemiologists) must perform a risk assessment to determine the appropriate number of AII rooms (negative pressure) and/or PE rooms (positive pressure) to serve the patient population. The AIA guidelines require a certain number of AII rooms as a minimum, and it is important to refer to the edition under which the building was built for appropriate guidance.120
In large health-care facilities with central HVAC systems, sealed windows help to ensure the efficient operation of the system, especially with respect to creating and maintaining pressure differentials. Sealing the windows in PE areas helps minimize the risk of airborne contamination from the outside. One outbreak of aspergillosis among immunosuppressed patients in a hospital was attributed in part to an open window in the unit during a time when both construction and a fire happened nearby; sealing the window prevented further entry of fungal spores into the unit from the outside air.111 Additionally, all emergency exits (e.g., fire escapes and emergency doors) in PE wards should be kept closed (except during emergencies) and equipped with alarms.
# e. Infection Control Impact of HVAC System Maintenance and Repair
A failure or malfunction of any component of the HVAC system may subject patients and staff to discomfort and exposure to airborne contaminants. Only limited information is available from formal studies on the infection-control implications of a complete air-handling system failure or shutdown for maintenance. Most experience has been derived from infectious disease outbreaks and adverse outcomes among high-risk patients when HVAC systems are poorly maintained. (See Table 7 for potential ventilation hazards, consequences, and correction measures.)
AIA guidelines prohibit U.S. hospitals and surgical centers from shutting down their HVAC systems for purposes other than required maintenance, filter changes, and construction.120 Airflow can be reduced; however, sufficient supply, return, and exhaust must be provided to maintain required pressure relationships when the space is not occupied. Maintaining these relationships can be accomplished with special drives on the air-handling units (i.e., a variable air ventilation [VAV] system).
Microorganisms proliferate in environments wherever air, dust, and water are present, and air-handling systems can be ideal environments for microbial growth.35 Properly engineered HVAC systems require routine maintenance and monitoring to provide acceptable indoor air quality efficiently and to minimize conditions that favor the proliferation of health-care-associated pathogens.35, 249 Performance monitoring of the system includes determining pressure differentials across filters, regular inspection of system filters, DOP testing of HEPA filters, testing of low-or medium efficiency filters, and manometer tests for positive-and negative-pressure areas in accordance with nationally recognized standards, guidelines, and manufacturers' recommendations. The use of hand-held, calibrated equipment that can provide a numerical reading on a daily basis is preferred for engineering purposes (A.Streifel, University of Minnesota, 2000). 256 Several methods that provide a visual, qualitative measure of pressure differentials (i.e., airflow direction) include smoke-tube tests or placing flutter strips, ping-pong balls, or tissue in the air stream.
Preventive filter and duct maintenance (e.g., cleaning ductwork vents, replacing filters as needed, and properly disposing spent filters into plastic bags immediately upon removal) is important to prevent potential exposures of patients and staff during HVAC system shut-down. The frequency of filter inspection and the parameters of this inspection are established by each facility to meet their unique needs. Ductwork in older health-care facilities may have insulation on the interior surfaces that can trap contaminants. This insulation material tends to break down over time to be discharged from the HVAC system. Additionally, a malfunction of the air-intake system can overburden the filtering system and permit aerosolization of fungal pathogens. Keeping the intakes free from bird droppings, especially those from pigeons, helps to minimize the concentration of fungal spores entering from the outside.98
Accumulation of dust and moisture within HVAC systems increases the risk for spread of health-careassociated environmental fungi and bacteria. Clusters of infections caused by Aspergillus spp., P. aeruginosa, S. aureus, and Acinetobacter spp. have been linked to poorly maintained and/or malfunctioning air conditioning systems.68, 161, 257, 258 Efforts to limit excess humidity and moisture in the infrastructure and on air-stream surfaces in the HVAC system can minimize the proliferation and dispersion of fungal spores and waterborne bacteria throughout indoor air.259-262 Within the HVAC system, water is present in water-wash units, humidifying boxes, or cooling units. The dual-duct system may also create conditions of high humidity and excess moisture that favor fungal growth in drain pans as well as in fibrous insulation material that becomes damp as a result of the humid air passing over the hot stream and condensing.
If moisture is present in the HVAC system, periods of stagnation should be avoided. Bursts of organisms can be released upon system start-up, increasing the risk of airborne infection.206 Proper engineering of the HVAC system is critical to preventing dispersal of airborne organisms. In one hospital, endophthalmitis caused by Acremonium kiliense infection following cataract extraction in an ambulatory surgical center was traced to aerosols derived from the humidifier water in the ventilation system.206 The organism proliferated because the ventilation system was turned off routinely when the center was not in operation; the air was filtered before humidification, but not afterwards.
Most health-care facilities have contingency plans in case of disruption of HVAC services. These plans include back-up power generators that maintain the ventilation system in high-risk areas (e.g., operating rooms, intensive-care units, negative-and positive-pressure rooms, transplantation units, and oncology units). Alternative generators are required to engage within 10 seconds of a loss of main power. If the ventilation system is out of service, rendering indoor air stagnant, sufficient time must be allowed to clean the air and re-establish the appropriate number of ACH once the HVAC system begins to function again. Air filters may also need to be changed, because reactivation of the system can dislodge substantial amounts of dust and create a transient burst of fungal spores.
Duct cleaning in health-care facilities has benefits in terms of system performance, but its usefulness for infection control has not been conclusively determined. Duct cleaning typically involves using specialized tools to dislodge dirt and a high-powered vacuum cleaner to clean out debris.263 Some duct cleaning services also apply chemical biocides or sealants to the inside surfaces of ducts to minimize fungal growth and prevent the release of particulate matter. The U.S. Environmental Protection Agency (EPA), however, has concerns with the use of sanitizers and/or disinfectants to treat the surfaces of ductwork, because the label indications for most of these products may not specifically include the use of the product in HVAC systems.264 Further, EPA has not evaluated the potency of disinfectants in such applications, nor has the agency examined the potential attendant health and safety risks. The EPA recommends that companies use only those chemical biocides that are registered for use in HVAC systems.264 Although infrequent cleaning of the exhaust ducts in AII areas has been documented as a cause of diminishing negative pressure and a decrease in the air exchange rates,214 no data indicate that duct cleaning, beyond what is recommended for optimal performance, improves indoor air quality or reduces the risk of infection. Exhaust return systems should be cleaned as part of routine system maintenance. Duct cleaning has not been shown to prevent any health problems,265 and EPA studies indicate that airborne particulate levels do not increase as a result of dirty air ducts, nor do they diminish after cleaning, presumably because much of the dirt inside air ducts adheres to duct surfaces and does not enter the conditioned space.265 Additional research is needed to determine if air-duct contamination can significantly increase the airborne infection risk in general areas of health-care facilities.
# Construction, Renovation, Remediation, Repair, and Demolition
# a. General Information
Environmental disturbances caused by construction and/or renovation and repair activities (e.g., disruption of the above-ceiling area, running cables through the ceiling, and structural repairs) in and near health-care facilities markedly increase the airborne Aspergillus spp. spore counts in the indoor air of such facilities, thereby increasing the risk for health-care-associated aspergillosis among high-risk patients. Although one case of health-care-associated aspergillosis is often difficult to link to a specific environmental exposure, the occurrence of temporarily clustered cases increase the likelihood that an environmental source within the facility may be identified and corrected. Construction, renovation, repair, and demolition activities in health-care facilities require substantial planning and coordination to minimize the risk for airborne infection both during projects and after their completion. Several organizations and experts have endorsed a multi-disciplinary team approach (Box 4) to coordinate the various stages of construction activities (e.g., project inception, project implementation, final walk-through, and completion).120, 249, 250, 273-276 Environmental services, employee health, engineering, and infection control must be represented in construction planning and design meetings should be convened with architects and design engineers. The number of members and disciplines represented is a function of the complexity of a project. Smaller, less complex projects and maintenance may require a minimal number of members beyond the core representation from engineering, infection control, environmental services, and the directors of the specialized departments.
# b. Preliminary Considerations
The three major topics to consider before initiating any construction or repair activity are as follows: a) design and function of the new structure or area, b) assessment of environmental risks for airborne disease and opportunities for prevention, and c) measures to contain dust and moisture during construction or repairs. A checklist of design and function considerations can help to ensure that a planned structure or area can be easily serviced and maintained for environmental infection control (Box 5) . , , , -Specifications for the construction, renovation, remodeling, and maintenance of health-care facilities are outlined in the AIA document, Guidelines for Design and Construction o f Hospitals and Health Care Facilities.120, 275
# Box 5. Construction design and function considerations for environmental infection control
Location of sinks and dispensers for handwashing products and hand hygiene products Types of faucets (e.g., aerated vs. non-aerated) Air-handling systems engineered for optimal performance, easy maintenance, and repair ACH and pressure differentials to accommodate special patient-care areas Location of fixed sharps containers Types of surface finishes (e.g., porous vs. non-porous) Well-caulked walls with minimal seams Location of adequate storage and supply areas Appropriate location of medicine preparations areas (e.g., >3 ft. from a sink) Appropriate location and type of ice machines (e.g., preferably ice dispensers rather than ice bins) Appropriate materials for sinks and wall coverings Appropriate traffic flow (e.g., no "dirty" movement through "clean" areas) Isolation rooms with anterooms as appropriate Appropriate flooring (e.g., seamless floors in dialysis units) Sensible use carpeting (e.g., avoiding use of carpeting in special care areas or areas likely to become wet)* Convenient location of soiled utility areas Properly engineered areas for linen services and solid waste management Location of main generator to minimize the risk of system failure from flooding or other emergency Installation guidelines for sheetrock Proactive strategies can help prevent environmentally mediated airborne infections in health-care facilities during demolition, construction, and renovation. The potential presence of dust and moisture and their contribution to health-care-associated infections must be critically evaluated early in the planning of any demolition, construction, renovation, and repairs.120, 250, 251, 273, 274, 276-279 Consideration must extend beyond dust generated by major projects to include dust that can become airborne if disturbed during routine maintenance and minor renovation activities (e.g., exposure of ceiling spaces for inspection; installation of conduits, cable, or sprinkler systems; rewiring; and structural repairs or replacement).273, 276, 277 Other projects that can compromise indoor air quality include construction and repair jobs that inadvertently allow substantial amounts of raw, unfiltered outdoor air to enter the facility (e.g., repair of elevators and elevator shafts) and activities that dampen any structure, area, or item made of porous materials or characterized by cracks and crevices (e.g., sink cabinets in need of repair, carpets, ceilings, floors, walls, vinyl wall coverings, upholstery, drapes, and countertops). , , Molds grow and proliferate on these surfaces when they become and remain wet.21, 120, 250, 266, 270, 272, 280 Scrubbable materials are preferred for use in patient-care areas.
Containment measures for dust and/or moisture control are dictated by the location of the construction site. Outdoor demolition and construction require actions to keep dust and moisture out of the facility (e.g., sealing windows and vents and keeping doors closed or sealed). Containment of dust and moisture generated from construction inside a facility requires barrier structures (either pre-fabricated or constructed of more durable materials as needed) and engineering controls to clean the air in and around the construction or repair site.
# c. Infection-Control Risk Assessment
An infection-control risk assessment (ICRA) conducted before initiating repairs, demolition, construction, or renovation activities can identify potential exposures of susceptible patients to dust and moisture and determine the need for dust and moisture containment measures. This assessment centers on the type and extent of the construction or repairs in the work area but may also need to include adjacent patient-care areas, supply storage, and areas on levels above and below the proposed project. An example of designing an ICRA as a matrix, the policy for performing an ICRA and implementing its results, and a sample permit form that streamlines the communication process are available.281 Knowledge of the air flow patterns and pressure differentials helps minimize or eliminate the inadvertent dispersion of dust that could contaminate air space, patient-care items, and surfaces. , , A recent aspergillosis outbreak among oncology patients was attributed to depressurization of the building housing the HSCT unit while construction was underway in an adjacent building. Pressure readings in the affected building (including 12 of 25 HSCT-patient rooms) ranged from 0.1 Pa-5.8 Pa. Unfiltered outdoor air flowed into the building through doors and windows, exposing patients in the HSCT unit to fungal spores.283 During long-term projects, providing temporary essential services (e.g., toilet facilities) and conveniences (e.g., vending machines) to construction workers within the site will help to minimize traffic in and out of the area. The type of barrier systems necessary for the scope of the project must be defined. 12,120,250,279,284 Depending on the location and extent of the construction, patients may need to be relocated to other areas in the facility not affected by construction dust.51, 285 Such relocation might be especially prudent when construction takes place within units housing immunocompromised patients (e.g., severely neutropenic patients and patients on corticosteroid therapy). Advance assessment of high-risk locations and planning for the possible transport of patients to other departments can minimize delays and waiting time in hallways.51 Although hospitals have provided immunocompromised patients with some form of respiratory protection for use outside their rooms, the issue is complex and remains unresolved until more research can be done. Previous guidance on this issue has been inconsistent.9 Protective respirators (i.e., N95) were well tolerated by patients when used to prevent further cases of constructionrelated aspergillosis in a recent outbreak.283 The routine use of the N95 respirator by patients, however, has not been evaluated for preventing exposure to fungal spores during periods of non-construction. Although health-care workers who would be using the N95 respirator for personal respiratory protect must be fit-tested, there is no indication that either patients or visitors should undergo fit-testing.
Surveillance activities should augment preventive strategies during construction projects. 3, 4 20, 110, 286, 287 By determining baseline levels of health-care-acquired airborne and waterborne infections, infectioncontrol staff can monitor changes in infection rates and patterns during and immediately after construction, renovations, or repairs.3
# d. Air Sampling
Air sampling in health-care facilities may be conducted both during periods of construction and on a periodic basis to determine indoor air quality, efficacy of dust-control measures, or air-handling system performance via parametric monitoring. Parametric monitoring consists of measuring the physical performance of the HVAC system in accordance with the system manufacturer's specifications. A periodic assessment of the system (e.g., air flow direction and pressure, ACH, and filter efficiency) can give assurance of proper ventilation, especially for special care areas and operating rooms.288
Air sampling is used to detect aerosols (i.e., particles or microorganisms). Particulate sampling (i.e., total numbers and size range of particulates) is a practical method for evaluating the infection-control performance of the HVAC system, with an emphasis on filter efficiency in removing respirable particles (<5 pm in diameter) or larger particles from the air. Particle size is reported in terms of the mass median aerodynamic diameter (MMAD), whereas count median aerodynamic diameter (CMAD) is useful with respect to particle concentrations.
Particle counts in a given air space within the health-care facility should be evaluated against counts obtained in a comparison area. Particle counts indoors are commonly compared with the particulate levels of the outdoor air. This approach determines the "rank order" air quality from "dirty" (i.e., the outdoor air) to "clean" (i.e., air filtered through high-efficiency filters [90%-95% filtration]) to "cleanest" (i.e., HEPA-filtered air).288 Comparisons from one indoor area to another may also provide useful information about the magnitude of an indoor air-quality problem. Making rank-order comparisons between clean, highly-filtered areas and dirty areas and/or outdoors is one way to interpret sampling results in the absence of air quality and action level standards.35, 289
In addition to verifying filter performance, particle counts can help determine if barriers and efforts to control dust dispersion from construction are effective. This type of monitoring is helpful when performed at various times and barrier perimeter locations during the project. Gaps or breaks in the barriers' joints or seals can then be identified and repaired. The American Conference of Governmental Industrial Hygienists (ACGIH) has set a threshold limit value-time weighted average (TLV®-TWA) of 10 mg/m3 for nuisance dust that contains no asbestos and <1% crystalline silica.290 Alternatively, OSHA has set permissible exposure limits (PELs) for inert or nuisance dust as follows: respirable fraction at 5 mg/m3 and total dust at 15 mg/m3.291 Although these standards are not measures of a bioaerosol, they are used for indoor air quality assessment in occupational settings and may be useful criteria in construction areas. Application of ACGIH guidance to health-care settings has not been standardized, but particulate counts in health-care facilities are likely to be well below this threshold value and approaching clean-room standards in certain care areas (e.g., operating rooms).100 Particle counters and anemometers are used in particulate evaluation. The anemometer measures air flow velocity, which can be used to determine sample volumes. Particulate sampling usually does not require microbiology laboratory services for the reporting of results.
Microbiologic sampling of air in health-care facilities remains controversial because of currently unresolved technical limitations and the need for substantial laboratory support (Box 6). Infectioncontrol professionals, laboratorians, and engineers should determine if microbiologic and/or particle sampling is warranted and assess proposed methods for sampling. The most significant technical limitation of air sampling for airborne fungal agents is the lack of standards linking fungal spore levels with infection rates. Despite this limitation, several health-care institutions have opted to use microbiologic sampling when construction projects are anticipated and/or underway in efforts to assess the safety of the environment for immunocompromised patients.35, 289 Microbiologic air sampling should be limited to assays for airborne fungi; of those, the thermotolerant fungi (i.e., those capable of growing at 95°F-98.6°F [35°C-37°C]) are of particular concern because of their pathogenicity in immunocompromised hosts.35 Use of selective media (e.g., Sabouraud dextrose agar and inhibitory mold agar) helps with the initial identification of recovered organisms.
Microbiologic sampling for fungal spores performed as part of various airborne disease outbreak investigations has also been problematic. 18, 49, 106, m ' 112, 289 The precise source of a fungus is often difficult to trace with certainty, and sampling conducted after exposure may neither reflect the circumstances that were linked to infection nor distinguish between health-care-acquired and community-acquired infections. Because fungal strains may fluctuate rapidly in the environment, health-care-acquired Aspergillus spp. infection cannot be confirmed or excluded if the infecting strain is not found in the health-care setting.287 Sensitive molecular typing methods (e.g., randomly amplified polymorphic DNA (RAPD) techniques and a more recent DNA fingerprinting technique that detects restriction fragment length polymorphisms in fungal genomic DNA) to identify strain differences among Aspergillus spp., however, are becoming increasingly used in epidemiologic investigations of health-care-acquired fungal infection (A.Streifel, University of Minnesota, 2000).68, 110, 286, 287, 292-296 During case cluster evaluation, microbiologic sampling may provide an isolate from the environment for molecular typing and comparison with patient isolates. Therefore, it may be prudent for the clinical laboratory to save Aspergillus spp. isolated from colonizations and invasive disease cases among patients in PE, oncology, and transplant services for these purposes. Sedimentation methods using settle plates and volumetric sampling methods using solid impactors are commonly employed when sampling air for bacteria and fungi. Settle plates have been used by numerous investigators to detect airborne bacteria or to measure air quality during medical procedures (e.g., surgery * Contamination of water pipes during demolition activities has been associated with health-care-associated transmission of Legionella spp.305 + When health-care facilities have immunosuppressed patients in their census, telephoning the city building department each month to find out if buildings are scheduled for demolition is prudent.
Minimizing the entry of outside dust into the HVAC system is crucial in reducing the risk for airborne contaminants. Facility engineers should be consulted about the potential impact of shutting down the system or increasing the filtration. Selected air handlers, especially those located close to excavation sites, may have to be shut off temporarily to keep from overloading the system with dust and debris.
Care is needed to avoid significant facility-wide reductions in pressure differentials that may cause the building to become negatively pressured relative to the outside. To prevent excessive particulate overload and subsequent reductions in effectiveness of intake air systems that cannot be shut off temporarily, air filters must be inspected frequently for proper installation and function. Excessive dust penetration can be avoided if recirculated air is maximally utilized while outdoor air intakes are shut down. Scheduling demolition and excavation during the winter, when Aspergillus spp. spores may be present in lower numbers, can help, although seasonal variations in spore density differ around the world.92, 287, 303 Dust control can be managed by misting the dirt and debris during heavy dust generating activities. To decrease the amount of aerosols from excavation and demolition projects, nearby windows, especially in areas housing immunocompromised patients, can be sealed and window and door frames caulked or weather-stripped to prevent dust intrusion.50, 301, 306 Monitoring for adherence to these control measures throughout demolition or excavation is crucial. Diverting pedestrian traffic away from the construction sites decreases the amount of dust tracked back into the health-care facility and minimizes exposure of high-risk patients to environmental pathogens. Additionally, closing entrances near construction or demolition sites might be beneficial; if this is not practical, creating an air lock (i.e., pressurizing the entry way) is another option.
# f. Internal Demolition, Construction, Renovations, and Repairs
The focus of a properly implemented infection-control program during interior construction and repairs is containment of dust and moisture. This objective is achieved by a) educating construction workers about the importance of control measures; b) preparing the site; c) notifying and issuing advisories for staff, patients, and visitors; d) moving staff and patients and relocating patients as needed; e) issuing standards of practice and precautions during activities and maintenance; f) monitoring for adherence to control measures during construction and providing prompt feedback about lapses in control; g) monitoring HVAC performance; h) implementing daily clean-up, terminal cleaning and removal of debris upon completion; and i) ensuring the integrity of the water system during and after construction. These activities should be coordinated with engineering staff and infection-control professionals.
Physical barriers capable of containing smoke and dust will confine dispersed fungal spores to the construction zone. , , , The specific type of physical barrier required depends on the project's scope and duration and on local fire codes. Short-term projects that result in minimal dust dispersion (e.g., installation of new cables or wiring above ceiling tiles) require only portable plastic enclosures with negative pressure and HEPA filtration of the exhaust air from the enclosed work area. The placement of a portable industrial-grade HEPA filter device capable of filtration rate of 300-800 ft3/min. adjacent to the work area will help to remove fungal spores, but its efficacy is dependent on the supplied ACH and size of the area. If the project is extensive but short-term, dust-abatement, fire-resistant plastic curtains (e.g., Visqueen®) may be adequate. These should be completely airtight and sealed from ceiling to floor with overlapping curtains;276, 277, 309 holes, tears, or other perforations should be repaired promptly with tape. A portable, industrial-grade HEPA filter unit on continuous operation is needed within the contained area, with the filtered air exhausted to the outside of the work zone. Patients should not remain in the room when dust-generating activities are performed. Tools to assist the decision-making process regarding selection of barriers based on an ICRA approach are available.281 More elaborate barriers are indicated for long-term projects that generate moderate to large amounts of dust. These barrier structures typically consist of rigid, noncombustible walls constructed from sheet rock, drywall, plywood, or plaster board and covered with sheet plastic (e.g., Visqueen®). Barrier requirements to prevent the intrusion of dust into patient-care areas include a) installing a plastic dust abatement curtain before construction of the rigid barrier; b) sealing and taping all joint edges including the top and bottom; c) extending the barrier from floor to floor, which takes into account the space [approximately 2-8 ft.] above the finished, lay-down ceiling; and d) fitting or sealing any temporary doors connecting the construction zone to the adjacent area. (See Box 7 for a list of the various construction and repair activities that require the use of some type of barrier.) Dust and moisture abatement and control rely primarily on the impermeable barrier containment approach; as construction continues, numerous opportunities can lead to dispersion of dust to other areas of the health-care facility. Infection-control measures that augment the use of barrier containment should be undertaken (Table 9). Dust-control measures for clinical laboratories are an essential part of the infection-control strategy during hospital construction or renovation. Use of plastic or solid barriers may be needed if the ICRA determines that air flow from construction areas may introduce airborne contaminants into the laboratory space. In one facility, pseudofungemia clusters attributed to Aspergillus spp. and Penicillium spp. were linked to improper air flow patterns and construction projects adjacent to the laboratory; intrusion of dust and spores into a biological safety cabinet from construction activity immediately next to the cabinet resulted in a cluster of cultures contaminated with Aspergillus niger310' 311 Reportedly, no barrier containment was used and the HEPA filtration system was overloaded with dust. In addition, an outbreak of pseudobacteremia caused by Bacillus spp. occurred in another hospital during construction above a storage area for blood culture bottles.207 Airborne spread of Bacillus spp. spores resulted in contamination of the bottles' plastic lids, which were not disinfected or handled with proper aseptic technique prior to collection of blood samples. Control dust in air and on surfaces. 1. Monitor the construction area daily for compliance with the infection-control plan. 2. Protective outer clothing for construction workers should be removed before entering clean areas. 3. Use mats with tacky surfaces within the construction zone at the entry; cover sufficient area so that both feet make contact with the mat while walking through the entry. 4. Construct an anteroom as needed where coveralls can be donned and removed. 5. Clean the construction zone and all areas used by construction workers with a wet mop. 6. If the area is carpeted, vacuum daily with a HEPA-filtered-equipped vacuum. 7. Provide temporary essential services (e.g., toilets) and worker conveniences (e.g, vending machines) in the construction zone as appropriate. 8. Damp-wipe tools if removed from the construction zone or left in the area. 9. Ensure that construction barriers remain well sealed; use particle sampling as needed. 10. Ensure that the clinical laboratory is free from dust contamination.
# 34
# Infection-control measure
Steps for implementation
# a. Protective Environments (PE)
Although the exact configuration and specifications of PEs might differ among hospitals, these care areas for high-risk, immunocompromised patients are designed to minimize fungal spore counts in air by maintaining a) filtration of incoming air by using central or point-of-use HEPA filters; b) directed room air flow [i.e., from supply on one side of the room, across the patient, and out through the exhaust on the opposite side of the room]; c) positive room air pressure of 2.5 Pa [0.01" water gauge] relative to the corridor; d) well-sealed rooms; and e) >12 ACH.44, 120, 251, 254, 316-319 Air flow rates must be adjusted accordingly to ensure sufficient ACH, and these rates vary depending on certain factors (e.g., room air leakage area). For example, to provide >12 ACH in a typical patient room with 0.5 sq. ft. air leakage, the air flow rate will be minimally 125 cubic feet/min (cfm). , Higher air flow rates may be needed. A general ventilation diagram for a positive-pressure room is given in Figure 2. Directed room air flow in PE rooms is not laminar; parallel air streams are not generated. Studies attempting to demonstrate patient benefit from laminar air flow in a PE setting are equivocal.316, 318, 319, 322 " 327
Air flow direction at the entrances to these areas should be maintained and verified, preferably on a daily basis, using either a visual means of indication (e.g., smoke tubes and flutter strips) or manometers. Permanent installation of a visual monitoring device is indicated for new PE construction and renovation.120 Facility service structures can interfere with the proper unidirectional air flow from the patients' rooms to the adjacent corridor. In one outbreak investigation, Aspergillus spp. infections in a critical care unit may have been associated with a pneumatic specimen transport system, a textile disposal duct system, and central vacuum lines for housekeeping, all of which disrupted proper air flow from the patients' rooms to the outside and allowed entry of fungal spores into the unit (M. McNeil, CDC, 2000). Appendix E).
Salient features of engineering controls for AII areas include a) use of negative pressure rooms with close monitoring of air flow direction using manometers or temporary or installed visual indicators [e.g., smoke tubes and flutter strips] placed in the room with the door closed; b) minimum 6 ACH for existing facilities, >12 ACH for areas under renovation or for new construction; and c) air from negative pressure rooms and treatment rooms exhausted directly to the outside if possible.4, 120, 248 As with PE, airflow rates need to be determined to ensure the proper numbers of ACH. , AII rooms can be constructed either with (Figure 3) or without (Figure 4) an anteroom. When the recirculation of air from AII rooms is unavoidable, HEPA filters should be installed in the exhaust duct leading from the room to the general ventilation system. In addition to UVGI fixtures in the room, UVGI can be placed in the ducts as an adjunct measure to HEPA filtration, but it can not replace the HEPA filter. The pressure differential of an anteroom can be positive or negative relative to the patient in the room.120 An anteroom can act as an airlock (Figure 4). If the anteroom is positive relative to the air space in the patient's room, staff members do not have to mask prior to entry into the anteroom if air is directly exhausted to the outside and a minimum of 10 ACH (Figure 4, top diagram).120 When an anteroom is negative relative to both the AII room and the corridor, health-care workers must mask prior to entering the anteroom (Figure 4, bottom diagram). If an AII room with an anteroom is not available, use of a portable, industrial-grade HEPA filter unit may help to increase the number of ACHs while facilitating the removal of fungal spores; however, a fresh air source must be present to achieve the proper air exchange rate. Incoming ambient air should receive HEPA filtration.
# c. Operating Rooms
Operating room air may contain microorganisms, dust, aerosol, lint, skin squamous epithelial cells, and respiratory droplets. The microbial level in operating room air is directly proportional to the number of people moving in the room.351 One study documented lower infection rates with coagulase-negative staphylococci among patients when operating room traffic during the surgical procedure was limited.352 Therefore, efforts should be made to minimize personnel traffic during operations. Outbreaks of SSIs caused by group A beta-hemolytic streptococci have been traced to airborne transmission from colonized operating-room personnel to patients.150154 Several potential health-care-associated pathogens (e.g., Staphylococcus aureus and Staphylococcus epidermidis) and drug-resistant organisms have also been recovered from areas adjacent to the surgical field,353 but the extent to which the presence of bacteria near the surgical field influences the development of postoperative SSIs is not clear. 354 Proper ventilation, humidity (<68%), and temperature control in the operating room is important for the comfort of surgical personnel and patients, but also in preventing environmental conditions that encourage growth and transmission of microorganisms.355 Operating rooms should be maintained at positive pressure with respect to corridors and adjacent areas.356 Operating rooms typically do not have a variable air handling system. Variable air handling systems are permitted for use in operating rooms only if they continue to provide a positive pressure with respect to the corridors and adjacent areas and the proper ACHs are maintained when the room is occupied. Conventional operating-room ventilation systems produce a minimum of about 15 ACH of filtered air for thermal control, three (20%) of which must be fresh air. , , Air should be introduced at the ceiling and exhausted near the floor. , Laminar airflow and UVGI have been suggested as adjunct measures to reduce SSI risk for certain operations. Laminar airflow is designed to move particle-free air over the aseptic operating field at a uniform velocity (0. The portable unit should be turned off while the surgical procedure is underway and turned on following extubation. Portable HEPA filter units previously placed in construction areas may be used in subsequent patient care, provided that all internal and external surfaces are cleaned and the filter's performance is verified with appropriate particle testing and is changed, if needed.
# Other Aerosol Hazards in Health-Care Facilities
In addition to infectious bioaerosols, several crucial non-infectious, indoor air-quality issues must be addressed by health-care facilities. The presence of sensitizing and allergenic agents and irritants in the workplace (e.g., ethylene oxide, glutaraldehyde, formaldehyde, hexachlorophene, and latex allergens375) is increasing. Asthma and dermatologic and systemic reactions often result with exposure to these chemicals. Anesthetic gases and aerosolized medications (e.g., ribavirin, pentamidine, and aminoglycosides) represent some of the emerging potentially hazardous exposures to health-care workers. Containment of the aerosol at the source is the first level of engineering control, but personal protective equipment (e.g., masks, respirators, and glove liners) that distances the worker from the hazard also may be needed.
Laser plumes and surgical smoke represent another potential risk for health-care workers.376-378 Lasers transfer electromagnetic energy into tissues, resulting in the release of a heated plume that includes particles, gases, tissue debris, and offensive smells. One concern is that aerosolized infectious material in the laser plume might reach the nasal mucosa of surgeons and adjacent personnel. Although some viruses (i.e., varicella-zoster virus, pseudorabies virus, and herpes simplex virus) do not aerosolize efficiently, , other viruses and bacteria (e.g., human papilloma virus [HPV], HIV, coagulasenegative Staphylococcus, Corynebacterium spp., and Neisseria spp.) have been detected in laser plumes. -The presence of an infectious agent in a laser plume may not, however, be sufficient to cause disease from airborne exposure, especially if the normal mode of transmission for the agent is not airborne. No evidence indicated that HIV or hepatitis B virus (HBV) has been transmitted via aerosolization and inhalation. 388 Although continuing studies are needed to fully evaluate the risk of laser plumes to surgical personnel, the prevention measures in these other guidelines should be followed: a) NIOSH recommendations,378 b) the Recommended Practices for Laser Safety in Practice Settings developed by the Association of periOperative Registered Nurses [AORN],389 c) the assessments of ECRI,390-392 and d) the ANSI standard.393 These guidelines recommend the use of a) respirators (N95 or N100) or full face shields and masks,260 b) central wall-suction units with in-line filters to collect particulate matter from minimal plumes, and c) dedicated mechanical smoke exhaust systems with a high-efficiency filter to remove large amounts of laser plume. Although transmission of TB has occurred as a result of abscess management practices that lacked airborne particulate control measures and respiratory protection, use of a smoke evacuator or needle aspirator and a high degree of clinical awareness can help protect health care workers when excising and draining an extrapulmonary TB abscess.137
# D. Water 1. Modes of Transmission of Waterborne Diseases
Moist environments and aqueous solutions in health-care settings have the potential to serve as reservoirs for waterborne microorganisms. Under favorable environmental circumstances (e.g., warm temperature and the presence of a source of nutrition), many bacterial and some protozoal microorganisms can either proliferate in active growth or remain for long periods in highly stable, environmentally resistant (yet infectious) forms. Modes of transmission for waterborne infections include a) direct contact [e.g., that required for hydrotherapy]; b) ingestion of water [e.g., through consuming contaminated ice]; c) indirect-contact transmission [e.g., from an improperly reprocessed medical device];6 d) inhalation of aerosols dispersed from water sources;3 and e) aspiration of contaminated water. The first three modes of transmission are commonly associated with infections caused by gram-negative bacteria and nontuberculous mycobacteria (NTM). Aerosols generated from water sources contaminated with Legionella spp. often serve as the vehicle for introducing legionellae to the respiratory tract.
# Waterborne Infectious Diseases in Health-Care Facilities a. Legionellosis
Legionellosis is a collective term describing infection produced by Legionella spp., whereas Legionnaires disease is a multi-system illness with pneumonia.395 The clinical and epidemiologic aspects of these diseases (Table 11) are discussed extensively in another guideline.3 Although Legionnaires disease is a respiratory infection, infection-control measures intended to prevent health care-associated cases center on the quality of water-the principal reservoir for Legionella spp. 12 and 13). Immunocompromised patients are at greatest risk of developing infection. Medical conditions associated with these bacterial agents range from colonization of the respiratory and urinary tracts to deep, disseminated infections that can result in pneumonia and bloodstream bacteremia. Colonization by any of these organisms often precedes the development of infection. The use of tap water in medical care (e.g., in direct patient care, as a diluent for solutions, as a water source for medical instruments and equipment, and during the final stages of instrument disinfection) therefore presents a potential risk for exposure. Colonized patients also can serve as a source of contamination, particularly for moist environments of medical equipment (e.g., ventilators).
In addition to Legionella spp., Pseudomonas aeruginosa and Pseudomonas spp. are among the most clinically relevant, gram-negative, health-care-associated pathogens identified from water. These and other gram-negative, non-fermentative bacteria have minimal nutritional requirements (i.e., these organisms can grow in distilled water) and can tolerate a variety of physical conditions. These attributes are critical to the success of these organisms as health-care-associated pathogens. Measures to prevent the spread of these organisms and other waterborne, gram-negative bacteria include hand hygiene, glove use, barrier precautions, and eliminating potentially contaminated environmental reservoirs.464, 465
# References
# Clinical syndromes and diseases
Septicemia, pneumonia (particularly ventilator-associated), chronic respiratory infections among cystic fibrosis patients, urinary tract infections, skin and soft-tissue infections (e.g., tissue necrosis and hemorrhage), burn-wound infections, folliculitis, endocarditis, central nervous system infections (e.g., meningitis and abscess), eye infections, and bone and joint infections 466-503 Patients and health-care workers contribute significantly to the environmental contamination of surfaces and equipment with Acinetobacter spp. and Enterobacter spp., especially in intensive care areas, because of the nature of the medical equipment (e.g., ventilators) and the moisture associated with this equipment.549, 571, 572, 585 Hand carriage and hand transfer are commonly associated with health-careassociated transmission of these organisms and for S. marcescens.586 Enterobacter spp. are primarily spread in this manner among patients by the hands of health-care workers.567, 587 Acinetobacter spp. have been isolated from the hands of 4%-33% of health-care workers in some studies,585-590 and transfer of an epidemic strain of Acinetobacter from patients' skin to health-care workers' hands has been demonstrated experimentally.591 Acinetobacter infections and outbreaks have also been attributed to medical equipment and materials (e.g., ventilators, cool mist humidifiers, vaporizers, and mist tents) that may have contact with water of uncertain quality (e.g., rinsing a ventilator circuit in tap water).549-556 Strict adherence to hand hygiene helps prevent the spread of both Acinetobacter spp. and 577, 592 Enterobacter spp. , Acinetobacter spp. have also been detected on dry environmental surfaces (e.g., bed rails, counters, sinks, bed cupboards, bedding, floors, telephones, and medical charts) in the vicinity of colonized or infected patients; such contamination is especially problematic for surfaces that are frequently touched.557-564 In two studies, the survival periods of Acinetobacter baumannii and Acinetobacter calcoaceticus on dry surfaces approximated that for S. aureus (e.g., 26-27 days).593, 594 Because Acinetobacter spp. may come from numerous sources at any given time, laboratory investigation of health-care-associated Acinetobacter infections should involve techniques to determine biotype, antibiotype, plasmid profile, and genomic fingerprinting (i.e., macrorestriction analysis) to accurately identify sources and modes of transmission of the organism(s).595 have also demonstrated some resistance to formaldehyde and glutaraldehyde, which has posed problems for reuse of hemodialyzers.31 The ability of NTM to form biofilms at fluid-surface interfaces (e.g., interior surfaces of water pipes) contributes to the organisms' resistance to chemical inactivation and provides a microenvironment for growth and proliferation.636, 637
# Modes of transmission
# c. Infections and Pseudo-Infections Due to Nontuberculous Mycobacteria
# d. Cryptosporidiosis
Cryptosporidium parvum is a protozoan parasite that causes self-limiting gastroenteritis in normal hosts but can cause severe, life-threatening disease in immunocompromised patients. First recognized as a human pathogen in 1976, C. parvum can be present in natural and finished waters after fecal contamination from either human or animal sources.638-641
The health risks associated with drinking potable water contaminated with minimal numbers of C. parvum oocysts are unknown.642 It remains to be determined if immunosuppressed persons are more susceptible to lower doses of oocysts than are immunocompetent persons. One study demonstrated that a median 50% infectious dose (ID50) of 132 oocysts of calf origin was sufficient to cause infection among healthy volunteers. 643 In a second study, the same researchers found that oocysts obtained from infected foals (newborn horses) were infectious for human volunteers at median ID50 of 10 oocysts, indicating that different strains or species of Cryptosporidium may vary in their infectivity for humans.644 In a small study population of 17 healthy adults with pre-existing antibody to C. parvum, the ID50 was determined to be 1,880 oocysts, more than 20-fold higher than in seronegative persons. 645 These data suggest that pre-existing immunity derived from previous exposures to Cryptosporidium offers some protection from infection and illness that ordinarily would result from exposure to low numbers of oocysts.645, 646
Oocysts, particularly those with thick walls, are environmentally resistant, but their survival under natural water conditions is poorly understood. Under laboratory conditions, some oocysts remain viable and infectious in cold (41°F [5°C]) for months. 641 The prevalence of Cryptosporidium in the U.S. drinking water supply is notable. Two surveys of approximately 300 surface water supplies revealed that 55%-77% of the water samples contained Cryptosporidium oocysts.647, 648 Because the oocysts are highly resistant to common disinfectants (e.g., chlorine) used to treat drinking water, filtration of the water is important in reducing the risk of waterborne transmission. Coagulation-floculation and sedimentation, when used with filtration, can collectively achieve approximately a 2.5 log10 reduction in the number of oocysts.649 However, outbreaks have been associated with both filtered and unfiltered drinking water systems (e.g., the 1993 outbreak in Milwaukee, Wisconsin that affected 400,000 people).641, 650-652 The presence of oocysts in the water is not an absolute indicator that infection will occur when the water is consumed, nor does the absence of detectable oocysts guarantee that infection will not occur. Health-care-associated outbreaks of cryptosporidiosis primarily have been described among groups of elderly patients and immunocompromised persons.653
# Water Systems in Health-Care Facilities a. Basic Components andPoint-of-Use Fixtures
Treated municipal water enters a health-care facility via the water mains and is distributed throughout the building(s) by a network of pipes constructed of galvanized iron, copper, and polyvinylchloride (PVC). The pipe runs should be as short as is practical. Where recirculation is employed, the pipe runs should be insulated and long dead legs avoided in efforts to minimize the potential for water stagnation, which favors the proliferation of Legionella spp. and NTM. In high-risk applications (e.g., PE areas for severely immunosuppressed patients), insulated recirculation loops should be incorporated as a design feature. Recirculation loops prevent stagnation and insulation maintains return water temperature with minimal loss.
Each water service main, branch main, riser, and branch (to a group of fixtures) has a valve and a means to reach the valves via an access panel.120 Each fixture has a stop valve. Valves permit the isolation of a portion of the water system within a facility during repairs or maintenance. Vacuum breakers and other similar devices in the lines prevent water from back-flowing into the system. All systems that supply water should be evaluated to determine risk for potential back siphonage and cross connections.
Health-care facilities generate hot water from municipal water using a boiler system. Hot water heaters and storage vessels for such systems should have a drainage facility at the lowest point, and the heating element should be located as close as possible to the bottom of the vessel to facilitate mixing and to prevent water temperature stratification. Those hot or cold water systems that incorporate an elevated holding tank should be inspected and cleaned annually. Lids should fit securely to exclude foreign materials.
The most common point-of-use fixtures for water in patient-care areas are sinks, faucets, aerators, showers, and toilets; eye-wash stations are found primarily in laboratories. The potential for these fixtures to serve as a reservoir for pathogenic microorganisms has long been recognized (Table 15). Although aerosols are produced with toilet flushing,662, 663 no epidemiologic evidence suggests that these aerosols pose a direct infection hazard.
Although not considered a standard point-of-use fixture, decorative fountains are being installed in increasing numbers in health-care facilities and other public buildings. Aerosols from a decorative fountain have been associated with transmission of Legionella pneumophila serogroup 1 infection to a small cluster of older adults.664 This hotel lobby fountain had been irregularly maintained, and water in the fountain may have been heated by submersed lighting, all of which favored the proliferation of Legionella in the system.664 Because of the potential for generations of infectious aerosols, a prudent prevention measure is to avoid locating these fixtures in or near high-risk patient-care areas and to adhere to written policies for routine fountain maintenance.120
# b. Water Temperature and Pressure
Hot water temperature is usually measured at the point of use or at the point at which the water line enters equipment requiring hot water for proper operation.120 Generally, the hot water temperature in hospital patient-care areas is no greater than a temperature within the range of 105°F-120°F (40.6°C-49°C), depending on the AIA guidance issued at the year in which the facility was built.120 Hot water temperature in patient-care areas of skilled nursing-care facilities is set within a slightly lower range of 95°F-110°F (35°C-43.3°C) depending on the AIA guidance at the time of facility construction.120 Many states have adopted a temperature setting in these ranges into their health-care regulations and building codes. ASHRAE, however, has recommended higher settings.661 Steam jets or booster heaters are usually needed to meet the hot water temperature requirements in certain service areas of the hospital (e.g., the kitchen [120°F (49°C)] or the laundry [160°F (71°C)]).120 Additionally, water lines may need to be heated to a particular temperature specified by manufacturers of specific hospital equipment. Hot-water distribution systems serving patient-care areas are generally operated under constant recirculation to provide continuous hot water at each hot-water outlet.120 If a facility is or has a hemodialysis unit, then continuously circulated, cold treated water is provided to that unit.120
To minimize the growth and persistence of gram-negative waterborne bacteria (e.g., thermophilic NTM and Legionella spp.),627, 703 709 cold water in health-care facilities should be stored and distributed at temperatures below 68°F (20°C); hot water should be stored above 140°F (60°C) and circulated with a minimum return temperature of 124°F (51°C),661 or the highest temperature specified in state regulations and building codes. If the return temperature setting of 124°F (51°C) is permitted, then installation of preset thermostatic mixing valves near the point-of-use can help to prevent scalding.
Valve maintenance is especially important in preventing valve failure, which can result in scalding. New shower systems in large buildings, hospitals, and nursing homes should be designed to permit mixing of hot and cold water near the shower head. The warm water section of pipe between the control valve and shower head should be self-draining. Where buildings can not be retrofitted, other approaches to minimize the growth of Legionella spp. include a) periodically increasing the temperature to at least 150°F [66°C] at the point of use [i.e., faucets] and b) adding additional chlorine and flushing the water.661, 710, 711 Systems should be inspected annually to ensure that thermostats are functioning properly.
Adequate water pressure ensures sufficient water supplies for a) direct patient care; b) operation of water-cooled instruments and equipment [e.g., lasers, computer systems, telecommunications systems, and automated endoscope reprocessors712]; c) proper function of vacuum suctioning systems; d) indoor climate control; and e) fire-protection systems. Maintaining adequate pressure also helps to ensure the integrity of the piping system.
# c. Infection-Control Impact of Water System Maintenance and Repair
Corrective measures for water-system failures have not been studied in well-designed experiments; these measures are instead based on empiric engineering and infection-control principles. Health-care facilities can occasionally sustain both intentional cut-offs by the municipal water authority to permit new construction project tie-ins and unintentional disruptions in service when a water main breaks as a result of aging infrastructure or a construction accident. Vacuum breakers or other similar devices can prevent backflow of water in the facility's distribution system during water-disruption emergencies.11 To be prepared for such an emergency, all health-care facilities need contingency plans that identify a) the total demand for potable water, b) the quantity of replacement water [e.g., bottled water] required for a minimum of 24 hours when the water system is down, c) mechanisms for emergency water distribution, and 4) procedures for correcting drops in water pressure that affect operation of essential devices and equipment that are driven or cooled by a water system [Table 16].713 * Arrange to have a contingency provision of these services from another resource, if possible (e.g., another health-care facility or contractor). + Some cooling towers may use a potable water source, but most units use non-potable water. § This item is included in the table under the assumption that electrical power is available during the water emergency.
Detailed, up-to-date plans for hot and cold water piping systems should be readily available for maintenance and repair purposes in case of system problems. Opening potable water systems for repair or construction and subjecting systems to water-pressure changes can result in water discoloration and dramatic increases in the concentrations of Legionella spp. and other gram-negative bacteria. The maintenance of a chlorine residual at all points within the piping system also offers some protection from entry of contamination to the pipes in the event of inadvertent cross-connection between potable and non-potable water lines. As a minimum preventive measure, ASHRAE recommends a thorough flushing of the system.661 High-temperature flushing or hyperchlorination may also be appropriate strategies to decrease potentially high concentrations of waterborne organisms. The decision to pursue either of these remediation strategies, however, should be made on a case-by-case basis. If only a portion of the system is involved, high temperature flushing or chlorination can be used on only that portion of the system.661
When shock decontamination of hot water systems is necessary (e.g., after disruption caused by construction and after cross-connections), the hot water temperature should be raised to 160°F-170°F (71°C-77°C) and maintained at that level while each outlet around the system is progressively flushed.
A minimum flush time of 5 minutes has been recommended;3 the optimal flush time is not known, however, and longer flush times may be necessary.714 The number of outlets that can be flushed simultaneously depends on the capacity of the water heater and the flow capability of the system. Appropriate safety procedures to prevent scalding are essential. When possible, flushing should be performed when the fewest building occupants are present (e.g., during nights and weekends).
When thermal shock treatment is not possible, shock chlorination may serve as an alternative method.661 Experience with this method of decontamination is limited, however, and high levels of free chlorine can corrode metals. Chlorine should be added, preferably overnight, to achieve a free chlorine residual of at least 2 mg/L (2 ppm) throughout the system.661 This may require chlorination of the water heater or tank to levels of 20-50 mg/L (20-50 ppm). The pH of the water should be maintained at 7.0-8.0.661 After completion of the decontamination, recolonization of the hot water system is likely to occur unless proper temperatures are maintained or a procedure such as continuous supplemental chlorination is continued.
Interruptions of the water supply and sewage spills are situations that require immediate recovery and remediation measures to ensure the health and safety of patients and staff.715 When delivery of potable water through the municipal distribution system has been disrupted, the public water supplier must issue a "boil water" advisory if microbial contamination presents an immediate public health risk to customers. The hospital engineer should oversee the restoration of the water system in the facility and clear it for use when appropriate. Hospitals must maintain a high level of surveillance for waterborne disease among patients and staff after the advisory is lifted.642
Flooding from either external (e.g., from a hurricane) or internal sources (e.g., a water system break) usually results in property damage and a temporary loss of water and sanitation.716-718 JCAHO requires all hospitals to have plans that address facility response for recovery from both internal and external disasters. , The plans are required to discuss a) general emergency preparedness, b) staffing, c) regional planning among area hospitals, d) emergency supply of potable water, e) infection control and medical services needs, f) climate control, and g) remediation. The basic principles of structural recovery from flooding are similar to those for recovery from sewage contamination (Box 9 and 10). Following a major event (e.g., flooding), facilities may elect to conduct microbial sampling of water after the system is restored to verify that water quality has been returned to safe levels (<500 CFU/mL, heterotrophic plate count). This approach may help identify point-of-use fixtures that may harbor contamination as a result of design or engineering features.720 Medical records should be allowed to dry and then either photocopied or placed in plastic covers before returning them to the record.
Moisture meters can be used to assess water-damaged structural materials. If porous structural materials for walls have a moisture content of >20% after 72 hours, the affected material should be removed.266, , The management of water-damaged structural materials is not strictly limited to major water catastrophes (e.g., flooding and sewage intrusions); the same principles are used to evaluate the damage from leaking roofs, point-of-use fixtures, and equipment. Additional sources of moisture include condensate on walls from boilers and poorly engineered humidification in HVAC systems.
An exception to these recommendations is made for hemodialysis units where water is further treated either by portable water treatment or large-scale water treatment systems usually involving reverse osmosis (RO). In the United States, >97% of dialysis facilities use RO treatment for their water.721 However, changing pre-treatment filters and disinfecting the system to prevent colonization of the RO membrane and microbial contamination down-stream of the pre-treatment filter are prudent measures.
# Box 10. Contingency planning for flooding G eneral em ergency preparedness
Ensure that emergency electrical generators are not located in flood-prone areas of the facility. Develop alternative strategies for moving patients, water containers, medical records, equipment, and supplies in the event that the elevators are inoperable. Establish in advance a centralized base of operations with batteries, flashlights, and cellular phones. Ensure sufficient supplies of sandbags to place at the entrances and the area around boilers, incinerators, and generators. Establish alternative strategies for bringing core employees to the facility if high water prevents travel.
# Staffing P atterns
Temporarily reassign licensed staff as needed to critical care areas to provide manual ventilation and to perform vital assessments on patients. Designate a core group of employees to remain on site to keep all services operational if the facility remains open. Train all employees in emergency preparedness procedures.
# R egional plan n in g am ong are facilities fo r d isaster m anagem ent
Incorporate community support and involvement (e.g., media alerts, news, and transportation). Develop in advance strategies for transferring patients, as needed. Develop strategies for sharing supplies and providing essential services among participating facilities (e.g., central sterile department services, and laundry services). Identify sources for emergency provisions (e.g., blood, emergency vehicles, and bottled water).
# M edical services and infection control
Use alcohol-based hand rubs in general patient-care areas. Postpone elective surgeries until full services are restored, or transfer these patients to other facilities. Consider using portable dialysis machines.+ Provide an adequate supply of tetanus and hepatitis A immunizations for patients and staff.
# C lim ate control
Provide adequate water for cooling towers. § * Material in this box was compiled from references 713, 716-719. + Portable dialysis machines require less water compared to the larger units situated in dialysis settings.
§ Water for cooling towers may need to be trucked in, especially if the tower uses a potable water source.
# Strategies for Controlling Waterborne Microbial Contamination a. Supplemental Treatment of Water with Heat and/or Chemicals
In addition to using supplemental treatment methods as remediation measures after inadvertent contamination of water systems, health-care facilities sometimes use special measures to control waterborne microorganisms on a sustained basis. This decision is most often associated with outbreaks of legionellosis and subsequent efforts to control legionellae,722 although some facilities have tried supplemental measures to better control thermophilic NTM.627
The primary disinfectant for both cold and hot water systems is chlorine. However, chlorine residuals are expected to be low, and possibly nonexistent, in hot water tanks because of extended retention time in the tank and elevated water temperature. Flushing, especially that which removes sludge from the bottom of the tank, probably provides the most effective treatment of water systems. Unlike the situation for disinfecting cooling towers, no equivalent recommendations have been made for potable water systems, although specific intervention strategies have been published. , The principal approaches to disinfection of potable systems are heat flushing using temperatures 160°F-170°F (71°-77°C), hyperchlorination, and physical cleaning of hot-water tanks.3, 403, 661 Potable systems are easily recolonized and may require continuous intervention (e.g., raising of hot water temperatures or continuous chlorination).403, 711 Chlorine solutions lose potency over time, thereby rendering the stocking of large quantities of chlorine impractical. Some hospitals with hot water systems identified as the source of Legionella spp. have performed emergency decontamination of their systems by pulse (i.e., one-time) thermal disinfection/superheating or hyperchlorination. , , , After either of these procedures, hospitals either maintain their heated water with a minimum return temperature of 124°F (51°C) and cold water at <68°F (<20°C) or chlorinate their hot water to achieve 1-2 mg/L (1-2 ppm) of free residual chlorine at the tap.26, 437, 709-711, 726, 727 Additional measures (e.g., physical cleaning or replacement of hot-water storage tanks, water heaters, faucets, and shower heads) may be required to help eliminate accumulations of scale and sediment that protect organisms from the biocidal effects of heat and chlorine.457, 711 Alternative methods for controlling and eradicating legionellae in water systems (e.g., treating water with chlorine dioxide, heavy metal ions [i.e., copper/silver ions], ozone, and UV light) have limited the growth of legionellae under laboratory and operating conditions.728-742 Further studies on the long-term efficacy of these treatments are needed before these methods can be considered standard applications.
Renewed interest in the use of chloramines stems from concerns about adverse health effects associated with disinfectants and disinfection by-products.743 Monochloramine usage minimizes the formation of disinfection by-products, including trihalomethanes and haloacetic acids. Monochloramine can also reach distal points in a water system and can penetrate into bacterial biofilms more effectively than free chlorine.744 However, monochloramine use is limited to municipal water treatment plants and is currently not available to health-care facilities as a supplemental water-treatment approach. A recent study indicated that 90% of Legionnaires disease outbreaks associated with drinking water could have been prevented if monochloramine rather than free chlorine has been used for residual disinfection.745 In a retrospective comparison of health-care-associated Legionnaires disease incidence in central Texas hospitals, the same research group documented an absence of cases in facilities located in communities with monochloramine-treated municipal water.746 Additional data are needed regarding the effectiveness of using monochloramine before its routine use as a disinfectant in water systems can be recommended. No data have been published regarding the effectiveness of monochloramine installed at the level of the health-care facility.
Additional filtration of potable water systems is not routinely necessary. Filters are used in water lines in dialysis units, however, and may be inserted into the lines for specific equipment (e.g., endoscope washers and disinfectors) for the purpose of providing bacteria-free water for instrument reprocessing. Additionally, an RO unit is usually added to the distribution system leading to PE areas.
# b. Primary Prevention of Legionnaires Disease (No Cases Identified)
The primary and secondary environmental infection-control strategies described in this section on the guideline pertain to health-care facilities without transplant units. Infection-control measures specific to PE or transplant units (i.e., patient-care areas housing patients at the highest risk for morbidity and mortality from Legionella spp. infection) are described in the subsection titled Preventing Legionnaires Disease in Protective Environments.
Health-care facilities use at least two general strategies to prevent health-care-associated legionellosis when no cases or only sporadic cases have been detected. The first is an environmental surveillance approach involving periodic culturing of water samples from the hospital's potable water system to monitor for Legionella spp.747 750 If any sample is culture-positive, diagnostic testing is recommended for all patients with health-care-associated pneumonia.748, 749 In-house testing is recommended for facilities with transplant programs as part of a comprehensive treatment/management program. If >30% of the samples are culture-positive for Legionella spp., decontamination of the facility's potable water system is warranted. 748 The premise for this approach is that no cases of health-care-associated legionellosis can occur if Legionella spp. are not present in the potable water system, and, conversely, cases of health-care-associated legionellosis could potentially occur if Legionella spp. are cultured from the water.26, 751 Physicians who are informed that the hospital's potable water system is culture-positive for Legionella spp. are more likely to order diagnostic tests for legionellosis.
A potential advantage of the environmental surveillance approach is that periodic culturing of water is less costly than routine laboratory diagnostic testing for all patients who have health-care-associated pneumonia. The primary argument against this approach is that, in the absence of cases, the relationship between water-culture results and legionellosis risk remains undefined.3 Legionnella spp. can be present in the water systems of buildings752 without being associated with known cases of disease.437, 707, 753 In a study of 84 hospitals in Québec, 68% of the water systems were found to be colonized with Legionella spp., and 26% were colonized at >30% of sites sampled; cases of Legionnaires disease, however, were infrequently reported from these hospitals.707
Other factors also argue against environmental surveillance. Interpretation of results from periodic water culturing might be confounded by differing results among the sites sampled in a single water system and by fluctuations in the concentration of Legionella spp. at the same site.709, 754 In addition, the risk for illness after exposure to a given source might be influenced by several factors other than the presence or concentration of organisms, including a) the degree to which contaminated water is aerosolized into respirable droplets, b) the proximity of the infectious aerosol to the potential host, c) the susceptibility of the host, and d) the virulence properties of the contaminating strain.755-757 Thus, data are insufficient to assign a level of disease risk even on the basis of the number of colony-forming units detected in samples from areas for immunocompetent patients. Conducting environmental surveillance would obligate hospital administrators to initiate water-decontamination programs if Legionella spp. are identified. Therefore, periodic monitoring of water from the hospital's potable water system and from aerosol-producing devices is not widely recommended in facilities that have not experienced cases of health-care-associated legionellosis.661, 758
The second strategy to prevent and control health-care-associated legionellosis is a clinical approach, in which providers maintain a high index of suspicion for legionellosis and order appropriate diagnostic tests (i.e., culture, urine antigen, and direct fluorescent antibody [DFA] serology) for patients with health-care-associated pneumonia who are at high risk for legionellosis and its complications.437, 759, 760 The testing of autopsy specimens can be included in this strategy should a death resulting from health care-associated pneumonia occur. Identification of one case of definite or two cases of possible health care-associated Legionnaires disease should prompt an epidemiologic investigation for a hospital source of Legionella spp., which may involve culturing the facility's water for Legionella. Routine maintenance of cooling towers, and use of sterile water for the filling and terminal rinsing of nebulization devices and ventilation equipment can help to minimize potential sources of contamination. Circulating potable water temperatures should match those outlined in the subsection titled Water Temperature and Pressure, as permitted by state code.
# c. Secondary prevention of Legionnaires Disease (With Identified Cases)
The indications for a full-scale environmental investigation to search for and subsequently decontaminate identified sources of Legionella spp. in health-care facilities without transplant units have not been clarified; these indications would likely differ depending on the facility. Case categories for health-care-associated Legionnaires disease in facilities without transplant units include definite cases (i.e., laboratory-confirmed cases of legionellosis that occur in patients who have been hospitalized continuously for >10 days before the onset of illness) and possible cases (i.e., laboratory-confirmed infections that occur 2-9 days after hospital admission). 3 In settings in which as few as one to three health-care-associated cases are recognized over several months, intensified surveillance for Legionnaires disease has frequently identified numerous additional cases.405, 408, 432, 453, 739, 759, 760 This finding suggests the need for a low threshold for initiating an investigation after laboratory confirmation of cases of health-care-associated legionellosis. When developing a strategy for responding to such a finding, however, infection-control personnel should consider the level of risk for health-care-associated acquisition of, and mortality from, Legionella spp. infection at their particular facility.
An epidemiologic investigation conducted to determine the source of Legionella spp. involves several important steps (Box 11). Laboratory assessment is crucial in supporting epidemiologic evidence of a link between human illness and a specific environmental source.761 Strain determination from subtype analysis is most frequently used in these investigations.410, 762-764 Once the environmental source is established and confirmed with laboratory support, supplemental water treatment strategies can be initiated as appropriate.
# Box 11. Steps in an epidemiologic investigation for legionellosis
Review medical and microbiologic records. Initiate active surveillance to identify all recent or ongoing cases. Develop a line listing of cases by time, place, and person. Determine the type of epidemiologic investigation needed for assessing risk factors:
• Case-control study,
• Cohort study. Gather and analyze epidemiologic information:
• Evaluate risk factors associated with potential environmental exposures (e.g., showers, cooling towers, and respiratory-therapy equipment). Collect water samples:
• Sample environmental sources implicated by epidemiologic investigation,
• Sample other potential source of water aerosols. Subtype strains of Legionella spp. cultured from both patients and environmental sources. Review autopsy records and include autopsy specimens in diagnostic testing.
# d. Preventing Legionnaires Disease in Protective Environments
This subsection outlines infection-control measures applicable to those health-care facilities providing care to severely immunocompromised patients. Indigenous microorganisms in the tap water of these facilities may pose problems for such patients. These measures are designed to prevent the generation of potentially infectious aerosols from water and the subsequent exposure of PE patients or other immunocompromised patients (e.g., transplant patients) (Table 17). Infection-control measures that address the use of water with medical equipment (e.g., ventilators, nebulizers, and equipment humidifiers) are described in other guidelines and publications. 3,455 If one case of laboratory-confirmed, health-care-associated Legionnaires disease is identified in a patient in a solid-organ transplant program or in PE (i.e., an inpatient in PE for all or part of the 2-10 days prior to onset of illness) or if two or more laboratory-confirmed cases occur among patients who had visited an outpatient PE setting, the hospital should report the cases to the local and state health departments. The hospital should then initiate a thorough epidemiologic and environmental investigation to determine the likely environmental sources of Legionella spp. 9 The source of Legionella should be decontaminated or removed. Isolated cases may be difficult to investigate. Because transplant recipients are at substantially higher risk for disease and death from legionellosis compared with other hospitalized patients, periodic culturing for Legionella spp. in water samples from the potable water in the solid-organ transplant and/or PE unit can be performed as part of an overall strategy to prevent Legionnaires disease in PE units.9, 431, 710, 769 The optimal methodology (i.e., frequency and number of sites) for environmental surveillance cultures in PE units has not been determined, and the cost-effectiveness of this strategy has not been evaluated. Because transplant recipients are at high risk for Legionnaires disease and because no data are available to determine a safe concentration of legionellae organisms in potable water, the goal of environmental surveillance for Legionella spp. should be to maintain water systems with no detectable organisms.9, 431 Culturing for legionellae may be used to assess the effectiveness of water treatment or decontamination methods, a practice that provides benefits to both patients and health-care workers.767, 770 • Use water that is not contaminated with Legionella spp. for patients' sponge baths.
• 9 • Provide sterile water for drinking, tooth brushing, or for flushing nasogastric tubes.
• 9, 412 • Perform supplemental treatment of the water for the unit.
• 732 • Consider periodic monitoring (i.e., culturing) of the unit water supply for Protecting patient-care devices and instruments from inadvertent tap water contamination during room cleaning procedures is also important in any immunocompromised patient-care area. In a recent outbreak of gram-negative bacteremias among open-heart-surgery patients, pressure-monitoring equipment that was assembled and left uncovered overnight prior to the next day's surgeries was inadvertently contaminated with mists and splashing water from a hose-disinfectant system used for cleaning.771
# Cooling Towers and Evaporative Condensers
Modern health-care facilities maintain indoor climate control during warm weather by use of cooling towers (large facilities) or evaporative condensers (smaller buildings). A cooling tower is a wet-type, evaporative heat transfer device used to discharge to the atmosphere waste heat from a building's air conditioning condensers (Figure 5).772, 773 Warm water from air-conditioning condensers is piped to the cooling tower where it is sprayed downward into a counter-or cross-current air flow. To accelerate heat transfer to the air, the water passes over the fill, which either breaks water into droplets or causes it to spread into a thin film.772, 773 Most systems use fans to move air through the tower, although some large industrial cooling towers rely on natural draft circulation of air. The cooled water from the tower is piped back to the condenser, where it again picks up heat generated during the process of chilling the system's refrigerant. The water is cycled back to the cooling tower to be cooled. Closed-circuit cooling towers and evaporative condensers are also evaporative heat-transfer devices. In these systems, the process fluid (e.g., water, ethylene glycol/water mixture, oil, or a condensing refrigerant) does not directly contact the cooling air, but is contained inside a coil assembly.661
# Figure 5. Diagram of a typical air conditioning (induced draft) cooling tower*
Water temperatures are approximate and may differ substantially according to system use and design. Warm water from the condenser (or chiller) is sprayed downward into a counter-or cross-current air flow. Water passes over the fill (a component of the system designed to increase the surface area of the water exposed to air), and heat from the water is transferred to the air. Some of the water becomes aerosolized during this process, although the volume of aerosol discharged to the air can be reduced by the placement of a drift eliminator. Water cooled in the tower returns to the heat source to cool refrigerant from the air conditioning unit. * This figure is reprinted with permission of the publisher of reference 773 (Plenum Medical).
Cooling towers and evaporative condensers incorporate inertial stripping devices called drift eliminators to remove water droplets generated within the unit. Although the effectiveness of these eliminators varies substantially depending on design and condition, some water droplets in the size range of <5 pm will likely leave the unit, and some larger droplets leaving the unit may be reduced to <5 pm by evaporation. Thus, even with proper operation, a cooling tower or evaporative condenser can generate and expel respirable water aerosols. If either the water in the unit's basin or the make-up water (added to replace water lost to evaporation) contains Legionella spp. or other waterborne microorganisms, these organisms can be aerosolized and dispersed from the unit.774 Clusters of both Legionnaires disease and Pontiac fever have been traced to exposure to infectious water aerosols originating from cooling towers and evaporative condensers contaminated with Legionella spp. Although most of these outbreaks have been community-acquired episodes of pneumonia, -health-care-associated Legionnaires disease has been linked to cooling tower aerosol exposure.404, 405 Contaminated aerosols from cooling towers on hospital premises gained entry to the buildings either through open windows or via air handling system intakes located near the tower equipment.
Cooling towers and evaporative condensers provide ideal ecological niches for Legionella spp. The typical temperature of the water in cooling towers ranges from 85°F-95°F (29°C-35°C), although temperatures can be above 120°F (49°C) and below 70°F (21°C) depending on system heat load, ambient temperature, and operating strategy.661 An Australian study of cooling towers found that legionellae colonized or multiplied in towers with basin temperatures above 60.8°F (16°C), and multiplication became explosive at temperatures above 73.4°F (23°C).783 Water temperature in closedcircuit cooling towers and evaporative condensers is similar to that in cooling towers. Considerable variation in the piping arrangement occurs. In addition, stagnant areas or dead legs may be difficult to clean or penetrate with biocides.
Several documents address the routine maintenance of cooling towers, evaporative condensers, and whirlpool spas.661, 784-787 They suggest following manufacturer's recommendations for cleaning and biocide treatment of these devices; all health-care facilities should ensure proper maintenance for their cooling towers and evaporative condensers, even in the absence of Legionella spp (Appendix C). Because cooling towers and evaporative condensers can be shut down during periods when air conditioning is not needed, this maintenance cleaning and treatment should be performed before starting up the system for the first time in the warm season.782 Emergency decontamination protocols describing cleaning procedures and hyperchlorination for cooling towers have been developed for towers implicated in the transmission of legionellosis.786, 787
# Dialysis Water Quality and Dialysate
# a. Rationale for Water Treatment in Hemodialysis
Hemodialysis, hemofiltration, and hemodiafiltration require special water-treatment processes to prevent adverse patient outcomes of dialysis therapy resulting from improper formulation of dialysate with water containing high levels of certain chemical or biological contaminants. The Association for the Advancement of Medical Instrumentation (AAMI) has established chemical and microbiologic standards for the water used to prepare dialysate, substitution fluid, or to reprocess hemodialyzers for renal replacement therapy. -
The AAMI standards address: a) equipment and processes used to purify water for the preparation of concentrates and dialysate and the reprocessing of dialyzers for multiple use and b) the devices used to store and distribute this water. Future revisions to these standards may include hemofiltration and hemodiafiltration.
Water treatment systems used in hemodialysis employ several physical and/or chemical processes either singly or in combination (Figure 6). These systems may be portable units or large systems that feed several rooms. In the United States, >97% of maintenance hemodialysis facilities use RO alone or in combination with deionization.793 Many acute-care facilities use portable hemodialysis machines with attached portable water treatment systems that use either deionization or RO. These machines were exempted from earlier versions of AAMI recommendations, but given current knowledge about toxic exposures to and inflammatory processes in patients new to dialysis, these machines should now come into compliance with current AAMI recommendations for hemodialysis water and dialysate quality.788, 789 Previous recommendations were based on the assumption that acute-care patients did not experience the same degree of adverse effects from short-term, cumulative exposures to either chemicals or microbiologic agents present in hemodialysis fluids compared with the effects encountered by patients during chronic, maintenance dialysis.788, 789 Additionally, JCAHO is reviewing inpatient practices and record-keeping for dialysis (acute and maintenance) for adherence to AAMI standards and recommended practices. Investigations of adverse outcomes among patients using reprocessed dialyzers have demonstrated a greater risk for developing pyrogenic reactions when the water used to reprocess these devices contained >6 ng/mL endotoxin and > 104 CFU/mL bacteria.820 In addition to the variability in endotoxin assays, host factors also are involved in determining whether a patient will mount a response to endotoxin.803 Outbreak investigations of pyrogenic reactions and bacteremias associated with hemodialyzer reuse have demonstrated that pyrogenic reactions are prevented once the endotoxin level in the water used to reprocess the dialyzers is returned to below the AAMI standard level.821
Reuse of dialyzers and use of bicarbonate dialysate, high-flux dialyzer membranes, or high-flux dialysis may increase the potential for pyrogenic reactions if the water in the dialysis setting does not meet standards.796-798 Although investigators have been unable to demonstrate endotoxin transfer across dialyzer membranes, , , the preponderance of reports now supports the ability of endotoxin to transfer across at least some high-flux membranes under some operating conditions. In addition to the acute risk of pyrogenic reactions, indirect evidence in increasingly demonstrating that chronic exposure to low amounts of endotoxin may play a role in some of the long-term complications of hemodialysis therapy. Patients treated with ultrafiltered dialysate for 5-6 months have demonstrated a decrease in serum p2 microglobulin concentrations and a decrease in markers of an inflammatory response.824-826 In studies of longer duration, use of microbiologically ultrapure dialysate has been associated with a 827, 828 decreased incidence of p2 microglobulin-associated amyloidosis. , Although patient benefit likely is associated with the use of ultrapure dialysate, no consensus has been reached regarding the potential adoption of this as standard in the United States. Debate continues regarding the bacterial and endotoxin limits for dialysate. As advances in water treatment and hemodialysis processes occur, efforts are underway to move improved technology from the manufacturer out into the user community. Cost-benefit studies, however, have not been done, and substantially increased costs to implement newer water treatment modalities are anticipated.
To reconcile AAMI documents with current International Organization for Standardization (ISO) format, AAMI has determined that its hemodialysis standards will be discussed in the following four installments: RD 5 for hemodialysis equipment, RD 62 for product water quality, RD 47 for dialyzer reprocessing, and RD 52 for dialysate quality. The Renal Diseases and Dialysis Committee of AAMI is expected to finalize and promulgated the dialysate standard pertinent to the user community (RD 52), adopting by reference the bacterial and endotoxin limits in product water as currently outlined in the AAMI standard that applies to systems manufacturers (RD 62). At present, the user community should continue to observe water quality and dialysate standards as outlined in AAMI RD 5 (Hemodialysis Systems, 1992) and AAMI RD 47 (Reuse of Hemodialyzers, 1993) until the new RD 52 standard becomes available (Table 18).789, 791 ) now specifies that all product water used to prepare dialysate or to reprocess dialyzers for multiple use should contain <2 endotoxin units per milliliter (EU/mL).792 A level of 2 EU/mL was chosen as the upper limit for endotoxin because this level is easily achieved with contemporary water treatment systems using RO and/or ultrafiltration. CDC has advocated monthly endotoxin testing along with microbiologic assays of water, because endotoxin activity may not correspond to the total heterotrophic plate counts.829 Additionally, the current AAMI standard RD 62 for manufacturers includes action levels for product water. Because 48 hours can elapse between the time of sampling water for microbial contamination and the time when results are received, and because bacterial proliferation can be rapid, action levels for microbial counts and endotoxin concentrations are reported as 50 CFU/mL and 1 EU/mL, respectively, in this revision of the standard.792 These recommendations will allow users to initiate corrective action before levels exceed the maximum levels established by the standard.
In hemodialysis, the net movement of water is from the blood to the dialysate, although within the dialyzer, local movement of water from the dialysate to the blood through the phenomenon of back filtration may occur, particularly in dialyzers with highly permeable membranes.830 In contrast, hemofiltration and hemodiaflltration feature infusion of large volumes of electrolyte solution (20-70 L) into the blood. Increasingly, this electrolyte solution is being prepared on-line from water and concentrate. Because of the large volumes of fluid infused, AAMI considered the necessity of setting more stringent requirements for water to be used in this application, but this organization has not yet established these because of lack of expert consensus and insufficient experience with on-line therapies in the United States. On-line hemofiltration and hemodiafiltration systems use sequential ultrafiltration as the final step in the preparation of infusion fluid. Several experts from AAMI concur that these point-of-use ultrafiltration systems should be capable of further reducing the bacteria and endotoxin burden of solutions prepared from water meeting the requirements of the AAMI standard to a safe level for infusion.
# b. Microbial Control Strategies
The strategy for controlling massive accumulations of gram-negative water bacteria and NTM in dialysis systems primarily involves preventing their growth through proper disinfection of watertreatment systems and hemodialysis machines. Gram-negative water bacteria, their associated lipopolysaccharides (bacterial endotoxins), and NTM ultimately come from the community water supply, and levels of these bacteria can be amplified depending on the water treatment system, dialysate distribution system, type of dialysis machine, and method of disinfection ( piping can act as bacterial reservoirs. Outlet taps should be located at the highest elevation to prevent loss of disinfectant; keep a recirculation loop in the system; flush unused ports routinely. Tanks are undesirable because they act as a reservoir for water bacteria; if tanks are present, they must be routinely scrubbed and disinfected.
# Dialysis machines
# Single-pass
Recirculating single-pass or recirculating (batch)
Disinfectant should have contact with a ll parts of the machine that are exposed to water or dialysis fluid. Recirculating pumps and machine design allow for massive contamination levels if not properly disinfected; overnight chemical germicide treatment is recommended.
Two components of hemodialysis water distribution systems -pipes (particularly those made of polyvinyl chloride [PVC]) and storage tanks -can serve as reservoirs of microbial contamination. Hemodialysis systems frequently use pipes that are wider and longer than are needed to handle the required flow, which slows the fluid velocity and increases both the total fluid volume and the wetted surface area of the system. Gram-negative bacteria in fluids remaining in pipes overnight multiply rapidly and colonize the wet surfaces, producing bacterial populations and endotoxin quantities in proportion to the volume and surface area. Such colonization results in formation of protective biofilm that is difficult to remove and protects the bacteria from disinfection.832 Routine (i.e., monthly), lowlevel disinfection of the pipes can help to control bacterial contamination of the distribution system. Additional measures to protect pipes from contaminations include a) situating all outlet taps at equal elevation and at the highest point of the system so that the disinfectant cannot drain from pipes by gravity before adequate contact time has elapsed and b) eliminating rough joints, dead-end pipes, and unused branches and taps that can trap fluid and serve as reservoirs of bacteria capable of continuously inoculating the entire volume of the system.800 Maintain a flow velocity of 3-5 ft/sec.
A storage tank in the distribution system greatly increases the volume of fluid and surface area available and can serve as a niche for water bacteria. Storage tanks are therefore not recommended for use in dialysis systems unless they are frequently drained and adequately disinfected, including scrubbing the sides of the tank to remove bacterial biofilm. An ultrafilter should be used distal to the storage tank.808, 833
Microbiologie sampling of dialysis fluids is recommended because gram-negative bacteria can proliferate rapidly in water and dialysate in hemodialysis systems; high levels of these organisms place patients at risk for pyrogenic reactions or health-care-associated infection.667, 668, 808
Health-care facilities are advised to sample dialysis fluids at least monthly using standard microbiologic assay methods for waterborne microorganisms.788, 793, 799, 834-836 Product water used to prepare dialysate and to reprocess hemodialyzers for reuse on the same patient should also be tested for bacterial endotoxin on a monthly basis. , , (See Appendix C for information about water sampling methods for dialysis.)
Cross-contamination of dialysis machines and inadequate disinfection measures can facilitate the spread of waterborne organisms to patients. Steps should be taken to ensure that dialysis equipment is performing correctly and that all connectors, lines, and other components are specific for the equipment, in good repair, and properly in place. A recent outbreak of gram-negative bacteremias among dialysis patients was attributed to faulty valves in a drain port of the machine that allowed backflow of saline used to flush the dialyzer before patient use.838, 839 This backflow contaminated the drain priming connectors, which contaminated the blood lines and exposed the patients to high concentrations of gram-negative bacteria. Environmental infection control in dialysis settings also includes low-level disinfection of housekeeping surfaces and spot decontamination of spills of blood (see Environmental Services in Part I of this guideline for further information).
# c. Infection-Control Issues in Peritoneal Dialysis
Peritoneal dialysis (PD), most commonly administered as continuous ambulatory peritoneal dialysis (CAPD) and continual cycling peritoneal dialysis (CCPD), is the third most common treatment for end stage renal disease (ESRD) in the United States, accounting for 12% of all dialysis patients.840 Peritonitis is the primary complication of CAPD, with coagulase-negative staphylococci the most clinically significant causative organisms.841 Other organisms that have been found to produce peritonitis include Staphylococcus aureus, Mycobacterium fortuitum, M. mucogenicum, Stenotrophomonas maltophilia, Burkholderia cepacia, Corynebacterium jeikeium, Candida spp., and other fungi.842-850 Substantial morbidity is associated with peritoneal dialysis infections. Removal of peritoneal dialysis catheters usually is required for treatment of peritonitis caused by fungi, NTM, or other bacteria that are not cleared within the first several days of effective antimicrobial treatment. Furthermore, recurrent episodes of peritonitis may lead to fibrosis and loss of the dialysis membrane.
Many reported episodes of peritonitis are associated with exit-site or tunneled catheter infections. Risk factors for the development of peritonitis in PD patients include a) under dialysis, b) immune suppression, c) prolonged antimicrobial treatment, d) patient age [more infections occur in younger patients and older hospitalized patients], e) length of hospital stay, and f) hypoalbuminemia.844, 851, 852 Concern has been raised about infection risk associated with the use of automated cyclers in both inpatient and outpatient settings; however, studies suggest that PD patients who use automated cyclers have much lower infection rates. 853 One study noted that a closed-drainage system reduced the incidence of system-related peritonitis among intermittent peritoneal dialysis (IPD) patients from 3.6 to 1.5 cases/100 patient days. 854 The association of peritonitis with management of spent dialysate fluids requires additional study. Therefore, ensuring that the tip of the waste line is not submerged beneath the water level in a toilet or in a drain is prudent.
# Ice Machines and Ice
Microorganisms may be present in ice, ice-storage chests, and ice-making machines. The two main sources of microorganisms in ice are the potable water from which it is made and a transferral of organisms from hands (Table 20). Ice from contaminated ice machines has been associated with patient colonization, blood stream infections, pulmonary and gastrointestinal illnesses, and pseudoinfections.602, 603, 683, 684, 854, 855 Microorganisms in ice can secondarily contaminate clinical specimens and medical solutions that require cold temperatures for either transport or holding.601, 620 An outbreak of surgicalsite infections was interrupted when sterile ice was used in place of tap water ice to cool cardioplegia solutions.601 In a study comparing the microbial populations of hospital ice machines with organisms recovered from ice samples gathered from the community, samples from 27 hospital ice machines yielded low numbers (<10 CFU/mL) of several potentially opportunistic microorganisms, mainly gram-negative bacilli.859 During the survey period, no health-care-associated infections were attributed to the use of ice. Ice from community sources had higher levels of microbial contamination (75%-95% of 194 samples had total heterotrophic plate counts <500 CFU/mL, with the proportion of positive cultures dependent on the incubation temperature) and showed evidence of fecal contamination from the source water.859 Thus, ice machines in health-care settings are no more heavily contaminated compared with ice machines in the community. If the source water for ice in a health-care facility is not fecally contaminated, then ice from clean ice machines and chests should pose no increased hazard for immunocompetent patients. Some waterborne bacteria found in ice could potentially be a risk to immunocompromised patients if they consume ice or drink beverages with ice. For example, Burkholderia cepacia in ice could present an infection risk for cystic fibrosis patients.859, 860 Therefore, protecting immunosuppressed and otherwise medically at-risk patients from exposure to tap water and ice potentially contaminated with opportunistic pathogens is prudent.9
No microbiologic standards for ice, ice-making machines, or ice storage equipment have been established, although several investigators have suggested the need for such standards.859, 866 Culturing of ice machines is not routinely recommended, but it may be useful as part of an epidemiologic investigation.867-869 Sampling might also help determine the best schedule for cleaning open ice-storage chests. Recommendations for a regular program of maintenance and disinfection have been published.866-869 Health-care facilities are advised to clean ice-storage chests on a regular basis. Open ice chests may require a more frequent cleaning schedule compared with chests that have covers.
Portable ice chests and containers require cleaning and low-level disinfection before the addition of ice intended for consumption. Ice-making machines may require less frequent cleaning, but their maintenance is important to proper performance. The manufacturer's instructions for both the proper method of cleaning and/or maintenance should be followed. These instructions may also recommend an EPA-registered disinfectant to ensure chemical potency, materials compatibility, and safety. In the event that instructions and suitable EPA-registered disinfectants are not available for this process, then a generic approach to cleaning, disinfecting, and maintaining ice machines and dispensers can be used (Box 12).
Ice and ice-making machines also may be contaminated via improper storage or handling of ice by patients and/or staff.684-686, 855-858, 870 Suggested steps to avoid this means of contamination include a) minimizing or avoiding direct hand contact with ice intended for consumption, b) using a hard-surface scoop to dispense ice, and c) installing machines that dispense ice directly into portable containers at the touch of a control.687, 869
# Hydrotherapy Tanks and Pools
# a. General Information
Hydrotherapy equipment (e.g., pools, whirlpools, whirlpool spas, hot tubs, and physiotherapy tanks) traditionally has been used to treat patients with certain medical conditions (e.g., burns, , septic ulcers, lesions, amputations,873 orthopedic impairments and injuries, arthritis,874 and kidney lithotripsy).654 Wound-care medicine is increasingly moving away from hydrotherapy, however, in favor of bedside pulsed-lavage therapy using sterile solutions for cleaning and irrigation.492, 875-878 Several episodes of health-care-associated infections have been linked to use of hydrotherapy equipment (Table 21). Potential routes of infection include incidental ingestion of the water, sprays and aerosols, and direct contact with wounds and intact skin (folliculitis). Risk factors for infection include a) age and sex of the patient, b) underlying medical conditions, c) length of time spent in the hydrotherapy water, and d) portals of entry.879 Although some facilities have used tub liners to minimize environmental contamination of the tanks, the use of a tub liner does not eliminate the need for cleaning and disinfection. Draining these small pools and tanks after each patient use, thoroughly cleaning with a detergent, and disinfecting according to manufacturers' instructions have reduced bacterial contamination levels in the water from 104 CFU/mL to <10 CFU/mL.892 A chlorine residual of 15 ppm in the water should be obtained prior to the patient's therapy session (e.g., by adding 15 grams of calcium hypochlorite 70% [e.g., HTH®] per 100 gallons of water).892 A study of commercial and residential whirlpools found that superchlorination or draining, cleaning, disinfection, and refilling of whirlpools markedly reduced densities of Pseudomonas aeruginosa in whirlpool water. 893 The bacterial populations were rapidly replenished, however, when disinfectant concentrations dropped below recommended levels for recreational use (i.e., chlorine at 3.0 ppm or bromine at 6.0 ppm). When using chlorine, however, knowing whether the community drinking-water system is disinfected with chloramine is important, because municipal utilities adjust the pH of the water to the basic side to enhance chloramine formation. Because chlorine is not very effective at pH levels above 8, it may be necessary to re-adjust the pH of the water to a more acidic level.894
A few reports describe the addition of antiseptic chemicals to hydrotherapy tank water, especially for burn patient therapy.895-897 One study involving a minimal number of participants demonstrated a reduction in the number of Pseudomonas spp. and other gram-negative bacteria from both patients and equipment surfaces when chloramine-T ("chlorazene") was added to the water.898 Chloramine-T has not, however, been approved for water treatment in the United States.
# c. Hydrotherapy Pools
Hydrotherapy pools typically serve large numbers of patients and are usually heated to 91.4°F-98.6°F (31°C-37°C). The temperature range is more narrow (94°F-96.8°F [35°C-36°C]) for pediatric and geriatric patient use.899 Because the size of hydrotherapy pools precludes draining after patient use, proper management is required to maintain the proper balance of water conditioning (i.e., alkalinity, hardness, and temperature) and disinfection. The most widely used chemicals for disinfection of pools are chlorine and chlorine compounds -calcium hypochlorite, sodium hypochlorite, lithium hypochlorite, chloroisocyanurates, and chlorine gas. Solid and liquid formulations of chlorine chemicals are the easiest and safest to use.900 Other halogenated compounds have also been used for pool-water disinfection, albeit on a limited scale. Bromine, which forms bactericidal bromamines in the presence of ammonia, has limited use because of its association with contact dermatitis.901 Iodine does not bleach hair, swim suits, or cause eye irritation, but when introduced at proper concentrations, it gives water a greenish-yellowish cast.892
In practical terms, maintenance of large hydrotherapy pools (e.g., those used for exercise) is similar to that for indoor public pools (i.e., continuous filtration, chlorine residuals no less than 0.4 ppm, and pH of 7.2-7.6).902, 903 Supply pipes and pumps also need to be maintained to eliminate the possibility of this equipment serving as a reservoir for waterborne organisms.904 Specific standards for chlorine residual and pH of the water are addressed in local and state regulations. Patients who are fecally incontinent or who have draining wounds should refrain from using these pools until their condition improves.
# d. Birthing Tanks and Other Equipment
The use of birthing tanks, whirlpool spas, and whirlpools is a recent addition to obstetrical practice.905 Few studies on the potential risks associated with these pieces of equipment have been conducted. In one study of 32 women, a newborn contracted a Pseudomonas infection after being birthed in such a tank, the strain of which was identical to the organism isolated from the tank water.906 Another report documented identical strains of P. aeruginosa isolates from a newborn with sepsis and on the environmental surfaces of a tub that the mother used for relaxation while in labor. 907 Other studies have shown no significant increases in the rates of post-immersion infections among mothers and infants.908, 909
Because the water and the tub surfaces routinely become contaminated with the mother's skin flora and blood during labor and delivery, birthing tanks and other tub equipment must be drained after each patient use and the surfaces thoroughly cleaned and disinfected. Health-care facilities are advised to follow the manufacturer's instructions for selection of disinfection method and chemical germicide. The range of chlorine residuals for public whirlpools and whirlpool spas is 2-5 ppm.910 Use of an inflatable tub is an alternative solution, but this item must be cleaned and disinfected between patients if it is not considered a single-use unit.
Recreational tanks and whirlpool spas are increasingly being used as hydrotherapy equipment.
Although such home equipment appears to be suitable for hydrotherapy, they are neither designed nor constructed to function in this capacity. Additionally, manufacturers generally are not obligated to provide the health-care facility with cleaning and disinfecting instructions appropriate for medical equipment use, and the U.S. Food and Drug Administration (FDA) does not evaluate recreational equipment. Health-care facilities should therefore carefully evaluate this "off-label" use of home equipment before proceeding with a purchase.
# Miscellaneous Medical/Dental Equipment Connected to Main Water Systems a. Automated Endoscope Reprocessors
The automated endoscopic reprocessor (AER) is classified by the FDA as an accessory for the flexible endoscope.654 A properly operating AER can provide a more consistent, reliable method of decontaminating and terminal reprocessing for endoscopes between patient procedures than manual reprocessing methods alone.911 An endoscope is generally subjected to high-level disinfection using a liquid chemical sterilant or a high-level disinfectant. Because the instrument is a semi-critical device, the optimal rinse fluid for a disinfected endoscope would be sterile water.3 Sterile water, however, is expensive and difficult to produce in sufficient quantities and with adequate quality assurance for instrument rinsing in an AER.912, 913 Therefore, one option to be used for AERs is rinse water that has been passed through filters with a pore size of 0.1-0.2 pm to render the water "bacteria-free." These filters usually are located in the water line at or near the port where the mains water enters the equipment. The product water (i.e., tap water passing through these filters) in these applications is not considered equivalent in microbial quality to that for membrane-filtered water as produced by pharmaceutical firms. Membrane filtration in pharmaceutical applications is intended to ensure the microbial quality of polished product water.
Water has been linked to the contamination of flexible fiberoptic endoscopes in the following two scenarios: a) rinsing a disinfected endoscope with unfiltered tap water, followed by storage of the instrument without drying out the internal channels and b) contamination of AERs from tap water inadvertently introduced into the equipment. In the latter instance, the machine's water reservoirs and fluid circuitry become contaminated with waterborne, heterotrophic bacteria (e.g., Pseudomonas aeruginosa and NTM), which can survive and persist in biofilms attached to these components.914-917 Colonization of the reservoirs and water lines of the AER becomes problematic if the required cleaning, disinfection, and maintenance are not performed on the equipment as recommended by the manufacturer.669, 916, 917 Use of the 0.1-0.2-pm filter in the water line helps to keep bacterial contamination to a minimum,670, 911, 917 but filters may fail and allow bacteria to pass through to the equipment and then to the instrument undergoing reprocessing.671-674, 913, 918 Filters also require maintenance for proper performance.670, 911, 912, 918, 919 Heightened awareness of the proper disinfection of the connectors that hook the instrument to the AER may help to further reduce the potential for contaminating endoscopes during reprocessing.920 An emerging issue in the field of endoscopy is that of the possible role of rinse water monitoring and its potential to help reduce endoscopy/bronchoscopyassociated infections.918
Studies have linked deficiencies in endoscope cleaning and/or disinfecting processes to the incidence of post-endoscopic adverse outcomes.921-924 Several clusters have been traced to AERs of older designs and these were associated with water quality.675, 914-916 Regardless of whether manual or automated terminal reprocessing is used for endoscopes, the internal channels of the instrument should be dried before storage.925 The presence of residual moisture in the internal channels encourages the proliferation of waterborne microorganisms, some of which may be pathogenic. One of the most frequently used methods employs 70% isopropyl alcohol to flush the internal channels, followed by forced air drying of these channels and hanging the endoscope vertically in a protected cabinet; this method ensures internal drying of the endoscope, lessens the potential for proliferation of waterborne microorganisms, 669
# b. Dental Unit Water Lines
Dental unit water lines (DUWLs) consist of small-bore plastic tubing that delivers water used for general, non-surgical irrigation and as a coolant to dental handpieces, sonic and ultrasonic scalers, and air-water syringes; municipal tap water is the source water for these lines. The presence of biofilms of waterborne bacteria and fungi (e.g., Legionella spp., Pseudomonas aeruginosa, and NTM) in DUWLs has been established.636, 637, 694, 695, 932-934 Biofilms continually release planktonic microorganisms into the water, the titers of which can exceed 1x106 CFU/mL.694 However, scientific evidence indicates that immunocompetent persons are only at minimal risk for substantial adverse health effects after contact with water from a dental unit. Nonetheless, exposing patients or dental personnel to water of uncertain microbiological quality is not consistent with universally accepted infection-control principles.935
In 1993, CDC issued guidelines relative to water quality in a dental setting. These guidelines recommend that all dental instruments that use water (including high-speed handpieces) should be run to discharge water for 20-30 seconds after each patient and for several minutes before the start of each clinic day.936 This practice can help to flush out any patient materials that many have entered the turbine, air, or waterlines.937, 938 The 1993 guidance also indicated that waterlines be flushed at the beginning of the clinic day. Although these guidelines are designed to help reduce the number of microorganisms present in treatment water, they do not address the issue of reducing or preventing biofilm formation in the waterlines. Research published subsequent to the 1993 dental infection control guideline suggests that flushing the lines at the beginning of the day has only minimal effect on the status of the biofilm in the lines and does not reliably improve the quality of water during dental treatment.939-941 Updated recommendations on infection-control practices for water line use in dentistry will be available in late 2003.942
The numbers of microorganisms in water used as coolant or irrigant for non-surgical dental treatment should be as low as reasonably achievable and, at a minimum, should meet nationally recognized standards for safe drinking water.935, 943 Only minimal evidence suggests that water meeting drinking water standards poses a health hazard for immunocompetent persons. The EPA, the American Public Health Association (APHA), and the American Water Works Association (AWWA) have set a maximum limit of 500 CFU/mL for aerobic, heterotrophic, mesophilic bacteria in drinking water in municipal distribution systems.944, 945 This standard is achievable, given improvements in water-line technology. Dentists should consult with the manufacturer of their dental unit to determine the best equipment and method for maintaining and monitoring good water quality.935, 946
# E. Environmental Services 1. Principles of Cleaning and Disinfecting Environmental Surfaces
Although microbiologically contaminated surfaces can serve as reservoirs of potential pathogens, these surfaces generally are not directly associated with transmission of infections to either staff or patients. The transferral of microorganisms from environmental surfaces to patients is largely via hand contact with the surface.947, 948 Although hand hygiene is important to minimize the impact of this transfer, cleaning and disinfecting environmental surfaces as appropriate is fundamental in reducing their potential contribution to the incidence of healthcare-associated infections.
The principles of cleaning and disinfecting environmental surfaces take into account the intended use of the surface or item in patient care. CDC retains the Spaulding classification for medical and surgical instruments, which outlines three categories based on the potential for the instrument to transmit infection if the instrument is microbiologically contaminated before use.949, 950 These categories are "critical," "semicritical," and "noncritical." In 1991, CDC proposed an additional category designated "environmental surfaces" to Spaulding's original classification951 to represent surfaces that generally do not come into direct contact with patients during care. Environmental surfaces carry the least risk of disease transmission and can be safely decontaminated using less rigorous methods than those used on medical instruments and devices. Environmental surfaces can be further divided into medical equipment surfaces (e.g., knobs or handles on hemodialysis machines, x-ray machines, instrument carts, and dental units) and housekeeping surfaces (e.g., floors, walls, and tabletops).951
The following factors influence the choice of disinfection procedure for environmental surfaces: a) the nature of the item to be disinfected, b) the number of microorganisms present, c) the innate resistance of those microorganisms to the inactivating effects of the germicide, d) the amount of organic soil present, e) the type and concentration of germicide used, f) duration and temperature of germicide contact, and 952 953 g) if using a proprietary product, other specific indications and directions for use. , Cleaning is the necessary first step of any sterilization or disinfection process. Cleaning is a form of decontamination that renders the environmental surface safe to handle or use by removing organic matter, salts, and visible soils, all of which interfere with microbial inactivation.954-960 The physical action of scrubbing with detergents and surfactants and rinsing with water removes large numbers of microorganisms from surfaces.957 If the surface is not cleaned before the terminal reprocessing procedures are started, the success of the sterilization or disinfection process is compromised.
Spaulding proposed three levels of disinfection for the treatment of devices and surfaces that do not require sterility for safe use. These disinfection levels are "high-level," "intermediate-level," and "lowlevel."949, 950 The basis for these levels is that microorganisms can usually be grouped according to their innate resistance to a spectrum of physical or chemical germicidal agents (Table 22). This information, coupled with the instrument/surface classification, determines the appropriate level of terminal disinfection for an instrument or surface. The process of high-level disinfection, an appropriate standard of treatment for heat-sensitive, semi critical medical instruments (e.g., flexible, fiberoptic endoscopes), inactivates all vegetative bacteria, mycobacteria, viruses, fungi, and some bacterial spores. High-level disinfection is accomplished with powerful, sporicidal chemicals (e.g., glutaraldehyde, peracetic acid, and hydrogen peroxide) that are not appropriate for use on housekeeping surfaces. These liquid chemical sterilants/high-level disinfectants are highly toxic.961-963 Use of these chemicals for applications other than those indicated in their label instructions (i.e., as immersion chemicals for treating heat-sensitive medical instruments) is not appropriate.964 Intermediate-level disinfection does not necessarily kill bacterial spores, but it does inactivate Mycobacterium tuberculosis var. bovis, which is substantially more resistant to chemical germicides than ordinary vegetative bacteria, fungi, and medium to small viruses (with or without lipid envelopes). Chemical germicides with sufficient potency to achieve intermediate-level disinfection include chlorine-containing compounds (e.g., sodium hypochlorite), alcohols, some phenolics, and some iodophors. Low-level disinfection inactivates vegetative bacteria, fungi, enveloped viruses (e.g., human immunodeficiency virus [HIV], and influenza viruses), and some non-enveloped viruses (e.g., adenoviruses). Low-level disinfectants include quaternary ammonium compounds, some phenolics, and some iodophors. Sanitizers are agents that reduce the numbers of bacterial contaminants to safe levels as judged by public health requirements, and are used in cleaning operations, particularly in food service and dairy applications. Germicidal chemicals that have been approved by FDA as skin antiseptics are not appropriate for use as environmental surface disinfectants.951
The selection and use of chemical germicides are largely matters ofjudgment, guided by product label instructions, information, and regulations. Liquid sterilant chemicals and high-level disinfectants intended for use on critical and semi-critical medical/dental devices and instruments are regulated exclusively by the FDA as a result of recent memoranda of understanding between FDA and the EPA that delineates agency authority for chemical germicide regulation.965, 966 Environmental surface germicides (i.e., primarily intermediate-and low-level disinfectants) are regulated by the EPA and labeled with EPA registration numbers. The labels and technical data or product literature of these germicides specify indications for product use and provide claims for the range of antimicrobial activity. The EPA requires certain pre-registration laboratory potency tests for these products to support product label claims. EPA verifies (through laboratory testing) manufacturers' claims to inactivate microorganisms for selected products and organisms. Germicides labeled as "hospital disinfectant" have passed the potency tests for activity against three representative microorganisms -Pseudomonas aeruginosa, Staphylococcus aureus, and Salmonella cholerae suis. Low-level disinfectants are often labeled "hospital disinfectant" without a tuberculocidal claim, because they lack the potency to inactivate mycobacteria. Hospital disinfectants with demonstrated potency against mycobacteria (i.e., intermediate-level disinfectants) may list "tuberculocidal" on the label as well. Other claims (e.g., "fungicidal," "pseudomonicidal," and "virucidal") may appear on labels of environmental surface germicides, but the designations of "tuberculocidal hospital disinfectant" and "hospital disinfectant" correlate directly to Spaulding's assessment of intermediate-level disinfectants and low-level disinfectants, respectively.951 A common misconception in the use of surface disinfectants in health-care settings relates to the underlying purpose for use of proprietary products labeled as a "tuberculocidal" germicide. Such products will not interrupt and prevent the transmission of TB in health-care settings because TB is not acquired from environmental surfaces. The tuberculocidal claim is used as a benchmark by which to measure germicidal potency. Because mycobacteria have the highest intrinsic level of resistance among the vegetative bacteria, viruses, and fungi, any germicide with a tuberculocidal claim on the label (i.e., an intermediate-level disinfectant) is considered capable of inactivating a broad spectrum of pathogens, including much less resistant organisms such the bloodborne pathogens (e.g., hepatitis B virus [HBV], hepatitis C virus [HCV], and HIV). It is this broad spectrum capability, rather than the product's specific potency against mycobacteria, that is the basis for protocols and OSHA regulations indicating the appropriateness of using tuberculocidal chemicals for surface disinfection.967
# General Cleaning Strategies for Patient-Care Areas
The number and types of microorganisms present on environmental surfaces are influenced by the following factors: a) number of people in the environment, b) amount of activity, c) amount of moisture, d) presence of material capable of supporting microbial growth, e) rate at which organisms suspended in the air are removed, and f) type of surface and orientation [i.e., horizontal or vertical].968 Strategies for cleaning and disinfecting surfaces in patient-care areas take into account a) potential for direct patient contact, b) degree and frequency of hand contact, and c) potential contamination of the surface with body substances or environmental sources of microorganisms (e.g., soil, dust, and water).
# a. Cleaning of Medical Equipment
Manufacturers of medical equipment should provide care and maintenance instructions specific to their equipment. These instructions should include information about a) the equipments' compatibility with chemical germicides, b) whether the equipment is water-resistant or can be safely immersed for cleaning, and c) how the equipment should be decontaminated if servicing is required.967 In the absence of manufacturers' instructions, non-critical medical equipment (e.g., stethoscopes, blood pressure cuffs, dialysis machines, and equipment knobs and controls) usually only require cleansing followed by low-to intermediate-level disinfection, depending on the nature and degree of contamination. Ethyl alcohol or isopropyl alcohol in concentrations of 60%-90% (v/v) is often used to disinfect small surfaces (e.g., rubber stoppers of multiple-dose medication vials, and thermometers)952, 969 and occasionally external surfaces of equipment (e.g., stethoscopes and ventilators). However, alcohol evaporates rapidly, which makes extended contact times difficult to achieve unless items are immersed, a factor that precludes its practical use as a large-surface disinfectant.951 Alcohol may cause discoloration, swelling, hardening, and cracking of rubber and certain plastics after prolonged and repeated use and may damage the shellac mounting of lenses in medical equipment. 970 Barrier protection of surfaces and equipment is useful, especially if these surfaces are a) touched frequently by gloved hands during the delivery of patient care, b) likely to become contaminated with body substances, or c) difficult to clean. Impervious-backed paper, aluminum foil, and plastic or fluidresistant covers are suitable for use as barrier protection. An example of this approach is the use of plastic wrapping to cover the handle of the operatory light in dental-care settings.936, 942 Coverings should be removed and discarded while the health-care worker is still gloved.936, 942 The health-care worker, after ungloving and performing hand hygiene, must cover these surfaces with clean materials before the next patient encounter.
# b. Cleaning Housekeeping Surfaces
Housekeeping surfaces require regular cleaning and removal of soil and dust. Dry conditions favor the persistence of gram-positive cocci (e.g., coagulase-negative Staphylococcus spp.) in dust and on surfaces, whereas moist, soiled environments favor the growth and persistence of gram-negative bacilli.948, 971, 972 Fungi are also present on dust and proliferate in moist, fibrous material.
Most, if not all, housekeeping surfaces need to be cleaned only with soap and water or a detergent/disinfectant, depending on the nature of the surface and the type and degree of contamination. Cleaning and disinfection schedules and methods vary according to the area of the health-care facility, type of surface to be cleaned, and the amount and type of soil present. Disinfectant/detergent formulations registered by EPA are used for environmental surface cleaning, but the actual physical removal of microorganisms and soil by wiping or scrubbing is probably as important, if not more so, than any antimicrobial effect of the cleaning agent used.973 Therefore, cost, safety, product-surface compatibility, and acceptability by housekeepers can be the main criteria for selecting a registered agent. If using a proprietary detergent/disinfectant, the manufacturers' instructions for appropriate use of the product should be followed.974 Consult the products' material safety data sheets (MSDS) to determine appropriate precautions to prevent hazardous conditions during product application. Personal protective equipment (PPE) used during cleaning and housekeeping procedures should be appropriate to the task.
Housekeeping surfaces can be divided into two groups -those with minimal hand-contact (e.g., floors, and ceilings) and those with frequent hand-contact ("high touch surfaces"). The methods, thoroughness, and frequency of cleaning and the products used are determined by health-care facility policy.6 However, high-touch housekeeping surfaces in patient-care areas (e.g., doorknobs, bedrails, light switches, wall areas around the toilet in the patient's room, and the edges of privacy curtains) should be cleaned and/or disinfected more frequently than surfaces with minimal hand contact. Infection-control practitioners typically use a risk-assessment approach to identify high-touch surfaces and then coordinate an appropriate cleaning and disinfecting strategy and schedule with the housekeeping staff.
Horizontal surfaces with infrequent hand contact (e.g., window sills and hard-surface flooring) in routine patient-care areas require cleaning on a regular basis, when soiling or spills occur, and when a patient is discharged from the facility.6 Regular cleaning of surfaces and decontamination, as needed, is also advocated to protect potentially exposed workers.967 Cleaning of walls, blinds, and window curtains is recommended when they are visibly soiled. , , Disinfectant fogging is not recommended for general infection control in routine patient-care areas.2, 976 Further, paraformaldehyde, which was once used in this application, is no longer registered by EPA for this purpose. Use of paraformaldehyde in these circumstances requires either registration or an exemption issued by EPA under the Federal Insecticide, Fungicide, and Rodenticide Act (FIFRA). Infection control, industrial hygienists, and environmental services supervisors should assess the cleaning procedures, chemicals used, and the safety issues to determine if a temporary relocation of the patient is needed when cleaning in the room.
Extraordinary cleaning and decontamination of floors in health-care settings is unwarranted. Studies have demonstrated that disinfection of floors offers no advantage over regular detergent/water cleaning and has minimal or no impact on the occurrence of health-care-associated infections.947, 948, 977-980 Additionally, newly cleaned floors become rapidly recontaminated from airborne microorganisms and those transferred from shoes, equipment wheels, and body substances.971, 975, 981 Nevertheless, health care institutions or contracted cleaning companies may choose to use an EPA-registered detergent/disinfectant for cleaning low-touch surfaces (e.g., floors) in patient-care areas because of the difficulty that personnel may have in determining if a spill contains blood or body fluids (requiring a detergent/disinfectant for clean-up) or when a multi-drug resistant organism is likely to be in the environment. Methods for cleaning non-porous floors include wet mopping and wet vacuuming, dry dusting with electrostatic materials, and spray buffing.973, 982-984 Methods that produce minimal mists and aerosols or dispersion of dust in patient-care areas are preferred.9, 20, 109, 272 Part of the cleaning strategy is to minimize contamination of cleaning solutions and cleaning tools. Bucket solutions become contaminated almost immediately during cleaning, and continued use of the solution transfers increasing numbers of microorganisms to each subsequent surface to be cleaned.971, 981, 985 Cleaning solutions should be replaced frequently. A variety of "bucket" methods have been devised to address the frequency with which cleaning solutions are replaced.986, 987 Another source of contamination in the cleaning process is the cleaning cloth or mop head, especially if left soaking in dirty cleaning solutions.971, 988-990 Laundering of cloths and mop heads after use and allowing them to dry before re-use can help to minimize the degree of contamination.990 A simplified approach to cleaning involves replacing soiled cloths and mop heads with clean items each time a bucket of detergent/disinfectant is emptied and replaced with fresh, clean solution (B. Stover, Kosair Children's Hospital, 2000). Disposable cleaning cloths and mop heads are an alternative option, if costs permit.
Another reservoir for microorganisms in the cleaning process may be dilute solutions of the detergents or disinfectants, especially if the working solution is prepared in a dirty container, stored for long periods of time, or prepared incorrectly.547 Gram-negative bacilli (e.g., Pseudomonas spp. and Serratia marcescens) have been detected in solutions of some disinfectants (e.g., phenolics and quaternary ammonium compounds).547, 991 Contemporary EPA registration regulations have helped to minimize this problem by asking manufacturers to provide potency data to support label claims for detergent/disinfectant properties under real-use conditions (e.g., diluting the product with tap water instead of distilled water). Application of contaminated cleaning solutions, particularly from smallquantity aerosol spray bottles or with equipment that might generate aerosols during operation, should be avoided, especially in high-risk patient areas.992, 993 Making sufficient fresh cleaning solution for daily cleaning, discarding any remaining solution, and drying out the container will help to minimize the degree of bacterial contamination. Containers that dispense liquid as opposed to spray-nozzle dispensers (e.g., quart-sized dishwashing liquid bottles) can be used to apply detergent/disinfectants to surfaces and then to cleaning cloths with minimal aerosol generation. A pre-mixed, "ready-to-use" detergent/disinfectant solution may be used if available.
# c. Cleaning Special Care Areas
Guidelines have been published regarding cleaning strategies for isolation areas and operating rooms.6, 7
The basic strategies for areas housing immunosuppressed patients include a) wet dusting horizontal surfaces daily with cleaning cloths pre-moistened with detergent or an EPA-registered hospital disinfectant or disinfectant wipes;94, 98463 b) using care when wet dusting equipment and surfaces above the patient to avoid patient contact with the detergent/disinfectant; c) avoiding the use of cleaning equipment that produces mists or aerosols; d) equipping vacuums with HEPA filters, especially for the exhaust, when used in any patient-care area housing immunosuppressed patients;9, 94, 986 and e) regular cleaning and maintenance of equipment to ensure efficient particle removal. When preparing the cleaning cloths for wet-dusting, freshly prepared solutions of detergents or disinfectants should be used rather than cloths that have soaked in such solutions for long periods of time. Dispersal of microorganisms in the air from dust or aerosols is more problematic in these settings than elsewhere in health-care facilities. Vacuum cleaners can serve as dust disseminators if they are not operating properly.994 Doors to immunosuppressed patients' rooms should be closed when nearby areas are being vacuumed.9 Bacterial and fungal contamination of filters in cleaning equipment is inevitable, and these filters should be cleaned regularly or replaced as per equipment manufacturer instructions.
Mats with tacky surfaces placed in operating rooms and other patient-care areas only slightly minimize the overall degree of contamination of floors and have little impact on the incidence rate of health-careassociated infection in general.351, 971, 983 An exception, however, is the use of tacky mats inside the entry ways of cordoned-off construction areas inside the health-care facility; these mats help to minimize the intrusion of dust into patient-care areas.
Special precautions for cleaning incubators, mattresses, and other nursery surfaces have been recommended to address reports of hyperbilirubinemia in newborns linked to inadequately diluted solutions of phenolics and poor ventilation.995-997 These medical conditions have not, however, been associated with the use of properly prepared solutions of phenolics. Non-porous housekeeping surfaces in neonatal units can be disinfected with properly diluted or pre-mixed phenolics, followed by rinsing with clean water.997 However, phenolics are not recommended for cleaning infant bassinets and incubators during the stay of the infant. Infants who remain in the nursery for an extended period should be moved periodically to freshly cleaned and disinfected bassinets and incubators.997 If phenolics are used for cleaning bassinets and incubators after they have been vacated, the surfaces should be rinsed thoroughly with water and dried before either piece of equipment is reused. Cleaning and disinfecting protocols should allow for the full contact time specified for the product used. Bassinet mattresses should be replaced, however, if the mattress cover surface is broken.997
# Cleaning Strategies for Spills of Blood and Body Substances
Neither HBV, HCV, nor HIV has ever been transmitted from a housekeeping surface (i.e., floors, walls, or countertops). Nonetheless, prompt removal and surface disinfection of an area contaminated by either blood or body substances are sound infection-control practices and OSHA requirements.967
Studies have demonstrated that HIV is inactivated rapidly after being exposed to commonly used chemical germicides at concentrations that are much lower than those used in practice.998 1003 HBV is readily inactivated with a variety of germicides, including quaternary ammonium compounds.1004 Embalming fluids (e.g., formaldehyde) are also capable of completely inactivating HIV and HBV.1005, 1006 OSHA has revised its regulation for disinfecting spills of blood or other potentially infectious material to include proprietary products whose label includes inactivation claims for HBV and HIV, provided that such surfaces have not become contaminated with agent(s) or volumes of or concentrations of agent(s) for which a higher level of disinfection is recommended. Sodium hypochlorite solutions are inexpensive and effective broad-spectrum germicidal solutions.1010, 1011 Generic sources of sodium hypochlorite include household chlorine bleach or reagent grade chemical. Concentrations of sodium hypochlorite solutions with a range of 5,000-6,150 ppm (1:10 v/v dilution of household bleaches marketed in the United States) to 500-615 ppm (1:100 v/v dilution) free chlorine are effective depending on the amount of organic material (e.g., blood, mucus, and urine) present on the surface to be cleaned and disinfected.1010, 1011 EPA-registered chemical germicides may be more compatible with certain materials that could be corroded by repeated exposure to sodium hypochlorite, especially the 1:10 dilution. Appropriate personal protective equipment (e.g., gloves and goggles) should be worn when preparing and using hypochlorite solutions or other chemical germicides.967
Despite laboratory evidence demonstrating adequate potency against bloodborne pathogens (e.g., HIV and HBV), many chlorine bleach products available in grocery and chemical-supply stores are not registered by the EPA for use as surface disinfectants. Use of these chlorine products as surface disinfectants is considered by the EPA to be an "unregistered use." EPA encourages the use of registered products because the agency reviews them for safety and performance when the product is used according to label instructions. When unregistered products are used for surface disinfection, users do so at their own risk.
Strategies for decontaminating spills of blood and other body fluids differ based on the setting in which they occur and the volume of the spill.1010 In patient-care areas, workers can manage small spills with cleaning and then disinfecting using an intermediate-level germicide or an EPA-registered germicide from the EPA List D or E.967, 1007 For spills containing large amounts of blood or other body substances, workers should first remove visible organic matter with absorbent material (e.g., disposable paper towels discarded into leak-proof, properly labeled containment) and then clean and decontaminate the area.1002, 1003, 1012 If the surface is nonporous and a generic form of a sodium hypochlorite solution is used (e.g., household bleach), a 1:100 dilution is appropriate for decontamination assuming that a) the worker assigned to clean the spill is wearing gloves and other personal protective equipment appropriate to the task, b) most of the organic matter of the spill has been removed with absorbent material, and c) the surface has been cleaned to remove residual organic matter. A recent study demonstrated that even strong chlorine solutions (i.e., 1:10 dilution of chlorine bleach) may fail to totally inactivate high titers of virus in large quantities of blood, but in the absence of blood these disinfectants can achieve complete viral inactivation.1011 This evidence supports the need to remove most organic matter from a large spill before final disinfection of the surface. Additionally, EPA-registered proprietary disinfectant label claims are based on use on a pre-cleaned surface.951, 954
Managing spills of blood, body fluids, or other infectious materials in clinical, public health, and research laboratories requires more stringent measures because of a) the higher potential risk of disease transmission associated with large volumes of blood and body fluids and b) high numbers of microorganisms associated with diagnostic cultures. The use of an intermediate-level germicide for routine decontamination in the laboratory is prudent.954 Recommended practices for managing large spills of concentrated infectious agents in the laboratory include a) confining the contaminated area, b) flooding the area with a liquid chemical germicide before cleaning, and c) decontaminating with fresh germicidal chemical of at least intermediate-level disinfectant potency.1010 A suggested technique when flooding the spill with germicide is to lay absorbent material down on the spill and apply sufficient germicide to thoroughly wet both the spill and the absorbent material.1013 If using a solution of household chlorine bleach, a 1:10 dilution is recommended for this purpose. EPA-registered germicides should be used according to the manufacturers' instructions for use dilution and contact time. Gloves should be worn during the cleaning and decontamination procedures in both clinical and laboratory settings. PPE in such a situation may include the use of respiratory protection (e.g., an N95 respirator) if clean-up procedures are expected to generate infectious aerosols. Protocols for cleaning spills should be developed and made available on record as part of good laboratory practice.1013 Workers in laboratories and in patient-care areas of the facility should receive periodic training in environmentalsurface infection-control strategies and procedures as part of an overall infection-control and safety curriculum.
# Carpeting and Cloth Furnishings
# a. Carpeting
Carpeting has been used for more than 30 years in both public and patient-care areas of health-care facilities. Advantages of carpeting in patient-care areas include a) its noise-limiting characteristics; b) the "humanizing" effect on health care; and c) its contribution to reductions in falls and resultant injuries, particularly for the elderly.10141016 Compared to hard-surface flooring, however, carpeting is harder to keep clean, especially after spills of blood and body substances. It is also harder to push equipment with wheels (e.g., wheelchairs, carts, and gurneys) on carpeting.
Several studies have documented the presence of diverse microbial populations, primarily bacteria and fungi, in carpeting;111, 10171024 the variety and number of microorganisms tend to stabilize over time. New carpeting quickly becomes colonized, with bacterial growth plateauing after about 4 weeks. 1019 Vacuuming and cleaning the carpeting can temporarily reduce the numbers of bacteria, but these populations soon rebound and return to pre-cleaning levels.1019, 1020, 1023 Bacterial contamination tends to increase with higher levels of activity.10181020, 1025 Soiled carpeting that is or remains damp or wet provides an ideal setting for the proliferation and persistence of gram-negative bacteria and fungi.1026 Carpeting that remains damp should be removed, ideally within 72 hours.
Despite the evidence of bacterial growth and persistence in carpeting, only limited epidemiologic evidence demonstrates that carpets influence health-care-associated infection rates in areas housing immunocompetent patients.1023, 1025, 1027 This guideline, therefore, includes no recommendations against the use of carpeting in these areas. Nonetheless, avoiding the use of carpeting is prudent in areas where spills are likely to occur (e.g., laboratories, areas around sinks, and janitor closets) and where patients may be at greater risk of infection from airborne environmental pathogens (e.g., HSCT units, burn units, ICUs, and ORs).111, 1028 An outbreak of aspergillosis in an HSCT unit was recently attributed to carpet contamination and a particular method of carpet cleaning.111 A window in the unit had been opened repeatedly during the time of a nearby building fire, which allowed fungal spore intrusion into the unit. After the window was sealed, the carpeting was cleaned using a "bonnet buffing" machine, which dispersed Aspergillus spores into the air.111 Wet vacuuming was instituted, replacing the dry cleaning method used previously; no additional cases of invasive aspergillosis were identified.
The care setting and the method of carpet cleaning are important factors to consider when attempting to minimize or prevent production of aerosols and dispersal of carpet microorganisms into the air.94, 111 Both vacuuming and shampooing or wet cleaning with equipment can disperse microorganisms to the air.111, 994 Vacuum cleaners should be maintained to minimize dust dispersal in general, and be equipped with HEPA filters, especially for use in high-risk patient-care areas.9, 94, 986 Some formulations of carpet-cleaning chemicals, if applied or used improperly, can be dispersed into the air as a fine dust capable of causing respiratory irritation in patients and staff.1029 Cleaning equipment, especially those that engage in wet cleaning and extraction, can become contaminated with waterborne organisms (e.g., Pseudomonas aeruginosa) and serve as a reservoir for these organisms if this equipment is not properly maintained. Substantial numbers of bacteria can then be transferred to carpeting during the cleaning process.1030 Therefore, keeping the carpet cleaning equipment in good repair and allowing such equipment to dry between uses is prudent.
Carpet cleaning should be performed on a regular basis determined by internal policy. Although spills of blood and body substances on non-porous surfaces require prompt spot cleaning using standard cleaning procedures and application of chemical germicides,967 similar decontamination approaches to blood and body substance spills on carpeting can be problematic from a regulatory perspective.1031 Most, if not all, modern carpet brands suitable for public facilities can tolerate the activity of a variety of liquid chemical germicides. However, according to OSHA, carpeting contaminated with blood or other potentially infectious materials can not be fully decontaminated.1032 Therefore, facilities electing to use carpeting for high-activity patient-care areas may choose carpet tiles in areas at high risk for spills.967, 1032 In the event of contamination with blood or other body substances, carpet tiles can be removed, discarded, and replaced. OSHA also acknowledges that only minimal direct skin contact occurs with carpeting, and therefore, employers are expected to make reasonable efforts to clean and sanitize carpeting using carpet detergent/cleaner products.1032
Over the last few years, some carpet manufacturers have treated their products with fungicidal and/or bactericidal chemicals. Although these chemicals may help to reduce the overall numbers of bacteria or fungi present in carpet, their use does not preclude the routine care and maintenance of the carpeting. Limited evidence suggests that chemically treated carpet may have helped to keep health-careassociated aspergillosis rates low in one HSCT unit,111 but overall, treated carpeting has not been shown to prevent the incidence of health-care-associated infections in care areas for immunocompetent patients.
# b. Cloth Furnishings
Upholstered furniture and furnishings are becoming increasingly common in patient-care areas. These furnishings range from simple cloth chairs in patients' rooms to a complete decorating scheme that gives the interior of the facility more the look of an elegant hotel.1033 Even though pathogenic microorganisms have been isolated from the surfaces of cloth chairs, no epidemiologic evidence suggests that general patient-care areas with cloth furniture pose increased risks of health-care-associated infection compared with areas that contain hard-surfaced furniture.1034, 1035 Allergens (e.g., dog and cat dander) have been detected in or on cloth furniture in clinics and elsewhere in hospitals in concentrations higher than those found on bed linens.1034, 1035 These allergens presumably are transferred from the clothing of visitors. Researchers have therefore suggested that cloth chairs should be vacuumed regularly to keep the dust and allergen levels to a minimum. This recommendation, however, has generated concerns that aerosols created from vacuuming could place immunocompromised patients or patients with preexisting lung disease (e.g., asthma) at risk for development of health-care-associated, environmental airborne disease.9, 20, 109, 988 Recovering worn, upholstered furniture (especially the seat cushion) with covers that are easily cleaned (e.g., vinyl), or replacing the item is prudent; minimizing the use of upholstered furniture and furnishings in any patientcare areas where immunosuppressed patients are located (e.g., HSCT units) reduces the likelihood of disease.9
# Flowers and Plants in Patient-Care Areas
Fresh flowers, dried flowers, and potted plants are common items in health-care facilities. In 1974, clinicians isolated an Erwinia sp. post mortem from a neonate diagnosed with fulminant septicemia, meningitis, and respiratory distress syndrome.1038 Because Erwinia spp. are plant pathogens, plants brought into the delivery room were suspected to be the source of the bacteria, although the case report did not definitively establish a direct link. Several subsequent studies evaluated the numbers and diversity of microorganisms in the vase water of cut flowers. These studies revealed that high concentrations of bacteria, ranging from 104-1010 CFU/mL, were often present, especially if the water was changed infrequently.515, 702, 1039 The major group of microorganisms in flower vase water was gram-negative bacteria, with Pseudomonas aeruginosa the most frequently isolated organism.515, 702, 1039, 1040 P. aeruginosa was also the primary organism directly isolated from chrysanthemums and other potted plants. 1041, 1042 However, flowers in hospitals were not significantly more contaminated with bacteria compared with flowers in restaurants or in the home.702 Additionally, no differences in the diversity and degree of antibiotic resistance of bacteria have been observed in samples isolated from hospital flowers versus those obtained from flowers elsewhere.702 Despite the diversity and large numbers of bacteria associated with flower-vase water and potted plants, minimal or no evidence indicates that the presence of plants in immunocompetent patient-care areas poses an increased risk of health-care-associated infection.515 In one study involving a limited number of surgical patients, no correlation was observed between bacterial isolates from flowers in the area and the incidence and etiology of postoperative infections among the patients.1040 Similar conclusions were reached in a study that examined the bacteria found in potted plants.1042 Nonetheless, some precautions for general patient-care settings should be implemented, including a) limiting flower and plant care to staff with no direct patient contact, b) advising health-care staff to wear gloves when handling plants, c) washing hands after handling plants, d) changing vase water every 2 days and discharging the water into a sink outside the immediate patient environment, and e) cleaning and disinfecting vases after use.702 Some researchers have examined the possibility of adding a chemical germicide to vase water to control bacterial populations. Certain chemicals (e.g., hydrogen peroxide and chlorhexidine) are well tolerated by plants.1040, 1043, 1044 Use of these chemicals, however, was not evaluated in studies to assess impact on health-care-associated infection rates. Modern florists now have a variety of products available to add to vase water to extend the life of cut flowers and to minimize bacterial clouding of the water.
Flowers (fresh and dried) and ornamental plants, however, may serve as a reservoir of Aspergillus spp., and dispersal of conidiospores into the air from this source can occur.109 Health-care-associated outbreaks of invasive aspergillosis reinforce the importance of maintaining an environment as free of Aspergillus spp. spores as possible for patients with severe, prolonged neutropenia. Potted plants, freshcut flowers, and dried flower arrangements may provide a reservoir for these fungi as well as other fungal species (e.g., Fusarium spp.).109, 1045, Researchers in one study of bacteria and flowers suggested that flowers and vase water should be avoided in areas providing care to medically at-risk patients (e.g., oncology patients and transplant patients), although this study did not attempt to correlate the observations of bacterial populations in the vase water with the incidence of health-care-associated infections.515 Another study using molecular epidemiology techniques demonstrated identical Aspergillus terreus types among environmental and clinical specimens isolated from infected patients with hematological malignancies.1046 Therefore, attempts should be made to exclude flowers and plants from areas where immunosuppressed patients are be located (e.g., HSCT units).9, 1046
# Pest Control
Cockroaches, flies and maggots, ants, mosquitoes, spiders, mites, midges, and mice are among the typical arthropod and vertebrate pest populations found in health-care facilities. Insects can serve as agents for the mechanical transmission of microorganisms, or as active participants in the disease transmission process by serving as a vector.1047-1049 Arthropods recovered from health-care facilities have been shown to carry a wide variety of pathogenic microorganisms.1050-1056 Studies have suggested that the diversity of microorganisms associated with insects reflects the microbial populations present in the indoor health-care environment; some pathogens encountered in insects from hospitals were either absent from or present to a lesser degree in insects trapped from residential settings.1057-1060 Some of the microbial populations associated with insects in hospitals have demonstrated resistance to antibiotics.1048, 1059, 1061-1063 Insect habitats are characterized by warmth, moisture, and availability of food.1064 Insects forage in and feed on substrates, including but not limited to food scraps from kitchens/cafeteria, foods in vending machines, discharges on dressings either in use or discarded, other forms of human detritis, medical wastes, human wastes, and routine solid waste.1057-1061 Cockroaches, in particular, have been known to feed on fixed sputum smears in laboratories.1065, 1066 Both cockroaches and ants are frequently found in the laundry, central sterile supply departments, and anywhere in the facility where water or moisture is present (e.g., sink traps, drains and janitor closets). Ants will often find their way into sterile packs of items as they forage in a warm, moist environment.1057 Cockroaches and other insects frequent loading docks and other areas with direct access to the outdoors.
Although insects carry a wide variety of pathogenic microorganisms on their surfaces and in their gut, the direct association of insects with disease transmission (apart from vector transmission) is limited, especially in health-care settings; the presence of insects in itself likely does not contribute substantially to health-care-associated disease transmission in developed countries. However, outbreaks of infection attributed to microorganisms carried by insects may occur because of infestation coupled with breaks in standard infection-control practices.1063 Studies have been conducted to examine the role of houseflies as possible vectors for shigellosis and other forms of diarrheal disease in non-health-care settings.1046, 1067 When control measures aimed at reducing the fly population density were implemented, a concomitant reduction in the incidence of diarrheal infections, carriage of Shigella organisms, and mortality caused by diarrhea among infants and young children was observed.
Myiasis is defined as a parasitosis in which the larvae of any of a variety of flies use living or necrotic tissue or body substances of the host as a nutritional source.1068 Larvae from health-care-acquired myiasis have been observed in nares, wounds, eyes, ears, sinuses, and the external urogenital structures.1069-1071 Patients with this rare condition are typically older adults with underlying medical conditions (e.g., diabetes, chronic wounds, and alcoholism) who have a decreased capacity to ward off the flies. Persons with underlying conditions who live or travel to tropical regions of the world are especially at risk.1070, 1071 Cases occur in the summer and early fall months in temperate climates when flies are most active.1071 An environmental assessment and review of the patient's history are necessary to verify that the source of the myiasis is health-care-acquired and to identify corrective measures.1069, 1072 Simple prevention measures (e.g., installing screens on windows) are important in reducing the incidence of myiasis.1072 From a public health and hygiene perspective, arthropod and vertebrate pests should be eradicated from all indoor environments, including health-care facilities.1073, 1074 Modern approaches to institutional pest management usually focus on a) eliminating food sources, indoor habitats, and other conditions that attract pests; b) excluding pests from the indoor environments; and c) applying pesticides as needed.1075 Sealing windows in modern health-care facilities helps to minimize insect intrusion. When windows need to be opened for ventilation, ensuring that screens are in good repair and closing doors to the outside can help with pest control. Insects should be kept out of all areas of the health-care facility, especially ORs and any area where immunosuppressed patients are located. A pest-control specialist with appropriate credentials can provide a regular insect-control program that is tailored to the needs of the facility and uses approved chemicals and/or physical methods. Industrial hygienists can provide information on possible adverse reactions of patients and staff to pesticides and suggest alternative methods for pest control, as needed. ) represent crucial and growing concerns for infection control. Although the term GISA is technically a more accurate description of the strains isolated to date (most of which are classified as having intermediate resistance to both vancomycin and teicoplanin), the term "glycopeptide" may not be recognized by many clinicians. Thus, the label of VISA, which emphasizes a change in minimum inhibitory concentration (MICs) to vancomycin, is similar to that of VRE and is more meaningful to clinicians.1076 According to National Nosocomial Infection Surveillance (NNIS) statistics for infections acquired among ICU patients in the United States in 1999, 52.3% of infections resulting from S. aureus were identified as MRSA infections, and 25.2% of enterococcal infections were attributed to VRE. These figures reflect a 37% and a 43% increase, respectively, since 1994-1998.1077
# Special Pathogen Concerns a. Antibiotic-Resistant Gram-Positive Cocci
People represent the primary reservoir of S. aureus.1078 Although S. aureus has been isolated from a variety of environmental surfaces (e.g., stethoscopes, floors, charts, furniture, dry mops, and hydrotherapy tanks), the role of environmental contamination in transmission of this organism in health care appears to be minimal.1079-1082 S. aureus contamination of surfaces and tanks within burn therapy units, however, may be a major factor in the transmission of infection among burn patients.1083
Colonized patients are the principal reservoir of VRE, and patients who are immunosuppressed (e.g., transplant patients) or otherwise medically at-risk (e.g., ICU patients, cardio-thoracic surgical patients, patients previously hospitalized for extended periods, and those having received multi-antimicrobial or vancomycin therapy) are at greatest risk for VRE colonization.1084-1087 The mechanisms by which cross-colonization take place are not well defined, although recent studies have indicated that both MRSA and VRE may be transmitted either a) directly from patient to patient, b) indirectly by transient carriage on the hands of health-care workers,1088-1091 or c) by hand transfer of these gram-positive organisms from contaminated environmental surfaces and patient-care equipment.1084, 1087, 1092-1097 In one survey, hand carriage of VRE in workers in a long-term care facility ranged from 13%-41%.1098 Many of the environmental surfaces found to be contaminated with VRE in outbreak investigations have been those that are touched frequently by the patient or the health-care worker.1099 Such high-touch surfaces include bedrails, doorknobs, bed linens, gowns, overbed tables, blood pressure cuffs, computer table, bedside tables, and various medical equipment.22, 1087, 1094, 1095, 1100-1102 Contamination of environmental surfaces with VRE generally occurs in clinical laboratories and areas where colonized patients are present,1087, 1092, 1094, 1095, 1103 but the potential for contamination increases when such patients have diarrhea1087 or have multiple body-site colonization.1104 Additional factors that can be important in the dispersion of these pathogens to environmental surfaces are misuse of glove techniques by health care workers (especially when cleaning fecal contamination from surfaces) and patient, family, and visitor hygiene.
Interest in the importance of environmental reservoirs of VRE increased when laboratory studies demonstrated that enterococci can persist in a viable state on dry environmental surfaces for extended periods of time (7 days to 4 months)1099, 1105 and multiple strains can be identified during extensive periods of surveillance.1104 VRE can be recovered from inoculated hands of health-care workers (with or without gloves) for up to 60 minutes. 22 The presence of either MRSA, VISA, or VRE on environmental surfaces, however, does not mean that patients in the contaminated areas will become colonized. Strict adherence to hand hygiene/handwashing and the proper use of barrier precautions help to minimize the potential for spread of these pathogens. Published recommendations for preventing the spread of vancomycin resistance address isolation measures, including patient cohorting and management of patient-care items.5 Direct patient-care items (e.g., blood pressure cuffs) should be disposable whenever possible when used in contact isolation settings for patients with multiply resistant microorganisms.1102 Careful cleaning of patient rooms and medical equipment contributes substantially to the overall control of MRSA, VISA, or VRE transmission. The major focus of a control program for either VRE or MRSA should be the prevention of hand transfer of these organisms. Routine cleaning and disinfection of the housekeeping surfaces (e.g., floors and walls) and patient-care surfaces (e.g., bedrails) should be adequate for inactivation of these organisms. Both MRSA and VRE are susceptible to several EPAregistered low-and intermediate-level disinfectants (e.g., alcohols, sodium hypochlorite, quaternary ammonium compounds, phenolics, and iodophors) at recommended use dilutions for environmental surface disinfection.1103, 1106-1109 Additionally, both VRE and vancomycin-sensitive enterococci are equally sensitive to inactivation by chemical germicides,1106, 1107, 1109 and similar observations have been made when comparing the germicidal resistance of MRSA to that of either methicillin-sensitive S. aureus (MSSA) or VISA.1110 The use of stronger solutions of disinfectants for inactivation of either VRE, MRSA, or VISA is not recommended based on the organisms' resistance to antibiotics.1110-1112 VRE from clinical specimens have exhibited some measure of increased tolerance to heat inactivation in temperature ranges <212°F (<100°C);1106, 1113 however, the clinical significance of these observations is unclear because the role of cleaning the surface or item prior to heat treatment was not evaluated. Although routine environmental sampling is not recommended, laboratory surveillance of environmental surfaces during episodes when VRE contamination is suspected can help determine the effectiveness of the cleaning and disinfecting procedures. Environmental culturing should be approved and supervised by the infection-control program in collaboration with the clinical laboratory.1084, 1087, 1088, 1092, 1096 Two cases of wound infections associated with vancomycin-resistant Staphylococcus aureus (VRSA) determined to be resistant by NCCLS standards for sensitivity/resistance testing were identified in Michigan and Pennsylvania in 2002.1114, 1115 These represented isolated cases, and neither the family members nor the health-care providers of these case-patients had evidence of colonization or infection with VRSA. Conventional environmental infection-control measures (i.e., cleaning and then disinfecting surfaces using EPA-registered disinfectants with label claims for S. aureus) were used during the environmental investigation of these two cases;11101112 however, studies have yet to evaluate the potential intrinsic resistance of these VRSA strains to surface disinfectants.
Standard procedures during terminal cleaning and disinfection of surfaces, if performed incorrectly, may be inadequate for the elimination of VRE from patient rooms.1113, 11161118 Given the sensitivity of VRE to hospital disinfectants, current disinfecting protocols should be effective if they are diligently carried out and properly performed. Health-care facilities should be sure that housekeeping staff use correct procedures for cleaning and disinfecting surfaces in VRE-contaminated areas, which include using sufficient amounts of germicide at proper use dilution and allowing adequate contact time.1118
# b. Clostridium difficile
Clostridium difficile is the most frequent etiologic agent for health-care-associated diarrhea.1119, 1120 In one hospital, 30% of adults who developed health-care-associated diarrhea were positive for C. difficile}121 One recent study employing PCR-ribotyping techniques demonstrated that cases of C. difiicile-acquired diarrhea occurring in the hospital included patients whose infections were attributed to endogenous C. difficile strains and patients whose illnesses were considered to be health-careassociated infections.1122 Most patients remain asymptomatic after infection, but the organism continues to be shed in their stools. Risk factors for acquiring C. difficile--associated infection include a) exposure to antibiotic therapy, particularly with beta-lactam agents;1123 b) gastrointestinal procedures and surgery;1124 c) advanced age; and d) indiscriminate use of antibiotics.1125-1128 Of all the measures that have been used to prevent the spread of C. difficile--associated diarrhea, the most successful has been the restriction of the use of antimicrobial agents.1129, 1130 C. difficile is an anaerobic, gram-positive bacterium. Normally fastidious in its vegetative state, it is capable of sporulating when environmental conditions no longer support its continued growth. The capacity to form spores enables the organism to persist in the environment (e.g., in soil and on dry surfaces) for extended periods of time. Environmental contamination by this microorganism is well known, especially in places where fecal contamination may occur. 1131 The environment (especially housekeeping surfaces) rarely serves as a direct source of infection for patients.1024, 1132-1136 However, direct exposure to contaminated patient-care items (e.g., rectal thermometers) and high-touch surfaces in patients' bathrooms (e.g., light switches) have been implicated as sources of infection.1130, 1135,1136,1138 Transfer of the pathogen to the patient via the hands of health-care workers is thought to be the most likely mechanism of exposure. , , Standard isolation techniques intended to minimize enteric contamination of patients, health-care-workers' hands, patient-care items, and environmental surfaces have been published.1140 Handwashing remains the most effective means of reducing hand contamination. Proper use of gloves is an ancillary measure that helps to further minimize transfer of these pathogens from one surface to another.
The degree to which the environment becomes contaminated with C. difficile spores is proportional to the number of patients with C. difficile-associated diarrhea, , , although asymptomatic, colonized patients may also serve as a source of contamination. Few studies have examined the use of specific chemical germicides for the inactivation of C. difficile spores, and no well-controlled trials have been conducted to determine efficacy of surface disinfection and its impact on health-care-associated diarrhea. Some investigators have evaluated the use of chlorine-containing chemicals (e.g., 1,000 ppm hypochlorite at recommended use-dilution, 5,000 ppm sodium hypochlorite [1:10 v/v dilution], 1:100 v/v dilutions of unbuffered hypochlorite, and phosphate-buffered hypochlorite [1,600 ppm]). One of the studies demonstrated that the number of contaminated environmental sites was reduced by half,1135 whereas another two studies demonstrated declines in health-care-associated C. difficile infections in a HSCT unit1141 and in two geriatric medical units1142 during a period of hypochlorite use. The presence of confounding factors, however, was acknowledged in one of these studies. 1142 The recommended approach to environmental infection control with respect to C. difficile is meticulous cleaning followed by disinfection using hypochlorite-based germicides as appropriate.952, 1130, 1143 However, because no EPA-registered surface disinfectants with label claims for inactivation of C. difficile spores are available, the recommendation is based on the best available evidence from the scientific literature.
# c. Respiratory and Enteric Viruses in Pediatric-Care Settings
Although the viruses mentioned in this guideline are not unique to the pediatric-care setting in health care facilities, their prevalence in these areas, especially during the winter months, is substantial. Children (particularly neonates) are more likely to develop infection and substantial clinical disease from these agents compared with adults and therefore are more likely to require supportive care during their illness.
Common respiratory viruses in pediatric-care areas include rhinoviruses, respiratory syncytial virus (RSV), adenoviruses, influenza viruses, and parainfluenza viruses. Transmission of these viruses occurs primarily via direct contact with small-particle aerosols or via hand contamination with respiratory secretions that are then transferred to the nose or eyes. Because transmission primarily requires close personal contact, contact precautions are appropriate to interrupt transmission.6 Hand contamination can occur from direct contact with secretions or indirectly from touching high-touch environmental surfaces that have become contaminated with virus from large droplets. The indirect transfer of virus from one persion to other via hand contact with frequently-touched fomites was demonstrated in a study using a bacteriophage whose environmental stability approximated that of human viral pathogens (e.g., poliovirus and parvovirus). 1144 The impact of this mode of transmission with respect to human respiratory-and enteric viruses is dependent on the ability of these agents to survive on environmental surfaces. Infectious RSV has been recovered from skin, porous surfaces, and non-porous surfaces after 30 minutes, 1 hour, and 7 hours, respectively.1145 Parainfluenza viruses are known to persist for up to 4 hours on porous surfaces and up to 10 hours on non-porous surfaces.1146 Rhinoviruses can persist on porous surfaces and non-porous surfaces for approximately 1 and 3 hours respectively; study participants in a controlled environment became infected with rhinoviruses after first touching a surface with dried secretions and then touching their nasal or conjunctival mucosa.1147 Although the efficiency of direct transmission of these viruses from surfaces in uncontrolled settings remains to be defined, these data underscore the basis for maintaining regular protocols for cleaning and disinfecting of high touch surfaces.
The clinically important enteric viruses encountered in pediatric care settings include enteric adenovirus, astroviruses, caliciviruses, and rotavirus. Group A rotavirus is the most common cause of infectious diarrhea in infants and children. Transmission of this virus is primarily fecal-oral, however, the role of fecally contaminated surfaces and fomites in rotavirus transmission is unclear. During one epidemiologic investigation of enteric disease among children attending day care, rotavirus contamination was detected on 19% of inanimate objects in the center. 1148,1149 In an outbreak in a pediatric unit, secondary cases of rotavirus infection clustered in areas where children with rotaviral diarrhea were located.1150 Astroviruses cause gastroenteritis and diarrhea in newborns and young children and can persist on fecally contaminated surfaces for several months during periods of relatively low humidity.1151, 1152 Outbreaks of small round-structured viruses (i.e., caliciviruses [Norwalk virus and Norwalk-like viruses]) can affect both patients and staff, with attack rates of >50%.1153 Routes of person-to-person transmission include fecal-oral spread and aerosols generated from vomiting.11541156 Fecal contamination of surfaces in care settings can spread large amounts of virus to the environment. Studies that have attempted to use low-and intermediate-level disinfectants to inactivate rotavirus suspended in feces have demonstrated a protective effect of high concentrations of organic matter.1157, 1158 Intermediate-level disinfectants (e.g., alcoholic quaternary ammonium compounds, and chlorine solutions) can be effective in inactivating enteric viruses provided that a cleaning step to remove most of the organic matter precedes terminal disinfection.1158 These findings underscore the need for proper cleaning and disinfecting procedures where contamination of environmental surfaces with body substances is likely. EPA-registered surface disinfectants with label claims for these viral agents should be used in these settings. Using disposable, protective barrier coverings may help to minimize the degree of surface contamination.936
# d. Severe Acute Respiratory Syndrome (SARS) Virus
In November 2002 an atypical pneumonia of unknown etiology emerged in Asia and subsequently developed into an international outbreak of respiratory illness among persons in 29 countries during the first six months of 2003. "Severe acute respiratory syndrome" (SARS) is a viral upper respiratory infection associated with a newly described coronavirus (SARS-associated Co-V [SARS-CoV]). SARS-CoV is an enveloped RNA virus. It is present in high titers in respiratory secretions, stool, and blood of infected persons. The modes of transmission determined from epidemiologic investigations were primarily forms of direct contact (i.e., large droplet aerosolization and person-to-person contact). Respiratory secretions were presumed to be the major source of virus in these situations; airborne transmission of virus has not been completely ruled out. Little is known about the impact of fecal-oral transmission and SARS.
The epidemiology of SARS-CoV infection is not completely understood, and therefore recommended infection control and prevention measures to contain the spread of SARS will evolve as new information becomes available.1159 At present there is no indication that established strategies for cleaning (i.e., to remove the majority of bioburden) and disinfecting equipment and environmental surfaces need to be changed for the environmental infection control of SARS. In-patient rooms housing SARS patients should be cleaned and disinfected at least daily and at the time of patient transfer or discharge. More frequent cleaning and disinfection may be indicated for high-touch surfaces and following aerosol-producing procedures (e.g., intubation, bronchoscopy, and sputum production). While there are presently no disinfectant products registered by EPA specifically for inactivation of SARS-CoV, EPA-registered hospital disinfectants that are equivalent to low-and intermediate-level germicides may be used on pre-cleaned, hard, non-porous surfaces in accordance with manufacturer's instructions for environmental surface disinfection. Monitoring adherence to guidelines established for cleaning and disinfection is an important component of environmental infection control to contain the spread of SARS.
# e. Creutzfeldt-Jakob Disease (CJD) in Patient-Care Areas
Creutzfeldt-Jakob disease (CJD) is a rare, invariably fatal, transmissible spongiform encephalopathy (TSE) that occurs worldwide with an average annual incidence of 1 case per million population.11601162 CJD is one of several TSEs affecting humans; other diseases in this group include kuru, fatal familial insomnia, and Gerstmann-Straussler-Scheinker syndrome. A TSE that affects a younger population (compared to the age range of CJD cases) has been described primarily in the United Kingdom since 1996.1163 This variant form of CJD (vCJD) is clinically and neuropathologically distinguishable from classic CJD; epidemiologic and laboratory evidence suggests a causal association for bovine spongiform encephalopathy (BSE [Mad Cow disease]) and vCJD.11631166
The agent associated with CJD is a prion, which is an abnormal isoform of a normal protein constituent of the central nervous system.11671169 The mechanism by which the normal form of the protein is converted to the abnormal, disease-causing prion is unknown. The tertiary conformation of the abnormal prion protein appears to confer a heightened degree of resistance to conventional methods of sterilization and disinfection.1170, 1171
Although about 90% of CJD cases occur sporadically, a limited number of cases are the result of a direct exposure to prion-containing material (usually central nervous system tissue or pituitary hormones) acquired as a result of health care (iatrogenic cases). These cases have been linked to a) pituitary hormone therapy [from human sources as opposed to hormones prepared through the use of recombinant technology],11701174 b) transplants of either dura mater or corneas,11751181 and c) neurosurgical instruments and depth electrodes.11821185 In the cases involving instruments and depth electrodes, conventional cleaning and terminal reprocessing methods of the day failed to fully inactivate the contaminating prions and are considered inadequate by today's standards.
Prion inactivation studies involving whole tissues and tissue homogenates have been conducted to determine the parameters of physical and chemical methods of sterilization or disinfection necessary for complete inactivation;1170, 1186 1191 however, the application of these findings to environmental infection control in health-care settings is problematic. No studies have evaluated the effectiveness of medical instrument reprocessing in inactivating prions. Despite a consensus that abnormal prions display some extreme measure of resistance to inactivation by either physical or chemical methods, scientists disagree about the exact conditions needed for sterilization. Inactivation studies utilizing whole tissues present extraordinary challenges to any sterilizing method.1192 Additionally, the experimental designs of these studies preclude the evaluation of surface cleaning as a part of the total approach to pathogen inactivation.951, 1192 Some researchers have recommended the use of either a 1:2 v/v dilution of sodium hypochorite (approximately 20,000 ppm), full-strength sodium hypochlorite (50,000-60,000 ppm), or 1-2 N sodium hydroxide (NaOH) for the inactivation of prions on certain surfaces (e.g., those found in the pathology laboratory).1170, 1188 Although these chemicals may be appropriate for the decontamination of laboratory, operating-room, or autopsy-room surfaces that come into contact with central nervous system tissue from a known or suspected patient, this approach is not indicated for routine or terminal cleaning of a room previously occupied by a CJD patient. Both chemicals pose hazards for the health care worker doing the decontamination. NaOH is caustic and should not make contact with the skin. Sodium hypochlorite solutions (i.e., chlorine bleach) can corrode metals (e.g., aluminum). MSDS information should be consulted when attempting to work with concentrated solutions of either chemical. Currently, no EPA-registered products have label claims for prion inactivation; therefore, this guidance is based on the best available evidence from the scientific literature.
Environmental infection-control strategies must based on the principles of the "chain of infection," regardless of the disease of concern.13 Although CJD is transmissible, it is not highly contagious. All iatrogenic cases of CJD have been linked to a direct exposure to prion-contaminated central nervous system tissue or pituitary hormones. The six documented iatrogenic cases associated with instruments and devices involved neurosurgical instruments and devices that introduced residual contamination directly to the recipient's brain. No evidence suggests that vCJD has been transmitted iatrogenically or that either CJD or vCJD has been transmitted from environmental surfaces (e.g., housekeeping surfaces). Therefore, routine procedures are adequate for terminal cleaning and disinfection of a CJD patient's room. Additionally, in epidemiologic studies involving highly transfused patients, blood was not identified as a source for prion transmission.1193-1198 Routine procedures for containing, decontaminating, and disinfecting surfaces with blood spills should be adequate for proper infection control in these situations. ' Guidance for environmental infection control in ORs and autopsy areas has been published.1197, 1199 Hospitals should develop risk-assessment procedures to identify patients with known or suspected CJD in efforts to implement prion-specific infection-control measures for the OR and for instrument reprocessing.1200 This assessment also should be conducted for older patients undergoing non-lesionous neurosurgery when such procedures are being done for diagnosis. Disposable, impermeable coverings should be used during these autopsies and neurosurgeries to minimize surface contamination. Surfaces that have become contaminated with central nervous system tissue or cerebral spinal fluid should be cleaned and decontaminated by a) removing most of the tissue or body substance with absorbent materials, b) wetting the surface with a sodium hypochlorite solution containing >5,000 ppm or a 1 N NaOH solution, and c) rinsing thoroughly.951, 1197-1199, 1201 The optimum duration of contact exposure in these instances is unclear. Some researchers recommend a 1-hour contact time on the basis of tissueinactivation studies,1197, 1198, 1201 whereas other reviewers of the subject draw no conclusions from this research.1199 Factors to consider before cleaning a potentially contaminated surface are a) the degree to which gross tissue/body substance contamination can be effectively removed and b) the ease with which the surface can be cleaned.
# F. Environmental Sampling
This portion of Part I addresses the basic principles and methods of sampling environmental surfaces and other environmental sources for microorganisms. The applied strategies of sampling with respect to environmental infection control have been discussed in the appropriate preceding subsections.
# General Principles: Microbiologie Sampling of the Environment
Before 1970, U.S. hospitals conducted regularly scheduled culturing of the air and environmental surfaces (e.g., floors, walls, and table tops).1202 By 1970, CDC and the American Hospital Association (AHA) were advocating the discontinuation of routine environmental culturing because rates of health care-associated infection had not been associated with levels of general microbial contamination of air or environmental surfaces, and because meaningful standards for permissible levels of microbial contamination of environmental surfaces or air did not exist. -During 1970-1975, 25% of U.S. hospitals reduced the extent of such routine environmental culturing -a trend that has continued.1206, 1207 Random, undirected sampling (referred to as "routine" in previous guidelines) differs from the current practice of targeted sampling for defined purposes.2, 1204 Previous recommendations against routine sampling were not intended to discourage the use of sampling in which sample collection, culture, and interpretation are conducted in accordance with defined protocols.2 In this guideline, targeted microbiologic sampling connotes a monitoring process that includes a) a written, defined, multidisciplinary protocol for sample collection and culturing; b) analysis and interpretation of results using scientifically determined or anticipatory baseline values for comparison; and c) expected actions based on the results obtained. Infection control, in conjunction with laboratorians, should assess the health-care facility's capability to conduct sampling and determine when expert consultation and/or services are needed.
Microbiologic sampling of air, water, and inanimate surfaces (i.e., environmental sampling) is an expensive and time-consuming process that is complicated by many variables in protocol, analysis, and interpretation. It is therefore indicated for only four situations. 1208 The first is to support an investigation of an outbreak of disease or infections when environmental reservoirs or fomites are implicated epidemiologically in disease transmission.161, 1209, 1210 It is important that such culturing be supported by epidemiologic data. Environmental sampling, as with all laboratory testing, should not be conducted if there is no plan for interpreting and acting on the results obtained. , , Linking microorganisms from environmental samples with clinical isolates by molecular epidemiology is crucial whenever it is possible to do so.
The second situation for which environmental sampling may be warranted is in research. Well-designed and controlled experimental methods and approaches can provide new information about the spread of health-care-associated diseases.126, 129 A classic example is the study of environmental microbial contamination that compared health-care-associated infection rates in an old hospital and a new facility before and shortly after occupancy.947
The third indication for sampling is to monitor a potentially hazardous environmental condition, confirm the presence of a hazardous chemical or biological agent, and validate the successful abatement of the hazard. This type of sampling can be used to: a) detect bioaerosols released from the operation of health-care equipment (e.g., an ultrasonic cleaner) and determine the success of repairs in containing the hazard,1213 b) detect the release of an agent of bioterrorism in an indoor environmental setting and determine its successful removal or inactivation, and c) sample for industrial hygiene or safety purposes (e.g., monitoring a "sick building").
The fourth indication is for quality assurance to evaluate the effects of a change in infection-control practice or to ensure that equipment or systems perform according to specifications and expected outcomes. Any sampling for quality-assurance purposes must follow sound sampling protocols and address confounding factors through the use of properly selected controls. Results from a single environmental sample are difficult to interpret in the absence of a frame of reference or perspective. Evaluations of a change in infection-control practice are based on the assumption that the effect will be measured over a finite period, usually of short duration. Conducting quality-assurance sampling on an extended basis, especially in the absence of an adverse outcome, is usually unjustified. A possible exception might be the use of air sampling during major construction periods to qualitatively detect breaks in environmental infection-control measures. In one study, which began as part of an investigation of an outbreak of health-care-associated aspergillosis, airborne concentrations of Aspergillus spores were measured in efforts to evaluate the effectiveness of sealing hospital doors and windows during a period of construction of a nearby building.50 Other examples of sampling for quality-assurance purposes may include commissioning newly constructed space in special care areas (i.e., ORs and units for immunosuppressed patients) or assessing a change in housekeeping practice. However, the only types of routine environmental microbiologic sampling recommended as part of a quality-assurance program are a) the biological monitoring of sterilization processes by using bacterial spores1214 and b) the monthly culturing of water used in hemodialysis applications and for the final dialysate use dilution. Some experts also advocate periodic environmental sampling to evaluate the microbial/particulate quality for regular maintenance of the air handling system (e.g., filters) and to verify that the components of the system meet manufacturer's specifications (A. Streifel, University of Minnesota, 2000). Certain equipment in health-care settings (e.g., biological safety cabinets) may also be monitored with air flow and particulate sampling to determine performance or as part of adherence to a certification program; results can then be compared with a predetermined standard of performance. These measurements, however, usually do not require microbiologic testing.
# Air Sampling
Biological contaminants occur in the air as aerosols and may include bacteria, fungi, viruses, and pollens.1215, 1216 Aerosols are characterized as solid or liquid particles suspended in air. Talking for 5 minutes and coughing each can produce 3,000 droplet nuclei; sneezing can generate approximately 40,000 droplets which then evaporate to particles in the size range of 0.5-12 pm. , Particles in a biological aerosol usually vary in size from <1 pm to >50 pm. These particles may consist of a single, unattached organism or may occur in the form of clumps composed of a number of bacteria. Clumps can also include dust and dried organic or inorganic material. Vegetative forms of bacterial cells and viruses may be present in the air in a lesser number than bacterial spores or fungal spores. Factors that determine the survival of microorganisms within a bioaerosol include a) the suspending medium, b) temperature, c) relative humidity, d) oxygen sensitivity, and e) exposure to UV or electromagnetic radiation.1215 Many vegetative cells will not survive for lengthy periods of time in the air unless the relative humidity and other factors are favorable for survival and the organism is enclosed within some protective cover (e.g., dried organic or inorganic matter).1216 Pathogens that resist drying (e.g., Staphylococcus spp., Streptococcus spp., and fungal spores) can survive for long periods and can be carried considerable distances via air and still remain viable. They may also settle on surfaces and become airborne again as secondary aerosols during certain activities (e.g., sweeping and bed making). 1216,1218 Microbiologic air sampling is used as needed to determine the numbers and types of microorganisms, or particulates, in indoor air.289 Air sampling for quality control is, however, problematic because of lack of uniform air-quality standards. Although airborne spores of Aspergillus spp. can pose a risk for neutropenic patients, the critical number (i.e., action level) of these spores above which outbreaks of aspergillosis would be expected to occur has not been defined. Health-care professionals considering the use of air sampling should keep in mind that the results represent indoor air quality at singular points in time, and these may be affected by a variety of factors, including a) indoor traffic, b) visitors entering the facility, c) temperature, d) time of day or year, e) relative humidity, f) relative concentration of particles or organisms, and g) the performance of the air-handling system components. To be meaningful, air-sampling results must be compared with those obtained from other defined areas, conditions, or time periods.
Several preliminary concerns must be addressed when designing a microbiologic air sampling strategy (Box 13). Because the amount of particulate material and bacteria retained in the respiratory system is largely dependent on the size of the inhaled particles, particle size should be determined when studying airborne microorganisms and their relation to respiratory infections. Particles >5 pm are efficiently trapped in the upper respiratory tract and are removed primarily by ciliary action.1219 Particles <5 pm in diameter reach the lung, but the greatest retention in the alveoli is of particles 1-2 pm in diameter.1220-1222 Bacteria, fungi, and particulates in air can be identified and quantified with the same methods and equipment (Table 23). The basic methods include a) impingement in liquids, b) impaction on solid surfaces, c) sedimentation, d) filtration, e) centrifugation, f) electrostatic precipitation, and g) thermal precipitation.1218 Of these, impingement in liquids, impaction on solid surfaces, and sedimentation (on settle plates) have been used for various air-sampling purposes in health-care settings.289 Several instruments are available for sampling airborne bacteria and fungi (Box 14). Some of the samplers are self-contained units requiring only a power supply and the appropriate collecting medium, but most require additional auxiliary equipment (e.g., a vacuum pump and an airflow measuring device [i.e., a flowmeter or anemometer]). Sedimentation or depositional methods use settle plates and therefore need no special instruments or equipment. Selection of an instrument for air sampling requires a clear understanding of the type of information desired and the particular determinations that must be made (Box 14). Information may be needed regarding a) one particular organism or all organisms that may be present in the air, b) the concentration of viable particles or of viable organisms, c) the change in concentration with time, and d) the size distribution of the collected particles. Before sampling begins, decisions should be made regarding whether the results are to be qualitative or quantitative. Comparing quantities of airborne microorganisms to those of outdoor air is also standard operating procedure. Infection-control professionals, hospital epidemiologists, industrial hygienists, and laboratory supervisors, as part of a multidisciplinary team, should discuss the potential need for microbial air sampling to determine if the capacity and expertise to conduct such sampling exists within the facility and when it is appropriate to enlist the services of an environmental microbiologist consultant.
# Box 14. Selecting an air sampling device*
The following factors must be considered when choosing an air sampling instrument: Liquid impinger and solid impactor samplers are the most practical for sampling bacteria, particles, and fungal spores, because they can sample large volumes of air in relatively short periods of time.289 Solid impactor units are available as either "slit" or "sieve" designs. Slit impactors use a rotating disc as support for the collecting surface, which allows determinations of concentration over time. Sieve impactors commonly use stages with calibrated holes of different diameters. Some impactor-type samplers use centrifugal force to impact particles onto agar surfaces. The interior of either device must be made sterile to avoid inadvertent contamination from the sampler. Results obtained from either sampling device can be expressed as organisms or particles per unit volume of air (CFU/m3).
• V
Sampling for bacteria requires special attention, because bacteria may be present as individual organisms, as clumps, or mixed with or adhering to dust or covered with a protective coating of dried organic or inorganic substances. Reports of bacterial concentrations determined by air sampling therefore must indicate whether the results represent individual organisms or particles bearing multiple cells. Certain types of samplers (e.g., liquid impingers) will completely or partially disintegrate clumps and large particles; the sampling result will therefore reflect the total number of individual organisms present in the air.
The task of sizing a bioaerosol is simplified through the use of sieves or slit impactors because these samplers will separate the particles and microorganisms into size ranges as the sample is collected. These samplers must, however, be calibrated first by sampling aerosols under similar use conditions.1225
The use of settle plates (i.e., the sedimentation or depositional method) is not recommended when sampling air for fungal spores, because single spores can remain suspended in air indefinitely.289 Settle plates have been used mainly to sample for particulates and bacteria either in research studies or during epidemiologic investigations.161, 1226 1229 Results of sedimentation sampling are typically expressed as numbers of viable particles or viable bacteria per unit area per the duration of sampling time (i.e., CFU/area/time); this method can not quantify the volume of air sampled. Because the survival of microorganisms during air sampling is inversely proportional to the velocity at which the air is taken into the sampler,1215 one advantage of using a settle plate is its reliance on gravity to bring organisms and particles into contact with its surface, thus enhancing the potential for optimal survival of collected organisms. This process, however, takes several hours to complete and may be impractical for some situations.
Air samplers are designed to meet differing measurement requirements. Some samplers are better suited for one form of measurement than others. No one type of sampler and assay procedure can be used to collect and enumerate 100% of airborne organisms. The sampler and/or sampling method chosen should, however, have an adequate sampling rate to collect a sufficient number of particles in a reasonable time period so that a representative sample of air is obtained for biological analysis. Newer analytical techniques for assaying air samples include PCR methods and enzyme-linked immunosorbent assays (ELISAs).
# Water Sampling
A detailed discussion of the principles and practices of water sampling has been published.945 Water sampling in health-care settings is used detect waterborne pathogens of clinical significance or to determine the quality of finished water in a facility's distribution system. Routine testing of the water in a health-care facility is usually not indicated, but sampling in support of outbreak investigations can help determine appropriate infection-control measures. Water-quality assessments in dialysis settings have been discussed in this guideline (see Water, Dialysis Water Quality and Dialysate, and Appendix C).
Health-care facilities that conduct water sampling should have their samples assayed in a laboratory that uses established methods and quality-assurance protocols. Water specimens are not "static specimens" at ambient temperature; potential changes in both numbers and types of microbial populations can occur during transport. Consequently, water samples should be sent to the testing laboratory cold (i.e., at approximately 39.2°F [4°C]) and testing should be done as soon as practical after collection (preferably within 24 hours).
Because most water sampling in health-care facilities involves the testing of finished water from the facility's distribution system, a reducing agent (i.e., sodium thiosulfate [Na2S2O3]) needs to be added to neutralize residual chlorine or other halogen in the collected sample. If the water contains elevated levels of heavy metals, then a chelating agent should be added to the specimen. The minimum volume of water to be collected should be sufficient to complete any and all assays indicated; 100 mL is considered a suitable minimum volume. Sterile collection equipment should always be used.
Sampling from a tap requires flushing of the water line before sample collection. If the tap is a mixing faucet, attachments (e.g., screens and aerators) must be removed, and hot and then cold water must be run through the tap before collecting the sample.945 If the cleanliness of the tap is questionable, disinfection with 500-600 ppm sodium hypochlorite (1:100 v/v dilution of chlorine bleach) and flushing the tap should precede sample collection.
Microorganisms in finished or treated water often are physically damaged ("stressed") to the point that growth is limited when assayed under standard conditions. Such situations lead to false-negative readings and misleading assessments of water quality. Appropriate neutralization of halogens and chelation of heavy metals are crucial to the recovery of these organisms. The choice of recovery media and incubation conditions will also affect the assay. Incubation temperatures should be closer to the ambient temperature of the water rather than at 98.6°F (37°C), and recovery media should be formulated to provide appropriate concentrations of nutrients to support organisms exhibiting less than rigorous growth.945 High-nutrient content media (e.g., blood agar and tryptic soy agar [TSA]) may actually inhibit the growth of these damaged organisms. Reduced nutrient media (e.g., diluted peptone and R2A) are preferable for recovery of these organisms.945
Use of aerobic, heterotrophic plate counts allows both a qualitative and quantitative measurement for water quality. If bacterial counts in water are expected to be high in number (e.g., during waterborne outbreak investigations), assaying small quantities using pour plates or spread plates is appropriate.945 Membrane filtration is used when low-count specimens are expected and larger sampling volumes are required (>100 mL). The sample is filtered through the membrane, and the filter is applied directly face-up onto the surface of the agar plate and incubated.
Unlike the testing of potable water supplies for coliforms (which uses standardized test and specimen collection parameters and conditions), water sampling to support epidemiologic investigations of disease outbreaks may be subjected to modifications dictated by the circumstances present in the facility. Assay methods for waterborne pathogens may also not be standardized. Therefore, control or comparison samples should be included in the experimental design. Any departure from a standard method should be fully documented and should be considered when interpreting results and developing strategies. Assay methods specific for clinically significant waterborne pathogens (e.g., Legionella spp., Aeromonas spp, Pseudomonas spp., and Acinetobacter spp.) are more complicated and costly compared with both methods used to detect coliforms and other standard indicators of water quality.
# Environmental Surface Sampling
Routine environmental-surface sampling (e.g., surveillance cultures) in health-care settings is neither 951 1225 cost-effective nor warranted. ,
When indicated, surface sampling should be conducted with multidisciplinary approval in adherence to carefully considered plans of action and policy (Box 15).
# Box 15. Undertaking environmental-surface sampling*
The following factors should be considered before engaging in environmental-surface sampling: Surface sampling is used currently for research, as part of an epidemiologic investigation, or as part of a comprehensive approach for specific quality assurance purposes. As a research tool, surface sampling has been used to determine a) potential environmental reservoirs of pathogens,564, 1230 1232 b) survival of microorganisms on surfaces, , and c) the sources of the environmental contamination. Some or all of these approaches can also be used during outbreak investigations.1232 Discussion of surface sampling of medical devices and instruments is beyond the scope of this document and is deferred to future guidelines on sterilization and disinfection issues.
Meaningful results depend on the selection of appropriate sampling and assay techniques.1214 The media, reagents, and equipment required for surface sampling are available from any well-equipped microbiology laboratory and laboratory supplier. For quantitative assessment of surface organisms, non-selective, nutrient-rich agar media and broth (e.g., TSA and brain-heart infusion broth [BHI] with or without 5% sheep or rabbit blood supplement) are used for the recovery of aerobic bacteria. Broth media are used with membrane-filtration techniques. Further sample work-up may require the use of selective media for the isolation and enumeration of specific groups of microorganisms. Examples of selective media are MacConkey agar (MAC [selects for gram-negative bacteria]), Cetrimide agar (selects for Pseudomonas aeruginosa), or Sabouraud dextrose-and malt extract agars and broths (select for fungi). Qualitative determinations of organisms from surfaces require only the use of selective or non-selective broth media.
Effective sampling of surfaces requires moisture, either already present on the surface to be sampled or via moistened swabs, sponges, wipes, agar surfaces, or membrane filters.1214, 1234-1236 Dilution fluids and rinse fluids include various buffers or general purpose broth media (Table 24). If disinfectant residuals are expected on surfaces being sampled, specific neutralizer chemicals should be used in both the growth media and the dilution or rinse fluids. Lists of the neutralizers, the target disinfectant active ingredients, and the use concentrations have been published. , Alternatively, instead of adding neutralizing chemicals to existing culture media (or if the chemical nature of the disinfectant residuals is unknown), the use of either a) commercially available media including a variety of specific and non specific neutralizers or b) double-strength broth media will facilitate optimal recovery of microorganisms. The inclusion of appropriate control specimens should be included to rule out both residual antimicrobial activity from surface disinfectants and potential toxicity caused by the presence of neutralizer chemicals carried over into the assay system.1214 Sample/rinse methods are frequently chosen because of their versatility. However, these sampling methods are the most prone to errors caused by manipulation of the swab, gauze pad, or sponge.1238 Additionally, no microbiocidal or microbiostatic agents should be present in any of these items when used for sampling.1238 Each of the rinse methods requires effective elution of microorganisms from the item used to sample the surface. Thorough mixing of the rinse fluids after elution (e.g., via manual or mechanical mixing using a vortex mixer, shaking with or without glass beads, and ultrasonic bath) will help to remove and suspend material from the sampling device and break up clumps of organisms for a more accurate count.1238 In some instances, the item used to sample the surface (e.g., gauze pad and sponge) may be immersed in the rinse fluids in a sterile bag and subjected to stomaching.1238 This technique, however, is suitable only for soft or absorbent items that will not puncture the bag during the elution process.
If sampling is conducted as part of an epidemiologic investigation of a disease outbreak, identification of isolates to species level is mandatory, and characterization beyond the species level is preferred.1214 When interpreting the results of the sampling, the expected degree of microbial contamination associated with the various categories of surfaces in the Spaulding classification must be considered. Environmental surfaces should be visibly clean; recognized pathogens in numbers sufficient to result in secondary transfer to other animate or inanimate surfaces should be absent from the surface being sampled.1214 Although the interpretation of a sample with positive microbial growth is self-evident, an environmental surface sample, especially that obtained from housekeeping surfaces, that shows no growth does not represent a "sterile" surface. Sensitivities of the sampling and assay methods (i.e., level of detection) must be taken into account when no-growth samples are encountered. Properly collected control samples will help rule out extraneous contamination of the surface sample.
# G. Laundry and Bedding
# General Information
Laundry in a health-care facility may include bed sheets and blankets, towels, personal clothing, patient apparel, uniforms, scrub suits, gowns, and drapes for surgical procedures.1245 Although contaminated textiles and fabrics in health-care facilities can be a source of substantial numbers of pathogenic microorganisms, reports of health-care-associated diseases linked to contaminated fabrics are so few in number that the overall risk of disease transmission during the laundry process likely is negligible.
When the incidence of such events are evaluated in the context of the volume of items laundered in health-care settings (estimated to be 5 billion pounds annually in the United States),1246 existing control measures (e.g., standard precautions) are effective in reducing the risk of disease transmission to patients and staff. Therefore, use of current control measures should be continued to minimize the contribution of contaminated laundry to the incidence of health-care-associated infections. The control measures described in this section of the guideline are based on principles of hygiene, common sense, and consensus guidance; they pertain to laundry services utilized by health-care facilities, either in house or contract, rather than to laundry done in the home.
# Epidemiology and General Aspects of Infection Control
Contaminated textiles and fabrics often contain high numbers of microorganisms from body substances, including blood, skin, stool, urine, vomitus, and other body tissues and fluids. When textiles are heavily contaminated with potentially infective body substances, they can contain bacterial loads of 106-108 CFU/100 cm2 of fabric.1247 Disease transmission attributed to health-care laundry has involved contaminated fabrics that were handled inappropriately (i.e., the shaking of soiled linens). Bacteria (Salmonella spp., Bacillus cereus), viruses (hepatitis B virus [HBV]), fungi (Microsporum canis), and ectoparasites (scabies) presumably have been transmitted from contaminated textiles and fabrics to workers via a) direct contact or b) aerosols of contaminated lint generated from sorting and handling contaminated textiles. -In these events, however, investigations could not rule out the possibility that some of these reported infections were acquired from community sources. Through a combination of soil removal, pathogen removal, and pathogen inactivation, contaminated laundry can be rendered hygienically clean. Hygienically clean laundry carries negligible risk to health-care workers and patients, provided that the clean textiles, fabric, and clothing are not inadvertently contaminated before use.
OSHA defines contaminated laundry as "laundry which has been soiled with blood or other potentially infectious materials or may contain sharps."967 The purpose of the laundry portion of the standard is to protect the worker from exposure to potentially infectious materials during collection, handling, and sorting of contaminated textiles through the use of personal protective equipment, proper work practices, containment, labeling, hazard communication, and ergonomics. Experts are divided regarding the practice of transporting clothes worn at the workplace to the health care worker's home for laundering. Although OSHA regulations prohibit home laundering of items that are considered personal protective apparel or equipment (e.g., laboratory coats),967 experts disagree about whether this regulation extends to uniforms and scrub suits that are not contaminated with blood or other potentially infectious material. Health-care facility policies on this matter vary and may be inconsistent with recommendations of professional organizations.1253, 1254 Uniforms without blood or body substance contamination presumably do not differ appreciably from street clothes in the degree and microbial nature of soilage. Home laundering would be expected to remove this level of soil adequately. However, if health-care facilities require the use of uniforms, they should either make provisions to launder them or provide information to the employee regarding infection control and cleaning guidelines for the item based on the tasks being performed at the facility. Health-care facilities should address the need to provide this service and should determine the frequency for laundering these items. In a recent study examining the microbial contamination of medical students' white coats, the students perceived the coats as "clean" as long as the garments were not visibly contaminated with body substances, even after wearing the coats for several weeks.1255 The heaviest bacterial load was found on the sleeves and the pockets of these garments; the organisms most frequently isolated were Staphylococcus aureus, diphtheroids, and Acinetobacter spp.1255 Presumably, the sleeves of the coat may make contact with a patient and potentially serve to transfer environmentally stable microorganisms among patients. In this study, however, surveillance was not conducted among patients to detect new infections or colonizations. The students did, however, report that they would likely replace their coats more frequently and regularly if clean coats were provided.1255 Apart from this study, which documents the presence of pathogenic bacteria on health-care facility clothing, reports of infections attributed to either the contact with such apparel or with home laundering have been rare.1256, 1257 Laundry services for health-care facilities are provided either in-house (i.e., on-premise laundry [OPL]), co-operatives (i.e., those entities owned and operated by a group of facilities), or by off-site commercial laundries. In the latter, the textiles may be owned by the health-care facility, in which case the processor is paid for laundering only. Alternatively, the textiles may be owned by the processor who is paid for every piece laundered on a "rental" fee. The laundry facility in a health-care setting should be designed for efficiency in providing hygienically clean textiles, fabrics, and apparel for patients and staff. Guidelines for laundry construction and operation for health-care facilities, including nursing facilities, have been published.120, 1258 The design and engineering standards for existing facilities are those cited in the AIA edition in effect during the time of the facility's construction.120 A laundry facility is usually partitioned into two separate areas -a "dirty" area for receiving and handling the soiled laundry and a "clean" area for processing the washed items.1259 To minimize the potential for recontaminating cleaned laundry with aerosolized contaminated lint, areas receiving contaminated textiles should be at negative air pressure relative to the clean areas.1260 1262 Laundry areas should have handwashing facilities readily available to workers. Laundry workers should wear appropriate personal protective equipment (e.g., gloves and protective garments) while sorting soiled fabrics and textiles.967 Laundry equipment should be used and maintained according to the manufacturer's instructions to prevent microbial contamination of the system.1250, 1263 Damp textiles should not be left in machines overnight.1250
# Collecting, Transporting, and Sorting Contaminated Textiles and Fabrics
The laundry process starts with the removal of used or contaminated textiles, fabrics, and/or clothing from the areas where such contamination occurred, including but not limited to patients' rooms, surgical/operating areas, and laboratories. Handling contaminated laundry with a minimum of agitation can help prevent the generation of potentially contaminated lint aerosols in patient-care areas.967, 1259 Sorting or rinsing contaminated laundry at the location where contamination occurred is prohibited by OSHA.967 Contaminated textiles and fabrics are placed into bags or other appropriate containment in this location; these bags are then securely tied or otherwise closed to prevent leakage.967 Single bags of sufficient tensile strength are adequate for containing laundry, but leak-resistant containment is needed if the laundry is wet and capable of soaking through a cloth bag.1264 Bags containing contaminated laundry must be clearly identified with labels, color-coding, or other methods so that health-care workers handle these items safely, regardless of whether the laundry is transported within the facility or destined for transport to an off-site laundry service.967 Typically, contaminated laundry originating in isolation areas of the hospital is segregated and handled with special practices; however, few, if any, cases of health-care-associated infection have been linked to this source.1265 Single-blinded studies have demonstrated that laundry from isolation areas is no more heavily contaminated with microorganisms than laundry from elsewhere in the hospital.1266 Therefore, adherence to standard precautions when handling contaminated laundry in isolation areas and minimizing agitation of the contaminated items are considered sufficient to prevent the dispersal of potentially infectious aerosols.6 Contaminated textiles and fabrics in bags can be transported by cart or chute.1258, 1262 Laundry chutes require proper design, maintenance, and use, because the piston-like action of a laundry bag traveling in the chute can propel airborne microbial contaminants throughout the facility.1267-1269 Laundry chutes should be maintained under negative air pressure to prevent the spread of microorganisms from floor to floor. Loose, contaminated pieces of laundry should not be tossed into chutes, and laundry bags should be closed or otherwise secured to prevent the contents from falling out into the chute.1270 Health-care facilities should determine the point in the laundry process at which textiles and fabrics should be sorted. Sorting after washing minimizes the exposure of laundry workers to infective material in soiled fabrics, reduces airborne microbial contamination in the laundry area, and helps to prevent potential percutaneous injuries to personnel.1271 Sorting laundry before washing protects both the machinery and fabrics from hard objects (e.g., needles, syringes, and patients' property) and reduces the potential for recontamination of clean textiles.1272 Sorting laundry before washing also allows for customization of laundry formulas based on the mix of products in the system and types of soils encountered. Additionally, if work flow allows, increasing the amount of segregation by specific product types will usually yield the greatest amount of work efficiency during inspection, folding, and pack-making operations.1253 Protective apparel for the workers and appropriate ventilation can minimize these exposures.967, 1258-1260 Gloves used for the task of sorting laundry should be of sufficient thickness to minimize sharps injuries.967 Employee safety personnel and industrial hygienists can help to determine the appropriate glove choice.
# Parameters of the Laundry Process
Fabrics, textiles, and clothing used in health-care settings are disinfected during laundering and generally rendered free of vegetative pathogens (i.e., hygienically clean), but they are not sterile.1273 Laundering cycles consist of flush, main wash, bleaching, rinsing, and souring.1274 Cleaned wet textiles, fabrics, and clothing are then dried, pressed as needed, and prepared (e.g., folded and packaged) for distribution back to the facility. Clean linens provided by an off-site laundry must be packaged prior to transport to prevent inadvertent contamination from dust and dirt during loading, delivery, and unloading. Functional packaging of laundry can be achieved in several ways, including a) placing clean linen in a hamper lined with a previously unused liner, which is then closed or covered; b) placing clean linen in a properly cleaned cart and covering the cart with disposable material or a properly cleaned reusable textile material that can be secured to the cart; and c) wrapping individual bundles of clean textiles in plastic or other suitable material and sealing or taping the bundles.
The antimicrobial action of the laundering process results from a combination of mechanical, thermal, and chemical factors.1271, 1275, 1276 Dilution and agitation in water remove substantial quantities of microorganisms. Soaps and detergents function to suspend soils and also exhibit some microbiocidal properties. Hot water provides an effective means of destroying microorganisms.1277 A temperature of at least 160°F (71°C) for a minimum of 25 minutes is commonly recommended for hot-water washing.2 Water of this temperature can be provided by steam jet or separate booster heater.120 The use of chlorine bleach assures an extra margin of safety. , A total available chlorine residual of 50-150 ppm is usually achieved during the bleach cycle.1277 Chlorine bleach becomes activated at water temperatures of 135°F-145°F (57.2°C-62.7°C). The last of the series of rinse cycles is the addition of a mild acid (i.e., sour) to neutralize any alkalinity in the water supply, soap, or detergent. The rapid shift in pH from approximately 12 to 5 is an effective means to inactivate some microorganisms.1247 Effective removal of residual alkali from fabrics is an important measure in reducing the risk for skin reactions among patients.
Chlorine bleach is an economical, broad-spectrum chemical germicide that enhances the effectiveness of the laundering process. Chlorine bleach is not, however, an appropriate laundry additive for all fabrics. Traditionally, bleach was not recommended for laundering flame-retardant fabrics, linens, and clothing because its use diminished the flame-retardant properties of the treated fabric.1273 However, some modern-day flame retardant fabrics can now tolerate chlorine bleach. Flame-retardant fabrics, whether topically treated or inherently flame retardant, should be thoroughly rinsed during the rinse cycles, because detergent residues are capable of supporting combustion. Chlorine alternatives (e.g., activated oxygen-based laundry detergents) provide added benefits for fabric and color safety in addition to antimicrobial activity. Studies comparing the antimicrobial potencies of chlorine bleach and oxygen-based bleach are needed. Oxygen-based bleach and detergents used in health-care settings should be registered by EPA to ensure adequate disinfection of laundry. Health-care workers should note the cleaning instructions of textiles, fabrics, drapes, and clothing to identify special laundering requirements and appropriate hygienic cleaning options.1278
Although hot-water washing is an effective laundry disinfection method, the cost can be substantial. Laundries are typically the largest users of hot water in hospitals. They consume 50%-75% of the total hot water,1280 representing an average of 10%-15% of the energy used by a hospital. Several studies have demonstrated that lower water temperatures of 71°F-77°F (22°C-25°C) can reduce microbial contamination when the cycling of the washer, the wash detergent, and the amount of laundry additive are carefully monitored and controlled.1247, 1281-1285 Low-temperature laundry cycles rely heavily on the presence of chlorine-or oxygen-activated bleach to reduce the levels of microbial contamination. The selection of hot-or cold-water laundry cycles may be dictated by state health-care facility licensing standards or by other regulation. Regardless of whether hot or cold water is used for washing, the temperatures reached in drying and especially during ironing provide additional significant microbiocidal action.1247 Dryer temperatures and cycle times are dictated by the materials in the fabrics. Man-made fibers (i.e., polyester and polyester blends) require shorter times and lower temperatures.
After washing, cleaned and dried textiles, fabrics, and clothing are pressed, folded, and packaged for transport, distribution, and storage by methods that ensure their cleanliness until use.2 State regulations and/or accrediting standards may dictate the procedures for this activity. Clean/sterile and contaminated textiles should be transported from the laundry to the health-care facility in vehicles (e.g., trucks, vans, and carts) that allow for separation of clean/sterile and contaminated items. Clean/sterile textiles and contaminated textiles may be transported in the same vehicle, provided that the use of physical barriers and/or space separation can be verified to be effective in protecting the clean/sterile items from contamination. Clean, uncovered/unwrapped textiles stored in a clean location for short periods of time (e.g., uncovered and used within a few hours) have not been demonstrated to contribute to increased levels of health-care-acquired infection. Such textiles can be stored in convenient places for use during the provision of care, provided that the textiles can be maintained dry and free from soil and bodysubstance contamination.
In the absence of microbiologic standards for laundered textiles, no rationale exists for routine microbiologic sampling of cleaned health-care textiles and fabrics.1286 Sampling may be used as part of an outbreak investigation if epidemiologic evidence suggests that textiles, fabrics, or clothing are a suspected vehicle for disease transmission. Sampling techniques include aseptically macerating the fabric into pieces and adding these to broth media or using contact plates (RODAC plates) for direct surface sampling.1271, 1286 When evaluating the disinfecting properties of the laundering process specifically, placing pieces of fabric between two membrane filters may help to minimize the contribution of the physical removal of microorganisms.1287
Washing machines and dryers in residential-care settings are more likely to be consumer items rather than the commercial, heavy-duty, large volume units typically found in hospitals and other institutional health-care settings. Although all washing machines and dryers in health-care settings must be properly maintained for performance according to the manufacturer's instructions, questions have been raised about the need to disinfect washers and dryers in residential-care settings. Disinfection of the tubs and tumblers of these machines is unnecessary when proper laundry procedures are followed; these procedures involve a) the physical removal of bulk solids (e.g., feces) before the wash/dry cycle and b) proper use of temperature, detergent, and laundry additives. Infection has not been linked to laundry procedures in residential-care facilities, even when consumer versions of detergents and laundry additives are used.
# Special Laundry Situations
Some textile items (e.g., surgical drapes and reusable gowns) must be sterilized before use and therefore require steam autoclaving after laundering.7 Although the American Academy of Pediatrics in previous guidelines recommended autoclaving for linens in neonatal intensive care units (NICUs), studies on the microbial quality of routinely cleaned NICU linen have not identified any increased risk for infection among the neonates receiving care.1288 Consequently, hygienically clean linens are suitable for use in this setting.997 The use of sterile linens in burn therapy units remains unresolved.
Coated or laminated fabrics are often used in the manufacture of PPE. When these items become contaminated with blood or other body substances, the manufacturer's instructions for decontamination and cleaning take into account the compatibility of the rubber backing with the chemical germicides or detergents used in the process. The directions for decontaminating these items should be followed as indicated; the item should be discarded when the backing develops surface cracks.
Dry cleaning, a cleaning process that utilizes organic solvents (e.g., perchloroethylene) for soil removal, is an alternative means of cleaning fabrics that might be damaged in conventional laundering and detergent washing. Several studies, however, have shown that dry cleaning alone is relatively ineffective in reducing the numbers of bacteria and viruses on contaminated linens;1289, 1290 microbial populations are significantly reduced only when dry-cleaned articles are heat pressed. Dry cleaning should therefore not be considered a routine option for health-care facility laundry and should be reserved for those circumstances in which fabrics can not be safely cleaned with water and detergent.1291
# Surgical Gowns, Drapes, and Disposable Fabrics
An issue of recent concern involves the use of disposable (i.e., single use) versus reusable (i.e., multiple use) surgical attire and fabrics in health-care settings.1292 Regardless of the material used to manufacture gowns and drapes, these items must be resistant to liquid and microbial penetration.7, 1293 1297 Surgical gowns and drapes must be registered with FDA to demonstrate their safety and effectiveness. Repellency and pore size of the fabric contribute to gown performance, but performance capability can be influenced by the item's design and construction.1298, 1299 Reinforced gowns (i.e., gowns with double-layered fabric) generally are more resistant to liquid strike-through.1300, 1301 Reinforced gowns may, however, be less comfortable. Guidelines for selection and use of barrier materials for surgical gowns and drapes have been published.1302 When selecting a barrier product, repellency level and type of barrier should be compatible for the exposure expected.967 However, data are limited regarding the association between gown or drape characteristics and risk for surgical site infections.7, 1303 Health-care facilities must ensure optimal protection of patients and health-care workers. Not all fabric items in health care lend themselves to single-use. Facilities exploring options for gowns and drapes should consider the expense of disposable items and the impact on the facility's waste-management costs once these items are discarded. Costs associated with the use of durable goods involve the fabric or textile items; staff expenses to collect, sort, clean, and package the laundry; and energy costs to operate the laundry if on-site or the costs to contract with an outside service.1304, 1305
# Antimicrobial-Impregnated Articles and Consumer Items Bearing Antimicrobial Labeling
Manufacturers are increasingly incorporating antibacterial or antimicrobial chemicals into consumer and health-care items. Some consumer products bearing labels that indicate treatment with antimicrobial chemicals have included pens, cutting boards, toys, household cleaners, hand lotions, cat litter, soaps, cotton swabs, toothbrushes, and cosmetics. The "antibacterial" label on household cleaning products, in particular, gives consumers the impression that the products perform "better" than comparable products without this labeling, when in fact all household cleaners have antibacterial properties.
In the health-care setting, treated items may include children's pajamas, mattresses, and bed linens with label claims of antimicrobial properties. These claims require careful evaluation to determine whether they pertain to the use of antimicrobial chemicals as preservatives for the fabric or other components or whether they imply a health claim.1306, 1307 No evidence is available to suggest that use of these products will make consumers and patients healthier or prevent disease. No data support the use of these items as part of a sound infection-control strategy, and therefore, the additional expense of replacing a facility's bedding and sheets with these treated products is unwarranted.
EPA has reaffirmed its position that manufacturers who make public health claims for articles containing antimicrobial chemicals must provide evidence to support those claims as part of the registration process.1308 Current EPA regulations outlined in the Treated Articles Exemption of the Federal Insecticide, Fungicide, and Rodenticide Act (FIFRA) require manufacturers to register both the antimicrobial chemical used in or on the product and the finished product itself if a public health claim is maintained for the item. The exemption applies to the use of antimicrobial chemicals for the purpose of preserving the integrity of the product's raw material(s). The U.S. Federal Trade Commission (FTC) is evaluating manufacturer advertising of products with antimicrobial claims.1309
# Standard Mattresses, Pillows, and Air-Fluidized Beds
Standard mattresses and pillows can become contaminated with body substances during patient care if the integrity of the covers of these items is compromised. The practice of sticking needles into the mattress should be avoided. A mattress cover is generally a fitted, protective material, the purpose of which is to prevent the mattress from becoming contaminated with body fluids and substances. A linen sheet placed on the mattress is not considered a mattress cover. Patches for tears and holes in mattress covers do not provide an impermeable surface over the mattress. Mattress covers should be replaced when torn; the mattress should be replaced if it is visibly stained. Wet mattresses, in particular, can be a substantial environmental source of microorganisms. Infections and colonizations caused by Acinetobacter spp., MRSA, and Pseudomonas aeruginosa have been described, especially among burn patients.13101315 In these reports, the removal of wet mattresses was an effective infection-control measure. Efforts were made to ensure that pads and covers were cleaned and disinfected between patients using disinfectant products compatible with mattress-cover materials to ensure that these covers remained impermeable to fluids.13101314 Pillows and their covers should be easily cleanable, preferably in a hot water laundry cycle.1315 These should be laundered between patients or if contaminated with body substances.
Air-fluidized beds are used for the care of patients immobilized for extended periods of time because of therapy or injury (e.g., pain, decubitus ulcers, and burns).1316 These specialized beds consist of a base unit filled with microsphere beads fluidized by warm, dry air flowing upward from a diffuser located at the bottom of the unit. A porous, polyester filter sheet separates the patient from direct contact with the beads but allows body fluids to pass through to the beads. Moist beads aggregate into clumps which settle to the bottom where they are removed as part of routine bed maintenance.
Because the beads become contaminated with the patient's body substances, concerns have been raised about the potential for these beds to serve as an environmental source of pathogens. Certain pathogens (e.g., Enterococcus spp., Serratia marcescens, Staphylococcus aureus, and Streptococcus fecalis) have been recovered either from the microsphere beads or the polyester sheet after cleaning.1317, 1318 Reports of cross-contamination of patients, however, are few.1318 Nevertheless, routine maintenance and between-patient decontamination procedures can minimize potential risks to patients. Regular removal of bead clumps, coupled with the warm, dry air of the bed, can help to minimize bacterial growth in the unit.13191321 Beads are decontaminated between patients by high heat (113°F-194°F [45°C-90°C], depending on the manufacturer's specifications) for at least 1 hour; this procedure is particularly important for the inactivation of Enterococcus spp. which are relatively resistant to heat. , The polyester filter sheet requires regular changing and thorough cleaning and disinfection, especially between patients.1317, 1318, 1322, 1323 Microbial contamination of the air space in the immediate vicinity of a properly maintained air-fluidized bed is similar to that found in air around conventional bedding, despite the air flow out of the base unit and around the patient. , , An operational air-fluidized bed can, however, interfere with proper pressure differentials, especially in negative-pressure rooms;1326 the effect varies with the location of the bed relative to the room's configuration and supply and exhaust vent locations. Use of an airfluidized bed in a negative-pressure room requires consultation with a facility engineer to determine appropriate placement of the bed.
# H. Animals in Health-Care Facilities I. General Information
Animals in health-care facilities traditionally have been limited to laboratories and research areas. However, their presence in patient-care areas is now more frequent, both in acute-care and long-term care settings, prompting consideration for the potential transmission of zoonotic pathogens from animals to humans in these settings. Although dogs and cats may be commonly encountered in health-care settings, other animals (e.g., fish, birds, non-human primates, rabbits, rodents, and reptiles) also can be present as research, resident, or service animals. These animals can serve as sources of zoonotic pathogens that could potentially infect patients and health-care workers (Table 26). -Animals potentially can serve as reservoirs for antibiotic-resistant microorganisms, which can be introduced to the health-care setting while the animal is present. VRE have been isolated from both farm animals and pets,1341 and a cat in a geriatric care center was found to be colonized with MRSA.1342 * The + symbol indicates that the pathogen associated with the infection has been isolated from animals and is considered to pose potential risk to humans.
Zoonoses can be transmitted from animals to humans either directly or indirectly via bites, scratches, aerosols, ectoparasites, accidental ingestion, or contact with contaminated soil, food, water, or unpasteurized milk. , , -Colonization and hand transferral of pathogens acquired from pets in health-care workers' homes represent potential sources and modes of transmission of zoonotic pathogens in health-care settings. An outbreak of infections caused by a yeast (Malassezia pachydermatis) among newborns was traced to transfer of the yeast from the hands of health-care workers with pet dogs at home.1346 In addition, an outbreak of ringworm in a NICU caused by Microsporum canis was associated with a nurse and her cat,1347 and an outbreak of Rhodococcus (Gordona) bronchialis sternal SSIs after coronary-artery bypass surgery was traced to a colonized nurse whose dogs were culture-positive for the organism.1348 In the latter outbreak, whether the dogs were the sole source of the organism and whether other environmental reservoirs contributed to the outbreak are unknown. Nonetheless, limited data indicate that outbreaks of infectious disease have occurred as a result of contact with animals in areas housing immunocompetent patients. However, the low frequency of outbreaks may result from a) the relatively limited presence of the animals in health-care facilities and b) the immunocompetency of the patients involved in the encounters. Formal scientific studies to evaluate potential risks of transmission of zoonoses in health-care settings outside of the laboratory are lacking.
# Animal-Assisted Activities, Animal-Assisted Therapy, and Resident Animals
Animal-Assisted Activities (AAA) are those programs that enhance the patients' quality of life. These programs allow patients to visit animals in either a common, central location in the facility or in individual patient rooms. A group session with the animals enhances opportunities for ambulatory patients and facility residents to interact with caregivers, family members, and volunteers.1349 1351 Alternatively, allowing the animals access to individual rooms provides the same opportunity to non ambulatory patients and patients for whom privacy or dignity issues are a consideration. The decision to allow this access to patients' rooms should be made on a case-by-case basis, with the consultation and consent of the attending physician and nursing staff.
Animal-Assisted Therapy (AAT) is a goal-directed intervention that incorporates an animal into the 1330, 1331 treatment process provided by a credentialed therapist. ,
The concept for AAT arose from the observation that some patients with pets at home recover from surgical and medical procedures more rapidly than patients without pets. , Contact with animals is considered beneficial for enhancing wellness in certain patient populations (e.g., children, the elderly, and extended-care hospitalized patients).1349, 1354 1357 However, evidence supporting this benefit is largely derived from anecdotal reports and observations of patient/animal interactions. -Guidelines for establishing AAT programs are available for facilities considering this option.1360
The incorporation of non-human primates into an AAA or AAT program is not encouraged because of concerns regarding potential disease transmission from and unpredictable behavior of these animals.1361, 1362 Animals participating in either AAA or AAT sessions should be in good health and up-to-date with recommended immunizations and prophylactic medications (e.g., heartworm prevention) as determined by a licensed veterinarian based on local needs and recommendations. Regular re-evaluation of the animal's health and behavior status is essential.1360 Animals should be routinely screened for enteric parasites and/or have evidence of a recently completed antihelminthic regimen.1363 They should also be free of ectoparasites (e.g., fleas and ticks) and should have no sutures, open wounds, or obvious dermatologic lesions that could be associated with bacterial, fungal, or viral infections or parasitic infestations. Incorporating young animals (i.e., those aged <1 year) into these programs is not encouraged because of issues regarding unpredictable behavior and elimination control. Additionally, the immune systems of very young puppies and kittens is not completely developed, thereby placing the health of these animals at risk. Animals should be clean and well-groomed. The visits must be supervised by persons who know the animals and their behavior. Animal handlers should be trained in these activities and receive site-specific orientation to ensure that they work efficiently with the staff in the specific health-care environment.1360 Additionally, animal handlers should be in good health.1360
The most important infection-control measure to prevent potential disease transmission is strict enforcement of hand-hygiene measures (e.g., using either soap and water or an alcohol-based hand rub) for all patients, staff, and residents after handling the animals.1355, 1364 Care should also be taken to avoid direct contact with animal urine or feces. Clean-up of these substances from environmental surfaces requires gloves and the use of leak-resistant plastic bags to discard absorbent material used in the process.2 The area must be cleaned after visits according to standard cleaning procedures.
The American Academy of Allergy, Asthma, and Immunology estimates that dog or cat allergies occur in approximately 15% of the population.1365 Minimizing contact with animal saliva, dander, and/or urine helps to mitigate allergic responses.1365 1367 Some facilities may not allow animal visitation for patients with a) underlying asthma, b) known allergies to cat or dog hair, c) respiratory allergies of unknown etiology, and d) immunosuppressive disorders. Hair shedding can be minimized by processes that remove dead hair (e.g., grooming) and that prevent the shedding of dead hair (e.g., therapy capes for dogs). Allergens can be minimized by bathing therapy animals within 24 hours of a visit. 1333,1368 Animal therapists and handlers must take precautions to prevent animal bites. Common pathogens associated with animal bites include Capnocytophaga canimorsus, Pasteurella spp., Staphylococcus spp., and Streptococcus spp. Selecting well-behaved and well-trained animals for these programs greatly decreases the incidence of bites. Rodents, exotic species, wild/domestic animals (i.e., wolf-dog hybrids), and wild animals whose behavior is unpredictable should be excluded from AAA or AAT programs. A well-trained animal handler should be able to recognize stress in the animal and to determine when to terminate a session to minimize risk. When an animal bites a person during AAA or AAT, the animal is to be permanently removed from the program. If a bite does occur, the wound must be cleansed immediately and monitored for subsequent infection. Most infections can be treated with antibiotics, and antibiotics often are prescribed prophylactically in these situations.
The health-care facility's infection-control staff should participate actively in planning for and coordinating AAA and AAT sessions. Many facilities do not offer AAA or AAT programs for severely immunocompromised patients (e.g., HSCT patients and patients on corticosteroid therapy).1339 The question of whether family pets or companion animals can visit terminally-ill HSCT patients or other severely immunosuppressed patients is best handled on a case-by-case basis, although animals should not be brought into the HSCT unit or any other unit housing severely immunosuppressed patients. An in-depth discussion of this issue is presented elsewhere.1366 Immunocompromised patients who have been discharged from a health-care facility may be at higher risk for acquiring some pet-related zoonoses. Although guidelines have been developed to minimize the risk of disease transmission to HIV-infected patients,8 these recommendations may be applicable for patients with other immunosuppressive disorders. In addition to handwashing or hand hygiene, these recommendations include avoiding contact with a) animal feces and soiled litter box materials, b) animals with diarrhea, c) very young animals (i.e., dogs <6 months of age and cats <1 year of age), and d) exotic animals and reptiles.8 Pets or companion animals with diarrhea should receive veterinary care to resolve their condition.
Many health-care facilities are adopting more home-like environments for residential-care or extendedstay patients in acute-care settings, and resident animals are one element of this approach.1369 One concept, the "Eden Alternative," incorporates children, plants, and animals (e.g., dogs, cats, fish, birds, rabbits, and rodents) into the daily care setting. ,
The concept of working with resident animals has not been scientifically evaluated. Several issues beyond the benefits of therapy must be considered before embarking on such a program, including a) whether the animals will come into direct contact with patients and/or be allowed to roam freely in the facility; b) how the staff will provide care for the animals; c) the management of patients' or residents' allergies, asthma, and phobias; d) precautionary measures to prevent bites and scratches; and e) measures to properly manage the disposal of animal feces and urine, thereby preventing environmental contamination by zoonotic microorganisms (e.g., Toxoplasma spp., Toxocara spp., and Ancylostoma spp.). , Few data document a link between health-care-acquired infection rates and frequency of cleaning fish tanks or rodent cages. Skin infections caused by Mycobacterium marinum have been described among persons who have fish aquariums at home. , Nevertheless, immunocompromised patients should avoid direct contact with fish tanks and cages and the aerosols that these items produce. Further, fish tanks should be kept clean on a regular basis as determined by facility policy, and this task should be performed by gloved staff members who are not responsible for patient care. The use of the infection-control risk assessment can help determine whether a fish tank poses a risk for patient or resident safety and health in these situations. No evidence, however, links the incidence of health-care-acquired infections among immunocompetent patients or residents with the presence of a properly cleaned and maintained fish tank, even in dining areas. As a general preventive measure, resident animal programs are advised to restrict animals from a) food preparation kitchens, b) laundries, c) central sterile supply and any storage areas for clean supplies, and d) medication preparation areas. Resident-animal programs in acute-care facilities should not allow the animals into the isolation areas, protective environments, ORs, or any area where immunocompromised patients are housed. Patients and staff routinely should wash their hands or use waterless, alcohol-based hand-hygiene products after contact with animals.
# Service Animals
Although this section provides an overview about service animals in health-care settings, it cannot address every situation or question that may arise (see Appendix E -Information Resources). A service animal is any animal individually trained to do work or perform tasks for the benefit of a person with a disability.1366, 1376 A service animal is not considered a pet but rather an animal trained to provide assistance to a person because of a disability. Title III of the "Americans with Disabilities Act" (ADA) of 1990 mandates that persons with disabilities accompanied by service animals be allowed access with their service animals into places of public accommodation, including restaurants, public transportation, schools, and health-care facilities.1366, 1376 In health-care facilities, a person with a disability requiring a service animal may be an employee, a visitor, or a patient.
An overview of the subject of service animals and their presence in health-care facilities has been published.1366 No evidence suggests that animals pose a more significant risk of transmitting infection than people; therefore, service animals should not be excluded from such areas, unless an individual patient's situation or a particular animal poses greater risk that cannot be mitigated through reasonable measures. If health-care personnel, visitors, and patients are permitted to enter care areas (e.g., in patient rooms, some ICUs, and public areas) without taking additional precautions to prevent transmission of infectious agents (e.g., donning gloves, gowns, or masks), a clean, healthy, wellbehaved service animal should be allowed access with its handler.1366 Similarly, if immunocompromised patients are able to receive visitors without using protective garments or equipment, an exclusion of service animals from this area would not be justified.1366
Because health-care facilities are covered by the ADA or the Rehabilitation Act, a person with a disability may be accompanied by a service animal within the facility unless the animal's presence or behavior creates a fundamental alteration in the nature of a facility's services in a particular area or a direct threat to other persons in a particular area.1366 A "direct threat" is defined as a significant risk to the health or safety of others that cannot be mitigated or eliminated by modifying policies, practices, or procedures.1376 The determination that a service animal poses a direct threat in any particular health care setting must be based on an individualized assessment of the service animal, the patient, and the health-care situation. When evaluating risk in such situations, health-care personnel should consider the nature of the risk (including duration and severity); the probability that injury will occur; and whether reasonable modifications of policies, practices, or procedures will mitigate the risk (J. Wodatch, U.S. Department of Justice, 2000). The person with a disability should contribute to the risk-assessment process as part of a pre-procedure health-care provider/patient conference.
Excluding a service animal from an OR or similar special care areas (e.g., burn units, some ICUs, PE units, and any other area containing equipment critical for life support) is appropriate if these areas are considered to have "restricted access" with regards to the general public. General infection-control measures that dictate such limited access include a) the area is required to meet environmental criteria to minimize the risk of disease transmission, b) strict attention to hand hygiene and absence of dermatologic conditions, and c) barrier protective measures [e.g., using gloves, wearing gowns and masks] are indicated for persons in the affected space. No infection-control measures regarding the use of barrier precautions could be reasonably imposed on the service animal. Excluding a service animal that becomes threatening because of a perceived danger to its handler during treatment also is appropriate; however, exclusion of such an animal must be based on the actual behavior of the particular animal, not on speculation about how the animal might behave.
Another issue regarding service animals is whether to permit persons with disabilities to be accompanied by their service animals during all phases of their stay in the health-care facility. Health care personnel should discuss all aspects of anticipatory care with the patient who uses a service animal. Health-care personnel may not exclude a service animal because health-care staff may be able to perform the same services that the service animal does (e.g., retrieving dropped items and guiding an otherwise ambulatory person to the restroom). Similarly, health-care personnel can not exclude service animals because the health-care staff perceive a lack of need for the service animal during the person's stay in the health-care facility. A person with a disability is entitled to independent access (i.e., to be accompanied by a service animal unless the animal poses a direct threat or a fundamental alteration in the nature of services); "need" for the animal is not a valid factor in either analysis. For some forms of care (e.g., ambulation as physical therapy following total hip replacement or knee replacement), the service animal should not be used in place of a credentialed health-care worker who directly provides therapy. However, service animals need not be restricted from being in the presence of its handler during this time; in addition, rehabilitation and discharge planning should incorporate the patient's future use of the animal. The health-care personnel and the patient with a disability should discuss both the possible need for the service animal to be separated from its handler for a period of time during non emergency care and an alternate plan of care for the service animal in the event the patient is unable or unwilling to provide that care. This plan might include family members taking the animal out of the facility several times a day for exercise and elimination, the animal staying with relatives, or boarding off-site. Care of the service animal, however, remains the obligation of the person with the disability, not the health-care staff.
Although animals potentially carry zoonotic pathogens transmissible to man, the risk is minimal with a healthy, clean, vaccinated, well-behaved, and well-trained service animal, the most common of which are dogs and cats. No reports have been published regarding infectious disease that affects humans originating in service dogs. Standard cleaning procedures are sufficient following occupation of an area by a service animal.1366 Clean-up of spills of animal urine, feces, or other body substances can be accomplished with blood/body substance procedures outlined in the Environmental Services section of this guideline. No special bathing procedures are required prior to a service animal accompanying its handler into a health-care facility.
Providing access to exotic animals (e.g., reptiles and non-human primates) that are used as service animals is problematic. Concerns about these animals are discussed in two published reviews.1331, 1366 Because some of these animals exhibit high-risk behaviors that may increase the potential for zoonotic disease transmission (e.g., herpes B infection), providing health-care facility access to nonhuman primates used as service animals is discouraged, especially if these animals might come into contact with the general public.1361, 1362 Health-care administrators should consult the Americans with Disabilities Act for guidance when developing policies about service animals in their facilities.1366, 1376
Requiring documentation for access of a service animal to an area generally accessible to the public would impose a burden on a person with a disability. When health-care workers are not certain that an animal is a service animal, they may ask the person who has the animal if it is a service animal required because of a disability; however, no certification or other documentation of service animal status can be required.1377
# Animals as Patients in Human Health-Care Facilities
The potential for direct and indirect transmission of zoonoses must be considered when rooms and equipment in human health-care facilities are used for the medical or surgical treatment or diagnosis of animals.1378 Inquiries should be made to veterinary medical professionals to determine an appropriate facility and equipment to care for an animal.
The central issue associated with providing medical or surgical care to animals in human health-care facilities is whether cross-contamination occurs between the animal patient and the human health-care workers and/or human patients. The fundamental principles of infection control and aseptic practice should differ only minimally, if at all, between veterinary medicine and human medicine. Health-careassociated infections can and have occurred in both patients and workers in veterinary medical facilities when lapses in infection-control procedures are evident.1379-1384 Further, veterinary patients can be at risk for acquiring infection from veterinary health-care workers if proper precautions are not taken. 1385 The issue of providing care to veterinary patients in human health-care facilities can be divided into the following three areas of infection-control concerns: a) whether the room/area used for animal care can be made safe for human patients, b) whether the medical/surgical instruments used on animals can be subsequently used on human patients, and c) which disinfecting or sterilizing procedures need to be done for these purposes. Studies addressing these concerns are lacking. However, with respect to disinfection or sterilization in veterinary settings, only minimal evidence suggests that zoonotic microbial pathogens are unusually resistant to inactivation by chemical or physical agents (with the exception of prions). Ample evidence supports the contrary observation (i.e., that pathogens from human-and animal sources are similar in their relative instrinsic resistance to inactivation).1386-1391 Further, no evidence suggests that zoonotic pathogens behave differently from human pathogens with respect to ventilation. Despite this knowledge, an aesthetic and sociologic perception that animal care must remain separate from human care persists. Health-care facilities, however, are increasingly faced with requests from the veterinary medical community for access to human health-care facilities for reasons that are largely economical (e.g., costs of acquiring sophisticated diagnostic technology and complex medical instruments). If hospital guidelines allow treatment of animals, alternate veterinary resources (including veterinary hospitals, clinics, and universities) should be exhausted before using human health-care settings. Additionally, the hospital's public/media relations should be notified of the situation. The goal is to develop policies and procedures to proactively and positively discuss and disclose this activity to the general public.
An infection-control risk assessment (ICRA) must be undertaken to evaluate the circumstances specific to providing care to animals in a human health-care facility. Individual hospital policies and guidelines should be reviewed before any animal treatment is considered in such facilities. Animals treated in human health-care facilities should be under the direct care and supervision of a licensed veterinarian; they also should be free of known infectious diseases, ectoparasites, and other external contaminants (e.g., soil, urine, and feces). Measures should be taken to avoid treating animals with a known or suspected zoonotic disease in a human health-care setting (e.g., lambs being treated for Q fever).
If human health-care facilities must be used for animal treatment or diagnostics, the following general infection-control actions are suggested: a) whenever possible, the use of ORs or other rooms used for invasive procedures should be avoided [e.g., cardiac catheterization labs and invasive nuclear medicine areas]; b) when all other space options are exhausted and use of the aforementioned rooms is unavoidable, the procedure should be scheduled late in the day as the last procedure for that particular area such that patients are not present in the department/unit/area; c) environmental surfaces should be thoroughly cleaned and disinfected using procedures discussed in the Environmental Services portion of this guideline after the animal is removed from the care area; d) sufficient time should be allowed for ACH to help prevent allergic reactions by human patients [Table B.1. in Appendix B]; e) only disposable equipment or equipment that can be thoroughly and easily cleaned, disinfected, or sterilized should be used; f) when medical or surgical instruments, especially those invasive instruments that are difficult to clean [e.g., endoscopes], are used on animals, these instruments should be reserved for future use only on animals; and g) standard precautions should be followed.
# Research Animals in Health-Care Facilities
The risk of acquiring a zoonotic infection from research animals has decreased in recent years because many small laboratory animals (e.g., mice, rats, and rabbits) come from quality stock and have defined microbiologic profiles.1392 Larger animals (e.g., nonhuman primates) are still obtained frequently from the wild and may harbor pathogens transmissible to humans. Primates, in particular, benefit from vaccinations to protect their health during the research period provided the vaccination does not interfere with the study of the particular agent. Animals serving as models for human disease studies pose some risk for transmission of infection to laboratory or health-care workers from percutaneous or mucosal exposure. Exposures can occur either through a) direct contact with an infected animal or its body substances and secretions or b) indirect contact with infectious material on equipment, instruments, surfaces, or supplies.1392 Uncontained aerosols generated during laboratory procedures can also transmit infection.
Infection-control measures to prevent transmission of zoonotic infections from research animals are largely derived from the following basic laboratory safety principles: a) purchasing pathogen-free animals, b) quarantining incoming animals to detect any zoonotic pathogens, c) treating infected animals or removing them from the facility, d) vaccinating animal carriers and high-risk contacts if possible, e) using specialized containment caging or facilities, and f) using protective clothing and equipment [e.g., gloves, face shields, gowns, and masks].1392 An excellent resource for detailed discussion of these safety measures has been published.1013
The animal research unit within a health-care facility should be engineered to provide a) adequate containment of animals and pathogens; b) daily decontamination and transport of equipment and waste; c) proper ventilation and air filtration, which prevents recirculation of the air in the unit to other areas of the facility; and d) negative air pressure in the animal rooms relative to the corridors. To ensure adequate security and containment, no through traffic to other areas of the health-care facility should flow through this unit; access should be restricted to animal-care staff, researchers, environmental services, maintenance, and security personnel.
Occupational health programs for animal-care staff, researchers, and maintenance staff should take into consideration the animals' natural pathogens and research pathogens. Components of such programs include a) prophylactic vaccines, b) TB skin testing when primates are used, c) baseline serums, and d) hearing and respiratory testing. Work practices, PPE, and engineering controls specific for each of the four animal biosafety levels have been published. , The facility's occupational or employee health clinic should be aware of the appropriate post-exposure procedures involving zoonoses and have available the appropriate post-exposure biologicals and medications.
# I. Regulated Medical Waste
# Epidemiology
No epidemiologic evidence suggests that most of the solid-or liquid wastes from hospitals, other health care facilities, or clinical/research laboratories is any more infective than residential waste. Several studies have compared the microbial load and the diversity of microorganisms in residential wastes and wastes obtained from a variety of health-care settings.1399 1402 Although hospital wastes had a greater number of different bacterial species compared with residential waste, wastes from residences were more heavily contaminated. , Moreover, no epidemiologic evidence suggests that traditional waste-disposal practices of health-care facilities (whereby clinical and microbiological wastes were decontaminated on site before leaving the facility) have caused disease in either the health-care setting or the general community.1400, 1401 This statement excludes, however, sharps injuries sustained during or immediately after the delivery of patient care before the sharp is "discarded." Therefore, identifying wastes for which handling and disposal precautions are indicated is largely a matter of judgment about the relative risk of disease transmission, because no reasonable standards on which to base these determinations have been developed. Aesthetic and emotional considerations (originating during the early years of the HIV epidemic) have, however, figured into the development of treatment and disposal policies, particularly for pathology and anatomy wastes and sharps.1402 1405 Public concerns have resulted in the promulgation of federal, state, and local rules and regulations regarding medical waste management and disposal.1406 1414
# Categories of Medical Waste
Precisely defining medical waste on the basis of quantity and type of etiologic agents present is virtually impossible. The most practical approach to medical waste management is to identify wastes that represent a sufficient potential risk of causing infection during handling and disposal and for which some precautions likely are prudent.2 Health-care facility medical wastes targeted for handling and disposal precautions include microbiology laboratory waste (e.g., microbiologic cultures and stocks of microorganisms), pathology and anatomy waste, blood specimens from clinics and laboratories, blood products, and other body-fluid specimens.2 Moreover, the risk of either injury or infection from certain sharp items (e.g., needles and scalpel blades) contaminated with blood also must be considered. Although any item that has had contact with blood, exudates, or secretions may be potentially infective, treating all such waste as infective is neither practical nor necessary. Federal, state, and local guidelines and regulations specify the categories of medical waste that are subject to regulation and outline the requirements associated with treatment and disposal. The categorization of these wastes has generated the term "regulated medical waste." This term emphasizes the role of regulation in defining the actual material and as an alternative to "infectious waste," given the lack of evidence of this type of waste's infectivity. State regulations also address the degree or amount of contamination (e.g., blood-soaked gauze) that defines the discarded item as a regulated medical waste. The EPA's Manual for Infectious Waste Management identifies and categorizes other specific types of waste generated in health-care facilities with research laboratories that also require handling precautions.1406
# Management of Regulated Medical Waste in Health-Care Facilities
Medical wastes require careful disposal and containment before collection and consolidation for treatment. OSHA has dictated initial measures for discarding regulated medical-waste items. These measures are designed to protect the workers who generate medical wastes and who manage the wastes from point of generation to disposal.967 A single, leak-resistant biohazard bag is usually adequate for containment of regulated medical wastes, provided the bag is sturdy and the waste can be discarded without contaminating the bag's exterior. The contamination or puncturing of the bag requires placement into a second biohazard bag. All bags should be securely closed for disposal. Punctureresistant containers located at the point of use (e.g., sharps containers) are used as containment for discarded slides or tubes with small amounts of blood, scalpel blades, needles and syringes, and unused sterile sharps.967 To prevent needlestick injuries, needles and other contaminated sharps should not be recapped, purposefully bent, or broken by hand. CDC has published general guidelines for handling sharps.6, 1415 Health-care facilities may need additional precautions to prevent the production of aerosols during the handling of blood-contaminated items for certain rare diseases or conditions (e.g.,
# Lassa fever and Ebola virus infection).203
Transporting and storing regulated medical wastes within the health-care facility prior to terminal treatment is often necessary. Both federal and state regulations address the safe transport and storage of on-and off-site regulated medical wastes.1406 1408 Health-care facilities are instructed to dispose medical wastes regularly to avoid accumulation. Medical wastes requiring storage should be kept in labeled, leak-proof, puncture-resistant containers under conditions that minimize or prevent foul odors. The storage area should be well ventilated and be inaccessible to pests. Any facility that generates regulated medical wastes should have a regulated medical waste management plan to ensure health and environmental safety as per federal, state, and local regulations.
# Treatment of Regulated Medical Waste
Regulated medical wastes are treated or decontaminated to reduce the microbial load in or on the waste and to render the by-products safe for further handling and disposal. From a microbiologic standpoint, waste need not be rendered "sterile" because the treated waste will not be deposited in a sterile site. In addition, waste need not be subjected to the same reprocessing standards as are surgical instruments. Historically, treatment methods involved steam-sterilization (i.e., autoclaving), incineration, or interment (for anatomy wastes). Alternative treatment methods developed in recent years include chemical disinfection, grinding/shredding/disinfection methods, energy-based technologies (e.g., microwave or radiowave treatments), and disinfection/encapsulation methods.1409 State medical waste regulations specify appropriate treatment methods for each category of regulated medical waste.
Of all the categories comprising regulated medical waste, microbiologic wastes (e.g., untreated cultures, stocks, and amplified microbial populations) pose the greatest potential for infectious disease transmission, and sharps pose the greatest risk for injuries. Untreated stocks and cultures of microorganisms are subsets of the clinical laboratory or microbiologic waste stream. If the microorganism must be grown and amplified in culture to high concentration to permit work with the specimen, this item should be considered for on-site decontamination, preferably within the laboratory unit. Historically, this was accomplished effectively by either autoclaving (steam sterilization) or incineration. If steam sterilization in the health-care facility is used for waste treatment, exposure of the waste for up to 90 minutes at 250°F (121°C) in a autoclave (depending on the size of the load and type container) may be necessary to ensure an adequate decontamination cycle.14161418 After steam sterilization, the residue can be safely handled and discarded with all other nonhazardous solid waste in accordance with state solid-waste disposal regulations. On-site incineration is another treatment option for microbiologic, pathologic, and anatomic waste, provided the incinerator is engineered to burn these wastes completely and stay within EPA emissions standards.1410 Improper incineration of waste with high moisture and low energy content (e.g., pathology waste) can lead to emission problems. State medical-waste regulatory programs identify acceptable methods for inactivating amplified stocks and cultures of microorganisms, some of which may employ technology rather than steam sterilization or incineration.
Concerns have been raised about the ability of modern health-care facilities to inactivate microbiologic wastes on-site, given that many of these institutions have decommissioned their laboratory autoclaves. Current laboratory guidelines for working with infectious microorganisms at biosafety level (BSL) 3 recommend that all laboratory waste be decontaminated before disposal by an approved method, preferably within the laboratory.1013 These same guidelines recommend that all materials removed from a BSL 4 laboratory (unless they are biological materials that are to remain viable) are to be decontaminated before they leave the laboratory.1013 Recent federal regulations for laboratories that handle certain biological agents known as "select agents" (i.e., those that have the potential to pose a severe threat to public health and safety) require these agents (and those obtained from a clinical specimen intended for diagnostic, reference, or verification purposes) to be destroyed on-site before disposal.1412 Although recommendations for laboratory waste disposal from BSL 1 or 2 laboratories (e.g., most health-care clinical and diagnostic laboratories) allow for these materials to be decontaminated off-site before disposal, on-site decontamination by a known effective method is preferred to reduce the potential of exposure during the handling of infectious material.
A recent outbreak of TB among workers in a regional medical-waste treatment facility in the United States demonstrated the hazards associated with aerosolized microbiologic wastes.1419, 1420 The facility received diagnostic cultures of Mycobacterium tuberculosis from several different health-care facilities before these cultures were chemically disinfected; this facility treated this waste with a grinding/shredding process that generated aerosols from the material. 1419, 1420 Several operational deficiencies facilitated the release of aerosols and exposed workers to airborne M. tuberculosis. Among the suggested control measures was that health-care facilities perform on-site decontamination of laboratory waste containing live cultures of microorganisms before release of the waste to a waste management company.1419, 1420 This measure is supported by recommendations found in the CDC/NIH guideline for laboratory workers.1013 This outbreak demonstrates the need to avoid the use of any medical-waste treatment method or technology that can aerosolize pathogens from live cultures and stocks (especially those of airborne microorganisms) unless aerosols can be effectively contained and workers can be equipped with proper p p e .14191421 Safe laboratory practices, including those addressing waste management, have been published.1013, 1422
In an era when local, state, and federal health-care facilities and laboratories are developing bioterrorism response strategies and capabilities, the need to reinstate in-laboratory capacity to destroy cultures and stocks of microorganisms becomes a relevant issue.1423 Recent federal regulations require health-care facility laboratories to maintain the capability of destroying discarded cultures and stocks on-site if these laboratories isolate from a clinical specimen any microorganism or toxin identified as a "select agent" from a clinical specimen (Table 27).1412, 1413 As an alternative, isolated cultures of select agents can be transferred to a facility registered to accept these agents in accordance with federal regulations.1412 State medical waste regulations can, however, complicate or completely prevent this transfer if these cultures are determined to be medical waste, because most states regulate the inter-facility transfer of untreated medical wastes. Crimean-Congo hemorrhagic fever virus; Ebola viruses; Cercopithecine herpesvirus 1 (herpes B virus); Lassa fever virus; Marburg virus; monkeypox virus; South American hemorrhagic fever viruses (Junin, Machupo, Sabia, Flexal, Guanarito); tick-borne encephalitis complex (flavi) viruses (Central European tick-borne encephalitis, Far Eastern tick-borne encephalitis [Russian spring and summer encephalitis, Kyasnaur Forest disease, Omsk hemorrhagic fever]); variola major virus (smallpox virus); and variola minor virus (alastrim)
# E x clu sio n s!
Vaccine strain of Junin virus (Candid. #1)
# B acteria
# Rickettsia prowazekii, R. rickettsii, Yersinia pestis
# Fungi
# Coccidioides posadasii T oxins
Abrin; conotoxins; diacetoxyscirpenol; ricin; saxitoxin; Shiga-like ribosome inactivating proteins; tetrodotoxin
# E x clu sio n s!
The following toxins (in purified form or in combinations of pure and impure forms) if the aggregate amount under the control of a principal investigator does not, at any time, exceed the amount specified: 100 mg of abrin; 100 mg of conotoxins; 1,000 mg of diacetoxyscirpenol; 100 mg of ricin; 100 mg of saxitoxin; 100 mg of Shiga-like ribosome inactivating proteins; or 100 mg of tetrodotoxin G enetic elem ents, recom binant nucleic acids, and recom binant o rg a n ism s!
• Select agent viral nucleic acids (synthetic or naturally-derived, contiguous or fragmented, in host chromosomes or in expression vectors) that can encode infectious and/or replication competent forms of any of the select agent viruses; • Nucleic acids (synthetic or naturally-derived) that encode for the functional form(s) of any of the toxins listed in this table if the nucleic acids: a) are in a vector or host chromosome; b) can be expressed in vivo or in vitro; or c) are in a vector or host chromosome and can be expressed in vivo or in vitro;
• Viruses, bacteria, fungi, and toxins listed in this table that have been genetically modified. The following toxins (in purified form or in combinations of pure and impure forms) if the aggregate amount under the control of a principal investigator does not, at any time, exceed the amount specified: 0.5 mg of botulinum neurotoxins; 100 mg of Clostridium perfringens epsilon toxin; 100 mg of Shigatoxin; 5 mg of staphylococcal enterotoxins; or 1,000 mg of T-2 toxin
# High consequence livestock pathogens and toxins/select agents (overlap agents) (42 CFR Part 73 §73.5 and USDA regulation 9 CFR Part 121) (continued)
G enetic elem ents, recom binant nucleic acids, and recom binant organism s^• Select agent viral nuclei acids (synthetic or naturally derived, contiguous or fragmented, in host chromosomes or in expression vectors) thatcan encode infectious and/or replication competent forms of any of the select agent viruses; • Nucleic acids (synthetic or naturally derived) that encode for the functional form(s) of any of the toxins listed in this table if the nucleic acids: a) are in a vector or host chromosome; b) can be expressed in vivo or in vitro; or c) are in a vector or host chromosome and can be expressed in vivo or in vitro;
• Viruses, bacteria, fungi, and toxins listed in this table that have been genetically modified * Material in this table is compiled from references 1412, 1413, and 1424. Reference 1424 also contains lists of select agents that include plant pathogens and pathogens affecting livestock. + 42 CFR 73 § §73.4 and 73.5 do not include any select agent or toxin that is in its naturally-occurring environment, provided it has not been intentionally introduced, cultivated, collected, or otherwise extracted from its natural source. These sections also do not include non-viable select agent organisms or nonfunctional toxins. This list of select agents is current as of 3 October 2003 and is subject to change pending the final adoption of 42 CFR Part 73. These table entries are listed in reference 1412 and 1413, but were not included in reference 1424.
# Discharging Blood, Fluids to Sanitary Sewers or Septic Tanks
The contents of all vessels that contain more than a few milliliters of blood remaining after laboratory procedures, suction fluids, or bulk blood can either be inactivated in accordance with state-approved treatment technologies or carefully poured down a utility sink drain or toilet.1414 State regulations may dictate the maximum volume allowable for discharge of blood/body fluids to the sanitary sewer. No evidence indicates that bloodborne diseases have been transmitted from contact with raw or treated sewage. Many bloodborne pathogens, particularly bloodborne viruses, are not stable in the environment for long periods of time;1425, 1426 therefore, the discharge of small quantities of blood and other body fluids to the sanitary sewer is considered a safe method of disposing of these waste materials.1414 The following factors increase the likelihood that bloodborne pathogens will be inactivated in the disposal process: a) dilution of the discharged materials with water; b) inactivation of pathogens resulting from exposure to cleaning chemicals, disinfectants, and other chemicals in raw sewage; and c) effectiveness of sewage treatment in inactivating any residual bloodborne pathogens that reach the treatment facility. Small amounts of blood and other body fluids should not affect the functioning of a municipal sewer system. However, large quantities of these fluids, with their high protein content, might interfere with the biological oxygen demand (BOD) of the system. Local municipal sewage treatment restrictions may dictate that an alternative method of bulk fluid disposal be selected. State regulations may dictate what quantity constitutes a small amount of blood or body fluids.
Although concerns have been raised about the discharge of blood and other body fluids to a septic tank system, no evidence suggests that septic tanks have transmitted bloodborne infections. A properly functioning septic system is adequate for inactivating bloodborne pathogens. System manufacturers' instructions specify what materials may be discharged to the septic tank without jeopardizing its proper operation.
# Medical Waste and CJD
Concerns also have been raised about the need for special handling and treatment procedures for wastes generated during the care of patients with CJD or other transmissible spongiform encephalopathies (TSEs). Prions, the agents that cause TSEs, have significant resistance to inactivation by a variety of physical, chemical, or gaseous methods.1427 No epidemiologic evidence, however, links acquisition of CJD with medical-waste disposal practices. Although handling neurologic tissue for pathologic examination and autopsy materials with care, using barrier precautions, and following specific procedures for the autopsy are prudent measures,1197 employing extraordinary measures once the materials are discarded is unnecessary. Regulated medical wastes generated during the care of the CJD patient can be managed using the same strategies as wastes generated during the care of other patients. After decontamination, these wastes may then be disposed in a sanitary landfill or discharged to the sanitary sewer, as appropriate.
# Part II. Recommendations for Environmental Infection Control in Health-Care Facilities
# A. Rationale for Recommendations
As in previous CDC guidelines, each recommendation is categorized on the basis of existing scientific data, theoretic rationale, applicability, and possible economic benefit. The recommendations are evidence-based wherever possible. However, certain recommendations are derived from empiric infection-control or engineering principles, theoretic rationale, or from experience gained from events that cannot be readily studied (e.g., floods).
The HICPAC system for categorizing recommendations has been modified to include a category for engineering standards and actions required by state or federal regulations. Guidelines and standards published by the American Institute of Architects (AIA), American Society of Heating, Refrigeration, and Air-Conditioning Engineers (ASHRAE), and the Association for the Advancement in Medical Instrumentation (AAMI) form the basis of certain recommendations. These standards reflect a consensus of expert opinions and extensive consultation with agencies of the U.S. Department of Health and Human Services. Compliance with these standards is usually voluntary. However, state and federal governments often adopt these standards as regulations. For example, the standards from AIA regarding construction and design of new or renovated health-care facilities, have been adopted by reference by >40 states. Certain recommendations have two category ratings (e.g., Categories IA and IC or Categories IB and IC), indicating the recommendation is evidence-based as well as a standard or regulation.
# B. Rating Categories
Recommendations are rated according to the following categories: Seal windows in work zones if practical; use window chutes for disposal of large pieces of debris as needed, but ensure that the negative pressure differential for the area is maintained.20, 120, 273 f.
•
Direct pedestrian traffic from construction zones away from patient-care areas to minimize the dispersion of dust.20, 49, 97, 109, 111, 120, 273-277 g.
Provide construction crews with 1) designated entrances, corridors, and elevators whenever practical; 2) essential services [e.g., toilet facilities], and convenience services [e.g., vending machines]; 3) protective clothing [e.g., coveralls, footgear, and headgear] for travel to patient-care areas; and 4) a space or anteroom for changing clothing and storing equipment. , ,h.
Clean work zones and their entrances daily by 1) wet-wiping tools and tool carts before their removal from the work zone; 2) placing mats with tacky surfaces inside the entrance; and 3) covering debris and securing this covering before removing debris from the work zone. , ,i.
In patient-care areas, for major repairs that include removal of ceiling tiles and disruption of the space above the false ceiling, use plastic sheets or prefabricated plastic units to contain dust; use a negative pressure system within this enclosure to remove dust; and either pass air through an industrial grade, portable HEPA filter capable of filtration rates ranging from 300-800 ft3/min., or exhaust air directly to the outside. Position the units appropriately so that all room air passes through the filter; obtain engineering consultation to determine the appropriate placement of the unit.4
Category II 2.
Switch the portable unit off during the surgical procedure. Category II 3.
Provide fresh air as per ventilation standards for operating rooms; portable units do not meet the requirements for the number of fresh ACH. , , Category II D.
If possible, schedule infectious TB patients as the last surgical cases of the day to maximize the time available for removal of airborne contamination. Category II E.
No recommendation is offered for performing orthopedic implant operations in rooms supplied with laminar airflow.362, 364 Unresolved issue F.
Maintain backup ventilation equipment (e.g., portable units for fans or filters) for emergency provision of ventilation requirements for operating rooms, and take immediate steps to restore the fixed ventilation system function. Maintain a high level of surveillance for waterborne disease among patients after a boil water advisory is lifted. Category II If the pH of the municipal water is in the basic range (e.g., when chloramine is used as the primary drinking water disinfectant in the community), consult the facility engineer regarding the possible need to adjust the pH of the water to a more acid level before disinfection, to enhance the biocidal activity of chlorine.894 Category II C.
Clean and disinfect hydrotherapy equipment after using tub liners. Category II D.
Clean and disinfect inflatable tubs unless they are single-use equipment.
# Category II E.
No recommendation is offered regarding the use of antiseptic chemicals (e.g., chloramine-T) in the water during hydrotherapy sessions. Unresolved issue F.
Conduct a risk assessment of patients prior to their use of large hydrotherapy pools, deferring patients with draining wounds or fecal incontinence from pool use until their condition resolves. Category II G.
For
# Part III. References
Note: The bold item in parentheses indicated the citation number or the location of this reference listed in the MMWR version of this guideline.
the degree of water pollution. The term is also referred to as Biological Oxygen Demand (BOD). Biological oxygen demand (BOD): an indirect measure of the concentration of biologically degradable material present in organic wastes (pertaining to water quality). It usually reflects the amount of oxygen consumed in five days by biological processes breaking down organic waste (BOD5). Biosafety level: a combination of microbiological practices, laboratory facilities, and safety equipment determined to be sufficient to reduce or prevent occupational exposures of laboratory personnel to the microbiological agents they work with. There are four biosafety levels based on the hazards associated with the various microbiological agents. BOD5: the amount of dissolved oxygen consumed in five days by biological processes breaking down organic matter. Bonneting: a floor cleaning method for either carpeted or hard surface floors that uses a circular motion of a large fibrous disc to lift and remove soil and dust from the surface. Capped spur: a pipe leading from the water recirculating system to an outlet that has been closed off ("capped"). A capped spur cannot be flushed, and it might not be noticed unless the surrounding wall is removed. CFU/m3: colony forming units per cubic meter (of air). Chlamydospores: thick-walled, typically spherical or ovoid resting spores asexually produced by certain types of fungi from cells of the somatic hyphae. Chloramines: compounds containing nitrogen, hydrogen, and chlorine. These are formed by the reaction between hypochlorous acid (HOCl) and ammonia (NH3) and/or organic amines in water. The formation of chloramines in drinking water treatment extends the disinfecting power of chlorine. The term is also referred to as Combined Available Chlorine. Cleaning: the removal of visible soil and organic contamination from a device or surface, using either the physical action of scrubbing with a surfactant or detergent and water, or an energy-based process (e.g., ultrasonic cleaners) with appropriate chemical agents. Coagulation-flocculation: coagulation is the clumping of particles that results in the settling of impurities. It may be induced by coagulants (e.g., lime, alum, and iron salts). Flocculation in water and wastewater treatment is the agglomeration or clustering of colloidal and finely-divided suspended matter after coagulation by gentle stirring by either mechanical or hydraulic means, such that they can be separated from water or sewage. Commissioning (a room): testing a system or device to ensure that it meets the pre-use specifications as indicated by the manufacturer or predetermined standard, or air sampling in a room to establish a pre occupancy baseline standard of microbial or particulate contamination. The term is also referred to as benchmarking at 77°F (25°C). Completely packaged: functionally packaged, as for laundry. Conidia: asexual spores of fungi borne externally. Conidiophores: specialized hyphae that bear conidia in fungi. Conditioned space: that part of a building that is heated or cooled, or both, for the comfort of the occupants.
Contaminant: an unwanted airborne constituent that may reduce the acceptibility of air. Convection: the transfer of heat or other atmospheric properties within the atmosphere or in the airspace of an enclosure by the circulation of currents from one region to another, especially by such motion directed upward.
Cooling tower: a structure engineered to receive accumulated heat from ventilation systems and equipment and transfer this heat to water, which then releases the stored heat to the atmosphere through evaporative cooling.
Critical item (medical instrument): a medical instrument or device that contacts normally sterile areas of the body or enters the vascular system. There is a high risk of infection from such devices if they are microbiologically contaminated prior to use. These devices must be sterilized before use. Dead legs: areas in the water system where water stagnates. A dead leg is a pipe or spur, leading from the water recirculating system to an outlet that is used infrequently, resulting in inadequate flow of water from the recirculating system to the outlet. This inadequate flow reduces the perfusion of heat or chlorine into this part of the water distribution system, thereby adversely affecting the disinfection of the water system in that area. Deionization: removal of ions from water by exchange with other ions associated with fixed charges on a resin bed. Cations are usually removed and H+ ions are exchanged; OH" ions are exchanged for anions. Detritis: particulate matter produced by or remaining after the wearing away or disintegration of a substance or tissue. Dew point: the temperature at which a gas or vapor condenses to form a liquid; the point at which moisture begins to condense out of the air. At dew point, air is cooled to the point where it is at 100% relative humidity or saturation. Dialysate: the aqueous electrolyte solution, usually containing dextrose, used to make a concentration gradient between the solution and blood in the hemodialyzer (dialyzer). Dialyzer: a device that consists of two compartments (blood and dialysate) separated by a semipermeable membrane. A dialyzer is usually referred to as an artificial kidney. Diffuser: the grille plate that disperses the air stream coming into the conditioned air space. Direct transmission: involves direct body surface-to-body surface contact and physical transfer of microorganisms between a susceptible host and an infected/colonized person, or exposure to cloud of infectious particles within 3 feet of the source; the aerosolized particles are >5 pm in size. Disability: as defined by the Americans with Disabilities Act, a disability is any physical or mental impairment that substantially limits one or more major life activities, including but not limited to walking, talking, seeing, breathing, hearing, or caring for oneself. Disinfection: a generally less lethal process of microbial inactivation (compared to sterilization) that eliminates virtually all recognized pathogenic microorganisms but not necessarily all microbial forms (e.g., bacterial spores). Drain pans: pans that collect water within the HVAC system and remove it from the system. Condensation results when air and steam come together. Drift: circulating water lost from the cooling tower in the form as liquid droplets entrained in the exhaust air stream (i.e., exhaust aerosols from a cooling tower). Drift eliminators: an assembly of baffles or labyrinth passages through which the air passes prior to its exit from the cooling tower. The purpose of a drift eliminator is to remove entrained water droplets from the exhaust air. Droplets: particles of moisture, such as are generated when a person coughs or sneezes, or when water is converted to a fine mist by a device such as an aerator or shower head. These particles may contain infectious microorganisms. Intermediate in size between drops and droplet nuclei, these particles tend to quickly settle out from the air so that any risk of disease transmission is generally limited to persons in close proximity to the droplet source. Droplet nuclei: sufficiently small particles (1-5 pm in diameter) that can remain airborne indefinitely and cause infection when a susceptible person is exposed at or beyond 3 feet of the source of these particles.
Dual duct system: an HVAC system that consists of parallel ducts that produce a cold air stream in one and a hot air stream in the other. Dust: an air suspension of particles (aerosol) of any solid material, usually with particle sizes <100 pm in diameter. Dust-spot test: a procedure that uses atmospheric air or a defined dust to measure a filter's ability to remove particles. A photometer is used to measure air samples on either side of the filter, and the difference is expressed as a percentage of particles removed. Effective leakage area: the area through which air can enter or leave the room. This does not include supply, return, or exhaust ducts. The smaller the effective leakage area, the better isolated the room. Endotoxin: the lipopolysaccharides of gram-negative bacteria, the toxic character of which resides in the lipid portion. Endotoxins generally produce pyrogenic reactions in persons exposed to these bacterial components. Enveloped virus: a virus whose outer surface is derived from a membrane of the host cell (either nuclear or the cell's outer membrane) during the budding phase of the maturation process. This membrane-derived material contains lipid, a component that makes these viruses sensitive to the action of chemical germicides. Evaporative condenser: a wet-type, heat-rejection unit that produces large volumes of aerosols during the process of removing heat from conditioned space air. Exhaust air: air removed from a space and not reused therein. Exposure: the condition of being subjected to something (e.g., infectious agents) that could have a harmful effect. Fastidious: having complex nutritional requirements for growth, as in microorganisms.
Fill: that portion of a cooling tower which makes up its primary heat transfer surface. Fill is alternatively known as "packing." Finished water: treated, or potable water. Fixed room-air HEPA recirculation systems: nonmobile devices or systems that remove airborne contaminants by recirculating air through a HEPA filter. These may be built into the room and permanently ducted or may be mounted to the wall or ceiling within the room. In either situation, they are fixed in place and are not easily movable.
Fomite: an inanimate object that may be contaminated with microorganisms and serves in their transmission.
Free and available chlorine: the term applied to the three forms of chlorine that may be found in solution (i.e., chlorine [Cl2] , hypochlorite [OCl], and hypochlorous acid [HOCl]). Germicide: a chemical that destroys microorganisms. Germicides may be used to inactivate microorganisms in or on living tissue (antiseptics) or on environmental surfaces (disinfectants). Health-care-associated: an outcome, usually an infection, that occurs in any health-care facility as a result of medical care. The term "health-care-associated" replaces "nosocomial," the latter term being limited to adverse infectious outcomes occurring only in hospitals. Hemodiafiltration: a form of renal replacement therapy in which waste solutes in the patient's blood are removed by both diffusion and convection through a high-flux membrane. Hemodialysis: a treatment for renal replacement therapy in which waste solutes in the patient's blood are removed by diffusion and/or convection through the semipermeable membrane of an artificial kidney or dialyzer. Hemofiltration: cleansing of waste products or other toxins from the blood by convection across a semipermeable, high-flux membrane where fluid balance is maintained by infusion of sterile, pyrogen free substitution fluid pre-or post-hemodialyzer. HEPA filter: High Efficiency Particulate Air filters capable of removing 99.97% of particles 0.3 pm in diameter and may assist in controlling the transmission of airborne disease agents. These filters may be used in ventilation systems to remove particles from the air or in personal respirators to filter air before it is inhaled by the person wearing the respirator. The use of HEPA filters in ventilation systems requires expertise in installation and maintenance. To test this type of filter, 0.3 pm particles of dioctylphthalate (DOP) are drawn through the filter. Efficiency is calculated by comparing the downstream and upstream particle counts. The optimal HEPA filter allows only three particles to pass through for every 10,000 particles that are fed to the filter. Heterotrophic (heterotroph): that which requires some nutrient components from exogenous sources. Heterotrophic bacteria cannot synthesize all of their metabolites and therefore require certain nutrients from other sources. High-efficiency filter: a filter with a particle-removal efficiency of 90%-95%. High flux: a type of dialyzer or hemodialysis treatment in which large molecules (>8,000 daltons [e.g., P2 microglobulin]) are removed from blood. High-level disinfection: a disinfection process that inactivates vegetative bacteria, mycobacteria, fungi, and viruses, but not necessarily high numbers of bacterial spores.
RODAC: Replicate Organism Direct Agar Contact. This term refers to a nutrient agar plate whose convex agar surface is directly pressed onto an environmental surface for the purpose of microbiologic sampling of that surface. Room-air HEPA recirculation systems and units: devices (either fixed or portable) that remove airborne contaminants by recirculating air through a HEPA filter. Routine sampling: environmental sampling conducted without a specific, intended purpose and with no action plan dependent on the results obtained.
Sanitizer: an agent that reduces microbial contamination to safe levels as judged by public health standards or requirements. Saprophytic: a naturally-occurring microbial contaminant. Sedimentation: the act or process of depositing sediment from suspension in water. The term also refers to the process whereby solids settle out of wastewater by gravity during treatment. Semicritical devices: medical devices that come into contact with mucous membranes or non-intact skin.
Service animal: any animal individually trained to do work or perform tasks for the benefit of a person with a disability. Shedding: the generation and dispersion of particles and spores by sources within the patient area, through activities such as patient movement and airflow over surfaces. Single-pass ventilation: ventilation in which 100% of the air supplied to an area is exhausted to the outside. Small, non-enveloped viruses: viruses whose particle diameter is <50 nm and whose outer surface is the protein of the particle itself and not that of host cell membrane components. Examples of small, non-enveloped viruses are polioviruses and hepatitis A virus. Spaulding Classification: the categorization of inanimate medical device surfaces in the medical environment as proposed in 1972 by Dr. Earle Spaulding. Surfaces are divided into three general categories, based on the theoretical risk of infection if the surfaces are contaminated at time of use. The categories are "critical," "semicritical," and "noncritical." Specific humidity: the mass of water vapor per unit mass of moist air. It is expressed as grains of water per pound of dry air, or pounds of water per pound of dry air. The specific humidity changes as moisture is added or removed. However, temperature changes do not change the specific humidity unless the air is cooled below the dew point. Splatter: visible drops of liquid or body fluid that are expelled forcibly into the air and settle out quickly, as distinguished from particles of an aerosol which remain airborne indefinitely. Steady state: the usual state of an area. Sterilization: the use of a physical or chemical procedure to destroy all microbial life, including large numbers of highly-resistant bacterial endospores. Stop valve: a valve that regulates the flow of fluid through a pipe. The term may also refer to a faucet. Substitution fluid: fluid that is used for fluid management of patients receiving hemodiafiltration. This fluid can be prepared on-line at the machine through a series of ultrafilters or with the use of sterile peritoneal dialysis fluid. Supply air: air that is delivered to the conditioned space and used for ventilation, heating, cooling, humidification, or dehumidification. Tensile strength: the resistance of a material to a force tending to tear it apart, measured as the maximum tension the material can withstand without tearing. Therapy animal: an animal (usually a personal pet) that, with their owners or handlers, provide supervised, goal-directed intervention to clients in hospitals, nursing homes, special-population schools, and other treatment sites. Thermophilic: capable of growing in environments warmer than body temperature. Thermotolerant: capable of withstanding high temperature conditions. TLV®: an exposure level under which most people can work consistently for 8 hours a day, day after day, without adverse effects. The term is used by the ACGIH to designate degree of exposure to contaminants. TLV® can be expressed as approximate milligrams of particulate per cubic meter of air (mg/m3). TLVs® are listed as either an 8-hour TWA (time weighted average) or a 15-minute STEL (short term exposure limit). TLV-TWA: Threshold Limit Value-Time Weighted Average. The term refers to the time-weighted average concentration for a normal 8-hour workday and a 40-hour workweek to which nearly all workers may be exposed repeatedly, day after day, without adverse effects. The TLV-TWA for "particulates (insoluble) not otherwise classified" (PNOC) -(sometimes referred to as nuisance dust)are those particulates containing no asbestos and <1% crystalline silica. A TLV-TWA of 10 mg/m3 for inhalable particulates and a TLV-TWA of 3 mg/m3 for respirable particulates (particulates <5 pm in aerodynamic diameter) have been established. Total suspended particulate matter: the mass of particles suspended in a unit of volume of air when collected by a high-volume air sampler.
Transient: a change in the condition of the steady state that takes a very short time compared with the steady state. Opening a door, and shaking bed linens are examples of transient activities.
TWA: average exposure for an individual over a given working period, as determined by sampling at given times during the period. TWA is usually presented as the average concentration over an 8-hour workday for a 40-hour workweek. Ultraclean air: air in laminar flow ventilation that has also passed through a bank of HEPA filters.
Ultrafilter: a membrane filter with a pore size in the range of 0.001-0.05 pm, the performance of which is usually rated in terms of a nominal molecular weight cut-off (defined as the smallest molecular weight species for which the filter membrance has more than 90% rejection).
Ultrafiltered dialysate: the process by which dialysate is passed through a filter having a molecular weight cut-off of approximately 1 kilodalton for the purpose of removing bacteria and endotoxin from the bath. Ultraviolet germicidal irradiation (UVGI): the use of ultraviolet radiation to kill or inactivate microorganisms. Ultraviolet germicidal irradiation lamps: lamps that kill or inactivate microorganisms by emitting ultraviolet germicidal radiation, predominantly at a wavelength of 254 nm. UVGI lamps can be used in ceiling or wall fixtures or within air ducts of ventilation systems.
Vapor pressure: the pressure exerted by free molecules at the surface of a solid or liquid. Vapor pressure is a function of temperature, increasing as the temperature rises.
Vegetative bacteria: bacteria that are actively growing and metabolizing, as opposed to a bacterial state of quiescence that is achieved when certain bacteria (gram-positive bacilli) convert to spores when the environment can no longer support active growth. Vehicle: any object, person, surface, fomite, or media that may carry and transfer infectious microorganisms from one site to another. Ventilation: the process of supplying and removing air by natural or mechanical means to and from any space. Such air may or may not be conditioned. Ventilation air: that portion of the supply air consisting of outdoor air plus any recirculated air that has been treated for the purpose of maintaining acceptable indoor air quality. Ventilation, dilution: an engineering control technique to dilute and remove airborne contaminants by the flow of air into and out of an area. Air that contains droplet nuclei is removed and replaced by contaminant-free air. If the flow is sufficient, droplet nuclei become dispersed, and their concentration in the air is diminished. Ventilation, local exhaust: ventilation used to capture and removed airborne contaminants by enclosing the contaminant source (the patient) or by placing an exhaust hood close to the contaminant source. v/v: volume to volume. This term is an expression of concentration of a percentage solution when the principle component is added as a liquid to the diluent. w/v: weight to volume. This term is an expression of concentration of a percentage solution when the principle component is added as a solid to the diluent.
Weight-arrestance: a measure of filter efficiency, used primarily when describing the performance of low-and medium-efficiency filters. The measurement of weight-arrestance is performed by feeding a standardized synthetic dust to the filter and weighing the fraction of the dust removed. T Values apply to an empty room with no aerosol-generating source. With a person present and generating aerosol, this table would not apply. Other equations are available that include a constant generating source. However, certain diseases (e.g., infectious tuberculosis) are not likely to be aerosolized at a constant rate. The times given assume perfect mixing of the air within the space (i.e., mixing factor = 1). However, perfect mixing usually does not occur. Removal times will be longer in rooms or areas with imperfect mixing or air stagnation.213 Caution should be exercised in using this table in such situations. For booths or other local ventilation enclosures, manufacturers' instructions should be consulted.
# Appendix B. Air 1. Airborne Contaminant Removal
# Air Sampling for Aerosols Containing Legionellae
Air sampling is an insensitive means of detecting Legionella pneumophila, and is of limited practical value in environmental sampling for this pathogen. In certain instances, however, it can be used to a) demonstrate the presence of legionellae in aerosol droplets associated with suspected bacterial reservoirs; b) define the role of certain devices [e.g., showers, faucets, decorative fountains, or evaporate condensers] in disease transmission; and c) quantitate and determine the size of the droplets containing legionellae.1436 Stringent controls and calibration are necessary when sampling is used to determine particle size and numbers of viable bacteria.1437 Samplers should be placed in locations where human exposure to aerosols is anticipated, and investigators should wear a NIOSH-approved respirator (e.g., N95 respirator) if sampling involves exposure to potentially infectious aerosols.
Methods used to sample air for legionellae include impingement in liquid, impaction on solid medium, and sedimentation using settle plates.1436 The Chemical Corps.-type all-glass impingers (AGI) with the stem 30 mm from the bottom of the flask have been used successfully to sample for legionellae.1436 Because of the velocity at which air samples are collected, clumps tend to become fragmented, leading to a more accurate count of bacteria present in the air. The disadvantages of this method are a) the velocity of collection tends to destroy some vegetative cells; b) the method does not differentiate particle sizes; and c) AGIs are easily broken in the field. Yeast extract broth (0.25%) is the recommended liquid medium for AGI sampling of legionellae;1437 standard methods for water samples can be used to culture these samples.
Andersen samplers are viable particle samplers in which particles pass through jet orifices of decreasing size in cascade fashion until they impact on an agar surface.1218 The agar plates are then removed and incubated. The stage distribution of the legionellae should indicate the extent to which the bacteria would have penetrated the respiratory system. The advantages of this sampling method are a) the equipment is more durable during use; b) the sampler can cetermine the number and size of droplets containing legionellae; c) the agar plates can be placed directly in an incubator with no further manipulations; and d) both selective and nonselective BCYE agar can be used. If the samples must be shipped to a laboratory, they should be packed and shipped without refrigeration as soon as possible.
# Calculation of Air Sampling Results
Assuming that each colony on the agar plate is the growth from a single bacteria-carrying particle, the contamination of the air being sampled is determined from the number of colonies counted. The airborne microorganisms may be reported in terms of the number per cubic foot of air sampled. The following formulas can be applied to convert colony counts to organisms per cubic foot of air sampled.1218
For solid agar impactor samplers: C / (R x P) = N where N = number of organisms collected per cubic foot of air sampled C = total plate count R = airflow rate in cubic feet per minute P = duration of sampling period in minutes For liquid impingers: (C x V) / (Q x P x R) = N where C = total number of colonies from all aliquots plated V = final volume in mL of collecting media Q = total number of mL plated P, R, and N are defined as above
# Ventilation Specifications for Health-Care Facilities
The 1. The ventilation rates in this table cover ventilation for comfort, as well as for asepsis and odor control in areas of acute care hospitals that directly affect patient care and are determined based on health-care facilities being predominantly "No Smoking" facilities. Where smoking may be allowed, ventilation rates will need adjustment. Areas where specific ventilation rates are not given in the table shall be ventilated in accordance Specialized patient care areas, including organ transplant units, burn units, specialty procedure rooms, etc., shall have additional ventilation provisions for air quality control as may be appropriate. OSHA standards and/or NIOSH criteria require special ventilation requirements for employee health and safety within health-care facilities.
2. Design of the ventilation system shall provide air movement which is generally from clean to less clean areas. If any form of variable air volume or load shedding system is used for energy conservation, it must not compromise the corridor-to-room pressure balancing relationships or the minimum air changes required by the table.
3. To satisfy exhaust needs, replacement air from the outside is necessary. Table B2 does not attempt to describe specific amounts of outside air to be supplied to individual spaces except for certain areas such as those listed. Distribution of the outside air, added to the system to balance required exhaust, shall be as required by good engineering practice. Minimum outside air quantities shall remain constant while the system is in operation.
4. Number of air changes may be reduced when the room is unoccupied if provisions are made to ensure that the number of air changes indicated is reestablished any time the space is being utilized. Adjustments shall include provisions so that the direction of air movement shall remain the same when the number of air changes is reduced. Areas not indicated as having continuous directional control may have ventilation systems shut down when space is unoccupied and ventilation is not otherwise needed, if the maximum infiltration or exfiltration permitted in Note 2 is not exceeded and if adjacent pressure balancing relationships are not compromised. Air quantity calculations must account for filter loading such that the indicated air change rates are provided up until the time of filter change-out.
5. Air change requirements indicated are minimum values. Higher values should be used when required to maintain indicated room conditions (temperature and jumidity), based on the cooling load of the space (lights, equipment, people, exterior walls and windows, etc.).
provided. Rooms with reversible airflow provisions for the purpose of switching between protective environment and airborne infection isolation functions are not acceptable.
18. The infectious disease isolation room described in these guidelines is to be used for isolating the airborne spread of infectious diseases, such as measles, varicella, or tuberculosis. The design of airborne infection isolation (AII) rooms should include the provision for normal patient care during periods not requiring isolation precautions. Supplemental recirculating devices may be used in the patient room to increase the equivalent room air exchanges; however, such recirculating devices do not provide the outside air requirements. Air may be recirculated within individual isolation rooms if HEPA filters are used. Rooms with reversible airflow provisions for the purpose of switching between protective environment and AII functions are not acceptable. 20. Food preparation centers shall have ventilation systems whose air supply mechanisms are interfaced appropriately with exhaust hood controls or relief vents so that exfiltration or infiltration to or from exit corridors does not compromise the exit corridor restrictions of NFPA 90A, the pressure requirements of NFPA 96, or the maximum defined in the table . The number of air changes may be reduced or varied to any extent required for odor control when the space is not in use. See Section 7.31.D1.p in the AIA guideline (reference 120).
# A ppendix I:
A7. Recirculating devices with HEPA filters may have potential uses in existing facilities as interim, supplemental environmental controls to meet requirements for the control of airborne infectious agents. Limitations in design must be recognized. The design of either portable or fixed systems should prevent stagnation and short circuiting of airflow. The supply and exhaust locations should direct clean air to areas where health-care workers are likely to work, across the infectious source, and then to the exhaust, so that the health care worker is not in position between the infectious source and the exhaust location. The design of such systems should also allow for easy access for scheduled preventative maintenance and cleaning.
A11. The verification of airflow direction can include a simple visual method such as smoke trail, ball-in-tube, or flutterstrip. These devices will require a minimum differential air pressure to indicate airflow direction. 1. The ventilation rates in this table cover ventilation for comfort, as well as for asepsis and odor control in areas of nursing facilities that directly affect resident care and are determined based on nursing facilities being predominantly "No Smoking" facilities. Where smoking may be allowed, ventilation rates will need adjustment. Areas where specific ventilation rates are not given in the table shall be ventilated in accordance with ASHRAE Standard 62, 2. Design of the ventilation system shall, insofar as possible, provide that air movement is from clean to less clean areas. However, continuous compliance may be impractical with full utilization of some forms of variable air volume and load shedding systems that may be used for energy conservation. Areas that do require positive and continuous control are noted with "Out" or "In" to indicate the required direction of air movement in relation to the space named. Rate of air movement may, of course, be varied as needed within the limits required for positive control. Where indication of air movement direction is enclosed in parentheses, continuous directional control is required only when the specialized equipment or device is in use or where room use may otherwise compromise the intent of movement from clean to less clean. Air movement for rooms with dashes and nonpatient areas may vary as necessary to satisfy the requirements of those spaces. Additional adjustments may be needed when space is unused or unoccupied and air systems are deenergized or reduced.
3. To satisfy exhaust needs, replacement air from outside is necessary. Table B.3 does not attempt to describe specific amounts of outside air to be supplied to individual spaces except for certain areas such as those listed. Distribution of the outside air, added to the system to balance required exhaust, shall be as required by good engineering practice.
4. Number of air changes may be reduced when the room is unoccupied if provisions are made to ensure that the number of air changes indicated is reestablished any time the space is being utilized. Adjustments shall include provisions so that the direction of air movement shall remain the same when the number of air changes is reduced. Areas not indicated as having continuous directional control may have ventilation systems shut down when space is unoccupied and ventilation is not otherwise needed.
5. Air from areas with contamination and/or odor problems shall be exhausted to the outside and not recirculated to other areas. Note that individual circumstances may require special consideration for air exhaust to outside. 6 7 8 9 1 0 All areas for patient care, treatment, and/or diagnosis, and those areas providing direct service or clean supplies such as sterile and clean processing, etc.
# Appendix C. Water 1. Biofilms
Microorganisms have a tendency to associate with and stick to surfaces. These adherent organisms can initiate and develop biofilms, which are comprised of cells embedded in a matrix of extracellularly produced polymers and associated abiotic particles.1438 It is inevitable that biofilms will form in most water systems. In the health-care facility environment, biofilms may be found in the potable water supply piping, hot water tanks, air conditioning cooling towers, or in sinks, sink traps, aerators, or shower heads. Biofilms, especially in water systems, are not present as a continuous slime or film, but are more often scanty and heterogeneous in nature.1439 Biofilms may form under stagnant as well as flowing conditions, so storage tanks, in addition to water system piping, may be vulnerable to the development of biofilm, especially if water temperatures are low enough to allow the growth of thermophilic bacteria (e.g., Legionella spp.). Favorable conditions for biofilm formation are present if these structures and equipment are not cleaned for extended periods of time.1440
Algae, protozoa, and fungi may be present in biofilms, but the predominant microorganisms of water system biofilms are gram-negative bacteria. Although most of these organisms will not normally pose a problem for healthy individuals, certain biofilm bacteria (e.g., Pseudomonas aeruginosa, Klebsiella spp., Pantoea agglomerans, and Enterobacter cloacae) all may be agents for opportunistic infections for immunocompromised individuals.1441, 1442 These biofilm organisms may easily contaminate indwelling medical devices or intravenous (IV) fluids, and they could be transferred on the hands of health-care workers.14411444 Biofilms may potentially provide an environment for the survival of pathogenic organisms, such as Legionella pneumophila and E. coli O157:H7. Although the association of biofilms and medical devices provides a plausible explanation for a variety of health-care-associated infections, it is not clear how the presence of biofilms in the water system may influence the rates of health-careassociated waterborne infection.
Organisms within biofilms behave quite differently than their planktonic (i.e., free floating) counterparts. Research has shown that biofilm-associated organisms are more resistant to antibiotics and disinfectants than are planktonic organisms, either because the cells are protected by the polymer matrix, or because they are physiologically different.1445-1450 Nevertheless, municipal water utilities attempt to maintain a chlorine residual in the distribution system to discourage microbiological growth.
Though chlorine in its various forms is a proven disinfectant, it has been shown to be less effective against biofilm bacteria.1448 Higher levels of chlorine for longer contact times are necessary to eliminate biofilms.
Routine sampling of health-care facility water systems for biofilms is not warranted. If an epidemiologic investigation points to the water supply system as a possible source of infection, then water sampling for biofilm organisms should be considered so that prevention and control strategies can be developed. An established biofilm is is difficult to remove totally in existing piping. Strategies to remediate biofilms in a water system would include flushing the system piping, hot water tank, dead legs, and those areas of the facility's water system subject to low or intermittent flow. The benefits of this treatment would include a) elimination of corrosion deposits and sludge from the bottom of hot water tanks, b) removal of biofilms from shower heads and sink aerators, and c) circulation of fresh water containing elevated chlorine residuals into the health-care facility water system.
The general strategy for evaluating water system biofilm depends on a comparision of the bacteriological quality of the incoming municipal water and that of water sampled from within facility's distribution system. Heterotrophic plate counts and coliform counts, both of which are routinely run by the municipal water utility, will at least provide in indication of the potential for biofilm formation. Heterotrophic plate count levels in potable water should be <500 CFU/mL. These levels may increase on occasion, but counts consistently >500 CFU/mL would indicate a general decrease in water quality.
A direct correlation between heterotrophic plate count and biofilm levels has been demonstrated.1450 Therefore, an increase in heterotrophic plate count would suggest a greater rate and extent of biofilm formation in a health-care facility water system. The water supplied to the facility should also contain <1 coliform bacteria/100 mL. Coliform bacteria are organisms whose presence in the distribution system could indicate fecal contamination. It has been shown that coliform bacteria can colonize biofilms within drinking water systems. Intermittant contamination of a water system with these organisms could lead to colonization of the system.
Water samples can be collected from throughout the health-care facility system, including both hot and cold water sources; samples should be cultured by standard methods.945 If heterotrophic plate counts in samples from the facility water system are higher than those from samples collected at the point of water entry to the building, it can be concluded that the facility water quality has diminished. If biofilms are detected in the facility water system and determined by an epidemiologic and environmental investigation to be a reservoir for health-care-associated pathogens, the municipal water supplier could be contacted with a request to provide higher chlorine residuals in the distribution system, or the health-care facility could consider installing a supplemental chlorination system.
Sample collection sites for biofilm in health-care facilities include a) hot water tanks; b) shower heads; and c) faucet aerators, especially in immunocompromised patient-care areas. Swabs should be placed into tubes containing phosphate buffered water, pH 7.2 or phosphate buffered saline, shipped to the laboratory under refrigeration and processed within 24 hrs. of collection. Samples are suspended by vortexing with sterile glass beads and plated onto a nonselective medium (e.g., Plate Count Agar or R2A medium) and selective media (e.g., media for Legionella spp. isolation) after serial dilution. If the plate counts are elevated above levels in the water (i.e. comparing the plate count per square centimeter of swabbed surface to the plate count per milliliter of water), then biofilm formation can be suspected.
In the case of an outbreak, it would be advisable to isolate organisms from these plates to determine whether the suspect organisms are present in the biofilm or water samples and compare them to the organisms isolated from patient specimens.
# Water and Dialysate Sampling Strategies in Dialysis
In order to detect the low, total viable heterotrophic plate counts outlined by the current AAMI standards for water and dialysate in dialysis settings, it is necessary to use standard quantitative culture techniques with appropriate sensitivity levels.792, 832, 833 The membrane filter technique is particularly suited for this application because it permits large volumes of water to be assayed.792, 834 Since the membrane filter technique may not be readily available in clinical laboratories, the spread plate assay can be used as an alternative.834 If the spread plate assay is used, however, the standard prohibits the use of a calibrated loop when applying sample to the plate.792 The prohibition is based on the low sensitivity of the calibrated loop. A standard calibrated loop transfers 0.001 mL of sample to the culture medium, so that the minimum sensitivity of the assay is 1,000 CFU/mL. This level of sensitivity is unacceptable when the maximum allowable limit for microorganisms is 200 CFU/mL. Therefore, when the spread plate method is used, a pipette must be used to place 0.1-0.5 mL of water on the culture medium.
The current AAMI standard specifically prohibits the use of nutrient-rich media (e.g., blood agar, and chocolate agar) in dialysis water and dialysate assays because these culture media are too rich for growth of the naturally occurring organisms found in water.792 Debate continues within AAMI, however, as to the most appropriate culture medium and incubation conditions to be used. The original clinical observations on which the microbiological requirements of this standard were based used Standard Methods Agar (SMA), a medium containing relatively few nutrients.666 The use of tryptic soy agar (TSA), a general purpose medium for isolating and cultivating microorganisms was recommended in later versions of the standard because it was thought to be more appropriate for culturing bicarbonatecontaining dialysate.788, 789, 835 Moreover, culturing systems based on TSA are readily available from commercial sources. Several studies, however, have shown that the use of nutrient-poor media, such as R2A, results in an increased recovery of bacteria from water.1451, 1452 The original standard also specified incubation for 48 hours at 95°F-98.6°F (35°C-37°C) before enumeration of bacterial colonies.
Extending the culturing time up to 168 hours, or 7 days and using incubation temperatures of 73.4°F-82.4°F (23°C-28°C) have also been shown to increase the recovery of bacteria.1451, 1452 Other investigators, however, have not found such clear cut differences between culturing techniques.835, 1453 After considerable discussion, the AAMI Committee has not reached a consensus regarding changes in the assay technique, and the use of TSA or its equivalent for 48 hours at 95°F-98.6°F (35°C-37°C) remains the recommended method. It should be recognized, however, that these culturing conditions may underestimate the bacterial burden in the water and fail to identify the presence of some organisms. Specifically, the recommended method may not detect the presence of various NTM that have been associated with several outbreaks of infection in dialysis units.31, 32 In these instances, however, the high numbers of mycobacteria in the water were related to the total heterotrophic plate counts, each of which was significantly greater than that allowable by the AAMI standard. Additionally, the recommended method will not detect fungi and yeast, which have been shown to contaminate water used for hemodialysis applications.1454 Biofilm on the surface of the pipes may hide viable bacterial colonies, even though no viable colonies are detected in the water using sensitive culturing techniques.1455 Many disinfection processes remove biofilm poorly, and a rapid increase in the level of bacteria in the water following disinfection may indicate significant biofilm formation. Therefore, although the results of microbiological surveillance obtained using the test methods outlined above may be useful in guiding disinfection schedules and in demonstrating compliance with AAMI standards, they should not be taken as an indication of the absolute microbiological purity of the water.792
Endotoxin can be tested by one of two types of assays a) a kinetic test method [e.g., colorimetric or turbidimetric] or b) a gel-clot assay. Endotoxin units are assayed by the Limulus Amebocyte Lysate (LAL) method. Because endotoxins differ in their activity on a mass basis, their activity is referred to a standard Escherichia coli endotoxin. The current standard (EC-6) is prepared from E. coli O113:H10. The relationship between mass of endotoxin and its activity varies with both the lot of LAL and the lot of control standard endotoxin used. Since standards for endotoxin were harmonized in 1983 with the introduction of EC-5, the relationship between mass and activity of endotoxin has been approximately 5-10 EU/ng. Studies to harmonize standards have led to the measurement of endotoxin units (EU) where 5 EU is equivalent to 1 ng E. coli O55:B5 endotoxin.1456
In summary, water used to prepare dialysate and to reprocess hemodialyzers should not contain a total microbial count >200 CFU/mL as determined by assay on TSA agar for 48 hrs. at 96.8°F (36°C), and <2 endotoxin units (EU) per mL. The dialysate at the end of a dialysis treatment should not contain >2,000 CFU/mL.31, 32, 668, 789, 792
# Water Sampling Strategies and Culture Techniques for Detecting Legionellae
Legionella spp. are ubiquitous and can be isolated from 20%-40% of freshwater environments, including man-made water systems.1457, 1458 In health-care facilities, where legionellae in potable water rarely result in disease among immunocompromised patients, courses of remedial action are unclear.
Scheduled microbiologic monitoring for legionellae remains controversial because the presence of legionellae is not necessarily evidence of a potential for causing disease.1459 CDC recommends aggressive disinfection measures for cleaning and maintaining devices known to transmit legionellae, but does not recommend regularly scheduled microbiologic assays for the bacteria.396 However, scheduled monitoring of potable water within a hospital might be considered in certain settings where persons are highly susceptible to illness and mortality from Legionella infection (e.g., hematopoietic stem cell transplantation units and solid organ transplant units).9 Also, after an outbreak of legionellosis, health officials agree monitoring is necessary to identify the source and to evaluate the efficacy of biocides or other prevention measures.
Examination of water samples is the most efficient microbiologic method for identifying sources of legionellae and is an integral part of an epidemiologic investigation into health-care-associated Legionnaires disease. Because of the diversity of plumbing and HVAC systems in health-care facilities, the number and types of sites to be tested must be determined before collection of water samples. One environmental sampling protocol that addresses sampling site selection in hospitals might serve as a prototype for sampling in other institutions.1209 Any water source that might be aerosolized should be considered a potential source for transmission of legionellae. The bacteria are rarely found in municipal water supplies and tend to colonize plumbing systems and point-of-use devices. To colonize, legionellae usually require a temperature range of 77°F-108°F (25°C-42.2°C) and are most commonly located in hot water systems.1460 Legionellae do not survive drying. Therefore, air-conditioning equipment condensate, which frequently evaporates, is not a likely source.1461
Water samples and swabs from point-of-use devices or system surfaces should be collected when sampling for legionellae (Box C.1).1437 Swabs of system surfaces allow sampling of biofilms, which frequently contain legionellae. When culturing faucet aerators and shower heads, swabs of surface areas should be collected first; water samples are collected after aerators or shower heads are removed from their pipes. Collection and culture techniques are outlined (Box C.2). Swabs can be streaked directly onto buffered charcoal yeast extract agar (BCYE) plates if the pates are available at the collection site.
If the swabs and water samples must be transported back to a laboratory for processing, immersing individual swabs in sample water minimizes drying during transit. Place swabs and water samples in insulated coolers to protect specimens from temperature extremes. incoming water main, water softener unit, holding tanks, cisterns, water heater tanks (at the inflows and outflows)
• P otable w ater outlets, especially th ose in o r near patient room s faucets or taps, showers
• C ooling tow ers and evaporative condensers makeup water (e.g., added to replace water lost because of evaporation, drift, or leakage), basin (i.e., area under the tower for collection of cooled water), sump (i.e., section of basin from which cooled water returns to heat source), heat sources (e.g., chillers)
• H um idfiers (e.g., nebullizers)
bubblers for oxygen, water used for respiratory therapy equipment
# Maintenance Procedures Used to Decrease Survival and Multiplications of L e g io n e lla spp. in Potable-Water Distribution Systems
Wherever allowable by state code, provide water at >124°F (>51°C) at all points in the heated water system, including the taps. This requires that water in calorifiers (e.g., water heaters) be maintained at >140°F (>60°C). In the United Kingdom, where maintenance of water temperatures at >122°F (>50°C) in hospitals has been mandated, installation of blending or mixing valves at or near taps to reduce the water temperature to <109.4°F (<63°C) has been recommended in certain settings to reduce the risk for scald injury to patients, visitors, and health care workers.726 However, Legionella spp. can multiply even in short segments of pipe containing water at this temperature. Increasing the flow rate from the hot-water-circulation system may help lessen the likelihood of water stagnation and cooling.711, 1465 Insulation of plumbing to ensure delivery of cold (<68°F [<20°C]) water to water heaters (and to coldwater outlets) may diminish the opportunity for bacterial multiplication.456 Both dead legs and capped spurs within the plumbing system provide areas of stagnation and cooling to <122°F (<50°C) regardless of the circulating water temperature; these segments may need to be removed to prevent colonization.704 Rubber fittings within plumbing systems have been associated with persistent colonization, and replacement of these fittings may be required for Legionella spp. eradication.1467
Continuous chlorination to maintain concentrations of free residual chlorine at 1-2 mg/L (1-2 ppm) at the tap is an alternative option for treatment. This requires the placement of flow-adjusted, continuous injectors of chlorine throughout the water distribution system. Adverse effects of continuous chlorination can include accelerated corrosion of plumbing (resulting in system leaks) and production of potentially carcinogenic trihalomethanes. However, when levels of free residual chlorine are below 3 mg/L (3 ppm), trihalomethane levels are kept below the maximum safety level recommended by the EPA 727, 1468, 1469
#
The recommendations in this guideline for Ebola Virus Disease has been superseded by CDC's Infection Prevention and Control Recommendations for Hospitalized Patients with Known or Suspected Ebola Virus Disease in U.S. Hospitals and by CDC's Interim Guidance for Environmental Infection Control in Hospitals for Ebola Virus issued on August 1,2014 Click here for current information on how Ebola virus is transmitted.
# Part IV. Appendices Appendix A. Glossary of Terms
Acceptable indoor air quality: air in which there are no known contaminants at harmful concentrations as determined by knowledgeble authorities and with which a substantial majority (>80%) of the people exposed do not express dissatisfaction. ACGIH: American Conference of Governmental Industrial Hygienists. Action level: the concentration of a contaminant at which steps should be taken to interrupt the trend toward higher, unacceptable levels. Aerosol: particles of respirable size generated by both humans and environmental sources and that have the capability of remaining viable and airborne for extended periods in the indoor environment. AIA: American Institute of Architects, a professional group responsible for publishing the Guidelines for Design and Construction o f Hospitals and Healthcare Facilities, a consensus document for design and construction of health-care facilities endorsed by the U.S. Department of Health and Human Services, health-care professionals, and professional organizations.
Air changes per hour (ACH): the ratio of the volume of air flowing through a space in a certain period of time (the airflow rate) to the volume of that space (the room volume). This ratio is expressed as the number of air changes per hour (ACH).
Air mixing: the degree to which air supplied to a room mixes with the air already in the room, usually expressed as a mixing factor. This factor varies from 1 (for perfect mixing) to 10 (for poor mixing). It is used as a multiplier to determine the actual airflow required (i.e., the recommended ACH multiplied by the mixing factor equals the actual ACH required). Airborne transmission: a means of spreading infection when airborne droplet nuclei (small particle residue of evaporated droplets <5 pm in size containing microorganisms that remain suspended in air for long periods of time) are inhaled by the susceptible host. Air-cleaning system: a device or combination of devices applied to reduce the concentration of airborne contaminants (e.g., microorganisms, dusts, fumes, aerosols, other particulate matter, and gases).
Air conditioning: the process of treating air to meet the requirements of a conditioned space by controlling its temperature, humidity, cleanliness, and distribution. Allogeneic: non-twin, non-self. The term refers to transplanted tissue from a donor closely matched to a recipient but not related to that person. Ambient air: the air surrounding an object. Anemometer: a flow meter which measures the wind force and velocity of air. An anemometer is often used as a means of determining the volume of air being drawn into an air sampler. Anteroom: a small room leading from a corridor into an isolation room. This room can act as an airlock, preventing the escape of contaminants from the isolation room into the corridor. ASHE: American Society for Healthcare Engineering, an association affiliated with the American Hospital Association. ASHRAE: American Society of Heating, Refrigerating, and Air-Conditioning Engineers Inc. Autologous: self. The term refers to transplanted tissue whose source is the same as the recipient, or an identical twin. Automated cycler: a machine used during peritoneal dialysis which pumps fluid into and out of the patient while he/she sleeps. Biochemical oxygen demand (BOD): a measure of the amount of oxygen removed from aquatic environments by aerobic microorganisms for their metabolic requirements. Measurement of BOD is used to determine the level of organic pollution of a stream or lake. The greater the BOD, the greater
# Procedure for Cleaning Cooling Towers and Related Equipment
I. Perform these steps prior to chemical disinfection and mechanical cleaning.
A. Provide protective equipment to workers who perform the disinfection, to prevent their exposure to chemicals used for disinfection and aerosolized water containing Legionella spp. Protective equipment may include full-length protective clothing, boots, gloves, goggles, and a full-or half-face mask that combines a HEPA filter and chemical cartridges to protect against airborne chlorine levels of up to 10 mg/L. B. Shut off cooling tower.
# Appendix D. Insects and Microorganisms
# Appendix E. Information Resources
The following sources of information may be helpful to the reader. Some of these are available at no charge, while others are available for purchase from the publisher.
Air andWater
# Appendix F. Areas of Future Research
# Air
• Standardize the methodology and interpretation of microbiologic air sampling (e.g., determine action levels or minimum infectious dose for aspergillosis, and evaluate the significance of airborne bacteria and fungi in the surgical field and the impact on postoperative SSI). • Develop new molecular typing methods to better define the epidemiology of health-care-associated outbreaks of aspergillosis and to associate isolates recovered from both clinical and environmental sources. • Develop new methods for the diagnosis of aspergillosis that can lead reliably to early recognition of infection. • Assess the value of laminar flow technology for surgeries other than for joint replacement surgery.
• Determine if particulate sampling can be routinely performed in lieu of microbiologic sampling for purposes such as determining air quality of clean environments (e.g., operating rooms, HSCT units).
# Water
• Evaluate new methods of water treatment, both in the facility and at the water utility (e.g., ozone, chlorine dioxide, copper/silver/monochloramine) and perform cost-benefit analyses of treatment in preventing health-care-associated legionellosis. • Evaluate the role of biofilms in overall water quality and determine the impact of water treatments for the control of biofilm in distribution systems. • Determine if the use of ultrapure fluids in dialysis is feasible and warranted, and determine the action level for the final bath. • Develop quality assurance protocols and validated methods for sampling filtered rinse water used with AERs and determine acceptable microbiologic quality of AER rinse water.
# Environmental Services
• Evaluate the innate resistance of microorganisms to the action of chemical germicides, and determine what, if any, linkage there may be between antibiotic resistance and resistance to disinfectants.
# Laundry and Bedding
• Evaluate the microbial inactivation capabilities of new laundry detergents, bleach substitutes, other laundry additives, and new laundry technologies.
# Animals in Health-Care Facilities
• Conduct surveillance to monitor incidence of infections among patients in facilities that use animal programs, and conduct investigations to determine new infection control strategies to prevent these infections. • Evaluate the epidemiologic impact of performing procedures on animals (e.g., surgery or imaging) in human health-care facilities.
# Regulated Medical Waste
• Determine the efficiency of current medical waste treatment technologies to inactivate emerging pathogens that may be present in medical waste (e.g., SARS-coV). • Explore options to enable health-care facilities to reinstate the capacity to inactivate microbiological cultures and stocks on-site. | None | None |
f45b5e0d58c0385603653d055aad6343ea015fe8 | cdc | None | Preventing Recreational Water Illnesses (RWIs) is a multifaceted issue that requires participation from aquatics facility designers as well as pool staff, swimmers, and health departments. Pool designers can ensure that operators are starting with the most current technology and design features. Although designers alone cannot completely prevent these complex problems, they play a key role in assuring that facilities have an RWI prevention foundation in place on opening day. By considering the following suggestions, based on contributing factors found during RWI outbreak investigations, designers can lead the way to a "Healthy Swimming" facility.#
- Install supplementary, optimally-designed, in-line disinfection (e.g., ultraviolet light, ozone) that can inactivate Cryptosporidium and potentially improve water quality.
- Install automatic chemical feeders to improve the uniformity of chemical addition.
- Install filters that are sized and optimized for particle and microbe removal.
- Avoid co-filtered pools. In particular, wading pools for young children should have dedicated filters to prevent cross-contamination of other general use pools.
- Adopt "kiddie" pool turnover rates that decrease the length of time that swimmers are exposed to germs and include safety considerations for avoiding suction injuries.
- Ensure adequate ventilation for indoor facilities to decrease exposure to chloramines and other pool water by-products.
- Provide adequate numbers of easily located, close, and safe restrooms, diaper changing areas, and shower facilities to promote good swimmer hygiene.
- Install diaper changing and hand washing facilities near children's pools to promote good hygiene and diaper changing practices among parents.
Healthy Swimming | Preventing Recreational Water Illnesses (RWIs) is a multifaceted issue that requires participation from aquatics facility designers as well as pool staff, swimmers, and health departments. Pool designers can ensure that operators are starting with the most current technology and design features. Although designers alone cannot completely prevent these complex problems, they play a key role in assuring that facilities have an RWI prevention foundation in place on opening day. By considering the following suggestions, based on contributing factors found during RWI outbreak investigations, designers can lead the way to a "Healthy Swimming" facility.#
• Install supplementary, optimally-designed, in-line disinfection (e.g., ultraviolet light, ozone) that can inactivate Cryptosporidium and potentially improve water quality.
• Install automatic chemical feeders to improve the uniformity of chemical addition.
• Install filters that are sized and optimized for particle and microbe removal.
• Avoid co-filtered pools. In particular, wading pools for young children should have dedicated filters to prevent cross-contamination of other general use pools.
• Adopt "kiddie" pool turnover rates that decrease the length of time that swimmers are exposed to germs and include safety considerations for avoiding suction injuries.
• Ensure adequate ventilation for indoor facilities to decrease exposure to chloramines and other pool water by-products.
• Provide adequate numbers of easily located, close, and safe restrooms, diaper changing areas, and shower facilities to promote good swimmer hygiene.
• Install diaper changing and hand washing facilities near children's pools to promote good hygiene and diaper changing practices among parents.
Healthy Swimming | None | None |
2c9464d282046ba0c25ab57109068aa88f660253 | cdc | None | ACIP is chartered as a federal advisory committee to provide expert external advice and guidance to the Director of the Centers for Disease Control and Prevention (CDC) on use of vaccines and related agents for the control of vaccine-preventable diseases in the civilian population of the United States. Recommendations for routine use of vaccines in children and adolescents are harmonized to the greatest extent possible with recommendations made by the American Academy of Pediatrics (AAP), the American Academy of Family Physicians (AAFP), and the American College of Obstetricians and Gynecologists. Recommendations for routine use of vaccines in adults are reviewed and approved by the American College of Physicians (ACP), AAFP, the American College of Obstetricians and Gynecologists, and the American College of Nurse-Midwives. ACIP recommendations adopted by the CDC Director become agency guidelines on the date published in the Morbidity and Mortality Weekly Report (MMWR).CDC, our planners, and our content experts disclose that they have no financial interests or other relationships with the manufacturers of commercial products, suppliers of commercial services, or commercial supporters. Presentations will not include any discussion of the unlabeled use of a product or a product under investigational use. CDC does not accept Recommendations and Reports# Introduction
Influenza viruses typically circulate widely in the United States annually from the late fall through early spring. Although most persons who become infected with influenza viruses will recover without sequelae, influenza can cause serious illness and death, particularly among persons aged ≥65 years and <2 years and those with medical conditions that confer high risk for complications from influenza (1)(2)(3)(4). During 30 seasons from the 1976-77 season through the 2005-06 season, estimated influenza-associated deaths ranged from 3,000 to 49,000 annually (4).
Annual influenza vaccination is the primary means of preventing influenza and its complications. There are many types of influenza vaccines, and the naming conventions have evolved over time (Box). Routine annual influenza vaccination for all persons aged ≥6 months who do not have contraindications has been recommended by the CDC and CDC's Advisory Committee on Immunization Practices (ACIP) since 2010 (5). This report provides updated recommendations and guidance for vaccination providers regarding the use of influenza vaccines for the 2013-14 season.
# Methods
ACIP provides annual recommendations for the prevention and control of influenza. The ACIP Influenza Work Group- meets by teleconference every 2-4 weeks throughout the year. Work Group membership includes several voting members of ACIP and representatives of ACIP Liaison Organizations. Discussions include topics such as influenza surveillance, vaccine effectiveness and safety, vaccine coverage, program feasibility, cost-effectiveness, and vaccine supply. Presentations are requested from invited experts, and published and unpublished data are discussed. For newly licensed influenza vaccines, discussion pertaining to new recommendations in this report included presentations of clinical data. For minor modifications to the recommendations for vaccination of persons with egg allergy, discussion included a review of influenza vaccine safety surveillance data from the Vaccine Adverse Event Reporting System (VAERS) for the 2012-13 season (see Surveillance for Anaphylaxis Following Influenza Vaccination).
Information presented in this report reflects recommendations presented during public meetings of the ACIP and approved on February 21, 2013, and on June 20, 2013. Meeting minutes and information on ACIP membership and conflicts of interest are available on the ACIP website (/ vaccines/acip/meetings/meetings-info.html). Modifications were made to the ACIP statement during subsequent review at CDC to update and clarify wording in the document. Further updates, if needed, will be posted at CDC's influenza website ().
# Primary Changes and Updates in the Recommendations
Routine annual influenza vaccination of all persons aged ≥6 months continues to be recommended. No preferential recommendation is made for one influenza vaccine product over another for persons for whom more than one product is otherwise appropriate. Updated information and guidance in this document include the following:
- 2013-14 U.S. trivalent influenza vaccines will contain an A/California/7/2009 (H1N1)-like virus, an H3N2 virus antigenically like the cell-propagated prototype virus
# BOX. Naming conventions for influenza vaccines
- The former abbreviation TIV (Trivalent Inactivated Influenza Vaccine, previously used for inactivated influenza vaccines) has been replaced with the new abbreviation IIV (Inactivated Influenza Vaccine). For the 2013-14 season, IIVs as a class will include: -egg-based and cell culture-based trivalent inactivated influenza vaccines (IIV3), and -egg-based quadrivalent inactivated influenza vaccine (IIV4). - RIV refers to recombinant hemagglutinin influenza vaccine, available as a trivalent formulation (RIV3) for the 2013-14 season. - LAIV refers to live-attenuated influenza vaccine, available as a quadrivalent formulation (LAIV4) for the 2013-14 season. - LAIV, IIV, and RIV denote vaccine categories; numeric suffix specifies the number of antigens in the vaccine. - When necessary to refer specifically to cell culturebased vaccine, the prefix "cc" is used (e.g., "ccIIV3").
Diagnostics, Cambridge, Massachusetts]) is indicated for persons aged ≥18 years. -A recombinant hemagglutinin (HA) vaccine (RIV3;
FluBlok ) is indicated for persons aged 18 through 49 years. - RIV3, an egg-free vaccine, is now an option for vaccination of persons aged 18 through 49 years with egg allergy of any severity. - For persons with egg allergy who have no known history of egg exposure but for whom results suggestive of egg allergy have been obtained on previous allergy testing, consultation with a physician with expertise in the management of allergic conditions is recommended before vaccination.
# Background and Epidemiology
# Biology of Influenza
Influenza A and B are the two types of influenza viruses that cause epidemic human disease. Influenza A viruses are categorized into subtypes based upon characterization of two surface antigens: hemagglutinin (HA) and neuraminidase (NA). Since 1977, influenza A(H1N1) viruses, influenza A(H3N2) viruses, and influenza B viruses have co-circulated globally. Influenza A virus subtypes and B viruses are further separated into groups on the basis of antigenic similarities. New influenza virus variants emerge via frequent antigenic change (i.e., antigenic drift), resulting from point mutations and recombination events that occur during viral replication (6). Immunity to surface antigens, HA and NA, reduces likelihood of infection (7,8). Antibody against one influenza virus type or subtype confers limited or no protection against another type or subtype. Moreover, antibody to one antigenic type or subtype of influenza virus might not confer immunity to a new antigenic variant of the same type or subtype (9). Frequent emergence of antigenic variants through antigenic drift is the virologic basis for seasonal epidemics, and necessitates consideration for adjustment of vaccine viruses each season.
Larger genetic changes, or antigenic shifts, occur among influenza A viruses, less frequently than antigenic drift events (6). The new or substantially different influenza A virus subtypes resulting from antigenic shifts have the potential to cause pandemics when they cause human illness, because they are efficiently transmitted from human to human in a sustained manner, and there is little or no pre-existing immunity among humans (6). In April 2009, human infections with a novel influenza A(H1N1) virus caused a worldwide pandemic. While not a new influenza A virus subtype, most humans had limited or no pre-existing antibody to key HA epitopes, and thus widespread transmission occurred. This virus is antigenically distinct from human influenza A(H1N1) viruses in circulation from 1977 through spring 2009. The HA gene is most closely related to that of contemporary influenza A viruses circulating among pigs during several preceding decades. This HA gene is believed to have evolved from the avian-origin 1918 pandemic influenza A(H1N1) virus, which is thought to have entered human and swine populations at about the same time (10,11).
Influenza B viruses are separated into two distinct genetic lineages (Yamagata and Victoria), but are not categorized into subtypes. Influenza B viruses undergo antigenic drift less rapidly than influenza A viruses (12). Influenza B viruses from both lineages have co-circulated in most recent influenza seasons (13,14). The trivalent influenza vaccines available in recent seasons have contained one influenza B virus, representing only one lineage. The proportion of circulating influenza B viruses that are of the lineage represented in the vaccine has varied. During the 10 seasons from 2001-02 through 2010-11, the predominant circulating influenza B virus lineage was represented in the trivalent vaccine in only five seasons (15).
# Health-Care Use, Hospitalizations, and Deaths Attributed to Influenza
In the United States, annual epidemics of influenza typically occur during the fall or winter months. Studies that report rates of clinical outcomes without laboratory confirmation of influenza (e.g., respiratory illness requiring hospitalization during influenza season) can be difficult to interpret because of coincident circulation of other respiratory pathogens (e.g., respiratory syncytial virus) (16)(17)(18). However, increases in health-care provider visits for acute febrile respiratory illness occur annually, coinciding with periods of increased influenza activity, making influenza-like illness surveillance systems valuable in understanding the seasonal and geographic occurrence of influenza each year (19).
In typical winter influenza seasons, increases in deaths and hospitalizations are observed during periods when influenza viruses are circulating. Excess deaths and hospitalizations occurring during influenza season have been estimated for decades. Although not all excess events occurring during periods when influenza viruses are circulating can be attributed to influenza, these estimates are useful for following season-toseason trends in influenza-associated outcomes. Estimates that include only outcomes attributed to pneumonia and influenza likely underestimate the burden of severe illnesses that are at least partly attributable to influenza because this category excludes deaths caused by exacerbations of underlying cardiac and pulmonary conditions that are associated with influenza virus infection (20)(21)(22). Thus, use of a broader category of respiratory and circulatory excess events are at times preferred for influenza burden estimates. During seasonal influenza epidemics from 1979-80 through 2000-01, the estimated annual overall number of influenza-associated hospitalizations in the United States ranged from approximately 55,000 to 431,000 per annual epidemic (mean: 226,000) (21). Between the 1976-77 season and 2006-07 season, estimated annual deaths attributable to influenza ranged from 3,000 to 49,000 each season (4).
Influenza viruses cause illness among persons of all ages (1)(2)(3)(23)(24)(25). Infection rates are highest among children, but complications, hospitalizations, and deaths from seasonal influenza are typically greatest among persons aged ≥65 years, children aged <5 years and particularly those aged <2 years, and persons of any age who have medical conditions that confer increased risk for complications from influenza (1,2,(25)(26)(27)(28)(29). Estimated rates of influenza-associated deaths vary substantially by age group. During 1990-1999, estimated average rates of influenza-associated pulmonary and circulatory deaths per 100,000 persons were 0.4-0.6 among persons aged 0 through 49 years, 7.5 among persons aged 50 through 64 years, and 98.3 among persons aged ≥65 years (20).
Children: Among children aged <5 years, influenza is a common cause of outpatient medical visits. During the 2002-03 and 2003-04 seasons, the percentage of visits among children aged <5 years with acute respiratory illness or fever caused by laboratory-confirmed influenza ranged from 10%-19% of medical office visits and 6%-29% of emergency department (ED) visits. From these data, the rate of clinic visits for influenza was estimated to be 50-95 visits per 1,000 children aged <5 years, and the rate of ED visits was 6-27 visits per 1,000 children aged <5 years (3). In a retrospective cohort study of children aged <15 years covering 19 consecutive seasons, an annual average of 6-15 additional outpatient visits and 3-9 additional antibiotic courses per 100 children were estimated to be attributable to influenza (29). During 1993During -2004 in the Boston area, the rate of ED visits for respiratory illness attributed to influenza based on viral surveillance data among children aged 6 months through 7 years during the winter respiratory illness season ranged from 22.1 per 1,000 children aged 6-23 months to 5.4 per 1,000 children aged 5 through 7 years (30).
Estimated rates of influenza-associated hospitalization are substantially higher among infants and younger children than among older children and are similar to rates for other groups considered at higher risk for influenza-related complications (31)(32)(33)(34)(35)(36), including persons aged ≥65 years. During 1993-2008, the estimated rate of influenza-associated hospitalizations was 91.5 per 100,000 for among children aged <1 year and 21.9 per 100,000 for children aged 1 through 4 years (37). Population-based studies that measured hospitalization rates for laboratory-confirmed influenza in young children have documented hospitalization rates that are similar to or higher than rates derived from studies that analyzed hospital discharge data (3,35,(38)(39)(40). Annual hospitalization rates for laboratoryconfirmed influenza decrease with increasing age, ranging from 240-720 hospitalizations per 100,000 children aged <6 months to approximately 20 hospitalizations per 100,000 children aged 2 through 5 years (3). Hospitalization rates for children aged <5 years with high-risk medical conditions are higher, with estimates of 250-500 hospitalizations per 100,000 children in some studies (27,41,42).
In the United States, death associated with laboratoryconfirmed influenza virus infection among children aged <18 years has been a nationally reportable condition since 2004 (43). Since reporting began, the annual number of influenza-associated pediatric deaths during regular influenza seasons has ranged from 34 deaths during the 2011-12 season to 122 deaths during the 2010-11 season (43,44). However, between April 15, 2009 and October 2, 2010 (the period of the 2009 H1N1 influenza pandemic), approximately 300 deaths attributed to laboratoryconfirmed 2009 H1N1 influenza occurred among children aged <18 years (44), the majority of whom had one or more underlying medical conditions previously associated with conferring a greater risk for influenza complications (45).
Adults: Hospitalization rates during typical influenza seasons are highest for adults aged ≥65 years. One retrospective analysis of data from managed-care organizations collected during 1996-2000 estimated that the risk during influenza season among persons aged ≥65 years with high-risk underlying medical conditions was approximately 560 influenzaassociated hospitalizations per 100,000 persons compared with approximately 190 per 100,000 among lower risk persons in this age group. Persons aged 50 through 64 years who have underlying medical conditions also were at substantially increased risk for hospitalization during influenza season compared with healthy adults aged 50 through 64 years (26).
Deaths associated with influenza are also most frequent among older adults. From the 1976-77 season through the 2006-07 season, an estimated yearly average of 21,098 influenza-related deaths occurred among adults aged ≥65 years, comprising approximately 90% of estimated annual average deaths across all age groups. In comparison, the average annual mortality was estimated to be 124 deaths among persons aged <19 years and 2,385 deaths among persons aged 19 through 64 years (4).
Among healthy younger adults, illness caused by seasonal influenza is typically less severe and results less frequently in hospitalization, as compared with children aged <5 years, adults aged ≥65 years, pregnant women, or persons with chronic medical conditions. However, influenza is an important cause of outpatient medical visits and worker absenteeism among healthy adults aged 19 through 49 years. In one economic modeling analysis, the average annual burden of seasonal influenza among adults aged 18 through 49 years without medical conditions that confer a higher risk for influenza complications was estimated to include approximately 5 million illnesses, 2.4 million outpatient visits, 32,000 hospitalizations, and 680 deaths (46). Studies of worker vaccination programs have reported lower rates of influenza like illness (ILI) (47,48), lost work time (47)(48)(49)(50), and healthcare visits (48,49) in association with vaccination.
During the 2009 H1N1 pandemic, adults aged <65 years appeared to be at higher risk for influenza-related complications (51,52) compared with typical influenza seasons. In addition, obesity (body-mass index ≥30) and particularly morbid obesity (BMI≥40) appeared to be risk factors for hospitalization and death in some studies (51)(52)(53)(54)(55). Other epidemiologic features of the 2009 H1N1 pandemic underscored racial and ethnic disparities in the risk for influenza-related complications among adults, including higher rates of hospitalization for blacks and higher rates of deaths among American Indians/Alaska Natives and indigenous populations in other countries (56)(57)(58)(59)(60)(61). These disparities might be attributable in part to the higher prevalence of underlying medical conditions or disparities in medical care among these racial/ethnic groups (61,62).
The duration of influenza symptoms might be prolonged and the severity of influenza illness increased among persons with human immunodeficiency virus (HIV) infection (63)(64)(65)(66). A retrospective study of women aged 15 through 64 years enrolled in Tennessee's Medicaid program determined that the attributable risk for cardiopulmonary hospitalizations and deaths among women with HIV infection was higher during influenza seasons than it was either before or after periods when influenza viruses were circulating. The risk for these events was higher for HIV-infected women (influenza attributable risk 152 per 10,000) than it was for women with other underlying medical conditions evaluated (including an influenza-attributable risk of 35 per 10,000 for chronic renal disease, 27 per 10,000 for chronic heart disease, and 25 per 10,000 for chronic lung disease) (67). Another study estimated that the excess death rate attributable to influenza was 94-146 deaths per 100,000 persons with acquired immune deficiency syndrome (AIDS) compared with 0.9-1.0 deaths per 100,000 persons aged 25 through 54 years and 64-70 deaths per 100,000 persons in the general population aged ≥65 years (68).
Increased severity of influenza among pregnant women was reported during the pandemics of 1918-1919, 1957-1958, and 2009-2010 (69-74). Severe infections among postpartum (delivered within previous 2 weeks) women also were observed in the 2009-10 pandemic (69,73). In a case series conducted during the 2009 H1N1 pandemic, 56 deaths were reported among 280 pregnant women admitted to intensive care units. Among the deaths, 36 (64%) occurred in the third trimester. Pregnant women who were treated with antivirals more than 4 days after symptom onset were more likely to be admitted to an intensive care unit (57% versus 9%; relative risk = 6.0; 95% confidence interval 3.5-10.6) than those treated within 2 days after symptom onset (75).
Case reports and some observational studies suggest that pregnancy also increases the risk for seasonal influenza complications for the mother (76)(77)(78). Most of these studies have measured changes in excess hospitalizations or outpatient visits for respiratory illness during influenza season rather than laboratory-confirmed influenza. A retrospective cohort study of approximately 134,000 pregnant women conducted in Nova Scotia during 1990-2002 compared medical record data for pregnant women to data from the same women during the year before pregnancy. Among 134,188 pregnant women, 510 (0.4%) were hospitalized, and 33,775 (25%) visited a clinician during pregnancy for a respiratory illness (78).
With regard to pregnancy outcomes, one cohort study noted that pregnant women with respiratory hospitalizations during the influenza season did not have an increase in adverse perinatal outcomes or delivery complications compared with pregnant controls without an influenza hospitalization (79); another study indicated an increase in delivery complications, including fetal distress, preterm labor, and cesarean delivery (80). However, infants born to women with laboratory-confirmed influenza during pregnancy do not have higher rates of low birthweight, congenital abnormalities, or lower Apgar scores compared with infants born to uninfected women (81,82).
# Influenza Vaccine Effectiveness Evaluating Influenza Vaccine Efficacy and Effectiveness Studies
Estimates of efficacy (i.e., prevention of illness among vaccinated persons enrolled in controlled clinical trials) and vaccine effectiveness (i.e., prevention of illness in vaccinated populations) of influenza vaccines depend on many factors, including the age and immunocompetence of the vaccine recipient, the degree of similarity between the viruses in the vaccine and those in circulation, study design, and the outcome being measured. Studies of influenza vaccine efficacy and effectiveness have used a variety of outcome measures, including the prevention of medically attended acute respiratory illness (MAARI), prevention of laboratory-confirmed influenza illness, prevention of influenza or pneumonia-associated hospitalizations or deaths, or prevention of seroconversion to circulating influenza virus strains. Efficacy or effectiveness for more specific outcomes such as laboratory-confirmed influenza typically will be higher than for less specific outcomes such as MAARI because the causes of MAARI include infections with other pathogens that influenza vaccination would not be expected to prevent (83). Observational studies that compare less-specific outcomes among vaccinated populations to those among unvaccinated populations might be more subject to biases than studies using laboratory outcomes. For example, an observational study that finds that influenza vaccination reduces overall mortality among elderly persons might be biased if healthier persons in the study are more likely to be vaccinated, and thus less likely to die for any reason (84,85). For studies assessing laboratory-confirmed outcomes, estimates of vaccine efficacy may also be affected be the sensitivity of the diagnostic tests used. A 2012 simulation study found that for each percentage point decrease in diagnostic test specificity for influenza virus infection, vaccine effectiveness would be underestimated by approximately 4% (86). Randomized controlled trials that measure laboratory-confirmed influenza virus infections as the outcome are the most persuasive evidence of vaccine efficacy, but such data are not available for all populations. Such trials might be difficult to conduct among groups recommended to receive vaccine annually.
# Immune Response Following Vaccination
Humoral and cell-mediated responses to influenza vaccination have been studied among children and adults. Serum antibodies (7,87) are considered to be correlates of vaccine-induced protection. Increased levels of antibody induced by vaccination decrease the risk for illness caused by strains that are antigenically similar to those strains of the same type or subtype included in the vaccine (8,(88)(89)(90). Most healthy children and adults have high titers of strainspecific antibody after vaccination (89,91). However, although immune correlates such as achievement of certain antibody titers after vaccination correlate well with immunity on a population level, reaching certain antibody threshold (typically defined as a hemagglutination inhibition antibody or HAI titer of 32 or 40) might not predict protection from infection on the individual level.
While LAIV induces lower levels of serum antibodies compared with IIV, LAIV more effectively induces cellular immune responses than IIV. The magnitude of this effect differs among adults and children. One study of children aged 6 months through 9 years and adults aged 22 through 49 years noted a significant increase in influenza A-specific interferon ϒ-producing CD4+ and CD8+ T-cells among children following LAIV but not following IIV. No significant increase in these parameters was noted among adults following either vaccine (92).
Antibody elicited by vaccination is generally strain-specific, such that antibody against one influenza virus type or subtype confers limited or no protection against another type or subtype, nor does it confer protection against antigenic variants of the same virus that arise by antigenic drift. Cellular immune responses might arise from more conserved viral epitopes and thus potentially provide broader heterosubtypic immunity. Administration of 2007-08 seasonal vaccine to adults boosted T-cell responses to both seasonal and pandemic 2009(H1N1) HA (93); this effect was significantly greater for LAIV. Among children aged 6 through 35 months, LAIV (but not IIV) induced T-cell responses to highly conserved viral peptides (94).
# Duration of Immunity
The composition of influenza vaccines is changed in most seasons, with one or more vaccine strains replaced annually to provide protection against viruses that are anticipated to circulate. Evidence from some clinical trials indicates that that protection against viruses that are antigenically similar to those contained in the vaccine extends at least for 6-8 months, particularly in nonelderly populations. In some situations, duration of immunity might be longer, and such effects can be detected if circulating influenza virus strains remain antigenically similar for multiple seasons. For example, 3 years after vaccination with the A/Hong Kong/68 vaccine (i.e., the 1968 pandemic vaccine), effectiveness was 67% for prevention of influenza caused by the A/Hong Kong/68 virus (95). In randomized trials conducted among healthy college students, immunization with IIV provided 92% and 100% efficacy against influenza H3N2 and H1N1 illnesses, respectively, during the first year after vaccination, and a 68% reduction against H1N1 illness during the second year after vaccination (when the predominant circulating virus was H1N1) without revaccination (96). In a similar study of young adults conducted in 1986-1987, IIV reduced influenza A(H1N1) illness by 75% in the first year after vaccination, reduced H3N2 illness by 45% in the second year, and reduced H1N1 illness by 61% during the third year after vaccination (96). Serum HAI influenza antibodies and nasal IgA elicited by vaccination remain detectable in children vaccinated with LAIV for >1 year after vaccination (97). In one community-based nonrandomized open-label trial, continued protection from MAARI during the 2000-01 influenza season was demonstrated in children who received only a single dose of LAIV during the previous 1999-00 season (98). A review of four trials (three randomized blinded and one open-label) of LAIV conducted among young children aged 6 months through 18 years reported that efficacy against A(H1N1) and A(H3N2) was similar at 9-12 months postvaccination to efficacy at 1-<5 months postvaccination; for B strains efficacy was still comparable at 5-7 months postvaccination. Two randomized trials and one open label study reported residual efficacy through a second season without revaccination, albeit at lower levels than observed in the first season (98)(99)(100)(101)(102).
Adults aged ≥65 years typically have diminished immune responses to influenza vaccination compared with healthy younger adults (103,104). One review of the published literature concluded that no clear evidence existed that vaccine-induced antibody declined more rapidly in the elderly (105). A case-control study conducted in Navarre, Spain during the 2011-12 season revealed a decline in vaccine effectiveness from 61% (95% CI = 5-84) in the first 100 days postvaccination, to 42% (95% CI = -39-75) for days 110-119 days postvaccination, to -35% (95% CI = -211-41) thereafter. This decline primarily affected persons aged ≥65 years, among whom effectiveness declined from 85% (95% CI = -8-98) to 24% (95% CI = -224-82) to -208 (95% CI = -1,563-43) over the same time intervals. However, most viruses isolated among infected vaccinees did not match the vaccine strains (106). In addition, the wide CIs surrounding the point estimates indicate that larger studies are needed to further characterize the magnitude of possible declines in vaccine effectiveness through the season. Limited available data suggest that administration of additional vaccine doses during the same season does not increase the antibody response among elderly vaccinees (107).
# Immunogenicity, Efficacy, and Effectiveness of IIV
Inactivated vaccines, which are administered by intramuscular or intradermal injection, contain nonreplicating virus. Immunogenicity, effectiveness, and efficacy have been evaluated in children and adults, although fewer data from randomized studies are available for some age groups (e.g., persons aged ≥65 years).
# Children
Children aged ≥6 months typically develop protective levels of antibodies against specific influenza virus strains after receiving the recommended number of doses of seasonal inactivated influenza vaccine (87,91,(108)(109)(110)(111). Immunogenicity studies using the influenza A(H1N1) 2009 monovalent vaccine indicated that 80%-95% of vaccinated children developed protective antibody levels to the 2009 H1N1 influenza virus after 2 doses (112,113); response after 1 dose was 50% for children aged 6 through 35 months and 75% for those aged 3 through 9 years (114). Studies involving seasonal inactivated influenza vaccine among young children have demonstrated that 2 vaccine doses provide better protection than 1 dose during the first season a child is vaccinated. In a study of children aged 5 through 8 years who received trivalent inactivated vaccine (TIV) for the first time, the proportion of children with protective antibody responses was significantly higher after 2 doses than after 1 dose and higher after 2 doses than after 1 dose of TIV for each antigen (p = 0.001 for influenza A; p = 0.01 for influenza A; and p = 0 0.001 for influenza B) (115). Vaccine effectiveness is lower among children aged <5 years who have never received influenza vaccine previously or who received only 1 dose in their first year of vaccination than it is among children who received 2 doses in their first year of being vaccinated. Two retrospective studies of children who had received only 1 dose of IIV in their first year of being vaccinated determined that no decrease was observed in ILI-related office visits compared with unvaccinated children (116,117). Similar results were reported in a case-control study of approximately 2,500 children aged 6 through 59 months in which laboratory-confirmed influenza was the outcome measured (118). The results of these studies support the recommendation that all children aged 6 months through 8 years who are being vaccinated for the first time should receive 2 vaccine doses separated by at least 4 weeks.
Some studies suggest that antibody responses among children at higher risk for influenza-related complications (i.e., children with chronic medical conditions) are lower than those reported typically among healthy children (119,120). However, another study found that antibody responses among children with asthma are similar to those of healthy children and are not substantially altered during asthma exacerbations requiring short-term prednisone treatment (121).
Estimates of the efficacy or effectiveness of inactivated vaccine among children aged ≥6 months vary by season and study design. Limited efficacy data are available for children from studies that used culture-or reverse transcriptionpolymerase chain reaction (RT-PCR)-confirmed influenza virus infections as the primary outcome. A recent large randomized trial compared rates of RT-PCR-confirmed influenza virus infections among 4,707 children aged 6 through 71 months who received inactivated vaccine, inactivated vaccine with MF59 oil-in-water adjuvant, or a control vaccine (meningococcal conjugate vaccine or tick-borne encephalitis vaccine). During the two seasons of the study (2007-08 and 2008-09), efficacy of inactivated vaccine versus control vaccine was 43% (95% CI = 15%-61%) and of inactivated vaccine plus MF59 versus control was 86% (95% CI = 74%-93%) (122). In a randomized trial conducted during five influenza seasons (1985)(1986)(1987)(1988)(1989)(1990) in the United States among children aged 1 through 15 years, receipt of inactivated vaccine reduced culture-confirmed influenza A by 77% (95% CI = 20%-93%) (89). A single season placebo-controlled study that enrolled 192 children aged 3 through 19 years found the efficacy of inactivated vaccine was 56% among healthy children aged 3 through 9 years and 100% among healthy children and adolescents aged 10 through 18 years (123); influenza infection was defined either by viral culture or, in the absence of a positive culture, by a postseason antibody rise in HI titer among symptomatic children from whom no other virus was isolated and whose symptoms began within 10 days of isolation of influenza from a household contact or during peak influenza activity in the community. In a randomized, double-blind, placebo-controlled trial conducted during two influenza seasons among 786 children aged 6 through 24 months, estimated efficacy was 66% (95% CI = 34%-82%) against culture-confirmed influenza illness during the 1999-00 influenza season but did not reduce culture-confirmed influenza illness significantly during the 2000-01 season, when influenza attack rates were lower (3% versus 16% during the 1999-00 season) (124).
Studies using a serological definition of influenza virus infection have raised concerns that dependence on a serological diagnosis of influenza in clinical trials might lead to overestimation of vaccine efficacy because of an "antibody ceiling" effect in adult subjects with historic exposures to both natural infections and vaccination. This could result in the decreased likelihood that antibody increases can be observed in vaccinated subjects after influenza infection with circulating viruses, as compared with adult subjects in control arms of trials. Thus, vaccinated subjects might be less likely to show a fourfold increase in antibody levels can after influenza infection with circulating viruses compared with unvaccinated subjects in such studies. Whether there is a substantial antibody ceiling effect in children, particularly younger children without extensive experience with influenza antigens, is not known.
Several observational studies to assess vaccine effectiveness were conducted during the 2003-04 influenza season, when the match between vaccine virus antigens and circulating viruses was suboptimal. A case-control study conducted during the 2003-04 season estimated vaccine effectiveness among fully vaccinated children aged 6 through 59 months to be 49% (95% CI = 30%-60%) against influenza diagnosed by a positive antigen-detection test with a specificity of 96% (125). An observational study among children aged 6 through 59 months with culture-or PCR-confirmed influenza compared with children who tested negative for influenza reported vaccine effectiveness of 44% (95% CI = -42%-78%) in the 2003-04 influenza season and 57% (95% CI = 28%-74%) during the 2004-05 season (118). Receipt of only 1 vaccine dose among children being vaccinated for the first time was not effective in either season. A retrospective cohort study conducted during the 2003-04 season among approximately 30,000 children aged 6 months through 8 years reported vaccine effectiveness of 51% (95% CI = 33%-64%) against medically attended, clinically diagnosed pneumonia or influenza (i.e., there was no laboratory confirmation of influenza infection). Estimated vaccine effectiveness was 49% (95% CI = 9%-71%) among children aged 6 through 23 months (117). Another retrospective cohort study of similar size that used a syndromically defined outcome and was conducted during the 2003-04 season among healthy children aged 6 through 21 months estimated effectiveness of 2 IIV doses to be 87% (95% CI = 78%-92%) against pneumonia/ influenza-related office visits (116). It is difficult to reconcile the high effectiveness estimate in this study with others from the same season because it focused on younger children and used a nonspecific outcome.
Among children, IIV effectiveness might be lower in very young children compared with older children (122,126). A 2012 systematic review of published studies estimated vaccine effectiveness among healthy children was 40% (95% CI = 6%-61%) for those aged 6 through 23 months and 60% (95% CI = 30%-78%) for those aged 24 through 59 month (127). However, during the 2010-11 season, when all three vaccine virus strains appeared antigenically similar to circulating strains, vaccine effectiveness among children was similar to that observed for those of all ages in a large multisite observational study that used RT-PCR-confirmed medically attended influenza virus infections as the outcome (all ages: 60%; 95% CI = 54%-66%; vaccine effectiveness among children aged 6 months through 2 years: 58%; 95% CI = 31%-74%; among children aged 3 through 8 years: 69%; 95% CI = 56%-77%) (128).
Because of the long-standing recommendation for annual influenza vaccination of immunosuppressed children and those with chronic medical conditions, randomized placebocontrolled studies to study efficacy specifically in these children are lacking. In a nonrandomized controlled trial among children aged 2 through 6 years and 7 through 14 years who had asthma, vaccine efficacy was 54% and 78% against laboratory-confirmed influenza A(H3N2) infection and 22% and 60% against laboratory-confirmed influenza B infection, respectively. However, vaccine effectiveness was not significant against B viruses for vaccinated children aged 2 through 6 years with asthma who did not have substantially fewer type B influenza virus infections compared with the control group in this study (129). The association between vaccination and prevention of asthma exacerbations is unclear.
One study suggested that vaccination might provide protection against asthma exacerbations (130).
Receipt of IIV was associated with a reduction in acute otitis media in some studies, but no effect was observed in others. Two studies reported that IIV decreases the risk for influenzarelated otitis media among children (131,132). However, a large study conducted among young children (mean age: 14 months) indicated that IIV did not reduce the proportion of children who developed acute otitis media during the study (124). Influenza vaccine effectiveness against a nonspecific clinical outcome such as acute otitis media, which is caused by a variety of pathogens and typically is not diagnosed by use of influenza virus detection methods, would be expected to be lower than effectiveness against laboratory-confirmed influenza.
# Adults Aged <65 Years
One dose of IIV tends to be highly immunogenic in healthy adults aged <65 years. For example, monovalent influenza A(H1N1)pdm09 (2009) vaccines were highly immunogenic, with approximately 90% of vaccinated adults aged 18 through 64 years demonstrating antibody levels considered protective (133,134). A 2012 meta-analysis found that IIV efficacy against RT-PCR or culture-confirmed influenza was 59% (95% CI = 51%-67%) among adults aged 18 through 65 years in eight of twelve seasons analyzed in ten randomized controlled trials (135). A 2010 meta-analysis of randomized clinical trial results among healthy adults aged 16 through 65 years suggested that when vaccine and circulating influenza viruses strains were well-matched, efficacy against influenza symptoms was 73% (95% CI = 54%-84%) whereas it was 44% (95% CI = 23%-59%) when they were not wellmatched. However, a standard definition of "matched" was not specified (136). Vaccination of healthy adults was associated with decreased work absenteeism and use of health-care resources in some studies, when the vaccine and circulating viruses are well-matched (48,137).
# Adults with Chronic Medical Conditions
There is some evidence to suggest that vaccine effectiveness among adults aged <65 years who have medical conditions conferring higher risk for influenza complications typically might be lower than that reported for healthy adults. In a case-control study conducted during the 2003-04 influenza season, when the vaccine was a suboptimal antigenic match to many circulating virus strains, effectiveness for prevention of laboratory-confirmed influenza (tests used not specified) illness among adults aged 50 through 64 years with high-risk conditions was 48% (95% CI = 21%-66%) compared with 60% (95% CI = 43%-72%) for healthy adults. By contrast, for the subset of cases who were hospitalized (n = 106), effectiveness varied more substantially by risk status: among those with high-risk conditions vaccine effectiveness was 36% (95% CI = 0-63%) while it was 90% (95% CI = 68%-97%) among healthy adults (138). Adults with immunocompromising conditions (e.g., solid organ transplant and HIV infection with low CD4 counts) have lower serum antibody responses after vaccination compared with healthy young adults (139,140).
A randomized controlled trial conducted among adults (median age: 68 years) in Thailand with chronic obstructive pulmonary disease (COPD) observed that vaccine efficacy was 76% (95% CI = 32%-93%) in preventing influenzaassociated acute respiratory infection (defined as respiratory illness associated with HAI titer increase and/or positive influenza antigen on indirect immunofluorescence testing) during a season when circulating influenza viruses were well-matched to vaccine viruses (141). A meta-analysis that examined effectiveness among persons with chronic obstructive pulmonary disease identified evidence of reduced risk for exacerbation from vaccination (142). However, another metaanalysis of published studies concluded that evidence was insufficient to demonstrate that persons with asthma benefit from vaccination (143).
A few randomized controlled trials have studied the effects of influenza vaccination on outcomes not usually associated with influenza virus infection. There is evidence suggesting that acute respiratory infections might trigger acute vascular events mediated by atherosclerosis (144). In particular, respiratory infections coded as influenza or occurring when influenza viruses were circulating transiently increase the risk for acute myocardial infarctions (145). A meta-analysis of two small randomized trials of influenza vaccination in persons with cardiovascular disease yielded a pooled efficacy estimate of 49% for prevention of acute myocardial infarction or cardiac death, although this effect was not statistically significant (95% CI = -76%-85%) (146).
Some observational studies that have provided estimates of vaccine effects for serious complications of influenza infections without laboratory confirmation of influenza have found large reductions in hospitalizations or deaths. For example, in a case-control study conducted during the 1999-00 season in the Netherlands among 75,227persons aged <65 years with underlying medical conditions, vaccination was reported to reduce deaths attributable to any cause by 78% and reduce hospitalizations attributable to respiratory infections or cardiopulmonary diseases by 87% (147). The benefit was greater among those who had been vaccinated previously than among first-time vaccinees (147). Among patients with diabetes mellitus, vaccination was associated with a 56% reduction in any complication, a 54% reduction in hospitalizations, and a 58% reduction in deaths (148). Effects of this magnitude on nonspecific outcomes might have been caused by confounding from unmeasured factors (e.g., dementia and difficulties with self-care) that are associated strongly with the measured outcomes (84,85). Recent studies using methods to account for unmeasured confounding have indicated that vaccine effectiveness among community-dwelling older persons for nonspecific serious outcomes such as pneumonia/influenza hospitalizations or all-cause mortality is <10%, which is much more plausible than higher estimates from earlier studies (149)(150)(151).
# Immunocompromised Persons
In general, HIV-infected persons with minimal AIDS-related symptoms and normal or near-normal CD4+ T-lymphocyte cell counts who receive IIV develop adequate antibody response (152)(153)(154). Among persons who have advanced HIV disease and low CD4+ T-lymphocyte cell counts, IIV might not induce protective antibody titers (154,155); a second dose of vaccine does not improve the immune response in these persons (155,156). A recent immunogenicity study of HIV-infected persons aged ≥18 years indicated that seroprotection rates were higher for persons given high-dose IIV (containing 60 µg of HA per vaccine virus) than those given standard-dose vaccine (which contains 15 µg of HA per vaccine virus); the high-dose vaccine is not licensed for persons aged 100 CD4+ cells and among those with <30,000 viral copies of HIV type-1/mL (64). In a randomized placebo-controlled trial conducted in South Africa among 506 HIV-infected adults, including 349 persons on antiretroviral treatment and 157 who were antiretroviral treatment-naïve, efficacy for culture-or RT-PCR-confirmed influenza illness was 75% (95% CI = 9%-96%) (158).
Several relatively small observational studies have suggested that immunogenicity among persons with solid organ transplants varies according to transplant type. Among persons with kidney or heart transplants, the proportion that developed seroprotective antibody concentrations was similar or slightly reduced compared with healthy persons (159)(160)(161). However, a study among persons with liver transplants indicated reduced immunologic responses to influenza vaccination (162)(163)(164), especially if vaccination occurred within the 4 months after the transplant procedure (162).
# Pregnant Women and Neonates
Pregnant women have protective levels of anti-influenza antibodies after vaccination (165). Passive transfer of antiinfluenza antibodies that might provide protection from vaccinated women to neonates has been reported (165)(166)(167)(168)(169). One randomized controlled trial conducted in Bangladesh that provided IIV3 vaccination to pregnant women during the third trimester demonstrated a 29% reduction in respiratory illness with fever among the infants and a 36% reduction in respiratory illness with fever among their mothers during the first 6 months after birth, compared with pregnant women receiving 23-valent pneumococcal polysaccharide vaccine. In addition, infants born to vaccinated women had a 63% reduction in laboratory-confirmed influenza illness during the first 6 months of life (170). All women in this trial breastfed their infants (mean duration: 14 weeks). Maternal influenza vaccination during pregnancy was associated with significantly reduced risk for influenza virus infection (relative risk: 0.59; 95% CI = 0.37-0.93) and hospitalization for influenza-like illness (ILI) (relative risk: 0.61; 95% CI = 0.45-0.84) among infants aged <6 months in a nonrandomized prospective cohort study; increased antibody titers were also noted in infants through age 2 to 3 months (171). However, a retrospective study conducted during 1997-2002 that used clinical records data did not indicate a reduction in ILI among vaccinated pregnant women or their infants (172). In a retrospective cohort study conducted during 1995-2001, medical visits for respiratory illness among the infants of vaccinated mothers were not substantially reduced (173).
# Older Adults
Most studies suggest that antibody responses to influenza vaccination are decreased in older adults, and it is likely that increasing dysregulation of the immune system with aging contributes to the increased likelihood of serious complications of influenza infection (174). A review of HAI antibody responses in 31 studies among adults aged ≥58 years found that 42%, 51%, and 35% of older persons seroconverted to H1N1, H3N2, and B vaccine antigens, respectively, compared with 60%, 62%, and 58% of younger persons (104). When seroprotection (defined as an HAI titer ≥40) was the outcome, 83%, 84%, and 78% of younger adults versus 69%, 74%, and 67% of older adults achieved protective titers to H1N1, H3N2, and B antigens, respectively (104). Although an HAI titer ≥40 is associated with approximately 50% clinical protection from infection, this standard was established in young healthy adults (8), and there are few data to suggest that such antibody titers represent a correlate of protection among elderly adults. Limited or no increase in antibody response is reported among elderly adults when a second dose is administered during the same season (175)(176)(177).
The desire to improve HI responses among adults aged ≥65 years led to the development and licensure of a vaccine with more antigen than standard-dose IIV. Immunogenicity data from 3 studies of high-dose IIV (Fluzone High-Dose, Sanofi Pasteur) among persons aged ≥65 years indicated that vaccine with four times the HA antigen content of standard-dose vaccine elicited substantially higher HAI titers (178)(179)(180). Pre-specified criteria for superiority in one clinical trial study was defined by a lower bound of a two-sided CI for the ratio of geometric mean HI titers >1.5 and a difference in fourfold rise of HI titers >10%. These criteria were met for influenza A(H1N1) and influenza A(H3N2) virus antigens (181), but not for the influenza B virus antigen (for which criteria for noninferiority were met) (179).
The only large randomized placebo-controlled trial conducted among community-dwelling persons aged ≥60 years reported a vaccine efficacy of 58% (95% CI = 26%-77%) against serologically confirmed clinical influenza illness during a season when the vaccine strains were considered to be well-matched to circulating strains (182). The outcome used for measuring the efficacy estimate was seroconversion to a circulating influenza virus and a symptomatic illness compatible with a clinical influenza infection. As noted previously, there is concern that seroconversion after symptomatic illness will be less likely among vaccinated persons who have higher levels of pre-existing anti-HA antibody that than among those not vaccinated. Such a situation would lead to an overestimate of the true vaccine efficacy, as was demonstrated in a recent clinical trial conducted among healthy adults aged 18 through 49 years (183). Additional information from this trial published after the main results indicated that efficacy among those aged ≥70 years was 57% (95% CI = -36%-87%), similar to the point estimate found among younger persons. However, few persons aged ≥70 years participated in this study, and the wide CI for the estimate of efficacy for persons in this age group included no efficacy (184). Influenza vaccine effectiveness in preventing MAARI among elderly persons residing in nursing homes has been estimated at 20%-40% (185,186), and reported outbreaks among well-vaccinated nursing-home populations have suggested that vaccination might not have any significant effectiveness when circulating strains are drifted from vaccine strains (187,188). Influenza vaccination might reduce the frequency of secondary complications and might reduce the risk for influenza-related hospitalization and death among community-dwelling adults aged ≥65 years with and without high-risk medical conditions (189)(190)(191)(192)(193). However, these studies demonstrating large reductions in hospitalizations and deaths among the vaccinated elderly have been conducted using medical record databases and have not measured reductions in laboratory-confirmed influenza illness. Such methods have been challenged because analyses might not be adjusted adequately to control for the possibility that healthier persons may be more likely to be vaccinated than less healthy persons (84,85,(194)(195)(196)(197)(198).
# Immunogenicity, Efficacy, and Effectiveness of LAIV
LAIV virus strains replicate in nasopharyngeal epithelial cells. The protective mechanisms induced by vaccination with LAIV are not understood completely but appear to involve both serum and nasal secretory antibodies, as well as cell-mediated immune responses. The immunogenicity of LAIV has been assessed in multiple studies (97,(199)(200)(201)(202)(203)(204)(205).
# Healthy Children
A randomized, double-blind, placebo-controlled trial among 1,602 healthy children aged 15 through 71 months assessed the efficacy of LAIV against culture-confirmed influenza during two seasons (206,207). During the first season (1996-97), when vaccine and circulating virus strains were well-matched, efficacy against culture-confirmed influenza was 94% for participants who received 2 doses of LAIV separated by >6 weeks, and 89% for those who received 1 dose. During the second season (1997-98), when the A(H3N2) component in the vaccine was not well-matched with circulating virus strains, efficacy for 1 dose was 86%. The overall efficacy during the two influenza seasons was 92%. Receipt of LAIV also resulted in 21% fewer febrile illnesses and a significant decrease in influenza A-associated otitis media (vaccine efficacy: 94%; 95% CI = 78%-99%) (206,207). In a randomized placebo-controlled trial among vaccine-naïve children aged 6 through <36 months which compared 1 versus 2 doses of LAIV, efficacy against culture-confirmed influenza was 58% (95% CI = 45%-68%) after 1 dose of LAIV and 74% (95% CI = 64%-81%) after 2 doses (100). Other randomized, placebo-controlled trials demonstrating the efficacy of LAIV in young children against culture-confirmed influenza include a study conducted among children aged 6 through 35 months attending child care centers during consecutive influenza seasons (208) in which 85%-89% efficacy was observed. Another study conducted among children aged 12 through 36 months living in Asia during consecutive influenza seasons reported efficacy of 64%-70% (101). In one communitybased, nonrandomized open-label study, reductions in MAARI were observed among children who received 1 dose of LAIV during the 1999-00 and 2000-01 influenza seasons even though antigenically drifted influenza A/H1N1 and B viruses were circulating during the latter season (98). LAIV efficacy in preventing laboratory-confirmed influenza also has been demonstrated in studies comparing the efficacy of LAIV with IIV rather than with a placebo (see Comparisons of LAIV and IIV Efficacy or Effectiveness).
A meta-analysis of six placebo-controlled studies concluded that the efficacy of LAIV against acute otitis media associated with culture-confirmed influenza among children aged 6 through 83 months was 85% (95% CI = 78%-90%) (209). In clinical trials, an increased risk for wheezing postvaccination was observed in LAIV recipients aged <24 months. An increase in hospitalizations was also observed in children aged <24 months after vaccination with LAIV (210).
# Healthy Adults
A randomized, double-blind, placebo-controlled trial of LAIV effectiveness among 4,561 healthy working adults aged 18 through 64 years assessed multiple endpoints, including reductions in self-reported respiratory tract illness without laboratory confirmation, work loss, health-care visits, and medication use during influenza outbreak periods. The study was conducted during the 1997-98 influenza season, when the vaccine and circulating A(H3N2) viruses were not wellmatched. The frequency of febrile illnesses was not significantly decreased among LAIV recipients compared with those who received placebo. However, vaccine recipients had significantly fewer severe febrile illnesses (19% reduction) and febrile upper respiratory tract illnesses (24% reduction); and significant reductions in days of illness, days of work lost, days with healthcare provider visits, and use of prescription antibiotics and overthe-counter medications (211). Estimated efficacy of LAIV against influenza confirmed by either culture or RT-PCR in a randomized, placebo-controlled study among approximately 2,000 young adults was 48% (95% CI = -7%-74%) in the 2004-05 influenza season, 8% (95% CI = -194%-67%) in the 2005-06 influenza season, and 36% (95% CI = 0-59%) in the 2007-08 influenza season; efficacy in the 2004-05 and 2005-06 seasons was not significant (212)(213)(214).
# Comparisons of LAIV and IIV Efficacy or Effectiveness
Both IIV and LAIV have been demonstrated to be effective in children and adults. Studies comparing the efficacy of IIV to that of LAIV have been conducted in a variety of settings and populations using several different outcomes. Among adults, most comparative studies have demonstrated either that LAIV and IIV were of similar efficacy or that IIV was more efficacious (215). One randomized, double-blind, placebo-controlled challenge study that was conducted among 92 healthy adults aged 18 through 41 years assessed the efficacy of both LAIV and IIV in preventing influenza infection when artificially challenged with wild-type strains that were antigenically similar to vaccine strains (205). The overall efficacy in preventing laboratory-documented influenza illness (defined as respiratory symptoms with either isolation of wild-type influenza virus from nasal secretions or fourfold and/or greater HAI antibody response to challenge) from all three influenza strains combined was 85% for LAIV and 71% for IIV when study participants were challenged 28 days after vaccination by viruses to which they were susceptible before vaccination. The difference in efficacy between the two vaccines was not statistically significant in this small study. No additional challenges were conducted to assess efficacy at time points later than 28 days (205). In a randomized, double-blind, placebo-controlled trial that was conducted among young adults during the 2004-05 influenza season, when the majority of circulating H3N2 viruses were antigenically drifted from that season's vaccine viruses, the efficacy of LAIV and IIV against cultureconfirmed influenza was 57% (95%CI = -3%-82%) and 77% (95% CI = 37%-92%), respectively. The difference in efficacy was not statistically significant and was attributable primarily to a difference in efficacy against influenza B (212) (216). However, in a retrospective cohort study comparing LAIV and IIV among 701,753 nonrecruit military personnel and 70,325 new recruits, among new recruits, incidence of ILI was lower among those who received LAIV than IIV. The previous vaccination status of the recruits was not known; it is possible that this population was relatively naïve to vaccination compared with previous service members who are vaccinated routinely each year (217).
Several studies have demonstrated superior efficacy of LAIV as compared with IIV among children (215). A randomized controlled clinical trial conducted among 7,852 children aged 6 through 59 months during the 2004-05 influenza season demonstrated a 55% reduction in cases of culture-confirmed influenza among children who received LAIV compared with those who received IIV (218). In this study, LAIV efficacy was higher compared with IIV against antigenically drifted viruses and well-matched viruses (218). An open-label, nonrandomized, community-based influenza vaccine trial conducted among 7,609 children aged 5 through 18 years during an influenza season when circulating H3N2 strains were poorly matched with strains contained in the vaccine also indicated that LAIV, but not IIV, was effective against antigenically drifted H3N2 viruses. In this study, children who received LAIV had significant protection against laboratoryconfirmed influenza (37%) and pneumonia/influenza events (50%) (219). LAIV provided 32% increased protection in preventing culture-confirmed influenza compared with IIV in one study conducted among children aged ≥6 years and adolescents with asthma (220) and 52% increased protection compared with IIV among children aged 6 through 71 months with recurrent respiratory tract infections (221).
# Safety of Influenza Vaccines Inactivated Influenza Vaccines
Children: A large postlicensure population-based study assessed IIV3 safety in 251,600 children aged <18 years (including 8,476 vaccinations in children aged 6 through 23 months) enrolled in one of five health-care organizations within the Vaccine Safety Datalink (VSD) (. gov/vaccinesafety/activities/vsd.html) during 1993-1999. This study indicated no increase in clinically important medically attended events during the 2 weeks after inactivated influenza vaccination compared with control periods 3-4 weeks before and after vaccination (222). In a retrospective cohort study using VSD data from 45,356 children aged 6 through 23 months during 1991-2003, IIV3 was not associated with statistically significant increases in any clinically important medically attended events other than gastritis/duodenitis during the 2 weeks after vaccination compared with control time periods before and after vaccination. Most vaccinated children with a diagnosis of gastritis/duodenitis had selflimited vomiting or diarrhea. Several diagnoses, including acute upper respiratory illness, otitis media and asthma, were significantly less common during the 2 weeks after influenza vaccination. Although there was a temporal relationship with vaccination, the vaccine did not necessarily cause nor prevent these conditions (223). A subsequent VSD study of 66,283 children aged 24 through 59 months noted diagnoses of fever, gastrointestinal tract symptoms, and gastrointestinal disorders to be significantly associated with IIV3. Upon medical record review, none of the events appeared to be serious, and none were associated with complications (224).
In a study of 791 healthy children aged 1 through 15 years, postvaccination fever was noted among 12% of those aged 1 through 5 years, 5% among those aged 6 through 10 years, and 5% among those aged 11 through 15 years (89). Fever, malaise, myalgia, and other systemic symptoms that can occur after vaccination with IIV most often affect persons who have had no previous exposure to the influenza virus antigens in the vaccine (e.g., young children) (225). These reactions are generally self-limited and subside after 1-2 days.
Febrile seizures associated with IIV and pneumococcal conjugate vaccine (PCV13): Febrile seizures are common in young children. At least one febrile seizure is experienced by 2%-5% of children aged 6 through 60 months; nearly all children who have a febrile seizure recover quickly and are healthy afterwards (226). Prior to the 2010-11 influenza season, an increased risk for febrile seizures following IIV3 had not been observed in the United States (223,227). During the 2010-11 influenza season, CDC and the Food and Drug Administration (FDA) conducted enhanced monitoring for febrile seizures following influenza vaccines after reports of an increased risk for fever and febrile seizures in young children in Australia associated with a 2010 Southern Hemisphere IIV3 produced by CSL Biotherapies (up to nine febrile seizures per 1,000 doses) (228). Because of the findings in Australia, ACIP does not recommend the U.S.-licensed CSL Biotherapies' IIV3, Afluria, for children aged <9 years (Table 1).
Surveillance among children receiving U.S.-licensed influenza vaccines during the 2010-11 influenza season subsequently detected safety concerns for febrile seizures in young children following IIV3 (229,230). Further assessment through a VSD study determined that the increased risk was in children aged 6 months through 4 years on the day of vaccination to the day after (risk window: Day 0-1). The risk was higher when children received concomitant PCV13 (i.e., when the two vaccines are given at the same health-care visit) and peaked at approximately age 16 months (230). No increased risk was observed in children aged >4 years after IIV3 or in children of any age after LAIV. The magnitude of the increased risk for febrile seizures in children aged 6 through 23 months in the United States observed in this study (<1 per 1,000 children vaccinated) was substantially lower than the risk observed in Australia in 2010 (228). Findings from surveillance for febrile seizures in young children following influenza vaccine for the 2011-12 influenza season (which had the same formulation as that of the 2010-11 season) were consistent with the 2010-11 influenza season; however, an increased risk for febrile seizures following IIV3 was not observed during the 2012-13 influenza season (CDC, unpublished data, 2013). After evaluating the data on febrile seizures from the 2010-11 influenza season and taking into consideration benefits and risks of vaccination, no policy change was recommended for use of IIV or PCV13 (231,232). Surveillance for febrile seizures after IIV is ongoing through VAERS. † For adults and older children, the recommended site of vaccination is the deltoid muscle. The preferred site for infants and young children is the anterolateral aspect of the thigh. Specific guidance regarding site and needle length for intramuscular administration may be found in the ACIP General Recommendations on Immunization (CDC. General recommendations on immunization: recommendations of the Advisory Committee on Immunization Practices, 2011. MMWR 2011;60). § The preferred site is over the deltoid muscle. Fluzone Intradermal is administered using the delivery system included with the vaccine. Inactivated influenza vaccine, high-dose: A 0.5-mL dose contains 60 µg of each vaccine antigen (180 µg total).
† † Inactivated influenza vaccine, intradermal: A 0.1-mL dose contains 9 µg of each vaccine antigen (27 µg total). § § It is anticipated that the quadrivalent formulation of FluMist will replace the trivalent formulation for the 2013-14 season. FluMist is shipped refrigerated and stored in the refrigerator at 35°F-46°F (2°C-8°C) after arrival in the vaccination clinic. The dose is 0.2 mL divided equally between each nostril. Health-care providers should consult the medical record, when available, to identify children aged 2 through 4 years with asthma or recurrent wheezing that might indicate asthma. In addition, to identify children who might be at greater risk for asthma and possibly at increased risk for wheezing after receiving LAIV, parents or caregivers of children aged 2 through 4 years should be asked, "In the past 12 months, has a health-care provider ever told you that your child had wheezing or asthma?" Children whose parents or caregivers answer "yes" to this question and children who have asthma or who had a wheezing episode noted in the medical record within the past 12 months should not receive FluMist. * Flumist is indicated for healthy, nonpregnant persons aged 2-49 years. Persons who care for severely immunosuppressed persons who require a protective environment should not receive FluMist given the theoretical risk of transmission of the live attenuated vaccine virus. † † † Age indication per package insert is ≥5 years; however, ACIP recommends that Afluria not be used in children aged 6 months through 8 years because of increased risk for febrile reactions noted in this age group with CSL's 2010 Southern Hemisphere IIV3. If no other age-appropriate, licensed inactivated seasonal influenza vaccine is available for a child aged 5-8 years who has a medical condition that increases the child's risk for influenza complications, Afluria can be used; however, providers should discuss with the parents or caregivers the benefits and risks of influenza vaccination with Afluria before administering this vaccine. Afluria may be used in persons aged ≥9 years. § § § Information not included in package insert. The total egg protein is estimated to be less than 50 femtograms (5x10-14 grams) total egg protein (of which a fraction is ovalbumin) per 0.5 mL dose of Flucelvax. ¶ ¶ ¶ Available on request from Sanofi Pasteur, telephone 1-800-822-2463 or e-mail [email protected].
# Adults:
In placebo-controlled studies among adults, the most frequent side effect of vaccination was soreness at the vaccination site (affecting 10%-64% of patients) that lasted <2 days (233,234). These local reactions typically were mild and rarely interfered with the recipients' ability to conduct usual daily activities. Placebo-controlled trials demonstrate that among older persons and healthy young adults, administration of IIV3 is not associated with higher rates for systemic symptoms (e.g., fever, malaise, myalgia, and headache) when compared with placebo injections (233)(234)(235). Adverse events in adults aged ≥18 years reported to VAERS during 1990-2005 were analyzed. The most common adverse events for adults described in 18,245 VAERS reports included injection site reactions, pain, fever, myalgia, and headache. The VAERS review identified no new safety concerns. Fourteen percent of the IIV3 VAERS reports in adults were classified as serious adverse events (defined as those involving death, life-threatening illness, hospitalization or prolongation of hospitalization, or permanent disability ), similar to proportions seen in VAERS for other adult vaccines. The most common serious adverse event reported after IIV3 in VAERS in adults was Guillain-Barré syndrome (GBS) (237). The potential association between IIV3 and GBS is an area of ongoing research (see Guillain-Barré Syndrome and IIV).
Injection site reactions and systemic adverse events were more frequent after vaccination with a vaccine containing 180 µg of HA antigen (Fluzone High-Dose, Sanofi Pasteur, Swiftwater, Pennsylvania) than after standard-dose (45 µg) (Fluzone, Sanofi Pasteur) but were typically mild and transient. In one study, 915 (36%) of 2,572 persons who received Fluzone High-Dose, compared with 306 (24%) of those who received Fluzone, reported injection site pain. Only 1.1% of Fluzone High Dose recipients reported moderate to severe fever, but this was significantly higher than the 0.3% of Fluzone recipients who reported this systemic adverse event (RR: 3.6, 95% CI = 1.3-10.1) (179). A randomized study of high-dose versus standard-dose vaccine including 9,172 participants found no difference in occurrence of serious adverse events or several specific adverse events of interest (including GBS, Bell's Palsy, encephalitis/myelitis, optic neuritis, Stevens-Johnson syndrome, and toxic epidermal necrolysis) (238). Safety monitoring of high-dose vaccine in VAERS during the first year after licensure indicated a higher than expected number of gastrointestinal events compared with standard-dose vaccine, but otherwise no new safety concerns were identified. Most of the reported gastrointestinal reports were nonserious (239). CDC and FDA will continue to monitor the safety of highdose vaccine through VAERS.
Intradermal IIV has been observed to be associated with higher rates of some injection site reactions as compared with intramuscularly administered influenza vaccines. In a randomized study of intradermal versus intramuscular vaccine among approximately 4,200 adults aged 18 through 64 years, erythema, induration, swelling, and pruritus occurred with greater frequency following intradermal vaccine compared with intramuscular vaccine; rates of injection site pain were not significantly different (240). A recent review of studies comparing intradermal and intramuscular vaccine similarly noted higher rates of erythema, induration, swelling, and pruritus among adults aged 18 through 60 years within the first 7 days after receiving intradermal vaccine; local pain and ecchymosis and systemic reactions occurred with similar frequency (241).
Pregnant women and neonates: Currently available IIVs are classified as either Pregnancy Category B or Category C † medications, depending upon whether adequate animal reproduction studies have been conducted. Available data indicate that influenza vaccine does not cause fetal harm when administered to a pregnant woman. However, data on the safety of influenza vaccination in the early first trimester are limited (242). One study of approximately 2,000 pregnant women who received IIV3 during pregnancy demonstrated no increase in malignancies during infancy or early childhood (243). A matched case-control study of 252 pregnant women who received IIV3 within the 6 months before delivery determined no adverse events after vaccination among pregnant women and no difference in pregnancy outcomes compared with 826 pregnant women who were not vaccinated (244). A case-control analysis of data from six health-care organizations participating in the VSD found no significant increase in the risk for pregnancy loss in the 4 weeks following seasonal influenza vaccination (245). A review of health registry data in Norway noted an increased risk for fetal death associated with pandemic 2009(H1N1) infection, but no increased risk of fetal mortality associated with vaccination (246). During 2000-2003, when an estimated 2 million pregnant women were vaccinated, only 20 adverse events among women who received IIV3 were reported to VAERS, including nine injection site reactions, eight systemic reactions (e.g., fever, headache, and myalgia), and three miscarriages (247). Background rates of miscarriage vary from 10.4% in women aged <25 years to 22.4% in women † Pregnancy Category B indicates that 1) animal reproduction studies have failed to demonstrate a risk to the fetus and there are no adequate and well-controlled studies in humans or 2) that animal studies have shown an adverse effect, but adequate and well-controlled studies in humans have failed to demonstrate a risk to the fetus in any trimester. Pregnancy Category C indicates that animal reproduction studies have shown an adverse effect on the fetus and there are no adequate and well-controlled studies in humans, but potential benefits may warrant use of the drug in pregnant women despite potential risks. Additional information about pregnancy categories is available at / Drugs/DevelopmentApprovalProcess/DevelopmentResources/Labeling/ ucm093307.htm.
aged >34 years (248); considering the number of pregnant women vaccinated, miscarriage following (but not attributable to) influenza vaccination would not be an unexpected event.
Recent reviews of studies pertaining to seasonal (249)(250)(251) and monovalent 2009(H1N1) (250,251) inactivated influenza vaccines in pregnancy concluded that no evidence exists to suggest harm to the fetus from maternal vaccination.
Persons with chronic medical conditions: In a blinded, randomized crossover study of 1,952 children and adults with asthma, no increase in asthma exacerbations was reported for either age group. Only myalgias were reported more frequently after IIV3 (25%) than placebo-injection (21%) (252). Among children with high-risk medical conditions, one study of 52 children aged 6 months through 3 years reported fever among 27% and irritability and insomnia among 25% (108); and a study among 33 children aged 6 through 18 months reported that one child had irritability and one had a fever and seizure after vaccination (253). No placebo comparison group was used in these studies. One prospective cohort study found that the rate of adverse events was similar among hospitalized persons who either were aged ≥65 years or were aged 18 through 64 years and had one or more chronic medical conditions compared with outpatients (254).
Immunocompromised persons: Data demonstrating safety of IIV3 for HIV-infected persons are limited, but no evidence exists that vaccination has a clinically important impact on HIV infection or immunocompetence. One study demonstrated a transient increase in HIV RNA (ribonucleic acid) levels in one HIV-infected person after influenza virus infection (255). While some earlier studies demonstrated a transient increase in replication of HIV-1 in the plasma or peripheral blood mononuclear cells of HIV-infected persons after vaccine administration (154,256), more recent and better-designed studies have not documented a substantial increase in the replication of HIV (257-260). CD4+ T-lymphocyte cell counts or progression of HIV disease have not been demonstrated to change substantially after influenza vaccination among HIV-infected persons compared with unvaccinated HIV-infected persons (154,261). Limited information is available about the effect of antiretroviral therapy on increases in HIV RNA levels after either influenza virus infection or influenza vaccination (63,262).
Data are similarly limited for persons with other immunocompromising conditions. In small studies, vaccination did not affect allograft function or cause rejection episodes in recipients of kidney transplants (159,160), heart transplants (161), or liver transplants (162). Limited data are available on influenza vaccination in the setting of solid organ transplantation. A recent literature review concluded that there is no convincing epidemiologic link between vaccination and allograft dysfunction (263). Case reports of corneal graft rejection have been reported following IIV (264)(265)(266), but no studies demonstrating an association have been conducted.
Immediate hypersensitivity reactions after influenza vaccines: Vaccine components can occasionally cause allergic reactions, also called immediate hypersensitivity reactions. Immediate hypersensitivity reactions are mediated by preformed immunoglobulin E (IgE) antibodies against a vaccine component and usually occur within minutes to hours of exposure (267). Symptoms of immediate hypersensitivity range from urticaria (hives) to angioedema and anaphylaxis. Anaphylaxis is a severe life-threatening reaction that involves multiple organ systems and can progress rapidly. Symptoms and signs of anaphylaxis can include but are not limited to generalized urticaria, wheezing, swelling of the mouth, tongue and throat, difficulty breathing, vomiting, hypotension, decreased level of consciousness, and shock. Minor symptoms such as red eyes or hoarse voice also might be present (267,268).
Allergic reactions might be caused by the vaccine antigen, residual animal protein, antimicrobial agents, preservatives, stabilizers, or other vaccine components (269). Manufacturers use a variety of compounds to inactivate influenza viruses and add antibiotics to prevent bacterial growth. Package inserts for specific vaccines of interest should be consulted for additional information. ACIP has recommended that all vaccine providers should be familiar with the office emergency plan and be certified in cardiopulmonary resuscitation (270). The Clinical Immunization Safety Assessment (CISA) network, a collaboration between CDC and medical research centers with expertise in vaccinology and vaccine safety, has developed an algorithm to guide evaluation and revaccination decisions for persons with suspected immediate hypersensitivity after vaccination (267).
Anaphylaxis after IIV and LAIV is rare. A study conducted in VSD during 2005-2008 observed that the incidence of anaphylaxis in the 0-2 days after IIV3 was 0.45-1.98 cases per million IIV3 doses administered in all ages (227). Anaphylaxis occurring after receipt of IIV3 and LAIV3 has rarely been reported to VAERS (237,271). A VSD study of children aged <18 years in four HMOs during 1991-1997 estimated the overall risk for postvaccination anaphylaxis after any type of childhood vaccine to be approximately 1.5 cases per million doses administered. In this study, no cases were identified in IIV3 recipients (272).
Some immediate hypersensitivity reactions after IIV or LAIV might be caused by the presence of residual egg protein in the vaccines (273). Although influenza vaccines contain only a limited quantity of egg protein, this protein can potentially induce immediate hypersensitivity reactions among persons who have severe egg allergy. Specific recommendations pertaining to the use of influenza vaccines for egg-allergic persons are provided (see Influenza Vaccination for Persons with a History of Egg Allergy).
Ocular and respiratory symptoms after receipt of IIV: Oculorespiratory syndrome (ORS), an acute, self-limited reaction to IIV with prominent ocular and respiratory symptoms, was first described during the 2000-01 influenza season in Canada. The initial case-definition for ORS was the onset of one or more of the following within 2-24 hours after receiving IIV, and resolving within 48 hours of onset: red eyes, cough, wheeze, chest tightness, difficulty breathing, sore throat, or facial swelling (274). ORS was strongly associated with one vaccine preparation (Fluviral S/F, Shire Biologics, Quebec, Canada) not available in the United States during the 2000-01 influenza season (275). Subsequent investigations identified persons with ocular or respiratory symptoms meeting an ORS case-definition in safety monitoring systems and trials that had been conducted before 2000 in Canada, the United States, and several European countries (276)(277)(278).
The cause of ORS has not been established; however, studies suggest that the reaction is not IgE-mediated (279). After changes in the manufacturing process of the vaccine preparation associated with ORS during the 2000-01 season, the incidence of ORS in Canada was reduced greatly (277). In one placebo-controlled study, only hoarseness, cough, and itchy or sore eyes (but not red eyes) were strongly associated with a reformulated Fluviral preparation. These findings indicated that ORS symptoms following use of the reformulated vaccine were mild, resolved within 24 hours, and might not typically be of sufficient concern to cause vaccine recipients to seek medical care (280).
Ocular and respiratory symptoms reported after IIV administration, including ORS, have some similarities with immediate hypersensitivity reactions. One study indicated that the risk for ORS recurrence with subsequent vaccination is low, and persons with ocular or respiratory symptoms (e.g., bilateral red eyes, cough, sore throat, or hoarseness) after receipt of IIV that did not involve the lower respiratory tract have been revaccinated without reports of serious adverse events after subsequent exposure to IIV (281).
When assessing whether a patient who experienced ocular and respiratory symptoms should be revaccinated, providers should determine if concerning signs and symptoms of IgE mediated immediate hypersensitivity are present (see Immediate Hypersensitivity after Influenza Vaccines). Health-care providers who are unsure whether symptoms reported or observed after receipt of IIV represent an IgE-mediated hypersensitivity immune response should seek advice from an allergist/ immunologist. Persons with symptoms of possible IgE-mediated hypersensitivity after receipt of IIV should not receive influenza vaccination unless hypersensitivity is ruled out or revaccination is administered under close medical supervision (267).
Ocular or respiratory symptoms observed after receipt of IIV often are coincidental and unrelated to IIV administration, as observed among placebo recipients in some randomized controlled studies. Determining whether ocular or respiratory symptoms are coincidental or related to possible ORS might not be possible. Persons who have had red eyes, mild upper facial swelling, or mild respiratory symptoms (e.g., sore throat, cough, or hoarseness) after receipt of IIV without other concerning signs or symptoms of hypersensitivity can receive IIV in subsequent seasons without further evaluation. Two studies indicated that persons who had symptoms of ORS after receipt of IIV were at a higher risk for ORS after subsequent IIV administration; however, these events usually were milder than the first episode (281,282).
Guillain-Barré syndrome and IIV: The annual incidence of GBS is 10-20 cases per 1 million adults (283). Evidence exists that multiple infectious illnesses, most notably Campylobacter jejuni gastrointestinal infections and upper respiratory tract infections, are associated with GBS (284)(285)(286). A recent study identified an association between serologically confirmed influenza virus infection and GBS, with time from onset of influenza illness to GBS of 3-30 days. The estimated frequency of influenza-related GBS was four to seven cases per 100,000 persons compared with one case per 1 million persons following vaccination with TIV) (287).
The 1976 swine influenza vaccine was associated with an increased frequency of GBS, estimated at one additional case of GBS per 100,000 persons vaccinated (288,289). The risk for influenza vaccine-associated GBS was higher among persons aged ≥25 years than among persons aged <25 years (290). No subsequent study conducted using influenza vaccines other than the 1976 swine influenza vaccine has demonstrated an increase in GBS associated with influenza vaccines on the order of magnitude seen in the 1976-77 season. During three of four influenza seasons studied during 1977-1991, the overall relative risk estimates for GBS after influenza vaccination were not statistically significant (291)(292)(293). However, in a study of the 1992-93 and 1993-94 seasons, the overall relative risk for GBS was 1.7 (95% CI = 1.0-2.8; p = 0.04) during the 6 weeks after vaccination, representing approximately one additional case of GBS per 1 million persons vaccinated. GBS cases peaked 2 weeks after vaccination (289). Results of a study that examined health-care data from Ontario, Canada, during 1992-2004 demonstrated a small but statistically significant temporal association between receiving influenza vaccination and subsequent hospital admission for GBS (relative incidence: 1.45; 95% CI = 1.05-1.99). However, no increase in cases of GBS at the population level was reported after introduction of a mass public influenza vaccination program in Ontario beginning in 2000 (294). Published data from the United Kingdom's General Practice Research Database (GPRD) found influenza vaccination to be associated with a decreased risk for GBS (odds ratio: 0.16; 95% CI = 0.02-1.25), although whether this was associated with protection against influenza or confounding because of a "healthy vaccinee" effect (e.g., healthier persons might be more likely to be vaccinated and also be at lower risk for GBS) is unclear (295). A separate GPRD analysis found no association between vaccination and GBS for a 9-year period; only three cases of GBS occurred within 6 weeks after administration of influenza vaccine (296). A third GPRD analysis found that GBS was associated with recent ILI, but not influenza vaccination (297).
The estimated risk for GBS (on the basis of the few studies that have demonstrated an association between seasonal IIV and GBS) is low; approximately one additional case per 1 million persons vaccinated (288,294). In addition, data from the systems monitoring influenza A(H1N1) 2009 monovalent vaccines suggest that the risk for GBS associated with these inactivated vaccines is approximately one or two additional cases per 1 million persons vaccinated, which is similar to that observed in some seasons for IIV (298)(299)(300)(301)(302)(303)(304).
The incidence of GBS among the general population is low (0.75 to 2 cases per 100,000 persons annually) ( 283), but persons with a history of GBS have a substantially greater likelihood of subsequently experiencing GBS than persons without such a history (283). Thus, the likelihood of coincidentally experiencing GBS after influenza vaccination is expected to be greater among persons with a history of GBS than among persons with no history of this syndrome. Whether influenza vaccination specifically might increase the risk for recurrence of GBS is unknown. Among 311 patients with GBS who responded to a survey, 11 (4%) reported some worsening of symptoms after influenza vaccination; however, some of these patients had received other vaccines at the same time, and recurring symptoms were generally mild (305). In a Kaiser Permanente Northern California database study among more than 3 million members conducted over an 11-year period, no cases of recurrent GBS were identified after influenza vaccination in 107 persons with a documented prior diagnosis of GBS, two of whom had initially developed GBS within 6 weeks of influenza vaccination (306).
As a precaution, persons who are not at high risk for severe influenza complications (see Persons at Risk for Medical Complications Attributable to Influenza) and who are known to have experienced GBS within 6 weeks of influenza vaccination generally should not be vaccinated. As an alternative, physicians might consider using influenza antiviral chemoprophylaxis for these persons. However, the benefits of influenza vaccination might outweigh the risks for certain persons who have a history of GBS and who also are at high risk for severe complications from influenza.
Thimerosal in multidose vials of IIV: Thimerosal, a mercury-containing antibacterial compound, is used in multidose vial preparations of IIV to reduce the likelihood of bacterial growth. While accumulating evidence shows no increased risks from exposure to thimerosal-containing vaccines (307-316), the U.S. Public Health Service and other organizations have recommended that efforts be made to eliminate or reduce the thimerosal content in vaccines as part of a strategy to reduce mercury exposures from all sources (307,308). LAIV, RIV, and most single-dose vial or syringe preparations of IIV are thimerosal-free. Persons recommended to receive IIV may receive any age-and risk factor-appropriate vaccine preparation, depending on availability.
# Live Attenuated Influenza Vaccines
# Shedding, transmission, and stability of vaccine viruses:
Data indicate that both children and adults vaccinated with LAIV can shed vaccine viruses after vaccination, although in lower amounts than occur typically with shedding of wild-type influenza viruses. Rarely, shed vaccine viruses can be transmitted from vaccine recipients to unvaccinated persons. However, serious illnesses have not been reported among unvaccinated persons who have been infected inadvertently with vaccine viruses. One study of 197 children aged 8 through 36 months in a child care center assessed transmissibility of vaccine viruses from 98 vaccinated children to the 99 unvaccinated children; 80% of vaccine recipients shed one or more virus strains (mean duration: 7.6 days). One influenza B vaccine virus strain isolate was recovered from a placebo recipient and was confirmed to be vaccine-type virus. The influenza B virus isolate retained the cold-adapted, temperature-sensitive, attenuated phenotype. The placebo recipient from whom the influenza B vaccine virus strain was isolated had symptoms of a mild upper respiratory illness. The estimated probability of acquiring vaccine virus after close contact with a single LAIV recipient in this population was 1%-2% (317).
Studies assessing shedding of vaccine virus have been based on viral cultures or RT-PCR detection of vaccine viruses in nasal aspirates from LAIV recipients. A study of 345 subjects aged 5 through 49 years who received LAIV indicated that 30% had detectable virus in nasal secretions obtained by nasal swabbing. The duration of virus shedding and the amount of virus shed was inversely correlated with age, and maximal shedding occurred within 2 days of vaccination. Symptoms reported after vaccination, including runny nose, headache, and sore throat, did not correlate with virus shedding (318).
Other smaller studies have reported similar findings (319,320). In an open-label study of 200 children aged 6 through 59 months who received a single dose of LAIV, shedding of at least one vaccine virus was detected on culture in 79% of children, and was more common among the younger recipients (89% of children aged 6 through 23 months compared with 69% of children aged 24 through 59 months) (321). The incidence of shedding was highest on day 2 postvaccination. Mean duration of shedding was 2.8 days (3.0 days and 2.7 days for the younger and older age groups, respectively); shedding detected after 11 days postvaccination was uncommon and nearly all instances occurred among children aged 6 through 23 months (an age group for which LAIV is not licensed). Titers of shed virus were low (321). Vaccine virus was detected from nasal secretions in one (2%) of 57 HIV-infected adults who received LAIV compared with none of 54 HIV-negative participants (322), and in three (13%) of 24 HIV-infected children compared with seven (28%) of 25 children who were not HIV-infected (323).
In clinical trials, viruses isolated from vaccine recipients have retained attenuated phenotypes. In one study, nasal and throat swab specimens were collected from 17 study participants for 2 weeks after vaccine receipt. Virus isolates were analyzed by multiple genetic techniques. All isolates retained the LAIV genotype after replication in the human host, and all retained the cold-adapted and temperature-sensitive phenotypes (324). A study conducted in a child care setting demonstrated that limited genetic change occurred in the LAIV strains following replication in the vaccine recipients (317).
Healthy children aged 2 through 18 years: In a subset of healthy children aged 60 through 71 months from one clinical trial, certain signs and symptoms were reported more often after the first dose among LAIV recipients (n = 214) than among placebo recipients (n = 95), including runny nose (48% and 44%, respectively); headache (18% and 12%, respectively); vomiting (5% and 3%, respectively); and myalgia (6% and 4%, respectively) (325). However, these differences were not statistically significant. In other trials, signs and symptoms reported after LAIV administration have included runny nose or nasal congestion (20%-75%), headache (2%-46%), fever (0-26%), vomiting (3%-13%), abdominal pain (2%), and myalgia (0-21%) (199,201,202,208,(326)(327)(328)(329). These symptoms were associated more often with the first dose and were self-limited. In a placebo-controlled trial in 9,689 children aged 1-17 years assessed pre-specified medically attended outcomes during the 42 days after vaccination, LAIV was associated with increased risk for asthma, upper respiratory infection, musculoskeletal pain, otitis media with effusion, and adenitis/adenopathy. The increased risk for wheezing events after LAIV was observed among children aged 18-35 months (RR: 4.06; 90% CI = 1.3-17.9). In this study, the proportion of serious adverse events was 0.2% in LAIV and placebo recipients; none of the serious adverse events was judged to be related to the vaccine by the study investigators (328).
In a randomized trial published in 2007, LAIV and IIV were compared among children aged 6 through 59 months (218). Children with medically diagnosed or treated wheezing in the 42 days before enrollment or with a history of severe asthma were excluded from participation. Among children aged 24 through 59 months who received LAIV, the proportion of children who experienced medically significant wheezing, using a prespecified definition, was not greater compared with those who received IIV (218). Wheezing was observed more frequently following the first dose among previously unvaccinated, younger LAIV recipients, primarily those aged <12 months; LAIV is not licensed for this age group. In a previous randomized placebo-controlled safety trial among children aged 12 months through 17 years without a history of asthma by parental report, an increased risk for asthma events (RR: 4.1; 95% CI = 1.3-17.9) was documented among 728 children aged 18 through 35 months who received LAIV. Of the 16 children with asthma-related events in this study, seven had a history of asthma on the basis of subsequent medical record review. None required hospitalization, and increased risk for asthma events were not observed in other age groups (328).
An open-label field trial was conducted among approximately 11,000 children aged 18 months through 18 years in which 18,780 doses of vaccine were administered between 1998-2002 For children aged 18 months through 4 years, no increase was reported in asthma visits 0-15 days after vaccination compared with the prevaccination period. A significant increase in asthma events was reported 15-42 days after vaccination, but only in vaccine year 1 (330). This trial later assessed LAIV safety among 2,196 children aged 18 months through 18 years with a history of intermittent wheezing who were otherwise healthy. Among these children, no increased risk was reported for medically attended acute respiratory illnesses, including acute asthma exacerbation, during the 0-14 or 0-42 days after LAIV compared with the pre-and postvaccination reference periods (331).
In a postlicensure observational study of 28,226 children aged 24 through 59 months, asthma and wheezing medically attended events were not statistically increased after LAIV during three influenza seasons (2007-08, 2008-09, and 2009-10) (332). Safety monitoring for wheezing events after LAIV is ongoing through VAERS.
Adults aged 19 through 49 years: In one clinical trial among a subset of healthy adults aged 18 through 49 years, signs and symptoms reported significantly more often (p<0.05; Fisher exact test) among LAIV recipients (n = 2,548) than placebo recipients (n = 1,290) within 7 days after each dose included cough (14% and 11%, respectively), runny nose (45% and 27%, respectively), sore throat (28% and 17%, respectively), chills (9% and 6%, respectively), and tiredness/weakness (26% and 22%, respectively) (325). A review of 460 reports to VAERS after distribution of approximately 2.5 million doses during the 2003-04 and 2004-05 influenza seasons did not indicate any new safety concerns (271). Few (9%) of the LAIV VAERS reports concerned serious adverse events; respiratory events were the most common conditions reported.
Persons at higher risk for influenza-related complications: Limited data assessing the safety of LAIV use for certain groups at higher risk for influenza-related complications are available. In one study of 57 HIV-infected persons aged 18 through 58 years with CD4+ counts >200 cells/mm3 who received LAIV, no serious adverse events attributable to vaccines were reported during a 1-month follow-up period (322). Similarly, one study demonstrated no significant difference in the frequency of adverse events or viral shedding among 24 HIV-infected children aged 1 through 8 years on effective antiretroviral therapy who were administered LAIV compared with 25 HIVuninfected children receiving LAIV (323). LAIV was welltolerated among adults aged ≥65 years with chronic medical conditions (333). Among 27 reports to VAERS involving inadvertent administration of LAIV to pregnant women during 1990-2009, no unusual patterns of maternal or fetal outcomes were observed (334); among 138 reports noted in a health insurance claims database, all outcomes occurred at similar rates to those observed in unvaccinated women (335). These findings suggest that persons at risk for influenza complications who have inadvertent exposure to LAIV are not expected to have significant adverse events or prolonged viral shedding and that persons who have contact with persons at higher risk for influenza-related complications may receive LAIV.
# Recombinant Influenza Vaccine
# Dosage, Administration, and Storage of Influenza Vaccines
The composition of influenza vaccines varies among different products. For all vaccines, package inserts should be consulted for authoritative guidance regarding storage conditions and administration. Influenza vaccine manufactured for a previous season should not be administered in any subsequent season and should not be administered after the expiration date.
# Inactivated Influenza Vaccine
IIVs are available in both single-dose and multidose formulations. Multidose vials contain the vaccine preservative thimerosal. Single-dose, unpreserved products should not be used for multiple doses. IIV should be stored at 35°F-46°F (2°C-8°C) and should not be frozen. IIV that has been frozen should be discarded. Dosage recommendations and schedules vary according to age group (Table 1). Vaccine prepared for a given influenza season should not be administered to provide protection for any subsequent season.
With the exception of Fluzone Intradermal (Sanofi Pasteur), IIV should be administered intramuscularly. For adults and older children, the deltoid is the preferred site. Infants and younger children should be vaccinated in the anterolateral thigh. Specific guidance regarding site and needle length for intramuscular administration can be found in the ACIP General Recommendations on Immunization (270). Fluzone Intradermal is administered intradermally, preferably over the deltoid muscle, using the delivery system included in the vaccine package. No influenza vaccines are licensed in the United States for administration via jet-injector device (336).
# Live Attenuated Influenza Vaccine (LAIV)
LAIV contains live, attenuated, cold-adapted, temperaturesensitive vaccine viruses which replicate efficiently only at temperatures present in the nasal mucosa. Providers should refer to the package insert, which contains additional information about the formulation of this vaccine and other vaccine components (210). LAIV does not contain thimerosal.
LAIV is shipped at 35°F-46°F (2°C-8°C). LAIV should be stored at 35°F-46°F (2°C-8°C) on receipt and can remain at that temperature until the expiration date is reached (210).
LAIV is intended for intranasal administration only. LAIV is supplied in a prefilled, single-use sprayer containing 0.2 mL of vaccine. Approximately 0.1 mL (i.e., half of the total sprayer contents) is sprayed into the first nostril while the recipient is in the upright position. An attached dose-divider clip is removed from the sprayer to administer the second half of the dose into the other nostril.
# Recombinant Influenza Vaccine
RIV should be stored refrigerated between 36°F-46°F (2°C-8°C). It should not be frozen. Vaccine which has frozen should be discarded. Vials should be protected from light. RIV has a shorter shelf life than IIV. Vaccine should not be used past its expiration date. RIV is administered intramuscularly.
# Influenza Vaccine Composition for the 2013-14 Season
All influenza vaccines licensed in the United States will contain hemagglutinin (HA) derived from influenza viruses antigenically identical to those recommended by FDA (337). This season, for the first time, both trivalent and quadrivalent influenza vaccines will be available in the United States Trivalent influenza vaccines will contain HA derived from three vaccine virus strains: one A(H1N1), one A(H3N2), and one B vaccine virus strain. Quadrivalent vaccines will contain the same the HA antigens as trivalent vaccines, but will also contain HA from a second B virus strain (one B virus strain from each lineage will be represented) (see Quadrivalent Influenza Vaccines).
Trivalent influenza vaccines will contain HA derived from the following:
- an A/California/7/2009 (H1N1)-like virus,
# New and Recently Approved Influenza Vaccine Products
Since early 2012, six new influenza vaccines have been approved for use by FDA. These include 1) Flumist Quadrivalent (MedImmune, Gaithersburg, Maryland), a quadrivalent live attenuated influenza vaccine (LAIV4);
# Quadrivalent Influenza Vaccines
All inactivated influenza vaccines available during recent seasons have been trivalent, containing A(H1N1), A(H3N2), and B viral antigens. There are two antigenically distinct lineages of influenza B viruses, referred to as Victoria and Yamagata lineages (13,14). Immunization against influenza B virus strains of one lineage provides only limited cross-protection against strains in the other lineage (338). Given this, and the challenge of predicting which B virus lineage will predominate during a given season, inclusion of two B virus strains (one from each lineage) in seasonal influenza vaccines may improve protection against circulating seasonal B virus strains. A recent modeling analysis indicates that the impact of a quadrivalent vaccine could result in a modest reduction in influenzaassociated outcomes (by 2,200-970,000 cases, 14-8,200 hospitalizations, and 1-485 deaths annually), depending upon adequate vaccine supply, coverage, effectiveness, and incidence of influenza associated with the two B lineages (339).
The World Health Organization (WHO) (340) and FDA (337) have made recommendations for inclusion of a second influenza B vaccine virus in quadrivalent influenza vaccines for the 2013-14 season. This strain will be included in addition to the A(H1N1), A(H3N2), and B vaccine virus strains contained in trivalent vaccines. For the 2013-14 season, quadrivalent influenza vaccines will include a Victoria lineage B/Brisbane/60/2008-like vaccine virus strain, in addition to the Yamagata lineage B/Massachusetts/2/2012-like virus strain contained in trivalent influenza vaccines.
As of August 15, 2013, four quadrivalent seasonal influenza vaccines are expected to be available for the 2013-14 influenza season. Other quadrivalent vaccines might become available in future seasons. New vaccines will be addressed in the ACIP influenza statement as they are approved and become commercially available.
Flumist Quadrivalent: Flumist Quadrivalent (MedImmune), an LAIV4, was approved by FDA in February 2012. All LAIV available in the United States for the 2013-14 season is expected to be the quadrivalent formulation. As with the prior trivalent formulation, Flumist Quadrivalent is approved for persons aged 2 through 49 years (210) and is an alternative for healthy, non-pregnant persons within this age range.
Flumist Quadrivalent contains 10 6.5 -10 7.5 fluorescent focus units (FFU) of live attenuated influenza virus reassortants of each of the four vaccine virus strains recommended for inclusion in quadrivalent influenza vaccines. It is supplied in a single-dose, 0.2 mL intranasal sprayer, and is administered intranasally (0.1 mL per nostril). Contraindications and precautions to the administration of FluMist are similar to those described for LAIV3 (see Contraindications and Precautions for the Use of LAIV; Table 2) (210).
In randomized trials comparing FluMist Quadrivalent with FluMist among children aged 2 through 17 years (210,341) and adults aged 18 through 49 years (210,342) with the exception of fever in children aged 2 through 8 years, similar rates of solicited adverse reactions were observed. Fever was more common after dose 1 in children aged 2 through 8 years following FluMist Quadrivalent (5.1%) compared with FluMist (3.1%). Assessment of the immunogenicity of Flumist Quadrivalent was based upon multicenter, randomized, double-blind, active-controlled non-inferiority studies of immunogenicity performed among children aged 2 through 17 years and adults. In immunogenicity assessments in each study, Flumist Quadrivalent was found to be non-inferior to FluMist. Comparison of the strain-specific serum HAI antibody geometric mean titers (GMTs) postvaccination indicated that the addition of the second B strain was not associated with immune interference to other strains included in the vaccine (344).
Fluarix Quadrivalent: Fluarix Quadrivalent (GlaxoSmithKline), an IIV4, was approved by FDA in December 2012. Fluarix Quadrivalent will be available alongside the trivalent formulation of Fluarix during the 2013-14 season. Both the trivalent and quadrivalent formulations of Fluarix are approved for persons aged ≥3 years (343). Fluarix Quadrivalent is formulated to contain 60 µg HA per 0.5 mL dose (15 µg HA of each of the four influenza virus strains recommended for inclusion in quadrivalent influenza vaccines). It is supplied in 0.5 mL single-dose prefilled syringes, and is administered by intramuscular injection. Contraindications and precautions to the administration of Fluarix Quadrivalent are similar to those described for the trivalent formulation of Fluarix (see Contraindications and Precautions for the Use of IIV; Table 2).
Two studies evaluated safety and immunogenicity of Fluarix Quadrivalent (343). Both involved subjects randomized to receive either Fluarix Quadrivalent or one of two formulations of comparator trivalent influenza vaccine (IIV3), each containing an influenza type B virus corresponding to one of the two type B viruses in Fluarix Quadrivalent. One study evaluated adults aged ≥18 years, and the other focused on children aged 3 through 17 years. In adults, the most common (≥10%) injection site adverse reaction was pain (36%); the most common systemic adverse events were muscle aches (16%), headache (16%), and fatigue (16%). Among children aged 3 through 17 years, the most common injection site adverse reactions were pain (44%), redness (23%), and swelling (19%). In children aged 3 through 5 years, the most common (≥10%) systemic adverse events were drowsiness (17%), irritability (17%), and loss of appetite (16%); in children aged 6 through 17 years, the most common systemic adverse events were fatigue (20%), muscle aches (18%), headache (16%), arthralgia (10%), and gastrointestinal symptoms (10%). Overall frequencies of most solicited adverse events associated with Fluzone Quadrivalent in these studies were generally similar to these reported for the comparator trivalent vaccines
In immunogenicity analyses, Fluarix Quadrivalent was noninferior to both comparator IIV3s based on adjusted GMTs and seroconversion rates. The antibody response to influenza B strains contained in Fluarix Quadrivalent was higher than the antibody response after vaccination with a trivalent IIV containing an influenza B strain from a different lineage. No evidence indicated that the addition of the second B strain resulted in immune interference to other strains included in the vaccine (343).
Fluzone Quadrivalent: Fluzone Quadrivalent (Sanofi Pasteur), an IIV4, was approved by FDA in June 2013. Fluzone Quadrivalent will be available alongside the trivalent formulation of Fluzone during the 2013-14 season. Both the trivalent and quadrivalent formulations of Fluzone are approved for persons aged ≥6 months (344).
Fluzone Quadrivalent is formulated to contain 60 µg HA per 0.5 mL dose (15 µg HA of each of the four influenza virus strains recommended for inclusion in quadrivalent influenza vaccines). It is available in three presentations (0.25 and 0.5 mL single-dose prefilled syringes and 0.5 mL single-dose vials), and is administered by intramuscular injection. Contraindications and precautions to the administration of Fluzone Quadrivalent are similar to those described for the trivalent formulation of Fluzone (see Contraindications and Precautions for the Use of IIV; Table 2).
Safety of Fluzone Quadrivalent was evaluated in three studies including participants aged ≥6 months who were randomized to receive either Fluzone Quadrivalent or one of two formulations of comparator trivalent influenza vaccine (IIV3), each containing an influenza type B virus corresponding to one of the two type B viruses in Fluzone Quadrivalent (344). Among children aged 6 through 35 months, the most common local reactions (reported in ≥10% of participants) included pain (57%), tenderness (54%), erythema (37%), and swelling (22%); the most common solicited systemic reactions were irritability (54%), abnormal crying (41%), drowsiness (38%), malaise (38%), myalgia (27%), appetite loss (32%), fever (14%), and vomiting (15%). Among children aged 3 through 8 years, the most frequently reported local reactions included pain (67%), erythema (34%), and swelling (25%); the most common solicited systemic reactions were malaise (32%), myalgia (39%), and headache (23%). Among adults aged ≥18 years, the most common injection site adverse reaction was pain (47% among those aged ≥18 years and 33% among those aged ≥65 years); the most common systemic adverse events were myalgia (24% among those aged ≥18 years and 18% among those aged ≥65 years), headache (16% among those aged ≥18 years and 13% among those aged ≥65 years), and malaise (11% among those in both age groups). Overall frequencies of most solicited adverse events associated with Fluzone Quadrivalent in these studies were generally similar to these reported for the comparator trivalent vaccines (344).
In immunogenicity analyses performed in these studies, Fluzone Quadrivalent was noninferior to both IIV3s based on adjusted GMTs and seroconversion rates for all four strains contained in the vaccine for children and for adults aged ≥18 years. For adults aged ≥65 years, GMTs were noninferior for all four strains; seroconversion rates were non-inferior to those for IIV3 for the included influenza A(H3N2), and both the Victoria and Yamagata B strains, but not for the included influenza A(H1N1). Overall, antibody response to influenza B strains contained in Fluzone Quadrivalent was higher than the antibody response after vaccination with a trivalent IIV containing an influenza B strain from a different lineage (344).
Flulaval Quadrivalent: Flulaval Quadrivalent (ID Biomedical Corporation/GlaxoSmithKline), an IIV4, was approved by FDA in August 2013. Fluarix Quadrivalent will be available alongside the trivalent formulation of Flulaval during the 2013-14 season. Both the trivalent and quadrivalent formulations of Flulaval are approved for persons aged ≥3 years (345).
Flulaval Quadrivalent is formulated to contain 60 µg HA per 0.5 mL dose (15 µg HA of each of the four influenza virus strains recommended for inclusion in quadrivalent influenza vaccines). It is supplied in 5.0 mL multi-dose vials and is administered by intramuscular injection. Contraindications and precautions to the administration of Fluarix Quadrivalent are similar to those described for the trivalent formulation of Flulaval (see Contraindications and Precautions for the Use of IIV; Table 2) (345).
In clinical studies, the most common (≥10%) solicited local adverse reaction to Flulaval Quadrivalent among adults was pain (60%); the most common solicited systemic adverse events were muscle aches (26%), headache (22%), fatigue (22%), and arthralgia (15%). Among children aged 3 through 17 years, the most common (≥10%) solicited local adverse reaction was pain (65%). Among children aged 3 through 4 years, the most common (≥10%) solicited systemic adverse events were irritability (26%), drowsiness (21%), and loss of appetite (17%). Among children aged 5 through 17 years, the most common (≥10%) solicited systemic adverse events were muscle aches (29%), fatigue (22%), headache (22%), arthralgia (13%), and gastrointestinal symptoms (10%) (345).
In immunogenicity studies, there was no evidence that the addition of a second B strain resulted in immune interference to other strains included in the vaccine. In a randomized, observer-blind, non-influenza vaccine-controlled study of FluLaval Quadrivakent vs. Havrix (hepatitis A vaccine, GlaxoSmithKline) conducted among children aged 3 through 8 years, vaccine efficacy was vaccine efficacy was vaccine efficacy was 55.4% (95% CI = 39.1-67.3) for RT-PCR-confirmed influenza, and 55.9% (97.5% CI = 35.4-69.9) for culture confirmed influenza (345).
# Vaccines Produced via Non-Egg Based Technologies
For the 2013-14 season, two new vaccines for adults will be available that are manufactured using newer technologies that minimize or avoid entirely the use of eggs. A primary advantage of these manufacturing methods is that they might permit more rapid scale up of vaccine production when needed (e.g., response to a pandemic). These include Flucelvax (Novartis, Cambridge, Massachusetts), which is produced using cell culture technology, and FluBlok (Protein Sciences, Meriden, Connecticut), which contains recombinant HA.
Flucelvax: Flucelvax, a ccIIV3, was approved by FDA in November 2012. It is a trivalent subunit IIV prepared from virus propagated in Madin Darby Canine Kidney (MDCK) cells. It is approved for persons aged ≥18 years (346).
Flucelvax contains a total of 45 µg HA (15 µg HA of each of the included influenza A(H1N1), influenza A(H3N2), and influenza B vaccine virus strains) per 0.5 mL dose. It is supplied in single-dose, prefilled syringes and is administered via intramuscular injection. Contraindications are similar to those for other IIVs (see Contraindications and Precautions for the Use of IIV; Table 2) (346).
In clinical studies of Flucelvax, the most common (≥10%) solicited adverse reactions among adults aged 18 through 64 years occurring within 7 days of vaccination were injection-site pain (28%), erythema at the injection site (13%), headache (16%), fatigue (12%), myalgia (11%), and malaise (10%). The most common (≥10%) solicited adverse reactions occurring in adults aged ≥65 years within 7 days of vaccination were erythema at the injection site (10%), fatigue (11%), headache (10%) and malaise (10%) (346)(347)(348). Injection site pain was reported significantly more frequently than with a licensed comparator egg-based IIV3 in one study, but was of mild or moderate severity in >99% of reports and usually resolved within 48 hours (348). In a multinational placebo-controlled study conducted during the 2007-08 influenza season among persons aged 18-49 years, Flucelvax was 83.8% effective (lower limit of one-sided 97% CI = 61%) against culture-confirmed influenza caused by viruses antigenically matched to the vaccine. In three studies in adults aged ≥18 years, Flucelvax demonstrated comparable immunogenicity to U.S.-licensed comparator vaccines for all three vaccine strains (346).
Although manufacture of the Flucelvax does not use eggs, the vaccine cannot be considered to be egg-free. Before beginning production, seed viruses are created using reference virus strains supplied by the World Health Organization that have been passaged in eggs. The total egg protein is estimated to be less than 50 femtograms (5x10 -14 grams or 5x10 -8 µg) total egg protein (of which a fraction is ovalbumin) per 0.5 mL dose of Flucelvax (Novartis, personal communication, 2013).
FluBlok: Approved in January 2013, FluBlok is a trivalent recombinant HA influenza vaccine (RIV3) containing purified HA proteins produced in a continuous insect cell line using a baculovirus vector. This process uses neither live influenza viruses nor eggs. Flublok is approved for persons aged 18 through 49 years (349).
FluBlok contains 135 µg HA per 0.5 mL dose (45 µg of each of the three HA antigens recommended for inclusion in trivalent influenza vaccines). It is supplied in 0.5 mL singledose vials and is administered by intramuscular injection. Contraindications include severe allergic reaction to any component of the vaccine (349).
Safety, immunogenicity, and efficacy of FluBlok were evaluated in randomized, double-blind, placebo-controlled studies (350,351) conducted among healthy adults aged 18 through 49 years that compared recombinant HA vaccines containing a total of 135 µg HA with placebo. The most frequently reported injection site reaction (reported in ≥10% of the 135 µg-dose recipients) was pain (>37%); the most common solicited systemic reactions were headache (>15%), fatigue (>15%), and myalgias (>11%) (349,351). Local pain and tenderness were reported significantly more frequently with FluBlok than placebo; however, 94% of reports of pain following FluBlok were rated as mild. In a randomized placebo-controlled efficacy study of the 135 µg HA dose of FluBlok conducted among healthy adults during the 2007-08 influenza season (349,351), estimated vaccine effectiveness for CDC-defined ILI with a positive culture for influenza virus was 75.4% (95% CI = -148.0%-99.5%) against matched strains; more precise estimation of vaccine effectiveness was not possible because 96% of isolates in this study did not antigenically match the strains represented in the vaccine (349). Estimated vaccine effectiveness without regard to match was 44.6% (95% CI = 18.8%-62.6%) (351).
# Recommendations for the Use of Influenza Vaccines, 2013-14 Influenza Season Groups Recommended for Vaccination
Routine annual influenza vaccination is recommended for all persons aged ≥6 months who do not have contraindications. Recommendations pertaining to the use of specific vaccines and populations are summarized below.
# Timing of Vaccination
In general, health-care providers should begin offering vaccination soon after vaccine becomes available and, if possible, by October. All children aged 6 months through 8 years who are recommended for 2 doses should receive their first dose as soon as possible after vaccine becomes available; these children should receive the second dose ≥4 weeks later. This practice increases the opportunity for both doses to be administered before or shortly after the onset of influenza activity. To avoid missed opportunities for vaccination, providers should offer vaccination during routine health-care visits or during hospitalizations whenever vaccine is available.
Vaccination efforts should be structured to ensure the vaccination of as many persons as possible before influenza activity in the community begins. In any given year, the optimal time to vaccinate cannot be determined precisely because influenza seasons vary in their timing and duration, and more than one outbreak might occur in a single community in a single year. In the United States, localized outbreaks that indicate the start of seasonal influenza activity can occur as early as October. However, in >80% of influenza seasons since 1976, peak influenza activity (which often is close to the midpoint of influenza activity for the season) has not occurred until January or later, and in >60% of seasons, the peak was in February or later (5).
In recent seasons, initial shipments of influenza vaccine have arrived to some vaccine providers as early as July. Very early availability of vaccine as compared with typical onset and peak of influenza activity raises questions related to the ideal time to begin vaccination. Antibody levels induced by vaccine decline over the months after vaccination (99,(352)(353)(354). Although a 2008 literature review found no clear evidence of more rapid decline among the elderly (105), a 2010 study noted significant decline in titers 6 months postvaccination among persons aged ≥65 years (though titers still met European Medicines Agency levels considered adequate for protection) (354). More recently, some investigators have estimated vaccine effectiveness over the course of a season, as a function of time since vaccination.
A case-control study conducted in Navarre, Spain, during the 2011-12 season revealed a decline in vaccine effectiveness from 61% (95% CI = 5-84) in the first 100 days postvaccination to 42% (95% CI = -39-75) for 100-119 days postvaccination and to -35% (95% CI = -211-41) thereafter. This decline primarily affected persons aged ≥65 years, among whom vaccine effectiveness declined from 85% (95% CI = -8-98) to 24% (95% CI = -224-82) to -208 (95% CI = -1,563-43) over these intervals. Most viruses isolated among those infected which were characterized did not match the vaccine strains (106). A case-control study conducted in the United Kingdom during the same season estimated an overall vaccine effectiveness against A(H3N2) of 53% (95% CI = 0-78) among those vaccinated less than 3 months, and 12% (95% CI = -31-41) for those vaccinated 3 months or more. The proportion of persons aged ≥65 years was too small to detect a substantial difference in vaccine effectiveness among this age group (355). Further evaluation of this effect in larger studies and in different seasons is needed. ACIP will continue to evaluate further data as they become available.
While delaying vaccination until later in the season might permit greater immunity later in the season, such deferral might result in missed opportunities to vaccinate, as well as difficulties in vaccinating a population within a more constrained time period. Community vaccination programs should balance maximizing likelihood of persistence of vaccineinduced protection through the season with avoiding missed opportunities to vaccinate or vaccinating after influenza circulation occurs.
Vaccination efforts should continue throughout the season, because the duration of the influenza season varies and influenza activity might not occur in certain communities until February or March. Providers should offer influenza vaccine routinely, and organized vaccination campaigns should continue throughout the influenza season, including after influenza activity has begun in the community. Vaccine administered in December or later, even if influenza activity has already begun, is likely to be beneficial in the majority of influenza seasons. The majority of adults have antibody protection against influenza virus infection within 2 weeks after vaccination (356,357).
# Available Vaccine Products and Indications
No preferential recommendation is made for one influenza vaccine product over another for persons for whom more than one product is otherwise appropriate. A variety of influenza vaccine products are available (Table 1), including (as of August 2013) six newly approved vaccines (see New and Recently Approved Influenza Vaccine Products). For many vaccine recipients, more than one type or brand of vaccine may be appropriate within indications and ACIP recommendations. Considerations for selection of a given vaccine when several appropriate options are available are discussed below. However, not all products are likely to be uniformly available in any practice setting or locality. For newer vaccines, supplies might be limited during the 2013-14 season; moreover, postmarketing safety and effectiveness data are as yet unavailable, prohibiting a full risk-benefit analysis of newer versus previously available products. Therefore, within these guidelines and approved indications, where more than one type of vaccine is appropriate and available, no preferential recommendation is made for use of any influenza vaccine product over another.
# Inactivated Influenza Vaccines
IIVs comprise a large group of products. For the 2013-14 season, most IIVs will be trivalent (IIV3), with some quadrivalent (IIV4) also available. Among IIV3 preparations, cell-culture based IIV will be available (ccIIV3). As a class, IIVs include products which might be administered to all persons aged ≥6 months. However, approved age indications for the various IIV products differ (Table 1). Only age-appropriate products should be administered. Providers should consult package inserts and updated CDC/ACIP guidance for current information. Of particular note, although Afluria (CSL Limited) is FDA-approved for children aged >5 years, CDC and ACIP recommend against use of Afluria in persons aged <9 years because of increased risk for febrile reactions noted in this age group with CSL's 2010 Southern Hemisphere IIV3 (228). If no other age-appropriate, licensed inactivated seasonal influenza vaccine is available for a child aged 5 through 8 years who has a medical condition that increases the child's risk for influenza complications, Afluria can be used; however, providers should discuss with the parents or caregivers the potential benefits and risks of influenza vaccination with Afluria in this age group before administering this vaccine (358).
All IIV preparations contain the same quantity of HA (15 µg per vaccine virus strain per 0.5 mL dose; 45 µg total), except Fluzone Intradermal and Fluzone High-Dose (Sanofi Pasteur). Fluzone Intradermal is approved for persons aged 18 through 64 years, and contains 9 µg of each HA per vaccine virus strain (27 µg total). Fluzone High-Dose is approved for persons aged ≥65 years and contains 60 µg of each HA per vaccine virus strain (180 µg total). Within specified age indications, ACIP expresses no preference for any given IIV over another.
The one IIV product licensed by FDA for children aged 6 through 36 months contains 0.25 mL/dose. The 0.25 mL dose may be administered from a prefilled single-dose syringe, single-use vial, or multi-dose vial of this age-appropriate formulation. Children aged 36 months through 18 years, and adults receiving IM preparations of IIV, should receive a 0.5 mL dose. If a pediatric vaccine dose (0.25 mL) is administered inadvertently to an adult, an additional pediatric dose (0.25 mL) should be administered to provide a full adult dose (0.5 mL). If the error is discovered later (after the patient has left the vaccination setting), an adult dose should be administered as soon as the patient can return. Vaccination with a formulation approved for adult use should be counted as a dose if inadvertently administered to a child (5).
With the exception of Fluzone Intradermal (Sanofi Pasteur), IIVs should be administered intramuscularly. For adults and older children, the deltoid is the preferred site. Infants and younger children should be vaccinated in the anterolateral thigh. Additional specific guidance regarding site selection and needle length for intramuscular administration are provided in ACIP's General Recommendations on Immunization (270). Fluzone Intradermal is administered intradermally, preferably over the deltoid muscle, using the included delivery system (240).
Trivalent versus Quadrivalent IIVs: For the first time, during the 2013-14 influenza season, both trivalent (IIV3) and quadrivalent (IIV4) IIVs will be available. The relative quantity of doses of IIV4 that will be available is not certain; however, it is expected that the supply of IIV4 might be limited. Quadrivalent vaccines are designed to provide broader protection against circulating influenza B viruses in seasons during which the B virus contained in trivalent vaccines is not an optimal match to the predominant circulating B viruses. However, vaccination should not be delayed if only IIV3 is available. No preference is expressed for IIV4 over IIV3.
IIVs and persons aged ≥65 years: For persons aged ≥65 years, either an age-appropriate standard-dose IIV (IIV3 or IIV4) or high-dose IIV3 are acceptable options. High-dose IIV3 (available as Fluzone High-Dose) is approved for persons aged ≥65 years. Immunogenicity data from three prelicensure studies among persons aged ≥65 years indicated that, compared with standard dose Fluzone, Fluzone High-Dose elicited higher HAI titers against all three influenza virus strains included in seasonal influenza vaccines recommended during the study period (178)(179)(180)359). Whether the higher postvaccination immune responses observed among Fluzone High-Dose vaccine recipients will result in greater protection against influenza illness is under study. Some solicited injection site and systemic adverse events were more frequent after vaccination with Fluzone High-Dose compared with standard Fluzone, but typically were mild and transient (178)(179)(180). No preferential recommendation is made for high-dose IIV over standard dose IIV for persons aged ≥65 years.
IIVs and egg allergy: With the exception of Flucelvax, IIVs are manufactured via propagation of virus in eggs and therefore might contain residual egg protein. Egg protein content (usually described as ovalbumin content as a surrogate measure) is not disclosed on all package inserts (Table 1); where not listed, this information generally can be obtained by contacting the manufacturer. Flucelvax is manufactured from virus propagated in Madin Darby Canine Kidney (MDCK) cells rather than embryonated eggs; however, before production seed virus is created using reference virus strains supplied by WHO, which have been passaged in eggs. Flucelvax can therefore not be considered egg-free. The total egg protein is estimated to be <50 femtograms (5x10 -14 grams) total egg protein (of which a fraction is ovalbumin) per 0.5 mL dose of Flucelvax (Novartis, unpublished data, 2013). Flucelvax can be administered to persons with a history of mild egg allergy (specifically, those who have experienced only hives following egg exposure; see Influenza Vaccination of Persons with Egg Allergy) who are aged ≥18 years and have no other contraindications. Because no data are available regarding the use of ccIIV among egg-allergic persons, and there is no established safe threshold for ovalbumin content in vaccines, ccIIV should be administered according to the guidance for other IIVs (see Influenza Vaccination of Persons with Egg Allergy).
Contraindications and precautions for use of IIVs: Manufacturer package inserts and updated CDC/ACIP guidance should be consulted for current information on contraindications and precautions for individual vaccine products. In general, IIV is contraindicated for, and should not be administered to, persons known to have anaphylactic hypersensitivity to eggs or to any vaccine components (Table 2). Prophylactic use of antiviral agents is an option for preventing influenza among such persons. Information about vaccine components is located in package inserts from each manufacturer.
Moderate or severe acute illness with or without fever is a general precaution for vaccination (270). GBS within 6 weeks following a previous dose of influenza vaccine is considered a precaution for use of influenza vaccines (Table 2).
# Recombinant Influenza Vaccine
One RIV product, FluBlok, a trivalent recombinant HA vaccine, is expected to be available for the 2013-14 influenza season. This RIV3 is administered by intramuscular injection, and is indicated for persons aged 18 through 49 years. RIV3 is manufactured without the use of influenza viruses; therefore, similarly to IIVs, no shedding of vaccine virus will occur. No preference is expressed for RIV versus IIV within specified indications.
RIV and egg allergy: The currently available RIV, FluBlok, is manufactured without the use of eggs, and does not carry a contraindication for egg allergy. Therefore, Flublok can be administered to persons with egg allergy of any severity who are aged 18 through 49 years and do not have other contraindications. Since 2011, ACIP has recommended that persons with a history of mild egg allergy (specifically, those who experience only hives following egg exposure) can receive IIV, with additional safety precautions. For such persons, vaccination should not be delayed if RIV is not available; IIV should be used in these settings, following the recommendations outlined (see Influenza Vaccination of Persons with Egg Allergy).
Contraindications and precautions for use of RIV: FluBlok is contraindicated in persons who have had a severe allergic reaction to any component of the vaccine. Moderate or severe acute illness with or without fever is a general precaution for vaccination (270). GBS within 6 weeks following a previous dose of influenza vaccine is considered a precaution for use of influenza vaccines (Table 2). FluBlok is not licensed for use in children aged 49 years.
# Live Attenuated Influenza Vaccine
One LAIV4 product, FluMist Quadrivalent (MedImmune), is expected to be available during the 2013-14 influenza season. Flumist is indicated for nonpregnant persons aged 2 through 49 years who do not have a medical condition that predisposes them to medical complications from influenza. No preference is indicated for LAIV versus other vaccines appropriate for this group.
LAIV is administered intranasally using the supplied 0.2 mL intranasal sprayer (0.1 mL in each nostril). If the vaccine recipient sneezes immediately after administration, the dose should not be repeated. However, if nasal congestion is present that might impede delivery of the vaccine to the nasopharyngeal mucosa, deferral of administration should be considered until resolution of the illness, or IIV should be administered instead.
LAIV versus IIV: Several randomized studies have evaluated the relative effectiveness of LAIV3 as compared with IIV3 (205,(212)(213)(214)218,220,221). Most studies conducted among adults have noted superior relative efficacy of IIV3 (205,(212)(213)(214). A significantly greater relative efficacy of LAIV3 as compared with IIV3 has been noted in several studies conducted among younger children, including a randomized, open label study among children aged 6 through 71 months (221), a randomized blinded trial of children aged 6 through 59 months (218), and a randomized blinded trial of children with asthma aged 6 through 17 years (220). However, no postmarketing safety data are yet available for the new quadrivalent formulation, LAIV4, which will be available for the first time during the 2013-14 season and is expected to replace LAIV3. Therefore, no preferential recommendation is made for LAIV4 over IIV for any age group at this time. This information will be updated as more data become available. Vaccination should not be delayed if LAIV is not available.
LAIV and egg allergy: Because of relative lack of data demonstrating safety of LAIV for persons with egg allergy, egg-allergic persons should receive IIV rather than LAIV (see Influenza Vaccination of Persons with Egg Allergy) (360).
Contraindications and precautions to the use of LAIV: LAIV is contraindicated for persons with a history of severe hypersensitivity reaction to any component of the vaccine or to a previous dose of any influenza vaccine, and in children and adolescents receiving concomitant aspirin therapy (Table 2). In addition, LAIV should not be administered to the following groups:
- children aged <2 years;
- adults aged ≥50 years;
- children aged 2 through 4 years whose parents or caregivers report that a health-care provider has told them during the preceding 12 months that their child had wheezing or asthma or whose medical record indicates a wheezing episode has occurred during the preceding 12 months (Table 1); - persons with asthma;
- children and adults who have chronic pulmonary, cardiovascular (except isolated hypertension), renal, hepatic, neurologic/neuromuscular, hematologic, or metabolic disorders; - children and adults who have immunosuppression (including immunosuppression caused by medications or by HIV); and - pregnant women. Moderate or severe acute illness with or without fever is a general precaution for vaccination (270). GBS within 6 weeks following a previous dose of influenza vaccine is considered a precaution for use of influenza vaccines.
# Persons at Risk for Medical Complications Attributable to Severe Influenza
Vaccination to prevent influenza is particularly important for persons who are at increased risk for severe complications from influenza, or at higher risk for influenza-related outpatient, ED, or hospital visits. When vaccine supply is limited, vaccination efforts should focus on delivering vaccination to the following persons (no hierarchy is implied by order of listing):
- all children aged 6 through 59 months;
- all persons aged ≥50 years;
# Vaccine Dose Considerations for Children Aged 6 Months Through 8 Years
Evidence from several studies indicates that children aged 6 months through 8 years require 2 doses of influenza vaccine (administered a minimum of 4 weeks apart) during their first season of vaccination to optimize immune response. In a study of children aged 5 through 8 years receiving trivalent inactivated influenza vaccine (IIV3) for the first time, the proportion of children with protective antibody responses was significantly higher (p<0.001 for influenza A(H1N1), p = 0.01 for influenza A(H3N2), and p<0.001 for influenza B) after 2 doses as compared with a single dose (115). Several studies have indicated that the time interval between two initial doses (from 4 weeks up to 1 year) of the same antigen may not be critical (363)(364)(365). However, because of the antigenic novelty of the 2009 influenza A(H1N1) pandemic virus, which is anticipated to continue circulating during the 2013-14 influenza season, exposure history to this vaccine virus antigen also must be considered. Children who last received seasonal (trivalent) influenza vaccine before the 2010-11 season but did not receive a vaccine containing 2009(H1N1) antigen (i.e., either in seasonal vaccine since July 2010 or monovalent 2009(H1N1) vaccine) will not have received this antigen. These children are recommended to receive 2 doses this season, even if 2 doses of seasonal influenza vaccine were received before the 2010-11 season. This recommendation is illustrated in the approaches outlined below. These recommendations are consistent with those of the American Academy of Pediatrics (366). Two approaches are recommended, both of which are acceptable.
The first approach (Figure 1), takes into consideration only doses of seasonal influenza vaccine received since July 1, 2010. This approach has the advantage of simplicity, particularly in settings in which it is difficult to ascertain vaccination history before the 2010-11 season. Using this approach, children aged In settings where adequate vaccination history from before the 2010-11 season is available, the second approach may be used. By this approach, if a child aged 6 months through 8 years is known to have received at least 2 doses of seasonal influenza vaccine during any prior season, and at least 1 dose of a 2009(H1N1)-containing vaccine (i.e., 2010-11, 2011-12, or 2012-13 seasonal vaccine or the monovalent 2009 vaccine) then the child needs only 1 dose for the 2013-14 season. Using this approach, children aged 6 months through 8 years need only 1 dose of vaccine in the 2013-14 season if they have received any of the following:
- 2 or more doses of seasonal influenza vaccine since July 1, 2010 or; - 2 or more doses of seasonal influenza vaccine before July 1, 2010 and 1 or more doses of monovalent 2009(H1N1) vaccine or; - 1 or more doses of seasonal influenza vaccine before July 1, 2010, and 1 or more doses of seasonal influenza vaccine since July 1, 2010. Children aged 6 months through 8 years for whom one of these conditions is not met require 2 doses in the 2013-14 season.
# Influenza Vaccination for Pregnant Women
Pregnant and postpartum women are at higher risk for severe illness and complications from influenza than women who are not pregnant because of changes in the immune system, heart, and lungs during pregnancy (367). Vaccination during pregnancy has been shown to protect infants from influenza (170,368), including infants aged <6 months, for whom no influenza vaccines are currently licensed (368)(369)(370). The ACIP and American College of Obstetricians and Gynecologists (ACOG) recommends that all women who are pregnant or who might be pregnant in the upcoming influenza season receive IIV because of this increased risk for serious illness and complications from influenza (371). Influenza vaccination can be administered at any time during pregnancy, before and during the influenza season.
Women who are or will be pregnant during influenza season should receive IIV. Live attenuated influenza vaccine (LAIV) is not recommended for use during pregnancy. Postpartum women can receive either LAIV or IIV. Pregnant and postpartum women do not need to avoid contact with persons recently vaccinated with LAIV.
# Influenza Vaccination of Persons With a History of Egg allergy
Severe allergic and anaphylactic reactions can occur in response to a number of influenza vaccine components, but such reactions are rare. With the exceptions of RIV and ccIIV3, currently available influenza vaccines are prepared by propagation of virus in embryonated eggs. A recent review of published data (including 4,172 patients, 513 of whom were reported to have a history of severe allergic reaction to egg) noted that no occurrences of anaphylaxis were reported, though some milder reactions did occur (372), suggesting that severe allergic reactions to egg-based influenza vaccines are unlikely. Vaccines containing as much as 0.7 µg/0.5 mL have been tolerated (360,373); however, a threshold below which no reactions would be expected is not known (360). Although ovalbumin content is not required to be disclosed on package inserts for vaccines used in the United States, manufacturers either report maximum albumin content in the package inserts or will provide this information on request. Among IIVs for which ovalbumin content was disclosed during the 2011-12 and 2012-13 seasons, reported maximum amounts were ≤1 µg/0.5 mL dose. Ovalbumin is not directly measured for Flucelvax, but it is estimated by calculation from the initial content in the reference virus strains to contain a maximum of 5x10 -8 µg/0.5 mL dose of total egg protein (Novartis, unpublished data, 2013). Flublok is egg-free. It should be noted, however, that neither Flucelvax nor Flublok are licensed for children aged <18 years.
# Surveillance for Anaphylaxis Following Influenza Vaccination
Following review of available data, since the 2011-12 influenza season, ACIP has recommended that persons with egg allergy who report only hives after egg exposure should receive IIV, with several additional safety measures (231); current FDA-approved packaging for influenza vaccines lists only severe hypersensitivity to egg protein as a contraindication to vaccination. Review of VAERS data for the 2011-12 and 2012-13 seasons indicated no disproportionate reporting of allergic reaction or anaphylaxis after influenza vaccination during the first two seasons the new recommendation was in place (374,375). However, during the 2012-13 influenza season, VAERS received one report containing a documented medical history of anaphylaxis following receipt of a first-ever split dose IIV in a child aged 12 months with atopy but no known prior egg ingestion in the past, who had a previous positive allergy skin prick test to ovalbumin. This child had previously received allergy testing attributed to a strong personal and family history of food allergies and other allergies (375). For the 2013-14 season, the recommendations which follow include guidance concerning persons who have no history of exposure to egg, but who have documented results potentially suggestive of egg allergy on previously performed allergy testing.
For the 2013-14 influenza season, ACIP recommends the following:
- Persons with a history of egg allergy who have experienced only hives after exposure to egg should receive influenza vaccine. Because relatively few data are available for use of LAIV in this setting, IIV or RIV should be used. RIV is egg-free and may be used for persons aged 18-49 years who have no other contraindications. However, IIV (egg-or cell-culture based) also may be used, with the following additional safety measures (Figure 2): -Vaccine should be administered by a health-care provider who is familiar with the potential manifestations of egg allergy; and -Vaccine recipients should be observed for at least 30 minutes for signs of a reaction after administration of each vaccine dose (360). - Other measures, such as dividing and administering the vaccine by a two-step approach and skin testing with vaccine, are not necessary (360). - Persons who report having had reactions to egg involving such symptoms as angioedema, respiratory distress, lightheadedness, or recurrent emesis; or who required epinephrine or another emergency medical intervention, particularly those that occurred immediately or within a short time (minutes to hours) after egg exposure, are more likely to have a serious systemic or anaphylactic reaction upon reexposure to egg proteins. These persons may receive RIV3, if aged 18 through 49 years and there are no other contraindications. If RIV3 is not available or the recipient is not within the indicated age range, such persons should be referred to a physician with expertise in the management of allergic conditions for further risk assessment before receipt of vaccine (Figure 2). - All vaccines should be administered in settings in which personnel and equipment for rapid recognition and treatment of anaphylaxis are available. ACIP recommends that all vaccination providers should be familiar with the office emergency plan (270). - Some persons who report allergy to egg might not be eggallergic. Those who are able to eat lightly cooked egg (e.g., scrambled egg) without reaction are unlikely to be allergic.
Egg-allergic persons might tolerate egg in baked products (e.g., bread or cake). Tolerance to egg-containing foods does not exclude the possibility of egg allergy (376). Egg allergy can be confirmed by a consistent medical history of adverse reactions to eggs and egg-containing foods, plus skin and/or blood testing for immunoglobulin E antibodies to egg proteins. - For persons who have no known history of exposure to egg, but who are suspected of being egg-allergic on the basis of previously performed allergy testing, consultation with a physician with expertise in the management of allergic conditions should be obtained before vaccination (Figure 2). Alternatively, RIV3 may be administered if the recipient is aged 18 through 49 years. - A previous severe allergic reaction to influenza vaccine, regardless of the component suspected to be responsible for the reaction, is a contraindication to future receipt of any influenza vaccine.
# Influenza Vaccines and Use of Influenza Antiviral Medications
Administration of IIV to persons receiving influenza antiviral drugs for treatment or chemoprophylaxis is acceptable. The effect on safety and effectiveness of LAIV co-administration with influenza antiviral medications has not been studied. However, because antiviral drugs reduce replication of influenza viruses, LAIV should not be administered until 48 hours after cessation of influenza antiviral therapy (210). If influenza antiviral medications are administered within 2 weeks after receipt of LAIV, the LAIV dose should be repeated 48 or more hours after the last dose of antiviral medication. Alternatively, persons receiving antiviral drugs within the period 2 days before to 14 days after vaccination with LAIV may be revaccinated another approved vaccine formulation (e.g., IIV or RIV).
# Concurrent Administration of Influenza Vaccine With Other Vaccines
Limited data are available on the concurrent administration of influenza vaccines with other live vaccines. Use of LAIV3 concurrently with measles, mumps, rubella (MMR) and varicella vaccine among children aged 12 through 15 months has been studied, and no interference with the immunogenicity to antigens in any of the vaccines was observed (210,377). Among adults aged ≥50 years, the safety and immunogenicity of zoster vaccine and IIV3 were similar whether administered simultaneously or sequentially spaced 4 weeks apart (378).
In the absence of specific data indicating interference, following ACIP's general recommendations for vaccination is prudent (270). Inactivated vaccines do not interfere with the immune response to other inactivated vaccines or to live vaccines. Inactivated or live vaccines can be administered simultaneously with LAIV. However, after administration of a live vaccine (such as LAIV), at least 4 weeks should pass before another live vaccine is administered.
# Sources of Information Regarding Influenza and Surveillance
Updated information regarding influenza surveillance, prevention, detection, and control is available at http:// www.cdc.gov/flu. U.S surveillance data are updated weekly during October-May on FluView (/ weekly). In addition, periodic updates regarding influenza are published in MMWR (). Additional information regarding influenza vaccine can be obtained from CDC by calling telephone 1-800-232-4636. State and local health departments should be consulted about availability of influenza vaccine, access to vaccination programs, information related to state or local influenza activity, reporting of influenza outbreaks and influenza-related pediatric deaths, and advice concerning outbreak control.
# Vaccine Adverse Event Reporting System
The National Childhood Vaccine Injury Act of 1986 requires health-care providers to report any adverse event listed by the vaccine manufacturer as a contraindication to further doses of the vaccine, or any adverse event listed in the VAERS Table of Reportable Events Following Vaccination (. hhs.gov/resources/VAERS_Table_of_Reportable_Events_ Following_Vaccination.pdf ) that occurs within the specified time period after vaccination. In addition to mandated reporting, health-care providers are encouraged to report any clinically significant adverse event following vaccination to VAERS. Information on how to report a vaccine adverse event is available at . Reports can be filed securely online, by mail, or by fax. A VAERS form can be downloaded from the VAERS website or requested by sending an e-mail message to [email protected], by calling telephone 1-800-822-7967, or by sending a request by facsimile to 1-877-721-0366. Additional information on VAERS or vaccine safety is available at or by calling telephone 1-800-822-7967.
# National Vaccine Injury Compensation Program
The National Vaccine Injury Compensation Program (VICP), established by the National Childhood Vaccine Injury Act of 1986, as amended, provides a mechanism through which compensation can be paid on behalf of a person determined to have been injured or to have died as a result of receiving a vaccine covered by VICP. The Vaccine Injury Table (available at . html) lists the vaccines covered by VICP and the associated injuries and conditions (including death) that may receive a legal presumption of causation. If the injury or condition is not on the Table, or does not occur within the specified time period on the Table, persons must prove that the vaccine caused the injury or condition. Eligibility for compensation is not affected by whether a covered vaccine is used off-label or inconsistently with recommendations.
For a claim to be eligible for compensation under the VICP, it must be filed within 3 years after the first symptom of the vaccine injury. Death claims must be filed within 2 years of the vaccine-related death and not more than 4 years after the start of the first symptom of the vaccine-related injury from which the death occurred. When a new vaccine is covered by VICP or when a new injury/condition is added to the Table, claims can be filed within 2 years from the date the vaccine or injury/condition is added to the Table for injuries or deaths that occurred up to 8 years before the Table change. Persons of all ages who receive a VICP-covered vaccine may be eligible to file a claim. Additional information is available at . hrsa.gov/vaccinecompensation or by calling 1-800-338-2382.
# Additional Information Regarding Prevention of Influenza in Specific Populations
- CDC. | ACIP is chartered as a federal advisory committee to provide expert external advice and guidance to the Director of the Centers for Disease Control and Prevention (CDC) on use of vaccines and related agents for the control of vaccine-preventable diseases in the civilian population of the United States. Recommendations for routine use of vaccines in children and adolescents are harmonized to the greatest extent possible with recommendations made by the American Academy of Pediatrics (AAP), the American Academy of Family Physicians (AAFP), and the American College of Obstetricians and Gynecologists. Recommendations for routine use of vaccines in adults are reviewed and approved by the American College of Physicians (ACP), AAFP, the American College of Obstetricians and Gynecologists, and the American College of Nurse-Midwives. ACIP recommendations adopted by the CDC Director become agency guidelines on the date published in the Morbidity and Mortality Weekly Report (MMWR).CDC, our planners, and our content experts disclose that they have no financial interests or other relationships with the manufacturers of commercial products, suppliers of commercial services, or commercial supporters. Presentations will not include any discussion of the unlabeled use of a product or a product under investigational use. CDC does not accept Recommendations and Reports# Introduction
Influenza viruses typically circulate widely in the United States annually from the late fall through early spring. Although most persons who become infected with influenza viruses will recover without sequelae, influenza can cause serious illness and death, particularly among persons aged ≥65 years and <2 years and those with medical conditions that confer high risk for complications from influenza (1)(2)(3)(4). During 30 seasons from the 1976-77 season through the 2005-06 season, estimated influenza-associated deaths ranged from 3,000 to 49,000 annually (4).
Annual influenza vaccination is the primary means of preventing influenza and its complications. There are many types of influenza vaccines, and the naming conventions have evolved over time (Box). Routine annual influenza vaccination for all persons aged ≥6 months who do not have contraindications has been recommended by the CDC and CDC's Advisory Committee on Immunization Practices (ACIP) since 2010 (5). This report provides updated recommendations and guidance for vaccination providers regarding the use of influenza vaccines for the 2013-14 season.
# Methods
ACIP provides annual recommendations for the prevention and control of influenza. The ACIP Influenza Work Group* meets by teleconference every 2-4 weeks throughout the year. Work Group membership includes several voting members of ACIP and representatives of ACIP Liaison Organizations. Discussions include topics such as influenza surveillance, vaccine effectiveness and safety, vaccine coverage, program feasibility, cost-effectiveness, and vaccine supply. Presentations are requested from invited experts, and published and unpublished data are discussed. For newly licensed influenza vaccines, discussion pertaining to new recommendations in this report included presentations of clinical data. For minor modifications to the recommendations for vaccination of persons with egg allergy, discussion included a review of influenza vaccine safety surveillance data from the Vaccine Adverse Event Reporting System (VAERS) for the 2012-13 season (see Surveillance for Anaphylaxis Following Influenza Vaccination).
Information presented in this report reflects recommendations presented during public meetings of the ACIP and approved on February 21, 2013, and on June 20, 2013. Meeting minutes and information on ACIP membership and conflicts of interest are available on the ACIP website (http://www.cdc.gov/ vaccines/acip/meetings/meetings-info.html). Modifications were made to the ACIP statement during subsequent review at CDC to update and clarify wording in the document. Further updates, if needed, will be posted at CDC's influenza website (http://www.cdc.gov/flu).
# Primary Changes and Updates in the Recommendations
Routine annual influenza vaccination of all persons aged ≥6 months continues to be recommended. No preferential recommendation is made for one influenza vaccine product over another for persons for whom more than one product is otherwise appropriate. Updated information and guidance in this document include the following:
• 2013-14 U.S. trivalent influenza vaccines will contain an A/California/7/2009 (H1N1)-like virus, an H3N2 virus antigenically like the cell-propagated prototype virus
# BOX. Naming conventions for influenza vaccines
• The former abbreviation TIV (Trivalent Inactivated Influenza Vaccine, previously used for inactivated influenza vaccines) has been replaced with the new abbreviation IIV (Inactivated Influenza Vaccine). For the 2013-14 season, IIVs as a class will include: -egg-based and cell culture-based trivalent inactivated influenza vaccines (IIV3), and -egg-based quadrivalent inactivated influenza vaccine (IIV4). • RIV refers to recombinant hemagglutinin influenza vaccine, available as a trivalent formulation (RIV3) for the 2013-14 season. • LAIV refers to live-attenuated influenza vaccine, available as a quadrivalent formulation (LAIV4) for the 2013-14 season. • LAIV, IIV, and RIV denote vaccine categories; numeric suffix specifies the number of antigens in the vaccine. • When necessary to refer specifically to cell culturebased vaccine, the prefix "cc" is used (e.g., "ccIIV3").
Diagnostics, Cambridge, Massachusetts]) is indicated for persons aged ≥18 years. -A recombinant hemagglutinin (HA) vaccine (RIV3;
FluBlok [Protein Sciences, Meriden, Connecticut]) is indicated for persons aged 18 through 49 years. • RIV3, an egg-free vaccine, is now an option for vaccination of persons aged 18 through 49 years with egg allergy of any severity. • For persons with egg allergy who have no known history of egg exposure but for whom results suggestive of egg allergy have been obtained on previous allergy testing, consultation with a physician with expertise in the management of allergic conditions is recommended before vaccination.
# Background and Epidemiology
# Biology of Influenza
Influenza A and B are the two types of influenza viruses that cause epidemic human disease. Influenza A viruses are categorized into subtypes based upon characterization of two surface antigens: hemagglutinin (HA) and neuraminidase (NA). Since 1977, influenza A(H1N1) viruses, influenza A(H3N2) viruses, and influenza B viruses have co-circulated globally. Influenza A virus subtypes and B viruses are further separated into groups on the basis of antigenic similarities. New influenza virus variants emerge via frequent antigenic change (i.e., antigenic drift), resulting from point mutations and recombination events that occur during viral replication (6). Immunity to surface antigens, HA and NA, reduces likelihood of infection (7,8). Antibody against one influenza virus type or subtype confers limited or no protection against another type or subtype. Moreover, antibody to one antigenic type or subtype of influenza virus might not confer immunity to a new antigenic variant of the same type or subtype (9). Frequent emergence of antigenic variants through antigenic drift is the virologic basis for seasonal epidemics, and necessitates consideration for adjustment of vaccine viruses each season.
Larger genetic changes, or antigenic shifts, occur among influenza A viruses, less frequently than antigenic drift events (6). The new or substantially different influenza A virus subtypes resulting from antigenic shifts have the potential to cause pandemics when they cause human illness, because they are efficiently transmitted from human to human in a sustained manner, and there is little or no pre-existing immunity among humans (6). In April 2009, human infections with a novel influenza A(H1N1) virus caused a worldwide pandemic. While not a new influenza A virus subtype, most humans had limited or no pre-existing antibody to key HA epitopes, and thus widespread transmission occurred. This virus is antigenically distinct from human influenza A(H1N1) viruses in circulation from 1977 through spring 2009. The HA gene is most closely related to that of contemporary influenza A viruses circulating among pigs during several preceding decades. This HA gene is believed to have evolved from the avian-origin 1918 pandemic influenza A(H1N1) virus, which is thought to have entered human and swine populations at about the same time (10,11).
Influenza B viruses are separated into two distinct genetic lineages (Yamagata and Victoria), but are not categorized into subtypes. Influenza B viruses undergo antigenic drift less rapidly than influenza A viruses (12). Influenza B viruses from both lineages have co-circulated in most recent influenza seasons (13,14). The trivalent influenza vaccines available in recent seasons have contained one influenza B virus, representing only one lineage. The proportion of circulating influenza B viruses that are of the lineage represented in the vaccine has varied. During the 10 seasons from 2001-02 through 2010-11, the predominant circulating influenza B virus lineage was represented in the trivalent vaccine in only five seasons (15).
# Health-Care Use, Hospitalizations, and Deaths Attributed to Influenza
In the United States, annual epidemics of influenza typically occur during the fall or winter months. Studies that report rates of clinical outcomes without laboratory confirmation of influenza (e.g., respiratory illness requiring hospitalization during influenza season) can be difficult to interpret because of coincident circulation of other respiratory pathogens (e.g., respiratory syncytial virus) (16)(17)(18). However, increases in health-care provider visits for acute febrile respiratory illness occur annually, coinciding with periods of increased influenza activity, making influenza-like illness surveillance systems valuable in understanding the seasonal and geographic occurrence of influenza each year (19).
In typical winter influenza seasons, increases in deaths and hospitalizations are observed during periods when influenza viruses are circulating. Excess deaths and hospitalizations occurring during influenza season have been estimated for decades. Although not all excess events occurring during periods when influenza viruses are circulating can be attributed to influenza, these estimates are useful for following season-toseason trends in influenza-associated outcomes. Estimates that include only outcomes attributed to pneumonia and influenza likely underestimate the burden of severe illnesses that are at least partly attributable to influenza because this category excludes deaths caused by exacerbations of underlying cardiac and pulmonary conditions that are associated with influenza virus infection (20)(21)(22). Thus, use of a broader category of respiratory and circulatory excess events are at times preferred for influenza burden estimates. During seasonal influenza epidemics from 1979-80 through 2000-01, the estimated annual overall number of influenza-associated hospitalizations in the United States ranged from approximately 55,000 to 431,000 per annual epidemic (mean: 226,000) (21). Between the 1976-77 season and 2006-07 season, estimated annual deaths attributable to influenza ranged from 3,000 to 49,000 each season (4).
Influenza viruses cause illness among persons of all ages (1)(2)(3)(23)(24)(25). Infection rates are highest among children, but complications, hospitalizations, and deaths from seasonal influenza are typically greatest among persons aged ≥65 years, children aged <5 years and particularly those aged <2 years, and persons of any age who have medical conditions that confer increased risk for complications from influenza (1,2,(25)(26)(27)(28)(29). Estimated rates of influenza-associated deaths vary substantially by age group. During 1990-1999, estimated average rates of influenza-associated pulmonary and circulatory deaths per 100,000 persons were 0.4-0.6 among persons aged 0 through 49 years, 7.5 among persons aged 50 through 64 years, and 98.3 among persons aged ≥65 years (20).
Children: Among children aged <5 years, influenza is a common cause of outpatient medical visits. During the 2002-03 and 2003-04 seasons, the percentage of visits among children aged <5 years with acute respiratory illness or fever caused by laboratory-confirmed influenza ranged from 10%-19% of medical office visits and 6%-29% of emergency department (ED) visits. From these data, the rate of clinic visits for influenza was estimated to be 50-95 visits per 1,000 children aged <5 years, and the rate of ED visits was 6-27 visits per 1,000 children aged <5 years (3). In a retrospective cohort study of children aged <15 years covering 19 consecutive seasons, an annual average of 6-15 additional outpatient visits and 3-9 additional antibiotic courses per 100 children were estimated to be attributable to influenza (29). During 1993During -2004 in the Boston area, the rate of ED visits for respiratory illness attributed to influenza based on viral surveillance data among children aged 6 months through 7 years during the winter respiratory illness season ranged from 22.1 per 1,000 children aged 6-23 months to 5.4 per 1,000 children aged 5 through 7 years (30).
Estimated rates of influenza-associated hospitalization are substantially higher among infants and younger children than among older children and are similar to rates for other groups considered at higher risk for influenza-related complications (31)(32)(33)(34)(35)(36), including persons aged ≥65 years. During 1993-2008, the estimated rate of influenza-associated hospitalizations was 91.5 per 100,000 for among children aged <1 year and 21.9 per 100,000 for children aged 1 through 4 years (37). Population-based studies that measured hospitalization rates for laboratory-confirmed influenza in young children have documented hospitalization rates that are similar to or higher than rates derived from studies that analyzed hospital discharge data (3,35,(38)(39)(40). Annual hospitalization rates for laboratoryconfirmed influenza decrease with increasing age, ranging from 240-720 hospitalizations per 100,000 children aged <6 months to approximately 20 hospitalizations per 100,000 children aged 2 through 5 years (3). Hospitalization rates for children aged <5 years with high-risk medical conditions are higher, with estimates of 250-500 hospitalizations per 100,000 children in some studies (27,41,42).
In the United States, death associated with laboratoryconfirmed influenza virus infection among children aged <18 years has been a nationally reportable condition since 2004 (43). Since reporting began, the annual number of influenza-associated pediatric deaths during regular influenza seasons has ranged from 34 deaths during the 2011-12 season to 122 deaths during the 2010-11 season (43,44). However, between April 15, 2009 and October 2, 2010 (the period of the 2009 H1N1 influenza pandemic), approximately 300 deaths attributed to laboratoryconfirmed 2009 H1N1 influenza occurred among children aged <18 years (44), the majority of whom had one or more underlying medical conditions previously associated with conferring a greater risk for influenza complications (45).
Adults: Hospitalization rates during typical influenza seasons are highest for adults aged ≥65 years. One retrospective analysis of data from managed-care organizations collected during 1996-2000 estimated that the risk during influenza season among persons aged ≥65 years with high-risk underlying medical conditions was approximately 560 influenzaassociated hospitalizations per 100,000 persons compared with approximately 190 per 100,000 among lower risk persons in this age group. Persons aged 50 through 64 years who have underlying medical conditions also were at substantially increased risk for hospitalization during influenza season compared with healthy adults aged 50 through 64 years (26).
Deaths associated with influenza are also most frequent among older adults. From the 1976-77 season through the 2006-07 season, an estimated yearly average of 21,098 influenza-related deaths occurred among adults aged ≥65 years, comprising approximately 90% of estimated annual average deaths across all age groups. In comparison, the average annual mortality was estimated to be 124 deaths among persons aged <19 years and 2,385 deaths among persons aged 19 through 64 years (4).
Among healthy younger adults, illness caused by seasonal influenza is typically less severe and results less frequently in hospitalization, as compared with children aged <5 years, adults aged ≥65 years, pregnant women, or persons with chronic medical conditions. However, influenza is an important cause of outpatient medical visits and worker absenteeism among healthy adults aged 19 through 49 years. In one economic modeling analysis, the average annual burden of seasonal influenza among adults aged 18 through 49 years without medical conditions that confer a higher risk for influenza complications was estimated to include approximately 5 million illnesses, 2.4 million outpatient visits, 32,000 hospitalizations, and 680 deaths (46). Studies of worker vaccination programs have reported lower rates of influenza like illness (ILI) (47,48), lost work time (47)(48)(49)(50), and healthcare visits (48,49) in association with vaccination.
During the 2009 H1N1 pandemic, adults aged <65 years appeared to be at higher risk for influenza-related complications (51,52) compared with typical influenza seasons. In addition, obesity (body-mass index [BMI]≥30) and particularly morbid obesity (BMI≥40) appeared to be risk factors for hospitalization and death in some studies (51)(52)(53)(54)(55). Other epidemiologic features of the 2009 H1N1 pandemic underscored racial and ethnic disparities in the risk for influenza-related complications among adults, including higher rates of hospitalization for blacks and higher rates of deaths among American Indians/Alaska Natives and indigenous populations in other countries (56)(57)(58)(59)(60)(61). These disparities might be attributable in part to the higher prevalence of underlying medical conditions or disparities in medical care among these racial/ethnic groups (61,62).
The duration of influenza symptoms might be prolonged and the severity of influenza illness increased among persons with human immunodeficiency virus (HIV) infection (63)(64)(65)(66). A retrospective study of women aged 15 through 64 years enrolled in Tennessee's Medicaid program determined that the attributable risk for cardiopulmonary hospitalizations and deaths among women with HIV infection was higher during influenza seasons than it was either before or after periods when influenza viruses were circulating. The risk for these events was higher for HIV-infected women (influenza attributable risk 152 per 10,000) than it was for women with other underlying medical conditions evaluated (including an influenza-attributable risk of 35 per 10,000 for chronic renal disease, 27 per 10,000 for chronic heart disease, and 25 per 10,000 for chronic lung disease) (67). Another study estimated that the excess death rate attributable to influenza was 94-146 deaths per 100,000 persons with acquired immune deficiency syndrome (AIDS) compared with 0.9-1.0 deaths per 100,000 persons aged 25 through 54 years and 64-70 deaths per 100,000 persons in the general population aged ≥65 years (68).
Increased severity of influenza among pregnant women was reported during the pandemics of 1918-1919, 1957-1958, and 2009-2010 (69-74). Severe infections among postpartum (delivered within previous 2 weeks) women also were observed in the 2009-10 pandemic (69,73). In a case series conducted during the 2009 H1N1 pandemic, 56 deaths were reported among 280 pregnant women admitted to intensive care units. Among the deaths, 36 (64%) occurred in the third trimester. Pregnant women who were treated with antivirals more than 4 days after symptom onset were more likely to be admitted to an intensive care unit (57% versus 9%; relative risk [RR] = 6.0; 95% confidence interval [CI] 3.5-10.6) than those treated within 2 days after symptom onset (75).
Case reports and some observational studies suggest that pregnancy also increases the risk for seasonal influenza complications for the mother (76)(77)(78). Most of these studies have measured changes in excess hospitalizations or outpatient visits for respiratory illness during influenza season rather than laboratory-confirmed influenza. A retrospective cohort study of approximately 134,000 pregnant women conducted in Nova Scotia during 1990-2002 compared medical record data for pregnant women to data from the same women during the year before pregnancy. Among 134,188 pregnant women, 510 (0.4%) were hospitalized, and 33,775 (25%) visited a clinician during pregnancy for a respiratory illness (78).
With regard to pregnancy outcomes, one cohort study noted that pregnant women with respiratory hospitalizations during the influenza season did not have an increase in adverse perinatal outcomes or delivery complications compared with pregnant controls without an influenza hospitalization (79); another study indicated an increase in delivery complications, including fetal distress, preterm labor, and cesarean delivery (80). However, infants born to women with laboratory-confirmed influenza during pregnancy do not have higher rates of low birthweight, congenital abnormalities, or lower Apgar scores compared with infants born to uninfected women (81,82).
# Influenza Vaccine Effectiveness Evaluating Influenza Vaccine Efficacy and Effectiveness Studies
Estimates of efficacy (i.e., prevention of illness among vaccinated persons enrolled in controlled clinical trials) and vaccine effectiveness (i.e., prevention of illness in vaccinated populations) of influenza vaccines depend on many factors, including the age and immunocompetence of the vaccine recipient, the degree of similarity between the viruses in the vaccine and those in circulation, study design, and the outcome being measured. Studies of influenza vaccine efficacy and effectiveness have used a variety of outcome measures, including the prevention of medically attended acute respiratory illness (MAARI), prevention of laboratory-confirmed influenza illness, prevention of influenza or pneumonia-associated hospitalizations or deaths, or prevention of seroconversion to circulating influenza virus strains. Efficacy or effectiveness for more specific outcomes such as laboratory-confirmed influenza typically will be higher than for less specific outcomes such as MAARI because the causes of MAARI include infections with other pathogens that influenza vaccination would not be expected to prevent (83). Observational studies that compare less-specific outcomes among vaccinated populations to those among unvaccinated populations might be more subject to biases than studies using laboratory outcomes. For example, an observational study that finds that influenza vaccination reduces overall mortality among elderly persons might be biased if healthier persons in the study are more likely to be vaccinated, and thus less likely to die for any reason (84,85). For studies assessing laboratory-confirmed outcomes, estimates of vaccine efficacy may also be affected be the sensitivity of the diagnostic tests used. A 2012 simulation study found that for each percentage point decrease in diagnostic test specificity for influenza virus infection, vaccine effectiveness would be underestimated by approximately 4% (86). Randomized controlled trials that measure laboratory-confirmed influenza virus infections as the outcome are the most persuasive evidence of vaccine efficacy, but such data are not available for all populations. Such trials might be difficult to conduct among groups recommended to receive vaccine annually.
# Immune Response Following Vaccination
Humoral and cell-mediated responses to influenza vaccination have been studied among children and adults. Serum antibodies (7,87) are considered to be correlates of vaccine-induced protection. Increased levels of antibody induced by vaccination decrease the risk for illness caused by strains that are antigenically similar to those strains of the same type or subtype included in the vaccine (8,(88)(89)(90). Most healthy children and adults have high titers of strainspecific antibody after vaccination (89,91). However, although immune correlates such as achievement of certain antibody titers after vaccination correlate well with immunity on a population level, reaching certain antibody threshold (typically defined as a hemagglutination inhibition antibody or HAI titer of 32 or 40) might not predict protection from infection on the individual level.
While LAIV induces lower levels of serum antibodies compared with IIV, LAIV more effectively induces cellular immune responses than IIV. The magnitude of this effect differs among adults and children. One study of children aged 6 months through 9 years and adults aged 22 through 49 years noted a significant increase in influenza A-specific interferon ϒ-producing CD4+ and CD8+ T-cells among children following LAIV but not following IIV. No significant increase in these parameters was noted among adults following either vaccine (92).
Antibody elicited by vaccination is generally strain-specific, such that antibody against one influenza virus type or subtype confers limited or no protection against another type or subtype, nor does it confer protection against antigenic variants of the same virus that arise by antigenic drift. Cellular immune responses might arise from more conserved viral epitopes and thus potentially provide broader heterosubtypic immunity. Administration of 2007-08 seasonal vaccine to adults boosted T-cell responses to both seasonal and pandemic 2009(H1N1) HA (93); this effect was significantly greater for LAIV. Among children aged 6 through 35 months, LAIV (but not IIV) induced T-cell responses to highly conserved viral peptides (94).
# Duration of Immunity
The composition of influenza vaccines is changed in most seasons, with one or more vaccine strains replaced annually to provide protection against viruses that are anticipated to circulate. Evidence from some clinical trials indicates that that protection against viruses that are antigenically similar to those contained in the vaccine extends at least for 6-8 months, particularly in nonelderly populations. In some situations, duration of immunity might be longer, and such effects can be detected if circulating influenza virus strains remain antigenically similar for multiple seasons. For example, 3 years after vaccination with the A/Hong Kong/68 vaccine (i.e., the 1968 pandemic vaccine), effectiveness was 67% for prevention of influenza caused by the A/Hong Kong/68 virus (95). In randomized trials conducted among healthy college students, immunization with IIV provided 92% and 100% efficacy against influenza H3N2 and H1N1 illnesses, respectively, during the first year after vaccination, and a 68% reduction against H1N1 illness during the second year after vaccination (when the predominant circulating virus was H1N1) without revaccination (96). In a similar study of young adults conducted in 1986-1987, IIV reduced influenza A(H1N1) illness by 75% in the first year after vaccination, reduced H3N2 illness by 45% in the second year, and reduced H1N1 illness by 61% during the third year after vaccination (96). Serum HAI influenza antibodies and nasal IgA elicited by vaccination remain detectable in children vaccinated with LAIV for >1 year after vaccination (97). In one community-based nonrandomized open-label trial, continued protection from MAARI during the 2000-01 influenza season was demonstrated in children who received only a single dose of LAIV during the previous 1999-00 season (98). A review of four trials (three randomized blinded and one open-label) of LAIV conducted among young children aged 6 months through 18 years reported that efficacy against A(H1N1) and A(H3N2) was similar at 9-12 months postvaccination to efficacy at 1-<5 months postvaccination; for B strains efficacy was still comparable at 5-7 months postvaccination. Two randomized trials and one open label study reported residual efficacy through a second season without revaccination, albeit at lower levels than observed in the first season (98)(99)(100)(101)(102).
Adults aged ≥65 years typically have diminished immune responses to influenza vaccination compared with healthy younger adults (103,104). One review of the published literature concluded that no clear evidence existed that vaccine-induced antibody declined more rapidly in the elderly (105). A case-control study conducted in Navarre, Spain during the 2011-12 season revealed a decline in vaccine effectiveness from 61% (95% CI = 5-84) in the first 100 days postvaccination, to 42% (95% CI = -39-75) for days 110-119 days postvaccination, to -35% (95% CI = -211-41) thereafter. This decline primarily affected persons aged ≥65 years, among whom effectiveness declined from 85% (95% CI = -8-98) to 24% (95% CI = -224-82) to -208 (95% CI = -1,563-43) over the same time intervals. However, most viruses isolated among infected vaccinees did not match the vaccine strains (106). In addition, the wide CIs surrounding the point estimates indicate that larger studies are needed to further characterize the magnitude of possible declines in vaccine effectiveness through the season. Limited available data suggest that administration of additional vaccine doses during the same season does not increase the antibody response among elderly vaccinees (107).
# Immunogenicity, Efficacy, and Effectiveness of IIV
Inactivated vaccines, which are administered by intramuscular or intradermal injection, contain nonreplicating virus. Immunogenicity, effectiveness, and efficacy have been evaluated in children and adults, although fewer data from randomized studies are available for some age groups (e.g., persons aged ≥65 years).
# Children
Children aged ≥6 months typically develop protective levels of antibodies against specific influenza virus strains after receiving the recommended number of doses of seasonal inactivated influenza vaccine (87,91,(108)(109)(110)(111). Immunogenicity studies using the influenza A(H1N1) 2009 monovalent vaccine indicated that 80%-95% of vaccinated children developed protective antibody levels to the 2009 H1N1 influenza virus after 2 doses (112,113); response after 1 dose was 50% for children aged 6 through 35 months and 75% for those aged 3 through 9 years (114). Studies involving seasonal inactivated influenza vaccine among young children have demonstrated that 2 vaccine doses provide better protection than 1 dose during the first season a child is vaccinated. In a study of children aged 5 through 8 years who received trivalent inactivated vaccine (TIV) for the first time, the proportion of children with protective antibody responses was significantly higher after 2 doses than after 1 dose and higher after 2 doses than after 1 dose of TIV for each antigen (p = 0.001 for influenza A[H1N1]; p = 0.01 for influenza A[H3N2]; and p = 0 0.001 for influenza B) (115). Vaccine effectiveness is lower among children aged <5 years who have never received influenza vaccine previously or who received only 1 dose in their first year of vaccination than it is among children who received 2 doses in their first year of being vaccinated. Two retrospective studies of children who had received only 1 dose of IIV in their first year of being vaccinated determined that no decrease was observed in ILI-related office visits compared with unvaccinated children (116,117). Similar results were reported in a case-control study of approximately 2,500 children aged 6 through 59 months in which laboratory-confirmed influenza was the outcome measured (118). The results of these studies support the recommendation that all children aged 6 months through 8 years who are being vaccinated for the first time should receive 2 vaccine doses separated by at least 4 weeks.
Some studies suggest that antibody responses among children at higher risk for influenza-related complications (i.e., children with chronic medical conditions) are lower than those reported typically among healthy children (119,120). However, another study found that antibody responses among children with asthma are similar to those of healthy children and are not substantially altered during asthma exacerbations requiring short-term prednisone treatment (121).
Estimates of the efficacy or effectiveness of inactivated vaccine among children aged ≥6 months vary by season and study design. Limited efficacy data are available for children from studies that used culture-or reverse transcriptionpolymerase chain reaction (RT-PCR)-confirmed influenza virus infections as the primary outcome. A recent large randomized trial compared rates of RT-PCR-confirmed influenza virus infections among 4,707 children aged 6 through 71 months who received inactivated vaccine, inactivated vaccine with MF59 oil-in-water adjuvant, or a control vaccine (meningococcal conjugate vaccine or tick-borne encephalitis vaccine). During the two seasons of the study (2007-08 and 2008-09), efficacy of inactivated vaccine versus control vaccine was 43% (95% CI = 15%-61%) and of inactivated vaccine plus MF59 versus control was 86% (95% CI = 74%-93%) (122). In a randomized trial conducted during five influenza seasons (1985)(1986)(1987)(1988)(1989)(1990) in the United States among children aged 1 through 15 years, receipt of inactivated vaccine reduced culture-confirmed influenza A by 77% (95% CI = 20%-93%) (89). A single season placebo-controlled study that enrolled 192 children aged 3 through 19 years found the efficacy of inactivated vaccine was 56% among healthy children aged 3 through 9 years and 100% among healthy children and adolescents aged 10 through 18 years (123); influenza infection was defined either by viral culture or, in the absence of a positive culture, by a postseason antibody rise in HI titer among symptomatic children from whom no other virus was isolated and whose symptoms began within 10 days of isolation of influenza from a household contact or during peak influenza activity in the community. In a randomized, double-blind, placebo-controlled trial conducted during two influenza seasons among 786 children aged 6 through 24 months, estimated efficacy was 66% (95% CI = 34%-82%) against culture-confirmed influenza illness during the 1999-00 influenza season but did not reduce culture-confirmed influenza illness significantly during the 2000-01 season, when influenza attack rates were lower (3% versus 16% during the 1999-00 season) (124).
Studies using a serological definition of influenza virus infection have raised concerns that dependence on a serological diagnosis of influenza in clinical trials might lead to overestimation of vaccine efficacy because of an "antibody ceiling" effect in adult subjects with historic exposures to both natural infections and vaccination. This could result in the decreased likelihood that antibody increases can be observed in vaccinated subjects after influenza infection with circulating viruses, as compared with adult subjects in control arms of trials. Thus, vaccinated subjects might be less likely to show a fourfold increase in antibody levels can after influenza infection with circulating viruses compared with unvaccinated subjects in such studies. Whether there is a substantial antibody ceiling effect in children, particularly younger children without extensive experience with influenza antigens, is not known.
Several observational studies to assess vaccine effectiveness were conducted during the 2003-04 influenza season, when the match between vaccine virus antigens and circulating viruses was suboptimal. A case-control study conducted during the 2003-04 season estimated vaccine effectiveness among fully vaccinated children aged 6 through 59 months to be 49% (95% CI = 30%-60%) against influenza diagnosed by a positive antigen-detection test with a specificity of 96% (125). An observational study among children aged 6 through 59 months with culture-or PCR-confirmed influenza compared with children who tested negative for influenza reported vaccine effectiveness of 44% (95% CI = -42%-78%) in the 2003-04 influenza season and 57% (95% CI = 28%-74%) during the 2004-05 season (118). Receipt of only 1 vaccine dose among children being vaccinated for the first time was not effective in either season. A retrospective cohort study conducted during the 2003-04 season among approximately 30,000 children aged 6 months through 8 years reported vaccine effectiveness of 51% (95% CI = 33%-64%) against medically attended, clinically diagnosed pneumonia or influenza (i.e., there was no laboratory confirmation of influenza infection). Estimated vaccine effectiveness was 49% (95% CI = 9%-71%) among children aged 6 through 23 months (117). Another retrospective cohort study of similar size that used a syndromically defined outcome and was conducted during the 2003-04 season among healthy children aged 6 through 21 months estimated effectiveness of 2 IIV doses to be 87% (95% CI = 78%-92%) against pneumonia/ influenza-related office visits (116). It is difficult to reconcile the high effectiveness estimate in this study with others from the same season because it focused on younger children and used a nonspecific outcome.
Among children, IIV effectiveness might be lower in very young children compared with older children (122,126). A 2012 systematic review of published studies estimated vaccine effectiveness among healthy children was 40% (95% CI = 6%-61%) for those aged 6 through 23 months and 60% (95% CI = 30%-78%) for those aged 24 through 59 month (127). However, during the 2010-11 season, when all three vaccine virus strains appeared antigenically similar to circulating strains, vaccine effectiveness among children was similar to that observed for those of all ages in a large multisite observational study that used RT-PCR-confirmed medically attended influenza virus infections as the outcome (all ages: 60%; 95% CI = 54%-66%; vaccine effectiveness among children aged 6 months through 2 years: 58%; 95% CI = 31%-74%; among children aged 3 through 8 years: 69%; 95% CI = 56%-77%) (128).
Because of the long-standing recommendation for annual influenza vaccination of immunosuppressed children and those with chronic medical conditions, randomized placebocontrolled studies to study efficacy specifically in these children are lacking. In a nonrandomized controlled trial among children aged 2 through 6 years and 7 through 14 years who had asthma, vaccine efficacy was 54% and 78% against laboratory-confirmed influenza A(H3N2) infection and 22% and 60% against laboratory-confirmed influenza B infection, respectively. However, vaccine effectiveness was not significant against B viruses for vaccinated children aged 2 through 6 years with asthma who did not have substantially fewer type B influenza virus infections compared with the control group in this study (129). The association between vaccination and prevention of asthma exacerbations is unclear.
One study suggested that vaccination might provide protection against asthma exacerbations (130).
Receipt of IIV was associated with a reduction in acute otitis media in some studies, but no effect was observed in others. Two studies reported that IIV decreases the risk for influenzarelated otitis media among children (131,132). However, a large study conducted among young children (mean age: 14 months) indicated that IIV did not reduce the proportion of children who developed acute otitis media during the study (124). Influenza vaccine effectiveness against a nonspecific clinical outcome such as acute otitis media, which is caused by a variety of pathogens and typically is not diagnosed by use of influenza virus detection methods, would be expected to be lower than effectiveness against laboratory-confirmed influenza.
# Adults Aged <65 Years
One dose of IIV tends to be highly immunogenic in healthy adults aged <65 years. For example, monovalent influenza A(H1N1)pdm09 (2009[H1N1]) vaccines were highly immunogenic, with approximately 90% of vaccinated adults aged 18 through 64 years demonstrating antibody levels considered protective (133,134). A 2012 meta-analysis found that IIV efficacy against RT-PCR or culture-confirmed influenza was 59% (95% CI = 51%-67%) among adults aged 18 through 65 years in eight of twelve seasons analyzed in ten randomized controlled trials (135). A 2010 meta-analysis of randomized clinical trial results among healthy adults aged 16 through 65 years suggested that when vaccine and circulating influenza viruses strains were well-matched, efficacy against influenza symptoms was 73% (95% CI = 54%-84%) whereas it was 44% (95% CI = 23%-59%) when they were not wellmatched. However, a standard definition of "matched" was not specified (136). Vaccination of healthy adults was associated with decreased work absenteeism and use of health-care resources in some studies, when the vaccine and circulating viruses are well-matched (48,137).
# Adults with Chronic Medical Conditions
There is some evidence to suggest that vaccine effectiveness among adults aged <65 years who have medical conditions conferring higher risk for influenza complications typically might be lower than that reported for healthy adults. In a case-control study conducted during the 2003-04 influenza season, when the vaccine was a suboptimal antigenic match to many circulating virus strains, effectiveness for prevention of laboratory-confirmed influenza (tests used not specified) illness among adults aged 50 through 64 years with high-risk conditions was 48% (95% CI = 21%-66%) compared with 60% (95% CI = 43%-72%) for healthy adults. By contrast, for the subset of cases who were hospitalized (n = 106), effectiveness varied more substantially by risk status: among those with high-risk conditions vaccine effectiveness was 36% (95% CI = 0-63%) while it was 90% (95% CI = 68%-97%) among healthy adults (138). Adults with immunocompromising conditions (e.g., solid organ transplant and HIV infection with low CD4 counts) have lower serum antibody responses after vaccination compared with healthy young adults (139,140).
A randomized controlled trial conducted among adults (median age: 68 years) in Thailand with chronic obstructive pulmonary disease (COPD) observed that vaccine efficacy was 76% (95% CI = 32%-93%) in preventing influenzaassociated acute respiratory infection (defined as respiratory illness associated with HAI titer increase and/or positive influenza antigen on indirect immunofluorescence testing) during a season when circulating influenza viruses were well-matched to vaccine viruses (141). A meta-analysis that examined effectiveness among persons with chronic obstructive pulmonary disease identified evidence of reduced risk for exacerbation from vaccination (142). However, another metaanalysis of published studies concluded that evidence was insufficient to demonstrate that persons with asthma benefit from vaccination (143).
A few randomized controlled trials have studied the effects of influenza vaccination on outcomes not usually associated with influenza virus infection. There is evidence suggesting that acute respiratory infections might trigger acute vascular events mediated by atherosclerosis (144). In particular, respiratory infections coded as influenza or occurring when influenza viruses were circulating transiently increase the risk for acute myocardial infarctions (145). A meta-analysis of two small randomized trials of influenza vaccination in persons with cardiovascular disease yielded a pooled efficacy estimate of 49% for prevention of acute myocardial infarction or cardiac death, although this effect was not statistically significant (95% CI = -76%-85%) (146).
Some observational studies that have provided estimates of vaccine effects for serious complications of influenza infections without laboratory confirmation of influenza have found large reductions in hospitalizations or deaths. For example, in a case-control study conducted during the 1999-00 season in the Netherlands among 75,227persons aged <65 years with underlying medical conditions, vaccination was reported to reduce deaths attributable to any cause by 78% and reduce hospitalizations attributable to respiratory infections or cardiopulmonary diseases by 87% (147). The benefit was greater among those who had been vaccinated previously than among first-time vaccinees (147). Among patients with diabetes mellitus, vaccination was associated with a 56% reduction in any complication, a 54% reduction in hospitalizations, and a 58% reduction in deaths (148). Effects of this magnitude on nonspecific outcomes might have been caused by confounding from unmeasured factors (e.g., dementia and difficulties with self-care) that are associated strongly with the measured outcomes (84,85). Recent studies using methods to account for unmeasured confounding have indicated that vaccine effectiveness among community-dwelling older persons for nonspecific serious outcomes such as pneumonia/influenza hospitalizations or all-cause mortality is <10%, which is much more plausible than higher estimates from earlier studies (149)(150)(151).
# Immunocompromised Persons
In general, HIV-infected persons with minimal AIDS-related symptoms and normal or near-normal CD4+ T-lymphocyte cell counts who receive IIV develop adequate antibody response (152)(153)(154). Among persons who have advanced HIV disease and low CD4+ T-lymphocyte cell counts, IIV might not induce protective antibody titers (154,155); a second dose of vaccine does not improve the immune response in these persons (155,156). A recent immunogenicity study of HIV-infected persons aged ≥18 years indicated that seroprotection rates were higher for persons given high-dose IIV (containing 60 µg of HA per vaccine virus) than those given standard-dose vaccine (which contains 15 µg of HA per vaccine virus); the high-dose vaccine is not licensed for persons aged <65 years (157). In an investigation of an influenza A outbreak at a residential facility for HIV-infected persons, vaccine was most effective at preventing ILI among persons with >100 CD4+ cells and among those with <30,000 viral copies of HIV type-1/mL (64). In a randomized placebo-controlled trial conducted in South Africa among 506 HIV-infected adults, including 349 persons on antiretroviral treatment and 157 who were antiretroviral treatment-naïve, efficacy for culture-or RT-PCR-confirmed influenza illness was 75% (95% CI = 9%-96%) (158).
Several relatively small observational studies have suggested that immunogenicity among persons with solid organ transplants varies according to transplant type. Among persons with kidney or heart transplants, the proportion that developed seroprotective antibody concentrations was similar or slightly reduced compared with healthy persons (159)(160)(161). However, a study among persons with liver transplants indicated reduced immunologic responses to influenza vaccination (162)(163)(164), especially if vaccination occurred within the 4 months after the transplant procedure (162).
# Pregnant Women and Neonates
Pregnant women have protective levels of anti-influenza antibodies after vaccination (165). Passive transfer of antiinfluenza antibodies that might provide protection from vaccinated women to neonates has been reported (165)(166)(167)(168)(169). One randomized controlled trial conducted in Bangladesh that provided IIV3 vaccination to pregnant women during the third trimester demonstrated a 29% reduction in respiratory illness with fever among the infants and a 36% reduction in respiratory illness with fever among their mothers during the first 6 months after birth, compared with pregnant women receiving 23-valent pneumococcal polysaccharide vaccine. In addition, infants born to vaccinated women had a 63% reduction in laboratory-confirmed influenza illness during the first 6 months of life (170). All women in this trial breastfed their infants (mean duration: 14 weeks). Maternal influenza vaccination during pregnancy was associated with significantly reduced risk for influenza virus infection (relative risk: 0.59; 95% CI = 0.37-0.93) and hospitalization for influenza-like illness (ILI) (relative risk: 0.61; 95% CI = 0.45-0.84) among infants aged <6 months in a nonrandomized prospective cohort study; increased antibody titers were also noted in infants through age 2 to 3 months (171). However, a retrospective study conducted during 1997-2002 that used clinical records data did not indicate a reduction in ILI among vaccinated pregnant women or their infants (172). In a retrospective cohort study conducted during 1995-2001, medical visits for respiratory illness among the infants of vaccinated mothers were not substantially reduced (173).
# Older Adults
Most studies suggest that antibody responses to influenza vaccination are decreased in older adults, and it is likely that increasing dysregulation of the immune system with aging contributes to the increased likelihood of serious complications of influenza infection (174). A review of HAI antibody responses in 31 studies among adults aged ≥58 years found that 42%, 51%, and 35% of older persons seroconverted to H1N1, H3N2, and B vaccine antigens, respectively, compared with 60%, 62%, and 58% of younger persons (104). When seroprotection (defined as an HAI titer ≥40) was the outcome, 83%, 84%, and 78% of younger adults versus 69%, 74%, and 67% of older adults achieved protective titers to H1N1, H3N2, and B antigens, respectively (104). Although an HAI titer ≥40 is associated with approximately 50% clinical protection from infection, this standard was established in young healthy adults (8), and there are few data to suggest that such antibody titers represent a correlate of protection among elderly adults. Limited or no increase in antibody response is reported among elderly adults when a second dose is administered during the same season (175)(176)(177).
The desire to improve HI responses among adults aged ≥65 years led to the development and licensure of a vaccine with more antigen than standard-dose IIV. Immunogenicity data from 3 studies of high-dose IIV (Fluzone High-Dose, Sanofi Pasteur) among persons aged ≥65 years indicated that vaccine with four times the HA antigen content of standard-dose vaccine elicited substantially higher HAI titers (178)(179)(180). Pre-specified criteria for superiority in one clinical trial study was defined by a lower bound of a two-sided CI for the ratio of geometric mean HI titers >1.5 and a difference in fourfold rise of HI titers >10%. These criteria were met for influenza A(H1N1) and influenza A(H3N2) virus antigens (181), but not for the influenza B virus antigen (for which criteria for noninferiority were met) (179).
The only large randomized placebo-controlled trial conducted among community-dwelling persons aged ≥60 years reported a vaccine efficacy of 58% (95% CI = 26%-77%) against serologically confirmed clinical influenza illness during a season when the vaccine strains were considered to be well-matched to circulating strains (182). The outcome used for measuring the efficacy estimate was seroconversion to a circulating influenza virus and a symptomatic illness compatible with a clinical influenza infection. As noted previously, there is concern that seroconversion after symptomatic illness will be less likely among vaccinated persons who have higher levels of pre-existing anti-HA antibody that than among those not vaccinated. Such a situation would lead to an overestimate of the true vaccine efficacy, as was demonstrated in a recent clinical trial conducted among healthy adults aged 18 through 49 years (183). Additional information from this trial published after the main results indicated that efficacy among those aged ≥70 years was 57% (95% CI = -36%-87%), similar to the point estimate found among younger persons. However, few persons aged ≥70 years participated in this study, and the wide CI for the estimate of efficacy for persons in this age group included no efficacy (184). Influenza vaccine effectiveness in preventing MAARI among elderly persons residing in nursing homes has been estimated at 20%-40% (185,186), and reported outbreaks among well-vaccinated nursing-home populations have suggested that vaccination might not have any significant effectiveness when circulating strains are drifted from vaccine strains (187,188). Influenza vaccination might reduce the frequency of secondary complications and might reduce the risk for influenza-related hospitalization and death among community-dwelling adults aged ≥65 years with and without high-risk medical conditions (189)(190)(191)(192)(193). However, these studies demonstrating large reductions in hospitalizations and deaths among the vaccinated elderly have been conducted using medical record databases and have not measured reductions in laboratory-confirmed influenza illness. Such methods have been challenged because analyses might not be adjusted adequately to control for the possibility that healthier persons may be more likely to be vaccinated than less healthy persons (84,85,(194)(195)(196)(197)(198).
# Immunogenicity, Efficacy, and Effectiveness of LAIV
LAIV virus strains replicate in nasopharyngeal epithelial cells. The protective mechanisms induced by vaccination with LAIV are not understood completely but appear to involve both serum and nasal secretory antibodies, as well as cell-mediated immune responses. The immunogenicity of LAIV has been assessed in multiple studies (97,(199)(200)(201)(202)(203)(204)(205).
# Healthy Children
A randomized, double-blind, placebo-controlled trial among 1,602 healthy children aged 15 through 71 months assessed the efficacy of LAIV against culture-confirmed influenza during two seasons (206,207). During the first season (1996-97), when vaccine and circulating virus strains were well-matched, efficacy against culture-confirmed influenza was 94% for participants who received 2 doses of LAIV separated by >6 weeks, and 89% for those who received 1 dose. During the second season (1997-98), when the A(H3N2) component in the vaccine was not well-matched with circulating virus strains, efficacy for 1 dose was 86%. The overall efficacy during the two influenza seasons was 92%. Receipt of LAIV also resulted in 21% fewer febrile illnesses and a significant decrease in influenza A-associated otitis media (vaccine efficacy: 94%; 95% CI = 78%-99%) (206,207). In a randomized placebo-controlled trial among vaccine-naïve children aged 6 through <36 months which compared 1 versus 2 doses of LAIV, efficacy against culture-confirmed influenza was 58% (95% CI = 45%-68%) after 1 dose of LAIV and 74% (95% CI = 64%-81%) after 2 doses (100). Other randomized, placebo-controlled trials demonstrating the efficacy of LAIV in young children against culture-confirmed influenza include a study conducted among children aged 6 through 35 months attending child care centers during consecutive influenza seasons (208) in which 85%-89% efficacy was observed. Another study conducted among children aged 12 through 36 months living in Asia during consecutive influenza seasons reported efficacy of 64%-70% (101). In one communitybased, nonrandomized open-label study, reductions in MAARI were observed among children who received 1 dose of LAIV during the 1999-00 and 2000-01 influenza seasons even though antigenically drifted influenza A/H1N1 and B viruses were circulating during the latter season (98). LAIV efficacy in preventing laboratory-confirmed influenza also has been demonstrated in studies comparing the efficacy of LAIV with IIV rather than with a placebo (see Comparisons of LAIV and IIV Efficacy or Effectiveness).
A meta-analysis of six placebo-controlled studies concluded that the efficacy of LAIV against acute otitis media associated with culture-confirmed influenza among children aged 6 through 83 months was 85% (95% CI = 78%-90%) (209). In clinical trials, an increased risk for wheezing postvaccination was observed in LAIV recipients aged <24 months. An increase in hospitalizations was also observed in children aged <24 months after vaccination with LAIV (210).
# Healthy Adults
A randomized, double-blind, placebo-controlled trial of LAIV effectiveness among 4,561 healthy working adults aged 18 through 64 years assessed multiple endpoints, including reductions in self-reported respiratory tract illness without laboratory confirmation, work loss, health-care visits, and medication use during influenza outbreak periods. The study was conducted during the 1997-98 influenza season, when the vaccine and circulating A(H3N2) viruses were not wellmatched. The frequency of febrile illnesses was not significantly decreased among LAIV recipients compared with those who received placebo. However, vaccine recipients had significantly fewer severe febrile illnesses (19% reduction) and febrile upper respiratory tract illnesses (24% reduction); and significant reductions in days of illness, days of work lost, days with healthcare provider visits, and use of prescription antibiotics and overthe-counter medications (211). Estimated efficacy of LAIV against influenza confirmed by either culture or RT-PCR in a randomized, placebo-controlled study among approximately 2,000 young adults was 48% (95% CI = -7%-74%) in the 2004-05 influenza season, 8% (95% CI = -194%-67%) in the 2005-06 influenza season, and 36% (95% CI = 0-59%) in the 2007-08 influenza season; efficacy in the 2004-05 and 2005-06 seasons was not significant (212)(213)(214).
# Comparisons of LAIV and IIV Efficacy or Effectiveness
Both IIV and LAIV have been demonstrated to be effective in children and adults. Studies comparing the efficacy of IIV to that of LAIV have been conducted in a variety of settings and populations using several different outcomes. Among adults, most comparative studies have demonstrated either that LAIV and IIV were of similar efficacy or that IIV was more efficacious (215). One randomized, double-blind, placebo-controlled challenge study that was conducted among 92 healthy adults aged 18 through 41 years assessed the efficacy of both LAIV and IIV in preventing influenza infection when artificially challenged with wild-type strains that were antigenically similar to vaccine strains (205). The overall efficacy in preventing laboratory-documented influenza illness (defined as respiratory symptoms with either isolation of wild-type influenza virus from nasal secretions or fourfold and/or greater HAI antibody response to challenge) from all three influenza strains combined was 85% for LAIV and 71% for IIV when study participants were challenged 28 days after vaccination by viruses to which they were susceptible before vaccination. The difference in efficacy between the two vaccines was not statistically significant in this small study. No additional challenges were conducted to assess efficacy at time points later than 28 days (205). In a randomized, double-blind, placebo-controlled trial that was conducted among young adults during the 2004-05 influenza season, when the majority of circulating H3N2 viruses were antigenically drifted from that season's vaccine viruses, the efficacy of LAIV and IIV against cultureconfirmed influenza was 57% (95%CI = -3%-82%) and 77% (95% CI = 37%-92%), respectively. The difference in efficacy was not statistically significant and was attributable primarily to a difference in efficacy against influenza B (212) (216). However, in a retrospective cohort study comparing LAIV and IIV among 701,753 nonrecruit military personnel and 70,325 new recruits, among new recruits, incidence of ILI was lower among those who received LAIV than IIV. The previous vaccination status of the recruits was not known; it is possible that this population was relatively naïve to vaccination compared with previous service members who are vaccinated routinely each year (217).
.
Several studies have demonstrated superior efficacy of LAIV as compared with IIV among children (215). A randomized controlled clinical trial conducted among 7,852 children aged 6 through 59 months during the 2004-05 influenza season demonstrated a 55% reduction in cases of culture-confirmed influenza among children who received LAIV compared with those who received IIV (218). In this study, LAIV efficacy was higher compared with IIV against antigenically drifted viruses and well-matched viruses (218). An open-label, nonrandomized, community-based influenza vaccine trial conducted among 7,609 children aged 5 through 18 years during an influenza season when circulating H3N2 strains were poorly matched with strains contained in the vaccine also indicated that LAIV, but not IIV, was effective against antigenically drifted H3N2 viruses. In this study, children who received LAIV had significant protection against laboratoryconfirmed influenza (37%) and pneumonia/influenza events (50%) (219). LAIV provided 32% increased protection in preventing culture-confirmed influenza compared with IIV in one study conducted among children aged ≥6 years and adolescents with asthma (220) and 52% increased protection compared with IIV among children aged 6 through 71 months with recurrent respiratory tract infections (221).
# Safety of Influenza Vaccines Inactivated Influenza Vaccines
Children: A large postlicensure population-based study assessed IIV3 safety in 251,600 children aged <18 years (including 8,476 vaccinations in children aged 6 through 23 months) enrolled in one of five health-care organizations within the Vaccine Safety Datalink (VSD) (http://www.cdc. gov/vaccinesafety/activities/vsd.html) during 1993-1999. This study indicated no increase in clinically important medically attended events during the 2 weeks after inactivated influenza vaccination compared with control periods 3-4 weeks before and after vaccination (222). In a retrospective cohort study using VSD data from 45,356 children aged 6 through 23 months during 1991-2003, IIV3 was not associated with statistically significant increases in any clinically important medically attended events other than gastritis/duodenitis during the 2 weeks after vaccination compared with control time periods before and after vaccination. Most vaccinated children with a diagnosis of gastritis/duodenitis had selflimited vomiting or diarrhea. Several diagnoses, including acute upper respiratory illness, otitis media and asthma, were significantly less common during the 2 weeks after influenza vaccination. Although there was a temporal relationship with vaccination, the vaccine did not necessarily cause nor prevent these conditions (223). A subsequent VSD study of 66,283 children aged 24 through 59 months noted diagnoses of fever, gastrointestinal tract symptoms, and gastrointestinal disorders to be significantly associated with IIV3. Upon medical record review, none of the events appeared to be serious, and none were associated with complications (224).
In a study of 791 healthy children aged 1 through 15 years, postvaccination fever was noted among 12% of those aged 1 through 5 years, 5% among those aged 6 through 10 years, and 5% among those aged 11 through 15 years (89). Fever, malaise, myalgia, and other systemic symptoms that can occur after vaccination with IIV most often affect persons who have had no previous exposure to the influenza virus antigens in the vaccine (e.g., young children) (225). These reactions are generally self-limited and subside after 1-2 days.
Febrile seizures associated with IIV and pneumococcal conjugate vaccine (PCV13): Febrile seizures are common in young children. At least one febrile seizure is experienced by 2%-5% of children aged 6 through 60 months; nearly all children who have a febrile seizure recover quickly and are healthy afterwards (226). Prior to the 2010-11 influenza season, an increased risk for febrile seizures following IIV3 had not been observed in the United States (223,227). During the 2010-11 influenza season, CDC and the Food and Drug Administration (FDA) conducted enhanced monitoring for febrile seizures following influenza vaccines after reports of an increased risk for fever and febrile seizures in young children in Australia associated with a 2010 Southern Hemisphere IIV3 produced by CSL Biotherapies (up to nine febrile seizures per 1,000 doses) (228). Because of the findings in Australia, ACIP does not recommend the U.S.-licensed CSL Biotherapies' IIV3, Afluria, for children aged <9 years (Table 1).
Surveillance among children receiving U.S.-licensed influenza vaccines during the 2010-11 influenza season subsequently detected safety concerns for febrile seizures in young children following IIV3 (229,230). Further assessment through a VSD study determined that the increased risk was in children aged 6 months through 4 years on the day of vaccination to the day after (risk window: Day 0-1). The risk was higher when children received concomitant PCV13 (i.e., when the two vaccines are given at the same health-care visit) and peaked at approximately age 16 months (230). No increased risk was observed in children aged >4 years after IIV3 or in children of any age after LAIV. The magnitude of the increased risk for febrile seizures in children aged 6 through 23 months in the United States observed in this study (<1 per 1,000 children vaccinated) was substantially lower than the risk observed in Australia in 2010 (228). Findings from surveillance for febrile seizures in young children following influenza vaccine for the 2011-12 influenza season (which had the same formulation as that of the 2010-11 season) were consistent with the 2010-11 influenza season; however, an increased risk for febrile seizures following IIV3 was not observed during the 2012-13 influenza season (CDC, unpublished data, 2013). After evaluating the data on febrile seizures from the 2010-11 influenza season and taking into consideration benefits and risks of vaccination, no policy change was recommended for use of IIV or PCV13 (231,232). Surveillance for febrile seizures after IIV is ongoing through VAERS. † For adults and older children, the recommended site of vaccination is the deltoid muscle. The preferred site for infants and young children is the anterolateral aspect of the thigh. Specific guidance regarding site and needle length for intramuscular administration may be found in the ACIP General Recommendations on Immunization (CDC. General recommendations on immunization: recommendations of the Advisory Committee on Immunization Practices, 2011. MMWR 2011;60[No. RR-2]). § The preferred site is over the deltoid muscle. Fluzone Intradermal is administered using the delivery system included with the vaccine. ** Inactivated influenza vaccine, high-dose: A 0.5-mL dose contains 60 µg of each vaccine antigen (180 µg total).
† † Inactivated influenza vaccine, intradermal: A 0.1-mL dose contains 9 µg of each vaccine antigen (27 µg total). § § It is anticipated that the quadrivalent formulation of FluMist will replace the trivalent formulation for the 2013-14 season. FluMist is shipped refrigerated and stored in the refrigerator at 35°F-46°F (2°C-8°C) after arrival in the vaccination clinic. The dose is 0.2 mL divided equally between each nostril. Health-care providers should consult the medical record, when available, to identify children aged 2 through 4 years with asthma or recurrent wheezing that might indicate asthma. In addition, to identify children who might be at greater risk for asthma and possibly at increased risk for wheezing after receiving LAIV, parents or caregivers of children aged 2 through 4 years should be asked, "In the past 12 months, has a health-care provider ever told you that your child had wheezing or asthma?" Children whose parents or caregivers answer "yes" to this question and children who have asthma or who had a wheezing episode noted in the medical record within the past 12 months should not receive FluMist. *** Flumist is indicated for healthy, nonpregnant persons aged 2-49 years. Persons who care for severely immunosuppressed persons who require a protective environment should not receive FluMist given the theoretical risk of transmission of the live attenuated vaccine virus. † † † Age indication per package insert is ≥5 years; however, ACIP recommends that Afluria not be used in children aged 6 months through 8 years because of increased risk for febrile reactions noted in this age group with CSL's 2010 Southern Hemisphere IIV3. If no other age-appropriate, licensed inactivated seasonal influenza vaccine is available for a child aged 5-8 years who has a medical condition that increases the child's risk for influenza complications, Afluria can be used; however, providers should discuss with the parents or caregivers the benefits and risks of influenza vaccination with Afluria before administering this vaccine. Afluria may be used in persons aged ≥9 years. § § § Information not included in package insert. The total egg protein is estimated to be less than 50 femtograms (5x10-14 grams) total egg protein (of which a fraction is ovalbumin) per 0.5 mL dose of Flucelvax. ¶ ¶ ¶ Available on request from Sanofi Pasteur, telephone 1-800-822-2463 or e-mail [email protected].
# Adults:
In placebo-controlled studies among adults, the most frequent side effect of vaccination was soreness at the vaccination site (affecting 10%-64% of patients) that lasted <2 days (233,234). These local reactions typically were mild and rarely interfered with the recipients' ability to conduct usual daily activities. Placebo-controlled trials demonstrate that among older persons and healthy young adults, administration of IIV3 is not associated with higher rates for systemic symptoms (e.g., fever, malaise, myalgia, and headache) when compared with placebo injections (233)(234)(235). Adverse events in adults aged ≥18 years reported to VAERS during 1990-2005 were analyzed. The most common adverse events for adults described in 18,245 VAERS reports included injection site reactions, pain, fever, myalgia, and headache. The VAERS review identified no new safety concerns. Fourteen percent of the IIV3 VAERS reports in adults were classified as serious adverse events (defined as those involving death, life-threatening illness, hospitalization or prolongation of hospitalization, or permanent disability [236]), similar to proportions seen in VAERS for other adult vaccines. The most common serious adverse event reported after IIV3 in VAERS in adults was Guillain-Barré syndrome (GBS) (237). The potential association between IIV3 and GBS is an area of ongoing research (see Guillain-Barré Syndrome and IIV).
Injection site reactions and systemic adverse events were more frequent after vaccination with a vaccine containing 180 µg of HA antigen (Fluzone High-Dose, Sanofi Pasteur, Swiftwater, Pennsylvania) than after standard-dose (45 µg) (Fluzone, Sanofi Pasteur) but were typically mild and transient. In one study, 915 (36%) of 2,572 persons who received Fluzone High-Dose, compared with 306 (24%) of those who received Fluzone, reported injection site pain. Only 1.1% of Fluzone High Dose recipients reported moderate to severe fever, but this was significantly higher than the 0.3% of Fluzone recipients who reported this systemic adverse event (RR: 3.6, 95% CI = 1.3-10.1) (179). A randomized study of high-dose versus standard-dose vaccine including 9,172 participants found no difference in occurrence of serious adverse events or several specific adverse events of interest (including GBS, Bell's Palsy, encephalitis/myelitis, optic neuritis, Stevens-Johnson syndrome, and toxic epidermal necrolysis) (238). Safety monitoring of high-dose vaccine in VAERS during the first year after licensure indicated a higher than expected number of gastrointestinal events compared with standard-dose vaccine, but otherwise no new safety concerns were identified. Most of the reported gastrointestinal reports were nonserious (239). CDC and FDA will continue to monitor the safety of highdose vaccine through VAERS.
Intradermal IIV has been observed to be associated with higher rates of some injection site reactions as compared with intramuscularly administered influenza vaccines. In a randomized study of intradermal versus intramuscular vaccine among approximately 4,200 adults aged 18 through 64 years, erythema, induration, swelling, and pruritus occurred with greater frequency following intradermal vaccine compared with intramuscular vaccine; rates of injection site pain were not significantly different (240). A recent review of studies comparing intradermal and intramuscular vaccine similarly noted higher rates of erythema, induration, swelling, and pruritus among adults aged 18 through 60 years within the first 7 days after receiving intradermal vaccine; local pain and ecchymosis and systemic reactions occurred with similar frequency (241).
Pregnant women and neonates: Currently available IIVs are classified as either Pregnancy Category B or Category C † medications, depending upon whether adequate animal reproduction studies have been conducted. Available data indicate that influenza vaccine does not cause fetal harm when administered to a pregnant woman. However, data on the safety of influenza vaccination in the early first trimester are limited (242). One study of approximately 2,000 pregnant women who received IIV3 during pregnancy demonstrated no increase in malignancies during infancy or early childhood (243). A matched case-control study of 252 pregnant women who received IIV3 within the 6 months before delivery determined no adverse events after vaccination among pregnant women and no difference in pregnancy outcomes compared with 826 pregnant women who were not vaccinated (244). A case-control analysis of data from six health-care organizations participating in the VSD found no significant increase in the risk for pregnancy loss in the 4 weeks following seasonal influenza vaccination (245). A review of health registry data in Norway noted an increased risk for fetal death associated with pandemic 2009(H1N1) infection, but no increased risk of fetal mortality associated with vaccination (246). During 2000-2003, when an estimated 2 million pregnant women were vaccinated, only 20 adverse events among women who received IIV3 were reported to VAERS, including nine injection site reactions, eight systemic reactions (e.g., fever, headache, and myalgia), and three miscarriages (247). Background rates of miscarriage vary from 10.4% in women aged <25 years to 22.4% in women † Pregnancy Category B indicates that 1) animal reproduction studies have failed to demonstrate a risk to the fetus and there are no adequate and well-controlled studies in humans or 2) that animal studies have shown an adverse effect, but adequate and well-controlled studies in humans have failed to demonstrate a risk to the fetus in any trimester. Pregnancy Category C indicates that animal reproduction studies have shown an adverse effect on the fetus and there are no adequate and well-controlled studies in humans, but potential benefits may warrant use of the drug in pregnant women despite potential risks. Additional information about pregnancy categories is available at http://www.fda.gov/ Drugs/DevelopmentApprovalProcess/DevelopmentResources/Labeling/ ucm093307.htm.
aged >34 years (248); considering the number of pregnant women vaccinated, miscarriage following (but not attributable to) influenza vaccination would not be an unexpected event.
Recent reviews of studies pertaining to seasonal (249)(250)(251) and monovalent 2009(H1N1) (250,251) inactivated influenza vaccines in pregnancy concluded that no evidence exists to suggest harm to the fetus from maternal vaccination.
Persons with chronic medical conditions: In a blinded, randomized crossover study of 1,952 children and adults with asthma, no increase in asthma exacerbations was reported for either age group. Only myalgias were reported more frequently after IIV3 (25%) than placebo-injection (21%) (252). Among children with high-risk medical conditions, one study of 52 children aged 6 months through 3 years reported fever among 27% and irritability and insomnia among 25% (108); and a study among 33 children aged 6 through 18 months reported that one child had irritability and one had a fever and seizure after vaccination (253). No placebo comparison group was used in these studies. One prospective cohort study found that the rate of adverse events was similar among hospitalized persons who either were aged ≥65 years or were aged 18 through 64 years and had one or more chronic medical conditions compared with outpatients (254).
Immunocompromised persons: Data demonstrating safety of IIV3 for HIV-infected persons are limited, but no evidence exists that vaccination has a clinically important impact on HIV infection or immunocompetence. One study demonstrated a transient increase in HIV RNA (ribonucleic acid) levels in one HIV-infected person after influenza virus infection (255). While some earlier studies demonstrated a transient increase in replication of HIV-1 in the plasma or peripheral blood mononuclear cells of HIV-infected persons after vaccine administration (154,256), more recent and better-designed studies have not documented a substantial increase in the replication of HIV (257-260). CD4+ T-lymphocyte cell counts or progression of HIV disease have not been demonstrated to change substantially after influenza vaccination among HIV-infected persons compared with unvaccinated HIV-infected persons (154,261). Limited information is available about the effect of antiretroviral therapy on increases in HIV RNA levels after either influenza virus infection or influenza vaccination (63,262).
Data are similarly limited for persons with other immunocompromising conditions. In small studies, vaccination did not affect allograft function or cause rejection episodes in recipients of kidney transplants (159,160), heart transplants (161), or liver transplants (162). Limited data are available on influenza vaccination in the setting of solid organ transplantation. A recent literature review concluded that there is no convincing epidemiologic link between vaccination and allograft dysfunction (263). Case reports of corneal graft rejection have been reported following IIV (264)(265)(266), but no studies demonstrating an association have been conducted.
Immediate hypersensitivity reactions after influenza vaccines: Vaccine components can occasionally cause allergic reactions, also called immediate hypersensitivity reactions. Immediate hypersensitivity reactions are mediated by preformed immunoglobulin E (IgE) antibodies against a vaccine component and usually occur within minutes to hours of exposure (267). Symptoms of immediate hypersensitivity range from urticaria (hives) to angioedema and anaphylaxis. Anaphylaxis is a severe life-threatening reaction that involves multiple organ systems and can progress rapidly. Symptoms and signs of anaphylaxis can include but are not limited to generalized urticaria, wheezing, swelling of the mouth, tongue and throat, difficulty breathing, vomiting, hypotension, decreased level of consciousness, and shock. Minor symptoms such as red eyes or hoarse voice also might be present (267,268).
Allergic reactions might be caused by the vaccine antigen, residual animal protein, antimicrobial agents, preservatives, stabilizers, or other vaccine components (269). Manufacturers use a variety of compounds to inactivate influenza viruses and add antibiotics to prevent bacterial growth. Package inserts for specific vaccines of interest should be consulted for additional information. ACIP has recommended that all vaccine providers should be familiar with the office emergency plan and be certified in cardiopulmonary resuscitation (270). The Clinical Immunization Safety Assessment (CISA) network, a collaboration between CDC and medical research centers with expertise in vaccinology and vaccine safety, has developed an algorithm to guide evaluation and revaccination decisions for persons with suspected immediate hypersensitivity after vaccination (267).
Anaphylaxis after IIV and LAIV is rare. A study conducted in VSD during 2005-2008 observed that the incidence of anaphylaxis in the 0-2 days after IIV3 was 0.45-1.98 cases per million IIV3 doses administered in all ages (227). Anaphylaxis occurring after receipt of IIV3 and LAIV3 has rarely been reported to VAERS (237,271). A VSD study of children aged <18 years in four HMOs during 1991-1997 estimated the overall risk for postvaccination anaphylaxis after any type of childhood vaccine to be approximately 1.5 cases per million doses administered. In this study, no cases were identified in IIV3 recipients (272).
Some immediate hypersensitivity reactions after IIV or LAIV might be caused by the presence of residual egg protein in the vaccines (273). Although influenza vaccines contain only a limited quantity of egg protein, this protein can potentially induce immediate hypersensitivity reactions among persons who have severe egg allergy. Specific recommendations pertaining to the use of influenza vaccines for egg-allergic persons are provided (see Influenza Vaccination for Persons with a History of Egg Allergy).
Ocular and respiratory symptoms after receipt of IIV: Oculorespiratory syndrome (ORS), an acute, self-limited reaction to IIV with prominent ocular and respiratory symptoms, was first described during the 2000-01 influenza season in Canada. The initial case-definition for ORS was the onset of one or more of the following within 2-24 hours after receiving IIV, and resolving within 48 hours of onset: red eyes, cough, wheeze, chest tightness, difficulty breathing, sore throat, or facial swelling (274). ORS was strongly associated with one vaccine preparation (Fluviral S/F, Shire Biologics, Quebec, Canada) not available in the United States during the 2000-01 influenza season (275). Subsequent investigations identified persons with ocular or respiratory symptoms meeting an ORS case-definition in safety monitoring systems and trials that had been conducted before 2000 in Canada, the United States, and several European countries (276)(277)(278).
The cause of ORS has not been established; however, studies suggest that the reaction is not IgE-mediated (279). After changes in the manufacturing process of the vaccine preparation associated with ORS during the 2000-01 season, the incidence of ORS in Canada was reduced greatly (277). In one placebo-controlled study, only hoarseness, cough, and itchy or sore eyes (but not red eyes) were strongly associated with a reformulated Fluviral preparation. These findings indicated that ORS symptoms following use of the reformulated vaccine were mild, resolved within 24 hours, and might not typically be of sufficient concern to cause vaccine recipients to seek medical care (280).
Ocular and respiratory symptoms reported after IIV administration, including ORS, have some similarities with immediate hypersensitivity reactions. One study indicated that the risk for ORS recurrence with subsequent vaccination is low, and persons with ocular or respiratory symptoms (e.g., bilateral red eyes, cough, sore throat, or hoarseness) after receipt of IIV that did not involve the lower respiratory tract have been revaccinated without reports of serious adverse events after subsequent exposure to IIV (281).
When assessing whether a patient who experienced ocular and respiratory symptoms should be revaccinated, providers should determine if concerning signs and symptoms of IgE mediated immediate hypersensitivity are present (see Immediate Hypersensitivity after Influenza Vaccines). Health-care providers who are unsure whether symptoms reported or observed after receipt of IIV represent an IgE-mediated hypersensitivity immune response should seek advice from an allergist/ immunologist. Persons with symptoms of possible IgE-mediated hypersensitivity after receipt of IIV should not receive influenza vaccination unless hypersensitivity is ruled out or revaccination is administered under close medical supervision (267).
Ocular or respiratory symptoms observed after receipt of IIV often are coincidental and unrelated to IIV administration, as observed among placebo recipients in some randomized controlled studies. Determining whether ocular or respiratory symptoms are coincidental or related to possible ORS might not be possible. Persons who have had red eyes, mild upper facial swelling, or mild respiratory symptoms (e.g., sore throat, cough, or hoarseness) after receipt of IIV without other concerning signs or symptoms of hypersensitivity can receive IIV in subsequent seasons without further evaluation. Two studies indicated that persons who had symptoms of ORS after receipt of IIV were at a higher risk for ORS after subsequent IIV administration; however, these events usually were milder than the first episode (281,282).
Guillain-Barré syndrome and IIV: The annual incidence of GBS is 10-20 cases per 1 million adults (283). Evidence exists that multiple infectious illnesses, most notably Campylobacter jejuni gastrointestinal infections and upper respiratory tract infections, are associated with GBS (284)(285)(286). A recent study identified an association between serologically confirmed influenza virus infection and GBS, with time from onset of influenza illness to GBS of 3-30 days. The estimated frequency of influenza-related GBS was four to seven cases per 100,000 persons compared with one case per 1 million persons following vaccination with TIV) (287).
The 1976 swine influenza vaccine was associated with an increased frequency of GBS, estimated at one additional case of GBS per 100,000 persons vaccinated (288,289). The risk for influenza vaccine-associated GBS was higher among persons aged ≥25 years than among persons aged <25 years (290). No subsequent study conducted using influenza vaccines other than the 1976 swine influenza vaccine has demonstrated an increase in GBS associated with influenza vaccines on the order of magnitude seen in the 1976-77 season. During three of four influenza seasons studied during 1977-1991, the overall relative risk estimates for GBS after influenza vaccination were not statistically significant (291)(292)(293). However, in a study of the 1992-93 and 1993-94 seasons, the overall relative risk for GBS was 1.7 (95% CI = 1.0-2.8; p = 0.04) during the 6 weeks after vaccination, representing approximately one additional case of GBS per 1 million persons vaccinated. GBS cases peaked 2 weeks after vaccination (289). Results of a study that examined health-care data from Ontario, Canada, during 1992-2004 demonstrated a small but statistically significant temporal association between receiving influenza vaccination and subsequent hospital admission for GBS (relative incidence: 1.45; 95% CI = 1.05-1.99). However, no increase in cases of GBS at the population level was reported after introduction of a mass public influenza vaccination program in Ontario beginning in 2000 (294). Published data from the United Kingdom's General Practice Research Database (GPRD) found influenza vaccination to be associated with a decreased risk for GBS (odds ratio: 0.16; 95% CI = 0.02-1.25), although whether this was associated with protection against influenza or confounding because of a "healthy vaccinee" effect (e.g., healthier persons might be more likely to be vaccinated and also be at lower risk for GBS) is unclear (295). A separate GPRD analysis found no association between vaccination and GBS for a 9-year period; only three cases of GBS occurred within 6 weeks after administration of influenza vaccine (296). A third GPRD analysis found that GBS was associated with recent ILI, but not influenza vaccination (297).
The estimated risk for GBS (on the basis of the few studies that have demonstrated an association between seasonal IIV and GBS) is low; approximately one additional case per 1 million persons vaccinated (288,294). In addition, data from the systems monitoring influenza A(H1N1) 2009 monovalent vaccines suggest that the risk for GBS associated with these inactivated vaccines is approximately one or two additional cases per 1 million persons vaccinated, which is similar to that observed in some seasons for IIV (298)(299)(300)(301)(302)(303)(304).
The incidence of GBS among the general population is low (0.75 to 2 cases per 100,000 persons annually) ( 283), but persons with a history of GBS have a substantially greater likelihood of subsequently experiencing GBS than persons without such a history (283). Thus, the likelihood of coincidentally experiencing GBS after influenza vaccination is expected to be greater among persons with a history of GBS than among persons with no history of this syndrome. Whether influenza vaccination specifically might increase the risk for recurrence of GBS is unknown. Among 311 patients with GBS who responded to a survey, 11 (4%) reported some worsening of symptoms after influenza vaccination; however, some of these patients had received other vaccines at the same time, and recurring symptoms were generally mild (305). In a Kaiser Permanente Northern California database study among more than 3 million members conducted over an 11-year period, no cases of recurrent GBS were identified after influenza vaccination in 107 persons with a documented prior diagnosis of GBS, two of whom had initially developed GBS within 6 weeks of influenza vaccination (306).
As a precaution, persons who are not at high risk for severe influenza complications (see Persons at Risk for Medical Complications Attributable to Influenza) and who are known to have experienced GBS within 6 weeks of influenza vaccination generally should not be vaccinated. As an alternative, physicians might consider using influenza antiviral chemoprophylaxis for these persons. However, the benefits of influenza vaccination might outweigh the risks for certain persons who have a history of GBS and who also are at high risk for severe complications from influenza.
Thimerosal in multidose vials of IIV: Thimerosal, a mercury-containing antibacterial compound, is used in multidose vial preparations of IIV to reduce the likelihood of bacterial growth. While accumulating evidence shows no increased risks from exposure to thimerosal-containing vaccines (307-316), the U.S. Public Health Service and other organizations have recommended that efforts be made to eliminate or reduce the thimerosal content in vaccines as part of a strategy to reduce mercury exposures from all sources (307,308). LAIV, RIV, and most single-dose vial or syringe preparations of IIV are thimerosal-free. Persons recommended to receive IIV may receive any age-and risk factor-appropriate vaccine preparation, depending on availability.
# Live Attenuated Influenza Vaccines
# Shedding, transmission, and stability of vaccine viruses:
Data indicate that both children and adults vaccinated with LAIV can shed vaccine viruses after vaccination, although in lower amounts than occur typically with shedding of wild-type influenza viruses. Rarely, shed vaccine viruses can be transmitted from vaccine recipients to unvaccinated persons. However, serious illnesses have not been reported among unvaccinated persons who have been infected inadvertently with vaccine viruses. One study of 197 children aged 8 through 36 months in a child care center assessed transmissibility of vaccine viruses from 98 vaccinated children to the 99 unvaccinated children; 80% of vaccine recipients shed one or more virus strains (mean duration: 7.6 days). One influenza B vaccine virus strain isolate was recovered from a placebo recipient and was confirmed to be vaccine-type virus. The influenza B virus isolate retained the cold-adapted, temperature-sensitive, attenuated phenotype. The placebo recipient from whom the influenza B vaccine virus strain was isolated had symptoms of a mild upper respiratory illness. The estimated probability of acquiring vaccine virus after close contact with a single LAIV recipient in this population was 1%-2% (317).
Studies assessing shedding of vaccine virus have been based on viral cultures or RT-PCR detection of vaccine viruses in nasal aspirates from LAIV recipients. A study of 345 subjects aged 5 through 49 years who received LAIV indicated that 30% had detectable virus in nasal secretions obtained by nasal swabbing. The duration of virus shedding and the amount of virus shed was inversely correlated with age, and maximal shedding occurred within 2 days of vaccination. Symptoms reported after vaccination, including runny nose, headache, and sore throat, did not correlate with virus shedding (318).
Other smaller studies have reported similar findings (319,320). In an open-label study of 200 children aged 6 through 59 months who received a single dose of LAIV, shedding of at least one vaccine virus was detected on culture in 79% of children, and was more common among the younger recipients (89% of children aged 6 through 23 months compared with 69% of children aged 24 through 59 months) (321). The incidence of shedding was highest on day 2 postvaccination. Mean duration of shedding was 2.8 days (3.0 days and 2.7 days for the younger and older age groups, respectively); shedding detected after 11 days postvaccination was uncommon and nearly all instances occurred among children aged 6 through 23 months (an age group for which LAIV is not licensed). Titers of shed virus were low (321). Vaccine virus was detected from nasal secretions in one (2%) of 57 HIV-infected adults who received LAIV compared with none of 54 HIV-negative participants (322), and in three (13%) of 24 HIV-infected children compared with seven (28%) of 25 children who were not HIV-infected (323).
In clinical trials, viruses isolated from vaccine recipients have retained attenuated phenotypes. In one study, nasal and throat swab specimens were collected from 17 study participants for 2 weeks after vaccine receipt. Virus isolates were analyzed by multiple genetic techniques. All isolates retained the LAIV genotype after replication in the human host, and all retained the cold-adapted and temperature-sensitive phenotypes (324). A study conducted in a child care setting demonstrated that limited genetic change occurred in the LAIV strains following replication in the vaccine recipients (317).
Healthy children aged 2 through 18 years: In a subset of healthy children aged 60 through 71 months from one clinical trial, certain signs and symptoms were reported more often after the first dose among LAIV recipients (n = 214) than among placebo recipients (n = 95), including runny nose (48% and 44%, respectively); headache (18% and 12%, respectively); vomiting (5% and 3%, respectively); and myalgia (6% and 4%, respectively) (325). However, these differences were not statistically significant. In other trials, signs and symptoms reported after LAIV administration have included runny nose or nasal congestion (20%-75%), headache (2%-46%), fever (0-26%), vomiting (3%-13%), abdominal pain (2%), and myalgia (0-21%) (199,201,202,208,(326)(327)(328)(329). These symptoms were associated more often with the first dose and were self-limited. In a placebo-controlled trial in 9,689 children aged 1-17 years assessed pre-specified medically attended outcomes during the 42 days after vaccination, LAIV was associated with increased risk for asthma, upper respiratory infection, musculoskeletal pain, otitis media with effusion, and adenitis/adenopathy. The increased risk for wheezing events after LAIV was observed among children aged 18-35 months (RR: 4.06; 90% CI = 1.3-17.9). In this study, the proportion of serious adverse events was 0.2% in LAIV and placebo recipients; none of the serious adverse events was judged to be related to the vaccine by the study investigators (328).
In a randomized trial published in 2007, LAIV and IIV were compared among children aged 6 through 59 months (218). Children with medically diagnosed or treated wheezing in the 42 days before enrollment or with a history of severe asthma were excluded from participation. Among children aged 24 through 59 months who received LAIV, the proportion of children who experienced medically significant wheezing, using a prespecified definition, was not greater compared with those who received IIV (218). Wheezing was observed more frequently following the first dose among previously unvaccinated, younger LAIV recipients, primarily those aged <12 months; LAIV is not licensed for this age group. In a previous randomized placebo-controlled safety trial among children aged 12 months through 17 years without a history of asthma by parental report, an increased risk for asthma events (RR: 4.1; 95% CI = 1.3-17.9) was documented among 728 children aged 18 through 35 months who received LAIV. Of the 16 children with asthma-related events in this study, seven had a history of asthma on the basis of subsequent medical record review. None required hospitalization, and increased risk for asthma events were not observed in other age groups (328).
An open-label field trial was conducted among approximately 11,000 children aged 18 months through 18 years in which 18,780 doses of vaccine were administered between 1998-2002 For children aged 18 months through 4 years, no increase was reported in asthma visits 0-15 days after vaccination compared with the prevaccination period. A significant increase in asthma events was reported 15-42 days after vaccination, but only in vaccine year 1 (330). This trial later assessed LAIV safety among 2,196 children aged 18 months through 18 years with a history of intermittent wheezing who were otherwise healthy. Among these children, no increased risk was reported for medically attended acute respiratory illnesses, including acute asthma exacerbation, during the 0-14 or 0-42 days after LAIV compared with the pre-and postvaccination reference periods (331).
In a postlicensure observational study of 28,226 children aged 24 through 59 months, asthma and wheezing medically attended events were not statistically increased after LAIV during three influenza seasons (2007-08, 2008-09, and 2009-10) (332). Safety monitoring for wheezing events after LAIV is ongoing through VAERS.
Adults aged 19 through 49 years: In one clinical trial among a subset of healthy adults aged 18 through 49 years, signs and symptoms reported significantly more often (p<0.05; Fisher exact test) among LAIV recipients (n = 2,548) than placebo recipients (n = 1,290) within 7 days after each dose included cough (14% and 11%, respectively), runny nose (45% and 27%, respectively), sore throat (28% and 17%, respectively), chills (9% and 6%, respectively), and tiredness/weakness (26% and 22%, respectively) (325). A review of 460 reports to VAERS after distribution of approximately 2.5 million doses during the 2003-04 and 2004-05 influenza seasons did not indicate any new safety concerns (271). Few (9%) of the LAIV VAERS reports concerned serious adverse events; respiratory events were the most common conditions reported.
Persons at higher risk for influenza-related complications: Limited data assessing the safety of LAIV use for certain groups at higher risk for influenza-related complications are available. In one study of 57 HIV-infected persons aged 18 through 58 years with CD4+ counts >200 cells/mm3 who received LAIV, no serious adverse events attributable to vaccines were reported during a 1-month follow-up period (322). Similarly, one study demonstrated no significant difference in the frequency of adverse events or viral shedding among 24 HIV-infected children aged 1 through 8 years on effective antiretroviral therapy who were administered LAIV compared with 25 HIVuninfected children receiving LAIV (323). LAIV was welltolerated among adults aged ≥65 years with chronic medical conditions (333). Among 27 reports to VAERS involving inadvertent administration of LAIV to pregnant women during 1990-2009, no unusual patterns of maternal or fetal outcomes were observed (334); among 138 reports noted in a health insurance claims database, all outcomes occurred at similar rates to those observed in unvaccinated women (335). These findings suggest that persons at risk for influenza complications who have inadvertent exposure to LAIV are not expected to have significant adverse events or prolonged viral shedding and that persons who have contact with persons at higher risk for influenza-related complications may receive LAIV.
# Recombinant Influenza Vaccine
# Dosage, Administration, and Storage of Influenza Vaccines
The composition of influenza vaccines varies among different products. For all vaccines, package inserts should be consulted for authoritative guidance regarding storage conditions and administration. Influenza vaccine manufactured for a previous season should not be administered in any subsequent season and should not be administered after the expiration date.
# Inactivated Influenza Vaccine
IIVs are available in both single-dose and multidose formulations. Multidose vials contain the vaccine preservative thimerosal. Single-dose, unpreserved products should not be used for multiple doses. IIV should be stored at 35°F-46°F (2°C-8°C) and should not be frozen. IIV that has been frozen should be discarded. Dosage recommendations and schedules vary according to age group (Table 1). Vaccine prepared for a given influenza season should not be administered to provide protection for any subsequent season.
With the exception of Fluzone Intradermal (Sanofi Pasteur), IIV should be administered intramuscularly. For adults and older children, the deltoid is the preferred site. Infants and younger children should be vaccinated in the anterolateral thigh. Specific guidance regarding site and needle length for intramuscular administration can be found in the ACIP General Recommendations on Immunization (270). Fluzone Intradermal is administered intradermally, preferably over the deltoid muscle, using the delivery system included in the vaccine package. No influenza vaccines are licensed in the United States for administration via jet-injector device (336).
# Live Attenuated Influenza Vaccine (LAIV)
LAIV contains live, attenuated, cold-adapted, temperaturesensitive vaccine viruses which replicate efficiently only at temperatures present in the nasal mucosa. Providers should refer to the package insert, which contains additional information about the formulation of this vaccine and other vaccine components (210). LAIV does not contain thimerosal.
LAIV is shipped at 35°F-46°F (2°C-8°C). LAIV should be stored at 35°F-46°F (2°C-8°C) on receipt and can remain at that temperature until the expiration date is reached (210).
LAIV is intended for intranasal administration only. LAIV is supplied in a prefilled, single-use sprayer containing 0.2 mL of vaccine. Approximately 0.1 mL (i.e., half of the total sprayer contents) is sprayed into the first nostril while the recipient is in the upright position. An attached dose-divider clip is removed from the sprayer to administer the second half of the dose into the other nostril.
# Recombinant Influenza Vaccine
RIV should be stored refrigerated between 36°F-46°F (2°C-8°C). It should not be frozen. Vaccine which has frozen should be discarded. Vials should be protected from light. RIV has a shorter shelf life than IIV. Vaccine should not be used past its expiration date. RIV is administered intramuscularly.
# Influenza Vaccine Composition for the 2013-14 Season
All influenza vaccines licensed in the United States will contain hemagglutinin (HA) derived from influenza viruses antigenically identical to those recommended by FDA (337). This season, for the first time, both trivalent and quadrivalent influenza vaccines will be available in the United States Trivalent influenza vaccines will contain HA derived from three vaccine virus strains: one A(H1N1), one A(H3N2), and one B vaccine virus strain. Quadrivalent vaccines will contain the same the HA antigens as trivalent vaccines, but will also contain HA from a second B virus strain (one B virus strain from each lineage will be represented) (see Quadrivalent Influenza Vaccines).
Trivalent influenza vaccines will contain HA derived from the following:
• an A/California/7/2009 (H1N1)-like virus,
•
# New and Recently Approved Influenza Vaccine Products
Since early 2012, six new influenza vaccines have been approved for use by FDA. These include 1) Flumist Quadrivalent (MedImmune, Gaithersburg, Maryland), a quadrivalent live attenuated influenza vaccine (LAIV4);
# Quadrivalent Influenza Vaccines
All inactivated influenza vaccines available during recent seasons have been trivalent, containing A(H1N1), A(H3N2), and B viral antigens. There are two antigenically distinct lineages of influenza B viruses, referred to as Victoria and Yamagata lineages (13,14). Immunization against influenza B virus strains of one lineage provides only limited cross-protection against strains in the other lineage (338). Given this, and the challenge of predicting which B virus lineage will predominate during a given season, inclusion of two B virus strains (one from each lineage) in seasonal influenza vaccines may improve protection against circulating seasonal B virus strains. A recent modeling analysis indicates that the impact of a quadrivalent vaccine could result in a modest reduction in influenzaassociated outcomes (by 2,200-970,000 cases, 14-8,200 hospitalizations, and 1-485 deaths annually), depending upon adequate vaccine supply, coverage, effectiveness, and incidence of influenza associated with the two B lineages (339).
The World Health Organization (WHO) (340) and FDA (337) have made recommendations for inclusion of a second influenza B vaccine virus in quadrivalent influenza vaccines for the 2013-14 season. This strain will be included in addition to the A(H1N1), A(H3N2), and B vaccine virus strains contained in trivalent vaccines. For the 2013-14 season, quadrivalent influenza vaccines will include a Victoria lineage B/Brisbane/60/2008-like vaccine virus strain, in addition to the Yamagata lineage B/Massachusetts/2/2012-like virus strain contained in trivalent influenza vaccines.
As of August 15, 2013, four quadrivalent seasonal influenza vaccines are expected to be available for the 2013-14 influenza season. Other quadrivalent vaccines might become available in future seasons. New vaccines will be addressed in the ACIP influenza statement as they are approved and become commercially available.
Flumist Quadrivalent: Flumist Quadrivalent (MedImmune), an LAIV4, was approved by FDA in February 2012. All LAIV available in the United States for the 2013-14 season is expected to be the quadrivalent formulation. As with the prior trivalent formulation, Flumist Quadrivalent is approved for persons aged 2 through 49 years (210) and is an alternative for healthy, non-pregnant persons within this age range.
Flumist Quadrivalent contains 10 6.5 -10 7.5 fluorescent focus units (FFU) of live attenuated influenza virus reassortants of each of the four vaccine virus strains recommended for inclusion in quadrivalent influenza vaccines. It is supplied in a single-dose, 0.2 mL intranasal sprayer, and is administered intranasally (0.1 mL per nostril). Contraindications and precautions to the administration of FluMist are similar to those described for LAIV3 (see Contraindications and Precautions for the Use of LAIV; Table 2) (210).
In randomized trials comparing FluMist Quadrivalent with FluMist among children aged 2 through 17 years (210,341) and adults aged 18 through 49 years (210,342) with the exception of fever in children aged 2 through 8 years, similar rates of solicited adverse reactions were observed. Fever was more common after dose 1 in children aged 2 through 8 years following FluMist Quadrivalent (5.1%) compared with FluMist (3.1%). Assessment of the immunogenicity of Flumist Quadrivalent was based upon multicenter, randomized, double-blind, active-controlled non-inferiority studies of immunogenicity performed among children aged 2 through 17 years and adults. In immunogenicity assessments in each study, Flumist Quadrivalent was found to be non-inferior to FluMist. Comparison of the strain-specific serum HAI antibody geometric mean titers (GMTs) postvaccination indicated that the addition of the second B strain was not associated with immune interference to other strains included in the vaccine (344).
Fluarix Quadrivalent: Fluarix Quadrivalent (GlaxoSmithKline), an IIV4, was approved by FDA in December 2012. Fluarix Quadrivalent will be available alongside the trivalent formulation of Fluarix during the 2013-14 season. Both the trivalent and quadrivalent formulations of Fluarix are approved for persons aged ≥3 years (343). Fluarix Quadrivalent is formulated to contain 60 µg HA per 0.5 mL dose (15 µg HA of each of the four influenza virus strains recommended for inclusion in quadrivalent influenza vaccines). It is supplied in 0.5 mL single-dose prefilled syringes, and is administered by intramuscular injection. Contraindications and precautions to the administration of Fluarix Quadrivalent are similar to those described for the trivalent formulation of Fluarix (see Contraindications and Precautions for the Use of IIV; Table 2).
Two studies evaluated safety and immunogenicity of Fluarix Quadrivalent (343). Both involved subjects randomized to receive either Fluarix Quadrivalent or one of two formulations of comparator trivalent influenza vaccine (IIV3), each containing an influenza type B virus corresponding to one of the two type B viruses in Fluarix Quadrivalent. One study evaluated adults aged ≥18 years, and the other focused on children aged 3 through 17 years. In adults, the most common (≥10%) injection site adverse reaction was pain (36%); the most common systemic adverse events were muscle aches (16%), headache (16%), and fatigue (16%). Among children aged 3 through 17 years, the most common injection site adverse reactions were pain (44%), redness (23%), and swelling (19%). In children aged 3 through 5 years, the most common (≥10%) systemic adverse events were drowsiness (17%), irritability (17%), and loss of appetite (16%); in children aged 6 through 17 years, the most common systemic adverse events were fatigue (20%), muscle aches (18%), headache (16%), arthralgia (10%), and gastrointestinal symptoms (10%). Overall frequencies of most solicited adverse events associated with Fluzone Quadrivalent in these studies were generally similar to these reported for the comparator trivalent vaccines
In immunogenicity analyses, Fluarix Quadrivalent was noninferior to both comparator IIV3s based on adjusted GMTs and seroconversion rates. The antibody response to influenza B strains contained in Fluarix Quadrivalent was higher than the antibody response after vaccination with a trivalent IIV containing an influenza B strain from a different lineage. No evidence indicated that the addition of the second B strain resulted in immune interference to other strains included in the vaccine (343).
Fluzone Quadrivalent: Fluzone Quadrivalent (Sanofi Pasteur), an IIV4, was approved by FDA in June 2013. Fluzone Quadrivalent will be available alongside the trivalent formulation of Fluzone during the 2013-14 season. Both the trivalent and quadrivalent formulations of Fluzone are approved for persons aged ≥6 months (344).
Fluzone Quadrivalent is formulated to contain 60 µg HA per 0.5 mL dose (15 µg HA of each of the four influenza virus strains recommended for inclusion in quadrivalent influenza vaccines). It is available in three presentations (0.25 and 0.5 mL single-dose prefilled syringes and 0.5 mL single-dose vials), and is administered by intramuscular injection. Contraindications and precautions to the administration of Fluzone Quadrivalent are similar to those described for the trivalent formulation of Fluzone (see Contraindications and Precautions for the Use of IIV; Table 2).
Safety of Fluzone Quadrivalent was evaluated in three studies including participants aged ≥6 months who were randomized to receive either Fluzone Quadrivalent or one of two formulations of comparator trivalent influenza vaccine (IIV3), each containing an influenza type B virus corresponding to one of the two type B viruses in Fluzone Quadrivalent (344). Among children aged 6 through 35 months, the most common local reactions (reported in ≥10% of participants) included pain (57%), tenderness (54%), erythema (37%), and swelling (22%); the most common solicited systemic reactions were irritability (54%), abnormal crying (41%), drowsiness (38%), malaise (38%), myalgia (27%), appetite loss (32%), fever (14%), and vomiting (15%). Among children aged 3 through 8 years, the most frequently reported local reactions included pain (67%), erythema (34%), and swelling (25%); the most common solicited systemic reactions were malaise (32%), myalgia (39%), and headache (23%). Among adults aged ≥18 years, the most common injection site adverse reaction was pain (47% among those aged ≥18 years and 33% among those aged ≥65 years); the most common systemic adverse events were myalgia (24% among those aged ≥18 years and 18% among those aged ≥65 years), headache (16% among those aged ≥18 years and 13% among those aged ≥65 years), and malaise (11% among those in both age groups). Overall frequencies of most solicited adverse events associated with Fluzone Quadrivalent in these studies were generally similar to these reported for the comparator trivalent vaccines (344).
In immunogenicity analyses performed in these studies, Fluzone Quadrivalent was noninferior to both IIV3s based on adjusted GMTs and seroconversion rates for all four strains contained in the vaccine for children and for adults aged ≥18 years. For adults aged ≥65 years, GMTs were noninferior for all four strains; seroconversion rates were non-inferior to those for IIV3 for the included influenza A(H3N2), and both the Victoria and Yamagata B strains, but not for the included influenza A(H1N1). Overall, antibody response to influenza B strains contained in Fluzone Quadrivalent was higher than the antibody response after vaccination with a trivalent IIV containing an influenza B strain from a different lineage (344).
Flulaval Quadrivalent: Flulaval Quadrivalent (ID Biomedical Corporation/GlaxoSmithKline), an IIV4, was approved by FDA in August 2013. Fluarix Quadrivalent will be available alongside the trivalent formulation of Flulaval during the 2013-14 season. Both the trivalent and quadrivalent formulations of Flulaval are approved for persons aged ≥3 years (345).
Flulaval Quadrivalent is formulated to contain 60 µg HA per 0.5 mL dose (15 µg HA of each of the four influenza virus strains recommended for inclusion in quadrivalent influenza vaccines). It is supplied in 5.0 mL multi-dose vials and is administered by intramuscular injection. Contraindications and precautions to the administration of Fluarix Quadrivalent are similar to those described for the trivalent formulation of Flulaval (see Contraindications and Precautions for the Use of IIV; Table 2) (345).
In clinical studies, the most common (≥10%) solicited local adverse reaction to Flulaval Quadrivalent among adults was pain (60%); the most common solicited systemic adverse events were muscle aches (26%), headache (22%), fatigue (22%), and arthralgia (15%). Among children aged 3 through 17 years, the most common (≥10%) solicited local adverse reaction was pain (65%). Among children aged 3 through 4 years, the most common (≥10%) solicited systemic adverse events were irritability (26%), drowsiness (21%), and loss of appetite (17%). Among children aged 5 through 17 years, the most common (≥10%) solicited systemic adverse events were muscle aches (29%), fatigue (22%), headache (22%), arthralgia (13%), and gastrointestinal symptoms (10%) (345).
In immunogenicity studies, there was no evidence that the addition of a second B strain resulted in immune interference to other strains included in the vaccine. In a randomized, observer-blind, non-influenza vaccine-controlled study of FluLaval Quadrivakent vs. Havrix (hepatitis A vaccine, GlaxoSmithKline) conducted among children aged 3 through 8 years, vaccine efficacy was vaccine efficacy was vaccine efficacy was 55.4% (95% CI = 39.1-67.3) for RT-PCR-confirmed influenza, and 55.9% (97.5% CI = 35.4-69.9) for culture confirmed influenza (345).
# Vaccines Produced via Non-Egg Based Technologies
For the 2013-14 season, two new vaccines for adults will be available that are manufactured using newer technologies that minimize or avoid entirely the use of eggs. A primary advantage of these manufacturing methods is that they might permit more rapid scale up of vaccine production when needed (e.g., response to a pandemic). These include Flucelvax (Novartis, Cambridge, Massachusetts), which is produced using cell culture technology, and FluBlok (Protein Sciences, Meriden, Connecticut), which contains recombinant HA.
Flucelvax: Flucelvax, a ccIIV3, was approved by FDA in November 2012. It is a trivalent subunit IIV prepared from virus propagated in Madin Darby Canine Kidney (MDCK) cells. It is approved for persons aged ≥18 years (346).
Flucelvax contains a total of 45 µg HA (15 µg HA of each of the included influenza A(H1N1), influenza A(H3N2), and influenza B vaccine virus strains) per 0.5 mL dose. It is supplied in single-dose, prefilled syringes and is administered via intramuscular injection. Contraindications are similar to those for other IIVs (see Contraindications and Precautions for the Use of IIV; Table 2) (346).
In clinical studies of Flucelvax, the most common (≥10%) solicited adverse reactions among adults aged 18 through 64 years occurring within 7 days of vaccination were injection-site pain (28%), erythema at the injection site (13%), headache (16%), fatigue (12%), myalgia (11%), and malaise (10%). The most common (≥10%) solicited adverse reactions occurring in adults aged ≥65 years within 7 days of vaccination were erythema at the injection site (10%), fatigue (11%), headache (10%) and malaise (10%) (346)(347)(348). Injection site pain was reported significantly more frequently than with a licensed comparator egg-based IIV3 in one study, but was of mild or moderate severity in >99% of reports and usually resolved within 48 hours (348). In a multinational placebo-controlled study conducted during the 2007-08 influenza season among persons aged 18-49 years, Flucelvax was 83.8% effective (lower limit of one-sided 97% CI = 61%) against culture-confirmed influenza caused by viruses antigenically matched to the vaccine. In three studies in adults aged ≥18 years, Flucelvax demonstrated comparable immunogenicity to U.S.-licensed comparator vaccines for all three vaccine strains (346).
Although manufacture of the Flucelvax does not use eggs, the vaccine cannot be considered to be egg-free. Before beginning production, seed viruses are created using reference virus strains supplied by the World Health Organization that have been passaged in eggs. The total egg protein is estimated to be less than 50 femtograms (5x10 -14 grams or 5x10 -8 µg) total egg protein (of which a fraction is ovalbumin) per 0.5 mL dose of Flucelvax (Novartis, personal communication, 2013).
FluBlok: Approved in January 2013, FluBlok is a trivalent recombinant HA influenza vaccine (RIV3) containing purified HA proteins produced in a continuous insect cell line using a baculovirus vector. This process uses neither live influenza viruses nor eggs. Flublok is approved for persons aged 18 through 49 years (349).
FluBlok contains 135 µg HA per 0.5 mL dose (45 µg of each of the three HA antigens recommended for inclusion in trivalent influenza vaccines). It is supplied in 0.5 mL singledose vials and is administered by intramuscular injection. Contraindications include severe allergic reaction to any component of the vaccine (349).
Safety, immunogenicity, and efficacy of FluBlok were evaluated in randomized, double-blind, placebo-controlled studies (350,351) conducted among healthy adults aged 18 through 49 years that compared recombinant HA vaccines containing a total of 135 µg HA with placebo. The most frequently reported injection site reaction (reported in ≥10% of the 135 µg-dose recipients) was pain (>37%); the most common solicited systemic reactions were headache (>15%), fatigue (>15%), and myalgias (>11%) (349,351). Local pain and tenderness were reported significantly more frequently with FluBlok than placebo; however, 94% of reports of pain following FluBlok were rated as mild. In a randomized placebo-controlled efficacy study of the 135 µg HA dose of FluBlok conducted among healthy adults during the 2007-08 influenza season (349,351), estimated vaccine effectiveness for CDC-defined ILI with a positive culture for influenza virus was 75.4% (95% CI = -148.0%-99.5%) against matched strains; more precise estimation of vaccine effectiveness was not possible because 96% of isolates in this study did not antigenically match the strains represented in the vaccine (349). Estimated vaccine effectiveness without regard to match was 44.6% (95% CI = 18.8%-62.6%) (351).
# Recommendations for the Use of Influenza Vaccines, 2013-14 Influenza Season Groups Recommended for Vaccination
Routine annual influenza vaccination is recommended for all persons aged ≥6 months who do not have contraindications. Recommendations pertaining to the use of specific vaccines and populations are summarized below.
# Timing of Vaccination
In general, health-care providers should begin offering vaccination soon after vaccine becomes available and, if possible, by October. All children aged 6 months through 8 years who are recommended for 2 doses should receive their first dose as soon as possible after vaccine becomes available; these children should receive the second dose ≥4 weeks later. This practice increases the opportunity for both doses to be administered before or shortly after the onset of influenza activity. To avoid missed opportunities for vaccination, providers should offer vaccination during routine health-care visits or during hospitalizations whenever vaccine is available.
Vaccination efforts should be structured to ensure the vaccination of as many persons as possible before influenza activity in the community begins. In any given year, the optimal time to vaccinate cannot be determined precisely because influenza seasons vary in their timing and duration, and more than one outbreak might occur in a single community in a single year. In the United States, localized outbreaks that indicate the start of seasonal influenza activity can occur as early as October. However, in >80% of influenza seasons since 1976, peak influenza activity (which often is close to the midpoint of influenza activity for the season) has not occurred until January or later, and in >60% of seasons, the peak was in February or later (5).
In recent seasons, initial shipments of influenza vaccine have arrived to some vaccine providers as early as July. Very early availability of vaccine as compared with typical onset and peak of influenza activity raises questions related to the ideal time to begin vaccination. Antibody levels induced by vaccine decline over the months after vaccination (99,(352)(353)(354). Although a 2008 literature review found no clear evidence of more rapid decline among the elderly (105), a 2010 study noted significant decline in titers 6 months postvaccination among persons aged ≥65 years (though titers still met European Medicines Agency levels considered adequate for protection) (354). More recently, some investigators have estimated vaccine effectiveness over the course of a season, as a function of time since vaccination.
A case-control study conducted in Navarre, Spain, during the 2011-12 season revealed a decline in vaccine effectiveness from 61% (95% CI = 5-84) in the first 100 days postvaccination to 42% (95% CI = -39-75) for 100-119 days postvaccination and to -35% (95% CI = -211-41) thereafter. This decline primarily affected persons aged ≥65 years, among whom vaccine effectiveness declined from 85% (95% CI = -8-98) to 24% (95% CI = -224-82) to -208 (95% CI = -1,563-43) over these intervals. Most viruses isolated among those infected which were characterized did not match the vaccine strains (106). A case-control study conducted in the United Kingdom during the same season estimated an overall vaccine effectiveness against A(H3N2) of 53% (95% CI = 0-78) among those vaccinated less than 3 months, and 12% (95% CI = -31-41) for those vaccinated 3 months or more. The proportion of persons aged ≥65 years was too small to detect a substantial difference in vaccine effectiveness among this age group (355). Further evaluation of this effect in larger studies and in different seasons is needed. ACIP will continue to evaluate further data as they become available.
While delaying vaccination until later in the season might permit greater immunity later in the season, such deferral might result in missed opportunities to vaccinate, as well as difficulties in vaccinating a population within a more constrained time period. Community vaccination programs should balance maximizing likelihood of persistence of vaccineinduced protection through the season with avoiding missed opportunities to vaccinate or vaccinating after influenza circulation occurs.
Vaccination efforts should continue throughout the season, because the duration of the influenza season varies and influenza activity might not occur in certain communities until February or March. Providers should offer influenza vaccine routinely, and organized vaccination campaigns should continue throughout the influenza season, including after influenza activity has begun in the community. Vaccine administered in December or later, even if influenza activity has already begun, is likely to be beneficial in the majority of influenza seasons. The majority of adults have antibody protection against influenza virus infection within 2 weeks after vaccination (356,357).
# Available Vaccine Products and Indications
No preferential recommendation is made for one influenza vaccine product over another for persons for whom more than one product is otherwise appropriate. A variety of influenza vaccine products are available (Table 1), including (as of August 2013) six newly approved vaccines (see New and Recently Approved Influenza Vaccine Products). For many vaccine recipients, more than one type or brand of vaccine may be appropriate within indications and ACIP recommendations. Considerations for selection of a given vaccine when several appropriate options are available are discussed below. However, not all products are likely to be uniformly available in any practice setting or locality. For newer vaccines, supplies might be limited during the 2013-14 season; moreover, postmarketing safety and effectiveness data are as yet unavailable, prohibiting a full risk-benefit analysis of newer versus previously available products. Therefore, within these guidelines and approved indications, where more than one type of vaccine is appropriate and available, no preferential recommendation is made for use of any influenza vaccine product over another.
# Inactivated Influenza Vaccines
IIVs comprise a large group of products. For the 2013-14 season, most IIVs will be trivalent (IIV3), with some quadrivalent (IIV4) also available. Among IIV3 preparations, cell-culture based IIV will be available (ccIIV3). As a class, IIVs include products which might be administered to all persons aged ≥6 months. However, approved age indications for the various IIV products differ (Table 1). Only age-appropriate products should be administered. Providers should consult package inserts and updated CDC/ACIP guidance for current information. Of particular note, although Afluria (CSL Limited) is FDA-approved for children aged >5 years, CDC and ACIP recommend against use of Afluria in persons aged <9 years because of increased risk for febrile reactions noted in this age group with CSL's 2010 Southern Hemisphere IIV3 (228). If no other age-appropriate, licensed inactivated seasonal influenza vaccine is available for a child aged 5 through 8 years who has a medical condition that increases the child's risk for influenza complications, Afluria can be used; however, providers should discuss with the parents or caregivers the potential benefits and risks of influenza vaccination with Afluria in this age group before administering this vaccine (358).
All IIV preparations contain the same quantity of HA (15 µg per vaccine virus strain per 0.5 mL dose; 45 µg total), except Fluzone Intradermal and Fluzone High-Dose (Sanofi Pasteur). Fluzone Intradermal is approved for persons aged 18 through 64 years, and contains 9 µg of each HA per vaccine virus strain (27 µg total). Fluzone High-Dose is approved for persons aged ≥65 years and contains 60 µg of each HA per vaccine virus strain (180 µg total). Within specified age indications, ACIP expresses no preference for any given IIV over another.
The one IIV product licensed by FDA for children aged 6 through 36 months contains 0.25 mL/dose. The 0.25 mL dose may be administered from a prefilled single-dose syringe, single-use vial, or multi-dose vial of this age-appropriate formulation. Children aged 36 months through 18 years, and adults receiving IM preparations of IIV, should receive a 0.5 mL dose. If a pediatric vaccine dose (0.25 mL) is administered inadvertently to an adult, an additional pediatric dose (0.25 mL) should be administered to provide a full adult dose (0.5 mL). If the error is discovered later (after the patient has left the vaccination setting), an adult dose should be administered as soon as the patient can return. Vaccination with a formulation approved for adult use should be counted as a dose if inadvertently administered to a child (5).
With the exception of Fluzone Intradermal (Sanofi Pasteur), IIVs should be administered intramuscularly. For adults and older children, the deltoid is the preferred site. Infants and younger children should be vaccinated in the anterolateral thigh. Additional specific guidance regarding site selection and needle length for intramuscular administration are provided in ACIP's General Recommendations on Immunization (270). Fluzone Intradermal is administered intradermally, preferably over the deltoid muscle, using the included delivery system (240).
Trivalent versus Quadrivalent IIVs: For the first time, during the 2013-14 influenza season, both trivalent (IIV3) and quadrivalent (IIV4) IIVs will be available. The relative quantity of doses of IIV4 that will be available is not certain; however, it is expected that the supply of IIV4 might be limited. Quadrivalent vaccines are designed to provide broader protection against circulating influenza B viruses in seasons during which the B virus contained in trivalent vaccines is not an optimal match to the predominant circulating B viruses. However, vaccination should not be delayed if only IIV3 is available. No preference is expressed for IIV4 over IIV3.
IIVs and persons aged ≥65 years: For persons aged ≥65 years, either an age-appropriate standard-dose IIV (IIV3 or IIV4) or high-dose IIV3 are acceptable options. High-dose IIV3 (available as Fluzone High-Dose) is approved for persons aged ≥65 years. Immunogenicity data from three prelicensure studies among persons aged ≥65 years indicated that, compared with standard dose Fluzone, Fluzone High-Dose elicited higher HAI titers against all three influenza virus strains included in seasonal influenza vaccines recommended during the study period (178)(179)(180)359). Whether the higher postvaccination immune responses observed among Fluzone High-Dose vaccine recipients will result in greater protection against influenza illness is under study. Some solicited injection site and systemic adverse events were more frequent after vaccination with Fluzone High-Dose compared with standard Fluzone, but typically were mild and transient (178)(179)(180). No preferential recommendation is made for high-dose IIV over standard dose IIV for persons aged ≥65 years.
IIVs and egg allergy: With the exception of Flucelvax, IIVs are manufactured via propagation of virus in eggs and therefore might contain residual egg protein. Egg protein content (usually described as ovalbumin content as a surrogate measure) is not disclosed on all package inserts (Table 1); where not listed, this information generally can be obtained by contacting the manufacturer. Flucelvax is manufactured from virus propagated in Madin Darby Canine Kidney (MDCK) cells rather than embryonated eggs; however, before production seed virus is created using reference virus strains supplied by WHO, which have been passaged in eggs. Flucelvax can therefore not be considered egg-free. The total egg protein is estimated to be <50 femtograms (5x10 -14 grams) total egg protein (of which a fraction is ovalbumin) per 0.5 mL dose of Flucelvax (Novartis, unpublished data, 2013). Flucelvax can be administered to persons with a history of mild egg allergy (specifically, those who have experienced only hives following egg exposure; see Influenza Vaccination of Persons with Egg Allergy) who are aged ≥18 years and have no other contraindications. Because no data are available regarding the use of ccIIV among egg-allergic persons, and there is no established safe threshold for ovalbumin content in vaccines, ccIIV should be administered according to the guidance for other IIVs (see Influenza Vaccination of Persons with Egg Allergy).
Contraindications and precautions for use of IIVs: Manufacturer package inserts and updated CDC/ACIP guidance should be consulted for current information on contraindications and precautions for individual vaccine products. In general, IIV is contraindicated for, and should not be administered to, persons known to have anaphylactic hypersensitivity to eggs or to any vaccine components (Table 2). Prophylactic use of antiviral agents is an option for preventing influenza among such persons. Information about vaccine components is located in package inserts from each manufacturer.
Moderate or severe acute illness with or without fever is a general precaution for vaccination (270). GBS within 6 weeks following a previous dose of influenza vaccine is considered a precaution for use of influenza vaccines (Table 2).
# Recombinant Influenza Vaccine
One RIV product, FluBlok, a trivalent recombinant HA vaccine, is expected to be available for the 2013-14 influenza season. This RIV3 is administered by intramuscular injection, and is indicated for persons aged 18 through 49 years. RIV3 is manufactured without the use of influenza viruses; therefore, similarly to IIVs, no shedding of vaccine virus will occur. No preference is expressed for RIV versus IIV within specified indications.
RIV and egg allergy: The currently available RIV, FluBlok, is manufactured without the use of eggs, and does not carry a contraindication for egg allergy. Therefore, Flublok can be administered to persons with egg allergy of any severity who are aged 18 through 49 years and do not have other contraindications. Since 2011, ACIP has recommended that persons with a history of mild egg allergy (specifically, those who experience only hives following egg exposure) can receive IIV, with additional safety precautions. For such persons, vaccination should not be delayed if RIV is not available; IIV should be used in these settings, following the recommendations outlined (see Influenza Vaccination of Persons with Egg Allergy).
Contraindications and precautions for use of RIV: FluBlok is contraindicated in persons who have had a severe allergic reaction to any component of the vaccine. Moderate or severe acute illness with or without fever is a general precaution for vaccination (270). GBS within 6 weeks following a previous dose of influenza vaccine is considered a precaution for use of influenza vaccines (Table 2). FluBlok is not licensed for use in children aged <18 years or adults aged >49 years.
# Live Attenuated Influenza Vaccine
One LAIV4 product, FluMist Quadrivalent (MedImmune), is expected to be available during the 2013-14 influenza season. Flumist is indicated for nonpregnant persons aged 2 through 49 years who do not have a medical condition that predisposes them to medical complications from influenza. No preference is indicated for LAIV versus other vaccines appropriate for this group.
LAIV is administered intranasally using the supplied 0.2 mL intranasal sprayer (0.1 mL in each nostril). If the vaccine recipient sneezes immediately after administration, the dose should not be repeated. However, if nasal congestion is present that might impede delivery of the vaccine to the nasopharyngeal mucosa, deferral of administration should be considered until resolution of the illness, or IIV should be administered instead.
LAIV versus IIV: Several randomized studies have evaluated the relative effectiveness of LAIV3 as compared with IIV3 (205,(212)(213)(214)218,220,221). Most studies conducted among adults have noted superior relative efficacy of IIV3 (205,(212)(213)(214). A significantly greater relative efficacy of LAIV3 as compared with IIV3 has been noted in several studies conducted among younger children, including a randomized, open label study among children aged 6 through 71 months (221), a randomized blinded trial of children aged 6 through 59 months (218), and a randomized blinded trial of children with asthma aged 6 through 17 years (220). However, no postmarketing safety data are yet available for the new quadrivalent formulation, LAIV4, which will be available for the first time during the 2013-14 season and is expected to replace LAIV3. Therefore, no preferential recommendation is made for LAIV4 over IIV for any age group at this time. This information will be updated as more data become available. Vaccination should not be delayed if LAIV is not available.
LAIV and egg allergy: Because of relative lack of data demonstrating safety of LAIV for persons with egg allergy, egg-allergic persons should receive IIV rather than LAIV (see Influenza Vaccination of Persons with Egg Allergy) (360).
Contraindications and precautions to the use of LAIV: LAIV is contraindicated for persons with a history of severe hypersensitivity reaction to any component of the vaccine or to a previous dose of any influenza vaccine, and in children and adolescents receiving concomitant aspirin therapy (Table 2). In addition, LAIV should not be administered to the following groups:
• children aged <2 years;
• adults aged ≥50 years;
• children aged 2 through 4 years whose parents or caregivers report that a health-care provider has told them during the preceding 12 months that their child had wheezing or asthma or whose medical record indicates a wheezing episode has occurred during the preceding 12 months (Table 1); • persons with asthma;
• children and adults who have chronic pulmonary, cardiovascular (except isolated hypertension), renal, hepatic, neurologic/neuromuscular, hematologic, or metabolic disorders; • children and adults who have immunosuppression (including immunosuppression caused by medications or by HIV); and • pregnant women. Moderate or severe acute illness with or without fever is a general precaution for vaccination (270). GBS within 6 weeks following a previous dose of influenza vaccine is considered a precaution for use of influenza vaccines.
# Persons at Risk for Medical Complications Attributable to Severe Influenza
Vaccination to prevent influenza is particularly important for persons who are at increased risk for severe complications from influenza, or at higher risk for influenza-related outpatient, ED, or hospital visits. When vaccine supply is limited, vaccination efforts should focus on delivering vaccination to the following persons (no hierarchy is implied by order of listing):
• all children aged 6 through 59 months;
• all persons aged ≥50 years;
•
# Vaccine Dose Considerations for Children Aged 6 Months Through 8 Years
Evidence from several studies indicates that children aged 6 months through 8 years require 2 doses of influenza vaccine (administered a minimum of 4 weeks apart) during their first season of vaccination to optimize immune response. In a study of children aged 5 through 8 years receiving trivalent inactivated influenza vaccine (IIV3) for the first time, the proportion of children with protective antibody responses was significantly higher (p<0.001 for influenza A(H1N1), p = 0.01 for influenza A(H3N2), and p<0.001 for influenza B) after 2 doses as compared with a single dose (115). Several studies have indicated that the time interval between two initial doses (from 4 weeks up to 1 year) of the same antigen may not be critical (363)(364)(365). However, because of the antigenic novelty of the 2009 influenza A(H1N1) pandemic virus, which is anticipated to continue circulating during the 2013-14 influenza season, exposure history to this vaccine virus antigen also must be considered. Children who last received seasonal (trivalent) influenza vaccine before the 2010-11 season but did not receive a vaccine containing 2009(H1N1) antigen (i.e., either in seasonal vaccine since July 2010 or monovalent 2009(H1N1) vaccine) will not have received this antigen. These children are recommended to receive 2 doses this season, even if 2 doses of seasonal influenza vaccine were received before the 2010-11 season. This recommendation is illustrated in the approaches outlined below. These recommendations are consistent with those of the American Academy of Pediatrics (366). Two approaches are recommended, both of which are acceptable.
The first approach (Figure 1), takes into consideration only doses of seasonal influenza vaccine received since July 1, 2010. This approach has the advantage of simplicity, particularly in settings in which it is difficult to ascertain vaccination history before the 2010-11 season. Using this approach, children aged In settings where adequate vaccination history from before the 2010-11 season is available, the second approach may be used. By this approach, if a child aged 6 months through 8 years is known to have received at least 2 doses of seasonal influenza vaccine during any prior season, and at least 1 dose of a 2009(H1N1)-containing vaccine (i.e., 2010-11, 2011-12, or 2012-13 seasonal vaccine or the monovalent 2009 [H1N1] vaccine) then the child needs only 1 dose for the 2013-14 season. Using this approach, children aged 6 months through 8 years need only 1 dose of vaccine in the 2013-14 season if they have received any of the following:
• 2 or more doses of seasonal influenza vaccine since July 1, 2010 or; • 2 or more doses of seasonal influenza vaccine before July 1, 2010 and 1 or more doses of monovalent 2009(H1N1) vaccine or; • 1 or more doses of seasonal influenza vaccine before July 1, 2010, and 1 or more doses of seasonal influenza vaccine since July 1, 2010. Children aged 6 months through 8 years for whom one of these conditions is not met require 2 doses in the 2013-14 season.
# Influenza Vaccination for Pregnant Women
Pregnant and postpartum women are at higher risk for severe illness and complications from influenza than women who are not pregnant because of changes in the immune system, heart, and lungs during pregnancy (367). Vaccination during pregnancy has been shown to protect infants from influenza (170,368), including infants aged <6 months, for whom no influenza vaccines are currently licensed (368)(369)(370). The ACIP and American College of Obstetricians and Gynecologists (ACOG) recommends that all women who are pregnant or who might be pregnant in the upcoming influenza season receive IIV because of this increased risk for serious illness and complications from influenza (371). Influenza vaccination can be administered at any time during pregnancy, before and during the influenza season.
Women who are or will be pregnant during influenza season should receive IIV. Live attenuated influenza vaccine (LAIV) is not recommended for use during pregnancy. Postpartum women can receive either LAIV or IIV. Pregnant and postpartum women do not need to avoid contact with persons recently vaccinated with LAIV.
# Influenza Vaccination of Persons With a History of Egg allergy
Severe allergic and anaphylactic reactions can occur in response to a number of influenza vaccine components, but such reactions are rare. With the exceptions of RIV and ccIIV3, currently available influenza vaccines are prepared by propagation of virus in embryonated eggs. A recent review of published data (including 4,172 patients, 513 of whom were reported to have a history of severe allergic reaction to egg) noted that no occurrences of anaphylaxis were reported, though some milder reactions did occur (372), suggesting that severe allergic reactions to egg-based influenza vaccines are unlikely. Vaccines containing as much as 0.7 µg/0.5 mL have been tolerated (360,373); however, a threshold below which no reactions would be expected is not known (360). Although ovalbumin content is not required to be disclosed on package inserts for vaccines used in the United States, manufacturers either report maximum albumin content in the package inserts or will provide this information on request. Among IIVs for which ovalbumin content was disclosed during the 2011-12 and 2012-13 seasons, reported maximum amounts were ≤1 µg/0.5 mL dose. Ovalbumin is not directly measured for Flucelvax, but it is estimated by calculation from the initial content in the reference virus strains to contain a maximum of 5x10 -8 µg/0.5 mL dose of total egg protein (Novartis, unpublished data, 2013). Flublok is egg-free. It should be noted, however, that neither Flucelvax nor Flublok are licensed for children aged <18 years.
# Surveillance for Anaphylaxis Following Influenza Vaccination
Following review of available data, since the 2011-12 influenza season, ACIP has recommended that persons with egg allergy who report only hives after egg exposure should receive IIV, with several additional safety measures (231); current FDA-approved packaging for influenza vaccines lists only severe hypersensitivity to egg protein as a contraindication to vaccination. Review of VAERS data for the 2011-12 and 2012-13 seasons indicated no disproportionate reporting of allergic reaction or anaphylaxis after influenza vaccination during the first two seasons the new recommendation was in place (374,375). However, during the 2012-13 influenza season, VAERS received one report containing a documented medical history of anaphylaxis following receipt of a first-ever split dose IIV in a child aged 12 months with atopy but no known prior egg ingestion in the past, who had a previous positive allergy skin prick test to ovalbumin. This child had previously received allergy testing attributed to a strong personal and family history of food allergies and other allergies (375). For the 2013-14 season, the recommendations which follow include guidance concerning persons who have no history of exposure to egg, but who have documented results potentially suggestive of egg allergy on previously performed allergy testing.
For the 2013-14 influenza season, ACIP recommends the following:
• Persons with a history of egg allergy who have experienced only hives after exposure to egg should receive influenza vaccine. Because relatively few data are available for use of LAIV in this setting, IIV or RIV should be used. RIV is egg-free and may be used for persons aged 18-49 years who have no other contraindications. However, IIV (egg-or cell-culture based) also may be used, with the following additional safety measures (Figure 2): -Vaccine should be administered by a health-care provider who is familiar with the potential manifestations of egg allergy; and -Vaccine recipients should be observed for at least 30 minutes for signs of a reaction after administration of each vaccine dose (360). • Other measures, such as dividing and administering the vaccine by a two-step approach and skin testing with vaccine, are not necessary (360). • Persons who report having had reactions to egg involving such symptoms as angioedema, respiratory distress, lightheadedness, or recurrent emesis; or who required epinephrine or another emergency medical intervention, particularly those that occurred immediately or within a short time (minutes to hours) after egg exposure, are more likely to have a serious systemic or anaphylactic reaction upon reexposure to egg proteins. These persons may receive RIV3, if aged 18 through 49 years and there are no other contraindications. If RIV3 is not available or the recipient is not within the indicated age range, such persons should be referred to a physician with expertise in the management of allergic conditions for further risk assessment before receipt of vaccine (Figure 2). • All vaccines should be administered in settings in which personnel and equipment for rapid recognition and treatment of anaphylaxis are available. ACIP recommends that all vaccination providers should be familiar with the office emergency plan (270). • Some persons who report allergy to egg might not be eggallergic. Those who are able to eat lightly cooked egg (e.g., scrambled egg) without reaction are unlikely to be allergic.
Egg-allergic persons might tolerate egg in baked products (e.g., bread or cake). Tolerance to egg-containing foods does not exclude the possibility of egg allergy (376). Egg allergy can be confirmed by a consistent medical history of adverse reactions to eggs and egg-containing foods, plus skin and/or blood testing for immunoglobulin E antibodies to egg proteins. • For persons who have no known history of exposure to egg, but who are suspected of being egg-allergic on the basis of previously performed allergy testing, consultation with a physician with expertise in the management of allergic conditions should be obtained before vaccination (Figure 2). Alternatively, RIV3 may be administered if the recipient is aged 18 through 49 years. • A previous severe allergic reaction to influenza vaccine, regardless of the component suspected to be responsible for the reaction, is a contraindication to future receipt of any influenza vaccine.
# Influenza Vaccines and Use of Influenza Antiviral Medications
Administration of IIV to persons receiving influenza antiviral drugs for treatment or chemoprophylaxis is acceptable. The effect on safety and effectiveness of LAIV co-administration with influenza antiviral medications has not been studied. However, because antiviral drugs reduce replication of influenza viruses, LAIV should not be administered until 48 hours after cessation of influenza antiviral therapy (210). If influenza antiviral medications are administered within 2 weeks after receipt of LAIV, the LAIV dose should be repeated 48 or more hours after the last dose of antiviral medication. Alternatively, persons receiving antiviral drugs within the period 2 days before to 14 days after vaccination with LAIV may be revaccinated another approved vaccine formulation (e.g., IIV or RIV).
# Concurrent Administration of Influenza Vaccine With Other Vaccines
Limited data are available on the concurrent administration of influenza vaccines with other live vaccines. Use of LAIV3 concurrently with measles, mumps, rubella (MMR) and varicella vaccine among children aged 12 through 15 months has been studied, and no interference with the immunogenicity to antigens in any of the vaccines was observed (210,377). Among adults aged ≥50 years, the safety and immunogenicity of zoster vaccine and IIV3 were similar whether administered simultaneously or sequentially spaced 4 weeks apart (378).
In the absence of specific data indicating interference, following ACIP's general recommendations for vaccination is prudent (270). Inactivated vaccines do not interfere with the immune response to other inactivated vaccines or to live vaccines. Inactivated or live vaccines can be administered simultaneously with LAIV. However, after administration of a live vaccine (such as LAIV), at least 4 weeks should pass before another live vaccine is administered.
# Sources of Information Regarding Influenza and Surveillance
Updated information regarding influenza surveillance, prevention, detection, and control is available at http:// www.cdc.gov/flu. U.S surveillance data are updated weekly during October-May on FluView (http://www.cdc.gov/flu/ weekly). In addition, periodic updates regarding influenza are published in MMWR (http://www.cdc.gov/mmwr). Additional information regarding influenza vaccine can be obtained from CDC by calling telephone 1-800-232-4636. State and local health departments should be consulted about availability of influenza vaccine, access to vaccination programs, information related to state or local influenza activity, reporting of influenza outbreaks and influenza-related pediatric deaths, and advice concerning outbreak control.
# Vaccine Adverse Event Reporting System
The National Childhood Vaccine Injury Act of 1986 requires health-care providers to report any adverse event listed by the vaccine manufacturer as a contraindication to further doses of the vaccine, or any adverse event listed in the VAERS Table of Reportable Events Following Vaccination (http://vaers. hhs.gov/resources/VAERS_Table_of_Reportable_Events_ Following_Vaccination.pdf ) that occurs within the specified time period after vaccination. In addition to mandated reporting, health-care providers are encouraged to report any clinically significant adverse event following vaccination to VAERS. Information on how to report a vaccine adverse event is available at http://vaers.hhs.gov/esub/index. Reports can be filed securely online, by mail, or by fax. A VAERS form can be downloaded from the VAERS website or requested by sending an e-mail message to [email protected], by calling telephone 1-800-822-7967, or by sending a request by facsimile to 1-877-721-0366. Additional information on VAERS or vaccine safety is available at http://vaers.hhs.gov/about/index or by calling telephone 1-800-822-7967.
# National Vaccine Injury Compensation Program
The National Vaccine Injury Compensation Program (VICP), established by the National Childhood Vaccine Injury Act of 1986, as amended, provides a mechanism through which compensation can be paid on behalf of a person determined to have been injured or to have died as a result of receiving a vaccine covered by VICP. The Vaccine Injury Table (available at http://www.hrsa.gov/vaccinecompensation/vaccinetable. html) lists the vaccines covered by VICP and the associated injuries and conditions (including death) that may receive a legal presumption of causation. If the injury or condition is not on the Table, or does not occur within the specified time period on the Table, persons must prove that the vaccine caused the injury or condition. Eligibility for compensation is not affected by whether a covered vaccine is used off-label or inconsistently with recommendations.
For a claim to be eligible for compensation under the VICP, it must be filed within 3 years after the first symptom of the vaccine injury. Death claims must be filed within 2 years of the vaccine-related death and not more than 4 years after the start of the first symptom of the vaccine-related injury from which the death occurred. When a new vaccine is covered by VICP or when a new injury/condition is added to the Table, claims can be filed within 2 years from the date the vaccine or injury/condition is added to the Table for injuries or deaths that occurred up to 8 years before the Table change. Persons of all ages who receive a VICP-covered vaccine may be eligible to file a claim. Additional information is available at http://www. hrsa.gov/vaccinecompensation or by calling 1-800-338-2382.
# Additional Information Regarding Prevention of Influenza in Specific Populations
• CDC. | None | None |
d95cbc4811cb72a3cbb495b10573fd1ed7e477ad | cdc | None | # Compendium of Animal Rabies Control, 1997 National Association of State Public Health
Veterinarians, Inc.*
This Compendium provides information on rabies control to veterinarians, public health officials, and others concerned with rabies control. These recommendations serve as the basis for animal rabies-control programs throughout the United States and facilitate standardization of procedures among jurisdictions, thereby contributing to an effective national rabies-control program. This document is reviewed annually and revised as necessary. Recommendations for immunization procedures are contained in Part I; all animal rabies vaccines licensed by the United States Department of Agriculture (USDA) and marketed in the United States are listed in Part II; Part III details the principles of rabies control.
# Part I: Recommendations for Immunization Procedures
# A. Vaccine Administration
All animal rabies vaccines should be restricted to use by, or under the direct supervision of, a veterinarian.
# B. Vaccine Selection
In comprehensive rabies-control programs, only vaccines with a 3-year duration of immunity should be used. This procedure constitutes the most effective method of increasing the proportion of immunized dogs and cats in any population. (See Part II.)
# C. Route of Inoculation
All vaccines must be administered in accordance with the specifications of the product label or package insert. If administered intramuscularly, it must be at one site in the thigh.
# D. Vaccination of Wildlife and Hybrids
The efficacy of parenteral rabies vaccination of wildlife and hybrids (i.e., the offspring of wild animals crossbred to domestic dogs and cats) has not been established, and no vaccine is licensed for these animals. Zoos or research institutions may establish vaccination programs that attempt to protect valuable animals, but these programs should not replace appropriate public health activities that protect humans. The use of licensed oral vaccines for the mass immunization of free-ranging wildlife should be considered in selected situations, with the approval of the state agency responsible for animal rabies control.
# E. Accidental Human Exposure to Vaccine
Accidental inoculation can occur during administration of animal rabies vaccine. Such exposure to inactivated vaccines constitutes no rabies hazard.
# F. Identification of Vaccinated Animals
All agencies and veterinarians should adopt the standard tag system. This practice will aid the administration of local, state, national, and international rabies-control procedures. Animal license tags should be distinguishable in shape and color from rabies tags. Anodized aluminum rabies tags should be no less than 0.064 inches in thickness.
1. Rabies Tags a. Licensure. Registration or licensure of all dogs and cats can be used to aid in rabies control. A fee frequently is charged for such licensure, and revenues collected are used to maintain rabies-or animal-control programs. Vaccination is an essential prerequisite to licensure. b. Canvassing of Area. House-to-house canvassing by animal-control personnel facilitates enforcement of vaccination and licensure requirements. c. Citations. Citations are legal summonses issued to owners for violations, including the failure to vaccinate or license their animals. The authority for officers to issue citations should be an integral part of each animal-control program. d. Animal Control. All communities should incorporate stray-animal control, leash laws, and training of personnel into their programs. 5. Postexposure Management. Any animal bitten or scratched by either a wild, carnivorous mammal or a bat that is not available for testing should be regarded as having been exposed to rabies. a. Dogs and Cats. Unvaccinated dogs and cats exposed to a rabid animal should be euthanized immediately. If the owner is unwilling to have this done, the animal should be placed in strict isolation for 6 months and vaccinated 1 month before being released. Animals with expired vaccinations need to be evaluated on a case-by-case basis. Dogs and cats that are currently vaccinated should be revaccinated immediately, kept under the owner's control, and observed for 45 days. b. Livestock. All species of livestock are susceptible to rabies; cattle and horses are among the most frequently infected. Livestock exposed to a rabid animal and currently vaccinated with a vaccine approved by USDA for that species should be revaccinated immediately and observed for 45 days. Unvaccinated livestock should be slaughtered immediately. If the owner is unwilling to have this done, the animal should be kept under close observation for 6 months.
The following are recommendations for owners of unvaccinated livestock exposed to rabid animals: 1) If the animal is slaughtered within 7 days of being bitten, its tissues may be eaten without risk of infection, provided liberal portions of the exposed area are discarded. Federal meat inspectors must reject for slaughter any animal known to have been exposed to rabies within 8 months. 2) Neither tissues nor milk from a rabid animal should be used for human or animal consumption. However, because pasteurization temperatures will inactivate rabies virus, drinking pasteurized milk or eating cooked meat does not constitute a rabies exposure.
3) It is rare to have more than one rabid animal in a herd or to have herbivoreto-herbivore transmission; therefore, it may not be necessary to restrict the rest of the herd if a single animal has been exposed to or infected by rabies. c. Other Animals. Other animals bitten by a rabid animal should be euthanized immediately. Such animals currently vaccinated with a vaccine approved by USDA for that species may be revaccinated immediately and placed in strict isolation for at least 90 days.
*Centers for Disease Control andPrevention. Rabies Prevention--United States, 1991. MMWR 1991;40(No. RR-3)1-19.
# Management of Animals that Bite Humans.
A healthy dog or cat that bites a person should be confined and observed for 10 days; it is recommended that rabies vaccine not be administered during the observation period. Such animals should be evaluated by a veterinarian at the first sign of illness during confinement. Any illness in the animal should be reported immediately to the local health department. If signs suggestive of rabies develop, the animal should be euthanized, its head removed, and the head shipped under refrigeration (not frozen) for examination of the brain by a qualified laboratory designated by the local or state health department. Any stray or unwanted dog or cat that bites a person may be euthanized immediately and the head submitted as described above for rabies examination. Other biting animals that might have exposed a person to rabies should be reported immediately to the local health department.
Prior vaccination of an animal may not preclude the necessity for euthanasia and testing if the period of virus shedding is unknown for that species. Management of animals other than dogs and cats depends on the species, the circumstances of the bite, the epidemiology of rabies in the area, and the biting animal's history, current health status, and potential for exposure to rabies.
# C. Control Methods in Wildlife
The public should be warned not to handle wildlife. Wild mammals and hybrids that bite or otherwise expose people, pets, or livestock should be considered for euthanasia and rabies examination. A person bitten by any wild mammal should immediately report the incident to a physician who can evaluate the need for antirabies treatment. (See current rabies prophylaxis recommendations of the ACIP.)- 1. Terrestrial Mammals. Continuous and persistent government-funded programs for trapping or poisoning wildlife are not cost effective in reducing wildlife rabies reservoirs on a statewide basis. However, limited control in high-contact areas (e.g., picnic grounds, camps, or suburban areas) might be indicated for the removal of selected high-risk species of wildlife. The state wildlife agency and state health department should be consulted for coordination of any proposed vaccination or population-reduction programs. 2. Bats. Indigenous rabid bats have been reported from every state except Alaska and Hawaii and have caused rabies in at least 24 humans in the United States. However, it is neither feasible nor desirable to control rabies in bats by programs to reduce bat populations. Bats should be excluded from houses and surrounding structures to prevent direct association with humans. Such structures should then be made bat-proof by sealing entrances used by bats.
The Morbidity and Mortality Weekly Report (MMWR) Series is prepared by the Centers for Disease Control and Prevention (CDC) and is available free of charge in electronic format and on a paid subscription basis for paper copy. To receive an electronic copy on Friday of each week, send an e-mail message to [email protected]. The body content should read subscribe mmwr-toc. Electronic copy also is available from CDC's World-Wide Web server at / or from CDC's file transfer protocol server at ftp.cdc.gov. To subscribe for paper copy, contact Superintendent of Documents, U.S. Government Printing Office, Washington, DC 20402; telephone (202) 512-1800.
Data in the weekly MMWR are provisional, based on weekly reports to CDC by state health departments. The reporting week concludes at close of business on Friday; compiled data on a national basis are officially released to the public on the following Friday. Address inquiries about the MMWR Series, including material to be considered for publication, to: Editor, MMWR Series, Mailstop C-08, CDC, 1600 Clifton Rd., N.E., Atlanta, GA 30333; telephone (404) 332-4555.
All material in the MMWR Series is in the public domain and may be used and reprinted without permission; citation as to source, however, is appreciated. 6U.S. Government Printing Office: 1997-532-228/47054 Region IV | # Compendium of Animal Rabies Control, 1997 National Association of State Public Health
Veterinarians, Inc.*
This Compendium provides information on rabies control to veterinarians, public health officials, and others concerned with rabies control. These recommendations serve as the basis for animal rabies-control programs throughout the United States and facilitate standardization of procedures among jurisdictions, thereby contributing to an effective national rabies-control program. This document is reviewed annually and revised as necessary. Recommendations for immunization procedures are contained in Part I; all animal rabies vaccines licensed by the United States Department of Agriculture (USDA) and marketed in the United States are listed in Part II; Part III details the principles of rabies control.
# Part I: Recommendations for Immunization Procedures
# A. Vaccine Administration
All animal rabies vaccines should be restricted to use by, or under the direct supervision of, a veterinarian.
# B. Vaccine Selection
In comprehensive rabies-control programs, only vaccines with a 3-year duration of immunity should be used. This procedure constitutes the most effective method of increasing the proportion of immunized dogs and cats in any population. (See Part II.)
# C. Route of Inoculation
All vaccines must be administered in accordance with the specifications of the product label or package insert. If administered intramuscularly, it must be at one site in the thigh.
# D. Vaccination of Wildlife and Hybrids
The efficacy of parenteral rabies vaccination of wildlife and hybrids (i.e., the offspring of wild animals crossbred to domestic dogs and cats) has not been established, and no vaccine is licensed for these animals. Zoos or research institutions may establish vaccination programs that attempt to protect valuable animals, but these programs should not replace appropriate public health activities that protect humans. The use of licensed oral vaccines for the mass immunization of free-ranging wildlife should be considered in selected situations, with the approval of the state agency responsible for animal rabies control.
# E. Accidental Human Exposure to Vaccine
Accidental inoculation can occur during administration of animal rabies vaccine. Such exposure to inactivated vaccines constitutes no rabies hazard.
# F. Identification of Vaccinated Animals
All agencies and veterinarians should adopt the standard tag system. This practice will aid the administration of local, state, national, and international rabies-control procedures. Animal license tags should be distinguishable in shape and color from rabies tags. Anodized aluminum rabies tags should be no less than 0.064 inches in thickness.
1. Rabies Tags a. Licensure. Registration or licensure of all dogs and cats can be used to aid in rabies control. A fee frequently is charged for such licensure, and revenues collected are used to maintain rabies-or animal-control programs. Vaccination is an essential prerequisite to licensure. b. Canvassing of Area. House-to-house canvassing by animal-control personnel facilitates enforcement of vaccination and licensure requirements. c. Citations. Citations are legal summonses issued to owners for violations, including the failure to vaccinate or license their animals. The authority for officers to issue citations should be an integral part of each animal-control program. d. Animal Control. All communities should incorporate stray-animal control, leash laws, and training of personnel into their programs. 5. Postexposure Management. Any animal bitten or scratched by either a wild, carnivorous mammal or a bat that is not available for testing should be regarded as having been exposed to rabies. a. Dogs and Cats. Unvaccinated dogs and cats exposed to a rabid animal should be euthanized immediately. If the owner is unwilling to have this done, the animal should be placed in strict isolation for 6 months and vaccinated 1 month before being released. Animals with expired vaccinations need to be evaluated on a case-by-case basis. Dogs and cats that are currently vaccinated should be revaccinated immediately, kept under the owner's control, and observed for 45 days. b. Livestock. All species of livestock are susceptible to rabies; cattle and horses are among the most frequently infected. Livestock exposed to a rabid animal and currently vaccinated with a vaccine approved by USDA for that species should be revaccinated immediately and observed for 45 days. Unvaccinated livestock should be slaughtered immediately. If the owner is unwilling to have this done, the animal should be kept under close observation for 6 months.
The following are recommendations for owners of unvaccinated livestock exposed to rabid animals: 1) If the animal is slaughtered within 7 days of being bitten, its tissues may be eaten without risk of infection, provided liberal portions of the exposed area are discarded. Federal meat inspectors must reject for slaughter any animal known to have been exposed to rabies within 8 months. 2) Neither tissues nor milk from a rabid animal should be used for human or animal consumption. However, because pasteurization temperatures will inactivate rabies virus, drinking pasteurized milk or eating cooked meat does not constitute a rabies exposure.
3) It is rare to have more than one rabid animal in a herd or to have herbivoreto-herbivore transmission; therefore, it may not be necessary to restrict the rest of the herd if a single animal has been exposed to or infected by rabies. c. Other Animals. Other animals bitten by a rabid animal should be euthanized immediately. Such animals currently vaccinated with a vaccine approved by USDA for that species may be revaccinated immediately and placed in strict isolation for at least 90 days.
*Centers for Disease Control andPrevention. Rabies Prevention--United States, 1991. MMWR 1991;40(No. RR-3)1-19.
# Management of Animals that Bite Humans.
A healthy dog or cat that bites a person should be confined and observed for 10 days; it is recommended that rabies vaccine not be administered during the observation period. Such animals should be evaluated by a veterinarian at the first sign of illness during confinement. Any illness in the animal should be reported immediately to the local health department. If signs suggestive of rabies develop, the animal should be euthanized, its head removed, and the head shipped under refrigeration (not frozen) for examination of the brain by a qualified laboratory designated by the local or state health department. Any stray or unwanted dog or cat that bites a person may be euthanized immediately and the head submitted as described above for rabies examination. Other biting animals that might have exposed a person to rabies should be reported immediately to the local health department.
Prior vaccination of an animal may not preclude the necessity for euthanasia and testing if the period of virus shedding is unknown for that species. Management of animals other than dogs and cats depends on the species, the circumstances of the bite, the epidemiology of rabies in the area, and the biting animal's history, current health status, and potential for exposure to rabies.
# C. Control Methods in Wildlife
The public should be warned not to handle wildlife. Wild mammals and hybrids that bite or otherwise expose people, pets, or livestock should be considered for euthanasia and rabies examination. A person bitten by any wild mammal should immediately report the incident to a physician who can evaluate the need for antirabies treatment. (See current rabies prophylaxis recommendations of the ACIP.)* 1. Terrestrial Mammals. Continuous and persistent government-funded programs for trapping or poisoning wildlife are not cost effective in reducing wildlife rabies reservoirs on a statewide basis. However, limited control in high-contact areas (e.g., picnic grounds, camps, or suburban areas) might be indicated for the removal of selected high-risk species of wildlife. The state wildlife agency and state health department should be consulted for coordination of any proposed vaccination or population-reduction programs. 2. Bats. Indigenous rabid bats have been reported from every state except Alaska and Hawaii and have caused rabies in at least 24 humans in the United States. However, it is neither feasible nor desirable to control rabies in bats by programs to reduce bat populations. Bats should be excluded from houses and surrounding structures to prevent direct association with humans. Such structures should then be made bat-proof by sealing entrances used by bats.
The Morbidity and Mortality Weekly Report (MMWR) Series is prepared by the Centers for Disease Control and Prevention (CDC) and is available free of charge in electronic format and on a paid subscription basis for paper copy. To receive an electronic copy on Friday of each week, send an e-mail message to [email protected]. The body content should read subscribe mmwr-toc. Electronic copy also is available from CDC's World-Wide Web server at http://www.cdc.gov/ or from CDC's file transfer protocol server at ftp.cdc.gov. To subscribe for paper copy, contact Superintendent of Documents, U.S. Government Printing Office, Washington, DC 20402; telephone (202) 512-1800.
Data in the weekly MMWR are provisional, based on weekly reports to CDC by state health departments. The reporting week concludes at close of business on Friday; compiled data on a national basis are officially released to the public on the following Friday. Address inquiries about the MMWR Series, including material to be considered for publication, to: Editor, MMWR Series, Mailstop C-08, CDC, 1600 Clifton Rd., N.E., Atlanta, GA 30333; telephone (404) 332-4555.
All material in the MMWR Series is in the public domain and may be used and reprinted without permission; citation as to source, however, is appreciated. 6U.S. Government Printing Office: 1997-532-228/47054 Region IV | None | None |
8cf0dc2e7dd023c4d2bf03efbc5c70d2d845acbc | cdc | None | This report contains CDC guidance that augments the 2011 recommendations of the Advisory Committee on Immunization Practices (ACIP) for evaluating hepatitis B protection among health-care personnel (HCP) and administering post-exposure prophylaxis. Explicit guidance is provided for persons working, training, or volunteering in health-care settings who have documented hepatitis B (HepB) vaccination years before hire or matriculation (e.g., when HepB vaccination was received as part of routine infant or catch-up adolescent In the United States, 2,890 cases of acute hepatitis B were reported to CDC in 2011, and an estimated 18,800 new cases of hepatitis B occurred after accounting for underreporting of cases and asymptomatic infection. Although the rate of acute hepatitis B virus (HBV) infections have declined approximately 89% during 1990-2011, from 8.5 to 0.9 cases per 100,000 population in the United States, the risk for occupationally acquired HBV among HCP persists, largely from exposures to patients with chronic HBV infection. ACIP recommends HepB vaccination for unvaccinated or incompletely vaccinated HCP with reasonably anticipated risk for blood or body fluid exposure. ACIP also recommends that vaccinated HCP receive postvaccination serologic testing (antibody to hepatitis B surface antigen ) 1-2 months after the final dose of vaccine is administered (CDC. Immunization of health-care personnel: recommendations of the Advisory Committee on Immunization Practices . MMWR 2011;60 ). Increasing numbers of HCP have received routine HepB vaccination either as infants (recommended since 1991) or as catch-up vaccination (recommended since 1995) in adolescence. HepB vaccination results in protective anti-HBs responses among approximately 95% of healthy-term infants. Certain institutions test vaccinated HCP by measuring anti-HBs upon hire or matriculation, even when anti-HBs testing occurs greater than 2 months after vaccination. This guidance can assist clinicians, occupational health and student health providers, infection-control specialists, hospital and health-care training program administrators, and others in selection of an approach for assessing HBV protection for vaccinated HCP. This report emphasizes the importance of administering HepB vaccination for all HCP, provides explicit guidance for evaluating hepatitis B protection among previously vaccinated HCP (particularly those who were vaccinated in infancy or adolescence), and clarifies recommendations for postexposure management of HCP exposed to blood or body fluids.# Introduction
Hepatitis B virus (HBV) has long been recognized as an occupational risk for health-care personnel (HCP), including HCP trainees (1,2). The virus remains infectious for prolonged periods on environmental surfaces and is transmissible in the absence of visible blood (1). HCP do not recognize all exposures to potentially infectious blood or body fluids (2) and, even if exposures are recognized, often do not seek postexposure prophylactic management (3). In serologic studies conducted in the United States during the 1970s, HCP had a prevalence of HBV infection approximately 10 times greater than the general population (1). In 1983, an estimated 17,000 HBV infections occurred among HCP (4).
Vaccines to prevent HBV became available in the United States in 1981 and were recommended by the Advisory Committee on Immunization Practices (ACIP) for HCP in 1982 (5). Although a high proportion of healthy vaccine recipients in clinical trials respond to hepatitis B (HepB) vaccination, the proportion of responders can be lower among the general population, particularly among persons with chronic medical conditions (6,7). Acute and chronic HBV infections are rare among HCP who respond to HepB vaccination, but HCP who do not respond to vaccination are thought to remain susceptible. Postvaccination serologic testing for antibody to hepatitis B surface antigen (anti-HBs) identifies vaccine nonresponders and guides the need for revaccination, additional testing for chronic HBV infection, and counseling for HCP who remain susceptible after failing to respond to vaccination.
In 1991, ACIP recommended consideration of postvaccination serologic testing for anti-HBs for HCP at risk for needlestick exposures (8). In 1997, ACIP recommended postvaccination serologic testing 1-2 months after completion of the HepB vaccine series for HCP who have contact with patients or blood and who are at ongoing risk for injuries with sharp instruments or needlesticks (9). Since 1982 (when HepB vaccine was recommended for HCP), major declines have occurred in reports of acute hepatitis B among HCP (10). In 2011, ACIP reaffirmed that unvaccinated and incompletely vaccinated HCP at reasonably anticipated risk for blood or body fluid exposure should receive HepB vaccination before potential exposure, and HCP at high risk for exposure should receive postvaccination serologic testing 1-2 months after completion of the vaccine series (11).
This report provides CDC guidance for persons working, training, or volunteering in health-care settings who have documented HepB vaccination received years before hire or matriculation (e.g., when HepB vaccination was received as part of routine infant or catch-up adolescent vaccination). No postvaccination serologic testing is recommended after routine infant or adolescent HepB vaccination. Although acute HBV infections have declined substantially since HepB vaccination was introduced in the United States, a risk for occupational exposure to HBV persists (10), largely from persons with chronic HBV infection. Because vaccine-induced anti-HBs wanes over time, testing HCP for anti-HBs years after vaccination might not distinguish vaccine nonresponders from responders. Pre-exposure assessment of current or past anti-HBs results upon hire or matriculation, followed by one or more additional doses of HepB vaccine for HCP with anti-HBs <10 mIU/mL, if necessary, helps to ensure that HCP will be protected if they have an exposure to HBV-containing blood or body fluids.
An expert panel convened by CDC acknowledged that the risk for HBV infection for vaccinated HCP can vary widely by setting and profession, and might be low enough in certain settings that assessment of anti-HBs status and appropriate follow-up can be done at the time of exposure to potentially infectious blood or body fluids. This approach relies on HCP recognizing and reporting blood and body fluid exposures and therefore might be applied on the basis of documented low risk, implementation, and cost considerations. Certain HCP occupations have lower risk for occupational blood and body fluid exposures (e.g., occupations involving counseling versus performing procedures), and nontrainees have lower risks for blood and body fluid exposures than trainees. Some settings also will have a lower prevalence of HBV infection in the patient population served than in other settings, which will influence the risk for HCP exposure to hepatitis B surface antigen (HBsAg)-positive blood and body fluids. All health-care institutions should ensure that HCP receive training to recognize and report exposures, have systems in place to facilitate reporting and postexposure assessment, and have prophylaxis readily accessible for timely administration. This report can guide clinicians, occupational health and student health clinicians, infection-control specialists, hospital and health-care training program administrators, and others in selection of an approach for assessing HBV protection for vaccinated HCP.
HCPs are defined as all paid and unpaid persons providing health care, or working or training in health-care settings, who have reasonably anticipated risks for exposure to infectious materials, including blood or body fluids, contaminated medical supplies and equipment, or contaminated environmental surfaces. HCP might include but are not limited to physicians, nurses, nursing assistants, nurse practitioners, physician assistants, therapists, technicians, emergency medical services personnel, dental personnel, pharmacists, laboratory personnel, autopsy personnel, health-care students and trainees, contractual staff not employed by the health-care facility, and persons not directly involved in patient care but with potential exposure to infectious agents that can be transmitted between patients and HCP (e.g., housekeeping, laundry, security, maintenance, and volunteers) (1,11).
This guidance applies but is not limited to HCP in acute-care hospitals, long-term-care facilities (e.g., nursing homes, skilled nursing facilities, and assisted living facilities), physician's offices, dental offices, rehabilitation centers, urgent-care centers, ambulatory surgical centers, dialysis centers, and outpatient clinics, and to persons who provide home health care and emergency medical services. Although this guidance pertains to HCP, the same principles might be applicable to persons in other professions with reasonably anticipated risk for blood or body fluid exposure (e.g., public safety workers, embalmers, and crime scene cleanup crews).
Recommendations for testing HCP in certain populations at risk for acquisition of HBV infection before matriculation or hire can be found elsewhere and will be reviewed only briefly in this document (11)(12)(13). HCP protection against hepatitis C virus (HCV), human immunodeficiency virus (HIV), and other infections also is covered elsewhere (1,11,14). Postvaccination serologic testing and the need for revaccination specific to HCP with immunocompromising conditions (e.g., HCP who are on dialysis, infected with HIV, hematopoietic stem-cell transplant recipients, and receiving chemotherapy) are addressed in separate recommendations (15). Additional guidance on the management of HCP with chronic HBV infection has been published (13). A list of frequently used abbreviations is provided (Box).
# New or Updated Information Provided in this Guidance
This document examines approaches for assessing HBV protection for vaccinated HCP and offers additional guidance for postexposure evaluation and testing of HCP in consideration of:
# Methods
In 2012, CDC identified and convened subject matter experts in the fields of HBV infection, health-care epidemiology, and evidence-based medicine to form an expert panel to address mechanisms for assessing HBV protection for vaccinated HCP.- The expert panel was comprised of professionals from academic medicine (e.g., pediatrics, family medicine, internal medicine, and infectious diseases) and occupational health; federal and state public health professionals with expertise in hepatitis and health-care associated infections; and liaisons from the Society for Healthcare Epidemiology of America (SHEA), Healthcare Infection Control Practices Advisory Committee (HICPAC), American Medical Directors Association (AMDA), American College Health Association (ACHA), American Academy of Family Physicians (AAFP), and the Society for Adolescent Health and Medicine (SAHM). The expert panel convened 21 teleconferences for deliberations during January 19, 2012-January 8, 2013. Materials for teleconference discussion were electronically distributed to members.
The expert panel reviewed relevant published literature identified through PubMed searches, citations, and personal files. Reference lists were reviewed to retrieve additional relevant information. The expert panel considered the changing epidemiology of hepatitis B infections from surveillance reports, which included follow-up with state health departments to obtain additional information on HCP with acute hepatitis B during (1,5,9,11,13,15,16), and results from an electronic survey administered to health-care institutions regarding current practices (see Hepatitis B Vaccination and Postvaccination Testing among HCP). Various members of the expert panel were consulted to address issues throughout the development of these guidelines. Evidence also was summarized in presentations discussed during expert panel teleconferences. The panel identified two approaches for assessing HBV protection for vaccinated HCP, on the basis of expert opinion, which form the foundation of this guidance. Members of the expert panel critically reviewed earlier drafts of this guidance document, which was developed by CDC, individually and as a group by teleconference. Names and affiliations of persons who provided input in the drafting of these recommendations are included at the beginning of this document and in the acknowledgments section.
# Changing Epidemiology of HBV Infection
Hepatitis B is a nationally reportable disease (17). In the United States, 2,890 cases of acute hepatitis B were reported to CDC in 2011, and an estimated 18,800 new cases of hepatitis B occurred after accounting for underreporting of cases and asymptomatic infection (Figure 1) (10). Among patients with reported cases of acute hepatitis B with information, approximately 55% were hospitalized and 1.3% died from hepatitis B (10). Acute HBV infection becomes chronic in 90% of infants, 30% of children aged <5 years, and <1%-12% of adults (18). Approximately 25% of persons who become chronically infected during childhood and 15% of those who become chronically infected after childhood die prematurely from cirrhosis or liver cancer (1,15). An estimated 800,000-1.4 million persons in the United States are living with chronic HBV infection; these persons serve as the main reservoir for HBV (12). In contrast to a decline in reports of acute hepatitis B, the prevalence of chronic HBV, which is often asymptomatic, remained relatively stable (Figure 2) (19) at 3 per 100,000 persons (95% confidence interval = 2-5 per 100,000) during 2005-2010, as did death certificate-registered deaths (20).
A national strategy to eliminate HBV transmission was implemented in 1991 (16). A key component was a recommendation for routine vaccination of infants (16). As a result, the rate of newly reported acute HBV infections in the United States declined approximately 89% during 1990-2011, from 8.5 to 0.9 cases per 100,000 population (10,11). The incidence was lowest (0.04 cases per 100,000 population) among persons aged ≤19 years (10), the population routinely vaccinated as infants and adolescents. Although HepB vaccine coverage rates in 2011 were high among infants, children, and adolescents (91.1% among children aged 19-35 months and 92.3% among adolescents aged 13-17 years) (21,22), self-reported ≥3-dose coverage remained considerably lower for adults (35.9% for adults aged 19-49 years in 2011) (23).
# Occupational Risk for HBV Exposure and Exposure Reporting
Blood from persons with HBV infection contains the highest HBV titers of all body fluids and is the most important vehicle of transmission in the health-care setting (1). The following body fluids also are considered potentially infectious: cerebrospinal fluid, synovial fluid, pleural fluid, peritoneal fluid, pericardial fluid, and amniotic fluid (1). Although studies have documented HBV in saliva and tears, these body fluids have generally not represented an occupational risk for HBV infection unless they contain blood (1). Semen and vaginal secretions have been implicated in the sexual transmission of HBV, but they have not been implicated in occupational transmission from patients to HCP (1). The presence of HBsAg, usually an indicator of active HBV infection, also is found in other body fluids (e.g., breast milk, bile, feces, nasopharyngeal washings, and sweat). However, most body fluids are not efficient vehicles of transmission (unless they contain blood) because they contain low quantities of infectious HBV (1). No.
# Year
Sputum, urine, and vomitus are not considered potentially infectious unless they contain blood (1).
HBV is highly infectious, can be transmitted in the absence of visible blood (1), and remains infectious on environmental surfaces for at least 7 days (24). HBV is transmitted through percutaneous (i.e., needlesticks), mucosal (i.e., direct contact with mucous membranes), or nonintact skin (e.g., psoriasis, eczema, burns, wounds, cuts, and scratches) exposure to infectious blood or body fluids. Although percutaneous exposures are among the most efficient modes of HBV transmission, these exposures might account for only a minority of HBV infections among HCP. In several investigations of HBV outbreaks, most infected HCP could not recall an overt percutaneous exposure (2,25).
Hepatitis B e antigen (HBeAg) is a marker for high HBV replication and viral load (15). Although testing occupational exposure source patients for HBeAg is not practical and is not recommended, the risk for acquiring HBV infection is particularly high in occupational exposures to blood or body fluids from source patients who are HBeAg-positive (4). In studies of HCP who sustained injuries from needles contaminated with blood containing HBV, the risk for developing clinical hepatitis if the blood was both HBsAg-positive and HBeAg-positive was 22%-31%; the risk for developing serologic evidence of HBV infection was 37%-62% (1,26). By comparison, the risk for developing clinical hepatitis from a needle contaminated with HBsAg-positive, HBeAg-negative blood was 1%-6%, and the risk for developing serologic evidence of HBV infection was 23%-37% (1,26).
The Needlestick Safety and Prevention Act of 2001 directed the Occupational Safety and Health Administration (OSHA) to revise the Occupational Exposure to Bloodborne Pathogens Standard and established in greater detail requirements for employers regarding the identification and use of effective and safer medical devices (27). Percutaneous injuries have since decreased from 39.6 injuries per 100 occupied beds in 1999 to 19.5 injuries per 100 occupied beds in 2011 (Figure 3) (28). Data since 2002 indicate that 18% of HCP trainees sustain a percutaneous exposure annually, and 54% of percutaneous exposures are reported to occupational health (3,(29)(30)(31)(32). Reluctance to report exposures to occupational health might be influenced by fear of being reprimanded, concerns regarding confidentiality, and the belief that reporting might be time consuming (29,31). The annual risk for a mucosal exposure among trainees is 22%, of which 17% are reported to occupational health (3,(29)(30)(31)(32). The risk for exposure is generally lower among nontrainees and varies by occupation and job duties (32,33). Surveillance data indicate nurses and physicians account for 41.9% and 22.8%, respectively, of HCP reporting percutaneous exposures (28). The purpose of the sharp item that resulted in the exposure was for intramuscular or subcutaneous injection in 30.5% of exposures and was for suturing in 18.7% of exposures (28). Medical students account for 44.3% of HCP reporting a mucosal exposure (28).
The probability of HBV infection among HCP trainees will vary by the prevalence of HBsAg-positivity of source patients and the approach to assessment (Figure 4). Exposure logs during 2000-2012 representing 7,170 exposures at three health-care systems in the United States indicated that 0.9% of source patients were HBsAg-positive (34). This figure likely varies substantially by setting; in some community screening programs among populations considered at higher risk, 11%-25% of persons screened are infected with HBV (35).
The source patient is identifiable in approximately 95% of exposures (28). The source patient might not be identifiable after exposure from an item protruding from a disposal container, an item disposed of in an inappropriate container, or from an item left in an inappropriate place (28).
# Vaccination HepB Vaccines
HepB vaccine is available as a single-antigen formulation and also in combination with other vaccines (Table 1) (15). Two single-antigen recombinant HBsAg vaccines are available in the United States: Recombivax HB (Merck and Co, Inc., - Chronic Hepatitis B is defined as the presence of both hepatitis B surface antigen (HBsAg) and antibody to hepatitis B core antigen (anti-HBc). † Represents 95% confidence interval.
# FIGURE 2. Weighted prevalence of chronic hepatitis B- -National Health and Nutrition Examination Survey, United States, 1976-2010
Whitehouse Station, NJ) and Engerix-B (GlaxoSmithKline Biologicals, Rixensart, Belgium) (15). Of the three licensed combination vaccines, one (Twinrix ) is available for persons aged ≥18 years. Twinrix contains recombinant HBsAg and inactivated hepatitis A virus (15).
Primary HepB vaccination of adults usually consists of 3 doses of 10 or 20 µg of recombinant HBsAg protein administered intramuscularly into the deltoid muscle on a 0, 1, and 6 month schedule (15). Alternative schedules (including a 4-dose schedule at 0, 1, 2, and 12 months) are U.S.-approved for routine vaccination for specific ages and vaccine formulations; vaccination according to these schedules elicits final rates of seroprotection similar to those obtained on a 0, 1, and 6 month schedule (15). Obese persons might require adjustment in the needle length for administering HepB vaccine to achieve optimal seroprotection (11,15).
# Vaccine Safety
HepB vaccines have been demonstrated to be safe among persons in all age groups (15). During 1982During -2004, an estimated 70 million adolescents and adults in the United States received ≥1 dose of HepB vaccine (15). The most frequently reported side effects are pain at the injection site (3%-29%) and temperature of >99.9°F (>37.7°C) (1%-6%) (15). In placebo-controlled studies, these side effects were reported no more frequently among persons receiving HepB vaccine than among persons receiving placebo (15). Administration of additional vaccine doses for nonresponders is not associated with an increase in adverse events (36).
Epidemiologic and mechanistic assessment by the Institute of Medicine for 27 adverse events supported a causal association with HepB vaccination only for anaphylaxis in persons who are sensitive to yeast (37). HepB vaccination is contraindicated for persons with a history of hypersensitivity to yeast or any vaccine component (15). Persons with a history of serious adverse events (e.g., anaphylaxis) after receipt of HepB vaccine should not receive additional doses. As with other vaccines, vaccination of persons with moderate or severe acute illness, with or without fever, should be deferred until illness resolves (15). Vaccination is not contraindicated in persons with a history of multiple sclerosis, Guillain-Barré Syndrome, autoimmune disease (e.g., systemic lupus erythematosis and rheumatoid arthritis), or other chronic diseases (15). HepB vaccination is not contraindicated for pregnant (15,38,39) or lactating (1) women. Available vaccines contain noninfectious HBsAg and do not pose a risk for infection to the fetus (15).
# Vaccine Seroprotection
Immunocompetent adults and children who have vaccineinduced anti-HBs levels of ≥10 mIU/mL 1-2 months after having received a complete, ≥3-dose HepB vaccine series are considered seroprotected and deemed vaccine responders (15). Vaccine efficacy studies have demonstrated protection against acute and chronic disease in immunocompetent vaccine responders (40,41). Vaccine-induced seroprotection is a useful surrogate of vaccine efficacy (42). Postvaccination seroprotection is achieved in approximately 95% of healthy infants (43,44), approximately 92% of HCP aged <40 years, and approximately 84% of HCP aged ≥40 years (6). Among infants vaccinated at birth, low birthweight is associated with a lower proportion of infants achieving seroprotection (45). Among persons vaccinated as adults, smoking, obesity, aging, chronic medical conditions, male sex, genetic factors, and immune suppression are associated with a decrease in proportions seroprotected (6,11,36,(46)(47)(48). Although immunogenicity is less among immunocompromised persons, those who achieve and maintain seroprotective antibody levels before exposure to HBV have a high level of protection (15).
# Persistence of Vaccine-Induced Antibody
Anti-HBs levels after vaccination decline over time. The persistence of detectable anti-HBs levels varies by age at vaccination. By 18 years after vaccination, approximately 16% of persons vaccinated at age <1 year have detectable antibody levels of ≥10 mIU/mL (49-54) (Figure 5), compared with 74% for those vaccinated at age ≥1 year (41,(54)(55)(56)(57)(58)(59)(60)(61)(62). In a study of matriculating health science students, 92.9% of those who had received 3 doses of HepB vaccine had anti-HBs ≥10 mIU/mL (58). Median age at receipt of the primary series was 14.5 years (interquartile range: 11.6-20.2 years) and at postvaccination testing was 23.2 years (interquartile range: 22.1-24.8 years) (58).
# Response to a Challenge Dose of Vaccine
To assess vaccine response in remotely vaccinated HCP, a challenge dose of HepB vaccine can be used to determine the presence of vaccine-induced immunologic memory through generation of an anamnestic response. The term "booster dose" has been used to refer to a dose of HepB vaccine administered after a primary vaccination series to provide rapid protective immunity against significant infection (i.e., infection resulting in serologic test results positive for HBV and/or clinically significant disease) (40). Among persons vaccinated 5.9-17.5 years previously at age <1 year who have anti-HBs levels <10 mIU/mL, approximately 60.0%-97.4% showed a response to a single challenge dose of HepB vaccine demonstrating protective levels of anti-HBs ≥10 mIU/mL (50)(51)(52)(53)(54). Among persons vaccinated 9-22 years previously at age ≥1 year who have anti-HBs levels <10 mIU/mL, 69.2%-96.4% showed a response to a single challenge dose of HepB vaccine demonstrating protective levels of anti-HBs ≥10 mIU/ mL (41,54,60,62). The proportion of responders to a challenge dose might vary by population and age at receiving the primary HepB series. HCP with a response ≥10 mIU/mL following a challenge dose are considered protected, regardless of future declines in anti-HBs. Conclusions about the response to a challenge dose are made on the basis of relatively few studies and might change as additional data become available.
# Duration of Vaccine Protection among Responders
Among immunocompetent HepB vaccine responders, studies suggest protection against acute symptomatic and chronic hepatitis B infection persists for ≥22 years (9,15,40). Three cohort studies that monitored 1,006 subjects for ≥20 years have been informative (41,63,64). In two of the cohorts from areas with high HBV endemicity, new chronic HBV infections were documented in 0.8% (0 and 1.0%) of 513 (109 and 404) subjects, respectively, who responded or presumably responded to HepB vaccination starting at birth (63,64). Approximately 20% of subjects had evidence of natural boosting of anti-HBs, presumably from exposure to HBV (63,64). A third cohort of 493 subjects in an area with intermediate HBV endemicity received HepB vaccination between ages 6 months and ≥50 years (41). Among vaccine responders, no acute or chronic HBV was detected, although 1% of subjects experienced subclinical HBV infection without chronic infection during ≥20 years of follow-up (41). The significance of subclinical breakthrough HBV infection without chronic HBV and transient HBV infection is unknown.
# HepB Vaccination and Postvaccination Testing among HCP
The Bloodborne Pathogens Standard issued in 1991 by OSHA mandates that HepB vaccination be made available at the employer's expense to employees who have reasonably anticipated skin, eye, mucous membrane, or parenteral contact with blood or other potentially infectious materials that might result from the performance of an employee's duties (27). HepB vaccination coverage data obtained through the National Health Interview Survey (NHIS) in 2011 demonstrated ≥3-dose coverage of 63.8% among HCP aged ≥19 years (23). NHIS 2010 data demonstrated ≥3-dose coverage of 74% for HCP with direct patient contact, and 46% for HCP without direct patient contact (65), substantially below the Healthy People 2020 target of 90% HepB vaccination coverage among HCP (objective no. IID-15.3) (66).
Postvaccination serologic testing for anti-HBs is recommended 1-2 months after the last vaccine dose for HCP at risk for occupational percutaneous or mucosal exposures (11). During 2012, a survey was administered to 389 California acute care hospitals or centers comprised of more than one hospital to assess current practices for ensuring HCP protection against HBV. Hospitals were identified from a listserv of 580 infection prevention and employee health staff (67). Responses (67). The majority of respondents (71.9%) indicated current practices at their institution consist of measuring anti-HBs on a pre-exposure basis, followed by HepB vaccination if anti-HBs is <10 mIU/mL (67). A smaller proportion of respondents (15.7%) indicated their institution follows an approach relying upon postexposure management (67). Postvaccination anti-HBs results were known for approximately 69% of HCP at these facilities (67).
# Revaccination for Vaccine Nonresponse
Revaccination with ≥1dose of HepB vaccine for nonresponse subsequent to the primary series increases the proportion of persons achieving vaccine-induced seroprotection (15). Among 178 persons with occupational risk for HBV infection, 47% of those without protective antibody levels after a primary vaccination series developed vaccine-induced seroprotection after one additional dose of HepB vaccine (6). An estimated 42% of 86 persons without protective anti-HBs levels after the first revaccination dose and who received 2 additional doses developed protective levels of anti-HBs representing a cumulative response rate of 69% among initial nonresponders after 3 revaccination doses (6). Persons who have measurable but low (i.e., 1-9 mIU/mL) levels of anti-HBs after the initial series have better response to revaccination than persons who have no measurable anti-HBs (36,62,68,69).
Single dose revaccination with a higher dosage has not been demonstrated to increase the proportion of healthy adult nonresponders (70,71) or previous responders revaccinated as part of a clinical trial (62) who achieve vaccine-induced seroprotection. However, 3-dose revaccination with a higher dosage (40 µg) did improve the proportion of nonresponders achieving anti-HBs levels of ≥10 mIU/mL in one study (100% among 17 persons receiving 40 µg dose versus 62.5% among 18 persons receiving 10 µg dose, p = 0.015, Fisher's exact test) (70). Revaccination with >3 doses (i.e., >6 total doses) is not recommended (11).
# HBV Infection among Vaccinated and Unvaccinated HCP
From 1983 to 2010, the number of HBV infections among HCP declined approximately 98%, from an estimated 17,000 infections to 263 acute HBV infections (considering that occupational history was assessed for 43.6% of cases and using a correction factor of 10.5 to account for underreporting and asymptomatic infection) (10). The decrease in acute HBV infection among HCP probably resulted from routine preexposure HepB vaccination and reduced risk for exposure through improvements in infection-control practices (28,72,73).
Although few studies have evaluated the vaccination history of persons with acute hepatitis B (74), some cases of acute hepatitis B and chronic HBV infection can be expected in unvaccinated persons and among vaccine nonresponders. During 2005-2010, a total of 203 cases of persons with acute hepatitis B among HCP were reported to CDC's National Notifiable Diseases Surveillance System (NNDSS) (75). Six of 17 patients with information on the development of chronic HBV infection developed chronic HBV infection (75). Follow-up of 67 (76.1%) of 88 HCP initially reported as having a positive or unknown HepB vaccination history indicated that 35 HCP reported vaccination with ≥3 HepB vaccine doses (seven had documentation to support the reported vaccination history) (75). Among the 35 HCP reporting vaccination with ≥3 HepB vaccine doses, one HCP demonstrated an immune response (i.e., anti-HBs ≥10 mlU/mL); the remaining 34 were nonresponders or had an unknown response status (75). Four of eight HCP with ≥3-dose HepB vaccination with information developed chronic HBV infection; none of the four had complete documentation of ≥3 HepB vaccine doses (75). Postvaccination serologic testing was available for only one of seven HCPs with documentation of ≥3-doses of HepB vaccine; this HCP had an anti-HBs level <10 mIU/mL after 4 doses of vaccine (75).
Although reported data did not enable identification of the modes of transmission or information on receipt of postexposure prophylaxis, 28 (16.7%) of 168 HCP for whom data were available reported an accidental stick or puncture with a needle or other object contaminated with blood during the 6 weeks through 6 months before illness, possibly representing occupational acquisition of infection (75). Unrecognized exposures might have resulted in HBV infections among HCP who did not report an exposure (2). Other risk factors for HBV exposure in the 6 weeks through 6 months before illness (i.e., injection drug use, men who have sex with men, multiple sex partners, contact with a hepatitis B case, dialysis patient, receipt of blood transfusion, surgery, acupuncture, and tattoo receipt) were present among 121 (59.6%) of 203 HCP, possibly suggesting their exposures were not occupational (75).
# Managing HCP Vaccination and Serologic Test Results
Immunization information systems (IIS) provide consolidated vaccination histories for use by vaccination providers in determining appropriate vaccinations (76). Accessing IIS for vaccination records might decrease unnecessary revaccination among HCP who no longer have records of HepB vaccination. IIS do not accept postvaccination anti-HBs test results (77). To reduce the cost and inconvenience of repeat anti-HBs testing when HCP are employed by different health-care facilities, CDC recommends that institutions consider systems for long-term management of anti-HBs and other hepatitis B serologic test results. Mechanisms for tracking vaccination and hepatitis B serologic test results in health information technology products could also reduce cost and inconvenience of repeat anti-HBs testing.
# Passive Prophylaxis of HBV Exposed Health Care Personnel Hepatitis B immune globulin
Hepatitis B immune globulin (HBIG) provides passive anti-HBs and temporary (i.e., 3-6 months) protection (15). HBIG is prepared from human plasma known to contain a high titer of anti-HBs. HBIG is typically used together with HepB vaccine for postexposure prophylaxis (15). For persons who do not respond to HepB vaccine, HBIG administered alone is the primary method of protection after HBV exposure (15). The standard adult dose of HBIG is 0.06 mL/kg. HBIG is administered by intramuscular injection; an appropriate muscle mass (i.e., deltoid or gluteal) should be chosen in which to deliver the large volume of HBIG required and a needle length appropriate for the HCP's size should be used. HBIG can be administered simultaneously with HepB vaccine but at a different injection site (15).
# Safety
The plasma from which HBIG is prepared is screened for HBsAg, HCV, and HIV (15). The process used to prepare HBIG inactivates HBV, HCV, and HIV from the final product. No evidence exists that HBV, HCV, or HIV has ever been transmitted by HBIG thar is commercially available in the United States (15).
Serious adverse effects from HBIG, when administered as recommended, are rare (1). Local pain and tenderness at the injection site, urticaria, and angioedema might occur; anaphylactic reactions, although rare, have been reported following the injection of human immune globulin (IG) preparations (1). HBIG is not contraindicated for pregnant (1,78) or lactating women (1).
# Efficacy
The effectiveness of HBIG and HepB vaccine in various postexposure settings has been evaluated by prospective studies. For perinatal exposure to a mother positive for both HBsAg and HBeAg, a regimen combining HBIG and initiation of the HepB vaccine series at birth is 85%-95% effective in preventing HBV infection (79,80). Regimens involving either multiple doses of HBIG alone or the HepB vaccine series alone are 70%-75% effective in preventing HBV infection when administered shortly after exposure (81). In the occupational setting, multiple doses of HBIG starting within 1 week following percutaneous exposure to HBsAg-positive blood provide an estimated 75% protection from HBV infection (82)(83)(84)(85)(86). Administration of HBIG might prolong the incubation period of HBV infection among persons who develop infection (82,85,87,88). A comparison of the postexposure efficacy of the combination of HBIG and the HepB vaccine series or HBIG alone has not been evaluated in the occupational setting (1). Whether the increased efficacy of HBIG added to HepB vaccine observed in the perinatal setting, compared with HBIG alone, applies to adults exposed occupationally remains unknown.
# Cost-Effectiveness Considerations
To examine the cost-effectiveness of various strategies for assessing HCP protection from hepatitis B, two economic models that yielded calculations of the incremental cost per quality-adjusted life-year (QALY) saved were developed. One model represented an approach in which anti-HBs is measured on a pre-exposure basis, and HCP with anti-HBs <10 mIU/mL receive an additional dose of HepB vaccine, followed by repeat anti-HBs measurement. If anti-HBs remains <10 mIU/mL after the first revaccination dose, the HCP receives two additional revaccination doses of HepB vaccine followed by repeat anti-HBs measurement. Another model represented a postexposure management approach; at the time of exposure, the HCP is tested for anti-HBs and the source patient is tested simultaneously for HBsAg, and postexposure prophylaxis would be administered on the basis of these results. Results from the two models were compared. A decision-tree analysis was used to combine all parameters and calculate the total intervention costs and probability of infection. In addition, HBV infection-related costs and QALY loss (accounting for acute and asymptomatic infections and a 6% probability of chronic infection) were determined from an existing model (89) and were considered for the HCP's remaining lifetime. The intervention time frame included a 1-year analysis and a multiyear analysis covering up to 10 years of exposure. A 3% annual discount rate was used, and all final cost figures were converted to 2010 U.S. dollars using the Medical Consumer Price Index.
The baseline cost-effectiveness models assumed that an ideal 95% of HCP have initial and sustained protection against HBV infection after a primary ≥3-dose HepB vaccine series, irrespective of the presence of detectable anti-HBs. Ninety-five percent protection was derived from the proportion of persons aged <40 years, including term newborns that have measurable anti-HBs ≥10 mIU/mL soon after a primary vaccination series. Approximately 18-25 years after vaccination, approximately 20% of HCP (vaccinated at age <1 year) or approximately 80% of HCP (vaccinated at age ≥1 year) retain anti-HBs ≥10 mIU/mL. The model did not account for unrecognized exposures, as probability data for unrecognized exposures are not available, or suboptimal vaccine coverage that exists among HCP.
For pre-exposure anti-HBs testing followed by revaccination and retesting, if necessary, compared with doing nothing, the incremental cost per QALY saved was $4,542,467 for trainees and $3,149,183 for nontrainees at year one, and decreased to $893,619 and $796,140, respectively, over 10 years. This approach is expected to result in 3.7 and 1.6 visits to occupational health for trainees and nontrainees, respectively. The expected number of infections is 0.7 per 100,000 and 0.4 per 100,000 for trainees and nontrainees, respectively. For an approach relying upon postexposure management, compared with doing nothing, the incremental cost per QALY saved was $2,270,801 for trainees and $1,610,998 for nontrainees at year one, and decreased to $917,859 and $1,114,364 respectively, over 10 years. The expected number of infections is 3.0 per 100,000 and 1.7 per 100,000 for trainees and nontrainees, respectively. Although an approach relying upon postexposure management might be less costly per QALY saved initially for many institutions, pre-exposure anti-HBs testing with possible revaccination becomes more cost-effective compared with a postexposure approach over time.
Sensitivity analyses demonstrated that cost-effectiveness improves in settings where a greater proportion of source patients are HBsAg-positive and among HCP with higher risk for exposure (e.g., surgeons). Cost-effectiveness can change as new antivirals become available for treatment of HBV infection. Vaccinating previously unvaccinated HCP trainees followed by postvaccination serologic testing, compared with doing nothing, has an incremental cost per QALY saved of $374,646 at year one and $51,537 over 10 years, accounting for direct costs to the health-care system and direct medical costs of hepatitis B-related illness and complications.
# Recommendations
# Pre-Exposure Management Education and Infrastructure
At the time of hire or matriculation, health-care providers and health-care institutions should provide training to HCP to improve recognition and encourage timely reporting of blood and body fluid exposures. The possibility that the postexposure evaluation will cause the HCP to have time lost from work should not be a barrier to reporting. Institutions should ensure that HCP have rapid access to postexposure testing and prophylaxis, including HBIG and HepB vaccine.
# Serologic Testing for HBV Infection
Testing unvaccinated HCP for HBV infection is not generally indicated for persons being evaluated for hepatitis B protection because of occupational risk. Prevaccination serologic testing is indicated for all persons born in geographic regions with HBsAg prevalence of ≥2% (e.g., much of Eastern Europe, Asia, Africa, the Middle East, and the Pacific Islands) and certain indigenous populations from countries with overall low HBV endemicity (<2%); persons with behavioral exposures to HBV (e.g., men who have sex with men and past or current injection drug users); persons receiving cytotoxic or immunosuppressive therapy; and persons with liver disease of unknown etiology.
HBV endemicity (HBsAg prevalence) can be described as low (<2%), moderate (2%-<8%), and high (≥8%). Because certain persons might have been infected with HBV before they received HepB vaccination, HBsAg testing is recommended regardless of vaccination history for persons born in geographic regions with HBsAg prevalence of ≥2%, U.S.-born persons not vaccinated as infants whose parents were born in regions with high HBV endemicity (HBsAg prevalence) (≥8%), persons who received HepB vaccination as adolescents or adults after the initiation of risk behaviors (12), and persons who are HIV-positive or who receive hemodialysis (11).
Testing HCP at risk for HBV infection should consist of a serologic assay for HBsAg, in addition to either anti-HBc or anti-HBs (11,12). For unvaccinated HCP at risk for previous HBV infection, blood should be drawn for testing before the first dose of vaccine is administered.
# Vaccination
All HCP whose work-, training-, and volunteer-related activities involve reasonably anticipated risk for exposure to blood or body fluids should be vaccinated with a complete, ≥3-dose HepB vaccine series. OSHA mandates that vaccination be available for employees within 10 days of initial assignment (27). HCP trainees should complete the series before the potential for exposure with blood or body fluids, when possible, as higher risk has been reported during professional training (e.g., residency training).
Incompletely vaccinated HCP should receive additional dose(s) to complete the vaccine series (15). The vaccine series does not need to be restarted for HCP with an incomplete series; however, minimum dosing intervals should be heeded (15). Minimum dosing intervals are 4 weeks between the first and second dose, 8 weeks between the second and third dose, and 16 weeks between the first and third dose (15).
HCP lacking documentation of HepB vaccination should be considered unvaccinated (when documentation for HepB vaccine doses is lacking) or incompletely vaccinated (when documentation for some HepB vaccine doses is lacking) and should receive additional doses to complete a documented HepB series. Health-care institutions are encouraged to seek documentation of "missing" HepB doses in IIS, when feasible, to avoid unnecessary vaccination.
OSHA mandates that HCP who refuse HepB vaccination sign a declination statement (/ oshaweb/owadisp.show_document?p_id=10052&p_ table=STANDARDS). HCP refusing HepB vaccination can obtain vaccination at a later date at no expense if the HCP is still covered under OSHA's Bloodborne Pathogens Standard. Health-care institutions should encourage HepB vaccination among HCP to improve HBV protection and to achieve the Healthy People 2020 target of 90% vaccination (66).
# Postvaccination Serologic Testing
HCP who have written documentation of a complete, ≥3-dose HepB vaccine series and subsequent postvaccination anti-HBs ≥10 mIU/mL are considered hepatitis B immune. Immunocompetent persons have long-term protection against HBV and do not need further periodic testing to assess anti-HBs levels (Figure 6).
All HCP recently vaccinated or recently completing HepB vaccination who are at risk for occupational blood or body fluid exposure should undergo anti-HBs testing. Anti-HBs testing should be performed 1-2 months after administration of the last dose of the vaccine series when possible. HCP with documentation of a complete ≥3-dose HepB vaccine series but no documentation of anti-HBs ≥10 mIU/mL who are at risk for occupational blood or body fluid exposure might undergo anti-HBs testing upon hire or matriculation. Testing should use a quantitative method that allows detection of the protective concentration of anti-HBs (≥10 mIU/mL) (e.g., enzyme-linked immunosorbent assay ).
- Completely vaccinated HCP with anti-HBs ≥10 mIU/mL are considered hepatitis B immune. Immunocompetent persons have long-term protection and do not need further periodic testing to assess anti-HBs levels. - Completely vaccinated HCP with anti-HBs <10 mIU/mL should receive an additional dose of HepB vaccine, followed by anti-HBs testing 1-2 months later. HCP whose anti-HBs remains <10 mIU/mL should receive 2 additional vaccine doses (usually 6 doses total), followed by repeat anti-HBs testing 1-2 months after the last dose. Alternatively, it might be more practical for very recently vaccinated HCP with anti-HBs <10 mIU/mL to receive 3 consecutive additional doses of HepB vaccine (usually 6 doses total), followed by anti-HBs testing 1-2 months after the last dose.
# Standard Precautions and Advising HCP to Report Exposures
All HCP should adhere to infection-control guidelines and follow Standard Precautions (90), including the use of engineering and work-practice controls, to reduce the risk for blood or body fluid exposure. All HCP, including those who have demonstrated protection against HBV, should be advised to immediately report blood or body fluid exposures to occupational health for evaluation of the appropriate measures to prevent transmission of bloodborne pathogens (including HIV, hepatitis C, and hepatitis B).
# Postexposure Management Initial Postexposure Management
Wounds and skin sites that have been in contact with blood or body fluids should be washed with soap and water; mucous membranes should be flushed with water. Using antiseptics (e.g., 2%-4% chlorhexidine) for wound care or expressing fluid by squeezing the wound further have not been shown to reduce the risk for HBV transmission; however, the use of antiseptics is not contraindicated. The application of caustic agents (e.g., bleach) or the injection of antiseptics or disinfectants into the wound is not recommended.
Procedures should be followed for testing known source persons, including obtaining informed consent, in accordance with applicable laws. Source patients determined to be HBsAg-positive should be referred for appropriate management and should be reported to the state or local health department. When a source patient is unknown (e.g., as occurs from a puncture with a needle in the trash), the exposed HCP should be managed as if the source patient were HBsAg-positive. Testing needles and other sharp instruments implicated in an exposure is not recommended, regardless of whether the source patient is known or unknown. The reliability and interpretation of findings in such circumstances are unknown, and testing could be hazardous to persons handling the sharp instrument. Exposures involving human bites should be managed with the knowledge that both the person being bitten and the person who engaged in biting were potentially exposed.
Institutions should ensure that HCP have timely access to postexposure management and prophylaxis, including - Should be performed 1-2 months after the last dose of vaccine using a quantitative method that allows detection of the protective concentration of anti-HBs (≥10 mIU/mL) (e.g., enzyme-linked immunosorbent assay ). † A nonresponder is defined as a person with anti-HBs <10 mIU/mL after ≥6 doses of HepB vaccine. Persons who do not have a protective concentration of anti-HBs after revaccination should be tested for HBsAg. If positive, the person should receive appropriate management or vaccination. (11). Anti-HBs testing should be performed using a method that allows detection of the protective concentration of anti-HBs (≥10 mIU/mL) (Table 2).
# Managing Vaccinated HCP
For vaccinated HCP (who have written documentation of a complete, ≥3-dose HepB vaccine series) with subsequent documented anti-HBs ≥10 mIU/mL, testing the source patient for HBsAg is unnecessary. No postexposure management for HBV is necessary, regardless of the source patient's HBsAg status.
For vaccinated HCP (who have written documentation of HepB vaccination) with anti-HBs <10 mIU/mL after two complete, ≥3-dose HepB vaccine series, the source patient should be tested for HBsAg as soon as possible after the exposure. If the source patient is HBsAg-positive or has unknown HBsAg status, the HCP should receive 2 doses of HBIG (1,11). The first dose should be administered as soon as possible after the exposure, and the second dose should be administered 1 month later. If the source patient is HBsAg-negative, neither HBIG nor HepB vaccine is necessary.
For vaccinated HCP (who have written documentation of a complete, ≥3-dose HepB vaccine series) without previous anti-HBs testing, the HCP should be tested for anti-HBs and the source patient (if known) should be tested for HBsAg as soon as possible after the exposure. Testing the source patient and the HCP should occur simultaneously; testing the source patient should not be delayed while waiting for the HCP anti-HBs test results, and likewise, testing the HCP should not be delayed while waiting for the source patient HBsAg results. - HBIG should be administered intramuscularly as soon as possible after exposure when indicated. The effectiveness of HBIG when administered >7 days after percutaneous, mucosal, or nonintact skin exposures is unknown. HBIG dosage is 0.06 mL/kg. † Should be performed 1-2 months after the last dose of the HepB vaccine series (and 4-6 months after administration of HBIG to avoid detection of passively administered anti-HBs) using a quantitative method that allows detection of the protective concentration of anti-HBs (≥10 mIU/mL). § A responder is defined as a person with anti-HBs ≥10 mIU/mL after ≥3 doses of HepB vaccine. ¶ A nonresponder is defined as a person with anti-HBs <10 mIU/mL after ≥6 doses of HepB vaccine. HCP who have anti-HBs <10mIU/mL, or who are unvaccinated or incompletely vaccinated, and sustain an exposure to a source patient who is HBsAg-positive or has unknown HBsAg status, should undergo baseline testing for HBV infection as soon as possible after exposure, and follow-up testing approximately 6 months later. Initial baseline tests consist of total anti-HBc; testing at approximately 6 months consists of HBsAg and total anti-HBc.
- If the HCP has anti-HBs <10 mIU/mL and the source patient is HBsAg-positive or has unknown HBsAg status, the HCP should receive 1 dose of HBIG and be revaccinated as soon as possible after the exposure. The HCP should then receive the second 2 doses to complete the second HepB vaccine series (6 doses total when accounting for the original 3-dose series) according to the vaccination schedule. To document the HCP's vaccine response status for future exposures, anti-HBs testing should be performed 1-2 months after the last dose of vaccine. - If the HCP has anti-HBs <10 mIU/mL and the source patient is HBsAg-negative, the HCP should receive an additional HepB vaccine dose, followed by repeat anti-HBs testing 1-2 months later. HCP whose anti-HBs remains <10 mIU/mL should undergo revaccination with 2 more doses (6 doses total when accounting for the original 3-dose series). To document the HCP's vaccine response status for future exposures, anti-HBs testing should be performed 1-2 months after the last dose of vaccine. - If the HCP has anti-HBs ≥10 mIU/mL at the time of the exposure, no postexposure HBV management is necessary, regardless of the source patient's HBsAg status.
# Managing HCP Who Lack Documentation of Vaccination, are Unvaccinated or Incompletely Vaccinated
For unvaccinated or incompletely vaccinated HCP (including those who refused vaccination), the source patient should be tested for HBsAg as soon as possible after the exposure. Testing unvaccinated or incompletely vaccinated HCP for anti-HBs is not necessary and is potentially misleading, because anti-HBs ≥10 mIU/mL as a correlate of vaccine-induced protection has only been determined for persons who have completed an approved vaccination series (15,42).
- If the source patient is HBsAg-positive or has unknown HBsAg status, the HCP should receive 1 dose of HBIG and 1 dose of HepB vaccine administered as soon as possible after the exposure. The HCP should complete the HepB vaccine series according to the vaccination schedule. To document the HCP's vaccine response status for future exposures, anti-HBs testing should be performed approximately 1-2 months after the last dose of vaccine. Because anti-HBs testing of HCP who received HBIG should be performed after anti-HBs from HBIG is no longer detectable (6 months after administration), it will likely be necessary to defer anti-HBs testing for a period longer than 1-2 months after the last vaccine dose.
-HCP with anti-HBs ≥10 mIU/mL after receipt of the primary vaccine series are considered immune. Immunocompetent persons have long-term protection and do not need further periodic testing to assess anti-HBs levels. -HCP with anti-HBs <10 mIU/mL after receipt of the primary series should be revaccinated. For these HCP, administration of a second complete 3-dose series on an appropriate schedule, followed by anti-HBs testing 1-2 months after the third dose, usually is more practical than conducting serologic testing after each additional dose of vaccine. To document the HCP's vaccine response status for future exposures, anti-HBs testing should be performed 1-2 months after the last dose of vaccine. - If the source patient is HBsAg-negative, the HCP should complete the HepB vaccine series according to the vaccination schedule. To document the HCP's vaccine response status for future exposures, anti-HBs testing should be performed approximately 1-2 months after the last dose of vaccine.
-HCP with anti-HBs ≥10 mIU/mL after receipt of the primary vaccine series are considered immune. Immunocompetent persons have long-term protection and do not need further periodic testing to assess anti-HBs levels. -HCP with anti-HBs <10 mIU/mL after receipt of the primary series should be revaccinated. For these HCP, administration of a second complete 3-dose series on an appropriate schedule, followed by anti-HBs testing 1-2 months after the third dose, usually is more practical than conducting serologic testing after each additional dose of vaccine. To document the HCP's vaccine response status for future exposures, anti-HBs testing should be performed 1-2 months after the last dose of vaccine.
# Testing of HCP Exposed to an HBsAg-Positive or Unknown Source
HCP who have anti-HBs <10 mIU/mL, or who are unvaccinated or incompletely vaccinated, and who sustain a percutaneous, mucosal, or nonintact skin exposure to a source patient who is HBsAg-positive or has unknown HBsAg status should undergo baseline testing for HBV infection as soon as possible after the exposure, and follow-up testing approximately 6 months later. Testing immediately after the exposure should consist of total anti-HBc, and follow-up testing approximately 6 months later should consist of HBsAg and total anti-HBc.
HCP exposed to a source patient who is HBsAg-positive or has unknown HBsAg status do not need to take special precautions to prevent secondary transmission during the follow-up period; however, they should refrain from donating blood, plasma, organs, tissue, or semen (1). The exposed HCP does not need to modify sexual practices or refrain from becoming pregnant (1). If an exposed HCP is breast feeding, she does not need to discontinue (1). No modifications to an exposed HCP's patient-care responsibilities are necessary to prevent transmission to patients based solely on exposure to a source patient who is HBsAg-positive or has unknown HBsAg status.
# Vaccine Nonresponders
Vaccinated HCP whose anti-HBs remains <10 mIU/mL after revaccination (i.e., after receiving a total of 6 doses) should be tested for HBsAg and anti-HBc to determine infection status. Those determined not to be HBV infected (vaccine nonresponders) should be considered susceptible to HBV infection. No specific work restrictions are recommended for vaccine nonresponders (91).
# Documentation
Health-care institutions should maintain records, ideally electronic records that are easily retrievable following exposures, of documented vaccination histories and serologic test results for reference in managing occupational exposures, and to provide to other health-care institutions if requested by the HCP. The vaccination information should be entered into an IIS accepting records from adult vaccination, if available. HCP should be provided a copy of HepB vaccination and anti-HBs testing results and encouraged to keep them with their personal health records so they can readily be made available to future employers.
# HCP with HBV Infection
HCP who are positive for HBsAg should be counseled how to prevent HBV transmission to others and referred for further evaluation (92). Those who perform exposure-prone procedures should be advised regarding the procedures they can perform safely as per updated CDC recommendations for the management of HBsAg-positive health-care providers and students (11,13). Chronic hepatitis B infection in itself should not preclude the practice or study of medicine, surgery, dentistry, or allied health professions (13).
# Future Studies
National surveillance systems to accurately assess the burden of hepatitis B among HCP and health-care facility databases tracking occupational exposures among HCP are important for monitoring the changing epidemiology of occupationally acquired HBV infections and other bloodborne pathogens. Systems and databases could ideally be electronically linked to employee health records and should include results that identify HepB vaccine responders and nonresponders, the nature and HBV status of the exposure source and postexposure management, and the HCP's anti-HBs level. Appropriate safeguards should be in place to protect the privacy of the health information. Data collection should be representative of HCP in a variety of settings (e.g., acute care, long-term care, and dialysis), including settings with frequent staff turnover. Studies assessing HBV transmission among all HCP exposed to an HBsAg-positive source, regardless of vaccination history or anti-HBs levels, approximately 6 months after an exposure will help to inform duration of vaccine protection. Surveillance activities for acute hepatitis B infection should continue to ascertain occupation among cases, in addition to HepB vaccination history. Long-term follow-up studies assessing disease incidence and duration of anti-HBs among persons vaccinated as infants and older adults, including persons who received booster doses subsequent to the primary vaccine series and persons from HBV-endemic areas, also might provide information on duration of vaccine-induced protection. Other subject areas that would benefit from research include efficacy and cost-effectiveness of antiviral agents for postexposure prophylaxis, immunogenicity of higher dosage or new vaccines for revaccinating vaccine nonresponders, and an examination of the future role of postexposure hepatitis B virus deoxyribonucleic acid (HBV DNA) testing. | This report contains CDC guidance that augments the 2011 recommendations of the Advisory Committee on Immunization Practices (ACIP) for evaluating hepatitis B protection among health-care personnel (HCP) and administering post-exposure prophylaxis. Explicit guidance is provided for persons working, training, or volunteering in health-care settings who have documented hepatitis B (HepB) vaccination years before hire or matriculation (e.g., when HepB vaccination was received as part of routine infant [recommended since 1991] or catch-up adolescent [recommended since 1995] In the United States, 2,890 cases of acute hepatitis B were reported to CDC in 2011, and an estimated 18,800 new cases of hepatitis B occurred after accounting for underreporting of cases and asymptomatic infection. Although the rate of acute hepatitis B virus (HBV) infections have declined approximately 89% during 1990-2011, from 8.5 to 0.9 cases per 100,000 population in the United States, the risk for occupationally acquired HBV among HCP persists, largely from exposures to patients with chronic HBV infection. ACIP recommends HepB vaccination for unvaccinated or incompletely vaccinated HCP with reasonably anticipated risk for blood or body fluid exposure. ACIP also recommends that vaccinated HCP receive postvaccination serologic testing (antibody to hepatitis B surface antigen [anti-HBs]) 1-2 months after the final dose of vaccine is administered (CDC. Immunization of health-care personnel: recommendations of the Advisory Committee on Immunization Practices [ACIP]. MMWR 2011;60 [No. RR-7]). Increasing numbers of HCP have received routine HepB vaccination either as infants (recommended since 1991) or as catch-up vaccination (recommended since 1995) in adolescence. HepB vaccination results in protective anti-HBs responses among approximately 95% of healthy-term infants. Certain institutions test vaccinated HCP by measuring anti-HBs upon hire or matriculation, even when anti-HBs testing occurs greater than 2 months after vaccination. This guidance can assist clinicians, occupational health and student health providers, infection-control specialists, hospital and health-care training program administrators, and others in selection of an approach for assessing HBV protection for vaccinated HCP. This report emphasizes the importance of administering HepB vaccination for all HCP, provides explicit guidance for evaluating hepatitis B protection among previously vaccinated HCP (particularly those who were vaccinated in infancy or adolescence), and clarifies recommendations for postexposure management of HCP exposed to blood or body fluids.# Introduction
Hepatitis B virus (HBV) has long been recognized as an occupational risk for health-care personnel (HCP), including HCP trainees (1,2). The virus remains infectious for prolonged periods on environmental surfaces and is transmissible in the absence of visible blood (1). HCP do not recognize all exposures to potentially infectious blood or body fluids (2) and, even if exposures are recognized, often do not seek postexposure prophylactic management (3). In serologic studies conducted in the United States during the 1970s, HCP had a prevalence of HBV infection approximately 10 times greater than the general population (1). In 1983, an estimated 17,000 HBV infections occurred among HCP (4).
Vaccines to prevent HBV became available in the United States in 1981 and were recommended by the Advisory Committee on Immunization Practices (ACIP) for HCP in 1982 (5). Although a high proportion of healthy vaccine recipients in clinical trials respond to hepatitis B (HepB) vaccination, the proportion of responders can be lower among the general population, particularly among persons with chronic medical conditions (6,7). Acute and chronic HBV infections are rare among HCP who respond to HepB vaccination, but HCP who do not respond to vaccination are thought to remain susceptible. Postvaccination serologic testing for antibody to hepatitis B surface antigen (anti-HBs) identifies vaccine nonresponders and guides the need for revaccination, additional testing for chronic HBV infection, and counseling for HCP who remain susceptible after failing to respond to vaccination.
In 1991, ACIP recommended consideration of postvaccination serologic testing for anti-HBs for HCP at risk for needlestick exposures (8). In 1997, ACIP recommended postvaccination serologic testing 1-2 months after completion of the HepB vaccine series for HCP who have contact with patients or blood and who are at ongoing risk for injuries with sharp instruments or needlesticks (9). Since 1982 (when HepB vaccine was recommended for HCP), major declines have occurred in reports of acute hepatitis B among HCP (10). In 2011, ACIP reaffirmed that unvaccinated and incompletely vaccinated HCP at reasonably anticipated risk for blood or body fluid exposure should receive HepB vaccination before potential exposure, and HCP at high risk for exposure should receive postvaccination serologic testing 1-2 months after completion of the vaccine series (11).
This report provides CDC guidance for persons working, training, or volunteering in health-care settings who have documented HepB vaccination received years before hire or matriculation (e.g., when HepB vaccination was received as part of routine infant [recommended since 1991] or catch-up adolescent [recommended since 1995] vaccination). No postvaccination serologic testing is recommended after routine infant or adolescent HepB vaccination. Although acute HBV infections have declined substantially since HepB vaccination was introduced in the United States, a risk for occupational exposure to HBV persists (10), largely from persons with chronic HBV infection. Because vaccine-induced anti-HBs wanes over time, testing HCP for anti-HBs years after vaccination might not distinguish vaccine nonresponders from responders. Pre-exposure assessment of current or past anti-HBs results upon hire or matriculation, followed by one or more additional doses of HepB vaccine for HCP with anti-HBs <10 mIU/mL, if necessary, helps to ensure that HCP will be protected if they have an exposure to HBV-containing blood or body fluids.
An expert panel convened by CDC acknowledged that the risk for HBV infection for vaccinated HCP can vary widely by setting and profession, and might be low enough in certain settings that assessment of anti-HBs status and appropriate follow-up can be done at the time of exposure to potentially infectious blood or body fluids. This approach relies on HCP recognizing and reporting blood and body fluid exposures and therefore might be applied on the basis of documented low risk, implementation, and cost considerations. Certain HCP occupations have lower risk for occupational blood and body fluid exposures (e.g., occupations involving counseling versus performing procedures), and nontrainees have lower risks for blood and body fluid exposures than trainees. Some settings also will have a lower prevalence of HBV infection in the patient population served than in other settings, which will influence the risk for HCP exposure to hepatitis B surface antigen (HBsAg)-positive blood and body fluids. All health-care institutions should ensure that HCP receive training to recognize and report exposures, have systems in place to facilitate reporting and postexposure assessment, and have prophylaxis readily accessible for timely administration. This report can guide clinicians, occupational health and student health clinicians, infection-control specialists, hospital and health-care training program administrators, and others in selection of an approach for assessing HBV protection for vaccinated HCP.
HCPs are defined as all paid and unpaid persons providing health care, or working or training in health-care settings, who have reasonably anticipated risks for exposure to infectious materials, including blood or body fluids, contaminated medical supplies and equipment, or contaminated environmental surfaces. HCP might include but are not limited to physicians, nurses, nursing assistants, nurse practitioners, physician assistants, therapists, technicians, emergency medical services personnel, dental personnel, pharmacists, laboratory personnel, autopsy personnel, health-care students and trainees, contractual staff not employed by the health-care facility, and persons not directly involved in patient care but with potential exposure to infectious agents that can be transmitted between patients and HCP (e.g., housekeeping, laundry, security, maintenance, and volunteers) (1,11).
This guidance applies but is not limited to HCP in acute-care hospitals, long-term-care facilities (e.g., nursing homes, skilled nursing facilities, and assisted living facilities), physician's offices, dental offices, rehabilitation centers, urgent-care centers, ambulatory surgical centers, dialysis centers, and outpatient clinics, and to persons who provide home health care and emergency medical services. Although this guidance pertains to HCP, the same principles might be applicable to persons in other professions with reasonably anticipated risk for blood or body fluid exposure (e.g., public safety workers, embalmers, and crime scene cleanup crews).
Recommendations for testing HCP in certain populations at risk for acquisition of HBV infection before matriculation or hire can be found elsewhere and will be reviewed only briefly in this document (11)(12)(13). HCP protection against hepatitis C virus (HCV), human immunodeficiency virus (HIV), and other infections also is covered elsewhere (1,11,14). Postvaccination serologic testing and the need for revaccination specific to HCP with immunocompromising conditions (e.g., HCP who are on dialysis, infected with HIV, hematopoietic stem-cell transplant recipients, and receiving chemotherapy) are addressed in separate recommendations (15). Additional guidance on the management of HCP with chronic HBV infection has been published (13). A list of frequently used abbreviations is provided (Box).
# New or Updated Information Provided in this Guidance
This document examines approaches for assessing HBV protection for vaccinated HCP and offers additional guidance for postexposure evaluation and testing of HCP in consideration of:
•
# Methods
In 2012, CDC identified and convened subject matter experts in the fields of HBV infection, health-care epidemiology, and evidence-based medicine to form an expert panel to address mechanisms for assessing HBV protection for vaccinated HCP.* The expert panel was comprised of professionals from academic medicine (e.g., pediatrics, family medicine, internal medicine, and infectious diseases) and occupational health; federal and state public health professionals with expertise in hepatitis and health-care associated infections; and liaisons from the Society for Healthcare Epidemiology of America (SHEA), Healthcare Infection Control Practices Advisory Committee (HICPAC), American Medical Directors Association (AMDA), American College Health Association (ACHA), American Academy of Family Physicians (AAFP), and the Society for Adolescent Health and Medicine (SAHM). The expert panel convened 21 teleconferences for deliberations during January 19, 2012-January 8, 2013. Materials for teleconference discussion were electronically distributed to members.
The expert panel reviewed relevant published literature identified through PubMed searches, citations, and personal files. Reference lists were reviewed to retrieve additional relevant information. The expert panel considered the changing epidemiology of hepatitis B infections from surveillance reports, which included follow-up with state health departments to obtain additional information on HCP with acute hepatitis B during [2005][2006][2007][2008][2009][2010] (1,5,9,11,13,15,16), and results from an electronic survey administered to health-care institutions regarding current practices (see Hepatitis B Vaccination and Postvaccination Testing among HCP). Various members of the expert panel were consulted to address issues throughout the development of these guidelines. Evidence also was summarized in presentations discussed during expert panel teleconferences. The panel identified two approaches for assessing HBV protection for vaccinated HCP, on the basis of expert opinion, which form the foundation of this guidance. Members of the expert panel critically reviewed earlier drafts of this guidance document, which was developed by CDC, individually and as a group by teleconference. Names and affiliations of persons who provided input in the drafting of these recommendations are included at the beginning of this document and in the acknowledgments section.
# Changing Epidemiology of HBV Infection
Hepatitis B is a nationally reportable disease (17). In the United States, 2,890 cases of acute hepatitis B were reported to CDC in 2011, and an estimated 18,800 new cases of hepatitis B occurred after accounting for underreporting of cases and asymptomatic infection (Figure 1) (10). Among patients with reported cases of acute hepatitis B with information, approximately 55% were hospitalized and 1.3% died from hepatitis B (10). Acute HBV infection becomes chronic in 90% of infants, 30% of children aged <5 years, and <1%-12% of adults (18). Approximately 25% of persons who become chronically infected during childhood and 15% of those who become chronically infected after childhood die prematurely from cirrhosis or liver cancer (1,15). An estimated 800,000-1.4 million persons in the United States are living with chronic HBV infection; these persons serve as the main reservoir for HBV (12). In contrast to a decline in reports of acute hepatitis B, the prevalence of chronic HBV, which is often asymptomatic, remained relatively stable (Figure 2) (19) at 3 per 100,000 persons (95% confidence interval = 2-5 per 100,000) during 2005-2010, as did death certificate-registered deaths (20).
A national strategy to eliminate HBV transmission was implemented in 1991 (16). A key component was a recommendation for routine vaccination of infants (16). As a result, the rate of newly reported acute HBV infections in the United States declined approximately 89% during 1990-2011, from 8.5 to 0.9 cases per 100,000 population (10,11). The incidence was lowest (0.04 cases per 100,000 population) among persons aged ≤19 years (10), the population routinely vaccinated as infants and adolescents. Although HepB vaccine coverage rates in 2011 were high among infants, children, and adolescents (91.1% among children aged 19-35 months and 92.3% among adolescents aged 13-17 years) (21,22), self-reported ≥3-dose coverage remained considerably lower for adults (35.9% for adults aged 19-49 years in 2011) (23).
# Occupational Risk for HBV Exposure and Exposure Reporting
Blood from persons with HBV infection contains the highest HBV titers of all body fluids and is the most important vehicle of transmission in the health-care setting (1). The following body fluids also are considered potentially infectious: cerebrospinal fluid, synovial fluid, pleural fluid, peritoneal fluid, pericardial fluid, and amniotic fluid (1). Although studies have documented HBV in saliva and tears, these body fluids have generally not represented an occupational risk for HBV infection unless they contain blood (1). Semen and vaginal secretions have been implicated in the sexual transmission of HBV, but they have not been implicated in occupational transmission from patients to HCP (1). The presence of HBsAg, usually an indicator of active HBV infection, also is found in other body fluids (e.g., breast milk, bile, feces, nasopharyngeal washings, and sweat). However, most body fluids are not efficient vehicles of transmission (unless they contain blood) because they contain low quantities of infectious HBV (1). No.
# Year
Sputum, urine, and vomitus are not considered potentially infectious unless they contain blood (1).
HBV is highly infectious, can be transmitted in the absence of visible blood (1), and remains infectious on environmental surfaces for at least 7 days (24). HBV is transmitted through percutaneous (i.e., needlesticks), mucosal (i.e., direct contact with mucous membranes), or nonintact skin (e.g., psoriasis, eczema, burns, wounds, cuts, and scratches) exposure to infectious blood or body fluids. Although percutaneous exposures are among the most efficient modes of HBV transmission, these exposures might account for only a minority of HBV infections among HCP. In several investigations of HBV outbreaks, most infected HCP could not recall an overt percutaneous exposure (2,25).
Hepatitis B e antigen (HBeAg) is a marker for high HBV replication and viral load (15). Although testing occupational exposure source patients for HBeAg is not practical and is not recommended, the risk for acquiring HBV infection is particularly high in occupational exposures to blood or body fluids from source patients who are HBeAg-positive (4). In studies of HCP who sustained injuries from needles contaminated with blood containing HBV, the risk for developing clinical hepatitis if the blood was both HBsAg-positive and HBeAg-positive was 22%-31%; the risk for developing serologic evidence of HBV infection was 37%-62% (1,26). By comparison, the risk for developing clinical hepatitis from a needle contaminated with HBsAg-positive, HBeAg-negative blood was 1%-6%, and the risk for developing serologic evidence of HBV infection was 23%-37% (1,26).
The Needlestick Safety and Prevention Act of 2001 directed the Occupational Safety and Health Administration (OSHA) to revise the Occupational Exposure to Bloodborne Pathogens Standard and established in greater detail requirements for employers regarding the identification and use of effective and safer medical devices (27). Percutaneous injuries have since decreased from 39.6 injuries per 100 occupied beds in 1999 to 19.5 injuries per 100 occupied beds in 2011 (Figure 3) (28). Data since 2002 indicate that 18% of HCP trainees sustain a percutaneous exposure annually, and 54% of percutaneous exposures are reported to occupational health (3,(29)(30)(31)(32). Reluctance to report exposures to occupational health might be influenced by fear of being reprimanded, concerns regarding confidentiality, and the belief that reporting might be time consuming (29,31). The annual risk for a mucosal exposure among trainees is 22%, of which 17% are reported to occupational health (3,(29)(30)(31)(32). The risk for exposure is generally lower among nontrainees and varies by occupation and job duties (32,33). Surveillance data indicate nurses and physicians account for 41.9% and 22.8%, respectively, of HCP reporting percutaneous exposures (28). The purpose of the sharp item that resulted in the exposure was for intramuscular or subcutaneous injection in 30.5% of exposures and was for suturing in 18.7% of exposures (28). Medical students account for 44.3% of HCP reporting a mucosal exposure (28).
The probability of HBV infection among HCP trainees will vary by the prevalence of HBsAg-positivity of source patients and the approach to assessment (Figure 4). Exposure logs during 2000-2012 representing 7,170 exposures at three health-care systems in the United States indicated that 0.9% of source patients were HBsAg-positive (34). This figure likely varies substantially by setting; in some community screening programs among populations considered at higher risk, 11%-25% of persons screened are infected with HBV (35).
The source patient is identifiable in approximately 95% of exposures (28). The source patient might not be identifiable after exposure from an item protruding from a disposal container, an item disposed of in an inappropriate container, or from an item left in an inappropriate place (28).
# Vaccination HepB Vaccines
HepB vaccine is available as a single-antigen formulation and also in combination with other vaccines (Table 1) (15). Two single-antigen recombinant HBsAg vaccines are available in the United States: Recombivax HB (Merck and Co, Inc., * Chronic Hepatitis B is defined as the presence of both hepatitis B surface antigen (HBsAg) and antibody to hepatitis B core antigen (anti-HBc). † Represents 95% confidence interval.
# FIGURE 2. Weighted prevalence of chronic hepatitis B* -National Health and Nutrition Examination Survey, United States, 1976-2010
Whitehouse Station, NJ) and Engerix-B (GlaxoSmithKline Biologicals, Rixensart, Belgium) (15). Of the three licensed combination vaccines, one (Twinrix [GlaxoSmithKline Biologicals]) is available for persons aged ≥18 years. Twinrix contains recombinant HBsAg and inactivated hepatitis A virus (15).
Primary HepB vaccination of adults usually consists of 3 doses of 10 or 20 µg of recombinant HBsAg protein administered intramuscularly into the deltoid muscle on a 0, 1, and 6 month schedule (15). Alternative schedules (including a 4-dose schedule at 0, 1, 2, and 12 months) are U.S.-approved for routine vaccination for specific ages and vaccine formulations; vaccination according to these schedules elicits final rates of seroprotection similar to those obtained on a 0, 1, and 6 month schedule (15). Obese persons might require adjustment in the needle length for administering HepB vaccine to achieve optimal seroprotection (11,15).
# Vaccine Safety
HepB vaccines have been demonstrated to be safe among persons in all age groups (15). During 1982During -2004, an estimated 70 million adolescents and adults in the United States received ≥1 dose of HepB vaccine (15). The most frequently reported side effects are pain at the injection site (3%-29%) and temperature of >99.9°F (>37.7°C) (1%-6%) (15). In placebo-controlled studies, these side effects were reported no more frequently among persons receiving HepB vaccine than among persons receiving placebo (15). Administration of additional vaccine doses for nonresponders is not associated with an increase in adverse events (36).
Epidemiologic and mechanistic assessment by the Institute of Medicine for 27 adverse events supported a causal association with HepB vaccination only for anaphylaxis in persons who are sensitive to yeast (37). HepB vaccination is contraindicated for persons with a history of hypersensitivity to yeast or any vaccine component (15). Persons with a history of serious adverse events (e.g., anaphylaxis) after receipt of HepB vaccine should not receive additional doses. As with other vaccines, vaccination of persons with moderate or severe acute illness, with or without fever, should be deferred until illness resolves (15). Vaccination is not contraindicated in persons with a history of multiple sclerosis, Guillain-Barré Syndrome, autoimmune disease (e.g., systemic lupus erythematosis and rheumatoid arthritis), or other chronic diseases (15). HepB vaccination is not contraindicated for pregnant (15,38,39) or lactating (1) women. Available vaccines contain noninfectious HBsAg and do not pose a risk for infection to the fetus (15).
# Vaccine Seroprotection
Immunocompetent adults and children who have vaccineinduced anti-HBs levels of ≥10 mIU/mL 1-2 months after having received a complete, ≥3-dose HepB vaccine series are considered seroprotected and deemed vaccine responders (15). Vaccine efficacy studies have demonstrated protection against acute and chronic disease in immunocompetent vaccine responders (40,41). Vaccine-induced seroprotection is a useful surrogate of vaccine efficacy (42). Postvaccination seroprotection is achieved in approximately 95% of healthy infants (43,44), approximately 92% of HCP aged <40 years, and approximately 84% of HCP aged ≥40 years (6). Among infants vaccinated at birth, low birthweight is associated with a lower proportion of infants achieving seroprotection (45). Among persons vaccinated as adults, smoking, obesity, aging, chronic medical conditions, male sex, genetic factors, and immune suppression are associated with a decrease in proportions seroprotected (6,11,36,(46)(47)(48). Although immunogenicity is less among immunocompromised persons, those who achieve and maintain seroprotective antibody levels before exposure to HBV have a high level of protection (15).
# Persistence of Vaccine-Induced Antibody
Anti-HBs levels after vaccination decline over time. The persistence of detectable anti-HBs levels varies by age at vaccination. By 18 years after vaccination, approximately 16% of persons vaccinated at age <1 year have detectable antibody levels of ≥10 mIU/mL (49-54) (Figure 5), compared with 74% for those vaccinated at age ≥1 year (41,(54)(55)(56)(57)(58)(59)(60)(61)(62). In a study of matriculating health science students, 92.9% of those who had received 3 doses of HepB vaccine had anti-HBs ≥10 mIU/mL (58). Median age at receipt of the primary series was 14.5 years (interquartile range: 11.6-20.2 years) and at postvaccination testing was 23.2 years (interquartile range: 22.1-24.8 years) (58).
# Response to a Challenge Dose of Vaccine
To assess vaccine response in remotely vaccinated HCP, a challenge dose of HepB vaccine can be used to determine the presence of vaccine-induced immunologic memory through generation of an anamnestic response. The term "booster dose" has been used to refer to a dose of HepB vaccine administered after a primary vaccination series to provide rapid protective immunity against significant infection (i.e., infection resulting in serologic test results positive for HBV and/or clinically significant disease) (40). Among persons vaccinated 5.9-17.5 years previously at age <1 year who have anti-HBs levels <10 mIU/mL, approximately 60.0%-97.4% showed a response to a single challenge dose of HepB vaccine demonstrating protective levels of anti-HBs ≥10 mIU/mL (50)(51)(52)(53)(54). Among persons vaccinated 9-22 years previously at age ≥1 year who have anti-HBs levels <10 mIU/mL, 69.2%-96.4% showed a response to a single challenge dose of HepB vaccine demonstrating protective levels of anti-HBs ≥10 mIU/ mL (41,54,60,62). The proportion of responders to a challenge dose might vary by population and age at receiving the primary HepB series. HCP with a response ≥10 mIU/mL following a challenge dose are considered protected, regardless of future declines in anti-HBs. Conclusions about the response to a challenge dose are made on the basis of relatively few studies and might change as additional data become available.
# Duration of Vaccine Protection among Responders
Among immunocompetent HepB vaccine responders, studies suggest protection against acute symptomatic and chronic hepatitis B infection persists for ≥22 years (9,15,40). Three cohort studies that monitored 1,006 subjects for ≥20 years have been informative (41,63,64). In two of the cohorts from areas with high HBV endemicity, new chronic HBV infections were documented in 0.8% (0 and 1.0%) of 513 (109 and 404) subjects, respectively, who responded or presumably responded to HepB vaccination starting at birth (63,64). Approximately 20% of subjects had evidence of natural boosting of anti-HBs, presumably from exposure to HBV (63,64). A third cohort of 493 subjects in an area with intermediate HBV endemicity received HepB vaccination between ages 6 months and ≥50 years (41). Among vaccine responders, no acute or chronic HBV was detected, although 1% of subjects experienced subclinical HBV infection without chronic infection during ≥20 years of follow-up (41). The significance of subclinical breakthrough HBV infection without chronic HBV and transient HBV infection is unknown.
# HepB Vaccination and Postvaccination Testing among HCP
The Bloodborne Pathogens Standard issued in 1991 by OSHA mandates that HepB vaccination be made available at the employer's expense to employees who have reasonably anticipated skin, eye, mucous membrane, or parenteral contact with blood or other potentially infectious materials that might result from the performance of an employee's duties (27). HepB vaccination coverage data obtained through the National Health Interview Survey (NHIS) in 2011 demonstrated ≥3-dose coverage of 63.8% among HCP aged ≥19 years (23). NHIS 2010 data demonstrated ≥3-dose coverage of 74% for HCP with direct patient contact, and 46% for HCP without direct patient contact (65), substantially below the Healthy People 2020 target of 90% HepB vaccination coverage among HCP (objective no. IID-15.3) (66).
Postvaccination serologic testing for anti-HBs is recommended 1-2 months after the last vaccine dose for HCP at risk for occupational percutaneous or mucosal exposures (11). During 2012, a survey was administered to 389 California acute care hospitals or centers comprised of more than one hospital to assess current practices for ensuring HCP protection against HBV. Hospitals were identified from a listserv of 580 infection prevention and employee health staff (67). Responses (67). The majority of respondents (71.9%) indicated current practices at their institution consist of measuring anti-HBs on a pre-exposure basis, followed by HepB vaccination if anti-HBs is <10 mIU/mL (67). A smaller proportion of respondents (15.7%) indicated their institution follows an approach relying upon postexposure management (67). Postvaccination anti-HBs results were known for approximately 69% of HCP at these facilities (67).
# Revaccination for Vaccine Nonresponse
Revaccination with ≥1dose of HepB vaccine for nonresponse subsequent to the primary series increases the proportion of persons achieving vaccine-induced seroprotection (15). Among 178 persons with occupational risk for HBV infection, 47% of those without protective antibody levels after a primary vaccination series developed vaccine-induced seroprotection after one additional dose of HepB vaccine (6). An estimated 42% of 86 persons without protective anti-HBs levels after the first revaccination dose and who received 2 additional doses developed protective levels of anti-HBs representing a cumulative response rate of 69% among initial nonresponders after 3 revaccination doses (6). Persons who have measurable but low (i.e., 1-9 mIU/mL) levels of anti-HBs after the initial series have better response to revaccination than persons who have no measurable anti-HBs (36,62,68,69).
Single dose revaccination with a higher dosage has not been demonstrated to increase the proportion of healthy adult nonresponders (70,71) or previous responders revaccinated as part of a clinical trial (62) who achieve vaccine-induced seroprotection. However, 3-dose revaccination with a higher dosage (40 µg) did improve the proportion of nonresponders achieving anti-HBs levels of ≥10 mIU/mL in one study (100% among 17 persons receiving 40 µg dose versus 62.5% among 18 persons receiving 10 µg dose, p = 0.015, Fisher's exact test) (70). Revaccination with >3 doses (i.e., >6 total doses) is not recommended (11).
# HBV Infection among Vaccinated and Unvaccinated HCP
From 1983 to 2010, the number of HBV infections among HCP declined approximately 98%, from an estimated 17,000 infections to 263 acute HBV infections (considering that occupational history was assessed for 43.6% of cases and using a correction factor of 10.5 to account for underreporting and asymptomatic infection) (10). The decrease in acute HBV infection among HCP probably resulted from routine preexposure HepB vaccination and reduced risk for exposure through improvements in infection-control practices (28,72,73).
Although few studies have evaluated the vaccination history of persons with acute hepatitis B (74), some cases of acute hepatitis B and chronic HBV infection can be expected in unvaccinated persons and among vaccine nonresponders. During 2005-2010, a total of 203 cases of persons with acute hepatitis B among HCP were reported to CDC's National Notifiable Diseases Surveillance System (NNDSS) (75). Six of 17 patients with information on the development of chronic HBV infection developed chronic HBV infection (75). Follow-up of 67 (76.1%) of 88 HCP initially reported as having a positive or unknown HepB vaccination history indicated that 35 HCP reported vaccination with ≥3 HepB vaccine doses (seven had documentation to support the reported vaccination history) (75). Among the 35 HCP reporting vaccination with ≥3 HepB vaccine doses, one HCP demonstrated an immune response (i.e., anti-HBs ≥10 mlU/mL); the remaining 34 were nonresponders or had an unknown response status (75). Four of eight HCP with ≥3-dose HepB vaccination with information developed chronic HBV infection; none of the four had complete documentation of ≥3 HepB vaccine doses (75). Postvaccination serologic testing was available for only one of seven HCPs with documentation of ≥3-doses of HepB vaccine; this HCP had an anti-HBs level <10 mIU/mL after 4 doses of vaccine (75).
Although reported data did not enable identification of the modes of transmission or information on receipt of postexposure prophylaxis, 28 (16.7%) of 168 HCP for whom data were available reported an accidental stick or puncture with a needle or other object contaminated with blood during the 6 weeks through 6 months before illness, possibly representing occupational acquisition of infection (75). Unrecognized exposures might have resulted in HBV infections among HCP who did not report an exposure (2). Other risk factors for HBV exposure in the 6 weeks through 6 months before illness (i.e., injection drug use, men who have sex with men, multiple sex partners, contact with a hepatitis B case, dialysis patient, receipt of blood transfusion, surgery, acupuncture, and tattoo receipt) were present among 121 (59.6%) of 203 HCP, possibly suggesting their exposures were not occupational (75).
# Managing HCP Vaccination and Serologic Test Results
Immunization information systems (IIS) provide consolidated vaccination histories for use by vaccination providers in determining appropriate vaccinations (76). Accessing IIS for vaccination records might decrease unnecessary revaccination among HCP who no longer have records of HepB vaccination. IIS do not accept postvaccination anti-HBs test results (77). To reduce the cost and inconvenience of repeat anti-HBs testing when HCP are employed by different health-care facilities, CDC recommends that institutions consider systems for long-term management of anti-HBs and other hepatitis B serologic test results. Mechanisms for tracking vaccination and hepatitis B serologic test results in health information technology products could also reduce cost and inconvenience of repeat anti-HBs testing.
# Passive Prophylaxis of HBV Exposed Health Care Personnel Hepatitis B immune globulin
Hepatitis B immune globulin (HBIG) provides passive anti-HBs and temporary (i.e., 3-6 months) protection (15). HBIG is prepared from human plasma known to contain a high titer of anti-HBs. HBIG is typically used together with HepB vaccine for postexposure prophylaxis (15). For persons who do not respond to HepB vaccine, HBIG administered alone is the primary method of protection after HBV exposure (15). The standard adult dose of HBIG is 0.06 mL/kg. HBIG is administered by intramuscular injection; an appropriate muscle mass (i.e., deltoid or gluteal) should be chosen in which to deliver the large volume of HBIG required and a needle length appropriate for the HCP's size should be used. HBIG can be administered simultaneously with HepB vaccine but at a different injection site (15).
# Safety
The plasma from which HBIG is prepared is screened for HBsAg, HCV, and HIV (15). The process used to prepare HBIG inactivates HBV, HCV, and HIV from the final product. No evidence exists that HBV, HCV, or HIV has ever been transmitted by HBIG thar is commercially available in the United States (15).
Serious adverse effects from HBIG, when administered as recommended, are rare (1). Local pain and tenderness at the injection site, urticaria, and angioedema might occur; anaphylactic reactions, although rare, have been reported following the injection of human immune globulin (IG) preparations (1). HBIG is not contraindicated for pregnant (1,78) or lactating women (1).
# Efficacy
The effectiveness of HBIG and HepB vaccine in various postexposure settings has been evaluated by prospective studies. For perinatal exposure to a mother positive for both HBsAg and HBeAg, a regimen combining HBIG and initiation of the HepB vaccine series at birth is 85%-95% effective in preventing HBV infection (79,80). Regimens involving either multiple doses of HBIG alone or the HepB vaccine series alone are 70%-75% effective in preventing HBV infection when administered shortly after exposure (81). In the occupational setting, multiple doses of HBIG starting within 1 week following percutaneous exposure to HBsAg-positive blood provide an estimated 75% protection from HBV infection (82)(83)(84)(85)(86). Administration of HBIG might prolong the incubation period of HBV infection among persons who develop infection (82,85,87,88). A comparison of the postexposure efficacy of the combination of HBIG and the HepB vaccine series or HBIG alone has not been evaluated in the occupational setting (1). Whether the increased efficacy of HBIG added to HepB vaccine observed in the perinatal setting, compared with HBIG alone, applies to adults exposed occupationally remains unknown.
# Cost-Effectiveness Considerations
To examine the cost-effectiveness of various strategies for assessing HCP protection from hepatitis B, two economic models that yielded calculations of the incremental cost per quality-adjusted life-year (QALY) saved were developed. One model represented an approach in which anti-HBs is measured on a pre-exposure basis, and HCP with anti-HBs <10 mIU/mL receive an additional dose of HepB vaccine, followed by repeat anti-HBs measurement. If anti-HBs remains <10 mIU/mL after the first revaccination dose, the HCP receives two additional revaccination doses of HepB vaccine followed by repeat anti-HBs measurement. Another model represented a postexposure management approach; at the time of exposure, the HCP is tested for anti-HBs and the source patient is tested simultaneously for HBsAg, and postexposure prophylaxis would be administered on the basis of these results. Results from the two models were compared. A decision-tree analysis was used to combine all parameters and calculate the total intervention costs and probability of infection. In addition, HBV infection-related costs and QALY loss (accounting for acute and asymptomatic infections and a 6% probability of chronic infection) were determined from an existing model (89) and were considered for the HCP's remaining lifetime. The intervention time frame included a 1-year analysis and a multiyear analysis covering up to 10 years of exposure. A 3% annual discount rate was used, and all final cost figures were converted to 2010 U.S. dollars using the Medical Consumer Price Index.
The baseline cost-effectiveness models assumed that an ideal 95% of HCP have initial and sustained protection against HBV infection after a primary ≥3-dose HepB vaccine series, irrespective of the presence of detectable anti-HBs. Ninety-five percent protection was derived from the proportion of persons aged <40 years, including term newborns that have measurable anti-HBs ≥10 mIU/mL soon after a primary vaccination series. Approximately 18-25 years after vaccination, approximately 20% of HCP (vaccinated at age <1 year) or approximately 80% of HCP (vaccinated at age ≥1 year) retain anti-HBs ≥10 mIU/mL. The model did not account for unrecognized exposures, as probability data for unrecognized exposures are not available, or suboptimal vaccine coverage that exists among HCP.
For pre-exposure anti-HBs testing followed by revaccination and retesting, if necessary, compared with doing nothing, the incremental cost per QALY saved was $4,542,467 for trainees and $3,149,183 for nontrainees at year one, and decreased to $893,619 and $796,140, respectively, over 10 years. This approach is expected to result in 3.7 and 1.6 visits to occupational health for trainees and nontrainees, respectively. The expected number of infections is 0.7 per 100,000 and 0.4 per 100,000 for trainees and nontrainees, respectively. For an approach relying upon postexposure management, compared with doing nothing, the incremental cost per QALY saved was $2,270,801 for trainees and $1,610,998 for nontrainees at year one, and decreased to $917,859 and $1,114,364 respectively, over 10 years. The expected number of infections is 3.0 per 100,000 and 1.7 per 100,000 for trainees and nontrainees, respectively. Although an approach relying upon postexposure management might be less costly per QALY saved initially for many institutions, pre-exposure anti-HBs testing with possible revaccination becomes more cost-effective compared with a postexposure approach over time.
Sensitivity analyses demonstrated that cost-effectiveness improves in settings where a greater proportion of source patients are HBsAg-positive and among HCP with higher risk for exposure (e.g., surgeons). Cost-effectiveness can change as new antivirals become available for treatment of HBV infection. Vaccinating previously unvaccinated HCP trainees followed by postvaccination serologic testing, compared with doing nothing, has an incremental cost per QALY saved of $374,646 at year one and $51,537 over 10 years, accounting for direct costs to the health-care system and direct medical costs of hepatitis B-related illness and complications.
# Recommendations
# Pre-Exposure Management Education and Infrastructure
At the time of hire or matriculation, health-care providers and health-care institutions should provide training to HCP to improve recognition and encourage timely reporting of blood and body fluid exposures. The possibility that the postexposure evaluation will cause the HCP to have time lost from work should not be a barrier to reporting. Institutions should ensure that HCP have rapid access to postexposure testing and prophylaxis, including HBIG and HepB vaccine.
# Serologic Testing for HBV Infection
Testing unvaccinated HCP for HBV infection is not generally indicated for persons being evaluated for hepatitis B protection because of occupational risk. Prevaccination serologic testing is indicated for all persons born in geographic regions with HBsAg prevalence of ≥2% (e.g., much of Eastern Europe, Asia, Africa, the Middle East, and the Pacific Islands) and certain indigenous populations from countries with overall low HBV endemicity (<2%); persons with behavioral exposures to HBV (e.g., men who have sex with men and past or current injection drug users); persons receiving cytotoxic or immunosuppressive therapy; and persons with liver disease of unknown etiology.
HBV endemicity (HBsAg prevalence) can be described as low (<2%), moderate (2%-<8%), and high (≥8%). Because certain persons might have been infected with HBV before they received HepB vaccination, HBsAg testing is recommended regardless of vaccination history for persons born in geographic regions with HBsAg prevalence of ≥2%, U.S.-born persons not vaccinated as infants whose parents were born in regions with high HBV endemicity (HBsAg prevalence) (≥8%), persons who received HepB vaccination as adolescents or adults after the initiation of risk behaviors (12), and persons who are HIV-positive or who receive hemodialysis (11).
Testing HCP at risk for HBV infection should consist of a serologic assay for HBsAg, in addition to either anti-HBc or anti-HBs (11,12). For unvaccinated HCP at risk for previous HBV infection, blood should be drawn for testing before the first dose of vaccine is administered.
# Vaccination
All HCP whose work-, training-, and volunteer-related activities involve reasonably anticipated risk for exposure to blood or body fluids should be vaccinated with a complete, ≥3-dose HepB vaccine series. OSHA mandates that vaccination be available for employees within 10 days of initial assignment (27). HCP trainees should complete the series before the potential for exposure with blood or body fluids, when possible, as higher risk has been reported during professional training (e.g., residency training).
Incompletely vaccinated HCP should receive additional dose(s) to complete the vaccine series (15). The vaccine series does not need to be restarted for HCP with an incomplete series; however, minimum dosing intervals should be heeded (15). Minimum dosing intervals are 4 weeks between the first and second dose, 8 weeks between the second and third dose, and 16 weeks between the first and third dose (15).
HCP lacking documentation of HepB vaccination should be considered unvaccinated (when documentation for HepB vaccine doses is lacking) or incompletely vaccinated (when documentation for some HepB vaccine doses is lacking) and should receive additional doses to complete a documented HepB series. Health-care institutions are encouraged to seek documentation of "missing" HepB doses in IIS, when feasible, to avoid unnecessary vaccination.
OSHA mandates that HCP who refuse HepB vaccination sign a declination statement (http://www.osha.gov/pls/ oshaweb/owadisp.show_document?p_id=10052&p_ table=STANDARDS). HCP refusing HepB vaccination can obtain vaccination at a later date at no expense if the HCP is still covered under OSHA's Bloodborne Pathogens Standard. Health-care institutions should encourage HepB vaccination among HCP to improve HBV protection and to achieve the Healthy People 2020 target of 90% vaccination (66).
# Postvaccination Serologic Testing
HCP who have written documentation of a complete, ≥3-dose HepB vaccine series and subsequent postvaccination anti-HBs ≥10 mIU/mL are considered hepatitis B immune. Immunocompetent persons have long-term protection against HBV and do not need further periodic testing to assess anti-HBs levels (Figure 6).
All HCP recently vaccinated or recently completing HepB vaccination who are at risk for occupational blood or body fluid exposure should undergo anti-HBs testing. Anti-HBs testing should be performed 1-2 months after administration of the last dose of the vaccine series when possible. HCP with documentation of a complete ≥3-dose HepB vaccine series but no documentation of anti-HBs ≥10 mIU/mL who are at risk for occupational blood or body fluid exposure might undergo anti-HBs testing upon hire or matriculation. Testing should use a quantitative method that allows detection of the protective concentration of anti-HBs (≥10 mIU/mL) (e.g., enzyme-linked immunosorbent assay [ELISA]).
• Completely vaccinated HCP with anti-HBs ≥10 mIU/mL are considered hepatitis B immune. Immunocompetent persons have long-term protection and do not need further periodic testing to assess anti-HBs levels. • Completely vaccinated HCP with anti-HBs <10 mIU/mL should receive an additional dose of HepB vaccine, followed by anti-HBs testing 1-2 months later. HCP whose anti-HBs remains <10 mIU/mL should receive 2 additional vaccine doses (usually 6 doses total), followed by repeat anti-HBs testing 1-2 months after the last dose. Alternatively, it might be more practical for very recently vaccinated HCP with anti-HBs <10 mIU/mL to receive 3 consecutive additional doses of HepB vaccine (usually 6 doses total), followed by anti-HBs testing 1-2 months after the last dose.
# Standard Precautions and Advising HCP to Report Exposures
All HCP should adhere to infection-control guidelines and follow Standard Precautions (90), including the use of engineering and work-practice controls, to reduce the risk for blood or body fluid exposure. All HCP, including those who have demonstrated protection against HBV, should be advised to immediately report blood or body fluid exposures to occupational health for evaluation of the appropriate measures to prevent transmission of bloodborne pathogens (including HIV, hepatitis C, and hepatitis B).
# Postexposure Management Initial Postexposure Management
Wounds and skin sites that have been in contact with blood or body fluids should be washed with soap and water; mucous membranes should be flushed with water. Using antiseptics (e.g., 2%-4% chlorhexidine) for wound care or expressing fluid by squeezing the wound further have not been shown to reduce the risk for HBV transmission; however, the use of antiseptics is not contraindicated. The application of caustic agents (e.g., bleach) or the injection of antiseptics or disinfectants into the wound is not recommended.
Procedures should be followed for testing known source persons, including obtaining informed consent, in accordance with applicable laws. Source patients determined to be HBsAg-positive should be referred for appropriate management and should be reported to the state or local health department. When a source patient is unknown (e.g., as occurs from a puncture with a needle in the trash), the exposed HCP should be managed as if the source patient were HBsAg-positive. Testing needles and other sharp instruments implicated in an exposure is not recommended, regardless of whether the source patient is known or unknown. The reliability and interpretation of findings in such circumstances are unknown, and testing could be hazardous to persons handling the sharp instrument. Exposures involving human bites should be managed with the knowledge that both the person being bitten and the person who engaged in biting were potentially exposed.
Institutions should ensure that HCP have timely access to postexposure management and prophylaxis, including * Should be performed 1-2 months after the last dose of vaccine using a quantitative method that allows detection of the protective concentration of anti-HBs (≥10 mIU/mL) (e.g., enzyme-linked immunosorbent assay [ELISA]). † A nonresponder is defined as a person with anti-HBs <10 mIU/mL after ≥6 doses of HepB vaccine. Persons who do not have a protective concentration of anti-HBs after revaccination should be tested for HBsAg. If positive, the person should receive appropriate management or vaccination. (11). Anti-HBs testing should be performed using a method that allows detection of the protective concentration of anti-HBs (≥10 mIU/mL) (Table 2).
# Managing Vaccinated HCP
For vaccinated HCP (who have written documentation of a complete, ≥3-dose HepB vaccine series) with subsequent documented anti-HBs ≥10 mIU/mL, testing the source patient for HBsAg is unnecessary. No postexposure management for HBV is necessary, regardless of the source patient's HBsAg status.
For vaccinated HCP (who have written documentation of HepB vaccination) with anti-HBs <10 mIU/mL after two complete, ≥3-dose HepB vaccine series, the source patient should be tested for HBsAg as soon as possible after the exposure. If the source patient is HBsAg-positive or has unknown HBsAg status, the HCP should receive 2 doses of HBIG (1,11). The first dose should be administered as soon as possible after the exposure, and the second dose should be administered 1 month later. If the source patient is HBsAg-negative, neither HBIG nor HepB vaccine is necessary.
For vaccinated HCP (who have written documentation of a complete, ≥3-dose HepB vaccine series) without previous anti-HBs testing, the HCP should be tested for anti-HBs and the source patient (if known) should be tested for HBsAg as soon as possible after the exposure. Testing the source patient and the HCP should occur simultaneously; testing the source patient should not be delayed while waiting for the HCP anti-HBs test results, and likewise, testing the HCP should not be delayed while waiting for the source patient HBsAg results. * HBIG should be administered intramuscularly as soon as possible after exposure when indicated. The effectiveness of HBIG when administered >7 days after percutaneous, mucosal, or nonintact skin exposures is unknown. HBIG dosage is 0.06 mL/kg. † Should be performed 1-2 months after the last dose of the HepB vaccine series (and 4-6 months after administration of HBIG to avoid detection of passively administered anti-HBs) using a quantitative method that allows detection of the protective concentration of anti-HBs (≥10 mIU/mL). § A responder is defined as a person with anti-HBs ≥10 mIU/mL after ≥3 doses of HepB vaccine. ¶ A nonresponder is defined as a person with anti-HBs <10 mIU/mL after ≥6 doses of HepB vaccine. ** HCP who have anti-HBs <10mIU/mL, or who are unvaccinated or incompletely vaccinated, and sustain an exposure to a source patient who is HBsAg-positive or has unknown HBsAg status, should undergo baseline testing for HBV infection as soon as possible after exposure, and follow-up testing approximately 6 months later. Initial baseline tests consist of total anti-HBc; testing at approximately 6 months consists of HBsAg and total anti-HBc.
• If the HCP has anti-HBs <10 mIU/mL and the source patient is HBsAg-positive or has unknown HBsAg status, the HCP should receive 1 dose of HBIG and be revaccinated as soon as possible after the exposure. The HCP should then receive the second 2 doses to complete the second HepB vaccine series (6 doses total when accounting for the original 3-dose series) according to the vaccination schedule. To document the HCP's vaccine response status for future exposures, anti-HBs testing should be performed 1-2 months after the last dose of vaccine. • If the HCP has anti-HBs <10 mIU/mL and the source patient is HBsAg-negative, the HCP should receive an additional HepB vaccine dose, followed by repeat anti-HBs testing 1-2 months later. HCP whose anti-HBs remains <10 mIU/mL should undergo revaccination with 2 more doses (6 doses total when accounting for the original 3-dose series). To document the HCP's vaccine response status for future exposures, anti-HBs testing should be performed 1-2 months after the last dose of vaccine. • If the HCP has anti-HBs ≥10 mIU/mL at the time of the exposure, no postexposure HBV management is necessary, regardless of the source patient's HBsAg status.
# Managing HCP Who Lack Documentation of Vaccination, are Unvaccinated or Incompletely Vaccinated
For unvaccinated or incompletely vaccinated HCP (including those who refused vaccination), the source patient should be tested for HBsAg as soon as possible after the exposure. Testing unvaccinated or incompletely vaccinated HCP for anti-HBs is not necessary and is potentially misleading, because anti-HBs ≥10 mIU/mL as a correlate of vaccine-induced protection has only been determined for persons who have completed an approved vaccination series (15,42).
• If the source patient is HBsAg-positive or has unknown HBsAg status, the HCP should receive 1 dose of HBIG and 1 dose of HepB vaccine administered as soon as possible after the exposure. The HCP should complete the HepB vaccine series according to the vaccination schedule. To document the HCP's vaccine response status for future exposures, anti-HBs testing should be performed approximately 1-2 months after the last dose of vaccine. Because anti-HBs testing of HCP who received HBIG should be performed after anti-HBs from HBIG is no longer detectable (6 months after administration), it will likely be necessary to defer anti-HBs testing for a period longer than 1-2 months after the last vaccine dose.
-HCP with anti-HBs ≥10 mIU/mL after receipt of the primary vaccine series are considered immune. Immunocompetent persons have long-term protection and do not need further periodic testing to assess anti-HBs levels. -HCP with anti-HBs <10 mIU/mL after receipt of the primary series should be revaccinated. For these HCP, administration of a second complete 3-dose series on an appropriate schedule, followed by anti-HBs testing 1-2 months after the third dose, usually is more practical than conducting serologic testing after each additional dose of vaccine. To document the HCP's vaccine response status for future exposures, anti-HBs testing should be performed 1-2 months after the last dose of vaccine. • If the source patient is HBsAg-negative, the HCP should complete the HepB vaccine series according to the vaccination schedule. To document the HCP's vaccine response status for future exposures, anti-HBs testing should be performed approximately 1-2 months after the last dose of vaccine.
-HCP with anti-HBs ≥10 mIU/mL after receipt of the primary vaccine series are considered immune. Immunocompetent persons have long-term protection and do not need further periodic testing to assess anti-HBs levels. -HCP with anti-HBs <10 mIU/mL after receipt of the primary series should be revaccinated. For these HCP, administration of a second complete 3-dose series on an appropriate schedule, followed by anti-HBs testing 1-2 months after the third dose, usually is more practical than conducting serologic testing after each additional dose of vaccine. To document the HCP's vaccine response status for future exposures, anti-HBs testing should be performed 1-2 months after the last dose of vaccine.
# Testing of HCP Exposed to an HBsAg-Positive or Unknown Source
HCP who have anti-HBs <10 mIU/mL, or who are unvaccinated or incompletely vaccinated, and who sustain a percutaneous, mucosal, or nonintact skin exposure to a source patient who is HBsAg-positive or has unknown HBsAg status should undergo baseline testing for HBV infection as soon as possible after the exposure, and follow-up testing approximately 6 months later. Testing immediately after the exposure should consist of total anti-HBc, and follow-up testing approximately 6 months later should consist of HBsAg and total anti-HBc.
HCP exposed to a source patient who is HBsAg-positive or has unknown HBsAg status do not need to take special precautions to prevent secondary transmission during the follow-up period; however, they should refrain from donating blood, plasma, organs, tissue, or semen (1). The exposed HCP does not need to modify sexual practices or refrain from becoming pregnant (1). If an exposed HCP is breast feeding, she does not need to discontinue (1). No modifications to an exposed HCP's patient-care responsibilities are necessary to prevent transmission to patients based solely on exposure to a source patient who is HBsAg-positive or has unknown HBsAg status.
# Vaccine Nonresponders
Vaccinated HCP whose anti-HBs remains <10 mIU/mL after revaccination (i.e., after receiving a total of 6 doses) should be tested for HBsAg and anti-HBc to determine infection status. Those determined not to be HBV infected (vaccine nonresponders) should be considered susceptible to HBV infection. No specific work restrictions are recommended for vaccine nonresponders (91).
# Documentation
Health-care institutions should maintain records, ideally electronic records that are easily retrievable following exposures, of documented vaccination histories and serologic test results for reference in managing occupational exposures, and to provide to other health-care institutions if requested by the HCP. The vaccination information should be entered into an IIS accepting records from adult vaccination, if available. HCP should be provided a copy of HepB vaccination and anti-HBs testing results and encouraged to keep them with their personal health records so they can readily be made available to future employers.
# HCP with HBV Infection
HCP who are positive for HBsAg should be counseled how to prevent HBV transmission to others and referred for further evaluation (92). Those who perform exposure-prone procedures should be advised regarding the procedures they can perform safely as per updated CDC recommendations for the management of HBsAg-positive health-care providers and students (11,13). Chronic hepatitis B infection in itself should not preclude the practice or study of medicine, surgery, dentistry, or allied health professions (13).
# Future Studies
National surveillance systems to accurately assess the burden of hepatitis B among HCP and health-care facility databases tracking occupational exposures among HCP are important for monitoring the changing epidemiology of occupationally acquired HBV infections and other bloodborne pathogens. Systems and databases could ideally be electronically linked to employee health records and should include results that identify HepB vaccine responders and nonresponders, the nature and HBV status of the exposure source and postexposure management, and the HCP's anti-HBs level. Appropriate safeguards should be in place to protect the privacy of the health information. Data collection should be representative of HCP in a variety of settings (e.g., acute care, long-term care, and dialysis), including settings with frequent staff turnover. Studies assessing HBV transmission among all HCP exposed to an HBsAg-positive source, regardless of vaccination history or anti-HBs levels, approximately 6 months after an exposure will help to inform duration of vaccine protection. Surveillance activities for acute hepatitis B infection should continue to ascertain occupation among cases, in addition to HepB vaccination history. Long-term follow-up studies assessing disease incidence and duration of anti-HBs among persons vaccinated as infants and older adults, including persons who received booster doses subsequent to the primary vaccine series and persons from HBV-endemic areas, also might provide information on duration of vaccine-induced protection. Other subject areas that would benefit from research include efficacy and cost-effectiveness of antiviral agents for postexposure prophylaxis, immunogenicity of higher dosage or new vaccines for revaccinating vaccine nonresponders, and an examination of the future role of postexposure hepatitis B virus deoxyribonucleic acid (HBV DNA) testing.
# Acknowledgments
The following persons were consulted during the drafting of these recommendations: Thomas J.
# Disclosure of Competing Interests
The developers of these guidelines wish to disclose that they have no financial interests or other relationships with the manufacturers of commercial products or suppliers of commercial services related to vaccines including any related to hepatitis B vaccines, with the following exceptions: David Weber, MD, wishes to disclose that he served as a consultant and on a speakers' bureau, whether paid or unpaid (e.g., travel related reimbursement, honoraria), for the following vaccine manufacturers: Merck, Sanofi, and Pfizer pharmaceutical companies. Amy B. Middleman, MD, also wishes to disclose that she received grant funding from the following pharmaceutical companies: MedImmune, Sanofi, and Merck.
# ISSN: 1057-5987
The Morbidity and Mortality Weekly Report (MMWR) Series is prepared by the Centers for Disease Control and Prevention (CDC) and is available free of charge in electronic format. To receive an electronic copy each week, visit MMWR's free subscription page at http://www.cdc.gov/mmwr/mmwrsubscribe. html. Paper copy subscriptions are available through the Superintendent of Documents, U.S. Government Printing Office, Washington, DC 20402; telephone 202-512-1800. | None | None |
4002b162b0b55f9b81f33d2c62a55faf8582c153 | cdc | None | Minor revisions were also made to correct typos, add references, and update content from cited guidelines and source materials.
# Disclaimers:
All material in this publication is in the public domain and may be used and reprinted without permission; citation as to source, however, is appreciated.
# Introduction
Recent findings from several clinical trials have demonstrated safety 1 and a substantial reduction in the rate of HIV acquisition for men who have sex with men (MSM) 2 , men and women in heterosexual discordant couples 3 , and heterosexual men and women recruited as individuals 4 who were prescribed daily oral antiretroviral preexposure prophylaxis (PrEP) with a fixed-dose combination of tenofovir disoproxil fumarate (TDF) and emtricitabine (FTC). The demonstrated efficacy of PrEP was in addition to the effects of repeated condom provision, sexual risk-reduction counseling, and the diagnosis and treatment of sexually transmitted infection (STI) that were provided to all trial participants. In July 2012, after reviewing these trial results, the U.S. Food and Drug Administration (FDA) approved an indication for the use of Truvada ® (TDF/FTC) "in combination with safer sex practices for pre-exposure prophylaxis (PrEP) to reduce the risk of sexually acquired HIV-1 in adults at high risk" 5,6 . In July 2013, an additional clinical trial found that daily oral TDF reduced the rate of HIV acquisition for persons who inject drugs (PWID) (also called injection drug users ) 7 .
On the basis of these trial results and the FDA approval, the U.S. Public Health Service has published a comprehensive clinical practice guideline for the use of PrEP for the prevention of HIV infection in the United States and updated it in 2017. This supplement to the PHS PrEP Clinical Practice Guidelines is intended to provide additional information that may be useful to clinicians providing PrEP. As additional materials become available, this document will be updated.
# Section 1
Contains a template checklist that clinicians can complete and share with patients to document the services provided to PrEP patients and the actions expected from patients to maximize the efficacy and safety of PrEP. Sections 2-4
Contain templates for informational handouts that can be provided to patients Section 5
Contains an information sheet for providers counseling patients about PrEP use during conception, pregnancy and breastfeeding. Section 6
Contains the HIV incidence Risk Index for MSM, a tool that clinicians may use to quickly and systematically determine which men are at especially high risk for acquiring HIV infection, for whom PrEP may be indicated. Section 7
Contains the HIV incidence Risk Index for PWID, a tool that clinicians may use to quickly determine which persons who inject drugs are at especially high risk for acquiring HIV infection, for whom PrEP may be indicated. Section 8
Contains more detailed information about the clinical management of patients who acquire HIV infection while on PrEP. Section 9
Contains more detailed information about the clinical management of transitioning patients from nPEP to PrEP. Sections 10-11 Contain more detailed information than that included in the guidelines about methods and resources for counseling patients receiving PrEP about medication adherence and HIV risk reduction behaviors.
# Sections 12
Contains information relevant to administrative and billing codes for PrEP related services. Section 13 Contains potential practice quality practice measures. Section 14 Documents the methods used to develop the PHS PrEP Clinical Practice Guidelines. Assessment for possible acute HIV infection Indicated laboratory screening to determine indications for these medications An HIV risk assessment to determine whether PrEP is indicated for this patient A medication fact sheet listing dosing instructions and side effects Counseling or a referral for counseling on condom use and any other HIV riskreduction methods this patient may need Advice on methods to help the patient to take medication daily as prescribed Information about PrEP use during conception and pregnancy (when indicated)
A prescription for Truvada (300 mg tenofovir disoproxil fumarate, 200 mg emtricitabine)
A follow-up appointment date
As the provider, I will:
- Limit refill periods to recommended intervals for repeat HIV testing (at least every 3 months)
- Conduct follow-up visits at least every 3 months that include the following:
- Assessment of HIV status (including signs or symptoms of acute HIV infection)
- Assessment of side effects and advice on how to manage them o Assessment of medication adherence and counseling to support adherence o Assessment of STI symptoms, HIV risk behavior and counseling support for riskreduction practices
- Inform the patient of any new information about PrEP and respond to questions
Patient Section
It has been explained to me that:
- Taking a dose of PrEP medication every day may lower my risk of getting HIV infection
- This medicine does not completely eliminate my risk of getting HIV infection, so I need to use condoms during sex
- This medicine may cause side effects so I should contact my provider for advice by calling ________________ if I have any health problems
- It is important for my health to find out quickly if I get HIV infection while I'm taking this medication, so o I will contact my provider right away if I have symptoms of possible HIV infection (fever with sore throat, rash, headache, or swollen glands)
- My provider will test for HIV infection at least once every 3 months Therefore, I will:
- Try my best to take the medication my provider has prescribed every day
- Talk to my provider about any problems I have in taking the medication every day
- Not share the medication with any other person
- Attend all my scheduled appointments
- Call _________________ to reschedule any appointments I cannot attend
# Give one copy to patient
Section 2 PrEP Information Sheet
# Pre-exposure Prophylaxis (PrEP) for HIV Prevention
Frequently Asked Questions What is PrEP? "PrEP" stands for preexposure prophylaxis. The word "prophylaxis" (pronounced pro fil ak sis) means to prevent or control the spread of an infection or disease. The goal of PrEP is to prevent HIV infection from taking hold if you are exposed to the virus. This is done by taking a pill that contains 2 HIV medications every day. These are the same medicines used to stop the virus from growing in people who are already infected.
# Why take PrEP?
The HIV epidemic in the United States is growing. About 50,000 people get infected with HIV each year. More of these infections are happening in some groups of people and some areas of the country than in others.
# Is PrEP a vaccine?
No. PrEP medication does not work the same way as a vaccine. When you take a vaccine, it trains the body's immune system to fight off infection for years. You will need to take a pill every day by mouth for PrEP medications to protect you from infection. PrEP does not work after you stop taking it. The medication that was shown to be safe and to help block HIV infection is called "Truvada" (pronounced tru va duh). Truvada is a combination of 2 drugs (tenofovir and emtricitabine). These medicines work by blocking important pathways that the HIV virus uses to set up an infection. If you take Truvada as PrEP daily, the presence of the medication in your bloodstream can often stop the HIV virus from establishing itself and spreading in your body. If you do not take the Truvada pills every day, there may not be enough medicine in your blood stream to block the virus.
# Should I consider taking PrEP?
PrEP is not for everyone. Doctors prescribe PrEP for some patients who have a very high risk of coming in contact with HIV by not using a condom when they have sex with a person who has HIV infection. You should consider PrEP if you are a man or woman who sometimes has sex without using a condom, especially if you have a sex partner who you know has HIV infection. You should also consider PrEP if you don't know whether your partner has HIV infection but you know that your partner is at risk (for example, your partner inject drugs or is having sex with other people in addition to you) or if you have recently been told by a health care provider that you had a sexually transmitted infection. If your partner has HIV infection, PrEP may be an option to help protect you from getting HIV infection while you try to get pregnant, during pregnancy, or while breastfeeding.
# How well does PrEP work?
PrEP was tested in several large studies with men who have sex with men, men who have sex with women, and women who have sex with men. All people in these studies (1) were tested at the beginning of the trial to be sure that they did not have HIV infection, (2) agreed to take an oral PrEP tablet daily,
(3) received intensive counseling on safer-sex behavior, (4) were tested regularly for sexually transmitted infections, and (5) were given a regular supply of condoms.
Several studies showed that PrEP reduced the risk of getting HIV infection.
- Men who have sex with men who were given PrEP medication to take, were 44% less likely to get HIV infection than were those men who took a pill without any PrEP medicine in it (a placebo). Forty-four percent was an average that included men who didn't take the medicine every day and those who did. Among the men who said they took most of their daily doses, PrEP reduced the risk of HIV infection by 73% or more, up to 92% for some.
- Among men and women in couples in which one partner had HIV infection and the other partner initially did not ("HIV-discordant" couples), those who received PrEP medication were 75% less likely to become infected than those who took a pill without any medicine in it (a placebo). Among those who said they took most of their daily doses, PrEP reduced the risk of HIV infection by up to 90%.
- In one study of men and women who entered the study as individuals (not as a couple), PrEP worked for both men and women in one study: those who received the medication were 62% less likely to get HIV infection; those who said they took most of their daily doses, were 85% less likely to get HIV infection. But in another study, only about 1 in 4 women (<26%) had PrEP medication found in their blood when it was checked. This indicated that few women were actually taking their medication and that study found no protection against HIV infection.
More information on the details of these studies can be found at .
# Is PrEP safe?
The clinical trials also provided safety information on PrEP. Some people in the trials had early side effects such as an upset stomach or loss of appetite but these were mild and usually went away within the first month. Some people also had a mild headache. No serious side effects were observed. You should tell your doctor if these or other symptoms become severe or do not go away.
# How can I start PrEP?
If you think you may be at high risk for HIV, talk to your doctor about PrEP. If you and your doctor agree that PrEP might reduce your risk of getting HIV infection, you will need to come in for a general health physical, blood tests for HIV, and tests for other infections that you can get from sex partners. Your blood will also be tested to see if your kidneys and liver are functioning well. If these tests show that PrEP medicines are likely to be safe for you to take and that you might benefit from PrEP, your doctor may give you a prescription after discussing it with you.
Taking PrEP medicines will require you to follow-up regularly with your doctor. You will receive counseling on sexual behaviors and blood tests for HIV infection and to see if your body is reacting well to Truvada. You should take your medicine every day as prescribed, and your doctor will advise you about ways to help you take it regularly so that it stands the best chance to help you avoid HIV infection. Why is this medication prescribed?
- Truvada is one of several medications that are currently used to treat human immunodeficiency virus (HIV) and hepatitis B virus infection. - Truvada is now being used to prevent HIV infection.
- Truvada is sometimes prescribed to some people who do not have HIV infection (for example, those who do not always use condoms or who have a sex partner that has HIV infection) to help reduce their chances of getting HIV infection - When you take Truvada to prevent HIV infection, doctors refer to this use as "pre-exposure prophylaxis" or "PrEP".
# How does Truvada (PrEP) help prevent HIV infection?
- HIV is a virus that attacks your body's immune cells (the cells that work to fight infections).
- The 2 medications that make up Truvada (tenofovir and emtricitabine) block important pathways that viruses use to set up infection. - If you take Truvada as PrEP daily, the presence of the medication in your bloodstream can sometimes stop the virus from establishing itself and slow the spread of HIV in your body. - By itself, PrEP with Truvada does not work all the time so you should also use condoms during sex for the most protection from HIV infection.
How should this medicine be used?
- You must take one tablet of Truvada by mouth every day.
- Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand.
# What other information should I know?
- Do not let anyone else take your medication.
- Ask your pharmacist if you have any questions about refilling your prescription.
- Write a list of all of your prescription and over-the-counter medicines, as well as any vitamins, minerals, or other dietary supplements that you take.
- Bring your medication list with you each time you visit a doctor or if you are admitted to a hospital. Keep it with you always in case of emergencies. These signs and symptoms of acute HIV infection can begin a few days after you are exposed to HIV and usually last for about 14 days. They could last for just a few days, or they could last for several months.
You might not realize your illness is acute HIV infection. For one thing, you may not have known that the person you had sex with had HIV infection. And the signs and symptoms of HIV infection may feel just like other common virus infections like flu, a cold, sore throat, or mononucleosis (mono).
# What tests can show that I have acute HIV infection?
When HIV enters your body, it moves inside white blood cells called CD4 lymphocytes. HIV takes over the CD4 cells and makes billions of copies of the virus each day. The virus spread through your body.
Your body tries to defend itself against HIV by making antibodies (these antibodies try to block the virus from spreading in your body And fourth, when people have lots of virus in their body during acute HIV infection, they are more likely to pass the virus on to people they have sex with, especially since they may not know yet that they have gotten infected. For example, if your last HIV test result was negative and your partner also had a recent negative HIV test result, you might choose to have sex without a condom just at the time when it's very likely you would pass the virus on. So the sooner you know you have become infected, the more careful you can be to protect others from getting HIV infection.
# How is HIV treated?
People who have HIV infection are treated with combinations of 3 or more medicines that fight HIV. Some doctors start people on treatment medications as soon as they become infected; other doctors wait for a while because the greatest benefits to a person's health are seen after they have been infected a while. Early treatment also reduces the chances that a person with HIV infection will pass the virus on to their sex partners.
# What do I do if I suspect I might have acute HIV infection?
First, contact your doctor's office and arrange to be examined and have the right blood tests.
Second, discuss with your doctor whether to stop your PrEP medications or continue them until your test results are back.
Third, be especially careful to use condoms and take other safer sex measures to protect your partner(s).
# Section 5 Provider Information Sheet -PrEP during Conception, Pregnancy, and Breastfeeding
# Information for Clinicians Counseling Patients about PrEP Use During Conception, Pregnancy, and Breastfeeding
PrEP use may be one of several options to help protect the HIV-negative male or female partner in a heterosexual HIV-discordant couple during attempts to conceive . Pregnancy care providers may not have access to the medical records of the partner with HIV infection to document their viral load status. The extent to which PrEP use further decreases risk of HIV acquisition when the partner with HIV infection has a documented current undetectable viral load is unknown.
# Based on DHHS Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission 9
Panel's Recommendations on Reproductive Options for HIV-Concordant and Serodiscordant Couples For Couples who Want to Conceive For Concordant (Both Partners are HIV-Infected) and Discordant Couples:
- Expert consultation is recommended so that approaches can be tailored to couples specific needs (AIII).
- Partners should be screened and treated for genital tract infections before attempting to conceive (AII).
- The HIV-infected partner(s) should attain maximum viral suppression before attempting conception (AIII). For Discordant Couples:
- The HIV-infected partner should be receiving combination antiretroviral therapy and demonstrate sustained suppression of plasma viral load below the limits of detection (AI). - Administration of antiretroviral pre-exposure prophylaxis (PrEP) for 30 days before attempting conception and for 30 days after conception is achieved for HIV-uninfected partners may offer an additional tool to reduce the risk of sexual transmission, particularly if the HIV-infected partner's plasma viral load is unknown or detectable (CIII). It is not known whether PrEP for the uninfected partner confers additional benefit when the infected partner receiving antiretroviral therapy has documented sustained viral suppression.
# Discordant Couples with HIV-Infected Women:
- The safest conception option is assisted insemination, at home or in a clinician's office with a partner's sperm during the peri-ovulatory period (AIII).
# Discordant Couples with HIV-Infected Men:
- The use of donor sperm from an HIV-uninfected man with artificial insemination is the safest option (AIII). - When the use of donor sperm is unacceptable, the use of sperm preparation techniques coupled with either intrauterine insemination or in vitro fertilization should be considered (BII).
# Based on DHHS Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission 9
Panel's Recommendations on Reproductive Options for HIV-Concordant and Serodiscordant Couples
- Semen analysis is recommended for HIV-infected men before conception is attempted to prevent unnecessary exposure to infectious genital fluid. Semen abnormalities appear to be more common among HIV-infected men than HIV-uninfected men (AIII). The following information is provided to help you inform your patients of current information about potential risks and benefits of PrEP use so that you and your patients can make an informed decision.
# Rating of Recommendations
# Key Points
Provide education about PrEP and other methods of conception that minimize the risk of HIV transmission to both members of an HIV-discordant couple whenever possible.
# Options
Reducing the risk of HIV acquisition by an HIV-negative man during conception can be achieved by use of the following, singly or ideally in combination :
- Antiretroviral treatment of the HIV-positive female partner to achieve an undetectable viral load 13 - STI diagnosis and any indicated treatment for both partners before conception attempts - Daily, oral doses of TDF/FTC beginning 1 month before a conception attempt and continuing for 1 month after a conception attempt. PrEP may be indicated when the partners recent viral load is unknown, reported to be detectable, or cannot be documented as undetectable 14 .
# AND EITHER
- Limit sex without a condom (natural conception) to peak fertility times identified by home or laboratory tests for ovulation 15. OR - Intravaginal insemination 13 (either at home or in the clinic) with a fresh semen sample
# Potential Benefits of PrEP use
In clinical trials with heterosexually active adults, daily oral PrEP with TDF/FTC was safe and reduced the risk of HIV acquisition by an average of 63%-75%. Higher levels of protection (≥90%) were found among persons whose drug levels in their blood indicated that they had consistently taken the medication 3,4 .
# Potential Risks of PrEP use
In PrEP trials, follow-up with persons taking medication has been conducted for an average of 1-4 years.
Although no serious health risks were associated with PrEP use by HIV-uninfected adults, the long-term safety of PrEP has not yet been determined.
# FOR AN HIV-NEGATIVE WOMAN PLANNING PREGNANCY WITH AN HIV-POSITIVE MALE PARTNER
# Options
Reducing the risk of HIV acquisition by an HIV-negative woman during conception can be achieved by use of the following, singly or ideally in combination 10,13 :
- Antiretroviral treatment of the HIV-positive male partner to achieve an undetectable viral load 13 - STI diagnosis and any indicated treatment for both partners before conception attempts - Daily, oral doses of TDF/FTC beginning 1 month before a conception attempt and continuing for 1 month after a conception attempt. PrEP may be indicated when the partners recent viral load is unknown, reported to be detectable, or cannot be documented as undetectable 14 .
# AND EITHER
- Limit sex without a condom (natural conception) to peak fertility times identified by home or laboratory tests for ovulation in the female partner 15 .
# OR
- Intravaginal 16 or intrauterine insemination, or intracytoplasmic sperm injection with a semen sample processed by "sperm washing" and confirmed to have a negative test result for the presence of remnant HIV . This option may be indicated for couples with fertility problems.
# Potential Benefits of PrEP use
In clinical trials with heterosexually active adults, daily oral PrEP with TDF/FTC was safe and reduced the risk of HIV acquisition by an average of 63%-75%. Higher levels of protection (≥90%) were found among persons whose drug levels in their blood indicated that they had consistently taken the medication 3,4 .
The risk of HIV acquisition increases during pregnancy 19 , as does the risk of HIV transmission to an infant born to a mother who becomes infected during pregnancy or breastfeeding 20 Therefore, an HIVnegative woman whose sexual partner/spouse has HIV infection may benefit from continuing PrEP use throughout her pregnancy and breastfeeding to protect herself and her infant a
# Potential Risks of PrEP use
In PrEP trials, follow-up with persons taking medication has been conducted for an average of 1-4 years.
Although no serious health risks were associated with PrEP use by HIV-uninfected adults, the long-term safety of PrEP has not yet been determined.
In PrEP trials women were taken off medication as soon as pregnancy was detected. During these trials, no health problems have been associated with PrEP use by women in early pregnancy or for their offspring. However, the long-term safety of PrEP taken by HIV-uninfected women after fetal (during pregnancy) or infant (during breastfeeding) exposure is not yet determined.
No adverse effects have been found among infants exposed to TDF/FTC when the medications were taken as part of a treatment regimen for HIV-infected women during pregnancy or during breastfeeding (for which data suggest limited drug exposure ).
If you prescribe PrEP to a woman while pregnant, you are encouraged to prospectively and anonymously submit information about the pregnancy to the Antiretroviral Use in Pregnancy Registry (/).
a Alth ugh the DHHS Perinatal HIV Guidelines state that "pregnancy and breastfeeding are n t c ntraindicati ns f r PrEP" 9 , the FDA-appr ved package insert 6 says, "If an uninfected individual bec mes pregnant while taking TRUVADA f r a PrEP indicati n, careful c nsiderati n sh uld be given t whether use f TRUVADA sh uld be c ntinued, taking int acc unt the p tential increased risk f HIV-1 infecti n during pregnancy" and "m thers sh uld be instructed n t t breastfeed if they are receiving TRUVADA, whether they are taking TRUVADA f r treatment r t reduce the risk f acquiring HIV-1.". Theref re b th are currently ff-label uses f Truvada.
# Section 6 MSM Risk Index
Epidemiologic studies have identified a wide range or personal, relationship, partner, social, cultural, network, and community factors that may be associated with the presence of HIV infection. However, to provide PrEP (or other intensive HIV prevention services), it is necessary to briefly and systematically screen for key information about those factors that are predictive of very high risk of acquiring HIV infection.
This section contains a tool that clinicians may use to quickly and systematically determine which MSM are at especially high risk of acquiring HIV infection, and for whom PrEP may be indicated.
# Section 7 PWID (IDU) Risk Index
Epidemiologic studies have identified a wide range or personal, relationship, partner, social, cultural, network, and community factors that may be associated with the presence of HIV infection. However, to provide PrEP (or other intensive HIV prevention services), it is necessary to briefly and systematically screen for key information about those factors that are predictive of very high risk of acquiring HIV infection.
This section contains a tool that clinicians can use to quickly and systematically determine which persons who inject drugs (PWID) (also called injection drug users ) are at especially high risk for acquiring HIV infection, and for whom PrEP may be indicated. Add the scores for age and methadone use to the Composite Injection Subscore to yield a Total Score _________ Total Score- - If the total score is 46 or greater, evaluate for PrEP or other intensive HIV prevention services for PWID. If score is 45 or less, provide indicated standard HIV prevention services for PWID. To identify active PWID in a clinician's practice, we recommend asking all their patients a routine question: "Have you ever injected drugs that were not prescribed for you by a physician?" If yes, ask, "When was the last time you injected any drugs?" Only complete PWID risk index if they have injected any nonprescription drug during the past 6 months.
# Section 8 Management of Patients Who Acquire HIV While on PrEP
Patients who are being prescribed PrEP might acquire HIV infection for several reasons. When HIV infection is detected at the first follow-up visit after PrEP initiation, it can indicate that the patient had undetected acute infection when PrEP was initiated. When infection is detected at later follow-up visits, as it most commonly occurs, it might be because patients have stopped taking PrEP, have been taking it infrequently, or have been stopping and restarting it without retesting for HIV infection before restarting. Rarely, despite high adherence to continuous daily dosing, patients taking PrEP have acquired HIV infection. This can occur because of exposure to a drug-resistant viral strain 30 or simply because, even with daily use, PrEP protection is high but not 100% 31 .
In all cases, when an HIV test during a follow-up visit indicates possible infection in a PrEP patient, the following steps should be taken:
- Counsel the patient about their HIV status and the resulting management plan:
- If a single rapid antibody blood test was positive, explain the need to confirm presumptive HIVpositive status with laboratory testing. o If a rapid 4 th generation (antigen/antibody) blood test was positive, explain high likelihood of HIV infection that will need to be confirmed with additional laboratory testing. o If a positive HIV test was based on laboratory testing with confirmatory results already known, explain certainty of HIV diagnosis. o Ask about signs and symptoms of acute infection since last clinic visit as well as PrEP medication adherence history.
- Conduct confirmatory HIV testing (if not completed already) and supplemental tests, if indicated:
- If one or more rapid tests were positive, draw blood for confirmatory laboratory-based HIV testing with adequate blood for reflex HIV viral load testing if confirmed to be HIV infected. o If laboratory-based testing was positive, draw blood for HIV viral load, CD4 cell count, and HIV resistance testing. o For persons with confirmed HIV infection, conduct the following supplemental testing indicated for initiation of HIV treatment, including but not necessarily limited to the following 32 : Chemistry screen, ALT, AST, bilirubin, CBC with differential, urinalysis, and pregnancy test (if female). Fasting lipid profile, glucose, and hemoglobin A1c are also indicated, on the day that seroconversion is detected, if possible.
- Convert the PrEP regimen to an HIV treatment regimen recommended by the DHHS Panel on Antiretroviral Guidelines for Adults and Adolescents 32 .
- It is not necessary to stop antiretrovirals entirely while waiting for additional laboratory test results. In the most likely event that the patient has HIV infection, immediate initiation of HIV treatment is indicated. The following regimens are recommended as of July 14, 2016 but the treatment guidelines should be consulted for updates 32 : o Continue the prescription of Truvada (TDF 300 mg/FTC 200 mg) once daily pending results of resistance tests o Add either: Dolutegravir (Tivicay) 50 mg once daily OR Darunavir (Prezista) 800 mg with Ritonavir (Norvir) 100 mg once daily.
In cases where a viral strain with significant resistance to tenofovir is later identified, the regimen can then be optimized. In cases where HIV infection is not confirmed, return to the PrEP regimen can be accomplished by dropping the additional treatment medication.
- Provide client education about time to viral load suppression:
- Reinforce the importance of medication adherence for the patient's long-term health.
- Discuss the importance of condom use to protect sexual partners and provide condoms. o Offer HIV testing for sex and drug injection partners and assistance with disclosure, if desired. o Ask if the patient had condomless sex or shared injection equipment during the past 72 hours, and if yes, offer nPEP for exposed partners.
- Consult with and transfer care to an experienced HIV care provider, if necessary. o Clinicians can call the National Clinical Consultation Center toll-free at (800) 933-3413.
- Discuss or complete insurance paperwork necessary for coverage of treatment medication. o Patients who are receiving medication through PrEP-specific medication assistance programs will need to switch to an HIV treatment assistance program. o Public or private insurance plans will generally not require additional paperwork but prior authorizations for PrEP may raise questions when switching to a prescription for a treatment regimen.
- Schedule follow-up visits (including social services, if required).
- Complete an HIV case report for the health department (completion of fields related to PrEP use at the time of seroconversion are highlighted in red below).
# Section 9 Transition of Patients From Nonoccupational Postexposure Prophylaxis (nPEP) to Preexposure Prophylaxis (PrEP)
Two types of patients may be considered candidates for PrEP use after a course of nonoccupational postexposure prophylaxis (nPEP):
- Patients who request PrEP and also have had a possible sexual or injection drug-related HIV exposure in the prior 72 hours (i.e., are within the recommended window to start nPEP)
- Patients who request repeated courses of nPEP, particularly over a relatively recent period (e.g., more than twice during the past 6 months)
If evaluation demonstrates nPEP is clinically indicated and that the patient is also eligible for PrEP (e.g., behavioral risk for repeated HIV exposure, recent bacterial STI diagnosis in a sexually active person), then these patients should both be provided a 28-day course of nPEP and be evaluated for transition to PrEP at the conclusion of their nPEP course.
# TRANSITIONING IMMEDIATELY FROM NPEP TO PREP
Transitioning from nPEP to PrEP without interruption at the completion of the 28-day nPEP course has the advantages of (1) maintaining satisfactory antiretroviral drug levels for PrEP (if nPEP adherence has been good); and (2) maximizing continuous prevention measures through continuity of nPEP to PrEP care. Essential steps include:
- At conclusion of 28 days of nPEP:
- Repeat a rapid HIV test (ideally with a fourth-generation antigen/antibody assay) and assess for signs and symptoms of acute HIV infection.
- If the rapid HIV test is positive or suspicion exists of possible acute HIV infection, draw blood for confirmatory testing and continue a 3-drug nPEP regimen pending confirmation of HIV status.
- If HIV infection is confirmed, see Section 8 of Clinical Providers' Supplement for indicated next steps.
- If the rapid HIV test is negative and no signs or symptoms of acute infection exist:
Stop the third medication in nPEP regimen and continue TDF/FTC daily as PrEP.
Complete any PrEP baseline laboratory testing not already performed as part of nPEP testing.
Provide medication adherence and risk-reduction support counseling.
Complete any insurance/medication assistance paperwork required to cover PrEP medications (might be different than nPEP medications).
Schedule follow-up visits for HIV, STI, and other laboratory testing as well as medication refills on the basis of standard PrEP clinical practice guidelines recommendations.
# INITIATING PREP AT
# Consultation
Consultation with local or regional experts in nPEP and PrEP, or with the toll-free national PrEPline at 855-448-7737 or PEPline at 888-448-4911, can be sought for clinical scenarios requiring additional information or management options.
# .Section 10 Supplemental Counseling Information -Medication Adherence MEDICATION EDUCATION AND ADHERENCE SUPPORT
Understanding what patients know about PrEP and why they are considering taking it can reveal important information about potential adherence facilitators or barriers. You may wish to begin discussion through a conversation (e.g., "Let's talk. Tell me what you know about PrEP" or "Why do you want to take PrEP?") that can help clarify whether the patient understands the risks and benefits of PrEP given their current sexual behavior and protection strategies, and how their reason(s) for taking PrEP may affect medication adherence.
Adherence to prophylactic regimens is strongly associated with patient understanding of drug information. Patients beginning a PrEP regimen need a very clear understanding of how to take their medications (i.e., when it is to be administered, how many pills to take at each dose) and what to do if they experience problems (e.g., how long outside the dosing window is a dose considered "missed", what to do if they miss a dose). Side effects are often a cause of nonadherence, so a plan for addressing them should be made. It is recommended that you and the patient develop a plan for addressing side effects that the patient would consider intolerable. The plan may include over-the-counter medications that can mitigate symptoms and should stress the need to use condoms consistently if the patient stops taking PrEP medication.
You should also discuss the need for the patient to be tested for HIV every 3 months. Although patients may feel anxious about such frequent testing, it is important that patients understand that frequent testing is needed to prevent drug resistance if they become infected while taking PrEP medication. Be prepared to answer other questions, such as,: "What if people see the medications and think I am HIV-positive?" "Do I need to tell my partner?" "Do I need to take the medication regularly when I am not having sex?"; "Will it help to take extra doses?" "How long can I take the medication?". When you begin a discussion around adherence, emphasize the normalcy of missing occasional doses and the importance of a plan to try to minimize missed doses (see Box 6.1 for an example of how to introduce this issue).
# Box 6.1: Adherence Discussion
You are going to have to take the pill once a day, every day. Although this seems easy, we know that people forget to take their medicines, especially when they are not sick. It will be easier to take your medicine if you think through now some plans about how you'll do it. First, let's briefly discuss your experiences other times you might have taken medicine.
*When you've taken medicines before, how did you remember to take them?
Please tell me about any problems you had taking your pill.
*What was most helpful for remembering to take them?
An adherence plan should include the following: (1) tailoring the dosing time to correspond with the patient's regularly scheduled activities so that medication taking becomes integrated into the patient's daily routine, (2) using reminders or technical devices (e.g., beepers, alarms) to minimize forgetfulness, (3) considering organizational needs and tools (e.g., calendars, strategies for weekends away from home) to address changes in routine and schedule, and (4) reviewing disclosure issues to identify those who can support the patient's intentions to adhere or barriers to adherence due to lack of disclosure/privacy at home. (See Box 6.2 for sample questions.)
# Box 6.2: Developing an adherence plan
OK, now let's come up with a plan for taking your medicine.
# Scheduling
What is your schedule like during a typical week day? At what point in the day do you think it would be easiest to take the pill? That is, is there a time when you are almost always at home, and not in too much of a rush? How does your schedule differ on weekends?
# Reminder devices
How will you remember to take the pill each day? One way to remember is to take the pill at the same time that you are doing another daily task, such as brushing your teeth or eating breakfast. Which of your daily tasks might be used for this purpose? Try to pick something that happens every day. Sometimes we might pick something that is not always done on the weekends or during other days, and then we are more likely to forget. (For example, … One potential example follows: sometimes I don't shave on Saturdays, but I always brush my teeth, so linking taking the medicine to brushing my teeth might be better than linking it to shaving.) It also helps to store the pills near the place where you perform this daily task. Some people use a reminder device to help them remember. Do you have any reminder devices that you have used in the past? For example, watches, beepers, or cell phones.
# Organizational skills
Where will you store the bottle of pills? When you travel or spend the night outside of your home, what will you do about taking the pill?
# Social support & disclosure
Who in your household will know the reason that you are taking the pills? Are they supportive of you taking them? Are there individuals who might make assumptions about your serostatus because you have these medicines?
You may wish to explore other potential barriers that emerged in initial conversations (e.g., beliefs and attitudes), including factors (e.g., as substance use, depression or unstable housing) known to negatively affect medication adherence, such. To adhere to PrEP medication well, some patients may need access to mental health or social services.
# MONITORING PREP PATIENTS: ASSESSING SIDE EFFECTS AND ADHERENCE
Assess medication adherence as well as adherence to HIV testing at every visit. Self-reported adherence is typically an overestimate of true adherence, but patients may over report their adherence when they fear that a more accurate report would results in a negative judgment from their clinician. When asking patients about their adherence, do your best to adopt a nonjudgmental attitude, giving the patient permission to share adherence difficulties without worrying that you will reproach them. Asking patients to help you understand how they are doing with their medications will provide more information and thus allow for a better diagnostic picture of a patient's needs than will a more prescriptive approach.
Begin follow-up visits by asking the patient how well they have been doing with taking all of their medicines as scheduled. Accept more general responses (e.g., "so so", "pretty good", "excellent", "perfect") before asking for specific information about the frequency and the context of missed doses. Provide reinforcement for patients who report that they are doing well: ask questions such as "What are you doing to keep this going so well?" or "That's great. Can you see anything getting in the way of this?" These exchanges can help solidify the factors that are supporting your patients' adherence while helping them prepare for any barriers that may arise in the future.
When talking with patients who are not reporting perfect adherence, ask as to how many doses they have missed during a specific period. Assessing a longer period (e.g., 30 days, 7 days) is preferred to shorter periods (e.g., 3 days), not only because adherence can vary with changes in schedule (e.g., weekends, holidays) that may not have occurred during the shorter assessment period, but because many patients increase medication-taking just before medical appointments, a phenomenon supported by blood level assessments in the iPrEx trial. 2 When asking about many doses were missed (e.g., "In the last 30 days, how many times have you missed your PrEP medication?"), also (1) ask whether this was typical since their last clinic visit in order to gain a sense of adherence patterns, (2) ask for specific information about when they most recently missed dose(s), and (4) determine the circumstances during which those missed doses occurred (e.g., "Where were you?" "Who were you with?" "What happened just before you were supposed to take your medicine?"). Asking what happened on the day the dose was missed, and getting the patient's perspective on what generally gets in the way of taking medications regularly, will facilitate a conversation that will help to identify the patient's specific adherence barriers as well as the type of adherence support the patient needs.
On the basis of this conversation, develop a plan to address adherence barriers. Questions such as "What do you think you can do differently?" "What things make it easier to take your medications?" "What things need to happen for you to take your medications regularly?" or "What might you try ?" bring the patient into the planning process and thus facilitate identification of the strategies most likely to be implemented. It's important for you to be familiar with a range of adherence strategies that can be shared with patients who require help with this task.
Finally, assess whether the patient is experiencing any side effects of medication, the severity of the side effects, and their role as an adherence barrier determined. Currently, most of what is known about antiretroviral therapy (ART) side effects is derived from patients with HIV. Healthy people may be more concerned about side effects than HIV patients. Try to determine whether clinical symptoms attributed to PrEP medication could possibly be due to other disorders (e.g., depression) or natural processes (e.g., aging). If necessary, include medications to treat side effects in the adherence plan.
# Section 11 Supplemental Counseling Information -HIV Risk Reduction
Determining whether the patient is a good candidate for PrEP is not strictly objective, and should be based on an ongoing discussion between you and your patient. Risk screening can be conducted using various approaches: face-to-face interviews, written forms, or computer-based tools. Written forms and computer-based tools are effective and can be conducted with fewer staff resources 33 . However, self-administered written forms are not recommended for persons with low literacy.
Using risk screening information and the HIV test results, provide your patients with services that are appropriate for their level of risk and are tailored to their prevention needs. Patients who report no or few risk factors, may have minimal prevention needs. In the absence of other information, these patients do not need PrEP. For patients for whom PrEP is appropriate, provide risk-reduction counseling and support services before, during, and after PrEP you prescribe PrEP.
# SEXUAL RISK REDUCTION COUNSELING
Address the sexual health of your patients, including risk behaviors that increase the likelihood of acquiring HIV or other sexually transmitted infections. Several discussion areas are recommended even in brief discussions of sexual risk behavior. For patients who demonstrate an elevated risk of sexual HIV acquisition, provide a brief risk reduction intervention onsite or link them to a program that provides those services (see ). For patients who are continuing to engage in high-risk sexual behaviors or who need additional prevention services (beyond a brief risk-reduction intervention), link them to a program that provides more intense interventions, such as those in the Compendium of Evidence-based HIV Prevention Interventions (see ) which are often provided by local health departments or community-based organizations. These patients may also be good candidates for continued use of PrEP until they are consistently practicing effective behavioral risk reduction.
Counseling patients who test HIV-negative. Guidelines have emphasized the importance of risk-reduction counseling for persons determined to be at substantial risk of sexual HIV acquisition 34 . It is recommended that you select the most appropriate brief sexual risk-reduction intervention that can address the immediate prevention needs of HIVnegative patients at substantial risk for acquiring HIV infection. One counseling approach designed for STD clinic providers, the RESPECT model 35 , can be used. The model consists of two brief, 20-minute, interactive, patient-focused counseling sessions that are conducted during HIV testing, and have been found to significantly reduce sexual risk behaviors and prevent new STDs among HIV-negative patients (although not HIV incidence). Besides RESPECT, there are now several other effective brief sexual riskreduction intervention models that should be considered when providing HIV-negative patients appropriate prevention counseling. Although no brief counseling models have yet proven effective for patients taking PrEP, some of the models developed for persons with HIV infection, (Partnership for Health 36 , and motivational interviewing 37,38) may be appropriate for adaptation to counseling patients who are taking PrEP.
Intensive sexual risk reduction interventions may be appropriate for some patients, who should be referred to appropriate providers. In general, HIV risk-reduction interventions have been shown through numerous systematic reviews, to be efficacious in reducing HIV sexual risk behaviors, promoting protective behaviors, and reducing the incidence of new sexually transmitted infections among high-risk populations from various demographic, racial/ethnic, or behavioral risk groups 39,40 .
Counseling patients who test HIV-positive. Provide emotional support and counseling to patients who receive preliminary or confirmed positive HIV test results to help them understand the test result, the benefits of initiating and remaining in HIV medical care, and the importance of reducing their HIV-related sexual and/or injection risk behaviors to help protect their health and the health of their partners. Link all HIV-positive patients to HIV medical care, prevention services that routinely offer risk screening and ongoing risk-reduction interventions, and other health services as needed.
# PREP FOLLOW-UP VISITS
Provide brief behavioral HIV risk assessment and supportive counseling at each follow-up visit while the patient is taking PrEP medication. For important components of these sessions, see Box 7.1. At least annually discuss with the patient whether discontinuation of PrEP is warranted.
If the decision is made to discontinue PrEP, a plan for periodic reassessment should be made and any indicated referrals to community programs or other support services should be arranged.
# Box 7.1: Elements of brief HIV risk-reduction counseling in clinical settings
Create and maintain a trusting and confidential environment for discussion of sexual or substance abuse behaviors.
Build an ongoing dialogue with the patient regarding their risk behavior (and document presence or absence of risk behaviors in the confidential medical record).
Reinforce the fact that PrEP is not always effective in preventing HIV infection particularly if used inconsistently, but that consistent use of PrEP together with other prevention methods (consistent condom use, discontinuing drug injection or never sharing injection equipment) confers very high levels of protection. Encounter for preprocedural laboratory examination (blood and urine tests prior to treatment or procedure) Z11. 3 Encounter for screening for infections with a predominantly sexual mode of transmission Z11. 4 Encounter for screening for human immunodeficiency virus (HIV) Z11.59
Encounter for screening for other viral diseases Z11. 8 Encounter for screening for other infectious and parasitic diseases Z13.89
Encounter for screening for other disorder (encounter for screening for genitourinary disorders) Z13.9
Encounter for screening unspecified
# Section 14 Methods for Developing the PrEP Clinical Practice Guideline
In 2009, in recognition of the lead time needed to develop clinical guidance for the safe and effective use of PrEP should clinical trials results support it, CDC initiated a formal guidelines development process to allow for early review of the relevant literature, discussion of potential guidelines content given scenarios of potential trial results, and fostering the development of expert and stakeholder consensus. This process was designed to provide a basis for the rapid issuance of interim guidance, to be followed by Public Health Service guidelines as soon as the earliest trial findings indicated sufficient PrEP efficacy and safety to merit its implementation for HIV prevention through one or more routes of transmission.
This guidelines development process was based on a review of experience with the development of other clinical and nonclinical guidelines at CDC, including those for STD treatment and antiretroviral prevention of mother-to-child transmission following the ACTG 076 trial results.
There were five basic components to the process for developing the 2014 PrEP guidelines:
1. An HHS Public Health Service (PHS) Working Group to develop interagency consensus on major points of implementation policy and provide agency review of guidelines. This working group included representatives from agencies that would formally clear PHS guidelines (FDA, HRSA, NIH, HHS/OHAP) as well as agencies that may implement such guidance (IHS, VA). The working groups and expert panels listed here were convened by teleconference before trial results were available (2009-2010) and some were reconvened after each trial results for each population group were published. As technical experts, prevention partners, and key stakeholders, they were asked to assist us to identify relevant scientific/medical literature and share thoughts on topics that would inform the Data from the clinical trial, human observational study, and laboratory human study results were added to the evidence tables. Study findings presented in the evidence tables were each assessed for quality of the study using GRADE criteria 39 (see guidelines Appendix 1, Table 13). Then all data supporting a specific recommendation were given a summary strength of evidence rating (across all studies relevant to that recommendation) using the same system as used for the DHHS antiretroviral treatment guidelines 32 (see PrEP clinical practice guidelines Appendix 1, Table 12).
# DRAFT GUIDELINE WRITING AND REVIEW PRIOR TO PUBLICATION
The draft was written to address guidelines standards for review of the strength of evidence (GRADE approach 41 ) as well as a format designed to promote guideline implementation (GLIA 42 ), dissemination (GEM 43 ), and adoption (AGREE 44,45 ).
The 2014 draft clinical practice guideline and clinical providers supplement were reviewed by CDC, FDA, NIH, HRSA, and HHS, and a series of webinars were held in 2012 and 2013 to obtain additional expert opinion and public engagement on draft recommendations for PrEP use.
The draft guideline and supplement were then reviewed by a panel of 6 external peer reviewers who had not been involved in their development. At each step, revisions were made in response to reviewer and public comments received.
For the 2017 update, the 2014 systematic review of published literature was updated through June 2017. Although no changes to the graded recommendations were indicated, additions to the evidence review tables were made; minor clarifying edits to the supporting text were made to enhance consistency with recently updated STD, nPEP, and perinatal guidelines sections relevant to PrEP; and updated references were added. These changes were shared with a group of 4 external peer reviewers for comment.
# Plans for Updates to the Guideline
PrEP is a rapidly changing field of HIV prevention with several additional clinical trials and studies are now underway or planned. Updates to these guidelines are anticipated as studies provide new information on PrEP efficacy, HIV testing, drug levels, adherence, longer term clinical safety, and changes in HIV risk behaviors associated with PrEP medication use for HIV uninfected MSM, heterosexuals, injection drug users, pregnant women and their newborns; as well as information on the efficacy and safety of other antiretroviral medications, and other routes and schedules of medication delivery for PrEP.
When significant new data become available that may affect patient safety or graded recommendations for PrEP use, an announcement with suggested revisions to the existing guidelines will be posted on the CDC web site and the public will be given a 2-week period to submit comments. These comments will be reviewed and a determination made as to whether additional revisions are indicated. Final updated guidelines will then be posted on the CDC web site.
This process allowed wide input, transparency in discussing the many issues involved, time for the evolution of awareness of PrEP and ideas for its possible implementation, in addition to facilitating the development of a consensus base for the eventual guidance. At the same time, it allowed for guidelines based on expert opinion, and recommendations deemed feasible by clinical providers and policymakers.
On the basis of results from the first 4 activities listed above and the publication in late November 2010 of results from the first clinical trial to show substantial efficacy and safety 2 , CDC issued interim guidance for PrEP use among men who have sex with men in January 2011. This interim guidance was followed by a face-to-face meeting of external in May 2011. As efficacy and safety results were published, additional interim guidance documents were issued for heterosexually active adults (August 2012) and injection drug users (July 2013).
# SYSTEMATIC LITERATURE REVIEW METHODS
For the 2014 guidelines, a systematic review was conducted of PrEP studies published from January 2010 through December 2013. For the 2017 guidelines, the same search strategy was run to update studies published through June 2017. Searches were conducted of MEDLINE, Embase, CINAHL, and Cochrane Library databases. The search strategy used the following criteria:
- Pre-Exposure Prophylaxis/ OR Chemoprevention/ OR (((Preexposure OR Pre-exposure) adjacent to prophylaxis) OR PrEP OR (topical adjacent to (prevention OR prophylaxis OR microbicide- OR gel OR pericoital OR precoital OR vaginal OR rectal OR anal)) OR chemoprophylaxis OR chemoprevention OR chemo-prophylaxis OR chemo-prevention OR iPrEX).mp. - AND - (exploded terms) Anti-HIV Agents/ OR Anti-Retroviral Agents/ OR HIV Infections/pc OR ((HIV OR human immunodeficiency virus) AND (antiretroviral- OR anti-retroviral- OR antiretrovirus- OR anti-retrovirus- OR Truvada OR tenofovir OR emtricitabine OR (TDF ADJ5 FTC))) - AND NOT animals - in the title, abstract, keyword heading word, subject heading fields Retrieved citations were provided in an Endnote reference file for deduplication. Then 2 scientists independently reviewed the citations and removed those that were not published in English, did not contain data (e.g., editorials, reviews, news reports), or did not contain data about oral TDF/FTC for PrEP. The next step was to screen citations to remove those that did not contain new data about oral PrEP (data/analyses not previously published). For the 2017 update, year of publication, author, and titles were compared with the 2014 Endnote library as necessary to identify already exiting entries. During this step, abstracts or full articles were read and publications were categorized into the following groups.
- New clinical trial results
- New human observational study results - New survey, focus group, or other behavioral study results
- New cost analysis results (e.g., program cost, cost benefit analysis)
- New modeling results (e.g., impact models)
- New laboratory human study results (e.g., drug levels, resistance)
- None of the above
The coding by the two reviewers was then compared and discrepancies were reconciled.
Citations with no new data about daily oral PrEP with TDF/FTC were deleted from the updated Endnote 2017 library. | #
Minor revisions were also made to correct typos, add references, and update content from cited guidelines and source materials.
# Disclaimers:
All material in this publication is in the public domain and may be used and reprinted without permission; citation as to source, however, is appreciated.
# Introduction
Recent findings from several clinical trials have demonstrated safety 1 and a substantial reduction in the rate of HIV acquisition for men who have sex with men (MSM) 2 , men and women in heterosexual discordant couples 3 , and heterosexual men and women recruited as individuals 4 who were prescribed daily oral antiretroviral preexposure prophylaxis (PrEP) with a fixed-dose combination of tenofovir disoproxil fumarate (TDF) and emtricitabine (FTC). The demonstrated efficacy of PrEP was in addition to the effects of repeated condom provision, sexual risk-reduction counseling, and the diagnosis and treatment of sexually transmitted infection (STI) that were provided to all trial participants. In July 2012, after reviewing these trial results, the U.S. Food and Drug Administration (FDA) approved an indication for the use of Truvada ® (TDF/FTC) "in combination with safer sex practices for pre-exposure prophylaxis (PrEP) to reduce the risk of sexually acquired HIV-1 in adults at high risk" 5,6 . In July 2013, an additional clinical trial found that daily oral TDF reduced the rate of HIV acquisition for persons who inject drugs (PWID) (also called injection drug users [IDU]) 7 .
On the basis of these trial results and the FDA approval, the U.S. Public Health Service has published a comprehensive clinical practice guideline for the use of PrEP for the prevention of HIV infection in the United States and updated it in 2017. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf This supplement to the PHS PrEP Clinical Practice Guidelines is intended to provide additional information that may be useful to clinicians providing PrEP. As additional materials become available, this document will be updated.
# Section 1
Contains a template checklist that clinicians can complete and share with patients to document the services provided to PrEP patients and the actions expected from patients to maximize the efficacy and safety of PrEP. Sections 2-4
Contain templates for informational handouts that can be provided to patients Section 5
Contains an information sheet for providers counseling patients about PrEP use during conception, pregnancy and breastfeeding. Section 6
Contains the HIV incidence Risk Index for MSM, a tool that clinicians may use to quickly and systematically determine which men are at especially high risk for acquiring HIV infection, for whom PrEP may be indicated. Section 7
Contains the HIV incidence Risk Index for PWID, a tool that clinicians may use to quickly determine which persons who inject drugs are at especially high risk for acquiring HIV infection, for whom PrEP may be indicated. Section 8
Contains more detailed information about the clinical management of patients who acquire HIV infection while on PrEP. Section 9
Contains more detailed information about the clinical management of transitioning patients from nPEP to PrEP. Sections 10-11 Contain more detailed information than that included in the guidelines about methods and resources for counseling patients receiving PrEP about medication adherence and HIV risk reduction behaviors.
# Sections 12
Contains information relevant to administrative and billing codes for PrEP related services. Section 13 Contains potential practice quality practice measures. Section 14 Documents the methods used to develop the PHS PrEP Clinical Practice Guidelines. Assessment for possible acute HIV infection Indicated laboratory screening to determine indications for these medications An HIV risk assessment to determine whether PrEP is indicated for this patient A medication fact sheet listing dosing instructions and side effects Counseling or a referral for counseling on condom use and any other HIV riskreduction methods this patient may need Advice on methods to help the patient to take medication daily as prescribed Information about PrEP use during conception and pregnancy (when indicated)
_________________________________
A prescription for Truvada (300 mg tenofovir disoproxil fumarate, 200 mg emtricitabine)
A follow-up appointment date
As the provider, I will:
• Limit refill periods to recommended intervals for repeat HIV testing (at least every 3 months)
• Conduct follow-up visits at least every 3 months that include the following:
o Assessment of HIV status (including signs or symptoms of acute HIV infection)
o Assessment of side effects and advice on how to manage them o Assessment of medication adherence and counseling to support adherence o Assessment of STI symptoms, HIV risk behavior and counseling support for riskreduction practices
• Inform the patient of any new information about PrEP and respond to questions
Patient Section
It has been explained to me that:
• Taking a dose of PrEP medication every day may lower my risk of getting HIV infection
• This medicine does not completely eliminate my risk of getting HIV infection, so I need to use condoms during sex
• This medicine may cause side effects so I should contact my provider for advice by calling ________________ if I have any health problems
• It is important for my health to find out quickly if I get HIV infection while I'm taking this medication, so o I will contact my provider right away if I have symptoms of possible HIV infection (fever with sore throat, rash, headache, or swollen glands)
• My provider will test for HIV infection at least once every 3 months Therefore, I will:
• Try my best to take the medication my provider has prescribed every day
• Talk to my provider about any problems I have in taking the medication every day
• Not share the medication with any other person
• Attend all my scheduled appointments
• Call _________________ to reschedule any appointments I cannot attend
# Give one copy to patient
Section 2 PrEP Information Sheet
# Pre-exposure Prophylaxis (PrEP) for HIV Prevention
Frequently Asked Questions What is PrEP? "PrEP" stands for preexposure prophylaxis. The word "prophylaxis" (pronounced pro fil ak sis) means to prevent or control the spread of an infection or disease. The goal of PrEP is to prevent HIV infection from taking hold if you are exposed to the virus. This is done by taking a pill that contains 2 HIV medications every day. These are the same medicines used to stop the virus from growing in people who are already infected.
# Why take PrEP?
The HIV epidemic in the United States is growing. About 50,000 people get infected with HIV each year. More of these infections are happening in some groups of people and some areas of the country than in others.
# Is PrEP a vaccine?
No. PrEP medication does not work the same way as a vaccine. When you take a vaccine, it trains the body's immune system to fight off infection for years. You will need to take a pill every day by mouth for PrEP medications to protect you from infection. PrEP does not work after you stop taking it. The medication that was shown to be safe and to help block HIV infection is called "Truvada" (pronounced tru va duh). Truvada is a combination of 2 drugs (tenofovir and emtricitabine). These medicines work by blocking important pathways that the HIV virus uses to set up an infection. If you take Truvada as PrEP daily, the presence of the medication in your bloodstream can often stop the HIV virus from establishing itself and spreading in your body. If you do not take the Truvada pills every day, there may not be enough medicine in your blood stream to block the virus.
# Should I consider taking PrEP?
PrEP is not for everyone. Doctors prescribe PrEP for some patients who have a very high risk of coming in contact with HIV by not using a condom when they have sex with a person who has HIV infection. You should consider PrEP if you are a man or woman who sometimes has sex without using a condom, especially if you have a sex partner who you know has HIV infection. You should also consider PrEP if you don't know whether your partner has HIV infection but you know that your partner is at risk (for example, your partner inject drugs or is having sex with other people in addition to you) or if you have recently been told by a health care provider that you had a sexually transmitted infection. If your partner has HIV infection, PrEP may be an option to help protect you from getting HIV infection while you try to get pregnant, during pregnancy, or while breastfeeding.
# How well does PrEP work?
PrEP was tested in several large studies with men who have sex with men, men who have sex with women, and women who have sex with men. All people in these studies (1) were tested at the beginning of the trial to be sure that they did not have HIV infection, (2) agreed to take an oral PrEP tablet daily,
(3) received intensive counseling on safer-sex behavior, (4) were tested regularly for sexually transmitted infections, and (5) were given a regular supply of condoms.
Several studies showed that PrEP reduced the risk of getting HIV infection.
• Men who have sex with men who were given PrEP medication to take, were 44% less likely to get HIV infection than were those men who took a pill without any PrEP medicine in it (a placebo). Forty-four percent was an average that included men who didn't take the medicine every day and those who did. Among the men who said they took most of their daily doses, PrEP reduced the risk of HIV infection by 73% or more, up to 92% for some.
• Among men and women in couples in which one partner had HIV infection and the other partner initially did not ("HIV-discordant" couples), those who received PrEP medication were 75% less likely to become infected than those who took a pill without any medicine in it (a placebo). Among those who said they took most of their daily doses, PrEP reduced the risk of HIV infection by up to 90%.
• In one study of men and women who entered the study as individuals (not as a couple), PrEP worked for both men and women in one study: those who received the medication were 62% less likely to get HIV infection; those who said they took most of their daily doses, were 85% less likely to get HIV infection. But in another study, only about 1 in 4 women (<26%) had PrEP medication found in their blood when it was checked. This indicated that few women were actually taking their medication and that study found no protection against HIV infection.
More information on the details of these studies can be found at http://www.cdc.gov/hiv/prep.
# Is PrEP safe?
The clinical trials also provided safety information on PrEP. Some people in the trials had early side effects such as an upset stomach or loss of appetite but these were mild and usually went away within the first month. Some people also had a mild headache. No serious side effects were observed. You should tell your doctor if these or other symptoms become severe or do not go away.
# How can I start PrEP?
If you think you may be at high risk for HIV, talk to your doctor about PrEP. If you and your doctor agree that PrEP might reduce your risk of getting HIV infection, you will need to come in for a general health physical, blood tests for HIV, and tests for other infections that you can get from sex partners. Your blood will also be tested to see if your kidneys and liver are functioning well. If these tests show that PrEP medicines are likely to be safe for you to take and that you might benefit from PrEP, your doctor may give you a prescription after discussing it with you.
Taking PrEP medicines will require you to follow-up regularly with your doctor. You will receive counseling on sexual behaviors and blood tests for HIV infection and to see if your body is reacting well to Truvada. You should take your medicine every day as prescribed, and your doctor will advise you about ways to help you take it regularly so that it stands the best chance to help you avoid HIV infection. Why is this medication prescribed?
• Truvada is one of several medications that are currently used to treat human immunodeficiency virus (HIV) and hepatitis B virus infection. • Truvada is now being used to prevent HIV infection.
• Truvada is sometimes prescribed to some people who do not have HIV infection (for example, those who do not always use condoms or who have a sex partner that has HIV infection) to help reduce their chances of getting HIV infection • When you take Truvada to prevent HIV infection, doctors refer to this use as "pre-exposure prophylaxis" or "PrEP".
# How does Truvada (PrEP) help prevent HIV infection?
• HIV is a virus that attacks your body's immune cells (the cells that work to fight infections).
• The 2 medications that make up Truvada (tenofovir and emtricitabine) block important pathways that viruses use to set up infection. • If you take Truvada as PrEP daily, the presence of the medication in your bloodstream can sometimes stop the virus from establishing itself and slow the spread of HIV in your body. • By itself, PrEP with Truvada does not work all the time so you should also use condoms during sex for the most protection from HIV infection.
How should this medicine be used?
• You must take one tablet of Truvada by mouth every day.
• Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand.
# What other information should I know?
• Do not let anyone else take your medication.
• Ask your pharmacist if you have any questions about refilling your prescription.
• Write a list of all of your prescription and over-the-counter medicines, as well as any vitamins, minerals, or other dietary supplements that you take.
• Bring your medication list with you each time you visit a doctor or if you are admitted to a hospital. Keep it with you always in case of emergencies. These signs and symptoms of acute HIV infection can begin a few days after you are exposed to HIV and usually last for about 14 days. They could last for just a few days, or they could last for several months.
You might not realize your illness is acute HIV infection. For one thing, you may not have known that the person you had sex with had HIV infection. And the signs and symptoms of HIV infection may feel just like other common virus infections like flu, a cold, sore throat, or mononucleosis (mono).
# What tests can show that I have acute HIV infection?
When HIV enters your body, it moves inside white blood cells called CD4 lymphocytes. HIV takes over the CD4 cells and makes billions of copies of the virus each day. The virus spread through your body.
Your body tries to defend itself against HIV by making antibodies (these antibodies try to block the virus from spreading in your body And fourth, when people have lots of virus in their body during acute HIV infection, they are more likely to pass the virus on to people they have sex with, especially since they may not know yet that they have gotten infected. For example, if your last HIV test result was negative and your partner also had a recent negative HIV test result, you might choose to have sex without a condom just at the time when it's very likely you would pass the virus on. So the sooner you know you have become infected, the more careful you can be to protect others from getting HIV infection.
# How is HIV treated?
People who have HIV infection are treated with combinations of 3 or more medicines that fight HIV. Some doctors start people on treatment medications as soon as they become infected; other doctors wait for a while because the greatest benefits to a person's health are seen after they have been infected a while. Early treatment also reduces the chances that a person with HIV infection will pass the virus on to their sex partners.
# What do I do if I suspect I might have acute HIV infection?
First, contact your doctor's office and arrange to be examined and have the right blood tests.
Second, discuss with your doctor whether to stop your PrEP medications or continue them until your test results are back.
Third, be especially careful to use condoms and take other safer sex measures to protect your partner(s).
# Section 5 Provider Information Sheet -PrEP during Conception, Pregnancy, and Breastfeeding
# Information for Clinicians Counseling Patients about PrEP Use During Conception, Pregnancy, and Breastfeeding
PrEP use may be one of several options to help protect the HIV-negative male or female partner in a heterosexual HIV-discordant couple during attempts to conceive [8][9][10] . Pregnancy care providers may not have access to the medical records of the partner with HIV infection to document their viral load status. The extent to which PrEP use further decreases risk of HIV acquisition when the partner with HIV infection has a documented current undetectable viral load is unknown.
# Based on DHHS Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission 9
Panel's Recommendations on Reproductive Options for HIV-Concordant and Serodiscordant Couples For Couples who Want to Conceive For Concordant (Both Partners are HIV-Infected) and Discordant Couples:
• Expert consultation is recommended so that approaches can be tailored to couples specific needs (AIII).
• Partners should be screened and treated for genital tract infections before attempting to conceive (AII).
• The HIV-infected partner(s) should attain maximum viral suppression before attempting conception (AIII). For Discordant Couples:
• The HIV-infected partner should be receiving combination antiretroviral therapy and demonstrate sustained suppression of plasma viral load below the limits of detection (AI). • Administration of antiretroviral pre-exposure prophylaxis (PrEP) for 30 days before attempting conception and for 30 days after conception is achieved for HIV-uninfected partners may offer an additional tool to reduce the risk of sexual transmission, particularly if the HIV-infected partner's plasma viral load is unknown or detectable (CIII). It is not known whether PrEP for the uninfected partner confers additional benefit when the infected partner receiving antiretroviral therapy has documented sustained viral suppression.
# Discordant Couples with HIV-Infected Women:
• The safest conception option is assisted insemination, at home or in a clinician's office with a partner's sperm during the peri-ovulatory period (AIII).
# Discordant Couples with HIV-Infected Men:
• The use of donor sperm from an HIV-uninfected man with artificial insemination is the safest option (AIII). • When the use of donor sperm is unacceptable, the use of sperm preparation techniques coupled with either intrauterine insemination or in vitro fertilization should be considered (BII).
# Based on DHHS Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission 9
Panel's Recommendations on Reproductive Options for HIV-Concordant and Serodiscordant Couples
• Semen analysis is recommended for HIV-infected men before conception is attempted to prevent unnecessary exposure to infectious genital fluid. Semen abnormalities appear to be more common among HIV-infected men than HIV-uninfected men (AIII). The following information is provided to help you inform your patients of current information about potential risks and benefits of PrEP use so that you and your patients can make an informed decision.
# Rating of Recommendations
# Key Points
Provide education about PrEP and other methods of conception that minimize the risk of HIV transmission to both members of an HIV-discordant couple whenever possible.
# Options
Reducing the risk of HIV acquisition by an HIV-negative man during conception can be achieved by use of the following, singly or ideally in combination [10][11][12][13] :
• Antiretroviral treatment of the HIV-positive female partner to achieve an undetectable viral load 13 • STI diagnosis and any indicated treatment for both partners before conception attempts • Daily, oral doses of TDF/FTC beginning 1 month before a conception attempt and continuing for 1 month after a conception attempt. PrEP may be indicated when the partners recent viral load is unknown, reported to be detectable, or cannot be documented as undetectable 14 .
# AND EITHER
• Limit sex without a condom (natural conception) to peak fertility times identified by home or laboratory tests for ovulation 15. OR • Intravaginal insemination 13 (either at home or in the clinic) with a fresh semen sample
# Potential Benefits of PrEP use
In clinical trials with heterosexually active adults, daily oral PrEP with TDF/FTC was safe and reduced the risk of HIV acquisition by an average of 63%-75%. Higher levels of protection (≥90%) were found among persons whose drug levels in their blood indicated that they had consistently taken the medication 3,4 .
# Potential Risks of PrEP use
In PrEP trials, follow-up with persons taking medication has been conducted for an average of 1-4 years.
Although no serious health risks were associated with PrEP use by HIV-uninfected adults, the long-term safety of PrEP has not yet been determined.
# FOR AN HIV-NEGATIVE WOMAN PLANNING PREGNANCY WITH AN HIV-POSITIVE MALE PARTNER
# Options
Reducing the risk of HIV acquisition by an HIV-negative woman during conception can be achieved by use of the following, singly or ideally in combination 10,13 :
• Antiretroviral treatment of the HIV-positive male partner to achieve an undetectable viral load 13 • STI diagnosis and any indicated treatment for both partners before conception attempts • Daily, oral doses of TDF/FTC beginning 1 month before a conception attempt and continuing for 1 month after a conception attempt. PrEP may be indicated when the partners recent viral load is unknown, reported to be detectable, or cannot be documented as undetectable 14 .
# AND EITHER
• Limit sex without a condom (natural conception) to peak fertility times identified by home or laboratory tests for ovulation in the female partner 15 .
# OR
• Intravaginal 16 or intrauterine insemination, or intracytoplasmic sperm injection with a semen sample processed by "sperm washing" and confirmed to have a negative test result for the presence of remnant HIV [16][17] . This option may be indicated for couples with fertility problems.
# Potential Benefits of PrEP use
In clinical trials with heterosexually active adults, daily oral PrEP with TDF/FTC was safe and reduced the risk of HIV acquisition by an average of 63%-75%. Higher levels of protection (≥90%) were found among persons whose drug levels in their blood indicated that they had consistently taken the medication 3,4 .
The risk of HIV acquisition increases during pregnancy 19 , as does the risk of HIV transmission to an infant born to a mother who becomes infected during pregnancy or breastfeeding 20 Therefore, an HIVnegative woman whose sexual partner/spouse has HIV infection may benefit from continuing PrEP use throughout her pregnancy and breastfeeding to protect herself and her infant a
# Potential Risks of PrEP use
In PrEP trials, follow-up with persons taking medication has been conducted for an average of 1-4 years.
Although no serious health risks were associated with PrEP use by HIV-uninfected adults, the long-term safety of PrEP has not yet been determined.
In PrEP trials women were taken off medication as soon as pregnancy was detected. During these trials, no health problems have been associated with PrEP use by women in early pregnancy or for their offspring. However, the long-term safety of PrEP taken by HIV-uninfected women after fetal (during pregnancy) or infant (during breastfeeding) exposure is not yet determined.
No adverse effects have been found among infants exposed to TDF/FTC when the medications were taken as part of a treatment regimen for HIV-infected women during pregnancy [21][22][23] or during breastfeeding (for which data suggest limited drug exposure [24][25][26][27] ).
If you prescribe PrEP to a woman while pregnant, you are encouraged to prospectively and anonymously submit information about the pregnancy to the Antiretroviral Use in Pregnancy Registry (http://www.apregistry.com/).
a Alth ugh the DHHS Perinatal HIV Guidelines state that "pregnancy and breastfeeding are n t c ntraindicati ns f r PrEP" 9 , the FDA-appr ved package insert 6 says, "If an uninfected individual bec mes pregnant while taking TRUVADA f r a PrEP indicati n, careful c nsiderati n sh uld be given t whether use f TRUVADA sh uld be c ntinued, taking int acc unt the p tential increased risk f HIV-1 infecti n during pregnancy" and "m thers sh uld be instructed n t t breastfeed if they are receiving TRUVADA, whether they are taking TRUVADA f r treatment r t reduce the risk f acquiring HIV-1.". Theref re b th are currently ff-label uses f Truvada.
# Section 6 MSM Risk Index
Epidemiologic studies have identified a wide range or personal, relationship, partner, social, cultural, network, and community factors that may be associated with the presence of HIV infection. However, to provide PrEP (or other intensive HIV prevention services), it is necessary to briefly and systematically screen for key information about those factors that are predictive of very high risk of acquiring HIV infection.
This section contains a tool that clinicians may use to quickly and systematically determine which MSM are at especially high risk of acquiring HIV infection, and for whom PrEP may be indicated.
# Section 7 PWID (IDU) Risk Index
Epidemiologic studies have identified a wide range or personal, relationship, partner, social, cultural, network, and community factors that may be associated with the presence of HIV infection. However, to provide PrEP (or other intensive HIV prevention services), it is necessary to briefly and systematically screen for key information about those factors that are predictive of very high risk of acquiring HIV infection.
This section contains a tool that clinicians can use to quickly and systematically determine which persons who inject drugs (PWID) (also called injection drug users [IDU]) are at especially high risk for acquiring HIV infection, and for whom PrEP may be indicated. Add the scores for age and methadone use to the Composite Injection Subscore to yield a Total Score _________ Total Score* * If the total score is 46 or greater, evaluate for PrEP or other intensive HIV prevention services for PWID. If score is 45 or less, provide indicated standard HIV prevention services for PWID. To identify active PWID in a clinician's practice, we recommend asking all their patients a routine question: "Have you ever injected drugs that were not prescribed for you by a physician?" If yes, ask, "When was the last time you injected any drugs?" Only complete PWID risk index if they have injected any nonprescription drug during the past 6 months.
# Section 8 Management of Patients Who Acquire HIV While on PrEP
Patients who are being prescribed PrEP might acquire HIV infection for several reasons. When HIV infection is detected at the first follow-up visit after PrEP initiation, it can indicate that the patient had undetected acute infection when PrEP was initiated. When infection is detected at later follow-up visits, as it most commonly occurs, it might be because patients have stopped taking PrEP, have been taking it infrequently, or have been stopping and restarting it without retesting for HIV infection before restarting. Rarely, despite high adherence to continuous daily dosing, patients taking PrEP have acquired HIV infection. This can occur because of exposure to a drug-resistant viral strain 30 or simply because, even with daily use, PrEP protection is high but not 100% 31 .
In all cases, when an HIV test during a follow-up visit indicates possible infection in a PrEP patient, the following steps should be taken:
• Counsel the patient about their HIV status and the resulting management plan:
o If a single rapid antibody blood test was positive, explain the need to confirm presumptive HIVpositive status with laboratory testing. o If a rapid 4 th generation (antigen/antibody) blood test was positive, explain high likelihood of HIV infection that will need to be confirmed with additional laboratory testing. o If a positive HIV test was based on laboratory testing with confirmatory results already known, explain certainty of HIV diagnosis. o Ask about signs and symptoms of acute infection since last clinic visit as well as PrEP medication adherence history.
• Conduct confirmatory HIV testing (if not completed already) and supplemental tests, if indicated:
o If one or more rapid tests were positive, draw blood for confirmatory laboratory-based HIV testing with adequate blood for reflex HIV viral load testing if confirmed to be HIV infected. o If laboratory-based testing was positive, draw blood for HIV viral load, CD4 cell count, and HIV resistance testing. o For persons with confirmed HIV infection, conduct the following supplemental testing indicated for initiation of HIV treatment, including but not necessarily limited to the following 32 : Chemistry screen, ALT, AST, bilirubin, CBC with differential, urinalysis, and pregnancy test (if female). Fasting lipid profile, glucose, and hemoglobin A1c are also indicated, on the day that seroconversion is detected, if possible.
• Convert the PrEP regimen to an HIV treatment regimen recommended by the DHHS Panel on Antiretroviral Guidelines for Adults and Adolescents 32 .
o It is not necessary to stop antiretrovirals entirely while waiting for additional laboratory test results. In the most likely event that the patient has HIV infection, immediate initiation of HIV treatment is indicated. The following regimens are recommended as of July 14, 2016 but the treatment guidelines should be consulted for updates 32 : o Continue the prescription of Truvada (TDF 300 mg/FTC 200 mg) once daily pending results of resistance tests o Add either: Dolutegravir (Tivicay) 50 mg once daily OR Darunavir (Prezista) 800 mg with Ritonavir (Norvir) 100 mg once daily.
In cases where a viral strain with significant resistance to tenofovir is later identified, the regimen can then be optimized. In cases where HIV infection is not confirmed, return to the PrEP regimen can be accomplished by dropping the additional treatment medication.
• Provide client education about time to viral load suppression:
o Reinforce the importance of medication adherence for the patient's long-term health.
o Discuss the importance of condom use to protect sexual partners and provide condoms. o Offer HIV testing for sex and drug injection partners and assistance with disclosure, if desired. o Ask if the patient had condomless sex or shared injection equipment during the past 72 hours, and if yes, offer nPEP for exposed partners.
• Consult with and transfer care to an experienced HIV care provider, if necessary. o Clinicians can call the National Clinical Consultation Center toll-free at (800) 933-3413.
• Discuss or complete insurance paperwork necessary for coverage of treatment medication. o Patients who are receiving medication through PrEP-specific medication assistance programs will need to switch to an HIV treatment assistance program. o Public or private insurance plans will generally not require additional paperwork but prior authorizations for PrEP may raise questions when switching to a prescription for a treatment regimen.
• Schedule follow-up visits (including social services, if required).
• Complete an HIV case report for the health department (completion of fields related to PrEP use at the time of seroconversion are highlighted in red below).
# Section 9 Transition of Patients From Nonoccupational Postexposure Prophylaxis (nPEP) to Preexposure Prophylaxis (PrEP)
Two types of patients may be considered candidates for PrEP use after a course of nonoccupational postexposure prophylaxis (nPEP):
• Patients who request PrEP and also have had a possible sexual or injection drug-related HIV exposure in the prior 72 hours (i.e., are within the recommended window to start nPEP)
• Patients who request repeated courses of nPEP, particularly over a relatively recent period (e.g., more than twice during the past 6 months)
If evaluation demonstrates nPEP is clinically indicated and that the patient is also eligible for PrEP (e.g., behavioral risk for repeated HIV exposure, recent bacterial STI diagnosis in a sexually active person), then these patients should both be provided a 28-day course of nPEP and be evaluated for transition to PrEP at the conclusion of their nPEP course.
# TRANSITIONING IMMEDIATELY FROM NPEP TO PREP
Transitioning from nPEP to PrEP without interruption at the completion of the 28-day nPEP course has the advantages of (1) maintaining satisfactory antiretroviral drug levels for PrEP (if nPEP adherence has been good); and (2) maximizing continuous prevention measures through continuity of nPEP to PrEP care. Essential steps include:
• At conclusion of 28 days of nPEP:
o Repeat a rapid HIV test (ideally with a fourth-generation antigen/antibody assay) and assess for signs and symptoms of acute HIV infection.
o If the rapid HIV test is positive or suspicion exists of possible acute HIV infection, draw blood for confirmatory testing and continue a 3-drug nPEP regimen pending confirmation of HIV status.
o If HIV infection is confirmed, see Section 8 of Clinical Providers' Supplement for indicated next steps.
o If the rapid HIV test is negative and no signs or symptoms of acute infection exist:
Stop the third medication in nPEP regimen and continue TDF/FTC daily as PrEP.
Complete any PrEP baseline laboratory testing not already performed as part of nPEP testing.
Provide medication adherence and risk-reduction support counseling.
Complete any insurance/medication assistance paperwork required to cover PrEP medications (might be different than nPEP medications).
Schedule follow-up visits for HIV, STI, and other laboratory testing as well as medication refills on the basis of standard PrEP clinical practice guidelines recommendations.
# INITIATING PREP AT
# Consultation
Consultation with local or regional experts in nPEP and PrEP, or with the toll-free national PrEPline at 855-448-7737 or PEPline at 888-448-4911, can be sought for clinical scenarios requiring additional information or management options.
# .Section 10 Supplemental Counseling Information -Medication Adherence MEDICATION EDUCATION AND ADHERENCE SUPPORT
Understanding what patients know about PrEP and why they are considering taking it can reveal important information about potential adherence facilitators or barriers. You may wish to begin discussion through a conversation (e.g., "Let's talk. Tell me what you know about PrEP" or "Why do you want to take PrEP?") that can help clarify whether the patient understands the risks and benefits of PrEP given their current sexual behavior and protection strategies, and how their reason(s) for taking PrEP may affect medication adherence.
Adherence to prophylactic regimens is strongly associated with patient understanding of drug information. Patients beginning a PrEP regimen need a very clear understanding of how to take their medications (i.e., when it is to be administered, how many pills to take at each dose) and what to do if they experience problems (e.g., how long outside the dosing window is a dose considered "missed", what to do if they miss a dose). Side effects are often a cause of nonadherence, so a plan for addressing them should be made. It is recommended that you and the patient develop a plan for addressing side effects that the patient would consider intolerable. The plan may include over-the-counter medications that can mitigate symptoms and should stress the need to use condoms consistently if the patient stops taking PrEP medication.
You should also discuss the need for the patient to be tested for HIV every 3 months. Although patients may feel anxious about such frequent testing, it is important that patients understand that frequent testing is needed to prevent drug resistance if they become infected while taking PrEP medication. Be prepared to answer other questions, such as,: "What if people see the medications and think I am HIV-positive?" "Do I need to tell my partner?" "Do I need to take the medication regularly when I am not having sex?"; "Will it help to take extra doses?" "How long can I take the medication?". When you begin a discussion around adherence, emphasize the normalcy of missing occasional doses and the importance of a plan to try to minimize missed doses (see Box 6.1 for an example of how to introduce this issue).
# Box 6.1: Adherence Discussion
You are going to have to take the pill once a day, every day. Although this seems easy, we know that people forget to take their medicines, especially when they are not sick. It will be easier to take your medicine if you think through now some plans about how you'll do it. First, let's briefly discuss your experiences other times you might have taken medicine.
*When you've taken medicines before, how did you remember to take them?
Please tell me about any problems you had taking your pill.
*What was most helpful for remembering to take them?
An adherence plan should include the following: (1) tailoring the dosing time to correspond with the patient's regularly scheduled activities so that medication taking becomes integrated into the patient's daily routine, (2) using reminders or technical devices (e.g., beepers, alarms) to minimize forgetfulness, (3) considering organizational needs and tools (e.g., calendars, strategies for weekends away from home) to address changes in routine and schedule, and (4) reviewing disclosure issues to identify those who can support the patient's intentions to adhere or barriers to adherence due to lack of disclosure/privacy at home. (See Box 6.2 for sample questions.)
# Box 6.2: Developing an adherence plan
OK, now let's come up with a plan for taking your medicine.
# Scheduling
What is your schedule like during a typical week day? At what point in the day do you think it would be easiest to take the pill? That is, is there a time when you are almost always at home, and not in too much of a rush? How does your schedule differ on weekends?
# Reminder devices
How will you remember to take the pill each day? One way to remember is to take the pill at the same time that you are doing another daily task, such as brushing your teeth or eating breakfast. Which of your daily tasks might be used for this purpose? Try to pick something that happens every day. Sometimes we might pick something that is not always done on the weekends or during other days, and then we are more likely to forget. (For example, … One potential example follows: sometimes I don't shave on Saturdays, but I always brush my teeth, so linking taking the medicine to brushing my teeth might be better than linking it to shaving.) It also helps to store the pills near the place where you perform this daily task. Some people use a reminder device to help them remember. Do you have any reminder devices that you have used in the past? For example, watches, beepers, or cell phones.
# Organizational skills
Where will you store the bottle of pills? When you travel or spend the night outside of your home, what will you do about taking the pill?
# Social support & disclosure
Who in your household will know the reason that you are taking the pills? Are they supportive of you taking them? Are there individuals who might make assumptions about your serostatus because you have these medicines?
You may wish to explore other potential barriers that emerged in initial conversations (e.g., beliefs and attitudes), including factors (e.g., as substance use, depression or unstable housing) known to negatively affect medication adherence, such. To adhere to PrEP medication well, some patients may need access to mental health or social services.
# MONITORING PREP PATIENTS: ASSESSING SIDE EFFECTS AND ADHERENCE
Assess medication adherence as well as adherence to HIV testing at every visit. Self-reported adherence is typically an overestimate of true adherence, but patients may over report their adherence when they fear that a more accurate report would results in a negative judgment from their clinician. When asking patients about their adherence, do your best to adopt a nonjudgmental attitude, giving the patient permission to share adherence difficulties without worrying that you will reproach them. Asking patients to help you understand how they are doing with their medications will provide more information and thus allow for a better diagnostic picture of a patient's needs than will a more prescriptive approach.
Begin follow-up visits by asking the patient how well they have been doing with taking all of their medicines as scheduled. Accept more general responses (e.g., "so so", "pretty good", "excellent", "perfect") before asking for specific information about the frequency and the context of missed doses. Provide reinforcement for patients who report that they are doing well: ask questions such as "What are you doing to keep this going so well?" or "That's great. Can you see anything getting in the way of this?" These exchanges can help solidify the factors that are supporting your patients' adherence while helping them prepare for any barriers that may arise in the future.
When talking with patients who are not reporting perfect adherence, ask as to how many doses they have missed during a specific period. Assessing a longer period (e.g., 30 days, 7 days) is preferred to shorter periods (e.g., 3 days), not only because adherence can vary with changes in schedule (e.g., weekends, holidays) that may not have occurred during the shorter assessment period, but because many patients increase medication-taking just before medical appointments, a phenomenon supported by blood level assessments in the iPrEx trial. 2 When asking about many doses were missed (e.g., "In the last 30 days, how many times have you missed your PrEP medication?"), also (1) ask whether this was typical since their last clinic visit in order to gain a sense of adherence patterns, (2) ask for specific information about when they most recently missed dose(s), and (4) determine the circumstances during which those missed doses occurred (e.g., "Where were you?" "Who were you with?" "What happened just before you were supposed to take your medicine?"). Asking what happened on the day the dose was missed, and getting the patient's perspective on what generally gets in the way of taking medications regularly, will facilitate a conversation that will help to identify the patient's specific adherence barriers as well as the type of adherence support the patient needs.
On the basis of this conversation, develop a plan to address adherence barriers. Questions such as "What do you think you can do differently?" "What things make it easier to take your medications?" "What things need to happen for you to take your medications regularly?" or "What might you try [to not forget your weekend doses]?" bring the patient into the planning process and thus facilitate identification of the strategies most likely to be implemented. It's important for you to be familiar with a range of adherence strategies that can be shared with patients who require help with this task.
Finally, assess whether the patient is experiencing any side effects of medication, the severity of the side effects, and their role as an adherence barrier determined. Currently, most of what is known about antiretroviral therapy (ART) side effects is derived from patients with HIV. Healthy people may be more concerned about side effects than HIV patients. Try to determine whether clinical symptoms attributed to PrEP medication could possibly be due to other disorders (e.g., depression) or natural processes (e.g., aging). If necessary, include medications to treat side effects in the adherence plan.
# Section 11 Supplemental Counseling Information -HIV Risk Reduction
Determining whether the patient is a good candidate for PrEP is not strictly objective, and should be based on an ongoing discussion between you and your patient. Risk screening can be conducted using various approaches: face-to-face interviews, written forms, or computer-based tools. Written forms and computer-based tools are effective and can be conducted with fewer staff resources 33 . However, self-administered written forms are not recommended for persons with low literacy.
Using risk screening information and the HIV test results, provide your patients with services that are appropriate for their level of risk and are tailored to their prevention needs. Patients who report no or few risk factors, may have minimal prevention needs. In the absence of other information, these patients do not need PrEP. For patients for whom PrEP is appropriate, provide risk-reduction counseling and support services before, during, and after PrEP you prescribe PrEP.
# SEXUAL RISK REDUCTION COUNSELING
Address the sexual health of your patients, including risk behaviors that increase the likelihood of acquiring HIV or other sexually transmitted infections. Several discussion areas are recommended even in brief discussions of sexual risk behavior. For patients who demonstrate an elevated risk of sexual HIV acquisition, provide a brief risk reduction intervention onsite or link them to a program that provides those services (see http://www.effectiveinterventions.org). For patients who are continuing to engage in high-risk sexual behaviors or who need additional prevention services (beyond a brief risk-reduction intervention), link them to a program that provides more intense interventions, such as those in the Compendium of Evidence-based HIV Prevention Interventions (see http://www.cdc.gov/hiv/topics/research/prs/evidence-basedinterventions.htm) which are often provided by local health departments or community-based organizations. These patients may also be good candidates for continued use of PrEP until they are consistently practicing effective behavioral risk reduction.
Counseling patients who test HIV-negative. Guidelines have emphasized the importance of risk-reduction counseling for persons determined to be at substantial risk of sexual HIV acquisition 34 . It is recommended that you select the most appropriate brief sexual risk-reduction intervention that can address the immediate prevention needs of HIVnegative patients at substantial risk for acquiring HIV infection. One counseling approach designed for STD clinic providers, the RESPECT model 35 , can be used. The model consists of two brief, 20-minute, interactive, patient-focused counseling sessions that are conducted during HIV testing, and have been found to significantly reduce sexual risk behaviors and prevent new STDs among HIV-negative patients (although not HIV incidence). Besides RESPECT, there are now several other effective brief sexual riskreduction intervention models that should be considered when providing HIV-negative patients appropriate prevention counseling. Although no brief counseling models have yet proven effective for patients taking PrEP, some of the models developed for persons with HIV infection, (Partnership for Health 36 , and motivational interviewing 37,38) may be appropriate for adaptation to counseling patients who are taking PrEP.
Intensive sexual risk reduction interventions may be appropriate for some patients, who should be referred to appropriate providers. In general, HIV risk-reduction interventions have been shown through numerous systematic reviews, to be efficacious in reducing HIV sexual risk behaviors, promoting protective behaviors, and reducing the incidence of new sexually transmitted infections among high-risk populations from various demographic, racial/ethnic, or behavioral risk groups 39,40 .
Counseling patients who test HIV-positive. Provide emotional support and counseling to patients who receive preliminary or confirmed positive HIV test results to help them understand the test result, the benefits of initiating and remaining in HIV medical care, and the importance of reducing their HIV-related sexual and/or injection risk behaviors to help protect their health and the health of their partners. Link all HIV-positive patients to HIV medical care, prevention services that routinely offer risk screening and ongoing risk-reduction interventions, and other health services as needed.
# PREP FOLLOW-UP VISITS
Provide brief behavioral HIV risk assessment and supportive counseling at each follow-up visit while the patient is taking PrEP medication. For important components of these sessions, see Box 7.1. At least annually discuss with the patient whether discontinuation of PrEP is warranted.
If the decision is made to discontinue PrEP, a plan for periodic reassessment should be made and any indicated referrals to community programs or other support services should be arranged.
# Box 7.1: Elements of brief HIV risk-reduction counseling in clinical settings
Create and maintain a trusting and confidential environment for discussion of sexual or substance abuse behaviors.
Build an ongoing dialogue with the patient regarding their risk behavior (and document presence or absence of risk behaviors in the confidential medical record).
Reinforce the fact that PrEP is not always effective in preventing HIV infection particularly if used inconsistently, but that consistent use of PrEP together with other prevention methods (consistent condom use, discontinuing drug injection or never sharing injection equipment) confers very high levels of protection. Encounter for preprocedural laboratory examination (blood and urine tests prior to treatment or procedure) Z11. 3 Encounter for screening for infections with a predominantly sexual mode of transmission Z11. 4 Encounter for screening for human immunodeficiency virus (HIV) Z11.59
Encounter for screening for other viral diseases Z11. 8 Encounter for screening for other infectious and parasitic diseases Z13.89
Encounter for screening for other disorder (encounter for screening for genitourinary disorders) Z13.9
Encounter for screening unspecified
# Section 14 Methods for Developing the PrEP Clinical Practice Guideline
In 2009, in recognition of the lead time needed to develop clinical guidance for the safe and effective use of PrEP should clinical trials results support it, CDC initiated a formal guidelines development process to allow for early review of the relevant literature, discussion of potential guidelines content given scenarios of potential trial results, and fostering the development of expert and stakeholder consensus. This process was designed to provide a basis for the rapid issuance of interim guidance, to be followed by Public Health Service guidelines as soon as the earliest trial findings indicated sufficient PrEP efficacy and safety to merit its implementation for HIV prevention through one or more routes of transmission.
This guidelines development process was based on a review of experience with the development of other clinical and nonclinical guidelines at CDC, including those for STD treatment and antiretroviral prevention of mother-to-child transmission following the ACTG 076 trial results.
There were five basic components to the process for developing the 2014 PrEP guidelines:
1. An HHS Public Health Service (PHS) Working Group to develop interagency consensus on major points of implementation policy and provide agency review of guidelines. This working group included representatives from agencies that would formally clear PHS guidelines (FDA, HRSA, NIH, HHS/OHAP) as well as agencies that may implement such guidance (IHS, VA). The working groups and expert panels listed here were convened by teleconference before trial results were available (2009-2010) and some were reconvened after each trial results for each population group were published. As technical experts, prevention partners, and key stakeholders, they were asked to assist us to identify relevant scientific/medical literature and share thoughts on topics that would inform the Data from the clinical trial, human observational study, and laboratory human study results were added to the evidence tables. Study findings presented in the evidence tables were each assessed for quality of the study using GRADE criteria 39 (see guidelines Appendix 1, Table 13). Then all data supporting a specific recommendation were given a summary strength of evidence rating (across all studies relevant to that recommendation) using the same system as used for the DHHS antiretroviral treatment guidelines 32 (see PrEP clinical practice guidelines Appendix 1, Table 12).
# DRAFT GUIDELINE WRITING AND REVIEW PRIOR TO PUBLICATION
The draft was written to address guidelines standards for review of the strength of evidence (GRADE approach 41 ) as well as a format designed to promote guideline implementation (GLIA 42 ), dissemination (GEM 43 ), and adoption (AGREE 44,45 ).
The 2014 draft clinical practice guideline and clinical providers supplement were reviewed by CDC, FDA, NIH, HRSA, and HHS, and a series of webinars were held in 2012 and 2013 to obtain additional expert opinion and public engagement on draft recommendations for PrEP use.
The draft guideline and supplement were then reviewed by a panel of 6 external peer reviewers who had not been involved in their development. At each step, revisions were made in response to reviewer and public comments received.
For the 2017 update, the 2014 systematic review of published literature was updated through June 2017. Although no changes to the graded recommendations were indicated, additions to the evidence review tables were made; minor clarifying edits to the supporting text were made to enhance consistency with recently updated STD, nPEP, and perinatal guidelines sections relevant to PrEP; and updated references were added. These changes were shared with a group of 4 external peer reviewers for comment.
# Plans for Updates to the Guideline
PrEP is a rapidly changing field of HIV prevention with several additional clinical trials and studies are now underway or planned. Updates to these guidelines are anticipated as studies provide new information on PrEP efficacy, HIV testing, drug levels, adherence, longer term clinical safety, and changes in HIV risk behaviors associated with PrEP medication use for HIV uninfected MSM, heterosexuals, injection drug users, pregnant women and their newborns; as well as information on the efficacy and safety of other antiretroviral medications, and other routes and schedules of medication delivery for PrEP.
When significant new data become available that may affect patient safety or graded recommendations for PrEP use, an announcement with suggested revisions to the existing guidelines will be posted on the CDC web site and the public will be given a 2-week period to submit comments. These comments will be reviewed and a determination made as to whether additional revisions are indicated. Final updated guidelines will then be posted on the CDC web site.
#
This process allowed wide input, transparency in discussing the many issues involved, time for the evolution of awareness of PrEP and ideas for its possible implementation, in addition to facilitating the development of a consensus base for the eventual guidance. At the same time, it allowed for guidelines based on expert opinion, and recommendations deemed feasible by clinical providers and policymakers.
On the basis of results from the first 4 activities listed above and the publication in late November 2010 of results from the first clinical trial to show substantial efficacy and safety 2 , CDC issued interim guidance for PrEP use among men who have sex with men in January 2011. This interim guidance was followed by a face-to-face meeting of external in May 2011. As efficacy and safety results were published, additional interim guidance documents were issued for heterosexually active adults (August 2012) and injection drug users (July 2013).
# SYSTEMATIC LITERATURE REVIEW METHODS
For the 2014 guidelines, a systematic review was conducted of PrEP studies published from January 2010 through December 2013. For the 2017 guidelines, the same search strategy was run to update studies published through June 2017. Searches were conducted of MEDLINE, Embase, CINAHL, and Cochrane Library databases. The search strategy used the following criteria:
• Pre-Exposure Prophylaxis/ OR Chemoprevention/ OR (((Preexposure OR Pre-exposure) adjacent to prophylaxis) OR PrEP OR (topical adjacent to (prevention OR prophylaxis OR microbicide* OR gel OR pericoital OR precoital OR vaginal OR rectal OR anal)) OR chemoprophylaxis OR chemoprevention OR chemo-prophylaxis OR chemo-prevention OR iPrEX).mp. • AND • (exploded terms) Anti-HIV Agents/ OR Anti-Retroviral Agents/ OR HIV Infections/pc OR ((HIV OR human immunodeficiency virus) AND (antiretroviral* OR anti-retroviral* OR antiretrovirus* OR anti-retrovirus* OR Truvada OR tenofovir OR emtricitabine OR (TDF ADJ5 FTC))) • AND NOT animals • in the title, abstract, keyword heading word, subject heading fields Retrieved citations were provided in an Endnote reference file for deduplication. Then 2 scientists independently reviewed the citations and removed those that were not published in English, did not contain data (e.g., editorials, reviews, news reports), or did not contain data about oral TDF/FTC for PrEP. The next step was to screen citations to remove those that did not contain new data about oral PrEP (data/analyses not previously published). For the 2017 update, year of publication, author, and titles were compared with the 2014 Endnote library as necessary to identify already exiting entries. During this step, abstracts or full articles were read and publications were categorized into the following groups.
• New clinical trial results
• New human observational study results • New survey, focus group, or other behavioral study results
• New cost analysis results (e.g., program cost, cost benefit analysis)
• New modeling results (e.g., impact models)
• New laboratory human study results (e.g., drug levels, resistance)
• None of the above
The coding by the two reviewers was then compared and discrepancies were reconciled.
Citations with no new data about daily oral PrEP with TDF/FTC were deleted from the updated Endnote 2017 library. | None | None |
eade2b551de2f21d6a1858106800003e16b92701 | cdc | None | C enters fo r D isease C o n tro l a n d P re v e n tio n MMWR M o r b id ity a n d M o r ta lity W e e k ly R e p o rt S u p ple m e nt / Vol. 60 A p ril 15, 2011 G u id e lin e s fo r Biosafety Laboratory C om petency C D C a n d th e A s s o c ia tio n o f P u b lic H e a lth L a b o ra to rie s# Competencies and Skill Domains
# Conclusion
T | C enters fo r D isease C o n tro l a n d P re v e n tio n MMWR M o r b id ity a n d M o r ta lity W e e k ly R e p o rt S u p ple m e nt / Vol. 60 A p ril 15, 2011 G u id e lin e s fo r Biosafety Laboratory C om petency C D C a n d th e A s s o c ia tio n o f P u b lic H e a lth L a b o ra to rie s# Competencies and Skill Domains
# Conclusion
T | None | None |
62fdfd9ff45809082da065f49cb2f1709ade71a4 | cdc | None | The effect of topical steroids on the aged human axilla, in Montagna V (ed): Advances in Biology of 8kin.#
I.
# RECOMMENDATIONS FOR AN ULTRAVIOLET RADIATION STANDARD
The National Institute for Occupational Safety and Health (NIOSH) recommends that occupational exposure to ultraviolet energy in the workplace be controlled by compliance with the following sections.
Ultraviolet radiation (ultraviolet energy) Is defined as that portion of the electromagnetic spectrum described by wavelengths from 200 to 400 nm. (For additional definitions and conversion factors, see Appendix II.) Adherence to the recommended standards will, it is believed, prevent occupational injury from ultraviolet radiation, that is, will prevent adverse acute and chronic cutaneous and ocular changes precipitated or aggravated by occupational exposure to ultraviolet radiation.
Sufficient technology exists to prevent adverse effects on workers, but technology to measure ultraviolet energy for compliance with the recommended standard is not now adequate, so work practices are recommended for control of exposure in cases where sufficient measurement or emission data are not available.
These criteria and the recommended standard will be reviewed and revised when relevant information warrants.
# Section 1 -Exposure Standards (a)
For the ultraviolet spectral region of 315 to 400 nm, total lrradiance incident on unprotected skin or eyes, based on either measurement data or on output data, shall not exceed 1.0 mW/cm^ for periods greater than 1000 seconds, and for exposure times of 1000 seconds or less the total radiant energy shall not exceed 1000 mW'sec/cm^ (1.0 J/cm^).
# (b)
For the ultraviolet spectral region of 200 to 315 nm, total lrradiance incident on unprotected skin or eyes, based on either measure ment data or on output data, shall not exceed levels described below.
Measurement techniques are discussed in Appendix I.
(1) If the ultraviolet energy is from a narrow-band or mono chromatic source, permissible dose levels for a daily 8-hour period can be read directly from Figure 1-1, or, for selected wavelengths, from (2) If the ultraviolet energy is from a broad-band source, the effective irradiance (I x ,) relative to a 270-nm monochromatic source exf shall be calculated from the formula below. From the permissible exposure time in seconds for unprotected skin or eyes shall be computed by dividing 0.003 J/cm , the permissible dose of 270-nm radiation, by I ,, in W/cm^. eff where I -effective irradiance relative to a monoe chromatic source at 270 nm. I spectral irradiance in W/cm^/nm. À - relative spectral effectiveness (unitless); see Table 1-1 for values of at different wavelengths.
band width in nm. If radiation intensity from a point source is known at some distance from the worker, for example, from measurement at another point or from output data at a known distance from the ultraviolet source, attenuation of radiation from that point to the worker can be calculated from the principle that radiation decreases with the square of the distance it must travel. For 1-2 example, an object 3 feet away from a radiation source receives 1/9 the energy of an object 1 foot away. This assumption is conservative
In some instances, since ultraviolet radiation, especially at very low wavelengths, may be absorbed by some components of the atmosphere.
Where information on atmospheric absorption of ultraviolet radiation is known, further correction may be applied. The calculation of intensity of radiation at any given point by use of the inverse square formula explained above does not take into consideration reflected energy.
The recommended standard is not proposed for application as a standard to lasers. It should be recognized that significant nonoccupatlonal exposure to ultraviolet radiation can occur from exposure to sunlight, particularly during the summer months.
(a) The worker's past medical history should be obtained to determine if the worker suffers from any condition that Is exacerbated or aggravated by exposure to sunlight. (b) A worker who gives a history of such a condition should not be permitted to work in an area exposed to ultraviolet radiation.
(c) The worker should be advised that any blemish that appears on skin exposed to long term ultraviolet radiation should be examined by a physician.
# Section 3 -Apprisal of Employees of Hazards From Exposure to
Ultraviolet Energy.
(a) Each employee who may be exposed to high Intensity artificial sources of ultraviolet energy shall be apprised of all hazards, relevant symptoms and precautions concerning exposure. This apprisal of hazards shall Include:
(1) Information as to the proper eye protection and protective clothing to be used.
(2) Instruction on how to recognize the symptoms of eye and skin damage due to ultraviolet radiation.
(3) Information as to special caution that shall be exercised in situations where employees are exposed to toxic agents and/or other stressful physical agents which may be present in addition to and simultaneously with ultraviolet radiation. All sources, work areas, and housings specified in
Worker exposure to ultraviolet energy from 200 to 400 nm shall be controlled by adherence to the standard set forth in Section 1 or the preventive procedures described in this Section, as applicable.
Compliance with the standard, based on measurement data or emission data, or adherence to the work practice procedures will protect against injury from ultraviolet energy.
Exposure to ultraviolet energy can be controlled by enclosures, shields, protective clothing, skin creams, gloves, goggles, or face shields.
Workers shall be protected from eye or skin exposure to ultraviolet radiation.
Specific protective measures to be used for various types of ultraviolet exposure are noted below. Additional hazards. There are other hazards from some ultraviolet sources that must also be prevented. There is a shock hazard in some operations involving arcs, because of the high starting voltages required;
wiring and connections must be adequately insulated, and persons handling the equipment must wear gloves and face shields. There must be adequate ventilation to prevent build-up of ozone and oxides of nitrogen. There may also be an explosion hazard from some ultraviolet operations, and the wearing of gloves and face shields will reduce the consequences of an explosion.
Arc welding on plates wet with unsaturated chlorinated hydrocarbons (perchloroethylene and trichloroethylene) must be avoided unless well vented, because of possible production of phosgene and hydrogen chloride.
# Section 6 -Recordkeeping
Because measurement of exposure of workers to ultraviolet energy Is not required, records are not required.
# Historical Reports
The light-induced, acute inflammatory reaction of the eye has been known since early times, as indicated by Xenophon's mention of "snowblindness" in his treatise Anabasis (ca. 375 BC), quoted by Duke-Elder.
Although more energetic than the visible portion of the electromagnetic III-l spectrum, most ultraviolet radiation is not detected by the visual receptors in mammals, including man. Thus, exposure to ultraviolet may result in ocular damage without the subject's being aware of the potential danger.
Cases of keratinization of the cornea and cataracts of the lens have been 2 3 observed since the early part of this century - from ultraviolet radiation levels associated with welding arcs, high-pressure pulsed lamps, and reflection of solar radiation from snow, desert and water.
# Effects on Humans
Reviews of the literature on the biologic effects of ultraviolet Ozone is produced principally at wavelengths less than 220 nm.
# Effects on eyes
Ordinary clinical photokeratitis has been described by Pitts and 9 Gibbons as characterized by a period of latency that tends to vary inversely with the severity of exposure. The latent period may be III-2 as short as 30 minutes or as long as 24 hours, but Is usually 6 to 12 hours. Conjunctivitis follows, often accompanied by erythema of the facial skin surrounding the eyelids. There is a sensation of a foreign body or "sand" in the eyes and varying degrees of photophobia, lacrlmation, and blepharospasm. These acute symptoms usually last from 6 to 24 hours with nearly all discomfort disappearing within 48 hours. The Individual is visually incapacitated for varying periods of time. It Is important to note that the ocular system, unlike the skin, does not develop tolerance 9 to repeated ultraviolet exposure.
Quantitative dose-response studies on eyes have been conducted in man and animals, and the two approaches have complemented each other; some of the following comments on effects on the human eye are amplified and compared with studies on animals in the section on Animal Toxicity.
Pitts and Tredici studied threshold intensities for production of photokeratitis. From animal studies, they predicted maximal sensitivity of humans to occur at 280 nm and exposed a few humans at this wavelength.
From the limited results, they estimated a threshold at 280 nm of to the difference in the absorption of the different wavebands. The lower wavebands were absorbed In the outer corneal epithelial layers and underwent rapid change whereas the higher wavebands were absorbed in the deeper epithelial layers and showed delayed changes because these cells were more viable. Thus, the response at shorter wavelengths was rapidly revised while at the longer wavelengths there was a delayed and more serious response.
# III-5
Through a series of graded determinations ranging from -to + +, the first + reaction is taken to be the MED. Melanin, the pigment responsible for varying degrees of skin coloration, is present in the epidermis of the skin.^ When it is present in high concentrations, the deeper levels of the skin are protected from damaging effects of ultraviolet radiation, the melanin acting somewhat as a supplementary epidermal biological filter. The process of melanin pigmentation in the skin is believed to be initiated from pigment granules present in melanocytes with transfer of the granules Oil to neighboring cells in the basal layers of the skin.
The number of 07 melanocytes in Negro and Caucasian skin is about the same, so that differences in degree of skin pigmentation result from differences in cell activities. Longer wavelengths than those required for erythema produce some suntanning, even wavelengths extending well into the visible range.3®
Miescher^O showed that the ratio of thresholds for mild sunburn was about 8 times as great for Negro skin as for Caucasian skin, and about 120 times as great for severe sunburn. Thus, though skin pigmentation does afford protection from sunburn, Fitzpatrick^1 III-7 demonstrated that erythema nevertheless does occur In deeply pigmented skin even though It is extremely difficult to measure.
The manner in which melanin affords protection is not entirely 42 understood. Daniels, in reviewing the relation between pigment and human adaptation to environmental radiation, stated that it was unlikely that a darkly pigmented skin was required solely as a shield against the ultraviolet radiation of sunlight.
The epidermis of the Bkln which has been exposed to mild doses of ultraviolet radiation becomes thickened, initially due to inter-and intra-cellular edema. After approximately 72 hours, the mitotic rate has accelerated and increased cellular production contributes to the epidermal thickening. All layers of the epidermis, except for the basal layer, are thickened and remain so with further stimulation. The thickened epidermal layer affords protection against damage by ultraviolet radiation. The potential protection afforded by the thickened epidermis is illustrated by the practical impossibility of eliciting an ultraviolet erythema in the palms of the hands or soles of the feet. Calculations based on the thickness of the horny layer have shown that a dose many thousandfold that of the MED for trunk skin would be required to produce erythema in such areas as the palms of the hands. a greater incidence of basal cell epithelioma and malignant melanoma than control groups. There was a 25 percent greater incidence of basal cell epithelioma among men than among women, most likely because men spend more hours outdoors for work or sport. Ninety-one percent of the basal cell epitheliomas were on sun-exposed parts. MW sec/cm^ was given to two groups of albino mice. Tumors developed in
# Worthy of brief mention is
the group exposed to 300 nm radiation but not in the group exposed to 310 nm. Winklemann^® found that 280 nm to 310 nm induced squamous cell carcinoma in the skin of hairless mice.
Prior to 1960, sarcoma was the primary tumor produced experi-49 mentally by ultraviolet radiation on the ears of albino mice and rats.
With the development of hairless mice, squamous cell carcinomas were 97 reported and further studies established that squamous cell carcinomas could be produced almost to the exclusion of connective tissue (sarcoma) 96,98 growths.
The hairless mouse has also provided an experimental sodel for demonstrating that benign pigmented lesions could be stimulated 99 to develop into malignant melanomas by ultraviolet radiation. This further emphasizes that exposure to the sun may play an important role The dose of ultraviolet radiation necessary to give a threshold erythema reaction at 253.7 nm wavelength is only about 50% of that necessary at 300 nm.
A limit of 0.1 yw/cm^(8.6 mJ/cmfor 24 hours 104 has been established.
Again, the proposed minimum hazard level is satisfactory at the 254 nm wavelength (6.0 mJ/cm^).
The comparative photokeratitic thresholds for the cornea shown in Above 300 nm, a trend toward decreased sensitivity is noted and would be expected to be quite marked as seen in the rabbit. The photo- 1000 ^U/cm at 253.7 nm and 400 PW/cm at 365.0 nm. The sunburn was followed by desquamation and pigmentation.
Cases of dermatitis and erythema have been reported from ultraviolet radiation below 320 nm produced by fluorescent lamps used for general lighting purposes. Irradiance levels were not known.
IV.
# ENVIRONMENTAL DATA
Although there is much information on Industrial applications of ultraviolet energy, there is little information on exposure levels. The Both of these values are substantially below the "standard" action spectrum to protect against erythema.
Recognizing that many factors affect Individual responses^, MateJ-sky11^suggested, based on the "standard" erythema action curve, the following threshold doses weighted on the basis of their action spectra:
(1) Minimum erythemal dose for previously non-exposed skin: 9 20 to 25 mJ/cm of erythemally-weighted ultraviolet.
(2) Minimum erythemal dose for previously exposed skin: 2 25 to 35 mJ/cm of erythemally-weighted ultraviolet.
(3) Minimum keratitic dose;_ 1.5 mJ/cm ^ of keratitically-weighted ultraviolet.
The American Conference of Governmental Industrial Hygienists has proposed Threshold Limit Values, for 320 to 400 nm, of 1.0 J/cm2 for periods greater than, and 1.0 mW/m^ for periods less than, 1000 seconds.
For the actinic spectral region of 200 to 315 nm, the Conference proposed limits described by a curve (see Figure 1-1) In which the maximum permissible doses range upward at both longer and shorter wavelengths from 3.0 mJ/cm^ at 270 nm.
# Basis for Recommended Standard
The environmental exposure standard recommended in this document is the same as that proposed by the American Conference of Governmental 120 Industrial Hygienists. The ACGIH has not published the documentation or reasoning behind their proposed standard. The NIOSH rationale for recommending the same environmental exposure standard is as follows:
The results of the early investigators were quite consistent in the 280 to 315 nm range, but were somewhat divergent in the lower wavelengths action spectra.
# V-3
There has been little uniformity in the choice of body sites irradiated by the different Investigators. Olson, Sayre, and Everett1^ have shown the trunk to be more sensitive than either the head or the extremities, and the abdomen (used by them to develop their action spectrum^) the most sensitive of three trunk locations tested. After exposing abdominal skin to ultraviolet radiation at nine wavelengths between 250 and 310 nm, they reported that, while erythema response was well developed for all wavelengths after 8 hours, the response had substantially decreased at the shorter wavelengths after 24 hours. Furthermore, the energy requirements for minimal perceptible erythema at 254 and 280 nm were lowest at 8 hours after irradiation and nearly twice as much at 24 hours. The energy requirements for minimal perceptible erythema at 297 nm, however, decreased about 5% between 8 and 24 hours. Thus, it is apparent that the recent erythema action spectra, indicative of minimal perceptible erythema doses determined 8 hours after irradiation of a sensitive part of the body should at least reflect lower energy requirements and possibly other differences as well, when compared to the traditional curve.
Relatively minor damage to the conjunctiva or cornea from ultraviolet results in photophobia, pain, epiphora, and blepharospasm. Although the response is acute and incapacitating at the time, it regresses after several days leaving no permanent damage.The action spectrum for photokeratitis developed by Pitts and Tredici,10 based on animal and human data, is slightly more conservative than the recent skin erythema curves and reflects maximum efficiency at 270 nm rather than 250 nm. Nevertheless, this curve and the recent erythema action spectra are In reasonably good agreement. This is in keeping with previous statements that the action spectrum for conjunctivitis V-4 is the same as that for skin erythema. 8 Sllney compared the action spectra, both for erythema and for photokeratltls, with the "standard" erythema action curve. Plotting energy versus wavelength, the recent action spectra are at considerably lower energies than is the traditional curve. Additionally, these action Second, the curve is, as mentioned, almost flat. This is in contrast to the animal photokeratltic curves reported by Pitts and Tredici1^ and 9 again in the Pitts and Gibbons paper. While it may well be true that the human response varies slightly, if at all, with wavelength, the present results alone are not strong enough to support such a conclusion. Consequently, g the curve drawn by Sliney is believed not to be invalidated by the data of Pitts and Gibbons.
Assigning a relative spectral effectiveness of 1.0 to 270 nm, the low point of the recommended standard, the relative spectral effectiveness of other wavelengths can be calculated (Table 1- The recommended standard (Figure 1-1) is based upon action spectra both for erythema and for keratoconjunctivitis and is intended to protect the skin and eyes against acute effects. Therefore, separate skin and eye standards are not recommended. The American Conference of Governmental Industrial Hygienists proposed the limits expressed In this recommended standard and they specified its applicability for protection of both eyes and skin. The recommended standard is more readily applicable to the eye since the eye, unlike the skin, does not acquire protective capabilities after repeated exposures.
On the other hand, the skin does acquire resistance to ultraviolet damage after repeated exposure. Additionally, individual variations in threshold 119 response are great. Matelsky states that, despite the extensive industrial exposures to ultraviolet radiation, no cases of industriallyinduced skin cancer or keratosis have been reported and concludes that protection against the painful acute effects adequately V-7 protects ag3ixi8f tumorigenic doses. Nevertheless, It is believed that there Is not enough information to be completely sure that Industrial exposures to ultraviolet energy will not cause chronic effects on eyes or skin, such as cataracts or skin tumors.
While erythematic and carcinogenic activity is limited to wavelengths 33 90 119 shorter than 320 nm, ' - the lens of the eye absorbs strongly in the 300 to 400 nm range. "Black-lights" have a powerful emission line of 366.3 nm, which can cause the lens to fluoresce. This apparently causes some people, when looking at "black-lights", to experience a "tired" feeling, blurred vision, discomfort, and sometimes headache, but apparently no permanent damage ensues.
There is some evidence from animal studies to implicate ultraviolet in 81 this range as contributing to cataract formation.
While few industrial sources emit strongly in this range, the standard for 320 to 400 nm is recommended to prevent occupational exposures in this range from exceeding levels normally encountered in the out-of-doors.
Normal individuals should be adequately protected by these standards.
Photosensitive individuals, however, may respond at extremely low energy levels and over very wide wavelength ranges, even into the visible w av e le n gth s.^22 Therefore, these standards may not be adequate for photosensitive Individuals. More research is needed before the adequacy of these standards in protecting against chronic effects on skin and eyes can be assured.
V-8
# VI. PROTECTION AND CONTROL MEASURES
Skin and eyes can be protected from the effects of ultraviolet radiation by shielding of sources of radiation, by goggles or face shields, by clothing, and, for special purposes, by absorbing or reflecting skin creams.
Principles and procedures in selecting suitable protection are summarized in this section, and studies of various protective measures are reviewed. Specific topics discussed are (1) sunscreens, (2) pro tective clothing and barrier creams, (3) transparent material for skin and eye protection and (4) reflection of ultraviolet radiation.
(1) Sunscreens
Sunscreening preparations are usually classified as chemical or physical. The former Include para-aminobenzoic acid and its esters, cinnamate8, and benzophenones, all of which act by absorbing radiation so that the energy can be dissipated as radiation of lower energy. The physical agents act as simple physical barriers, reflecting, blocking, or scattering light. They include titanium dioxide, talc, and zinc oxide.
Largely because of cosmetic objections, the physical barriers are infrequently used In sunscreen formulations.
Sunscreen protection from absorbing chemicals depends on maintenance 127 of film thickness. Robertson reported that a series of sunscreens of 0.0 1 mm thickness protected fair skin during four to five hours of sunshine if the protective layer was fully maintained for the whole period.
When the thickness of the layer was halved, erythema occurred within a maximum of one hour.
# VI-1
Pathak, Fitzpatrick and Frenk produced evidence suggesting that para-aminobenzoic acid and its esters in ethanol afforded protection against the sunburn range (290 to 320 nm) for several hours with one application and that the protective action was unaffected by bathing, swimming, or vigorous exercise. MacLeod and Frain-Bell1^ confirmed the effectiveness of para-aminobenzoic acid in ethanol and observed that protection was provided for up to seven hours after the initial application.
They found, however, that the agent was easily removed as a result of 130 bathing or exercising. Katz also noted that para-aminobenzoic acid is not water-resistant; he found that a consistently satisfactory protection against the erythematogenic rays of the sun was lost after a 10-minute swim.
Goldman and E p s t e i n -^l reported that a commercial sunscreening agent containing the ultraviolet-absorbing chemical glyceryl para-aminobenzoate was a photosensitizer and that it had produced severe dermatitis in a patient who applied it prior to exposure to sunlight. The agent was an ordinary contact allergen as well as a photosensitizer. Turner, Barnes and Greene-32 found that a preparation containing vitamin A and calcium carbonate reduced the unpleasant effects of solar radiation without affecting normal tanning. The beneficial effect was most marked in subjects with blond hair. This observation could not be repeated, according to Findlay.^3
Red veterinary petrolatum is cosmetically less acceptable than other agents, but has a long history of effective protection of normal skin from the damaging effects of the ultraviolet sunburn spectrum. Like the benzophenones, it also gives some protection in the long ultraviolet doubted Its efficacy with their patients.
For Individuals with chronic photosensitivity diseases, It Is desirable to add a light-scattering and reflecting agent (e.g., titanium dioxide, talc, and zinc oxide) In combination with a light absorber in a hydrophilic ointment.
(2) Clothing and Barrier Creams Protective clothing consists of long-sleeved garments to protect the arms while a small cape sewed to the cap protects the back of the neck and the sides of the face. Flannelette and poplin give maximum protection, while other materials give less protection (Table X -4).
Where it is impossible to shield the skin by clothing, polyvinyl chloride gloves, masks, shields or by redirecting the radiation by suitable reflectors, a barrier cream should be applied to the skin before Irradiation. Ordinary soft paraffin is an excellent barrier, but its greasiness will often preclude its use on hands. Barrier creams contain ingredients which absorb ultraviolet radiation. The benzophenones are the best compounds for this purpose because of their great absorption capability 139 throughout most of the near and far ultraviolet spectrum (Parrish et al.
VI-3 As can be seen from the curve, the transmission falls off rapidly with wavelength below 360 nm.
Window glass 1/8 In. in thickness is adequate protection for the eyes and skin against ultraviolet radiation from ordinary ultraviolet sources. In the case of very intense sources of ultraviolet radiation, It may not be sufficient.
# VI-4
Full protection against 253. Glass workers, arc welders and people engaged In similar types of work may be exposed to infrared radiation as well as ultraviolet radiation, and may need eye protection from both types of radiation. Such people should wear goggles with an infrared absorbing glass and an infrared reflecting surface. Ordinary glass, plastics and other materials are usually transparent to Infrared rays which can cause thermal damage to the eye. A glass that absorbs in both the ultraviolet and infrared regions of the spectrum will be needed in such cases. For listings of absorbing 142 glasses refer to ANSI-Z 49.1.
# (4) Reflection of Ultraviolet Radiation
When a number of ultraviolet generators are operating in one room, protection of personnel poses several problems. In many applications, little difficulty is encountered in properly shielding the source so that most, or all, of the output is restricted to the exposed material. Stray radiation can be reduced, but reflection from glass, polished metal, and VI-5 high-gloss ceramic surfaces can be harmful to people working In the room.
Absorption of ultraviolet radiation therefore becomes an Important Item to consider In planning a safe work environment. Since painted walls and ceilings can be a significant source of ultraviolet reflection, It Is necessary to consider the ultraviolet reflective properties of the paint used.
The reflection of Incident ultraviolet radiation from pigments can range from negligible to more than 90%. A given material's ability to reflect visible light is no indication of its ability to perform similarly with ultraviolet. Table X-7 gives the reflection from a number of white pigments and other materials at several wavelengths In the ultra violet. The table shows that ordinary white wall plaster has a reflection of 46% at 253.7 nm, whereas zinc and titanium oxides, which are equally good reflectors for visible light, reflect only 2.5% and 6%, respectively, at this wavelength. 0 11-vehicle paints usually have low reflectances because of the absorption by the oil. However, some paints using synthetic plastic vehicles with high ultraviolet transmission may have high reflectances.
Walls surfaced with gypsum products tend to have high reflectances.
Table X-8 shows the ultraviolet reflectance of a number of dry white pigments in the region between 280 and 320 nm. These measurements were made with the unresolved radiation from a S-l lamp as a source and a cadmium phototube as a detector. These measurements may be assumed to be predominantly at the wavelength 302.4 nm.
# VI-6
No assumptions regarding the reflections of white pigments should be made without investigating their composition. The reason for this is demonstrated by the difference between two white pigments, zinc oxide and white lead. Although both of the pigments are very good reflectors of visible radiation, zinc oxide reflects only 3% of the ultraviolet, whereas white lead reflects about 60%. Colored pigments are almost invariably poor reflectors of ultraviolet. Stutz1^ studied 38 colored pigments and found that only turquoise blue had a reflectance of as much as 25% at 331.1 nm. At 253.6 nm turquoise blue had a reflectance of 22%, whereas none of the others exceeded 7.5%.
Table X-9 shows the ultraviolet reflectance of a number of paints with different white pigments suspended in silicone.
The basic requirements which determine the reflecting power of an 141 ultraviolet-reflecting paint have been given by Roller :
1. Particles of the pigment must be low in absorption (except metallic pigments), so that a large portion of the Incident radiation Is returned by multiple reflection and refractions.
2. The binder or vehicle must be transparent to the radiation to be reflected.
3. The difference in refractive index between pigment and medium must be large so that reflection and refraction at pigment-medium interfaces will be appreciable. the availability of measuring devices to cover these specific areas of the ultraviolet spectrum.
The band between 320 to 280 nm is referred to as the erythemal region with 295 to 298 nm being the wavelengths of maximal effect.
This area is also the one which has been Identified as having a carcinogenic effect upon the skin.
Slightly overlapping these wavelengths is a germicidal band between 280 and 220 nm with a maximum germicidal effective wavelength at 265 nm with some erythemal effect noted between 250 and 260 nm. In order to avoid errors of major magnitude In assessing ultraviolet energy, the following must be given serious consideration:
1. The spectral output of the specific source being evaluated and the spectral response of the phosphor or phototube that Is being utilized in measurement of ultraviolet energy. The selection of a meter or phototube should be one that is sensitive in the range most nearly covering that part of the spectrum under consideration.
Response curves of various phototubes are shown in Figure X-9.
2. Solarlzation and aging of lenses, tube envelopes, or cells.
This can be accomplished only by calibration against a source of known wavelengths and intensity.
3. Water vapor in the atmosphere may cause absorption of ultraviolet energy as well as affecting the electronic circuitry. There are several sources of commercial measuring devices available. These devices are primarily designed to measure output from specific sources. They are not in frequency ranges that can be satisfactorily utilized for purposes of evaluating exposures from wide band sources. An attempt to use these measuring devices with specific phototubes or phosphors can be extremely hazardous and give erroneous results when attempts are made to utilize them for wide-band ultraviolet energy.
Most of the devices are marketed as being sensitive at a specific wavelength. However, it should be pointed out that the ultraviolet response may be much wider than the one wavelength indicated; and the relative spectral response of each filter or phototube must be known to reasonably assess the exposure to ultraviolet energy. Examples of spectral response of several phototubes and filters are included in Figures X-9, X-10 and X-ll.
An ultraviolet device to measure broad-band ultraviolet energy is not presently available. However, it is possible to construct through a series of filters and phototubes a reasonable assessment of the levels of ultraviolet energy to which a worker may be exposed. | The effect of topical steroids on the aged human axilla, in Montagna V (ed): Advances in Biology of 8kin.#
I.
# RECOMMENDATIONS FOR AN ULTRAVIOLET RADIATION STANDARD
The National Institute for Occupational Safety and Health (NIOSH) recommends that occupational exposure to ultraviolet energy in the workplace be controlled by compliance with the following sections.
Ultraviolet radiation (ultraviolet energy) Is defined as that portion of the electromagnetic spectrum described by wavelengths from 200 to 400 nm. (For additional definitions and conversion factors, see Appendix II.) Adherence to the recommended standards will, it is believed, prevent occupational injury from ultraviolet radiation, that is, will prevent adverse acute and chronic cutaneous and ocular changes precipitated or aggravated by occupational exposure to ultraviolet radiation.
Sufficient technology exists to prevent adverse effects on workers, but technology to measure ultraviolet energy for compliance with the recommended standard is not now adequate, so work practices are recommended for control of exposure in cases where sufficient measurement or emission data are not available.
These criteria and the recommended standard will be reviewed and revised when relevant information warrants.
# Section 1 -Exposure Standards (a)
For the ultraviolet spectral region of 315 to 400 nm, total lrradiance incident on unprotected skin or eyes, based on either measurement data or on output data, shall not exceed 1.0 mW/cm^ for periods greater than 1000 seconds, and for exposure times of 1000 seconds or less the total radiant energy shall not exceed 1000 mW'sec/cm^ (1.0 J/cm^).
# (b)
For the ultraviolet spectral region of 200 to 315 nm, total lrradiance incident on unprotected skin or eyes, based on either measure ment data or on output data, shall not exceed levels described below.
# 1-1
Measurement techniques are discussed in Appendix I.
(1) If the ultraviolet energy is from a narrow-band or mono chromatic source, permissible dose levels for a daily 8-hour period can be read directly from Figure 1-1, or, for selected wavelengths, from (2) If the ultraviolet energy is from a broad-band source, the effective irradiance (I x ,) relative to a 270-nm monochromatic source exf shall be calculated from the formula below. From the permissible exposure time in seconds for unprotected skin or eyes shall be computed by dividing 0.003 J/cm , the permissible dose of 270-nm radiation, by I ,, in W/cm^. eff where I -effective irradiance relative to a monoe chromatic source at 270 nm. I ■ spectral irradiance in W/cm^/nm. À * relative spectral effectiveness (unitless); see Table 1-1 for values of at different wavelengths.
■ band width in nm. If radiation intensity from a point source is known at some distance from the worker, for example, from measurement at another point or from output data at a known distance from the ultraviolet source, attenuation of radiation from that point to the worker can be calculated from the principle that radiation decreases with the square of the distance it must travel. For 1-2 example, an object 3 feet away from a radiation source receives 1/9 the energy of an object 1 foot away. This assumption is conservative
In some instances, since ultraviolet radiation, especially at very low wavelengths, may be absorbed by some components of the atmosphere.
Where information on atmospheric absorption of ultraviolet radiation is known, further correction may be applied. The calculation of intensity of radiation at any given point by use of the inverse square formula explained above does not take into consideration reflected energy.
The recommended standard is not proposed for application as a standard to lasers. It should be recognized that significant nonoccupatlonal exposure to ultraviolet radiation can occur from exposure to sunlight, particularly during the summer months.
# 1-6
(a) The worker's past medical history should be obtained to determine if the worker suffers from any condition that Is exacerbated or aggravated by exposure to sunlight. (b) A worker who gives a history of such a condition should not be permitted to work in an area exposed to ultraviolet radiation.
(c) The worker should be advised that any blemish that appears on skin exposed to long term ultraviolet radiation should be examined by a physician.
# Section 3 -Apprisal of Employees of Hazards From Exposure to
Ultraviolet Energy.
(a) Each employee who may be exposed to high Intensity artificial sources of ultraviolet energy shall be apprised of all hazards, relevant symptoms and precautions concerning exposure. This apprisal of hazards shall Include:
(1) Information as to the proper eye protection and protective clothing to be used.
(2) Instruction on how to recognize the symptoms of eye and skin damage due to ultraviolet radiation.
(3) Information as to special caution that shall be exercised in situations where employees are exposed to toxic agents and/or other stressful physical agents which may be present in addition to and simultaneously with ultraviolet radiation. All sources, work areas, and housings specified in
# 1-8
Worker exposure to ultraviolet energy from 200 to 400 nm shall be controlled by adherence to the standard set forth in Section 1 or the preventive procedures described in this Section, as applicable.
Compliance with the standard, based on measurement data or emission data, or adherence to the work practice procedures will protect against injury from ultraviolet energy.
Exposure to ultraviolet energy can be controlled by enclosures, shields, protective clothing, skin creams, gloves, goggles, or face shields.
Workers shall be protected from eye or skin exposure to ultraviolet radiation.
Specific protective measures to be used for various types of ultraviolet exposure are noted below. Additional hazards. There are other hazards from some ultraviolet sources that must also be prevented. There is a shock hazard in some operations involving arcs, because of the high starting voltages required;
wiring and connections must be adequately insulated, and persons handling the equipment must wear gloves and face shields. There must be adequate ventilation to prevent build-up of ozone and oxides of nitrogen. There may also be an explosion hazard from some ultraviolet operations, and the wearing of gloves and face shields will reduce the consequences of an explosion.
Arc welding on plates wet with unsaturated chlorinated hydrocarbons (perchloroethylene and trichloroethylene) must be avoided unless well vented, because of possible production of phosgene and hydrogen chloride.
# Section 6 -Recordkeeping
Because measurement of exposure of workers to ultraviolet energy Is not required, records are not required.
# Historical Reports
The light-induced, acute inflammatory reaction of the eye has been known since early times, as indicated by Xenophon's mention of "snowblindness" in his treatise Anabasis (ca. 375 BC), quoted by Duke-Elder.
Although more energetic than the visible portion of the electromagnetic III-l spectrum, most ultraviolet radiation is not detected by the visual receptors in mammals, including man. Thus, exposure to ultraviolet may result in ocular damage without the subject's being aware of the potential danger.
Cases of keratinization of the cornea and cataracts of the lens have been 2 3 observed since the early part of this century * from ultraviolet radiation levels associated with welding arcs, high-pressure pulsed lamps, and reflection of solar radiation from snow, desert and water.
# Effects on Humans
Reviews of the literature on the biologic effects of ultraviolet Ozone is produced principally at wavelengths less than 220 nm.
# Effects on eyes
Ordinary clinical photokeratitis has been described by Pitts and 9 Gibbons as characterized by a period of latency that tends to vary inversely with the severity of exposure. The latent period may be III-2 as short as 30 minutes or as long as 24 hours, but Is usually 6 to 12 hours. Conjunctivitis follows, often accompanied by erythema of the facial skin surrounding the eyelids. There is a sensation of a foreign body or "sand" in the eyes and varying degrees of photophobia, lacrlmation, and blepharospasm. These acute symptoms usually last from 6 to 24 hours with nearly all discomfort disappearing within 48 hours. The Individual is visually incapacitated for varying periods of time. It Is important to note that the ocular system, unlike the skin, does not develop tolerance 9 to repeated ultraviolet exposure.
Quantitative dose-response studies on eyes have been conducted in man and animals, and the two approaches have complemented each other; some of the following comments on effects on the human eye are amplified and compared with studies on animals in the section on Animal Toxicity.
# 10
Pitts and Tredici studied threshold intensities for production of photokeratitis. From animal studies, they predicted maximal sensitivity of humans to occur at 280 nm and exposed a few humans at this wavelength.
From the limited results, they estimated a threshold at 280 nm of to the difference in the absorption of the different wavebands. The lower wavebands were absorbed In the outer corneal epithelial layers and underwent rapid change whereas the higher wavebands were absorbed in the deeper epithelial layers and showed delayed changes because these cells were more viable. Thus, the response at shorter wavelengths was rapidly revised while at the longer wavelengths there was a delayed and more serious response.
# III-5
Through a series of graded determinations ranging from -to + +, the first + reaction is taken to be the MED. Melanin, the pigment responsible for varying degrees of skin coloration, is present in the epidermis of the skin.^ When it is present in high concentrations, the deeper levels of the skin are protected from damaging effects of ultraviolet radiation, the melanin acting somewhat as a supplementary epidermal biological filter. The process of melanin pigmentation in the skin is believed to be initiated from pigment granules present in melanocytes with transfer of the granules Oil to neighboring cells in the basal layers of the skin.
The number of 07 melanocytes in Negro and Caucasian skin is about the same, so that differences in degree of skin pigmentation result from differences in cell activities. Longer wavelengths than those required for erythema produce some suntanning, even wavelengths extending well into the visible range.3®
Miescher^O showed that the ratio of thresholds for mild sunburn was about 8 times as great for Negro skin as for Caucasian skin, and about 120 times as great for severe sunburn. Thus, though skin pigmentation does afford protection from sunburn, Fitzpatrick^1 III-7 demonstrated that erythema nevertheless does occur In deeply pigmented skin even though It is extremely difficult to measure.
The manner in which melanin affords protection is not entirely 42 understood. Daniels, in reviewing the relation between pigment and human adaptation to environmental radiation, stated that it was unlikely that a darkly pigmented skin was required solely as a shield against the ultraviolet radiation of sunlight.
The epidermis of the Bkln which has been exposed to mild doses of ultraviolet radiation becomes thickened, initially due to inter-and intra-cellular edema. After approximately 72 hours, the mitotic rate has accelerated and increased cellular production contributes to the epidermal thickening. All layers of the epidermis, except for the basal layer, are thickened and remain so with further stimulation. The thickened epidermal layer affords protection against damage by ultraviolet radiation. The potential protection afforded by the thickened epidermis is illustrated by the practical impossibility of eliciting an ultraviolet erythema in the palms of the hands or soles of the feet. Calculations based on the thickness of the horny layer have shown that a dose many thousandfold that of the MED for trunk skin would be required to produce erythema in such areas as the palms of the hands. a greater incidence of basal cell epithelioma and malignant melanoma than control groups. There was a 25 percent greater incidence of basal cell epithelioma among men than among women, most likely because men spend more hours outdoors for work or sport. Ninety-one percent of the basal cell epitheliomas were on sun-exposed parts. MW sec/cm^ was given to two groups of albino mice. Tumors developed in
# Worthy of brief mention is
# 111-18
the group exposed to 300 nm radiation but not in the group exposed to 310 nm. Winklemann^® found that 280 nm to 310 nm induced squamous cell carcinoma in the skin of hairless mice.
Prior to 1960, sarcoma was the primary tumor produced experi-49 mentally by ultraviolet radiation on the ears of albino mice and rats.
With the development of hairless mice, squamous cell carcinomas were 97 reported and further studies established that squamous cell carcinomas could be produced almost to the exclusion of connective tissue (sarcoma) 96,98 growths.
The hairless mouse has also provided an experimental sodel for demonstrating that benign pigmented lesions could be stimulated 99 to develop into malignant melanomas by ultraviolet radiation. This further emphasizes that exposure to the sun may play an important role The dose of ultraviolet radiation necessary to give a threshold erythema reaction at 253.7 nm wavelength is only about 50% of that necessary at 300 nm.
A limit of 0.1 yw/cm^(8.6 mJ/cmfor 24 hours 104 has been established.
Again, the proposed minimum hazard level is satisfactory at the 254 nm wavelength (6.0 mJ/cm^).
The comparative photokeratitic thresholds for the cornea shown in Above 300 nm, a trend toward decreased sensitivity is noted and would be expected to be quite marked as seen in the rabbit. The photo- 1000 ^U/cm at 253.7 nm and 400 PW/cm at 365.0 nm. The sunburn was followed by desquamation and pigmentation.
Cases of dermatitis and erythema have been reported from ultraviolet radiation below 320 nm produced by fluorescent lamps used for general lighting purposes. Irradiance levels were not known.
# 111-23
IV.
# ENVIRONMENTAL DATA
Although there is much information on Industrial applications of ultraviolet energy, there is little information on exposure levels. The Both of these values are substantially below the "standard" action spectrum to protect against erythema.
Recognizing that many factors affect Individual responses^, MateJ-sky11^suggested, based on the "standard" erythema action curve, the following threshold doses weighted on the basis of their action spectra:
(1) Minimum erythemal dose for previously non-exposed skin: 9 20 to 25 mJ/cm of erythemally-weighted ultraviolet.
(2) Minimum erythemal dose for previously exposed skin: 2 25 to 35 mJ/cm of erythemally-weighted ultraviolet.
(3) Minimum keratitic dose;_ 1.5 mJ/cm ^ of keratitically-weighted ultraviolet.
The American Conference of Governmental Industrial Hygienists has proposed Threshold Limit Values, for 320 to 400 nm, of 1.0 J/cm2 for periods greater than, and 1.0 mW/m^ for periods less than, 1000 seconds.
For the actinic spectral region of 200 to 315 nm, the Conference proposed limits described by a curve (see Figure 1-1) In which the maximum permissible doses range upward at both longer and shorter wavelengths from 3.0 mJ/cm^ at 270 nm.
# Basis for Recommended Standard
The environmental exposure standard recommended in this document is the same as that proposed by the American Conference of Governmental 120 Industrial Hygienists. The ACGIH has not published the documentation or reasoning behind their proposed standard. The NIOSH rationale for recommending the same environmental exposure standard is as follows:
The results of the early investigators were quite consistent in the 280 to 315 nm range, but were somewhat divergent in the lower wavelengths action spectra.
# V-3
There has been little uniformity in the choice of body sites irradiated by the different Investigators. Olson, Sayre, and Everett1^ have shown the trunk to be more sensitive than either the head or the extremities, and the abdomen (used by them to develop their action spectrum^) the most sensitive of three trunk locations tested. After exposing abdominal skin to ultraviolet radiation at nine wavelengths between 250 and 310 nm, they reported that, while erythema response was well developed for all wavelengths after 8 hours, the response had substantially decreased at the shorter wavelengths after 24 hours. Furthermore, the energy requirements for minimal perceptible erythema at 254 and 280 nm were lowest at 8 hours after irradiation and nearly twice as much at 24 hours. The energy requirements for minimal perceptible erythema at 297 nm, however, decreased about 5% between 8 and 24 hours. Thus, it is apparent that the recent erythema action spectra, indicative of minimal perceptible erythema doses determined 8 hours after irradiation of a sensitive part of the body should at least reflect lower energy requirements and possibly other differences as well, when compared to the traditional curve.
Relatively minor damage to the conjunctiva or cornea from ultraviolet results in photophobia, pain, epiphora, and blepharospasm. Although the response is acute and incapacitating at the time, it regresses after several days leaving no permanent damage.The action spectrum for photokeratitis developed by Pitts and Tredici,10 based on animal and human data, is slightly more conservative than the recent skin erythema curves and reflects maximum efficiency at 270 nm rather than 250 nm. Nevertheless, this curve and the recent erythema action spectra are In reasonably good agreement. This is in keeping with previous statements that the action spectrum for conjunctivitis V-4 is the same as that for skin erythema. 8 Sllney compared the action spectra, both for erythema and for photokeratltls, with the "standard" erythema action curve. Plotting energy versus wavelength, the recent action spectra are at considerably lower energies than is the traditional curve. Additionally, these action Second, the curve is, as mentioned, almost flat. This is in contrast to the animal photokeratltic curves reported by Pitts and Tredici1^ and 9 again in the Pitts and Gibbons paper. While it may well be true that the human response varies slightly, if at all, with wavelength, the present results alone are not strong enough to support such a conclusion. Consequently, g the curve drawn by Sliney is believed not to be invalidated by the data of Pitts and Gibbons.
Assigning a relative spectral effectiveness of 1.0 to 270 nm, the low point of the recommended standard, the relative spectral effectiveness of other wavelengths can be calculated (Table 1- The recommended standard (Figure 1-1) is based upon action spectra both for erythema and for keratoconjunctivitis and is intended to protect the skin and eyes against acute effects. Therefore, separate skin and eye standards are not recommended. The American Conference of Governmental Industrial Hygienists proposed the limits expressed In this recommended standard and they specified its applicability for protection of both eyes and skin. The recommended standard is more readily applicable to the eye since the eye, unlike the skin, does not acquire protective capabilities after repeated exposures.
On the other hand, the skin does acquire resistance to ultraviolet damage after repeated exposure. Additionally, individual variations in threshold 119 response are great. Matelsky states that, despite the extensive industrial exposures to ultraviolet radiation, no cases of industriallyinduced skin cancer or keratosis have been reported and concludes that protection against the painful acute effects adequately V-7 protects ag3ixi8f tumorigenic doses. Nevertheless, It is believed that there Is not enough information to be completely sure that Industrial exposures to ultraviolet energy will not cause chronic effects on eyes or skin, such as cataracts or skin tumors.
While erythematic and carcinogenic activity is limited to wavelengths 33 90 119 shorter than 320 nm, ' * the lens of the eye absorbs strongly in the 300 to 400 nm range. "Black-lights" have a powerful emission line of 366.3 nm, which can cause the lens to fluoresce. This apparently causes some people, when looking at "black-lights", to experience a "tired" feeling, blurred vision, discomfort, and sometimes headache, but apparently no permanent damage ensues.
There is some evidence from animal studies to implicate ultraviolet in 81 this range as contributing to cataract formation.
While few industrial sources emit strongly in this range, the standard for 320 to 400 nm is recommended to prevent occupational exposures in this range from exceeding levels normally encountered in the out-of-doors.
Normal individuals should be adequately protected by these standards.
Photosensitive individuals, however, may respond at extremely low energy levels and over very wide wavelength ranges, even into the visible w av e le n gth s.^22 Therefore, these standards may not be adequate for photosensitive Individuals. More research is needed before the adequacy of these standards in protecting against chronic effects on skin and eyes can be assured.
V-8
# VI. PROTECTION AND CONTROL MEASURES
Skin and eyes can be protected from the effects of ultraviolet radiation by shielding of sources of radiation, by goggles or face shields, by clothing, and, for special purposes, by absorbing or reflecting skin creams.
Principles and procedures in selecting suitable protection are summarized in this section, and studies of various protective measures are reviewed. Specific topics discussed are (1) sunscreens, (2) pro tective clothing and barrier creams, (3) transparent material for skin and eye protection and (4) reflection of ultraviolet radiation.
(1) Sunscreens
Sunscreening preparations are usually classified as chemical or physical. The former Include para-aminobenzoic acid and its esters, cinnamate8, and benzophenones, all of which act by absorbing radiation so that the energy can be dissipated as radiation of lower energy. The physical agents act as simple physical barriers, reflecting, blocking, or scattering light. They include titanium dioxide, talc, and zinc oxide.
Largely because of cosmetic objections, the physical barriers are infrequently used In sunscreen formulations.
Sunscreen protection from absorbing chemicals depends on maintenance 127 of film thickness. Robertson reported that a series of sunscreens of 0.0 1 mm thickness protected fair skin during four to five hours of sunshine if the protective layer was fully maintained for the whole period.
When the thickness of the layer was halved, erythema occurred within a maximum of one hour.
# VI-1
Pathak, Fitzpatrick and Frenk produced evidence suggesting that para-aminobenzoic acid and its esters in ethanol afforded protection against the sunburn range (290 to 320 nm) for several hours with one application and that the protective action was unaffected by bathing, swimming, or vigorous exercise. MacLeod and Frain-Bell1^ confirmed the effectiveness of para-aminobenzoic acid in ethanol and observed that protection was provided for up to seven hours after the initial application.
They found, however, that the agent was easily removed as a result of 130 bathing or exercising. Katz also noted that para-aminobenzoic acid is not water-resistant; he found that a consistently satisfactory protection against the erythematogenic rays of the sun was lost after a 10-minute swim.
Goldman and E p s t e i n -^l reported that a commercial sunscreening agent containing the ultraviolet-absorbing chemical glyceryl para-aminobenzoate was a photosensitizer and that it had produced severe dermatitis in a patient who applied it prior to exposure to sunlight. The agent was an ordinary contact allergen as well as a photosensitizer. Turner, Barnes and Greene-32 found that a preparation containing vitamin A and calcium carbonate reduced the unpleasant effects of solar radiation without affecting normal tanning. The beneficial effect was most marked in subjects with blond hair. This observation could not be repeated, according to Findlay.^3
Red veterinary petrolatum is cosmetically less acceptable than other agents, but has a long history of effective protection of normal skin from the damaging effects of the ultraviolet sunburn spectrum. Like the benzophenones, it also gives some protection in the long ultraviolet doubted Its efficacy with their patients.
For Individuals with chronic photosensitivity diseases, It Is desirable to add a light-scattering and reflecting agent (e.g., titanium dioxide, talc, and zinc oxide) In combination with a light absorber in a hydrophilic ointment.
(2) Clothing and Barrier Creams Protective clothing consists of long-sleeved garments to protect the arms while a small cape sewed to the cap protects the back of the neck and the sides of the face. Flannelette and poplin give maximum protection, while other materials give less protection (Table X -4).
Where it is impossible to shield the skin by clothing, polyvinyl chloride gloves, masks, shields or by redirecting the radiation by suitable reflectors, a barrier cream should be applied to the skin before Irradiation. Ordinary soft paraffin is an excellent barrier, but its greasiness will often preclude its use on hands. Barrier creams contain ingredients which absorb ultraviolet radiation. The benzophenones are the best compounds for this purpose because of their great absorption capability 139 throughout most of the near and far ultraviolet spectrum (Parrish et al.
).
VI-3 As can be seen from the curve, the transmission falls off rapidly with wavelength below 360 nm.
Window glass 1/8 In. in thickness is adequate protection for the eyes and skin against ultraviolet radiation from ordinary ultraviolet sources. In the case of very intense sources of ultraviolet radiation, It may not be sufficient.
# VI-4
Full protection against 253. Glass workers, arc welders and people engaged In similar types of work may be exposed to infrared radiation as well as ultraviolet radiation, and may need eye protection from both types of radiation. Such people should wear goggles with an infrared absorbing glass and an infrared reflecting surface. Ordinary glass, plastics and other materials are usually transparent to Infrared rays which can cause thermal damage to the eye. A glass that absorbs in both the ultraviolet and infrared regions of the spectrum will be needed in such cases. For listings of absorbing 142 glasses refer to ANSI-Z 49.1.
# (4) Reflection of Ultraviolet Radiation
When a number of ultraviolet generators are operating in one room, protection of personnel poses several problems. In many applications, little difficulty is encountered in properly shielding the source so that most, or all, of the output is restricted to the exposed material. Stray radiation can be reduced, but reflection from glass, polished metal, and VI-5 high-gloss ceramic surfaces can be harmful to people working In the room.
Absorption of ultraviolet radiation therefore becomes an Important Item to consider In planning a safe work environment. Since painted walls and ceilings can be a significant source of ultraviolet reflection, It Is necessary to consider the ultraviolet reflective properties of the paint used.
The reflection of Incident ultraviolet radiation from pigments can range from negligible to more than 90%. A given material's ability to reflect visible light is no indication of its ability to perform similarly with ultraviolet. Table X-7 gives the reflection from a number of white pigments and other materials at several wavelengths In the ultra violet. The table shows that ordinary white wall plaster has a reflection of 46% at 253.7 nm, whereas zinc and titanium oxides, which are equally good reflectors for visible light, reflect only 2.5% and 6%, respectively, at this wavelength. 0 11-vehicle paints usually have low reflectances because of the absorption by the oil. However, some paints using synthetic plastic vehicles with high ultraviolet transmission may have high reflectances.
Walls surfaced with gypsum products tend to have high reflectances.
Table X-8 shows the ultraviolet reflectance of a number of dry white pigments in the region between 280 and 320 nm. These measurements were made with the unresolved radiation from a S-l lamp as a source and a cadmium phototube as a detector. These measurements may be assumed to be predominantly at the wavelength 302.4 nm.
# VI-6
No assumptions regarding the reflections of white pigments should be made without investigating their composition. The reason for this is demonstrated by the difference between two white pigments, zinc oxide and white lead. Although both of the pigments are very good reflectors of visible radiation, zinc oxide reflects only 3% of the ultraviolet, whereas white lead reflects about 60%. Colored pigments are almost invariably poor reflectors of ultraviolet. Stutz1^ studied 38 colored pigments and found that only turquoise blue had a reflectance of as much as 25% at 331.1 nm. At 253.6 nm turquoise blue had a reflectance of 22%, whereas none of the others exceeded 7.5%.
Table X-9 shows the ultraviolet reflectance of a number of paints with different white pigments suspended in silicone.
The basic requirements which determine the reflecting power of an 141 ultraviolet-reflecting paint have been given by Roller :
1. Particles of the pigment must be low in absorption (except metallic pigments), so that a large portion of the Incident radiation Is returned by multiple reflection and refractions.
2. The binder or vehicle must be transparent to the radiation to be reflected.
3. The difference in refractive index between pigment and medium must be large so that reflection and refraction at pigment-medium interfaces will be appreciable. the availability of measuring devices to cover these specific areas of the ultraviolet spectrum.
The band between 320 to 280 nm is referred to as the erythemal region with 295 to 298 nm being the wavelengths of maximal effect.
This area is also the one which has been Identified as having a carcinogenic effect upon the skin.
Slightly overlapping these wavelengths is a germicidal band between 280 and 220 nm with a maximum germicidal effective wavelength at 265 nm with some erythemal effect noted between 250 and 260 nm. In order to avoid errors of major magnitude In assessing ultraviolet energy, the following must be given serious consideration:
1. The spectral output of the specific source being evaluated and the spectral response of the phosphor or phototube that Is being utilized in measurement of ultraviolet energy. The selection of a meter or phototube should be one that is sensitive in the range most nearly covering that part of the spectrum under consideration.
Response curves of various phototubes are shown in Figure X-9.
2. Solarlzation and aging of lenses, tube envelopes, or cells.
This can be accomplished only by calibration against a source of known wavelengths and intensity.
3. Water vapor in the atmosphere may cause absorption of ultraviolet energy as well as affecting the electronic circuitry. There are several sources of commercial measuring devices available. These devices are primarily designed to measure output from specific sources. They are not in frequency ranges that can be satisfactorily utilized for purposes of evaluating exposures from wide band sources. An attempt to use these measuring devices with specific phototubes or phosphors can be extremely hazardous and give erroneous results when attempts are made to utilize them for wide-band ultraviolet energy.
Most of the devices are marketed as being sensitive at a specific wavelength. However, it should be pointed out that the ultraviolet response may be much wider than the one wavelength indicated; and the relative spectral response of each filter or phototube must be known to reasonably assess the exposure to ultraviolet energy. Examples of spectral response of several phototubes and filters are included in Figures X-9, X-10 and X-ll.
An ultraviolet device to measure broad-band ultraviolet energy is not presently available. However, it is possible to construct through a series of filters and phototubes a reasonable assessment of the levels of ultraviolet energy to which a worker may be exposed. | None | None |
9e96e516516901e0135eb66c32a8750c810be7a7 | cdc | None | Version 1.0 is a set of recommendations designed to promote consistent terminology and data collection related to child maltreatment. This document was developed through an extensive consultation process. It is published by the National Center for Injury Prevention and Control (NCIPC), part of Centers for Disease Control and Prevention (CDC).# INTRODUCTION The Problem of Child Maltreatment
Child maltreatment is a considerable social and public health problem in the United States. In 2004, data collected from Child Protective Services (CPS) determined approximately 900,000 children in the United States were victims of child maltreatment and about 1,500 children died because of abuse or neglect (US DHHS, 2006). Unfortunately, these numbers likely underestimate the number of children affected by maltreatment due to underreporting and focus on a single data source.
Research into the consequences of child maltreatment has identified various acute and severe negative outcomes such as death, injury, and traumatic brain injury. Research has also uncovered many deleterious long-term developmental outcomes: academic problems, anxiety, conduct disorder, childhood aggression, delinquency, depression, increased risk for suicide, high-risk sexual behavior, interpersonal problems, poor physical health, posttraumatic stress disorder, risky health behaviors, substance abuse, and youth violence (e.g., Bolger, Patterson, and Kupersmidt 1998;Cerezo and Frias 1994;Felitti et al. 1998;Kang et al. 1999;Mannarino and Cohen 1996;Widom 1999). Along with the legal and medical consequences, these substantial short-and long-term sequelae make prevention, early identification, and intervention a necessity.
# The Need for Consistent Definitions and Data Elements
Calculation of child victimization rates for maltreatment depends on how the definition of maltreatment is operationalized. To date, the multiple sectors addressing this issue (CPS, legal and medical communities, public health officials, researchers, practitioners, and advocates) often use their own definitions, thus limiting communication across disciplines and hampering efforts to identify, assess, track, treat, and prevent child abuse and neglect effectively. In addition, victimization rates are often based on reports from a single source, for example, vital statistics or CPS (e.g., National Child Abuse and Neglect Data System ). The most recent NCANDS estimate is 11.9 per 1,000 children, or 872,000 victims per year in 2004 (US DHHS, 2006). However, the Third National Incidence Study, with its more inclusive ascertainment methods (e.g., multiple sources), suggests CPS may investigate fewer than half the actual number of maltreatment cases (Sedlak and Broadhurst 1996).
Estimates for child fatalities due to maltreatment vary to an even greater extent depending on the methodologies, definitions, and sources used (Crume et al. 2002;Herman-Giddens et al. 1999;McClain, Sacks, Frohlke, and Ewigman 1993). On the one hand, death certificate data from 2002 suggest rates as low as 0.28 per 100,000 children 0 to 17 years of age (N = 204) (CDC Wonder website: . cdc.gov/). On the other hand, the NCANDS Child Maltreatment 2004 report estimates 2.0 per 100,000 children 0 to 17 years of age (N ~ 1,500). Fatality rates vary inversely by age as well, with the rate for infants varying by source from 2.4 per 100,000 for vital statistics to 17.5 per 100,000 for CPS sources. This lack of consistent information about the number of children affected by maltreatment limits the ability of the public health community to respond to the problem in several ways. First, it limits ability to gauge the magnitude of child maltreatment in relation to other public health problems. Second, it limits ability to identify those groups at highest risk who might benefit from focused intervention or increased services. Finally, it limits ability to monitor changes in the incidence and prevalence of child maltreatment over time. In turn, this limits the ability to monitor the effectiveness of child maltreatment prevention and intervention activities (Saltzman et al. 1999).
# The Public Health Approach to Child Maltreatment
The mission of the Centers for Disease Control and Prevention (CDC) is to promote health and quality of life by preventing and controlling disease, injury, and disability. Child maltreatment can result in direct physical, behavioral, social, and emotional harm and disability and is a risk factor for a range of other health risk factors that contribute to acute and chronic health problems. For example, research has shown that individuals who experienced multiple forms of child maltreatment early in life are more likely to engage in health risk behaviors such as smoking and heavy alcohol use. These health risk behaviors have been linked to poor health outcomes such as respiratory illness, liver damage, and cancer later in life (Edwards 2004). The ultimate goal of CDC's child maltreatment prevention activities is to prevent child maltreatment before it occurs. To do this, CDC uses the public health model in which surveillance is the first step.
Surveillance is defined as the ongoing, systematic collection, analysis, and interpretation of outcomespecific data for use in the planning, implementation, and evaluation of public health practice (Thacker and Berkelman 1988). Public health based child maltreatment surveillance systems rely on a variety of unique data sources, for example, hospital in-patient records, emergency department records, police and homicide reports, child death review findings, and medical examiner and coroner reports. These surveillance systems also use traditional CPS data that have been used by databases such as NCANDS and the Adoption and Foster Care Analysis Reporting System (AFCARS).
Although the research and legal communities have attempted to develop consistent and uniform definitions of child abuse and neglect, none of these definitions is adequate for use in public health surveillance. Research definitions such as the Maltreatment Coding Scheme for Abuse Allegations (MCS) Cicchetti 1991, 1993) and the "harm" and "endangerment" standards from the National Incidence Study (NIS) rely on interview data from a variety of sources that are not available to state and local health departments. Also, legal definitions vary from state to state, making comparisons across states and the collection of national data difficult. Users of this document are strongly encouraged to familiarize themselves with the child abuse and neglect laws in their state when designing surveillance systems because the differences may affect the language used to find cases and interpret data.
Because no public health based definitions for child maltreatment exist, public health officials continue to use terms related to child maltreatment in different ways and use different terms to describe the same acts. Not surprising, these inconsistencies have contributed to varied conclusions about the incidence and prevalence of child abuse and neglect.
# CDC Development of Uniform Definitions and Recommended Data Elements
In 1999, CDC published Version 1.0 of Intimate Partner Violence Surveillance: Uniform Definitions and Recommended Data Elements (Saltzman et al. 1999;revised 2002). That document was intended to guide data collection for public health surveillance of intimate partner violence. In 2002, CDC published Version 1.0 of Sexual Violence Surveillance: Uniform Definitions and Recommended Data Elements (Basile and Saltzman 2002). It covered sexual violence committed by all perpetrators and was intended for surveillance of sexual violence against both adult and child victims.
This document is the third in the series of Uniform Definitions and Recommended Data Elements. We used a process and format similar to that of the other two documents and focused on all types of child maltreatment, including sexual abuse. To maintain consistency and ease of use, we have drawn heavily from the sexual violence definitions in our definitions of sexual abuse. However, the definition of sexual abuse in this document covers only sexual violence against children that occurs in the context of a caregiver relationship.
# Development Process
Professionals in child maltreatment research, prevention, and surveillance from settings including universities, state health departments, hospitals, contract research firms, and federal agencies served as panelists for this project. The panelists first met in March 2003. At this meeting, panelists were charged with generating initial drafts of operational definitions of child maltreatment overall and the individual types of child maltreatment. The results of this meeting were compiled and refined and sent to the panelists for feedback in December 2003. Expanded and revised documents were presented to the panel in June 2004 and November 2004. The final draft of the document was sent to the panelists and other child maltreatment experts for review in May 2005.
# Purpose
This document defines child maltreatment, presents associated terms, and recommends data elements for voluntary use by individuals and organizations in the public health community. It is designed to aid state and local health department staff in the collection of public health surveillance data on child maltreatment. This document is not intended to be a set of mandates; rather, it is intended to promote and improve consistency of child maltreatment surveillance for public health practices.
The recommended data elements are designed to help people collect information of value for public health surveillance of child maltreatment and to serve as a technical reference for the collection of surveillance data. Developers of surveillance systems may choose to include as many or as few of the recommended data elements as they deem feasible. If the recommended data elements can be uniformly recorded and the data made available to numerous users, information about the characteristics and risk factors for child maltreatment will become more comparable and problems such as data incompatibility and the high cost of collecting, linking, and using data can be substantially reduced. The data elements in this document may be most useful for systematic, on-going collection, analysis, and interpretation of data already available from sources such as emergency departments, police departments, or CPS records. These data are typically collected for other agency-related purposes, but can later be extracted and used for surveillance.
Other approaches to surveillance exist that can be potentially viable options for measuring the incidence and prevalence of child maltreatment. Surveys, for example, involve systematic data collection from a representative sample of the population of interest for analysis and interpretation. Survey data are collected directly from individuals such as parents, caregivers, and children. Although the definitions and data elements contained in this document apply to some surveys, they were not designed specifically for use in surveys and discussion of these definitions and elements in this context is beyond the scope of the current document.
# Content and Scope
This document contains definitions and data elements that can be used to create instruments for surveillance. Users should be aware that its contents neither represent instruments for surveillance nor provide clinical information for identifying child maltreatment. The document is divided into two major sections:
- Uniform Definitions (for child maltreatment) - Recommended Data Elements for Child Maltreatment Surveillance In the first section, we provide a conceptual definition of child maltreatment and associated terms. In the second section, we provide recommended data elements for surveillance. The recommended data elements are divided into basic data elements and expanded data elements. The basic data elements represent fundamental information that should be collected in a child maltreatment surveillance system. Although not mandatory, these data elements should be relatively easy to collect. Some basic data elements may not be available or may be inappropriate to collect from certain data sources. If users of a surveillance system are unable to collect some basic data elements, the system is by no means inadequate. If resources allow, collection of the expanded data elements-which includes the basic data elements-will yield additional beneficial information. This information will provide richer dataset that includes contextual variables which may be more difficult to collect than the basic data elements.
An example of information that may be difficult to obtain is Injury Characteristics. Depending on the data sources used, the linkage across different data systems, and the completeness of available records, data for this element can be difficult or time-consuming to collect. Although not included in the list of basic data elements, we do not imply that injury characteristics are unimportant; rather, we acknowledge that these data are difficult to capture in a surveillance system.
Although we recommend definitions and data elements for use in child maltreatment surveillance systems, this document does not specify a database structure for the elements, preferring to leave the decision and choice of software to the database designer. However, the elements in this document can be used either in a flat file format, where one child record links to each incident, or in a relational database format, where multiple incident records may be linked to each child record. Examples of these database types can be found in existing data systems: death certificate data is stored in a flat file format, whereas both the FBI's National Incident Based Reporting System and the CDC's National Violent Death Reporting System use relational databases.
The flat file format is easier to implement and analyze. However, if a file in this format is set up with one record for each incident, it will be necessary to link multiple incidents for the same child in some fashion. A flat format also requires that the designer include enough fields to handle the most complicated incidents (e.g., those with multiple caregivers) or else force the user to choose among several caregivers for the one or two to be recorded. Either way, a flat file format will require relabeling the repeated variables (e.g., caregiver1 and caregiver2).
On the other hand, the relational database format can accommodate multiple records linked to a single record, whether those are multiple caregivers in one incident or multiple incidents for one child. A relational database tends to require more programming assistance to implement. Each surveillance system should use the format that best matches the available technical resources. For the most part, data from two systems that share the same data elements but use different database structures should be comparable. This document's order of presentation for various types of child maltreatment does not imply a hierarchy of risk or harm to the child; all abuse and neglect can have serious negative consequences for the victims.
# Caveats to the Use of this Document
- As with all research on children, ethical and safety issues are paramount. No data should be collected or stored in a way that would jeopardize a child's safety. Those interested in developing a surveillance system for child maltreatment must be particularly conscious of the need to preserve confidentiality. The issue of confidentiality must also be balanced with the need for data linkage across multiple data sources, perhaps through mechanisms such as encryption designed to preserve confidentiality and individual anonymity.
- Recognize that the parent and child behaviors and child outcomes which can be markers for child maltreatment are diverse and can result from other stressors or trauma. For example, infants and toddlers who present subdural hemotoma in emergency rooms could have suffered the injury from a fall or as a result of being unintentionally struck on the head-not as a consequence of shaken baby syndrome. Users should rely on multiple sources for data and consider available contextual information to determine whether a behavior or injury is, in fact, an indicator of child maltreatment.
- Because identification and documentation of child maltreatment is not standard across the many sources that collect data on abuse and neglect, data from multiple sources may be needed to better estimate the number of children who experience maltreatment. However, use of multiple data sources can present logistical and economic challenges. Data collection from multiple data sources can be costly, and these data will need to be linked once collected. As such, developers of surveillance systems may want to explore the viability of various approaches to determine the most efficacious and cost-effective method of child maltreatment surveillance. The recommendations in this document provide suggested means for organizing information whether it comes from a single source or a variety of sources.
- The definitions in this document include discrete types of violence: physical abuse, sexual abuse, psychological abuse, and neglect (Failure to Provide and Failure to Supervise). We recommend that users of the document take several approaches to assess the incidence and prevalence of child maltreatment when designing their surveillance system.
- First, research has demonstrated that experiencing maltreatment of any type can have deleterious consequences on development (Bolger, Patterson, and Kupersmidt 1998;Cerezo and Frias 1994;Felitti et al. 1998;Kang et al. 1999;Mannarino and Cohen 1996;Widom 1999). For this reason, we recommend that surveillance systems be designed to capture whether a child has experienced any maltreatment-regardless of the type experienced. o Second, research on child maltreatment has demonstrated that the various types of maltreatment often co-occur (Cicchetti and Barnett 1991;Clausen and Crittenden 1991;Higgins and McCabe 2000;Lewis, Mallouh, and Webb 1989;McGee and Wolfe 1991;Straus and Gelles 1986). As such, we recommend that the incidence of each type of maltreatment be documented separately to gauge its magnitude relative to other types of maltreatment.
- Many issues covered in this document fall into a grey area where it is difficult to delineate or encompass every possibility. Surveillance allows for error and interpretation by the individuals involved and does not strive for the same precision as research.
# Next Steps
As users of this document apply these definitions and data elements, we hope that most acts of child maltreatment will be captured. This document serves as a starting point, and revisions may become necessary as the definitions and data elements are used.
# UNIFORM DEFINITIONS
# CHILD MALTREATMENT AND ASSOCIATED TERMS
# Child Maltreatment
Any act or series of acts of commission 1 or omission by a parent 2 or other caregiver that results in harm, potential for harm, or threat of harm to a child 3 .
# Acts of Commission (Child Abuse 4 )
Words or overt actions that cause harm, potential harm, or threat of harm to a child. Acts of commission are deliberate and intentional; however, harm to a child may or may not be the intended consequence. Intentionality only applies to the caregivers' acts-not the consequences of those acts. For example, a caregiver may intend to hit a child as punishment (i.e., hitting the child is not accidental or unintentional) but not intend to cause the child to have a concussion. The following types of maltreatment involve acts of commission:
- Physical abuse - Sexual abuse - Psychological abuse
# Acts of Omission (Child Neglect)
The failure to provide for a child's basic physical, emotional, or educational needs or to protect a child from harm or potential harm 5 . Like acts of commission, harm to a child may or may not be the intended consequence.The following types of maltreatment involve acts of omission: 1 Words in boldface type will be defined. 2 The term "parent" includes custodial and noncustodial parents. 3 The terms "maltreatment" and "abuse" are often used interchangeably in the literature. However, in this document, "maltreatment" is a general term that includes both abuse and neglect; "abuse" refers explicitly to acts of commission. 4 In this document, the term "abuse" includes single acts and repeated, ongoing acts. 5 Adapted from Administration for Children and Families (ACF), What is Child Maltreatment?
Caregiver A caregiver 6 is a person, or people, who at the time of the maltreatment is in a permanent (primary caregiver) or temporary (substitute caregiver) custodial role. In a custodial role, the person is responsible for care and control of the child and for the child's overall health and welfare.
- Primary caregivers must live with the child at least part of the time and can include, but are not limited to, a relative or biological, adoptive, step-, or foster parent(s); a legal guardian(s); or their intimate partner 7 .
- Substitute caregivers may or may not reside with the child and can include clergy, coaches, teachers, relatives, babysitters, residential facility staff, or others who are not the child's primary caregiver(s).
# Harm
Any acute disruption caused by the threatened or actual acts of commission or omission to a child's physical or emotional health (ISPCAN 2003). Disruptions can affect the child's physical, cognitive, or emotional development.
Threat of harm occurs when a parent or caregiver expresses an intention or gives signs or warnings through the use of words, gestures, or weapons to communicate the likelihood of inflicting harm to the child. Threat of harm can be explicit or implicit. Explicit threats would include such acts as pointing a gun at the child or raising a hand as if to strike the child. Implicit threats would include such acts as kicking holes in walls or breaking down doors.
Disruption of physical health includes, but is not exclusive to, physical injuries, avoidable illnesses, and inadequate nutrition.
- Physical injuries are physical harm, including death, occurring to the body from exposure to thermal, mechanical, electrical, or chemical energy interacting with the body in amounts or rates that exceed the threshold of physiological tolerance, or from the absence of such essentials as oxygen or heat (Holder et al. 2001 (Saltzman, Fanslow et al. 1999).
Disruption of emotional health can include anxiety problems, disruption of social functioning, impaired relationships, depression and depressive symptoms, eating disorders, posttraumatic stress (including posttraumatic stress disorder ), externalizing behaviors (e.g., aggression), lack of education, school failure, delinquency, or substance abuse.
Harm can be immediate (e.g., broken bones) or delayed (e.g., depression, PTSD).
# Child
Any individual from birth through 17 years of age 8 at the time of maltreatment.
For the purposes of this document, maltreatment of an adult (age 18 or older) is not considered child maltreatment regardless of the emotional or intellectual age of the person.
For the purposes of this document the following are irrelevant to determining whether child maltreatment has occurred:
- Caregiver's intent to harm the child.
- Caregiver's legal liability for the maltreatment. - Caregiver's economic means.
- Caregiver's religious or cultural norms.
# DEFINITIONS OF ACTS OF COMMISSION (CHILD ABUSE)
For the purposes of this document, an incident of child maltreatment is defined as an event documented by CPS, law enforcement, the medical system, or other reporting source (e.g.,school) in which child maltreatment is alleged or confirmed 9 .
# Physical Abuse
Physical abuse is defined as the intentional use of physical force against a child that results in, or has the potential to result in, physical injury.
Physical abuse includes physical acts ranging from those which do not leave a physical mark on the child to physical acts which cause permanent disability, disfigurement, or death (Barnett, Manly, and Cicchetti 1993). Physical abuse can result from discipline or physical punishment (ACF 2002).
Physical acts can include hitting, kicking, punching, beating, stabbing, biting, pushing, shoving, throwing, pulling, dragging, dropping, shaking, strangling/choking, smothering, burning, scalding, and poisoning.
# Exceptions
Physical injuries to the anal or genital area or surrounding areas (e.g., anal or genital bruising or tearing; internal injuries resulting from penetration by a penis, hand, finger, or other object) that occur during attempted or completed sexual abuse, or other physical injuries that result from attempted or completed sexual abuse (e.g., bruises due to restraint, hitting, pushing) are considered sexual abuse and do not constitute physical abuse.
# Sexual Abuse
Any completed or attempted (non-completed) sexual act, sexual contact with, or exploitation (i.e., noncontact sexual interaction) of a child by a caregiver.
# Sexual Act
Sexual acts include contact involving penetration, however slight, between the mouth, penis, vulva, or anus of the child and another individual. Sexual acts also include penetration, however slight, of the anal or genital opening by a hand, finger, or other object (Basile and Saltzman 2002). Genital on genital contact includes:
# Noncontact Sexual Abuse
Noncontact sexual abuse does not include physical contact of a sexual nature between the caregiver and the child.
Noncontact sexual abuse can include the following:
1. Acts which expose a child to sexual activity (e.g., pornography; voyeurism of the child by an adult; intentional exposure of a child to exhibitionism); 2. Filming 10 of a child in a sexual manner (e.g., depiction, either photographic or cinematic, of a child in a sexual act); 3. Sexual harassment of a child (e.g., quid pro quo; creating a hostile environment because of comments or attention of a sexual nature by a caregiver to a child); 4. Prostitution of a child (e.g., employing, using, persuading, inducing, enticing, encouraging, allowing, or permitting a child to engage in or assist any other person to engage in, prostitution 11 , or sexual trafficking. Sexual trafficking is defined as the act of transporting children across international borders through deception for forced sexual activity such as prostitution or sexual slavery (Miller and Jayasundara 2001).
# Psychological Abuse
Intentional caregiver behavior (i.e., act of commission) that conveys to a child that he/she is worthless, flawed, unloved, unwanted, endangered, or valued only in meeting another's needs 12 . Psychological abuse can be continual (e.g., chronic and pervasive) or episodic (e.g., triggered by a specific context or situation: caregiver substance use/abuse) (Kairys and Johnson 2002).
Psychologically abusive behaviors may include blaming, belittling, degrading, intimidating, terrorizing, isolating, restraining, confining, corrupting, exploiting, spurning, or otherwise behaving in a manner that is harmful, potentially harmful, or insensitive to the child's developmental needs, or can potentially damage the child psychologically or emotionally (Barnett, Manly, and Cicchetti 1991;McGee and Wolfe 1991a, b).
# Terrorizing
Terrorizing includes caregiver behavior that is life-threatening; makes a child feel unsafe (e.g., situations that are likely to physically hurt, kill, or abandon the child) (Myers et al. 2002); sets unrealistic expectations of the child with threat of loss, harm, or danger if expectations are not met; and threatens or perpetrates violence against a child or a child's loved ones or objects (including toys, pets, or other possessions) (Kairys and Johnson 2002). For example, placing a child in unpredictable or chaotic circumstances would be considered terrorizing as would be placing a child in a situation reasonably considered dangerous by either the child or another adult.
# Isolating
Psychological isolation occurs when a caregiver forbids, prevents, or minimizes a child's contact with others.
# DEFINITIONS OF ACTS OF OMISSION (CHILD NEGLECT)
Failure to Provide (Barnett, Manly, and Cicchetti 1993) Failure by a caregiver to meet a child's basic physical, emotional, medical/dental, or educational needs-or combination thereof. Failure to provide includes the following:
# Physical Neglect
Caregiver fails to provide adequate nutrition, hygiene, or shelter; or, caregiver fails to provide clothing that is adequately clean, appropriate size, or adequate for the weather. Several examples follow (Barnett, Manly, and Cicchetti 1993):
- Nutrition: A 9-year-old child makes dinner several times per week because the caregiver(s) are sleeping, away, or otherwise unavailable; a child misses or is denied meals on numerous occasions over time; a child is diagnosed as being severely malnourished.
- Hygiene: Child is dirty, smells bad, or has unwashed hair. Child's living situation is unsanitary; dirty dishes and spoiled food are left on the kitchen table and counter.
- Shelter: Living arrangements for the child and family are unstable for two weeks or more; the residence is infested with roaches or vermin; residence in unheated or inadequately heated because caregivers have failed to ensure heat available.
- Clothing: The child always wears clothing that is too small; the child is not given a warm coat and gloves when the weather is cold.
# Emotional Neglect
Caregiver ignores the child, or denies emotional responsiveness or adequate access to mental health care (e.g., caregiver does not respond to infant cries or older child's attempt to interact) (Barnett, Manly, and Cicchetti 1993).
# Medical/Dental Neglect
Caregiver fails to provide adequate access to medical, vision, or dental care for the child. Examples include the following:
- Caregiver does not administer prescribed medications;
- Caregiver refuses to take the child for needed medical attention or seek timely medical attention (Barnett, Manly, and Cicchetti 1993).
# Educational Neglect
Caregiver fails to provide access to adequate education. Examples include:
- Caregiver allows child to miss 25 or more school days in one academic year without excuse;
- Caregiver does not enroll the child in school; caregiver encourages a child (under 16 years of age) to drop out of school (Barnett, Manly, and Cicchetti 1993).
# Failure to Supervise
Failure by the caregiver to ensure a child's safety within and outside the home given the child's emotional and developmental needs (Barnett, Manly, and Cicchetti 1993).
# Inadequate Supervision
Failure by the caregiver to ensure that the child engages in safe activities and uses appropriate safety devices; to ensure that the child is not exposed to unnecessary hazards; or to ensure appropriate supervision by an adequate substitute caregiver (Barnett, Manly, and Cicchetti 1993).
Inadequate supervision (sometimes called "supervisional neglect ") includes occasions when a caregiver knowingly fails to protect a child from maltreatment perpetrated by a substitute caregiver. Under such conditions, the primary caregiver's behavior would be considered neglectful only if the maltreatment was recognized and allowed to occur. Regardless of the primary caregiver's knowledge of the maltreatment, the substitute caregiver's behavior would be considered maltreatment.
# Exposure to Violent Environments
Caregiver intentionally 13 fails to take available measures to protect the child from pervasive violence within the home, neighborhood, or community (Kairys and Johnson 2002). For example, a caregiver who sells illicit drugs out of the child's home exposes the child to a violent environment; or, a school bus driver (temporary caregiver) who allows a student to be routinely victimized by another student while riding the bus without taking steps to intervene (e.g., notifying school administrators) also exposes a child to a violent environment.
Exposure of a child to violence between caregivers in the home may also qualify as exposure to a violent environment, particularly if the caregivers do not take available measures to protect the child from exposure. But, in instances where the caregiver is being victimized by a partner, and alternatives to protect the child are not available, or the caregiver is unaware of alternatives, the caregiver is not maltreating the child.
# CO-OCCURRENCE OF MULTIPLE TYPES OF ABUSE AND NEGLECT 14
Multiple forms of maltreatment often coexist, as described in these examples:
- Police find a 20-month-old child with bruises on extremities, cigarette burns to the forehead and upper chest, and signs of dehydration. The child was at home with the male caregiver who was high on opium. In this instance, physical abuse, failure to provide (adequate nutrition), failure to protect (caregiver is under the influence of drugs and unable to care for the child), and psychological abuse have occurred.
- Paramedics find a two-and-a-half-year-old child. The undressed child was walking outside in the winter and had belt-patterned bruises on the legs and trunk. The child also had ethyl alcohol in his blood system. In this example, physical abuse, failure to provide (adequate clothing), and failure to protect (unaccompanied child) have occurred.
- Upon reading a school report card, the caregiver/parent slaps the child's face, withholds food, and berates the child's ability until "better marks" are produced. In this scenario, physical abuse, failure to provide, and psychological abuse have occurred.
# INTRODUCTION
Each section describes the recommended data elements that can be included in a surveillance system designed to collect information on child maltreatment. The order in which the data elements are presented is not intended to suggest a hierarchy; users may select data elements that best fit their surveillance needs.
Depending on the applicability of the information, some or all of the following categories of information are listed for each data element:
- Description or definition of the data element;
- Uses/data element type describes how the data element should be used and whether it is a basic or expanded data element;
- Discussion of relevant conceptual or operational issues;
- Allow for multiple responses indicates when it is appropriate to include all applicable answers or response options;
- Field values/coding instructions indicate how to enter data in the field and what each represents;
- Data standards or guidelines used to define the data elements and its field values;
- Other references consulted in developing the data elements.
# BASIC AND EXPANDED DATA ELEMENTS FOR CHILD MALTREATMENT SURVEILLANCE
# Discussion
The data elements in this section relate directly to information about the index child.
Creators of surveillance systems should be mindful of confidentiality and safety issues as they develop and use their system. No data should be collected or stored that could potentially jeopardize a child's safety. When developing a surveillance system for child maltreatment, the issue of confidentiality must be balanced with the need for data linkage across multiple data sets. Data elements containing identifying information may be stripped once data from all records related to the child have been identified and entered into the surveillance system.
# *Expanded data element
Case ID 1.01
# Description/Definition
A required, unique identification code used by the agency compiling child maltreatment surveillance data.
# Uses/Data Element Type
Ensures that entered or accessed records correspond with the proper child. It also facilitates data linkage for administrative and research purposes.
Data element type: Basic.
# Discussion
Case ID may be assigned by the agency compiling child maltreatment (CM) surveillance data, or it may be an identifier previously assigned by the contributing data source. Case ID can be identical to the identifier created to allow linkage across multiple sources.
Because identification and documentation of CM is not standard across the many sources that may collect data on abuse and neglect, data from multiple sources may be needed to better estimate the number of children who experience maltreatment. As such, developers of surveillance systems may want to explore the viability of a variety of approaches to child maltreatment surveillance. One method is to include data from multiple sources (e.g. The mechanics of how to set up a database that accommodates data from multiple sources are not discussed in this document. Users should refer to other sources for information on how to set up a database.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
For recommended field values and coding instructions, please refer to Data Standards or Guidelines listed below.
# Data Standards or Guidelines
Health Level 7, Version 3.0 (HL7 2003); www.HL7.org
Child's Name 1.02
# Description/Definition
Child's first, middle, and last name.
# Uses/Data Element Type
Allows for linking data on a particular child across records, thus reducing the chance of duplicate records on the same child.
Can be used with 1.03 Alternate Name for Child to ensure that records related to the child are correctly linked to the child.
Data element type: Basic.
# Discussion
The practice of including names in public health surveillance systems is not uncommon. Most state-level surveillance systems for infectious diseases include names, as do surveillance systems such as the National Violent Death Reporting System. Additionally, inclusion of the index child's name(s) in a surveillance system to track child maltreatment allows for a unique identifier that can facilitate data linkage across sources.
These data are not intended for tracking victims or offenders. Protection of individuals' privacy is paramount; to protect child victim privacy and confidentiality, access to this data element must be limited to authorized personnel.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
Record child's name as follows: Î f the child's name does not conform to the coding instructions above, please refer to the Data Standards or Guidelines listed below.
Alternate Name for Child 1.03
# Description/Definition
Other first, middle, and last name by which child is known.
# Uses/Data Element Type
Allows for linking data on a particular child across records, thus reducing the chance of duplicate records on the same child.
Can be used with 1.02 Child's Name to ensure that records related to the child are correctly linked to the child.
Data element type: Basic.
# Discussion
The practice of including names in public health surveillance systems is not uncommon. Most state-level surveillance systems for infectious diseases include names, as do surveillance systems such as the National Violent Death Reporting System. Additionally, inclusion of the index child's name(s) in a surveillance system to track child maltreatment allows for a unique identifier that can facilitate data linkage across sources.
These data are not intended for tracking victims or offenders. Protection of individuals' privacy is paramount; to protect child victim privacy and confidentiality, access to this data element must be limited to authorized personnel.
# Allow for Multiple Responses
No.
# Discussion
Because developmental changes occur rapidly in the first three years of life, record the child's age in months for ages 3 years (36 months) and younger . Age in months allows for greater precision and a better understanding of the child's physical, cognitive, and emotional abilities at the time of the incident of maltreatment.
If the child's exact age is not available, an estimated age can be used.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
Record age in months and round to the nearest month. For example, a child who is 2 years and 3 months would be coded as 27 months of age. If the child is 2 years, 3 months, and 15 or fewer days, the age would be coded as 27 months. On the other hand, if the child is 2 years, 3 months, and 16 or more days, the age would be coded as 28 months.
# Data Standards or Guidelines
Common Data Elements Implementation Guide, Version 2.4 (CDC 2000); www.cdc.gov/data/index.htm
Age (in Years) of Child Older Than 3 years 1.06
# Description/Definition
Age of child, if the child is older than 3 years, at the time of the incident on which data are being collected.
# Uses/Data Element Type
Can be used if child's date of birth (see 1.04) is not available or is in question.
Data element type: Expanded.
# Discussion
If the child's exact age is not available, an estimated age can be used.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
Record age in years. If fractional ages (e.g., 7.5 years or 7 ½ years) are provided, round to the nearest year. For example, a child who is 7.5 years of age would be coded as 8 years.
# Data Standards or Guidelines
Common Data Elements Implementation Guide, Version 2.4 (CDC 2000); www.cdc.gov/data/index.htm
Sex of Child 1.07
# Description/Definition
Sex of child.
# Uses/Data Element Type
Standard demographic and identifying information.
Data element type: Basic.
# Allow for Multiple Responses
No. Data element type: Basic.
# Field Values/Coding Instructions
# Discussion
The categories below represent a social-political construct designed for collecting data on the race and ethnicity of broad population groups in the United States. For more than 20 years, the Federal government has promoted the use of a common language to ensure uniformity and comparability of data on race and ethnicity. Development of the data standards stemmed in large measure from new responsibilities to enforce civil rights laws. Data were needed to monitor equal access in housing, education, employment, and other areas for populations that historically had experienced discrimination and differential treatment because of their race or ethnicity. The standards are used not only in the decennial census (which provides data for the "denominator" for many measures), but also in household surveys, on administrative forms (e.g., school registration and mortgage-lending applications), and in medical and other research.
Race is a concept used to differentiate population groups largely by physical characteristics transmitted by descent. This concept lacks clear scientific definition, as racial categories are neither precise nor mutually exclusive. The common use of race in the United States draws upon differences not only in physical attributes, but also in ancestry and geographic origins. (OMB 1997) was developed to meet Federal legislative and program requirements, and these standards are used widely in the public and private sectors. The directive provides five basic racial categories but states that collection of race data need not be limited to these categories. However, additional reporting that uses more detail must be organized in such a way that the additional categories can be aggregated into the five basic groups. Although the directive does not specify a method for determining an individual's race, OMB prefers self-identification to identification by an observer whenever possible. The directive states that persons of multiple racial origins should be coded using multiple categories, not a multiracial category.
# Allow for Multiple Responses
Yes. If the agency providing the data to the child maltreatment surveillance system uses multiple racial categories, the child maltreatment surveillance system also allows for multiple racial categories to be coded. Uses/Data Element Type Provides information on preexisting disabilities or health conditions that the child may have which are not likely to have resulted from abuse or neglect. Differentiates between conditions existing before the onset of maltreatment, comorbid conditions, and conditions resulting from maltreatment.
# Field Values/Coding Instructions
Data element type: Expanded.
# Discussion
Access to data on preexisting disabilities or health conditions will allow for more accurate prevalence rates of risk factors for maltreatment and for specific points of intervention.
Children with physical, behavioral, health, and cognitive disabilities are at higher risk for maltreatment than children without such conditions Knutson 1998, 2000). These children comprise more than one third of the maltreated children between birth and 18 years of age.
# Allow for Multiple Responses
Yes.
# Field Values/Coding Instructions
# Discussion
As defined previously, an incident of child maltreatment is an event documented by CPS, law enforcement, the medical system, or other reporting sources (e.g., school) where child maltreatment is alleged or confirmed.
# Date of Incident 2.01
# Description/Definition
Date of the current incident of child maltreatment.
# Uses/Data Element Type
Provides information on when the incident occurred.
Date of Incident can be used with data element 1.04 Birth Date of Child to calculate the child's age at the time of the current incident.
If date of incident is not available, 2.02 Date of Report to Child Protective Services can be used instead.
Data element type: Basic.
# Discussion
If the incident of maltreatment exceeded one day, code the date that the incident ended. If the date of the incident is unknown, use the date of record (report).
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
For recommended field values and coding instructions, please refer to Data Standards and Guidelines listed below.
# Data Standards or Guidelines E1384-96 (ASTM 1996)
Health Level 7, Version 3.0 (HL7 2003); www.HL7.org
Date of Report to Child Protective Services (CPS) 2.02
# Description/Definition
Date on which the current incident of child maltreatment was reported to CPS.
# Uses/Data Element Type
Provides information on when the incident came to the attention of CPS.
If the actual date of incident is not available, Date of Report to Child Protective Services can be used as a proxy for data element 2.01 Date of Incident.
Data element type: Basic.
# Discussion
If the date of incident is unknown, use the date of record (report).
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
For recommended field values and coding instructions, please refer to Data Standards and Guidelines listed below.
# Data Standards or Guidelines E1384-96 (ASTM 1996).
Health Level 7, Version 3.0 (HL7 2003); www.HL7.org
Location where Maltreatment Occurred 2.03
# Description/Definition
Where did the maltreatment occur?
# Uses/Data Element Type
Describes the context in which the maltreatment took place.
Can be used with 2.04.03 Type of Residence to determine the specific type of location or residence if the response below is "Child's residence".
Data element type: Expanded.
# Discussion
Child maltreatment does not always occur in the child's home. The location(s) where child maltreatment occurs is beneficial for designing effective prevention programs.
# Allow for Multiple Responses
Yes.
# Field Values/Coding Instructions
# Uses/Data Element Type
Provides the location at which the index child resides at least most of the time.
Can be used with 2.04.02 Child's Second Address at Time of Incident to determine where the child was living at the time of the incident of maltreatment.
Data element type: Basic.
# Discussion
When child custody is shared due to parental divorce or legal separation, a child can have more than one official address. The first address should be the one where the index child was staying at the time of the incident. The other address, where the child spends some or most of the time, may be entered in 2.04.02 Child's Second Address at Time of Incident.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
For recommended field values and coding instructions, please refer to Data Standards and Guidelines listed below.
# Data Standards or Guidelines
Health Level 7, Version 3.0 (HL7 2003); www.HL7.org
Child's Second Address at Time of Incident 2.04.02
# Description/Definition
Address of the index child's second official residence at time of incident.
# Uses/Data Element Type
Provides the second location at which the index child resides when not at the first address (see 2.04.01 Child's First Address at Time of Incident).
Can be used with 2.04.01 Child's First Address at Time of Incident to determine where the child was living at the time of the incident of maltreatment.
Data element type: Basic.
# Discussion
In cases where custody of a child is shared due to parental divorce or legal separation, a child can have more than one official address. The other address at which the child spends some or most of the time may be entered in 2.04.01 Child's First Address at Time of Incident.
# Data Type (and Field Length)
XAD -extended address ( 106)
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
For recommended field values and coding instructions, please refer to Data Standards and Guidelines listed below.
# Data Standards or Guidelines
Health Level 7, Version 3.0 (HL7 2003); www.HL7.org
Type of Residence 2.04.03
# Description/Definition
Type of residence or living arrangement in which the index child resides at the time of the incident.
# Uses/Data Element Type
Provides information on the context and environment in which the child lives at the time of the incident.
Data element type: Expanded.
# Discussion
If the index child has more than one address, as indicated by data in 2. 04
# Uses/Data Element Type
The length of time the child has lived at the current address can provide information on the stability of the child's living situation.
Data element type: Expanded.
# Discussion
See discussion under 2.04.04 Time in First Residence.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
Record time in residence in number of months, rounded to the nearest month.
Physical Abuse
# Discussion
Physical abuse is the intentional use of physical force against a child that results in or has the potential to result in physical injury. Physical abuse includes physical acts ranging from those which do not leave a physical mark on the child to those which cause permanent disability, disfigurement, or death.
Physical abuse can result from discipline or physical punishment and is coded regardless of the caregiver's intent to harm or injure the child.
The following are considered sexual abuse and should be coded accordingly:
- Physical injuries to the anal, genital, or surrounding areas that occur during attempted or completed sexual abuse (e.g., anal or genital bruising or tear; internal injuries resulting from penetration by a penis, hand, finger, or other object) - Other physical injuries that result from attempted or completed sexual abuse (e.g., bruises due to restraint, hitting, or pushing)
Notation of Physical Abuse 2.04.06
# Description/Definition
Is physical abuse noted in any record of this incident of maltreatment?
# Uses/Data Element Type
Used to describe whether the child experienced physical abuse.
Data element type: Basic.
# Discussion
Noted physical abuse includes any mention of the term "physical abuse" or "child physical abuse" or intentionally inflicted injury of the child by a caregiver in the child's record. Noted physical abuse also includes suspected abuse or an indication that an abuse-related referral was made (e.g., to CPS).
If the record has a notation that physical abuse is suspected, code physical abuse as noted in that record. Other terms that can be used include but are not limited to "substantiated," "indicated," "reason to suspect," "suspected," "reported," "documented," "founded," "supported," "credible evidence exists," "suspected-confirmation unknown," or "suspected-confirmed."
Do not note physical abuse if the record indicated that the abuse was "unsubstantiated," "unsubstantiated due to intentionally false report," "ruled out," or "suspected-ruled out" (NCANDS 2004;DePanfilis and Salus 2003).
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
Code Description
No, physical abuse is not noted in any record of this incident of maltreatment. 02Yes, physical abuse is noted in one or more records of this incident of maltreatment. 99It is unknown if physical abuse occurred in this incident of maltreatment.
Abusive Head Trauma/Shaken Baby Syndrome 2.04.07
# Description/Definition
Describes a constellation of injuries related to violently shaking an infant or toddler and can include impact to the head if the infant is subsequently thrown down onto a crib or other surface.
# Uses/Data Element Type
Can be used to determine whether the child is a victim of Shaken Baby Syndrome (SBS)/Abusive Head Trauma (AHT).
Data element type: Basic.
# Discussion
SBS/AHT is defined as the violent shaking of an infant or child with sufficient vigor to produce whiplash forces which can result in subdural and retinal bleeding, seizures, paralysis, and death. SBS commonly occurs in the context of an inconsistent or inappropriate history given by the caregiver and can be accompanied by other injuries such as posterior rib fractures and retinal hemorrhages.
SBS/AHT is commonly observed in children under 1 year of age, but it has been documented in children as old as 3 to 4 years of age.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
# Description/Definition
Archival data sources from which child maltreatment surveillance information is abstracted.
# Uses/Data Element Type
Identifies the data source(s) documenting physical abuse in the current incident of maltreatment.
Data element type: Basic.
# Allow for Multiple Responses
Yes. Repetition is allowed to identify all sources containing data on physical abuse in the current incident. Sexual acts comprise acts in which contact involves penetration, however slight, between the caregiver and the child. A caregiver can also force or coerce a child to commit a sexual act on another individual (either adult or child).
# Field Values/Coding Instructions
Abusive sexual contact includes acts in which penetration is not attempted, but intentional touching occurs either directly or through the clothing of the genitalia, anus, groin, breast, inner thigh, or buttocks. Sexual contact can be performed by the caregiver on the child, by the child on the caregiver, or by the child on another adult or child through force or coercion by the caregiver. Sexual contact does not include touching required for normal care or attention to day-to-day needs of the child.
Noncontact sexual abuse does not require physical contact of a sexual nature between the caregiver and the child. However, it does include acts which expose a child to sexual activity such as filming of a child in a sexual manner, sexual harassment of a child, or prostitution of a child.
Notation of Sexual Abuse 2.04.09
# Description/Definition
Is sexual abuse noted in any record of this incident of maltreatment?
Uses/Data Element Type Describes whether the child experienced sexual abuse.
Data element type: Basic.
# Discussion
Noted sexual abuse includes any mention of the term "sexual abuse," "child sexual abuse," or similar variation in the child's record. Noted sexual abuse also includes suspected abuse or an indication that an abuse-related referral was made (e.g., to CPS). If a notation in the record states that sexual abuse is suspected, code sexual abuse as documented in that record. Other terms that can be used include, but are not limited to, "substantiated," "indicated," "reason to suspect," "suspected," "reported," "documented," "founded," "supported," "credible evidence exists," "suspected-confirmation unknown," or "suspected-confirmed."
Sexual abuse would not be noted if the record indicated that the sexual abuse was "unsubstantiated," "unsubstantiated due to intentionally false report," "ruled out," or "suspected-ruled out" (NCANDS 2004;DePanfilis and Salus 2003).
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
Code Description
No, sexual abuse is not noted in any record of this incident of maltreatment. 02Yes, sexual abuse is noted in one or more records of this incident of maltreatment. 99It is unknown if sexual abuse occurred in this incident of maltreatment.
Data Source(s) Documenting Sexual Abuse 2.04.10
# Description/Definition
Archival data sources from which child maltreatment surveillance information is abstracted.
# Uses/Data Element Type
Identifies the data source(s) documenting sexual abuse in the current incident of maltreatment.
Data element type: Basic.
# Allow for Multiple Responses
Yes. Repetition is allowed to identify all sources containing data on sexual abuse in the current incident.
# Field Values/Coding Instructions
# Discussion
Sexual acts include penetration, however slight, between the mouth, penis, vulva, or anus of the child and the adult. Sexual acts can also include penetration, however slight, of the anal or genital opening by a hand, finger, or other object.
Sexual acts can be performed by the caregiver on the child or by the child on the caregiver. A caregiver can also force or coerce a child to commit a sexual act on another individual (either child or adult).
Penetration Status 2.04.11
# Description/Definition
Describes whether the sexual abuse involved penetration or attempted penetration of either the child or the adult.
# Uses/Data Element Type
If used with 2.04.12 Object Used for Sexual Act(s) and 2.04.13 Part of the Body Affected by Sexual Act(s) information can be gathered regarding the process by which the abusive sexual contact occurred.
Data element type: Expanded.
# Discussion
Penetration is defined as sexual contact involving penetration, however slight, of the mouth, penis, vulva, or anus. Penetration status is either all or nothing. That is, even slight penetration should be included as "penetration."
No penetration includes intentional touching, either directly or through the clothing.
# Allow for Multiple Responses
No. Object Used for Sexual Act(s) 2.04.12
# Field Values/Coding Instructions
# Description/Definition
Describes the object used for penetration or attempted penetration.
# Uses/Data Element Type
If used with 2. 04.11 Penetration Status and 2.04.13 Part of the Body Affected by Sexual Act(s) information can be gathered regarding the process by which the abusive sexual contact occurred.
Data element type: Expanded.
# Allow for Multiple Responses
Yes. Part of the Body Affected by Sexual Act(s) 2.04.13
# Field Values/Coding Instructions
# Description/Definition
Describes the body part penetrated or attempted to be penetrated during the sexual act and whether the penetration was done by the adult or child.
# Uses/Data Element Type
If used with 2.04.11 Penetration Status and 2.04.12 Object Used for Sexual Act(s) information can be gathered regarding the process by which the abusive sexual contact occurred.
Data element type: Expanded.
# Allow for Multiple Responses
Yes. Sexually Transmitted Disease Diagnosed 2.04.14
# Field Values/Coding Instructions
# Description/Definition
Whether a sexually transmitted disease (STD) was found in the context of the current incident of sexual abuse.
Uses/Data Element Type Documents sexually transmitted disease infection related to the current incident of sexual abuse. Identification of the STD can precede or follow the discovery of sexual abuse.
Data element type: Expanded.
# Discussion
STDs in children, particularly ages 0 to 9 years, are a signal that sexual abuse may be occurring.
With older children and teenagers who could be sexually active, it is important to differentiate between STDs resulting from sexual abuse and STDs resulting from other sexual behavior.
In addition, if the incident of sexual abuse was within 3 to 6 months of the date of record, possible STD infection can be unknown or undetectable.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
# Uses/Data Element Type
Indicates whether the index child experienced abusive sexual contact in this incident of maltreatment.
Data element type: Expanded.
# Discussion
Abusive sexual contact includes intentional touching, either directly or through the clothing, that does not involve penetration.
Abusive sexual contact can be performed by the caregiver on the child or by the child on the caregiver. A caregiver can also force or coerce a child to engage in sexual contact with another individual (child or adult).
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
Code Description
No, abusive sexual contact did not occur in this incident of maltreatment. 02Yes, abusive sexual contact occurred in this incident of maltreatment. 99It is unknown/not documented whether abusive sexual contact occurred.
# Other References Basile and Saltzman 2002
Object Used for Abusive Sexual Contact 2.04.16
# Description/Definition
Describes the object used for sexual contact.
# Uses/Data Element Type
If used with 2. 04.11 Penetration Status and 2.04.17 Part of the Body Affected by Abusive Sexual Contact information can be gathered regarding the process by which the abusive sexual contact occurred.
Data element type: Expanded.
# Allow for Multiple Responses
Yes.
# Field Values/Coding Instructions
# Uses/Data Element Type
Indicates whether the index child experienced noncontact sexual abuse in this incident of maltreatment.
Data element type: Expanded.
# Discussion
Noncontact sexual abuse includes acts such as:
- Voyeurism of the child by an adult;
- Intentional exposure of a child to exhibitionism;
- Exposure to pornography;
- Photograph(s) of a child in a sexual manner or act;
- Filming of a child engaged in a sexual manner or act;
- Sexual harassment of a child;
- Sexual trafficking of a child;
- Employing, using, persuading, inducing, enticing, encouraging, allowing, or permitting a child to engage in or assist any other person to engage in prostitution.
Noncontact sexual abuse does not include physical contact of a sexual nature between the caregiver and the child.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
Code Description
No, noncontact sexual abuse did not occur in this incident of maltreatment. 02Yes, noncontact sexual abuse occurred in this incident of maltreatment (specify). 99
It is unknown/not documented whether noncontact sexual abuse occurred.
Method of Noncontact Sexual Abuse 2.04.19
# Description/Definition
Describes the method by which noncontact sexual abuse occurred.
# Uses/Data Element Type
Describes the process(es) by which the child experienced noncontact sexual abuse.
Data element type: Expanded.
# Discussion
Noncontact sexual abuse includes acts such as:
- Voyeurism of the child by an adult;
- Intentional exposure of a child to exhibitionism;
- Exposure to pornography;
- Photograph(s) of a child in a sexual manner or act;
- Filming of a child engaged in a sexual manner or act;
- Sexual harassment of a child;
- Sexual trafficking of a child;
- Employing, using, persuading, inducing, enticing, encouraging, allowing, or permitting a child to engage in or assist any other person to engage in prostitution.
# Allow for Multiple Responses
Yes.
# Field Values/Coding Instructions
# Discussion
It can be argued that all forms of child maltreatment include psychological abuse because all forms of child maltreatment have emotional consequences for the child. However, specific caregiver behaviors that involve trauma to the child caused by acts, threats of acts, or coercive tactics such as those listed below constitute a form of child maltreatment that is unique. This list is not exhaustive.
Psychological/emotional maltreatment can include but is not limited tothe following: - Behaving in a manner that is harmful, potentially harmful, or insensitive to the child's developmental needs; - Behaving in a manner that can potentially damage the child psychologically or emotionally.
Because psychological abuse is often difficult to detect and is unlikely to be picked up by data systems used in traditional public health surveillance, the number of children who experience psychological abuse will likely exceed those counted in traditional surveillance.
# Notation of Psychological Abuse
# Description/Definition
Is psychological abuse noted in any record of this incident of maltreatment?
Uses/Data Element Type Describes whether the child experienced psychological abuse.
Data element type: Basic.
# Discussion
Noted psychological abuse includes any mention of the terms "psychological abuse," "emotional abuse," "psychological maltreatment," or similar variation in the child's record. Noted psychological abuse also includes suspected abuse. If there is a notation in the record that psychological abuse is suspected, then code psychological abuse as documented in that record. Other terms that can be used include but are not limited to "substantiated," "indicated," "reason to suspect," "suspected," "reported," "documented," "founded," "supported," "credible evidence exists," "suspected-confirmation unknown," or "suspectedconfirmed."
Psychological abuse would not be noted if the record indicated that the psychological abuse was "unsubstantiated," "unsubstantiated due to intentionally false report," "ruled out," or "suspectedruled out" (NCANDS 2004;DePanfilis and Salus 2003).
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
Code Description
No, psychological abuse is not noted in any record of this incident of maltreatment. 02Yes, psychological abuse is noted in one or more records of this incident of maltreatment. 99It is unknown whether psychological abuse occurred in this incident of maltreatment.
Data Source(s) Documenting Psychological Abuse 2.04.21
# Description/Definition
Archival data sources from which child maltreatment surveillance information is abstracted.
# Uses/Data Element Type
Identifies the data source(s) documenting psychological abuse in the current incident of maltreatment.
Data element type: Basic.
# Allow for Multiple Responses
Yes. Repetition is allowed to identify all sources containing data on psychological abuse in the current incident. Method of Psychological Abuse 2.04.22
# Field Values/Coding Instructions
# Description/Definition
Describes the process by which psychological abuse occurred.
# Uses/Data Element Type
Describes the process(es) by which the child was psychologically abused.
Data element type: Expanded.
# Discussion
Psychologically abusive behaviors can include blaming, belittling, degrading, intimidating, terrorizing, isolating, restraining, confining, corrupting, exploiting, spurning or behaving in a manner that is harmful, potentially harmful, or insensitive to the child's developmental needs or may potentially damage the child psychologically or emotionally. (Barnett, Manly, and Cicchetti 1993;McGee and Wolfe 1991a, b) Terrorizing includes caregiver behavior that is life-threatening or makes a child feel unsafe (e.g., situations in which a child is likely to be hurt, killed, or abandoned) (Myers et al. 2002); sets unrealistic expectations of the child with threat of loss, harm, or danger if not met; and threatens or perpetrates violence against a child or a child's loved ones or objects (toys, pets, other possessions) (Kairys and Johnson 2002). For example, placing a child in unpredictable or chaotic circumstances would be considered terrorizing as would be placing a child in a situation that would reasonably be considered dangerous by the child or another adult.
Isolating (psychological) occurs when a caregiver forbids, prevents, or minimizes a child's contact with others.
# Allow for Multiple Responses
Yes.
# Field Values/Coding Instructions
# Discussion
Neglect encompasses a multitude of caregiver behaviors that can be divided into two types:
1. Failure to provide or meet the basic physical, emotional, or educational needs of the child. Failure to provide includes physical, emotional, medical/dental, and educational neglect;
2. Failure to supervise or ensure a child's safety within and outside the residence, given the emotional and developmental needs of the child. Failure to supervise includes inadequate supervision and exposure of the child to violent environments.
Although neglect comprises most maltreatment cases (DHHS 2003), neglect is less likely than physical or sexual abuse to be captured by data systems used in traditional public health surveillance. For example, emergency departments and hospitals are likely to see only the most egregious cases of medical, dental, or supervisional neglect. Few, if any, cases of physical, emotional, or educational neglect are seen. Consequently, physicians may fail to recognize and document cases of neglect. For this reason, traditional surveillance systems may undercount cases of neglect.
Failure to provide 2.04.23 Notation of failure to provide 2.04.24 Data source(s) documenting failure to provide 2.04.25 Mitigating circumstances for failure to provide*
# Discussion
Neglect-failure to provide includes the following types of neglect:
- Physical neglect: Caregiver fails to provide adequate nutrition, hygiene, shelter, or clothing that is adequately clean, appropriate size, or adequate for the weather.
Examples (Barnett, Manly, and Cicchetti 1993):
Nutrition: A 9-year-old makes dinner several times per week because the caregiver(s) are away, sleeping, or otherwise unavailable; a child misses or is denied meals on a number of occasions over time; a child is diagnosed as being severely malnourished.
Hygiene: Child is dirty, smells bad, or has unwashed hair. Child's living situation is unsanitary; dirty dishes and spoiled food are left on the kitchen table and counter.
Shelter: Child and family are without stable living arrangements for two weeks or more; child's residence is infested with roaches or vermin; residence is unheated because caregiver(s) failed to ensure availability of adequate heating.
Clothing: Child always wears clothing that is too small; child is not given a warm coat and gloves when the weather is cold.
- Emotional neglect: Caregiver ignores or denies emotional responsiveness to the child or provides inadequate access to mental health care for the child. Example: Caregiver does not respond to infant cries or older child's attempts to initiate interaction (Barnett, Manly, and Cicchetti 1993).
- Medical/dental neglect: Caregiver fails to provide adequate access to medical, vision, or dental care. Example: The caregiver does not administer prescribed medications. The caregiver refuses to take the child for needed medical attention (Barnett, Manly, and Cicchetti 1993).
- Educational neglect: Caregiver fails to provide access to adequate education. Examples: Caregiver allows child to miss 25 or more school days in one academic year without excuse; caregiver does not enroll the child in school; caregiver encourages a child (under 16 years of age) to drop out of school (Barnett, Manly, and Cicchetti 1993).
*Expanded data element Notation of Failure to Provide 2.04.23
# Description/Definition
Is failure to provide on the part of the caregiver noted in any record of this incident of maltreatment?
Uses/Data Element Type Describes whether the caregiver failed to provide for the child's basic needs.
Data element type: Basic.
# Discussion
Noted neglect-failure to provide includes any mention of the term "neglect," "denial," or "withholding" of basic necessities or "failure to provide." Examples of failure to provide are found in 2.04.34 Mechanism of Harm/Injury. Noted neglect-failure to provide also includes suspected neglect. If there is a notation in the record that "neglect-failure to provide" is suspected, then code neglect as documented in that record. Other terms that can be used include but are not limited to "substantiated," "indicated," "reason to suspect," "suspected," "reported," "documented," "founded," "supported," "credible evidence exists," "suspected-confirmation unknown," or "suspectedconfirmed."
Failure to provide would not be noted if the record indicated that the failure to provide was "unsubstantiated," "unsubstantiated due to intentionally false report," "ruled out," or "suspectedruled out" (NCANDS 2004;DePanfilis and Salus 2003).
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
Code Description
No, failure to provide is not noted in any record of this incident of maltreatment. 02Yes, failure to provide is noted in one or more records of this incident of maltreatment. 99It is unknown if failure to provide occurred in this incident of maltreatment.
# Discussion
Neglect-failure to supervise includes the following:
- Inadequate supervision. Failure by the caregiver to ensure that the child engages in safe activities, uses appropriate safety devices, is not exposed to unnecessary hazards, or is supervised by an adequate substitute caregiver.
Inadequate supervision includes occasions when a caregiver knowingly fails to protect the child from maltreatment perpetrated by a substitute caregiver. When this occurs, the primary caregiver's behavior would be considered neglectful only if the maltreatment was recognized and allowed to occur or recur.
- Exposure to violent environments. Failure by the caregiver to take available measures to protect the child from violence within the residence, neighborhood, or community. Uses/Data Element Type Describes whether the child experienced a lack of supervision by the caregiver.
Data element type: Basic.
# Discussion
Noted neglect-failure to supervise includes any mention of the term "neglect" or "failure to supervise" in addition to terms listed in 2.04.29 Method of Harm/Injury Related to Failure to Supervise. Noted neglect-failure to supervise also includes suspected neglect. If the record notes that neglect-failure to supervise is suspected, code as neglect. Other terms that can be used include but are not limited to "substantiated," "indicated," "reason to suspect," "suspected," "reported," "documented," "founded," "supported," "credible evidence exists," "suspected-confirmation unknown," or "suspected-confirmed."
Failure to supervise would not be noted if the record indicated that the failure to supervise was "unsubstantiated," "unsubstantiated due to intentionally false report," "ruled out," or "suspectedruled out" (NCANDS 2004;DePanfilis and Salus 2003).
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
Code Description
No, failure to supervise is not noted in any record of this incident of maltreatment. 02Yes, failure to supervise is noted in one or more records of this incident of maltreatment. 99It is unknown if failure to supervise occurred in this incident of maltreatment.
Harm Resulting from Failure to Supervise 2.04.28
# Description/Definition
Describes whether the child was harmed because of the caregiver's failure to supervise.
# Uses/Data Element Type
When used with data element 3.13 Factors Affecting Caregiver at Time of Incident, it is possible to examine the reason(s) the child was unsupervised and whether this lack of supervision resulted in harm or injury.
Data element type: Expanded.
# Discussion
An example of a child inadequately supervised with no harm or injury resulting would be a toddler who is left alone to play in an unfenced yard for several hours.
An example of a child inadequately supervised with harm but no injury resulting would be a toddler who wanders away at a park and is located later by the park rangers who transport the child to safety. The child is traumatized, but uninjured, by the experience.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
# Description/Definition
Describes the process by which the caregiver failed to supervise the child.
# Uses/Data Element Type
Determines the processes by which the caregiver failed to supervise the child.
Can be used with section 3.13 Factors Affecting Caregiver at Time of Incident to determine specific caregiver factors that may have contributed to failure to ensure the safety of the child.
Data element type: Expanded.
# Allow for Multiple Responses
Yes. Cicchetti 1991, 1993.
# Field Values/Coding Instructions
Child Fatality Related to Maltreatment Incident 2.04.30
# Description/Definition
Did the child die as a result of the incident of maltreatment?
Uses/Data Element Type Provides information about child mortality due to child maltreatment.
Data element type: Basic.
# Discussion
No time frame for death is specified for this data element. Include a death if the original incident/ injury qualifies as maltreatment based on the case definition outlined in this document and the medical examiner/coroner or death certificate classify the subsequent death as due to the incident.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
# Description/Definition
Was the child under the influence of alcohol or drugs at the time of the current incident of maltreatment?
Uses/Data Element Type Provides information about the child's behavior and susceptibility to influence at the time of the incident.
Data element type: Expanded.
# Discussion
Alcohol and drug use by a child is a risk factor for child maltreatment, particularly sexual abuse (Martino, Collins, and Ellickson 2004). Additionally, adults who abuse children have been known to give children drugs or alcohol.
Drugs prescribed for the child and over-the-counter medications used as directed should not be included unless given to the child in excess.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
# Code Description
Injury Characteristics 2.04.33
# Description/Definition
Characteristics that may prompt suspicion of child maltreatment by health care providers or others responsible for the care of children.
# Uses/Data Element Type
Provides indicators that maltreatment may have, or did, occur.
Data element type: Expanded.
# Allow for Multiple Responses
Yes.
# Field Values/Coding Instructions
# Description/Definition
Describes the mechanism by which the maltreatment occurred.
# Uses/Data Element Type
Describes the mechanism(s) by which the child was harmed or injured.
Data element type: Expanded.
# Allow for Multiple Responses
Yes.
# Field Values/Coding Instructions
# Description/Definition
Existence and location of external physical injury to child resulting from maltreatment.
# Uses/Data Element Type
Describes external physical injuries resulting from maltreatment sustained by the child.
May be used with data elements 2.04. Failure to Supervise to provide information on injuries related to different types of abuse.
Can provide information on the severity of the injury sustained by the child.
Data element type: Expanded.
# Discussion
To develop prevention strategies and advance the recognition of physical child maltreatment, it recommended that is the description of the injury include, when possible, whether the injury was inflicted by the caregiver or resulted from the caregiver's failure to protect or supervise the child.
# Allow for Multiple Responses
Yes.
# Field Values/Coding Instructions
# Description/Definition
Were ICD 9/10 codes for child abuse or neglect assigned to the case?
Uses/Data Element Type Provides information on the ICD 9/10 codes assigned to the case. Codes can be used for descriptive purposes and as a potential measure of the application of these codes. Application of these codes can be compared to reports of child maltreatment and to other sources and thus may be used to determine the extent of under-ascertainment of child maltreatment if these codes are used as the sole source of maltreatment data.
Data element type: Expanded.
# Discussion
Use of ICD 9/10 codes varies by hospital and region. As such, physicians may or may not use the ICD 9/10 codes for child maltreatment.
The ICD 9 code for general child maltreatment is 995.5X Child maltreatment syndrome.
The ICD 9 code for child abuse is E967 Child battering and other maltreatment, which includes:
- E967.0 Child battering and other maltreatment by parent - E967.1 Child battering and other maltreatment by other specified person - E967.2 Child battering and other maltreatment by unspecified person
The ICD 9 code for child neglect is E968.4 Assault by other and unspecified means-criminal neglect ("Abandonment of child, infant, or other helpless person with intent to injure or kill" WHO 1991, p.1045).
Additional ICD 9 codes for Homicide and injury purposely inflicted by other persons are commonly used for cases of maltreatment in which the victim fits the age criteria for a child and the perpetrator is designated as a caregiver. For the purpose of the document, incident is defined as any contact with CPS, law enforcement, the medical system, or other reporting sources where child maltreatment is alleged or confirmed Information for some data elements in this section may not be available for non-primary caregivers; therefore, developers of the surveillance system will need to decide how missing data should be handled.
Prior CPS Involvement with Family/Household 4.03
# Description/Definition
Describes prior contact between CPS and the index child's family or household.
# Uses/Data Element Type
Provides information on whether the index child's family or household is known to CPS.
Data element type: Expanded.
# Discussion
Prior CPS involvement with the family is a known risk factor for subsequent CPS involvement.
Exercise caution when using this data element as a risk factor for maltreatment in the light of potential biases found in reports to CPS. Some researchers have found racial, cultural, and socioeconomic disparities among children and families who are reported to CPS relative to those who are not (Cohen, DeVos, and Newberger 1997;Minnesota DHS 2002;Roberts 2002;Tsang 2001), whereas other researchers have not found these disparities (Sedlak and Broadhurst 1996). Nevertheless, knowing whether prior contact has occurred between the family and CPS is useful.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions | Version 1.0 is a set of recommendations designed to promote consistent terminology and data collection related to child maltreatment. This document was developed through an extensive consultation process. It is published by the National Center for Injury Prevention and Control (NCIPC), part of Centers for Disease Control and Prevention (CDC).# INTRODUCTION The Problem of Child Maltreatment
Child maltreatment is a considerable social and public health problem in the United States. In 2004, data collected from Child Protective Services (CPS) determined approximately 900,000 children in the United States were victims of child maltreatment and about 1,500 children died because of abuse or neglect (US DHHS, 2006). Unfortunately, these numbers likely underestimate the number of children affected by maltreatment due to underreporting and focus on a single data source.
Research into the consequences of child maltreatment has identified various acute and severe negative outcomes such as death, injury, and traumatic brain injury. Research has also uncovered many deleterious long-term developmental outcomes: academic problems, anxiety, conduct disorder, childhood aggression, delinquency, depression, increased risk for suicide, high-risk sexual behavior, interpersonal problems, poor physical health, posttraumatic stress disorder, risky health behaviors, substance abuse, and youth violence (e.g., Bolger, Patterson, and Kupersmidt 1998;Cerezo and Frias 1994;Felitti et al. 1998;Kang et al. 1999;Mannarino and Cohen 1996;Widom 1999). Along with the legal and medical consequences, these substantial short-and long-term sequelae make prevention, early identification, and intervention a necessity.
# The Need for Consistent Definitions and Data Elements
Calculation of child victimization rates for maltreatment depends on how the definition of maltreatment is operationalized. To date, the multiple sectors addressing this issue (CPS, legal and medical communities, public health officials, researchers, practitioners, and advocates) often use their own definitions, thus limiting communication across disciplines and hampering efforts to identify, assess, track, treat, and prevent child abuse and neglect effectively. In addition, victimization rates are often based on reports from a single source, for example, vital statistics or CPS (e.g., National Child Abuse and Neglect Data System [NCANDS]). The most recent NCANDS estimate is 11.9 per 1,000 children, or 872,000 victims per year in 2004 (US DHHS, 2006). However, the Third National Incidence Study, with its more inclusive ascertainment methods (e.g., multiple sources), suggests CPS may investigate fewer than half the actual number of maltreatment cases (Sedlak and Broadhurst 1996).
Estimates for child fatalities due to maltreatment vary to an even greater extent depending on the methodologies, definitions, and sources used (Crume et al. 2002;Herman-Giddens et al. 1999;McClain, Sacks, Frohlke, and Ewigman 1993). On the one hand, death certificate data from 2002 suggest rates as low as 0.28 per 100,000 children 0 to 17 years of age (N = 204) (CDC Wonder website: http://wonder. cdc.gov/). On the other hand, the NCANDS Child Maltreatment 2004 report estimates 2.0 per 100,000 children 0 to 17 years of age (N ~ 1,500). Fatality rates vary inversely by age as well, with the rate for infants varying by source from 2.4 per 100,000 for vital statistics to 17.5 per 100,000 for CPS sources. This lack of consistent information about the number of children affected by maltreatment limits the ability of the public health community to respond to the problem in several ways. First, it limits ability to gauge the magnitude of child maltreatment in relation to other public health problems. Second, it limits ability to identify those groups at highest risk who might benefit from focused intervention or increased services. Finally, it limits ability to monitor changes in the incidence and prevalence of child maltreatment over time. In turn, this limits the ability to monitor the effectiveness of child maltreatment prevention and intervention activities (Saltzman et al. 1999).
# The Public Health Approach to Child Maltreatment
The mission of the Centers for Disease Control and Prevention (CDC) is to promote health and quality of life by preventing and controlling disease, injury, and disability. Child maltreatment can result in direct physical, behavioral, social, and emotional harm and disability and is a risk factor for a range of other health risk factors that contribute to acute and chronic health problems. For example, research has shown that individuals who experienced multiple forms of child maltreatment early in life are more likely to engage in health risk behaviors such as smoking and heavy alcohol use. These health risk behaviors have been linked to poor health outcomes such as respiratory illness, liver damage, and cancer later in life (Edwards 2004). The ultimate goal of CDC's child maltreatment prevention activities is to prevent child maltreatment before it occurs. To do this, CDC uses the public health model in which surveillance is the first step.
Surveillance is defined as the ongoing, systematic collection, analysis, and interpretation of outcomespecific data for use in the planning, implementation, and evaluation of public health practice (Thacker and Berkelman 1988). Public health based child maltreatment surveillance systems rely on a variety of unique data sources, for example, hospital in-patient records, emergency department records, police and homicide reports, child death review findings, and medical examiner and coroner reports. These surveillance systems also use traditional CPS data that have been used by databases such as NCANDS and the Adoption and Foster Care Analysis Reporting System (AFCARS).
Although the research and legal communities have attempted to develop consistent and uniform definitions of child abuse and neglect, none of these definitions is adequate for use in public health surveillance. Research definitions such as the Maltreatment Coding Scheme for Abuse Allegations (MCS) Cicchetti 1991, 1993) and the "harm" and "endangerment" standards from the National Incidence Study (NIS) rely on interview data from a variety of sources that are not available to state and local health departments. Also, legal definitions vary from state to state, making comparisons across states and the collection of national data difficult. Users of this document are strongly encouraged to familiarize themselves with the child abuse and neglect laws in their state when designing surveillance systems because the differences may affect the language used to find cases and interpret data.
Because no public health based definitions for child maltreatment exist, public health officials continue to use terms related to child maltreatment in different ways and use different terms to describe the same acts. Not surprising, these inconsistencies have contributed to varied conclusions about the incidence and prevalence of child abuse and neglect.
# CDC Development of Uniform Definitions and Recommended Data Elements
In 1999, CDC published Version 1.0 of Intimate Partner Violence Surveillance: Uniform Definitions and Recommended Data Elements (Saltzman et al. 1999;revised 2002). That document was intended to guide data collection for public health surveillance of intimate partner violence. In 2002, CDC published Version 1.0 of Sexual Violence Surveillance: Uniform Definitions and Recommended Data Elements (Basile and Saltzman 2002). It covered sexual violence committed by all perpetrators and was intended for surveillance of sexual violence against both adult and child victims.
This document is the third in the series of Uniform Definitions and Recommended Data Elements. We used a process and format similar to that of the other two documents and focused on all types of child maltreatment, including sexual abuse. To maintain consistency and ease of use, we have drawn heavily from the sexual violence definitions in our definitions of sexual abuse. However, the definition of sexual abuse in this document covers only sexual violence against children that occurs in the context of a caregiver relationship.
# Development Process
Professionals in child maltreatment research, prevention, and surveillance from settings including universities, state health departments, hospitals, contract research firms, and federal agencies served as panelists for this project. The panelists first met in March 2003. At this meeting, panelists were charged with generating initial drafts of operational definitions of child maltreatment overall and the individual types of child maltreatment. The results of this meeting were compiled and refined and sent to the panelists for feedback in December 2003. Expanded and revised documents were presented to the panel in June 2004 and November 2004. The final draft of the document was sent to the panelists and other child maltreatment experts for review in May 2005.
# Purpose
This document defines child maltreatment, presents associated terms, and recommends data elements for voluntary use by individuals and organizations in the public health community. It is designed to aid state and local health department staff in the collection of public health surveillance data on child maltreatment. This document is not intended to be a set of mandates; rather, it is intended to promote and improve consistency of child maltreatment surveillance for public health practices.
The recommended data elements are designed to help people collect information of value for public health surveillance of child maltreatment and to serve as a technical reference for the collection of surveillance data. Developers of surveillance systems may choose to include as many or as few of the recommended data elements as they deem feasible. If the recommended data elements can be uniformly recorded and the data made available to numerous users, information about the characteristics and risk factors for child maltreatment will become more comparable and problems such as data incompatibility and the high cost of collecting, linking, and using data can be substantially reduced. The data elements in this document may be most useful for systematic, on-going collection, analysis, and interpretation of data already available from sources such as emergency departments, police departments, or CPS records. These data are typically collected for other agency-related purposes, but can later be extracted and used for surveillance.
Other approaches to surveillance exist that can be potentially viable options for measuring the incidence and prevalence of child maltreatment. Surveys, for example, involve systematic data collection from a representative sample of the population of interest for analysis and interpretation. Survey data are collected directly from individuals such as parents, caregivers, and children. Although the definitions and data elements contained in this document apply to some surveys, they were not designed specifically for use in surveys and discussion of these definitions and elements in this context is beyond the scope of the current document.
# Content and Scope
This document contains definitions and data elements that can be used to create instruments for surveillance. Users should be aware that its contents neither represent instruments for surveillance nor provide clinical information for identifying child maltreatment. The document is divided into two major sections:
• Uniform Definitions (for child maltreatment) • Recommended Data Elements for Child Maltreatment Surveillance In the first section, we provide a conceptual definition of child maltreatment and associated terms. In the second section, we provide recommended data elements for surveillance. The recommended data elements are divided into basic data elements and expanded data elements. The basic data elements represent fundamental information that should be collected in a child maltreatment surveillance system. Although not mandatory, these data elements should be relatively easy to collect. Some basic data elements may not be available or may be inappropriate to collect from certain data sources. If users of a surveillance system are unable to collect some basic data elements, the system is by no means inadequate. If resources allow, collection of the expanded data elements-which includes the basic data elements-will yield additional beneficial information. This information will provide richer dataset that includes contextual variables which may be more difficult to collect than the basic data elements.
An example of information that may be difficult to obtain is Injury Characteristics. Depending on the data sources used, the linkage across different data systems, and the completeness of available records, data for this element can be difficult or time-consuming to collect. Although not included in the list of basic data elements, we do not imply that injury characteristics are unimportant; rather, we acknowledge that these data are difficult to capture in a surveillance system.
Although we recommend definitions and data elements for use in child maltreatment surveillance systems, this document does not specify a database structure for the elements, preferring to leave the decision and choice of software to the database designer. However, the elements in this document can be used either in a flat file format, where one child record links to each incident, or in a relational database format, where multiple incident records may be linked to each child record. Examples of these database types can be found in existing data systems: death certificate data is stored in a flat file format, whereas both the FBI's National Incident Based Reporting System and the CDC's National Violent Death Reporting System use relational databases.
The flat file format is easier to implement and analyze. However, if a file in this format is set up with one record for each incident, it will be necessary to link multiple incidents for the same child in some fashion. A flat format also requires that the designer include enough fields to handle the most complicated incidents (e.g., those with multiple caregivers) or else force the user to choose among several caregivers for the one or two to be recorded. Either way, a flat file format will require relabeling the repeated variables (e.g., caregiver1 and caregiver2).
On the other hand, the relational database format can accommodate multiple records linked to a single record, whether those are multiple caregivers in one incident or multiple incidents for one child. A relational database tends to require more programming assistance to implement. Each surveillance system should use the format that best matches the available technical resources. For the most part, data from two systems that share the same data elements but use different database structures should be comparable. This document's order of presentation for various types of child maltreatment does not imply a hierarchy of risk or harm to the child; all abuse and neglect can have serious negative consequences for the victims.
# Caveats to the Use of this Document
• As with all research on children, ethical and safety issues are paramount. No data should be collected or stored in a way that would jeopardize a child's safety. Those interested in developing a surveillance system for child maltreatment must be particularly conscious of the need to preserve confidentiality. The issue of confidentiality must also be balanced with the need for data linkage across multiple data sources, perhaps through mechanisms such as encryption designed to preserve confidentiality and individual anonymity.
• Recognize that the parent and child behaviors and child outcomes which can be markers for child maltreatment are diverse and can result from other stressors or trauma. For example, infants and toddlers who present subdural hemotoma in emergency rooms could have suffered the injury from a fall or as a result of being unintentionally struck on the head-not as a consequence of shaken baby syndrome. Users should rely on multiple sources for data and consider available contextual information to determine whether a behavior or injury is, in fact, an indicator of child maltreatment.
• Because identification and documentation of child maltreatment is not standard across the many sources that collect data on abuse and neglect, data from multiple sources may be needed to better estimate the number of children who experience maltreatment. However, use of multiple data sources can present logistical and economic challenges. Data collection from multiple data sources can be costly, and these data will need to be linked once collected. As such, developers of surveillance systems may want to explore the viability of various approaches to determine the most efficacious and cost-effective method of child maltreatment surveillance. The recommendations in this document provide suggested means for organizing information whether it comes from a single source or a variety of sources.
• The definitions in this document include discrete types of violence: physical abuse, sexual abuse, psychological abuse, and neglect (Failure to Provide and Failure to Supervise). We recommend that users of the document take several approaches to assess the incidence and prevalence of child maltreatment when designing their surveillance system.
o First, research has demonstrated that experiencing maltreatment of any type can have deleterious consequences on development (Bolger, Patterson, and Kupersmidt 1998;Cerezo and Frias 1994;Felitti et al. 1998;Kang et al. 1999;Mannarino and Cohen 1996;Widom 1999). For this reason, we recommend that surveillance systems be designed to capture whether a child has experienced any maltreatment-regardless of the type experienced. o Second, research on child maltreatment has demonstrated that the various types of maltreatment often co-occur (Cicchetti and Barnett 1991;Clausen and Crittenden 1991;Higgins and McCabe 2000;Lewis, Mallouh, and Webb 1989;McGee and Wolfe 1991;Straus and Gelles 1986). As such, we recommend that the incidence of each type of maltreatment be documented separately to gauge its magnitude relative to other types of maltreatment.
• Many issues covered in this document fall into a grey area where it is difficult to delineate or encompass every possibility. Surveillance allows for error and interpretation by the individuals involved and does not strive for the same precision as research.
# Next Steps
As users of this document apply these definitions and data elements, we hope that most acts of child maltreatment will be captured. This document serves as a starting point, and revisions may become necessary as the definitions and data elements are used.
# UNIFORM DEFINITIONS
# CHILD MALTREATMENT AND ASSOCIATED TERMS
# Child Maltreatment
Any act or series of acts of commission 1 or omission by a parent 2 or other caregiver that results in harm, potential for harm, or threat of harm to a child 3 .
# Acts of Commission (Child Abuse 4 )
Words or overt actions that cause harm, potential harm, or threat of harm to a child. Acts of commission are deliberate and intentional; however, harm to a child may or may not be the intended consequence. Intentionality only applies to the caregivers' acts-not the consequences of those acts. For example, a caregiver may intend to hit a child as punishment (i.e., hitting the child is not accidental or unintentional) but not intend to cause the child to have a concussion. The following types of maltreatment involve acts of commission:
• Physical abuse • Sexual abuse • Psychological abuse
# Acts of Omission (Child Neglect)
The failure to provide for a child's basic physical, emotional, or educational needs or to protect a child from harm or potential harm 5 . Like acts of commission, harm to a child may or may not be the intended consequence.The following types of maltreatment involve acts of omission: 1 Words in boldface type will be defined. 2 The term "parent" includes custodial and noncustodial parents. 3 The terms "maltreatment" and "abuse" are often used interchangeably in the literature. However, in this document, "maltreatment" is a general term that includes both abuse and neglect; "abuse" refers explicitly to acts of commission. 4 In this document, the term "abuse" includes single acts and repeated, ongoing acts. 5 Adapted from Administration for Children and Families (ACF), What is Child Maltreatment?
Caregiver A caregiver 6 is a person, or people, who at the time of the maltreatment is in a permanent (primary caregiver) or temporary (substitute caregiver) custodial role. In a custodial role, the person is responsible for care and control of the child and for the child's overall health and welfare.
• Primary caregivers must live with the child at least part of the time and can include, but are not limited to, a relative or biological, adoptive, step-, or foster parent(s); a legal guardian(s); or their intimate partner 7 .
• Substitute caregivers may or may not reside with the child and can include clergy, coaches, teachers, relatives, babysitters, residential facility staff, or others who are not the child's primary caregiver(s).
# Harm
Any acute disruption caused by the threatened or actual acts of commission or omission to a child's physical or emotional health (ISPCAN 2003). Disruptions can affect the child's physical, cognitive, or emotional development.
Threat of harm occurs when a parent or caregiver expresses an intention or gives signs or warnings through the use of words, gestures, or weapons to communicate the likelihood of inflicting harm to the child. Threat of harm can be explicit or implicit. Explicit threats would include such acts as pointing a gun at the child or raising a hand as if to strike the child. Implicit threats would include such acts as kicking holes in walls or breaking down doors.
Disruption of physical health includes, but is not exclusive to, physical injuries, avoidable illnesses, and inadequate nutrition.
• Physical injuries are physical harm, including death, occurring to the body from exposure to thermal, mechanical, electrical, or chemical energy interacting with the body in amounts or rates that exceed the threshold of physiological tolerance, or from the absence of such essentials as oxygen or heat (Holder et al. 2001 (Saltzman, Fanslow et al. 1999).
Disruption of emotional health can include anxiety problems, disruption of social functioning, impaired relationships, depression and depressive symptoms, eating disorders, posttraumatic stress (including posttraumatic stress disorder [PTSD]), externalizing behaviors (e.g., aggression), lack of education, school failure, delinquency, or substance abuse.
Harm can be immediate (e.g., broken bones) or delayed (e.g., depression, PTSD).
# Child
Any individual from birth through 17 years of age 8 at the time of maltreatment.
For the purposes of this document, maltreatment of an adult (age 18 or older) is not considered child maltreatment regardless of the emotional or intellectual age of the person.
For the purposes of this document the following are irrelevant to determining whether child maltreatment has occurred:
• Caregiver's intent to harm the child.
• Caregiver's legal liability for the maltreatment. • Caregiver's economic means.
• Caregiver's religious or cultural norms.
# DEFINITIONS OF ACTS OF COMMISSION (CHILD ABUSE)
For the purposes of this document, an incident of child maltreatment is defined as an event documented by CPS, law enforcement, the medical system, or other reporting source (e.g.,school) in which child maltreatment is alleged or confirmed 9 .
# Physical Abuse
Physical abuse is defined as the intentional use of physical force against a child that results in, or has the potential to result in, physical injury.
Physical abuse includes physical acts ranging from those which do not leave a physical mark on the child to physical acts which cause permanent disability, disfigurement, or death (Barnett, Manly, and Cicchetti 1993). Physical abuse can result from discipline or physical punishment (ACF 2002).
Physical acts can include hitting, kicking, punching, beating, stabbing, biting, pushing, shoving, throwing, pulling, dragging, dropping, shaking, strangling/choking, smothering, burning, scalding, and poisoning.
# Exceptions
Physical injuries to the anal or genital area or surrounding areas (e.g., anal or genital bruising or tearing; internal injuries resulting from penetration by a penis, hand, finger, or other object) that occur during attempted or completed sexual abuse, or other physical injuries that result from attempted or completed sexual abuse (e.g., bruises due to restraint, hitting, pushing) are considered sexual abuse and do not constitute physical abuse.
# Sexual Abuse
Any completed or attempted (non-completed) sexual act, sexual contact with, or exploitation (i.e., noncontact sexual interaction) of a child by a caregiver.
# Sexual Act
Sexual acts include contact involving penetration, however slight, between the mouth, penis, vulva, or anus of the child and another individual. Sexual acts also include penetration, however slight, of the anal or genital opening by a hand, finger, or other object (Basile and Saltzman 2002). Genital on genital contact includes:
# Noncontact Sexual Abuse
Noncontact sexual abuse does not include physical contact of a sexual nature between the caregiver and the child.
Noncontact sexual abuse can include the following:
1. Acts which expose a child to sexual activity (e.g., pornography; voyeurism of the child by an adult; intentional exposure of a child to exhibitionism); 2. Filming 10 of a child in a sexual manner (e.g., depiction, either photographic or cinematic, of a child in a sexual act); 3. Sexual harassment of a child (e.g., quid pro quo; creating a hostile environment because of comments or attention of a sexual nature by a caregiver to a child); 4. Prostitution of a child (e.g., employing, using, persuading, inducing, enticing, encouraging, allowing, or permitting a child to engage in or assist any other person to engage in, prostitution 11 , or sexual trafficking. Sexual trafficking is defined as the act of transporting children across international borders through deception for forced sexual activity such as prostitution or sexual slavery (Miller and Jayasundara 2001).
# Psychological Abuse
Intentional caregiver behavior (i.e., act of commission) that conveys to a child that he/she is worthless, flawed, unloved, unwanted, endangered, or valued only in meeting another's needs 12 . Psychological abuse can be continual (e.g., chronic and pervasive) or episodic (e.g., triggered by a specific context or situation: caregiver substance use/abuse) (Kairys and Johnson 2002).
Psychologically abusive behaviors may include blaming, belittling, degrading, intimidating, terrorizing, isolating, restraining, confining, corrupting, exploiting, spurning, or otherwise behaving in a manner that is harmful, potentially harmful, or insensitive to the child's developmental needs, or can potentially damage the child psychologically or emotionally (Barnett, Manly, and Cicchetti 1991;McGee and Wolfe 1991a, b).
# Terrorizing
Terrorizing includes caregiver behavior that is life-threatening; makes a child feel unsafe (e.g., situations that are likely to physically hurt, kill, or abandon the child) (Myers et al. 2002); sets unrealistic expectations of the child with threat of loss, harm, or danger if expectations are not met; and threatens or perpetrates violence against a child or a child's loved ones or objects (including toys, pets, or other possessions) (Kairys and Johnson 2002). For example, placing a child in unpredictable or chaotic circumstances would be considered terrorizing as would be placing a child in a situation reasonably considered dangerous by either the child or another adult.
# Isolating
Psychological isolation occurs when a caregiver forbids, prevents, or minimizes a child's contact with others.
# DEFINITIONS OF ACTS OF OMISSION (CHILD NEGLECT)
Failure to Provide (Barnett, Manly, and Cicchetti 1993) Failure by a caregiver to meet a child's basic physical, emotional, medical/dental, or educational needs-or combination thereof. Failure to provide includes the following:
# Physical Neglect
Caregiver fails to provide adequate nutrition, hygiene, or shelter; or, caregiver fails to provide clothing that is adequately clean, appropriate size, or adequate for the weather. Several examples follow (Barnett, Manly, and Cicchetti 1993):
• Nutrition: A 9-year-old child makes dinner several times per week because the caregiver(s) are sleeping, away, or otherwise unavailable; a child misses or is denied meals on numerous occasions over time; a child is diagnosed as being severely malnourished.
• Hygiene: Child is dirty, smells bad, or has unwashed hair. Child's living situation is unsanitary; dirty dishes and spoiled food are left on the kitchen table and counter.
• Shelter: Living arrangements for the child and family are unstable for two weeks or more; the residence is infested with roaches or vermin; residence in unheated or inadequately heated because caregivers have failed to ensure heat available.
• Clothing: The child always wears clothing that is too small; the child is not given a warm coat and gloves when the weather is cold.
# Emotional Neglect
Caregiver ignores the child, or denies emotional responsiveness or adequate access to mental health care (e.g., caregiver does not respond to infant cries or older child's attempt to interact) (Barnett, Manly, and Cicchetti 1993).
# Medical/Dental Neglect
Caregiver fails to provide adequate access to medical, vision, or dental care for the child. Examples include the following:
• Caregiver does not administer prescribed medications;
• Caregiver refuses to take the child for needed medical attention or seek timely medical attention (Barnett, Manly, and Cicchetti 1993).
# Educational Neglect
Caregiver fails to provide access to adequate education. Examples include:
• Caregiver allows child to miss 25 or more school days in one academic year without excuse;
• Caregiver does not enroll the child in school; caregiver encourages a child (under 16 years of age) to drop out of school (Barnett, Manly, and Cicchetti 1993).
# Failure to Supervise
Failure by the caregiver to ensure a child's safety within and outside the home given the child's emotional and developmental needs (Barnett, Manly, and Cicchetti 1993).
# Inadequate Supervision
Failure by the caregiver to ensure that the child engages in safe activities and uses appropriate safety devices; to ensure that the child is not exposed to unnecessary hazards; or to ensure appropriate supervision by an adequate substitute caregiver (Barnett, Manly, and Cicchetti 1993).
Inadequate supervision (sometimes called "supervisional neglect ") includes occasions when a caregiver knowingly fails to protect a child from maltreatment perpetrated by a substitute caregiver. Under such conditions, the primary caregiver's behavior would be considered neglectful only if the maltreatment was recognized and allowed to occur. Regardless of the primary caregiver's knowledge of the maltreatment, the substitute caregiver's behavior would be considered maltreatment.
# Exposure to Violent Environments
Caregiver intentionally 13 fails to take available measures to protect the child from pervasive violence within the home, neighborhood, or community (Kairys and Johnson 2002). For example, a caregiver who sells illicit drugs out of the child's home exposes the child to a violent environment; or, a school bus driver (temporary caregiver) who allows a student to be routinely victimized by another student while riding the bus without taking steps to intervene (e.g., notifying school administrators) also exposes a child to a violent environment.
Exposure of a child to violence between caregivers in the home may also qualify as exposure to a violent environment, particularly if the caregivers do not take available measures to protect the child from exposure. But, in instances where the caregiver is being victimized by a partner, and alternatives to protect the child are not available, or the caregiver is unaware of alternatives, the caregiver is not maltreating the child.
# CO-OCCURRENCE OF MULTIPLE TYPES OF ABUSE AND NEGLECT 14
Multiple forms of maltreatment often coexist, as described in these examples:
• Police find a 20-month-old child with bruises on extremities, cigarette burns to the forehead and upper chest, and signs of dehydration. The child was at home with the male caregiver who was high on opium. In this instance, physical abuse, failure to provide (adequate nutrition), failure to protect (caregiver is under the influence of drugs and unable to care for the child), and psychological abuse have occurred.
• Paramedics find a two-and-a-half-year-old child. The undressed child was walking outside in the winter and had belt-patterned bruises on the legs and trunk. The child also had ethyl alcohol in his blood system. In this example, physical abuse, failure to provide (adequate clothing), and failure to protect (unaccompanied child) have occurred.
• Upon reading a school report card, the caregiver/parent slaps the child's face, withholds food, and berates the child's ability until "better marks" are produced. In this scenario, physical abuse, failure to provide, and psychological abuse have occurred.
# INTRODUCTION
Each section describes the recommended data elements that can be included in a surveillance system designed to collect information on child maltreatment. The order in which the data elements are presented is not intended to suggest a hierarchy; users may select data elements that best fit their surveillance needs.
Depending on the applicability of the information, some or all of the following categories of information are listed for each data element:
• Description or definition of the data element;
• Uses/data element type describes how the data element should be used and whether it is a basic or expanded data element;
• Discussion of relevant conceptual or operational issues;
• Allow for multiple responses indicates when it is appropriate to include all applicable answers or response options;
• Field values/coding instructions indicate how to enter data in the field and what each represents;
• Data standards or guidelines used to define the data elements and its field values;
• Other references consulted in developing the data elements.
# BASIC AND EXPANDED DATA ELEMENTS FOR CHILD MALTREATMENT SURVEILLANCE
# Discussion
The data elements in this section relate directly to information about the index child.
Creators of surveillance systems should be mindful of confidentiality and safety issues as they develop and use their system. No data should be collected or stored that could potentially jeopardize a child's safety. When developing a surveillance system for child maltreatment, the issue of confidentiality must be balanced with the need for data linkage across multiple data sets. Data elements containing identifying information may be stripped once data from all records related to the child have been identified and entered into the surveillance system.
# *Expanded data element
Case ID 1.01
# Description/Definition
A required, unique identification code used by the agency compiling child maltreatment surveillance data.
# Uses/Data Element Type
Ensures that entered or accessed records correspond with the proper child. It also facilitates data linkage for administrative and research purposes.
Data element type: Basic.
# Discussion
Case ID may be assigned by the agency compiling child maltreatment (CM) surveillance data, or it may be an identifier previously assigned by the contributing data source. Case ID can be identical to the identifier created to allow linkage across multiple sources.
Because identification and documentation of CM is not standard across the many sources that may collect data on abuse and neglect, data from multiple sources may be needed to better estimate the number of children who experience maltreatment. As such, developers of surveillance systems may want to explore the viability of a variety of approaches to child maltreatment surveillance. One method is to include data from multiple sources (e.g. The mechanics of how to set up a database that accommodates data from multiple sources are not discussed in this document. Users should refer to other sources for information on how to set up a database.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
For recommended field values and coding instructions, please refer to Data Standards or Guidelines listed below.
# Data Standards or Guidelines
Health Level 7, Version 3.0 (HL7 2003); www.HL7.org
Child's Name 1.02
# Description/Definition
Child's first, middle, and last name.
# Uses/Data Element Type
Allows for linking data on a particular child across records, thus reducing the chance of duplicate records on the same child.
Can be used with 1.03 Alternate Name for Child to ensure that records related to the child are correctly linked to the child.
Data element type: Basic.
# Discussion
The practice of including names in public health surveillance systems is not uncommon. Most state-level surveillance systems for infectious diseases include names, as do surveillance systems such as the National Violent Death Reporting System. Additionally, inclusion of the index child's name(s) in a surveillance system to track child maltreatment allows for a unique identifier that can facilitate data linkage across sources.
These data are not intended for tracking victims or offenders. Protection of individuals' privacy is paramount; to protect child victim privacy and confidentiality, access to this data element must be limited to authorized personnel.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
Record child's name as follows: <Family Name>< Given Name>< Middle Name or Initial>Î f the child's name does not conform to the coding instructions above, please refer to the Data Standards or Guidelines listed below.
Alternate Name for Child 1.03
# Description/Definition
Other first, middle, and last name by which child is known.
# Uses/Data Element Type
Allows for linking data on a particular child across records, thus reducing the chance of duplicate records on the same child.
Can be used with 1.02 Child's Name to ensure that records related to the child are correctly linked to the child.
Data element type: Basic.
# Discussion
The practice of including names in public health surveillance systems is not uncommon. Most state-level surveillance systems for infectious diseases include names, as do surveillance systems such as the National Violent Death Reporting System. Additionally, inclusion of the index child's name(s) in a surveillance system to track child maltreatment allows for a unique identifier that can facilitate data linkage across sources.
These data are not intended for tracking victims or offenders. Protection of individuals' privacy is paramount; to protect child victim privacy and confidentiality, access to this data element must be limited to authorized personnel.
# Allow for Multiple Responses
No.
# Discussion
Because developmental changes occur rapidly in the first three years of life, record the child's age in months for ages 3 years (36 months) and younger . Age in months allows for greater precision and a better understanding of the child's physical, cognitive, and emotional abilities at the time of the incident of maltreatment.
If the child's exact age is not available, an estimated age can be used.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
Record age in months and round to the nearest month. For example, a child who is 2 years and 3 months would be coded as 27 months of age. If the child is 2 years, 3 months, and 15 or fewer days, the age would be coded as 27 months. On the other hand, if the child is 2 years, 3 months, and 16 or more days, the age would be coded as 28 months.
# Data Standards or Guidelines
Common Data Elements Implementation Guide, Version 2.4 (CDC 2000); www.cdc.gov/data/index.htm
Age (in Years) of Child Older Than 3 years 1.06
# Description/Definition
Age of child, if the child is older than 3 years, at the time of the incident on which data are being collected.
# Uses/Data Element Type
Can be used if child's date of birth (see 1.04) is not available or is in question.
Data element type: Expanded.
# Discussion
If the child's exact age is not available, an estimated age can be used.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
Record age in years. If fractional ages (e.g., 7.5 years or 7 ½ years) are provided, round to the nearest year. For example, a child who is 7.5 years of age would be coded as 8 years.
# Data Standards or Guidelines
Common Data Elements Implementation Guide, Version 2.4 (CDC 2000); www.cdc.gov/data/index.htm
Sex of Child 1.07
# Description/Definition
Sex of child.
# Uses/Data Element Type
Standard demographic and identifying information.
Data element type: Basic.
# Allow for Multiple Responses
No. Data element type: Basic.
# Field Values/Coding Instructions
# Discussion
The categories below represent a social-political construct designed for collecting data on the race and ethnicity of broad population groups in the United States. For more than 20 years, the Federal government has promoted the use of a common language to ensure uniformity and comparability of data on race and ethnicity. Development of the data standards stemmed in large measure from new responsibilities to enforce civil rights laws. Data were needed to monitor equal access in housing, education, employment, and other areas for populations that historically had experienced discrimination and differential treatment because of their race or ethnicity. The standards are used not only in the decennial census (which provides data for the "denominator" for many measures), but also in household surveys, on administrative forms (e.g., school registration and mortgage-lending applications), and in medical and other research.
Race is a concept used to differentiate population groups largely by physical characteristics transmitted by descent. This concept lacks clear scientific definition, as racial categories are neither precise nor mutually exclusive. The common use of race in the United States draws upon differences not only in physical attributes, but also in ancestry and geographic origins. (OMB 1997) was developed to meet Federal legislative and program requirements, and these standards are used widely in the public and private sectors. The directive provides five basic racial categories but states that collection of race data need not be limited to these categories. However, additional reporting that uses more detail must be organized in such a way that the additional categories can be aggregated into the five basic groups. Although the directive does not specify a method for determining an individual's race, OMB prefers self-identification to identification by an observer whenever possible. The directive states that persons of multiple racial origins should be coded using multiple categories, not a multiracial category.
# Allow for Multiple Responses
Yes. If the agency providing the data to the child maltreatment surveillance system uses multiple racial categories, the child maltreatment surveillance system also allows for multiple racial categories to be coded. Uses/Data Element Type Provides information on preexisting disabilities or health conditions that the child may have which are not likely to have resulted from abuse or neglect. Differentiates between conditions existing before the onset of maltreatment, comorbid conditions, and conditions resulting from maltreatment.
# Field Values/Coding Instructions
Data element type: Expanded.
# Discussion
Access to data on preexisting disabilities or health conditions will allow for more accurate prevalence rates of risk factors for maltreatment and for specific points of intervention.
Children with physical, behavioral, health, and cognitive disabilities are at higher risk for maltreatment than children without such conditions Knutson 1998, 2000). These children comprise more than one third of the maltreated children between birth and 18 years of age.
# Allow for Multiple Responses
Yes.
# Field Values/Coding Instructions
# Discussion
As defined previously, an incident of child maltreatment is an event documented by CPS, law enforcement, the medical system, or other reporting sources (e.g., school) where child maltreatment is alleged or confirmed.
# Date of Incident 2.01
# Description/Definition
Date of the current incident of child maltreatment.
# Uses/Data Element Type
Provides information on when the incident occurred.
Date of Incident can be used with data element 1.04 Birth Date of Child to calculate the child's age at the time of the current incident.
If date of incident is not available, 2.02 Date of Report to Child Protective Services can be used instead.
Data element type: Basic.
# Discussion
If the incident of maltreatment exceeded one day, code the date that the incident ended. If the date of the incident is unknown, use the date of record (report).
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
For recommended field values and coding instructions, please refer to Data Standards and Guidelines listed below.
# Data Standards or Guidelines E1384-96 (ASTM 1996)
Health Level 7, Version 3.0 (HL7 2003); www.HL7.org
Date of Report to Child Protective Services (CPS) 2.02
# Description/Definition
Date on which the current incident of child maltreatment was reported to CPS.
# Uses/Data Element Type
Provides information on when the incident came to the attention of CPS.
If the actual date of incident is not available, Date of Report to Child Protective Services can be used as a proxy for data element 2.01 Date of Incident.
Data element type: Basic.
# Discussion
If the date of incident is unknown, use the date of record (report).
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
For recommended field values and coding instructions, please refer to Data Standards and Guidelines listed below.
# Data Standards or Guidelines E1384-96 (ASTM 1996).
Health Level 7, Version 3.0 (HL7 2003); www.HL7.org
Location where Maltreatment Occurred 2.03
# Description/Definition
Where did the maltreatment occur?
# Uses/Data Element Type
Describes the context in which the maltreatment took place.
Can be used with 2.04.03 Type of Residence to determine the specific type of location or residence if the response below is "Child's residence".
Data element type: Expanded.
# Discussion
Child maltreatment does not always occur in the child's home. The location(s) where child maltreatment occurs is beneficial for designing effective prevention programs.
# Allow for Multiple Responses
Yes.
# Field Values/Coding Instructions
# Uses/Data Element Type
Provides the location at which the index child resides at least most of the time.
Can be used with 2.04.02 Child's Second Address at Time of Incident to determine where the child was living at the time of the incident of maltreatment.
Data element type: Basic.
# Discussion
When child custody is shared due to parental divorce or legal separation, a child can have more than one official address. The first address should be the one where the index child was staying at the time of the incident. The other address, where the child spends some or most of the time, may be entered in 2.04.02 Child's Second Address at Time of Incident.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
For recommended field values and coding instructions, please refer to Data Standards and Guidelines listed below.
# Data Standards or Guidelines
Health Level 7, Version 3.0 (HL7 2003); www.HL7.org
Child's Second Address at Time of Incident 2.04.02
# Description/Definition
Address of the index child's second official residence at time of incident.
# Uses/Data Element Type
Provides the second location at which the index child resides when not at the first address (see 2.04.01 Child's First Address at Time of Incident).
Can be used with 2.04.01 Child's First Address at Time of Incident to determine where the child was living at the time of the incident of maltreatment.
Data element type: Basic.
# Discussion
In cases where custody of a child is shared due to parental divorce or legal separation, a child can have more than one official address. The other address at which the child spends some or most of the time may be entered in 2.04.01 Child's First Address at Time of Incident.
# Data Type (and Field Length)
XAD -extended address ( 106)
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
For recommended field values and coding instructions, please refer to Data Standards and Guidelines listed below.
# Data Standards or Guidelines
Health Level 7, Version 3.0 (HL7 2003); www.HL7.org
Type of Residence 2.04.03
# Description/Definition
Type of residence or living arrangement in which the index child resides at the time of the incident.
# Uses/Data Element Type
Provides information on the context and environment in which the child lives at the time of the incident.
Data element type: Expanded.
# Discussion
If the index child has more than one address, as indicated by data in 2. 04
# Uses/Data Element Type
The length of time the child has lived at the current address can provide information on the stability of the child's living situation.
Data element type: Expanded.
# Discussion
See discussion under 2.04.04 Time in First Residence.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
Record time in residence in number of months, rounded to the nearest month.
Physical Abuse
# Discussion
Physical abuse is the intentional use of physical force against a child that results in or has the potential to result in physical injury. Physical abuse includes physical acts ranging from those which do not leave a physical mark on the child to those which cause permanent disability, disfigurement, or death.
Physical abuse can result from discipline or physical punishment and is coded regardless of the caregiver's intent to harm or injure the child.
The following are considered sexual abuse and should be coded accordingly:
• Physical injuries to the anal, genital, or surrounding areas that occur during attempted or completed sexual abuse (e.g., anal or genital bruising or tear; internal injuries resulting from penetration by a penis, hand, finger, or other object) • Other physical injuries that result from attempted or completed sexual abuse (e.g., bruises due to restraint, hitting, or pushing)
Notation of Physical Abuse 2.04.06
# Description/Definition
Is physical abuse noted in any record of this incident of maltreatment?
# Uses/Data Element Type
Used to describe whether the child experienced physical abuse.
Data element type: Basic.
# Discussion
Noted physical abuse includes any mention of the term "physical abuse" or "child physical abuse" or intentionally inflicted injury of the child by a caregiver in the child's record. Noted physical abuse also includes suspected abuse or an indication that an abuse-related referral was made (e.g., to CPS).
If the record has a notation that physical abuse is suspected, code physical abuse as noted in that record. Other terms that can be used include but are not limited to "substantiated," "indicated," "reason to suspect," "suspected," "reported," "documented," "founded," "supported," "credible evidence exists," "suspected-confirmation unknown," or "suspected-confirmed."
Do not note physical abuse if the record indicated that the abuse was "unsubstantiated," "unsubstantiated due to intentionally false report," "ruled out," or "suspected-ruled out" (NCANDS 2004;DePanfilis and Salus 2003).
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
Code Description
# 01
No, physical abuse is not noted in any record of this incident of maltreatment. 02Yes, physical abuse is noted in one or more records of this incident of maltreatment. 99It is unknown if physical abuse occurred in this incident of maltreatment.
Abusive Head Trauma/Shaken Baby Syndrome 2.04.07
# Description/Definition
Describes a constellation of injuries related to violently shaking an infant or toddler and can include impact to the head if the infant is subsequently thrown down onto a crib or other surface.
# Uses/Data Element Type
Can be used to determine whether the child is a victim of Shaken Baby Syndrome (SBS)/Abusive Head Trauma (AHT).
Data element type: Basic.
# Discussion
SBS/AHT is defined as the violent shaking of an infant or child with sufficient vigor to produce whiplash forces which can result in subdural and retinal bleeding, seizures, paralysis, and death. SBS commonly occurs in the context of an inconsistent or inappropriate history given by the caregiver and can be accompanied by other injuries such as posterior rib fractures and retinal hemorrhages.
SBS/AHT is commonly observed in children under 1 year of age, but it has been documented in children as old as 3 to 4 years of age.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
# Description/Definition
Archival data sources from which child maltreatment surveillance information is abstracted.
# Uses/Data Element Type
Identifies the data source(s) documenting physical abuse in the current incident of maltreatment.
Data element type: Basic.
# Allow for Multiple Responses
Yes. Repetition is allowed to identify all sources containing data on physical abuse in the current incident. Sexual acts comprise acts in which contact involves penetration, however slight, between the caregiver and the child. A caregiver can also force or coerce a child to commit a sexual act on another individual (either adult or child).
# Field Values/Coding Instructions
Abusive sexual contact includes acts in which penetration is not attempted, but intentional touching occurs either directly or through the clothing of the genitalia, anus, groin, breast, inner thigh, or buttocks. Sexual contact can be performed by the caregiver on the child, by the child on the caregiver, or by the child on another adult or child through force or coercion by the caregiver. Sexual contact does not include touching required for normal care or attention to day-to-day needs of the child.
Noncontact sexual abuse does not require physical contact of a sexual nature between the caregiver and the child. However, it does include acts which expose a child to sexual activity such as filming of a child in a sexual manner, sexual harassment of a child, or prostitution of a child.
Notation of Sexual Abuse 2.04.09
# Description/Definition
Is sexual abuse noted in any record of this incident of maltreatment?
Uses/Data Element Type Describes whether the child experienced sexual abuse.
Data element type: Basic.
# Discussion
Noted sexual abuse includes any mention of the term "sexual abuse," "child sexual abuse," or similar variation in the child's record. Noted sexual abuse also includes suspected abuse or an indication that an abuse-related referral was made (e.g., to CPS). If a notation in the record states that sexual abuse is suspected, code sexual abuse as documented in that record. Other terms that can be used include, but are not limited to, "substantiated," "indicated," "reason to suspect," "suspected," "reported," "documented," "founded," "supported," "credible evidence exists," "suspected-confirmation unknown," or "suspected-confirmed."
Sexual abuse would not be noted if the record indicated that the sexual abuse was "unsubstantiated," "unsubstantiated due to intentionally false report," "ruled out," or "suspected-ruled out" (NCANDS 2004;DePanfilis and Salus 2003).
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
Code Description
# 01
No, sexual abuse is not noted in any record of this incident of maltreatment. 02Yes, sexual abuse is noted in one or more records of this incident of maltreatment. 99It is unknown if sexual abuse occurred in this incident of maltreatment.
Data Source(s) Documenting Sexual Abuse 2.04.10
# Description/Definition
Archival data sources from which child maltreatment surveillance information is abstracted.
# Uses/Data Element Type
Identifies the data source(s) documenting sexual abuse in the current incident of maltreatment.
Data element type: Basic.
# Allow for Multiple Responses
Yes. Repetition is allowed to identify all sources containing data on sexual abuse in the current incident.
# Field Values/Coding Instructions
# Discussion
Sexual acts include penetration, however slight, between the mouth, penis, vulva, or anus of the child and the adult. Sexual acts can also include penetration, however slight, of the anal or genital opening by a hand, finger, or other object.
Sexual acts can be performed by the caregiver on the child or by the child on the caregiver. A caregiver can also force or coerce a child to commit a sexual act on another individual (either child or adult).
Penetration Status 2.04.11
# Description/Definition
Describes whether the sexual abuse involved penetration or attempted penetration of either the child or the adult.
# Uses/Data Element Type
If used with 2.04.12 Object Used for Sexual Act(s) and 2.04.13 Part of the Body Affected by Sexual Act(s) information can be gathered regarding the process by which the abusive sexual contact occurred.
Data element type: Expanded.
# Discussion
Penetration is defined as sexual contact involving penetration, however slight, of the mouth, penis, vulva, or anus. Penetration status is either all or nothing. That is, even slight penetration should be included as "penetration."
No penetration includes intentional touching, either directly or through the clothing.
# Allow for Multiple Responses
No. Object Used for Sexual Act(s) 2.04.12
# Field Values/Coding Instructions
# Description/Definition
Describes the object used for penetration or attempted penetration.
# Uses/Data Element Type
If used with 2. 04.11 Penetration Status and 2.04.13 Part of the Body Affected by Sexual Act(s) information can be gathered regarding the process by which the abusive sexual contact occurred.
Data element type: Expanded.
# Allow for Multiple Responses
Yes. Part of the Body Affected by Sexual Act(s) 2.04.13
# Field Values/Coding Instructions
# Description/Definition
Describes the body part penetrated or attempted to be penetrated during the sexual act and whether the penetration was done by the adult or child.
# Uses/Data Element Type
If used with 2.04.11 Penetration Status and 2.04.12 Object Used for Sexual Act(s) information can be gathered regarding the process by which the abusive sexual contact occurred.
Data element type: Expanded.
# Allow for Multiple Responses
Yes. Sexually Transmitted Disease Diagnosed 2.04.14
# Field Values/Coding Instructions
# Description/Definition
Whether a sexually transmitted disease (STD) was found in the context of the current incident of sexual abuse.
Uses/Data Element Type Documents sexually transmitted disease infection related to the current incident of sexual abuse. Identification of the STD can precede or follow the discovery of sexual abuse.
Data element type: Expanded.
# Discussion
STDs in children, particularly ages 0 to 9 years, are a signal that sexual abuse may be occurring.
With older children and teenagers who could be sexually active, it is important to differentiate between STDs resulting from sexual abuse and STDs resulting from other sexual behavior.
In addition, if the incident of sexual abuse was within 3 to 6 months of the date of record, possible STD infection can be unknown or undetectable.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
# Uses/Data Element Type
Indicates whether the index child experienced abusive sexual contact in this incident of maltreatment.
Data element type: Expanded.
# Discussion
Abusive sexual contact includes intentional touching, either directly or through the clothing, that does not involve penetration.
Abusive sexual contact can be performed by the caregiver on the child or by the child on the caregiver. A caregiver can also force or coerce a child to engage in sexual contact with another individual (child or adult).
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
Code Description
# 01
No, abusive sexual contact did not occur in this incident of maltreatment. 02Yes, abusive sexual contact occurred in this incident of maltreatment. 99It is unknown/not documented whether abusive sexual contact occurred.
# Other References Basile and Saltzman 2002
Object Used for Abusive Sexual Contact 2.04.16
# Description/Definition
Describes the object used for sexual contact.
# Uses/Data Element Type
If used with 2. 04.11 Penetration Status and 2.04.17 Part of the Body Affected by Abusive Sexual Contact information can be gathered regarding the process by which the abusive sexual contact occurred.
Data element type: Expanded.
# Allow for Multiple Responses
Yes.
# Field Values/Coding Instructions
# Uses/Data Element Type
Indicates whether the index child experienced noncontact sexual abuse in this incident of maltreatment.
Data element type: Expanded.
# Discussion
Noncontact sexual abuse includes acts such as:
• Voyeurism of the child by an adult;
• Intentional exposure of a child to exhibitionism;
• Exposure to pornography;
• Photograph(s) of a child in a sexual manner or act;
• Filming of a child engaged in a sexual manner or act;
• Sexual harassment of a child;
• Sexual trafficking of a child;
• Employing, using, persuading, inducing, enticing, encouraging, allowing, or permitting a child to engage in or assist any other person to engage in prostitution.
Noncontact sexual abuse does not include physical contact of a sexual nature between the caregiver and the child.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
Code Description
# 01
No, noncontact sexual abuse did not occur in this incident of maltreatment. 02Yes, noncontact sexual abuse occurred in this incident of maltreatment (specify). 99
It is unknown/not documented whether noncontact sexual abuse occurred.
Method of Noncontact Sexual Abuse 2.04.19
# Description/Definition
Describes the method by which noncontact sexual abuse occurred.
# Uses/Data Element Type
Describes the process(es) by which the child experienced noncontact sexual abuse.
Data element type: Expanded.
# Discussion
Noncontact sexual abuse includes acts such as:
• Voyeurism of the child by an adult;
• Intentional exposure of a child to exhibitionism;
• Exposure to pornography;
• Photograph(s) of a child in a sexual manner or act;
• Filming of a child engaged in a sexual manner or act;
• Sexual harassment of a child;
• Sexual trafficking of a child;
• Employing, using, persuading, inducing, enticing, encouraging, allowing, or permitting a child to engage in or assist any other person to engage in prostitution.
# Allow for Multiple Responses
Yes.
# Field Values/Coding Instructions
# Discussion
It can be argued that all forms of child maltreatment include psychological abuse because all forms of child maltreatment have emotional consequences for the child. However, specific caregiver behaviors that involve trauma to the child caused by acts, threats of acts, or coercive tactics such as those listed below constitute a form of child maltreatment that is unique. This list is not exhaustive.
Psychological/emotional maltreatment can include but is not limited tothe following: • Behaving in a manner that is harmful, potentially harmful, or insensitive to the child's developmental needs; • Behaving in a manner that can potentially damage the child psychologically or emotionally.
Because psychological abuse is often difficult to detect and is unlikely to be picked up by data systems used in traditional public health surveillance, the number of children who experience psychological abuse will likely exceed those counted in traditional surveillance.
# Notation of Psychological Abuse
2.04.20
# Description/Definition
Is psychological abuse noted in any record of this incident of maltreatment?
Uses/Data Element Type Describes whether the child experienced psychological abuse.
Data element type: Basic.
# Discussion
Noted psychological abuse includes any mention of the terms "psychological abuse," "emotional abuse," "psychological maltreatment," or similar variation in the child's record. Noted psychological abuse also includes suspected abuse. If there is a notation in the record that psychological abuse is suspected, then code psychological abuse as documented in that record. Other terms that can be used include but are not limited to "substantiated," "indicated," "reason to suspect," "suspected," "reported," "documented," "founded," "supported," "credible evidence exists," "suspected-confirmation unknown," or "suspectedconfirmed."
Psychological abuse would not be noted if the record indicated that the psychological abuse was "unsubstantiated," "unsubstantiated due to intentionally false report," "ruled out," or "suspectedruled out" (NCANDS 2004;DePanfilis and Salus 2003).
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
Code Description
# 01
No, psychological abuse is not noted in any record of this incident of maltreatment. 02Yes, psychological abuse is noted in one or more records of this incident of maltreatment. 99It is unknown whether psychological abuse occurred in this incident of maltreatment.
Data Source(s) Documenting Psychological Abuse 2.04.21
# Description/Definition
Archival data sources from which child maltreatment surveillance information is abstracted.
# Uses/Data Element Type
Identifies the data source(s) documenting psychological abuse in the current incident of maltreatment.
Data element type: Basic.
# Allow for Multiple Responses
Yes. Repetition is allowed to identify all sources containing data on psychological abuse in the current incident. Method of Psychological Abuse 2.04.22
# Field Values/Coding Instructions
# Description/Definition
Describes the process by which psychological abuse occurred.
# Uses/Data Element Type
Describes the process(es) by which the child was psychologically abused.
Data element type: Expanded.
# Discussion
Psychologically abusive behaviors can include blaming, belittling, degrading, intimidating, terrorizing, isolating, restraining, confining, corrupting, exploiting, spurning or behaving in a manner that is harmful, potentially harmful, or insensitive to the child's developmental needs or may potentially damage the child psychologically or emotionally. (Barnett, Manly, and Cicchetti 1993;McGee and Wolfe 1991a, b) Terrorizing includes caregiver behavior that is life-threatening or makes a child feel unsafe (e.g., situations in which a child is likely to be hurt, killed, or abandoned) (Myers et al. 2002); sets unrealistic expectations of the child with threat of loss, harm, or danger if not met; and threatens or perpetrates violence against a child or a child's loved ones or objects (toys, pets, other possessions) (Kairys and Johnson 2002). For example, placing a child in unpredictable or chaotic circumstances would be considered terrorizing as would be placing a child in a situation that would reasonably be considered dangerous by the child or another adult.
Isolating (psychological) occurs when a caregiver forbids, prevents, or minimizes a child's contact with others.
# Allow for Multiple Responses
Yes.
# Field Values/Coding Instructions
# Discussion
Neglect encompasses a multitude of caregiver behaviors that can be divided into two types:
1. Failure to provide or meet the basic physical, emotional, or educational needs of the child. Failure to provide includes physical, emotional, medical/dental, and educational neglect;
2. Failure to supervise or ensure a child's safety within and outside the residence, given the emotional and developmental needs of the child. Failure to supervise includes inadequate supervision and exposure of the child to violent environments.
Although neglect comprises most maltreatment cases (DHHS 2003), neglect is less likely than physical or sexual abuse to be captured by data systems used in traditional public health surveillance. For example, emergency departments and hospitals are likely to see only the most egregious cases of medical, dental, or supervisional neglect. Few, if any, cases of physical, emotional, or educational neglect are seen. Consequently, physicians may fail to recognize and document cases of neglect. For this reason, traditional surveillance systems may undercount cases of neglect.
Failure to provide 2.04.23 Notation of failure to provide 2.04.24 Data source(s) documenting failure to provide 2.04.25 Mitigating circumstances for failure to provide*
# Discussion
Neglect-failure to provide includes the following types of neglect:
• Physical neglect: Caregiver fails to provide adequate nutrition, hygiene, shelter, or clothing that is adequately clean, appropriate size, or adequate for the weather.
Examples (Barnett, Manly, and Cicchetti 1993):
Nutrition: A 9-year-old makes dinner several times per week because the caregiver(s) are away, sleeping, or otherwise unavailable; a child misses or is denied meals on a number of occasions over time; a child is diagnosed as being severely malnourished.
Hygiene: Child is dirty, smells bad, or has unwashed hair. Child's living situation is unsanitary; dirty dishes and spoiled food are left on the kitchen table and counter.
Shelter: Child and family are without stable living arrangements for two weeks or more; child's residence is infested with roaches or vermin; residence is unheated because caregiver(s) failed to ensure availability of adequate heating.
Clothing: Child always wears clothing that is too small; child is not given a warm coat and gloves when the weather is cold.
• Emotional neglect: Caregiver ignores or denies emotional responsiveness to the child or provides inadequate access to mental health care for the child. Example: Caregiver does not respond to infant cries or older child's attempts to initiate interaction (Barnett, Manly, and Cicchetti 1993).
• Medical/dental neglect: Caregiver fails to provide adequate access to medical, vision, or dental care. Example: The caregiver does not administer prescribed medications. The caregiver refuses to take the child for needed medical attention (Barnett, Manly, and Cicchetti 1993).
• Educational neglect: Caregiver fails to provide access to adequate education. Examples: Caregiver allows child to miss 25 or more school days in one academic year without excuse; caregiver does not enroll the child in school; caregiver encourages a child (under 16 years of age) to drop out of school (Barnett, Manly, and Cicchetti 1993).
*Expanded data element Notation of Failure to Provide 2.04.23
# Description/Definition
Is failure to provide on the part of the caregiver noted in any record of this incident of maltreatment?
Uses/Data Element Type Describes whether the caregiver failed to provide for the child's basic needs.
Data element type: Basic.
# Discussion
Noted neglect-failure to provide includes any mention of the term "neglect," "denial," or "withholding" of basic necessities or "failure to provide." Examples of failure to provide are found in 2.04.34 Mechanism of Harm/Injury. Noted neglect-failure to provide also includes suspected neglect. If there is a notation in the record that "neglect-failure to provide" is suspected, then code neglect as documented in that record. Other terms that can be used include but are not limited to "substantiated," "indicated," "reason to suspect," "suspected," "reported," "documented," "founded," "supported," "credible evidence exists," "suspected-confirmation unknown," or "suspectedconfirmed."
Failure to provide would not be noted if the record indicated that the failure to provide was "unsubstantiated," "unsubstantiated due to intentionally false report," "ruled out," or "suspectedruled out" (NCANDS 2004;DePanfilis and Salus 2003).
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
Code Description
# 01
No, failure to provide is not noted in any record of this incident of maltreatment. 02Yes, failure to provide is noted in one or more records of this incident of maltreatment. 99It is unknown if failure to provide occurred in this incident of maltreatment.
# Discussion
Neglect-failure to supervise includes the following:
• Inadequate supervision. Failure by the caregiver to ensure that the child engages in safe activities, uses appropriate safety devices, is not exposed to unnecessary hazards, or is supervised by an adequate substitute caregiver.
Inadequate supervision includes occasions when a caregiver knowingly fails to protect the child from maltreatment perpetrated by a substitute caregiver. When this occurs, the primary caregiver's behavior would be considered neglectful only if the maltreatment was recognized and allowed to occur or recur.
• Exposure to violent environments. Failure by the caregiver to take available measures to protect the child from violence within the residence, neighborhood, or community. Uses/Data Element Type Describes whether the child experienced a lack of supervision by the caregiver.
Data element type: Basic.
# Discussion
Noted neglect-failure to supervise includes any mention of the term "neglect" or "failure to supervise" in addition to terms listed in 2.04.29 Method of Harm/Injury Related to Failure to Supervise. Noted neglect-failure to supervise also includes suspected neglect. If the record notes that neglect-failure to supervise is suspected, code as neglect. Other terms that can be used include but are not limited to "substantiated," "indicated," "reason to suspect," "suspected," "reported," "documented," "founded," "supported," "credible evidence exists," "suspected-confirmation unknown," or "suspected-confirmed."
Failure to supervise would not be noted if the record indicated that the failure to supervise was "unsubstantiated," "unsubstantiated due to intentionally false report," "ruled out," or "suspectedruled out" (NCANDS 2004;DePanfilis and Salus 2003).
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
Code Description
# 01
No, failure to supervise is not noted in any record of this incident of maltreatment. 02Yes, failure to supervise is noted in one or more records of this incident of maltreatment. 99It is unknown if failure to supervise occurred in this incident of maltreatment.
Harm Resulting from Failure to Supervise 2.04.28
# Description/Definition
Describes whether the child was harmed because of the caregiver's failure to supervise.
# Uses/Data Element Type
When used with data element 3.13 Factors Affecting Caregiver at Time of Incident, it is possible to examine the reason(s) the child was unsupervised and whether this lack of supervision resulted in harm or injury.
Data element type: Expanded.
# Discussion
An example of a child inadequately supervised with no harm or injury resulting would be a toddler who is left alone to play in an unfenced yard for several hours.
An example of a child inadequately supervised with harm but no injury resulting would be a toddler who wanders away at a park and is located later by the park rangers who transport the child to safety. The child is traumatized, but uninjured, by the experience.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
# Description/Definition
Describes the process by which the caregiver failed to supervise the child.
# Uses/Data Element Type
Determines the processes by which the caregiver failed to supervise the child.
Can be used with section 3.13 Factors Affecting Caregiver at Time of Incident to determine specific caregiver factors that may have contributed to failure to ensure the safety of the child.
Data element type: Expanded.
# Allow for Multiple Responses
Yes. Cicchetti 1991, 1993.
# Field Values/Coding Instructions
Child Fatality Related to Maltreatment Incident 2.04.30
# Description/Definition
Did the child die as a result of the incident of maltreatment?
Uses/Data Element Type Provides information about child mortality due to child maltreatment.
Data element type: Basic.
# Discussion
No time frame for death is specified for this data element. Include a death if the original incident/ injury qualifies as maltreatment based on the case definition outlined in this document and the medical examiner/coroner or death certificate classify the subsequent death as due to the incident.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
# Description/Definition
Was the child under the influence of alcohol or drugs at the time of the current incident of maltreatment?
Uses/Data Element Type Provides information about the child's behavior and susceptibility to influence at the time of the incident.
Data element type: Expanded.
# Discussion
Alcohol and drug use by a child is a risk factor for child maltreatment, particularly sexual abuse (Martino, Collins, and Ellickson 2004). Additionally, adults who abuse children have been known to give children drugs or alcohol.
Drugs prescribed for the child and over-the-counter medications used as directed should not be included unless given to the child in excess.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
# Code Description
Injury Characteristics 2.04.33
# Description/Definition
Characteristics that may prompt suspicion of child maltreatment by health care providers or others responsible for the care of children.
# Uses/Data Element Type
Provides indicators that maltreatment may have, or did, occur.
Data element type: Expanded.
# Allow for Multiple Responses
Yes.
# Field Values/Coding Instructions
# Description/Definition
Describes the mechanism by which the maltreatment occurred.
# Uses/Data Element Type
Describes the mechanism(s) by which the child was harmed or injured.
Data element type: Expanded.
# Allow for Multiple Responses
Yes.
# Field Values/Coding Instructions
# Description/Definition
Existence and location of external physical injury to child resulting from maltreatment.
# Uses/Data Element Type
Describes external physical injuries resulting from maltreatment sustained by the child.
May be used with data elements 2.04. Failure to Supervise to provide information on injuries related to different types of abuse.
Can provide information on the severity of the injury sustained by the child.
Data element type: Expanded.
# Discussion
To develop prevention strategies and advance the recognition of physical child maltreatment, it recommended that is the description of the injury include, when possible, whether the injury was inflicted by the caregiver or resulted from the caregiver's failure to protect or supervise the child.
# Allow for Multiple Responses
Yes.
# Field Values/Coding Instructions
# Description/Definition
Were ICD 9/10 codes for child abuse or neglect assigned to the case?
Uses/Data Element Type Provides information on the ICD 9/10 codes assigned to the case. Codes can be used for descriptive purposes and as a potential measure of the application of these codes. Application of these codes can be compared to reports of child maltreatment and to other sources and thus may be used to determine the extent of under-ascertainment of child maltreatment if these codes are used as the sole source of maltreatment data.
Data element type: Expanded.
# Discussion
Use of ICD 9/10 codes varies by hospital and region. As such, physicians may or may not use the ICD 9/10 codes for child maltreatment.
The ICD 9 code for general child maltreatment is 995.5X Child maltreatment syndrome.
The ICD 9 code for child abuse is E967 Child battering and other maltreatment, which includes:
• E967.0 Child battering and other maltreatment by parent • E967.1 Child battering and other maltreatment by other specified person • E967.2 Child battering and other maltreatment by unspecified person
The ICD 9 code for child neglect is E968.4 Assault by other and unspecified means-criminal neglect ("Abandonment of child, infant, or other helpless person with intent to injure or kill" WHO 1991, p.1045).
Additional ICD 9 codes for Homicide and injury purposely inflicted by other persons are commonly used for cases of maltreatment in which the victim fits the age criteria for a child and the perpetrator is designated as a caregiver. For the purpose of the document, incident is defined as any contact with CPS, law enforcement, the medical system, or other reporting sources where child maltreatment is alleged or confirmed Information for some data elements in this section may not be available for non-primary caregivers; therefore, developers of the surveillance system will need to decide how missing data should be handled.
Prior CPS Involvement with Family/Household 4.03
# Description/Definition
Describes prior contact between CPS and the index child's family or household.
# Uses/Data Element Type
Provides information on whether the index child's family or household is known to CPS.
Data element type: Expanded.
# Discussion
Prior CPS involvement with the family is a known risk factor for subsequent CPS involvement.
Exercise caution when using this data element as a risk factor for maltreatment in the light of potential biases found in reports to CPS. Some researchers have found racial, cultural, and socioeconomic disparities among children and families who are reported to CPS relative to those who are not (Cohen, DeVos, and Newberger 1997;Minnesota DHS 2002;Roberts 2002;Tsang 2001), whereas other researchers have not found these disparities (Sedlak and Broadhurst 1996). Nevertheless, knowing whether prior contact has occurred between the family and CPS is useful.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
# Acknowledgements vi
# ACKNOWLEDGEMENTS
We thank the experts and panel members who took time from their busy schedules to review and provide feedback on numerous drafts of this publication. Their valuable input helped guide us through the lengthy development process. We also thank the staff members of CDC's National Center for Injury Prevention
We welcome comments and feedback from users. Please e-mail or send suggestions for improving this document to:
# Data Standards or Guidelines
Health Level 7, Version 3.0 (HL7 2003); www.HL7.org Common Data Elements Implementation Guide, Version 2.4 (CDC 2000); www.cdc.gov/data/index.htm
# Data Standards or Guidelines
Health Level 7, Version 3.0 (HL7 2003); www.HL7.org Common Data Elements Implementation Guide, Version 2.4 (CDC 2000); www.cdc.gov/data/index.htm Data element type: Expanded.
# Discussion
Research has demonstrated a link between family residential mobility and child maltreatment (e.g., McCloskey and Bailey 2000;Reppucci, Fried, and Schmidt 2002). For example, McCloskey and colleagues found that families in which sexual abuse occurred had a higher mean number of residential moves than families in which no sexual abuse was reported.
If time in residences is split (e.g., joint custody of a child), consecutive time is defined as the total time spent at each address individually in the same 12-month period.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
Record time in residence in number of months, rounded to the nearest month.
Data Source(s) Documenting Failure to Provide 2.04.24
# Description/Definition
Archival data sources from which child maltreatment surveillance information is abstracted.
# Uses/Data Element Type
Identifies the data source(s) documenting failure to provide in the current incident of maltreatment.
Data element type: Basic.
# Allow for Multiple Responses
Yes. Repetition is allowed to identify all of the sources containing data on failure to provide in the current incident. Mitigating Circumstances for Failure to Provide 2.04.25
# Field Values/Coding Instructions
# Description/Definition
Presents possible rationale for caregiver's failure to provide for the child's basic needs.
# Uses/Data Element Type
Examines mitigating circumstances that make the caregiver unable or unwilling to provide for the child's basic needs.
Data element type: Expanded.
# Discussion
Note circumstances where caregiver(s) provide explanations or mitigating circumstances for failing to provide for the child's basic needs. However, the case still fits the definition of neglect-failure to provide.
# Allow for Multiple Responses
Yes.
# Field Values/Coding Instructions
Code Description
# 01
No mitigating circumstances for neglect-failure to provide. 02 Caregiver failed to seek or provide care for child due to religious reasons. 03 Caregiver failed to seek or provide care for child due to cultural reasons. 04 Caregiver lacked access to adequate financial resources to provide for child. 05 Caregiver lacked access to transportation to provide for child.
# 06
Caregiver lacked access to adequate or appropriate health insurance to provide for child.
# 07
Caregiver lacked access to adequate or appropriate other resources to provide for child (specify). 88 Other (specify) 99
Unknown/not documented Data Source(s) Documenting Failure to Supervise 2.04.27
# Description/Definition
Archival data sources from which child maltreatment surveillance information is abstracted.
# Uses/Data Element Type
Identifies the data source(s) documenting failure to supervise in the current incident of maltreatment.
Data element type: Basic.
# Allow for Multiple Responses
Yes. Repetition is allowed to identify all sources containing data on failure to supervise in the current incident. Internal Physical Injury 2.04.36
# Field Values/Coding Instructions
# Description/Definition
Existence and location of internal physical injury to child resulting from maltreatment.
# Uses/Data Element Type
Describes internal physical injuries resulting from maltreatment sustained by the child.
Can provide information on the severity of the injury sustained by the child.
Data element type: Expanded.
# Discussion
Numerous diverse internal physical injuries can result from maltreatment. The injuries listed below include some of the more common internal injuries, but it is impossible to list all potential injuries. Users of this document should be aware that injuries can occur that are not listed.
Similarly, it is possible that internal injuries may not be documented in the child's record. In cases where no injuries are documented, abuse may still have occurred.
Detailed descriptions of injuries can inform and aid prevention strategies while advancing the recognition of physical child maltreatment. When possible, describe whether the injury was inflicted by the caregiver or resulted from a caregiver's failure to protect or supervise the child.
# Allow for Multiple Responses
Yes.
# Field Values/Coding Instructions
# Description/Definition
Illnesses or other related health conditions that may prompt suspicion of previously undetected child maltreatment by health care providers or others responsible for the care of children.
# Uses/Data Element Type
Provides indicators that maltreatment occurred.
Data element type: Expanded.
# Discussion
Documented illnesses, when used with other contextual information, may prompt suspicion of maltreatment that might otherwise go unrecognized. The illnesses listed below often result from a caregiver's neglectful behavior. Typically, children who receive proper care and recommended vaccinations do not have these illnesses. These outcomes alone do not constitute cases, and all available information should be used to determine whether the illness is the result of maltreatment.
Illness should be coded if a causal link to maltreatment is suspected.
# Allow for Multiple Responses
Yes.
# Field Values/Coding Instructions
# Uses/Data Element Type
In combination with 2.01 Date of Incident, information can be gathered regarding the delay between the incident and care provided for the child.
Data element type: Expanded.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
Code Description
# 01
Child not brought to hospital for treatment of injuries or harm (including psychological reactions to maltreatment) related to current incident of child maltreatment 02
Child brought to hospital for treatment of injuries or harm (including psychological reactions to maltreatment) related to current incident of child maltreatment (specify date) 99Unknown/not documented For recommended specifications for coding date, please refer to Data Standards and Guidelines listed below.
# Data Standards or Guidelines E1384-96 (ASTM 1996)
Health Level 7, Version 3.0 (HL7 2003); www.HL7.org
# Discussion
We recommend collecting data on all the index child's primary caregivers and any adults who were responsible for the child at the time of the maltreatment incident. Individuals responsible for the child at the time of the incident can include a single caregiver or multiple caregivers depending on the context, and can include the primary caregiver(s) or a substitute caregiver selected by the child's primary caregiver.
Primary caregivers must live with the child at least part of the time and may include, but are not limited to a relative or biological, adoptive, step-, or foster parent(s); legal guardian(s); or the caregiver's intimate partner.
Caregivers responsible for the index child at the time of the maltreatment may or may not live with the child.
A substitute caregiver is defined as having a temporary caregiving role, care and control of the child, and responsibility for the child's health and welfare. Caregiver's Name 3.01
# Description/Definition
First, middle, and last name of index child's primary or substitute caregiver at the time of maltreatment.
# Uses/Data Element Type
Allows data about a particular caregiver to be linked across records to a specific child, thus reducing the chance of duplication.
Can be used with 1.02 Child's Name, 1.03 Alternate Name for Child, and 3.02 Alternate Name for Caregiver to ensure that records related to the child are correctly linked.
Can also be used with 3.11 Primary Caregiver Status and 3.12 Responsibility for Maltreatment to determine whether this person is the primary caregiver for the index child and is responsible for the current incident of maltreatment.
Data element type: Basic.
# Discussion
Names are commonly included in public health surveillance systems. Most state-level surveillance systems for infectious diseases include names, as do surveillance systems such as the National Violent Death Reporting System. Inclusion of the caregiver's names in a surveillance system to track child maltreatment allows a unique identifier that can facilitate data linkage across sources.
These data are not intended to be used to track victims or offenders; further, protection of individuals' privacy is paramount. To protect victim and caregiver privacy and confidentiality, access to this data element must be limited to authorized personnel.
# Allow for Multiple Responses
No. Alternate Name for Caregiver 3.02
# Description/Definition
Other first, middle, and last name of index child's primary or substitute caregiver at the time of maltreatment.
# Uses/Data Element Type
Allows data on a particular caregiver to be linked across records to a particular child, thus reducing the chance of duplication.
Can be used with 1.02 Child's Name, 1.03 Alternate Name for Child, and 3.01 Caregiver's Name to ensure that all records related to the child are correctly linked to the child.
Can also be used with 3.11 Primary Caregiver Status and 3.12 Responsibility for Maltreatment to determine whether this person is the primary caregiver for the index child and is responsible for the current incident of maltreatment.
# Data element type: Basic
# Discussion
Names are commonly included in public health surveillance systems. Most state-level surveillance systems for infectious diseases include names, as do surveillance systems such as the National Violent Death Reporting System. Inclusion of the caregiver's names in a surveillance system to track child maltreatment allows a unique identifier that can facilitate data linkage across sources.
These data are not intended to be used to track victims or offenders; further, protection of individuals' privacy is paramount. To protect victim and caregiver privacy and confidentiality, access to this data element must be limited to authorized personnel.
# Allow for Multiple Responses
No.
# Uses/Data Element Type
Can be used to calculate the caregiver's age and to distinguish between caregivers with the same name.
Data element type: Expanded.
# Discussion
If date of birth is not known, the year can be estimated from the caregiver's age.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
For recommended field values and coding instructions, please refer to Data Standards and Guidelines listed below.
# Data Standards or Guidelines E1384-96 (ASTM 1996)
Health Level 7, Version 3.0 (HL7 2003); www.HL7.org
Age of Caregiver 3.04
# Description/Definition
Age of caregiver at the time of the maltreatment incident for which data are being collected.
# Uses/Data Element Type
Can be used if caregiver date of birth (see data element 3.03) is not available or is unreliable.
Data element type: Basic.
# Discussion
Standard demographic information.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
Ages should be given in years.
# Data Standards or Guidelines
Common Data Elements Implementation Guide, Version 2.4 (CDC 2000); www.cdc.gov/data/index.htm
Sex of Caregiver 3.05
# Description/Definition
Sex of the caregiver.
# Uses/Data Element Type
Standard demographic and identifying information.
Data element type: Basic.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
# Discussion
See discussion under data element 1.08 Race of Child.
# Allow for Multiple Responses
Yes. If the agency providing the data to the child maltreatment surveillance system uses multiple racial categories, the child maltreatment surveillance system also allows for multiple racial categories to be coded. Marital Status of Caregiver 3.08
# Field Values/Coding Instructions
# Description/Definition
Caregiver's legal marital status at the time of the child maltreatment incident.
# Uses/Data Element Type
Allows for examination of the association between risk of child maltreatment and the caregiver's marital status.
Data element type: Expanded.
# Discussion
Some unmarried partners may be cohabiting. Depending on the state laws, cohabitation may qualify as common-law marriage. But in cases where cohabitating unmarried partners do not qualify as common-law marriage, the adult should be coded as Single. Similarly, same-sex cohabiting couples should only be coded as Married if same-sex marriage is allowed by the state in which they live.
This data element does not provide information on whether the caregiver or adult identified in 3.01 Caregiver's Name is cohabiting with a partner or significant other. That information can be extrapolated from 3.09 Relationship of Caregiver to the Child, 3.10 Caregiver Residential Status, and 3.11 Primary Caregiver Status.
# Allow for Multiple Responses
No. However, if the child has more than one primary caregiver, code the marital status of each caregiver. Relationship of Caregiver to the Child 3.09
# Field Values/Coding Instructions
# Description/Definition
Describes the caregiver's relationship to the index child.
# Uses/Data Element Type
Provides information about the child-caregiver relationship.
Can be use with 3.10 Caregiver Residential Status, 3.11 Primary Caregiver Status, and 3.12 Responsibility for Maltreatment to determine where the individual lives, whether he or she is a primary caregiver for the index child, and whether this person is responsible for the current incident of maltreatment.
Data element type: Basic.
# Allow for Multiple Responses
Yes.
# Field Values/Coding Instructions
# Description/Definition
Describes whether the person identified in 3.01 Caregiver's Name lives in the same residence with the index child at least part of the time when the incident of maltreatment occurred.
# Uses/Data Element Type
Provides information about the place of residence of important adults in the index child's environment.
When used with 4. 01 Other Adult(s) in Residence and 4. 02 Other Children/Siblings in Residence, the number of individuals who reside with the index child can be examined.
Data element type: Expanded.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
# Description/Definition
Describes whether the person identified in 3.01 Caregiver's Name is the index child's primary caregiver.
# Uses/Data Element Type
Provides information about who has primary responsibility for the care, custody, and control of the child.
When used with 4. 01 Other Adult(s) in Residence and 4. 02 Other Children/Siblings in Residence, the number of individuals who reside with the index child can be examined.
Data element type: Basic.
# Discussion
A primary caregiver can be one or more persons in a permanent custodial role who reside with the child. This person is responsible for the child's health and welfare and has the ultimate authority for the care and control of the child.
In cases where custody of a child is shared, more than one primary caregiver can be identified. When more than one primary caregiver is identified, all data elements in this section should be repeated for each primary caregiver.
# Description/Definition
Identifies whether the person described in 3.01 Caregiver's Name is the individual responsible for the current incident of maltreatment.
# Uses/Data Element Type
Provides information on who is responsible for the current incident of maltreatment.
Data element type: Basic.
# Allow for Multiple Responses
No. Factors Affecting Caregiver at Time of Incident 3.13
# Field Values/Coding Instructions
# Description/Definition
Describes conditions that may have affected the behavior or ability of the caregiver to provide care for the child at the time of the incident of child maltreatment.
# Uses/Data Element Type
Provides information on the caregiver's behavior and ability to provide care at the time of the incident.
Data element type: Expanded.
# Allow for Multiple Responses
Yes. Repeat coding is allowed for identification of multiple factors affecting the caregiver's ability to care for the index child.
# Field Values/Coding Instructions Code Description
Prior Termination of Parental Rights to the Index Child 3.14
# Description/Definition
Describes whether the caregiver(s) of the index child ever had parental rights to the index child terminated.
# Uses/Data Element Type
Provides information on possible history of maltreatment.
Data element type: Expanded.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
# Discussion
The language used to describe the notification of CPS about maltreatment and possible maltreatment is complex and varies among agencies and states. However, research has demonstrated that a family environment which necessitates CPS involvement, regardless of the outcome, can have long-term harmful consequences on a child's health and development (Hussey et al. 2005).
For surveillance of child maltreatment, a complaint to CPS can include, but is not exclusive to, the following language: a "referral" to CPS, a "report" to CPS, an "investigation" of the child/family by a CPS caseworker, an "allegation" of maltreatment, "substantiated" maltreatment, "founded" maltreatment, "suspected" maltreatment, and "indicated" maltreatment.
Other Adult(s) in Residence 4.01
# Description/Definition
Presence and relationship of other adults (not primary caregivers) living in the same residence as the index child at least part of the time when the incident of child maltreatment occurred.
Adults are individuals age 18 years or older.
# Uses/Data Element Type
Allows for examination of the extent to which risk of child maltreatment increases with the number of people living in the child's residence and the presence of adults not responsible for the child's health and well-being.
Data element type: Expanded.
# Discussion
To be included in this category, the person must live at least part of the time in the same residence as the child and not be a primary caregiver.
# Allow for Multiple Responses
Yes.
# Field Values/Coding Instructions
# Description/Definition
Presence of other children, including siblings of the maltreated child, living in the residence of the index child at the time of the maltreatment.
A child is defined as anyone from birth through 17 years of age.
# Uses/Data Element Type
Describes the demographic characteristics of families in which child maltreatment has occurred.
Data element type: Expanded.
# Discussion
Risk of child maltreatment increases with the number of people, specifically the number of children, living in the same residence as the child (Zuravin 1986).
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
# Description/Definition
Describes whether CPS was notified of one or more complaints of maltreatment against the index child by the primary caregiver(s) prior to the current incident.
# Uses/Data Element Type
Provides information about the relationship between the index child and the primary caregiver on whom a prior complaint was made.
Data element type: Expanded.
# Discussion
Prior complaints to CPS about the child's primary caregiver are a known risk factor for future maltreatment of the index child and other children in the home. This data element can be used with 3. 09 Relationship of Caregiver to the Child,3.10 Caregiver Residential Status,3.11 Primary Caregiver Status,and 3.12 Responsibility for Maltreatment to determine whether the adults responsible for the current incident of maltreatment also have a history with CPS related to the index child.
See discussion on racial disparities in 4.03 Prior CPS Involvement with Family/Household.
# Allow for Multiple Responses
Yes.
# Field Values/Coding Instructions
# Code Description
Prior CPS Complaint(s) on Other Adult(s) Associated with Index Child 4.05
# Description/Definition
Describes whether CPS was notified of one or more complaints of maltreatment prior to the current incident against a non-primary caregiving adult associated with the index child.
# Uses/Data Element Type
Provides information about the relationship between the index child and the non-primary caregiving adult on whom the prior complaint was made.
Data element type: Expanded.
# Discussion
Prior complaints to CPS about other adults living in or outside the child's home are a known risk factor for future maltreatment of the index child and other children in the home. This data element can be used with 3. 09 Relationship of Caregiver to the Child,3.11 Primary Caregiver Status,3.12 Responsibility for Maltreatment, and 4. 01 Other Adult(s) in Residence to determine whether the adult(s) responsible for the current incident of maltreatment also has a history with CPS related to the index child.
Can also be used with 4.06 Residency Status of Other Adult(s) with Prior CPS Complaints to determine whether the adult currently lives with the index child.
# Allow for Multiple Responses
Yes.
# Field Values/Coding Instructions
# Code Description
Prior CPS Complaint(s) Involving Index Child 4.07
# Description/Definition
Describes whether CPS reports were filed on the index child prior to the current incident of maltreatment.
# Uses/Data Element Type
Provides information on whether the index child was known to CPS prior to the current incident of maltreatment Can be used with 4.08 Types of Maltreatment in Prior Complaint(s) Involving Index Child to determine past type(s) of maltreatment the child has experienced.
Data element type: Expanded.
# Discussion
Children with a history of maltreatment are at high risk for future maltreatment, especially if they still live with the adult(s) who previously maltreated them.
# Allow for Multiple Responses
No.
# Field Values/Coding Instructions
# Description/Definition
Describes whether CPS reports were filed on other children living in the same residence as the index child prior to the current incident of maltreatment.
# Uses/Data Element Type
Provides information about whether other children living in the same residence with the index child were known to CPS prior to the current incident of maltreatment. Can be used with 4.10 Types of Maltreatment in Prior Complaint(s) Involving Other Children in Residence to determine the type(s) of maltreatment other children in the index child's environment have experienced.
Data element type: Expanded.
# Discussion
Information about prior maltreatment of other children living in the residence helps estimate the scope of violence in the index child's residence. It is useful to know whether other children in the residence have also experienced maltreatment.
# Allow for Multiple Responses
No. Data element type: Expanded.
# Field Values/Coding Instructions
Code
# Discussion
Information on prior maltreatment of other children living in the residence provides an estimate of the scope of violence in the index child's residence. It is useful to know whether other children in the residence have also experienced maltreatment.
# Allow for Multiple Responses
Yes.
# Field Values/Coding Instructions
| None | None |
d71f1562bd3352ed0ef03ffda6047e38af08d250 | cdc | None | These revised recommendations of the Advisory Committee on Immunization Practices (ACIP) on measles, mumps, and rubella prevention supersede recommendations published in 1989 and 1990. This statement summarizes the goals and current strategies for measles, rubella, and congenital rubella syndrome (CRS) elimination and for mumps reduction in the United States. Changes from previous recommendations include - Updated information on adverse events and contraindications, particularly for persons with severe HIV infection, persons with a history of egg allergy or gelatin allergy, persons with a history of thrombocytopenia, and persons receiving steroid therapy.#
- Emphasis on the use of combined MMR vaccine for most indications; - A change in the recommended age for routine vaccination to 12-15 months for the first dose of MMR, and to 4-6 years for the second dose of MMR;
- A recommendation that all states take immediate steps to implement a two dose MMR requirement for school entry and any additional measures needed to ensure that all school-aged children are vaccinated with two doses of MMR by 2001;
- A clarification of the role of serologic screening to determine immunity; - A change in the criteria for determining acceptable evidence of rubella immunity;
- A recommendation that all persons who work in health-care facilities have acceptable evidence of measles and rubella immunity;
- Changes in the recommended interval between administration of immune globulin and measles vaccination; and
# INTRODUCTION
Since monovalent vaccines containing measles, rubella, and mumps vaccine viruses-and subsequently combined measles-mumps-rubella (MMR) vaccine-were licensed, the numbers of reported cases of measles, mumps, rubella, and congenital rubella syndrome (CRS) have decreased by more than 99%. In 1993, the Childhood Immunization Initiative established goals of eliminating indigenous transmission of measles and rubella in the United States by 1996. Subsequently, the goals of the initiative were extended to include reducing the number of reported mumps cases to ≤1600 by 1996. U.S. Public Health Service year 2000 objectives include eliminating measles, rubella, and congenital rubella syndrome, and reducing mumps incidence to <500 reported cases per year. Since 1995, fewer cases of measles, rubella, and mumps have been reported than at any time since nationwide disease reporting began, and elimination of indigenous transmission appears feasible. These recommendations are intended to hasten the achievement of these disease elimination goals.
# Measles Clinical Characteristics
The incubation period of measles (rubeola) averages 10-12 days from exposure to prodrome and 14 days from exposure to rash (range: 7-18 days). The disease can be severe and is most frequently complicated by diarrhea, middle ear infection, or bronchopneumonia. Encephalitis occurs in approximately one of every 1,000 reported cases; survivors of this complication often have permanent brain damage and mental retardation. Death occurs in 1-2 of every 1,000 reported measles cases in the United States. The risk for death from measles or its complications is greater for infants, young children, and adults than for older children and adolescents. The most common causes of death are pneumonia and acute encephalitis. In developing countries, measles is often more severe and the case-fatality rate can be as high as 25%.
Subacute sclerosing panencephalitis (SSPE) is a rare degenerative disease of the central nervous system associated with measles virus. Signs and symptoms of the disease appear years after measles infection. Widespread use of measles vaccine has essentially eliminated SSPE from the United States (1 ).
Measles illness during pregnancy leads to increased rates of premature labor, spontaneous abortion, and low birth weight among affected infants (2)(3)(4)(5). Birth defects, with no definable pattern of malformation, have been reported among infants born to women infected with measles during pregnancy, but measles infection has not been confirmed as the cause of the malformations.
Measles can be severe and prolonged among immunocompromised persons, particularly those who have certain leukemias, lymphomas, or human immunodeficiency virus (HIV) infection. Among these persons, measles may occur without the typical rash and a patient may shed measles virus for several weeks after the acute illness (6,7 ).
# Measles Elimination
Before measles vaccine was licensed in 1963, an average of 400,000 measles cases were reported each year in the United States (8 ). However, because virtually all children acquired measles, the number of cases probably approached 3.5 million per year (i.e., an entire birth cohort).
Since measles vaccine became available, professional and voluntary medical and public health organizations have collaborated in vaccination programs that have reduced the reported incidence of measles by >99%. During the late 1960s and early 1970s, the number of reported cases decreased to approximately 22,000-75,000 cases per year. Although measles incidence decreased substantially in all age groups, the greatest decrease occurred among children aged <10 years. A less marked decrease also occurred among older children.
During 1978, the Department of Health, Education, and Welfare (DHEW) initiated a Measles Elimination Program with the goal of eliminating indigenous measles from the United States by October 1, 1982. The three components of this program were a) maintenance of high levels of immunity with a single dose of measles vaccine, b) enhanced surveillance of disease, and c) aggressive outbreak control. As a result of this program, the number of cases reported annually decreased from 26,871 during 1978 to 1,497 during 1983. However, an average of 3,750 cases was reported each year during 1984-1988; 58% of these cases occurred among children aged ≥10 years, most of whom had received only one dose of measles vaccine (9 ). Recurrent measles outbreaks among vaccinated school-aged children prompted both the Advisory Committee on Immunization Practices (ACIP) and the American Academy of Pediatrics (AAP) in 1989 to recommend that all children receive two doses of measles-containing vaccine, preferably as MMR. Although administration of the second dose was originally recommended either at entry to primary school (ACIP) or middle/ secondary school (AAP), ACIP, the AAP, and the American Academy of Family Physicians (AAFP) now recommend that a child receive the second dose before school entry, rather than delaying it until the child is aged 11-12 years.
During 1989-1991, a major resurgence of measles occurred in the United States. More than 55,000 cases and >120 measles-related deaths were reported. The resurgence was characterized by an increasing proportion of cases among unvaccinated preschool-aged children, particularly those resident in urban areas (10)(11)(12).
Multiple barriers to timely vaccination of preschool-aged children were identified during investigation of the 1989-1991 measles resurgence. Efforts to increase vaccination coverage among preschool-aged children emphasized vaccination as close to the recommended age as possible. These efforts, coupled with ongoing implementation of the two-dose MMR recommendation, reduced reported measles cases from 2,237 in 1992 to 312 in 1993 (9 ). Although 963 measles cases were reported in 1994, measles incidence again declined in 1995, when 309 cases were reported (13 ). In 1996, 508 cases were reported, of which 65 were classified as international importations (14 ).
In 1993, the Childhood Immunization Initiative called for the elimination from the United States by 1996 of indigenous transmission of six childhood diseases, including rubella, congenital rubella syndrome (CRS), and measles (10 ). In September 1994, the Pan American Health Organization (PAHO) adopted a similar goal of eliminating measles throughout the Americas by 2000 (15 ). Both epidemiologic and laboratory evidence suggest that the transmission of indigenous measles was interrupted in the United States for the first time during 1993 (16,17 ).
However, even after indigenous measles transmission has been eliminated, measles cases caused by the importation of the virus from other countries will continue to occur. Sustaining measles elimination will require continuing efforts. Enhanced surveillance for measles must be maintained and disease control activities must be undertaken immediately when suspected cases of measles are reported. The major challenges to sustaining the elimination of measles from the United States are a) continuing to vaccinate all children aged 12-15 months with a first dose of MMR, b) ensuring that all school-aged children receive a second dose of MMR vaccine, and c) working with other countries to set and achieve national measles elimination goals.
# Rubella And Congenital Rubella Syndrome (CRS) Clinical Characteristics
Rubella is an exanthematous illness characterized by nonspecific signs and symptoms including transient erythematous and sometimes pruritic rash, postauricular or suboccipital lymphadenopathy, arthralgia, and low-grade fever. Clinically similar exanthematous illnesses are caused by parvovirus, adenoviruses, and enteroviruses. Moreover, 25%-50% of rubella infections are subclinical. The incubation period ranges from 12 to 23 days. Before rubella vaccine was available, the disease was common among children and young adults.
Among adults infected with rubella, transient polyarthralgia or polyarthritis occur frequently. These manifestations are particularly common among women (18 ). Central nervous system complications (i.e., encephalitis) occur at a ratio of 1 per 6,000 cases and are more likely to affect adults. Thrombocytopenia occurs at a ratio of 1 per 3,000 cases and is more likely to affect children.
The most important consequences of rubella are the miscarriages, stillbirths, fetal anomalies, and therapeutic abortions that result when rubella infection occurs during early pregnancy, especially during the first trimester. An estimated 20,000 cases of CRS occurred during 1964-1965 during the last U.S. rubella epidemic before rubella vaccine became available.
The anomalies most commonly associated with CRS are auditory (e.g., sensorineural deafness), ophthalmic (e.g., cataracts, microphthalmia, glaucoma, chorioretinitis), cardiac (e.g., patent ductus arteriosus, peripheral pulmonary artery stenosis, atrial or ventricular septal defects), and neurologic (e.g., microcephaly, meningoencephalitis, mental retardation). In addition, infants with CRS frequently exhibit both intrauterine and postnatal growth retardation. Other conditions sometimes observed among patients who have CRS include radiolucent bone defects, hepatosplenomegaly, thrombocytopenia, and purpuric skin lesions.
Infants who are moderately or severely affected by CRS are readily recognizable at birth, but mild CRS (e.g., slight cardiac involvement or deafness) may be detected months or years after birth, or not at all. Although CRS has been estimated to occur among 20%-25% of infants born to women who acquire rubella during the first 20 weeks of pregnancy, this figure may underestimate the risk for fetal infection and birth defects. When infants born to mothers who were infected during the first 8 weeks of gestation were followed for 4 years, 85% were found to be affected (19 ). The risk for any defect decreases to approximately 52% for infections that occur during the ninth to twelfth weeks of gestation. Infection after the twentieth week of gestation rarely causes defects. Inapparent (subclinical) maternal rubella infection can also cause congenital malformations. Fetal infection without clinical signs of CRS can occur during any stage of pregnancy.
# Rubella Elimination
Before rubella vaccine was licensed during 1969, rubella incidence was greatest among preschool and elementary school children. Therefore, vaccination campaigns initially targeted children in kindergarten and the early grades of elementary school, with the aim of interrupting circulation of the virus and eliminating the risk for exposure among susceptible pregnant women. The risks associated with administering a potentially teratogenic live virus vaccine to young women of childbearing age were not known. During 1969During -1976, reported rubella cases decreased from 57,600 to 12,400. However, during 197512,400. However, during -1977, 62% of reported rubella cases occurred among persons aged >15 years compared with 23% of cases occurring during 1966-1968, and serologic studies suggested that 10%-15% of adults remained susceptible to rubella (20 ).
The number of CRS cases reported nationwide decreased by 69% from 69 in 1970 to 22 in 1976. Rubella outbreaks continued to occur among older adolescents and young adults (e.g, in military camps, high schools, colleges, and universities). In 1977, ACIP modified its recommendations to include the vaccination of susceptible postpubertal girls and women. During the same year, the DHEW undertook the National Childhood Immunization Initiative, which sought to immunize >90% of the nation's children against all vaccine-preventable diseases. Enforcement of requirements for vaccination before school entry was part of the initiative. The number of reported rubella and CRS cases decreased after these programs were implemented, from 20,395 rubella cases and 29 CRS cases in 1977 to 752 rubella cases and 2 CRS cases in 1984. In 1988, 225 cases of rubella were reported in the United States, the fewest since national reporting began.
However, because of outbreaks among unvaccinated adults (e.g., in prisons, colleges, and workplaces), >1000 rubella cases were reported in 1990 and again in 1991. The largest outbreak and the greatest number of CRS cases occurred among children and adults in religious communities that do not accept vaccination. Since 1992, reported indigenous rubella and CRS have continued to occur at a low but relatively constant endemic level with an annual average of <200 rubella cases (128 cases in 1995 and 213 cases in 1996). Four confirmed CRS cases occurred in 1995 and 2 in 1996. However, in the United States, surveillance for CRS relies on a passive system. Consequently, the reported annual totals of CRS are regarded as minimum figures, representing an estimated 40%-70% of all cases (21,22 ).
During 1992-1997, 65% of reported cases of rubella occurred among persons aged ≥20 years. In addition, recent evidence suggests that the risk for both rubella and CRS is increased among persons of Hispanic ethnicity, particularly those born outside the United States. Outbreaks of rubella in California (1990California ( -1991, Massachusetts (1993Massachusetts ( -1994, Connecticut (1995), and North Carolina (1996 and 1997) have occurred primarily among persons of Hispanic origin. During 1985-1995, the ethnicity of a total of 89 children with laboratory-confirmed or clinically compatible cases of CRS was known; 35 (39%) were of Hispanic origin (23)(24)(25)(26)(27).
Recent data indicate that the rate of rubella susceptibility and risk for rubella infection are highest among young adults. During 1992-94, approximately 8% of persons aged 15-29 years were estimated to lack serologic evidence of immunity to rubella (CDC, unpublished data). Data from two recent studies indicate that vaccine-induced rubella antibody levels among adolescents may have decreased during the 9-14 years that had elapsed since they were initially vaccinated. However, recent rubella surveillance data do not indicate that rubella and CRS are increasing among vaccinated persons (28 ) (CDC, unpublished data).
The primary objective of the rubella immunization program is the prevention of CRS. The major components of the rubella and CRS elimination strategy are achieving and maintaining high immunization levels for children and adults, especially women of childbearing age; conducting accurate surveillance for rubella and CRS; and undertaking control measures promptly when a rubella outbreak occurs. Since the late 1970s, this strategy has effectively prevented major epidemics of rubella and CRS in the United States.
# Mumps Clinical Characteristics
Persons in whom "classical" mumps develops have bilateral or (less commonly) unilateral parotitis, with onset an average of 16-18 days after exposure. Parotitis may be preceded by fever, headache, malaise, myalgia, and anorexia. Only 30%-40% of mumps infections produce typical acute parotitis; 15%-20% of infections are asymptomatic and up to 50% of infections are associated with nonspecific or primarily respiratory symptoms (29,30 ). Inapparent infection may be more common among adults than children; parotitis occurs more commonly among children aged 2-9 years (30,31 ). Serious complications of mumps infection can occur without evidence of parotitis (29,32,33 ).
Most serious complications of mumps are more common among adults than among children (29,34 ). Although orchitis may occur among up to 38% of postpubertal men in whom mumps develops, sterility is thought to occur only rarely (35 ).
Aseptic meningitis affects 4%-6% of persons with clinical cases of mumps and typically is mild (29,(36)(37)(38). However, mumps meningoencephalitis can cause permanent sequelae, including paralysis, seizures, cranial nerve palsies, aqueductal stenosis, and hydrocephalus (39)(40)(41). In the prevaccine era, mumps was a major cause of sensorineural deafness among children. Deafness may be sudden in onset, bilateral, and permanent (42)(43)(44).
Among women in whom mumps develops during the first trimester of pregnancy, an increased risk for fetal death has been observed (45 ). However, mumps infection during pregnancy is not associated with congenital malformations (46 ).
# Mumps Control
In the United States, the reported incidence of mumps decreased steadily after the introduction of live mumps vaccine in 1967 and the recommendation for its routine use in 1977. In 1995, 906 cases were reported, representing a 99% decrease from the 185,691 cases reported in 1968. The enactment and enforcement of state vaccination laws requiring that students be vaccinated before school entry has contributed more to reducing mumps incidence than any other measure (47 ). During the 1980s and early 1990s, mumps incidence was lowest in states where comprehensive vaccination laws were enforced. States where vaccination laws were less comprehensive reported intermediate mumps incidence, and the highest incidence was reported in states did not have such laws (47)(48)(49)(50)(51).
Mumps incidence is now very low in all areas of the United States. The substantial reduction in mumps incidence during the past few years may reflect the change in the recommendations for use of MMR vaccine. The implementation of the two-dose MMR vaccination schedule likely decreased mumps incidence further by immunizing children among whom the first dose of mumps antigen did not elicit an immune response (52,53 ). The principal strategy to prevent mumps is to achieve and maintain high immunization levels by routinely vaccinating all children with two doses of MMR.
# VACCINE PREPARATIONS
# Measles Component
Since 1963, when both inactivated and live attenuated (Edmonston B strain) vaccines were licensed, the type of measles vaccine used in the United States has changed several times. Distribution of the inactivated and live Edmonston B vaccines ceased after 1967 and 1975, respectively. Distribution in the United States of a live, further attenuated vaccine (Schwarz strain) first introduced in 1965 has also ceased. A live, further attenuated preparation of the Enders-Edmonston virus strain that is grown in chick embryo fibroblast cell culture, licensed in 1968, is the only measles virus vaccine now available in the United States. This further attenuated vaccine (formerly called "Moraten") causes fewer adverse reactions than the Edmonston B vaccine.
Measles vaccine produces an inapparent or mild, noncommunicable infection. Measles antibodies develop among approximately 95% of children vaccinated at age 12 months and 98% of children vaccinated at age 15 months (CDC, unpublished data). Studies indicate that, if the first dose is administered no earlier than the first birthday, >99% of persons who receive two doses of measles vaccine develop serologic evidence of measles immunity (54 )(CDC, unpublished data). Although vaccination produces lower antibody levels than natural disease, both serologic and epidemiologic evidence indicate that the vaccine induces long-term-probably lifelong-immunity, in most persons (55 ). Most vaccinated persons who appear to lose antibody show an anamnestic immune response upon revaccination, indicating that they are probably still immune (56 ). Although revaccination elicits increased antibody levels in some persons, these increased levels may not be sustained (57 ). Findings of some studies indicate that immunity can wane after successful vaccination (secondary vaccine failure), but this phenomenon appears to occur rarely and to have little effect on measles transmission and the occurrence of outbreaks (55,58,59 ).
# Rubella Component
The live rubella virus vaccine currently distributed in the United States is prepared in human diploid cell culture. This vaccine, containing virus strain RA 27/3, was licensed in the United States in January, 1979 and replaced previous rubella vaccines (e.g., HPV-77 and Cendehill) because it induced an increased and more persistent antibody response and was associated with fewer adverse events.
In clinical trials, ≥95% of susceptible persons aged ≥12 months who received a single dose of strain RA 27/3 rubella vaccine developed serologic evidence of immunity (60)(61)(62). Clinical efficacy and challenge studies indicate that >90% of vaccinated persons have protection against both clinical rubella and viremia for at least 15 years (63)(64)(65)(66). Follow-up studies indicate that one dose of vaccine confers long-termprobably lifelong-protection (67 ). Although antibody titers induced by the vaccine are generally lower than those stimulated by rubella infection, vaccine-induced immunity protects, in nearly all instances, against both clinical illness and viremia after natural exposure (68,69 ). In studies that attempted artificial reinfection of persons who received RA 27/3 vaccine, resistance to reinfection was similar to the resistance that follows natural infection (70 ). However, several reports indicate that viremic reinfection following exposure may occur among vaccinated persons who have low levels of detectable antibody (64 ). The frequency and consequences of this phenomenon are unknown but it is believed to be uncommon. Clinical reinfection and fetal infection among persons who developed immunity as a consequence of infection with wild virus have been documented, but are apparently rare (71 ). Rarely, clinical reinfection and fetal infection have been reported among women with vaccine-induced immunity. Rare cases of CRS have occurred among infants born to mothers who had documented serologic evidence of rubella immunity before they became pregnant.
# Mumps Component
The only mumps vaccine now available in the United States is a live virus vaccine (Jeryl-Lynn strain) that is prepared in chick-embryo cell culture. The vaccine produces a subclinical, noncommunicable infection with very few side effects.
More than 97% of persons who are susceptible to mumps develop measurable antibody following vaccination and, in controlled clinical trials, one dose of vaccine was approximately 95% efficacious in preventing mumps disease (72)(73)(74). However, field studies have documented lower estimates of vaccine efficacy, ranging from 75% to 95% (47,75 ). Antibody levels induced by the vaccine are lower than antibody levels resulting from natural infection (72,76,77 ). The duration of vaccine-induced immunity is unknown, but serologic and epidemiologic data collected during 30 years of live vaccine use indicate both the persistence of antibody and continuing protection against infection (33,78,79 ).
# Vaccine Shipment and Storage
Administration of improperly stored vaccine may fail to provide protection against disease from measles, rubella, and/or mumps. These live virus vaccines are supplied in lyophilized form and should be stored at 2-8 C (35.6-46.4 F) or colder. They must be shipped at 10 C (50 F) or colder and may be shipped on dry ice. The vaccines must be protected from light, which may inactivate the vaccine viruses. Reconstituted vaccine also must be protected from light, must be stored at 2-8 C (35.6-46.4 F), and must not be frozen. Reconstituted vaccine must be discarded if not used within 8 hours.
# VACCINE USAGE
Two doses of MMR vaccine separated by at least 1 month (i.e., a minimum of 28 days) and administered on or after the first birthday are recommended for all children and for certain high-risk groups of adolescents and adults. The recommended 1 month interval between successive doses of MMR or other measles-containing vaccine is based on the principle that live virus vaccines not administered at the same time should be separated by at least 1 month (80 ).
MMR is the vaccine of choice when protection against any of these three diseases is required on or after the first birthday, unless any of its component vaccines is contraindicated. The purpose of the two-dose vaccination schedule is to produce immunity in the small proportion of persons who fail to respond immunologically to one or more of the components of the first dose. Studies indicate that two doses of measles vaccine are necessary to develop adequate population immunity to prevent measles outbreaks among school-aged and older persons. Mumps can occur in highly vaccinated populations; in these outbreaks, substantial numbers of cases have occurred among persons who had previously received a single dose of mumpscontaining vaccine (33,81 ). Although primary rubella vaccine failure rarely occurs, the potential consequences of failure (i.e., CRS) are substantial.
Almost all persons who do not respond to the measles component of the first dose of MMR vaccine will respond to the second dose (82 ) (CDC, unpublished data). Few data regarding the immune response to the rubella and mumps components of a second dose of MMR vaccine are available, but most persons who do not respond to the rubella or mumps components of the first dose would be expected to respond to the second (82-84 ) (CDC, unpublished data). The second dose is not generally considered a booster dose because a primary immune response to the first dose provides longterm protection. Although some persons who develop normal antibody titers in response to a single dose of MMR vaccine will develop higher antibody titers to the three component vaccines when administered a second dose of vaccine, these increased antibody levels typically do not persist (57 ).
Use of combined MMR vaccine for both measles doses and all other indications should provide an additional safeguard against primary vaccine failures and facilitate elimination of rubella and CRS and continued reduction of mumps incidence. Data also indicate that the favorable benefit/cost ratio for routine measles, rubella, and mumps vaccination is even greater when the vaccines are administered as combined MMR vaccine (85,86 ).
# Dosage and Route of Administration
The lyophilized live MMR vaccine (and its component vaccines) should be reconstituted and administered as recommended by the manufacturer. All measles-, rubella-, or mumps-containing vaccines available in the United States should be administered subcutaneously in the recommended standard single-dose volume of 0.5 mL.
# Simultaneous Administration of Vaccines
In general, simultaneous administration of the most widely used live and inactivated vaccines does not impair antibody responses or increase rates of adverse reactions (80 ). The antibody responses of persons vaccinated with MMR are similar to those of persons vaccinated with single-antigen measles, mumps, and rubella vaccines at different sites or at different times.
ACIP encourages routine simultaneous administration of MMR, diphtheria and tetanus toxoids and acellular pertussis (DTaP) or diphtheria and tetanus toxoids and whole-cell pertussis (DTP) vaccine, Haemophilus influenzae type b (Hib) vaccine, and oral poliovirus vaccine (OPV) or inactivated poliovirus vaccine (IPV) to children who are at the recommended age to receive these vaccines. Antibody responses were equivalent and no clinically significant increases in the frequency of adverse events occurred when MMR vaccine, DTaP (or DTP), Hib vaccine, hepatitis B vaccine, and IPV or OPV were administered either simultaneously at different sites or at separate times (87 ). Likewise, seroconversion rates, antibody levels, and frequencies of adverse reactions were similar in two groups, one of which was administered MMR and varicella vaccines simultaneously at separate sites and the other of which received the vaccines 6 weeks apart (88 )(Merck Research Laboratories, unpublished data).
Live measles and yellow fever vaccines can be administered simultaneously at separate anatomical sites in separate syringes (89 ). Limited data also indicate that the immunogenicity and safety of inactivated Japanese encephalitis vaccine are not compromised by simultaneous administration with live measles vaccine (90 ). Limited data exist concerning concurrent administration of MMR vaccine and other vaccines that are often recommended for international travelers (e.g., meningococcal vaccine, typhoid vaccines). However, neither theoretical considerations nor practical experience indicate that the simultaneous administration at separate anatomic sites of MMR and other live or inactivated vaccines will produce a diminished immune response or increase the incidence of adverse events among vaccinated persons.
# DOCUMENTATION OF IMMUNITY
Only doses of vaccine for which written documentation of the date of administration is presented should be considered valid. Neither a self-reported dose nor a history of vaccination provided by a parent is, by itself, considered adequate documentation. No health-care worker should provide a vaccination record for a patient unless that health-care worker has administered the vaccine or has seen a record that documents vaccination. Persons who may be immune to measles, mumps, or rubella but who lack either adequate documentation of vaccination or other acceptable evidence of immunity (Table 1) should be vaccinated. Vaccination status and date of . Facilities that provide care exclusively for elderly patients who are at minimal risk for measles and rubella and complications of these diseases are a possible exception. † The first dose should be administered on or after the first birthday; the second dose of measles-containing vaccine should be administered no earlier than one month (i.e., minimum of 28 days) after the first dose. Combined measles-mumps-rubella (MMR) vaccine generally should be used whenever any of its component vaccines is indicated. § May vary depending on current state or local requirements. ¶ Health-care facilities should consider recommending a dose of MMR vaccine for unvaccinated workers born before 1957 who are at risk for occupational exposure to measles and who do not have a history of measles disease or laboratory evidence of measles immunity. Children aged 6-11 months should receive a dose of monovalent measles vaccine (or MMR, if monovalent vaccine is not available) before departure. Children who receive a dose of measles-containing vaccine before their first birthdays should be revaccinated with two doses of MMR vaccine, the first of which should be administered when the child is aged 12-15 months (12 months if the child remains in a high-risk area) and the second at least 28 days later. † † Women of childbearing age are adolescent girls and premenopausal adult women. Because rubella can occur in some persons born before 1957 and because congenital rubella and congenital rubella syndrome can occur in the offspring of women infected with rubella virus during pregnancy, birth before 1957 is not acceptable evidence of rubella immunity for women who could become pregnant.
administration of all vaccinations should be documented in the patient's permanent medical record. Serologic screening for measles, rubella, or mumps immunity generally is neither necessary nor recommended if a person has other acceptable evidence of immunity to the disease (Table 1). Serologic screening can be a barrier to vaccination. With the exception of women who are known to be pregnant (see Women of Childbearing Age), persons who lack acceptable evidence of immunity generally should be vaccinated without serologic testing. Serologic screening is appropriate only when persons identified as susceptible are subsequently vaccinated in a timely manner. Screening is most applicable when the return and vaccination of those tested can be ensured (e.g., hiring of new health-care workers). If these conditions are not met, serologic screening is inappropriate (91 ). Likewise, during an outbreak of measles, rubella, or mumps, serologic screening before vaccination generally is not recommended because waiting for results, contacting, and then vaccinating persons identified as susceptible can impede the rapid vaccination needed to curb the outbreak.
Serologic screening for antibodies to measles, rubella, or mumps alone will not identify persons who are susceptible to the other diseases for which screening is not done. Post-vaccination serologic testing to verify an immune response to MMR or its component vaccines is not recommended.
The criteria for acceptable evidence of immunity to measles, rubella, and mumps (Table 1) provide presumptive rather than absolute evidence of immunity. Occasionally, a person who meets the criteria for presumptive immunity can contract and transmit disease. Specific criteria for documentation of immunity have been established for certain persons (e.g., health-care workers, international travelers, and students at post-high school educational institutions) who are at increased risk for exposure to measles, rubella, and mumps (Table 1). Criteria accepted as evidence of immunity for the purpose of meeting school or college entry requirements or other government regulations may vary among state and local jurisdictions.
# Measles
Persons generally can be presumed immune to measles (Table 1) if they have documentation of adequate vaccination, laboratory evidence of immunity to measles, documentation of physician-diagnosed measles, or were born before 1957. Criteria for adequate vaccination currently vary depending on state and local vaccination policy because of differences in the way states have implemented the two-dose measles vaccination schedule. All states are strongly encouraged to take immediate steps to implement the two-dose MMR vaccination schedule so that, by 2001, adequate vaccination of children will be defined in all 50 states as follows:
- For preschool-aged children: documentation of at least one dose of MMR vaccine administered on or after the first birthday.
- For children in kindergarten through grade 12: documentation of two doses of MMR vaccine separated by at least 28 days (i.e., 1 month), with the first dose administered no earlier than the first birthday. Doses of MMR and other measles-containing vaccines administered before the first birthday should not be counted when determining adequacy of measles vaccination.
When measles virus is introduced into a community, persons who work in healthcare facilities are at greater risk for acquiring measles than the general population (92 ). Because persons working in medical settings have been infected with and have transmitted measles to patients and coworkers, rigorous criteria for immunity among health-care workers have been established. For persons born during or after 1957 who work in health-care facilities, adequate vaccination consists of two doses of MMR or other live measles-containing vaccine separated by at least 28 days, with the first dose administered no earlier than the first birthday (Table 1). In addition, although birth before 1957 is generally considered acceptable evidence of measles immunity (Table 1), measles has occurred in some unvaccinated persons born before 1957 who worked in health-care facilities. Therefore, health-care facilities should consider recommending a dose of MMR vaccine for unvaccinated workers born before 1957 who lack a history of measles disease or laboratory evidence of measles immunity (see Health-Care Facilities).
The previously described criteria apply only to routine vaccination. During measles outbreaks, evidence of adequate vaccination for school-aged children, adolescents, and adults born during or after 1957 who are at risk for measles exposure and infection consists of two doses of measles-containing vaccine separated by at least 28 days, with the first dose administered no earlier than the first birthday (see Measles Outbreak Control). During outbreaks involving preschool-aged children, authorities should consider extending this criterion to all children aged ≥12 months.
In the past, the most commonly used laboratory test for assessing immunity to measles was the hemagglutination-inhibition (HI) test but more sensitive assays (e.g., the enzyme immunoassay or enzyme-linked immunosorbent assay ) are now used in most laboratories. Persons who have measles-specific antibody that is detectable by any serologic test are considered immune. Persons with an "equivocal" test result should be considered susceptible unless they have other evidence of measles immunity (Table 1) or subsequent testing indicates they are immune. All new cases of suspected measles should be confirmed by laboratory testing (see Measles Case Investigation-Laboratory Diagnosis).
# Rubella
Persons generally can be presumed immune to rubella (Table 1) if they have documentation of vaccination with at least one dose of MMR or other live rubellacontaining vaccine administered on or after the first birthday, laboratory evidence of rubella immunity, or were born before 1957 (except women who could become pregnant). Birth before 1957 is not acceptable evidence of rubella immunity for women who could become pregnant because it provides only presumptive evidence of rubella immunity and does not guarantee that a person is immune (see Women of Childbearing Age). Rubella can occur among some unvaccinated persons born before 1957 and congenital rubella and CRS can occur among the offspring of women infected with rubella during pregnancy.
Persons who have an "equivocal" serologic test result should be considered susceptible to rubella unless they have evidence of adequate vaccination or a subsequent serologic test result indicates rubella immunity. Although only one dose of rubellacontaining vaccine is required as acceptable evidence of immunity to rubella, children should receive two doses of MMR vaccine. The first dose is administered routinely when the child is aged 12-15 months and the second before the child enters school (i.e., at age 4-6 years)(see Routine Vaccination).
The clinical diagnosis of rubella is unreliable and should not be considered in assessing immune status. Because many rash illnesses may mimic rubella infection and many rubella infections are unrecognized, the only reliable evidence of previous rubella infection is the presence of serum rubella immunoglobulin G (IgG). Laboratories that regularly perform antibody testing generally provide the most reliable results because their reagents and procedures are more likely to be strictly standardized (see Rubella Case Investigation and Outbreak Control).
Postinfection immunity to rubella appears to be long-lasting and is probably lifelong. However, as with other viral diseases, re-exposure to natural rubella occasionally leads to reinfection without clinical illness or detectable viremia. The risk for CRS among infants born to women reinfected with rubella during pregnancy is minimal (93,94 ). Although data from several studies indicate that levels of vaccineinduced rubella antibodies may decline with time, data from surveillance of rubella and CRS suggest that waning immunity with increased susceptibility to rubella disease does not occur (28 )(CDC, unpublished data).
HI antibody testing was formerly the method most frequently used to screen for rubella antibodies. However, the HI test has been supplanted by other assays of equal or greater sensitivity. EIAs are the most commonly used of these newer commercial assays, but latex agglutination, immunofluorescence assay (IFA), passive hemagglutination, hemolysis-in-gel, and virus neutralization tests are also available.
Any antibody level above the standard positive cutoff value of the assay with which it is measured can be considered evidence of immunity, if the assay is licensed. When serum specimens from adults who did not produce antibodies detectable by HI after vaccination were examined with an equivalently specific but more sensitive test, almost all had detectable antibody (95,96 ). A few children who initially developed antibody detectable by HI apparently "lost" this antibody during follow-up intervals of up to 16 years (77,97,98 ). However, almost all had antibody detectable by more sensitive tests. In several of these cases, immunity was confirmed by documenting a booster response (i.e., absence of IgM antibody and a rapid rise in IgG antibody) after revaccination (62,99 ).
Occasionally, persons with documented histories of rubella vaccination have rubella serum IgG levels that are not clearly positive by ELISA. Such persons can be administered a dose of MMR vaccine and need not be retested for serologic evidence of rubella immunity.
# Mumps
Persons generally can be presumed immune to mumps (Table 1) if they have documentation of vaccination with live mumps virus vaccine on or after the first birthday, laboratory evidence of mumps immunity, documentation of physician-diagnosed mumps, or were born before 1957.
The demonstration of mumps IgG antibody by any commonly used serologic assay is acceptable evidence of mumps immunity. Persons who have an "equivocal" serologic test result should be considered susceptible to mumps unless they have other evidence of mumps immunity (Table 1) or subsequent testing indicates they are immune. All new cases of suspected mumps should be confirmed by an appropriate serologic assay (see Mumps Case Investigation, Laboratory Diagnosis).
Live mumps vaccine was not used routinely before 1977. Before the vaccine was introduced, the age-specific incidence of the disease peaked among children aged 5-9 years. Therefore, most persons born before 1957 are likely to have been infected naturally between 1957 and 1977 and may be presumed immune, even if they have not had clinically recognizable mumps disease. However, birth before 1957 does not guarantee mumps immunity. Therefore, during mumps outbreaks, MMR vaccination should be considered for persons born before 1957 who may be exposed to mumps and who may be susceptible. Laboratory testing for mumps susceptibility before vaccination is not necessary.
# ROUTINE VACCINATION
# Preschool-Aged Children
Children should receive the first dose of MMR vaccine at age 12-15 months (i.e., on or after the first birthday). In areas where risk for measles is high, initial vaccination with MMR vaccine is recommended for all children as soon as possible upon reaching the first birthday (i.e., at age 12 months). An area where measles risk is high is defined as:
- a county with a large inner city population,
- a county where a recent measles outbreak has occurred among unvaccinated preschool-aged children, or
- a county in which more than five cases of measles have occurred among preschool-aged children during each of the last 5 years. These recommendations may be implemented for an entire county or only within defined areas of a county. This strategy assumes that the benefit of preventing measles cases among children aged 12-15 months outweighs the slightly reduced efficacy of the vaccine when administered to children aged <15 months. In addition, almost all children who do not respond immunologically to the first dose of MMR vaccine will develop measles immunity after receiving a second dose. HIV-infected children should receive MMR vaccine at age 12 months, if not otherwise contraindicated (see Special Considerations for Vaccination-Persons Infected with Human Immunodeficiency Virus (HIV)).
# School-Aged Children and Adolescents
The second dose of MMR vaccine is recommended when children are aged 4-6 years (i.e., before a child enters kindergarten or first grade). This recommended timing for the second dose of MMR vaccine has been adopted jointly by ACIP, the American Academy of Pediatrics (AAP), and the American Academy of Family Physicians (AAFP). Evidence now indicates that a) the major benefit of administering the second dose is a reduction in the proportion of persons who remain susceptible because of primary vaccine failure, b) waning immunity is not a major cause of vaccine failure and has little influence on measles transmission, and c) revaccination of children who have low levels of measles antibody produces only a transient rise in antibody levels (55,(57)(58)(59)100,101 ).
Because approximately 5% of children who receive only one dose of MMR vaccine fail to develop immunity to measles, ACIP recommends that all states implement a requirement that all children entering school have received two doses of MMR vaccine (with the first dose administered no earlier than the first birthday) or have other evidence of immunity to measles, rubella, and mumps (see Documentation of Immunity). In addition, to achieve complete immunization of all school-aged children and hasten progress toward measles elimination, states are strongly encouraged to take immediate steps to ensure that, by 2001, all children in grades kindergarten through 12 have received two doses of MMR vaccine.
As part of comprehensive health services for all adolescents, ACIP, AAP, and AAFP recommend a health maintenance visit at age 11-12 years. This visit should serve as an opportunity to evaluate vaccination status and administer MMR vaccine to all persons who have not received two doses at the recommended ages.
Children who do not have documentation of adequate vaccination against measles, rubella, and mumps or other acceptable evidence of immunity to these diseases (see Documentation of Immunity) should be admitted to school only after administration of the first dose of MMR vaccine. If required, the second MMR dose should be administered as soon as possible, but no sooner than 28 days after the first dose. Children who have already received two doses of MMR vaccine at least 1 month apart, with the first dose administered no earlier than the first birthday, do not need an additional dose when they enter school.
# Adults
Persons born in 1957 or later who are aged ≥18 years and who do not have a medical contraindication should receive at least one dose of MMR vaccine unless they have a) documentation of vaccination with at least one dose of measles-, rubella-, and mumps-containing vaccine or b) other acceptable evidence of immunity to these three diseases (Table 1). Persons born before 1957 generally can be considered immune to measles and mumps. In addition, persons born before 1957, except women who could become pregnant, generally can be considered immune to rubella.
MMR vaccine (one dose or two doses administered at least 28 days apart) may be administered to any person born before 1957 for whom the vaccine is not contraindicated. Adults who may be at increased risk for exposure to and transmission of measles, mumps, and rubella should receive special consideration for vaccination. These persons include international travelers, persons attending colleges and other post-high school educational institutions, and persons who work at health-care facilities. In addition, all women of childbearing age should be considered susceptible to rubella unless they have received at least one dose of MMR or other live rubella virus vaccine on or after the first birthday or have serologic evidence of immunity. Vaccination recommendations for these high-risk groups follow.
# Women of Childbearing Age
MMR vaccine should be offered to all women of childbearing age (i.e., adolescent girls and premenopausal adult women) who do not have acceptable evidence of rubella immunity whenever they make contact with the health-care system. Opportunities to vaccinate susceptible women include occasions when their children undergo routine examinations or vaccinations. The continuing occurrence of rubella among women of childbearing age indicates the need to continue vaccination of susceptible adolescent and adult women of childbearing age, and the absence of evidence of vaccine teratogenicity indicates that the practice is safe (102 ). Vaccination of susceptible women of childbearing age should - be part of routine general medical and gynecologic outpatient care;
- take place in all family-planning settings; and - be provided routinely before discharge from any hospital, birthing center, or other medical facility, unless a specific contraindication exists (see Precautions and Contraindications).
Outbreaks of rubella in the United States recently have occurred among women of Hispanic ethnicity, many of whom were born outside the fifty states. Efforts should be made to ensure that all susceptible women of childbearing age, especially those who grew up outside the fifty states in areas where routine rubella vaccination may not occur, are vaccinated with MMR vaccine or have other acceptable evidence of immunity (Table 1). Ascertainment of rubella-immune status of women of childbearing age and the availability of rubella vaccination should be components of the health-care program in places where the risks for disease exposure and transmission are substantial (e.g., day care facilities, schools, colleges, jails, and prisons).
No evidence indicates that administration of rubella-containing vaccine virus to a pregnant woman presents a risk for her fetus, although such a risk cannot be excluded on theoretical grounds. Therefore, women of childbearing age should receive rubellacontaining vaccines (i.e., rubella, MR, or MMR vaccine) only if they state that they are not pregnant and only if they are counseled not to become pregnant for 3 months after vaccination. Because of the importance of protecting women of childbearing age against rubella, reasonable practices in any immunization program include a) asking women if they are pregnant, b) not vaccinating women who state that they are pregnant, c) explaining the potential risk for the fetus to women who state that they are not pregnant, and d) counseling women who are vaccinated not to become pregnant during the 3 months following MMR vaccination.
Routine Vaccination of Women Who Are Not Pregnant. Women of childbearing age who do not have documentation of rubella vaccination or serologic evidence of rubella immunity should be vaccinated with MMR, if they have no contraindications to the vaccine. Birth before 1957 is not acceptable evidence of immunity for women who could become pregnant (Table 1). The use of MMR vaccine provides the potential additional benefit of protection against measles and mumps. Serologic testing before vaccination is not necessary and might present a barrier to timely vaccination. Routine testing for rubella antibody during clinic visits for routine health care, premarital evaluation, family planning, or diagnosis and treatment of sexually transmitted diseases may identify women who are not immune to rubella before they become pregnant. Such routine serologic testing is not useful unless it is linked to timely follow-up and vaccination of women who are susceptible (103 ).
Prenatal Screening and Postpartum Vaccination. Prenatal serologic screening of women who have acceptable evidence of rubella immunity is generally not necessary, but is indicated for all pregnant women who lack acceptable evidence of rubella immunity (Table 1). Upon completion or termination of their pregnancies, women who do not have serologic evidence of rubella immunity or documentation of rubella vaccination should be vaccinated with MMR before discharge from the hospital, birthing center, or abortion clinic (104 ). They should be counseled to avoid conception for 3 months after vaccination. Postpartum rubella vaccination of all women not known to be immune could prevent up to half of CRS cases (105-108 ) ( CDC, unpublished data).
# Colleges and Other Post-High School Educational Institutions
Risks for transmission of measles, rubella, and mumps at post-high school educational institutions can be high because these institutions may bring together large concentrations of persons susceptible to these diseases (109)(110)(111)(112)(113). Therefore, colleges, universities, technical and vocational schools, and other institutions for post-high school education should require that all undergraduate and graduate students have received two doses of MMR vaccine or have other acceptable evidence of measles, rubella, and mumps immunity (Table 1) before enrollment.
College entry requirements for measles immunity substantially reduce the risk for measles outbreaks on college campuses where they are implemented and enforced (111 ). State requirements for pre-enrollment vaccination ensure the best protection against widespread measles transmission among students at college campuses and other post-high school educational institutions. States are strongly encouraged to adopt such regulations. Students who do not have documentation of live measles, rubella, or mumps vaccination or other acceptable evidence of immunity at the time of enrollment (Table 1) should be admitted to classes only after receiving the first dose of MMR vaccine. These students should be administered a second dose of MMR vaccine 1 month (i.e., at least 28 days) later. Students who have documentation of having received only one dose of measles-containing vaccine on or after the first birthday should receive a second dose of MMR before enrollment, provided at least 1 month has elapsed since the previous dose. Students who have a medical contraindication to receiving any of the components of MMR vaccine should be given a letter of explanation to present to the health officials of their educational institution.
# Health-Care Facilities
When measles virus is introduced into a community, persons who work in healthcare facilities are at increased risk for acquiring measles compared with the general population (92,114,115 ). During 1985-1991, at least 795 measles cases (1.1% of all reported cases) occurred among adult health-care workers. Of these, 29% occurred among nurses, 15% among physicians, 11% among persons in other health-care occupations (e.g., laboratory and radiology technicians, etc.), 11% among clerks, 4% among nursing assistants, and 4% among medical and nursing students (115 ) (CDC, unpublished data). A general decline in measles incidence occurred after 1991. However, 15 of the 75 measles outbreaks reported during 1993-1996 involved transmission in a medical facility, and a total of 36 measles cases (1.8% of all reported cases) occurred among persons working in health-care facilities (CDC, unpublished data). Although similar surveillance data are not available for rubella, outbreaks have occurred in health-care settings, and health-care workers have transmitted rubella to patients (116 ) (CDC, unpublished data).
All persons who work in health-care facilities should be immune to measles and rubella (Table 1). Because any health-care worker (i.e., medical or nonmedical, paid or volunteer, full-or part-time, student or nonstudent, with or without patient-care responsibilities) who is not immune to measles and rubella can contract and transmit these diseases, all health-care facilities (i.e., inpatient and outpatient, private and public) should ensure that those who work in their facilities are immune to measles and rubella (Table 1)*.
Health-care workers have a responsibility to avoid transmitting these diseases and thereby causing harm to patients. Adequate vaccination for health-care workers born during or after 1957 consists of two doses of a live measles-containing vaccine and at least one dose of a live rubella-containing vaccine (Table 1). Health-care workers who need a second dose of measles-containing vaccine should be revaccinated 1 month (at least 28 days) after their first dose.
Although birth before 1957 is generally considered acceptable evidence of measles and rubella immunity (Table 1), health-care facilities should consider recommending a dose of MMR vaccine to unvaccinated workers born before 1957 who do not have a history of physician-diagnosed measles or laboratory evidence of measles immunity AND laboratory evidence of rubella immunity.
Rubella vaccination or laboratory evidence of rubella immunity is particularly important for female health-care workers who could become pregnant, including those born before 1957. In addition, during rubella outbreaks, health-care facilities should strongly consider recommending a dose of MMR vaccine to unvaccinated health-care workers born before 1957 who do not have serologic evidence of immunity. Serologic surveys of hospital workers indicate that 5%-9% of those born before 1957 do not have detectable measles antibody (117,118 ) and about 6% do not have detectable rubella antibody (119 ). In addition, during 1985-1992, 643 measles cases were reported among health-care workers whose year of birth was known; 27% of these persons were born before 1957 (CDC, unpublished data). Comparable surveillance data are not available for rubella.
Serologic screening need not be done before vaccinating for measles and rubella unless the medical facility considers it cost-effective (91,120,121 ). Serologic testing is appropriate only if persons who are identified as susceptible are subsequently vaccinated in a timely manner. Serologic screening ordinarily is not necessary for persons who have documentation of appropriate vaccination or other acceptable evidence of immunity (Table 1). During outbreaks of measles or rubella, serologic screening before vaccination is not generally recommended because rapid vaccination is necessary to halt disease transmission. *Facilities that provide care exclusively for elderly patients who are at minimal risk for measles and rubella and complications of these diseases are a possible exception.
Transmission of mumps has occurred in medical settings (122 ). Therefore, immunity to mumps is highly desirable for all health-care workers (Table 1). Adequate mumps vaccination for health-care workers born during or after 1957 consists of one dose of live mumps-containing vaccine.
MMR vaccine generally should be used whenever any of its component vaccines is indicated. However, if the prospective vaccinee has acceptable evidence of immunity to one or two of the components of MMR vaccine (Table 1), a monovalent or bivalent vaccine can be used.
# International Travel
Measles, rubella, and mumps are endemic in many countries. Protection against measles is especially important for persons planning foreign travel, including adolescents and adults who have not had measles disease and have not been adequately vaccinated, and infants aged 6-11 months. Similarly, protection against rubella is especially important for women of childbearing age who are not immune to the disease. Although proof of vaccination is not required for entry into the United States, persons traveling or living abroad should ensure that they are immune to measles, rubella, and mumps.
Persons who travel or live abroad and who do not have acceptable evidence of measles, rubella, and mumps immunity (Table 1) should be vaccinated with MMR. Children who travel or live abroad should be vaccinated at an earlier age than recommended for children remaining in the United States. Before their departure from the United States, children aged ≥12 months should have received two doses of MMR vaccine separated by at least 28 days, with the first dose administered on or after the first birthday. Children aged 6-11 months should receive a dose of monovalent measles vaccine before departure. If monovalent measles vaccine is not available, no specific contraindication exists to administering MMR to children aged 6-11 months. However, because the risk for serious disease from either mumps or rubella infection among infants is relatively low and because children aged <12 months are less likely to develop serologic evidence of immunity when vaccinated with measles, mumps, and rubella antigens than are older children, mumps vaccine and rubella vaccine generally are administered only to children aged ≥12 months. Children administered monovalent measles vaccine or MMR before the first birthday should be considered potentially susceptible to all three diseases and should be revaccinated with two doses of MMR, the first of which should be administered when the child is aged 12-15 months (12 months if the child remains in an area where disease risk is high) and the second at least 28 days later.
Parents who travel or reside abroad with infants aged <12 months should have acceptable evidence of immunity to rubella and mumps (Table 1), as well as measles, so they will not become infected if their infants contract these diseases. Infants aged <6 months are usually protected against measles, rubella, and mumps by maternally derived antibodies and ordinarily do not require additional protection unless the infant's mother is diagnosed with measles (see Use of Vaccine and Immune Globulin Among Persons Exposed to Measles, Rubella, or Mumps).
# SPECIAL CONSIDERATIONS FOR VACCINATION Persons Infected with Human Immunodeficiency Virus (HIV)
Although the risk for measles exposure is currently low in most areas of the United States and the Western Hemisphere, this risk remains high in many other regions and measles continues to be imported into the United States. HIV-infected persons are at increased risk for severe complications if infected with measles (126,127 ). Among HIV-infected persons who did not have evidence of severe immunosuppression (Table 2), no serious or unusual adverse events have been reported after measles vaccination (123)(124)(125)(126). Therefore, MMR vaccination is recommended for all asymptomatic HIV-infected persons who do not have evidence of severe immunosuppression and for whom measles vaccination would otherwise be indicated. MMR vaccination should also be considered for all symptomatic HIV-infected persons who do not have evidence of severe immunosuppression (Table 2) (128,129 ). Testing asymptomatic persons for HIV infection is not necessary before administering MMR or other measles-containing vaccine (130 ).
Transient increases in HIV viral load have been observed after administration of other vaccines to HIV-infected persons (131,132 ). The clinical significance of these increases is not known. Theoretically, a similar increase also may occur after MMR vaccination of HIV-infected persons.
Because the immunologic response to live and killed-antigen vaccines may decrease as HIV disease progresses, vaccination early in the course of HIV infection may be more likely to induce an immune response (133 ). Therefore, HIV-infected infants without severe immunosuppression should routinely receive MMR vaccine as soon as possible upon reaching the first birthday (i.e., at age 12 months) (130 ). Consideration should be given to administering the second dose of MMR vaccine as soon as 28 days (i.e., 1 month) after the first dose rather than waiting until the child is ready to enter kindergarten or first grade. In addition, if at risk for exposure to measles, HIV-infected infants who are not severely immunocompromised should be administered singleantigen measles vaccine or MMR vaccine at age 6-11 months. These children should receive another dose, administered as MMR vaccine, as soon as possible upon reaching the first birthday, provided at least 1 month has elapsed since the administration of the previous dose of measles-containing vaccine. An additional dose of MMR vaccine can be administered as early as 1 month after the second dose. If otherwise indicated, newly diagnosed HIV-infected children and adults without acceptable evidence of measles immunity (Table 1) should receive MMR vaccine as soon as possible after diagnosis, unless they have evidence of severe immunosuppression (Table 2). Data indicate that, of the HIV-infected infants born in the United States annually, approximately 5% (i.e., 50 children per year) would be classified as severely immunocompromised at age 12 months, when the first dose of MMR vaccine is recommended.
Measles vaccine is not recommended for HIV-infected persons with evidence of severe immunosuppression (Table 2) for several reasons:
- a case of progressive measles pneumonitis occurred in a person with AIDS and severe immunosuppression to whom MMR vaccine was administered (134 );
- evidence indicates a diminished antibody response to measles vaccine among severely immunocompromised HIV-infected persons (133 );
- morbidity related to measles vaccination has been reported among persons with severe immunosuppression unrelated to HIV infection (135)(136)(137)(138); and
- in the United States, the incidence of measles is presently very low.
Serious illness associated with administration of rubella or mumps vaccines to HIVinfected persons has not been reported. MMR vaccine is not contraindicated for the close contacts of immunocompromised persons. All family and other close contacts of HIV-infected persons should be vaccinated with MMR vaccine, unless they have acceptable evidence of measles immunity.
Severely immunocompromised patients and other symptomatic HIV-infected patients who are exposed to measles should receive immune globulin (IG) prophylaxis regardless of vaccination status because they may not be protected by the vaccine. For patients receiving intravenous immune globulin (IGIV) therapy, a standard dose of 100-400 mg/kg should be sufficient to prevent measles infection after exposures occurring within 3 weeks after administration of IGIV; for patients exposed to measles >3 weeks after receiving a standard IGIV dose, an additional dose should be considered. Although no data are available concerning the effectiveness of IGIV in preventing measles, high dose IGIV may be as effective as immune globulin administered intramuscularly. Persons receiving regular (e.g., monthly) IGIV therapy for HIV infection or other indications may not respond to MMR or its component vaccines because of the continued presence of high levels of passively acquired antibody (see Precautions and Contraindications, Recent Administration of Immune Globulin). If indicated, MMR vaccine should be administered at least 2 weeks before beginning IGIV therapy.
# Use of Vaccine and Immune Globulin Among Persons Exposed to Measles, Rubella, or Mumps
# Use of Vaccine
Exposure to measles is not a contraindication to vaccination. MMR or measles vaccine, if administered within 72 hours of initial measles exposure, may provide some protection (139)(140)(141)(142)(143). For most persons aged ≥12 months who are exposed to measles in most settings (e.g., day care facilities, schools, colleges, health-care facilities), administration of MMR or measles vaccine is preferable to using immune globulin (IG). For susceptible persons aged ≥6 months who are household contacts of measles patients, use of vaccine within 72 hours of initial exposure is also acceptable. However, measles often is not recognized as such until >72 hours after onset. Therefore, administration of IG to susceptible household contacts who are not vaccinated within 72 hours of initial exposure is recommended (see Use of Immune Globulin). Infants vaccinated before age 12 months must be revaccinated on or after the first birthday with two doses of MMR vaccine separated by at least 28 days (see Routine Vaccination). Measles-containing vaccine is not recommended for postexposure measles prophylaxis in immunocompromised persons or pregnant women (see Contraindications).
Postexposure MMR vaccination does not prevent or alter the clinical severity of rubella or mumps. However, widespread vaccination during a mumps outbreak may help terminate such outbreaks (144 ).
If exposure to measles, rubella, or mumps does not cause infection, postexposure vaccination with MMR should induce protection against subsequent infection. If the exposure results in infection, no evidence indicates that administration of MMR vaccine during the presymptomatic or prodromal stage of illness increases the risk for vaccine-associated adverse events.
# Use of Immune Globulin
If administered within 6 days of exposure, IG can prevent or modify measles in a nonimmune person. However, any immunity conferred is temporary unless modified or typical measles occurs (139 ). The usual recommended dose of IG is 0.25 mL/kg (0.11 mL/lb) of body weight (maximum dose = 15 mL). However, the recommended dose of IG for immunocompromised persons is 0.5 mL/kg of body weight (maximum dose = 15 mL). For persons receiving IGIV therapy, administration of at least 100 mg/kg within 3 weeks before measles exposure should be sufficient to prevent measles infection.
IG is indicated for susceptible household contacts of measles patients, particularly those for whom the risk for complications is increased (i.e., infants aged ≤12 months, pregnant women, or immunocompromised persons). Infants <6 months of age are usually immune because of passively acquired maternal antibodies. However, if measles is diagnosed in a mother, unvaccinated children of all ages in the household who lack other evidence of measles immunity should receive IG. IG prophylaxis is not indicated for household contacts who have received a dose of measles vaccine on or after the first birthday, unless they are immunocompromised. Only if administered within 72 hours of initial measles exposure is MMR vaccine acceptable for postexposure prophylaxis in household contacts aged ≥6 months except pregnant women, immunocompromised patients, and others for whom vaccine is contraindicated (see Use of Vaccine). IG should not be used to control measles outbreaks.
Any person exposed to measles who lacks evidence of measles immunity (Table 1) and to whom IG is administered should subsequently receive MMR vaccine, which should be administered no earlier than 5-6 months after IG administration, provided the person is then aged ≥12 months and the vaccine is not otherwise contraindicated. Kawasaki disease 2 g/kg IV (as IGIV) 11 *This table is not intended for determining the correct indications and dosage for the use of immune globulin preparations. Unvaccinated persons may not be fully protected against measles during the entire suggested time interval, and additional doses of immune globulin and/or measles vaccine may be indicated after measles exposure. The concentration of measles antibody in a particular immune globulin preparation can vary by lot. The rate of antibody clearance after receipt of an immune globulin preparation can vary. The recommended intervals are extrapolated from an estimated half life of 30 days for passively acquired antibody and an observed interference with the immune response to measles vaccine for months after a dose of 80 Passively acquired measles antibodies can interfere with the immune response to measles vaccination (see Recent Administration of Immune Globulins). The interval required to avoid such interference varies (Table 3).
# TABLE 3. Suggested intervals between administration of immune globulin preparations for various indications and vaccines containing live-measles virus*
Indications
IG does not prevent rubella or mumps infection after exposure and is not recommended for that purpose. Although administration of IG after exposure to rubella will not prevent infection or viremia, it may modify or suppress symptoms and create an unwarranted sense of security. Therefore, IG is not recommended for routine postexposure prophylaxis of rubella in early pregnancy or any other circumstance. Infants with congenital rubella have been born to women who received IG shortly after exposure. Administration of IG should be considered only if a pregnant woman who has been exposed to rubella will not consider termination of pregnancy under any circumstances. In such cases, intramuscular administration of 20 mL of immune globulin within 72 hours of rubella exposure may reduce-but will not eliminate-the risk for rubella (145,146 ).
# Revaccination of Persons Vaccinated According to Earlier Recommendations
Some persons vaccinated according to earlier recommendations for use of measles, rubella, mumps, and MMR vaccines should be revaccinated to ensure that they are adequately protected. Unless one of its component vaccines is contraindicated, MMR vaccine should be used for this purpose.
# Previous vaccination with live measles, rubella, and mumps vaccines.
Persons vaccinated with live measles, rubella, or mumps vaccines before the first birthday who were not revaccinated on or after the first birthday should be considered unvaccinated. Unless they have other acceptable evidence of immunity to measles, rubella, and mumps (Table 1), these persons should be revaccinated with MMR.
Live attenuated Edmonston B measles vaccine (distributed from 1963 to 1975) was usually administered with IG or high-titer measles immune globulin (MIG; no longer available in the United States). Vaccination with this product, administered on or after the first birthday, is considered an effective first dose of vaccine. If indicated, a second dose of MMR vaccine should be administered (see Documentation of Immunity).
IG or MIG administered simultaneously with further attenuated measles vaccines (i.e., vaccines containing the Schwarz or Moraten virus strains) may have impaired the immune response to vaccination. Persons who received measles vaccine of unknown type or further attenuated measles vaccine accompanied by IG or MIG should be considered unvaccinated and should be administered two doses of MMR vaccine. Persons vaccinated with other previously licensed live rubella vaccines that were not administered with IG or MIG (i.e., HPV-77 or Cendehill vaccines) need not be revaccinated against rubella.
# Previous vaccination with inactivated measles vaccine or measles vaccine of unknown type. Inactivated (killed) measles vaccine was available in the United
States only from 1963 to 1967 but was available through the early 1970s in some other countries. It was frequently administered as a series of two or three injections. Because persons who received inactivated vaccine are at risk for developing severe atypical measles syndrome when exposed to the natural virus, they should receive two doses of MMR or other live measles vaccine, separated by at least 28 days (147 ). Persons who received inactivated vaccine followed within 3 months by live virus vaccine should also be revaccinated with two more doses of MMR or other live measles vaccine. Revaccination is particularly important when the risk for exposure to natural measles virus is increased (e.g., during international travel).
Persons vaccinated during 1963-1967 with vaccine of unknown type may have received inactivated vaccine and also should be revaccinated. Persons who received a vaccine of unknown type after 1967 need not be revaccinated unless the original vaccination occurred before the first birthday or was accompanied by IG or MIG. However, such persons should receive a second dose before entering college, beginning work in a health-care facility, or undertaking international travel. Some recipients of inactivated measles vaccine who were later revaccinated with live measles vaccine have had adverse reactions to the live vaccine; the percentage who reported adverse reactions ranges from 4% to 55% (148 ). In most cases, these reactions were mild (e.g., local swelling and erythema, low-grade fever lasting 1-2 days), but rarely more severe reactions (e.g., prolonged high fevers, extensive local reactions) have been reported. However, natural measles infection is more likely to cause serious illness among recipients of inactivated measles vaccine than is live measles virus vaccine.
# Previous vaccination with inactivated mumps vaccine or mumps vaccine of unknown type.
A killed mumps virus vaccine was licensed for use in the United States from 1950 through 1978. Although this vaccine induced antibody, the immunity was transient. The number of doses of killed mumps vaccine administered between licensure of live attenuated mumps vaccine in 1967 until the killed vaccine was withdrawn in 1978 is unknown but appears to have been limited.
Revaccination with MMR should be considered for certain persons vaccinated before 1979 with either killed mumps vaccine or mumps vaccine of unknown type who are at high risk for mumps infection (e.g., persons who work in health-care facilities during a mumps outbreak). No evidence exists that persons who have had mumps disease or who have previously received mumps vaccine (killed or live) are at increased risk for local or systemic reactions upon receiving MMR or live mumps vaccine.
# ADVERSE EVENTS AFTER MMR VACCINATION
Adverse events associated with administration of MMR vaccine range from local pain, induration, and edema to rare systemic reactions such as anaphylaxis. Side effects tend to occur among vaccine recipients who are nonimmune and therefore are very rare after revaccination (see Revaccination). Expert committees at the Institute of Medicine (IOM) recently reviewed all evidence concerning the causal relationship between MMR vaccination and various adverse events (149,150 ). The IOM determined that evidence establishes a causal relation between MMR vaccination and anaphylaxis, thrombocytopenia, febrile seizures, and acute arthritis. Although vasculitis, otitis media, conjunctivitis, optic neuritis, ocular palsies, Guillain-Barré syndrome, and ataxia have been reported after administration of MMR or its component vaccines and are listed in the manufacturer's package insert, no causal relationship has been established between these events and MMR vaccination.
Evidence does not support a causal association of administration of measlescontaining vaccine with risk for Crohn disease, a hypothesis proposed by some researchers in the United Kingdom and Sweden (151)(152)(153)(154)(155)(156). Other researchers have been unable to replicate the laboratory findings that were reported to support this hypothesized association (157,158 ). Concerns also have been raised about the methods used in the epidemiologic studies that suggested an association between Crohn disease and measles vaccination (159)(160)(161)(162)(163). Other data do not support an association between measles vaccination and risk for Crohn disease or other inflammatory bowel disease (164,165 ).
Infection with mumps virus may trigger the onset of diabetes mellitus in some persons. However, no association has been established between vaccination with MMR or other mumps virus vaccine and pancreatic damage or subsequent development of diabetes mellitus (150 ).
# Fever, Rash, Lymphadenopathy, or Parotitis
Measles, rubella, and mumps vaccines may cause fever after vaccination; the measles component of MMR vaccine is most often associated with this adverse event. Approximately 5% of children develop a temperature of ≥103 F (≥39.4 C) after MMR vaccination. Such febrile reactions usually occur 7-12 days after vaccination and generally last 1-2 days (166 ). Most persons with fever are otherwise asymptomatic.
Measles-and rubella-containing vaccines (including MMR) can cause transient rashes, which usually appear 7-10 days after vaccination, in approximately 5% of vaccinated persons. Transient lymphadenopathy sometimes occurs following administration of MMR or other rubella-containing vaccine, and parotitis has been reported rarely following administration of MMR or other mumps-containing vaccine.
# Allergic Reactions
Hypersensitivity reactions, usually consisting of urticaria or a wheal and flare at the injection site, occur rarely after administration of MMR or any of its component vaccines. Immediate anaphylactic reactions to these vaccines are very rare. More than 70 million doses of MMR vaccine have been distributed in the United States since the Vaccine Adverse Events Reporting System (VAERS) was implemented in 1990. The reported rate of possible anaphylaxis after vaccination with measles-containing vaccine is <1 case per 1 million doses distributed (CDC, unpublished data). Allergic reactions including rash, pruritus, and purpura have been temporally associated with mumps vaccination but are uncommon, usually mild, and of brief duration.
# Thrombocytopenia
Surveillance of adverse reactions in the United States and other countries indicates that MMR vaccine can, in rare instances, cause clinically apparent thrombocytopenia within 2 months after vaccination. In prospective studies, the reported frequency of clinically apparent thrombocytopenia after MMR vaccination ranged from 1 case per 30,000 vaccinated children in Finland and Great Britain (167,168 ) to 1 case per 40,000 in Sweden (169 ), with a temporal clustering of cases occurring 2-3 weeks after vaccination. Based on passive surveillance, the reported frequency of thrombocytopenia was approximately 1 case per 100,000 vaccine doses distributed in Canada (170 ) and France (171 ), and approximately 1 case per 1 million doses distributed in the United States (172 ). The clinical course of these cases was usually transient and benign, although hemorrhage occurred rarely (172 ). The risk for thrombocytopenia during rubella or measles infection is much greater than the risk after vaccination (173 ). Based on case reports, the risk for MMR-associated thrombocytopenia may be increased for persons who have previously had immune thrombocytopenic purpura, particularly for those who had thrombocytopenic purpura after an earlier dose of MMR vaccine (150,174,175 ).
# Neurological Events
Adverse neurological events after administration of MMR vaccine are rare. Reports of nervous system illness following MMR vaccination do not necessarily denote an etiologic relationship between the illness and the vaccine. Although several cases of sensorineural deafness have been reported after administration of MMR vaccine, evidence from these case reports (e.g., timing of onset and other features) is inadequate to accept or reject a causal relation between MMR vaccination and sensorineural deafness.
# Aseptic Meningitis
Aseptic meningitis has been clearly associated with administration of the Urabe strain mumps vaccine virus but not with the Jeryl Lynn strain, which is the only mumps vaccine used in the United States (176)(177)(178). Sentinel surveillance laboratories in the United Kingdom identified thirteen aseptic meningitis cases (91 cases per 1 million doses distributed) that occurred after administration of the Urabe strain vaccine during 1988-1992 (168 ). Since the United Kingdom switched to Jeryl Lynn strain vaccine in 1992, no mumps vaccine-associated aseptic meningitis cases have been reported by the surveillance laboratories (178 ).
# Subacute Sclerosing Panencephalitis (SSPE)
Measles vaccination substantially reduces the occurrence of SSPE as evidenced by the near elimination of SSPE cases after widespread measles vaccination. SSPE has been reported rarely among children who had no history of natural measles infection, but who had received measles vaccine. Evidence indicates that at least some of these children had unrecognized measles infection before they were vaccinated and that the SSPE was directly related to the natural measles infection. The administration of live measles vaccine does not increase the risk for SSPE, even among persons who have previously had measles disease or received live measles vaccine (150,179 ).
# Encephalopathy/Encephalitis
Encephalitis with resultant residual permanent central nervous system (CNS) impairment (encephalopathy) develops in approximately 1 per 1,000 persons infected with measles virus. Whether attenuated live viral measles vaccine can also produce such a syndrome has been a concern since the earliest days of measles vaccine use.
In 1994, the IOM noted that most data were from case reports, case series, or uncontrolled observational studies, and concluded that the evidence was inadequate to accept or reject a causal relation (150 ).
The British National Childhood Encephalopathy Study (NCES) identified a fourfold elevation in risk for encephalopathy or convulsions among children who received measles vaccine during 1976-1979, compared with the risk for these conditions among unvaccinated children (180). Among previously normal children, the attributable risk for acute encephalopathy or convulsions was 1 case per 87,000 vaccinations. Findings of a subsequent 10-year follow-up study of persons diagnosed with convulsions or acute encephalopathy in the NCES indicated little difference in risk for persisting neurological abnormality among those who had received measles vaccine compared with those who had not (E. Miller, personal communication).
Although cases of encephalopathy have been reported after administration of measles-containing vaccine (181 ), lack of a unique clinical syndrome or specific laboratory test has hampered causality assessment. However, four independent passive surveillance systems in the United States (i.e., CDC measles surveillance from 1963 to 1971, the Monitoring System for Adverse Events Following Immunizations from 1979 to 1990, the Vaccine Adverse Event Reporting System from 1991 to 1996, and the Vaccine Injury Compensation Program ) have reported cases of encephalopathy in which a similar timing of reported events following vaccine administration is apparent. In all four case series, onset of encephalopathies follows a non-random distribution with onset approximately 10 days after vaccination, a timing consistent with onset of encephalopathy after infection with wild measles virus (182 ). Although this pattern may be in part attributable to consistent biases of these passive surveillance systems, it is also consistent with a causal relationship between measles vaccine and encephalopathies (183 ). During the period these four systems have collected data, 166 cases of encephalopathy occurring 6-15 days after vaccination have been identified and an estimated 313 million doses of measles-containing vaccines have been distributed (i.e., approximately 1 case per 2 million doses distributed). Thus, encephalopathy occurs much less frequently after administration of measles vaccine than after measles infection.
# Febrile Seizures and Personal and Family History of Convulsions
MMR vaccination, like other causes of fever, may cause febrile seizures. The risk for such seizures is approximately 1 case per 3,000 doses of MMR vaccine administered (168 ). Studies have not established an association between MMR vaccination and residual seizure disorders (150 ). Although children with personal or family histories of seizures are at increased risk for idiopathic epilepsy, febrile seizures after vaccinations do not increase the probability that epilepsy or other neurologic disorders will subsequently develop in these children. Most convulsions that occur after measles vaccination are simple febrile seizures, which affect children who do not have other known risk factors for seizure disorders.
Antipyretics may prevent febrile seizures after MMR vaccination if administered before the onset of fever and continued for 5-7 days. However, antipyretics are difficult to use for this purpose because the onset of fever is often sudden and occurs unpredictably. Seizures can occur early in the course of fever. Parents should be vigilant for fever that occurs after vaccination and should be counseled regarding its appropriate treatment. Use of aspirin during some illnesses in childhood is associated with the occurrence of Reye syndrome. Therefore, aspirin generally should not be used to prevent or control fever among children and adolescents.
The 5%-7% of children who have either a personal history of convulsions or a parent or sibling with history of convulsions may be at increased risk for febrile convulsions after MMR vaccination (184 ). The precise risk has not been measured, but appears to be minimal. On the other hand, febrile seizures occur commonly among children in whom measles disease develops, and the risk for acquiring measles is substantial. Therefore, the benefits of administering MMR vaccine to children with a personal or family history of convulsions substantially outweigh the risks and these children should be vaccinated following the recommendations for children who have no contraindications.
Children who are being treated with anticonvulsants should continue to take them after measles vaccination. Because protective levels of most currently available anticonvulsant drugs (e.g., phenobarbital) are not achieved for some time after therapy is initiated, prophylactic use of these drugs is not feasible.
The parents of children who have either a personal or family history of seizures should be advised of the benefits of vaccination and the minimal increased risk for seizures, which generally occur 5-14 days after measles vaccination.
# Guillain-Barré Syndrome (GBS)
Cases of GBS occurring after administration of MMR or its component vaccines have been reported, but the IOM judged the evidence insufficient to accept or reject a causal relationship (150 ). Recent studies provide evidence against this potential association (185,186 ). After recent mass vaccination campaigns that involved approximately eight million doses of measles-rubella vaccine in the United Kingdom and >70 million doses of measles vaccine in Latin America, evaluations of GBS incidence demonstrated no increases over background rates.
# Arthralgia, Arthritis, and Persistent or Recurrent Arthropathy
Joint symptoms are associated with the rubella component of MMR. Among susceptible persons who receive rubella vaccine, arthralgia and transient arthritis occur more frequently among adults than among children and more frequently among postpubertal females than among males. Acute arthralgia or arthritis are rare among children who receive RA 27/3 vaccine (187 ). By contrast, arthralgia develops among approximately 25% of susceptible postpubertal females after RA 27/3 vaccination and approximately 10% have acute arthritis-like signs and symptoms (188,189 ). Although rare reports of transient peripheral neuritic complaints have occurred, insufficient evidence exists to indicate a causal relation between RA 27/3 vaccine and peripheral neuropathies (149,190 ). When acute joint symptoms occur, or when pain and/or paresthesias not associated with joints occur, they generally begin 1-3 weeks after vaccination, persist for 1 day to 3 weeks, and rarely recur. Adults who experienced acute joint symptoms after rubella vaccination usually have not had to disrupt work activities (189,190,191 ).
A 1991 report by the IOM stated that although some data were consistent with a causal relation between RA27/3 rubella vaccine and chronic arthritis among adult women, the evidence was limited in scope and confined to reports from a single institution (149 ). Several more recently published studies have found no evidence of increased risk for new onset of chronic arthropathies among women vaccinated with RA 27/3 vaccine (192)(193)(194). In addition, data from a recent prospective, randomized, placebo-controlled trial by the same group that initially reported chronic arthropathy after rubella vaccination demonstrated only a small excess risk for persistent joint symptoms among persons who received rubella vaccine (relative risk = 1.58; 95% confidence interval = 1.01-2.45) (195 ). Neither the duration of arthropathy nor timing of onset was reported. The occurrence of arthropathy described as moderate or severe did not differ between vaccine and placebo recipients and was rare in both groups.
# Interference with Tuberculin Skin Tests
Tuberculin testing is not a prerequisite for vaccination with MMR or any of its component vaccines. MMR vaccine may interfere with the response to a tuberculin test (196)(197)(198). Therefore, tuberculin testing, if otherwise indicated, can be done either on the same day MMR vaccine is administered or 4-6 weeks later.
# Revaccination
No evidence indicates that administration of live measles, mumps, or rubella vaccine increases the risk for adverse reactions among persons who are already immune to these diseases as a result of previous vaccination or natural disease. Data indicate that only persons who are not immune when vaccinated tend to have postvaccination side effects similar to the disease symptoms (139 ). No evidence exists that persons who have previously received killed mumps vaccine or had mumps disease are at increased risk for local or systemic reactions from receiving live mumps vaccine. Some recipients of inactivated measles vaccine who were later revaccinated with live measles vaccines have had adverse reactions to the live vaccine (see Revaccination of Persons Vaccinated According to Earlier Recommendations).
# REPORTING ADVERSE EVENTS
Reporting of serious adverse events that occur after administration of MMR or its component vaccines helps identify adverse events that may be caused by these vaccines. The National Childhood Vaccine Injury Act of 1986 requires health-care providers to report serious adverse events that occur after vaccination with MMR and its component vaccines to the Vaccine Adverse Events Reporting System (VAERS). Persons other than health-care workers can also report adverse events to VAERS. Events that must be reported after MMR vaccination are listed in the reportable events table within the Act and include anaphylaxis or anaphylactic shock occurring within 7 days of vaccination, encephalopathy (or encephalitis) occurring within 7 days of vaccination, and any events described in the manufacturer's package insert as contraindications to additional doses of vaccine (199 ). Other adverse events occurring after administration of a vaccine, especially events that are serious or unusual, also should be reported to VAERS, regardless of the provider's opinion of the causality of the association. VAERS reporting forms and information are available 24 hours a day by calling 1-800-822-7967 or via the World Wide Web at http:\\www.cdc.gov/nip/ vaers.htm.
# VACCINE INJURY COMPENSATION
The National Vaccine Injury Compensation Program, established by the National Childhood Vaccine Injury Act of 1986, is a system under which compensation may be paid on behalf of a person thought to have been injured or to have died as a result of receiving a vaccine covered by the program. The program is intended as an alternative to civil litigation under the traditional tort system because negligence need not be proven.
The Act establishes a) a Vaccine Injury Compensation Table that lists the vaccines covered by the program; b) the injuries, disabilities, and conditions (including death) for which compensation may be paid without proof of causation; and c) the period after vaccination during which the first symptom or substantial aggravation of the injury must appear. Modifications to the Vaccine Injury Table became effective March 24, 1997 (199 ). Persons may be compensated for an injury listed in the established table or one that can be demonstrated to result from administration of a listed vaccine. Additional information about the program is available.*
# PRECAUTIONS AND CONTRAINDICATIONS Pregnancy
MMR and its component vaccines should not be administered to women known to be pregnant. Because a risk to the fetus from administration of these live virus vaccines cannot be excluded for theoretical reasons, women should be counseled to avoid becoming pregnant for 30 days after vaccination with measles or mumps vaccines and for 3 months after administration of MMR or other rubella-containing vaccines. Routine precautions for vaccinating postpubertal women with MMR should be followed in all vaccination programs (see Routine Vaccination-Women of Childbearing Age). If a pregnant woman is vaccinated or if she becomes pregnant within 3 months after vaccination, she should be counseled about the theoretical basis of concern for the fetus, but MMR vaccination during pregnancy should not ordinarily be a reason to consider termination of pregnancy. Rubella-susceptible women who are not vaccinated because they state they are or may be pregnant should be counseled about the potential risk for CRS and the importance of being vaccinated as soon as they are no longer pregnant.
Because birth defects are noted in 3%-5% of all births, confusion about the etiology of birth defects may result if vaccine is administered during pregnancy. Although of theoretical concern, no cases of congenital rubella syndrome or abnormalities attributable to infection with measles, rubella, or mumps vaccine virus infection have been observed among infants born to susceptible mothers who received any of these vaccines during pregnancy. From January 1971 through April 1989, CDC followed to term 321 known rubella-susceptible pregnant women who had been vaccinated with live rubella vaccine within 3 months before or 3 months after conception. Ninety-four women received HPV-77 or Cendehill vaccines, one received vaccine of unknown strain, and 226 received RA 27/3 vaccine (the only rubella vaccine presently used in the United States). None of the 324 infants born to these mothers had malformations compatible with congenital rubella infection. This total included five infants who had serologic evidence of subclinical infection; three of the infants were exposed to HPV-77 or Cendehill vaccine and two were exposed to RA 27/3 vaccine. Based on these data, the estimated risk for serious malformations attributable to RA 27/3 rubella vaccine ranges from zero to 1.6%. If the infants exposed to other rubella vaccines are included, the estimated risk is zero to 1.2%, substantially less than the ≥20% risk for CRS associated with maternal infection during the first trimester of pregnancy (200 ). Moreover, the observed risk for CRS with both the HPV-77 or Cendehill and RA 27/3 strains of vaccine is zero. Rubella vaccine virus has been isolated from the aborted fetus of one (3%) of 35 rubella-susceptible women who received RA 27/3 strain vaccine during pregnancy. In contrast, vaccine virus was isolated from the fetuses of 17 (20%) of 85 women to whom HPV-77 or Cendehill vaccines were administered (201). This finding provides additional evidence that the RA 27/3 vaccine poses no greater risk for teratogenicity than did the HPV-77 or Cendehill vaccines.
Breast feeding is not a contraindication to vaccination. Although a woman can excrete rubella vaccine virus in breast milk and transmit the virus to her infant, the infection remains asymptomatic (202)(203)(204)(205). Otherwise, persons who receive MMR or its component vaccines do not transmit measles, rubella, or mumps vaccine viruses (206,207 ). Thus, MMR vaccine can be administered safely to susceptible children or other persons with household contacts who are pregnant to help protect these pregnant women from exposure to wild rubella virus.
All suspected cases of CRS, whether presumed to be due to wild-virus or vaccinevirus infection, should be reported to state and local health departments. Suspected or confirmed cases of CRS can also be reported to the VAERS (see Reporting Adverse Events).
# Severe Illness
Because of the importance of protecting susceptible children against measles, mumps, and rubella, medical personnel should use every opportunity to vaccinate susceptible persons. The decision to vaccinate or postpone vaccination of a person who currently has or recently has had an acute febrile illness depends largely on the cause of the illness and the severity of symptoms. Minor illnesses, with or without fever (e.g., diarrhea, upper respiratory infection, otitis media) are not contraindications for vaccination and vaccination should not be postponed because of them. Data indicate that seroconversion rates for each component of MMR vaccine among persons with mild febrile illness are similar to those among healthy persons (208,209 ). Similarly, performing routine physical examinations or measuring temperatures are not prerequisites for vaccinating persons who appear to be in good health. In childhood vaccination programs, appropriate procedures include a) asking the parent or guardian if the child is ill, b) postponing vaccination of children who have moderate or severe febrile illnesses, and c) vaccinating children who do not have other contraindications.
Vaccination of persons with moderate or severe febrile illnesses should generally be deferred until they have recovered from the acute phase of their illness. This wait avoids superimposing adverse effects of vaccination on the underlying illness or mistakenly attributing a manifestation of the underlying illness to the vaccine. Data are generally not available regarding the safety and immunogenicity of MMR vaccine among persons with moderate or severe febrile illness.
Persons under treatment for tuberculosis have not experienced exacerbations of the disease when vaccinated with MMR. Although no studies have been reported concerning the effect of MMR vaccine on persons with untreated tuberculosis, a theoretical basis exists for concern that measles vaccine might exacerbate tuberculosis. Consequently, before administering MMR to persons with untreated active tuberculosis, initiating antituberculous therapy is advisable. Tuberculin testing is not a prerequisite for routine vaccination with MMR or other measles-containing vaccines.
# Allergies
Among persons who are allergic to eggs, the risk for serious allergic reactions such as anaphylaxis following administration of measles-or mumps-containing vaccines is extremely low and skin-testing with vaccine is not predictive of allergic reaction to vaccination (210)(211)(212). Therefore, skin testing is not required before administering MMR (or other measles-and mumps-containing vaccines) to persons who are allergic to eggs. Similarly, the administration of gradually increasing doses of vaccine is not required. In the past, persons with a history of anaphylactic reactions (i.e., hives, swelling of the mouth or throat, difficulty breathing, hypotension, and shock) following egg ingestion were considered to be at increased risk for serious reactions after administration of measles-or mumps-containing vaccines, which are produced in chick embryo fibroblasts. Although protocols have been developed for skin testing and vaccination of persons who experience anaphylactic reactions to egg ingestion, data indicate that most anaphylactic reactions to measles-and mumps-containing vaccines are not associated with hypersensitivity to egg antigens but to other components of the vaccines (213)(214)(215)(216)(217).
The literature contains several case reports of persons with an anaphylactic sensitivity to gelatin who had anaphylactic reactions after receiving MMR vaccine (218)(219)(220). MMR and its component vaccines contain hydrolyzed gelatin as a stabilizer. Therefore, extreme caution should be exercised when administering MMR or its component vaccines to persons who have a history of an anaphylactic reaction to gelatin or gelatin-containing products. Before administering MMR or its component vaccines to such persons, skin testing for sensitivity to gelatin can be considered. However, no specific protocols for this purpose have been published.
Because MMR and its component vaccines contain trace amounts of neomycin (25 µg), persons who have experienced anaphylactic reactions to topically or systemically administered neomycin should not receive these vaccines. However, neomycin allergy is most often manifested as a delayed or cell-mediated immune response (i.e., a contact dermatitis), rather than anaphylaxis. In persons who have such a sensitivity, the adverse reaction to the neomycin in the vaccine is an erythematous, pruritic nodule or papule appearing 48-96 hours after vaccination. A history of contact dermatitis to neomycin is not a contraindication to receiving MMR vaccine. MMR vaccine does not contain penicillin and therefore a history of penicillin allergy is not a contraindication to MMR vaccination.
Although anaphylaxis after vaccination is extremely rare and no anaphylaxis deaths associated with administration of MMR vaccine have been reported, this adverse event can be life threatening (150 ). Epinephrine should be available for immediate use at any site where vaccines are administered in case symptoms of anaphylaxis occur.
# Thrombocytopenia
Children who have a history of thrombocytopenia or thrombocytopenic purpura may be at increased risk for developing clinically significant thrombocytopenia after MMR vaccination (172,175 ). Although thrombocytopenia can be life threatening, no deaths have been reported as a direct consequence of vaccine-induced thrombocytopenia. The decision to vaccinate with MMR should depend on the benefits of immunity to measles, mumps, and rubella and the risks for recurrence or exacerbation of thrombocytopenia after vaccination or during natural infection with measles or rubella. The benefits of primary immunization are usually greater than the potential risks, and administration of MMR vaccine is justified, particularly with regard to the even greater risk for thrombocytopenia after measles or rubella disease. However, avoiding a subsequent dose of MMR vaccine may be prudent if an episode of thrombocytopenia occurred within approximately 6 weeks after a previous dose of the vaccine. Serologic evidence of measles immunity among such persons may be sought in lieu of MMR vaccination.
# Recent Administration of Immune Globulins
Recent evidence indicates that high doses of immune globulins can inhibit the immune response to measles and rubella vaccine for 3 or more months (221,222 ). The duration of this interference with the immune response depends on the dose of immune globulin administered. The effect of immune globulin preparations on the response to mumps vaccine is unknown. Blood (e.g., whole blood, packed red blood cells, and plasma) and other antibody-containing blood products (e.g., IG, specific immune globulins, and IGIV) can reduce the immune response to MMR or its component vaccines. Therefore, these vaccines should be administered to persons who have received an immune globulin preparation only after the recommended intervals have elapsed (Table 3) (80 ). However, postpartum administration of MMR or rubella vaccine to women who are susceptible to rubella should not be delayed because anti-Rho(D) immune globulin (human) or any other blood product was received during the last trimester of pregnancy or at delivery. Such rubella-susceptible women should be vaccinated immediately after delivery and tested at least 3 months later to ensure that they are immune to rubella and measles.
Immune globulin preparations generally should not be administered simultaneously with MMR or its component vaccines. If administration of an immune globulin preparation becomes necessary because of imminent exposure to disease, MMR or its component vaccines can be administered simultaneously with the IG preparation, although vaccine-induced immunity may be compromised. Usually, vaccine virus replication and stimulation of immunity will occur 1-2 weeks after vaccination. Thus, if the interval between administration of any of these vaccines and administration of an IG preparation is <14 days, vaccination should be repeated after the recommended interval (Table 3), unless serologic testing indicates that the vaccinated person's immune system has produced antibodies to each vaccine component (i.e., measles, rubella, and mumps). The vaccine should be administered at an anatomic site remote from that chosen for the IG injection.
# Altered Immunocompetence
Enhanced replication of vaccine viruses may occur in persons who have immune deficiency diseases and in other persons who are immunosuppressed. Severe immunosuppression may be caused by many disease conditions (e.g., congenital immunodeficiency, HIV infection, hematologic or generalized malignancy) and by therapy with immunosuppressive agents, including large doses of corticosteroids. For some of these conditions, all affected persons are severely immunocompromised. For other conditions (e.g., HIV infection), the degree to which the immune system is compromised depends on the severity of the condition, which in turn depends on the disease or treatment stage. Ultimately, the patient's physician must assume responsibility for determining whether the patient is severely immunocompromised based on clinical and laboratory assessment.
Case reports have linked vaccine-associated measles infection to the deaths of some severely immunocompromised persons (150,223 ). Therefore, MMR vaccine should not be administered to severely immunocompromised persons. To reduce the risk for measles, rubella, and mumps exposure of immunocompromised patients, their susceptible close contacts should be vaccinated with MMR. No case reports exist linking MMR or mumps-or rubella-containing vaccines with clinically significant infection caused by mumps or rubella vaccine virus among immunocompromised vaccine recipients.
# HIV-Infected Persons
Among asymptomatic and symptomatic HIV-infected patients who are not severely immunosuppressed, MMR vaccination has been associated with variable antibody responses but not with severe or unusual adverse events. Asymptomatic persons do not need to be evaluated and tested for HIV infection before MMR and other measlescontaining vaccines are administered. MMR vaccine is recommended for all asymptomatic HIV-infected persons who are not severely immunosuppressed and who lack evidence of measles immunity. MMR vaccination of symptomatic HIV-infected persons should be considered if they a) do not have evidence of severe immunosuppression and b) lack evidence of measles immunity. MMR and other measles-containing vaccines are not recommended for HIV-infected persons with evidence of severe immunosuppression (see Special Considerations for Vaccination-Persons Infected with Human Immunodeficiency Virus ) (Table 2).
# Steroids
Systemically absorbed corticosteroids can suppress the immune system of an otherwise healthy person. However, neither the minimum dose nor the duration of therapy sufficient to cause immune suppression are well defined. Most experts agree that steroid therapy usually does not contraindicate administration of live virus vaccines such as MMR and its component vaccines when therapy is: a) short term (i.e., <14 days) low-to-moderate dose; b) low-to-moderate dose administered daily or on alternate days; c) long term alternate day treatment with short-acting preparations; d) physiologic maintenance doses (replacement therapy); or e) administered topically (skin or eyes), by aerosol, or by intra-articular, bursal, or tendon injection. Although the immunosuppressive effects of steroid treatment vary, many clinicians consider a steroid dose that is equivalent to or greater than a prednisone dose of 2 mg/kg of body weight per day or a total of 20 mg per day sufficiently immunosuppressive to raise concern about the safety of administration of live virus vaccines. Persons who have received systemic corticosteroids in these or greater doses daily or on alternate days for an interval of ≥14 days should avoid vaccination with MMR and its component vaccines for at least 1 month after cessation of steroid therapy. Persons who have received prolonged or extensive topical, aerosol, or other local corticosteroid therapy that causes clinical or laboratory evidence of systemic immunosuppression should also avoid vaccination with MMR for at least 1 month after cessation of therapy. Persons who receive doses of systemic corticosteroids equivalent to a prednisone dose of ≥2 mg/kg of body weight or ≥20 mg total daily or on alternate days during an interval of <14 days generally can receive MMR or its component vaccines immediately after cessation of treatment, although some experts prefer waiting until 2 weeks after completion of therapy. MMR or its component vaccines generally should not be administered to persons who have a disease that, in itself, suppresses the immune response and who are receiving either systemic or locally administered corticosteroids.
# Leukemia
Persons with leukemia in remission who were not immune to measles, rubella, or mumps when diagnosed with leukemia may receive MMR or its component vaccines. At least 3 months should elapse after termination of chemotherapy before administration of the first dose of MMR vaccine.
# Management of Patients with Contraindications to Measles Vaccine
If immediate protection against measles is required for persons with contraindications to measles vaccination, 0.25 mL/kg (0.11 mL/lb) of body weight (maximum dose = 15 mL) of IG should be administered as soon as possible after known exposure (See Use of Vaccine and Immune Globulin Among Persons Exposed to Measles, Rubella, or Mumps). Exposed symptomatic HIV-infected and other immunocompromised persons should receive IG regardless of their previous vaccination status. Because IG in usual doses may not be effective for immunocompromised persons, the recommended dose is 0.5 mL/kg of body weight if IG is administered intramuscularly (maximum dose = 15 mL). This corresponds to a dose of IgG protein of approximately 82.5 mg/kg (maximum dose = 2,475 mg). Intramuscular IG may not be needed if a patient is receiving at least 100-400 mg/kg IGIV at regular intervals and exposure occurs within 3 weeks after administration of the last dose of IGIV. Because the amounts of protein administered are similar, high-dose IGIV may be as effective as intramuscular IG. However, no data are available concerning the effectiveness of IGIV in preventing measles.
The effectiveness of IG or IGIV for preventing mumps or rubella is unknown. These products should not be used for prophylaxis among immunocompromised persons exposed to these diseases.
# SURVEILLANCE AND OUTBREAK CONTROL
Surveillance for vaccine preventable diseases has four primary purposes: a) to provide important data on program progress and long term trends, b) to provide the basis for changes in disease prevention strategies, c) to help define groups in greatest need of vaccination, and d) to evaluate vaccine safety and effectiveness (e.g., protective efficacy, duration of vaccine-induced immunity, and occurrence of adverse effects). As the incidence of measles, rubella, and mumps declines in the United States, enhanced surveillance becomes increasingly important.
Any person aware of a suspected or known cases of measles, rubella, congenital rubella syndrome, or mumps should report the case to the local or state health department. The designated public health authorities should investigate the case immediately. The purpose of the investigation is to classify the case, identify the characteristics of the case and the source of exposure, and prevent further spread.
Cases of measles, rubella, and congenital rubella syndrome are reportable in all states, and mumps is reportable in most states. Data from measles, rubella, congenital rubella syndrome, and mumps cases are routinely reported by state and local health departments to CDC and published weekly in the Morbidity and Mortality Weekly Report.
# Measles Case Investigation and Outbreak Control Case Definition
A suspected measles case is defined as any febrile illness accompanied by rash. Suspected and known cases of measles should be reported immediately to the local or state health department. The designated public health authorities should quickly initiate an investigation of the reported case. Rapid case reporting and investigation can help limit further transmission.
A clinical case of measles is defined as an illness characterized by
- a generalized rash lasting ≥3 days, and - a temperature of ≥38.3 C (≥101 F), and - cough, coryza, or conjunctivitis.
A probable case of measles
- meets the clinical case definition for measles, and
- is not epidemiologically linked to a confirmed case, and - has not been serologically or virologically tested or has noncontributory serologic or virologic results.
A confirmed case of measles
- meets the laboratory criteria for measles or
- meets the clinical case definition and is epidemiologically linked to a confirmed case.
Confirmed measles cases are routinely reported to CDC by state health departments.
# Laboratory Diagnosis
The laboratory criteria for measles diagnosis are:
- a positive serologic test for measles IgM antibody, or - a significant rise in measles antibody level by any standard serologic assay, or - isolation of measles virus from a clinical specimen.
A laboratory-confirmed case need not meet the clinical case definition. Serologic confirmation should be attempted for every suspected case of measles and is particularly important for any case that cannot be epidemiologically linked through a chain of transmission to a confirmed case. However, reporting of suspected or probable cases, investigation of cases, and the implementation of control activities should not be delayed pending laboratory results.
Blood for serologic testing should be collected during the first clinical encounter with a person who has suspected or probable measles. The serum should be tested for measles IgM antibody as soon as possible using an assay that is both sensitive and specific (e.g., direct-capture IgM EIA method). Correct interpretation of serologic data depends on the timing of specimen collection in relation to rash onset and on the characteristics of the antibody assay used. This timing is especially important for interpreting negative results because IgM antibody may not be detectable with some less sensitive assays until at least 72 hours after rash onset. Measles IgM may be detectable at the time of rash onset, peaks approximately 10 days after rash onset, and is usually undetectable 30-60 days after rash onset. In general, if measles IgM is not detected in a serum specimen obtained in the first 72 hours after rash onset from a person whose illness meets the clinical case definition for measles, another specimen should be obtained at least 72 hours after rash onset and tested for measles IgM antibody. Measles IgM is detectable for at least 1 month after rash onset. Persons with febrile rash illnesses who are seronegative for measles should be tested for rubella.
As measles becomes rare in the United States, the likelihood of obtaining false positive serologic results from measles IgM antibody testing increases. False positive results have been obtained by using a commercially available ELISA assay for measles IgM in persons with parvovirus infection (fifth disease) (224 ). Confirmatory testing by using an assay that is both sensitive and specific (e.g., direct-capture IgM EIA method) should be considered when IgM is detected in a patient with suspected measles who has no identified source of infection and no epidemiologic linkage to another confirmed case. The Measles Virus Laboratory of CDC's National Center for Infectious Diseases has provided training to all state public health laboratories to perform such testing.
Serologic diagnosis of measles can also be confirmed by a significant rise in antibody titer between acute-and convalescent-phase serum specimens. Typically, the acute-phase serum specimen is obtained within 1-3 days after rash onset and the convalescent-phase specimen is obtained approximately 2-4 weeks later. This method has been largely supplanted by IgM assays which can be done on a single serum specimen obtained soon after rash onset.
Asymptomatic measles reinfection can occur among persons who have previously developed antibodies from vaccination or from natural disease. Symptomatic reinfections accompanied by rises in measles antibody titers are rare, and those resulting in detectable measles IgM antibody occur even more rarely.
Molecular characterization of measles virus isolates has become an important tool for defining the epidemiologic features of measles during periods of low disease incidence and for documenting the impact of measles elimination efforts (16 ). In addition to serologic confirmation, a specimen (e.g., urine or nasopharyngeal mucus) for measles virus isolation and genetic characterization should be collected as close to the time of rash onset as possible. Delay in collection of these clinical specimens reduces the chance of isolating measles virus. Clinicians who have a patient with suspected measles should immediately contact their local or state health departments concerning additional information about collecting and shipping urine and nasal specimens for measles virus isolation. Molecular characterization of the measles virus isolated from urine or nasopharyngeal specimens requires considerable time and cannot be used for diagnosis of measles. Use of oral fluid in tests for detecting measles IgM and IgG antibodies is being investigated (225 ).
# Measles Outbreak Control
The local or state health department should be contacted immediately when suspected cases of measles occur in a community. All reports of suspected measles cases should be investigated promptly. Because of the potential for rapid spread of the disease, one confirmed case of measles in a community is an urgent public health situation. Once a case is confirmed, prompt vaccination of susceptible persons at risk for exposure may help prevent dissemination of measles. Control activities should not be delayed pending the return of laboratory results from persons with suspected or probable cases. Persons who cannot readily provide acceptable evidence of measles immunity (Table 1) should be vaccinated or excluded from the setting of the outbreak (e.g., school, day care facility, hospital, clinic). Almost all persons who are excluded from an outbreak area because they lack acceptable evidence of immunity quickly comply with vaccination requirements. Persons exempted from measles vaccination for medical, religious, or other reasons should be excluded from involved institutions in the outbreak area until 21 days after the onset of rash in the last case of measles. Mass revaccination of entire communities generally is not necessary. Staff of the National Immunization Program, CDC, are available to assist health departments in developing an outbreak control strategy.
# Measles Outbreaks Among Preschool-Aged Children
Although most infants are protected from measles by maternal antibody, the disease is often more severe when it affects children aged <12 months. If cases are occurring among infants aged <12 months, measles vaccination of infants aged as young as 6 months may be undertaken as an outbreak control measure. Monovalent measles vaccine is preferred, but MMR vaccine may be administered if the monovalent vaccine is not readily available (see Routine Vaccination-International Travel). Children vaccinated with measles or MMR vaccine before the first birthday should be revaccinated at age 12-15 months and again before entering school.
Passive immunization with IG may be preferred for infants aged 72 hours before diagnosis of the disease in the household member and because they are at highest risk for complications from the disease (see Use of Vaccine and Immune Globulin Among Persons Exposed to Measles, Rubella, or Mumps). IG should not be used to control measles outbreaks.
# Measles Outbreaks in Day Care Facilities, Schools, and Other Educational Institutions
During an outbreak in a day care facility, revaccination with MMR is recommended for all attendees and their siblings who have not received two doses of measles-containing vaccine on or after the first birthday and who do not have other evidence of measles immunity. Facility personnel (e.g., employees, volunteers, service providers) who cannot provide acceptable evidence of immunity (Table 1) also should be vaccinated with MMR. Revaccination also should be considered for unaffected child care facilities in the community that may be at risk for measles exposure and transmission.
During outbreaks in schools (elementary, middle, junior and senior high schools, colleges and other institutions of higher education), a program of revaccination with MMR vaccine is recommended in the involved schools. Revaccination of students and personnel of unaffected schools in the same geographic area who may be at risk for measles transmission also should be considered. Revaccination should include all students and their siblings and all school personnel born during or after 1957 who cannot provide documentation of adequate measles vaccination or other acceptable evidence of measles immunity. For persons born in 1957 or later, adequate vaccination consists of two doses of measles-containing vaccine separated by at least 28 days with the first dose administered no earlier than the first birthday (Table 1) ( see Documentation of Immunity). Persons who cannot readily provide documentation of acceptable evidence of measles immunity should be vaccinated or excluded from the day care facility, school, or other educational institution. Revaccinated persons, as well as persons who receive their first dose as part of the outbreak control program, may be readmitted to school immediately. Persons exempted from measles vaccination for medical, religious, or other reasons, and those who refuse vaccination for any reason, should be excluded from the day care facility, school, or other educational institution until 21 days after the onset of rash in the last case of measles.
# Measles Outbreaks in Health-Care Settings
If a measles outbreak occurs within a health-care facility (e.g., hospital, clinic, physician office) or in the areas served by the facility, all persons working at the facility who cannot provide documentation of two doses of measles-containing vaccine separated by at least 28 days with the first dose administered on or after the first birthday, or who do not have other evidence of measles immunity (Table 1), should receive a dose of MMR vaccine. If indicated, health-care workers born during or after 1957 should receive a second dose of MMR vaccine at least 28 days after the previous dose (see Documentation of Immunity). Some health-care workers born before 1957 have acquired measles in health-care facilities and have transmitted the disease to patients or coworkers (see Health-care Facilities). Therefore, during outbreaks, health-care facilities also should strongly consider recommending a dose of MMR vaccine to unvaccinated health-care workers born before 1957 who do not have serologic evidence of immunity or a history of measles disease.
Serologic testing of health-care workers before vaccination is not generally recommended during an outbreak because arresting measles transmission requires rapid vaccination of susceptible health-care workers. The need to screen, wait for results, and then contact and vaccinate susceptible persons can impede the rapid vaccination needed to curb the outbreak.
Susceptible health-care workers (Table 1) exposed to measles should receive a dose of MMR vaccine and should be removed from all patient contact and excluded from the facility from the fifth to the 21st day after the exposure. They may return to work on the 22nd day after exposure. However, susceptible health-care workers who are not vaccinated after exposure should be removed from all patient contact and excluded from the facility from the fifth day after their first exposure to the 21st day after the last exposure, even if they receive postexposure IG. Personnel who become ill with prodromal symptoms or rash should be removed from all patient contact and excluded immediately from the facility until 4 days after the onset of their rash.
# Use of Quarantine
Imposing quarantine measures for outbreak control is usually both difficult and disruptive to schools and other organizations. Under special circumstances (i.e., during outbreaks in schools attended by large numbers of persons who refuse vaccination), restriction of an event or other quarantine measures might be warranted (226). However, such action is not recommended as a routine measure for control of most outbreaks.
# Rubella Case Investigation and Outbreak Control Case Definition
A suspected rubella case is any generalized rash illness of acute onset. A clinical case of rubella is defined as an illness characterized by all of the following clinical features:
- acute onset of generalized maculopapular rash; and - a temperature of >37.2 C (>99 F), if measured; and - arthralgia/arthritis, or lymphadenopathy, or conjunctivitis.
Cases meeting the measles case definition are excluded, as are cases with serologic findings compatible with recent measles virus infection.
A probable case of rubella
- meets the clinical case definition for rubella, and - has no or noncontributory serologic or virologic testing, and - is not epidemiologically linked to a laboratory-confirmed case.
A confirmed rubella case
- meets the laboratory criteria for rubella, or
- meets the clinical case definition and is epidemiologically linked to a laboratory confirmed case.
Suspected and known rubella cases should be reported immediately to local health departments. Aggressive case finding and intensified surveillance for CRS should follow. Rubella surveillance is complicated by the nonspecific nature of the symptoms of the clinical disease. Rubella can be confused with other illnesses, including measles. Thus, all rubella cases, particularly isolated cases that do not occur as part of an outbreak, should be confirmed by laboratory testing. Confirmed rubella cases are reported to the CDC by state health departments. Cases of febrile rash illness that are laboratory-negative for rubella may be measles (rubeola) and the patients should be tested for measles IgM.
Laboratory confirmation of suspected cases of CRS also is necessary because the constellation of findings of CRS varies. Case reports of indigenous congenital rubella syndrome are sentinel events, indicating the presence of rubella infections in the community that may previously have been unrecognized. The diagnosis of one or more indigenous CRS cases in a community should trigger intensified rubella and CRS surveillance.
A confirmed case of CRS has laboratory confirmation of rubella infection and at least one defect in each of the two following categories: a) cataracts/congenital glaucoma (either or both count as one), congenital heart disease, loss of hearing, pigmentary retinopathy; and, b) purpura, splenomegaly, jaundice, microcephaly, mental retardation, meningoencephalitis, radiolucent bone disease.
A probable case of CRS has any two conditions listed in category a) or one from category a) and one from category b) and lacks evidence of any other etiology. A case with laboratory evidence of rubella infection but no clinical symptoms or signs of CRS is classified "infection only."
# Laboratory Diagnosis
The criteria for laboratory diagnosis of rubella are - the isolation of rubella virus from an appropriately collected clinical specimen.
The clinical diagnosis of acute rubella should be confirmed by laboratory testing (230 ). The demonstration of rubella-specific IgM antibody is the most commonly used method to obtain serologic confirmation of acute rubella infection. Rubella-specific IgM antibody usually becomes detectable shortly after rash onset. The IgM antibody peaks approximately 7 days after rash onset and remains detectable for 4-12 weeks, although it is more likely to be detectable if the serum specimen is obtained within 4-5 weeks after rash onset. Occasionally, rubella-specific IgM antibody can be detected up to 1 year after acute infection.
To test for IgM, one serum specimen can be obtained as early as 1-2 days after rash onset. If IgM is not detectable in this first specimen, a second serum specimen should be collected 5 days after the onset of rash or as soon as possible thereafter. Falsenegative rubella IgM antibody test results may sometimes occur even if the specimen is appropriately drawn. False-positive IgM test results may occur among persons with certain viral infections (e.g., acute infectious mononucleosis, cytomegalovirus, or parvovirus) and among persons who are rheumatoid factor positive.
For IgG assays, the criteria for a significant rise in rubella antibody level vary by type of assay and by laboratory. For HI assays, a fourfold rise in the titer of antibody indicates recent infection. The acute-phase serum specimen should be obtained as soon after rash onset as possible, preferably within 7 days. The convalescentphase serum specimen should be drawn at least 10 days after the acute-phase serum specimen. The acute-and convalescent-phase serum specimens should be tested simultaneously in the same laboratory. If the acute-phase serum specimen is drawn >7 days (and occasionally even if obtained within 7 days) after rash onset, a significant rise in antibody titer may not be detected by most commonly used IgG assays.
In the absence of rash illness, the diagnosis of subclinical cases of rubella can be facilitated by obtaining the acute-phase serum specimen as soon as possible after exposure. The convalescent-phase specimen should be drawn at least 28 days after exposure. If acute-and convalescent-phase paired sera provide inconclusive results, rubella-specific IgM antibody testing can be performed. Expert consultation may be necessary to interpret the data.
Among pregnant women of unknown immune status who experience a rash illness or who are exposed to rubella, laboratory confirmation of rubella infection may be difficult. A serum specimen should be obtained as soon as possible. Unfortunately, serologic results are often nonconfirmatory. Such situations can be avoided by performing routine prenatal serologic screening of women who do not have acceptable evidence of rubella immunity (see Documentation of Immunity and Women of Childbearing Age). In addition, health-care providers should request that laboratories performing prenatal serologic screening retain such specimens until delivery, in case retesting is necessary.
# Congenital Rubella
Suspected cases of CRS should be managed with contact isolation (228 ). While diagnostic confirmation is pending, children with suspected CRS should be cared for only by personnel known to be immune to rubella. Confirmation of diagnosis by virus isolation can be done by culturing nasopharyngeal and urine specimens. Serologic confirmation can be obtained by testing cord blood for the presence of rubella-specific IgM antibodies. An alternative method for infants aged ≥3 months is to document rubella-specific antibody levels that do not decline at the rate expected from passive transfer of maternal antibody (i.e., the equivalent of a twofold decline in HI titer per month). However, some infected infants may have low antibody levels because of agammaglobulinemia or dysgammaglobulinemia.
In some infants with CRS, rubella virus can persist and can be isolated from nasopharyngeal and urine cultures throughout the first year of life or longer (229 ). Children with CRS should be presumed infectious at least through the first year of life unless nasopharyngeal and urine cultures are negative for virus after age 3 months (230 ). Some authorities suggest that an infant who has CRS should be considered infectious until two cultures of clinical specimens obtained 1 month apart are negative for rubella virus (230 ). Precautions should be taken to ensure that infants with CRS do not cause additional rubella outbreaks. Specifically, all persons who have contact with a child with CRS (e.g., care givers, household contacts, medical personnel, laboratory workers) should be immune to rubella (Table 1) (see Documentation of Immunity and Routine Vaccination).
# Rubella Outbreak Control
Outbreak control is important for eliminating CRS. Aggressive responses to outbreaks may interrupt chains of transmission and can increase vaccination coverage among persons who might not be protected otherwise. Although methods for controlling rubella outbreaks are evolving, the main strategy should be to define target populations for rubella vaccination, ensure that susceptible persons within the target populations are vaccinated rapidly (or excluded from exposure if a contraindication to vaccination exists), and maintain active surveillance to permit modification of control measures as needed.
Control measures should be implemented as soon as a case of rubella is confirmed in a community. This approach is especially important in any outbreak setting involving pregnant women (e.g., obstetric-gynecologic and prenatal clinics). All persons at risk who cannot readily provide laboratory evidence of immunity or a documented history of vaccination on or after the first birthday should be considered susceptible and should be vaccinated unless vaccination is contraindicated (Table 1) (see Documentation of Immunity).
# Rubella Outbreaks in Schools or Other Educational Institutions
An effective means of terminating rubella outbreaks and increasing rates of vaccination quickly is to exclude from possible contact persons who cannot provide valid evidence of immunity. Experience with measles outbreak control indicates that almost all students who are excluded from school because they lack evidence of immunity quickly comply with vaccination requirements and are promptly readmitted to school. Persons exempted from rubella vaccination for medical, religious, or other reasons should also be excluded from attendance. Exclusion should continue for 3 weeks after the onset of rash of the last reported case in the outbreak setting. Less rigorous approaches (e.g., voluntary appeals for vaccination) have not been effective in terminating outbreaks.
# Rubella Outbreaks in Health-Care Settings
During rubella outbreaks in health-care settings where pregnant women may be exposed, mandatory exclusion and vaccination of health-care workers who lack evidence of rubella immunity (Table 1) should be practiced. Exposed health-care workers who lack evidence of immunity should be excluded from duty from the seventh day after first exposure through the twenty-first day after their last exposure or until 5 days after the rash appears. In addition, because birth before 1957 does not guarantee rubella immunity, health-care facilities should strongly consider recommending a dose of MMR vaccine to unvaccinated health-care workers born before 1957 who do not have serologic evidence of immunity. Although rubella vaccination during an outbreak has not been associated with substantial personnel absenteeism (116,191 ), vaccination of susceptible persons before an outbreak occurs is preferable because vaccination causes far less absenteeism and disruption of routine work activities than does rubella infection.
# Mumps Case Investigation and Outbreak Control Case Definition
A clinical case of mumps is defined as an illness characterized by acute onset of unilateral or bilateral tender, self-limited swelling of the parotid or other salivary gland lasting ≥2 days, and without other apparent cause (as reported by a health professional).
A probable case of mumps
- meets the clinical case definition of mumps, and - is not epidemiologically linked to a confirmed or probable case, and - has noncontributory or no serologic or virologic testing.
A confirmed case of mumps
- meets the laboratory criteria for mumps, or
- meets the clinical case definition and is epidemiologically linked to a confirmed or probable case.
A laboratory-confirmed case need not meet the clinical case definition. Two probable cases that are epidemiologically linked are considered confirmed, even in the absence of laboratory confirmation.
Reporting of mumps often has been based solely on clinical diagnosis without laboratory confirmation. However, parotitis may have other infectious and noninfectious causes. Therefore, serologic confirmation of the diagnosis is preferred. Use of criteria for clinical diagnosis that are both stricter and more reliable, combined with laboratory confirmation, can be expected to decrease the number of false positive mumps cases reported and allow a more accurate assessment of mumps incidence.
Probable or confirmed cases of mumps should be reported immediately to state and local health departments. Recommended procedures to enhance the comprehensiveness of reporting include identification of all contacts, follow-up of susceptible contacts, and serologic testing of all probable cases to confirm the diagnosis.
# Laboratory Diagnosis
The laboratory criteria for the diagnosis of mumps are - isolation of the mumps virus from a clinical specimen, or - a significant rise between acute and convalescent-phase titers in serum mumps IgG antibody level by any standard serologic assay, or
- a positive serologic test for mumps IgM antibody.
In a prospective study in the practices of family practitioners in a Canadian community, one-third of persons with clinically diagnosed cases of mumps had no serologic evidence of recent mumps infection (28 ). Serum mumps IgM IFA tests are commercially available. However, until more data are available concerning the use and interpretation of these tests, laboratory confirmation of mumps should be based on tests of demonstrated reliability. State health department laboratories can provide guidance when testing for acute mumps infection is necessary.
# Mumps Outbreak Control
The strategy for outbreak control includes three main elements. The target population (transmission setting) must be defined. Persons within the population who are susceptible to mumps must be identified and vaccinated. Consideration should be given to excluding susceptible persons who are exempt from vaccination (for medical, religious, or other reasons) from the affected institution or setting until the outbreak is terminated. Active surveillance for mumps should be conducted until two incubation periods (i.e., 5-6 weeks) have elapsed since onset of the last case.
# School-based Mumps Outbreaks
Exclusion of susceptible students from schools affected by a mumps outbreak (and other, unaffected schools judged by local public health authorities to be at risk for transmission of the disease) should be considered among the means to control mumps outbreaks. Excluded students can be readmitted immediately after they are vaccinated. Experience with outbreak control for other vaccine-preventable diseases indicates that almost all students who are excluded from the outbreak area because they lack evidence of immunity quickly comply with requirements and can be readmitted to school. Pupils who have been exempted from mumps vaccination for medical, religious, or other reasons should be excluded until at least 26 days after the onset of parotitis in the last person with mumps in the affected school.
# Mumps Outbreaks in Health-Care Settings
Sporadic nosocomial cases of mumps have occurred in long-term care facilities housing adolescents and young adults (122 ). However, mumps virus is less transmissible than measles and other respiratory viruses. The low level of mumps transmission in the community results in a low risk for introduction of the disease into health-care facilities. Because mumps is shed by infected persons before clinical symptoms become evident and because infected persons often remain asymptomatic, an effective routine MMR vaccination program for health-care workers is the best approach to prevent nosocomial transmission.
To prevent droplet transmission of the disease, respiratory isolation precautions for persons with mumps should be maintained for 9 days after onset of symptoms (e.g., parotitis). If exposed to mumps, health-care workers who lack acceptable evidence of immunity (Table 1) should be excluded from the health-care facility from the 12th day after the first exposure through the 26th day after the last exposure. Workers in whom the disease develops should be excluded from work until 9 days after the onset of symptoms.
# The Morbidity and Mortality Weekly Report (MMWR) Series is prepared by the Centers for Disease Control and Prevention (CDC) and is available free of charge in electronic format and on a paid subscription basis for paper copy. To receive an electronic copy on | These revised recommendations of the Advisory Committee on Immunization Practices (ACIP) on measles, mumps, and rubella prevention supersede recommendations published in 1989 and 1990. This statement summarizes the goals and current strategies for measles, rubella, and congenital rubella syndrome (CRS) elimination and for mumps reduction in the United States. Changes from previous recommendations include • Updated information on adverse events and contraindications, particularly for persons with severe HIV infection, persons with a history of egg allergy or gelatin allergy, persons with a history of thrombocytopenia, and persons receiving steroid therapy.#
• Emphasis on the use of combined MMR vaccine for most indications; • A change in the recommended age for routine vaccination to 12-15 months for the first dose of MMR, and to 4-6 years for the second dose of MMR;
• A recommendation that all states take immediate steps to implement a two dose MMR requirement for school entry and any additional measures needed to ensure that all school-aged children are vaccinated with two doses of MMR by 2001;
• A clarification of the role of serologic screening to determine immunity; • A change in the criteria for determining acceptable evidence of rubella immunity;
• A recommendation that all persons who work in health-care facilities have acceptable evidence of measles and rubella immunity;
• Changes in the recommended interval between administration of immune globulin and measles vaccination; and
# INTRODUCTION
Since monovalent vaccines containing measles, rubella, and mumps vaccine viruses-and subsequently combined measles-mumps-rubella (MMR) vaccine-were licensed, the numbers of reported cases of measles, mumps, rubella, and congenital rubella syndrome (CRS) have decreased by more than 99%. In 1993, the Childhood Immunization Initiative established goals of eliminating indigenous transmission of measles and rubella in the United States by 1996. Subsequently, the goals of the initiative were extended to include reducing the number of reported mumps cases to ≤1600 by 1996. U.S. Public Health Service year 2000 objectives include eliminating measles, rubella, and congenital rubella syndrome, and reducing mumps incidence to <500 reported cases per year. Since 1995, fewer cases of measles, rubella, and mumps have been reported than at any time since nationwide disease reporting began, and elimination of indigenous transmission appears feasible. These recommendations are intended to hasten the achievement of these disease elimination goals.
# Measles Clinical Characteristics
The incubation period of measles (rubeola) averages 10-12 days from exposure to prodrome and 14 days from exposure to rash (range: 7-18 days). The disease can be severe and is most frequently complicated by diarrhea, middle ear infection, or bronchopneumonia. Encephalitis occurs in approximately one of every 1,000 reported cases; survivors of this complication often have permanent brain damage and mental retardation. Death occurs in 1-2 of every 1,000 reported measles cases in the United States. The risk for death from measles or its complications is greater for infants, young children, and adults than for older children and adolescents. The most common causes of death are pneumonia and acute encephalitis. In developing countries, measles is often more severe and the case-fatality rate can be as high as 25%.
Subacute sclerosing panencephalitis (SSPE) is a rare degenerative disease of the central nervous system associated with measles virus. Signs and symptoms of the disease appear years after measles infection. Widespread use of measles vaccine has essentially eliminated SSPE from the United States (1 ).
Measles illness during pregnancy leads to increased rates of premature labor, spontaneous abortion, and low birth weight among affected infants (2)(3)(4)(5). Birth defects, with no definable pattern of malformation, have been reported among infants born to women infected with measles during pregnancy, but measles infection has not been confirmed as the cause of the malformations.
Measles can be severe and prolonged among immunocompromised persons, particularly those who have certain leukemias, lymphomas, or human immunodeficiency virus (HIV) infection. Among these persons, measles may occur without the typical rash and a patient may shed measles virus for several weeks after the acute illness (6,7 ).
# Measles Elimination
Before measles vaccine was licensed in 1963, an average of 400,000 measles cases were reported each year in the United States (8 ). However, because virtually all children acquired measles, the number of cases probably approached 3.5 million per year (i.e., an entire birth cohort).
Since measles vaccine became available, professional and voluntary medical and public health organizations have collaborated in vaccination programs that have reduced the reported incidence of measles by >99%. During the late 1960s and early 1970s, the number of reported cases decreased to approximately 22,000-75,000 cases per year. Although measles incidence decreased substantially in all age groups, the greatest decrease occurred among children aged <10 years. A less marked decrease also occurred among older children.
During 1978, the Department of Health, Education, and Welfare (DHEW) initiated a Measles Elimination Program with the goal of eliminating indigenous measles from the United States by October 1, 1982. The three components of this program were a) maintenance of high levels of immunity with a single dose of measles vaccine, b) enhanced surveillance of disease, and c) aggressive outbreak control. As a result of this program, the number of cases reported annually decreased from 26,871 during 1978 to 1,497 during 1983. However, an average of 3,750 cases was reported each year during 1984-1988; 58% of these cases occurred among children aged ≥10 years, most of whom had received only one dose of measles vaccine (9 ). Recurrent measles outbreaks among vaccinated school-aged children prompted both the Advisory Committee on Immunization Practices (ACIP) and the American Academy of Pediatrics (AAP) in 1989 to recommend that all children receive two doses of measles-containing vaccine, preferably as MMR. Although administration of the second dose was originally recommended either at entry to primary school (ACIP) or middle/ secondary school (AAP), ACIP, the AAP, and the American Academy of Family Physicians (AAFP) now recommend that a child receive the second dose before school entry, rather than delaying it until the child is aged 11-12 years.
During 1989-1991, a major resurgence of measles occurred in the United States. More than 55,000 cases and >120 measles-related deaths were reported. The resurgence was characterized by an increasing proportion of cases among unvaccinated preschool-aged children, particularly those resident in urban areas (10)(11)(12).
Multiple barriers to timely vaccination of preschool-aged children were identified during investigation of the 1989-1991 measles resurgence. Efforts to increase vaccination coverage among preschool-aged children emphasized vaccination as close to the recommended age as possible. These efforts, coupled with ongoing implementation of the two-dose MMR recommendation, reduced reported measles cases from 2,237 in 1992 to 312 in 1993 (9 ). Although 963 measles cases were reported in 1994, measles incidence again declined in 1995, when 309 cases were reported (13 ). In 1996, 508 cases were reported, of which 65 were classified as international importations (14 ).
In 1993, the Childhood Immunization Initiative called for the elimination from the United States by 1996 of indigenous transmission of six childhood diseases, including rubella, congenital rubella syndrome (CRS), and measles (10 ). In September 1994, the Pan American Health Organization (PAHO) adopted a similar goal of eliminating measles throughout the Americas by 2000 (15 ). Both epidemiologic and laboratory evidence suggest that the transmission of indigenous measles was interrupted in the United States for the first time during 1993 (16,17 ).
However, even after indigenous measles transmission has been eliminated, measles cases caused by the importation of the virus from other countries will continue to occur. Sustaining measles elimination will require continuing efforts. Enhanced surveillance for measles must be maintained and disease control activities must be undertaken immediately when suspected cases of measles are reported. The major challenges to sustaining the elimination of measles from the United States are a) continuing to vaccinate all children aged 12-15 months with a first dose of MMR, b) ensuring that all school-aged children receive a second dose of MMR vaccine, and c) working with other countries to set and achieve national measles elimination goals.
# Rubella And Congenital Rubella Syndrome (CRS) Clinical Characteristics
Rubella is an exanthematous illness characterized by nonspecific signs and symptoms including transient erythematous and sometimes pruritic rash, postauricular or suboccipital lymphadenopathy, arthralgia, and low-grade fever. Clinically similar exanthematous illnesses are caused by parvovirus, adenoviruses, and enteroviruses. Moreover, 25%-50% of rubella infections are subclinical. The incubation period ranges from 12 to 23 days. Before rubella vaccine was available, the disease was common among children and young adults.
Among adults infected with rubella, transient polyarthralgia or polyarthritis occur frequently. These manifestations are particularly common among women (18 ). Central nervous system complications (i.e., encephalitis) occur at a ratio of 1 per 6,000 cases and are more likely to affect adults. Thrombocytopenia occurs at a ratio of 1 per 3,000 cases and is more likely to affect children.
The most important consequences of rubella are the miscarriages, stillbirths, fetal anomalies, and therapeutic abortions that result when rubella infection occurs during early pregnancy, especially during the first trimester. An estimated 20,000 cases of CRS occurred during 1964-1965 during the last U.S. rubella epidemic before rubella vaccine became available.
The anomalies most commonly associated with CRS are auditory (e.g., sensorineural deafness), ophthalmic (e.g., cataracts, microphthalmia, glaucoma, chorioretinitis), cardiac (e.g., patent ductus arteriosus, peripheral pulmonary artery stenosis, atrial or ventricular septal defects), and neurologic (e.g., microcephaly, meningoencephalitis, mental retardation). In addition, infants with CRS frequently exhibit both intrauterine and postnatal growth retardation. Other conditions sometimes observed among patients who have CRS include radiolucent bone defects, hepatosplenomegaly, thrombocytopenia, and purpuric skin lesions.
Infants who are moderately or severely affected by CRS are readily recognizable at birth, but mild CRS (e.g., slight cardiac involvement or deafness) may be detected months or years after birth, or not at all. Although CRS has been estimated to occur among 20%-25% of infants born to women who acquire rubella during the first 20 weeks of pregnancy, this figure may underestimate the risk for fetal infection and birth defects. When infants born to mothers who were infected during the first 8 weeks of gestation were followed for 4 years, 85% were found to be affected (19 ). The risk for any defect decreases to approximately 52% for infections that occur during the ninth to twelfth weeks of gestation. Infection after the twentieth week of gestation rarely causes defects. Inapparent (subclinical) maternal rubella infection can also cause congenital malformations. Fetal infection without clinical signs of CRS can occur during any stage of pregnancy.
# Rubella Elimination
Before rubella vaccine was licensed during 1969, rubella incidence was greatest among preschool and elementary school children. Therefore, vaccination campaigns initially targeted children in kindergarten and the early grades of elementary school, with the aim of interrupting circulation of the virus and eliminating the risk for exposure among susceptible pregnant women. The risks associated with administering a potentially teratogenic live virus vaccine to young women of childbearing age were not known. During 1969During -1976, reported rubella cases decreased from 57,600 to 12,400. However, during 197512,400. However, during -1977, 62% of reported rubella cases occurred among persons aged >15 years compared with 23% of cases occurring during 1966-1968, and serologic studies suggested that 10%-15% of adults remained susceptible to rubella (20 ).
The number of CRS cases reported nationwide decreased by 69% from 69 in 1970 to 22 in 1976. Rubella outbreaks continued to occur among older adolescents and young adults (e.g, in military camps, high schools, colleges, and universities). In 1977, ACIP modified its recommendations to include the vaccination of susceptible postpubertal girls and women. During the same year, the DHEW undertook the National Childhood Immunization Initiative, which sought to immunize >90% of the nation's children against all vaccine-preventable diseases. Enforcement of requirements for vaccination before school entry was part of the initiative. The number of reported rubella and CRS cases decreased after these programs were implemented, from 20,395 rubella cases and 29 CRS cases in 1977 to 752 rubella cases and 2 CRS cases in 1984. In 1988, 225 cases of rubella were reported in the United States, the fewest since national reporting began.
However, because of outbreaks among unvaccinated adults (e.g., in prisons, colleges, and workplaces), >1000 rubella cases were reported in 1990 and again in 1991. The largest outbreak and the greatest number of CRS cases occurred among children and adults in religious communities that do not accept vaccination. Since 1992, reported indigenous rubella and CRS have continued to occur at a low but relatively constant endemic level with an annual average of <200 rubella cases (128 cases in 1995 and 213 cases in 1996). Four confirmed CRS cases occurred in 1995 and 2 in 1996. However, in the United States, surveillance for CRS relies on a passive system. Consequently, the reported annual totals of CRS are regarded as minimum figures, representing an estimated 40%-70% of all cases (21,22 ).
During 1992-1997, 65% of reported cases of rubella occurred among persons aged ≥20 years. In addition, recent evidence suggests that the risk for both rubella and CRS is increased among persons of Hispanic ethnicity, particularly those born outside the United States. Outbreaks of rubella in California (1990California ( -1991, Massachusetts (1993Massachusetts ( -1994, Connecticut (1995), and North Carolina (1996 and 1997) have occurred primarily among persons of Hispanic origin. During 1985-1995, the ethnicity of a total of 89 children with laboratory-confirmed or clinically compatible cases of CRS was known; 35 (39%) were of Hispanic origin (23)(24)(25)(26)(27).
Recent data indicate that the rate of rubella susceptibility and risk for rubella infection are highest among young adults. During 1992-94, approximately 8% of persons aged 15-29 years were estimated to lack serologic evidence of immunity to rubella (CDC, unpublished data). Data from two recent studies indicate that vaccine-induced rubella antibody levels among adolescents may have decreased during the 9-14 years that had elapsed since they were initially vaccinated. However, recent rubella surveillance data do not indicate that rubella and CRS are increasing among vaccinated persons (28 ) (CDC, unpublished data).
The primary objective of the rubella immunization program is the prevention of CRS. The major components of the rubella and CRS elimination strategy are achieving and maintaining high immunization levels for children and adults, especially women of childbearing age; conducting accurate surveillance for rubella and CRS; and undertaking control measures promptly when a rubella outbreak occurs. Since the late 1970s, this strategy has effectively prevented major epidemics of rubella and CRS in the United States.
# Mumps Clinical Characteristics
Persons in whom "classical" mumps develops have bilateral or (less commonly) unilateral parotitis, with onset an average of 16-18 days after exposure. Parotitis may be preceded by fever, headache, malaise, myalgia, and anorexia. Only 30%-40% of mumps infections produce typical acute parotitis; 15%-20% of infections are asymptomatic and up to 50% of infections are associated with nonspecific or primarily respiratory symptoms (29,30 ). Inapparent infection may be more common among adults than children; parotitis occurs more commonly among children aged 2-9 years (30,31 ). Serious complications of mumps infection can occur without evidence of parotitis (29,32,33 ).
Most serious complications of mumps are more common among adults than among children (29,34 ). Although orchitis may occur among up to 38% of postpubertal men in whom mumps develops, sterility is thought to occur only rarely (35 ).
Aseptic meningitis affects 4%-6% of persons with clinical cases of mumps and typically is mild (29,(36)(37)(38). However, mumps meningoencephalitis can cause permanent sequelae, including paralysis, seizures, cranial nerve palsies, aqueductal stenosis, and hydrocephalus (39)(40)(41). In the prevaccine era, mumps was a major cause of sensorineural deafness among children. Deafness may be sudden in onset, bilateral, and permanent (42)(43)(44).
Among women in whom mumps develops during the first trimester of pregnancy, an increased risk for fetal death has been observed (45 ). However, mumps infection during pregnancy is not associated with congenital malformations (46 ).
# Mumps Control
In the United States, the reported incidence of mumps decreased steadily after the introduction of live mumps vaccine in 1967 and the recommendation for its routine use in 1977. In 1995, 906 cases were reported, representing a 99% decrease from the 185,691 cases reported in 1968. The enactment and enforcement of state vaccination laws requiring that students be vaccinated before school entry has contributed more to reducing mumps incidence than any other measure (47 ). During the 1980s and early 1990s, mumps incidence was lowest in states where comprehensive vaccination laws were enforced. States where vaccination laws were less comprehensive reported intermediate mumps incidence, and the highest incidence was reported in states did not have such laws (47)(48)(49)(50)(51).
Mumps incidence is now very low in all areas of the United States. The substantial reduction in mumps incidence during the past few years may reflect the change in the recommendations for use of MMR vaccine. The implementation of the two-dose MMR vaccination schedule likely decreased mumps incidence further by immunizing children among whom the first dose of mumps antigen did not elicit an immune response (52,53 ). The principal strategy to prevent mumps is to achieve and maintain high immunization levels by routinely vaccinating all children with two doses of MMR.
# VACCINE PREPARATIONS
# Measles Component
Since 1963, when both inactivated and live attenuated (Edmonston B strain) vaccines were licensed, the type of measles vaccine used in the United States has changed several times. Distribution of the inactivated and live Edmonston B vaccines ceased after 1967 and 1975, respectively. Distribution in the United States of a live, further attenuated vaccine (Schwarz strain) first introduced in 1965 has also ceased. A live, further attenuated preparation of the Enders-Edmonston virus strain that is grown in chick embryo fibroblast cell culture, licensed in 1968, is the only measles virus vaccine now available in the United States. This further attenuated vaccine (formerly called "Moraten") causes fewer adverse reactions than the Edmonston B vaccine.
Measles vaccine produces an inapparent or mild, noncommunicable infection. Measles antibodies develop among approximately 95% of children vaccinated at age 12 months and 98% of children vaccinated at age 15 months (CDC, unpublished data). Studies indicate that, if the first dose is administered no earlier than the first birthday, >99% of persons who receive two doses of measles vaccine develop serologic evidence of measles immunity (54 )(CDC, unpublished data). Although vaccination produces lower antibody levels than natural disease, both serologic and epidemiologic evidence indicate that the vaccine induces long-term-probably lifelong-immunity, in most persons (55 ). Most vaccinated persons who appear to lose antibody show an anamnestic immune response upon revaccination, indicating that they are probably still immune (56 ). Although revaccination elicits increased antibody levels in some persons, these increased levels may not be sustained (57 ). Findings of some studies indicate that immunity can wane after successful vaccination (secondary vaccine failure), but this phenomenon appears to occur rarely and to have little effect on measles transmission and the occurrence of outbreaks (55,58,59 ).
# Rubella Component
The live rubella virus vaccine currently distributed in the United States is prepared in human diploid cell culture. This vaccine, containing virus strain RA 27/3, was licensed in the United States in January, 1979 and replaced previous rubella vaccines (e.g., HPV-77 and Cendehill) because it induced an increased and more persistent antibody response and was associated with fewer adverse events.
In clinical trials, ≥95% of susceptible persons aged ≥12 months who received a single dose of strain RA 27/3 rubella vaccine developed serologic evidence of immunity (60)(61)(62). Clinical efficacy and challenge studies indicate that >90% of vaccinated persons have protection against both clinical rubella and viremia for at least 15 years (63)(64)(65)(66). Follow-up studies indicate that one dose of vaccine confers long-termprobably lifelong-protection (67 ). Although antibody titers induced by the vaccine are generally lower than those stimulated by rubella infection, vaccine-induced immunity protects, in nearly all instances, against both clinical illness and viremia after natural exposure (68,69 ). In studies that attempted artificial reinfection of persons who received RA 27/3 vaccine, resistance to reinfection was similar to the resistance that follows natural infection (70 ). However, several reports indicate that viremic reinfection following exposure may occur among vaccinated persons who have low levels of detectable antibody (64 ). The frequency and consequences of this phenomenon are unknown but it is believed to be uncommon. Clinical reinfection and fetal infection among persons who developed immunity as a consequence of infection with wild virus have been documented, but are apparently rare (71 ). Rarely, clinical reinfection and fetal infection have been reported among women with vaccine-induced immunity. Rare cases of CRS have occurred among infants born to mothers who had documented serologic evidence of rubella immunity before they became pregnant.
# Mumps Component
The only mumps vaccine now available in the United States is a live virus vaccine (Jeryl-Lynn strain) that is prepared in chick-embryo cell culture. The vaccine produces a subclinical, noncommunicable infection with very few side effects.
More than 97% of persons who are susceptible to mumps develop measurable antibody following vaccination and, in controlled clinical trials, one dose of vaccine was approximately 95% efficacious in preventing mumps disease (72)(73)(74). However, field studies have documented lower estimates of vaccine efficacy, ranging from 75% to 95% (47,75 ). Antibody levels induced by the vaccine are lower than antibody levels resulting from natural infection (72,76,77 ). The duration of vaccine-induced immunity is unknown, but serologic and epidemiologic data collected during 30 years of live vaccine use indicate both the persistence of antibody and continuing protection against infection (33,78,79 ).
# Vaccine Shipment and Storage
Administration of improperly stored vaccine may fail to provide protection against disease from measles, rubella, and/or mumps. These live virus vaccines are supplied in lyophilized form and should be stored at 2-8 C (35.6-46.4 F) or colder. They must be shipped at 10 C (50 F) or colder and may be shipped on dry ice. The vaccines must be protected from light, which may inactivate the vaccine viruses. Reconstituted vaccine also must be protected from light, must be stored at 2-8 C (35.6-46.4 F), and must not be frozen. Reconstituted vaccine must be discarded if not used within 8 hours.
# VACCINE USAGE
Two doses of MMR vaccine separated by at least 1 month (i.e., a minimum of 28 days) and administered on or after the first birthday are recommended for all children and for certain high-risk groups of adolescents and adults. The recommended 1 month interval between successive doses of MMR or other measles-containing vaccine is based on the principle that live virus vaccines not administered at the same time should be separated by at least 1 month (80 ).
MMR is the vaccine of choice when protection against any of these three diseases is required on or after the first birthday, unless any of its component vaccines is contraindicated. The purpose of the two-dose vaccination schedule is to produce immunity in the small proportion of persons who fail to respond immunologically to one or more of the components of the first dose. Studies indicate that two doses of measles vaccine are necessary to develop adequate population immunity to prevent measles outbreaks among school-aged and older persons. Mumps can occur in highly vaccinated populations; in these outbreaks, substantial numbers of cases have occurred among persons who had previously received a single dose of mumpscontaining vaccine (33,81 ). Although primary rubella vaccine failure rarely occurs, the potential consequences of failure (i.e., CRS) are substantial.
Almost all persons who do not respond to the measles component of the first dose of MMR vaccine will respond to the second dose (82 ) (CDC, unpublished data). Few data regarding the immune response to the rubella and mumps components of a second dose of MMR vaccine are available, but most persons who do not respond to the rubella or mumps components of the first dose would be expected to respond to the second (82-84 ) (CDC, unpublished data). The second dose is not generally considered a booster dose because a primary immune response to the first dose provides longterm protection. Although some persons who develop normal antibody titers in response to a single dose of MMR vaccine will develop higher antibody titers to the three component vaccines when administered a second dose of vaccine, these increased antibody levels typically do not persist (57 ).
Use of combined MMR vaccine for both measles doses and all other indications should provide an additional safeguard against primary vaccine failures and facilitate elimination of rubella and CRS and continued reduction of mumps incidence. Data also indicate that the favorable benefit/cost ratio for routine measles, rubella, and mumps vaccination is even greater when the vaccines are administered as combined MMR vaccine (85,86 ).
# Dosage and Route of Administration
The lyophilized live MMR vaccine (and its component vaccines) should be reconstituted and administered as recommended by the manufacturer. All measles-, rubella-, or mumps-containing vaccines available in the United States should be administered subcutaneously in the recommended standard single-dose volume of 0.5 mL.
# Simultaneous Administration of Vaccines
In general, simultaneous administration of the most widely used live and inactivated vaccines does not impair antibody responses or increase rates of adverse reactions (80 ). The antibody responses of persons vaccinated with MMR are similar to those of persons vaccinated with single-antigen measles, mumps, and rubella vaccines at different sites or at different times.
ACIP encourages routine simultaneous administration of MMR, diphtheria and tetanus toxoids and acellular pertussis (DTaP) or diphtheria and tetanus toxoids and whole-cell pertussis (DTP) vaccine, Haemophilus influenzae type b (Hib) vaccine, and oral poliovirus vaccine (OPV) or inactivated poliovirus vaccine (IPV) to children who are at the recommended age to receive these vaccines. Antibody responses were equivalent and no clinically significant increases in the frequency of adverse events occurred when MMR vaccine, DTaP (or DTP), Hib vaccine, hepatitis B vaccine, and IPV or OPV were administered either simultaneously at different sites or at separate times (87 ). Likewise, seroconversion rates, antibody levels, and frequencies of adverse reactions were similar in two groups, one of which was administered MMR and varicella vaccines simultaneously at separate sites and the other of which received the vaccines 6 weeks apart (88 )(Merck Research Laboratories, unpublished data).
Live measles and yellow fever vaccines can be administered simultaneously at separate anatomical sites in separate syringes (89 ). Limited data also indicate that the immunogenicity and safety of inactivated Japanese encephalitis vaccine are not compromised by simultaneous administration with live measles vaccine (90 ). Limited data exist concerning concurrent administration of MMR vaccine and other vaccines that are often recommended for international travelers (e.g., meningococcal vaccine, typhoid vaccines). However, neither theoretical considerations nor practical experience indicate that the simultaneous administration at separate anatomic sites of MMR and other live or inactivated vaccines will produce a diminished immune response or increase the incidence of adverse events among vaccinated persons.
# DOCUMENTATION OF IMMUNITY
Only doses of vaccine for which written documentation of the date of administration is presented should be considered valid. Neither a self-reported dose nor a history of vaccination provided by a parent is, by itself, considered adequate documentation. No health-care worker should provide a vaccination record for a patient unless that health-care worker has administered the vaccine or has seen a record that documents vaccination. Persons who may be immune to measles, mumps, or rubella but who lack either adequate documentation of vaccination or other acceptable evidence of immunity (Table 1) should be vaccinated. Vaccination status and date of . Facilities that provide care exclusively for elderly patients who are at minimal risk for measles and rubella and complications of these diseases are a possible exception. † The first dose should be administered on or after the first birthday; the second dose of measles-containing vaccine should be administered no earlier than one month (i.e., minimum of 28 days) after the first dose. Combined measles-mumps-rubella (MMR) vaccine generally should be used whenever any of its component vaccines is indicated. § May vary depending on current state or local requirements. ¶ Health-care facilities should consider recommending a dose of MMR vaccine for unvaccinated workers born before 1957 who are at risk for occupational exposure to measles and who do not have a history of measles disease or laboratory evidence of measles immunity. ** Children aged 6-11 months should receive a dose of monovalent measles vaccine (or MMR, if monovalent vaccine is not available) before departure. Children who receive a dose of measles-containing vaccine before their first birthdays should be revaccinated with two doses of MMR vaccine, the first of which should be administered when the child is aged 12-15 months (12 months if the child remains in a high-risk area) and the second at least 28 days later. † † Women of childbearing age are adolescent girls and premenopausal adult women. Because rubella can occur in some persons born before 1957 and because congenital rubella and congenital rubella syndrome can occur in the offspring of women infected with rubella virus during pregnancy, birth before 1957 is not acceptable evidence of rubella immunity for women who could become pregnant.
administration of all vaccinations should be documented in the patient's permanent medical record. Serologic screening for measles, rubella, or mumps immunity generally is neither necessary nor recommended if a person has other acceptable evidence of immunity to the disease (Table 1). Serologic screening can be a barrier to vaccination. With the exception of women who are known to be pregnant (see Women of Childbearing Age), persons who lack acceptable evidence of immunity generally should be vaccinated without serologic testing. Serologic screening is appropriate only when persons identified as susceptible are subsequently vaccinated in a timely manner. Screening is most applicable when the return and vaccination of those tested can be ensured (e.g., hiring of new health-care workers). If these conditions are not met, serologic screening is inappropriate (91 ). Likewise, during an outbreak of measles, rubella, or mumps, serologic screening before vaccination generally is not recommended because waiting for results, contacting, and then vaccinating persons identified as susceptible can impede the rapid vaccination needed to curb the outbreak.
Serologic screening for antibodies to measles, rubella, or mumps alone will not identify persons who are susceptible to the other diseases for which screening is not done. Post-vaccination serologic testing to verify an immune response to MMR or its component vaccines is not recommended.
The criteria for acceptable evidence of immunity to measles, rubella, and mumps (Table 1) provide presumptive rather than absolute evidence of immunity. Occasionally, a person who meets the criteria for presumptive immunity can contract and transmit disease. Specific criteria for documentation of immunity have been established for certain persons (e.g., health-care workers, international travelers, and students at post-high school educational institutions) who are at increased risk for exposure to measles, rubella, and mumps (Table 1). Criteria accepted as evidence of immunity for the purpose of meeting school or college entry requirements or other government regulations may vary among state and local jurisdictions.
# Measles
Persons generally can be presumed immune to measles (Table 1) if they have documentation of adequate vaccination, laboratory evidence of immunity to measles, documentation of physician-diagnosed measles, or were born before 1957. Criteria for adequate vaccination currently vary depending on state and local vaccination policy because of differences in the way states have implemented the two-dose measles vaccination schedule. All states are strongly encouraged to take immediate steps to implement the two-dose MMR vaccination schedule so that, by 2001, adequate vaccination of children will be defined in all 50 states as follows:
• For preschool-aged children: documentation of at least one dose of MMR vaccine administered on or after the first birthday.
• For children in kindergarten through grade 12: documentation of two doses of MMR vaccine separated by at least 28 days (i.e., 1 month), with the first dose administered no earlier than the first birthday. Doses of MMR and other measles-containing vaccines administered before the first birthday should not be counted when determining adequacy of measles vaccination.
When measles virus is introduced into a community, persons who work in healthcare facilities are at greater risk for acquiring measles than the general population (92 ). Because persons working in medical settings have been infected with and have transmitted measles to patients and coworkers, rigorous criteria for immunity among health-care workers have been established. For persons born during or after 1957 who work in health-care facilities, adequate vaccination consists of two doses of MMR or other live measles-containing vaccine separated by at least 28 days, with the first dose administered no earlier than the first birthday (Table 1). In addition, although birth before 1957 is generally considered acceptable evidence of measles immunity (Table 1), measles has occurred in some unvaccinated persons born before 1957 who worked in health-care facilities. Therefore, health-care facilities should consider recommending a dose of MMR vaccine for unvaccinated workers born before 1957 who lack a history of measles disease or laboratory evidence of measles immunity (see Health-Care Facilities).
The previously described criteria apply only to routine vaccination. During measles outbreaks, evidence of adequate vaccination for school-aged children, adolescents, and adults born during or after 1957 who are at risk for measles exposure and infection consists of two doses of measles-containing vaccine separated by at least 28 days, with the first dose administered no earlier than the first birthday (see Measles Outbreak Control). During outbreaks involving preschool-aged children, authorities should consider extending this criterion to all children aged ≥12 months.
In the past, the most commonly used laboratory test for assessing immunity to measles was the hemagglutination-inhibition (HI) test but more sensitive assays (e.g., the enzyme immunoassay [EIA] or enzyme-linked immunosorbent assay [ELISA]) are now used in most laboratories. Persons who have measles-specific antibody that is detectable by any serologic test are considered immune. Persons with an "equivocal" test result should be considered susceptible unless they have other evidence of measles immunity (Table 1) or subsequent testing indicates they are immune. All new cases of suspected measles should be confirmed by laboratory testing (see Measles Case Investigation-Laboratory Diagnosis).
# Rubella
Persons generally can be presumed immune to rubella (Table 1) if they have documentation of vaccination with at least one dose of MMR or other live rubellacontaining vaccine administered on or after the first birthday, laboratory evidence of rubella immunity, or were born before 1957 (except women who could become pregnant). Birth before 1957 is not acceptable evidence of rubella immunity for women who could become pregnant because it provides only presumptive evidence of rubella immunity and does not guarantee that a person is immune (see Women of Childbearing Age). Rubella can occur among some unvaccinated persons born before 1957 and congenital rubella and CRS can occur among the offspring of women infected with rubella during pregnancy.
Persons who have an "equivocal" serologic test result should be considered susceptible to rubella unless they have evidence of adequate vaccination or a subsequent serologic test result indicates rubella immunity. Although only one dose of rubellacontaining vaccine is required as acceptable evidence of immunity to rubella, children should receive two doses of MMR vaccine. The first dose is administered routinely when the child is aged 12-15 months and the second before the child enters school (i.e., at age 4-6 years)(see Routine Vaccination).
The clinical diagnosis of rubella is unreliable and should not be considered in assessing immune status. Because many rash illnesses may mimic rubella infection and many rubella infections are unrecognized, the only reliable evidence of previous rubella infection is the presence of serum rubella immunoglobulin G (IgG). Laboratories that regularly perform antibody testing generally provide the most reliable results because their reagents and procedures are more likely to be strictly standardized (see Rubella Case Investigation and Outbreak Control).
Postinfection immunity to rubella appears to be long-lasting and is probably lifelong. However, as with other viral diseases, re-exposure to natural rubella occasionally leads to reinfection without clinical illness or detectable viremia. The risk for CRS among infants born to women reinfected with rubella during pregnancy is minimal (93,94 ). Although data from several studies indicate that levels of vaccineinduced rubella antibodies may decline with time, data from surveillance of rubella and CRS suggest that waning immunity with increased susceptibility to rubella disease does not occur (28 )(CDC, unpublished data).
HI antibody testing was formerly the method most frequently used to screen for rubella antibodies. However, the HI test has been supplanted by other assays of equal or greater sensitivity. EIAs are the most commonly used of these newer commercial assays, but latex agglutination, immunofluorescence assay (IFA), passive hemagglutination, hemolysis-in-gel, and virus neutralization tests are also available.
Any antibody level above the standard positive cutoff value of the assay with which it is measured can be considered evidence of immunity, if the assay is licensed. When serum specimens from adults who did not produce antibodies detectable by HI after vaccination were examined with an equivalently specific but more sensitive test, almost all had detectable antibody (95,96 ). A few children who initially developed antibody detectable by HI apparently "lost" this antibody during follow-up intervals of up to 16 years (77,97,98 ). However, almost all had antibody detectable by more sensitive tests. In several of these cases, immunity was confirmed by documenting a booster response (i.e., absence of IgM antibody and a rapid rise in IgG antibody) after revaccination (62,99 ).
Occasionally, persons with documented histories of rubella vaccination have rubella serum IgG levels that are not clearly positive by ELISA. Such persons can be administered a dose of MMR vaccine and need not be retested for serologic evidence of rubella immunity.
# Mumps
Persons generally can be presumed immune to mumps (Table 1) if they have documentation of vaccination with live mumps virus vaccine on or after the first birthday, laboratory evidence of mumps immunity, documentation of physician-diagnosed mumps, or were born before 1957.
The demonstration of mumps IgG antibody by any commonly used serologic assay is acceptable evidence of mumps immunity. Persons who have an "equivocal" serologic test result should be considered susceptible to mumps unless they have other evidence of mumps immunity (Table 1) or subsequent testing indicates they are immune. All new cases of suspected mumps should be confirmed by an appropriate serologic assay (see Mumps Case Investigation, Laboratory Diagnosis).
Live mumps vaccine was not used routinely before 1977. Before the vaccine was introduced, the age-specific incidence of the disease peaked among children aged 5-9 years. Therefore, most persons born before 1957 are likely to have been infected naturally between 1957 and 1977 and may be presumed immune, even if they have not had clinically recognizable mumps disease. However, birth before 1957 does not guarantee mumps immunity. Therefore, during mumps outbreaks, MMR vaccination should be considered for persons born before 1957 who may be exposed to mumps and who may be susceptible. Laboratory testing for mumps susceptibility before vaccination is not necessary.
# ROUTINE VACCINATION
# Preschool-Aged Children
Children should receive the first dose of MMR vaccine at age 12-15 months (i.e., on or after the first birthday). In areas where risk for measles is high, initial vaccination with MMR vaccine is recommended for all children as soon as possible upon reaching the first birthday (i.e., at age 12 months). An area where measles risk is high is defined as:
• a county with a large inner city population,
• a county where a recent measles outbreak has occurred among unvaccinated preschool-aged children, or
• a county in which more than five cases of measles have occurred among preschool-aged children during each of the last 5 years. These recommendations may be implemented for an entire county or only within defined areas of a county. This strategy assumes that the benefit of preventing measles cases among children aged 12-15 months outweighs the slightly reduced efficacy of the vaccine when administered to children aged <15 months. In addition, almost all children who do not respond immunologically to the first dose of MMR vaccine will develop measles immunity after receiving a second dose. HIV-infected children should receive MMR vaccine at age 12 months, if not otherwise contraindicated (see Special Considerations for Vaccination-Persons Infected with Human Immunodeficiency Virus (HIV)).
# School-Aged Children and Adolescents
The second dose of MMR vaccine is recommended when children are aged 4-6 years (i.e., before a child enters kindergarten or first grade). This recommended timing for the second dose of MMR vaccine has been adopted jointly by ACIP, the American Academy of Pediatrics (AAP), and the American Academy of Family Physicians (AAFP). Evidence now indicates that a) the major benefit of administering the second dose is a reduction in the proportion of persons who remain susceptible because of primary vaccine failure, b) waning immunity is not a major cause of vaccine failure and has little influence on measles transmission, and c) revaccination of children who have low levels of measles antibody produces only a transient rise in antibody levels (55,(57)(58)(59)100,101 ).
Because approximately 5% of children who receive only one dose of MMR vaccine fail to develop immunity to measles, ACIP recommends that all states implement a requirement that all children entering school have received two doses of MMR vaccine (with the first dose administered no earlier than the first birthday) or have other evidence of immunity to measles, rubella, and mumps (see Documentation of Immunity). In addition, to achieve complete immunization of all school-aged children and hasten progress toward measles elimination, states are strongly encouraged to take immediate steps to ensure that, by 2001, all children in grades kindergarten through 12 have received two doses of MMR vaccine.
As part of comprehensive health services for all adolescents, ACIP, AAP, and AAFP recommend a health maintenance visit at age 11-12 years. This visit should serve as an opportunity to evaluate vaccination status and administer MMR vaccine to all persons who have not received two doses at the recommended ages.
Children who do not have documentation of adequate vaccination against measles, rubella, and mumps or other acceptable evidence of immunity to these diseases (see Documentation of Immunity) should be admitted to school only after administration of the first dose of MMR vaccine. If required, the second MMR dose should be administered as soon as possible, but no sooner than 28 days after the first dose. Children who have already received two doses of MMR vaccine at least 1 month apart, with the first dose administered no earlier than the first birthday, do not need an additional dose when they enter school.
# Adults
Persons born in 1957 or later who are aged ≥18 years and who do not have a medical contraindication should receive at least one dose of MMR vaccine unless they have a) documentation of vaccination with at least one dose of measles-, rubella-, and mumps-containing vaccine or b) other acceptable evidence of immunity to these three diseases (Table 1). Persons born before 1957 generally can be considered immune to measles and mumps. In addition, persons born before 1957, except women who could become pregnant, generally can be considered immune to rubella.
MMR vaccine (one dose or two doses administered at least 28 days apart) may be administered to any person born before 1957 for whom the vaccine is not contraindicated. Adults who may be at increased risk for exposure to and transmission of measles, mumps, and rubella should receive special consideration for vaccination. These persons include international travelers, persons attending colleges and other post-high school educational institutions, and persons who work at health-care facilities. In addition, all women of childbearing age should be considered susceptible to rubella unless they have received at least one dose of MMR or other live rubella virus vaccine on or after the first birthday or have serologic evidence of immunity. Vaccination recommendations for these high-risk groups follow.
# Women of Childbearing Age
MMR vaccine should be offered to all women of childbearing age (i.e., adolescent girls and premenopausal adult women) who do not have acceptable evidence of rubella immunity whenever they make contact with the health-care system. Opportunities to vaccinate susceptible women include occasions when their children undergo routine examinations or vaccinations. The continuing occurrence of rubella among women of childbearing age indicates the need to continue vaccination of susceptible adolescent and adult women of childbearing age, and the absence of evidence of vaccine teratogenicity indicates that the practice is safe (102 ). Vaccination of susceptible women of childbearing age should • be part of routine general medical and gynecologic outpatient care;
• take place in all family-planning settings; and • be provided routinely before discharge from any hospital, birthing center, or other medical facility, unless a specific contraindication exists (see Precautions and Contraindications).
Outbreaks of rubella in the United States recently have occurred among women of Hispanic ethnicity, many of whom were born outside the fifty states. Efforts should be made to ensure that all susceptible women of childbearing age, especially those who grew up outside the fifty states in areas where routine rubella vaccination may not occur, are vaccinated with MMR vaccine or have other acceptable evidence of immunity (Table 1). Ascertainment of rubella-immune status of women of childbearing age and the availability of rubella vaccination should be components of the health-care program in places where the risks for disease exposure and transmission are substantial (e.g., day care facilities, schools, colleges, jails, and prisons).
No evidence indicates that administration of rubella-containing vaccine virus to a pregnant woman presents a risk for her fetus, although such a risk cannot be excluded on theoretical grounds. Therefore, women of childbearing age should receive rubellacontaining vaccines (i.e., rubella, MR, or MMR vaccine) only if they state that they are not pregnant and only if they are counseled not to become pregnant for 3 months after vaccination. Because of the importance of protecting women of childbearing age against rubella, reasonable practices in any immunization program include a) asking women if they are pregnant, b) not vaccinating women who state that they are pregnant, c) explaining the potential risk for the fetus to women who state that they are not pregnant, and d) counseling women who are vaccinated not to become pregnant during the 3 months following MMR vaccination.
Routine Vaccination of Women Who Are Not Pregnant. Women of childbearing age who do not have documentation of rubella vaccination or serologic evidence of rubella immunity should be vaccinated with MMR, if they have no contraindications to the vaccine. Birth before 1957 is not acceptable evidence of immunity for women who could become pregnant (Table 1). The use of MMR vaccine provides the potential additional benefit of protection against measles and mumps. Serologic testing before vaccination is not necessary and might present a barrier to timely vaccination. Routine testing for rubella antibody during clinic visits for routine health care, premarital evaluation, family planning, or diagnosis and treatment of sexually transmitted diseases may identify women who are not immune to rubella before they become pregnant. Such routine serologic testing is not useful unless it is linked to timely follow-up and vaccination of women who are susceptible (103 ).
Prenatal Screening and Postpartum Vaccination. Prenatal serologic screening of women who have acceptable evidence of rubella immunity is generally not necessary, but is indicated for all pregnant women who lack acceptable evidence of rubella immunity (Table 1). Upon completion or termination of their pregnancies, women who do not have serologic evidence of rubella immunity or documentation of rubella vaccination should be vaccinated with MMR before discharge from the hospital, birthing center, or abortion clinic (104 ). They should be counseled to avoid conception for 3 months after vaccination. Postpartum rubella vaccination of all women not known to be immune could prevent up to half of CRS cases (105-108 ) ( CDC, unpublished data).
# Colleges and Other Post-High School Educational Institutions
Risks for transmission of measles, rubella, and mumps at post-high school educational institutions can be high because these institutions may bring together large concentrations of persons susceptible to these diseases (109)(110)(111)(112)(113). Therefore, colleges, universities, technical and vocational schools, and other institutions for post-high school education should require that all undergraduate and graduate students have received two doses of MMR vaccine or have other acceptable evidence of measles, rubella, and mumps immunity (Table 1) before enrollment.
College entry requirements for measles immunity substantially reduce the risk for measles outbreaks on college campuses where they are implemented and enforced (111 ). State requirements for pre-enrollment vaccination ensure the best protection against widespread measles transmission among students at college campuses and other post-high school educational institutions. States are strongly encouraged to adopt such regulations. Students who do not have documentation of live measles, rubella, or mumps vaccination or other acceptable evidence of immunity at the time of enrollment (Table 1) should be admitted to classes only after receiving the first dose of MMR vaccine. These students should be administered a second dose of MMR vaccine 1 month (i.e., at least 28 days) later. Students who have documentation of having received only one dose of measles-containing vaccine on or after the first birthday should receive a second dose of MMR before enrollment, provided at least 1 month has elapsed since the previous dose. Students who have a medical contraindication to receiving any of the components of MMR vaccine should be given a letter of explanation to present to the health officials of their educational institution.
# Health-Care Facilities
When measles virus is introduced into a community, persons who work in healthcare facilities are at increased risk for acquiring measles compared with the general population (92,114,115 ). During 1985-1991, at least 795 measles cases (1.1% of all reported cases) occurred among adult health-care workers. Of these, 29% occurred among nurses, 15% among physicians, 11% among persons in other health-care occupations (e.g., laboratory and radiology technicians, etc.), 11% among clerks, 4% among nursing assistants, and 4% among medical and nursing students (115 ) (CDC, unpublished data). A general decline in measles incidence occurred after 1991. However, 15 of the 75 measles outbreaks reported during 1993-1996 involved transmission in a medical facility, and a total of 36 measles cases (1.8% of all reported cases) occurred among persons working in health-care facilities (CDC, unpublished data). Although similar surveillance data are not available for rubella, outbreaks have occurred in health-care settings, and health-care workers have transmitted rubella to patients (116 ) (CDC, unpublished data).
All persons who work in health-care facilities should be immune to measles and rubella (Table 1). Because any health-care worker (i.e., medical or nonmedical, paid or volunteer, full-or part-time, student or nonstudent, with or without patient-care responsibilities) who is not immune to measles and rubella can contract and transmit these diseases, all health-care facilities (i.e., inpatient and outpatient, private and public) should ensure that those who work in their facilities are immune to measles and rubella (Table 1)*.
Health-care workers have a responsibility to avoid transmitting these diseases and thereby causing harm to patients. Adequate vaccination for health-care workers born during or after 1957 consists of two doses of a live measles-containing vaccine and at least one dose of a live rubella-containing vaccine (Table 1). Health-care workers who need a second dose of measles-containing vaccine should be revaccinated 1 month (at least 28 days) after their first dose.
Although birth before 1957 is generally considered acceptable evidence of measles and rubella immunity (Table 1), health-care facilities should consider recommending a dose of MMR vaccine to unvaccinated workers born before 1957 who do not have a history of physician-diagnosed measles or laboratory evidence of measles immunity AND laboratory evidence of rubella immunity.
Rubella vaccination or laboratory evidence of rubella immunity is particularly important for female health-care workers who could become pregnant, including those born before 1957. In addition, during rubella outbreaks, health-care facilities should strongly consider recommending a dose of MMR vaccine to unvaccinated health-care workers born before 1957 who do not have serologic evidence of immunity. Serologic surveys of hospital workers indicate that 5%-9% of those born before 1957 do not have detectable measles antibody (117,118 ) and about 6% do not have detectable rubella antibody (119 ). In addition, during 1985-1992, 643 measles cases were reported among health-care workers whose year of birth was known; 27% of these persons were born before 1957 (CDC, unpublished data). Comparable surveillance data are not available for rubella.
Serologic screening need not be done before vaccinating for measles and rubella unless the medical facility considers it cost-effective (91,120,121 ). Serologic testing is appropriate only if persons who are identified as susceptible are subsequently vaccinated in a timely manner. Serologic screening ordinarily is not necessary for persons who have documentation of appropriate vaccination or other acceptable evidence of immunity (Table 1). During outbreaks of measles or rubella, serologic screening before vaccination is not generally recommended because rapid vaccination is necessary to halt disease transmission. *Facilities that provide care exclusively for elderly patients who are at minimal risk for measles and rubella and complications of these diseases are a possible exception.
Transmission of mumps has occurred in medical settings (122 ). Therefore, immunity to mumps is highly desirable for all health-care workers (Table 1). Adequate mumps vaccination for health-care workers born during or after 1957 consists of one dose of live mumps-containing vaccine.
MMR vaccine generally should be used whenever any of its component vaccines is indicated. However, if the prospective vaccinee has acceptable evidence of immunity to one or two of the components of MMR vaccine (Table 1), a monovalent or bivalent vaccine can be used.
# International Travel
Measles, rubella, and mumps are endemic in many countries. Protection against measles is especially important for persons planning foreign travel, including adolescents and adults who have not had measles disease and have not been adequately vaccinated, and infants aged 6-11 months. Similarly, protection against rubella is especially important for women of childbearing age who are not immune to the disease. Although proof of vaccination is not required for entry into the United States, persons traveling or living abroad should ensure that they are immune to measles, rubella, and mumps.
Persons who travel or live abroad and who do not have acceptable evidence of measles, rubella, and mumps immunity (Table 1) should be vaccinated with MMR. Children who travel or live abroad should be vaccinated at an earlier age than recommended for children remaining in the United States. Before their departure from the United States, children aged ≥12 months should have received two doses of MMR vaccine separated by at least 28 days, with the first dose administered on or after the first birthday. Children aged 6-11 months should receive a dose of monovalent measles vaccine before departure. If monovalent measles vaccine is not available, no specific contraindication exists to administering MMR to children aged 6-11 months. However, because the risk for serious disease from either mumps or rubella infection among infants is relatively low and because children aged <12 months are less likely to develop serologic evidence of immunity when vaccinated with measles, mumps, and rubella antigens than are older children, mumps vaccine and rubella vaccine generally are administered only to children aged ≥12 months. Children administered monovalent measles vaccine or MMR before the first birthday should be considered potentially susceptible to all three diseases and should be revaccinated with two doses of MMR, the first of which should be administered when the child is aged 12-15 months (12 months if the child remains in an area where disease risk is high) and the second at least 28 days later.
Parents who travel or reside abroad with infants aged <12 months should have acceptable evidence of immunity to rubella and mumps (Table 1), as well as measles, so they will not become infected if their infants contract these diseases. Infants aged <6 months are usually protected against measles, rubella, and mumps by maternally derived antibodies and ordinarily do not require additional protection unless the infant's mother is diagnosed with measles (see Use of Vaccine and Immune Globulin Among Persons Exposed to Measles, Rubella, or Mumps).
# SPECIAL CONSIDERATIONS FOR VACCINATION Persons Infected with Human Immunodeficiency Virus (HIV)
Although the risk for measles exposure is currently low in most areas of the United States and the Western Hemisphere, this risk remains high in many other regions and measles continues to be imported into the United States. HIV-infected persons are at increased risk for severe complications if infected with measles (126,127 ). Among HIV-infected persons who did not have evidence of severe immunosuppression (Table 2), no serious or unusual adverse events have been reported after measles vaccination (123)(124)(125)(126). Therefore, MMR vaccination is recommended for all asymptomatic HIV-infected persons who do not have evidence of severe immunosuppression and for whom measles vaccination would otherwise be indicated. MMR vaccination should also be considered for all symptomatic HIV-infected persons who do not have evidence of severe immunosuppression (Table 2) (128,129 ). Testing asymptomatic persons for HIV infection is not necessary before administering MMR or other measles-containing vaccine (130 ).
Transient increases in HIV viral load have been observed after administration of other vaccines to HIV-infected persons (131,132 ). The clinical significance of these increases is not known. Theoretically, a similar increase also may occur after MMR vaccination of HIV-infected persons.
Because the immunologic response to live and killed-antigen vaccines may decrease as HIV disease progresses, vaccination early in the course of HIV infection may be more likely to induce an immune response (133 ). Therefore, HIV-infected infants without severe immunosuppression should routinely receive MMR vaccine as soon as possible upon reaching the first birthday (i.e., at age 12 months) (130 ). Consideration should be given to administering the second dose of MMR vaccine as soon as 28 days (i.e., 1 month) after the first dose rather than waiting until the child is ready to enter kindergarten or first grade. In addition, if at risk for exposure to measles, HIV-infected infants who are not severely immunocompromised should be administered singleantigen measles vaccine or MMR vaccine at age 6-11 months. These children should receive another dose, administered as MMR vaccine, as soon as possible upon reaching the first birthday, provided at least 1 month has elapsed since the administration of the previous dose of measles-containing vaccine. An additional dose of MMR vaccine can be administered as early as 1 month after the second dose. If otherwise indicated, newly diagnosed HIV-infected children and adults without acceptable evidence of measles immunity (Table 1) should receive MMR vaccine as soon as possible after diagnosis, unless they have evidence of severe immunosuppression (Table 2). Data indicate that, of the HIV-infected infants born in the United States annually, approximately 5% (i.e., 50 children per year) would be classified as severely immunocompromised at age 12 months, when the first dose of MMR vaccine is recommended.
Measles vaccine is not recommended for HIV-infected persons with evidence of severe immunosuppression (Table 2) for several reasons:
• a case of progressive measles pneumonitis occurred in a person with AIDS and severe immunosuppression to whom MMR vaccine was administered (134 );
• evidence indicates a diminished antibody response to measles vaccine among severely immunocompromised HIV-infected persons (133 );
• morbidity related to measles vaccination has been reported among persons with severe immunosuppression unrelated to HIV infection (135)(136)(137)(138); and
• in the United States, the incidence of measles is presently very low.
Serious illness associated with administration of rubella or mumps vaccines to HIVinfected persons has not been reported. MMR vaccine is not contraindicated for the close contacts of immunocompromised persons. All family and other close contacts of HIV-infected persons should be vaccinated with MMR vaccine, unless they have acceptable evidence of measles immunity.
Severely immunocompromised patients and other symptomatic HIV-infected patients who are exposed to measles should receive immune globulin (IG) prophylaxis regardless of vaccination status because they may not be protected by the vaccine. For patients receiving intravenous immune globulin (IGIV) therapy, a standard dose of 100-400 mg/kg should be sufficient to prevent measles infection after exposures occurring within 3 weeks after administration of IGIV; for patients exposed to measles >3 weeks after receiving a standard IGIV dose, an additional dose should be considered. Although no data are available concerning the effectiveness of IGIV in preventing measles, high dose IGIV may be as effective as immune globulin administered intramuscularly. Persons receiving regular (e.g., monthly) IGIV therapy for HIV infection or other indications may not respond to MMR or its component vaccines because of the continued presence of high levels of passively acquired antibody (see Precautions and Contraindications, Recent Administration of Immune Globulin). If indicated, MMR vaccine should be administered at least 2 weeks before beginning IGIV therapy.
# Use of Vaccine and Immune Globulin Among Persons Exposed to Measles, Rubella, or Mumps
# Use of Vaccine
Exposure to measles is not a contraindication to vaccination. MMR or measles vaccine, if administered within 72 hours of initial measles exposure, may provide some protection (139)(140)(141)(142)(143). For most persons aged ≥12 months who are exposed to measles in most settings (e.g., day care facilities, schools, colleges, health-care facilities), administration of MMR or measles vaccine is preferable to using immune globulin (IG). For susceptible persons aged ≥6 months who are household contacts of measles patients, use of vaccine within 72 hours of initial exposure is also acceptable. However, measles often is not recognized as such until >72 hours after onset. Therefore, administration of IG to susceptible household contacts who are not vaccinated within 72 hours of initial exposure is recommended (see Use of Immune Globulin). Infants vaccinated before age 12 months must be revaccinated on or after the first birthday with two doses of MMR vaccine separated by at least 28 days (see Routine Vaccination). Measles-containing vaccine is not recommended for postexposure measles prophylaxis in immunocompromised persons or pregnant women (see Contraindications).
Postexposure MMR vaccination does not prevent or alter the clinical severity of rubella or mumps. However, widespread vaccination during a mumps outbreak may help terminate such outbreaks (144 ).
If exposure to measles, rubella, or mumps does not cause infection, postexposure vaccination with MMR should induce protection against subsequent infection. If the exposure results in infection, no evidence indicates that administration of MMR vaccine during the presymptomatic or prodromal stage of illness increases the risk for vaccine-associated adverse events.
# Use of Immune Globulin
If administered within 6 days of exposure, IG can prevent or modify measles in a nonimmune person. However, any immunity conferred is temporary unless modified or typical measles occurs (139 ). The usual recommended dose of IG is 0.25 mL/kg (0.11 mL/lb) of body weight (maximum dose = 15 mL). However, the recommended dose of IG for immunocompromised persons is 0.5 mL/kg of body weight (maximum dose = 15 mL). For persons receiving IGIV therapy, administration of at least 100 mg/kg within 3 weeks before measles exposure should be sufficient to prevent measles infection.
IG is indicated for susceptible household contacts of measles patients, particularly those for whom the risk for complications is increased (i.e., infants aged ≤12 months, pregnant women, or immunocompromised persons). Infants <6 months of age are usually immune because of passively acquired maternal antibodies. However, if measles is diagnosed in a mother, unvaccinated children of all ages in the household who lack other evidence of measles immunity should receive IG. IG prophylaxis is not indicated for household contacts who have received a dose of measles vaccine on or after the first birthday, unless they are immunocompromised. Only if administered within 72 hours of initial measles exposure is MMR vaccine acceptable for postexposure prophylaxis in household contacts aged ≥6 months except pregnant women, immunocompromised patients, and others for whom vaccine is contraindicated (see Use of Vaccine). IG should not be used to control measles outbreaks.
Any person exposed to measles who lacks evidence of measles immunity (Table 1) and to whom IG is administered should subsequently receive MMR vaccine, which should be administered no earlier than 5-6 months after IG administration, provided the person is then aged ≥12 months and the vaccine is not otherwise contraindicated. Kawasaki disease 2 g/kg IV (as IGIV) 11 *This table is not intended for determining the correct indications and dosage for the use of immune globulin preparations. Unvaccinated persons may not be fully protected against measles during the entire suggested time interval, and additional doses of immune globulin and/or measles vaccine may be indicated after measles exposure. The concentration of measles antibody in a particular immune globulin preparation can vary by lot. The rate of antibody clearance after receipt of an immune globulin preparation can vary. The recommended intervals are extrapolated from an estimated half life of 30 days for passively acquired antibody and an observed interference with the immune response to measles vaccine for months after a dose of 80 Passively acquired measles antibodies can interfere with the immune response to measles vaccination (see Recent Administration of Immune Globulins). The interval required to avoid such interference varies (Table 3).
# TABLE 3. Suggested intervals between administration of immune globulin preparations for various indications and vaccines containing live-measles virus*
Indications
IG does not prevent rubella or mumps infection after exposure and is not recommended for that purpose. Although administration of IG after exposure to rubella will not prevent infection or viremia, it may modify or suppress symptoms and create an unwarranted sense of security. Therefore, IG is not recommended for routine postexposure prophylaxis of rubella in early pregnancy or any other circumstance. Infants with congenital rubella have been born to women who received IG shortly after exposure. Administration of IG should be considered only if a pregnant woman who has been exposed to rubella will not consider termination of pregnancy under any circumstances. In such cases, intramuscular administration of 20 mL of immune globulin within 72 hours of rubella exposure may reduce-but will not eliminate-the risk for rubella (145,146 ).
# Revaccination of Persons Vaccinated According to Earlier Recommendations
Some persons vaccinated according to earlier recommendations for use of measles, rubella, mumps, and MMR vaccines should be revaccinated to ensure that they are adequately protected. Unless one of its component vaccines is contraindicated, MMR vaccine should be used for this purpose.
# Previous vaccination with live measles, rubella, and mumps vaccines.
Persons vaccinated with live measles, rubella, or mumps vaccines before the first birthday who were not revaccinated on or after the first birthday should be considered unvaccinated. Unless they have other acceptable evidence of immunity to measles, rubella, and mumps (Table 1), these persons should be revaccinated with MMR.
Live attenuated Edmonston B measles vaccine (distributed from 1963 to 1975) was usually administered with IG or high-titer measles immune globulin (MIG; no longer available in the United States). Vaccination with this product, administered on or after the first birthday, is considered an effective first dose of vaccine. If indicated, a second dose of MMR vaccine should be administered (see Documentation of Immunity).
IG or MIG administered simultaneously with further attenuated measles vaccines (i.e., vaccines containing the Schwarz or Moraten virus strains) may have impaired the immune response to vaccination. Persons who received measles vaccine of unknown type or further attenuated measles vaccine accompanied by IG or MIG should be considered unvaccinated and should be administered two doses of MMR vaccine. Persons vaccinated with other previously licensed live rubella vaccines that were not administered with IG or MIG (i.e., HPV-77 or Cendehill vaccines) need not be revaccinated against rubella.
# Previous vaccination with inactivated measles vaccine or measles vaccine of unknown type. Inactivated (killed) measles vaccine was available in the United
States only from 1963 to 1967 but was available through the early 1970s in some other countries. It was frequently administered as a series of two or three injections. Because persons who received inactivated vaccine are at risk for developing severe atypical measles syndrome when exposed to the natural virus, they should receive two doses of MMR or other live measles vaccine, separated by at least 28 days (147 ). Persons who received inactivated vaccine followed within 3 months by live virus vaccine should also be revaccinated with two more doses of MMR or other live measles vaccine. Revaccination is particularly important when the risk for exposure to natural measles virus is increased (e.g., during international travel).
Persons vaccinated during 1963-1967 with vaccine of unknown type may have received inactivated vaccine and also should be revaccinated. Persons who received a vaccine of unknown type after 1967 need not be revaccinated unless the original vaccination occurred before the first birthday or was accompanied by IG or MIG. However, such persons should receive a second dose before entering college, beginning work in a health-care facility, or undertaking international travel. Some recipients of inactivated measles vaccine who were later revaccinated with live measles vaccine have had adverse reactions to the live vaccine; the percentage who reported adverse reactions ranges from 4% to 55% (148 ). In most cases, these reactions were mild (e.g., local swelling and erythema, low-grade fever lasting 1-2 days), but rarely more severe reactions (e.g., prolonged high fevers, extensive local reactions) have been reported. However, natural measles infection is more likely to cause serious illness among recipients of inactivated measles vaccine than is live measles virus vaccine.
# Previous vaccination with inactivated mumps vaccine or mumps vaccine of unknown type.
A killed mumps virus vaccine was licensed for use in the United States from 1950 through 1978. Although this vaccine induced antibody, the immunity was transient. The number of doses of killed mumps vaccine administered between licensure of live attenuated mumps vaccine in 1967 until the killed vaccine was withdrawn in 1978 is unknown but appears to have been limited.
Revaccination with MMR should be considered for certain persons vaccinated before 1979 with either killed mumps vaccine or mumps vaccine of unknown type who are at high risk for mumps infection (e.g., persons who work in health-care facilities during a mumps outbreak). No evidence exists that persons who have had mumps disease or who have previously received mumps vaccine (killed or live) are at increased risk for local or systemic reactions upon receiving MMR or live mumps vaccine.
# ADVERSE EVENTS AFTER MMR VACCINATION
Adverse events associated with administration of MMR vaccine range from local pain, induration, and edema to rare systemic reactions such as anaphylaxis. Side effects tend to occur among vaccine recipients who are nonimmune and therefore are very rare after revaccination (see Revaccination). Expert committees at the Institute of Medicine (IOM) recently reviewed all evidence concerning the causal relationship between MMR vaccination and various adverse events (149,150 ). The IOM determined that evidence establishes a causal relation between MMR vaccination and anaphylaxis, thrombocytopenia, febrile seizures, and acute arthritis. Although vasculitis, otitis media, conjunctivitis, optic neuritis, ocular palsies, Guillain-Barré syndrome, and ataxia have been reported after administration of MMR or its component vaccines and are listed in the manufacturer's package insert, no causal relationship has been established between these events and MMR vaccination.
Evidence does not support a causal association of administration of measlescontaining vaccine with risk for Crohn disease, a hypothesis proposed by some researchers in the United Kingdom and Sweden (151)(152)(153)(154)(155)(156). Other researchers have been unable to replicate the laboratory findings that were reported to support this hypothesized association (157,158 ). Concerns also have been raised about the methods used in the epidemiologic studies that suggested an association between Crohn disease and measles vaccination (159)(160)(161)(162)(163). Other data do not support an association between measles vaccination and risk for Crohn disease or other inflammatory bowel disease (164,165 ).
Infection with mumps virus may trigger the onset of diabetes mellitus in some persons. However, no association has been established between vaccination with MMR or other mumps virus vaccine and pancreatic damage or subsequent development of diabetes mellitus (150 ).
# Fever, Rash, Lymphadenopathy, or Parotitis
Measles, rubella, and mumps vaccines may cause fever after vaccination; the measles component of MMR vaccine is most often associated with this adverse event. Approximately 5% of children develop a temperature of ≥103 F (≥39.4 C) after MMR vaccination. Such febrile reactions usually occur 7-12 days after vaccination and generally last 1-2 days (166 ). Most persons with fever are otherwise asymptomatic.
Measles-and rubella-containing vaccines (including MMR) can cause transient rashes, which usually appear 7-10 days after vaccination, in approximately 5% of vaccinated persons. Transient lymphadenopathy sometimes occurs following administration of MMR or other rubella-containing vaccine, and parotitis has been reported rarely following administration of MMR or other mumps-containing vaccine.
# Allergic Reactions
Hypersensitivity reactions, usually consisting of urticaria or a wheal and flare at the injection site, occur rarely after administration of MMR or any of its component vaccines. Immediate anaphylactic reactions to these vaccines are very rare. More than 70 million doses of MMR vaccine have been distributed in the United States since the Vaccine Adverse Events Reporting System (VAERS) was implemented in 1990. The reported rate of possible anaphylaxis after vaccination with measles-containing vaccine is <1 case per 1 million doses distributed (CDC, unpublished data). Allergic reactions including rash, pruritus, and purpura have been temporally associated with mumps vaccination but are uncommon, usually mild, and of brief duration.
# Thrombocytopenia
Surveillance of adverse reactions in the United States and other countries indicates that MMR vaccine can, in rare instances, cause clinically apparent thrombocytopenia within 2 months after vaccination. In prospective studies, the reported frequency of clinically apparent thrombocytopenia after MMR vaccination ranged from 1 case per 30,000 vaccinated children in Finland and Great Britain (167,168 ) to 1 case per 40,000 in Sweden (169 ), with a temporal clustering of cases occurring 2-3 weeks after vaccination. Based on passive surveillance, the reported frequency of thrombocytopenia was approximately 1 case per 100,000 vaccine doses distributed in Canada (170 ) and France (171 ), and approximately 1 case per 1 million doses distributed in the United States (172 ). The clinical course of these cases was usually transient and benign, although hemorrhage occurred rarely (172 ). The risk for thrombocytopenia during rubella or measles infection is much greater than the risk after vaccination (173 ). Based on case reports, the risk for MMR-associated thrombocytopenia may be increased for persons who have previously had immune thrombocytopenic purpura, particularly for those who had thrombocytopenic purpura after an earlier dose of MMR vaccine (150,174,175 ).
# Neurological Events
Adverse neurological events after administration of MMR vaccine are rare. Reports of nervous system illness following MMR vaccination do not necessarily denote an etiologic relationship between the illness and the vaccine. Although several cases of sensorineural deafness have been reported after administration of MMR vaccine, evidence from these case reports (e.g., timing of onset and other features) is inadequate to accept or reject a causal relation between MMR vaccination and sensorineural deafness.
# Aseptic Meningitis
Aseptic meningitis has been clearly associated with administration of the Urabe strain mumps vaccine virus but not with the Jeryl Lynn strain, which is the only mumps vaccine used in the United States (176)(177)(178). Sentinel surveillance laboratories in the United Kingdom identified thirteen aseptic meningitis cases (91 cases per 1 million doses distributed) that occurred after administration of the Urabe strain vaccine during 1988-1992 (168 ). Since the United Kingdom switched to Jeryl Lynn strain vaccine in 1992, no mumps vaccine-associated aseptic meningitis cases have been reported by the surveillance laboratories (178 ).
# Subacute Sclerosing Panencephalitis (SSPE)
Measles vaccination substantially reduces the occurrence of SSPE as evidenced by the near elimination of SSPE cases after widespread measles vaccination. SSPE has been reported rarely among children who had no history of natural measles infection, but who had received measles vaccine. Evidence indicates that at least some of these children had unrecognized measles infection before they were vaccinated and that the SSPE was directly related to the natural measles infection. The administration of live measles vaccine does not increase the risk for SSPE, even among persons who have previously had measles disease or received live measles vaccine (150,179 ).
# Encephalopathy/Encephalitis
Encephalitis with resultant residual permanent central nervous system (CNS) impairment (encephalopathy) develops in approximately 1 per 1,000 persons infected with measles virus. Whether attenuated live viral measles vaccine can also produce such a syndrome has been a concern since the earliest days of measles vaccine use.
In 1994, the IOM noted that most data were from case reports, case series, or uncontrolled observational studies, and concluded that the evidence was inadequate to accept or reject a causal relation (150 ).
The British National Childhood Encephalopathy Study (NCES) identified a fourfold elevation in risk for encephalopathy or convulsions among children who received measles vaccine during 1976-1979, compared with the risk for these conditions among unvaccinated children (180). Among previously normal children, the attributable risk for acute encephalopathy or convulsions was 1 case per 87,000 vaccinations. Findings of a subsequent 10-year follow-up study of persons diagnosed with convulsions or acute encephalopathy in the NCES indicated little difference in risk for persisting neurological abnormality among those who had received measles vaccine compared with those who had not (E. Miller, personal communication).
Although cases of encephalopathy have been reported after administration of measles-containing vaccine (181 ), lack of a unique clinical syndrome or specific laboratory test has hampered causality assessment. However, four independent passive surveillance systems in the United States (i.e., CDC measles surveillance from 1963 to 1971, the Monitoring System for Adverse Events Following Immunizations [MSAEFI] from 1979 to 1990, the Vaccine Adverse Event Reporting System [VAERS] from 1991 to 1996, and the Vaccine Injury Compensation Program [VICP]) have reported cases of encephalopathy in which a similar timing of reported events following vaccine administration is apparent. In all four case series, onset of encephalopathies follows a non-random distribution with onset approximately 10 days after vaccination, a timing consistent with onset of encephalopathy after infection with wild measles virus (182 ). Although this pattern may be in part attributable to consistent biases of these passive surveillance systems, it is also consistent with a causal relationship between measles vaccine and encephalopathies (183 ). During the period these four systems have collected data, 166 cases of encephalopathy occurring 6-15 days after vaccination have been identified and an estimated 313 million doses of measles-containing vaccines have been distributed (i.e., approximately 1 case per 2 million doses distributed). Thus, encephalopathy occurs much less frequently after administration of measles vaccine than after measles infection.
# Febrile Seizures and Personal and Family History of Convulsions
MMR vaccination, like other causes of fever, may cause febrile seizures. The risk for such seizures is approximately 1 case per 3,000 doses of MMR vaccine administered (168 ). Studies have not established an association between MMR vaccination and residual seizure disorders (150 ). Although children with personal or family histories of seizures are at increased risk for idiopathic epilepsy, febrile seizures after vaccinations do not increase the probability that epilepsy or other neurologic disorders will subsequently develop in these children. Most convulsions that occur after measles vaccination are simple febrile seizures, which affect children who do not have other known risk factors for seizure disorders.
Antipyretics may prevent febrile seizures after MMR vaccination if administered before the onset of fever and continued for 5-7 days. However, antipyretics are difficult to use for this purpose because the onset of fever is often sudden and occurs unpredictably. Seizures can occur early in the course of fever. Parents should be vigilant for fever that occurs after vaccination and should be counseled regarding its appropriate treatment. Use of aspirin during some illnesses in childhood is associated with the occurrence of Reye syndrome. Therefore, aspirin generally should not be used to prevent or control fever among children and adolescents.
The 5%-7% of children who have either a personal history of convulsions or a parent or sibling with history of convulsions may be at increased risk for febrile convulsions after MMR vaccination (184 ). The precise risk has not been measured, but appears to be minimal. On the other hand, febrile seizures occur commonly among children in whom measles disease develops, and the risk for acquiring measles is substantial. Therefore, the benefits of administering MMR vaccine to children with a personal or family history of convulsions substantially outweigh the risks and these children should be vaccinated following the recommendations for children who have no contraindications.
Children who are being treated with anticonvulsants should continue to take them after measles vaccination. Because protective levels of most currently available anticonvulsant drugs (e.g., phenobarbital) are not achieved for some time after therapy is initiated, prophylactic use of these drugs is not feasible.
The parents of children who have either a personal or family history of seizures should be advised of the benefits of vaccination and the minimal increased risk for seizures, which generally occur 5-14 days after measles vaccination.
# Guillain-Barré Syndrome (GBS)
Cases of GBS occurring after administration of MMR or its component vaccines have been reported, but the IOM judged the evidence insufficient to accept or reject a causal relationship (150 ). Recent studies provide evidence against this potential association (185,186 ). After recent mass vaccination campaigns that involved approximately eight million doses of measles-rubella vaccine in the United Kingdom and >70 million doses of measles vaccine in Latin America, evaluations of GBS incidence demonstrated no increases over background rates.
# Arthralgia, Arthritis, and Persistent or Recurrent Arthropathy
Joint symptoms are associated with the rubella component of MMR. Among susceptible persons who receive rubella vaccine, arthralgia and transient arthritis occur more frequently among adults than among children and more frequently among postpubertal females than among males. Acute arthralgia or arthritis are rare among children who receive RA 27/3 vaccine (187 ). By contrast, arthralgia develops among approximately 25% of susceptible postpubertal females after RA 27/3 vaccination and approximately 10% have acute arthritis-like signs and symptoms (188,189 ). Although rare reports of transient peripheral neuritic complaints have occurred, insufficient evidence exists to indicate a causal relation between RA 27/3 vaccine and peripheral neuropathies (149,190 ). When acute joint symptoms occur, or when pain and/or paresthesias not associated with joints occur, they generally begin 1-3 weeks after vaccination, persist for 1 day to 3 weeks, and rarely recur. Adults who experienced acute joint symptoms after rubella vaccination usually have not had to disrupt work activities (189,190,191 ).
A 1991 report by the IOM stated that although some data were consistent with a causal relation between RA27/3 rubella vaccine and chronic arthritis among adult women, the evidence was limited in scope and confined to reports from a single institution (149 ). Several more recently published studies have found no evidence of increased risk for new onset of chronic arthropathies among women vaccinated with RA 27/3 vaccine (192)(193)(194). In addition, data from a recent prospective, randomized, placebo-controlled trial by the same group that initially reported chronic arthropathy after rubella vaccination demonstrated only a small excess risk for persistent joint symptoms among persons who received rubella vaccine (relative risk [RR] = 1.58; 95% confidence interval = 1.01-2.45) (195 ). Neither the duration of arthropathy nor timing of onset was reported. The occurrence of arthropathy described as moderate or severe did not differ between vaccine and placebo recipients and was rare in both groups.
# Interference with Tuberculin Skin Tests
Tuberculin testing is not a prerequisite for vaccination with MMR or any of its component vaccines. MMR vaccine may interfere with the response to a tuberculin test (196)(197)(198). Therefore, tuberculin testing, if otherwise indicated, can be done either on the same day MMR vaccine is administered or 4-6 weeks later.
# Revaccination
No evidence indicates that administration of live measles, mumps, or rubella vaccine increases the risk for adverse reactions among persons who are already immune to these diseases as a result of previous vaccination or natural disease. Data indicate that only persons who are not immune when vaccinated tend to have postvaccination side effects similar to the disease symptoms (139 ). No evidence exists that persons who have previously received killed mumps vaccine or had mumps disease are at increased risk for local or systemic reactions from receiving live mumps vaccine. Some recipients of inactivated measles vaccine who were later revaccinated with live measles vaccines have had adverse reactions to the live vaccine (see Revaccination of Persons Vaccinated According to Earlier Recommendations).
# REPORTING ADVERSE EVENTS
Reporting of serious adverse events that occur after administration of MMR or its component vaccines helps identify adverse events that may be caused by these vaccines. The National Childhood Vaccine Injury Act of 1986 requires health-care providers to report serious adverse events that occur after vaccination with MMR and its component vaccines to the Vaccine Adverse Events Reporting System (VAERS). Persons other than health-care workers can also report adverse events to VAERS. Events that must be reported after MMR vaccination are listed in the reportable events table within the Act and include anaphylaxis or anaphylactic shock occurring within 7 days of vaccination, encephalopathy (or encephalitis) occurring within 7 days of vaccination, and any events described in the manufacturer's package insert as contraindications to additional doses of vaccine (199 ). Other adverse events occurring after administration of a vaccine, especially events that are serious or unusual, also should be reported to VAERS, regardless of the provider's opinion of the causality of the association. VAERS reporting forms and information are available 24 hours a day by calling 1-800-822-7967 or via the World Wide Web at http:\\www.cdc.gov/nip/ vaers.htm.
# VACCINE INJURY COMPENSATION
The National Vaccine Injury Compensation Program, established by the National Childhood Vaccine Injury Act of 1986, is a system under which compensation may be paid on behalf of a person thought to have been injured or to have died as a result of receiving a vaccine covered by the program. The program is intended as an alternative to civil litigation under the traditional tort system because negligence need not be proven.
The Act establishes a) a Vaccine Injury Compensation Table that lists the vaccines covered by the program; b) the injuries, disabilities, and conditions (including death) for which compensation may be paid without proof of causation; and c) the period after vaccination during which the first symptom or substantial aggravation of the injury must appear. Modifications to the Vaccine Injury Table became effective March 24, 1997 (199 ). Persons may be compensated for an injury listed in the established table or one that can be demonstrated to result from administration of a listed vaccine. Additional information about the program is available.*
# PRECAUTIONS AND CONTRAINDICATIONS Pregnancy
MMR and its component vaccines should not be administered to women known to be pregnant. Because a risk to the fetus from administration of these live virus vaccines cannot be excluded for theoretical reasons, women should be counseled to avoid becoming pregnant for 30 days after vaccination with measles or mumps vaccines and for 3 months after administration of MMR or other rubella-containing vaccines. Routine precautions for vaccinating postpubertal women with MMR should be followed in all vaccination programs (see Routine Vaccination-Women of Childbearing Age). If a pregnant woman is vaccinated or if she becomes pregnant within 3 months after vaccination, she should be counseled about the theoretical basis of concern for the fetus, but MMR vaccination during pregnancy should not ordinarily be a reason to consider termination of pregnancy. Rubella-susceptible women who are not vaccinated because they state they are or may be pregnant should be counseled about the potential risk for CRS and the importance of being vaccinated as soon as they are no longer pregnant.
Because birth defects are noted in 3%-5% of all births, confusion about the etiology of birth defects may result if vaccine is administered during pregnancy. Although of theoretical concern, no cases of congenital rubella syndrome or abnormalities attributable to infection with measles, rubella, or mumps vaccine virus infection have been observed among infants born to susceptible mothers who received any of these vaccines during pregnancy. From January 1971 through April 1989, CDC followed to term 321 known rubella-susceptible pregnant women who had been vaccinated with live rubella vaccine within 3 months before or 3 months after conception. Ninety-four women received HPV-77 or Cendehill vaccines, one received vaccine of unknown strain, and 226 received RA 27/3 vaccine (the only rubella vaccine presently used in the United States). None of the 324 infants born to these mothers had malformations compatible with congenital rubella infection. This total included five infants who had serologic evidence of subclinical infection; three of the infants were exposed to HPV-77 or Cendehill vaccine and two were exposed to RA 27/3 vaccine. Based on these data, the estimated risk for serious malformations attributable to RA 27/3 rubella vaccine ranges from zero to 1.6%. If the infants exposed to other rubella vaccines are included, the estimated risk is zero to 1.2%, substantially less than the ≥20% risk for CRS associated with maternal infection during the first trimester of pregnancy (200 ). Moreover, the observed risk for CRS with both the HPV-77 or Cendehill and RA 27/3 strains of vaccine is zero. Rubella vaccine virus has been isolated from the aborted fetus of one (3%) of 35 rubella-susceptible women who received RA 27/3 strain vaccine during pregnancy. In contrast, vaccine virus was isolated from the fetuses of 17 (20%) of 85 women to whom HPV-77 or Cendehill vaccines were administered (201). This finding provides additional evidence that the RA 27/3 vaccine poses no greater risk for teratogenicity than did the HPV-77 or Cendehill vaccines.
Breast feeding is not a contraindication to vaccination. Although a woman can excrete rubella vaccine virus in breast milk and transmit the virus to her infant, the infection remains asymptomatic (202)(203)(204)(205). Otherwise, persons who receive MMR or its component vaccines do not transmit measles, rubella, or mumps vaccine viruses (206,207 ). Thus, MMR vaccine can be administered safely to susceptible children or other persons with household contacts who are pregnant to help protect these pregnant women from exposure to wild rubella virus.
All suspected cases of CRS, whether presumed to be due to wild-virus or vaccinevirus infection, should be reported to state and local health departments. Suspected or confirmed cases of CRS can also be reported to the VAERS (see Reporting Adverse Events).
# Severe Illness
Because of the importance of protecting susceptible children against measles, mumps, and rubella, medical personnel should use every opportunity to vaccinate susceptible persons. The decision to vaccinate or postpone vaccination of a person who currently has or recently has had an acute febrile illness depends largely on the cause of the illness and the severity of symptoms. Minor illnesses, with or without fever (e.g., diarrhea, upper respiratory infection, otitis media) are not contraindications for vaccination and vaccination should not be postponed because of them. Data indicate that seroconversion rates for each component of MMR vaccine among persons with mild febrile illness are similar to those among healthy persons (208,209 ). Similarly, performing routine physical examinations or measuring temperatures are not prerequisites for vaccinating persons who appear to be in good health. In childhood vaccination programs, appropriate procedures include a) asking the parent or guardian if the child is ill, b) postponing vaccination of children who have moderate or severe febrile illnesses, and c) vaccinating children who do not have other contraindications.
Vaccination of persons with moderate or severe febrile illnesses should generally be deferred until they have recovered from the acute phase of their illness. This wait avoids superimposing adverse effects of vaccination on the underlying illness or mistakenly attributing a manifestation of the underlying illness to the vaccine. Data are generally not available regarding the safety and immunogenicity of MMR vaccine among persons with moderate or severe febrile illness.
Persons under treatment for tuberculosis have not experienced exacerbations of the disease when vaccinated with MMR. Although no studies have been reported concerning the effect of MMR vaccine on persons with untreated tuberculosis, a theoretical basis exists for concern that measles vaccine might exacerbate tuberculosis. Consequently, before administering MMR to persons with untreated active tuberculosis, initiating antituberculous therapy is advisable. Tuberculin testing is not a prerequisite for routine vaccination with MMR or other measles-containing vaccines.
# Allergies
Among persons who are allergic to eggs, the risk for serious allergic reactions such as anaphylaxis following administration of measles-or mumps-containing vaccines is extremely low and skin-testing with vaccine is not predictive of allergic reaction to vaccination (210)(211)(212). Therefore, skin testing is not required before administering MMR (or other measles-and mumps-containing vaccines) to persons who are allergic to eggs. Similarly, the administration of gradually increasing doses of vaccine is not required. In the past, persons with a history of anaphylactic reactions (i.e., hives, swelling of the mouth or throat, difficulty breathing, hypotension, and shock) following egg ingestion were considered to be at increased risk for serious reactions after administration of measles-or mumps-containing vaccines, which are produced in chick embryo fibroblasts. Although protocols have been developed for skin testing and vaccination of persons who experience anaphylactic reactions to egg ingestion, data indicate that most anaphylactic reactions to measles-and mumps-containing vaccines are not associated with hypersensitivity to egg antigens but to other components of the vaccines (213)(214)(215)(216)(217).
The literature contains several case reports of persons with an anaphylactic sensitivity to gelatin who had anaphylactic reactions after receiving MMR vaccine (218)(219)(220). MMR and its component vaccines contain hydrolyzed gelatin as a stabilizer. Therefore, extreme caution should be exercised when administering MMR or its component vaccines to persons who have a history of an anaphylactic reaction to gelatin or gelatin-containing products. Before administering MMR or its component vaccines to such persons, skin testing for sensitivity to gelatin can be considered. However, no specific protocols for this purpose have been published.
Because MMR and its component vaccines contain trace amounts of neomycin (25 µg), persons who have experienced anaphylactic reactions to topically or systemically administered neomycin should not receive these vaccines. However, neomycin allergy is most often manifested as a delayed or cell-mediated immune response (i.e., a contact dermatitis), rather than anaphylaxis. In persons who have such a sensitivity, the adverse reaction to the neomycin in the vaccine is an erythematous, pruritic nodule or papule appearing 48-96 hours after vaccination. A history of contact dermatitis to neomycin is not a contraindication to receiving MMR vaccine. MMR vaccine does not contain penicillin and therefore a history of penicillin allergy is not a contraindication to MMR vaccination.
Although anaphylaxis after vaccination is extremely rare and no anaphylaxis deaths associated with administration of MMR vaccine have been reported, this adverse event can be life threatening (150 ). Epinephrine should be available for immediate use at any site where vaccines are administered in case symptoms of anaphylaxis occur.
# Thrombocytopenia
Children who have a history of thrombocytopenia or thrombocytopenic purpura may be at increased risk for developing clinically significant thrombocytopenia after MMR vaccination (172,175 ). Although thrombocytopenia can be life threatening, no deaths have been reported as a direct consequence of vaccine-induced thrombocytopenia. The decision to vaccinate with MMR should depend on the benefits of immunity to measles, mumps, and rubella and the risks for recurrence or exacerbation of thrombocytopenia after vaccination or during natural infection with measles or rubella. The benefits of primary immunization are usually greater than the potential risks, and administration of MMR vaccine is justified, particularly with regard to the even greater risk for thrombocytopenia after measles or rubella disease. However, avoiding a subsequent dose of MMR vaccine may be prudent if an episode of thrombocytopenia occurred within approximately 6 weeks after a previous dose of the vaccine. Serologic evidence of measles immunity among such persons may be sought in lieu of MMR vaccination.
# Recent Administration of Immune Globulins
Recent evidence indicates that high doses of immune globulins can inhibit the immune response to measles and rubella vaccine for 3 or more months (221,222 ). The duration of this interference with the immune response depends on the dose of immune globulin administered. The effect of immune globulin preparations on the response to mumps vaccine is unknown. Blood (e.g., whole blood, packed red blood cells, and plasma) and other antibody-containing blood products (e.g., IG, specific immune globulins, and IGIV) can reduce the immune response to MMR or its component vaccines. Therefore, these vaccines should be administered to persons who have received an immune globulin preparation only after the recommended intervals have elapsed (Table 3) (80 ). However, postpartum administration of MMR or rubella vaccine to women who are susceptible to rubella should not be delayed because anti-Rho(D) immune globulin (human) or any other blood product was received during the last trimester of pregnancy or at delivery. Such rubella-susceptible women should be vaccinated immediately after delivery and tested at least 3 months later to ensure that they are immune to rubella and measles.
Immune globulin preparations generally should not be administered simultaneously with MMR or its component vaccines. If administration of an immune globulin preparation becomes necessary because of imminent exposure to disease, MMR or its component vaccines can be administered simultaneously with the IG preparation, although vaccine-induced immunity may be compromised. Usually, vaccine virus replication and stimulation of immunity will occur 1-2 weeks after vaccination. Thus, if the interval between administration of any of these vaccines and administration of an IG preparation is <14 days, vaccination should be repeated after the recommended interval (Table 3), unless serologic testing indicates that the vaccinated person's immune system has produced antibodies to each vaccine component (i.e., measles, rubella, and mumps). The vaccine should be administered at an anatomic site remote from that chosen for the IG injection.
# Altered Immunocompetence
Enhanced replication of vaccine viruses may occur in persons who have immune deficiency diseases and in other persons who are immunosuppressed. Severe immunosuppression may be caused by many disease conditions (e.g., congenital immunodeficiency, HIV infection, hematologic or generalized malignancy) and by therapy with immunosuppressive agents, including large doses of corticosteroids. For some of these conditions, all affected persons are severely immunocompromised. For other conditions (e.g., HIV infection), the degree to which the immune system is compromised depends on the severity of the condition, which in turn depends on the disease or treatment stage. Ultimately, the patient's physician must assume responsibility for determining whether the patient is severely immunocompromised based on clinical and laboratory assessment.
Case reports have linked vaccine-associated measles infection to the deaths of some severely immunocompromised persons (150,223 ). Therefore, MMR vaccine should not be administered to severely immunocompromised persons. To reduce the risk for measles, rubella, and mumps exposure of immunocompromised patients, their susceptible close contacts should be vaccinated with MMR. No case reports exist linking MMR or mumps-or rubella-containing vaccines with clinically significant infection caused by mumps or rubella vaccine virus among immunocompromised vaccine recipients.
# HIV-Infected Persons
Among asymptomatic and symptomatic HIV-infected patients who are not severely immunosuppressed, MMR vaccination has been associated with variable antibody responses but not with severe or unusual adverse events. Asymptomatic persons do not need to be evaluated and tested for HIV infection before MMR and other measlescontaining vaccines are administered. MMR vaccine is recommended for all asymptomatic HIV-infected persons who are not severely immunosuppressed and who lack evidence of measles immunity. MMR vaccination of symptomatic HIV-infected persons should be considered if they a) do not have evidence of severe immunosuppression and b) lack evidence of measles immunity. MMR and other measles-containing vaccines are not recommended for HIV-infected persons with evidence of severe immunosuppression (see Special Considerations for Vaccination-Persons Infected with Human Immunodeficiency Virus [HIV]) (Table 2).
# Steroids
Systemically absorbed corticosteroids can suppress the immune system of an otherwise healthy person. However, neither the minimum dose nor the duration of therapy sufficient to cause immune suppression are well defined. Most experts agree that steroid therapy usually does not contraindicate administration of live virus vaccines such as MMR and its component vaccines when therapy is: a) short term (i.e., <14 days) low-to-moderate dose; b) low-to-moderate dose administered daily or on alternate days; c) long term alternate day treatment with short-acting preparations; d) physiologic maintenance doses (replacement therapy); or e) administered topically (skin or eyes), by aerosol, or by intra-articular, bursal, or tendon injection. Although the immunosuppressive effects of steroid treatment vary, many clinicians consider a steroid dose that is equivalent to or greater than a prednisone dose of 2 mg/kg of body weight per day or a total of 20 mg per day sufficiently immunosuppressive to raise concern about the safety of administration of live virus vaccines. Persons who have received systemic corticosteroids in these or greater doses daily or on alternate days for an interval of ≥14 days should avoid vaccination with MMR and its component vaccines for at least 1 month after cessation of steroid therapy. Persons who have received prolonged or extensive topical, aerosol, or other local corticosteroid therapy that causes clinical or laboratory evidence of systemic immunosuppression should also avoid vaccination with MMR for at least 1 month after cessation of therapy. Persons who receive doses of systemic corticosteroids equivalent to a prednisone dose of ≥2 mg/kg of body weight or ≥20 mg total daily or on alternate days during an interval of <14 days generally can receive MMR or its component vaccines immediately after cessation of treatment, although some experts prefer waiting until 2 weeks after completion of therapy. MMR or its component vaccines generally should not be administered to persons who have a disease that, in itself, suppresses the immune response and who are receiving either systemic or locally administered corticosteroids.
# Leukemia
Persons with leukemia in remission who were not immune to measles, rubella, or mumps when diagnosed with leukemia may receive MMR or its component vaccines. At least 3 months should elapse after termination of chemotherapy before administration of the first dose of MMR vaccine.
# Management of Patients with Contraindications to Measles Vaccine
If immediate protection against measles is required for persons with contraindications to measles vaccination, 0.25 mL/kg (0.11 mL/lb) of body weight (maximum dose = 15 mL) of IG should be administered as soon as possible after known exposure (See Use of Vaccine and Immune Globulin Among Persons Exposed to Measles, Rubella, or Mumps). Exposed symptomatic HIV-infected and other immunocompromised persons should receive IG regardless of their previous vaccination status. Because IG in usual doses may not be effective for immunocompromised persons, the recommended dose is 0.5 mL/kg of body weight if IG is administered intramuscularly (maximum dose = 15 mL). This corresponds to a dose of IgG protein of approximately 82.5 mg/kg (maximum dose = 2,475 mg). Intramuscular IG may not be needed if a patient is receiving at least 100-400 mg/kg IGIV at regular intervals and exposure occurs within 3 weeks after administration of the last dose of IGIV. Because the amounts of protein administered are similar, high-dose IGIV may be as effective as intramuscular IG. However, no data are available concerning the effectiveness of IGIV in preventing measles.
The effectiveness of IG or IGIV for preventing mumps or rubella is unknown. These products should not be used for prophylaxis among immunocompromised persons exposed to these diseases.
# SURVEILLANCE AND OUTBREAK CONTROL
Surveillance for vaccine preventable diseases has four primary purposes: a) to provide important data on program progress and long term trends, b) to provide the basis for changes in disease prevention strategies, c) to help define groups in greatest need of vaccination, and d) to evaluate vaccine safety and effectiveness (e.g., protective efficacy, duration of vaccine-induced immunity, and occurrence of adverse effects). As the incidence of measles, rubella, and mumps declines in the United States, enhanced surveillance becomes increasingly important.
Any person aware of a suspected or known cases of measles, rubella, congenital rubella syndrome, or mumps should report the case to the local or state health department. The designated public health authorities should investigate the case immediately. The purpose of the investigation is to classify the case, identify the characteristics of the case and the source of exposure, and prevent further spread.
Cases of measles, rubella, and congenital rubella syndrome are reportable in all states, and mumps is reportable in most states. Data from measles, rubella, congenital rubella syndrome, and mumps cases are routinely reported by state and local health departments to CDC and published weekly in the Morbidity and Mortality Weekly Report.
# Measles Case Investigation and Outbreak Control Case Definition
A suspected measles case is defined as any febrile illness accompanied by rash. Suspected and known cases of measles should be reported immediately to the local or state health department. The designated public health authorities should quickly initiate an investigation of the reported case. Rapid case reporting and investigation can help limit further transmission.
A clinical case of measles is defined as an illness characterized by
• a generalized rash lasting ≥3 days, and • a temperature of ≥38.3 C (≥101 F), and • cough, coryza, or conjunctivitis.
A probable case of measles
• meets the clinical case definition for measles, and
• is not epidemiologically linked to a confirmed case, and • has not been serologically or virologically tested or has noncontributory serologic or virologic results.
A confirmed case of measles
• meets the laboratory criteria for measles or
• meets the clinical case definition and is epidemiologically linked to a confirmed case.
Confirmed measles cases are routinely reported to CDC by state health departments.
# Laboratory Diagnosis
The laboratory criteria for measles diagnosis are:
• a positive serologic test for measles IgM antibody, or • a significant rise in measles antibody level by any standard serologic assay, or • isolation of measles virus from a clinical specimen.
A laboratory-confirmed case need not meet the clinical case definition. Serologic confirmation should be attempted for every suspected case of measles and is particularly important for any case that cannot be epidemiologically linked through a chain of transmission to a confirmed case. However, reporting of suspected or probable cases, investigation of cases, and the implementation of control activities should not be delayed pending laboratory results.
Blood for serologic testing should be collected during the first clinical encounter with a person who has suspected or probable measles. The serum should be tested for measles IgM antibody as soon as possible using an assay that is both sensitive and specific (e.g., direct-capture IgM EIA method). Correct interpretation of serologic data depends on the timing of specimen collection in relation to rash onset and on the characteristics of the antibody assay used. This timing is especially important for interpreting negative results because IgM antibody may not be detectable with some less sensitive assays until at least 72 hours after rash onset. Measles IgM may be detectable at the time of rash onset, peaks approximately 10 days after rash onset, and is usually undetectable 30-60 days after rash onset. In general, if measles IgM is not detected in a serum specimen obtained in the first 72 hours after rash onset from a person whose illness meets the clinical case definition for measles, another specimen should be obtained at least 72 hours after rash onset and tested for measles IgM antibody. Measles IgM is detectable for at least 1 month after rash onset. Persons with febrile rash illnesses who are seronegative for measles should be tested for rubella.
As measles becomes rare in the United States, the likelihood of obtaining false positive serologic results from measles IgM antibody testing increases. False positive results have been obtained by using a commercially available ELISA assay for measles IgM in persons with parvovirus infection (fifth disease) (224 ). Confirmatory testing by using an assay that is both sensitive and specific (e.g., direct-capture IgM EIA method) should be considered when IgM is detected in a patient with suspected measles who has no identified source of infection and no epidemiologic linkage to another confirmed case. The Measles Virus Laboratory of CDC's National Center for Infectious Diseases has provided training to all state public health laboratories to perform such testing.
Serologic diagnosis of measles can also be confirmed by a significant rise in antibody titer between acute-and convalescent-phase serum specimens. Typically, the acute-phase serum specimen is obtained within 1-3 days after rash onset and the convalescent-phase specimen is obtained approximately 2-4 weeks later. This method has been largely supplanted by IgM assays which can be done on a single serum specimen obtained soon after rash onset.
Asymptomatic measles reinfection can occur among persons who have previously developed antibodies from vaccination or from natural disease. Symptomatic reinfections accompanied by rises in measles antibody titers are rare, and those resulting in detectable measles IgM antibody occur even more rarely.
Molecular characterization of measles virus isolates has become an important tool for defining the epidemiologic features of measles during periods of low disease incidence and for documenting the impact of measles elimination efforts (16 ). In addition to serologic confirmation, a specimen (e.g., urine or nasopharyngeal mucus) for measles virus isolation and genetic characterization should be collected as close to the time of rash onset as possible. Delay in collection of these clinical specimens reduces the chance of isolating measles virus. Clinicians who have a patient with suspected measles should immediately contact their local or state health departments concerning additional information about collecting and shipping urine and nasal specimens for measles virus isolation. Molecular characterization of the measles virus isolated from urine or nasopharyngeal specimens requires considerable time and cannot be used for diagnosis of measles. Use of oral fluid in tests for detecting measles IgM and IgG antibodies is being investigated (225 ).
# Measles Outbreak Control
The local or state health department should be contacted immediately when suspected cases of measles occur in a community. All reports of suspected measles cases should be investigated promptly. Because of the potential for rapid spread of the disease, one confirmed case of measles in a community is an urgent public health situation. Once a case is confirmed, prompt vaccination of susceptible persons at risk for exposure may help prevent dissemination of measles. Control activities should not be delayed pending the return of laboratory results from persons with suspected or probable cases. Persons who cannot readily provide acceptable evidence of measles immunity (Table 1) should be vaccinated or excluded from the setting of the outbreak (e.g., school, day care facility, hospital, clinic). Almost all persons who are excluded from an outbreak area because they lack acceptable evidence of immunity quickly comply with vaccination requirements. Persons exempted from measles vaccination for medical, religious, or other reasons should be excluded from involved institutions in the outbreak area until 21 days after the onset of rash in the last case of measles. Mass revaccination of entire communities generally is not necessary. Staff of the National Immunization Program, CDC, are available to assist health departments in developing an outbreak control strategy.
# Measles Outbreaks Among Preschool-Aged Children
Although most infants are protected from measles by maternal antibody, the disease is often more severe when it affects children aged <12 months. If cases are occurring among infants aged <12 months, measles vaccination of infants aged as young as 6 months may be undertaken as an outbreak control measure. Monovalent measles vaccine is preferred, but MMR vaccine may be administered if the monovalent vaccine is not readily available (see Routine Vaccination-International Travel). Children vaccinated with measles or MMR vaccine before the first birthday should be revaccinated at age 12-15 months and again before entering school.
Passive immunization with IG may be preferred for infants aged <12 months who are household contacts of measles patients, both because it is likely they will have been exposed >72 hours before diagnosis of the disease in the household member and because they are at highest risk for complications from the disease (see Use of Vaccine and Immune Globulin Among Persons Exposed to Measles, Rubella, or Mumps). IG should not be used to control measles outbreaks.
# Measles Outbreaks in Day Care Facilities, Schools, and Other Educational Institutions
During an outbreak in a day care facility, revaccination with MMR is recommended for all attendees and their siblings who have not received two doses of measles-containing vaccine on or after the first birthday and who do not have other evidence of measles immunity. Facility personnel (e.g., employees, volunteers, service providers) who cannot provide acceptable evidence of immunity (Table 1) also should be vaccinated with MMR. Revaccination also should be considered for unaffected child care facilities in the community that may be at risk for measles exposure and transmission.
During outbreaks in schools (elementary, middle, junior and senior high schools, colleges and other institutions of higher education), a program of revaccination with MMR vaccine is recommended in the involved schools. Revaccination of students and personnel of unaffected schools in the same geographic area who may be at risk for measles transmission also should be considered. Revaccination should include all students and their siblings and all school personnel born during or after 1957 who cannot provide documentation of adequate measles vaccination or other acceptable evidence of measles immunity. For persons born in 1957 or later, adequate vaccination consists of two doses of measles-containing vaccine separated by at least 28 days with the first dose administered no earlier than the first birthday (Table 1) ( see Documentation of Immunity). Persons who cannot readily provide documentation of acceptable evidence of measles immunity should be vaccinated or excluded from the day care facility, school, or other educational institution. Revaccinated persons, as well as persons who receive their first dose as part of the outbreak control program, may be readmitted to school immediately. Persons exempted from measles vaccination for medical, religious, or other reasons, and those who refuse vaccination for any reason, should be excluded from the day care facility, school, or other educational institution until 21 days after the onset of rash in the last case of measles.
# Measles Outbreaks in Health-Care Settings
If a measles outbreak occurs within a health-care facility (e.g., hospital, clinic, physician office) or in the areas served by the facility, all persons working at the facility who cannot provide documentation of two doses of measles-containing vaccine separated by at least 28 days with the first dose administered on or after the first birthday, or who do not have other evidence of measles immunity (Table 1), should receive a dose of MMR vaccine. If indicated, health-care workers born during or after 1957 should receive a second dose of MMR vaccine at least 28 days after the previous dose (see Documentation of Immunity). Some health-care workers born before 1957 have acquired measles in health-care facilities and have transmitted the disease to patients or coworkers (see Health-care Facilities). Therefore, during outbreaks, health-care facilities also should strongly consider recommending a dose of MMR vaccine to unvaccinated health-care workers born before 1957 who do not have serologic evidence of immunity or a history of measles disease.
Serologic testing of health-care workers before vaccination is not generally recommended during an outbreak because arresting measles transmission requires rapid vaccination of susceptible health-care workers. The need to screen, wait for results, and then contact and vaccinate susceptible persons can impede the rapid vaccination needed to curb the outbreak.
Susceptible health-care workers (Table 1) exposed to measles should receive a dose of MMR vaccine and should be removed from all patient contact and excluded from the facility from the fifth to the 21st day after the exposure. They may return to work on the 22nd day after exposure. However, susceptible health-care workers who are not vaccinated after exposure should be removed from all patient contact and excluded from the facility from the fifth day after their first exposure to the 21st day after the last exposure, even if they receive postexposure IG. Personnel who become ill with prodromal symptoms or rash should be removed from all patient contact and excluded immediately from the facility until 4 days after the onset of their rash.
# Use of Quarantine
Imposing quarantine measures for outbreak control is usually both difficult and disruptive to schools and other organizations. Under special circumstances (i.e., during outbreaks in schools attended by large numbers of persons who refuse vaccination), restriction of an event or other quarantine measures might be warranted (226). However, such action is not recommended as a routine measure for control of most outbreaks.
# Rubella Case Investigation and Outbreak Control Case Definition
A suspected rubella case is any generalized rash illness of acute onset. A clinical case of rubella is defined as an illness characterized by all of the following clinical features:
• acute onset of generalized maculopapular rash; and • a temperature of >37.2 C (>99 F), if measured; and • arthralgia/arthritis, or lymphadenopathy, or conjunctivitis.
Cases meeting the measles case definition are excluded, as are cases with serologic findings compatible with recent measles virus infection.
A probable case of rubella
• meets the clinical case definition for rubella, and • has no or noncontributory serologic or virologic testing, and • is not epidemiologically linked to a laboratory-confirmed case.
A confirmed rubella case
• meets the laboratory criteria for rubella, or
• meets the clinical case definition and is epidemiologically linked to a laboratory confirmed case.
Suspected and known rubella cases should be reported immediately to local health departments. Aggressive case finding and intensified surveillance for CRS should follow. Rubella surveillance is complicated by the nonspecific nature of the symptoms of the clinical disease. Rubella can be confused with other illnesses, including measles. Thus, all rubella cases, particularly isolated cases that do not occur as part of an outbreak, should be confirmed by laboratory testing. Confirmed rubella cases are reported to the CDC by state health departments. Cases of febrile rash illness that are laboratory-negative for rubella may be measles (rubeola) and the patients should be tested for measles IgM.
Laboratory confirmation of suspected cases of CRS also is necessary because the constellation of findings of CRS varies. Case reports of indigenous congenital rubella syndrome are sentinel events, indicating the presence of rubella infections in the community that may previously have been unrecognized. The diagnosis of one or more indigenous CRS cases in a community should trigger intensified rubella and CRS surveillance.
A confirmed case of CRS has laboratory confirmation of rubella infection and at least one defect in each of the two following categories: a) cataracts/congenital glaucoma (either or both count as one), congenital heart disease, loss of hearing, pigmentary retinopathy; and, b) purpura, splenomegaly, jaundice, microcephaly, mental retardation, meningoencephalitis, radiolucent bone disease.
A probable case of CRS has any two conditions listed in category a) or one from category a) and one from category b) and lacks evidence of any other etiology. A case with laboratory evidence of rubella infection but no clinical symptoms or signs of CRS is classified "infection only."
# Laboratory Diagnosis
The criteria for laboratory diagnosis of rubella are • the isolation of rubella virus from an appropriately collected clinical specimen.
The clinical diagnosis of acute rubella should be confirmed by laboratory testing (230 ). The demonstration of rubella-specific IgM antibody is the most commonly used method to obtain serologic confirmation of acute rubella infection. Rubella-specific IgM antibody usually becomes detectable shortly after rash onset. The IgM antibody peaks approximately 7 days after rash onset and remains detectable for 4-12 weeks, although it is more likely to be detectable if the serum specimen is obtained within 4-5 weeks after rash onset. Occasionally, rubella-specific IgM antibody can be detected up to 1 year after acute infection.
To test for IgM, one serum specimen can be obtained as early as 1-2 days after rash onset. If IgM is not detectable in this first specimen, a second serum specimen should be collected 5 days after the onset of rash or as soon as possible thereafter. Falsenegative rubella IgM antibody test results may sometimes occur even if the specimen is appropriately drawn. False-positive IgM test results may occur among persons with certain viral infections (e.g., acute infectious mononucleosis, cytomegalovirus, or parvovirus) and among persons who are rheumatoid factor positive.
For IgG assays, the criteria for a significant rise in rubella antibody level vary by type of assay and by laboratory. For HI assays, a fourfold rise in the titer of antibody indicates recent infection. The acute-phase serum specimen should be obtained as soon after rash onset as possible, preferably within 7 days. The convalescentphase serum specimen should be drawn at least 10 days after the acute-phase serum specimen. The acute-and convalescent-phase serum specimens should be tested simultaneously in the same laboratory. If the acute-phase serum specimen is drawn >7 days (and occasionally even if obtained within 7 days) after rash onset, a significant rise in antibody titer may not be detected by most commonly used IgG assays.
In the absence of rash illness, the diagnosis of subclinical cases of rubella can be facilitated by obtaining the acute-phase serum specimen as soon as possible after exposure. The convalescent-phase specimen should be drawn at least 28 days after exposure. If acute-and convalescent-phase paired sera provide inconclusive results, rubella-specific IgM antibody testing can be performed. Expert consultation may be necessary to interpret the data.
Among pregnant women of unknown immune status who experience a rash illness or who are exposed to rubella, laboratory confirmation of rubella infection may be difficult. A serum specimen should be obtained as soon as possible. Unfortunately, serologic results are often nonconfirmatory. Such situations can be avoided by performing routine prenatal serologic screening of women who do not have acceptable evidence of rubella immunity (see Documentation of Immunity and Women of Childbearing Age). In addition, health-care providers should request that laboratories performing prenatal serologic screening retain such specimens until delivery, in case retesting is necessary.
# Congenital Rubella
Suspected cases of CRS should be managed with contact isolation (228 ). While diagnostic confirmation is pending, children with suspected CRS should be cared for only by personnel known to be immune to rubella. Confirmation of diagnosis by virus isolation can be done by culturing nasopharyngeal and urine specimens. Serologic confirmation can be obtained by testing cord blood for the presence of rubella-specific IgM antibodies. An alternative method for infants aged ≥3 months is to document rubella-specific antibody levels that do not decline at the rate expected from passive transfer of maternal antibody (i.e., the equivalent of a twofold decline in HI titer per month). However, some infected infants may have low antibody levels because of agammaglobulinemia or dysgammaglobulinemia.
In some infants with CRS, rubella virus can persist and can be isolated from nasopharyngeal and urine cultures throughout the first year of life or longer (229 ). Children with CRS should be presumed infectious at least through the first year of life unless nasopharyngeal and urine cultures are negative for virus after age 3 months (230 ). Some authorities suggest that an infant who has CRS should be considered infectious until two cultures of clinical specimens obtained 1 month apart are negative for rubella virus (230 ). Precautions should be taken to ensure that infants with CRS do not cause additional rubella outbreaks. Specifically, all persons who have contact with a child with CRS (e.g., care givers, household contacts, medical personnel, laboratory workers) should be immune to rubella (Table 1) (see Documentation of Immunity and Routine Vaccination).
# Rubella Outbreak Control
Outbreak control is important for eliminating CRS. Aggressive responses to outbreaks may interrupt chains of transmission and can increase vaccination coverage among persons who might not be protected otherwise. Although methods for controlling rubella outbreaks are evolving, the main strategy should be to define target populations for rubella vaccination, ensure that susceptible persons within the target populations are vaccinated rapidly (or excluded from exposure if a contraindication to vaccination exists), and maintain active surveillance to permit modification of control measures as needed.
Control measures should be implemented as soon as a case of rubella is confirmed in a community. This approach is especially important in any outbreak setting involving pregnant women (e.g., obstetric-gynecologic and prenatal clinics). All persons at risk who cannot readily provide laboratory evidence of immunity or a documented history of vaccination on or after the first birthday should be considered susceptible and should be vaccinated unless vaccination is contraindicated (Table 1) (see Documentation of Immunity).
# Rubella Outbreaks in Schools or Other Educational Institutions
An effective means of terminating rubella outbreaks and increasing rates of vaccination quickly is to exclude from possible contact persons who cannot provide valid evidence of immunity. Experience with measles outbreak control indicates that almost all students who are excluded from school because they lack evidence of immunity quickly comply with vaccination requirements and are promptly readmitted to school. Persons exempted from rubella vaccination for medical, religious, or other reasons should also be excluded from attendance. Exclusion should continue for 3 weeks after the onset of rash of the last reported case in the outbreak setting. Less rigorous approaches (e.g., voluntary appeals for vaccination) have not been effective in terminating outbreaks.
# Rubella Outbreaks in Health-Care Settings
During rubella outbreaks in health-care settings where pregnant women may be exposed, mandatory exclusion and vaccination of health-care workers who lack evidence of rubella immunity (Table 1) should be practiced. Exposed health-care workers who lack evidence of immunity should be excluded from duty from the seventh day after first exposure through the twenty-first day after their last exposure or until 5 days after the rash appears. In addition, because birth before 1957 does not guarantee rubella immunity, health-care facilities should strongly consider recommending a dose of MMR vaccine to unvaccinated health-care workers born before 1957 who do not have serologic evidence of immunity. Although rubella vaccination during an outbreak has not been associated with substantial personnel absenteeism (116,191 ), vaccination of susceptible persons before an outbreak occurs is preferable because vaccination causes far less absenteeism and disruption of routine work activities than does rubella infection.
# Mumps Case Investigation and Outbreak Control Case Definition
A clinical case of mumps is defined as an illness characterized by acute onset of unilateral or bilateral tender, self-limited swelling of the parotid or other salivary gland lasting ≥2 days, and without other apparent cause (as reported by a health professional).
A probable case of mumps
• meets the clinical case definition of mumps, and • is not epidemiologically linked to a confirmed or probable case, and • has noncontributory or no serologic or virologic testing.
A confirmed case of mumps
• meets the laboratory criteria for mumps, or
• meets the clinical case definition and is epidemiologically linked to a confirmed or probable case.
A laboratory-confirmed case need not meet the clinical case definition. Two probable cases that are epidemiologically linked are considered confirmed, even in the absence of laboratory confirmation.
Reporting of mumps often has been based solely on clinical diagnosis without laboratory confirmation. However, parotitis may have other infectious and noninfectious causes. Therefore, serologic confirmation of the diagnosis is preferred. Use of criteria for clinical diagnosis that are both stricter and more reliable, combined with laboratory confirmation, can be expected to decrease the number of false positive mumps cases reported and allow a more accurate assessment of mumps incidence.
Probable or confirmed cases of mumps should be reported immediately to state and local health departments. Recommended procedures to enhance the comprehensiveness of reporting include identification of all contacts, follow-up of susceptible contacts, and serologic testing of all probable cases to confirm the diagnosis.
# Laboratory Diagnosis
The laboratory criteria for the diagnosis of mumps are • isolation of the mumps virus from a clinical specimen, or • a significant rise between acute and convalescent-phase titers in serum mumps IgG antibody level by any standard serologic assay, or
• a positive serologic test for mumps IgM antibody.
In a prospective study in the practices of family practitioners in a Canadian community, one-third of persons with clinically diagnosed cases of mumps had no serologic evidence of recent mumps infection (28 ). Serum mumps IgM IFA tests are commercially available. However, until more data are available concerning the use and interpretation of these tests, laboratory confirmation of mumps should be based on tests of demonstrated reliability. State health department laboratories can provide guidance when testing for acute mumps infection is necessary.
# Mumps Outbreak Control
The strategy for outbreak control includes three main elements. The target population (transmission setting) must be defined. Persons within the population who are susceptible to mumps must be identified and vaccinated. Consideration should be given to excluding susceptible persons who are exempt from vaccination (for medical, religious, or other reasons) from the affected institution or setting until the outbreak is terminated. Active surveillance for mumps should be conducted until two incubation periods (i.e., 5-6 weeks) have elapsed since onset of the last case.
# School-based Mumps Outbreaks
Exclusion of susceptible students from schools affected by a mumps outbreak (and other, unaffected schools judged by local public health authorities to be at risk for transmission of the disease) should be considered among the means to control mumps outbreaks. Excluded students can be readmitted immediately after they are vaccinated. Experience with outbreak control for other vaccine-preventable diseases indicates that almost all students who are excluded from the outbreak area because they lack evidence of immunity quickly comply with requirements and can be readmitted to school. Pupils who have been exempted from mumps vaccination for medical, religious, or other reasons should be excluded until at least 26 days after the onset of parotitis in the last person with mumps in the affected school.
# Mumps Outbreaks in Health-Care Settings
Sporadic nosocomial cases of mumps have occurred in long-term care facilities housing adolescents and young adults (122 ). However, mumps virus is less transmissible than measles and other respiratory viruses. The low level of mumps transmission in the community results in a low risk for introduction of the disease into health-care facilities. Because mumps is shed by infected persons before clinical symptoms become evident and because infected persons often remain asymptomatic, an effective routine MMR vaccination program for health-care workers is the best approach to prevent nosocomial transmission.
To prevent droplet transmission of the disease, respiratory isolation precautions for persons with mumps should be maintained for 9 days after onset of symptoms (e.g., parotitis). If exposed to mumps, health-care workers who lack acceptable evidence of immunity (Table 1) should be excluded from the health-care facility from the 12th day after the first exposure through the 26th day after the last exposure. Workers in whom the disease develops should be excluded from work until 9 days after the onset of symptoms.
# The Morbidity and Mortality Weekly Report (MMWR) Series is prepared by the Centers for Disease Control and Prevention (CDC) and is available free of charge in electronic format and on a paid subscription basis for paper copy. To receive an electronic copy on
| None | None |
45d6cab00907c364476652bb68fb4caa01c49fac | cdc | None | The recommended standard is measurable by techniques that are valid, reproducible, and available to industry and governmental agencies. Sufficient technology exists to permit compliance with the recommended standard. Pertinent new information will be reviewed periodically and the recommendations will be revised as necessary.
Section 1 -Environmental (Workplace air) (a) Concentration
(1) Occupational exposure to trichloroethylene shall be controlled so that workers will not be exposed to trichloroethylene at a concentration in excess of 100 ppm determined as a time-weighted average (TWA) exposure for an 8-hour workday, as measured by a minimum sampling time of 10 minutes.
(2) No worker shall be exposed to a peak concentration of trichloroethylene in excess of 150 ppm, as measured by a maximum sampling time of 10 minutes.
(b) Sampling, Calibration, and Analysis
Procedures for collection of environmental samples shall be as provided in Appendix I, or by an equivalent method. Analysis of samples shall be as provided in Appendix II, or by any method shown to be equivalent in precision, sensitivity, and accuracy to the method specified in Appendix II.
Section 2 -Medical (a) Medical surveillance as specified in this section shall be made available to workers who are exposed to trichloroethylene.
(1) A preplacement examination shall be made available to all workers who will be exposed to trichloroethylene and within 6 months to all workers who are exposed to trichloroethylene on the effective date of this standard, and it shall consist of:
(A) A comprehensive medical history of each work applicant shall be taken. The history should be directed towards but not limited to the incidence of headaches, nausea, and dizziness; particular attention should be focused on complaints and evidence of eye, mucous membrane and skin irritation. Workers who complain of chronic eye irritation should have an ophthalmic (eye) examination.
(B) A comprehensive physical examination shall be made available, with emphasis on cardiac, pulmonary, liver, and kidney examinations.
(2) Periodic medical examinations shall be made available to workers exposed to trichloroethylene annually. (1) Only appropriate respirators, as defined below, shall be provided and used when a variance which allows the use of respirators as a means of controlling exposure for routine operations has been granted or while action on application for a variance is pending.
(2) The requirements set forth in this section shall apply for nonroutine operations such as a brief exposure to concentrations in excess of the environmental standard as a result of maintenance or repair activities or in emergency situations.
(3) A respiratory protection program meeting the general requirements outlined in section 3.5 of American National Standard Practices for Respiratory Protection Z88.2-1969 shall be established and enforced by the employer. This program shall include instructions on the selection, fitting, use, testing for leakage, cleaning, and maintenance of the respiratory protective devices.
(4) For the purpose of determining the class of respirator to be used, the employer shall measure the atmospheric concentration of trichloroethylene in the workplace when the initial application for variance is made and thereafter whenever process, worksite, climate or control changes occur which are likely to affect the concentrations of airborne trichloroethylene. Only appropriate respirators as described in (5) Employees who experience breathing difficulty while wearing a respirator shall be medically examined to determine their ability to wear the respirator. Greater than 10000 ppm Chemical cartridge respirator with organic vapor cartridge(s).
Type C demand type supplied air res pirator with half mask facepiece.
Gas mask, chin type, with organic vapor canister.
Type C demand type supplied air res pirator with full facepiece.
Type C continuous flow supplied air respirator.
Self-contained breathing apparatus in pressure-demand mode (positive pressure)
The self-contained breathing apparatus shall be made available and used for emergencies. (a) Each employee exposed to trichloroethylene and its decomposition products shall be apprised of all hazards, the consequences of overexposure, appropriate emergency procedures, proper conditions for safe use, and precautions to minimize exposure. This apprisal shall include, as a minimum, all information set forth in Appendix III which is applicable to that specific product or material containing trichloroethylene.
(b) Each employee shall be apprised of the location of the information prescribed in paragraph (c) of this section. This information shall be kept on file and shall be readily accessible to all employees at each establishment where exposure to trichloro ethylene occurs. (1) Disposal of small quantities of trichloroethylene call be accomplished by pouring the liquid onto a mixture of 10% soda aSh and sand and placing the mixed material in a paper container and incinerating.
(2) Waste from cleaning contaminated with trichloroethylene should be stored in a ventilated area until ready for disposal and may be burned in an incinerator. (2) Smoking should not be permitted in areas where vapor of trichloroethylene is present.
(3) Powdered metals or turnings shall not be used or stored in any area where trichloroethylene liquid is in use or stored.
Section 7 -Sanitation Practices Showers, hand-washing facilities, soap, and water shall be available.
# Section 8 -Monitoring and Recordkeeping Requirements
Workroom areas where it has been determined, on the basis of an industrial hygiene survey or the judgment of a compliance officer, that environmental levels of trichloroethylene are less than half of the TWA limit shall not be considered to have trichloroethylene exposure.
Records of these surveys, including the basis for concluding that air levels of trichloroethylene are below half of the Later in the 1930's it was used as a surgical anesthetic and proposed for use as the basis for treatment of various nervous disorders.
The first reported evidence of acute overexposure to trichloroethylene in industrial applications resulted from its use as a grease solvent.
This first report of chronic poisoning from trichloroethylene in industrial situations suggested that the observed effects were more likely due to impurities in the material rather than to trichloroethylene itself. From 1963 to 1967 the common manufacturing process for trichloroethylene produced as an intermediate chemical They noted that the daily excretion of trichloroacetic acid reached a maximum at 1:00 pm daily, irrespective of the quantity of urine excreted. Excretion of trichloroethanol began soon after the initial inhalation and rose rapidly to its maximum a few hours after the end of exposure; the total excreted was equivalent to 32 to 59% (average, 50) of the retained trichloroethylene. Excretion of trichloroethanol also appeared to fall as the sum of two exponential rates, the first phase lasting 3 or 4 days, the second lasting 7 to 9 days. Trichloroethanol excretion did not exhibit fluctuations related to time of day. In these studies, the total amount of metabolites excreted amounted to 43% to 100% (average, 73) of the trichloroethylene absorbed and the three metabolites, monochloroacetic acid, trichloroacetic acid, and trichloroethanol were found in the ratios of 1:5:12, respectively.
Bartonicek, using eight resting volunteers exposed to a concentration of 1 milligram per liter (186 ppm) of trichloroethylene in five-hour periods, found that they excreted an average of 45.4% of the retained trichloroethylene as trichloroethanol and 31.9% as trichloroacetic acid, thus accounting for 77.3% of the retained trichloroethylene. Expired air analyses were performed to estimate retained trichloroethylene. Three days after exposure, the average concentration of trichloroacetic acid was 2.4 milligrams per 100 milliliters of blood plasma and 0.5 milligram per 100 milliliters red blood cells. These studies indicated that a small amount of trichloroacetic acid was excreted in sweat and in feces and, on the third day after exposure, 0.23 milligram per 100 milliliters of saliva was measured. They showed that 58% (a range of 51 to 64) of trichloroethylene inhaled at a concentration of 186 ppm was retained.
Trichloroethanol excretion was maximal at the first post-exposure test (within the first 24 hours after exposure) and decreased exponentially while the rate of trichloroacetic acid excretion reached its peak 3 days after exposure and decreased more gradually for 18 days. This test was shown to be a less sensitive indicator of effects of trichloroethylene than of effects of alcohol.
Todd reported the case of a man who had ingested unknown amounts of trichloroethylene.
After prolonged unconsciousness and some cyanosis, the result was a temporary paranoid psychosis and a distortion of both vertical and horizontal vision so that persons appeared 12-18 inches high, an effect described as "Lilliputian hallucinations". (e) Other Effects
Friborska showed that leukocyte alkaline phosphatase levels increase in persons repeatedly exposed to trichloroethylene. The acid phosphatase in blood also increased. These increases persisted after two weeks without exposure. The investigator considered that these findings might signify a defense mechanism or an increased capacity to metabolize alcohols, might be a response to changing pH of the blood, or be related to glycogen metabolism in the liver. For the workers studied, the following percentages of complaints were indicated: dizziness, 88%; headache, 74%; nausea, 43%; euphoria, 31%; palpitation, 29%; disturbances of vision, 21%; and sleepiness at the end of the shift, 29%. The study further showed an insidious onset after some months, up to one or two years, of the following complaints: fatigue, 68%; irritability, 56%; disturbed sleep, 46%; anxiety, 27%; loss of appetite, 50%; alcohol intolerance, 21%.
Accompanying findings included excessive sweating in 39%, palpitation in 29%, nausea in 19%, and some parasthesias. While the percentage of workers that indicated complaints are in excess of the percentage of samples at or below 50 mg/cu m (about 10 ppm), a direct relationship can not be established since the sampling protocol is unknown. and the description of the bone marrow led the authors to the conclusion that chronic intoxication to trichloroethylene has a direct action on the bone marrow and thus causes myelotoxic anemia.
Another factor studied was dehydration before trichloroethylene exposures. Baetjer, in careful hypothalamic self-stimulation performance tests, showed that a three-day dehydration caused rats to make fewer responses than nondehydrated rats. After exposure to trichloroethylene, neither group performed as well as before exposure.
The dehydrated rats performed better than the nondehydrated rats, although some tolerance for trichloroethylene developed in both groups. Recovery of nondehydrated rats was prompt after moderate exposures but was not completed in 24 hours, suggesting that either the trichloroethylene concentration in the brain was greater or the dehydrated brains were more resistant to trichloroethylene or both.
Ten-day dehydration tests and trichloroethylene exposure resulted in further decrements in performance after the fifth day of exposure, suggesting that high concentration of trichloroethylene combined with dehydration may have produced some residual brain damage. to produce lighter anesthesia but it lasted two to three hours.
Bartonicek and Brun made extensive studies of brain tissue, EEG, acid phosphatase levels, and erythrocyte sedimentation rates in two groups of rabbits. In one group, rabbits were injected with 3 ml trichloroethylene into the muscle three times per week for 29 days (a total of 53 g per rabbit).
The second group was given 2 ml trichloroethylene twice a week for periods lasting from 41 to 247 days, or a total of 18-133 g per rabbit. Controls were also studied. acid was also excreted but in much smaller quantity. Friberg et al showed that rats exposed for four hours to 640, 1150 or 2500 ppm excreted trichloroacetic acid increasingly up to 24 hours after exposure then decreasingly for up to six days irrespective of dosage.
Studies by Forssman and Holmquist showed that rats exposed for studied rabbits' metabolism for a year and concluded that their metabolism was qualitatively like humans and only the relative quantities differed. Rabbits excreted 10 times more trichloroethanol than trichloroacetic acid and about 50 times less trichloroacetic acid than man, but equally slowly.
Fabre and Truhaut studied tissue homogenate. They found trichloroethylene in all tissues obtained during exposure, greatest in fat, then in lungs, spleen, liver, and least in brain and kidney.
Trichloroacetic acid was present in greatest concentration in fresh spleen, suprarenal glands, reproductive organs, and urine. In vitro studies of tissue homogenates exposed to trichloroethylene showed the most active conversion of the substance to its metabolites in the spleen, and decreasing activity in the lung, brain, liver, and kidney tissues.
In 1967 Leibman and McAllister reported studies with liver microsomal tissue extracts. They were able to show that there was an increase in the ability to metabolize trichloroethylene to chloral and to trichloroethanol when the animals from which the tissue extracts were obtained had been previously treated with phénobarbital. Rats pretreated with phénobarbital and then exposed to trichloroethylene also excreted more metabolites in the first few hours than the similarly exposed but not pretreated controls.
The authors pointed out that drug intake might vitiate conclusions drawn from levels of trichloroacetic acid urinary excretion based on single samples.
# Correlation of Exposure and Effects
The most meaningful studies for purposes of establishing a welldefined cause-and-effect relationship are those in which an attempt has been made to relate the environmental exposures with subsequent effects in the exposed population.
Longley and Jones reported that unconsciousness suddenly occurred in a worker who entered a tank in which a paint containing in excess of 75% trichloroethylene had been recently used. An attempt was made to simulate conditions which produced the unconsciousness and air sampling was conducted within the tank after application of some of the paint. Concentrations of trichloroethylene within the tank varied by location between 1700 and 3300 ppm. The authors estimated that a concentration of 3000 ppm would cause unconsciousness in human subjects after a 10-minute exposure. Their studies indicated no significant effect on psychomotor performance at the 100 ppm level.
There was a slight decline in performance at the 200 ppm level which became progressively more pronounced at the 300 and 500 ppm concentrations. A relatively high frequency of subjective complaints, alterations of the involuntary nervous system and of neurological and psychiatric symptoms were reported. The frequency showed a good relationship with total duration of exposure (months on the job). A total of 96 air samples were collected during the study, the results of which ranged between 1 and 335 ppm, many of them lying between 20 and 40 ppm. The authors stated that a series of consecu tive samples collected during a period of 3 to 4 hours in one workplace showed a great variation in concentrations due to the actual degree of ventilation and utilization of the degreasing apparatus.
The authors admitted that air measurements provided Insufficient indication of the total exposure. Laboratory tests of hepatic function showed no significant changes. On that basis they stated that they could not conclude that there was any causal relationship between liver troubles and exposure to trichloroethylene. In the case in question, the workman emptied the tank, rinsed it with water from a powerful hose pipe, then got inside the tank and spent half an hour cleaning with a scrubbing brush. Analyses of the air showed a concentration of 1,120 ppm outside the tank while the hose pipe was in action, with 815 and 395 ppm inside the apparatus during and after the scrubbing respectively."
Skinner reported the use of baffles on windows near degreasers in the plant to control high velocity drafts.
Trichloroethylene concentrations of 170 to 230 ppm were reduced to 30 to 40 ppm with this approach to control.
Hargarten et al reported results of tests carried out from 1952 to 1957 around 43 degreaser operations. Ninety-three percent of the operators' breathing zone samples taken during the cleaning cycle of the degreasers were 100 ppm or less. Methods of sampling and analysis were not stated.
In a 1963 report Ahlmark et al found that during the preceding decade, when 570 degreasing plants were inspected in Sweden,
# Process ventilation
Ventilation is by far the most common engineering method for controlling solvent vapors. Vapor recovery sytems are sometimes used when a high airflow exhaust system is required for good ventilation. In 1967 this standard was revised by the Z-37 Committee.
The revision established 100 ppm as an acceptable time-weighted average concentration for an 8-hour workday. In addition, an accept able ceiling concentration of 200 ppm, provided that the time-weighted average is kept at or below 100 ppm, was recommended. Furthermore, a concentration of 300 ppm for a duration of not more than 5 minutes was judged acceptable if encountered not more than once in 2 hours during In summary, deaths of several workers from exposure to trichloroothylene have been reported ; in the. best documented case, exposure was at levels estimated to be between 1700 and 3300 ppm for ten minutes. Exposures at 1000 ppm for even short periods of time have resulted in effects on the central nervous system. Subjective complaints by one of 8 male volunteers was reported at exposure levels of 300 ppm for two hours. No adverse effects were noted by psychophysiological testing of the same subjects at 100 ppm. In another paper, results of psychophysiological testing of one subject for 2-1/2 hours indicated no significant effect on psychomotor performance from exposure at 100 ppm, but a slight effect was noted at 200 ppm. Adverse effects were reported by 3 of 7 subjects exposed at 160 ppm for less than 83 minutes. These effects, subjective in nature, included headache, drowsiness and mild eye irritation. trichloroethylene except when it is contaminated by other compounds, especially tetrachloroethane, is the correct explanation.
As discussed above, the study by Salvini et al indicates that exposures of approximately 100 ppm may interfere with the psychophysiological efficiency of the worker. Therefore, a TWA limit of 100 ppm will protect most of the workers but with probably very little margin of safety at this level of exposure. The effects of short exposures to trichloro ethylene on swimming performances and motor activity of rats. Am Ind Hyg Assoc J 24:376-79, 1963 (1) Air sampling instruments shall be calibrated after making any repairs or modifications to the sampling system and at least once a year with a reference such as a wet test meter over a normal range of flowrates and pressure drops.
(2) The wet test meter shall be in good working condition and shall have been calibrated against a spirometer (or other primary standard) upon procurement, after each repair, and at least annually. (2) The charcoal in the tube is transferred to a small test tube and desorbed with carbon disulfide.
(3) An aliquot of the desorbed sample is injected into a gas chromatograph. If a particular atmosphere is suspected of containing a large amount of trichloroethylene, it is recommended that a smaller sampling volume be taken.
# (c) Interferences
(1) When the amount of water in the air is so great that condensation actually occurs in the tube, organic vapors will not be trapped.
Water vapor does not seem to be a problem, only water present as a mist.
(2) Any compound which has the same retention time as trichloroethylene at the operating conditions described in this method could be considered an interference. This type of interference can be overcome by changing the operating conditions of the instrument.
# (d) Precision and Accuracy
(1) Precision of the analytical method: plus or minus 4.8%.
(2) Precision of the analytical method plus field sampling with the personal sampling pump has not been established.
(3) The accuracy of the sampling and analytical method, as established during breakthrough testing of the front section of activated charcoal: 91%.
# (e) Advantages and Disadvantages of the Method
This method is advantageous in that it provides one basic method for determining many different organic solvents. The sampling device is small, portable, and involves no liquids. Interferences are minimal, and most of those which do occur can be eliminated by altering chromatographic conditions. The analysis of the tubes is accomplished using a quick instrumental method.
One disadvantage of the method is that the amount of sample which can be taken is limited by the weight of sample which the tube will hold before overloading. Also the precision of the method is limited by the reproducibility of the pressure drop across the tubes.
Variability in this pressure drop w^Lll affect the flowrate, causing the volume to be imprecise since the pump is usually calibrated for one tube only.
(f) Apparatus consists of:
(1) An approved coal mine dust personal sampling pump for personal samples or any vacuum pump whose flow can accurately be determined at 1 liter per minute or less. (3) Gas chromatograph equipped with a flame ionization detector.
(4) Column (20 ft x 1/8 in) with 10% FFAP stationary phase on 80/100 mesh acid washed DMCS Chromosorb W solid support.
One liter per minute is the recommended sampling rate. A 10-liter sample is normally adequate. The tube must be supported in a vertical position for sampling. Due to the high resistance of the charcoal tube, this sampling method places a heavy load on the personal sampling pump. Therefore, it should not be assumed that this pump will run a full 8 hours without recharging the battery. After the sample is collected, the tube must be capped; caps are provided with commercial tubes.
One charcoal tube should be treated in the same manner as the sample tubes (break, seal, ship) with the exception that no air be drawn through it. This tube will serve as a blank.
If bulk samples are submitted in addition to charcoal tubes, the tubes should be shipped in a separate container from the bulk sample. It is convenient to prepare standards in terms of mg/0.5 ml of carbon disulfide because samples are desorbed in this amount of carbon disulfide.
To minimize error due to the volatility of carbon disulfide, twenty times the weight can be injected into 10 ml of carbon disulfide. For example, to prepare a 0.3 mg/0.5 ml standard- 6.0 mg is injected into exactly 10 ml of carbon disulfide in a glassstoppered flask. The density for trichloroethylene is used to convert 6.0 mg into microliters for easy measurements with a microliter The first method is used because of its simplicity.
Because desorption efficiencies may vary from one laboratory to another and with different batches of charcoal, each laboratory should determine its own. However, for comparison, NIOSH determined a value of 97% for trichloroethylene, with one lot of activated charcoal.
# (j) Calculations
(1) The first step in calculating the results is to read the weight in milligrams corresponding to each peak area from the standard curve. The standard curve is based on mg/0.5 ml of carbon disulfide, and therefore, no correction need be made for the volume of the sample injected, since this is identical to the volume of the standards injected.
(2) The weight of trichloroethylene in the front section of the blank tube is subtracted from the weight determined for the front section of each sample; a similar procedure is followed for the backup sections.
(3) Amounts present on the front and backup sections of the same tube are then added to calculate the total amount in the sample.
(4) This total weight of trichloroethylene in the tube is corrected by dividing by the desorption factor to determine the total number of milligrams in the sample. (1) Toxic level for total compound or mixture, relevant symptoms of exposure, skin and eye irritation properties, principal routes of absorption, effects of chronic (long-term) exposure, and emergency arid first aid procedures.
(g) Section VI. Reactivity Data.
(1) Chemical stability, incompatibility, hazardous decomposition products, and hazardous polymerization.
(h) Section VII. Spill or Leak Procedures.
(1) Detailed procedures to be followed with emphasis on precautions to be taken in cleaning up and safe disposal of materials leaked or spilled. This includes proper labeling and disposal of containers containing residues, contaminated absorbents, etc.
(i) Section VIII. Special Protection Information.
(1) Requirements for personal protective equipment, such as respirators, eye protection, protective clothing, and ventilation, such as local exhaust (at site of product use or application), general, or other special types.
(j) Section IX. Special Precautions.
(1) Any other general precautionary information such as personal protective equipment for exposure to the thermal decomposition products listed in Section VI, and to particulates formed by abrading a dry coating, such as by a power sanding disc.
(k) The signature of the responsible person filling out the data sheet, his address, and the data on which it is filled out. 1 ppm = 5.38 mg/m3 @25 C 1 mg/liter = 186.1 ppm Mean time spent by each operator at the various locations. It is understood that an operator may perform at a given location with greater frequency than another operator.
(1) Breathing zone samples shall be collected as near as practicable to the worker's face without interfering with his freedom of movement and shall characterize the exposure from each job or specific operation in each production area.
(2) A portable battery-operated personal sampling pump plus an activated charcoal tube shall be used to collect the sample.
(3) The activated charcoal tube shall be attached to the worker's clothing; the shirt collar is convenient for this purpose.
(5) A mechanical or electronic integrator or a recorder and some method for determining peak area.
(6) Small glass-stoppered test tubes or equivalent.
(7) Micro syringes: 10 pi, and convenient sizes for making standards.
(g) Reagents
(1) Spectroquality carbon disulfide.
(2) Trichloroethylene, preferably chromatoquality grade.
(3) Bureau of Mines Grade A helium.
(4) Prepurified hydrogen.
(5) Filtered compressed air.
(h) Procedure
(1) Cleaning of Equipment All equipment used for the laboratory analysis should be washed in detergent followed by tap and distilled water rinses.
(2) Collection and Shipping of Samples Both ends of the charcoal tube should be broken to provide openings of at least 2 mm which is one-half the I.D. of the tube. A smaller opening causes a limiting orifice effect which reduces the flow through the tube.
The smaller section of charcoal in the tube is used as a backup section and should therefore be placed nearest the sampling pump. Tubing may be used to connect the back of the tube to the pump, but no tubing must ever be put in front of the charcoal tube. Values in parentheses are approximate conversions where the standard was published in only one of the two units listed above.
From | #
The recommended standard is measurable by techniques that are valid, reproducible, and available to industry and governmental agencies. Sufficient technology exists to permit compliance with the recommended standard. Pertinent new information will be reviewed periodically and the recommendations will be revised as necessary.
Section 1 -Environmental (Workplace air) (a) Concentration
(1) Occupational exposure to trichloroethylene shall be controlled so that workers will not be exposed to trichloroethylene at a concentration in excess of 100 ppm determined as a time-weighted average (TWA) exposure for an 8-hour workday, as measured by a minimum sampling time of 10 minutes.
(2) No worker shall be exposed to a peak concentration of trichloroethylene in excess of 150 ppm, as measured by a maximum sampling time of 10 minutes.
(b) Sampling, Calibration, and Analysis
Procedures for collection of environmental samples shall be as provided in Appendix I, or by an equivalent method. Analysis of samples shall be as provided in Appendix II, or by any method shown to be equivalent in precision, sensitivity, and accuracy to the method specified in Appendix II.
Section 2 -Medical (a) Medical surveillance as specified in this section shall be made available to workers who are exposed to trichloroethylene.
(1) A preplacement examination shall be made available to all workers who will be exposed to trichloroethylene and within 6 months to all workers who are exposed to trichloroethylene on the effective date of this standard, and it shall consist of:
(A) A comprehensive medical history of each work applicant shall be taken. The history should be directed towards but not limited to the incidence of headaches, nausea, and dizziness; particular attention should be focused on complaints and evidence of eye, mucous membrane and skin irritation. Workers who complain of chronic eye irritation should have an ophthalmic (eye) examination.
(B) A comprehensive physical examination shall be made available, with emphasis on cardiac, pulmonary, liver, and kidney examinations.
(2) Periodic medical examinations shall be made available to workers exposed to trichloroethylene annually. (1) Only appropriate respirators, as defined below, shall be provided and used when a variance which allows the use of respirators as a means of controlling exposure for routine operations has been granted or while action on application for a variance is pending.
(2) The requirements set forth in this section shall apply for nonroutine operations such as a brief exposure to concentrations in excess of the environmental standard as a result of maintenance or repair activities or in emergency situations.
(3) A respiratory protection program meeting the general requirements outlined in section 3.5 of American National Standard Practices for Respiratory Protection Z88.2-1969 shall be established and enforced by the employer. This program shall include instructions on the selection, fitting, use, testing for leakage, cleaning, and maintenance of the respiratory protective devices.
(4) For the purpose of determining the class of respirator to be used, the employer shall measure the atmospheric concentration of trichloroethylene in the workplace when the initial application for variance is made and thereafter whenever process, worksite, climate or control changes occur which are likely to affect the concentrations of airborne trichloroethylene. Only appropriate respirators as described in (5) Employees who experience breathing difficulty while wearing a respirator shall be medically examined to determine their ability to wear the respirator. Greater than 10000 ppm Chemical cartridge respirator with organic vapor cartridge(s).
Type C demand type supplied air res pirator with half mask facepiece.
Gas mask, chin type, with organic vapor canister.
Type C demand type supplied air res pirator with full facepiece.
Type C continuous flow supplied air respirator.
Self-contained breathing apparatus in pressure-demand mode (positive pressure)
The self-contained breathing apparatus shall be made available and used for emergencies. (a) Each employee exposed to trichloroethylene and its decomposition products shall be apprised of all hazards, the consequences of overexposure, appropriate emergency procedures, proper conditions for safe use, and precautions to minimize exposure. This apprisal shall include, as a minimum, all information set forth in Appendix III which is applicable to that specific product or material containing trichloroethylene.
(b) Each employee shall be apprised of the location of the information prescribed in paragraph (c) of this section. This information shall be kept on file and shall be readily accessible to all employees at each establishment where exposure to trichloro ethylene occurs. (1) Disposal of small quantities of trichloroethylene call be accomplished by pouring the liquid onto a mixture of 10% soda aSh and sand and placing the mixed material in a paper container and incinerating.
(2) Waste from cleaning contaminated with trichloroethylene should be stored in a ventilated area until ready for disposal and may be burned in an incinerator. (2) Smoking should not be permitted in areas where vapor of trichloroethylene is present.
(3) Powdered metals or turnings shall not be used or stored in any area where trichloroethylene liquid is in use or stored.
Section 7 -Sanitation Practices Showers, hand-washing facilities, soap, and water shall be available.
# Section 8 -Monitoring and Recordkeeping Requirements
Workroom areas where it has been determined, on the basis of an industrial hygiene survey or the judgment of a compliance officer, that environmental levels of trichloroethylene are less than half of the TWA limit shall not be considered to have trichloroethylene exposure.
Records of these surveys, including the basis for concluding that air levels of trichloroethylene are below half of the Later in the 1930's it was used as a surgical anesthetic [12] and proposed for use as the basis for treatment of various nervous disorders.
[13] The first reported evidence of acute overexposure to trichloroethylene in industrial applications [2] resulted from its use as a grease solvent.
This first report of chronic poisoning from trichloroethylene in industrial situations [2] suggested that the observed effects were more likely due to impurities in the material rather than to trichloroethylene itself. From 1963 to 1967 the common manufacturing process for trichloroethylene [5] produced as an intermediate chemical They noted that the daily excretion of trichloroacetic acid reached a maximum at 1:00 pm daily, irrespective of the quantity of urine excreted. Excretion of trichloroethanol began soon after the initial inhalation and rose rapidly to its maximum a few hours after the end of exposure; the total excreted was equivalent to 32 to 59% (average, 50) of the retained trichloroethylene. Excretion of trichloroethanol also appeared to fall as the sum of two exponential rates, the first phase lasting 3 or 4 days, the second lasting 7 to 9 days. Trichloroethanol excretion did not exhibit fluctuations related to time of day. In these studies, the total amount of metabolites excreted amounted to 43% to 100% (average, 73) of the trichloroethylene absorbed and the three metabolites, monochloroacetic acid, trichloroacetic acid, and trichloroethanol were found in the ratios of 1:5:12, respectively.
Bartonicek, [20] using eight resting volunteers exposed to a concentration of 1 milligram per liter (186 ppm) of trichloroethylene in five-hour periods, found that they excreted an average of 45.4% of the retained trichloroethylene as trichloroethanol and 31.9% as trichloroacetic acid, thus accounting for 77.3% of the retained trichloroethylene. Expired air analyses were performed to estimate retained trichloroethylene. Three days after exposure, the average concentration of trichloroacetic acid was 2.4 milligrams per 100 milliliters of blood plasma and 0.5 milligram per 100 milliliters red blood cells. These studies indicated that a small amount of trichloroacetic acid was excreted in sweat and in feces and, on the third day after exposure, 0.23 milligram per 100 milliliters of saliva was measured. They showed that 58% (a range of 51 to 64) of trichloroethylene inhaled at a concentration of 186 ppm was retained.
Trichloroethanol excretion was maximal at the first post-exposure test (within the first 24 hours after exposure) and decreased exponentially while the rate of trichloroacetic acid excretion reached its peak 3 days after exposure and decreased more gradually for 18 days. This test was shown to be a less sensitive indicator of effects of trichloroethylene than of effects of alcohol.
Todd [47] reported the case of a man who had ingested unknown amounts of trichloroethylene.
After prolonged unconsciousness and some cyanosis, the result was a temporary paranoid psychosis and a distortion of both vertical and horizontal vision so that persons appeared 12-18 inches high, an effect described as "Lilliputian hallucinations". (e) Other Effects
Friborska [61] showed that leukocyte alkaline phosphatase levels increase in persons repeatedly exposed to trichloroethylene. The acid phosphatase in blood also increased. These increases persisted after two weeks without exposure. The investigator considered that these findings might signify a defense mechanism or an increased capacity to metabolize alcohols, might be a response to changing pH of the blood, or be related to glycogen metabolism in the liver. For the workers studied, the following percentages of complaints were indicated: dizziness, 88%; headache, 74%; nausea, 43%; euphoria, 31%; palpitation, 29%; disturbances of vision, 21%; and sleepiness at the end of the shift, 29%. The study further showed an insidious onset after some months, up to one or two years, of the following complaints: fatigue, 68%; irritability, 56%; disturbed sleep, 46%; anxiety, 27%; loss of appetite, 50%; alcohol intolerance, 21%.
Accompanying findings included excessive sweating in 39%, palpitation in 29%, nausea in 19%, and some parasthesias. While the percentage of workers that indicated complaints are in excess of the percentage of samples at or below 50 mg/cu m (about 10 ppm), a direct relationship can not be established since the sampling protocol is unknown. and the description of the bone marrow led the authors to the conclusion that chronic intoxication to trichloroethylene has a direct action on the bone marrow and thus causes myelotoxic anemia.
Another factor studied was dehydration before trichloroethylene exposures. Baetjer, [77] in careful hypothalamic self-stimulation performance tests, showed that a three-day dehydration caused rats to make fewer responses than nondehydrated rats. After exposure to trichloroethylene, neither group performed as well as before exposure.
The dehydrated rats performed better than the nondehydrated rats, although some tolerance for trichloroethylene developed in both groups. Recovery of nondehydrated rats was prompt after moderate exposures but was not completed in 24 hours, suggesting that either the trichloroethylene concentration in the brain was greater or the dehydrated brains were more resistant to trichloroethylene or both.
Ten-day dehydration tests and trichloroethylene exposure resulted in further decrements in performance after the fifth day of exposure, suggesting that high concentration of trichloroethylene combined with dehydration may have produced some residual brain damage. to produce lighter anesthesia but it lasted two to three hours.
Bartonicek and Brun [84] made extensive studies of brain tissue, EEG, acid phosphatase levels, and erythrocyte sedimentation rates in two groups of rabbits. In one group, rabbits were injected with 3 ml trichloroethylene into the muscle three times per week for 29 days (a total of 53 g per rabbit).
The second group was given 2 ml trichloroethylene twice a week for periods lasting from 41 to 247 days, or a total of 18-133 g per rabbit. Controls were also studied. acid was also excreted but in much smaller quantity. Friberg et al [24] showed that rats exposed for four hours to 640, 1150 or 2500 ppm excreted trichloroacetic acid increasingly up to 24 hours after exposure then decreasingly for up to six days irrespective of dosage.
Studies by Forssman and Holmquist [85] showed that rats exposed for studied rabbits' metabolism for a year and concluded that their metabolism was qualitatively like humans and only the relative quantities differed. Rabbits excreted 10 times more trichloroethanol than trichloroacetic acid and about 50 times less trichloroacetic acid than man, but equally slowly.
Fabre and Truhaut [88] studied tissue homogenate. They found trichloroethylene in all tissues obtained during exposure, greatest in fat, then in lungs, spleen, liver, and least in brain and kidney.
Trichloroacetic acid was present in greatest concentration in fresh spleen, suprarenal glands, reproductive organs, and urine. In vitro studies of tissue homogenates exposed to trichloroethylene showed the most active conversion of the substance to its metabolites in the spleen, and decreasing activity in the lung, brain, liver, and kidney tissues.
In 1967 Leibman and McAllister [89] reported studies with liver microsomal tissue extracts. They were able to show that there was an increase in the ability to metabolize trichloroethylene to chloral and to trichloroethanol when the animals from which the tissue extracts were obtained had been previously treated with phénobarbital. Rats pretreated with phénobarbital and then exposed to trichloroethylene also excreted more metabolites in the first few hours than the similarly exposed but not pretreated controls.
The authors pointed out that drug intake might vitiate conclusions drawn from levels of trichloroacetic acid urinary excretion based on single samples.
# Correlation of Exposure and Effects
The most meaningful studies for purposes of establishing a welldefined cause-and-effect relationship are those in which an attempt has been made to relate the environmental exposures with subsequent effects in the exposed population.
Longley and Jones [90] reported that unconsciousness suddenly occurred in a worker who entered a tank in which a paint containing in excess of 75% trichloroethylene had been recently used. An attempt was made to simulate conditions which produced the unconsciousness and air sampling was conducted within the tank after application of some of the paint. Concentrations of trichloroethylene within the tank varied by location between 1700 and 3300 ppm. The authors estimated that a concentration of 3000 ppm would cause unconsciousness in human subjects after a 10-minute exposure. Their studies indicated no significant effect on psychomotor performance at the 100 ppm level.
There was a slight decline in performance at the 200 ppm level which became progressively more pronounced at the 300 and 500 ppm concentrations. A relatively high frequency of subjective complaints, alterations of the involuntary nervous system and of neurological and psychiatric symptoms were reported. The frequency showed a good relationship with total duration of exposure (months on the job). A total of 96 air samples were collected during the study, the results of which ranged between 1 and 335 ppm, many of them lying between 20 and 40 ppm. The authors stated that a series of consecu tive samples collected during a period of 3 to 4 hours in one workplace showed a great variation in concentrations due to the actual degree of ventilation and utilization of the degreasing apparatus.
The authors admitted that air measurements provided Insufficient indication of the total exposure. Laboratory tests of hepatic function showed no significant changes. On that basis they stated that they could not conclude that there was any causal relationship between liver troubles and exposure to trichloroethylene. In the case in question, the workman emptied the tank, rinsed it with water from a powerful hose pipe, then got inside the tank and spent half an hour cleaning with a scrubbing brush. Analyses of the air showed a concentration of 1,120 ppm outside the tank while the hose pipe was in action, with 815 and 395 ppm inside the apparatus during and after the scrubbing respectively."
Skinner [109] reported the use of baffles on windows near degreasers in the plant to control high velocity drafts.
Trichloroethylene concentrations of 170 to 230 ppm were reduced to 30 to 40 ppm with this approach to control.
Hargarten et al [110] reported results of tests carried out from 1952 to 1957 around 43 degreaser operations. Ninety-three percent of the operators' breathing zone samples taken during the cleaning cycle of the degreasers were 100 ppm or less. Methods of sampling and analysis were not stated.
In a 1963 report Ahlmark et al [111] found that during the preceding decade, when 570 degreasing plants were inspected in Sweden,
# Process ventilation
Ventilation is by far the most common engineering method for controlling solvent vapors. Vapor recovery sytems are sometimes used when a high airflow exhaust system is required for good ventilation. In 1967 this standard was revised by the Z-37 Committee.
[116] The revision established 100 ppm as an acceptable time-weighted average concentration for an 8-hour workday. In addition, an accept able ceiling concentration of 200 ppm, provided that the time-weighted average is kept at or below 100 ppm, was recommended. Furthermore, a concentration of 300 ppm for a duration of not more than 5 minutes was judged acceptable if encountered not more than once in 2 hours during In summary, deaths of several workers from exposure to trichloroothylene have been reported [36,90]; in the. best documented case, exposure was at levels estimated to be between 1700 and 3300 ppm for ten minutes. Exposures at 1000 ppm for even short periods of time have resulted in effects on the central nervous system. Subjective complaints by one of 8 male volunteers was reported [91] at exposure levels of 300 ppm for two hours. No adverse effects were noted by psychophysiological testing of the same subjects at 100 ppm. In another paper, [92] results of psychophysiological testing of one subject for 2-1/2 hours indicated no significant effect on psychomotor performance from exposure at 100 ppm, but a slight effect was noted at 200 ppm. Adverse effects were reported by 3 of 7 subjects exposed at 160 ppm for less than 83 minutes. These effects, subjective in nature, included headache, drowsiness and mild eye irritation. trichloroethylene except when it is contaminated by other compounds, especially tetrachloroethane, is the correct explanation.
As discussed above, the study by Salvini et al [93] indicates that exposures of approximately 100 ppm may interfere with the psychophysiological efficiency of the worker. Therefore, a TWA limit of 100 ppm will protect most of the workers but with probably very little margin of safety at this level of exposure. The effects of short exposures to trichloro ethylene on swimming performances and motor activity of rats. Am Ind Hyg Assoc J 24:376-79, 1963 (1) Air sampling instruments shall be calibrated after making any repairs or modifications to the sampling system and at least once a year with a reference such as a wet test meter over a normal range of flowrates and pressure drops.
(2) The wet test meter shall be in good working condition and shall have been calibrated against a spirometer (or other primary standard) upon procurement, after each repair, and at least annually. (2) The charcoal in the tube is transferred to a small test tube and desorbed with carbon disulfide.
(3) An aliquot of the desorbed sample is injected into a gas chromatograph. If a particular atmosphere is suspected of containing a large amount of trichloroethylene, it is recommended that a smaller sampling volume be taken.
# (c) Interferences
(1) When the amount of water in the air is so great that condensation actually occurs in the tube, organic vapors will not be trapped.
Water vapor does not seem to be a problem, only water present as a mist.
(2) Any compound which has the same retention time as trichloroethylene at the operating conditions described in this method could be considered an interference. This type of interference can be overcome by changing the operating conditions of the instrument.
# (d) Precision and Accuracy
(1) Precision of the analytical method: plus or minus 4.8%.
(2) Precision of the analytical method plus field sampling with the personal sampling pump has not been established.
(3) The accuracy of the sampling and analytical method, as established during breakthrough testing of the front section of activated charcoal: 91%.
# (e) Advantages and Disadvantages of the Method
This method is advantageous in that it provides one basic method for determining many different organic solvents. The sampling device is small, portable, and involves no liquids. Interferences are minimal, and most of those which do occur can be eliminated by altering chromatographic conditions. The analysis of the tubes is accomplished using a quick instrumental method.
One disadvantage of the method is that the amount of sample which can be taken is limited by the weight of sample which the tube will hold before overloading. Also the precision of the method is limited by the reproducibility of the pressure drop across the tubes.
Variability in this pressure drop w^Lll affect the flowrate, causing the volume to be imprecise since the pump is usually calibrated for one tube only.
(f) Apparatus consists of:
(1) An approved coal mine dust personal sampling pump for personal samples or any vacuum pump whose flow can accurately be determined at 1 liter per minute or less. (3) Gas chromatograph equipped with a flame ionization detector.
(4) Column (20 ft x 1/8 in) with 10% FFAP stationary phase on 80/100 mesh acid washed DMCS Chromosorb W solid support.
One liter per minute is the recommended sampling rate. A 10-liter sample is normally adequate. The tube must be supported in a vertical position for sampling. Due to the high resistance of the charcoal tube, this sampling method places a heavy load on the personal sampling pump. Therefore, it should not be assumed that this pump will run a full 8 hours without recharging the battery. After the sample is collected, the tube must be capped; caps are provided with commercial tubes.
One charcoal tube should be treated in the same manner as the sample tubes (break, seal, ship) with the exception that no air be drawn through it. This tube will serve as a blank.
If bulk samples are submitted in addition to charcoal tubes, the tubes should be shipped in a separate container from the bulk sample. It is convenient to prepare standards in terms of mg/0.5 ml of carbon disulfide because samples are desorbed in this amount of carbon disulfide.
To minimize error due to the volatility of carbon disulfide, twenty times the weight can be injected into 10 ml of carbon disulfide. For example, to prepare a 0.3 mg/0.5 ml standard* 6.0 mg is injected into exactly 10 ml of carbon disulfide in a glassstoppered flask. The density for trichloroethylene is used to convert 6.0 mg into microliters for easy measurements with a microliter The first method is used because of its simplicity.
Because desorption efficiencies may vary from one laboratory to another and with different batches of charcoal, each laboratory should determine its own. However, for comparison, NIOSH determined a value of 97% for trichloroethylene, with one lot of activated charcoal.
# (j) Calculations
(1) The first step in calculating the results is to read the weight in milligrams corresponding to each peak area from the standard curve. The standard curve is based on mg/0.5 ml of carbon disulfide, and therefore, no correction need be made for the volume of the sample injected, since this is identical to the volume of the standards injected.
(2) The weight of trichloroethylene in the front section of the blank tube is subtracted from the weight determined for the front section of each sample; a similar procedure is followed for the backup sections.
(3) Amounts present on the front and backup sections of the same tube are then added to calculate the total amount in the sample.
(4) This total weight of trichloroethylene in the tube is corrected by dividing by the desorption factor to determine the total number of milligrams in the sample. (1) Toxic level for total compound or mixture, relevant symptoms of exposure, skin and eye irritation properties, principal routes of absorption, effects of chronic (long-term) exposure, and emergency arid first aid procedures.
(g) Section VI. Reactivity Data.
(1) Chemical stability, incompatibility, hazardous decomposition products, and hazardous polymerization.
(h) Section VII. Spill or Leak Procedures.
(1) Detailed procedures to be followed with emphasis on precautions to be taken in cleaning up and safe disposal of materials leaked or spilled. This includes proper labeling and disposal of containers containing residues, contaminated absorbents, etc.
(i) Section VIII. Special Protection Information.
(1) Requirements for personal protective equipment, such as respirators, eye protection, protective clothing, and ventilation, such as local exhaust (at site of product use or application), general, or other special types.
(j) Section IX. Special Precautions.
(1) Any other general precautionary information such as personal protective equipment for exposure to the thermal decomposition products listed in Section VI, and to particulates formed by abrading a dry coating, such as by a power sanding disc.
(k) The signature of the responsible person filling out the data sheet, his address, and the data on which it is filled out. 1 ppm = 5.38 mg/m3 @25 C 1 mg/liter = 186.1 ppm [111] **Mean time spent by each operator at the various locations. It is understood that an operator may perform at a given location with greater frequency than another operator.
#
(1) Breathing zone samples shall be collected as near as practicable to the worker's face without interfering with his freedom of movement and shall characterize the exposure from each job or specific operation in each production area.
(2) A portable battery-operated personal sampling pump plus an activated charcoal tube shall be used to collect the sample.
(3) The activated charcoal tube shall be attached to the worker's clothing; the shirt collar is convenient for this purpose.
(5) A mechanical or electronic integrator or a recorder and some method for determining peak area.
(6) Small glass-stoppered test tubes or equivalent.
(7) Micro syringes: 10 pi, and convenient sizes for making standards.
(g) Reagents
(1) Spectroquality carbon disulfide.
(2) Trichloroethylene, preferably chromatoquality grade.
(3) Bureau of Mines Grade A helium.
(4) Prepurified hydrogen.
(5) Filtered compressed air.
(h) Procedure
(1) Cleaning of Equipment All equipment used for the laboratory analysis should be washed in detergent followed by tap and distilled water rinses.
(2) Collection and Shipping of Samples Both ends of the charcoal tube should be broken to provide openings of at least 2 mm which is one-half the I.D. of the tube. A smaller opening causes a limiting orifice effect which reduces the flow through the tube.
The smaller section of charcoal in the tube is used as a backup section and should therefore be placed nearest the sampling pump. Tubing may be used to connect the back of the tube to the pump, but no tubing must ever be put in front of the charcoal tube. Values in parentheses are approximate conversions where the standard was published in only one of the two units listed above.
From [118] | None | None |
7d2a57a18a542da7949b54d6e2be2fab88cfa1b5 | cdc | None | CDC Editorial Note: Asthma is a chronic respiratory illness often associated with familial, allergenic, socioeconomic, psychological, and environmental factors. 3 Although recent reports suggest asthma-related mortality has been declining since 1996, a disparity remains between rates for non-Hispanic whites and those for non-Hispanic blacks and other racial/ethnic populations. 4 Non-Hispanic blacks experience higher rates than non-Hispanic whites for ED visits, hospitalizations, and deaths; these trends are not explained entirely by higher asthma prevalence among non-Hispanic blacks. 4 Other racial/ethnic populations experience higher asthma mortality and hospitalization rates than non-Hispanic whites while also reporting lower asthma prevalence and fewer outpatient and ED visits. The asthma-control characteristics described in this report can contribute to increased mortality and higher hospitalization rates.
In 2002, the BRFSS adult lifetime asthma prevalence estimate and the adult current asthma prevalence estimate for the 50 states and DC were higher than in 2001 3 The findings in this report are subject to at least four limitations. First, the median response rate for the survey was 58.3%. However, BRFSS asthma prevalence is similar to estimates from other surveys with higher response rates, such as the National Health Interview Survey. 5 Second, BRFSS does not measure asthma prevalence among institutionalized adults, military personnel, persons aged Ͻ18 years, and residents without telephones. Third, the validity of selfreported asthma or asthma-control characteristics in BRFSS is unknown. 6 Actual adherence to prescribed medication or asthma treatment plans in respondents with current asthma is unknown. Finally, the asthma-control questions were asked in 19 of the 54 BRFSS reporting areas and might not accurately reflect the asthma-control characteristics of other reporting areas or accurately represent their racial/ethnic distribution.
States and territories using the BRFSS Adult Asthma History module can direct asthma management within their jurisdictions and address disparities in asthma risk and control characteristics among racial/ethnic populations. Use of comprehensive state-specific asthma surveillance data to identify populations with poorly controlled asthma is instrumental in developing, implementing, and evaluating asthma-control programs and interventions. MMWR. 2004;53:154-157 WEST NILE VIRUS (WNV) IS A SINGLEstranded RNA flavivirus with antigenic similarities to Japanese encephalitis and St. Louis encephalitis viruses. It is transmitted to humans primarily through the bites of infected mosquitoes. Flavivirus infection during pregnancy has been associated rarely with both spontaneous abortion and neonatal illness but has not been known to cause birth defects in humans. During 2002, a total of 4,156 cases of WNV illness in humans, including 2,946 cases of neuroinvasive disease, were reported to CDC by state health departments. In 2002, a woman who had WNV encephalitis during the 27th week of her pregnancy delivered a full-term infant with chorioretinitis, cystic destruction of cerebral tissue, and FROM THE CENTERS FOR DISEASE CONTROL AND PREVENTION laboratory evidence of congenitally acquired WNV infection. 5,6 Although this case demonstrated intrauterine WNV infection in an infant with congenital abnormalities, it did not prove a causal relation between WNV infection and these abnormalities. During 2002, CDC investigated three other instances of maternal WNV infection. In all three cases, the infants were born at full term with normal appearance and negative laboratory tests for WNV infection; cranial imaging studies and ophthalmologic examinations were not performed. During 2003, CDC received reports of approximately 9,100 cases of WNV illness, including approximately 2,600 cases of neuroinvasive disease. - CDC is gathering data on pregnancy outcomes for approximately 70 women with WNV illness during pregnancy (CDC, unpublished data, 2003).
# Interim Guidelines for the Evaluation of Infants Born to Mothers Infected With West Nile Virus During Pregnancy
To develop guidelines for evaluating infants born to mothers who acquire WNV infection during pregnancy, on December 2, 2003, CDC convened a meeting of specialists in the evaluation of congenital infections. This report summarizes the interim guidelines established during that meeting.
# Screening for WNV During Pregnancy
No specific treatment for WNV infection exists, and the consequences of WNV infection during pregnancy have not been well defined. For these reasons, screening of asymptomatic pregnant women for WNV infection is not recommended.
# Diagnosis of WNV Infection During Pregnancy
Pregnant women who have meningitis, encephalitis, acute flaccid paralysis, or unexplained fever in an area of ongoing WNV transmission should have serum (and cerebrospinal fluid , if clinically indicated) tested for antibody to WNV. If serologic or other laboratory tests indicate recent infection with WNV, these infections should be reported to the local or state health department, and the women should be followed to determine the outcomes of their pregnancies.
# Evaluation of the Fetus in Pregnant Women with WNV Infection
If WNV illness is diagnosed during pregnancy, a detailed ultrasound examination of the fetus to evaluate for structural abnormalities should be considered no soonerthan2-4weeksafteronsetofWNV illness in the mother, unless earlier examination is otherwise indicated. Amniotic fluid, chorionic villi, or fetal serum can be tested for evidence of WNV infec-tion. However, the sensitivity, specificity,andpredictivevalueofteststhatmight be used to evaluate fetal WNV infection are not known, and the clinical consequences of fetal infection have not been determined. In case of miscarriage or induced abortion, testing of all products of conception (e.g., the placenta and umbilical cord) for evidence of WNV infection is advised to document the effects of WNV infection on pregnancy outcome.
# FROM THE CENTERS FOR DISEASE CONTROL AND PREVENTION
# Evaluation of Infants Born to Mothers Infected With WNV During Pregnancy
When an infant is born to a mother who was known or suspected to have WNV infection during pregnancy, clinical evaluation is recommended (see sidebar 1). Further evaluation should be considered if any clinical abnormality is identified or if laboratory testing indicates that an infant might have congenital WNV infection (see sidebar 2).
# Prevention of WNV Infection During Pregnancy
Pregnant women who live in areas with WNV-infected mosquitoes should ap-ply insect repellent to skin and clothes when exposed to mosquitoes and wear clothing that will help protect against mosquito bites. In addition, whenever possible, pregnant women should avoid being outdoors during peak mosquitofeeding times (i.e., usually dawn and dusk). CDC Editorial Note: Neither the proportion of WNV infections during pregnancy that result in congenital infection nor the spectrum of clinical abnormalities associated with congenital WNV infection is known. However, one case reported in 2002 suggests that intrauterine transmission of WNV in certain instances might affect the newborn adversely. To evaluate the possible effects of WNV infection during pregnancy, CDC is gathering clinical and laboratory data on outcomes of pregnancies of women who were known or suspected to be infected with WNV during pregnancy. Guidance on diagnosis of WNV can be obtained from local or state health departments and from CDC, telephone 970-221-6400. Guidance also is available at .gov/ncidod/dvbid/westnile/resources /fact_sheet_clinician.htm. Clinicians are encouraged to report cases of WNV infections in pregnant women to their state or local health departments or CDC. | #
CDC Editorial Note: Asthma is a chronic respiratory illness often associated with familial, allergenic, socioeconomic, psychological, and environmental factors. 3 Although recent reports suggest asthma-related mortality has been declining since 1996, a disparity remains between rates for non-Hispanic whites and those for non-Hispanic blacks and other racial/ethnic populations. 4 Non-Hispanic blacks experience higher rates than non-Hispanic whites for ED visits, hospitalizations, and deaths; these trends are not explained entirely by higher asthma prevalence among non-Hispanic blacks. 4 Other racial/ethnic populations experience higher asthma mortality and hospitalization rates than non-Hispanic whites while also reporting lower asthma prevalence and fewer outpatient and ED visits. The asthma-control characteristics described in this report can contribute to increased mortality and higher hospitalization rates.
In 2002, the BRFSS adult lifetime asthma prevalence estimate and the adult current asthma prevalence estimate for the 50 states and DC were higher than in 2001 3 The findings in this report are subject to at least four limitations. First, the median response rate for the survey was 58.3%. However, BRFSS asthma prevalence is similar to estimates from other surveys with higher response rates, such as the National Health Interview Survey. 5 Second, BRFSS does not measure asthma prevalence among institutionalized adults, military personnel, persons aged Ͻ18 years, and residents without telephones. Third, the validity of selfreported asthma or asthma-control characteristics in BRFSS is unknown. 6 Actual adherence to prescribed medication or asthma treatment plans in respondents with current asthma is unknown. Finally, the asthma-control questions were asked in 19 of the 54 BRFSS reporting areas and might not accurately reflect the asthma-control characteristics of other reporting areas or accurately represent their racial/ethnic distribution.
States and territories using the BRFSS Adult Asthma History module can direct asthma management within their jurisdictions and address disparities in asthma risk and control characteristics among racial/ethnic populations. Use of comprehensive state-specific asthma surveillance data to identify populations with poorly controlled asthma is instrumental in developing, implementing, and evaluating asthma-control programs and interventions. MMWR. 2004;53:154-157 WEST NILE VIRUS (WNV) IS A SINGLEstranded RNA flavivirus with antigenic similarities to Japanese encephalitis and St. Louis encephalitis viruses. It is transmitted to humans primarily through the bites of infected mosquitoes. Flavivirus infection during pregnancy has been associated rarely with both spontaneous abortion and neonatal illness but has not been known to cause birth defects in humans. [1][2][3][4] During 2002, a total of 4,156 cases of WNV illness in humans, including 2,946 cases of neuroinvasive disease, were reported to CDC by state health departments. In 2002, a woman who had WNV encephalitis during the 27th week of her pregnancy delivered a full-term infant with chorioretinitis, cystic destruction of cerebral tissue, and FROM THE CENTERS FOR DISEASE CONTROL AND PREVENTION laboratory evidence of congenitally acquired WNV infection. 5,6 Although this case demonstrated intrauterine WNV infection in an infant with congenital abnormalities, it did not prove a causal relation between WNV infection and these abnormalities. During 2002, CDC investigated three other instances of maternal WNV infection. In all three cases, the infants were born at full term with normal appearance and negative laboratory tests for WNV infection; cranial imaging studies and ophthalmologic examinations were not performed. During 2003, CDC received reports of approximately 9,100 cases of WNV illness, including approximately 2,600 cases of neuroinvasive disease. * CDC is gathering data on pregnancy outcomes for approximately 70 women with WNV illness during pregnancy (CDC, unpublished data, 2003).
# Interim Guidelines for the Evaluation of Infants Born to Mothers Infected With West Nile Virus During Pregnancy
To develop guidelines for evaluating infants born to mothers who acquire WNV infection during pregnancy, on December 2, 2003, CDC convened a meeting of specialists in the evaluation of congenital infections. This report summarizes the interim guidelines established during that meeting.
# Screening for WNV During Pregnancy
No specific treatment for WNV infection exists, and the consequences of WNV infection during pregnancy have not been well defined. For these reasons, screening of asymptomatic pregnant women for WNV infection is not recommended.
# Diagnosis of WNV Infection During Pregnancy
Pregnant women who have meningitis, encephalitis, acute flaccid paralysis, or unexplained fever in an area of ongoing WNV transmission should have serum (and cerebrospinal fluid [CSF], if clinically indicated) tested for antibody to WNV. If serologic or other laboratory tests indicate recent infection with WNV, these infections should be reported to the local or state health department, and the women should be followed to determine the outcomes of their pregnancies.
# Evaluation of the Fetus in Pregnant Women with WNV Infection
If WNV illness is diagnosed during pregnancy, a detailed ultrasound examination of the fetus to evaluate for structural abnormalities should be considered no soonerthan2-4weeksafteronsetofWNV illness in the mother, unless earlier examination is otherwise indicated. Amniotic fluid, chorionic villi, or fetal serum can be tested for evidence of WNV infec-tion. However, the sensitivity, specificity,andpredictivevalueofteststhatmight be used to evaluate fetal WNV infection are not known, and the clinical consequences of fetal infection have not been determined. In case of miscarriage or induced abortion, testing of all products of conception (e.g., the placenta and umbilical cord) for evidence of WNV infection is advised to document the effects of WNV infection on pregnancy outcome.
# FROM THE CENTERS FOR DISEASE CONTROL AND PREVENTION
# Evaluation of Infants Born to Mothers Infected With WNV During Pregnancy
When an infant is born to a mother who was known or suspected to have WNV infection during pregnancy, clinical evaluation is recommended (see sidebar 1). Further evaluation should be considered if any clinical abnormality is identified or if laboratory testing indicates that an infant might have congenital WNV infection (see sidebar 2).
# Prevention of WNV Infection During Pregnancy
Pregnant women who live in areas with WNV-infected mosquitoes should ap-ply insect repellent to skin and clothes when exposed to mosquitoes and wear clothing that will help protect against mosquito bites. In addition, whenever possible, pregnant women should avoid being outdoors during peak mosquitofeeding times (i.e., usually dawn and dusk). CDC Editorial Note: Neither the proportion of WNV infections during pregnancy that result in congenital infection nor the spectrum of clinical abnormalities associated with congenital WNV infection is known. However, one case reported in 2002 suggests that intrauterine transmission of WNV in certain instances might affect the newborn adversely. To evaluate the possible effects of WNV infection during pregnancy, CDC is gathering clinical and laboratory data on outcomes of pregnancies of women who were known or suspected to be infected with WNV during pregnancy. Guidance on diagnosis of WNV can be obtained from local or state health departments and from CDC, telephone 970-221-6400. Guidance also is available at http://www.cdc .gov/ncidod/dvbid/westnile/resources /fact_sheet_clinician.htm. Clinicians are encouraged to report cases of WNV infections in pregnant women to their state or local health departments or CDC.
# Acknowledgment
This report is based on data contributed by state BRFSS coordinators.
# Acknowledgments
| None | None |
23f80621ad395234592a5014595f402b911b7c5f | cdc | None | This document examines the occupational health risks associated with welding, brazing, and thermal cutting, and it provides criteria for eliminating or minimizing the risks encountered by workers in these occupations. The main health concerns are increased risks of lung cancer and acute or chronic respiratory disease.# FOREWORD
The purpose of the Occupational Safety and Health Act of 1970 (Public Law 91-596) is to ensure safe and healthful working conditions for every working person and to preserve our human resources by providing medical and other criteria that will ensure, insofar as practicable, that no worker will suffer diminished health, functional capacity, or life expectancy as a result of his or her work experience. The Act authorizes the National Institute for Occupational Safety and Health (NIOSH) to develop and recommend occupational safety and health standards and to develop criteria for improving them. By this means, NIOSH communicates these criteria both to regulatory agencies and others in the community of occupational safety and health.
Criteria documents provide the basis for the occupational health and safety standards sought by Congress. These documents generally contain a critical review of the scientific and technical information available on the prevalence of hazards, the existence of safety and health risks, and the adequacy of control methods. NIOSH distributes these documents to health professionals in academia, industry, organized labor, public interest groups, and other appropriate government agencies. This criteria document on welding, brazing, and thermal cutting reviews available information on the health risks for workers in these occupations and provides criteria for eliminating or minimizing the occupational risks these workers may encounter. Evidence from epidemiologic studies and case reports of workers exposed to welding emissions clearly establishes the risk of acute and chronic respiratory disease. The major concern, however, is the excessive incidence of lung cancer among welders. A large body of evidence from regional occupational mortality data, case control studies, and cohort studies indicates that welders generally have a 40% increase in relative risk of developing lung cancer as a result of their work experiences. The basis of this excess risk is difficult to determine given uncertainties about smoking habits, possible interactions among the various components of welding emissions, and possible exposures to other occupational carcinogens, including asbestos. The severity and prevalence of other respiratory conditions such as chronic bronchitis, pneumonia, and decrements in pulmonary function are not well characterized among welders, but these effects have been observed in both smoking and nonsmoking workers in this occupation. Excesses in morbidity and mortality among welders appear to exist even when exposures have been reported to be below current Occupational Safety and Health Administration (OSHA) permissible exposure limits (PELs) for the many individual components of welding emissions.
An exposure limit for total welding emissions cannot be established because the composition of welding fumes and gases varies for different welding processes and because the various components of the emissions may interact to produce adverse health effects. NIOSH therefore recommends that exposures to all welding emissions be reduced to the lowest feasible concentrations using state-of-the-art engineering controls and work practices. Exposure limits for individual chemical or physical agents are to be considered upper boundaries of exposure. Presently it is not possible to associate a particular health hazard with a specific component of total welding emissions; however, the risk of lung cancer for workers who weld on stainless steel appears to be associated with exposure to fumes that contain nickel and chromium. NIOSH has previously recommended to OSHA that exposures to specific forms of these metals be treated as exposures to occupational carcinogens. Future research may make it possible to differentiate risks associated with a particular exposure. NIOSH will evaluate such data as they become available and revise this recommended standard as appropriate.
The Institute takes sole responsibility for the conclusions and recommendations presented in this document. All reviewers' comments are being sent with this document to the Occupational Safety and Health Administration (OSHA) for consideration in standard setting.
The data in this document indicate that welders have a 40% increase in relative risk of developing lung cancer as a result of their work experience. The basis for this excess risk is difficult to determine because of uncertainties about smoking habits, possible interactions among the various components of welding emissions, and possible exposures to other occupational carcinogens. However, the risk of lung cancer for workers who weld on stainless steel appears to be associated with exposure to fumes that contain nickel and chromium.
The severity and prevalence of noncarcinogenic respiratory conditions are not well characterized among welders, but they have been observed in both smoking and nonsmoking workers in occupations associated with welding. Excesses in morbidity and mortality among welders exist even when reported exposures are below current Occupational Safety and Health Administration (OSHA) permissible exposure limits (PELs) for the many individual components of welding emissions.
An exposure limit for total welding emissions cannot be established because the composition of welding fumes and gases varies for different welding processes and because the various components of a welding emission may interact to produce adverse health effects. NIOSH therefore recommends that exposures to all welding emissions be reduced to the lowest feasible concentrations using state-of-the-art engineering controls and work practices. Exposure limits for individual chemical or physical agents are to be considered upper boundaries of exposure.
# . E. NIOSH Recommendations that Differ from Current
OSHA R e gu la ti on s. 1. Arc W e l d i n g 2. Oxyfuel Gas W e l d i n g 5. Thermal C u t t i n g 1. Fumes and Other .. c. Bery 11 .. d . Cadm i u . 38 IV. Health and Safety H a z a r d s . B. Health H a z a r d s
# III. Characteristics of Welding
1. Animal T o x i c i t y . 42 d. Mu .. d. Cardiovascular
1. F i r e s . .. 139 v i i i CONTENTS (continued) 3. Toxicological .. a. Epidemiological Studies........ b. Toxicological .. c. Dermal E f f e c t s . .. d. Eye I n j u ri es. .. c. Monitoring 1. Medical .. b. Periodic Medical 1. Optical (Radiation) .. 167 2. Chemical Hazards (Gases,Vapors,and
# Electric S h o c k
# V. Basis for the Recommended
# Other Adverse Health
# Physical Agent
# I. RECOMMENDATIONS FOR A STANDARD
The National Institute for Occupational Safety and Health (NIOSH) recommends that worker exposure to hazards associated with welding processes in the workplace be controlled by complying with the provisions presented in Chapter I of this document. Chapters VI and VII provide additional detail concerning the implementation of these provisions. Adherence to these recommendations should prevent or greatly reduce the risk of adverse health effects among exposed workers. These recommendations are designed to protect the health and provide for the safety of workers engaged in welding over a working lifetime; they are to be used as an adjunct to existing NIOSH recommendations. The following sections shall replace or modify the provisions for welding, cutting, and brazing contained in 29 CFR- 191029 CFR- .251-254, 191529 CFR- .51-57, and 1926 Other specific requirements contained in those regulations and not addressed in the NIOSH recommended standard shall be retained.
Section 1 -Definitions (a) Worker is any person who is or may reasonably be expected to be exposed to chemical and physical hazards associated with welding processes.
(b) Exposure Limit is the concentration of a chemical or physical agent emitted during welding that shall not be exceeded in the workplace. The NIOSH recommended exposure limit (REL) shall be used when available for any chemical or physical agent.
In the absence of a NIOSH REL, the Occupational Safety and Health Administration (OSHA) permissible exposure limit (PEL) shall be used unless a more restrictive limit has been recommended by a recognized voluntary consensus group or committee. When neither a NIOSH REL nor an OSHA PEL exists, an appropriate consensus-groupor committee-recommended exposure limit shall be used. Although NIOSH has not evaluated the adequacy of such exposure limits, their adoption would be a prudent public health measure and would afford a greater degree of protection than using no limit.
The OSHA PELs shall not be exceeded under any circumstances. Appendix A lists some of the more common chemical and physical agents that may be found in the workplace or near workers engaged in welding.
(c) Welding includes those processes that join or cut pieces of metal by heat, pressure, or both. These processes differ in the way heat is created and applied to the parts being joined; they comprise a group of processes referred to as welding, brazing, and thermal cutting (see explanation of terms in Chapter III).
# Section 2 -Recommended Exposure Limits
Exposures to chemical and physical agents shall be controlled so that workers are not exposed to concentrations above the exposure limits (see Definitions, Section 1(b)).
An exposure limit for total welding emissions cannot be established because the composition of welding emissions (chemical and physical agents) varies for different welding processes and because the various components of a welding emission may interact to produce adverse health effects. Thus even compliance with specific chemical or physical agent exposure limits may not ensure complete protection against an adverse health effect. Therefore, as a prudent public health measure, the employer shall reduce worker exposures to all chemical and physical agents associated with welding to the lowest concentrations technically feasible using current state-of-the-art engineering and good work practice controls. Exposure limits for individual chemical or physical agents are to be considered upper boundaries of exposure.
# Section 3 -Medical Monitoring
The following requirements supplement existing medical monitoring measures that NIOSH recommends for workers exposed to specific chemical or physical agents. The objective of these requirements is to provide an additional level of monitoring for workers who may be exposed to welding emissions or who may have been adversely affected by them in the past. NIOSH recommended standards and existing OSHA standards shall be used to determine the need for specific medical tests. Appendix B lists published sources of NIOSH recommended standards for some specific chemical and physical agents.
(a) General (1) The employer shall institute a medical monitoring program for all workers who are or may reasonably be expected to be exposed to hazards from welding processes.
(2) The employer shall ensure that all medical examinations and procedures are performed by or under the direction of a licensed physician.
(3) The employer shall provide the required medical monitoring without loss of pay or other cost to the workers, and at a reasonable time and place.
# (b) Preplacement Medical Examination
The preplacement medical examination shall include the following items at a minimum:
(1) A comprehensive work and medical history that emphasizes identification of existing medical conditions and previous occupational exposure to chemical or physical health hazards, particularly those associated with welding processes.
(2) A comprehensive physical examination.
(3) A thorough examination of the respiratory system, including baseline pulmonary function tests (at a minimum, forced vital capacity and forced expiratory volume in one second ) using the current recommendations of the American Thoracic Society regarding testing procedures and equipment. Guidelines are given in Appendix C.
(4) A posterio-anterior chest radiograph that is interpreted by qualified B readers (i.e., those who have passed the NIOSH proficiency examination) using the current recommendations of the International Labour Office (ILO) regarding the classification of pneumocon i os i s .
(5) An examination of the skin and eyes for scars that appear to have been caused by burns. The locations of such scars should be noted.
(6) A baseline cardiovascular evaluation.
(7) A baseline audiogram.
(8) A thorough ophthalmologic evaluation.
# (c) Periodic Medical Examination
A periodic medical examination shall be provided at least annually to all workers. The following conditions may shorten the interval between examinations and the need for special medical tests:
(1) Workers reporting signs or symptoms associated with exposure to welding emissions, and
(2) Airborne concentrations of specific agents that exceed exposure limits.
Periodic medical examinations shall include the following:
(1) Updates of medical and occupational histories. These shall include a description of the following items based on an interview of the worker and records maintained by the employer: the type of welding performed, metals worked and fluxes used, locations and conditions (e.g., confined spaces and hot environments), and potentially hazardous exposures not directly related to welding (e.g., chlorinated hydrocarbons).
(2) An evaluation of the respiratory system. Because of the potential for chronic respiratory disease, this evaluation shall include spirometry at intervals indicated by the judgment of the examining physician. Workers with symptomatic, spirometric, or radiographic evidence of pulmonary impairment or disease shall be counseled about the risks of further exposure. Smokers shall be counseled about how smoking may enhance the adverse effects of other respiratory hazards.
(3) Posterio-anterior chest radiographs interpreted by qualified B readers (i.e., those who have passed the NIOSH proficiency examination) using the current recommendations of the International Labour Office (ILO) regarding the classification of pneumoconiosis. These radiographs shall be performed at intervals determined by the examining physician. Periodic chest radiographs are recommended for monitoring workers exposed to fibrogenic respiratory hazards (e.g., quartz). At a minimum, chest radiographs should be obtained at 1-to 5-year intervals, depending on the nature and intensity of exposures and the related health risks. A recent chest radiograph obtained for other purposes (e.g., upon hospitalization) may be substituted for the periodic chest radiograph if it is made available and is of acceptable qua Ii ty.
(4) An examination of the skin and eyes for scars that appear to have been caused by burns. The locations of such scars should be noted.
(5) An evaluation of the cardiovascular system.
(6) An ophthalmological evaluation. (7) An audiogram. (8) Other tests deemed appropriate by the attending physician.
# Section 4 -Labeling and Posting
Workers shall be informed of exposure hazards, of potential adverse health effects, and of methods to protect themselves in accordance with 29 CFR 191029 CFR .1200, Hazard Communication. Manufacturers of welding materials shall warn employers and workers of the potentially hazardous components of the filler metals, electrodes, and flux materials by applying precautionary labels to the packing containers. Such labels shall indicate the identity of the hazardous agents and the adverse health effects that may result from exposure.
In addition, the employer must comply with the labeling and posting requirements contained in the following subsections.
# (a) Labeling
All labels and warning signs shall be printed in both English and in the predominant language of non-English-reading workers. Workers who cannot read the language used on labels and posted signs shall be identified so that they may receive information regarding hazardous areas and be informed of the instructions printed on labels and signs.
(1) Containers of filler metal, electrodes, and flux materials shall bear warning labels containing the following information at a mini mum :
- The following warning: WARNING Welding produces hazardous fumes and gases.
Avoid breathing them. Use adequate ventilation.
- Instructions for emergency first aid - Instructions for safe use - Instructions for the type of personal protective clothing or equipment to be worn (2) Labels shall identify the hazardous constituents of the container's contents.
(3) The following information shall be included on the labels of containers holding filler metal, electrodes, and flux materials that contain agents identified as carcinogens by NIOSH and OSHA:
- The name of the potential occupational carcinogen and a description of its health hazards. For materials containing carcinogens, the warning label listed in Section 3(a)(1) above shall include the following statement:
Fumes or gases from this may cause cancer.
- Instructions for avoiding inhalation of fumes and excessive skin or eye contact with them.
(4) Base metals that contain or are coated with materials containing carcinogens or other toxic metals (e.g., lead or mercury) shall be clearly labeled or marked to indicate their contents before being welded.
(b) Post i ng (1) In areas where welding is conducted, the following sign shall be posted in readily visible locations: WARNING Welding produces hazardous fumes, gases, and radiation. Appropriate personal protective equipment is required. 00 NOT LOOK AT ARC. EYE INJURY MAY OCCUR.
(2) Signs posted in work areas where emissions contain carcinogens shall differ from the preceding example, as follows:
- The word "DANGER" shall be used instead of "WARNING."
- The name of the carcinogen shall be included along with a warning describing its health hazards.
If a carcinogen is contained in the base or filler metals, electrodes, or fluxes, the warning shall include the statement, "Fumes or gases from may cause cancer," with the type(s) of base or filler metals, electrodes, or fluxes specified.
- Any requirements for personal protective clothing and equipment shall also be stated.
# Section 5 -Protective Clothing and Equipment
Engineering controls and safe work practices shall be used to keep the emissions from welding processes below the exposure limits specified in Chapter I, Section 2 of this document.
In addition, the employer shall provide protective clothing and equipment to workers as follows:
(a) Clothing (1) The employer shall provide and require the use of appropriate protective clothing as follows:
- Fire-resistant gauntlet gloves and shirts with sleeves of sufficient length and construction to protect the arms from heat, UV radiation, and sparks. Wool and leather clothing are preferable because they are more resistant to deterioration and flames than cotton or synthetics.
Fire-resistant aprons, coveralls, and leggings or high boots.
Fire-resistant shoulder covers (e.g., capes), head covers (e.g., skullcaps), and ear covers for workers doing overhead work.
(2) The employer shall do the following for workers welding with highly toxic materials (e.g., carcinogens, lead, fluorides):
- Provide and require the use of work uniforms, coveralls, or similar full-body coverings.
- Provide lockers or other closed areas to store work clothing separately from street clothing.
- Collect work clothing at the end of each work shift and provide for laundering. Clothing treated for fire resistance may need to be retreated after laundering. Laundry personnel shall be adequately informed of the potential hazards and protected from any contaminants on the work clothing.
(3) The employer shall ensure that protective clothing is inspected, maintained, and worn to preserve its effectiveness.
- Clothing shall be kept reasonably free of oil or grease.
- Clothing treated for fire resistance shall be retreated after laundering if necessary.
- Upturned sleeves or cuffs shall be prohibited.
- Sleeves and collars shall be kept buttoned.
# (b) Eye and Face Protection
(1) The employer shall provide and require the use of the following protective gear for the eyes and face:
- Welding helmets that meet the requirements of 29 CFR 1910.252(e)(2)(ii), Specifications for Protectors.
- Welding helmets with approved ultraviolet radiation (UV) filter plates, or safety spectacles with side-shields, or goggles for all workers exposed to arc welding or cutting processes.
- Goggles or similar eye protectors with filter lenses for workers exposed to oxyfuel gas welding, brazing, or cutting.
- Goggles or similar eye protectors with transparent lenses shall be used for workers exposed to resistance welding or to mechanical cleaning or chipping operations.
(2) The shade numbers used for filter plates or lenses shall meet the requirements of 29 CFR 1910.252(e) (i i).
(3) Eye and face protectors shall be maintained and periodically cleaned and inspected by the employer. Eye and face protectors shall be sanitized before being used by another worker.
# (c) Respiratory Protection
Engineering controls and good work practices shall be used to control respiratory exposure to airborne contaminants. Workers shall use respiratory protection only when controls are not technically feasible, when certain routine or nonroutine short-term operations (e.g., maintenance and repair or emergencies) are performed, or when engineering and work practice controls do not reduce the concentration of the contaminant below the exposure limit.
(1) When respirators are used, a complete respiratory protection program shall be instituted as set forth in 29 CFR 1910.134. This program shall include the following elements at a minimum:
- A written program for respiratory protection (e.g., standard operating procedures governing the selection and use of respi rators).
- Regular worker training.
- Routine air monitoring and work surveillance.
- Routine maintenance, proper storage, inspection, cleaning, and evaluation of respirators.
- Testing of each respirator while it is worn by an individual to confirm that the protection factor expected for that class of respirators is being achieved.
(2) Selecting the appropriate respirator depends on the specific contaminants and their concentration in the worker's breathing zone. Before a respirator can be selected, an assessment of the work environment is usually necessary to determine the concentration of the specific metal fume and other particulates, gases, or vapors that may be present. Until an environmental assessment is completed, however, the employer should review the precautionary labels on filler metals, electrodes, and flux materials and make a best estimate of the appropriate class of respirators. Only the most protective types of respirators shall be used if exposure to a carcinogen is likely (e.g., cadmium, chromium, nickel contained in filler metals, electrodes, fluxes, or during stainless steel welding) or confirmed by environmental measurements. Respirators shall be selected in accordance with the most recent edition of the NIOSH Respirator Decision Logic ,
(3) When workers are exposed to a combination of contaminants in different physical forms, combination cartridge and particulate filter air-purifying respirators may be acceptable under specific conditions as long as none of the agents are considered to be carcinogenic.
In such cases, a qualified individual shall select the respirator, taking into account the specific use conditions, which include the interaction of contaminants with the filter medium, space restrictions caused by the work location, and the use of welding helmets or other face and eye protective devices.
(4) A self-contained breathing apparatus or a supplied-air respirator with an auxiliary self-contained breathing apparatus shall be used when welding in confined spaces. Such welding may reduce ambient oxygen concentration, especially if an inert-gas, shielded-arc welding process is used.
# (d) Hearing Protection
The employer shall provide and require the use of ear protectors whenever there is a potential for noise levels to exceed the NIOSH REL or OSHA PEL.
- Insert-type ear protectors shall be fitted by a person trained in this procedure.
- Inspection procedures shall be established to assure proper issuance, maintenance, and use of ear protectors.
- Workers shall be trained in the proper care and use of all ear protectors.
# Section 6 -Informing Workers of the Hazard (a) Frequency of Hazard Communication
Before assignment and at least annually thereafter, the employer shall provide information about workplace hazards to all workers assigned to work in welding areas.
In addition, employers shall follow the OSHA regulations in 29 CFR 191029 CFR .1200, Hazard Communication.
# (b) Training Program
Hazard information shall be disseminated through a training program that describes how a task is properly done, how each work practice reduces potential exposure, and how it benefits the worker to use such a practice. Workers who are able to recognize hazards and who know how to control them are better equipped to protect themselves from unnecessary exposure. Frequent reinforcement of the training and supervision of work practices are essential.
# (c) File of Written Hazard Information
Appropriate written hazard information and records of training shall be kept on file and made readily available to workers. This information shall include the following:
(1) Identification of the various health hazards, including specific metal fumes, gases released or formed by the processes, heat, noise and vibration, optical radiation, and X-radiation.
(2) Instructions for preventing accidents such as explosion, fire, and electrocut ion.
(3) An explanation of the hazards of working in confined spaces, including the risk of oxygen-deficient atmospheres, exposure to toxic or explosive chemicals, and the potential for heat stress.
(4) An explanation of the potential health effects of exposure to chemical and physical agents generated by welding (e.g., a warning of the increased cancer risk for workers exposed to carcinogens or fumes and gases during stainless steel welding).
(5) Information on precautionary measures for minimizing hazards, including work practices, engineering controls, and personal protective equipment. (6) A description of the environmental and medical surveillance procedures and their benefits.
# (d) Instruction about Sanitation
Workers shall also be instructed about their responsibilities for following proper sanitation procedures to protect their own health and safety and that of their fellow workers.
# (e) Tobacco Use
Workers should be counseled against the use of tobacco products.
# Section 7 -Engineering Controls and Work Practices (a) Engineering Controls
The following engineering controls shall be used whenever welding is performed, unless they can be demonstrated to be infeasible.
# (1) Optical Radiation
Welding shall be performed in booths or screened areas constructed of materials that are noncombustible, opaque, and minimally reflective to light in the range of 200 to 3,000 nm. The booths and screens shall be arranged in a manner that does not restrict ventilation. Such equipment shall conform to the requirements of 29 CFR 1910.252(f)(1)(i i i), Screens.
(2) Chemicals (Gases, Fumes, and Particulates) Fixed-station local exhaust ventilation shall be used whenever possible (e.g., at the workbench). In some situations where fixed local exhaust is not feasible, a movable hood with a flexible duct may be used. For gas-shielded arc welding processes, contaminants can be removed by means of a low-volume, high-velocity exhaust (extracting gun).
General ventilation may be necessary where local exhaust ventilation cannot be used; it may also be used to supplement local exhaust ventilation.
When exhaust ventilation systems are used to control emissions, the following requirements shall apply:
- Exhaust hoods and ductwork shall be constructed of fire-resistant materials.
- Ventilation systems shall be equipped with alarms, flowmeters, or other devices to indicate malfunction or blockage of the systems. These systems shall be inspected at the beginning of each shift to ensure their effect iveness.
- The ventilating airflow shall be directed to carry contaminants from the process away from the breathing zone of the process operator or other workers. For local exhaust systems, this usually entails placement of the fume source between the operator and the face of the exhaust duct.
- The hood design, capture velocity, and flow rate must be chosen to capture the emissions effectively.
- Clean make-up air shall be provided in accordance with 29 CFR 1910.252(f)(4)(i).
- Local exhaust systems used to control welding fumes shall have in-line duct velocities of at least 3,000 feet per minute (fpm) to prevent particulates from settling in horizontal duct runs.
- Canopy hoods may be used under limited conditions. For example, they may be advisable for collecting the heated fumes from automated welding operations and preventing their dissipation into the general work environment.
If a canopy hood is used, however, the worker must not work directly over the welding process and there must be no cross currents beneath the hood.
- Cooling fans shall be considered only when local exhaust is not possible (e.g., remote work areas or outdoor work settings). Cooling fans can remove welding fumes from the breathing zone when properly placed at the side of the worker, but their use is rather limited and they may cause dispersion. Any use of a cooling fan at an indoor worksite requires supplemental general ventilation.
# 3) X-Rays
Electron beam welding processes shall be enclosed and shielded with lead or other suitable materials of sufficient mass to prevent the emission of X-rays. All doors, ports, and other openings shall be checked and maintained to ensure that they have proper seals that prevent X-ray emission.
# (4) Oxyfuel Equipment
Oxyfuel equipment for welding shall be installed, maintained, and used in a manner that prevents leakage, explosion, or accidental fire. Such equipment shall conform to the requirements of 29 CFR 1910.252(a), Installation and Operation of Oxygen-Fuel Gas Systems for Welding and Cutting.
# 5) Fires or Electric Shocks
Arc and resistance welding equipment shall be installed, maintained, and used in a manner that prevents fire or electric shock. Such equipment shall conform to the requirements of 29 CFR 1910.252(b), Application, Installation, and Operation of Arc Welding and Cutting Equipment, and to 29 CFR 1910.252(c), Installation and Operation of Resistance Welding Equipment.
# (b) Work Practices
Work practices shall, at a minimum, conform to 29 CFR 1910.251-254, Welding, Cutting, and Brazing. Specific work requirements include the foI lowing:
(1) Workers shall use welding helmets. Hand-held screens shall be prohibited during welding.
(2) Workers shall adhere to the following safety procedures:
- Workers shall observe the fire precautions prescribed in 29 CFR 1910.252(d).
- Workers shall not conduct welding on materials that may produce toxic pyrolysis or combustion products.
- Workers shall use personal protective clothing and equipment selected specifically for the hazard. Whenever possible, the workpieces to be welded should be positioned to minimize worker exposure to molten metal, sparks, and fumes.
# Section 8 -Sanitation (a) Food, Cosmetics, and Tobacco
The storage, preparation, dispensing, or consumption of food or beverages; the storage or application of cosmetics; and the storage or use of all tobacco products shall be prohibited in areas where welding is conducted.
# (b) Handwash i ng
The employer shall provide handwashing facilities and encourage workers to use them before eating, smoking, using the toilet, or leaving the worksi te.
# (c) Cleaning of Clothes and Equipment
Protective clothing, equipment, and tools shall be cleaned periodically.
# (d) Toxic Waste Disposal
Toxic wastes shall be collected and disposed of in a manner that is not hazardous to workers or others.
# (e) Cleanup of Work Area
The work area shall be cleaned at the end of each shift (or more frequently if needed) using vacuum pickup. Dry sweeping or air hoses shall not be used to clean the work area. Collected wastes shall be placed in sealed containers with labels that indicate the contents.
Cleanup and disposal shall be conducted in a manner that prevents worker contact with wastes and complies with all applicable Federal, State, and local regulations.
# (f) Showering and Changing Facilities
Workers shall be provided with and advised to use facilities for showering and changing clothes at the end of each work shift.
# (g) Flammable Materials
Work areas shall be kept free of flammable debris. Flammable work materials (rags, solvents, etc.) shall be stored in approved safety containers.
# Section 9 -Exposure Monitoring (a) General
(1) Exposure monitoring shall be conducted as specified in parts (b), (c), and (d) of this section for all workers performing welding and for all other workers who may be occupationally exposed through their proximity to these processes.
(2) Air from the worker's breathing zone shall be sampled for fumes and gases. Samples for workers performing welding shall be collected in the welding helmet; samples for other workers shall be collected as close to the mouth and nose as possible.
(3) Results of all exposure monitoring (e.g., of fumes, gases, and physical agents) shall be recorded and retained as specified in Chapter I, Section 10 of this document.
# (b) Determination of Exposures
(1) The employer shall conduct industrial hygiene surveys to determine whether exposures to any air contaminant exceed the applicable exposure limit (see definition in Section 1(b)).
(2) The employer shall keep records of these surveys as defined in Chapter I, Section 10 of this document.
If the employer concludes that exposures are below NIOSH exposure limits, the records must show the basis for this conclusion.
(3) Surveys shall be performed semiannually or whenever changes in work processes or conditions are likely to produce increased concentrations of any air contaminant.
# (c) Routine Monitoring
(1) If the occupational exposure to any air contaminant is at or above the exposure limit (see definition in Section 1(b)), a program of personal monitoring shall be instituted to permit calculation of each worker's exposure. Source and area monitoring may be a useful supplement to personal monitoring.
In all personal monitoring, samples representative of a time-weighted average (TWA) and/or ceiling exposure (depending on the specific agent) shall be collected in the breathing zone of the worker. Sampling and analysis shall be done in accordance with the methods given in Chapter VI, Table VI-1. For each determination of an occupational exposure, a sufficient number of samples shall be collected to characterize each worker's exposure during each work shift. Though not all workers have to be monitored, sufficient samples should be collected to characterize the exposures of all workers who may be potentially exposed. Variations in work habits and production schedules, worker locations, and job functions shall be considered when deciding on sampling locations, times, and frequencies.
A worker exposed to any specific fume or gas at concentrations below its exposure limit shall be monitored at least once every 6 months; more frequent monitoring may be indicated by a professional industrial hygienist.
If a worker is exposed to any specific fume or gas in excess of the exposure limit, controls shall be initiated as specified in Chapter I, Section 7 of this document.
In addition, the worker shall be notified of the exposure and of the control measures being implemented. The worker's exposure shall be evaluated at least once a month. Such monitoring shall continue until two consecutive determinations at least 1 week apart are below the exposure limit. After that point, monitoring shall be conducted at least semiannually or whenever the work process or conditions change.
# (d) Physical Agent Monitoring
(1) Exposure to UV radiation shall be prevented by means of a management control program. The program shall require the use of barriers wherever possible. Where barriers cannot be used, workers shall use personal protective devices, including proper clothing, sunscreens with a sun protection factor (SPF) >15, and body and face shields. The use of barriers and protective devices shall be evaluated every month.
(2) Noise exposures shall be evaluated for all workers performing welding. Plasma arc, metal spraying, and arc air gouging processes are likely to result in excessive noise exposures. Employers shall meet the requirements of 29 CFR 1910.95(c), Hearing Conservation Program, whenever a worker's noise exposure is >85 decibels measured on the A scale (dBA) as an 8-hr TWA. All monitoring instruments shall conform to the requirements of 29 CFR 1910.95(d)(2), Monitoring; they shall have a Type II microphone at a minimum. Such noise monitoring surveys must be repeated whenever a change in the work process or environment increases the potential for worker noise exposures.
(3) Electron beam welding equipment shall be surveyed periodically to detect any leakage of X-radiation. A preliminary survey shall be conducted at the time of installation while operating at maximum current and voltage levels. Subsequent surveys should be made whenever the equipment is moved or repaired. Operators of such equipment shall use film badges or some other means of monitoring X-ray exposure.
(4) Environmental heat exposures shall be assessed whenever the potential exists for workers to be exposed to elevated ambient temperatures (e.g., when working in confined spaces or subjected to poor ventilation). Monitoring practices shall be those specified in Criteria for a Recommended Standard. ...OccupationaI Exposure to Hot Environments .
# Section 10 -Recordkeeping (a) Exposure Monitoring
The employer shall establish and maintain an accurate record of all exposure measurements as required in Chapter I, Section 9 of this document. These records shall include the name of the worker being monitored, social security number, duties performed and job locations, dates and times of measurements, sampling and analytical methods used, type of personal protection used (if any), and number, duration, and results of samples taken.
# (b) Medical Monitoring
The employer shall establish and maintain an accurate record for each worker subject to the medical monitoring specified in Chapter I, Section 3 of this document.
# (c) Record Retention
In accordance with the requirements of 29 CFR 1910.20(d), Preservation of Records, the employer shall retain the records described in Chapter I, Sections 3, 6, and 9 of this document for at least the following per iods:
(1) Thirty years for exposure monitoring records, and
(2) Duration of employment plus 30 years for medical surveillance records.
# (d) Availability of Records
(1) In accordance with 29 CFR 1910.20, Access to Employee Exposure and Medical Records, the employer shall upon request allow examination and copying of exposure monitoring records by the subject worker, the former worker, or anyone having the specific written consent of the subject or former worker.
(2) Any medical records that are required by this recommended standard shall be provided upon request for examination and copying to the subject worker, the former worker, or anyone having the specific written consent of the subject or former worker.
# (e) Transfer of Records
The employer shall comply with the requirements for the transfer of records as set forth in 29 CFR 1910.20(h), Transfer of Records.
# II. INTRODUCTION
# A. Scope
NIOSH has formalized a system for developing criteria on which to base standards for ensuring the health and safety of workers exposed to hazardous chemical and physical agents. The criteria and recommended standards are intended to enable management and labor to develop better engineering controls and more healthful work practices. This document presents the criteria and recommended standards for preventing health impairment from exposures associated with welding. The criteria document was developed by the National Institute for Occupational Safety and Health (NIOSH) in response to Section 20(a)(3) of the Occupational Safety and Health Act of 1970. In this act, NIOSH is charged with the responsibility of developing criteria for toxic materials and harmful physical agents to describe exposure concentrations at which no worker will suffer impaired health or functional capacities or diminished life expectancy as a result of work experience.
This document contains information on workplace exposures that may occur during welding and the adverse health effects associated with these exposures (e.g., gastrointestinal disorders, cancer, and ocular, dermatological, reproductive, musculoskeletal, and chronic and acute respiratory diseases. For the purpose of this recommended standard, "welding" is defined as those processes that join or cut pieces of metal by heat, pressure, or both (e.g., arc welding, brazing, and cutting) , These processes differ only in the way heat is created and applied to the parts being joined and in the type of filler material used. Chapter III describes these processes. 11-1 lists specific welding processes and some of the potentially hazardous agents associated with them. This table should be used as a reference guide and not as a complete inventory of possible emissions. Chapter III contains more complete discussion of these agents. Laser and underwater welding processes are not included since they require specific control procedures that are beyond the scope of this document.
# B. Number of Workers Potentially Exposed to Welding
The 1972-74 National Occupational Hazard Survey showed that an estimated 176,000 workers had a primary occupation of welder, brazer, or thermal cutter . A follow-up survey in 1981-83 indicated that 185,000 workers were employed in these occupations . These NIOSH surveys were limited to facilities that employed eight or more workers and did not account for any welding conducted at mining sites or government fac i Ii t i e s .
Estimates indicate that the duties of more than 700,000 U.S. workers involve the welding of various types of materials within many different industries (e.g., manufacturing and construction) . Census data from 1980 indicated that 673,357 males and 39,242 females were employed as welders and cutters. Note that brazers were classified along with solderers in the census data and thus are not included in these employment figures.
# C. Special Considerations for Controlling Welding Hazards
The hazards associated with welding can be divided into two categories:
(1) the hazardous chemicals (e.g., fumes and gases) that are formed or released by the processes, and ( 2) the physical hazards such as ionizing and nonionizing radiation, noise, vibration, high temperatures, and electricity. Because of the many techniques applied in welding and the various types of materials used, it is often difficult to characterize exposures completely at any given time. However, as noted in Table 11-1, specific gases and fumes are typically generated when certain welding processes are applied to known base metals. This knowledge can be used to implement good industrial hygiene practices before any comprehensive evaluation of the workplace is initiated.
This document discusses the adverse health effects that have been observed among workers who perform welding, but many of these effects cannot be attributed to any specific agent because of the possible additive or synergistic effects from mixed exposures. For example, welders have historically been exposed to asbestos as a result of using asbestoscontaining materials or working in industries where asbestos was used as an insulation material. Many of the morbidity and mortality studies conducted on welders demonstrate an increased risk in respiratory diseases, including cancer. Because of the absence of exposure data for many of these studies, the etiology of the reported disease is unknown but often clinically resembles the diseases associated with workers exposed to asbestos. Although the potential for an asbestos exposure has decreased with the elimination of asbestos-containing materials used by welders, it still remains a possible concomitant exposure in some work environments (e.g., asbestos insulation around pipes). , ship repairing , shipbuilding , longshoring , and general industry , Most of the Federal standards were adopted from consensus standards developed by a variety of organizations, including the American Conference of Governmental Industrial Hygienists (ACGIH), AWS, ANSI, the National Fire Protection Association (NFPA), the Compressed Gas Association (CGA), the American Petroleum Institute (API), and the Rubber Manufacturers Association (RMA).
The Federal standards covering welding, cutting, and brazing are generally process-or design-oriented rather than performance-or exposure-Iimitoriented. That is, though the standards refer to allowable limits of exposure, they actually prescribe work procedures or practices that are intended to minimize health and safety risks. Some of the potential hazards to which the standards are directed include fire, explosion, electric shock, UV radiation, infrared (IR) radiation, oxygen-deficient atmospheres, decomposition products of chlorinated solvents, fluorides, nitrogen dioxide, and toxic metals such as beryllium, cadmium, chromium, lead, mercury, and zinc .
Environmental monitoring is prescribed to evaluate confined spaces for sufficient oxygen, to monitor exposures resulting from the heating of greased metals, and to check for the presence of flammable gases. Labeling is required on the packages holding fluoride-containing flux or filler metals to warn that ventilation is required to control the fumes and gases that may be produced. No sanitation procedures are specified. Some types of personal protective equipment are specified, including eye protectors, helmets, gloves, boots, aprons, and other clothing. Requirements for specific work practices are covered for a number of particularly hazardous operations, including working in confined spaces, handling compressed-gas cylinders, welding or cutting metal containers, and working on elevated surfaces. The engineering controls required are screens or booths to protect against UV radiation, and ventilation for enclosed areas and confined spaces. The general industry standards for welding, cutting, and brazing refer to the PELs as stated in 29 CFR 191029 CFR .1000. The construction standards for welding and cutting incorporate by reference the ACGIH Threshold Limit Values (TLVs®). The maritime employment standards for welding, brazing, and thermal cutting [29 CFR 1915[29 CFR .31-36, 1916[29 CFR .31-36, 1917 do not specify or refer to environmental limits.
Since 1970, the ACGIH has recommended a TLV of 5 mg/m^ for total particulates in welding fumes. In addition, the ACGIH recommends that specific constituents of the fumes and toxic gases also be considered in assessing airborne exposures from welding . For example, a TLV of 0.05 mg/m3 (as Cr) is recommended for exposures to chromium(VI) by the ACGIH.
NIOSH has RELs for individual substances and physical agents found in the welding environment. These RELs are listed in Appendix A along with the current OSHA PELs and ACGIH TLVs.
# E. NIOSH Recommendations That Differ From Current OSHA Regulations
Many of the exposure limits and program requirements recommended in this document are not currently required by OSHA, and other recommendations are intended to augment existing OSHA requirements. NIOSH recommendations that differ from current OSHA regulations include those that pertain to the following items:
- Adoption of NIOSH RELs (or in some instances, other limits proposed by voluntary consensus groups) for specific chemical and physical agents (see Chapter I, Section 1, Definitions).
- Initial and periodic medical surveillance.
- Labeling and posting for potential carcinogens.
- Warning of eye damage from looking at a welding arc.
- Warning of high noise areas.
- Criteria for heat stress.
- Recommendations for personal protective clothing and equipment, including the criteria for selecting appropriate types of respirators.
- Information to supplement the Hazard Communication Standard (29 CFR 1910(29 CFR .1200).
- Engineering controls and work practices.
- Requirements for food storage and consumption, use of tobacco products, use of cosmetics, and personal hygiene (availability of shower and locker facilities).
- Exposure monitoring, both initial and periodic.
- Recordkeeping.
# III.
# CHARACTERISTICS OF WELDING PROCESSES
# A. Identification of Processes
More than 80 different types of welding and allied processes are in commercial use, including brazing and thermal cutting (Figure 111-1). The most commonly used processes are briefly discussed in this section. Definitions for types of welding processes appear in the Glossary. Appendix D lists industries that employ welders, brazers, and cutters, along with their respective standard industrial classification (SIC) codes.
# Arc Welding
In arc welding, heat is created as electricity flows across a gap between the tip of the welding electrode and the metal. Arc welding is the most frequently used process. It encompasses numerous variations, depending on the types of electrodes, fluxes, shielding gases, and other equipment that may be used. The arc welding process involves the melting of an electrode by an electric current to form a molten puddle in the base metal. Because of the generated heat, the base metal also becomes molten at the joining surfaces, which bond upon cooling.
Electrodes are manufactured as bare wire or as wire lightly to heavily coated with flux material. Bare wire electrodes are the least expensive, but they are difficult to maintain, and they produce an inferior weld. Also, a coating of copper on filler materials may be used in place of a flux to prevent oxidation of the material before use. Flux material generally consists of asbestos, feldspar, fluorine compounds, mica, steatite (a form of talc), titanium dioxide, calcium carbonate, magnesium carbonate, or various aluminas. The flux prevents or removes oxides or other undesirable substances from the weld.
Inert shielding gases such as helium, argon, or carbon dioxide are used in some variations of arc welding. These variations of arc welding are often referred to as shielded metal arc, metal inert gas, and plasma arc welding. The inert gas prevents oxygen and active chemicals in the atmosphere from reacting with the hot metal .
# Oxyfuei Gas Welding
Oxyfuel gas welding is the process by which heat from burning gases is used to melt the base metal without the use of welding rods; however, rods are used when extra metal is needed as a filler to obtain a complete bond. The composition of these consumable rods is very similar to that of the base metals. Some are coated with flux, the composition of which depends on the application. . . CAW S -tw . . LBC IG -o x y g e n .
# MASTER CHART OF WELDING AND ALLIED P R O C E SSES
# . CAW T electrogas w eld in
# R e sista n c e W elding
Resistance welding is a process in which pieces of metal are pressed together and an electric current is passed through them. At the contact point, there is sufficient resistance to cause an increase in temperature and melting of the metal.
# Brazing
Brazing is the process by which metals are heated and joined together by a molten filler metal at temperatures exceeding 450°C (840°F) . Soldering, which is not included in this document, is similar to brazing, but it uses filler metals that have melting points below 450°C. The filler metal used in brazing may be in the form of wire, foil, filings, slugs, powder, paste, or tape. Fluxes must be used unless the process is performed in a vacuum, since oxidation of the brazed area will weaken the bond. The most common ingredients of fluxes are borates (e.g., lithium, potassium, and sodium), fused borax, fluoroborates (e.g., potassium and sodium), fluorides (e.g., lithium, potassium, and sodium), chlorides (e.g., lithium, potassium, and sodium), acids (e.g., boric acid and calcined boric acid), alkalis (e.g., potassium hydroxide and sodium hydroxide), and water (either as water of hydration or as an addition for paste fluxes) .
# Thermal Cutting
Thermal cutting includes processes that cut the metal by melting. These processes are divided into two main groups: oxygen and arc cutting. Oxygen cutting is performed on plain carbon, manganese, and lowchromium-content steels. When the metal is heated and exposed to oxygen, it oxidizes and melts. Flame cutting uses a fuel gas (or a combination of gases) such as acetylene, hydrogen, natural gas, or propane that burns and produces sufficient heat to vaporize and separate the metal. Arc cutting is used with nonferrous metals, stainless steels, or steels with a high chromium or tungsten content .
# B. Potential for Exposure
Welding, brazing, and thermal cutting processes generate exposures to many chemical and physical agents. Chemical and physical agents produced by these processes are described in the following sections, which identify the source, mechanism of production, disposition, and exposure concentrations found in many occupational environments. The potential exists for other confounding exposures (e.g., asbestos and heat) in the work environment of welders and needs to be assessed for each welding process.
# Fumes and Other Particulates
A fume is generated by volatilization of melted substances with subsequent condensation of solid particles from the gaseous state . For the processes discussed in this document, temperatures may range from about 450°C (840°F) for brazing to well above 15,000°C (27,000°F) for plasma arc cutting . The single largest source of fumes is the filler metal being used .
Fumes may also originate from the base metal , from coatings applied to the base metal , and from the flux or electrode coating . Fume particles typically have a diameter of less than 1 micrometer (fxm) .
Fumes are not the only sources of airborne particulates. Fluxes and filler metals used in powdered form (e.g., in submerged arc welding and furnace brazing) may enter the air as fugitive dusts. Mineral and metal dusts may also be produced when material is pulverized during the cleaning of welds and brazes by surface brushing or grinding . Historically, the potential has also existed for asbestos exposure during welding processes. These exposures often occurred as a result of using materials that contained asbestos, disturbing asbestos insulation while welding, or working near other operations that used asbestos. Steel and Sanderson investigated the composition of welding fumes to determine the extent of impurities that may be present in fluxes. Flux that is formulated into a coating for stick electrodes may generate shielding gas, produce slag, alloy with rods, or act as binders.
In one of their experiments, these investigators conducted shielded metal arc welding on mild steel in a test chamber using 12 different commercial electrodes. Air samples were collected at a distance from the source of exposure that corresponded to the breathing zone of a welder standing upright. On several occasions, fume concentrations exceeded NIOSH RELs for lead and vanadium pentoxide. Chromium(VI), copper, and manganese were also detected.
The chemical composition of the airborne fumes generally reflects the elemental composition of the base and filler metals and the flux, but the fume components may have different chemical forms. Thus concentrations of the various fume components may vary for each job and process and are best determined on a case-by-case basis.
# a. Alkali Metals and Alkaline Earths
The airborne concentrations of calcium, magnesium, potassium, and sodium are significantly greater in the emissions from lime (low-hydrogen) electrodes than in those from nonlime electrodes . Although concentrations vary greatly within the two classes, low-hydrogen electrodes generally produce higher concentrations of calcium, magnesium, potassium, and sodium in their fumes.
# b. Aluminum
Aluminum is generally found in small quantities in the fumes from all types of electrodes, both low-hydrogen and non-low-hydrogen. Morita and Tanigaki reported a range of 0.21% to 1.44% aluminum (as AI2O3 ), and Kimura et al. noted a range of 0 .1% to 0 .8% in the fumes for all electrodes tested. -Pushkin evaluated the composition of fumes produced by the electron beam welding of beryllium bronze. The welding was done in a vacuum chamber that was flushed with air before opening. The purged air was filtered, and the collected fumes were analyzed for beryllium. As in most electron beam welding, two pieces of base metal (2% beryllium content) were joined without the use of a filler metal. Samples of the purged air contained detectable amounts of beryllium in only 5 of the 44 samples. However, periodic cleaning by dry scrubbing of the vacuum chamber walls caused redispersion of fumes that contained beryllium concentrations of 130 to 150 jug/m»- in the chamber and 4 /ng/m^ in the breathing zones of welders working outside the chamber.
# c. Beryllium
# Bobrishchev
# d . Cadmi um
Cadmium concentrations in the breathing zone have been reported to be 10 to 250 ¡xg/rn^ during shipboard brazing with a silver-and cadmium-based filler metal . Cadmiumbearing alloys are used in more than 50% of all brazed joints .
# e. Chromium
Both the chromium concentration and its oxidative state vary within the fumes depending on the welding or cutting process and the base metal. Virtamo compared fume composition in shielded metal arc welding, gas tungsten arc welding, gas metal arc welding, and plasma arc cutting. These operations were performed on high-alloy, nieke I-chromium stainless steel to determine the relative amounts of nickel, chromium(VI), and total chromium evolved in the fumes. Analysis of breathing zone samples indicated the following:
- Shielded metal arc welding produced the highest water-soluble chromium(VI) fume concentrations-as high as 720 jug/m^.
- Gas tungsten arc welding produced chromium(VI) concentrations below the 10-^g/m^ detection limit in 8 of 10 samples (the highest concentration found was 45 jug/m^).
- No chromium(VI) was detected during plasma arc cutting or gas metal arc welding.
While surveying Swedish worksites, Ulfvarson found higher chromium concentrations with shielded metal arc welding than with gas metal arc welding on stainless steel. The median breathing zone concentration of chromium was 150 ng/m3 at 86 worksites where shielded metal arc welding was performed. For gas metal arc welding, the median breathing zone concentration of chromium (mostly insoluble) was about 20 jug/m^ at 41 worksites.
At a large maintenance shop, Arnold assessed the exposures of three groups of welders. The first group performed gas tungsten arc and gas metal arc welding. Their breathing zone samples all contained <6 jug/m^ of chromium(VI). Group II performed shielded metal arc welding and had breathing zone concentrations of chromium(VI) that averaged 14 |ug/m3, with a high of 90 pig/m^. Group III used a variety of welding methods-mostly shielded metal arc welding (including flux cored arc and gas metal arc welding). Within this group, the average chromium(VI) concentration was 64 |jg/m3, with a high of 329 jug/m^.
Both Lautner et al. and Ulfvarson found that shielded metal arc welding produced the highest percentage of chromium(VI) in the fumes. When electron spectroscopy was used for chemical analysis (ESCA), gas metal arc and gas tungsten arc welding of stainless steel produced only traces of chromium(VI) (concentrations too small to be quantified). Shielded metal arc welding generated 73% of the total chromium in the fumes as chromium(VI) (mean net mass = 1,016 ¡xq chromium(VI )/f i I ter).
# f . FIuor i des
The inclusion of fluorspar in low-hydrogen (lime) electrodes produces significant amounts of fluoride compounds in welding fumes. In a study conducted by Kimura et al. , welding fumes contained 11% to 18% fluoride. Another study reports that the fumes contained 14% to 23% fluoride when low-hydrogen electrodes were used for shielded metal arc welding on mild and high-tensile steel. Tebbens and Drinker found that high-alloy electrodes containing 1 to 5 mg fluoride per electrode generated fumes that contained 9% to 26% fluoride compounds. This high percentage was partly due to the low melting points of the fluoride compounds. Only negligible amounts of hydrogen fluoride were detected in the welding emissions.
# g . Iron
Iron is the main constituent of the fume when welding is performed on non-alloy steel. Dreesen et al. studied arc welders in steel ship construction and reported welding fumes with iron concentrations above 20 mg/m^. Ulfvarson collected breathing zone samples for welders performing shielded metal arc and gas metal arc welding. The geometric mean concentration for iron was 14 mg/m^ during the welding of unpainted non-alloy steel and 30 mg/nr- during the welding of painted non-alloy steel. Akbarkhanzadeh surveyed British worksites (mostly shipyards) where shielded metal arc welding was being performed on mild steel. The mean concentration of iron (ferric oxide) from 209 breathing zone samples was mg/m^. The iron concentration increased linearly with increasing arc current (correlation coefficient = 0.323, p<0.001). KleinfeId et al. sampled welders while they performed oxyfuel cutting and shielded metal arc welding; they found concentrations of iron oxide ranging from 0.65 to 1.7 mg/nr- inside the welders' face shields and from 1.6 to 12 mg/m^ outside the face shield.
# h . Lead
Because zinc may contain lead as an impurity, significant amounts of lead can be generated when welding zinc-primed steel or steel that has been hot-dipped in zinc. Pegues determined lead concentrations from air samples collected in the breathing zone of workers performing oxyacetylene cutting and arc welding on zinc-coated steel. Welding was performed in a confined space without ventilation on steel that was protected by hot-dip galvanization and on steel that was painted with zinc silicate.
During arc welding, breathing zone concentrations of lead ranged from 0.9 to 15.2 mg/m^ with the zinc-silicate-coated steel, and from 0.4 to 0.7 mg/m^ with the galvanized steel. During oxyacetylene welding, lead concentrations ranged from 1.2 to 3.5 mg/m^ with the zinc-silicate-coated steel, and from 0.2 to 0.7 mg/m^ with the galvanized steel.
# i. Manganese
Akbarkhanzadeh collected breathing zone samples from welders performing shielded metal arc welding of mild steel coated with an unspecified primer and found average manganese fume concentrations of 0.14 mg/nw. By comparison, breathing zone samples from welders performing shielded metal arc and gas metal arc welding had average manganese concentrations of 3.1 mg/m^ during welding on primed mild steel and 1.4 mg/m^ during welding on unprimed mild steel .
The percentage of manganese in welding fumes was reported to be relatively independent of the type of electrode , In a study of 61 brands of electrodes of different composition , the level of manganese oxide (MnO) in the fume ranged from 2.5% to 9.5%. In a similar study of 25 brands of electrodes, Kimura et al. observed fumes containing 3.3% to 11.2% manganese as MnO. Fumes from ilmenite electrodes tended to have higher concentrations of manganese compared with those generated from lime electrodes.
# j . N i ekeI
Virtamo assessed the nickel content of fumes generated from shielded metal arc welding, gas metal arc welding, and plasma arc cutting of stainless steel. Shielded metal arc welding produced nickel concentrations that ranged from trace amounts to 160 jiig/m^; gas metal arc welding produced concentrations as high as 60 and plasma arc cutting produced concentrations up to 470 /^g/m3. When Ulfvarson et a l . surveyed welders who were performing shielded metal arc and gas metal arc welding of stainless steel, a median breathing zone concentration of approximately 25 n g nickel/m^ was determined for shielded metal arc and approximately 5 /ug nickel/m^ for gas metal arc welding. Bernacki et al. reported an average airborne concentration of 6 /ug nickel/m^ (with a high of 46 jug nickel/m^) from welding nickel-alloyed steel. Wilson et al. examined various maintenance welding operations at a chemical plant and found that the highest nickel concentrations were produced when welding was conducted on stainless steel inside distillation towers. Airborne concentrations of nickel from 22 of 23 samples exceeded the NIOSH REL of 15 /ug/m3. The mean concentration of nickel was 3.65 /¿g/m^, with a high of 17.6 /Lig/m^.
# k. Silica
Silica in welding fumes originates from the coating on the electrode, which varies in quantity depending on the type of electrode used. Twenty-six brands of ilmenite and lime titania electrodes produced fumes containing 18% to 22% silicon as silicon dioxide (Si02); two brands of iron powder/iron oxide electrodes produced fumes containing 8% and 12% SiO2 ; and 10 brands of lime electrodes produced fumes containing 4% to 11% SiO2 .
In a study of 61 brands of electrodes, Morita and Tanigaki observed that the mean silica contents of fumes were as follows:
(1) 33% for 7 high-titania and iron powder/iron oxide electrodes, (2 ) 22% for 26 brands of ilmenite and lime titania electrodes, (3) 12% for 1 high-cellulose electrode produced, and (4) 6% for 27 low-hydrogen electrodes. Tebbens and Drinker observed the presence of silica in fumes generated from the shielded metal arc welding of mild steel. Silica and silicates are commonly used ingredients in fluxes on mild-steelcovered electrodes. When two such electrodes were tested, one generated fumes containing 15% crystalline silica plus a high silicate content; fumes from the other contained no crystalline silica but were high in silicates. The two electrodes generated comparable amounts of silicon (18% to 22% of the total fume), which was present as soluble silicates or amorphous silica. X-ray diffraction was used to confirm the absence of crystalline silica.
# I. Titanium
In two studies , ilmenite, lime titania, and high-titania electrodes generated similar percentages of titanium in fumes.
In the first study, 30 of these types of electrodes produced a range of 0.6% to 2.3% titanium as titanium dioxide (Ti02). When 30 different brands of iron oxide/iron powder and low-hydrogen electrodes were tested in that same study, a range of 0.1% to 0.4% TiOo was found in the fume. The second study examined 25 brands of electrodes. Thirteen brands of ilmenite, lime titania, and titania electrodes produced a range of 0.6% to 5.5% Ti02 in the fume; the remaining 12 iron powder/iron oxide and lime electrodes generated fumes containing 0.2% to 0.9% Ti02m . Z i nc In a study of oxypropane flame cutting and shielded metal arc welding in a shipyard , fumes containing zinc were generated from the protective coating on the metal. Breathing zone concentrations ranged from no detectable zinc to 8.6 mg/m^. Shielded metal arc welding of metal plate treated with zinc powder and zinc chromate primers produced fumes containing up to 74 mg zinc/m^ when ventilation was poor. A report on fumes from welding and flame cutting processes in the shipbuilding and ship-repairing industry collected breathing zone samples from welders who were gas metal arc welding on mild steel that was either untreated or coated with a zinc tetraoxychromate/iron oxide primer. Samples collected during the welding of untreated steel had a mean zinc concentration of 0.11 mg/m^, and those collected during the welding of primer-coated steel had a mean zinc concentration of 0.43 mg/nr*. Dreesen et al. reported zinc concentrations in area samples that exceeded 12 mg/m^ (15 mg/m^ expressed as zinc oxide) in welding fumes produced from arc welding on steel during ship repair. Pegues (see subsection 1,h, Lead, of this chapter) analyzed fume samples collected from workers performing oxyacetylene cutting and arc welding on zinc-coated steel in a confined space without ventilation. Steel that had two types of zinc-coatings (e.g., zinc silicate and galvanized steel) were evaluated to determine the generation of zinc in the fumes. The zinc-silicatecoated steel produced a mean zinc concentration of 19.81 mg/m^ during electric arc welding and 12.28 mg/m^ during oxyacetylene cutting. Electric arc welding of galvanized steel produced a mean zinc concentration of 6.63 mg/m^. No exposures to zinc were detected during oxyacetylene cutting.
# Spec i f i c Gases
A number of toxic gases such as carbon monoxide, oxides of nitrogen, ozone, and various photochemical and pyrolytic decomposition products of halogenated hydrocarbons are present or produced by chemical reactions during welding. Fuel gases that may be released (such as propane, acetylene, and hydrogen) are asphyxiants. These gases and oxygen may combust during use . The lower explosive limits (LELs) for some of these gases are quite low-for example, 2.3% for propane, 4.1% for hydrogen, and 2.5% for acetylene.
Oxygen is hazardous at higher than normal concentrations because it increases the flammability of materials (e.g., clothes) .
Shielding gases such as argon, nitrogen, helium, and carbon dioxide (CO2 ) may also be present. Alone, these gases do not normally pose a hazard; however, in confined spaces they may displace the oxygen-containing air and give no warning of oxygen deficiency because they are odorless and colorless.
Many of the gases that may be encountered during various welding processes are listed below with information on their source of generation and reported concentrations.
# a. Carbon Monoxide
Carbon monoxide CO exposures often result from the reduction of CO2 used for shielding in gas metal arc welding, de Kretser et al. found CO concentrations often approaching 300 ppm when CO2 exposures were measured at 1400 parts per million (ppm) during gas metal arc welding. Ulfvarson found CO exposures to be sporadic and at low concentrations in many Swedish work sites except where gas metal arc welding was being done. At the latter sites, about 10% of the measurements had CO readings above 50 ppm, with peak readings of 150 ppm. Press and Florian found that for gas metal arc welding, CO concentrations increased as the percentage of carbon dioxide was increased in the shielding gas.
Erman et a l . measured CO concentrations in poorly ventilated confined spaces during shipbuilding operations. Welding was done on steel with CO2 gas metal arc welding. CO concentrations increased as the duration of welding increased.
In a space of 4.9 m3, CO concentrations exceeded 160 mg/m^ (145 ppm) within 40 min. Ulfvarson et al. assessed the generation of CO during flame cutting of primed steel. They found that in a laboratory setting, CO concentrations up to 35 ppm were generated when the ventilation was poor. Flame cutting of primed steel during ship repair and construction in confined spaces produced CO concentrations exceeding 100 ppm.
# b. Oxides of Nitrogen
An arc or a very high-temperature flame may cause the oxygen and nitrogen in the air to combine and form oxides of nitrogen. One combustion product, nitrogen dioxide (NO2 ), has been detected in shielded arc welding, oxyacetylene welding, arc gouging , gas metal arc welding , submerged arc welding, and oxyacetylene and oxypropane cutting .
Tests performed with tungsten electrodes produced 0.3 to 0.5 ppm of nitrogen oxides with helium shielding and 2.5 to 3.0 ppm with argon shielding. The higher concentrations for both were obtained when the shield gas flow rate was doubled. Ferry and Ginther found lower NO2 concentrations for oxyacetylene welding, argon-shielded gas metal arc welding, and carbon arc gouging. The authors speculated that the increase in current for gas metal arc welding produced the higher NO2 concentrations. Akbarkhanzadeh , however, found no relationship between the current and the generation rates for nitrogen oxides when shielded metal arc welding was performed on mild steel. Ferry and Ginther observed that nitrogen dioxide concentrations were always greatest in the area of visible fume (within 0.15 m of the arc). At greater distances from the arc, the concentrations decreased in all directions except in the direction of the fume stream. The authors suggested that NO2 is formed thermally and diffuses away from the arc.
In a study that used oxyacetylene welding, flame size was an important factor in the generation of nitrogen oxides. Generation rates for nitrogen oxides were 10 times higher with an unrestricted flame length than with a 10-mm flame. In addition, increasing blowpipe size from 1 to 8 produced dramatic increases in nitrogen oxide concentrations.
Ventilation that is adequate to control exposures to total fumes is sufficient to control nitrogen oxide exposures .
Octavian and Nicolae observed that nitrogen oxides are formed at a distance from plasma arc cutting or argon-shielded arc welding, with maximum formation rates at 1.75 to 2.5 m and 4 m, respectively. Nitrogen oxide concentrations were determined by drawing air through a quartz tube at various distances from the welding operations and therefore measuring only those oxides formed by UV radiation.
Press found that for plasma arc cutting of aluminum alloys with an argon/hydrogen mixture, the highest measured concentrations were 2 ppm for NO2 and 9 ppm for nitrous oxide (N2O). Both concentrations were determined in the absence of ventilation. Siekierzynska and Paluch examined emission rates of nitrogen oxides for plasma arc cutting on various base metals that were 0.5 mm thick. Although N2O concentrations were not given, generation rates were reported to be very similar for cutting mild steel (150 mg/sec), alloy steel (140 mg/sec), copper (70 mg/sec), brass (80 mg/sec), and aluminum (70 mg/sec). The NO2 emission rates were 50 mg/sec for mild steel, 40 mg/sec for alloy steel, 45 mg/sec for copper, 50 mg/sec for brass, and 40 mg/sec for aluminum. Concentrations as high as 100 ppm have been reported .
# c . Ozone
In the presence of UV light, atmospheric oxygen can convert to ozone . Among the various welding processes, gas metal arc and gas tungsten arc welding produce the highest ozone concentrations, especially when aluminum is used as a base metal .
In studies of argon-shielded arc welding of aluminum, Lunau found that after 3 to 5 min with a 200-ampere (A) current density, ozone concentrations averaged 5.1 ppm; with a 250-A current density, ozone was 7.5 ppm; and with a 300-A current, ozone was 8.4 ppm. All concentrations decreased over time because of strong thermal upcurrents formed from the heat during welding. Shironin and Dorosheva also found an increase in ozone concentrations with increasing current density. With continuous argon-shielded arc welding, breathing zone samples collected from welders indicated an average ozone concentration of 0.6 mg/m^ when an 80-A current density was used. This concentration increased to 1.0 mg/m^ at a 300-A current density; with pulsed arcing, the concentrations were 0.5 mg/m^ for a 50% duty cycle and 0.7 mg/m^ for a 75% duty cycle. When Ditschun and Sahoo assessed the generation of ozone during gas metal arc welding of copper-nickel and nickel-aluminum bronze alloys, ozone concentrations varied from 0.07 to 0 .19 ppm. Ferry and Ginther found that when argon-shielded gas tungsten arc welding was performed on a copper block, the breathing zone concentration of ozone was 0.1 ppm with a 55-A current and 0.5 to 0.6 ppm with a 110-A current. When a helium shield was used, the ozone concentration was 0.1 ppm with either current level.
The spatial distribution of ozone concentrations has been studied under various conditions . Ozone generation diminished as the distance from the arc increased . In argon-shielded gas tungsten arc welding of aluminum, ozone concentrations were consistently higher than with argon-shielded gas metal arc welding. The author postulated that the high-energy (short-wavelength) UV rays resulting from gas tungsten arc welding caused more ozone formation.
Fay et al. also found that ozone concentrations were higher at 0.15 m from the arc in argon-shielded gas metal arc welding than at 0.60 m. However, the opposite was observed with argon-shielded gas tungsten arc welding, regardless of the metal welded or the current used. Frant also studied ozone concentrations in argon-shielded gas tungsten arc welding but found that the rate of ozone formation measured in a quartz tube was 10 times higher at 0.2 m than at 0.5 m from the arc.
Ferry and Ginther found that the shielding gas had a decided effect on ozone formation. Changing from argon to helium in gas tungsten arc welding caused ozone concentrations in the breathing zone to decrease from 0.5-0.6 ppm to 0.1 ppm regardless of the current level. Frant observed a similar reduction when using a CO2 shield. In gas metal arc welding of steel, argon shielding produced 33 /xg ozone/min, and carbon dioxide shielding produced 7 jug ozone/m in when measured in a quartz tube placed 30 cm from the arc.
Several authors have shown that the type of base metal can affect the rate of ozone production. Frant found that ozone was produced at a concentration of 300 jug/min during argon-shielded gas metal arc welding on aluminum, compared with only 33 jLig/min during argon-shielded gas metal arc welding on steel. Lunau showed large variations in ozone concentrations depending on the particular aluminum alloy being welded. Argon-shielded gas metal arc welding on pure aluminum produced 6.1 ppm ozone at 0.15 m from the arc; welding under the same conditions on a 5% magnesium alloy of aluminum produced only 2.3 ppm ozone; and welding on a 5% silicon alloy of aluminum produced 14.5 ppm ozone. Press and Florian observed that shielded metal arc welding of aluminum produced ozone concentrations 10 times higher than shielded metal arc welding of mild steel.
In addition, much higher ozone concentrations occurred when a silicon alloy electrode was used for welding aluminum than when a magnesium alloy electrode was used.
# d. Decomposition Products of Organics
Trichloroethylene and tetrachloroethylene are solvents commonly used to degrease metals. They may therefore be present on the surface of recently cleaned metal parts or in the atmosphere where welding processes are being performed. Ultraviolet radiation may react with the vapors of those solvents and produce a number of irritating and toxic gases as a result of photooxidation. Dahl berg and Myrin assessed 10 welding workshops and found that roughly five times as much dichloroacetyI chloride as phosgene was formed where welding was done in the presence of trichloroethylene vapor. There was almost a complete conversion of trichloroethylene vapor to phosgene (1.5 ppm) and dichloroacetyI chloride (10 ppm) at 30 cm from an argon-shielded aluminum welding arc located 4 m from a degreaser.
In other workshop environments, Dahlberg and Myrin found 0.01 to 0.3 ppm of phosgene and 0.03 to 13 ppm of dichloroacety I chloride.
Andersson et a l . studied the formation of trichloroacetyl chloride and phosgene from tetrachloroethylene vapor during shielded metal arc and gas metal arc welding. These two hazardous products were formed in equal proportions. The authors recommended that welding be avoided in work environments contaminated with tetrachloroethylene.
A variety of other potentially toxic gases may be produced when the welding process inadvertently heats certain other materials. For instance, residual oil on steel may emit acrolein during welding .
# Physical Agents
The potential exists for exposure to a variety of physical agents during the welding process. Workers may be subjected to excessive heat in the welding environment , radiation emitted from the welding processes (including ionizing radiation and nonionizing radiation in the IR, visible, and UV ranges , noise, and electricity. The following types of exposures are representative of those that have been specifically documented in the work environments of welders.
# a. Electromagnetic Radiation
Optical radiation may be produced by electric or plasma arcs. Radiation from a 50-A arc ranges from a wavelength of 200 to 800 nm . Levels produced from oxyfuel welding, torch brazing, and oxygen cutting are lower than levels produced by other welding methods .
Sliney et a l . conducted a study to determine the effectiveness of transparent welding curtains that were designed to block exposure to "blue light." The transparent curtains were most effective in blocking the wavelengths between 400 and 500 nm. These wavelengths are known to cause photochemical injury to the retina. The energy emitted from shielded metal arc welding was determined by van Someren and Rollason using a 4-gauge covered electrode operating at a 280-A current. The relative spectral distribution of emitted optical radiation was 5% in the UV range, 26% in the visible range, and 69% in the IR range.
Various factors can affect the radiation intensity from welding and cutting arcs .
Increasing current flow causes a sharp increase in UV emissions. Gas metal arc welding of aluminum produces much greater UV intensity than gas tungsten arc welding. UV emissions increase by a factor of 10 when using magnesium instead of aluminum as an alloying material. The use of argon gas for shielding significantly increases the intensity of the optical radiation compared with carbon dioxide or helium as a shielding gas. As the amount of fume increases, the amount of radiation is reduced proportionately. When gas tungsten arc welding is performed on aluminum-magnesium alloys, the amount of UV emitted decreases as the arc length increases. Tip size, flame type, and filler metal composition are other variables that affect the amount of UV, visible, and IR radiation produced by oxyfuel welding . Marshall et al. assessed the amount of optical radiation that was generated from carbon arc cutting. The results of those tests demonstrated that other physical agents such as sparks and noise present more serious hazards than optical radiation. The authors stated that the observed low level of optical radiation produced was probably due to the removal of particulate material from the air, which left no material to become luminescent.
IR radiation can be absorbed by a worker's clothing and skin and can elevate the skin temperature and contribute to the body's heat load. Light-colored, loose clothing reduces the heating of the skin.
# b. Electricity
Electrical shock from arc and resistance welding is a common hazard and can be sufficient to paralyze the respiratory system or to cause ventricular fibrillation and death. This risk is highest when equipment is in disrepair (e.g., worn insulation) or when electrical resistance through the welder is decreased (e.g., by sweat or standing in water) . Even minor electrical shocks can cause serious secondary accidents (e.g., muscular reaction to the shock can cause a worker to fall).
# c. Noise
Although high noise levels can occur during several types of welding processes (e.g., torch brazing and chipping), they are more often associated with plasma arcs than with any other . The high noise levels with plasma arc occur from the passage of heated gas through the constricted throat of the nozzle at supersonic velocities. Noise levels have been measured in the 2,400 to 4,800-Hz range and often exceed 100 dBA. Low-velocity nozzles greatly reduce the noise emitted. The use of induction-coupled plasma jets also greatly reduces the level of noise . Levels exceeding 90 dBA have been found in torch brazing operations . Cresswell [1971 described noise levels of only 70 to 80 dBA from torches using argon-hydrogen mixtures; however, nitrogen and nitrogenhydrogen mixtures produced levels of 100 to 120 dBA. The same author also noted that cutting materials up to 50 mm thick did not usually pose a noise problem but that thicker materials produced more intense noise levels (levels not given) that required hearing protect ion.
# d . I on i z i ng Rad i at i on
X-rays are produced as secondary radiation by electron beam welding equipment. The configuration and operating principles of this equipment are similar to those of an X-ray tube . The electrons are generated at the cathode, which is a heated tungsten filament. The electrons are accelerated toward a target by a difference in potential and are focused by using a magnetic field. X-rays are produced when high-speed electrons strike the workpiece, its metal base, or other materials. The intensity and energy of the X-rays are functions of the beam current, the accelerating voltage, and the atomic number of the material on which the beam impinges . X-radiation may be produced in the electron beam gun itself, at the anode, or in the work chamber wherever the beam strikes a surface. The radiation may be produced any time that power is applied to the high-voltage portion of the equipment.
Radiation may be emitted from the welding equipment at vacuum ports, door flanges, or windows, or from motor shaft and power conduit openings .
Nonconsumable thoriated tungsten electrodes are usually used in gas tungsten arc welding. The electrodes may contain 1% to 3% thorium oxide, which may potentially emit alpha radiation . Although the electrodes are considered nonconsumable, they are gradually used up. Breslin and Harris investigated the potential exposure to alpha radiation from thorium during various types of gas tungsten arc welding. Commercially available equipment was used to weld with a 2% thorium oxide electrode; welding operations were performed according to manufacturers' recommendations but without any ventilation. Personal air samples were collected in the operator's breathing zone at the lowest part of the welding helmet. General air samples were also taken at a distance of 1 ft (0.3 m) from the arc. Alpha activity was measured using alpha scintillation counters. No detectable alpha activity was found in the samples. The authors concluded that welding with thoriated tungsten electrodes poses no significant radiation hazard.
# e. Radiofrequency Radiation
Radiofrequency (RF) radiation can be used in tungsten inert gas welding to start or continue an arc between the base metal and a nonconsumable tungsten electrode. The frequency of RF radiation in this application is reported to be less than or equal to 5 megahertz (MHz) with a power output of 20 to 30 kilowatts (kW). Since no one has measured the exposure of welders to electric or magnetic field radiation from this type of welding, potential exposure levels cannot be estimated .
# IV. HEALTH AND SAFETY HAZARDS
# A. Introduction
Welding processes are potentially hazardous because they require intense energy to change the physical state of metals. The chemical changes associated with such energy may result in emissions of various toxic fumes, dusts, gases, and vapors; they may also generate exposures to physical agents that include noise, vibration, heat, electrical current, and infrared (IR), visible, ultraviolet (UV), ionizing, and radiofrequency (RF) radiation.
The degree of risk varies with the method and control measures employed, work practices used, metals and fluxes involved, and duration of exposure permitted. Safety hazards encountered on a daily basis complicate working conditions for welders. These conditions have resulted in both major and minor traumatic injuries and in death. Introduction
Over the past 40 years, a number of animal studies have examined the acute and subchronic effects of welding fumes and the mutagenic potential of total airborne welding emissions (gases plus fumes). However, only one animal study has investigated the carcinogenicity of welding fumes as a result of long-term exposures . In this document, the term "welding emissions" refers to a combination of gases plus fumes. Unless otherwise reported, these exposures were generated from shielded metal arc or gas metal arc we Id i n g .
# b. Acute Effects
In a series of experiments, Titus et a l . exposed groups of animals (1 to 4 cats, 1 to 5 rabbits) for 0.8 to 8.5 hr to iron oxide or to the welding emissions produced during electric arc cutting of iron with iron electrodes. Exposure concentrations ranged from 10 to 350 mg/m^ (0.3-jum particle size) of fumes, which contained mostly ferric oxide. Concentrations above 275 mg/m^ were difficult to maintain, since at these increased concentrations, the particles from the fumes aggregated as rapidly as they were produced. To accentuate the effect of fume exposure, carbon dioxide (1% to 14%) was added to chamber air to increase respiration. An additional four groups of rabbits were exposed to arc cutting gases alone, and two other groups were exposed to ferric oxide alone at concentrations comparable with those contained in the fumes. When exposed to high concentrations of either the arc cutting emissions (320 mg/m^) or gases, animals exhibited severe pulmonary edema, dilation of alveoli, hemorrhage of the lungs, and death. Since higher air concentrations of ferric oxide alone did not cause acute lung pathology or death in exposed animals, the arc cutting gases (unidentified) were considered the probable cause of the observed toxicity. The authors noted that these pulmonary effects induced by the gaseous components of the emissions were similar to those caused by such irritating gases as nitrogen peroxide, ozone, or chlorine.
Senczuk administered 0.5-ml saline suspensions of welding fumes generated from either acid-, basic-, or rutile-coated electrodes into the stomachs of six white female mice (strain unspecified) per treatment group. The type of metal welded was not stated. The suspension from basic electrode fumes produced lethality at lower doses than did suspensions from acid or rutile fumes. The dose capable of killing 50% of the animals within 48 hr after treatment (LD50) was 755, 5,000, or 5,000 mg/kg for suspended fumes generated from basic-, acid-, or ruti le-coated electrodes, respectively. When similar suspensions were intratracheally injected into groups of six white female Wistar rats, the LD5q's for basic, acid, or rutile welding fumes were 132, 762, or 792 mg/kg, respectively. Welding fume composition was analytically determined by an unreported method. The author theorized that the increased toxicity associated with basic electrode fumes was caused by fluorine, which was not present in the other test electrode fumes. Manganese, silicon, and aluminum compounds were considered the toxic components of acid or rutile dusts, whereas sodium and magnesium carbonates and titanium compounds were considered much less toxic. Chromium content was neither determined nor discussed. Kawada and Iwano used several animal species to study the acute lethality of emissions from basic and rutile (ilmenite) electrode welding of a steel (composition undefined) plate. Unknown strains of mature male mice, white rats, rabbits, and guinea pigs were subjected to a 1-hr inhalation exposure to emissions from a 1-min burn with a basic electrode. The group sizes and chamber emission concentrations were unspecified. Since lethality was observed only in the guinea pig, the guinea pig was chosen as the test species for further study. A 1-hr inhalation of emissions from a 1-min burn of a basic electrode produced death within 24 hr in 10 of 12 guinea pigs and in 2 of 10 guinea pigs when exposure was to rutile emissions under the same conditions. Upon sacrifice of the survivors from the group exposed to basic fumes (time unspecified), the collective histopathology for the lungs revealed deposits of fumes, blood stasis, edema, pneumonia, atelectasis, and emphysema. However, when an additional group of guinea pigs was exposed only to the gaseous components of basic electrode emission, no deaths occurred. The disposition of these animals was not stated. Kawada and Iwano also used additional groups of guinea pigs that were intraperitoneally injected with a constant volume of 2 ml of either a water suspension containing 150 mg of basic or rutile fumes or the supernate or insoluble sediment fractions of a similar suspension. The aqueous suspension of basic electrode fumes killed 15 of 15 guinea pigs within 3.5 hr after injection, whereas the suspension of rutile fumes was nonlethal in 6 of 6 treated guinea pigs. Because rutile fumes were not lethal in guinea pigs, no further testing of soluble or insoluble fractions was conducted.
Intraperitoneal injection of the water soluble fraction from basic electrode fumes resulted in the deaths of all six treated animals within 1 hr after injection, but six of six animals survived administration of the water-insoluble fraction. Each active compound present in the water-soluble fraction of basic welding fumes was tested and ranked by decreasing lethal potential as follows: potassium fluoride, potassium acid fluoride, potassium hydroxide, sodium hydroxide, sodium fluoride, and calcium si I icofluoride. Since the water-insoluble metal oxides (aluminum, barium, calcium, iron, magnesium, manganese, silicon, or titanium) in these two fumes were not lethal to injected animals, the authors did not consider them to be toxicologically active.
Hewitt and Hicks exposed male albino SCE strain rats by inhalation to rutile welding emissions at an average concentration of 1,500 mg/m3. The lungs were analyzed with neutron activation to assess tissue concentrations, rates of uptake, and elimination of inhaled metals. Metal uptake in liver and blood was also assessed.
The rutile iron electrode used was coated with limestone, manganese dioxide, kaolin, cellulose powder, and sodium and potassium silicate binders. Two rats were exposed for 30 min, while seven rats were exposed for 4 hr. Tissue concentrations at 24-hr post-exposure were expressed as Mg compound/g of freeze-dried tissue. The rats exposed for 30 min had a statistically significant increase (p<0.05) of iron (1,175 Mg) and cobalt (0.22 m9) in the lung but not chromium (0.01 (jg) or antimony (0.01 ¡xg) when compared with controls. The seven rats exposed for 4 hr had a statistically significant increase (p<0.05) in iron (7,175 jug), cobalt (0.32 p.g), chromium (0.03 ¡¿g), and antimony (0.25 Mg) in the lung. Additionally, the cobalt concentrations in the liver (0.6 m 9) ar|d blood (0.2 Mg) were statistically increased (p<0.05) after a 4-hr exposure when compared to the controls. Microscopic examination of the treated lungs revealed large numbers of particulate-loaded macrophages in the alveoli and alveolar ducts, slight alveolar epithelial thickening, and peribronchial edema. In a subsequent experiment, eight rats were exposed to welding emissions for 4 hr. Pairs of these animals (and pairs of control rats) were killed 1, 7, 28, or 75 days after exposure. The iron, cobalt, chromium, and antimony contents in the lung progressively decreased over the 75-day period.
The histopathological lung changes that were observed within the first 4 hr of exposure returned to normal following 75 days of no exposure. However, macrophages that contained particulate material continued to be present.
# c. Subchronic E ffe c t s
The effects of welding emissions on animals have been summarized in Table IV- 1. Tollman et al. performed an inhalation study in which 2 groups of 12 young adult guinea pigs and 10 young adult white rats were exposed for 4 hr/day, 6 days/week. One group was exposed for approximately 29 weeks to partially filtered carbon arc welding emissions, and the other group was exposed for approximately 33 weeks to oxides of nitrogen only. This was followed by a 1-month nonexposure period for guinea pigs. The type of metal welded and filter used were not reported. Fumes passing through the filter were less than 25 mg/m^ during the total study period. The authors reported that the average concentration of oxides of nitrogen was 107 ppm in the gas phase of the welding emissions. This concentration was comparable to the average concentration of oxides of nitrogen (125 ppm) when administered alone. The investigators found a consistent response in all test groups regardless of the parameter studied. Guinea pigs in both groups had an average loss of 11% to 15% in terminal body weights when compared with their maximum weights attained during the experiment. Similar weight loss data for rats were not given. At the end of 7-1/2 months of treatment, guinea pig mortality reached 67% in the filtered emissions group and 92% in the oxides of nitrogen group, whereas all rats were dead within the first 3.4 months of exposure. Histopathologic examination of tissues revealed the lungs as the primary target organ for both species and all treatment groups. Pulmonary pathology included: epithelial desquamation and necrosis, atelectasis, edema, and pneumonia. The principal differences observed were thicker alveolar walls and more macrophages in the lungs of those animals exposed to filtered welding emissions. No histopathology was specifically cited for the guinea pigs that survived the exposure period. The authors concluded that the effects were primarily due to exposure to oxides of nitrogen rather than to any other component present in carbon arc welding emissions. McCord et al. reported on the inhalation exposure of 24 albino rats and 16 rabbits of both sexes (strains, ages, and numbers of each sex not given) to the emissions produced during shielded metal arc welding (unspecified metal) from electrodes that contained mostly silicon (21%) and titanium (42%) dioxides. An equal number of nonexposed rats and rabbits were used as controls. Exposures were for 6 hr/day, 5 days/week for a total of 46 days. This was followed by 43 days of nonexposure before study termination. The total fume concentration was not given; however, four components accounted for over 97%: iron oxide (79%), manganese oxide (5%), silicon dioxide (8.4%), and titanium dioxide (5.4%). The average chamber concentration of nitrogen dioxide was 20-24 ppm, and the average nitrous oxide concentration was 3 ppm, while the average concentrations of ferric oxide, manganese, and silicon dioxide were 465, 16, and 61 mg/m^, respectively. Titanium dioxide values were not cited. Average weight gains for exposed versus nonexposed groups were 272 g versus 366 g for rabbits and 2.9 g versus 32 g for rats. Siderosis of the lungs was the only biologically significant pathology present in all of the exposed animals sacrificed at the end of the experiment, with the earliest detection of siderosis observed in a rat that died after 22 days of exposure. No silicosis was found in any of these animals.
Byczkowski et a l . reported on the metal concentrations in the lungs of 290 rats and 30 rabbits exposed by inhalation to emissions generated during the melting of basic or rutile electrodes. The effect of exercise on the retention of inhaled metals from rutile welding emissions was also studied in rats. Baseline metal concentrations were determined in an unstated number of animals from each treatment group before the start of the exposure period. Groups of young adult male Wistar rats and 1-year-old albino rabbits (group sizes not specified) were exposed to approximately 60 mg/m^ of basic welding emissions, while a group of rats was exposed to 198-222 mg/m3 of rutile welding emissions.
In addition, one similarly exposed rutile welding group was exercised by being housed in cages that rotated during two of the 3-hr daily exposures. Exposures for the remaining groups were 3 hr/day, 7 days/week for 91 to 95 days for rats and 110 days for rabbits. During the period of time in which the animals were being exposed, an undefined number of surviving animals in each treatment group were withdrawn from exposure for terminal assessment of changes in lung metal content. Final sacrifices occurred 130 days after termination of exposures for rats and rabbits in the basic welding emissions groups and after 182 days for rats in the rutile welding emissions group.
Rats sacrificed after 95 days of exposure to welding emissions from basic electrodes had total lung tissue contents of 0.57 mg fluorine, 4.95 mg manganese, and 223 mg iron. Similarly exposed rabbits sacrificed at the end of 110 days had lower total lung contents of 0.32 mg fluorine, 4.2 mg manganese, and 103 mg iron when compared to the rats. Tracheal tissue concentrations for fluorine in rats and rabbits were five times higher (2.79 mg and 1.76 mg, respectively) than those found in the lung tissue. The groups of rats and rabbits that were exposed to the same basic welding emissions and removed from exposure for 130 days, had up to a 50% decrease in fluorine and iron levels and over an 80% decrease in manganese from those determined after 95 and 110 days. The group of rats exposed to rutile welding emissions had the following total lung metal contents at the end of the 91-to 95-day exposure period: silicon, 0.45 mg; titanium, 0.117 mg; manganese, 0.495 mg; and iron, 9.3 mg. When these values for the rutile exposure group were compared to those in a similarly exposed but exercised group, exercise increased the metal concentrations by approximately 50%. No analysis was performed for lung metal content during the 182 days that followed the termination of exposure. However, unexercised rats withdrawn from rutile fume exposure for 182 days had approximately a 50% decrease in silicon, titanium, and manganese concentrations but only a 23% decrease in iron. Kalliomaki et al. exposed adult male Wistar rats (300+15g) to emissions generated from shielded metal arc welding of either mild steel with basic electrodes or stainless steel with rutile electrodes. The purpose of the study was to determine which metals (iron, manganese, chromium, or nickel) contained in the two types of welding emissions were retained by or cleared from the lung. A total of 52 rats in groups of 2 rats or less was used in 14 treatment and 14 control groups. Each treatment group was exposed to 43 mg/m3 of emissions. Four of the treatment groups were designed to determine retention of metals in animals exposed for 1 hr/day, 5 days/week for 1, 2, 3, or 4 weeks with sacrifice of a treatment group and a control group 24 hr after last exposure. The animals in the remaining 10 groups were exposed for 1 hr/day, 5 days/week for 4 weeks and were evaluated for clearance of metals. Following the last exposure, a treatment group and a control group were sacrificed at the following time intervals: 1, 3, or 8 hr and 1, 4, 8 , 14, 28, 56, or 106 days.
Basic electrode welding of mild steel produced emissions that contained 20% iron and 2.8% manganese by weight but only trace amounts of chromium and nickel (remaining fraction unstated).
In rats exposed to these emissions, the lung tissue retention rates for iron and manganese each became saturated by the third week of exposure with initial retention rates of 28 and 4 jug/g dry lung tissue/hr, respectively. Clearance time was measured as the time required to decrease the tissue load of a metal by 50% (T-j/2 )-These metals had fast and slow clearance times for their curves. Rutile electrode welding of stainless steel produced emissions which contained 4.0% iron, 2.2% manganese, 3.0% chromium, and 0.4% nickel by weight (remaining composition unstated).
In rats exposed to these rutile emissions, the retention curves were linear with initial rates of 4.8 (iron), 2.8 (chromium), and 0.3 (nickel) n q / g dry lung tissue/hr. The retention of manganese reached saturation after 19 hr of exposure, with an initial retention rate of 1.5 ¡ jlg/g dry lung tissue/hr. Slow clearance T -|/2 times were 50 days for iron, 40 days for chromium and manganese, and 30 days for nickel. These metals did not have fast clearance times.
Senczuk used 3-to 4-month-old Wistar rats to study the toxicity of inhaled emissions produced by welding (metal unspecified) with rutile electrodes. A treatment group of 120 male rats was exposed to an average emission concentration of 222 mg/m^ for 3 hr/day for 13 weeks. The control group consisted of 30 nonexposed young adult male rats. Interim sacrifices within the exposure group occurred after 2, 4, 6 , 8 , 11, and 13 weeks, and 2 and 5 weeks postexposure. Similar interim sacrifice intervals were used for the control group with the omission of those during exposure weeks 2, , and 11 and postexposure week 2. Twenty-six weeks after cessation of exposure, the remaining survivors (number unstated) were sacrificed. Mortality within the groups was not reported. Analysis of chamber emissions demonstrated concentrations of 102 mg/m3 ferric oxide, 15.2 mg/m^ silicon, 9.4 mg/m^ manganese, 3.5 mg/m^ titanium dioxide, and 8 mg/m3 oxides of nitrogen. Examination of the growth curves showed that the exposed rats progressively lost 2% body weight during the 13-week treatment period. During the 5 weeks following the 13-week exposure period, their body weight gain was parallel to that of the controls, after which it began to decrease. Twenty-six weeks after the 13-week exposure period, the animals' terminal body weights were compared with their preexposure weights. The results showed that the treated rats had a 2% gain while the controls had a 29% gain. Lung weights (dry) from treated and control rats were approximately equal at the end of the exposure period; however, the lung weights (dry) of the treated rats sacrificed 26 weeks following the exposure period were 18% heavier than those of the corresponding controls. Because the lungs were desiccated for weighing, histopathologic evaluations were not performed. Garnuszewski and Dobrzynski compared the pulmonary effects of inhalation of welding emissions on guinea pigs and rabbits (strain, age, and sex unreported). Two types of electrodes were used to generate the test emissions, but the type of metal welded was not reported. One type, EP52-28p, had high silicon oxide (25.5%) and high ferric oxide (18%) contents, while the other, EP47-28p, had low silicon oxide (7.8%) but high ferric oxide (23%) levels. Comparative pathology of animal tissues was used to determine if exposure to the welding emissions from the low silicon oxide electrode was biologically safer than that from the high silicon oxide electrode.
The first experiment included a total of 72 guinea pigs exposed to high si I icon oxide emissions; half of the group was exposed to emission concentrations of 18 mg/m^, while the other half was exposed to 36 mg/m^. The emissions were generated from the high silicon oxide electrode and the experiments carried out 4 hr/day, 6 days/week for 110 days. A total of 10 guinea pigs comprised the nonexposed (undefined) control group. Although the number of animal deaths per treatment group was not stated, the combined total was 30 of 72. Guinea pigs exposed to either emission concentration had a mixed type of pneumoconiosis (e.g., siderosis coexisting with silicosis as manifested by pneumoconiotic nodules containing collagenous fibers and silica particles). Phagocytes containing silica and iron oxide particles were found in abundance throughout the trachea, bronchi, and interalveolar septa and lumen. The above findings were all concentration-related in intensity.
In the second experiment, 50 guinea pigs and 10 rabbits were exposed to the emissions from the low silicon oxide electrode. The animals were divided into 2 equal groups and exposed 4 hr/day, 6 days/week for 6 months to the same emission concentrations as in the first experiment. Scheduled sacrifices occurred after 6 months of exposure followed by 1 and 4 months of nonexposure. The control groups included 10 guinea pigs and 2 rabbits. During exposure, the combined mortality for both guinea pig exposure groups was 25 of 50. These low silicon oxide exposures produced fewer and milder pulmonary effects than those observed in the animals of the high silicon groups for the first experiment. The changes were limited to the alveolar septa and alveoli which were thin and sometimes ruptured. All exposed guinea pigs were found to have siderosis, but little silicosis.
If nodules were present, they were small and few in number when compared to those induced by high silicon oxide electrode emissions. These small nodules contained fibroblasts, histiocytes, and cells with low amounts of silicon, but did not contain pronounced amounts of collagenous fibers. Because similar histopathology effects were present in tissues from guinea pigs sacrificed after the nonexposure periods, the induced effects were not considered readily reversible. The exposed rabbits had siderosis including slightly thickened interalveolar septa that had few dust-containing cells. Neither collagenous fiber proliferation, silicotic nodules, nor silica particles were observed in rabbit lung tissues. The authors concluded that the emissions from the low silicon oxide electrode were biologically less hazardous than those from the high silicon oxide electrode.
# d. Mutagenicity
Welding emissions from shielded metal arc and gas metal arc welding on mild and stainless steels as well as some of the individual metals contained in the emissions have been tested for their potential to induce adverse mutagenic changes in DNA through use of in vitro (bacterial or cell culture) assays, or in vivo (animal) test systems. In bacterial and cell culture tests, the test agent is added to microbiological or tissue culture media, respectively, while in animal tests the agent is administered to live animals. The in vitro and in vivo tests are used as predictors of a chemical agent's potential to induce cancer through genetic changes in exposed animals or humans.
(1) Mild Steel-Bacterial and Cell Culture Studies Hedenstedt et al. found the fumes to be nonmutagenic from basic or rutile electrode for shielded metal arc welding and the solid wire or powder-filled rutile electrode for gas metal arc welding of mild steel. E . co I i W3110 (pol A+ ) and E . coIi p3478 (a pol A" derivate) and S. typhimurium (TA 100), with and without metabolic activation were used in the study. The weight of fume tested per plate ranged from 100 to 1,250 jug.
Maxi Id et al. also found that the fumes from rutile shielded metal arc and gas metal arc welding on mild steel were nonmutagenic in the TA 98 and TA 100 test strains of S. typhimurium with or without metabolic activation. The dry weight of fume suspended in dimethylsulfoxide (DMSO) solvent and added to each test plate ranged from 0.1 to 8 mg.
Shielded metal arc fume from mild steel welding was also confirmed to be nonmutagenic by Stern et al. following testing in S. typhimurium TA 100 with and without metabolic activation. The types of electrodes used to generate the fume and the weight of fume tested per plate were not reported.
Niebuhr et a l . collected gas metal arc fume from the welding of mild steel when solid nickel electrodes were used. A modified sister chromatid exchange (SCE) assay was used to detect mutations. The presence of nickel in the welding fume induced increases in SCEs that were directly proportional to the amount of nickel biologically available in the test media. Concentrations of water-or serum-soluble nickel that ranged from 2.5 to 10 ptg/mI yielded SCEs that ranged from 7.3 to 9.4/cell compared to a control value of 8.4/cell.
Although mild steel welding fumes devoid of nickel and chromium(VI) compounds were inactive in bacterial mutagenesis assays , the addition of nickel into the fumes produced a slight increase in mutagenic activity in the SCE assay.
Hansen and Stern used the baby hamster kidney cel I (BHK-21) assay to determine the ability of gas metal arc fumes generated from welding with a pure nickel wire electrode to transform colonies.
In addition, pure nickel oxides, water soluble nickel acetate, and water insoluble nickel subsulfide were tested. They found that welding fumes and all the tested nickel compounds transformed the BHK-21 cell line.
(2) Stainless Steel (a) Bacterial and Cell Culture Studies Hedenstedt et al. studied the mutagenic potential of fumes generated during either shielded metal arc welding (rutile electrodes) or gas metal arc (solid wire electrodes) welding of stainless steels in E . coIi and S. typhimurium bacterial test systems. E . coIi W3110 (pol A+ ) and E . coIi p3478 (a pol A-derivate), and S. typhimurium (TA 98 and TA 100 strains) were used. All bacterial test systems were studied with and without a liver microsomal metabolizing system (S-9 mix). Both types of welding fumes were mutagenic in the absence of S-9 mix, regardless of bacterial strain employed; however, at equal plate concentrations shielded metal arc welding fumes were more mutagenic than gas metal arc fumes.
In addition, all water soluble fume fractions were mutagenic. The magnitude of these mutagenic effects were proportional to the degree of water solubility of the hexavalent chromium compounds present in the two types of stainless steel welding fumes.
The hexavalent chromium content in shielded metal arc welding fumes was significantly higher (10 to 1000 times) than that present in gas metal arc fumes.
In S. typhimurium, metabolic inactivation of the mutagenic effects for shielded metal arc fumes required both S-9 mix plus an NADP generating system. For all bacterial strains tested, similar inactivation of gas metal arc fumes required the S-9 mix alone. The authors suggested that the mutagenic potential for both types of stainless steel welding fumes may have been due to their water soluble hexavalent chromium content. However, if different chromium compounds were present in shielded rather than gas metal arc fumes, it would explain why they had dissimilar metabolic requirements for mutagenic inactivation.
Maxi Id et al. investigated the mutagenic potential of stainless steel welding fumes by utilizing TA 98 and TA 100 strains of S. typhimurium with and without metabolic activation. The dry weight of shielded metal arc welding fume suspended in DMSO solvent and added to each test plate ranged from 0.1 to 8 mg. Based on the weight of fumes required to double the mutation frequency in these bacterial strains, with or without a liver microsome metabolizing system (S-9 mix), shielded welding fumes were more mutagenic than gas metal arc fumes. The mutagenic activity was reduced for both types of fumes when S-9 mix was used. Regardless of the state of activation, the number of mutations induced by these fumes was increased in a dose-related manner. The authors stated that the amount of fumes produced by shielded metal arc welding was 3 to 6 times greater than that produced by gas metal arc welding. Fume analyses revealed that the fumes from shielded metal arc welding contained 330 times more soluble chromium (valence state unspecified) than did gas metal arc welding fumes.
The amount of welding fumes required to double the mutation rate of the S. typhimurium TA 100 (LT2) bacterial strain was also studied by Pedersen et al. . The activity was equalized on the basis of the chromium content of aqueous extracts (assumed to be chromium) of shielded and gas metal arc welding fume versus a chromium(VI) positive control solution (sodium dichromate). The authors did not define the types of welding electrodes used to generate the fume. They established that 9 ¿¿g of watersoluble chromium(VI) in shielded metal arc welding fumes, 5 /j.g of water-soluble chromium(VI) in gas metal arc fumes, and 10 ftg of water-soluble sodium dichromate (chromium) per plate caused mutations to double. The authors concluded that the mutagenic potential of stainless steel welding fumes can be completely accounted for on the basis of their chromium(VI) content. Stern et al. used the S. typhimurium TA 100 assay in dose-response experiments and factorial design studies to show that the mutagenic activity present in welding fumes is caused by its soluble chromium(VI) content. When mutagenic activity was expressed as revertants/mg/plate, shielded metal arc welding fumes were more mutagenic than gas metal arc fumes. However, when it was expressed as specific activity (number revertants/^g soluble chromium(VI)/plate), gas metal arc fumes were the more mutagenic of the two types of fumes. The authors concluded that the soluble chromium(VI) content of gas metal arc fumes could be partially reduced to insoluble chromium(VI), and to chromium(111) when reducing substances (aluminium and magnesium) were present. When compared to gas metal arc fumes, the specific activity of chromium(VI) in shielded metal arc welding fumes was reduced by components unique to these fumes. They also observed that when fumes containing chromium(VI) were suspended in water, chromium(VI) was contained in both the water soluble and insoluble phases; however, only the water soluble phase was mutagenically active. The authors stated that data from experiments with synthetic fumes demonstrated that neither the manganese nor the nickel content of stainless steel welding fumes was mutagenic nor did these metal compounds act in an antagonistic or synergistic manner when in the presence of fumes containing chromium(VI). Hedenstedt et al. used mammalian cells-the V-79 Chinese hamster cell assay-to detect the mutagenic potential (6-thioguanine resistance) of stainless steel welding fumes. The water soluble fraction of rutile electrode fumes from stainless steel welding produced a significant increase (p<.01) in the number of 6-thioguanine resistant mutants when compared to the negative controls. Koshi also used a mammalian cell assay-a pseudo-diploid Chinese Hamster cell line-to investigate the mutagenic effect of shielded metal arc versus gas metal arc welding fumes from mild and stainless steels, respectively. This assay was used to determine the frequencies of SCEs.
In addition, Koshi studied the metallic composition of these two types of generated fumes and their solubilities in water and in culture medium. Koshi found dose-related increases for SCEs for both shielded and gas metal arc welding fumes; however, it took 50 times more weight for the gas metal arc fumes than for shielded metal arc fumes to produce a doubling of the control background rate (5.3 SCE/cell). The lower potency of gas metal arc fumes was directly proportional to the decreased water solubility of its chromium(VI) component. When the frequency of SCEs/cell was compared for equivalent chromium contents, the authors stated chromic acid, a chromium(VI) component, was the most active followed by shielded metal arc fumes and then gas metal arc fumes; however, they presented other data which support equal activities also. Since water soluble nickel, manganese, or chromium(lll) compounds present in the two types of fumes were mutagenically inactive, the authors concluded that the active mutagen was chromium(VI). The induction of increased chromosome aberrations in the form of chromatid gaps and chromatin exchanges were similarly ascribed to the chromium(VI) content in both types of welding fumes tested.
# (b) Animal Studies
Knudsen performed a mammalian spot test in female mice to detect genetic mutations through changes in hair color. T-stock males (homozygous for four recessive coat-color mutations) were mated with C57BL females (homozygous wiId-type for the mutations carried by T-stock males). The pregnant C57BL mice were administered suspensions of shielded metal arc welding fumes from stainless steel or doses of potassium chromate (positive control) containing approximately 0.5 to 1.5 times the chromium(VI) content of the fume fraction tested. The type of electrode used for fume generation was not described. The mice were intraperitoneally injected with the test materials on days 8 , 9, and 10 of gestation. The offspring were checked for spots of recessive hair color at the end of 2, 3, 4, and 5 weeks of age. The shielded metal arc welding fumes produced the same number of spots as approximately equivalent doses of chromium(VI). The authors suggested that the positive mutagenic effect induced by shielded metal arc welding fumes was primarily caused by its chromium(VI) content.
# e. Carcinogenicity
Reuzel et a l . investigated the toxicity of welding fumes intratracheally instilled into the lungs of hamsters. Fumes were produced either from shielded electrodes used during metal arc welding or from wire metal electrodes used during gas metal arc welding of stainless steel. The welding fumes were collected onto filters. Each of five treatment groups contained 35 male Syrian golden hamsters. Dosage quantities of fumes were suspended in 0.2 ml of saline for intratracheal injection. The treatment concentrations were 0.5 and 2.0 mg for two shielded welding groups, 2.0 mg for one gas metal arc welding group, 0.1 mg calcium chromate for a "positive control" group (calcium chromate has not been shown to be carcinogenic in this test system), and 0.2 ml of saline for the unexposed control group. The treatment groups were dosed once weekly for 56 weeks, except that the 2.0 mg shielded welding group developed early body weight loss and a few hamsters died; therefore, from weeks 26 through 56, single doses were injected only on every fourth week. Autopsies for all groups were performed after 100 experimental weeks. The chromium contents of the fume from shielded metal arc and gas metal arc welding fumes were 5% and 0.4%, respectively. The nickel content in shielded metal arc fumes was 0.4% while that for gas metal arc fumes was 2.4%. Although not stated by the authors, the total amount (mg/hamster) of chromium injected during the study was calculated as 1.4 (low dose) and 3.3 (high dose) for the shielded metal arc welding fume groups; 0.45 (low dose) and 5.6 (high dose) for the gas metal arc fume groups, and 1.85 for the calcium chromate positive controls.
Although lung weights of hamsters treated with either 2 mg shielded metal arc fumes or 2 mg gas metal arc fumes were significantly heavier (level unstated) than control lung weights; the heaviest lung weights occurred in the gas metal arc fume group. Regardless of treatment or dose level, hamsters that died and those that survived through the nonexposure period following treatment differed little in histopathology or in the number of dust particles present in lungs. This indicated that little recovery had occurred during this period. However, those hamsters in the 2 mg treatment group exposed to gas metal arc welding fumes had the greatest degree of induced pulmonary pathology. This included moderate to severe nonspecific pneumonia, slight to moderate interstitial pneumonia, moderate alveolar bronchiolization, and slight emphysema. Animals dosed with 0.5 mg shielded metal arc welding fumes and those that received calcium chromate showed similar but less pronounced changes.
Two lung cancers were found in the shielded metal arc welding treatment groups. One cancer (a we Il-differentiated combined epidermoid and adenocarcinoma type) was found in the lung of an animal that was treated with 2.0 mg of shielded metal arc fumes and sacrificed at the end of the 100-week study. The second cancer (an anaplastic tumor, probably a carcinoma, which had metastasized to the surrounding lung parenchyma and mediastinum) was found in the lung of a hamster that died after one year of treatment with 0.5 mg of shielded metal arc fumes. The investigators believed these two tumors were induced by the shielded metal arc welding fumes and were toxicologically significant because neither noncancerous nor cancerous tumors had been observed either in the concurrent controls or in nearly 800 historical laboratory controls. Because pulmonary tumors were not present in the positive control (calcium chromate) animals, the investigators theorized that compounds other than chromium in welding fumes were probably responsible for the induction of the cancers in the shielded metal arc welding fume groups.
# f. Summary-Animal Toxicity
Shielded metal arc welding fumes and gases have caused severe acute lung damage (e.g., edema, hemorrhage, pneumonia, and atelectasis) . Basic electrode welding of nonstainless steels that did not contain chromium or nickel has produced fumes that are potentially more lethal than those produced by welding of the same metal with acid or rutile electrodes .
It appears that the increased toxic potential of the fumes generated while welding with basic electrodes can be ascribed to the high fluoride content that is absent in either acid or rutile-type electrodes.
Subacute toxicologic studies have demonstrated that irreversible chronic lung disease can result in animals repeatedly exposed by inhalation to welding fumes and gases. Tollman et a l . investigated the pulmonary effects in animals repeatedly exposed to welding gases (oxides of nitrogen). Concentrations which induced mortality also caused lung tissue damage (edema, atelectasis, pneumonia, and necrosis).
In addition, the subacute effects of total welding emissions (gases plus fumes) generated during the welding of nonstainless steels were studied in animals by Garnuszewski and Oobrzynski and Senczuk .
In general, these investigators found that exposure of animals to welding emissions induced premature mortality, suppression of weight gain, fibrotic lung disease, and pneumoconiosis in surviving animals. Siderosis and silicosis resulted from exposures to emissions which contained iron or silicon, respectively. This fibrotic pulmonary pathology was found irreversible during nonexposed periods despite recovery times that sometimes exceeded the length of treatment.
Pulmonary deposition and clearance rates for metals contained in emissions generated during the welding of nonstainless and stainless steels were investigated in animals by several authors (McCord et al. 1941, Byczkowski et a l . 1970Kalliomaki et a l . 1983). They found the rates of metal deposition in exposed lungs to be proportional to the metal contents in the emissions. These deposition rates were further increased in animals with concomitant exercise during exposure. For some metals with slow clearance rates, even prolonged periods of nonexposure did not permit complete elimination.
In a wide variety of in vi t ro and in vivo mutagenesis assays, mild steel welding fumes had little to no mutagenic potential, whereas stainless steel welding fumes were consistently mutagenic.
Shielded metal arc welding of stainless steel produced three to six times more fumes "per mass of weld metal" than gas metal arc welding. The shielded metal arc welding fumes were more water soluble than the gas metal arc welding fumes . The water-soluble fraction of these fumes was shown to be mutagenically active , but the water-insoluble fraction had no significant mutagenic activity . Assays have demonstrated that much of the mutagenic activity may be ascribed to the chromium(VI) in the water-soluble fraction . However, when the mutagenic potentials for these fumes were compared on an equivalent chromium(VI) basis, gas metal arc welding fumes produced four times more mutations in bacteria than did shielded metal arc welding fumes . Yet SCE data were equivocal for these two types of fumes .
In addition, it appears that compounds other than chromium(VI) could also be active in the water soluble fractions of fumes generated from the two welding processes. This is based on the fact that when the water soluble fractions of both fumes were tested in a metabolically activated S. typhimurium mutagenicity assay, only shielded metal arc fumes lost their metabolic potency .
One 2-year carcinogenicity study has been reported for Syrian golden hamsters that were intratracheally injected with saline suspensions of stainless steel welding fumes . Lung cancer was observed in one animal from each of the two dose groups that were intratracheally injected with shielded metal arc welding fumes. No cancers were observed in the gas metal arc fume treatment group or the calcium chromate, saline, and historical control groups. Despite the fact that there were only two cancers observed, the authors concluded that these tumors were biologically significant based on the absence of tumors in the calcium chromate (positive control) group and the concurrent and historical nonexposed control groups. However, some question exists concerning calcium chromate being considered as a positive control since:
(1) no published experimental data shows the induction of any kind of cancers in hamsters when calcium chromate is intratracheal ly administered, and ( 2) the number of animals and dose used for the calcium chromate positive control group may not have been large enough to detect a positive carcinogenic response in these animals.
# Hunan Toxicity a. Pulmonary Effects
This section evaluates case reports and epidemiologic studies that document the adverse respiratory effects reported for workers who are associated with various types of welding processes. The studies are presented in order of the severity of the effects they report, beginning with those that discuss the acute effects associated with exposure to welding fumes and gases (e.g., metal fume fever and pneumonitis) and ending with studies that suggest a risk of respiratory cancer. The data from these investigations are summarized in Tables IV-2, IV-3, and IV-4. Although many of the studies have shortcomings (e.g., the absence of information on types and concentrations of specific chemical agents or on smoking habits), they collectively demonstrate the consistency of the many respiratory diseases in welders.
# (1) NonmaIi gnant PuImonary D i seases (a) Metal Fume Fever
Metal fume fever is an acute respiratory disease that is usually of short duration; it is caused by the inhalation of metal oxide fumes that are typically 0.2 to 1.0 /¿m in particle size (Papp 1968). Although several metals are In addition, it appears that compounds other than chromium(VI) could also be active in the water soluble fractions of fumes generated from the two welding processes. This is based on the fact that when the water soluble fractions of both fumes were tested in a metabolically activated S. typhimurium mutagenicity assay, only shielded metal arc fumes lost their metabolic potency .
One 2-year carcinogenicity study has been reported for Syrian golden hamsters that were intratracheally injected with saline suspensions of stainless steel welding fumes . Lung cancer was observed in one animal from each of the two dose groups that were intratracheally injected with shielded metal arc welding fumes. No cancers were observed in the gas metal arc fume treatment group or the calcium chromate, saline, and historical control groups. Despite the fact that there were only two cancers observed, the authors concluded that these tumors were biologically significant based on the absence of tumors in the calcium chromate (positive control) group and the concurrent and historical nonexposed control groups. However, some question exists concerning calcium chromate being considered as a positive control since:
(1) no published experimental data shows the induction of any kind of cancers in hamsters when calcium chromate is intratracheal ly administered, and ( 2) the number of animals and dose used for the calcium chromate positive control group may not have been large enough to detect a positive carcinogenic response in these animals.
# Hunan Toxicity a. Pulmonary Effects
This section evaluates case reports and epidemiologic studies that document the adverse respiratory effects reported for workers who are associated with various types of welding processes. The studies are presented in order of the severity of the effects they report, beginning with those that discuss the acute effects associated with exposure to welding fumes and gases (e.g., metal fume fever and pneumonitis) and ending with studies that suggest a risk of respiratory cancer. The data from these investigations are summarized in Tables IV-2, IV-3, and IV-4. Although many of the studies have shortcomings (e.g., the absence of information on types and concentrations of specific chemical agents or on smoking habits), they collectively demonstrate the consistency of the many respiratory diseases in welders.
# (1) NonmaIi gnant PuImonary D i seases (a) Metal Fume Fever
Metal fume fever is an acute respiratory disease that is usually of short duration; it is caused by the inhalation of metal oxide fumes that are typically 0.2 to 1.0 /¿m in particle size (Papp 1968). Although several metals are Respiratory distress, fever, c h ills , and pulmonary edema occurring over a period of several days and sometimes resulting in death.
(Continued) I t was estimated that 10% more welders smoked than did members of the control group (Swedish male population). 1.15n (Continued)
Logistic analysis indicating a s t a t is t ic a lly sign ifican t interaction observed between welding and y e a r-firstemployed for lung cancer. ' Analysis of welders for lung cancer risk using internal non-exposed comparison group and two types of regression analysis. A total of 137 lung cancer deaths (50 welders, 87 controls). m Logistic analysis indicating a s t a t is t ic a lly sign ifican t interaction between cumulative exposure of welders and lung cancer. n Cox regression analysis indicating elevated lung cancer risk among welders when analyzed by cumulative exposure.
# No
# Yes
x Proportional mortality ratio. Y SMR adjusted for the welder's incidence of smoking, which was 22% higher than that expected in the general population. Mean age of death for these cases was several years older than that for controls. capable of causing this disease, exposure to zinc oxide has been the most common cause in welders (Drinker 1922;Drinker et al. 1927). The clinical signs and symptoms of metal fume fever resemble those of an upper respiratory infection such as influenza, acute bronchitis, or pneumonia, or an upper gastrointestinal infection (Papp 1968). Chills, shivering, trembling, nausea, and vomiting may occur (Rohrs 1957). The attack usually lasts 6 to 12 hr and in some instances up to 24 hr. Weakness and mild prostration follow but recovery is usually complete.
With repeated exposure, an increased resistance develops but this apparent tolerance is lost within a short time (e.g., during a weekend).
The attacks tend to be more frequent and prevalent on Mondays (Drinker 1922;AGA 1978).
Although other reports exist, the studies of Ross and Johnson and KiIburn are typical examples of symptomatic effects reported in welders.
Ross reported a case of metal fume fever in a shielded metal arc welder exposed to mixed fumes. Although the covered electrode contained primarily nickel, the fume contained iron, calcium, fluoride, manganese, silica, titanium, aluminum, copper, nickel, and traces of other metals.
The welder experienced a severe headache and felt cold and shivery.
The next day he experienced tightness of the chest, profuse sweating, and unusual thirst.
Chest examination revealed wheezing.
His temperature varied between 99.5° and 101.5°F (37.5° and 38.6°C).
On the basis of occupational history and clinical findings, he was diagnosed as having metal fume fever complicated by pneumonia and was removed from further exposure. Two months later he was completely recovered and returned to work. Johnson and KiIburn described the illness of a 30-year-old male Caucasian who had welded for 9 years and who became ill following torch brazing. Several filler metals that contained zinc, cadmium, copper, or mild steel were used in the process. To assist in the diagnosis, the welder was asked to braze with a silver-based filler metal containing 24% cadmium.
Shortly after he started to weld, he complained of eye irritation and headache.
The worker's blood leukocyte count increased 6 hours after exposure and peaked at 13 hours (increase not reported).
Nine hours after onset of exposure, he developed muscular pain, chills, feverish feelings, headache, backache, chest tightness, malaise, and shortness of breath.
Ten hours later, his body temperature rose and peaked at 100°F (37.7°C) for about 13 hours. A chest radiograph taken 13 hours after exposure indicated the presence of nodular densities that were not apparent in radiographs taken before exposure or after recovery (time of examination not given).
As a result of these observed effects, the welder discontinued brazing with silver-based filler metals; a 6-month follow-up examination revealed no further subjective symptoms.
The authors concluded that cadmium, which was present in the silver-based filler metal the welder was using, was the causative agent in this case of metal fume fever.
# (b) Pneumon i t i s
Pneumonitis and pulmonary edema have been frequently reported among welders who use various types of welding processes (e.g., gas and shielded metal arc, silver brazing, and oxyacetylene) in which exposures to the following have been identified:
nitrogen dioxide (Maddock 1970;Mangold and Beckett 1971), ozone (Molos and Collins 1957; Klein feId et al. 1957; Challen et a 1 . 1958), cadmium fumes (Patwardhan and Finckh 1976;Blejer and Caplan 1969;Townshend 1968), chromium and nickel fumes (Jindrichova 1976), and aluminum and iron fumes (Herbert et al. 1982).
# (i) Exposure to Metal Fumes
Cases of acute cadmium fume pneumonitis and death have been reported among welders who were exposed to cadmium fumes by either brazing with siIver-cadmium alloy or cutting or welding cadmium-coated metal in poorly ventilated areas (Christensen and Olson 1957;Beton et al. 1966;Patwardhan and Finckh 1976). Beton et al. reported the death of a welder who was cutting cadmium-plated bolts with an oxyacetylene torch in a confined space.
Although exposure measurements for cadmium fumes were not taken, the authors estimated that exposure to cadmium oxide may have averaged 8.6 mg/m^ based on the amount of cadmium oxide found in the welder's lungs during a postmortem examination. Patwardhan and Finckh reported on another fatality that occurred in a 38-year-old man who was exposed to cadmium fumes while welding handles onto cadmium-plated drums.
No respiratory protection or local exhaust ventilation was used.
He developed respiratory distress, fever, and chills the first night after exposure.
On the third day of his illness, he was admitted to the hospital, where chest X-rays revealed heart enlargement and pulmonary edema. He died of cardiac arrest approximately 3-1/2 days after exposure to cadmium fumes.
Postmortem examination revealed lung changes consistent with pulmonary edema and diffuse congestion of alveolar capillaries.
The liver contained 0.23 mg cadmium and the lungs contained 0.15 mg cadmium per 100 g of wet tissue. Townshend reported on a 4-year evaluation of a 51-year-old welder who had suffered from acute pneumonitis following exposure to fumes from the welding of a siIver-cadmium alloy.
On the day of the incident, the welder had been using an argon arc to weld plates composed of an alloy of 91% silver and 9% cadmium. The night after exposure, he developed a burning pain in the chest, dyspnea, and dry cough and was hospitalized.
The first chest radiograph was taken 23 days after the incident and showed extensive bilateral shadows, suggesting severe pulmonary edema. Eight weeks after the incident, extensive patchy shadowing was still evident.
For 6 months after the exposure, lung function tests showed a progressive improvement in the forced vital capacity (FVC) to just under 80% of the predicted value, after which there was no further improvement.
After 4 years, the chest X-ray showed faint nodulation.
No information on smoking habits or exposure concentrations were reported. Jindrichova and Herbert et a l . reported on pneumonitis that occurred in welders exposed to fumes composed of various types of metals. Jindrichova used nose, throat, and neurologic examinations and chromium determinations from the urine to study 31 welders who welded with shielded metal arc on metals containing chromium. These welders were compared with 26 workers who were not exposed to welding fumes or chromium.
All welders were divided into three groups.
Group 1 consisted of 9 welders who spent about 13% of their time working with electrodes containing chromium.
Group 2 consisted of 11 welders who spent half of their time using electrodes containing either 18% chromium and 9% nickel, or 23% chromium and 19% nickel.
Group 3 consisted of 11 welders who used electrodes containing 19% chromium and 9% nickel for 70% of their welding time. Welders in Group 3 were exposed to a concentration of 0.75 m g / m^ of chromium (0.62 mg/m3 soluble chromium) oxide measured inside a container (1.1 x 3.3 m) that had no local exhaust. The same work performed with local exhaust ventilation produced a chromium concentration of 0.16 mg/m3 (0.12 m g / m^ soluble chromium(VI) oxide. No exposure data were given for Groups 1 and 2, but chromium exposures for Group 2 were reported to be the same as for the control group.
Group 1 had no evidence of chronic bronchitis, but one welder had a chronic atrophic rhinitis with acute nosebleeds.
In Group 2, one welder with 25 years of experience had pulmonary fibrosis associated with siderosis.
In Group 3, all of the welders had coughs and respiratory problems.
Seven of the 11 welders smoked.
In Group 3, erosion of the nasal septum was found in 35% of the welders, atrophic rhinitis in 54%, pharyngitis in 45%, chronic laryngitis in 11%, and bronchitis in 72%.
The findings of nasal erosion in Group 3 were consistent with chromate-induced lesions.
Concentrations of chromium in urine (122-128 fxg/\i ter of urine) for welders in Group 3 were significantly higher than either the control group or Groups 1 and 2 (concentrations not reported).
Although these differences were reported to be statistically significant, no statistical methods were discussed.
Herbert et a l . described chronic interstitial pneumonitis in a 35-year-old male electric arc welder who had been employed as a welder for 16 years.
A biopsy of the lung revealed unspecified quantities of iron and aluminum particles and occasional asbestos bodies.
Chest X-rays revealed bilateral basal infiltrates with a more discrete opacity on one side. Lung function tests showed diminished forced expiratory volume (FEV), FVC, and total lung capacity.
The welder had smoked for a short period but had not smoked for the past 20 years.
No exposure data were reported.
# (11) Exposure to Gases
Cases of pneumonitis and acute pulmonary edema in welders have been attributed to the inhalation of nitrogen dioxide and ozone .
Mangold and Beckett reported on two silver brazers who were assembling a cupronickel firemain in the overhead of a 2-by 3-by 4.6-m storage compartment aboard a ship. The workers used a "silver solder" containing 80% copper, 15% silver, and 5% flux.
The flux contained 27% potassium fluoride and 72% potassium borate.
No local exhaust ventilation was used. Respiratory irritation forced the men to stop working after 30 min, and both were hospitalized 6 to 8 hr later with acute pulmonary edema and lung damage.
One worker returned to work in a few days, whereas the other retired because of respiratory impairment. Reconstruction of the event indicated that no cadmium-bearing solders were used but that nitrogen dioxide concentrations increased from 0.38 to 122 ppm in 30 min. Maddock reported a fatality resulting from pulmonary edema in a boilermaker who used two oxyacetylene torches with multiple jets to repair a rudder post in an enclosed compartment.
He worked for several hours without complaint but developed a cough that evening.
The worker was admitted to a hospital and died the following day. Death was attributed to pulmonary edema resulting from nitrogen dioxide poisoning.
Reconstruction of the event revealed that a blower had dispersed the fumes throughout the compartment instead of ventilating it. The nitrogen dioxide concentration was found to exceed 20 ppm within 3 min of lighting the torches.
The boilermaker had been exposed to nitrogen dioxide at an estimated concentration greater than 100 ppm.
Case reports described by Molos and Collins , KleinfeId et al. , and Challen et al. document how pneumonitis can occur from the inhalation of ozone during argon-oxygen shielded and gas metal arc welding.
Molos and Collins described respiratory irritation in a welder who performed argon-oxygen shielded gas metal arc welding on mild steel tanks using a mixture of 98% argon and 2% oxygen.
From time to time, the welder and other workers complained of respiratory and eye irritation. Occasionally, the irritation became so severe that welding had to be discontinued.
The welder continued to complain of discomfort and described symptoms of chest cramps, fatigue, headaches, impaired appetite, shortness of breath, difficulty in sleeping, and a persistent cough with occasional blood-tinged sputum. The mean ozone concentration was 2.6 ppm during welding activities.
Substitution of pure argon or carbon dioxide eliminated worker complaints, but the resulting welds proved to be unacceptable and gas shielded metal arc welding was discontinued.
Pneumonitis was also reported by KleinfeId et al. in eight welders who used gas metal and gas tungsten arc welding machines that were located in a corner of a room measuring 60 by 27 by 3 m. No supplementary ventilation was provided.
The work was performed on various metal parts that contained nickel.
The ozone concentration in the breathing zones of the welders was 9.2 ppm; nickel carbonyl and oxides of nitrogen were not detected.
A trichloroethylene degreaser was located about 15 m from the welding area, but air measurements were negative for phosgene, a photodecomposition product of trichloroethylene. One welder was admitted to a hospital with pulmonary edema an hour after leaving work.
Chest X-rays revealed diffuse peribronchial infiltration consistent with multilobular pneumonia. He remained in critical condition for 2 days with persistent pulmonary congestion, and he recovered after weeks.
Two of the eight welders developed dyspnea, and X-ray examination revealed scattered radiographic densities over both lung fields. Both workers were hospitalized and recovered within 9 days.
Four of the remaining five welders complained of severe headaches and throat irritation.
Challen et a l . also described symptoms of upper respiratory tract irritation in 11 of 14 welders who were exposed to ozone at concentrations of 0.8 to 1.7 ppm while performing gas tungsten arc welding on aluminum.
These symptoms ceased when the concentrations of ozone were reduced to approximately 0.2 ppm; no mention of aluminum concentration was made.
# (c) Pneumoconiosis, Including Siderosis
In 1936, clinical, radiographic, and pathologic changes in welders' lungs were first described by Doig and McLaughlin .
They reported nodulations in the lungs of eight electric arc welders employed for 7 to 12 years. Similar findings were reported 2 years later on a group of 26 electric welders who used bare metal electrodes and were exposed to iron oxide. Microscopic examination of a lung tissue biopsy from 5 of the 26 welders revealed no parenchymatous changes or fibrosis, but it did reveal a large quantity of iron deposited in the bronchi, the lymphatic vessels, and the alveolar septa-a condition that is characteristic of siderosis.
Numerous other reports described similar findings of asymptomatic, benign, and radiologically detectable lung changes attributed to the deposition of iron oxide fume particles in the lung (Britton and Walsh 1940;Sander 1944;Sander 1947;Doig and McLaughlin 1948;Mignolet 1950). Although no exposure conditions were reported in these studies, the respiratory effects noted were in electric welders who were employed before 1950, when bare metal electrodes were primarily used.
To a large extent, bare metal electrodes have been replaced by covered electrodes.
In addition to iron, covered electrodes often contain silicon, silicates, fluorides, titanium, manganese, copper, and other metals.
With the increased use of covered electrodes, there have also been increases in reports of fibrosis, respiratory impairment, and active lesions at the site of accumulation of iron particles in the lungs.
The following reports are representative of such observations in welders exposed to fumes of mixed composition. Dreesen et al. reported an investigation on the health status of arc welders in steel ship construction 90 from seven shipyards.
Medical examinations were made of 4,650 workers, 70% of whom were welders.
Less than 6% of the welders had more than 3 years of shipyard experience. The study population was divided into three groups: welders (Group 1); persons who did not have a clearly defined welding or nonwelding work history (Group 2); and nonwelders, including electricians, machinists, and sheet metal workers who did not have an exposure to welding fumes (Group 3). Arc welder's siderosis was diagnosed in 61 (3%) of the welders in Group 1 and in 10 (3%) of the persons in Group 2. All welders in Group 1 had a lower mean systolic blood pressure that was unrelated to age and no appreciable difference in the hematocrit and erythrocyte sedimentation rate.
Approximately 25% of the welders had slag burns or scars.
Welders (Group 1) had approximately the same visual acuity as those persons in Groups 2 and 3 when the data were adjusted for age.
Conjunctival irritation was slightly more prevalent among welders when compared to the other two groups.
Greater incidences of nasal congestion, pharyngitis, and upper respiratory symptoms were reported in welders from Group 1, with tobacco-using welders in this group showing even greater incidences; however, these differences were not reported to be statistically different when compared to those persons in Groups 2 and 3.
In the chest X-rays of welders, a slight increase in lung field markings was observed as length of welding experience increased.
A total of 1,761 welding fume samples were collected and analyzed for iron and total fume.
Zinc was evaluated in 278 and lead in 25 of these samples.
Iron fume concentrations in excess of 20 mg/m^ (>30 mg/m^ expressed as ferric oxide) were found in all welding locations.
The highest average iron and total fume concentrations were found in confined spaces where no ventilation was installed.
Zinc concentrations in excess of 12 mg/m^ (>15 mg/m^ expressed as zinc oxide) were reported. No exposure data were given for total fume or lead.
To determine the frequency of siderosis, Mignolet examined and assessed the medical histories of 216 workers who were classified into the following groups:
32 oxyfuel gas welders, 99 oxyacetylene cutters, and 85 arc welders. These groups were compared with 100 workers selected from other occupations; the types of occupations and their potential for exposure to welding fumes were not stated. The number of abnormal X-rays was much higher among arc welders (61%) than among the oxyacetylene cutters (41%), the oxyfuel gas welders (18%), and the comparison group (17%). The changes included pleural adhesions, distinct diffuse sclerosis, and enlarged hilar shadows.
The changes were attributed to the inhalation of iron oxide and other metals from the coverings of electrodes.
In all cases, the siderosis was a localized sclerosis, not granular.
Based on these findings, the author concluded that arc welding was more hazardous than oxyacetylene cutting and oxyfuel gas welding.
Marchand et a l . and Attfield and Ross have likewise reported on the radiological examination of arc welders.
Marchand et a l . reported on the incidence of pneumopathy in 402 arc welders.
Of this total, 192 had worked for 5 to 10 years, 137 had worked for 11 to 15 years, 54 had worked for 16 to 25 years, and 19 had worked for more than 25 years.
Pneumoconiosis was radiological ly demonstrable in 25 (7%) of the 402 welders, with 13 of the 25 cases found in the group that had worked for 11 to 15 years (the remaining 12 cases not identified). Of the 25 cases of pneumoconiosis, 7 (6 of which were in the group exposed for 11 to 15 years) were classified as siderosis.
Attfield and Ross studied radiological abnormalities in 661 electric arc welders who were engaged in many types of arc welding, including gas metal arc and gas tungsten arc processes.
No exposure data were given, but 264 (40%) of the welders said they had worked near locations where asbestos was being used. Results from radiological examination of the welders indicated that 53 (8%) of them had small rounded lung opacities.
Of those 53 welders, 41 (78%) had opacities that measured from 1.5 to 3 mm in diameter.
One film showed lung opacities with diameters of 3 to 10 mm, while the balance of the films revealed opacities that ranged from just visible up to 1.5 mm in d i a m e t e r .
The clinical findings reported by Meyer et al. of a 55-year-old arc welder who had been employed at a shipyard for 24 years were consistent with the findings previously reported by Dreesen et a l . on other shipyard welders.
The welder had worn a welding helmet only intermittently and frequently worked in confined areas. Both ferrous (cast, zinc-coated, and stainless) and nonferrous (aluminum, cupronickel, copper, brass, and bronze) welding materials were used.
All electrodes apparently were covered.
For 8 to 10 years, the welder's chest X-rays demonstrated mottling, and a lung lobectomy revealed dark pigmentation on the visceral pleural surface.
The iron concentration (10 jug/m I of tissue) was 20 times the normal amount, and the silica concentration (2.8 ng/ml of tissue) was 30% of the total mineral content.
Mild functional impairment was noted in the following pulmonary function parameters (% decrease from predicted values):
vital capacity (VC), 4%; inspiratory capacity (IC), 15%; residual volume (RV), 52%; and functional residual capacity (FRC), 29%. A massive conglomerate fibrosis was diagnosed.
Tuberculosis was suspected but not confirmed because lung cultures were not taken.
The pulmonary changes were attributed to the iron and silica in the electrode coatings.
Levy and Margolis described the case of a 35-year-old man with siderosiIicosis of the lung, diffuse interstitial fibrosis, and atypical alveolar epithelium associated with cancer of the lung.
The subject was employed as an oxyacetylene cutter in a steel foundry for 5 years; he wore a welder's helmet for eye protection but used no specific respiratory protection.
The torch-cutting was performed approximately 4 m from sandblasting operations. Within the work area, the concentration of respirable silica was reported to be 6.82 mg/m^ and the quantity of iron oxide was 19.4 m g / m^.
The welder had no previous occupational exposure to fibrogenic dusts.
A lung X-ray revealed a fine reticular pattern in both lung fields.
Pulmonary function studies indicated an obstructive and restrictive ventilatory impairment accompanied by arterial hypoxemia and compensated respiratory alkalosis.
X-ray diffraction analysis of lung biopsy tissue revealed iron oxide and silica.
A lung biopsy analysis reported by Brun et al. of an arc welder who had worked for 16 years on stainless steel in an area with poor ventilation indicated the presence of diffuse fibrosis.
Prior medical history revealed that he had suffered dyspnea combined with an asthma-like bronchitis.
Examination at the time of the report revealed rales at both lung bases, fine bilateral micronodular reticulation, and the presence of numerous macrophages laden with ferric oxide (siderophages) in the sputum. Respiratory function tests revealed a moderate respiratory deficit: vital capacity (VC) was 73% of the predicted value, and the forced expiratory volume in 1 second (FEV-)> was 65% of the predicted value.
Microscopic examination of biopsy material revealed intra-alveolar fibrosis.
Numerous histiocytes and macrophages filled with iron were present in the fibrositic wall.
Stettler et al. reported two cases of siderosis in which the severity of disease appeared to be associated with the welding fume composition.
One worker arc welded primarily in open spaces, whereas the second worker arc welded primarily in confined spaces.
The authors did not state the age of the workers, the length of employment, or the base metal(s) welded by the two workers.
Lung biopsy specimens from both welders, and air samples from the workplace environments were analyzed by electron microscopy using energy dispersive X-ray analysis to determine the chemical composition of the observed particulate matter. The majority of particles in the lungs of both welders were determined to be from stainless steel welding fumes and were comprised mostly of iron with some chromium, manganese, and nickel.
In addition, silica, aluminum, and various silicate particles were found in each biopsy preparation.
The same types of particles were also found in air samples collected at the worksite during arc welding operations.
Although both welders were considered to have siderosis, the first welder had moderate lung disease with minimal interstitial fibrosis, while the second welder had severe respiratory impairment with extensive interstitial fibrosis.
The authors concluded that the severity of the disease in the second welder may have been due to the concentration of aluminum particles found in this welder's lungs, which was six times that of the other welder.
The authors attributed this increase to his working in a confined space. Stanescu et al. examined 16 arc welders (12.1 years average exposure) who had chest X-rays suggestive of siderosis and who had more than 7 years of experience.
He found that seven suffered from exertional dyspnea. Although spirometric values (i.e., VC, FEV-), total lung capacity , and RV) were generally within normal limits, the authors found a statistically significant (p<0.05) decrement in pulmonary compliance when these 7 welders were compared with 13 workers who were not exposed to welding fumes. The authors attributed this decrease either to iron deposits per se or to associated fibrosis caused by other chemical exposures.
No mention was made as to whether or not the welders' smoking habits or ages were considered.
In contrast to the decrements in pulmonary compliance found in welders by Stanescu et al. , Kleinfeld et al. found no differences between welders and a comparison group when they were given a series of pulmonary function tests.
Twenty-five welders were compared with a group of 20 men who resided in the same area but who were not exposed to welding fumes. Occupational histories were obtained from all workers in the study, and clinical examinations were performed, including chest X-rays. The average age of the welders was 48.8 years, and the average age of the comparison group was 46.7 years.
Fifty-six percent of the welders and 55% of the comparison group were smokers.
The average work experience of the welders was 18.7 years, with a range of 3 to 32 years.
Their work included oxyfuel cutting and shielded metal arc welding.
Eight (32%) of the 25 welders showed lung changes on X-rays that were characterized by reticular nodular shadows in both lungs.
These changes were absent in members of the comparison group.
Pulmonary function values, including FEV, FEV-|, RV, and TLC, were normal for both groups. In addition, none of the clinical tests showed statistically significant differences between welders exposed for more than 20 years and those exposed for fewer than 20 years. At the time of the study, environmental sampling was conducted at the sheet metal fabrication facility where the welders were employed. Concentrations of iron oxide ranged from 0.65 to 1.7 mg/m^ inside the welders' face shields and from 1.6 to 12 mg/m^ outside the face shields. Exposure to other fume constituents was not reported. Eight years before the study and just before an improved ventilation system was installed, iron oxide concentrations had ranged from 30 to 47 mg/m«- in the breathing zones of other welders working at the facility.
# (d) Bronchitis/Pulmonary Function
The inhalation of welding fumes and gases have been shown to cause decrements in pulmonary function and the development of other chronic nonmalignant respiratory diseases. Many studies (Doig and Challen 1964;Hunnicutt et al. 1964;Kujawska 1968; Ulrich et a 1 . 1974;Antti-Poika et al. 1977;Akbarkhanzadeh 1980;Keimig et a l . 1983;Sjogren and Ulfvarson 1985;Oleru and Ademiluyi 1987) have reported the potential health risk to welders from exposure to fumes and gases of unknown composition.
Other studies (Doig and Challen 1964;Glass et al. 1971) have shown a risk of exposure to phosgene resulting from the decomposition of trichloroethylene that may be present in the welding work environment.
Several other studies (Hunnicutt et al. 1964;Fogh et al. 1969;Akbarkhanzadeh 1980;Sjogren and Ulfvarson 1985) have demonstrated an association between smoking by welders and an increased risk of developing respiratory disease.
The following studies are representative of those collective data. Kujawska reported on a study of workers aged 35 to 45 who had been arc welding for at least 10 years, had never been employed in trades that would have exposed them to fibrosis-producing dusts, and had acquired no respiratory diseases before starting work as welders.
Two equal groups of welders were randomly selected (total group size not given) and placed in a group according to radiologic changes in the lung. One group of 30 had radiologic changes indicative of siderosis and the other group of 30 had normal lung radiographs.
The welders of both these groups performed about half their work in small and confined spaces (e.g., inside boiler tanks).
Covered acid electrodes were used most often; basic and rutile electrodes were occasionally used.
No identification of potential exposures was reported.
The comparison group (controls) consisted of 30 healthy pipefitters, mechanics, and turners.
Each of the 90 workers (welders and controls) was given a physical examination including medical history, X-ray, ECG, and lung function tests such as lung volumes and capacities, pulmonary ventilation, and examination of alveolar ventilation.
No significant differences in age, height, weight, or length of service were found between groups.
The distribution of smokers and nonsmokers was also similar.
Complaints of labored breathing (86%) and dry cough (40%) were more frequent in the group of welders with siderotic changes than in the other group of welders (37% and 3%) or controls (10% and 7%). Chronic bronchitis was found only in the two groups of welders, indicating a statistically significant difference (p<0.05) from controls.
In addition, reduced pulmonary function parameters (including lower values of the VC and FEV-| and an increase in the ratio of residual volume to TLC) were found in the group of welders with siderotic changes.
Antti-Poika et a l . found simple chronic bronchitis to be more prevalent (p<0.01) among 157 electric arc welders than among 108 controls who were employed at the same facility but not exposed to welding fumes.
The controls were matched to welders with respect to age, smoking habits, and social class.
The prevalence of simple chronic bronchitis was compared with the length and concentration of exposure, but no dose-response relationships were noted.
The welders (average age was 36.1 + 10.1 years) mainly used covered electrodes and had been welding for 3 or more years for at least 3 hours a day. Most worked in engineering shops.
Samples of total fumes were collected outside the helmet at the time of the study, and concentrations ranged from 1.0 to 9.0 mg/m 3 as an 8-hour TWA.
No historical exposure data were reported.
# (i) Phosgene Poisoning
Several cases of respiratory distress and pulmonary function impairment have been attributed to phosgene exposure.
For example, Doig and Challen described seven workers who had been complaining for several months about periodic attacks of mild to severe respiratory distress, cough, chest constriction, and breathlessness while they performed gas metal arc welding.
The cause of the problem was attributed to vapors from an inadequately ventilated degreasing tank that contained trichloroethylene.
The tank was positioned next to open doors so that air currents carried the trichloroethylene vapor 46 m or more to the welding bay, where it decomposed (as a result of heat and ultraviolet radiation from the arc) and formed phosgene.
In another case of phosgene poisoning, a welder experienced chest congestion, difficult breathing, and coughing while welding metal studs to metal links using gas metal arc welding with carbon dioxide .
The studs were cleaned in an open bucket of trichloroethylene adjacent to the welding bench, and the still-damp studs were placed on the bench and welded.
By the end of the morning, the welder's gloves were soaked with trichloroethylene. Examination of the welder 24 hours after exposure revealed reduced vital capacity and FEV-j, airway obstruction, arterial hypoxia, and impaired carbon monoxide transfer.
No exposure measurements were reported.
# (ii) Interactive Effects of Smoking and Welding
Hunnicutt et al. reported on one of the first cross-sectional studies that took into account the smoking habits of welders.
The study group consisted of 100 electric arc welders and an equal number of nonwelding workers employed at the same plant who were not exposed to welding fumes.
The welders were under 60 years of age and had 10 or more years of welding experience in shipyards.
Arc welding was the predominant process that was used.
However, no exposure data were reported.
The following pulmonary tests were conducted on all individuals: FVC, FEV-j, maximum expiratory flow rate (MEFR), maximum mid-expiratory flow rate (MMF), and maximum breathing capacity (MBC). A statistically significant (p=0.01) decrement in welders compared to controls was noted for FEV-|, MEFR, and MMF.
Seventy-one percent of the welders and 59% of the controls had a history of cigarette smoking.
The combined effects of cigarette smoking and exposure to welding fumes increased the likelihood of impaired pulmonary function. Among smokers, the incidence of abnormal pulmonary function in welders was twice that observed in controls. Complaints of shortness of breath, coughs, expectoration, and wheezing occurred twice as often among welders who smoked as among welders who did not smoke.
Radiographic evidence of siderosis was found in 34% of the welders (smokers and nonsmokers combined), but the authors found no correlation between degree of respiratory impairment and radiographic abnormality.
Siderosis was not observed in the controls.
Fogh et al. reported on the examination of a group of 154 electric arc welders (more than half were shipyard welders while the remaining were engine/boiler welders), 2 oxyacetylene cutters, and 152 nonexposed comparison workers from the same locations.
The authors found an increased incidence of chronic bronchitis with increased tobacco smoking in welders as well as in the comparison group when compared to those workers from both groups who did not smoke.
Decreased pulmonary function (i.e., FEV'j) was found to be statistically significant among nonsmoking welders when compared with either the welders or controls that smoked (i.e., 10 cigarettes/day, p=<0.01). No statistically significant difference was shown when welders who smoked were compared with the control group of smokers.
Among all the controls, symptoms did not increase with age.
However, in welders under and over 50 years of age the prevalence of symptoms was 25% and 55%, respectively (p<0.05). Among the welders who smoked, 26% of those under the age of 50 and 55% of those over 50 displayed increases in bronchitic symptoms.
Neither age group differed significantly when compared to the same age groups of smokers in the comparison group.
Chest X-rays revealed a fine mottling indicative of siderosis in five welders (3%). No exposure data were reported. Barhad et al. reported on the prevalence of respiratory symptoms and the impairment of ventilatory function in a group of 173 shipyard welders who had 5 or more years of welding experience.
The average age was 34.1 years (range: 22 to 57). Cough was found to be increased 22% and chronic bronchitis 20% in welders when compared to a control group of workers from the same shipyard but with no welding fume exposure.
The prevalence of chronic bronchitis was 1.5 times more frequent among welders when compared to controls; the difference in prevalence tended to be larger in nonsmokers (12% of welders versus 3% of controls) as compared to smokers (26% of welders versus 21% of controls) but the limited number of observations precluded any statistical analysis.
Dyspnea and wheezing (p<0.001) and paroxysmal dyspnea (p<0.005) were approximately two times more common among welders (smokers, ex-smokers, and nonsmokers) when compared to controls matched for age and smoking habits.
The major type of welding was arc with some oxyacetylene torch and shielded welding.
At the time of the study, breathing zone welding fume concentrations were found to range from 6 to 36 mg/m^ while welding in open work areas and 48 to 92 mg/m^ in confined spaces. Nitrogen oxide exposures averaged I.7 mg /m^ for shielded and 1.1 mg/m for arc welding.
Carbon monoxide exposures averaged 17 mg/m3 for torch welding, 8.4 mg/m^ for electrical, and 6.3 mg/nr- for flux welding.
No historical exposure data were reported.
A similar type of analysis of shipyard welders was performed by Akbarkhanzadeh .
A study was initiated to determine the influence of welding fumes and cigarette smoke on the bronchopulmonary system. The study included 209 welders with 1 or more years of welding experience (mostly shielded metal arc) and a comparison group of 109 shipyard workers who were not exposed to welding fume and who worked for at least 10 years in the same work environment.
The welders and the comparison group were divided into smokers, ex-smokers, and nonsmokers.
The durations of exposure for welders who smoked (22.5 years) and those who did not smoke (20.9 years) were similar.
The smoking habits of the welders and the comparison group were reported to be identical.
Persistent cough and phlegm were found to be twice as frequent among welders who smoked (16.7%) as among the comparison workers who smoked (8.3%).
Chronic bronchitis was found only in welders (12.4%) who smoked or had smoked.
The mean duration of exposure for these welders was 30 years.
For all welders the FEV^ was less (3.77) than that of the total comparison group (4.03) and less for the nonsmoking welders (3.92) when compared to the controls who did not smoke (4.27).
Differences observed for both groups were statistically significant (p<0.025).
Although the FEV-j was lower among welders who smoked when compared to controls who smoked (3.63 versus 3.82), the difference was not statistically significant.
The FVCs for smoking (4.91) and nonsmoking (5.10) welders were lower than the corresponding smoking/nonsmoking (5.07 and 5.40, respectively) comparison groups.
These differences were not statistically significant.
With advancing years of exposure, all lung function parameters of welders deteriorated more than those of workers in the comparison group.
No exposure data were reported.
A cross-sectional study was reported by Keimig et al. on the prevalence of respiratory symptoms or impaired lung function in welders exposed to fumes and gases from gas metal arc welding and flux core welding on mild steel. Welders and controls were white males, aged 25 to 49 and were employed for at least 4 years at a plant that manufactured heavy construction equipment.
The study group was comprised of 91 welders (46 nonsmokers, 45 smokers) with a mean welding exposure of 108 months, and 80 controls (35 nonsmokers, 45 smokers) who were employed at the same plant but had jobs with minimal exposure to respiratory irritants.
Occupational and smoking histories were collected from all subjects.
The types of pulmonary function tests given and the questionnaire administered to all subjects were in accordance with the guidelines of the American Thoracic Society.
Measurements of pulmonary function were made on each subject before and after each work sh i f t .
As expected, welders and controls that smoked reported a higher frequency of respiratory symptoms (e.g., bronchitis, pneumonia, cough) than corresponding nonsmokers.
Although welders who did not smoke reported higher frequencies of symptoms than nonsmoking controls, the differences were statistically significant (p<0.05) for only the symptoms of increased phlegm and episodes of cough and phlegm.
Pulmonary function measurements were compared both within and between welders and controls, and by smoking status.
Predicted normals were not used in the statistical analysis.
The only statistically significant differences noted were decreases in forced vital capacity (FVC) measurements at the end of the work shift for nonsmoking welders, nonsmoking controls, and smoking controls.
The authors concluded that these differences were not attributable to welding exposure, because controls as well as welders showed a significant decrease.
Nonsmoking welders and smoking welders compared to respective controls did not have significantly decreased mean values of FVC or forced expired volume in 1 sec (FEV-|). The mean expiratory flow rates and forced expiratory flow rates measured at 75% of the FVC were found to be lower but not significantly different for welders when compared to controls.
Breathing zone air samples collected near welders at the time of the study indicated iron oxide concentrations of 1.3 to 8.5 mg/m^.
No detectable amounts of chromium, copper, fluoride, and lead were found in any of the air samples.
A more detailed cross-sectional study was described by Sjogren and Ulfvarson who assessed the respiratory symptoms of cough, phlegm, and irritation; chronic bronchitis; and pulmonary function of male welders in Sweden.
Welders were identified from the Swedish Register of Enterprises, Bureau of Statistics, and placed into three study groups: those who welded using gas metal or tungsten arc on aluminum (Group 1); those who welded with coated electrodes on stainless steel (Group 2); and those who welded on railroad tracks (Group 3).
To be included in the study, each welder must have worked at least 1 year, spending at least 3.5 hours per workday performing the type of work identified above.
No specific restrictions on the amount of welding time per day were applied to Group 3. All workers who were asked to be in Groups 1 (64 welders) and 2 (46 welders) agreed to participate.
The median exposure time was 5 years (range: 1 to 24) in Group 1 and 15 years (range: 1 to 39) in Group 2. A total of 149 welders who were asked to be in Group 3 agreed to participate.
A nonwelding comparison group was chosen for Groups 1 and 2 from the same companies and were matched by age (with a variance of 4 years) and smoking habits.
The comparison group for Group 3 included 70 railroad workers who did not weld.
This group was not matched for age or smoking habits.
All three groups of welders had higher frequencies of chronic bronchitis than their respective comparisons, but the differences were statistically nonsignificant and appeared to be more dependent on smoking than on welding fumes .
However, overall respiratory symptoms were more prevalent for welders working with gas-shielded welding on aluminum (Group 1) than the comparison group, and were statistically significant (p=0.03) with increasing exposure to ozone.
Exposure to ozone rather than to aluminum fumes appeared to be responsible for the excess in the observed respiratory symptoms of Group 1 welders .
Almost 50% of the exposures to ozone exceeded 0.1 ppm when gas metal arc welding was performed on aluminum.
Likewise, welders in Groups 2 and 3 displayed more respiratory symptoms with increasing chromium exposures, but the difference was not statistically significant.
More than 80% of the hexavalent chromium exposures exceeded 20 y.q/m3 when stainless steel was welded with coated electrodes.
According to the authors, respiratory symptoms were not related to total fume concentrations (concentrations not stated) or nitrogen oxides (<5 ppm).
No differences were observed regarding FVC or FEV-j between the three groups of welders and their respective comparison groups. Oleru and Ademiluyi reported the results of pulmonary function measurements made on workers engaged in welding and thermal cutting of window and door frames made from medium and high alloy steel and aluminum.
A group of 67 (36.8%) from a total of 182 men in the workforce were evaluated for decrements in pulmonary function.
Of the 67 subjects, 16 were maintenance workers who were indirectly exposed to welding fumes and gases;
13 were engaged in mild steel welding and 7 were engaged in mild steel cutting; 18 were involved in aluminum cutting operations; and 13 were responsible for the paint dipping of metal frames.
A modified British Medical Council respiratory disease questionnaire was administered to all subjects.
Lung function assessments including peak expiratory flow rate (PEFR), one second forced expiratory volume (FEV-|), and forced vital capacity (FVC) were made with a Wright's peak flow meter for PEFR and a Vitalograph spirometer for FEV-j and FVC.
To assess the potential acute respiratory effects that may have occurred over a work-week (40 hours) 8 of the 13 mild steel welders were given spirometric tests on Monday morning and after the work shift on Friday.
To measure possible pulmonary function changes that may have occurred after an 8-hour work shift and 3 consecutive work shifts, the peak flow test was administered to all 13 welders and 13 paint dippers before and after the work shifts on Wednesday and Friday.
The expected lung function parameters of the subjects were calculated from the pulmonary function equations developed for a group of normal, non-industrially exposed Nigerian subjects.
Only 9 of the 67 subjects were found to have ever smoked with an average cigarette comsumption of less than 5 per day and an average duration of about 4 years.
Although not statistically significant, those workers classified as maintenance workers had higher lung function measurements (FEV-j and FVC) than the other groups of workers.
However, there was no evidence of obstructive lung disease among any of the groups as supported by the high FEV-|/FVC ratios observed for all subjects, with the lowest 95% confidence interval for any group being 87.6% to 84.2% found for the maintenance workers.
Seven cases of restrictive lung impairment were observed among the subjects-3 paint dippers, 2 aluminum workers, and 2 welders. All complained of coughing, chest pains, and difficulty in breathing.
The length of employment for these cases ranged from 3 to 7 years.
The eight welders who were given spirometric lung function tests to assess the effects of exposure over a work week (40 hours) demonstrated statistically significant (p<0.05) decrements in all parameters measured.
Peak flow measurements made on this group after an 8-hour work shift showed acute changes in pulmonary function that were statistically significant (p<0.05); however, these changes in pulmonary function were not found to be significantly different when welders were tested at the end of three consecutive work shifts. Statistically significant (p<0.005) changes in peak flow measurements were observed for the 13 paint dippers when tested after either an 8-hour work shift or 3 consecutive work shifts.
The absence of any obstructive lung disease among the exposed subjects is consistent with the low number of subjects who smoked.
The analysis of spirometric and peak flow rate data gathered on a small number of welders and paint dippers after 8-, 24-, and 40-hour work shifts did demonstrate statistically significant changes in lung function.
However, because of the low participation rate (36.8%) it is not possible to determine the significance of these data.
Although no exposure data were collected, the authors hypothesized that based on the amount of settled dust that had accumulated in the work area, airborne dust concentrations probably exceeded 5 mg/m^.
# (e) Summary-Nonmalignant Pulmonary Diseases
The acute respiratory diseases metal fume fever and pneumonitis have been observed in workers involved in many types of welding processes.
Several studies have shown the occurrence of metal fume fever in workers exposed to mixed fume compositions and to specific metals .
In all cases, workers experienced nonspecific systemic reactions, including eye and throat irritation, headache, shortness of breath, and nausea that usually ceased within 24 hr after removal from exposure.
Likewise, welders' pneumonitis has been documented in several case reports and cross-sectional morbidity studies that have shown exposures to the mixed fume composition and gases to be a causative factor in the observed cases of respiratory distress, pulmonary edema, and diminished pulmonary function.
Except for limited exposure data reported by KleinfeId et al. , Molos and Collins , and Challen et al. , all the above studies lacked quantitative exposure data and reported workers being exposed to welding fumes and gases in confined spaces or poorly ventilated work areas.
Several fatalities have been observed among workers acutely exposed to cadmium fumes and nitrogen dioxide .
The occurrence of pneumoconiosis, including siderosis, was first recognized in 1936 among a group of welders .
Since then, many case and epidemiologic reports have described similar clinical findings of asymptomatic, benign, and radiologically detectable lung changes in welders.
Before 1950, much of the welding was performed with bare metal electrodes that produced high concentrations of iron oxide.
Since the replacement of bare metal electrodes with covered electrodes, the potential for mixed exposure to other metal fumes has increased.
As a result of these mixed exposures, there have been subsequent reports of welders in which the complications of fibrosis , pulmonary impairment , and reticular nodular shadows were identified with siderosis.
Bronchitis and decrements in pulmonary function have been reported in welders who have been involved in many types of welding processes.
Welders employed in shipyards have shown statistically significant decrements in pulmonary function and increases in chronic bronchitis . With the exception of one study , in which exposures to welding fume were measured at 6 to 36 mg/m^ in welders' breathing zones and 48 to 92 mg/m^ in confined spaces, no exposure data were reported.
The interpretation of these studies is complicated by the heterogeneity of welding exposures and the possible presence of asbestos as a concomitant respiratory hazard.
Studies reported by Keimig et. al and Oleru and Ademi luyi on welders exposed to mild steel fume and gases in industries other than shipyards observed differences in pulmonary function measurements between welders and nonexposed groups but could not differentiate between smoking and welding exposure on the observed changes. Keimig et al. found a higher frequency of reported symptoms of phlegm and episodes of cough and phlegm for welders who smoked compared to nonsmoking welders.
Decrements in pulmonary function parameters were reported by Oleru and Ademiluyi for welders after an 8-hr work shift and at the end of a 40-hr workweek.
Although these differences were statistically significant, there was a low participation rate (36.8%) in the study.
Several other studies have shown a statistically significant increase in chronic bronchitis in welders performing different welding tasks when compared to nonexposed comparison groups.
In all the studies where chronic bronchitis occurred, the prevalence of the disease increased with the increasing use of tobacco.
# 2) Respiratory Cancer
The following assessment of epidemiologic investigations provides information about the possible association between cancer and occupational exposure to welding fumes and gases .
Many of the studies report standard mortality ratios (SMRs) greater than 100 or odds ratios (ORs) above 1.0, which suggests an increased risk of respiratory cancer. However, some of these studies are not statistically significant and many do not account for the confounding factors of smoking or possible asbestos exposure.
To facilitate discussion, the studies have been grouped as cohort mortality or case-control studies.
To permit comparison of study results, summaries of these studies (including information on study design, observed/expected numbers, SMRs, ORs, etc.) are presented in Tables IV-3 and IV-4.
# (a) Cohort Mortality Studies
The study reported by Sjogren of Swedish welders has been the only cohort mortality study to specifically assess the association between lung cancer mortality and exposure from welding on stainless steel.
The study cohort included 234 nonasbestos-exposed stainless steel welders who had a minimum of 5 years exposure between 1950 and 1965.
The cohort was followed through December 1977. Of the 234 welders, 207 welded with covered electrodes most of the time. An OR of 4.4, based on three lung cancer deaths (p<0.03), was observed among the stainless steel welders when compared to Swedish death rates. All three welders who died of lung cancer were cigarette smokers.
The O R was still statistically significant at p<0.05 after adjusting for a theoretical 10% increase in cigarette smoking among stainless steel welders.
No exposure data were available for the study cohort; however, measurements of chromium taken in 1975 at a similar stainless steel welding process revealed median TWA chromium concentrations of 210 jug/m^ while welding with covered electrodes and 20 /ng/m^ during gas-shielded welding.
The author stated that only a minor fraction of the exposure was in the hexavalent form; therefore, the concentrations were an overestimate of hexavalent chromium exposure.
In 1987, Sjogren et a l . reported on the follow-up analysis of these 234 stainless steel welders who were exposed to high concentrations of chromium.
After 7 years of additional follow-up, the mortality of this cohort was reanalyzed and the results compared to another cohort that consisted of 208 railway track welders exposed to low concentrations of chromium (<10 mg/mg3).
The participants of both cohorts had welded for at least 5 years sometime between 1950 and 1965 and were followed for mortality until December 1984.
The expected number of deaths in the two cohorts were calculated by the multiplication of the person-years of observation within 5-year age categories during 1955-1984 by cause-, gender-, age-, and calendar-year-specific national death rates of Sweden.
An increase in deaths (SMR=249) from respiratory cancer was observed for the cohort of welders who were exposed to high concentrations of chromium.
In contrast, deaths from respiratory cancer in the low-exposure cohort of welders were less than expected (1 death observed, 3 deaths expected).
When welders who had high exposures to chromium were compared with those who had low exposures, the number of deaths from respiratory cancer was significantly elevated in the high exposure group, which had a relative risk of 7.01 (95% Cl = 1.32-37.3).
No other statistically significant increase in deaths from other causes was observed in either cohort.
The authors noted that the expected number of deaths from respiratory cancer reported in the earlier analysis by Sjogren were incorrectly calculated as 0.7 instead of 0.9, resulting in an OR of approximately 3.3 (estimated by NIOSH).
No correction for smoking habits was made when either cohort was compared with the expected national death rates. However, smoking as a confounder was not considered to have a significant influence on the comparison of lung cancer risk between the two cohorts of welders.
Becker et a l . reported on a retrospective mortality study of 1,224 welders and 1,694 turners (machinists) who were employed in 25 German factories from 1950-1970 and followed until 1983.
The death rates of welders were compared with the death rates from internal and external comparison groups.
The internal comparison, based on the death rates of turners not exposed to nickel or chromium, yielded a statistically significant OR of 2.4 for welders (p<0.05) for all cancers and a statistically nonsignificant OR of 1.7 for cancer of the trachea, bronchus, and lung. External analyses (German National death rates) showed that the SMRs for all cancers; cancer of the trachea, bronchus, and lung; and respiratory diseases were statistically less than expected (p<0.05).
Increases in ORs and SMRs for welders who used covered electrodes and who had greater than 20 or 30 years latency were observed for all cancers, including cancer of the trachea, bronchus, and lung, when compared to the internal comparison group.
Since the method of age adjustment was not given, it was impossible to determine what bias the difference in age distribution of the internal comparison group may have contributed to the results.
No historical exposure data were reported.
A retrospective mortality study of 3,247 welders from Seattle, Washington, was reported by Beaumont and Weiss .
The cohort of welders was selected from local union records of the International Brotherhood of Boilermakers, Iron Ship Builders, Blacksmiths, Forgers, and Helpers.
The welders had a minimum of 3 years of union membership and had worked between 1950 and 1973. A majority of them had been employed at shipyards or metal fabrication shops.
An SMR of 132 (p=0.06) for lung cancer was observed when death rates for U.S. white males were used for comparison.
The SMR for lung cancer in welders rose to 174 (p<0.001) when the investigators considered the 39 deaths that occurred 20 or more years after first employment. No historical exposure data were reported, especially data regarding exposure to asbestos in shipyards.
Likewise, the potential effect of cigarette smoking on the observed excess in lung cancer was not determined.
Internal comparison of welders and nonwelders revealed an excess lung cancer risk that was found to be greater among welders employed 20 or more years following fi rst exposure. In 1986, Steenland et al. study using the Cox and logistic regression analyses to compare lung cancer risk of welders.
These analyses were thought to be preferable because they use an internal nonexposed comparison group that is more likely to have lifestyles (e.g., smoking habits) similar to the exposed group.
The Cox regression analysis compared welding as either a dichotomous or continuous variable with time-since-first-employment and year-first-employed.
The logistic regression was used to analyze the 137 lung cancer deaths (cases) and the remaining 8,542 study subjects (controls).
Of the total number of controls, 3110 were welders while the remaining 5,432 were other members (e.g., shipfitters, riggers) of the same union who were frequently employed in the same place as the welders. Men who died of lung cancer were compared to men who did not and an OR for lung cancer was determined for welders versus nonwelders.
When welding was analyzed as a dichotomous variable, a statistically significant interaction was observed with year-first-employed (0R=152, p=0.03).
An OR of 1.29 (p=0.03) for lung cancer was observed among welders when welding was considered as a cumulative dose in the logistic analysis.
An elevated OR of 1.15 still remained for lung cancer among welders when cumulative dose was analyzed in the Cox regression.
In a mortality analysis of 1,027 shipyard welders employed from 1940 to 1968 in Northeast England, Newhouse et al. reported elevated SMRs for all cancers (SMR=114), and for lung cancer (SMR=113) after excluding mesothelioma.
Accurate dates of employment were not available, so analysis by latency and duration of employment was not made.
No smoking histories or information on exposures were cited.
Another mortality study of 2,190 Italian shipyard workers in Genoa, Italy was reported by Puntoni et al. .
The study population consisted of working or retired workers as of January 1, 1960 and followed until December 31, 1975 (duration of employment not given).
Age-and sex-specific mortality ORs were calculated for 19 occupational groups including electric and gas welders and compared with two comparison groups:
the entire male population of Genoa and the male staff of St. Martin's Hospital in Genoa.
Overall, the shipyard workers had statistically significant ORs for total deaths and several specific causes of death including all cancers and cancer of the trachea, bronchus, lung, and larynx when compared to the male population of Genoa, Italy. Gas welders had statistically significant increased ORs for total deaths (p<0.0005) and respiratory diseases (p<0.05), when compared with the same comparison group.
No statistically significant excess in lung cancer was noted for either electric or gas welders.
Although no exposure data were reported, the authors cited exposures to other potential carcinogens (e.g., asbestos, aromatic and halogenated hydrocarbons) in the work environment.
The smoking habits of the workers were not assessed nor was the study population age-adjusted.
The study consisted of a survivor population, with terminated workers not included in the analysis.
The absence of terminated workers probably biased the distribution of deaths because of the many long-term workers.
Polednak reported on a study of 1,059 white male welders from 3 nuclear facilities in Tennessee.
Increases of SMRs were found for lung cancer (SMR=150) and diseases of the respiratory system (SMR=133) that were not statistically significant when compared to U.S. white male death rates.
Welders were selected for the cohort if they were hired between 1943 and 1973.
SMRs for lung cancer (SMR=175) and respiratory disease (SMR=167) were higher among welders not exposed to nickel oxides than for welders exposed to nickel oxides (SMR=124 for lung cancer, SMR=101 for respiratory disease).
Two smoking surveys conducted in 1955 and 1966 showed that cigarette smoking among the group of welders who were not exposed to nickel oxides was 2.5 times more prevalent than the nickel oxide exposed group. About 20% of the welders exposed to nickel oxide smoked cigarettes during the years surveyed.
The difference in smoking habits may account for the higher SMRs for lung cancer and respiratory disease among the nonexposed group of welders.
In relation to duration of employment in all welders, the lung cancer SMR was elevated for those who worked more than 50 weeks, while the respiratory disease SMRs were higher for those with shorter durations of employment.
The fume exposures of welders were causally implicated in the increased risk of respiratory diseases, including pneumoconiosis and bronchitis.
At the facility where nickel alloy pipes were welded, time-weighted average (TWA) air concentrations of nickel found in 1975-1977 were all higher than 0.015 mg/m^ (range of concentrations not given).
The sample size of the two subgroups of welders was small, and 8.3% of the study cohort was of unknown vital status at the end of the study period.
The nonexposed welders were slightly older than those exposed which may have contributed a negative bias to the SMRs.
In a prospective mortality study reported by Dunn and Weir a slight, but not statistically significant, excess of lung cancer deaths (0R=1.05) was observed for welders and burners studied over an 8-year period.
The study design, which included 13 other occupational groups ascertained from California union records, was based on the information gained from 121,314 mailed questionnaires (85% response rate).
Statistical analyses were conducted using age-and smoking-specific death rates, and compared with the death rates of the total union population.
No exposure measurements were made and employment records were unavailable.
Potential exposures were estimated from the general occupational information that appeared on the questionnaire provided by the respondent.
Mi lham reported a statistically significant increase in proportional mortality ratios (PMRs) observed for male welders and flamecutters for several causes of death.
The proportional mortality study was based on death certificates collected over a 29-year period (1950-1979) in Washington State.
The statistically significant PMRs are reported in Table IV-5. Occupations were derived from death certificates, which were reported to be inaccurate for as many as 30% of the deaths.
The study consisted of a survivor population with deaths of terminated workers not included in the study analysis.
Smoking and the potential exposure to asbestos were not accounted for and could have had an effect on the outcome of the study.
In a review of lung cancer rates (by occupation) for Los Angeles County, Menck and Henderson observed a significantly increased SMR of 137 (p<0.05) for welders when compared to the age-, race-, and sex-adjusted Los Angeles County employed population.
A total of 2,161 death certificates cited lung cancer as the cause of death in white males, ages 20 to 64, during the periods 1968 to 1970.
In addition, 1,777 cases of lung cancer in white males during 1972 and 1973 in Los Angeles County were used.
Neither the potential effect of asbestos exposure nor smoking habits were assessed in the study analysis. Occupation and type of industry were ascertained from death certificates (which only listed last job held) and medical records.
Thus a clear delineation of all jobs held, years of employment, and potential occupational exposures could not be made.
In the report published by Her Majesty's Stationary Office of England and Wales, increased mortality caused by pneumonia, lung cancer, and other and unspecified respiratory cancer was observed for gas and electric welders, cutters, and brazers during the period 1970-72. An overall increase (22%) in deaths was recorded even after adjustment for smoking, age, and social class.
This was more than was expected for this occupational group.
A statistically significant increase (p<0.01) in the PMR for lung cancer mortality was found among smokers and nonsmokers.
This risk remained statistically significant with an SMR of 116 (p<0.01) when controlled for smoking. The number of lung cancer cases recorded in 1966-1967 and 1968-1969 were noted as "particularly" high.
In 1968-1969, seven cancer cases were recorded for other and unspecified respiratory organs, whereas only one was expected. Although no explanation was provided, the authors attributed the excess in lung cancer to an association with asbestos exposure.
Possible errors in the analysis could have resulted from differences in the occupational classifications used for the numerator and denominator in determining PMRs.
Numerator estimates were based on occupations given in death certificates, whereas the denominator used occupations found in the national census data.
Therefore, the rates reflect some bias (unknown direction) in their estimation of risk.
Although this type of mortality study (which relies on routinely collected data) is useful for identifying associations between occupation and mortality, it is imprecise for detecting complex relationships between cause of death, exposure, and occupation.
No information on the types of exposures were available for analysis.
Smoking habits were not assessed but were controlled by using a 22% over-incidence for smoking in the analysis. Ott et al. reported on a cohort mortality study of 8,171 male workers employed at a chemical facility.
The study population was subdivided into two cohorts; the one cohort consisted of those workers (5,994) hired before 1950 and the other consisted of workers (2,177) hired between January 1950 and March 1954.
The vital status of all workers was followed until 1973.
Analysis of malignant neoplasms was ascertained for 15 job categories including welders and lead burners.
Based on 12 malignant neoplasm deaths, welders and lead burners had an elevated but not statistically significant SMR of 162 when compared to U.S. white male death rates.
It was not possible to validate the increase of lung cancer based on two observed lung cancer deaths.
Although workers who were potentially exposed to arsenicals or asbestos were eliminated from the study, no further characterization of other potential exposures was provided.
A potential misclassification bias could have been introduced because workers were assigned job categories based on their job titles the day they were hired; subsequent job changes were not taken into account.
# (b) Case-Control Studies
Gerin et al. reported on a case-comparison study of hospital cancer patients and their possible occupational exposure to nickel.
Lung cancer risk was determined on case ascertainment from 17 hospitals in Montreal, Canada. A statistically significant dose-related OR of 3.3 (95% CI =1.2 to 9.2) was reported for patients who were classified as stainless steel welders "exposed to nickel." Welders identified as having no nickel exposures did not have a statistically significant excess risk.
Lung cancer patients identified as nonwelders, but who were exposed to nickel, had a statistically significant OR of 2.9 (95% CI=1.3 to 5.7).
The potential for exposure to nickel and chromium were highly correlated, with 78 out of 79 cases exposed to both nickel and chromium.
Analyses were controlled for age, smoking history, socioeconomic status, ethnicity, and unknown hospital referral patterns. Occupational exposure to nickel was derived from the patients' responses to a semi-structured questionnaire administered by a team of chemists and industrial hygienists who were unaware of the cancer status. The cases were not controlled for a potential asbestos exposure.
A similar case comparison study was conducted by Breslow et al. of 518 lung cancer patients from 11 California hospitals during 1949-1952.
Of the 518 lung cancer patients, 14 (10 welders and 4 sheet metal workers) were classified as having occupations that exposed them to welding fumes.
Although no exposure data were presented, the 14 lung cancer patients were probably exposed to welding fumes associated with the use of arc welding and bare metal electrodes, because this was the primary method of welding prior to 1950.
An equal number of patients admitted to the same hospital but whose diagnosis was not cancer or respiratory disease, were used as controls and matched for age, race, and sex.
A questionnaire was given to lung cancer patients and the controls to determine occupations, tobacco use, and exposure to toxic materials. The 14 lung cancer patients who were probably exposed to welding fume represented a statistically significant (p<0.05) occupational group even after adjustment for cigarette smoking. Gottlieb observed a statistically significant OR of 1.19 for white and black males (combined) in a case-control study of lung cancer mortality among all workers employed in the Louisiana petroleum industry between 1960-1975. When the relative risks were determined for welders and were stratified by age at death, only the relative risk for welders under age 60 remained elevated at 0R=1.89 (95% Cl=0.5 to 7.4), suggesting an occupational etiology. Controls were selected from noncancer deaths and matched to the cases individually by sex, race, year of death, parish of residence, and age at death.
A survivor bias may have existed because of death certificate identification of the study population.
Smoking habits and the potential for asbestos exposure were not included in the analysis.
In an effort to determine the cause of the high rate of lung cancer among male residents of 11 coastal counties of Georgia, a case control incidence study was conducted by Blot et a l . .
Cases were identified from hospital records, and death certificates were obtained for lung cancer patients.
Controls were selected from hospital admissions and death certificates, and were matched (two controls for every case) closely by sex, race, age, residence, and vital status.
A questionnaire was given to patients and controls (or the next of kin) to determine place, type, and length of employment for any job held for 6 months.
Patients who had been employed in a shipyard, had an OR of 1.6 (95% CI=1.1 to 2.3, p=0.006) for lung cancer.
The 11 patients who were welders or who were exposed to welding fumes had a crude relative risk of 0.7. Although the relative risk of those employed at shipyards was adjusted for cigarette smoking, asbestos exposure, age, race, and sex, the crude relative risk among welders was not adjusted and, therefore, may not be a reliable estimate of cancer incidence.
In contrast to the study reported by Blot et a l . , Schoenberg et al. found an increased risk of lung cancer among welders employed in shipyards who had no reported asbestos exposure.
These results were observed in a case-control study that included 763 white males with histologically confirmed primary cancer of the trachea, bronchus, and lung and 900 general population white male controls.
All cases and controls were selected from six geographical areas of New Jersey with risk estimates determined by either job title or industry job title category.
The effects of smoking and other potential confounders were examined.
A more detailed analyses was conducted for shipbuilding workers and included comparisons of risk by job category and by reported exposure to asbestos.
Personal interviews of all cases and controls, or their next of kin, were conducted to collect demographic data, information on personal and environment risk factors, smoking history, and diet.
Of the 42 job title categories examined, 15 were considered to be at high risk, with printing workers, janitors, and cleaners having statistically significant (p>0.05) increased smoking-adjusted ORs; 11 had smoking-adjusted ORs of 1.3 or greater, while 4 categories with small numbers of subjects had crude ORs greater than 1.3. Of the 34 industry job title categories examined, 13 were considered to be at high risk.
Shipbuilding workers, as well as trucking service warehousing and storage workers, had statistically significant (p>0.05) increased smoking-adjusted ORs.
The risk for lung cancer among shipbuilding workers was found primarily among subjects with reported nonincidental asbestos exposure.
An increased OR both for latency of less than 30 years (OR of 3.9) and for latency of 30-39 years (OR of 1.7) was observed for these workers.
When shipbuilding workers were further analyzed by shipyard job category, welders were observed to have a statistically significant increased OR of 3.8 (95% Cl=1.8 to 7.8).
Of the 33 cases and 18 controls classified as welders, 16 cases and 7 controls were reported to have been exposed to asbestos.
When the remaining 17 cases and 11 controls who had no reported asbestos exposure were analyzed, an increased smoking-adjusted OR of 2.5 (95% Cl=1.1 to 5.5) remai n e d .
A case-control study was conducted by Olsen et al. to assess the elevated laryngeal cancer risk found among white males in Denmark, and to determine if any association existed between these cases and exposure to welding fumes. The study population was composed of 271 incident cases of cancer of the larynx and 971 population controls matched on date of birth, sex, and residence.
Patients and controls were interviewed to determine occupations, potential exposures, and tobacco and alcohol usage.
Based on the analysis of 271 cancer patients during 1980-1982, workers exposed to welding fumes had a statistically significant increased OR of 6.3 (95% C I =1.8 to 21.6) for cancer of the subglottic area of the larynx.
An elevated but not statistically significant OR of 1.3 (95% Cl=0.9 to 2.0) was observed for cancer of the larynx.
After adjustment for quantified tobacco and alcohol usage, the relative risks persisted.
When the study was restricted to 12 stainless steel welders, only the relative risk for subglottic cancer remained elevated with an OR of 6.7 (95% Cl=1.0 to 33.3).
Several of the epidemiologic studies demonstrated statistically significant increased risks for lung cancer among male welding populations .
Four of these studies showed statistically significant dose-response relationships, one with an increasing observation period and duration of welding exposure , two with exposures to nickel and chromium during welding of stainless steel , and a case control study of shipyard welders that was controlled for smoking and accounted for possible asbestos exposure.
In one study , the contribution of cigarette smoking habits to lung cancer risks was used as a control, while the other study used a crude estimate of smoking habits (10% more welders who smoke) as the control.
The two other studies reaffirmed the excess risk of lung cancer observed by Beaumont and Weiss and Sjogren . Steenland et al. found an elevated risk of lung cancer among the study cohort reported by Beaumont and Weiss when they used an internal comparison group that shared similar lifestyles (e.g., smoking) and occupational exposures (e.g., asbestos).
Likewise, Sjogren et al. observed that the risk of lung cancer remained increased when the study group that was used in a previous study was compared to another group of welders who were exposed to lower concentrations of chromium.
The remaining three studies support an association between welding exposures and increased risk of lung cancer.
One of these three studies made adjustments for the contribution of cigarette smoking to the proportion of welders with lung cancer ,
The other two studies , although based on national data sets, are relevant since analyses of these types of data are usually not considered sensitive enough to detect the kinds of complex relationships (exposure and effect) observed unless the disease is rare and the occupational association considerable.
In addition to the above cited studies, a study of welders in the Louisiana petroleum industry also showed a statistically significant lung cancer risk .
However, when the study group was adjusted for age, the OR was not statistically significant.
# (c) Summary-Respiratory Cancer
Five other mortality studies found elevated risks for lung cancer among male welders.
Two of the five were cohort studies conducted on subgroups of white males who worked as welders at nuclear facilities and at sanitary installations and power plants .
The larger of the two studies indicated an OR of 1.7 for lung cancer that, although based on small numbers, remained increased in those workers with greater than 20 and 30 years employment.
The smaller cohort study showed elevated SMRs for the two groups of welders who were exposed and not exposed to nickel oxides.
Although the welders not exposed to nickel oxides had a higher SMR, this increase could have been attributed to the higher prevalence rate (2.5 times) of smokers within the group as compared to the exposed group of welders.
Two of the mortality studies were conducted on welders in shipyards.
These studies indicated elevated relative risks and SMRs for subgroups of welders and other occupational groups potentially exposed to welding fumes and gases.
However, neither smoking habits nor the potential for exposure to asbestos were taken into consideration in these two studies.
The last of the five mortality studies that showed an elevated risk of dying from lung cancer was a prospective study that used mortality data collected from questionnaires and union records over a 5-year period.
A slightly elevated OR of 1.05 was observed when adjusted for age and smoking and compared with the death rates of the total union population.
No employment records were available and any potential exposures had to be derived from the questionnaires.
In a case control study conducted to investigate the high rate of lung cancer among male residents of 11 Georgia coastal counties, a statistically significant increased OR of 1.6 was found for shipyard workers.
However, when cases were analyzed by occupations within the shipyard, a crude OR of 0.7 was observed for w e l d e r s .
An unusually high elevated risk of cancer (OR = 6.3) of the subglottic area of the larynx was found among 271 cancer patients of whom 42 had been exposed to welding fumes .
The high OR persisted after adjustment for tobacco and alcohol use but was found not to be statistically significant when restricted to twelve stainless steel workers.
None of the other epidemiologic studies found an elevated risk of larynx cancer.
Several of the studies that explored the relationship between exposure to welding fumes and gases and the incidence of mortality from lung cancer among welders, suffered from one or more of the following methodologic problems:
(1) incomplete information on the extent of exposure, requiring estimations of these exposures from job titles, (2) insufficient cohort size and person years to observe elevated risks of lung cancer, and ( 3) confounding variables such as smoking and exposure to asbestos.
These limitations make it difficult to draw definitive conclusions about the cause of cancer excesses observed within each study.
However, collectively these studies demonstrate an elevated risk of lung cancer among welders that is not completely accounted for by smoking or asbestos exposure, and that appears to increase with the latent period from onset of first exposure and duration of employment.
Additionally, a few of the studies suggest a strong association between lung cancer risk and exposures generated while welding on stainless steel. This association could be attributed to the carcinogenic properties of the nickel and chromium found in the fume.
An overview of each evaluated study is presented in Tables IV-2 through IV-4.
# b. Kidney and Other Urinary Tract Cancers
The cohort mortality studies conducted by Puntoni et a l . , Milham have shown a statistically significant increased risk of kidney or other urinary tract cancers in welders.
The study by Puntoni et al. of shipyard workers showed ORs of 5.06 (p<0.05) and 5.88 (p<0.05) for cancer of the kidney and other urinary organs in gas welders when compared to the male population of Genoa, Italy and the male staff at St. Martino Hospital, respectively.
Although the ORs were elevated for these cancers in electric welders, they were not statistically significant.
When all shipyard workers were grouped and compared with either comparison population, the elevated ORs for these cancers were found to be statistically significant (p<0.0005).
Similarly, the study reported by Milham showed statistically significant (p<0.01) increased PMRs for kidney cancer in male welders and flamecutters who had been employed in Washington State. Welders and flamecutters analyzed during the period 1970-1979 and for the total observation period 1950-1979 had PMRs of 234 and 182, respectively.
The observations of Becker et al. were consistent with these findings with an OR of 15.0 (3 observed versus 0.2 expected) for kidney and other urinary tract cancers in welders when compared with the German national death rates.
Although it was not reported by the authors, NIOSH calculated a p value of 0.002 (95% C l =3.09- 43.83).
Several of the studies that explored the relationship between exposure to welding fumes and gases and the incidence of mortality from lung cancer among welders, suffered from one or more of the following methodologic problems:
(1) incomplete information on the extent of exposure, requiring estimations of these exposures from job titles, (2) insufficient cohort size and person years to observe elevated risks of lung cancer, and ( 3) confounding variables such as smoking and exposure to asbestos.
These limitations make it difficult to draw definitive conclusions about the cause of cancer excesses observed within each study.
However, collectively these studies demonstrate an elevated risk of lung cancer among welders that is not completely accounted for by smoking or asbestos exposure, and that appears to increase with the latent period from onset of first exposure and duration of employment.
Additionally, a few of the studies suggest a strong association between lung cancer risk and exposures generated while welding on stainless steel. This association could be attributed to the carcinogenic properties of the nickel and chromium found in the fume.
An overview of each evaluated study is presented in Tables IV-2 through IV-4.
# b. Kidney and Other Urinary Tract Cancers
The cohort mortality studies conducted by Puntoni et a l . , Milham have shown a statistically significant increased risk of kidney or other urinary tract cancers in welders.
The study by Puntoni et al. of shipyard workers showed ORs of 5.06 (p<0.05) and 5.88 (p<0.05) for cancer of the kidney and other urinary organs in gas welders when compared to the male population of Genoa, Italy and the male staff at St. Martino Hospital, respectively.
Although the ORs were elevated for these cancers in electric welders, they were not statistically significant.
When all shipyard workers were grouped and compared with either comparison population, the elevated ORs for these cancers were found to be statistically significant (p<0.0005).
Similarly, the study reported by Milham showed statistically significant (p<0.01) increased PMRs for kidney cancer in male welders and flamecutters who had been employed in Washington State. Welders and flamecutters analyzed during the period 1970-1979 and for the total observation period 1950-1979 had PMRs of 234 and 182, respectively.
The observations of Becker et al. were consistent with these findings with an OR of 15.0 (3 observed versus 0.2 expected) for kidney and other urinary tract cancers in welders when compared with the German national death rates.
Although it was not reported by the authors, NIOSH calculated a p value of 0.002 (95% C l =3.09- 43.83).
As described earlier in this Chapter in Section B,2,a(2)(a), these three studies had a number of methodologic problems, including a lack of information on potential occupational exposures.
Because of these limitations, the possible etiology for these observed cancers is difficult to assess.
# c. Reproductive Effects
Adverse reproductive effects (e.g., infertility or spontaneous abortions) have been reported by Rachootin and Olsen and Lindbohm et al. for both men and women who were either employed as welders or who were potentially exposed to metals.
A case-control study was conducted by Rachootin and Olsen to determine whether an association existed between delayed conception or infertility and the occupations of women and their husbands.
The study population was identified from the inpatient register at a large Danish hospital; 1,069 case couples and 4,305 comparison couples were identified as study candidates.
Case couples were undergoing evaluation for fertility problems, and the female partner had been admitted to the hospital for testing during the period 1977 to 1980. Comparison couples had had a healthy child born at the same hospital during the period 1977 to 1979.
A questionnaire was mailed, and responses were received from 87% of each group (927 case and 3,728 comparison couples).
All information on a couple was solicited from the woman.
Three types of analyses were conducted.
The first analysis compared the reported occupational exposures of the case and comparison couples residing in the hospital's direct catchment area (Table IV -6).
In this analysis, comparison couples were limited to those of the 3,728 comparison couples who were the parents of a healthy child conceived within 1 year.
The case couples were restricted to those of the 927 case couples who were examined or treated for infertility of at least 1 year's duration. This analysis examined three subgroups of case couples:
(1) those with a male partner having abnormal sperm number, motility, or shape, (2) those with a female partner having hormonal disturbances, and (3) those with idiopathic infertility.
The first two subgroups had medical histories that were potentially related to occupational ex p o s u r e s .
The second analysis compared the reported occupational exposures of case couples (Table IV-7).
The three subgroups from the first analysis were compared with infertile case couples having conditions that were unlikely to be caused directly by occupational exposures (e.g., varicocele or history of mumps as an adult in the male, or blocked fallopian tubes or endometriosis in the female).
The third analysis compared two subgroups within the original comparison group of couples who had had a healthy child born at the study hospital during the period 1977 to 1979. One subgroup was made up of comparison couples who had given birth to a healthy child after a conception delay of more than 1 year, and the second subgroup comprised the remaining comparison couples who had conceived a healthy child within 1 year.
A variety of potentially important occupational exposures were considered in the analysis, and those relevant to the welding environment are shown in Tables IV-6, IV-7, and IV-8.
In both the first analysis (Table IV-6) and the third analysis (Table IV-8), significantly elevated ORs were seen for a variety of occupational exposures associated with welding.
Exposure to heat and noise was consistently associated with elevated ORs.
Exposure to heavy metals and welding (either on stainless steel or other metals) was also associated with elevated ORs.
Both men and women who were assigned to the exposure category "Welding of Other Metals" in the third analysis (Table IV-8) had a statistically significant increase (p<0.05) in delayed conception, with ORs of 1.4 (95% C I =1.1-1.8) for men and 2.4 (95% CI=1. 1-5.1) for women.
This risk was still statistically significant for women after adjustment for age and education, parity, area of residence, smoking habits, alcohol consumption, and past use of oral contraceptives.
In contrast, men and women who were assigned to the exposure category "Welding of Stainless Steel" had no statistically significant increase in delayed conception.
In the second analysis (Table IV-7), none of the exposures potentially encountered in the welding environment were associated with elevated ORs. Lindbohm et al. evaluated possible influences of paternal or maternal occupations and exposures on spontaneous abortion by linking discharge records from Finnish hospitals with national census data.
For the period 1973 to 1976, data were available for 294,309 pregnancies.
Census data on occupations were used to form seven categories of presumed exposure to specific agents (animal microorganisms, solvents, polycyclic aromatic hydrocarbons, automobile exhaust fumes, other chemicals, metals, textile dust). Because the census data referred to occupations in 1975, the analysis of spontaneous abortion was limited to pregnancies in 1976. Women in these exposure categories were compared with all other "economically active" women, and wives of exposed men were compared with wives of nonexposed men. A logistic regression model was used to control for age, place of residence, parity, marital status, and age-parity interaction.
None of the specific exposures were associated with a significantly increased odds ratio.
The odds ratio was 0.78 (95% C I =0. 54-1.13) for women exposed to metals (iron and metalware workers; smelting, metallurgic, and foundry workers; miners and quarry workers).
For the wives of similarly exposed men, the OR was significantly reduced to 0.86 (95% C I = 0 . 7 5 -0 . 9 5 ) . Lindbohm et al. also used the pregnancy data for the period 1973 to 1976 to investigate spontaneous abortion by occupation. Women in five occupations had elevated ORs, but none appeared to be related to the welding environment. One of four occupations associated with increased ORs for the wives of exposed men was "metal-plate and constructional steel workers" with an OR of ).
This occupational category was not described in any further detail except for the comment that these men "are occasionally exposed to chromates and nickel." No information was available on smoking habits and alcohol consumption. Potential occupational exposures were assigned based on employment history.
The significance of the results from these two studies is questionable given the studies' limitations (e.g., estimation of exposures and confounding exposures of smoking or alcohol consumption).
# d. Cardiovascular Effects
A few case reports indicated that exposure to welding fumes and gases may cause acute cardiac episodes or aggravate preexisting cardiovascular diseases in welders . In these case reports, welders worked in confined spaces with poor ventilation. No information was given as to the types of metal being welded or exposures being generated.
Two of four mortality studies cited previously in this Chapter in Section B, 2, a,( 2),(a) reported increased risks of cardiovascular disease in welders employed at shipyards . Newhouse et al. observed an increased SMR of 130 (90% CI=104-156) for ischemic heart disease in welders, whereas Puntoni et al. reported ORs greater than 1.00 for a similar cohort of welders.
Neither study was adjusted for smoking and no conclusions were drawn by the authors as to the relevance of the elevated risks. One of the other two mortality studies reported a PMR of 97 for welders and flame cutters when analyzed for the total study period of 1950-79; the other study showed SMRs of 70 and 82 for welders exposed and nonexposed to nickel oxide fumes, respectively.
The slightly higher SMR of the nonexposed group of welders could be attributed to the 2.5 times greater percentage of cigarette smokers reported among this group.
# e. Gastrointestinal Effects
Gastrointestinal disorders in welders experiencing metal fume fever usually take the form of nausea, vomiting, and gastrointestinal cramps .
These effects appear to subside within 24 to 48 hr after acute exposure to welding fumes.
Two cases of gastrointestinal disorders were reported by Rieke in workers performing oxyacetylene torch cutting of scrap metal.
Both men had been employed in a ferrous metal scrap yard where they disassembled and cut large (often painted) metal parts. The men complained of back and lower abdominal pains, poor appetite, and constipation after being exposed for several days to metal fumes. Urinary lead analysis revealed markedly elevated lead levels (e.g., 0.44 and 0.43 mg lead/liter) and both men were treated for lead intoxication and given calcium disodium edetate for several days.
Following this period of treatment all gastrointestinal disorders ceased.
The workers' health problems were attributed to exposure to lead contained in the paints.
In three epidemiologic studies , an increased incidence of digestive disorders in welders was reported.
Rozera et al. reported that 22% of a population of 620 welders had digestive system disorders compared with 12% found in the general industrial population. Mignolet reported similar finding among 216 welders who were placed into three groups according to the welding process they used.
Thirty-five out of 85 (41%) shielded metal arc welders complained of digestive disorders, including loss of appetite, slow digestion, and nausea.
Two out of 99 (2%) oxyfuel gas welders had gastric ulcers.
Two out of 32 (6.3%) oxyacetylene cutters had symptoms of gastrointestinal disorders.
These disorders were attributed to the inhalation of fumes from certain types (unspecified) of covered electrodes because no similar effects were noted in welders who used bare metal electrodes. Most of the symptoms associated with digestive disorders disappeared during weekends and vacations.
Gastroduodenopathies were reported by Stancari and Amorati in 264 arc welders aged 17 to 58 years.
Of the 264 arc welders, 67% of those with over 10 years work experience, 43% of those with 3 to 10 years work experience, and 15% of those with less than 2 years exper i ence had gast r i t i s , gast roduoden i t i s , or gast roduodenaI ulcer.
The authors concluded that the inhalation of fumes and gases associated with arc welding caused the gradual development of chronic gastritis and gastroduodenitis among welders.
These ulcers were described as moderate and responded well to treatment; as soon as welding was discontinued, regression occurred.
The authors further stated that the specific cause of these ulcers was unknown.
Houten and Bross reported on the relative risk of cancer among male patients at a regional cancer institute.
Cancer patients were compared with other admitted male patients who did not have neoplastic disease in an attempt to ascertain if specific types of cancers were associated with certain occupations.
Three cases of stomach cancer were noted among welders and flamecutters, for an OR of 2. 5. This cancer incidence was not statistically significant due to the small number of observed cases.
In contrast, several of the mortality studies discussed previously in this Chapter in Section B, 2, a,( 2),(a) reported no increases in welder mortality as a result of cancer or other diseases of the digestive system.
# f. Ophthalmologic Effects
Persons who are involved in or working near welding processes are at risk of eye injury from metal spatter and exposure to nonionizing electromagnetic radiation in the UV to IR wavelengths .
Exposure to UV radiation from the welding arc can result in acute keratoconjunctivitis, also known as arc eye, welder's flash, or actinic ray photokeratitis. This inflammatory disorder affects the outer structure of the eye (cornea, conjunctiva, iris) and causes blurred vision, lacrimation, burning pain, and headache . These symptoms usually appear within 4 to 12 hr after the beginning of the exposure and last up to 2 days.
The visible radiation emitted during welding can penetrate the eye and be absorbed by the retina and choroid causing retinal injury .
Similarly, exposure to the IR radiation wavelength can cause thermal damage to the cornea and aqueous humor of the eye and has been associated with the formation of lenticular cataracts .
These types of adverse ocular effects have been reported in welders who were wearing improper eye protection or no protection at all .
In one study , 31 eye injuries were reported that were caused by contact with hot slag, metal chips, sparks, and hot electrodes.
Several of the injuries involved workers assisting welders, and others involved welders who had been provided with approved types of faceshields but did not use them properly. Golychev and Nikatina also reported that because eye protection was not used, cataracts occurred in a 42-year-old welder's helper who had regularly assisted electric arc welders for 19 years.
This worker reportedly suffered from welder's flash and conjunctivitis 3 to 4 times a month.
Other studies have reported similar cases of retinitis and dendritic keratitis in welders who did not protect their eyes while igniting their arcs.
In a case control study of 118 welders, a statistically significant (p<0.05) increase was observed in damage to the corneal epithelium and endothelium of the eye when compared to 85 nonwelders .
The increase in eye injuries was attributed to exposure to ultraviolet radiation.
Two studies have reported on the evaluation of visual acuity of welders.. The visual acuity was evaluated in a group of 520 welders, of whom approximately 76% were under 40 years of age; 23% of the study group worked for 20 years and 20% worked up to 30 years .
Eye complaints that included watering, blurred vision, burning, soreness, and haziness were reported by 60% of the welders.
The principal clinical conditions, reported in descending order of frequency, were conjunctivitis (45%), keratoconjunctivitis (11%), pterygium (7%), incipient cataract (7%), edema of the lids (5%), brown pigmentation around the cornea (4%), trachoma (2%), corneal opacity (2%), and dilated pupils (2%).
The two most common eye injuries were imbedded foreign bodies in the eye (21%) and burns of the conjunctiva (4%). Almost all the welders had suffered from arc flash at least once.
Visual acuity in 33% of the welders was at the minimum accepted acuity for welders (20/30).
Serious visual impairment was observed in 20%; substandard acuity of 20/60 or less was present in 59% of the welders; and defective muscle balance of the eyes was noted in 78%.
# The percentage of welders with defective visual performance increased with age.
A similar investigation of visual acuity was made in a group of 216 welders . Although the types of tests conducted were not stated, unilateral and bilateral alterations in visual acuity were reported for 41% of the oxyfuel gas welders, 47% of the oxyacetylene cutters, and 58% of the arc welders.
Two cases of cataracts were also noted. No control groups were used in either study for comparison of visual acu i t y .
# g. Dermatologic Effects
Dermal effects related to welding processes may result from exposure to UV radiation and IR radiation , from hot metal spatter , and from sensitization to metals .
Exposure of the welder's skin to UV radiation can result in skin burns similar to sunburn.
According to a review by Pattee et al. , the most common sites for such burns are the arms, hands, neck, and chin. Ross also noted that the front and sides of the neck were the most common sites for such burns.
In a clinical investigation conducted by Dreesen et al. , 25% of 3,255 arc welders had burns or scars from burns on their bodies.
Similar findings were noted by Entwistle who reported that over 50 cases of burned fingers, wrists, hands, elbows, arms, and legs occurred among welders during an 8-month period.
The cause of those burns was attributed to metal spatter, hot slag, and the flame from oxyacetylene torches.
Several case reports have documented the occurrence of chronic dermatitis among welders and other persons working near welding processes . Balabanow et al. [1967 reported a case of dermatitis in a welder who had been in this occupation for 35 years.
He suffered from edema of the eyelids and redness of the face and neck, the scalp, upper chest, back of hands, forearms, and the lower extremities.
A series of clinical tests revealed no pathologic cause for these effects other than welding.
A similar finding was reported by Shelley for a 40-year-old crane operator who worked near welding operations and had had recurrent eczematous eruptions on both hands for 14 years.
Roquet-Doffiny et al. reported a severe case of chronic actinic dermatitis, erythema, atrophic plaques, telangiectasis, and pruritic keratotic lesions for a welder who had been performing oxyacetylene gas welding for 30 years.
In addition, over a 4-year period, eight tumors were removed from his face and neck-five basal cell carcinomas and three squamous cell carcinomas.
Exposure to radiation and welding fumes and gases was reported in all three reports as the causative factor in the observed skin diseases.
When workers discontinued welding or were removed from the work environment where welding was being performed, dermatitis ceased. Among welders, a number of cases involving chromium skin sensitization have been reported . Kalliomaki et a l . reported a case of chromium sensitivity involving dermal allergy and asthma for a welder who typically welded on stainless steel. After the individual welded on stainless steel for about 1 hr, bronchial obstruction was observed that, according to the investigator, demonstrated severe sensitivity to the fume exposure. Measurements of airborne hexavalent chromium revealed concentrations of 0.02 to 1.7 mg/m^. A similar finding was reported by Fregert and Ovrum for a welder who experienced repeated episodes of facial contact dermatitis while welding. The welder was found to be sensitized to chromium that was emitted while he welded on stainless steel or from the welding rod that contained trace amounts of chromium.
The dermatitis disappeared after the welder ceased his exposure to welding fumes that contained chromium.
# h. Auditory Effects
Hearing loss among welders has usually been due to traumatic injury or to excessive sound pressure . Frenkiel andAlberti reviewed 11 cases of middle ear trauma resulting from burns, including 5 such cases in welders.
The eardrums of the welders were perforated by flying sparks or pieces of metal during welding processes.
In four of the five cases, hearing loss was permanent.
Auditory impairment from exposure to excessive noise levels may occur during arc air gouging of metal, and plasma torch processes . Bell reported that a considerable risk of noise-induced deafness was possible among a group of welders during arc air gouging in which sound level measurements exceeded 115 dbA. Hickish and Challen noted a mean temporary hearing loss in both ears of 19 dB at 4,000 Hz and up to 35 dB at 8,000 Hz in three persons who were exposed to the noise from a plasma torch for 1 hr. In one person, recovery of normal hearing took 48 hr.
# i. Musculoskeletal Effects
Welding is a static type of work that usually requires customary postures and considerable shoulder joint motion.
Shoulder pain may be caused or aggravated by welding.
Complaints of shoulder pain are very common among older welders, according to observations by Herberts and Kadefors , who investigated the clinical and radiological features of shoulder pain in 10 shipyard welders aged 50 to 65 years.
An electromyographic (EMG) evaluation of the impact of static loading on their shoulder muscles was also conducted.
The most consistent finding was reduced muscle power and shoulder pain. All subjects had normal shoulders upon inspection, but mild local tenderness of the rotator cuff was always present. Measurement of the isometric muscle power revealed reduced power in the painful shoulder in abduction, outward rotation, and flexion.
The radiographic appearance was normal in only 3 of the 10 subjects. Analysis of EMG signals recorded during actual overhead welding revealed significant changes in the action potential of the supraspinatus muscle, implying that this muscle is under sustained heavy strain in this working situation. Kadefors et al. also studied the effect of overhead welding on muscles of the shoulder in 20 welders aged 20 to 35 years.
An inexperienced group consisted of 10 men with less than 1 year of welding experience, and the experienced group consisted of 10 men who had been working for more than 1 but less than 5 years. Among the inexperienced workers, overhead welding resulted in EMG changes indicative of localized fatigue in the deltoid, upper trapezius, and supraspinatus muscles.
Experienced welders demonstrated some adaptation but still had abnormal EMG readings for the supraspinatus muscles.
The authors concluded that overhead welding places considerable amounts of strain on this muscle, which cannot be overcome by experience and training. Petersen et al. reported similar findings in a third study. Those observed included 10 experienced workers with at least 5 years of experience and 10 inexperienced welders with less than 1 year of training. After overhead welding, all experienced welders and a few inexperienced welders (number not given) showed increased fatigue of the supraspinatus muscle.
A subset of older welders complaining of shoulder pain was tested further.
Clinical examination (X-ray) showed diminished strength in shoulder movements in which the supraspinatus was active, and clear signs of supraspinatus tendinitis.
However, it was emphasized that the tendinitis may have been caused by long exposure or as a consequence of natural changes from age in combination with overhead welding.
Ross reported on the results of medical examinations of 926 shielded metal arc welders; all were male, had heavy engineering and shipbuilding experience, and had been observed for 6 years. These findings were compared with the results of medical examinations of 755 nonwelders who were used as controls.
Chronic conditions encountered included occupational hearing loss, Raynaud's phenomenon, and Dupuytren's contracture.
Raynaud's phenomenon, also called white finger disease, affected 102 (11%) of the welders, compared with 7 (1%) of the nonwelders.
It was associated with the use of vibratory tools but was considered by the author to be relatively minor in nature.
Dupuytren's contracture, a flexion deformity of the finger, which the author reported as not usually occupational in origin, was found in 38 (4%) of the welders and 4 (0.5%) of the controls.
The author speculated that it could be caused by tightly gripping the electrode holders. Nauwald studied knee joint changes in 100 welders (type not stated) in the shipbuilding industry.
Sixty-nine of the 100 welders complained of spontaneous pains in the knee joints.
These included pain during motion, pain when starting to move, pain during hypercompression of the joint, and the so-called "giving-away" phenomenon.
Arthritis, proliferation of fatty tissue in knee joint, and fluid sac diseases were observed with increasing frequency in welders who were older than 25 and had a minimum exposure time of 6 years.
The author stated several potential causative factors in the development of the observed knee joint diseases:
(1) the static-mechanical stress on the bent knee while working, (2) the chronic, persistent pressure on the soft parts of the joint, and ( 3) thermal effects such as cooling due to kneeling on cold iron for an extended period of time.
# C. Safety Hazards
In addition to being exposed to chemical and physical agents, welders are also exposed to potential safety hazards that may result in injury or death. In a cross analysis, the source of injury was cross-tabulated with type of accident, nature of injury, and body part. The analysis of the SDS accident/injury data was performed for the top 10 source-of-injury categories that identified tools, tasks, or equipment used by welders and thermal cutters.
A total of 166,907 injuries were reported to the SDS data base from welders and thermal cutters during the period 1976-1981; 109,774 of these injuries were included in the cross analysis and reported in Table IV-9. The SDS data do not include any information on the cause of the injury.
The Bureau of Labor Statistics obtained data from 18 States on welding-and cutting-related injuries for 1,364 workers that occurred during a 5-month period in 1978.
Forty-two percent of the reported injuries during this period occurred in welders or cutters who had 5 or more years of experience; 92% of these welders and cutters had received safety training in the form of classroom or on-the-job safety training or written material about welding or cutting safety measures.
Arc welding or cutting was being performed when two-thirds of these injuries occurred, and 83% had received safety training in the use of this equipment.
Sixty-seven percent of the reported injuries were to the eye(s); 58% of the burns to the eyes resulted from welding being performed in the nearby work area; 50% of all eye injuries occurred as a result of not wearing filtering lenses to protect the e y e s .
Injury of workers by industrial welding robots has also occurred. Specific types and the number of injuries reported for welders involved in these types of processes are not available; however, this kind of information is being gathered by the Division of Safety Research, NI0SH . According to Percival [1984, the six main sources of hazards from industrial robots are as follows:
(1) control errors caused by errors in the software, faults within the control system, or electrical interference;
(2) unauthorized access to robot enclosures; (3) human error when working close to a robot; (4) electrical, hydraulic, and pneumatic faults;
(5) mechanical hazards from the function of the robot (e.g., welding hazards); and (6) environmental hazards (e.g., dust, fumes, radiation). Although specific controls for these hazards are not addressed in this document, many of the measures recommended for controlling emissions generated at other welding processes can be applied to industrial welding robot operations. Some of the specific safety hazards associated with welding processes are fires, explosions, or electric shocks.
The following are case reports of injuries and fatalities resulting from such hazards.
# F i res
The fire hazards caused by either the welding flame itself or flying sparks have been responsible for injuries and fatalities of workers .
Fires associated with oxygen-enriched atmospheres provide dramatic examples of the risks involved when there is either enrichment of the air by oxygen in enclosed spaces or leakage of oxygen.
Accidents have also been reported when air has been intentionally enriched (sweetened) before welding to purge the air of contaminants.
Three fires in oxygen-enriched atmospheres were reported by Rames .
The first occurred inside a storage tank where a welder was making repairs by electric arc welding.
He enriched the inside atmosphere with oxygen from a cylinder outside the tank.
His assistant went inside to help instead of keeping watch outside.
After 20 min, their clothing suddenly ignited, and although they succeeded in getting out of the tank, they both died on the way to the hospital.
The second case report was of a welder who went down a deep well to cut a rusty suction basket from a pump.
Before he descended, he fed oxygen instead of compressed air into the well because he thought there might be dangerous gases present. When he started to cut, his clothing burst into flames and he fell into the water.
His assistant, who was watching, was unable to help.
The welder was dead when he was removed from the well.
The third case was that of a welder and his assistant who were arc welding while repairing pipelines inside a small channel. Their clothing suddenly caught fire, and even though they were being observed from the outside by others, they died before they could be rescued.
Investigation of the accident revealed that they were using oxygen from the cutting equipment to sweeten the air.
The National Fire Protection Association (NFPA) reviewed reports of several fires caused by cutting and welding equipment. During repairs of an underground missile silo, a welder struck and caused a rupture to a temporarily installed, high pressure hose containing hydraulic oil.
The oil escaped as a fine mist and ignited at the electric arc.
Although the fire was of short duration, it killed 53 of the construction workers trapped in the confined silo space.
The California Division of Labor Statistics and Research (CDLSR) also described several fires resulting from welding.
An auto dismantler was using an acetylene torch to cut the metal straps holding a fuel tank in place.
The tank fell to the ground and pulled off the filler spout.
Sparks from the torch ignited the fuel in the tank. The dismantler sustained second-degree burns on his hands and face.
In another occurrence, a man was burning and cutting scrap metal.
The oxygen hose caught fire and caused the worker to drop the torch, breaking the fitting. Oxygen went up his pants leg, which ignited.
In another incident, a ladle helper was holding an oxygen hose while another worker was cutting with a torch. The oxygen accumulated in the worker's glove, ignited the glove, and burned his right hand.
# Explosions
Explosions caused by welding sparks igniting flammable or explosive materials are a potential problem associated with all welding processes.
A mixture of acetylene with air containing more than 2.5% or less than 80% acetylene is explosive .
Fire resulting from an explosion occurred in the cooling plant located in the basement of a newly erected hospital .
A chief electrician and an electrical fitter were installing wiring for an electrical plant.
The chief electrician who had on-the-job experience had not received any formal welding training. While cable supports were being welded from a ladder, sparks fell to the floor igniting a rag lying on a varnish can. An explosion occurred and both workers were immediately surrounded by flames.
The welder on the ladder was able to escape.
His coworker who was unable to escape suffered extensive burns.
The NFPA described several explosions caused by welding that resulted in death.
In one case, a workman using a torch to cut an object on the top of a drum containing kerosene cut into the drum and the oil exploded, fatally burning him.
In another case, after partially unloading a tanker of asphalt stored at a temperature of about 143°C (290°F), two workmen went to the top of the tank to straighten the pipe through which they measured the oil level. They were using an acetylene torch that ignited the leaking vapors and caused an explosion that killed both men.
In another reported incident, three welders were killed as a result of an explosion that occurred while they were repairing a leak in an odor-scrubbing system.
Heat from the torch had ignited flammable vapors within a connecting pipe, and the flame was propagated to the tank that contained naphthalene.
The tank ruptured, killing all three workmen.
Several explosions were reported in the CDLSR description of welding accidents .
Some of these occurred in atmospheres enriched by oxygen and some occurred when sparks caused the ignition of flammable vapors or liquids that had leaked from hoses or containers.
# Electric Shocks
Because currents of 100 to 600 A at 30 to 60 V, either AC or DC, are used in welding, shocks to workers have resulted in falls causing serious injuries or deaths .
The usual practice in welding operations is to have the work grounded to one terminal of the power supply while the electrode holder is connected to the other terminal.
Fatalities have resulted from a current passing through the body when the worker stepped on the "live" electrode, while in contact with the other terminal of the current. Careless handling or changing of electrodes has also resulted in serious injuries and fatalities.
Five welding-related deaths from electrocution occurring between 1956 and 1975 were reported by Simonsen and Petersen . One case involved a 37-year-old electric arc welder who was working in a confined space where the temperature was 35° to 40°C (95° to 104°F). He had perspired heavily and had removed one glove.
The welder developed severe spasms, apparently from an electrical contact, was hospitalized, and died a short time later. Burnlike lesions were found on his lower right cheek, left thigh, and left hand.
Another welder was presumably attempting to ignite his cutting torch by drawing a spark from the welding apparatus while the transformer was operating.
He suddenly fell and died a short time later. The authors provided no information on the type of protective clothing worn. Electrical malfunction of the welding machine was not a factor in this fatali t y .
In a third reported fatality, a 22-year-old man was welding a metal plate onto the hull of a ship while standing on a platform located about 50 cm above the water surface.
He had been working for 4 hr when he lay down to weld on the edge of the plate.
A large wave immersed the platform, and the welder's hand holding the welding device was submerged in water.
He died from electric shock.
In 1974, a 47-year-old welder was found dead at his workplace. He had been welding on the floor of a small compartment that measured 70 x 73 x 105 cm.
There was a small amount of water on the floor of the compartment.
When he was found, the welding tool was in his right hand and the end of the welding electrode had slid under the face mask and up under his glasses near the left eye. At autopsy, a burnlike perforation of the median sclera of the left eye was found.
In 1975, a 47-year-old man was found dead in a section of a ship where he had been welding.
He was found lying on his back against the side of the ship with the welding tool in his left hand and the tip of the electrode pointing toward his throat.
His helmet and mask lay beside him.
It was very hot in the area where he had been working, and his clothing was soaked with perspiration.
# V. BASIS FOR THE STANDARD
# A. Introduction
This chapter summarizes the studies used by NIOSH to form the basis of its recommended standard for welding, brazing, and thermal cutting. NIOSH believes that the studies discussed here provide the best available evidence of the association between adverse health effects and welding.
The results of these studies are summarized briefly in the following subsection; they are described and fully referenced later in the chapter.
# B . Summary
Analysis of data obtained from welders reveals several types of adverse effects associated with various welding processes.
The respiratory system is the primary target of injury. Metal fume fever and pneumonitis are the most common acute respiratory diseases associated with welding as a result of short-term exposures to high concentrations of fumes and gases.
Chronic respiratory diseases such as cancer, pneumoconiosis, and bronchitis have been observed among welders exposed to welding fumes and gases (and possibly to asbestos in some instances over long periods).
In addition to respiratory diseases, cancers of the kidney, and other urinary tract organs, and the subglottic area of the larynx have been described in such workers. Other health effects and injuries reported include cardiovascular and gastrointestinal diseases, skin sensitization, hearing loss, and eye and musculoskeletal injury.
Some evidence indicates a possible relationship between adverse reproductive outcomes and exposure to welding fumes. Because of the diversity of welding techniques, processes, and materials used, most of these studies lack sufficient information to associate a specific chemical or physical agent with a particular health effect.
# C. Malignant Diseases
# Lung Cancer-Epidemiologic Studies a. Exposure to Fumes from Welding on Stainless Steel and Other Metal Alloys
Statistically significant increases in the rates of lung cancer have occurred among welders exposed to fumes and gases generated from welding on stainless steel and other metal alloys .
In four of these studies, exposure-response relationships were demonstrated . Steenland et al. reaffirmed the excess lung cancer risk when they reanalyzed the studies by Beaumont and Weiss and Sjogren , respectively. Beaumont and Weiss reported excess cancer rates that increased with the duration of welding exposure and the length of time from onset of first exposure.
A standard mortality ratio (SMR) of 132 (p=0.06) was observed for deaths from lung cancer among welders compared with those for U.S. white males.
The SMR for deaths from lung cancer was 174 (p<0.001) when calculated on the basis of deaths that occurred 20 or more years after first welding exposure or initial employment as a welder.
This study cohort was reanalyzed by Steenland et al. using an internal comparison group who more closely matched the lifestyles (e.g., smoking habits) of the welders and who were potentially exposed to the same occupational hazards (e.g., asbestos).
The lung cancer risk remained statistically significant, with an OR of 152 (p=0.03) when duration of exposure was measured using the year the worker was first employed as a welder.
An OR of 1.29 (p=0.03) for lung cancer was also observed for welders as a function of increasing cumulative exposure.
Two studies reported increased incidences of lung cancer among welders who were exposed to stainless steel welding fumes that contained nickel and chromium. Sjogren reported an OR of 4.4 (p<0.03), and Gerin et al. found an OR of 3.3 (95% C I =1.2 to 9.2) among another group of stainless steel welders.
Deaths from lung cancer remained statistically significant in both studies after adjustment for smoking habits.
Although no exposure data were available for either study, measurements of airborne chromium were taken by Sjogren at similar stainless steel welding sites.
They revealed median TWA chromium (trivalent and hexavalent) concentrations of 210 g/m3 during welding with covered electrodes and 20 during gas-shielded welding. Sjogren et al. reported on a reanalysis of these stainless steel welders to determine lung cancer risk after 7 years of additional followup.
The lung cancer risk remained high for the stainless steel welders, who had an SMR of 249 when their death rates were compared with national death rates.
This cohort was also compared with another group of welders who did not weld on stainless steel but were exposed to low concentrations of chromium. These welders had a relative risk of 7.01 (95% C I =1.32 to 37.3) for lung cancer compared with stainless steel welders, which suggests that emissions typically produced during the welding of stainless steel (e.g., chromium, nickel) may be associated with excess lung cancer risk.
# b. Exposure to Welding Fumes in General
Studies reported by Breslow et a l . , HMS0 , and Schoenberg et a l . , provide evidence of an association between exposure to various compositions of welding fumes and gases and an increased risk of lung cancer.
A statistically significant (p<0.05) OR of 1.56 was reported by Breslow et al. in a case control study of 518 lung cancer patients that included 10 welders and 4 sheet metal workers exposed to welding fumes.
The OR remained statistically significant after adjustment for smoking habits.
Mi lham reported on the proportional mortality of lung cancer among welders and flame cutters employed in the State of Washington.
The study used death certificates collected over a 29-year period; proportional mortality ratios (PMRs) were determined at 10-year intervals.
A statistically significant (p<0.01) PMR of 136 was observed for the period 1970-79, and a PMR of 135 (p<0.01) was observed for the total study period .
In another study , statistically significant (p<0.01) SMRs of 151 (not controlled for smoking) and of 116 (controlled for smoking) were found for a group of workers classified as "gas and electric welders, cutters, and braziers."
The study cohort was made up of workers employed in different industries and potentially exposed to various compositions of fumes and gases.
A study of welders in the Louisiana petroleum industry also showed a statistically significant lung cancer risk . However, when the cohort was adjusted for age, the OR was no longer statistically significant.
Although an increased risk of lung cancer was found for welders in these studies , the absence of specific exposure information, type of welding performed, and possible concomitant exposures (e.g., asbestos) makes it difficult to associate exposure with the risk of lung cancer. However, in a case control study reported by Schoenberg et al. , shipyard welders had a statistically significant increase in the rate of lung cancer, with an OR of 3.8 (95% C I =1.8 to 7.8). This risk remained high after adjustment for smoking and exposure to asbestos. Of the 33 cases and 18 controls classified as welders, 16 cases and 7 controls were reported to have been exposed to asbestos.
The remaining 17 cases and 11 controls who had no reported asbestos exposure, showed an increased smoking-adjusted OR of 2.5 (95% C l =1.1 to 5.5).
Four other mortality studies reported increased risks for lung cancer among male welders.
Although the increases were not statistically significant, the studies collectively demonstrate the possible association between classification as a welder and an increased risk of developing lung cancer.
Two of the four studies were conducted on white males who worked as welders at nuclear facilities or at sanitary installations and power plants .
The larger of those studies revealed an OR of 2.4 (p0.05) for cancer of the trachea, bronchus, and lung when compared with a control group that was not exposed to welding fumes. When an external analysis was performed (i.e., comparison with the German national death rates), SMRs for deaths from malignant neoplasms and lung cancer were not markedly increased over the general population.
However, when welders were analyzed by 10-year intervals since first exposure, an upward trend in SMRs was observed.
The incidence of malignant neoplasms was statistically significant (p 30 years since first exposure).
In the smaller cohort study , welders were analyzed according to their potential exposure to nickel oxides. Increased SMRs were observed for lung cancer deaths among both exposed (SMR=124) and unexposed (SMR=175) welders.
The SMRs were not statistically significant when compared with death rates for U.S. white males.
The welders who were not exposed to nickel oxides had a prevalence of smoking that was 2.5 times that of the exposed group.
The difference in smoking habits and the fact that the study groups were small (N=536 exposed, N=523 unexposed) contribute to uncertainty in the interpretation of the results.
Although the SMRs did not reach statistical significance, the risk of death from lung cancer increased among both groups of welders with increasing years of exposure to welding fumes and gases.
Studies of welders in shipyards demonstrate an increased risk of lung cancer.
Although neither study showed statistically significant increases, Puntoni et a l . found elevated ORs for lung cancer in gas welders (0R=2.12) and electric welders (0R=2.54) when compared with the male staff of a local hospital.
An elevated OR of 1.25 for gas welders and an OR of 1.60 for electric welders were observed when the groups were compared with the male population of Genoa, Italy. Newhouse et al. found an elevated SMR of 113 for deaths from lung cancer among a group of welders who performed various welding tasks during ship repair.
Latency and duration of employment were not analyzed in either study, and no attempt was made to account for the confounding exposure of asbestos.
# Other Cancer-Epidemiologic Studies
Several studies indicate a possible association between classification as a welder and an increased risk of cancer of the larynx and of the kidney or other urinary tract organs .
Skin cancer has also been reported among welders employed for more than 30 years in this occupation .
A case-control study conducted by Olsen et al. reported an unusually high risk of cancer (0R=6.3) of the subglottic area of the larynx among 271 cancer patients who had been occupationally exposed to welding fumes and gases.
The high OR for this type of cancer persisted after adjustment for tobacco and alcohol use, but it was not high for those patients (N=12) reported to have been exposed to fumes from stainless steel welding.
Other epidemiologic studies revealed no elevated risk of larynx cancer.
Several cohort mortality studies have reported increased incidences of kidney or other urinary tract cancers among welders.
The study of shipyard workers by Puntoni et a l . reported ORs of 5.06 (p<0.05) and 5.88 (p<0.05) for cancer of the kidney and other urinary tract organs in gas welders compared with two different external control populations. Elevated but statistically insignificant ORs were also reported for electric arc welders.
An increased risk of kidney cancer was also noted by Milham in welders and flame cutters (PMR=182, p<0.01), and Becker et a l . reported a statistically significant (p<0.002) OR of 15.0 (3 observed versus 0.2 expected) for kidney and other urinary tract cancers among welders.
No exposure data were reported in any of the three studies, but Becker et al. reported that most of the welders in his study performed arc welding with coated chromium-nickel alloy electrodes.
Although these studies associated classification as a welder with an increased risk of dying from kidney or other urinary tract cancers, other mortality studies indicated no increased incidences of death from these causes.
# Toxicological Evidence
The risk of cancer noted among welders is consistent with the findings of in vitro and in vivo mutagenesis assays that have demonstrated various mutagenic potentials for welding fumes, depending on their composition . Results of assays have shown that most of the mutagenic activity of stainless steel welding fumes can be ascribed to chromium(VI) in the water-soluble fraction . Maxi Id et al. [1978 reported that shielded metal arc welding of stainless steel produces 3 to 6 times more fumes (per mass of weld metal) than gas metal arc welding.
When the mutagenic potentials for shielded metal and gas metal arc fumes were compared on an equivalent chromium(VI) basis, gas metal arc welding fumes produced four times more mutations in bacteria than shielded metal arc welding fumes . Other data reported by Hedenstedt et al . and Stern et al. suggest that compounds other than chromium(VI) may be active in the water-soluble fractions of fumes generated from shielded or gas metal arc welding of stainless steel.
When water-soluble fractions of both fumes were tested in an assay using metabolically activated S. typhimurium, arc welding fumes were less mutagenic.
In a 2-year study reported by Reuzel et al. , evidence of carcinogenicity was found in animals exposed to stainless steel fumes. Syrian golden hamsters were intratracheally injected with saline suspensions of stainless steel fumes from shielded metal arc welding. One lung cancer resulted from each of two dose groups.
No cancers were observed in the untreated control groups or in animals treated with gas metal arc fumes, calcium chromate (positive control), or saline. Because these tumors are extremely rare in Syrian golden hamsters, the authors concluded that the lung tumors were induced by welding fumes.
# D. Other Diseases
# Acute Respiratory Diseases a. Epidemiological Studies
One of the more frequently reported health effects from exposure to welding fumes is metal fume fever, which often resembles an upper respiratory infection such as influenza, acute bronchitis, pneumonia, or upper gastrointestinal infections .
These conditions usually last 6 to 24 hr and are often accompanied by chills, trembling, nausea, and vomiting . Exposure to specific metals such as zinc in zinc oxide fumes and to fumes of mixed composition have been associated with metal fume fever. Although no specific exposure concentrations have been associated with metal fume fever, most reported cases have occurred in workers exposed to welding fumes while working in confined or other poorly ventilated spaces.
Pneumonitis and pulmonary edema have been reported in welders who performed various welding processes (e.g., gas and shielded metal arc welding, silver brazing, or oxyacetylene welding) and were exposed over short periods to high concentrations of nitrogen dioxide , ozone , cadmium fumes , chromium and nickel fumes , or aluminum and iron oxide fumes . Cases of acute cadmium fume pneumonitis and death have been reported among welders exposed either by brazing with siIver-cadmium alloy or by cutting or welding cadmium-coated metal in poorly ventilated areas . Beton et al. reported on the death of a welder who was cutting cadmium-plated bolts with an oxyacetylene torch.
Based on the amount of cadmium oxide found in the welder's lung during a postmortem examination, the authors estimated that his exposure to cadmium oxide averaged 8.6 mg/m^.
Several other fatalities have resulted from pulmonary edema in welders exposed to nitrogen dioxide concentrations above 100 ppm .
# b. Toxicological Evidence
Pathological lung changes observed in welders acutely exposed to welding fumes and gases have also been documented in exposed animals .
Animals exposed to welding fumes and gases for short periods suffered severe lung damage (e.g., edema, hemorrhage, pneumonia, and atelectasis) and death.
In one experimental study , cats and rabbits were exposed to iron oxide fumes for up to 8.5 hr at concentrations of 10 to 350 mg/m^.
All animals developed pulmonary edema.
Their alveoli became dilated, their lungs hemorrhaged, and several died.
Similar results were reported by Hewitt and Hicks in albino rats exposed to rutile welding fumes and gases at an average concentration of 1,500 mg/m^. Rats exposed for either 30 min or 4 hr demonstrated a statistically significant (p<0.05) increase in uptake of chromium and antimony by the lungs, and of cobalt by the liver and blood. Microscopic examination of the lungs revealed peribronchial edema and large numbers of particulate-laden macrophages in the alveoli and alveolar ducts.
Histopathological lung changes were reversed following 75 days with no exposure; only the particulate material remained within the macrophages.
Pulmonary deposition and clearance rates in animals exposed to fumes from welding nonstainless and stainless steels were investigated by McCord et al. andByczkowski et al. .
The rates of metal deposition in the lungs were proportional to the metal content of the emissions; these rates increased in animals that exercised during exposure.
# Chronic Respiratory Diseases a. Epidemiologic Studies
Pneumoconiosis, including siderosis, has been reported among welders exposed to iron oxide fumes from bare metal electrodes . Although quantitative data on exposures are lacking for most of these studies, Dreesen et al. provide some data on the extent of exposures before 1950.
Samples collected during arc welding of mild steel in a shipyard revealed iron oxide concentrations above 30 mg/nr- and zinc oxide concentrations above 15 mg/m^.
The highest exposure concentrations were found in poorly ventilated work areas.
Approximately 50% of the samples contained less than 5 ppm oxides of nitrogen, and 10% of the samples exceeded 25 ppm.
Other studies have described siderosis complicated by fibrosis .
These findings appear to be associated with the replacement of bare metal electrodes by covered electrodes. Clinical evaluations were made of workers who were exposed to iron oxides and silica and who welded both ferrous and nonferrous materials using covered electrodes.
These evaluations revealed diffuse interstitial fibrosis and siderosilicosis . Levy and Margolis reported peak airborne concentrations of 19.4 mg/m^ for iron oxide and 6.82 mg/m^ for respirable silica among steel foundry welders who had evidence of siderosi Iicosis.
Welders have also shown decrements in pulmonary function and increases in the prevalence of chronic bronchitis .
The only exposure data reported are those cited in the studies by Barhad et al. , Sjogren and Ulfvarson , and Keimig et al. . Barhad et al. reported that shipyard welders were exposed to total fume concentrations of 6 to 36 mg/m^ in open work areas and 48 to 92 mg/m^ in confined spaces during arc welding with covered electrodes.
Oxides of nitrogen averaged concentrations of 1.7 mg/m^ during shielded arc welding and 1.1 mg/m^ during arc welding.
Regardless of the welding process, carbon monoxide concentrations ranged from 6.3 to 17 mg/m^.
In the study by Sjogren and Ulfvarson , exposures to ozone exceeded 0.1 ppm in 50% of the samples collected during gas metal arc welding of aluminum.
During stainless steel welding with covered electrodes, 80% of the chromium(VI) concentrations exceeded 20 ug/m3.
Concentrations of nitrogen oxides were less than 5 ppm for all welding processes .
Breathing zone air samples collected near welders at the time of the study reported by Keimig et al. indicated iron oxide concentrations of 1.3 to 8.5 mg/m3, with no detectable amounts of chromium, copper, fluoride, or lead in any of the air samples.
The cross-sectional study reported by Keimig et al. found that welders and controls who smoked had higher frequencies of reported respiratory symptoms (e.g., bronchitis, pneumonia, and cough) than corresponding nonsmokers.
Although welders who did not smoke reported higher frequencies of symptoms than nonsmoking controls, the differences were statistically significant (p<0.05) only for the symptoms of increased phlegm and episodes of cough and phlegm.
The only statistically significant differences noted in pulmonary function tests were decreases in forced vital capacity (FVC) at the end of the work shift for nonsmoking welders, nonsmoking controls, and smoking controls.
Similar findings were reported by Oleru and Ademi luyi for a group of workers engaged in the welding of medium-and high-alloy steel.
Although no evidence of obstructive lung disease was found, 7 of 67 persons tested had restrictive lung impairment.
Welders given pulmonary function tests to assess the effects of exposure over a 40-hr work week demonstrated statistically significant (p<0.05) decrements in all parameters measured.
Peak flow measurements made on this group after an 8-hr work shift showed acute changes in pulmonary function that were statistically significant (p<0.05).
However, these changes were not statistically significant when the group was retested after 3 additional days of welding.
In the studies by Hunnicutt et al . , Fogh et al. , andAkbarkhanzadeh , the increased prevalence in decrements of pulmonary function or chronic bronchitis were observed only in welders who smoked.
# b. Toxicological Evidence
Siderosis has been produced by exposing animals to mixed compositions of fumes .
All rats and rabbits developed siderosis when they were exposed to shielded metal arc welding fumes for 6 hr/day, 5 days/week for 46 days followed by an additional 43 days without exposure .
Animals were exposed to average concentrations of 465 mg/m^ (ferric oxide), 61 mg/m^ (silicon dioxide), and 16 mg/m^ (manganese).
Similar results were produced by Garnuszewski and Dobrzynski , who exposed groups of guinea pigs and rabbits to fumes that were either high in silicon oxide (25.5%) and low in ferric oxide (18%), or low in silicon oxide (7.8%) and high in ferric oxide (23%).
Each experimental group of animals was subdivided into a high-exposure group (36 mg of total fumes/m^ of air) or low-exposure group (18 mg of total fumes/m^ of air).
All animals were exposed 4 hr/day, 6 days/week for 110 days.
All exposed guinea pigs developed a mixed type of pneumoconiosis (e.g., siderosis with silicosis manifested by pneumoconiotic nodules containing collagenous fibers and silica particles).
No pneumoconiosis was observed in the exposed rabbits.
# Other Adverse Health Effects a. Auditory Impairment
Auditory impairment has been reported among welders as a result of traumatic injury or excessive sound pressure . Several cases of eardrum injury and permanent hearing loss were reported by Frenkiel and Alberti among welders who did not wear ear protection and were injured by sparks and molten metal that entered the ear while welding.
Studies conducted by Hickish and Challen and Bell described the risk of noise-induced hearing loss in welders performing arc air gouging or plasma torch welding of metals. Mean temporary hearing losses of 19 dB at 4,000 Hz and up to 35 dB at 8.000 Hz were reported by Hickish and Challen among a group of welders who were performing plasma torch welding for 1 hr without wearing hearing protection.
# b. Cardiovascular Disease
Studies that have assessed cardiovascular disease in welders have produced equivocal results.
Two mortality studies indicate increased risks of death from cardiovascular disease among shipyard welders . Newhouse et al. reported an increased SMR of 130 (p=0.10) for ischemic heart disease, and Puntoni et a l . reported ORs greater than 1.00 for cardiovascular disease.
Neither study adjusted for smoking habits, and no information was provided on other possible risk factors.
Two other studies analyzed deaths from cardiovascular disease:
An SMR reported by Polednak and a PMR by Milham were both less than 100. Although the association between welding and an increased risk of cardiovascular disease remains equivocal, the data do provide cause for concern.
# c. Dermal Effects
Several types of dermal conditions observed in welders have been attributed to exposure to physical agents, including UV radiation , IR radiation , and metals to which workers can become sensitized .
Chronic dermatitis and other skin diseases have been documented in several case reports that described welders whose skin came into contact with many types of metals (e.g., nickel, cadmium, and chromium) and fluxes.
Welders exposed to welding fumes from stainless steel have experienced episodes of facial contact dermatitis .
In these cases, removal of the worker from exposure or the use of protective clothing eliminated or greatly minimized the severity of the d i s o r d e r .
# d. Eye Injuries
Welders or others working near welding processes risk eye injury from metal spatter, foreign bodies in the eyes, and exposure to nonionizing electromagnetic radiation .
Exposure to ultraviolet radiation (UV) from welding arcs has caused acute keratoconjunctivitis, also known as welder's flash or actinic ray photokeratitis .
Repeated episodes of welder's flash over a long period have caused cataracts , Similarly, exposure to infrared radiation (IR) has caused thermal damage to the cornea and aqueous humor of the eye and has been associated with the formation of lenticular cataracts .
Such adverse ocular effects have been attributed to the improper use or absence of eye protection .
According to Bureau of Labor Statistics (BLS) data for the period 1976-81, eye injury was the type of injury that welders reported most frequently.
Such injuries were associated with exposure to radiation or foreign bodies in the eyes among welders and flame cutters .
These recent data are consistent with earlier data .
For the 1983 BLS report, data were collected over a 5-month period in 1978 from welders in 18 states (BLS 1983). Sixty-seven percent of the reported injuries were to the eyes.
No information was given in either report as to whether eye protection was being worn at the time of the injury.
# e. Gastrointestinal Disorders
Gastrointestinal disorders (e.g., nausea, vomiting, and gastro intestinal cramps) are often experienced by welders with metal fume fever, but they are reversible following treatment and removal of the worker from additional exposure . Studies by Mignolet , Stancari and Amorati , andRozera et al. reported digestive system disorders in welders that included gastritis, gastroduodenitis, and gastroduodenal ulcers. The authors attributed these conditions to long-term exposures to welding fumes and gases.
Epidemiological studies of welders conducted by Puntoni et al. , Polednak , and Becker et al. found no increases in mortality as a result of diseases of the digestive system.
# f. Musculoskeletal Effects
Reports of musculoskeletal injuries involving the shoulders, back, and knees have been noted in several studies of welders .
Complaints of shoulder pain and reduced muscle power, particularly of the supraspinatus muscle, have been frequently attributed to overhead welding performed by both inexperienced and experienced welders. Knee joint problems (including fluid sac diseases, arthritis, and proliferation of fatty tissue) have also been observed, primarily in welders with more than 6 years of experience.
# g. Reproductive Effects
Studies conducted by Rachootin and Olsen and Lindbohm et a l . suggest a possible association between adverse reproductive outcomes and the subject's status as a welder or as the wife of a metal plate worker.
A statistically significant increase (p<0.05) in spontaneous abortions was observed for wives of metal plate workers ,
The authors suggested that this increase was caused by exposure to chromium or nickel.
The case-control study by Rachootin and Olsen indicated a statistically significant increase (p<0.05) in delayed conception, with ORs of 1.4 for male welders and 2.4 for female welders.
The risk remained statistically significant for women after adjustment for age, smoking habits, alcohol consumption, and past use of oral contraceptives.
Men and women assigned to the subgroup "Welding of Stainless Steel" had no statistically significant increase in their risk of delayed conception.
Although the studies suggest a reproductive risk, several méthodologie problems exist, including the inability to accurately estimate possible exposures based on employment history , the lack of information on smoking habits or alcohol consumption , and possible data collection biases resulting from the use of self-administered questionnaires .
No experimental animal studies have been conducted to determine the effects of welding fumes and gases on the reproductive system.
# E. Safety
Fires, explosions, and electric shocks are common welding hazards that have caused many disabling injuries and fatalities .
Fires caused by the welding flame itself or by flying sparks have been responsible for many injuries and fatalities of welders .
Injuries have also been reported as a result of accidental fires caused by welding in oxygen-enriched atmospheres in confined spaces or by oxygen leaks from welding tanks .
Fires and explosions have also been caused by welding or cutting tanks and drums that have not been properly emptied and cleaned of flammable liquids .
Electric shocks have occurred in welders using alternating or direct currents of 120 to 600 A at 30 to 60 volts.
Even if the shock itself was harmless, resulting falls have caused serious injury or death .
Many of these incidents have occurred from improper grounding of the welding electrode or careless handling and changing of electrodes.
# F . Cone I us i ons
Epidemiologic studies and case reports of workers exposed to welding fumes and gases provide adequate evidence that these workers are at an increased risk of contracting acute respiratory diseases such as metal fume fever and pneumonitis . Chronic respiratory diseases such as pneumoconiosis and bronchitis have also been documented in workers exposed to welding emissions . Some studies report that an increased risk of lung cancer is associated with welding on stainless steel , and the study reported by Polednak observed an increased risk in welders exposed to nickel oxides.
Studies of welders exposed to fumes of mixed composition have also reported an increased risk of lung cancer , An exposure limit for total welding emissions cannot be established because the composition of welding emissions (chemical and physical agents) varies for different welding processes and because the various components of a welding emission may interact to produce adverse health effects, including cancer.
Thus even compliance with specific chemical or physical agent exposure limits may not ensure complete protection against an adverse health effect.
Therefore, exposures to all chemical and physical agents associated with welding should be reduced to the lowest concentrations technically feasible using current state-of-the-art engineering controls and good work practices.
Individual exposure limits for chemical or physical agents are to be considered upper boundaries of exposure.
Equivocal evidence exists to show the effects of welding emissions on ( 1) the increased risk of cancer at sites other than the lung , (2) the cardiovascular system , and (3) the reproductive system . However, following the recommendations in this document should prevent or greatly reduce a welder's risk of developing these diseases.
Following the recommendations should also reduce injuries and deaths resulting from unsafe work conditions.
# VI. HAZARD IDENTIFICATION
An occupational health program should include methods for thoroughly identifying and assessing all potential hazards if it is to protect welders from the adverse health effects of chemical and physical agents in their work environment.
Information provided by monitoring and analysis is needed to determine whether controls (e.g.
# Airborne Contaminants
Routine air monitoring of the workplace helps to determine whether a worker is exposed to any individual chemical at or above its exposure limit.
These data must be obtained for all workers involved in welding activities and for all other persons working near welding sites.
If a worker's exposure can be accurately characterized, and if concentrations of specific agents are found to be below their exposure limits (or below their action limits if the agents have established NIOSH RELs), further characterization of the work environment is not needed as long as the process or work conditions do not change.
No safe exposure concentration has been established for chemicals that NIOSH has identified as potential occupational carcinogens.
An effective air monitoring program should include the following components to accurately assess each worker's exposure:
A procedure to assess the worker's potential for exposure. This procedure should include collection of data on the types of materials being used (e.g., welding rods and fluxes) and the composition of the base metals,
- Knowledge of air sampling and analytical method(s) required to determine concentrations of airborne chemical and physical agents, and
- Information on the number of workers potentially exposed and the duration of their exposure.
# A. Workplace Monitoring and Analytical Methods a. Determining the Potential for Exposure
The first step in determining the potential for exposure to a specific agent is the preparation of a hazard inventory. This inventory should include information on the type of welding process that will be performed, the possible chemical and physical agents that may be encountered, and the composition of the base metal, coatings on the metal, fillers, and fluxes.
This initial assessment should include a review of all precautionary labels on containers of filler metals, electrodes, and flux materials and any material safety data sheets.
Refer to Chapter III, B (Potential for Exposure) for a more detailed description of contaminants that may be encountered during welding.
After an initial assessment of potential airborne exposures, employers should identify workers whose exposures to a specific agent may be at or above its exposure limit (or action limit if the agent has an established NIOSH REL).
To determine which workers may be at increased risk of exposure, the following work conditions should be evaluated: the location of the welding process with respect to the worker(s), frequency of the welding being performed, the use of engineering controls, and the type of work practices employed.
If some uncertainty exists about a worker's exposure (regardless of job title), the worker should be included in the air monitoring program, at least initially.
# b. Sampling Strategy (Location, Number, and Frequency of Sampling)
The following subsections provide some basic criteria for establishing and implementing a sampling strategy.
# (1) Sampling Location
The sampling location is important in achieving an accurate characterization of the suspected exposure.
The preferred sampling location is within the breathing zone of the worker and is referred to as a personal sample.
The concentration of fumes or gases in the welder's breathing zone for a given process varies depending on the specific work practices of the welder and the type of exhaust ventilation used.
For example, if a welder leans over the work, exposure for that worker will be greater than for a welder in an upright position. Moreton et al. reported that exposure concentrations varied by a factor of six among welders who performed the same task but used different work practices.
In addition, the concentration of airborne contaminants typically varies as a function of distance from the worksite.
The type of ventilation, convective drafts, and location of the operation further increase the variability of contaminant concentrations with distance from the source.
If personal samples are collected on a worker wearing a welding helmet, the inlet to the sampling device should be correctly positioned within the helmet.
The helmet reduces to some degree the amount of contaminant in the breathing zone. Johnson sampled outside and inside a welding helmet simultaneously during production welding.
Concentrations of iron fumes were compared for the two sample locations.
The ratio of outside to inside concentrations ranged from 1.03:1 to 7.55:1, with an average of 3.5:1. Based on this and similar experimental studies, the American Welding Society (AWS) Standard F1.1-76, "Method for Sampling Airborne Particulates Generated by Welding and Allied Processes," specifies that air samples should be taken within the welding helmet 50 millimeters (mm) to the left or right of the welder's mouth.
In a similar study measuring the performance of full-facepiece respirators, Myers and Hornung found that sampling errors in the facepiece were minimized by placing the inlet of the sampling probe to within 1/2 to 3/4 inch (in.) of the wearer's mouth.
Because welding emissions often consist of fumes and gases, different sampling media are often required.
However, space is restricted in the welding helmet, and wearing several air sampling instruments can cause discomfort.
Thus a given worker may have to be monitored over a period of several days, or different types of samples may have to be collected on various workers at the same worksite.
# (2) Number of Samples Required
Once the sampling location has been identified, employers should select the number and type of workers to be sampled by considering which workers have the highest potential for exposure and which workers are potentially exposed despite working some distance from the welding process.
For a more detailed discussion on the selection of workers and a strategy for sample collection, consult the NIOSH Occupational Exposure Sampling Strategy Manual ,
This manual also provides guidance on the length of time needed for sample collection, number of samples required for statistical validity, and the scheduling of sample collection (i.e., on one or multiple days) to accurately define workers' exposures.
# (3) Sampling Frequency
Unless welding is performed under product ion-1ine conditions, sampling should be conducted at frequent intervals to characterize exposures adequately and determine the need for controls.
However, when the welding process is repetitive (as it is on a production line), exposure conditions may be characterized and quantified by an initial sampling survey.
It can be assumed that conditions will remain relatively constant during future welding activities if there is no change in the process or type of welding.
Under these circumstances, routine sampling should not be necessary.
This strategy applies only when the survey results indicate that workers are not being exposed to any agent at or above its exposure limit (or action limit if the agent has an established NIOSH REL).
With these survey results, no further sampling is necessary as long as no change occurs in the conditions that existed during sampling.
Unfortunately, it is not always possible to note when conditions change.
For example, if debris accumulates in the ventilation system, the collection efficiency of the system may decrease, and workers' exposures could increase without any visible signs of change.
Although this type of potential problem may not necessitate routine air sample monitoring, it does require periodic examination of the ventilation system to ensure that it is operating at optimum efficiency.
If the potential exists for any condition to change (e.g., malfunction of ventilation system) without apparent warning, then a routine monitoring program should be implemented and continued until all such conditions can be standardized.
For a more detailed discussion on determining the need for additional sampling, consult the NIOSH Occupational Exposure Sampling Strategy Manual ,
# c. Analytical Methods
Analytical methods for assessing samples of most welding emissions have been developed by NIOSH and are listed in
# Physical Agent Monitoring
Physical hazards associated with welding include electromagnetic radiation, X-radiation, and noise.
The following guidance is provided to assist in the initial assessment of these potential hazards.
# a. Monitoring UV Radiation Levels
Quantifying exposure to optical radiation is difficult, and the NIOSH criteria document on radiation does not include specific recommendations for monitoring UV radiation.
The following guidelines are provided to assist in the recognition and control of any potential exposure to UV radiation.
Many welding processes generate radiation from the entire UV spectrum or from parts of the UV spectrum.
Most commercially available UV measuring devices (with the exception of the thermopile) are wavelength selective.
Thus measuring a welder's exposures to UV radiation can be difficult.
Other problems in accurately measuring worker exposures include measurement errors caused by water vapor in the air, errors caused by the directionality of exposure meters, reflection errors, and equipment problems such as solarization and aging of lenses and other components . Control of UV radiation exposure is best ensured through a management control program that relies on the containment of UV emissions through barriers.
Where barriers cannot be used, personal protective devices such as appropriate clothing and barrier creams should be used to protect the skin; proper safety glasses should be worn to protect the eyes.
# b. Monitoring X-Radiation
Electron beam welding equipment produces X-rays that are normally contained by the welding chamber.
The AWS recommendations outlined in F2.1-78, "Recommended Safe Practice for Electron Beam Welding and Cutting" , specify that periodic surveys be made to detect any leakage of X-radiation.
The electron beam should be grossly unfocused and aimed at a tungsten target.
A preliminary assessment of the equipment should be made while it is operating at maximum current and voltage levels to detect leakage.
Thereafter, periodic surveys can be made when the equipment is moved or repaired.
Film badges or some other means of X-ray exposure monitoring should be provided for equipment operators.
# c. Monitoring Noise Levels
Excessive noise may be produced in a number of welding and allied processes including plasma arc, metal spraying, and arc air gouging processes.
The potential for a given process to generate excessive noise can quickly be determined using a sound level meter with an A-weighted scale and a type II microphone.
However, these meters do not accurately measure impact noise.
Operations that generate significant noise levels during a full work shift require a comprehensive exposure evaluation.
With the exception of routine "assembly line" operations, where sound level meters can be used to characterize exposures, most processes are best evaluated using dosimeters.
Also, an octave band analysis can be useful in determining the source and frequency of the noise so that appropriate sound-absorptive materials or a barrier for controlling the path of the sound can be selected.
The NIOSH criteria document on noise discusses equipment and procedures for monitoring noise levels, along with recommendations for reducing exposures and implementing a hearing conservation program.
# Biological Monitoring
Biological indicators may be useful for assessing human exposures to certain contaminants in the welding environment.
Further information may be found in Section B,2 of this chapter (Biological Monitoring).
# B. Medical Monitoring
Workers exposed to chemical and physical agents associated with welding processes are at risk of suffering adverse health effects.
The respiratory system, eyes, and skin require particular attention during medical examinations conducted for preplacement, periodic monitoring, emergencies, or employment termination.
Medical monitoring as described below should be made available to a 11 workers.
The employer should provide the following information to the physician responsible for the medical monitoring program:
- Any specific requirements of the applicable OSHA standard or NIOSH recommended standard
- Identification of and extent of exposure to physical and chemical agents that may be encountered by the worker
- Any available workplace sampling results that characterize exposures for job categories previously and currently held by the worker - A description of any protective devices or equipment the worker may be requ i red to use
The composition and toxic properties of the materials used in welding
The frequency and nature of any reported illness or injury of a worker
# Med i caI Exam i nat i ons
The objectives of a medical monitoring program are to augment the primary preventive measures, which include industrial hygiene monitoring of the workplace, the implementation of engineering controls, and the use of proper work practices and personal protective equipment. Medical monitoring data may also be used for epidemiologic analysis within large plants and on an industry-wide basis; they should be compared with exposure data from industrial hygiene monitoring.
The preplacement medical examination allows the physician to assess the applicant's functional capacity and, insofar as possible, to match these capabilities with the physical demands and risks of the job.
Fu rt he r more, it provides baseline medical data that can be compared with any subsequent health changes. This preplacement examination should also provide information on prior occupational exposures.
The following factors should be considered at the time of the preplacement medical evaluation and during ongoing medical monitoring of the worker:
(a) exposure to chemical and physical agents that may exert independent and/or interactive adverse effects on the worker's health (including exacerbation of certain preexisting health problems and synergism with nonoccupational risk factors such as cigarette smoking), (b) ancillary activities involved in welding (e.g., climbing and lifting), and (c) potentially hazardous characteristics of the worksite (e.g., confined spaces, heat, and proximity to hazards such as explosive atmospheres, toxic chemicals, and noise).
The specific types of information that should be gathered are discussed in the following subsect ions.
# a. Preplacement Examination (1) Medical History
The medical history should include information on work, social activities, family, and tobacco-smoking habits .
Special attention should be given to any history of previous occupational exposure to chemical and physical agents that may be potentially hazardous.
# (2) Clinical Examination
The preplacement examination should ascertain the worker's general fitness to engage in strenuous, hot work.
Welding processes entail the use of equipment that is often heavy and that may generate potentially harmful levels of UV radiation, heat, noise, fumes, and gases.
The preplacement examination should be directed toward determining the fitness of the worker to perform the intended job assignment.
Appropriate pulmonary and musculoskeletal evaluation should be given to workers whose jobs may require extremes of physical exertion or stamina (e.g., heavy lifting), especially those who must wear personal respiratory protection.
Because the standard 12-lead electrocardiogram is of little practical value in monitoring for nonsymptomatic cardiovascular disease, it is not recommended. More valuable diagnostic information is provided by physician interviews of workers that elicit reports of the occurrence and work-relatedness of angina, breathlessness, and other symptoms of chest illnesses.
Special attention should also be given to workers who require the use of eye glasses; to assure that these workers must be able to wear simultaneously any equipment needed for respiratory protection, eye protection, and visual acuity, and they must be able to maintain their concurrent use during work activities.
Specific welding processes entail potential exposure to diverse chemical agents known to cause specific occupationally related adverse health effects.
These are known as sentinel health events (occupational), or SHE(0)s .
For example, heating of metals with low-boiling points (such as zinc and cadmium) may result in metal fume fever.
Exposure to cadmium fumes may result in delayed onset of pulmonary edema and may lead to pulmonary fibrosis and cancer.
Nickel and chrome are both found in stainless steel and may cause allergic sensitization as a result of an acute exposure or cancer as a result of chronic exposure.
Welding processes that involve the use of flux may generate irritating concentrations of fluorides. Welding on painted metal may result in exposure to lead or other chemical agents, and welding on materials cleaned with a chlorinated solvent may cause photodecomposition of the solvent with resulting exposure.
In addition, the worker's duties may be performed in proximity to unrelated operations that generate potentially harmful exposures (e.g., asbestos or cleaning or degreasing solvents).
The physician must be aware of these potential exposures to evaluate possible hazards to the individual worker.
# (3) Special Examinations and Laboratory Tests
A pulmonary function test (PFT) and a 14-by 1 7 -in. (36-by 43-cm) postero-anterior chest radiograph should be taken and kept as part of the worker's medical record .
The preplacement chest radiograph and PFT gives the physician objective information with which to assess a worker's fitness for a specific job; it may also prevent confusion or misinterpretation of any subsequent lung tissue c h a n g e s .
The International Labour Office (ILO) stresses the importance of radiographic technique in the detection of early pneumoconiosis.
High-speed and miniature films are not recommended.
Films should be interpreted using the current recommendations of the ILO .
Classification of films should be made by NIOSH-certified B readers . Although the short classification may be useful for clinical purposes, films that are obtained in a workplace program of medical monitoring for respiratory hazards must be read and recorded by the complete classification .
Preplacement audiograms of all workers are recommended, since welders, brazers, and thermal cutters may be exposed to noise intensities exceeding prescribed levels.
i A periodic medical examination should be conducted at least annually or more frequently, depending on age, health status at the time of a prior examination, and reported signs or symptoms associated with exposure to welding emissions.
The purpose of these examinations is to detect any work-related changes in health at an early stage.
The physician should note any trends in health changes revealed by epidemiologic analyses of examination results.
The occurrence of an occupationally related disease or other work-related adverse health effects should prompt an immediate evaluation of industrial hygiene control measures and an assessment of the workplace to determine the presence of a previously unrecognized or potential hazard.
The physician's interview with the worker is an essential part of a periodic medical examination.
The interview gives the physician the opportunity to learn of changes in (a) the type of welding performed by the worker, (b) metals and/or fluxes being used, (c) the work setting (e.g., confined spaces), and (d) potentially hazardous workplace exposures that are in the vicinity of the worker but are not attributable to the worker's on-the-job activities.
Because radiographic abnormalities may appear before pulmonary impairment is clinically manifested or otherwise detectable, periodic chest radiographs are routinely recommended for monitoring workers exposed to fibrogenic respiratory hazards .
However, the chest radiograph may not distinguish between a relatively benign disease such as siderosis (caused by iron oxide exposure) and a disease that may be of greater medical importance such as pneumoconiosis.
Under ordinary conditions, chest radiographs may be obtained for workers at 1-to 5-year intervals, depending on the nature and intensity of specific exposures and related health risks. Workers with 10 years or more of exposure and workers previously employed in dusty jobs may require chest radiographs at more frequent intervals.
These intervals may be changed as called for by other regulatory requirements or at the discretion of the examining physician.
For example, a previous radiograph (e.g., one taken at the time of hospitalization) may be substituted for one of the periodic chest radiographs if it is made available and is of acceptable quality.
If a worker has radiographic evidence of pneumoconiosis or spirometric/symptomatic evidence of pulmonary impairment, the physician should counsel the worker and employer about the potential risks of further exposure and the benefits of removing the worker from exposure.
Smokers should be counseled about how smoking may enhance the adverse effects of other respiratory hazards.
Epidemiologic studies suggest an association between exposure to airborne welding fumes and gases and an excessive risk of lung cancer.
Because routine chest radiographs and sputum cytology are inadequate for detecting bronchogenic carcinoma early enough to
# b. Periodic Medical Examination
alter the course of the disease, they are not currently recommended as part of regular medical monitoring for lung cancer in workers.
During the periodic medical examination of individual welders, the physician should reexamine the skin, eyes, and other organ systems at risk to note changes from the previous examination.
The physician should direct special attention to evidence of burns and effects from exposure to UV radiation and solvents.
This evidence may suggest inadequate industrial hygiene control measures, improper work practices, or malfunctioning equipment (e.g., exposure to metal spatter, flying sparks, UV light flashes, or degreaser solvents).
In addition, the physician should be vigilant for musculoskeletal morbidity attributable to ergonomic problems caused by inadequate worker training on the handling of equipment or by improper working position (e.g., kneeling and overhead welding).
When welders are exposed to agents for which there is an existing OSHA standard or for which NIOSH has recommended medical monitoring, physicians should refer to the appropriate standard or recommendation for guidance on specific medical examinations. Appendix B lists published sources of NIOSH RELs for hazardous agents associated with various welding operations.
Hazardous agents that are commonly associated with welding processes are listed in Table VI-3 along with their potential toxic effects and recommendations for additional tests.
# Biological Monitoring
Urinary or blood concentrations of lead, cadmium, chromium, and aluminum, and urinary concentrations of fluoride ions may be useful biological indicators of worker exposure to welding emissions.
Several studies have correlated exposures to welding fumes containing chromium , aluminum , or fluoride with their urinary or blood concentrations.
However, biological monitoring may not be sensitive enough to use as a primary monitoring measure.
For example, Tola et al. found no increase in urinary chromium concentrations when environmental chromium concentrations were within the NIOSH REL. Biological monitoring has the potential for assessing total exposure when the work load (physical activity) and the routes of exposure are taken into account. Mutti et al. and Pantucek showed that urinary levels of chromium and fluoride can provide information on either current exposure or body burden, depending on the timing of the sample collection. Schaller and Valentin concluded that aluminum concentration in serum seemed to be an indicator of body burden, and that aluminum concentration in urine seemed to be an indicator of current exposure.
Thus biological monitoring may be a useful adjunct for detecting accidental exposure or a failure of primary control m e a s u r e s . "Distinction between short-term and long-term effects is not clear-cut and is somewhat arbitrary. Short-term effects are usually the result of acute exposure(s) and may appear immediately to several days or weeks after the exposure.
Long-term effects are usually the result of chronic, repeated low-close exposures extending from several months to many years.
However, long-term effects may also include the aftereffects of single or repeated acute expo su re s. "Tests to be considered at the discretion of the attending physician.
--May contain toxic impurities such as arsine, carbon disulfide, carbon monoxide, hydrogen sulfide, and phosphine. "Toxicity information is mostly from chromium plating operation and chromium pigment manufacturing. ®Metal fume fever is manifested by fever, chills, cough, joint and muscle pains, and general malaise.
Reports of health effects of tungsten come almost exclusively from the studies of workers exposed to tungsten carbide, which usually contains cobalt. SRenal functions should be evaluated because renal dysfunctions are known to hinder urinary excretion of fluorides.
# Recordkeeping
Medical records and exposure monitoring results must be maintained for workers as specified in Chapter I, Section 10(c) of this document. Such records must be kept for at least 30 years after termination of employment.
Copies of environmental exposure records for each worker must be included with the medical records.
These records must be made available to the worker or former worker or to anyone having the specific written consent of the worker, as specified in Chapter I, Section 10(d) of this document.
# Ergonomic Monitoring
Ergonomic factors in the workplace should be assessed to determine the need for changes in the work environment, equipment, or work practices, or compensating exercises to avoid fatigue or injury. Work postures, vibrating equipment, and moving of heavy objects may all strain the muscles and joints of welders.
The static positions frequently used in welding and similar processes may also create ergonomic problems that require analysis.
For example, several studies have indicated that overhead welding may severely strain the supraspinatus muscle of the shoulder, leading to tendinitis.
The movement of workpieces and distribution of workloads may also require study and planning. Ilner-Paine reported the use of video monitoring to observe and record the physical exertion of welders while they worked. This technique was useful in diagnosing the causes of back and shoulder pain among shipyard welders. Grandjean has published additional information on ergonomic principles that can be adapted to jobs typically performed by welders.
# VII. METHODS FOR PROTECTING WORKERS
# A. Informing Workers of Hazards
Employers should provide information about workplace hazards before assignment and at least annually thereafter to all workers assigned to work in welding, brazing, and thermal cutting areas.
The OSHA "Hazard Communication" regulation must be followed .
Appropriate written information on hazards (including material safety data sheets) should be kept on file and should be readily available to workers. This information should include a description of the potential health hazards associated with welding (e.g., exposures to noise, vibration, hot metal, optical and X-radiation, and carcinogenic agents such as chromium, nickel, and cadmium) and their possible adverse health effects (e.g., hearing loss, eye injury, burns, and cancer).
Workers should also be informed of the most common types of accidents encountered while welding (e.g., explosions, fires, electrocution, and asphyxiation from oxygendeficient environments).
This information should list precautionary measures for minimizing exposure and injury, including work practices, engineering controls, and personal protective equipment.
The file should also include a description of the environmental, medical monitoring, and emergency first aid procedures that have been implemented.
Workers should also be instructed about their responsibilities for following proper sanitation procedures to help protect their health and provide for their safety as well as that of their fellow workers.
Information on hazards should be disseminated to all workers through a training program that describes how a task is properly performed, how specific work practices reduce exposures or minimize the risk of injury, and how compliance with these procedures will benefit the worker.
Frequent reinforcement of this training and routine monitoring of work practices are essent ial.
# B. Engineering Controls
Because welding processes involve many chemical and physical agents, the hazards they pose cannot always be controlled using current engineering control methods.
The processes are usually dynamic, making it difficult to use fixed systems to control exposures.
In addition, because of the various characteristics of welding emissions (e.g., fumes, gases, radiation) and the extent and fluctuation of exposure at different processes, the evaluation of exposures is often imprecise, and appropriate controls are difficult to implement.
Despite these limitations, engineering controls should be implemented wherever they can minimize the risk of exposure.
# Optical (Radiation) Hazards
When feasible, welding should be performed in booths or screened areas constructed of one of the following materials:
(1) metal, ( 2) flameresistant fabric that is opaque to most optical radiation, or (3) transparent colored polyvinyl chloride material that is formulated with a flame retardant and a UV-visible absorber in the range of 200 to 3,000 nanometers (nm) .
The booths and screens should be arranged so that they do not restrict ventilation.
Such equipment must conform to requirements of 29 CFR 1910.252(f )(1)(i i i), "Screens."
To minimize ozone production, an opaque shroud should be placed around the arc to minimize the interaction between the optical radiation and the oxides of nitrogen that are generated during the process .
# Chemical Hazards (Gases and Fumes)
Gases and fumes generated during welding may necessitate both local and general exhaust ventilation.
Although local exhaust ventilation is preferred wherever possible, general ventilation may be used in some cases where the exposures are well characterized and local exhaust ventilation cannot be placed close to the source of emissions , Ventilation systems should meet the following minimum specifications:
- Exhaust hoods and ductwork should be constructed of fireresistant materials.
- Systems should be equipped with alarms, flowmeters, or other devices to indicate malfunction or blockage of ductwork.
The air velocity at the face of the duct should be sufficient to capture the emissions. Hood design should be such that captured emissions are carried away from the breathing zone of the worker.
Provision should be made for clean make-up air; 29 CFR 1910.25 2( f)(4)(i) states, "All air replacing that withdrawn shall be clean and respirable."
Various designs of exhaust ventilation systems can provide effective control of fume and gas emissions.
In general, local exhaust ventilation works well for welding processes that are conducted at a fixed location such as a workbench, or that are performed on parts of the same size and shape.
The degree of effectiveness depends on the distance between the face of the duct inlet and the work, the design of the system, and the flow rate and volume of air exhausted.
The use of side baffles or flanges at the duct inlet can increase the capture velocity.
The effectiveness of the exhaust ventilation system declines as the distance between the work and the duct inlet increases; a distance of about 9 to 14 in. (24 to 36 cm) is adequate for capturing fumes and gases.
After optimizing the design of the duct hood so that it can be placed as close as possible to the work, the flow rate should be adjusted to ensure an effective capture velocity.
When welding is performed at remote sites or with different-sized or very large parts, a flanged hood with a flexible duct may be appropriate.
The hood face should be placed at a 0-to 45-degree angle to the work surface and positioned on the side opposite the welder.
The use of a flexible duct system requires that the welder be properly instructed to keep the duct hood close to the emission source and to ensure that the duct is not twisted or bent.
An alternative to using an exhaust hood for gas-shielded arc welding processes is to exhaust the emissions by means of an extracting gun. Such extraction systems can reduce breathing zone concentrations by 70% or more . These systems require that the gun and shielding gas flow rates be carefully balanced to maintain weld quality and still provide good exhaust flow.
General ventilation can be used to supplement local exhaust ventilation.
General ventilation may be necessary where local exhausts cannot be placed close enough to the work to be completely effective.
The ACGIH recommends that where local exhaust cannot be used, 800 cubic feet per minute (cfm) of air be exhausted for every pound of welding rod used per hour.
In-line duct velocities for local exhaust systems that are used to control welding emissions should exceed 3,000 feet per minute (fpm) to prevent particulates from settling in horizontal duct runs.
The recirculation of air from local exhaust systems may be appropriate depending on the potential toxicity of the emissions and the efficiency of the filter collection system.
The recirculation of air from local exhaust systems is not recommended when the collected emissions are unknown or contain extremely toxic agents.
Local exhaust systems must be equipped with flow or vacuum meters or other devices to monitor air flow. These exhaust systems should not be used if their failure to work properly will result in bodily harm before remedial action can be taken .
For automated welding processes where the worker does not work directly over the source of emissions and there are no cross currents, canopy hoods could be used for collecting heated fumes and gases.
When properly placed at the side of the worker and operated at a relatively low velocity, cooling fans can be used in some work environments to remove welding fumes from the breathing zone. Cooling fans have limited use and should be considered only when local exhaust is not possible. The use of a cooling fan in an indoor situation requires supplemental general ventilation.
# X-Radiation
Electron beam welding processes should be enclosed and shielded with lead or other suitable materials that have a mass sufficient to prevent the emission of X-rays. All doors, ports, and other openings should be checked for X-ray emissions to ensure that all seals are working prop er ly.
# Noise
During plasma arc welding and cutting and during arc air gouging processes, a water table or other method of similar effectiveness should be used to control noise and airborne emissions.
# a. Acoustic Shields
An effective noise reduction of up to 8 decibels (dB) can be achieved by placing an acoustic shield between the worker and the source of the noise usually constructed of safety glass or clear plastic (polycarbonate or polymethyl methacrylate), is placed.
This shield is most effective when its thickness is at least three times the wavelength of the sound that is contributing to the noise.
Thus shields can be effective barriers against the high-frequency sound emitted from the air ejection systems of plasma and metal spray guns.
# b. Total Enclosure
A reduction of up to 20 dB can result when the machinery or process is totally enclosed.
However, heat buildup is a potential problem and may require the installation of adequate ventilation.
Vibration within these enclosures should be isolated from the floor.
The enclosure must have ports for possible servicing of electrical, water, oil, and other systems.
These ports should be sealed with sound-dampening materials (e.g., 1/8-in. or heavier rubber washers).
# c. Other Recommendations
Personal hearing protection devices are recommended if engineering controls cannot maintain worker exposures at 85 dBA as an 8-hr TWA. Ear plugs (molded, foam, or acoustic wool) and earmuffs can significantly reduce a worker's noise exposure.
To determine whether the hearing protection device will be adequate, the manufacturers' data on noise attenuation should be compared with the actual reduction required.
Employers can also use one of three methods developed by NIOSH and reported in the List of Personal Hearing Protectors and Attenuation Data .
Additional information on hearing protection devices may be found in the Compendium of Hearing Protection Devices .
Extreme care must be taken in using the manufacturers' data, as it represents the maximum protection possible under ideal conditions. In a NIOSH study to determine the noise reduction provided by insert-type hearing protectors, 50% of the workers tested were receiving less than one-half the expected noise attenuation . Noise reduction was also less than expected when the Mine Safety and Health Administration (MSHA) conducted a study in which microphones were placed inside and outside the protective cup on muff-type protectors while the workers performed their normal tasks .
Whenever workers are exposed to noise levels exceeding 85 dBA as an 8-hr TWA, the employer must administer a continuing, effective hearing conservation program .
The program must include monitoring, worker notification, an audiometric testing program, availability of hearing protectors for workers, record keeping, and a training program.
Hearing protection becomes mandatory when workers' exposures exceed 90 dBA as an 8-hr TWA .
# Oxyfuel Equipment
Ventilation systems and other control devices for oxyfuel equipment should be inspected at least weekly to ensure their effectiveness. Oxyfuel equipment for welding should be installed and maintained in a manner that prevents leakage, explosion, or accidental fire. Such equipment must conform to the requirements of 29 CFR 1910.252(a), "Installation and operation of oxygen-fuel gas systems for welding and cutt i n g ."
Fire or Electric Shock
Arc and resistance welding equipment should be installed and maintained in a manner that prevents fire or electric shock. Such equipment must conform to the requirements of 29 CFR 1910.252(b), "Application, installation, and operation of arc welding and cutting equipment," and to 29 CFR 1910.252(c), "Installation and operation of resistance welding e q u i pm en t."
# C. Work Practices
The prevention of occupational illness and injury while welding requires the use of well-designed work practices.
These include wearing personal protective clothing; using safe work procedures for process operations; practicing good housekeeping, sanitation, and personal hygiene; handling compressed gases safely; and being informed on how to handle emergency situations.
Together with engineering controls, such practices can reduce the health risks to workers.
At a minimum, work practices must conform to OSHA standards (e.g., 29 CFR 1910.251-254, "Welding, Cutting, and Brazing" ).
Additional information on proper work practices is available in the ANSI Z49.1 standard, "Safety in welding and cutting"
# Specific Work Procedures
The manner in which a worker prepares for and carries out welding processes has a direct bearing on the type and extent of the exposure hazard.
For example, Moreton et al. found that variations in the size of work area, ventilation, and work practices caused welders performing the same welding task to be exposed to breathing zone concentrations of fumes and gases that varied by a factor of up to six.
Other factors that affect the generation of fumes, gases, and optical radiation include the operating current and voltage, the diameter and angle of the electrode, and the type of shielding gas used.
Some of these factors may not be up to the worker's discretion to change, and others may depend on product specifications or production schedules.
The type of welding process used on steel can affect fume generation rates. Flux-cored arc and shielded metal arc welding generate many more fumes than gas metal arc and gas tungsten arc welding.
When shielded metal arc welding must be used, low-fuming electrodes may be acceptable substitutes for conventional types.
The electrical current and the position of the electrode while welding both affect fume generation .
An increase in the welding current tends to increase the rate of fuming, gas production, and optical radiation emission.
Manufacturers of consumable electrodes usually specify a range of amperages that should be used during welding.
The welder can minimize emissions by using the lowest acceptable amperage.
In addition, holding the electrode as close to the work surface as possible and perpendicular to it will minimize the arc voltage used and thus decrease the rate of fuming . Pattee et al. noted that when the contact-tube-to-work distance is increased, a greater metal deposition rate occurs, which in effect decreases the fume generation rate. However, fume rate tends to increase when the polarity is dc+ (i.e., reverse polarity) rather than dc-or ac or when the thickness of the metal increases .
The type and moisture content of flux coating used on electrodes also affects the fume generation rate , as does the composition of the shielding or plasma gas . Special precautions should be taken when working in areas not specifically designed for welding.
Such precautions must include (1) observing fire precautions prescribed in 29 CFR 1910.252(d), (2) removing, shielding, or cooling any materials present that may produce toxic pyrolysis or combustion products, and (3) using appropriate personal protective clothing and equipment required for the specific hazard. Whenever possible, the workpieces to be welded should be positioned to minimize worker exposure to molten metal, sparks, and fu me s.
# Confi ned Spaces
Working in confined spaces can be extremely hazardous as a result of explosive, toxic, or oxygen-deficient atmospheres . Although a confined space may initially have good air quality, any subsequent welding in this space can cause a rapid buildup of toxic air contaminants, a displacement of oxygen by an inert or asphyxiating gas, or an excess of oxygen that might explode. Only by careful preparation can a worker be assured of working safely within a confined space. A complete set of recommendations for working in a confined space is presented in the NIOSH document Criteria for a Recommended Standard: Working in Confined Spaces .
Some of the more pertinent recommendations are given below. a. Before workers enter a tank, reaction vessel, ship compartment, or other confined space, a permit entry procedure should be set up. Authorization to permit entry should be assigned to a qualified person, and access should be permitted only when all necessary measures have been taken to protect the worker.
The following precautions must be taken before permission is given: All pipes, ducts, and power lines connected to the space but not necessary to the operation must be disconnected or shut off.
All shutoff valves and switches must be tagged and secured with a safety lockout device.
Continuous mechanical ventilation must be provided when welding or thermal cutting is done in confined spaces. Oxygen must never be used for ventilation purposes .
Initial air monitoring must be performed to determine the presence of flammable or explosive materials and toxic chemicals, and to determine if there is sufficient or excessive oxygen.
Depending on the monitoring results and the adequacy of the mechanical ventilation, continuous monitoring may be necessary during welding.
Prohibit entry when tests indicate flammable concentrations greater than 10% of the lower flammable limit.
Gas cylinders and power sources for welding processes must be located in a secure position outside the space.
- A designated worker must be stationed outside the confined work space to maintain visual and voice contact and to assist or rescue the entering worker if necessary.
The designated worker must be equipped with appropriate protective gear and must remain in position throughout the time that any worker is within the enclosed space.
The worker entering the confined space must be outfitted with a safety harness, a lifeline, and appropriate personal protective clothing and equipment, including a respirator.
- Lifelines must be attached so that the welder's body cannot become jammed in a small exit opening.
- When not in use, torches and other gas-or oxygen-supplied equipment must be removed from the confined space [29 CFR 1910.2 5 2 ( d )( 4)
(i i)].
- All welders and persons supporting those workers shall be trained in the following areas: emergency entry and exit procedures, use of applicable respirators, first aid, lockout procedures, safety equipment use, rescue procedures, permit system, and good work practices.
The type of respirator required depends on the concentration of oxygen and the contaminants that might be generated.
Respirator requirements may range from none to a self-contained breathing apparatus with a full facepiece operated in pressure-demand or positive-pressure mode. Respirators must be selected in accordance with the most recent edition of the NIOSH Respirator Decision Logic .
Even though continuous mechanical ventilation is required during welding processes in confined spaces, initial and continuous environmental monitoring is extremely important.
Equipment used for monitoring of fumes and gases should be ex pl os io np ro of, and continuous monitoring equipment should have an audible alarm or danger-signaling device to alert workers when a hazardous situation develops.
All instruments should be calibrated periodically in accordance with the manufacturers' instructions. The results of each calibration must be recorded, filed by the employer, and made available for inspection for 1 year after the calibration date. Monitoring equipment must be reliable and have sufficient sensitivity to clearly identify a hazardous condition.
Oxygen deficiencies are of particular concern when welding in confined spaces.
The normal 21% concentration of oxygen in air may be decreased in confined spaces by chemical or biological processes.
When oxygen concentrations fall below 16.8% by volume, a worker may have difficulty remaining alert. Whenever the oxygen content falls below 19.5%, appropriate respirators must be used.
NIOSH respirator certification requires that only self-contained breathing apparatuses or supplied-air respirators with auxiliary self-contained breathing apparatuses be used in atmospheres below 19.5% oxygen.
# Preparation for Work
Before welding is performed in any work area, the worker should be aware of any potentially hazardous materials or conditions that may exist in that area.
Before striking an arc or lighting a flame the worker must remove all nearby flammable materials if the piece to be welded or cut is not readily movable.
A number of companies have a "permit system" that requires the supervisor's approval before welding is performed ,
Before issuing such a permit, the supervisor must check for conformance to OSHA regulations (such as 29 CFR 1910.252) and any specific company rules. Some of the most common company requirements include checking the serviceability of local firefighting equipment, moving all combustible materials at least 35 ft (10.7 m) from the work site, and assigning a worker (equipped with a suitable extinguisher and trained in its use) to perform a fire watch from outside the workspace.
Combustibles that cannot be removed should be shielded with a nonflammable material.
Shielding should also be provided to cover openings or cracks in floors, walls, and windows to prevent other workers from being exposed to sparks, hot metal and slag, and opt ical radiat io n.
The fire watch should be continued for at least 30 min after job completion to guard against smoldering fires.
The workpiece and work area should also be free of substances that may be rendered more hazardous by the work.
These include any halogenated hydrocarbons in the atmosphere that can be decomposed to phosgene or other harmful products by an arc or a flame .
Polymer materials may also form hazardous fumes or gases when exposed to heat .
Finally, the worker should be informed of ( 1) any unusually hazardous constituents of the work materials such as beryllium, cadmium, chromium, nickel, etc., (2) any hazardous coatings such as lead paint, mercury, or zinc, and ( 3) any precautions and control measures necessary for minimizing potential health risks.
# Containers
Drums, containers, pipes, jackets, and other hollow structures should be properly prepared and tested before welding .
Preparation of hollow structures varies depending on their contents.
At a minimum, the following procedures should be undertaken to minimize the risk of accidental injury or exposure to toxic agents: remove all ignition sources; disconnect the structure from any pipes, hoses, or other connections; examine the interior for waste or debris; and cleanse the structure of flammable materials or materials that could produce flammable or toxic vapors upon heating.
The appropriate cleaning process for containers depends on the materials present.
For many types of materials, an adequate cleaning process consists of steaming the container, washing with caustic soda, and rinsing with boiling water. The container should be dried and inspected.
Check for the presence of flammable or toxic gases or vapors. Vent the container to prevent a buildup of pressure in the interior.
Further protection may be given by filling the container with water to within an inch or two of the area to be welded or cut, and/or purging the interior of the container with inert gas. Before cutting or welding is permitted, the area must be inspected by the individual responsible for authorizing welding processes .
Preferably, such authorization should be in the form of a written permit.
# Emergencies
The employer should formulate a set of written procedures covering fire, explosion, electrical shock, asphyxiation, and any other foreseeable emergency that may arise in welding processes.
All potentially affected workers should receive training in evacuation procedures to be used in the event of fire or explosion.
All workers who are involved in welding processes should be thoroughly trained in the proper work practices to reduce the potential for starting fires and causing explosions.
# D. Personal Protective Clothing and Equipment
# Clothing
The employer should provide and require the use of protective clothing as fo ll ow s:
All welders should wear flame-resistant gauntlet gloves and shirts with sleeves of sufficient length and construction to protect the arms from heat, UV radiation, and sparks.
In most cases, wool and leather clothes are preferable because they are more resistant to deterioration and flames than cotton or synthetics. Welders should not wear light-weight, translucent fabrics and fabrics that show severe wear with holes .
All welders should wear fire-resistant aprons, coveralls, and leggings or high boots.
- Welders performing overhead work should wear fire-resistant shoulder covers (e.g., capes), head covers (e.g., skullcaps), and ear covers.
- Workers welding on metal alloys that contain highly toxic elements (e.g., beryllium, cadmium, chromium, lead, mercury, or nickel), should wear work uniforms, coveralls, or similar full-body coverings that are laundered each day. Employers should provide lockers or other closed areas to store work and street clothing separately.
Employers should collect work clothing at the end of each work shift and provide for its laundering.
Any clothing treated for fire resistance should be retreated after each laundering.
Laundry personnel should be informed about the potential hazards of handling contaminated clothing and instructed on measures to minimize their health risk.
Employers should ensure that protective clothing is inspected and maintained to preserve its effectiveness.
Clothing should be kept reasonably free of oil or grease.
Front pockets and upturned sleeves or cuffs should be prohibited, and sleeves and collars should be kept buttoned to prevent hot metal slag or sparks from contacting the skin.
Workers and persons responsible for worker health and safety should be informed that protective clothing may interfere with the body's heat dissipation, especially during hot weather or in hot industries or work situations (e.g., confined spaces).
Therefore, additional monitoring is required to prevent heatrelated illness when protective clothing is worn under these condi t ions.
# Eye and Face Protection
The employer should provide and require the use of welding helmets with the following eye and face protection: approved UV filter plates and safety spectacles with side shields or goggles for workers exposed to arc welding or cutting processes; goggles or similar eye protectors with filter lenses for oxyfuel gas welding, brazing, or cutting; and goggles or similar eye protectors with transparent lenses for resistance welding and brazing.
Hand-held screens for shielding the face and eyes should not be used since they may inadvertently be held incorrectly.
A report prepared by C.E. Moss provides a compendium of protective eyeware that may be helpful in choosing appropriate eye protection.
All welding helmets must meet the requirements of 29 CFR 1910.252(e)( 2) (ii), "Specifications for protectors."
Eye and face protectors should be periodically inspected and maintained by the employer.
Eye and face protectors should be sanitized before being used by another worker.
In addition, submerged arc welders must, where the work permits, be enclosed in an individual booth coated on the inside with a nonreflective material as set forth in 29 CFR 1910.252(e)(2)(ii).
# Respiratory Protection
Engineering controls should be the primary method used to control exposure to airborne contaminants.
Respiratory protection should be used by workers only in the following circumstances:
- During the development, installation, or testing of required engineering controls
- When engineering controls are not feasible to control exposure to airborne contaminants during short-duration operations such as maintenance and repair
# During emergencies
Respiratory protection is the least preferred method of controlling worker exposures and should not be used routinely to prevent or minimize exposures.
When respirators are used, employers should institute a complete respiratory protection program that includes worker training at regular intervals in the use and limitations of respirators, routine air monitoring, and maintenance, inspection, cleaning, and evaluation of the respirator.
Respirators should be used in accordance with the manufacturer's instructions.
Each respirator user should be fit tested and, if possible, receive a quantitative, on-the-job evaluation of his or her respirator protection factor to confirm the protection factor assumed for that class of respirator.
For additional information on the use of respiratory protection, refer to the NIOSH Guide to Industrial Respiratory Protection .
Selection of the appropriate respirator depends on the types of contaminants and their concentration in the worker's breathing zone. Before a respirator can be selected, an assessment of the work environment is typically necessary to determine the concentrations of specific metal fumes and other particulates, gases, or vapors that may be present.
As an interim measure until the environmental assessment has been made, the evaluator should conduct an initial review of precautionary labels on filler metals, electrodes, and flux materials to make a best estimate of the appropriate class of respirators. Respirator types shall be selected in accordance with the most recent edition of the NIOSH Respirator Decision Logic .
The following respirators should be used if a carcinogen is present at any detectable concentration, or if any other conditions are present that are considered to be immediately dangerous to life or health (IDLH):
- A self-contained breathing apparatus with a full facepiece operated in a pressure-demand or other positive-pressure mode.
- A combination respirator that includes a supplied-air respirator with a full facepiece operated in pressure-demand or positivepressure mode and an auxiliary self-contained breathing apparatus operated in a pressure-demand or other positive-pressure mode.
When respirators must be selected for combinations of contaminants in different physical forms, combination cartridge and particulate filter air-purifying respirators may be acceptable under specific conditions as long as none of the agents are considered carcinogenic.
The actual respirator selection should be made by a qualified individual, taking into account specific use conditions including the interaction of contaminants with the filter medium, space restrictions caused by the work location, and the use of welding helmets or other face and eye protect ive devices.
When welding is performed in confined spaces, the potential exists for a reduction in ambient oxygen concentrations.
A self-contained breathing apparatus or supplied-air respirator with an auxiliary self-contained breathing apparatus must be used for oxygen concentrations below 19.5% (at sea level).
# E. Labeling and Posting
In accordance with 29 CFR 191029 CFR .1200, "Hazard Communication," workers must be informed of exposure hazards, of potential adverse health effects, and of methods to protect themselves. Though all workers associated with welding processes should have received such information as part of their training, labels and signs serve as important reminders.
Labels and signs also provide an initial warning to other workers who may not normally work near those processes.
Depending on the process, warning signs may state a need to wear eye protection, hearing protectors, or a respirator; or they may be used to limit entry to an area without protective equipment.
For transient nonproduction work, it may be necessary to display warning signs at the worksite to inform other workers of the potential hazards.
Labels on containers of filler metal, electrodes, and flux materials that are toxic shall include the following information:
(1) the name of the metal and a warning describing its health hazards (for materials containing carcinogens, the warning should include a statement that fumes or gases from these materials may cause cancer), (2) instructions to avoid inhalation of or excessive skin or eye contact with the fumes of the materials, (3) instructions for emergency first aid in case of exposure, ( 4) appropriate instructions for the safe use of the materials, and ( 5) instructions for the type of personal protective clothing or equipment to be worn.
Base metals that contain or are coated with materials containing carcinogens or other toxic metals (e.g., lead or mercury) should be clearly labeled or marked to indicate their contents before being welded.
This same type of information must be posted in areas where welding is being performed.
All labels and warning signs should be printed in both English and the predominant language of non-English-reading workers.
Workers who cannot read labels or posted signs should be identified so that they may receive information about hazardous areas and be informed of the instructions printed on labels and signs.
# F. Sanitation
The preparation, storage, or consumption of food should not be permitted in areas where welding takes place.
The employer should make handwashing facilities available and encourage the workers to use them before eating, smoking, using the toilet, or leaving the work site.
Tools and protective clothing and equipment should be cleaned as needed to maintain a sanitary condition.
Toxic wastes should be collected and disposed of in a manner that is not hazardous to workers or surrounding environments.
No dry sweeping or blowing should be permitted in areas where welding is performed with materials containing carcinogens or other highly toxic metals.
Vacuum pickup or wet mopping should be used to clean the work area at the end of each work shift or more frequently as needed to maintain good housekeeping practices.
Collected wastes should be placed in sealed containers that are labeled as to their contents.
Cleanup and disposal should be conducted in a manner that enables workers to avoid contact with the waste and to observe applicable Federal, State, or local regulations.
Uncovered tobacco products should not be permitted to be carried or used for smoking or chewing. Workers should be provided with and advised to use facilities for showering and changing clothes at the end of each work shift. Work areas should be kept free of flammable debris.
Flammable work materials (rags, solvents, etc.) should be stored in approved safety cans.
# G. Availability of Substitutes
Fume and gas composition may be affected by material substitution. Toxic agents in welding fumes and gases may require remedial action such as changing the electrodes, fluxes, or type of welding process if appropriate control measures cannot be implemented.
Materials that may come into contact with welding processes (e.g., metals coated with oil and paint) should always be cleaned to prevent exposure to other toxic agents . Because impurities or contaminants are often contained in fluxes or base metal coatings , substitutions should be done cautiously to avoid introducing other toxic exposures.
In practice, however, substitution is not always an alternative to minimizing exposures, since material and process selection usually depend on the type of weld required and the quality of the finished product.
# VIM. RESEARCH NEEDS
Research is needed in several areas to evaluate the work-relatedness of disease symptoms in exposed workers who are associated with welding processes.
The various chemical agents (fumes and gases) and physical agents generated during these processes need to be characterized, and their possible interactions need to be assessed.
Long-term inhalation studies in animals, and morbidity and mortality studies of welders are needed to better define the relationship between exposure and respiratory disease, including lung cancer.
Several studies have indicated that workers who smoke and weld have an increased incidence and severity of respiratory disease. This association should be clarified.
Several epidemiologic studies have shown statistically significant increases in the risk of lung cancer for workers who weld stainless steel.
Thus the carcinogenic potential of stainless steel welding emissions needs to be better defined.
Research is particularly needed to assess the carcinogenicity of chromium and nickel in the forms generated during this process.
Comprehensive industrial hygiene evaluations are needed to quantitate exposure concentrations and ascertain past exposures.
To make such evaluations, investigators must gather information on the types of welding performed, work practices and controls used, and composition of base metals, fluxes, and electrodes.
To simplify the task of repetitively characterizing work environments where welding processes are performed, researchers should pursue a means of indexing exposures by job type or process. Workplace exposures should be characterized by representative jobs and job sites with the use of personal and stationary samplers.
The various components of the fumes and gases should be identified and quantified as a fraction of the total or respirable fumes.
In addition, information should be gathered on the type of welding technology and welding consumables used.
This information should take the form of a list of processes and their applications, the types of material they use, the nature of the workplace, and the type of job. Furthermore, the intensity of the work should be determined by estimates of arcing time per job shift, the number of electrodes consumed per unit of time, or the quantity of consumables purchased.
Also, the use of any specific work practices or local exhaust ventilation should be recorded along with their effects on the extent and composition of the fume exposure.
Better control technology should be developed in the form of new welding processes and worker-protective measures to assure that the worker is protected to the greatest extent possible.
The use of new metals, alloys, and complex composites of materials should be closely monitored and assessed for their potential to cause adverse health effects.
Recordkeeping and medical monitoring requirements proposed in this document need to be assessed for welders who change jobs frequently (e.g., welders in job shops or construction).
Because of the short-term nature of these jobs, the recordkeeping and monitoring provisions of this document may not be readily implemented. Methods are also needed to prevent the replication of medical examination and monitoring records among various employers.
ACGIH .
Industrial ventilation, a manual of recommended practice, 18th ed.
Lansing, Ml: American Conference of Governmental Industrial H y g i e n i s t s . R a tio n a le . For the M W maneuver, the fre q u e n c y content of the volume-time signal is high (28,29). Results are depe n d e n t o n the patient effort as well as the frequency response characteristics of the spirometer (21,(30)(31)(32). (
- SUBJECT/PATIENT MANEUVERS 1 ----- MEASUREMENT PROCEDURES I ACCEPTABILITY | 1 ---- REPRODUCIBILITY 1 ----------- REFERENCE VALUE/ INTERPRETATION - ----
# CLINICAL ASSESSMENT
# D e fin itio n s
# II. EQUIPMENT RECOMMENDATIONS
# R e c o m m e n d a tio n -V C E q u ip m e n t
# Recommendation-Forced Vital Capacity (FVC)
# Recommendation-Timed Forced Expiratory Volume (FEVt)
F E V t = T h e v
# General Background-Spirometry Recorders/Displays
# ) H A N D M E A S U R E M E N T fu n c tio n -
# Recommendation-FVC Maneuver Time Scale (1) D I A G N O S T I C function: time scale, A T L E A S T 1 cm/s.
( 2 give further specifi cation details.
# ) V A L I D A T I O N a n d H A N D M E A S U R E M E N T functions: time scale, A T L E A S T
# Recommendation-Flow-Volume Curves
# III. EQUIPMENT VALIDATION Recommendation-FVC Validation of Test Equipment
# Recommendation-MW Validation Equipment
# IV. EQUIPMENT QUALITY CONTROL
Routine e q u i p m e n t preventive maintenance, cleaning, calibration checks, verification, a n d quality control are important to assure ac curate spirometry results (38). A spirometry procedure m a n u a l is a n important base for a quality assurance program. T h e m a n u a l should contain a quality control plan, guide lines for ordering spirometry, guidelines for performing spirometry, a n d guidelines for reporting spirometry results. See the d o c u m e n t "A T S Quality Assurance for P u l m o n a r y Laboratories" for m o r e details (38).
T h e role o f spirometric e q u i p m e n t in the transmission o f infections has not b e e n es tablished (39) 7) m a i n t e n a n c e o f equipment, ( 8) protection of patients f r o m other infected/colonized p a tients or staff, a n d ( 9) microbiologic m o n i t o r ing (39). (6,45), the A T S has published "C o m p u t e r Guidelines for P u l m o n a r y Laboratories" (46), w h i c h should b e followed.
# Recommendation-Equipment Quality Control
# Recommendation-FVC Subject Instruction and Maneuver
# Recommendation-FVC End of Test Criteria
Subjects should be verbally exhorted to c o n tinue to squeeze out the air at the e n d of the maneuver. "E n d of list" will occur w h e n there is:
# Recommendation -Minimum FVC Exhalation Time
A m i n i m u m exhalation time of 6 s, unless there is a n obvious plateau, is required to o b tain m a x i m a l F V C results. L o n g e r times are often required to achieve "e n d o f test," par ticularly in obstructed individuals. 15) h ave reported that for adults a n d children, 8 m a n e u v e r s is a practical u p p e r limit.
# Recommendation-FVC Satisfactory Start of Test Criteria
# Recommendation-FVC: Maximum Number of Maneuvers
# Recommendation-FVC Environmental Conditions
# Recommendation-FVC Use of Nose Clips
U s e o f nose clips is encouraged.
# R a tio n a le .
# Recommendation-FVC Sitting Versus Standing
Subjects m a y be studied in the sitting or standing position. Indication o f position is necessary. In fact, these regulations are already in place a n d will not likely change.
# VI. MEASUREMENT PROCEDURES Measurement
# Recommendation-Test Result Selection/Reporting of Results
Because the average differences between the 2 m e t h o d s are so small ( < 10 ml), a n y refer ence value studies ( 63) o r epidemiologic studies previously d o n e with the "best test" m e t h o d are still valid.
# VII. ACCEPTABILITY AND REPRODUCIBILITY Recommendation-FVC Maneuver Acceptability
# Recommendation-FVC Test Result Reproducibility
# VIII. REFERENCE VALUES AND INTERPRETATION STANDARDIZATION
This area of spirometry standardization is.at a n early stage in its development. T h e standardization of interpretive proce dures is also in nee d of further investigation (70). T h e present situation allows e n o u g h in terpretive variability to cause identical data f r o m a patient to be interpreted differently in different laboratories (71).
# IX. CLINICAL ASSESSMENT Clinical/Epidemiologic Considerations
# TIMI (HO
# APPENDIX B-Standard Waveforms for Spirometer Validation
A recent study using the standard spirometry w a v e f o r m s ( 6 . 6,7, 8,11,12,15, 17, 21, 23)
-1 -1 -t i ' -1 -1 -1 -iT -'-1
# OXYFUEL GAS WELDING
# PLASMA ARC CUTTING
An arc cu ttin g process that severs metal by m elting a lo c a lize d area with a co n stricte d arc and removing the molten m aterial w ith a h ig h -v e lo c ity je t of hot ionized gas issuing from the o r i f ic e .
# PLASMA ARC WELDING
An arc welding process that produces coalescence of metals by heating them with a co n stricte d arc between an electro de and the workpiece (tra n sfe rre d a rc ) or the electrode and the c o n s tric tin g nozzle (nontransferred a r c ) . Shield ing is obtained from the hot ionized gas issuing from the o r i f i c e , which may be supplemented by an a u x ilia r y source of sh ie ld in g gas. S hield ing gas may be an in e rt gas or a m ixture of gases. Pressure may or may not be used, and f i l l e r metal may or may not be supp I i ed.
# RESISTANCE WELDING
Welding processes that produce coalescence of metals with the a p p lic a tio n of pressure and with the heat obtained from re sista n c e of the work to e le c t r ic current in a c ir c u it that includes the work.
# SHIELDED METAL ARC WELDING
An arc welding process that produces coalescence of metals by heating them with an arc between a covered metal electro de and the work. S hield ing is obtained from decomposition of the electro de co vering . Pressure is not used, and filler metal is obtained from the e le ctro d e .
# SUBMERGED ARC WELDING
An arc welding process that produces coalescence of metals by heating them with an arc or a rcs between a bare metal electro de or electro d es and the work. The a rc and molten metal are shielded by a blanket of granular fusible m aterial on the work. Pressure is not used, and filler metal is obtained from the electro de or sometimes from a supplemental source (welding rod, flux, or metal g ra n u le s).
# TIG WELDING
See p referred term-GAS TUNGSTEN ARC WELDING.
# TORCH BRAZING
A brazing process in which the heat required is furnished by a fuel gas flame.
Welding processes that produce coalescence by heating materials with an oxyfuel gas flame, with or without the application of pressure and with or without the use of filler metal.
The authors stated that the welding apparatus was not defective and the maximum voltage at idle was 86.0 V. The autopsy revealed an electrical burn on the right side of the throat.
Beton DC, Andrew GS, Davies HJ, Howells L, Smith GF . 25. Blot RH, Harrington JM, Toledo A, Hover R, Heath CW, Fraumenti JR, . Lung cancer after employment in shipyards during World War II. N Engl J Med 299:620-624.
BLS .
Survey of welding and cutting accidents resulting in injuries, 1978.
Washington, DC: U.S. Department of Labor, Bureau of Labor Statistics.
NT IS PB 83 -2 0 8 0 0 1 7 , p. 33. BLS . SDS data base available from NTIS. Washington, DC: U.S. Department of Labor, Office of Occupational Safety and Health Statistics, Bureau of Labor Statistics. Bobrishchev-Pushkin DM .
Health assessment of electron-beam welding of beryllium bronze (in Russian).
Weld Prod 19 ( 1 1 ) :72-74.
Breslin AJ, Harris WB .
Use of thoriated tungsten electrodes in inert gas shielded arc welding-investigation of potential hazard.
Am Ind Hyg Assoc Q 13 (4):191-195. Breslow L, Hoaglin L, Rasmussen G, Abrams HK .
Occupations and cigarette smoking as factors in lung cancer.
Am J Public Health 44:171-181.
Britton JA, Walsh EL .
Health hazards of electric and gas welding: (1) review of the literature; (2) results of examination of 286 welders; (3) preventive measures.
J Ind Hyg 22(4): 125-151.
Brun J, Cassan G, Kofman J, Gi Ily J . Siderosclerosis of arc welders with diffuse interstitial fibrosis and a pseudo-tumoral conglomerative picture (in French).
Poumon Coeur 2 8 ( 1 ) :7-14.
Buhrer P, Brunschwiler P . Some cases of fire caused by welding or cutting fires caused by welding sparks (in Swedish). Document No. VIII-790-78.
London, England: International Institute of Welding, p. 12.
Bureau of the Census . 1980 Byczkowski S, Cempel M, Gadomska J .
Studies Challen PJR, Hickish DE, Bedford J .
An investigation of some health hazards in an inert-gas tungsten-arc welding shop.
Br J Ind Med 15:276-282.
Christensen FC, Olson EC . Cadmium poisoning.
# AMA Arch
Ind Health 1 6 ( 1 ) :8-13.
Compressed Gas Association .
Acetylene, Pamphlet G-1. New York, NY: Compressed Gas Association, Inc. Cresswell RA .
Health and safety aspects of plasma cutting (in French). Document No.
V I 1 1-433-71.
London, England: International Institute of Welding, pp. 73-81. Dahlberg JA .
The intensity and spectral distribution of ultraviolet emission from welding arcs in relation to the photodecomposition of gases. Ann Occup Hyg 14:259-267.
Dahlberg JA, Myrin LM .
The formation of dichloroacetyI chloride and phosgene from trichloroethylene in the atmosphere of welding shops.
Ann Occup Hyg 14:269-274.
Gerin M, Siemiatycki J, Richardson L, Pellerin J, Lakhani R, Dewar R .
Nickel Particulate fume generation in arc welding processes. Weld J 54(7)(Suppl):201s-210s.
Herbert A, Sterling G, Abraham J, Abraham J, Corrin B .
Desquamative interstitial pneumonia in an aluminum welder.
Hum Pathol 13( 8):694-699.
Herberts P, Kadefors R .
A study of painful shoulder in welders. Acta Orthop Scand 4 7 ( 4 ) :381-387.
Hewitt PJ, Hicks R .
An investigation of the effects of inhaled welding fume in the rat. Ann Occup Hyg 16:213-221. Hickish DE, Challen PJR .
A preliminary study of some health hazards in the plasma jet process.
Br J Ind Med 20:95-99. The effect of new welding processes on health (in Czechoslovakian).
Pracov Lek 2 9 ( 2 ) :47-50. USAEHA .
Nonionizing radiation protection study no. 25-42-0328-84. Transmission of potentially hazardous actinic ultraviolet radiation through fabrics.
January 1981-March 1982.
Aberdeen Proving Ground, MD: United States Army Environmental Hygiene Agency.
van Someren E, R o M a s o n EC .
Radiation from the welding arc. Its effect on the eye. Weld J (Suppl) 2 7 ( 9) :448s-452s.
Virtamo M .
Fumes from welding of stainless and acid resistant Cr-Ni-steels (in Finnish Reprints m a y be requested from your state or local lung associations.
# VII. Acceptability and Reproducibility
Reproduced by permission of the American Review of Respiratory Disease. 1987Disease. , 136:1285Disease. -1298. V o l u m e sam p l i n g techniques with optical
# ARC CUTTING
Cutting processes that melt the metals to be cut with the heat of an a rc between an electrode and the base m etal.
# ARC WELDING
Welding processes that produce coalescence of m etals by heating them w ith an a r c , with or without the a p p lic a tio n of p re ssu re , and w ith or without the use of in e rt gases or f i l l e r m etal.
# CARBON ARC CUTTING
An arc cu ttin g process in which m etals are severed by m elting them with the heat of an a rc between a carbon electro de and the base m etal.
# CARBON ARC WELDING
An arc welding process that produces fusion of m etals by heating them with an a rc between a carbon electro d e and the work. No sh ie ld in g is used. Pressure and f i l l e r metal may or may not be used.
# COLD WELDING
A s o lid -s ta te welding process in which pressure is used at room temperature to produce coalescence of metals w ith su b sta n tia l deformation at the weld.
# ELECTRON BEAM WELDING
A welding process that produces coalescence of metals w ith the heat obtained from a concentrated beam composed p rim a rily of h ig h -v e lo c ity electro n s impinging on the jo in t to be welded.
# FLUX-CORED ARC WELDING
An a rc welding process that produces coalescence of metals by heating them w ith an a rc between a continuous f i l l e r metal (consumable) electro d e and the work. S h ie ld in g is provided by a flu x contained w ith in the tubular e le c tro d e . A dd itio nal sh ie ld in g may or may not be obtained from an e x te rn a lly supplied gas or gas m ixtu re.
# FURNACE BRAZING
A brazing process in which the p a rts to be joined are placed in a furnace heated to a s u ita b le temperature.
# GAS METAL ARC WELDING
An a rc welding process that produces coalescence of metals by heating them w ith an a rc between a continuous f i l l e r metal (consumable) electro d e and the work. Sh ie ld in g is obtained e n t ir e ly from an e x te rn a lly supplied gas or gas m ixtu re . Some v a ria tio n s of th is process are c a lle d MIG or CO2 welding (nonpreferred term s).
# GAS TUNGSTEN ARC WELDING
An a rc welding process that produces coalescence of metals by heating them w ith an a rc between a tungsten (nonconsumable) electro de and the work. Sh ield in g is obtained from a gas or gas m ixtu re. Pressure and f i l l e r metal may or may not be used.
# GOUGING
The forming of a bevel or groove by m aterial removal.
# LASER BEAM WELDING
A welding process that produces coalescence of m a te ria ls w ith the heat obtained from the a p p lic a tio n of a concentrated coherent lig h t beam impinging on the members to be jo in e d .
# MIG WELDING
See p referred terms-GAS METAL ARC WELDING and FLUX-CORED ARC WELDING.
# OXYACETYLENE WELDING
An oxyfuel gas welding process that produces coalescence of metals by heating them with a gas flame obtained from the combustion of acetylene with oxygen. The process may be used with or without the a p p lic a tio n of pressure and with or without the use of f i l l e r m etal. | This document examines the occupational health risks associated with welding, brazing, and thermal cutting, and it provides criteria for eliminating or minimizing the risks encountered by workers in these occupations. The main health concerns are increased risks of lung cancer and acute or chronic respiratory disease.# FOREWORD
The purpose of the Occupational Safety and Health Act of 1970 (Public Law 91-596) is to ensure safe and healthful working conditions for every working person and to preserve our human resources by providing medical and other criteria that will ensure, insofar as practicable, that no worker will suffer diminished health, functional capacity, or life expectancy as a result of his or her work experience. The Act authorizes the National Institute for Occupational Safety and Health (NIOSH) to develop and recommend occupational safety and health standards and to develop criteria for improving them. By this means, NIOSH communicates these criteria both to regulatory agencies and others in the community of occupational safety and health.
Criteria documents provide the basis for the occupational health and safety standards sought by Congress. These documents generally contain a critical review of the scientific and technical information available on the prevalence of hazards, the existence of safety and health risks, and the adequacy of control methods. NIOSH distributes these documents to health professionals in academia, industry, organized labor, public interest groups, and other appropriate government agencies. This criteria document on welding, brazing, and thermal cutting reviews available information on the health risks for workers in these occupations and provides criteria for eliminating or minimizing the occupational risks these workers may encounter. Evidence from epidemiologic studies and case reports of workers exposed to welding emissions clearly establishes the risk of acute and chronic respiratory disease. The major concern, however, is the excessive incidence of lung cancer among welders. A large body of evidence from regional occupational mortality data, case control studies, and cohort studies indicates that welders generally have a 40% increase in relative risk of developing lung cancer as a result of their work experiences. The basis of this excess risk is difficult to determine given uncertainties about smoking habits, possible interactions among the various components of welding emissions, and possible exposures to other occupational carcinogens, including asbestos. The severity and prevalence of other respiratory conditions such as chronic bronchitis, pneumonia, and decrements in pulmonary function are not well characterized among welders, but these effects have been observed in both smoking and nonsmoking workers in this occupation. Excesses in morbidity and mortality among welders appear to exist even when exposures have been reported to be below current Occupational Safety and Health Administration (OSHA) permissible exposure limits (PELs) for the many individual components of welding emissions.
An exposure limit for total welding emissions cannot be established because the composition of welding fumes and gases varies for different welding processes and because the various components of the emissions may interact to produce adverse health effects. NIOSH therefore recommends that exposures to all welding emissions be reduced to the lowest feasible concentrations using state-of-the-art engineering controls and work practices. Exposure limits for individual chemical or physical agents are to be considered upper boundaries of exposure. Presently it is not possible to associate a particular health hazard with a specific component of total welding emissions; however, the risk of lung cancer for workers who weld on stainless steel appears to be associated with exposure to fumes that contain nickel and chromium. NIOSH has previously recommended to OSHA that exposures to specific forms of these metals be treated as exposures to occupational carcinogens. Future research may make it possible to differentiate risks associated with a particular exposure. NIOSH will evaluate such data as they become available and revise this recommended standard as appropriate.
The Institute takes sole responsibility for the conclusions and recommendations presented in this document. All reviewers' comments are being sent with this document to the Occupational Safety and Health Administration (OSHA) for consideration in standard setting.
The data in this document indicate that welders have a 40% increase in relative risk of developing lung cancer as a result of their work experience. The basis for this excess risk is difficult to determine because of uncertainties about smoking habits, possible interactions among the various components of welding emissions, and possible exposures to other occupational carcinogens. However, the risk of lung cancer for workers who weld on stainless steel appears to be associated with exposure to fumes that contain nickel and chromium.
The severity and prevalence of noncarcinogenic respiratory conditions are not well characterized among welders, but they have been observed in both smoking and nonsmoking workers in occupations associated with welding. Excesses in morbidity and mortality among welders exist even when reported exposures are below current Occupational Safety and Health Administration (OSHA) permissible exposure limits (PELs) for the many individual components of welding emissions.
An exposure limit for total welding emissions cannot be established because the composition of welding fumes and gases varies for different welding processes and because the various components of a welding emission may interact to produce adverse health effects. NIOSH therefore recommends that exposures to all welding emissions be reduced to the lowest feasible concentrations using state-of-the-art engineering controls and work practices. Exposure limits for individual chemical or physical agents are to be considered upper boundaries of exposure.
# . E. NIOSH Recommendations that Differ from Current
OSHA R e gu la ti on s. 1. Arc W e l d i n g 2. Oxyfuel Gas W e l d i n g 5. Thermal C u t t i n g 1. Fumes and Other .. c. Bery 11 .. d . Cadm i u . 38 IV. Health and Safety H a z a r d s . B. Health H a z a r d s
# III. Characteristics of Welding
1. Animal T o x i c i t y . 42 d. Mu .. d. Cardiovascular
1. F i r e s . .. 139 v i i i CONTENTS (continued) 3. Toxicological .. a. Epidemiological Studies........ b. Toxicological .. c. Dermal E f f e c t s . .. d. Eye I n j u ri es. .. c. Monitoring 1. Medical .. b. Periodic Medical 1. Optical (Radiation) .. 167 2. Chemical Hazards (Gases,Vapors,and
# Electric S h o c k
# V. Basis for the Recommended
# Other Adverse Health
# Physical Agent
# I. RECOMMENDATIONS FOR A STANDARD
The National Institute for Occupational Safety and Health (NIOSH) recommends that worker exposure to hazards associated with welding processes in the workplace be controlled by complying with the provisions presented in Chapter I of this document. Chapters VI and VII provide additional detail concerning the implementation of these provisions. Adherence to these recommendations should prevent or greatly reduce the risk of adverse health effects among exposed workers. These recommendations are designed to protect the health and provide for the safety of workers engaged in welding over a working lifetime; they are to be used as an adjunct to existing NIOSH recommendations. The following sections shall replace or modify the provisions for welding, cutting, and brazing contained in 29 CFR* 191029 CFR* .251-254, 191529 CFR* .51-57, and 1926 Other specific requirements contained in those regulations and not addressed in the NIOSH recommended standard shall be retained.
Section 1 -Definitions (a) Worker is any person who is or may reasonably be expected to be exposed to chemical and physical hazards associated with welding processes.
(b) Exposure Limit is the concentration of a chemical or physical agent emitted during welding that shall not be exceeded in the workplace. The NIOSH recommended exposure limit (REL) shall be used when available for any chemical or physical agent.
In the absence of a NIOSH REL, the Occupational Safety and Health Administration (OSHA) permissible exposure limit (PEL) shall be used unless a more restrictive limit has been recommended by a recognized voluntary consensus group or committee. When neither a NIOSH REL nor an OSHA PEL exists, an appropriate consensus-groupor committee-recommended exposure limit shall be used. Although NIOSH has not evaluated the adequacy of such exposure limits, their adoption would be a prudent public health measure and would afford a greater degree of protection than using no limit.
The OSHA PELs shall not be exceeded under any circumstances. Appendix A lists some of the more common chemical and physical agents that may be found in the workplace or near workers engaged in welding.
(c) Welding includes those processes that join or cut pieces of metal by heat, pressure, or both. These processes differ in the way heat is created and applied to the parts being joined; they comprise a group of processes referred to as welding, brazing, and thermal cutting (see explanation of terms in Chapter III).
# Section 2 -Recommended Exposure Limits
Exposures to chemical and physical agents shall be controlled so that workers are not exposed to concentrations above the exposure limits (see Definitions, Section 1(b)).
An exposure limit for total welding emissions cannot be established because the composition of welding emissions (chemical and physical agents) varies for different welding processes and because the various components of a welding emission may interact to produce adverse health effects. Thus even compliance with specific chemical or physical agent exposure limits may not ensure complete protection against an adverse health effect. Therefore, as a prudent public health measure, the employer shall reduce worker exposures to all chemical and physical agents associated with welding to the lowest concentrations technically feasible using current state-of-the-art engineering and good work practice controls. Exposure limits for individual chemical or physical agents are to be considered upper boundaries of exposure.
# Section 3 -Medical Monitoring
The following requirements supplement existing medical monitoring measures that NIOSH recommends for workers exposed to specific chemical or physical agents. The objective of these requirements is to provide an additional level of monitoring for workers who may be exposed to welding emissions or who may have been adversely affected by them in the past. NIOSH recommended standards and existing OSHA standards shall be used to determine the need for specific medical tests. Appendix B lists published sources of NIOSH recommended standards for some specific chemical and physical agents.
(a) General (1) The employer shall institute a medical monitoring program for all workers who are or may reasonably be expected to be exposed to hazards from welding processes.
(2) The employer shall ensure that all medical examinations and procedures are performed by or under the direction of a licensed physician.
(3) The employer shall provide the required medical monitoring without loss of pay or other cost to the workers, and at a reasonable time and place.
# (b) Preplacement Medical Examination
The preplacement medical examination shall include the following items at a minimum:
(1) A comprehensive work and medical history that emphasizes identification of existing medical conditions and previous occupational exposure to chemical or physical health hazards, particularly those associated with welding processes.
(2) A comprehensive physical examination.
(3) A thorough examination of the respiratory system, including baseline pulmonary function tests (at a minimum, forced vital capacity [FVC] and forced expiratory volume in one second [FEV-j]) using the current recommendations of the American Thoracic Society regarding testing procedures and equipment. Guidelines are given in Appendix C.
(4) A posterio-anterior chest radiograph that is interpreted by qualified B readers (i.e., those who have passed the NIOSH proficiency examination) using the current recommendations of the International Labour Office (ILO) regarding the classification of pneumocon i os i s .
(5) An examination of the skin and eyes for scars that appear to have been caused by burns. The locations of such scars should be noted.
(6) A baseline cardiovascular evaluation.
(7) A baseline audiogram.
(8) A thorough ophthalmologic evaluation.
# (c) Periodic Medical Examination
A periodic medical examination shall be provided at least annually to all workers. The following conditions may shorten the interval between examinations and the need for special medical tests:
(1) Workers reporting signs or symptoms associated with exposure to welding emissions, and
(2) Airborne concentrations of specific agents that exceed exposure limits.
Periodic medical examinations shall include the following:
(1) Updates of medical and occupational histories. These shall include a description of the following items based on an interview of the worker and records maintained by the employer: the type of welding performed, metals worked and fluxes used, locations and conditions (e.g., confined spaces and hot environments), and potentially hazardous exposures not directly related to welding (e.g., chlorinated hydrocarbons).
(2) An evaluation of the respiratory system. Because of the potential for chronic respiratory disease, this evaluation shall include spirometry at intervals indicated by the judgment of the examining physician. Workers with symptomatic, spirometric, or radiographic evidence of pulmonary impairment or disease shall be counseled about the risks of further exposure. Smokers shall be counseled about how smoking may enhance the adverse effects of other respiratory hazards.
(3) Posterio-anterior chest radiographs interpreted by qualified B readers (i.e., those who have passed the NIOSH proficiency examination) using the current recommendations of the International Labour Office (ILO) regarding the classification of pneumoconiosis. These radiographs shall be performed at intervals determined by the examining physician. Periodic chest radiographs are recommended for monitoring workers exposed to fibrogenic respiratory hazards (e.g., quartz). At a minimum, chest radiographs should be obtained at 1-to 5-year intervals, depending on the nature and intensity of exposures and the related health risks. A recent chest radiograph obtained for other purposes (e.g., upon hospitalization) may be substituted for the periodic chest radiograph if it is made available and is of acceptable qua Ii ty.
(4) An examination of the skin and eyes for scars that appear to have been caused by burns. The locations of such scars should be noted.
(5) An evaluation of the cardiovascular system.
(6) An ophthalmological evaluation. (7) An audiogram. (8) Other tests deemed appropriate by the attending physician.
# Section 4 -Labeling and Posting
Workers shall be informed of exposure hazards, of potential adverse health effects, and of methods to protect themselves in accordance with 29 CFR 191029 CFR .1200, Hazard Communication. Manufacturers of welding materials shall warn employers and workers of the potentially hazardous components of the filler metals, electrodes, and flux materials by applying precautionary labels to the packing containers. Such labels shall indicate the identity of the hazardous agents and the adverse health effects that may result from exposure.
In addition, the employer must comply with the labeling and posting requirements contained in the following subsections.
# (a) Labeling
All labels and warning signs shall be printed in both English and in the predominant language of non-English-reading workers. Workers who cannot read the language used on labels and posted signs shall be identified so that they may receive information regarding hazardous areas and be informed of the instructions printed on labels and signs.
(1) Containers of filler metal, electrodes, and flux materials shall bear warning labels containing the following information at a mini mum :
• The following warning: WARNING Welding produces hazardous fumes and gases.
Avoid breathing them. Use adequate ventilation.
• Instructions for emergency first aid • Instructions for safe use • Instructions for the type of personal protective clothing or equipment to be worn (2) Labels shall identify the hazardous constituents of the container's contents.
(3) The following information shall be included on the labels of containers holding filler metal, electrodes, and flux materials that contain agents identified as carcinogens by NIOSH and OSHA:
• The name of the potential occupational carcinogen and a description of its health hazards. For materials containing carcinogens, the warning label listed in Section 3(a)(1) above shall include the following statement:
Fumes or gases from this [filler metal, electrode, or flux material] may cause cancer.
• Instructions for avoiding inhalation of fumes and excessive skin or eye contact with them.
(4) Base metals that contain or are coated with materials containing carcinogens or other toxic metals (e.g., lead or mercury) shall be clearly labeled or marked to indicate their contents before being welded.
(b) Post i ng (1) In areas where welding is conducted, the following sign shall be posted in readily visible locations: WARNING Welding produces hazardous fumes, gases, and radiation. Appropriate personal protective equipment is required. 00 NOT LOOK AT ARC. EYE INJURY MAY OCCUR.
(2) Signs posted in work areas where emissions contain carcinogens shall differ from the preceding example, as follows:
• The word "DANGER" shall be used instead of "WARNING."
• The name of the carcinogen shall be included along with a warning describing its health hazards.
If a carcinogen is contained in the base or filler metals, electrodes, or fluxes, the warning shall include the statement, "Fumes or gases from [the base metal(s), filler metal, electrode, or flux] may cause cancer," with the type(s) of base or filler metals, electrodes, or fluxes specified.
• Any requirements for personal protective clothing and equipment shall also be stated.
# Section 5 -Protective Clothing and Equipment
Engineering controls and safe work practices shall be used to keep the emissions from welding processes below the exposure limits specified in Chapter I, Section 2 of this document.
In addition, the employer shall provide protective clothing and equipment to workers as follows:
(a) Clothing (1) The employer shall provide and require the use of appropriate protective clothing as follows:
• Fire-resistant gauntlet gloves and shirts with sleeves of sufficient length and construction to protect the arms from heat, UV radiation, and sparks. Wool and leather clothing are preferable because they are more resistant to deterioration and flames than cotton or synthetics.
Fire-resistant aprons, coveralls, and leggings or high boots.
Fire-resistant shoulder covers (e.g., capes), head covers (e.g., skullcaps), and ear covers for workers doing overhead work.
(2) The employer shall do the following for workers welding with highly toxic materials (e.g., carcinogens, lead, fluorides):
• Provide and require the use of work uniforms, coveralls, or similar full-body coverings.
• Provide lockers or other closed areas to store work clothing separately from street clothing.
• Collect work clothing at the end of each work shift and provide for laundering. Clothing treated for fire resistance may need to be retreated after laundering. Laundry personnel shall be adequately informed of the potential hazards and protected from any contaminants on the work clothing.
(3) The employer shall ensure that protective clothing is inspected, maintained, and worn to preserve its effectiveness.
• Clothing shall be kept reasonably free of oil or grease.
• Clothing treated for fire resistance shall be retreated after laundering if necessary.
• Upturned sleeves or cuffs shall be prohibited.
• Sleeves and collars shall be kept buttoned.
# (b) Eye and Face Protection
(1) The employer shall provide and require the use of the following protective gear for the eyes and face:
• Welding helmets that meet the requirements of 29 CFR 1910.252(e)(2)(ii), Specifications for Protectors.
• Welding helmets with approved ultraviolet radiation (UV) filter plates, or safety spectacles with side-shields, or goggles for all workers exposed to arc welding or cutting processes.
• Goggles or similar eye protectors with filter lenses for workers exposed to oxyfuel gas welding, brazing, or cutting.
• Goggles or similar eye protectors with transparent lenses shall be used for workers exposed to resistance welding or to mechanical cleaning or chipping operations.
(2) The shade numbers used for filter plates or lenses shall meet the requirements of 29 CFR 1910.252(e) (i i).
(3) Eye and face protectors shall be maintained and periodically cleaned and inspected by the employer. Eye and face protectors shall be sanitized before being used by another worker.
# (c) Respiratory Protection
Engineering controls and good work practices shall be used to control respiratory exposure to airborne contaminants. Workers shall use respiratory protection only when controls are not technically feasible, when certain routine or nonroutine short-term operations (e.g., maintenance and repair or emergencies) are performed, or when engineering and work practice controls do not reduce the concentration of the contaminant below the exposure limit.
(1) When respirators are used, a complete respiratory protection program shall be instituted as set forth in 29 CFR 1910.134. This program shall include the following elements at a minimum:
• A written program for respiratory protection (e.g., standard operating procedures governing the selection and use of respi rators).
• Regular worker training.
• Routine air monitoring and work surveillance.
• Routine maintenance, proper storage, inspection, cleaning, and evaluation of respirators.
• Testing of each respirator while it is worn by an individual to confirm that the protection factor expected for that class of respirators is being achieved.
(2) Selecting the appropriate respirator depends on the specific contaminants and their concentration in the worker's breathing zone. Before a respirator can be selected, an assessment of the work environment is usually necessary to determine the concentration of the specific metal fume and other particulates, gases, or vapors that may be present. Until an environmental assessment is completed, however, the employer should review the precautionary labels on filler metals, electrodes, and flux materials and make a best estimate of the appropriate class of respirators. Only the most protective types of respirators shall be used if exposure to a carcinogen is likely (e.g., cadmium, chromium, nickel contained in filler metals, electrodes, fluxes, or during stainless steel welding) or confirmed by environmental measurements. Respirators shall be selected in accordance with the most recent edition of the NIOSH Respirator Decision Logic [NIOSH 1987],
(3) When workers are exposed to a combination of contaminants in different physical forms, combination cartridge and particulate filter air-purifying respirators may be acceptable under specific conditions as long as none of the agents are considered to be carcinogenic.
In such cases, a qualified individual shall select the respirator, taking into account the specific use conditions, which include the interaction of contaminants with the filter medium, space restrictions caused by the work location, and the use of welding helmets or other face and eye protective devices.
(4) A self-contained breathing apparatus or a supplied-air respirator with an auxiliary self-contained breathing apparatus shall be used when welding in confined spaces. Such welding may reduce ambient oxygen concentration, especially if an inert-gas, shielded-arc welding process is used.
# (d) Hearing Protection
The employer shall provide and require the use of ear protectors whenever there is a potential for noise levels to exceed the NIOSH REL or OSHA PEL.
• Insert-type ear protectors shall be fitted by a person trained in this procedure.
• Inspection procedures shall be established to assure proper issuance, maintenance, and use of ear protectors.
• Workers shall be trained in the proper care and use of all ear protectors.
# Section 6 -Informing Workers of the Hazard (a) Frequency of Hazard Communication
Before assignment and at least annually thereafter, the employer shall provide information about workplace hazards to all workers assigned to work in welding areas.
In addition, employers shall follow the OSHA regulations in 29 CFR 191029 CFR .1200, Hazard Communication.
# (b) Training Program
Hazard information shall be disseminated through a training program that describes how a task is properly done, how each work practice reduces potential exposure, and how it benefits the worker to use such a practice. Workers who are able to recognize hazards and who know how to control them are better equipped to protect themselves from unnecessary exposure. Frequent reinforcement of the training and supervision of work practices are essential.
# (c) File of Written Hazard Information
Appropriate written hazard information and records of training shall be kept on file and made readily available to workers. This information shall include the following:
(1) Identification of the various health hazards, including specific metal fumes, gases released or formed by the processes, heat, noise and vibration, optical radiation, and X-radiation.
(2) Instructions for preventing accidents such as explosion, fire, and electrocut ion.
(3) An explanation of the hazards of working in confined spaces, including the risk of oxygen-deficient atmospheres, exposure to toxic or explosive chemicals, and the potential for heat stress.
(4) An explanation of the potential health effects of exposure to chemical and physical agents generated by welding (e.g., a warning of the increased cancer risk for workers exposed to carcinogens or fumes and gases during stainless steel welding).
(5) Information on precautionary measures for minimizing hazards, including work practices, engineering controls, and personal protective equipment. (6) A description of the environmental and medical surveillance procedures and their benefits.
# (d) Instruction about Sanitation
Workers shall also be instructed about their responsibilities for following proper sanitation procedures to protect their own health and safety and that of their fellow workers.
# (e) Tobacco Use
Workers should be counseled against the use of tobacco products.
# Section 7 -Engineering Controls and Work Practices (a) Engineering Controls
The following engineering controls shall be used whenever welding is performed, unless they can be demonstrated to be infeasible.
# (1) Optical Radiation
Welding shall be performed in booths or screened areas constructed of materials that are noncombustible, opaque, and minimally reflective to light in the range of 200 to 3,000 nm. The booths and screens shall be arranged in a manner that does not restrict ventilation. Such equipment shall conform to the requirements of 29 CFR 1910.252(f)(1)(i i i), Screens.
(2) Chemicals (Gases, Fumes, and Particulates) Fixed-station local exhaust ventilation shall be used whenever possible (e.g., at the workbench). In some situations where fixed local exhaust is not feasible, a movable hood with a flexible duct may be used. For gas-shielded arc welding processes, contaminants can be removed by means of a low-volume, high-velocity exhaust (extracting gun).
General ventilation may be necessary where local exhaust ventilation cannot be used; it may also be used to supplement local exhaust ventilation.
When exhaust ventilation systems are used to control emissions, the following requirements shall apply:
• Exhaust hoods and ductwork shall be constructed of fire-resistant materials.
• Ventilation systems shall be equipped with alarms, flowmeters, or other devices to indicate malfunction or blockage of the systems. These systems shall be inspected at the beginning of each shift to ensure their effect iveness.
• The ventilating airflow shall be directed to carry contaminants from the process away from the breathing zone of the process operator or other workers. For local exhaust systems, this usually entails placement of the fume source between the operator and the face of the exhaust duct.
• The hood design, capture velocity, and flow rate must be chosen to capture the emissions effectively.
• Clean make-up air shall be provided in accordance with 29 CFR 1910.252(f)(4)(i).
• Local exhaust systems used to control welding fumes shall have in-line duct velocities of at least 3,000 feet per minute (fpm) to prevent particulates from settling in horizontal duct runs.
• Canopy hoods may be used under limited conditions. For example, they may be advisable for collecting the heated fumes from automated welding operations and preventing their dissipation into the general work environment.
If a canopy hood is used, however, the worker must not work directly over the welding process and there must be no cross currents beneath the hood.
• Cooling fans shall be considered only when local exhaust is not possible (e.g., remote work areas or outdoor work settings). Cooling fans can remove welding fumes from the breathing zone when properly placed at the side of the worker, but their use is rather limited and they may cause dispersion. Any use of a cooling fan at an indoor worksite requires supplemental general ventilation.
(
# 3) X-Rays
Electron beam welding processes shall be enclosed and shielded with lead or other suitable materials of sufficient mass to prevent the emission of X-rays. All doors, ports, and other openings shall be checked and maintained to ensure that they have proper seals that prevent X-ray emission.
# (4) Oxyfuel Equipment
Oxyfuel equipment for welding shall be installed, maintained, and used in a manner that prevents leakage, explosion, or accidental fire. Such equipment shall conform to the requirements of 29 CFR 1910.252(a), Installation and Operation of Oxygen-Fuel Gas Systems for Welding and Cutting.
(
# 5) Fires or Electric Shocks
Arc and resistance welding equipment shall be installed, maintained, and used in a manner that prevents fire or electric shock. Such equipment shall conform to the requirements of 29 CFR 1910.252(b), Application, Installation, and Operation of Arc Welding and Cutting Equipment, and to 29 CFR 1910.252(c), Installation and Operation of Resistance Welding Equipment.
# (b) Work Practices
Work practices shall, at a minimum, conform to 29 CFR 1910.251-254, Welding, Cutting, and Brazing. Specific work requirements include the foI lowing:
(1) Workers shall use welding helmets. Hand-held screens shall be prohibited during welding.
(2) Workers shall adhere to the following safety procedures:
• Workers shall observe the fire precautions prescribed in 29 CFR 1910.252(d).
• Workers shall not conduct welding on materials that may produce toxic pyrolysis or combustion products.
• Workers shall use personal protective clothing and equipment selected specifically for the hazard. Whenever possible, the workpieces to be welded should be positioned to minimize worker exposure to molten metal, sparks, and fumes.
# Section 8 -Sanitation (a) Food, Cosmetics, and Tobacco
The storage, preparation, dispensing, or consumption of food or beverages; the storage or application of cosmetics; and the storage or use of all tobacco products shall be prohibited in areas where welding is conducted.
# (b) Handwash i ng
The employer shall provide handwashing facilities and encourage workers to use them before eating, smoking, using the toilet, or leaving the worksi te.
# (c) Cleaning of Clothes and Equipment
Protective clothing, equipment, and tools shall be cleaned periodically.
# (d) Toxic Waste Disposal
Toxic wastes shall be collected and disposed of in a manner that is not hazardous to workers or others.
# (e) Cleanup of Work Area
The work area shall be cleaned at the end of each shift (or more frequently if needed) using vacuum pickup. Dry sweeping or air hoses shall not be used to clean the work area. Collected wastes shall be placed in sealed containers with labels that indicate the contents.
Cleanup and disposal shall be conducted in a manner that prevents worker contact with wastes and complies with all applicable Federal, State, and local regulations.
# (f) Showering and Changing Facilities
Workers shall be provided with and advised to use facilities for showering and changing clothes at the end of each work shift.
# (g) Flammable Materials
Work areas shall be kept free of flammable debris. Flammable work materials (rags, solvents, etc.) shall be stored in approved safety containers.
# Section 9 -Exposure Monitoring (a) General
(1) Exposure monitoring shall be conducted as specified in parts (b), (c), and (d) of this section for all workers performing welding and for all other workers who may be occupationally exposed through their proximity to these processes.
(2) Air from the worker's breathing zone shall be sampled for fumes and gases. Samples for workers performing welding shall be collected in the welding helmet; samples for other workers shall be collected as close to the mouth and nose as possible.
(3) Results of all exposure monitoring (e.g., of fumes, gases, and physical agents) shall be recorded and retained as specified in Chapter I, Section 10 of this document.
# (b) Determination of Exposures
(1) The employer shall conduct industrial hygiene surveys to determine whether exposures to any air contaminant exceed the applicable exposure limit (see definition in Section 1(b)).
(2) The employer shall keep records of these surveys as defined in Chapter I, Section 10 of this document.
If the employer concludes that exposures are below NIOSH exposure limits, the records must show the basis for this conclusion.
(3) Surveys shall be performed semiannually or whenever changes in work processes or conditions are likely to produce increased concentrations of any air contaminant.
# (c) Routine Monitoring
(1) If the occupational exposure to any air contaminant is at or above the exposure limit (see definition in Section 1(b)), a program of personal monitoring shall be instituted to permit calculation of each worker's exposure. Source and area monitoring may be a useful supplement to personal monitoring.
In all personal monitoring, samples representative of a time-weighted average (TWA) and/or ceiling exposure (depending on the specific agent) shall be collected in the breathing zone of the worker. Sampling and analysis shall be done in accordance with the methods given in Chapter VI, Table VI-1. For each determination of an occupational exposure, a sufficient number of samples shall be collected to characterize each worker's exposure during each work shift. Though not all workers have to be monitored, sufficient samples should be collected to characterize the exposures of all workers who may be potentially exposed. Variations in work habits and production schedules, worker locations, and job functions shall be considered when deciding on sampling locations, times, and frequencies.
A worker exposed to any specific fume or gas at concentrations below its exposure limit shall be monitored at least once every 6 months; more frequent monitoring may be indicated by a professional industrial hygienist.
If a worker is exposed to any specific fume or gas in excess of the exposure limit, controls shall be initiated as specified in Chapter I, Section 7 of this document.
In addition, the worker shall be notified of the exposure and of the control measures being implemented. The worker's exposure shall be evaluated at least once a month. Such monitoring shall continue until two consecutive determinations at least 1 week apart are below the exposure limit. After that point, monitoring shall be conducted at least semiannually or whenever the work process or conditions change.
# (d) Physical Agent Monitoring
(1) Exposure to UV radiation shall be prevented by means of a management control program. The program shall require the use of barriers wherever possible. Where barriers cannot be used, workers shall use personal protective devices, including proper clothing, sunscreens with a sun protection factor (SPF) >15, and body and face shields. The use of barriers and protective devices shall be evaluated every month.
(2) Noise exposures shall be evaluated for all workers performing welding. Plasma arc, metal spraying, and arc air gouging processes are likely to result in excessive noise exposures. Employers shall meet the requirements of 29 CFR 1910.95(c), Hearing Conservation Program, whenever a worker's noise exposure is >85 decibels measured on the A scale (dBA) as an 8-hr TWA. All monitoring instruments shall conform to the requirements of 29 CFR 1910.95(d)(2), Monitoring; they shall have a Type II microphone at a minimum. Such noise monitoring surveys must be repeated whenever a change in the work process or environment increases the potential for worker noise exposures.
(3) Electron beam welding equipment shall be surveyed periodically to detect any leakage of X-radiation. A preliminary survey shall be conducted at the time of installation while operating at maximum current and voltage levels. Subsequent surveys should be made whenever the equipment is moved or repaired. Operators of such equipment shall use film badges or some other means of monitoring X-ray exposure.
(4) Environmental heat exposures shall be assessed whenever the potential exists for workers to be exposed to elevated ambient temperatures (e.g., when working in confined spaces or subjected to poor ventilation). Monitoring practices shall be those specified in Criteria for a Recommended Standard. ...OccupationaI Exposure to Hot Environments [NIOSH 1986].
# Section 10 -Recordkeeping (a) Exposure Monitoring
The employer shall establish and maintain an accurate record of all exposure measurements as required in Chapter I, Section 9 of this document. These records shall include the name of the worker being monitored, social security number, duties performed and job locations, dates and times of measurements, sampling and analytical methods used, type of personal protection used (if any), and number, duration, and results of samples taken.
# (b) Medical Monitoring
The employer shall establish and maintain an accurate record for each worker subject to the medical monitoring specified in Chapter I, Section 3 of this document.
# (c) Record Retention
In accordance with the requirements of 29 CFR 1910.20(d), Preservation of Records, the employer shall retain the records described in Chapter I, Sections 3, 6, and 9 of this document for at least the following per iods:
(1) Thirty years for exposure monitoring records, and
(2) Duration of employment plus 30 years for medical surveillance records.
# (d) Availability of Records
(1) In accordance with 29 CFR 1910.20, Access to Employee Exposure and Medical Records, the employer shall upon request allow examination and copying of exposure monitoring records by the subject worker, the former worker, or anyone having the specific written consent of the subject or former worker.
(2) Any medical records that are required by this recommended standard shall be provided upon request for examination and copying to the subject worker, the former worker, or anyone having the specific written consent of the subject or former worker.
# (e) Transfer of Records
The employer shall comply with the requirements for the transfer of records as set forth in 29 CFR 1910.20(h), Transfer of Records.
# II. INTRODUCTION
# A. Scope
NIOSH has formalized a system for developing criteria on which to base standards for ensuring the health and safety of workers exposed to hazardous chemical and physical agents. The criteria and recommended standards are intended to enable management and labor to develop better engineering controls and more healthful work practices. This document presents the criteria and recommended standards for preventing health impairment from exposures associated with welding. The criteria document was developed by the National Institute for Occupational Safety and Health (NIOSH) in response to Section 20(a)(3) of the Occupational Safety and Health Act of 1970. In this act, NIOSH is charged with the responsibility of developing criteria for toxic materials and harmful physical agents to describe exposure concentrations at which no worker will suffer impaired health or functional capacities or diminished life expectancy as a result of work experience.
This document contains information on workplace exposures that may occur during welding and the adverse health effects associated with these exposures (e.g., gastrointestinal disorders, cancer, and ocular, dermatological, reproductive, musculoskeletal, and chronic and acute respiratory diseases. For the purpose of this recommended standard, "welding" is defined as those processes that join or cut pieces of metal by heat, pressure, or both (e.g., arc welding, brazing, and cutting) [ILO 1972], These processes differ only in the way heat is created and applied to the parts being joined and in the type of filler material used. Chapter III describes these processes. 11-1 lists specific welding processes and some of the potentially hazardous agents associated with them. This table should be used as a reference guide and not as a complete inventory of possible emissions. Chapter III contains more complete discussion of these agents. Laser and underwater welding processes are not included since they require specific control procedures that are beyond the scope of this document.
# B. Number of Workers Potentially Exposed to Welding
The 1972-74 National Occupational Hazard Survey showed that an estimated 176,000 workers had a primary occupation of welder, brazer, or thermal cutter [Sundin 1972]. A follow-up survey in 1981-83 indicated that 185,000 workers were employed in these occupations [Sundin 1981]. These NIOSH surveys were limited to facilities that employed eight or more workers and did not account for any welding conducted at mining sites or government fac i Ii t i e s .
Estimates indicate that the duties of more than 700,000 U.S. workers involve the welding of various types of materials within many different industries (e.g., manufacturing and construction) [Bureau of the Census 1984]. Census data from 1980 [Bureau of the Census 1984] indicated that 673,357 males and 39,242 females were employed as welders and cutters. Note that brazers were classified along with solderers in the census data and thus are not included in these employment figures.
# C. Special Considerations for Controlling Welding Hazards
The hazards associated with welding can be divided into two categories:
(1) the hazardous chemicals (e.g., fumes and gases) that are formed or released by the processes, and ( 2) the physical hazards such as ionizing and nonionizing radiation, noise, vibration, high temperatures, and electricity. Because of the many techniques applied in welding and the various types of materials used, it is often difficult to characterize exposures completely at any given time. However, as noted in Table 11-1, specific gases and fumes are typically generated when certain welding processes are applied to known base metals. This knowledge can be used to implement good industrial hygiene practices before any comprehensive evaluation of the workplace is initiated.
This document discusses the adverse health effects that have been observed among workers who perform welding, but many of these effects cannot be attributed to any specific agent because of the possible additive or synergistic effects from mixed exposures. For example, welders have historically been exposed to asbestos as a result of using asbestoscontaining materials or working in industries where asbestos was used as an insulation material. Many of the morbidity and mortality studies conducted on welders demonstrate an increased risk in respiratory diseases, including cancer. Because of the absence of exposure data for many of these studies, the etiology of the reported disease is unknown but often clinically resembles the diseases associated with workers exposed to asbestos. Although the potential for an asbestos exposure has decreased with the elimination of asbestos-containing materials used by welders, it still remains a possible concomitant exposure in some work environments (e.g., asbestos insulation around pipes). [29 CFR 1926.350-54], ship repairing [29 CFR 1915.31-36], shipbuilding [29 CFR 1916.31-36], longshoring [29 CFR 1917.31-36], and general industry [29 CFR 1910.251-54], Most of the Federal standards were adopted from consensus standards developed by a variety of organizations, including the American Conference of Governmental Industrial Hygienists (ACGIH), AWS, ANSI, the National Fire Protection Association (NFPA), the Compressed Gas Association (CGA), the American Petroleum Institute (API), and the Rubber Manufacturers Association (RMA).
The Federal standards covering welding, cutting, and brazing are generally process-or design-oriented rather than performance-or exposure-Iimitoriented. That is, though the standards refer to allowable limits of exposure, they actually prescribe work procedures or practices that are intended to minimize health and safety risks. Some of the potential hazards to which the standards are directed include fire, explosion, electric shock, UV radiation, infrared (IR) radiation, oxygen-deficient atmospheres, decomposition products of chlorinated solvents, fluorides, nitrogen dioxide, and toxic metals such as beryllium, cadmium, chromium, lead, mercury, and zinc [29 CFR 1910[29 CFR .1915[29 CFR -17, 1910[29 CFR .1926].
Environmental monitoring is prescribed to evaluate confined spaces for sufficient oxygen, to monitor exposures resulting from the heating of greased metals, and to check for the presence of flammable gases. Labeling is required on the packages holding fluoride-containing flux or filler metals to warn that ventilation is required to control the fumes and gases that may be produced. No sanitation procedures are specified. Some types of personal protective equipment are specified, including eye protectors, helmets, gloves, boots, aprons, and other clothing. Requirements for specific work practices are covered for a number of particularly hazardous operations, including working in confined spaces, handling compressed-gas cylinders, welding or cutting metal containers, and working on elevated surfaces. The engineering controls required are screens or booths to protect against UV radiation, and ventilation for enclosed areas and confined spaces. The general industry standards for welding, cutting, and brazing [29 CFR 1910.251-54] refer to the PELs as stated in 29 CFR 191029 CFR .1000. The construction standards for welding and cutting [29 CFR 1926.350-54] incorporate by reference the ACGIH Threshold Limit Values (TLVs®). The maritime employment standards for welding, brazing, and thermal cutting [29 CFR 1915[29 CFR .31-36, 1916[29 CFR .31-36, 1917 do not specify or refer to environmental limits.
Since 1970, the ACGIH has recommended a TLV of 5 mg/m^ for total particulates in welding fumes. In addition, the ACGIH recommends that specific constituents of the fumes and toxic gases also be considered in assessing airborne exposures from welding [ACGIH 1987-88]. For example, a TLV of 0.05 mg/m3 (as Cr) is recommended for exposures to chromium(VI) by the ACGIH.
NIOSH has RELs for individual substances and physical agents found in the welding environment. These RELs are listed in Appendix A along with the current OSHA PELs and ACGIH TLVs.
# E. NIOSH Recommendations That Differ From Current OSHA Regulations
Many of the exposure limits and program requirements recommended in this document are not currently required by OSHA, and other recommendations are intended to augment existing OSHA requirements. NIOSH recommendations that differ from current OSHA regulations include those that pertain to the following items:
• Adoption of NIOSH RELs (or in some instances, other limits proposed by voluntary consensus groups) for specific chemical and physical agents (see Chapter I, Section 1, Definitions).
• Initial and periodic medical surveillance.
• Labeling and posting for potential carcinogens.
• Warning of eye damage from looking at a welding arc.
• Warning of high noise areas.
• Criteria for heat stress.
• Recommendations for personal protective clothing and equipment, including the criteria for selecting appropriate types of respirators.
• Information to supplement the Hazard Communication Standard (29 CFR 1910(29 CFR .1200).
• Engineering controls and work practices.
• Requirements for food storage and consumption, use of tobacco products, use of cosmetics, and personal hygiene (availability of shower and locker facilities).
• Exposure monitoring, both initial and periodic.
• Recordkeeping.
# III.
# CHARACTERISTICS OF WELDING PROCESSES
# A. Identification of Processes
More than 80 different types of welding and allied processes are in commercial use, including brazing and thermal cutting (Figure 111-1). The most commonly used processes are briefly discussed in this section. Definitions for types of welding processes appear in the Glossary. Appendix D lists industries that employ welders, brazers, and cutters, along with their respective standard industrial classification (SIC) codes.
# Arc Welding
In arc welding, heat is created as electricity flows across a gap between the tip of the welding electrode and the metal. Arc welding is the most frequently used process. It encompasses numerous variations, depending on the types of electrodes, fluxes, shielding gases, and other equipment that may be used. The arc welding process involves the melting of an electrode by an electric current to form a molten puddle in the base metal. Because of the generated heat, the base metal also becomes molten at the joining surfaces, which bond upon cooling.
Electrodes are manufactured as bare wire or as wire lightly to heavily coated with flux material. Bare wire electrodes are the least expensive, but they are difficult to maintain, and they produce an inferior weld. Also, a coating of copper on filler materials may be used in place of a flux to prevent oxidation of the material before use. Flux material generally consists of asbestos, feldspar, fluorine compounds, mica, steatite (a form of talc), titanium dioxide, calcium carbonate, magnesium carbonate, or various aluminas. The flux prevents or removes oxides or other undesirable substances from the weld.
Inert shielding gases such as helium, argon, or carbon dioxide are used in some variations of arc welding. These variations of arc welding are often referred to as shielded metal arc, metal inert gas, and plasma arc welding. The inert gas prevents oxygen and active chemicals in the atmosphere from reacting with the hot metal [AWS 1976].
# Oxyfuei Gas Welding
Oxyfuel gas welding is the process by which heat from burning gases is used to melt the base metal without the use of welding rods; however, rods are used when extra metal is needed as a filler to obtain a complete bond. The composition of these consumable rods is very similar to that of the base metals. Some are coated with flux, the composition of which depends on the application. . . CAW S -tw . . LBC IG -o x y g e n .
# MASTER CHART OF WELDING AND ALLIED P R O C E SSES
# . CAW T electrogas w eld in
# R e sista n c e W elding
Resistance welding is a process in which pieces of metal are pressed together and an electric current is passed through them. At the contact point, there is sufficient resistance to cause an increase in temperature and melting of the metal.
# Brazing
Brazing is the process by which metals are heated and joined together by a molten filler metal at temperatures exceeding 450°C (840°F) [AWS 1980]. Soldering, which is not included in this document, is similar to brazing, but it uses filler metals that have melting points below 450°C. The filler metal used in brazing may be in the form of wire, foil, filings, slugs, powder, paste, or tape. Fluxes must be used unless the process is performed in a vacuum, since oxidation of the brazed area will weaken the bond. The most common ingredients of fluxes are borates (e.g., lithium, potassium, and sodium), fused borax, fluoroborates (e.g., potassium and sodium), fluorides (e.g., lithium, potassium, and sodium), chlorides (e.g., lithium, potassium, and sodium), acids (e.g., boric acid and calcined boric acid), alkalis (e.g., potassium hydroxide and sodium hydroxide), and water (either as water of hydration or as an addition for paste fluxes) [AWS 1963].
# Thermal Cutting
Thermal cutting includes processes that cut the metal by melting. These processes are divided into two main groups: oxygen and arc cutting. Oxygen cutting is performed on plain carbon, manganese, and lowchromium-content steels. When the metal is heated and exposed to oxygen, it oxidizes and melts. Flame cutting uses a fuel gas (or a combination of gases) such as acetylene, hydrogen, natural gas, or propane that burns and produces sufficient heat to vaporize and separate the metal. Arc cutting is used with nonferrous metals, stainless steels, or steels with a high chromium or tungsten content [AWS 1980].
# B. Potential for Exposure
Welding, brazing, and thermal cutting processes generate exposures to many chemical and physical agents. Chemical and physical agents produced by these processes are described in the following sections, which identify the source, mechanism of production, disposition, and exposure concentrations found in many occupational environments. The potential exists for other confounding exposures (e.g., asbestos and heat) in the work environment of welders and needs to be assessed for each welding process.
# Fumes and Other Particulates
A fume is generated by volatilization of melted substances with subsequent condensation of solid particles from the gaseous state [Dinman 1978]. For the processes discussed in this document, temperatures may range from about 450°C (840°F) for brazing [AWS 1980] to well above 15,000°C (27,000°F) for plasma arc cutting [Grimm and Kusnetz 1962;Siekierzynska and Paluch 1972]. The single largest source of fumes is the filler metal being used [Jones 1967;Hei le and Hill 1975].
Fumes may also originate from the base metal [Jones 1967], from coatings applied to the base metal [Pegues 1960;Oliver and Molyneux 1975], and from the flux or electrode coating [Thrysin et al. 1952]. Fume particles typically have a diameter of less than 1 micrometer (fxm) [Hewitt and Hicks 1973;Heile and Hill 1975;Akselsson et a l . 1976].
Fumes are not the only sources of airborne particulates. Fluxes and filler metals used in powdered form (e.g., in submerged arc welding and furnace brazing) may enter the air as fugitive dusts. Mineral and metal dusts may also be produced when material is pulverized during the cleaning of welds and brazes by surface brushing or grinding [Moreton et al. 1975]. Historically, the potential has also existed for asbestos exposure during welding processes. These exposures often occurred as a result of using materials that contained asbestos, disturbing asbestos insulation while welding, or working near other operations that used asbestos. Steel and Sanderson [1966] investigated the composition of welding fumes to determine the extent of impurities that may be present in fluxes. Flux that is formulated into a coating for stick electrodes may generate shielding gas, produce slag, alloy with rods, or act as binders.
In one of their experiments, these investigators conducted shielded metal arc welding on mild steel in a test chamber using 12 different commercial electrodes. Air samples were collected at a distance from the source of exposure that corresponded to the breathing zone of a welder standing upright. On several occasions, fume concentrations exceeded NIOSH RELs for lead and vanadium pentoxide. Chromium(VI), copper, and manganese were also detected.
The chemical composition of the airborne fumes generally reflects the elemental composition of the base and filler metals and the flux, but the fume components may have different chemical forms. Thus concentrations of the various fume components may vary for each job and process and are best determined on a case-by-case basis.
# a. Alkali Metals and Alkaline Earths
The airborne concentrations of calcium, magnesium, potassium, and sodium are significantly greater in the emissions from lime (low-hydrogen) electrodes than in those from nonlime electrodes [Morita and Tanigaki 1977;Kimura et a l . 1974]. Although concentrations vary greatly within the two classes, low-hydrogen electrodes generally produce higher concentrations of calcium, magnesium, potassium, and sodium in their fumes.
# b. Aluminum
Aluminum is generally found in small quantities in the fumes from all types of electrodes, both low-hydrogen and non-low-hydrogen. Morita and Tanigaki [1977] reported a range of 0.21% to 1.44% aluminum (as AI2O3 ), and Kimura et al. [1974] noted a range of 0 .1% to 0 .8% in the fumes for all electrodes tested. -Pushkin [1972] evaluated the composition of fumes produced by the electron beam welding of beryllium bronze. The welding was done in a vacuum chamber that was flushed with air before opening. The purged air was filtered, and the collected fumes were analyzed for beryllium. As in most electron beam welding, two pieces of base metal (2% beryllium content) were joined without the use of a filler metal. Samples of the purged air contained detectable amounts of beryllium in only 5 of the 44 samples. However, periodic cleaning by dry scrubbing of the vacuum chamber walls caused redispersion of fumes that contained beryllium concentrations of 130 to 150 jug/m»* in the chamber and 4 /ng/m^ in the breathing zones of welders working outside the chamber.
# c. Beryllium
# Bobrishchev
# d . Cadmi um
Cadmium concentrations in the breathing zone have been reported to be 10 to 250 ¡xg/rn^ during shipboard brazing with a silver-and cadmium-based filler metal [Oliver and Molyneux 1974]. Cadmiumbearing alloys are used in more than 50% of all brazed joints [Timmins et a l . 1977].
# e. Chromium
Both the chromium concentration and its oxidative state vary within the fumes depending on the welding or cutting process and the base metal. Virtamo [1975] compared fume composition in shielded metal arc welding, gas tungsten arc welding, gas metal arc welding, and plasma arc cutting. These operations were performed on high-alloy, nieke I-chromium stainless steel to determine the relative amounts of nickel, chromium(VI), and total chromium evolved in the fumes. Analysis of breathing zone samples indicated the following:
• Shielded metal arc welding produced the highest water-soluble chromium(VI) fume concentrations-as high as 720 jug/m^.
• Gas tungsten arc welding produced chromium(VI) concentrations below the 10-^g/m^ detection limit in 8 of 10 samples (the highest concentration found was 45 jug/m^).
• No chromium(VI) was detected during plasma arc cutting or gas metal arc welding.
While surveying Swedish worksites, Ulfvarson [1981b] found higher chromium concentrations with shielded metal arc welding than with gas metal arc welding on stainless steel. The median breathing zone concentration of chromium [almost all soluble chromium(VI)] was 150 ng/m3 at 86 worksites where shielded metal arc welding was performed. For gas metal arc welding, the median breathing zone concentration of chromium (mostly insoluble) was about 20 jug/m^ at 41 worksites.
At a large maintenance shop, Arnold [1983] assessed the exposures of three groups of welders. The first group performed gas tungsten arc and gas metal arc welding. Their breathing zone samples all contained <6 jug/m^ of chromium(VI). Group II performed shielded metal arc welding and had breathing zone concentrations of chromium(VI) that averaged 14 |ug/m3, with a high of 90 pig/m^. Group III used a variety of welding methods-mostly shielded metal arc welding (including flux cored arc and gas metal arc welding). Within this group, the average chromium(VI) concentration was 64 |jg/m3, with a high of 329 jug/m^.
Both Lautner et al. [1978] and Ulfvarson [1981b] found that shielded metal arc welding produced the highest percentage of chromium(VI) in the fumes. When electron spectroscopy was used for chemical analysis (ESCA), gas metal arc and gas tungsten arc welding of stainless steel produced only traces of chromium(VI) (concentrations too small to be quantified). Shielded metal arc welding generated 73% of the total chromium in the fumes as chromium(VI) (mean net mass = 1,016 ¡xq chromium(VI )/f i I ter).
# f . FIuor i des
The inclusion of fluorspar in low-hydrogen (lime) electrodes produces significant amounts of fluoride compounds in welding fumes. In a study conducted by Kimura et al. [1974], welding fumes contained 11% to 18% fluoride. Another study [Persinger et al. 1973] reports that the fumes contained 14% to 23% fluoride when low-hydrogen electrodes were used for shielded metal arc welding on mild and high-tensile steel. Tebbens and Drinker [1941] found that high-alloy electrodes containing 1 to 5 mg fluoride per electrode generated fumes that contained 9% to 26% fluoride compounds. This high percentage was partly due to the low melting points of the fluoride compounds. Only negligible amounts of hydrogen fluoride were detected in the welding emissions.
# g . Iron
Iron is the main constituent of the fume when welding is performed on non-alloy steel. Dreesen et al. [1947] studied arc welders in steel ship construction and reported welding fumes with iron concentrations above 20 mg/m^. Ulfvarson [1981b] collected breathing zone samples for welders performing shielded metal arc and gas metal arc welding. The geometric mean concentration for iron was 14 mg/m^ during the welding of unpainted non-alloy steel and 30 mg/nr* during the welding of painted non-alloy steel. Akbarkhanzadeh [1979] surveyed British worksites (mostly shipyards) where shielded metal arc welding was being performed on mild steel. The mean concentration of iron (ferric oxide) from 209 breathing zone samples was mg/m^. The iron concentration increased linearly with increasing arc current (correlation coefficient = 0.323, p<0.001). KleinfeId et al. [1969] sampled welders while they performed oxyfuel cutting and shielded metal arc welding; they found concentrations of iron oxide ranging from 0.65 to 1.7 mg/nr* inside the welders' face shields and from 1.6 to 12 mg/m^ outside the face shield.
# h . Lead
Because zinc may contain lead as an impurity, significant amounts of lead can be generated when welding zinc-primed steel or steel that has been hot-dipped in zinc. Pegues [1960] determined lead concentrations from air samples collected in the breathing zone of workers performing oxyacetylene cutting and arc welding on zinc-coated steel. Welding was performed in a confined space without ventilation on steel that was protected by hot-dip galvanization and on steel that was painted with zinc silicate.
During arc welding, breathing zone concentrations of lead ranged from 0.9 to 15.2 mg/m^ with the zinc-silicate-coated steel, and from 0.4 to 0.7 mg/m^ with the galvanized steel. During oxyacetylene welding, lead concentrations ranged from 1.2 to 3.5 mg/m^ with the zinc-silicate-coated steel, and from 0.2 to 0.7 mg/m^ with the galvanized steel.
# i. Manganese
Akbarkhanzadeh [1979] collected breathing zone samples from welders performing shielded metal arc welding of mild steel coated with an unspecified primer and found average manganese fume concentrations of 0.14 mg/nw. By comparison, breathing zone samples from welders performing shielded metal arc and gas metal arc welding had average manganese concentrations of 3.1 mg/m^ during welding on primed mild steel and 1.4 mg/m^ during welding on unprimed mild steel [Ulfvarson 1981].
The percentage of manganese in welding fumes was reported to be relatively independent of the type of electrode [Kimura et a l . 1974;Morita and Tanigaki 1977], In a study of 61 brands of electrodes of different composition [Morita and Tanigaki 1977], the level of manganese oxide (MnO) in the fume ranged from 2.5% to 9.5%. In a similar study of 25 brands of electrodes, Kimura et al. [1974] observed fumes containing 3.3% to 11.2% manganese as MnO. Fumes from ilmenite electrodes tended to have higher concentrations of manganese compared with those generated from lime electrodes.
# j . N i ekeI
Virtamo [1975] assessed the nickel content of fumes generated from shielded metal arc welding, gas metal arc welding, and plasma arc cutting of stainless steel. Shielded metal arc welding produced nickel concentrations that ranged from trace amounts to 160 jiig/m^; gas metal arc welding produced concentrations as high as 60 and plasma arc cutting produced concentrations up to 470 /^g/m3. When Ulfvarson et a l . [1981] surveyed welders who were performing shielded metal arc and gas metal arc welding of stainless steel, a median breathing zone concentration of approximately 25 n g nickel/m^ was determined for shielded metal arc and approximately 5 /ug nickel/m^ for gas metal arc welding. Bernacki et al. [1978] reported an average airborne concentration of 6 /ug nickel/m^ (with a high of 46 jug nickel/m^) from welding nickel-alloyed steel. Wilson et al. [1981] examined various maintenance welding operations at a chemical plant and found that the highest nickel concentrations were produced when welding was conducted on stainless steel inside distillation towers. Airborne concentrations of nickel from 22 of 23 samples exceeded the NIOSH REL of 15 /ug/m3. The mean concentration of nickel was 3.65 /¿g/m^, with a high of 17.6 /Lig/m^.
# k. Silica
Silica in welding fumes originates from the coating on the electrode, which varies in quantity depending on the type of electrode used. Twenty-six brands of ilmenite and lime titania electrodes produced fumes containing 18% to 22% silicon as silicon dioxide (Si02); two brands of iron powder/iron oxide electrodes produced fumes containing 8% and 12% SiO2 ; and 10 brands of lime electrodes produced fumes containing 4% to 11% SiO2 [Kimura et a l . 1974].
In a study of 61 brands of electrodes, Morita and Tanigaki [1977] observed that the mean silica contents of fumes were as follows:
(1) 33% for 7 high-titania and iron powder/iron oxide electrodes, (2 ) 22% for 26 brands of ilmenite and lime titania electrodes, (3) 12% for 1 high-cellulose electrode produced, and (4) 6% for 27 low-hydrogen electrodes. Tebbens and Drinker [1941] observed the presence of silica in fumes generated from the shielded metal arc welding of mild steel. Silica and silicates are commonly used ingredients in fluxes on mild-steelcovered electrodes. When two such electrodes were tested, one generated fumes containing 15% crystalline silica plus a high silicate content; fumes from the other contained no crystalline silica but were high in silicates. The two electrodes generated comparable amounts of silicon (18% to 22% of the total fume), which was present as soluble silicates or amorphous silica. X-ray diffraction was used to confirm the absence of crystalline silica.
# I. Titanium
In two studies [Morita and Tanigaki 1977], ilmenite, lime titania, and high-titania electrodes generated similar percentages of titanium in fumes.
In the first study, 30 of these types of electrodes produced a range of 0.6% to 2.3% titanium as titanium dioxide (Ti02). When 30 different brands of iron oxide/iron powder and low-hydrogen electrodes were tested in that same study, a range of 0.1% to 0.4% TiOo was found in the fume. The second study [Kimura et al. 1974] examined 25 brands of electrodes. Thirteen brands of ilmenite, lime titania, and titania electrodes produced a range of 0.6% to 5.5% Ti02 in the fume; the remaining 12 iron powder/iron oxide and lime electrodes generated fumes containing 0.2% to 0.9% Ti02m . Z i nc In a study of oxypropane flame cutting and shielded metal arc welding in a shipyard [Bell 1976], fumes containing zinc were generated from the protective coating on the metal. Breathing zone concentrations ranged from no detectable zinc to 8.6 mg/m^. Shielded metal arc welding of metal plate treated with zinc powder and zinc chromate primers produced fumes containing up to 74 mg zinc/m^ when ventilation was poor. A report on fumes from welding and flame cutting processes in the shipbuilding and ship-repairing industry [IIW 19701 showed breathing zone zinc concentrations as high as 44 mg/m^. Ulfvarson [1981b] collected breathing zone samples from welders who were gas metal arc welding on mild steel that was either untreated or coated with a zinc tetraoxychromate/iron oxide primer. Samples collected during the welding of untreated steel had a mean zinc concentration of 0.11 mg/m^, and those collected during the welding of primer-coated steel had a mean zinc concentration of 0.43 mg/nr*. Dreesen et al. [1947] reported zinc concentrations in area samples that exceeded 12 mg/m^ (15 mg/m^ expressed as zinc oxide) in welding fumes produced from arc welding on steel during ship repair. Pegues [1960] (see subsection 1,h, Lead, of this chapter) analyzed fume samples collected from workers performing oxyacetylene cutting and arc welding on zinc-coated steel in a confined space without ventilation. Steel that had two types of zinc-coatings (e.g., zinc silicate and galvanized steel) were evaluated to determine the generation of zinc in the fumes. The zinc-silicatecoated steel produced a mean zinc concentration of 19.81 mg/m^ during electric arc welding and 12.28 mg/m^ during oxyacetylene cutting. Electric arc welding of galvanized steel produced a mean zinc concentration of 6.63 mg/m^. No exposures to zinc were detected during oxyacetylene cutting.
# Spec i f i c Gases
A number of toxic gases such as carbon monoxide, oxides of nitrogen, ozone, and various photochemical and pyrolytic decomposition products of halogenated hydrocarbons are present or produced by chemical reactions during welding. Fuel gases that may be released (such as propane, acetylene, and hydrogen) are asphyxiants. These gases and oxygen may combust during use [Occupational Health (London) 1975]. The lower explosive limits (LELs) for some of these gases are quite low-for example, 2.3% for propane, 4.1% for hydrogen, and 2.5% for acetylene.
Oxygen is hazardous at higher than normal concentrations because it increases the flammability of materials (e.g., clothes) [Jefferson 1970].
Shielding gases such as argon, nitrogen, helium, and carbon dioxide (CO2 ) may also be present. Alone, these gases do not normally pose a hazard; however, in confined spaces they may displace the oxygen-containing air and give no warning of oxygen deficiency because they are odorless and colorless.
Many of the gases that may be encountered during various welding processes are listed below with information on their source of generation and reported concentrations.
# a. Carbon Monoxide
Carbon monoxide CO exposures often result from the reduction of CO2 used for shielding in gas metal arc welding, de Kretser et al. [1964] found CO concentrations often approaching 300 ppm when CO2 exposures were measured at 1400 parts per million (ppm) during gas metal arc welding. Ulfvarson [1981b] found CO exposures to be sporadic and at low concentrations in many Swedish work sites except where gas metal arc welding was being done. At the latter sites, about 10% of the measurements had CO readings above 50 ppm, with peak readings of 150 ppm. Press and Florian [1983] found that for gas metal arc welding, CO concentrations increased as the percentage of carbon dioxide was increased in the shielding gas.
Erman et a l . [1968] measured CO concentrations in poorly ventilated confined spaces during shipbuilding operations. Welding was done on steel with CO2 gas metal arc welding. CO concentrations increased as the duration of welding increased.
In a space of 4.9 m3, CO concentrations exceeded 160 mg/m^ (145 ppm) within 40 min. Ulfvarson et al. [1981a] assessed the generation of CO during flame cutting of primed steel. They found that in a laboratory setting, CO concentrations up to 35 ppm were generated when the ventilation was poor. Flame cutting of primed steel during ship repair and construction in confined spaces produced CO concentrations exceeding 100 ppm.
# b. Oxides of Nitrogen
An arc or a very high-temperature flame may cause the oxygen and nitrogen in the air to combine and form oxides of nitrogen. One combustion product, nitrogen dioxide (NO2 ), has been detected in shielded arc welding, oxyacetylene welding, arc gouging [Fay et al. 1957], gas metal arc welding [Erman et a l . 1968], submerged arc welding, and oxyacetylene and oxypropane cutting [IIW 1970].
Tests performed with tungsten electrodes produced 0.3 to 0.5 ppm of nitrogen oxides with helium shielding and 2.5 to 3.0 ppm with argon shielding. The higher concentrations for both were obtained when the shield gas flow rate was doubled. Ferry and Ginther [1953] found lower NO2 concentrations for oxyacetylene welding, argon-shielded gas metal arc welding, and carbon arc gouging. The authors speculated that the increase in current for gas metal arc welding produced the higher NO2 concentrations. Akbarkhanzadeh [1979], however, found no relationship between the current and the generation rates for nitrogen oxides when shielded metal arc welding was performed on mild steel. Ferry and Ginther [1953] observed that nitrogen dioxide concentrations were always greatest in the area of visible fume (within 0.15 m of the arc). At greater distances from the arc, the concentrations decreased in all directions except in the direction of the fume stream. The authors suggested that NO2 is formed thermally and diffuses away from the arc.
In a study [IIW 1980] that used oxyacetylene welding, flame size was an important factor in the generation of nitrogen oxides. Generation rates for nitrogen oxides were 10 times higher with an unrestricted flame length than with a 10-mm flame. In addition, increasing blowpipe size from 1 to 8 produced dramatic increases in nitrogen oxide concentrations.
Ventilation that is adequate to control exposures to total fumes is sufficient to control nitrogen oxide exposures [Ferry and Ginther 1953;Akbarkhanzadeh 1979;IIW 1980].
Octavian and Nicolae [1968] observed that nitrogen oxides are formed at a distance from plasma arc cutting or argon-shielded arc welding, with maximum formation rates at 1.75 to 2.5 m and 4 m, respectively. Nitrogen oxide concentrations were determined by drawing air through a quartz tube at various distances from the welding operations and therefore measuring only those oxides formed by UV radiation.
Press [1976] found that for plasma arc cutting of aluminum alloys with an argon/hydrogen mixture, the highest measured concentrations were 2 ppm for NO2 and 9 ppm for nitrous oxide (N2O). Both concentrations were determined in the absence of ventilation. Siekierzynska and Paluch [1972] examined emission rates of nitrogen oxides for plasma arc cutting on various base metals that were 0.5 mm thick. Although N2O concentrations were not given, generation rates were reported to be very similar for cutting mild steel (150 mg/sec), alloy steel (140 mg/sec), copper (70 mg/sec), brass (80 mg/sec), and aluminum (70 mg/sec). The NO2 emission rates were 50 mg/sec for mild steel, 40 mg/sec for alloy steel, 45 mg/sec for copper, 50 mg/sec for brass, and 40 mg/sec for aluminum. Concentrations as high as 100 ppm have been reported [Maddock 1970;Mangold and Beckett 1971].
# c . Ozone
In the presence of UV light, atmospheric oxygen can convert to ozone [Lunau 1967]. Among the various welding processes, gas metal arc and gas tungsten arc welding produce the highest ozone concentrations, especially when aluminum is used as a base metal [Lunau 1967;Press and Florian 1983;Ditschun and Sahoo 1983].
In studies of argon-shielded arc welding of aluminum, Lunau [1967] found that after 3 to 5 min with a 200-ampere (A) current density, ozone concentrations averaged 5.1 ppm; with a 250-A current density, ozone was 7.5 ppm; and with a 300-A current, ozone was 8.4 ppm. All concentrations decreased over time because of strong thermal upcurrents formed from the heat during welding. Shironin and Dorosheva [1976] also found an increase in ozone concentrations with increasing current density. With continuous argon-shielded arc welding, breathing zone samples collected from welders indicated an average ozone concentration of 0.6 mg/m^ when an 80-A current density was used. This concentration increased to 1.0 mg/m^ at a 300-A current density; with pulsed arcing, the concentrations were 0.5 mg/m^ for a 50% duty cycle and 0.7 mg/m^ for a 75% duty cycle. When Ditschun and Sahoo [1983] assessed the generation of ozone during gas metal arc welding of copper-nickel and nickel-aluminum bronze alloys, ozone concentrations varied from 0.07 to 0 .19 ppm. Ferry and Ginther [1953] found that when argon-shielded gas tungsten arc welding was performed on a copper block, the breathing zone concentration of ozone was 0.1 ppm with a 55-A current and 0.5 to 0.6 ppm with a 110-A current. When a helium shield was used, the ozone concentration was 0.1 ppm with either current level.
The spatial distribution of ozone concentrations has been studied under various conditions [Fay et al. 1957;Frant 1963;Lunau 1967]. Ozone generation diminished as the distance from the arc increased [Lunau 1967]. In argon-shielded gas tungsten arc welding of aluminum, ozone concentrations were consistently higher than with argon-shielded gas metal arc welding. The author postulated that the high-energy (short-wavelength) UV rays resulting from gas tungsten arc welding caused more ozone formation.
Fay et al. [1957] also found that ozone concentrations were higher at 0.15 m from the arc in argon-shielded gas metal arc welding than at 0.60 m. However, the opposite was observed with argon-shielded gas tungsten arc welding, regardless of the metal welded or the current used. Frant [1963] also studied ozone concentrations in argon-shielded gas tungsten arc welding but found that the rate of ozone formation measured in a quartz tube was 10 times higher at 0.2 m than at 0.5 m from the arc.
Ferry and Ginther [1953] found that the shielding gas had a decided effect on ozone formation. Changing from argon to helium in gas tungsten arc welding caused ozone concentrations in the breathing zone to decrease from 0.5-0.6 ppm to 0.1 ppm regardless of the current level. Frant [1963] observed a similar reduction when using a CO2 shield. In gas metal arc welding of steel, argon shielding produced 33 /xg ozone/min, and carbon dioxide shielding produced 7 jug ozone/m in when measured in a quartz tube placed 30 cm from the arc.
Several authors have shown that the type of base metal can affect the rate of ozone production. Frant [1963] found that ozone was produced at a concentration of 300 jug/min during argon-shielded gas metal arc welding on aluminum, compared with only 33 jLig/min during argon-shielded gas metal arc welding on steel. Lunau [1967] showed large variations in ozone concentrations depending on the particular aluminum alloy being welded. Argon-shielded gas metal arc welding on pure aluminum produced 6.1 ppm ozone at 0.15 m from the arc; welding under the same conditions on a 5% magnesium alloy of aluminum produced only 2.3 ppm ozone; and welding on a 5% silicon alloy of aluminum produced 14.5 ppm ozone. Press and Florian [1983] observed that shielded metal arc welding of aluminum produced ozone concentrations 10 times higher than shielded metal arc welding of mild steel.
In addition, much higher ozone concentrations occurred when a silicon alloy electrode was used for welding aluminum than when a magnesium alloy electrode was used.
# d. Decomposition Products of Organics
Trichloroethylene and tetrachloroethylene are solvents commonly used to degrease metals. They may therefore be present on the surface of recently cleaned metal parts or in the atmosphere where welding processes are being performed. Ultraviolet radiation may react with the vapors of those solvents and produce a number of irritating and toxic gases as a result of photooxidation. Dahl berg and Myrin [1971] assessed 10 welding workshops and found that roughly five times as much dichloroacetyI chloride as phosgene was formed where welding was done in the presence of trichloroethylene vapor. There was almost a complete conversion of trichloroethylene vapor to phosgene (1.5 ppm) and dichloroacetyI chloride (10 ppm) at 30 cm from an argon-shielded aluminum welding arc located 4 m from a degreaser.
In other workshop environments, Dahlberg and Myrin [1971] found 0.01 to 0.3 ppm of phosgene and 0.03 to 13 ppm of dichloroacety I chloride.
Andersson et a l . [1975] studied the formation of trichloroacetyl chloride and phosgene from tetrachloroethylene vapor during shielded metal arc and gas metal arc welding. These two hazardous products were formed in equal proportions. The authors recommended that welding be avoided in work environments contaminated with tetrachloroethylene.
A variety of other potentially toxic gases may be produced when the welding process inadvertently heats certain other materials. For instance, residual oil on steel may emit acrolein during welding [de Kretser et al. 1964].
# Physical Agents
The potential exists for exposure to a variety of physical agents during the welding process. Workers may be subjected to excessive heat in the welding environment [NIOSH 1986], radiation emitted from the welding processes (including ionizing radiation and nonionizing radiation in the IR, visible, and UV ranges [Fannick and Corn 1969], noise, and electricity. The following types of exposures are representative of those that have been specifically documented in the work environments of welders.
# a. Electromagnetic Radiation
Optical radiation may be produced by electric or plasma arcs. Radiation from a 50-A arc ranges from a wavelength of 200 to 800 nm [Marshall et al. 1977]. Levels produced from oxyfuel welding, torch brazing, and oxygen cutting are lower than levels produced by other welding methods [Moss and Murray 1979].
Sliney et a l . [1981] conducted a study to determine the effectiveness of transparent welding curtains that were designed to block exposure to "blue light." The transparent curtains were most effective in blocking the wavelengths between 400 and 500 nm. These wavelengths are known to cause photochemical injury to the retina. The energy emitted from shielded metal arc welding was determined by van Someren and Rollason [1948] using a 4-gauge covered electrode operating at a 280-A current. The relative spectral distribution of emitted optical radiation was 5% in the UV range, 26% in the visible range, and 69% in the IR range.
Various factors can affect the radiation intensity from welding and cutting arcs [Dahlberg 1971;Lyon et al. 1976;Bartley et a l . 1979;Bennett and Harlan 1980].
Increasing current flow causes a sharp increase in UV emissions. Gas metal arc welding of aluminum produces much greater UV intensity than gas tungsten arc welding. UV emissions increase by a factor of 10 when using magnesium instead of aluminum as an alloying material. The use of argon gas for shielding significantly increases the intensity of the optical radiation compared with carbon dioxide or helium as a shielding gas. As the amount of fume increases, the amount of radiation is reduced proportionately. When gas tungsten arc welding is performed on aluminum-magnesium alloys, the amount of UV emitted decreases as the arc length increases. Tip size, flame type, and filler metal composition are other variables that affect the amount of UV, visible, and IR radiation produced by oxyfuel welding [Moss andMurray 1979]. Marshall et al. [1980] assessed the amount of optical radiation that was generated from carbon arc cutting. The results of those tests demonstrated that other physical agents such as sparks and noise present more serious hazards than optical radiation. The authors stated that the observed low level of optical radiation produced was probably due to the removal of particulate material from the air, which left no material to become luminescent.
IR radiation can be absorbed by a worker's clothing and skin [Moss et al. 1985] and can elevate the skin temperature and contribute to the body's heat load. Light-colored, loose clothing reduces the heating of the skin.
# b. Electricity
Electrical shock from arc and resistance welding is a common hazard and can be sufficient to paralyze the respiratory system or to cause ventricular fibrillation and death. This risk is highest when equipment is in disrepair (e.g., worn insulation) or when electrical resistance through the welder is decreased (e.g., by sweat or standing in water) [Simonsen and Peterson 1977;Ostgaard 1981]. Even minor electrical shocks can cause serious secondary accidents (e.g., muscular reaction to the shock can cause a worker to fall).
# c. Noise
Although high noise levels can occur during several types of welding processes (e.g., torch brazing and chipping), they are more often associated with plasma arcs than with any other [National Safety Council 1964]. The high noise levels with plasma arc occur from the passage of heated gas through the constricted throat of the nozzle at supersonic velocities. Noise levels have been measured in the 2,400 to 4,800-Hz range and often exceed 100 dBA. Low-velocity nozzles greatly reduce the noise emitted. The use of induction-coupled plasma jets also greatly reduces the level of noise [National Safety Council 1964]. Levels exceeding 90 dBA have been found in torch brazing operations [NIOSH 1978]. Cresswell [1971 described noise levels of only 70 to 80 dBA from torches using argon-hydrogen mixtures; however, nitrogen and nitrogenhydrogen mixtures produced levels of 100 to 120 dBA. The same author also noted that cutting materials up to 50 mm thick did not usually pose a noise problem but that thicker materials produced more intense noise levels (levels not given) that required hearing protect ion.
# d . I on i z i ng Rad i at i on
X-rays are produced as secondary radiation by electron beam welding equipment. The configuration and operating principles of this equipment are similar to those of an X-ray tube [Taylor 1964]. The electrons are generated at the cathode, which is a heated tungsten filament. The electrons are accelerated toward a target by a difference in potential and are focused by using a magnetic field. X-rays are produced when high-speed electrons strike the workpiece, its metal base, or other materials. The intensity and energy of the X-rays are functions of the beam current, the accelerating voltage, and the atomic number of the material on which the beam impinges [Voltkova et al. 1969]. X-radiation may be produced in the electron beam gun itself, at the anode, or in the work chamber wherever the beam strikes a surface. The radiation may be produced any time that power is applied to the high-voltage portion of the equipment.
Radiation may be emitted from the welding equipment at vacuum ports, door flanges, or windows, or from motor shaft and power conduit openings [AWS 1978].
Nonconsumable thoriated tungsten electrodes are usually used in gas tungsten arc welding. The electrodes may contain 1% to 3% thorium oxide, which may potentially emit alpha radiation [Breslin and Harris 1952;Bergtholdt 1961]. Although the electrodes are considered nonconsumable, they are gradually used up. Breslin and Harris [1952] investigated the potential exposure to alpha radiation from thorium during various types of gas tungsten arc welding. Commercially available equipment was used to weld with a 2% thorium oxide electrode; welding operations were performed according to manufacturers' recommendations but without any ventilation. Personal air samples were collected in the operator's breathing zone at the lowest part of the welding helmet. General air samples were also taken at a distance of 1 ft (0.3 m) from the arc. Alpha activity was measured using alpha scintillation counters. No detectable alpha activity was found in the samples. The authors concluded that welding with thoriated tungsten electrodes poses no significant radiation hazard.
# e. Radiofrequency Radiation
Radiofrequency (RF) radiation can be used in tungsten inert gas welding to start or continue an arc between the base metal and a nonconsumable tungsten electrode. The frequency of RF radiation in this application is reported to be less than or equal to 5 megahertz (MHz) with a power output of 20 to 30 kilowatts (kW). Since no one has measured the exposure of welders to electric or magnetic field radiation from this type of welding, potential exposure levels cannot be estimated [OSHA 1982].
# IV. HEALTH AND SAFETY HAZARDS
# A. Introduction
Welding processes are potentially hazardous because they require intense energy to change the physical state of metals. The chemical changes associated with such energy may result in emissions of various toxic fumes, dusts, gases, and vapors; they may also generate exposures to physical agents that include noise, vibration, heat, electrical current, and infrared (IR), visible, ultraviolet (UV), ionizing, and radiofrequency (RF) radiation.
The degree of risk varies with the method and control measures employed, work practices used, metals and fluxes involved, and duration of exposure permitted. Safety hazards encountered on a daily basis complicate working conditions for welders. These conditions have resulted in both major and minor traumatic injuries and in death. Introduction
Over the past 40 years, a number of animal studies have examined the acute and subchronic effects of welding fumes and the mutagenic potential of total airborne welding emissions (gases plus fumes). However, only one animal study has investigated the carcinogenicity of welding fumes as a result of long-term exposures [Reuzel et al. 1986]. In this document, the term "welding emissions" refers to a combination of gases plus fumes. Unless otherwise reported, these exposures were generated from shielded metal arc or gas metal arc we Id i n g .
# b. Acute Effects
In a series of experiments, Titus et a l . [1935] exposed groups of animals (1 to 4 cats, 1 to 5 rabbits) for 0.8 to 8.5 hr to iron oxide or to the welding emissions produced during electric arc cutting of iron with iron electrodes. Exposure concentrations ranged from 10 to 350 mg/m^ (0.3-jum particle size) of fumes, which contained mostly ferric oxide. Concentrations above 275 mg/m^ were difficult to maintain, since at these increased concentrations, the particles from the fumes aggregated as rapidly as they were produced. To accentuate the effect of fume exposure, carbon dioxide (1% to 14%) was added to chamber air to increase respiration. An additional four groups of rabbits were exposed to arc cutting gases alone, and two other groups were exposed to ferric oxide alone at concentrations comparable with those contained in the fumes. When exposed to high concentrations of either the arc cutting emissions (320 mg/m^) or gases, animals exhibited severe pulmonary edema, dilation of alveoli, hemorrhage of the lungs, and death. Since higher air concentrations of ferric oxide alone did not cause acute lung pathology or death in exposed animals, the arc cutting gases (unidentified) were considered the probable cause of the observed toxicity. The authors noted that these pulmonary effects induced by the gaseous components of the emissions were similar to those caused by such irritating gases as nitrogen peroxide, ozone, or chlorine.
Senczuk [1967] administered 0.5-ml saline suspensions of welding fumes generated from either acid-, basic-, or rutile-coated electrodes into the stomachs of six white female mice (strain unspecified) per treatment group. The type of metal welded was not stated. The suspension from basic electrode fumes produced lethality at lower doses than did suspensions from acid or rutile fumes. The dose capable of killing 50% of the animals within 48 hr after treatment (LD50) was 755, 5,000, or 5,000 mg/kg for suspended fumes generated from basic-, acid-, or ruti le-coated electrodes, respectively. When similar suspensions were intratracheally injected into groups of six white female Wistar rats, the LD5q's for basic, acid, or rutile welding fumes were 132, 762, or 792 mg/kg, respectively. Welding fume composition was analytically determined by an unreported method. The author theorized that the increased toxicity associated with basic electrode fumes was caused by fluorine, which was not present in the other test electrode fumes. Manganese, silicon, and aluminum compounds were considered the toxic components of acid or rutile dusts, whereas sodium and magnesium carbonates and titanium compounds were considered much less toxic. Chromium content was neither determined nor discussed. Kawada and Iwano [1964] used several animal species to study the acute lethality of emissions from basic and rutile (ilmenite) electrode welding of a steel (composition undefined) plate. Unknown strains of mature male mice, white rats, rabbits, and guinea pigs were subjected to a 1-hr inhalation exposure to emissions from a 1-min burn with a basic electrode. The group sizes and chamber emission concentrations were unspecified. Since lethality was observed only in the guinea pig, the guinea pig was chosen as the test species for further study. A 1-hr inhalation of emissions from a 1-min burn of a basic electrode produced death within 24 hr in 10 of 12 guinea pigs and in 2 of 10 guinea pigs when exposure was to rutile emissions under the same conditions. Upon sacrifice of the survivors from the group exposed to basic fumes (time unspecified), the collective histopathology for the lungs revealed deposits of fumes, blood stasis, edema, pneumonia, atelectasis, and emphysema. However, when an additional group of guinea pigs was exposed only to the gaseous components of basic electrode emission, no deaths occurred. The disposition of these animals was not stated. Kawada and Iwano [1964] also used additional groups of guinea pigs that were intraperitoneally injected with a constant volume of 2 ml of either a water suspension containing 150 mg of basic or rutile fumes or the supernate or insoluble sediment fractions of a similar suspension. The aqueous suspension of basic electrode fumes killed 15 of 15 guinea pigs within 3.5 hr after injection, whereas the suspension of rutile fumes was nonlethal in 6 of 6 treated guinea pigs. Because rutile fumes were not lethal in guinea pigs, no further testing of soluble or insoluble fractions was conducted.
Intraperitoneal injection of the water soluble fraction from basic electrode fumes resulted in the deaths of all six treated animals within 1 hr after injection, but six of six animals survived administration of the water-insoluble fraction. Each active compound present in the water-soluble fraction of basic welding fumes was tested and ranked by decreasing lethal potential as follows: potassium fluoride, potassium acid fluoride, potassium hydroxide, sodium hydroxide, sodium fluoride, and calcium si I icofluoride. Since the water-insoluble metal oxides (aluminum, barium, calcium, iron, magnesium, manganese, silicon, or titanium) in these two fumes were not lethal to injected animals, the authors did not consider them to be toxicologically active.
Hewitt and Hicks [1973] exposed male albino SCE strain rats by inhalation to rutile welding emissions at an average concentration of 1,500 mg/m3. The lungs were analyzed with neutron activation to assess tissue concentrations, rates of uptake, and elimination of inhaled metals. Metal uptake in liver and blood was also assessed.
The rutile iron electrode used was coated with limestone, manganese dioxide, kaolin, cellulose powder, and sodium and potassium silicate binders. Two rats were exposed for 30 min, while seven rats were exposed for 4 hr. Tissue concentrations at 24-hr post-exposure were expressed as Mg compound/g of freeze-dried tissue. The rats exposed for 30 min had a statistically significant increase (p<0.05) of iron (1,175 Mg) and cobalt (0.22 m9) in the lung but not chromium (0.01 (jg) or antimony (0.01 ¡xg) when compared with controls. The seven rats exposed for 4 hr had a statistically significant increase (p<0.05) in iron (7,175 jug), cobalt (0.32 p.g), chromium (0.03 ¡¿g), and antimony (0.25 Mg) in the lung. Additionally, the cobalt concentrations in the liver (0.6 m 9) ar|d blood (0.2 Mg) were statistically increased (p<0.05) after a 4-hr exposure when compared to the controls. Microscopic examination of the treated lungs revealed large numbers of particulate-loaded macrophages in the alveoli and alveolar ducts, slight alveolar epithelial thickening, and peribronchial edema. In a subsequent experiment, eight rats were exposed to welding emissions for 4 hr. Pairs of these animals (and pairs of control rats) were killed 1, 7, 28, or 75 days after exposure. The iron, cobalt, chromium, and antimony contents in the lung progressively decreased over the 75-day period.
The histopathological lung changes that were observed within the first 4 hr of exposure returned to normal following 75 days of no exposure. However, macrophages that contained particulate material continued to be present.
# c. Subchronic E ffe c t s
The effects of welding emissions on animals have been summarized in Table IV- 1. Tollman et al. [1941] performed an inhalation study in which 2 groups of 12 young adult guinea pigs and 10 young adult white rats were exposed for 4 hr/day, 6 days/week. One group was exposed for approximately 29 weeks to partially filtered carbon arc welding emissions, and the other group was exposed for approximately 33 weeks to oxides of nitrogen only. This was followed by a 1-month nonexposure period for guinea pigs. The type of metal welded and filter used were not reported. Fumes passing through the filter were less than 25 mg/m^ during the total study period. The authors reported that the average concentration of oxides of nitrogen was 107 ppm in the gas phase of the welding emissions. This concentration was comparable to the average concentration of oxides of nitrogen (125 ppm) when administered alone. The investigators found a consistent response in all test groups regardless of the parameter studied. Guinea pigs in both groups had an average loss of 11% to 15% in terminal body weights when compared with their maximum weights attained during the experiment. Similar weight loss data for rats were not given. At the end of 7-1/2 months of treatment, guinea pig mortality reached 67% in the filtered emissions group and 92% in the oxides of nitrogen group, whereas all rats were dead within the first 3.4 months of exposure. Histopathologic examination of tissues revealed the lungs as the primary target organ for both species and all treatment groups. Pulmonary pathology included: epithelial desquamation and necrosis, atelectasis, edema, and pneumonia. The principal differences observed were thicker alveolar walls and more macrophages in the lungs of those animals exposed to filtered welding emissions. No histopathology was specifically cited for the guinea pigs that survived the exposure period. The authors concluded that the effects were primarily due to exposure to oxides of nitrogen rather than to any other component present in carbon arc welding emissions. McCord et al. [1941] reported on the inhalation exposure of 24 albino rats and 16 rabbits of both sexes (strains, ages, and numbers of each sex not given) to the emissions produced during shielded metal arc welding (unspecified metal) from electrodes that contained mostly silicon (21%) and titanium (42%) dioxides. An equal number of nonexposed rats and rabbits were used as controls. Exposures were for 6 hr/day, 5 days/week for a total of 46 days. This was followed by 43 days of nonexposure before study termination. The total fume concentration was not given; however, four components accounted for over 97%: iron oxide (79%), manganese oxide (5%), silicon dioxide (8.4%), and titanium dioxide (5.4%). The average chamber concentration of nitrogen dioxide was 20-24 ppm, and the average nitrous oxide concentration was 3 ppm, while the average concentrations of ferric oxide, manganese, and silicon dioxide were 465, 16, and 61 mg/m^, respectively. Titanium dioxide values were not cited. Average weight gains for exposed versus nonexposed groups were 272 g versus 366 g for rabbits and 2.9 g versus 32 g for rats. Siderosis of the lungs was the only biologically significant pathology present in all of the exposed animals sacrificed at the end of the experiment, with the earliest detection of siderosis observed in a rat that died after 22 days of exposure. No silicosis was found in any of these animals.
Byczkowski et a l . [1970] reported on the metal concentrations in the lungs of 290 rats and 30 rabbits exposed by inhalation to emissions generated during the melting of basic or rutile electrodes. The effect of exercise on the retention of inhaled metals from rutile welding emissions was also studied in rats. Baseline metal concentrations were determined in an unstated number of animals from each treatment group before the start of the exposure period. Groups of young adult male Wistar rats and 1-year-old albino rabbits (group sizes not specified) were exposed to approximately 60 mg/m^ of basic welding emissions, while a group of rats was exposed to 198-222 mg/m3 of rutile welding emissions.
In addition, one similarly exposed rutile welding group was exercised by being housed in cages that rotated during two of the 3-hr daily exposures. Exposures for the remaining groups were 3 hr/day, 7 days/week for 91 to 95 days for rats and 110 days for rabbits. During the period of time in which the animals were being exposed, an undefined number of surviving animals in each treatment group were withdrawn from exposure for terminal assessment of changes in lung metal content. Final sacrifices occurred 130 days after termination of exposures for rats and rabbits in the basic welding emissions groups and after 182 days for rats in the rutile welding emissions group.
Rats sacrificed after 95 days of exposure to welding emissions from basic electrodes had total lung tissue contents of 0.57 mg fluorine, 4.95 mg manganese, and 223 mg iron. Similarly exposed rabbits sacrificed at the end of 110 days had lower total lung contents of 0.32 mg fluorine, 4.2 mg manganese, and 103 mg iron when compared to the rats. Tracheal tissue concentrations for fluorine in rats and rabbits were five times higher (2.79 mg and 1.76 mg, respectively) than those found in the lung tissue. The groups of rats and rabbits that were exposed to the same basic welding emissions and removed from exposure for 130 days, had up to a 50% decrease in fluorine and iron levels and over an 80% decrease in manganese from those determined after 95 and 110 days. The group of rats exposed to rutile welding emissions had the following total lung metal contents at the end of the 91-to 95-day exposure period: silicon, 0.45 mg; titanium, 0.117 mg; manganese, 0.495 mg; and iron, 9.3 mg. When these values for the rutile exposure group were compared to those in a similarly exposed but exercised group, exercise increased the metal concentrations by approximately 50%. No analysis was performed for lung metal content during the 182 days that followed the termination of exposure. However, unexercised rats withdrawn from rutile fume exposure for 182 days had approximately a 50% decrease in silicon, titanium, and manganese concentrations but only a 23% decrease in iron. Kalliomaki et al. [1983] exposed adult male Wistar rats (300+15g) to emissions generated from shielded metal arc welding of either mild steel with basic electrodes or stainless steel with rutile electrodes. The purpose of the study was to determine which metals (iron, manganese, chromium, or nickel) contained in the two types of welding emissions were retained by or cleared from the lung. A total of 52 rats in groups of 2 rats or less was used in 14 treatment and 14 control groups. Each treatment group was exposed to 43 mg/m3 of emissions. Four of the treatment groups were designed to determine retention of metals in animals exposed for 1 hr/day, 5 days/week for 1, 2, 3, or 4 weeks with sacrifice of a treatment group and a control group 24 hr after last exposure. The animals in the remaining 10 groups were exposed for 1 hr/day, 5 days/week for 4 weeks and were evaluated for clearance of metals. Following the last exposure, a treatment group and a control group were sacrificed at the following time intervals: 1, 3, or 8 hr and 1, 4, 8 , 14, 28, 56, or 106 days.
Basic electrode welding of mild steel produced emissions that contained 20% iron and 2.8% manganese by weight but only trace amounts of chromium and nickel (remaining fraction unstated).
In rats exposed to these emissions, the lung tissue retention rates for iron and manganese each became saturated by the third week of exposure with initial retention rates of 28 and 4 jug/g dry lung tissue/hr, respectively. Clearance time was measured as the time required to decrease the tissue load of a metal by 50% (T-j/2 )-These metals had fast and slow clearance times for their curves. Rutile electrode welding of stainless steel produced emissions which contained 4.0% iron, 2.2% manganese, 3.0% chromium, and 0.4% nickel by weight (remaining composition unstated).
In rats exposed to these rutile emissions, the retention curves were linear with initial rates of 4.8 (iron), 2.8 (chromium), and 0.3 (nickel) n q / g dry lung tissue/hr. The retention of manganese reached saturation after 19 hr of exposure, with an initial retention rate of 1.5 ¡ jlg/g dry lung tissue/hr. Slow clearance T -|/2 times were 50 days for iron, 40 days for chromium and manganese, and 30 days for nickel. These metals did not have fast clearance times.
Senczuk [1967] used 3-to 4-month-old Wistar rats to study the toxicity of inhaled emissions produced by welding (metal unspecified) with rutile electrodes. A treatment group of 120 male rats was exposed to an average emission concentration of 222 mg/m^ for 3 hr/day for 13 weeks. The control group consisted of 30 nonexposed young adult male rats. Interim sacrifices within the exposure group occurred after 2, 4, 6 , 8 , 11, and 13 weeks, and 2 and 5 weeks postexposure. Similar interim sacrifice intervals were used for the control group with the omission of those during exposure weeks 2, , and 11 and postexposure week 2. Twenty-six weeks after cessation of exposure, the remaining survivors (number unstated) were sacrificed. Mortality within the groups was not reported. Analysis of chamber emissions demonstrated concentrations of 102 mg/m3 ferric oxide, 15.2 mg/m^ silicon, 9.4 mg/m^ manganese, 3.5 mg/m^ titanium dioxide, and 8 mg/m3 oxides of nitrogen. Examination of the growth curves showed that the exposed rats progressively lost 2% body weight during the 13-week treatment period. During the 5 weeks following the 13-week exposure period, their body weight gain was parallel to that of the controls, after which it began to decrease. Twenty-six weeks after the 13-week exposure period, the animals' terminal body weights were compared with their preexposure weights. The results showed that the treated rats had a 2% gain while the controls had a 29% gain. Lung weights (dry) from treated and control rats were approximately equal at the end of the exposure period; however, the lung weights (dry) of the treated rats sacrificed 26 weeks following the exposure period were 18% heavier than those of the corresponding controls. Because the lungs were desiccated for weighing, histopathologic evaluations were not performed. Garnuszewski and Dobrzynski [1966] compared the pulmonary effects of inhalation of welding emissions on guinea pigs and rabbits (strain, age, and sex unreported). Two types of electrodes were used to generate the test emissions, but the type of metal welded was not reported. One type, EP52-28p, had high silicon oxide (25.5%) and high ferric oxide (18%) contents, while the other, EP47-28p, had low silicon oxide (7.8%) but high ferric oxide (23%) levels. Comparative pathology of animal tissues was used to determine if exposure to the welding emissions from the low silicon oxide electrode was biologically safer than that from the high silicon oxide electrode.
The first experiment included a total of 72 guinea pigs exposed to high si I icon oxide emissions; half of the group was exposed to emission concentrations of 18 mg/m^, while the other half was exposed to 36 mg/m^. The emissions were generated from the high silicon oxide electrode and the experiments carried out 4 hr/day, 6 days/week for 110 days. A total of 10 guinea pigs comprised the nonexposed (undefined) control group. Although the number of animal deaths per treatment group was not stated, the combined total was 30 of 72. Guinea pigs exposed to either emission concentration had a mixed type of pneumoconiosis (e.g., siderosis coexisting with silicosis as manifested by pneumoconiotic nodules containing collagenous fibers and silica particles). Phagocytes containing silica and iron oxide particles were found in abundance throughout the trachea, bronchi, and interalveolar septa and lumen. The above findings were all concentration-related in intensity.
In the second experiment, 50 guinea pigs and 10 rabbits were exposed to the emissions from the low silicon oxide electrode. The animals were divided into 2 equal groups and exposed 4 hr/day, 6 days/week for 6 months to the same emission concentrations as in the first experiment. Scheduled sacrifices occurred after 6 months of exposure followed by 1 and 4 months of nonexposure. The control groups included 10 guinea pigs and 2 rabbits. During exposure, the combined mortality for both guinea pig exposure groups was 25 of 50. These low silicon oxide exposures produced fewer and milder pulmonary effects than those observed in the animals of the high silicon groups for the first experiment. The changes were limited to the alveolar septa and alveoli which were thin and sometimes ruptured. All exposed guinea pigs were found to have siderosis, but little silicosis.
If nodules were present, they were small and few in number when compared to those induced by high silicon oxide electrode emissions. These small nodules contained fibroblasts, histiocytes, and cells with low amounts of silicon, but did not contain pronounced amounts of collagenous fibers. Because similar histopathology effects were present in tissues from guinea pigs sacrificed after the nonexposure periods, the induced effects were not considered readily reversible. The exposed rabbits had siderosis including slightly thickened interalveolar septa that had few dust-containing cells. Neither collagenous fiber proliferation, silicotic nodules, nor silica particles were observed in rabbit lung tissues. The authors concluded that the emissions from the low silicon oxide electrode were biologically less hazardous than those from the high silicon oxide electrode.
# d. Mutagenicity
Welding emissions from shielded metal arc and gas metal arc welding on mild and stainless steels as well as some of the individual metals contained in the emissions have been tested for their potential to induce adverse mutagenic changes in DNA through use of in vitro (bacterial or cell culture) assays, or in vivo (animal) test systems. In bacterial and cell culture tests, the test agent is added to microbiological or tissue culture media, respectively, while in animal tests the agent is administered to live animals. The in vitro and in vivo tests are used as predictors of a chemical agent's potential to induce cancer through genetic changes in exposed animals or humans.
(1) Mild Steel-Bacterial and Cell Culture Studies Hedenstedt et al. [1977] found the fumes to be nonmutagenic from basic or rutile electrode for shielded metal arc welding and the solid wire or powder-filled rutile electrode for gas metal arc welding of mild steel. E . co I i W3110 (pol A+ ) and E . coIi p3478 (a pol A" derivate) and S. typhimurium (TA 100), with and without metabolic activation were used in the study. The weight of fume tested per plate ranged from 100 to 1,250 jug.
Maxi Id et al. [1978] also found that the fumes from rutile shielded metal arc and gas metal arc welding on mild steel were nonmutagenic in the TA 98 and TA 100 test strains of S. typhimurium with or without metabolic activation. The dry weight of fume suspended in dimethylsulfoxide (DMSO) solvent and added to each test plate ranged from 0.1 to 8 mg.
Shielded metal arc fume from mild steel welding was also confirmed to be nonmutagenic by Stern et al. [1982] following testing in S. typhimurium TA 100 with and without metabolic activation. The types of electrodes used to generate the fume and the weight of fume tested per plate were not reported.
Niebuhr et a l . [1980] collected gas metal arc fume from the welding of mild steel when solid nickel electrodes were used. A modified sister chromatid exchange (SCE) assay was used to detect mutations. The presence of nickel in the welding fume induced increases in SCEs that were directly proportional to the amount of nickel biologically available in the test media. Concentrations of water-or serum-soluble nickel that ranged from 2.5 to 10 ptg/mI yielded SCEs that ranged from 7.3 to 9.4/cell compared to a control value of 8.4/cell.
Although mild steel welding fumes devoid of nickel and chromium(VI) compounds were inactive in bacterial mutagenesis assays [Hedenstedt et al. 1977;Maxi Id et al. 1978;Stern et a l . 1982], the addition of nickel into the fumes produced a slight increase in mutagenic activity in the SCE assay.
Hansen and Stern [1983] used the baby hamster kidney cel I (BHK-21) assay to determine the ability of gas metal arc fumes generated from welding with a pure nickel wire electrode to transform colonies.
In addition, pure nickel oxides, water soluble nickel acetate, and water insoluble nickel subsulfide were tested. They found that welding fumes and all the tested nickel compounds transformed the BHK-21 cell line.
(2) Stainless Steel (a) Bacterial and Cell Culture Studies Hedenstedt et al. [1977] studied the mutagenic potential of fumes generated during either shielded metal arc welding (rutile electrodes) or gas metal arc (solid wire electrodes) welding of stainless steels in E . coIi and S. typhimurium bacterial test systems. E . coIi W3110 (pol A+ ) and E . coIi p3478 (a pol A-derivate), and S. typhimurium (TA 98 and TA 100 strains) were used. All bacterial test systems were studied with and without a liver microsomal metabolizing system (S-9 mix). Both types of welding fumes were mutagenic in the absence of S-9 mix, regardless of bacterial strain employed; however, at equal plate concentrations shielded metal arc welding fumes were more mutagenic than gas metal arc fumes.
In addition, all water soluble fume fractions were mutagenic. The magnitude of these mutagenic effects were proportional to the degree of water solubility of the hexavalent chromium compounds present in the two types of stainless steel welding fumes.
The hexavalent chromium content in shielded metal arc welding fumes was significantly higher (10 to 1000 times) than that present in gas metal arc fumes.
In S. typhimurium, metabolic inactivation of the mutagenic effects for shielded metal arc fumes required both S-9 mix plus an NADP generating system. For all bacterial strains tested, similar inactivation of gas metal arc fumes required the S-9 mix alone. The authors suggested that the mutagenic potential for both types of stainless steel welding fumes may have been due to their water soluble hexavalent chromium content. However, if different chromium compounds were present in shielded rather than gas metal arc fumes, it would explain why they had dissimilar metabolic requirements for mutagenic inactivation.
Maxi Id et al. [1978] investigated the mutagenic potential of stainless steel welding fumes by utilizing TA 98 and TA 100 strains of S. typhimurium with and without metabolic activation. The dry weight of shielded metal arc welding fume suspended in DMSO solvent and added to each test plate ranged from 0.1 to 8 mg. Based on the weight of fumes required to double the mutation frequency in these bacterial strains, with or without a liver microsome metabolizing system (S-9 mix), shielded welding fumes were more mutagenic than gas metal arc fumes. The mutagenic activity was reduced for both types of fumes when S-9 mix was used. Regardless of the state of activation, the number of mutations induced by these fumes was increased in a dose-related manner. The authors stated that the amount of fumes produced by shielded metal arc welding was 3 to 6 times greater than that produced by gas metal arc welding. Fume analyses revealed that the fumes from shielded metal arc welding contained 330 times more soluble chromium (valence state unspecified) than did gas metal arc welding fumes.
The amount of welding fumes required to double the mutation rate of the S. typhimurium TA 100 (LT2) bacterial strain was also studied by Pedersen et al. [1983]. The activity was equalized on the basis of the chromium content of aqueous extracts (assumed to be chromium[VI]) of shielded and gas metal arc welding fume versus a chromium(VI) positive control solution (sodium dichromate). The authors did not define the types of welding electrodes used to generate the fume. They established that 9 ¿¿g of watersoluble chromium(VI) in shielded metal arc welding fumes, 5 /j.g of water-soluble chromium(VI) in gas metal arc fumes, and 10 ftg of water-soluble sodium dichromate (chromium[VI]) per plate caused mutations to double. The authors concluded that the mutagenic potential of stainless steel welding fumes can be completely accounted for on the basis of their chromium(VI) content. Stern et al. [1982] used the S. typhimurium TA 100 assay in dose-response experiments and factorial design studies to show that the mutagenic activity present in welding fumes is caused by its soluble chromium(VI) content. When mutagenic activity was expressed as revertants/mg/plate, shielded metal arc welding fumes were more mutagenic than gas metal arc fumes. However, when it was expressed as specific activity (number revertants/^g soluble chromium(VI)/plate), gas metal arc fumes were the more mutagenic of the two types of fumes. The authors concluded that the soluble chromium(VI) content of gas metal arc fumes could be partially reduced to insoluble chromium(VI), and to chromium(111) when reducing substances (aluminium and magnesium) were present. When compared to gas metal arc fumes, the specific activity of chromium(VI) in shielded metal arc welding fumes was reduced by components unique to these fumes. They also observed that when fumes containing chromium(VI) were suspended in water, chromium(VI) was contained in both the water soluble and insoluble phases; however, only the water soluble phase was mutagenically active. The authors stated that data from experiments with synthetic fumes demonstrated that neither the manganese nor the nickel content of stainless steel welding fumes was mutagenic nor did these metal compounds act in an antagonistic or synergistic manner when in the presence of fumes containing chromium(VI). Hedenstedt et al. [1977] used mammalian cells-the V-79 Chinese hamster cell assay-to detect the mutagenic potential (6-thioguanine resistance) of stainless steel welding fumes. The water soluble fraction of rutile electrode fumes from stainless steel welding produced a significant increase (p<.01) in the number of 6-thioguanine resistant mutants when compared to the negative controls. Koshi [1979] also used a mammalian cell assay-a pseudo-diploid Chinese Hamster cell line-to investigate the mutagenic effect of shielded metal arc versus gas metal arc welding fumes from mild and stainless steels, respectively. This assay was used to determine the frequencies of SCEs.
In addition, Koshi studied the metallic composition of these two types of generated fumes and their solubilities in water and in culture medium. Koshi [1979] found dose-related increases for SCEs for both shielded and gas metal arc welding fumes; however, it took 50 times more weight for the gas metal arc fumes than for shielded metal arc fumes to produce a doubling of the control background rate (5.3 SCE/cell). The lower potency of gas metal arc fumes was directly proportional to the decreased water solubility of its chromium(VI) component. When the frequency of SCEs/cell was compared for equivalent chromium contents, the authors stated chromic acid, a chromium(VI) component, was the most active followed by shielded metal arc fumes and then gas metal arc fumes; however, they presented other data which support equal activities also. Since water soluble nickel, manganese, or chromium(lll) compounds present in the two types of fumes were mutagenically inactive, the authors concluded that the active mutagen was chromium(VI). The induction of increased chromosome aberrations in the form of chromatid gaps and chromatin exchanges were similarly ascribed to the chromium(VI) content in both types of welding fumes tested.
# (b) Animal Studies
Knudsen [1980] performed a mammalian spot test in female mice to detect genetic mutations through changes in hair color. T-stock males (homozygous for four recessive coat-color mutations) were mated with C57BL females (homozygous wiId-type for the mutations carried by T-stock males). The pregnant C57BL mice were administered suspensions of shielded metal arc welding fumes from stainless steel or doses of potassium chromate (positive control) containing approximately 0.5 to 1.5 times the chromium(VI) content of the fume fraction tested. The type of electrode used for fume generation was not described. The mice were intraperitoneally injected with the test materials on days 8 , 9, and 10 of gestation. The offspring were checked for spots of recessive hair color at the end of 2, 3, 4, and 5 weeks of age. The shielded metal arc welding fumes produced the same number of spots as approximately equivalent doses of chromium(VI). The authors suggested that the positive mutagenic effect induced by shielded metal arc welding fumes was primarily caused by its chromium(VI) content.
# e. Carcinogenicity
Reuzel et a l . [1986] investigated the toxicity of welding fumes intratracheally instilled into the lungs of hamsters. Fumes were produced either from shielded electrodes used during metal arc welding or from wire metal electrodes used during gas metal arc welding of stainless steel. The welding fumes were collected onto filters. Each of five treatment groups contained 35 male Syrian golden hamsters. Dosage quantities of fumes were suspended in 0.2 ml of saline for intratracheal injection. The treatment concentrations were 0.5 and 2.0 mg for two shielded welding groups, 2.0 mg for one gas metal arc welding group, 0.1 mg calcium chromate for a "positive control" group (calcium chromate has not been shown to be carcinogenic in this test system), and 0.2 ml of saline for the unexposed control group. The treatment groups were dosed once weekly for 56 weeks, except that the 2.0 mg shielded welding group developed early body weight loss and a few hamsters died; therefore, from weeks 26 through 56, single doses were injected only on every fourth week. Autopsies for all groups were performed after 100 experimental weeks. The chromium contents of the fume from shielded metal arc and gas metal arc welding fumes were 5% and 0.4%, respectively. The nickel content in shielded metal arc fumes was 0.4% while that for gas metal arc fumes was 2.4%. Although not stated by the authors, the total amount (mg/hamster) of chromium injected during the study was calculated as 1.4 (low dose) and 3.3 (high dose) for the shielded metal arc welding fume groups; 0.45 (low dose) and 5.6 (high dose) for the gas metal arc fume groups, and 1.85 for the calcium chromate positive controls.
Although lung weights of hamsters treated with either 2 mg shielded metal arc fumes or 2 mg gas metal arc fumes were significantly heavier (level unstated) than control lung weights; the heaviest lung weights occurred in the gas metal arc fume group. Regardless of treatment or dose level, hamsters that died and those that survived through the nonexposure period following treatment differed little in histopathology or in the number of dust particles present in lungs. This indicated that little recovery had occurred during this period. However, those hamsters in the 2 mg treatment group exposed to gas metal arc welding fumes had the greatest degree of induced pulmonary pathology. This included moderate to severe nonspecific pneumonia, slight to moderate interstitial pneumonia, moderate alveolar bronchiolization, and slight emphysema. Animals dosed with 0.5 mg shielded metal arc welding fumes and those that received calcium chromate showed similar but less pronounced changes.
Two lung cancers were found in the shielded metal arc welding treatment groups. One cancer (a we Il-differentiated combined epidermoid and adenocarcinoma type) was found in the lung of an animal that was treated with 2.0 mg of shielded metal arc fumes and sacrificed at the end of the 100-week study. The second cancer (an anaplastic tumor, probably a carcinoma, which had metastasized to the surrounding lung parenchyma and mediastinum) was found in the lung of a hamster that died after one year of treatment with 0.5 mg of shielded metal arc fumes. The investigators believed these two tumors were induced by the shielded metal arc welding fumes and were toxicologically significant because neither noncancerous nor cancerous tumors had been observed either in the concurrent controls or in nearly 800 historical laboratory controls. Because pulmonary tumors were not present in the positive control (calcium chromate) animals, the investigators theorized that compounds other than chromium in welding fumes were probably responsible for the induction of the cancers in the shielded metal arc welding fume groups.
# f. Summary-Animal Toxicity
Shielded metal arc welding fumes and gases have caused severe acute lung damage (e.g., edema, hemorrhage, pneumonia, and atelectasis) [Titus et a l . 1935;Kawada and Iwano 1964;Hewitt and Hicks 1973]. Basic electrode welding of nonstainless steels that did not contain chromium or nickel has produced fumes that are potentially more lethal than those produced by welding of the same metal with acid or rutile electrodes [Senczuk 1967].
It appears that the increased toxic potential of the fumes generated while welding with basic electrodes can be ascribed to the high fluoride content that is absent in either acid or rutile-type electrodes.
Subacute toxicologic studies have demonstrated that irreversible chronic lung disease can result in animals repeatedly exposed by inhalation to welding fumes and gases. Tollman et a l . [1941] investigated the pulmonary effects in animals repeatedly exposed to welding gases (oxides of nitrogen). Concentrations which induced mortality also caused lung tissue damage (edema, atelectasis, pneumonia, and necrosis).
In addition, the subacute effects of total welding emissions (gases plus fumes) generated during the welding of nonstainless steels were studied in animals by Garnuszewski and Oobrzynski [1966] and Senczuk [1967].
In general, these investigators found that exposure of animals to welding emissions induced premature mortality, suppression of weight gain, fibrotic lung disease, and pneumoconiosis in surviving animals. Siderosis and silicosis resulted from exposures to emissions which contained iron or silicon, respectively. This fibrotic pulmonary pathology was found irreversible during nonexposed periods despite recovery times that sometimes exceeded the length of treatment.
Pulmonary deposition and clearance rates for metals contained in emissions generated during the welding of nonstainless and stainless steels were investigated in animals by several authors (McCord et al. 1941, Byczkowski et a l . 1970Kalliomaki et a l . 1983). They found the rates of metal deposition in exposed lungs to be proportional to the metal contents in the emissions. These deposition rates were further increased in animals with concomitant exercise during exposure. For some metals with slow clearance rates, even prolonged periods of nonexposure did not permit complete elimination.
In a wide variety of in vi t ro and in vivo mutagenesis assays, mild steel welding fumes had little to no mutagenic potential, whereas stainless steel welding fumes were consistently mutagenic.
Shielded metal arc welding of stainless steel produced three to six times more fumes "per mass of weld metal" than gas metal arc welding. The shielded metal arc welding fumes were more water soluble than the gas metal arc welding fumes [Maxi Id et al. 1978]. The water-soluble fraction of these fumes was shown to be mutagenically active [Hedenstedt et al. 1977;Koshi 1979;Stern et al. 1982;Pedersen et al. 1983], but the water-insoluble fraction had no significant mutagenic activity [Stern et al. 1982]. Assays have demonstrated that much of the mutagenic activity may be ascribed to the chromium(VI) in the water-soluble fraction [Stern et al. 1982]. However, when the mutagenic potentials for these fumes were compared on an equivalent chromium(VI) basis, gas metal arc welding fumes produced four times more mutations in bacteria than did shielded metal arc welding fumes [Stern et al. 1982]. Yet SCE data were equivocal for these two types of fumes [Koshi 1979].
In addition, it appears that compounds other than chromium(VI) could also be active in the water soluble fractions of fumes generated from the two welding processes. This is based on the fact that when the water soluble fractions of both fumes were tested in a metabolically activated S. typhimurium mutagenicity assay, only shielded metal arc fumes lost their metabolic potency [Hedenstedt et al. 1977;Stern et a l . 1982].
One 2-year carcinogenicity study has been reported for Syrian golden hamsters that were intratracheally injected with saline suspensions of stainless steel welding fumes [Reuzel et a l . 1986]. Lung cancer was observed in one animal from each of the two dose groups that were intratracheally injected with shielded metal arc welding fumes. No cancers were observed in the gas metal arc fume treatment group or the calcium chromate, saline, and historical control groups. Despite the fact that there were only two cancers observed, the authors concluded that these tumors were biologically significant based on the absence of tumors in the calcium chromate (positive control) group and the concurrent and historical nonexposed control groups. However, some question exists concerning calcium chromate being considered as a positive control since:
(1) no published experimental data shows the induction of any kind of cancers in hamsters when calcium chromate is intratracheal ly administered, and ( 2) the number of animals and dose used for the calcium chromate positive control group may not have been large enough to detect a positive carcinogenic response in these animals.
# Hunan Toxicity a. Pulmonary Effects
This section evaluates case reports and epidemiologic studies that document the adverse respiratory effects reported for workers who are associated with various types of welding processes. The studies are presented in order of the severity of the effects they report, beginning with those that discuss the acute effects associated with exposure to welding fumes and gases (e.g., metal fume fever and pneumonitis) and ending with studies that suggest a risk of respiratory cancer. The data from these investigations are summarized in Tables IV-2, IV-3, and IV-4. Although many of the studies have shortcomings (e.g., the absence of information on types and concentrations of specific chemical agents or on smoking habits), they collectively demonstrate the consistency of the many respiratory diseases in welders.
# (1) NonmaIi gnant PuImonary D i seases (a) Metal Fume Fever
Metal fume fever is an acute respiratory disease that is usually of short duration; it is caused by the inhalation of metal oxide fumes that are typically 0.2 to 1.0 /¿m in particle size (Papp 1968). Although several metals are In addition, it appears that compounds other than chromium(VI) could also be active in the water soluble fractions of fumes generated from the two welding processes. This is based on the fact that when the water soluble fractions of both fumes were tested in a metabolically activated S. typhimurium mutagenicity assay, only shielded metal arc fumes lost their metabolic potency [Hedenstedt et al. 1977;Stern et a l . 1982].
One 2-year carcinogenicity study has been reported for Syrian golden hamsters that were intratracheally injected with saline suspensions of stainless steel welding fumes [Reuzel et a l . 1986]. Lung cancer was observed in one animal from each of the two dose groups that were intratracheally injected with shielded metal arc welding fumes. No cancers were observed in the gas metal arc fume treatment group or the calcium chromate, saline, and historical control groups. Despite the fact that there were only two cancers observed, the authors concluded that these tumors were biologically significant based on the absence of tumors in the calcium chromate (positive control) group and the concurrent and historical nonexposed control groups. However, some question exists concerning calcium chromate being considered as a positive control since:
(1) no published experimental data shows the induction of any kind of cancers in hamsters when calcium chromate is intratracheal ly administered, and ( 2) the number of animals and dose used for the calcium chromate positive control group may not have been large enough to detect a positive carcinogenic response in these animals.
# Hunan Toxicity a. Pulmonary Effects
This section evaluates case reports and epidemiologic studies that document the adverse respiratory effects reported for workers who are associated with various types of welding processes. The studies are presented in order of the severity of the effects they report, beginning with those that discuss the acute effects associated with exposure to welding fumes and gases (e.g., metal fume fever and pneumonitis) and ending with studies that suggest a risk of respiratory cancer. The data from these investigations are summarized in Tables IV-2, IV-3, and IV-4. Although many of the studies have shortcomings (e.g., the absence of information on types and concentrations of specific chemical agents or on smoking habits), they collectively demonstrate the consistency of the many respiratory diseases in welders.
# (1) NonmaIi gnant PuImonary D i seases (a) Metal Fume Fever
Metal fume fever is an acute respiratory disease that is usually of short duration; it is caused by the inhalation of metal oxide fumes that are typically 0.2 to 1.0 /¿m in particle size (Papp 1968). Although several metals are Respiratory distress, fever, c h ills , and pulmonary edema occurring over a period of several days and sometimes resulting in death.
(Continued) I t was estimated that 10% more welders smoked than did members of the control group (Swedish male population). 1.15n (Continued)
Logistic analysis indicating a s t a t is t ic a lly sign ifican t interaction observed between welding and y e a r-firstemployed for lung cancer. ' Analysis of welders for lung cancer risk using internal non-exposed comparison group and two types of regression analysis. A total of 137 lung cancer deaths (50 welders, 87 controls). m Logistic analysis indicating a s t a t is t ic a lly sign ifican t interaction between cumulative exposure of welders and lung cancer. n Cox regression analysis indicating elevated lung cancer risk among welders when analyzed by cumulative exposure.
# No
# Yes
x Proportional mortality ratio. Y SMR adjusted for the welder's incidence of smoking, which was 22% higher than that expected in the general population. Mean age of death for these cases was several years older than that for controls. capable of causing this disease, exposure to zinc oxide has been the most common cause in welders (Drinker 1922;Drinker et al. 1927). The clinical signs and symptoms of metal fume fever resemble those of an upper respiratory infection such as influenza, acute bronchitis, or pneumonia, or an upper gastrointestinal infection (Papp 1968). Chills, shivering, trembling, nausea, and vomiting may occur (Rohrs 1957). The attack usually lasts 6 to 12 hr and in some instances up to 24 hr. Weakness and mild prostration follow but recovery is usually complete.
With repeated exposure, an increased resistance develops but this apparent tolerance is lost within a short time (e.g., during a weekend).
The attacks tend to be more frequent and prevalent on Mondays (Drinker 1922;AGA 1978).
Although other reports exist, the studies of Ross [1974] and Johnson and KiIburn [1983] are typical examples of symptomatic effects reported in welders.
Ross [1974] reported a case of metal fume fever in a shielded metal arc welder exposed to mixed fumes. Although the covered electrode contained primarily nickel, the fume contained iron, calcium, fluoride, manganese, silica, titanium, aluminum, copper, nickel, and traces of other metals.
The welder experienced a severe headache and felt cold and shivery.
The next day he experienced tightness of the chest, profuse sweating, and unusual thirst.
Chest examination revealed wheezing.
His temperature varied between 99.5° and 101.5°F (37.5° and 38.6°C).
On the basis of occupational history and clinical findings, he was diagnosed as having metal fume fever complicated by pneumonia and was removed from further exposure. Two months later he was completely recovered and returned to work. Johnson and KiIburn [1983] described the illness of a 30-year-old male Caucasian who had welded for 9 years and who became ill following torch brazing. Several filler metals that contained zinc, cadmium, copper, or mild steel were used in the process. To assist in the diagnosis, the welder was asked to braze with a silver-based filler metal containing 24% cadmium.
Shortly after he started to weld, he complained of eye irritation and headache.
The worker's blood leukocyte count increased 6 hours after exposure and peaked at 13 hours (increase not reported).
Nine hours after onset of exposure, he developed muscular pain, chills, feverish feelings, headache, backache, chest tightness, malaise, and shortness of breath.
Ten hours later, his body temperature rose and peaked at 100°F (37.7°C) for about 13 hours. A chest radiograph taken 13 hours after exposure indicated the presence of nodular densities that were not apparent in radiographs taken before exposure or after recovery (time of examination not given).
As a result of these observed effects, the welder discontinued brazing with silver-based filler metals; a 6-month follow-up examination revealed no further subjective symptoms.
The authors concluded that cadmium, which was present in the silver-based filler metal the welder was using, was the causative agent in this case of metal fume fever.
# (b) Pneumon i t i s
Pneumonitis and pulmonary edema have been frequently reported among welders who use various types of welding processes (e.g., gas and shielded metal arc, silver brazing, and oxyacetylene) in which exposures to the following have been identified:
nitrogen dioxide (Maddock 1970;Mangold and Beckett 1971), ozone (Molos and Collins 1957; Klein feId et al. 1957; Challen et a 1 . 1958), cadmium fumes (Patwardhan and Finckh 1976;Blejer and Caplan 1969;Townshend 1968), chromium and nickel fumes (Jindrichova 1976), and aluminum and iron fumes (Herbert et al. 1982).
# (i) Exposure to Metal Fumes
Cases of acute cadmium fume pneumonitis and death have been reported among welders who were exposed to cadmium fumes by either brazing with siIver-cadmium alloy or cutting or welding cadmium-coated metal in poorly ventilated areas (Christensen and Olson 1957;Beton et al. 1966;Patwardhan and Finckh 1976). Beton et al. [1966] reported the death of a welder who was cutting cadmium-plated bolts with an oxyacetylene torch in a confined space.
Although exposure measurements for cadmium fumes were not taken, the authors estimated that exposure to cadmium oxide may have averaged 8.6 mg/m^ based on the amount of cadmium oxide found in the welder's lungs during a postmortem examination. Patwardhan and Finckh [1976] reported on another fatality that occurred in a 38-year-old man who was exposed to cadmium fumes while welding handles onto cadmium-plated drums.
No respiratory protection or local exhaust ventilation was used.
He developed respiratory distress, fever, and chills the first night after exposure.
On the third day of his illness, he was admitted to the hospital, where chest X-rays revealed heart enlargement and pulmonary edema. He died of cardiac arrest approximately 3-1/2 days after exposure to cadmium fumes.
Postmortem examination revealed lung changes consistent with pulmonary edema and diffuse congestion of alveolar capillaries.
The liver contained 0.23 mg cadmium and the lungs contained 0.15 mg cadmium per 100 g of wet tissue. Townshend [1968] reported on a 4-year evaluation of a 51-year-old welder who had suffered from acute pneumonitis following exposure to fumes from the welding of a siIver-cadmium alloy.
On the day of the incident, the welder had been using an argon arc to weld plates composed of an alloy of 91% silver and 9% cadmium. The night after exposure, he developed a burning pain in the chest, dyspnea, and dry cough and was hospitalized.
The first chest radiograph was taken 23 days after the incident and showed extensive bilateral shadows, suggesting severe pulmonary edema. Eight weeks after the incident, extensive patchy shadowing was still evident.
For 6 months after the exposure, lung function tests showed a progressive improvement in the forced vital capacity (FVC) to just under 80% of the predicted value, after which there was no further improvement.
After 4 years, the chest X-ray showed faint nodulation.
No information on smoking habits or exposure concentrations were reported. Jindrichova [1976] and Herbert et a l . [1982] reported on pneumonitis that occurred in welders exposed to fumes composed of various types of metals. Jindrichova [1976] used nose, throat, and neurologic examinations and chromium determinations from the urine to study 31 welders who welded with shielded metal arc on metals containing chromium. These welders were compared with 26 workers who were not exposed to welding fumes or chromium.
All welders were divided into three groups.
Group 1 consisted of 9 welders who spent about 13% of their time working with electrodes containing chromium.
Group 2 consisted of 11 welders who spent half of their time using electrodes containing either 18% chromium and 9% nickel, or 23% chromium and 19% nickel.
Group 3 consisted of 11 welders who used electrodes containing 19% chromium and 9% nickel for 70% of their welding time. Welders in Group 3 were exposed to a concentration of 0.75 m g / m^ of chromium (0.62 mg/m3 soluble chromium[VI]) oxide measured inside a container (1.1 x 3.3 m) that had no local exhaust. The same work performed with local exhaust ventilation produced a chromium concentration of 0.16 mg/m3 (0.12 m g / m^ soluble chromium(VI) oxide. No exposure data were given for Groups 1 and 2, but chromium exposures for Group 2 were reported to be the same as for the control group.
Group 1 had no evidence of chronic bronchitis, but one welder had a chronic atrophic rhinitis with acute nosebleeds.
In Group 2, one welder with 25 years of experience had pulmonary fibrosis associated with siderosis.
In Group 3, all of the welders had coughs and respiratory problems.
Seven of the 11 welders smoked.
In Group 3, erosion of the nasal septum was found in 35% of the welders, atrophic rhinitis in 54%, pharyngitis in 45%, chronic laryngitis in 11%, and bronchitis in 72%.
The findings of nasal erosion in Group 3 were consistent with chromate-induced lesions.
Concentrations of chromium in urine (122-128 fxg/\i ter of urine) for welders in Group 3 were significantly higher than either the control group or Groups 1 and 2 (concentrations not reported).
Although these differences were reported to be statistically significant, no statistical methods were discussed.
Herbert et a l . [1982] described chronic interstitial pneumonitis in a 35-year-old male electric arc welder who had been employed as a welder for 16 years.
A biopsy of the lung revealed unspecified quantities of iron and aluminum particles and occasional asbestos bodies.
Chest X-rays revealed bilateral basal infiltrates with a more discrete opacity on one side. Lung function tests showed diminished forced expiratory volume (FEV), FVC, and total lung capacity.
The welder had smoked for a short period but had not smoked for the past 20 years.
No exposure data were reported.
# (11) Exposure to Gases
Cases of pneumonitis and acute pulmonary edema in welders have been attributed to the inhalation of nitrogen dioxide [Maddock 1970;Mangold and Beckett 1971] and ozone [Mo I os and Collins 1957;Kleinfeld et al. 1957;Challen et a l . 1958].
Mangold and Beckett [1971] reported on two silver brazers who were assembling a cupronickel firemain in the overhead of a 2-by 3-by 4.6-m storage compartment aboard a ship. The workers used a "silver solder" containing 80% copper, 15% silver, and 5% flux.
The flux contained 27% potassium fluoride and 72% potassium borate.
No local exhaust ventilation was used. Respiratory irritation forced the men to stop working after 30 min, and both were hospitalized 6 to 8 hr later with acute pulmonary edema and lung damage.
One worker returned to work in a few days, whereas the other retired because of respiratory impairment. Reconstruction of the event indicated that no cadmium-bearing solders were used but that nitrogen dioxide concentrations increased from 0.38 to 122 ppm in 30 min. Maddock [1970] reported a fatality resulting from pulmonary edema in a boilermaker who used two oxyacetylene torches with multiple jets to repair a rudder post in an enclosed compartment.
He worked for several hours without complaint but developed a cough that evening.
The worker was admitted to a hospital and died the following day. Death was attributed to pulmonary edema resulting from nitrogen dioxide poisoning.
Reconstruction of the event revealed that a blower had dispersed the fumes throughout the compartment instead of ventilating it. The nitrogen dioxide concentration was found to exceed 20 ppm within 3 min of lighting the torches.
The boilermaker had been exposed to nitrogen dioxide at an estimated concentration greater than 100 ppm.
Case reports described by Molos and Collins [1957], KleinfeId et al. [1957], and Challen et al. [1958] document how pneumonitis can occur from the inhalation of ozone during argon-oxygen shielded and gas metal arc welding.
Molos and Collins [1957] described respiratory irritation in a welder who performed argon-oxygen shielded gas metal arc welding on mild steel tanks using a mixture of 98% argon and 2% oxygen.
From time to time, the welder and other workers complained of respiratory and eye irritation. Occasionally, the irritation became so severe that welding had to be discontinued.
The welder continued to complain of discomfort and described symptoms of chest cramps, fatigue, headaches, impaired appetite, shortness of breath, difficulty in sleeping, and a persistent cough with occasional blood-tinged sputum. The mean ozone concentration was 2.6 ppm during welding activities.
Substitution of pure argon or carbon dioxide eliminated worker complaints, but the resulting welds proved to be unacceptable and gas shielded metal arc welding was discontinued.
Pneumonitis was also reported by KleinfeId et al. [1957] in eight welders who used gas metal and gas tungsten arc welding machines that were located in a corner of a room measuring 60 by 27 by 3 m. No supplementary ventilation was provided.
The work was performed on various metal parts that contained nickel.
The ozone concentration in the breathing zones of the welders was 9.2 ppm; nickel carbonyl and oxides of nitrogen were not detected.
A trichloroethylene degreaser was located about 15 m from the welding area, but air measurements were negative for phosgene, a photodecomposition product of trichloroethylene. One welder was admitted to a hospital with pulmonary edema an hour after leaving work.
Chest X-rays revealed diffuse peribronchial infiltration consistent with multilobular pneumonia. He remained in critical condition for 2 days with persistent pulmonary congestion, and he recovered after weeks.
Two of the eight welders developed dyspnea, and X-ray examination revealed scattered radiographic densities over both lung fields. Both workers were hospitalized and recovered within 9 days.
Four of the remaining five welders complained of severe headaches and throat irritation.
Challen et a l . [1958] also described symptoms of upper respiratory tract irritation in 11 of 14 welders who were exposed to ozone at concentrations of 0.8 to 1.7 ppm while performing gas tungsten arc welding on aluminum.
These symptoms ceased when the concentrations of ozone were reduced to approximately 0.2 ppm; no mention of aluminum concentration was made.
# (c) Pneumoconiosis, Including Siderosis
In 1936, clinical, radiographic, and pathologic changes in welders' lungs were first described by Doig and McLaughlin [1936].
They reported nodulations in the lungs of eight electric arc welders employed for 7 to 12 years. Similar findings were reported 2 years later [Enzer and Sander 1938] on a group of 26 electric welders who used bare metal electrodes and were exposed to iron oxide. Microscopic examination of a lung tissue biopsy from 5 of the 26 welders revealed no parenchymatous changes or fibrosis, but it did reveal a large quantity of iron deposited in the bronchi, the lymphatic vessels, and the alveolar septa-a condition that is characteristic of siderosis.
Numerous other reports described similar findings of asymptomatic, benign, and radiologically detectable lung changes attributed to the deposition of iron oxide fume particles in the lung (Britton and Walsh 1940;Sander 1944;Sander 1947;Doig and McLaughlin 1948;Mignolet 1950). Although no exposure conditions were reported in these studies, the respiratory effects noted were in electric welders who were employed before 1950, when bare metal electrodes were primarily used.
To a large extent, bare metal electrodes have been replaced by covered electrodes.
In addition to iron, covered electrodes often contain silicon, silicates, fluorides, titanium, manganese, copper, and other metals.
With the increased use of covered electrodes, there have also been increases in reports of fibrosis, respiratory impairment, and active lesions at the site of accumulation of iron particles in the lungs.
The following reports are representative of such observations in welders exposed to fumes of mixed composition. Dreesen et al. [1947] reported an investigation on the health status of arc welders in steel ship construction 90 from seven shipyards.
Medical examinations were made of 4,650 workers, 70% of whom were welders.
Less than 6% of the welders had more than 3 years of shipyard experience. The study population was divided into three groups: welders (Group 1); persons who did not have a clearly defined welding or nonwelding work history (Group 2); and nonwelders, including electricians, machinists, and sheet metal workers who did not have an exposure to welding fumes (Group 3). Arc welder's siderosis was diagnosed in 61 (3%) of the welders in Group 1 and in 10 (3%) of the persons in Group 2. All welders in Group 1 had a lower mean systolic blood pressure that was unrelated to age and no appreciable difference in the hematocrit and erythrocyte sedimentation rate.
Approximately 25% of the welders had slag burns or scars.
Welders (Group 1) had approximately the same visual acuity as those persons in Groups 2 and 3 when the data were adjusted for age.
Conjunctival irritation was slightly more prevalent among welders when compared to the other two groups.
Greater incidences of nasal congestion, pharyngitis, and upper respiratory symptoms were reported in welders from Group 1, with tobacco-using welders in this group showing even greater incidences; however, these differences were not reported to be statistically different when compared to those persons in Groups 2 and 3.
In the chest X-rays of welders, a slight increase in lung field markings was observed as length of welding experience increased.
A total of 1,761 welding fume samples were collected and analyzed for iron and total fume.
Zinc was evaluated in 278 and lead in 25 of these samples.
Iron fume concentrations in excess of 20 mg/m^ (>30 mg/m^ expressed as ferric oxide) were found in all welding locations.
The highest average iron and total fume concentrations were found in confined spaces where no ventilation was installed.
Zinc concentrations in excess of 12 mg/m^ (>15 mg/m^ expressed as zinc oxide) were reported. No exposure data were given for total fume or lead.
To determine the frequency of siderosis, Mignolet [1950] examined and assessed the medical histories of 216 workers who were classified into the following groups:
32 oxyfuel gas welders, 99 oxyacetylene cutters, and 85 arc welders. These groups were compared with 100 workers selected from other occupations; the types of occupations and their potential for exposure to welding fumes were not stated. The number of abnormal X-rays was much higher among arc welders (61%) than among the oxyacetylene cutters (41%), the oxyfuel gas welders (18%), and the comparison group (17%). The changes included pleural adhesions, distinct diffuse sclerosis, and enlarged hilar shadows.
The changes were attributed to the inhalation of iron oxide and other metals from the coverings of electrodes.
In all cases, the siderosis was a localized sclerosis, not granular.
Based on these findings, the author concluded that arc welding was more hazardous than oxyacetylene cutting and oxyfuel gas welding.
Marchand et a l . [1964] and Attfield and Ross [1978] have likewise reported on the radiological examination of arc welders.
Marchand et a l . [1964] reported on the incidence of pneumopathy in 402 arc welders.
Of this total, 192 had worked for 5 to 10 years, 137 had worked for 11 to 15 years, 54 had worked for 16 to 25 years, and 19 had worked for more than 25 years.
Pneumoconiosis was radiological ly demonstrable in 25 (7%) of the 402 welders, with 13 of the 25 cases found in the group that had worked for 11 to 15 years (the remaining 12 cases not identified). Of the 25 cases of pneumoconiosis, 7 (6 of which were in the group exposed for 11 to 15 years) were classified as siderosis.
Attfield and Ross [1978] studied radiological abnormalities in 661 electric arc welders who were engaged in many types of arc welding, including gas metal arc and gas tungsten arc processes.
No exposure data were given, but 264 (40%) of the welders said they had worked near locations where asbestos was being used. Results from radiological examination of the welders indicated that 53 (8%) of them had small rounded lung opacities.
Of those 53 welders, 41 (78%) had opacities that measured from 1.5 to 3 mm in diameter.
One film showed lung opacities with diameters of 3 to 10 mm, while the balance of the films revealed opacities that ranged from just visible up to 1.5 mm in d i a m e t e r .
The clinical findings reported by Meyer et al. [1967] of a 55-year-old arc welder who had been employed at a shipyard for 24 years were consistent with the findings previously reported by Dreesen et a l . [1947] on other shipyard welders.
The welder had worn a welding helmet only intermittently and frequently worked in confined areas. Both ferrous (cast, zinc-coated, and stainless) and nonferrous (aluminum, cupronickel, copper, brass, and bronze) welding materials were used.
All electrodes apparently were covered.
For 8 to 10 years, the welder's chest X-rays demonstrated mottling, and a lung lobectomy revealed dark pigmentation on the visceral pleural surface.
The iron concentration (10 jug/m I of tissue) was 20 times the normal amount, and the silica concentration (2.8 ng/ml of tissue) was 30% of the total mineral content.
Mild functional impairment was noted in the following pulmonary function parameters (% decrease from predicted values):
vital capacity (VC), 4%; inspiratory capacity (IC), 15%; residual volume (RV), 52%; and functional residual capacity (FRC), 29%. A massive conglomerate fibrosis was diagnosed.
Tuberculosis was suspected but not confirmed because lung cultures were not taken.
The pulmonary changes were attributed to the iron and silica in the electrode coatings.
Levy and Margolis [1974] described the case of a 35-year-old man with siderosiIicosis of the lung, diffuse interstitial fibrosis, and atypical alveolar epithelium associated with cancer of the lung.
The subject was employed as an oxyacetylene cutter in a steel foundry for 5 years; he wore a welder's helmet for eye protection but used no specific respiratory protection.
The torch-cutting was performed approximately 4 m from sandblasting operations. Within the work area, the concentration of respirable silica was reported to be 6.82 mg/m^ and the quantity of iron oxide was 19.4 m g / m^.
The welder had no previous occupational exposure to fibrogenic dusts.
A lung X-ray revealed a fine reticular pattern in both lung fields.
Pulmonary function studies indicated an obstructive and restrictive ventilatory impairment accompanied by arterial hypoxemia and compensated respiratory alkalosis.
X-ray diffraction analysis of lung biopsy tissue revealed iron oxide and silica.
A lung biopsy analysis reported by Brun et al. [1972] of an arc welder who had worked for 16 years on stainless steel in an area with poor ventilation indicated the presence of diffuse fibrosis.
Prior medical history revealed that he had suffered dyspnea combined with an asthma-like bronchitis.
Examination at the time of the report revealed rales at both lung bases, fine bilateral micronodular reticulation, and the presence of numerous macrophages laden with ferric oxide (siderophages) in the sputum. Respiratory function tests revealed a moderate respiratory deficit: vital capacity (VC) was 73% of the predicted value, and the forced expiratory volume in 1 second (FEV-)> was 65% of the predicted value.
Microscopic examination of biopsy material revealed intra-alveolar fibrosis.
Numerous histiocytes and macrophages filled with iron were present in the fibrositic wall.
Stettler et al. [1977] reported two cases of siderosis in which the severity of disease appeared to be associated with the welding fume composition.
One worker arc welded primarily in open spaces, whereas the second worker arc welded primarily in confined spaces.
The authors did not state the age of the workers, the length of employment, or the base metal(s) welded by the two workers.
Lung biopsy specimens from both welders, and air samples from the workplace environments were analyzed by electron microscopy using energy dispersive X-ray analysis to determine the chemical composition of the observed particulate matter. The majority of particles in the lungs of both welders were determined to be from stainless steel welding fumes and were comprised mostly of iron with some chromium, manganese, and nickel.
In addition, silica, aluminum, and various silicate particles were found in each biopsy preparation.
The same types of particles were also found in air samples collected at the worksite during arc welding operations.
Although both welders were considered to have siderosis, the first welder had moderate lung disease with minimal interstitial fibrosis, while the second welder had severe respiratory impairment with extensive interstitial fibrosis.
The authors concluded that the severity of the disease in the second welder may have been due to the concentration of aluminum particles found in this welder's lungs, which was six times that of the other welder.
The authors attributed this increase to his working in a confined space. Stanescu et al. [1967] examined 16 arc welders (12.1 years average exposure) who had chest X-rays suggestive of siderosis and who had more than 7 years of experience.
He found that seven suffered from exertional dyspnea. Although spirometric values (i.e., VC, FEV-), total lung capacity [ T L C ] , and RV) were generally within normal limits, the authors found a statistically significant (p<0.05) decrement in pulmonary compliance when these 7 welders were compared with 13 workers who were not exposed to welding fumes. The authors attributed this decrease either to iron deposits per se or to associated fibrosis caused by other chemical exposures.
No mention was made as to whether or not the welders' smoking habits or ages were considered.
In contrast to the decrements in pulmonary compliance found in welders by Stanescu et al. [1967], Kleinfeld et al. [1969] found no differences between welders and a comparison group when they were given a series of pulmonary function tests.
Twenty-five welders were compared with a group of 20 men who resided in the same area but who were not exposed to welding fumes. Occupational histories were obtained from all workers in the study, and clinical examinations were performed, including chest X-rays. The average age of the welders was 48.8 years, and the average age of the comparison group was 46.7 years.
Fifty-six percent of the welders and 55% of the comparison group were smokers.
The average work experience of the welders was 18.7 years, with a range of 3 to 32 years.
Their work included oxyfuel cutting and shielded metal arc welding.
Eight (32%) of the 25 welders showed lung changes on X-rays that were characterized by reticular nodular shadows in both lungs.
These changes were absent in members of the comparison group.
Pulmonary function values, including FEV, FEV-|, RV, and TLC, were normal for both groups. In addition, none of the clinical tests showed statistically significant differences between welders exposed for more than 20 years and those exposed for fewer than 20 years. At the time of the study, environmental sampling was conducted at the sheet metal fabrication facility where the welders were employed. Concentrations of iron oxide ranged from 0.65 to 1.7 mg/m^ inside the welders' face shields and from 1.6 to 12 mg/m^ outside the face shields. Exposure to other fume constituents was not reported. Eight years before the study and just before an improved ventilation system was installed, iron oxide concentrations had ranged from 30 to 47 mg/m«* in the breathing zones of other welders working at the facility.
# (d) Bronchitis/Pulmonary Function
The inhalation of welding fumes and gases have been shown to cause decrements in pulmonary function and the development of other chronic nonmalignant respiratory diseases. Many studies (Doig and Challen 1964;Hunnicutt et al. 1964;Kujawska 1968; Ulrich et a 1 . 1974;Antti-Poika et al. 1977;Akbarkhanzadeh 1980;Keimig et a l . 1983;Sjogren and Ulfvarson 1985;Oleru and Ademiluyi 1987) have reported the potential health risk to welders from exposure to fumes and gases of unknown composition.
Other studies (Doig and Challen 1964;Glass et al. 1971) have shown a risk of exposure to phosgene resulting from the decomposition of trichloroethylene that may be present in the welding work environment.
Several other studies (Hunnicutt et al. 1964;Fogh et al. 1969;Akbarkhanzadeh 1980;Sjogren and Ulfvarson 1985) have demonstrated an association between smoking by welders and an increased risk of developing respiratory disease.
The following studies are representative of those collective data. Kujawska [1968] reported on a study of workers aged 35 to 45 who had been arc welding for at least 10 years, had never been employed in trades that would have exposed them to fibrosis-producing dusts, and had acquired no respiratory diseases before starting work as welders.
Two equal groups of welders were randomly selected (total group size not given) and placed in a group according to radiologic changes in the lung. One group of 30 had radiologic changes indicative of siderosis and the other group of 30 had normal lung radiographs.
The welders of both these groups performed about half their work in small and confined spaces (e.g., inside boiler tanks).
Covered acid electrodes were used most often; basic and rutile electrodes were occasionally used.
No identification of potential exposures was reported.
The comparison group (controls) consisted of 30 healthy pipefitters, mechanics, and turners.
Each of the 90 workers (welders and controls) was given a physical examination including medical history, X-ray, ECG, and lung function tests such as lung volumes and capacities, pulmonary ventilation, and examination of alveolar ventilation.
No significant differences in age, height, weight, or length of service were found between groups.
The distribution of smokers and nonsmokers was also similar.
Complaints of labored breathing (86%) and dry cough (40%) were more frequent in the group of welders with siderotic changes than in the other group of welders (37% and 3%) or controls (10% and 7%). Chronic bronchitis was found only in the two groups of welders, indicating a statistically significant difference (p<0.05) from controls.
In addition, reduced pulmonary function parameters (including lower values of the VC and FEV-| and an increase in the ratio of residual volume to TLC) were found in the group of welders with siderotic changes.
Antti-Poika et a l . [1977] found simple chronic bronchitis to be more prevalent (p<0.01) among 157 electric arc welders than among 108 controls who were employed at the same facility but not exposed to welding fumes.
The controls were matched to welders with respect to age, smoking habits, and social class.
The prevalence of simple chronic bronchitis was compared with the length and concentration of exposure, but no dose-response relationships were noted.
The welders (average age was 36.1 + 10.1 years) mainly used covered electrodes and had been welding for 3 or more years for at least 3 hours a day. Most worked in engineering shops.
Samples of total fumes were collected outside the helmet at the time of the study, and concentrations ranged from 1.0 to 9.0 mg/m 3 as an 8-hour TWA.
No historical exposure data were reported.
# (i) Phosgene Poisoning
Several cases of respiratory distress and pulmonary function impairment have been attributed to phosgene exposure.
For example, Doig and Challen [1964] described seven workers who had been complaining for several months about periodic attacks of mild to severe respiratory distress, cough, chest constriction, and breathlessness while they performed gas metal arc welding.
The cause of the problem was attributed to vapors from an inadequately ventilated degreasing tank that contained trichloroethylene.
The tank was positioned next to open doors so that air currents carried the trichloroethylene vapor 46 m or more to the welding bay, where it decomposed (as a result of heat and ultraviolet radiation from the arc) and formed phosgene.
In another case of phosgene poisoning, a welder experienced chest congestion, difficult breathing, and coughing while welding metal studs to metal links using gas metal arc welding with carbon dioxide [Glass et al. 1971].
The studs were cleaned in an open bucket of trichloroethylene adjacent to the welding bench, and the still-damp studs were placed on the bench and welded.
By the end of the morning, the welder's gloves were soaked with trichloroethylene. Examination of the welder 24 hours after exposure revealed reduced vital capacity and FEV-j, airway obstruction, arterial hypoxia, and impaired carbon monoxide transfer.
No exposure measurements were reported.
# (ii) Interactive Effects of Smoking and Welding
Hunnicutt et al. [1964] reported on one of the first cross-sectional studies that took into account the smoking habits of welders.
The study group consisted of 100 electric arc welders and an equal number of nonwelding workers employed at the same plant who were not exposed to welding fumes.
The welders were under 60 years of age and had 10 or more years of welding experience in shipyards.
Arc welding was the predominant process that was used.
However, no exposure data were reported.
The following pulmonary tests were conducted on all individuals: FVC, FEV-j, maximum expiratory flow rate (MEFR), maximum mid-expiratory flow rate (MMF), and maximum breathing capacity (MBC). A statistically significant (p=0.01) decrement in welders compared to controls was noted for FEV-|, MEFR, and MMF.
Seventy-one percent of the welders and 59% of the controls had a history of cigarette smoking.
The combined effects of cigarette smoking and exposure to welding fumes increased the likelihood of impaired pulmonary function. Among smokers, the incidence of abnormal pulmonary function in welders was twice that observed in controls. Complaints of shortness of breath, coughs, expectoration, and wheezing occurred twice as often among welders who smoked as among welders who did not smoke.
Radiographic evidence of siderosis was found in 34% of the welders (smokers and nonsmokers combined), but the authors found no correlation between degree of respiratory impairment and radiographic abnormality.
Siderosis was not observed in the controls.
Fogh et al. [1969] reported on the examination of a group of 154 electric arc welders (more than half [number not given] were shipyard welders while the remaining were engine/boiler welders), 2 oxyacetylene cutters, and 152 nonexposed comparison workers from the same locations.
The authors found an increased incidence of chronic bronchitis with increased tobacco smoking in welders as well as in the comparison group when compared to those workers from both groups who did not smoke.
Decreased pulmonary function (i.e., FEV'j) was found to be statistically significant among nonsmoking welders when compared with either the welders or controls that smoked (i.e., <10 cigarettes/day, p=<0.05; >10 cigarettes/day, p=<0.01). No statistically significant difference was shown when welders who smoked were compared with the control group of smokers.
Among all the controls, symptoms did not increase with age.
However, in welders under and over 50 years of age the prevalence of symptoms was 25% and 55%, respectively (p<0.05). Among the welders who smoked, 26% of those under the age of 50 and 55% of those over 50 displayed increases in bronchitic symptoms.
Neither age group differed significantly when compared to the same age groups of smokers in the comparison group.
Chest X-rays revealed a fine mottling indicative of siderosis in five welders (3%). No exposure data were reported. Barhad et al. [1975] reported on the prevalence of respiratory symptoms and the impairment of ventilatory function in a group of 173 shipyard welders who had 5 or more years of welding experience.
The average age was 34.1 years (range: 22 to 57). Cough was found to be increased 22% and chronic bronchitis 20% in welders when compared to a control group of workers from the same shipyard but with no welding fume exposure.
The prevalence of chronic bronchitis was 1.5 times more frequent among welders when compared to controls; the difference in prevalence tended to be larger in nonsmokers (12% of welders versus 3% of controls) as compared to smokers (26% of welders versus 21% of controls) but the limited number of observations precluded any statistical analysis.
Dyspnea and wheezing (p<0.001) and paroxysmal dyspnea (p<0.005) were approximately two times more common among welders (smokers, ex-smokers, and nonsmokers) when compared to controls matched for age and smoking habits.
The major type of welding was arc with some oxyacetylene torch and shielded welding.
At the time of the study, breathing zone welding fume concentrations were found to range from 6 to 36 mg/m^ while welding in open work areas and 48 to 92 mg/m^ in confined spaces. Nitrogen oxide exposures averaged I.7 mg /m^ for shielded and 1.1 mg/m** for arc welding.
Carbon monoxide exposures averaged 17 mg/m3 for torch welding, 8.4 mg/m^ for electrical, and 6.3 mg/nr* for flux welding.
No historical exposure data were reported.
A similar type of analysis of shipyard welders was performed by Akbarkhanzadeh [1980].
A study was initiated to determine the influence of welding fumes and cigarette smoke on the bronchopulmonary system. The study included 209 welders with 1 or more years of welding experience (mostly shielded metal arc) and a comparison group of 109 shipyard workers who were not exposed to welding fume and who worked for at least 10 years in the same work environment.
The welders and the comparison group were divided into smokers, ex-smokers, and nonsmokers.
The durations of exposure for welders who smoked (22.5 years) and those who did not smoke (20.9 years) were similar.
The smoking habits of the welders and the comparison group were reported to be identical.
Persistent cough and phlegm were found to be twice as frequent among welders who smoked (16.7%) as among the comparison workers who smoked (8.3%).
Chronic bronchitis was found only in welders (12.4%) who smoked or had smoked.
The mean duration of exposure for these welders was 30 years.
For all welders the FEV^ was less (3.77) than that of the total comparison group (4.03) and less for the nonsmoking welders (3.92) when compared to the controls who did not smoke (4.27).
Differences observed for both groups were statistically significant (p<0.025).
Although the FEV-j was lower among welders who smoked when compared to controls who smoked (3.63 versus 3.82), the difference was not statistically significant.
The FVCs for smoking (4.91) and nonsmoking (5.10) welders were lower than the corresponding smoking/nonsmoking (5.07 and 5.40, respectively) comparison groups.
These differences were not statistically significant.
With advancing years of exposure, all lung function parameters of welders deteriorated more than those of workers in the comparison group.
No exposure data were reported.
A cross-sectional study was reported by Keimig et al. [1983] on the prevalence of respiratory symptoms or impaired lung function in welders exposed to fumes and gases from gas metal arc welding and flux core welding on mild steel. Welders and controls were white males, aged 25 to 49 and were employed for at least 4 years at a plant that manufactured heavy construction equipment.
The study group was comprised of 91 welders (46 nonsmokers, 45 smokers) with a mean welding exposure of 108 months, and 80 controls (35 nonsmokers, 45 smokers) who were employed at the same plant but had jobs with minimal exposure to respiratory irritants.
Occupational and smoking histories were collected from all subjects.
The types of pulmonary function tests given and the questionnaire administered to all subjects were in accordance with the guidelines of the American Thoracic Society.
Measurements of pulmonary function were made on each subject before and after each work sh i f t .
As expected, welders and controls that smoked reported a higher frequency of respiratory symptoms (e.g., bronchitis, pneumonia, cough) than corresponding nonsmokers.
Although welders who did not smoke reported higher frequencies of symptoms than nonsmoking controls, the differences were statistically significant (p<0.05) for only the symptoms of increased phlegm and episodes of cough and phlegm.
Pulmonary function measurements were compared both within and between welders and controls, and by smoking status.
Predicted normals were not used in the statistical analysis.
The only statistically significant differences noted were decreases in forced vital capacity (FVC) measurements at the end of the work shift for nonsmoking welders, nonsmoking controls, and smoking controls.
The authors concluded that these differences were not attributable to welding exposure, because controls as well as welders showed a significant decrease.
Nonsmoking welders and smoking welders compared to respective controls did not have significantly decreased mean values of FVC or forced expired volume in 1 sec (FEV-|). The mean expiratory flow rates and forced expiratory flow rates measured at 75% of the FVC were found to be lower but not significantly different for welders when compared to controls.
Breathing zone air samples collected near welders at the time of the study indicated iron oxide concentrations of 1.3 to 8.5 mg/m^.
No detectable amounts of chromium, copper, fluoride, and lead were found in any of the air samples.
A more detailed cross-sectional study was described by Sjogren and Ulfvarson [1985] who assessed the respiratory symptoms of cough, phlegm, and irritation; chronic bronchitis; and pulmonary function of male welders in Sweden.
Welders were identified from the Swedish Register of Enterprises, Bureau of Statistics, and placed into three study groups: those who welded using gas metal or tungsten arc on aluminum (Group 1); those who welded with coated electrodes on stainless steel (Group 2); and those who welded on railroad tracks (Group 3).
To be included in the study, each welder must have worked at least 1 year, spending at least 3.5 hours per workday performing the type of work identified above.
No specific restrictions on the amount of welding time per day were applied to Group 3. All workers who were asked to be in Groups 1 (64 welders) and 2 (46 welders) agreed to participate.
The median exposure time was 5 years (range: 1 to 24) in Group 1 and 15 years (range: 1 to 39) in Group 2. A total of 149 welders who were asked to be in Group 3 agreed to participate.
A nonwelding comparison group was chosen for Groups 1 and 2 from the same companies and were matched by age (with a variance of 4 years) and smoking habits.
The comparison group for Group 3 included 70 railroad workers who did not weld.
This group was not matched for age or smoking habits.
All three groups of welders had higher frequencies of chronic bronchitis than their respective comparisons, but the differences were statistically nonsignificant and appeared to be more dependent on smoking than on welding fumes [Sjogren and Ulfvarson 1985].
However, overall respiratory symptoms were more prevalent for welders working with gas-shielded welding on aluminum (Group 1) than the comparison group, and were statistically significant (p=0.03) with increasing exposure to ozone.
Exposure to ozone rather than to aluminum fumes appeared to be responsible for the excess in the observed respiratory symptoms of Group 1 welders [Sjogren and Ulfvarson 1985].
Almost 50% of the exposures to ozone exceeded 0.1 ppm when gas metal arc welding was performed on aluminum.
Likewise, welders in Groups 2 and 3 displayed more respiratory symptoms with increasing chromium exposures, but the difference was not statistically significant.
More than 80% of the hexavalent chromium exposures exceeded 20 y.q/m3 when stainless steel was welded with coated electrodes.
According to the authors, respiratory symptoms were not related to total fume concentrations (concentrations not stated) or nitrogen oxides (<5 ppm).
No differences were observed regarding FVC or FEV-j between the three groups of welders and their respective comparison groups. Oleru and Ademiluyi [1987] reported the results of pulmonary function measurements made on workers engaged in welding and thermal cutting of window and door frames made from medium and high alloy steel and aluminum.
A group of 67 (36.8%) from a total of 182 men in the workforce were evaluated for decrements in pulmonary function.
Of the 67 subjects, 16 were maintenance workers who were indirectly exposed to welding fumes and gases;
13 were engaged in mild steel welding and 7 were engaged in mild steel cutting; 18 were involved in aluminum cutting operations; and 13 were responsible for the paint dipping of metal frames.
A modified British Medical Council respiratory disease questionnaire was administered to all subjects.
Lung function assessments including peak expiratory flow rate (PEFR), one second forced expiratory volume (FEV-|), and forced vital capacity (FVC) were made with a Wright's peak flow meter for PEFR and a Vitalograph spirometer for FEV-j and FVC.
To assess the potential acute respiratory effects that may have occurred over a work-week (40 hours) 8 of the 13 mild steel welders were given spirometric tests on Monday morning and after the work shift on Friday.
To measure possible pulmonary function changes that may have occurred after an 8-hour work shift and 3 consecutive work shifts, the peak flow test was administered to all 13 welders and 13 paint dippers before and after the work shifts on Wednesday and Friday.
The expected lung function parameters of the subjects were calculated from the pulmonary function equations developed for a group of normal, non-industrially exposed Nigerian subjects.
Only 9 of the 67 subjects were found to have ever smoked with an average cigarette comsumption of less than 5 per day and an average duration of about 4 years.
Although not statistically significant, those workers classified as maintenance workers had higher lung function measurements (FEV-j and FVC) than the other groups of workers.
However, there was no evidence of obstructive lung disease among any of the groups as supported by the high FEV-|/FVC ratios observed for all subjects, with the lowest 95% confidence interval for any group being 87.6% to 84.2% found for the maintenance workers.
Seven cases of restrictive lung impairment were observed among the subjects-3 paint dippers, 2 aluminum workers, and 2 welders. All complained of coughing, chest pains, and difficulty in breathing.
The length of employment for these cases ranged from 3 to 7 years.
The eight welders who were given spirometric lung function tests to assess the effects of exposure over a work week (40 hours) demonstrated statistically significant (p<0.05) decrements in all parameters measured.
Peak flow measurements made on this group after an 8-hour work shift showed acute changes in pulmonary function that were statistically significant (p<0.05); however, these changes in pulmonary function were not found to be significantly different when welders were tested at the end of three consecutive work shifts. Statistically significant (p<0.005) changes in peak flow measurements were observed for the 13 paint dippers when tested after either an 8-hour work shift or 3 consecutive work shifts.
The absence of any obstructive lung disease among the exposed subjects is consistent with the low number of subjects who smoked.
The analysis of spirometric and peak flow rate data gathered on a small number of welders and paint dippers after 8-, 24-, and 40-hour work shifts did demonstrate statistically significant changes in lung function.
However, because of the low participation rate (36.8%) it is not possible to determine the significance of these data.
Although no exposure data were collected, the authors hypothesized that based on the amount of settled dust that had accumulated in the work area, airborne dust concentrations probably exceeded 5 mg/m^.
# (e) Summary-Nonmalignant Pulmonary Diseases
The acute respiratory diseases metal fume fever and pneumonitis have been observed in workers involved in many types of welding processes.
Several studies have shown the occurrence of metal fume fever in workers exposed to mixed fume compositions [Ross 1972;Johnson and Ki Iburn 1983] and to specific metals [Drinker 1922;Drinker et a l . 1927].
In all cases, workers experienced nonspecific systemic reactions, including eye and throat irritation, headache, shortness of breath, and nausea that usually ceased within 24 hr after removal from exposure.
Likewise, welders' pneumonitis has been documented in several case reports and cross-sectional morbidity studies that have shown exposures to the mixed fume composition [KleinfeId et al. 1957;Beton et al. 1966;Townshend 1968;Blejer and Caplan 1969;Patwardhan and Finckh 1976;Jindrichova 1976;Herbert et al. 1982] and gases [Mo I os and Collins 1957;Challen et al. 1958;Maddock 1970;Mangold and Beckett 1971] to be a causative factor in the observed cases of respiratory distress, pulmonary edema, and diminished pulmonary function.
Except for limited exposure data reported by KleinfeId et al. [1957], Molos and Collins [1957], and Challen et al. [1958], all the above studies lacked quantitative exposure data and reported workers being exposed to welding fumes and gases in confined spaces or poorly ventilated work areas.
Several fatalities have been observed among workers acutely exposed to cadmium fumes [Beton et al. 1966;Patwardhan and Finckh 1976] and nitrogen dioxide [Maddock 1970].
The occurrence of pneumoconiosis, including siderosis, was first recognized in 1936 among a group of welders [Doig and McLaughlin 1936].
Since then, many case and epidemiologic reports [Britton and Walsh 1940;Sander 1944;Sander 1947;Doig and McLaughlin 1948;Mignolet 1950] have described similar clinical findings of asymptomatic, benign, and radiologically detectable lung changes in welders.
Before 1950, much of the welding was performed with bare metal electrodes that produced high concentrations of iron oxide.
Since the replacement of bare metal electrodes with covered electrodes, the potential for mixed exposure to other metal fumes has increased.
As a result of these mixed exposures, there have been subsequent reports of welders in which the complications of fibrosis [Stettler et al. 1977;Meyer et al. 1967], pulmonary impairment [Meyer et al. 1967;Brun 1972;Levy and Margolis 1974], and reticular nodular shadows [Klein fe Id et al. 1969;Attfield and Ross 1978] were identified with siderosis.
Bronchitis and decrements in pulmonary function have been reported in welders who have been involved in many types of welding processes.
Welders employed in shipyards have shown statistically significant decrements in pulmonary function [Hunnicutt et al. 1964;Fogh et al. 1969] and increases in chronic bronchitis [Fogh et al. 1969;Barhad et al. 1975;Akbarkhanzadeh 1980]. With the exception of one study [Barhad et al. 1975], in which exposures to welding fume were measured at 6 to 36 mg/m^ in welders' breathing zones and 48 to 92 mg/m^ in confined spaces, no exposure data were reported.
The interpretation of these studies is complicated by the heterogeneity of welding exposures and the possible presence of asbestos as a concomitant respiratory hazard.
Studies reported by Keimig et. al [1983] and Oleru and Ademi luyi [1987] on welders exposed to mild steel fume and gases in industries other than shipyards observed differences in pulmonary function measurements between welders and nonexposed groups but could not differentiate between smoking and welding exposure on the observed changes. Keimig et al. [1983] found a higher frequency of reported symptoms of phlegm and episodes of cough and phlegm for welders who smoked compared to nonsmoking welders.
Decrements in pulmonary function parameters were reported by Oleru and Ademiluyi for welders after an 8-hr work shift and at the end of a 40-hr workweek.
Although these differences were statistically significant, there was a low participation rate (36.8%) in the study.
Several other studies [Mangold and Beckett 1971;Antti-Poika et al. 1977;ACGIH 1986] have shown a statistically significant increase in chronic bronchitis in welders performing different welding tasks when compared to nonexposed comparison groups.
In all the studies where chronic bronchitis occurred, the prevalence of the disease increased with the increasing use of tobacco.
(
# 2) Respiratory Cancer
The following assessment of epidemiologic investigations provides information about the possible association between cancer and occupational exposure to welding fumes and gases [Breslow et al. 1954;Dunn and Weir 1968;Ott et al. 1976;HMSO 1978;Blot et al. 1978;Gottlieb 1980;Sjogren 1980;Milham 1983;Beaumont and Weiss 1981;Polednak 1981;Becker et al. 1985;Newhouse et al. 1985;Steenland et a l . 1986;Schoenberg et al. 1987;Sjogren et al. 1987].
Many of the studies report standard mortality ratios (SMRs) greater than 100 or odds ratios (ORs) above 1.0, which suggests an increased risk of respiratory cancer. However, some of these studies are not statistically significant and many do not account for the confounding factors of smoking or possible asbestos exposure.
To facilitate discussion, the studies have been grouped as cohort mortality or case-control studies.
To permit comparison of study results, summaries of these studies (including information on study design, observed/expected numbers, SMRs, ORs, etc.) are presented in Tables IV-3 and IV-4.
# (a) Cohort Mortality Studies
The study reported by Sjogren [1980] of Swedish welders has been the only cohort mortality study to specifically assess the association between lung cancer mortality and exposure from welding on stainless steel.
The study cohort included 234 nonasbestos-exposed stainless steel welders who had a minimum of 5 years exposure between 1950 and 1965.
The cohort was followed through December 1977. Of the 234 welders, 207 welded with covered electrodes most of the time. An OR of 4.4, based on three lung cancer deaths (p<0.03), was observed among the stainless steel welders when compared to Swedish death rates. All three welders who died of lung cancer were cigarette smokers.
The O R was still statistically significant at p<0.05 after adjusting for a theoretical 10% increase in cigarette smoking among stainless steel welders.
No exposure data were available for the study cohort; however, measurements of chromium taken in 1975 at a similar stainless steel welding process revealed median TWA chromium concentrations of 210 jug/m^ while welding with covered electrodes and 20 /ng/m^ during gas-shielded welding.
The author stated that only a minor fraction of the exposure was in the hexavalent form; therefore, the concentrations were an overestimate of hexavalent chromium exposure.
In 1987, Sjogren et a l . [1987] reported on the follow-up analysis of these 234 stainless steel welders who were exposed to high concentrations of chromium.
After 7 years of additional follow-up, the mortality of this cohort was reanalyzed and the results compared to another cohort that consisted of 208 railway track welders exposed to low concentrations of chromium (<10 mg/mg3).
The participants of both cohorts had welded for at least 5 years sometime between 1950 and 1965 and were followed for mortality until December 1984.
The expected number of deaths in the two cohorts were calculated by the multiplication of the person-years of observation within 5-year age categories during 1955-1984 by cause-, gender-, age-, and calendar-year-specific national death rates of Sweden.
An increase in deaths (SMR=249) from respiratory cancer was observed for the cohort of welders who were exposed to high concentrations of chromium.
In contrast, deaths from respiratory cancer in the low-exposure cohort of welders were less than expected (1 death observed, 3 deaths expected).
When welders who had high exposures to chromium were compared with those who had low exposures, the number of deaths from respiratory cancer was significantly elevated in the high exposure group, which had a relative risk of 7.01 (95% Cl = 1.32-37.3).
No other statistically significant increase in deaths from other causes was observed in either cohort.
The authors noted that the expected number of deaths from respiratory cancer reported in the earlier analysis by Sjogren [1980] were incorrectly calculated as 0.7 instead of 0.9, resulting in an OR of approximately 3.3 (estimated by NIOSH).
No correction for smoking habits was made when either cohort was compared with the expected national death rates. However, smoking as a confounder was not considered to have a significant influence on the comparison of lung cancer risk between the two cohorts of welders.
Becker et a l . [1985] reported on a retrospective mortality study of 1,224 welders and 1,694 turners (machinists) who were employed in 25 German factories from 1950-1970 and followed until 1983.
The death rates of welders were compared with the death rates from internal and external comparison groups.
The internal comparison, based on the death rates of turners not exposed to nickel or chromium, yielded a statistically significant OR of 2.4 for welders (p<0.05) for all cancers and a statistically nonsignificant OR of 1.7 for cancer of the trachea, bronchus, and lung. External analyses (German National death rates) showed that the SMRs for all cancers; cancer of the trachea, bronchus, and lung; and respiratory diseases were statistically less than expected (p<0.05).
Increases in ORs and SMRs for welders who used covered electrodes and who had greater than 20 or 30 years latency were observed for all cancers, including cancer of the trachea, bronchus, and lung, when compared to the internal comparison group.
Since the method of age adjustment was not given, it was impossible to determine what bias the difference in age distribution of the internal comparison group may have contributed to the results.
No historical exposure data were reported.
A retrospective mortality study of 3,247 welders from Seattle, Washington, was reported by Beaumont and Weiss [1981].
The cohort of welders was selected from local union records of the International Brotherhood of Boilermakers, Iron Ship Builders, Blacksmiths, Forgers, and Helpers.
The welders had a minimum of 3 years of union membership and had worked between 1950 and 1973. A majority of them had been employed at shipyards or metal fabrication shops.
An SMR of 132 (p=0.06) for lung cancer was observed when death rates for U.S. white males were used for comparison.
The SMR for lung cancer in welders rose to 174 (p<0.001) when the investigators considered the 39 deaths that occurred 20 or more years after first employment. No historical exposure data were reported, especially data regarding exposure to asbestos in shipyards.
Likewise, the potential effect of cigarette smoking on the observed excess in lung cancer was not determined.
Internal comparison of welders and nonwelders revealed an excess lung cancer risk that was found to be greater among welders employed 20 or more years following fi rst exposure. In 1986, Steenland et al. [1986 reported on a reanalysis of the Beaumont and Weiss [1981] study using the Cox and logistic regression analyses to compare lung cancer risk of welders.
These analyses were thought to be preferable because they use an internal nonexposed comparison group that is more likely to have lifestyles (e.g., smoking habits) similar to the exposed group.
The Cox regression analysis compared welding as either a dichotomous or continuous variable with time-since-first-employment and year-first-employed.
The logistic regression was used to analyze the 137 lung cancer deaths (cases) and the remaining 8,542 study subjects (controls).
Of the total number of controls, 3110 were welders while the remaining 5,432 were other members (e.g., shipfitters, riggers) of the same union who were frequently employed in the same place as the welders. Men who died of lung cancer were compared to men who did not and an OR for lung cancer was determined for welders versus nonwelders.
When welding was analyzed as a dichotomous variable, a statistically significant interaction was observed with year-first-employed (0R=152, p=0.03).
An OR of 1.29 (p=0.03) for lung cancer was observed among welders when welding was considered as a cumulative dose in the logistic analysis.
An elevated OR of 1.15 still remained for lung cancer among welders when cumulative dose was analyzed in the Cox regression.
In a mortality analysis of 1,027 shipyard welders employed from 1940 to 1968 in Northeast England, Newhouse et al. [1985] reported elevated SMRs for all cancers (SMR=114), and for lung cancer (SMR=113) after excluding mesothelioma.
Accurate dates of employment were not available, so analysis by latency and duration of employment was not made.
No smoking histories or information on exposures were cited.
Another mortality study of 2,190 Italian shipyard workers in Genoa, Italy was reported by Puntoni et al. [1979].
The study population consisted of working or retired workers as of January 1, 1960 and followed until December 31, 1975 (duration of employment not given).
Age-and sex-specific mortality ORs were calculated for 19 occupational groups including electric and gas welders and compared with two comparison groups:
the entire male population of Genoa and the male staff of St. Martin's Hospital in Genoa.
Overall, the shipyard workers had statistically significant ORs for total deaths and several specific causes of death including all cancers and cancer of the trachea, bronchus, lung, and larynx when compared to the male population of Genoa, Italy. Gas welders had statistically significant increased ORs for total deaths (p<0.0005) and respiratory diseases (p<0.05), when compared with the same comparison group.
No statistically significant excess in lung cancer was noted for either electric or gas welders.
Although no exposure data were reported, the authors cited exposures to other potential carcinogens (e.g., asbestos, aromatic and halogenated hydrocarbons) in the work environment.
The smoking habits of the workers were not assessed nor was the study population age-adjusted.
The study consisted of a survivor population, with terminated workers not included in the analysis.
The absence of terminated workers probably biased the distribution of deaths because of the many long-term workers.
Polednak [1981] reported on a study of 1,059 white male welders from 3 nuclear facilities in Tennessee.
Increases of SMRs were found for lung cancer (SMR=150) and diseases of the respiratory system (SMR=133) that were not statistically significant when compared to U.S. white male death rates.
Welders were selected for the cohort if they were hired between 1943 and 1973.
SMRs for lung cancer (SMR=175) and respiratory disease (SMR=167) were higher among welders not exposed to nickel oxides than for welders exposed to nickel oxides (SMR=124 for lung cancer, SMR=101 for respiratory disease).
Two smoking surveys conducted in 1955 and 1966 showed that cigarette smoking among the group of welders who were not exposed to nickel oxides was 2.5 times more prevalent than the nickel oxide exposed group. About 20% of the welders exposed to nickel oxide smoked cigarettes during the years surveyed.
The difference in smoking habits may account for the higher SMRs for lung cancer and respiratory disease among the nonexposed group of welders.
In relation to duration of employment in all welders, the lung cancer SMR was elevated for those who worked more than 50 weeks, while the respiratory disease SMRs were higher for those with shorter durations of employment.
The fume exposures of welders were causally implicated in the increased risk of respiratory diseases, including pneumoconiosis and bronchitis.
At the facility where nickel alloy pipes were welded, time-weighted average (TWA) air concentrations of nickel found in 1975-1977 were all higher than 0.015 mg/m^ (range of concentrations not given).
The sample size of the two subgroups of welders was small, and 8.3% of the study cohort was of unknown vital status at the end of the study period.
The nonexposed welders were slightly older than those exposed which may have contributed a negative bias to the SMRs.
In a prospective mortality study reported by Dunn and Weir [1968] a slight, but not statistically significant, excess of lung cancer deaths (0R=1.05) was observed for welders and burners studied over an 8-year period.
The study design, which included 13 other occupational groups ascertained from California union records, was based on the information gained from 121,314 mailed questionnaires (85% response rate).
Statistical analyses were conducted using age-and smoking-specific death rates, and compared with the death rates of the total union population.
No exposure measurements were made and employment records were unavailable.
Potential exposures were estimated from the general occupational information that appeared on the questionnaire provided by the respondent.
Mi lham [1983] reported a statistically significant increase in proportional mortality ratios (PMRs) observed for male welders and flamecutters for several causes of death.
The proportional mortality study was based on death certificates collected over a 29-year period (1950-1979) in Washington State.
The statistically significant PMRs are reported in Table IV-5. Occupations were derived from death certificates, which were reported to be inaccurate for as many as 30% of the deaths.
The study consisted of a survivor population with deaths of terminated workers not included in the study analysis.
Smoking and the potential exposure to asbestos were not accounted for and could have had an effect on the outcome of the study.
In a review of lung cancer rates (by occupation) for Los Angeles County, Menck and Henderson [1976] observed a significantly increased SMR of 137 (p<0.05) for welders when compared to the age-, race-, and sex-adjusted Los Angeles County employed population.
A total of 2,161 death certificates cited lung cancer as the cause of death in white males, ages 20 to 64, during the periods 1968 to 1970.
In addition, 1,777 cases of lung cancer in white males during 1972 and 1973 in Los Angeles County were used.
Neither the potential effect of asbestos exposure nor smoking habits were assessed in the study analysis. Occupation and type of industry were ascertained from death certificates (which only listed last job held) and medical records.
Thus a clear delineation of all jobs held, years of employment, and potential occupational exposures could not be made.
In the report published by Her Majesty's Stationary Office [HMSO 1978] of England and Wales, increased mortality caused by pneumonia, lung cancer, and other and unspecified respiratory cancer was observed for gas and electric welders, cutters, and brazers during the period 1970-72. An overall increase (22%) in deaths was recorded even after adjustment for smoking, age, and social class.
This was more than was expected for this occupational group.
A statistically significant increase (p<0.01) in the PMR for lung cancer mortality was found among smokers and nonsmokers.
This risk remained statistically significant with an SMR of 116 (p<0.01) when controlled for smoking. The number of lung cancer cases recorded in 1966-1967 and 1968-1969 were noted as "particularly" high.
In 1968-1969, seven cancer cases were recorded for other and unspecified respiratory organs, whereas only one was expected. Although no explanation was provided, the authors attributed the excess in lung cancer to an association with asbestos exposure.
Possible errors in the analysis could have resulted from differences in the occupational classifications used for the numerator and denominator in determining PMRs.
Numerator estimates were based on occupations given in death certificates, whereas the denominator used occupations found in the national census data.
Therefore, the rates reflect some bias (unknown direction) in their estimation of risk.
Although this type of mortality study (which relies on routinely collected data) is useful for identifying associations between occupation and mortality, it is imprecise for detecting complex relationships between cause of death, exposure, and occupation.
No information on the types of exposures were available for analysis.
Smoking habits were not assessed but were controlled by using a 22% over-incidence for smoking in the analysis. Ott et al. [1976] reported on a cohort mortality study of 8,171 male workers employed at a chemical facility.
The study population was subdivided into two cohorts; the one cohort consisted of those workers (5,994) hired before 1950 and the other consisted of workers (2,177) hired between January 1950 and March 1954.
The vital status of all workers was followed until 1973.
Analysis of malignant neoplasms was ascertained for 15 job categories including welders and lead burners.
Based on 12 malignant neoplasm deaths, welders and lead burners had an elevated but not statistically significant SMR of 162 when compared to U.S. white male death rates.
It was not possible to validate the increase of lung cancer based on two observed lung cancer deaths.
Although workers who were potentially exposed to arsenicals or asbestos were eliminated from the study, no further characterization of other potential exposures was provided.
A potential misclassification bias could have been introduced because workers were assigned job categories based on their job titles the day they were hired; subsequent job changes were not taken into account.
# (b) Case-Control Studies
Gerin et al. [1984] reported on a case-comparison study of hospital cancer patients and their possible occupational exposure to nickel.
Lung cancer risk was determined on case ascertainment from 17 hospitals in Montreal, Canada. A statistically significant dose-related OR of 3.3 (95% CI =1.2 to 9.2) was reported for patients who were classified as stainless steel welders "exposed to nickel." Welders identified as having no nickel exposures did not have a statistically significant excess risk.
Lung cancer patients identified as nonwelders, but who were exposed to nickel, had a statistically significant OR of 2.9 (95% CI=1.3 to 5.7).
The potential for exposure to nickel and chromium were highly correlated, with 78 out of 79 cases exposed to both nickel and chromium.
Analyses were controlled for age, smoking history, socioeconomic status, ethnicity, and unknown hospital referral patterns. Occupational exposure to nickel was derived from the patients' responses to a semi-structured questionnaire administered by a team of chemists and industrial hygienists who were unaware of the cancer status. The cases were not controlled for a potential asbestos exposure.
A similar case comparison study was conducted by Breslow et al. [1954] of 518 lung cancer patients from 11 California hospitals during 1949-1952.
Of the 518 lung cancer patients, 14 (10 welders and 4 sheet metal workers) were classified as having occupations that exposed them to welding fumes.
Although no exposure data were presented, the 14 lung cancer patients were probably exposed to welding fumes associated with the use of arc welding and bare metal electrodes, because this was the primary method of welding prior to 1950.
An equal number of patients admitted to the same hospital but whose diagnosis was not cancer or respiratory disease, were used as controls and matched for age, race, and sex.
A questionnaire was given to lung cancer patients and the controls to determine occupations, tobacco use, and exposure to toxic materials. The 14 lung cancer patients who were probably exposed to welding fume represented a statistically significant (p<0.05) occupational group even after adjustment for cigarette smoking. Gottlieb [1980] observed a statistically significant OR of 1.19 for white and black males (combined) in a case-control study of lung cancer mortality among all workers employed in the Louisiana petroleum industry between 1960-1975. When the relative risks were determined for welders and were stratified by age at death, only the relative risk for welders under age 60 remained elevated at 0R=1.89 (95% Cl=0.5 to 7.4), suggesting an occupational etiology. Controls were selected from noncancer deaths and matched to the cases individually by sex, race, year of death, parish of residence, and age at death.
A survivor bias may have existed because of death certificate identification of the study population.
Smoking habits and the potential for asbestos exposure were not included in the analysis.
In an effort to determine the cause of the high rate of lung cancer among male residents of 11 coastal counties of Georgia, a case control incidence study was conducted by Blot et a l . [1978].
Cases were identified from hospital records, and death certificates were obtained for lung cancer patients.
Controls were selected from hospital admissions and death certificates, and were matched (two controls for every case) closely by sex, race, age, residence, and vital status.
A questionnaire was given to patients and controls (or the next of kin) to determine place, type, and length of employment for any job held for 6 months.
Patients who had been employed in a shipyard, had an OR of 1.6 (95% CI=1.1 to 2.3, p=0.006) for lung cancer.
The 11 patients who were welders or who were exposed to welding fumes had a crude relative risk of 0.7. Although the relative risk of those employed at shipyards was adjusted for cigarette smoking, asbestos exposure, age, race, and sex, the crude relative risk among welders was not adjusted and, therefore, may not be a reliable estimate of cancer incidence.
In contrast to the study reported by Blot et a l . [1978], Schoenberg et al. [1987] found an increased risk of lung cancer among welders employed in shipyards who had no reported asbestos exposure.
These results were observed in a case-control study that included 763 white males with histologically confirmed primary cancer of the trachea, bronchus, and lung and 900 general population white male controls.
All cases and controls were selected from six geographical areas of New Jersey with risk estimates determined by either job title or industry job title category.
The effects of smoking and other potential confounders were examined.
A more detailed analyses was conducted for shipbuilding workers and included comparisons of risk by job category and by reported exposure to asbestos.
Personal interviews of all cases and controls, or their next of kin, were conducted to collect demographic data, information on personal and environment risk factors, smoking history, and diet.
Of the 42 job title categories examined, 15 were considered to be at high risk, with printing workers, janitors, and cleaners having statistically significant (p>0.05) increased smoking-adjusted ORs; 11 had smoking-adjusted ORs of 1.3 or greater, while 4 categories with small numbers of subjects had crude ORs greater than 1.3. Of the 34 industry job title categories examined, 13 were considered to be at high risk.
Shipbuilding workers, as well as trucking service warehousing and storage workers, had statistically significant (p>0.05) increased smoking-adjusted ORs.
The risk for lung cancer among shipbuilding workers was found primarily among subjects with reported nonincidental asbestos exposure.
An increased OR both for latency of less than 30 years (OR of 3.9) and for latency of 30-39 years (OR of 1.7) was observed for these workers.
When shipbuilding workers were further analyzed by shipyard job category, welders were observed to have a statistically significant increased OR of 3.8 (95% Cl=1.8 to 7.8).
Of the 33 cases and 18 controls classified as welders, 16 cases and 7 controls were reported to have been exposed to asbestos.
When the remaining 17 cases and 11 controls who had no reported asbestos exposure were analyzed, an increased smoking-adjusted OR of 2.5 (95% Cl=1.1 to 5.5) remai n e d .
A case-control study was conducted by Olsen et al. [1984] to assess the elevated laryngeal cancer risk found among white males in Denmark, and to determine if any association existed between these cases and exposure to welding fumes. The study population was composed of 271 incident cases of cancer of the larynx and 971 population controls matched on date of birth, sex, and residence.
Patients and controls were interviewed to determine occupations, potential exposures, and tobacco and alcohol usage.
Based on the analysis of 271 cancer patients during 1980-1982, workers exposed to welding fumes had a statistically significant increased OR of 6.3 (95% C I =1.8 to 21.6) for cancer of the subglottic area of the larynx.
An elevated but not statistically significant OR of 1.3 (95% Cl=0.9 to 2.0) was observed for cancer of the larynx.
After adjustment for quantified tobacco and alcohol usage, the relative risks persisted.
When the study was restricted to 12 stainless steel welders, only the relative risk for subglottic cancer remained elevated with an OR of 6.7 (95% Cl=1.0 to 33.3).
Several of the epidemiologic studies demonstrated statistically significant increased risks for lung cancer among male welding populations [Breslow et al. 1954;HMSO 1978;Sjogren 1980;Beaumont and Weiss 1981;Milham 1983;Gerin et al. 1984;Steenland et al. 1986;Schoenberg et al. 1987;Sjogren et al. 1987].
Four of these studies showed statistically significant dose-response relationships, one with an increasing observation period and duration of welding exposure [Beaumont and Weiss 1981], two with exposures to nickel and chromium during welding of stainless steel [Sjogren 1980;Gerin et al. 1984;Steenland et al. 1986;Schoenberg et al. 1987;Sjogren et al. 1987], and a case control study [Schoenberg et al. 1987] of shipyard welders that was controlled for smoking and accounted for possible asbestos exposure.
In one study [Gerin et al. 1984], the contribution of cigarette smoking habits to lung cancer risks was used as a control, while the other study [Sjogren 1980] used a crude estimate of smoking habits (10% more welders who smoke) as the control.
The two other studies [Steenland et al. 1986;Sjogren et al. 1987] reaffirmed the excess risk of lung cancer observed by Beaumont and Weiss [1981] and Sjogren [1980]. Steenland et al. [1986] found an elevated risk of lung cancer among the study cohort reported by Beaumont and Weiss [1981] when they used an internal comparison group that shared similar lifestyles (e.g., smoking) and occupational exposures (e.g., asbestos).
Likewise, Sjogren et al. [1987] observed that the risk of lung cancer remained increased when the study group that was used in a previous study [Sjogren 1980] was compared to another group of welders who were exposed to lower concentrations of chromium.
The remaining three studies [Breslow et a l . 1954;HMSO 1978;Milham 1983] support an association between welding exposures and increased risk of lung cancer.
One of these three studies made adjustments for the contribution of cigarette smoking to the proportion of welders with lung cancer [Breslow et al. 1954],
The other two studies [HMSO 1978;Milham 1983], although based on national data sets, are relevant since analyses of these types of data are usually not considered sensitive enough to detect the kinds of complex relationships (exposure and effect) observed unless the disease is rare and the occupational association considerable.
In addition to the above cited studies, a study of welders in the Louisiana petroleum industry also showed a statistically significant lung cancer risk [Gottlieb 1980].
However, when the study group was adjusted for age, the OR was not statistically significant.
# (c) Summary-Respiratory Cancer
Five other mortality studies [Dunn and Weir 1968;Puntoni et al. 1979;Polednak 1981;Becker et al. 1985;Newhouse et al. 1985] found elevated risks for lung cancer among male welders.
Two of the five were cohort studies conducted on subgroups of white males who worked as welders at nuclear facilities [Polednak 1981] and at sanitary installations and power plants [Becker et al. 1985].
The larger of the two studies [Becker et al. 1985] indicated an OR of 1.7 for lung cancer that, although based on small numbers, remained increased in those workers with greater than 20 and 30 years employment.
The smaller cohort study [Polednak 1981] showed elevated SMRs for the two groups of welders who were exposed and not exposed to nickel oxides.
Although the welders not exposed to nickel oxides had a higher SMR, this increase could have been attributed to the higher prevalence rate (2.5 times) of smokers within the group as compared to the exposed group of welders.
Two of the mortality studies [Puntoni et Newhouse et al. 1985] were conducted on welders in shipyards.
These studies indicated elevated relative risks [Puntoni et al. 1979] and SMRs [Newhouse et al. 1985] for subgroups of welders and other occupational groups potentially exposed to welding fumes and gases.
However, neither smoking habits nor the potential for exposure to asbestos were taken into consideration in these two studies.
The last of the five mortality studies that showed an elevated risk of dying from lung cancer was a prospective study [Dunn and Weir 1968] that used mortality data collected from questionnaires and union records over a 5-year period.
A slightly elevated OR of 1.05 was observed when adjusted for age and smoking and compared with the death rates of the total union population.
No employment records were available and any potential exposures had to be derived from the questionnaires.
In a case control study [Blot et al. 1978] conducted to investigate the high rate of lung cancer among male residents of 11 Georgia coastal counties, a statistically significant increased OR of 1.6 was found for shipyard workers.
However, when cases were analyzed by occupations within the shipyard, a crude OR of 0.7 was observed for w e l d e r s .
An unusually high elevated risk of cancer (OR = 6.3) of the subglottic area of the larynx was found among 271 cancer patients of whom 42 had been exposed to welding fumes [Olsen et al. 1984].
The high OR persisted after adjustment for tobacco and alcohol use but was found not to be statistically significant when restricted to twelve stainless steel workers.
None of the other epidemiologic studies found an elevated risk of larynx cancer.
Several of the studies that explored the relationship between exposure to welding fumes and gases and the incidence of mortality from lung cancer among welders, suffered from one or more of the following methodologic problems:
(1) incomplete information on the extent of exposure, requiring estimations of these exposures from job titles, (2) insufficient cohort size and person years to observe elevated risks of lung cancer, and ( 3) confounding variables such as smoking and exposure to asbestos.
These limitations make it difficult to draw definitive conclusions about the cause of cancer excesses observed within each study.
However, collectively these studies demonstrate an elevated risk of lung cancer among welders that is not completely accounted for by smoking or asbestos exposure, and that appears to increase with the latent period from onset of first exposure and duration of employment.
Additionally, a few of the studies suggest a strong association between lung cancer risk and exposures generated while welding on stainless steel. This association could be attributed to the carcinogenic properties of the nickel and chromium found in the fume.
An overview of each evaluated study is presented in Tables IV-2 through IV-4.
# b. Kidney and Other Urinary Tract Cancers
The cohort mortality studies conducted by Puntoni et a l . [ ], Milham [1983, and Becker et al. [1985] have shown a statistically significant increased risk of kidney or other urinary tract cancers in welders.
The study by Puntoni et al. [1979] of shipyard workers showed ORs of 5.06 (p<0.05) and 5.88 (p<0.05) for cancer of the kidney and other urinary organs in gas welders when compared to the male population of Genoa, Italy and the male staff at St. Martino Hospital, respectively.
Although the ORs were elevated for these cancers in electric welders, they were not statistically significant.
When all shipyard workers were grouped and compared with either comparison population, the elevated ORs for these cancers were found to be statistically significant (p<0.0005).
Similarly, the study reported by Milham [1983] showed statistically significant (p<0.01) increased PMRs for kidney cancer in male welders and flamecutters who had been employed in Washington State. Welders and flamecutters analyzed during the period 1970-1979 and for the total observation period 1950-1979 had PMRs of 234 and 182, respectively.
The observations of Becker et al. [1985] were consistent with these findings with an OR of 15.0 (3 observed versus 0.2 expected) for kidney and other urinary tract cancers in welders when compared with the German national death rates.
Although it was not reported by the authors, NIOSH calculated a p value of 0.002 (95% C l =3.09- 43.83).
Several of the studies that explored the relationship between exposure to welding fumes and gases and the incidence of mortality from lung cancer among welders, suffered from one or more of the following methodologic problems:
(1) incomplete information on the extent of exposure, requiring estimations of these exposures from job titles, (2) insufficient cohort size and person years to observe elevated risks of lung cancer, and ( 3) confounding variables such as smoking and exposure to asbestos.
These limitations make it difficult to draw definitive conclusions about the cause of cancer excesses observed within each study.
However, collectively these studies demonstrate an elevated risk of lung cancer among welders that is not completely accounted for by smoking or asbestos exposure, and that appears to increase with the latent period from onset of first exposure and duration of employment.
Additionally, a few of the studies suggest a strong association between lung cancer risk and exposures generated while welding on stainless steel. This association could be attributed to the carcinogenic properties of the nickel and chromium found in the fume.
An overview of each evaluated study is presented in Tables IV-2 through IV-4.
# b. Kidney and Other Urinary Tract Cancers
The cohort mortality studies conducted by Puntoni et a l . [ ], Milham [1983, and Becker et al. [1985] have shown a statistically significant increased risk of kidney or other urinary tract cancers in welders.
The study by Puntoni et al. [1979] of shipyard workers showed ORs of 5.06 (p<0.05) and 5.88 (p<0.05) for cancer of the kidney and other urinary organs in gas welders when compared to the male population of Genoa, Italy and the male staff at St. Martino Hospital, respectively.
Although the ORs were elevated for these cancers in electric welders, they were not statistically significant.
When all shipyard workers were grouped and compared with either comparison population, the elevated ORs for these cancers were found to be statistically significant (p<0.0005).
Similarly, the study reported by Milham [1983] showed statistically significant (p<0.01) increased PMRs for kidney cancer in male welders and flamecutters who had been employed in Washington State. Welders and flamecutters analyzed during the period 1970-1979 and for the total observation period 1950-1979 had PMRs of 234 and 182, respectively.
The observations of Becker et al. [1985] were consistent with these findings with an OR of 15.0 (3 observed versus 0.2 expected) for kidney and other urinary tract cancers in welders when compared with the German national death rates.
Although it was not reported by the authors, NIOSH calculated a p value of 0.002 (95% C l =3.09- 43.83).
As described earlier in this Chapter in Section B,2,a(2)(a), these three studies had a number of methodologic problems, including a lack of information on potential occupational exposures.
Because of these limitations, the possible etiology for these observed cancers is difficult to assess.
# c. Reproductive Effects
Adverse reproductive effects (e.g., infertility or spontaneous abortions) have been reported by Rachootin and Olsen [1983] and Lindbohm et al. [1984] for both men and women who were either employed as welders or who were potentially exposed to metals.
A case-control study was conducted by Rachootin and Olsen [1983] to determine whether an association existed between delayed conception or infertility and the occupations of women and their husbands.
The study population was identified from the inpatient register at a large Danish hospital; 1,069 case couples and 4,305 comparison couples were identified as study candidates.
Case couples were undergoing evaluation for fertility problems, and the female partner had been admitted to the hospital for testing during the period 1977 to 1980. Comparison couples had had a healthy child born at the same hospital during the period 1977 to 1979.
A questionnaire was mailed, and responses were received from 87% of each group (927 case and 3,728 comparison couples).
All information on a couple was solicited from the woman.
Three types of analyses were conducted.
The first analysis compared the reported occupational exposures of the case and comparison couples residing in the hospital's direct catchment area (Table IV -6).
In this analysis, comparison couples were limited to those of the 3,728 comparison couples who were the parents of a healthy child conceived within 1 year.
The case couples were restricted to those of the 927 case couples who were examined or treated for infertility of at least 1 year's duration. This analysis examined three subgroups of case couples:
(1) those with a male partner having abnormal sperm number, motility, or shape, (2) those with a female partner having hormonal disturbances, and (3) those with idiopathic infertility.
The first two subgroups had medical histories that were potentially related to occupational ex p o s u r e s .
The second analysis compared the reported occupational exposures of case couples (Table IV-7).
The three subgroups from the first analysis were compared with infertile case couples having conditions that were unlikely to be caused directly by occupational exposures (e.g., varicocele or history of mumps as an adult in the male, or blocked fallopian tubes or endometriosis in the female).
The third analysis compared two subgroups within the original comparison group of couples who had had a healthy child born at the study hospital during the period 1977 to 1979. One subgroup was made up of comparison couples who had given birth to a healthy child after a conception delay of more than 1 year, and the second subgroup comprised the remaining comparison couples who had conceived a healthy child within 1 year.
A variety of potentially important occupational exposures were considered in the analysis, and those relevant to the welding environment are shown in Tables IV-6, IV-7, and IV-8.
In both the first analysis (Table IV-6) and the third analysis (Table IV-8), significantly elevated ORs were seen for a variety of occupational exposures associated with welding.
Exposure to heat and noise was consistently associated with elevated ORs.
Exposure to heavy metals and welding (either on stainless steel or other metals) was also associated with elevated ORs.
Both men and women who were assigned to the exposure category "Welding of Other Metals" in the third analysis (Table IV-8) had a statistically significant increase (p<0.05) in delayed conception, with ORs of 1.4 (95% C I =1.1-1.8) for men and 2.4 (95% CI=1. 1-5.1) for women.
This risk was still statistically significant for women after adjustment for age and education, parity, area of residence, smoking habits, alcohol consumption, and past use of oral contraceptives.
In contrast, men and women who were assigned to the exposure category "Welding of Stainless Steel" had no statistically significant increase in delayed conception.
In the second analysis (Table IV-7), none of the exposures potentially encountered in the welding environment were associated with elevated ORs. Lindbohm et al. [1984] evaluated possible influences of paternal or maternal occupations and exposures on spontaneous abortion by linking discharge records from Finnish hospitals with national census data.
For the period 1973 to 1976, data were available for 294,309 pregnancies.
Census data on occupations were used to form seven categories of presumed exposure to specific agents (animal microorganisms, solvents, polycyclic aromatic hydrocarbons, automobile exhaust fumes, other chemicals, metals, textile dust). Because the census data referred to occupations in 1975, the analysis of spontaneous abortion was limited to pregnancies in 1976. Women in these exposure categories were compared with all other "economically active" women, and wives of exposed men were compared with wives of nonexposed men. A logistic regression model was used to control for age, place of residence, parity, marital status, and age-parity interaction.
None of the specific exposures were associated with a significantly increased odds ratio.
The odds ratio was 0.78 (95% C I =0. 54-1.13) for women exposed to metals (iron and metalware workers; smelting, metallurgic, and foundry workers; miners and quarry workers).
For the wives of similarly exposed men, the OR was significantly reduced to 0.86 (95% C I = 0 . 7 5 -0 . 9 5 ) . Lindbohm et al. [1984] also used the pregnancy data for the period 1973 to 1976 to investigate spontaneous abortion by occupation. Women in five occupations had elevated ORs, but none appeared to be related to the welding environment. One of four occupations associated with increased ORs for the wives of exposed men was "metal-plate and constructional steel workers" with an OR of ).
This occupational category was not described in any further detail except for the comment that these men "are occasionally exposed to chromates and nickel." No information was available on smoking habits and alcohol consumption. Potential occupational exposures were assigned based on employment history.
The significance of the results from these two studies [Rachootin and Olsen 1983;Lindbohm et a l . 1984] is questionable given the studies' limitations (e.g., estimation of exposures and confounding exposures of smoking or alcohol consumption).
# d. Cardiovascular Effects
A few case reports indicated that exposure to welding fumes and gases may cause acute cardiac episodes or aggravate preexisting cardiovascular diseases in welders [Beintker 1932;Jacobi 1934]. In these case reports, welders worked in confined spaces with poor ventilation. No information was given as to the types of metal being welded or exposures being generated.
Two of four mortality studies cited previously in this Chapter in Section B, 2, a,( 2),(a) reported increased risks of cardiovascular disease in welders employed at shipyards [Puntoni et a l . 1979;Newhouse et al. 1985]. Newhouse et al. [1985] observed an increased SMR of 130 (90% CI=104-156) for ischemic heart disease in welders, whereas Puntoni et al. [1979] reported ORs greater than 1.00 for a similar cohort of welders.
Neither study was adjusted for smoking and no conclusions were drawn by the authors as to the relevance of the elevated risks. One of the other two mortality studies [Mi I ham 1983] reported a PMR of 97 for welders and flame cutters when analyzed for the total study period of 1950-79; the other study [Polednak 1981] showed SMRs of 70 and 82 for welders exposed and nonexposed to nickel oxide fumes, respectively.
The slightly higher SMR of the nonexposed group of welders could be attributed to the 2.5 times greater percentage of cigarette smokers reported among this group.
# e. Gastrointestinal Effects
Gastrointestinal disorders in welders experiencing metal fume fever usually take the form of nausea, vomiting, and gastrointestinal cramps [Rohrs 1957;Papp 1968].
These effects appear to subside within 24 to 48 hr after acute exposure to welding fumes.
Two cases of gastrointestinal disorders were reported by Rieke [1969] in workers performing oxyacetylene torch cutting of scrap metal.
Both men had been employed in a ferrous metal scrap yard where they disassembled and cut large (often painted) metal parts. The men complained of back and lower abdominal pains, poor appetite, and constipation after being exposed for several days to metal fumes. Urinary lead analysis revealed markedly elevated lead levels (e.g., 0.44 and 0.43 mg lead/liter) and both men were treated for lead intoxication and given calcium disodium edetate for several days.
Following this period of treatment all gastrointestinal disorders ceased.
The workers' health problems were attributed to exposure to lead contained in the paints.
In three epidemiologic studies [Mignolet 1950;Stancari and Amorati 1963;Rozera et al. 1966], an increased incidence of digestive disorders in welders was reported.
Rozera et al. [1966] reported that 22% of a population of 620 welders had digestive system disorders compared with 12% found in the general industrial population. Mignolet [1950] reported similar finding among 216 welders who were placed into three groups according to the welding process they used.
Thirty-five out of 85 (41%) shielded metal arc welders complained of digestive disorders, including loss of appetite, slow digestion, and nausea.
Two out of 99 (2%) oxyfuel gas welders had gastric ulcers.
Two out of 32 (6.3%) oxyacetylene cutters had symptoms of gastrointestinal disorders.
These disorders were attributed to the inhalation of fumes from certain types (unspecified) of covered electrodes because no similar effects were noted in welders who used bare metal electrodes. Most of the symptoms associated with digestive disorders disappeared during weekends and vacations.
Gastroduodenopathies were reported by Stancari and Amorati [1963] in 264 arc welders aged 17 to 58 years.
Of the 264 arc welders, 67% of those with over 10 years work experience, 43% of those with 3 to 10 years work experience, and 15% of those with less than 2 years exper i ence had gast r i t i s , gast roduoden i t i s , or gast roduodenaI ulcer.
The authors concluded that the inhalation of fumes and gases associated with arc welding caused the gradual development of chronic gastritis and gastroduodenitis among welders.
These ulcers were described as moderate and responded well to treatment; as soon as welding was discontinued, regression occurred.
The authors further stated that the specific cause of these ulcers was unknown.
Houten and Bross [1971] reported on the relative risk of cancer among male patients at a regional cancer institute.
Cancer patients were compared with other admitted male patients who did not have neoplastic disease in an attempt to ascertain if specific types of cancers were associated with certain occupations.
Three cases of stomach cancer were noted among welders and flamecutters, for an OR of 2. 5. This cancer incidence was not statistically significant due to the small number of observed cases.
In contrast, several of the mortality studies [Milham 1983;Puntoni et al. 1979;Polednak 1981;Becker et al. 1985] discussed previously in this Chapter in Section B, 2, a,( 2),(a) reported no increases in welder mortality as a result of cancer or other diseases of the digestive system.
# f. Ophthalmologic Effects
Persons who are involved in or working near welding processes are at risk of eye injury from metal spatter and exposure to nonionizing electromagnetic radiation in the UV to IR wavelengths [NIOSH 1972a;Marshall et a l . 1977].
Exposure to UV radiation from the welding arc can result in acute keratoconjunctivitis, also known as arc eye, welder's flash, or actinic ray photokeratitis. This inflammatory disorder affects the outer structure of the eye (cornea, conjunctiva, iris) and causes blurred vision, lacrimation, burning pain, and headache [NIOSH 1972a;Palmer 1983]. These symptoms usually appear within 4 to 12 hr after the beginning of the exposure and last up to 2 days.
The visible radiation emitted during welding can penetrate the eye and be absorbed by the retina and choroid causing retinal injury [Palmer 1983;Marshall et al. 1977].
Similarly, exposure to the IR radiation wavelength can cause thermal damage to the cornea and aqueous humor of the eye and has been associated with the formation of lenticular cataracts [Palmer 1983].
These types of adverse ocular effects have been reported in welders who were wearing improper eye protection or no protection at all [Minton 1949;Sykowski 1951;Entwistle 1964;Karai et al. 1984].
In one study [Entwistle 1964], 31 eye injuries were reported that were caused by contact with hot slag, metal chips, sparks, and hot electrodes.
Several of the injuries involved workers assisting welders, and others involved welders who had been provided with approved types of faceshields but did not use them properly. Golychev and Nikatina [1974] also reported that because eye protection was not used, cataracts occurred in a 42-year-old welder's helper who had regularly assisted electric arc welders for 19 years.
This worker reportedly suffered from welder's flash and conjunctivitis 3 to 4 times a month.
Other studies [Minton 1949;Sykowski 1951] have reported similar cases of retinitis and dendritic keratitis in welders who did not protect their eyes while igniting their arcs.
In a case control study of 118 welders, a statistically significant (p<0.05) increase was observed in damage to the corneal epithelium and endothelium of the eye when compared to 85 nonwelders [Karai et a l . 1984].
The increase in eye injuries was attributed to exposure to ultraviolet radiation.
Two studies [Mignolet 1950;Gupta and Singh 1968] have reported on the evaluation of visual acuity of welders.. The visual acuity was evaluated in a group of 520 welders, of whom approximately 76% were under 40 years of age; 23% of the study group worked for 20 years and 20% worked up to 30 years [Gupta and Singh 1968].
Eye complaints that included watering, blurred vision, burning, soreness, and haziness were reported by 60% of the welders.
The principal clinical conditions, reported in descending order of frequency, were conjunctivitis (45%), keratoconjunctivitis (11%), pterygium (7%), incipient cataract (7%), edema of the lids (5%), brown pigmentation around the cornea (4%), trachoma (2%), corneal opacity (2%), and dilated pupils (2%).
The two most common eye injuries were imbedded foreign bodies in the eye (21%) and burns of the conjunctiva (4%). Almost all the welders had suffered from arc flash at least once.
Visual acuity in 33% of the welders was at the minimum accepted acuity for welders (20/30).
Serious visual impairment was observed in 20%; substandard acuity of 20/60 or less was present in 59% of the welders; and defective muscle balance of the eyes was noted in 78%.
# The percentage of welders with defective visual performance increased with age.
A similar investigation of visual acuity was made in a group of 216 welders [Mignolet 1950]. Although the types of tests conducted were not stated, unilateral and bilateral alterations in visual acuity were reported for 41% of the oxyfuel gas welders, 47% of the oxyacetylene cutters, and 58% of the arc welders.
Two cases of cataracts were also noted. No control groups were used in either study for comparison of visual acu i t y .
# g. Dermatologic Effects
Dermal effects related to welding processes may result from exposure to UV radiation [Grimm and Kusnetz 1962;Pattee et al. 1973;Balabanow et al. 1967;Roquet-Doffiny et al. 1977;Ross 1978] and IR radiation [Lydahl 1984;Moss et al. 1985], from hot metal spatter [Britton and Walsh 1940;Entwistle 1964;CDLSR 1975], and from sensitization to metals [Kaplan and Zeligman 1963;Fregert and Ovrum 1963;Shelley 1964;Kalliomaki et al. 1977].
Exposure of the welder's skin to UV radiation can result in skin burns similar to sunburn.
According to a review by Pattee et al. [1973], the most common sites for such burns are the arms, hands, neck, and chin. Ross [1978] also noted that the front and sides of the neck were the most common sites for such burns.
In a clinical investigation conducted by Dreesen et al. [1947], 25% of 3,255 arc welders had burns or scars from burns on their bodies.
Similar findings were noted by Entwistle [1964] who reported that over 50 cases of burned fingers, wrists, hands, elbows, arms, and legs occurred among welders during an 8-month period.
The cause of those burns was attributed to metal spatter, hot slag, and the flame from oxyacetylene torches.
Several case reports have documented the occurrence of chronic dermatitis among welders and other persons working near welding processes [Shelley 1964;Balabanow et a l . 1967;Roquet-Doffiny et al. 1977]. Balabanow et al. [1967 reported a case of dermatitis in a welder who had been in this occupation for 35 years.
He suffered from edema of the eyelids and redness of the face and neck, the scalp, upper chest, back of hands, forearms, and the lower extremities.
A series of clinical tests revealed no pathologic cause for these effects other than welding.
A similar finding was reported by Shelley [1964] for a 40-year-old crane operator who worked near welding operations and had had recurrent eczematous eruptions on both hands for 14 years.
Roquet-Doffiny et al. [1977] reported a severe case of chronic actinic dermatitis, erythema, atrophic plaques, telangiectasis, and pruritic keratotic lesions for a welder who had been performing oxyacetylene gas welding for 30 years.
In addition, over a 4-year period, eight tumors were removed from his face and neck-five basal cell carcinomas and three squamous cell carcinomas.
Exposure to radiation and welding fumes and gases was reported in all three reports as the causative factor in the observed skin diseases.
When workers discontinued welding or were removed from the work environment where welding was being performed, dermatitis ceased. Among welders, a number of cases involving chromium skin sensitization have been reported [Fregert and Ovrum 1963;Kalliomaki et al.1977]. Kalliomaki et a l . [1977] reported a case of chromium sensitivity involving dermal allergy and asthma for a welder who typically welded on stainless steel. After the individual welded on stainless steel for about 1 hr, bronchial obstruction was observed that, according to the investigator, demonstrated severe sensitivity to the fume exposure. Measurements of airborne hexavalent chromium revealed concentrations of 0.02 to 1.7 mg/m^. A similar finding was reported by Fregert and Ovrum [1963] for a welder who experienced repeated episodes of facial contact dermatitis while welding. The welder was found to be sensitized to chromium that was emitted while he welded on stainless steel or from the welding rod that contained trace amounts of chromium.
The dermatitis disappeared after the welder ceased his exposure to welding fumes that contained chromium.
# h. Auditory Effects
Hearing loss among welders has usually been due to traumatic injury [Frenkiel and Alberti 1977] or to excessive sound pressure [Hickish and Challen 1963;Bell 1976]. Frenkiel andAlberti [1977] reviewed 11 cases of middle ear trauma resulting from burns, including 5 such cases in welders.
The eardrums of the welders were perforated by flying sparks or pieces of metal during welding processes.
In four of the five cases, hearing loss was permanent.
Auditory impairment from exposure to excessive noise levels may occur during arc air gouging of metal, and plasma torch processes [Hickish and Challen 1963;Bell 1976]. Bell [1976] reported that a considerable risk of noise-induced deafness was possible among a group of welders during arc air gouging in which sound level measurements exceeded 115 dbA. Hickish and Challen [1963] noted a mean temporary hearing loss in both ears of 19 dB at 4,000 Hz and up to 35 dB at 8,000 Hz in three persons who were exposed to the noise from a plasma torch for 1 hr. In one person, recovery of normal hearing took 48 hr.
# i. Musculoskeletal Effects
Welding is a static type of work that usually requires customary postures and considerable shoulder joint motion.
Shoulder pain may be caused or aggravated by welding.
Complaints of shoulder pain are very common among older welders, according to observations by Herberts and Kadefors [1976], who investigated the clinical and radiological features of shoulder pain in 10 shipyard welders aged 50 to 65 years.
An electromyographic (EMG) evaluation of the impact of static loading on their shoulder muscles was also conducted.
The most consistent finding was reduced muscle power and shoulder pain. All subjects had normal shoulders upon inspection, but mild local tenderness of the rotator cuff was always present. Measurement of the isometric muscle power revealed reduced power in the painful shoulder in abduction, outward rotation, and flexion.
The radiographic appearance was normal in only 3 of the 10 subjects. Analysis of EMG signals recorded during actual overhead welding revealed significant changes in the action potential of the supraspinatus muscle, implying that this muscle is under sustained heavy strain in this working situation. Kadefors et al. [1976] also studied the effect of overhead welding on muscles of the shoulder in 20 welders aged 20 to 35 years.
An inexperienced group consisted of 10 men with less than 1 year of welding experience, and the experienced group consisted of 10 men who had been working for more than 1 but less than 5 years. Among the inexperienced workers, overhead welding resulted in EMG changes indicative of localized fatigue in the deltoid, upper trapezius, and supraspinatus muscles.
Experienced welders demonstrated some adaptation but still had abnormal EMG readings for the supraspinatus muscles.
The authors concluded that overhead welding places considerable amounts of strain on this muscle, which cannot be overcome by experience and training. Petersen et al. [1977] reported similar findings in a third study. Those observed included 10 experienced workers with at least 5 years of experience and 10 inexperienced welders with less than 1 year of training. After overhead welding, all experienced welders and a few inexperienced welders (number not given) showed increased fatigue of the supraspinatus muscle.
A subset of older welders complaining of shoulder pain was tested further.
Clinical examination (X-ray) showed diminished strength in shoulder movements in which the supraspinatus was active, and clear signs of supraspinatus tendinitis.
However, it was emphasized that the tendinitis may have been caused by long exposure or as a consequence of natural changes from age in combination with overhead welding.
Ross [1978] reported on the results of medical examinations of 926 shielded metal arc welders; all were male, had heavy engineering and shipbuilding experience, and had been observed for 6 years. These findings were compared with the results of medical examinations of 755 nonwelders who were used as controls.
Chronic conditions encountered included occupational hearing loss, Raynaud's phenomenon, and Dupuytren's contracture.
Raynaud's phenomenon, also called white finger disease, affected 102 (11%) of the welders, compared with 7 (1%) of the nonwelders.
It was associated with the use of vibratory tools but was considered by the author to be relatively minor in nature.
Dupuytren's contracture, a flexion deformity of the finger, which the author reported as not usually occupational in origin, was found in 38 (4%) of the welders and 4 (0.5%) of the controls.
The author speculated that it could be caused by tightly gripping the electrode holders. Nauwald [1980] studied knee joint changes in 100 welders (type not stated) in the shipbuilding industry.
Sixty-nine of the 100 welders complained of spontaneous pains in the knee joints.
These included pain during motion, pain when starting to move, pain during hypercompression of the joint, and the so-called "giving-away" phenomenon.
Arthritis, proliferation of fatty tissue in knee joint, and fluid sac diseases were observed with increasing frequency in welders who were older than 25 and had a minimum exposure time of 6 years.
The author stated several potential causative factors in the development of the observed knee joint diseases:
(1) the static-mechanical stress on the bent knee while working, (2) the chronic, persistent pressure on the soft parts of the joint, and ( 3) thermal effects such as cooling due to kneeling on cold iron for an extended period of time.
# C. Safety Hazards
In addition to being exposed to chemical and physical agents, welders are also exposed to potential safety hazards that may result in injury or death. In a cross analysis, the source of injury was cross-tabulated with type of accident, nature of injury, and body part. The analysis of the SDS accident/injury data was performed for the top 10 source-of-injury categories that identified tools, tasks, or equipment used by welders and thermal cutters.
A total of 166,907 injuries were reported to the SDS data base from welders and thermal cutters during the period 1976-1981; 109,774 of these injuries were included in the cross analysis and reported in Table IV-9. The SDS data do not include any information on the cause of the injury.
The Bureau of Labor Statistics [1983] obtained data from 18 States on welding-and cutting-related injuries for 1,364 workers that occurred during a 5-month period in 1978.
Forty-two percent of the reported injuries during this period occurred in welders or cutters who had 5 or more years of experience; 92% of these welders and cutters had received safety training in the form of classroom or on-the-job safety training or written material about welding or cutting safety measures.
Arc welding or cutting was being performed when two-thirds of these injuries occurred, and 83% had received safety training in the use of this equipment.
Sixty-seven percent of the reported injuries were to the eye(s); 58% of the burns to the eyes resulted from welding being performed in the nearby work area; 50% of all eye injuries occurred as a result of not wearing filtering lenses to protect the e y e s .
Injury of workers by industrial welding robots has also occurred. Specific types and the number of injuries reported for welders involved in these types of processes are not available; however, this kind of information is being gathered by the Division of Safety Research, NI0SH [NI0SH 1985]. According to Percival [1984, the six main sources of hazards from industrial robots are as follows:
(1) control errors caused by errors in the software, faults within the control system, or electrical interference;
(2) unauthorized access to robot enclosures; (3) human error when working close to a robot; (4) electrical, hydraulic, and pneumatic faults;
(5) mechanical hazards from the function of the robot (e.g., welding hazards); and (6) environmental hazards (e.g., dust, fumes, radiation). Although specific controls for these hazards are not addressed in this document, many of the measures recommended for controlling emissions generated at other welding processes can be applied to industrial welding robot operations. Some of the specific safety hazards associated with welding processes are fires, explosions, or electric shocks.
The following are case reports of injuries and fatalities resulting from such hazards.
# F i res
The fire hazards caused by either the welding flame itself or flying sparks have been responsible for injuries and fatalities of workers [NFPA 1977;Buhrer and Brunschwiler 1978].
Fires associated with oxygen-enriched atmospheres provide dramatic examples of the risks involved when there is either enrichment of the air by oxygen in enclosed spaces or leakage of oxygen.
Accidents have also been reported when air has been intentionally enriched (sweetened) before welding to purge the air of contaminants.
Three fires in oxygen-enriched atmospheres were reported by Rames [1976].
The first occurred inside a storage tank where a welder was making repairs by electric arc welding.
He enriched the inside atmosphere with oxygen from a cylinder outside the tank.
His assistant went inside to help instead of keeping watch outside.
After 20 min, their clothing suddenly ignited, and although they succeeded in getting out of the tank, they both died on the way to the hospital.
The second case report was of a welder who went down a deep well to cut a rusty suction basket from a pump.
Before he descended, he fed oxygen instead of compressed air into the well because he thought there might be dangerous gases present. When he started to cut, his clothing burst into flames and he fell into the water.
His assistant, who was watching, was unable to help.
The welder was dead when he was removed from the well.
The third case was that of a welder and his assistant who were arc welding while repairing pipelines inside a small channel. Their clothing suddenly caught fire, and even though they were being observed from the outside by others, they died before they could be rescued.
Investigation of the accident revealed that they were using oxygen from the cutting equipment to sweeten the air.
The National Fire Protection Association (NFPA) [NFPA 1977] reviewed reports of several fires caused by cutting and welding equipment. During repairs of an underground missile silo, a welder struck and caused a rupture to a temporarily installed, high pressure hose containing hydraulic oil.
The oil escaped as a fine mist and ignited at the electric arc.
Although the fire was of short duration, it killed 53 of the construction workers trapped in the confined silo space.
The California Division of Labor Statistics and Research (CDLSR) [CDLSR 1975] also described several fires resulting from welding.
An auto dismantler was using an acetylene torch to cut the metal straps holding a fuel tank in place.
The tank fell to the ground and pulled off the filler spout.
Sparks from the torch ignited the fuel in the tank. The dismantler sustained second-degree burns on his hands and face.
In another occurrence, a man was burning and cutting scrap metal.
The oxygen hose caught fire and caused the worker to drop the torch, breaking the fitting. Oxygen went up his pants leg, which ignited.
In another incident, a ladle helper was holding an oxygen hose while another worker was cutting with a torch. The oxygen accumulated in the worker's glove, ignited the glove, and burned his right hand.
# Explosions
Explosions caused by welding sparks igniting flammable or explosive materials are a potential problem associated with all welding processes.
A mixture of acetylene with air containing more than 2.5% or less than 80% acetylene is explosive [Compressed Gas Association 1966].
Fire resulting from an explosion occurred in the cooling plant located in the basement of a newly erected hospital [Buhrer and Brunschwiler 1978].
A chief electrician and an electrical fitter were installing wiring for an electrical plant.
The chief electrician who had on-the-job experience had not received any formal welding training. While cable supports were being welded from a ladder, sparks fell to the floor igniting a rag lying on a varnish can. An explosion occurred and both workers were immediately surrounded by flames.
The welder on the ladder was able to escape.
His coworker who was unable to escape suffered extensive burns.
The NFPA [1977] described several explosions caused by welding that resulted in death.
In one case, a workman using a torch to cut an object on the top of a drum containing kerosene cut into the drum and the oil exploded, fatally burning him.
In another case, after partially unloading a tanker of asphalt stored at a temperature of about 143°C (290°F), two workmen went to the top of the tank to straighten the pipe through which they measured the oil level. They were using an acetylene torch that ignited the leaking vapors and caused an explosion that killed both men.
In another reported incident, three welders were killed as a result of an explosion that occurred while they were repairing a leak in an odor-scrubbing system.
Heat from the torch had ignited flammable vapors within a connecting pipe, and the flame was propagated to the tank that contained naphthalene.
The tank ruptured, killing all three workmen.
Several explosions were reported in the CDLSR description of welding accidents [CDLSR 1975].
Some of these occurred in atmospheres enriched by oxygen and some occurred when sparks caused the ignition of flammable vapors or liquids that had leaked from hoses or containers.
# Electric Shocks
Because currents of 100 to 600 A at 30 to 60 V, either AC or DC, are used in welding, shocks to workers have resulted in falls causing serious injuries or deaths [Britton and Walsh 1940].
The usual practice in welding operations is to have the work grounded to one terminal of the power supply while the electrode holder is connected to the other terminal.
Fatalities have resulted from a current passing through the body when the worker stepped on the "live" electrode, while in contact with the other terminal of the current. Careless handling or changing of electrodes has also resulted in serious injuries and fatalities.
Five welding-related deaths from electrocution occurring between 1956 and 1975 were reported by Simonsen and Petersen [1977]. One case involved a 37-year-old electric arc welder who was working in a confined space where the temperature was 35° to 40°C (95° to 104°F). He had perspired heavily and had removed one glove.
The welder developed severe spasms, apparently from an electrical contact, was hospitalized, and died a short time later. Burnlike lesions were found on his lower right cheek, left thigh, and left hand.
Another welder was presumably attempting to ignite his cutting torch by drawing a spark from the welding apparatus while the transformer was operating.
He suddenly fell and died a short time later. The authors provided no information on the type of protective clothing worn. Electrical malfunction of the welding machine was not a factor in this fatali t y .
In a third reported fatality, a 22-year-old man was welding a metal plate onto the hull of a ship while standing on a platform located about 50 cm above the water surface.
He had been working for 4 hr when he lay down to weld on the edge of the plate.
A large wave immersed the platform, and the welder's hand holding the welding device was submerged in water.
He died from electric shock.
In 1974, a 47-year-old welder was found dead at his workplace. He had been welding on the floor of a small compartment that measured 70 x 73 x 105 cm.
There was a small amount of water on the floor of the compartment.
When he was found, the welding tool was in his right hand and the end of the welding electrode had slid under the face mask and up under his glasses near the left eye. At autopsy, a burnlike perforation of the median sclera of the left eye was found.
In 1975, a 47-year-old man was found dead in a section of a ship where he had been welding.
He was found lying on his back against the side of the ship with the welding tool in his left hand and the tip of the electrode pointing toward his throat.
His helmet and mask lay beside him.
It was very hot in the area where he had been working, and his clothing was soaked with perspiration.
# V. BASIS FOR THE STANDARD
# A. Introduction
This chapter summarizes the studies used by NIOSH to form the basis of its recommended standard for welding, brazing, and thermal cutting. NIOSH believes that the studies discussed here provide the best available evidence of the association between adverse health effects and welding.
The results of these studies are summarized briefly in the following subsection; they are described and fully referenced later in the chapter.
# B . Summary
Analysis of data obtained from welders reveals several types of adverse effects associated with various welding processes.
The respiratory system is the primary target of injury. Metal fume fever and pneumonitis are the most common acute respiratory diseases associated with welding as a result of short-term exposures to high concentrations of fumes and gases.
Chronic respiratory diseases such as cancer, pneumoconiosis, and bronchitis have been observed among welders exposed to welding fumes and gases (and possibly to asbestos in some instances over long periods).
In addition to respiratory diseases, cancers of the kidney, and other urinary tract organs, and the subglottic area of the larynx have been described in such workers. Other health effects and injuries reported include cardiovascular and gastrointestinal diseases, skin sensitization, hearing loss, and eye and musculoskeletal injury.
Some evidence indicates a possible relationship between adverse reproductive outcomes and exposure to welding fumes. Because of the diversity of welding techniques, processes, and materials used, most of these studies lack sufficient information to associate a specific chemical or physical agent with a particular health effect.
# C. Malignant Diseases
# Lung Cancer-Epidemiologic Studies a. Exposure to Fumes from Welding on Stainless Steel and Other Metal Alloys
Statistically significant increases in the rates of lung cancer have occurred among welders exposed to fumes and gases generated from welding on stainless steel [Sjogren 1980;Gerin et al. 1984;Sjogren et al. 1987] and other metal alloys [Breslow et al. 1954;HMSO 1978;Beaumont and Weiss 1981;Milham 1983;Steenland et al. 1986;Schoenberg et al. 1987].
In four of these studies, exposure-response relationships were demonstrated [Sjogren 1980;Beaumont and Weiss 1981;Gerin et a l . 1984;Schoenberg et al. 1987]. Steenland et al. [1986 and Sjogren et al. [1987] reaffirmed the excess lung cancer risk when they reanalyzed the studies by Beaumont and Weiss [1981] and Sjogren [1980], respectively. Beaumont and Weiss [1981] reported excess cancer rates that increased with the duration of welding exposure and the length of time from onset of first exposure.
A standard mortality ratio (SMR) of 132 (p=0.06) was observed for deaths from lung cancer among welders compared with those for U.S. white males.
The SMR for deaths from lung cancer was 174 (p<0.001) when calculated on the basis of deaths that occurred 20 or more years after first welding exposure or initial employment as a welder.
This study cohort was reanalyzed by Steenland et al. [1986] using an internal comparison group who more closely matched the lifestyles (e.g., smoking habits) of the welders and who were potentially exposed to the same occupational hazards (e.g., asbestos).
The lung cancer risk remained statistically significant, with an OR of 152 (p=0.03) when duration of exposure was measured using the year the worker was first employed as a welder.
An OR of 1.29 (p=0.03) for lung cancer was also observed for welders as a function of increasing cumulative exposure.
Two studies [Sjogren 1980;Gerin et al. 1984] reported increased incidences of lung cancer among welders who were exposed to stainless steel welding fumes that contained nickel and chromium. Sjogren [1980] reported an OR of 4.4 (p<0.03), and Gerin et al. [1984] found an OR of 3.3 (95% C I =1.2 to 9.2) among another group of stainless steel welders.
Deaths from lung cancer remained statistically significant in both studies after adjustment for smoking habits.
Although no exposure data were available for either study, measurements of airborne chromium were taken by Sjogren [1980] at similar stainless steel welding sites.
They revealed median TWA chromium (trivalent and hexavalent) concentrations of 210 g/m3 during welding with covered electrodes and 20 during gas-shielded welding. Sjogren et al. [1987] reported on a reanalysis of these stainless steel welders [Sjogren 1980] to determine lung cancer risk after 7 years of additional followup.
The lung cancer risk remained high for the stainless steel welders, who had an SMR of 249 when their death rates were compared with national death rates.
This cohort was also compared with another group of welders who did not weld on stainless steel but were exposed to low concentrations of chromium. These welders had a relative risk of 7.01 (95% C I =1.32 to 37.3) for lung cancer compared with stainless steel welders, which suggests that emissions typically produced during the welding of stainless steel (e.g., chromium, nickel) may be associated with excess lung cancer risk.
# b. Exposure to Welding Fumes in General
Studies reported by Breslow et a l . [1954[ ], HMS0 [1978, Mi I ham [1983], and Schoenberg et a l . [1987], provide evidence of an association between exposure to various compositions of welding fumes and gases and an increased risk of lung cancer.
A statistically significant (p<0.05) OR of 1.56 was reported by Breslow et al. [1954] in a case control study of 518 lung cancer patients that included 10 welders and 4 sheet metal workers exposed to welding fumes.
The OR remained statistically significant after adjustment for smoking habits.
Mi lham [1983] reported on the proportional mortality of lung cancer among welders and flame cutters employed in the State of Washington.
The study used death certificates collected over a 29-year period; proportional mortality ratios (PMRs) were determined at 10-year intervals.
A statistically significant (p<0.01) PMR of 136 was observed for the period 1970-79, and a PMR of 135 (p<0.01) was observed for the total study period .
In another study [HMSO 1978], statistically significant (p<0.01) SMRs of 151 (not controlled for smoking) and of 116 (controlled for smoking) were found for a group of workers classified as "gas and electric welders, cutters, and braziers."
The study cohort was made up of workers employed in different industries and potentially exposed to various compositions of fumes and gases.
A study of welders in the Louisiana petroleum industry also showed a statistically significant lung cancer risk [Gottlieb 1980]. However, when the cohort was adjusted for age, the OR was no longer statistically significant.
Although an increased risk of lung cancer was found for welders in these studies [Breslow et al. 1954;HMSO 1978;Gottlieb 1980;Milham 1983], the absence of specific exposure information, type of welding performed, and possible concomitant exposures (e.g., asbestos) makes it difficult to associate exposure with the risk of lung cancer. However, in a case control study reported by Schoenberg et al. [1987], shipyard welders had a statistically significant increase in the rate of lung cancer, with an OR of 3.8 (95% C I =1.8 to 7.8). This risk remained high after adjustment for smoking and exposure to asbestos. Of the 33 cases and 18 controls classified as welders, 16 cases and 7 controls were reported to have been exposed to asbestos.
The remaining 17 cases and 11 controls who had no reported asbestos exposure, showed an increased smoking-adjusted OR of 2.5 (95% C l =1.1 to 5.5).
Four other mortality studies [Puntoni et a l . 1979;Polednak 1981;Becker et al. 1985;Newhouse et al. 1985] reported increased risks for lung cancer among male welders.
Although the increases were not statistically significant, the studies collectively demonstrate the possible association between classification as a welder and an increased risk of developing lung cancer.
Two of the four studies were conducted on white males who worked as welders at nuclear facilities [Polednak 1981] or at sanitary installations and power plants [Becker et a l . 1985].
The larger of those studies [Becker et al. 1985] revealed an OR of 2.4 (p<0.05) for all cancers and an elevated OR of 1.7 (p>0.05) for cancer of the trachea, bronchus, and lung when compared with a control group that was not exposed to welding fumes. When an external analysis was performed (i.e., comparison with the German national death rates), SMRs for deaths from malignant neoplasms and lung cancer were not markedly increased over the general population.
However, when welders were analyzed by 10-year intervals since first exposure, an upward trend in SMRs was observed.
The incidence of malignant neoplasms was statistically significant (p<0.05) only for the last interval (> 30 years since first exposure).
In the smaller cohort study [Polednak 1981], welders were analyzed according to their potential exposure to nickel oxides. Increased SMRs were observed for lung cancer deaths among both exposed (SMR=124) and unexposed (SMR=175) welders.
The SMRs were not statistically significant when compared with death rates for U.S. white males.
The welders who were not exposed to nickel oxides had a prevalence of smoking that was 2.5 times that of the exposed group.
The difference in smoking habits and the fact that the study groups were small (N=536 exposed, N=523 unexposed) contribute to uncertainty in the interpretation of the results.
Although the SMRs did not reach statistical significance, the risk of death from lung cancer increased among both groups of welders with increasing years of exposure to welding fumes and gases.
Studies of welders in shipyards [Puntoni et al. 1979;Newhouse et al. 1985] demonstrate an increased risk of lung cancer.
Although neither study showed statistically significant increases, Puntoni et a l . [1979] found elevated ORs for lung cancer in gas welders (0R=2.12) and electric welders (0R=2.54) when compared with the male staff of a local hospital.
An elevated OR of 1.25 for gas welders and an OR of 1.60 for electric welders were observed when the groups were compared with the male population of Genoa, Italy. Newhouse et al. [1985] found an elevated SMR of 113 for deaths from lung cancer among a group of welders who performed various welding tasks during ship repair.
Latency and duration of employment were not analyzed in either study, and no attempt was made to account for the confounding exposure of asbestos.
# Other Cancer-Epidemiologic Studies
Several studies indicate a possible association between classification as a welder and an increased risk of cancer of the larynx [Olsen et al. 1984] and of the kidney or other urinary tract organs [Puntoni et al. 1979;Mi I ham 1983;Becker et al. 1985].
Skin cancer has also been reported among welders employed for more than 30 years in this occupation [Roquet-Doffiny et al. 1977].
A case-control study conducted by Olsen et al. [1984] reported an unusually high risk of cancer (0R=6.3) of the subglottic area of the larynx among 271 cancer patients who had been occupationally exposed to welding fumes and gases.
The high OR for this type of cancer persisted after adjustment for tobacco and alcohol use, but it was not high for those patients (N=12) reported to have been exposed to fumes from stainless steel welding.
Other epidemiologic studies [Dunn and Weir 1968;Ott et a l . 1976;HMSO 1978;Puntoni et a l . 1979;Sjogren 1980;Polednak 1981;Milham 1983] revealed no elevated risk of larynx cancer.
Several cohort mortality studies [Puntoni et a l . 1979;Milham 1983;Becker et al. 1985] have reported increased incidences of kidney or other urinary tract cancers among welders.
The study of shipyard workers by Puntoni et a l . [1979] reported ORs of 5.06 (p<0.05) and 5.88 (p<0.05) for cancer of the kidney and other urinary tract organs in gas welders compared with two different external control populations. Elevated but statistically insignificant ORs were also reported for electric arc welders.
An increased risk of kidney cancer was also noted by Milham [1983] in welders and flame cutters (PMR=182, p<0.01), and Becker et a l . [1985] reported a statistically significant (p<0.002) OR of 15.0 (3 observed versus 0.2 expected) for kidney and other urinary tract cancers among welders.
No exposure data were reported in any of the three studies, but Becker et al. [1985] reported that most of the welders in his study performed arc welding with coated chromium-nickel alloy electrodes.
Although these studies associated classification as a welder with an increased risk of dying from kidney or other urinary tract cancers, other mortality studies [Dunn and Weir 1968;Ott et a l . 1976;HMSO 1978;Polednak 1981;Newhouse et a l . 1985] indicated no increased incidences of death from these causes.
# Toxicological Evidence
The risk of cancer noted among welders is consistent with the findings of in vitro and in vivo mutagenesis assays that have demonstrated various mutagenic potentials for welding fumes, depending on their composition [Hedenstedt et a l . 1977;Koshi 1979;Stern et a l . 1982;Pedersen et al. 1983]. Results of assays have shown that most of the mutagenic activity of stainless steel welding fumes can be ascribed to chromium(VI) in the water-soluble fraction [Stern et a l . 1982]. Maxi Id et al. [1978 reported that shielded metal arc welding of stainless steel produces 3 to 6 times more fumes (per mass of weld metal) than gas metal arc welding.
When the mutagenic potentials for shielded metal and gas metal arc fumes were compared on an equivalent chromium(VI) basis, gas metal arc welding fumes produced four times more mutations in bacteria than shielded metal arc welding fumes [Stern et a l . 1982]. Other data reported by Hedenstedt et al . [1977] and Stern et al. [1982] suggest that compounds other than chromium(VI) may be active in the water-soluble fractions of fumes generated from shielded or gas metal arc welding of stainless steel.
When water-soluble fractions of both fumes were tested in an assay using metabolically activated S. typhimurium, arc welding fumes were less mutagenic.
In a 2-year study reported by Reuzel et al. [1986], evidence of carcinogenicity was found in animals exposed to stainless steel fumes. Syrian golden hamsters were intratracheally injected with saline suspensions of stainless steel fumes from shielded metal arc welding. One lung cancer resulted from each of two dose groups.
No cancers were observed in the untreated control groups or in animals treated with gas metal arc fumes, calcium chromate (positive control), or saline. Because these tumors are extremely rare in Syrian golden hamsters, the authors concluded that the lung tumors were induced by welding fumes.
# D. Other Diseases
# Acute Respiratory Diseases a. Epidemiological Studies
One of the more frequently reported health effects from exposure to welding fumes is metal fume fever, which often resembles an upper respiratory infection such as influenza, acute bronchitis, pneumonia, or upper gastrointestinal infections [Papp 1968].
These conditions usually last 6 to 24 hr and are often accompanied by chills, trembling, nausea, and vomiting [Rohrs 1957]. Exposure to specific metals such as zinc in zinc oxide fumes [Drinker 1922;Drinker et a l . 1927] and to fumes of mixed composition [Ross 1974;Johnson and Ki Iburn 1983] have been associated with metal fume fever. Although no specific exposure concentrations have been associated with metal fume fever, most reported cases have occurred in workers exposed to welding fumes while working in confined or other poorly ventilated spaces.
Pneumonitis and pulmonary edema have been reported in welders who performed various welding processes (e.g., gas and shielded metal arc welding, silver brazing, or oxyacetylene welding) and were exposed over short periods to high concentrations of nitrogen dioxide [Maddock 1970;Mangold and Beckett 1971], ozone [Mo I os and Collin 1957;Kleinfeld et al. 1957;Challen et al. 1958], cadmium fumes [Patwardhan and Finckh 1976;Blejer and Cap I an 1969;Townshend 1968], chromium and nickel fumes [Jindrichova 1976], or aluminum and iron oxide fumes [Herbert et al. 1982]. Cases of acute cadmium fume pneumonitis and death have been reported among welders exposed either by brazing with siIver-cadmium alloy or by cutting or welding cadmium-coated metal in poorly ventilated areas [Christensen and Olson 1957;Beton et al. 1966;Patwardhan andFinckh 1976]. Beton et al. [1966] reported on the death of a welder who was cutting cadmium-plated bolts with an oxyacetylene torch.
Based on the amount of cadmium oxide found in the welder's lung during a postmortem examination, the authors estimated that his exposure to cadmium oxide averaged 8.6 mg/m^.
Several other fatalities have resulted from pulmonary edema in welders exposed to nitrogen dioxide concentrations above 100 ppm [Maddock 1970].
# b. Toxicological Evidence
Pathological lung changes observed in welders acutely exposed to welding fumes and gases have also been documented in exposed animals [Titus et al. 1935;Kawada and Iwano 1964;Hewitt and Hicks 1973].
Animals exposed to welding fumes and gases for short periods suffered severe lung damage (e.g., edema, hemorrhage, pneumonia, and atelectasis) and death.
In one experimental study [Titus et al. 1935], cats and rabbits were exposed to iron oxide fumes for up to 8.5 hr at concentrations of 10 to 350 mg/m^.
All animals developed pulmonary edema.
Their alveoli became dilated, their lungs hemorrhaged, and several died.
Similar results were reported by Hewitt and Hicks [1973] in albino rats exposed to rutile welding fumes and gases at an average concentration of 1,500 mg/m^. Rats exposed for either 30 min or 4 hr demonstrated a statistically significant (p<0.05) increase in uptake of chromium and antimony by the lungs, and of cobalt by the liver and blood. Microscopic examination of the lungs revealed peribronchial edema and large numbers of particulate-laden macrophages in the alveoli and alveolar ducts.
Histopathological lung changes were reversed following 75 days with no exposure; only the particulate material remained within the macrophages.
Pulmonary deposition and clearance rates in animals exposed to fumes from welding nonstainless and stainless steels were investigated by McCord et al. [1941] andByczkowski et al. [1970].
The rates of metal deposition in the lungs were proportional to the metal content of the emissions; these rates increased in animals that exercised during exposure.
# Chronic Respiratory Diseases a. Epidemiologic Studies
Pneumoconiosis, including siderosis, has been reported among welders exposed to iron oxide fumes from bare metal electrodes [Britton and Walsh 1940;Sander 1944;Sander 1947;Doig and McLaughlin 1948;Mignolet 1950]. Although quantitative data on exposures are lacking for most of these studies, Dreesen et al. [1947] provide some data on the extent of exposures before 1950.
Samples collected during arc welding of mild steel in a shipyard revealed iron oxide concentrations above 30 mg/nr* and zinc oxide concentrations above 15 mg/m^.
The highest exposure concentrations were found in poorly ventilated work areas.
Approximately 50% of the samples contained less than 5 ppm oxides of nitrogen, and 10% of the samples exceeded 25 ppm.
Other studies have described siderosis complicated by fibrosis [Marchand et al. 1964;Meyer et al. 1967;Stettler et al. 1977;Kleinfeld et al. 1969;Brun 1972;Levy and Margolis 1974;Attfield and Ross 1978].
These findings appear to be associated with the replacement of bare metal electrodes by covered electrodes. Clinical evaluations were made of workers who were exposed to iron oxides and silica and who welded both ferrous and nonferrous materials using covered electrodes.
These evaluations revealed diffuse interstitial fibrosis [Meyer et a l . 1967] and siderosilicosis [Levy and Margolis 1974]. Levy and Margolis [1974] reported peak airborne concentrations of 19.4 mg/m^ for iron oxide and 6.82 mg/m^ for respirable silica among steel foundry welders who had evidence of siderosi Iicosis.
Welders have also shown decrements in pulmonary function [Hunnicutt et al. 1964;Fogh et a l . 1969;Keimig et a l . 1983;Oleru and Ademiluyi 1987] and increases in the prevalence of chronic bronchitis [Kujawska 1968;Fogh et al. 1969;Barhad et al. 1975;Antti-Poika et al. 1977;Akbarkhanzadeh 1980;Sjogren and Ulfvarson 1985].
The only exposure data reported are those cited in the studies by Barhad et al. [1975], Sjogren and Ulfvarson [1985], and Keimig et al. [1983]. Barhad et al. [1975] reported that shipyard welders were exposed to total fume concentrations of 6 to 36 mg/m^ in open work areas and 48 to 92 mg/m^ in confined spaces during arc welding with covered electrodes.
Oxides of nitrogen averaged concentrations of 1.7 mg/m^ during shielded arc welding and 1.1 mg/m^ during arc welding.
Regardless of the welding process, carbon monoxide concentrations ranged from 6.3 to 17 mg/m^.
In the study by Sjogren and Ulfvarson [1985], exposures to ozone exceeded 0.1 ppm in 50% of the samples collected during gas metal arc welding of aluminum.
During stainless steel welding with covered electrodes, 80% of the chromium(VI) concentrations exceeded 20 ug/m3.
Concentrations of nitrogen oxides were less than 5 ppm for all welding processes [Sjogren and Ulfvarson 1985].
Breathing zone air samples collected near welders at the time of the study reported by Keimig et al. [1983] indicated iron oxide concentrations of 1.3 to 8.5 mg/m3, with no detectable amounts of chromium, copper, fluoride, or lead in any of the air samples.
The cross-sectional study reported by Keimig et al. [1983] found that welders and controls who smoked had higher frequencies of reported respiratory symptoms (e.g., bronchitis, pneumonia, and cough) than corresponding nonsmokers.
Although welders who did not smoke reported higher frequencies of symptoms than nonsmoking controls, the differences were statistically significant (p<0.05) only for the symptoms of increased phlegm and episodes of cough and phlegm.
The only statistically significant differences noted in pulmonary function tests were decreases in forced vital capacity (FVC) at the end of the work shift for nonsmoking welders, nonsmoking controls, and smoking controls.
Similar findings were reported by Oleru and Ademi luyi [1987] for a group of workers engaged in the welding of medium-and high-alloy steel.
Although no evidence of obstructive lung disease was found, 7 of 67 persons tested had restrictive lung impairment.
Welders given pulmonary function tests to assess the effects of exposure over a 40-hr work week demonstrated statistically significant (p<0.05) decrements in all parameters measured.
Peak flow measurements made on this group after an 8-hr work shift showed acute changes in pulmonary function that were statistically significant (p<0.05).
However, these changes were not statistically significant when the group was retested after 3 additional days of welding.
In the studies by Hunnicutt et al . [1964], Fogh et al. [1969], andAkbarkhanzadeh [1980], the increased prevalence in decrements of pulmonary function or chronic bronchitis were observed only in welders who smoked.
# b. Toxicological Evidence
Siderosis has been produced by exposing animals to mixed compositions of fumes [McCord et a l . 1941;Garnuszewski and Dobrzynski 1966].
All rats and rabbits developed siderosis when they were exposed to shielded metal arc welding fumes for 6 hr/day, 5 days/week for 46 days followed by an additional 43 days without exposure [McCord et al. 1941].
Animals were exposed to average concentrations of 465 mg/m^ (ferric oxide), 61 mg/m^ (silicon dioxide), and 16 mg/m^ (manganese).
Similar results were produced by Garnuszewski and Dobrzynski [1966], who exposed groups of guinea pigs and rabbits to fumes that were either high in silicon oxide (25.5%) and low in ferric oxide (18%), or low in silicon oxide (7.8%) and high in ferric oxide (23%).
Each experimental group of animals was subdivided into a high-exposure group (36 mg of total fumes/m^ of air) or low-exposure group (18 mg of total fumes/m^ of air).
All animals were exposed 4 hr/day, 6 days/week for 110 days.
All exposed guinea pigs developed a mixed type of pneumoconiosis (e.g., siderosis with silicosis manifested by pneumoconiotic nodules containing collagenous fibers and silica particles).
No pneumoconiosis was observed in the exposed rabbits.
# Other Adverse Health Effects a. Auditory Impairment
Auditory impairment has been reported among welders as a result of traumatic injury [Frenkiel and Alberti 1977] or excessive sound pressure [Hickish and Challen 1963;Bell 1976]. Several cases of eardrum injury and permanent hearing loss were reported by Frenkiel and Alberti [1977] among welders who did not wear ear protection and were injured by sparks and molten metal that entered the ear while welding.
Studies conducted by Hickish and Challen [1963] and Bell [1976] described the risk of noise-induced hearing loss in welders performing arc air gouging or plasma torch welding of metals. Mean temporary hearing losses of 19 dB at 4,000 Hz and up to 35 dB at 8.000 Hz were reported by Hickish and Challen [1963] among a group of welders who were performing plasma torch welding for 1 hr without wearing hearing protection.
# b. Cardiovascular Disease
Studies that have assessed cardiovascular disease in welders have produced equivocal results.
Two mortality studies indicate increased risks of death from cardiovascular disease among shipyard welders [Newhouse et al. 1985;Puntoni et al. 1979]. Newhouse et al. [1985] reported an increased SMR of 130 (p=0.10) for ischemic heart disease, and Puntoni et a l . [1979] reported ORs greater than 1.00 for cardiovascular disease.
Neither study adjusted for smoking habits, and no information was provided on other possible risk factors.
Two other studies analyzed deaths from cardiovascular disease:
An SMR reported by Polednak [1981] and a PMR by Milham [1983] were both less than 100. Although the association between welding and an increased risk of cardiovascular disease remains equivocal, the data do provide cause for concern.
# c. Dermal Effects
Several types of dermal conditions observed in welders have been attributed to exposure to physical agents, including UV radiation [Grimm and Kusnetz 1962;Pattee et al. 1973;Balabanow et a l . 1967;Roquet-Doffiny et al. 1977;Ross 1978], IR radiation [Lydahl and Philipson 1984;Moss et al. 1985], and metals to which workers can become sensitized [Kaplan and Zeligman 1963;Fregert and Ovrum 1963;Shelley 1964;Kalliomaki et al. 1977].
Chronic dermatitis and other skin diseases have been documented in several case reports [Shelley 1964;Balabanow et al. 1967;Roquet-Doffiny et a l . 1977] that described welders whose skin came into contact with many types of metals (e.g., nickel, cadmium, and chromium) and fluxes.
Welders exposed to welding fumes from stainless steel have experienced episodes of facial contact dermatitis [Fregert and Ovrum 1963].
In these cases, removal of the worker from exposure or the use of protective clothing eliminated or greatly minimized the severity of the d i s o r d e r .
# d. Eye Injuries
Welders or others working near welding processes risk eye injury from metal spatter, foreign bodies in the eyes, and exposure to nonionizing electromagnetic radiation [NIOSH 1972a;Marshall et al. 1977;Palmer 1983;BLS 1985].
Exposure to ultraviolet radiation (UV) from welding arcs has caused acute keratoconjunctivitis, also known as welder's flash or actinic ray photokeratitis [Minton 1949;Sykowski 1951].
Repeated episodes of welder's flash over a long period have caused cataracts [Golychev and Nikitina 1974], Similarly, exposure to infrared radiation (IR) has caused thermal damage to the cornea and aqueous humor of the eye and has been associated with the formation of lenticular cataracts [Palmer 1983].
Such adverse ocular effects have been attributed to the improper use or absence of eye protection [Minton 1949;Sykowski 1951;Entwistle 1964;Karai et a l . 1984].
According to Bureau of Labor Statistics (BLS) data for the period 1976-81, eye injury was the type of injury that welders reported most frequently.
Such injuries were associated with exposure to radiation or foreign bodies in the eyes among welders and flame cutters [BLS 1985].
These recent data are consistent with earlier data [BLS 1983].
For the 1983 BLS report, data were collected over a 5-month period in 1978 from welders in 18 states (BLS 1983). Sixty-seven percent of the reported injuries were to the eyes.
No information was given in either report as to whether eye protection was being worn at the time of the injury.
# e. Gastrointestinal Disorders
Gastrointestinal disorders (e.g., nausea, vomiting, and gastro intestinal cramps) are often experienced by welders with metal fume fever, but they are reversible following treatment and removal of the worker from additional exposure [Rohrs 1957;Papp 1968]. Studies by Mignolet [1950], Stancari and Amorati [1963], andRozera et al. [1966] reported digestive system disorders in welders that included gastritis, gastroduodenitis, and gastroduodenal ulcers. The authors attributed these conditions to long-term exposures to welding fumes and gases.
Epidemiological studies of welders conducted by Puntoni et al. [ ], Polednak [1981, Mi I ham [1983], and Becker et al. [1985] found no increases in mortality as a result of diseases of the digestive system.
# f. Musculoskeletal Effects
Reports of musculoskeletal injuries involving the shoulders, back, and knees have been noted in several studies of welders [Herberts and Kadefors 1976;Kadefors et al. 1976;Nauwald 1980].
Complaints of shoulder pain and reduced muscle power, particularly of the supraspinatus muscle, have been frequently attributed to overhead welding performed by both inexperienced and experienced welders. Knee joint problems (including fluid sac diseases, arthritis, and proliferation of fatty tissue) have also been observed, primarily in welders with more than 6 years of experience.
# g. Reproductive Effects
Studies conducted by Rachootin and Olsen [1983] and Lindbohm et a l . [1984] suggest a possible association between adverse reproductive outcomes and the subject's status as a welder or as the wife of a metal plate worker.
A statistically significant increase (p<0.05) in spontaneous abortions was observed for wives of metal plate workers [Lindbohm et al. 1984],
The authors suggested that this increase was caused by exposure to chromium or nickel.
The case-control study by Rachootin and Olsen [1983] indicated a statistically significant increase (p<0.05) in delayed conception, with ORs of 1.4 for male welders and 2.4 for female welders.
The risk remained statistically significant for women after adjustment for age, smoking habits, alcohol consumption, and past use of oral contraceptives.
Men and women assigned to the subgroup "Welding of Stainless Steel" had no statistically significant increase in their risk of delayed conception.
Although the studies suggest a reproductive risk, several méthodologie problems exist, including the inability to accurately estimate possible exposures based on employment history [Lindbohm et al. 1984;Rachootin and Olsen 1983], the lack of information on smoking habits or alcohol consumption [Lindbohm et al. 1984], and possible data collection biases resulting from the use of self-administered questionnaires [Rachootin and Olsen 1983].
No experimental animal studies have been conducted to determine the effects of welding fumes and gases on the reproductive system.
# E. Safety
Fires, explosions, and electric shocks are common welding hazards that have caused many disabling injuries and fatalities [BLS 1985].
Fires caused by the welding flame itself or by flying sparks have been responsible for many injuries and fatalities of welders [NFPA 1977;Buhrer and Brunschwi ler 1978].
Injuries have also been reported as a result of accidental fires caused by welding in oxygen-enriched atmospheres in confined spaces or by oxygen leaks from welding tanks [Rames 1976].
Fires and explosions have also been caused by welding or cutting tanks and drums that have not been properly emptied and cleaned of flammable liquids [CDLSR 1975;NFPA 1977].
Electric shocks have occurred in welders using alternating or direct currents of 120 to 600 A at 30 to 60 volts.
Even if the shock itself was harmless, resulting falls have caused serious injury or death [Britton and Walsh 1940].
Many of these incidents have occurred from improper grounding of the welding electrode or careless handling and changing of electrodes.
# F . Cone I us i ons
Epidemiologic studies and case reports of workers exposed to welding fumes and gases provide adequate evidence that these workers are at an increased risk of contracting acute respiratory diseases such as metal fume fever and pneumonitis [Drinker 1922;Drinker et al. 1927;Christensen and Olson 1957;Kleinfeld et al. 1957;Molos and Collins 1957;Rohrs 1957;Challen et al. 1958;Beton et al. 1966;Papp 1968;Townshend 1968;Blejer and Caplan 1969;Maddock 1970;Mangold and Beckett 1971;Ross 1974;Jindrichova 1976;Patwardhan and Finckh 1976;Herbert 1982;Johnson and Kilburn 1983]. Chronic respiratory diseases such as pneumoconiosis and bronchitis have also been documented in workers exposed to welding emissions [Britton and Walsh 1940;Sander 1944;Dreesen et a l . 1947;Sander 1947;Doig and McLaughlin 1948;Mignolet 1950;Hunnicutt et al. 1964;Marchand et al. 1964;Meyer et a l . 1967;Kujawska 1968;Fogh et al. 1969;Kleinfeld et al. 1969;Brun et a l . 1972;Levy and Margolis 1974;Barhad et al. 1975;Antti-Poika et al. 1977;Stettler et a l . 1977;Attfield and Ross 1978;Akbarkhanzadeh 1980;Sjogren and Ulfvarson 1985;Keimig et al. 1986;Oleru and Ademiluyi 1987]. Some studies report that an increased risk of lung cancer is associated with welding on stainless steel [Sjogren 1980;Polednak 1981;Gerin et al. 1984;Sjogren et al. 1987], and the study reported by Polednak [1981] observed an increased risk in welders exposed to nickel oxides.
Studies of welders exposed to fumes of mixed composition have also reported an increased risk of lung cancer [Beaumont and Weiss 1981;Breslow et al. 1954;HMSO 1978;Milham 1983;Puntoni et al. 1979;Becker et al. 1985;Newhouse et al. 1985;Steen I and et al. 1986;Schoenberg et al. 1987], An exposure limit for total welding emissions cannot be established because the composition of welding emissions (chemical and physical agents) varies for different welding processes and because the various components of a welding emission may interact to produce adverse health effects, including cancer.
Thus even compliance with specific chemical or physical agent exposure limits may not ensure complete protection against an adverse health effect.
Therefore, exposures to all chemical and physical agents associated with welding should be reduced to the lowest concentrations technically feasible using current state-of-the-art engineering controls and good work practices.
Individual exposure limits for chemical or physical agents are to be considered upper boundaries of exposure.
Equivocal evidence exists to show the effects of welding emissions on ( 1) the increased risk of cancer at sites other than the lung [Olsen et al. 1984;Puntoni et al. 1979;Mi lham 1983;Becker et a l . 1985;Roquet-Doffiny et a l . 1977], (2) the cardiovascular system [Newhouse et al. 1985;Puntoni et al. 1979], and (3) the reproductive system [Rachootin and Olsen 1983;Lindbohm et a l . 1984]. However, following the recommendations in this document should prevent or greatly reduce a welder's risk of developing these diseases.
Following the recommendations should also reduce injuries and deaths resulting from unsafe work conditions.
# VI. HAZARD IDENTIFICATION
An occupational health program should include methods for thoroughly identifying and assessing all potential hazards if it is to protect welders from the adverse health effects of chemical and physical agents in their work environment.
Information provided by monitoring and analysis is needed to determine whether controls (e.g.
# Airborne Contaminants
Routine air monitoring of the workplace helps to determine whether a worker is exposed to any individual chemical at or above its exposure limit.
These data must be obtained for all workers involved in welding activities and for all other persons working near welding sites.
If a worker's exposure can be accurately characterized, and if concentrations of specific agents are found to be below their exposure limits (or below their action limits if the agents have established NIOSH RELs), further characterization of the work environment is not needed as long as the process or work conditions do not change.
No safe exposure concentration has been established for chemicals that NIOSH has identified as potential occupational carcinogens.
An effective air monitoring program should include the following components to accurately assess each worker's exposure:
•
A procedure to assess the worker's potential for exposure. This procedure should include collection of data on the types of materials being used (e.g., welding rods and fluxes) and the composition of the base metals,
• Knowledge of air sampling and analytical method(s) required to determine concentrations of airborne chemical and physical agents, and
• Information on the number of workers potentially exposed and the duration of their exposure.
# A. Workplace Monitoring and Analytical Methods a. Determining the Potential for Exposure
The first step in determining the potential for exposure to a specific agent is the preparation of a hazard inventory. This inventory should include information on the type of welding process that will be performed, the possible chemical and physical agents that may be encountered, and the composition of the base metal, coatings on the metal, fillers, and fluxes.
This initial assessment should include a review of all precautionary labels on containers of filler metals, electrodes, and flux materials and any material safety data sheets.
Refer to Chapter III, B (Potential for Exposure) for a more detailed description of contaminants that may be encountered during welding.
After an initial assessment of potential airborne exposures, employers should identify workers whose exposures to a specific agent may be at or above its exposure limit (or action limit if the agent has an established NIOSH REL).
To determine which workers may be at increased risk of exposure, the following work conditions should be evaluated: the location of the welding process with respect to the worker(s), frequency of the welding being performed, the use of engineering controls, and the type of work practices employed.
If some uncertainty exists about a worker's exposure (regardless of job title), the worker should be included in the air monitoring program, at least initially.
# b. Sampling Strategy (Location, Number, and Frequency of Sampling)
The following subsections provide some basic criteria for establishing and implementing a sampling strategy.
# (1) Sampling Location
The sampling location is important in achieving an accurate characterization of the suspected exposure.
The preferred sampling location is within the breathing zone of the worker and is referred to as a personal sample.
The concentration of fumes or gases in the welder's breathing zone for a given process varies depending on the specific work practices of the welder and the type of exhaust ventilation used.
For example, if a welder leans over the work, exposure for that worker will be greater than for a welder in an upright position. Moreton et al. [1975] reported that exposure concentrations varied by a factor of six among welders who performed the same task but used different work practices.
In addition, the concentration of airborne contaminants typically varies as a function of distance from the worksite.
The type of ventilation, convective drafts, and location of the operation further increase the variability of contaminant concentrations with distance from the source.
If personal samples are collected on a worker wearing a welding helmet, the inlet to the sampling device should be correctly positioned within the helmet.
The helmet reduces to some degree the amount of contaminant in the breathing zone. Johnson [1959] sampled outside and inside a welding helmet simultaneously during production welding.
Concentrations of iron fumes were compared for the two sample locations.
The ratio of outside to inside concentrations ranged from 1.03:1 to 7.55:1, with an average of 3.5:1. Based on this and similar experimental studies, the American Welding Society (AWS) Standard F1.1-76, "Method for Sampling Airborne Particulates Generated by Welding and Allied Processes," specifies that air samples should be taken within the welding helmet 50 millimeters (mm) to the left or right of the welder's mouth.
In a similar study measuring the performance of full-facepiece respirators, Myers and Hornung [1987] found that sampling errors in the facepiece were minimized by placing the inlet of the sampling probe to within 1/2 to 3/4 inch (in.) of the wearer's mouth.
Because welding emissions often consist of fumes and gases, different sampling media are often required.
However, space is restricted in the welding helmet, and wearing several air sampling instruments can cause discomfort.
Thus a given worker may have to be monitored over a period of several days, or different types of samples may have to be collected on various workers at the same worksite.
# (2) Number of Samples Required
Once the sampling location has been identified, employers should select the number and type of workers to be sampled by considering which workers have the highest potential for exposure and which workers are potentially exposed despite working some distance from the welding process.
For a more detailed discussion on the selection of workers and a strategy for sample collection, consult the NIOSH Occupational Exposure Sampling Strategy Manual [Leidel et al . 1977],
This manual also provides guidance on the length of time needed for sample collection, number of samples required for statistical validity, and the scheduling of sample collection (i.e., on one or multiple days) to accurately define workers' exposures.
# (3) Sampling Frequency
Unless welding is performed under product ion-1ine conditions, sampling should be conducted at frequent intervals to characterize exposures adequately and determine the need for controls.
However, when the welding process is repetitive (as it is on a production line), exposure conditions may be characterized and quantified by an initial sampling survey.
It can be assumed that conditions will remain relatively constant during future welding activities if there is no change in the process or type of welding.
Under these circumstances, routine sampling should not be necessary.
This strategy applies only when the survey results indicate that workers are not being exposed to any agent at or above its exposure limit (or action limit if the agent has an established NIOSH REL).
With these survey results, no further sampling is necessary as long as no change occurs in the conditions that existed during sampling.
Unfortunately, it is not always possible to note when conditions change.
For example, if debris accumulates in the ventilation system, the collection efficiency of the system may decrease, and workers' exposures could increase without any visible signs of change.
Although this type of potential problem may not necessitate routine air sample monitoring, it does require periodic examination of the ventilation system to ensure that it is operating at optimum efficiency.
If the potential exists for any condition to change (e.g., malfunction of ventilation system) without apparent warning, then a routine monitoring program should be implemented and continued until all such conditions can be standardized.
For a more detailed discussion on determining the need for additional sampling, consult the NIOSH Occupational Exposure Sampling Strategy Manual [Leidel et al. 1977],
# c. Analytical Methods
Analytical methods for assessing samples of most welding emissions have been developed by NIOSH and are listed in
# Physical Agent Monitoring
Physical hazards associated with welding include electromagnetic radiation, X-radiation, and noise.
The following guidance is provided to assist in the initial assessment of these potential hazards.
# a. Monitoring UV Radiation Levels
Quantifying exposure to optical radiation is difficult, and the NIOSH criteria document on radiation [NIOSH 1972b] does not include specific recommendations for monitoring UV radiation.
The following guidelines are provided to assist in the recognition and control of any potential exposure to UV radiation.
Many welding processes generate radiation from the entire UV spectrum or from parts of the UV spectrum.
Most commercially available UV measuring devices (with the exception of the thermopile) are wavelength selective.
Thus measuring a welder's exposures to UV radiation can be difficult.
Other problems in accurately measuring worker exposures include measurement errors caused by water vapor in the air, errors caused by the directionality of exposure meters, reflection errors, and equipment problems such as solarization and aging of lenses and other components [NIOSH 1972a]. Control of UV radiation exposure is best ensured through a management control program that relies on the containment of UV emissions through barriers.
Where barriers cannot be used, personal protective devices such as appropriate clothing and barrier creams should be used to protect the skin; proper safety glasses should be worn to protect the eyes.
# b. Monitoring X-Radiation
Electron beam welding equipment produces X-rays that are normally contained by the welding chamber.
The AWS recommendations outlined in F2.1-78, "Recommended Safe Practice for Electron Beam Welding and Cutting" [AWS 1978], specify that periodic surveys be made to detect any leakage of X-radiation.
The electron beam should be grossly unfocused and aimed at a tungsten target.
A preliminary assessment of the equipment should be made while it is operating at maximum current and voltage levels to detect leakage.
Thereafter, periodic surveys can be made when the equipment is moved or repaired.
Film badges or some other means of X-ray exposure monitoring should be provided for equipment operators.
# c. Monitoring Noise Levels
Excessive noise may be produced in a number of welding and allied processes including plasma arc, metal spraying, and arc air gouging processes.
The potential for a given process to generate excessive noise can quickly be determined using a sound level meter with an A-weighted scale and a type II microphone.
However, these meters do not accurately measure impact noise.
Operations that generate significant noise levels during a full work shift require a comprehensive exposure evaluation.
With the exception of routine "assembly line" operations, where sound level meters can be used to characterize exposures, most processes are best evaluated using dosimeters.
Also, an octave band analysis can be useful in determining the source and frequency of the noise so that appropriate sound-absorptive materials or a barrier for controlling the path of the sound can be selected.
The NIOSH criteria document on noise [NIOSH 1972b] discusses equipment and procedures for monitoring noise levels, along with recommendations for reducing exposures and implementing a hearing conservation program.
# Biological Monitoring
Biological indicators may be useful for assessing human exposures to certain contaminants in the welding environment.
Further information may be found in Section B,2 of this chapter (Biological Monitoring).
# B. Medical Monitoring
Workers exposed to chemical and physical agents associated with welding processes are at risk of suffering adverse health effects.
The respiratory system, eyes, and skin require particular attention during medical examinations conducted for preplacement, periodic monitoring, emergencies, or employment termination.
Medical monitoring as described below should be made available to a 11 workers.
The employer should provide the following information to the physician responsible for the medical monitoring program:
• Any specific requirements of the applicable OSHA standard or NIOSH recommended standard
• Identification of and extent of exposure to physical and chemical agents that may be encountered by the worker
• Any available workplace sampling results that characterize exposures for job categories previously and currently held by the worker • A description of any protective devices or equipment the worker may be requ i red to use
The composition and toxic properties of the materials used in welding
The frequency and nature of any reported illness or injury of a worker
# Med i caI Exam i nat i ons
The objectives of a medical monitoring program are to augment the primary preventive measures, which include industrial hygiene monitoring of the workplace, the implementation of engineering controls, and the use of proper work practices and personal protective equipment. Medical monitoring data may also be used for epidemiologic analysis within large plants and on an industry-wide basis; they should be compared with exposure data from industrial hygiene monitoring.
The preplacement medical examination allows the physician to assess the applicant's functional capacity and, insofar as possible, to match these capabilities with the physical demands and risks of the job.
Fu rt he r more, it provides baseline medical data that can be compared with any subsequent health changes. This preplacement examination should also provide information on prior occupational exposures.
The following factors should be considered at the time of the preplacement medical evaluation and during ongoing medical monitoring of the worker:
(a) exposure to chemical and physical agents that may exert independent and/or interactive adverse effects on the worker's health (including exacerbation of certain preexisting health problems and synergism with nonoccupational risk factors such as cigarette smoking), (b) ancillary activities involved in welding (e.g., climbing and lifting), and (c) potentially hazardous characteristics of the worksite (e.g., confined spaces, heat, and proximity to hazards such as explosive atmospheres, toxic chemicals, and noise).
The specific types of information that should be gathered are discussed in the following subsect ions.
# a. Preplacement Examination (1) Medical History
The medical history should include information on work, social activities, family, and tobacco-smoking habits [Guidotti et al. 1983].
Special attention should be given to any history of previous occupational exposure to chemical and physical agents that may be potentially hazardous.
# (2) Clinical Examination
The preplacement examination should ascertain the worker's general fitness to engage in strenuous, hot work.
Welding processes entail the use of equipment that is often heavy and that may generate potentially harmful levels of UV radiation, heat, noise, fumes, and gases.
The preplacement examination should be directed toward determining the fitness of the worker to perform the intended job assignment.
Appropriate pulmonary and musculoskeletal evaluation should be given to workers whose jobs may require extremes of physical exertion or stamina (e.g., heavy lifting), especially those who must wear personal respiratory protection.
Because the standard 12-lead electrocardiogram is of little practical value in monitoring for nonsymptomatic cardiovascular disease, it is not recommended. More valuable diagnostic information is provided by physician interviews of workers that elicit reports of the occurrence and work-relatedness of angina, breathlessness, and other symptoms of chest illnesses.
Special attention should also be given to workers who require the use of eye glasses; to assure that these workers must be able to wear simultaneously any equipment needed for respiratory protection, eye protection, and visual acuity, and they must be able to maintain their concurrent use during work activities.
Specific welding processes entail potential exposure to diverse chemical agents known to cause specific occupationally related adverse health effects.
These are known as sentinel health events (occupational), or SHE(0)s [Rutstein et al. 1983].
For example, heating of metals with low-boiling points (such as zinc and cadmium) may result in metal fume fever.
Exposure to cadmium fumes may result in delayed onset of pulmonary edema and may lead to pulmonary fibrosis and cancer.
Nickel and chrome are both found in stainless steel and may cause allergic sensitization as a result of an acute exposure or cancer as a result of chronic exposure.
Welding processes that involve the use of flux may generate irritating concentrations of fluorides. Welding on painted metal may result in exposure to lead or other chemical agents, and welding on materials cleaned with a chlorinated solvent may cause photodecomposition of the solvent with resulting exposure.
In addition, the worker's duties may be performed in proximity to unrelated operations that generate potentially harmful exposures (e.g., asbestos or cleaning or degreasing solvents).
The physician must be aware of these potential exposures to evaluate possible hazards to the individual worker.
# (3) Special Examinations and Laboratory Tests
A pulmonary function test (PFT) and a 14-by 1 7 -in. (36-by 43-cm) postero-anterior chest radiograph should be taken and kept as part of the worker's medical record [American Thoracic Society 1982].
The preplacement chest radiograph and PFT gives the physician objective information with which to assess a worker's fitness for a specific job; it may also prevent confusion or misinterpretation of any subsequent lung tissue c h a n g e s .
The International Labour Office (ILO) stresses the importance of radiographic technique in the detection of early pneumoconiosis.
High-speed and miniature films are not recommended.
Films should be interpreted using the current recommendations of the ILO [ILO 1980].
Classification of films should be made by NIOSH-certified B readers [Martin 1985]. Although the short classification may be useful for clinical purposes, films that are obtained in a workplace program of medical monitoring for respiratory hazards must be read and recorded by the complete classification [Martin 1985].
Preplacement audiograms of all workers are recommended, since welders, brazers, and thermal cutters may be exposed to noise intensities exceeding prescribed levels.
i A periodic medical examination should be conducted at least annually or more frequently, depending on age, health status at the time of a prior examination, and reported signs or symptoms associated with exposure to welding emissions.
The purpose of these examinations is to detect any work-related changes in health at an early stage.
The physician should note any trends in health changes revealed by epidemiologic analyses of examination results.
The occurrence of an occupationally related disease or other work-related adverse health effects should prompt an immediate evaluation of industrial hygiene control measures and an assessment of the workplace to determine the presence of a previously unrecognized or potential hazard.
The physician's interview with the worker is an essential part of a periodic medical examination.
The interview gives the physician the opportunity to learn of changes in (a) the type of welding performed by the worker, (b) metals and/or fluxes being used, (c) the work setting (e.g., confined spaces), and (d) potentially hazardous workplace exposures that are in the vicinity of the worker but are not attributable to the worker's on-the-job activities.
Because radiographic abnormalities may appear before pulmonary impairment is clinically manifested or otherwise detectable, periodic chest radiographs are routinely recommended for monitoring workers exposed to fibrogenic respiratory hazards [American Thoracic Society 1982].
However, the chest radiograph may not distinguish between a relatively benign disease such as siderosis (caused by iron oxide exposure) and a disease that may be of greater medical importance such as pneumoconiosis.
Under ordinary conditions, chest radiographs may be obtained for workers at 1-to 5-year intervals, depending on the nature and intensity of specific exposures and related health risks. Workers with 10 years or more of exposure and workers previously employed in dusty jobs may require chest radiographs at more frequent intervals.
These intervals may be changed as called for by other regulatory requirements or at the discretion of the examining physician.
For example, a previous radiograph (e.g., one taken at the time of hospitalization) may be substituted for one of the periodic chest radiographs if it is made available and is of acceptable quality.
If a worker has radiographic evidence of pneumoconiosis or spirometric/symptomatic evidence of pulmonary impairment, the physician should counsel the worker and employer about the potential risks of further exposure and the benefits of removing the worker from exposure.
Smokers should be counseled about how smoking may enhance the adverse effects of other respiratory hazards.
Epidemiologic studies suggest an association between exposure to airborne welding fumes and gases and an excessive risk of lung cancer.
Because routine chest radiographs and sputum cytology are inadequate for detecting bronchogenic carcinoma early enough to
# b. Periodic Medical Examination
alter the course of the disease, they are not currently recommended as part of regular medical monitoring for lung cancer in workers.
During the periodic medical examination of individual welders, the physician should reexamine the skin, eyes, and other organ systems at risk to note changes from the previous examination.
The physician should direct special attention to evidence of burns and effects from exposure to UV radiation and solvents.
This evidence may suggest inadequate industrial hygiene control measures, improper work practices, or malfunctioning equipment (e.g., exposure to metal spatter, flying sparks, UV light flashes, or degreaser solvents).
In addition, the physician should be vigilant for musculoskeletal morbidity attributable to ergonomic problems caused by inadequate worker training on the handling of equipment or by improper working position (e.g., kneeling and overhead welding).
When welders are exposed to agents for which there is an existing OSHA standard or for which NIOSH has recommended medical monitoring, physicians should refer to the appropriate standard or recommendation for guidance on specific medical examinations. Appendix B lists published sources of NIOSH RELs for hazardous agents associated with various welding operations.
Hazardous agents that are commonly associated with welding processes are listed in Table VI-3 along with their potential toxic effects and recommendations for additional tests.
# Biological Monitoring
Urinary or blood concentrations of lead, cadmium, chromium, and aluminum, and urinary concentrations of fluoride ions may be useful biological indicators of worker exposure to welding emissions.
Several studies have correlated exposures to welding fumes containing chromium [Tola et a l . 1977;Mutti et al. 1979;Kalliomaki et al. 1981;Sjogren et al. 1983a], aluminum [Sjogren 1983b;Mussi et al. 1984], or fluoride [Krechniak 1969;Pantucek 1975] with their urinary or blood concentrations.
However, biological monitoring may not be sensitive enough to use as a primary monitoring measure.
For example, Tola et al. [1977] found no increase in urinary chromium concentrations when environmental chromium concentrations were within the NIOSH REL. Biological monitoring has the potential for assessing total exposure when the work load (physical activity) and the routes of exposure are taken into account. Mutti et al. [1979] and Pantucek [1975] showed that urinary levels of chromium and fluoride can provide information on either current exposure or body burden, depending on the timing of the sample collection. Schaller and Valentin [1984] concluded that aluminum concentration in serum seemed to be an indicator of body burden, and that aluminum concentration in urine seemed to be an indicator of current exposure.
Thus biological monitoring may be a useful adjunct for detecting accidental exposure or a failure of primary control m e a s u r e s . "Distinction between short-term and long-term effects is not clear-cut and is somewhat arbitrary. Short-term effects are usually the result of acute exposure(s) and may appear immediately to several days or weeks after the exposure.
Long-term effects are usually the result of chronic, repeated low-close exposures extending from several months to many years.
However, long-term effects may also include the aftereffects of single or repeated acute expo su re s. "Tests to be considered at the discretion of the attending physician.
•-May contain toxic impurities such as arsine, carbon disulfide, carbon monoxide, hydrogen sulfide, and phosphine. "Toxicity information is mostly from chromium plating operation and chromium pigment manufacturing. ®Metal fume fever is manifested by fever, chills, cough, joint and muscle pains, and general malaise.
Reports of health effects of tungsten come almost exclusively from the studies of workers exposed to tungsten carbide, which usually contains cobalt. SRenal functions should be evaluated because renal dysfunctions are known to hinder urinary excretion of fluorides.
# Recordkeeping
Medical records and exposure monitoring results must be maintained for workers as specified in Chapter I, Section 10(c) of this document. Such records must be kept for at least 30 years after termination of employment.
Copies of environmental exposure records for each worker must be included with the medical records.
These records must be made available to the worker or former worker or to anyone having the specific written consent of the worker, as specified in Chapter I, Section 10(d) of this document.
# Ergonomic Monitoring
Ergonomic factors in the workplace should be assessed to determine the need for changes in the work environment, equipment, or work practices, or compensating exercises to avoid fatigue or injury. Work postures, vibrating equipment, and moving of heavy objects may all strain the muscles and joints of welders.
The static positions frequently used in welding and similar processes may also create ergonomic problems that require analysis.
For example, several studies [Herberts and Kadefors 1976;Kadefors et a l . 1976;Petersen et a l . 1977] have indicated that overhead welding may severely strain the supraspinatus muscle of the shoulder, leading to tendinitis.
The movement of workpieces and distribution of workloads may also require study and planning. Ilner-Paine [1977] reported the use of video monitoring to observe and record the physical exertion of welders while they worked. This technique was useful in diagnosing the causes of back and shoulder pain among shipyard welders. Grandjean [1981] has published additional information on ergonomic principles that can be adapted to jobs typically performed by welders.
# VII. METHODS FOR PROTECTING WORKERS
# A. Informing Workers of Hazards
Employers should provide information about workplace hazards before assignment and at least annually thereafter to all workers assigned to work in welding, brazing, and thermal cutting areas.
The OSHA "Hazard Communication" regulation must be followed [29 CFR 1910[29 CFR .1200].
Appropriate written information on hazards (including material safety data sheets) should be kept on file and should be readily available to workers. This information should include a description of the potential health hazards associated with welding (e.g., exposures to noise, vibration, hot metal, optical and X-radiation, and carcinogenic agents such as chromium, nickel, and cadmium) and their possible adverse health effects (e.g., hearing loss, eye injury, burns, and cancer).
Workers should also be informed of the most common types of accidents encountered while welding (e.g., explosions, fires, electrocution, and asphyxiation from oxygendeficient environments).
This information should list precautionary measures for minimizing exposure and injury, including work practices, engineering controls, and personal protective equipment.
The file should also include a description of the environmental, medical monitoring, and emergency first aid procedures that have been implemented.
Workers should also be instructed about their responsibilities for following proper sanitation procedures to help protect their health and provide for their safety as well as that of their fellow workers.
Information on hazards should be disseminated to all workers through a training program that describes how a task is properly performed, how specific work practices reduce exposures or minimize the risk of injury, and how compliance with these procedures will benefit the worker.
Frequent reinforcement of this training and routine monitoring of work practices are essent ial.
# B. Engineering Controls
Because welding processes involve many chemical and physical agents, the hazards they pose cannot always be controlled using current engineering control methods.
The processes are usually dynamic, making it difficult to use fixed systems to control exposures.
In addition, because of the various characteristics of welding emissions (e.g., fumes, gases, radiation) and the extent and fluctuation of exposure at different processes, the evaluation of exposures is often imprecise, and appropriate controls are difficult to implement.
Despite these limitations, engineering controls should be implemented wherever they can minimize the risk of exposure.
# Optical (Radiation) Hazards
When feasible, welding should be performed in booths or screened areas constructed of one of the following materials:
(1) metal, ( 2) flameresistant fabric that is opaque to most optical radiation, or (3) transparent colored polyvinyl chloride material that is formulated with a flame retardant and a UV-visible absorber in the range of 200 to 3,000 nanometers (nm) [Tola et al. 1977;Moss and Gawenda 1978;Sliney et al. 1981].
The booths and screens should be arranged so that they do not restrict ventilation.
Such equipment must conform to requirements of 29 CFR 1910.252(f )(1)(i i i), "Screens."
To minimize ozone production, an opaque shroud should be placed around the arc to minimize the interaction between the optical radiation and the oxides of nitrogen that are generated during the process [Ferry and Ginther 1953;Ditschun and Sahoo 1983].
# Chemical Hazards (Gases and Fumes)
Gases and fumes generated during welding may necessitate both local and general exhaust ventilation.
Although local exhaust ventilation is preferred wherever possible, general ventilation may be used in some cases where the exposures are well characterized and local exhaust ventilation cannot be placed close to the source of emissions [ACGIH 1984], Ventilation systems should meet the following minimum specifications:
• Exhaust hoods and ductwork should be constructed of fireresistant materials.
• Systems should be equipped with alarms, flowmeters, or other devices to indicate malfunction or blockage of ductwork.
•
The air velocity at the face of the duct should be sufficient to capture the emissions. Hood design should be such that captured emissions are carried away from the breathing zone of the worker.
# •
Provision should be made for clean make-up air; 29 CFR 1910.25 2( f)(4)(i) states, "All air replacing that withdrawn shall be clean and respirable."
Various designs of exhaust ventilation systems can provide effective control of fume and gas emissions.
In general, local exhaust ventilation works well for welding processes that are conducted at a fixed location such as a workbench, or that are performed on parts of the same size and shape.
The degree of effectiveness depends on the distance between the face of the duct inlet and the work, the design of the system, and the flow rate and volume of air exhausted.
The use of side baffles or flanges at the duct inlet can increase the capture velocity.
The effectiveness of the exhaust ventilation system declines as the distance between the work and the duct inlet increases; a distance of about 9 to 14 in. (24 to 36 cm) is adequate for capturing fumes and gases.
After optimizing the design of the duct hood so that it can be placed as close as possible to the work, the flow rate should be adjusted to ensure an effective capture velocity.
When welding is performed at remote sites or with different-sized or very large parts, a flanged hood with a flexible duct may be appropriate.
The hood face should be placed at a 0-to 45-degree angle to the work surface and positioned on the side opposite the welder.
The use of a flexible duct system requires that the welder be properly instructed to keep the duct hood close to the emission source and to ensure that the duct is not twisted or bent.
An alternative to using an exhaust hood for gas-shielded arc welding processes is to exhaust the emissions by means of an extracting gun. Such extraction systems can reduce breathing zone concentrations by 70% or more [Hughes and Amendola 1982]. These systems require that the gun and shielding gas flow rates be carefully balanced to maintain weld quality and still provide good exhaust flow.
General ventilation can be used to supplement local exhaust ventilation.
General ventilation may be necessary where local exhausts cannot be placed close enough to the work to be completely effective.
The ACGIH [1984] recommends that where local exhaust cannot be used, 800 cubic feet per minute (cfm) of air be exhausted for every pound of welding rod used per hour.
In-line duct velocities for local exhaust systems that are used to control welding emissions should exceed 3,000 feet per minute (fpm) to prevent particulates from settling in horizontal duct runs.
The recirculation of air from local exhaust systems may be appropriate depending on the potential toxicity of the emissions and the efficiency of the filter collection system.
The recirculation of air from local exhaust systems is not recommended when the collected emissions are unknown or contain extremely toxic agents.
Local exhaust systems must be equipped with flow or vacuum meters or other devices to monitor air flow. These exhaust systems should not be used if their failure to work properly will result in bodily harm before remedial action can be taken [Hughes and Amendola 1982].
For automated welding processes where the worker does not work directly over the source of emissions and there are no cross currents, canopy hoods could be used for collecting heated fumes and gases.
When properly placed at the side of the worker and operated at a relatively low velocity, cooling fans can be used in some work environments to remove welding fumes from the breathing zone. Cooling fans have limited use and should be considered only when local exhaust is not possible. The use of a cooling fan in an indoor situation requires supplemental general ventilation.
# X-Radiation
Electron beam welding processes should be enclosed and shielded with lead or other suitable materials that have a mass sufficient to prevent the emission of X-rays. All doors, ports, and other openings should be checked for X-ray emissions to ensure that all seals are working prop er ly.
# Noise
During plasma arc welding and cutting and during arc air gouging processes, a water table or other method of similar effectiveness should be used to control noise and airborne emissions.
# a. Acoustic Shields
An effective noise reduction of up to 8 decibels (dB) can be achieved by placing an acoustic shield between the worker and the source of the noise [Salmon et al. 1975] usually constructed of safety glass or clear plastic (polycarbonate or polymethyl methacrylate), is placed.
This shield is most effective when its thickness is at least three times the wavelength of the sound that is contributing to the noise.
Thus shields can be effective barriers against the high-frequency sound emitted from the air ejection systems of plasma and metal spray guns.
# b. Total Enclosure
A reduction of up to 20 dB can result when the machinery or process is totally enclosed.
However, heat buildup is a potential problem and may require the installation of adequate ventilation.
Vibration within these enclosures should be isolated from the floor.
The enclosure must have ports for possible servicing of electrical, water, oil, and other systems.
These ports should be sealed with sound-dampening materials (e.g., 1/8-in. or heavier rubber washers).
# c. Other Recommendations
Personal hearing protection devices are recommended if engineering controls cannot maintain worker exposures at 85 dBA as an 8-hr TWA. Ear plugs (molded, foam, or acoustic wool) and earmuffs can significantly reduce a worker's noise exposure.
To determine whether the hearing protection device will be adequate, the manufacturers' data on noise attenuation should be compared with the actual reduction required.
Employers can also use one of three methods developed by NIOSH and reported in the List of Personal Hearing Protectors and Attenuation Data [NIOSH 1976].
Additional information on hearing protection devices may be found in the Compendium of Hearing Protection Devices [Lempert 1984].
Extreme care must be taken in using the manufacturers' data, as it represents the maximum protection possible under ideal conditions. In a NIOSH study to determine the noise reduction provided by insert-type hearing protectors, 50% of the workers tested were receiving less than one-half the expected noise attenuation [Lempert and Edwards 1983]. Noise reduction was also less than expected when the Mine Safety and Health Administration (MSHA) conducted a study in which microphones were placed inside and outside the protective cup on muff-type protectors while the workers performed their normal tasks [Bureau of the Census 1984].
Whenever workers are exposed to noise levels exceeding 85 dBA as an 8-hr TWA, the employer must administer a continuing, effective hearing conservation program [29 CFR 1910.95(c)].
The program must include monitoring, worker notification, an audiometric testing program, availability of hearing protectors for workers, record keeping, and a training program.
Hearing protection becomes mandatory when workers' exposures exceed 90 dBA as an 8-hr TWA [29 CFR 1910.95(b)].
# Oxyfuel Equipment
Ventilation systems and other control devices for oxyfuel equipment should be inspected at least weekly to ensure their effectiveness. Oxyfuel equipment for welding should be installed and maintained in a manner that prevents leakage, explosion, or accidental fire. Such equipment must conform to the requirements of 29 CFR 1910.252(a), "Installation and operation of oxygen-fuel gas systems for welding and cutt i n g ."
# 6.
Fire or Electric Shock
Arc and resistance welding equipment should be installed and maintained in a manner that prevents fire or electric shock. Such equipment must conform to the requirements of 29 CFR 1910.252(b), "Application, installation, and operation of arc welding and cutting equipment," and to 29 CFR 1910.252(c), "Installation and operation of resistance welding e q u i pm en t."
# C. Work Practices
The prevention of occupational illness and injury while welding requires the use of well-designed work practices.
These include wearing personal protective clothing; using safe work procedures for process operations; practicing good housekeeping, sanitation, and personal hygiene; handling compressed gases safely; and being informed on how to handle emergency situations.
Together with engineering controls, such practices can reduce the health risks to workers.
At a minimum, work practices must conform to OSHA standards (e.g., 29 CFR 1910.251-254, "Welding, Cutting, and Brazing" [OSHA]).
Additional information on proper work practices is available in the ANSI Z49.1 standard, "Safety in welding and cutting" [AWS 1973]
# Specific Work Procedures
The manner in which a worker prepares for and carries out welding processes has a direct bearing on the type and extent of the exposure hazard.
For example, Moreton et al. [1975] found that variations in the size of work area, ventilation, and work practices caused welders performing the same welding task to be exposed to breathing zone concentrations of fumes and gases that varied by a factor of up to six.
Other factors that affect the generation of fumes, gases, and optical radiation include the operating current and voltage, the diameter and angle of the electrode, and the type of shielding gas used.
Some of these factors may not be up to the worker's discretion to change, and others may depend on product specifications or production schedules.
The type of welding process used on steel can affect fume generation rates. Flux-cored arc and shielded metal arc welding generate many more fumes than gas metal arc and gas tungsten arc welding.
When shielded metal arc welding must be used, low-fuming electrodes may be acceptable substitutes for conventional types.
The electrical current and the position of the electrode while welding both affect fume generation [Thrysin et al. 1952;Morita and Tanigaki 1977;Pattee et al . 1978].
An increase in the welding current tends to increase the rate of fuming, gas production, and optical radiation emission.
Manufacturers of consumable electrodes usually specify a range of amperages that should be used during welding.
The welder can minimize emissions by using the lowest acceptable amperage.
In addition, holding the electrode as close to the work surface as possible and perpendicular to it will minimize the arc voltage used and thus decrease the rate of fuming [Kobayashi et al. 1976;Pattee et a l . 1978]. Pattee et al. [1978] noted that when the contact-tube-to-work distance is increased, a greater metal deposition rate occurs, which in effect decreases the fume generation rate. However, fume rate tends to increase when the polarity is dc+ (i.e., reverse polarity) rather than dc-or ac [Kobayashi et al. 1976;Pattee et al. 1978] or when the thickness of the metal increases [Heile and Hill 1975;Kobayashi et al. 1976;Siekierzynska and Paluch 1972;Ulrich et al. 1977].
The type and moisture content of flux coating used on electrodes also affects the fume generation rate [Kobayashi et al. 1976], as does the composition of the shielding or plasma gas [Pattee et a l . 1978]. Special precautions should be taken when working in areas not specifically designed for welding.
Such precautions must include (1) observing fire precautions prescribed in 29 CFR 1910.252(d), (2) removing, shielding, or cooling any materials present that may produce toxic pyrolysis or combustion products, and (3) using appropriate personal protective clothing and equipment required for the specific hazard. Whenever possible, the workpieces to be welded should be positioned to minimize worker exposure to molten metal, sparks, and fu me s.
# Confi ned Spaces
Working in confined spaces can be extremely hazardous as a result of explosive, toxic, or oxygen-deficient atmospheres [NIOSH 1979]. Although a confined space may initially have good air quality, any subsequent welding in this space can cause a rapid buildup of toxic air contaminants, a displacement of oxygen by an inert or asphyxiating gas, or an excess of oxygen that might explode. Only by careful preparation can a worker be assured of working safely within a confined space. A complete set of recommendations for working in a confined space is presented in the NIOSH document Criteria for a Recommended Standard: Working in Confined Spaces [NIOSH 1979].
Some of the more pertinent recommendations are given below. a. Before workers enter a tank, reaction vessel, ship compartment, or other confined space, a permit entry procedure should be set up. Authorization to permit entry should be assigned to a qualified person, and access should be permitted only when all necessary measures have been taken to protect the worker.
The following precautions must be taken before permission is given: All pipes, ducts, and power lines connected to the space but not necessary to the operation must be disconnected or shut off.
All shutoff valves and switches must be tagged and secured with a safety lockout device.
Continuous mechanical ventilation must be provided when welding or thermal cutting is done in confined spaces. Oxygen must never be used for ventilation purposes [29 CFR 1910.252].
Initial air monitoring must be performed to determine the presence of flammable or explosive materials and toxic chemicals, and to determine if there is sufficient or excessive oxygen.
Depending on the monitoring results and the adequacy of the mechanical ventilation, continuous monitoring may be necessary during welding.
Prohibit entry when tests indicate flammable concentrations greater than 10% of the lower flammable limit.
# •
Gas cylinders and power sources for welding processes must be located in a secure position outside the space.
• A designated worker must be stationed outside the confined work space to maintain visual and voice contact and to assist or rescue the entering worker if necessary.
The designated worker must be equipped with appropriate protective gear and must remain in position throughout the time that any worker is within the enclosed space.
# •
The worker entering the confined space must be outfitted with a safety harness, a lifeline, and appropriate personal protective clothing and equipment, including a respirator.
• Lifelines must be attached so that the welder's body cannot become jammed in a small exit opening.
• When not in use, torches and other gas-or oxygen-supplied equipment must be removed from the confined space [29 CFR 1910.2 5 2 ( d )( 4)
(i i)].
• All welders and persons supporting those workers shall be trained in the following areas: emergency entry and exit procedures, use of applicable respirators, first aid, lockout procedures, safety equipment use, rescue procedures, permit system, and good work practices.
The type of respirator required depends on the concentration of oxygen and the contaminants that might be generated.
Respirator requirements may range from none to a self-contained breathing apparatus with a full facepiece operated in pressure-demand or positive-pressure mode. Respirators must be selected in accordance with the most recent edition of the NIOSH Respirator Decision Logic [NIOSH 1987].
Even though continuous mechanical ventilation is required during welding processes in confined spaces, initial and continuous environmental monitoring is extremely important.
Equipment used for monitoring of fumes and gases should be ex pl os io np ro of, and continuous monitoring equipment should have an audible alarm or danger-signaling device to alert workers when a hazardous situation develops.
All instruments should be calibrated periodically in accordance with the manufacturers' instructions. The results of each calibration must be recorded, filed by the employer, and made available for inspection for 1 year after the calibration date. Monitoring equipment must be reliable and have sufficient sensitivity to clearly identify a hazardous condition.
Oxygen deficiencies are of particular concern when welding in confined spaces.
The normal 21% concentration of oxygen in air may be decreased in confined spaces by chemical or biological processes.
When oxygen concentrations fall below 16.8% by volume, a worker may have difficulty remaining alert. Whenever the oxygen content falls below 19.5%, appropriate respirators must be used.
NIOSH respirator certification [30 CFR 11] requires that only self-contained breathing apparatuses or supplied-air respirators with auxiliary self-contained breathing apparatuses be used in atmospheres below 19.5% oxygen.
# Preparation for Work
Before welding is performed in any work area, the worker should be aware of any potentially hazardous materials or conditions that may exist in that area.
Before striking an arc or lighting a flame the worker must remove all nearby flammable materials if the piece to be welded or cut is not readily movable.
A number of companies have a "permit system" that requires the supervisor's approval before welding is performed [Shell Chemical Company 1974;Toleen 1977],
Before issuing such a permit, the supervisor must check for conformance to OSHA regulations (such as 29 CFR 1910.252) and any specific company rules. Some of the most common company requirements include checking the serviceability of local firefighting equipment, moving all combustible materials at least 35 ft (10.7 m) from the work site, and assigning a worker (equipped with a suitable extinguisher and trained in its use) to perform a fire watch from outside the workspace.
Combustibles that cannot be removed should be shielded with a nonflammable material.
Shielding should also be provided to cover openings or cracks in floors, walls, and windows to prevent other workers from being exposed to sparks, hot metal and slag, and opt ical radiat io n.
The fire watch should be continued for at least 30 min after job completion to guard against smoldering fires.
The workpiece and work area should also be free of substances that may be rendered more hazardous by the work.
These include any halogenated hydrocarbons in the atmosphere that can be decomposed to phosgene or other harmful products by an arc or a flame [Frant 1974].
Polymer materials may also form hazardous fumes or gases when exposed to heat [Robbins and Ware 1964].
Finally, the worker should be informed of ( 1) any unusually hazardous constituents of the work materials such as beryllium, cadmium, chromium, nickel, etc., (2) any hazardous coatings such as lead paint, mercury, or zinc, and ( 3) any precautions and control measures necessary for minimizing potential health risks.
# Containers
Drums, containers, pipes, jackets, and other hollow structures should be properly prepared and tested before welding [McElroy 1980].
Preparation of hollow structures varies depending on their contents.
At a minimum, the following procedures should be undertaken to minimize the risk of accidental injury or exposure to toxic agents: remove all ignition sources; disconnect the structure from any pipes, hoses, or other connections; examine the interior for waste or debris; and cleanse the structure of flammable materials or materials that could produce flammable or toxic vapors upon heating.
The appropriate cleaning process for containers depends on the materials present.
For many types of materials, an adequate cleaning process consists of steaming the container, washing with caustic soda, and rinsing with boiling water. The container should be dried and inspected.
Check for the presence of flammable or toxic gases or vapors. Vent the container to prevent a buildup of pressure in the interior.
Further protection may be given by filling the container with water to within an inch or two of the area to be welded or cut, and/or purging the interior of the container with inert gas. Before cutting or welding is permitted, the area must be inspected by the individual responsible for authorizing welding processes [29 CFR 1910.252].
Preferably, such authorization should be in the form of a written permit.
# Emergencies
The employer should formulate a set of written procedures covering fire, explosion, electrical shock, asphyxiation, and any other foreseeable emergency that may arise in welding processes.
All potentially affected workers should receive training in evacuation procedures to be used in the event of fire or explosion.
All workers who are involved in welding processes should be thoroughly trained in the proper work practices to reduce the potential for starting fires and causing explosions.
# D. Personal Protective Clothing and Equipment
# Clothing
The employer should provide and require the use of protective clothing as fo ll ow s:
•
All welders should wear flame-resistant gauntlet gloves and shirts with sleeves of sufficient length and construction to protect the arms from heat, UV radiation, and sparks.
In most cases, wool and leather clothes are preferable because they are more resistant to deterioration and flames than cotton or synthetics. Welders should not wear light-weight, translucent fabrics and fabrics that show severe wear with holes [USAEHA 1984].
# •
All welders should wear fire-resistant aprons, coveralls, and leggings or high boots.
• Welders performing overhead work should wear fire-resistant shoulder covers (e.g., capes), head covers (e.g., skullcaps), and ear covers.
• Workers welding on metal alloys that contain highly toxic elements (e.g., beryllium, cadmium, chromium, lead, mercury, or nickel), should wear work uniforms, coveralls, or similar full-body coverings that are laundered each day. Employers should provide lockers or other closed areas to store work and street clothing separately.
Employers should collect work clothing at the end of each work shift and provide for its laundering.
Any clothing treated for fire resistance should be retreated after each laundering.
Laundry personnel should be informed about the potential hazards of handling contaminated clothing and instructed on measures to minimize their health risk.
# •
Employers should ensure that protective clothing is inspected and maintained to preserve its effectiveness.
Clothing should be kept reasonably free of oil or grease.
Front pockets and upturned sleeves or cuffs should be prohibited, and sleeves and collars should be kept buttoned to prevent hot metal slag or sparks from contacting the skin.
# •
Workers and persons responsible for worker health and safety should be informed that protective clothing may interfere with the body's heat dissipation, especially during hot weather or in hot industries or work situations (e.g., confined spaces).
Therefore, additional monitoring is required to prevent heatrelated illness when protective clothing is worn under these condi t ions.
# Eye and Face Protection
The employer should provide and require the use of welding helmets with the following eye and face protection: approved UV filter plates and safety spectacles with side shields or goggles for workers exposed to arc welding or cutting processes; goggles or similar eye protectors with filter lenses for oxyfuel gas welding, brazing, or cutting; and goggles or similar eye protectors with transparent lenses for resistance welding and brazing.
Hand-held screens for shielding the face and eyes should not be used since they may inadvertently be held incorrectly.
A report prepared by C.E. Moss [1985] provides a compendium of protective eyeware that may be helpful in choosing appropriate eye protection.
All welding helmets must meet the requirements of 29 CFR 1910.252(e)( 2) (ii), "Specifications for protectors."
Eye and face protectors should be periodically inspected and maintained by the employer.
Eye and face protectors should be sanitized before being used by another worker.
In addition, submerged arc welders must, where the work permits, be enclosed in an individual booth coated on the inside with a nonreflective material as set forth in 29 CFR 1910.252(e)(2)(ii).
# Respiratory Protection
Engineering controls should be the primary method used to control exposure to airborne contaminants.
Respiratory protection should be used by workers only in the following circumstances:
• During the development, installation, or testing of required engineering controls
• When engineering controls are not feasible to control exposure to airborne contaminants during short-duration operations such as maintenance and repair
# • During emergencies
Respiratory protection is the least preferred method of controlling worker exposures and should not be used routinely to prevent or minimize exposures.
When respirators are used, employers should institute a complete respiratory protection program that includes worker training at regular intervals in the use and limitations of respirators, routine air monitoring, and maintenance, inspection, cleaning, and evaluation of the respirator.
Respirators should be used in accordance with the manufacturer's instructions.
Each respirator user should be fit tested and, if possible, receive a quantitative, on-the-job evaluation of his or her respirator protection factor to confirm the protection factor assumed for that class of respirator.
For additional information on the use of respiratory protection, refer to the NIOSH Guide to Industrial Respiratory Protection [NIOSH 1987a].
Selection of the appropriate respirator depends on the types of contaminants and their concentration in the worker's breathing zone. Before a respirator can be selected, an assessment of the work environment is typically necessary to determine the concentrations of specific metal fumes and other particulates, gases, or vapors that may be present.
As an interim measure until the environmental assessment has been made, the evaluator should conduct an initial review of precautionary labels on filler metals, electrodes, and flux materials to make a best estimate of the appropriate class of respirators. Respirator types shall be selected in accordance with the most recent edition of the NIOSH Respirator Decision Logic [NIOSH 1987b].
The following respirators should be used if a carcinogen is present at any detectable concentration, or if any other conditions are present that are considered to be immediately dangerous to life or health (IDLH):
• A self-contained breathing apparatus with a full facepiece operated in a pressure-demand or other positive-pressure mode.
• A combination respirator that includes a supplied-air respirator with a full facepiece operated in pressure-demand or positivepressure mode and an auxiliary self-contained breathing apparatus operated in a pressure-demand or other positive-pressure mode.
When respirators must be selected for combinations of contaminants in different physical forms, combination cartridge and particulate filter air-purifying respirators may be acceptable under specific conditions as long as none of the agents are considered carcinogenic.
The actual respirator selection should be made by a qualified individual, taking into account specific use conditions including the interaction of contaminants with the filter medium, space restrictions caused by the work location, and the use of welding helmets or other face and eye protect ive devices.
When welding is performed in confined spaces, the potential exists for a reduction in ambient oxygen concentrations.
A self-contained breathing apparatus or supplied-air respirator with an auxiliary self-contained breathing apparatus must be used for oxygen concentrations below 19.5% (at sea level).
# E. Labeling and Posting
In accordance with 29 CFR 191029 CFR .1200, "Hazard Communication," workers must be informed of exposure hazards, of potential adverse health effects, and of methods to protect themselves. Though all workers associated with welding processes should have received such information as part of their training, labels and signs serve as important reminders.
Labels and signs also provide an initial warning to other workers who may not normally work near those processes.
Depending on the process, warning signs may state a need to wear eye protection, hearing protectors, or a respirator; or they may be used to limit entry to an area without protective equipment.
For transient nonproduction work, it may be necessary to display warning signs at the worksite to inform other workers of the potential hazards.
Labels on containers of filler metal, electrodes, and flux materials that are toxic shall include the following information:
(1) the name of the metal and a warning describing its health hazards (for materials containing carcinogens, the warning should include a statement that fumes or gases from these materials may cause cancer), (2) instructions to avoid inhalation of or excessive skin or eye contact with the fumes of the materials, (3) instructions for emergency first aid in case of exposure, ( 4) appropriate instructions for the safe use of the materials, and ( 5) instructions for the type of personal protective clothing or equipment to be worn.
Base metals that contain or are coated with materials containing carcinogens or other toxic metals (e.g., lead or mercury) should be clearly labeled or marked to indicate their contents before being welded.
This same type of information must be posted in areas where welding is being performed.
All labels and warning signs should be printed in both English and the predominant language of non-English-reading workers.
Workers who cannot read labels or posted signs should be identified so that they may receive information about hazardous areas and be informed of the instructions printed on labels and signs.
# F. Sanitation
The preparation, storage, or consumption of food should not be permitted in areas where welding takes place.
The employer should make handwashing facilities available and encourage the workers to use them before eating, smoking, using the toilet, or leaving the work site.
Tools and protective clothing and equipment should be cleaned as needed to maintain a sanitary condition.
Toxic wastes should be collected and disposed of in a manner that is not hazardous to workers or surrounding environments.
No dry sweeping or blowing should be permitted in areas where welding is performed with materials containing carcinogens or other highly toxic metals.
Vacuum pickup or wet mopping should be used to clean the work area at the end of each work shift or more frequently as needed to maintain good housekeeping practices.
Collected wastes should be placed in sealed containers that are labeled as to their contents.
Cleanup and disposal should be conducted in a manner that enables workers to avoid contact with the waste and to observe applicable Federal, State, or local regulations.
Uncovered tobacco products should not be permitted to be carried or used for smoking or chewing. Workers should be provided with and advised to use facilities for showering and changing clothes at the end of each work shift. Work areas should be kept free of flammable debris.
Flammable work materials (rags, solvents, etc.) should be stored in approved safety cans.
# G. Availability of Substitutes
Fume and gas composition may be affected by material substitution. Toxic agents in welding fumes and gases may require remedial action such as changing the electrodes, fluxes, or type of welding process if appropriate control measures cannot be implemented.
Materials that may come into contact with welding processes (e.g., metals coated with oil and paint) should always be cleaned to prevent exposure to other toxic agents [DWI 1977]. Because impurities or contaminants are often contained in fluxes [Steel and Sanderson 1966] or base metal coatings [Pegues 1960], substitutions should be done cautiously to avoid introducing other toxic exposures.
In practice, however, substitution is not always an alternative to minimizing exposures, since material and process selection usually depend on the type of weld required and the quality of the finished product.
# VIM. RESEARCH NEEDS
Research is needed in several areas to evaluate the work-relatedness of disease symptoms in exposed workers who are associated with welding processes.
The various chemical agents (fumes and gases) and physical agents generated during these processes need to be characterized, and their possible interactions need to be assessed.
Long-term inhalation studies in animals, and morbidity and mortality studies of welders are needed to better define the relationship between exposure and respiratory disease, including lung cancer.
Several studies have indicated that workers who smoke and weld have an increased incidence and severity of respiratory disease. This association should be clarified.
Several epidemiologic studies have shown statistically significant increases in the risk of lung cancer for workers who weld stainless steel.
Thus the carcinogenic potential of stainless steel welding emissions needs to be better defined.
Research is particularly needed to assess the carcinogenicity of chromium and nickel in the forms generated during this process.
Comprehensive industrial hygiene evaluations are needed to quantitate exposure concentrations and ascertain past exposures.
To make such evaluations, investigators must gather information on the types of welding performed, work practices and controls used, and composition of base metals, fluxes, and electrodes.
To simplify the task of repetitively characterizing work environments where welding processes are performed, researchers should pursue a means of indexing exposures by job type or process. Workplace exposures should be characterized by representative jobs and job sites with the use of personal and stationary samplers.
The various components of the fumes and gases should be identified and quantified as a fraction of the total or respirable fumes.
In addition, information should be gathered on the type of welding technology and welding consumables used.
This information should take the form of a list of processes and their applications, the types of material they use, the nature of the workplace, and the type of job. Furthermore, the intensity of the work should be determined by estimates of arcing time per job shift, the number of electrodes consumed per unit of time, or the quantity of consumables purchased.
Also, the use of any specific work practices or local exhaust ventilation should be recorded along with their effects on the extent and composition of the fume exposure.
Better control technology should be developed in the form of new welding processes and worker-protective measures to assure that the worker is protected to the greatest extent possible.
The use of new metals, alloys, and complex composites of materials should be closely monitored and assessed for their potential to cause adverse health effects.
Recordkeeping and medical monitoring requirements proposed in this document need to be assessed for welders who change jobs frequently (e.g., welders in job shops or construction).
Because of the short-term nature of these jobs, the recordkeeping and monitoring provisions of this document may not be readily implemented. Methods are also needed to prevent the replication of medical examination and monitoring records among various employers.
ACGIH [1984].
Industrial ventilation, a manual of recommended practice, 18th ed.
Lansing, Ml: American Conference of Governmental Industrial H y g i e n i s t s . R a tio n a le . For the M W maneuver, the fre q u e n c y content of the volume-time signal is high (28,29). Results are depe n d e n t o n the patient effort as well as the frequency response characteristics of the spirometer (21,(30)(31)(32). (
* SUBJECT/PATIENT MANEUVERS 1 ----- MEASUREMENT PROCEDURES I ACCEPTABILITY | 1 ---- REPRODUCIBILITY 1 ----------- REFERENCE VALUE/ INTERPRETATION * ----
# CLINICAL ASSESSMENT
# D e fin itio n s
# II. EQUIPMENT RECOMMENDATIONS
# R e c o m m e n d a tio n -V C E q u ip m e n t
# Recommendation-Forced Vital Capacity (FVC)
# Recommendation-Timed Forced Expiratory Volume (FEVt)
F E V t = T h e v
# General Background-Spirometry Recorders/Displays
# ) H A N D M E A S U R E M E N T fu n c tio n -
# Recommendation-FVC Maneuver Time Scale (1) D I A G N O S T I C function: time scale, A T L E A S T 1 cm/s.
( 2 give further specifi cation details.
# ) V A L I D A T I O N a n d H A N D M E A S U R E M E N T functions: time scale, A T L E A S T
# Recommendation-Flow-Volume Curves
# III. EQUIPMENT VALIDATION Recommendation-FVC Validation of Test Equipment
# Recommendation-MW Validation Equipment
# IV. EQUIPMENT QUALITY CONTROL
Routine e q u i p m e n t preventive maintenance, cleaning, calibration checks, verification, a n d quality control are important to assure ac curate spirometry results (38). A spirometry procedure m a n u a l is a n important base for a quality assurance program. T h e m a n u a l should contain a quality control plan, guide lines for ordering spirometry, guidelines for performing spirometry, a n d guidelines for reporting spirometry results. See the d o c u m e n t "A T S Quality Assurance for P u l m o n a r y Laboratories" for m o r e details (38).
T h e role o f spirometric e q u i p m e n t in the transmission o f infections has not b e e n es tablished (39) 7) m a i n t e n a n c e o f equipment, ( 8) protection of patients f r o m other infected/colonized p a tients or staff, a n d ( 9) microbiologic m o n i t o r ing (39). (6,45), the A T S has published "C o m p u t e r Guidelines for P u l m o n a r y Laboratories" (46), w h i c h should b e followed.
.
# Recommendation-Equipment Quality Control
# Recommendation-FVC Subject Instruction and Maneuver
# Recommendation-FVC End of Test Criteria
Subjects should be verbally exhorted to c o n tinue to squeeze out the air at the e n d of the maneuver. "E n d of list" will occur w h e n there is:
(
# Recommendation -Minimum FVC Exhalation Time
A m i n i m u m exhalation time of 6 s, unless there is a n obvious plateau, is required to o b tain m a x i m a l F V C results. L o n g e r times are often required to achieve "e n d o f test," par ticularly in obstructed individuals. 15) h ave reported that for adults a n d children, 8 m a n e u v e r s is a practical u p p e r limit.
# Recommendation-FVC Satisfactory Start of Test Criteria
# Recommendation-FVC: Maximum Number of Maneuvers
# Recommendation-FVC Environmental Conditions
# Recommendation-FVC Use of Nose Clips
U s e o f nose clips is encouraged.
# R a tio n a le .
# Recommendation-FVC Sitting Versus Standing
Subjects m a y be studied in the sitting or standing position. Indication o f position is necessary. In fact, these regulations are already in place a n d will not likely change.
# VI. MEASUREMENT PROCEDURES Measurement
# Recommendation-Test Result Selection/Reporting of Results
Because the average differences between the 2 m e t h o d s are so small ( < 10 ml), a n y refer ence value studies ( 63) o r epidemiologic studies previously d o n e with the "best test" m e t h o d are still valid.
# VII. ACCEPTABILITY AND REPRODUCIBILITY Recommendation-FVC Maneuver Acceptability
# Recommendation-FVC Test Result Reproducibility
# VIII. REFERENCE VALUES AND INTERPRETATION STANDARDIZATION
This area of spirometry standardization is.at a n early stage in its development. T h e standardization of interpretive proce dures is also in nee d of further investigation (70). T h e present situation allows e n o u g h in terpretive variability to cause identical data f r o m a patient to be interpreted differently in different laboratories (71).
# IX. CLINICAL ASSESSMENT Clinical/Epidemiologic Considerations
# TIMI (HO
# APPENDIX B-Standard Waveforms for Spirometer Validation
A recent study using the standard spirometry w a v e f o r m s ( 6 . 6,7, 8,11,12,15, 17, 21, 23)
-1 -1 -t i ' -1 -1 -1 -iT -'-1
# OXYFUEL GAS WELDING
# PLASMA ARC CUTTING
An arc cu ttin g process that severs metal by m elting a lo c a lize d area with a co n stricte d arc and removing the molten m aterial w ith a h ig h -v e lo c ity je t of hot ionized gas issuing from the o r i f ic e .
# PLASMA ARC WELDING
An arc welding process that produces coalescence of metals by heating them with a co n stricte d arc between an electro de and the workpiece (tra n sfe rre d a rc ) or the electrode and the c o n s tric tin g nozzle (nontransferred a r c ) . Shield ing is obtained from the hot ionized gas issuing from the o r i f i c e , which may be supplemented by an a u x ilia r y source of sh ie ld in g gas. S hield ing gas may be an in e rt gas or a m ixture of gases. Pressure may or may not be used, and f i l l e r metal may or may not be supp I i ed.
# RESISTANCE WELDING
Welding processes that produce coalescence of metals with the a p p lic a tio n of pressure and with the heat obtained from re sista n c e of the work to e le c t r ic current in a c ir c u it that includes the work.
# SHIELDED METAL ARC WELDING
An arc welding process that produces coalescence of metals by heating them with an arc between a covered metal electro de and the work. S hield ing is obtained from decomposition of the electro de co vering . Pressure is not used, and filler metal is obtained from the e le ctro d e .
# SUBMERGED ARC WELDING
An arc welding process that produces coalescence of metals by heating them with an arc or a rcs between a bare metal electro de or electro d es and the work. The a rc and molten metal are shielded by a blanket of granular fusible m aterial on the work. Pressure is not used, and filler metal is obtained from the electro de or sometimes from a supplemental source (welding rod, flux, or metal g ra n u le s).
# TIG WELDING
See p referred term-GAS TUNGSTEN ARC WELDING.
# TORCH BRAZING
A brazing process in which the heat required is furnished by a fuel gas flame.
# 230
Welding processes that produce coalescence by heating materials with an oxyfuel gas flame, with or without the application of pressure and with or without the use of filler metal.
#
The authors stated that the welding apparatus was not defective and the maximum voltage at idle was 86.0 V. The autopsy revealed an electrical burn on the right side of the throat.
#
Beton DC, Andrew GS, Davies HJ, Howells L, Smith GF [1966]. 25. Blot RH, Harrington JM, Toledo A, Hover R, Heath CW, Fraumenti JR, . Lung cancer after employment in shipyards during World War II. N Engl J Med 299:620-624.
BLS [1983].
Survey of welding and cutting accidents resulting in injuries, 1978.
Washington, DC: U.S. Department of Labor, Bureau of Labor Statistics.
NT IS PB 83 -2 0 8 0 0 1 7 , p. 33. BLS [1985]. SDS data base available from NTIS. Washington, DC: U.S. Department of Labor, Office of Occupational Safety and Health Statistics, Bureau of Labor Statistics. Bobrishchev-Pushkin DM [1972].
Health assessment of electron-beam welding of beryllium bronze (in Russian).
Weld Prod 19 ( 1 1 ) :72-74.
Breslin AJ, Harris WB [1952].
Use of thoriated tungsten electrodes in inert gas shielded arc welding-investigation of potential hazard.
Am Ind Hyg Assoc Q 13 (4):191-195. Breslow L, Hoaglin L, Rasmussen G, Abrams HK [1954].
Occupations and cigarette smoking as factors in lung cancer.
Am J Public Health 44:171-181.
Britton JA, Walsh EL [1940].
Health hazards of electric and gas welding: (1) review of the literature; (2) results of examination of 286 welders; (3) preventive measures.
J Ind Hyg 22(4): 125-151.
Brun J, Cassan G, Kofman J, Gi Ily J [1972]. Siderosclerosis of arc welders with diffuse interstitial fibrosis and a pseudo-tumoral conglomerative picture (in French).
Poumon Coeur 2 8 ( 1 ) :7-14.
Buhrer P, Brunschwiler P [1978]. Some cases of fire caused by welding or cutting fires caused by welding sparks (in Swedish). Document No. VIII-790-78.
London, England: International Institute of Welding, p. 12.
Bureau of the Census [1984]. 1980 Byczkowski S, Cempel M, Gadomska J [1970].
Studies Challen PJR, Hickish DE, Bedford J [1958].
An investigation of some health hazards in an inert-gas tungsten-arc welding shop.
Br J Ind Med 15:276-282.
Christensen FC, Olson EC [1957]. Cadmium poisoning.
# AMA Arch
Ind Health 1 6 ( 1 ) :8-13.
Compressed Gas Association [1966].
Acetylene, Pamphlet G-1. New York, NY: Compressed Gas Association, Inc. Cresswell RA [1971].
Health and safety aspects of plasma cutting (in French). Document No.
V I 1 1-433-71.
London, England: International Institute of Welding, pp. 73-81. Dahlberg JA [1971].
The intensity and spectral distribution of ultraviolet emission from welding arcs in relation to the photodecomposition of gases. Ann Occup Hyg 14:259-267.
Dahlberg JA, Myrin LM [1971].
The formation of dichloroacetyI chloride and phosgene from trichloroethylene in the atmosphere of welding shops.
Ann Occup Hyg 14:269-274.
Gerin M, Siemiatycki J, Richardson L, Pellerin J, Lakhani R, Dewar R [1984].
Nickel Particulate fume generation in arc welding processes. Weld J 54(7)(Suppl):201s-210s.
Herbert A, Sterling G, Abraham J, Abraham J, Corrin B [1982].
Desquamative interstitial pneumonia in an aluminum welder.
Hum Pathol 13( 8):694-699.
Herberts P, Kadefors R [1976].
A study of painful shoulder in welders. Acta Orthop Scand 4 7 ( 4 ) :381-387.
Hewitt PJ, Hicks R [1973].
An investigation of the effects of inhaled welding fume in the rat. Ann Occup Hyg 16:213-221. Hickish DE, Challen PJR [1963].
A preliminary study of some health hazards in the plasma jet process.
Br J Ind Med 20:95-99. The effect of new welding processes on health (in Czechoslovakian).
Pracov Lek 2 9 ( 2 ) :47-50. USAEHA [1984].
Nonionizing radiation protection study no. 25-42-0328-84. Transmission of potentially hazardous actinic ultraviolet radiation through fabrics.
January 1981-March 1982.
Aberdeen Proving Ground, MD: United States Army Environmental Hygiene Agency.
van Someren E, R o M a s o n EC [1948].
Radiation from the welding arc. Its effect on the eye. Weld J (Suppl) 2 7 ( 9) :448s-452s.
Virtamo M [1975].
Fumes from welding of stainless and acid resistant Cr-Ni-steels (in Finnish Reprints m a y be requested from your state or local lung associations.
# VII. Acceptability and Reproducibility
Reproduced by permission of the American Review of Respiratory Disease. 1987Disease. , 136:1285Disease. -1298. V o l u m e sam p l i n g techniques with optical
# ARC CUTTING
Cutting processes that melt the metals to be cut with the heat of an a rc between an electrode and the base m etal.
# ARC WELDING
Welding processes that produce coalescence of m etals by heating them w ith an a r c , with or without the a p p lic a tio n of p re ssu re , and w ith or without the use of in e rt gases or f i l l e r m etal.
# CARBON ARC CUTTING
An arc cu ttin g process in which m etals are severed by m elting them with the heat of an a rc between a carbon electro de and the base m etal.
# CARBON ARC WELDING
An arc welding process that produces fusion of m etals by heating them with an a rc between a carbon electro d e and the work. No sh ie ld in g is used. Pressure and f i l l e r metal may or may not be used.
# COLD WELDING
A s o lid -s ta te welding process in which pressure is used at room temperature to produce coalescence of metals w ith su b sta n tia l deformation at the weld.
# ELECTRON BEAM WELDING
A welding process that produces coalescence of metals w ith the heat obtained from a concentrated beam composed p rim a rily of h ig h -v e lo c ity electro n s impinging on the jo in t to be welded.
# FLUX-CORED ARC WELDING
An a rc welding process that produces coalescence of metals by heating them w ith an a rc between a continuous f i l l e r metal (consumable) electro d e and the work. S h ie ld in g is provided by a flu x contained w ith in the tubular e le c tro d e . A dd itio nal sh ie ld in g may or may not be obtained from an e x te rn a lly supplied gas or gas m ixtu re.
# FURNACE BRAZING
A brazing process in which the p a rts to be joined are placed in a furnace heated to a s u ita b le temperature.
# GAS METAL ARC WELDING
An a rc welding process that produces coalescence of metals by heating them w ith an a rc between a continuous f i l l e r metal (consumable) electro d e and the work. Sh ie ld in g is obtained e n t ir e ly from an e x te rn a lly supplied gas or gas m ixtu re . Some v a ria tio n s of th is process are c a lle d MIG or CO2 welding (nonpreferred term s).
# GAS TUNGSTEN ARC WELDING
An a rc welding process that produces coalescence of metals by heating them w ith an a rc between a tungsten (nonconsumable) electro de and the work. Sh ield in g is obtained from a gas or gas m ixtu re. Pressure and f i l l e r metal may or may not be used.
# GOUGING
The forming of a bevel or groove by m aterial removal.
# LASER BEAM WELDING
A welding process that produces coalescence of m a te ria ls w ith the heat obtained from the a p p lic a tio n of a concentrated coherent lig h t beam impinging on the members to be jo in e d .
# MIG WELDING
See p referred terms-GAS METAL ARC WELDING and FLUX-CORED ARC WELDING.
# OXYACETYLENE WELDING
An oxyfuel gas welding process that produces coalescence of metals by heating them with a gas flame obtained from the combustion of acetylene with oxygen. The process may be used with or without the a p p lic a tio n of pressure and with or without the use of f i l l e r m etal. | None | None |
8da29ddb71bca4071159dc1eb481dc56802c2912 | cdc | None | depar depar depar depar department of health and human ser tment of health and human ser tment of health and human ser tment of health and human ser tment of health and human services vices vices vices vices# Background
This report presents CDC's recommendations for case definitions for Acute Idiopathic Pulmonary Hemorrhage (AIPH) among infants and CDC's plan for retrospective surveillance for AIPH among infants, including a study to evaluate the feasibility of using International Classification of Diseases (ICD) (1) codes for surveillance for AIPH.
In 1994 and 1997, CDC reported clusters of acute pulmonary hemorrhage (APH) among infants (2,3) in Cleveland, Ohio. During 1992, a similar cluster occurred in the Chicago area (4). In Cleveland, risk factors for illness included male sex; lack of breast-feeding; residence in households with smokers; residence in homes where water damage had occurred during the previous 6 months; and residence in homes with increased quantities of fungi, including Stachybotrys atra.
Reviews by CDC staff and external consultants of these investigations identified shortcomings in the conduct of the studies (5). These panels concluded that the investigations did not prove an association between APH among infants and exposure to molds, specifically S. chartarum (atra). These reviewers recommended that CDC, pediatric pulmonologists, and state and local public health officials collaborate to
- develop a standard surveillance case definition;
- develop standard protocols for data collection and environmental assessment; - implement surveillance for AIPH; - investigate cases of AIPH among infants, particularly when clusters are identified, considering associations with multiple possible etiologies; and - enhance sampling and laboratory analytic methods to improve assessment of environmental exposures to molds and fungi (5). In response to the reviewers' recommendations, CDC staff developed a plan to conduct surveillance for AIPH, investigate clusters of cases, and conduct studies. In formulating this response, CDC convened three meetings to establish a case definition and classification scheme for public health surveillance for AIPH, recommend a standard home environmental investigation protocol, and outline a plan for surveillance and investigation of AIPH among infants. As a consequence of these meetings, CDC has determined that a series of surveillance activities should be initiated to direct future efforts. In addition to providing an overview of the results of the three meetings, this report describes surveillance activities and how results from those activities can guide efforts to investigate the burden and etiology of AIPH among infants.
AIPH among infants is a diagnosis of exclusion. Certain syndromes (Box 1) and other disease states can occur with pulmonary hemorrhage. Thus, differential diagnoses and neonatal medical problems that can cause pulmonary hemorrhage should be ruled out.
# Meeting Panelists and Goals
Three meetings of panelists were convened to advise CDC staff regarding investigation of AIPH among infants. The Case Definition Panel included three pediatric pulmonologists, one pediatric intensive care specialist, one pediatric pathologist, two epidemiologists, and one environmental epidemiologist. The purpose of this panel was to recommend a case definition for use in public health surveillance for AIPH to facilitate case finding. Case finding will facilitate documentation of the burden of the condition and identification of possible etiologic agents or risk factors.
The Surveillance Implementation Panel included one pediatrician, one pediatric pulmonologist, one forensic pathologist, three epidemiologists (including one state epidemiologist), and four environmental epidemiologists (including one state epidemiologist and one toxicologist). Its purpose was to recommend a standard approach for public health surveillance for AIPH.
The Home/Indoor Environment and Laboratory Investigation Panel included two mycologists, one biochemist, two microbiologists, two industrial hygienists, two toxicologists, and one environmental epidemiologist. Its purpose was to recommend standard approaches and protocols for environmental data collection, laboratory analysis, and data interpretation during public health surveillance for AIPH.
For each of the three areas, group discussion led by a moderator was based on prepared questions. Participants produced written summaries, which form the basis of the recommendations provided in this report.
# BOX 1. Pulmonary hemorrhage terminology
The term used for the cluster of cases reported in Cleveland- was pediatric idiopathic pulmonary hemorrhage and hemosiderosis. The term pulmonary hemorrhage has been used to describe situations with identifiable causes of bleeding. † Idiopathic pulmonary hemosiderosis (IPH) § or primary hemosiderosis ¶ has been used to denote presumably idiopathic bleeds or the accumulation of iron as hemosiderin. § The terms pulmonary hemorrhage and primary hemosiderosis are often used interchangeably. The new International Classification of Diseases, Tenth Revision (ICD-10) mortality coding system † † has no code for idiopathic pulmonary hemosiderosis. The CDC definition of a case of AIPH in an infant uses the term pulmonary hemosid-erosis as a pathological finding to denote the possible occurrence of pulmonary hemorrhage, and not to describe a clinical syndrome.
The term pulmonary hemorrhage encompasses multiple clinical syndromes, including - diffuse pulmonary hemorrhage; § § - pulmonary hemorrhage of the newborn (ICD-9: 770.3; ICD-10: P26) ¶ ¶ or hemoptysis; - cough with hemorrhage; - pulmonary hemorrhage not otherwise specified 786.3; ICD-10 R04, R04.2); and - idiopathic pulmonary hemosiderosis (ICD-9: 516.1, no ICD-10 code).
# Case Definition Case Classification and Severity Criteria
AIPH is the sudden onset of pulmonary hemorrhage in a previously healthy infant in whom differential diagnoses and neonatal medical problems that might cause pulmonary hemorrhage have been ruled out. Pulmonary hemorrhage can appear as hemoptysis or blood in the nose or airway with no evidence of upper respiratory or gastrointestinal bleeding. Patients have acute, severe respiratory distress or failure, requiring mechanical ventilation and chest radiograph (CXR), and usually demonstrate bilateral infiltrates.
AIPH among infants and sudden infant death syndrome (SIDS) potentially share similar risk factors (e.g., age group and maternal cigarette smoking). Also, in certain cases, SIDS is associated with pulmonary hemorrhage found at autopsy (6,7). Thus, factors that are known risk factors for SIDS should be identified when evaluating an infant possibly having AIPH. Potential information sources for case-identification and casestatus classification during an investigation of pulmonary hemorrhage are provided (Table 1).
# Clinically Confirmed Cases of AIPH Among Infants
Criteria for a confirmed case include pulmonary hemorrhage in a previously healthy infant aged 32 weeks, with no history of neonatal medical problems that might cause pulmonary hemorrhage, and whose condition meets all of the following three criteria:
- Abrupt or sudden onset of overt bleeding or obvious evidence of blood in the airway, including -epistaxis, hemoptysis, or frank blood in the airway below the larynx at visualization, not caused by any medical procedure (e.g., laryngoscopy or intubation); or -identification of hemosiderin-laden macrophages (>20% of pulmonary macrophages containing hemosiderin on bronchoalveolar lavage or biopsy specimen).
A source of bleeding from the nose and oropharynx should be ruled out at the time of admission. - Severe-appearing illness leading to acute respiratory distress or respiratory failure, resulting in hospitalization in a pediatric intensive care unit (PICU) or neonatal intensive care unit (NICU) with intubation and mechanical ventilation. - Diffuse unilateral or bilateral pulmonary infiltrates visible on CXR or computerized tomography (CT) of the chest. CXR or chest CT findings should be documented within 48 hours of examination of the infant. A previously healthy infant should
- have been discharged from the hospital after birth with an uneventful course before the occurrence of bronchoalveolar hemorrhage; - never have been previously intubated, nor required respiratory support with oxygen; - not have evidence of physical abuse;
- not have any abnormality identified on admission or follow-up bronchoscopy that would explain the bleeding; and - not have neonatal medical problems that can cause pulmonary hemorrhage. CDC will adhere closely to this case definition, requiring that all the criteria be met for a confirmed case. The definition for a clinically confirmed case excludes pulmonary hemorrhage among older children and infants with restricted access to a PICU. Because no criteria exist for postmortem examinations, this definition excludes infants who die before hospital and PICU admission, whose illness might have met the case definition. However, the definitions for probable and suspect cases (see the following) will capture the majority of these cases and allow identification of illness among infants who die before examination by a physician.
# Probable Cases of AIPH Among Infants
Criteria for a probable case include a previously healthy infant aged 32 weeks,
- who has a sudden onset of bleeding from the airway, with or without respiratory distress, with or without intubation, and with or without pulmonary infiltrates on CXR or chest CT; or - who died and had evidence of bleeding from the airway found on autopsy or postmortem; had been in respiratory distress; would or should have been intubated in the opinion of a clinician; and would have had infiltrates on CXR or chest CT.
# Suspected Cases of AIPH Among Infants
Criteria for a suspected case include a previously healthy infant,
- who died and had evidence of bleeding from the airway found on autopsy or postmortem or who - either did not have chest imaging studies or had imaging studies that indicated no pulmonary infiltrates. Respiratory distress or intubation is not required for a suspected case.
# Severity Classification Scheme for AIPH Among Infants
Because of the potential for variation in symptoms among infants for each of the criteria, different case combinations might be related to the timing or duration of symptoms, disease severity, pathologic processes, or etiologic agents associated with AIPH among infants. A discussion of the proposed case-classification categories for AIPH among infants is provided (Tables 2 and 3).
# Discussion
- Bleeding might begin in a localized region of one lung with dispersion of blood to other areas of the lung through the airways - Initial chest radiograph (CXR) might indicate unilateral infiltrates, but following dispersion indicates diffuse infiltrates - Infants with unilateral infiltrates are considered confirmed for AIPH, but their characteristics might be different from infants with diffuse infiltrates
- Not considered confirmed because identification depends on lavage or biopsy finding of hemosiderin-laden macrophages and not on active bleeding or recovering blood from below the larynx - Work of breathing might vary for infants with a similar pathology (e.g., resulting from different body temperature, serum glucose levels, and duration of respiratory distress) - Infants who do not need intubation would not have acute bleeding directly identified from below the glottis - Upon initial examination, infants' circumstances might vary; information should be collected to identify these circumstances as best as possible during data abstraction so that the categories can be expanded if needed during data analysis - The circumstances might be that 1) the attending physician intended to intubate an infant who died; 2) the clinician who reviewed the death of an infant with postmortem findings consistent with pulmonary hemorrhage secondary to clinical respiratory failure thought the infant should have been intubated; 3) the infant died before arrival at the hospital and therefore was not intubated nor received thoracic imaging studies - Age-specific normochromic, normocytic, or microangiopathic anemia might indicate different pathophysiologic processes and in conjunction with appropriate clinical signs and symptoms might be supportive of a diagnosis of AIPH - Rankings of 1-5 represent categories with decreasing levels of certainty; 1 = highly probable, and 5 = least probable. The letter designations a, b, and c represent approximately equivalent levels within each category (see also Table 2).
# MMWR March 12, 2004
A summary of clinical features of AIPH among infants (Table 4) (Box 2) and neonatal medical problems and differential diagnoses that should be ruled out before classifying a case as AIPH among infants (Box 3) are included. Other differential diagnoses associated with pulmonary hemorrhage are listed (Table 5).
# Feasibility Study To Determine the Concordance of ICD Codes for Pulmonary Hemorrhage with the CDC Case Definition
Prospective nationwide surveillance for cases of AIPH among infants is difficult to justify on the basis of the available epidemiologic data. In addition to the limitations reported for the Cleveland study (5), no risk factors were conclusively linked to disease in the Chicago investigation ( 4), and only one other cluster (in Detroit) was reported during 1992-1996 (7).
CDC will retrospectively review cases of pulmonary hemorrhage to determine the public health impact of AIPH among infants and to generate hypotheses regarding the importance of risk factors possibly associated with AIPH among infants. If that review indicates that AIPH among infants is a separate clinical entity and that these cases have occurred in clusters, or that an increase in incidence or mortality is associated with these cases, CDC will initiate prospective surveillance and case ascertainment to identify cases for epidemiologic studies designed to confirm or disprove associations between pulmonary hemorrhage host factors, environmental factors, and biologic agents, including such molds as S. chartarum (5).
# Retrospective Review by Using Existing Data Sources
The ability to use existing data sources should substantially facilitate both determining the public health impact of AIPH among infants. However, the reliable data regarding mortality from pulmonary hemorrhage is only available at the national level. CDC conducted a preliminary evaluation of ICD codes for surveillance of pulmonary hemorrhage among infants to determine whether existing data sources can be used to estimate the magnitude of the problem of AIPH among infants. CDC examined data from the National Hospital Discharge Survey (NHDS) and National Mortality Data. Possible cases of AIPH among infants were identified by using ICD-9 codes 770. 3, 784.7, 784.8, 786.3, and 516.1 (Table 6).
Infants identified by ICD-9 codes 770.3 and 786.3 differ from the cases reported in Cleveland. In the national datasets, the majority of cases of pulmonary hemorrhage had diagnoses such as prematurity or immaturity and death occurring within the first 7 days of life. The Cleveland cases occurred among stable, healthy, mature infants who had been discharged from the hospital to their homes after birth and subsequently experienced pulmonary hemorrhage (8)(9)(10). Thus, the estimates of deaths and hospital admissions for cases of pulmonary hemorrhage using ICD codes 770.3 and 786.3 does not distinctly identify infants with AIPH as defined by CDC. In addition, these national datasets do not determine if infants had identifiable etiologies or complications before their discharge from the hospital or their death. Because the estimated number of hospitalized cases with a primary diagnosis of pulmonary hemorrhage was less than the number of deaths, these national datasets might not be reliable for surveillance for infantile pulmonary hemorrhage. These analyses might be better performed by using state-based data.
A retrospective review for AIPH among infants will be performed in metropolitan cities in those states with the highest death rates and with >100 deaths associated with pulmonary hemorrhage among infants, on the basis of relevant ICD-9 and ICD-10 codes used from 1979 to the most recent available data. By focusing on PICUs and NICUs with substantial numbers of deaths, cases from innercity catchment areas, where the incidence of AIPH among infants is suspected to be higher, will be captured. Potential cases will be identified by using standardized methods of case ascertainment and data collection from hospital discharge and mortality data sources, based on ICD codes. Potential cases will be compared with the recommended case definition by reviewing medical records related to all cases of pulmonary hemorrhage observed since 1979 among children aged <2 years.
This retrospective review of AIPH among infants will - determine whether AIPH among infants is a distinct clinical entity within existing ICD-9/ICD-10 diagnostic codes for pulmonary hemorrhage; - describe the epidemiology of pulmonary hemorrhage; - identify trends in the frequency of cases and the geographic distribution and clustering of cases; - estimate the public health impact of AIPH among infants;
- identify groups at high risk for AIPH among infants; and - determine the need for prospective surveillance as a source of cases for a case-control study. The data will be reviewed to determine how these cases, including the apparent case clusters of AIPH among infants in Cleveland and Chicago, have been coded on hospital discharge abstracts, and how deaths attributed to the syndrome have been characterized on death certificates. Both Ohio and Illinois meet the criteria of >100 deaths from pulmonary hemorrhage. In Cleveland and Chicago, this review also will
# TABLE 4. Clinical features of acute idiopathic pulmonary hemorrhage (AIPH) among infants Finding
No evidence of cow milk protein allergy or associated respiratory, heart, kidney, or pancreatic disease- Abrupt cessation of crying or unusual crying or irritability hours to days before the initial recognition of blood in the airway † Not observed § Decreased muscle tone and dusky pallor minutes to hours before progressing to sudden onset of hypoxemic respiratory distress or failure ¶ Hours to days before onset of respiratory failure Accompanies or immediately precedes respiratory failure † † Acute and appears to be idiopathic § § Characterized by tachypnea, grunting, and chest retractions ¶ ¶ Diffusely diminished breath sounds without the presence of rales or rhonchi* Often requires intubation and mechanical ventilation; intubation when required is for 2-7 days † † † Often demonstrates bilateral pulmonary infiltrates within the first 24 hours § § § Typically, alveolar infiltrates begin to clear within the first 24-48 hours ¶ ¶ ¶ Atraumatic intubation; bronchoscopy including inspection of upper airway Typically, no source from the lung or gastrointestinal tract; presumed to be from diffuse alveolar capillary injury † † † † Typically, found in bronchoalveolar lavage fluid; might not be present in an infant experiencing an acute, initial pulmonary bleed § § § § Indicates evidence of bleeding into the lungs; finding >20% of total pulmonary macrophages containing hemosiderin can be consistent with pulmonary hemorrhage that occurred >48 hours before examination ¶ ¶ ¶ ¶ First 48 hours, fragmented or damaged red blood cells, hemoglobinuria; microangiopathic anemia might be indicative of a hemolytic process; normochromic normocytic might be consistent with acute, abrupt blood loss* Serum negative for antiglomerular basement membrane antibody, anticytoplasmic neutrophilic antibody, complement titers, serum immune complexes, and antinuclear antibody † † † † † None; spontaneous recovery with or without supportive care indicates these pathophysiologic processes are not the cause of bleeding
# BOX 2. Clinical descriptions of pulmonary hemorrhage
In early texts, pulmonary hemorrhage was not commonly described in children, although it was noted to occur.- Blood found in the airways or alveoli of humans can result from different anatomic sites. Specific sites can include alveoli, large or small conducting airways, or the nasopharynx and gastrointestinal tract with pulmonary aspiration. Regardless of the origin of blood entering the lung, substantial amounts of blood lead to impaired gas exchange, altered pulmonary mechanics, and respiratory distress. Different pathophysiologic processes are associated with pulmonary hemorrhage. These can be divided into - conditions where bleeding occurs at sites of normal tissue with mechanical disruption causing a loss of vascular integrity (e.g., intentional suffocation and mitral valve disease); - vascular inflammation, whereby the inflammatory process causes a loss of vascular integrity (e.g., vasculitis secondary to such conditions as collagen vascular diseases); - vascular malformations, whereby a combination of altered vascular integrity and physical influences (e.g., Laplace's law † ) lead to disruption of the blood vessel; and - coagulopathies, which usually also require additional physical disruption of the blood vessel through greater than normal transpulmonary vascular pressures.
The manifestations of pulmonary hemorrhage can be classified into different syndromes. Diffuse pulmonary hemorrhage is usually diagnosed by bronchoscopy, either by virtue of grossly bloody lavage fluid or by the presence of hemosiderin-laden macrophages in bronchoalveolar lavage. In biopsy and autopsy tissue, the diagnosis is made on the basis of the presence of recent blood and hemosiderin in the alveolar spaces or the interstitium. § In the immunocompromised host, intra-alveolar bleeding can result from thrombocytopenia often associated with other factors. Diffuse pulmonary hemorrhage (DPH) can either be secondary to other disease states, associated with other organ dysfunction, or be isolated. Isolated causes of DPH include lung immaturity, cow milk hypersensitivity, pulmonary capillary hemangiomatosis, and idiopathic causes. ¶ Pulmonary hemorrhage of the newborn (ICD-9: 770.3; ICD-10: P26) is manifested by focal hemorrhage into airspaces or the interstitium in the lungs of infants with hyaline membrane disease, bronchopulmonary dysplasia, and other neonatal pulmonary disorders. These infants are most often male, preterm, small for gestational age, and have a history of perinatal stress. † † The etiology and pathogenesis of the disorder has not been elucidated.
Hemoptysis, cough with hemorrhage, pulmonary hemorrhage not otherwise specified (ICD-9: 786.3; ICD-10 R04, R04.2) is an acute manifestation of bleeding from the airway. This ICD category captures all the nonneonatal (and certain neonatal) diagnoses of pulmonary hemorrhage. Children with pulmonary hemorrhage might not appear to have hemoptysis if they swallow their sputum.
Consensus is lacking on the meaning of the term idiopathic pulmonary hemosiderosis (ICD-9: 516.1, no ICD-10 code). One pathology text states that the term denotes a separate clinical entity of which diffuse pulmonary hemorrhage is the major manifestation. § § A later edition of the same text ¶ ¶ notes that the presence of hemosiderin in lung macrophages indicates degradation products of hemoglobin. Hemosiderin is thus a pathologic state indicative of bleeding of any type into the lungs* secondary to the processing of hemoglobin in the red blood cells in the airway by alveolar macrophages. † † † Adults with active alveolar hemorrhage have high hemosiderin scores in bronchoalveolar lavage fluid, § § § but hemosiderin-containing macrophages have limited differential diagnostic value. ¶ ¶ ¶ In one clinical text, the term means diffuse recurrent intrapulmonary hemorrhage that is not secondary to bleeding from trauma, bleeding from the airways, tumors, or left ventricular failure. Another author † † † † describes variants of primary and secondary pulmonary hemosiderosis.
On review of National Hospital Discharge Survey data for 1979-1996 and national mortality data for 1979-1998 for ICD-9 code 516.1 for infants, no instances were found in either dataset where ICD-9 code 516.1 was the primary listed diagnosis. However, in 207 cases, this code was the other listed diagnosis. This indicates that idiopathic pulmonary hemorrhage is usually an accompanying diagnosis to other diagnoses that result in hospitalization or death among infants. If performed, environmental assessment of the home to gather pertinent risk-assessment data should use standard protocols designed by trained environmental health professionals. At a minimum, the assessment should involve visual inspection, including checks for dampness, water damage, obvious mold, evidence of pests, and environmental tobacco smoke. Depending on the assessed need for further evaluation and the resources available, additional investigation might include determining moisture content, settled dust sampling, air sampling for different allergens, and biologically active compounds, and other investigations as needed.
# Conclusion
CDC recommends a definition for a clinically confirmed case of AIPH among infants on the basis of 1) evidence of blood in the airway; 2.) age <1 year; 3) absence of medical conditions related to pulmonary hemorrhage; and 4) severe acute respiratory distress or respiratory failure, requiring admission to a PICU with intubation and mechanical ventilation. CDC recommends that PICUs report cases that meet the CDC case definition to state health departments and to CDC.
CDC will retrospectively analyze state-level mortality and hospitalization data based on ICD codes and will retrospec- tively review discharges for pulmonary hemorrhage in selected PICUs. These studies will - distinguish between the clinical findings associated with different symptoms of AIPH among infants; - determine whether ICD codes capture cases that meet the CDC-recommended case definition for AIPH among infants; - determine whether AIPH among infants is a distinct recognizable clinical entity; - determine the proportion of cases ascertained retrospectively through ICD-9 codes that meet the clinical case definition by estimating PPV of ICD-coded data; and - define the magnitude of AIPH among infants and the need for conducting etiologic studies. CDC will review the Cleveland and Chicago case series to determine the degree to which the present case definition applies to them. In addition, CDC will evaluate the present case definition on the basis of data from initial surveillance findings and modify it as appropriate.
If these reviews establish that AIPH among infants is a public health problem on the basis of increasing numbers or clusters of cases geographically or temporally, targeted prospective case surveillance will be initiated. If prospective surveillance is initiated, CDC will maintain a database of current cases of AIPH among infants, reported by PICUs that meet the case definition. The database will serve as a source of cases for casecontrol studies to determine etiology. CDC will work with state and local health departments to investigate clusters of AIPH among infants cases. ('tr st-"w r-the) e e | depar depar depar depar department of health and human ser tment of health and human ser tment of health and human ser tment of health and human ser tment of health and human services vices vices vices vices# Background
This report presents CDC's recommendations for case definitions for Acute Idiopathic Pulmonary Hemorrhage (AIPH) among infants and CDC's plan for retrospective surveillance for AIPH among infants, including a study to evaluate the feasibility of using International Classification of Diseases (ICD) (1) codes for surveillance for AIPH.
In 1994 and 1997, CDC reported clusters of acute pulmonary hemorrhage (APH) among infants (2,3) in Cleveland, Ohio. During 1992, a similar cluster occurred in the Chicago area (4). In Cleveland, risk factors for illness included male sex; lack of breast-feeding; residence in households with smokers; residence in homes where water damage had occurred during the previous 6 months; and residence in homes with increased quantities of fungi, including Stachybotrys atra.
Reviews by CDC staff and external consultants of these investigations identified shortcomings in the conduct of the studies (5). These panels concluded that the investigations did not prove an association between APH among infants and exposure to molds, specifically S. chartarum (atra). These reviewers recommended that CDC, pediatric pulmonologists, and state and local public health officials collaborate to
• develop a standard surveillance case definition;
• develop standard protocols for data collection and environmental assessment; • implement surveillance for AIPH; • investigate cases of AIPH among infants, particularly when clusters are identified, considering associations with multiple possible etiologies; and • enhance sampling and laboratory analytic methods to improve assessment of environmental exposures to molds and fungi (5). In response to the reviewers' recommendations, CDC staff developed a plan to conduct surveillance for AIPH, investigate clusters of cases, and conduct studies. In formulating this response, CDC convened three meetings to establish a case definition and classification scheme for public health surveillance for AIPH, recommend a standard home environmental investigation protocol, and outline a plan for surveillance and investigation of AIPH among infants. As a consequence of these meetings, CDC has determined that a series of surveillance activities should be initiated to direct future efforts. In addition to providing an overview of the results of the three meetings, this report describes surveillance activities and how results from those activities can guide efforts to investigate the burden and etiology of AIPH among infants.
AIPH among infants is a diagnosis of exclusion. Certain syndromes (Box 1) and other disease states can occur with pulmonary hemorrhage. Thus, differential diagnoses and neonatal medical problems that can cause pulmonary hemorrhage should be ruled out.
# Meeting Panelists and Goals
Three meetings of panelists were convened to advise CDC staff regarding investigation of AIPH among infants. The Case Definition Panel included three pediatric pulmonologists, one pediatric intensive care specialist, one pediatric pathologist, two epidemiologists, and one environmental epidemiologist. The purpose of this panel was to recommend a case definition for use in public health surveillance for AIPH to facilitate case finding. Case finding will facilitate documentation of the burden of the condition and identification of possible etiologic agents or risk factors.
The Surveillance Implementation Panel included one pediatrician, one pediatric pulmonologist, one forensic pathologist, three epidemiologists (including one state epidemiologist), and four environmental epidemiologists (including one state epidemiologist and one toxicologist). Its purpose was to recommend a standard approach for public health surveillance for AIPH.
The Home/Indoor Environment and Laboratory Investigation Panel included two mycologists, one biochemist, two microbiologists, two industrial hygienists, two toxicologists, and one environmental epidemiologist. Its purpose was to recommend standard approaches and protocols for environmental data collection, laboratory analysis, and data interpretation during public health surveillance for AIPH.
For each of the three areas, group discussion led by a moderator was based on prepared questions. Participants produced written summaries, which form the basis of the recommendations provided in this report.
# BOX 1. Pulmonary hemorrhage terminology
The term used for the cluster of cases reported in Cleveland* was pediatric idiopathic pulmonary hemorrhage and hemosiderosis. The term pulmonary hemorrhage has been used to describe situations with identifiable causes of bleeding. † Idiopathic pulmonary hemosiderosis (IPH) § or primary hemosiderosis ¶ has been used to denote presumably idiopathic bleeds or the accumulation of iron as hemosiderin. § The terms pulmonary hemorrhage and primary hemosiderosis are often used interchangeably.** The new International Classification of Diseases, Tenth Revision (ICD-10) mortality coding system † † has no code for idiopathic pulmonary hemosiderosis. The CDC definition of a case of AIPH in an infant uses the term pulmonary hemosid-erosis as a pathological finding to denote the possible occurrence of pulmonary hemorrhage, and not to describe a clinical syndrome.
The term pulmonary hemorrhage encompasses multiple clinical syndromes, including • diffuse pulmonary hemorrhage; § § • pulmonary hemorrhage of the newborn (ICD-9: 770.3; ICD-10: P26) ¶ ¶ or hemoptysis; • cough with hemorrhage; • pulmonary hemorrhage not otherwise specified 786.3; ICD-10 R04, R04.2); and • idiopathic pulmonary hemosiderosis (ICD-9: 516.1, no ICD-10 code).
# Case Definition Case Classification and Severity Criteria
AIPH is the sudden onset of pulmonary hemorrhage in a previously healthy infant in whom differential diagnoses and neonatal medical problems that might cause pulmonary hemorrhage have been ruled out. Pulmonary hemorrhage can appear as hemoptysis or blood in the nose or airway with no evidence of upper respiratory or gastrointestinal bleeding. Patients have acute, severe respiratory distress or failure, requiring mechanical ventilation and chest radiograph (CXR), and usually demonstrate bilateral infiltrates.
AIPH among infants and sudden infant death syndrome (SIDS) potentially share similar risk factors (e.g., age group and maternal cigarette smoking). Also, in certain cases, SIDS is associated with pulmonary hemorrhage found at autopsy (6,7). Thus, factors that are known risk factors for SIDS should be identified when evaluating an infant possibly having AIPH. Potential information sources for case-identification and casestatus classification during an investigation of pulmonary hemorrhage are provided (Table 1).
# Clinically Confirmed Cases of AIPH Among Infants
Criteria for a confirmed case include pulmonary hemorrhage in a previously healthy infant aged <1 year with a gestational age of >32 weeks, with no history of neonatal medical problems that might cause pulmonary hemorrhage, and whose condition meets all of the following three criteria:
• Abrupt or sudden onset of overt bleeding or obvious evidence of blood in the airway, including -epistaxis, hemoptysis, or frank blood in the airway below the larynx at visualization, not caused by any medical procedure (e.g., laryngoscopy or intubation); or -identification of hemosiderin-laden macrophages (>20% of pulmonary macrophages containing hemosiderin on bronchoalveolar lavage or biopsy specimen).
A source of bleeding from the nose and oropharynx should be ruled out at the time of admission. • Severe-appearing illness leading to acute respiratory distress or respiratory failure, resulting in hospitalization in a pediatric intensive care unit (PICU) or neonatal intensive care unit (NICU) with intubation and mechanical ventilation. • Diffuse unilateral or bilateral pulmonary infiltrates visible on CXR or computerized tomography (CT) of the chest. CXR or chest CT findings should be documented within 48 hours of examination of the infant. A previously healthy infant should
• have been discharged from the hospital after birth with an uneventful course before the occurrence of bronchoalveolar hemorrhage; • never have been previously intubated, nor required respiratory support with oxygen; • not have evidence of physical abuse;
• not have any abnormality identified on admission or follow-up bronchoscopy that would explain the bleeding; and • not have neonatal medical problems that can cause pulmonary hemorrhage. CDC will adhere closely to this case definition, requiring that all the criteria be met for a confirmed case. The definition for a clinically confirmed case excludes pulmonary hemorrhage among older children and infants with restricted access to a PICU. Because no criteria exist for postmortem examinations, this definition excludes infants who die before hospital and PICU admission, whose illness might have met the case definition. However, the definitions for probable and suspect cases (see the following) will capture the majority of these cases and allow identification of illness among infants who die before examination by a physician.
# Probable Cases of AIPH Among Infants
Criteria for a probable case include a previously healthy infant aged <1 year with a gestational age of >32 weeks,
• who has a sudden onset of bleeding from the airway, with or without respiratory distress, with or without intubation, and with or without pulmonary infiltrates on CXR or chest CT; or • who died and had evidence of bleeding from the airway found on autopsy or postmortem; had been in respiratory distress; would or should have been intubated in the opinion of a clinician; and would have had infiltrates on CXR or chest CT.
# Suspected Cases of AIPH Among Infants
Criteria for a suspected case include a previously healthy infant,
• who died and had evidence of bleeding from the airway found on autopsy or postmortem or who • either did not have chest imaging studies or had imaging studies that indicated no pulmonary infiltrates. Respiratory distress or intubation is not required for a suspected case.
# Severity Classification Scheme for AIPH Among Infants
Because of the potential for variation in symptoms among infants for each of the criteria, different case combinations might be related to the timing or duration of symptoms, disease severity, pathologic processes, or etiologic agents associated with AIPH among infants. A discussion of the proposed case-classification categories for AIPH among infants is provided (Tables 2 and 3).
# Discussion
• Bleeding might begin in a localized region of one lung with dispersion of blood to other areas of the lung through the airways • Initial chest radiograph (CXR) might indicate unilateral infiltrates, but following dispersion indicates diffuse infiltrates • Infants with unilateral infiltrates are considered confirmed for AIPH, but their characteristics might be different from infants with diffuse infiltrates
• Not considered confirmed because identification depends on lavage or biopsy finding of hemosiderin-laden macrophages and not on active bleeding or recovering blood from below the larynx • Work of breathing might vary for infants with a similar pathology (e.g., resulting from different body temperature, serum glucose levels, and duration of respiratory distress) • Infants who do not need intubation would not have acute bleeding directly identified from below the glottis • Upon initial examination, infants' circumstances might vary; information should be collected to identify these circumstances as best as possible during data abstraction so that the categories can be expanded if needed during data analysis • The circumstances might be that 1) the attending physician intended to intubate an infant who died; 2) the clinician who reviewed the death of an infant with postmortem findings consistent with pulmonary hemorrhage secondary to clinical respiratory failure thought the infant should have been intubated; 3) the infant died before arrival at the hospital and therefore was not intubated nor received thoracic imaging studies • Age-specific normochromic, normocytic, or microangiopathic anemia might indicate different pathophysiologic processes and in conjunction with appropriate clinical signs and symptoms might be supportive of a diagnosis of AIPH * Rankings of 1-5 represent categories with decreasing levels of certainty; 1 = highly probable, and 5 = least probable. The letter designations a, b, and c represent approximately equivalent levels within each category (see also Table 2).
# MMWR March 12, 2004
A summary of clinical features of AIPH among infants (Table 4) (Box 2) and neonatal medical problems and differential diagnoses that should be ruled out before classifying a case as AIPH among infants (Box 3) are included. Other differential diagnoses associated with pulmonary hemorrhage are listed (Table 5).
# Feasibility Study To Determine the Concordance of ICD Codes for Pulmonary Hemorrhage with the CDC Case Definition
Prospective nationwide surveillance for cases of AIPH among infants is difficult to justify on the basis of the available epidemiologic data. In addition to the limitations reported for the Cleveland study (5), no risk factors were conclusively linked to disease in the Chicago investigation ( 4), and only one other cluster (in Detroit) was reported during 1992-1996 (7).
CDC will retrospectively review cases of pulmonary hemorrhage to determine the public health impact of AIPH among infants and to generate hypotheses regarding the importance of risk factors possibly associated with AIPH among infants. If that review indicates that AIPH among infants is a separate clinical entity and that these cases have occurred in clusters, or that an increase in incidence or mortality is associated with these cases, CDC will initiate prospective surveillance and case ascertainment to identify cases for epidemiologic studies designed to confirm or disprove associations between pulmonary hemorrhage host factors, environmental factors, and biologic agents, including such molds as S. chartarum (5).
# Retrospective Review by Using Existing Data Sources
The ability to use existing data sources should substantially facilitate both determining the public health impact of AIPH among infants. However, the reliable data regarding mortality from pulmonary hemorrhage is only available at the national level. CDC conducted a preliminary evaluation of ICD codes for surveillance of pulmonary hemorrhage among infants to determine whether existing data sources can be used to estimate the magnitude of the problem of AIPH among infants. CDC examined data from the National Hospital Discharge Survey (NHDS) and National Mortality Data. Possible cases of AIPH among infants were identified by using ICD-9 codes 770. 3, 784.7, 784.8, 786.3, and 516.1 (Table 6).
Infants identified by ICD-9 codes 770.3 and 786.3 differ from the cases reported in Cleveland. In the national datasets, the majority of cases of pulmonary hemorrhage had diagnoses such as prematurity or immaturity and death occurring within the first 7 days of life. The Cleveland cases occurred among stable, healthy, mature infants who had been discharged from the hospital to their homes after birth and subsequently experienced pulmonary hemorrhage (8)(9)(10). Thus, the estimates of deaths and hospital admissions for cases of pulmonary hemorrhage using ICD codes 770.3 and 786.3 does not distinctly identify infants with AIPH as defined by CDC. In addition, these national datasets do not determine if infants had identifiable etiologies or complications before their discharge from the hospital or their death. Because the estimated number of hospitalized cases with a primary diagnosis of pulmonary hemorrhage was less than the number of deaths, these national datasets might not be reliable for surveillance for infantile pulmonary hemorrhage. These analyses might be better performed by using state-based data.
A retrospective review for AIPH among infants will be performed in metropolitan cities in those states with the highest death rates and with >100 deaths associated with pulmonary hemorrhage among infants, on the basis of relevant ICD-9 and ICD-10 codes used from 1979 to the most recent available data. By focusing on PICUs and NICUs with substantial numbers of deaths, cases from innercity catchment areas, where the incidence of AIPH among infants is suspected to be higher, will be captured. Potential cases will be identified by using standardized methods of case ascertainment and data collection from hospital discharge and mortality data sources, based on ICD codes. Potential cases will be compared with the recommended case definition by reviewing medical records related to all cases of pulmonary hemorrhage observed since 1979 among children aged <2 years.
This retrospective review of AIPH among infants will • determine whether AIPH among infants is a distinct clinical entity within existing ICD-9/ICD-10 diagnostic codes for pulmonary hemorrhage; • describe the epidemiology of pulmonary hemorrhage; • identify trends in the frequency of cases and the geographic distribution and clustering of cases; • estimate the public health impact of AIPH among infants;
• identify groups at high risk for AIPH among infants; and • determine the need for prospective surveillance as a source of cases for a case-control study. The data will be reviewed to determine how these cases, including the apparent case clusters of AIPH among infants in Cleveland and Chicago, have been coded on hospital discharge abstracts, and how deaths attributed to the syndrome have been characterized on death certificates. Both Ohio and Illinois meet the criteria of >100 deaths from pulmonary hemorrhage. In Cleveland and Chicago, this review also will
# TABLE 4. Clinical features of acute idiopathic pulmonary hemorrhage (AIPH) among infants Finding
No evidence of cow milk protein allergy or associated respiratory, heart, kidney, or pancreatic disease* Abrupt cessation of crying or unusual crying or irritability hours to days before the initial recognition of blood in the airway † Not observed § Decreased muscle tone and dusky pallor minutes to hours before progressing to sudden onset of hypoxemic respiratory distress or failure ¶ Hours to days before onset of respiratory failure** Accompanies or immediately precedes respiratory failure † † Acute and appears to be idiopathic § § Characterized by tachypnea, grunting, and chest retractions ¶ ¶ Diffusely diminished breath sounds without the presence of rales or rhonchi*** Often requires intubation and mechanical ventilation; intubation when required is for 2-7 days † † † Often demonstrates bilateral pulmonary infiltrates within the first 24 hours § § § Typically, alveolar infiltrates begin to clear within the first 24-48 hours ¶ ¶ ¶ Atraumatic intubation; bronchoscopy including inspection of upper airway**** Typically, no source from the lung or gastrointestinal tract; presumed to be from diffuse alveolar capillary injury † † † † Typically, found in bronchoalveolar lavage fluid; might not be present in an infant experiencing an acute, initial pulmonary bleed § § § § Indicates evidence of bleeding into the lungs; finding >20% of total pulmonary macrophages containing hemosiderin can be consistent with pulmonary hemorrhage that occurred >48 hours before examination ¶ ¶ ¶ ¶ First 48 hours, fragmented or damaged red blood cells, hemoglobinuria; microangiopathic anemia might be indicative of a hemolytic process; normochromic normocytic might be consistent with acute, abrupt blood loss***** Serum negative for antiglomerular basement membrane antibody, anticytoplasmic neutrophilic antibody, complement titers, serum immune complexes, and antinuclear antibody † † † † † None; spontaneous recovery with or without supportive care indicates these pathophysiologic processes are not the cause of bleeding
# BOX 2. Clinical descriptions of pulmonary hemorrhage
In early texts, pulmonary hemorrhage was not commonly described in children, although it was noted to occur.* Blood found in the airways or alveoli of humans can result from different anatomic sites. Specific sites can include alveoli, large or small conducting airways, or the nasopharynx and gastrointestinal tract with pulmonary aspiration. Regardless of the origin of blood entering the lung, substantial amounts of blood lead to impaired gas exchange, altered pulmonary mechanics, and respiratory distress. Different pathophysiologic processes are associated with pulmonary hemorrhage. These can be divided into • conditions where bleeding occurs at sites of normal tissue with mechanical disruption causing a loss of vascular integrity (e.g., intentional suffocation and mitral valve disease); • vascular inflammation, whereby the inflammatory process causes a loss of vascular integrity (e.g., vasculitis secondary to such conditions as collagen vascular diseases); • vascular malformations, whereby a combination of altered vascular integrity and physical influences (e.g., Laplace's law † ) lead to disruption of the blood vessel; and • coagulopathies, which usually also require additional physical disruption of the blood vessel through greater than normal transpulmonary vascular pressures.
The manifestations of pulmonary hemorrhage can be classified into different syndromes. Diffuse pulmonary hemorrhage is usually diagnosed by bronchoscopy, either by virtue of grossly bloody lavage fluid or by the presence of hemosiderin-laden macrophages in bronchoalveolar lavage. In biopsy and autopsy tissue, the diagnosis is made on the basis of the presence of recent blood and hemosiderin in the alveolar spaces or the interstitium. § In the immunocompromised host, intra-alveolar bleeding can result from thrombocytopenia often associated with other factors. Diffuse pulmonary hemorrhage (DPH) can either be secondary to other disease states, associated with other organ dysfunction, or be isolated. Isolated causes of DPH include lung immaturity, cow milk hypersensitivity, pulmonary capillary hemangiomatosis, and idiopathic causes. ¶ Pulmonary hemorrhage of the newborn (ICD-9: 770.3; ICD-10: P26) is manifested by focal hemorrhage into airspaces or the interstitium in the lungs of infants with hyaline membrane disease, bronchopulmonary dysplasia, and other neonatal pulmonary disorders.** These infants are most often male, preterm, small for gestational age, and have a history of perinatal stress. † † The etiology and pathogenesis of the disorder has not been elucidated.
Hemoptysis, cough with hemorrhage, pulmonary hemorrhage not otherwise specified (ICD-9: 786.3; ICD-10 R04, R04.2) is an acute manifestation of bleeding from the airway. This ICD category captures all the nonneonatal (and certain neonatal) diagnoses of pulmonary hemorrhage. Children with pulmonary hemorrhage might not appear to have hemoptysis if they swallow their sputum.
Consensus is lacking on the meaning of the term idiopathic pulmonary hemosiderosis (ICD-9: 516.1, no ICD-10 code). One pathology text states that the term denotes a separate clinical entity of which diffuse pulmonary hemorrhage is the major manifestation. § § A later edition of the same text ¶ ¶ notes that the presence of hemosiderin in lung macrophages indicates degradation products of hemoglobin. Hemosiderin is thus a pathologic state indicative of bleeding of any type into the lungs*** secondary to the processing of hemoglobin in the red blood cells in the airway by alveolar macrophages. † † † Adults with active alveolar hemorrhage have high hemosiderin scores in bronchoalveolar lavage fluid, § § § but hemosiderin-containing macrophages have limited differential diagnostic value. ¶ ¶ ¶ In one clinical text, the term means diffuse recurrent intrapulmonary hemorrhage that is not secondary to bleeding from trauma, bleeding from the airways, tumors, or left ventricular failure.**** Another author † † † † describes variants of primary and secondary pulmonary hemosiderosis.
On review of National Hospital Discharge Survey data for 1979-1996 and national mortality data for 1979-1998 for ICD-9 code 516.1 for infants, no instances were found in either dataset where ICD-9 code 516.1 was the primary listed diagnosis. However, in 207 cases, this code was the other listed diagnosis. This indicates that idiopathic pulmonary hemorrhage is usually an accompanying diagnosis to other diagnoses that result in hospitalization or death among infants. If performed, environmental assessment of the home to gather pertinent risk-assessment data should use standard protocols designed by trained environmental health professionals. At a minimum, the assessment should involve visual inspection, including checks for dampness, water damage, obvious mold, evidence of pests, and environmental tobacco smoke. Depending on the assessed need for further evaluation and the resources available, additional investigation might include determining moisture content, settled dust sampling, air sampling for different allergens, and biologically active compounds, and other investigations as needed.
# Conclusion
CDC recommends a definition for a clinically confirmed case of AIPH among infants on the basis of 1) evidence of blood in the airway; 2.) age <1 year; 3) absence of medical conditions related to pulmonary hemorrhage; and 4) severe acute respiratory distress or respiratory failure, requiring admission to a PICU with intubation and mechanical ventilation. CDC recommends that PICUs report cases that meet the CDC case definition to state health departments and to CDC.
CDC will retrospectively analyze state-level mortality and hospitalization data based on ICD codes and will retrospec- tively review discharges for pulmonary hemorrhage in selected PICUs. These studies will • distinguish between the clinical findings associated with different symptoms of AIPH among infants; • determine whether ICD codes capture cases that meet the CDC-recommended case definition for AIPH among infants; • determine whether AIPH among infants is a distinct recognizable clinical entity; • determine the proportion of cases ascertained retrospectively through ICD-9 codes that meet the clinical case definition by estimating PPV of ICD-coded data; and • define the magnitude of AIPH among infants and the need for conducting etiologic studies. CDC will review the Cleveland and Chicago case series to determine the degree to which the present case definition applies to them. In addition, CDC will evaluate the present case definition on the basis of data from initial surveillance findings and modify it as appropriate.
If these reviews establish that AIPH among infants is a public health problem on the basis of increasing numbers or clusters of cases geographically or temporally, targeted prospective case surveillance will be initiated. If prospective surveillance is initiated, CDC will maintain a database of current cases of AIPH among infants, reported by PICUs that meet the case definition. The database will serve as a source of cases for casecontrol studies to determine etiology. CDC will work with state and local health departments to investigate clusters of AIPH among infants cases. ('tr st-"w r-the) e e
# Acknowledgments
The following CDC staff provided program support for this report: Wesley J. Hodgson, James A. Rifenburg, Tammy T. Rowe, and Sala S. Sharp, Division of Environmental Hazards and Health Effects, National Center for Environmental Health. We also thank Dorr Dearborn, M.D., for reviewing draft manuscripts and for his feedback regarding portions of this report. We also thank Roy Baron, M.D., for sharing background documents from the internal and external panels that prepared the March 2001 CDC report regarding pulmonary hemorrhage.
#
determine the positive predictive value (PPV) between the clusters of pulmonary hemorrhage cases previously reported and the CDC definition of AIPH among infants. Because the relation between IPH, pulmonary hemorrhage, and AIPH among infants is not clearly understood in terms of rate, etiology, and risk factors, this analysis will define basic demographics of cases among infants and whether the proposed case definition for AIPH among infants is clearly distinguish-able from other conditions. The magnitude and dimensions of AIPH among infants will be determined by describing the distribution of cases on the basis of ICD codes and the CDC case definition. This will involve enumerating cases, determining hospital discharge and mortality rates, and describing the distributions for available demographic variables (e.g., temporal and urban versus rural differences), if any.
# Investigation of Suspected Clusters of AIPH Among Infants
If an apparent cluster of cases of pulmonary hemorrhage occurs, CDC recommends that state health departments initiate an investigation. CDC staff will work with each state, upon request, to evaluate case reports to assist the epidemiologic and environmental investigation, if any. State health departments can use existing protocols for outbreak or cluster investigations and collect information to determine if cases meet the CDC case definition for AIPH among infants. Because these cases probably will be identified in PICUs, CDC recommends that if PICU staff identify any suspected cases, they report them to their state epidemiologist.
For each case of AIPH in an infant, CDC recommends that PICU and NICU staff collect clinical information to certify case status, demographic information, and reports regarding the status of the patient's home. PICU and NICU staff also should carefully document illnesses that are similar clinically to AIPH, even if another specific etiology is confirmed, because they might offer additional information or indicate the need to re-assess the case definition. † Unexplained or repeated injuries (e.g., welts, bruises, or burns); injuries in the shape of an object (e.g., belt buckle or electric cord); injuries not likely to happen given the age or ability of the child (e.g., broken bones in a child too young to walk or climb). § From parental or guardian history or injuries that are possible given the age or ability of the child. ¶ Rare among infants. | None | None |
7f12df2d082523849741d78d0a2c6c9ec4510cae | cdc | None | depar depar depar depar department of health and human ser tment of health and human ser tment of health and human ser tment of health and human ser tment of health and human services vices vices vices vices# Part I: Rabies Prevention and Control
A. Principles of Rabies Prevention and Control. 1. . . . . Rabies Exposure. Rabies is transmitted only when the virus is introduced into bite wounds, open cuts in skin, or onto mucous membranes from saliva or other potentially infectious material such as neural tissue (2). Questions about possible exposures should be directed to state or local public health authorities.
# Human Rabies Prevention. Rabies in humans can be
prevented either by eliminating exposures to rabid animals or by providing exposed persons with prompt local treatment of wounds combined with the administration of human rabies immune globulin and vaccine.
The rationale for recommending preexposure and postexposure rabies prophylaxis and details of their administration can be found in the current recommendations of the Advisory Committee on Immunization Practices (ACIP) (2). These recommendations, along with information concerning the current local and regional epidemiology of animal rabies and the availability of human rabies biologics, are available from state health departments.
# Domestic Animals.
Local governments should initiate and maintain effective programs to ensure vaccination of all dogs, cats, and ferrets and to remove strays and unwanted animals. Such procedures in the United States have reduced laboratory-confirmed cases of rabies in dogs from 6,949 in 1947 to 94 in 2004 (3). Because more rabies cases are reported annually involving cats (281 in 2004) than dogs, vaccination of cats should be required. Animal shelters and animal control authorities should establish policies to ensure that adopted animals are vaccinated against rabies. The recommended vaccination procedures and the licensed animal vaccines are specified in Parts II and III of the compendium, respectively. 4. Rabies in Vaccinated Animals. Rabies is rare in vaccinated animals (4)
# Compendium of Animal Rabies Prevention and Control, 2006- National Association of State Public Health Veterinarians, Inc. (NASPHV)
Rabies is a fatal viral zoonosis and a serious public health problem (1). The recommendations in this compendium serve as a basis for animal rabies prevention and control programs throughout the United States and facilitate standardization of procedures among jurisdictions, thereby contributing to an effective national rabies-control program. This document is reviewed annually and revised as necessary. These recommendations do not supersede state and local laws or requirements. Principles of rabies prevention and control are detailed in Part I; Part II contains recommendations for parenteral vaccination procedures; all animal rabies vaccines licensed by the United States Department of Agriculture (USDA) and marketed in the United States are listed in Part III. Rabies vaccinations may also be administered under the supervision of a veterinarian to animals held in animal control shelters prior to release. Any veterinarian signing a rabies certificate must ensure that the person administering vaccine is identified on the certificate and is appropriately trained in vaccine storage, handling, and administration and in the management of adverse events. This practice assures that a qualified and responsible person can be held accountable to ensure that the animal has been properly vaccinated. Within 28 days after primary vaccination, a peak rabies antibody titer is reached and the animal can be considered immunized. An animal is currently vaccinated and is considered immunized if the primary vaccination was administered at least 28 days previously and vaccinations have been administered in accordance with this compendium.
Regardless of the age of the animal at initial vaccination, a booster vaccination should be administered 1 year later (see Parts II and III for vaccines and procedures). No laboratory or epidemiologic data exist to support the annual or biennial administration of 3-year vaccines following the initial series. Because a rapid anamnestic response is expected, an animal is considered currently vaccinated immediately after a booster vaccination. a. Dogs, Cats, and Ferrets. All dogs, cats, and ferrets should be vaccinated against rabies and revaccinated in accordance with Part III of this compendium. If a previously vaccinated animal is overdue for a booster, it should be revaccinated. Immediately following the booster, the animal is considered currently vaccinated and should be placed on an annual or triennial schedule depending on the type of vaccine used. b. Livestock. Consideration should be given to vaccinating livestock that are particularly valuable or that might have frequent contact with humans (e.g., in petting zoos, fairs, and other public exhibitions) (11,12). Horses traveling interstate should be currently vaccinated against rabies. c. Confined Animals. The following are recommendations for owners of livestock exposed to rabid animals: 1) If the animal is slaughtered within 7 days of being bitten, its tissues may be eaten without risk of infection, provided that liberal portions of the exposed area are discarded. Federal guidelines for meat inspectors require that any animal known to have been exposed to rabies within 8 months be rejected for slaughter. 2) Neither tissues nor milk from a rabid animal should be used for human or animal consumption (20). Pasteurization temperatures will inactivate rabies virus; therefore, drinking pasteurized milk or eating cooked meat does not constitute a rabies exposure. 3) Having more than one rabid animal in a herd or having herbivore-to-herbivore transmission is uncommon; therefore, restricting the rest of the herd if a single animal has been exposed to or infected by rabies might not be necessary. c. Other Animals. Other mammals bitten by a rabid animal should be euthanized immediately. Animals maintained in USDA-licensed research facilities or accredited zoological parks should be evaluated on a case-by-case basis.
6. Management of Animals that Bite Humans. a. Dogs, Cats, and Ferrets. Rabies virus may be excreted in the saliva of infected dogs, cats, and ferrets during illness and/or for only a few days prior to illness or death (21)(22)(23)(24). A healthy dog, cat, or ferret that bites a person should be confined and observed daily for 10 days; administration of rabies vaccine to the animal is not recommended during the observation period to avoid confusing signs of rabies with possible side effects of vaccine administration. Such animals should be evaluated by a veterinarian at the first sign of illness during confinement. Any illness in the animal should be reported immediately to the local health department.
If signs suggestive of rabies develop, the animal should be euthanized and the head shipped for testing as described in Part I.A.7. Any stray or unwanted dog, cat, or ferret that bites a person may be euthanized immediately and the head submitted for rabies examination. b. Other Biting Animals. Other biting animals which might have exposed a person to rabies should be reported immediately to the local health department. Management of animals other than dogs, cats, and ferrets depends on the species, the circumstances of the bite, the epidemiology of rabies in the area, the biting animal's history, current health status, and potential for exposure to rabies. Prior vaccination of these animals may not preclude the necessity for euthanasia and testing. 7. Outbreak Prevention and Control. The emergence of new rabies virus variants or the introduction of non indigenous viruses poses a significant risk to humans, domestic animals and wildlife (25)(26)(27)(28)(29)(30)(31). A rapid and comprehensive response should include all or some of the following measures: a. Characterize the virus at a national or regional reference laboratory. b. Identify and control the source of the introduction. c. Enhance laboratory-based surveillance in wild and domestic animals. d. Increase animal rabies vaccination rates. e. Restrict the movement of animals. f. Evaluate the need for vector population reduction. g. Coordinate a multi-agency response. h. Provide public and professional outreach and education. (41). No laboratory or epidemiologic data exist to support the annual or biennial administration of 3-year vaccines following the initial series. C. Adverse Events. Currently, no epidemiologic association exists between a particular licensed vaccine product and adverse events, including vaccine failure (42,43 Computer-generated forms containing the same information are also acceptable. | depar depar depar depar department of health and human ser tment of health and human ser tment of health and human ser tment of health and human ser tment of health and human services vices vices vices vices# Part I: Rabies Prevention and Control
A. Principles of Rabies Prevention and Control. 1. . . . . Rabies Exposure. Rabies is transmitted only when the virus is introduced into bite wounds, open cuts in skin, or onto mucous membranes from saliva or other potentially infectious material such as neural tissue (2). Questions about possible exposures should be directed to state or local public health authorities.
# Human Rabies Prevention. Rabies in humans can be
prevented either by eliminating exposures to rabid animals or by providing exposed persons with prompt local treatment of wounds combined with the administration of human rabies immune globulin and vaccine.
The rationale for recommending preexposure and postexposure rabies prophylaxis and details of their administration can be found in the current recommendations of the Advisory Committee on Immunization Practices (ACIP) (2). These recommendations, along with information concerning the current local and regional epidemiology of animal rabies and the availability of human rabies biologics, are available from state health departments.
# Domestic Animals.
Local governments should initiate and maintain effective programs to ensure vaccination of all dogs, cats, and ferrets and to remove strays and unwanted animals. Such procedures in the United States have reduced laboratory-confirmed cases of rabies in dogs from 6,949 in 1947 to 94 in 2004 (3). Because more rabies cases are reported annually involving cats (281 in 2004) than dogs, vaccination of cats should be required. Animal shelters and animal control authorities should establish policies to ensure that adopted animals are vaccinated against rabies. The recommended vaccination procedures and the licensed animal vaccines are specified in Parts II and III of the compendium, respectively. 4. Rabies in Vaccinated Animals. Rabies is rare in vaccinated animals (4)
.
# Compendium of Animal Rabies Prevention and Control, 2006* National Association of State Public Health Veterinarians, Inc. (NASPHV)
Rabies is a fatal viral zoonosis and a serious public health problem (1). The recommendations in this compendium serve as a basis for animal rabies prevention and control programs throughout the United States and facilitate standardization of procedures among jurisdictions, thereby contributing to an effective national rabies-control program. This document is reviewed annually and revised as necessary. These recommendations do not supersede state and local laws or requirements. Principles of rabies prevention and control are detailed in Part I; Part II contains recommendations for parenteral vaccination procedures; all animal rabies vaccines licensed by the United States Department of Agriculture (USDA) and marketed in the United States are listed in Part III. Rabies vaccinations may also be administered under the supervision of a veterinarian to animals held in animal control shelters prior to release. Any veterinarian signing a rabies certificate must ensure that the person administering vaccine is identified on the certificate and is appropriately trained in vaccine storage, handling, and administration and in the management of adverse events. This practice assures that a qualified and responsible person can be held accountable to ensure that the animal has been properly vaccinated. Within 28 days after primary vaccination, a peak rabies antibody titer is reached and the animal can be considered immunized. An animal is currently vaccinated and is considered immunized if the primary vaccination was administered at least 28 days previously and vaccinations have been administered in accordance with this compendium.
Regardless of the age of the animal at initial vaccination, a booster vaccination should be administered 1 year later (see Parts II and III for vaccines and procedures). No laboratory or epidemiologic data exist to support the annual or biennial administration of 3-year vaccines following the initial series. Because a rapid anamnestic response is expected, an animal is considered currently vaccinated immediately after a booster vaccination. a. Dogs, Cats, and Ferrets. All dogs, cats, and ferrets should be vaccinated against rabies and revaccinated in accordance with Part III of this compendium. If a previously vaccinated animal is overdue for a booster, it should be revaccinated. Immediately following the booster, the animal is considered currently vaccinated and should be placed on an annual or triennial schedule depending on the type of vaccine used. b. Livestock. Consideration should be given to vaccinating livestock that are particularly valuable or that might have frequent contact with humans (e.g., in petting zoos, fairs, and other public exhibitions) (11,12). Horses traveling interstate should be currently vaccinated against rabies. c. Confined Animals. The following are recommendations for owners of livestock exposed to rabid animals: 1) If the animal is slaughtered within 7 days of being bitten, its tissues may be eaten without risk of infection, provided that liberal portions of the exposed area are discarded. Federal guidelines for meat inspectors require that any animal known to have been exposed to rabies within 8 months be rejected for slaughter. 2) Neither tissues nor milk from a rabid animal should be used for human or animal consumption (20). Pasteurization temperatures will inactivate rabies virus; therefore, drinking pasteurized milk or eating cooked meat does not constitute a rabies exposure. 3) Having more than one rabid animal in a herd or having herbivore-to-herbivore transmission is uncommon; therefore, restricting the rest of the herd if a single animal has been exposed to or infected by rabies might not be necessary. c. Other Animals. Other mammals bitten by a rabid animal should be euthanized immediately. Animals maintained in USDA-licensed research facilities or accredited zoological parks should be evaluated on a case-by-case basis.
6. Management of Animals that Bite Humans. a. Dogs, Cats, and Ferrets. Rabies virus may be excreted in the saliva of infected dogs, cats, and ferrets during illness and/or for only a few days prior to illness or death (21)(22)(23)(24). A healthy dog, cat, or ferret that bites a person should be confined and observed daily for 10 days; administration of rabies vaccine to the animal is not recommended during the observation period to avoid confusing signs of rabies with possible side effects of vaccine administration. Such animals should be evaluated by a veterinarian at the first sign of illness during confinement. Any illness in the animal should be reported immediately to the local health department.
If signs suggestive of rabies develop, the animal should be euthanized and the head shipped for testing as described in Part I.A.7. Any stray or unwanted dog, cat, or ferret that bites a person may be euthanized immediately and the head submitted for rabies examination. b. Other Biting Animals. Other biting animals which might have exposed a person to rabies should be reported immediately to the local health department. Management of animals other than dogs, cats, and ferrets depends on the species, the circumstances of the bite, the epidemiology of rabies in the area, the biting animal's history, current health status, and potential for exposure to rabies. Prior vaccination of these animals may not preclude the necessity for euthanasia and testing. 7. Outbreak Prevention and Control. The emergence of new rabies virus variants or the introduction of non indigenous viruses poses a significant risk to humans, domestic animals and wildlife (25)(26)(27)(28)(29)(30)(31). A rapid and comprehensive response should include all or some of the following measures: a. Characterize the virus at a national or regional reference laboratory. b. Identify and control the source of the introduction. c. Enhance laboratory-based surveillance in wild and domestic animals. d. Increase animal rabies vaccination rates. e. Restrict the movement of animals. f. Evaluate the need for vector population reduction. g. Coordinate a multi-agency response. h. Provide public and professional outreach and education. (41). No laboratory or epidemiologic data exist to support the annual or biennial administration of 3-year vaccines following the initial series. C. Adverse Events. Currently, no epidemiologic association exists between a particular licensed vaccine product and adverse events, including vaccine failure (42,43 Computer-generated forms containing the same information are also acceptable. | None | None |
2b408f518713d945e78eacac21d675d602f14054 | cdc | None | Enrolled participants were randomized to receive either daily doses of TDF/FTC or a placebo pill. Participants were seen every 4 weeks for an interview, HIV testing, risk-reduction and PrEP medication adherence counseling, pill count, and dispensing of pills and condoms. Every 3 months, participants received physical examinations with collection of blood and urine samples for evaluation of renal and liver function, and were tested for sexually transmitted infections and treated as needed. Positive HIV rapid tests were confirmed by Western blot. The cohort was followed for an average 1.2 years with a maximum of 2.8 years. Participants were tested for hepatitis B infection at enrollment, and those found to be susceptible to hepatitis B infection were offered vaccination; 94% accepted.
Based on analysis of data from visits through May 1, 2010, for 2,499 enrolled participants (including 29 male-to-female transgender persons) in the modified "intent to treat" analysis (excluding 10 participants found to be HIV-infected at enrollment and 48 who did not have an HIV test after enrollment), 36 of 1,224 participants in the PrEP arm and 64 of 1,217 participants in the placebo arm who were followed for acquisition of HIV infection. Enrollment in the PrEP arm was associated with a 44% reduction in HIV acquisition (95% confidence interval = 15%-63%). The reduction was greater in the "as treated" analysis; participants at visits with ≥50% adherence by An estimated 56,000 human immunodeficiency virus (HIV) infections occur each year in the United States (1). Men who have sex with men (MSM) account for 53% of the estimated incident infections, and surveillance data suggest that the annual number of new HIV infections among MSM has been rising since the mid-1990s (1). Strategies for reducing acquisition of HIV infection by MSM have included 1) expanded HIV testing so that infected persons can be treated and their risk for transmitting infection minimized; 2) individual, small-group, and community-level behavioral interventions to reduce risk behaviors (2); 3) promotion of condom use; 4) detection and treatment of sexually transmitted infections (3); and 5) mental health and substance abuse counseling when needed. On November 23, 2010, investigators for the Pre-Exposure Prophylaxis Initiative (iPrEX) study announced results from a multinational, randomized, double-blind, placebo-controlled, phase III clinical trial of daily oral antiretrovirals (tenofovir disoproxil fumarate and emtricitabine ) to prevent acquisition of HIV infection among uninfected but exposed MSM (4). This report provides interim guidance to health-care providers based on the reported results of that trial, which indicated that TDF plus FTC taken orally once a day as preexposure prophylaxis (PrEP) is safe and partially effective in reducing HIV acquisition among MSM when provided with regular monitoring of HIV status and ongoing risk-reduction and PrEP medication adherence counseling.
The iPrEx study was conducted in Peru, Ecuador, Brazil, Thailand, South Africa, and the United States. Eligible participants were consenting HIV-uninfected men and male-tofemale transgender adults (aged ≥18 years) who reported sex with a man and reported engaging in high-risk sexual behaviors during the preceding 6 months, and had no clinical contraindication to taking a combined formulation of 300 mg TDF and 200 mg FTC (TDF/FTC).- self-report and pill count/dispensing had a 50% reduction in HIV acquisition (CI = 18%-70%). Reduction in risk for HIV acquisition was 21% among participants at visits with <90% adherence (CI = -31%-52%) and 73% at visits with ≥90% adherence (CI = 41%-88%). Among those randomly assigned to the TDF/FTC arm, drug level testing was performed for all HIV seroconverters and a matched subset of participants who remained uninfected; a 92% reduction in risk for HIV acquisition (CI = 40%-99%) was found in participants with detectable levels of TDF/FTC versus those with no drug detected. TDF/FTC generally was well tolerated, although nausea in the first month was more common among those taking medication than among those on placebo (9% versus 5%). No differences in severe (grade 3) or life-threatening (grade 4) laboratory abnormalities were observed between the active and placebo arms, and no drug-resistant virus was found in the 100 participants infected after enrollment. Among 10 participants who were seronegative at enrollment but later found to have been infected before enrollment, two cases of FTC resistance occurred in the active arm, and one occurred in the placebo arm. Participants in both arms reported lower total numbers of sex partners with whom the participants had receptive anal intercourse and higher percentages of partners who used condoms than reported at baseline.
# Editorial Note
This clinical trial demonstrated the safety and efficacy of daily TDF/FTC, in conjunction with behavioral interventions, in reducing sexual HIV acquisition in a multinational population of MSM exposed to HIV through high-risk sex (4). A recent safety study of PrEP with TDF among 400 MSM in the United States also revealed few safety concerns (5). As a component of a comprehensive HIV prevention intervention, PrEP showed a significant added benefit, although effectiveness was highly dependent on medication adherence.
The findings in this report are subject to at least five limitations. First, the trial was not large enough to evaluate efficacy in each of the sites, and the majority of the participants were in South America; only 10% were in the United States, making it impossible to determine effects on incidence in the United States trial sites specifically. Second, the assessment of adherence by drug-level testing was not performed for all trial participants and was performed for seroconverters at the first clinical visit in which infection was diagnosed; therefore, the findings might not reflect drug levels at the time of infection. Third, the study does not provide information about long-term health effects of TDF/FTC in HIV-uninfected men or men who became HIV-infected while on PrEP medications. Fourth, results of drug-level testing showed that adherence measures in the trial might overstate levels of actual adherence; many of those with high levels of adherence to the daily regimen by self-report, pill count, and bottles dispensed had low levels or no drug measured in their blood (4). Finally, sexual risk behavior and adherence to PrEP medications among MSM taking TDF/FTC for PrEP outside of a trial setting, and with awareness of trial results, might be different from what was observed for men in the iPrEx trial.
Based on the results of this study, CDC and other U.S. Public Health Service (PHS) agencies have begun to develop PHS guidelines on the use of PrEP for MSM at high risk for HIV acquisition in the United States as part of a comprehensive set of HIV prevention services. Completing the guidelines and obtaining expert input and public comment will take several months before they can be published. Concerns exist that without early guidance, various unsafe and potentially less effective PrEP-related practices could develop among health-care providers and MSM beginning to use PrEP in the coming weeks and months. These concerns include 1) use of other antiretrovirals than those so far proven safe for uninfected persons (e.g., more than two drugs or protease inhibitors); 2) use of dosing schedules of unproven efficacy (e.g., "intermittent" dosing just before and/or after sex); 3) not screening for acute infection before beginning PrEP or long intervals without retesting for HIV infection; and 4) providing prescriptions without other HIV prevention support (e.g., condom access and risk-reduction counseling). Until the more detailed PHS guidelines are available, CDC is providing interim recommendations to help guide clinical practice (3,(6)(7)(8)(9)
# (Box).
Until the safety and efficacy of PrEP is determined in trials now under way with populations at high risk for HIV acquisition by other routes of transmission (10), PrEP should be considered only for MSM. The iPrEX trial results provide strong evidence that support for adherence to the prescribed medication regimen must be a routine component of any PrEP program. To minimize the risk for drug resistance, PrEP should not be started in persons with signs or symptoms of acute viral infection unless HIV-uninfected status is confirmed by HIV RNA testing or a repeat antibody test performed after the viral syndrome resolves (6). When evaluating MSM for the prescription of PrEP medications, it is important to establish whether other effective risk-reduction measures (e.g., condom use) are not being used consistently and to ascertain that the risk for HIV acquisition is high (e.g., frequent partner change or concurrent partners in a geographic setting with high HIV prevalence) because these patients might benefit most from the addition of PrEP to their HIV prevention regimen. Health-care providers and patients should be aware that HIV prevention is not a labeled indication for the use of Truvada † and that its long-term safety in HIV-uninfected persons is not yet known. Health-care providers should report any serious adverse events resulting from prescribed TDF/FTC for PrEP to the Food and Drug Administration's MedWatch. § In addition, because the medication is costly, ensuring that patients understand the financial implications of starting PrEP is critical.
PrEP has the potential to contribute to effective and safe HIV prevention for MSM if 1) it is targeted to MSM at high risk for HIV acquisition; 2) it is delivered as part of a comprehensive set of prevention services, including risk-reduction and PrEP medication adherence counseling, ready access to condoms, and diagnosis and treatment of sexually transmitted infections; and 3) it is accompanied by monitoring of HIV status, side effects, adherence, and risk behaviors at regular intervals.
BOX. CDC interim guidance for health-care providers electing to provide preexposure prophylaxis (PrEP) for the prevention of HIV infection in adult men who have sex with men and who are at high risk for sexual acquisition of HIV | #
Enrolled participants were randomized to receive either daily doses of TDF/FTC or a placebo pill. Participants were seen every 4 weeks for an interview, HIV testing, risk-reduction and PrEP medication adherence counseling, pill count, and dispensing of pills and condoms. Every 3 months, participants received physical examinations with collection of blood and urine samples for evaluation of renal and liver function, and were tested for sexually transmitted infections and treated as needed. Positive HIV rapid tests were confirmed by Western blot. The cohort was followed for an average 1.2 years with a maximum of 2.8 years. Participants were tested for hepatitis B infection at enrollment, and those found to be susceptible to hepatitis B infection were offered vaccination; 94% accepted.
Based on analysis of data from visits through May 1, 2010, for 2,499 enrolled participants (including 29 male-to-female transgender persons) in the modified "intent to treat" analysis (excluding 10 participants found to be HIV-infected at enrollment and 48 who did not have an HIV test after enrollment), 36 of 1,224 participants in the PrEP arm and 64 of 1,217 participants in the placebo arm who were followed for acquisition of HIV infection. Enrollment in the PrEP arm was associated with a 44% reduction in HIV acquisition (95% confidence interval [CI] = 15%-63%). The reduction was greater in the "as treated" analysis; participants at visits with ≥50% adherence by An estimated 56,000 human immunodeficiency virus (HIV) infections occur each year in the United States (1). Men who have sex with men (MSM) account for 53% of the estimated incident infections, and surveillance data suggest that the annual number of new HIV infections among MSM has been rising since the mid-1990s (1). Strategies for reducing acquisition of HIV infection by MSM have included 1) expanded HIV testing so that infected persons can be treated and their risk for transmitting infection minimized; 2) individual, small-group, and community-level behavioral interventions to reduce risk behaviors (2); 3) promotion of condom use; 4) detection and treatment of sexually transmitted infections (3); and 5) mental health and substance abuse counseling when needed. On November 23, 2010, investigators for the Pre-Exposure Prophylaxis Initiative (iPrEX) study announced results from a multinational, randomized, double-blind, placebo-controlled, phase III clinical trial of daily oral antiretrovirals (tenofovir disoproxil fumarate [TDF] and emtricitabine [FTC]) to prevent acquisition of HIV infection among uninfected but exposed MSM (4). This report provides interim guidance to health-care providers based on the reported results of that trial, which indicated that TDF plus FTC taken orally once a day as preexposure prophylaxis (PrEP) is safe and partially effective in reducing HIV acquisition among MSM when provided with regular monitoring of HIV status and ongoing risk-reduction and PrEP medication adherence counseling.
The iPrEx study was conducted in Peru, Ecuador, Brazil, Thailand, South Africa, and the United States. Eligible participants were consenting HIV-uninfected men and male-tofemale transgender adults (aged ≥18 years) who reported sex with a man and reported engaging in high-risk sexual behaviors during the preceding 6 months, and had no clinical contraindication to taking a combined formulation of 300 mg TDF and 200 mg FTC (TDF/FTC).* self-report and pill count/dispensing had a 50% reduction in HIV acquisition (CI = 18%-70%). Reduction in risk for HIV acquisition was 21% among participants at visits with <90% adherence (CI = -31%-52%) and 73% at visits with ≥90% adherence (CI = 41%-88%). Among those randomly assigned to the TDF/FTC arm, drug level testing was performed for all HIV seroconverters and a matched subset of participants who remained uninfected; a 92% reduction in risk for HIV acquisition (CI = 40%-99%) was found in participants with detectable levels of TDF/FTC versus those with no drug detected. TDF/FTC generally was well tolerated, although nausea in the first month was more common among those taking medication than among those on placebo (9% versus 5%). No differences in severe (grade 3) or life-threatening (grade 4) laboratory abnormalities were observed between the active and placebo arms, and no drug-resistant virus was found in the 100 participants infected after enrollment. Among 10 participants who were seronegative at enrollment but later found to have been infected before enrollment, two cases of FTC resistance occurred in the active arm, and one occurred in the placebo arm. Participants in both arms reported lower total numbers of sex partners with whom the participants had receptive anal intercourse and higher percentages of partners who used condoms than reported at baseline.
# Editorial Note
This clinical trial demonstrated the safety and efficacy of daily TDF/FTC, in conjunction with behavioral interventions, in reducing sexual HIV acquisition in a multinational population of MSM exposed to HIV through high-risk sex (4). A recent safety study of PrEP with TDF among 400 MSM in the United States also revealed few safety concerns (5). As a component of a comprehensive HIV prevention intervention, PrEP showed a significant added benefit, although effectiveness was highly dependent on medication adherence.
The findings in this report are subject to at least five limitations. First, the trial was not large enough to evaluate efficacy in each of the sites, and the majority of the participants were in South America; only 10% were in the United States, making it impossible to determine effects on incidence in the United States trial sites specifically. Second, the assessment of adherence by drug-level testing was not performed for all trial participants and was performed for seroconverters at the first clinical visit in which infection was diagnosed; therefore, the findings might not reflect drug levels at the time of infection. Third, the study does not provide information about long-term health effects of TDF/FTC in HIV-uninfected men or men who became HIV-infected while on PrEP medications. Fourth, results of drug-level testing showed that adherence measures in the trial might overstate levels of actual adherence; many of those with high levels of adherence to the daily regimen by self-report, pill count, and bottles dispensed had low levels or no drug measured in their blood (4). Finally, sexual risk behavior and adherence to PrEP medications among MSM taking TDF/FTC for PrEP outside of a trial setting, and with awareness of trial results, might be different from what was observed for men in the iPrEx trial.
Based on the results of this study, CDC and other U.S. Public Health Service (PHS) agencies have begun to develop PHS guidelines on the use of PrEP for MSM at high risk for HIV acquisition in the United States as part of a comprehensive set of HIV prevention services. Completing the guidelines and obtaining expert input and public comment will take several months before they can be published. Concerns exist that without early guidance, various unsafe and potentially less effective PrEP-related practices could develop among health-care providers and MSM beginning to use PrEP in the coming weeks and months. These concerns include 1) use of other antiretrovirals than those so far proven safe for uninfected persons (e.g., more than two drugs or protease inhibitors); 2) use of dosing schedules of unproven efficacy (e.g., "intermittent" dosing just before and/or after sex); 3) not screening for acute infection before beginning PrEP or long intervals without retesting for HIV infection; and 4) providing prescriptions without other HIV prevention support (e.g., condom access and risk-reduction counseling). Until the more detailed PHS guidelines are available, CDC is providing interim recommendations to help guide clinical practice (3,(6)(7)(8)(9)
# (Box).
Until the safety and efficacy of PrEP is determined in trials now under way with populations at high risk for HIV acquisition by other routes of transmission (10), PrEP should be considered only for MSM. The iPrEX trial results provide strong evidence that support for adherence to the prescribed medication regimen must be a routine component of any PrEP program. To minimize the risk for drug resistance, PrEP should not be started in persons with signs or symptoms of acute viral infection unless HIV-uninfected status is confirmed by HIV RNA testing or a repeat antibody test performed after the viral syndrome resolves (6). When evaluating MSM for the prescription of PrEP medications, it is important to establish whether other effective risk-reduction measures (e.g., condom use) are not being used consistently and to ascertain that the risk for HIV acquisition is high (e.g., frequent partner change or concurrent partners in a geographic setting with high HIV prevalence) because these patients might benefit most from the addition of PrEP to their HIV prevention regimen. Health-care providers and patients should be aware that HIV prevention is not a labeled indication for the use of Truvada † and that its long-term safety in HIV-uninfected persons is not yet known. Health-care providers should report any serious adverse events resulting from prescribed TDF/FTC for PrEP to the Food and Drug Administration's MedWatch. § In addition, because the medication is costly, ensuring that patients understand the financial implications of starting PrEP is critical.
PrEP has the potential to contribute to effective and safe HIV prevention for MSM if 1) it is targeted to MSM at high risk for HIV acquisition; 2) it is delivered as part of a comprehensive set of prevention services, including risk-reduction and PrEP medication adherence counseling, ready access to condoms, and diagnosis and treatment of sexually transmitted infections; and 3) it is accompanied by monitoring of HIV status, side effects, adherence, and risk behaviors at regular intervals.
#
BOX. CDC interim guidance for health-care providers electing to provide preexposure prophylaxis (PrEP) for the prevention of HIV infection in adult men who have sex with men and who are at high risk for sexual acquisition of HIV | None | None |
adecc935b127f91f6ea3a84beb1d220b5039a2b9 | cdc | None | # I. RECOMMENDATIONS FOR CYANIDE STANDARDS
The National Institute for Occupational Safety and Health recommends that employee exposure to hydrogen cyanide (HCN) and the cyanide salts in the workplace be controlled by adherence to the following sections. The standards are designed to protect the health of workers for up to a 10-hour workday, and a 40-hour workweek over a working lifetime. Compliance with the standard should therefore prevent adverse effects of HCN and cyanide salts on the health of workers. The standards are measurable by techniques that are valid, reproducible, and available to industry and government agencies.
Sufficient technology exists to permit compliance with the recommended standards. The standards will be subject to review and revision as necessary.
These criteria and recommended standards apply to occupational exposure of workers to HCN and cyanide salts. Synonyms for HCN are hydrocyanic acid, prussic acid, and formonitrile. For the purpose of this document, cyanide salts are defined as sodium cyanide (NaCN), potassium cyanide (KCN), or calcium cyanide (Ca(CN)2). The word, cyanide, or the symbol, "CN", is used to designate salts as well as hydrogen cyanide.
The "action level" for hydrogen cyanide or a cyanide salt is defined as one-half the corresponding recommended ceiling environmental exposure limit. "Occupational exposure" to these compounds is defined as exposure to airborne concentrations greater than the corresponding action levels.
The criteria and recommended standards apply to any area in which HCN, any of the cyanide salts or materials containing any of them, alone or in combination with other substances, is used, produced, packaged, processed, mixed, blended, handled, stored in large quantities, or applied.
Exposure to cyanide at concentrations less than or equal to the respective action levels will not require adherence to the recommended standards except for sections 2-7, and 8(c). If "exposure" to other chemicals also occurs, for example to a combination of cyanide and methyl alcohol, provisions of any applicable standards for such other chemicals shall be followed also.
# Section 1 -Environmental (Workplace Air) (a) Concentration
Employee exposure to HCN shall be controlled so as not to exceed 5 milligrams per cubic meter of air expressed as CN (4.7 ppm), determined as a ceiling concentration based on a 10-minute sampling period.
Employee exposure to cyanide salts shall be controlled so as not to exceed 5 milligrams per cubic meter of air expressed as CN, determined as a ceiling value based upon a 10-minute sampling period.
Whenever the air is analyzed for cyanide salts, a concurrent analysis shall be made for HCN. Neither of the respective ceiling values may be exceeded nor may the combined values exceed 5 mg/cu m measured as CN during a 10-minute sampling period.
# (b) Sampling and Analysis
Procedures for sampling, calibration of equipment, and analysis of air samples for HCN and cyanide salts shall be as provided in Appendices I and II, or by any method shown to be equivalent in precision, accuracy and sensitivity to those specified. A sampling period of about 10 minutes is necessary to provide an amount of cyanide readily amenable to analysis by the cyanide selective electrode.
Section 2 -Medical Medical surveillance shall be made available as specified below for all workers occupationally exposed to HCN or cyanide salts.
(a) Preplacement and annual medical examinations shall include:
(1) An initial or interim work and medical history with special attention to skin disorders and those non-specific symptoms, such as headache, nausea, vomiting, dizziness or weakness, that may be associated with chronic exposure.
(2) A physical examination giving particular attention to skin, thyroid, and the cardiovascular and upper respiratory systems.
(3) An evaluation of the advisability of the worker's use of negative-or positive-pressure respirators.
(b) Initial medical examinations shall be made available to presently employed workers within six months of the promulgation of a standard.
# (c)
The responsible physician and the employer shall be aware of the material contained in Appendix V and shall ensure that employees trained in these first-aid measures are on duty whenever there is occupational exposure to HCN or a cyanide salt.
(d) Two physician's treatment kits shall be immediately available to trained medical personnel at each plant where there is a potential for the release of, accidental or otherwise, or for contact with, hydrogen cyanide or cyanide salts. One kit should be portable in order that it may be carried by medical personnel while accompanying a patient to the hospital. The other kit should be kept under lock and key to assure that it is intact and available when and if needed. The key should be readily available at all times to the work supervisor on duty and the storage place should be of such construction as to allow accessibility in the event of loss of the key.
(e) First-aid kits shall be immediately available at workplaces where there is a potential for the release, accidental or otherwise, of hydrogen cyanide or a potential for exposure to cyanide salts. This kit shall contain as a minimum two (2) boxes of ampules (2 dozen), each containing 0.3 ml of amyl nitrite. Ampules shall be replaced biannually or sooner if needed to ensure their potency. The amyl nitrite ampules should be protected from high temperatures. In all cases, the contents of the medical and first-aid kits shall be replaced before the manufacturer's assigned expiration dates. Suggested contents for these kits are listed in Appendix V. In case of contact, immediately flush skin or eyes with plenty of water for at least 15 minutes; get medical attention. Remove contaminated clothing and wash before reuse.
# POISON First Aid
Carry patient to fresh air. Have the patient lie down. Remove contaminated clothing but keep patient warm. Start artificial respiration if breathing stops. Administer antidote (amyl nitrite ampule). Call a physician.
# Temporary Antidote
If cyanide gas is inhaled: Break an amyl nitrite ampule in a cloth and hold lightly under nose for 15 seconds. Repeat at about 15-second intervals.
If cyanide is swallowed:
Break an amyl nitrite ampule in a cloth and hold lightly under nose for 15 seconds.
Repeat inhalation of amyl nitrite 5 times at about 15 second intervals. If patient is conscious or when consciousness returns, give emetic (1 tablespoonful of salt to each glass of warm water) and repeat until vomit fluid is clear. Do not give an emetic to an unconscious or barely conscious person.
# (b)
The following warning sign shall be affixed in a readily visible location at or near entrances to areas containing HCN and where there is reasonable potential for emergencies: (1) location of gas masks and other emergency equipment,
(2) instructions for sounding emergency alarm,
(3) location of first-aid equipment and supplies, and
(4) instructions for summoning medical aid.)
The sign shall be printed both in English and in the predominant language of non-English-reading workers. All workers shall receive training and information on the hazards and safe work practices in handling HCN and cyanide salts, and on first-aid procedures in poisoning by these compounds.
(c) When HCN gas is used as a fumigant, warning signs shall be prominently displayed about the area and at all entries to the area as Temporary Antidote
If aerosolized salt has been inhaled or if solid or dissolved salt has caused poisoning after contact with the skin: Break an amyl nitrite ampule in a cloth and hold lightly under nose for 15 seconds. Repeat 5 times at about 15-second intervals. Repeat as necessary using a fresh amyl nitrite ampule every three minutes. Use artificial respiration if breathing stops.
If cyanide salt in any form is swallowed: proceed as above. If the victim is conscious and capable of some activity, give an emetic (1 tablespoonful of table salt in a glass of warm water) in repeated doses until the vomit fluid is clear. Never give anything by mouth to an unconscious person.
(e) Containers of Ca(CN)2 shall be labeled in the same manner as other solid cyanide salts, except that an additional warning is necessary because this material will react with water to release hydrogen cyanide.
The statement of the hazard shall read as follows for Ca(CN)2:
# DANGER! MAY BE FATAL IF SWALLOWED OR INHALED CONTACT WITH WATER OR ACID LIBERATES POISONOUS GAS CAUSES EYE BURNS AND MAY IRRITATE SKIN (f)
All containers of solutions of cyanide salts shall bear the following labeling in addition to, or in combination with, labels required by other statutes, regulations, or ordinances. The proper chemical name of the specific inorganic cyanide compound followed by the word "solution"
shall appear in large, bold face type at the top of the label.
(insert name of compound) SOLUTION (Inorganic Cyanide Solution) DANGER! MAY BE FATAL IF SWALLOWED OR ABSORBED THROUGH SKIN CAUSES BURNS CONTACT WITH ACID LIBERATES POISONOUS GAS Do not breathe gas. Do not get in eyes, on skin, on clothing. Wash thoroughly after handling. Keep container closed and away from acids. In case of contact, immediately flush skin or eyes with plenty of water for at least J.5 minutes and call a physician. Treat spillage with strong calcium hypochlorite solution and flush to sewer.
# POISON First Aid
Always have on hand a Cyanide First-Aid Kit. Carry patient to fresh air, have him lie down.
Remove contaminated clothing but keep patient warm. Start treatment immediately. Call a physician.
# Temporary Antidote
If gas is inhaled: Break an amyl nitrite ampule in a cloth and hold lightly under nose for 15 seconds. Repeat 5 times at about 15-second intervals. Repeat as necessary, using a fresh amyl nitrite ampule every three minutes. Use artificial respiration if breathing stops. If swallowed: Break an amyl nitrite ampule in a cloth and hold lightly under nose for 15 seconds. If patient is conscious, or when consciousness returns, give emetic (1 tablespoonful of salt in a glass of warm water) and repeat until vomit fluid is clear. Repeat inhalation of amyl nitrite ampule every three minutes. Use artificial respiration if breathing stops. Never give anything by mouth to an unconscious person. Engineering controls and safe work practices shall be used to maintain exposures to HCN and cyanide salts below the prescribed limits.
Administrative controls may also be used to reduce exposure. However, because the inhalation of cyanides or their absorption through the skin may be immediately dangerous to life, the added protection of personal protective equipment and clothing must be provided for work procedures and for emergency situations as discussed below. Such equipment and clothing must be provided to the workers engaged in work with cyanide. Emergency equipment shall be located at well marked and identified stations within the cyanide work areas. This equipment must allow each and every worker to escape the area in case of a cyanide emergency.
# (a) Respiratory Protection
Engineering controls shall be used whenever feasible to maintain airborne cyanide concentrations at or below the environmental limits recommended in Section 1 above. Compliance with the permissible exposure limits by the use of respirators is only allowed when airborne cyanide concentrations are in excess of the workplace environmental limits while required engineering controls are being installed or tested, when nonroutine maintenance or repair is being accomplished, or during emergencies. Appropriate respirators as described in Table 1-1 for HCN and Table 1-2 for cyanide salts shall be used only when permitted by the above restrictions. Respirators shall be selected and used in accordance with the following requirements:
(1) For the purpose of determining the type of respirator to be used, the employer shall measure, when possible, the airborne concentration of HCN or cyanide salt in the workplace initially and thereafter whenever process, worksite, climate, or control changes occur which are likely to increase the airborne concentration of these cyanides.
The employer shall ensure that no worker is being exposed to cyanide in excess of the standards either because of improper respirator selection, fit, use, or maintenance.
The employer shall provide respirators in accordance with Tables 1-1 and 1-2 and shall ensure that the employee uses the respirator provided.
(4) Respiratory protective devices shall be those approved under the provisions of 30 CFR 11, published in the Federal Register, March 25, 1972, as amended.
(5) Respirators specified for use in higher concentrations of HCN may be used in atmospheres of lower concentrations. Likewise, respirators specified for use in higher concentrations of cyanide salts are permitted in atmospheres of lower concentrations.
The employer shall ensure that the respirators are adequately cleaned, maintained, and stored when not in use, and that employees are instructed in the use of respirators assigned to them and in testing for facepiece leakage before each use.
Cartridges or canisters shall be discarded and replaced with fresh canisters after each use. Unused canisters shall be discarded and replaced when seals are broken, after three years if seals are unbroken, or on the manufacturer's recommendation, whichever is first.
Cartridges and canisters shall not be used for periods of time in excess of those indicated in Tables 1-1 and 1-2.
(8) Emergency and escape-type respirators shall be made immediately available at the work stations for each worker when there is potential for exposure to concentrations of the various cyanides above the ceiling values.
For purpose of selection of respiratory protective equipment, entry into areas containing unknown and/or suspected dangerous atmospheric concentrations of HCN or cyanide salts shall be treated as an emergency. Less than or equal to 90 ppm (1) Type C supplied-air respirator, demand or continuous-flow type (negative or positive pressure), with half or full facepiece.
(2) Full facepiece gas mask, chin-style canister specific for HCN. The maximum service life of canisters is one hour.
Less than or equal to 200 ppm Full facepiece gas mask, front-or backmounted type canister specific for hydrogen cyanide. The maximum service life of canisters is one hour.
(1) Self-contained breathing apparatus in pressure-demand mode (positive pressure) with full facepiece worn under gas-tight suit providing whole body protection.
(2) Combination supplied-air respirator, pressure-demand type (positive pressure), with auxiliary self-contained air supply and full facepiece; all worn under gas tight suit providing whole body protection.
(1) Positive pressure self-contained breathing apparatus worn under a gas-tight suit providing whole body protection.
(2) Combination supplied-air respirator, pressure-demand type, with auxiliary selfcontained air supply; all worn under gastight suit providing whole body protection.
(1) Self-contained breathing apparatus in demand or pressure-demand mode (negative or positive pressure).
(2) Gas mask, full facepiece or mouthpiece type, with canister specific for HCN.
# NOTE:
During the use of any respirator with half mask, full facepiece or hood, protective clothing should be worn if there is a chance that liquid HCN may contact any part of the body.
Greater than 200 ppm Emergency (no concentration limit)
Evacuation or Escape (no concentration limit) Less than or equal to (1) Filter type respirators, approved for 25 mg/cu m toxic dust, with half-mask (not appli cable for Ca(CN)2).
(2) Chemical cartridge respirators with replaceable cartridge for toxic dusts and acid gases; with half-mask. Maximum service life 4 hours.
(1) Full-face gas mask, chest or back mounted type, with industrial size canister for toxic dust and hydro cyanic acid gas. Maximum service life 2 hours.
(2) Type C supplied air-respirator, continuous-flow or pressure-demand type (positive pressure) with full facepiece.
(3) Type A supplied-air respirator, (hose mask with blower) with full facepiece.
Greater than 50 mg/cu m (1) Self-contained breathing apparatus with positive pressure in full facepiece.
(2) Combination supplied-air respirator pressure-demand type with auxiliary self-contained air supply.
(1) Self-contained breathing apparatus with positive pressure in facepiece.
(2) Combination supplied-air respirator, pressure-demand type, with auxiliary self-contained air supply.
Evacuation or Escape (no (1) Self-contained breathing apparatus in concentration limit) demand or pressure-demand mode (negative or positive pressure).
(2) Full-face gas mask, front or back mount type with industrial size canister for toxic dust and hydro cyanic acid gas.
# Emergency (no concentration limit)
Less than or equal to 50 mg/cu m (b)
Protective Clothing
Because HCN and cyanide salts, dry or in solution, may be absorbed readily through the skin or any break in the skin, the provision and use of protective clothing are necessary for the protection of workers in most operations where HCN and cyanide salts are used in pure or diluted condition.
(1) When entering a HCN gas-filled area in emergency situations, when the airborne concentration of HCN is unknown, or when the known airborne concentration is greater than 200 ppm, employees shall wear gas-tight suits in addition to the required respiratory protection. The gas-tight suits shall provide full body protection.
(2) Employees engaged in maintenance, repair, or other work on equipment, or in circumstances whereby they may be exposed to HCN liquid or gas, shall wear protective garments or suits made of material impervious to HCN and providing full body protection.
(3) Employees shall wear rubber gloves when engaged in any activity which may involve the handling of, or possible contact with, HCN.
Employees shall wear gloves when handling dry cyanide salts and when using or handling equipment whose surfaces may be contaminated with these salts in such manner that contact of the chemical with the employee's hands is possible or likely.
Employees shall wear gloves made of rubber or other impervious material when engaged in any operation wherein contact of the hands with solutions of cyanide salts is possible or likely.
Employees shall wear protective sleeves, aprons, and/or full body protective clothing as needed to protect their skin from contact with cyanide salts, dry or in solution. When handling solutions, the outer garment shall be of rubber or other material impervious to the solutions involved in the exposures. The garments shall fit snugly about the wrist, arm, neck, waist, and/or ankle (as appropriate to the particular garment) and shall have closures which will exclude dust, powder, mist, and/or splashes of cyanide salts in either dry or liquid formulations.
(10) In areas where spills or splashes of solutions of cyanide salts are likely to occur, the employees shall wear shoes, boots, or overshoes made of rubber or other material impervious to these solutions.
(11) Chemical safety goggles shall be worn by employees engaged in any operation wherein there is danger or likelihood that dusts or solutions of cyanide salts will come into contact with the eye.
Full-length face shields with forehead protection shall be worn by employees engaged in any operation wherein there is danger or likelihood that dusts, molten salts, or solutions of cyanide salts may contact the face.
The employer shall be responsible for maintaining all devices and clothing to be used for personal protection in a clean and effective condition. (2) Buildings in which HCN is to be stored, handled, or used must be designed to prevent fire and explosion hazards and to minimize the release of the highly toxic liquid or gas. Equipment and vessels containing or using HCN should be isolated in rooms or buildings designed for, and devoted to, these purposes.
Building construction shall be fire-and explosion-resistant and shall meet the requirements of the National Fire Protection Association codes and of the local codes, regulations, and ordinances. Explosion vents and fire doors shall be provided in accordance with codes and good practice.
Each room or building shall have no less than two means of exit, with doors opening outward and provided with "panic bar" release latches.
Exits shall be provided so that no location within the room or building is more than 75 feet from an exit and personnel can be evacuated in less than 1 minute.
(3) All regular work areas where HCN is handled or used must be adequately ventilated so that, under normal or reasonably anticipated operating conditions, the airborne concentrations of HCN will not exceed the standard recommended in Section 1.
Local exhaust ventilation shall be used at points or areas of regular or anticipated release of HCN gas.
Equipment for very high rates of ventilation of an area may be provided for the rapid reduction of contamination of air by HCN when emergency situations arise.
The HCN-contaminated air from an exhaust ventilation system must either be passed through a suitable collector to remove the HCN or be discharged at a location or in a manner such that persons or animals will not be endangered by the toxic gas.
Ventilation equipment must meet the applicable codes for explosionproof and fireproof installation of such equipment. where applicable, shall be followed.
# (b) Cyanide Salts
(1) All necessary precautions must be taken to prevent cyanide salts from coming into contact with liquid or airborne acids. In addition, precautions must be exercised to prevent Ca(CN)2 from coming into contact with water or humid atmospheres.
Cyanide salts must be protected also from contact with large concentrations of carbon dioxide. Carbon dioxide fire extinguishers must not be used where cyanide salts are present.
In any circumstance in which there is probable contact of cyanide salts with liquid or airborne acids such as Cr03, S02, C02, HC1 etc, or of Ca(CN)2 with a high concentration of water vapor or with liquid water, the standards and requirements applicable to exposures to HCN shall also apply.
( All containers of cyanide salts must be labeled in accordance
with the recommendations in Section 3.
Areas in which cyanides are stored must be posted in accordance with the recommendations in Section 3.
(3) When containers of cyanide salts are removed or unloaded from trucks, boxcars, or poorly ventilated spaces, these should be thoroughly ventilated, purged, and tested before a worker enters.
When cyanide salts are placed in other containers for transport or temporary storage, such containers must be properly covered and labeled.
(A) Mechanical exhaust ventilation by local exhaust shall be provided for all operations producing, or likely to produce, dust or mists of cyanide salts in excess of the limit recommended in Section 1, or to vaporize HCN in excess of the recommended limit for that vapor.
Examples of such operations are: there is evolution of mist from the bath, the employees shall be encouraged to wear at least a filter type respiratory protective device as a measure of protection in addition to that provided by ventilation.
Nonreturnable containers and other containers or equipment contaminated with cyanides before being discarded should be washed thoroughly with alkalinized water to remove cyanide residues.
(10) When cyanide salts are used in fused salt baths, mechanical local exhaust ventilation should be provided to control any cyanide emissions.
Care in operation of the bath and in housekeeping must be exercised so that the area around the bath does not become covered with cyanide-containing powder or dust. Employees working at baths of fused cyanide salts should wear face shields and appropriate protective clothing to protect them from burns and skin contact with cyanides in the event of splashes. A shovel or similar tool should be used to add cyanide salts to a fused salt bath. The cyanide salt should not be added directly by hand.
(11) Inspection, cleaning, or repairing of tanks or other equipment used with solutions of cyanide salts should be performed only by properly trained workmen under careful supervision.
(A) The tank should be drained of all cyanide solution as completely as possible, then filled with alkalinized water and allowed to stand for 15 minutes, preferably with agitation. This procedure should be repeated; then a preliminary inspection may be made. Any encrustation should be removed by mechanical means and/or by means of a stream of water from a hose.
# (B)
If the tank is to be entered, the atmosphere in the tank should be tested for the presence of hydrogen cyanide and cyanide salts, to be certain it does not contain a dangerous airborne concentration of these or other materials.
(C) The tank should be purged with fresh air to ensure an adequate oxygen supply and air should be supplied to the tank while the worker is in the tank.
# (D)
Equipment other than tanks should be washed and vented similarly, as applicable.
In the event of finding airborne concentrations of cyanide salts in excess of the limit, immediate action must be taken to eliminate the cause of the elevated airborne cyanide concentration. In case of any emergency situation (spills, leaks, or other unusual emissions of cyanide which result or potentially may result in dangerous airborn concentrations), all personnel shall be evacuated from the area. The personnel required to return to the area to institute corrective measures shall wear approved respiratory protective gear while entering and working in the area until the situation is corrected.
(13) Any area in which there is the potential of an emergency involving HCN or a cyanide salt shall be posted in accordance with the provisions of Section 3, and emergency equipment stations shall be established. These stations shall be sufficient in number and so located as to be readily and immediately accessible to the workers in the area.
The stations shall be provided with first-aid supplies and instructions for first-aid treatment of any persons suffering excessive exposure to cyanide.
Approved type respiratory protective devices, as indicated in Section 4, shall be available at designated emergency stations. These devices shall be sufficient in number for the workers in the area and readily accessible. Occurrence and Use HCN is a colorless gas or a colorless or bluish-white liquid with a faint, characteristic odor of bitter almonds perceptible to some people. Kirk and Stenhouse reported that 88% of 244 persons tested could smell hydrogen cyanide but that in a fourth of these, the determination was made only with difficulty.
The glucoside amygdalin which occurs in nature in some plants, notably almonds, readily yields HCN upon hydrolysis. Recently, attention has been brought to the presence of HCN in automobile emissions. HCN is manufactured in the United States from coke-oven gas by reaction with sodium carbonate, from cyanide salts by reaction with acid, by the decomposition of formamide, from the reaction of ammonia, air, and natural gas, or, most commonly, from the reaction of methane and ammonia under specific controlled conditions. The great bulk of the HCN synthesized is used directly in the same process system. In 1973, the estimated consumption of HCN in the United States was approximately 310,000 short tons. HCN is used primarily in the production of chemical intermediates for the manufacture of synthetic fibers, plastics, cyanide salts and nitrites; in the fumigation of ships, In the presence of any source of hydrogen ions in quantity, eg, strong mineral acid, the production of HCN from cyanide salts becomes both rapid and large. Above 50 degrees C, an irreversible decomposition to formate and ammonia, as shown below, becomes important. In the presence of NaCl, the hydrolysis of NaCN to HCN is increased at temperatures below 80 C, but decomposition to ammonia and formate is retarded. Sodium cyanide is marketed as a powder, granule, flake or block in pillow-shaped pieces weighing about 1 oz, and as a 30% aqueous solution.
Solid sodium cyanide is packed in steel or fiber drums, and the aqueous solution is shipped in tanks by truck or rail. Potassium cyanide, KCN, is a white crystalline, deliquescent, solid. KCN is produced by methods similar to those for NaCN. The chemical reactivity of KCN is similar to that of NaCN. Hydrolysis to HCN, as was the case with NaCN, is slight (Kh = 2.54 x 10 exp(-5)). Potassium cyanide is sold in forms similar to those of NaCN but because KCN is more expensive, its world production for 1963 was only 5,000 tons. Calcium cyanide, Ca(CN)2, is also called "black cyanide" and is the only commercially important alkaline earth cyanide.
The hydrolysis of Ca(CN)2, which takes place in two steps, as shown below, is complete.
The resulting calcium hydroxide has dissociation constants of 3.74 x 10 exp (-3) and 4.0 x 10 exp (-2) but is much less soluble in water at 0 degrees C than sodium hydroxide so that its aqueous solutions are not as alkaline.
For example, the pH of an aqueous solution of Ca(0H)2 in an electric furnace above 1000 C in the presence of sodium chloride.
saturated
Rapid cooling apparently prevents the reversion to calcium cyanamide.
It is manufactured primarily in Canada, South Africa, and East Germany and sold as flakes or blocks.
There is also some production elsewhere in Europe and Japan.
in 1898 to kill vermin in railway cars, in to kill bed bugs in prisons, and, after 1910, for the fumigation of the holds of ships. Stock and Monier-Williams Cytochrome c absorbs radiation at 550 nanometers (nm). In the presence of cytochrome oxidase, the optical density at 550 nm decreases at a rate directly proportional to the activity of cytochrome oxidase. This rate of change was determined in the presence of cyanide, demonstrating the ability of cyanide to inhibit cytochrome oxidase activity. Additions of methemoglobin, in which the iron had been oxidized electronically to the ferric state, to a solution containing cytochrome c, cytochrome oxidase, and cyanide were found to increase the activity of cytochrome oxidase, thus reversing the inhibitory effect of cyanide. The authors also found that the addition of cyanmethemoglobin to a solution of cytochrome c and cytochrome oxidase had no immediate effect on enzyme activity, but after a few minutes the enzyme became increasingly inhibited. Thus, the authors demonstrated in vitro the abilities of cytochrome oxidase and methemoglobin to compete in a reversible fashion for the cyanide ion.
In a 1958 survey, Dixon and Webb found that the concentration of cyanide necessary for inhibition of cytochrome oxidase was 2-6 orders of magnitude less than those required for inhibition of other enzymes. The interference of CN with many different enzyme systems other than those involved in respiration may thus contribute to its toxicity.
Schubert and Brill in 1968 measured the inhibition and recovery of liver cytochrome oxidase in mice, rats, and gerbils after the intraperitoneal administration of KCN. Inhibition of the enzyme was found to reach a maximum 5 to 10 minutes after the cyanide injection. Depending on the dose, the enzyme activity returned to normal 5 to 20 minutes after maximal inhibition in mice but required up to 1 hour or more in the rat and gerbil. Interestingly, they found that the abilities of mice and rats to tolerate divided doses of cyanide depended on the total dose as well as on the time-dependent degree of enzyme inhibition. For example, they found that mice invariably survived a single sublethal dose of 6 mg/kg of KCN but not two doses of 3 mg/kg given 6 minutes apart or three doses of 2 mg/kg given at 6 minute intervals. They further showed that sodium thiosulfate and nitrite were able to reactivate liver cytochrome oxidase within minutes when administered to cyanide-treated rats and mice. Both men complained of headache and weakness or fatigability and were observed to have slight lid lag, enlarged thyroids, and excessive perspiration. One of the two also experienced dizziness and mental confusion, slurring of speech, coughing, sneezing, and occasional abdominal cramps, nausea, vomiting, and coarse tremor of the extremities followed by their temporary paralysis. Both men were exposed to cyanide aerosols generated by case hardening. Some exposure to HCN may have occurred.
Wuthrich in 1954 described a 39-year-old German blacksmith who was exposed to cyanide in case hardening on a sporadic basis for 2 years and then more frequently for the next 4 years. The worker noticed some initial irritation, followed by a general worsening of health. He experienced loss of appetite, nervousness, vertigo, headaches, nausea, and vomiting.
During 2-3 week vacations, the symptoms disappeared but reappeared within a month after returning to work. His thyroid gland was slightly enlarged. After exposure to cyanide had ceased for about 14 days, the man was given a placebo of NaCl, iv, for three days during which time he reported an improvement in his condition. On the 4th day, 1.4 g of sodium thiocyanate was substituted for NaCl in the daily injections. The thiocyanate concentration in the blood serum increased rapidly following these injections and did not decay to normal between injections. From the day of the first NaSCN injection, the man began to complain of nausea, lack of appetite and nervousness. After three NaSCN injections, he reported nausea and vomiting and spontaneously stated that he felt the same symptoms as at his workplace.
If there are 5200 ml of blood in the average man, then a dose of and eventually by complete disappearance of P waves. A secondary increase in rate, but not to the rate prior to administration of HCN, was observed during the 3rd and 4th minutes along with the irregular reappearance of P waves, some of which were not conducted. All subjects showed A-V dissociation with a secondary decrease in rate during the 5th minute.
During the 6th and 7th minutes, the heart rates again showed a slight increase and a return to normal sinus rhythm. Thereafter, the heart rates slowed progressively. Normal A-V conduction in one man and incomplete A-V block in another were maintained throughout the period of observation (approximately 13 minutes).
A third subject developed Wenckebach's phenomenon, (2:1 block), and, finally, complete heart block. The fourth subject's heart had normal A-V conduction until the 14th minute, when it developed ventricular tachycardia and ventricular fibrillation. It must be remembered that the concentrations of HCN to which these men were exposed were huge, so that the details of the changes in their ECG recordings may not be entirely typical of those to be expected in occupational exposures.
Wexler's observations do seem to demonstrate that cyanide has no specific action on the heart but rather exerts on the myocardium actions that are typical of hypoxia and anoxia.
There have been several reports of exposure to HCN which included both the airborne concentration of HCN and the human physiological response. However, in many cases no additional information relating to worker exposure was provided. These reports are summarized in Table XIV-5.
In many cases it is difficult to attribute a specific concentration range directly to a group of investigators since many of the citations involve reference to the work of others with no additional supporting information.
Therefore, the validities of concentrations presented only by secondary references may be questioned. In large part they appear to be based on the unreferenced work of Lehmann and Hess. However, the application of
# Lehmann's data to man has been questioned by McNamara because
Lehmann's work was apparently done entirely with rabbits, which McNamara considers to be more sensitive to a given dose (product of concentration and time) of HCN than man. He concluded that man has a susceptibility to HCN more like those of the comparatively resistant goat and monkey and on
this assumption (and one that the LCt50 for man is four times that for the mouse) has estimated that 3,404 mg/cu m will cause 50% mortality in humans exposed to it for one minute. McNamara estimated that a concentration of HCN of 607 mg/cu m would kill 50% of men after a 10-minute exposure.
The various fatal doses of HCN seen in Table XIV had just returned from a 13-month leave of absence 5 months prior to this episode.
In use, the solution was heated to boiling whereupon 50 ml of hydrogen peroxide were added. The gold articles were cleaned in a manner causing splashing on the skin and the production of a visible aerosol.
There may have been some exposure to HCN. A study of plant records revealed another plater who developed typical signs and symptoms in 1 month. The man had been treated for 7 weeks, was removed from exposure, and recovered. An investigation of the plant was made and these 19 illnesses were attributed to aerosols emitted by the improperly operated plating tanks. After engineering controls and housekeeping procedures had been instituted, there were no recurrences of these illnesses. No airborne concentrations of contaminants were reported.
Elkins in reported that in a plant where there was considerable brass plating the ambient air contained a mist. The mist was reported to have contained NaCN in a concentration not greatly exceeding 5 ppm, expressed as HCN. Severe irritation was a widespread complaint and there were some incidents of ulceration of the nasal septum. The author noted that other alkalies of undetermined concentration in the air may have contributed to the irritating action of the mist. with the exception of one with a perforated septum who gave a history suggestive of previous exposure to chromates. The cyanides were not described but they were likely a mixture of NaCN, KCN, and some alkaline complex of CuCN in the copper plating tanks, and alkaline NaCN in the zinc bath.
In None of the four unexposed men had evidence of disease of the stomach or duodenum. The author reported that three of the exposed and two of the unexposed men had erythrocyte counts above 5,000,000 but below 6,100,000/cu mm and that seven of the exposed and none of the unexposed men had a percentage of lymphocytes above 40 but below 49%. He attributed the latter change to stress resulting from repeated exposure to small doses of HCN. He concluded that his results demonstrated that not all the effects of repeated acute or subacute exposures to HCN are entirely reversible.
In Exposure was continued until the animals became apneic, their heart beats became irregular and weak, and distinct cyanosis was apparent. Administration of oxygen through a plaster of Paris mask, modelled to fit the rabbit's muzzle, by hand pressure applied to a rubber bag connected to the mask succeeded in reviving 18 of the 36 rabbits. The authors stated that the hearts of the other 18 rabbits had become too weak when oxygen administration was started to be able to perform the necessary movement of oxygenated blood to the important organs.
In 1951, Moss et al exposed 16 rats to HCN at 24-465 ppm for up at 22 minutes. The rats exposed at 25-50 ppm survived, except for one exposed at 50 ppm. This rat was violently agitated after 1 minute 49 seconds, paralyzed after 2 minutes 30 seconds, unconscious after 3 minutes, and dead after 8 minutes.
In experiments reported in 1952 by Haymaker et al, six dogs were exposed at concentrations of 620, 590, 700, 700, 165, and 690 mg/cu m, for periods of 2.0, 2.0, 1.75, 1.75, 10.0, and 2.0 minutes, respectively.
The first three dogs died in 20 hours or less and the others were killed 24, 26, and 28 hours after exposure. Four of the six dogs had convulsive seizures. The dog exposed at 620 mg/cu m had marked proliferation of histiocytes in the leptomeninges and in the perivascular spaces of the molecular layer of the cerebellum. Only shadows of the Purkinje cells remained. Some of these dogs suffered necrosis of gray matter. Definite alterations of structure were not seen in dogs that died within 21 minutes after being exposed to HCN; they were found in dogs that died 2.5 or more hours after exposure. At these comparatively early times, there was subpial edema of the cerebrum and the cerebellum. Dogs that survived for as long as 16 hours had cellular damage, particularly in the cerebral cortex.
The frontal and parietal lobes were more likely to be affected than the temporal or occipital.
Cortical damage was concentrated frequently in the trough of a sulcus in the form of massive coagulation necrosis.
Valade in 1952 exposed four dogs to HCN at 50 mg/cu m for 12 30-minute periods, conducted at 8-day intervals. Of these dogs, two survived, one died after 38 days, and one died of an intercurrent disease.
In a second experiment, four dogs were subjected to 19 30-minute inhalation periods at 2-day intervals and at the same HCN concentration. One died after 73 days, the other after 77 days. Another group of five dogs went through seven 30-minute inhalations at 2-day intervals, but this experiment was interrupted when pulmonary inflammation occurred, causing the death of three dogs. Still another group of four dogs were subjected to fourteen 30-minute inhalation periods at 2-day intervals; one of these died after 34 days.
The first signs were dyspnea, nausea, exaggerated intestinal peristalsis, and diarrhea. Later, the dogs developed tremors followed by loss of equilibrium and convulsions. These observations tend to support the hypothesis of a cumulative effect from exposure to HCN.
Valade autopsied the dogs immediately after they died or were
killed and observed similar central nervous system lesions in each of them.
Vascular changes were vasodilatation and hemorrhages which were most pronounced in the central gray nuclei, brain stem, bulb, and medulla cervicalis.
Cellular lesions manifested themselves by glial reactions throughout the central nervous system and by cytologic changes in the Purkinje cells of the cerebellum and in the bulbar gray nuclei. These histopathologic examinations led the author to conclude that the lesions resulted from anoxia caused by inhibition of cytochrome oxidase or from a selective effect of the poison. To support the contention that the latter cause was the more significant, the author noted that the dogs were very quickly affected by respiratory disorders before the onset of other signs.
He thought there was reason to believe that the suddenness with which these disorders appeared was linked to a particular sensitivity of these animals' bulbar cells to cyanide, rather than to an inhibition of cytochrome oxidase. In 1955, Howard and Hanzal reported a feeding study with HCNfumigated food. Thirty male and 30 female weanling albino rats were divided into 3 groups of 10 males and 10 females each. Two of the groups were given dog meal containing 300 ppm and 100 ppm of HCN, respectively. A third, similar group was fed unfumigated food as a control. At the end of a 2-year feeding period, no gross signs of cyanide toxicity were observed.
Autopsies revealed the same general abnormalities and signs of senility in control and experimental rats. Microscopic examination of heart, lungs, liver, spleen, stomach, small and large intestines, kidneys, adrenal, thyroid, testes or uterus and ovary, and the cerebrum and cerebellum revealed no evidence of pathology due to HCN feeding. All findings were compatible with those usually seen in aging animals, and the same general changes were found in both the control and the experimental animals.
Thiocyanate concentrations in plasmas, RBC's, and kidneys, but not in the livers, of rats given food containing 300 or 100 ppm HCN were about twice as high as those in controls.
In 1959, Levine and Stypulkowski reported lesions in several areas of the brains of rats which survived exposure for 20-45 minutes at an unknown concentration of airborne HCN. The concentration of the airborne cyanide aerosol, which the authors presumed to be HCN, was not determined but was sufficient to debilitate the rats in 10 minutes. Earlier, Flury
and Zernik found that persisting prostration occurred in 9.5 minutes at 127 ppm and, thus, it may be estimated that the rats in this experiment had exposures to HCN at approximately 127 ppm. Below this concentration (127 ppm), exposure to HCN for 2 hours did not produce brain lesions.
Above this concentration at which persisting prostration occurred, brain lesions were produced readily in 20-30 minutes. These lesions involved a multiplicity of sites in the brain although they were not universal in distribution.
For example, the cord, most of the stem, cerebellum, diencephalon, and portions of the cerebrum were spared. A predominance of isolated lesions appeared in the callosum and striatum. Later that same year, Levine and Weinstein, using the same technique described above, reported that high concentrations of HCN generally caused the death of rats without causing brain damage. Low concentrations did not produce either, but moderate concentrations (perhaps 100-150 ppm) caused brain lesions while consciousness was maintained for an hour or so, followed by sudden unconsciousness and death. Unfortunately, in neither of these studies was the airborne concentration reported. Wistar albino rats receiving 0.5 mg of KCN subcutaneously once weekly for 22 weeks. They reported some pallid myelin but found it difficult to estimate whether or not there was demyelination. The animals appeared to be without other ill-effects from these small doses. The authors suggested that these lesions were due to excessive utilization of hydroxocobalamin to form cyanocobalamin. Whether these effects on nervous tissue are due to a specific action of the cyanide ion or of the thiocyanate ion, or to general histotoxic anoxia, is not clear.
Moss et al in 1951 subjected from one to three rats to mixtures of CO and HCN. Atmospheres containing either HCN or CO alone were generally lethal to rats at concentrations of 50 or 5000 ppm, respectively.
A mixture of 10-20 ppm of HCN and 2000 ppm of CO was lethal to some.
Mixtures of 30 ppm of HCN and 1000 ppm of CO and of 5 ppm of HCN and 2000 ppm of CO were not lethal.
Hirner in 1969 subjected male rats weighing about 250 g to subcutaneous injections of 0.2% KCN.
The daily dose, which averaged between 3 and 5 mg/rat, was divided into parts, which were injected within the span of 1 hour. Five rats received single daily doses and were killed 2 or 3 days later. Six rats received 4 to 12 daily doses, two received 14, and four received 20. All the multiply dosed rats were killed at the end of 9 weeks from the first daily dose. These rats were perfused through the left ventricle with a sodium cacodylate-glutaraldehyde solution;
appropriate samples of nervous tissue were ultrasectioned and examined electronmicroscopically as well as by conventional optical microscopy. The principal lesion found in this study was necrosis in the caudal part of the corpus callosum, with spongy alteration at the margin of the necrotic area.
Phagocytes invaded the necrotic area 2 days after the last dose of KCN; astrocytic gliosis followed. In the area of spongy change, there was vacuolization of axons and swelling of the astrocytes and oligodendroglia.
Demyelination was visible in the later stages of the study. Hirner considered that the effects on glial cells were primary effects of cyanide, but that disintegration of myelin and axonal degeneration were secondary effects, the axon remaining intact when swelling of the glia had occurred.
He stated the belief that the oligodendroglia are particularly susceptible to injury by cyanide. Unfortunately, neither report sought to quantify the dose of either HCN or KCN.
In the first study, Levine and Stypulkowski In the second study, Levi and Amaducci in 1968 brought their animals through the first two stages, after which they were allowed to partially recover, and were then killed by decapitation. The meninges appeared congested. Some rats had hemorrhagic pulmonary infarctions. In some animals trypan blue was injected iv to test the integrity of the blood-brain barrier. Subsequent examination of the brains did not show any abnormal passage of the trypan blue into the nervous tissue. Brain slices of other rats were used to study the active transport of amino acids.
Initial and steady state accumulation of amino acids and rates of amino acid exit were identical in brain slices from control and treated animals when a glucose-containing incubation medium was used. Tissue respiration rates were also measured in vitro and found to be identical in both control and treated animals. Thereafter, the analytical method selected determines cyanide radical content, and it is impossible to say what fraction of the total was attributable to any particular compound.
In order to differentiate between HCN gas and other cyanide compounds, it is necessary to first remove particulates by passing the air through an efficient filter, then absorb HCN from the stream by passage through an alkaline absorbing solution.
The filtered cyanides can subsequently be leached from the filter by treatment with alkaline solution, and the same analytical technique applied to both portions of the sample.
The presence of small quantities of cyanide in water was of concern long before relatively recent ecologic considerations led to an awareness that many other substances were toxic at trace concentrations. As a result, there exists substantial literature dealing with the qualitative and quantitative detection of cyanides in air and water, with at least one method (the titrimetric estimation of cyanide with silver nitrate published by Liebig in 1851) still in use today, more than a century after its origination. Almost all the methods proposed for the analysis of water or other materials have been, or can be, applied to the analysis of cyanides in air, for most air methods ultimately involve the determination of cyanide ion in solution. One of the most widely used colorimetric methods is the so-called pyridine-pyrazolone method, an example of the Konig synthesis for pyridine dyes, first published by Aldridge in 1944 (using pyridine and benzidine) and subsequently modified by various authors.
In this method, cyanides are converted to cyanogen bromide or cyanogen chloride, which then reacts with pyridine to form a glutaconic aldehyde.
Next, a primary aromatic amine reacts with the aldehyde to yield a colored Schiff's base. In the original procedure of Aldridge, the aromatic amine used was benzidine, but the more frequently used modification of Epstein voltammetry , amperometry , coulometry potentiometry and others. The most recently introduced and probably mosc useful in its application to air analysis, is the eleccrometric technique relying on specific ion electrodes, or ion selective electrodes which respond only to cyanide ion concentrations, Cohen A -novel approach to determining cyanide levels has been described by OancniK and Br/lr.z involving Indirect atomic absorption " spectrometric analysis.
In the first of two methods, the complex dicyano-bis-(l,10phenanthroline)-iron(II) is formed and then ¿-.:tracted into chloroform. The
- iaiororG-ia is evaporated and the residue is taken ap m ethanol. The
- -.thaiioi. solution is aspirated directly into the flame, and iron equivalent 99 i to a known amount of cyanide is then determined. The second method is based on precipitating silver cyanide, then determining the excess silver ion in the supernatant by atomic absorption spectrometry.
In place of titrimetric techniques, several investigators have described methods in which turbidity resulting from the formation of silver cyanide, or the reduction in turbidity due to the formation of a cyanide complex with silver iodide, are measured.
, a specific ion electrode method , and a blood method using microdiffusion , first used by Conway.
A respired air method based on the pyridine-pyrazolone reagent , as well as more general methods applicable to biologic samples using this same reagent are also used.
The rationale used in making a forensic diagnosis of cyanide poisoning have also received some attention. Many of the methods listed have also been used for water and waste water analyses, and currently the methods most favored appear to be colorimetric, using some version of the pyridine-pyrazolone method, or modifications of the titrimetric determination with silver nitrate.
Specific ion electrodes , and picric acid have also been used.
Recently, an opto-acoustic infrared absorption technique as well as the titrimetric method utilizing silver nitrate have been used in the analysis of HCN in automobile exhaust. Virtually every method used for cyanide analyses is subject to some interferences, usually due to the presence of certain metals which may form complexes, other anions, particularly sulfide, and a host of oxidizing and reducing agents. It is, therefore, frequently necessary to isolate the cyanide by some means, most frequently by a distillation from strongly acid solution, where all but the most tightly bound metal complexes are dis sociated to release hydrogen cyanide which is then absorbed in alkaline solution.
The recommended sampling and analytical method for the cyanides covered by this document is essentially that of the standard NIOSH method for cyanide in air as published in the NIOSH Manual of Analytical Methods. should be followed.
High ventilation rate systems for the rapid dilution or removal of HCN gas and aerosols may be useful in some areas.
Control of the hazard of potential release of hydrogen cyanide from cyanide salts requires constant care and attention to good work practices.
The cyanide salts should be kept well apart from, and protected from contact with, acids, moisture, or elevated concentrations of carbon dioxide.
# Basis for Recommended Environmental Standard
Cyanide is well known as an acute, fast acting poison which can be described as insidious in that its toxic action at high concentrations is so rapid that its odor has no value as a warning.
At lower concentrations the sense of smell may provide forewarning. For HCN, the primary routes of entry from occupational exposure are inhalation and absorption through the skin.
Thus, it may be presumed by analogy that if 90 ppm of HCN is fatal, 96 mg/cu m of CN, derived from cyanide salts, may be also. Extending this analogy to threshold levels, presumably 11 mg/cu m of CN would be equivalent to the current Federal standard of 10 ppm of HCN and restriction of exposures to 11 mg/cu m of CN would protect against acute toxicity from cyanide salts.
However, taking into account the irritant effects observed from exposure to cyanide salts, the current Federal standard of 5 mg/cu m of CN as an 8-hour time-weighted average appears to be too high in that it allows substantial excesses above that concentration for short periods of time.
Therefore, NIOSH recommends that the current value of 5 mg/cu m of CN be retained, but that its basis be changed from an 8-hour time-weighted average to a 10-minute ceiling. This action should provide the employee with adequate protection from the systemic effects of cyanide and prevent the erosional effects produced by the alkalinity associated with the cyanide salts.
A review of the cases involving exposure to cyanide reveals that they fall into three general categories. First are those cases in which there was an acute or subacute exposure followed immediately by an acute illness. [11,13,20,26,27 ppm. They also stated that it was difficult to give reliable limits for normal levels of cyanide and thiocyanate in the urine. However, in order to assess the hazards of occupational exposure, they considered it safe to state that nonsmokers who have greater than 400 #ig/100 ml of free thiocyanate in the urine, or smokers with urinary concentrations exceeding It is recognized that many workers are exposed to cyanides in concentrations considerably below the recommended occupational limits.
Under these conditions, it should not be necessary to comply with many of the provisions of the recommended standards. However, concern for worker health and well-being requires that protective measures be instituted below the enforceable limits to ensure that exposures do not exceed the standard.
Is given the super.vi sion necessary to assure that all safety tP'lii p r ;} r f \ c p c rn f-»V. I (7) is instructed to shower before removing any respirator or gas-tight suit if prior contact with HCN liquid has occurred or is suspected; (preferably sight contact) in a safe area or at a distance so as not to be affected by an emergency situation at the site of the first employee. The second employee ("buddy") should be alert and equipped to summon help and render aid, if needed.
The employee should carefully and precisely follow all operational procedures specified for the handling of HCN in containers, transfer operations, or other equipment. Suppliers' and manufacturers' instructions should be carefully followed.
When HCN is used for fumigation purposes, the space should be sealed to prevent the gas from leaking into surrounding spaces or areas. Warning signs should be posted and guards placed to keep unauthorized persons at a safe distance. All laws, regulations, ordinances, and codes applicable should be followed. Only licensed fumigators should do Such work. Open containers of any solid cyanide salts or of solutions of cyanide salts should be limited to those necessary for operational requirements and procedures. Such open containers must be used only in adequately ventilated spaces so that the recommended standards for the airborne concentration of cyanide are not exceeded. Good practice dictates that, in so far as practical, covers be provided for such containers and used whenever possible.
Solutions of cyanides should be maintained as basic as practical to prevent any evolution of hydrogen cyanide. When weakly basic or neutral solutions are used, ventilation must be provided sufficient to prevent accumulation of the HCN evolved from exceeding the recommended standard for HCN in the work room air. When the addition of an acid to a cyanide solution may be necessary, the process should be fully enclosed and ventilated.
Respiratory protection should be provided for all workers potentially exposed to any release of hydrogen cyanide.
Fused salt baths containing cyanide salts should be provided with local exhaust ventilation. Care should be exercised in the operation of such baths to avoid spills and splashes. Addition of salts should be made carefully, using a shovel or special tool. The area about the bath should be regularly cleaned to prevent accumulation and encrustation of cyanide salts on adjacent areas. Workers at fused salt baths should wear safety goggles with side shields.
Local exhaust ventilation must be used for all operations emitting dusts or mists of cyanide salts. Tanks and other equipment which must be entered for inspection, maintenance or repair, should be drained as completely as possible and then filled with water and agitated. After 15 minutes, they should be drained again and refilled for another 15 minutes, then drained again. The tanks should then be inspected for residue and encrustation of cyanides. These should be broken loose mechanically or by the force of a water stream and flushed away.
The tank should then be purged with fresh air, followed by testing for the absence of cyanide in the air before anyone enters. Cyanide waste solutions and cyanide-contaminated rinse or wash waters should be treated to destroy the cyanide before being discarded.
Treatment of cyanide waste is achieved by oxidation of the cyanide in alkaline solution by addition of chlorine or other oxidizing agents.
# IN AIR AND CALIBRATION
The same sampling and analytical methods are used for atmospheric hydrogen cyanide and the particulate cyanides. They can be collected and analyzed separately or by insertion of a filter can be simultaneously collected and individually analyzed. A sampling period of about 10 minutes is necessary to provide an amount of cyanide readily amenable to analysis by the cyanide selective electrode.
# Sampling
All glassware is washed in detergent solution, rinsed in tap water, and then rinsed with distilled or deionized water. Ten ml of an absorbing solution (0.1 M NaOH) is poured into an all-glass midget impinger using a graduated cylinder to measure the volume.
The fritted inlet of the impinger should have a porosity approximately equal to that of Corning EC (170-220 micron maximum pore diameter). A membrane prefilter (0.45 / u r n pore size) should be inserted (by means of an in-line cassette or similar device) before the impinger when sampling for particulate cyanides is to be performed.
Sampling for HCN and/or the particulate cyanides is performed for at least 10 minutes at a rate of 2 liters/minute, but the total volume of air sampled should not exceed 200 liters. A personal sampling pump or other satisfactory source of suction may be used for sampling provided it is calibrated as outlined below. Alternate sampling systems may be used, providing the required volume of air is sampled from the breathing zone of the worker.
Certain cyanide compounds, especially calcium cyanide, may hydrolyze at sufficiently high relative humidities, resulting in losses of collected sample as HCN gas. In such cases, it may be advisable to minimize losses by keeping the sampling time as short as possible, then storing it in a refrigerator until analysis.
It should be noted that when sampling for HCN without a prefilter, particulates will pass through the midget impinger. Likewise, when sampling for particulate cyanides by means of a midget impinger without a prefilter, HCN gas will also be collected and will constitute a positive interference.
# Calibration
Since the accuracy of an analysis can be no greater than the accuracy of measurement of the volume of air sampled, the accurate calibration of a sampling device is essential to the correct interpretation of an instrument's indication. The frequency of calibration is dependent upon the use, care, and handling to which the pump is subjected. Pumps should be calibrated if they have been subjected to misuse or if they have just been repaired or received from a manufacturer. If the pump receives hard usage, more frequent calibration may be necessary.
Ordinarily, pumps should be calibrated in the laboratory both before they are used in the field and after they have been used to collect a large number of field samples. The accuracy of calibration is dependent on the type of instrument used as a reference. The choice of calibration instrument will depend largely upon where the calibration is to be performed. For laboratory testing, a soapbubble flow meter or wet-test meter is recommended, although other standard calibrating instruments, such as a spirometer or dry-gas meter, can be used. The actual setup will be connected in sequence to the filter cassette or fritted impinger unit which will be followed by the sampler pump.
In this way, the calibration instrument will be at atmospheric pressure. If the personal sampler pump is used, each pump must be calibrated separately. If the buret is used, it should be set up so that the flow is toward the narrow end of the unit.
Care must be exercised in the assembly procedure to ensure that seals at the joints are airtight and that the length of connecting tubing is kept to a minimum. Calibration should be performed under the same conditions of pressure and temperature as those encountered in use. The calibrated pump rotameter should be used to set the flow rate in the field. Samples are analyzed using the cyanide ion selective electrode.
# Range and Sensitivity
The ultimate range and sensitivity of the method have not been established at this time. The recommended range of the method is 0.013-13 mg/cu m in air (approximately 0.0117-11.7 ppm of HCN).
# Interference
Sulfide ion irreversibly poisons the cyanide ion selective electrode and must be removed if found in the sample. Check for the presence of sulfide ion by touching a drop of sample to a piece of lead acetate paper.
The presence of sulfide is indicated by discoloration of the paper.
Sulfide is removed by the addition of a small amount (spatula tip) of powdered cadmium carbonate to the sample at pH 11-13. Swirl to disperse the solid, and recheck the liquid by again touching a drop to a piece of lead acetate paper. If sulfide ion has not been removed completely, add more cadmium carbonate. Avoid a large excess of cadmium carbonate and long contact time with the solution.
# METHOD FOR ANALYSIS OF CYANIDE SAMPLES
When a drop of liquid no longer discolors a strip of lead acetate paper, remove the solid by filtering the sample through a small plug of glass wool and proceed with the analysis.
# Precision and Accuracy
The precision and accuracy of this method have not been completely determined at this time. No collaborative tests have been performed on this method.
# Apparatus (a) Sampling and Calibration Equipment
(1) A filter unit (if needed) consisting of the filter media and cassette filter holder.
(2) A midget fritted impinger containing the absorbing solution or reagent.
(3) A pump suitable for delivering desired flow rates.
The sampling pump is protected from splashover or water condensation by an absorption tube loosely packed with a plug of glass wool and inserted between the exit arm of the impinger and the pump.
(A) An integrating volume meter such as a dry-gas or wet test meter.
(5) Thermometer ( 6) Manometer
# (f)
Precision and repeatability must be plus or minus 2% of full scale.
(g) It is desirable that the instrument respond only to HCN, but instruments which respond to other gases not normally present in the atmosphere may be acceptable.
In general, it is probable that any gas which causes a reading sufficiently high to set off the alarm will itself be present at a concentration sufficiently high to warrant corrective actions. Whenever there is a possibility that gases or vapors such as hydrogen chloride, chlorine, etc, may be present, it would be desirable to determine the response of the instrument to such gases in advance.
(h) An operating range of 0-100 ppm HCN is optimal, but other ranges may be selected to suit individual needs.
(i) The device should be capable of 7 days of continuous unattended operation.
# (j)
The device and alarm should be intrinsically safe for use in hazardous locations.
# Discussion
The principal requirements for such monitors in addition to responding to HCN gas are that they be sufficiently rugged to withstand normal extremes of temperature, pressure, vibration, etc, and not be susceptible to plugging or interferences due to contaminants likely to be encountered in most work places. They should be so constructed that it is possible to quickly check the zero setting of the instrument and the response at 25 ppm in a rapid routine manner. Chemical substances should be listed according to their complete name derived from a recognized system of nomenclature. Where possible, avoid using common names and general class names such as "aromatic amine,"
"safety solvent," or "aliphatic hydrocarbon" when the specific name is known.
The "%" may be the approximate percentage by weight or volume (indicate basis) which each hazardous ingredient of the mixture bears to the whole mixture. This may be indicated as a range or maximum amount, ie, "10-40% vol" or "10% max wt" to avoid disclosure of trade secrets.
# IX S P E C IA L PREC A U TIO N S P R E C A U T I O N A R Y S T A T E M E N T S O T H E R H A N D L I N G A N O S T O R A G E R E Q U I R E M E N T S P R E P A R E D B Y A O O R E S S O A T E
# XIII. APPENDIX V
First Aid and Treatment Kits Two physician's treatment kits should be immediately available to trained medical personnel at each plant where there is a potential for the release of, accidental or otherwise, or for contact with, hydrogen cyanide or cyanide salts. One kit should be portable in order that it may be carried by medical personnel while accompanying a patient to the hospital.
The other kit should be kept under lock and key to assure that it is intact and available when and if needed. The key should be readily available at all times to the work supervisor on duty and the storage place should be of such construction as to allow accessibility in the event of loss of the key.
Both kits for use by the medical personnel servicing each firm should contain the following as a minimum.
(1) Two (2) boxes (2 dozen) ampules; each ampule containing 0.3 ml of amyl nitrite.
(2) Two (2) ampules of sterile sodium nitrite solution (10 ml of a 3% solution in each).
(3) Two (2) ampules of sterile sodium thiosulfate solution (50 ml of a 25% solution in each).
(4) 2 sterile 10-ml syringe with intravenous needles.
(5) 1 sterile 50-ml syringe with intravenous needle.
(6) 1 tourniquet (7) 1 gastric tube (rubber).
(8) 1 non-sterile 100 ml syringe.
The medical personnel servicing a firm where there is a potential for hydrogen cyanide release or a potential for exposure to inorganic cyanide should be familiarized with the use of these kits.
First-aid kits should be immediately available at work places where there is a potential for the release, accidental or otherwise, of hydrogen cyanide or a potential for exposure to inorganic cyanide. This kit should contain as a minimum two (2) boxes of ampules ( 2 dozen), each containing 0.3 ml of amyl nitrite. Ampules should be replaced biannually or sooner if needed to ensure their potency.
The amyl nitrite ampules should be protected from high temperatures. In all cases, the contents of the medical and first-aid kits should be replaced before the manufacturer's assigned expiration dates.
First-Aid Procedure Speed in the rendering of first-aid treatment is of the utmost importance. The patient should be removed at once to an area free from HCN. The rescuer should wear respiratory protective equipment in order not to be overcome or weakened by the gas.
Many victims will have stopped breathing.
In this case, it is imperative that efforts at resuscitation be instituted at once and continued without interruption even while other treatment is being administered.
A physician should be summoned immediately.
First-aid kits should be readily available at all times. They should be quickly accessible but should not be kept only in operating areas mixtures with air may be explosive if a source of ignition is present.
# (B) Resuscitation
Before instituting artificial resuscitation, dentures and foreign objects, such as gum and tobacco, and any accumulated oropharyngeal fluids (saliva, etc) should be removed from the patient's mouth and pharynx and the tongue pulled forward.
If the patient's breathing is weak or has stopped, artificial resuscitation should be started at the earliest possible moment and continued without interruption until normal breathing has been established or the patient is pronounced dead.
Mouth-to-mouth resuscitation is the method of choice because of its simplicity and effectiveness. It is, however, impossible to administer amyl nitrite while using this method. Therefore, it is advisable to switch to other methods of artificial respiration, such as the Holger-Nielsen arm-lift back pressure method, during the periods when the amyl nitrite is being given.
If a mechanical resuscitator and personnel skilled in its use are available, this equipment may be used instead of other forms of resuscitation.
(C) The patient should be kept comfortably warm but not hot. Other drugs and stimulants are rarely necessary and should be administered only by a physician or trained medical personnel under the direction of a physician. Step -Through the formation of a relatively stable coordination complex with ferric iron, cyanide tends to keep this metal in its higher oxidation state and thus reduces its efficacy as an electron carrier in ferric to ferrous iron transitions.
By such a complexation of iron, the respiratory enzyme ferricytochrome oxidase is changed to ferricytochrome oxidasecyanide and its ability to catalyze the reaction of reduced cytochrome with oxygen is inhibited, with consequent impairment of cellular oxygen utilization
Step -Since numerous metabolic pathways converge at the cytochrome system, the impairment of the cells' ability to utilize oxygen reduces or even stops aerobic metabolism. True histotoxic (cytotoxic) hypoxia results with a shift to anaerobic metabolism with accumulation of lactate, pyruvate, and glucose.
Step -The cells are thus unable to use the oxygen brought to them as 02Hb by the arterial blood. The oxyhemoglobin continues into the veins, the arteriovenous oxygen difference diminishes, and the venous blood is almost as bright a red as the arterial blood.
Step 4 -The chemoreceptors in the carotid and aortic bodies, which are the tissues most sensitive to cellular hypoxia, trigger an inspiratory gasp and hyperpnea as an almost instantaneous path ophysiologic effect of cyanide absorption.
Current concepts about the treatment of selected poisonings-nitrite, cyanide, sulfide, barium, and quinidine. Ann Rev Pharmacol Toxicol 16:189 -199, 1976 109.
Carmelo, S: Rass Med Ind 24: 254-71, 1955 (Ita) 110.
El Ghawabi SH, Gaafar MA, El-Saharti AA, Ahmed SH, Malash KK, Fanes R: Chronic cyanide exposure: a clinical, radioisotope, and laboratory study. Br J Ind Med 32: 1975 111.
Wollman SH: Nature of the inhibition by thiocyanate of the iodide concentrating mechanism of the thyroid gland. Amer J Physiol 186: 1956 112.
Heymans JF, Masoin P:
Arch Int Pharmacodyn Ther 7:297-306, 1900 (Fre) After sampling, the fritted impinger stem can be removed and cleaned in the following manner. Tap the stem gently against the inside wall of the impinger bottle to recover as much of the sampling solution as possible. Wash the stem with a small amount (1-2 ml) of unused absorbing solution and add the wash to the impinger bottle. Then the impinger bottle is sealed with a hard, non-reactive stopper (preferably Teflon) and an appropriate identifying number attached to it. Do not seal with rubber.
The stoppers on the impinger bottle should be tightly sealed to prevent leakage during shipping. If it is preferred to ship the fritted impingers with the stems in, the outlets of the stem should be sealed with Parafilm or other nonrubber covers, and the ground glass joints should be sealed, ie, taped to secure the top tightly. Upon completion of sampling for the particulate cyanides, plastic caps should be replaced on the inlet and outlet tubes of the cassette and an appropriate identifying number attached to it.
Care should be taken to minimize spillage or loss by evaporation at all times. Refrigerate samples if analysis cannot be done within a day. Whenever possible, hand delivery of the samples is recommended. Otherwise, special impinger shipping cases should be used to ship the samples.
A "blank" fritted impinger should be handled as the other samples (fill, seal, and transport) except that no air is sampled through this fritted impinger.
Where a prefilter has been used for the collection of particulate cyanides, the filter cassettes are capped and placed in an appropriate cassette shipping container. One filter disc should be handled like the other samples (seal and transport) except that no air is sampled through it, and this is labeled as a blank.
# M A TERIA L SAFETY DATA SHEET 1 PRO D U CT IDENTIFICATIO N M A N U F A C T U R E R 'S N A M E R E G U L A R T E L E P H O N E N O . E M E R G E N C Y T E L E P H O N E N O A D O R E S S
# TRADE N AM E S Y N O N Y M S II H A ZA R D O U S IN G R E D IE N T S M A T E R I A L O R C O M P O N E N T % H A Z A R D D A T A
# III P H Y SIC A L DATA
# O L E V A P O R A T I O N R A T E ( B U T Y L A C E T A T E M ) A P P E A R A N C E A N O O D O R
where they may not be available in case of a spill.
( (3) Inhalation (A) Administer amyl nitrite A pearl (ampule), if not provided with a fabric sleeve, should be wrapped lightly in a handkerchief or gauze pad, broken, and held about 1 inch from the patient's mouth and nostrils for 15 seconds.
Repeat 5 times at 15-second intervals. Use a fresh pearl every 5 minutes until 3 or 4 pearls have been administered.
# WARNING:
First-aiders should keep the pearls away from their own mouths and noses lest they become weak and dizzy and unable to give proper assistance to the victim. Amyl nitrite is flammable and | # I. RECOMMENDATIONS FOR CYANIDE STANDARDS
The National Institute for Occupational Safety and Health recommends that employee exposure to hydrogen cyanide (HCN) and the cyanide salts in the workplace be controlled by adherence to the following sections. The standards are designed to protect the health of workers for up to a 10-hour workday, and a 40-hour workweek over a working lifetime. Compliance with the standard should therefore prevent adverse effects of HCN and cyanide salts on the health of workers. The standards are measurable by techniques that are valid, reproducible, and available to industry and government agencies.
Sufficient technology exists to permit compliance with the recommended standards. The standards will be subject to review and revision as necessary.
These criteria and recommended standards apply to occupational exposure of workers to HCN and cyanide salts. Synonyms for HCN are hydrocyanic acid, prussic acid, and formonitrile. For the purpose of this document, cyanide salts are defined as sodium cyanide (NaCN), potassium cyanide (KCN), or calcium cyanide (Ca(CN)2). The word, cyanide, or the symbol, "CN", is used to designate salts as well as hydrogen cyanide.
The "action level" for hydrogen cyanide or a cyanide salt is defined as one-half the corresponding recommended ceiling environmental exposure limit. "Occupational exposure" to these compounds is defined as exposure to airborne concentrations greater than the corresponding action levels.
The criteria and recommended standards apply to any area in which HCN, any of the cyanide salts or materials containing any of them, alone or in combination with other substances, is used, produced, packaged, processed, mixed, blended, handled, stored in large quantities, or applied.
Exposure to cyanide at concentrations less than or equal to the respective action levels will not require adherence to the recommended standards except for sections 2-7, and 8(c). If "exposure" to other chemicals also occurs, for example to a combination of cyanide and methyl alcohol, provisions of any applicable standards for such other chemicals shall be followed also.
# Section 1 -Environmental (Workplace Air) (a) Concentration
Employee exposure to HCN shall be controlled so as not to exceed 5 milligrams per cubic meter of air expressed as CN (4.7 ppm), determined as a ceiling concentration based on a 10-minute sampling period.
Employee exposure to cyanide salts shall be controlled so as not to exceed 5 milligrams per cubic meter of air expressed as CN, determined as a ceiling value based upon a 10-minute sampling period.
Whenever the air is analyzed for cyanide salts, a concurrent analysis shall be made for HCN. Neither of the respective ceiling values may be exceeded nor may the combined values exceed 5 mg/cu m measured as CN during a 10-minute sampling period.
# (b) Sampling and Analysis
Procedures for sampling, calibration of equipment, and analysis of air samples for HCN and cyanide salts shall be as provided in Appendices I and II, or by any method shown to be equivalent in precision, accuracy and sensitivity to those specified. A sampling period of about 10 minutes is necessary to provide an amount of cyanide readily amenable to analysis by the cyanide selective electrode.
Section 2 -Medical Medical surveillance shall be made available as specified below for all workers occupationally exposed to HCN or cyanide salts.
(a) Preplacement and annual medical examinations shall include:
(1) An initial or interim work and medical history with special attention to skin disorders and those non-specific symptoms, such as headache, nausea, vomiting, dizziness or weakness, that may be associated with chronic exposure.
(2) A physical examination giving particular attention to skin, thyroid, and the cardiovascular and upper respiratory systems.
(3) An evaluation of the advisability of the worker's use of negative-or positive-pressure respirators.
(b) Initial medical examinations shall be made available to presently employed workers within six months of the promulgation of a standard.
# (c)
The responsible physician and the employer shall be aware of the material contained in Appendix V and shall ensure that employees trained in these first-aid measures are on duty whenever there is occupational exposure to HCN or a cyanide salt.
(d) Two physician's treatment kits shall be immediately available to trained medical personnel at each plant where there is a potential for the release of, accidental or otherwise, or for contact with, hydrogen cyanide or cyanide salts. One kit should be portable in order that it may be carried by medical personnel while accompanying a patient to the hospital. The other kit should be kept under lock and key to assure that it is intact and available when and if needed. The key should be readily available at all times to the work supervisor on duty and the storage place should be of such construction as to allow accessibility in the event of loss of the key.
(e) First-aid kits shall be immediately available at workplaces where there is a potential for the release, accidental or otherwise, of hydrogen cyanide or a potential for exposure to cyanide salts. This kit shall contain as a minimum two (2) boxes of ampules (2 dozen), each containing 0.3 ml of amyl nitrite. Ampules shall be replaced biannually or sooner if needed to ensure their potency. The amyl nitrite ampules should be protected from high temperatures. In all cases, the contents of the medical and first-aid kits shall be replaced before the manufacturer's assigned expiration dates. Suggested contents for these kits are listed in Appendix V. In case of contact, immediately flush skin or eyes with plenty of water for at least 15 minutes; get medical attention. Remove contaminated clothing and wash before reuse.
# POISON First Aid
Carry patient to fresh air. Have the patient lie down. Remove contaminated clothing but keep patient warm. Start artificial respiration if breathing stops. Administer antidote (amyl nitrite ampule). Call a physician.
# Temporary Antidote
If cyanide gas is inhaled: Break an amyl nitrite ampule in a cloth and hold lightly under nose for 15 seconds. Repeat at about 15-second intervals.
If cyanide is swallowed:
Break an amyl nitrite ampule in a cloth and hold lightly under nose for 15 seconds.
Repeat inhalation of amyl nitrite 5 times at about 15 second intervals. If patient is conscious or when consciousness returns, give emetic (1 tablespoonful of salt to each glass of warm water) and repeat until vomit fluid is clear. Do not give an emetic to an unconscious or barely conscious person.
# (b)
The following warning sign shall be affixed in a readily visible location at or near entrances to areas containing HCN and where there is reasonable potential for emergencies: (1) location of gas masks and other emergency equipment,
(2) instructions for sounding emergency alarm,
(3) location of first-aid equipment and supplies, and
(4) instructions for summoning medical aid.)
The sign shall be printed both in English and in the predominant language of non-English-reading workers. All workers shall receive training and information on the hazards and safe work practices in handling HCN and cyanide salts, and on first-aid procedures in poisoning by these compounds.
(c) When HCN gas is used as a fumigant, warning signs shall be prominently displayed about the area and at all entries to the area as Temporary Antidote
If aerosolized salt has been inhaled or if solid or dissolved salt has caused poisoning after contact with the skin: Break an amyl nitrite ampule in a cloth and hold lightly under nose for 15 seconds. Repeat 5 times at about 15-second intervals. Repeat as necessary using a fresh amyl nitrite ampule every three minutes. Use artificial respiration if breathing stops.
If cyanide salt in any form is swallowed: proceed as above. If the victim is conscious and capable of some activity, give an emetic (1 tablespoonful of table salt in a glass of warm water) in repeated doses until the vomit fluid is clear. Never give anything by mouth to an unconscious person.
(e) Containers of Ca(CN)2 shall be labeled in the same manner as other solid cyanide salts, except that an additional warning is necessary because this material will react with water to release hydrogen cyanide.
The statement of the hazard shall read as follows for Ca(CN)2:
# DANGER! MAY BE FATAL IF SWALLOWED OR INHALED CONTACT WITH WATER OR ACID LIBERATES POISONOUS GAS CAUSES EYE BURNS AND MAY IRRITATE SKIN (f)
All containers of solutions of cyanide salts shall bear the following labeling in addition to, or in combination with, labels required by other statutes, regulations, or ordinances. The proper chemical name of the specific inorganic cyanide compound followed by the word "solution"
shall appear in large, bold face type at the top of the label.
(insert name of compound) SOLUTION (Inorganic Cyanide Solution) DANGER! MAY BE FATAL IF SWALLOWED OR ABSORBED THROUGH SKIN CAUSES BURNS CONTACT WITH ACID LIBERATES POISONOUS GAS Do not breathe gas. Do not get in eyes, on skin, on clothing. Wash thoroughly after handling. Keep container closed and away from acids. In case of contact, immediately flush skin or eyes with plenty of water for at least J.5 minutes and call a physician. Treat spillage with strong calcium hypochlorite solution and flush to sewer.
# POISON First Aid
Always have on hand a Cyanide First-Aid Kit. Carry patient to fresh air, have him lie down.
Remove contaminated clothing but keep patient warm. Start treatment immediately. Call a physician.
# Temporary Antidote
If gas is inhaled: Break an amyl nitrite ampule in a cloth and hold lightly under nose for 15 seconds. Repeat 5 times at about 15-second intervals. Repeat as necessary, using a fresh amyl nitrite ampule every three minutes. Use artificial respiration if breathing stops. If swallowed: Break an amyl nitrite ampule in a cloth and hold lightly under nose for 15 seconds. If patient is conscious, or when consciousness returns, give emetic (1 tablespoonful of salt in a glass of warm water) and repeat until vomit fluid is clear. Repeat inhalation of amyl nitrite ampule every three minutes. Use artificial respiration if breathing stops. Never give anything by mouth to an unconscious person. Engineering controls and safe work practices shall be used to maintain exposures to HCN and cyanide salts below the prescribed limits.
Administrative controls may also be used to reduce exposure. However, because the inhalation of cyanides or their absorption through the skin may be immediately dangerous to life, the added protection of personal protective equipment and clothing must be provided for work procedures and for emergency situations as discussed below. Such equipment and clothing must be provided to the workers engaged in work with cyanide. Emergency equipment shall be located at well marked and identified stations within the cyanide work areas. This equipment must allow each and every worker to escape the area in case of a cyanide emergency.
# (a) Respiratory Protection
Engineering controls shall be used whenever feasible to maintain airborne cyanide concentrations at or below the environmental limits recommended in Section 1 above. Compliance with the permissible exposure limits by the use of respirators is only allowed when airborne cyanide concentrations are in excess of the workplace environmental limits while required engineering controls are being installed or tested, when nonroutine maintenance or repair is being accomplished, or during emergencies. Appropriate respirators as described in Table 1-1 for HCN and Table 1-2 for cyanide salts shall be used only when permitted by the above restrictions. Respirators shall be selected and used in accordance with the following requirements:
(1) For the purpose of determining the type of respirator to be used, the employer shall measure, when possible, the airborne concentration of HCN or cyanide salt in the workplace initially and thereafter whenever process, worksite, climate, or control changes occur which are likely to increase the airborne concentration of these cyanides.
The employer shall ensure that no worker is being exposed to cyanide in excess of the standards either because of improper respirator selection, fit, use, or maintenance.
(
The employer shall provide respirators in accordance with Tables 1-1 and 1-2 and shall ensure that the employee uses the respirator provided.
(4) Respiratory protective devices shall be those approved under the provisions of 30 CFR 11, published in the Federal Register, March 25, 1972, as amended.
(5) Respirators specified for use in higher concentrations of HCN may be used in atmospheres of lower concentrations. Likewise, respirators specified for use in higher concentrations of cyanide salts are permitted in atmospheres of lower concentrations.
The employer shall ensure that the respirators are adequately cleaned, maintained, and stored when not in use, and that employees are instructed in the use of respirators assigned to them and in testing for facepiece leakage before each use.
Cartridges or canisters shall be discarded and replaced with fresh canisters after each use. Unused canisters shall be discarded and replaced when seals are broken, after three years if seals are unbroken, or on the manufacturer's recommendation, whichever is first.
Cartridges and canisters shall not be used for periods of time in excess of those indicated in Tables 1-1 and 1-2.
(8) Emergency and escape-type respirators shall be made immediately available at the work stations for each worker when there is potential for exposure to concentrations of the various cyanides above the ceiling values.
For purpose of selection of respiratory protective equipment, entry into areas containing unknown and/or suspected dangerous atmospheric concentrations of HCN or cyanide salts shall be treated as an emergency. Less than or equal to 90 ppm (1) Type C supplied-air respirator, demand or continuous-flow type (negative or positive pressure), with half or full facepiece.
(2) Full facepiece gas mask, chin-style canister specific for HCN. The maximum service life of canisters is one hour.
Less than or equal to 200 ppm Full facepiece gas mask, front-or backmounted type canister specific for hydrogen cyanide. The maximum service life of canisters is one hour.
(1) Self-contained breathing apparatus in pressure-demand mode (positive pressure) with full facepiece worn under gas-tight suit providing whole body protection.
(2) Combination supplied-air respirator, pressure-demand type (positive pressure), with auxiliary self-contained air supply and full facepiece; all worn under gas tight suit providing whole body protection.
(1) Positive pressure self-contained breathing apparatus worn under a gas-tight suit providing whole body protection.
(2) Combination supplied-air respirator, pressure-demand type, with auxiliary selfcontained air supply; all worn under gastight suit providing whole body protection.
(1) Self-contained breathing apparatus in demand or pressure-demand mode (negative or positive pressure).
(2) Gas mask, full facepiece or mouthpiece type, with canister specific for HCN.
# NOTE:
During the use of any respirator with half mask, full facepiece or hood, protective clothing should be worn if there is a chance that liquid HCN may contact any part of the body.
Greater than 200 ppm Emergency (no concentration limit)
Evacuation or Escape (no concentration limit) Less than or equal to (1) Filter type respirators, approved for 25 mg/cu m toxic dust, with half-mask (not appli cable for Ca(CN)2).
(2) Chemical cartridge respirators with replaceable cartridge for toxic dusts and acid gases; with half-mask. Maximum service life 4 hours.
(1) Full-face gas mask, chest or back mounted type, with industrial size canister for toxic dust and hydro cyanic acid gas. Maximum service life 2 hours.
(2) Type C supplied air-respirator, continuous-flow or pressure-demand type (positive pressure) with full facepiece.
(3) Type A supplied-air respirator, (hose mask with blower) with full facepiece.
Greater than 50 mg/cu m (1) Self-contained breathing apparatus with positive pressure in full facepiece.
(2) Combination supplied-air respirator pressure-demand type with auxiliary self-contained air supply.
(1) Self-contained breathing apparatus with positive pressure in facepiece.
(2) Combination supplied-air respirator, pressure-demand type, with auxiliary self-contained air supply.
Evacuation or Escape (no (1) Self-contained breathing apparatus in concentration limit) demand or pressure-demand mode (negative or positive pressure).
(2) Full-face gas mask, front or back mount type with industrial size canister for toxic dust and hydro cyanic acid gas.
# Emergency (no concentration limit)
Less than or equal to 50 mg/cu m (b)
Protective Clothing
Because HCN and cyanide salts, dry or in solution, may be absorbed readily through the skin or any break in the skin, the provision and use of protective clothing are necessary for the protection of workers in most operations where HCN and cyanide salts are used in pure or diluted condition.
(1) When entering a HCN gas-filled area in emergency situations, when the airborne concentration of HCN is unknown, or when the known airborne concentration is greater than 200 ppm, employees shall wear gas-tight suits in addition to the required respiratory protection. The gas-tight suits shall provide full body protection.
(2) Employees engaged in maintenance, repair, or other work on equipment, or in circumstances whereby they may be exposed to HCN liquid or gas, shall wear protective garments or suits made of material impervious to HCN and providing full body protection.
(3) Employees shall wear rubber gloves when engaged in any activity which may involve the handling of, or possible contact with, HCN.
Employees shall wear gloves when handling dry cyanide salts and when using or handling equipment whose surfaces may be contaminated with these salts in such manner that contact of the chemical with the employee's hands is possible or likely.
Employees shall wear gloves made of rubber or other impervious material when engaged in any operation wherein contact of the hands with solutions of cyanide salts is possible or likely.
Employees shall wear protective sleeves, aprons, and/or full body protective clothing as needed to protect their skin from contact with cyanide salts, dry or in solution. When handling solutions, the outer garment shall be of rubber or other material impervious to the solutions involved in the exposures. The garments shall fit snugly about the wrist, arm, neck, waist, and/or ankle (as appropriate to the particular garment) and shall have closures which will exclude dust, powder, mist, and/or splashes of cyanide salts in either dry or liquid formulations.
(10) In areas where spills or splashes of solutions of cyanide salts are likely to occur, the employees shall wear shoes, boots, or overshoes made of rubber or other material impervious to these solutions.
(11) Chemical safety goggles shall be worn by employees engaged in any operation wherein there is danger or likelihood that dusts or solutions of cyanide salts will come into contact with the eye.
Full-length face shields with forehead protection shall be worn by employees engaged in any operation wherein there is danger or likelihood that dusts, molten salts, or solutions of cyanide salts may contact the face.
The employer shall be responsible for maintaining all devices and clothing to be used for personal protection in a clean and effective condition. (2) Buildings in which HCN is to be stored, handled, or used must be designed to prevent fire and explosion hazards and to minimize the release of the highly toxic liquid or gas. Equipment and vessels containing or using HCN should be isolated in rooms or buildings designed for, and devoted to, these purposes.
Building construction shall be fire-and explosion-resistant and shall meet the requirements of the National Fire Protection Association codes and of the local codes, regulations, and ordinances. Explosion vents and fire doors shall be provided in accordance with codes and good practice.
Each room or building shall have no less than two means of exit, with doors opening outward and provided with "panic bar" release latches.
Exits shall be provided so that no location within the room or building is more than 75 feet from an exit and personnel can be evacuated in less than 1 minute.
(3) All regular work areas where HCN is handled or used must be adequately ventilated so that, under normal or reasonably anticipated operating conditions, the airborne concentrations of HCN will not exceed the standard recommended in Section 1.
Local exhaust ventilation shall be used at points or areas of regular or anticipated release of HCN gas.
Equipment for very high rates of ventilation of an area may be provided for the rapid reduction of contamination of air by HCN when emergency situations arise.
The HCN-contaminated air from an exhaust ventilation system must either be passed through a suitable collector to remove the HCN or be discharged at a location or in a manner such that persons or animals will not be endangered by the toxic gas.
Ventilation equipment must meet the applicable codes for explosionproof and fireproof installation of such equipment. where applicable, shall be followed.
# (b) Cyanide Salts
(1) All necessary precautions must be taken to prevent cyanide salts from coming into contact with liquid or airborne acids. In addition, precautions must be exercised to prevent Ca(CN)2 from coming into contact with water or humid atmospheres.
Cyanide salts must be protected also from contact with large concentrations of carbon dioxide. Carbon dioxide fire extinguishers must not be used where cyanide salts are present.
In any circumstance in which there is probable contact of cyanide salts with liquid or airborne acids such as Cr03, S02, C02, HC1 etc, or of Ca(CN)2 with a high concentration of water vapor or with liquid water, the standards and requirements applicable to exposures to HCN shall also apply.
( All containers of cyanide salts must be labeled in accordance
# «
with the recommendations in Section 3.
Areas in which cyanides are stored must be posted in accordance with the recommendations in Section 3.
(3) When containers of cyanide salts are removed or unloaded from trucks, boxcars, or poorly ventilated spaces, these should be thoroughly ventilated, purged, and tested before a worker enters.
When cyanide salts are placed in other containers for transport or temporary storage, such containers must be properly covered and labeled.
(A) Mechanical exhaust ventilation by local exhaust shall be provided for all operations producing, or likely to produce, dust or mists of cyanide salts in excess of the limit recommended in Section 1, or to vaporize HCN in excess of the recommended limit for that vapor.
Examples of such operations are: there is evolution of mist from the bath, the employees shall be encouraged to wear at least a filter type respiratory protective device as a measure of protection in addition to that provided by ventilation.
Nonreturnable containers and other containers or equipment contaminated with cyanides before being discarded should be washed thoroughly with alkalinized water to remove cyanide residues.
(10) When cyanide salts are used in fused salt baths, mechanical local exhaust ventilation should be provided to control any cyanide emissions.
Care in operation of the bath and in housekeeping must be exercised so that the area around the bath does not become covered with cyanide-containing powder or dust. Employees working at baths of fused cyanide salts should wear face shields and appropriate protective clothing to protect them from burns and skin contact with cyanides in the event of splashes. A shovel or similar tool should be used to add cyanide salts to a fused salt bath. The cyanide salt should not be added directly by hand.
(11) Inspection, cleaning, or repairing of tanks or other equipment used with solutions of cyanide salts should be performed only by properly trained workmen under careful supervision.
(A) The tank should be drained of all cyanide solution as completely as possible, then filled with alkalinized water and allowed to stand for 15 minutes, preferably with agitation. This procedure should be repeated; then a preliminary inspection may be made. Any encrustation should be removed by mechanical means and/or by means of a stream of water from a hose.
# (B)
If the tank is to be entered, the atmosphere in the tank should be tested for the presence of hydrogen cyanide and cyanide salts, to be certain it does not contain a dangerous airborne concentration of these or other materials.
(C) The tank should be purged with fresh air to ensure an adequate oxygen supply and air should be supplied to the tank while the worker is in the tank.
# (D)
Equipment other than tanks should be washed and vented similarly, as applicable.
In the event of finding airborne concentrations of cyanide salts in excess of the limit, immediate action must be taken to eliminate the cause of the elevated airborne cyanide concentration. In case of any emergency situation (spills, leaks, or other unusual emissions of cyanide which result or potentially may result in dangerous airborn concentrations), all personnel shall be evacuated from the area. The personnel required to return to the area to institute corrective measures shall wear approved respiratory protective gear while entering and working in the area until the situation is corrected.
(13) Any area in which there is the potential of an emergency involving HCN or a cyanide salt shall be posted in accordance with the provisions of Section 3, and emergency equipment stations shall be established. These stations shall be sufficient in number and so located as to be readily and immediately accessible to the workers in the area.
The stations shall be provided with first-aid supplies and instructions for first-aid treatment of any persons suffering excessive exposure to cyanide.
Approved type respiratory protective devices, as indicated in Section 4, shall be available at designated emergency stations. These devices shall be sufficient in number for the workers in the area and readily accessible. Occurrence and Use HCN is a colorless gas [1] or a colorless or bluish-white liquid [1,2] with a faint, characteristic odor of bitter almonds [2, 3,4] perceptible to some people. [3,4] Kirk and Stenhouse [5] reported that 88% of 244 persons tested could smell hydrogen cyanide but that in a fourth of these, the determination was made only with difficulty.
The glucoside amygdalin which occurs in nature in some plants, notably almonds, [3] readily yields HCN upon hydrolysis. Recently, attention has been brought to the presence of HCN in automobile emissions. [6,7] HCN is manufactured in the United States from coke-oven gas by reaction with sodium carbonate, from cyanide salts by reaction with acid, by the decomposition of formamide, from the reaction of ammonia, air, and natural gas, or, most commonly, from the reaction of methane and ammonia under specific controlled conditions. [8] The great bulk of the HCN synthesized is used directly in the same process system. [8] In 1973, the estimated consumption of HCN in the United States was approximately 310,000 short tons. [9] HCN is used primarily in the production of chemical intermediates for the manufacture of synthetic fibers, [8,10] plastics, [8] cyanide salts [8,10] and nitrites; in the fumigation of ships, [11,12,13,14,15] In the presence of any source of hydrogen ions in quantity, eg, strong mineral acid, the production of HCN from cyanide salts becomes both rapid and large. Above 50 degrees C, an irreversible decomposition to formate and ammonia, as shown below, becomes important. [28] In the presence of NaCl, the hydrolysis of NaCN to HCN is increased at temperatures below 80 C, but decomposition to ammonia and formate is retarded. [28] Sodium cyanide is marketed as a powder, granule, flake or block in pillow-shaped pieces weighing about 1 oz, and as a 30% aqueous solution.
[28] Solid sodium cyanide is packed in steel or fiber drums, and the aqueous solution is shipped in tanks by truck or rail. [28,30] Potassium cyanide, KCN, is a white crystalline, deliquescent, solid. KCN is produced by methods similar to those for NaCN. [28,29] The chemical reactivity of KCN is similar to that of NaCN. [28] Hydrolysis to HCN, as was the case with NaCN, is slight (Kh = 2.54 x 10 exp(-5)). [28] Potassium cyanide is sold in forms similar to those of NaCN but because KCN is more expensive, its world production for 1963 was only 5,000 tons. [28] Calcium cyanide, Ca(CN)2, is also called "black cyanide" and is the only commercially important alkaline earth cyanide.
[31] The hydrolysis of Ca(CN)2, which takes place in two steps, as shown below, is complete.
[31] The resulting calcium hydroxide has dissociation constants of 3.74 x 10 exp (-3) and 4.0 x 10 exp (-2) but is much less soluble in water at 0 degrees C than sodium hydroxide [1,32] so that its aqueous solutions are not as alkaline.
For example, the pH of an aqueous solution of Ca(0H)2 in an electric furnace above 1000 C in the presence of sodium chloride.
saturated
[31] Rapid cooling apparently prevents the reversion to calcium cyanamide.
[31] It is manufactured primarily in Canada, South Africa, and East Germany and sold as flakes or blocks.
There is also some production elsewhere in Europe and Japan.
[ The first uses of the gas as a fumigant were in 1886 to control scale on citrus trees in California, [19] in 1898 to kill vermin in railway cars, [11] in to kill bed bugs in prisons, [11] and, after 1910, for the fumigation of the holds of ships. [11] Stock and Monier-Williams [11] Cytochrome c absorbs radiation at 550 nanometers (nm). In the presence of cytochrome oxidase, the optical density at 550 nm decreases at a rate directly proportional to the activity of cytochrome oxidase. This rate of change was determined in the presence of cyanide, demonstrating the ability of cyanide to inhibit cytochrome oxidase activity. Additions of methemoglobin, in which the iron had been oxidized electronically to the ferric state, to a solution containing cytochrome c, cytochrome oxidase, and cyanide were found to increase the activity of cytochrome oxidase, thus reversing the inhibitory effect of cyanide. The authors also found that the addition of cyanmethemoglobin to a solution of cytochrome c and cytochrome oxidase had no immediate effect on enzyme activity, but after a few minutes the enzyme became increasingly inhibited. Thus, the authors demonstrated in vitro the abilities of cytochrome oxidase and methemoglobin to compete in a reversible fashion for the cyanide ion.
In a 1958 survey, Dixon and Webb [56] found that the concentration of cyanide necessary for inhibition of cytochrome oxidase was 2-6 orders of magnitude less than those required for inhibition of other enzymes. The interference of CN with many different enzyme systems other than those involved in respiration may thus contribute to its toxicity.
Schubert and Brill [57] in 1968 measured the inhibition and recovery of liver cytochrome oxidase in mice, rats, and gerbils after the intraperitoneal administration of KCN. Inhibition of the enzyme was found to reach a maximum 5 to 10 minutes after the cyanide injection. Depending on the dose, the enzyme activity returned to normal 5 to 20 minutes after maximal inhibition in mice but required up to 1 hour or more in the rat and gerbil. Interestingly, they found that the abilities of mice and rats to tolerate divided doses of cyanide depended on the total dose as well as on the time-dependent degree of enzyme inhibition. For example, they found that mice invariably survived a single sublethal dose of 6 mg/kg of KCN but not two doses of 3 mg/kg given 6 minutes apart or three doses of 2 mg/kg given at 6 minute intervals. They further showed that sodium thiosulfate and nitrite were able to reactivate liver cytochrome oxidase within minutes when administered to cyanide-treated rats and mice. Both men complained of headache and weakness or fatigability and were observed to have slight lid lag, enlarged thyroids, and excessive perspiration. One of the two also experienced dizziness and mental confusion, slurring of speech, coughing, sneezing, and occasional abdominal cramps, nausea, vomiting, and coarse tremor of the extremities followed by their temporary paralysis. Both men were exposed to cyanide aerosols generated by case hardening. Some exposure to HCN may have occurred.
Wuthrich [25] in 1954 described a 39-year-old German blacksmith who was exposed to cyanide in case hardening on a sporadic basis for 2 years and then more frequently for the next 4 years. The worker noticed some initial irritation, followed by a general worsening of health. He experienced loss of appetite, nervousness, vertigo, headaches, nausea, and vomiting.
During 2-3 week vacations, the symptoms disappeared but reappeared within a month after returning to work. His thyroid gland was slightly enlarged. After exposure to cyanide had ceased for about 14 days, the man was given a placebo of NaCl, iv, for three days during which time he reported an improvement in his condition. On the 4th day, 1.4 g of sodium thiocyanate was substituted for NaCl in the daily injections. The thiocyanate concentration in the blood serum increased rapidly following these injections and did not decay to normal between injections. From the day of the first NaSCN injection, the man began to complain of nausea, lack of appetite and nervousness. After three NaSCN injections, he reported nausea and vomiting and spontaneously stated that he felt the same symptoms as at his workplace.
If there are 5200 ml of blood in the average man, then a dose of and eventually by complete disappearance of P waves. A secondary increase in rate, but not to the rate prior to administration of HCN, was observed during the 3rd and 4th minutes along with the irregular reappearance of P waves, some of which were not conducted. All subjects showed A-V dissociation with a secondary decrease in rate during the 5th minute.
During the 6th and 7th minutes, the heart rates again showed a slight increase and a return to normal sinus rhythm. Thereafter, the heart rates slowed progressively. Normal A-V conduction in one man and incomplete A-V block in another were maintained throughout the period of observation (approximately 13 minutes).
A third subject developed Wenckebach's phenomenon, (2:1 block), and, finally, complete heart block. The fourth subject's heart had normal A-V conduction until the 14th minute, when it developed ventricular tachycardia and ventricular fibrillation. It must be remembered that the concentrations of HCN to which these men were exposed were huge, so that the details of the changes in their ECG recordings may not be entirely typical of those to be expected in occupational exposures.
Wexler's observations do seem to demonstrate that cyanide has no specific action on the heart but rather exerts on the myocardium actions that are typical of hypoxia and anoxia.
There have been several reports of exposure to HCN which included both the airborne concentration of HCN and the human physiological response. However, in many cases no additional information relating to worker exposure was provided. These reports are summarized in Table XIV-5.
In many cases it is difficult to attribute a specific concentration range directly to a group of investigators since many of the citations involve reference to the work of others with no additional supporting information.
Therefore, the validities of concentrations presented only by secondary references may be questioned. In large part they appear to be based on the unreferenced work of Lehmann and Hess. However, the application of
# Lehmann's data to man has been questioned by McNamara [68] because
Lehmann's work was apparently done entirely with rabbits, which McNamara considers to be more sensitive to a given dose (product of concentration and time) of HCN than man. He concluded that man has a susceptibility to HCN more like those of the comparatively resistant goat and monkey and on
this assumption (and one that the LCt50 for man is four times that for the mouse) has estimated that 3,404 mg/cu m will cause 50% mortality in humans exposed to it for one minute. McNamara estimated that a concentration of HCN of 607 mg/cu m would kill 50% of men after a 10-minute exposure.
The various fatal doses of HCN seen in Table XIV had just returned from a 13-month leave of absence 5 months prior to this episode.
In use, the solution was heated to boiling whereupon 50 ml of hydrogen peroxide were added. The gold articles were cleaned in a manner causing splashing on the skin and the production of a visible aerosol.
There may have been some exposure to HCN. A study of plant records revealed another plater who developed typical signs and symptoms in 1 month. The man had been treated for 7 weeks, was removed from exposure, and recovered. An investigation of the plant was made and these 19 illnesses were attributed to aerosols emitted by the improperly operated plating tanks. After engineering controls and housekeeping procedures had been instituted, there were no recurrences of these illnesses. No airborne concentrations of contaminants were reported.
Elkins [91] in reported that in a plant where there was considerable brass plating the ambient air contained a mist. The mist was reported to have contained NaCN in a concentration not greatly exceeding 5 ppm, expressed as HCN. Severe irritation was a widespread complaint and there were some incidents of ulceration of the nasal septum. The author noted that other alkalies of undetermined concentration in the air may have contributed to the irritating action of the mist. with the exception of one with a perforated septum who gave a history suggestive of previous exposure to chromates. The cyanides were not described but they were likely a mixture of NaCN, KCN, and some alkaline complex of CuCN in the copper plating tanks, and alkaline NaCN in the zinc bath.
[93]
In None of the four unexposed men had evidence of disease of the stomach or duodenum. The author reported that three of the exposed and two of the unexposed men had erythrocyte counts above 5,000,000 but below 6,100,000/cu mm and that seven of the exposed and none of the unexposed men had a percentage of lymphocytes above 40 but below 49%. He attributed the latter change to stress resulting from repeated exposure to small doses of HCN. He concluded that his results demonstrated that not all the effects of repeated acute or subacute exposures to HCN are entirely reversible.
In Exposure was continued until the animals became apneic, their heart beats became irregular and weak, and distinct cyanosis was apparent. Administration of oxygen through a plaster of Paris mask, modelled to fit the rabbit's muzzle, by hand pressure applied to a rubber bag connected to the mask succeeded in reviving 18 of the 36 rabbits. The authors stated that the hearts of the other 18 rabbits had become too weak when oxygen administration was started to be able to perform the necessary movement of oxygenated blood to the important organs.
In 1951, Moss et al [124] exposed 16 rats to HCN at 24-465 ppm for up at 22 minutes. The rats exposed at 25-50 ppm survived, except for one exposed at 50 ppm. This rat was violently agitated after 1 minute 49 seconds, paralyzed after 2 minutes 30 seconds, unconscious after 3 minutes, and dead after 8 minutes.
In experiments reported in 1952 by Haymaker et al, [125] six dogs were exposed at concentrations of 620, 590, 700, 700, 165, and 690 mg/cu m, for periods of 2.0, 2.0, 1.75, 1.75, 10.0, and 2.0 minutes, respectively.
The first three dogs died in 20 hours or less and the others were killed 24, 26, and 28 hours after exposure. Four of the six dogs had convulsive seizures. The dog exposed at 620 mg/cu m had marked proliferation of histiocytes in the leptomeninges and in the perivascular spaces of the molecular layer of the cerebellum. Only shadows of the Purkinje cells remained. Some of these dogs suffered necrosis of gray matter. Definite alterations of structure were not seen in dogs that died within 21 minutes after being exposed to HCN; they were found in dogs that died 2.5 or more hours after exposure. At these comparatively early times, there was subpial edema of the cerebrum and the cerebellum. Dogs that survived for as long as 16 hours had cellular damage, particularly in the cerebral cortex.
The frontal and parietal lobes were more likely to be affected than the temporal or occipital.
Cortical damage was concentrated frequently in the trough of a sulcus in the form of massive coagulation necrosis.
Valade [126] in 1952 exposed four dogs to HCN at 50 mg/cu m for 12 30-minute periods, conducted at 8-day intervals. Of these dogs, two survived, one died after 38 days, and one died of an intercurrent disease.
In a second experiment, four dogs were subjected to 19 30-minute inhalation periods at 2-day intervals and at the same HCN concentration. One died after 73 days, the other after 77 days. Another group of five dogs went through seven 30-minute inhalations at 2-day intervals, but this experiment was interrupted when pulmonary inflammation occurred, causing the death of three dogs. Still another group of four dogs were subjected to fourteen 30-minute inhalation periods at 2-day intervals; one of these died after 34 days.
The first signs were dyspnea, nausea, exaggerated intestinal peristalsis, and diarrhea. Later, the dogs developed tremors followed by loss of equilibrium and convulsions. These observations tend to support the hypothesis of a cumulative effect from exposure to HCN.
Valade [126] autopsied the dogs immediately after they died or were
killed and observed similar central nervous system lesions in each of them.
Vascular changes were vasodilatation and hemorrhages which were most pronounced in the central gray nuclei, brain stem, bulb, and medulla cervicalis.
Cellular lesions manifested themselves by glial reactions throughout the central nervous system and by cytologic changes in the Purkinje cells of the cerebellum and in the bulbar gray nuclei. These histopathologic examinations led the author to conclude that the lesions resulted from anoxia caused by inhibition of cytochrome oxidase or from a selective effect of the poison. To support the contention that the latter cause was the more significant, the author noted that the dogs were very quickly affected by respiratory disorders before the onset of other signs.
He thought there was reason to believe that the suddenness with which these disorders appeared was linked to a particular sensitivity of these animals' bulbar cells to cyanide, rather than to an inhibition of cytochrome oxidase. In 1955, Howard and Hanzal [127] reported a feeding study with HCNfumigated food. Thirty male and 30 female weanling albino rats were divided into 3 groups of 10 males and 10 females each. Two of the groups were given dog meal containing 300 ppm and 100 ppm of HCN, respectively. A third, similar group was fed unfumigated food as a control. At the end of a 2-year feeding period, no gross signs of cyanide toxicity were observed.
Autopsies revealed the same general abnormalities and signs of senility in control and experimental rats. Microscopic examination of heart, lungs, liver, spleen, stomach, small and large intestines, kidneys, adrenal, thyroid, testes or uterus and ovary, and the cerebrum and cerebellum revealed no evidence of pathology due to HCN feeding. All findings were compatible with those usually seen in aging animals, and the same general changes were found in both the control and the experimental animals.
Thiocyanate concentrations in plasmas, RBC's, and kidneys, but not in the livers, of rats given food containing 300 or 100 ppm HCN were about twice as high as those in controls.
In 1959, Levine and Stypulkowski [128] reported lesions in several areas of the brains of rats which survived exposure for 20-45 minutes at an unknown concentration of airborne HCN. The concentration of the airborne cyanide aerosol, which the authors presumed to be HCN, was not determined but was sufficient to debilitate the rats in 10 minutes. Earlier, Flury
and Zernik [118] found that persisting prostration occurred in 9.5 minutes at 127 ppm and, thus, it may be estimated that the rats in this experiment had exposures to HCN at approximately 127 ppm. Below this concentration (127 ppm), exposure to HCN for 2 hours did not produce brain lesions.
Above this concentration at which persisting prostration occurred, brain lesions were produced readily in 20-30 minutes. These lesions involved a multiplicity of sites in the brain although they were not universal in distribution.
For example, the cord, most of the stem, cerebellum, diencephalon, and portions of the cerebrum were spared. A predominance of isolated lesions appeared in the callosum and striatum. Later that same year, Levine and Weinstein, [129] using the same technique described above, reported that high concentrations of HCN generally caused the death of rats without causing brain damage. Low concentrations did not produce either, but moderate concentrations (perhaps 100-150 ppm) caused brain lesions while consciousness was maintained for an hour or so, followed by sudden unconsciousness and death. Unfortunately, in neither of these studies was the airborne concentration reported. Wistar albino rats receiving 0.5 mg of KCN subcutaneously once weekly for 22 weeks. They reported some pallid myelin but found it difficult to estimate whether or not there was demyelination. The animals appeared to be without other ill-effects from these small doses. The authors suggested that these lesions were due to excessive utilization of hydroxocobalamin to form cyanocobalamin. Whether these effects on nervous tissue are due to a specific action of the cyanide ion or of the thiocyanate ion, or to general histotoxic anoxia, is not clear.
Moss et al [124] in 1951 subjected from one to three rats to mixtures of CO and HCN. Atmospheres containing either HCN or CO alone were generally lethal to rats at concentrations of 50 or 5000 ppm, respectively.
A mixture of 10-20 ppm of HCN and 2000 ppm of CO was lethal to some.
Mixtures of 30 ppm of HCN and 1000 ppm of CO and of 5 ppm of HCN and 2000 ppm of CO were not lethal.
Hirner [132] in 1969 subjected male rats weighing about 250 g to subcutaneous injections of 0.2% KCN.
The daily dose, which averaged between 3 and 5 mg/rat, was divided into parts, which were injected within the span of 1 hour. Five rats received single daily doses and were killed 2 or 3 days later. Six rats received 4 to 12 daily doses, two received 14, and four received 20. All the multiply dosed rats were killed at the end of 9 weeks from the first daily dose. These rats were perfused through the left ventricle with a sodium cacodylate-glutaraldehyde solution;
appropriate samples of nervous tissue were ultrasectioned and examined electronmicroscopically as well as by conventional optical microscopy. The principal lesion found in this study was necrosis in the caudal part of the corpus callosum, with spongy alteration at the margin of the necrotic area.
Phagocytes invaded the necrotic area 2 days after the last dose of KCN; astrocytic gliosis followed. In the area of spongy change, there was vacuolization of axons and swelling of the astrocytes and oligodendroglia.
Demyelination was visible in the later stages of the study. Hirner considered that the effects on glial cells were primary effects of cyanide, but that disintegration of myelin and axonal degeneration were secondary effects, the axon remaining intact when swelling of the glia had occurred.
He stated the belief that the oligodendroglia are particularly susceptible to injury by cyanide. Unfortunately, neither report sought to quantify the dose of either HCN or KCN.
In the first study, Levine and Stypulkowski [128] In the second study, Levi and Amaducci [137] in 1968 brought their animals through the first two stages, after which they were allowed to partially recover, and were then killed by decapitation. The meninges appeared congested. Some rats had hemorrhagic pulmonary infarctions. In some animals trypan blue was injected iv to test the integrity of the blood-brain barrier. Subsequent examination of the brains did not show any abnormal passage of the trypan blue into the nervous tissue. Brain slices of other rats were used to study the active transport of amino acids.
Initial and steady state accumulation of amino acids and rates of amino acid exit were identical in brain slices from control and treated animals when a glucose-containing incubation medium was used. Tissue respiration rates were also measured in vitro and found to be identical in both control and treated animals. Thereafter, the analytical method selected determines cyanide radical content, and it is impossible to say what fraction of the total was attributable to any particular compound.
In order to differentiate between HCN gas and other cyanide compounds, it is necessary to first remove particulates by passing the air through an efficient filter, then absorb HCN from the stream by passage through an alkaline absorbing solution.
The filtered cyanides can subsequently be leached from the filter by treatment with alkaline solution, and the same analytical technique applied to both portions of the sample.
The presence of small quantities of cyanide in water was of concern long before relatively recent ecologic considerations led to an awareness that many other substances were toxic at trace concentrations. As a result, there exists substantial literature dealing with the qualitative and quantitative detection of cyanides in air and water, with at least one method (the titrimetric estimation of cyanide with silver nitrate published by Liebig [156] in 1851) still in use today, more than a century after its origination. [6,7] Almost all the methods proposed for the analysis of water or other materials have been, or can be, applied to the analysis of cyanides in air, for most air methods ultimately involve the determination of cyanide ion in solution. One of the most widely used colorimetric methods is the so-called pyridine-pyrazolone method, an example of the Konig synthesis for pyridine dyes, first published by Aldridge [174] in 1944 (using pyridine and benzidine) and subsequently modified by various authors.
[78,175-181] In this method, cyanides are converted to cyanogen bromide or cyanogen chloride, which then reacts with pyridine to form a glutaconic aldehyde.
Next, a primary aromatic amine reacts with the aldehyde to yield a colored Schiff's base. In the original procedure of Aldridge, the aromatic amine used was benzidine, but the more frequently used modification of Epstein voltammetry [191], amperometry [192,193], coulometry [194] potentiometry [195] and others. [196,197] The most recently introduced and probably mosc useful in its application to air analysis, is the eleccrometric technique relying on specific ion electrodes, or ion selective electrodes which respond only to cyanide ion concentrations, [198][199][200][201][202][203][204][205] Cohen A -novel approach to determining cyanide levels has been described by OancniK and Br/lr.z [209] involving Indirect atomic absorption " spectrometric analysis.
In the first of two methods, the complex dicyano-bis-(l,10phenanthroline)-iron(II) is formed and then ¿-.:tracted into chloroform. The
• iaiororG-ia is evaporated and the residue is taken ap m ethanol. The
• -.thaiioi. solution is aspirated directly into the flame, and iron equivalent 99 i to a known amount of cyanide is then determined. The second method is based on precipitating silver cyanide, then determining the excess silver ion in the supernatant by atomic absorption spectrometry.
In place of titrimetric techniques, several investigators have described methods in which turbidity resulting from the formation of silver cyanide, or the reduction in turbidity due to the formation of a cyanide complex with silver iodide, are measured.
[ [170], a specific ion electrode method [198], and a blood method using microdiffusion [77], first used by Conway.
[226] A respired air method based on the pyridine-pyrazolone reagent [227], as well as more general methods applicable to biologic samples using this same reagent are also used.
[
# 220,228]
The rationale used in making a forensic diagnosis of cyanide poisoning have also received some attention. [21,229] Many of the methods listed have also been used for water and waste water analyses, and currently the methods most favored appear to be colorimetric, using some version of the pyridine-pyrazolone method, or modifications of the titrimetric determination with silver nitrate.
[177,178,186,187] Specific ion electrodes [198], and picric acid [184] have also been used.
Recently, an opto-acoustic infrared absorption technique as well as the titrimetric method utilizing silver nitrate have been used in the analysis of HCN in automobile exhaust. [6,7] Virtually every method used for cyanide analyses is subject to some interferences, usually due to the presence of certain metals which may form complexes, other anions, particularly sulfide, and a host of oxidizing and reducing agents. It is, therefore, frequently necessary to isolate the cyanide by some means, most frequently by a distillation from strongly acid solution, where all but the most tightly bound metal complexes are dis sociated to release hydrogen cyanide which is then absorbed in alkaline solution.
The recommended sampling and analytical method for the cyanides covered by this document is essentially that of the standard NIOSH method for cyanide in air as published in the NIOSH Manual of Analytical Methods. [232] should be followed.
High ventilation rate systems for the rapid dilution or removal of HCN gas and aerosols may be useful in some areas.
Control of the hazard of potential release of hydrogen cyanide from cyanide salts requires constant care and attention to good work practices.
The cyanide salts should be kept well apart from, and protected from contact with, acids, moisture, or elevated concentrations of carbon dioxide.
[
# Basis for Recommended Environmental Standard
Cyanide is well known as an acute, fast acting poison which can be described as insidious in that its toxic action at high concentrations is so rapid that its odor has no value as a warning.
[2] At lower concentrations the sense of smell may provide forewarning. For HCN, the primary routes of entry from occupational exposure are inhalation and absorption through the skin.
[ It appears to be generally accepted that HCN and cyanide salts act by the same mechanism, namely, the release of the cyanide ion, which inhibits cytochrome oxidase and results in histotoxic anoxia. [107] Thus, it may be presumed by analogy that if 90 ppm of HCN is fatal, 96 mg/cu m of CN, derived from cyanide salts, may be also. Extending this analogy to threshold levels, presumably 11 mg/cu m of CN would be equivalent to the current Federal standard of 10 ppm of HCN and restriction of exposures to 11 mg/cu m of CN would protect against acute toxicity from cyanide salts.
However, taking into account the irritant effects observed from exposure to cyanide salts, [90,91] the current Federal standard of 5 mg/cu m of CN as an 8-hour time-weighted average appears to be too high in that it allows substantial excesses above that concentration for short periods of time.
Therefore, NIOSH recommends that the current value of 5 mg/cu m of CN be retained, but that its basis be changed from an 8-hour time-weighted average to a 10-minute ceiling. This action should provide the employee with adequate protection from the systemic effects of cyanide and prevent the erosional effects produced by the alkalinity associated with the cyanide salts.
A review of the cases involving exposure to cyanide reveals that they fall into three general categories. First are those cases in which there was an acute or subacute exposure followed immediately by an acute illness. [11,13,20,26,27 ppm. They also stated that it was difficult to give reliable limits for normal levels of cyanide and thiocyanate in the urine. However, in order to assess the hazards of occupational exposure, they considered it safe to state that nonsmokers who have greater than 400 #ig/100 ml of free thiocyanate in the urine, or smokers with urinary concentrations exceeding It is recognized that many workers are exposed to cyanides in concentrations considerably below the recommended occupational limits.
Under these conditions, it should not be necessary to comply with many of the provisions of the recommended standards. However, concern for worker health and well-being requires that protective measures be instituted below the enforceable limits to ensure that exposures do not exceed the standard.
Is given the super.vi sion necessary to assure that all safety tP'lii p r ;} r f \ c p c rn f-»V. I (7) is instructed to shower before removing any respirator or gas-tight suit if prior contact with HCN liquid has occurred or is suspected; (preferably sight contact) in a safe area or at a distance so as not to be affected by an emergency situation at the site of the first employee. The second employee ("buddy") should be alert and equipped to summon help and render aid, if needed.
The employee should carefully and precisely follow all operational procedures specified for the handling of HCN in containers, transfer operations, or other equipment. Suppliers' and manufacturers' instructions should be carefully followed.
[2]
When HCN is used for fumigation purposes, the space should be sealed to prevent the gas from leaking into surrounding spaces or areas. Warning signs should be posted and guards placed to keep unauthorized persons at a safe distance. All laws, regulations, ordinances, and codes applicable should be followed. Only licensed fumigators should do Such work. [246] Open containers of any solid cyanide salts or of solutions of cyanide salts should be limited to those necessary for operational requirements and procedures. Such open containers must be used only in adequately ventilated spaces so that the recommended standards for the airborne concentration of cyanide are not exceeded. Good practice dictates that, in so far as practical, covers be provided for such containers and used whenever possible.
Solutions of cyanides should be maintained as basic as practical to prevent any evolution of hydrogen cyanide. When weakly basic or neutral solutions are used, ventilation must be provided sufficient to prevent accumulation of the HCN evolved from exceeding the recommended standard for HCN in the work room air. When the addition of an acid to a cyanide solution may be necessary, the process should be fully enclosed and ventilated.
Respiratory protection should be provided for all workers potentially exposed to any release of hydrogen cyanide.
Fused salt baths containing cyanide salts should be provided with local exhaust ventilation. Care should be exercised in the operation of such baths to avoid spills and splashes. Addition of salts should be made carefully, using a shovel or special tool. The area about the bath should be regularly cleaned to prevent accumulation and encrustation of cyanide salts on adjacent areas. Workers at fused salt baths should wear safety goggles with side shields.
Local exhaust ventilation must be used for all operations emitting dusts or mists of cyanide salts. [80,232] Tanks and other equipment which must be entered for inspection, maintenance or repair, should be drained as completely as possible and then filled with water and agitated. After 15 minutes, they should be drained again and refilled for another 15 minutes, then drained again. The tanks should then be inspected for residue and encrustation of cyanides. These should be broken loose mechanically or by the force of a water stream and flushed away.
The tank should then be purged with fresh air, followed by testing for the absence of cyanide in the air before anyone enters. Cyanide waste solutions and cyanide-contaminated rinse or wash waters should be treated to destroy the cyanide before being discarded.
Treatment of cyanide waste is achieved by oxidation of the cyanide in alkaline solution by addition of chlorine or other oxidizing agents.
[
# IN AIR AND CALIBRATION
The same sampling and analytical methods are used for atmospheric hydrogen cyanide and the particulate cyanides. They can be collected and analyzed separately or by insertion of a filter can be simultaneously collected and individually analyzed. A sampling period of about 10 minutes is necessary to provide an amount of cyanide readily amenable to analysis by the cyanide selective electrode.
# Sampling
All glassware is washed in detergent solution, rinsed in tap water, and then rinsed with distilled or deionized water. Ten ml of an absorbing solution (0.1 M NaOH) is poured into an all-glass midget impinger using a graduated cylinder to measure the volume.
The fritted inlet of the impinger should have a porosity approximately equal to that of Corning EC (170-220 micron maximum pore diameter). A membrane prefilter (0.45 / u r n pore size) should be inserted (by means of an in-line cassette or similar device) before the impinger when sampling for particulate cyanides is to be performed.
Sampling for HCN and/or the particulate cyanides is performed for at least 10 minutes at a rate of 2 liters/minute, but the total volume of air sampled should not exceed 200 liters. A personal sampling pump or other satisfactory source of suction may be used for sampling provided it is calibrated as outlined below. Alternate sampling systems may be used, providing the required volume of air is sampled from the breathing zone of the worker.
Certain cyanide compounds, especially calcium cyanide, may hydrolyze at sufficiently high relative humidities, resulting in losses of collected sample as HCN gas. In such cases, it may be advisable to minimize losses by keeping the sampling time as short as possible, then storing it in a refrigerator until analysis.
It should be noted that when sampling for HCN without a prefilter, particulates will pass through the midget impinger. Likewise, when sampling for particulate cyanides by means of a midget impinger without a prefilter, HCN gas will also be collected and will constitute a positive interference.
# Calibration
Since the accuracy of an analysis can be no greater than the accuracy of measurement of the volume of air sampled, the accurate calibration of a sampling device is essential to the correct interpretation of an instrument's indication. The frequency of calibration is dependent upon the use, care, and handling to which the pump is subjected. Pumps should be calibrated if they have been subjected to misuse or if they have just been repaired or received from a manufacturer. If the pump receives hard usage, more frequent calibration may be necessary.
Ordinarily, pumps should be calibrated in the laboratory both before they are used in the field and after they have been used to collect a large number of field samples. The accuracy of calibration is dependent on the type of instrument used as a reference. The choice of calibration instrument will depend largely upon where the calibration is to be performed. For laboratory testing, a soapbubble flow meter or wet-test meter is recommended, although other standard calibrating instruments, such as a spirometer or dry-gas meter, can be used. The actual setup will be connected in sequence to the filter cassette or fritted impinger unit which will be followed by the sampler pump.
In this way, the calibration instrument will be at atmospheric pressure. If the personal sampler pump is used, each pump must be calibrated separately. If the buret is used, it should be set up so that the flow is toward the narrow end of the unit.
Care must be exercised in the assembly procedure to ensure that seals at the joints are airtight and that the length of connecting tubing is kept to a minimum. Calibration should be performed under the same conditions of pressure and temperature as those encountered in use. The calibrated pump rotameter should be used to set the flow rate in the field. Samples are analyzed using the cyanide ion selective electrode.
# Range and Sensitivity
The ultimate range and sensitivity of the method have not been established at this time. The recommended range of the method is 0.013-13 mg/cu m in air (approximately 0.0117-11.7 ppm of HCN).
# Interference
Sulfide ion irreversibly poisons the cyanide ion selective electrode and must be removed if found in the sample. Check for the presence of sulfide ion by touching a drop of sample to a piece of lead acetate paper.
The presence of sulfide is indicated by discoloration of the paper.
Sulfide is removed by the addition of a small amount (spatula tip) of powdered cadmium carbonate to the sample at pH 11-13. Swirl to disperse the solid, and recheck the liquid by again touching a drop to a piece of lead acetate paper. If sulfide ion has not been removed completely, add more cadmium carbonate. Avoid a large excess of cadmium carbonate and long contact time with the solution.
# METHOD FOR ANALYSIS OF CYANIDE SAMPLES
When a drop of liquid no longer discolors a strip of lead acetate paper, remove the solid by filtering the sample through a small plug of glass wool and proceed with the analysis.
# Precision and Accuracy
The precision and accuracy of this method have not been completely determined at this time. No collaborative tests have been performed on this method.
# Apparatus (a) Sampling and Calibration Equipment
(1) A filter unit (if needed) consisting of the filter media and cassette filter holder.
(2) A midget fritted impinger containing the absorbing solution or reagent.
(3) A pump suitable for delivering desired flow rates.
The sampling pump is protected from splashover or water condensation by an absorption tube loosely packed with a plug of glass wool and inserted between the exit arm of the impinger and the pump.
(A) An integrating volume meter such as a dry-gas or wet test meter.
(5) Thermometer ( 6) Manometer
# (f)
Precision and repeatability must be plus or minus 2% of full scale.
(g) It is desirable that the instrument respond only to HCN, but instruments which respond to other gases not normally present in the atmosphere may be acceptable.
In general, it is probable that any gas which causes a reading sufficiently high to set off the alarm will itself be present at a concentration sufficiently high to warrant corrective actions. Whenever there is a possibility that gases or vapors such as hydrogen chloride, chlorine, etc, may be present, it would be desirable to determine the response of the instrument to such gases in advance.
(h) An operating range of 0-100 ppm HCN is optimal, but other ranges may be selected to suit individual needs.
(i) The device should be capable of 7 days of continuous unattended operation.
# (j)
The device and alarm should be intrinsically safe for use in hazardous locations.
# Discussion
The principal requirements for such monitors in addition to responding to HCN gas are that they be sufficiently rugged to withstand normal extremes of temperature, pressure, vibration, etc, and not be susceptible to plugging or interferences due to contaminants likely to be encountered in most work places. They should be so constructed that it is possible to quickly check the zero setting of the instrument and the response at 25 ppm in a rapid routine manner. Chemical substances should be listed according to their complete name derived from a recognized system of nomenclature. Where possible, avoid using common names and general class names such as "aromatic amine,"
"safety solvent," or "aliphatic hydrocarbon" when the specific name is known.
The "%" may be the approximate percentage by weight or volume (indicate basis) which each hazardous ingredient of the mixture bears to the whole mixture. This may be indicated as a range or maximum amount, ie, "10-40% vol" or "10% max wt" to avoid disclosure of trade secrets.
# 168
# IX S P E C IA L PREC A U TIO N S P R E C A U T I O N A R Y S T A T E M E N T S O T H E R H A N D L I N G A N O S T O R A G E R E Q U I R E M E N T S P R E P A R E D B Y A O O R E S S O A T E
# XIII. APPENDIX V
First Aid and Treatment Kits Two physician's treatment kits should be immediately available to trained medical personnel at each plant where there is a potential for the release of, accidental or otherwise, or for contact with, hydrogen cyanide or cyanide salts. One kit should be portable in order that it may be carried by medical personnel while accompanying a patient to the hospital.
The other kit should be kept under lock and key to assure that it is intact and available when and if needed. The key should be readily available at all times to the work supervisor on duty and the storage place should be of such construction as to allow accessibility in the event of loss of the key.
Both kits for use by the medical personnel servicing each firm should contain the following as a minimum.
(1) Two (2) boxes (2 dozen) ampules; each ampule containing 0.3 ml of amyl nitrite.
(2) Two (2) ampules of sterile sodium nitrite solution (10 ml of a 3% solution in each).
(3) Two (2) ampules of sterile sodium thiosulfate solution (50 ml of a 25% solution in each).
(4) 2 sterile 10-ml syringe with intravenous needles.
(5) 1 sterile 50-ml syringe with intravenous needle.
(6) 1 tourniquet (7) 1 gastric tube (rubber).
(8) 1 non-sterile 100 ml syringe.
The medical personnel servicing a firm where there is a potential for hydrogen cyanide release or a potential for exposure to inorganic cyanide should be familiarized with the use of these kits.
First-aid kits should be immediately available at work places where there is a potential for the release, accidental or otherwise, of hydrogen cyanide or a potential for exposure to inorganic cyanide. This kit should contain as a minimum two (2) boxes of ampules ( 2 dozen), each containing 0.3 ml of amyl nitrite. Ampules should be replaced biannually or sooner if needed to ensure their potency.
The amyl nitrite ampules should be protected from high temperatures. In all cases, the contents of the medical and first-aid kits should be replaced before the manufacturer's assigned expiration dates.
First-Aid Procedure Speed in the rendering of first-aid treatment is of the utmost importance. The patient should be removed at once to an area free from HCN. The rescuer should wear respiratory protective equipment in order not to be overcome or weakened by the gas.
Many victims will have stopped breathing.
In this case, it is imperative that efforts at resuscitation be instituted at once and continued without interruption even while other treatment is being administered.
A physician should be summoned immediately.
First-aid kits should be readily available at all times. They should be quickly accessible but should not be kept only in operating areas mixtures with air may be explosive if a source of ignition is present.
# (B) Resuscitation
Before instituting artificial resuscitation, dentures and foreign objects, such as gum and tobacco, and any accumulated oropharyngeal fluids (saliva, etc) should be removed from the patient's mouth and pharynx and the tongue pulled forward.
If the patient's breathing is weak or has stopped, artificial resuscitation should be started at the earliest possible moment and continued without interruption until normal breathing has been established or the patient is pronounced dead.
Mouth-to-mouth resuscitation is the method of choice because of its simplicity and effectiveness. It is, however, impossible to administer amyl nitrite while using this method. Therefore, it is advisable to switch to other methods of artificial respiration, such as the Holger-Nielsen arm-lift back pressure method, during the periods when the amyl nitrite is being given.
If a mechanical resuscitator and personnel skilled in its use are available, this equipment may be used instead of other forms of resuscitation.
(C) The patient should be kept comfortably warm but not hot. Other drugs and stimulants are rarely necessary and should be administered only by a physician or trained medical personnel under the direction of a physician. Step -Through the formation of a relatively stable coordination complex with ferric iron, cyanide tends to keep this metal in its higher oxidation state and thus reduces its efficacy as an electron carrier in ferric to ferrous iron transitions.
By such a complexation of iron, the respiratory enzyme ferricytochrome oxidase is changed to ferricytochrome oxidasecyanide and its ability to catalyze the reaction of reduced cytochrome with oxygen is inhibited, with consequent impairment of cellular oxygen utilization
Step -Since numerous metabolic pathways converge at the cytochrome system, the impairment of the cells' ability to utilize oxygen reduces or even stops aerobic metabolism. True histotoxic (cytotoxic) hypoxia results with a shift to anaerobic metabolism with accumulation of lactate, pyruvate, and glucose.
Step -The cells are thus unable to use the oxygen brought to them as 02Hb by the arterial blood. The oxyhemoglobin continues into the veins, the arteriovenous oxygen difference diminishes, and the venous blood is almost as bright a red as the arterial blood.
Step 4 -The chemoreceptors in the carotid and aortic bodies, which are the tissues most sensitive to cellular hypoxia, trigger an inspiratory gasp and hyperpnea as an almost instantaneous path ophysiologic effect of cyanide absorption.
#
Current concepts about the treatment of selected poisonings-nitrite, cyanide, sulfide, barium, and quinidine. Ann Rev Pharmacol Toxicol 16:189 -199, 1976 109.
Carmelo, S: [New contributions to the study of subacute-chronic hydrocyanic acid intoxication in man.] Rass Med Ind 24: 254-71, 1955 (Ita) 110.
El Ghawabi SH, Gaafar MA, El-Saharti AA, Ahmed SH, Malash KK, Fanes R: Chronic cyanide exposure: a clinical, radioisotope, and laboratory study. Br J Ind Med 32: 1975 111.
Wollman SH: Nature of the inhibition by thiocyanate of the iodide concentrating mechanism of the thyroid gland. Amer J Physiol 186: [453][454][455][456][457][458][459]1956 112.
Heymans JF, Masoin P:
[The diachronic toxicity of some cyanogen compounds.] Arch Int Pharmacodyn Ther 7:297-306, 1900 (Fre) After sampling, the fritted impinger stem can be removed and cleaned in the following manner. Tap the stem gently against the inside wall of the impinger bottle to recover as much of the sampling solution as possible. Wash the stem with a small amount (1-2 ml) of unused absorbing solution and add the wash to the impinger bottle. Then the impinger bottle is sealed with a hard, non-reactive stopper (preferably Teflon) and an appropriate identifying number attached to it. Do not seal with rubber.
The stoppers on the impinger bottle should be tightly sealed to prevent leakage during shipping. If it is preferred to ship the fritted impingers with the stems in, the outlets of the stem should be sealed with Parafilm or other nonrubber covers, and the ground glass joints should be sealed, ie, taped to secure the top tightly. Upon completion of sampling for the particulate cyanides, plastic caps should be replaced on the inlet and outlet tubes of the cassette and an appropriate identifying number attached to it.
Care should be taken to minimize spillage or loss by evaporation at all times. Refrigerate samples if analysis cannot be done within a day. Whenever possible, hand delivery of the samples is recommended. Otherwise, special impinger shipping cases should be used to ship the samples.
A "blank" fritted impinger should be handled as the other samples (fill, seal, and transport) except that no air is sampled through this fritted impinger.
Where a prefilter has been used for the collection of particulate cyanides, the filter cassettes are capped and placed in an appropriate cassette shipping container. One filter disc should be handled like the other samples (seal and transport) except that no air is sampled through it, and this is labeled as a blank.
# M A TERIA L SAFETY DATA SHEET 1 PRO D U CT IDENTIFICATIO N M A N U F A C T U R E R 'S N A M E R E G U L A R T E L E P H O N E N O . E M E R G E N C Y T E L E P H O N E N O A D O R E S S
# TRADE N AM E S Y N O N Y M S II H A ZA R D O U S IN G R E D IE N T S M A T E R I A L O R C O M P O N E N T % H A Z A R D D A T A
# III P H Y SIC A L DATA
# O L E V A P O R A T I O N R A T E ( B U T Y L A C E T A T E M ) A P P E A R A N C E A N O O D O R
where they may not be available in case of a spill.
( (3) Inhalation (A) Administer amyl nitrite A pearl (ampule), if not provided with a fabric sleeve, should be wrapped lightly in a handkerchief or gauze pad, broken, and held about 1 inch from the patient's mouth and nostrils for 15 seconds.
Repeat 5 times at 15-second intervals. Use a fresh pearl every 5 minutes until 3 or 4 pearls have been administered.
# WARNING:
First-aiders should keep the pearls away from their own mouths and noses lest they become weak and dizzy and unable to give proper assistance to the victim. Amyl nitrite is flammable and | None | None |
2857d4af0e0aa874619ed7388b63c2d27aae9b29 | cdc | None | On December 13, 2007, certain lots of Haemophilus influenzae type b (Hib) vaccine marketed as PedvaxHIB (monovalent Hib vaccine) and Comvax (Hib-HepB vaccine), and manufactured by Merck & Co., Inc., were recalled voluntarily, and the company temporarily suspended production of these vaccines. To conserve the limited supply of Hib-containing vaccines, CDC, in consultation with the Advisory Committee on Immunization Practices (ACIP), the American Academy of Family Physicians (AAFP), and the American Academy of Pediatrics (AAP), on December 18, 2007, recommended that vaccination providers temporarily defer the routine Hib vaccine booster dose administered to most healthy children at age 12--15 months (1--5). Production of Merck Hib vaccine products is still suspended. However, two other Hib-containing vaccines manufactured by Sanofi Pasteur have been available for use in the United States during this shortage: monovalent Hib vaccine (ActHIB) and DTaP-IPV/Hib (Pentacel). Beginning in July 2009, the manufacturer of these two vaccines will increase the number of doses of these two products available for use in the United States, which will result in the supply being sufficient to reinstate the Hib vaccine booster dose.# Reinstatement of Hib Booster Dose
Effective immediately, CDC, in consultation with ACIP, AAFP, and AAP, is recommending reinstatement of the booster dose of Hib vaccine for children aged 12--15 months who have completed the primary 3-dose series. Infants should continue to receive the primary Hib vaccine series at ages 2, 4, and 6 months. Children aged 12--15 months should receive the booster dose on time. Older children for whom the booster dose was deferred should receive their Hib booster dose at the next routinely scheduled visit or medical encounter. Although supply is sufficient to reinstate the booster dose and begin catch-up vaccination, supply is not yet ample enough to support a mass notification process to contact all children with deferred Hib booster doses. Sufficient vaccine will be available to administer the primary series at ages 2, 4, and 6 months and a booster dose on time to children aged 12--15 months. As part of delivering the booster dose to those children for whom it was deferred at the next routinely scheduled appointment or medical encounter, practices should discuss with parents the reasons for the change in recommendation and might consider 1) reviewing electronic or paper medical records or immunization information system records to identify children in need of a booster dose before physician encounters, 2) evaluating children's vaccination status during their scheduled visit, and 3) sharing immunization schedules with parents to make them aware of this plan.
# Use of Combination Vaccines | On December 13, 2007, certain lots of Haemophilus influenzae type b (Hib) vaccine marketed as PedvaxHIB (monovalent Hib vaccine) and Comvax (Hib-HepB vaccine), and manufactured by Merck & Co., Inc., were recalled voluntarily, and the company temporarily suspended production of these vaccines. To conserve the limited supply of Hib-containing vaccines, CDC, in consultation with the Advisory Committee on Immunization Practices (ACIP), the American Academy of Family Physicians (AAFP), and the American Academy of Pediatrics (AAP), on December 18, 2007, recommended that vaccination providers temporarily defer the routine Hib vaccine booster dose administered to most healthy children at age 12--15 months (1--5). Production of Merck Hib vaccine products is still suspended. However, two other Hib-containing vaccines manufactured by Sanofi Pasteur have been available for use in the United States during this shortage: monovalent Hib vaccine (ActHIB) and DTaP-IPV/Hib (Pentacel). Beginning in July 2009, the manufacturer of these two vaccines will increase the number of doses of these two products available for use in the United States, which will result in the supply being sufficient to reinstate the Hib vaccine booster dose.# Reinstatement of Hib Booster Dose
Effective immediately, CDC, in consultation with ACIP, AAFP, and AAP, is recommending reinstatement of the booster dose of Hib vaccine for children aged 12--15 months who have completed the primary 3-dose series. Infants should continue to receive the primary Hib vaccine series at ages 2, 4, and 6 months. Children aged 12--15 months should receive the booster dose on time. Older children for whom the booster dose was deferred should receive their Hib booster dose at the next routinely scheduled visit or medical encounter. Although supply is sufficient to reinstate the booster dose and begin catch-up vaccination, supply is not yet ample enough to support a mass notification process to contact all children with deferred Hib booster doses. Sufficient vaccine will be available to administer the primary series at ages 2, 4, and 6 months and a booster dose on time to children aged 12--15 months. As part of delivering the booster dose to those children for whom it was deferred at the next routinely scheduled appointment or medical encounter, practices should discuss with parents the reasons for the change in recommendation and might consider 1) reviewing electronic or paper medical records or immunization information system records to identify children in need of a booster dose before physician encounters, 2) evaluating children's vaccination status during their scheduled visit, and 3) sharing immunization schedules with parents to make them aware of this plan.
# Use of Combination Vaccines
| None | None |
70b97abad68805443af28746c6871cf26b7c9cd4 | cdc | None | depar depar depar depar department of health and human ser tment of health and human ser tment of health and human ser tment of health and human ser tment of health and human services vices vices vices vices# Background
In the United States, the incidence and mortality from cutaneous malignant melanoma (CMM) have increased rapidly in the last few decades (1,2). In 2003, approximately 54,200 persons will have new diagnoses of melanoma, and 7,600 will die from the disease (3). The incidence of the other two skin cancers, basal cell carcinoma (BCC) and squamous cell carcinoma (SCC), is estimated to be >1 million new cases per year (3). According to the data from the Surveillance, Epidemiology and End Results (SEER) cancer registry of the National Cancer Institute, during 1995-1999, average annual age-adjusted incidence rates for melanoma per 100,000 population were 23.5 for men and 15.7 for women for non-Hispanic whites; 3.8 for men and 3.7 for women for Hispanics; 1.8 for men and 1.3 for women for Asians; 1.5 for men and 0.9 for Ameri-
# Introduction
The Task Force on Community Preventive Services (the Task Force) is developing the Guide to Community Preventive Services (the Community Guide), a resource that will include multiple systematic reviews, each focusing on a preventive health topic. The Community Guide is being developed with the support of the U.S. Department of Health and Human Services (DHHS) in collaboration with public and private partners. Although CDC provides staff support to the Task Force for development of the Community Guide, the recommendations presented in this report were developed by the Task Force and are not necessarily the recommendations of DHHS or CDC. This report is one in a series of topics included in the Community Guide. It provides an overview of the process used by the Task Force to select and review evidence and summarize its recommendations regarding interventions to reduce UV exposure and increase UV protective behaviors for prevention of skin cancer. A full report on the recommendations, additional evidence (i.e., discussions of applicability, additional benefits, potential harms, existing barriers to implementation, costs, cost benefit, and cost effectiveness of the interventions ), and remaining research questions will be published in the American Journal of Preventive Medicine.
Community Guide topics are prepared and released as each is completed. The findings from systematic reviews on vaccinepreventable diseases, tobacco use prevention and reduction, motor vehicle occupant injury, physical activity, diabetes, oral health, and the effects of the social environment on health have already been published. A compilation of systematic reviews will be published in book form. Additional information regarding the Task Force and the Community Guide and a list of published articles are available on the Internet at http:/ /www.thecommunityguide.org.
# Methods
The methods used by the Community Guide for conducting systematic reviews and linking evidence to recommendations have been described elsewhere (20). In brief, for each Community Guide topic, a multidisciplinary team (the systematic review development team) conducts a review consisting of the following steps:
- developing an approach to organizing, grouping, and selecting the interventions; - systematically searching for and retrieving evidence;
- assessing the quality of and summarizing the strength of the body of evidence of effectiveness; - assessing cost and cost effectiveness evidence, identifying applicability and barriers to implementation (if the effectiveness of the intervention has been established); - summarizing information regarding other evidence; and - identifying and summarizing research gaps. For each review of interventions regarding skin cancer prevention, the systematic review development team developed a conceptual model (or analytic framework) to show the relationship of the intervention to relevant intermediate outcomes (e.g., knowledge, attitudes and beliefs, and intentions regarding sun-protective behaviors), to implementing key sunprotective behaviors, and to the assumed relationships of improvements in sun-protective behaviors to skin cancer prevention. A representative example of an analytic framework for mass media interventions is illustrated (Figure). The analytic frameworks for the other interventions were similar to this example except that they included environmental and policy components.
The analytic frameworks focused on key health outcomes (e.g., sunburn or nevi*) and sun-protective behaviors:
- avoiding peak sun; -seeking shade, and -avoiding the sun during peak UV hours. - covering up; -wearing a hat, -wearing a long-sleeved shirt, and -wearing pants.
- sunscreen use. The team also examined intermediate outcomes that were postulated to be associated with sun-protective behaviors (e.g., knowledge, attitudes, and intentions). Recommendations were based either on better health outcomes (rare with this subject matter because relevant cancer outcomes would become apparent long after the time of the intervention) or risk behaviors that were thought to be established proxies for cancer outcomes (in this case, avoiding peak UV hours or covering up).
The team considered sunscreen use to be a key secondary outcome of sun protection programs because sunscreens prevent sunburn (a marker of unprotected UV exposure and a health outcome associated with increased risk of skin cancer in epidemiologic studies) and reduce the incidence of SCC, and better alternatives are not always available (e.g., when swimming). Sunscreen's role in preventing skin cancer has been demonstrated to be complex, according to information in recent reports from national and international groups (18,21) and summarized in the last section of this report.
Epidemiologic studies suggest that sunscreen use could be considered harmful if it increased a person's total time in the sun and total UV exposure. Partly for that reason, suncreen use alone might not protect against melanoma despite its protective effect on SCC. The International Agency for Research on Cancer (IARC) recommends that sunscreens not be used as the sole method for skin cancer prevention and not be used as a means to extend the duration of UV exposure (21). The team therefore did not consider sunscreen use, by itself, to be an established proxy for better health. - Nevi are lesions of pigment-forming skin cells that can be a risk factor for melanoma.
# Intervention
# FIGURE. Analytic framework for media interventions to reduce ultraviolet (UV) exposure and increase sun-protective behaviors.
Major stratification variables were type of media (e.g., small media versus large media ); characteristics of target population (e.g., age, sex, skin color, skin type, baseline risk, socioeconomic status, sunburn incidence, occupation); intervention intensity (i.e., comparison, some intervention, high level of intervention); geographic or environmental characteristics (e.g., urban, rural, climate of location ); intervention characteristics (e.g., size, access to media).
# MMWR October 17, 2003
The coordination team, † which conducted the systematic review, and their consultants § generated a comprehensive list of interventions to reduce skin cancer. From this, a priority list of interventions for review was developed through a process of polling the coordination team, the consultants, and other specialists in the field regarding their perception of the public health importance (number of persons affected), the practicality of application, and the need of those promoting UV protective behaviors for information regarding each intervention.
To conduct the review, the team organized interventions into three groups: setting-specific, target population-specific, and communitywide (Table ). Setting was used as an organizing structure because it was a convenient proxy for key characteristics of the target populations and the implementers of the interventions. The majority of the interventions in this group involved diverse activities -provision of information, environmental approaches (e.g., planting shade trees), or policy approaches (e.g., implementing a policy to reschedule outdoor activities or a requirement to wear hats when outside). Interventions in the setting-specific group consisted of educational and policy approaches in the following settings:
- child care centers, - primary schools,
- secondary schools and colleges,
- recreational or tourism settings,
- occupational settings, and - health-care settings and for health-care providers.
The target population of interest category included one intervention: children's parents or caregivers (some of these interventions might have already been examined in settingspecific groups).
The category of communitywide interventions included two types of interventions and a subgroup:
- media campaigns alone, and - communitywide multicomponent interventions that include at least two interventions in an integrated manner. (Comprehensive communitywide programs, a subset of communitywide multicomponent interventions, include interventions at several levels and last longer than 1 year.) Interventions reviewed were either single component (i.e., using only one activity to achieve desired outcomes) or multicomponent (i.e., using more than one activity, such as a policy or environmental intervention with a media campaign). Certain studies provided results relevant to more than one intervention and were included in each of the reviews to which they were applicable. Studies and outcome measures were classified according to definitions developed as part of the review process. The nomenclature used in this report sometimes differs from that used in the original studies.
To be included in the reviews of effectiveness, studies had to 1) be primary investigations of interventions selected for evaluation rather than, for example, guidelines or reviews; 2) be published in English during the years 1966-2000; 3) be conducted in established market economies ¶ ; and 4) compare outcomes among groups of persons exposed to the intervention with outcomes among groups of persons not exposed or less exposed to the intervention (i.e., the study design included a concurrent or before-and-after comparison.) ¶ Searches of three computerized databases (MEDLINE, PsychINFO, CINAHL) were conducted. Team members also reviewed reference lists and consulted with other specialists in the field (e.g., participants in a skin cancer prevention listserv) to identify relevant studies. Each included study was evaluated by using a standardized abstraction form and was assessed for suitability of the study design and threats to validity (22). Studies were characterized as having good, fair, or limited execution based on the number of threats to validity (20).
Results for each outcome of interest were obtained from each study that met the minimum quality criteria. Net effects were derived when appropriate by calculating the difference between the changes observed in the intervention and comparison groups relative to the respective baseline levels. † † The median was used to summarize a typical measure of effect across the body of evidence for each outcome of interest; both the median and the range are reported. For bodies of evidence consisting of four or more studies, an interquartile range was used to represent variability.
The strength of the body of evidence of effectiveness was characterized as strong, sufficient, or insufficient on the basis of the number of available studies, the suitability of study designs for evaluating effectiveness, the quality of execution of the studies as defined by the Community Guide (20), the consistency of the results, and the effect size.
The Task Force uses these systematic reviews to evaluate the evidence of intervention effectiveness and makes recommendations based on the findings of the reviews (20). The strength of each recommendation is based on the evidence of effectiveness (i.e., an intervention is recommended on the basis of either strong or sufficient evidence of effectiveness) (20). Other types of evidence can also affect a recommendation. For example, harms resulting from an intervention that outweigh benefits might lead to a recommendation that the intervention not be used even if it is effective in improving some outcomes.
A finding of insufficient evidence to determine effectiveness should not be interpreted as evidence of ineffectiveness. Insufficient evidence may be found for any of a number of reasons, alone or in combination, including an insufficient number of studies; too many threats to the validity of the available studies based on their design, execution, or both; conflicts in the results of the studies that preclude a coherent summary of effectiveness; or no indication that the outcomes measured to date, by themselves, represent success in improving health. In all these situations, a finding of insufficient evidence to determine effectiveness is important for identifying areas of uncertainty and continuing research needs. In contrast, sufficient or strong evidence of ineffectiveness would lead to a recommendation against use of the intervention.
# Results
Database searches and bibliographic reviews yielded a list of 6,373 potentially relevant titles. After review of the abstracts and consultation with specialists in the field, a total of 313 reports were retrieved. Of these, 154 were not used in the review because they did not provide results, did not refer to an intervention, or reported on noncomparative studies. The remaining 159 were retained for full review. On the basis of limitations in execution or design or because they provided only background information on studies that were already included, 74 of these were excluded and were not considered further. The remaining 85 studies were considered qualifying studies. The Task Force recommendations in this report are based on the systematic review and evaluation of these qualifying studies, all of which had good or fair quality of execution.
The Task Force recommended two interventions, both in the setting-specific category (Table ):
- educational and policy approaches in primary schoolschanging children's covering-up behavior (wearing protective clothing); and - educational and policy approaches in recreational or tourism settings -changing adults' covering-up behaviors. Interventions in primary school settings were designed to increase sun-protective knowledge, attitudes, intentions, and behavior among children from kindergarten through eighth grade. The interventions ranged from a curriculum that included interactive classroom and take-home activities to staff education, brochures for parents, and a working session to develop skin protection plans for schools. All interventions focused on some combination of increasing application of sunscreen, scheduling activities to avoid peak sun hours, increasing availability of shade and encouraging children to play in shady areas, and encouraging children to wear sunprotective clothing. Interventions in this category included at least one of the following activities:
- provision of information to children (e.g., instruction or small media or both); - additional activities to influence children's behavior (e.g., modeling, demonstration, role playing); - activities intended to change the knowledge, attitudes, or behavior of caregivers (i.e., teachers or parents); or - environmental or policy approaches (e.g., provision of sunscreen, provision of shade, or scheduling outdoor activities to avoid hours of peak sunlight). Single-and multicomponent interventions in recreational settings were designed to increase knowledge; influence attitudes, beliefs, and intentions; and change behavior of adults and children. Interventions included one or more of the following: educational brochures, including culturally relevant materials and photographs of skin cancer lesions; sun-safety training for lifeguards, aquatic instructors, and outdoor recreation staff and role-modeling by these groups; sun-safety lessons, interactive activities, and incentives for parents and children; increasing available shaded areas; providing sunscreen; and point-of-purchase prompts.
The recommended interventions had small to moderate behavior change scores. In primary schools, the median net relative increase was 25% (interquartile range: 1%-40%, six studies). In recreational settings, the median net relative increase was 11.2% (interquartile range: 5.1%-12.9%, five studies).
It should be noted that the interventions were targeted to populations rather than single persons. Small changes in behavior in large populations can result in substantial public health benefits.
The Task Force found insufficient evidence on which to make recommendations for or against the following interventions: educational and policy approaches in child care centers; educational and policy approaches in secondary schools and colleges; educational and policy approaches in recreational or tourism settings for children; educational and policy approaches in occupational settings; interventions oriented to health-care settings and providers; interventions oriented to children's parents or caregivers; media campaigns alone; and communitywide multicomponent interventions (Table ). The finding of insufficient evidence to determine effectiveness was most often based on the limited numbers of studies that measured behavioral or health outcomes, inconsistent evidence among studies that measured changes in sun-protective behaviors, and limitations in the design and execution of available studies.
Summary tables of the reviews will be available at http:// www.thecommunityguide.org/cancer when the full evidence is published in a supplement to the American Journal of Preventive Medicine.
# Use of Recommendations in Communities and Health-Care Settings
Malignant melanoma is the deadliest of the skin cancers, and its incidence in the United States has increased rapidly in the past 2 decades. Melanoma accounts for approximately three fourths of all skin cancer deaths. Basal cell and squamous cell skin cancers are seldom fatal but, if advanced, can cause severe disfigurement and morbidity (3). UV exposure in childhood and intense intermittent UV exposures are the major environmental risk factors for melanoma and BCC, and cumulative UV exposure is the major preventable risk factor for SCC (23). National surveys indicate that only one third of Americans practice sun-protective behaviors, and their practices vary greatly, depending on age, sex, and their ability to tan and burn (9,12,13).
The two Task Force recommendations -educational and policy approaches in primary schools, and educational and policy approaches for adults in outdoor recreational or tourism settings -are based on improving covering-up behaviors. These recommendations represent tested interventions that promote decreased UV exposure at the community level. They can be used for planning interventions to promote UV protection or to evaluate existing programs.
Several of the studies reviewed included multiple components that could not be evaluated separately. For example, a school-based program might involve components of policy, such as establishing school guidelines, in tandem with implementation of one-on-one didactic and interactive sessions regarding adapting sun-protective behaviors. Although sunprotective behaviors were increased by school-based programs, the specific effect could not be attributed to one specific intervention characteristic. In selecting and implementing interventions, the potential for an unintended increase in the duration and intensity of UV exposure must be considered. Also, communities should strive to develop comprehensive programs that include a wide range of activities suitable for their local resources, population characteristics, and settings.
The other interventions reviewed, for which evidence was insufficient to determine effectiveness, could also prove useful. They provide a broader taxonomy of interventions that deserve further testing and evaluation, and the documentation of research gaps in these reviews could potentially help to improve the next generation of research. Additional information on research gaps will be provided in the report in the American Journal of Preventive Medicine.
Choosing interventions that are well matched to local needs and capabilities, and then carefully implementing those interventions, are vital steps for increasing UV protection. Several factors can affect the attitudes, ability, and behaviors of a community regarding taking sun safety precautions. Some of the most important are program priorities, location of the community, and population. Establishing skin cancer prevention as a priority might be difficult because skin cancer is but one of many health topics, and for certain communities, may not be as high a priority as other cancers or diseases. Although it might be a higher priority in areas where UV radiation is more intense, even in areas with lower UV intensity, education about UV exposure during times of episodic exposure (e.g., during winter sports, when the sun comes out, and when traveling to higher UV intensity regions) could be helpful. Likewise, although skin cancer prevention might be a higher priority for populations at an increased risk (e.g., light-skinned, sunsensitive), even darker-skinned or less sun-sensitive persons need to take precautions when exposed to UV radiation. To meet local objectives, recommendations and other evidence provided in the Community Guide should be supplemented with local information such as skin cancer incidence, skin cancer mortality, prevalence of sun-protective behaviors, latitude, UV index, resource availability, administrative structures, and economic and social environments of organizations and practitioners.
These reviews by themselves do not provide advice regarding implementation of effective programs; the referenced articles, however, provide additional detail. Implementation advice is also available elsewhere (24)(25)(26)(27)(28).
# Introduction
This statement summarizes the current U.S. Preventive Services Task Force (USPSTF) recommendation on counseling to prevent skin cancer and the supporting scientific evidence, and updates the 1996 recommendation contained in the Guide to Clinical Preventive Services, Second Edition (1). The USPSTF, an independent panel of private sector experts in primary care and prevention, systematically reviews the evidence of effectiveness of a wide range of clinical preventive services, including screening tests, counseling, and chemoprevention. The Task Force grades its recommendations according to one of five classifications (A, B, C, D, I), reflecting the strength of evidence and magnitude of net benefit (benefits minus harms) (Box 1). The USPSTF grades the quality of the overall evidence for a service on a 3-point scale (good, fair, poor) (Box 2).
This recommendation and rationale statement and complete information on which this statement is based, including evidence tables and references, are available at . gov/clinic/uspstfix.htm (2) and in print by subscription through the AHRQ Clearinghouse (1-800-358-9295 or e-mail at [email protected]) and through the National Guideline Clearinghouse ™ at .
# Summary of Recommendation
The U.S. Preventive Services Task Force concludes that the evidence is insufficient to recommend for or against routine counseling by primary care clinicians to prevent skin cancer.
# I recommendation.
The USPSTF found insufficient evidence to determine whether clinician counseling is effective in changing patient behaviors to reduce skin cancer risk. Counseling parents may increase the use of sunscreen for children, but there is little evidence to determine the effects of counseling on other preventive behaviors (such as wearing protective clothing, reducing excessive sun exposure, avoiding sun lamps/tanning beds, or practicing skin self-examination) and little evidence on potential harms.
# Clinical Considerations
- Using sunscreen has been shown to prevent squamous cell skin cancer. The evidence for the effect of sunscreen use in preventing melanoma, however, is mixed. Sunscreens that block both ultraviolet A (UV-A) and ultraviolet B (UV-B) light may be more effective in preventing squamous cell cancer and its precursors than those that block only UV-B light. However, people who use sunscreen alone could increase their risk for melanoma if they increase the time they spend in the sun. - UV exposure increases the risk for skin cancer among people with all skin types, but especially fair-skinned people. Those who sunburn readily and tan poorly, namely those with red or blond hair and fair skin that freckles or burns easily, are at highest risk for developing skin cancer and would benefit most from sun protection behaviors. The incidence of melanoma among whites is 20 times higher than it is among blacks; the incidence of melanoma among whites is approximately four times higher than it is among Hispanics. - Observational studies indicate that intermittent or intense sun exposure is a greater risk factor for melanoma than chronic exposure. These studies support the hypothesis that preventing sunburn, especially in childhood, may reduce the lifetime risk for melanoma. - Other measures for preventing skin cancer include avoiding direct exposure to midday sun (between the hours of 10:00 a.m. and 4:00 p.m.) to reduce exposure to ultraviolet (UV) rays and covering skin exposed to the sun (by wearing protective clothing such as broad-brimmed hats, long-sleeved shirts, long pants, and sunglasses). - The effects of sunlamps and tanning beds on the risk for melanoma are unclear because of limited study design and conflicting results from retrospective studies. - Only a single case-control study of skin self-examination has reported a lower risk for melanoma among patients who reported ever examining their skin over 5 years.
Although results from this study suggest that skin selfexamination may be effective in preventing skin cancer, these results are not definitive.
# Scientific Evidence Epidemiology and Clinical Consequences
Melanoma is a leading cause of cancer death in the United States. The lifetime risk for dying of melanoma is 0.36% in white men and 0.21% in white women (3). Between 1973 and 1995, the age-adjusted incidence of melanoma increased more than 100%, from 5.7 per 100,000 people to 13.3 per 100,000 people. The increase in annual incidence rates is likely due to several factors, including increased sun exposure and possibly earlier detection of melanoma. Although primary prevention efforts have focused on young people, the elderly (especially elderly men) bear a disproportionate burden of morbidity and mortality from melanoma and nonmelanoma skin cancer. Men older than age 65 account for 22% of the newly diagnosed cases of malignant melanoma each year and women in the same age group account for 14%. Basal cell and squa-mous cell carcinomas are more than 10 times as common as melanoma but account for less morbidity and mortality. Squamous cell cancers, however, may account for 20% of all deaths from skin cancer.
# Effectiveness of Available Interventions
Preventive strategies include reducing sun exposure (e.g., by wearing protective clothing and using sunscreen regularly), avoiding sunlamps and tanning equipment, and practicing skin self-examination. There is little direct evidence, however, that any of these interventions reduce skin cancer morbidity or mortality.
# Reducing Sun Exposure
Avoiding direct sunlight by staying indoors or in the shade or by wearing protective clothing is the most effective measure for reducing exposure to ultraviolet light, but there are no randomized trials of sun avoidance to prevent skin cancer. In numerous observational studies, increased sun exposure in childhood and adolescence is associated with increased risk for nonmelanoma skin cancer, which usually occurs in sunexposed areas such as the face.
Recent studies provide a more complex picture of the relationship between sun exposure and melanoma, however. Although melanoma incidence is higher in regions near the equator where ultraviolet exposure is most intense, melanoma often occurs in areas of the body not exposed to the sun. In observational studies, intermittent or intense sun exposure was associated with increased risk for melanoma; chronic exposure was associated with lower risk, as was the ability to tan (4-7).
# Sunlamp and Tanning Bed Avoidance
Six of 19 case-control studies found a positive association between use of sun lamps and melanoma risk, but most did not adjust for recreational sun exposure or for the dosage and timing of sunlamp exposure (8). Among nine studies that examined the duration, frequency, or timing of sunlamp or tanning bed exposure, four found a positive association, particularly if the dose of exposure was high and if it caused burning.
# Sunscreen Use
Daily sunscreen use on the hands and face reduced the total incidence of squamous cell cancer in a randomized trial of 1,621 residents in Australia (rate ratio : 0.61; 95% confidence interval = 0.46-0.81) (9). Sunscreen had no effect on basal cell cancer. Based on this trial, 140 people would need to use sunscreen daily for 4½ years to prevent one case of squamous cell cancer. An earlier randomized trial demonstrated that sunscreen use reduced solar keratoses, precursors of squamous cell cancers (10). There are no direct data about the effect of sunscreen on melanoma incidence. An unblinded randomized trial showed that children at high risk for skin cancers who used sunscreen developed fewer nevi than those who did not. Several epidemiologic studies have found higher risk for melanoma among users of sunscreens than among nonusers (11)(12)(13). A recent meta-analysis of population-based casecontrol studies found no effect of sunscreen use on risk for melanoma (14). The conflicting results may reflect the fact that sunscreen use is more common among fair-skinned people, who are at higher risk for melanoma, than it is among darkerskinned people; or, this finding may reflect the fact that sunscreen use could be harmful if it encourages longer stays in the sun without protecting completely against cancer-causing radiation.
# Skin Self-Examination
The only evidence for the effectiveness of skin self-examination comes from a single case-control study (1,15). After adjustment for other risk factors, skin self-examination was associated with lower incidence of melanoma (odds ratio : 0.66; 95% CI = 0.44-0.99) and lower mortality from melanoma (OR: 0.37; 95% CI = 0.16-0.84), although the definition of "self-examination" was limited. This study did not provide sufficient evidence that skin self-examination would reduce the incidence of melanoma or improve outcomes of melanoma.
# Effectiveness of Counseling
Community and worksite educational interventions have demonstrated effectiveness for increasing the use of skin protection measures, such as wearing hats and long-sleeve shirts and staying in the shade; however, evidence addressing the effectiveness of clinician counseling to prevent skin cancer is extremely limited. Most studies of counseling have examined intermediate outcomes such as knowledge and attitudes rather than changes in behavior. In a recent survey, 60% of pediatricians said that they usually or always counsel patients about skin protection, but advice to use sunscreen is more common than advice about wearing protective clothing or avoiding the midday sun (16).
Simple reminders and instructional materials for clinicians can overcome some of the barriers to regular counseling. A randomized trial of a community-based intervention involving 10 towns in New Hampshire suggests that office-based counseling by physicians may be an effective component of a multimodal program to promote skin protection (17). The proportion of children using some sun protection increased significantly in the intervention towns (from 78% to 87%) compared to a decrease in the control communities (from 85% to 80%). More parents reported receiving some sun protection information from a clinician in the intervention towns. However, most of the change was due to increased sunscreen use rather than to reduced sun exposure.
# Potential Harms of Skin Protection Behaviors
There are limited data regarding potential harms of counseling or of specific skin protection behaviors. Skin cancer counseling that focuses on the use of sunscreen could possibly lead to a false sense of security, which might lead to more time in the sun. For example, a randomized trial with young adults found that those who used sunscreen with a high sun protection factor (SPF) stayed longer in the sun than those who used sunscreen with a lower SPF (18). There has been some concern that use of SPF of 15 results in vitamin D deficiency. However, a randomized trial among people over 40 years of age found that sunscreen use over the summer had no effect on 25-hydroxyvitamin D3 levels. Concerns related to sun avoidance include reduced physical activity levels among children and negative effects on mental health. However, no studies have evaluated the effects of sun protection behaviors on these outcomes.
# Recommendations Of Others
The American Cancer Society (19), the American Academy of Dermatology (20), the American Academy of Pediatrics (21), the American College of Obstetricians and Gynecologists (22), and a National Institutes of Health consensus panel (23) all recommend patient education concerning sun avoidance and sunscreen use. The American Academy of Family Physicians recommends sun protection for all with increased sun exposure (24). The American College of Preventive Medicine (ACPM) concluded that sun-protective measures (e.g., clothing, hats, opaque sunscreens) are probably effective in reducing skin cancer but that the evidence does not support discussion of sunscreen and sun protection with every patient. ACPM concluded that evidence is insufficient to advise patients that chemical sunscreens protect against malignant melanoma and that their use may actually lead to increased risk (25). Recently, the International Agency for Research on Cancer (IARC), part of the World Health Organization, qualified their recommendation for sunscreen use in ways that address the importance of learning more about potential harms of counseling for sunscreen use as follows:
# MMWR October 17, 2003
Sunscreens probably prevent squamous-cell carcinoma of the skin when used mainly during unintentional sun exposure. No conclusion can be drawn about the cancerpreventive activity of topical use of sunscreens against basalcell carcinoma and cutaneous melanoma. Use of sunscreens can extend the duration of intentional sun exposure, such as sunbathing. Such an extension may increase the risk for cutaneous melanoma (26). The Task Force on Community Preventive Services found insufficient evidence to determine the effectiveness of a range of population-based interventions to reduce unprotected UV light exposure and recommended additional research on educational policy approaches, media campaigns, and both health-care setting and community-based interventions (27).
# U.S. Preventive Services Task Force
# BOX 1. U.S. Preventive Services Task Force (USPSTF) recommendations and ratings
The Task Force grades its recommendations according to one of five classifications (A, B, C, D, I) reflecting the strength of evidence and magnitude of net benefit (benefits minus harms): The USPSTF grades the quality of the overall evidence for a service on a 3-point scale (good, fair, poor):
A.
Good: Evidence includes consistent results from welldesigned, well-conducted studies in representative populations that directly assess effects on health outcomes.
Fair: Evidence is sufficient to determine effects on health outcomes, but the strength of the evidence is limited by the number, quality, or consistency of the individual studies, generalizability to routine practice, or indirect nature of the evidence on health outcomes.
Poor: Evidence is insufficient to assess the effects on health outcomes because of limited number or power of studies, important flaws in their design or conduct, gaps in the chain of evidence, or lack of information on important health outcomes. | depar depar depar depar department of health and human ser tment of health and human ser tment of health and human ser tment of health and human ser tment of health and human services vices vices vices vices# Background
In the United States, the incidence and mortality from cutaneous malignant melanoma (CMM) have increased rapidly in the last few decades (1,2). In 2003, approximately 54,200 persons will have new diagnoses of melanoma, and 7,600 will die from the disease (3). The incidence of the other two skin cancers, basal cell carcinoma (BCC) and squamous cell carcinoma (SCC), is estimated to be >1 million new cases per year (3). According to the data from the Surveillance, Epidemiology and End Results (SEER) cancer registry of the National Cancer Institute, during 1995-1999, average annual age-adjusted incidence rates for melanoma per 100,000 population were 23.5 for men and 15.7 for women for non-Hispanic whites; 3.8 for men and 3.7 for women for Hispanics; 1.8 for men and 1.3 for women for Asians; 1.5 for men and 0.9 for Ameri-
# Introduction
The Task Force on Community Preventive Services (the Task Force) is developing the Guide to Community Preventive Services (the Community Guide), a resource that will include multiple systematic reviews, each focusing on a preventive health topic. The Community Guide is being developed with the support of the U.S. Department of Health and Human Services (DHHS) in collaboration with public and private partners. Although CDC provides staff support to the Task Force for development of the Community Guide, the recommendations presented in this report were developed by the Task Force and are not necessarily the recommendations of DHHS or CDC. This report is one in a series of topics included in the Community Guide. It provides an overview of the process used by the Task Force to select and review evidence and summarize its recommendations regarding interventions to reduce UV exposure and increase UV protective behaviors for prevention of skin cancer. A full report on the recommendations, additional evidence (i.e., discussions of applicability, additional benefits, potential harms, existing barriers to implementation, costs, cost benefit, and cost effectiveness of the interventions [when available]), and remaining research questions will be published in the American Journal of Preventive Medicine.
Community Guide topics are prepared and released as each is completed. The findings from systematic reviews on vaccinepreventable diseases, tobacco use prevention and reduction, motor vehicle occupant injury, physical activity, diabetes, oral health, and the effects of the social environment on health have already been published. A compilation of systematic reviews will be published in book form. Additional information regarding the Task Force and the Community Guide and a list of published articles are available on the Internet at http:/ /www.thecommunityguide.org.
# Methods
The methods used by the Community Guide for conducting systematic reviews and linking evidence to recommendations have been described elsewhere (20). In brief, for each Community Guide topic, a multidisciplinary team (the systematic review development team) conducts a review consisting of the following steps:
• developing an approach to organizing, grouping, and selecting the interventions; • systematically searching for and retrieving evidence;
• assessing the quality of and summarizing the strength of the body of evidence of effectiveness; • assessing cost and cost effectiveness evidence, identifying applicability and barriers to implementation (if the effectiveness of the intervention has been established); • summarizing information regarding other evidence; and • identifying and summarizing research gaps. For each review of interventions regarding skin cancer prevention, the systematic review development team developed a conceptual model (or analytic framework) to show the relationship of the intervention to relevant intermediate outcomes (e.g., knowledge, attitudes and beliefs, and intentions regarding sun-protective behaviors), to implementing key sunprotective behaviors, and to the assumed relationships of improvements in sun-protective behaviors to skin cancer prevention. A representative example of an analytic framework for mass media interventions is illustrated (Figure). The analytic frameworks for the other interventions were similar to this example except that they included environmental and policy components.
The analytic frameworks focused on key health outcomes (e.g., sunburn or nevi*) and sun-protective behaviors:
• avoiding peak sun; -seeking shade, and -avoiding the sun during peak UV hours. • covering up; -wearing a hat, -wearing a long-sleeved shirt, and -wearing pants.
• sunscreen use. The team also examined intermediate outcomes that were postulated to be associated with sun-protective behaviors (e.g., knowledge, attitudes, and intentions). Recommendations were based either on better health outcomes (rare with this subject matter because relevant cancer outcomes would become apparent long after the time of the intervention) or risk behaviors that were thought to be established proxies for cancer outcomes (in this case, avoiding peak UV hours or covering up).
The team considered sunscreen use to be a key secondary outcome of sun protection programs because sunscreens prevent sunburn (a marker of unprotected UV exposure and a health outcome associated with increased risk of skin cancer in epidemiologic studies) and reduce the incidence of SCC, and better alternatives are not always available (e.g., when swimming). Sunscreen's role in preventing skin cancer has been demonstrated to be complex, according to information in recent reports from national and international groups (18,21) and summarized in the last section of this report.
Epidemiologic studies suggest that sunscreen use could be considered harmful if it increased a person's total time in the sun and total UV exposure. Partly for that reason, suncreen use alone might not protect against melanoma despite its protective effect on SCC. The International Agency for Research on Cancer (IARC) recommends that sunscreens not be used as the sole method for skin cancer prevention and not be used as a means to extend the duration of UV exposure (21). The team therefore did not consider sunscreen use, by itself, to be an established proxy for better health. * Nevi are lesions of pigment-forming skin cells that can be a risk factor for melanoma.
# Intervention
# FIGURE. Analytic framework for media interventions to reduce ultraviolet (UV) exposure and increase sun-protective behaviors.
Major stratification variables were type of media (e.g., small media [posters, brochures] versus large media [television, radio] ); characteristics of target population (e.g., age, sex, skin color, skin type, baseline risk, socioeconomic status, sunburn incidence, occupation); intervention intensity (i.e., comparison, some intervention, high level of intervention); geographic or environmental characteristics (e.g., urban, rural, climate of location [e.g., sunny versus cloudy] ); intervention characteristics (e.g., size, access to media).
# MMWR October 17, 2003
The coordination team, † which conducted the systematic review, and their consultants § generated a comprehensive list of interventions to reduce skin cancer. From this, a priority list of interventions for review was developed through a process of polling the coordination team, the consultants, and other specialists in the field regarding their perception of the public health importance (number of persons affected), the practicality of application, and the need of those promoting UV protective behaviors for information regarding each intervention.
To conduct the review, the team organized interventions into three groups: setting-specific, target population-specific, and communitywide (Table ). Setting was used as an organizing structure because it was a convenient proxy for key characteristics of the target populations and the implementers of the interventions. The majority of the interventions in this group involved diverse activities -provision of information, environmental approaches (e.g., planting shade trees), or policy approaches (e.g., implementing a policy to reschedule outdoor activities or a requirement to wear hats when outside). Interventions in the setting-specific group consisted of educational and policy approaches in the following settings:
• child care centers, • primary schools,
• secondary schools and colleges,
• recreational or tourism settings,
• occupational settings, and • health-care settings and for health-care providers.
The target population of interest category included one intervention: children's parents or caregivers (some of these interventions might have already been examined in settingspecific groups).
The category of communitywide interventions included two types of interventions and a subgroup:
• media campaigns alone, and • communitywide multicomponent interventions that include at least two interventions in an integrated manner. (Comprehensive communitywide programs, a subset of communitywide multicomponent interventions, include interventions at several levels [individual, setting, whole community] and last longer than 1 year.) Interventions reviewed were either single component (i.e., using only one activity to achieve desired outcomes) or multicomponent (i.e., using more than one activity, such as a policy or environmental intervention with a media campaign). Certain studies provided results relevant to more than one intervention and were included in each of the reviews to which they were applicable. Studies and outcome measures were classified according to definitions developed as part of the review process. The nomenclature used in this report sometimes differs from that used in the original studies.
To be included in the reviews of effectiveness, studies had to 1) be primary investigations of interventions selected for evaluation rather than, for example, guidelines or reviews; 2) be published in English during the years 1966-2000; 3) be conducted in established market economies ¶ ; and 4) compare outcomes among groups of persons exposed to the intervention with outcomes among groups of persons not exposed or less exposed to the intervention (i.e., the study design included a concurrent or before-and-after comparison.) ¶ Searches of three computerized databases (MEDLINE, PsychINFO, CINAHL)** were conducted. Team members also reviewed reference lists and consulted with other specialists in the field (e.g., participants in a skin cancer prevention listserv) to identify relevant studies. Each included study was evaluated by using a standardized abstraction form and was assessed for suitability of the study design and threats to validity (22). Studies were characterized as having good, fair, or limited execution based on the number of threats to validity (20).
Results for each outcome of interest were obtained from each study that met the minimum quality criteria. Net effects were derived when appropriate by calculating the difference between the changes observed in the intervention and comparison groups relative to the respective baseline levels. † † The median was used to summarize a typical measure of effect across the body of evidence for each outcome of interest; both the median and the range are reported. For bodies of evidence consisting of four or more studies, an interquartile range was used to represent variability.
The strength of the body of evidence of effectiveness was characterized as strong, sufficient, or insufficient on the basis of the number of available studies, the suitability of study designs for evaluating effectiveness, the quality of execution of the studies as defined by the Community Guide (20), the consistency of the results, and the effect size.
The Task Force uses these systematic reviews to evaluate the evidence of intervention effectiveness and makes recommendations based on the findings of the reviews (20). The strength of each recommendation is based on the evidence of effectiveness (i.e., an intervention is recommended on the basis of either strong or sufficient evidence of effectiveness) (20). Other types of evidence can also affect a recommendation. For example, harms resulting from an intervention that outweigh benefits might lead to a recommendation that the intervention not be used even if it is effective in improving some outcomes.
A finding of insufficient evidence to determine effectiveness should not be interpreted as evidence of ineffectiveness. Insufficient evidence may be found for any of a number of reasons, alone or in combination, including an insufficient number of studies; too many threats to the validity of the available studies based on their design, execution, or both; conflicts in the results of the studies that preclude a coherent summary of effectiveness; or no indication that the outcomes measured to date, by themselves, represent success in improving health. In all these situations, a finding of insufficient evidence to determine effectiveness is important for identifying areas of uncertainty and continuing research needs. In contrast, sufficient or strong evidence of ineffectiveness would lead to a recommendation against use of the intervention.
# Results
Database searches and bibliographic reviews yielded a list of 6,373 potentially relevant titles. After review of the abstracts and consultation with specialists in the field, a total of 313 reports were retrieved. Of these, 154 were not used in the review because they did not provide results, did not refer to an intervention, or reported on noncomparative studies. The remaining 159 were retained for full review. On the basis of limitations in execution or design or because they provided only background information on studies that were already included, 74 of these were excluded and were not considered further. The remaining 85 studies were considered qualifying studies. The Task Force recommendations in this report are based on the systematic review and evaluation of these qualifying studies, all of which had good or fair quality of execution.
The Task Force recommended two interventions, both in the setting-specific category (Table ):
• educational and policy approaches in primary schoolschanging children's covering-up behavior (wearing protective clothing); and • educational and policy approaches in recreational or tourism settings -changing adults' covering-up behaviors. Interventions in primary school settings were designed to increase sun-protective knowledge, attitudes, intentions, and behavior among children from kindergarten through eighth grade. The interventions ranged from a curriculum that included interactive classroom and take-home activities to staff education, brochures for parents, and a working session to develop skin protection plans for schools. All interventions focused on some combination of increasing application of sunscreen, scheduling activities to avoid peak sun hours, increasing availability of shade and encouraging children to play in shady areas, and encouraging children to wear sunprotective clothing. Interventions in this category included at least one of the following activities:
• provision of information to children (e.g., instruction or small media [brochures, flyers, newsletters, informational letters or videos] or both); • additional activities to influence children's behavior (e.g., modeling, demonstration, role playing); • activities intended to change the knowledge, attitudes, or behavior of caregivers (i.e., teachers or parents); or • environmental or policy approaches (e.g., provision of sunscreen, provision of shade, or scheduling outdoor activities to avoid hours of peak sunlight). Single-and multicomponent interventions in recreational settings were designed to increase knowledge; influence attitudes, beliefs, and intentions; and change behavior of adults and children. Interventions included one or more of the following: educational brochures, including culturally relevant materials and photographs of skin cancer lesions; sun-safety training for lifeguards, aquatic instructors, and outdoor recreation staff and role-modeling by these groups; sun-safety lessons, interactive activities, and incentives for parents and children; increasing available shaded areas; providing sunscreen; and point-of-purchase prompts.
The recommended interventions had small to moderate behavior change scores. In primary schools, the median net relative increase was 25% (interquartile range: 1%-40%, six studies). In recreational settings, the median net relative increase was 11.2% (interquartile range: 5.1%-12.9%, five studies).
It should be noted that the interventions were targeted to populations rather than single persons. Small changes in behavior in large populations can result in substantial public health benefits.
The Task Force found insufficient evidence on which to make recommendations for or against the following interventions: educational and policy approaches in child care centers; educational and policy approaches in secondary schools and colleges; educational and policy approaches in recreational or tourism settings for children; educational and policy approaches in occupational settings; interventions oriented to health-care settings and providers; interventions oriented to children's parents or caregivers; media campaigns alone; and communitywide multicomponent interventions (Table ). The finding of insufficient evidence to determine effectiveness was most often based on the limited numbers of studies that measured behavioral or health outcomes, inconsistent evidence among studies that measured changes in sun-protective behaviors, and limitations in the design and execution of available studies.
Summary tables of the reviews will be available at http:// www.thecommunityguide.org/cancer when the full evidence is published in a supplement to the American Journal of Preventive Medicine.
# Use of Recommendations in Communities and Health-Care Settings
Malignant melanoma is the deadliest of the skin cancers, and its incidence in the United States has increased rapidly in the past 2 decades. Melanoma accounts for approximately three fourths of all skin cancer deaths. Basal cell and squamous cell skin cancers are seldom fatal but, if advanced, can cause severe disfigurement and morbidity (3). UV exposure in childhood and intense intermittent UV exposures are the major environmental risk factors for melanoma and BCC, and cumulative UV exposure is the major preventable risk factor for SCC (23). National surveys indicate that only one third of Americans practice sun-protective behaviors, and their practices vary greatly, depending on age, sex, and their ability to tan and burn (9,12,13).
The two Task Force recommendations -educational and policy approaches in primary schools, and educational and policy approaches for adults in outdoor recreational or tourism settings -are based on improving covering-up behaviors. These recommendations represent tested interventions that promote decreased UV exposure at the community level. They can be used for planning interventions to promote UV protection or to evaluate existing programs.
Several of the studies reviewed included multiple components that could not be evaluated separately. For example, a school-based program might involve components of policy, such as establishing school guidelines, in tandem with implementation of one-on-one didactic and interactive sessions regarding adapting sun-protective behaviors. Although sunprotective behaviors were increased by school-based programs, the specific effect could not be attributed to one specific intervention characteristic. In selecting and implementing interventions, the potential for an unintended increase in the duration and intensity of UV exposure must be considered. Also, communities should strive to develop comprehensive programs that include a wide range of activities suitable for their local resources, population characteristics, and settings.
The other interventions reviewed, for which evidence was insufficient to determine effectiveness, could also prove useful. They provide a broader taxonomy of interventions that deserve further testing and evaluation, and the documentation of research gaps in these reviews could potentially help to improve the next generation of research. Additional information on research gaps will be provided in the report in the American Journal of Preventive Medicine.
Choosing interventions that are well matched to local needs and capabilities, and then carefully implementing those interventions, are vital steps for increasing UV protection. Several factors can affect the attitudes, ability, and behaviors of a community regarding taking sun safety precautions. Some of the most important are program priorities, location of the community, and population. Establishing skin cancer prevention as a priority might be difficult because skin cancer is but one of many health topics, and for certain communities, may not be as high a priority as other cancers or diseases. Although it might be a higher priority in areas where UV radiation is more intense, even in areas with lower UV intensity, education about UV exposure during times of episodic exposure (e.g., during winter sports, when the sun comes out, and when traveling to higher UV intensity regions) could be helpful. Likewise, although skin cancer prevention might be a higher priority for populations at an increased risk (e.g., light-skinned, sunsensitive), even darker-skinned or less sun-sensitive persons need to take precautions when exposed to UV radiation. To meet local objectives, recommendations and other evidence provided in the Community Guide should be supplemented with local information such as skin cancer incidence, skin cancer mortality, prevalence of sun-protective behaviors, latitude, UV index, resource availability, administrative structures, and economic and social environments of organizations and practitioners.
These reviews by themselves do not provide advice regarding implementation of effective programs; the referenced articles, however, provide additional detail. Implementation advice is also available elsewhere (24)(25)(26)(27)(28).
# Introduction
This statement summarizes the current U.S. Preventive Services Task Force (USPSTF) recommendation on counseling to prevent skin cancer and the supporting scientific evidence, and updates the 1996 recommendation contained in the Guide to Clinical Preventive Services, Second Edition (1). The USPSTF, an independent panel of private sector experts in primary care and prevention, systematically reviews the evidence of effectiveness of a wide range of clinical preventive services, including screening tests, counseling, and chemoprevention. The Task Force grades its recommendations according to one of five classifications (A, B, C, D, I), reflecting the strength of evidence and magnitude of net benefit (benefits minus harms) (Box 1). The USPSTF grades the quality of the overall evidence for a service on a 3-point scale (good, fair, poor) (Box 2).
This recommendation and rationale statement and complete information on which this statement is based, including evidence tables and references, are available at http://www.ahrq. gov/clinic/uspstfix.htm (2) and in print by subscription through the AHRQ Clearinghouse (1-800-358-9295 or e-mail at [email protected]) and through the National Guideline Clearinghouse ™ at http://www.guideline.gov.
# Summary of Recommendation
The U.S. Preventive Services Task Force concludes that the evidence is insufficient to recommend for or against routine counseling by primary care clinicians to prevent skin cancer.
# I recommendation.
The USPSTF found insufficient evidence to determine whether clinician counseling is effective in changing patient behaviors to reduce skin cancer risk. Counseling parents may increase the use of sunscreen for children, but there is little evidence to determine the effects of counseling on other preventive behaviors (such as wearing protective clothing, reducing excessive sun exposure, avoiding sun lamps/tanning beds, or practicing skin self-examination) and little evidence on potential harms.
# Clinical Considerations
• Using sunscreen has been shown to prevent squamous cell skin cancer. The evidence for the effect of sunscreen use in preventing melanoma, however, is mixed. Sunscreens that block both ultraviolet A (UV-A) and ultraviolet B (UV-B) light may be more effective in preventing squamous cell cancer and its precursors than those that block only UV-B light. However, people who use sunscreen alone could increase their risk for melanoma if they increase the time they spend in the sun. • UV exposure increases the risk for skin cancer among people with all skin types, but especially fair-skinned people. Those who sunburn readily and tan poorly, namely those with red or blond hair and fair skin that freckles or burns easily, are at highest risk for developing skin cancer and would benefit most from sun protection behaviors. The incidence of melanoma among whites is 20 times higher than it is among blacks; the incidence of melanoma among whites is approximately four times higher than it is among Hispanics. • Observational studies indicate that intermittent or intense sun exposure is a greater risk factor for melanoma than chronic exposure. These studies support the hypothesis that preventing sunburn, especially in childhood, may reduce the lifetime risk for melanoma. • Other measures for preventing skin cancer include avoiding direct exposure to midday sun (between the hours of 10:00 a.m. and 4:00 p.m.) to reduce exposure to ultraviolet (UV) rays and covering skin exposed to the sun (by wearing protective clothing such as broad-brimmed hats, long-sleeved shirts, long pants, and sunglasses). • The effects of sunlamps and tanning beds on the risk for melanoma are unclear because of limited study design and conflicting results from retrospective studies. • Only a single case-control study of skin self-examination has reported a lower risk for melanoma among patients who reported ever examining their skin over 5 years.
Although results from this study suggest that skin selfexamination may be effective in preventing skin cancer, these results are not definitive.
# Scientific Evidence Epidemiology and Clinical Consequences
Melanoma is a leading cause of cancer death in the United States. The lifetime risk for dying of melanoma is 0.36% in white men and 0.21% in white women (3). Between 1973 and 1995, the age-adjusted incidence of melanoma increased more than 100%, from 5.7 per 100,000 people to 13.3 per 100,000 people. The increase in annual incidence rates is likely due to several factors, including increased sun exposure and possibly earlier detection of melanoma. Although primary prevention efforts have focused on young people, the elderly (especially elderly men) bear a disproportionate burden of morbidity and mortality from melanoma and nonmelanoma skin cancer. Men older than age 65 account for 22% of the newly diagnosed cases of malignant melanoma each year and women in the same age group account for 14%. Basal cell and squa-mous cell carcinomas are more than 10 times as common as melanoma but account for less morbidity and mortality. Squamous cell cancers, however, may account for 20% of all deaths from skin cancer.
# Effectiveness of Available Interventions
Preventive strategies include reducing sun exposure (e.g., by wearing protective clothing and using sunscreen regularly), avoiding sunlamps and tanning equipment, and practicing skin self-examination. There is little direct evidence, however, that any of these interventions reduce skin cancer morbidity or mortality.
# Reducing Sun Exposure
Avoiding direct sunlight by staying indoors or in the shade or by wearing protective clothing is the most effective measure for reducing exposure to ultraviolet light, but there are no randomized trials of sun avoidance to prevent skin cancer. In numerous observational studies, increased sun exposure in childhood and adolescence is associated with increased risk for nonmelanoma skin cancer, which usually occurs in sunexposed areas such as the face.
Recent studies provide a more complex picture of the relationship between sun exposure and melanoma, however. Although melanoma incidence is higher in regions near the equator where ultraviolet exposure is most intense, melanoma often occurs in areas of the body not exposed to the sun. In observational studies, intermittent or intense sun exposure was associated with increased risk for melanoma; chronic exposure was associated with lower risk, as was the ability to tan (4-7).
# Sunlamp and Tanning Bed Avoidance
Six of 19 case-control studies found a positive association between use of sun lamps and melanoma risk, but most did not adjust for recreational sun exposure or for the dosage and timing of sunlamp exposure (8). Among nine studies that examined the duration, frequency, or timing of sunlamp or tanning bed exposure, four found a positive association, particularly if the dose of exposure was high and if it caused burning.
# Sunscreen Use
Daily sunscreen use on the hands and face reduced the total incidence of squamous cell cancer in a randomized trial of 1,621 residents in Australia (rate ratio [RR]: 0.61; 95% confidence interval [CI] = 0.46-0.81) (9). Sunscreen had no effect on basal cell cancer. Based on this trial, 140 people would need to use sunscreen daily for 4½ years to prevent one case of squamous cell cancer. An earlier randomized trial demonstrated that sunscreen use reduced solar keratoses, precursors of squamous cell cancers (10). There are no direct data about the effect of sunscreen on melanoma incidence. An unblinded randomized trial showed that children at high risk for skin cancers who used sunscreen developed fewer nevi than those who did not. Several epidemiologic studies have found higher risk for melanoma among users of sunscreens than among nonusers (11)(12)(13). A recent meta-analysis of population-based casecontrol studies found no effect of sunscreen use on risk for melanoma (14). The conflicting results may reflect the fact that sunscreen use is more common among fair-skinned people, who are at higher risk for melanoma, than it is among darkerskinned people; or, this finding may reflect the fact that sunscreen use could be harmful if it encourages longer stays in the sun without protecting completely against cancer-causing radiation.
# Skin Self-Examination
The only evidence for the effectiveness of skin self-examination comes from a single case-control study (1,15). After adjustment for other risk factors, skin self-examination was associated with lower incidence of melanoma (odds ratio [OR]: 0.66; 95% CI = 0.44-0.99) and lower mortality from melanoma (OR: 0.37; 95% CI = 0.16-0.84), although the definition of "self-examination" was limited. This study did not provide sufficient evidence that skin self-examination would reduce the incidence of melanoma or improve outcomes of melanoma.
# Effectiveness of Counseling
Community and worksite educational interventions have demonstrated effectiveness for increasing the use of skin protection measures, such as wearing hats and long-sleeve shirts and staying in the shade; however, evidence addressing the effectiveness of clinician counseling to prevent skin cancer is extremely limited. Most studies of counseling have examined intermediate outcomes such as knowledge and attitudes rather than changes in behavior. In a recent survey, 60% of pediatricians said that they usually or always counsel patients about skin protection, but advice to use sunscreen is more common than advice about wearing protective clothing or avoiding the midday sun (16).
Simple reminders and instructional materials for clinicians can overcome some of the barriers to regular counseling. A randomized trial of a community-based intervention involving 10 towns in New Hampshire suggests that office-based counseling by physicians may be an effective component of a multimodal program to promote skin protection (17). The proportion of children using some sun protection increased significantly in the intervention towns (from 78% to 87%) compared to a decrease in the control communities (from 85% to 80%). More parents reported receiving some sun protection information from a clinician in the intervention towns. However, most of the change was due to increased sunscreen use rather than to reduced sun exposure.
# Potential Harms of Skin Protection Behaviors
There are limited data regarding potential harms of counseling or of specific skin protection behaviors. Skin cancer counseling that focuses on the use of sunscreen could possibly lead to a false sense of security, which might lead to more time in the sun. For example, a randomized trial with young adults found that those who used sunscreen with a high sun protection factor (SPF) stayed longer in the sun than those who used sunscreen with a lower SPF (18). There has been some concern that use of SPF of 15 results in vitamin D deficiency. However, a randomized trial among people over 40 years of age found that sunscreen use over the summer had no effect on 25-hydroxyvitamin D3 levels. Concerns related to sun avoidance include reduced physical activity levels among children and negative effects on mental health. However, no studies have evaluated the effects of sun protection behaviors on these outcomes.
# Recommendations Of Others
The American Cancer Society (19), the American Academy of Dermatology (20), the American Academy of Pediatrics (21), the American College of Obstetricians and Gynecologists (22), and a National Institutes of Health consensus panel (23) all recommend patient education concerning sun avoidance and sunscreen use. The American Academy of Family Physicians recommends sun protection for all with increased sun exposure (24). The American College of Preventive Medicine (ACPM) concluded that sun-protective measures (e.g., clothing, hats, opaque sunscreens) are probably effective in reducing skin cancer but that the evidence does not support discussion of sunscreen and sun protection with every patient. ACPM concluded that evidence is insufficient to advise patients that chemical sunscreens protect against malignant melanoma and that their use may actually lead to increased risk (25). Recently, the International Agency for Research on Cancer (IARC), part of the World Health Organization, qualified their recommendation for sunscreen use in ways that address the importance of learning more about potential harms of counseling for sunscreen use as follows:
# MMWR October 17, 2003
Sunscreens probably prevent squamous-cell carcinoma of the skin when used mainly during unintentional sun exposure. No conclusion can be drawn about the cancerpreventive activity of topical use of sunscreens against basalcell carcinoma and cutaneous melanoma. Use of sunscreens can extend the duration of intentional sun exposure, such as sunbathing. Such an extension may increase the risk for cutaneous melanoma (26). The Task Force on Community Preventive Services found insufficient evidence to determine the effectiveness of a range of population-based interventions to reduce unprotected UV light exposure and recommended additional research on educational policy approaches, media campaigns, and both health-care setting and community-based interventions (27).
# U.S. Preventive Services Task Force
# BOX 1. U.S. Preventive Services Task Force (USPSTF) recommendations and ratings
The Task Force grades its recommendations according to one of five classifications (A, B, C, D, I) reflecting the strength of evidence and magnitude of net benefit (benefits minus harms): The USPSTF grades the quality of the overall evidence for a service on a 3-point scale (good, fair, poor):
A.
Good: Evidence includes consistent results from welldesigned, well-conducted studies in representative populations that directly assess effects on health outcomes.
Fair: Evidence is sufficient to determine effects on health outcomes, but the strength of the evidence is limited by the number, quality, or consistency of the individual studies, generalizability to routine practice, or indirect nature of the evidence on health outcomes.
Poor: Evidence is insufficient to assess the effects on health outcomes because of limited number or power of studies, important flaws in their design or conduct, gaps in the chain of evidence, or lack of information on important health outcomes. | None | None |
9cc3520b5248a34dfa45b5c6a4c56ac9b7f1a843 | cdc | None | This schedule includes recommendations in effect as of January 1, 2017. Any dose not administered at the recommended age should be administered at a subsequent visit, when indicated and feasible. The use of a combination vaccine generally is preferred over separate injections of its equivalent component vaccines. Vaccination providers should consult the relevant Advisory Committee on Immunization Practices (ACIP) statement for detailed recommendations, available online at www.cdc.gov/vaccines/hcp/acip-recs/index.html. Clinically significant adverse events that follow vaccination should be reported to the Vaccine Adverse Event Reporting System (VAERS) online (www.vaers.hhs.gov) or by telephone (800-822-7967). Suspected cases of vaccinepreventable diseases should be reported to the state or local health department. Additional information, including precautions and contraindications for vaccination, is available from CDC online (www.cdc.gov/vaccines/hcp/admin/ contraindications.html) or by telephone (800-CDC- ).#
). These recommendations must be read with the footnotes that follow. For those who fall behind or start late, provide catch-up vaccination at the earliest opportunity as indicated by the green bars in Figure 1. To determine minimum intervals between doses, see the catch-up schedule (Figure 2). School entry and adolescent vaccine age groups are shaded in gray.
# NOTE:
The above recommendations must be read along with the footnotes of this schedule. No recommendation Range of recommended ages for certain high-risk groups Range of recommended ages for all children Range of recommended ages for catch-up immunization Range of recommended ages for non-high-risk groups that may receive vaccine, subject to individual clinical decision making FIGURE 2. Catch-up immunization schedule for persons aged 4 months through 18 years who start late or who are more than 1 month behind-United States, 2017.
The figure below provides catch-up schedules and minimum intervals between doses for children whose vaccinations have been delayed. A vaccine series does not need to be restarted, regardless of the time that has elapsed between doses. Use the section appropriate for the child's age. Always use this table in conjunction with Figure 1 and the footnotes that follow.
# Additional information
- For information on contraindications and precautions for the use of a vaccine and for additional information regarding that vaccine, vaccination providers should consult the ACIP General Recommendations on Immunization and the relevant ACIP statement, available online at www.cdc.gov/vaccines/hcp/acip-recs/index.html. - For purposes of calculating intervals between doses, 4 weeks = 28 days. Intervals of 4 months or greater are determined by calendar months.
- Vaccine doses administered ≤4 days before the minimum interval are considered valid. Doses of any vaccine administered ≥5 days earlier than the minimum interval or minimum age should not be counted as valid doses and should be repeated as age-appropriate. The repeat dose should be spaced after the invalid dose by the recommended minimum interval. For further details, see - Administer monovalent HepB vaccine to all newborns within 24 hours of birth. - For infants born to hepatitis B surface antigen (HBsAg)positive mothers, administer HepB vaccine and 0.5 mL of hepatitis B immune globulin (HBIG) within 12 hours of birth. These infants should be tested for HBsAg and antibody to HBsAg (anti-HBs) at age 9 through 12 months (preferably at the next well-child visit) or 1 to 2 months after completion of the HepB series if the series was delayed. - If mother's HBsAg status is unknown, within 12 hours of birth, administer HepB vaccine regardless of birth weight. For infants weighing less than 2,000 grams, administer HBIG in addition to HepB vaccine within 12 hours of birth. Determine mother's HBsAg status as soon as possible and, if mother is HBsAg-positive, also administer HBIG to infants weighing 2,000 grams or more as soon as possible, but no later than age 7 days.
# Doses following the birth dose:
- The second dose should be administered at age 1 or 2 months. Monovalent HepB vaccine should be used for doses administered before age 6 weeks. - Infants who did not receive a birth dose should receive 3 doses of a HepB-containing vaccine on a schedule of 0, 1 to 2 months, and 6 months, starting as soon as feasible (see figure 2). - Administer the second dose 1 to 2 months after the first dose (minimum interval of 4 weeks); administer the third dose at least 8 weeks after the second dose AND at least 16 weeks after the first dose. The final (third or fourth) dose in the HepB vaccine series should be administered no earlier than age 24 weeks.
- Administration of a total of 4 doses of HepB vaccine is permitted when a combination vaccine containing HepB is administered after the birth dose.
# Catch-up vaccination:
- Unvaccinated persons should complete a 3-dose series. - Administer a 4-dose series of IPV at ages 2, 4, 6 through 18 months, and 4 through 6 years. The final dose in the series should be administered on or after the fourth birthday and at least 6 months after the previous dose.
# Catch-up vaccination:
- In the first 6 months of life, minimum age and minimum intervals are only recommended if the person is at risk of imminent exposure to circulating poliovirus (i.e., travel to a polio-endemic region or during an outbreak). - If 4 or more doses are administered before age 4 years, an additional dose should be administered at age 4 through 6 years and at least 6 months after the previous dose. - A fourth dose is not necessary if the third dose was administered at age 4 years or older and at least 6 months after the previous dose. - If both oral polio vaccine (OPV) and IPV were administered as part of a series, a total of 4 doses should be administered, regardless of the child's current age.
If only OPV was administered, and all doses were given prior to age 4 years, 1 dose of IPV should be given at 4 years or older, at least 4 weeks after the last OPV dose. - IPV is not routinely recommended for U.S. residents aged 18 years or older. - For other catch-up guidance, see Figure 2.
For further guidance on the use of the vaccines mentioned below, see: www.cdc.gov/vaccines/hcp/acip-recs/index.html. - Administer a 2-dose series of MMR vaccine at ages 12 through 15 months and 4 through 6 years. The second dose may be administered before age 4 years, provided at least 4 weeks have elapsed since the first dose. - Administer 1 dose of MMR vaccine to infants aged 6 through 11 months before departure from the United States for international travel. These children should be revaccinated with 2 doses of MMR vaccine, the first at age 12 through 15 months (12 months if the child remains in an area where disease risk is high), and the second dose at least 4 weeks later. - Administer 2 doses of MMR vaccine to children aged 12 months and older before departure from the United States for international travel. The first dose should be administered on or after age 12 months and the second dose at least 4 weeks later.
# Catch-up vaccination:
- Ensure that all school-aged children and adolescents have had 2 doses of MMR vaccine; the minimum interval between the 2 doses is 4 weeks.
# Varicella (VAR) vaccine. (Minimum age: 12 months)
Routine vaccination:
- Administer a 2-dose series of VAR vaccine at ages 12 through 15 months and 4 through 6 years. The second dose may be administered before age 4 years, provided at least 3 months have elapsed since the first dose. If the second dose was administered at least 4 weeks after the first dose, it can be accepted as valid.
# Catch-up vaccination:
- Ensure that all persons aged 7 through 18 years without evidence of immunity (see MMWR 2007;56, available at www.cdc.gov/mmwr/pdf/rr/rr5604.pdf ) have 2 doses of varicella vaccine. For children aged 7 through 12 years, the recommended minimum interval between doses is 3 months (if the second dose was administered at least 4 weeks after the first dose, it can be accepted as valid); for persons aged 13 years and older, the minimum interval between doses is 4 weeks. For further guidance on the use of the vaccines mentioned below, see: www.cdc.gov/vaccines/hcp/acip-recs/index.html.
# CS270457-C
Menactra ɱ Children with anatomic or functional asplenia or HIV infection ʲ Children 24 months and older who have not received a complete series. Administer 2 primary doses at least 8 weeks apart. If Menactra is administered to a child with asplenia (including sickle cell disease) or HIV infection, do not administer Menactra until age 2 years and at least 4 weeks after the completion of all PCV13 doses. ɱ Children with persistent complement component deficiency ʲ Children 9 through 23 months. Administer 2 primary doses at least 12 weeks apart. ʲ Children 24 months and older who have not received a complete series. Administer 2 primary doses at least 8 weeks apart. ɱ All high-risk children ʲ If Menactra is to be administered to a child at high risk for meningococcal disease, it is recommended that Menactra be given either before or at the same time as DTaP. Bexsero or Trumenba ɱ Persons 10 years or older who have not received a complete series. Administer a 2-dose series of Bexsero, with doses at least 1 month apart, or a 3-dose series of Trumenba, with the second dose at least 1-2 months after the first and the third dose at least 6 months after the first. The two MenB vaccines are not interchangeable; the same vaccine product must be used for all doses. For children who travel to or reside in countries in which meningococcal disease is hyperendemic or epidemic, including countries in the African meningitis belt or the Hajj:
Administer an age-appropriate formulation and series of Menactra or Menveo for protection against serogroups A and W meningococcal disease. Prior receipt of MenHibrix is not sufficient for children traveling to the meningitis belt or the Hajj because it does not contain serogroups A or W. For children at risk during an outbreak attributable to a vaccine serogroup: For serogroup A, C, W, or Y: Administer or complete an age-and formulation-appropriate series of MenHibrix, Menactra, or Menveo.
For serogroup B: Administer a 2-dose series of Bexsero, with doses at least 1 month apart, or a 3-dose series of Trumenba, with the second dose at least 1-2 months after the first and the third dose at least 6 months after the first. The two MenB vaccines are not interchangeable; the same vaccine product must be used for all doses. For MenACWY booster doses among persons with high-risk conditions, refer to MMWR 2013;62(RR02):1-22, at www.cdc.gov/mmwr/preview/mmwrhtml/rr6202a1.htm, MMWR June 20, 2014 / 63( 24 - Administer a 2-dose series of HPV vaccine on a schedule of 0, 6-12 months to all adolescents aged 11 or 12 years. The vaccination series can start at age 9 years. - Administer HPV vaccine to all adolescents through age 18 years who were not previously adequately vaccinated. The number of recommended doses is based on age at administration of the first dose. - For persons initiating vaccination before age 15, the recommended immunization schedule is 2 doses of HPV vaccine at 0, 6-12 months. - For persons initiating vaccination at age 15 years or older, the recommended immunization schedule is 3 doses of HPV vaccine at 0, 1-2, 6 months. - A vaccine dose administered at a shorter interval should be readministered at the recommended interval. In a 2-dose schedule of HPV vaccine, the minimum interval is 5 months between the first and second dose.
If the second dose is administered at a shorter interval, a third dose should be administered a minimum of 12 weeks after the second dose and a minimum of 5 months after the first dose. In a 3-dose schedule of HPV vaccine, the minimum intervals are 4 weeks between the first and second dose, 12 weeks between the second and third dose, and 5 months between the first and third dose. If a vaccine dose is administered at a shorter interval, it should be readministered after another minimum interval has been met since the most recent dose.
# Special populations:
- For children with history of sexual abuse or assault, administer HPV vaccine beginning at age 9 years. - Immunocompromised persons*, including those with human immunodeficiency virus (HIV) infection, should receive a 3-dose series at 0, 1-2, and 6 months, regardless of age at vaccine initiation. - Note: HPV vaccination is not recommended during pregnancy, although there is no evidence that the vaccine poses harm. If a woman is found to be pregnant after initiating the vaccination series, no intervention is needed; the remaining vaccine doses should be delayed until after the pregnancy. | This schedule includes recommendations in effect as of January 1, 2017. Any dose not administered at the recommended age should be administered at a subsequent visit, when indicated and feasible. The use of a combination vaccine generally is preferred over separate injections of its equivalent component vaccines. Vaccination providers should consult the relevant Advisory Committee on Immunization Practices (ACIP) statement for detailed recommendations, available online at www.cdc.gov/vaccines/hcp/acip-recs/index.html. Clinically significant adverse events that follow vaccination should be reported to the Vaccine Adverse Event Reporting System (VAERS) online (www.vaers.hhs.gov) or by telephone (800-822-7967). Suspected cases of vaccinepreventable diseases should be reported to the state or local health department. Additional information, including precautions and contraindications for vaccination, is available from CDC online (www.cdc.gov/vaccines/hcp/admin/ contraindications.html) or by telephone (800-CDC- ).#
2]
). These recommendations must be read with the footnotes that follow. For those who fall behind or start late, provide catch-up vaccination at the earliest opportunity as indicated by the green bars in Figure 1. To determine minimum intervals between doses, see the catch-up schedule (Figure 2). School entry and adolescent vaccine age groups are shaded in gray.
# NOTE:
The above recommendations must be read along with the footnotes of this schedule. No recommendation Range of recommended ages for certain high-risk groups Range of recommended ages for all children Range of recommended ages for catch-up immunization Range of recommended ages for non-high-risk groups that may receive vaccine, subject to individual clinical decision making FIGURE 2. Catch-up immunization schedule for persons aged 4 months through 18 years who start late or who are more than 1 month behind-United States, 2017.
The figure below provides catch-up schedules and minimum intervals between doses for children whose vaccinations have been delayed. A vaccine series does not need to be restarted, regardless of the time that has elapsed between doses. Use the section appropriate for the child's age. Always use this table in conjunction with Figure 1 and the footnotes that follow.
# Additional information
• For information on contraindications and precautions for the use of a vaccine and for additional information regarding that vaccine, vaccination providers should consult the ACIP General Recommendations on Immunization and the relevant ACIP statement, available online at www.cdc.gov/vaccines/hcp/acip-recs/index.html. • For purposes of calculating intervals between doses, 4 weeks = 28 days. Intervals of 4 months or greater are determined by calendar months.
• Vaccine doses administered ≤4 days before the minimum interval are considered valid. Doses of any vaccine administered ≥5 days earlier than the minimum interval or minimum age should not be counted as valid doses and should be repeated as age-appropriate. The repeat dose should be spaced after the invalid dose by the recommended minimum interval. For further details, see • Administer monovalent HepB vaccine to all newborns within 24 hours of birth. • For infants born to hepatitis B surface antigen (HBsAg)positive mothers, administer HepB vaccine and 0.5 mL of hepatitis B immune globulin (HBIG) within 12 hours of birth. These infants should be tested for HBsAg and antibody to HBsAg (anti-HBs) at age 9 through 12 months (preferably at the next well-child visit) or 1 to 2 months after completion of the HepB series if the series was delayed. • If mother's HBsAg status is unknown, within 12 hours of birth, administer HepB vaccine regardless of birth weight. For infants weighing less than 2,000 grams, administer HBIG in addition to HepB vaccine within 12 hours of birth. Determine mother's HBsAg status as soon as possible and, if mother is HBsAg-positive, also administer HBIG to infants weighing 2,000 grams or more as soon as possible, but no later than age 7 days.
# Doses following the birth dose:
• The second dose should be administered at age 1 or 2 months. Monovalent HepB vaccine should be used for doses administered before age 6 weeks. • Infants who did not receive a birth dose should receive 3 doses of a HepB-containing vaccine on a schedule of 0, 1 to 2 months, and 6 months, starting as soon as feasible (see figure 2). • Administer the second dose 1 to 2 months after the first dose (minimum interval of 4 weeks); administer the third dose at least 8 weeks after the second dose AND at least 16 weeks after the first dose. The final (third or fourth) dose in the HepB vaccine series should be administered no earlier than age 24 weeks.
• Administration of a total of 4 doses of HepB vaccine is permitted when a combination vaccine containing HepB is administered after the birth dose.
# Catch-up vaccination:
• Unvaccinated persons should complete a 3-dose series. • Administer a 4-dose series of IPV at ages 2, 4, 6 through 18 months, and 4 through 6 years. The final dose in the series should be administered on or after the fourth birthday and at least 6 months after the previous dose.
# Catch-up vaccination:
• In the first 6 months of life, minimum age and minimum intervals are only recommended if the person is at risk of imminent exposure to circulating poliovirus (i.e., travel to a polio-endemic region or during an outbreak). • If 4 or more doses are administered before age 4 years, an additional dose should be administered at age 4 through 6 years and at least 6 months after the previous dose. • A fourth dose is not necessary if the third dose was administered at age 4 years or older and at least 6 months after the previous dose. • If both oral polio vaccine (OPV) and IPV were administered as part of a series, a total of 4 doses should be administered, regardless of the child's current age.
If only OPV was administered, and all doses were given prior to age 4 years, 1 dose of IPV should be given at 4 years or older, at least 4 weeks after the last OPV dose. • IPV is not routinely recommended for U.S. residents aged 18 years or older. • For other catch-up guidance, see Figure 2.
For further guidance on the use of the vaccines mentioned below, see: www.cdc.gov/vaccines/hcp/acip-recs/index.html. • Administer a 2-dose series of MMR vaccine at ages 12 through 15 months and 4 through 6 years. The second dose may be administered before age 4 years, provided at least 4 weeks have elapsed since the first dose. • Administer 1 dose of MMR vaccine to infants aged 6 through 11 months before departure from the United States for international travel. These children should be revaccinated with 2 doses of MMR vaccine, the first at age 12 through 15 months (12 months if the child remains in an area where disease risk is high), and the second dose at least 4 weeks later. • Administer 2 doses of MMR vaccine to children aged 12 months and older before departure from the United States for international travel. The first dose should be administered on or after age 12 months and the second dose at least 4 weeks later.
# Catch-up vaccination:
• Ensure that all school-aged children and adolescents have had 2 doses of MMR vaccine; the minimum interval between the 2 doses is 4 weeks.
# Varicella (VAR) vaccine. (Minimum age: 12 months)
Routine vaccination:
• Administer a 2-dose series of VAR vaccine at ages 12 through 15 months and 4 through 6 years. The second dose may be administered before age 4 years, provided at least 3 months have elapsed since the first dose. If the second dose was administered at least 4 weeks after the first dose, it can be accepted as valid.
# Catch-up vaccination:
• Ensure that all persons aged 7 through 18 years without evidence of immunity (see MMWR 2007;56[No. RR-4], available at www.cdc.gov/mmwr/pdf/rr/rr5604.pdf ) have 2 doses of varicella vaccine. For children aged 7 through 12 years, the recommended minimum interval between doses is 3 months (if the second dose was administered at least 4 weeks after the first dose, it can be accepted as valid); for persons aged 13 years and older, the minimum interval between doses is 4 weeks. For further guidance on the use of the vaccines mentioned below, see: www.cdc.gov/vaccines/hcp/acip-recs/index.html.
# CS270457-C
▪ Menactra ɱ Children with anatomic or functional asplenia or HIV infection ʲ Children 24 months and older who have not received a complete series. Administer 2 primary doses at least 8 weeks apart. If Menactra is administered to a child with asplenia (including sickle cell disease) or HIV infection, do not administer Menactra until age 2 years and at least 4 weeks after the completion of all PCV13 doses. ɱ Children with persistent complement component deficiency ʲ Children 9 through 23 months. Administer 2 primary doses at least 12 weeks apart. ʲ Children 24 months and older who have not received a complete series. Administer 2 primary doses at least 8 weeks apart. ɱ All high-risk children ʲ If Menactra is to be administered to a child at high risk for meningococcal disease, it is recommended that Menactra be given either before or at the same time as DTaP. ▪ Bexsero or Trumenba ɱ Persons 10 years or older who have not received a complete series. Administer a 2-dose series of Bexsero, with doses at least 1 month apart, or a 3-dose series of Trumenba, with the second dose at least 1-2 months after the first and the third dose at least 6 months after the first. The two MenB vaccines are not interchangeable; the same vaccine product must be used for all doses. For children who travel to or reside in countries in which meningococcal disease is hyperendemic or epidemic, including countries in the African meningitis belt or the Hajj:
▪ Administer an age-appropriate formulation and series of Menactra or Menveo for protection against serogroups A and W meningococcal disease. Prior receipt of MenHibrix is not sufficient for children traveling to the meningitis belt or the Hajj because it does not contain serogroups A or W. For children at risk during an outbreak attributable to a vaccine serogroup: ▪ For serogroup A, C, W, or Y: Administer or complete an age-and formulation-appropriate series of MenHibrix, Menactra, or Menveo.
#
▪ For serogroup B: Administer a 2-dose series of Bexsero, with doses at least 1 month apart, or a 3-dose series of Trumenba, with the second dose at least 1-2 months after the first and the third dose at least 6 months after the first. The two MenB vaccines are not interchangeable; the same vaccine product must be used for all doses. For MenACWY booster doses among persons with high-risk conditions, refer to MMWR 2013;62(RR02):1-22, at www.cdc.gov/mmwr/preview/mmwrhtml/rr6202a1.htm, MMWR June 20, 2014 / 63( 24 • Administer a 2-dose series of HPV vaccine on a schedule of 0, 6-12 months to all adolescents aged 11 or 12 years. The vaccination series can start at age 9 years. • Administer HPV vaccine to all adolescents through age 18 years who were not previously adequately vaccinated. The number of recommended doses is based on age at administration of the first dose. • For persons initiating vaccination before age 15, the recommended immunization schedule is 2 doses of HPV vaccine at 0, 6-12 months. • For persons initiating vaccination at age 15 years or older, the recommended immunization schedule is 3 doses of HPV vaccine at 0, 1-2, 6 months. • A vaccine dose administered at a shorter interval should be readministered at the recommended interval. ▪ In a 2-dose schedule of HPV vaccine, the minimum interval is 5 months between the first and second dose.
If the second dose is administered at a shorter interval, a third dose should be administered a minimum of 12 weeks after the second dose and a minimum of 5 months after the first dose. ▪ In a 3-dose schedule of HPV vaccine, the minimum intervals are 4 weeks between the first and second dose, 12 weeks between the second and third dose, and 5 months between the first and third dose. If a vaccine dose is administered at a shorter interval, it should be readministered after another minimum interval has been met since the most recent dose.
# Special populations:
• For children with history of sexual abuse or assault, administer HPV vaccine beginning at age 9 years. • Immunocompromised persons*, including those with human immunodeficiency virus (HIV) infection, should receive a 3-dose series at 0, 1-2, and 6 months, regardless of age at vaccine initiation. • Note: HPV vaccination is not recommended during pregnancy, although there is no evidence that the vaccine poses harm. If a woman is found to be pregnant after initiating the vaccination series, no intervention is needed; the remaining vaccine doses should be delayed until after the pregnancy. | None | None |
79d22442c180f2a08eb777d92530249cfd6c0c6a | cdc | African Tick Bite Fever | African Tick Bite Fever | Disease Directory | Travelers' Health | CDC
### African Tick Bite Fever
### What is African tick bite fever?
African tick bite fever is a disease caused by a bacteria. You can get infected if you are bitten by an infected tick.
Symptoms usually appear within two weeks after a tick bite. The first sign is often a red sore that develops a dark crust, called an eschar. Eschars are found at the site of tick bite; multiple eschars may be present if you have multiple tick bites. Later symptoms may include fever, headache, muscle soreness, swollen lymph nodes, and a rash.
African tick bite fever is the most common disease travelers report getting from tick bites.
### Who is at risk?
Travelers to sub-Saharan Africa, parts of the Caribbean, and Oceania (Australia, New Zealand, Melanesia, Micronesia, and Polynesia are at risk for African tick bite fever. You are at higher risk if your travel plans include outdoor activities such as camping, hiking, and game hunting in wooded, brushy, or grassy areas.
Ticks that are infected with bacteria that cause African tick bite fever are usually most active from November through April.
### What can travelers do to prevent African tick bite fever?
There are no vaccines that prevent African tick bite fever. Travelers can protect themselves from infection by taking the following precautions:
Prevent Tick Bites
- Know where to expect ticks. Ticks live in grassy, brushy, or wooded areas, or even on animals. Spending time outside camping, gardening, or hunting could bring you in close contact with ticks. Many people get ticks in their own yard or neighborhood.
- Treat clothing and gear with products containing 0.5% permethrin. Permethrin can be used to treat boots, clothing and camping gear and remain protective through several washings. Alternatively, you can buy permethrin-treated clothing and gear.
- Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) containing DEET, picaridin, IR3535, Oil of Lemon Eucalyptus (OLE), para-menthane-diol (PMD), or 2-undecanone. EPA’s helpful [search tool](https://www.epa.gov/insect-repellents/find-insect-repellent-right-you) can help you find the product that best suits your needs. Always follow product instructions. Do not use products containing OLE or PMD on children under 3 years old.
- Avoid Contact with Ticks
- Avoid wooded and brushy areas with high grass and leaf litter.
- Walk in the center of trails.
Find and Remove Ticks
- Check your clothing for ticks. Ticks may be carried into the house on clothing. Any ticks that are found should be removed. When possible, tumble dry clothes in a dryer on high heat for 10 minutes to kill ticks on dry clothing after you come indoors. If the clothes are damp, additional time may be needed. If the clothes require washing first, hot water is recommended. Cold and medium temperature water will not kill ticks.
- Examine gear and pets. Ticks can ride on clothing and pets, then attach to a person later, so carefully examine pets, coats, and daypacks.
- Shower soon after being outdoors. Showering within two hours of coming indoors has been shown to reduce your risk of getting tick-borne diseases. Showering may help wash off unattached ticks and it is a good opportunity to do a tick check.
- Check your body for ticks. Conduct a full body check upon return from potentially tick-infested areas. Use a hand-held or full-length mirror to view all parts of your body. Check these parts of your body for ticks:
- Under the arms
- In and around the ears
- Inside belly button
- Back of the knees
- In and around the hair
- Between the legs
- Around the waist
- If you find a tick attached to your skin, simply remove the tick as soon as possible.
|
### African Tick Bite Fever
### What is African tick bite fever?
African tick bite fever is a disease caused by a bacteria. You can get infected if you are bitten by an infected tick.
Symptoms usually appear within two weeks after a tick bite. The first sign is often a red sore that develops a dark crust, called an eschar. Eschars are found at the site of tick bite; multiple eschars may be present if you have multiple tick bites. Later symptoms may include fever, headache, muscle soreness, swollen lymph nodes, and a rash.
African tick bite fever is the most common disease travelers report getting from tick bites.
### Who is at risk?
Travelers to sub-Saharan Africa, parts of the Caribbean, and Oceania (Australia, New Zealand, Melanesia, Micronesia, and Polynesia are at risk for African tick bite fever. You are at higher risk if your travel plans include outdoor activities such as camping, hiking, and game hunting in wooded, brushy, or grassy areas.
Ticks that are infected with bacteria that cause African tick bite fever are usually most active from November through April.
### What can travelers do to prevent African tick bite fever?
There are no vaccines that prevent African tick bite fever. Travelers can protect themselves from infection by taking the following precautions:
**Prevent Tick Bites**
* **Know where to expect ticks.** Ticks live in grassy, brushy, or wooded areas, or even on animals. Spending time outside camping, gardening, or hunting could bring you in close contact with ticks. Many people get ticks in their own yard or neighborhood.
* **Treat clothing and gear** with products containing 0.5% permethrin. Permethrin can be used to treat boots, clothing and camping gear and remain protective through several washings. Alternatively, you can buy permethrin-treated clothing and gear.
* **Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents)** containing DEET, picaridin, IR3535, Oil of Lemon Eucalyptus (OLE), para-menthane-diol (PMD), or 2-undecanone. EPA’s helpful [search tool](https://www.epa.gov/insect-repellents/find-insect-repellent-right-you) can help you find the product that best suits your needs. Always follow product instructions. Do not use products containing OLE or PMD on children under 3 years old.
* **Avoid Contact with Ticks**
+ Avoid wooded and brushy areas with high grass and leaf litter.
+ Walk in the center of trails.

**Find and Remove Ticks**
* **Check your clothing for ticks.** Ticks may be carried into the house on clothing. Any ticks that are found should be removed. When possible, tumble dry clothes in a dryer on high heat for 10 minutes to kill ticks on dry clothing after you come indoors. If the clothes are damp, additional time may be needed. If the clothes require washing first, hot water is recommended. Cold and medium temperature water will not kill ticks.
* **Examine gear and pets.** Ticks can ride on clothing and pets, then attach to a person later, so carefully examine pets, coats, and daypacks.
* **Shower soon after being outdoors.** Showering within two hours of coming indoors has been shown to reduce your risk of getting tick-borne diseases. Showering may help wash off unattached ticks and it is a good opportunity to do a tick check.
* **Check your body for ticks.** Conduct a full body check upon return from potentially tick-infested areas. Use a hand-held or full-length mirror to view all parts of your body. Check these parts of your body for ticks:
+ Under the arms
+ In and around the ears
+ Inside belly button
+ Back of the knees
+ In and around the hair
+ Between the legs
+ Around the waist
* If you find a tick attached to your skin, simply remove the tick as soon as possible.
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [Avoid Bug Bites](/travel/page/avoid-bug-bites)
* [Preventing Tick Bites](https://www.cdc.gov/ticks/avoid/on_people.html)
* [Other Tick-borne Spotted Fever Rickettsial Infections](http://www.cdc.gov/otherspottedfever/)
* CDC Yellow Book: [Rickettsial Diseases](/travel/yellowbook/2012/chapter-3-infectious-diseases-related-to-travel/rickettsial-spotted-and-typhus-fevers-and-related-infections-anaplasmosis-and-ehrlichiosis.htm)
| None | None |
0c5338103fa83aa1c9eb3b9530149c3fd784db5d | cdc | African Trypanosomiasis (African Sleeping Sickness) | African Trypanosomiasis (African Sleeping Sickness) | Disease Directory | Travelers' Health | CDC
### African Trypanosomiasis (African Sleeping Sickness)
### What is African trypanosomiasis?
African trypanosomiasis, also called sleeping sickness, is a disease caused by a parasite. People can get this parasite when an infected Tsetse fly bites them.
Symptoms include fatigue, high fever, headaches, and muscle aches. If the disease is not treated, it can cause death.
### Who is at risk?
Tsetse flies are found in sub-Saharan Africa. Travelers spending a lot of time outdoors or visiting game parks in these areas can be bitten by tsetse flies and get infected.
### What can travelers do to prevent African trypanosomiasis?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" - value;
if (value == '0'){
window.location = "/travel/destinations/list";
window.location = url;
There is no vaccine or medicine that prevents African trypanosomiasis. Travelers can protect themselves by preventing tsetse fly bites.
Prevent tsetse fly bites by taking the following steps:
- Cover exposed skin by wearing long-sleeved shirts, long pants, and hats.
- Clothing fabric should be at least medium weight because the tsetse fly can bite through thin fabric.
- Wear neutral-colored clothing. The tsetse fly is attracted to bright colors, very dark colors, metallic fabric, particularly the colors blue and black.
- Avoid bushes during the day; the fly rests in bushes and will bite if disturbed.
- Inspect vehicles for tsetse flies before entering. The flies are attracted to the motion and dust from moving vehicles.
- Although, there is limited evidence that insect repellent works against tsetse flies, you should still use insect repellent as it can prevent other diseases spread by bug bites. [Learn more about how to avoid other bug bites.](/travel/page/avoid-bug-bites)
|
### African Trypanosomiasis (African Sleeping Sickness)
### What is African trypanosomiasis?

African trypanosomiasis, also called sleeping sickness, is a disease caused by a parasite. People can get this parasite when an infected Tsetse fly bites them.
Symptoms include fatigue, high fever, headaches, and muscle aches. If the disease is not treated, it can cause death.
### Who is at risk?
Tsetse flies are found in sub-Saharan Africa. Travelers spending a lot of time outdoors or visiting game parks in these areas can be bitten by tsetse flies and get infected.
### What can travelers do to prevent African trypanosomiasis?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
function goSelectPage(){
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" + value;
if (value == '0'){
window.location = "/travel/destinations/list";
}else{
window.location = url;
}
}
There is no vaccine or medicine that prevents African trypanosomiasis. Travelers can protect themselves by preventing tsetse fly bites.
**Prevent tsetse fly bites by taking the following steps****:**
* Cover exposed skin by wearing long-sleeved shirts, long pants, and hats.
+ Clothing fabric should be at least medium weight because the tsetse fly can bite through thin fabric.
+ Wear neutral-colored clothing. The tsetse fly is attracted to bright colors, very dark colors, metallic fabric, particularly the colors blue and black.
* Avoid bushes during the day; the fly rests in bushes and will bite if disturbed.
* Inspect vehicles for tsetse flies before entering. The flies are attracted to the motion and dust from moving vehicles.
* Although, there is limited evidence that insect repellent works against tsetse flies, you should still use insect repellent as it can prevent other diseases spread by bug bites. [Learn more about how to avoid other bug bites.](/travel/page/avoid-bug-bites)
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [African Trypanosomiasis](http://www.cdc.gov/parasites/sleepingsickness/)
* [Avoid Bug Bites](/travel/page/avoid-bug-bites)
* CDC Yellow Book: [Trypanosomiasis-African](/travel/yellowbook/2020/travel-related-infectious-diseases/trypanosomiasis-african-sleeping-sickness) in CDC Yellow Book
| None | None |
4027ce748d26a248496ee0d429829b89222df893 | cdc | Avian Flu (Bird Flu) | Avian Flu (Bird Flu) | Disease Directory | Travelers' Health | CDC
### Avian Flu (Bird Flu)
### What is avian flu (bird flu)?
Avian influenza, also called bird flu, is caused by a virus that usually infects wild and domestic birds. Wild birds that carry bird flu viruses include migratory waterbirds, like ducks, geese and swans, and shorebirds, like storks. Bird flu viruses can easily spread from wild birds to domestic poultry, like chickens, turkeys, geese, and pheasants. The virus is found in an infected bird’s feces (poop) and fluids from the bird’s eyes, nose, or mouth.
Bird flu viruses don’t usually infect people. However, this can happen if you:
- Touch your eyes, nose, or mouth after handling infected live or dead birds.
- Touch surfaces or handle items contaminated by bird flu viruses and touch your eyes, nose, or mouth.
- Breathe in droplets or dust contaminated with the virus.
People who get sick with bird flu can have no symptoms to severe illness. Some people have mild symptoms, including eye redness (conjunctivitis), cough, sore throat, runny or stuffy nose, muscle or body aches, headaches, and tiredness. More serious symptoms include high fever, shortness of breath, and difficulty breathing. People with severe disease can develop pneumonia that may require hospitalization. Less common signs and symptoms include diarrhea, nausea, vomiting, or seizures.
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" - value;
if (value == '0'){
window.location = "/travel/destinations/list";
window.location = url;
### Can travelers get bird flu?
Most travelers are unlikely to get bird flu. However, travelers who work with animals, such as veterinarians, farmers, animal industry experts, and wildlife professionals, or people who visit poultry farms or live-animal markets may be at higher risk.
### What can travelers do to prevent bird flu?
Do not touch birds and avoid visiting places where birds live
- Avoid visiting poultry farms, live animal markets, and other places where live poultry are raised, kept, slaughtered, or sold. If you must visit such places, wear a well-fitting facemask and avoid touching poultry or other birds.
- If you visit wetlands or other outdoor places where birds live, make sure you take steps to [avoid germs](#germs) during and after your visit.
- Avoid touching sick or dead wild birds or poultry.
- Wash your hands often with soap and water for at least 20 seconds, especially after having contact with or being around birds or places where birds are kept or touching uncooked poultry.
- If soap and water aren’t available, clean hands with hand sanitizer containing at least 60% alcohol.
- Avoid touching your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean.
- Avoid close contact, such as kissing, hugging, or sharing eating utensils or cups with people who are sick.
|
### Avian Flu (Bird Flu)
### What is avian flu (bird flu)?
Avian influenza, also called bird flu, is caused by a virus that usually infects wild and domestic birds. Wild birds that carry bird flu viruses include migratory waterbirds, like ducks, geese and swans, and shorebirds, like storks. Bird flu viruses can easily spread from wild birds to domestic poultry, like chickens, turkeys, geese, and pheasants. The virus is found in an infected bird’s feces (poop) and fluids from the bird’s eyes, nose, or mouth.

Bird flu viruses don’t usually infect people. However, this can happen if you:
* Touch your eyes, nose, or mouth after handling infected live or dead birds.
* Touch surfaces or handle items contaminated by bird flu viruses and touch your eyes, nose, or mouth.
* Breathe in droplets or dust contaminated with the virus.
People who get sick with bird flu can have no symptoms to severe illness. Some people have mild symptoms, including eye redness (conjunctivitis), cough, sore throat, runny or stuffy nose, muscle or body aches, headaches, and tiredness. More serious symptoms include high fever, shortness of breath, and difficulty breathing. People with severe disease can develop pneumonia that may require hospitalization. Less common signs and symptoms include diarrhea, nausea, vomiting, or seizures.
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
function goSelectPage(){
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" + value;
if (value == '0'){
window.location = "/travel/destinations/list";
}else{
window.location = url;
}
}
### Can travelers get bird flu?
Most travelers are unlikely to get bird flu. However, travelers who work with animals, such as veterinarians, farmers, animal industry experts, and wildlife professionals, or people who visit poultry farms or live-animal markets may be at higher risk.
### What can travelers do to prevent bird flu?
**Do not touch birds and avoid visiting places where birds live**
* Avoid visiting poultry farms, live animal markets, and other places where live poultry are raised, kept, slaughtered, or sold. If you must visit such places, wear a well-fitting facemask and avoid touching poultry or other birds.
* If you visit wetlands or other outdoor places where birds live, make sure you take steps to [avoid germs](#germs) during and after your visit.
* Avoid touching sick or dead wild birds or poultry.
**Avoid Germs**
* Wash your hands often with soap and water for at least 20 seconds, especially after having contact with or being around birds or places where birds are kept or touching uncooked poultry.
* If soap and water aren’t available, clean hands with hand sanitizer containing at least 60% alcohol.
* Avoid touching your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean.
* Avoid close contact, such as kissing, hugging, or sharing eating utensils or cups with people who are sick.
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. Avoid contact with other people while you are sick.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [Avian Influenza](https://www.cdc.gov/flu/avianflu/index.htm)
* [Bird Flu Virus Infections in Humans](https://wwwdev.cdc.gov/flu/avianflu/avian-in-humans.htm#symptoms)
* CDC Yellow Book: [Influenzas (including Avian)](/travel/yellowbook/2020/travel-related-infectious-diseases/influenza)
| None | None |
9669850841423f59ed63ccbc6a1cef67c3cb1e40 | cdc | COVID-19 | COVID-19 | Disease Directory | Travelers' Health | CDC
As of 12:01 am EDT May 12, 2023, noncitizen nonimmigrant air passengers no longer need to show proof of being fully vaccinated with an accepted COVID-19 vaccine to board a flight to the United States. [See more information](https://www.cdc.gov/quarantine/order-safe-travel.html).
### What is COVID-19?
Coronavirus disease 2019 (COVID-19) is a respiratory illness caused by the virus SARS-CoV-2. The virus spreads mainly from person to person through respiratory droplets and small particles produced when an infected person coughs, sneezes, or talks. The virus spreads easily in crowded or poorly ventilated indoor settings.
People with COVID-19 have reported a [wide range of symptoms](https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html) – ranging from no or mild symptoms to severe illness. Symptoms may appear 2–14 days after exposure to the virus. Possible symptoms include fever, chills, cough, shortness of breath, fatigue, muscle aches, headache, new loss of taste and smell, sore throat, runny nose, nausea, vomiting, or diarrhea.
### Who can get COVID-19?
Anyone can get COVID-19. However, some people are more likely than others to get very sick if they get COVID-19. These include people who are older, are [immunocompromised](https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-who-are-immunocompromised.html), or have certain [disabilities](https://www.cdc.gov/ncbddd/humandevelopment/covid-19/people-with-disabilities.html), or have [underlying health conditions](https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html). Vaccination, past infection, and timely access to testing and treatment can help protect you from getting very sick from COVID-19.
### Can I travel if I recently had COVID-19?
Yes, you can travel once you have ended [isolation](https://www.cdc.gov/coronavirus/2019-ncov/your-health/isolation.html). Check [CDC guidance](https://www.cdc.gov/coronavirus/2019-ncov/your-health/isolation.html#removing-mask) for additional precautions, including testing and wearing a mask around others. If you recently had COVID-19 and are recommended to wear a mask, do not travel on public transportation such as airplanes, buses, and trains if you are unable to wear a mask whenever around others.
### What can travelers do to prevent COVID-19?
Get [up to date](https://www.cdc.gov/coronavirus/2019-ncov/vaccines/stay-up-to-date.html) with your COVID-19 vaccines before you travel and take steps to [protect yourself and others](https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html). Consider [wearing a mask](/travel/page/masks) in crowded or poorly ventilated indoor areas, including on public transportation and in transportation hubs. Take [additional precautions](https://www.cdc.gov/coronavirus/2019-ncov/your-health/if-you-were-exposed.html) if you were recently exposed to a person with COVID-19. Don’t travel while sick.
If you have a [weakened immune system](https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-who-are-immunocompromised.html) or [are at increased risk for severe disease](https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html) talk to a healthcare professional before you decide to travel. If you travel, take multiple prevention steps to provide additional layers of protection from COVID-19, even if you are up to date with your COVID-19 vaccines. These include improving ventilation and spending more time outdoors, avoiding sick people, [getting tested for COVID-19](https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/testing.html) if you develop symptoms, staying home if you have or think you have COVID-19, and seeking treatment if you have COVID-19.
Consider getting a COVID-19 test if you:
- Develop COVID-19 symptoms before, during, or after travel.
- Will be traveling to visit someone who is at higher risk of getting very sick from COVID-19.
- Were in a situation with a greater risk of exposure during travel (e.g., in an indoor, crowded space like an airport terminal while not wearing a mask).
If you traveled and feel sick, particularly if you have a fever, talk to a healthcare professional, and tell them about your recent travel.
|
### COVID-19
As of 12:01 am EDT May 12, 2023, noncitizen nonimmigrant air passengers no longer need to show proof of being fully vaccinated with an accepted COVID-19 vaccine to board a flight to the United States. [See more information](https://www.cdc.gov/quarantine/order-safe-travel.html).
### What is COVID-19?
Coronavirus disease 2019 (COVID-19) is a respiratory illness caused by the virus SARS-CoV-2. The virus spreads mainly from person to person through respiratory droplets and small particles produced when an infected person coughs, sneezes, or talks. The virus spreads easily in crowded or poorly ventilated indoor settings.
People with COVID-19 have reported a [wide range of symptoms](https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html) – ranging from no or mild symptoms to severe illness. Symptoms may appear 2–14 days after exposure to the virus. Possible symptoms include fever, chills, cough, shortness of breath, fatigue, muscle aches, headache, new loss of taste and smell, sore throat, runny nose, nausea, vomiting, or diarrhea.
### Who can get COVID-19?
Anyone can get COVID-19. However, some people are more likely than others to get very sick if they get COVID-19. These include people who are older, are [immunocompromised](https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-who-are-immunocompromised.html), or have certain [disabilities](https://www.cdc.gov/ncbddd/humandevelopment/covid-19/people-with-disabilities.html), or have [underlying health conditions](https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html). Vaccination, past infection, and timely access to testing and treatment can help protect you from getting very sick from COVID-19.
### Can I travel if I recently had COVID-19?
Yes, you can travel once you have ended [isolation](https://www.cdc.gov/coronavirus/2019-ncov/your-health/isolation.html). Check [CDC guidance](https://www.cdc.gov/coronavirus/2019-ncov/your-health/isolation.html#removing-mask) for additional precautions, including testing and wearing a mask around others. If you recently had COVID-19 and are recommended to wear a mask, do not travel on public transportation such as airplanes, buses, and trains if you are unable to wear a mask whenever around others.
### What can travelers do to prevent COVID-19?
Get [**up to date**](https://www.cdc.gov/coronavirus/2019-ncov/vaccines/stay-up-to-date.html) with your COVID-19 vaccines before you travel and take steps to [protect yourself and others](https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html). Consider [wearing a mask](/travel/page/masks) in crowded or poorly ventilated indoor areas, including on public transportation and in transportation hubs. Take [additional precautions](https://www.cdc.gov/coronavirus/2019-ncov/your-health/if-you-were-exposed.html) if you were recently exposed to a person with COVID-19. Don’t travel while sick.
If you have a [weakened immune system](https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-who-are-immunocompromised.html) or [are at increased risk for severe disease](https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html) talk to a healthcare professional before you decide to travel. If you travel, take multiple prevention steps to provide additional layers of protection from COVID-19, even if you are up to date with your COVID-19 vaccines. These include improving ventilation and spending more time outdoors, avoiding sick people, [getting tested for COVID-19](https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/testing.html) if you develop symptoms, staying home if you have or think you have COVID-19, and seeking treatment if you have COVID-19.
**Consider getting [travel insurance](/travel/page/insurance)** in case you need [medical care abroad](/travel/page/health-care-during-travel).
**Consider getting a COVID-19 test if you:**
* Develop COVID-19 symptoms before, during, or after travel.
* Will be traveling to visit someone who is at higher risk of getting very sick from COVID-19.
* Were in a situation with a greater risk of exposure during travel (e.g., in an indoor, crowded space like an airport terminal while not wearing a mask).
**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare professional, and tell them about your recent travel.
### More Information
* [COVID-19](https://www.cdc.gov/coronavirus/2019-ncov/index.html)
* [Masking During Travel](/travel/page/masks)
| None | None |
0ad0c9f56d5636aae816878b659ebb4b49d3f6f9 | cdc | Chagas Disease (American Trypanosomiasis) | Chagas Disease (American Trypanosomiasis) | Disease Directory | Travelers' Health | CDC
### Chagas Disease (American Trypanosomiasis)
### What is Chagas Disease (American Trypanosomiasis)?
American trypanosomiasis, also known as Chagas disease, is caused by a parasite. This parasite lives in the poop of [triatomine (kissing) bugs](https://www.cdc.gov/parasites/chagas/gen_info/vectors/index.html). The bug often poops when it bites. Most people get Chagas disease by unknowingly rubbing triatomine bug poop into the bug bite when they scratch the bite. People may also accidentally get triatomine bug poop in their eyes and mouth.
A few people experience swelling around the bite area. However, most people never have symptoms, but remain infected throughout their lives.
About 1 out of 3 people who get Chagas disease will develop more serious symptoms later in life, including heart conditions or gastrointestinal problems. These later symptoms can occur whether a person has early symptoms or not.
### Who is at risk?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" - value;
if (value == '0'){
window.location = "/travel/destinations/list";
window.location = url;
Chagas disease is spread by triatomine bugs in parts of Mexico, Central America, and South America, especially rural areas.
Most travelers to these areas don’t need to worry about Chagas disease. Travelers who sleep outdoors or stay in poorly constructed housing are more likely to get bitten by triatomine bugs.
### What can travelers do to prevent Chagas disease?
There is no vaccine or medicine to prevent Chagas disease. Travelers can protect themselves by taking a few steps.
Avoid Bug Bites
- Stay and sleep in screened or air-conditioned rooms.
- Avoid sleeping in thatch, mud, and adobe housing in areas with triatomine bugs; use insecticides in and around such homes. Insecticide-treated bed nets are helpful
- Cover exposed skin by wearing long-sleeved shirts, long pants, and hats.
- Use EPA-registered insect repellents with one of the following active ingredients: DEET, picaridin, IR3535, oil of lemon eucalyptus (OLE), para-menthane-diol (PMD), or 2-undecanone. [Find an EPA-registered insect repellent that’s right for you.](https://www.epa.gov/insect-repellents/find-repellent-right-you)
- Always follow product directions and reapply as directed.
- If you are also using sunscreen, apply sunscreen first and insect repellent second.
- When using insect repellent on children
- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.
- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.
- Adults: Spray insect repellent onto your hands and then apply to a child’s face.
- Use [permethrin-treated](http://npic.orst.edu/pest/mosquito/ptc.html) clothing and gear (such as boots, pants, socks, and tents). You can buy pre-treated clothing and gear or treat them yourself:
- Treated clothing remains protective after multiple washings. See the product information to find out how long the protection will last.
- If treating items yourself, follow the product instructions carefully.
- Do not use permethrin directly on skin.
|
### Chagas Disease (American Trypanosomiasis)
### What is Chagas Disease (American Trypanosomiasis)?

American trypanosomiasis, also known as Chagas disease, is caused by a parasite. This parasite lives in the poop of [triatomine (kissing) bugs](https://www.cdc.gov/parasites/chagas/gen_info/vectors/index.html). The bug often poops when it bites. Most people get Chagas disease by unknowingly rubbing triatomine bug poop into the bug bite when they scratch the bite. People may also accidentally get triatomine bug poop in their eyes and mouth.
A few people experience swelling around the bite area. However, most people never have symptoms, but remain infected throughout their lives.
About 1 out of 3 people who get Chagas disease will develop more serious symptoms later in life, including heart conditions or gastrointestinal problems. These later symptoms can occur whether a person has early symptoms or not.
### Who is at risk?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
function goSelectPage(){
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" + value;
if (value == '0'){
window.location = "/travel/destinations/list";
}else{
window.location = url;
}
}
Chagas disease is spread by triatomine bugs in parts of Mexico, Central America, and South America, especially rural areas.
Most travelers to these areas don’t need to worry about Chagas disease. Travelers who sleep outdoors or stay in poorly constructed housing are more likely to get bitten by triatomine bugs.
### What can travelers do to prevent Chagas disease?
There is no vaccine or medicine to prevent Chagas disease. Travelers can protect themselves by taking a few steps.
**Avoid Bug Bites**
* Stay and sleep in screened or air-conditioned rooms.
+ Avoid sleeping in thatch, mud, and adobe housing in areas with triatomine bugs; use insecticides in and around such homes. Insecticide-treated bed nets are helpful
* Cover exposed skin by wearing long-sleeved shirts, long pants, and hats.
* Use EPA-registered insect repellents with one of the following active ingredients: DEET, picaridin, IR3535, oil of lemon eucalyptus (OLE), para-menthane-diol (PMD), or 2-undecanone. [Find an EPA-registered insect repellent that’s right for you.](https://www.epa.gov/insect-repellents/find-repellent-right-you)
+ Always follow product directions and reapply as directed.
+ If you are also using sunscreen, apply sunscreen first and insect repellent second.
* When using insect repellent on children
+ Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.
+ Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.
+ Adults: Spray insect repellent onto your hands and then apply to a child’s face.
* Use [permethrin-treated](http://npic.orst.edu/pest/mosquito/ptc.html) clothing and gear (such as boots, pants, socks, and tents). You can buy pre-treated clothing and gear or treat them yourself:
+ Treated clothing remains protective after multiple washings. See the product information to find out how long the protection will last.
+ If treating items yourself, follow the product instructions carefully.
+ Do **not** use permethrin directly on skin.
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [Chagas disease FAQs](http://www.cdc.gov/parasites/chagas/gen_info/detailed.html)
* [Avoid Bug Bites](/travel/page/avoid-bug-bites)
* CDC Yellow Book: [Trypanosomiasis-American](/travel/yellowbook/2020/travel-related-infectious-diseases/trypanosomiasis-american-chagas-disease)
| None | None |
5988115fc031f78f112c25d8b06db12bf01075ba | cdc | Chikungunya | Chikungunya | Disease Directory | Travelers' Health | CDC
### What is chikungunya?

Chikungunya virus is spread to people by the bite of an infected mosquito. Mosquitoes become infected when they feed on a person already infected with the virus. Infected mosquitoes can then spread the virus to other people through bites.
Symptoms usually begin 3–7 days after being bitten by an infected mosquito. The most common [symptoms](http://www.cdc.gov/chikungunya/symptoms/index.html) of chikungunya are fever and joint pain. Other symptoms include headache, muscle pain, joint swelling, or rash. Most people feel better within a week. In some people the joint pain may persist for months.
### Who is at risk?
The mosquitoes that spread chikungunya virus are found in many countries throughout the world. Travelers going to countries in Africa, Asia, the Americas, and islands in the Indian and Pacific Oceans might be at risk for infection.
Mosquitoes that spread chikungunya bite during the day and at night.
### What can travelers do to prevent chikungunya?
There are no vaccines or medicines that prevent chikungunya. Travelers can protect themselves against infection by taking the following steps.
Use an EPA-registered insect repellent
- Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.
- Picaridin (known as KBR 3023 and icaridin outside the US)
- Oil of lemon eucalyptus (OLE)
- Para-menthane-diol (PMD)
Find the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).

- Insect Repellent Tips for Babies and Children
- Dress your child in clothing that covers arms and legs.
- Cover strollers and baby carriers with mosquito netting.
- When using insect repellent on your child:
- Always follow label instructions.
- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.
- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.
- Adults: Spray insect repellent onto your hands and then apply to a child’s face.
- If also using sunscreen, always apply insect repellent after sunscreen.
Wear long-sleeved shirts and long pants
Treat clothing and gear with permethrin
- Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.
- Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.
- Permethrin-treated clothing provides protection after multiple washings.
- Read product information to find out how long the protection will last.
- If treating items yourself, follow the product instructions.
- Do not use permethrin products directly on skin.
- Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).
Keep mosquitoes out of your hotel room or lodging
- Choose a hotel or lodging with air conditioning or window and door screens.
- Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.
Sleep under a mosquito net

- Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.
- Buy a mosquito net at your local outdoor store or online before traveling overseas.
- Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.
- [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.
- Permethrin is an insecticide that kills mosquitoes and other insects.
- To determine if you can wash a treated mosquito net, follow the label instructions.
If you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).
If you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment.](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html)
|
### Chikungunya
### What is chikungunya?

Chikungunya virus is spread to people by the bite of an infected mosquito. Mosquitoes become infected when they feed on a person already infected with the virus. Infected mosquitoes can then spread the virus to other people through bites.
Symptoms usually begin 3–7 days after being bitten by an infected mosquito. The most common [symptoms](http://www.cdc.gov/chikungunya/symptoms/index.html) of chikungunya are fever and joint pain. Other symptoms include headache, muscle pain, joint swelling, or rash. Most people feel better within a week. In some people the joint pain may persist for months.
### Who is at risk?
The mosquitoes that spread chikungunya virus are found in many countries throughout the world. Travelers going to countries in Africa, Asia, the Americas, and islands in the Indian and Pacific Oceans might be at risk for infection.
Mosquitoes that spread chikungunya bite during the day and at night.
### What can travelers do to prevent chikungunya?
There are no vaccines or medicines that prevent chikungunya. Travelers can protect themselves against infection by taking the following steps.
**Use an EPA-registered insect repellent**

* Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.
+ DEET
+ Picaridin (known as KBR 3023 and icaridin outside the US)
+ IR3535
+ Oil of lemon eucalyptus (OLE)
+ Para-menthane-diol (PMD)
+ 2-undecanone
Find the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).

* Insect Repellent Tips for Babies and Children
+ Dress your child in clothing that covers arms and legs.
+ Cover strollers and baby carriers with mosquito netting.
+ When using insect repellent on your child:
- Always follow label instructions.
- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.
- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.
* Adults: Spray insect repellent onto your hands and then apply to a child’s face.
- If also using sunscreen, always apply insect repellent after sunscreen.
**Wear long-sleeved shirts and long pants**
**Treat clothing and gear with permethrin**

* Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.
+ Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.
+ Permethrin-treated clothing provides protection after multiple washings.
+ Read product information to find out how long the protection will last.
* If treating items yourself, follow the product instructions.
* Do not use permethrin products directly on skin.
* Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).
**Keep mosquitoes out of your hotel room or lodging**
* Choose a hotel or lodging with air conditioning or window and door screens.
* Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.
**Sleep under a mosquito net**

* Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.
* Buy a mosquito net at your local outdoor store or online before traveling overseas.
* Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.
* [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.
+ Permethrin is an insecticide that kills mosquitoes and other insects.
+ To determine if you can wash a treated mosquito net, follow the label instructions.
If you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).
If you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment.](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html)
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### Traveler Information
* [Avoid Bug Bites](/travel/page/avoid-bug-bites)
* [Chikungunya Prevention](https://www.cdc.gov/chikungunya/prevention/index.html)
* [CDC Chikungunya website](http://www.cdc.gov/chikungunya/)
### Clinician Information
* [Chikungunya](/travel/yellowbook/2012/chapter-3-infectious-diseases-related-to-travel/chikungunya.htm) in CDC Yellow Book
| None | None |
690cc6098820658c544492c061c73016e6fc4032 | cdc | Cholera | Cholera | Disease Directory | Travelers' Health | CDC
### What is cholera?

Cholera can be a life-threatening disease caused by bacteria called - Vibrio cholerae- .
A person can get cholera from unsafe food or water. This can happen when cholera bacteria spread from a person into drinking water or water used to grow food or prepare food. This can also happen when stool (poop) in sewage gets into the water supply.
Most people who get Cholera will have mild or no symptoms. About 1 in 10 people with cholera will experience severe symptoms. Early [cholera symptoms](https://www.cdc.gov/cholera/illness.html) include the following:
- Profuse watery diarrhea, sometimes described as “rice-water stools”
- Increased thirst
- Leg cramps
- Restlessness or irritability
People who are seriously ill with cholera can develop severe dehydration, leading to kidney failure and death.
### Who is at risk?
People who live in or travel to places where cholera is common are at the highest risk of getting the disease. Cholera in travelers is extremely rare but can occur in some situations such as among people visiting friends or family, health care workers, and response workers in outbreak settings.
CDC considers the countries below to have areas of active cholera transmission. For information about the level of cholera transmission and where it is occurring in a country, check the cholera section on an affected country’s [destination page](/travel/destinations/list).
- Africa: [Burundi](/travel/destinations/traveler/none/burundi), [Cameroon](/travel/destinations/traveler/none/cameroon), [Democratic Republic of the Congo](/travel/destinations/traveler/none/democratic-republic-of-congo), [Ethiopia](/travel/destinations/traveler/none/ethiopia), [Kenya](/travel/destinations/traveler/none/kenya), [Malawi](/travel/destinations/traveler/none/malawi), [Mozambique](/travel/destinations/traveler/none/mozambique), [Niger](/travel/destinations/traveler/none/niger), [Nigeria](/travel/destinations/traveler/none/nigeria), [Somalia](/travel/destinations/traveler/none/somalia), [South Africa](/travel/destinations/traveler/none/south-africa), [South Sudan](/travel/destinations/traveler/none/south-sudan), [Tanzania](/travel/destinations/traveler/none/tanzania), [Zambia](/travel/destinations/traveler/none/zambia), [Zimbabwe](/travel/destinations/traveler/none/zimbabwe)
- Asia: [Afghanistan](/travel/destinations/traveler/none/afghanistan), [Bangladesh](/travel/destinations/traveler/none/bangladesh), [India](/travel/destinations/traveler/none/india), [Nepal](/travel/destinations/traveler/none/nepal), [Pakistan](/travel/destinations/traveler/none/pakistan), [Philippines](/travel/destinations/traveler/none/philippines)
- Middle East: [Iraq](/travel/destinations/traveler/none/iraq), [Lebanon](/travel/destinations/traveler/none/lebanon), [Syria](/travel/destinations/traveler/none/syria), [Yemen](/travel/destinations/traveler/none/yemen)
- Americas: [Dominican Republic](/travel/destinations/traveler/none/dominican-republic), [Haiti](/travel/destinations/traveler/none/haiti)
- Pacific: none
### What can travelers do to prevent cholera?
You can protect yourself against cholera by taking the following steps.
#### Choose safer food and drinks while traveling
Follow [food and drink safety tips](/travel/page/food-water-safety) to lower your chance of getting cholera through unsafe food and drinks.
#### Wash your hands often
- Wash your hands with soap and water. If soap and water aren’t available, clean hands with hand sanitizer (containing at least 60% alcohol).
- Don’t touch your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean.
- Cover your mouth and nose with a tissue or your sleeve (not your hands) when coughing or sneezing.
### How is cholera treated?
The most important step in treating cholera is to drink plenty of fluids. People who are severely ill might need intravenous (IV) fluids. Antibiotics are recommended for people who are severely ill or may become severely ill, such as pregnant people and children. [Zinc treatment](https://www.cdc.gov/cholera/treatment/zinc-treatment.html) has also been shown to help improve cholera symptoms among children 3 to 14 years of age and shorten acute diarrhea for children more than six months of age.
|
### Cholera
### What is cholera?

Cholera can be a life-threatening disease caused by bacteria called *Vibrio cholerae*.
A person can get cholera from unsafe food or water. This can happen when cholera bacteria spread from a person into drinking water or water used to grow food or prepare food. This can also happen when stool (poop) in sewage gets into the water supply.
Most people who get Cholera will have mild or no symptoms. About 1 in 10 people with cholera will experience severe symptoms. Early [cholera symptoms](https://www.cdc.gov/cholera/illness.html) include the following:
* Profuse watery diarrhea, sometimes described as “rice-water stools”
* Vomiting
* Increased thirst
* Leg cramps
* Restlessness or irritability
People who are seriously ill with cholera can develop severe dehydration, leading to kidney failure and death.
### Who is at risk?
People who live in or travel to places where cholera is common are at the highest risk of getting the disease. Cholera in travelers is extremely rare but can occur in some situations such as among people visiting friends or family, health care workers, and response workers in outbreak settings.
CDC considers the countries below to have areas of active cholera transmission. For information about the level of cholera transmission and where it is occurring in a country, check the cholera section on an affected country’s [destination page](/travel/destinations/list).
* **Africa:** [Burundi](/travel/destinations/traveler/none/burundi), [Cameroon](/travel/destinations/traveler/none/cameroon), [Democratic Republic of the Congo](/travel/destinations/traveler/none/democratic-republic-of-congo), [Ethiopia](/travel/destinations/traveler/none/ethiopia), [Kenya](/travel/destinations/traveler/none/kenya), [Malawi](/travel/destinations/traveler/none/malawi), [Mozambique](/travel/destinations/traveler/none/mozambique), [Niger](/travel/destinations/traveler/none/niger), [Nigeria](/travel/destinations/traveler/none/nigeria), [Somalia](/travel/destinations/traveler/none/somalia), [South Africa](/travel/destinations/traveler/none/south-africa), [South Sudan](/travel/destinations/traveler/none/south-sudan), [Tanzania](/travel/destinations/traveler/none/tanzania), [Zambia](/travel/destinations/traveler/none/zambia), [Zimbabwe](/travel/destinations/traveler/none/zimbabwe)
* **Asia:** [Afghanistan](/travel/destinations/traveler/none/afghanistan), [Bangladesh](/travel/destinations/traveler/none/bangladesh), [India](/travel/destinations/traveler/none/india), [Nepal](/travel/destinations/traveler/none/nepal), [Pakistan](/travel/destinations/traveler/none/pakistan), [Philippines](/travel/destinations/traveler/none/philippines)
* **Middle East:** [Iraq](/travel/destinations/traveler/none/iraq), [Lebanon](/travel/destinations/traveler/none/lebanon), [Syria](/travel/destinations/traveler/none/syria), [Yemen](/travel/destinations/traveler/none/yemen)
* **Americas:** [Dominican Republic](/travel/destinations/traveler/none/dominican-republic), [Haiti](/travel/destinations/traveler/none/haiti)
* **Pacific:** none
### What can travelers do to prevent cholera?
You can protect yourself against cholera by taking the following steps.
#### Choose safer food and drinks while traveling
Follow [food and drink safety tips](/travel/page/food-water-safety) to lower your chance of getting cholera through unsafe food and drinks.
#### Wash your hands often
* Wash your hands with soap and water. If soap and water aren’t available, clean hands with hand sanitizer (containing at least 60% alcohol).
* Don’t touch your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean.
* Cover your mouth and nose with a tissue or your sleeve (not your hands) when coughing or sneezing.
### How is cholera treated?
The most important step in treating cholera is to drink plenty of fluids. People who are severely ill might need intravenous (IV) fluids. Antibiotics are recommended for people who are severely ill or may become severely ill, such as pregnant people and children. [Zinc treatment](https://www.cdc.gov/cholera/treatment/zinc-treatment.html) has also been shown to help improve cholera symptoms among children 3 to 14 years of age and shorten acute diarrhea for children more than six months of age.
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. Avoid contact with other people while you are sick.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [CDC Cholera Homepage](https://www.cdc.gov/cholera/index.html)
* [Information for Travelers](https://www.cdc.gov/cholera/travelers.html)
* CDC Yellow Book: [Cholera](/travel/yellowbook/2020/travel-related-infectious-diseases/cholera)
* [Cholera Information for Health Care Professionals](/travel/page/cholera-travel-information)
| None | None |
34d38fe147bab8d82cf165961b66b61bdeca791b | cdc | Crimean-Congo Hemorrhagic fever | Crimean-Congo Hemorrhagic fever | Disease Directory | Travelers' Health | CDC
### Crimean-Congo Hemorrhagic fever
window.location.href = 'https://www.cdc.gov/vhf/crimean-congo/index.html';
|
### Crimean-Congo Hemorrhagic fever
setTimeout(function(){
window.location.href = 'https://www.cdc.gov/vhf/crimean-congo/index.html';
}, 1);
| None | None |
2046c4bcfab71f0e176be77351af6fbd5128ffed | cdc | Dengue | Dengue | Disease Directory | Travelers' Health | CDC
### What is dengue?
Dengue viruses are spread to people through the bite of an infected mosquito.
Dengue symptoms usually start within a few days of being bitten but can take up to 2 weeks to develop. Symptoms can be mild or severe and can include fever with nausea, vomiting, rash, headache, eye pain, joint and muscle pain. In severe cases, dengue can cause shock, internal bleeding, and even death. [Learn more about severe dengue](https://www.cdc.gov/dengue/symptoms/index.htm).
Not everyone who gets infected with dengue will feel sick, only about 1 out of 4 infected people get sick. You are more likely to develop severe dengue if you were infected before. Infants and pregnant women are more likely to develop severe dengue.
### Who is at risk?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" - value;
if (value == '0'){
window.location = "/travel/destinations/list";
window.location = url;
Mosquitoes that spread dengue bite during the day and less frequently at night. They are found in tropical and subtropical areas of the Americas, Africa, the Middle East, Asia, and the Pacific Islands. Check if dengue is a concern at your [destination](/travel/destinations/list).
The following activities can increase a traveler’s chance of getting infected:
- Spending a lot of time outdoors
- Traveling to [destinations with risk of dengue](https://www.cdc.gov/dengue/areaswithrisk/around-the-world.html) during times of the year when mosquitoes are more common, such as during warm weather.
### What can travelers do to prevent dengue?
Travelers can protect themselves from dengue by taking the following steps.
Use an EPA-registered insect repellent
- Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.
- Picaridin (known as KBR 3023 and icaridin outside the US)
- Oil of lemon eucalyptus (OLE)
- Para-menthane-diol (PMD)
Find the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).

- Insect Repellent Tips for Babies and Children
- Dress your child in clothing that covers arms and legs.
- Cover strollers and baby carriers with mosquito netting.
- When using insect repellent on your child:
- Always follow label instructions.
- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.
- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.
- Adults: Spray insect repellent onto your hands and then apply to a child’s face.
- If also using sunscreen, always apply insect repellent after sunscreen.
Wear long-sleeved shirts and long pants
Treat clothing and gear with permethrin
- Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.
- Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.
- Permethrin-treated clothing provides protection after multiple washings.
- Read product information to find out how long the protection will last.
- If treating items yourself, follow the product instructions.
- Do not use permethrin products directly on skin.
- Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).
Keep mosquitoes out of your hotel room or lodging
- Choose a hotel or lodging with air conditioning or window and door screens.
- Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.
Sleep under a mosquito net

- Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.
- Buy a mosquito net at your local outdoor store or online before traveling overseas.
- Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.
- [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.
- Permethrin is an insecticide that kills mosquitoes and other insects.
- To determine if you can wash a treated mosquito net, follow the label instructions.
If you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).
#### Dengue Vaccine and Travel
Currently there are no dengue vaccine recommendations for travelers.
|
### Dengue
### What is dengue?
Dengue viruses are spread to people through the bite of an infected mosquito.
Dengue symptoms usually start within a few days of being bitten but can take up to 2 weeks to develop. Symptoms can be mild or severe and can include fever with nausea, vomiting, rash, headache, eye pain, joint and muscle pain. In severe cases, dengue can cause shock, internal bleeding, and even death. [Learn more about severe dengue](https://www.cdc.gov/dengue/symptoms/index.htm).
Not everyone who gets infected with dengue will feel sick, only about 1 out of 4 infected people get sick. You are more likely to develop severe dengue if you were infected before. Infants and pregnant women are more likely to develop severe dengue.
### Who is at risk?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
function goSelectPage(){
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" + value;
if (value == '0'){
window.location = "/travel/destinations/list";
}else{
window.location = url;
}
}
Mosquitoes that spread dengue bite during the day and less frequently at night. They are found in tropical and subtropical areas of the Americas, Africa, the Middle East, Asia, and the Pacific Islands. Check if dengue is a concern at your [destination](/travel/destinations/list).
The following activities can increase a traveler’s chance of getting infected:
* Spending a lot of time outdoors
* Traveling to [destinations with risk of dengue](https://www.cdc.gov/dengue/areaswithrisk/around-the-world.html) during times of the year when mosquitoes are more common, such as during warm weather.
### What can travelers do to prevent dengue?
Travelers can protect themselves from dengue by taking the following steps.
**Use an EPA-registered insect repellent**

* Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.
+ DEET
+ Picaridin (known as KBR 3023 and icaridin outside the US)
+ IR3535
+ Oil of lemon eucalyptus (OLE)
+ Para-menthane-diol (PMD)
+ 2-undecanone
Find the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).

* Insect Repellent Tips for Babies and Children
+ Dress your child in clothing that covers arms and legs.
+ Cover strollers and baby carriers with mosquito netting.
+ When using insect repellent on your child:
- Always follow label instructions.
- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.
- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.
* Adults: Spray insect repellent onto your hands and then apply to a child’s face.
- If also using sunscreen, always apply insect repellent after sunscreen.
**Wear long-sleeved shirts and long pants**
**Treat clothing and gear with permethrin**

* Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.
+ Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.
+ Permethrin-treated clothing provides protection after multiple washings.
+ Read product information to find out how long the protection will last.
* If treating items yourself, follow the product instructions.
* Do not use permethrin products directly on skin.
* Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).
**Keep mosquitoes out of your hotel room or lodging**
* Choose a hotel or lodging with air conditioning or window and door screens.
* Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.
**Sleep under a mosquito net**

* Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.
* Buy a mosquito net at your local outdoor store or online before traveling overseas.
* Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.
* [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.
+ Permethrin is an insecticide that kills mosquitoes and other insects.
+ To determine if you can wash a treated mosquito net, follow the label instructions.
If you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).
#### Dengue Vaccine and Travel
Currently there are no dengue vaccine recommendations for travelers.
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [CDC Dengue page](http://www.cdc.gov/dengue/)
* CDC Yellow Book: [Dengue](/travel/yellowbook/2016/infectious-diseases-related-to-travel/dengue)
* [D](http://www.cdc.gov/dengue/)[engue Map](https://www.healthmap.org/dengue/en/)
| None | None |
4afb484139cda61f460dcc2c142dfee8024e5f92 | cdc | Diphtheria | Diphtheria | Disease Directory | Travelers' Health | CDC
### What is diphtheria?
Diphtheria is a disease caused by bacteria called - Corynebacterium diphtheriae (C. diphtheriae).- These bacteria cause respiratory and skin infections. People with diphtheria can spread the bacteria to others when they cough or sneeze, or if others come into contact with their infected wounds.
Symptoms of respiratory diphtheria include weakness, fever, sore throat, and swollen glands in the neck. A thick, grey coating in the throat or nose can also appear, making it very hard to breathe and swallow. In severe respiratory disease, there can be damage to the heart and nerves. Skin infections caused by - C. diphtheriae- typically consist of shallow ulcers (sores) and does not result in severe disease.
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" - value;
if (value == '0'){
window.location = "/travel/destinations/list";
window.location = url;
### Who is at risk?
Due to childhood vaccination, high income countries don’t have many cases of diphtheria. The disease still exists in parts of the world where diphtheria vaccines are not used or where few people get vaccinated. Travelers going to Asia, the South Pacific, the Middle East, and Eastern Europe, who are not up to date with diphtheria vaccines, can become infected.
### What can travelers do to prevent diphtheria?
Getting vaccinated is the best way to protect against diphtheria. Diphtheria vaccines are combination vaccines. These vaccines protect against diphtheria and tetanus, and some also protect against pertussis (whooping cough). These vaccines are often called [DTaP, Tdap, or Td](https://www.cdc.gov/vaccines/vpd/dtap-tdap-td/public/index.html).
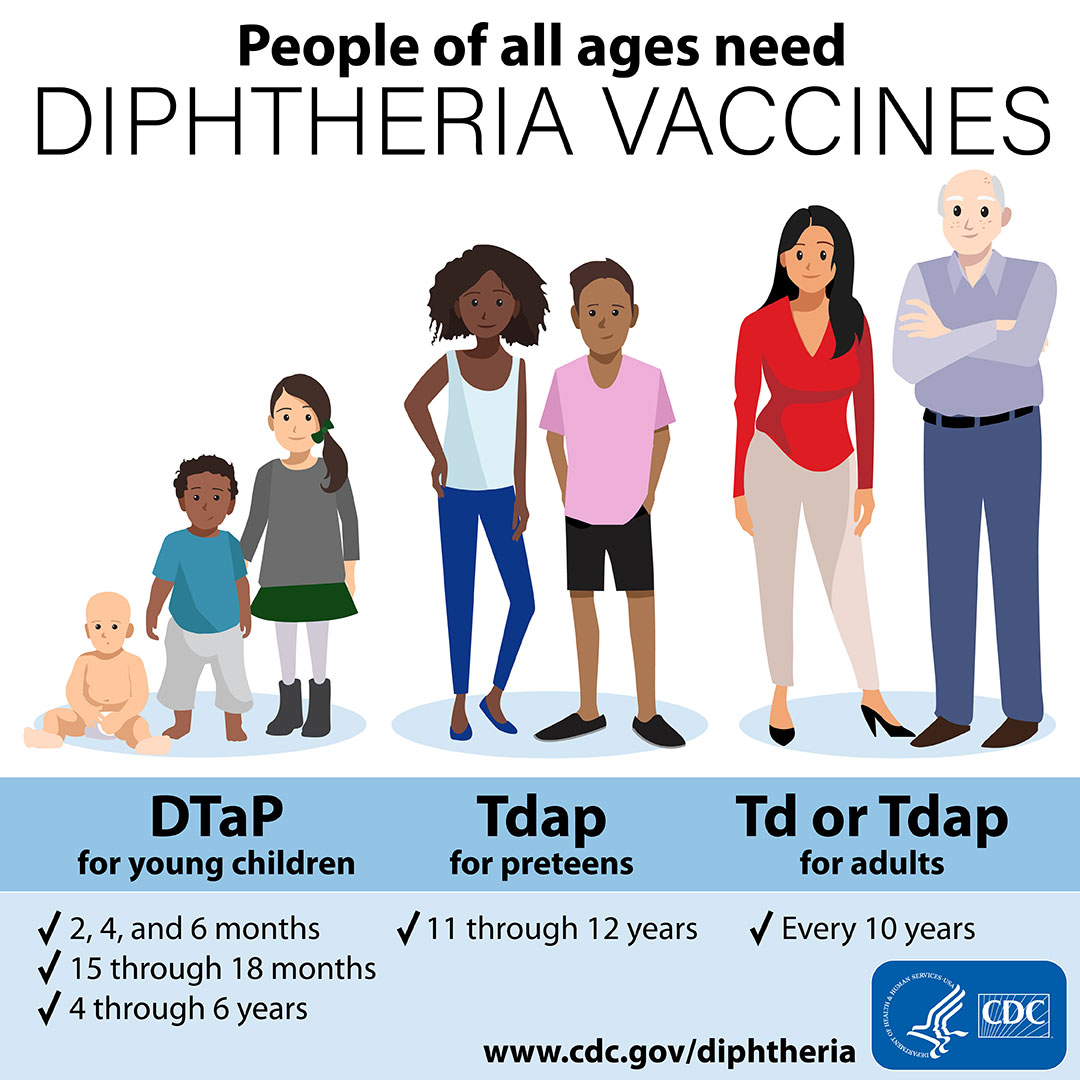
#### Babies and Children
Babies need three shots of DTaP to build up high levels of protection against diphtheria, tetanus, and whooping cough. Then, young children need two booster shots to maintain protection through early childhood. CDC recommends doses at the following ages:
- 2 months
- 4 months
- 6 months
- 15 through 18 months
- 4 through 6 years
#### Preteens and Teens
Preteens should get one shot of Tdap between the ages of 11 and 12 years to boost their immunity. Teens who didn’t get Tdap as a preteen should get one shot the next time they visit their healthcare provider.
All adults should get a Td or Tdap diphtheria shot every 10 years after getting their most recent dose as an adolescent. All adults who have never received Tdap should get one shot followed by either a Td or Tdap shot every 10 years.
|
### Diphtheria
### What is diphtheria?
Diphtheria is a disease caused by bacteria called *Corynebacterium diphtheriae (C. diphtheriae).* These bacteria cause respiratory and skin infections. People with diphtheria can spread the bacteria to others when they cough or sneeze, or if others come into contact with their infected wounds.
Symptoms of respiratory diphtheria include weakness, fever, sore throat, and swollen glands in the neck. A thick, grey coating in the throat or nose can also appear, making it very hard to breathe and swallow. In severe respiratory disease, there can be damage to the heart and nerves. Skin infections caused by *C. diphtheriae*typically consist of shallow ulcers (sores) and does not result in severe disease.
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
function goSelectPage(){
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" + value;
if (value == '0'){
window.location = "/travel/destinations/list";
}else{
window.location = url;
}
}
### Who is at risk?
Due to childhood vaccination, high income countries don’t have many cases of diphtheria. The disease still exists in parts of the world where diphtheria vaccines are not used or where few people get vaccinated. Travelers going to Asia, the South Pacific, the Middle East, and Eastern Europe, who are not up to date with diphtheria vaccines, can become infected.
### What can travelers do to prevent diphtheria?
Getting vaccinated is the best way to protect against diphtheria. Diphtheria vaccines are combination vaccines. These vaccines protect against diphtheria and tetanus, and some also protect against pertussis (whooping cough). These vaccines are often called [DTaP, Tdap, or Td](https://www.cdc.gov/vaccines/vpd/dtap-tdap-td/public/index.html).
#### Babies and Children
Babies need three shots of DTaP to build up high levels of protection against diphtheria, tetanus, and whooping cough. Then, young children need two booster shots to maintain protection through early childhood. CDC recommends doses at the following ages:
* 2 months
* 4 months
* 6 months
* 15 through 18 months
* 4 through 6 years
#### Preteens and Teens
Preteens should get one shot of Tdap between the ages of 11 and 12 years to boost their immunity. Teens who didn’t get Tdap as a preteen should get one shot the next time they visit their healthcare provider.
#### Adults
All adults should get a Td or Tdap diphtheria shot every 10 years after getting their most recent dose as an adolescent. All adults who have never received Tdap should get one shot followed by either a Td or Tdap shot every 10 years.
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [Diphtheria Homepage](http://www.cdc.gov/diphtheria/)
* [Diphtheria Vaccine Information](https://www.cdc.gov/vaccines/vpd/dtap-tdap-td/public/index.html#should-get-vaccines)
* CDC Yellow Book: [Diphtheria](/travel/yellowbook/2020/travel-related-infectious-diseases/diphtheria)
* Pink Book: [Diphtheria](http://www.cdc.gov/vaccines/pubs/pinkbook/dip.html)
| None | None |
20e47661fda21d53c87df397157fa1c61b981d15 | cdc | Ebola and Marburg | Ebola and Marburg | Disease Directory | Travelers' Health | CDC
### Ebola and Marburg
### What are Ebola and Marburg?
Ebola disease and Marburg virus disease [are viral hemorrhagic fevers](https://www.cdc.gov/vhf/about.html). These diseases damage organs and blood vessels and may cause death. A person can get infected with Ebola or Marburg viruses if they touch or handle the following:
- Body fluids from an infected person (alive or dead), such as blood, urine, saliva, sweat, feces, vomit, breast milk, semen, and others.
- Objects such as clothes, bedding, needles, and medical equipment contaminated with the body fluids of an infected person or a person who died of Ebola or Marburg.
- Infected wild animals, for example bats and non-human primates, or their body fluids or meat ([bushmeat](https://www.cdc.gov/importation/bushmeat.html)).
Ebola and Marburg symptoms may start 2 to 21 days after a person is infected (for Ebola, the average is 8-10 days) and may include sudden onset of fever, chills, headache, body aches, and a rash on the chest, back, and stomach. As the person gets sicker, they can have nausea, vomiting, chest pain, sore throat, abdominal pain, and diarrhea.
People with Ebola or Marburg are at risk for internal bleeding, critically low blood pressure (shock), damage to multiple organs and organ systems (liver, pancreas, kidneys, brain), and death.
Who is at risk?
Most travelers are unlikely to be exposed to Ebola or Marburg viruses.
Ebola and Marburg viruses are found in sub-Saharan Africa.
Travelers to sub-Saharan Africa who work closely with or visit areas with bats or non-human primates, such as monkeys, chimpanzees, and gorillas, may be more likely to get infected. For example, two tourists visiting Uganda in 2008 were infected with Marburg virus and likely exposed while visiting a cave known for its large bat population. People who care for patients with Ebola or Marburg may also be more likely to get infected because of exposure to blood or body fluids.
What can travelers do to prevent Ebola and Marburg?
You can protect yourself from infection by taking the following steps:
- Avoid close contact with sick people and blood or body fluids from all people
- Do not kiss, hug, or share eating utensils or cups.
- Don't touch items that may have blood or body fluids on them.
- Avoid animals when traveling
- Don't touch live or dead animals.
- Avoid markets or farms with animals.
- Don't eat or handle meat from wild animals ([bushmeat](https://www.cdc.gov/importation/bushmeat.html)).
- If you are traveling for work that involves animals, wear appropriate protective gear.
- Wash your hands
- Wash hands often with soap and water. If soap and water aren’t available, use an alcohol-based hand sanitizer containing at least 60% alcohol.
- Keep your hands away from your eyes, nose, and mouth. If you need to touch your face, make sure your hands are clean.
- Avoid touching dead bodies
- Don’t participate in funeral activities that involve touching dead bodies, or touch items that have been in contact with dead bodies or have blood or body fluids on them.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/health-care-during-travel).
|
### Ebola and Marburg
### What are Ebola and Marburg?
Ebola disease and Marburg virus disease [are viral hemorrhagic fevers](https://www.cdc.gov/vhf/about.html). These diseases damage organs and blood vessels and may cause death. A person can get infected with Ebola or Marburg viruses if they touch or handle the following:
* Body fluids from an infected person (alive or dead), such as blood, urine, saliva, sweat, feces, vomit, breast milk, semen, and others.
* Objects such as clothes, bedding, needles, and medical equipment contaminated with the body fluids of an infected person or a person who died of Ebola or Marburg.
* Infected wild animals, for example bats and non-human primates, or their body fluids or meat ([bushmeat](https://www.cdc.gov/importation/bushmeat.html)).
Ebola and Marburg symptoms may start 2 to 21 days after a person is infected (for Ebola, the average is 8-10 days) and may include sudden onset of fever, chills, headache, body aches, and a rash on the chest, back, and stomach. As the person gets sicker, they can have nausea, vomiting, chest pain, sore throat, abdominal pain, and diarrhea.
People with Ebola or Marburg are at risk for internal bleeding, critically low blood pressure (shock), damage to multiple organs and organ systems (liver, pancreas, kidneys, brain), and death.
Who is at risk?
Most travelers are unlikely to be exposed to Ebola or Marburg viruses.
Ebola and Marburg viruses are found in sub-Saharan Africa.
Travelers to sub-Saharan Africa who work closely with or visit areas with bats or non-human primates, such as monkeys, chimpanzees, and gorillas, may be more likely to get infected. For example, two tourists visiting Uganda in 2008 were infected with Marburg virus and likely exposed while visiting a cave known for its large bat population. People who care for patients with Ebola or Marburg may also be more likely to get infected because of exposure to blood or body fluids.
What can travelers do to prevent Ebola and Marburg?
You can protect yourself from infection by taking the following steps:
* **Avoid close contact with sick people and blood or body fluids from all people**
+ Do not kiss, hug, or share eating utensils or cups.
+ Don't touch items that may have blood or body fluids on them.
* **Avoid animals when traveling**
+ Don't touch live or dead animals.
+ Avoid markets or farms with animals.
+ Don't eat or handle meat from wild animals ([bushmeat](https://www.cdc.gov/importation/bushmeat.html)).
+ If you are traveling for work that involves animals, wear appropriate protective gear.
* **Wash your hands**
+ Wash hands often with soap and water. If soap and water aren’t available, use an alcohol-based hand sanitizer containing at least 60% alcohol.
+ Keep your hands away from your eyes, nose, and mouth. If you need to touch your face, make sure your hands are clean.
* **Avoid touching dead bodies**
+ Don’t participate in funeral activities that involve touching dead bodies, or touch items that have been in contact with dead bodies or have blood or body fluids on them.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/health-care-during-travel).
### After Travel
**If you traveled to an area where there is an Ebola or Marburg outbreak and feel sick,** particularly if you have a fever, contact your local health department or a healthcare professional immediately and tell them about your symptoms and where you traveled. Avoid contact with other people while you are sick.
Follow [additional recommendations](https://www.cdc.gov/quarantine/vhf/after-you-travel.html) after returning to the United States.
### More Information
* [CDC Ebola website](https://www.cdc.gov/vhf/ebola/)
* [CDC Marburg website](https://www.cdc.gov/vhf/marburg/index.html)
* CDC Yellow Book: [Viral Hemorrhagic Fevers](/travel/yellowbook/2020/travel-related-infectious-diseases/viral-hemorrhagic-fevers)
| None | None |
9f2b25ab5427a2fc5654db59ea3458b129ede272 | cdc | Flu (Influenza) | Flu (Influenza) | Disease Directory | Travelers' Health | CDC
### Flu (Influenza)

The best way to reduce the risk of flu and possible flu complications is to get vaccinated each year, learn about special considerations for travel.
#### You may need a flu vaccine before travel at other times of the year, depending on your destination .
- In the Northern Hemisphere, flu season can begin as early as October and can last until April or May.
- In the temperate regions (areas with seasons) in the Southern Hemisphere, flu activity typically occurs from April to September.
- In the tropics, flu activity occurs throughout the year.
- Travelers who are part of large tourist groups that include people from other parts of the world, such as on cruise ships, may be at risk.
- People should get vaccinated at least 2 weeks before travel because it takes 2 weeks for immunity to develop after vaccination.
- Getting a flu vaccine is very important for [people at higher risk of serious flu complications](https://www.cdc.gov/flu/highrisk/index.htm).
- If you already got your annual flu vaccine, you usually don't need to get vaccinated again during the same season.
#### Do not travel if you are sick
- If you are sick with flu-like symptoms, do not travel. Stay home until you are fever-free for at least 24 hours without using a fever-reducing medicine, such as acetaminophen.
- Flu symptoms include:
- Fever (Not everyone with flu will have a fever.)
- Cough o Sore throat
- Runny or stuffy nose
- Muscle or body aches
- Some people may have vomiting and diarrhea, though this is more common in children.
### During Travel
During your trip, follow local guidelines and practice healthy habits.
- Avoid close contact with sick people.
- Wash your hands often with soap and running water, especially after coughing or sneezing.
- If soap and water are not readily available, use a hand sanitizer that contains at least 60% alcohol. Cover all surfaces of your hands and rub them together until they feel dry.
- Cover your mouth and nose with a tissue when you cough or sneeze and put the used tissue in the trash. If you don’t have a tissue, cough or sneeze into your upper sleeve, not your hands.
#### What to do if you feel sick
Most people with flu will recover without needing medical care. However, if you have severe illness or are [at risk of getting serious flu complications](https://www.cdc.gov/flu/highrisk/index.htm), seek medical care.
A U.S. consular officer can help you find local medical care in a foreign country. To contact the U.S. Embassy or consulate in the country you are visiting, call Overseas Citizens Services at 1-888-407-4747 if calling from the U.S. or Canada, 00-1-202-501-4444 if calling from other countries. You can also visit the [websites of U.S. Embassies, consulates, and diplomatic missionsExternal Link](https://www.usembassy.gov/) to find the contact information for the local U.S. Embassy of the country you are visiting.
Follow all local health recommendations
|
### Flu (Influenza)

The best way to reduce the risk of flu and possible flu complications is to get vaccinated each year, learn about special considerations for travel.
#### You may need a flu vaccine before travel at other times of the year, depending on your destination .
* In the Northern Hemisphere, flu season can begin as early as October and can last until April or May.
* In the temperate regions (areas with seasons) in the Southern Hemisphere, flu activity typically occurs from April to September.
* In the tropics, flu activity occurs throughout the year.
* Travelers who are part of large tourist groups that include people from other parts of the world, such as on cruise ships, may be at risk.
* People should get vaccinated at least 2 weeks before travel because it takes 2 weeks for immunity to develop after vaccination.
* Getting a flu vaccine is very important for [people at higher risk of serious flu complications](https://www.cdc.gov/flu/highrisk/index.htm).
* If you already got your annual flu vaccine, you usually don't need to get vaccinated again during the same season.
#### Do not travel if you are sick
* **If you are sick with flu-like symptoms, do not travel.** Stay home until you are fever-free for at least 24 hours without using a fever-reducing medicine, such as acetaminophen.
* Flu symptoms include:
+ Fever (Not everyone with flu will have a fever.)
+ Cough o Sore throat
+ Runny or stuffy nose
+ Muscle or body aches
+ Headache
+ Fatigue
+ Some people may have vomiting and diarrhea, though this is more common in children.
### During Travel
During your trip, follow local guidelines and practice healthy habits.
* Avoid close contact with sick people.
* Wash your hands often with soap and running water, especially after coughing or sneezing.
* If soap and water are not readily available, use a hand sanitizer that contains at least 60% alcohol. Cover all surfaces of your hands and rub them together until they feel dry.
* Cover your mouth and nose with a tissue when you cough or sneeze and put the used tissue in the trash. If you don’t have a tissue, cough or sneeze into your upper sleeve, not your hands.
#### What to do if you feel sick
Most people with flu will recover without needing medical care. However, if you have severe illness or are [at risk of getting serious flu complications](https://www.cdc.gov/flu/highrisk/index.htm), seek medical care.
A U.S. consular officer can help you find local medical care in a foreign country. To contact the U.S. Embassy or consulate in the country you are visiting, call Overseas Citizens Services at 1-888-407-4747 if calling from the U.S. or Canada, 00-1-202-501-4444 if calling from other countries. You can also visit the [websites of U.S. Embassies, consulates, and diplomatic missionsExternal Link](https://www.usembassy.gov/) to find the contact information for the local U.S. Embassy of the country you are visiting.
Follow all local health recommendations
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* CDC: [Travelers’ Health Website](/travel/) (General)
* CDC: [Traveler Information Center](/travel/page/resources-for-travelers)
| None | None |
f3efaab4e14521d0497deea936ef720c26170ed1 | cdc | HIV | HIV | Disease Directory | Travelers' Health | CDC
### What is HIV?
[HIV](https://www.cdc.gov/actagainstaids/basics/whatishiv.html) (human immunodeficiency virus) is a virus that attacks the body’s immune system. It is [spread](https://www.cdc.gov/actagainstaids/basics/transmission.html) through certain body fluids, including blood, sexual fluids (like semen and vaginal or rectal fluids) and breast milk. Most people get HIV from having unprotected sex (including vaginal or anal sex) with someone who has HIV, or from sharing needles or other drug injection equipment with someone who has HIV.
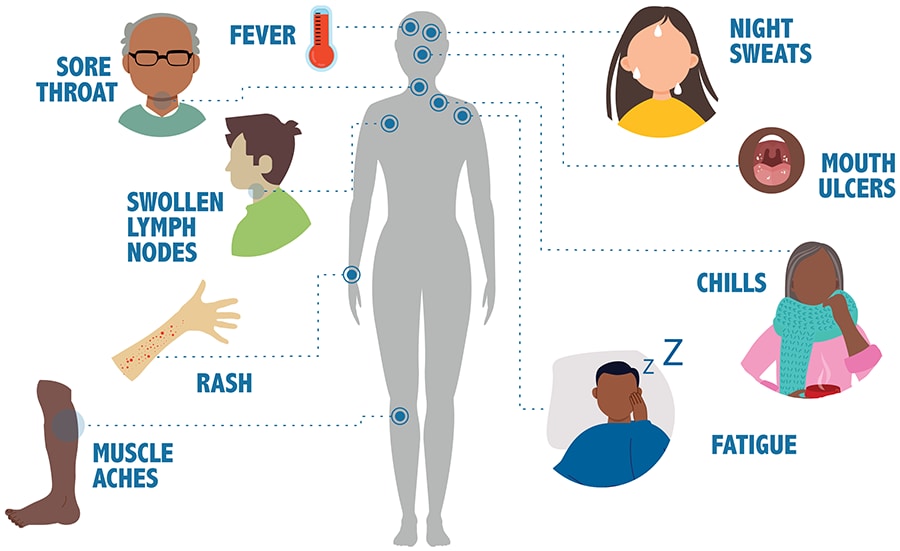
Early symptoms of HIV infection may include cough, body aches, headaches, nasal congestion, and sore throat. These symptoms usually go away on their own and can be mistaken for flu-like illness. Some people may have no early symptoms at all and may feel healthy. The only way to know for sure whether you have HIV is to get tested.
Over time, HIV infection damages the immune system, making it harder for the body to fight off infections and other diseases, including heart disease, kidney disease, liver disease, and cancer. Left untreated, HIV infection can lead to AIDS (acquired immune deficiency syndrome). AIDS is the most severe phase of HIV infection. People with AIDS have such badly damaged immune systems that they get severe infections that don’t normally infect healthy people, called opportunistic infections, and eventually the infection leads to death. No effective cure exists, but with early diagnosis and proper medical care, HIV can be managed and controlled.
### Who is at risk?
Travelers are generally at low risk for getting HIV unless they engage in activities that could put them at risk, such as having unprotected sex or sharing needles.
A person can get HIV by being stuck with a contaminated needle or another sharp object, though this is more of a risk for healthcare workers. Some low-income countries may not adequately screen their blood supplies or properly sterilize medical equipment used in medical clinics, dental clinics, and hospitals. There is a small chance that travelers to these countries who receive medical care could get infected.
HIV infection affects people globally. Sub-Saharan Africa remains the most affected part of the world. Still, other regions significantly affected by HIV include Asia and the Pacific, Latin America, the Caribbean, Eastern Europe, and Central Asia.
### What can travelers do to prevent HIV?
- Talk with your health care provider about PrEP or [pre-exposure prophylaxis](https://www.cdc.gov/hiv/risk/prep/). It is usually a pill or a shot. PrEP is most effective when it is prescribed by your healthcare provider
- Before having sex for the first time with a new partner, you and your partner should talk about your sexual and drug-use history, disclose your HIV status, and get tested for HIV and other sexually transmitted infections.
- If you have sex, [use condoms the right way](https://www.cdc.gov/hiv/basics/hiv-transmission/ways-people-get-hiv.html) every time you have vaginal, oral, or anal sex, from start to finish.
- Do not inject drugs or share needles or other devices that can break the skin. If you do inject drugs, use only new, sterile syringes and needles.
- If you get tattoos, piercings, or acupuncture abroad, make sure a new, sterile needle is used each time.
- If you get medical or dental care abroad, make sure the equipment is unused or properly sterilized.
If you have HIV and are traveling, your destination may increase your risk of getting [opportunistic infections](https://www.cdc.gov/hiv/basics/livingwithhiv/opportunisticinfections.html) or more severe illnesses from infections like travelers’ diarrhea. Bring enough of your medications to last your entire trip since not all countries have all HIV medication.
Consult your doctor or travel medicine specialist at least 4 weeks before leaving as you may not be eligible for certain travel vaccines required at your destination, or you may need to take additional precautions.
Check the [Department of State websiteExternal Link](https://travel.state.gov/content/travel/en/international-travel/International-Travel-Country-Information-Pages.html) for any restrictions on travel for people with HIV at your destination
|
### HIV
### What is HIV?
[HIV](https://www.cdc.gov/actagainstaids/basics/whatishiv.html) (human immunodeficiency virus) is a virus that attacks the body’s immune system. It is [spread](https://www.cdc.gov/actagainstaids/basics/transmission.html) through certain body fluids, including blood, sexual fluids (like semen and vaginal or rectal fluids) and breast milk. Most people get HIV from having unprotected sex (including vaginal or anal sex) with someone who has HIV, or from sharing needles or other drug injection equipment with someone who has HIV.
**HIV symptoms**
Early symptoms of HIV infection may include cough, body aches, headaches, nasal congestion, and sore throat. These symptoms usually go away on their own and can be mistaken for flu-like illness. Some people may have no early symptoms at all and may feel healthy. The only way to know for sure whether you have HIV is to get tested.
Over time, HIV infection damages the immune system, making it harder for the body to fight off infections and other diseases, including heart disease, kidney disease, liver disease, and cancer. Left untreated, HIV infection can lead to AIDS (acquired immune deficiency syndrome). AIDS is the most severe phase of HIV infection. People with AIDS have such badly damaged immune systems that they get severe infections that don’t normally infect healthy people, called opportunistic infections, and eventually the infection leads to death. No effective cure exists, but with early diagnosis and proper medical care, HIV can be managed and controlled.
### Who is at risk?
Travelers are generally at low risk for getting HIV unless they engage in activities that could put them at risk, such as having unprotected sex or sharing needles.
A person can get HIV by being stuck with a contaminated needle or another sharp object, though this is more of a risk for healthcare workers. Some low-income countries may not adequately screen their blood supplies or properly sterilize medical equipment used in medical clinics, dental clinics, and hospitals. There is a small chance that travelers to these countries who receive medical care could get infected.
HIV infection affects people globally. Sub-Saharan Africa remains the most affected part of the world. Still, other regions significantly affected by HIV include Asia and the Pacific, Latin America, the Caribbean, Eastern Europe, and Central Asia.
### What can travelers do to prevent HIV?

* Talk with your health care provider about PrEP or [pre-exposure prophylaxis](https://www.cdc.gov/hiv/risk/prep/). It is usually a pill or a shot. PrEP is most effective when it is prescribed by your healthcare provider
* Before having sex for the first time with a new partner, you and your partner should talk about your sexual and drug-use history, disclose your HIV status, and get tested for HIV and other sexually transmitted infections.
* If you have sex, [use condoms the right way](https://www.cdc.gov/hiv/basics/hiv-transmission/ways-people-get-hiv.html) every time you have vaginal, oral, or anal sex, from start to finish.
* Do not inject drugs or share needles or other devices that can break the skin. If you do inject drugs, use only new, sterile syringes and needles.
* If you get tattoos, piercings, or acupuncture abroad, make sure a new, sterile needle is used each time.
* If you get medical or dental care abroad, make sure the equipment is unused or properly sterilized.
If you have HIV and are traveling, your destination may increase your risk of getting [opportunistic infections](https://www.cdc.gov/hiv/basics/livingwithhiv/opportunisticinfections.html) or more severe illnesses from infections like travelers’ diarrhea. Bring enough of your medications to last your entire trip since not all countries have all HIV medication.
Consult your doctor or travel medicine specialist at least 4 weeks before leaving as you may not be eligible for certain travel vaccines required at your destination, or you may need to take additional precautions.
Check the [Department of State websiteExternal Link](https://travel.state.gov/content/travel/en/international-travel/International-Travel-Country-Information-Pages.html) for any restrictions on travel for people with HIV at your destination
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [About HIV](https://www.cdc.gov/hiv/basics/whatishiv.html)
* [CDC HIV Homepage](https://www.cdc.gov/hiv/)
* CDC Yellow Book: [HIV Infection](/travel/yellowbook/2018/infectious-diseases-related-to-travel/hiv-infection) in CDC Yellow Book
* [HIV Guidelines](https://www.cdc.gov/hiv/guidelines/index.html)
| None | None |
92680a73c5fcfbdde2d61f6411211972fcf182c1 | cdc | Hand, Foot, and Mouth Disease | Hand, Foot, and Mouth Disease | Disease Directory | Travelers' Health | CDC
### Hand, Foot, and Mouth Disease
### What is hand, foot, and mouth disease?
Hand, foot, and mouth disease is a contagious disease that is caused by different viruses. It usually affects infants and children under 5 years old, occasionally adults will also get the disease. [Symptoms](http://www.cdc.gov/hand-foot-mouth/about/signs-symptoms.html) of hand, foot, and mouth disease include fever, painful blister-like sores in the mouth, and a rash that may appear as blisters. It is usually a mild disease, and nearly all infected people recover in 7 to 10 days.
Hand, foot, and mouth disease spreads through close personal contact, such as kissing or hugging, coughing and sneezing, contact with feces (poop), and touching objects or surfaces that have the virus on them then putting your fingers in your eyes, nose or mouth.
### Who is at risk?

Viruses that cause hand, foot, and mouth disease occur worldwide and are more common in summer and fall in temperate climates. Large, severe outbreaks affecting thousands of people occur frequently in some countries in Asia.
### What can travelers do to prevent hand, foot, and mouth disease?
There is no vaccine to prevent hand, foot, and mouth disease but you can take steps to lower your risk of getting it.
#### Wash your hands:
- Wash your hands often with soap and water, especially after using the bathroom and before eating. If soap and water aren't available, use an alcohol-based hand sanitizer.
- Don’t touch your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean.
- Cover your mouth and nose with a tissue or your sleeve (not your hands) when coughing or sneezing.
- Try to avoid close contact, such as kissing, hugging, or sharing eating utensils or cups with people who are sick.
#### Disinfect dirty surfaces and soiled items:
- If you are able, first wash items with soap and water, then disinfect them with a solution of chlorine bleach (made by mixing 1 tablespoon of bleach with 4 cups of water) or a cleaning product that contains bleach.
#### If you develop mouth sores and think you have hand, foot, and mouth disease:
- Take over-the-counter medications to relieve pain and fever.
- Children should not take aspirin.
- Use mouthwashes or sprays that numb mouth pain.
- Drink plenty of liquids to stay hydrated.
- Seek medical care if
- Your child is not drinking enough to stay hydrated
- Symptoms do not improve after 10 days
- Your child has a weakened immune system
- Symptoms are severe
- Your child is very young, especially younger than 6 months
|
### Hand, Foot, and Mouth Disease
### What is hand, foot, and mouth disease?
Hand, foot, and mouth disease is a contagious disease that is caused by different viruses. It usually affects infants and children under 5 years old, occasionally adults will also get the disease. [Symptoms](http://www.cdc.gov/hand-foot-mouth/about/signs-symptoms.html) of hand, foot, and mouth disease include fever, painful blister-like sores in the mouth, and a rash that may appear as blisters. It is usually a mild disease, and nearly all infected people recover in 7 to 10 days.
Hand, foot, and mouth disease spreads through close personal contact, such as kissing or hugging, coughing and sneezing, contact with feces (poop), and touching objects or surfaces that have the virus on them then putting your fingers in your eyes, nose or mouth.
### Who is at risk?

Viruses that cause hand, foot, and mouth disease occur worldwide and are more common in summer and fall in temperate climates. Large, severe outbreaks affecting thousands of people occur frequently in some countries in Asia.
### What can travelers do to prevent hand, foot, and mouth disease?
There is no vaccine to prevent hand, foot, and mouth disease but you can take steps to lower your risk of getting it.
#### Wash your hands:
* Wash your hands often with soap and water, especially after using the bathroom and before eating. If soap and water aren't available, use an alcohol-based hand sanitizer.
* Don’t touch your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean.
* Cover your mouth and nose with a tissue or your sleeve (not your hands) when coughing or sneezing.
* Try to avoid close contact, such as kissing, hugging, or sharing eating utensils or cups with people who are sick.
#### Disinfect dirty surfaces and soiled items:
* If you are able, first wash items with soap and water, then disinfect them with a solution of chlorine bleach (made by mixing 1 tablespoon of bleach with 4 cups of water) or a cleaning product that contains bleach.
#### If you develop mouth sores and think you have hand, foot, and mouth disease:
* Take over-the-counter medications to relieve pain and fever.
+ Children should not take aspirin.
* Use mouthwashes or sprays that numb mouth pain.
* Drink plenty of liquids to stay hydrated.
* Seek medical care if
+ Your child is not drinking enough to stay hydrated
+ Symptoms do not improve after 10 days
+ Your child has a weakened immune system
+ Symptoms are severe
+ Your child is very young, especially younger than 6 months
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [CDC Hand Foot Mouth Disease webpage](http://www.cdc.gov/hand-foot-mouth/index.html)
* [CDC Yellow Book: Hand, Foot, and Mouth Disease](/travel/yellowbook/2020/travel-related-infectious-diseases/hand-foot-and-mouth-disease)
| None | None |
a9355b1b34eb56f7d9c180f37be671812cc0ca47 | cdc | Hantavirus | Hantavirus | Disease Directory | Travelers' Health | CDC
### What is Hantavirus?
Hantaviruses are viruses that can spread from animals to people that can cause serious disease in people. You can be infected with a hantavirus if you
- Breathe air or eat food contaminated with the urine, droppings, or saliva of infected rodents
- Are bitten by an infected rodent, typically a mouse or a rat
[Andes virus](https://www.cdc.gov/hantavirus/resources/andes-virus.html), found in South America, is the only hantavirus known to spread from person to person.
Hantaviruses in North and South America most commonly cause a serious lung disease known as [hantavirus pulmonary syndrome.](https://www.cdc.gov/hantavirus/hps/index.html)
Hantaviruses in Europe and Asia cause organ damage, especially to the kidneys and blood vessels. This is known as [hemorrhagic fever with renal syndrome](https://www.cdc.gov/hantavirus/hfrs/index.html). Recovery can take weeks to months. In some cases hantavirus can cause death.
Symptoms of hantavirus disease usually develop three to four weeks after infection but can occur as early as one week and, in rare cases, not start until eight weeks after infection. Early symptoms include fatigue, fever, and muscle aches. There may also be headaches, dizziness, chills, nausea, vomiting, diarrhea, and abdominal pain.
### Who is at risk?
Hantaviruses are found throughout the world. Cases of hantavirus disease are rare among travelers, but some activities increase a traveler’s chances of being exposed to rodents, rodent nests, rodent urine and droppings. These activities include the following:
- Working with animals (veterinarians and wildlife professionals)
- Working on farms
- Traveling to rural areas
### What can travelers do to prevent hantavirus infection?
There are no vaccines or medicines to prevent hantavirus disease. Travelers can protect themselves by taking the following steps.
#### Avoid rodents when traveling
- Disinfect droppings and nesting materials by spraying with a disinfectant, wearing kitchen gloves. Dispose of sprayed materials in a plastic bag.
- Avoid touching live or dead rodents. Do not disturb rodents, burrows, or nests.
- Before occupying abandoned or unused cabins, open them up to air out. Inspect for rodents and do not use cabins if you find signs of rodent infestation such as droppings or nests.
- If you sleep outdoors, check potential campsites for rodent droppings and burrows.
- Avoid sleeping near woodpiles or garbage areas. These may be frequented by rodents.
- Avoid sleeping on bare ground; use a tent with a floor, mat or elevated cots if they are available.
- Do not leave pet food in feeding dishes.
- Store foods in rodent-proof containers and promptly discard, bury, or burn all garbage in accordance with campsite regulations.
#### Wash your hands
- Wash hands often with soap and water. If soap and water aren’t available, use an alcohol-based hand sanitizer containing at least 60% alcohol.
- Keep your hands away from your eyes, nose, and mouth. If you need to touch your face, make sure your hands are clean.
#### Avoid close contact with people who are sick
- Do not kiss, hug, or share eating utensils or cups.
- Do not touch the bedding or clothing of a sick person.
|
### Hantavirus
### What is Hantavirus?

Hantaviruses are viruses that can spread from animals to people that can cause serious disease in people. You can be infected with a hantavirus if you
* Breathe air or eat food contaminated with the urine, droppings, or saliva of infected rodents
* Are bitten by an infected rodent, typically a mouse or a rat
[Andes virus](https://www.cdc.gov/hantavirus/resources/andes-virus.html), found in South America, is the only hantavirus known to spread from person to person.
Hantaviruses in North and South America most commonly cause a serious lung disease known as [hantavirus pulmonary syndrome.](https://www.cdc.gov/hantavirus/hps/index.html)
Hantaviruses in Europe and Asia cause organ damage, especially to the kidneys and blood vessels. This is known as [hemorrhagic fever with renal syndrome](https://www.cdc.gov/hantavirus/hfrs/index.html). Recovery can take weeks to months. In some cases hantavirus can cause death.
Symptoms of hantavirus disease usually develop three to four weeks after infection but can occur as early as one week and, in rare cases, not start until eight weeks after infection. Early symptoms include fatigue, fever, and muscle aches. There may also be headaches, dizziness, chills, nausea, vomiting, diarrhea, and abdominal pain.
### Who is at risk?
Hantaviruses are found throughout the world. Cases of hantavirus disease are rare among travelers, but some activities increase a traveler’s chances of being exposed to rodents, rodent nests, rodent urine and droppings. These activities include the following:
* Working with animals (veterinarians and wildlife professionals)
* Working on farms
* Camping
* Traveling to rural areas
### What can travelers do to prevent hantavirus infection?
There are no vaccines or medicines to prevent hantavirus disease. Travelers can protect themselves by taking the following steps.
#### Avoid rodents when traveling
* Disinfect droppings and nesting materials by spraying with a disinfectant, wearing kitchen gloves. Dispose of sprayed materials in a plastic bag.
* Avoid touching live or dead rodents. Do not disturb rodents, burrows, or nests.
* Before occupying abandoned or unused cabins, open them up to air out. Inspect for rodents and do not use cabins if you find signs of rodent infestation such as droppings or nests.
* If you sleep outdoors, check potential campsites for rodent droppings and burrows.
* Avoid sleeping near woodpiles or garbage areas. These may be frequented by rodents.
* Avoid sleeping on bare ground; use a tent with a floor, mat or elevated cots if they are available.
* Do not leave pet food in feeding dishes.
* Store foods in rodent-proof containers and promptly discard, bury, or burn all garbage in accordance with campsite regulations.
#### Wash your hands
* Wash hands often with soap and water. If soap and water aren’t available, use an alcohol-based hand sanitizer containing at least 60% alcohol.
* Keep your hands away from your eyes, nose, and mouth. If you need to touch your face, make sure your hands are clean.
#### Avoid close contact with people who are sick
* Do not kiss, hug, or share eating utensils or cups.
* Do not touch the bedding or clothing of a sick person.
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [CDC Website: Hantavirus](https://www.cdc.gov/hantavirus/index.html)
* [Hantavirus Guide for Tourists, Campers, and Hikers](https://www.cdc.gov/hantavirus/resources/guide-for-tourists-campers-and-hikers.html)
* CDC Yellow Book: [Viral Hemorrhagic Fevers](/travel/yellowbook/2020/travel-related-infectious-diseases/viral-hemorrhagic-fevers)
| None | None |
4992227c5db2e9774d0aa2fd1ad039382d0e966e | cdc | Hepatitis A | Hepatitis A | Disease Directory | Travelers' Health | CDC
### Hepatitis A
### What is hepatitis A?
Hepatitis A virus can cause liver disease. Hepatitis A virus is found in the stool (poop) and blood of infected people. People infected with hepatitis A virus can spread it to others.
You can be infected with hepatitis A virus if you
- Eat food or drink beverages contaminated with hepatitis A virus
- Touch objects with the virus on it and then put your hands in your mouth
- Have close, personal contact with an infected person, such as caring for them
- Have sex with an infected person
Symptoms can appear quickly and may include fever, fatigue, loss of appetite, nausea, vomiting, abdominal pain, dark urine, diarrhea, clay-colored bowel movements, joint pain, and yellowing of the skin and eyes (jaundice). Most older children and adults who get hepatitis A feel sick for several weeks, but usually recover and do not have lasting liver damage. Children younger than age six usually do not have symptoms.
In rare cases, hepatitis A virus can cause liver failure and death. This is more common in older people and people with existing liver diseases.
### Who is at risk?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" - value;
if (value == '0'){
window.location = "/travel/destinations/list";
window.location = url;
Hepatitis A is a common disease in countries throughout the world. Anyone who has not been vaccinated or had hepatitis A infection before can get infected.
Travelers are more likely to get infected with hepatitis A if they visit rural areas, travel in backcountry areas, or frequently eat or drink in settings of poor sanitation. However, even travelers who stay in urban areas, resorts, or luxury hotels, who wash their hands regularly, and who choose food and drinks carefully have been infected when visiting countries where hepatitis A is common.
### What can travelers do to prevent hepatitis A?
Getting vaccinated is the best way to protect against hepatitis A. The hepatitis A vaccine is very effective and has been a routine childhood vaccine since 1996. The vaccine is recommended for international travelers 6 months of age or older going to countries where hepatitis A infection is common. Check if hepatitis A vaccine is recommended for [your destination.](/travel/destinations/list)
Hepatitis A vaccine is given in two doses. If your plans don’t allow you to get all doses before your trip, get at least 1 dose, as soon as possible before you travel.
Infants 6 to 11 months old should be vaccinated when protection against hepatitis A is recommended for the [destination.](/travel/destinations/list) This dose does not count toward the routine 2-dose series.
Travelers allergic to a vaccine component or 6 months of age or younger should receive a single dose of immune globulin, which provides effective protection for up to 2 months depending on dosage given. Talk to your doctor to see if this is the best option for you.
Additional protection against hepatitis B can be given using the combination hepatitis A and hepatitis B vaccine, usually given in 3 doses. If your trip is soon, talk to your doctor about accelerated dosing of the combination hepatitis A and hepatitis B vaccine.
|
### Hepatitis A
### What is hepatitis A?
Hepatitis A virus can cause liver disease. Hepatitis A virus is found in the stool (poop) and blood of infected people. People infected with hepatitis A virus can spread it to others.
You can be infected with hepatitis A virus if you
* Eat food or drink beverages contaminated with hepatitis A virus
* Touch objects with the virus on it and then put your hands in your mouth
* Have close, personal contact with an infected person, such as caring for them
* Have sex with an infected person
Symptoms can appear quickly and may include fever, fatigue, loss of appetite, nausea, vomiting, abdominal pain, dark urine, diarrhea, clay-colored bowel movements, joint pain, and yellowing of the skin and eyes (jaundice). Most older children and adults who get hepatitis A feel sick for several weeks, but usually recover and do not have lasting liver damage. Children younger than age six usually do not have symptoms.
In rare cases, hepatitis A virus can cause liver failure and death. This is more common in older people and people with existing liver diseases.
### Who is at risk?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
function goSelectPage(){
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" + value;
if (value == '0'){
window.location = "/travel/destinations/list";
}else{
window.location = url;
}
}
Hepatitis A is a common disease in countries throughout the world. Anyone who has not been vaccinated or had hepatitis A infection before can get infected.
Travelers are more likely to get infected with hepatitis A if they visit rural areas, travel in backcountry areas, or frequently eat or drink in settings of poor sanitation. However, even travelers who stay in urban areas, resorts, or luxury hotels, who wash their hands regularly, and who choose food and drinks carefully have been infected when visiting countries where hepatitis A is common.
### What can travelers do to prevent hepatitis A?
Getting vaccinated is the best way to protect against hepatitis A. The hepatitis A vaccine is very effective and has been a routine childhood vaccine since 1996. The vaccine is recommended for international travelers 6 months of age or older going to countries where hepatitis A infection is common. Check if hepatitis A vaccine is recommended for [your destination.](/travel/destinations/list)
Hepatitis A vaccine is given in two doses. If your plans don’t allow you to get all doses before your trip, get at least 1 dose, as soon as possible before you travel.
Infants 6 to 11 months old should be vaccinated when protection against hepatitis A is recommended for the [destination.](/travel/destinations/list) This dose does not count toward the routine 2-dose series.
Travelers allergic to a vaccine component or 6 months of age or younger should receive a single dose of immune globulin, which provides effective protection for up to 2 months depending on dosage given. Talk to your doctor to see if this is the best option for you.
Additional protection against hepatitis B can be given using the combination hepatitis A and hepatitis B vaccine, usually given in 3 doses. If your trip is soon, talk to your doctor about accelerated dosing of the combination hepatitis A and hepatitis B vaccine.
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [Hepatitis A](http://www.cdc.gov/hepatitis/A/index.htm)
* [Vaccine Information Statement](http://www.cdc.gov/vaccines/pubs/vis/default.htm#hepa)
* [Choose Food and Drinks Carefully](/travel/page/food-water-safety)
* CDC Yellow Book: [Hepatitis A](/travel/yellowbook/2020/travel-related-infectious-diseases/hepatitis-a)
| None | None |
8f90f70f2f869ebd42a4c22df32ce3b7cc166ed5 | cdc | Hepatitis B | Hepatitis B | Disease Directory | Travelers' Health | CDC
### Hepatitis B
### What is hepatitis B?
Hepatitis B is a vaccine-preventable liver disease. Hepatitis B virus is found in the blood and body fluids of infected people. People with hepatitis B virus infection can spread it to others.
You can get hepatitis B virus if you
- Have sex with an infected partner.
- Share needles, syringes, or drug preparation equipment with an infected person.
- Share personal care items such as razors, toothbrushes, or medical equipment, such as a glucose monitor, with an infected person.
- Get cut with a sharp instrument or have a needlestick injury in a health care setting.
- Touch the blood or open sores of an infected person.
- Hepatitis B can be spread from mother to baby during pregnancy or childbirth.
Early symptoms of hepatitis B may include fever, fatigue, loss of appetite, nausea, vomiting, abdominal pain, dark urine, clay-colored bowel movements, joint pain, and jaundice (yellow color in the skin or the eyes).
For some people, hepatitis B can become a chronic infection. The long-term health effects of chronic hepatitis B can cause early death from liver disease and liver cancer.
### Who is at risk?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" - value;
if (value == '0'){
window.location = "/travel/destinations/list";
window.location = url;
Hepatitis B occurs in nearly every part of the world but is more common in some countries in Asia, Africa, South America and the Caribbean.
Although the risk to most travelers is low, people who travel for medical purposes ([medical tourists](/travel/yellowbook/2020/travel-for-work-other-reasons/medical-tourism)) or people who need emergency medical care while traveling may be more likely to get infected.
### What can travelers do to prevent disease?
The best way to protect yourself against hepatitis B is by getting vaccinated. Hepatitis B vaccine is a routine vaccination that infants in the United States receive at birth. The hepatitis B vaccine is over 90% effective and has been routinely recommended for infants since 1991. The vaccine is given in 2, 3, or 4 shots, and the series of shots is usually completed by 6 months of age.
Hepatitis B vaccine is recommended for all unvaccinated travelers under 60 years old and is also recommended for travelers 60 years and older going to a country where hepatitis B virus infection is common. The vaccine is given in 2 or 3 doses. To find the hepatitis B vaccine recommendations for your destination check [CDC's destination pages.](/travel/destinations/list)
It usually takes 6 months to be fully vaccinated against hepatitis B so if you’ll be traveling internationally within 6 months talk to your doctor about accelerated vaccination options including the 2-dose series (Heplisav-B) and [accelerated dosing](https://www.cdc.gov/hepatitis/hbv/hbvfaq.htm#D4) of the combination hepatitis A and hepatitis B vaccine.
|
### Hepatitis B
### What is hepatitis B?
Hepatitis B is a vaccine-preventable liver disease. Hepatitis B virus is found in the blood and body fluids of infected people. People with hepatitis B virus infection can spread it to others.
You can get hepatitis B virus if you
* Have sex with an infected partner.
* Share needles, syringes, or drug preparation equipment with an infected person.
* Share personal care items such as razors, toothbrushes, or medical equipment, such as a glucose monitor, with an infected person.
* Get cut with a sharp instrument or have a needlestick injury in a health care setting.
* Touch the blood or open sores of an infected person.
* Hepatitis B can be spread from mother to baby during pregnancy or childbirth.
Early symptoms of hepatitis B may include fever, fatigue, loss of appetite, nausea, vomiting, abdominal pain, dark urine, clay-colored bowel movements, joint pain, and jaundice (yellow color in the skin or the eyes).
For some people, hepatitis B can become a chronic infection. The long-term health effects of chronic hepatitis B can cause early death from liver disease and liver cancer.
### Who is at risk?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
function goSelectPage(){
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" + value;
if (value == '0'){
window.location = "/travel/destinations/list";
}else{
window.location = url;
}
}
Hepatitis B occurs in nearly every part of the world but is more common in some countries in Asia, Africa, South America and the Caribbean.
Although the risk to most travelers is low, people who travel for medical purposes ([medical tourists](/travel/yellowbook/2020/travel-for-work-other-reasons/medical-tourism)) or people who need emergency medical care while traveling may be more likely to get infected.
### What can travelers do to prevent disease?
The best way to protect yourself against hepatitis B is by getting vaccinated. Hepatitis B vaccine is a routine vaccination that infants in the United States receive at birth. The hepatitis B vaccine is over 90% effective and has been routinely recommended for infants since 1991. The vaccine is given in 2, 3, or 4 shots, and the series of shots is usually completed by 6 months of age.
Hepatitis B vaccine is recommended for all unvaccinated travelers under 60 years old and is also recommended for travelers 60 years and older going to a country where hepatitis B virus infection is common. The vaccine is given in 2 or 3 doses. To find the hepatitis B vaccine recommendations for your destination check [CDC's destination pages.](/travel/destinations/list)
It usually takes 6 months to be fully vaccinated against hepatitis B so if you’ll be traveling internationally within 6 months talk to your doctor about accelerated vaccination options including the 2-dose series (Heplisav-B) and [accelerated dosing](https://www.cdc.gov/hepatitis/hbv/hbvfaq.htm#D4) of the combination hepatitis A and hepatitis B vaccine.
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [Hepatitis B Homepage](http://www.cdc.gov/hepatitis/HBV/index.htm)
* CDC Yellow Book: [Hepatitis B](/travel/yellowbook/2020/travel-related-infectious-diseases/hepatitis-b)
| None | None |
192a349dfbc829a9922d85ce603a8cb0e57e4f4f | cdc | Hepatitis C | Hepatitis C | Disease Directory | Travelers' Health | CDC
### Hepatitis C
### What is hepatitis C?
Hepatitis C virus can cause liver disease. Most people who get infected with hepatitis C virus will have it the rest of their life, this is called a chronic infection. Hepatitis C virus is found in the blood of infected people, who can spread it to others.
You can be infected with the hepatitis C virus if you
- Share needles, syringes, or drug preparation equipment with an infected person
- Share personal care items such as razors, toothbrushes, or medical equipment, such as a glucose monitor, with an infected person
- Get a tattoo, body piercing, or acupuncture with unsterile equipment
- Get cut with a sharp instrument or a needlestick injury in a health care setting
- Have sex with an infected partner
- Accidentally get stuck by a contaminated needle
Many people infected with hepatitis C virus have no symptoms. Those with symptoms may have fever, fatigue, dark urine, clay-colored bowel movements, abdominal pain, loss of appetite, nausea, vomiting, joint pain, and yellow color in the skin or eyes (jaundice).
An infected person with or without symptoms may develop long-term complications of chronic infection that can result in serious liver damage, such as cirrhosis (scarring), liver failure, or liver cancer.
### Who is at risk?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" - value;
if (value == '0'){
window.location = "/travel/destinations/list";
window.location = url;
Hepatitis C occurs in nearly every part of the world but is most common in some countries in Asia and Africa. This map shows the [global prevalence of hepatitis C virus infection](/travel/yellowbook/2020/travel-related-infectious-diseases/hepatitis-c#5521).
Although the risk to most travelers is low, your chances of infection increase if you get a transfusion of unscreened blood, have medical or dental procedures abroad, get tattoos or piercings or receive acupuncture with unsterile needles, or have sex with a person infected with hepatitis C.
### What can travelers do to prevent hepatitis C infection?
There is no vaccine to prevent hepatitis C. Although there are treatments for chronic hepatitis, it is better to prevent infection by taking the following steps:
- Don’t inject drugs
- Make sure tattoo, piercing, and acupuncture equipment has been sterilized
- Don’t share toothbrushes or devices that can break the skin, including needles for tattoos, piercings, and acupuncture
- Make sure medical and dental equipment has been sterilized
- Use latex condoms correctly when having sex, especially with new partners
|
### Hepatitis C
### What is hepatitis C?
Hepatitis C virus can cause liver disease. Most people who get infected with hepatitis C virus will have it the rest of their life, this is called a chronic infection. Hepatitis C virus is found in the blood of infected people, who can spread it to others.
You can be infected with the hepatitis C virus if you
* Share needles, syringes, or drug preparation equipment with an infected person
* Share personal care items such as razors, toothbrushes, or medical equipment, such as a glucose monitor, with an infected person
* Get a tattoo, body piercing, or acupuncture with unsterile equipment
* Get cut with a sharp instrument or a needlestick injury in a health care setting
* Have sex with an infected partner
* Accidentally get stuck by a contaminated needle
Many people infected with hepatitis C virus have no symptoms. Those with symptoms may have fever, fatigue, dark urine, clay-colored bowel movements, abdominal pain, loss of appetite, nausea, vomiting, joint pain, and yellow color in the skin or eyes (jaundice).
An infected person with or without symptoms may develop long-term complications of chronic infection that can result in serious liver damage, such as cirrhosis (scarring), liver failure, or liver cancer.
### Who is at risk?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
function goSelectPage(){
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" + value;
if (value == '0'){
window.location = "/travel/destinations/list";
}else{
window.location = url;
}
}
Hepatitis C occurs in nearly every part of the world but is most common in some countries in Asia and Africa. This map shows the [global prevalence of hepatitis C virus infection](/travel/yellowbook/2020/travel-related-infectious-diseases/hepatitis-c#5521).
Although the risk to most travelers is low, your chances of infection increase if you get a transfusion of unscreened blood, have medical or dental procedures abroad, get tattoos or piercings or receive acupuncture with unsterile needles, or have sex with a person infected with hepatitis C.
### What can travelers do to prevent hepatitis C infection?
There is no vaccine to prevent hepatitis C. Although there are treatments for chronic hepatitis, it is better to prevent infection by taking the following steps:
* Don’t inject drugs
* Make sure tattoo, piercing, and acupuncture equipment has been sterilized
* Don’t share toothbrushes or devices that can break the skin, including needles for tattoos, piercings, and acupuncture
* Make sure medical and dental equipment has been sterilized
* Use latex condoms correctly when having sex, especially with new partners
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [Hepatitis C Information](https://www.cdc.gov/hepatitis/hcv/index.htm)
* CDC Yellow Book: [Hepatitis C](/travel/yellowbook/2020/travel-related-infectious-diseases/hepatitis-c)
| None | None |
451914a549d8be0cee384bd49829657413c18150 | cdc | Hepatitis E | Hepatitis E | Disease Directory | Travelers' Health | CDC
### Hepatitis E
### What is hepatitis E?
Hepatitis E virus can cause liver disease. Hepatitis E virus is mainly found in places around the world where sanitation is poor and there is limited access to safe drinking water.
You can get infected with hepatitis E virus if you
- Eat food or drink beverages contaminated with hepatitis E virus
- Eat shellfish or uncooked or undercooked products made from deer, boar, and pig
Some people who get hepatitis E never feel sick. Others have symptoms that may include fever, tiredness, loss of appetite, nausea, vomiting, stomach pain, dark urine, clay-colored bowel movements, joint pain, and yellow color in the skin or eyes (jaundice). Symptoms usually last less than two months but can last for up to six months.
Most people infected with hepatitis E virus recover with no lasting liver damage. However, people with preexisting liver disease can get seriously ill. Infected pregnant women can get seriously ill and have pregnancy complications.
### Who is at risk?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" - value;
if (value == '0'){
window.location = "/travel/destinations/list";
window.location = url;
Hepatitis E is found worldwide. Hepatitis E is more widespread in low- and middle-income countries, specifically in Asia and Africa, that do not have adequate food and water safety standards. Travelers to these countries are more likely to get infected.
In addition, travelers working in health care settings or refugee camps may be more at risk of infection. Many large hepatitis E outbreaks have occurred among refugees and internally displaced people living in camps.
### What can travelers do to prevent hepatitis E?
There is no approved vaccine in the United States to prevent hepatitis E. Travelers can help prevent hepatitis E by taking the following steps:
Choose food and drinks carefully
- Only drink beverages from factory-sealed containers
- Avoid ice because it may have been made from unclean water
- Only drink pasteurized milk
- Only eat foods that are cooked and served hot
- Avoid food that has been sitting on a buffet
- Only eat raw fruits and vegetables if you have washed them in clean water or peeled them
|
### Hepatitis E
### What is hepatitis E?

Hepatitis E virus can cause liver disease. Hepatitis E virus is mainly found in places around the world where sanitation is poor and there is limited access to safe drinking water.
You can get infected with hepatitis E virus if you
* Eat food or drink beverages contaminated with hepatitis E virus
* Eat shellfish or uncooked or undercooked products made from deer, boar, and pig
Some people who get hepatitis E never feel sick. Others have symptoms that may include fever, tiredness, loss of appetite, nausea, vomiting, stomach pain, dark urine, clay-colored bowel movements, joint pain, and yellow color in the skin or eyes (jaundice). Symptoms usually last less than two months but can last for up to six months.
Most people infected with hepatitis E virus recover with no lasting liver damage. However, people with preexisting liver disease can get seriously ill. Infected pregnant women can get seriously ill and have pregnancy complications.
### Who is at risk?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
function goSelectPage(){
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" + value;
if (value == '0'){
window.location = "/travel/destinations/list";
}else{
window.location = url;
}
}
Hepatitis E is found worldwide. Hepatitis E is more widespread in low- and middle-income countries, specifically in Asia and Africa, that do not have adequate food and water safety standards. Travelers to these countries are more likely to get infected.
In addition, travelers working in health care settings or refugee camps may be more at risk of infection. Many large hepatitis E outbreaks have occurred among refugees and internally displaced people living in camps.
### What can travelers do to prevent hepatitis E?
There is no approved vaccine in the United States to prevent hepatitis E. Travelers can help prevent hepatitis E by taking the following steps:
**Choose food and drinks carefully**
* Only drink beverages from factory-sealed containers
* Avoid ice because it may have been made from unclean water
* Only drink pasteurized milk
* Only eat foods that are cooked and served hot
* Avoid food that has been sitting on a buffet
* Only eat raw fruits and vegetables if you have washed them in clean water or peeled them
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [Hepatitis E](https://www.cdc.gov/hepatitis/hev/index.htm)
* [Hepatitis E—WHO Fact SheetExternal Link](http://www.who.int/mediacentre/factsheets/fs280/en/)
* CDC Yellow Book: [Hepatitis E](/travel/yellowbook/2020/travel-related-infectious-diseases/hepatitis-e)
| None | None |
ac2fa3a1c74034ff37f3cae52a2e2dc39ff619e0 | cdc | Japanese Encephalitis | Japanese Encephalitis | Disease Directory | Travelers' Health | CDC
### Japanese Encephalitis
### What is Japanese encephalitis?

Japanese encephalitis virus is spread to people through the bite of an infected mosquito.
Most people who get infected experience mild or no symptoms. In people who develop severe disease, early symptoms include fever, headache, and vomiting. These symptoms may be followed by disorientation, coma, and seizures. Seizures are more common in children.
### Who is at risk?
Travelers to some parts of Asia and the Western Pacific can get infected if bitten by an infected mosquito. However, for most travelers the chance of getting infected with Japanese encephalitis virus is low.
Activities that can increase a traveler’s chance of getting Japanese encephalitis include:
- Spending a lot of time outdoors in rural areas
- Traveling during times of the year when mosquitoes are more common, such as during the summer
- Traveling for long periods of time in a place that has Japanese encephalitis
In places with four seasons, your chances of getting Japanese encephalitis are greatest in the summer and fall. In tropical and subtropical areas, mosquitoes spread the virus all year long.
### What can travelers do to prevent Japanese encephalitis?
Travelers can protect themselves against Japanese encephalitis by taking the following steps.
Get vaccinated if recommended:
Japanese encephalitis vaccine is recommended for travelers who
- Are moving to an area with Japanese encephalitis to live
- Spend long periods of time, such as a month or more, in areas with Japanese encephalitis
- Frequently travel to areas with Japanese encephalitis
Consider vaccination for travelers
- Spending less than a month in areas with Japanese encephalitis but will be doing activities that increase risk of infection, such as visiting rural areas, hiking or camping, or staying in places without air conditioning, screens, or bed nets
- Going to areas with Japanese encephalitis who are uncertain of their activities or how long they will be there
Not recommended for travelers planning short-term travel to urban areas or travel to areas with no clear Japanese encephalitis season.
Use an EPA-registered insect repellent
- Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.
- Picaridin (known as KBR 3023 and icaridin outside the US)
- Oil of lemon eucalyptus (OLE)
- Para-menthane-diol (PMD)
Find the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).

- Insect Repellent Tips for Babies and Children
- Dress your child in clothing that covers arms and legs.
- Cover strollers and baby carriers with mosquito netting.
- When using insect repellent on your child:
- Always follow label instructions.
- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.
- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.
- Adults: Spray insect repellent onto your hands and then apply to a child’s face.
- If also using sunscreen, always apply insect repellent after sunscreen.
Wear long-sleeved shirts and long pants
Treat clothing and gear with permethrin
- Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.
- Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.
- Permethrin-treated clothing provides protection after multiple washings.
- Read product information to find out how long the protection will last.
- If treating items yourself, follow the product instructions.
- Do not use permethrin products directly on skin.
- Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).
Keep mosquitoes out of your hotel room or lodging
- Choose a hotel or lodging with air conditioning or window and door screens.
- Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.
Sleep under a mosquito net

- Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.
- Buy a mosquito net at your local outdoor store or online before traveling overseas.
- Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.
- [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.
- Permethrin is an insecticide that kills mosquitoes and other insects.
- To determine if you can wash a treated mosquito net, follow the label instructions.
If you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).
|
### Japanese Encephalitis
### What is Japanese encephalitis?

Japanese encephalitis virus is spread to people through the bite of an infected mosquito.
Most people who get infected experience mild or no symptoms. In people who develop severe disease, early symptoms include fever, headache, and vomiting. These symptoms may be followed by disorientation, coma, and seizures. Seizures are more common in children.
### Who is at risk?
Travelers to some parts of Asia and the Western Pacific can get infected if bitten by an infected mosquito. However, for most travelers the chance of getting infected with Japanese encephalitis virus is low.
Activities that can increase a traveler’s chance of getting Japanese encephalitis include:
* Spending a lot of time outdoors in rural areas
* Traveling during times of the year when mosquitoes are more common, such as during the summer
* Traveling for long periods of time in a place that has Japanese encephalitis
In places with four seasons, your chances of getting Japanese encephalitis are greatest in the summer and fall. In tropical and subtropical areas, mosquitoes spread the virus all year long.
### What can travelers do to prevent Japanese encephalitis?
Travelers can protect themselves against Japanese encephalitis by taking the following steps.
**Get vaccinated if recommended:**
Japanese encephalitis vaccine is recommended for travelers who
* Are moving to an area with Japanese encephalitis to live
* Spend long periods of time, such as a month or more, in areas with Japanese encephalitis
* Frequently travel to areas with Japanese encephalitis
Consider vaccination for travelers
* Spending less than a month in areas with Japanese encephalitis but will be doing activities that increase risk of infection, such as visiting rural areas, hiking or camping, or staying in places without air conditioning, screens, or bed nets
* Going to areas with Japanese encephalitis who are uncertain of their activities or how long they will be there
Not recommended for travelers planning short-term travel to urban areas or travel to areas with no clear Japanese encephalitis season.
**Use an EPA-registered insect repellent**

* Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.
+ DEET
+ Picaridin (known as KBR 3023 and icaridin outside the US)
+ IR3535
+ Oil of lemon eucalyptus (OLE)
+ Para-menthane-diol (PMD)
+ 2-undecanone
Find the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).

* Insect Repellent Tips for Babies and Children
+ Dress your child in clothing that covers arms and legs.
+ Cover strollers and baby carriers with mosquito netting.
+ When using insect repellent on your child:
- Always follow label instructions.
- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.
- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.
* Adults: Spray insect repellent onto your hands and then apply to a child’s face.
- If also using sunscreen, always apply insect repellent after sunscreen.
**Wear long-sleeved shirts and long pants**
**Treat clothing and gear with permethrin**

* Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.
+ Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.
+ Permethrin-treated clothing provides protection after multiple washings.
+ Read product information to find out how long the protection will last.
* If treating items yourself, follow the product instructions.
* Do not use permethrin products directly on skin.
* Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).
**Keep mosquitoes out of your hotel room or lodging**
* Choose a hotel or lodging with air conditioning or window and door screens.
* Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.
**Sleep under a mosquito net**

* Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.
* Buy a mosquito net at your local outdoor store or online before traveling overseas.
* Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.
* [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.
+ Permethrin is an insecticide that kills mosquitoes and other insects.
+ To determine if you can wash a treated mosquito net, follow the label instructions.
If you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* CDC's [Japanese encephalitis page](http://www.cdc.gov/japaneseencephalitis/)
* [Avoid Bug Bites](/travel/page/avoid-bug-bites)
* [JE Vaccine Information Statement (VIS)](http://www.cdc.gov/vaccines/hcp/vis/vis-statements/je-ixiaro.pdf)
* CDC Yellow Book: [Japanese Encephalitis](/travel/yellowbook/2012/chapter-3-infectious-diseases-related-to-travel/japanese-encephalitis.htm)
| None | None |
8b09643e639a8a2d8b031d8afc35b28ba1b1d866 | cdc | Leishmaniasis | Leishmaniasis | Disease Directory | Travelers' Health | CDC
### What is leishmaniasis?
Leishmaniasis is a disease caused by a parasite. Sand flies can spread this parasite to people when the sand fly bites them.
Two common forms of leishmaniasis are - cutaneous- and - visceral- .
The most common symptom of - cutaneous leishmaniasis- is skin sores that can change in size and appearance over time. These sores may be closed, like a lump or a bump, or open (ulcer). Some people have swollen glands near the sores.
Common symptoms of - visceral leishmaniasis- are fever and weight loss. People with visceral leishmaniasis can also have an enlarged spleen and liver, low red blood cell count (anemia), low white blood cell count (leukopenia), and low platelet count (thrombocytopenia).
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" - value;
if (value == '0'){
window.location = "/travel/destinations/list";
window.location = url;
Some people with leishmaniasis never have symptoms.
### Who is at risk?
Sand flies are found in certain parts of Asia, the Middle East, Africa, Southern Europe, Mexico, Central America, and South America. Travelers going to these areas are at risk of being bitten by sand flies and getting infected.
See if leishmaniasis is a concern at [your destination](/travel/destinations/list).
### What can travelers do to prevent leishmaniasis?
There is no vaccine or medicine that prevents leishmaniasis. Travelers can take the following steps to prevent sand fly bites:
Use an EPA-registered insect repellent
- Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.
- Picaridin (known as KBR 3023 and icaridin outside the US)
- Oil of lemon eucalyptus (OLE)
- Para-menthane-diol (PMD)
Find the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).

- Insect Repellent Tips for Babies and Children
- Dress your child in clothing that covers arms and legs.
- Cover strollers and baby carriers with mosquito netting.
- When using insect repellent on your child:
- Always follow label instructions.
- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.
- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.
- Adults: Spray insect repellent onto your hands and then apply to a child’s face.
- If also using sunscreen, always apply insect repellent after sunscreen.
Wear long-sleeved shirts and long pants
Treat clothing and gear with permethrin
- Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.
- Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.
- Permethrin-treated clothing provides protection after multiple washings.
- Read product information to find out how long the protection will last.
- If treating items yourself, follow the product instructions.
- Do not use permethrin products directly on skin.
- Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).
Keep mosquitoes out of your hotel room or lodging
- Choose a hotel or lodging with air conditioning or window and door screens.
- Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.
Sleep under a mosquito net

- Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.
- Buy a mosquito net at your local outdoor store or online before traveling overseas.
- Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.
- [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.
- Permethrin is an insecticide that kills mosquitoes and other insects.
- To determine if you can wash a treated mosquito net, follow the label instructions.
If you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).
|
### Leishmaniasis

### What is leishmaniasis?
Leishmaniasis is a disease caused by a parasite. Sand flies can spread this parasite to people when the sand fly bites them.
Two common forms of leishmaniasis are *cutaneous* and *visceral*.
The most common symptom of *cutaneous leishmaniasis* is skin sores that can change in size and appearance over time. These sores may be closed, like a lump or a bump, or open (ulcer). Some people have swollen glands near the sores.
Common symptoms of *visceral leishmaniasis* are fever and weight loss. People with visceral leishmaniasis can also have an enlarged spleen and liver, low red blood cell count (anemia), low white blood cell count (leukopenia), and low platelet count (thrombocytopenia).
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
function goSelectPage(){
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" + value;
if (value == '0'){
window.location = "/travel/destinations/list";
}else{
window.location = url;
}
}
Some people with leishmaniasis never have symptoms.
### Who is at risk?
Sand flies are found in certain parts of Asia, the Middle East, Africa, Southern Europe, Mexico, Central America, and South America. Travelers going to these areas are at risk of being bitten by sand flies and getting infected.
See if leishmaniasis is a concern at [your destination](/travel/destinations/list).
### What can travelers do to prevent leishmaniasis?
There is no vaccine or medicine that prevents leishmaniasis. **Travelers can take the following steps to prevent sand fly bites:**
**Use an EPA-registered insect repellent**

* Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.
+ DEET
+ Picaridin (known as KBR 3023 and icaridin outside the US)
+ IR3535
+ Oil of lemon eucalyptus (OLE)
+ Para-menthane-diol (PMD)
+ 2-undecanone
Find the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).

* Insect Repellent Tips for Babies and Children
+ Dress your child in clothing that covers arms and legs.
+ Cover strollers and baby carriers with mosquito netting.
+ When using insect repellent on your child:
- Always follow label instructions.
- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.
- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.
* Adults: Spray insect repellent onto your hands and then apply to a child’s face.
- If also using sunscreen, always apply insect repellent after sunscreen.
**Wear long-sleeved shirts and long pants**
**Treat clothing and gear with permethrin**

* Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.
+ Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.
+ Permethrin-treated clothing provides protection after multiple washings.
+ Read product information to find out how long the protection will last.
* If treating items yourself, follow the product instructions.
* Do not use permethrin products directly on skin.
* Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).
**Keep mosquitoes out of your hotel room or lodging**
* Choose a hotel or lodging with air conditioning or window and door screens.
* Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.
**Sleep under a mosquito net**

* Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.
* Buy a mosquito net at your local outdoor store or online before traveling overseas.
* Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.
* [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.
+ Permethrin is an insecticide that kills mosquitoes and other insects.
+ To determine if you can wash a treated mosquito net, follow the label instructions.
If you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [Leishmaniasis Information](https://www.cdc.gov/parasites/leishmaniasis/)
* CDC Yellow Book: [Cutaneous Leishmaniasis](/travel/yellowbook/2020/travel-related-infectious-diseases/leishmaniasis-cutaneous)
| None | None |
3fb3bb853b27e5743c7881280068f558fe470937 | cdc | Leptospirosis | Leptospirosis | Disease Directory | Travelers' Health | CDC
### What is leptospirosis?

Leptospirosis is a disease caused by bacteria. Infected animals spread the bacteria through their urine (pee). When infected animals pee, the bacteria get into the water or soil and can live there for weeks to months.
You can be infected if you touch fresh water, soil, or other objects contaminated with infected animal urine. The most common ways to get infected is urine or contaminated water getting in your eyes, nose, mouth, or broken skin (such as a cut or scratch). You can also get infected by eating contaminated food or drinking contaminated water.
Some people with leptospirosis do not have any symptoms. When symptoms occur, they can include fever, headache, chills, muscle aches, vomiting, jaundice (yellow eyes and skin), red eyes, stomach pain, diarrhea, and sometimes a rash. Without proper treatment with antibiotics, people with leptospirosis may develop serious problems with their kidneys, liver, or lining of the brain and spinal cord (meningitis). In some cases, leptospirosis can cause death.
### Who is at risk?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" - value;
if (value == '0'){
window.location = "/travel/destinations/list";
window.location = url;
Leptospirosis is found in countries around the world. It is most common in temperate or tropical climate regions that include South and Southeast Asia, Oceania, the Caribbean, parts of sub-Saharan Africa, and parts of Latin America.
Travelers are more likely to get leptospirosis if they
- Visit flooded or recently flooded areas
- [Swim, wade, kayak, or raft](http://www.cdc.gov/leptospirosis/features/adventure-racing.html) in potentially contaminated fresh water like lakes and rivers
- Visit urban areas with poor sanitation
- Touch animals or their body fluids. Animals that can be infected are mammals, including rodents, cows, sheep/goats, pigs, horses, dogs, and wildlife.
### What can travelers do to prevent leptospirosis?
There is no vaccine approved for use in the United States to prevent leptospirosis in people.
Travelers can take the following steps to protect themselves:
- Avoid touching fresh water or soil that may be contaminated with animal urine
- Avoid touching objects that may be contaminated with animal urine, such as animal bedding
- Don't wade, swim, or put your head in floodwaters or water from lakes, rivers, or swamps. Especially avoid freshwater contact after flooding or heavy rain.
- If it is not possible to avoid wading in floodwaters or other fresh water, wear protective clothing like footwear and cover cuts and wounds with waterproof bandages or dressing.
- Make water [safe to drink](https://www.cdc.gov/disasters/foodwater/facts.html) by boiling or using an appropriate chemical treatment
For some travelers, taking medicine before you travel to prevent leptospirosis might be an option. Talk to your health care provider before you travel and tell them about all your planned activities.
|
### Leptospirosis
### What is leptospirosis?

Leptospirosis is a disease caused by bacteria. Infected animals spread the bacteria through their urine (pee). When infected animals pee, the bacteria get into the water or soil and can live there for weeks to months.
You can be infected if you touch fresh water, soil, or other objects contaminated with infected animal urine. The most common ways to get infected is urine or contaminated water getting in your eyes, nose, mouth, or broken skin (such as a cut or scratch). You can also get infected by eating contaminated food or drinking contaminated water.
Some people with leptospirosis do not have any symptoms. When symptoms occur, they can include fever, headache, chills, muscle aches, vomiting, jaundice (yellow eyes and skin), red eyes, stomach pain, diarrhea, and sometimes a rash. Without proper treatment with antibiotics, people with leptospirosis may develop serious problems with their kidneys, liver, or lining of the brain and spinal cord (meningitis). In some cases, leptospirosis can cause death.
### Who is at risk?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
function goSelectPage(){
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" + value;
if (value == '0'){
window.location = "/travel/destinations/list";
}else{
window.location = url;
}
}
Leptospirosis is found in countries around the world. It is most common in temperate or tropical climate regions that include South and Southeast Asia, Oceania, the Caribbean, parts of sub-Saharan Africa, and parts of Latin America.
Travelers are more likely to get leptospirosis if they
* Visit flooded or recently flooded areas
* [Swim, wade, kayak, or raft](http://www.cdc.gov/leptospirosis/features/adventure-racing.html) in potentially contaminated fresh water like lakes and rivers
* Visit urban areas with poor sanitation
* Touch animals or their body fluids. Animals that can be infected are mammals, including rodents, cows, sheep/goats, pigs, horses, dogs, and wildlife.
### What can travelers do to prevent leptospirosis?
There is no vaccine approved for use in the United States to prevent leptospirosis in people.
Travelers can take the following steps to protect themselves:
* Avoid touching fresh water or soil that may be contaminated with animal urine
* Avoid touching objects that may be contaminated with animal urine, such as animal bedding
* Don't wade, swim, or put your head in floodwaters or water from lakes, rivers, or swamps. Especially avoid freshwater contact after flooding or heavy rain.
* If it is not possible to avoid wading in floodwaters or other fresh water, wear protective clothing like footwear and cover cuts and wounds with waterproof bandages or dressing.
* Make water [safe to drink](https://www.cdc.gov/disasters/foodwater/facts.html) by boiling or using an appropriate chemical treatment
For some travelers, taking medicine before you travel to prevent leptospirosis might be an option. Talk to your health care provider before you travel and tell them about all your planned activities.
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* CDC Website: [Leptospirosis](http://www.cdc.gov/leptospirosis/index.html)
* CDC Yellow Book: [Leptospriosis](/travel/yellowbook/2018/infectious-diseases-related-to-travel/leptospirosis)
| None | None |
cfeedbae41c33dd6cbd313991bbc221ecaa66916 | cdc | Middle East Respiratory Syndrome (MERS) | Middle East Respiratory Syndrome (MERS) | Disease Directory | Travelers' Health | CDC
### Middle East Respiratory Syndrome (MERS)
### What is Middle East Respiratory Syndrome (MERS)?
Middle East respiratory syndrome (MERS) is an illness caused by a coronavirus called MERS-CoV. Scientists do not yet fully understand how the virus spreads. It is likely that a person can get infected with the virus if they:
- Have close contact with someone or touch the body fluids of a person sick with MERS, for example living with or caring for a person sick with MERS.
- Breathe in infectious droplets released into the air when a person sick with MERS coughs or sneezes.
The virus can also spread from camels to people, although it is unclear how that occurs. Touching camels or being around infected camels or their body fluids (milk, feces/poop, urine/pee, saliva/spit, etc.) can increase a person’s chances of becoming infected with MERS-CoV.
Common MERS symptoms include fever, cough, and shortness of breath. Some people also get diarrhea, nausea, and vomiting. Severe complications include pneumonia and kidney failure. MERS can cause death, and most people who died have been older adults or people with a weakened immune system or an existing illness or disease (e.g., diabetes, cancer, lung disease, heart disease, or kidney disease).
### Who can get MERS?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" - value;
if (value == '0'){
window.location = "/travel/destinations/list";
window.location = url;
Though MERS is rare, MERS has been found in countries on or near the Arabian Peninsula. These countries include Bahrain, Iran, Jordan, Kuwait, Lebanon, Oman, Qatar, Saudi Arabia, United Arab Emirates (UAE), and Yemen.
### What can travelers do to prevent MERS?
There is no vaccine to prevent MERS, but you can take steps to protect yourself.
Avoid touching animals when traveling:
- Avoid touching live animals, especially camels, when traveling.
- Avoid visiting markets or farms with animals, including camels.
- Do not touch dead animals.
- Do not use products made from camels or wild animals.
- Avoid drinking raw (unpasteurized) camel milk or camel urine or eating undercooked camel meat (cook to 145°F).
- Do not touch materials, such as bedding, that animals use.
People with diabetes, kidney failure, chronic lung disease, and weakened immune systems are more likely to get severe MERS. People with these health conditions should pay extra attention to the guidelines above and avoid close contact with sick people and camels.
Here are some good tips on how to stay healthy when you travel to avoid getting sick
- Wash your hands often with soap and water for at least 20 seconds.
- If soap and water aren’t available, clean hands with hand sanitizer containing at least 60% alcohol.
- Avoid touching your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean.
- Cover your mouth and nose with a tissue or your sleeve (not your hands) when coughing or sneezing.
- Try to avoid close contact (e.g., kissing, hugging, or sharing eating utensils or cups) with people who are sick.
|
### Middle East Respiratory Syndrome (MERS)
### What is Middle East Respiratory Syndrome (MERS)?
Middle East respiratory syndrome (MERS) is an illness caused by a coronavirus called MERS-CoV. Scientists do not yet fully understand how the virus spreads. It is likely that a person can get infected with the virus if they:
* Have close contact with someone or touch the body fluids of a person sick with MERS, for example living with or caring for a person sick with MERS.
* Breathe in infectious droplets released into the air when a person sick with MERS coughs or sneezes.
The virus can also spread from camels to people, although it is unclear how that occurs. Touching camels or being around infected camels or their body fluids (milk, feces/poop, urine/pee, saliva/spit, etc.) can increase a person’s chances of becoming infected with MERS-CoV.
Common MERS symptoms include fever, cough, and shortness of breath. Some people also get diarrhea, nausea, and vomiting. Severe complications include pneumonia and kidney failure. MERS can cause death, and most people who died have been older adults or people with a weakened immune system or an existing illness or disease (e.g., diabetes, cancer, lung disease, heart disease, or kidney disease).
### Who can get MERS?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
function goSelectPage(){
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" + value;
if (value == '0'){
window.location = "/travel/destinations/list";
}else{
window.location = url;
}
}
Though MERS is rare, MERS has been found in countries on or near the Arabian Peninsula. These countries include Bahrain, Iran, Jordan, Kuwait, Lebanon, Oman, Qatar, Saudi Arabia, United Arab Emirates (UAE), and Yemen.
### What can travelers do to prevent MERS?
There is no vaccine to prevent MERS, but you can take steps to protect yourself.
**Avoid touching animals when traveling:**
* Avoid touching live animals, especially camels, when traveling.
* Avoid visiting markets or farms with animals, including camels.
* Do not touch dead animals.
* Do not use products made from camels or wild animals.
* Avoid drinking raw (unpasteurized) camel milk or camel urine or eating undercooked camel meat (cook to 145°F).
* Do not touch materials, such as bedding, that animals use.
People with diabetes, kidney failure, chronic lung disease, and weakened immune systems are more likely to get severe MERS. People with these health conditions should pay extra attention to the guidelines above and avoid close contact with sick people and camels.
**Here are some good tips on how to stay healthy when you travel to avoid getting sick**
* Wash your hands often with soap and water for at least 20 seconds.
* If soap and water aren’t available, clean hands with hand sanitizer containing at least 60% alcohol.
* Avoid touching your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean.
* Cover your mouth and nose with a tissue or your sleeve (not your hands) when coughing or sneezing.
* Try to avoid close contact (e.g., kissing, hugging, or sharing eating utensils or cups) with people who are sick.
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. Avoid contact with other people while you are sick.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [CDC MERS Guidance for Travel](https://www.cdc.gov/coronavirus/mers/travel.html)
* CDC Yellow Book: [MERS](/travel/yellowbook/2020/travel-related-infectious-diseases/middle-east-respiratory-syndrome-mers)
| None | None |
b7c33f2d57672db304090b9d76d531942f26b005 | cdc | Malaria | Malaria | Disease Directory | Travelers' Health | CDC
### What is malaria?
Malaria is a disease caused by a parasite. Mosquitoes spread the parasite to people when they bite them.
Malaria symptoms usually appear within in 7 to 30 days but can take up to one year to develop. Symptoms may include high fevers and shaking chills, flu-like illness. Without treatment, malaria can cause severe illness and death.
### Who is at risk?
The mosquitoes that spread malaria are found in Africa, Central and South America, parts of the Caribbean, Asia, Eastern Europe, and the South Pacific (See maps: [Eastern Hemisphere](/travel/yellowbook/2020/travel-related-infectious-diseases/malaria#5544) and [Western Hemisphere](/travel/yellowbook/2020/travel-related-infectious-diseases/malaria#5542)). Travelers going to these countries may get bit by mosquitoes and get infected.
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" - value;
if (value == '0'){
window.location = "/travel/destinations/list";
window.location = url;
About 2,000 cases of malaria are diagnosed in the United States annually, mostly among returned travelers.
### What can travelers do to prevent malaria?
Travelers can protect themselves from malaria by taking prescription medicine and preventing mosquito bites. There is no malaria vaccine.
Take Malaria Medicine
Check your [destination](/travel/destinations/list) to see if you should take prescription malaria medication. Depending on the medicine you take, you will need to start taking this medicine multiple days before your trip, as well as during and after your trip. Talk to your doctor about [which medicine you should take](https://www.cdc.gov/malaria/travelers/drugs.html).
Travelers should also take steps to prevent mosquito bites.
Use an EPA-registered insect repellent
- Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.
- Picaridin (known as KBR 3023 and icaridin outside the US)
- Oil of lemon eucalyptus (OLE)
- Para-menthane-diol (PMD)
Find the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).

- Insect Repellent Tips for Babies and Children
- Dress your child in clothing that covers arms and legs.
- Cover strollers and baby carriers with mosquito netting.
- When using insect repellent on your child:
- Always follow label instructions.
- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.
- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.
- Adults: Spray insect repellent onto your hands and then apply to a child’s face.
- If also using sunscreen, always apply insect repellent after sunscreen.
Wear long-sleeved shirts and long pants
Treat clothing and gear with permethrin
- Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.
- Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.
- Permethrin-treated clothing provides protection after multiple washings.
- Read product information to find out how long the protection will last.
- If treating items yourself, follow the product instructions.
- Do not use permethrin products directly on skin.
- Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).
Keep mosquitoes out of your hotel room or lodging
- Choose a hotel or lodging with air conditioning or window and door screens.
- Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.
Sleep under a mosquito net

- Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.
- Buy a mosquito net at your local outdoor store or online before traveling overseas.
- Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.
- [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.
- Permethrin is an insecticide that kills mosquitoes and other insects.
- To determine if you can wash a treated mosquito net, follow the label instructions.
If you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).
|
### Malaria
### What is malaria?

Malaria is a disease caused by a parasite. Mosquitoes spread the parasite to people when they bite them.
Malaria symptoms usually appear within in 7 to 30 days but can take up to one year to develop. Symptoms may include high fevers and shaking chills, flu-like illness. Without treatment, malaria can cause severe illness and death.
### Who is at risk?
The mosquitoes that spread malaria are found in Africa, Central and South America, parts of the Caribbean, Asia, Eastern Europe, and the South Pacific (See maps: [Eastern Hemisphere](/travel/yellowbook/2020/travel-related-infectious-diseases/malaria#5544) and [Western Hemisphere](/travel/yellowbook/2020/travel-related-infectious-diseases/malaria#5542)). Travelers going to these countries may get bit by mosquitoes and get infected.
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
function goSelectPage(){
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" + value;
if (value == '0'){
window.location = "/travel/destinations/list";
}else{
window.location = url;
}
}
About 2,000 cases of malaria are diagnosed in the United States annually, mostly among returned travelers.
### What can travelers do to prevent malaria?
Travelers can protect themselves from malaria by taking prescription medicine and preventing mosquito bites. There is no malaria vaccine.
**Take Malaria Medicine**
Check your [destination](/travel/destinations/list) to see if you should take prescription malaria medication. Depending on the medicine you take, you will need to start taking this medicine multiple days before your trip, as well as during and after your trip. Talk to your doctor about [which medicine you should take](https://www.cdc.gov/malaria/travelers/drugs.html).
**Travelers should also take steps to prevent mosquito bites.**
**Use an EPA-registered insect repellent**

* Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.
+ DEET
+ Picaridin (known as KBR 3023 and icaridin outside the US)
+ IR3535
+ Oil of lemon eucalyptus (OLE)
+ Para-menthane-diol (PMD)
+ 2-undecanone
Find the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).

* Insect Repellent Tips for Babies and Children
+ Dress your child in clothing that covers arms and legs.
+ Cover strollers and baby carriers with mosquito netting.
+ When using insect repellent on your child:
- Always follow label instructions.
- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.
- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.
* Adults: Spray insect repellent onto your hands and then apply to a child’s face.
- If also using sunscreen, always apply insect repellent after sunscreen.
**Wear long-sleeved shirts and long pants**
**Treat clothing and gear with permethrin**

* Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.
+ Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.
+ Permethrin-treated clothing provides protection after multiple washings.
+ Read product information to find out how long the protection will last.
* If treating items yourself, follow the product instructions.
* Do not use permethrin products directly on skin.
* Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).
**Keep mosquitoes out of your hotel room or lodging**
* Choose a hotel or lodging with air conditioning or window and door screens.
* Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.
**Sleep under a mosquito net**

* Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.
* Buy a mosquito net at your local outdoor store or online before traveling overseas.
* Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.
* [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.
+ Permethrin is an insecticide that kills mosquitoes and other insects.
+ To determine if you can wash a treated mosquito net, follow the label instructions.
If you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [Malaria](https://www.cdc.gov/parasites/malaria/index.html)
* CDC Yellow Book: [Malaria](/travel/yellowbook/2020/travel-related-infectious-diseases/malaria)
* [Malaria Hotline](https://www.cdc.gov/media/releases/2019/s0328-artesunate-first-line-treatment.html)—770-488-7788 or 770-488-7100
* [Malaria Risk Assessment for Travelers](http://www.cdc.gov/malaria/travelers/risk_assessment.html)
* [Choosing the Right Drug to Prevent Malaria](http://www.cdc.gov/malaria/travelers/drugs.html)
| None | None |
e91cc1d7c39a5580d4c3a60c61fdc18f6a89a1a6 | cdc | Measles | Measles | Disease Directory | Travelers' Health | CDC
### What is measles?
Measles is a disease caused by a highly contagious virus. People with measles spread the virus through the air when they cough, sneeze, or breathe.
[Symptoms](https://www.cdc.gov/measles/symptoms/signs-symptoms.html) of measles include high fever, cough, runny nose, red and watery eyes, and rash. Koplik spots (tiny white spots inside the mouth) can appear 2 to 3 days after symptoms begin. Some people who become sick with measles also get a serious lung infection, such as pneumonia. Although severe cases are rare, measles can cause swelling of the brain and even death. Measles can be especially severe in infants and in people who are malnourished or who have weakened immune systems.
### Who is at risk?
Anyone who has not been fully vaccinated or had measles before can get measles. Measles remains a common disease in many parts of the world, including Europe, the Middle East, Asia, the Pacific, and Africa.
In the United States, most measles cases occur among unvaccinated travelers who get infected while traveling internationally and spread measles to people who are not fully vaccinated in the United States.
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" - value;
if (value == '0'){
window.location = "/travel/destinations/list";
window.location = url;
### What can travelers do to prevent measles?
Getting vaccinated is the best way to protect yourself and others against measles. Measles vaccine is a routine vaccination given to children in the United States. Measles vaccine is usually given in two doses. It’s recommended that children get the first dose when they are 12 to 15 months old and the second dose when they are 4 to 6 years old. Measles vaccine is a combination vaccine that also protects against mumps and rubella (MMR vaccine) or mumps, rubella, and varicella (MMRV vaccine).
If you were born in or after 1957 and have never had measles or have never been vaccinated against measles, you should get vaccinated with two doses of MMR vaccine before you travel. The second dose is given at least 28 days after the first dose. People born before 1957 were likely exposed to measles as children and do not need to be vaccinated with the MMR vaccine.
Infants 6 to 11 months old traveling internationally should get one dose of MMR vaccine before travel. This dose does not count as part of the routine childhood vaccination series.
CAUTION: Pregnant people should NOT get the MMR vaccine. Any unvaccinated person should get the MMR vaccine immediately after their pregnancy.
Avoid getting pregnant for at least 4 weeks after receiving the MMR vaccine.
|
### Measles
### What is measles?

Measles is a disease caused by a highly contagious virus. People with measles spread the virus through the air when they cough, sneeze, or breathe.
[Symptoms](https://www.cdc.gov/measles/symptoms/signs-symptoms.html) of measles include high fever, cough, runny nose, red and watery eyes, and rash. Koplik spots (tiny white spots inside the mouth) can appear 2 to 3 days after symptoms begin. Some people who become sick with measles also get a serious lung infection, such as pneumonia. Although severe cases are rare, measles can cause swelling of the brain and even death. Measles can be especially severe in infants and in people who are malnourished or who have weakened immune systems.
### Who is at risk?
Anyone who has not been fully vaccinated or had measles before can get measles. Measles remains a common disease in many parts of the world, including Europe, the Middle East, Asia, the Pacific, and Africa.
**In the United States, most measles cases occur among unvaccinated travelers who get infected while traveling internationally and spread measles to people who are not fully vaccinated in the United States.**
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
function goSelectPage(){
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" + value;
if (value == '0'){
window.location = "/travel/destinations/list";
}else{
window.location = url;
}
}
### What can travelers do to prevent measles?
Getting vaccinated is the best way to protect yourself and others against measles. Measles vaccine is a routine vaccination given to children in the United States. Measles vaccine is usually given in two doses. It’s recommended that children get the first dose when they are 12 to 15 months old and the second dose when they are 4 to 6 years old. Measles vaccine is a combination vaccine that also protects against mumps and rubella (MMR vaccine) or mumps, rubella, and varicella (MMRV vaccine).
If you were born in or after 1957 and have never had measles or have never been vaccinated against measles, you should get vaccinated with two doses of MMR vaccine before you travel. The second dose is given at least 28 days after the first dose. People born before 1957 were likely exposed to measles as children and do not need to be vaccinated with the MMR vaccine.
Infants 6 to 11 months old traveling internationally should get one dose of MMR vaccine before travel. This dose does not count as part of the routine childhood vaccination series.
**CAUTION:** Pregnant people should NOT get the MMR vaccine. Any unvaccinated person should get the MMR vaccine immediately after their pregnancy.
Avoid getting pregnant for at least 4 weeks after receiving the MMR vaccine.
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [Measles Homepage](http://www.cdc.gov/measles/index.html)
* [Measles Webpage for Travelers](https://www.cdc.gov/measles/plan-for-travel.html)
* [Measles Vaccination Information](http://www.cdc.gov/measles/vaccination.html)
* CDC Yellow Book: [Measles](/travel/yellowbook/2020/travel-related-infectious-diseases/measles-rubeola)
* [Guidance on Measles during the Summer Travel Season](https://emergency.cdc.gov/han/2023/han00493.asp)
| None | None |
aa2c9b5e782560de3989ec25a3b223f433e3490e | cdc | Meningococcal Disease | Meningococcal Disease | Disease Directory | Travelers' Health | CDC
### Meningococcal Disease
### What is meningococcal disease?
Meningococcal disease is caused by bacteria called - Neisseria meningitidis- . People with meningococcal disease spread the bacteria to others through close personal contact such as living together or kissing. A person with meningococcal disease needs immediate medical attention.
The symptoms of meningococcal disease can vary based on the type of illness. Common symptoms of meningococcal [meningitis](https://www.cdc.gov/meningococcal/about/symptoms.html#meningitis) include sudden fever, headache, and stiff neck. Other symptoms may include nausea, vomiting, increased sensitivity to light, and confusion. Children and infants may show different signs and symptoms, such as inactivity, irritability, vomiting, or poor reflexes.
Bacteria that cause meningococcal disease can also infect the blood, causing [septicemia](https://www.cdc.gov/meningococcal/about/symptoms.html#septicemia). Symptoms of septicemia include tiredness, vomiting, chills, severe aches and pain, fast breathing, diarrhea, and a dark rash. Meningococcal disease can lead to death in as little as a few hours.
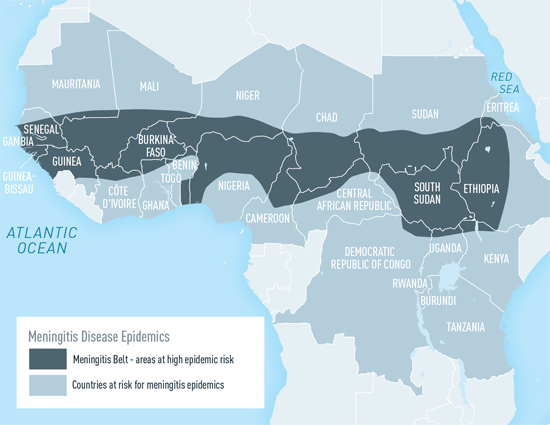
Map: Areas with frequent epidemics of meningococcal meningitis
### Who is at risk?
Anyone can get meningococcal disease, but people who live in or travel to certain areas of the world are more likely to get it.
The [“meningitis belt” of sub-Saharan Africa](/travel/yellowbook/2020/travel-related-infectious-diseases/meningococcal-disease#5559) has the highest rates of meningococcal disease in the world. The disease is more common in this part of Africa from December to June, during the dry season.
Travelers who spend a lot of time with local populations in the meningitis belt, especially during outbreaks of meningococcal disease, are more likely to get this disease.
Participants in the Hajj or Umrah pilgrimages in Saudi Arabia are also more likely to get sick.
### What can travelers do to prevent meningococcal disease?
Getting a meningococcal vaccine is the best way to protect against meningococcal disease. There are two types of meningococcal vaccines available in the United States:
- Meningococcal ACWY (MenACWY) vaccine
- Serogroup B meningococcal (MenB) vaccine
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" - value;
if (value == '0'){
window.location = "/travel/destinations/list";
window.location = url;
MenACWY vaccine is a routine vaccination given to pre-teens and teens in the United States. All 11 to 12-year-olds should get a dose of a MenACWY vaccine and a booster shot at age 16. Teens and young adults may also get a MenB vaccine, preferably at 16 to 18 years old.
Younger children and adults may also need a MenACWY vaccine depending on their travel plans. Some people who have been vaccinated before may need a booster shot. It takes 7 to 10 days after a person has been vaccinated before they have maximum protection against the disease. See your doctor as soon as possible before travel to make sure you are protected.
See if a MenACWY vaccine is recommended for your [destination.](/travel/destinations/list) There are currently no recommendations to receive MenB vaccine before traveling.
Those traveling to Saudi Arabia to participate in the Hajj or Umrah pilgrimages must show proof of MenACWY vaccination. It may also be referred to as tetravalent or quadrivalent meningococcal vaccine.
|
### Meningococcal Disease
### What is meningococcal disease?
Meningococcal disease is caused by bacteria called *Neisseria meningitidis*. People with meningococcal disease spread the bacteria to others through close personal contact such as living together or kissing. A person with meningococcal disease needs immediate medical attention.
The symptoms of meningococcal disease can vary based on the type of illness. Common symptoms of meningococcal [meningitis](https://www.cdc.gov/meningococcal/about/symptoms.html#meningitis) include sudden fever, headache, and stiff neck. Other symptoms may include nausea, vomiting, increased sensitivity to light, and confusion. Children and infants may show different signs and symptoms, such as inactivity, irritability, vomiting, or poor reflexes.
Bacteria that cause meningococcal disease can also infect the blood, causing [septicemia](https://www.cdc.gov/meningococcal/about/symptoms.html#septicemia). Symptoms of septicemia include tiredness, vomiting, chills, severe aches and pain, fast breathing, diarrhea, and a dark rash. Meningococcal disease can lead to death in as little as a few hours.
**Map: Areas with frequent epidemics of meningococcal meningitis**
### Who is at risk?
Anyone can get meningococcal disease, but people who live in or travel to certain areas of the world are more likely to get it.
The [“meningitis belt” of sub-Saharan Africa](/travel/yellowbook/2020/travel-related-infectious-diseases/meningococcal-disease#5559) has the highest rates of meningococcal disease in the world. The disease is more common in this part of Africa from December to June, during the dry season.
Travelers who spend a lot of time with local populations in the meningitis belt, especially during outbreaks of meningococcal disease, are more likely to get this disease.
Participants in the Hajj or Umrah pilgrimages in Saudi Arabia are also more likely to get sick.
### What can travelers do to prevent meningococcal disease?
Getting a meningococcal vaccine is the best way to protect against meningococcal disease. There are two types of meningococcal vaccines available in the United States:
* Meningococcal ACWY (MenACWY) vaccine
* Serogroup B meningococcal (MenB) vaccine
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
function goSelectPage(){
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" + value;
if (value == '0'){
window.location = "/travel/destinations/list";
}else{
window.location = url;
}
}
MenACWY vaccine is a routine vaccination given to pre-teens and teens in the United States. All 11 to 12-year-olds should get a dose of a MenACWY vaccine and a booster shot at age 16. Teens and young adults may also get a MenB vaccine, preferably at 16 to 18 years old.
Younger children and adults may also need a MenACWY vaccine depending on their travel plans. Some people who have been vaccinated before may need a booster shot. It takes 7 to 10 days after a person has been vaccinated before they have maximum protection against the disease. See your doctor as soon as possible before travel to make sure you are protected.
See if a MenACWY vaccine is recommended for your [destination.](/travel/destinations/list) There are currently no recommendations to receive MenB vaccine before traveling.
Those traveling to Saudi Arabia to participate in the Hajj or Umrah pilgrimages must show proof of MenACWY vaccination. It may also be referred to as tetravalent or quadrivalent meningococcal vaccine.
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [Meningococcal Disease](http://www.cdc.gov/meningococcal/)
* [Meningococcal Vaccination](https://www.cdc.gov/meningococcal/vaccine-info.html)
* CDC Yellow Book: [Meningococcal Disease](/travel/yellowbook/2020/travel-related-infectious-diseases/meningococcal-disease)
| None | None |
bcf2cfc9c8e1c4645b212e119ef4114365892b2a | cdc | Mpox | Mpox | Disease Directory | Travelers' Health | CDC
### What is Mpox?
[Mpox](https://www.cdc.gov/poxvirus/mpox/index.html) is a disease caused by infection with mpox virus. In 2022, an outbreak began around the world in areas where mpox is not usually found. Previously, mpox was found mainly in Central and West Africa, often in forested areas.
People infected with mpox develop a rash that can initially look like pimples or blisters. The rash is usually painful.
### What are the symptoms?
[Symptoms](https://www.cdc.gov/poxvirus/mpox/symptoms/index.html) of mpox can include:
- A rash that may:
- Initially look like pimples or blisters
- be painful or itch
- be located on or near the genitals (penis, testicle, labia, and vagina) or anus (butthole) or other areas like the hands, feet, chest, face, or mouth.
The rash will go through several stages, including scabs, before healing. The illness typically lasts 2–4 weeks.
- Muscle aches and backache
- Swollen lymph nodes
- Respiratory symptoms (e.g. sore throat, nasal congestion, or cough)
### How does mpox spread?
Mpox [spreads](https://www.cdc.gov/poxvirus/mpox/if-sick/transmission.html) in a few ways.
Mpox can spread to anyone through close, personal, often skin-to-skin contact, including:
- Direct contact with mpox rash and scabs from a person with mpox, as well as contact with their saliva, upper respiratory secretions (snot, mucus), and areas around the anus, rectum, or vagina
This direct contact can happen during intimate contact, including:
- Oral, anal, or vaginal sex, or touching the genitals (penis, testicles, labia, and vagina) or anus of a person with mpox
- Hugging, massage, and kissing
- Prolonged face-to-face contact
The risk for getting mpox is considered relatively low by touching objects, fabrics, and surfaces that have been used by someone with mpox and not disinfected, such as clothing, bedding, or towels.
### Who is at risk?
Anyone in close contact with a person with mpox can get it and should take steps to protect themselves, especially vaccination. At this time, [data](https://www.cdc.gov/mmwr/volumes/71/wr/mm7132e3.htm) suggest that gay, bisexual, and other men who have sex with men make up the majority of cases in the mpox outbreak that began in 2022.
Travelers who plan to attend [gatherings](https://www.cdc.gov/poxvirus/mpox/prevention/sexual-health.html) that may place them in close, skin-to-skin contact with someone who has mpox are at higher risk of getting infected.
Caregivers of persons with mpox should avoid close skin-to-skin contact with persons who have a rash, wash hands regularly and use proper PPE (mask, gloves) when providing care. Do not share eating utensils or cups and do no handle bedding, towels, or clothing of persons with mpox. Caregivers should consider getting the mpox vaccine.
Travelers such as veterinarians and wildlife professionals may be at risk if they work with infected animals including in areas where wild animals are known to be infected such as Central and West Africa.
### What can travelers do to avoid getting mpox?
Mpox is often transmitted through close, sustained physical contact, and during the outbreak that began in 2022, most frequently, sexual contact.
Travelers can [protect themselves](https://www.cdc.gov/poxvirus/mpox/prevention/protect-yourself.html) against infection by taking the following steps.
- If you are [eligible to get vaccinated](https://www.cdc.gov/poxvirus/mpox/vaccines/index.html) for mpox, get two doses of vaccine before you travel. Use the [Mpox Vaccine Locator](https://mpoxvaxmap.org/) to find out where you can get vaccinated.
- Avoid close, skin-to-skin contact with people who have a rash that looks like mpox.
- Do not touch the rash or scabs of a person with mpox.
- Do not kiss, hug, cuddle or have sex with someone with mpox.
- Avoid contact with objects and materials that a person with mpox has used.
- Do not share eating utensils or cups with a person with mpox.
- Do not handle or touch the bedding, towels, clothing, fetish gear, or sex toys of a person with mpox.
- Wash your hands often with soap and water or use an alcohol-based hand sanitizer, especially before eating or touching your face and after you use the bathroom.
### What to do if you have mpox symptoms or have been around someone with mpox?
If you have [mpox symptoms](https://www.cdc.gov/poxvirus/mpox/symptoms/index.html) or had close contact with someone who has mpox, talk to your healthcare provider about [testing](https://www.cdc.gov/poxvirus/mpox/testing/testing-basics.html) and [treatment](https://www.cdc.gov/poxvirus/mpox/if-sick/treatment.html). CDC [recommends vaccination](https://www.cdc.gov/poxvirus/mpox/vaccines/index.html) for people who have been exposed to mpox and for [people who are at higher risk of being exposed to mpox](https://www.cdc.gov/poxvirus/mpox/prevention/index.html).
Do Not Travel if You Have Mpox
- [Isolate](https://www.cdc.gov/poxvirus/mpox/clinicians/isolation-procedures.html) at home or in another location until your symptoms are gone and your rash has healed; this means all scabs have fallen off and a fresh layer of skin has formed.
- If you have mpox and must travel:
- Make sure that you do not have fever or respiratory symptoms such as sore throat, nasal congestion, or cough.
- Cover your rash and wear a well-fitting mask.
- Take additional steps to [prevent spread to others](https://www.cdc.gov/poxvirus/mpox/if-sick/preventing-spread.html).
Additional Travel Considerations
- If you test positive for mpox while at your international destination, you may be subject to local public health laws and regulations. These could include requirements to isolate and not being allowed travel until you are no longer considered contagious.
- If you have been in contact with a person who has mpox and travel internationally, you may be subject to local public health laws and regulations. These could include requirements to [quarantine](https://www.cdc.gov/quarantine/quarantineisolation.html) and not being allowed travel until you are no longer at risk for developing mpox.
- If you have symptoms of mpox, you may be required to isolate and be tested for mpox. Check your destination’s ministry of health or [US embassyExternal Link](https://www.usembassy.gov/) website to learn about arrival procedures.
|
### Mpox
### What is Mpox?
[Mpox](https://www.cdc.gov/poxvirus/mpox/index.html) is a disease caused by infection with mpox virus. In 2022, an outbreak began around the world in areas where mpox is not usually found. Previously, mpox was found mainly in Central and West Africa, often in forested areas.
People infected with mpox develop a rash that can initially look like pimples or blisters. The rash is usually painful.
### What are the symptoms?
[Symptoms](https://www.cdc.gov/poxvirus/mpox/symptoms/index.html) of mpox can include:
* A rash that may:
+ Initially look like pimples or blisters
+ be painful or itch
+ be located on or near the genitals (penis, testicle, labia, and vagina) or anus (butthole) or other areas like the hands, feet, chest, face, or mouth.
The rash will go through several stages, including scabs, before healing. The illness typically lasts 2–4 weeks.
* Fever
* Headache
* Muscle aches and backache
* Swollen lymph nodes
* Chills
* Exhaustion
* Respiratory symptoms (e.g. sore throat, nasal congestion, or cough)
### How does mpox spread?
Mpox [spreads](https://www.cdc.gov/poxvirus/mpox/if-sick/transmission.html) in a few ways.
Mpox can spread to anyone through close, personal, often skin-to-skin contact, including:
* Direct contact with mpox rash and scabs from a person with mpox, as well as contact with their saliva, upper respiratory secretions (snot, mucus), and areas around the anus, rectum, or vagina
This direct contact can happen during intimate contact, including:
* Oral, anal, or vaginal sex, or touching the genitals (penis, testicles, labia, and vagina) or anus of a person with mpox
* Hugging, massage, and kissing
* Prolonged face-to-face contact
The risk for getting mpox is considered relatively low by touching objects, fabrics, and surfaces that have been used by someone with mpox and not disinfected, such as clothing, bedding, or towels.
### Who is at risk?
Anyone in close contact with a person with mpox can get it and should take steps to protect themselves, especially vaccination. At this time, [data](https://www.cdc.gov/mmwr/volumes/71/wr/mm7132e3.htm) suggest that gay, bisexual, and other men who have sex with men make up the majority of cases in the mpox outbreak that began in 2022.
Travelers who plan to attend [gatherings](https://www.cdc.gov/poxvirus/mpox/prevention/sexual-health.html) that may place them in close, skin-to-skin contact with someone who has mpox are at higher risk of getting infected.
Caregivers of persons with mpox should avoid close skin-to-skin contact with persons who have a rash, wash hands regularly and use proper PPE (mask, gloves) when providing care. Do not share eating utensils or cups and do no handle bedding, towels, or clothing of persons with mpox. Caregivers should consider getting the mpox vaccine.
Travelers such as veterinarians and wildlife professionals may be at risk if they work with infected animals including in areas where wild animals are known to be infected such as Central and West Africa.
### What can travelers do to avoid getting mpox?
Mpox is often transmitted through close, sustained physical contact, and during the outbreak that began in 2022, most frequently, sexual contact.
Travelers can [protect themselves](https://www.cdc.gov/poxvirus/mpox/prevention/protect-yourself.html) against infection by taking the following steps.
* If you are [eligible to get vaccinated](https://www.cdc.gov/poxvirus/mpox/vaccines/index.html) for mpox, get two doses of vaccine before you travel. Use the [Mpox Vaccine Locator](https://mpoxvaxmap.org/) to find out where you can get vaccinated.
* Avoid close, skin-to-skin contact with people who have a rash that looks like mpox.
+ Do not touch the rash or scabs of a person with mpox.
+ Do not kiss, hug, cuddle or have sex with someone with mpox.
* Avoid contact with objects and materials that a person with mpox has used.
+ Do not share eating utensils or cups with a person with mpox.
+ Do not handle or touch the bedding, towels, clothing, fetish gear, or sex toys of a person with mpox.
* Wash your hands often with soap and water or use an alcohol-based hand sanitizer, especially before eating or touching your face and after you use the bathroom.
### What to do if you have mpox symptoms or have been around someone with mpox?
If you have [mpox symptoms](https://www.cdc.gov/poxvirus/mpox/symptoms/index.html) or had close contact with someone who has mpox, talk to your healthcare provider about [testing](https://www.cdc.gov/poxvirus/mpox/testing/testing-basics.html) and [treatment](https://www.cdc.gov/poxvirus/mpox/if-sick/treatment.html). CDC [recommends vaccination](https://www.cdc.gov/poxvirus/mpox/vaccines/index.html) for people who have been exposed to mpox and for [people who are at higher risk of being exposed to mpox](https://www.cdc.gov/poxvirus/mpox/prevention/index.html).
Do Not Travel if You Have Mpox
* [Isolate](https://www.cdc.gov/poxvirus/mpox/clinicians/isolation-procedures.html) at home or in another location until your symptoms are gone and your rash has healed; this means all scabs have fallen off and a fresh layer of skin has formed.
* If you have mpox and must travel:
+ Make sure that you do not have fever or respiratory symptoms such as sore throat, nasal congestion, or cough.
+ Cover your rash and wear a well-fitting mask.
+ Take additional steps to [prevent spread to others](https://www.cdc.gov/poxvirus/mpox/if-sick/preventing-spread.html).
Additional Travel Considerations
* **If you test positive for mpox while at your international destination,** you may be subject to local public health laws and regulations. These could include requirements to isolate and not being allowed travel until you are no longer considered contagious.
* If you have been in contact with a person who has mpox and travel internationally, you may be subject to local public health laws and regulations. These could include requirements to [quarantine](https://www.cdc.gov/quarantine/quarantineisolation.html) and not being allowed travel until you are no longer at risk for developing mpox.
* If you have symptoms of mpox, you may be required to isolate and be tested for mpox. Check your destination’s ministry of health or [US embassyExternal Link](https://www.usembassy.gov/) website to learn about arrival procedures.
* If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/health-care-during-travel). Consider [travel health and medical evacuation insurance](/travel/page/insurance). Options for [treatment](https://www.cdc.gov/poxvirus/mpox/if-sick/treatment.html) may not be available in some countries.
### More Information
* [2022 Mpox Outbreak Cases and Data](https://www.cdc.gov/poxvirus/mpox/response/2022/index.html)
* CDC Website: [Mpox](https://www.cdc.gov/poxvirus/mpox/index.html)
| None | None |
253f187c1374679033e8256c92508c3356bf91f6 | cdc | Mumps | Mumps | Disease Directory | Travelers' Health | CDC
### What is mumps?
Mumps is a contagious disease caused by a virus. People with mumps can spread the virus to others when they
- Cough, sneeze, or talk.
- Share items that have saliva on them (e.g., water bottles or cups).
- Participate in close-contact activities (e.g., playing sports, dancing, or kissing).
Mumps [symptoms](http://www.cdc.gov/mumps/about/signs-symptoms.html) may include fever, headache, muscle aches, tiredness, loss of appetite, and swollen and tender glands under the ears or jaw on one or both sides of the face (parotitis). Most people with mumps recover fully. However, mumps infection can occasionally cause complications, such as swelling of the brain, testicles, ovaries, or breasts. It can also cause temporary or permanent hearing loss.
### Who is at risk?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" - value;
if (value == '0'){
window.location = "/travel/destinations/list";
window.location = url;
Mumps remains a common disease in many countries therefore travelers who are not vaccinated are at risk for getting mumps. Mumps outbreaks are more common among groups of people who have frequent, close contact with each other, such as college students, sports teams, or community groups (e.g., church members).
### What can travelers do to prevent mumps?
Getting vaccinated is the best way to protect yourself against mumps. Mumps vaccine is routinely given to children in the United States. The vaccine is given in two doses: children usually get the first dose at 12 to 15 months old and the second dose when they are 4 to 6 years old. Mumps vaccine is a combination vaccine that also protects against measles and rubella (MMR vaccine) or measles, rubella, and varicella (MMRV vaccine).
If you were born in or after 1957 and have never had mumps or have never been vaccinated against mumps, you should get vaccinated with two doses of MMR vaccine before you travel, with the second dose given at least 28 days after the first dose.
Infants 6 to 11 months old traveling internationally should get one dose MMR vaccine before travel. This dose does not count as part of the routine childhood vaccination series.
Sometimes, vaccine protection can decrease over time. Disease symptoms for previously vaccinated people who get mumps are milder and complications are less frequent.
CAUTION: Pregnant people should NOT get MMR vaccine. Any unvaccinated person should get the MMR vaccine immediately after their pregnancy.
Avoid getting pregnant for at least 4 weeks after receiving MMR vaccine.
|
### Mumps
### What is mumps?
Mumps is a contagious disease caused by a virus. People with mumps can spread the virus to others when they
* Cough, sneeze, or talk.
* Share items that have saliva on them (e.g., water bottles or cups).
* Participate in close-contact activities (e.g., playing sports, dancing, or kissing).
Mumps [symptoms](http://www.cdc.gov/mumps/about/signs-symptoms.html) may include fever, headache, muscle aches, tiredness, loss of appetite, and swollen and tender glands under the ears or jaw on one or both sides of the face (parotitis). Most people with mumps recover fully. However, mumps infection can occasionally cause complications, such as swelling of the brain, testicles, ovaries, or breasts. It can also cause temporary or permanent hearing loss.
### Who is at risk?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
function goSelectPage(){
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" + value;
if (value == '0'){
window.location = "/travel/destinations/list";
}else{
window.location = url;
}
}
Mumps remains a common disease in many countries therefore travelers who are not vaccinated are at risk for getting mumps. Mumps outbreaks are more common among groups of people who have frequent, close contact with each other, such as college students, sports teams, or community groups (e.g., church members).
### What can travelers do to prevent mumps?
Getting vaccinated is the best way to protect yourself against mumps. Mumps vaccine is routinely given to children in the United States. The vaccine is given in two doses: children usually get the first dose at 12 to 15 months old and the second dose when they are 4 to 6 years old. Mumps vaccine is a combination vaccine that also protects against measles and rubella (MMR vaccine) or measles, rubella, and varicella (MMRV vaccine).
If you were born in or after 1957 and have never had mumps or have never been vaccinated against mumps, you should get vaccinated with two doses of MMR vaccine before you travel, with the second dose given at least 28 days after the first dose.
Infants 6 to 11 months old traveling internationally should get one dose MMR vaccine before travel. This dose does not count as part of the routine childhood vaccination series.
Sometimes, vaccine protection can decrease over time. Disease symptoms for previously vaccinated people who get mumps are milder and complications are less frequent.
**CAUTION:** Pregnant people should NOT get MMR vaccine. Any unvaccinated person should get the MMR vaccine immediately after their pregnancy.
Avoid getting pregnant for at least 4 weeks after receiving MMR vaccine.
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [Mumps](http://www.cdc.gov/mumps/)
* [Mumps Vaccination Information](http://www.cdc.gov/mumps/vaccination.html)
* CDC Yellow Book:[Mumps](http://wwwnc.cdc.gov/travel/yellowbook/2012/chapter-3-infectious-diseases-related-to-travel/mumps.htm)
| None | None |
b70cba10dd09c0d4152856721be84e51ada3123c | cdc | Murray Valley Encephalitis virus | Murray Valley Encephalitis virus | Disease Directory | Travelers' Health | CDC
### Murray Valley Encephalitis virus
### What is Murray Valley encephalitis?
Murray Valley encephalitis virus is spread to people through the bite of an infected mosquito.
Most people who get infected never have symptoms. Symptoms of Murray Valley encephalitis can include fever, headache, nausea, vomiting, and tiredness. Some people may develop severe symptoms including confusion, trouble speaking, seizures, and lack of coordination.
### Who is at risk?
Travelers to parts of Australia, Papua New Guinea, or Indonesia are at risk for being infected with Murray Valley encephalitis virus.
Activities that can increase a traveler’s risk of being infected include
- Spending a lot of time outdoors
- Traveling during times of the year when mosquitoes are more common, such as during the summer.
### What can travelers do to prevent Murray Valley encephalitis?
There are no vaccines or medicines that prevent Murray Valley encephalitis. Travelers can protect themselves by taking the following steps.
Use an EPA-registered insect repellent
- Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.
- Picaridin (known as KBR 3023 and icaridin outside the US)
- Oil of lemon eucalyptus (OLE)
- Para-menthane-diol (PMD)
Find the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).

- Insect Repellent Tips for Babies and Children
- Dress your child in clothing that covers arms and legs.
- Cover strollers and baby carriers with mosquito netting.
- When using insect repellent on your child:
- Always follow label instructions.
- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.
- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.
- Adults: Spray insect repellent onto your hands and then apply to a child’s face.
- If also using sunscreen, always apply insect repellent after sunscreen.
Wear long-sleeved shirts and long pants
Treat clothing and gear with permethrin
- Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.
- Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.
- Permethrin-treated clothing provides protection after multiple washings.
- Read product information to find out how long the protection will last.
- If treating items yourself, follow the product instructions.
- Do not use permethrin products directly on skin.
- Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).
Keep mosquitoes out of your hotel room or lodging
- Choose a hotel or lodging with air conditioning or window and door screens.
- Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.
Sleep under a mosquito net

- Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.
- Buy a mosquito net at your local outdoor store or online before traveling overseas.
- Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.
- [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.
- Permethrin is an insecticide that kills mosquitoes and other insects.
- To determine if you can wash a treated mosquito net, follow the label instructions.
If you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).
|
### Murray Valley Encephalitis virus
### What is Murray Valley encephalitis?
Murray Valley encephalitis virus is spread to people through the bite of an infected mosquito.
Most people who get infected never have symptoms. Symptoms of Murray Valley encephalitis can include fever, headache, nausea, vomiting, and tiredness. Some people may develop severe symptoms including confusion, trouble speaking, seizures, and lack of coordination.
### Who is at risk?
Travelers to parts of Australia, Papua New Guinea, or Indonesia are at risk for being infected with Murray Valley encephalitis virus.
Activities that can increase a traveler’s risk of being infected include
* Spending a lot of time outdoors
* Traveling during times of the year when mosquitoes are more common, such as during the summer.
### What can travelers do to prevent Murray Valley encephalitis?
There are no vaccines or medicines that prevent Murray Valley encephalitis. Travelers can protect themselves by taking the following steps.
**Use an EPA-registered insect repellent**

* Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.
+ DEET
+ Picaridin (known as KBR 3023 and icaridin outside the US)
+ IR3535
+ Oil of lemon eucalyptus (OLE)
+ Para-menthane-diol (PMD)
+ 2-undecanone
Find the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).

* Insect Repellent Tips for Babies and Children
+ Dress your child in clothing that covers arms and legs.
+ Cover strollers and baby carriers with mosquito netting.
+ When using insect repellent on your child:
- Always follow label instructions.
- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.
- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.
* Adults: Spray insect repellent onto your hands and then apply to a child’s face.
- If also using sunscreen, always apply insect repellent after sunscreen.
**Wear long-sleeved shirts and long pants**
**Treat clothing and gear with permethrin**

* Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.
+ Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.
+ Permethrin-treated clothing provides protection after multiple washings.
+ Read product information to find out how long the protection will last.
* If treating items yourself, follow the product instructions.
* Do not use permethrin products directly on skin.
* Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).
**Keep mosquitoes out of your hotel room or lodging**
* Choose a hotel or lodging with air conditioning or window and door screens.
* Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.
**Sleep under a mosquito net**

* Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.
* Buy a mosquito net at your local outdoor store or online before traveling overseas.
* Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.
* [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.
+ Permethrin is an insecticide that kills mosquitoes and other insects.
+ To determine if you can wash a treated mosquito net, follow the label instructions.
If you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [Avoid Bug Bites](/travel/page/avoid-bug-bites)
* [Information on Arboviral Diseases](https://www.cdc.gov/ncezid/dvbd/)
| None | None |
cd5134dd4ed81b3df6b2a541bbb2ff2a0a889665 | cdc | Pertussis (Whooping Cough) | Pertussis (Whooping Cough) | Disease Directory | Travelers' Health | CDC
### Pertussis (Whooping Cough)
### What is pertussis?
Whooping cough, also known as pertussis, is a highly contagious respiratory disease caused by bacteria called - Bordetella pertussis- . Whooping cough is known for uncontrollable, violent coughing, which often makes it hard to breathe. Pertussis can affect people of all ages, but can be very serious, even deadly, for babies less than a year old. People with whooping cough can spread the bacteria to others when they cough, sneeze, or share the same breathing space.
Early symptoms are typically mild, like a cold, and can include runny nose, low fever, and mild cough. Later symptoms of the disease may include “fits” of many rapid coughs followed by a high-pitched “whoop,” vomiting, and exhaustion. The coughing fits can continue for up to 10 weeks or more. In babies, the cough can be minimal or not even there. Instead, babies may have pauses in breathing known as apnea.
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" - value;
if (value == '0'){
window.location = "/travel/destinations/list";
window.location = url;
### Who is at risk?
Whooping cough is found worldwide. More whooping cough is seen in developing countries where very few people get vaccinated. Each year, it is estimated that worldwide there are about 24.1 million whooping cough cases and 160,700 deaths in children younger than 5 years old.
### What can travelers do to prevent whooping cough?
Being up to date on whooping cough vaccines is the best way to protect against disease. Whooping cough vaccines are combination vaccines, that also protect against diphtheria and tetanus. These vaccines are often called [DTaP and Tdap](https://www.cdc.gov/vaccines/vpd/dtap-tdap-td/public/index.html).
Babies and Children
Babies need 3 shots of DTaP to build up high levels of protection against diphtheria, tetanus, and whooping cough. Then, young children need 2 booster shots to maintain that protection through early childhood. CDC recommends shots at the following ages:
- 2 months
- 4 months
- 6 months
- 15 through 18 months
- 4 through 6 years
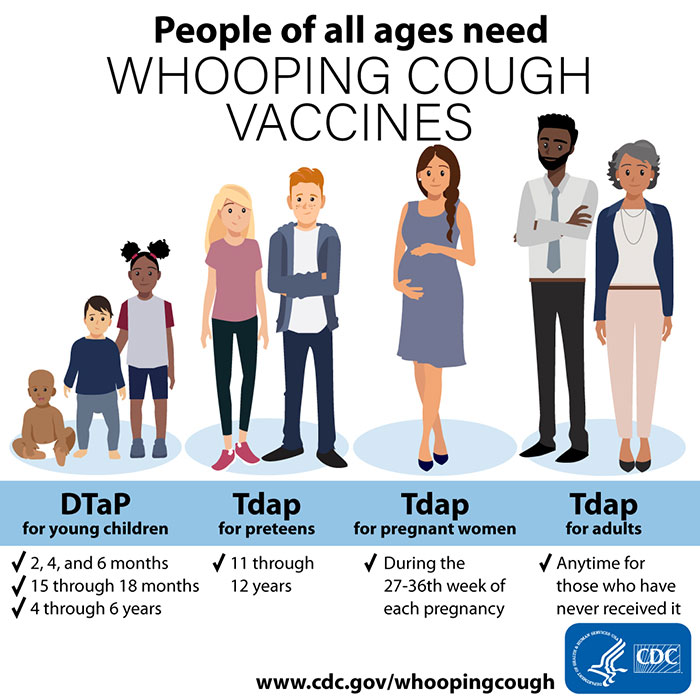
Preteens and Teens
Preteens should get one shot of Tdap between the ages of 11 and 12 years to boost their immunity. Teens who didn’t get Tdap as a preteen should get one shot the next time they visit their healthcare professional.
Pregnant women should get Tdap during the early part of the 3rd trimester of every pregnancy. By doing so, she helps protect her baby from whooping cough in the first few months of life. [Find out more about the Tdap pregnancy recommendation](https://www.cdc.gov/pertussis/pregnant/).
All adults who have never received one should get a shot of Tdap. This can be given at any time, regardless of when they last got Td. This should be followed by either a Td or Tdap shot every 10 years.
|
### Pertussis (Whooping Cough)
### What is pertussis?
Whooping cough, also known as pertussis, is a highly contagious respiratory disease caused by bacteria called *Bordetella pertussis*. Whooping cough is known for uncontrollable, violent coughing, which often makes it hard to breathe. Pertussis can affect people of all ages, but can be very serious, even deadly, for babies less than a year old. People with whooping cough can spread the bacteria to others when they cough, sneeze, or share the same breathing space.
Early symptoms are typically mild, like a cold, and can include runny nose, low fever, and mild cough. Later symptoms of the disease may include “fits” of many rapid coughs followed by a high-pitched “whoop,” vomiting, and exhaustion. The coughing fits can continue for up to 10 weeks or more. In babies, the cough can be minimal or not even there. Instead, babies may have pauses in breathing known as apnea.
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
function goSelectPage(){
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" + value;
if (value == '0'){
window.location = "/travel/destinations/list";
}else{
window.location = url;
}
}
### Who is at risk?
Whooping cough is found worldwide. More whooping cough is seen in developing countries where very few people get vaccinated. Each year, it is estimated that worldwide there are about 24.1 million whooping cough cases and 160,700 deaths in children younger than 5 years old.
### What can travelers do to prevent whooping cough?
Being up to date on whooping cough vaccines is the best way to protect against disease. Whooping cough vaccines are combination vaccines, that also protect against diphtheria and tetanus. These vaccines are often called [DTaP and Tdap](https://www.cdc.gov/vaccines/vpd/dtap-tdap-td/public/index.html).
**Babies and Children**
Babies need 3 shots of DTaP to build up high levels of protection against diphtheria, tetanus, and whooping cough. Then, young children need 2 booster shots to maintain that protection through early childhood. CDC recommends shots at the following ages:
* 2 months
* 4 months
* 6 months
* 15 through 18 months
* 4 through 6 years
**Preteens and Teens**
Preteens should get one shot of Tdap between the ages of 11 and 12 years to boost their immunity. Teens who didn’t get Tdap as a preteen should get one shot the next time they visit their healthcare professional.
**Pregnant Women**
Pregnant women should get Tdap during the early part of the 3rd trimester of every pregnancy. By doing so, she helps protect her baby from whooping cough in the first few months of life. [Find out more about the Tdap pregnancy recommendation](https://www.cdc.gov/pertussis/pregnant/).
**Adults**
All adults who have never received one should get a shot of Tdap. This can be given at any time, regardless of when they last got Td. This should be followed by either a Td or Tdap shot every 10 years.
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [Pertussis](http://www.cdc.gov/pertussis/index.html)
* [Pertussis Vaccine Information](https://www.cdc.gov/vaccines/vpd/dtap-tdap-td/public/index.html)
* CDC Yellow Book: [Pertussis](/travel/yellowbook/2020/travel-related-infectious-diseases/pertussis)
| None | None |
5463b202da0af282c9c7b18e83c031d84f61950b | cdc | Plague | Plague | Disease Directory | Travelers' Health | CDC
### What is plague?
Plague is a rare disease caused by bacteria that can infect people and animals. People can get plague after being bitten by infected fleas, handling an infected animal, or breathing in infectious droplets from an infected person or animal.
Plague symptoms depend on how the patient was exposed to the bacteria. Plague can present with different clinical forms, but the most common forms in humans are bubonic, septicemic, and pneumonic plague.
Type of Plague
How it Spreads
Type of Plague
How it Spreads
Bites from infected fleas and handling infected animals
Fever, headache, chills, and painful, swollen, and tender lymph nodes
Type of Plague
How it Spreads
Bites from infected fleas and handling infected animals
Fever, chills, weakness, stomach pain, and sometimes bleeding into the skin and other organs. Skin and other tissues may turn black and die, especially on fingers, toes, and the nose
Type of Plague
How it Spreads
Breathe in infectious droplets from people or animals. A person can develop pneumonic plague if they get bubonic or septicemic plague and don't treat it
Fever, weakness, shortness of breath, chest pain, cough with bloody or watery mucous
### Who is at risk?
Plague is found in certain regions of Africa, central Asia, the Indian subcontinent, the northern part of South America, and the Southwest United States. Though rare, urban outbreaks of plague have been reported in Madagascar.
Though plague is found in countries around the world, the risk to travelers is low. However, camping, hunting, hiking, or working outdoors can increase your risk.
### What can travelers do to prevent plague?
There is no vaccine to prevent plague available in the United States. However, travelers can protect themselves from plague by taking the following precautions
Wear insect repellent
- Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women.
- Picaridin (known as KBR 3023 and icaridin outside the US)
- Oil of lemon eucalyptus (OLE)
- Para-menthane-diol (PMD)
- Find the right insect repellent for you by using EPA’s search tool.
Treat clothing and gear with permethrin
- Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.
- Permethrin is an insecticide that kills or repels insects.
- Permethrin-treated clothing provides protection after multiple washings..
- Read product information to find out how long the protection will last.
- If treating items yourself, follow the product instructions.
- Do not apply permethrin products directly to skin.
- Watch the video [What You Need to Know About Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).
Do not touch sick or dead animals. Infected fleas can jump from a live or dead animal onto a person. People can also become infected when handling tissue or body fluids of an infected animal. For example, a hunter skinning an infected animal without using proper precautions could become infected with plague.
- If you must handle a sick or dead animal, wear gloves, pants, and long sleeves to cover your skin, and use additional personal protective equipment.
Additional steps to take if visiting or living in an area with plague
- Store food, including pet food, in rodent-proof containers.
- Keep rodents out of the house and make living spaces rodent proof.
- Protect yourself and your pets
- Do not allow pets that roam free in known plague areas to sleep on your bed.
- Protect your pet from fleas. Talk to a veterinarian.
Plague is a very serious illness but is treatable with commonly available antibiotics. The earlier a patient seeks medical care and receives treatment that is appropriate for plague, the better their chances are of a full recovery.
|
### Plague
### What is plague?
Plague is a rare disease caused by bacteria that can infect people and animals. People can get plague after being bitten by infected fleas, handling an infected animal, or breathing in infectious droplets from an infected person or animal.
Plague symptoms depend on how the patient was exposed to the bacteria. Plague can present with different clinical forms, but the most common forms in humans are bubonic, septicemic, and pneumonic plague.
Type of Plague
How it Spreads
[Symptoms](http://www.cdc.gov/plague/symptoms/index.html)
Type of Plague
Bubonic
How it Spreads
Bites from infected fleas and handling infected animals
[Symptoms](http://www.cdc.gov/plague/symptoms/index.html)
Fever, headache, chills, and painful, swollen, and tender lymph nodes
Type of Plague
Septicemic
How it Spreads
Bites from infected fleas and handling infected animals
[Symptoms](http://www.cdc.gov/plague/symptoms/index.html)
Fever, chills, weakness, stomach pain, and sometimes bleeding into the skin and other organs. Skin and other tissues may turn black and die, especially on fingers, toes, and the nose
Type of Plague
Pneumonic
How it Spreads
Breathe in infectious droplets from people or animals. A person can develop pneumonic plague if they get bubonic or septicemic plague and don't treat it
[Symptoms](http://www.cdc.gov/plague/symptoms/index.html)
Fever, weakness, shortness of breath, chest pain, cough with bloody or watery mucous
### Who is at risk?
Plague is found in certain regions of Africa, central Asia, the Indian subcontinent, the northern part of South America, and the Southwest United States. Though rare, urban outbreaks of plague have been reported in Madagascar.
Though plague is found in countries around the world, the risk to travelers is low. However, camping, hunting, hiking, or working outdoors can increase your risk.
### What can travelers do to prevent plague?
There is no vaccine to prevent plague available in the United States. However, travelers can protect themselves from plague by taking the following precautions
**Wear insect repellent**
* Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women.
+ DEET
+ Picaridin (known as KBR 3023 and icaridin outside the US)
+ IR3535
+ Oil of lemon eucalyptus (OLE)
+ Para-menthane-diol (PMD)
+ 2-undecanone
* Find the right insect repellent for you by using EPA’s search tool.
**Treat clothing and gear with permethrin**
* Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.
+ Permethrin is an insecticide that kills or repels insects.
+ Permethrin-treated clothing provides protection after multiple washings..
+ Read product information to find out how long the protection will last.
* If treating items yourself, follow the product instructions.
* Do not apply permethrin products directly to skin.
* Watch the video [What You Need to Know About Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).
**Do not touch sick or dead animals.** Infected fleas can jump from a live or dead animal onto a person. People can also become infected when handling tissue or body fluids of an infected animal. For example, a hunter skinning an infected animal without using proper precautions could become infected with plague.
* If you must handle a sick or dead animal, wear gloves, pants, and long sleeves to cover your skin, and use additional personal protective equipment.
**Additional steps to take if visiting or living in an area with plague**
* Store food, including pet food, in rodent-proof containers.
* Keep rodents out of the house and make living spaces rodent proof.
* Protect yourself and your pets
+ Do not allow pets that roam free in known plague areas to sleep on your bed.
+ Protect your pet from fleas. Talk to a veterinarian.
Plague is a very serious illness but is treatable with commonly available antibiotics. The earlier a patient seeks medical care and receives treatment that is appropriate for plague, the better their chances are of a full recovery.
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [Plague](http://www.cdc.gov/Plague/)
* [Avoid Bug Bites](/travel/page/avoid-bug-bites)
* CDC Yellow Book: [Plague](/travel/yellowbook/2012/chapter-3-infectious-diseases-related-to-travel/plague-bubonic-pneumonic-septicemic.htm)
| None | None |
fdf70d5fb5fe88e66cae3332c20a0bb759e0535d | cdc | Pneumococcal Disease | Pneumococcal Disease | Disease Directory | Travelers' Health | CDC
### Pneumococcal Disease
### What is pneumococcal disease?
Pneumococcal disease is caused by bacteria called - Streptococcus pneumoniae- (pneumococcus). People with pneumococcal disease can spread the bacteria to others when they cough or sneeze.
Pneumococcus bacteria can cause infections in many parts of the body, including
- Lungs (pneumonia)
- Ears (otitis)
- Sinuses (sinusitis)
- The lining of the brain and spinal cord (meningitis)
- Blood (bacteremia)
Symptoms of pneumococcal infection depend on the part of the body affected. Symptoms can include fever, cough, shortness of breath, chest pain, stiff neck, confusion, increased sensitivity to light, joint pain, chills, ear pain, sleeplessness, and irritability. In severe cases, pneumococcal disease can cause hearing loss, brain damage, or death. You can find a full list of symptoms for each part of the body that is affected on the [symptoms and complications of pneumococcal disease page](https://www.cdc.gov/pneumococcal/about/symptoms-complications.html).
### Who is at risk?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" - value;
if (value == '0'){
window.location = "/travel/destinations/list";
window.location = url;
Pneumococcal disease occurs around the world but is more common in low- and middle-income countries where fewer people get vaccinated against pneumococcal disease. In places with four seasons, pneumococcal disease is more common during winter and early spring. In tropical climates with dry and rainy seasons, pneumococcal disease tends to occur more in the dry season.
### What can travelers do to prevent pneumococcal disease?
Getting vaccinated is the best way to protect against pneumococcal disease. Pneumococcal vaccines are routinely recommended in the United States.
CDC recommends [PCV13 or PCV15](https://www.cdc.gov/vaccines/hcp/vis/vis-statements/pcv.html) for
- All children younger than 5 years old
- Children 2 through 18 years old with certain medical conditions
For those who have never received any pneumococcal conjugate vaccine, CDC recommends PCV15 or PCV20 for
- Adults 65 years or older
- Adults 19 through 64 years old with certain medical conditions or other risk factors
CDC reocmmends [PPSV23](https://www.cdc.gov/vaccines/hcp/vis/vis-statements/ppv.html) for
- Children 2 through 18 years old with certain medical conditions
- Adults 19 years or older who receive PCV15
Some groups may need multiple doses or booster shots. Talk with your or your child’s clinician about what is best for your specific situation.
|
### Pneumococcal Disease
### What is pneumococcal disease?
Pneumococcal disease is caused by bacteria called *Streptococcus pneumoniae* (pneumococcus). People with pneumococcal disease can spread the bacteria to others when they cough or sneeze.
Pneumococcus bacteria can cause infections in many parts of the body, including
* Lungs (pneumonia)
* Ears (otitis)
* Sinuses (sinusitis)
* The lining of the brain and spinal cord (meningitis)
* Blood (bacteremia)
Symptoms of pneumococcal infection depend on the part of the body affected. Symptoms can include fever, cough, shortness of breath, chest pain, stiff neck, confusion, increased sensitivity to light, joint pain, chills, ear pain, sleeplessness, and irritability. In severe cases, pneumococcal disease can cause hearing loss, brain damage, or death. You can find a full list of symptoms for each part of the body that is affected on the [symptoms and complications of pneumococcal disease page](https://www.cdc.gov/pneumococcal/about/symptoms-complications.html).
### Who is at risk?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
function goSelectPage(){
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" + value;
if (value == '0'){
window.location = "/travel/destinations/list";
}else{
window.location = url;
}
}
Pneumococcal disease occurs around the world but is more common in low- and middle-income countries where fewer people get vaccinated against pneumococcal disease. In places with four seasons, pneumococcal disease is more common during winter and early spring. In tropical climates with dry and rainy seasons, pneumococcal disease tends to occur more in the dry season.
### What can travelers do to prevent pneumococcal disease?
Getting vaccinated is the best way to protect against pneumococcal disease. Pneumococcal vaccines are routinely recommended in the United States.
CDC recommends [PCV13 or PCV15](https://www.cdc.gov/vaccines/hcp/vis/vis-statements/pcv.html) for
* All children younger than 5 years old
* Children 2 through 18 years old with certain medical conditions
For those who have never received any pneumococcal conjugate vaccine, CDC recommends PCV15 or PCV20 for
* Adults 65 years or older
* Adults 19 through 64 years old with certain medical conditions or other risk factors
CDC reocmmends [PPSV23](https://www.cdc.gov/vaccines/hcp/vis/vis-statements/ppv.html) for
* Children 2 through 18 years old with certain medical conditions
* Adults 19 years or older who receive PCV15
Some groups may need multiple doses or booster shots. Talk with your or your child’s clinician about what is best for your specific situation.
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [Pneumococcal Disease](http://www.cdc.gov/pneumococcal/)
* CDC Yellow Book: [Pneumococcal Disease](/travel/yellowbook/2020/travel-related-infectious-diseases/pneumococcal-disease) in CDC Yellow Book
| None | None |
a1325da97b25f82faebb42529d767f9a6b9a60b1 | cdc | Polio | Polio | Disease Directory | Travelers' Health | CDC
### What is polio?
Polio is a life-threatening disease caused by a virus that affects the nervous system and is usually spread from one person to another when stool (poop) or, less commonly, droplets from a sneeze or cough of an infected person gets into the mouth of another person. For example, you can get polio if you:
- Eat raw or undercooked food or drink water or other drinks that are contaminated with the stool of an infected person.
- Put a contaminated object such as a toy in your mouth.
- Touch a contaminated object and put your fingers in your mouth.
- Have close contact with a person sick with polio, for example when caring for them.
Most people with polio do not feel sick. Some people have only minor symptoms, such as fever, tiredness, nausea, headache, nasal congestion, sore throat, cough, stiffness in the neck and back, and pain in the stomach, arms, and legs. Most people recover completely. In rare cases, polio infection can affect the brain and spinal cord and cause permanent loss of muscle function (paralysis) in the arms or legs (usually the legs). Death can occur if there is a loss of function of the muscles used for breathing or an infection of the brain.
### Who is at risk?
Polio is still a concern in some places. If you are not up to date with your polio vaccines, you are at risk of getting polio. If you are up to date on your polio vaccines but traveling to a polio-affected country, you may need a one-time polio adult booster. Check your [destination’s travel health page](/travel/destinations/list) and talk to your healthcare professional to learn what vaccines you may need before your trip.
### What can travelers do to prevent polio?
#### Get the polio vaccine:
- Make sure you are [up to date](https://www.cdc.gov/vaccines/schedules/hcp/imz/child-adolescent.html#note-polio) on your polio vaccines. If you are up to date on your polio vaccines and traveling to a polio-affected country, you may need a one-time polio adult booster. Check your [destination’s travel health page](/travel/destinations/list) and talk to your healthcare professional to learn which vaccines you may need before traveling.
- Make sure children are vaccinated. For best protection, children should get four doses of polio vaccine. Ideally, children should receive a dose at ages
- 2 months;
- 4 months;
- 6 through 18 months; and
- a booster dose at age 4 through 6 years.
- For information about adults who may not have received sufficient vaccine protection, see the [adult polio vaccination schedule](https://www.cdc.gov/vaccines/vpd/polio/public/index.html).
- See [Polio Vaccine Information Statement (VIS)](http://www.cdc.gov/vaccines/hcp/vis/vis-statements/ipv.html) for more information.
#### Choose safer food and drinks while traveling
Follow the [food and drink safety](/travel/page/food-water-safety) tips to avoid exposure to any food and drinks that could be contaminated by the stool of a person infected with polio.
#### Wash your hands often
- Wash your hands often with soap and water, especially after using the bathroom or changing a child’s diaper and before eating or preparing food. Alcohol-based hand sanitizers do not kill poliovirus.
- Don’t touch your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean.
- Cover your mouth and nose with a tissue or your sleeve (not your hands) when coughing or sneezing.
|
### Polio
### What is polio?
Polio is a life-threatening disease caused by a virus that affects the nervous system and is usually spread from one person to another when stool (poop) or, less commonly, droplets from a sneeze or cough of an infected person gets into the mouth of another person. For example, you can get polio if you:
* Eat raw or undercooked food or drink water or other drinks that are contaminated with the stool of an infected person.
* Put a contaminated object such as a toy in your mouth.
* Touch a contaminated object and put your fingers in your mouth.
* Have close contact with a person sick with polio, for example when caring for them.
Most people with polio do not feel sick. Some people have only minor symptoms, such as fever, tiredness, nausea, headache, nasal congestion, sore throat, cough, stiffness in the neck and back, and pain in the stomach, arms, and legs. Most people recover completely. In rare cases, polio infection can affect the brain and spinal cord and cause permanent loss of muscle function (paralysis) in the arms or legs (usually the legs). Death can occur if there is a loss of function of the muscles used for breathing or an infection of the brain.
### Who is at risk?
Polio is still a concern in some places. If you are not up to date with your polio vaccines, you are at risk of getting polio. If you are up to date on your polio vaccines but traveling to a polio-affected country, you may need a one-time polio adult booster. Check your [destination’s travel health page](/travel/destinations/list) and talk to your healthcare professional to learn what vaccines you may need before your trip.
### What can travelers do to prevent polio?
#### Get the polio vaccine:
* Make sure you are [up to date](https://www.cdc.gov/vaccines/schedules/hcp/imz/child-adolescent.html#note-polio) on your polio vaccines. If you are up to date on your polio vaccines and traveling to a polio-affected country, you may need a one-time polio adult booster. Check your [destination’s travel health page](/travel/destinations/list) and talk to your healthcare professional to learn which vaccines you may need before traveling.
* Make sure children are vaccinated. For best protection, children should get four doses of polio vaccine. Ideally, children should receive a dose at ages
+ 2 months;
+ 4 months;
+ 6 through 18 months; and
+ a booster dose at age 4 through 6 years.
* For information about adults who may not have received sufficient vaccine protection, see the [adult polio vaccination schedule](https://www.cdc.gov/vaccines/vpd/polio/public/index.html).
* See [Polio Vaccine Information Statement (VIS)](http://www.cdc.gov/vaccines/hcp/vis/vis-statements/ipv.html) for more information.
#### Choose safer food and drinks while traveling
Follow the [food and drink safety](/travel/page/food-water-safety) tips to avoid exposure to any food and drinks that could be contaminated by the stool of a person infected with polio.
#### Wash your hands often
* Wash your hands often with soap and water, especially after using the bathroom or changing a child’s diaper and before eating or preparing food. Alcohol-based hand sanitizers do not kill poliovirus.
* Don’t touch your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean.
* Cover your mouth and nose with a tissue or your sleeve (not your hands) when coughing or sneezing.
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel. Avoid contact with other people while you are sick.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [CDC Travel Health Notice: Polio in Multiple Countries](/travel/notices/alert/global-polio)
* [What is Polio?](https://www.cdc.gov/polio/what-is-polio/index.htm)
* [Polio: For Travelers](https://www.cdc.gov/polio/what-is-polio/travelers.html)
* [Choose Safe Food and Drinks When Traveling](/travel/page/food-water-safety)
* CDC Yellow Book: [Polio](/travel/yellowbook/2012/chapter-3-infectious-diseases-related-to-travel/poliomyelitis.htm)
* [World Health Organization: PolioExternal Link](https://www.who.int/health-topics/poliomyelitis#tab=tab_1)
| None | None |
8310a6caf57014d6a8d381df0e8154b7c4b691bd | cdc | Rabies | Rabies | Disease Directory | Travelers' Health | CDC
### What is rabies?
Rabies is a deadly disease caused by a virus. You can get rabies if you are bitten or scratched by an animal with rabies.
In the United States, rabies is mostly found in wild animals like bats, raccoons, skunks, and foxes. However, in many other countries around the world, bites from dogs (including puppies) are the main source of rabies infections in people. Most people who die of rabies were bitten by a dog with rabies.
Rabies affects the central nervous system (the brain and spinal cord). Without appropriate medical care, rabies causes brain disease and death. Once symptoms of rabies appear, the disease is nearly always fatal. For this reason, preventing animal bites and receiving prompt medical care is especially important.
Early rabies symptoms include weakness or discomfort, fever, and headache. There may be discomfort or a prickling or itching sensation at the place of the bite. Within days, an infected person may become anxious, confused, and agitated. As a person gets sicker, they may become delirious, hallucinate, be unable to sleep, and unable to swallow or quench their thirst.
### Who is at risk?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" - value;
if (value == '0'){
window.location = "/travel/destinations/list";
window.location = url;
Rabid dogs are a problem in many countries around the world, including most of Africa, Asia, and parts of Central and South America. Although any mammal can transmit rabies, dog bites are how most travelers get rabies.
Activities that may increase a traveler’s chances of rabies infection include:
- Camping or exploring caves (spelunkers)
- Working with animals (veterinarians, animal handlers, field biologists, or laboratory workers handling animal specimens)
- Long-term travelers and expatriates
Children are more likely to get infected because they often play with animals and may not report bites.
Rabies in dogs is rare in the United States, Australia, Canada, Japan, and most European countries.
### What can travelers do to prevent rabies?
Travelers can protect themselves from rabies by taking the following steps:
Avoid animals when traveling
- Don’t touch dogs, puppies, or other animals. This goes for strays as well as pets. Not all countries require pets to be vaccinated against rabies. Even animals that appear healthy can spread rabies.
- Supervise children closely, especially around dogs and puppies, cats and kittens, and wildlife.
- If you travel with your pet, watch it closely. Do not allow it around other local pets or wild animals.
- Avoid bringing animals home to the United States. Dogs and cats may be infected with rabies but not show signs until several days or months later. If you do decide to bring an animal with you to the United States, be aware of [CDC’s](https://www.cdc.gov/importation/bringing-an-animal-into-the-united-states/index.html) and [USDA’s](https://www.aphis.usda.gov/aphis/ourfocus/animalhealth/animal-and-animal-product-import-information/live-animal-imports/import-live-animals) [animal importation regulations](https://www.cdc.gov/importation/bringing-an-animal-into-the-united-states/index.html).
- If you are traveling to work with animals, bring and wear appropriate protective gear.
- For more information, see [Be Safe Around Animals](/travel/page/be-safe-around-animals).
Act quickly if you are bitten or scratched by a dog or other animal
- Immediately wash all bites and scratches well. Use plenty of soap and running water.
- Seek medical care immediately, even if you don’t feel sick or the wound does not look serious.
- To prevent rabies, start treatment immediately. Treatment for rabies includes getting a vaccine after you have been bitten. Even if you were vaccinated before your trip, you still need to seek care if you get bitten or scratched by an animal.
- Be prepared to travel back to the United States or to another area to receive treatment. Vaccination and medicine for rabies exposure is not available everywhere in the world.
Pre-travel rabies vaccine
For some travelers, it may make sense to get the rabies vaccine before your trip. Check if rabies vaccine is recommended for [your destination](/travel/destinations/list).
The rabies vaccine is given in two shots. The second dose is given seven days after the first dose. Even if you are vaccinated against rabies, if you are bitten or scratched by an [animal that may have rabies](https://www.cdc.gov/rabies/animals/index.html) while traveling, you need to seek medical care immediately and get two booster doses of the vaccine.
|
### Rabies
### What is rabies?

Rabies is a deadly disease caused by a virus. You can get rabies if you are bitten or scratched by an animal with rabies.
In the United States, rabies is mostly found in wild animals like bats, raccoons, skunks, and foxes. However, in many other countries around the world, bites from dogs (including puppies) are the main source of rabies infections in people. Most people who die of rabies were bitten by a dog with rabies.
Rabies affects the central nervous system (the brain and spinal cord). Without appropriate medical care, rabies causes brain disease and death. Once symptoms of rabies appear, the disease is nearly always fatal. For this reason, preventing animal bites and receiving prompt medical care is especially important.
Early rabies symptoms include weakness or discomfort, fever, and headache. There may be discomfort or a prickling or itching sensation at the place of the bite. Within days, an infected person may become anxious, confused, and agitated. As a person gets sicker, they may become delirious, hallucinate, be unable to sleep, and unable to swallow or quench their thirst.
### Who is at risk?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
function goSelectPage(){
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" + value;
if (value == '0'){
window.location = "/travel/destinations/list";
}else{
window.location = url;
}
}
Rabid dogs are a problem in many countries around the world, including most of Africa, Asia, and parts of Central and South America. Although any mammal can transmit rabies, dog bites are how most travelers get rabies.
Activities that may increase a traveler’s chances of rabies infection include:
* Camping or exploring caves (spelunkers)
* Working with animals (veterinarians, animal handlers, field biologists, or laboratory workers handling animal specimens)
* Long-term travelers and expatriates
Children are more likely to get infected because they often play with animals and may not report bites.
Rabies in dogs is rare in the United States, Australia, Canada, Japan, and most European countries.
### What can travelers do to prevent rabies?
Travelers can protect themselves from rabies by taking the following steps:
**Avoid animals when traveling**
* Don’t touch dogs, puppies, or other animals. This goes for strays as well as pets. Not all countries require pets to be vaccinated against rabies. Even animals that appear healthy can spread rabies.
* Supervise children closely, especially around dogs and puppies, cats and kittens, and wildlife.
* If you travel with your pet, watch it closely. Do not allow it around other local pets or wild animals.
* Avoid bringing animals home to the United States. Dogs and cats may be infected with rabies but not show signs until several days or months later. If you do decide to bring an animal with you to the United States, be aware of [CDC’s](https://www.cdc.gov/importation/bringing-an-animal-into-the-united-states/index.html) and [USDA’s](https://www.aphis.usda.gov/aphis/ourfocus/animalhealth/animal-and-animal-product-import-information/live-animal-imports/import-live-animals) [animal importation regulations](https://www.cdc.gov/importation/bringing-an-animal-into-the-united-states/index.html).
* If you are traveling to work with animals, bring and wear appropriate protective gear.
* For more information, see [Be Safe Around Animals](/travel/page/be-safe-around-animals).
**Act quickly if you are bitten or scratched by a dog or other animal**
* Immediately wash all bites and scratches well. Use plenty of soap and running water.
* Seek medical care immediately, even if you don’t feel sick or the wound does not look serious.
* To prevent rabies, start treatment immediately. Treatment for rabies includes getting a vaccine after you have been bitten. Even if you were vaccinated before your trip, you still need to seek care if you get bitten or scratched by an animal.
* Be prepared to travel back to the United States or to another area to receive treatment. Vaccination and medicine for rabies exposure is not available everywhere in the world.
**Pre-travel rabies vaccine**
For some travelers, it may make sense to get the rabies vaccine before your trip. Check if rabies vaccine is recommended for [your destination](/travel/destinations/list).
The rabies vaccine is given in two shots. The second dose is given seven days after the first dose. Even if you are vaccinated against rabies, if you are bitten or scratched by an [animal that may have rabies](https://www.cdc.gov/rabies/animals/index.html) while traveling, you need to seek medical care immediately and get two booster doses of the vaccine.
**Consider medical evacuation insurance**
Rabies vaccine is not available in all countries. Medical evacuation insurance can cover the cost of transferring you home or to the nearest destination where care can be obtained. For more information, see [Travel Insurance: Peace of Mind While You Travel](/travel/page/insurance) and [Travel Insurance, Travel Health Insurance & Medical Evacuation Insurance](/travel/yellowbook/2020/health-care-abroad/travel-insurance-travel-health-insurance-and-medical-evacuation-insurance).
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### Traveler Information
* CDC Website: [Rabies](http://www.cdc.gov/rabies/)
* [Be Safe Around Animals](/travel/page/be-safe-around-animals)
* [Vaccine Information Statements (VIS)](http://www.cdc.gov/vaccines/pubs/vis/downloads/vis-rabies.pdf)
### Clinician Information
* [Rabies](/travel/yellowbook/2012/chapter-3-infectious-diseases-related-to-travel/rabies.htm) in CDC Yellow Book
* [R](http://www.cdc.gov/rabies/)[abies Information for Doctors](https://www.cdc.gov/rabies/specific_groups/doctors/index.html)
* [Rabies: Notifiable Disease](http://c.ymcdn.com/sites/www.cste.org/resource/resmgr/PDFs/CSTENotifiableConditionListA.pdf)
* [Rabies Diagnosis](http://www.cdc.gov/rabies/diagnosis/index.html)
| None | None |
8c1c4ef7879454bbd96b716e98517d2c35c22704 | cdc | Ross River virus disease | Ross River virus disease | Disease Directory | Travelers' Health | CDC
### Ross River virus disease
### What is Ross River virus disease?

Ross River virus disease is spread to people by the bite of an infected mosquito.
Most people who get Ross River virus do not feel sick. For those who do get sick, symptoms include joint pain and swelling, muscle pain, fever, tiredness, and rash. Most patients recover within a few weeks, but some people experience joint pain, joint stiffness, or tiredness for many months.
### Who is at risk?
Travelers to Australia and Papua New Guinea can get Ross River virus disease if bitten by an infected mosquito. It is the most common mosquito-borne disease in Australia.
The following activities can increase a traveler’s chance of getting infected:
- Spending a lot of time outdoors
- Traveling during times of the year when mosquitoes are more common, such as during the summer.
### What can travelers do to prevent Ross River virus disease?
There are no vaccines or medicines that prevent Ross River virus disease. Travelers can protect themselves by taking the following steps.
Use an EPA-registered insect repellent
- Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.
- Picaridin (known as KBR 3023 and icaridin outside the US)
- Oil of lemon eucalyptus (OLE)
- Para-menthane-diol (PMD)
Find the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).

- Insect Repellent Tips for Babies and Children
- Dress your child in clothing that covers arms and legs.
- Cover strollers and baby carriers with mosquito netting.
- When using insect repellent on your child:
- Always follow label instructions.
- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.
- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.
- Adults: Spray insect repellent onto your hands and then apply to a child’s face.
- If also using sunscreen, always apply insect repellent after sunscreen.
Wear long-sleeved shirts and long pants
Treat clothing and gear with permethrin
- Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.
- Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.
- Permethrin-treated clothing provides protection after multiple washings.
- Read product information to find out how long the protection will last.
- If treating items yourself, follow the product instructions.
- Do not use permethrin products directly on skin.
- Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).
Keep mosquitoes out of your hotel room or lodging
- Choose a hotel or lodging with air conditioning or window and door screens.
- Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.
Sleep under a mosquito net

- Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.
- Buy a mosquito net at your local outdoor store or online before traveling overseas.
- Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.
- [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.
- Permethrin is an insecticide that kills mosquitoes and other insects.
- To determine if you can wash a treated mosquito net, follow the label instructions.
If you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).
If you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment.](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html)
|
### Ross River virus disease
### What is Ross River virus disease?

Ross River virus disease is spread to people by the bite of an infected mosquito.
Most people who get Ross River virus do not feel sick. For those who do get sick, symptoms include joint pain and swelling, muscle pain, fever, tiredness, and rash. Most patients recover within a few weeks, but some people experience joint pain, joint stiffness, or tiredness for many months.
### Who is at risk?
Travelers to Australia and Papua New Guinea can get Ross River virus disease if bitten by an infected mosquito. It is the most common mosquito-borne disease in Australia.
The following activities can increase a traveler’s chance of getting infected:
* Spending a lot of time outdoors
* Traveling during times of the year when mosquitoes are more common, such as during the summer.
### What can travelers do to prevent Ross River virus disease?
There are no vaccines or medicines that prevent Ross River virus disease. Travelers can protect themselves by taking the following steps.
**Use an EPA-registered insect repellent**

* Use [Environmental Protection Agency (EPA)-registered insect repellents](https://www.epa.gov/insect-repellents) with one of the active ingredients below. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women. If also using sunscreen, always apply insect repellent after sunscreen.
+ DEET
+ Picaridin (known as KBR 3023 and icaridin outside the US)
+ IR3535
+ Oil of lemon eucalyptus (OLE)
+ Para-menthane-diol (PMD)
+ 2-undecanone
Find the right insect repellent for you by using [EPA's search tool](https://www.epa.gov/insect-repellents/find-repellent-right-you).

* Insect Repellent Tips for Babies and Children
+ Dress your child in clothing that covers arms and legs.
+ Cover strollers and baby carriers with mosquito netting.
+ When using insect repellent on your child:
- Always follow label instructions.
- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.
- Do not apply insect repellent to a child’s hands, eyes, mouth, cuts, or irritated skin.
* Adults: Spray insect repellent onto your hands and then apply to a child’s face.
- If also using sunscreen, always apply insect repellent after sunscreen.
**Wear long-sleeved shirts and long pants**
**Treat clothing and gear with permethrin**

* Use 0.5% permethrin to treat clothing and gear (such as boots, pants, socks, and tents) or buy permethrin-treated clothing and gear.
+ Permethrin is an insecticide that kills or repels insects like mosquitoes and sand flies.
+ Permethrin-treated clothing provides protection after multiple washings.
+ Read product information to find out how long the protection will last.
* If treating items yourself, follow the product instructions.
* Do not use permethrin products directly on skin.
* Watch the CDC video [How to Use Permethrin](https://www.cdc.gov/mosquitoes/mosquito-bites/how-to-use-permethrin.html).
**Keep mosquitoes out of your hotel room or lodging**
* Choose a hotel or lodging with air conditioning or window and door screens.
* Use a mosquito net if you are unable to stay in a place with air conditioning or window and door screens or if you are sleeping outside.
**Sleep under a mosquito net**

* Sleep under a mosquito net if you are outside or when screened rooms are not available. Mosquitoes can live indoors and bite during the day and night.
* Buy a mosquito net at your local outdoor store or online before traveling overseas.
* Choose a mosquito net that is compact, white, rectangular, with 156 holes per square inch, and long enough to tuck under the mattress.
* [Permethrin-treated mosquito nets](https://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html) provide more protection than untreated nets.
+ Permethrin is an insecticide that kills mosquitoes and other insects.
+ To determine if you can wash a treated mosquito net, follow the label instructions.
If you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html).
If you are bitten by mosquitoes, avoid scratching the bites and apply over-the-counter anti-itch or antihistamine cream to relieve itching. See [Mosquito Bite Symptoms and Treatment.](https://www.cdc.gov/mosquitoes/mosquito-bites/symptoms.html)
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### Traveler Information
* [Avoid Bug Bites](/travel/page/avoid-bug-bites)
* [Ross River Virus](/travel/yellowbook/2020/travel-related-infectious-diseases/chikungunya)
| None | None |
c2d4b3c089a44ff67b5a834ec837ac92aefcd79a | cdc | Routine Vaccines | Routine Vaccines | Travelers' Health | CDC
### Routine Vaccines

### What are "routine vaccines"?
Routine vaccines are those recommended for everyone in the United States, depending on age and vaccine history. Most people think of these as [childhood vaccines](https://www.cdc.gov/vaccines/parents/protecting-children/index.html) that you get before starting school, but but there are also routine vaccines for [adolescents](https://www.cdc.gov/vaccines/schedules/hcp/imz/child-adolescent.html) and [adults](https://www.cdc.gov/vaccines/schedules/hcp/imz/adult.html).
### Why are routine vaccines important for travelers?
Because most U.S. children get routine vaccines, many vaccine-preventable diseases, such as measles, mumps, or chickenpox, are not common in the United States. If you are not vaccinated, international travel increases your chances of getting and spreading diseases that are not common in the United Sates. Popular destinations, including Europe, still have outbreaks of [measles](https://www.cdc.gov/measles/travelers.html) and other vaccine-preventable diseases.
Make sure you are up-to-date on all of your [routine vaccines](/travel/page/routine-vaccines). Routine vaccinations protect you from infectious diseases such as measles that can spread quickly in groups of unvaccinated people. Many diseases prevented by routine vaccination are not common in the United States but are still common in other countries.
[Check CDC’s destination pages for travel health information](/travel/destinations/list). Check CDC’s webpage for your destination to see what vaccines or medicines you may need and what diseases or health risks are a concern at your destination.
Make an appointment with your healthcare provider or a [travel health specialist](/travel/page/find-clinic) that takes place at least one month before you leave. They can help you get destination-specific vaccines, medicines, and information. Discussing your health concerns, itinerary, and planned activities with your provider allows them to give more specific advice and recommendations.
### What routine vaccines do I need?
The routine vaccines you need before travel may depend on your age, health, and vaccine history. You may need to get an accelerated dose of a vaccine or a booster dose before traveling.
Routine vaccinations related to travel may include the following:
- Chickenpox (Varicella)
- Hepatitis A
- Hepatitis B
- Human Papilloma Virus (HPV)
- Measles, mumps, Rubella
- Tetanus, diphtheria, pertussis
- Shingles (Zoster)
The following are CDC immunization schedules for by age group:
- [Recommended Vaccinations or Infants and Children (birth through 6 years)](https://www.cdc.gov/vaccines/schedules/easy-to-read/adolescent-easyread.html)
- [Recommended Vaccinations for Children (7-18 years old)](https://www.cdc.gov/vaccines/schedules/easy-to-read/adolescent-easyread.html)
- [Recommended Adult Immunization Schedule for ages 19 years or older](https://www.cdc.gov/vaccines/schedules/hcp/imz/adult.html)
|
### Routine Vaccines

### What are "routine vaccines"?
Routine vaccines are those recommended for everyone in the United States, depending on age and vaccine history. Most people think of these as [childhood vaccines](https://www.cdc.gov/vaccines/parents/protecting-children/index.html) that you get before starting school, but but there are also routine vaccines for [adolescents](https://www.cdc.gov/vaccines/schedules/hcp/imz/child-adolescent.html) and [adults](https://www.cdc.gov/vaccines/schedules/hcp/imz/adult.html).
### Why are routine vaccines important for travelers?
Because most U.S. children get routine vaccines, many vaccine-preventable diseases, such as measles, mumps, or chickenpox, are not common in the United States. If you are not vaccinated, international travel increases your chances of getting and spreading diseases that are not common in the United Sates. Popular destinations, including Europe, still have outbreaks of [measles](https://www.cdc.gov/measles/travelers.html) and other vaccine-preventable diseases.
**Make sure you are up-to-date on all of your [routine vaccines](/travel/page/routine-vaccines).** Routine vaccinations protect you from infectious diseases such as measles that can spread quickly in groups of unvaccinated people. Many diseases prevented by routine vaccination are not common in the United States but are still common in other countries.
**[Check CDC’s destination pages for travel health information](/travel/destinations/list).** Check CDC’s webpage for your destination to see what vaccines or medicines you may need and what diseases or health risks are a concern at your destination.
**Make an appointment** with your healthcare provider or a [travel health specialist](/travel/page/find-clinic) that takes place at least one month before you leave. They can help you get destination-specific vaccines, medicines, and information. Discussing your health concerns, itinerary, and planned activities with your provider allows them to give more specific advice and recommendations.
### What routine vaccines do I need?
The routine vaccines you need before travel may depend on your age, health, and vaccine history. You may need to get an accelerated dose of a vaccine or a booster dose before traveling.
Routine vaccinations related to travel may include the following:
* COVID-19
* Chickenpox (Varicella)
* Hepatitis A
* Hepatitis B
* Human Papilloma Virus (HPV)
* Influenza
* Measles, mumps, Rubella
* Meningococcal
* Pneumococcal
* Polio
* Rotavirus
* Tetanus, diphtheria, pertussis
* Shingles (Zoster)
The following are CDC immunization schedules for by age group:
* [Recommended Vaccinations or Infants and Children (birth through 6 years)](https://www.cdc.gov/vaccines/schedules/easy-to-read/adolescent-easyread.html)
* [Recommended Vaccinations for Children (7-18 years old)](https://www.cdc.gov/vaccines/schedules/easy-to-read/adolescent-easyread.html)
* [Recommended Adult Immunization Schedule for ages 19 years or older](https://www.cdc.gov/vaccines/schedules/hcp/imz/adult.html)
### More Information
* [Immunization Schedules](https://www.cdc.gov/vaccines/schedules/index.html)
* [Travel Vaccines](/travel/page/travel-vaccines)
| None | None |
a82e54543cf819eb163023f5f851c4a858edbd8b | cdc | Rubella | Rubella | Disease Directory | Travelers' Health | CDC
### What is rubella?
Rubella, also called German measles, is a contagious disease caused by a virus. People with rubella can spread it when they cough or sneeze. Pregnant women infected with rubella can pass it on to their developing babies.
Many people who get rubella never have symptoms or have only mild symptoms. For people who have symptoms, they may include a red rash that starts on the face and spreads to the rest of the body. Other symptoms include low-grade fever, headache, mild pink eye, general discomfort, swollen and enlarged lymph nodes, cough, and runny nose.
While most adults who get rubella have only mild symptoms, rubella infection is especially dangerous during pregnancy. Pregnant women who get rubella can have miscarriages or stillbirths, and their developing babies are at risk for severe birth defects with devastating, lifelong consequences
### Who is at risk?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" - value;
if (value == '0'){
window.location = "/travel/destinations/list";
window.location = url;
Rubella has been eliminated through vaccination in South and North America, including the United States. It still exists in other parts of the world. Travelers going to areas with rubella who have not been vaccinated can get infected.
### What can travelers do to prevent rubella?
Getting vaccinated is the best way to protect yourself against rubella. Rubella vaccine is routinely given to children in the United States. The vaccine is given in two doses: children usually get the first dose when they are 12 to 15 months old and the second dose when they are 4 to 6 years old. Rubella vaccine is a combination vaccine that also protects against measles and mumps (MMR vaccine) or measles, mumps, and varicella (MMRV vaccine).
If you were born after 1956 and do not have evidence of immunity, you should get vaccinated with two doses of MMR vaccine before you travel. The second dose is given at least 28 days after the first dose. People born before 1957 do not need to be vaccinated with the MMR vaccine.
Infants 6 to 11 months old traveling internationally should get one dose of MMR vaccine before travel. This dose does not count as part of the routine childhood vaccination series.
CAUTION: Pregnant people should avoid all exposures to the rubella virus. This means NOT getting the MMR vaccine during pregnancy. It also means that anyone who is pregnant and not already vaccinated against rubella should not travel to countries with rubella or areas with known rubella outbreaks. This is especially true during the first 20 weeks of pregnancy when the risk for a miscarriage or severe birth defects from rubella virus infection is greatest. Any pregnant person not already vaccinated against rubella should get the MMR vaccine immediately after the pregnancy.
Avoid getting pregnant for at least 4 weeks after receiving the MMR vaccine.
|
### Rubella
### What is rubella?
Rubella, also called German measles, is a contagious disease caused by a virus. People with rubella can spread it when they cough or sneeze. Pregnant women infected with rubella can pass it on to their developing babies.
Many people who get rubella never have symptoms or have only mild symptoms. For people who have symptoms, they may include a red rash that starts on the face and spreads to the rest of the body. Other symptoms include low-grade fever, headache, mild pink eye, general discomfort, swollen and enlarged lymph nodes, cough, and runny nose.
While most adults who get rubella have only mild symptoms, rubella infection is especially dangerous during pregnancy. Pregnant women who get rubella can have miscarriages or stillbirths, and their developing babies are at risk for severe birth defects with devastating, lifelong consequences
### Who is at risk?
Information by Destination

Where are you going?
-- Select One --AfghanistanAlbaniaAlgeriaAmerican SamoaAndorraAnegadaAngolaAnguilla (U.K.)AntarcticaAntigua and BarbudaArgentinaArmeniaArubaAustral IslandsAustraliaAustriaAzerbaijanAzoresBahamas, TheBahrainBangladeshBarbadosBarbudaBelarusBelgiumBelizeBeninBermuda (U.K.)BhutanBoliviaBonaireBora-BoraBosnia and HerzegovinaBotswanaBrazilBritish Indian Ocean Territory (U.K.)BruneiBulgariaBurkina FasoBurma (Myanmar)BurundiCaicos IslandsCambodiaCameroonCanadaCanary Islands (Spain)Cape VerdeCayman Islands (U.K.)Central African RepublicChadChileChinaChristmas Island (Australia)Cocos (Keeling) Islands (Australia)ColombiaComorosCongo, Republic of theCook Islands (New Zealand)Costa RicaCôte d'IvoireCroatiaCubaCuraçaoCyprusCzech RepublicDemocratic Republic of the CongoDenmarkDjiboutiDominicaDominican RepublicDubaiEaster Island (Chile)EcuadorEgyptEl SalvadorEnglandEquatorial GuineaEritreaEstoniaEswatini (Swaziland)EthiopiaFalkland Islands (Islas Malvinas)Faroe Islands (Denmark)FijiFinlandFranceFrench Guiana (France)French Polynesia (France)GabonGalápagos IslandsGambia, TheGeorgiaGermanyGhanaGibraltar (U.K.)GreeceGreenland (Denmark)GrenadaGrenadinesGuadeloupeGuam (U.S.)GuatemalaGuernseyGuineaGuinea-BissauGuyanaHaitiHoly SeeHondurasHong Kong SAR (China)HungaryIcelandIndiaIndonesiaIranIraqIrelandIsle of ManIsrael, including the West Bank and GazaItalyIvory CoastJamaicaJapanJerseyJordanJost Van DykeKazakhstanKenyaKiribatiKosovoKuwaitKyrgyzstanLaosLatviaLebanonLesothoLiberiaLibyaLiechtensteinLithuaniaLuxembourgMacau SAR (China)MadagascarMadeira Islands (Portugal)MalawiMalaysiaMaldivesMaliMaltaMarquesas IslandsMarshall IslandsMartinique (France)MauritaniaMauritiusMayotte (France)MexicoMicronesia, Federated States ofMoldovaMonacoMongoliaMontenegroMontserrat (U.K.)MooreaMoroccoMozambiqueMyanmar (Burma)NamibiaNauruNepalNetherlands, TheNew Caledonia (France)New ZealandNicaraguaNigerNigeriaNiue (New Zealand)Norfolk Island (Australia)North KoreaNorth MacedoniaNorthern IrelandNorthern Mariana Islands (U.S.)NorwayOmanPakistanPalauPanamaPapua New GuineaParaguayPeruPhilippinesPitcairn Islands (U.K.)PolandPortugalPuerto Rico (U.S.)QatarRéunion (France)RomaniaRotaRurutuRussiaRwandaSabaSaint BarthelemySaint CroixSaint Helena (U.K.)Saint JohnSaint Kitts and NevisSaint LuciaSaint MartinSaint Pierre and Miquelon (France)Saint ThomasSaint Vincent and the GrenadinesSaipanSamoaSan MarinoSão Tomé and PríncipeSaudi ArabiaScotlandSenegalSerbiaSeychellesSierra LeoneSingaporeSint EustatiusSint MaartenSlovakiaSloveniaSociety IslandsSolomon IslandsSomaliaSouth AfricaSouth Georgia and the South Sandwich Islands (U.K.)South KoreaSouth Sandwich IslandsSouth SudanSpainSri LankaSudanSurinameSwaziland (Eswatini)SwedenSwitzerlandSyriaTahitiTaiwanTajikistanTanzaniaThailandTimor-Leste (East Timor)TinianTobagoTogoTokelau (New Zealand)TongaTortolaTrinidad and TobagoTubuaiTunisiaTurkeyTurkmenistanTurks and Caicos Islands (U.K.)TuvaluUgandaUkraineUnited Arab EmiratesUnited KingdomUnited StatesUruguayUzbekistanVanuatuVatican CityVenezuelaVietnamVirgin GordaVirgin Islands, BritishVirgin Islands, U.S.Wake IslandWalesYemenZambiaZanzibarZimbabweGo
function goSelectPage(){
var e = document.getElementById("thlrdssl-traveler");
var value = e.options[e.selectedIndex].value;
var url = "/travel/destinations/traveler/none/" + value;
if (value == '0'){
window.location = "/travel/destinations/list";
}else{
window.location = url;
}
}
Rubella has been eliminated through vaccination in South and North America, including the United States. It still exists in other parts of the world. Travelers going to areas with rubella who have not been vaccinated can get infected.
### What can travelers do to prevent rubella?
Getting vaccinated is the best way to protect yourself against rubella. Rubella vaccine is routinely given to children in the United States. The vaccine is given in two doses: children usually get the first dose when they are 12 to 15 months old and the second dose when they are 4 to 6 years old. Rubella vaccine is a combination vaccine that also protects against measles and mumps (MMR vaccine) or measles, mumps, and varicella (MMRV vaccine).
If you were born after 1956 and do not have evidence of immunity, you should get vaccinated with two doses of MMR vaccine before you travel. The second dose is given at least 28 days after the first dose. People born before 1957 do not need to be vaccinated with the MMR vaccine.
Infants 6 to 11 months old traveling internationally should get one dose of MMR vaccine before travel. This dose does not count as part of the routine childhood vaccination series.
**CAUTION**: Pregnant people should avoid all exposures to the rubella virus. This means NOT getting the MMR vaccine during pregnancy. It also means that anyone who is pregnant and not already vaccinated against rubella should not travel to countries with rubella or areas with known rubella outbreaks. This is especially true during the first 20 weeks of pregnancy when the risk for a miscarriage or severe birth defects from rubella virus infection is greatest. Any pregnant person not already vaccinated against rubella should get the MMR vaccine immediately after the pregnancy.
Avoid getting pregnant for at least 4 weeks after receiving the MMR vaccine.
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* CDC Yellow Book: [Rubella](/travel/yellowbook/2020/travel-related-infectious-diseases/rubella)
* [Rubella](http://www.cdc.gov/rubella/)
| None | None |
78c6ddf16720a812e4375f5d3219f5a3f648733a | cdc | Scabies | Scabies | Disease Directory | Travelers' Health | CDC
### What is scabies?
Scabies is a skin condition in people caused by the human itch mite. The mite burrows into the upper layer of skin to live and lay eggs.
Common scabies symptoms include intense itching and a skin rash. Scabies can occur anywhere on the body but are more common on the following parts of the body:
- Between the fingers
- Genitals (Penis and Vagina)
- Shoulder blades
Children are often more likely to get scabies. For babies and very young children scabies is often found on the head, face, neck, palms, and soles of the feet.
For people who have never had scabies before, symptoms usually take 4-6 weeks to appear. Symptoms appear more quickly in people who have had scabies before, in as few as 1 to 4 days. Scabies mites can spread to other parts of the body and from one person to another person even before symptoms start.
The same mite that causes scabies also causes crusted scabies. Crusted scabies is severe scabies that happens in people who have weakened immune systems. People with crusted scabies are infested with very large numbers of mites. This increases their risk of spreading mites to others, either from brief skin-to-skin contact or from contact with items such as bedding, clothing, furniture, rugs, and carpeting.
### Who is at risk?
Scabies is found worldwide and can spread rapidly under crowded conditions where close skin-to-skin contact is frequent. Child-care facilities, nursing homes, extended-care facilities, and prisons are often sites of scabies outbreaks. Scabies is more common in long-term travelers than in those who travel for less than 8 weeks at a time.
Animals do not have scabies and cannot spread scabies to people.
### What can travelers do to prevent scabies?
There is no vaccine or medicine to prevent scabies. Effective medicine to treat scabies is only available with a doctor's prescription.
Travelers can avoid scabies by not touching or having close skin-to-skin contact with a person who has a rash or who is itching. Avoid touching or handling a sick person’s clothing or bedding.
Scabies mites die when you wash bedding and clothing using hot water and hot dryer cycles or dry-clean the items. Items that cannot be dry-cleaned or laundered can be disinfested by storing them in a closed plastic bag for more than 72 hours. Scabies mites generally do not survive more than 2 to 3 days away from human skin.
|
### Scabies
### What is scabies?
Scabies is a skin condition in people caused by the human itch mite. The mite burrows into the upper layer of skin to live and lay eggs.
Common scabies symptoms include intense itching and a skin rash. Scabies can occur anywhere on the body but are more common on the following parts of the body:
* Between the fingers
* Wrist
* Elbow
* Armpit
* Genitals (Penis and Vagina)
* Nipple
* Waist
* Buttocks
* Shoulder blades
Children are often more likely to get scabies. For babies and very young children scabies is often found on the head, face, neck, palms, and soles of the feet.
For people who have never had scabies before, symptoms usually take 4-6 weeks to appear. Symptoms appear more quickly in people who have had scabies before, in as few as 1 to 4 days. Scabies mites can spread to other parts of the body and from one person to another person even before symptoms start.
The same mite that causes scabies also causes crusted scabies. Crusted scabies is severe scabies that happens in people who have weakened immune systems. People with crusted scabies are infested with very large numbers of mites. This increases their risk of spreading mites to others, either from brief skin-to-skin contact or from contact with items such as bedding, clothing, furniture, rugs, and carpeting.
### Who is at risk?
Scabies is found worldwide and can spread rapidly under crowded conditions where close skin-to-skin contact is frequent. Child-care facilities, nursing homes, extended-care facilities, and prisons are often sites of scabies outbreaks. Scabies is more common in long-term travelers than in those who travel for less than 8 weeks at a time.
Animals do not have scabies and cannot spread scabies to people.
### What can travelers do to prevent scabies?
There is no vaccine or medicine to prevent scabies. Effective medicine to treat scabies is only available with a doctor's prescription.
Travelers can avoid scabies by not touching or having close skin-to-skin contact with a person who has a rash or who is itching. Avoid touching or handling a sick person’s clothing or bedding.
Scabies mites die when you wash bedding and clothing using hot water and hot dryer cycles or dry-clean the items. Items that cannot be dry-cleaned or laundered can be disinfested by storing them in a closed plastic bag for more than 72 hours. Scabies mites generally do not survive more than 2 to 3 days away from human skin.
### After Travel

**If you traveled and feel sick,** particularly if you have a fever, talk to a healthcare provider and tell them about your travel.
If you need medical care abroad, see [Getting Health Care During Travel](/travel/page/getting-health-care-abroad).
### More Information
* [Scabies](http://www.cdc.gov/parasites/scabies/)
* [Scabies FAQs](http://www.cdc.gov/parasites/scabies/gen_info/faqs.html)
* CDC Yellow Book: [Scabies](/travel/yellowbook/2012/chapter-3-infectious-diseases-related-to-travel/scabies-sarcoptic-itch-sarcoptic-acariasis.htm)
* [Scabies Treatment](http://www.cdc.gov/parasites/scabies/treatment.html)
| None | None |
Subsets and Splits